Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 14/185/13. The contractual start date was in May 2016. The final report began editorial review in December 2018 and was accepted for publication in May 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Peymane Adab reports grants from the National Institute for Health Research (NIHR), Birmingham City Council and Zhejiang Yongning Pharmaceutical Co. Ltd (Taizhou, China) during the conduct of the study, and is a member of the NIHR Public Health Research (PHR) funding committee. Clare Collins reports being involved in the development of the original Healthy Dads, Healthy Kids (HDHK) intervention and previous evaluations. Furthermore, she is supported by an Australian National Health and Medical Research Council Senior Research Fellowship and a Faculty of Health and Medicine Gladys M Brawn Senior Research Fellowship at the University of Newcastle. Amanda Daley reports being a member of the NIHR Health Technology Assessment (HTA) Clinical Trials Committee, from July 2014 to July 2015. Emma Frew reports grants from NIHR and Birmingham City Council, outside the submitted work. Kate Jolly reports grants from NIHR and funding for the intervention from local authorities in the West Midlands and the South West during the conduct of the study; she is part funded by the NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRC) West Midlands and is a subpanel chairperson of the NIHR Programme Grants for Applied Research panel. Laura Jones reports grants from the NIHR PHR programme during the conduct of the study and personal fees from North 51Bionical (Willington, UK), outside the submitted work. Miranda Pallan reports grants from NIHR during the conduct of the study for HTA 12/137/05: cultural adaptation of an existing children’s weight management programme: the Child weigHt mANaGement for Ethnically diverse communities (CHANGE) intervention and feasibility randomised controlled trial. Philip Morgan reports that he developed the Healthy Dads, Healthy Kids programme.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Jolly et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
The epidemiology of overweight and obesity in men
Overweight and obesity are major public health challenges. Obesity is associated with an increased risk of diseases including type 2 diabetes mellitus, cardiovascular disease, cancers (e.g. of the colon) and osteoarthritis. 1 It is also associated with higher rates of depression. 2 For each increase in body mass index (BMI) of 5 kg/m2, mortality increases by 30% and median survival reduces by 2–4 years for people with a BMI of 30–35 kg/m2 compared with those with a BMI of 22.5–25 kg/m2. 3 Owing to its associations with many long-term medical conditions, the cost of obesity is high. Public Health England estimated that obesity cost the NHS in England £6.1B in the year 2014–15 and the wider costs to society were estimated at £27B. 4
Men are at a higher risk of overweight and obesity than women. 5 Inequalities are evident, with a higher proportion of men in the lowest income quintile having a very raised waist circumference (> 102 cm) (38%, vs. 32% in the highest income quintile), which puts them at high risk of the long-term conditions associated with obesity. 6 In addition, compared with white Europeans, people of South Asian ethnicity living in England tend to have a higher percentage of body fat at the same BMI and more features of the metabolic syndrome at the same waist circumference. 7 The proportion of men who want to lose weight varies by age group, with the highest proportions among those aged 35–44 years (46%) compared with 39% of those aged 25–34 years and 44% of those aged 54–64 years. 6 Entrance into fatherhood is associated with an increase in BMI trajectory for both fathers who reside and fathers who do not reside with their children. 8 In the 2016 Health Survey for England,6 39% of men reported using some form of weight management aid: the most popular were gyms or another form of exercise (31%), 7% used websites or mobile phone applications, 6% used activity trackers or fitness monitors and only 2% attended dieting clubs. 6
In terms of dietary behaviours, men and women have suboptimal diets for long-term health. 9 Only 24% of men in England report eating at least the recommended five portions of fruit and vegetables each day5 and only 13% of men aged 19–64 years consume below the recommended amount of free sugars. 9
In conjunction with the high rates of overweight and obesity and poor dietary practices, men have become less physically active. Although 66% of men self-report meeting the UK government guidelines10 of achieving at least 150 minutes of moderate physical activity or 75 minutes of vigorous activity per week,11 objective measurement shows this to be an overestimate. 12 The most recent comparison of population-based objective measurement of physical activity by the Health Survey for England was in 2008,13 which found that only 5% of men aged 35–64 years achieved the recommended activity level. Overall, 26% of men in England are classified as inactive, namely undertaking < 30 minutes of physical activity each week. 11 People from Asian, black and Chinese ethnic groups were more likely to be inactive than those from white or mixed ethnic groups. 14 After having children, men’s physical activity levels generally reduce. 15–17
Evidence of the effectiveness of weight management programmes for men
In a series of systematic reviews, Robertson and colleagues collated the evidence for the management of obesity in men. 18 Fewer men than women joined weight management programmes, but, once they joined, they had higher retention rates and a similar or greater percentage weight loss than women. A meta-analysis of male-only weight loss interventions revealed a clinically significant difference in weight change favouring interventions over no-intervention controls at the last reported assessment [–5.66 kg, 95% confidence interval (CI) –6.35 to –4.97 kg]. 19 Successful men-only weight loss programmes have been run in football clubs20 and workplaces,21 tapping into a shared identity associated with their club or workplace. 18
Robertson et al.’s18 reviews identified no eligible studies that looked at how to increase the engagement of men in weight management interventions. However, many men said that a health concern motivated them to lose weight, rather than a concern about their appearance. 18 A qualitative synthesis of 22 studies18 identified that men felt an individual responsibility for their weight gain, and that men from socioeconomically disadvantaged communities were often constrained by economic circumstances from healthy eating and exercise. To date, few studies have explored the beliefs of men from minority ethnic groups in the UK. 22 The qualitative review18 also identified the features associated with successful weight loss programmes in men. These included group-based programmes and social support, promoting engagement with the use of humour, accountability and adherence, and goal setting. 18 Men also valued a personalised approach that took account of their individual needs, and individual tailoring of advice assisted weight loss.
The epidemiology of overweight and obesity and physical activity in children
Overweight and obesity in children (aged 2–15 years) has generally increased since the 1990s, with a rise from 1995 to 2005, but an overall levelling off in recent years, with a childhood obesity prevalence of 16% in 2016. 5 However, underlying this is a widening trend in inequalities, with overweight and obesity prevalence continuing to increase in more socioeconomically deprived communities. In 2017–18, 9.5% of children aged 4 or 5 years in England were classified as obese, with a further 12.8% classified as overweight. 23 The prevalence of overweight and obesity increases during the primary school years, with 20.1% of children aged 10 or 11 years classified as obese and a further 14.2% classified as overweight. 23 Ethnic differences in the prevalence of obesity have been shown in children aged 10 or 11 years, with 29.0% of black Caribbean and African children and 24.8% of South Asian children (originating from the Indian subcontinent) living with obesity, compared with 18.4% of white British children. There are socioeconomic differences in childhood obesity, with prevalence in the most socioeconomically deprived areas double that of the least deprived areas for children aged 4 or 5 years (5.7% of children in the least deprived decile were obese, compared with 12.8% of those in the most deprived decile) and 10 or 11 years (11.7% in the least deprived decile vs. 26.8% in the most deprived decile). 23
Engaging in adequate levels of physical activity is important for children in the short, medium and long term. 24 Apart from the increased risk of obesity with physical inactivity, there are many other negative physical and mental health consequences. 25,26 Active children are less likely to suffer the adverse health consequences of physical inactivity in adulthood, as habits formed in childhood track forward into adulthood. 26 In children, physical activity is essential for motor development, cognitive improvement, psychosocial health and cardiometabolic health; physical activity reduces body fat and can increase academic achievement. 25
Current UK recommendations27 for physical activity in children aged ≥ 5 years are that they should be at least moderately active for a minimum of 60 minutes every day. This is the minimum level, and there is a recommendation that children should engage in moderate to vigorous physical activity for up to several hours each day. It is also recommended that vigorous intensity activity, including muscle- and bone-strengthening activities, should be undertaken at least 3 days each week. 27
However, national objectively measured data using accelerometry shows that, in 2008, the proportion of boys and girls classified as meeting the minimum recommendations27 were 33% and 21%, respectively. 13 In children aged 4–10 years, 51% of boys and 34% of girls met the recommendations, compared with 7% of boys and no girls aged 11–15 years. Data from England’s 2016 Report Card on Physical Activity28 suggest that overall physical activity levels in children and young people has declined. Recent objective data on children’s physical activity come from regional studies. 29 A study from Bristol reported that boys and girls aged 5 or 6 years undertook a mean of 72.4 [standard deviation (SD) 20.7] and 62.3 (SD 16.2) minutes, respectively, of physical activity daily, and that there was a decrease in physical activity and increase in sedentary time in boys and girls between the ages of 5 or 6 and 8 or 9 years. 30 This demonstrates the importance of strategies to encourage and promote physical activity into later childhood and beyond.
Family physical activity and eating behaviours
Parental support, direct help from parents, support from significant others and perceived and actual physical competence have been shown to be positively associated with children’s physical activity levels, although the association with parental physical activity is inconsistent. 31 Promising strategies to involve parents in interventions to increase their children’s physical activity include engaging family members in a family physical activity programme, parent training, family counselling or preventative messages during family visits. 32 A systematic review of interventions to promote physical activity in children highlighted the limited evidence of the effect of interventions targeting low socioeconomic populations and interventions aimed at the home environment. 33
Family eating practices are associated with child eating behaviours. 34 Eating meals together as a family, parents role modelling healthy eating behaviours and having healthy foods available in the home have been shown to be positively related to the eating habits of children. 35–39 In addition, parents who have an involved and caring parenting style rather than a controlling style have children who eat healthier diets. 40,41 UK evidence from the National Diet and Nutrition Survey shows that whether or not families eat together is influenced by parents’ work schedules, children’s age and appetite for earlier eating than their parents, their child-care regimes, their extracurricular activities and the problem of co-ordinating different food preferences and tastes. 42
The health inequalities in obesity experienced by people from minority ethnic groups is likely to be, in part, affected by different dietary practices and beliefs about physical activity. 43,44 However, food practices of minority ethnic groups are heterogeneous and, although affected by ethnic background, they are also affected by age, religion, socioeconomic circumstances, geographical area and generation. 43 Factors that influence food practices in minority ethnic groups include sociocultural norms and affordability and accessibility of food; these need to be seen in the context of poverty and there have been calls for culturally sensitive interventions that build on positive food practices and adopt a family- and community-centred approach. 43 A systematic review44 of qualitative literature relating to the health beliefs of British South Asians on lifestyle diseases highlights the primacy of social and cultural norms over an individualised approach to lifestyle change, and many barriers to physical activity and exercise.
The Healthy Dads, Healthy Kids intervention
The Healthy Dads, Healthy Kids (HDHK) programme was developed by a team of researchers in Australia, including some of authors of this report (PM, CC and MY), and was established to address weight management in fathers, but in the context of their families, such that changes in their health behaviours would positively affect their children. A highly novel aspect to the intervention was that children also play a major role in motivating and helping their father to maintain his behaviour change.
The HDHK programme has been rigorously evaluated in two randomised controlled trials (RCTs) in Australia. 45,46 In the community RCT with trained facilitators in disadvantaged areas, the authors reported a mean difference in weight of the fathers of 3.4 kg (95% CI 2.1 to 4.7 kg) in favour of the intervention at 14 weeks, compared with a wait-list control. They also observed significant group-by-time reductions in children’s BMI z-scores (–0.10, 95% CI –0.21 to 0.00), physical activity levels and diet quality, favouring the intervention group. 45 A larger-scale community roll-out has demonstrated clinically meaningful weight loss sustained to 1 year in fathers (3.8 kg loss; 95% CI 3.1 to 4.6 kg), and a significant mean reduction in BMI z-scores (–0.12, 95% CI –0.17 to –0.07) in children. 47 Positive effects reported via qualitative research were improved family relationships and involvement of the fathers and children in joint activities. 47 In additional, the quantitative findings showed that participation in the HDHK programme positively affected fathers’ co-physical activity with their child and beliefs about healthy eating, which mediated changes in children’s diet and physical activity behaviours. 48 Although the intervention has been evaluated in Australia, its transferability to a multiethnic UK setting needs to be tested.
The existing Healthy Dads, Healthy Kids programme
Since the initial evaluation of the Australian HDHK programme, it has undergone a number of iterations, with changes to the number of sessions and the inclusion of mothers. At the time of commencing HDHK-UK, it had a format of nine sessions of 90 minutes’ duration, delivered at weekly intervals. Mothers/partners were invited to attend two sessions, fathers attended all nine and the children attended seven. In the joint sessions, the children and fathers separated for 20–25 minutes for a discussion session followed by a 1-hour joint physical activity session. The physical activity session aimed to be interactive, highly active and fun, focusing on elements associated with optimal child development outcomes across physical, cognitive and social–emotional domains. This included fundamental movement skills, health-related fitness-based activities and rough-and-tumble play.
The HDHK programme is based on social cognitive theory (SCT)49 and family systems theory (FST). 50 SCT constructs targeted in the HDHK programme are self-efficacy, goals/intention, outcome expectations, perceived facilitators of and barriers to changes, and social support. 49 The FST postulates a framework of reciprocal relationships between family members. 50 Thus, when a father changes his dietary behaviours and physical activity levels, this will be reflected in his child’s behaviour and the child will help to sustain their father’s behaviour change. 51
The HDHK programme aims to provide fathers with the knowledge and skills for long-term behaviour change. It teaches fathers about the importance of engaging with their children and uses healthy eating and physical activity as media to engage fathers with their children. The children’s engagement and enthusiasm for the HDHK programme’s father–child activity aims to reinforce the change in family lifestyle. During the programme, fathers come to understand the profound influence that their parenting, actions, behaviours and attitudes have on their children; this realisation becomes a driving force behind their motivation to get fit and become more engaged in their children’s lives.
The individual session content is summarised in Box 1. Resources include handbooks for fathers and children; a logbook for dads; and a website for self-monitoring, with an instruction guide for use.
Highlights the unique influence of dads in contributing to the physical and mental health of children.
Weight management for menExplores the challenges of healthy eating in the modern world, outlines the mathematics of weight loss and sets SMART goals to achieve activity and dietary ambitions.
Healthy eating for familiesProvides advice on appropriate portion sizes for the whole family, and discusses strategies for implementing the trust paradigm to encourage their children to eat healthily at home.
Being a healthy dad: strategies to enhance you and your family’s lifeHighlights the eight weight loss tips for men, tells dads how to ‘stay on track’ and provides advice on sustainable approaches to weight loss.
The unique and powerful influence of fathersExplains to dads why they have such a powerful influence over their children and the importance of being a good role model, and outlines the most effective parenting style.
Raising active kids in an inactive worldExplains the growing issues of childhood obesity and why physical activity is so important for children; highlights key strategies for dads to be physical activity leaders.
‘Switching on’ your child’s mind by ‘switching off’Highlights the physical and mental health issues created by excessive screen time and provides strategies for ‘switching off’.
‘Healthy’ fathering in a busy worldEncourages discussion of barriers to achieving SMART goals, and solutions for those barriers; highlights opportunities to create family traditions and maximise the time dads can spend with their children.
Continuing the ‘healthy dad’ journeyReviews the key messages of the programme, provides tips for staying on track after the programme, awards children with their certificates and awards dads with a card.
Children’s sessions Rough-and-tumble funChildren learn about their mission to ‘get dad fit and healthy’ and are taught about rough-and-tumble activities.
Turning dad into a healthy eaterThrough fun activities, children learn about ‘sometimes’ foods and ‘any time’ foods and how they can encourage dad to eat more healthily.
The Healthy Dads, Healthy Kids rainbow plateThrough fun activities, children learn about different fruits and vegetables and are challenged to make their plates ‘rainbows’ with a variety of healthy fruits and vegetables.
Quality time with dadChildren are given activities to help them think about games they can play with dad to spend quality time together.
Helping dad ‘switch off’Children think about activities they could enjoy with dad instead of playing on the computer or watching television.
Becoming dad’s personal trainerChildren develop an activity board with games and exercises the family can complete at home.
Helping dad stay on trackChildren review the programme and receive their HDHK certificate for achieving their mission to get dad fit and healthy. Dads receive a card from their children for their commitment to the programme.
SMART, specific, measurable, achievable, relevant, time-bound.
Rationale for the Healthy Dads, Healthy Kids UK study
This study addressed a commissioned call from the National Institute for Health Research (NIHR) Public Health Research programme for research on weight loss services for men. The recruitment of fathers with their children, and the involvement of mothers/partners in the intervention, meant that meaningful health gains were possible for the whole family. There was the potential for sustained behaviour change as a result of family behaviour change, which would help to break the cycle of intergenerational obesity.
A patient and public involvement (PPI) group was consulted in the development of the research proposal and, through this group and the research team, it was identified that there would be a need to adapt the Australian version of the HDHK programme.
As a result of changes in migration patterns over the previous 20 years, urban populations, such as that of the West Midlands, have become more complex and ‘superdiverse’. Superdiversity is characterised by overlapping variables including country of origin, ethnicity, language, religion, regional/local identities, migration history and experience (influenced by sex, age, education, specific social networks and economic factors) and immigration status (encompassing a variety of entitlements and restrictions). 52,53 Such complexity in the population has created unique challenges with regard to how we identify and respond to the health needs of all members of a superdiverse society.
Cultural adaptations have been described by Resnicow et al. 54 with regard to different dimensions of cultural sensitivity: surface and deep structure. An intervention that addresses surface-structure adaptations would match intervention materials or messages to ‘fit’ within a specified culture – be it by matching on language, food, music or location, and including items of familiarity to the target population to help them engage with the intervention. Deep-structure adaptations would address the core cultural values or ethnic, cultural, historical, social or environmental factors that may influence specific health behaviours. 54
In relation to the delivery of the HDHK programme, a number of issues to be addressed in the adaptations were known to the research team from the outset, namely awareness of certain cultural barriers to engagement with behaviour change activities in some black, Asian and minority ethnic (BAME) groups. For example, participation in sports and physical activity outside the home may be discouraged among girls, and cultural dress codes can restrict physical activity.
In addition, the Australian programme was predominantly delivered by teachers, and this model was considered unlikely to be replicable in the UK owing to different incentives to deliver after-school activities in the two countries. In the Australian studies, the HDHK programme was delivered mainly in schools, often by a physical education teacher who was able to use the initial training towards their continuing professional development requirement. Our experience of working with UK schools suggested that teachers are overburdened and schools are regularly approached to take part in projects and initiatives. 55 There are similarities between Australia and the UK in the proportion of men who are overweight or living with obesity. 5,56 Australian guidance for adult fruit and vegetable intake is five or six portions each day, whereas the UK’s guidance is five portions. 57 About one in four men in the UK report adequate fruit and vegetable consumption,58 but < 5% of Australian men have an adequate intake. 59 Australian guidelines also separate fruit and vegetable portions, unlike the UK. 57 Guidance in relation to alcohol consumption is similar. Given these relatively modest differences, we considered that the intervention should be transferable with some adaptions.
However, it was also agreed that, as part of the study, cultural adaptation would need to be informed by the community and that changes would need to be made before implementing the HDHK programme in the UK setting.
Potential benefits of the adapted Healthy Dads, Health Kids UK programme
The potential benefits to the men of the adapted HDHK-UK programme are weight loss, improved physical activity levels and improved diet quality, which can result in a reduction in risk for a wide range of health conditions including type 2 diabetes mellitus, cardiovascular disease, certain cancers, arthritis and other musculoskeletal symptoms. 60 Increased physical activity is also associated with mental well-being61 and joint activities with their children may result in closer relationships and bonding. 62 For the children, there are the benefits of healthier eating patterns and increased physical activity, resulting in a lowered risk of developing obesity,63 potentially improved attention and outcomes at school,64 improved social–emotional well-being and a shared activity with their father potentially leading to a closer relationship. 65
Chapter 2 Overview of study design and aims and objectives
Study aims
The overall aim of HDHK-UK study was to modify an existing weight management and healthy lifestyle programme for fathers and their children (aged 5–11 years) to be culturally acceptable in a UK multiethnic population and to assess the feasibility of conducting a RCT. The study was delivered in two phases.
Phase 1: adaptation of the existing programme
The aim of phase 1 was to modify an existing weight management and healthy lifestyle programme for fathers and their primary school-aged children45,46 so that it is culturally acceptable in a multiethnic population in the UK. The cultural adaptation (phase 1a) drew on the findings of qualitative interviews and focus groups from an ethnically diverse population in areas of socioeconomic disadvantage, as well as findings from a study that was culturally adapting a weight management programme for children in the same population. 53 The specific objectives for phase 1a were to:
-
explore the cultural (ethnic, religious and socioeconomic) acceptability of the programme elements and proposed questionnaires with fathers from a range of ethnic, religious and socioeconomic groups
-
increase the cultural acceptability of the programme using theoretically informed adaptations so that it is acceptable and accessible to a UK population with ethnic, religious and socioeconomic diversity.
In phase 1b, an uncontrolled feasibility trial was undertaken at two sites to explore the acceptability of the adapted programme and research methods. The specific objectives for phase 1b were to assess the:
-
feasibility of delivering the adapted intervention and the feasibility of recruitment and follow-up
-
acceptability of the HDHK-UK programme in an ethnically diverse population and make refinements to the programme based on the facilitators’ and participants’ feedback.
Phase 2: feasibility randomised controlled trial
The aim of phase 2 was to assess the feasibility of delivering the adapted intervention, the feasibility of recruitment and follow-up and the feasibility of a future definitive RCT. This was achieved using a two-arm RCT. Participants were randomised to the intervention or control arm in a ratio of 2 : 1, respectively. Data were collected from participants [fathers and their child(ren)] at baseline and at 3 and 6 months from the start of the intervention. Qualitative methods were also used as part of the evaluation. The specific objectives were to:
-
assess the acceptability of a UK-adapted weight management and healthy lifestyle programme for overweight/obese fathers of primary school-aged children in an ethnically diverse population and make refinements to the programme based on facilitator and participant feedback
-
determine levels of adherence to the programme
-
assess fidelity of intervention delivery and feedback from facilitators and modify the facilitator training programme if required
-
assess whether or not participants are willing to be randomised
-
assess whether or not the expected recruitment rate for a subsequent full-scale RCT is feasible and to identify successful recruitment strategies
-
explore the ability to obtain educational attainment data for children
-
explore participants’ and facilitators’ perceptions of the intervention, trial participation and processes
-
provide estimates of the variability in the primary outcome
-
test the components of the proposed RCT to determine the feasibility of the protocol.
Study partners
The feasibility study had two key study partners that were closely involved in the set-up and delivery of the trial.
University of Newcastle, NSW, Australia
Ranked in the top 1% of universities worldwide, the University of Newcastle (UoN) is a leading global institution that is distinguished by a commitment to equity and excellence.
Professor Philip Morgan is co-director of the Priority Research Centre for Physical Activity and Nutrition (PRC-PAN) at UoN, theme leader of the obesity research programme and founder of the original HDHK programme. The PRC-PAN investigates physical activity and nutrition for population health across the lifespan, with a particular emphasis on education and health promotion strategies for chronic disease prevention, treatment and well-being. Professor Morgan delivered training to the Fatherhood Institute, which later trained the HDHK programme facilitators. He also reviewed the UK cultural adaptations to the HDHK programme, ensuring that changes were in keeping with the original programme, and contributed to the intervention implementation, evaluation and research output.
Professor Clare Collins is co-director of UoN’s PRC-PAN, theme leader of the Nutrition and Dietetics research programme and a senior research fellow. In this study, Professor Collins advised on nutrition assessment and reviewed programme cultural adaptations to nutrition and dietary elements, ensuring consistency with the original programme.
Dr Myles Young is a post-doctoral researcher at UoN’s PRC-PAN who assisted on the original HDHK intervention. Dr Young assisted with training of the Fatherhood Institute, advised on practical aspects of the intervention implementation and contributed to research output.
The UoN team also provided support through the provision of resources and advice on all aspects of the trial, including recruitment, training, implementation and evaluation, for the duration of the project.
The Fatherhood Institute
The Fatherhood Institute (registered charity number 1075104) is a world leader in research, policy and practice with fathers. Activities include collating, undertaking and publicising research; lobbying for policy changes; and training and supporting public services, employers and others to approach families in a more father-inclusive manner. The Fatherhood Institute also works directly with fathers, mothers and children in a range of settings, including in health, education, the community and workplaces. The Fatherhood Institute’s mission is to give all children a strong and positive relationship with their father and any father figures, to support both mothers and fathers as earners and carers, and to prepare boys and girls for a future shared role in caring for children.
The Fatherhood Institute supported the adaptation of the HDHK programme materials to make them suitable for a UK audience and contributed to the father research materials. They also developed and delivered a number of training sessions for HDHK-UK facilitators. Report author Adrienne Burgess (Joint Chief Executive and Head of Research) was a member of the Study Management Group (SMG).
Study management
The study was overseen by two groups: the Study Steering Committee (SSC) and the SMG.
Study Steering Committee
The SSC included three independent academic members and an independent lay member. The committee convened at regular intervals throughout the study (October 2016, April and November 2017 and May and November 2018). The SSC monitored progress, recommended and agreed changes to protocol and monitored safety.
Study Management Group
The SMG consisted of the study co-investigators and research staff and met to oversee the research, to interpret findings and to agree the dissemination strategy. The SMG met at regular intervals (February and November 2016, April and October 2017 and March and September 2018).
Patient and public involvement
Patient and public involvement was integrated throughout the study and is described in detail in Chapter 7. The aim of PPI in the HDHK-UK study was to gain insight from fathers and their partners from the diverse communities where the study was to take place into issues that might affect the uptake and acceptability of the HDHK programme, methods of communication with fathers, participant-facing documents, data collection and how we might address the issue of an eligibility criterion of being ‘overweight or obese’. The PPI group was brought together by the Fatherhood Institute in one of the localities (site A) where the HDHK study was planned to take place. The first meeting took place during the development of the research proposal and seven fathers from diverse ethnic backgrounds were asked to comment on key features of the proposed protocol. This group agreed to support the study if funded. A male lay representative (AE) was invited to comment on the Plain English summary and was invited to be a member of the SMG. One male lay representative was recruited to be an independent member of the SSC.
Funding, ethics approval and study registration
Study funding was granted in October 2015 by the NIHR Public Health Research programme (reference number 14/185/13). The randomised trial was registered with the International Standard Randomised Controlled Trial Number (ISRCTN) registry January 2017.
Ethics approval for the two phases of the study was obtained from The University of Birmingham Science, Technology, Engineering and Mathematics Ethics Review Committee. Phase 1a was approved on 22 April 2016 (ethics reference number ERN_15–1287), phases 1b and 2 were approved on 16 January 2017 (ethics reference number ERN_16–1323). A number of amendments were submitted for review throughout the study, as detailed in Appendix 1. Important changes to the original protocol were (1) the widening of the eligibility criteria for phases 1b and 2 to include men categorised as overweight or with a waist circumference of ≥ 94 cm, (2) the inclusion of the Strengths and Difficulties Questionnaire at follow-up for phase 2 and (3) stratification of the randomisation.
Chapter 3 Phase 1a: cultural adaptation methods and results
This phase of the study addressed the development stage of the UK Medical Research Council framework for the development and evaluation of complex health interventions. 66 Information from three main sources was used in the adaptation process:
-
data from a qualitative study with fathers and other family members from a range of ethnic, religious and socioeconomic groups
-
findings emerging from another NIHR-funded family-based weight management study designed for BAME communities in the UK, called CHild weight mAnaGement for Ethnically diverse communities (CHANGE),53 targeted at Bangladeshi and Pakistani children and their families, which was led by members of the HDHK-UK research team (MP and PA)
-
findings from the Dads And Daughters Exercising and Empowered (DADEE) programme67 for fathers and daughters, developed by the Australian HDHK team.
Qualitative study methods
Qualitative data collection with fathers and other family members
The qualitative study addressed the first of our aims, which was to explore the cultural acceptability of the programme elements and proposed questionnaires with fathers and other family members from a range of ethnic, religious and socioeconomic groups through qualitative interviews and focus groups.
We aimed to conduct up to five focus groups and 15 one-to-one interviews; focus groups were the preferred method of data collection as they use group interaction as a way to stimulate discussion. 68 However, individual interviews were also offered as a way to maximise participation.
Theoretical underpinning
We used Liu et al. ’s69 typology of cultural adaptations to make the programme culturally responsive and appropriate for multiethnic populations living in socioeconomically disadvantaged communities. The typology was the result of a comprehensive study69 that explored the adaptation of health promotion programmes that targeted diet, physical activity and smoking for minority ethnic groups. As part of this work, Liu et al. 69 undertook a systematic review of health promotion programmes that had been adapted for minority ethnic groups and included international literature, from which they developed a 46-item typology. Liu et al. 69 also highlighted the importance of taking a systematic approach to cultural adaptation and recommended that a generic theory of the health promotion cycle be used alongside the typology when adapting health promotion interventions. This programme cycle has eight stages: conception/planning, promotion, recruitment, implementation, retention, evaluation, outcome and dissemination. We started by considering each of the items in the typology, at which stage of the programme theory it might apply and how it might be relevant to our cultural adaptation. It was clear that the adaptations would apply both to the content and delivery of the intervention and to the research processes (see Appendix 2). The findings were used to inform the development of the topic guide for qualitative interviews and it supported the analysis of our qualitative interviews and focus groups (see Data analysis).
Finally, we used individual items in the typology to consider what adaptations to the intervention and to the research processes could and should be made, drawing on the findings from the qualitative interviews/focus groups, the findings from the CHANGE study70 and insights from the Australian HDHK programme team from the DADEE study. 67
Setting/context
Phase 1a was undertaken in three urban local authority areas in the West Midlands, UK. In these local authority areas, a high proportion of the populations are from BAME communities (32–48%) and > 50% live in the 20% most deprived neighbourhoods (lower-layer super output areas) in England; deprivation is measured by the Index of Multiple Deprivation (IMD). 71 The West Midlands has the highest proportion of children aged < 16 years of all the English regions. 72
Inclusion/exclusion criteria
People were eligible to take part in phase 1a if they were a father/male guardian or family member from the Bangladeshi and Pakistani communities or from socioeconomically deprived communities (e.g. white British, African Caribbean and other ethnic groups). The focus on Bangladeshi/Pakistani ethnic groups was due to the particularly high rates of obesity in the adults and children from these communities,73 together with low attendance of members of these ethnic groups at weight management programmes for adults and children. 53
Sampling and recruitment
We used a purposeful sampling approach based on maximum variation. 74,75 The HDHK-UK intervention was to be evaluated in men with children of primary school age. Therefore, our intention was to recruit fathers and male guardians of primary school-aged children to phase 1a, as well as other family members who may act as gatekeepers to fathers/male guardians, namely mothers/significant female others (e.g. grandmothers). In relation to our recruitment strategies, we targeted socioeconomically disadvantaged locations and sampling was undertaken to include a range of ethnicities.
Multiple pathways were employed to identify suitable participants to take part and share their views in qualitative interviews or focus groups. We aimed to identify participants through community networks, including primary schools, and gatekeepers in local communities who acted as advocates on behalf of the research team. We approached a range of organisations for permission to canvas parents at their facilities or at the activities they ran. The following is a summary of the organisations approached and how the HDHK study was advertised via that organisation:
-
primary schools across the West Midlands – mail-out to pupils, canvassing parents at school gates during pick-up/drop-off, promotion via school media (website, text messages to parents)
-
after-school/youth organisations – approaching parents at after-school clubs and martial arts groups during pick-up/drop-off, and working with local Scouts organisations (district and local leaders were to identify interested parents)
-
parent and child classes – local child and parent groups at Sure Start centres
-
leisure and well-being centres – canvassing parents after popular child activity classes, for example swimming
-
charities and volunteer services – advertising the study on the Birmingham Volunteer Services website/e-newsletter sent to all members
-
research advocates in business districts – identifying prominent business people located in multiethnic business districts to approach customers on the research team’s behalf to share information about the study
-
contacts of the research team – e-mails to staff at the University of Birmingham.
At first approach, potential participants were given an invitation letter with details of how to contact the research team. People who expressed an interest in taking part in phase 1a were then sent a participant information leaflet and a time was booked for the interview/focus group.
Data collection
We conducted 18 one-to-one interviews with 14 fathers, two grandfathers and one mother, one paired interview with a couple (father and mother) and two focus groups consisting of 10 mothers overall. Overall, 30 participants took part. Eighteen interviews and one focus group were conducted in English, and one interview and one focus group were conducted in Urdu. Data collection was stopped when no new core themes were interpreted from the data. However, owing to difficulties in recruiting Bangladeshi and Pakistani fathers, we did not achieve saturation in the different ethnic groups.
All interviews were completed by Manbinder Sidhu (a male qualitative researcher in applied health sciences); focus groups and a single interview were completed in conjunction with a female qualitative researcher (Farina Kokab) from a South Asian background with the necessary language skills (Urdu). Prior to the start of each interview or focus group, participants were asked to provide written informed consent and complete a short demographic questionnaire to facilitate description of the sample. Participants were informed of their right to withdraw from the study at any time (although any data collected prior to withdrawal would be used in our analysis) and were assured that their personal details would be kept confidential.
We developed topic guides for the focus groups and interviews, which were informed by the typology of cultural adaptation,69 literature on facilitators of and potential barriers to men and children to attending weight management programmes, and discussions between the research team and PPI group. In addition, there was iterative development of topic guides, as certain topics that arose in earlier interviews were explored in greater depth in later interviews (i.e. gender considerations in an ethnocultural context).
The objectives of the interviews and focus groups were to explore a range of issues including but not limited to:
-
family- and community-embedded attitudes towards group participation in a physical activity programme with members from outside and within their own community
-
the cultural acceptability of girls and their fathers partaking in ‘rough and tumble’ and other physical activities together
-
acceptable locations and timing of sessions
-
any cultural issues related to fathers being more involved in food preparation
-
how fathers would like to be invited to take part, including the ‘hook’ that would encourage them to take part (e.g. personal weight loss, health, role modelling to improve children’s health, time with children)
-
any potential barriers to changes in diet and physical activity.
Our approach to interviewing, facilitating group discussions, topic guides and participant-facing material was developed with input from the study PPI group. Specifically, this group commented on the wording on the invitation flyers and raised issues about the HDHK programme and resources. We explored these issues further in the interviews and focus group discussions.
To provide context and facilitate discussions with our participants, we shared original resources from the intervention developed in Australia; these included presentation of information on PowerPoint® (Microsoft Corporation, Redmond, WA, USA) slides, printed images of physical activities with fathers and children, written resources to support the programme and details about the activities children and fathers would be expected to complete between the programme sessions. The intention of the researchers conducting data collection was to generate discussion, by providing a ‘space’ for participants to elaborate on points openly with the support of materials from the intervention. 76 Interviews lasted, on average, 50 minutes (range 35–67 minutes) and focus groups lasted, on average, 71 minutes (range 61–81 minutes). Interviews and focus groups were conducted in participant’s homes (n = 16), places of employment (n = 3) and recognised and trusted locations in their community (i.e. primary school and hair/beauty salon) (n = 2).
In carrying out interviews and focus groups, researchers emphasised and ensured that participants understood the overall purpose and why certain questions were being asked, while paying ongoing reflexive and critical attention to interpreting the social context behind accounts. 77,78 All participants received a £10 shopping voucher to cover their time/travel expenses and as a thank-you for taking part.
Data analysis
Interviews and focus groups were audio-recorded and transcribed clean verbatim for analysis by an external transcription company (The Transcription Company, Sutton Coldfield, UK). Transcripts of interviews conducted in Urdu were translated into English for conceptual equivalence, determined by FK and Manbinder Sidhu. 79
We used Braun and Clarke’s80 thematic analysis to inductively develop a coding framework informed by Liu et al. ’s69 typology, and surface and deep structural levels. We explored similarities and differences in narratives across the different groups of interest (e.g. gender, ethnicity and migration status). 81,82 Two members (MS and LJ) of the qualitative research team independently coded a batch of transcripts and then developed a descriptive framework to allow for inductive coding in each domain. 82,83 The Liu et al. 69 typology informed the coding and the development of a descriptive coding framework. Transcripts were coded using NVivo 10 (QSR International, Warrington, UK). The team met regularly to discuss themes identified in the data linked to adaptions that could influence the modified design of the programme. We then undertook further interrogation of the data81 to explore cultural adaption at (1) surface level and (2) deeper structural levels.
Findings of the qualitative component
Participant characteristics
Participant characteristics are presented in Table 1. We were able to achieve reasonable ethnic diversity, with over half of our sample comprising South Asian community members. Furthermore, aligning with the overall aim of the HDHK-UK trial, 20 participants (two-thirds of the sample) resided in locations in the highest quintile of socioeconomic deprivation nationally.
| Characteristic | Total sample (N = 30) |
|---|---|
| Gender, n (%) | |
| Male | 17 (56.7) |
| Female | 13 (43.3) |
| Age (years), n (%) | |
| 20–29 | 3 (10.0) |
| 30–39 | 10 (33.3) |
| 40–49 | 7 (23.3) |
| 50–59 | 5 (16.7) |
| ≥ 60 | 1 (3.3) |
| Missing | 4 (13.3) |
| Ethnicity, n (%) | |
| White | 7 (23.3) |
| Black Caribbean | 2 (6.7) |
| Indian | 9 (30.0) |
| Pakistani | 9 (30.0) |
| Bangladeshi | 3 (10.0) |
| Parental status, n (%) | |
| Father | 15 (50.0) |
| Grandfather | 2 (6.7) |
| Mother | 13 (43.3) |
| Marital status, n (%) | |
| Married | 29 (96.7) |
| Co-habiting | 1 (3.3) |
| Age (years) of childa | |
| < 4 | 1 |
| 4–11 (primary) | 52 |
| ≥ 11 | 15 |
| IMD, n (%) | |
| 1 and 2 (least deprived) | 2 (6.7) |
| 3 | 4 (13.3) |
| 4 | 4 (13.3) |
| 5 (most deprived) | 20 (66.7) |
All participants were recruited from inner-city locations. Participants were part of families with primary school-aged children, with some also having secondary school-aged children. Of our non-white sample, the majority were second-generation migrants, who were born in the UK. One participant, who used a wheelchair, discussed the potential for incapacitated adults to take part in a lifestyle programme with young children.
Relevance of the theory underpinning the Healthy Dads, Healthy Kids programme
As highlighted in Chapter 1, the HDHK programme has two underpinning theories: FST50 and SCT. 49 The relevance of FST to the lives of the families was confirmed by reports of the importance of the reciprocal relationships within families. Parents described the importance of being a good role model to their children, a key component of the theory [quotation sources include the work package number and the participants identifier (ID) number, followed by either ‘interview’ or ‘FG’ (focus group) and the participant’s ethnicity)]:
Just to be a good example to the children and to be a good role model and also to ensure that they’re to provide, first of all, and secondly to, er, like I said be a good role model, show them the rights and wrongs.
WP1a-06, interview, Pakistani mother
Parents described trying to ensure that they were setting good examples to their children around snacking behaviour, for example replacing high sugar treats like chocolate and crisps with healthier alternatives such as fruit and vegetables. Nevertheless, there were challenges in implementing and sustaining these behaviours. Mothers described a continuum of role models from a discordance between the dietary practices of fathers and the mothers’ desire for their children to eat healthily, to fathers being a positive influence:
I can eat fruit and veg and the kids can eat fruit and veg, but my husband will never touch fruit and veg. He just won’t touch it.
WP1a-FG1, Pakistani mother
So we look at the healthy options but my daughter now will reach for a yoghurt or carrots or grapes or strawberries, which are her favourite snacks. Whereas I, as a child, wouldn’t have done that so, and that’s my husband’s influence.
WP1a-06 interview, Pakistani mother
Family systems theory views the family as an emotional unit; therefore, the behaviours of one individual cannot be viewed in isolation. The importance of the family undertaking activities together was confirmed:
I think it’s a very good idea getting the kids and the parents to do activities together.
WP1a-59, interview, British Asian Indian father
If my little one pushes his dad, ‘You have to come, you have to come’, then he probably will.
WP1a-FG1, Pakistani mother
Lifestyle changes in people of Pakistani and Bangladeshi ethnicity needed to consider multiple family members living in a single household, that is grandparents (acting as matriarchs or patriarchs) who also influenced child behaviour:
. . . we’ll cap that time on the TV and we’ll cap their time [yeah] on the Xbox [Microsoft Corporation] so it will be half an hour, 20 minutes, 30 minutes, whatever it is that we’ve got [yeah]. Erm, so the grandparents, you know, they’re like, ‘No, we’ll just let them play’.
WP1a-064, interview, Bangladeshi father
The other theory underpinning HDHK was SCT. The relevance of the associated behaviour change techniques based on social cognitive constructs such as goal-setting and self-monitoring was not questioned by the fathers. There were examples of a lack of knowledge of important skills in weight management, such as calorie counting. Fathers reported setting goals in relation to exercise to manage their weight and acknowledged considerable barriers to behaviour change because of family constraints in relation to time for activity:
Well, I’d rather have somebody give me information face to face or in a group, then I know what to do, basically. How to do activities with the kids.
WP1a-03, interview, Bangladeshi father
I’ve never done calorie-counting, and it’s not, er, something I’ve ever pursued.
