Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 12/180/20. The contractual start date was in April 2015. The final report began editorial review in May 2018 and was accepted for publication in February 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Sharon Anne Simpson reports membership of the National Institute for Health Research (NIHR) Health Technology Assessment programme, Clinical Evaluation and Trials funding committee from January 2017 to present. She also reports membership of the NIHR Policy Research Programme committee and the Chief Scientist Office Health Improvement, Protection and Services funding committee. Emma McIntosh reports membership of the NIHR Public Health Research funding board from January 2016 to present. There are no other competing interests in relation to personal, developer or institutional proprietorship of the current app or potential future product.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Simpson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Obesity: a key public health problem
Obesity is typically defined as a condition of excess or abnormal accumulation of body fat at a level that impairs health. 1 Individuals with a body mass index (BMI) of ≥ 30 kg/m2 are considered obese. Obesity has been highlighted as one of the top 10 risk factors for global burden of disease. 2,3 In 2017, the UK prevalence of obesity was 24.9%, one of the highest rates in Europe. 4 In Scotland, where this study was undertaken, the prevalence of obesity increased from approximately 15% in the mid-1990s to 29% in 2017. 5 This high prevalence of obesity places a significant burden on health services, with individuals with increased BMI using greater health-care resources than those with healthy BMI. 6
Obesity, alongside poor diet and physical inactivity, is a significant contributor to diseases such as diabetes, cancer, heart disease, hypertension and stroke. 7 Preventative interventions that are accessible and engaging and successfully improve health behaviours are necessary to reverse current trends. Interventions to date have had limited impact and approaches that are known to work are not always adopted. 8 Therefore, novel interventions that incorporate effective approaches are needed.
To inform the background to this study, a literature search was completed on the MEDLINE and PsycINFO databases from inception to 2017 using keywords including obesity, overweight, weight loss, social support, social network, digital health, ehealth, mhealth, physical activity, exercise and diet. A summary of the findings is presented in Chapter 2, Overarching approach: 6SQuID to The HelpMeDoIt! intervention content.
Previous weight loss research
Although obesity has been a major public health issue for years, there is still no consensus on the most cost-effective approach to support individuals to lose weight. The obesity system map9 highlights the complex layers of influence acting to create and maintain current levels of obesity. This links with the multiple interacting domains of the socioecological model that contribute to the problem. 10 Research has demonstrated that tackling multiple health behaviours, such as diet and physical activity, can be effective. However, interventions to date have had mostly small or no effects, with longer-term maintenance remaining a key challenge. 11
Previous research has shown that theory-based interventions, which specifically link elements of an intervention to outcomes, generally have greater success. 12 Despite this, many interventions are not theory based and most do not attempt to take account of the complexity of influences contributing to the development and maintenance of obesity. 12 Evidence indicates that intervention effectiveness generally increases with the intensity or amount of intervention delivered (total contact time or number of contacts). 13,14 The challenge is how this can be achieved while keeping the intervention cost-effective, as successful interventions often employ intensive, high-cost, one-to-one approaches. 13 These interventions have low reach as the intervention is deliverable to only a small proportion of the population. Given the scale of the problem of lifestyle-related illness, it is clear that alternative, cost-effective approaches need to be developed and tested.
Behaviour change: goal–setting, self-monitoring and social support
Guidance from the National Institute for Health and Care Excellence (NICE)15 highlights the importance of developing interventions that are based on theory and identify specific intervention components. A refined taxonomy of 40 behaviour change techniques for physical activity and healthy eating, by Michie et al. ,16 highlighted the wide range of approaches used in studies aiming to change lifestyle behaviours. The NICE guidance identified three of these techniques as showing promise for behaviour change, including setting goals, monitoring progress and harnessing social support. Studies employing these techniques have been associated with better outcomes. 11,17 Goal-setting and self-monitoring are techniques associated with intrapersonal processes, whereas engaging social support is linked with interpersonal processes. These techniques derive, in the main, from social cognitive theory18 and control theory,19 two of the key theories on which the HelpMeDoIt! intervention is based (described further in Chapter 2).
Goal-setting and self-monitoring (intrapersonal processes)
The important role of goal-setting and self-monitoring is well established in behaviour change research. In a meta-analysis of behaviour change interventions for physical activity and healthy eating, more effective interventions were shown to combine self-monitoring with at least one other technique derived from control theory (e.g. intention formation, specific goal-setting). 17 Goal-setting and self-monitoring are two of the most commonly used behaviour change strategies in weight loss interventions, and are typically used in conjunction. 20,21 A recent meta-analysis of behaviour change techniques in 48 weight loss interventions found that goal-setting and self-monitoring were the most effective components of the interventions. 21 Other intrapersonal processes, which we planned to address within our intervention, included intrinsic motivation, self-efficacy, action-planning22 and implementation intentions23 (described further in Chapter 2).
Social support (interpersonal process)
Social support and its relation to health behaviour change is undertheorised. This is partly because social support is a broad and somewhat loosely used concept; for example, it is an element in the widely used terms of ‘social capital’ and ‘social networks’, which are used to frame ideas about social support. 24,25
Social support is multifaceted: there are various types of social support (e.g. emotional, instrumental, informational)26,27 and there are different kinds of support-giving/-receiving behaviours (e.g. reinforcement, encouragement, motivation, feedback, empathy, role-modelling). 28 Although it is generally used as a positive construct, social support may also have negative elements, such as bullying or co-dependency. 24,29 Minimising negative support, as well as promoting positive support, should be a consideration of behaviour change interventions. 29
Social support is also conceptualised in varied ways in terms of who provides the support. Family,30 friends and colleagues,31 influential people within existing social networks,32 and fellow members of groups with a shared behavioural goal (e.g. weight loss, exercise)33 have been found to be effective in supporting behaviour change in alcohol consumption, smoking prevention and cessation, physical activity, diet and sexual behaviour.
There is evidence that using a ‘buddy’ or ‘helper’ can be effective for weight loss. One trial31 found that when people came with a friend to a weight loss programme they were more likely to adhere to the programme, have greater weight loss and maintain weight loss than those who came alone. Another study34 exploring predictors of adherence to a weight loss programme found that having a buddy (family member or friend) led to an increase in programme adherence from 79.9% to 96.1%. In a study35 of 704 participants in a 15-week online weight loss programme, 54% of participants chose to use a buddy, and they lost more weight than those who did not have a buddy. The same level of effectiveness was found whether the buddies were romantic or non-romantic. A systematic review36 of 21 studies supported these findings, reporting that spousal support could be effective for weight loss. These findings identify the important role that a buddy, or helper, could have in supporting weight loss.
Individuals draw on different types of support from different people in their network. For example, they may derive emotional support from a close friend in their network but may choose to recruit a more distant friend for that person’s expertise in a particular area. Family and friends are significant social influences on health behaviour as a result of factors such as intimacy, influence and proximity to day-to-day health behaviours. They are also immediately accessible to participants because this type of support does not entail joining any kind of formal group.
Social support is important in the initiation and longer-term maintenance of behaviour change,13,31,37 and is typically employed and theorised as one of several elements of behaviour change interventions. 38 In reviews13,17 it has been identified as one contributing factor to effectiveness, alongside goal-setting and self-monitoring. Common intervention elements theorised to operate in conjunction with social support are self-efficacy,39 perceived control39,40 and social norms. 41 Ferranti et al. 42 found that social support is positively correlated with healthy diet. Social support is also associated with increased physical activity40,43 and can improve weight loss maintenance,31 encourage health-promoting behaviours and promote well-being. 44 There is also evidence that unhealthy lifestyle behaviours are correlated with less social support. 15 For many of us, a significant proportion of our social contact is now via digital technologies, and therefore an intervention using this medium to facilitate social support may be useful. In one study45 of an online intervention, despite social support not being specifically promoted as part of the intervention, findings demonstrated that perceived social support from existing social networks and the use of self-regulatory behaviours were strong predictors of improved physical activity and nutrition behaviour. Similarly, Neuhauser and Kreps46 argue that communication that is interpersonal, affective (not just rational), interactive, individually tailored and set within an individual’s social context is more likely than other forms of communication to be effective in changing health behaviour, and that this should be incorporated within new technology- and internet-based interventions. This type and quality of social support would be better facilitated through contact with family and existing friends, rather than anonymous online groups. However, social support from friends and families tends not to be incorporated into the formal design of online behaviour change interventions.
Using technology to influence lifestyle
Emerging evidence in this field suggests that technology-based interventions can be effective, for example texting to promote healthy behaviours. 47 A growing body of evidence on web-based interventions employing goal-setting and self-monitoring has demonstrated positive effects on programme engagement and health behaviours. 12,48 Mobile apps in particular could be a convenient, potentially cost-effective and wide-reaching weight management strategy. 49 There is also evidence that new technologies can be effective with both young and older people. 50,51 However, interventions have often been rather simplistic and not based on the best evidence or theory of effective behaviour change. 52 The effectiveness of these interventions could be enhanced by incorporating well-evidenced behaviour change techniques and promoting support from an individual’s social network to assist them to achieve health-related goals.
A key driving force behind digital health is the need to move to more cost-effective health-care delivery models. Reviews53,54 of digital health interventions have demonstrated that few evaluations have captured data that sufficiently allow for consideration of economic outcomes and the overall effectiveness and cost-effectiveness of interventions. NICE55 plans to develop a new evaluation system for digital health apps to respond to the recent growth in digital health.
The growing accessibility of internet and smartphones
Technology offers opportunities to deliver behaviour change interventions that can reach a large proportion of the population at a low cost. 56 In particular, smartphone apps and web-based interventions can be effective in reaching large numbers of people. 47,57,58 In 2017, internet access was available in 88% of UK households. 59 Smartphones were owned by 85% of adults, of whom 55% reported checking their phone within 15 minutes of waking. 60 Interventions delivered via these technologies have the potential to reach large numbers of people, including ‘Silver Swipers’ (those aged 55–75 years), who were the fastest-growing adopters of smartphones in 2017;60 and those from lower socioeconomic groups, with 73% of people living in Scotland’s 20% most deprived areas having access to the internet. 61
Previous research
There are many smartphone apps (and accompanying websites) for weight loss available that incorporate some or all of the key behaviour change features of goal-setting, self-monitoring and social support [e.g. StickK (Brooklyn, NY, USA), www.stickk.com (accessed 1 June 2016);62 MyFitnessPal (Under Armour, Inc., Baltimore, MD, USA), www.myfitnesspal.com (accessed 1 June 2016)63]. However, a systematic review64 of the most popular apps for weight loss (n = 28) found that the majority were of inadequate quality, lacked evidence-based information on weight loss and lacked appropriate behaviour change techniques. Furthermore, although evidence from research-based interventions using new technologies suggested that they could be effective,47,57,58 the interventions were often simplistic and not based on the best evidence and theory of effective behaviour change. 52 The effectiveness of these interventions could be enhanced by incorporating well-evidenced behaviour change techniques and promoting support through an individual’s social network (family, friends and colleagues).
There is a need to improve our understanding of how interventions involving new technologies effectively facilitate changes, for example factors such as optimal website design, how to maximise exposure to websites or what type of prompting works best are areas that still require development. 65 Particular aspects of new technologies may enhance interventions, such as through higher intensity (e.g. more frequent contact with people in an individual’s social network). This may increase the success of an intervention13 but at a lower cost than traditional methods. Some applications may also allow for more personalisation or individual tailoring of an intervention to suit individual needs, which may also improve success rates. 66 However, the evidence base is limited and, to date, somewhat mixed. 67 Therefore, although there have been promising signs in this emerging field, such as the potential for high reach and for engaging hard-to-reach groups, there is a need to address research gaps in understanding how new technologies might support or enhance known health behaviour change mechanisms.
Currently available websites or apps for weight loss use various strategies for behaviour change, including elements such as monetary incentives or prizes, competing with others and behavioural goals. Some apps provide an element of social support, such as a chat forum. 63 There is some evidence to suggest that online social networks can have a positive impact on health behaviour change. 68 However, online users are typically not known to each other and the apps are not designed to harness the ‘offline world’ and the immediate support of family, friends and colleagues. Evidence indicates that support from key individuals in a person’s life is more effective than that provided by anonymous online contacts. 13
The perceived value of, and demand for, social support has resulted in many health behaviour change websites having chat forums or bulletin boards, which facilitate support from other users. These provide empathy and encouragement, but may not be able to build on evidence of the importance of who provides the social support and the many mechanisms through which social support can facilitate and sustain behaviour change. None of the resources we explored focused on the combination of elements that we used in our intervention, most importantly social support from key individuals within that person’s social network. These are individuals whom they know well, and who are part of their everyday lives and available to support them when needed, in a sustainable ongoing way.
The summary above has identified goal-setting, self-monitoring and social support as promising behaviour change techniques. 69 Although they have featured in a number of apps, for which there is mixed evidence, we have not identified any existing intervention that specifically aims to mobilise support from existing social networks using an application- (app) and web-based intervention. This is the unique aspect of the HelpMeDoIt! intervention, and this is the first study to our knowledge to explore the feasibility of engaging social support from existing social networks, in combination with goal-setting and self-monitoring, in a digital health intervention for weight loss. If brief engagement with an app could catalyse input from existing social connections to support longer-term change, then this could offer a sustainable approach to behaviour change.
Rationale for the current study
Policy
Improving health behaviours is a priority for government. However, current health behaviour change initiatives require improvements in their reach and effectiveness to have a significant impact on the population’s health. The House of Lords Science and Technology Select Committee report on behaviour change8 highlighted that no single approach is likely to be effective in tackling priority health behaviours and that complex interventions addressing multiple levels of behavioural determinants are likely to be needed to bring about sustained change. HelpMeDoIt! is a complex intervention addressing two of these levels: the intrapersonal and the interpersonal.
Economy
Lifestyle-related illness represents a significant cost to the NHS. One-to-one individualised lifestyle interventions are unlikely to yield substantial population-level improvements at a realistic cost to the public purse unless they are highly effective. In comparison, web- and app-based behaviour change interventions can reach substantial numbers at a lower cost. New technologies, such as smartphone apps, present opportunities to promote healthy lifestyles cost-effectively on a large scale. 70 Content, covering evidence-based behaviour change components with the engagement of community-based social support resources, can be delivered in an engaging and accessible way.
Evidence base
Although the intervention elements of goal-setting, monitoring and social support are well established, and although new technologies have shown promise, the evidence base is limited and theoretically underdeveloped. 50,52 Studies are often limited by small, short-term effects71 and high attrition. 12,72 There are significant gaps in understanding how these elements work together, for example how social support operates through personal networks mediated by new technologies, and what impact this has on mechanisms such as monitoring and goal-setting. There is a need to (1) explore the application and mechanisms of goal-setting, monitoring and social support via web and app-based interventions; (2) explore how they interact with each other: and (3) test this type of intervention in both a feasibility and a full-scale effectiveness trial. Feasibility trials of this nature are a necessary first step in developing public health improvement interventions, particularly where mechanisms, such as social support, are not well understood and where technological innovations present new possibilities.
Future impact
The proposed intervention has the potential to have both reach and effectiveness in all socioeconomic groups including those who are traditionally hard to reach. If the intervention were proven effective in a future powered trial, it could be applied to other behaviour change areas and would be universally available through a free-to-access website and/or promoted in specific NHS and community settings across the UK.
Study aims and objectives
The principal element of the HelpMeDoIt! intervention is social support from members of an individual’s close social network. This study explored the promising role of social support in successful health behaviour change, and developed theory concerning the types of social support that participants seek within their personal networks, which individuals they choose, the types of support provided in the context of a web- and app-based environment, the interaction with known behaviour change mechanisms such as goal-setting and monitoring, and the impact that this has on health behaviour change.
The aims of the study were to develop and test the feasibility of an intervention (HelpMeDoIt!) to promote health behaviour change for adults with obesity delivered via an app and website, which (1) incorporated evidence-based behaviour change techniques (goal-setting, self-monitoring and social support) and evidence-based information on weight loss strategies; and (2) delivered this information via a platform that was both usable for and acceptable to participants.
The study was completed in two stages (Figure 1):
-
In stage 1 the intervention was developed and piloted with the help of a panel of user representatives to address (1) the engagement and ease of use of the website and app and its success in promoting realistic goal-setting; (2) the acceptability of the social support content; (3) the functionality of the technology and its facilitation of social support from helpers; and (4) the views of the panel on how the intervention might attract and support helpers.
-
Stage 2 was a feasibility trial, with an accompanying process and economic evaluation, which aimed to examine reach, feasibility, acceptability and trial parameters for a future effectiveness trial. Findings from stage 2 will help to assess whether or not a larger randomised controlled trial (RCT) is warranted.
FIGURE 1.
The two stages of the HelpMeDoIt! study.

Key objectives of the study
-
To develop an app- and web-based intervention that enables participants to set and monitor goals and facilitate effective social support (see Chapter 2).
-
To investigate recruitment and retention as well as feasibility and acceptability of the intervention (see Chapters 4–6).
-
To explore the potential of the intervention to reach traditionally ‘hard-to-reach’ groups (e.g. lower socioeconomic groups) (see Chapters 4 and 6).
-
To explore the barriers to and facilitators of implementing the intervention (see Chapter 5).
-
To assess the feasibility and acceptability of different outcome measures for diet and physical activity in this population (see Chapters 4 and 5).
-
To use outcome data (diet, physical activity, BMI) to help decide on a primary outcome and to estimate the potential effect size of the intervention to facilitate the calculation of an appropriate sample size for a full trial (see Chapters 4 and 7).
-
To assess data collection tools and obtain estimates of key cost drivers to inform the design of a future cost-effectiveness analysis (see Chapter 4).
-
To investigate how participants and helpers engage with goal-setting, monitoring and social support using new technologies and how these elements interact within a behaviour change intervention (see Chapters 5 and 6).
-
To develop a conceptual model of how the key mechanisms of goal-setting, monitoring by self and others, social support and behaviour change are facilitated by the intervention (see Chapter 6).
-
To test the logic model and theoretical basis of the intervention in stages 1 and 2 (see Chapter 6).
-
To explore the characteristics of participants’ social networks and the influence social networks have on participant experiences and outcomes of the intervention (note that this was not part of the original funding application and will be published at a later date).
-
To assess whether or not an effectiveness trial is warranted (see Chapter 7).
Chapter 2 Stage 1: intervention development, methods and findings
An adapted version of the following methods was published open access in Matthews et al. 73 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The HelpMeDoIt! study was undertaken in two stages: stage 1, an intervention development and formative evaluation phase; and stage 2, a feasibility RCT. This chapter describes stage 1, and is split into three key sections:
-
overarching approach to stage 1 intervention development
-
findings from stage 1
-
progression criteria from stage 1 to stage 2.
Multimethod approach to intervention development
The aim of stage 1 was to design the HelpMeDoIt! app and website with the help of users and to explore initial usability and acceptability. It was important that the development of the intervention was guided by the target audience, and was theory based built on the best available evidence for behaviour change. In addition to the app and website, the goal of stage 1 was to develop a comprehensive programme theory and logic model. This programme theory was tested and refined as part of both stage 1 and stage 2 of the study.
We took a novel approach to the design of the HelpMeDoIt! app and website by combining four approaches to intervention development. These were general intervention development methods in the form of the ‘6SQuID model’ (6 Steps in Quality Intervention Development);74 digital health-focused methods using the Person-Based Approach75 and the Behaviour Intervention Technology model;76 and identification of appropriate behaviour change theories and techniques using the behaviour change taxonomy16 and current theoretical evidence base.
A brief overview of each approach is provided below. The key components of each approach, and how they complement each other, are outlined in Appendix 1.
Approach 1: the 6 Steps in Quality Intervention Development (6SQuID) model
This model by Wight et al. 74 was developed to address gaps in current guidance for the development of interventions. For example, the Medical Research Council (MRC) guidance on developing and evaluating complex interventions77 is primarily devoted to evaluation and does not provide sufficient detail on actual intervention development. The 6SQuID method involved six steps:
(1) defining and understanding the problem and its causes; (2) identifying which causal or contextual factors are modifiable: which have the greatest scope for change and who would benefit most; (3) deciding on the mechanisms of change; (4) clarifying how these will be delivered; (5) testing and adapting the intervention; and (6) collecting sufficient evidence of effectiveness to proceed to a rigorous evaluation.
We adhered to this six-step process, and used it as the overarching approach throughout our intervention development from initial idea to testing in the feasibility trial.
Approach 2: the Person-Based Approach
The Person-Based Approach is a framework for developing digital interventions that are based on a comprehensive understanding of the social, psychological and environmental context of the target group. 75 This approach involves potential users in the development of the intervention and incorporates their perspectives. As well as focusing on the views of users about engagement, content and usability, crucially it also addresses the behaviour change techniques included in the intervention. We considered the Person-Based Approach complementary to the approaches we were already using to identify theory- and evidence-based approaches to changing weight-related behaviours. The Person-Based Approach provided a systematic approach to intervention development, relying on qualitative methods throughout the whole process to inform intervention design. This type of iterative, consultation approach, understanding user perspectives and incorporating key contextual influences, was key to developing an intervention that could be engaging and have a chance of being effective.
Approach 3: the Behaviour Intervention Technology model
Another digital health-related framework is the Behaviour Intervention Technology (BIT) model. 76 The BIT model was developed to fill a gap in the literature on the design of behavioural intervention technologies, such as lifestyle interventions using web-based technology and mobile phones. The BIT model helps answer the questions why, what, how and when. For example, ‘why’ was reflective of the intervention aims; ‘what’ includes the BIT elements such as app notifications and report logs; ‘how’ includes behaviour change strategies, such as goal-setting, and technical characteristics, such as personalisation of the app; and ‘when’ refers to the navigation through the app/website as determined by either the software or the user. This model was particularly helpful in guiding the development of software characteristics.
Approach 4: utilising theory and behaviour change techniques
Between 36% and 89% of interventions that seek to change health behaviours are not clearly theory based. 78 Interventions based on theories of behaviour change have been shown to be more effective, although reviews relating the impact of using theory to the success of interventions have shown mixed results, and theory is often poorly applied. 79 The use of behaviour change techniques and how they relate to theoretical concepts is also often inadequately reported. 80 We sought to address both of these issues by exploring multiple behaviour change theories and identifying the most appropriate candidate theories and associated behaviour change techniques that could be useful in the HelpMeDoIt! intervention. We used these theoretical underpinnings to develop a programme theory, identifying multiple causal mechanisms describing how the HelpMeDoIt! intervention could lead to positive outcomes for weight management in adults with obesity.
Figure 2 presents how these four approaches were combined. This involved the 6SQuID model being used as an overarching cradle-to-grave process, with the Person-Based Approach, the BIT model and behaviour theory approaches being incorporated to address more specific development issues. The other elements represented in Figure 2 will be described in detail throughout this chapter.
FIGURE 2.
The combined framework for the development of the HelpMeDoIt! intervention.

Overarching approach: 6SQuID
The remainder of this section is structured using the six steps of our overarching approach, the 6SQuID model. We describe under each step how and when we incorporated the other three approaches: the Person-Based Approach, the BIT model and behaviour change theories and techniques.
6SQuID step 1: ‘define and understand the problem and its cause’
The initial step of intervention development involved undertaking a literature review to identify up-to-date evidence on obesity. This involved gathering data on the prevalence, causes and associated risks. Obesity is a well-researched area, so there was extensive evidence providing insights into this public health problem. The causes of obesity are complex and multilayered, and the solutions are likely to involve intervening at multiple levels, including individual, interpersonal, organisational, community and policy. The HelpMeDoIt! intervention focused on the first two of these levels. An overview of our literature review findings was provided in Chapter 1. Further detail can be found in our study protocol (see Report Supplementary Material 1).
6SQuID step 2: ‘clarify which causal or contextual factors are malleable and have greatest scope for change’
As part of the above review, we explored causal and contextual factors that could be influenced as part of the intervention. The key influencing factors associated with weight loss are diet and physical activity. Harnessing positive social support was identified as an important factor, as were motivation and self-efficacy. These have already been discussed in Chapter 1.
6SQuID step 3: ‘identify how to bring about change: the change mechanism’
Identifying the potential mechanisms of change was a critical step in the development of the intervention. It was at this stage that we incorporated the first of our other intervention development approaches by identifying relevant behaviour change theories and techniques. We conducted a search to identify the intervention components most likely to contribute to successful weight loss, as well as components associated with successful and unsuccessful interventions. We also conducted a search for web-based and other technology-based interventions and those involving any kind of social support, whether from friends, family, colleagues or groups such as Weight Watchers. We also conducted an internet search for websites or apps aimed at changing health behaviours around diet and physical activity. We found many sites that utilised monetary incentives or prizes, competition with others, behavioural goals, and social support elements such as chat forums. However, we did not identify any that included family members and friends to encourage and promote weight-related behaviour change in the way we envisaged. Our review of the literature and 6SQuID steps 1 and 2 provided us with the rationale to develop an intervention for adults with obesity, using technology in the form of an app/website, to facilitate social support for weight loss. The resulting intervention is, thus, a combination of (1) individual behaviour change approaches, (2) social support and (3) the use of technology.
Behaviour change theories and techniques
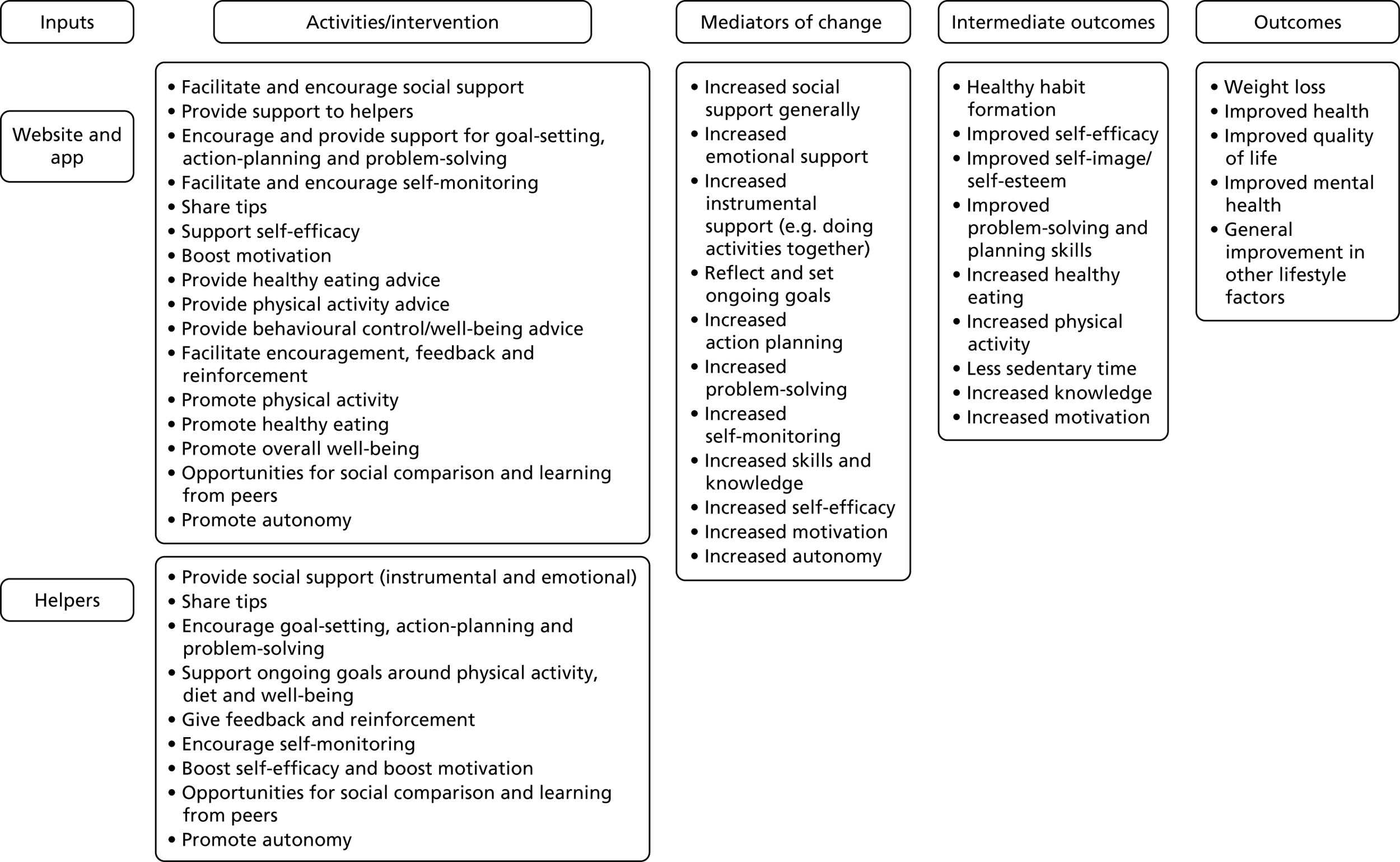
The literature review identified the most appropriate candidate theories and associated behaviour change techniques that could inform the early-stage development of the ‘version 1.0’ programme theory and logic model (Figure 3). This initial logic model broadly focused on goal-setting, self-monitoring and social support,as these techniques have been shown to be effective for weight loss. 11,81 It also included a number of other evidence-based techniques, such as boosting motivation and increasing autonomy. We mapped these behaviour change techniques to behaviour change theories relevant to our intervention. 82,83 These were Social Cognitive Theory,18 Self-Determination Theory,84 Control Theory19 and Social Support Theories. 27,85 Elements of the version 1.0 logic model that related to each of these theories are highlighted in Table 1.
FIGURE 3.
Version 1.0 of the HelpMeDoIt! programme theory and logic model.
| Source of input | Behaviour change technique | Behaviour change theory |
|---|---|---|
| HelpMeDoIt! website and app | Facilitate and encourage social support | Social support theories |
| Provide general encouragement and instruction (support) to helpers | Social cognitive theory | |
| Encourage and provide support for goal-setting, action-planning and problem-solving | Social cognitive theory | |
| Facilitate and encourage self-monitoring | Control theory/social cognitive theory | |
| Share tips | Social cognitive theory | |
| Support self-efficacy | Social cognitive theory | |
| Boost (intrinsic) motivation | Self-determination theory | |
| Provide healthy eating advice | Social cognitive theory | |
| Provide physical activity advice | Social cognitive theory | |
| Provide behavioural control/well-being advice | Social cognitive theory | |
| Facilitate encouragement, feedback and reinforcement | Social cognitive theory | |
| Promote physical activity | Social cognitive theory | |
| Promote healthy eating | Social cognitive theory | |
| Give feedback and reinforcement (app only) | Control theory/social cognitive theory | |
| Promote autonomy | Self-determination theory | |
| Opportunities for social comparison and learning from peers | Social cognitive theory | |
| Promote problem-solving | Social cognitive theory | |
| Support from helpers | Provide social support (instrumental and emotional) | Social cognitive theory/social support theories |
| Share tips | Social cognitive theory | |
| Encourage goal-setting, action-planning and problem-solving | Social cognitive theory | |
| Support ongoing goals around physical activity, diet, etc. | Social support theories | |
| Give feedback and reinforcement | Social cognitive theory | |
| Encourage self-monitoring | Control theory/social cognitive theory | |
| Boost self-efficacy | Social cognitive theory | |
| Boost (intrinsic) motivation | Self-determination theory | |
| Opportunities for social comparison and learning from peers | Social cognitive theory |
Table 1 presents the mapping of individual behaviour change techniques used in the intervention to these four behaviour change theories.
6SQuID step 4: ‘identify how to deliver the change mechanism’
Version 1.0 of the logic model was based on the research evidence, using 6SQuID steps 1–3. The logic model was used as a starting point for then engaging with stakeholders, with a view to further refining the mechanisms of change and intervention content. At this point we began developing the intervention alongside potential users and technical experts from a software company. This was a critical stage in our intervention development and involved the use of the two other approaches: (1) the Person-Based Approach75 and (2) the BIT model. 76 Each of these explored how to effectively deliver the mechanisms of change and specific content of the interventions.
The Person-Based Approach
We adopted the Person-Based Approach as an appropriate method of involving key stakeholders in the development of the intervention, allowing us to iteratively explore usability, engagement and content, including relevant behaviour change techniques. The first step of the Person-Based Approach was to develop guiding principles on which to base the intervention. Our HelpMeDoIt! guiding principles are outlined in Appendix 2. The second step was to gather insights from key stakeholders, namely potential users of the app/website and members of the software company (described below). The Person-Based Approach helped identify which key components should be included, taking into account context and implementation, in a way that was acceptable and convincing to the target group.
The Behaviour Intervention Technology model
The purpose of using the BIT model was to guide the practical build of the intervention in relation to its conceptual aim of weight loss using social support. The BIT model was crucial in providing us with a digital health-focused framework for ensuring that the intervention’s technical aspects aligned with its objectives of goal-setting, self-monitoring and social support via helper interaction. The model is based on five elements: (1) why the software is being developed, for example to promote weight loss; (2) how the software is conceptually considered to achieve the overall goal of weight loss, for example via goal-setting, self-monitoring and social support; (3) what elements the software requires to ensure that these aspects of the intervention are achieved, for example use of notifications and reminders to use the app; (4) how these features will technically be delivered by the software to meet the needs of the participant, for example specific requirements, such as choosing days of the week, for the goal-setting feature; and (5) when the various elements of the intervention are delivered; for example, the timing of some features will be led by participants, compared with other features that will be time-based and set by the software, such as push notifications. Table 2 provides examples of how the BIT model helped develop the technical build of the app and website. For this phase, we worked alongside a software company, ensuring that we captured their expertise in and insights into developing the intervention into an app and website.
| BIT component | Examples | |
|---|---|---|
| Why | Intervention aims (informed by our previous scoping work under 6SQuID step 1) | Weight loss:
|
| How (conceptual) | Behaviour change strategies (informed by our previous scoping work under 6SQuID steps 2 and 3) |
Goal-setting Self-monitoring Social support Action-planning Problem-solving |
| What | Elements |
Information delivery Messaging Notifications Rewards Passive data collection Reports App-to-app contact |
| How (technical) | Characteristics |
Medium – app and website Complexity – option to use free text or templated goals Aesthetics – friendly-looking, bright Personalisation |
| When | Workflow |
User defined Frequency – reminders Conditions |
Methods for involving users in the development phase
We recruited a development panel of 10 users. An overview of the methods used with the development panel is provided in Table 3. The development panel was instrumental in helping us develop features of the app and website that were evidence based but user led. It allowed the study team to gather critical insights into the psychosocial context as well as the perspectives of potential users. It enabled us to explore ideas for engagement, and helped refine the key elements and delivery mechanism of the app and website. Findings are presented in Results of stage 1 intervention development.
| Study aspect | Methods used |
|---|---|
| Sample | 10 user representatives who were adults aged ≥ 18 years, owned a smartphone and were interested in losing weight |
| Recruitment | Posters in large organisations; adverts via Gumtree; frequent tweets using our HelpMeDoIt! Twitter account (Twitter, Inc., San Francisco, CA, USA; www.twitter.com); and frequent posts on our HelpMeDoIt! Facebook page (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) |
| Sampling frame | Based on age, gender, postcode and current experience of using apps |
| Role | To contribute to the concept, design and development of the intervention, and to test the beta version of the app and website |
| Method |
Invited to three evening focus groups Focus group 1 was held in June 2015 and involved participants discussing potential key features of the intervention. The study team and the software company subsequently worked on developing initial plans for the intervention based on these findings Focus group 2 was held in September 2015 and involved participants sharing their feedback on the initial designs and key features Focus group 3 was held in December 2015 and involved participants giving feedback after having had the opportunity to test the app and website on their telephone/PC for 1 week. At this point they also completed the USE questionnaire, which collects data on acceptability. 86 The study team and the software company subsequently used the findings from this group to refine and strengthen the software ready for implementation in stage 2 |
| Analysis |
Focus groups were audio-recorded and transcribed verbatim. Although a full thematic analysis was not carried out at this stage, two members of the study team analysed the transcripts for key data to inform the software development, including the scope, intervention content and design. This involved separately extracting key points from the transcripts related to potential key elements of the intervention. These data were tabulated and discussed in detail both among the study team and with the software company. Further analysis and discussion included comparing key points with evidence from the literature and current software capabilities This analysis categorised potential software features into three groups: (1) definitely to be included (i.e. evidence based, feasible to implement and welcomed by participants); (2) maybe to be included (i.e. some evidence base, feasible to implement but with challenges and disadvantages, and welcomed by majority of participants); or (3) not to be included (i.e. limited evidence base, challenging to implement, welcomed by some participants). Decisions on software development were presented and discussed with the development panel at each focus group, following which the key elements of the intervention were developed further |
| Software development | Software was refined based on these findings |
6SQuID step 5: ‘test and refine on a small scale’
In addition to our development panel, we used a separate testing group to gather feedback at various points throughout the development process.
Methods for involving users in the testing phase
An overview of the methods used with our testing group is provided in Table 4. In addition to gathering feedback on the content, look and navigation of the app and website, this testing stage helped identify technical bugs, software issues such as navigation errors, and areas of the app/website that could be strengthened further. Findings are presented in Results of stage 1 intervention development.
| Study aspect | Methods used |
|---|---|
| Sample | 28 user representatives who were adults aged ≥ 18 years. Unlike the development panel, it was not necessary for this group to own a smartphone or have an interest in losing weight. This phase of testing focused on operational aspects of the app and website, and not on the behaviour change content |
| Recruitment | The methods were the same as for the development panel, with the addition of (1) inviting individuals who were not selected for the development panel to join our testing group and (2) word of mouth (by members of the original development panel to people in their social network) |
| Sampling frame | Based on age, gender and socioeconomic status |
| Role | To test the app and website prior to their delivery in the trial |
| Method | Conducted over a 4-month period using two methods. (1) Individual semistructured interviews between August and November 2015. Users were presented with initial software designs for the app and website (either printed as a hard copy on A4 paper or presented as a digital copy on a PC/television screen) and asked to provide feedback in relation to the look, feel, key features, wording and content. (2) Think-aloud interviews87 were undertaken about the prototype version of the app and website in late November–December 2015. During these interviews, users were asked to work their way through the software and share their immediate feedback by speaking out loud their thoughts while using it, and with the interviewer present. The interviewer asked questions throughout the process to probe further into the thought process of participants (e.g. ‘You’ve been quiet for a few moments. Can you tell me what you are thinking?’). This helped to assess the clarity and ease of use of the app and website interface and also to identify ‘sticking points’ |
| Analysis | All sessions were audio-recorded and analysed by two members of the study team. Analysis included collating (1) a list of positive and negative feedback on participants’ test runs of the app; (2) feedback on the look, feel, key features, wording and content; and (3) insights from participants on using the intervention in the context of their daily lives. Data from these interviews and think-aloud sessions were fed back to the software company and this led to further refinement of the app, website and programme theory |
Heuristic evaluation
Further testing was performed via a heuristic evaluation. This standardised process involved the app and website being assessed by two independent technology experts. 88 Each expert applied and assessed set heuristic criteria to both the app and the website (see Appendix 3). The aim of the heuristic evaluation was to identify strengths and limitations of the software and highlight areas for further refinement.
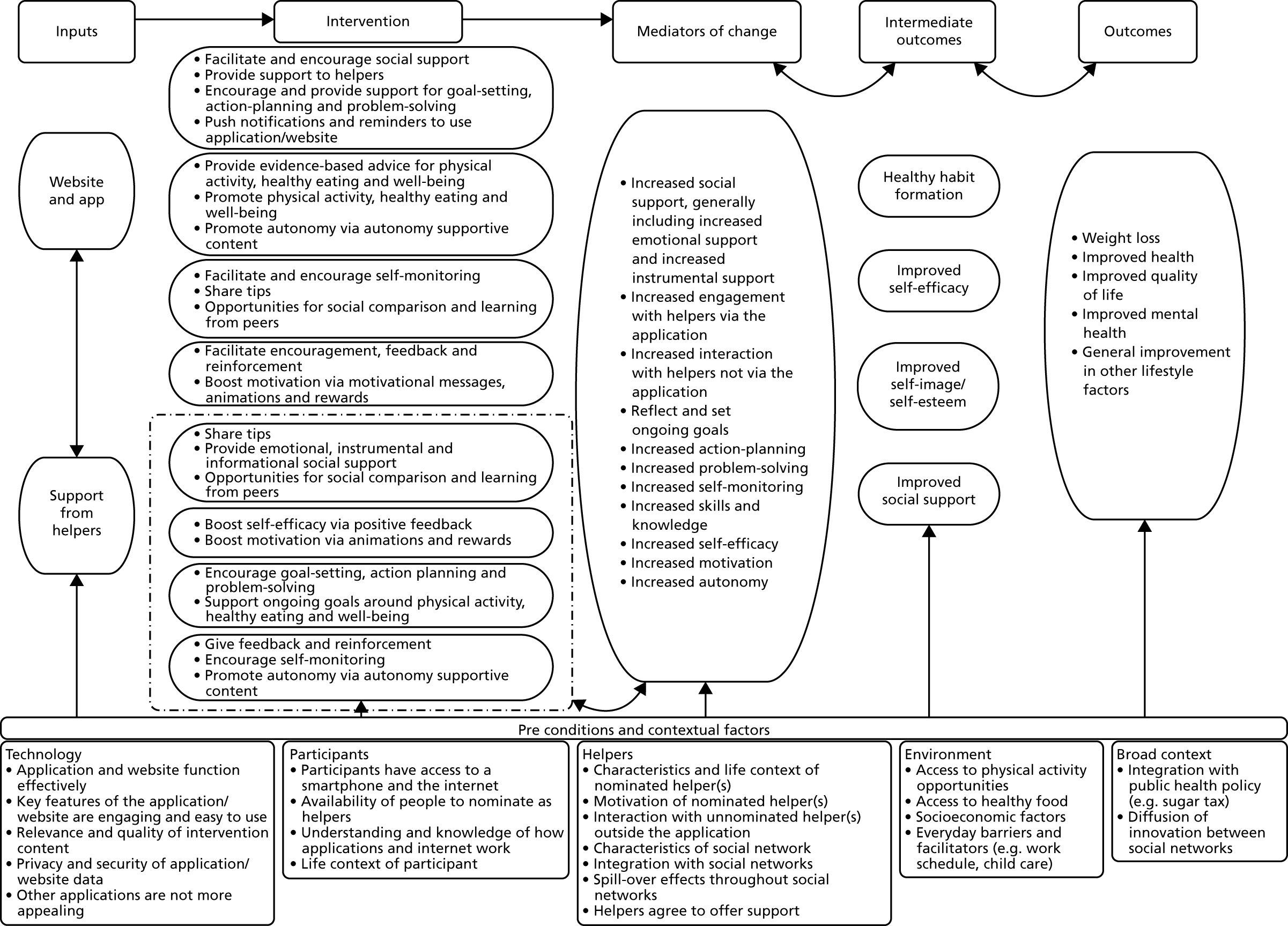
Logic model and programme theory development
The valuable insights gathered by 6SQuID steps 1–5, incorporating the Person-Based Approach, BIT model and behaviour theory/technique exploration, helped refine and strengthen the HelpMeDoIt! programme theory and logic model. We developed and continually updated the programme theory used to design our intervention and plan the evaluation, and this is represented in the logic model. The original version 1.0 of the programme theory logic model (see Figure 3) identified general links between the software elements of the intervention and the proposed outcomes. The ongoing user involvement and feedback throughout stage 1 allowed us to consider additional contextual factors and further refine ‘version 2.0’ of the programme theory and logic model. The revised logic model now included (1) further mechanisms of action (e.g. increased motivation and increased autonomy); (2) a reduced number of intermediate outcomes (e.g. less sedentary time and increased physical activity and healthy eating were condensed into healthy habit formation); and (3) multiple contextual factors (e.g. availability of people in participants’ social network to act as helpers) (Figure 4).
FIGURE 4.
Version 2.0 of the HelpMeDoIt! programme theory and logic model.
6SQuID step 6: ‘collect sufficient evidence of effectiveness to justify rigorous evaluation/implementation’
In step 6 of the 6SQuID process, the resulting version 2.0 logic model and intervention were ready for implementation and testing in a feasibility RCT with accompanying process and health economic evaluation (stage 2). The methods and findings for this stage are presented in Chapters 3–6.
Results of stage 1 intervention development
As described above, the intervention was developed in collaboration with a development panel of users, a testing group of users and a software company and used evaluation feedback from software experts. Details of how this input helped inform the development of the HelpMeDoIt! intervention are presented below in the following order:
-
findings from the development panel
-
findings from the testing group
-
usage statistics for the app and website
-
findings from the heuristic evaluation
-
findings from the USE questionnaire.
Findings from the development panel
We recruited 10 individuals with a range of characteristics to our development panel. We had a good gender balance (female, n = 6; male, n = 4) and spread of ages (18–70 years). All participants were interested in losing weight. We also attempted to include individuals with characteristics associated with a higher likelihood of obesity, and thus included participants of non-white ethnicity (n = 2) and a greater number of individuals from areas of lower socioeconomic status (n = 7). We included two individuals with limited experience of using smartphone apps (the majority of people who responded to the study advert were experienced in this). When participants were unable to attend one of the focus groups, their feedback was collected via a one-to-one interview (n = 1) or by e-mail (n = 2).
Insights and feedback from the development panel were useful and informative at all data collection time points. Participants were engaged, motivated and creative in their approach to the software development and many of their ideas and suggestions were incorporated into the prototype of the app and website. Some suggestions were not included as they were beyond the scope of the app, such as taking photographs of a meal and the app providing an accurate nutritional analysis.
Thematic analyses of the focus groups identified three main themes and related subthemes. These are detailed in Table 5 along with examples of how the different themes were addressed within the app and website.
| Theme | Subtheme | Description | Examples of how theme was addressed |
|---|---|---|---|
| 1. Software design | Avoiding non-adherence | Barriers to and facilitators of using the app and website, and ongoing engagement using various methods (e.g. autonomous wording and gamification) | Participants can earn medals and trophies for engaging with the app |
| Adaptability of the app | Issues related to flexibility and individual tailoring of the app | Options for setting unit of measurement for inputting weight (e.g. kg or lb) | |
| Usability of the app | Technical-related factors, such as the app interface, colour and font, and software issues | Colour palette was chosen to be unintimidating, friendly and fun | |
| 2. Intervention content and features | Key features of the app | Insight related to the three key features of the app: (1) goal-setting, (2) self-monitoring and (3) helper interaction | Animated smileys created for participants and their helpers to interact via the app |
| Feedback from the app | Issues related to app engagement around progress graphs, reminders, prompts and rewards | Weight change graph included in the app so participants could see progress | |
| Key features of the website | Issues related to the purpose and content of the website compared with the app | Website information provided on the emotional benefits of weight loss | |
| 3. People and context | Characteristics of social support for lifestyle change | Issues related to peer modelling, characteristics of helpers, types of social support offered, and barriers to and facilitators of being a helper | Website offered examples of what type of person might make a good helper |
| Person-centred motivations | Motivations for using the app, making and sustaining lifestyle change, and types of motivations (e.g. intrinsic vs. extrinsic) | Promotion of intrinsic motivation via app (e.g. template well-being goals and well-being messages) | |
| Context of using the app and website | Insight into how participants might fit the intervention into their everyday life, including working patterns; child care; memory problems; comparison with other apps; and previous experiences of app use | Appropriate font size used for both app and website |
Theme 1: software design
This theme included discussion around how the design of the app and website could influence whether or not it was adopted and used successfully.
Subtheme 1.1: avoiding non-adherence
This included discussion on barriers to and facilitators of using the app and website, and how to facilitate ongoing engagement. Our review of the literature had highlighted that ongoing engagement with apps was a significant challenge for software designers. Therefore, the development panel were asked for their insights on what features might help maintain their engagement with the app. Various methods were discussed, such as wording that boosted intrinsic motivation, as well as gamification, daily messages/tips from the app, and a method of receiving instant feedback from their helper(s). These ideas were explored further in the three focus groups. The agreed features were (1) gamification, where participants and helpers could earn points (which would convert to medals and trophies); (2) regular tips via the app or e-mail, which included tips for weight loss, physical activity, well-being, SMART (specific, measurable, attainable, relevant and time-bound) goal-setting, self-monitoring and social support; (3) daily messages via the app or e-mail, which provided motivation, inspiration and encouragement; and (4) instant feedback between participants and helpers via fun animations, for example an animated ‘high five’ from helpers to participants when the latter achieved a goal.
The development panel also discussed likely barriers to and facilitators of using the app. For example, when they were asked to identify reasons they might not use the app, their responses included having trouble with the login process; not having in-app rewards; if the app shows adverts or asks for money; a lack of engagement from the nominated helper; difficulties with using the interface; or if they found another app that performed better.
Subtheme 1.2: adaptability of the app
Here, issues about flexibility and the individual’s ability to tailor certain aspects of the app to suit their routine were discussed. Participants provided useful insights into contextual factors that might encourage use, for example being able to personalise the time and frequency of notifications to match their work schedule:
You could also change it, like if you do get a reminder, you can set snooze for 1 hour, 2 hours. I don’t know if that’s possible. I don’t know, but it’s an option. Because you may think, ‘I am at work just now, but maybe when I get in I want to be reminded’ and you can upload that information.
DP02, male, 40 years
Not all members of the development panel viewed the use of short message service (SMS) text messaging positively. Although some participants did not mind receiving text messages, others felt that this was ‘intrusive’:
I don’t like that [receiving messages via text]. The same as you get text messages from all these companies, stuff like that . . . I feel like junk spam kinda text messages.
DP01, male, 40 years
It was agreed that the main method of communication from HelpMeDoIt! would be set as a preference by the participant (i.e. they would have the choice of receiving push notifications via the app or by e-mail). Several participants indicated they would choose to receive notifications via the app, with some stating that they enjoyed logging into an app each day and seeing a different message. This provided variety and helped with ongoing engagement. However, SMS text messaging was not considered intrusive in the context of helper interaction. Participants liked the idea of receiving supportive text messages from their helper(s). It was agreed that a ‘quick access’ icon would be included in the app to allow participants and helpers to send text messages to each other.
Subtheme 1.3: usability of the app
This related to technical issues such as the app interface, colour and font, and the software itself. The development panel provided feedback on the initial designs and then finally on the prototype of the app and website. Overall, their feedback was positive. The majority of participants liked the layout, colour scheme, design and key features. The development panel also shared critical feedback of the app and website that identified areas for further consideration and refinement. Criticisms of the intervention included difficulties with the initial login via the third-party test app; numerous software bugs affecting their ability to test run the app (e.g. absence of screen animations, buttons obscured by text); not having enough guidance on how to initially use the app or earn rewards; and not having the ability to earn points, and, thus, rewards, during the early stages of testing.
Theme 2: intervention content and features
This theme included the actual intervention elements, what they might look like within the app and website, and how they could help or hinder the process of adopting a healthy lifestyle change.
Subtheme 2.1: key features of the app
This consisted of insights related to goal-setting, self-monitoring and helper interaction.
Participants agreed that having template goals developed by the research team would be useful to help them understand what an appropriate and manageable goal was. They felt that it was important that the template goal could be edited so that they could tailor it to their own circumstances. They also suggested that focusing on a small number of goals would be beneficial, and that goals should focus on sustainable lifestyle change rather than simply weight loss:
It was good that it [the app] gave you the option of already made goals, if that makes sense. Something you struggle to think of. Having one there and being able to work on it gives you more ideas. It’s a good idea.
DP05, female, 70 years
Graphs were unanimously participants’ preferred method of viewing and monitoring progress. Participants shared positive experiences of using graphs on other apps and requested that the HelpMeDoIt! app use a simple yet informative style similar to that of apps they had previously used. They understood that monitoring their progress could help them ‘learn to succeed’:
. . . you are proving to the app like I can do this. Not saying something like ‘I am going to change the world’ but at least like ‘to walk more’, ‘take one bus stop less’. Yes, more like lifestyle changes.
DP08, male, 51 years
Early discussion highlighted that participants were engaged with the concept of helpers, and in particular with helpers interacting via an app. They felt that the intervention could be helpful and effective but they spoke about other lifestyle apps that they used (e.g. MyFitnessPal) and emphasised that HelpMeDoIt! needed to identify its uniqueness in relation to the helper interaction. They shared numerous ideas in relation to interaction with their helper(s). This included insight into the motivation of helpers, who potentially would be more willing to log on to the app and support their friend initially for the fun and novelty. Some shared thoughts on how they imagined the helper would use the app for instant feedback (e.g. a husband or wife messaging their partner from across the room). Participants agreed that having a ‘pat on the back’ from their helper would be encouraging and motivating, and they thought they would enjoy receiving motivating messages from their helper(s). To maximise the support that helpers provide, it was recommended that as much information as possible was shared with them, with helpers basically seeing the same version of the app as the participant. This would allow helpers to see the achievement of small goals, as well as larger weight loss goals. Helpers should therefore receive notifications of new goals, goal progress and goal lapses; however, participants recognised that the frequency of notifications should be limited to avoid their helper(s) becoming annoyed and disengaged with the app:
[I like] having other people helping you. No one pats you on your back unless you go around [saying] ‘I reached my target weight’. All right there are no like celebrations, no cake, no anything like that.
DP04, female, 34 years
Subtheme 2.2: feedback from the app
This related to app engagement around progress graphs, reminders, prompts and rewards. Participants were aware that receiving too many push notifications and e-mails could be a potential barrier to engagement. The majority agreed that either a weekly or a fortnightly summary e-mail of their progress would be useful and non-intrusive. They also agreed that push notifications were a good method of receiving feedback, as these reminded them to use the apps on their phone:
I think in Fitbit [Fitbit, Inc., San Francisco, CA, USA] every week you get an e-mail to see how many steps you’ve done and your overall progress or whatever, which is I suppose it saves you being bombarded.
DP01, male, 40 years
Subtheme 2.3: key features of the website
This addressed content that participants considered useful and informative to have on the accompanying website. The majority considered that they would use the website as a source of information, but would use the app as the main source of the intervention. They did not want all of the information on the app, a suggestion that was also supported by the software company, which also suggested trying to keep the app simple and develop any extra detail for inclusion on the website. Ongoing discussion with the development panel identified that the website should provide guidance (1) for participants on how to safely and effectively lose weight and get the most out of their social support; and (2) for helpers on how to be a good helper and how to support their friend when they experience setbacks, etc.:
. . . maybe for some web page maybe some particular advice, I don’t know . . . What to eat? Or . . . I don’t know. Because that would . . . for me reinforcement is you would go to a web page for reinforcement. For me it’s some sort of psychological reinforcement.
DP08, male, 35 years
Theme 3: people and context
This theme covered social support and contextual factors in the participant’s life that could affect the likelihood that they would be able to make lifestyle changes. This theme included how people in the participants’ social network could help them achieve their goals and what that their social network looked like in terms of supportive and less supportive individuals. It also touched on factors related to the motivation needed to effect change. Finally, this theme included discussion of contextual factors in terms of work obligations, family responsibilities and friends, and the participants’ own histories of health and attempts to lose weight.
Subtheme 3.1: social support for lifestyle change
This related to peer modelling, characteristics of helpers, types of social support offered, and barriers to and facilitators of being a helper. Participants discussed the different people they had in their social network and how some of them might be good helpers because they would be good at motivating them, while others might be supportive because they too were embarking on lifestyle change. Some were reluctant to choose helpers who had an active healthy lifestyle, feeling that these helpers might lack empathy and understanding of a weight loss journey. Most participants liked the idea of nominating helpers from their social network rather than strangers:
I think having someone who can push me would be very good because I lack motivation on my own. But I think it is better to have one single person than different persons.
DP05, female, 65 years
Subtheme 3.2: motivation
This encompassed participants’ motivations for using the app, lifestyle change, sustaining lifestyle changes, and whether motivation was intrinsic or extrinsic. Some participants were motivated by recently diagnosed health problems, for which their lifestyle change was a form of disease management. Others described how they were motivated by the change in lifestyle rather than setting goals, and therefore sustained lifestyle change was the ultimate goal. They also shared important insight into their motivation for continuing to use the app, which typically involved the app being simple, engaging and fun to use:
. . . from my perspective, I am not looking to achieve my target weight. I am looking to generally improve my lifestyle [. . .] drinking water rather than Irn Bru [AG Barr, Cumbernauld, UK]. Rather than actual 18, 15, 10 stone. The rest of it is no target for me [. . .] ideally I would like it to be sustainable for the rest of my life.
DP08, male, 35 years
Subtheme 3.3: context
This included insights into how participants might fit the intervention into their everyday life, including working patterns, childcare, problems with their short-term memory, comparison with other apps and previous experiences of app use. Participants described how they used apps on their phone daily, and typically checked their phone when they woke up in the morning. Others noted how their busy work day made it difficult to manage apps during the day; however, they used their evenings to ‘catch up’ on notifications. Some participants described the challenges of sustaining lifestyle change around shift work, and how weekly rather than daily goals were likely to have greater chance of success:
I don’t have some apps on my phone, because I don’t have time during the day. I only do it on my iPad [Apple Inc., Cupertino, CA, USA] at night-time so I am not harassed by notifications. But I like to be harassed at night. That’s when I fill everything in.
DP04, female, 34 years
First thing I do is check my phone when I get up.
DP03, female, 26 years
Table 6 presents a summary of the key features agreed by the development panel for inclusion in the app and/or website.
| Intervention component | Specific intervention strategies |
|---|---|
| Goal-setting |
|
| Self-monitoring |
|
| Helper interaction |
|
| Settings |
|
Findings from the testing group
Feasibility of the app and website was also evaluated by the 28 participants recruited to the testing group. We purposely aimed to recruit participants with a range of characteristics: 19 were women and 9 were men; age range was 18–64 years; nine participants were from the top two quintiles of socioeconomic deprivation; two participants were from minority ethnic backgrounds; and two individuals had limited experience of using apps (the majority of people who responded to the study advert were experienced in the use of smartphone apps). Participants were recruited via word of mouth (n = 15) (e.g. by members of the original developmental panel to people in their social network), study adverts on Gumtree (www.gumtree.com) or Facebook (Facebook, Inc., Menlo Park, CA, USA) (n = 8), and a university-wide staff e-mail announcement (n = 4). Although feedback was collected on an ongoing basis between August and December 2015, participants provided feedback on only one occasion as a ‘user’ (n = 11), a ‘helper’ (n = 11) or both (n = 6). Detailed feedback from the testing group is presented in Appendix 4. A brief overview is provided below. Overall, feedback from the testing group was constructively critical.
Early feedback at the first time point (August and September 2015) focused on gathering feedback on the initial ideas and designs for the app and website. Feedback was positive, with participants in agreement about the proposed key features of goal-setting, self-monitoring and helper interaction, as well as how these would be delivered. They provided feedback on the initial design, look and feel of the app, and the majority of responses were positive comments on the simple design and colour scheme. Helpful suggestions related to grammar were received to help make the app more engaging. They also provided insights to help the team refine the initial design, for example guidance to choose from more than one goal category.
Feedback collected at time point 2 (October and November 2015) focused on participant insights on our refined app and website ideas. Feedback highlighted that some guidance was required to help participants choose and set goals using the app. This phase of testing also identified useful content to support helpers in their supportive role. Ideas participants provided for the helper section of the website included (1) example conversations between the helper and their friend; (2) guidance on what a helper could do if their friend was struggling to meet their goals; (3) things not to say to their friend; and (4) an online quiz to engage and motivate helpers:
When mentoring at my work it’s about trying to be encouraging so maybe some examples of encouraging dialogue.