WP1a-37, interview, white British father
Logistical and pragmatic considerations of delivering the intervention
All participants reported that they would like the intervention to be delivered close to their homes for various reasons. For mothers, reasons were linked to familiarity, which was usually interlinked with issues of safety, that is knowing where their child would be for a given period of time even when attending with their father. The school was considered ideal for programme delivery, had ongoing relationships with parents and was a trusted location. Some mothers expressed concern about dropping their children back to school in the light of other commitments siblings may have, for example tutoring, scouts, religious readings or other physical activities. For fathers, attendance and likelihood of continuing to attend centred on working hours, travel time and the intervention having a degree of ‘in-built’ flexibility to account for traffic or unintended events:
I just think for me the school is the nub – is the nub, is the hub; it’s the place to start because that’s where you can engage with the families.
WP1a-23, interview, white British grandfather
Local, erm, and they have the space. You know, you open up the school hall, erm, school’s easy to get to. I don’t know if it’s gonna be linked to schools or, erm, but, you know, also if it does come from the school and the fathers are going along there, erm, then, you know, there might be less barriers to break down in terms of the – you know, they might know each other.
WP1a-37, interview, white British father
Although nearly all participants recognised the convenience and familiarity of delivering services in the school, some parents questioned whether or not young children would be happy returning to school in the evenings, having spent the majority of the day learning in the same location. Logistically, venues that accommodated travel by car were preferred, with availability of parking a key factor for many; otherwise, ease of access was important if travelling by public transport. The issue of parking was contextualised by expressing fears of having to travel to unfamiliar locations, or even known locations perceived to be areas with high rates of crime:
Somewhere close with, with, with somewhere you actually park. A, a busy road, you can do it by public transport or parking is hard to get to [OK].
WP1a-24, interview, white British father
Well, the place of where I live in, [place] to be specific, we don’t have much things going around. We just have, it’s, it’s more of a council estate area. Whenever you go out with your kids you have to watch your back, it’s not very safe . . .
WP1a-63, interview, Bangladeshi father
Views about the timing of the programme varied, largely because of child-related commitments with respect to child care or attending other extracurricular activities. Parents varied in their preferences for attending the programme on weekends or during evening weekdays, mornings or afternoons or evenings. For some, timing of the programme was strongly linked to continued attendance, with some suggesting that reminders would be helpful:
Because he [father] works in the morning. He goes at 8:30 and doesn’t come home until 7:00 in the evening. So he’s got no time to come.
WP1a-FG1, interview, Pakistani mother
They [children] go to school and they finish and they’ve got homework to do and I suppose one of the days in the evening wouldn’t be too bad. Weekend would be better . . .
WP1a-45, interview, British black Caribbean father
Programme structure and delivery
Programme length and commitment
Parents shared concerns that the programme might be too long in duration for their children to maintain concentration and interest, and fathers (particularly those with alternating working patterns) expressed concerns about the time commitment. With travel time and completing weekly tasks as part of the programme, as well as remembering to bring resources, the programme would take up a significant amount of time in a single day. Therefore, a shorter intervention (time allocated per session) was preferred by some:
I think the length of time will cause a problem to people because 90 minutes is an hour and a half. You’ve got to realise that you’ve got time to get there and time to get back. If it’s a weekday, then you’ve also got – depending on the child’s age, you’ve got to take into account homework and things like that as well. So, that might cause an issue.
WP1a-59, interview, British Asian Indian father
If it’s in the weekday, then 90 minutes is too long . . . activities that they have, they don’t last more than 45 minutes anywhere, so say 45 minutes, 1 hour on a weekday is maximum that somebody would, er, tend to give.
WP1a-61, interview, Indian father
Session delivery
Fathers questioned elements of the programme. Although the 90 minutes was broken into three subsessions, the fathers’ session in particular drew the greatest criticism; criticism highlighted the drawbacks of using PowerPoint and, therefore, the perception that speakers would be lecturing rather than teaching. As the majority of our participants in this study were British-born, discussion of language issues as a barrier to attending or understanding content was limited (note that ‘school mothers’ indicates mothers who attended a focus group at a school and ‘salon mothers’ indicates mothers who took part in a focus group in a hairdressing salon):
I think, personally, it’s too long. I would switch off. 20 minutes for me, I’d think, ‘What am I doing here?’ That is too long for me. If they can break it down.
WP1a-FG1, Pakistani school mothers
I always find, honestly, in my educational as well experience, I hated lectures with a passion. That lecturer standing in the front with that PowerPoint presentation, I actually wanted to die. Really I did.
WP1a-FG1, Pakistani mother
The visual presentation of material was welcomed, with appreciation of novel methods to convey well-known public health messages, although the method of using PowerPoint so extensively was a deterrent; instead, there was a desire for more demonstration-based learning.
The programme materials
The programme resources (manuals for the fathers, children and mothers; activity cards and homework slips) were welcomed and considered a useful addition to the programme, potentially enhancing the take-home messages from each session. Nevertheless, parents felt cautious and some overwhelmed with the quantity of information and concepts used in it. Many struggled to understand certain terminology without initial explanation; this could be interpreted as a barrier to engagement. As this was highlighted by British-born participants, this was not an issue of a language barrier due to having English as a second language, but an issue of plain English at an appropriate reading level. This further coincided with the use of terms such as ‘manual’, with some finding this slightly condescending and others suggesting they would be unlikely to read such a document:
How many times have you, man, read a manual?
WP1A-61, interview, Indian father
Nevertheless, the fathers welcomed the extensive use of visual representation in the Dad’s manual to present ideas and information to help challenge established parental messages/habits/practices common among families that are culturally ingrained and to convey new ones, for example praising a child for finishing all the food on a plate:
See, the thing is, the language is quite complicated in general. Family strategies I’ll understanding, ‘To make the Trust paradigm work’, what do they mean by, ‘paradigm work’? [Mmm]. So, I would personally say it’s too complicated for the Bangladeshi community [OK] to understand that.
WP1a-63, interview, Bangladeshi father
It’s like a manual made for people who like reading [yeah] and look how big it is – erm, who like reading, who’ve got time, who are keen . . . it’s way too much, too much information [yeah] – I would switch off, I would switch off. I wouldn’t read this.
WP1a-39, interview, British Asian Indian father
Manual for Dads. Erm it may be a bit sort of – not patronising’s the word, may be a bit for suggesting, ‘Oh, I know how to be a dad. You’re telling me how to be a dad!’
WP1a-41, interview, British Asian Indian father
Notably, when shown the Australian materials, nearly all non-white participants (as well as some white participants) identified the lack of ethnic representation in materials, namely images of non-white families taking part in the programme were missing throughout. Hence, many felt that it was important that images of ethnic minority families were embedded in the materials to help them relate to the content and imagine their own families performing tasks and activities promoted as part of the programme:
What is noticeable is the ethnicity of the, err, the males in the pictures. Erm yeah. And I just think it would definitely have to be relevant for me.
WP1a-45, interview, black British Caribbean father
Right, the images aren’t multicultural; I’ll tell you that straightaway at the start off. They are – if you’re gonna aim at a broad range of people within the community, these are just aiming at the European ones, so you need to have more multicultural images. That will then help people associate with it and recognise – say that they can recognise that lifestyle and go from there.
WP1a-59, interview, British Asian Indian father
Facilitator characteristics
Overall, men welcomed the group nature of the fathers’ session, which was then followed by physical activity play with children. Some mothers expressed the desire for more information about the activities that their children would be taking part in and in the presence of whom:
The person delivering the programme would never be one-to-one interacting with my child anyway. If that did happen, that would concern me quite a bit. I’m assuming that they are CRB [Criminal Records Bureau] checked and all that. So as long as you’ve done all your background checks, that person’s safe to work with children and things like that.
WP1a-FG1, interview, Pakistani school mothers
For non-white men, some stated the preference for cultural and gender-based concordance, whereas others stated that they would feel more comfortable if the intervention was delivered by a fellow father. Notably, there was little importance placed on ethnic concordance between facilitator and fathers:
The big no-no is if you give an Asian lady, a Bangladeshi lady with a bunch of Bangladeshi guys . . . So you need probably a male with a male and definitely a female with a female.
WP1a-63, interview, Bangladeshi father
I’d say another father, certainly somebody that you can say ‘well at least they know what they’re talking about’ because, you know, they’ve been in those shoes that I’m in so they’d understand it.
WP1a-06, interview, Pakistani mother
People have issues with it, if they’re obviously from a nationality [mmm], possibly or especially a different religion [mmm], I don’t know. But that, to me, that wouldn’t make a difference at all with that [mmm]. It’s, it, the same things would work whichever way you go [yeah]. The same things apply to anybody no matter where they’re from.
WP1a-24, interview, white British father
Group delivery
In general, fathers welcomed the face-to-face nature of their specific sessions, but shared concerns about the nature of group and how supportive the interactions would be, not only with the facilitator but other fathers in the group, and whether or not they would be confident sharing personal anecdotes from their family experiences. Furthermore, many of the older fathers questioned whether or not their experiences would be relatable to younger fathers present in the group. Some shared concerns about being stigmatised for being obese, even when in a group where all participants are overweight:
I think it would depend on the makeup of the group. Erm, if I felt – if I felt there were similar to me then I’d be comfortable, obviously, but I’m probably – I’m on the older side for parenting, really. I was fairly old when the children came into my life, compared with most, so if I felt I was way older than everybody there, I’d be uncomfortable with it. If I felt I was from a different kind of social background, I’d be uncomfortable with it.
WP1a-36, interview, white British father
There were mixed feelings about taking part with a group of men of different weights, sizes and body image, some of whom were perceived as potentially being ‘competitive’ men:
I don’t want to be there with the rest of the dads and they’re going to be . . . because, you know, the competitive dads and they’ll be, ‘Oh, I’ve lost weight.’ Then it turns into them rather than them and the kids.
WP1a-41, interview, British Asian Indian father
I think it would depend on the makeup of the group. Erm, if I felt – if I felt there were similar [size] to me then I’d be comfortable.
WP1a-36, interview, white British father
Content of the programme
Weight
Mothers welcomed the nature of focusing on calories; South Asian mothers, who predominantly prepared meals, stated that they would like to know more about how health promotion information, such as calories and portion control, could be applied to South Asian cuisine, inclusive of halal practices for Muslims. Men also recognised the need to know more about calories, portion control and healthier alternative foods/drinks, yet the greatest concern was how best to incorporate these changes in their family routines. If this could be achieved over the long term, it was clear to many that there would be benefits to their health and well-being, as well as financial benefits:
It doesn’t say anywhere how many calories are in a chapatti or how many calories are in a curry. Maybe because to know the calorie of a curry you’d have to make it word by word from a recipe.
WP1a-FG1, Pakistani school mothers
. . . never been interested, really, in counting calories. I’m more interested in my own weight issues, if you like. I know I’m overweight a bit, but I don’t focus on what I’m eating and drinking. I would rather focus on increasing the time I spend at the gym and trying to work it out that way.
WP1a-36, interview, white British father
Nutrition
There was an awareness that family nutrition was often not as good as it could be. All participants reported that their families consumed a varied diet where traditional staples, regardless of heritage, were being replaced by more unhealthy Western foods, combined with dining out, as well as regularly purchasing takeaway either as snacks or to replace cooked evening meals:
My daughter, she’s very fussy. She only likes chicken nuggets and pizza, and it has to be a particular pizza.
WP1a-FG1, Pakistani school mothers
Men described the challenges they faced in keeping to a healthy lifestyle:
You start having a few beers, you start having the odd takeaway.
WP1a-23, interview, white British grandfather
Physical activity
Fathers understood physical activity as an important element of building a closer bond with their children, rather than as a method for them to lose weight or become healthier. Working fathers questioned how easy it would be for them to engage in physical activity with their children if they did not already have some form of close relationship prior to beginning the programme. Furthermore, owing to gender–cultural considerations, the programme was considered more appropriate for younger children in the eligible bracket (4–8 years), as opposed to children aged 9–11 years:
It’s nice to have that time with your kids and there’s – they know it’s – I know it’s for me and I also know they know it’s for them too and it’s for us together, you know, an activity together or time together.
WP1a-45, interview, British black Caribbean father
Gender considerations
Gender considerations in both delivery and within-programme active play was a focal theme among parent narratives. In particular, South Asian participants who took part in the earlier interviews raised the issue, and the remainder of participants were directly questioned on this topic.
Through analysis of subgroups, there were notable differences between participants who were either migrants or married to migrant partners from South Asia. First, these participants felt that sport or engaging in physical activity, particularly outdoors or away from home, were activities exclusive to boys or men. This was particularly acute when girls reached the end of primary school. 84
For Pakistani and Bangladeshi Muslim participants, there were clear distinctions between female and male obligations: certain practices, in particular household tasks, needed to be encouraged in girls from a young age. In conjunction, migrant parents recognised the lack of sporting/physical activity role models for both girls and boys, while parents also recognised that they too were poor role models. Notably, some migrant Pakistani mothers felt that it was culturally appropriate to prepare their daughters to be Pakistani women. There was the perception of greater stigma attached to girls’ behaviour in comparison with that of boys:
I mean, being from an Asian background, you know, we have certain cultures and traditions and everything, so up to the age of probably, of probably like, 7, 8 I’d say, would be OK with [mmm] their daughters [mmm]. Anything more than that, I don’t think a lot of dads would be comfortable [OK] so I, personally, I wouldn’t be comfortable [mmm]. So, I mean, with boys it’s OK, I mean, you know.
WP1a-03, interview, Bangladeshi father
I have seen that there is so many burdens on women, that even if the men aren’t doing anything, their mothers say nothing, it’s their son, but if it comes to their daughter, yes it is important . . . some kids say ‘daddy doesn’t do it, so why should I do it?’
WP1a-FG2, Pakistani salon mothers
South Asian migrant mothers and fathers were very clear that, from a certain age (ranging from approximately 7 years to the start of menstruation), there should be a culturally determined distance between fathers and their daughters, based largely on limiting tactile contact:
We have certain cultures and traditions and everything, so up to the age of probably, of probably like 7, 8 I’d say, would be OK with [mmm] their daughters. Anything more than that, I don’t think a lot of dads would be comfortable. So I, personally, I wouldn’t be comfortable.
WP1a-03, Bangladeshi father
There are a lot of problems; we watch the news, and so, as a Muslim, Islam teaches us about the gap, when the daughter starts her periods, keep a gap [in contact between the daughter and her father].
WP1a-04, Pakistani mother
Some parents expressed concern about children engaging in inappropriate rough-and-tumble play outside the intervention; hence, there was an implicit need to establish ground rules for both children and adults to adhere to about when and with whom rough-and-tumble play was acceptable:
With my daughter, she’s very smart. She’ll understand that we’re doing this here. It’s a little activity. We’re not going to continue to do it at home or maybe I’m not going to continue to do this with my friend, male friend at school.
WP1a-FG1, Pakistani school mothers
In addition, one mother raised the issue of girls mixing with boys, once they had reached the age of 11 years:
You know, you said 4- to 11-year-old kids as well, didn’t you? And I think there’s some barriers around– sometimes don’t want their daughters of 11 to mix with boys of 11. I mean, I think that might be an issue as well . . .
P1a-06, interview, Pakistani mother
Alcohol
Pakistani and Bangladeshi participants acknowledged that some members of their community may drink alcohol, but still felt that it would be awkward for those who drink privately:
It wouldn’t mean much because I don’t drink, I’m, I’ve come from a Muslim background, so that wouldn’t mean anything, but then again, a lot of Bangladeshi people do drink [yeah] and they probably drink heavier than the people that are allowed to drink [yeah].
WP1a-63, interview, Bangladeshi father
Screen time
A topic covered in the HDHK programme is the amount and nature of screen time that children spend on electronic gadgets. This resonated with the parents who were concerned about the amount of time their children spent playing computer games and looking at their phones and electronic tablets. Fathers also expressed concern about not knowing what their children were reading/watching and the nature of the activity itself, which is often in isolation away from the family:
Our kids are coming to a teenage time, we didn’t know they know how to play iPad [Apple Inc., Cupertino, CA, USA] and PlayStation [Sony Corporation, Tokyo, Japan], we had the proper childhood, we could run around and play games.
The electronic media that our children have, we never sat still or indoors.
Electronics have stolen their childhood. They sit on their phones all day now.
WP1a-FG2, Pakistani salon mothers
My son came back, my oldest son, well, middle son, came back from school and he was supposed to sit down and do some reading and he wasn’t interested at all. All he wanted to do was sit on his iPad . . . it’s when they seem more interested in what’s going on on YouTube [YouTube, LLC, San Bruno, CA, USA] and whatever else then actually their own development, that’s when I think it’s a problem.
WP1a-45, interview, British black Caribbean father
Nowadays, what the kids are doing, especially my one, they’ve got this, erm, iPad in front of them, they’ve got a TV in front of them, hardly any exercise, hardly any running around.
WP1a-63, interview, Bangladeshi father
Parenting
South Asian mothers felt that their husbands took a laissez-faire attitude to fatherhood, conforming to traditional working-class masculine ideals of male breadwinner and provider. Nevertheless, there were notable exceptions in the accounts between Indian and Pakistani/Bangladeshi mothers, with the former sharing accounts of men playing a greater role in household duties. However, all recognised and understood the value of men as fathers and the importance of being good role models for their children. South Asian fathers, in particular, were less likely to narrate experiences of spending significant periods engaging with their children in either home-based or outdoor activity without the supervision of their partner. For South Asian mothers, particularly Muslim Pakistani mothers, it was imperative that there was a bond between fathers and their children:
Nothing, praise be to Allah; my husband is very friendly, he’s very attached to my kids. I have nothing to worry about nor do I desire anything else; he is ready to do something before I am.
WP1a-FG2, Pakistani salon mothers
We want equal bonding that mother and father should play an equal role.
WP1a-FG2, Pakistani salon mothers
In general, participants highlighted that the nature of communication between parent and child was key to raising children, that is listening and discussing whether or not their child has any issues at school and, ultimately, whether or not their child was happy. Compared with the mothers, fathers focused more on their child’s personality traits and how they envisage their children when they become adults. Ensuring that the transition to adulthood was ‘successful’ was influenced by instilling values, building confidence and self-esteem, while also instilling discipline and control, with the discipline and control at times derived from religious beliefs. These resonated well with the HDHK programme objectives, whereby South Asian fathers may be more inclined to engage if they believe the intervention provides an opportunity to build a closer relationship with their child, while equipping them with the necessary traits to be ‘successful’ later in adulthood:
The challenges are just getting them to do things in a timely manner because kids don’t wanna do it. Getting them to do their homework . . . Realising that, OK, they might want to watch TV, but you’re the dad and you have to say that they can’t. You have to be quite strict about it.
WP1a-59, interview, British Asian Indian father
I want him to be happy. I want him to be good-natured. I want him to be humorous, and have a laugh. Erm, and be hard-working and conscientious. Erm, I think – I think that’s it. I’d never – I’ve never tried to mould him into something, or on the odd occasion that – that I have, I realised, you know, you can’t do that with kids.
WP1a-37, interview, white British father
Participants expressed interest in the HDHK programme’s section on parenting styles. In general, they felt that their parenting style converged with definitions of being authoritative, telling their children what was and was not acceptable behaviour and monitoring their tone and demeanour to ensure that children understood that they, as parents, were the ones making decisions. However, a common vignette used in accounts was parents depicting the good cop, bad cop role, namely bad cop being the stricter coercive parent, whereas the good cop was the softer, approachable parent who would lessen the punishment or authoritative action decided by the bad cop. Fathers described facing personal challenges in keeping a balance between being strict and fair, with the latter being associated with more permissive parenting:
The one thing that’s grabbed me already is I’m just looking at one – two characteristics best describe an authoritative parenting style.
WP1a-45, interview, British black Caribbean father
I think, erm, we’re probably – wouldn’t say good cop, bad cop, but it’s probably one day maybe she is – I’m bad cop and she’s good cop, if you know what I mean.
WP1a-41, interview, British Asian Indian father
Healthy Dads, Healthy Kids programme ‘hook’: getting families to attend and continue to attend the programme
Participants noted a number of factors and features of the programme that would encourage them to attend, continue with and complete the programme. As mentioned in Logistical and pragmatic considerations of delivering the intervention, the timing of the programme to accommodate father’s working patterns and children’s extracurricular activities was essential.
Key to attracting parents to attend was the nature of how the programme was branded. Fathers would be encouraged to attend if the programme was publicised as being about improving child development (e.g. health, well-being, personal development) rather than as a weight management programme designed for fathers or even as a parenting class; mothers would also be supportive if the programme was publicised this way. Hence, better parenting and establishing closer relationships with children should be the advertised outcome of the programme. Notably, fathers expressed a need for a space to meet other fathers and share their thoughts about being a parent and for support; often this was discussed in the context of a dearth of fathers’ parenting groups and how many more services are provided for women:
The sports lines, if there was a sports focus to it, or a – stuff that can transfer into sport, like physical activity that will improve fitness and so on.
WP1a-36, interview, white British father
If there was a social element to it [the HDHK programme].
WP1a-39, interview, British Asian Indian father
Making it more about the kids. Erm, like, my kids go to Beavers and all that, so it’s like – they enjoy it themselves, so maybe, you know, it’s gotta be more – the children relationship kind of thing. Not that ‘you’re the dad, you need to lose a few pounds’.
WP1a-42, interview, British Indian father
The main attraction would be, erm, just having some time with the kids, I guess, er, whilst there’s other dads there with their kids.
WP1a-64, interview, British Bangladeshi father
The operative word to prevent attrition and encourage completion for many participants was ‘fun’ embedded in a social environment, rather than purely learning based. The greatest concern was children losing interest in the programme, as fathers were willing to attend as long as their children wanted to; thus, activities need to maintain children’s interest and fathers want clear take-home messages:
I think making it fun for the children. That kind of thing. Making it more about the kids.
WP1a-42, interview, British Indian father
To make it work, I think it’d have to be – the main focus – I don’t know, 90% at least, needs to be about the fun and the activities, with just a general kind of overview of, kind of, reasoning behind it. I wouldn’t have thought people would want to know the detail. They don’t wanna feel like they’re back at school, I don’t think.
WP1a-36, interview, white British father
It was imperative that both fathers and children were gaining something from the programme in the form of small incentives, such as t-shirts and reusable resources, or even an incentive to complete the full 9 weeks.
Summary of the qualitative findings
In summary, the design of the programme was well received, including the opportunity to meet other fathers, the novelty of a group format, ‘rough-and-tumble’ play and the chance to pick up parenting, nutrition and physical activity skills that could be used outside the programme. There was strong agreement among fathers and mothers that the intervention would be beneficial for fathers and children to build closer relationships and increase the amount of time that they spent with each other. Support was greatest among Pakistani and Bangladeshi mothers who felt that their husbands struggled to spend enough time with their children. There was limited preference for ethnic concordance between fathers and facilitators and there was not a strong preference for participants to be from the same ethnic group or community. Some concerns were expressed about the ability to commit to a 9-week programme owing to employment and child care commitments.
There were a number of issues that needed to be considered to successfully deliver the HDHK programme for a UK population. Many of these were features that are associated with best practice for the delivery of a community-based group programme for parents and children. These included the logistical features of the programme, namely identifying a safe, close, well-known location and delivering the programme on a day and time that suits both parents (in the light of, for example, children’s extracurricular activities and parents’ work). Many of the features described are those that are already integral to the HDHK programme that is currently delivered in Australia, for example branding the programme as being about quality time spent between fathers and their children, a preference for the facilitator leading the programme to be a father, and focusing on how families can make behavioural changes, rather than just providing information.
There were some more specific cultural issues identified, although these were limited. Some participants of Bangladeshi and Pakistani heritage reported that there would be an issue with fathers and older daughters taking part in ‘rough-and-tumble’ activities. In addition, although physical activities would be done in family groups, there were some concerns about older daughters mixing with boys in the groups. The physical activities in the HDHK programme are all adaptable, with more and less tactile options available; it was noted that this would be an important part of facilitator training. With regard to content, it was clear that assumptions should not be made about foods consumed or methods of cooking based on cultural heritage. However, participants did highlight the need for the dietary components of the programme to include images of and information about foods that are traditionally consumed by different cultural groups. Participants also highlighted the need for the images in the programme materials to reflect the cultural diversity of the UK.
One important issue was the view that the programme should not be advertised as a men’s weight management programme, but should focus more on being a children’s activity programme supported by fathers with the opportunity to build a stronger father–child bond through learning and play.
The findings of the qualitative research comprise beliefs at both the surface level and the deep structural level. We identified surface structural-level beliefs, such as the need for the programme materials to depict images reflecting the ethnic diversity of the community and foods consumed by different cultural groups. The deep structural-level beliefs related to the importance of the benefits of children and fathers spending more time together to build closer relationships, concerns about physical contact between fathers and their daughters, concerns about older girls and boys spending time together and the importance of not branding the programme as a weight loss programme.
The considerations for delivery and adaptation of the HDHK-UK programme are summarised in Appendix 2, Table 31. Many of these components were part of the HDHK programme and others needed to be considered in the implementation of any group behaviour change programme, but are included here for completeness.
Summary of recommendations arising from the qualitative findings for delivery of the Healthy Dads, Healthy Kids UK programme
-
For a UK context, the HDHK programme needs to be branded as an activity programme for fathers and their children rather than as a weight management programme.
-
Avoid a stigmatised approach to recruitment, that is not simply targeting overweight/obese fathers.
-
There needs to be pragmatic considerations on the timing and location of the programme delivery that account for both parent and child commitments. Evening and weekend times in nearby, familiar locations are preferred.
-
The multicomponent content (diet, physical, parenting, screen time) was welcomed, as was the focus on implementing and sustaining lifestyle changes.
-
Interventions need to limit the extent of didactic presentation and ensure a facilitative approach to group-based learning.
-
Encourage co-physical activity between fathers and children while being sensitive to what individual families may consider acceptable play according to age, ability and culture, both within and outside the programme.
-
Provision of additional resources with clear take-home messages [e.g. food diaries; specific, measurable, achievable, relevant and time-bound (SMART) goal sheets; local information about physical activity opportunities]. These should be easy to use and take into account local population literacy. Resources can act as incentives.
-
Facilitators need to be knowledgeable and enthusiastic and be able to establish and build rapport with families.
-
Facilitators need to be trained to deal with large groups comprising adults and children, deliver evidence-based content and demonstrate and supervise physical activity learning experiences safely to attendees of different weights and physical abilities.
Findings from the CHANGE study
We also drew on findings from the CHANGE study, led by one of the study team (MP). The CHANGE study was a cultural adaptation and feasibility trial of a children’s weight management programme attended by parents and children in Birmingham, UK. 53 This included a detailed process of cultural adaptation of an existing weight management programme for overweight children aged 4–11 years. The CHANGE study included interviews/focus groups with 43 parents of Bangladeshi or Pakistani heritage who had either completed the programme, partially attended or not attended the programme.
Many of the findings from the CHANGE study supported those from the interviews and focus groups in phase 1a of HDHK-UK. The CHANGE study participants, who were all parents (predominantly mothers) of overweight children of Pakistani or Bangladeshi heritage, confirmed the importance of the programme taking place in a close, familiar location and at a convenient time. They supported a programme that involved children in all of the sessions, rather than just some, as it was felt that they need to learn how to change their behaviour first hand and would respond differently to messages given by someone other than their parents. Parents reported that the nutritional content should be relevant to traditional South Asian diets, while acknowledging the importance of also talking about Western foods, as, typically, their children’s diets consisted of a mixture of foods. Other key findings were the value of sharing experiences and supporting each other in the group environment and the need for assistance with making behavioural changes at home.
Adaptations recommended as a result of the Dads And Daughters Exercising and Empowered programme
At the time of HDHK-UK, the Australian team that developed the HDHK programme recommended changes to the HDHK programme as a result of a new programme they had developed and were evaluating for fathers and their daughters: the DADEE programme. 67 HDHK had nine sessions, with the children attending seven of the sessions, whereas the children in the DADEE programme attended all of the sessions. Feedback from the participants and those delivering the DADEE programme was that fathers and children attending every session was an improvement on the HDHK programme.
Another difference in the DADEE programme was to start the session with a 15-minute joint session with the fathers and children together in which they recapped the previous session and discussed how they had got on with homework tasks. Again, this was felt to be a successful adaptation from the HDHK programme, in which the fathers and children immediately went into separate sessions.
Adaptation process
We then took the findings from the qualitative study and applied the Liu et al. 69 typology to consider which of the items in the typology these factors addressed and then considered how this could be operationalised. This final stage drew on the qualitative findings, the CHANGE study,53,70 previous experience from the Australian delivery of the HDHK programme and the delivery of the DADEE programme. 67
The adaptation process was undertaken by two members of the research team (MS and KJ). An example of how the process was undertaken is as follows. We identified, through the qualitative data, that the facilitator needed to be able to adapt physical activities to reduce physical contact between fathers and daughters for some families of Bangladeshi or Pakistani heritage. This fitted within the Liu et al. 69 typology as ‘gender considerations’. We then ensured that the facilitators had training that included adaptations to the physical activities to limit the amount of close physical contact.
Changes to the Healthy Dads, Healthy Kids programme
Adaptations were made in three key areas of the programme: (1) programme promotion, recruitment and follow up; (2) programme delivery; and (3) programme content. No changes were made to the theoretical underpinning of the programme; most changes were at the surface structure level, but some, such as branding the programme as a father–child activity programme and acceptability of physical activities for fathers and daughters, were deep structural adaptations.
However, it is important to note that we were unable to remove the inclusion criterion of obese or overweight, despite the qualitative research recommending that this was changed, given that men’s weight management was the objective of the funding call. Most of the components interpreted as important in the qualitative data were already built into the programme. As a research team, our main concerns were whether or not the content of the resources were too difficult to be delivered with fidelity by a facilitator who was not a teacher and whether or not the supporting workbook was too detailed. Given the very positive findings from the Australian studies, the research team took the approach of making fairly limited changes before running the uncontrolled feasibility trial, then assessing whether or not further changes were required.
Programme promotion, recruitment and follow-up
Key to the promotion of the HDHK-UK programme was not to advertise the programme as a weight management intervention but as a father–child activity programme with the added benefits of addressing weight loss and becoming healthier. As a result, participant-facing promotional material tried to minimise weight-focused phrases/terminology.
To encourage easier recruitment and follow-up, and to limit the number of visits made to participants’ homes for data collection, we planned to hold baseline recruitment events at local, well-known community/youth organisations while offering follow-up at children’s soft play centres.
Programme delivery
The session format was amended to include a 15-minute introduction to each session for the fathers and children together, and children were invited to all nine sessions, rather than seven as in the original HDHK programme. The format of separate sessions for fathers and children, followed by co-activity with parents/children, was kept the same, as well as the 90-minute duration. However, programmes were designated to be delivered at both after school and weekend times. To ensure that programmes were delivered locally to communities, we planned to deliver the intervention in schools, youth centres and leisure centres.
Programme content
First, content was adapted to make it applicable to UK families, which included removing Australian terminology and images (e.g. Australian branded food/drink products). After this, content was reduced in the fathers’ sessions by reducing the number of PowerPoint slides and limiting the evidence-based information. Images were altered to include a mix of cultural foods as well as foods from well-known restaurants/takeaway providers known to local communities. The language on the PowerPoint slides and in the fathers’ manual was simplified.
Resources were altered to include some images (where possible) of non-white families throughout; however, these were limited owing to availability, cost and the nature of the image itself (i.e. few images of South Asian fathers engaging in physical play with children).
The name of the ‘Dad’s manual’ was changed to ‘Dad’s Handbook’ to reflect the feedback from fathers. In keeping with the desire for some form of inducement to take part, the giving of HDHK-UK branded t-shirts for the fathers and children was maintained.
Details of the changes to the programme by item described in the Liu et al. 69 typology are in Table 2.
| Factors to address identified from qualitative data and other studies | Liu et al.69 typology item | Cultural adaptations made |
|---|---|---|
| Programme delivery | ||
| Convenient and familiar programme location | 24. Intervention delivered in culturally appropriate or preferred format |
|
| 33. Located in ethnically/culturally appropriate/familiar location | Delivery in schools, leisure centres and community centres in local communities | |
| Convenient timing of programme | 25. Consider target population’s employment situations | Intervention to be delivered in evenings/weekends |
| Incentives to attend and continue | 29. Utilise appropriate incentives and timing of the programme | Use of incentives: t-shirts, evening and weekend sessions to avoid Islamic education and other children’s activities |
| 39. Address physical/financial (structural) barriers to participation | Use of local sites, high-street vouchers at end, programme merchandise. Possibility of bringing slightly younger or older children along | |
| Male preferred for delivery of fathers’ session | 46. Gender considerations | Preferentially have male facilitator for Dad’s sessions |
| Programme content | ||
| Programme materials reflect the ethnic diversity of the UK in images of people and of foods commonly consumed by BAME communities | 12. Material depicts individuals from target population | Adaption of HDHK programme using UK ethnically suitable families (fathers, mothers children); use UK ethnic faces in participant facing material; images of relevant food, cooking practices and recreational activities |
| 18. Material depicts appropriate graphics and scenarios (this can be heterogeneous) |
|
|
| 19. Material/guidance based on preferences of target population | Material refers to foods commonly eaten by members of BAME communities | |
| 26. Intervention addresses health behaviour patterns found in target population | Address high fat, convenience foods, preparing food in multigenerational households, and low physical activity | |
| 43. Maintaining cultural significance of food | Incorporate calorie information for cultural foods; incorporate references to and images of cultural foods | |
| Need to remove Australian activities and foods | 14. Reflect target population’s language (usage: concepts, vocabulary) | Programme materials anglicised |
| Need to remove Australian statistics | 17. Material presents ethnic-specific data | UK statistics in HDHK PowerPoint slides |
| Written materials need to reflect the literacy levels of the population | 15. Match reading level and literacy | Language in programme material for participants plus PowerPoint slides to be simplified |
| 24. Intervention delivered in culturally appropriate or preferred format | Use of visual material | |
| Reduce focus on weight in promotion of the programme; focus on father–child activity programme | 23. Intervention goals and outcomes are culturally appropriate |
|
| Need to enable adaptation of physical activities to reduce physical contact | 46. Gender considerations | Provide a range of activities in physical activity sessions to enable more/less tactile activities |
The adapted Healthy Dads, Healthy Kids UK programme
Detail of the final adapted HDHK-UK programme is described using the Template for Intervention Description and Replication (TIDieR) checklist (Table 3).
| Item | Item description |
|---|---|
| 1. Name | HDHK-UK |
| 2. Why |
|
| 3 and 4: Materials and procedures | Fathers, of primary school-aged children, who were classed as overweight or obese (BMI of > 25 kg/m2 or of > 23 kg/m2 for fathers of South Asian origin) were invited to take part in the HDHK study with their primary school-aged children (aged 4–11 years). Participants randomised to the intervention group were asked to attend the HDHK intervention programme with their children. The intervention programme involved a 90-minute session once per week for 9 weeks with weekly goals and activities to be completed in their own time |
|
Materials provided to the participants Fathers and children were provided with an intervention pack |
|
|
Materials provided to the facilitators0–15 minutes. Father and children review of their weekly goals with facilitators15–45 minutes. Fathers (‘father-only’) and children (‘children-only’) participate in separate education sessionsFathers’ sessions:Children’s sessions:45–90 minutes. Fathers and children joint physical activity session Each week the joint father-and-child physical activity session covered three components: |
|
| 5. Who provided? |
Three facilitators were required to deliver the HDHK programme. One facilitator to deliver the father-only education sessions and two facilitators delivered the child-only education and joint father-and-child activity sessions Staff were recruited from four organisations to deliver the programme across the different courses. A face-to-face training session, a course manual and all materials required for delivery were provided The fathers-only education sessions were delivered by:For successful delivery, father-education facilitators were required to have presentation and group facilitation skills. The programme was designed for this section to be delivered by male facilitators; however, as a result of staff availability, this was not always possible The child-only education sessions and joint child and family activity sessions were delivered by:Although not essential for delivery, sports coaching skills supported successful delivery to the physical activity elements of the programme. For child protection and ease of facilitation, it was recommended that two facilitators run the child-only education sessions. The second facilitator does not need to lead the session; this role could be undertaken by research staff or work experience students |
| 6: How | HDHK-UK is a group-based programme; the optimum group size is 8–15 fathers |
| 7. Where? | The programme is delivered in community venues, such as community, youth or leisure centres and schools. The venue must have classroom (or equivalent) space for an educational session with PowerPoint projection facilities and a sports hall (or equivalent) for the physical activity session |
| 8. When and how often? | The programme is 9-weeks long with one 90-minute session delivered each week. Sessions need to be delivered at a time when fathers and their children (aged 4–11 years) can attend. Of the four courses delivered, two were on a weekday evening and two were on a weekend. The weekend sessions were more popular |
| 9. Tailoring | Each week throughout the education session, fathers were encouraged to reflect on the session content and apply the key messages in context to their own personal circumstances. Similarly, participants were asked to tailor their weekly goals and set home activities to meet their own needs and their family needs |
| Modifications | Details of the programme adaptation from the original Australian programme are presented earlier in this chapter. Throughout the delivery of the adapted programme, small modifications were made between courses, mainly when delivery of the father-only education session took longer than the allocated 30 minutes, the material was shortened to ensure that there was sufficient time for the physical activity session |
| How well the programme was delivered – planned | The university research team completed observations of intervention delivery, completing a checklist to report on items of fidelity, including session timings, the delivery of key messages, facilitator skills and enthusiasm and participants’ responsiveness |
| How well the programme was delivered – actual | Researcher observations of programme delivery showed that it was delivered with good fidelity. The main challenge was keeping the father-only education session to the allotted 30 minutes. This was improved throughout the courses. The fidelity of intervention delivery is described in Chapter 6 |
Discussion and conclusions
The aim of this work package was to adapt an existing weight management programme for overweight fathers and their children for superdiverse communities living in socially/economically disadvantaged communities in the UK, particularly encouraging members from the Pakistani and Bangladeshi communities. As a result, we sought the views of potential service users (fathers/grandfathers) and those who may act as gatekeepers (mothers/grandmothers). Our adaption process was theoretically informed with the use of the Liu et al. 69 typology of cultural adaptation.
Through our collection of qualitative data, we were able to identify a number of cultural adaptations to encourage attendance from both BAME and white British communities. As a result, our suggested cultural adaptations are not aimed to address specific community beliefs or practices, but to accommodate members from a range of communities. Many of the issues identified as important are those that apply to any group-based activity involving children, although there were some deep structural adaptations.
However, the application of the taxonomy was difficult for a number of reasons. First, the taxonomy focuses on ‘ethnic matching’ in the conception, planning and implementation phases, which can be complex given the changing nature of designing and adapting weight management programmes in a UK context. In addition, our data showed very little support for ethnic concordance. Second, there is an overemphasis on surface-level adaptations (addressing language needs, culturally matched foods, visual images) that are specific to catering to non-white groups that have well-established lifestyle practices, rather than recent migrant groups or second-/third-generation families. Third, limited consideration is given to wider social determinants affecting families, rather than individuals, for example, mixed employment practices in a single household, single-parent families or those who are reliant on the support of extended family (social networks). Hence, the cultural adaptations that we have listed and implemented as part of the intervention are responsive to a ‘family context’.
In a systematic review of the effectiveness of cultural adaptations for interventions aimed at smoking cessation, diet or physical activity in ethnic minorities, Nierkens et al. 85 reported that culturally targeted behavioural interventions may be more effective if they are implemented as a package of adaptations, at a family level, and where the adaptation results in a higher intensity of the intervention than the original unadapted version. This resonates well with the family focus of the HDHK programme and the adaptations made to programme delivery and content. In addition, the Nierkens et al. 85 review found no evidence that the level of adaptation (deep/surface) influenced effectiveness; our adaptation resulted mainly in surface-level changes. 85
There are very few pilot or feasibility studies that have evaluated the process of culturally adapting lifestyle intervention programmes in the UK, with the majority completed in the USA with Latino, Hispanic and African-American minority communities. 86–88 Findings from these studies are not wholly applicable to populations living in the UK. In addition, Sidhu et al. 89 found that cultural adaptations to lay-led, group-based lifestyle interventions were inconclusive with regard to increased effectiveness, although structural adaptations were successful in increasing attendance, albeit mostly among women. 90,91 Nevertheless, there is poor reporting of cultural adaptations and their theoretical justifications for being used.
Notably, the CHANGE study,53 described earlier, played a fundamental role in theoretically guiding the early stages of our study and informed the nature of our cultural adaptation. 53 Lessons learned from the previous application of the Liu et al. 69 typology in the cultural adaptation for the CHANGE study were brought forward into the cultural adaptation of the HDHK intervention. Many of our surface-level suggestions for altering content and presentation of material, such as inclusion of BAME foods and images, were also supported by the findings of the CHANGE study.
There were a number of challenges during the completion of this study phase. Recruitment of fathers to take part in interviews or focus groups was difficult. As a result, recruitment was prolonged and labour intensive, as a result of travel, postal mail-out and predominantly using a face-to-face approach (canvassing) to identify eligible participants. Furthermore, we struggled to engage with Pakistani and Bangladeshi fathers, but were successful in engaging mothers from these communities using an approach by means of research advocates in high ethnic density areas. The fact that almost half of those interviewed were women does mean that there may have been issues relevant to men that we missed. Furthermore, along with providing an incentive to complete interviews (e.g. high-street voucher) and collecting data in participants’ places of employment, beauty salons, a meeting room in a school and homes, we were able to reach saturation overall, although not for specific ethnic groups.