TG08, female, 33 years
At the final time point (December 2015), participants were presented with the prototype version of the app. This was accessed using a third-party testing platform. This enabled participants to access and use the app in its beta version and sync to the latest version as features were updated and errors were rectified.
Feedback was gathered via the ‘think-aloud’ approach. 87 This approach facilitated identification of software bugs and errors, which the software company worked on rectifying immediately (e.g. icons obscured by text, inconsistent display of progress graphs). Many of the software bugs were caused by the interaction of our software with a third-party testing platform. Some of these were addressed when the third-party testing platform released an update near the end of our testing phase. In addition to software issues, the feedback helped highlight navigation issues, things that were not intuitive in the design and areas of the app that could be strengthened further. One key suggestion was the need for tutorial guidance to help first-time users understand the process of choosing template versus custom goals:
I’m not sure what I’m meant to do here [on goal-setting screen]. Do I press this button? How do I go back and see the list of goals again?
TG18, female, 39 years
When time allowed, some participants in the testing group also provided feedback on the website (n = 8). Feedback for the website was very positive, with the majority of participants commenting on the simple layout, easy navigation, clear display of information and fun animations. Several suggestions were made to strengthen the website further, for example embedding hyperlinks within the text and simplifying some of the grammar.
Usage statistics for the app and website
There were 498 individual logins recorded for the app, showing that the development panel accessed the software regularly during the testing period. All key features of the app were used. The website was accessed by the development panel on 70 occasions, with 687 web page views in total. The average login for each member of the development panel was four sessions of around 10 minutes’ duration. During this initial testing phase, a number of software issues and bugs were identified and several participants had difficulty logging in. This is normal and expected when beta-testing software.
Findings from the heuristic evaluation
A heuristic evaluation was undertaken by two independent technical experts. The aim of the evaluation was to identify strengths and limitations of the software and to highlight areas for further refinement. This involved applying and assessing set heuristic criteria to both the app and the website. The heuristic criteria were scored on a scale of 1–5 (1, very poor; 5, excellent).
Overall, the findings of the heuristic evaluation were positive. The full heuristic report is presented in Appendix 3. The majority of criteria for the website (71%; n = 35 of 49 criteria) and the app (71%; n = 24 of 34 criteria) were assessed as either ‘good’ or ‘excellent’. Eleven issues were identified as needing improvement. Most of these were minor, for example slowing down the images on the website homepage, and clarifying the goal template headings in the app. Two issues with the app were rated as ‘poor’ and related to a lack of a clear method of returning to (1) the main navigation menu and (2) the main dashboard. All issues highlighted by the heuristic evaluation were addressed by the study team and the software company.
Findings from the Usefulness, Satisfaction, and Ease of Use questionnaire
During the final focus group, participants were asked to complete the Usefulness, Satisfaction, and Ease of Use (USE) questionnaire. 86 This explored the acceptability of the software and also allowed the study team to assess the feasibility of using this questionnaire as a process measure in the trial. Overall, the questionnaire was quick and simple to complete and it was identified as useful for stage 2. Participants responded to 30 individual statements on a scale of 1 (strongly disagree) to 7 (strongly agree). The results are presented in Appendix 5. Despite the app being a prototype, all of the mean responses (with the exception of question 29) had a score of ≥ 4 [i.e. all mean participant responses were greater than or equal to a score of 4 (neutral)]. However, it should be noted that in this initial test run some of the USE questions were difficult to answer as participants did not have access to the software over a longer period of time to be able to assess items such as ‘the software helps me be more effective’. In addition, some participants had access to the software for less than 1 week (owing to difficulties with the login process caused by third-party software), which affected their ability to answer all of the USE questions, as some were not applicable because they referred to longer-term use. The USE questionnaire would therefore benefit from a ‘not applicable’ response option.
The HelpMeDoIt! intervention content
The findings from stage 1 informed the resulting intervention. HelpMeDoIt! was delivered via smartphone app and website. The list of app and website features, and how they map to individual components of the logic model, is presented in Appendix 6. Social support was the unique aspect of this intervention. The core element involved participants nominating one or more ‘helpers’ from their social network (friends, family or colleagues). Participants could nominate one or more people to be an official helper. There was no limit to the number of the helpers they could nominate; however, the website suggested one to five helpers as a manageable number. They were not restricted to choosing helpers from the UK.
The app and website had different functions that complemented each other; therefore, participants and their nominated helpers were encouraged to make use of both the app and the website. This combined approach was agreed with user representatives during our initial intervention development phase. Substantial amounts of text or content on apps were identified as a barrier to engagement. Users from our development phase highlighted the preference for a separate website that contained more detailed information. The website was designed to be accessible and viewable from both desktop computers and smartphone devices. Example screenshots of our app and website content are available online. 73
The HelpMeDoIt! website
The website presented evidence-based information for participants on healthy eating, physical activity and weight loss, and guidance on how to select and/or be a good helper.
Participant information included:
-
guidance on how to use the app to set SMART goals and monitor progress (tracking goals achieved and recording weight) and how to identify appropriate helpers using helpful hints to evaluate the support around them
-
evidence-based information on healthy eating (e.g. daily portions of fruit and vegetables, reading food labels), physical activity (current UK guidelines) and behavioural strategies to support weight loss (e.g. regular sleep pattern)
-
‘top tips’ for weight loss (based on the key points of the evidence-based information, e.g. ‘add volume to your meal with liquid or fibre)
-
‘helpful links’ to other relevant pages [e.g. NHS Eat Well (www.nhs.uk/live-well/eat-well/; formerly NHS Food Mixer) for healthy recipe ideas].
Helper information aimed to provide helpers with the guidance needed to be an effective helper for the participant who was trying to lose weight. This information included:
-
tips on how to be a good helper (e.g. ‘be a cheerleader not a coach’)
-
methods of positive feedback and encouragement to the participant (e.g. the option to send animated smiles or send a well-done text message when their friend completed a goal)
-
examples of non-food rewards to help motivate the participant [e.g. new music for their friend’s iPod (Apple Inc., Cupertino, CA, USA)]
-
examples of dialogue and motivational language to support the participant (e.g. helpful phrases for helpers to use when their friend had experienced a difficult week)
-
Helpers could interact with participants over the telephone, in person, by sending a text message or by sending ‘smiles’ via the app.
The HelpMeDoIt! app
The app focused on the three key elements of the intervention: social support, goal-setting and self-monitoring.
The participant version of the app included the following features.
-
Goal-setting: participants were encouraged to set goals for healthy eating, physical activity and other lifestyle factors, such as sleep. There was no maximum goal limit; however, participants were advised that five or more goals could be difficult to manage. They could either choose predefined template goals or write their own custom goals. Custom goal-setting was a two-step process that encouraged participants to action plan and problem-solve as they set their goals. This involved setting a short title for each custom goal, followed by adding SMART goal detail; for example, ‘stand up more’ – watching evening television (TV) on Monday and Wednesday I will stand up each time there is an advert break’.
-
Monitor progress: participants could update the app to either log their most recent weight or report when a goal had been achieved. Personal progress was presented over several graphs, including one that showed their change in weight over the past month and also their change in weight since they started using the app; a figure showing their most recent weight; and a list of all set goals, each with a ‘% completed’ bar.
-
Nominate helpers: participants could enter the contact details of one or more individuals from their social network that they wanted to invite to be a helper. Nominated helpers received an invitation by e-mail. Participants could also use this feature of the app to remove a helper, for example if the helper was not supportive.
-
Helper interaction: the app provided several ways to interact with helpers. These included sending animated smiles (e.g. ‘Great help this week’), sending text messages and making telephone calls.
The helper version of the app included the following features:
-
display of the participant’s goals, where they were able to view new, completed and missed goals
-
display of the participant’s progress for weight and goals completed
-
methods of giving positive feedback and encouragement to the participant, for example sending animated smiles (e.g. ‘Keep up the good work’), sending text messages and making telephone calls.
An element of ‘gamification’ was used within the app to encourage frequent use and to support the ongoing engagement of both participants and helpers. This involved both participants and helpers receiving points for (1) regularly inputting progress data, (2) interacting with each other and (3) achieving goals. Once participants and/or helpers had accumulated a certain number of points, they were awarded virtual medals (i.e. bronze, silver or gold) or a trophy. Ongoing engagement was also supported through the use of (1) push and e-mail notifications (e.g. informative messages, progress summaries and notifications of new badges); (2) daily motivating messages (e.g. ‘Doing well? Think about how you can progress one of your goals this week’); and (3) weekly reminders for uncompleted goals. Helpers were sent (1) daily messages (e.g. ‘A kind word can do wonders for motivation’) and (2) regular prompts via push and e-mail notifications to remind them to provide encouragement, celebration or further support (e.g. ‘Your friend hasn’t set any goals recently. Get in touch to find out how you can help them’).
Overall, the guidance given to participants and their helpers regarding how to establish social support for weight loss was not prescriptive or structured. Participants and their helpers were encouraged to use strategies that worked best for them, and as part of this feasibility study we were interested to find out what the range of approaches were. Participants and their helpers were encouraged to interact with each other either via or outside the app and examples of how they could do this were given in both the app and the website.
Progression criteria from intervention development (stage 1) to feasibility trial (stage 2)
The HelpMeDoIt! study was overseen by an independent Trial Steering Committee. To progress to the stage 2 feasibility RCT, the intervention needed to demonstrate successful achievement of the stage 1 progression criteria, which the Trial Steering Committee had previously approved. The progression criteria are listed in Table 7, along with key associated findings. The results of stage 1 were discussed with the Trial Steering Committee, which agreed that the progression criteria had been met and approved progression to the stage 2 feasibility study.
| Criterion 1: development of the intervention | |
|---|---|
| (a) Was the software developed to a good standard in the timescale available? | Yes |
|
|
| (b) Did the software company produce the intervention as specified in the detailed design document? | Yes |
|
|
| (c) Did the software include the appropriate intervention elements to facilitate social support and behaviour change? | Yes |
|
|
| Criterion 2: implementation of the intervention | |
| (a) Was it feasible to implement the HelpMeDoIt! intervention via the web-based platform, app and text? | Yes |
|
|
| (b) If there were issues with the app, the website or other technical problems were the company responsive and able to provide solutions to any issues? | Yes |
|
|
| Criterion 3: acceptability of the intervention | |
| Was the intervention acceptable and did the majority of the development group members find the intervention usable and acceptable? | Yes |
|
|
Stage 1 conclusions
This rigorous multimethod approach facilitated the development of an intervention that was developed with input from the target audience. A comprehensive programme theory was developed, incorporating behaviour change techniques and relevant theory, and addressing multiple contextual factors. Stage 1 progressed well and resulted in an app and a website that were both feasible and acceptable to participants and their helpers. All stage 1 progression criteria were achieved and no significant threats or weaknesses were identified.
Chapter 3 Stage 2 methods
An adapted version of the following methods was published open access in Matthews et al. 73 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The development of the HelpMeDoIt! website and app (stage 1) has been described in Chapter 2, as have the methods and findings. This chapter describes the methods for the feasibility RCT (stage 2). The study protocol can be found online (see Report Supplementary Material 1). Amendments to the original protocol are presented in Appendix 7. The following description of the methods adheres to the TIDieR (Template for Intervention Description and Replication) guidelines. 89
Study design and setting
HelpMeDoIt! was a feasibility RCT conducted with adults with obesity living in Greater Glasgow and Clyde Health Board area of Scotland (April 2016–February 2018).
Participants
Participants were eligible for the trial if they met all of the following inclusion criteria and none of the following exclusion criteria. All queries about eligibility were directed to the HelpMeDoIt! trial manager, and discussed among the study team as needed, before randomisation took place.
The inclusion criteria were:
-
being an adult aged 18–70 years
-
having a BMI of ≥ 30 kg/m2
-
trying to lose weight
-
having access to a smartphone and the internet.
The exclusion criteria were:
-
having a terminal illness
-
having had previous bariatric surgery
-
living with dementia
-
being pregnant
-
having poor competence in English (resulting in inability to complete study materials)
-
having contraindications to physical activity
-
having previously been a participant in stage 1 intervention development
-
already being a nominated helper in the trial.
Potential participants were briefly screened by the trial manager over the telephone or by e-mail. Any individual who did not meet the initial criteria for age and BMI (e.g. they had a BMI of 27 kg/m2) was thanked for their interest and directed to other publicly available, evidence-based resources for weight loss. The contact details of individuals who met these initial criteria were passed to a field worker, who then liaised with the participant for the remainder of the eligibility checking process and follow-on steps.
Contraindications to physical activity were assessed using an adapted Physical Activity Readiness Questionnaire. 90 Anyone with a medical condition or taking medication or who thought they may have a contraindication to physical activity was advised to check with their GP before commencing any physical activity. We asked women of childbearing age to let the study team know if they became pregnant at any point during the trial. Women already recruited were not excluded from the study if they became pregnant, as the intervention could still help them make healthy lifestyle choices. They were given a leaflet on diet and safe physical activity during pregnancy. In a future trial, the analysis would be intention to treat and we would not exclude women who become pregnant.
Sample size
This was a feasibility study, and the main focus was to assess the acceptability of the intervention and the feasibility of the evaluation methods and to estimate parameters for a larger study. We intended to recruit 120 participants. As we were most interested in the acceptability of the intervention, we recruited using a 2 : 1 ratio, with 80 participants in the intervention group and 40 participants in the control group. We expected a dropout rate of 30%. This final sample size of 84 for analysis was not powered to detect differences between groups for the proposed effectiveness outcomes (BMI, physical activity and diet) but it allowed an estimation of any feasibility proportion (e.g. proportions retained/found the study acceptable/provided outcome data) across the whole sample with a 95% confidence interval (CI) of plus or minus 11 percentage points. This would also allow for the estimation of the mean of a continuous outcome (such as BMI) in the intervention arm with a 95% CI of 0.262 of a standard deviation.
Recruitment and retention
A multipoint recruitment strategy was employed to target a broad range of participants (e.g. age, gender, socioeconomic status). This primarily involved recruiting via (1) primary care, (2) online sources and (3) community sources.
-
Primary care recruitment: we collaborated with the Scottish Primary Care Research Network (SPCRN) to recruit participants. The SPCRN staff liaised with GP practices and searched patient databases for potentially eligible participants based on the inclusion/exclusion criteria. Practice staff excluded vulnerable patients based on other known information, for example having dementia or receiving social work input for drug dependency. The SPCRN posted the recruitment pack to the agreed list of patients. The recruitment pack included (1) a GP cover letter informing patients that they had been identified as eligible for this study, (2) a study information sheet, (3) a contact details form and (4) a prepaid envelope. After reading the information, individuals who were interested in taking part were asked to complete the contact details form and return it to the study team using the prepaid envelope.
-
Online recruitment: regular adverts were placed on the Glasgow hub of Gumtree (Gumtree.com Limited, London, UK; www.gumtree.com) (a free online community advertising website). The advert was brief, highlighting the key points of the study and the eligibility criteria, and directing interested individuals to contact the trial manager for full details. We also established a HelpMeDoIt! Facebook page and Twitter account for posting up-to-date information and we advertised on online forums, for example new-mother groups and local weight loss groups. People were encouraged to express their interest to the study team.
-
Community recruitment: we advertised in the local press and through slimming clubs, weight management clinics and exercise-on-referral services, and by placing study posters in multiple community locations. In addition to the strategies already mentioned, we had planned to target men through barbershops and football grounds, as recruiting men into weight loss trials is known to be challenging, but owing to resource restrictions we were unable do this. 91
All individuals who expressed an interest in the study received a participant information sheet (see Report Supplementary Material 2) and had at least 1 week to consider taking part. After individuals were screened for initial eligibility by the trial manager, a trained field worker contacted them by telephone to check their full eligibility and to arrange a face-to-face appointment for baseline data collection. Prior to any data being collected, participants had the opportunity to ask questions before signing an informed consent form (see Report Supplementary Material 3). Field workers met with participants at a place of their choice, which included their home (in which case our lone-working policy was followed) or a room at our research unit. All field workers were trained in study procedures, had undertaken recent training in good clinical practice,92 and held NHS Research Passports allowing them to liaise with participants who were recruited via primary care.
A key aspect of the HelpMeDoIt! intervention was the recruitment of ‘helpers’. A helper was an individual whom participants nominated as someone they thought could support them with their weight loss goals. If an individual agreed to be a helper, they were directed to a web link via which they were able to access an information sheet about the study (see Report Supplementary Material 4) and provide informed consent using an online form (see Report Supplementary Material 5). This indicated their consent to be a helper and for the study team to keep their contact details (for the purposes described below), and to signify whether they were willing to be contacted with regard to completing an interview at a later date (for which they would be given separate information and give separate consent). Contact details for the study team were available via the web link and information sheet so that helpers could call or e-mail if they had any queries or needed further information. After providing consent to be a helper, they were asked to enter brief demographic and contact details. We asked for their postal address, mobile phone number and e-mail address (where available); this information was required so that we could give them updates on participants’ progress and send them reminders as well as voucher payment for interviews. The demographic data were used to describe the characteristics of the helpers and to sample them for the qualitative interviews according to gender, age and relationship with participant.
We developed a retention strategy to optimise the number of participants with data at follow-up. This included offering flexibility regarding where data collection took place; sending newsletters and birthday cards; obtaining mobile numbers and alternative contact details; offering a reduced data collection (‘minimum data set’) to participants who were reluctant to complete the full follow-up; and giving £20 voucher payments as a thank you for each point of data collection.
Randomisation
We were most interested in exploring the feasibility of the intervention and so randomised participants in a 2 : 1 ratio into intervention and control groups. Participants were allocated using a mixed randomisation/minimisation algorithm to ensure balance with respect to gender and BMI (< 40 and ≥ 40 kg/m2). In blocks of 15 participants, 12 were assigned according to the minimisation algorithm (designed to maintain as close to a 2 : 1 allocation ratio within strata defined by each minimisation factor) and three were allocated (in a 2 : 1 ratio) at random. The minimisation/randomisation schedule (the order in which participants were allocated by minimisation or randomisation) was prepared by a statistician in the Robertson Centre for Biostatistics (University of Glasgow) using the method of randomised permuted blocks. This statistician did not carry out the final analysis for the study. Participants were remotely allocated by field workers using an automated telephone service operational 24 hours per day. Allocation was undertaken in the presence of the participant after they had completed the relevant baseline data collection procedures. On group allocation, participants were allocated a unique randomisation number.
The intervention group
Participants in the intervention group received access to the HelpMeDoIt! smartphone app and website for 12 months. The app and website content has been described in detail in Chapter 2. Participants were advised that they could continue to access other sources of lifestyle change/support external to the app, such as attending weight loss groups and fitness classes.
Exploring the feasibility of participants also acting as helpers
The HelpMeDoIt! study aimed to explore how the intervention might work in a real-world setting. Because the intervention had a social support focus, it was possible that two or more friends/relatives would wish to lose weight together and support each other. It was unknown if participants would choose to act as helpers, but it was important to allow for and explore this for several reasons, including the following: (1) this approach may have potential benefits for participants as a result of increased support and motivation; (2) participants who also act as helpers might have more beneficial outcomes than participants who do not act as helpers; and (3) it would allow the identification of a spillover effect in line with the diffusion of innovation theory. 93 Our study therefore allowed participants in the intervention group to act as helpers for a friend or relative. Their helper would then also have access to the participant aspect of the intervention (i.e. so that they could be both participants and helpers to each other). Participants in the control group could not act as helpers as this would enable them to view the intervention content. In addition, individuals who were already helpers for someone else could not sign up as a participant as they might have been randomised to the control group and therefore would have already seen the intervention content.
The control group
The control group received leaflets about the health benefits associated with healthy eating and physical activity behaviour change (see Report Supplementary Material 6 and 7). They did not receive any prompted advice on social support or personalised content. They were not restricted in any way regarding their involvement in other weight loss activities, for example joining a slimming club. We collected data on this as part of the process evaluation. Control participants were offered access to the website and app after follow-up was complete at 12 months.
Progression criteria from feasibility to full trial
The feasibility of the evaluation methods, the feasibility and acceptability of the intervention, and the intervention’s potential to be further developed and delivered in a fully powered RCT were the key questions addressed by this study. Feasibility was assessed using the progression criteria outlined in Table 8. These criteria were finalised within the Trial Management Group and approved by the Trial Steering Committee at the end of stage 1, prior to beginning stage 2. There was substantial debate around criterion 5. On the one hand, current research on app use indicates that around 21% of users engage with an app only once. 94 However, if only a minority of participants engage with the app and it is effective for them, then it may have a cost-effective and worthwhile impact on public health when rolled out across the population. On the other hand, we wanted to see a reasonable proportion of participants engaging with the app sufficiently to set goals and identify helpers, even if the subsequent interactions with their helpers were not made via the app. The cut-off point of visiting the app at least twice was chosen as we felt that, with this level of engagement, participants could have exposure to the key intervention components, in particular the idea of goal-setting, monitoring and recruiting helpers to aid in weight loss goals, and that this level of exposure may be enough to kick start the process of behaviour change. 95
| Progression criterion | Method of assessment |
|---|---|
| 1. Are appropriate and effective routes of recruitment available to achieve a powered sample size in a full trial? | Coming close to the sample size, as judged by the TSC, with reasonable expectations of being able to address any recruitment issues |
| 2. Are participants willing to be randomised to the intervention? |
Recruitment experiences of the study team and field workers Insight from qualitative interviews with participants |
| 3. Are appropriate retention rates achieved at 12-month follow-up? | Measured using the following scale in both the intervention and the control group at 12 months: if ≥ 70% are followed up, proceed; if 50–69% are followed up, discuss with TSC; if ≤ 49% are followed up, do not proceed |
| 4. Is the intervention feasible to deliver and acceptable to participants and their helpers? |
|
| 5. Do the majority (> 50%) of participants within the intervention group visit the app at least twice OR do 25% of participants randomised use it three or more times? |
|
| 6. Are identified barriers and challenges to implementation of the intervention planned for and surmountable? |
|
| 7. Do the data collection procedures effectively collect the data required for a full trial? – Successful completion of at least one data collection outcome measure (BMI, physical activity or healthy eating) at both baseline and at 12 months in those retained measured using the following scale |
|
| 8. Are the intervention costs of a full trial covered? |
|
The results of the study are reported in Chapters 4–6 and were used to assess whether or not the progression criteria had been achieved. Final assessment of the study results against the progression criteria was completed by the Trial Steering Committee.
Feasibility measures and exploratory outcomes
All feasibility measures and exploratory outcomes are outlined in Table 9. These were collected using a case report form (CRF) and questionnaire completed face to face with a study researcher in the participant’s home or an interview room in the university (with the exception of one measure collected over the telephone; see Table 9). Data were collected using hard-copy documentation (see Report Supplementary Material 8 and 9).
| Measure | Method of measurement | Time point | Findings presented in |
|---|---|---|---|
| Demographics | |||
| Case report form: gender, age, socioeconomic status, employment and education status, current weight loss status, current health status, current computer and phone use | Baseline and 12 months | Chapters 4 and 6 | |
| Feasibility measures (reflecting progression criteria) | |||
| Recruitment |
Sample size and rate of recruitment Sources of recruitment |
Post baseline | Chapters 4 and 6 (assessed by progression criterion 1) |
| Randomisation | Interviews with participants and insight from study team | 6 months | Chapters 4 and 5 (assessed by progression criterion 2) |
| Retention | Retention rates for data collection at 12-month follow-up | 12 months | Chapters 4–6 (assessed by progression criterion 3) |
| Feasibility of app/website (intervention) |
Interviews with participants Interviews with helpers App and website use statistics USE29 questionnaire |
6 and 12 months 12 months 12 months 12 months |
Chapters 5 and 6 (assessed by progression criteria 4–6) |
| Data collection | Rates of completion for different measures | Baseline and 12 months | Chapters 4 and 5 (assessed by progression criterion 7) |
| Exploratory primary outcomes | |||
| BMI (kg/m2) | Physical measurement of height (m) and weight (kg) | Baseline and 12 months | Chapter 4 |
| Diet |
DINE questionnaire96 (via telephone) 4 days of 24-hour dietary recall97 |
Baseline and 12 months | Chapter 4 |
| Physical activity |
7-day accelerometry98 7-day Physical Activity Recall Questionnaire99 |
Baseline and 12 months | Chapter 4 |
| Secondary outcomes | |||
| Anthropometric changes | Waist and hip circumference (cm) | Baseline and 12 months | Chapter 4 |
| Health-related quality of life |
EQ-5D-3L questionnaire100 ICECAP-A scale101 |
Baseline and 12 months | Chapter 4 |
| Mental health | General Health Questionnaire – 12 items102 | Baseline and 12 months | Chapter 4 |
| NHS resource use and participant-borne costs | Specially designed resource use questionnaire | Baseline and 12 months | Chapter 4 |
| Social support | Exercise and Eating Habits Social Support Scales103 | Baseline and 12 months | Chapter 4 |
| Self-efficacy | Weight104 and Exercise Efficacy Lifestyle Scales105,106 | Baseline and 12 months | Chapter 4 |
| Motivation | Treatment Self-Regulation Questionnaire107 | Baseline and 12 months | Chapter 4 |
| Smoking use | HSI108 | 12-months | Chapter 4 |
| Alcohol use | Alcohol Use Disorders Identification Test109 | 12-months | Chapter 4 |
Feasibility measures
Feasibility and acceptability of the HelpMeDoIt! intervention and study methods was the key focus of this trial. These relate to the overall progression criteria (see Table 8) and are summarised in Table 9. The majority of these measures will be discussed further in the qualitative and process evaluation methods sections below.
Exploratory primary outcomes
We explored the feasibility of assessing multiple outcome measures, including potential primary outcomes for a future trial. We collected data in relation to three outcomes that could be used as the primary outcome: BMI, physical activity and diet (see Table 9). We explored which of these was the most feasible by assessing acceptability and data completeness. BMI was expected to be the most appropriate measure because it is objective, cheap to measure and more accurately measured than diet and physical activity, and has higher response rates. As measuring diet110 and physical activity111 in community-based trials is challenging, we assessed two ways of measuring these outcomes. Each outcome was measured at baseline and 12 months. Twelve months was chosen as the primary outcome point for the feasibility trial, which would be the same for any future effectiveness trial. This longer-term follow-up is important as, although there may be some benefits of short-term weight loss, weight loss maintenance is key to longer-term health benefits and cost savings to the NHS and society. 112
Body mass index (kg/m2) was calculated from measures of height and weight. Height was measured using a Seca Leicester Height Measuring Stadiometer (Seca GmbH & Co., Hamburg, Germany), with the participant facing forward, wearing no shoes and with their head in the Frankfort plane (parallel to the floor). Height was recorded once, in centimetres, to one decimal point. Weight was measured, without shoes on, using Tanita HD 352 High Capacity Low Profile Electronic Weighing Scales (Tanita Europe BV, Amsterdam, the Netherlands). Scales were calibrated before first use. Weight was recorded once, in kilograms, to one decimal point.
Physical activity was measured using ActiGraph GT3X (ActiGraph, LLC, Pensacola, FL, USA) accelerometers, objective activity monitors that measure the duration, intensity and frequency of physical activity. Participants were asked to wear the accelerometer on their right hip for 7 days during waking hours (except when swimming or bathing). Participants received their accelerometer during a face-to-face visit; this enabled the researcher to demonstrate the correct placement of the device. Data were collected in 1-second epochs at a sample rate of 100 Hz, and converted to 15-second epochs for analysis using ActiLife 6 software (ActiGraph, LLC, Pensacola, FL, USA). 113 Non-wear time was identified by > 60 minutes of continuous 0 counts and removed before analysis. Data were included for analysis when the accelerometer had been worn for a minimum of 4 days, and with a minimum wear time of 10 hours per day. Freedson cut-off points98 were used to determine the amount of time spent sedentary and in moderate to vigorous physical activity. The 7-day Physical Activity Recall questionnaire114 was used to measure physical activity by self-report. Participants, guided by the researcher, reported their activity over the previous 7 days in relation to moderate, hard and very hard exercise. This measure has been validated for use in adult populations,99 and researchers adhered to the protocol published by Sallis et al. 114
Diet was measured with the Dietary Instrument for Nutrition Education (DINE) questionnaire,96 a validated seven-item questionnaire that explores the frequency of consumption of different food types, for example bread and rolls, cereals and meats. Field workers asked participants to report the frequency with which they ate specific foods. The frequencies were scored using DINE guidelines96 to produce an overall score for fat and fibre. Diet was also measured using repeat 24-hour dietary recall97 collected by a researcher over the telephone on 4 separate days within a 10-day period (including one weekend day). Participants self-reported their food intake, prompted by the researcher, for the previous 24 hours. Researchers were guided by photographic and textual examples of portion sizes, which they could use as prompts over the telephone. Participants’ food intake was entered into weighed intake software programme (WISP) dietary analysis software (version 4.0; Tinuviel Software, www.tinuvielsoftware.co.uk/wisp4.htm; accessed 1 May 2018)115 and analysed for energy intake, macronutrients and fibre. The 24-hour dietary recall measure was found to be a poor method of data collection at baseline and, therefore, it was not used at follow-up. Full details of this decision are provided in Chapter 6.
Secondary outcomes
Waist circumference was measured using a 2-metre flexible tape measure with a buckle around the mid-point between the iliac crest and the inferior margin of the lower rib. Hip circumference was measured around the widest point of the buttocks. Measurements were recorded twice in centimetres to one decimal point (e.g. 95.2 cm). A third measure was taken if the difference was > 0.5 cm.