We were successful in gathering data from a heterogeneous sample in our non-white cohort, including non-English-speaking first-generation parents, second-generation parents and those in mixed-heritage marriages. To accommodate non-English-speaking participants (exclusively Pakistani mothers), we sought to involve a researcher with substantial experience of completing qualitative data collection in the West Midlands Pakistani community. Nevertheless, among this group, there was greater preference to complete a one-to-one interview rather than taking part in a focus group, with fewer members attending scheduled focus groups despite confirming attendance by telephone. This was more time-consuming and costly than originally planned for.
Our approach of showing participants material from the Australian version of the intervention was successful in narrowing the focus of conversations to the intervention as a whole, the activities involved (both physical play and education sessions) and the supplementary materials given to attendees to take away from the sessions. This was appropriate in the context of this study because we were not looking to redevelop the programme, but instead preserve the essence of the Australian programme while making it suitable to be delivered in a local context. As a result, we felt that our findings were useful and relevant for making suggested cultural adaptations to the intervention. Hence, we successfully achieved our aim of a theoretically guided cultural adaptation of the HDHK programme for the UK context, keeping changes to the programme to the minimum necessary.
Although we were able to recruit a diverse sample, we may have benefited from greater participation from Pakistani and Bangladeshi fathers, either migrant or British-born, given that the literature identifies these as groups who could benefit most from attending the intervention. Participants may have benefited from viewing Australian materials for a longer period of time, having the opportunity to view video clips of the HDHK sessions or even viewing the materials before the interview/focus group. Importantly, greater consideration needs to be given to recruitment strategies to engage with fathers/families from superdiverse communities, as this can be time-consuming and requires considerable effort from members of the research team.
An additional approach to elicit preferences in relation to the importance of individual components or modes of delivery of a new or adapted intervention would be to use preference elicitation techniques. We were not funded to do this, but it would have identified the trade-offs between characteristics such as timing of delivery and session length, for example.
Chapter 4 Phases 1b and 2: methods
The aim of phase 1b was to explore the acceptability of the adapted programme and research methods in preparation for the delivery of the randomised controlled feasibility trial in phase 2. Therefore, there was significant overlap in the methods for both work packages so this chapter presents these together to avoid duplication; if a section refers to only one of the work packages, this is indicated in the heading. Phase 2 is reported according to the Consolidated Standards of Reporting Trials (CONSORT) extension for pilot and feasibility trials. 92
Study setting
The study took place in two local authority areas of the West Midlands in the UK. Both areas are ranked to be within the 20% most deprived authorities in England, with lower life expectancy than the national average and around one-third of children living with families of low income. 71,93 Census data collected in 2011 showed that unemployment was higher at both sites (7.5% and 7.3%) than the overall national unemployment rate for England (4.4%). Both areas were ethnically diverse: site A – white British (66.7%), Asian and Asian British (18.9%); site B – white British (69.9%), Asian and Asian British (19.2%) (overall ethnic diversity in England: white British, 85.4%; Asian/Asian British, 7.8%). 93
Facilitator recruitment and training
At each of the study sites, the local authority public health teams were asked to propose or recommend facilitators to deliver the HDHK intervention programme, considering the required characteristics. Each course required two facilitators for delivery: one facilitator for the father-only education session and the other for both the children-only education session and the joint father-and-child physical activity session. An additional support facilitator/helper was also needed for the children-only sessions, as recommended by UK child supervision guidelines. 94 Training was to be provided, but HDHK facilitators ideally needed to have previous experience of working with children and families. The HDHK programme training materials advise that a successful programme facilitator should be credible, relatable and likeable, and that it would be preferable for the father-only session to be delivered by a male facilitator. Facilitators were required for the delivery of six courses across two sites: two courses for phase 1b (courses A and B) and four courses for phase 2 (courses 1–4).
At site A, the programme was delivered by the local authority Healthy Lifestyles Team (‘lifestyles team’) and an independent fitness instructor, with support from the study researchers. The lifestyles team, employed by the city council, had experience in delivering a range of health promotion programmes and support to adults and, in some cases, children across the region, including programmes such as weight management and smoking cessation. The lifestyles team delivered the father-only education session. The fitness instructor delivered the child-only education sessions and the joint father-and-child physical activity sessions.
At site B, the physical activity project manager in the public health commissioning team was keen that the HDHK programme should be delivered by a third-sector organisation that, at the time, delivered physical activity education and after-school clubs in schools in the region. This was to avoid a plethora of different organisations interacting with schools with different offers. The staff from this organisation (referred to hereafter as the ‘coaching organisation’) were qualified children’s activity professionals with extensive experience of activity coaching.
Owing to unexpected delays [described in Chapter 5, Site B (course B)], in addition to the coaching organisation, the university research team appointed staff of a local leisure centre to deliver three HDHK courses (courses B, 2 and 3) at site B. At these courses, the father-only education sessions were delivered by three different staff (personal trainer, health and well-being manager and gym manager). The children-only education session and joint physical activity sessions were delivered by a team of sports coaches. Two of the leisure centre sports coaches worked for both the leisure centre and the coaching organisation; therefore, the courses were delivered at two venues: the leisure centre (courses B, 2 and 3 – employed by the leisure centre) and a community centre (course 4 – employed by the coaching organisation).
The intention was to recruit and train facilitators who would deliver courses during both phase 1b and phase 2; however, changes experienced at local authority level and limitations to staff availability resulted in a change of facilitators throughout the study, meaning that several facilitator training sessions were delivered. The facilitator training was mainly undertaken by staff from the Fatherhood Institute who were experienced in offering other training programmes to fathers. They had themselves undergone a bespoke 2-day training-the-trainer course delivered by Philip Morgan, who developed the Australian HDHK programme. The training involved the modelling of the intervention by the trainers, opportunities to practise session delivery with feedback and a half-day session on the physical activity component. This training took place before the research grant was awarded, so there was an 18-month gap between training the Fatherhood Institute and the Fatherhood Institute’s delivery of the training. The Fatherhood Institute, in turn, trained some of the University of Birmingham research team that subsequently delivered facilitator training. The facilitator training programme drew on training slides developed by the Australian research team and included modelling of delivery of the programme and opportunities to practise delivery of both the father-only education sessions and the physical activity sessions. Facilitators were provided with a delivery manual and access to video-recordings of the delivery of the various activities by the Australian team. The physical activity sessions were omitted from the facilitator training when the trainees were experienced sports coaches. Training sessions are summarised in Table 4 and further detail around the circumstances that led to a high turnover in staff are presented in Chapter 5, Set-up and delivery of Healthy Dads, Healthy Kids sessions for the uncontrolled feasibility trial.
| Date | Site | Attendees | Training location | Delivered by | Training set-upa | Sessions the team delivered |
|---|---|---|---|---|---|---|
| January 2017 | A | Healthy Lifestyles Team (n = 8) | Community venue at site A | Fatherhood Institute | Two days: desk-based learning and physical activity session; 1 day refresher | Five of the team were unable to deliver the sessions. Three of the team attended refresher training in July (see ‘July 2017’ row of this table) |
| January 2017 | B | Coaching organisation (n = 2) | Community venue at site B | Fatherhood Institute | Two days: desk-based learning and physical activity session | Both members of staff left the coaching organisation before delivery commenced |
| July 2017 | A | Healthy Lifestyles Team (n = 3) and independent fitness instructor (n = 1) | University of Birmingham | Fatherhood Institute | One day: desk-based learning and physical activity session |
|
| August 2017 | B | Health manager | Leisure centre | Research team: TG | Desk-based learning session (90 minutes) and weekly consultations with TG |
|
| August 2017 | B | Sports coaches (n = 2) | Leisure centre | Research team: TG | Review of materials with research team (TG) and observations of phase 1b in action |
|
| November 2017 | B | Gym manager | Leisure centre | Health manager and research team TG | Observations of phase 1b in action and weekly consultations with TG |
|
| January 2018 | B | Coaching organisation staff (n = 4) | University of Birmingham | Research team: TG | Desk-based learning session (120 minutes) and weekly consultations with TG |
|
Delivery venues
The intervention programme was delivered at a number of community venues across the two sites, depending on the availability, accessibility and location of the facilitators. The venues were required to have a classroom or conference room with a computer projection facility to deliver the father-only education sessions, and a safe and comfortable sports hall with an available range of play equipment for the child-only and father-and-child physical activity sessions. At site A, phase 1b (course A) was delivered in a primary school and phase 2 (course 1) was delivered at a youth centre. At site B, three of the courses were delivered in a leisure centre (courses B, 2 and 3) and one course was delivered in a community centre (course 4).
Participant recruitment
Recruitment was ongoing from July 2017 to January 2018. The target was to recruit 30 participants for phase 1b and 90 participants for phase 2. A number of different recruitment methods were used to identify participants for both phase 1b and phase 2, including recruitment stands at local venues (shopping, leisure and community centres) and speaking at school assemblies, parent evenings and teacher meetings. Bright, attractive flyers were distributed at school gates, community centres, places of worship and large workplace organisations. Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) and Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) pages were set up for the study, promoted by the youth centre at site A and by the local authority public health team and leisure centre at site B.
Potential participants who were interested in the study either provided their details to a research team member at a recruitment event or were encouraged to contact the team using the details that were shown on the flyer or social media pages. When contact was made, interested participants were asked if they had any further questions and their eligibility was discussed according to the inclusion and exclusion criteria. To take part in the study the participants had to be:
-
Men who were overweight or living with obesity, aged 18–65 years with a BMI of ≥ 25 kg/m2 (23 kg/m2 for minority ethnic groups) and/or a waist circumference of ≥ 94 cm (37 inches).
-
Fathers/stepfathers/father figures of primary school-aged children (4–11 years). Fathers did not have to be resident in the same household as the child(ren) to take part.
-
Willing to lose weight.
Participants were asked to complete the Physical Activity Readiness Questionnaire [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/1418513/#/ (accessed 25 November 2019)], which screens for conditions that might preclude safe exercise. If any question responses were positive, they were advised to seek advice from their general practitioner (GP) for direction to alternative local weight management pathways. Further exclusion criteria were as follows:
-
angina or other cardiovascular disease
-
orthopaedic or joint problems that would be a barrier to vigorous physical activity
-
weight loss of 3 kg or 7 lbs in the 3 months prior to the programme
-
fathers with diabetes who were not confident in managing their condition during exercise
-
unable to speak and/or understand English
-
families involved in ongoing custody or access disputes and/or any contexts with a risk of domestic violence (if a parent or other person who knew the family raised this as an issue).
Eligible participants who agreed to take part in the study were provided with information sheets for both adults and children and were required to provide written informed consent on behalf of themselves and their child (or children) aged 4–11 years. Children over 8 years of age were asked to complete an assent form to confirm that they understood the study and were happy to take part.
Data collection and randomisation
As part of the feasibility study, data were collected to test whether or not the processes of data collection that would be used in a randomised trial were acceptable to participants and researchers. In a definitive trial, the primary outcome would be the difference in fathers’ weight between the groups at 12 months’ follow-up, whereas in this study the final follow-up was at 6 months.
Appointments for baseline data collection measurements for both phase 1b and phase 2 were mainly conducted in participants’ homes. Alternative measurement locations were offered if participants were uncomfortable with a researcher visiting their home. The anthropometric measurements and questionnaire data collected are summarised in Table 5 and further detailed in the next section. Copies of the baseline questionnaire booklets are available on the project web page [www.journalslibrary.nihr.ac.uk/programmes/phr/1418513/#/ (accessed 25 November 2019)].
| Data collection item | Details | Data collection time point | ||
|---|---|---|---|---|
| Baseline | 3 months | 6 months | ||
| Father measurements | ||||
| Ethnicity | Reported by participant | ✓ | ||
| Date of birth | ✓ | |||
| Name and address of GP | ✓ | |||
| Highest educational attainment | ✓ | |||
| Marital status | ✓ | |||
| Composition of household | ✓ | |||
| Employment status | ✓ | |||
| Religion | ✓ | |||
| Main spoken language | ✓ | |||
| Health service utilisation | Participant use of health services (i.e. GP, pharmacy, A&E) | ✓ | ✓ | ✓ |
| Weight and percentage body fat | TANITA (Tokyo, Japan) BC-420MA body composition scales | ✓ | ✓ | ✓ |
| Height | Marsden (Marsden Weighing Machine Group Ltd, Rotherham, UK) Leicester Height Measure | ✓ | ||
| Waist circumference | Tape measure | ✓ | ✓ | ✓ |
| Objectively measured 7-day physical activity record | Wrist-worn GENEActiv™ (Activinsights Ltd, Kimbolton, UK) on non-dominant side of body | ✓ | ✓ | ✓ |
| Self-reported physical activity | International Physical Activity Questionnaire (short)95 | ✓ | ✓ | ✓ |
| Dietary questionnaires | Food frequency items | ✓ | ✓ | ✓ |
| Alcohol consumption | ✓ | ✓ | ✓ | |
| Health-related quality of life | EQ-5D-5L96 | ✓ | ✓ | ✓ |
| Adult capability and well-being measure | ICECAP-A97 | ✓ | ✓ | ✓ |
| Parenting for physical activity |
Physical Activity Modelling subscale of the ACTS-MG98 Parenting for physical activity99 |
✓ | ✓ | ✓ |
| Parent–child relationship | Parent–Child Relationships Questionnaire100 | ✓ | ✓ | ✓ |
| Child measurements | ||||
| Weight and percentage body fat | TANITA BC-420MA body composition scales | ✓ | ✓ | ✓ |
| Height | Marsden Leicester Height Measure HM-250P (two measures taken) | ✓ | ✓ | ✓ |
| Objectively measured 7-day physical activity record (eldest child only) | Wrist-worn GENEActiv on non-dominant side of body | ✓ | ✓ | ✓ |
| Parent-reported dietary questionnaire | Food frequency items | ✓ | ✓ | ✓ |
| Quality of life | CHU-9D101–103 | ✓ | ✓ | ✓ |
| Family nutrition and physical activity | Family Nutrition and Physical Activity questionnaire104 | ✓ | ✓ | ✓ |
| Health service utilisation | Parent reported child’s use of health services (i.e. GP, pharmacy, A&E) | ✓ | ✓ | ✓ |
| Parent-reported Strengths and Difficulties Questionnaire | Strengths and Difficulties Questionnaire105 | ✓ | ||
Anthropometric assessments
Anthropometric assessments of fathers and their children were collected by trained researchers. Height measures were collected using a Marsden Leicester Height Measure. Two measurements were taken to ensure accuracy; if the first two measures differed by > 0.4 cm, a third measurement was taken. The average of the two closest readings was used as definitive height. Body weight and percentage body fat were assessed using body composition scales (TANITA BC-420MA body composition scales). The BMI of adults was calculated by dividing weight (kg) by height squared (m2). For children’s BMI, z-scores were calculated using the LMS method106 and UK reference data. 107
Fathers’ waist circumference was measured at the level of the umbilicus. Two measurements were taken; a third was taken if the first two differed by > 0.4 cm. The two closest readings were averaged for the definitive value.
Questionnaire data collection
Fathers and children were asked to complete a number of questionnaires. Fathers completed the items on their own, with researchers providing clarification if requested. For the children, questions were read aloud to the children by the researcher and their verbal answers recorded. All children in the family aged 4–11 years were invited to complete questionnaires.
Personal information and demographic data
Fathers were asked to self-report information on date of birth, ethnicity, religion, spoken language, educational attainment, employment, marital status and household composition. The address of their (and their children’s) GP was requested in case of an incident at the session that would need to be reported.
Alcohol consumption
Alcohol consumption was measured using a frequency questionnaire used in the evaluations of the Australian programme. This asked about the number of days alcohol was consumed, average consumption per day and maximum consumption in a 24-hour period.
Dietary questionnaires
Two dietary questionnaires were used: a questionnaire developed and used by the local dietetic service that was sensitive to dietary behaviour changes in clinical practice and a food frequency questionnaire. The food frequency questionnaire assessed the type of milk consumed, the frequency of consumption of fruit, vegetables, soft drinks, fruit juice-based drinks as well as frequency of certain food-related behaviours: takeaway meals, eating in front of the television and consumption of snacks. In the local questionnaire, both fathers and children were asked to report whether or not they had eaten any fruit and vegetables in the previous 24 hours and, if they had, to estimate the portion size(s).
Father–child relationship
Father–child relationship was measured using the Parent–Child Relationships Questionnaire. 100 This has seven scales: prosocial, praise, intimacy, nurturance, shared decision-making, companionship and rationale, which are collapsed into two subscales: disciplinary warmth (six items) and personal relationships (eight items).
Parenting for physical activity
Parenting for physical activity was measured using items from two different questionnaires. Domains relating to family physical activity, screen use and eating patterns were from the Physical Activity Modelling subscale of the Activity Support Scale for Multiple Groups (ACTS-MG). 98 Items relating to physical activity and screen time were taken from the Parenting strategies for Eating and Activity Scale (PEAS). 99 Four subscales are reported: limit-setting, control, monitoring and disciplining in relation to eating and physical activity.
Family Nutrition and Physical Activity
The Family Nutrition and Physical Activity (FNPA) questionnaire was designed to assess family behaviours and environments related to children’s nutrition and physical activity. 104 It was completed by a parent or carer. The questionnaire has 20 items, composed of 10 subscales of two items each: (1) family meals, (2) family eating practices, (3) family food choices, (4) family beverage choices, (5) restriction and reward, (6) screen time, (7) creating a healthy environment, (8) family activity, (9) child activity and (10) family schedule/sleep routine. A low FNPA score may indicate an increased risk for the development of obesity.
Strengths and Difficulties Questionnaire
The Strengths and Difficulties Questionnaire is a parent- or carer-completed questionnaire that relates to child emotions and behaviours. 105 The scale has 25 items, with five subscales each of five items. The subscales are: (1) emotional symptoms, (2) conduct problems, (3) hyperactivity/inattention, (4) peer relationship problems and (5) prosocial behaviour. Total difficulties score is generated by summing scores from all the scales except the prosocial scale. The resultant score ranges from 0 to 40, and is counted as missing if one of the four component scores is missing.
Physical activity questionnaire
Fathers were asked to self-report physical activity using the short-form International Physical Activity Questionnaire (IPAQ). 95 The questionnaires asked fathers to report how much time they had spent doing vigorous and moderate physical activity, walking and being sedentary in the previous 7 days. The total minutes of walking and moderate and vigorous intensity activity per week was calculated by multiplying the minutes of an activity per day by the number of days per week the activity was reported. Metabolic equivalent of task scores of 3.3, 4.0 and 8.0 for walking, moderate intensity activity and vigorous intensity activity, respectively, were assigned as per the IPAQ scoring protocol. Total minutes of physical activity and minutes of moderate or vigorous activity were calculated.
Objective physical activity assessment
An objective measure of physical activity was recorded with participants and their eldest child using wrist-worn GENEActiv triaxial accelerometers. Participants wore the device on their non-dominant wrist for 7 days. Data were extracted from the devices using a bulk import Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) macro-enabled spreadsheet provided by the device developers. 108 Activity levels were assigned as ‘sedentary’, ‘light’, ‘moderate’ or ‘vigorous’ using previously published child- and adult-specific thresholds. 109,110 The data were then processed using Stata® 15 (StataCorp LP, College Station, TX, USA). A valid day’s wear was defined as > 10 hours’ wear time in a 24-hour period for all participants111 and pragmatic limits were set for valid activity levels: no more than 16 hours spent in sleep or sedentary or light activity and no more than 6 hours (children) or 8 hours (fathers) in moderate or vigorous activity. All data exceeding these limits were excluded from the analyses. Data were reported as median total minutes of physical activity and moderate or vigorous activity per week.
Participant randomisation (phase 2 only)
Father participants were block randomised using a 2 : 1 ratio of intervention-to-control group with stratification for the father’s ethnicity (white British or Irish/other ethnic group). The randomisation list was developed by the trial statistician and held in a secure database.
To ensure allocation concealment, after consent was taken and baseline measurements were complete, researchers entered the participant details into a secure, web-based randomisation website designed and maintained by the data programmers at the Birmingham Clinical Trials Unit and the system provided the participant’s treatment allocation. Participants were advised whether they were in the control or the intervention group first by text message then by a follow-up telephone call.
Control group (phase 2 only)
Participants allocated to the control group were provided with a voucher for one free family swim or use of a badminton court at their local leisure centre.
Intervention group
Participants of phase 1b and the intervention group of phase 2 were invited to attend the 9-week intervention programme detailed in Chapter 3. The times and locations of each session for both phase 1b and phase 2 are presented in Table 6.
| Phase | Venue | Course label | Session time | Facilitators | |
|---|---|---|---|---|---|
| Father-only education session | Children-only education session and joint father-and-child activity session | ||||
| Site A | |||||
| 1b | Primary school | Course A | Tuesdays, 16.00–17.30 | Local authority Healthy Lifestyles Team | Independent fitness instructor |
| 2 | Youth centre | Course 1 | Sundays, 13.00–14.30 | ||
| Site B | |||||
| 1b | Leisure centre | Course B | Wednesdays, 17.15–18.45 | University research team and leisure centre staffa | Leisure centre sport coaches |
| 2 | Course 2 | Leisure centre staff | |||
| 2 | Course 3 | ||||
| 2 | Community centre | Course 4 | Saturdays, 10.00–11.30 | Coaching organisation | |
Follow-up appointments to collect outcome data
Follow-up data collection appointments were completed with participants 3 and 6 months after the start of the intervention programme. The appointments were conducted using the same methods as at baseline, and were conducted either at the participants’ home or at the intervention venue. Table 5 shows the time points when each measure was collected. It was not always possible for the researcher undertaking the follow-up assessment to be blinded to a participant’s allocation group, as the research team that undertook measurements also completed observation of intervention sessions.
Iterative intervention adaptations during delivery
Between phase 1b and phase 2, the session materials were further developed and adapted based on researcher observations and participant and facilitator feedback. Session feedback and guidance was also provided during the course to the facilitators to ensure that delivery was optimised throughout.
Process measures
Collection of data measuring the fidelity of intervention delivery was a key component in assessing the feasibility. Three main methods were used for information capture; these were as follows.
Session observations and researcher reports
Observation checklists, completed by the research team, reported on factors such as timing of the session, involvement and engagement of participants in the sessions, quality of delivery and whether or not key components in the intervention were delivered as intended. The checklists were tested in phase 1b and refined for phase 2. The final checklist is shown in Appendix 3. The observation target was for researchers to observe at least two sessions of each intervention programme. Researchers also kept a reflexive log of their experiences or comments made by facilitators and participants that would not have been captured by the observation checklists.
Session feedback forms
After each session, participants and facilitators were asked to complete a feedback form to evaluate the session. Participants were asked to rate five statements on a five-point scale: ‘The session was enjoyable’, ‘I learnt a lot from this session’, ‘the information presented was easy to understand’, ‘the session motivated me to improve my family’s health’ (answer scale ranged from strongly disagree to strongly agree) and the ‘overall rating of the session’ (answer scale ranged from poor to excellent). There was also space to add additional comments. Facilitators were asked to report on the same questions, but their opinions related to the participants, that is ‘the fathers appeared to enjoy the session’, ‘the fathers appeared to learn a lot from this session’, etc. Responses were assessed numerically (1–5) with a higher score indicating a more positive rating. Facilitators were also asked to report on attendance at the session and confirm whether or not they had delivered the key elements of the session (presented in a list) and evaluate what went well, whether or not they encountered any significant barriers in delivery and their overall rating of the session.
Qualitative interviews
All facilitators and participants were invited to take part in a semistructured interview following the intervention. Interviews were conducted in participants’ homes or the venue of the intervention, or by telephone, based on participant preference. Interviews with facilitators were conducted at their place of work. A topic guide was used to guide the interviews [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/phr/1418513/#/ (accessed 25 November 2019)]. Informed consent was obtained before the interview and participants received a £10 gift voucher on completion. Audio files were transcribed verbatim, checked for quality and anonymised. Data were analysed following the framework approach112 and supported by NVivo 12. This approach allowed the research team to explore experiences of the HDHK among fathers and between fathers and facilitators, as well as across the different courses of the programme. Transcripts were coded inductively, bearing in mind the feasibility objectives, and summarised into an initial framework matrix. Themes and subthemes interpreted in the data set were discussed between the researchers (TG and KH) throughout the process to allow clarification and consensus of themes and the final analytic matrix.
Synthesis of process data
The process data were predominantly used to assess the feasibility of delivering the HDHK intervention sessions. Data to inform this research aim were organised under four themes: (1) the ability to recruit and train facilitators, (2) the ability to deliver sessions at a time and location convenient for participants, (3) the fidelity of session delivery and (4) the acceptability of the programme to participants. This section shows how each of the process data (shown in italic font) were used across the different assessment themes:
-
The ability to recruit and train facilitators, which was assessed by –
-
researcher experience – study team summary of their experiences of recruitment and training
-
facilitator interviews – facilitator experience of their training sessions
-
participant interviews and researcher observations of session delivery – as a proxy measure of participant and researcher experiences of facilitators’ delivery to reflect the ability to recruit and train facilitators who were acceptable and credible to participants.
-
-
The ability to deliver sessions at a time and location convenient for participants, which was assessed by –
-
researcher experience – study team summary of their experiences in organising session delivery
-
participant and facilitator interviews and observation checklists – facilitator and participant experiences of session timings and location and details on difficulties of venue and timings reported in observation checklists
-
attendance data – as a proxy measure for the ability to deliver sessions at a convenient time evidenced by attendance rates.
-
-
The acceptability of the programme to participants, which was assessed by –
-
participant interviews – participant experiences of the programme and their views of the content
-
participant and facilitator session feedback forms – participant feedback and facilitator-reported perception of participant enjoyment of the sessions
-
observation checklists – researcher observations reporting on perceived participant enjoyment and engagement with sessions.
-
-
The fidelity of delivery, which was assessed by –
-
observation checklists – researcher observations reporting whether or not key components of the intervention were delivered
-
facilitator session feedback forms – facilitator descriptions of what they delivered well or less well and any difficulties experienced
-
participant interviews – as a proxy for fidelity, the impact of the sessions on participant lifestyle changes to assess whether or not the key messages were delivered (and then implemented) by participants.
-
Sample size
As a feasibility study, a formal sample size calculation was not performed because it was not designed or powered to detect a statistically significant difference in weight change between the two treatment arms; rather, the aim was to assess if the adapted HDHK intervention is acceptable and deliverable, and also to assess whether or not the whole trial could be run as planned. Therefore, only some reasonably estimated recruitment figures were adopted to enable estimation of the feasibility outcomes with reasonable precision.
Non-randomised study (phase 1b) sample size
The total sample size for the non-randomised study was 30 fathers plus their children.
Two HDHK programmes with up to 15 fathers in each were conducted to explore the acceptability of the amended HDHK programme and trial processes.
Feasibility randomised controlled trial (phase 2) sample size
The total sample size for the feasibility RCT was 90 fathers plus their children.
Each HDHK programme aimed to recruit 15 fathers; thus, we aimed to randomise 60 fathers to the HDHK groups and 30 to the control group.
Qualitative research sample size
-
Phase 1b: the aim was to undertake two focus groups (n = 6–8 per group) with fathers who participated, individual interviews with fathers who dropped out of the programme before completion and interviews with the group facilitators (n = 4).
-
Phase 2: it was planned to interview fathers who dropped out during the intervention (up to n = 10), participants who completed the programme and participants who had a range of sociodemographic characteristics and family structures, as well as their partners and child(ren) (independently from the fathers when possible). We planned to interview up to 20 family groups on two occasions at 3 and 6 months, ensuring that they were sampled from across the different HDHK programmes delivered. We also planned to undertake one or two focus groups (or interviews if focus groups were not feasible) with programme facilitators at the end of the programmes with the aim of exploring experiences and perspectives of the trial. We also planned to interview up to 10 fathers who were randomised to the control group to ascertain their experiences and identify any behaviour change made as a family after joining the study.
Data analysis/statistical analysis
The statistical analysis plan provides details about the presentation and analysis for the quantitative results from phases 1b and 2. This report follows the statistical analysis plan dated 8 November 2018, apart from deviations from the plan, which are described and justified in Appendix 4.
All comparisons for phase 2 were made for (1) the HDHK-UK programme versus (2) minimum intervention (information about local opportunities for physical activity plus a voucher for the family to attend a leisure centre) control group. All analyses were performed by intention to treat. Participants were analysed in the intervention group to which they were randomised and all participants were included whether or not they received the allocated intervention.
We summarised categorical data by number of responses, frequencies and percentages. Continuous data are summarised by the number of responses, mean and SD, median and interquartile range (IQR).
We present baseline demographics for the fathers in phase 1b, and by allocated group and overall for the fathers, the eldest child and all children in phase 2. Baseline questionnaire scores are presented for fathers and the eldest child by allocated group and overall for phase 2.
We analysed feasibility outcomes by pooling the two groups and presenting overall estimates with 95% CIs, as well as by allocated group. The number of responses and percentages are provided with 95% CIs when relevant. We also present the number of forms completed and the form completion rate. We summarise weight change in fathers at the 3- and 6-month follow-ups using means, SDs and within-group 95% CIs.
All clinical outcomes are summarised by allocated group only. As the study is not powered to detect any treatment effects on clinical outcomes, we do not report p-values and 95% CIs.
We define adherence according to ‘completion of the intervention programme’ and evaluate it by the number of sessions that a family attended. A family that attended at least five out of the nine planned sessions is classified as completing the programme.
We present the number and percentage of fathers and children experiencing any serious adverse event (SAE) and suspected unexpected serious adverse reaction by group. Only overnight admissions to hospital due to injury or sudden illness during a HDHK session are reported as a SAE.
No subgroup analyses were planned for this feasibility study.
All analyses were undertaken in Stata version 12.
Health economics
The economic evaluation focused on the feasibility of cost and outcome data collection to inform a future trial evaluating the cost-effectiveness of the HDHK programme. An exploratory analysis was undertaken to assess the incremental cost of the interventions. The evaluation of the intervention effectiveness was not the focus; however, we measured the mean and SD of the Child Health Utility-9 Dimensions (CHU-9D) at various time points and assessed the level of completion for other resource use and outcome questionnaires detailed below.
Costs
For the interventions, resource use data were collected to capture all resources used for the delivery of the programme materials including costs related to handbooks and logbooks, additional information provided, room hire and staff training.
Utilisation of health services
Utilisation of health services for both fathers and their children was ascertained by asking fathers to report on the number of times in the previous 3 months that they, or their children, had seen their GP, practice nurse or pharmacist, attended an accident and emergency department, attended hospital as an outpatient or been admitted to hospital.
Health-related quality of life
Health-related quality of life was assessed in fathers using the EuroQol-5 Dimensions, five-level version (EQ-5D-5L) and in children the CHU-9D. The EQ-5D-5L96 is a standardised measure of health-related quality of life with five multiple-choice questions concerning different aspects of health: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each question requires the participant to select one of five ordered responses to indicate their level of problem with each domain. The permitted responses are chosen from one of the following: no problems = 1, slight problems = 2, moderate problems = 3, severe problems = 4, extreme problems/unable to perform activity = 5. The numbers assigned to each five-digit health state are then converted into an index value on a scale of 0 (representing death) to 1 (full health), with negative values permitted. These index values can then be used to construct quality-adjusted life-years (QALYs). The CHU-9D questionnaire was used to measure child quality of life; this is a validated,101–103 preference-based measure administered for use in health economic analyses. It comprises a descriptive system and a set of preference weights allowing the calculation of QALYs for use in a cost–utility analysis. The nine multiple-choice questions concern different aspects about how the child is today (worried, sad, in pain, tired, annoyed), school work/homework, sleep, daily routine and ability to join in activities; each requires the child to select one of five ordered responses to indicate their level of problem with each domain. The index score ranges from 0.33 to 1; higher scores are better.
Adult capability and well-being
The ICEpop CAPability measure for Adults (ICECAP-A) is a measure of capability for adults. 97 It focuses on well-being rather than health and comprises five attributes of wellbeing: (1) attachment (an ability to have love, friendship and support), (2) stability (an ability to feel settled and secure), (3) achievement (an ability to achieve and progress in life), (4) enjoyment (an ability to experience enjoyment and pleasure) and (5) autonomy (an ability to be independent). Coding is such that the ‘top’ level (full capability for an attribute) should take the value ‘4’, down to the bottom level (no capability), which should take the value ‘1’. Thus ‘44444’ represents the state described by full capability on all five attributes. A tariff value for an overall state can be calculated by summing the values across the individual attributes, whereby the values for each individual state are fixed and based on an official scoring method. The score ranges from –0.001 to 1; higher scores are better.
Both the EQ-5D-5L and ICECAP-A questionnaires were assessed for feasibility in this population to inform methods of an economic evaluation alongside a future trial.
Changes to the protocol
Changes to the protocol are described in Appendix 1 (see Table 30) and were all approved by the funder. Changes to the eligibility criteria for phases 1b and 2 were in response to recruitment challenges.
Chapter 5 Phase 1b: results
Despite overlap of processes for phases 1b and 2, the results of phase 1b are presented separately, as phase 1b informed processes used in phase 2. Much of this chapter is descriptive and, in places, presents methodological processes, which are included to provide context that would otherwise be lost.
Set-up and delivery of Healthy Dads, Healthy Kids sessions for the uncontrolled feasibility trial
Successfully aligning participant, venue and facilitator availability for the delivery of a course (courses A and B) at each site was a significant challenge. The process of recruiting sites for programme delivery, identifying and training facilitators who were then able to deliver the programme at the sites at the allotted time and recruiting participants is summarised in Figures 1 and 2.
FIGURE 1.
Descriptive timeline of processes in setting up delivery of the HDHK programme for WP1b at site A.
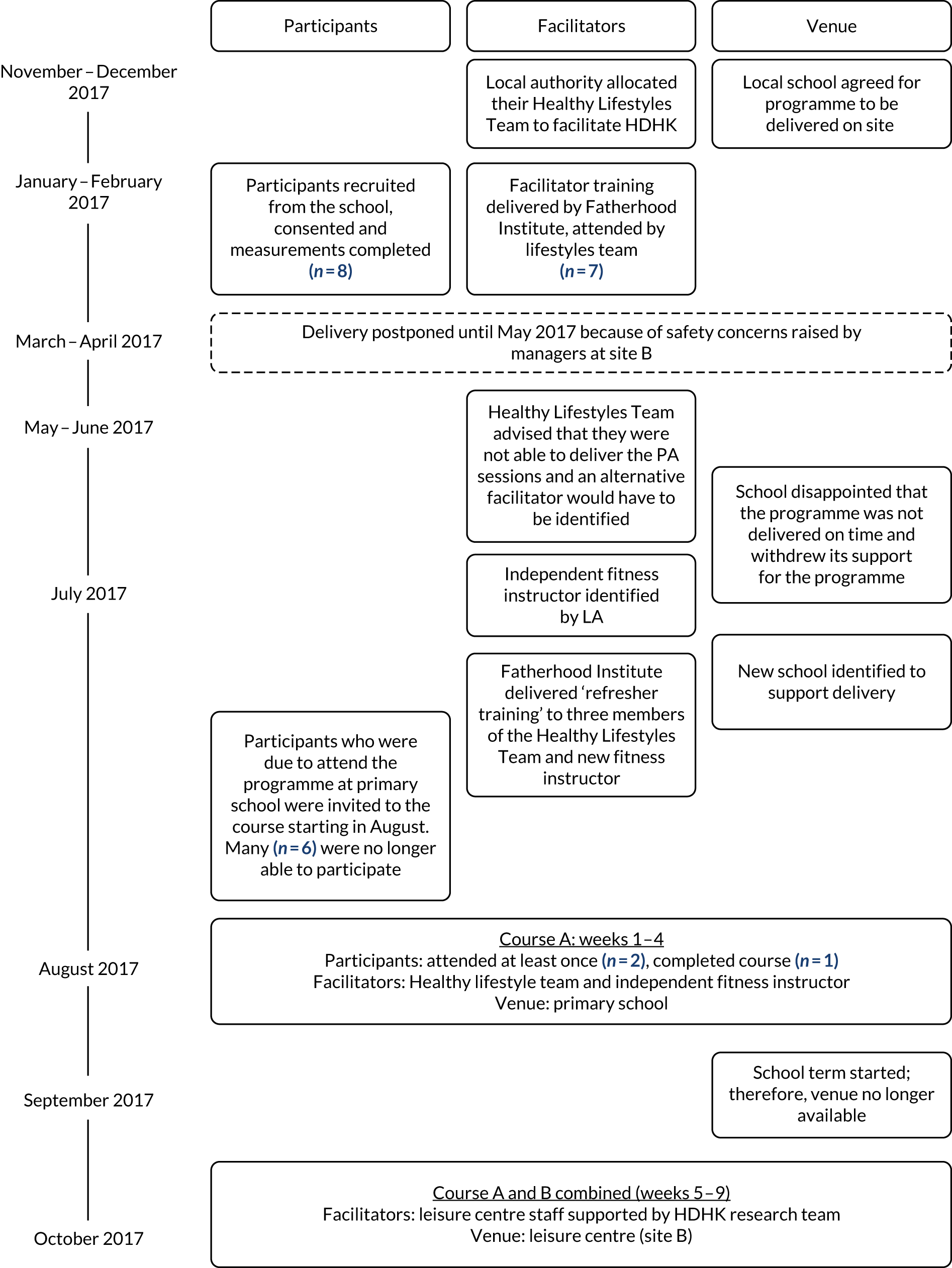
FIGURE 2.
Descriptive timeline of processes in setting up delivery of the HDHK for WP1b at site B.
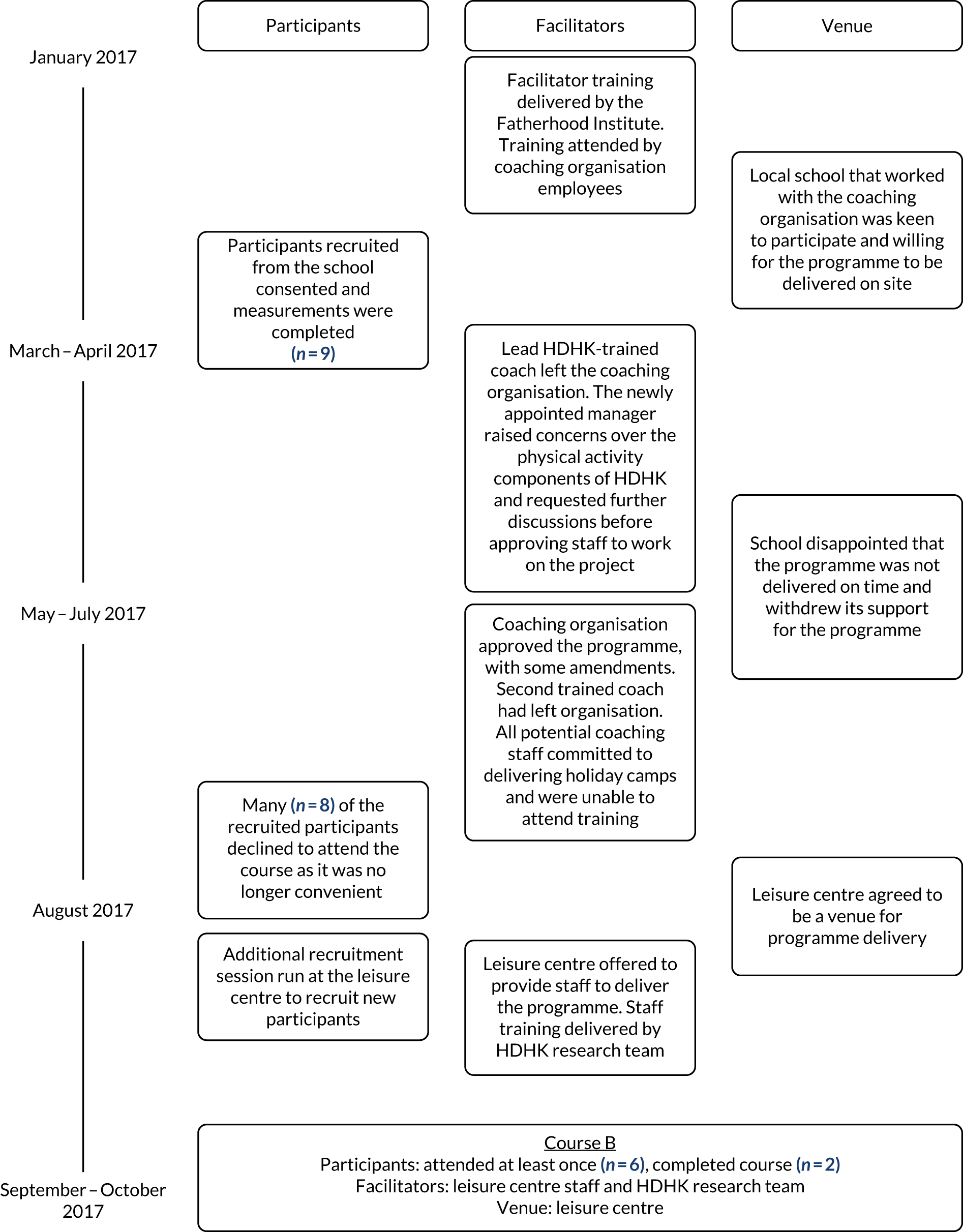
Site A (course A)
In November 2016, a local school was recruited to offer the HDHK programme as an after-school club commencing at 15.30, to their children’s parents with the programme delivered by the local authority Healthy Lifestyles Team. Following training of seven members of the Healthy Lifestyles Team as HDHK facilitators, there were a number of challenges:
-
Few of the staff trained as facilitators were able to add the extra commitment of HDHK-UK programme delivery within their working hours.