Health-related quality of life was measured using the five-item EuroQol-5 Dimensions, three-level version (EQ-5D-3L), questionnaire and quality-of-life thermometer. 100 This measure is used frequently in health-related research to explore five dimensions: mobility, self-care, usual activities, pain and anxiety/depression. An additional measure of capability well-being was carried out using the ICEpop CAPability measure for Adults (ICECAP-A)101 scale. This is a new scale which, compared with the EQ-5D-3L, explores less clinically related changes in quality of life over four dimensions: feeling settled and secure, being independent, achievement and progress, and enjoyment and pleasure. This was considered an appropriate measure in our population owing to the potentially large range of participant characteristics. Mental health was measured using the General Health Questionnaire – 12 items (GHQ-12),102 a validated and frequently used 12-item self-report questionnaire. We gathered data on NHS resource use and participant-borne costs using a specially designed resource questionnaire. These data helped us establish key cost drivers of the intervention.
Questionnaires assessing potential mediators of change were used to explore their feasibility in a future trial. These included the Exercise and Eating Habits Social Support Scales (social support),103 the Weight104 and Exercise Efficacy Lifestyle Scales (self-efficacy)105,106 and the Treatment Self-Regulation Questionnaire (motivation). 107
At 12 months we administered the USE questionnaire86 to assess the usefulness, ease of use, ease of learning and satisfaction with the app and website. We also asked participants to complete the Heaviness of Smoking Index (HSI)108 and Alcohol Use Disorders Identification Test (AUDIT-C)109 questionnaires at 12 months, using this opportunity to assess the feasibility of additional questionnaires for data collection. These may be helpful in identifying other potential lifestyle changes made by participants in a future trial related to ‘spillover’ effects of the intervention.
Process evaluation
The process evaluation explored, in detail, the feasibility and acceptability of both the intervention and the study design. The process evaluation was conducted following the MRC guidelines for process evaluation of complex interventions116 and examined the following elements: (1) intervention-related findings on context, fidelity, exposure, reach, programme theory and logic model; and (2) study-related findings on recruitment, retention and contamination. Report Supplementary Material 10 illustrates the different domains of the process evaluation, as well as examples of key questions and the methods for addressing those questions. In brief, some quantitative data informed the process evaluation (e.g. intervention use statistics); the remaining process data were gathered from qualitative interviews with participants and helpers.
Quantitative process data
Web/app analytics
App and website use data were collected for both helpers and participants to assess engagement with the intervention. Key use data included the number of logins to the website and app by the helper and participant; the duration of logins; the average sessions per user; which web pages were viewed and how often; the number of goals set using the app; the frequency of weight updates; the number of helpers nominated; contacts between helpers and participants via the app; the number of views of ‘progress charts’ by participant and helper; and patterns of use over time. Demographic data on the helpers, including their relationship to the participant, were also included in the process evaluation.
Qualitative process data
Qualitative interviews with participants
We planned to interview up to 30 participants at 6 months and up to 20 participants at 12 months (dependent on data saturation). Participants were purposively sampled for a range of characteristics (e.g. level of app/website use, age, gender). We also specifically interviewed participants who did not take up the intervention to explore their reasons for this. Semistructured interview guides were used at both time points to explore participants’ insights into the acceptability of the outcome measures, the acceptability and usability of the app and website, patterns of use, the impact of the intervention on behaviour, the support received from helpers, and the barriers to use (see Report Supplementary Material 11). Interview schedules were guided by the HelpMeDoIt! programme theory and helped us explore potential mediators of change. All participants at baseline were guided to draw a sociogram (a diagrammatic representation of their social network). This was used as a prompt with interview participants to explore the potential sources of social support they had in their social network. This also informed a social network analysis, which was not part of the initial funding bid or timeline, and will be published at a later date.
Qualitative interviews with helpers
At 6 months we planned to interview up to 20 helpers, purposively sampled for a range of characteristics (e.g. level of app/website use, age, gender). A semistructured interview guide was used to explore helper insights related to acceptability; guidance provided for being a helper; types of support they provided to their friend; challenges of supporting their friend and/or using the app and website; and changes in their own health behaviour as a result of being a helper (see Report Supplementary Material 12).
All interviews were completed by trained researchers over the telephone or face to face in a meeting room in the university. Interviews were audio-recorded and transcribed verbatim. A separate informed consent process was undertaken for the qualitative interviews, whereby participants and helpers were sent a separate information sheet detailing what was expected of them during the interview. They were also sent a copy of the consent form, which they were asked to read. Prior to beginning the interview, the researcher checked if the participant had any queries and gained (1) verbal consent if over the telephone (audio-recorded) or (2) written consent if face to face.
Economic evaluation
The economic evaluation aimed to (1) identify and measure the key cost drivers of the intervention and control arms, including health, social care and societal resource use; and (2) identify suitable outcome measures and summarise mean costs to inform the design of an economic evaluation in a definitive trial. The following costs were collected at baseline and 12-month follow-up.
Intervention costs
Intervention costs were identified and measured for the development of the intervention. The cost of the design of the mobile application and maintenance for the purposes of the feasibility study are reported.
Health, social care and personal resource use
All resource use data were collected from participants with a specially designed resource use questionnaire (see Report Supplementary Material 8 and 9). This collected information on (1) primary care services provided in the NHS (e.g. GP visits, practical nurse, dietitian); (2) secondary care services provided in the NHS [e.g. accident and emergency (A&E) attendances, hospital stay, visit by consultant]; (3) and personal costs (e.g. household income spent on different food and drinks items, including groceries, alcohol, takeaway food, meals out and lifestyle activities). Medication use at baseline and follow-up was also recorded. Mean group costs were calculated by attaching the unit costs to frequency of resource use per group participant. Medians and ranges for resource use quantities and costs are reported.
Reference costs
Reference costs for items of resource use were identified from readily available UK reference sources including the Personal Social Services Research Unit reference cost book. 117
Health economics outcomes
The economic analysis assessed the feasibility of using the EQ-5D-3L instrument100 and the ICECAP-A101 instrument as a means of capturing any short-term effects on health-related quality of life or capability well-being. This involved exploring data completeness and response rates. Participant responses were converted to a utility score using the value set elicited from UK general population. The EQ-5D-3L is the preferred measure of health-related quality of life in adults by NICE technology appraisal. 118 The ICECAP-A is a complementary measure of capability well-being.
The economic evaluation adhered to guidelines for good economic evaluation practice as outlined by Gold et al. 119 Specific guidance was also sought from the NICE economic evaluation public health reference case120 as it was anticipated that this intervention was likely to have an impact on costs and outcomes beyond the NHS and Personal Social Services and thus require a broader public sector evaluative perspective.
Quantitative analysis
A statistical analysis plan (see Report Supplementary Material 13) was drafted by the Robertson Centre for Biostatistics, University of Glasgow, and reviewed by the Trial Management Group and Trial Steering Committee during the trial. It was finalised and approved by the principal investigator and trial statistician before the analyses commenced. All quantitative analyses were carried out using R1 for Microsoft Windows v3.2.2 or higher (Microsoft Corporation, Redmond, WA, USA). 121 The mice122 and interplot123 packages were also used. A summary of the analyses is as follows.
Baseline characteristics
These were summarised overall and by randomised group. Participant characteristics were summarised in relation to sociodemographic, lifestyle, occupational, health status and quality-of-life variables.
Feasibility measures
These were the primary focus of the analysis. Study-related data, including recruitment, randomisation and retention at 12-month follow-up, were reported overall and by randomised group, with 95% CIs. The association between baseline factors and follow-up was assessed using logistic regression, with follow-up (yes/no) as the response variable. Intervention-related data, including use of the intervention, was summarised for the intervention group, overall and in relation to selected baseline characteristics. The availability and utility of data relating to use of the app and website was explored, and a range of summary measures was presented in the final statistical outputs.
Exploratory outcomes
These were summarised overall and by randomised group, and compared using linear regression models, with randomised group, the baseline measurement of the outcome, age and gender as predictor variables. Regression models also adjusted for the minimisation factors. The residuals from each regression model were assessed for normality. When necessary, the outcome measure (at follow-up and at baseline) was transformed to improve model fit. All analyses were conducted under intention-to-treat principles and complete-case analysis used, unless > 20% of cases were lost as a result of missing data, in which case multiple imputation was also performed. These analyses were exploratory and underpowered, so no formal hypothesis testing was performed. P-values are presented for descriptive purposes as a guide to the interpretation of the magnitude of reported associations. Effect sizes were reported in line with CONSORT guidelines for reporting feasibility and pilot studies. 124
Process evaluation measures
These were descriptively analysed to summarise use of the app and website. A per-protocol analysis was conducted using simple proxies for adherence (e.g. website login) to explore the treatment effect associated with adherence.
Health economics cost data
These were analysed as follows. Resource use data were summarised and described using mean values and variation around these estimates. Key fixed and variable costs of developing the intervention were described and summarised. EQ-5D-3L and ICECAP-A outcome data were reported by within-attribute response rates, mean values and associated variance. Within-trial economic analyses were performed using Stata® 12.0 (StataCorp, College Station, TX, USA).
Qualitative analysis
Qualitative data analysis explored the feasibility and acceptability of the intervention, the extent to which participants and helpers engaged with it, the perceptions of how the intervention influenced behaviour, the value of helpers’ support, and contextual factors. Qualitative data were analysed by two researchers who independently coded using an adapted version of Braun and Clark’s125 approach to thematic analysis. Twenty per cent of the interviews were double-coded by two researchers, who resolved disagreements by discussion. The resultant coding framework was discussed between the researchers and also within the larger study team to finalise the themes and subthemes. The results of the qualitative analyses were combined with intervention use data to explore and refine the HelpMeDoIt! programme theory. The aim of analysing the programme theory in this way was to better understand the mechanisms and key contextual factors to consider when refining the intervention and evaluation design. A refined version of the programme theory and updated logic model can be found in Chapter 6. Qualitative analyses were supported by NVivo 10 (QSR International, Warrington, UK).
Withdrawal of participants
Participants had the right to withdraw consent to participate in any aspect of the HelpMeDoIt! study at any time. Participants had three options for withdrawing from the study: (1) withdrawal from the study intervention, (2) withdrawal from study follow-up or (3) withdrawal from the entire study and removal of their data from analysis. A participant withdrawal form was completed by the participant, field worker or trial manager, noting the withdrawal option and also the reason for withdrawal (if given).
Data management
A data management plan was developed to ensure safe and accurate data management. All study data were gathered by trained researchers using hard-copy paper questionnaires and stored in a locked filing cabinet in our secure research unit. Hard-copy data were anonymised using participant study ID. Data were entered by approved study personnel into a secure online database using a unique participant ID, so that study personnel remained blinded to group allocation. Appropriate elements of the database had automated error-checking facilities to ensure that only valid data were entered. We performed single data entry, 10% of which was cross-checked by double entry. Full double data entry would have been undertaken had a > 5% error rate been detected. Our error rate was 2% and so additional data entry verification was not performed. Audio-recordings were stored on a password-protected server. Files were then shared for transcription via a secure password-protected online cloud, where files were available for only 24 hours. Identifiable information was removed from the transcripts of the qualitative data.
All data will be kept for 10 years in line with University of Glasgow Research Governance Framework Regulations for clinical research. These data will be stored confidentially on password-protected servers. The final data set was accessed only by approved members of staff from the research team and Robertson Centre for Biostatistics, University of Glasgow. Approved members of the software company, who had signed a data protection agreement, had access to limited participant contact details to enable them to effectively manage software errors. The low-risk nature of this study meant that a Data Monitoring and Ethics Committee (DMEC) was not required. Our Trial Steering Committee covered the functions of the DMEC, particularly in relation to ethical issues, patient safety and continuation of the trial.
Assessment of harms
The intervention was low risk to participants. Participants were advised to discuss any health concerns with their GP. We encouraged field workers, participants and helpers to report negative outcomes or experiences to the study team. The issue of ‘harm’ was also explored in the interviews. We developed a standardised operating procedure for dealing with adverse events should these be reported.
Ethics approval
Ethics approval for stage 1 (see Chapter 2) was granted by the University of Glasgow Medical, Veterinary and Life Sciences College Ethics Committee (reference 200140108). Ethics approval for stage 2 was granted by the NHS West of Scotland Research Ethics Committee (reference 15/WS/0288) (see Report Supplementary Material 14). Research governance approval was given by NHS Greater Glasgow and Clyde Health Board.
Patient and public involvement
Patient and public involvement (PPI) was central to all aspects of the HelpMeDoIt! study, including the design and management of the research and the development of participant information resources, as well as contributing to the reporting and dissemination of the research findings.
Patient and public involvement informed the planning stage and preparation of the grant application. Patient representatives who had been involved in other behaviour change trials provided insights related to feasibility, outcomes, content and target population. They reported that this type of intervention had the potential to overcome some issues faced in other studies, for example cost and time to attend intervention groups and other family members or friends undermining behaviour change efforts. They felt that some questionnaires used to collect physical activity and diet data were burdensome and that testing out different measures in this study would be useful. They also felt that it would be important to explore engagement and motivation in the longer term.
Once the study commenced, one PPI member, Selin Campbell, was recruited to join our Trial Management Group and attended monthly meetings. Selin was an active contributor and provided valuable input into the ongoing management of the study and the development of participant information resources. She also helped with piloting the interview schedule, and provided ongoing feedback related to the intervention development and delivery, evaluation methods and interpretation of data. Selin also provided feedback on the interim report of the stage 1 findings and helped the Trial Management Group finalise the HelpMeDoIt! dissemination strategy.
We also had one active PPI member, Kenneth Wallace, on our Trial Steering Committee. Kenneth helped finalise and approve the progression criteria and contributed to assessment of both sets of criteria, namely from stage 1 to stage 2, and from stage 2 to a full trial. He was involved in the ongoing governance and oversight of the study, as well as providing feedback on the interim report of stage 1 findings. He also provided helpful recommendations on how to improve the HelpMeDoIt! app and website for a future trial.
Presentation of the findings
Although feasibility and acceptability in relation to the progression criteria was the focus of the feasibility trial, the remainder of the report presents the findings, beginning with the standard quantitative outcomes and economic analysis results (see Chapter 4), followed by the qualitative results (see Chapter 5), and the process evaluation results (see Chapter 6). In the final discussion chapter (see Chapter 7), the findings are integrated and considered in relation to the overall progression criteria and the research questions.
Chapter 4 Results
Part 1: stage 2 outcome results
The key feasibility outcomes are reported in this chapter as well as in Chapters 5 and 6. In this section, we describe the recruitment rates and retention in the trial (progression criteria 1–3), as well as the characteristics of participants. The quantitative analyses relating to the exploratory primary outcomes and secondary outcomes are presented, followed by the health economic analyses. Key data are provided in this chapter, with the full statistical outputs presented in Appendix 8.
Recruitment
One hundred and eighty-eight individuals were screened for inclusion in the study, of whom 156 were identified as eligible. A total of 109 participants (70% of those eligible) proceeded to be randomised between 22 April 2016 and 22 October 2016 (Figure 5). This was slightly short of the target of 120 participants randomised. Of the 109 participants, 73 participants were allocated to the intervention group and 36 participants were allocated to the control group. Figure 6 shows the cumulative numbers randomised over time during this period. Although initially a slow start, the recruitment rate continued in line with or quicker than target, which is positive sign for a future trial. No individual signed up as both a participant and a helper.
FIGURE 5.
The CONSORT flow diagram for the HelpMeDoIt! study.
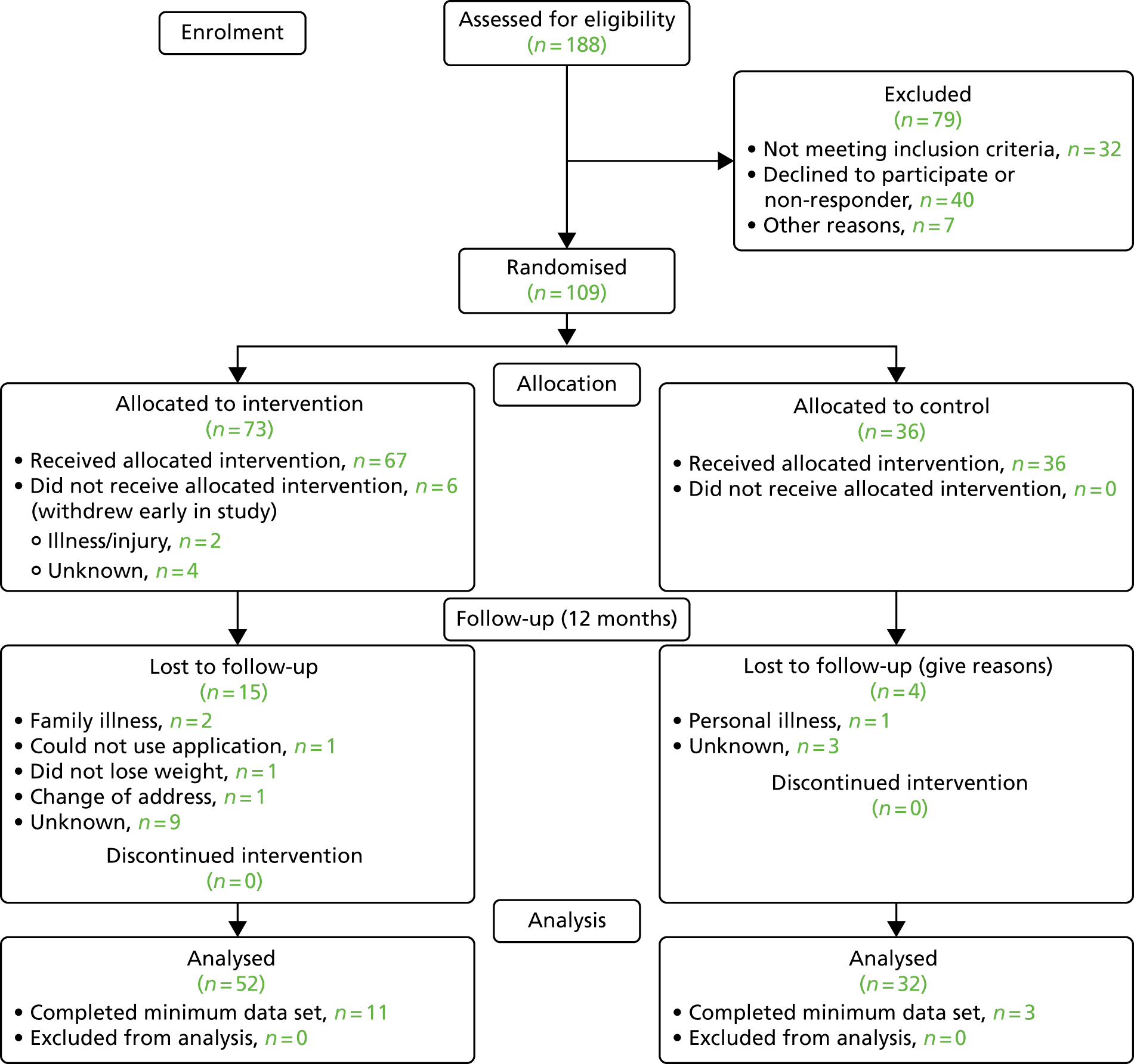
FIGURE 6.
Recruitment rate in comparison with target rate (dashed line) over 6 months.
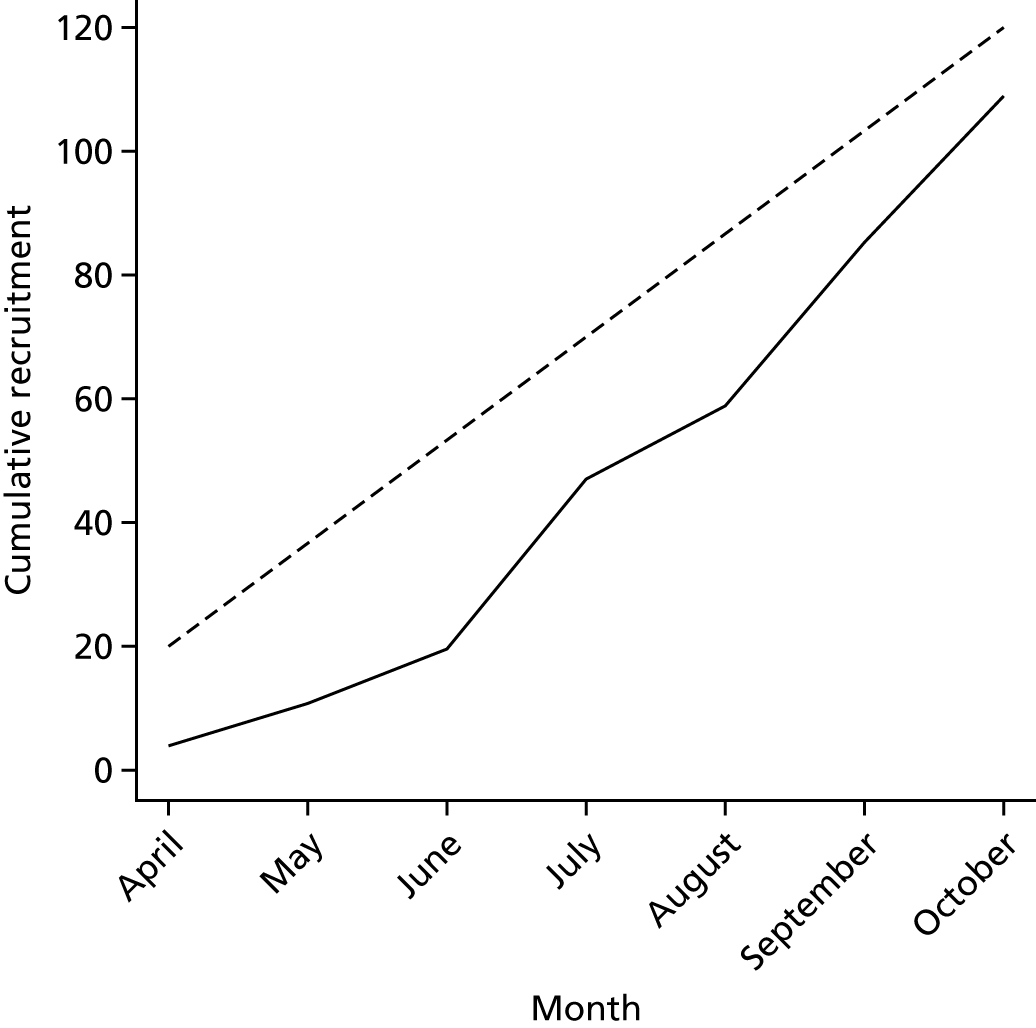
Baseline characteristics
Key baseline characteristics of the randomised population are reported in Tables 10–12 (see Appendix 8, Tables 49–65, for additional baseline summaries). Overall, more women (69.7%, n = 76) than men were recruited, and the average age was 47 years [standard deviation (SD) 10.7 years]. The average BMI was 37.6 kg/m2 (SD 5.9 kg/m2) and just over one-quarter were currently attending a weight loss group. We recruited across the spectrum of levels of deprivation, with over one-third being from the highest quintile of socioeconomic deprivation. Most participants were employed and the majority were married. Over 60% had received higher education. Participants’ daily moderate to vigorous activity was a mean of 45 minutes per day (SD 32.9 minutes per day).
| Characteristic | All, n (%) (N = 109) | Intervention, n (%) (N = 73) | Control, n (%) (N = 36) |
|---|---|---|---|
| Participant age (years), mean (SD) | 47.3 (10.7) | 46.2 (10.6) | 49.4 (10.7) |
| Participant sex | |||
| Female | 76 (69.7) | 49 (67.1) | 27 (75.0) |
| Male | 33 (30.3) | 24 (32.9) | 9 (25.0) |
| SIMD quintile | |||
| 1: most deprived | 36 (36.4) | 25 (37.9) | 11 (33.3) |
| 2 | 21 (21.2) | 15 (22.7) | 6 (18.2) |
| 3 | 13 (13.1) | 7 (10.6) | 6 (18.2) |
| 4 | 16 (16.2) | 10 (15.2) | 6 (18.2) |
| 5: least deprived | 13 (13.1) | 9 (13.6) | 4 (12.1) |
| Marital statusa | |||
| Living with partner | 61 (59.2) | 41 (60.3) | 20 (57.1) |
| Single | 42 (40.8) | 27 (39.7) | 15 (42.9) |
| Ethnicity | |||
| White British/Irish | 91 (84.3) | 57 (79.2) | 34 (94.4) |
| White Other | 6 (5.6) | 5 (6.9) | 1 (2.8) |
| Indian | 2 (1.9) | 1 (1.4) | 1 (2.8) |
| Pakistani | 2 (1.9) | 2 (2.8) | 0 (0.0) |
| Chinese | 1 (0.9) | 1 (1.4) | 0 (0.0) |
| Other | 6 (5.6) | 6 (8.3) | 0 (0.0) |
| Educationb | |||
| Higher education | 64 (61.5) | 47 (67.1) | 17 (50.0) |
| Other | 40 (38.5) | 23 (32.9) | 17 (50.0) |
| Employment | |||
| Employee | 86 (78.9) | 57 (78.1) | 29 (80.6) |
| Self-employed | 16 (14.7) | 12 (16.4) | 4 (11.1) |
| Not employed | 7 (6.4) | 4 (5.5) | 3 (8.3) |
| Access to computer at home | 103 (95.4) | 68 (94.4) | 35 (97.2) |
| Use internet every day | 105 (97.2) | 69 (95.8) | 36 (100.0) |
| Characteristic | All, mean (SD) (N = 109) | Intervention, mean (SD) (N = 73) | Control, mean (SD) (N = 36) |
|---|---|---|---|
| Weight (kg) | 104.6 (20.7) | 105.7 (21.4) | 102.2 (19.4) |
| BMI (kg/m2) | 37.6 (5.9) | 37.8 (6.0) | 37.1 (5.7) |
| Waist circumference (cm) | 114.1 (14.7) | 113.9 (15.4) | 114.6 (13.2) |
| Hip circumference (cm) | 124.3 (13.4) | 125.0 (14.2) | 122.7 (11.7) |
| Characteristic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|
| Physical activity monitor worn, n (%) | 81 (74.3) | 55 (75.3) | 26 (72.2) |
| Minimum wear time achieved (for those who wore monitor), n (%) | 74 (91.4) | 51 (92.7) | 23 (88.5) |
| Activity monitor data, mean (SD) | |||
| MVPA time as percentage of wear time | 5.3 (3.4) | 5.8 (3.8) | 4.1 (2.1) |
| Average daily MVPA time (minutes) | 45.6 (32.9) | 50.1 (37.2) | 35.6 (17.5) |
| Average daily sedentary time (minutes) | 685.2 (306.1) | 693.3 (360.7) | 667.3 (121.0) |
| Average daily step count | 6569.8 (3971.0) | 7017.5 (4633.9) | 5577.0 (1423.4) |
| Self-reported average daily energy expenditure, mean (SD) | |||
| Total (kcal/day) | 3867.4 (870.9) | 3857.4 (752.3) | 3887.3 (1081.8) |
| Per kg body weight (kcal/kg/day) | 37.1 (5.3) | 36.7 (4.4) | 38.0 (6.8) |
| DINE questionnaire, mean (SD) | |||
| Fibre scorea | 19.7 (11.2) | 20.3 (11.4) | 18.6 (10.8) |
| Fat scorea | 28.7 (12.3) | 29.5 (12.4) | 27.0 (12.2) |
| Healthy eating scoreb | –9.0 (15.4) | –9.2 (15.6) | –8.4 (15.3) |
Randomised groups were generally well matched, although intervention group participants were more likely to have higher levels of education. They were also more likely to have higher levels of physical activity (measured objectively), as well as more variability between participants. They also had more sedentary time. Slightly more people in the control group were attending a weight loss group and those in the control group were more likely to weigh themselves regularly (see Appendix 8, Table 50).
Retention
Table 13 shows the follow-up rates at 12 months in each group. Overall, 77.1% of participants were followed up, achieving the progression criterion of at least 70%. Both randomised groups achieved the overall target of 70%.
| All (N = 109) | Intervention (N = 73) | Control (N = 36) | |
|---|---|---|---|
| Followed up, n (%); 95% CI | 84 (77.1); 68.0 to 84.6 | 52 (71.2); 59.4 to 81.2 | 32 (88.9); 73.9 to 96.9 |
Table 14 shows selected baseline data for those who were successfully followed up at 12 months compared with those who were not followed up. Also reported are the odds ratios for being successfully followed up associated with these baseline characteristics, derived from univariate logistic regression models (see Appendix 8, Tables 68–84 and 85–100, for additional summaries).
| Follow-up status at 12 months, n (%) | OR of being followed up | ||||
|---|---|---|---|---|---|
| Followed up (N = 84) | Not followed up (N = 25) | Effect | OR | 95% CI | |
| Study group | |||||
| Control | 32 (88.9) | 4 (11.1) | Reference | – | – |
| Intervention | 52 (71.2) | 21 (28.8) | vs. control | 0.31 | 0.10 to 0.98 |
| Age, mean (SD) | 48.3 (10.4) | 43.9 (11.2) | Per 10 years | 1.47 | 0.96 to 2.26 |
| Sex | |||||
| Male | 22 (66.7) | 11 (33.3) | Reference | – | – |
| Female | 62 (81.6) | 14 (18.4) | vs. male | 2.21 | 0.88 to 5.60 |
| SIMD quintile | |||||
| 1: most deprived | 24 (66.7) | 12 (33.3) | Reference | – | – |
| 2–5 | 52 (82.5) | 11 (17.5) | vs. Q1 | 2.36 | 0.91 to 6.11 |
| Employment | |||||
| Employed | 71 (82.6) | 15 (17.4) | Reference | – | – |
| Self-employed | 8 (50.0) | 8 (50.0) | vs. employed | 0.21 | 0.07 to 0.65 |
| Not employed | 5 (71.4) | 2 (28.6) | vs. employed | 0.53 | 0.09 to 2.98 |
| Height (m), mean (SD) | 165.6 (9.3) | 169.6 (8.9) | Per 10 cm | 0.95 | 0.91 to 1.00 |
| Weight (kg), mean (SD) | 101.9 (19.7) | 113.7 (21.8) | Per kg | 0.97 | 0.95 to 1.00 |
| BMI (kg/m2), mean (SD) | 37.0 (5.4) | 39.5 (7.0) | Per kg/m2 | 0.93 | 0.87 to 1.00 |
| Waist (cm), mean (SD) | 112.2 (13.8) | 120.7 (16.0) | Per cm | 0.96 | 0.93 to 0.99 |
| Attending weight loss groupa | |||||
| No | 57 (72.2) | 22 (27.8) | Reference | – | – |
| Yes | 26 (89.7) | 3 (10.3) | vs. no | 3.35 | 0.92 to 12.2 |
| Physical activity monitor wornb | |||||
| No | 18 (64.3) | 10 (35.7) | Reference | – | – |
| Yes | 66 (81.5) | 15 (18.5) | vs. no | 2.44 | 0.94 to 6.35 |
Those in the intervention group were less likely to be followed up at 12 months. This may reflect a tendency for those who disengaged from the intervention to be disinclined to continue to participate in the trial. Older participants, and women, were more likely to be followed up, as expected. Those who were self-employed at baseline were less likely to be followed up, as were those living in one of the 20% most deprived areas of Scotland. Follow-up rates were lower for those who had higher weight, BMI or waist circumference, perhaps reflecting a greater tendency for these participants to withdraw from the intervention. Those currently attending a weight loss group were more likely to be followed up, as were those who complied with the baseline physical activity assessment by wearing a physical activity monitor. Both of these factors may represent markers of increased motivation to take part in the trial.