-
Delays resulted from concerns about the safety of some of the activities in the programme, which were raised by the organisation planning to deliver the intervention at the second local authority site (site B).
-
Delays resulted from concerns raised by a manager in the local authority about the ability of the Healthy Lifestyles Team to deliver the physical activity component.
-
It was difficult to recruit fathers.
-
Delays in programme delivery led to the need to provide top-up facilitator training.
-
One school was not willing to allow families who did not attend the school to join an after-school club.
-
A school withdrew support because of delivery delays.
-
A second school did not have availability of facilities for the full 9 weeks of the programme.
The first 4 weeks of course A were delivered at a primary school (16.00–17.30) by a member of the local authority Healthy Lifestyles Team (male) and an independent fitness instructor (female) (supported by the research team). Two participants attended the session: one father attended the first session only and one father attended weeks 1–4. As only one participant was attending by the fourth week, to try to facilitate his experience of a group setting, he was invited to attend weeks 5–9 of the course at site B (course B). Additional travel costs incurred by the participant were covered by the research study funding.
Site B (course B)
Two male staff members from the coaching organisation attended a facilitator training session delivered by the Fatherhood Institute in January 2017. Owing to existing links that the coaches had with local schools, one of them proposed delivery of the programme in one of his assigned schools. The school was supportive and the research team recruited nine participants by March 2017. Subsequent challenges encountered are summarised in the following list and in Figure 2:
-
The lead coach left the coaching organisation shortly after the training.
-
The new manager of the coaching organisation raised concerns about the safety and appropriateness of the HDHK programme.
-
A second coach who was trained to facilitate the HDHK programme left the coaching organisation.
-
A school that had agreed to host programme delivery was disappointed that the programme had been delayed and withdrew its support.
-
An alternative venue for programme delivery had to be identified; a leisure centre was chosen.
-
The coaching organisation’s staff were fully employed in holiday clubs over summer and unable to attend training.
-
There was a need to train new facilitators from the leisure centre quickly to meet time pressures.
-
Some recruited participants were no longer interested/available, additional participants needed to be identified.
Owing to time and cost limitations of running an additional training session delivered by the Fatherhood Institute, a pragmatic decision was made for one of the research team (TG) to run a training session with the leisure centre staff. There was a short turnaround between training and delivery of course B, so the father-education sessions were initially delivered by both the researcher (TG) and the leisure centre facilitators, with the leisure centre staff taking over full delivery as they became more confident. The first child-only and joint physical activity session of course B was delivered by the independent fitness instructor from site A with the leisure centre staff present. Although joint delivery was arranged for the first 3 weeks as a minimum, the leisure centre staff were qualified sports coaches and picked up the programme quickly, and were confidently running the sessions independently from week 2 onwards.
Owing to the delays, many of the recruited participants were no longer available to join the programme and only one participant confirmed attendance. Additional recruitment sessions were needed; however, finding time to complete baseline measurement appointments would have delayed the programme even further. Pragmatically, it was agreed that recruitment and measurement had already been tested with the originally recruited participants. Therefore, fathers who were recruited in August 2017 completed informed consent for the study but did not complete the baseline measurements or questionnaires. Observations showed that the leisure centre staff delivered the sessions to a high standard and were asked to continue delivery of the programmes for phase 2.
Delivery venues
Courses A and B were delivered in a primary school and leisure centre, respectively. Despite initial expectations that primary schools would be an ideal delivery venue, in practice they proved challenging to work with. The timing of session delivery was restricted by school opening hours, which meant that the sessions could not run on a weekend or after 18.00 (making attendance difficult for working parents). The availability of equipment in the schools at site A was limited, which made it more challenging to deliver the physical activity sessions. At site B, once the sports coach from the coaching organisation was no longer involved, the links with the school broke down and communication became difficult. In addition, access to school sports equipment was restricted unless the member of the coaching organisation was delivering the session. The leisure centre proved to be an ideal venue for delivery. The sports hall was bright and welcoming and there was a plethora of equipment to support the delivery of the physical activity sessions.
Participant recruitment
Participant recruitment was another significant challenge of this study. At site A, the local authority recommended schools that served ethnically diverse, socioeconomically deprived populations. These schools were approached to ask if they would be interested in taking part; three expressed an interest, and one of these three took part. The school that agreed to take part had approximately 500 pupils. Recruitment took place at the school gates at school pick-up times, and the school sent e-mails to parents and included information in school newsletters. A recruitment session was offered on the school premises after school. In site B, the school was identified by the coaching organisation. The school (with 450 pupils) that agreed to take part actively facilitated recruitment and fathers were approached at a parents evening, via e-mails to parents, at the school gate and during a school assembly. Despite extensive efforts, recruitment was challenging: communication with schools was slow, with delayed responses to e-mails and telephone calls from the identified links in the schools. Fathers’ interest in the study was low, with feedback primarily being that the course timings did not suit. We did not initially extend recruitment to other settings, such as other community and religious settings, because the school was not willing for families who did not attend the school to join the HDHK sessions.
Similarly, the recruitment sessions for course B that took place in August 2017 at the leisure centre were difficult. Few fathers were willing to engage with the research recruitment team, and others were not available to attend the sessions because of other commitments.
Data collection: baseline appointments
It was difficult to book appointments for baseline data collection that suited both fathers and their children. Many of the appointments were after work, when congestion on the roads is at its greatest, adding significant travel time outside typical working hours for the research team. Weekend appointments were offered to participants, but often these clashed with family weekend activities. Despite repeated reminders to the participants of the appointment slot and encouragement for them to contact the team to rearrange if they were no longer available, there were still many failed appointments where researchers would attend the participant’s house to find that they were no longer available, did not have enough time to complete the measurements or had forgotten about the appointment and were not at home. This added significant time and financial costs to the study.
Characteristics of recruited participants
We collected baseline data on 17 fathers (Table 7). We successfully recruited participants from BAME groups (52.9%) and fathers living in socioeconomically disadvantaged communities (70.6% lived in the 20% most deprived of localities in England). Participants’ mean BMI was 31.8 kg/m2 (SD 3.3 kg/m2) and 12 (70.6%) were married or in a civil partnership.
| Characteristic | HDHK-UK programme (N = 17) |
|---|---|
| Ethnicity, n (%) | |
| British | 8 (47.1) |
| Latvian | 1 (5.9) |
| Indian | 2 (11.8) |
| Afghani | 1 (5.9) |
| African | 4 (23.5) |
| Caribbean | 1 (5.9) |
| Missing | 0 (0) |
| Age (years) | |
| Mean (SD) | 41.1 (7.5) |
| Minimum, maximum | 29.4, 63.0 |
| Missing (n) | 0 |
| BMI (kg/m2) | |
| Mean (SD) | 31.8 (3.3) |
| Minimum, maximum | 26.3, 38.4 |
| Missing (n) | 0 |
| Percentage body fat (%) | |
| Mean (SD) | 30.2 (5.1) |
| Minimum, maximum | 22.5, 42.3 |
| Missing (n) | 0 |
| Waist circumference (cm) | |
| Mean (SD) | 104.9 (9.3) |
| Minimum, maximum | 88.0, 125.0 |
| Missing (n) | 5 |
| Highest level of qualification, n (%) | |
| No formal qualification | 1 (5.9) |
| GCSE, CSE, O level or equivalent | 5 (29.4) |
| A level/AS level or equivalent | 2 (11.8) |
| Degree level or higher | 8 (47.1) |
| Other | 0 (0.0) |
| Missing | 1 (5.9) |
| Age (years) when completed continuous full-time education | |
| Mean (SD), n | 20.1 (5.1), 15 |
| Minimum, maximum | 15.0, 31.0 |
| Never went to school, n (%) | 1 (5.9) |
| Missing, n (%) | 1 (5.9) |
| Legal marital or civil partnership status, n (%) | |
| Married or in a registered civil partnership | 12 (70.6) |
| Separated, but still legally married or in a civil partnership | 0 (0.0) |
| Divorced or formerly in a civil partnership that is now legally dissolved | 2 (11.8) |
| Widowed or surviving partner from a civil partnership | 0 (0.0) |
| Never married and never registered in a civil partnership | 2 (11.8) |
| Missing | 1 (5.9) |
| Number of additional adults (aged ≥ 18 years) living in the same household as participant, n (%) | |
| 0 | 2 (11.8) |
| 1 | 13 (76.5) |
| 2 | 0 (0.0) |
| 3 | 1 (5.9) |
| Missing | 1 (5.9) |
| Number of children living in the same household as participant, n (%) | |
| 1 | 4 (23.5) |
| 2 | 7 (41.2) |
| 3 | 4 (23.5) |
| 4 | 0 (0.0) |
| 5 | 1 (5.9) |
| Missing | 1 (5.9) |
| Number of children (not necessarily co-resident), n (%) | |
| 1 | 2 (11.8) |
| 2 | 7 (41.2) |
| 3 | 5 (29.4) |
| 4 | 0 (0.0) |
| 5 | 2 (11.8) |
| Missing | 1 (5.9) |
| Number of children of preschool age, n (%) | |
| 0 | 9 (52.9) |
| 1 | 5 (29.4) |
| 2 | 2 (11.8) |
| Missing | 1 (5.9) |
| Number of children of primary school age, n (%) | |
| Reception, school years 1 and 2 | |
| 0 | 7 (41.2) |
| 1 | 8 (47.1) |
| 2 | 1 (5.9) |
| Missing | 1 (5.9) |
| School years 3–6 | |
| 0 | 8 (47.1) |
| 1 | 4 (23.5) |
| 2 | 4 (23.5) |
| Missing | 1 (5.9) |
| Number of children of secondary school age (school years 7–11), n (%) | |
| 0 | 11 (64.7) |
| 1 | 4 (23.5) |
| 2 | 1 (5.9) |
| Missing | 1 (5.9) |
| Number of children in college/sixth form, n (%) | |
| 0 | 15 (88.2) |
| 1 | 1 (5.9) |
| Missing | 1 (5.9) |
| Number of children aged ≥ 18 years, n (%) | |
| 0 | 15 (88.2) |
| 1 | 0 (0.0) |
| 2 | 1 (5.9) |
| Missing | 1 (5.9) |
| Religion, n (%) | |
| None | 3 (17.7) |
| Christian | 12 (70.6) |
| Islam/Muslim | 1 (5.9) |
| Missing | 1 (5.9) |
| Main spoken language, n (%) | |
| English | 13 (76.5) |
| Lithuanian | 1 (5.9) |
| Latvian | 1 (5.9) |
| Ghanaian | 1 (5.9) |
| Missing | 1 (5.9) |
| IMD quintile, n (%) | |
| 1 (least deprived) | 0 (0.0) |
| 2 | 0 (0.0) |
| 3 | 1 (5.9) |
| 4 | 4 (23.5) |
| 5 (most deprived) | 12 (70.6) |
| Missing | 0 (0.0) |
Intervention session attendance
Attendance and completion of sessions is shown in Figure 3. In total, across both sites, eight participants attended at least one session and two participants (25%) completed the programme, that is they attended at least five of the sessions.
FIGURE 3.
Session attendance for WP1b. a, Owing to small numbers, the participant was invited to complete the course at site B.

Participant experiences of the programme
Participant experiences of the programme were collected through qualitative interviews with three fathers, two of whom completed the programme (father 1 and father 2), and one who had attended only one session. Feedback was also collected from session feedback forms. The data were collected to test the interview schedule and session feedback forms ahead of phase 2, but some of the participant feedback was also used to inform the implementation of phase 2. Owing to the small sample size, the data are not presented thematically but as a narrative of findings that informed the delivery of phase 2.
The overall feedback on the course was positive, which confirmed that, overall, the course was acceptable to the participants and there were no major concerns taking it forward to phase 2:
I’ve just found it quite . . . quite a powerful experience in terms of yeah, just being able to, I guess just reassess where we were with it all and the things that we’ve let slip . . . and yeah, the value for me especially has come from seeing my children thriving in sports . . . I think it was a brilliant scheme and I can really see the value of a scheme like this in, yeah, in any dad’s life.
Father 1
It’s been a great experience, I can’t say that I’ve kind of done 100% of what I’ve learned, but I’ve definitely made a start and seen the benefits of it in terms of lost some extra pounds and got a bit more fitter and run a bit longer, a bit better, a bit further and spent some quality time with the kids.
Father 2
When asked about the facilitators, one participant preferred the more discursive approach that was adopted by the facilitators as the programme progressed; similarly, the researchers observed this to be a good approach. Therefore, the discursive approach was recommended for facilitators in phase 2:
I think they got better throughout the weeks . . . there was definite progression . . . at the start, a couple of weeks it was very much things were read off the projector . . . But towards the end there was a real shift . . . it went from just presenting the material to using the material as a prompt and a platform to inspire discussion and inspire the sharing of experience, which was a really positive, for me anyway, a really positive outcome of the sessions.
Father 1
The facilitator’s upbeat supportive demeanour was appreciated, and emphasised the importance the role the facilitators had in helping the participants to feel at ease. Facilitators were encouraged as part of the conversations with the research team ahead of phase 2 to be positive and welcoming for the subsequent courses:
. . . it was quite nice that [facilitator name] was always there well in advance and would always welcome us in. And again, he was just brilliant with the kids and the kids enjoyed going in and they’d race up to him and give him a high five.
Father 1
The one that jumps out to me is the openness from the get-go really. There was no awkwardness in communication, there was no kind of, there was no like settling in period, it felt very welcoming and it’s true for all of them [facilitators] really; they really made a good effort.
Father 2
Similarly, the feedback for the sports coaches was positive. One participant was exceptionally positive about the coaching skills, and the benefit of their experience and skill set for the programme was also observed by the researchers. This was carried across to WP2 and emphasised the importance of recruiting facilitators with coaching skills to deliver the physical activity elements of the programme, a key reason continued efforts were made (despite the delays) to engage with the coaching organisation for delivery of at least one course in phase 2:
The two guys were brilliant . . . the quality of the coaching was there enough that the kids made some brilliant progress . . . they [participant’s children] both now own a tennis racket each ‘cause they really enjoyed playing tennis. They try and get to the park regularly and knock a ball around and they still talk about kind of the hints and tips and the coaching methods that were used. And on the way to school they try and jump over everything and leap over things and again kind of refer back to the kind of coaching that was given within the sessions. So it’s been something we’ve been able to really take forward and build on, those coach sessions.
Father 1
The four children of the fathers who took part in courses A and B were all aged < 7 years. Researchers and facilitators observed that some of the elements of the children’s workbook were too advanced for the younger children, but the younger children still engaged well with the facilitators. One father commented that they really appreciated that they were actively involved in the programme:
The reward system I think for my two children, being slightly younger. They really enjoyed each week filling up their chart and going off then and feeling like there was a real value to completing the tasks and completing the kind of homework elements, that they came back next week ready and eager to be able to show what they’ve done and earn their next sticker on their chart . . . They loved trying a new sport and bits like that, but I think they also enjoyed having a, yeah, having a responsibility and a specific role within the process that they knew that they had targets that they had to get Daddy to do and for them they really enjoyed that.
Father 1
The timing of sessions was a challenge, and was the main reason that the non-attenders could not complete the programme:
Just the timing yeah, I just I couldn’t get away from work early enough to get to [venue name] for five.
Father 3
Another participant who was not interviewed was also not able to complete the course for the same reason: it clashed with other evening commitments. It was also noted that the evening sessions were late for young children, although the challenge of finding a suitable time was acknowledged:
Timing, again having younger children was a bit of a challenge as the kind of sessions didn’t tend to finish till quarter to seven, seven o’clock and my children’s bedtime kind of starts about seven o’clock . . . it was a bit of a challenge but it was still knowing it was only 9 weeks and we’d planned in for that. But again, I don’t know how else it would have been done because if it started earlier I’d have struggled to feed them tea before we got there. And it felt like the hour and a half did just race by and I think if it was any shorter a session then we wouldn’t have got the same value from it for the two sections to work as well as they did. So there is, whilst it was a bit of a challenge finishing later, it was workable and I couldn’t offer a better solution than the solution that is.
Father 1
Neither of the participants could think of any significant negatives to the programme and most of the changes made to the session content ahead of phase 2 were based on researcher observations. One participant did mention that at times the PowerPoint presentation did not match the handbook (also identified by the researchers and the facilitators) and this was remedied for WP2. Similarly, the importance of the facilitators being comfortable with delivery and familiar with the materials from session 1 of the courses was important and highlighted the benefit of running the courses in phase 1b:
I think there was those first couple of weeks where it was just, it felt, yeah, that it was just going to be a bit of a presentation of literally what we were reading on the screen. But easy to see now that was just everybody getting used to the kind of programme but then once you going, no, I thoroughly enjoyed the sessions and enjoyed the discussion.
Father 1
Both participants spoke positively of lifestyle changes that they had made as a result of the programme, suggesting that the key messages of the programme were being delivered with impact. Both participants spoke about making more efforts to increase the amount of walking:
I’m moving throughout the day and more consciously choose to kind of go for a walk at lunchtime and just to get my steps up a bit.
Father 1
I’ve made good use of my fitness well app that the facilitator suggested and I’ve started looking after what I eat, how much I eat, when and planned my food intake as opposed to not doing it at all. And personally for me it’s helped, I’ve lost a bit of weight and it’s still coming down close to where it should be.
Father 2
One of the things that we’d started doing, doing Healthy Dads, from the challenges that we’re set was to walk more . . . once a week on the way home from school . . . we’ll go on a big long walk and go and find and do an adventure somewhere and that’s something the kids have really enjoyed and I’ve really valued, actually finding that time in the week . . . it’s become more of a tradition now that we do . . . and have really grown to value the time that we spend together doing these walks which has come, yeah, straight off the back of the Healthy Dads programme.
Father 1
Further monitoring of participant feedback for sessions were the weekly session feedback forms, which were completed at all but one session (in error, forms were not handed out at session 5) by the participants. The forms were well completed, suggesting that they were acceptable to the participants and were carried forward to be used in phase 2. The results of the feedback again highlighted that the participants rated the sessions highly (Tables 8 and 9).
| Statement | Mean scorea |
|---|---|
| This session was enjoyableb | 4.76 |
| I learnt a lot from this sessionb | 4.59 |
| The information presented in this session was easy to understandb | 4.70 |
| The session motivated me to improve my family’s healthb | 4.69 |
| Overall I would rate this session asc | 4.70 |
| Session number | Comments |
|---|---|
| 1 | Conversations with kids, finding out more about their interests was something I rarely have had time to do so I enjoyed this session |
| 2 | Very fun and enjoyable, kids got a little tiredReally enjoying time spent with children and the skills they are gainingI particular enjoyed the concept of SMART goals that could make it easier to lose weight and change bad habits |
| 3 | I liked tips on how to lose weight – simple to implement and maintainPhysical activities was varied and enjoyable |
| 4 | Enjoyed finding about things to do and not to do to get kids eating healthy at home – definitely an area we can improve on |
| 6 | Good session, difficult to always match slides to handbook. Good to see the children trying new skills and enjoying themselves |
| 7 | Very thought-provoking session, bit more discussion which was good. Love seeing the progression the kids are making in the FMSFocusing on certain areas of physical development catching/throwing etc. That helps me to identify which games to play more at home |
| 8 | This lesson has helped me to understand that I need to focus more on meaningful conversations and interaction with my kidsThought-provoking session, good practical elements to take away. Well presented without too much reliance on slides. Enjoyed the discussion time |
| 9 | Good recap and time to reflect on all the changes made. Really enjoyable and positive experienceA great experience, it has helped me to identify the opportunities in everyday life to spend more time with my children |
Iterative intervention adaptations during delivery
Researchers attended and observed every session for phase 1b (courses A and B), often assisting with delivery as previously described. The first 4 weeks of the programme were delivered in course A before course B; therefore, it was possible to make changes and test these out in course B for the first four sessions. Researcher observations and experience of delivery, and facilitator feedback, formed the basis for much of the amendments made throughout the programme delivery. Facilitator feedback was obtained informally through discussions between the researchers and facilitators following each session and also in a formal facilitator interview. However, all but one of the facilitators who were interviewed post intervention had delivered courses for both phase 1b and phase 2. Therefore, when interviewed, they mostly spoke of their experiences of the programme as a whole, rather than separately by work package. Many of the findings from these interviews are presented in Chapter 6. One facilitator only presented phase 1b; some findings from his interview are presented here. The identification code to indicate their quotations are, for example, ‘P1b.B-FE1.M’, to denote the work package (phase 1b or 2) delivered, the site (A or B), section of session delivered (FE: father-only education), ID number (1) and the facilitators gender (M: male).
The main change for the father-only education sessions was to reduce the volume and complexity of information delivered, as these sessions were challenging to deliver for the facilitators and often ran over time, which meant that there was less time for the joint physical activity sessions. This was mainly picked up by researcher observations but also commented on by both a facilitator and a participant during their interviews:
There was a bit too much information and probably going into a little bit too much depth, I’d say, for the type of clientele that we get to the groups but then I do think you need a bit of a wide variety. I do feel that when we’re delivering the presentations that sometimes, we were rushing at times and yet we still ended up going over by quite a bit of time.
P1b.A-FE1.M
Sometimes, and this is when we kind of over-run the presentation part, time wise, when they had prepared some game and not always they have the chance to play with me during the activity part because we run out of time. So that’s what they [participant’s children] were sometimes slightly down about, but other than that, they were really happy, really enjoyed it.
Father 2
Some content of the session was also considered by researchers and facilitators to be unnecessarily complex for the audience. The facilitator drew on his experience of working in the community to consider the suitability of the materials:
. . . I think for this particular area, going back to what I said, I think it might have been a little bit too complex for some of the dads. In terms of the people that we see day to day with healthy lifestyles, I think some of them may have struggled to take in the information that we were working with and we were delivering to them. In terms of the parent that we saw, it was no problem for him.
P1b.A-FE1.M
Therefore, the research team simplified some sections to ensure that participants remained engaged with the programme. An example of this change is a component of the week-2 session, which asked participants to calculate their daily energy needs using maths equations. The materials were changed such that the participants’ daily energy needs were explained, but much of the calculation was completed for them and they were signposted to a website that could do the calculation for them in the future.
In general, the child-only sessions required little amendment. Small changes were made to the children’s handbook, mainly to make it simpler for completing, especially in the tasks that children were asked to select for participation with their fathers. The content of the physical activity sessions worked well and, similarly, required little amendment. The most pressing challenge was fitting the session into the allocated time slot, compounded by the father’s education sessions running over time.
Key learning points from phase 1b
While acknowledging the limitations of the small number of participants who attended the intervention and were interviewed, there were learning points for the delivery of phase 2. In summary, phase 1b helped to inform phase 2; the key findings are detailed in the following sections.
Facilitator skill requirements and training
-
A strong skill set of presentation skills (for father-education sessions) and physical education skills (for the physical activity sessions) were important for successful session delivery.
-
The skills of a facilitator to be positive, enthusiastic, professional and welcoming were seen as important by the participants.
Delivery venues
-
Schools were challenging to work with because of the restrictions of their opening hours combined with fathers’ working patterns.
-
Leisure centres were a good location for delivery.
Participant recruitment and retention
-
Recruiting fathers to take part in the programme was more challenging and time-consuming than anticipated; thus, more resources and a wider network would be needed for future recruitment. A key challenge was the researchers obtaining direct contact with potential participants.
-
The participant measurement process was challenging and resource intensive because of many failed appointments and participants not being available at pre-agreed times.
-
Once recruited, participants completed the measurement assessment sessions without difficulty.
Intervention delivery and content
-
It was necessary to reduce the quantity of, and simplify, the content of the father-only education sessions to try to keep the sessions to 30 minutes’ duration.
-
Participants preferred a more interactive, rather than directive, style for the father-only education sessions.
-
Identifying suitable session times to meet participant, facilitator and venue availability was challenging.
Chapter 6 Phase 2: results
The results are presented using synthesised data from several different sources to address each research objective. This chapter presents the results in three sections:
-
the feasibility of delivering an adapted HDHK programme
-
the feasibility of recruitment and follow-up
-
the feasibility of a definitive trial.
Data collected
As explained in Chapter 4, the findings from different data sources are integrated into each section of the results; therefore, for clarity, this section presents the availability and summary of data from the different sources used to inform the results section.
Qualitative data
Thirteen interviews with 12 participants from phase 2 were completed at either 3 or 6 months post intervention; one participant completed an interview at both time points. The average interview duration was 16 minutes (range 7–29 minutes) and interviews were completed either face to face (n = 4) or by telephone (n = 9). Identifying participants to take part in an interview proved challenging: most participants declined to be interviewed, citing being too busy, or repeated attempts to contact them to arrange the interview time were unsuccessful. Although it was intended that children would be interviewed with their fathers, for pragmatic reasons this was not possible as the children were too young to take part in the qualitative evaluation. The preferred interview method was face to face, but many participants chose to be interviewed by telephone for their own convenience. All facilitators who delivered the sessions, including the father- and children-only educational sessions and the joint physical activity sessions, were interviewed post intervention. The characteristics of participants who were interviewed are shown in Table 10. The letter preceding the participant IDs indicates the site (A or B). The facilitator ID codes indicate which section of the HDHK sessions a facilitator delivered as follows: FE – fathers-only education session; CEFPA – child-only education session and family physical activity; and M or F – male or female. As with participants, the letter preceding a facilitator’s code indicates at which site they delivered sessions.
| ID | Time point of interview (post intervention) (months) | Interview method | Number of HDHK sessions attended/delivered | Timing of session attended/delivered |
|---|---|---|---|---|
| Participant interviews | ||||
| B-008 | 6 | Telephone | 6 | Weekday evening |
| B-040 | 6 | In person | 9 | Weekday evening |
| B-041 | 3 and 6 | Telephone and in person | 6 | Weekday evening |
| B-066 | 3 | Telephone | 0 | – |
| B-068 | 3 | Telephone | 8 | Weekday evening |
| B-074 | 3 | In person | 7 | Weekday evening |
| B-075 | 6 | Telephone | 0 | – |
| B-082 | 3 | Telephone | 7 | Weekend |
| B-089 | 3 | In person | 9 | Weekday evening |
| A-058 | 3 | Telephone | 5 | Weekend |
| A-072 | 3 | Telephone | 8 | Weekend |
| A-077 | 3 | Telephone | 9 | Weekend |
| Facilitator interviews | ||||
| B-FE1.M | 3 | In person | 13 | Weekday evening |
| B-FE2.M | 3 | In person | 11 | Weekday evening |
| B-FE3.F | 3 | In person | 9 | Weekend |
| B-CEFPA1&2.M | 3 | In person | 21 and 17 | Weekday evening and weekend |
| A-FE1.F | 3 | In person | 5 | Weekend |
| A-CEFPA1.F | 3 | In person | 7 | Weekend |
Observation checklist data
Researcher-completed observation checklists were available for 16 sessions (Table 11). In most cases, only one researcher attended the session; therefore, when the fathers and children were in separate sessions, they could observe only one of the two. Six father-only educational session observations were completed and 12 children-only educational sessions were completed. There were more children session observations as three of the research team completing observations were female and it was seen that their presence in the father-only education sessions, when these were delivered by male facilitators, affected the dynamics of the session.
| Course | Session | Total, n/N (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| 1 | ✓ | ✓ | ✓ | ✓ | * | 4/8 (50.0) | ||||
| 2 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6/9 (66.7) | |||
| 3 | ✓ | ✓ | ✓ | 3/9 (33.3) | ||||||
| 4 | ✓ | ✓ | ✓ | 3/9 (3.3) | ||||||
| Total (n) | 3 | 3 | 2 | 2 | 1 | 0 | 1 | 1 | 3 | 16/35 (45.7) |
Participant and facilitator feedback forms
Based on the number of participants attending each session, 144 participant feedback forms should have been distributed across all four courses. Of the possible 144 forms, 118 were completed (81.9%). The facilitators delivering the fathers-only educational session completed 26 of a possible 36 forms (72.2%) and the facilitators delivering the joint physical activity session completed 41 of a possible 55 forms (74.5%). (Further details are available in Appendix 5.) Facilitators advised that reasons for non-completion of feedback forms were that they forgot to give out the forms at the end of the session or participants were in a rush to leave.
The Healthy Dads, Healthy Kids session attendance data
Facilitators of each course were asked to complete attendance registers for each session; this was done.
Study recruitment
Owing to the wide range of methods used for recruitment, including recruitment stands, leaflet distribution and social media posts, it was not possible to identify a denominator for reach-in recruitment.
Questionnaires and anthropometric data
Questionnaire and anthropometric data were available from participants at baseline and at the 3- and 6-month follow-ups.
The feasibility of delivering an adapted Healthy Dads, Healthy Kids programme
Ability to recruit and train facilitators
Researcher experience
Facilitator recruitment
Phase 2 was implemented by facilitators who were mainly recruited and trained in phase 1b; the description of this process is presented in Chapter 5. The one exception was that the new staff from the coaching organisation were not identified until December 2017; therefore, they received their training in January 2018, ready for the delivery of course 4. The delays in recruiting facilitators from the coaching organisation were due to unique barriers [see Chapter 5, Site B (course B)], staff turnover and changes in local managers. During the delivery of course 1 (site A), the local authority level underwent a restructure, which meant that, a few weeks after course 1 finished, the trained facilitators from the Healthy Lifestyles Team were no longer employed by the local authority (and were therefore not available to deliver any more courses), and the independent physical activity facilitator was leaving the area. Recruitment of new facilitators at such a late stage of the study was attempted, but without success, and the facilitators from site B were not able to travel to site A because of the distance of travel. In addition, researcher experience of participant recruitment at site A was exceptionally challenging; schools were not willing to engage with the study and participant interest through all methods of recruitment was poor. Despite extensive recruitment efforts for the second course at site A, only one participant was recruited. Compounded by long travel time from the University of Birmingham to site A (often > 70 minutes), there was significant strain on researcher’s time and capacity at a key time when recruitment at site B needed to be optimised. After considering the possible options, the research team took the decision to cease delivery of the HDHK programme at site A and deliver an extra course at site B.
Facilitator training
As outlined in Chapter 4, owing to the changeover of staff and significant delays experienced during the training phase, several different training sessions were delivered. The original intention was that all of the facilitators would complete a training course with the Fatherhood Institute, delivery of phase 1b would identify difficulties with the content and then phase 2 would be delivered with just light support from the research team. The reality, with the staff turnover and shortened time scales, was that it was necessary to retain support for facilitators from the research team through both work packages, which added significantly to the workload of the research team. This was not a reflection of the facilitators, who worked admirably in difficult circumstances, but rather a result of shortened time scales due to the delays experienced in delivering phase 1b and evolving programme materials in a short time frame between phases 1b and 2.
Facilitator interviews
Facilitators’ experiences of their training were obtained from qualitative interviews, by asking ‘what did you think of the training you received?’, and are presented in Table 12.
| Training session | Facilitator feedback |
|---|---|
| Central training session delivered by Fatherhood Institute | I think the training was fine for such as myself because I am used to working with children and all types of peoples from myself . . . I don’t think I needed any more training, I think that I was fine, yeah, I was fine with itA-CEFPA1.F |
| One-to-one session with researcher (TG) followed by observation of researcher delivery and week-by-week consultations with research team | Honestly, because we had that quick turnaround, it was quite rushed. So you came to site and did the, ‘Here’s the basic introduction’, a lot of information quite quickly. But the ongoing stuff of, ‘OK, here’s how I want this week to feel. Here’s the theme of it. You’ve read the pre-pack now let’s have a chat about it,’ that worked a lot betterB-FE1.M |
| One-to-one session with researcher (TG) followed by observation of colleague delivery and week-by-week consultation with colleague and research team | It was really good so I shadowed [B-FE1.M] for I think it was half of the last session before I started in and then each week me and [B-FE1.M] would sit down together, go through the presentation. He’d give me kind of the feedback on how he got on and then he’d give me things that he thought worked well when he did it that I could use to implement when I didB-FE2.M |
| One-to-one session with researcher (TG) followed by week-by-week consultation with research team for first course. Central researcher delivered training session at University of Birmingham | Yeah, so, like, the first part when I was doing on job it was like, it’s kind of like, not thrown in at the deep end but like I kind of just had to learn as I was doing it. But it was good . . . And because I was familiar with the surroundings and I’d kind of done a lot of coaching before, we kind of looked at lesson plans, adapted it a little bit and it was fine. On top of the training I did attend uni[versity], that was obviously really helpful . . . [second programme] was a lot more structured and I think it ran better and it was because of the training. The training were good, couldn’t have faulted it at all. Obviously the 4 weeks, the first 9 weeks was obviously a bit of a learning curve, but it was fine, so yeah, I can’t fault the training at allB-CEFPA1.M |
| Central researcher delivered training session at University of Birmingham and weekly consultations | Training was great. I was quite worried when I agreed, no, I wasn’t worried, I was excited, but you feel like, you know, what am I doing?, what is it all going to be about?, and once it came to the training, you kind of gave us all the information we needed and that really settled me and got me excited for it. Instead of that stomach ‘oh, what’s going to happen?, am I going to be OK?’. But yeah, after the training, I didn’t feel like that at allB-FE3.F |
Participant interviews
As a proxy measure, participants’ experiences of facilitators during the courses are presented, reflecting on the ability to recruit and train suitable facilitators for session delivery. Participant comments on the father-only facilitators showed that they appreciated the relaxed and interactive delivery style:
They were good and interactive.
D B-041
I think it was really informative. I think they were really clear. They encouraged a lot and they gave alternative ideas if you might be stuck. They were really good. Yeah, really good.
ID B-068
Fantastic, very well presented, well engaging, knowledgeable.
ID A-058
She was really good and she’d happily take time out to meet you after the sessions or before the sessions; she was always there on time so she was really good and it varied.
ID B-082
Great. You could have a laugh with him but he brought it down when he needed to bring it down.
ID B-008
Comments were equally positive in reference to the facilitators who ran the child-and-father physical activity sessions:
Yeah, brilliant, again. I think the kids benefitted more from that than I did, but they were very friendly. Again, they were very informative. I think they were able to present from a child-friendly perspective, that was good.
ID B-068
They were excellent, really good lads. They explained things, they never made it dry, it didn’t seem to go on for ages. We were always busy, always sweating, it was all good, all the way around.
ID B-089
I thought they were good. It’s quite difficult when you’ve got a mixed-ability group with the Healthy Dads, Healthy Kids, but because it was more a circuit training it allowed you to almost progress at your own pace.
ID A-077
Researcher observations
Data from the observation checklists are also positive; researchers reported that the facilitators delivering the father-only sessions were approachable and friendly (‘strongly agree’, n = 5; ‘agree’, n = 1) and had ‘excellent’ (n = 4) or ‘good’ (n = 2) rapport with the group. For ‘clarity of communication’, four observations rated the facilitator as ‘excellent’, one rated the facilitator as ‘good’ and one as ‘OK’. Five observations reported the facilitator to be ‘fully prepared’ and one reported ‘somewhat prepared’.
Observations were similar for staff facilitating the child-and-father physical activity sessions, who were rated as being approachable and friendly (‘strongly agree’, n = 10; ‘agree’, n = 2) and clear in their communication (six observations rated the facilitator as ‘excellent’, three rated the facilitator as ‘good’ and three as ‘OK’). Eight observations reported the facilitator to be ‘fully prepared’, three observations reported the facilitator to be ‘somewhat prepared’ and one observation reported ‘not at all prepared’.
The free-text notes section of the checklist were, in the main, positive, but highlighted a few sessions for which it was felt that the facilitators’ preparation needed improvement.
Comments from researcher observations on the facilitators who delivered the fathers-only sessions were as follows:
Facilitator was slightly nervous, however very engaging.
Facilitator was very enthusiastic and encouraging. Drew on her stories and ideas, had clearly learnt the session inside out and referred back to previous weeks. The session was a little repetitive but that was the slides rather than facilitator’s delivery (fathers-only session).
Comments from researcher observations on the facilitators who delivered the physical activity sessions were as follows:
Really good session – all very happy and engaged. Children remained engaged – none drifted off.
Dads all really happy at the end of the session and very grateful to us for the course.
Great preparation – well-run session. Good coaching skills but also good fun and interactive for all.
Very impressed with delivery. Facilitator spoke a lot but was high energy. The physical activity session was energetic and fun and everyone left smiling.
Facilitator not really prepared – seemed a bit distracted (children and dads physical activity session facilitator).
Summary: ability to recruit and train facilitators
In summary, the process data triangulates well, suggesting that facilitators who delivered the programme considered their training to be appropriate and suitable, and they were well received by participants. However, the process was not without challenge. Owing to the change of facilitators throughout the delivery period, the workload for the research team in training each new staff member and monitoring their delivery was significant. The repeated process of recruiting and training facilitators was time and labour intensive, which is an important finding when considering feasibility. Although, in part, this was a reflection of study circumstances, the changeover of staff in the sports coaching industry is not unusual, and this would need to be considered in future planning.
Ability to deliver sessions at a time and location convenient for participants
Researcher experience
As experienced in phase 1b, successfully aligning venue, participant and facilitator availability remained one of the biggest challenges in setting up the HDHK intervention programme. For participants, the session times had to accommodate parent working patterns, child bedtime routines for evening sessions and weekend commitments for weekend sessions. This also had to be matched to venue and staff availability. Suitable venues for the HDHK programme were those in an easily accessible community setting with space to deliver both the father-only education session (including computer projection facilities) and the physical activity sessions. It was ascertained during phase 1b that ‘after school’ was not suitable for working fathers and, although primary schools are an ideal location in terms of equipment facilities and locality, they are not able to open on weekends and close at 18.00. The leisure centre worked well in phase 1b; therefore, it was used again as a venue in phase 2. However, researchers noted that the evening session time became even more of a challenge: phase 1b was delivered in summer/autumn, whereas phase 2 was delivered in winter. The evenings were darker and colder and the roads were more congested. Some of the children were half way through their first term at school and it was clear that tiredness became more of a factor for some of the younger children. It was not possible to move the session time to the weekend at this venue, as significant income is generated from hall bookings for children’s parties at weekends, which the management were not keen to displace for the temporary HDHK programme.
Another challenge for weekend delivery was staff availability. Only a small number of the lifestyles team who were trained to deliver the HDHK programme at site A were available to work on weekends, thereby limiting the pool of potential facilitators from which to select for delivery of the programme (and only female staff were available). The delivery teams at site B were often involved in other coaching sessions at a weekend or were asked to add the HDHK session to their weekend in addition to their weekly work commitments, which meant that they were often committing to working long hours.
Participant and facilitator interviews
As in phase 1b, the challenges of session timings and the subsequent impact on attendance were acknowledged in qualitative interviews. Researcher observations at the evening sessions identified that it was common for the sessions to start late owing to the late arrival of participants, the most common reasons being traffic and working hours, which were also reported by the participants:
It started at half past five, which is obviously rush-hour time. Dads are leaving work . . . In the end, what happened was it went from a group of six dads and their children to the last session being just three dads . . . I think that wasn’t due to their motivation but their work time commitments.
ID B-068
I’m not knocking anyone because I know what it’s like to get across [name of town] this time of night, but sometimes when there was literally, like, 30 minutes between one person arriving and the next, that person missed a bit.
ID B-074
In comparison, participants of the Sunday session tended to find it convenient:
Yeah ideal for me because you know . . . mid-afternoon yeah, we went to church, come back.
ID B-058
Yes, it was fine. Absolutely no problem at all.
ID A-072
Despite the difficulties described, both participants and facilitators recognised the challenge of finding a suitable time for session delivery:
It’s about timing it right, isn’t it? Are the dad’s home from work or will the school allow you to open on a Sunday and go in?
ID A-PPT.1 – facilitator
I wasn’t finishing work until 5 o’clock and then I was having to fight my way through the traffic to get there. If it had been any later, it’s harder for the kids then, because they’ve got to get up for school the next week . . . and weekends wouldn’t be any good because the leisure centre would be packed. You’ve got to put it in mid-week, haven’t you?
ID B-008
The sessions that you ran were (a) contradicted my fathers’ group session which I’ve been doing for some years and didn’t want to give up and (b) the week sessions you gave, with kids, there are always clubs and other stuff they’re involved in and so the time scale didn’t suit mine or my kids’ availability.
ID B-075
Researcher observations and participants
Both researcher observations and participants reported the venues to be largely suitable and acceptable for session delivery. Both the community and youth centre had difficulties with the projection equipment, which caused delays to programme timings, and, at the weekends, the centres lacked staff who were able to quickly resolve the technical faults. The youth centre was open to members at the time of delivery; researchers observed that this created a slightly chaotic and noisy environment, but the facilitators dealt with it well and the participants did not pass comment. The community centre had a small sports hall, which was identified several times in researcher observations and the facilitator feedback to be a challenge for delivery:
The space was a bit small and there was a lot of stuff around the edges, which was quite dangerous at times.
B-PA2.M facilitator
An additional challenge to the timing of delivery of sessions was that the programmes were being delivered during the UK winter. This was not only a challenge of attendance but also for implementing the lifestyle recommendations of the programme. One session had to be cancelled as a result of unsafe travelling conditions and several sessions were poorly attended for similar reasons:
The weather had been against us a lot of the times. I think if we had done it now in the summer, I think it would have been a lot better for us.
ID B-089
. . . although we’ve been out Saturdays and Sundays, it’s trying to fit it into darker nights, when it’s been cold and it’s been wet or it’s been snowing or whatever else, that’s been difficult . . . it’s almost like all the hard work and we were like, ‘Yes, let’s go out,’ and then suddenly it was cold nights and wet nights and it was very dark, so it lost a bit in that timing of the year.
ID A-072
We missed a few sessions with the snow, which didn’t help, so that lost a little bit of momentum.
ID B-082
Attendance data
Session timings and their associated attendance rates are shown in Table 13; 29 participants were allocated to the intervention group and, when contacted, 25 agreed to attend a course (four advised that they were no longer available to attend). Of these 25 participants, 80% of participants attended at least once and 60% completed the course (n = 15). Of those who attended at least once, 75% completed the intervention. Overall, 69% of those allocated to the intervention group attended at least once.
| Attendance characteristics | All participants | Course | |||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Venue | Youth centre (site A) | Leisure centre (site B) | Leisure centre (site B) | Community centre (site B) | |
| Session timings and start date | Sundays, 13.00–14.30, 1 October 2017 | Wednesdays, 17.15–19.00, 1 November 2017 | Wednesdays, 17.15–19.00, 17 January 2018 | Saturdays, 10.00–11.30, 20 January 2018 | |
| Randomised (n) | 29 | ||||
| Participants who agreed to attend an intervention programme (n) | 25 | 8 | 4 | 4 | 9 |
| Participants who attended at least once (n) | 20 | 6 | 3 | 4 | 7 |
| Participants who completed the programme (5/9 sessions) (n) | 15 | 4 | 3 | 3 | 5 |
Summary: ability to deliver session at a time and location convenient for participants
In summary, identifying a suitable venue and delivery time for the programme remained a key challenge throughout the whole study and was often the reason for non-attendance or non-completion of the course. Evening courses were challenging to fit in around father working patterns and children’s bedtime routines. Weekends were more popular with participants, but it was more of a challenge to identify suitable venues and facilitator availability for weekends. The key constraints are summarised in Appendix 6.
Fidelity of intervention delivery
Observation checklists
The detailed observation checklist was the main source of data to assess fidelity; researchers completed a checklist of session components that were to be delivered, details of which are presented in Table 14. Overall delivery fidelity of the individual components was good. Reasons for not delivering a number of components were limited time due to participants arriving late, the fathers’ education session running over and shortening the physical activity session, and the age of the children making completion of the children’s educational activities challenging.
| Were the following sections delivered? | Fidelity (n) | ||
|---|---|---|---|
| Yes | No | N/A | |
| Dads and kids welcome section | |||
| Welcome back | 13 | 2 | 1 |
| Review of the week: dads and kids activities | 12 | 1 | 3 |
| Dads and kids ‘bonding’ activity | 13 | 3 | – |
| Dads-only educational session | |||
| Review of the previous week’s green slip? | 5 | 1 | |
| Reminder for next week’s green slip activities? | 4 | 2 | |
| Weight review | 6 | ||
| Step count review | 6 | ||
| Monthly goals/weekly targets review | 3 | 1 | 2 |
| Summary of last week’s session | 6 | ||
| Is all relevant session content covered? | 6 | ||
| Is there reference to the dad’s handbook? | 4 | 2 | |
| Are dads completing the logbook when asked? | 5 | 1 | |
| Are the group engaged in spot quiz active responses? | 5 | 1 | |
| Are men talking to each other in brainstorm activities? | 6 | ||
| Do the dads share and discuss? | 6 | ||
| Is there a clear use of behaviour change techniques? | 6 | ||
| Do you think the content is relatable to group’s cultural norms and practices? | 6 | ||
| Children-only educational session | |||
| Was there a review of the previous week’s tasks? | 7 | 3 | 2 |
| Did all children have their handbook with them? | 6 | 5 | 1 |
| Were the session handbook tasks completed? | 11 | 1 | |
| Did the children pick tasks to work on with dad this week? | 9 | 1 | 2 |
| Joint physical activity session | |||
| Was there a rough-and-tumble activity? | 12 | 4 | |
| Was there a FMS activity? | 15 | 1 | |
| Was there a dad’s fitness activity? | 12 | 4 | |
| Was there a review at the end to tell dads what the children had done in their session? | 8 | 3 | 4 |
The observers also rated the quality of the physical activity sessions: delivery of 10 out of 12 of the rough-and-tumble elements, 11 out of 14 of the fundamental movement skills and 8 out of 12 of the fitness components were rated as good or excellent.
Facilitator feedback forms
Facilitator session feedback forms assessed fidelity of delivery asking the facilitators to report ‘what did you do well during the session and did you encounter any significant barriers/issues?’ A selection of comments written in response to this question by facilitators are presented below.
Overall, the facilitators delivering the fathers-only educational sessions felt that the sessions had gone well and that they had dealt with the challenges of fathers arriving late well:
I explained the intervention programme and their journey to weight loss and kids to push fathers to lose weight. One father came in really late but I dealt with that correctly and the session ran smoothly.
Course 1, session 1
I delivered slides very well and had great feedback from two dads.
Course 4, session 1
The challenges they faced were the amount of material to deliver and small numbers in some sessions:
Again timing is off – need more time. Great understanding from dads.
Course 4, session 6
Kept to time. Low numbers meant discussion was hard.
Course 2, session 7
There were some challenges in the delivery of messages about managing anger and parenting:
Trust paradigm did not seem to ‘land’.
Course 2, session 4
How important role of dad is the content led to a very negative atmosphere in room. Not sure keep your anger in check is a useful message. Felt like this session was not fun.
Course 2, session 5
Some of the children were too young to cope with the activities in the children’s education sessions:
Children too young to do the activity booklet.
Course 1, session 4
Overall, the facilitators felt that they delivered the joint physical activity sessions well and that they were well received. There were challenges in one location where the room was rather small and often the father-only educational sessions over-ran time, curtailing the time for the physical activity sessions:
Enjoyable, safe, effective, lack of time.
Course 1, session 2
Kept everyone motivated and engaged.
Course 2, session 4
Kept structure to the session. Small space, lack of equipment.
Course 4, session 3
Summary: fidelity of intervention delivery
There is agreement across researcher observations and facilitator session feedback showing that, overall, the sessions were delivered with good fidelity. There were some issues that were consistently reported across data sources, the most frequent being challenges with timing and delivering the full session content. Although this will have had a significant impact on fidelity, the data still suggest that the key points were delivered according to the facilitators and participants, who noted the positive lifestyle changes made as a result of the programme.
Acceptability of the programme to participants
Participant interviews
Programme acceptability was primarily assessed through qualitative interviews with participants and researcher-reported observations. This is presented in the following themes identified during data analyses.
Overall experiences and feedback of the intervention
Participants were positive about their overall experiences of the programme, stating how they thought:
It was brilliant overall. I really enjoyed it. The kids enjoyed it.
ID B-068
Or that they:
Loved it. The kids loved it as well. We looked forward to it on Wednesdays.
ID B-074
Several participants spoke about appreciating the ‘relaxed environment’ and the informal approach allowing the group to feel at ease:
It was well put together. It was a good laugh as well, which was a good thing.
ID B-074
Despite being directly asked as part of the interview, participants struggled to come up with their least enjoyed sections of the course:
Least enjoy? I don’t know. I don’t think there was anything that I didn’t enjoy about it.
ID B-041
One participant noted that, on the first course to be delivered, there were some areas for improvement. This was the first course and owing to delivery difficulties had several different facilitators delivering the fathers-only educational sessions:
I think some of the PowerPoint stuff was . . . I think that could have been done a lot better and it felt a bit disjointed and it felt a bit like the continuity wasn’t there. And it did feel like some of the people who were doing it were trying to deliver the bits of the information but didn’t really know what they were talking about. So I found some of that wasn’t great and I think that could be a lot better.
ID A-072
One important finding was that participants appreciated the opportunity to spend quality time with their children:
I’m working during the week and it’s just nice to have that dad-and-daughter time when, just for a couple of hours, it was just us and I think we’ve really benefited from that.
ID A-072
The activity time with my son and actually engaging in the physical activity, whether it was dodge ball or sock wrestling or whatever we were playing, that was something that we really enjoyed, that time together.
ID B-082
Group sessions
Many fathers reported enjoying the group setting:
. . . the group were a lovely bunch of people you didn’t feel embarrassed, you didn’t feel worried.
ID A-058
Some participants explained how they found it useful to:
. . . learn a lot of other ideas from other parents and how they do what they do.
ID B-068
They also enjoyed the peer support and motivation that the group setting facilitated:
I enjoyed the group-based elements . . . it allowed to people to bounce off, talk about – and also the blokes, a little bit of competitive edge, especially when the weight round was coming. So I think it benefited me and I preferred the group format rather than just individually between me and my children.
ID A-077
Some of the dads, we kept in touch even by Facebook and stuff like that so we used to encourage each other. There was myself and another dad, who was quite competitive and the kids were quite competitive so it was nice and we used to do the weigh-in and stuff together, just to not compete against each other, as such, personally, but just to have a monitor and talk about what we’d done during the week, how we’d got on and how the kids had got on, so I think the group environment was really good.
ID B-082
Father perception of children’s enjoyment of the session
Fathers were enthusiastic about their children’s enjoyment of the programme, and the positivity of the theme suggested that it was likely to be a strong motivator for continued attendance at the programme:
You could see by the kids’ faces they were loving it and they would talk about it for a day or two after as well and look forward to it.
ID B-074
The fundamental movement skills taught throughout the programme were also seen positively by the fathers, with many noticing significant improvements in their children. These comments were from participants who attended the courses at site B, which were delivered by experienced, qualified sports coaches:
They both catch, throw and kick better now.
ID B-074
I think it helped me and [child’s name] to learn how to do things. There was one on throwing and I had been trying to teach [child’s name] ways to throw, I think they explained it a bit more to him and he does it now. You can see the point in his arm and stuff like that.
ID B-089
Mums attending
The invitation for mums/partners to attend one of the sessions was seen to be a positive component of the programme:
I remember one day when my wife turned up that was nice to have her to see what went on.
ID A-072
I think it was nice to call the mums in; I thought that was useful because obviously we talk about it with them.
ID B-082
She really enjoyed it and she will use things against me, if I ever want to have a takeaway or anything like that. I think it was a good thing to bring her in. She was a bit wary when she first came in, she didn’t know what to expect. But when she got here, she was straight in and it was really good.
ID B-089
Session content and information received
The session content of the father-only education sessions was well received and appreciated:
It was an eye-opener in some things. Like with the yoghurts that are fat free, you have to read the labels to find out more stuff. I’m encouraged to do that now and I find myself reading the labels on our foods.
ID B-089
I felt like it was informal but you’d definitely say it was researched evidence, but it was presented in an informal way, which I was pleased with.
ID B-068
. . . there were things that were brought up on the PowerPoint slideshows that I thought, ‘I do that but I don’t do that,’ and it was good having it illustrated and making you take a step back and think.
ID B-074
Participants spoke positively regarding the physical activity sessions. Their simplicity was noted by some but this was also suggested to be a positive and encouraging approach to get involved in active play with their children:
It catered for everyone, really. It was, like I said, the first time it was nerve racking. When I got here and we were told to wear appropriate clothing and we’d be going upstairs, I was thinking, ‘I’m going to end up sweating and panting and struggling in front of maybe far healthier dads’, but it was nothing – some of it was exerting but it was nothing to be worried about.
ID B-074
Myself and some of the dads that I know, you tend to more watch and observe them [children] and supervise them rather than actually getting involved. So it was nice to do some of the games ourselves as well.
ID A-072
By comparison, one participant was less positive regarding the activity sessions with the feeling that they were ‘more geared towards the children’:
I didn’t really break a sweat. From a bonding perspective, it’s quite good but from a physical perspective, maybe not so good, for the adults anyway. For the children, they’re running around and having fun.
ID B-041
Children’s age
One emerging theme noted across the interviews (and researcher observations) was questioning the suitability of the programme elements for children as young as 4 years. The child-only sessions involved completing workbooks, which was more challenging for the younger children:
I think with my youngest one [aged 4 years], with the learning stuff, I think he was liking that but with [child’s name – aged 6], I think he was taking it more in.
ID B-089
I think when I asked her, because she’s only 4, so some of the writing and things at the time, because she’s only just learning to write now, so I think that some of that she wouldn’t have engaged with very well.
ID A-072
The physical activity session facilitators who had a lot of coaching experience coped well with delivering to a range of age groups, which is probably a reflection of their extensive coaching experience. One facilitator commented:
Even though we had, kind of like, a few older ones and younger ones, there wasn’t really, usually it is a problem, but it wasn’t really a problem in this project from my opinion. I mean, like, so the first one, we had the younger sister and older sister and we thought it could have been a struggle; it wasn’t, everyone kind of just got involved.
ID B-PA1M
Lifestyle changes
Despite there being some difficulties in keeping programme delivery to time, which could have challenged fidelity of delivery, the reports from participants imply that the key messages were delivered, prompting changes in lifestyle behaviours:
My youngest daughter, for example, who isn’t really keen on fruit and vegetables has increased her intake. Our 30-minute sessions of cardio play, we’ve been doing that a bit and getting out more and making use of outdoor spaces.
ID B-068
Certainly we’ve looked at some of the foods that we eat and try not to reward – so for my daughter for good behaviour we’d always have some sweets or we’d have some chocolate, so it really made you think about the way that you interact with regards to food and try not to have almost like food shouldn’t be either a reward or a punishment.
ID A-072
It made me focus more on my health and the interaction with my children, which I was lucky that I was able to make that adjustment.
ID A-077
My children are choosing healthy options voluntarily as a result of the course.
ID A-077
It’s changed our shopping habits massively. The main thing that I’ve got out of this is I thought that I understood how many calories were in food and I didn’t and I was absolutely horrified at the amount of calories in a custard cream because I would think nothing of eating eight custard creams in a night. So one of the biggest changes that we’ve done is we’ve altered our diet.
ID A-077
We spend more family time doing activities; I have continued to motivate myself to try and go to the gym 5 days a week and I think we watch what we eat and we’re a little bit more mindful of what we eat so it has changed our perspective of how we do things.
ID B-082
Participant and facilitator session feedback forms
Data from the participant feedback forms showed high acceptability of the programme. The facilitator feedback forms from both the father-only session and the child-only session (and father-and-child physical activity sessions) show that the facilitators also perceived the acceptability of the course to participants to be high. Feedback by session is shown in Appendix 7, Tables 34 and 35. Overall feedback that is summarised for all four courses is presented in Table 15 and a selection of comments provided by the participants in the free-text box of the feedback form is shown in Box 2.
| Participant feedback (118 responses) | Father-only education session facilitator feedback (25 responses) | Child-only education session and father-and-child activity session facilitator feedback (41 responses) | |||
|---|---|---|---|---|---|
| Statement | Mean score | Statement | Mean score | Statement | Mean score |
| This session was enjoyablea | 4.74 | The dads enjoyed the sessiona | 4.24 | The children enjoyed the sessiona | 4.52 |
| I learnt a lot from this sessiona | 4.39 | The dads learnt a lot from the sessiona | 4.10 | The children learnt a lot from the sessiona | 4.50 |
| The information presented in this session was easy to understanda | 4.59 | The dads understood the information in the sessiona | 4.88 | The children understood the information in the sessiona | 4.49 |
| The session motivated me to improve my family’s healtha | 4.62 | The dads appeared motivated to use the recommended strategies at homea | 4.50 | The children appeared motivated to use the recommended strategies for Dad at homea | 4.48 |
| Overall, I would rate this session asb | 4.56 | Overall, I would rate this session asb | 4.00 | Overall I would rate this session asb | 4.11 |
Excellent structure to session. Great info. Enjoyed it.
Course 3
My son liked rough-and-tumble play.
Course 4
Very enjoyable, learnt a lot, it was fun things we can take away for family life.
Course 4
Session 2
Group sessions excellent.
Course 1
Good laugh! Calculating Kcals was tricky. Was dressed appropriately and in better condition following minor surgery.
Course 2
Session 3
Needs more time for Dads to share their experiences during the week.
Course 1
Got weighed – have lost weight.
Course 2
I enjoyed it a lot I am very proud of how much weight I have lost. Very Happy. Well done.
Course 2 (child, aged 10 years)
Session 4
Thought it was brilliant wish there were more regular sessions like this for family fun/fitness.
Course 1
It was good to have moms/partners involved.
Course 2
More delivery time required for material and discussions to allow more physical activity.
Course 4
Session 5
My sister was tired and moaning but it was very fun and enjoyable.
Course 2 (child, aged 10 years)
Too much classroom not enough play with the kids.
Course 4
Shorter theory session more fun time this session which was great.
Course 4
Session 6
Excellent as its building a good/strong bond.
Course 3
Not enough physical activity due to time!!
Course 4
Great session. Had more time for dads and kids activities.
Course 4
Session 7
Great activities today.
Course 4
Good understanding and fun. Great PE session.
Course 4
Session 8
Great sport session today.
Course 4
Session 9
Loved it all! Thank you!
Course 2
Thank you very much we liked it we will miss the fun.
Course 3 (child, aged 6 years)
Great finish to an amazing programme.
Course 4
PE, physical education.
Detail (not presented in Table 15) highlighted that week 5 (the session on parenting) was scored the lowest by father-only education session facilitators (the average score of the overall session was 2.5). However, only two facilitators completed the feedback form and the participant feedback for this week remained positive, thereby not reflecting the facilitators’ experiences.
Observation checklists
Data from the observation checklists relating to researcher perception of programme acceptability were also positive. For the father-only sessions, five observations reported on elements around programme acceptability (one missing data item). The rapport among participants in the father-only sessions was rated ‘excellent’ in four observations and ‘good’ in one. Four observations stated ‘strongly agree’ and one stated ‘agree’ that the fathers appeared to enjoy the session, engaged with the content and understood the information. When observed in the joint father-and-child physical activity sessions, fathers were reported to ‘appear engaged with session content’ (strongly agree, n = 14; agree, n = 1; neutral, n = 1) and to work well with their children (strongly agree, n = 14).
Similar to the participant interviews, observations identified that, despite facilitator efforts to integrate all of the children into the sessions, some of the younger children struggled to engage with the education session materials. An additional challenge and probable contributor to younger child engagement was tiredness owing to the late timing of the evening sessions.
Summary: acceptability of the programme to participants
There is consistency across the data sources that suggests that the programme had high acceptability among participants. Participants enjoyed attending the sessions and reported positively on both the father education sessions and the joint father-and-child physical activity sessions. Few comments were made about the child-only education sessions except some of the content was too advanced for the younger children.
A full summary is presented in Table 16.
| Feasibility outcomes | Research team experience | Qualitative data from interviews | Participant and facilitator HDHK session feedback questionnaires | HDHK session observation data | HDHK session attendance data |
|---|---|---|---|---|---|
| Ability to recruit and train facilitators | Challenging because of changing workforce throughout programme delivery |
Facilitators rated their training experiences positively Participants rated the facilitators to be skilled in delivery |
Mainly positive reports. At times, facilitators were not sufficiently prepared, but more often than not the observations were positive | ||
| Ability to deliver sessions at a time and location convenient for participants | A key challenge working around parent working patterns, child routines and other activity commitments | Participants recognised the challenges of finding a suitable time for delivery. Weekend sessions were preferred to weekday evening sessions |
|
||
| Acceptability of the programme to participants | Participants were very positive about the programme and enjoyed attending the programme | Course was rated positively by participants | Researchers’ observations suggested high acceptability of the course to participants | ||
| Fidelity of intervention delivery | Participants reported on lifestyle changes associated with the main messages delivered from the programme | Programmes were delivered with high fidelity |
The feasibility of recruitment and follow-up
Recruitment rates
Despite having a range of recruitment pathways, only 43 fathers and 61 children were recruited in WP2. Overall, 92 men expressed an interest in the study; most did not proceed to recruitment because of loss of interest or the research team being unable to make contact, six had too low a BMI and four did not have children in the correct age range. Further details are in Figure 4.
FIGURE 4.
Participant flow through HDHK-UK for fathers. a, One participant followed up by completing questionnaire only; b, lost to follow-up out of those participants who completed follow-up at month 3; c, 15 participants continued from the previous 17 who completed the follow-up at month 3 – two of them were not able to complete the 6-month follow-up appointments, but offered to send in measurements only. In addition, two participants returned from lost to follow-up at month 3; d, eight participants continued from the previous 10 who completed the follow-up at month 3 (one completed the questionnaire only at month 3 but completed the follow-up visit at month 6, and another completed follow-up visit at month 3 but changed to send measurement in only at month 6). In addition, two participants returned from lost to follow-up at month 3. Reproduced from Griffin et al. 113 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. Minor formatting changes have been made to this figure.
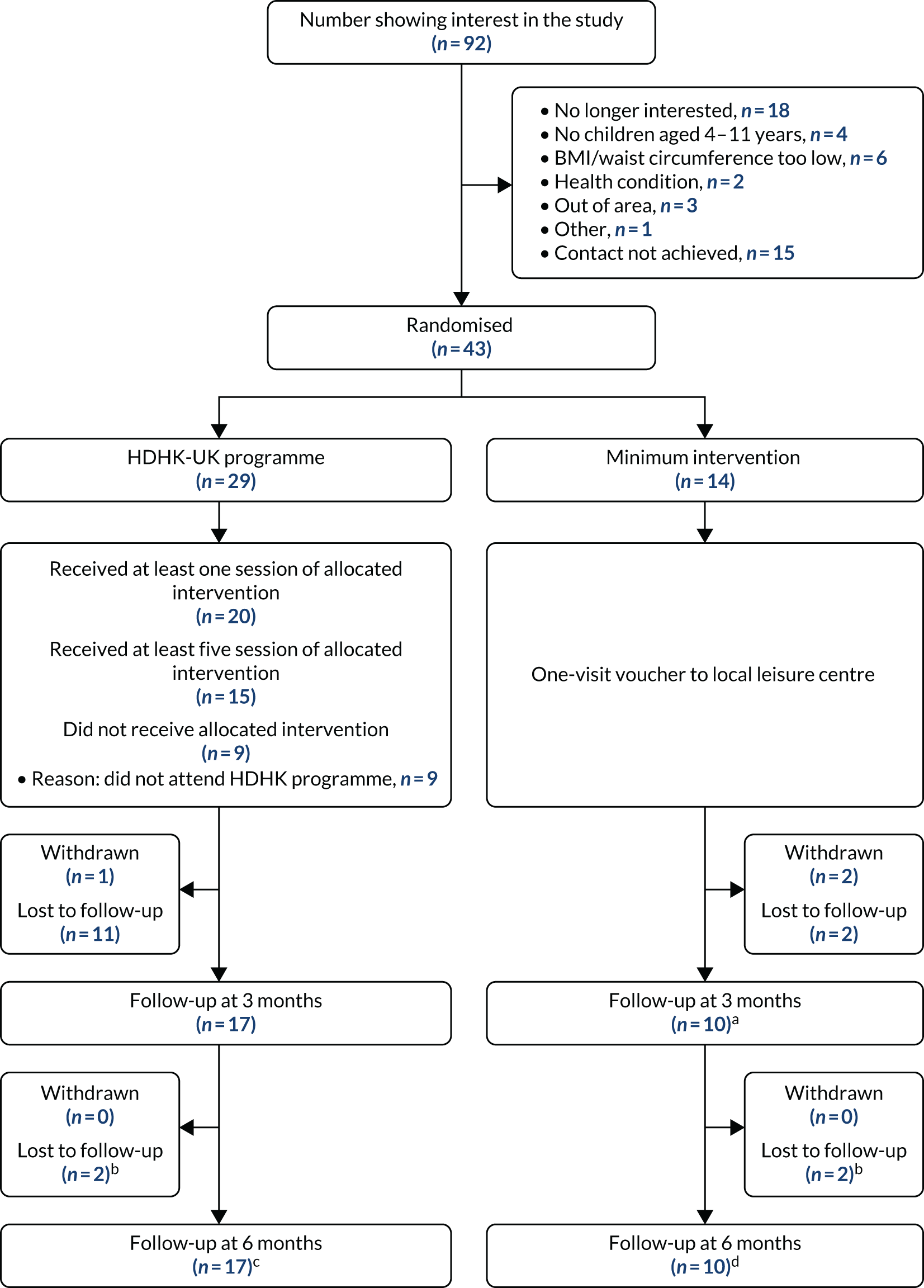
Participants’ willingness to be randomised
All participants who completed baseline measurements and were eligible accepted randomisation.
Follow-up rates at 3 and 6 months
Follow-up rates at 3 and 6 months are presented in Table 17 and in the CONSORT flow diagram (see Figure 4). Follow-up of fathers at 3 and 6 months was 62.8%.
| Time point | Treatment arm, n (%) | Total, n (%) | |
|---|---|---|---|
| HDHK-UK programme | Minimum intervention | ||
| Baseline | 29 (100) | 14 (100) | 43 (100) |
| 3-month follow-up | 17 (58.6) | 10 (71.4) | 27 (62.8) |
| 6-month follow-up | 17 (58.6) | 10 (71.4) | 27 (62.8) |
The rate of follow-up at 3 months in the intervention group was 62.5% for participants who attended no HDHK sessions (5/8), 20% for those who attended once or twice (1/5) and 68.8% for those who attended at least three times (11/16).
Summary: the feasibility of recruitment and follow-up
Recruitment was challenging and very time-consuming; however, the demographic characteristics of the recruited fathers demonstrated that, with more resources, it was possible to recruit BAME groups and people living in socioeconomically deprived localities.
The feasibility of a future definitive trial
Collection of outcome data: baseline data
Similar to experiences during phase 1b, finding appointment times for consent and baseline measurements that suited both father and child(ren) was challenging. As would be expected, fathers tended to request appointments for the evening, which significantly extended travelling time by up to 70 minutes each way for the research team owing to congestion on the roads, particularly for appointments at site A. There were also numerous occasions when, despite confirming the appointment time by telephone call and/or text message, the participant and/or their children were not at home. ‘Failed’ appointments were a significant financial and time burden on the research team. Questionnaire completion and measurement processes took 30–45 minutes and researchers reported that the measurements were acceptable to the participants, although a number of fathers declined the waist measurement.
For follow-up appointments, the team ran several measurement days, often at the site of intervention delivery, offering participants individual appointment slots. These sessions were of mixed success: some were well attended, but on two occasions up to five participants had confirmed attendance but one or none attended on the day. To encourage attendance at the final 6-month follow-up (March 2018), participants were offered free access to the soft play or a free swim for attending the measurement appointment. This helped to encourage attendance at the measurement session.
Baseline data: fathers
The mean age of participants recruited to WP2 was 40.0 years (SD 6.4 years), 60.5% were from a black, Asian or other minority ethnic group; 53.5% lived in one of the 20% most deprived English localities, as measured by the IMD; and 74.4% lived in one of the 40% most deprived localities. Despite living in areas of socioeconomic deprivation, 48.8% were educated to degree level. The fathers’ mean weight was 90.8 kg (SD 15.3 kg) and mean BMI was 30.2 kg/m2 (SD 5.1 kg/m2), and they were a moderately active group with a mean of 110 minutes of weekly moderate/vigorous physical activity, measured objectively using GENEactiv accelerometers. One-third of fathers self-reported low levels of physical activity on the IPAQ. Further detail is given in Table 18 and in Appendix 8, Table 36. Additional data on the ages of the children are reported in Appendix 8, Table 38.
| Characteristic | Treatment arm | ||
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | Overall (N = 43) | |
| Minimisation variables | |||
| Ethnicity, n (%) | |||
| White British | 12 (41.4) | 5 (35.7) | 17 (39.5) |
| Non-white British | 17 (58.6) | 9 (64.3) | 26 (60.5) |
| Weight characteristics | |||
| BMI (kg/m2) | |||
| Mean (SD), n | 30.1 (4.8), 29 | 30.2 (5.8), 14 | 30.2 (5.1), 43 |
| Minimum, maximum | 25.1, 50.9 | 23.8, 45.5 | 23.8, 50.9 |
| Weight (kg) | |||
| Mean (SD), n | 90.1 (13.2), 29 | 92.2 (19.3), 14 | 90.8 (15.3), 43 |
| Minimum, maximum | 70.9, 136.9 | 64.0, 142.5 | 64.0, 142.5 |
| Percentage body fat (%) | |||
| Mean (SD), n | 28.3 (7.6), 28 | 29.8 (9.0), 14 | 28.8 (8.0), 42 |
| Minimum, maximum | 19.5, 59.9 | 17.9, 51.8 | 17.9, 59.9 |
| Missing (n) | 1 | 0 | 1 |
| Waist circumference (cm) | |||
| Mean (SD), n | 101.8 (8.5), 19 | 103.1 (15.0), 14 | 102.3 (11.5), 33 |
| Minimum, maximum | 88.0, 127.0 | 72.0, 135.0 | 72.0, 135.0 |
| Missing (n) | 10 | 0 | 10 |
| Demographics | |||
| Age (years) | |||
| Mean (SD), n | 39.4 (6.3), 29 | 41.1 (6.6), 14 | 40.0 (6.4), 43 |
| Minimum, maximum | 23.6, 56.0 | 26.8, 52.8 | 23.6, 56.0 |
| Highest level of qualification, n (%) | |||
| No formal qualification | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| GCSE, CSE, O level or equivalent | 7 (24.1) | 6 (42.9) | 13 (30.2) |
| A level/AS level or equivalent | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| Degree level or higher | 15 (51.7) | 6 (42.9) | 21 (48.8) |
| Other | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Missing | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Age completed continuous full time education (years) | |||
| Mean (SD), n | 21.8 (6.5), 24 | 20.1 (3.2), 14 | 21.1 (5.5), 38 |
| Minimum, maximum | 15.0, 44.0 | 16.0, 27.0 | 15.0, 44.0 |
| Missing (n) | 5 | 0 | 5 |
| Legal marital or civil partnership status, n (%) | |||
| Married or in a registered civil partnership | 25 (86.2) | 13 (92.9) | 38 (88.4) |
| Separated, but still legally married or in a civil partnership | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Divorced or formerly in a civil partnership that is now legally dissolved | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Widowed or surviving partner from a civil partnership | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Never married and never registered in a civil partnership | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| Missing | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Number of adults aged ≥ 18 years living in the same household, n (%) | |||
| 0 | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| 1 | 17 (58.6) | 11 (78.6) | 28 (65.1) |
| 2 | 6 (20.7) | 2 (14.3) | 8 (18.6) |
| 3 | 0 (0.0) | 1 (7.1) | 1 (2.3) |
| 4 | 2 (6.9) | 1 (0.0) | 2 (4.6) |
| Missing | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| Number of children living in the same household, n (%) | |||
| 1 | 8 (27.6) | 2 (14.3) | 10 (23.3) |
| 2 | 11 (37.9) | 6 (42.9) | 17 (39.5) |
| 3 | 5 (17.2) | 2 (14.3) | 7 (16.3) |
| 4 | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| 5 | 0 (0.0) | 1 (7.1) | 1 (2.3) |
| Missing | 2 (6.9) | 1 (7.1) | 3 (7.0) |
| Number of children (not necessarily co-resident), n (%) | |||
| 1 | 4 (13.8) | 2 (14.3) | 6 (14.0) |
| 2 | 12 (41.4) | 7 (50.0) | 19 (44.2) |
| 3 | 6 (20.7) | 2 (14.3) | 8 (18.6) |
| 4 | 5 (17.2) | 1 (7.1) | 6 (14.0) |
| 5 | 0 (0.0) | 2 (14.3) | 2 (4.7) |
| Missing | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Religion, n (%) | |||
| None | 7 (28.1) | 1 (7.1) | 8 (18.6) |
| Hinduism/Hindu | 2 (6.9) | 1 (7.1) | 3 (7.0) |
| Christian | 8 (27.6) | 4 (28.6) | 12 (27.9) |
| Islam/Muslim | 6 (20.7) | 6 (42.9) | 12 (27.9) |
| Sikhism/Sikh | 4 (13.8) | 0 (0.0) | 4 (9.3) |
| Ad-Dharm | 0 (0.0) | 1 (7.1) | 1 (2.3) |
| I do not wish to answer | 1 (3.5) | 1 (7.1) | 2 (4.6) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Main spoken language, n (%) | |||
| English | 23 (79.3) | 14 (100.0) | 37 (86.1) |
| Urdu | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Punjabi | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Spanish | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Turkish | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Missing | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| IMD quintile, n (%) | |||
| 1 (least deprived) | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| 2 | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| 3 | 5 (17.2) | 1 (7.1) | 6 (14.0) |
| 4 | 5 (17.2) | 4 (28.6) | 9 (20.9) |
| 5 (most deprived) | 17 (58.6) | 6 (42.9) | 23 (53.5) |
| Missing | 0 (0.0) | 2 (14.3) | 2 (4.7) |
Data on the eating practices, alcohol consumption, parenting and general health at baseline are reported in Table 19. Fathers reported dietary practices that were associated with weight gain, such as consumption of sugar-sweetened beverages on a daily basis (n = 35, 81.4%), eating in front of the television on a daily basis (n = 9, 20.9%) and consuming takeaway food at least weekly (n = 25, 58%). About one-third of participants consumed vegetables or salad with their evening meal fewer than three times per week. Data on fathers’ use of health services are given in Appendix 8, Table 37.
| Questionnaire | Treatment arm | ||
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | Overall (N = 43) | |
| IPAQ-short | |||
| Total physical activity, MET-minutes/week (continuous) | |||
| Median (IQR) | 2017.5 (1032.0–3573.0) | 1098.8 (410.0–4158.0) | 1980.0 (810.0–3573.0) |
| Missing (n) | 6 | 4 | 10 |
| Categorical score, n (%) | |||
| Low activity | 8 (27.6) | 6 (42.9) | 14 (32.6) |
| Moderate activity | 10 (34.5) | 4 (28.6) | 14 (32.6) |
| Vigorous activity | 10 (34.5) | 3 (21.4) | 13 (30.2) |
| Missing | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| GENEACTIV measurement | |||
| Total activity (minutes) | |||
| Median (IQR) | 207.3 (175.8–270.1) | 213.6 (157.4–248.9) | 210.4 (167.7–264.6) |
| Missing (n) | 4 | 1 | 5 |
| Moderate/vigorous activity (minutes) | |||
| Median (IQR) | 110.8 (88.4–141.3) | 87.0 (75.9–148.4) | 109.7 (83.8–148.4) |
| Missing (n) | 4 | 1 | 5 |
| Food and drink intake, n (%) | |||
| Type of milk | |||
| Normal full-fat milk | 11 (37.9) | 4 (28.6) | 15 (34.9) |
| Semi-skimmed milk | 10 (34.5) | 7 (50.0) | 17 (39.5) |
| Skimmed milk | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| Soy milk | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Rice milk | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not sure | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| I don’t drink milk | 4 (13.8) | 3 (21.4) | 7 (16.3) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Pieces of fruit | |||
| None | 4 (13.8) | 0 (0.0) | 4 (9.3) |
| Fewer than 1 per week | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| 1 or 2 per week | 9 (31.0) | 2 (14.3) | 11 (25.6) |
| 3 or 4 per week | 4 (13.8) | 5 (35.7) | 9 (20.9) |
| 5 or 6 per week | 2 (6.9) | 3 (21.4) | 5 (11.6) |
| Once per day | 2 (6.9) | 2 (14.3) | 4 (9.3) |
| 2 or 3 per day | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| ≥ 4 per day | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Vegetables or salad consumption with evening meal | |||
| Never | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Less than once per week | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Once or twice per week | 9 (31.0) | 5 (35.7) | 14 (32.6) |
| 3 or 4 times per week | 10 (34.5) | 6 (42.9) | 16 (37.2) |
| ≥ 5 times per week | 8 (27.6) | 3 (21.4) | 11 (25.6) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Takeaway foods | |||
| Never | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Fewer than once per week | 9 (31.0) | 8 (57.1) | 17 (39.5) |
| Once or twice per week | 11 (37.9) | 4 (28.6) | 15 (34.9) |
| 3 or 4 times per week | 7 (24.1) | 2 (14.3) | 9 (20.9) |
| 5 or 6 times per week | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Once a day | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Twice or more per day | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Eating in front of the television | |||
| Never | 4 (13.8) | 7 (50.0) | 11 (25.6) |
| Fewer times than once per week | 2 (6.9) | 3 (21.4) | 5 (11.6) |
| Once or twice per week | 8 (27.6) | 3 (21.4) | 11 (25.6) |
| 3 or 4 times per week | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| 5 or 6 times per week | 4 (13.8) | 0 (0.0) | 4 (9.3) |
| Every day | 9 (31.0) | 0 (0.0) | 9 (20.9) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Sugary drinks | |||
| Never | 3 (10.3) | 3 (21.4) | 6 (14.0) |
| < 1 per day | 9 (31.0) | 2 (14.3) | 11 (25.6) |
| 1 per day | 4 (13.8) | 3 (21.4) | 7 (16.3) |
| 2 or 3 per day | 8 (27.6) | 6 (42.9) | 14 (32.6) |
| 4–6 per day | 4 (13.8) | 0 (0.0) | 14 (32.6) |
| ≥ 7 per day | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Fruit juice-based drinks | |||
| Never | 2 (6.9) | 1 (7.1) | 3 (7.0) |
| < 1 per month | 4 (13.8) | 3 (21.4) | 7 (16.3) |
| 1–3 per month | 5 (17.2) | 2 (14.3) | 7 (16.3) |
| 1 per week | 7 (24.1) | 3 (21.4) | 10 (23.3) |
| 2–6 per week | 5 (17.2) | 3 (21.4) | 8 (18.6) |
| 1 per day | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| ≥ 2 per day | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Snacks consumed | |||
| < 1 per day | 7 (24.1) | 4 (28.6) | 11 (25.6) |
| 1 or 2 per day | 12 (41.4) | 8 (57.1) | 20 (46.5) |
| 3 or 4 per day | 9 (31.0) | 2 (14.3) | 11 (25.6) |
| 5 or 6 per day | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| ≥ 7 per day | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Ever drink alcohol | |||
| Yes | 19 (65.5) | 7 (50.0) | 26 (60.5) |
| No | 8 (27.6) | 7 (50.0) | 15 (34.9) |
| Missing | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| If Yes to the above question, then answer the following three questions | |||
| Total number of days of alcohol consumed over the previous 3 months, n (%) | |||
| ≥ 1a | 19 (100.0) | 7 (100.0) | 26 (100.0) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Average number of glasses of alcohol consumed per day | |||
| ≥ 1a | 19 (100.0) | 7 (100.0) | 26 (100.0) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Maximum number of glasses of alcohol consumed in 24 hours | |||
| ≥ 1a | 18 (94.7) | 7 (100.0) | 25 (96.2) |
| Missing | 1 (5.3) | 0 (0.0) | 1 (3.9) |
| General health | |||
| EQ-5D-5L index score | |||
| Mean (SD) | 0.91 (0.16) | 0.95 (0.07) | 0.93 (0.13) |
| Minimum, maximum | 0.24, 1.00 | 0.82, 1.00 | 0.24, 1.00 |
| Missing (n) | 2 | 0 | 2 |
| ICECAP-A total capability score | |||
| Mean (SD) | 0.86 (0.15) | 0.95 (0.06) | 0.89 (0.13) |
| Minimum, maximum | 0.51, 1.00 | 0.81, 1.00 | 0.51, 1.00 |
| Missing (n) | 1 | 0 | 1 |
| Parenting for physical activity | |||
| ACTS-MG | |||
| Mean (SD) | 14.0 (3.5) | 13.5 (3.1) | 13.9 (3.3) |
| Minimum, maximum | 5.0, 20.0 | 8.0, 19.0 | 5.0, 20.0 |
| Missing (n) | 1 | 0 | 1 |
| Limit-setting | |||
| Mean (SD) | 7.1 (2.3) | 8.6 (1.5) | 7.6 (2.1) |
| Minimum, maximum | 2.0, 10.0 | 6.0, 10.0 | 2.0, 10.0 |
| Missing (n) | 1 | 0 | 1 |
| Control | |||
| Mean (SD) | 3.0 (1.4) | 2.4 (1.4) | 2.8 (1.4) |
| Minimum, maximum | 1.0, 5.0 | 1.0, 5.0 | 1.0, 5.0 |
| Missing (n) | 2 | 0 | 2 |
| Monitoring | |||
| Mean (SD) | 6.9 (1.9) | 7.4 (1.1) | 7.0 (1.7) |
| Minimum, maximum | 2.0, 10.0 | 6.0, 9.0 | 2.0, 10.0 |
| Missing (n) | 1 | 0 | 1 |
| Disciplining | |||
| Mean (SD) | 5.8 (2.2) | 5.8 (2.3) | 5.8 (2.2) |
| Minimum, maximum | 2.0, 10.0 | 2.0, 10.0 | 2.0, 10.0 |
| Missing (n) | 2 | 0 | 2 |
| Co-physical activity | |||
| Mean (SD) | 3.6 (0.9) | 2.8 (0.8) | 3.3 (1.0) |
| Minimum, maximum | 2.0, 5.0 | 1.0, 4.0 | 1.0, 5.0 |
| Missing (n) | 1 | 0 | 1 |
| Father–child relationship | |||
| Disciplinary warmth (subscale) | |||
| Mean (SD) | 22.8 (4.1) | 23.9 (2.4) | 23.2 (3.6) |
| Minimum, maximum | 15.0, 30.0 | 18.0, 27.0 | 15.0, 30.0 |
| Missing (n) | 3 | 0 | 3 |
| Personal relationships (subscale) | |||
| Mean (SD) | 31.4 (4.9) | 30.6 (4.1) | 31.1 (4.6) |
| Minimum, maximum | 22.0, 40.0 | 22.0, 37.0 | 22.0, 40.0 |
| Missing (n) | 4 | 0 | 4 |
| Prosocial | |||
| Mean (SD) | 7.8 (1.2) | 7.6 (1.3) | 7.7 (1.3) |
| Minimum, maximum | 5.0, 10.0 | 5.0, 10.0 | 5.0, 10.0 |
| Missing (n) | 3 | 0 | 3 |
| Praise | |||
| Mean (SD) | 7.9 (1.3) | 8.3 (1.2) | 8.1 (1.3) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 10.0 | 6.0, 10.0 |
| Missing (n) | 3 | 0 | 3 |
| Intimacy | |||
| Mean (SD) | 7.0 (1.8) | 7.4 (1.3) | 7.2 (1.6) |
| Minimum, maximum | 3.0, 10.0 | 5.0, 10.0 | 3.0, 10.0 |
| Missing (n) | 2 | 0 | 2 |
| Nurturance | |||
| Mean (SD) | 8.3 (1.2) | 7.8 (1.2) | 8.1 (1.2) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 10.0 | 6.0, 10.0 |
| Missing (n) | 3 | 0 | 3 |
| Shared decision-making | |||
| Mean (SD) | 7.2 (1.6) | 7.5 (1.2) | 7.3 (1.5) |
| Minimum, maximum | 5.0, 10.0 | 5.0, 9.0 | 5.0, 10.0 |
| Missing (n) | 2 | 0 | 2 |
| Companionship | |||
| Mean (SD) | 8.2 (1.4) | 7.8 (1.3) | 8.0 (1.3) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 10.0 | 6.0, 10.0 |
| Missing (n) | 1 | 0 | 1 |
| Rationale | |||
| Mean (SD) | 7.7 (1.7) | 8.1 (0.5) | 7.8 (1.4) |
| Minimum, maximum | 4.0, 10.0 | 7.0, 9.0 | 4.0, 10.0 |
| Missing (n) | 2 | 0 | 2 |
Baseline data: children
The 61 children who were recruited had a mean age of 7.7 years (range 4.01–11.67 years); 39 (63.9%) were male and 20 (32.8%) were overweight or obese (Table 20). The baseline characteristics of the eldest child in each family are reported in Table 21 and their eating and physical activity behaviours, health-related quality of life and health service utilisation are reported in Appendix 8, Table 41. Thirty (70%) of the children reported consumption of sugary drinks on a daily basis.