Exploratory primary outcomes
As a feasibility study, the trial was powered not to detect statistically significant changes, but to explore the feasibility and potential sensitivity of measures for use in a definitive trial. This study explored the use of three primary outcomes: (1) physical activity (2) dietary measures and (3) BMI.
Physical activity
Table 15 summarises physical activity measures derived from the 7-day physical activity recall, and from accelerometers, in the randomised groups, along with estimated between-group differences, with 95% CIs and p-values, derived from linear regression models of 12-month outcomes, with randomised group, baseline score, age, gender and BMI of ≥ 40 kg/m2 as predictor variables.
| Measure | n | Baseline | 12 months | Change | Between-group difference (intervention – control) | ||
|---|---|---|---|---|---|---|---|
| Estimate (95% CI) | ES (95% CI) | ||||||
| MVPA time as % of wear time (from activity monitor) | |||||||
| Control | 15 | 4.1 (2.3) | 3.5 (2.3) | –0.6 (1.0) | Unadjusted | –0.3 (–2.2 to 1.7) | –0.08 (–0.73 to 0.56) |
| Intervention | 24 | 6.5 (4.0) | 5.6 (2.5) | –0.9 (3.8) | Adjusted | 1.3 (–0.1 to 2.7) | 0.44 (–0.02 to 0.90) |
| Average daily MVPA time (minutes, from activity monitor) | |||||||
| Control | 15 | 35.5 (19.4) | 31.3 (20.3) | –4.3 (10.5) | Unadjusted | –4.2 (–21.1 to 12.7) | –0.16 (–0.81 to 0.48) |
| Intervention | 24 | 54.8 (34.3) | 46.3 (20.2) | –8.5 (32.2) | Adjusted | 9.3 (–2.3 to 20.9) | 0.35 (–0.09 to 0.80) |
| Average daily sedentary time (minutes, from activity monitor) | |||||||
| Control | 15 | 661.7 (138.2) | 703.4 (166.6) | 41.7 (83.5) | Unadjusted | –52.9(–104.4 to –1.4) | –0.66 (–1.31 to –0.02) |
| Intervention | 24 | 642.7 (94.0) | 631.5 (82.8) | –11.2 (77.6) | Adjusted | –60.8 (–110.5 to –11.0) | –0.76 (–1.38 to –0.14) |
| Average daily step count (from activity monitor) | |||||||
| Control | 15 | 5650 (1526) | 5335 (1844) | –315 (1130) | Unadjusted | 43 (–1876 to 1963) | 0.01 (–0.63 to 0.66) |
| Intervention | 24 | 7232 (3712) | 6960 (2568) | –272 (3669) | Adjusted | 1187 (–180 to 2555) | 0.40 (–0.06 to 0.86) |
| Average daily energy expenditure (kcal/day, self-report) | |||||||
|
Control Intervention |
32 49 |
3879 (1121) 3717 (715) |
3606 (750) 3557 (779) |
–273 (828) –160 (502) |
Unadjusted Adjusted |
113 (–179 to 404) 62 (–180 to 304) |
0.17 (–0.27 to 0.62) 0.09 (–0.28 to 0.47) |
| Average daily energy expenditure per kg of body weight (kcal/kg/day, self-report) | |||||||
|
Control Intervention |
32 49 |
38.2 (7.1) 37.2 (4.9) |
36.7 (4.1) 36.7 (3.7) |
–1.6 (6.5) –0.6 (5.3) |
Unadjusted Adjusted |
1.0 (–1.6 to 3.6) 0.0 (–1.7 to 1.6) |
0.17 (–0.27 to 0.62) 0.00 (–0.29 to 0.28) |
For each estimated intervention effect estimate, the standardised effect size is reported with a 95% CI. The original plan had been to derive this effect size estimate by dividing the intervention effect estimate and confidence limits on the original scale by the standard deviation of the outcome measure at baseline in the total study population. However, it was recognised that for some measures, there was considerably more variability between individuals in baseline scores (or follow-up scores) than there was between individuals in the change from baseline. For an individual, a change in outcome equal to the standard deviation in the whole population might be an unachievable goal, but a change in outcome equal to the standard deviation of the distribution of within-person changes may be much more attainable, so it was felt that standardising between-group differences relative to the pooled standard deviation of changes from baseline would be more relevant.
As part of the modelling process, outcomes were initially analysed on their original scale. The residuals from each regression model were visually assessed for normality. For those measures where substantial non-normality was observed, data transformations (at follow-up and at baseline) were attempted to improve model fit; if no suitable transformation could be found, then changes from baseline to follow-up are compared between groups using the Wilcoxon–Mann–Whitney test. See Appendix 8, Tables 105 and 106, for additional summaries.
Only 39 participants (36% of those randomised, 46% of those followed up at 12 months) provided valid activity monitor data at both baseline and 12 months, in comparison with 81 (74% of those randomised, 96% of those followed up) who provided self-report physical activity data at both time points.
Both groups showed reductions in objectively measured physical activity (moderate to vigorous physical activity and step counts), but the intervention group had higher mean values, and showed greater variation, at each time point. Adjusted analyses suggest effect sizes of around 0.4, but unadjusted analyses give effect size estimates close to zero. Similar reductions in physical activity in both groups were seen in self-reported energy expenditure data, with intervention effect estimates close to zero. The intervention group had lower objectively measured sedentary times at 12 months, with 50–60 fewer minutes per day spent in sedentary activities relative to the control group. This represents an effect size estimate of around 0.7. We also examined whether self-report physical activity differed between those who did and those who did not provide valid accelerometry data (Table 16). There was no difference.
| Achieved minimum wear time at follow-up | ||
|---|---|---|
| No | Yes | |
| Total 7-day PAR/kg | 255.6 | 257.17 |
| Total day PAR/kg | 36.5 | 36.7 |
| Total day PAR | 3668.7 | 3511.2 |
The results seem to offer evidence that self-report physical activity was no different between those who did and those who did not provide accelerometry data. This increases confidence in the differences found between the groups in the accelerometry data.
Diet
Table 17 summarises dietary outcome measures derived from the DINE questionnaire. These have been analysed in the same way as the physical activity data. Additional data summaries can be found in Appendix 8, Tables 107 and 108.
| Measure | n | Baseline | 12 months | Change | Between-group difference (intervention – control) | ||
|---|---|---|---|---|---|---|---|
| Estimate (95% CI) | ES (95% CI) | ||||||
| Fibre score (score of < 30 = low fibre) | |||||||
| Control | 32 | 18.6 (10.6) | 19.2 (11.6) | 0.6 (12.6) | Unadjusted | –4.1 (–9.2 to 0.9) | –0.36 (–0.81 to 0.08) |
| Intervention | 49 | 19.8 (9.7) | 16.3 (11.8) | –3.6 (10.6) | Adjusted | –3.3 (–8.1 to 1.5) | –0.29 (–0.71 to 0.13) |
| Fat score (score of < 30 = low fat) | |||||||
| Control | 32 | 27.1 (12.6) | 22.9 (9.6) | –4.1 (10.8) | Unadjusted | –1.4 (–6.4 to 3.6) | –0.13 (–0.57 to 0.32) |
| Intervention | 49 | 28.4 (11.6) | 22.9 (12.7) | –5.5 (11.4) | Adjusted | –0.4 (–4.8 to 4.0) | –0.04 (–0.43 to 0.36) |
| Healthy eating score (score = fibre – fat; negative score indicates unhealthy diet) | |||||||
| Control | 32 | –8.5 (16.1) | –3.8 (13.2) | 4.7 (16.6) | Unadjusted | –2.7 (–8.9 to 3.4) | –0.20 (–0.64 to 0.25) |
| Intervention | 49 | –8.6 (13.3) | –6.6 (12.9) | 2.0 (11.7) | Adjusted | –2.9 (–8.0 to 2.2) | –0.21 (–0.58 to 0.16) |
| Unsaturated fat score (score of 6–9 = moderate unsaturated fat intake) | |||||||
| Control | 32 | 9.3 (1.8) | 8.2 (3.7) | –1.1 (3.5) | Unadjusted | –2.3 (–4.3 to –0.3) | –0.45 (–0.85 to –0.06) |
| Intervention | 49 | 9.2 (2.2) | 5.8 (5.0) | –3.3 (5.6) | Adjusted | –2.2 (–4.0 to –0.4) | –0.44 (–0.80 to –0.07) |
| Fruit and vegetable score (score = portions per day) | |||||||
| Control | 32 | 5.0 (3.4) | 4.9 (2.9) | –0.1 (3.4) | Unadjusted | 0.7 (–0.6 to 1.9) | 0.24 (–0.21 to 0.69) |
| Intervention | 49 | 4.7 (2.6) | 5.2 (2.5) | 0.5 (2.2) | Adjusted | 0.4 (–0.6 to 1.5) | 0.16 (–0.23 to 0.55) |
| Fizzy drink score (score = cans per day) | |||||||
| Control | 32 | 0.2 (0.6) | 0.3 (0.9) | 0.1 (0.4) | Non-parametric testa | ||
| Intervention | 49 | 0.0 (0.0) | 0.2 (0.6) | 0.2 (0.6) | |||
| Sugar score (score = teaspoons of sugar per day) | |||||||
| Control | 32 | 0.9 (5.3) | 0.8 (3.5) | –0.2 (1.9) | Non-parametric testa | ||
| Intervention | 49 | 0.5 (1.3) | 0.3 (0.8) | –0.2 (0.9) | |||
Dietary scores were available for 81 (74% of those randomised, 96% of those followed up) participants at baseline and 12 months. These generally improved or remained stable in both groups between baseline and 12 months, with the exception of the fibre score in the intervention group. Both groups achieved an increase in healthy eating score (difference between fibre score and fat score), although this was greater in the control group, with an effect size in favour of control. The intervention appeared most promising in terms of the unsaturated fat score, with an effect size of approximately 0.45. Fruit and vegetable scores were slightly higher in the intervention group, but fizzy drink and sugar scores were skewed towards zero and changed little in both groups during the study, and therefore show little promise as outcomes for a future study.
Body mass index
Table 18 summarises BMI data, which were analysed in the same way as the other primary outcomes (see also Appendix 8, Table 109). Data were available for 82 participants (75% of those randomised, 98% of those followed up). Both groups showed similar reductions in BMI during the study of approximately 1 kg/m2.
| Measure | n | Baseline | 12 months | Change | Between-group difference (intervention – control) | ||
|---|---|---|---|---|---|---|---|
| Estimate (95% CI) | ES (95% CI) | ||||||
| BMI (kg/m2) | |||||||
| Control | 32 | 36.9 (5.7) | 36.0 (6.3) | –0.9 (3.3) | Unadjusted | –0.3 (–1.5 to 0.9) | –0.11 (–0.56 to 0.33) |
| Intervention | 50 | 36.9 (5.3) | 35.7 (5.4) | –1.2 (2.4) | Adjusted | –0.2 (–1.4 to 1.0) | –0.08 (–0.52 to 0.37) |
Table 19 presents thresholds of weight loss for each group. A greater proportion of participants in the control group gained weight than in the intervention group (47% vs. 34%). A greater proportion of participants in the intervention group lost < 10 kg than in the control group (52% vs. 31%). However, weight loss of > 10 kg was more frequent in the control group than in the intervention group (22% vs. 14%).
| Control | Intervention | |
|---|---|---|
| Weight gain | 15 (47%) | 17 (34%) |
| < 5 kg weight loss | 9 (28%) | 19 (38%) |
| ≥ 5 and < 10 kg weight loss | 1 (3%) | 7 (14%) |
| ≥ 10 kg weight loss | 7 (22%) | 7 (14%) |
Per-protocol analyses
Per-protocol analyses were carried out after excluding those who had either failed to provide follow-up data or failed to comply with the intervention (for those in the intervention group). Twenty-five participants did not provide any outcome data at the 12-month follow-up, although for objectively measured physical activity measures the follow-up rates were much lower (70 participants failed to provide valid activity monitor data for analysis). Fifteen participants in the intervention group showed a lack of adherence to the intervention, defined as failure to use the app at least twice.
Tables 20 and 21 show the intervention effect estimates for each primary outcome measure using the full analysis set and the per-protocol population.
| Measure | Full analysis set | p-value | Per-protocol population | ||
|---|---|---|---|---|---|
| Estimate (ES) | 95% CI (ES CI) | Estimate (ES) | 95% CI (ES CI) | ||
| MVPA time as % of wear time (from activity monitor) | 1.3 (0.44) | –0.1 to 2.7 (–0.02 to 0.90) | 0.068 | 1.4 (0.69) | 0.2 to 2.7 (0.09 to 1.28) |
| Average daily MVPA time (minutes, from activity monitor) | 9.3 (0.35) | –2.3 to 20.9 (–0.09 to 0.80) | 0.127 | 10.4 (0.56) | 0.0 to 20.8 (0.00 to 1.13) |
| Average daily sedentary time (minutes, from activity monitor) | –60.8 (–0.76) | –110.5 to –11.0 (–1.38 to –0.14) | 0.022 | –73.2 (–0.95) | –126.0 to –20.5 (–1.64 to –0.27) |
| Average daily step count (from activity monitor) | 1187 (0.40) | –180 to 2555 (–0.06 to 0.86) | 0.098 | 1397.4 (0.72) | 179.6 to 2615.2 (0.09 to 1.34) |
| Average daily energy expenditure (kcal/day, self-report) | 62 (0.09) | –180 to 304 (–0.28 to 0.47) | 0.619 | 117.7 (0.17) | –142.4 to 377.9 (–0.21 to 0.55) |
| Average daily energy expenditure per kg of body weight (kcal/kg/day, self-report) | 0.0 (0.00) | –1.7 to 1.6 (–0.29 to 0.28) | 0.974 | 0.1 (0.02) | –1.7 to 1.9 (–0.28 to 0.31) |
| Measure | Full analysis set | Per-protocol population | ||
|---|---|---|---|---|
| Estimate (ES) | 95% CI (ES CI) | Estimate (ES) | 95% CI (ES CI) | |
| DINE fibre score | –3.3 (–0.29) | –8.1 to 1.5 (–0.71 to 0.13) | –2.2 (–0.20) | –7.3 to 2.9 (–0.65 to 0.26) |
| DINE fat score | –0.4 (–0.04) | –4.8 to 4.0 (–0.43 to 0.36) | 0.0 (0.00) | –4.6 to 4.6 (–0.42 to 0.42) |
| DINE healthy eating score | –2.9 (–0.21) | –8.0 to 2.2 (–0.58 to 0.16) | –2.3 (–0.16) | –7.9 to 3.3 (–0.55 to 0.23) |
| DINE unsaturated fat score | –2.2 (–0.44) | –4.0 to –0.4 (–0.80 to –0.07) | –1.8 (–0.40) | –3.6 to 0.1 (–0.83 to 0.02) |
| DINE fruit and vegetable score | 0.4 (0.16) | –0.6 to 1.5 (–0.23 to 0.55) | 0.4 (0.14) | –0.8 to 1.6 (–0.27 to 0.55) |
| BMI (kg/m2) | –0.2 (–0.08) | –1.4 to 1.0 (–0.52 to 0.37) | –0.4 (–0.14) | –1.6 to 0.9 (–0.62 to 0.34) |
Objective physical activity measures collected with an activity monitor showed greater between-group differences in the per-protocol population, with effect sizes increasing from 0.35–0.76 to 0.56–0.95. In particular, the average daily step count showed an increase of approximately 1400 steps per day (p = 0.033), and average sedentary time was reduced by approximately 70 minutes per day (p = 0.011), suggesting clinically relevant changes in physical activity among those who engaged with the intervention. However, self-reported physical activity continued to show little effect of the intervention in the per-protocol analysis.
For dietary outcomes and BMI, the per-protocol analysis showed little evidence of positive intervention effects.
Multiple imputation analyses
Because fewer than 80% of participants provided data for all primary outcome measures, multiple imputation analysis was carried out, as specified in the statistical analysis plan. Multiple imputation was implemented using chained equations. For each outcome studied, 10 imputed data sets were generated, imputed using the outcome variable at 12 months, age, gender, baseline BMI, and the baseline value of the relevant outcome measure.
Table 22 shows the results of the adjusted analyses from the original analysis and the analysis using multiple imputation (see Appendix 8, Table 132).
| Measure | Original analysis | Multiple imputation | ||
|---|---|---|---|---|
| Estimate | 95% CI | Estimate | 95% CI | |
| Physical activity from activity monitor | ||||
| MVPA (%) | 1.3 | –0.1 to 2.7 | 0.7 | –0.5 to 2.0 |
| MVPA time (minutes/day) | 9.3 | –2.3 to 20.9 | 4.3 | –6.1 to 14.6 |
| Sedentary time (minutes/day) | –60.8 | –110.5 to –11.0 | –42.9 | –108.0 to 22.2 |
| Daily step count | 1187 | –180 to 2555 | 593 | –702 to 1888 |
| Self-reported physical activity (energy expenditure) | ||||
| Per kg (kcal/kg/day) | 0.0 | –1.7 to 1.6 | 0.0 | –1.7 to 1.7 |
| Total (kcal/day) | 62 | –180 to 304 | 84 | –131 to 299 |
| Dietary measures (DINE questionnaire scores) | ||||
| Fibre | –3.3 | –8.1 to 1.5 | –2.7 | –7.6 to 2.1 |
| Fat | –0.4 | –4.8 to 4.0 | –0.2 | –4.4 to 4.0 |
| Healthy eating | –2.9 | –8.0 to 2.2 | –2.4 | –7.5 to 2.8 |
| Unsaturated fat | –2.2 | –4.0 to –0.4 | –2.2 | –4.1 to –0.3 |
| Fruit and vegetables | 0.4 | –0.6 to 1.5 | 0.4 | –1.0 to 1.7 |
| Physical measures | ||||
| BMI (kg/m2) | –0.2 | –1.4 to 1.0 | –0.2 | –1.5 to 1.0 |
The estimated intervention effects for objectively measured physical activity were reduced in the multiple imputation analyses, generally by about half. This suggests that these results are sensitive to missing data; there was a large number of missing data for these outcomes. Other outcome measures were much less affected by missing data, with results using multiple imputation being generally similar to those of the original analyses.
Secondary outcomes
Tables 23 and 24 report the other outcome measures at baseline and follow-up and model estimates (see Appendix 8, Tables 110–120, for additional summaries).
| Measure | n | Baseline | 12 months | Change | Between-group difference (intervention – control) | ||
|---|---|---|---|---|---|---|---|
| Estimate (95% CI) | ES (95% CI) | ||||||
| Weight (kg) | |||||||
| Control | 32 | 101.2 (19.7) | 98.7 (20.3) | –2.5 (9.3) | Unadjusted | –0.7 (–4.2 to 2.7) | –0.10 (–0.54 to 0.35) |
| Intervention | 50 | 101.4 (19.8) | 98.1 (19.7) | –3.3 (6.5) | Adjusted | –0.6 (–4.1 to 2.9) | –0.08 (–0.53 to 0.37) |
| Waist circumference (cm) | |||||||
| Control | 32 | 114.0 (13.9) | 107.7 (15.1) | –6.4 (18.5) | Unadjusted | 4.3 (–2.1 to 10.7) | 0.32 (–0.16 to 0.80) |
| Intervention | 50 | 110.1 (13.3) | 108.0 (15.5) | –2.1 (8.1) | Adjusted | 3.2 (–3.0 to 9.4) | 0.24 (–0.22 to 0.70) |
| Waist-to-hip ratio | |||||||
| Control | 32 | 0.94 (0.09) | 0.92 (0.08) | –0.02 (0.04) | Unadjusted | 0.02 (0.00 to 0.04) | 0.39 (–0.08 to 0.87) |
| Intervention | 50 | 0.90 (0.09) | 0.90 (0.09) | 0.00 (0.05) | Adjusted | 0.01 (–0.01 to 0.04) | 0.30 (–0.12 to 0.73) |
| Measure | n | Baseline | 12 months | Change | Between-group difference (intervention – control) | ||
|---|---|---|---|---|---|---|---|
| Estimate (95% CI) | ES (95% CI) | ||||||
| EQ-5D-3L health utility score | |||||||
| Control | 32 | 0.894 (0.095) | 0.858 (0.123) | –0.037 (0.100) | Unadjusted | 0.022 (–0.017 to 0.061) | 0.26 (–0.20 to 0.71) |
| Intervention | 45 | 0.924 (0.079) | 0.910 (0.082) | –0.015 (0.071) | Adjusted | 0.032 (–0.007 to 0.070) | 0.37 (–0.08 to 0.83) |
| EQ-5D-3L VAS | |||||||
| Control | 32 | 64.8 (18.3) | 68.0 (18.6) | 3.2 (18.3) | Unadjusted | 4.4 (–3.6 to 12.4) | 0.25 (–0.20 to 0.70) |
| Intervention | 45 | 67.3 (16.1) | 74.9 (14.8) | 7.6 (17.0) | Adjusted | 5.3 (–1.4 to 12.0) | 0.30 (–0.08 to 0.68) |
| ICECAP-A total score | |||||||
| Control | 32 | 11.6 (1.9) | 12.0 (2.5) | 0.4 (2.1) | Unadjusted | –0.2 (–1.0 to 0.6) | –0.11 (–0.57 to 0.34) |
| Intervention | 45 | 12.7 (1.9) | 12.9 (2.1) | 0.2 (1.5) | Adjusted | 0.0 (–0.8 to 0.8) | 0.01 (–0.45 to 0.47) |
| GHQ score | |||||||
| Control | 28 | 3.2 (2.7) | 3.5 (3.8) | 0.4 (4.4) | Unadjusted | –0.8 (–2.8 to 1.1) | –0.20 (–0.69 to 0.29) |
| Intervention | 38 | 2.9 (3.5) | 2.4 (3.5) | –0.4 (3.7) | Adjusted | –0.8 (–2.5 to 0.9) | –0.21 (–0.63 to 0.21) |
| GHQ Likert score | |||||||
| Control | 28 | 13.6 (5.2) | 13.2 (6.2) | –0.4 (7.9) | Unadjusted | –1.5 (–4.8 to 1.8) | –0.22 (–0.70 to 0.27) |
| Intervention | 38 | 13.4 (5.3) | 11.5 (6.8) | –1.9 (5.8) | Adjusted | –1.4 (–4.2 to 1.5) | –0.20 (–0.63 to 0.22) |
| GHQ case (Likert score of ≥ 12); data reported as n (%); intervention effect estimate reported as odds ratio | |||||||
|
Control Intervention |
28 38 |
18 (64.3%) 21 (55.3%) |
14 (50.0%) 19 (50.0%) |
Unadjusted Adjusted |
1.0 (0.4 to 2.7) 1.2 (0.3 to 4.0) |
||
Weight showed similar results to BMI, with slight reductions in both study groups, and little to suggest a greater reduction in the intervention group. Waist circumference and waist-to-hip ratio demonstrated similar patterns within groups, with larger reductions observed in the control group.
General Health Questionnaire (GHQ) scores were slightly in favour of the intervention group, although the effect sizes were small (around 0.2). GHQ caseness was 50% in both groups at follow-up. Quality of life (EQ-5D-3L) health utility scores reduced slightly in both groups, but EQ-5D-3L visual analogue scale (VAS) scores increased slightly in both groups. Between-group differences were in favour of the intervention, with effect size estimates of around 0.25–0.30. ICECAP-A scores changed little during the study and showed no signs of between-group differences (see Table 24). The feasibility of the EQ-5D-3L and ICECAP-A measures is reported in Part 2: health economics analysis.
There was no clear pattern of positive benefits across the other questionnaire measures used in the study (see Appendix 8, Table 99), with the possible exception of questionnaires measuring motivation to eat a healthy diet [Treatment Self-Regulation Questionnaire Concerning the Motivation for Eating a Healthy Diet (TSRD), effect size approximately 0.4] or to exercise regularly [Treatment Self-Regulation Questionnaire Concerning the Motivation for Exercising Regularly (TSRE), effect size approximately 0.2].
Alcohol use (AUDIT-C score) and smoking status (HSI) were collected at 12 months only. This was to explore their feasibility and potential use in a definitive trial. AUDIT-C scores were generally low and smoking was uncommon in both groups, with no evidence of any differences between the groups (see Appendix 8, Table 114).
Potential moderators
For primary outcome measures, intervention effect moderation was assessed with respect to age, gender, socioeconomic status and the baseline measurement of the outcome. This was limited to analyses of the objective measures of physical activity (average daily sedentary time and average daily step count), as these showed the largest effect sizes in earlier analyses. This was achieved by fitting regression models with main effects for randomised group and the moderator variable of interest, plus their interaction. All models were adjusted for the baseline measurement of the outcome, age, gender and BMI, if these were not already included in the model.
Table 25 shows the interaction test p-values in relation to each potential moderator. There was no evidence to suggest any effect moderation with respect to age, gender or socioeconomic status. For sedentary time (p = 0.021), and to a lesser extent daily step counts (p = 0.11), there was some evidence that any intervention effect was moderated by the baseline activity measurement.
| Age | Gender | SES | Baseline | |
|---|---|---|---|---|
| Sedentary time (minutes per day) | p = 0.208 | p = 0.736 | p = 0.891 | p = 0.021 |
| Daily step count | p = 0.406 | p = 0.220 | p = 0.742 | p = 0.110 |
Figure 7 shows the nature of the interactions identified in Table 25. For those with higher levels of sedentary time at baseline, the intervention appears to reduce sedentary time relative to the control group, while having less of an effect in those with low sedentary times at baseline. For those with low step counts at baseline, the intervention appears to increase step counts relative to the control group, whereas outcomes appear to be less affected by the intervention for those with higher baseline step counts.
FIGURE 7.
Intervention effect moderation by baseline measures. (a) Estimated intervention effect for daily sedentary time, in relation to baseline daily sedentary time; and (b) estimated intervention effect for daily step counts, in relation to baseline daily step count.

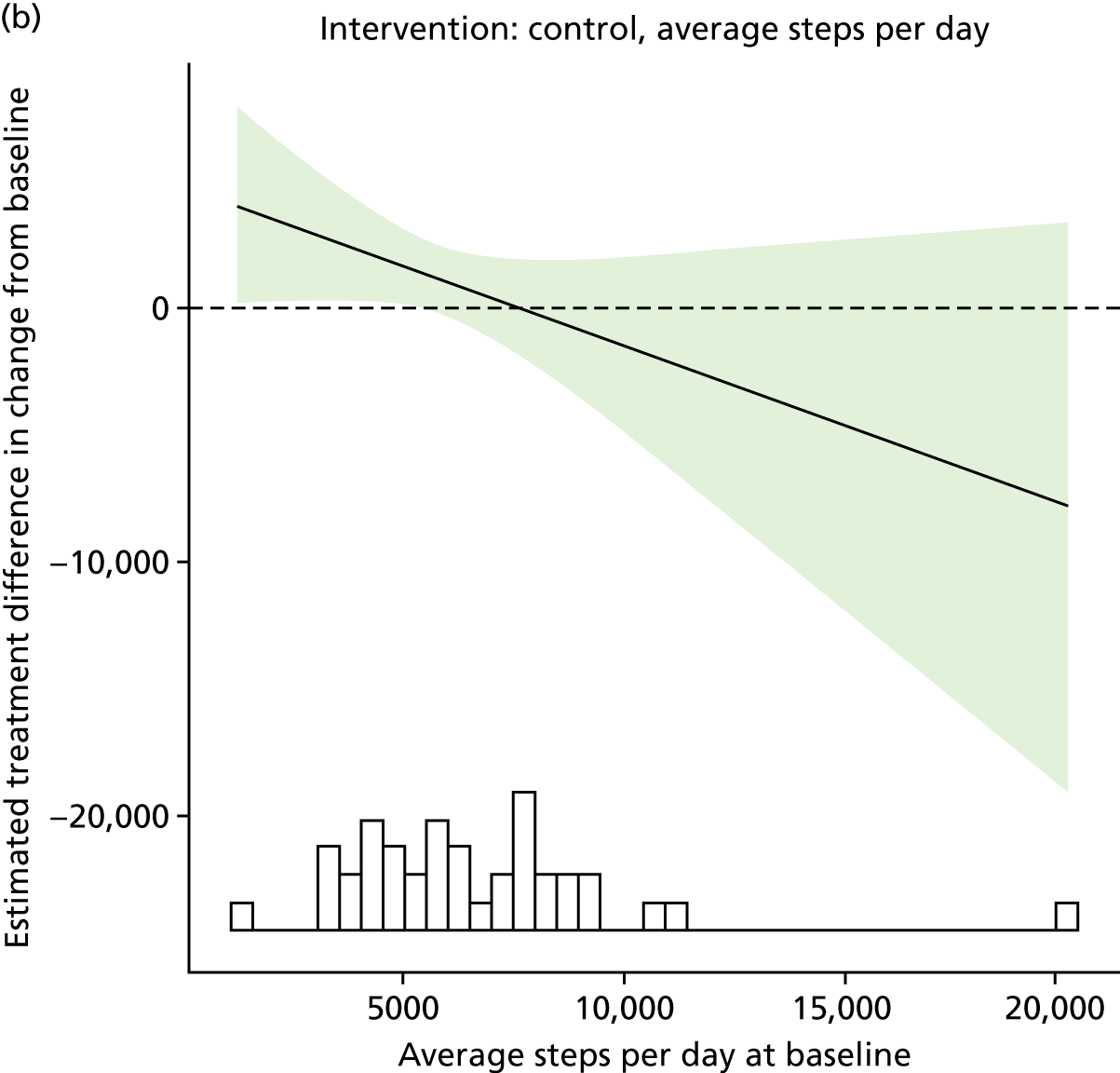
These figures highlighted the presence of some outliers at baseline, which may have an undue influence on these findings. Figure 8 shows the results of these analyses after two individuals were removed from the sedentary time analysis (with the highest and lowest baseline values) and one individual was removed from the step count analysis (with the highest baseline value). In general, the patterns of results are much the same, with the intervention showing most evidence of an effect for those with high levels of sedentary behaviour and low levels of physical activity at baseline.
FIGURE 8.
Intervention effect moderation by baseline measures, sensitivity analyses. Individuals with extreme baseline values were removed from the analysis. (a) Sedentary minutes per day (highest and lowest baseline values removed); and (b) step count per day (highest baseline value removed).

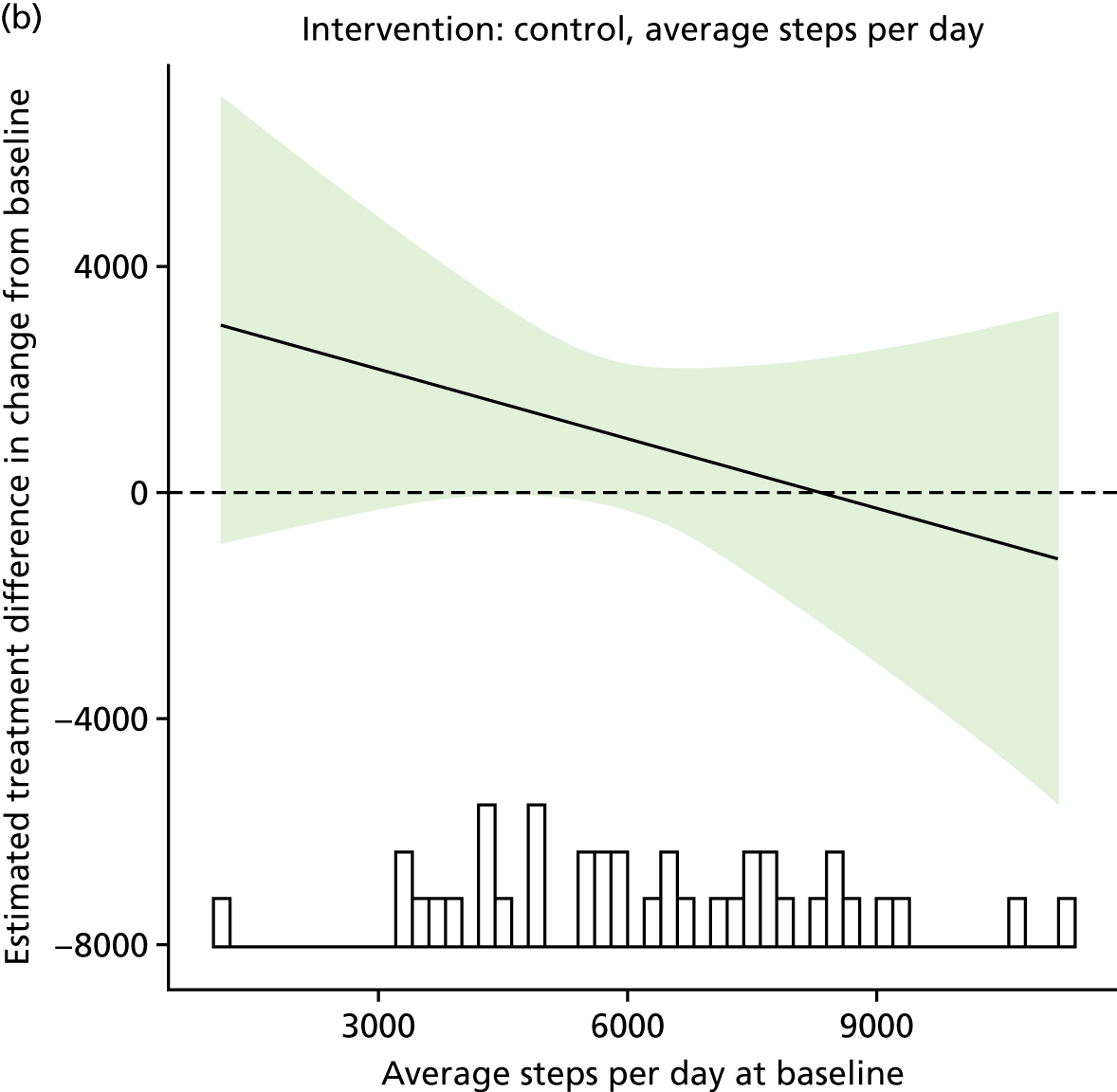
These apparent interactions may reflect floor (for sedentary time) and ceiling (for step counts) effects, with those who are more physically active, or less sedentary, having less room for improvement through the intervention.
Safety outcomes
There were no serious adverse events reported during the study.
Summary of quantitative analyses results
Recruitment was close (91%) to the target of 120 participants over 6 months, suggesting that the study could recruit large numbers of participants if run over a longer period at multiple study sites. In terms of sample characteristics, more than twice as many women as men were recruited, with an average age of 47 (range 25–68) years; most were employed and married. The average BMI was 37.6 kg/m2. One-third of those recruited were from the most deprived quintile and over 60% had received higher education.
Retention at 12 months was above the target of 70% overall, and in both randomised groups, although it was lower in the intervention group, with a lower 95% confidence limit of approximately 60%. Any future study may require measures to increase follow-up of participants who become disengaged from the intervention.
Collection of data was good for self-reported outcomes, with > 90% of those followed up providing data for weight, and physical activity and dietary questionnaires. Data on objectively measured physical activity using an accelerometer were poorly collected, with fewer than half of those followed up providing valid data at both baseline and 12 months.
The study was underpowered to detect effects, so caution is required when interpreting these results. Point estimates of standardised intervention effect sizes were generally small (often less than ± 0.3), or small and in favour of the control group. However, CIs were generally wide and were therefore consistent with clinically relevant benefits. The one exception to this was the objective physical activity data, which showed moderate to large effect size estimates across several measures, particularly the daily step count and sedentary time. These findings were amplified in per-protocol analyses, and appeared strongest in those with lower levels of physical activity at baseline. There was no evidence to suggest that self-report physical activity was different between those who did and those who did not provide valid accelerometry data, which increases confidence in these results. However, these outcomes were poorly completed, and these findings were sensitive to missing data, being greatly reduced in multiple imputation analyses.
Part 2: health economics analysis
Data were collected for 109 participants at baseline: 36 in the control group and 73 in the intervention group. All costs were collected, with the exception of five participants who did not provide expenditure on food purchases. At 12-month follow-up, data were collected for 78 participants (72% of baseline sample) in relation to the EQ-5D-3L, ICECAP-A and expenditure on food purchases. Fewer participants (n = 69) provided data on health, social and personal resource use, which were gathered using a CRF. This was because a proportion of participants at follow-up, who were at risk of dropping out of the study, completed a ‘minimum data set’ that omitted the additional questions linked to resource use. The following section summarises the health economics findings in relation to (1) intervention costs; (2) health, social and personal resource use; and (3) quality-of-life and capability well-being measures.
Figure 9 shows the enrolment for the resource use CRF, food cost questionnaire and EQ-5D-3L and ICECAP-A data.
FIGURE 9.
Flow chart of enrolment and follow-up of participants.
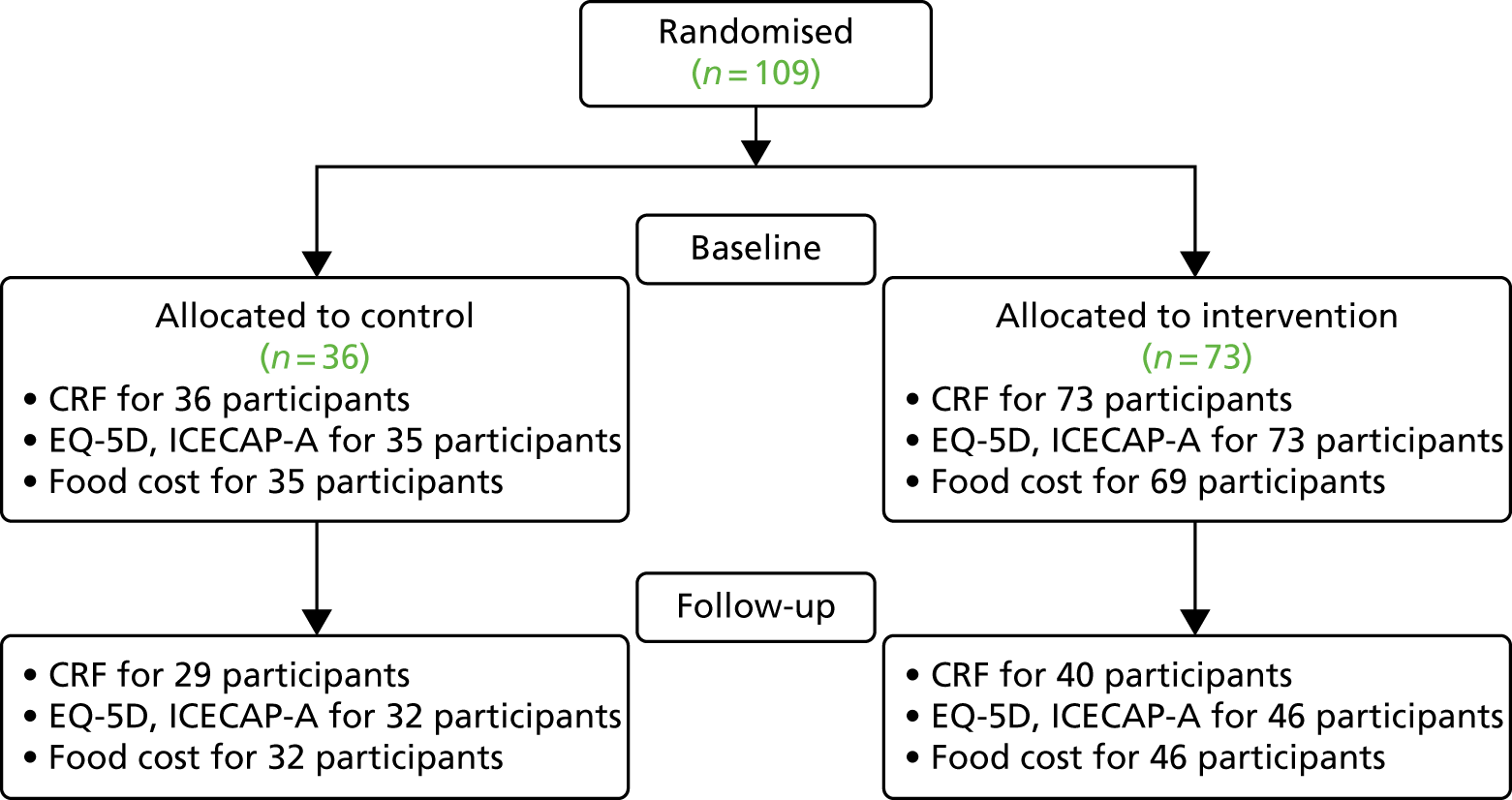
Table 26 shows the number of participants taking weight loss medication in both groups at baseline and follow-up.
| Baseline, n (%) | Follow-up, n (%) | |||
|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |
| Weight loss medication in past 12 months | 3 (8.33) | 5 (6.85) | 1 (3.45) | 1 (2.5) |
| Current weight loss medication | 0 (0) | 1 (1.37) | 0 (0) | 1 (2.5) |
Intervention costs
The intervention cost comprised the cost of developing a mobile app and website and the cost of maintaining and updating the app. Table 27 shows the cost of the intervention, including app development and maintenance, alongside the research costs. The cost per participant for the current study was high, at £740 (see Table 27: calculated by the fixed cost of the study plus variable cost of the study divided between 109 participants); however, these costs involved the upfront cost of intervention and software development. Now that the app and website are developed, a future trial would simply need some refinement based on the feasibility results (£10,000), ongoing costs for hosting and support (£10,000), and costs of the study (variable depending on sample size). This would mean a low cost per participant in a future trial, at approximately £370 per participant for a sample of 400 or £220 per participant for a sample of 1000. If rolled out ‘in the real world’, only hosting (£10,000) and maintenance costs (£10,000) would be required, resulting in a low cost, for example, of £2 per participant per 10,000 users.
| Description | Quantity | Cost (£) | Total cost (£) |
|---|---|---|---|
| Fixed cost | |||
| Development of app and website for current study | 1 | 60,000 | 60,000 |
| Maintenance and hosting cost of software for current study | 1 | 300 | 300 |
| Training of field workers including baseline and follow-up refresher training (eight field workers × hourly rate) | 8 | 140 | 1120 |
| Costs of field worker data collection: approximately 4 hours per participant at both baseline and follow-up (eight field workers × approximately 20 participants × hourly rate) | 8 | 1500 | 12,000 |
| Total | 73,420 | ||
| Variable cost | |||
| Promotion and marketing of study (printing and media adverts) | 1 | 700 | 700 |
| Recruitment support via the SPCRN | 1 | 440 | 440 |
| Retention resources for participants (e.g. newsletters, birthday cards) | 1 | 500 | 500 |
| Incentives for participants (i.e. £20 thank-you vouchers at both time points) | 109 | 40 | 4360 |
| Cost of posting information to participants | 109 | 3 | 327 |
| Printing of data collection resources | 1 | 1000 | 1000 |
| Total | 7327 | ||
| Estimation of future cost | |||
| Quote for updating app for a future trial | 1 | 10,000 | 10,000 |
| Quote for 3-year maintenance and hosting cost of software for future trial | 1 | 10,000 | 10,000 |
| Total | 20,000 | ||
Health, social and personal resource use
Health and social resource use
The most frequently used health and social resources within the 3-month period prior to data collection were visits to GP, practice nurse and physiotherapy (see Appendix 9). The data identified individual participants with high attendances at GP, practice nurse and physiotherapy; these outliers giving rise to right-skewed data are a typical pattern occurring in resource use data. The mean cost of baseline health service resource use for the control and intervention groups at baseline was £285 (SD £571) and £80 (SD £119), respectively. The mean cost of follow-up health service resource use for the control and intervention groups was £553 (SD £1554) and £152 (SD £224), respectively. No formal statistical tests of the difference in costs were conducted owing to lack of power.
Data revealed that the HelpMeDoIt! resource use data collection instrument identified and measured resource use items across a range of health services in both arms including GP, nurse, physiotherapist, hospital consultants for various specialties, community psychiatric nurse, A&E and hospital inpatient stay. NHS weight management services were also used by both control and intervention arm participants at follow-up only.
Personal resource use
The total weekly cost of participant food and drink at baseline for the control and intervention groups was £98.93 and £104.75, respectively (see Appendix 9). Overall, grocery costs were the highest component of weekly costs at baseline and follow-up (64% and 58% at baseline for the control and intervention groups, respectively; 67% and 61% at follow-up for the control and intervention groups, respectively). Meals out constituted between 20–22% and 18–24% of weekly food expenditure at baseline and follow-up for control and intervention, respectively. Alcohol spend was the smallest component of weekly food and drink cost, at between 5% and 8% at baseline and follow-up, in both arms. Overall, these weekly food and drink data collection questions appeared feasible for gathering information on food and drink spend.
The mean spend on lifestyle activities (including slimming clubs, health clubs, gyms, swimming pools and exercise classes) in the 3 months prior to baseline and follow-up was £43.29 and £30.08 at baseline for the control and intervention groups, respectively. At follow-up this spend was £51.46 and £55.23 in the control and intervention groups, respectively. These lifestyle costs exhibited the same pattern of right skewness as health services data, including a small number of high values. This method of directly collecting lifestyle spend, pre-empted by a closed-ended yes/no question, proved acceptable to participants.
Quality-of-life and capability well-being measures
EuroQoL measure of quality of life
Responses to each level of all domains of the EQ-5D-3L are shown in Table 28. The majority of responses are in the level 1 (no problems) category across all five attributes, with the exception of the attributes ‘pain and discomfort’ and ‘anxiety’. These two are the only attributes that report higher responses in values in the level 2 and 3 categories (some/extreme problems). The EQ-5D-3L health index and visual analogue (VAS) values for each treatment group at baseline and follow-up are shown in Table 29. Table 29 shows that the EQ-5D-3L index values from baseline to follow-up are in the range 0.67–0.79 across control and intervention groups. These index and VAS values are slightly lower than the population norms reported for this age group. 126
| EQ-5D-3L dimension | Baseline, n (%) | Follow-up, n (%) | ||
|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |
| Mobility | ||||
| No problems | 24 (0.67) | 54 (0.75) | 22 (0.69) | 35 (0.76) |
| Problems | 12 (0.33) | 18 (0.25) | 10 (0.31) | 11 (0.24) |
| Self-care | ||||
| No problems | 33 (0.92) | 66 (0.92) | 25 (0.78) | 45 (0.98) |
| Problems | 3 (0.08) | 6 (0.08) | 7 (0.22) | 1 (0.02) |
| Usual activities | ||||
| No problems | 25 (0.69) | 56 (0.78) | 21 (0.66) | 36 (0.78) |
| Problems | 11 (0.31) | 16 (0.22) | 11 (0.34) | 10 (0.22) |
| Pain/discomfort | ||||
| No problems | 10 (0.28) | 37 (0.51) | 13 (0.41) | 26 (0.57) |
| Problems | 26 (0.72) | 35 (0.49) | 19 (0.59) | 20 (0.43) |
| Anxiety | ||||
| No problems | 21 (0.58) | 38 (0.53) | 19 (0.59) | 27 (0.59) |
| Problems | 15 (0.42) | 34 (0.47) | 13 (0.41) | 19 (0.41) |
| Baseline | Follow-up | |||
|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |
| EQ-5D-3L VAS | ||||
| Mean (SD) | 62.86 (20.49) | 65.29 (18.02) | 67.97 (18.56) | 73.89 (16.07) |
| Median (25th–75th) | 65 (57.5 to 75) | 65 (60 to 77.5) | 70 (60.5 to 80) | 80 (65 to 80) |
| EQ-5D-3L utility index | ||||
| Mean (SD) | 0.71 (0.28) | 0.79 (0.22) | 0.67 (0.36) | 0.79 (0.25) |
| Median (25th–75th) | 0.73 (0.67 to 0.92) | 0.8 (0.73 to 1) | 0.8 (0.59 to 1) | 0.85 (0.73 to 1) |
ICECAP-A measure of capability well-being
The ICECAP-A instrument feasibly identified and measured responses across all levels of capability well-being across the control and intervention groups. The highest percentage of responses typically lie in level 3, with few responses in level 1 (see Appendix 9). These results reveal that the ICECAP-A instrument is able to distinguish between different levels of self-reported capability well-being in this population group. No data were collected for the domain ‘love, friendship and support’. This question had been omitted from the questionnaire in error.
Summary of health economics feasibility findings
The aim of this feasibility study was to assess procedures, validity and reliability of tools, estimation of the recruitment rate, and prior estimation of parameters such as the variance of the outcome variable. 127 The resource use patterns were similar between the groups; the main items of resource use were GP, practice nurse, physiotherapist, A&E and hospitalisations. In reviewing the data, three cases had outlier cost as a result of hospitalisation. Such outlier observations can have a strong influence on the results of an economic evaluation. The cost of lifestyle activities in the 3 months prior to follow-up was in the range £50–55. The mean weekly cost of food and drink at follow-up was in the range of £75–100 across both groups, with the majority of food expenditure on groceries, followed by meals out, takeaways and alcohol spend. This pattern was the same across both groups at baseline and at follow-up.
The EQ-5D-3L and VAS and utility index values reported values on the lower end of typical ‘healthy population’ values when compared with published population norms126 and revealed expected variation in values between the measures, with the VAS (non-preference weighted) reporting lower values. There were no implausible data for the EQ-5D-3L. An improvement is observed in both groups for EQ-5D-3L. Given the high completeness rates, the EQ-5D-3L appears to be an appropriate tool for detecting changes in quality of life in a weight loss intervention. As above, although data for the ‘love, friendship and support’ domain of the ICECAP-A questionnaire were accidentally omitted, all other ICECAP-A domains were collected correctly, with no implausible data.
The appropriateness of the data collection method was assessed by completion rates, missing data and implausible values. Response rate at baseline was high, with only one and four participants in the control and intervention groups, respectively, not completing questionnaires. Loss to follow-up was seven (22%) and four (12%) for cost data and outcome data, respectively, in the control group (n = 32), and 23 (31%) and 17 (23%) in the intervention group (n = 73). At follow-up, some participants in both groups were ‘at risk of dropping out’; these participants agreed to complete a shorter follow-up (minimum data set) over the telephone (n = 14). These participants completed the EQ-5D-3L, ICECAP-A and food/grocery expenditure, but did not include the additional CRF questions linked to resource use. However, loss to follow-up was not specific to the health economic aspect of the study. Implausible values in our results regarding resource use and outcome measures were not identified. Data were collected by interview, so the participants who attended an interview responded to all questions; however, one challenging issue for data processing was blank responses in the questionnaire. For many responders, if their response was ‘no’ or if they had used no resource they left the response section blank; this blank response can be misleading with respect to the type of missingness, so a re-design of this section is advised for any future study. Such a re-design would involve asking the participant to write answers for responses such as ‘no’ or ‘not applicable’ or adding a zero value. Some data for ‘other health staff’ were collected using open-ended questions and in some cases the exact meaning of the response was unclear. In the design of a full study, the questions should not be open-ended.
Overall, the results of the health economics feasibility study showed that the questionnaires designed for measuring resource use, lifestyle and grocery spend, EQ-5D-3L and ICECAP-A would be suitable for inclusion in a full study, with some minor re-design of the resource use questions. Although the per-participant costs of the intervention were high, this cost of development is mostly upfront. The intervention refinement and ongoing hosting in a future trial will deliver a low cost per participant intervention.
Chapter 5 Stage 2 qualitative findings
Overview
Interviews were conducted to explore participants’ experiences with the HelpMeDoIt! intervention, app and website. In addition, helpers were interviewed about their experiences of using the app and website and of providing social support to the participants. The interviews also explored fidelity, recruitment and retention, and contributed to testing the logic model as part of the study process evaluation.
Thirty-five individuals were interviewed: 22 participants and nine helpers at 6 months, and another four participants at 12 months. Only four participants were interviewed at 12 months (from a proposed maximum of 20). This was a result of challenges in contacting participants and recruiting people to complete the interview and does not reflect a decision about data saturation. Table 30 presents the interviewee characteristics. The findings are presented below in three sections: (1) interviews with participants, (2) interviews with helpers and (3) how these findings map onto the overall study objectives.
| Characteristic | Participant | Helper | Total |
|---|---|---|---|
| Time of interview | |||
| 6 months | 22 | 9 | 31 |
| 12 months | 4 | 0 | 4 |
| Total | 26 | 9 | 35 |
| Gender | |||
| Female | 19 | 7 | 26 |
| Male | 7 | 2 | 9 |
| Age (years) | |||
| 18–34 | 5 | N/A | 5 |
| 35–50 | 10 | 10 | |
| 51–69 | 11 | 11 | |
| App use | |||
| No use (0) | 9 | N/A | 9 |
| Low use (1) | 3 | 3 | |
| High use (≥ 2) | 14 | 14 | |
Findings from interviews with participants
Participant data at 6 and 12 months were combined for analysis. Thematic analysis identified five key themes and accompanying subthemes (Table 31). These will be described in turn below. Quotations from participants are identified using an identification number, gender (M/F), age in years, extent of app use, and time since randomisation (6 months/12 months).
| Overarching themes | Subthemes |
|---|---|
| 1. Contextual factors | 1.1 Relapse or previous experience |
| 1.2 Life change | |
| 1.3 Insight into self | |
| 1.4 Concern for health | |
| 1.5 Social or group norms | |
| 1.6 Barriers to lifestyle change | |
| 2. Software and barriers to use | 2.1 The HelpMeDoIt! app |
| 2.2 The HelpMeDoIt! website | |
| 2.3 Barriers to using the app | |
| 3. Mechanisms of change | 3.1 Goal-setting and self-monitoring |
| 3.2 Motivation | |
| 3.3 Social support | |
| 3.4 Diet and physical activity | |
| 4. Impact of the HelpMeDoIt! intervention | 4.1 Change in behaviour |
| 4.2 Change in weight | |
| 5. Study- and intervention-related insights | 5.1 Data collection tools |
| 5.2 Retention strategies | |
| 5.3 Recommendations and suggestions | |
| 5.4 Negative aspects of study | |
| 5.5 Best things about the study |
Theme 1: contextual factors
Participants described contextual factors that influenced their behaviour with regard to losing weight, physical activity and diet. These including the importance of social influences and their own traits and preferences. Life context was seen as influencing both past and current experience with weight loss.
Subtheme 1.1: relapse or previous experience
Participants talked about relapse and the difficulties of maintaining weight loss over time, as well as a history of trying different approaches to weight loss:
. . . over the years I’ve sorta tried an awful lot of things. I’ve had hypnotherapy, I’ve gone to women’s clubs, slimming clubs, I’ve had lots of ways that I’ve been trying to lose weight.
122, F, 59 years, no use, 6 months
Subtheme 1.2: life change
Substantial life change, especially around jobs, could influence participants’ weight:
My main thing was I was walking 15 mile a day to and from work and then I changed jobs and that went from 15 miles to nothing since November, so since November I’ve put on a stone.
076, M, 56 years, no use, 6 months
Subtheme 1.3: insight into self
Participants commented on how their mood and personality traits or preferences might affect their decisions around healthy lifestyle choices:
It might be appropriate to know just in general that I am often very angry . . . that angriness seems to be very related to the way that I eat.
124, F, 59 years, no use, 6 months
Subtheme 1.4: concern for health
Some participants explained how concerns about their health influenced when they exercised and why they started exercising:
I was diagnosed with type 2 diabetes . . . You go along to the doctor and basically first thing they say is that it’s your weight. If you lost all this weight, everything will be hunky-dory [laughing] and you will be able to do everything you would love to do.
023, F, 60 years, high use, 6 months
This woman describes the reasons why she wanted to lose weight, specifying that her appearance was not a driving factor:
I know some people who are much more kind of, em, focused on their look and their appearance and things but, ya know, I’m somebody who doesn’t use hair product in the hair, ya know, it’s just . . . it just doesn’t, it’s not that important. It would be for health reasons.
007, F, 45 years, high use, 6 months
Subtheme 1.5: social or group norms
Participants commented on how social or group norms can influence their ability to make healthy lifestyle choices. They were most affected by family and workplace norms around eating:
I’ll just say, ‘Well, I’ll have a cup of tea’. And then they’ll give me a cup of tea and the cake with it. And they’ll say, ‘Oh just have it, we can’t eat all of them’.
119, F, 53 years, high use, 6 months
Subtheme 1.6: barriers to lifestyle change
In addition to discussing barriers to using the app, participants provided insight into barriers to making healthy lifestyle change and otherwise engaging with the HelpMeDoIt! intervention.
Contextual/environmental barriers
Participants spoke about contextual or environmental factors, such as the weather, the workplace, lack of routine, injury, and the cost of gym memberships, which contributed to difficulties in maintaining healthy lifestyle behaviours:
When I am on a routine it works fine, I seem to kind of drop a couple of pounds every week, you know, at lunch time I’ll have a light dinner and so on. If I’m careful with the amount of wine I drink then it’ll come down and I also get exercise as well. I do walking as a part of exercise, but it’s difficult when I am on the road, which is probably about 70% of my time, really.
015, M, 64 years, high use, 6 months
The price of food, and the time it could take to prepare healthy food, tempted individuals to make unhealthy purchases instead of healthy purchases:
Pound Shop sweeties are so cheap or biscuits in the Pound shop, that’s my big downfall. And it’s quick and fast, and you can eat it on the move.
053, F, 50 years, high use, 6 months
Participant-related barriers
Factors to do with self-control, willpower, wanting to eat, routines and motivation were identified as barriers to making, and sticking to, healthy lifestyle changes:
Probably another challenge would be self-control. Whenever I am sitting down, watching TV I just continue eating a lot of crisps.
064, M, 25 years, low use, 6 months
Although I eat an enormous amount, well quite a lot, I also have to be thoughtful that at the right times I’m actually eating enough so I’m not extremely hungry or you know so there’s a tension between the two things.
124, F, 59 years, no use, 6 months
Social context
Five participants felt uncomfortable having to ask people to be helpers. They were concerned that this would be a burden for helpers or wondered if they should be able to manage on their own:
. . . maybe you feel a bit guilty having to ask someone [to be a helper], maybe I should just be able to do it you know?