| Characteristic | Treatment arm | ||
|---|---|---|---|
| HDHK-UK programme (N = 42) | Minimum intervention (N = 19) | Overall (N = 61) | |
| Age (years) | |||
| Mean (SD) | 7.7 (2.0) | 7.78 (2.2) | 7.7 (2.1) |
| Minimum, maximum | 4.2, 11. 5 | 4.0, 11. 7 | 4.0, 11. 7 |
| Missing (n) | 0 | 0 | 0 |
| BMI (kg/m2), n (%) | |||
| Underweight/healthy | 20 (47.6) | 13 (68.4) | 33 (54.1) |
| Overweight/obese | 16 (38.1) | 4 (21.1) | 20 (32.8) |
| Missing | 6 (14.3) | 2 (10.5) | 8 (13.1) |
| Percentage body fat (%) | |||
| Mean (SD) | 24.0 (5.8) | 22.9 (4.9) | 23.6 (5.5) |
| Minimum, maximum | 10.3, 36.7 | 16.9, 37.3 | 10.3, 37.3 |
| Missing (n) | 6 | 3 | 9 |
| Sex, n (%) | |||
| Female | 16 (38.1) | 6 (31.6) | 22 (36.1) |
| Male | 26 (61.9) | 13 (68.4) | 39 (63.9) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Characteristic | Treatment arm | ||
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | Overall (N = 43) | |
| Age (years) | |||
| Mean (SD) | 8.1 (2.2) | 8.2 (2.2) | 8.1 (2.1) |
| Minimum, maximum | 4.2, 11.5 | 4.0, 11. 7 | 4.0, 11.7 |
| Missing (n) | 0 | 0 | 0 |
| BMI (kg/m2), n (%) | |||
| Underweight/healthy | 13 (44.8) | 9 (64.3) | 22 (51.2) |
| Overweight/obese | 14 (48.3) | 3 (21.4) | 17 (39.5) |
| Missing | 2 (6.9) | 2 (14.3) | 4 (9.3) |
| Percentage body fat (%) | |||
| Mean (SD) | 24.7 (6.0) | 22.8 (5.2) | 24.1 (5. 8) |
| Minimum, maximum | 10.3, 36.7 | 16.9, 37.3 | 10.3, 37.3 |
| Missing (n) | 3 | 2 | 5 |
| Sex, n (%) | |||
| Female | 11 (37.9) | 5 (35.7) | 16 (37.2) |
| Male | 18 (62.1) | 9 (64.3) | 27 (62.8) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Weight data at 3 and 6 months: fathers
The primary outcome of a definitive RCT would be weight loss in fathers. Table 22 reports these data at the 3- and 6-month follow-ups. Among the 25 fathers who provided weight data at 6 months, there was a mean weight loss of 2.9 kg (95% CI 0.6 kg to 5.1 kg, n = 15) in the intervention arm and a mean weight loss of 2.0 kg (95% CI –0.6 kg to 4.6 kg, n = 10) in the control arm.
| Weight change | Treatment arm | |
|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | |
| Weight change at 3 months | ||
| Mean (SD) (kg) | –1.8 (2.5) | –1.2 (3.3) |
| 95% CI (kg) | –3.1 to –0.5 | –3.7 to 1.3 |
| Minimum, maximum (kg) | –5.7, 4.2 | –6.3, 2.6 |
| Missing (n) | 12 | 5 |
| Weight change at 6 months | ||
| Mean (SD) (kg) | –2.9 (4.1) | –2.0 (3.6) |
| 95% CI (kg) | –5.1 to –0.6 | –4.6 to 0.6 |
| Minimum, maximum (kg) | –7.2, 3.3 | –9.1, 3.2 |
| Missing (n) | 14 | 4 |
Outcomes of a future definitive trial
Fathers’ secondary outcomes
Table 23 and Appendix 8, Table 39, present the secondary outcomes of a future definitive trial for fathers. More detail is presented in Appendix 8, Table 42. At the 6-month follow-up, 9 (60%) of the 15 fathers with weight data had lost at least 5% of their baseline weight, which was 31% of the total participants randomised to the intervention.
| Outcome measure | Time point | |||
|---|---|---|---|---|
| 3 months | 6 months | |||
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | |
| Change from baseline in waist circumference (cm) | ||||
| Mean (SD), n | –10.8 (18.0), 9 | 3.4 (9.3), 6 | –5.2 (5.0), 6 | –2.8 (6.4), 5 |
| Change from baseline in % body fat (%) | ||||
| Mean (SD), n | –1.5 (3.1), 26 | –0.3 (2.6), 9 | –2.2 (3.2), 14 | –2.3 (3.9), 9 |
| Self-reported physical activity measured by the IPAQ-short (MET-minutes/week) | ||||
| Median (IQR), n | 3276.0 (2556.0–4685.4), 15 | 2678.0 (520.0–3732.0), 9 | 2931.0 (1455.0–4158.0), 10 | 1866.0 (693.0–3465.0), 7 |
| Physical activity measured by a GENEactive accelerometer (minutes) | ||||
| Median for total activity (IQR), n | 208.8 (185.6–287.0), 17 | 168.3 (147.8–194.0), 9 | 239.6 (194.3–287.0), 11 | 146.2 (125.0–230.6), 9 |
| Median for moderate/vigorous activity (IQR), n | 113.3 (99.3–151.3), 17 | 84.2 (69.4–106.2), 9 | 125.6 (101.3–163.1), 11 | 68.2 (59.1–86.5), 9 |
| Parenting for physical activity | ||||
| ACTS-MG | ||||
| Mean (SD), n | 15.6 (3.5), 17 | 13.0 (2.3), 9 | 16.4 (2.2), 12 | 13.7 (1.5), 9 |
| Limit-setting | ||||
| Mean (SD), n | 8.4 (1.9), 17 | 8.8 (1.4), 9 | 7.5 (2.1), 13 | 9.1 (1.2), 9 |
| Control | ||||
| Mean (SD), n | 2.7 (1.6), 17 | 2.1 (1.3), 9 | 3.4 (1.3), 13 | 2.6 (1.7), 9 |
| Monitoring | ||||
| Mean (SD), n | 7.3 (1.5), 17 | 7.4 (1.1), 9 | 7.4 (1.5), 14 | 7.7 (0.7), 9 |
| Disciplining | ||||
| Mean (SD), n | 5.2 (2.3), 17 | 4.7 (2.4), 9 | 5.2 (2.7), 14 | 6.3 (2.2), 9 |
| Co-physical activity | ||||
| Mean (SD), n | 3.5 (0.9), 17 | 2.7 (0.7), 9 | 3.8 (1.3), 14 | 3.2 (0.8), 9 |
| Father–child relationship | ||||
| Disciplinary warmth (praise + shared decision-making + rationale) | ||||
| Mean (SD), n | 22.9 (4.0), 16 | 23.0 (1.6), 9 | 23.8 (3.6), 12 | 23.3 (3.0), 9 |
| Personal relationships (prosocial + intimacy + nurturance + companionship) | ||||
| Mean (SD), n | 31.4 (5.0), 16 | 28.9 (2.6), 9 | 30.6 (4.8), 12 | 30.0 (2.9), 9 |
| Prosocial | ||||
| Mean (SD), n | 7.8 (1.2), 17 | 7.0 (0.7), 9 | 7.1 (1.2), 12 | 7.6 (1.4), 9 |
| Praise | ||||
| Mean (SD), n | 7.9 (1.3), 16 | 7.8 (1.2), 9 | 8.2 (1.3), 12 | 8.0 (1.2), 9 |
| Intimacy | ||||
| Mean (SD), n | 6.8 (2.0), 16 | 6.4 (0.9), 9 | 7.0 (1.8), 12 | 6.9 (1.3), 9 |
| Nurturance | ||||
| Mean (SD), n | 8.4 (1.2), 17 | 7.8 (0.8), 9 | 8.0 (1.4), 12 | 8.1 (0.8), 9 |
| Shared decision-making | ||||
| Mean (SD), n | 7.3 (1.6), 17 | 7.2 (1.1), 9 | 7.6 (1.7), 12 | 7.1 (1.5), 9 |
| Companionship | ||||
| Mean (SD), n | 8.2 (1.3), 17 | 7.7 (0.9), 9 | 8.4 (1.3), 12 | 7.4 (0.9), 9 |
| Rationale | ||||
| Mean (SD), n | 7.8 (1.7), 17 | 8.0 (0.5), 9 | 8.0 (1.5), 15 | 8.2 (1.6), 9 |
| EQ-5D-5L | ||||
| Mean (SD), n | 0.870 (0.188), 15 | 0.939 (0.096), 9 | 0.917 (0.141), 12 | 0.937 (0.127), 9 |
| ICECAP-A | ||||
| Mean (SD), n | 0.92 (0.09), 17 | 0.95 (0.05), 9 | 0.89 (0.13), 14 | 0.92 (0.07), 9 |
| Lost ≥ 5% of body mass, n (%) | ||||
| Yes | 2 (6.9) | 1 (7.1) | 9 (31.0) | 1 (7.1) |
| No | 15 (51.7) | 8 (57.1) | 6 (20.7) | 9 (64.3) |
Children’s secondary outcomes
Tables 24 and 25 report the data completeness for the children’s questionnaires at the 3- and 6-month follow-ups. Incomplete data were largely due to loss to follow-up; the level of partial completion of individual questionnaires was low.
| Questionnaire | Treatment arm, n (%) | Overall (N = 43), n (%) [95% CI] | |
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | ||
| Food and drink intake (8 items) | |||
| Fully completed | 16 (55.2) | 9 (64.3) | 25 (58.1) [95% CI 42.1% to 73.0%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 13 (44.8) | 5 (35.7) | 18 (41.9) |
| CHU-9D (9 items) | |||
| Fully completed | 15 (51.7) | 9 (64.3) | 24 (55.8) [95% CI 39.9% to 70.9%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 14 (48.3) | 5 (35.7) | 19 (44.2) |
| Family nutrition and physical activity (20 items) | |||
| Fully completed | 16 (55.2) | 9 (64.3) | 25 (58.1) [95% CI 42.1% to 73.0%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 13 (44.8) | 5 (35.7) | 18 (41.9) |
| Questionnaire | Treatment arm, n (%) | Overall (N = 43), n (%) [95% CI] | |
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | ||
| Food and drink intake (8 items) | |||
| Fully completed | 13 (44.8) | 9 (64.3) | 22 (51.2) [95% CI 35.5% to 66.7%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 16 (55.2) | 5 (35.7) | 21 (48.8) |
| CHU-9D (9 items) | |||
| Fully completed | 11 (37.9) | 8 (57.1) | 19 (44.2) [95% CI 29.1% to 60.1%] |
| Partially completed | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Not completed at all | 17 (58.6) | 6 (42.9) | 23 (53.5) |
| Family nutrition and physical activity (20 items) | |||
| Fully completed | 9 (31.0) | 8 (57.1) | 17 (39.5) [95% CI 25.0% to 55.6%] |
| Partially completed | 4 (13.8) | 0 (0.0) | 4 (9.3) |
| Not completed at all | 16 (55.2) | 6 (42.9) | 22 (51.2) |
The secondary outcomes for the eldest child of a future definitive RCT are reported in Table 26 and the weight outcomes for all children are in Table 27. At 3 months’ follow-up, the BMI z-score in the intervention group reduced by 0.13 points (SD 0.27 points) from that at baseline; at the 6-month follow-up, it reduced by 0.016 points (SD 0.3 points) from that at baseline.
| Outcome measure | Time point | |||
|---|---|---|---|---|
| 3 months | 6 months | |||
| HDHK-UK programme | Minimum intervention | HDHK-UK programme | Minimum intervention | |
| Change from baseline in BMI z-score (points) | ||||
| Mean (SD), n | –0.131 (0.272), 14 | 0.016 (0.346), 8 | –0.016 (0.299), 12 | 0.039 (0.449),10 |
| Change from baseline in % body fat (%) | ||||
| Mean (SD), n | –0.577 (1.172), 13 | 0.037 (2.843), 8 | –0.800 (1.481), 11 | –0.875 (3.071), 8 |
| Categorised as overweight or obese, n (%) | ||||
| Underweight/healthy | 8 (27.6) | 6 (42.9) | 7 (24.1) | 6 (42.9) |
| Overweight/obese | 7 (24.1) | 3 (21.4) | 6 (20.7) | 4 (28.6) |
| Missing | 14 (48.3) | 5 (35.7) | 16 (55.2) | 4 (28.6) |
| Physical activity measured by a GENEactive accelerometer (minutes) | ||||
| Median for total activity (IQR), n | 342.29 (262.71–427.71), 17 | 277.00 (272.50–314.25), 9 | 347.33 (321.63–384.00), 10 | 312.79 (245.43–456.83), 8 |
| Median for moderate/vigorous activity (IQR), n | 73.50 (34.71–99.29), 17 | 57.00 (26.75–73.00), 9 | 73.19 (49.00–105.67), 10 | 56.00 (32.43–110.58), 8 |
| Family nutrition and physical activity | ||||
| Mean (SD), n | 62.25 (7.68), 16 | 61.11 (5.21), 9 | 61.22 (6.48), 9 | 62.13 (3.04), 8 |
| CHU-9D | ||||
| Mean (SD), n | 0.89 (0.09), 15 | 0.93 (0.04), 9 | 0.92 (0.09), 11 | 0.92 (0.11), 8 |
| SDQ,a mean (SD), n | ||||
| Total SDQ scale | – | – | 7.4 (3.8), 12 | 11.2 (6.1), 6 |
| Emotional problems scale | – | – | 1.5 (1.8), 12 | 2.0 (1.4), 6 |
| Conduct problems scale | – | – | 1.0 (1.1), 12 | 1.3 (1.5), 6 |
| Hyperactivity scale | – | – | 3.4 (2.1), 12 | 5.5 (2.7), 6 |
| Peer problems scale | – | – | 1.4 (1.3), 12 | 2.3 (1.5), 6 |
| Prosocial scale | – | – | 8.1 (1.9), 12 | 8.3 (1.8), 6 |
| Outcome measure | Time point | |||
|---|---|---|---|---|
| 3 months | 6 months | |||
| HDHK-UK programme | Minimum intervention | HDHK-UK programme | Minimum intervention | |
| Change from baseline in BMI z-score (points) | ||||
| Mean (SD), n | –0.134 (0.265), 19 | –0.018 (0.335), 12 | –0.096 (0.350), 18 | 0.039 (0.449), 10 |
| Change from baseline in % body fat (%) | ||||
| Mean (SD), n | –0.388 (1.185), 16 | –0.183 (2.297), 12 | –0.842 (1.419), 12 | –0.875 (3.071), 8 |
Level of data completeness at 3 and 6 months
The level of data completion of the questionnaires by the fathers at 3 and 6 months was acceptable. Missing questionnaire data were highest for the IPAQ, for which a missing item can result in an inability to compute a continuous outcome measure. There was also a high level of missing data for fathers’ waist circumference, with many men preferring not to have this measured. The level of data completion is reported in detail in Appendix 8, Tables 40 and 41. The ability to collect the Strengths and Difficulties Questionnaire data at the 6-month follow-up for the eldest child is reported in Table 28; most of the missing data were due to loss to follow-up of participants, missing items were few.
| Strengths and Difficulties Questionnaire (25 items) | Treatment arm, n (%) | Overall (N = 43), n (%) [95% CI] | |
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | ||
| Fully completed | 11 (37.9) | 6 (42.9) | 17 (39.5) [95% CI 25.0% to 55.6%] |
| Partially completed | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Not completed at all | 17 (58.6) | 8 (57.1) | 25 (58.1) |
| Five scales of five items each | |||
| Emotional problems scale | |||
| At least 3 items completed | 12 (41.4) | 6 (42.9) | 18 (41.9) [95% CI 27.0% to 57.9%] |
| 1 or 2 items completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 17 (58.6) | 8 (57.1) | 25 (58.1) |
| Conduct problems scale | |||
| At least 3 items completed | 12 (41.4) | 6 (42.9) | 18 (41.9) [95% CI 27.0% to 57.9%] |
| 1 or 2 items completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 17 (58.6) | 8 (57.1) | 25 (58.1) |
| Hyperactivity scale | |||
| At least 3 items completed | 12 (41.4) | 6 (42.9) | 18 (41.9) [95% CI 27.0% to 57.9%] |
| 1 or 2 items completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 17 (58.6) | 8 (57.1) | 25 (58.1) |
| Peer problems scale | |||
| At least 3 items completed | 12 (41.4) | 6 (42.9) | 18 (41.9) [95% CI 27.0% to 57.9%] |
| 1 or 2 items completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 17 (58.6) | 8 (57.1) | 25 (58.1) |
| Prosocial scale | |||
| At least 3 items completed | 12 (41.4) | 6 (42.9) | 18 (41.9) [95% CI 27.0% to 57.9%] |
| 1 or 2 items completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 17 (58.6) | 8 (57.1) | 25 (58.1) |
We were able to collect the data required for a health economic analysis in a future full-scale RCT; the data completeness levels were good for the EQ-5D-5L and for the reports of health service utilisation (see Appendix 8, Tables 40 and 41).
Adverse events
There were no serious adverse events necessitating hospital admission or adverse events necessitating medical attention during the intervention. There were three minor events: two children had incidents in which they bumped their heads and one father felt unwell during the exercise component and stopped. He reported the next day that he felt better and had not sought medical attention.
Costs of programme delivery
We have estimated the costs of the HDHK-UK programme delivery (details are in Appendix 9, Tables 42–44). The costs exceeded those estimated and varied according to the site and provider. Using 2018 prices, the delivery model using Healthy Lifestyles staff and an independent physical activity coach cost a total of £1881 for the entire programme, excluding training. If take-up had been higher and the programme had included 15 families attending, then the cost per family would be £150. The marginal cost per family rises as the number of participating families falls; for example, the equivalent per-family cost for eight families participating would be £235. Appendix 9 describes the variance in these costs according to the design and provider of the programme.
Summary: the feasibility of trial data collection
Overall, the level of missing data from the participants at baseline and at follow-up was acceptable.
Chapter 7 Discussion and conclusions
Introduction to discussion
In this section, we provide a summary and an interpretation of the main findings of the study; compare our findings with those of other studies, particularly the original reports of the HDHK study from Australia; discuss strengths and limitations; describe public involvement in the study; discuss the criteria for progression to a full trial; and provide recommendations for future research.
Summary of findings
Feasibility of delivery and acceptability of the adapted Healthy Dads, Healthy Kids programme
The main aims of the HDHK-UK study were to adapt the Australian HDHK programme to be culturally acceptable in a UK ethnically diverse population, to explore the acceptability of the adapted programme and to assess the feasibility of delivering the adapted intervention and the feasibility of recruitment and follow-up.
To achieve the first of these aims, we undertook qualitative interviews and focus groups with participants from a range of ethnic, religious and socioeconomic groups and drew on a typology of adaptation of health promotion interventions to make changes to the programme and to inform the evaluation methods. The changes were largely superficial in nature, for example change to the content to be relevant to the UK, use of images of people from ethnic minority groups in participant-facing materials, reference to foods from ethnically diverse communities, the identification of primary schools as a suitable place for programme delivery and simplification of the language and terminology contained in the written HDHK materials. There were some structural adaptations, which included the branding of the intervention and ensuring that all of the physical activities included less tactile options between the fathers and children.
To assess the acceptability and feasibility of delivering the adapted programme, we undertook an uncontrolled feasibility study in two localities. We faced major challenges in aligning the three essential components of delivery: (1) a suitable setting for delivery with a large space for safe family exercise and a room for delivery of the fathers’ education session with projection facilities to display PowerPoint slides, (2) appropriately trained facilitators with the skills to deliver the fathers-only and children-only education sessions and the physical activity element that required sports and fitness coaching training and (3) both of these available at a time suitable for young children and their fathers, who had to be recruited in a timely manner so that they did not have to wait long for the programme to commence. Despite very low attendance at the sessions for this phase, we did identify changes to the programme materials required before we progressed to the randomised feasibility trial, particularly in relation to the quantity and complexity of content in the fathers’ educational sessions. We were also able to confirm the required skill set of the facilitators. Despite concerns raised by one organisation prior to delivery about the difficulties of delivering the physical activity component, and potential risks associated with the activities, these were delivered well and enjoyed by the participants.
Finally, we undertook a randomised feasibility trial in two sites to assess the feasibility of delivering the adapted intervention by assessing the ability to recruit intervention facilitators and overweight fathers and their children to the intervention, and to assess fidelity of delivery and acceptability through interviews with the participants, observations and feedback from participants and facilitators after sessions. To assess the feasibility of a future trial, we measured the ability to recruit participants to the trial and follow-up rates.
Overall, we found that we were able to recruit and train facilitators to the randomised feasibility trial, who could deliver the intervention with reasonable fidelity, and the intervention was highly acceptable to the participants who attended, although non-attendance at the programme was high (31%). The very positive feedback from the fathers who attended the programme contrasted with some of the concerns raised by parents during the adaptations phase. However, we were unable to recruit to target and follow-up rates were low.
Interpretation of these findings
We have reported challenges in bringing an effective intervention, the HDHK programme, from Australia and implementing it in socioeconomically deprived and ethnically diverse areas of the UK. Other interventions have failed to transfer across high-income settings with a failure to replicate the outcomes, such as the lack of effectiveness of an intervention to increase physical activity and diet in children,114,115 the lack of effectiveness of the Family Nurse Partnership in the UK,116 compared with its effectiveness in the USA,117–119 or the failure of breastfeeding peer support interventions in the UK, compared with other settings. 120
Although there have been many adaptations of health promotion activities to meet the needs of ethnic minority populations, Liu et al. 69 reported the findings of a systematic review in which it was possible to link effectiveness to the adaptations in only 9 out of 107 primary studies of adapted interventions. 69 Our adaptation aimed to produce an intervention that was acceptable to general multiethnic, socioeconomically diverse populations, not just one minority group. Methods of cultural adaptation generally focus on adapting an intervention that has been effective in the majority population to one homogenous minority ethnic group;85,121,122 this does not address the needs of the super-diverse populations of large cities. This is an area requiring further research. We used a typology of cultural adaptation,69 which included components that related both to the intervention adaptation and to ensuring that the research processes were also culturally acceptable. This was challenging to operationalise.
We had significant difficulties in recruiting overweight and obese men. A systematic review18 of what motivated men to participate in a weight management programme reported difficulties recruiting men to weight-loss trials. Trials of interventions to manage obesity in men are still relatively sparse,18 compared with the literature for weight loss overall, in which women are the predominant participants. 123,124 No recent trials have specifically targeted ethnic minority males, who make up only 1.8% of the total participants of US studies of weight management interventions. 123 However, weight management trials in men have previously reported findings of effectiveness in the context of work places21,125 and football supporters. 20 There is a need to explore alternative settings for delivery, as the reach of interventions in sports venues and workplaces is not clear18 and many men will be excluded from interventions that recruit through these routes through unemployment or through financial circumstances making attendance at sports events less likely. We hoped that trying to recruit overweight and obese men through other routes that involved their children would be an inclusive recruitment method. Consistent with previous research,126 we found that active recruitment strategies whereby we engaged with the fathers were more successful than passive advertising strategies or recruitment via leaflets given to children or mothers. A potential explanation may have been the sensitivity of inviting an overweight partner/father to the HDHK programme, which was raised by our PPI group. Despite our attempts to brand the programme as being about healthy family lifestyles and quality time between fathers and their children, we did have to mention the lower BMI threshold on the promotional leaflet, which may have been a barrier. Other potential barriers may have been the need for attendance at a recruitment session either at home or a convenient venue, and the challenges of finding a convenient time for the father and child(ren). Recruitment to group-based interventions can be difficult owing to the accessibility and comfort of the venue, the meanings attributed to the setting and the sociodemographic characteristics of the participants and facilitators of a group. 127
Once recruited, 31% of the participants who were randomised to the intervention group did not commence the programme. This is consistent with other RCTs of group-based weight management, but much higher than the Australian HDHK evaluation (2%). 128 In other contexts, such as cardiac rehabilitation, which is offered after a cardiac event, uptake to the group-based rehabilitation is low, with only 51% of eligible people taking up the programme in the UK. 129 Attrition from the intervention was high: of those who attended a session, 75% attended five or more, but only 45% attended seven or more sessions, which may reflect issues of convenience and timing. Participant attrition in HDHK-UK was high, with only 63% of participants followed up at 6 months. Intervention participants who attended only one or two sessions had the lowest follow-up rates at 3 months (20%; 1/5); this might be as a result of the group climate or group cohesiveness, which have been associated with increased attendance and self-efficacy in exercise classes. 130 High levels of attrition have also been seen in a trial of children’s weight management in a similar population;53 in others trials of child weight management,131,132 trials of men’s weight management18,19 and weight management interventions overall;124 and in trials of physical activity promotion in socioeconomically disadvantaged communities. 133 However, the majority of the research on behaviour change interventions in people from black and ethnic minority groups and from socioeconomically disadvantaged communities comes from research conducted in the USA, with a predominance of research in African American and Hispanic populations133 and conducted in faith-based settings, which may not be transferable to a UK context.
One challenge we faced was that the research funding for the study was from a call to address men’s weight management. Other studies have reported that parents are more likely to enrol on programmes that focus on a healthy lifestyle, rather than on weight loss. 134 Although the HDHK programme in Australia was designed as a weight management programme, in its community roll-out, it used a more inclusive approach and focused on family healthy lifestyle practices. Our public involvement panel reinforced the difficulty and power imbalance in families, whereby a child or partner might suggest their father/partner joined the programme. Although our initial flyer focused on lifestyle change and fun physical activities with their children, we had eligibility criteria of a high BMI value or large waist circumference. We had interest from fathers who were interested in taking part, but were not overweight. Any future roll-out of the HDHK programme in the UK would be better placed if an inclusive approach is taken with fathers/father figures without a weight eligibility criterion.
The findings from the qualitative interviews and feedback from the fathers who attended the programme support those reported by Robertson et al. 18 The men liked the physical activity component and the interactions within the group. The measures of acceptability of the HDHK-UK intervention fulfil a number of the component constructs of acceptability as described by Sekhon et al. 135 Fathers described their feelings about the intervention (affective attitude), the burden, the intervention coherence, opportunity costs, the intervention’s perceived effectiveness and their self-efficacy in performing the behaviours. 135
Costs of programme delivery
The aims of the feasibility study in relation to health economics were to determine whether or not the quality-of-life and well-being questionnaires were acceptable and completed with sufficient completeness to determine utility and capability scores in fathers and children, and to collect data on the costs of delivering the programme and on health-care resource utilisation. The feasibility study highlighted the differential costs depending on delivery and setting. Per-family costs (dependent on the number of families per group) ranged substantially from £150 (15 families) to £235 (8 families), excluding training. In any future definitive trial, it would be important to collect data on the costs to the participants in terms of time, as well as financial costs, to inform a wider perspective for a health economic analysis. For the feasibility study, we were trying to minimise questionnaire burden.
Furthermore, for the economic evaluation, although the generic utility-based instruments might not be as sensitive to change as weight-focused quality-of-life measures, they are a generic measure of outcome and therefore relevant for informing resource allocation decisions across different sectors and disease areas. For a comprehensive economic evaluation alongside a weight-loss trial, we would recommend the use of utility instruments such as the EuroQol-5 Dimensions (EQ-5D) and the CHU-9D to place the analysis in this broader context, as well as more specific weight-focused instruments to facilitate a cost-effectiveness analysis.
Comparison with the Australian Healthy Dads, Healthy Kids research findings
The Australian RCTs of the HDHK programme had positive outcomes, reporting a mean difference in weight loss in the fathers of 3.4 kg (95% CI 2.1 kg to 4.7 kg) in favour of the intervention at 14 weeks, compared with a wait-list control in a community trial,45 and a mean weight loss in the fathers of 7.6 kg (95% CI 6.0 kg to 9.2 kg) in an efficacy trial at the 6-month follow-up. 46 In this section, we explore the differences between the delivery and context of the Australian trials and HDHK-UK programme (Table 29). The efficacy trial was delivered by Philip Morgan, who developed the programme, in a university setting with highly engaged participants; thus, the findings are unlikely to be replicable. Therefore, we have compared the findings of the HDHK-UK study with that of the randomised controlled community trial. 45 Overall weight loss in the intervention group of the Australian HDHK study was 3.3 kg (95% CI 2.4 kg to 4.3 kg) at the 14-week follow-up, similar to the 2.9 kg (95% CI 0.6 kg to 5.1 kg) at the 6-month follow-up in our UK study.
| Site | UK | Australia |
|---|---|---|
| Organisation | University with local authorities | University with schools for HDHK community RCT (2010–11)45 |
| Intervention funding | Local authorities in time of austerity and reductions in funding to traditional ‘lifestyles’ public health | Industry partner/community fund |
| Localities | Socioeconomically deprived localities with high proportion of the population from black and minority ethnic groups | Rural areas with high rates of mining and shift work |
| Delivery sites |
|
Schools |
| Timing of groups |
|
|
| Size of groups | Two to six families per group | RCT: two groups of 25 families in each trial arm |
| Age of eligible children | Primary school: 4–11 years | Primary school: 5–12 years |
| Support infrastructure | University of Birmingham research team and Fatherhood Institute | HDHK research team at the UoN, Australia |
| Training |
|
|
| Programme facilitators | A number of different facilitators across the delivery sites:
|
University-qualified and experienced primary school teachers and high school health and physical education teachers were employed as programme facilitators |
| Skill set of facilitators |
|
|
| Delivery style | Challenge to deliver the 30-minute fathers’ session within the time, even after reducing the slides; facilitatory style, possibly reflecting relatively small groups | Delivery more ‘lecture’ style, with brief opportunities for interactions between the dads |
| Gender of deliverers of fathers’ session | Variable owing to staff availability; two programmes led by male facilitators, two by female facilitators | Male |
| Continuity | Three programmes achieved mostly good continuity in the facilitator team; one programme had frequent changes owing to availability of staff | Continuity of facilitator of fathers session |
| Fitting HDHK into existing role |
|
Completed in own time as a paid role |
| Population |
|
Mix of socioeconomic status levels (low, middle and high); 3% in lowest two quintiles of socioeconomic status based on the SEIFA Index of Relative Socioeconomic Advantage and Disadvantage. High shift-working population in a coal-mining region |
| Recruitment methods |
|
|
| Study allocation | Only intervention group offered HDHK programme; comparator group received leisure centre voucher | All participants received HDHK either initially or as wait-list control |
| Other challenges faced |
|
High rates of shift-work employment were the most common barrier to programme attendance (on average, participants attended five of seven sessions) |
| Relationship between university and commissioning/delivery organisations | Local authorities provided contacts to potential delivery settings and potential facilitators; turnover of staff | University recruited, employed and trained programme facilitators directly |
Key differences relate to the setting and context: the UK programmes were delivered in a public health context in socioeconomically disadvantaged localities and among populations with high ethnic diversity. The populations invited to the Australian HDHK programme were more sociodemographically heterogeneous, with people from high and low socioeconomic circumstances and a large proportion doing shift work. In our UK sample, 74.4% lived in localities in the two most disadvantaged quintiles of socioeconomic deprivation, compared with 3% of the Australian sample being in the lowest two quintiles of socioeconomic status. The Australian programme was funded by an industry partner and community fund, whereas the UK intervention was funded by the local authority public health budget, which was resource constrained.
The training in the UK took a ‘train-the-trainer’ approach, with training manuals and additional video clips of the physical activity sessions and activities for facilitators to watch before the sessions. Owing to difficulties in recruitment, planning training and delivery issues, some of the facilitators were trained several months prior to the start of the programme, whereas others had a few hours of training then support for the early weeks of delivery. By contrast, all of the Australian facilitators were trained by PM 2–3 weeks before the start of the programme. This may have affected the fidelity and style of delivery in the UK.
The UK study randomised participants to the HDHK programme or to a control group with a minimal intervention with follow-up at 6 months, whereas the Australian programme had a wait-list control and a follow-up at 14 weeks. The wait-list control meant that the trial could be promoted as offering a fun programme for children and their fathers, whereas we could not promote the HDHK programme, as some of the participants would not receive the intervention. This made the first approach to recruitment substantially more difficult.
Recruitment in the UK was a huge challenge, with difficulties engaging with schools and other organisations to gain access to fathers of primary school-aged children. Schools had a large number of competing demands and communication was slow. In addition, despite schools being identified in the cultural adaptation as an ideal place for the programmes to take place, constraints in opening hours and availability of school halls made it difficult to align availability with the times when fathers could manage to attend sessions after they had finished work and commuted through a very congested urban area. Once we had interest from schools, we invited their teachers to the HDHK training; however, there was no interest from teachers in the schools. Therefore, we sought alternative people to deliver the programme. It became apparent that a high degree of skill was required to deliver the content of the fathers-only educational sessions and the physical activity component. The HDHK programme in Australia was delivered by qualified teachers; a male facilitator (who was a father) led the fathers-only education session. Furthermore, continuity of facilitators was maintained. We identified lower satisfaction in the group for which we were unable to have a consistent facilitator and we also had feedback from the male facilitators of two of the groups that the interactions between the participants changed when a female observer attended the sessions. However, previous research has not identified that the sex of the person delivering a weight loss intervention to men affected men’s outcomes. 18 During our adaptation phase, phase 1a, participants highlighted the importance of having someone who is a father himself delivering the fathers-only educational sessions. This was something that we were unable to accommodate.
There were differences in delivery in terms of the time of the year, with the UK programme taking place over the winter and the Australian programme taking place over summer, when evenings are brighter. Feedback from fathers in our feasibility study highlighted the dark evenings and poor weather as deterring attendance.
The HDHK programme had also changed by the time we adapted it. The subsequent community roll-out in Australia had extended the programme to nine sessions and included mothers for one session; this longer duration may have affected engagement with the UK programme. The small number of attendees at each session in the UK meant that the programme was delivered in a more participatory and discursive manner than was the case in Australia, where the groups were much larger.
These differences provide some insights into how the programme would be best delivered in the UK context, as discussed below.
Strengths and limitations
This study had many strengths. The intervention adaptation process was multifaceted and drew on a typology of cultural adaptation. 69 We also drew on other family-based programmes that were being developed in a similar UK locality53 and a new family-based programme developed by the Australian team for fathers and their daughters. 67 We did not find any evidence from our qualitative interviews and focus groups in phase 1a that the underpinning theories of the HDHK programme were not relevant to our population. We did identify a number of surface and deep structural adaptations, which were implemented and then further tested in phase 1b, the uncontrolled feasibility trial. We undertook two iterations of the feasibility trial, so we were able to test recruitment and delivery strategies, as well as content acceptability, during the uncontrolled trial (phase 1b). In addition, we included a robust process evaluation with data from qualitative interviews, observations, feedback after sessions from both facilitators and participants alongside both the uncontrolled feasibility trial (phase 1b) and the randomised feasibility trial (phase 2).
However, the study had limitations. The small numbers of participants attending the programme in phase 1b means that we may not have gained as much learning about the acceptability of the programme and delivery as would have been optimal. If there had not been challenges with venues and staff to deliver the programme, we may have reached different conclusions about the acceptability and adaptations needed following phase 1b. Many of the limitations were as a result of challenges we faced, particularly the difficulty in recruiting overweight fathers from ethnically diverse, socioeconomically disadvantaged communities to a group-based healthy lifestyles programme. The study was made more challenging by the need for the intervention to be funded by the local authority, which has responsibility for delivering public health interventions. However, weight management is not one of the mandated activities that local authorities have to deliver and the context of the study period was a financial tightening of public health activities in local authorities. One of the planned partner local authorities close to the university ceased to offer adult weight management, and so was unable to support the intervention. This resulted in a considerable increase in travel costs and time to locate the study in other sites, which may have affected our recruitment and delivery challenges. We had less local knowledge about these areas and had to rely on our local authority partners to help identify delivery sites. Financial constraints also led to the need to use the staff employed by one of the local authorities rather than select from a wider pool of potential HDHK programme facilitators, as these staff were already paid and there were limited funds available to fund the intervention costs. During the delivery of the HDHK-UK programme, one of the local authorities had a reorganisation of their public health department, which resulted in loss of staff who were trained to deliver the programme. Staff changes were also an issue in the coaching organisation; indeed, none of the nine facilitators trained in January 2016 by the Fatherhood Institute were in the same post or organisation 12 months after training. Consequently, our training needed to be more flexible and ongoing to cope with staff changes, which may have affected fidelity.
Another issue that may have affected fidelity in the delivery of the programme to the children was that many of the children failed to bring their handbook with them to sessions. In addition, owing to delays in starting, we ended up delivering the programmes over the winter, which was a particularly harsh UK winter (2017–18). This contrasts with delivery of the HDHK programmes in Australia that have all been delivered over the summer months. Although our adaptation work directed us towards delivery in primary schools, we found primary schools challenging to work with: communication was slow, as our link was sometimes classroom-based with limited time to respond to e-mail requests; and permissions, for example to speak to parents at school pick-up time, often required us to go up through a chain of people to gain approval.
We had planned to interview the children as well as the fathers at the 3-month follow-up point of the feasibility trial, but many of the children were too young to take part in an interview, so we do not have feedback directly from the children. Participant attrition was high, and was higher in the intervention group than in the comparison group; we can speculate that families that did not enjoy or perceive benefit from the programme were less likely to attend follow-up. With the small participant numbers, we have been careful to report data completion rates and, in keeping with good practice for feasibility studies, not to make any comparisons between the study arms.
Lessons in delivery of the Healthy Dads, Healthy Kids programme in the UK
We have identified a number of issues relating to the delivery of the programme that would need to be addressed to successfully deliver the HDHK programme in a UK community context:
-
The facilitators need to have been trained in sport and fitness coaching and have the ability to deliver an educational session.
-
The timing of the sessions should avoid the evenings in winter and should include the option of weekend daytime sessions, as these were popular.
-
Children in the UK start school younger than in Australia and we found that the 4-year-olds struggled with the structure of the sessions; the programme is probably best suited to children aged 5–11 years.
-
To deliver the fathers-educational sessions in a discursive and participatory manner, the number of slides needs to be reduced further to keep this part to 30 minutes.