064, M, 25 years, low use, 6 months
A small minority of participants said that they did not have people in their social network whom they felt they could ask to take on the task of helping them make lifestyle changes. These participants were usually worried that their potential helpers had too much going on to ask them to do something else:
I felt kind of ashamed because I couldn’t come up with a friend to help me do it. I have friends but nobody that I felt that I could call on to do this sort of thing. This seemed to be a very difficult thing . . . my daughter works 12-hour days, she’s really tired, my stepbrother is in Canada, erm you know he also gets tired, and I don’t . . . yeah, I don’t know someone that I feel I could ask for that kind of day-to-day [support].
124, F, 59 years, no use, 6 months
Theme 2: software and barriers to use
Subtheme 2.1: the HelpMeDoIt! app
Participants were asked for feedback about the HelpMeDoIt! app. Feedback covered the design of the app (i.e. how it was set up and how it looked) and the functionality of the app (i.e. how it worked).
Design of the app
We asked participants what they thought of the app design, and most gave positive feedback. Part of the app design included push notifications and reminders to thank helpers or to remind participants to update their goals. Most participants valued the reminders and said that they were an important part of engaging with the app and helping them adhere to their weight loss goals:
I do like the reminders coming up . . . as well as weight loss tips and things.
053, F, 50 years, high use, 6 months
Functionality of the app
Some participants reported that the app was easy to use right away but others found it more challenging and requested further guidance. For example, using the app to set goals was difficult for some participants:
I didn’t find it easy [laugh]. No, because it was asking you to set a target and then it told you to change your target. And I didn’t understand what weekly targets were and what daily targets were. It wasn’t clear for me what I was doing.
043, F, 61 years, high use, 6 months
Regarding push notifications, one participant suggested it would be better to set the default push setting to ‘on’. As most participants wanted push notifications, we made this change. There were a number of initial technical problems with the app that affected some participants’ ability to use it. Some of the discussion around functionality centred on these technical issues, which are reported separately under the ‘barriers’ theme below.
Subtheme 2.2: the HelpMeDoIt! website
Participants did not access the website regularly. Many participants reported looking at it once or twice, while others did not use it at all. However, a couple of visits to the website is likely all that is needed to give the participants the information they need. The app also delivered some of the key website information via daily messages and push notifications. Some participants did not realise there was an accompanying website. Individuals who did visit the website often did not return for subsequent visits, either because they forgot about it or because they did not feel that they needed the information again:
I didn’t see any point in going back onto the web page tae tell me tae go tae the gym . . . I think if sometimes if you were feeling that you needed a wee boost, the web page could’ve been a wee bit helpful. The other stuff on the webpage was OK, but it wasnae for me.
080, M, 61 years, no use, 12 months
The majority of participants who did visit the website provided positive feedback:
. . . it was quite friendly. I liked the clean interface. Sometimes I can get annoyed with websites that are overly complicated, but that one’s quite clean. I liked it.
032, F, 37 years, high use, 6 months
I just liked the whole idea that you could go in [to the website] and it wasnae preaching to you, ‘You will lose weight’. It was kinda doing it in a fun way that, you know, you thought, ‘Well, aye, maybe . . . that’s quite a good idea’.
167, F, 49 years, high use, 12 months
Subtheme 2.3: barriers to using the app
We explored participants’ barriers to engaging with the HelpMeDoIt! app.
App-related barriers
Participants’ barriers to engaging with the app primarily revolved around technical problems with the app when it was first implemented. Despite a 3-month testing period prior to launch, the software company continued to resolve many ongoing technical issues and software bugs during the initial months of the intervention (see Chapter 6). Problems for participants included difficulty downloading the app, the app not remembering login passwords, and other issues highlighted in the quotes below. The majority of these issues were resolved, after which participants were more likely to give positive feedback about the app, especially related to features that did not initially work, such as push notifications. Several minor issues were not resolved for several participants, as the app was otherwise working well for them, and we were keen to avoid new software bugs:
. . . it [the app] made me set up more goals and then when I was hitting the back button it would send me back through all the forms I completed for the previous goals.
161, M, 38 years, no use, 6 months
I think the worst part was probably being quite frustrated with the app at first, and that probably led me not to use it as much because there wasn’t really any point in using it because I couldn’t really do anything with it at first, and then I think I got more correspondence just after Christmas about it and reset it and everything and it was working much better after that so, but I think if the app had been better at first I might have you know used it more often if that makes sense?
150, F, 41 years, high use, 6 months
Beyond technical problems with the app, a minority of participants had other criticisms.
. . . it was just so basic . . . I think because things are so sophisticated these days it was kind of childish.
063, F, 53 years, high use, 6 months
The HelpMeDoIt! app seemed a little old-fashioned and so I thought it would be a bit better.
064, M, 25 years, low use, 6 months
Participant-related barriers
A small number of participants admitted that their reasons for not engaging with the app had more to do with themselves, rather than the app. For example, they were embarrassed to share their eating habits with helpers, had low confidence in their ability to make lifestyle changes, were not very good with technology, or were embarrassed to start using the app again after a long period of non-use:
I haven’t done it for so long and I’m thinking I don’t want to look as though I am just starting this again.
120, F, 69 years, high use, 6 months
So though even discussing like even putting in just people in the app to me meant eventually I would have to get in touch with them about why I’ve been binging, to not eat and erm like it just felt, no, I just couldn’t and I just couldn’t picture myself doing it.
161, M, 37 years, no use, 6 months
Helper-related barriers
Participants occasionally reported that it was their helper who was having problems engaging with the app. This was sometimes because of technical problems with the app, or because helpers felt that they had received no incentive to provide support:
. . . she [helper] just thought it [the app] wasn’t really much . . . she didn’t think there was anything about it that would help her, like giving her an incentive to lose weight, or giving her any incentive to help me lose weight. So she just wasn’t impressed, that’s what her words were.
043, F, 61 years, high use, 6 months
Some participants found it challenging when their helpers were not giving feedback through the app:
I had problems initially . . . so I think maybe that put me off a bit and also the fact that I wasn’t getting any feedback from my friends.
063, F, 53 years, high use, 6 months
One participant felt that it was difficult to ask the helper to use the app:
Finding a helper is not challenging, but kind of telling the helper to use the app and monitor the app as well it is probably a bit difficult and a bit different to just having a chat.
064, M, 25 years, low use, 6 months
Other technology-related barriers
Barriers to using the app were sometimes outside the control of the study team, including problems with participants’ phones, such as insufficient memory or needing to replace a phone.
Theme 3: mechanisms of change
Subtheme 3.1: goal-setting and self-monitoring
Two main features of the HelpMeDoIt! intervention were goal-setting and self-monitoring. Most of the interview participants who logged in set goals using either the template or the custom goals feature. Only one participant said that they had not set goals. Participants discussed goal-setting using the app, the kind of goals they had been setting, and what was or was not working for them. Participants made goals for weight loss:
My goal was to be under 20 [stone]. I have been under 20 for the last 3–4 years. So my goal was to be back under 20 by Christmas. By the time of the end of the study I would like to be under 18 stone.
015, M, 64 years, high use, 6 months
A few participants said that it was easy to forget their set goals as they did not receive reminders from the app to update them. This mainly affected participants early in the intervention when technical issues prevented participants from receiving reminder messages. This issue was resolved by the software company:
I would forget that the goals, because the goals you have to set manually and maybe people because we are busy we will forget, we may forget so it could be good if like the app could have like a reminder.
074, F, 34 years, low use, 6 months
Most participants liked the template goals that were included in the app, for example ‘stand more – when watching TV I will stand up at each advert break’:
I thought the goals that were already inputted were quite good ideas, so I quite liked them and it was quite easy to add your own if you wanted to.
150, F, 41 years, high use, 6 months
Most participants set goals and monitored progress towards their goals via the app. They liked being able to monitor their progress towards multiple goals at the same time. They also said that they used self-monitoring outside the app, such as weighing themselves regularly. Feedback from those who did record their weight on the app suggested that progress on this was not displayed in a very engaging way.
Participants frequently made use of other devices, apps and programmes to help them achieve their weight loss goals using goal-setting and self-monitoring. These included scales, the FitBit (FitBit Inc., San Francisco, CA, USA) or other activity tracker, and food diary apps such as MyFitnessPal.
Subtheme 3.2: motivation
Motivation was an element of the intervention that was highlighted by the many participants. Motivation was identified for several different categories.
Motivation for joining the study
Many participants joined the study because they wanted to lose weight, with some explaining that they had hoped that the study would help them get started with the positive changes they wanted to make:
I was at that point where I think I had been to an away day and I felt really overweight and I just thought I need to do something.
063, F, 53 years, high use, 6 months
Motivation for lifestyle change
Participants talked about what motivated them to begin making healthy lifestyle changes. Some of the reasons included enjoying positive comments from others, wanting to be a healthier person, and avoiding the same health problems as other family members:
People were saying to me, ‘Oh, you’re losing weight, I can see it comin’ off your face’. So that was quite good.
007, F, 45 years, high use, 6 months
. . . my mum . . . she had to get operated on her stomach because she was overweight or obese I don’t know which. Really overweight and it was really bad so . . . that’s what I think and I don’t want to be like her. And my sister is getting fatter. I don’t want to become like that, I want to . . . yeah, I want to change.
074, F, 34 years, low use, 6 months
Motivation provided by helper
Participants talked about the helper as a source of encouragement and motivation to keep them working towards healthy lifestyle goals. Some found this particularly helpful when they were struggling to sustain positive changes. Motivation was also discussed by some as being reciprocal:
I would say probably me [I’m my helper’s helper] you know she will say to me, ‘Thanks for motivating me’ or ‘Thanks for saying that’ so we probably motivate each other.
063, F, 53 years, high use, 6 months
Subtheme 3.3: social support
Social support was the key aspect of the HelpMeDoIt! intervention. In the interviews we discussed helper support and other lifestyle influences within the participant’s wider social network. Participants drew a sociogram (diagram of their social network) at baseline, which illustrated the 5–10 people they were in most contact with (see Chapter 3). Participants also gave information on whether they perceived individuals in their sociogram to be healthy or likely to be a positive (or negative) influence for the participant making healthy changes. Discussion of the sociogram gave us insight into the social support available to participants and the influence of those people in their network.
Broader social context
We asked participants about their broader social network before asking for specific information about the individual(s) they had identified to be their helper(s).
We explored whether participants’ social networks had changed during the 6 months since they drew their first sociogram. Almost all participants said that their social network remained unchanged. Only two participants reported some changes, one because of a recent move and the other because of a job change. A change in the sociogram presented a change, either positive or negative, to the levels of social support received by the participant:
The sociogram thing that I done . . . a few of my supports were work colleagues who worked with me an all that, I’m away from three of them right now. But I moved jobs and I wasn’t expecting it, but I moved jobs very quickly.
076, M, 56 years, no use, 6 months
Although many participants had very good support from friends, partners, or family, about one-third of interview participants struggled to get the help that they wanted or needed. In addition, sometimes friends, families or coworkers showed a lack of support for or interest in what the participant was trying to achieve:
[Interviewer: Did you actually ask, ‘Would you help me do this’?] . . . Yeah . . . I talked to her then a wee bit . . . and then she seemed to . . . [Interviewer: OK, so even though you asked, ‘Will you help me?’ she wasn’t really interested.] . . . Nah [indicating that his wife was not interested in being his helper].
147, M, 44 years, no use, 6 months
Other times, although rarely reported, there was an active attempt to derail the participant from their healthy lifestyle goals:
They [participant’s parents] would say, ‘Ah, that wee cake, it won’t do you any harm.’ [Interviewer: So they actually encourage you to eat more?] [Laughing] Definitely or they’ll like, I’ll just say, ‘Well, I’ll have a cup of tea’ and then they’ll give me a cup of tea and the cake with it. And they’ll say, ‘Oh just have it we can’t eat all of them’.
119, F, 53 years, high use, 6 months
Support from helpers
All participants interviewed used a helper to help them achieve their weight loss goals. However, quite a few participants did not use helpers formally nominated through the app. Some participants encountered technical issues when trying to nominate their helpers and some helpers were either not technically minded or did not receive their invitations. Despite not using the app, these participant–helper pairs engaged with the concept of the HelpMeDoIt! intervention:
I didn’t take on the help through the app of a buddy, I think he [helper] were supposed to but he’s just not technology-minded, he’s just no got a clue – knows how to answer his phone and that’s it. He supported me all the way through and obviously he still supports me today.
132, F, 44 years, high use, 12 months
Yeah my auntie actually, I mean she is one of my helpers I tried to put in the app. She didn’t join, anyway she helped me to send me, we shared some pictures, some healthy food and she helped me a lot but she didn’t join the app.
074, F, 34 years, low use, 6 months
Participants usually asked someone to be their helper when they felt close to that person. In general, this was a partner, a friend or a family member, but it could also be a coworker with whom the participant got on well. Participants also considered whether their potential helper needed support himself/herself, whether the helper had time to help them, how often they met up, and whether the helper would understand what they were going through:
I think you need somebody who has walked your shoes and has an idea of what you are going through or what the difficulties can be or what you are struggling with when you might just go ‘Aaarrggghhh, I’m just going to have 10 pizzas’ you know what I mean?
171, F, 36 years, high use, 12 months
Helpers provided different kinds of support in different ways. They gave support through the app (e.g. sending ‘smiles’), by texts or telephone calls or in person. We identified three categories of support given by helpers: (1) informational, (2) emotional and (3) instrumental.
Informational help could take the form of sharing recipes or tips for weight loss and primarily involved giving the participant useful information:
[Interviewer: What would you say was the most helpful things your helpers did for you?] I would say, show me how to eat properly, like quantities of food and discover that you don’t need to be on a diet because you can eat healthy and enjoy the food.
074, F, 34 years, low use, 6 months
Much of the support that participants received was instrumental, which meant offering support in a tangible or physical way. This could be helping to pay for a gym membership, not buying or offering junk food, or supporting the participant to do more physical activity by doing an activity together:
. . . if it’s a nice day he is like ‘come on, get your shoes on’ and we go for a walk.
070, F, 63 years, no use, 6 months
Emotional help took the form of encouragement to make and sustain healthy changes. Some participants found this to be the most helpful type of support given by their helpers:
. . . one of my nominees is a health nut and she was good because she kept on at the background, you know? ‘You can do it!’ That’s, I think part of what you need when you’re losing weight is somebody tae say tae you, ‘You know, aye it’s gonnae be hard, but you’re no’ daft. You can dae it’. And that was her.
167, F, 49 years, high use, 12 months
Participants described contextual factors in the lives of helpers that influenced the helper’s ability to provide support. This usually came up when participants were discussing why they might not have received as much support from their helper as they had hoped. Sometimes participants felt that their helpers were too busy or perhaps had their own health issues to contend with:
Well, I did speak with my friend who was going to help me with it. She is quite healthy herself and she was quite interested to do it. But then unfortunately she had kind of health issues herself so I just did it all in my own.
070, F, 63 years, no use, 6 months
We asked participants if there were instances when the healthy lifestyle choices they made influenced their helpers or others. Participants talked about the mutual benefit they often felt from having a helper and that encouragement went both ways in the relationship:
Definitely I think, like, we both [participant and helper] have been trying to eat a bit more healthier and just sort of be a bit more active as well.
150, F, 41 years, high use, 6 months
Ma wee girl she eats healthier, she tracks, well she tries to keep up with what we are eating as well erm, I’d say it has had a whole effect on the family, like ma partner and ma wee girl.
132, F, 44 years, high use, 12 months
Most participants did not experience any negative aspects of helper support. Of those few who did, some had expected more help but realised that their helpers had too much going on in their own lives to give the desired level of support. Only one participant mentioned that her helper pushed a bit too much:
About the only [negative] thing is the daughter keeps insisting that she knows better than me. Like you shouldn’t be eating this or that. You are eating far too many potatoes! And I say to her, ‘Well I am allowed . . . We have been given a personal plan with an amount of calories’.
023, F, 60 years, high use, 6 months
Subtheme 3.4: diet and physical activity
All participants talked about diet and physical activity as being an important part of their healthy lifestyle change. Most participants said that they were trying to make small adjustments to their diet. Overall, there was a focus on drinking water rather than sugary or alcoholic beverages and on eating more fruit and vegetables. Participants also discussed how price, convenience and the time of day factored into their dietary choices. Many participants said that they had made small changes around eating more fruit and vegetables:
. . . [reducing] the amount of red meat that I’m eating and trying to improve ma fish and ma fruit and vegetable and that’s it.
122, F, 59 years, no use, 6 months
Alcohol, fizzy drinks and sugary drinks were regularly part of the discussion about diet:
I have tried to cut down on how much I drink, like, I mean I’m in a pub every week but . . . I’d say I’ve cut down on how much I drink. ‘Cause it used to be that I’d maybe drink, not all the time, but a beer in the house a couple nights a week, like one or two bottles and you know, I’ve stopped doing that for the most part.
032, F, 37 years, high use, 6 months
Increasing physical activity was an important part of participants’ attempts to make healthy lifestyle changes. Participants frequently increased their walking or cycling but also used classes and gyms to do more physical activity. All participants valued physical activity and believed that it was important to their weight loss goals:
I’ve started cycling to work and I don’t drive.
032, F, 37 years, high use, 6 months
I am going for walks a bit more and doing some exercise you know using the stairs as an exercise thing.
102, F, 31 years, low use, 6 months
Theme 4: impact of the HelpMeDoIt! study
Subtheme 4.1: change in behaviour
HelpMeDoIt! inspired participants to do things such as join a weight loss group, get a personal trainer, sign up for a gym, start using a physical activity tracker, and set up a weight loss challenge with family members. It inspired one woman to seek out a helper who gave her the positive support she had been missing before:
I don’t really think I had very much in the way of support. Probably sort of more the negative type, you know from people like my parents kind of nagging me, ‘oh you need to lose weight, you need to lose weight’, but that would be all that they would say really so I think it has been quite different having a helper that . . . he doesn’t ever say it about ‘oh you need to lose weight’ because you are overweight, it is more let’s sort of like try and eat healthily or let’s try and be more active, not in a negative way more in a positive way so I think that’s been a big change just having somebody kind of more positive about it all.
150, F, 41 years, high use, 6 months
Participants discussed changes had they had made in their efforts to lose weight and be healthier. Reporting actual behaviour change was more common than simply thinking about making a change or reporting a change that they planned to make in the future. Few participants had not yet implemented any actual behaviour change. Most participants had made changes to diet or physical activity, usually both:
I still binge, I mean I still enjoy food because I love food, but I have smaller portions now like and healthy amounts, switched to lentils, changed my diet slightly, things like that.
010, M, 28 years, no use, 6 months
I was cycling to work, home and back every day and I was doing at least 10 miles a day back and forth to work . . . um . . . I would say on top of that I started swimming once a week and also doing a core strength class which is like, that’s like using a bit of weight and lunges and doing some upper body strength. And then I’ve been doing Zumba on a Sunday because I like it and I’ve also started a spin class, it’s like stationary cycling. Those are kind of the three main activities I’ve added.
032, F, 37 years, high use, 6 months
Subtheme 4.2: change in weight
We asked participants if they had experienced a change in their weight as a result of making healthy lifestyle changes as part of the HelpMeDoIt! study. Many participants reported losing weight but some had not been able to maintain their weight loss, especially around the holidays. A few had not been able to lose weight and fewer still reported gaining weight:
To date I have probably lost about 2 stone . . . because you know somebody is goin’ to be comin’ out and weighing you and measuring you, so you’ve got to try and achieve something.
132, F, 44 years, high use, 12 months
I weighed myself . . . But over the Christmas period it was all back on again.
043, F, 61 years, high use, 6 months
Theme 5: study- and intervention-related insights
Participants were also asked about their views of the study evaluation methods.
Subtheme 5.1: data collection tools
The data collection tools were considered acceptable and even enjoyable. Initially we had concerns about the time it would take participants to complete the questionnaires but none said that this process was burdensome.
Subtheme 5.2: retention strategies
To optimise retention rates at 12-month follow-up, we sent all participants a newsletter at 3, 6 and 9 months post baseline. This included an update on the study, as well as evidence-based tips for weight loss. The newsletter was popular with participants. They also liked receiving thank-you vouchers, but most said that they would have participated without this incentive:
I think if it caught my eye I would have done it regardless of the vouchers but I think the newsletters it was a good way of getting people that are straying off the path to have another wee look at it.
122, F, 59 years, no use, 6 months
Subtheme 5.3: recommendations and suggestions
Most of the recommendations made related to the intervention rather than the HelpMeDoIt! study methods. Participants gave suggestions to improve the app, mostly about fixing the technical glitches in the initial roll-out. Some participants liked the idea of the app integrating with other popular fitness-related apps. A HelpMeDoIt! community was also suggested:
. . . maybe the only other thing I would say is the level of contact in the beginning was good. But I do think a little bit more, actually would be helpful. I don’t know if you could manage it, but more a sense of community, knowing how others are getting on.
032, F, 37 years, high use, 6 months
I think what would’ve been good is if you have peer support. So maybe actually rather than asking somebody outwith the study to help you, maybe having somebody else on the study to be a kind of peer support, would’ve been quite good.
007, F, 45 years, high use, 6 months
Subtheme 5.4: negative aspects of study
Negative aspects related to the intervention have been reported under Subtheme 3.3: social support, Lack of or negative social support and Subtheme 2.3: barriers to using the app, App-related barriers. Participants did not report any other negative aspects of taking part in HelpMeDoIt!. However, a few participants had misunderstood the aim of the intervention when they first joined:
I liked the title, HelpMeDoIt, I didn’t at that time fully appreciate that the ‘help me’ bit had to do with, you know, another person that I needed to find.
124, F, 59 years, no use, 6 months
Subtheme 5.5: best things about the study
Some of the participants reported that they had really benefited from having a helper:
I think the best thing has probably been my helper getting involved, I think that has been a huge help, you know . . . I think it has been good to have somebody prod you a wee bit.
150, F, 41 years, high use, 6 months
Many participants said that they liked the baseline questionnaire session at which they received their measurements:
Well the best thing about taking part in the study is when they measure us and all the information about my fat percentage.
074, F, 34 years, low use, 6 months
Other participants liked knowing that there was a follow-up session in 1 year to help keep them on track. For one participant, joining the HelpMeDoIt! study had helped him realise that he needed to make some changes:
The best thing’s been it was making me more aware . . . that everythin’ in ma life just went . . . haywire so I’d say that’s definitely the best thing.
147, M, 44 years, no use, 6 months
Findings from interviews with helpers
Interviews with nine helpers provided useful feedback on the helper aspect of the intervention. Thematic analysis identified five key themes and accompanying subthemes (Table 32). Quotations from helpers are identified using their linked participant identification number and gender (M/F).
| Overarching theme | Subthemes |
|---|---|
| 6. The helper experience | 6.1 Helper nomination process |
| 6.2 Guidance provided for helpers | |
| 6.3 Facilitating change | |
| 6.4 Impact on helper | |
| 6.5 Negative aspects of the helper experience | |
| 6.6 Positive aspects of the helper experience | |
| 7. The HelpMeDoIt! software and barriers to use | 7.1 The HelpMeDoIt! app |
| 7.2 Barriers to using the app | |
| 7.3 The HelpMeDoIt! website | |
| 7.4 Barriers to using the website | |
| 8. Helpers’ impact on participants | 8.1 Change in behaviour or awareness |
| 8.2 Diet and physical activity | |
| 8.3 Motivation | |
| 9. Social support | 9.1 Ways of interacting between helper and friend |
| 9.2 Types of support given | |
| 9.3 Context of and insights into the helper–friend relationship | |
| 10. The HelpMeDoIt! study and intervention | 10.1 Recommendations and suggestions |
| 10.2 Negative aspects of the intervention | |
| 10.3 Impact of the HelpMeDoIt! intervention | |
| 10.4 Best things about the intervention |
Theme 6: the helper experience
Subtheme 6.1: helper nomination process
Feedback about the helper nomination process was variable, with some helpers saying that it was time-consuming (which may have been related to the initial technical glitches) and others finding it to be straightforward. Some helpers could not remember what the process involved and others had agreed to be helpers without formally accepting the nomination via e-mail and app.
Subtheme 6.2: guidance provided for helpers
Views on whether or not the app/website provided sufficient guidance to the helper. Many helpers thought that the guidance provided to them by the app and website was sufficient. Not everyone had visited the website so some were uncertain about what guidance was available. However, these helpers also felt that it was easy and intuitive to actually provide help. One helper said that she would have liked more guidance (she did not realise there was a website with information on this topic).
Subtheme 6.3: facilitating change
Helpers primarily facilitated change by providing emotional support, encouraging more physical activity, joining the participant in doing activities and improving healthy eating through recipe sharing or cooking lessons:
She sits just down the corridor and me and my other colleague will say are you coming on the stair walk? We are doing a stair walk and she will usually join us. Yeah, I definitely think there is some motivation there from having some help.
Helper-027-F
I walk a lot up on the moors and that’s the benefit of having a dog. That’s why today, you know normally I would pick her up at the station but I thought, ‘No, no, it’s dry. Let her walk up’. You know. I was trying to encourage her to do more.
Helper-053a-F
Subtheme 6.4: impact on helper
Helpers said that being a helper influenced them to make healthy lifestyle changes. Some attended new fitness classes or did more walking and others improved their diet. Several helpers said that they were already leading healthy lives and that they had not made further changes as a result of being a helper:
She made me focus, possibly, on the fact that even in this stage it is really possible and it’s really good to set yourself a challenge and a change.
Helper-053b-F
. . . even from the very start this [being a helper] could motivate me as well . . . but I think if I had been able to use the app I’m pretty sure it would have motivated me that little bit more than I have been, so yeah, you know, I definitely think there is a case there of helping the helper.
Helper-027-M
Subtheme 6.5: negative aspects of the helper experience
Most helpers reported no negative aspects of being a helper. Among the comments made, most were about initial problems with the app (which are described under the ‘Barriers/App/App-related’ theme). One woman said that it was difficult for her and her son to get their participant active and engaged in making changes:
I think that my son and I are frustrated, my son goes to the gym four or five nights a week and he is frustrated with his dad [participant], they were talking about joining the gym and going with him and I think once they sign up for the gym rather than the money going to waste because they’ve already paid for that, I know that will be an incentive for [participant’s name] to actually go to the gym.
Helper-076-F
Another participant struggled with knowing how to support change in her partner, who experienced depression. She also described the struggle to help her partner eat better. She said that she cooked healthy food from scratch using lots of vegetables but still could not make her partner eat more healthily:
I’m still cooking, I can hear the rustling of the crisp bags cause he’s at his desk at his computer or he’ll eat a bag of Skittles and he’ll eat crap, before I can even get the dinner out. I can’t control any of that.
Helper-097-F
Subtheme 6.6: positive aspects of the helper experience
Helpers described how happy they were to have supported healthy lifestyle changes in their friend and contributed to their success. They felt good knowing that they had been trusted to help:
I think it’s nice to know that that person kind of trusts you to be supportive and have access to kind of their personal information in that way.
Helper-032-F
Theme 7: the HelpMeDoIt! software and barriers to use
Subtheme 7.1: the HelpMeDoIt! app
Design and functionality
We received limited helper feedback on the app. Several of the interviewed helpers did not use the app because of initial technical problems in attempting to download or use it; these issues are described in the section ‘Barriers/App/App related’. Most helpers provided support outside the app.
Goal-setting and self-monitoring
This helper liked the idea of being able to see her mother’s goals as it helped her follow up as the helper:
I think it is good to be able to see if they have completed their goals because then you’ve got, you know, if I can see it then I can text her and say, ‘Right mum, you’ve no done this, chop, chop’. Whereas if I couldn’t see it then she could just say, ‘Oh yeah I did that’. I mean, she just might not have inputted it but no I think that’s good to see the goals.
Helper-119-F
Messaging
Helpers liked the idea of receiving reminders from the app regarding progress and rewards received by their friend. Push notifications went directly to helpers’ phones to notify them of relevant updates. Lack of notifications was an initial technical issue affecting some helpers. This was later resolved by the software company.
Patterns of use
Patterns of use among helpers varied from no use to regular use. Initial technical issues prevented helpers from using it more regularly:
Yeah, it’s hard to say on average. I think the first few weeks I was certainly using it once a day.
Helper-032-F
Positive aspects of the app
Helpers liked the concept of the app and thought it could help participants if the technical issues could be minimised:
. . . I think the app is still that something, that little extra, you know, you can go that little extra mile with it.
Helper-027a-F
Subtheme 7.2: barriers to using the app
App-related barriers
Helpers cited initial problems with the app, including problems logging on, the app not remembering their assigned unique ID, the app being very slow, problems sending smiles, and push notifications or messages from the app coming in repetitively or sporadically. The helpers who downloaded the app said that they would have used it more if it had functioned better. We did not interview any helpers who used the app after the technical issues had been resolved (this was because of the ethical constraints on contacting helpers):
I couldn’t actually log on, it wouldn’t hold the information and every time I tried to go onto the HelpMeDoIt! app it wanted me to enter my unique ID so unless I had memorised it I’d have to go back to the original e-mail that told me that.
Helper-053b-F
Participant-related barriers
Helpers found it difficult to engage with the app if their friend was not also engaged:
. . . when she wasn’t using [the app] that much then I didn’t use it quite as much . . . Perhaps if I’d seen more activity more progress, em I would have definitely kind of been more active myself I think on the app.
Helper-032-F
Helper-related barriers
A few helpers admitted to not being very experienced or interested in using technology and apps:
I’m not intae gadgety technology . . . I cannae think of an app, an actual app that I use on my phone. I use it for calling, texting.
Helper-027b-M
Other technology-related barriers
As with participants, a few helpers said that they did not have the storage on their phone to get the app. In some phone models, typically older Android phones, the app did not work well.