-
The focus should be on family lifestyle change, benefits to the children and the father–child relationship, and fun, not weight management of the fathers.
-
Given the high turnover of staff in the organisations that provided facilitators, any future intervention delivery needs to plan repeated training. Consideration should be given to the development of a training video to support implementation.
Consideration of progression to a trial to assess the effectiveness and cost-effectiveness of the Healthy Dads, Healthy Kids programme in the UK context
In the HDHK-UK study protocol, we specified that we would consider the following factors when making the decision to proceed to a full trial of the effectiveness and cost-effectiveness of the HDHK programme in the UK:
-
a process evaluation suggests that the intervention is acceptable to a majority of fathers and families from differing BAME and socioeconomic backgrounds
-
randomisation occurs and > 80% of those assessed accept randomisation
-
recruitment of at least 68 out of the planned 90 fathers (75%) within the 4-month time frame
-
intervention implemented with fidelity in 75% of observations
-
attendance – 70% attending at least five out of nine of the planned sessions
-
> 70% follow-up at 3 and 6 months
-
mean weight loss in the intervention arm of ≥ 3 kg.
There were high levels of acceptability among those who attended the programme; however, only 69% (20/29) of the fathers allocated to the HDHK-UK programme attended at least once. Participants who attended reported changes to their own and their family’s dietary and physical activity. All of the fathers who were assessed and eligible were randomised and we delivered the intervention achieving the acceptable level of fidelity. However, our challenges to delivery of the programme in the current UK public health context were as follows: low recruitment rate of only 43 of the planned 90 fathers and high attrition with only 63% follow-up at 6 months. These suggest that, at present, it would not be feasible to progress to a full-scale trial of the effectiveness and cost-effectiveness of the HDHK programme in the UK. Although 75% of fathers who attended at least one HDHK session ‘completed’ (i.e. attended at least five of the nine sessions) the programme, overall, only 52% of the fathers randomised to the intervention completed the programme. Mean weight loss in the intervention arm was 2.9 kg (95% CI 0.6 kg to 5.1 kg) at the 6-month follow-up, but based on the 25 (58%) participants who provided weight data at this follow-up point.
However, the programme may be feasible in a different context. The randomisation to a control group made the recruitment more difficult and the comparison to a wait-list control may well have enhanced our recruitment, as we could have ‘sold’ the potential benefits of the HDHK programme, as seen in the Australian studies. Recruitment and delivery through an organisation such as a professional sports club’s community arm would be more feasible and would remove the delivery challenges, but the programme is unlikely to be funded by such a club in the current financial climate.
Patient and public involvement in the study
In this section, we describe PPI in the HDHK-UK study, using the Guidance for Reporting Involvement of Patients and the Public 2 (GRIPP2)-Short Form as a guide to content. 136 The aims of PPI and a brief description of the methods used are described in Chapter 2.
Methods used for patient and public involvement in the study
Prior to the start of the study we convened one PPI meeting, and two were convened during the study period in July 2017 and June 2018. Between these meetings, we had an e-mail discussion about the challenges that we were facing. Overall, eight fathers and two mothers attended the groups: seven fathers and one mother at session one, five fathers and two mothers at session two (July 2017) and three fathers and one mother at session three (June 2018). The sessions all took place on Sundays.
At the first two sessions, we asked the PPI group to suggest ways that we could promote the study (both the cultural adaptation phase and the feasibility trials), to comment on participant-facing documents, for their thoughts about the issues raised in the cultural adaptation of the programme, about issues in relation to programme delivery that would affect their willingness to take part in a programme and to suggest potential modes of recruitment and local organisations that we might approach for recruitment of fathers.
Reimbursement was provided for PPI input. The PPI representative for the Trial Steering Committee was reimbursed the equivalent of £150 per day. Attendees at PPI sessions were provided with a £20 shopping voucher as a thank-you and refreshments were provided at the sessions. The PPI member of the SMG was reimbursed at the equivalent of £150 per day for attending a meeting.
Results of patient and public involvement in the study (including both positive and negative outcomes)
During the cultural adaptation phase and the development of feasibility trials, the PPI group advised on the overall approach to approaching and recruiting overweight fathers, particularly in relation to the sensitivity of the issue of the eligibility criterion of being overweight or obese. The PPI group suggested that the attraction to fathers was more likely to be in relation to benefits for the children and time spent with their children. Therefore, the PPI group suggested altering our proposed participant-facing documentation to be less about health and instead to promote how the intervention encourages greater quality time between fathers and children. We altered the invitation brochure to reflect their comments.
The PPI group also suggested that parents may wish to know more about the programme to appease any safety concerns (i.e. who would be present/responsible for children at the location where the programme was to be delivered). As a result, we ensured that details about who would be delivering the intervention and its nature were clearly explained at the recruitment meeting.
The group stated that participant-facing material (participant information leaflet and invitation brochure) were not inclusive enough for all ‘father figures’ (e.g. stepfathers). The material in question was changed to be more inclusive.
To boost recruitment to the trial, the PPI group suggested organisations that might be accessed by our target population and that might be interested in supporting the study (e.g. youth clubs, after-school clubs and sports centres). Therefore, we approached and successfully recruited fathers from after-school and martial arts clubs and Scouts groups for the cultural adaptation phase.
When asked about dissemination of study results, PPI representatives thought that it was important to report the findings back to the local authorities that funded the HDHK programmes and to include the use of the local authorities’ social media channels for dissemination. The group encouraged the research team to be fully open about the challenges faced in delivering the HDHK programme and the research study.
In considering any future implementation of the HDHK intervention, there were suggestions that fathers might contribute to the cost of the programme, but be refunded if they completed the programme.
The PPI representative on the Study Steering Group either attended the meetings or contributed by e-mail. He offered a useful perspective and ensured that we remained participant-focused.
The independent lay member of the SSC attended all of the meetings and offered a lay perspective.
Reflections on use of patient and public involvement in the study
The PPI in the HDHK study offered a very useful father perspective. However, organising meetings was difficult because of the commitments of the parents and the researchers and the need to meet at a weekend. Several meetings were rearranged owing to difficulties in bringing the group together.
In addition, the PPI group suggested that the intervention should not focus on addressing overweight and obesity, but should instead highlight the benefits to the children and to father–child relationships; this directly clashed with the motivation for funding the trial, which was to address overweight and obesity in men, meaning that there was a need for the eligibility criteria to include a minimum BMI. This was not a resolvable issue.
Research recommendations
Given that we did not meet the progression criteria for a future definitive RCT, we do not recommend a RCT of HDHK-UK for men’s weight loss in a community context in this specific UK context at present. However, we have the following areas that merit further research:
-
research to explore the optimal ways to engage fathers from ethnically diverse, socioeconomically deprived populations in research
-
an evaluation of the HDHK programme outside the context of weight management
-
research into the best methods to recruit men to trials of weight management interventions
-
research into the effect on recruitment and generalisability of public health interventions with a wait-list control compared with a no/minimal intervention control.
Conclusions
Men have high rates of overweight and obesity in the UK and in many other countries internationally. Although there is a need for systems approaches to tackling obesity through social, economic, political and structural environments,137–139 there is also a need for individualised approaches to supporting weight management. The evidence base for effective interventions is limited and we sought to address this gap in the literature by evaluating the feasibility of adapting a successful programme from Australia for fathers and their children aged 4–11 years to the UK context.
The randomised feasibility trial and process evaluation showed that, although well received and enjoyed, it was not feasible to deliver the HDHK programme to overweight and obese fathers in ethnically diverse, socioeconomically deprived communities in the UK in the current context. The lack of feasibility was largely due to implementation issues and our failure to recruit overweight and obese fathers to the study. Other challenges related to the relatively low retention rate at follow-up and high attrition from the intervention. Among those who attended the programme, there was a good completion rate and positive feedback about the programme from the fathers. We cannot comment on the feasibility of recruiting to the study outside the context of a men’s weight management intervention.
Acknowledgements
We would like to acknowledge and thank a number of people and organisations for their support and/or participation in this study: the NIHR Health Technology Assessment programme (project number 14/185/13) for funding the study; all the participants of the study – the fathers, their children and other family members; the local authorities for their support and direction; and all the facilitators who were involved in session delivery.
We would like to thank Dr Khaled Ahmed and Felicity Brant for their contribution to recruitment, follow-up and study administration; Dr Farina Kokab for help with the qualitative interviews in phase 1a; and the casual research staff who supported data collection: David Sardar and Meanaz Akhtar.
We acknowledge members of the SSC who oversaw the running of the study: Professor John Wright, Bradford Institute for Health Research (chairperson); Professor Pat Hoddinott, University of Stirling; Dr Elaine Nicholls, Keele University; and Mr Ray Fiveash, PPI representative.
Fatherhood Institute: we would like to thank Kathy Jones and Cassius Campbell who developed and led the training programme; and Jeremy Davies who contributed to father-facing materials and the adaptation of the HDHK programme.
We would also like to thank Jeszemma Garratt from the Fatherhood Institute and the Parent Advisory Panel.
We acknowledge the academics Professor David Lubans and Kristen Saunders from the UoN, Australia, who developed the original HDHK programme and who supported the study through the development of training materials and shared their experience of delivery in the Australian setting.
Contributions of authors
Kate Jolly (https://orcid.org/0000-0002-6224-2115) (Professor of Public Health and Primary Care) was the principal investigator, leading the study from design to delivery, and wrote the study report.
Tania Griffin (https://orcid.org/0000-0003-0146-4440) (Research Fellow) was the study co-ordinator for 14 months (July 2017–September 2018) and was a member of the study management team. She oversaw the delivery of phase 1b and the set-up and delivery of phase 2, and led the writing of Chapters 4–6.
Manbinder Sidhu (https://orcid.org/0000-0001-5663-107X) (Research Fellow) was the study co-ordinator from the start of the study to July 2017. He led phase 1a, the cultural adaptation, and the set-up of phase 2. He led the writing of Chapter 3.
Peymane Adab (https://orcid.org/0000-0001-9087-3945) (Professor of Chronic Disease Epidemiology and Public Health) was a co-investigator and contributed to the study design and interpretation of findings.
Adrienne Burgess (https://orcid.org/0000-0003-0965-365X) (Joint Chief Executive and Head of Research at the Fatherhood Institute) was a co-investigator and contributed to the study design, advised about recruitment of fathers, and contributed to the adaptation of the original HDHK materials and to the interpretation of findings.
Clare Collins (https://orcid.org/0000-0003-3298-756X) (Professor of Nutrition and Dietetics) was a co-investigator and contributed to the study design and collection of dietary data.
Amanda Daley (https://orcid.org/0000-0002-4866-8726) (Professor of Behavioural Medicine) was a co-investigator and contributed to the study design and interpretation of findings.
Andrew Entwistle (https://orcid.org/0000-0001-9745-3556) (Public Member) was a co-investigator, provided a PPI perspective and contributed to the Plain English summary.
Emma Frew (https://orcid.org/0000-0002-5462-1158) (Reader in Health Economics) was a co-investigator, contributed to the study design and interpretation of findings and advised on the health economic data collection.
Pollyanna Hardy (https://orcid.org/0000-0003-2937-8368) (Senior Statistician) advised on the statistical analysis and contributed to the interpretation of findings.
Kiya Hurley (https://orcid.org/0000-0002-5084-5410) (Research Fellow) led the physical activity accelerometry data analysis, contributed to study management and undertook qualitative interviews in phase 2.
Laura Jones (https://orcid.org/0000-0002-4018-3855) (Senior Lecturer in Qualitative and Mixed-Methods Applied Health Research) oversaw the qualitative components, was a co-investigator and contributed to the study design and interpretation of findings.
Eleanor McGee (https://orcid.org/0000-0002-8497-9927) (Dietitian, Birmingham Community Healthcare Trust, NHS) was a co-investigator, and contributed to the study design and interpretation of findings.
Miranda Pallan (https://orcid.org/0000-0002-2868-4892) (Senior Lecturer in Public Health) was a co-investigator. She led the CHANGE study and advised on the cultural adaptation, and contributed to the study design and interpretation of findings.
Yongzhong Sun (https://orcid.org/0000-0003-0659-9811) (Statistician) developed the statistical analysis plan, undertook the statistical analysis and contributed to the interpretation of findings.
Myles Young (https://orcid.org/0000-0001-7670-9196) (Research Fellow) was a co-investigator, he advised on implementation and contributed to the study design and interpretation of findings.
Philip Morgan (https://orcid.org/0000-0002-5632-8529) (Professor of Education) designed the original HDHK programme. He was a co-investigator, and contributed to the study design, delivered training materials, advised on implementation and contributed to interpretation of findings.
All authors read and approved the final version of the report.
Publications
Griffin T, Hurley K, Sidhu M, Adab P, Pallan M, Daley A, et al. Recruitment and Delivery of a Weight Management Programme for Fathers of Primary School Aged Children: Challenges Experienced in the Healthy Dads, Healthy Kids-UK Feasibility Study. 5th UK Congress on Obesity, Newcastle, 6–7 September 2018.
Griffin T, Hurley K, Sidhu M, Jones L, Morgan P, Adab P, et al. A Weight Management Programme for Fathers of Primary School Aged Children: Qualitative Findings from Healthy Dads, Healthy Kids-UK. 5th UK Congress on Obesity, Newcastle, 6–7 September 2018.
Jolly K, Griffin T, Sidhu M, Hurley K, Adab P, Burgess A, et al. Healthy Dads, Healthy Kids. Adapting an Australian Group Based Weight Management Programme for Fathers of Young Children in a UK setting; a Feasibility Study. UK Society for Behavioural Medicine Annual Meeting, Birmingham, 13 December 2018.
Griffin T, Sun Y, Sidhu M, Adab P, Burgess A, Collins C, et al. Healthy Dads, Healthy Kids UK, a weight management programme for fathers: feasibility RCT. BMJ Open 2019;9:e033534.
Data-sharing statement
All data are available on request from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Kopelman P. Health risks associated with overweight and obesity. Obes Rev 2007;8:13-7. https://doi.org/10.1111/j.1467-789X.2007.00311.x.
- Gatineau M, Dent M. Obesity and Mental Health. Oxford: National Obesity Observatory; 2011.
- Prospective Studies Collaboration . Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083-96. https://doi.org/10.1016/S0140-6736(09)60318-4.
- Public Health England . Health Matters: Obesity and the Food Environment 2017. www.gov.uk/government/publications/health-matters-obesity-and-the-food-environment/health-matters-obesity-and-the-food-environment--2 (accessed 28 May 2018).
- NHS Digital . Statistics on Obesity, Physical Activity and Diet. England 2017 2017. https://files.digital.nhs.uk/publicationimport/pub23xxx/pub23742/obes-phys-acti-diet-eng-2017-rep.pdf (accessed 28 May 2018).
- NHS Digital . Health Survey for England 2016. Adult Overweight and Obesity 2016. https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/health-survey-for-england-2016 (accessed 28 May 2018).
- National Institute for Health and Care Excellence (NICE) . BMI: Preventing Ill Health and Premature Death in Black, Asian and Other Minority Ethnic Groups 2013.
- Garfield CF, Duncan G, Gutina A, Rutsohn J, McDade TW, Adam EK, et al. Longitudinal study of body mass index in young males and the transition to fatherhood. Am J Mens Health 2016;10:NP158-NP167. https://doi.org/10.1177/1557988315596224.
- Roberts C ST, Maplethorpe N, Cox L, Meadows S, Nicholson S, Page P, et al. National Diet and Nutrition Survey: Results from Years 7 and 8 (Combined) of the Rolling Programme (2014/2015 to 2015/2016). London: Public Health England, Food Standards Agency; 2018.
- Department of Health and Social Care . UK Physical Activity Guidelines n.d. www.gov.uk/government/publications/uk-physical-activity-guidelines (accessed 14 December 2018).
- NHS Digital . Health Survey for England 2016: Physical Activity in Adults 2017.
- Steene-Johannessen J, Anderssen SA, van der Ploeg HP, Hendriksen IJ, Donnelly AE, Brage S, et al. Are self-report measures able to define individuals as physically active or inactive?. Med Sci Sports Exerc 2015;48:235-44. https://doi.org/10.1249/MSS.0000000000000760.
- Craig R, Mindell J, Hirani V. Health Survey for England 2008. Volume 1. Physical Activity and Fitness 2008. https://files.digital.nhs.uk/publicationimport/pub00xxx/pub00430/heal-surv-phys-acti-fitn-eng-2008-rep-v2.pdf (accessed 25 November 2019).
- Sport England . Active Lives Adult Survey: May 17 18 Report 2018.
- Allender S, Cowburn G, Foster C. Understanding participation in sport and physical activity among children and adults: a review of qualitative studies. Health Educ Res 2006;21:826-35. https://doi.org/10.1093/her/cyl063.
- Hull EE, Rofey DL, Robertson RJ, Nagle EF, Otto AD, Aaron DJ. Influence of marriage and parenthood on physical activity: a 2-year prospective analysis. J Phys Act Health 2010;7:577-83. https://doi.org/10.1123/jpah.7.5.577.
- Pot N, Keizer R. Physical activity and sport participation: a systematic review of the impact of fatherhood. Prev Med Rep 2016;4:121-7. https://doi.org/10.1016/j.pmedr.2016.05.018.
- Robertson C, Archibald D, Avenell A, Douglas F, Hoddinott P, van Teijlingen E, et al. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18350.
- Young MD, Morgan PJ, Plotnikoff RC, Callister R, Collins CE. Effectiveness of male-only weight loss and weight loss maintenance interventions: a systematic review with meta-analysis. Obes Rev 2012;13:393-408. https://doi.org/10.1111/j.1467-789X.2011.00967.x.
- Hunt K, Wyke S, Gray CM, Anderson AS, Brady A, Bunn C, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet 2014;383:1211-21. https://doi.org/10.1016/S0140-6736(13)62420-4.
- Morgan PJ, Callister R, Collins CE, Plotnikoff RC, Young MD, Berry N, et al. The SHED-IT community trial: a randomized controlled trial of internet- and paper-based weight loss programs tailored for overweight and obese men. Ann Behav Med 2013;45:139-52. https://doi.org/10.1007/s12160-012-9424-z.
- Sidhu M, Aiyegbusi OL, Daley A, Jolly K. Older men’s experience of weight loss maintenance interventions: qualitative findings from the Lighten Up Plus trial. J Obes Weight Loss 2016;1. https://doi.org/10.24966/OWL-7372/1000003.
- NHS Digital . National Child Measurement Programme: England – 2017 18 School Year [PAS] 2018.
- Boreham C, Riddoch C. The physical activity, fitness and health of children. J Sports Sci 2001;19:915-29. https://doi.org/10.1080/026404101317108426.
- Donnelly JE, Hillman CH, Castelli D, Etnier JL, Lee S, Tomporowski P, et al. Physical activity, fitness, cognitive function, and academic achievement in children: a systematic review. Med Sci Sports Exerc 2016;48:1197-222. https://doi.org/10.1249/MSS.0000000000000901.
- Telama R. Tracking of physical activity from childhood to adulthood: a review. Obes Facts 2009;2:187-95. https://doi.org/10.1159/000222244.
- Chief Medical Officers of the UK . Factsheet 3. Physical Activity Guidelines for Children and Young People (5–18 Years) 2011.
- Wilkie H, Standage M, Sherar L, Cumming S, Parnell C, Davis A, et al. Results from England’s 2016 report card on physical activity for children and youth. J Phys Act Health 2016;13:143-9. https://doi.org/10.1123/jpah.2016-0298.
- Standage M, Sherar L, Curran T, Wilkie HJ, Jago R, Davis A, et al. Results from England’s 2018 report card on physical activity for children and youth. J Phys Act Health 2018;15:S347-s9. https://doi.org/10.1123/jpah.2018-0537.
- Jago R, Solomon-Moore E, Macdonald-Wallis C, Sebire SJ, Thompson JL, Lawlor DA. Change in children’s physical activity and sedentary time between year 1 and year 4 of primary school in the B-PROACT1V cohort. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966-017-0492-0.
- Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc 2000;32:963-75. https://doi.org/10.1097/00005768-200005000-00014.
- O’Connor TM, Jago R, Baranowski T. Engaging parents to increase youth physical activity a systematic review. Am J Prev Med 2009;37:141-9. https://doi.org/10.1016/j.amepre.2009.04.020.
- van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ 2007;335. https://doi.org/10.1136/bmj.39320.843947.BE.
- Lytle LA, Hearst MO, Fulkerson J, Murray DM, Martinson B, Klein E, et al. Examining the relationships between family meal practices, family stressors, and the weight of youth in the family. Ann Behav Med 2011;41:353-62. https://doi.org/10.1007/s12160-010-9243-z.
- Oliveria SA, Ellison RC, Moore LL, Gillman MW, Garrahie EJ, Singer MR. Parent–child relationships in nutrient intake: the Framingham Children’s Study. Am J Clin Nutr 1992;56:593-8. https://doi.org/10.1093/ajcn/56.3.593.
- Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr 2005;24:83-92. https://doi.org/10.1080/07315724.2005.10719448.
- Neumark-Sztainer D, Hannan PJ, Story M, Croll J, Perry C. Family meal patterns: associations with sociodemographic characteristics and improved dietary intake among adolescents. J Am Diet Assoc 2003;103:317-22. https://doi.org/10.1053/jada.2003.50048.
- Videon TM, Manning CK. Influences on adolescent eating patterns: the importance of family meals. J Adolesc Health 2003;32:365-73. https://doi.org/10.1016/S1054-139X(02)00711-5.
- Gillman MW, Rifas-Shiman SL, Frazier AL, Rockett HR, Camargo CA, Field AE, et al. Family dinner and diet quality among older children and adolescents. Arch Fam Med 2000;9:235-40. https://doi.org/10.1001/archfami.9.3.235.
- Nicklas TA, Baranowski T, Baranowski JC, Cullen K, Rittenberry L, Olvera N. Family and child-care provider influences on preschool children’s fruit, juice, and vegetable consumption. Nutr Rev 2001;59:224-35. https://doi.org/10.1111/j.1753-4887.2001.tb07014.x.
- Kremers SP, Brug J, de Vries H, Engels RC. Parenting style and adolescent fruit consumption. Appetite 2003;41:43-50. https://doi.org/10.1016/S0195-6663(03)00038-2.
- Brannen J, O’Connell R, Mooney A. Families, meals and synchronicity: eating together in British dual earner families. Community Work Fam 2013;16:417-34. https://doi.org/10.1080/13668803.2013.776514.
- Chowbey P, Harrop D. Healthy Eating in UK Minority Ethnic Households: Influences and Way Forward. London: Race Equality Foundation; 2016.
- Lucas A, Murray E, Kinra S. Heath beliefs of UK South Asians related to lifestyle diseases: a review of qualitative literature. J Obes 2013;2013. https://doi.org/10.1155/2013/827674.
- Morgan PJ, Collins CE, Plotnikoff RC, Callister R, Burrows T, Fletcher R, et al. The ’Healthy Dads, Healthy Kids’ community randomized controlled trial: a community-based healthy lifestyle program for fathers and their children. Prev Med 2014;61:90-9. https://doi.org/10.1016/j.ypmed.2013.12.019.
- Morgan PJ, Lubans DR, Callister R, Okely AD, Burrows TL, Fletcher R, et al. The ’Healthy Dads, Healthy Kids’ randomized controlled trial: efficacy of a healthy lifestyle program for overweight fathers and their children. Int J Obes 2011;35:436-47. https://doi.org/10.1038/ijo.2010.151.
- Morgan P, Lloyd A, Barnes A, Young M, Miller A, Lubans D, et al. Engaging fathers to improve family physical and mental health: the impact of the ’Healthy Dads, Healthy Kids’ community program. Edinburgh, UK: International Society for Behavioural Nutrition and Physical Activity; 2015.
- Lloyd AB, Lubans DR, Plotnikoff RC, Morgan PJ. Paternal lifestyle-related parenting practices mediate changes in children’s dietary and physical activity behaviors: findings from the Healthy Dads, Healthy Kids community randomized controlled trial. J Phys Act Health 2015;12:1327-35. https://doi.org/10.1123/jpah.2014-0367.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory (Prentice-Hall Series in Social Learning Theory). Englewood Cliffs, NJ: Prentice-Hall, Inc.; 1986.
- Golan M, Weizman A. Familial approach to the treatment of childhood obesity: conceptual mode. J Nutr Educ 2001;33:102-7. https://doi.org/10.1016/S1499-4046(06)60173-5.
- Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treatment of childhood obesity. Am J Clin Nutr 1998;67:1130-5. https://doi.org/10.1093/ajcn/67.6.1130.
- Vertovec S. Super-diversity and its implications. Ethnic Racial Studies 2007;30:1024-54. https://doi.org/10.1080/01419870701599465.
- Pallan M, Griffin T, Hurley KL, Lancashire E, Blissett J, Frew E, et al. Cultural adaptation of an existing children’s weight management programme: the CHANGE intervention and feasibility RCT. Health Technol Assess 2019;23. https://doi.org/10.3310/hta23330.
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis 1999;9:10-21.
- Griffin TL, Clarke JL, Lancashire ER, Pallan MJ, Passmore S, Adab P. Teacher experiences of delivering an obesity prevention programme (The WAVES study intervention) in a primary school setting. Health Educ J 2015;74:655-67. https://doi.org/10.1177/0017896914556907.
- Australian Institute of Health and Welfare . Australia’s Health 2018 2018. www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/indicators-of-australias-health/proportion-of-people-obese-and-overweight (accessed 3 April 2019).
- National Health and Medical Research Council, Department of Health and Ageing . Australian Dietary Guidelines 2013.
- NHS Digital . Health Survey for England 2017. Fruit and Vegetables 2017. http://healthsurvey.hscic.gov.uk/data-visualisation/data-visualisation/explore-the-trends/fruit-vegetables.aspx (accessed 25 November 2019).
- Australian Bureau of Statistics . Daily Intake of Fruit and Vegetables 2014. www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.001∼2014-15∼Main%20Features∼Daily%20intake%20of%20fruit%20and%20vegetables∼28 (accessed 3 April 2019).
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Lancet Physical Activity Series Working Group . Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219-29. https://doi.org/10.1016/S0140-6736(12)61031-9.
- Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, et al. Exercise for depression. Cochrane Database Syst Rev 2013;9. https://doi.org/10.1002/14651858.CD004366.pub6.
- Fagan J, Iglesias A. Father involvement program effects on fathers, father figures, and their head start children: a quasi-experimental study. Early Child Res Q 1999;14:243-69. https://doi.org/10.1016/S0885-2006(99)00008-3.
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010;7. https://doi.org/10.1186/1479-5868-7-40.
- Singh A, Uijtdewilligen L, Twisk JW, van Mechelen W, Chinapaw MJ. Physical activity and performance at school: a systematic review of the literature including a methodological quality assessment. Arch Pediatr Adolesc Med 2012;166:49-55. https://doi.org/10.1001/archpediatrics.2011.716.
- Forrest S, Lloyd T. Results of an Evaluation of Outcomes and Impact for FRED. Boys Development Project 2014. www.fatherhoodinstitute.org/wp-content/uploads/2014/10/FRED-evaluation-report-Sep-2014.pdf (accessed 25 November 2019).
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Morgan PJ, Young MD, Barnes AT, Eather N, Pollock ER, Lubans DR. Engaging fathers to increase physical activity in girls: the ’Dads And Daughters Exercising and Empowered’ (DADEE) randomized controlled trial. Ann Behav Med 2019;53:39-52. https://doi.org/10.1093/abm/kay015.
- Kitzinger J, Holloway I. Qualitative Research in Health Care. Maidenhead: Open University Press; 2005.
- Liu J, Davidson E, Bhopal R, White M, Johnson M, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technol Assess 2012;16. https://doi.org/10.3310/hta16440.
- Pallan M, Parry J, Cheng KK, Adab P. Development of a childhood obesity prevention programme with a focus on UK South Asian communities. Prev Med 2013;57:948-54. https://doi.org/10.1016/j.ypmed.2013.08.025.
- Department for Communities and Local Government . The English Indices of Deprivation 2015 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/465791/English_Indices_of_Deprivation_2015_-_Statistical_Release.pdf (accessed 22 September 2018).
- Medland A. Portrait of the West Midlands. Newport: Office for National Statistics; 2011.
- Gatineau M, Mathrani S. Obesity and Ethnicity. Oxford: National Obesity Observatory; 2011.
- Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries?. J Adv Nurs 1997;26:623-30. https://doi.org/10.1046/j.1365-2648.1997.t01-25-00999.x.
- Marshall MN. Sampling for qualitative research. Fam Pract 1996;13:522-5. https://doi.org/10.1093/fampra/13.6.522.
- Elwood SA, Martin DG. ’Placing’ interviews: location and scales of power in qualitative research. Prof Geogr 2000;52:649-57. https://doi.org/10.1111/0033-0124.00253.
- Sword W. Accounting for presence of self: reflections on doing qualitative research. Qual Health Res 1999;9:270-8. https://doi.org/10.1177/104973299129121839.
- Berger R. Now I see it, now I don’t: researcher’s position and reflexivity in qualitative research. Qual Res 2015;15:219-34. https://doi.org/10.1177/1468794112468475.
- Sidhu MS, Kokab F, Jolly K, Marshall T, Gale NK, Gill P. Methodological challenges of cross-language qualitative research with South Asian communities living in the UK. Fam Med Community Health 2016;4:16-28. https://doi.org/10.15212/FMCH.2015.0146.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Timmermans S, Tavory I. Theory construction in qualitative research: from grounded theory to abductive analysis. Sociol Theory 2012;30:167-86. https://doi.org/10.1177/0735275112457914.
- Saldana J. The Coding Manual for Qualitative Researchers. London: Sage Publications Ltd; 2009.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage Publications, Inc.; 1998.
- Farooq MA, Parkinson KN, Adamson AJ, Pearce MS, Reilly JK, Hughes AR, et al. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. BR J Sports Med 2018;52:1002-6. https://doi.org/10.1136/bjsports-2016-096933.
- Nierkens V, Hartman MA, Nicolaou M, Vissenberg C, Beune EJ, Hosper K, et al. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. A systematic review. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0073373.
- Lagisetty PA, Priyadarshini S, Terrell S, Hamati M, Landgraf J, Chopra V, et al. Culturally targeted strategies for diabetes prevention in minority population. Diabetes Educ 2017;43:54-77. https://doi.org/10.1177/0145721716683811.
- Lofton S, Julion WA, McNaughton DB, Bergren MD, Keim KS. A systematic review of literature on culturally adapted obesity prevention interventions for African American youth. J Sch Nurs 2016;32:32-46. https://doi.org/10.1177/1059840515605508.
- Barr-Anderson DJ, Adams-Wynn AW, DiSantis KI, Kumanyika S. Family-focused physical activity, diet and obesity interventions in African-American girls: a systematic review. Obes Rev 2013;14:29-51. https://doi.org/10.1111/j.1467-789X.2012.01043.x.
- Sidhu MS, Gale NK, Gill P, Marshall T, Taylor B, Jolly K. A systematic review of lay-led group-based self-management interventions for minority ethnic populations diagnosed with long term conditions in high income countries. Divers Equal Health Care 2014;11:225-36.
- Auslander W, Haire-Joshu D, Houston C, Rhee CW, Williams JH. A controlled evaluation of staging dietary patterns to reduce the risk of diabetes in African-American women. Diabetes Care 2002;25:809-14. https://doi.org/10.2337/diacare.25.5.809.
- Williams JH, Auslander WF, de Groot M, Robinson AD, Houston C, Haire-Joshu D. Cultural relevancy of a diabetes prevention nutrition program for African American women. Health Promot Pract 2006;7:56-67. https://doi.org/10.1177/1524839905275393.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- Office for National Statistics . Local Area Report for Areas in England and Wales 2017. www.nomisweb.co.uk/reports/localarea (accessed 9 October 2018).
- National Society for the Prevention of Cruelty to Children . Recommended Adult to Child Ratios for Working With Children 2018. https://learning.nspcc.org.uk/research-resources/briefings/recommended-adult-child-ratios-working-with-children/ (accessed 9 October 2018).
- Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381-95. https://doi.org/10.1249/01.MSS.0000078924.61453.FB.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res 2012;21:167-76. https://doi.org/10.1007/s11136-011-9927-2.
- Lampard AM, Nishi A, Baskin ML, Carson TL, Davison KK. The Activity Support Scale for Multiple Groups (ACTS-MG): child-reported physical activity parenting in African American and non-Hispanic white families. Behav Med 2016;42:112-19. https://doi.org/10.1080/08964289.2014.979757.
- Larios SE, Ayala GX, Arredondo EM, Baquero B, Elder JP. Development and validation of a scale to measure Latino parenting strategies related to children’s obesigenic behaviors. The Parenting strategies for Eating and Activity Scale (PEAS). Appetite 2009;52:166-72. https://doi.org/10.1016/j.appet.2008.09.011.
- Furman W, Giberson RS, Shulman S. Close Relationships in Socioemotional Development. Stamford, CT: Ablex Publishing Corporation; 1995.
- Stevens K. Developing a descriptive system for a new preference-based measure of health-related quality of life for children. Qual Life Res 2009;18:1105-13. https://doi.org/10.1007/s11136-009-9524-9.
- Stevens KJ. Working with children to develop dimensions for a preference-based, generic, pediatric, health-related quality-of-life measure. Qual Health Res 2010;20:340-51. https://doi.org/10.1177/1049732309358328.
- Stevens K. Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy 2011;9:157-69. https://doi.org/10.2165/11587350-000000000-00000.
- Ihmels MA, Welk GJ, Eisenmann JC, Nusser SM. Development and preliminary validation of a Family Nutrition and Physical Activity (FNPA) screening tool. Int J Behav Nutr Phys Act 2009;6. https://doi.org/10.1186/1479-5868-6-14.
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45. https://doi.org/10.1097/00004583-200111000-00015.
- Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr 1990;44:46-60.
- McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0–16.9 y. Eur J Clin Nutr 2001;55:902-7. https://doi.org/10.1038/sj.ejcn.1601240.
- GENEActiv . How to Use Macros 2018. https://open.geneactiv.org/geneactiv_macros.html (accessed 9 October 2018).
- Phillips LR, Parfitt G, Rowlands AV. Calibration of the GENEA accelerometer for assessment of physical activity intensity in children. J Sci Med Sport 2013;16:124-8. https://doi.org/10.1016/j.jsams.2012.05.013.
- Esliger DW, Rowlands AV, Hurst TL, Catt M, Murray P, Eston RG. Validation of the GENEA Accelerometer. Med Sci Sports Exerc 2011;43:1085-93. https://doi.org/10.1249/MSS.0b013e31820513be.
- Fairclough SJ, Noonan R, Rowlands AV, Van Hees V, Knowles Z, Boddy LM. Wear compliance and activity in children wearing wrist- and hip-mounted accelerometers. Med Sci Sports Exerc 2016;48:245-53. https://doi.org/10.1249/MSS.0000000000000771.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13.
- Griffin T, Sun Y, Sidhu MS, Adab P, Burgess A, Collins C, et al. Healthy Dads, Healthy Kids UK, a weight management programme for fathers: feasibility RCT. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-033534.
- Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med 1999;153:409-18. https://doi.org/10.1001/archpedi.153.4.409.
- Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014;348. https://doi.org/10.1136/bmj.g3256.
- Robling M, Bekkers MJ, Bell K, Butler CC, Cannings-John R, Channon S, et al. Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (Building Blocks): a pragmatic randomised controlled trial. Lancet 2016;387:146-55. https://doi.org/10.1016/S0140-6736(15)00392-X.
- Olds DL, Henderson CR, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics 1986;78:65-78.
- Kitzman H, Olds DL, Henderson CR, Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. JAMA 1997;278:644-52. https://doi.org/10.1001/jama.1997.03550080054039.
- Olds DL, Robinson J, O’Brien R, Luckey DW, Pettitt LM, Henderson CR, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics 2002;110:486-96. https://doi.org/10.1542/peds.110.3.486.
- Jolly K, Ingram L, Khan KS, Deeks JJ, Freemantle N, MacArthur C. Systematic review of peer support for breastfeeding continuation: metaregression analysis of the effect of setting, intensity, and timing. BMJ 2012;344. https://doi.org/10.1136/bmj.d8287.
- Netto G, Bhopal R, Lederle N, Khatoon J, Jackson A. How can health promotion interventions be adapted for minority ethnic communities? Five principles for guiding the development of behavioural interventions. Health Promot Int 2010;25:248-57. https://doi.org/10.1093/heapro/daq012.
- Barrera M, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol 2013;81:196-205. https://doi.org/10.1037/a0027085.
- Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity 2012;20:1234-9. https://doi.org/10.1038/oby.2011.140.
- National Institute for Health and Care Excellence (NICE) . Weight Management: Lifestyle Services for Overweight or Obese Adults 2014.
- Morgan PJ, Collins CE, Plotnikoff RC, Cook AT, Berthon B, Mitchell S, et al. The impact of a workplace-based weight loss program on work-related outcomes in overweight male shift workers. J Occup Environ Med 2012;54:122-7. https://doi.org/10.1097/JOM.0b013e31824329ab.
- Chu JTW, Wan A, Stewart SM, Ng KT, Lam TH, Chan SS. Recruitment and lessons learned from a community-based intervention program: the Learning Families Project in Hong Kong. Front Public Health 2018;6. https://doi.org/10.3389/fpubh.2018.00016.
- Hoddinott P, Allan K, Avenell A, Britten J. Group interventions to improve health outcomes: a framework for their design and delivery. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-800.
- Jolly K, Lewis A, Beach J, Denley J, Adab P, Deeks JJ, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: Lighten Up randomised controlled trial. BMJ 2011;343. https://doi.org/10.1136/bmj.d6500.
- British Heart Foundation . The National Audit of Cardiac Rehabilitation (NACR) Annual Statistical Report 2017 2018.
- Estabrooks PA, Carron AV. The Physical Activity Group Environment Questionnaire: an instrument for the assessment of cohesion in exercise classes. Group Dyn Theory Res Pract 2000;4:230-43. https://doi.org/10.1037/1089-2699.4.3.230.
- Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev 2017;6. https://doi.org/10.1002/14651858.CD012651.
- Colquitt JL, Loveman E, O’Malley C, Azevedo LB, Mead E, Al-Khudairy L, et al. Diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database Syst Rev 2016;3. https://doi.org/10.1002/14651858.CD012105.
- Cleland CL, Tully MA, Kee F, Cupples ME. The effectiveness of physical activity interventions in socioeconomically disadvantaged communities: a systematic review. Prev Med 2012;54:371-80. https://doi.org/10.1016/j.ypmed.2012.04.004.
- Kelleher E, Davoren MP, Harrington JM, Shiely F, Perry IJ, McHugh SM. Barriers and facilitators to initial and continued attendance at community-based lifestyle programmes among families of overweight and obese children: a systematic review. Obes Rev 2017;18:183-94. https://doi.org/10.1111/obr.12478.
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2031-8.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- Lee BY, Bartsch SM, Mui Y, Haidari LA, Spiker ML, Gittelsohn J. A systems approach to obesity. Nutr Rev 2017;75:94-106. https://doi.org/10.1093/nutrit/nuw049.
- Economos CD, Hatfield DP, King AC, Ayala GX, Pentz MA. Food and physical activity environments: an energy balance approach for research and practice. Am J Prev Med 2015;48:620-9. https://doi.org/10.1016/j.amepre.2014.12.007.
- Rutter H, Savona N, Glonti K, Bibby J, Cummins S, Finegood DT, et al. The need for a complex systems model of evidence for public health. Lancet 2017;390:2602-4. https://doi.org/10.1016/S0140-6736(17)31267-9.
- Youth Employment UK . Health Trainer Jobs n.d. www.youthemployment.org.uk/careers-hub-job-role/health-trainer/ (accessed 6 December 2019).
- University of Birmingham . Salary Scales n.d. www.birmingham.ac.uk/staff/jobs/pay.aspx (accessed 25 November 2019).
Appendix 1 The Healthy Dads, Healthy Kids programme: ethics approvals and amendments to the protocol
| Study phase | Reference ID | Date | Details |
|---|---|---|---|
| Phase 1a | ERN_15_1287 | 22 April 2016 | Study approved |
| ERN_15–1287A | 22 March 2017 | Eligibility criteria for fathers taking part in phase 1a (qualitative study) broadened to allow for interviews to be conducted with parents of children aged 4–16 years and from socially disadvantaged, ethnically diverse communities across the UK (i.e. not restricted to the West Midlands) | |
| Phases 1b and 2 | ERN_16–1323A | 16 January 2017 | Study approved |
| ERN_16–1323A | 6 February 2017 | Change of eligibility criteria for fathers recruited to phase 1b from ‘obese’ to ‘overweight and obese’ | |
| ERN_16–1323B | 24 July 2017 |
|
|
| ERN_16–1323C | 11 September 2017 | Use of social media for recruitment | |
| ERN_16–1323D | 18 December 2017 |
|
Appendix 2 Potential cultural adaptions and their relevance to adapting the Healthy Dads, Healthy Kids programme
| Liu et al.69 adaptation | Stages of programme theory | Relevant phase in HDHK-UK | How will it be explored in HDHK-UK? |
|---|---|---|---|
| 1. Exploratory phase with target population (same group as intervention group) |
|
|
|
| 2. Exploratory phase with target population (different group from intervention group or unknown) |
|
|
|
| 3. Exploratory phase with community leaders |
|
|
|
| 4. Ethnically matched intervention staff or facilitators (with qualifications) |
|
|
|
| 5. Ethnically matched peer role models or peer education |
|
|
|
| 6. Ethnically matched facilitators and peer role models who have successfully changed their behaviour |
|
|
|
| 7. Ethnically matched high-level/respected individuals to increase salience of programme goals |
|
|
|
| 8. Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages |
|
|
|
| 9. Ethnically matched leadership within the study |
|
|
|
| 10. Utilise local/respected religious/spiritual leaders |
|
|
|
| 11. Collaboration with ethnic-specific institutions and professional organisations (formal) |
|
|
|
| 12. Material depicts individuals from target population |
|
|
|
| 13. Material (video, booklet, skits, handouts, games) in target population’s language |
|
|
|
| 14. Reflect target population’s language (usage – concepts, vocabulary) |
|
|
|
| 15. Match reading level and literacy |
|
|
|
| 16. Reflect target population’s preferred method of communication |
|
|
|
| 17. Material presents ethnic-specific data |
|
|
|
| 18. Material depicts appropriate graphics and scenarios (this can be heterogeneous) |
|
|
|
| 19. Material/guidance based on preferences of target population |
|
|
|
| 20. Material developed specifically for target population (by project investigators, expert opinion, tools) |
|
|
|
| 21. Material created by members of the target population |
|
|
|
| 22. Intervention content targets population’s social and cultural values |
|
|
|
| 23. Intervention goals and outcomes are culturally appropriate |
|
|
|
| 24. Intervention delivered in culturally appropriate or preferred format |
|
|
|
| 25. Consider target population’s employment situations |
|
|
|
| 26. Intervention addresses health behaviour patterns found in target population |
|
|
|
| 27. Dietary issues unique to their context |
|
|
|
| 28. Utilise resources from target population |
|
|
|
| 29. Utilise appropriate incentives and timing of programme |
|
|
|
| 30. Utilise and addresses appropriate norms |
|
|
|
| 31. Address concerns with medical programmes, procedures and medication |
|
|
|
| 32. Utilise appropriate evaluation instruments and tools |
|
|
|
| 33. Located in ethnically/culturally appropriate/familiar location |
|
|
|
| 34. Utilise ethnically/culturally appropriate media sources |
|
|
|
| 35. Utilise ethnically/culturally appropriate formal and informal networks |
|
|
|
| 36. Provide ethnically/culturally appropriate food/activities/music |
|
|
|
| 37. Present a pro-ethnic/race approach |
|
|
|
| 38. Address emotional barriers and stressors |
|
|
|
| 39. Address physical/financial (structural) barriers to participation |
|
|
|
| 40. Teach appropriate communication skills |
|
|
|
| 41. Encourage/involve social support |
|
|
|
| 42. Purposefully maintaining an exclusive or open intervention environment |
|
|
|
| 43. Maintaining cultural significance of food |
|
|
|
| 44. Cross-cultural training for all study personnel |
|
|
|
| 45. Address discrimination and mistrust |
|
|
|
| 46. Gender considerations |
|
|
|
Appendix 3 Observation checklist for Healthy Dads, Healthy Kids programme sessions
Appendix 4 Deviations from the statistical analysis plan
Section of report not following the statistical analysis plan: ‘appendix D2, table 2’
In Table 20, baseline demographic information is presented for all children of the fathers who participated in phase 2, in addition to just the eldest child, as specified in the dummy tables.
Section of report not following the statistical analysis plan: ‘appendix D5, table 14’
In Table 27, change in BMI z-score and change in percentage of body fat from baseline to 3 months and 6 months are presented for all children of the fathers who participated in phase 2, in addition to just the eldest child, as specified in the dummy tables.
Appendix 5 Data availability of participant and facilitator feedback questionnaires
| Form of feedback | Week, forms returned/forms expected (n/N) | Total, n/N (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| Course 1 | ||||||||||
| Participant feedback | 6/6 | 4/4 | 4/4 | 6/6 | 0/2 | 0/3 | 1/3 | 3/3 | a | 24/31 (77.4) |
| PPT facilitator feedback | 1/1 | 1/1 | 0/1 | 1/1 | 0/1 | 1/1 | 0/1 | 1/1 | a | 5/8 (62.5) |
| PA facilitator forms | 1/1 | 1/1 | 0/1 | 1/1 | 0/1 | 0/1 | 0/1 | 1/1 | a | 4/8 (50.0) |
| Course 2 | ||||||||||
| Participant feedback | 4/4 | 3/4 | 1/4 | 9/9 | 4/4 | 4/4 | 1/1 | 0/3 | 3/3 | 29/36 (80.6) |
| PPT facilitator feedback | 1/1 | 0/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 0/1 | 1/1 | 7/9 (77.8) |
| PA facilitator forms | 2/2 | 0/2 | 1/2 | 2/2 | 2/2 | 1/1 | 1/2 | 0/2 | 2/2 | 11/17 (64.7) |
| Course 3 | ||||||||||
| Participant feedback | 4/4 | 3/3 | 0/4 | 2/6 | 0/2 | 3/3 | 1/1 | 2/2 | 2/2 | 17/27 (63.0) |
| PPT facilitator feedback | 2/2 | 0/1 | 0/1 | 1/1 | 0/1 | 1/1 | 0/1 | 1/1 | 1/1 | 6/10 (60.0) |
| PA facilitator forms | 2/2 | 2/2 | 0/2 | 2/2 | 0/2 | 2/2 | 2/2 | 2/2 | 2/2 | 14/18 (77.8) |
| Course 4 | ||||||||||
| Participant feedback | 6/6 | 6/6 | 6/6 | 9/11 | 4/4 | 4/4 | 5/5 | 4/4 | 4/4 | 48/50 (96.0) |
| PPT facilitator feedback | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 0/1 | 1/1 | 8/9 (88.8) |
| PA facilitator forms | 2/2 | 1/1 | 2/2 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 2/2 | 12/12 (100.0) |
Appendix 6 Challenges to planning session timings
| Session component | Sessions: challenge | |
|---|---|---|
| Weekday evening | Weekend | |
| Participants | ||
| Participant availability |
|
|
| Venue | ||
| Schools |
|
|
| Leisure centre |
|
|
| Community centre |
|
|
| Facilitator | ||
| Facilitator availability |
|
|
Appendix 7 Session observation checklists and facilitator feedback forms: results
| Checklist | Response (n) | |||||
|---|---|---|---|---|---|---|
| Very poor | Poor | OK | Good | Excellent | Missing | |
| Dads-only session | ||||||
| The rapport among the dads in the session was . . . | – | – | – | 1 | 4 | 1 |
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | Missing | |
| The dads appeared to enjoy the session | 1 | 4 | 1 | |||
| The dads appeared well engaged with session content | 1 | 4 | 1 | |||
| The dads appeared to understand information from the session | 1 | 4 | 1 | |||
| The dads appeared motivated to use recommended strategies at home | 1 | 4 | 1 | |||
| Kids-only session | ||||||
| What proportion of the children . . . | None | A few | Some | Most | All | Missing |
| . . . were ‘on task’ for at least some of the session? | 6 | 6 | ||||
| . . . were ‘on task’ for most of the session? | 6 | 6 | ||||
| . . . understood the session content? | 1 | 6 | 5 | |||
| . . . seemed to enjoy the session? | 4 | 8 | ||||
| Dads and kids joint physical activity session | ||||||
| What proportion of the . . . | None | A few | Some | Most | All | Missing |
| . . . children seemed to enjoy the session? | 2 | 13 | 1 | |||
| . . . children seemed to engage with the session? (following instruction, joining in activities) | 3 | 13 | ||||
| . . . dads seemed to enjoy the session? | 1 | 15 | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | N/A | |
| The dads appeared well engaged with session content | 1 | 1 | 14 | |||
| The dads and kids worked well together | 1 | 15 | ||||
| Fathers educational session facilitators | Physical activity facilitators |
|---|---|
| What did you do well during the session and did you encounter any significant barriers/issues? | |
| Session 1 | |
| Explained the intervention programme and their journey to weight loss and kids to push fathers to lose weight. No – however one father came in really late but I dealt with that correctly and the session ran smoothly (1)Men being late, time pushed and no target set as not time to scale (2)All (participants) knew what to expect (3)Delivered slides very well and had great feedback from two dads (4) | Motivated and had fun (1)Kept all children engaged (2)Motivate, coaching points (3)Kept everyone engaged throughout the session (3)Went through everything well (3)Discussion within group covered all presentation slides. Discovered why the Dads were here, most here to improve lifestyle/better role model. Got the whole group into the programme they really took to the idea and showed a lot of interest. Ran out of time in activity session to cover all 4 elements. Balls didn’t bounce well enough (4)The delivery was good, No, ran out of time but had a session that was planned (4) |
| Session 2 | |
| Motivate fathers to lose weight (1)Delivered the slides well, timing – need to try to keep to this (4) | Enjoyable, safe, effective, lack of time (1)Refreshed knowledge from past sessions (3)Explained the fundamental elements (3)Explain the elements of throwing (4) |
| Session 3 | |
| Kept it moving, integrating men, good banter (2)Enthusiasm, fun – Dads had lots of time to discuss (4) | Motivate (2)Kept structure to the session. Small space, lack of equipmentExplained the rules of each activity |
| Session 4 | |
| Explain the importance of family meal times and children having choices – no (1)Kept it moving, engaged, trust paradigm did not seem to ‘land’ (2)Kept discussion flowing, good engagement with Dads and Mom (3)Not enough time (4) | Kept children engaged. Children too young to do the activity booklet (1)Motivate (2)Kept everyone motivated and engaged (2)Explained the rules (3)Kept the group engaged and interested (3)Explained. Not enough time (4) |
| Session 5 | |
| Recap last week went well. You are your kids PT and vice versa. How important role of Dad is, the content led to a very negative atmosphere in room. Not sure keep your anger in check is a useful message. Felt like this session was not fun (2)Timing was perfect. Discussion element. Facilitator is not a parent so hard to relate. Also examples need to be changed to English examples, more realistic (4) | Utilise teaching points. Hoops aren’t best equipment for jumping (2)Helped the children with teaching points, technicalities of jumping. Quite a few falls within the session (2)Discussed the elements (4) |
| Session 6 | |
| Deliver the session with conviction and valid reasons why screen time should be reduced. Dads pointed out that schools now send homework or children do their homework on computers/tablets suggesting screen time is a normal part of life. (1)Lots of the content had been covered in talking. Session did not start until 17.30–17.40 due to Dad/kid running late (2)Delivery flowing. Kept conversation positive (course 3) HAMM slide – needs to be workshop where we almost spoonfeed ideas. Better to have options and simplify (3)Again timing is off – need more time. Great understanding from Dads (4) | Led the session single handedly. Showed good leadership throughout. (2)Went through the skills for the session (3)Kept everyone engaged (3)Explained the rules and specific skills for the game (4) |
| Session 7 | |
| The flow, kept to time, low numbers meant discussion was hard. The dad was already taking steps to lower screen time (2)Delivered the session well – 30 mins for PA. Great discussions during the session (enjoyed by all), all Dads seemed motivated (4) | Kept children engaged. Really enjoyed it. (2)Kept everyone engaged and enjoyed it. Limited amount of participants (3)Made it fun even with 1 kid and 1 Dad. Yes, no more people turned up (3)Engaged the session (4) |
| Session 8 | |
| Deliver the message and motivate and send out the message that staying healthy is a lifelong goal (1) | Explained the rules (3)Kept everyone engaged (3)The activity with the children, teamwork element and choice was good. The session 8 booklet task didn’t take long as the space was limited to draw their family so they all wrote it which was a lot quickerGet the children to put their ideas into action with games and exercises they have learnt (1) |
| Session 9 | |
| Gained positive feedback and examples of how course helped the Dads (3)Overview of all session - delivery went well and had PA time (4)Motivate and focus on positives (2) | Good games in the session and incorporated all of the fundamental movement skills (2)Summarised all core skills, enjoyed by all (2)Explained the elementary (3)Everyone had fun and really enjoyed it (3)Ran the session going through the elements (4)Very structured, enjoyable session (4) |
Appendix 8 Baseline characteristics for fathers by treatment arm: number of children
| Number of children | Treatment arm, n (%) | Overall (N = 43), n (%) | |
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | ||
| How old are your children? | |||
| Number of children at preschool age | |||
| 0 | 18 (62.1) | 8 (57.1) | 26 (60.5) |
| 1 | 8 (27.6) | 5 (35.7) | 13 (30.2) |
| 2 | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| Missinga | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Number of children at primary school age | |||
| Reception, school years 1 and 2 | |||
| 0 | 12 (41.4) | 6 (42.9) | 18 (41.9) |
| 1 | 13 (44.8) | 7 (50.0) | 20 (46.5) |
| 2 | 2 (6.9) | 1 (7.1) | 3 (7.0) |
| Missinga | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| School years 3–6 | |||
| 0 | 9 (31.0) | 7 (50.0) | 16 (37.2) |
| 1 | 15 (51.7) | 7 (50.0) | 22 (51.2) |
| 2 | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| Missinga | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Number of children at secondary school age: school years 7–11 | |||
| 0 | 20 (69.0) | 7 (50.0) | 27 (62.8) |
| 1 | 5 (17.2) | 2 (14.3) | 7 (16.3) |
| 2 | 2 (6.9) | 5 (35.7) | 7 (16.3) |
| Missinga | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Number of children at college/sixth form age | |||
| 0 | 25 (86.2) | 14 (100.0) | 39 (90.7) |
| 1 | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Missinga | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Number of children aged ≥ 18 years | |||
| 0 | 23 (79.3) | 13 (92.9) | 36 (83.7) |
| 1 | 2 (6.9) | 1 (7.1) | 3 (7.0) |
| 2 | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| 3 | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Missinga | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Use of health services | Treatment arm, n (%) | Overall (N = 43), n (%) | |
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | ||
| Number of times consulted a health-care professional | |||
| GP | |||
| 0 | 11 (37.9) | 9 (64.3) | 20 (46.5) |
| 1 | 8 (27.6) | 3 (21.4) | 11 (25.6) |
| > 2 | 8 (27.6) | 2 (14.3) | 10 (23.3) |
| Missing | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Practice nurse | |||
| 0 | 20 (69.0) | 14 (100.0) | 34 (79.1) |
| 1 | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| > 2 | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| Missing | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| Pharmacist | |||
| 0 | 21 (72.4) | 13 (92.9) | 34 (79.1) |
| 1 | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| > 2 | 3 (10.3) | 1 (7.1) | 4 (9.3) |
| Missing | 4 (13.8) | 0 (0.0) | 4 (9.3) |
| Admitted to hospital in the previous 12 months | |||
| Yes | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| No | 25 (86.2) | 14 (100.0) | 39 (90.7) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Attended the casualty or A&E department of a hospital in the previous 12 months | |||
| Yes | 9 (31.0) | 3 (21.4) | 12 (27.9) |
| No | 19 (65.5) | 11 (78.6) | 30 (69.8) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Attended an outpatient appointment at a hospital in the previous 12 months | |||
| Yes | 10 (34.5) | 3 (21.4) | 13 (30.2) |
| No | 18 (62.1) | 11 (78.6) | 29 (67.4) |
| Missing | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Questionnaire | Treatment arm | Overall (N = 43) | |
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | ||
| Food and drink intake, n (%) | |||
| Type of milk | |||
| Normal full-fat milk | 12 (41.4) | 7 (50.0) | 19 (44.2) |
| Semi-skimmed milk | 11 (37.9) | 5 (35.7) | 16 (37.2) |
| Skimmed milk | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Soy milk | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Rice milk | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not sure | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| I don’t drink milk | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Missing | 2 (6.9) | 2 (14.3) | 4 (9.3) |
| Pieces of fruit | |||
| None | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Fewer than 1 per week | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 1 or 2 per week | 4 (13.8) | 0 (0.0) | 4 (9.3) |
| 3 or 4 per week | 3 (10.3) | 1 (7.1) | 4 (9.3) |
| 5 or 6 per week | 7 (24.1) | 1 (7.1) | 8 (18.6) |
| Once per day | 4 (13.8) | 4 (28.6) | 8 (18.6) |
| 2 or 3 per day | 8 (27.6) | 5 (35.7) | 13 (30.2) |
| ≥ 4 per day | 0 (0.0) | 1 (7.1) | 1 (2.3) |
| Missing | 1 (3.5) | 2 (14.3) | 3 (7.0) |
| Vegetables or salad consumption with evening meal | |||
| Never | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Less than once per week | 0 (0.0) | 1 (7.1) | 1 (2.3) |
| Once or twice per week | 6 (20.7) | 3 (21.4) | 9 (20.9) |
| 3 or 4 times per week | 9 (31.0) | 4 (28.6) | 13 (30.2) |
| ≥ 5 times per week | 12 (41.4) | 4 (28.6) | 16 (37.2) |
| Missing | 2 (6.9) | 2 (14.3) | 4 (9.3) |
| Takeaway foods | |||
| Never | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Less than once per week | 15 (51.7) | 9 (64.3) | 24 (55.8) |
| Once or twice per week | 10 (34.5) | 2 (14.3) | 12 (27.9) |
| 3 or 4 times per week | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| 5 or 6 times per week | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| Once per day | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Twice or more per day | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 1 (3.5) | 2 (14.3) | 3 (7.0) |
| Eating in front of the television | |||
| Never | 6 (20.7) | 8 (57.1) | 14 (32.6) |
| Fewer times than once per week | 3 (10.3) | 0 (0.0) | 3 (7.0) |
| Once or twice per week | 6 (20.7) | 3 (21.4) | 9 (20.9) |
| 3 or 4 times per week | 4 (13.8) | 1 (7.1) | 5 (11.6) |
| 5 or 6 times per week | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Every day | 6 (20.7) | 0 (0.0) | 6 (14.0) |
| Missing | 2 (6.9) | 2 (14.3) | 4 (9.3) |
| Sugary drinks | |||
| Never | 1 (3.5) | 2 (14.3) | 3 (7.0) |
| < 1 per day | 6 (20.7) | 1 (7.1) | 7 (16.3) |
| 1 per day | 7 (24.1) | 7 (50.0) | 14 (32.6) |
| 2 or 3 per day | 9 (31.0) | 1 (7.1) | 10 (23.3) |
| 4–6 per day | 4 (13.8) | 1 (7.1) | 5 (11.6) |
| ≥ 7 per day | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Missing | 1 (3.5) | 2 (14.3) | 3 (7.0) |
| Fruit juice-based drinks | |||
| Never | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| < 1 per month | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| 1–3 per month | 6 (20.7) | 1 (7.1) | 7 (16.3) |
| 1 per week | 1 (3.5) | 2 (14.3) | 3 (7.0) |
| 2–6 per week | 7 (24.1) | 4 (28.6) | 11 (25.6) |
| 1 per day | 4 (13.8) | 1 (7.1) | 5 (11.6) |
| ≥ 2 per day | 7 (24.1) | 2 (14.3) | 9 (20.9) |
| Missing | 2 (6.9) | 2 (14.3) | 4 (9.3) |
| Snacks | |||
| < 1 per day | 1 (3.5) | 3 (21.4) | 4 (9.3) |
| 1 or 2 per day | 16 (55.2) | 6 (42.9) | 22 (51.2) |
| 3 or 4 per day | 9 (31.0) | 2 (14.3) | 11 (25.6) |
| 5 or 6 per day | 2 (6.9) | 1 (7.1) | 3 (7.0) |
| ≥ 7 per day | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 1 (3.5) | 2 (14.3) | 3 (7.0) |
| CHU-9D | |||
| Mean score (SD) | 0.92 (0.09) | 0.91 (0.11) | 0.92 (0.09) |
| Minimum, maximum | 0.60, 1.00 | 0.67, 1.00 | 0.60, 1.00 |
| Missing (n) | 3 | 4 | 7 |
| Family nutrition & physical activity | |||
| Mean score (SD) | 61.13 (9.24) | 62.09 (4.57) | 61.44 (7.96) |
| Minimum, maximum | 44.00, 77.00 | 56.00, 72.00 | 44.00, 77.00 |
| Missing | 6 | 3 | 9 |
| Your child’s use of health services, n (%) | |||
| Number of times consulted a health-care professional in the previous 3 months | |||
| GP | |||
| 0 | 18 (62.1) | 8 (57.1) | 26 (60.5) |
| 1 | 6 (20.7) | 3 (21.4) | 9 (20.9) |
| > 2 | 2 (6.9) | 1 (7.1) | 3 (7.0) |
| Missing | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| Practice nurse | |||
| 0 | 26 (89.7) | 11 (78.6) | 37 (86.1) |
| 1 | 0 (0.0) | 1 (7.1) | 1 (2.3) |
| > 2 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| Pharmacist | |||
| 0 | 23 (79.3) | 11 (78.6) | 34 (79.1) |
| 1 | 3 (10.3) | 1 (7.1) | 4 (9.3) |
| > 2 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| Admitted to hospital in the previous 3 months | |||
| Yes | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| No | 25 (86.2) | 10 (71.4) | 35 (81.4) |
| Missing | 3 (10.3) | 3 (21.4) | 6 (14.0) |
| Attended the casualty or A&E department of a hospital in the previous 12 months | |||
| Yes | 1 (3.5) | 1 (7.1) | 2 (4.7) |
| No | 25 (86.2) | 11 (78.6) | 36 (83.7) |
| Missing | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| Attended an outpatient appointment at a hospital in the previous 3 months | |||
| Yes | 3 (10.3) | 1 (7.1) | 4 (9.3) |
| No | 23 (79.3) | 11 (78.6) | 34 (79.1) |
| Missing | 3 (10.3) | 2 (14.3) | 5 (11.6) |
| Outcome measure | Treatment arm | |
|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | |
| Change in waist circumference from baseline (cm) | ||
| 3 months | ||
| Mean (SD) | –10.8 (18.0) | 3.4 (9.3) |
| Minimum, maximum | –56.5, 2.0 | –3.6, 22.0 |
| Missing (n) | 20 | 8 |
| 6 months | ||
| Mean (SD) | –5.2 (5.0) | –2.8 (6.4) |
| Minimum, maximum | –15, –1.0 | –10, 7.2 |
| Missing (n) | 23 | 9 |
| Change in % body fat from baseline (%) | ||
| 3 months | ||
| Mean (SD) | –1.5 (3.1) | –0.3 (2.6) |
| Minimum, maximum | –5.6, 4.0 | –6.0, 2.1 |
| Missing (n) | 13 | 5 |
| 6 months | ||
| Mean (SD) | –2.2 (3.2) | –2.3 (3.9) |
| Minimum, maximum | –8.2, 3.3 | –10.8, 1.4 |
| Missing (n) | 15 | 5 |
| Self-reported physical activity measured by the IPAQ-Short Form (MET-minutes/week) | ||
| 3 months | ||
| Median (IQR) | 3818.3 (2475.0–4901.7) | 918.0 (495.0–4158.0) |
| Minimum, maximum | 396.0, 17838.0 | 0.0, 9135.0 |
| Missing (n) | 17 | 7 |
| 6 months | ||
| Median (IQR) | 1731.0 (1731.0–1731.0) | |
| Minimum, maximum | 1731.0, 1731.0 | |
| Missing (n) | 28 | 14 |
| Physical activity measured by a GENEactive accelerometer (minutes) | ||
| 3 months | ||
| Median for total activity (IQR) | 208.8 (185.6–287.0) | 168.3 (147.8–194.0) |
| Minimum, maximum | 56.0, 319.0 | 88.3, 420.0 |
| Missing (n) | 12 | 5 |
| Median for moderate/vigorous activity (IQR) | 113.3 (99.3–151.3) | 84.2 (69.4–106.2) |
| Minimum, maximum | 29.0, 187.9 | 46.7, 253.6 |
| Missing (n) | 12 | 5 |
| 6 months | ||
| Median for total activity (IQR) | 239.6 (194.3–287.0) | 146.2 (125.0–230.6) |
| Minimum, maximum | 162.7, 313.8 | 62.8, 421.7 |
| Missing (n) | 18 | 5 |
| Median for moderate/vigorous activity (IQR) | 125.6 (101.3–163.1) | 68.2 (59.1–86.5) |
| Minimum, maximum | 87.7, 205.5 | 30.8, 208.4 |
| Missing (n) | 18 | 5 |
| Parenting for physical activity | ||
| 3 months | ||
| ACTS-MG (the first five items) | ||
| Mean (SD) | 15.6 (3.5) | 13.0 (2.3) |
| Minimum, maximum | 5.0, 20.0 | 10.0, 17.0 |
| Missing (n) | 12 | 5 |
| Limit-setting (first box, items a and b) | ||
| Mean (SD) | 8.4 (1.9) | 8.8 (1.4) |
| Minimum, maximum | 4.0, 10.0 | 6.0, 10.0 |
| Missing (n) | 12 | 5 |
| Control (first box, item c) | ||
| Mean (SD) | 2.7 (1.6) | 2.1 (1.3) |
| Minimum, maximum | 1.0, 5.0 | 1.0, 5.0 |
| Missing (n) | 12 | 5 |
| Monitoring (second box, items a and b) | ||
| Mean (SD) | 7.3 (1.5) | 7.4 (1.1) |
| Minimum, maximum | 4.0, 10.0 | 6.0, 9.0 |
| Missing (n) | 12 | 5 |
| Disciplining (third box, items a and b) | ||
| Mean (SD) | 5.2 (2.3) | 4.7 (2.4) |
| Minimum, maximum | 2.0, 10.0 | 2.0, 8.0 |
| Missing (n) | 12 | 5 |
| Co-physical activity (the final item) | ||
| Mean (SD) | 3.5 (0.9) | 2.7 (0.7) |
| Minimum, maximum | 1.0, 5.0 | 2.0, 4.0 |
| Missing (n) | 12 | 5 |
| 6 months | ||
| ACTS-MG (the first five items) | ||
| Mean (SD) | 16.4 (2.2) | 13.7 (1.5) |
| Minimum, maximum | 13.0, 20.0 | 11.0, 16.0 |
| Missing (n) | 15 | 5 |
| Limit-setting (first box, items a and b) | ||
| Mean (SD) | 7.5 (2.1) | 9.1 (1.2) |
| Minimum, maximum | 2.0, 10.0 | 7.0, 10.0 |
| Missing (n) | 16 | 5 |
| Control (first box, item c) | ||
| Mean (SD) | 3.4 (1.3) | 2.6 (1.7) |
| Minimum, maximum | 2.0, 5.0 | 1.0, 5.0 |
| Missing (n) | 16 | 5 |
| Monitoring (second box, items a and b) | ||
| Mean (SD) | 7.4 (1.5) | 7.7 (0.7) |
| Minimum, maximum | 4.0, 9.0 | 7.0, 9.0 |
| Missing (n) | 15 | 5 |
| Disciplining (third box, items a and b) | ||
| Mean (SD) | 5.2 (2.7) | 6.3 (2.2) |
| Minimum, maximum | 2.0, 10.0 | 3.0, 10.0 |
| Missing (n) | 15 | 5 |
| Co-physical activity (the final item) | ||
| Mean (SD) | 3.8 (1.3) | 3.2 (0.8) |
| Minimum, maximum | 1.0, 5.0 | 2.0, 5.0 |
| Missing (n) | 15 | 5 |
| Father–child relationship | ||
| 3 months | ||
| Disciplinary warmth (praise + shared decision-making + rationale) | ||
| Mean (SD) | 22.9 (4.0) | 23.0 (1.6) |
| Minimum, maximum | 16.0, 30.0 | 20.0, 25.0 |
| Missing (n) | 13 | 5 |
| Personal relationships (prosocial + intimacy + nurturance + companionship) | ||
| Mean (SD) | 31.4 (5.0) | 28.9 (2.6) |
| Minimum, maximum | 24.0, 39.0 | 26.0, 33.0 |
| Missing (n) | 13 | 5 |
| Prosocial (items 1 and 8) | ||
| Mean (SD) | 7.8 (1.2) | 7.0 (0.7) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 8.0 |
| Missing (n) | 12 | 5 |
| Praise (items 2 and 9) | ||
| Mean (SD) | 7.9 (1.3) | 7.8 (1.2) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 10.0 |
| Missing (n) | 13 | 5 |
| Intimacy (items 3 and 10) | ||
| Mean (SD) | 6.8 (2.0) | 6.4 (0.9) |
| Minimum, maximum | 3.0, 10.0 | 5.0, 8.0 |
| Missing (n) | 13 | 5 |
| Nurturance (items 4 and 11) | ||
| Mean (SD) | 8.4 (1.2) | 7.8 (0.8) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 9.0 |
| Missing (n) | 12 | 5 |
| Shared decision-making (items 5 and 12) | ||
| Mean (SD) | 7.3 (1.6) | 7.2 (1.1) |
| Minimum, maximum | 5.0, 10.0 | 5.0, 8.0 |
| Missing (n) | 12 | 5 |
| Companionship (items 6 and 13) | ||
| Mean (SD) | 8.2 (1.3) | 7.7 (0.9) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 9.0 |
| Missing (n) | 12 | 5 |
| Rationale (items 7 and 14) | ||
| Mean (SD) | 7.8 (1.7) | 8.0 (0.5) |
| Minimum, maximum | 5.0, 10.0 | 7.0, 9.0 |
| Missing (n) | 12 | 5 |
| 6 months | ||
| Disciplinary warmth (praise + shared decision-making + rationale) | ||
| Mean (SD) | 23.8 (3.6) | 23.3 (3.0) |
| Minimum, maximum | 18.0, 30.0 | 18.0, 27.0 |
| Missing (n) | 15 | 5 |
| Personal relationships (prosocial + intimacy + nurturance + companionship) | ||
| Mean (SD) | 30.6 (4.8) | 30.0 (2.9) |
| Minimum, maximum | 25.0, 39.0 | 24.0, 33.0 |
| Missing (n) | 15 | 5 |
| Prosocial (items 1 and 8) | ||
| Mean (SD) | 7.1 (1.2) | 7.6 (1.4) |
| Minimum, maximum | 5.0, 9.0 | 6.0, 10.0 |
| Missing (n) | 15 | 5 |
| Praise (items 2 and 9) | ||
| Mean (SD) | 8.2 (1.3) | 8.0 (1.2) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 10.0 |
| Missing (n) | 15 | 5 |
| Intimacy (items 3 and 10) | ||
| Mean (SD) | 7.0 (1.8) | 6.9 (1.3) |
| Minimum, maximum | 4.0, 10.0 | 5.0, 9.0 |
| Missing (n) | 15 | 5 |
| Nurturance (items 4 and 11) | ||
| Mean (SD) | 8.0 (1.4) | 8.1 (0.8) |
| Minimum, maximum | 6.0, 10.0 | 7.0, 10.0 |
| Missing (n) | 15 | 5 |
| Shared decision-making (items 5 and 12) | ||
| Mean (SD) | 7.6 (1.7) | 7.1 (1.5) |
| Minimum, maximum | 5.0, 10.0 | 5.0, 9.0 |
| Missing (n) | 15 | 5 |
| Companionship (items 6 and 13) | ||
| Mean (SD) | 8.4 (1.3) | 7.4 (0.9) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 9.0 |
| Missing (n) | 15 | 5 |
| Rationale (items 7 and 14) | ||
| Mean (SD) | 8.0 (1.5) | 8.2 (1.6) |
| Minimum, maximum | 6.0, 10.0 | 6.0, 10.0 |
| Missing (n) | 12 | 5 |
| EQ-5D-5L | ||
| 3 months | ||
| Mean (SD) | 0.870 (0.188) | 0.939 (0.096) |
| Minimum, maximum | 0.331, 1.000 | 0.725, 1.000 |
| Missing (n) | 12 | 5 |
| 6 months | ||
| Mean (SD) | 0.917 (0.141) | 0.937 (0.127) |
| Minimum, maximum | 0.508, 1.000 | 0.622, 1.000 |
| Missing (n) | 15 | 5 |
| ICECAP-A | ||
| 3 months | ||
| Mean (SD) | 0.92 (0.09) | 0.95 (0.05) |
| Minimum, maximum | 0.62, 1.00 | 0.88, 1.00 |
| Missing (n) | 12 | 5 |
| 6 months | ||
| Mean (SD) | 0.89 (0.13) | 0.92 (0.07) |
| Minimum, maximum | 0.63, 1.00 | 0.81, 1.00 |
| Missing (n) | 15 | 5 |
| Lost ≥ 5% of body mass, n (%) | ||
| 3 months | ||
| Yes | 2 (6.9) | 1 (7.1) |
| No | 15 (51.7) | 8 (57.1) |
| Missing | 12 (41.4) | 5 (35.7) |
| 6 months | ||
| Yes | 9 (31.0) | 1 (7.1) |
| No | 6 (20.7) | 9 (64.3) |
| Missing | 14 (48.3) | 4 (28.6) |
| Questionnaire | Treatment arm, n (%) | Overall (N = 43), n (%) [95% CI] | |
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | ||
| IPAQ-Short Form (7 items) | |||
| Fully completed | 7 (24.1) | 1 (7.1) | 8 (18.6) [95% CI 8.4% to 33.4%] |
| Partially completed | 10 (34.5) | 8 (57.1) | 18 (41.9) |
| Not completed at all | 12 (41.4) | 5 (35.7) | 17 (39.5) |
| Food and drink intake (8 items) | |||
| Fully completed | 16 (55.2) | 9 (64.3) | 25 (58.1) [95% CI 42.1% to 73.0%] |
| Partially completed | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Not completed at all | 12 (41.4) | 5 (35.7) | 17 (39.5) |
| EQ-5D-5L questionnaire (5 items) | |||
| Fully completed | 17 (58.6) | 9 (64.3) | 26 (60.5) [95% CI 44.4% to 75.0%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 12 (41.4) | 5 (35.7) | 17 (39.5) |
| ICECAP-A questionnaire (5 items) | |||
| Fully completed | 17 (58.6) | 9 (64.3) | 26 (60.5) [95% CI 44.4% to 75.0%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 12 (41.4) | 5 (35.7) | 17 (39.5) |
| Parenting for physical activity (13 items) | |||
| Fully completed | 17 (58.6) | 9 (64.3) | 26 (60.5) [95% CI 44.4% to 75.0%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 12 (41.4) | 5 (35.7) | 17 (39.5) |
| Father–child relationship (14 items) | |||
| Fully completed | 15 (51.7) | 9 (64.3) | 24 (55.8) [95% CI 39.9% to 70.9%] |
| Partially completed | 2 (6.9) | 0 (0.0) | 2 (4.7) |
| Not completed at all | 12 (41.4) | 5 (35.7) | 17 (39.5) |
| Questionnaire | Treatment arm, n (%) | Overall (N = 43), n (%) [95% CI] | |
|---|---|---|---|
| HDHK-UK programme (N = 29) | Minimum intervention (N = 14) | ||
| IPAQ-Short Form (7 items) | |||
| Fully completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Partially completed | 14 (48.3) | 9 (64.3) | 23 (53.5) |
| Not completed at all | 15 (51.7) | 5 (35.7) | 20 (46.5) |
| Food and drink intake (9 items) | |||
| Fully completed | 14 (48.3) | 7 (50.0) | 21 (48.8) [95% CI 33.3 % to 64.5%] |
| Partially completed | 0 (0.0) | 2 (14.3) | 2 (4.7) |
| Not completed at all | 15 (51.7) | 5 (35.7) | 20 (46.5) |
| EQ-5D-5L questionnaire (5 items) | |||
| Fully completed | 14 (48.3) | 9 (64.3) | 23 (53.5) [95% CI 37.7 % to 68.8%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 15 (51.7) | 5 (35.7) | 20 (46.5) |
| ICECAP-A questionnaire (5 items) | |||
| Fully completed | 14 (48.3) | 9 (64.3) | 23 (53.5) [95% CI 37.7 % to 68.8%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 15 (51.7) | 5 (35.7) | 20 (46.5) |
| Parenting for physical activity (13 items) | |||
| Fully completed | 13 (44.8) | 9 (64.3) | 22 (51.2) [95% CI 35.5 % to 66.7%] |
| Partially completed | 1 (3.5) | 0 (0.0) | 1 (2.3) |
| Not completed at all | 15 (51.7) | 5 (35.7) | 20 (46.5) |
| Father–child relationship (14 items) | |||
| Fully completed | 14 (48.3) | 9 (64.3) | 23 (53.5) [95% CI 37.7 % to 68.8%] |
| Partially completed | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not completed at all | 15 (51.7) | 5 (35.7) | 20 (46.5) |
Appendix 9 Total costs and cost per family to deliver the Healthy Dads, Healthy Kids UK programme
| Type of cost | Unit | Unit cost (£) | Total cost (£) based on 15 families per group | Total cost (£) based on 8 families per group |
|---|---|---|---|---|
| Equipment costs | ||||
| T-shirts | Per family: 2 × 2.5 for dad and 1.5 for children | 3 | ||
| Pedometers | 1 | 16.50 | ||
| Stickers | 1 pack | 0.50 | ||
| Handbook for dad | 1 | 8.40 | ||
| Handbook for child | 1 | 2.50 | ||
| Handbook for mum | 1 | 4.25 | ||
| Logbook | 1 | 4.60 | ||
| Play card | 1 | 1.85 | ||
| Spinner | 1 | 0.50 | ||
| Subtotal (per family pack) | 52.35 | |||
| Set up/training costs | ||||
| Room hire for training | 2 days | 40.00 per day | 80.00 | 80.00 |
| Training the health trainers | 2-day training | 1000.00 per day | 2000.00 (for nine trainers) | 2000.00 (for nine trainers) |
| Training the sports coach | 1-day training | 250.00 per day | 250.00 (for one sports coach) | 250.00 (for one sports coach) |
| Subtotal | 2330.00 | 2330.00 | ||
| Delivery | ||||
| Equipment | 1 pack per family | 52.35 | 785.00 | 419.00 |
| Room hire | Provided free of charge | 0.00 | 0.00 | 0.00 |
| Preparation time for 2 × health trainers | 1 hour per weekly session × 9 weeks | 18.00 (hourly wage)a | 324.00 | 324.00 |
| Delivery time for 2 × health trainers | 1.5 hours per weekly session × 9 weeks | 18.00 (hourly wage) | 486.00 | 486.00 |
| Delivery time for 1 × sports coach | 1.5 hours per weekly session × 9 weeks | 50.00 per weekly session | 450.00 | 450.00 |
| Delivery time for grade 6 researcher | 1.5 hours per weekly session × 9 weeks | 15.00 (hourly wage)b | 203.00 | 203.00 |
| Subtotal | 2248.00 | 1881.00 | ||
| Total | ||||
| Total (including training costs) | 4578.00 | 4211.00 | ||
| Total (excluding training costs) | 2248.00 | 1881.00 | ||
| Type of cost | Unit | Unit cost (£) | Total cost (£) based on 15 families per group | Total cost (£) based on 8 families per group |
|---|---|---|---|---|
| Training and delivery | Whole package including training and delivery | 3444.00 (for 9 weeks) | 3444.00 | 3444.00 |
| Room hire | Per week | 40.00 | 360.00 | 360.00 |
| Total | 3804.00 | 3804.00 | ||
| Type of cost | Unit | Unit cost (£) | Total cost (£) based on 15 families per group | Total cost (£) based on 8 families per group |
|---|---|---|---|---|
| Training and delivery | Whole package including training and delivery | 1530.00 (for 9 weeks) | 1530.00 | 1530.00 |
| Room hire | Per week | 40.00 | 360.00 | 360.00 |
| Total | 1890.00 | 1890.00 | ||
| Cost per family | Delivery component | Cost (£) for 9-week programme |
|---|---|---|
| Based on 15 families per group | Local authority delivery (including training costs) | 305.00 |
| Local authority delivery (excluding training costs) | 150.00 | |
| Coaching organisation | 254.00 | |
| Leisure centre | 126.00 | |
| Based on 8 families per group | Local authority delivery (including training costs) | 526.00 |
| Local authority delivery (excluding training costs) | 235.00 | |
| Coaching organisation | 476.00 | |
| Leisure centre | 236.00 |
List of abbreviations
- BAME
- black, Asian and minority ethnic
- BMI
- body mass index
- CHANGE
- CHild weight mAnaGement for Ethnically diverse communities
- CHU-9D
- Child Health Utility-9 Dimensions
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DADEE
- Dads And Daughters Exercising and Empowered
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FG
- focus group
- FNPA
- Family Nutrition and Physical Activity
- FST
- family systems theory
- GP
- general practitioner
- HDHK
- Healthy Dads, Healthy Kids
- ICECAP-A
- ICEpop CAPability measure for Adults
- ID
- identifier
- IMD
- Index of Multiple Deprivation
- IPAQ
- International Physical Activity Questionnaire
- IQR
- interquartile range
- NIHR
- National Institute for Health Research
- PPI
- patient and public involvement
- PRC-PAN
- Priority Research Centre for Physical Activity and Nutrition
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SAE
- serious adverse event
- SCT
- social cognitive theory
- SD
- standard deviation
- SMART
- specific, measurable, achievable, relevant, time-bound
- SMG
- Study Management Group
- SSC
- Study Steering Committee
- UoN
- University of Newcastle