Subtheme 7.3: the HelpMeDoIt! website
Most helpers did not use the website, while others used it at the very beginning once or twice. High use of the website was not anticipated, as once helpers had read the guidance they did not necessarily need to revisit. The reasons for not using the website are reported in the ‘Barriers/Website’ section below. Among those who did see the website, comments were neutral or positive, with some helpers admitting that they did not remember much about it:
I went into it initially to look at it and . . . I think the whole concept of it is a really good idea.
Helper-053b-F
Subtheme 7.4: barriers to using the website
There were many similarities between participants and helpers in terms of the barriers to website use. As with participants, low website use was reported by helpers. Some helpers felt that they got the information they needed from the website from one visit. However, there was not a lot of awareness among helpers about the website content or how it could be helpful. If a helper was not engaged with the app, they tended to not use the website. Some helpers said the need for their password, tucked away in an old e-mail, was a barrier to accessing the website.
These two helpers described why they did not use the website:
I think because it’s mostly, or that I felt that it [the intervention] was mostly an app-based exercise if you like.
Helper-027a-F
I didn’t really go back to the website. And I think I understood, I understood what it [the intervention] was all about.
Helper-053b-F
Theme 8: helpers’ impact on participants
Subtheme 8.1: change in behaviour or awareness
Helpers mentioned that they had observed changes in the behaviour or awareness of their friends, such as being more active and making a conscious effort to improve their diets:
We probably did [attempt lifestyle changes] to a certain extent but I think using the app made us both aware of what we do on a daily basis, you know. [Interviewer: So you did a little but it maybe brought it more to the front of your mind?] Yes, and just added that little bit of motivation perhaps.
Helper-027a-F
Subtheme 8.2: diet and physical activity
Helpers reported a number of ways they supported their friends with healthy eating and physical activity, including sharing recipes, teaching healthy cooking, buying fresh fruits and vegetables and avoiding junk food in the house, preparing healthy meals, and going for walks together. Helper and friend accounts were similar.
Subtheme 8.3: motivation
Helpers talked about motivation and the role it played in facilitating change. They believed that their help contributed to their friend’s motivation to make healthy changes. Many helpers found that they were more motivated to eat well and be active themselves because of their role:
Being a helper, I think it kind of motivated me to continue doing my walking and doing my healthy eating in order to get [participant’s name] to go with me.
Helper-076-F
Theme 9: social support
Subtheme 9.1: ways of interacting between helper and friend
We asked helpers how they preferred to communicate and engage with their friend. Helpers usually used a combination of text, phone, app, and in-person meet-ups. The distance between friend and helper was a major determinant of how they chose to keep in touch.
Subtheme 9.2: types of support given
Helpers reported giving types of help that we categorised as informational, instrumental or emotional. The following quotations are examples of each of those three types of support, respectively:
I was happy to e-mail her recipes.
Helper-053a-F
Yeah, yeah, well, I’d go over to her house and say, ‘Come on!’ and we’ll go for walk.
Helper-027-M
I tend to usually go into it [the app] kind of after she’d been to the gym or kind of done something along those lines, you know, and send her one of the stickers [smiles]. Kind of a ‘Well done’ or ‘Keep going’ type of thing.
Helper-150-M
Subtheme 9.3: context of and insights into the helper–friend relationship
There was a fine balance for some helpers as to how much advice they could give their friend, especially when their friend was also their partner. One helper felt that being part of the HelpMeDoIt! intervention made their partner more receptive to gentle encouragement and advice. Part of being a good helper was understanding the person they were trying to help and working within the constraints of that relationship. Helpers also acknowledged that if they lived with the person they were helping that factors into how much and what type of support they can give:
[Interviewer: . . . the first thing you said, was it that sometimes it was difficult . . . to provide help?] Yeah, because you know, let’s not eat this because it is not healthy and not good for us, and he gets fed up of me keep telling him what to do. You have to get a balance.
Helper-076-F
Helpers had further insights into the relationship between the helper and participant and how this might affect the ability for success:
I was really well supported by my husband and that really showed me that if you are supported by someone it can absolutely make a difference to do something, to have the power to do something to help yourself.
Helper-053b-F
Theme 10: the HelpMeDoIt! study and intervention
Subtheme 10.1: recommendations and suggestions
We received a range of recommendations from helpers. Most of these comments were about the HelpMeDoIt! app. For example, they wanted the app to remember their assigned password, to receive an app notification when their friend achieved a goal, to have more example goals and to have automatic syncing with FitBit or other activity trackers, and one helper suggested that the friend’s weight be hidden and only weight change be visible to helper. Finally, one helper had this to say about the app and encouraging messages:
Almost having somewhere where you can record progress and you can, you know . . . everything or your messaging is kind of captured in the app. Then if somebody is logged in and feeling a little bit low then they can maybe look back and see all the encouragement and support that they’d had from people at one point.
Helper-032-F
Subtheme 10.2: negative aspects of the intervention
Feedback from helpers was mostly very positive. When helpers described negative aspects of the intervention, these mostly revolved around the initial technical glitches in the app, which were most pronounced at the beginning of the study. One helper said that it could sometimes be challenging to encourage their friend (their partner in this case) who might be negative:
When you are trying to say to him or advise him not to eat certain stuff he would moan you know, ‘But I want to eat it!’ kind of thing.
Helper-076-F
Subtheme 10.3: impact of the HelpMeDoIt! intervention
Helpers believed that the intervention made them and their friends more aware of their healthy lifestyle behaviours and also influenced helpers themselves to be healthier. One helper said that the intervention had made her partner more receptive to following her advice and encouragement and reported that the whole household was eating more healthily as result of her partner participating in the study:
I don’t know if he [participant] would have listened to me if he hadn’t been taking part in the study, because I have always been a healthy eater and always been very active . . . I think the fact that [participant’s name] was doing the programme with yourself encouraged him to try and be active and do healthy eating and . . . before getting on the programme he wasn’t keen to do it alongside me.
Helper-076-F
Subtheme 10.4: best things about the intervention
Helpers had many positive things to say about the HelpMeDoIt! intervention. They enjoyed making healthy lifestyle changes along with their friend. They liked the idea of the app and helping their friend make healthy changes. Helpers believed that being part of the intervention helped their friend become and stay motivated to make positive changes. Helper–friend pairs who were also partners felt that the HelpMeDoIt! intervention had helped them become closer:
I think it’s probably brought us close together. I just . . . having her being, I don’t know, I hate using the word ‘journey’ but this kind of ehh kind of following her goals to kind of lose weight and get fitter I think it’s because I’ve been her helper and she’s been doing the same for me as well. It’s . . . I’d say it’s certainly brought us a bit closer.
Helper-150-M
Further exploratory analysis
For those interview participants with follow-up data (n = 21), we compared those who lost weight (n = 14) with those who had gained weight (n = 7) to explore whether or not there were differences in their accounts. The interview participants who lost the most weight (8–19% of their body weight) reported receiving excellent social support from more than one person in their social network. Many said that they had a strong helper or two but also reported getting support from other family members or friends. They usually described receiving all three types of social support: emotional, instrumental and informational.
Participants who lost the most weight (≥ 5% of their body weight; 7/14) also reported rigorous diet and physical activity-related goal-setting and self-monitoring, usually relying on more than one app (e.g. MyFitnessPal) or device (FitBit or another pedometer) and participating in weekly weigh-ins in a group setting [e.g. Weight Watchers (New York, NY, USA)]. These participants were also more likely to engage with the HelpMeDoIt! app for longer, despite technical problems that eventually led them to taper their use and move to apps that functioned more smoothly. Participants who lost more weight typically said that they had joined the study to be healthier rather than simply to lose weight.
Participants who gained weight (n = 7) also reported some good social support but a few described a lack of, or a change in, social support in some aspect of their life. For example, one woman who gained weight said that her nominated helpers had a significant language barrier and that they did not engage with the app or the idea. One male participant described having great support from his wife and son but said that he had recently changed jobs, which prevented him from walking as much and had removed him from supportive coworkers. Another participant who gained weight reported making goals, monitoring them, and having a helper who was supportive. However, this participant had recently moved to a new city so he did not have as much support as he was used to, had some difficult and unsupportive family members, and said that his goals differed quite a bit from those of his sole helper, who was also a workout buddy. Among participants who gained weight, one said that he never used goal-setting or monitoring, another said that he focused on diet only and not on physical activity, and another said that she regularly forgot to set goals. Participants who gained weight were more likely to say that they had joined the HelpMeDoIt! study because their GP suggested it.
Participants, whether they lost or gained weight, said that they faced barriers to making healthy lifestyle changes, but these were more pronounced in the participants who gained weight, who were less successful in finding workarounds for their barriers. One woman did not like doing things by herself, but her helpers had too much going on to exercise with her and she was unable to find other helpers. Conversely, participants who lost weight said that they tried other ways to find the support they needed, such as joining a weight loss group that met in person or online (e.g. on Facebook). Similarly, both gainers and losers said that motivation to implement and maintain healthy lifestyle changes was a challenge, but participants who lost weight found ways to sustain that motivation, usually by using a supportive helper or community (e.g. a Facebook weight loss group). Similar life contextual factors were identified by weight losers and gainers. These included health issues, habits and past experiences of trying to lose weight.
Mapping the qualitative themes to the HelpMeDoIt! study objectives
We mapped themes from our qualitative interview analysis onto our HelpMeDoIt! objectives (Table 33) to illustrate how the data helped answer the study objectives.
| HelpMeDoIt! objectives that qualitative interviews aimed to address | Addressed by participant themes . . . | Addressed by helper themes . . . |
|---|---|---|
| 1. To develop an internet- and app-based intervention that enables participants to set and monitor goals and facilitate effective social support | 1, 2, 3 | 6, 7, 8, 9 |
| 2. To investigate recruitment and retention as well as feasibility and acceptability of the intervention | 5 | n/a |
| 3. To explore the potential of the intervention to reach traditionally ‘hard to reach’ groups (e.g. lower socioeconomic groups) | 4 | 6 |
| 4. To explore the barriers to and facilitators of implementing the intervention | 1, 2, 3 | 6, 7, 8, 10 |
| 5. To assess the feasibility and acceptability of different outcome measures for diet and physical activity in this population | 5 | n/a |
| 6. To use outcome data (diet, physical activity, BMI) to help decide on a primary outcome and to estimate the potential effect size of the intervention to facilitate the calculation of an appropriate sample size for a full trial | n/a | n/a |
| 7. To assess data collection tools and obtain estimates of key cost drivers to inform the design of a future cost-effectiveness analysis | n/a | n/a |
| 8. To investigate how participants and helpers engage with goal-setting, monitoring and social support using new technologies and how these elements interact within a behaviour change intervention | 1, 2, 3 | 6, 7, 9 |
| 9. To develop a conceptual model of how the key mechanisms of goal-setting, monitoring by self and others, social support and behaviour change are facilitated by the intervention | 1, 3, 4 | 6, 7, 8, 9 |
| 10. To test the logic model and theoretical basis of the intervention in stages 1 and 2 | 1, 3, 4 | 7, 8, 9 |
| 11. To explore the characteristics of participants’ social networks and the influence social networks have on participant experiences and outcomes of the intervention | 3 | 9 |
| 12. To assess whether or not an effectiveness trial is warranted | 4, 5 | 8, 10 |
Summary of interview findings
Although there were issues with both helper and, to some extent, participant engagement with the app, partly due to technical issues that were subsequently resolved, overall the social support concept of the HelpMeDoIt! intervention was well received. Both participants and helpers engaged with the idea of having a helper, or being a helper, even if they were unable to do so via the app.
A different level of app engagement was observed between participants and helpers. Participants, who were enrolled into the study, spent more time trying to make the app work and feeding back problems they had with it. Helpers were less likely to try as hard to make the app work and were happy to provide support as helpers even if they did not access the website or download the app.
Helpers enjoyed the role of supporting their friend in making healthy lifestyle changes and felt flattered to have been asked. Different types of support were given by helpers, including instrumental, informational and emotional. Participants seemed to benefit most from emotional support and encouragement. Participant–helper pairings between partners were usually beneficial, although helpers in these situations were more likely to report not always knowing how much to push their partner and dismay over their partner continuing to make less healthy decisions, which they were more aware of because they lived together.
There were differences between interview participants who lost weight and those who gained weight in terms of social support, goal-setting and self-monitoring. In general, the participants who lost the most weight had excellent and varied social support and were enthusiastic about and consistent with goal-setting and self-monitoring. Participants who lost or gained weight had many similarities in motivation, barriers and life context. However, individuals who lost weight found ways to work around barriers, lapses in motivation and life contextual factors, compared with participants that gained weight.
The findings from participants and helpers have identified several key issues for us to consider in a future study. These include ensuring that the app functions effectively on a large scale prior to implementation, having better signposting to the guidance and information on the accompanying website and continuing to provide the positive features that engage participants and helpers with each other. The interview data also addresses questions related to the programme theory and mechanisms of change of the intervention. These are considered further in Chapter 6.
Chapter 6 Process evaluation findings
The process evaluation employed mixed methods to provide insight into the programme theory, logic model and evaluation design. Qualitative data presented in Chapter 5, and some quantitative data presented in Chapter 4, informed the process evaluation. Data are presented below in relation to (1) intervention-related findings on context, fidelity, exposure, reach, programme theory and logic model; and (2) evaluation design-related findings on recruitment, retention, contamination and researcher insights. A summary of how these findings address the HelpMeDoIt! progression criteria is presented in Chapter 7.
Part 1: intervention-related findings
Contextual factors
Contextual factors influencing the effect of the intervention include (1) the context in which the intervention itself takes place and (2) contextual factors that have either a negative or a positive impact on various pathways of the intervention (see Figure 4).
The HelpMeDoIt! intervention was designed to be implemented with minimal contact with the study team or health professionals, so it was delivered as an app and accompanying information website. The HelpMeDoIt! app was designed for use on both the Apple (Apple, Inc., Cupertino, CA, USA) and the Android (Google, Google Inc., Mountain View, CA, USA) operating system. Slightly more than half of participants used Android software (n = 38, 52%) on numerous different versions of smartphones (e.g. Samsung, LG, Huawei), and the remainder used Apple operating systems on iPhone devices (Apple Inc., Cupertino, CA, USA) (n = 35, 48%). The HelpMeDoIt! website was accessible from smartphones, desktop computers or tablets. Of those who accessed the website (n = 55), the majority of participants used a desktop computer (n = 35, 64.1%), followed by a smartphone (n = 17, 30.6%) and a tablet device (n = 3, 5.4%).
Contextual factors influencing the intervention have already been described in Chapter 5. In brief, these included (1) participants’ previous experience of weight loss and relapse; (2) significant life change, such as new job or moving house; (3) the influence of personality traits and mood; (4) influence and/or motivation of health issues; (5) social and group norms; and (6) multiple barriers to lifestyle change, for example environmental, participant-related, helper-related and/or social context barriers.
Fidelity of delivery of the intervention
Although the app was tested for a 3-month period using a testing group, some technical issues arose when it was initially launched via the app stores. The testing phase used a third-party platform allowing the app to be test-run before it was submitted to the app stores for release. This helped identify numerous bugs, which the software company resolved. There was no built-in testing phase after the app was available for download from the app stores. This unfortunately resulted in many technical issues being detected after the app had ‘gone live’. The majority of technical problems were associated with (1) the app crashing or working slowly because database information was downloaded to phones on each login; (2) elements of the key features not displaying correctly, which had an impact on how effectively participants could operate the app; and (3) the frequent emergence of new software bugs as a result of ‘app updates’ intended to solve previous issues. The software company had difficulty resolving software bugs for Android phones, which, unlike iPhones, are designed by numerous companies, using multiple combinations of operation systems. After several months of trying to stabilise the app, the software company carried out a ‘technical rebuild’. This did not change the content of the app but resolved the key issues and improved the overall quality of the app.
These issues had an impact on initial fidelity of the intervention being delivered as some participants were not able to access the key intervention components of the intervention via the app (i.e. goal-setting, self-monitoring and social support) and some of the app features did not work as intended. However, qualitative findings demonstrated that participants received the social support elements outside the app (e.g. meeting helpers face to face), which was in keeping with our programme theory and was not always because of technical issues but sometimes was participant and/or helper preference. Qualitative findings also indicated that some helpers did not access the website, which contained guidance on being a good helper, so they may not have delivered the social support elements as we had intended, for example using language that supported their friend’s autonomy.
Facilitators that might promote future fidelity of the intervention delivery include (1) resolving software bugs using both a ‘pre-live’ and a ‘post-live’ testing phase; (2) further streamlining the app and website based on findings from this feasibility study; (3) installation of the app on participants’ phones and a run-through with field workers at the baseline face-to-face visit (relevant for the study but not for wider roll-out); and (4) ensuring better signposting to the website.
Exposure to the intervention
As part of this feasibility study, we were interested in exploring how the intervention was used by participants and their helpers. One way of measuring this is through data use statistics; these were gathered and analysed to explore which features of the app and website were used, and how often they were used. The analysis of app and website use provided us with some meaningful insights into how the intervention was used and what elements of the intervention were potentially effective. A summary of app/website use is presented for participants in Table 34 and for helpers in Table 35. Engagement with the intervention was also explored in the qualitative work (see Chapter 5).
| Software component | Total | Range | Mean per participant (SD) | Median (IQR) |
|---|---|---|---|---|
| App use | ||||
| Number of logins | 955 | 1–408 | 17.7 (56.3) | 4.5 (2.0–11.0) |
| Number of views of main dashboard | 715 | 1–412 | 13.2 (57.1) | 1.5 (1.0–3.0) |
| Number of views of progress charts | 213 | 1–96 | 3.9 (13.7) | 1.0 (0.0–2.0) |
| Number of ‘enter your weight’ updates | 108 | 1–21 | 2.0 (4.2) | 1.0 (0.0–2.0) |
| Number of views of ‘smiles’ feature | 76 | 1–43 | 1.4 (6.0) | 0.0 (0.0–1.0) |
| Number of views of ‘rewards’ feature | 86 | 1–32 | 1.6 (5.0) | 0.0 (0.0–1.0) |
| Number of template goals created | 59 | 1–16 | 1.1 (3.0) | 0.0 (0.0–1.0) |
| Number of custom goals created | 898 | 1–143 | 16.6 (24.9) | 9.5 (4.0–18.0) |
| Number of goals deleted | 30 | 1–12 | 0.6 (2.0) | 0.0 (0.0–0.0) |
| Number of goals completed | 580 | 1–109 | 10.7 (23.1) | 3.0 (0.0–21.0) |
| Number of goals updated | 244 | 1–181 | 4.5 (24.7) | 0.0 (0.0–2.0) |
| Number of helpers invited | 45 | 1–8 | 0.8 (1.5) | 1.0 (1.0–2.0) |
| Number of uses of ‘contact helper’ feature | 27 | 1–8 | 0.5 (1.6) | 1.0 (1.0–2.0) |
| Number of smile sent to helper | 87 | 1–24 | 1.6 (6.3) | 0.0 (0.0–3.0) |
| Read summary e-mail | 150 | 1–40 | 2.8 (5.9) | 1.0 (0.0–3.0) |
| Website use | ||||
| Number of website sessions | 172 | 1–12 | 3.1 (2.6) | 2.0 (1.0–4.0) |
| Number of page views | 677 | 1–45 | 12.4 (11.1) | 8.0 (5.0–18.0) |
| Total duration of website sessions (minutes) | 372 | 1.6–43.8 | 6.8 (8.5) | 3.8 (1.2–7.5) |
| Software component | Total | Range | Mean per participant (SD) | Median (IQR) |
|---|---|---|---|---|
| App use | ||||
| Number of logins | 122 | 1–48 | 4.9 (9.5) | 2.0 (1.0–4.0) |
| Number of views of progress charts | 0 | 0 | 0.0 (0.0) | 0.0 (0.0–0.0) |
| Number of views of ‘smiles’ feature | 9 | 1–5 | 0.4 (1.0) | 0.0 (0.0–0.0) |
| Number of views of ‘rewards’ feature | 13 | 1–4 | 0.5 (1.0) | 0.0 (0.0–1.0) |
| Number of times goals viewed | 27 | 1–7 | 1.1 (1.5) | 0.0 (0.0–1.0) |
| Number of times goals liked | 21 | 1–8 | 0.8 (1.8) | 0.0 (0.0–1.0) |
| Number of uses of ‘contact friend’ feature | 9 | 1–2 | 0.4 (0.6) | 0.0 (0.0–1.0) |
| Number of smiles sent to participant | 95 | 1–46 | 3.8 (9.0) | 2.0 (1.0–3.0) |
| Website use | ||||
| Number of website sessions | 23 | 1–2 | 1.2 (0.4) | 1.0 (1.0–1.0) |
| Number of page views | 54 | 1–8 | 2.8 (2.0) | 2.0 (1.0–4.0) |
| Total duration of website sessions (minutes) | 111.7 | 1–27.3 | 5.9 (6.5) | 3.8 (2.4–5.6) |
Participant engagement with the HelpMeDoIt! app
Participant engagement with the app varied widely. Nineteen participants (26%) did not use the app at all. We assessed engagement with the app in comparison with 2017 use statistics for commercial apps, which reported that 21% of users will engage with an app only once. 94 In our study, of the 54 (74%) participants who downloaded the app, six (11%) used the app only once, 48 (89%) used it twice or more, 38 (70%) used it three times or more, and six (11%) people used it ≥ 30 times. Thus, there was greater engagement with the HelpMeDoIt! app than the current standard within the app industry.
Data use statistics explored how often participants engaged with key features of the app (see Table 34). After logging in to the app, the top five activities were (1) creating custom goals, (2) viewing the main dashboard, (3) completing goals, (4) updating goals and (5) viewing progress charts. Of the 957 goals created by participants, 94% were custom goals, compared with 6% template goals, and 61% were recorded as completed.
A key feature of the intervention was the nomination by participants of one or more helpers from their social network. In total, 19 participants (36%) invited at least one helper via the app. In total, 45 helpers were invited, ranging from one to eight helpers per participant. Of the 45 invited helpers, 25 (56%) accepted the invitation and downloaded the app (helper use is reported below). Table 34 also demonstrates that participants used the social support elements of the app: the ‘send a smile’ feature; and ‘contact helper’ feature. Qualitative findings demonstrated that participants and helpers also interacted outside the app, either face to face or with a telephone call, text message or e-mail (see Chapter 5).
Participant engagement with the HelpMeDoIt! website
Of the 73 participants in the intervention group, 18 (25%) participants did not visit the website (similar to the number of participants who did not use the app). Among those who did use the website (n = 55, 75%) the number of visits ranged from 1 to 12 individual sessions, each session lasting 18 seconds to 44 minutes, with a total of 1–45 individual web pages viewed (see Table 34). Qualitative findings suggested that some participants were unclear about the purpose of the website, forgot about the website or did not find it helpful. More effective signposting of the website and the help that it can provide is an important consideration for a future trial. Although website use was limited, participants and helpers may have gathered sufficient information to proceed with the intervention from one or two visits.
Helper engagement with the HelpMeDoIt! app
App use by helpers is presented in Table 35. Forty-five individuals were invited as helpers. Twenty-eight (62%) accepted the invitation, of whom 25 (56% of nominated helpers) used the app at least once. Overall engagement was assessed against similar criteria to those used for participants: eight helpers (29% of accepted helpers) used the app only once; 17 (61%) used it twice or more; 10 (36%) used it three times or more; and only two (7%) used it 10 times or more. In total, there were 122 logins by helpers (ranging from 1 to 48). The top three features used by helpers were sending smiles to participants, viewing participant goals and liking participant goals. Qualitative findings suggested that helpers were uncertain how to help the participant using the app, with many providing support outside the app with face-to-face chats, text messages or telephone calls (see Chapter 5). The level of helper engagement with the social support element was therefore higher than indicated by the app use data.
Helper engagement with the HelpMeDoIt! website
Of the 28 helpers who accepted a participant invitation, 19 (68%) used the website at least once, and nine (32%) used the website twice. No helper visited the website more than twice. The number of pages viewed by helpers ranged from one to eight, with a session duration of 1.5 minutes to 27 minutes (see Table 35). Similar to insights from participants, qualitative findings showed that helpers were unaware either that a website was available or of how it could help them. Signposting the website more effectively to helpers should be considered for a future trial. A consideration is that helpers may not need to revisit the website often after reading the ‘helper guidance’.
Characteristics of app and website use
Table 36 shows summaries of selected measures of app use in relation to participant gender. Complete summary tables are provided in Appendix 8. Women were higher users of the app than men, but app use by helpers did not vary between helpers of male and female participants. Apart from gender, there were no other associations between participant baseline characteristics and app use. Participant age, Scottish Index of Multiple Deprivation (SIMD), BMI, physical activity and diet showed no correlation with the number of logins by participants or their helpers, or the number of goals set by the participants.
| App use | Participant gender | p-value | |
|---|---|---|---|
| Female (n = 49) | Male (n = 24) | ||
| Number of app logins (participant), median (IQR) | 4 (1, 10) | 2 (0, 3) | 0.042 |
| Number of goals created (participant), median (IQR) | 10 (0, 19) | 0.5 (0, 4) | 0.002 |
| Number of app logins (helper), median (IQR) | 2 (1, 3) | 2.5 (0, 3) | 0.947 |
Although participants were informed that this was an option, no participants enquired about the potential to be both a participant and a helper for someone else in their social network.
Potential mediating effects of intervention use
Within the intervention group, the potential mediating effects of measures of app/website use were assessed by testing the correlation between each measure of app/website use and each primary outcome measure (Table 37).
| App use | BMI (kg/m2) | Physical activity monitor | DINE questionnaire scores | |||
|---|---|---|---|---|---|---|
| Steps per day | Sedentary time | Healthy eating | Unsaturated fat | Fruit and vegetables | ||
| Number of logins (subject) | –0.381; p = 0.006 | 0.405; p = 0.050 | –0.408; p = 0.048 | 0.262; p = 0.069 | 0.273; p = 0.019 | 0.091; p = 0.551 |
| Number of goals created (subject) | –0.237; p = 0.098 | 0.332; p = 0.113 | –0.223; p = 0.295 | 0.276; p = 0.054 | 0.255; p = 0.029 | 0.266; p = 0.077 |
| Number of logins (helper) | –0.276; p = 0.182 | –0.134; p = 0.649 | 0.218; p = 0.453 | –0.056; p = 0.786 | 0.229; p = 0.242 | –0.352; p = 0.078 |
Those who made greater use of the app, as measured by the number of logins and goals created, showed greater reductions in BMI. Objectively measured physical activity (step counts and time spent in sedentary activities) was correlated with the number of logins, more than with the number of goals created. Healthy eating scores from the DINE questionnaire were correlated with increased app use, as were fruit and vegetable scores, particularly with the number of goals created. There was also a positive correlation between app use and DINE unsaturated fat scores. Helpers’ use of the app demonstrated less association with participants’ outcomes, with only fruit and vegetable scores showing some signs of a (counter-intuitive) negative association with the number of helper logins.
It is important to note that, although these identified associations could indicate mediating effects, these results could also be found as a result of reverse causality or be artefacts of another predictor of success; for example, people who are losing weight will maintain engagement with HelpMeDoIt! as it is going well, but they may have been successful anyway.
Dose–response relationship: illustrative case studies
Given the range of engagement with the app, and the possibility that for some individuals the intervention might be particularly helpful, we explored use characteristics and outcomes for the six (8%) intervention participants who used the app most frequently (range 30–408 logins). All of these participants lost weight (between 3% and 19% of their starting weight) and that weight loss typically increased as app use increased. In addition to having the largest number of logins, these six participants also had the highest engagement with the three key features of the intervention: goal-setting, self-monitoring and helper interaction. Interestingly, the participant who had greatest success with weight loss (a clinically significant weight loss of 19% body weight) was the individual who used the app most frequently, completed the greatest number of goals, had the greatest number of helpers using the app and had the greatest number of helper interactions. However, while it may be the case that using the app leads to more weight loss, it could also be that individuals may use the app more because they are being successful and losing weight.
Participant insights on Usability, Satisfaction and Ease of Use questionnaire
Overall, the response rate for the 30 individual USE questions ranged from 40% to 49% (n = 21–24 of the intervention group at follow-up). This response rate was lower than that for other measures in the questionnaire and was probably due to participants who had never, or rarely, used the app/website feeling that they could not provide informed responses. For example, it was difficult for participants to respond to ‘I can use it without written instructions’ if they had never used the app/website or had logged in only once. A ‘not applicable’ or ‘don’t know’ option should be included for a future study to improve data completeness. It is also possible that participants who did not enjoy using the app did not complete all of the USE questions, potentially skewing the data.
The USE questionnaire presented summed scores over four categories: (1) ease of use, (2) ease of learning, (3) usefulness and (4) satisfaction. Lower scores indicate more positive results. Among those participants who did respond, the mean ease of use score was 52.1 (range 14–77 from a potential range of 11–77), the mean ease of learning score was 15.2 (range 4–28 from a potential score range of 4–28), the mean usefulness score was 41.9 (range 8–56 from a potential range of 7–56) and the mean satisfaction score was 36.8 (range 7–49 from a potential range of 7–49). These findings suggest that, although the majority of participants found the app/website moderately easy to use and quite easy to learn, the majority did not find the app/website useful and were moderately unsatisfied. Qualitative findings suggest that the reasons for dissatisfaction and lack of usefulness were related to the technical issues experienced with the app. Importantly, better scores were demonstrated in participants who started using the app after the technical issues had been resolved. For example, the first five users of the app (in the presence of technical issues) reported a mean total USE score of 146 (range 113–210), compared with the final five users of the app (in the absence of technical issues), who had an improved mean total USE score of 136 (range 108–173). In addition, participants who used the app most frequently, and experienced no technical issues, provided the most positive scores. This demonstrates that when the app operated effectively it was perceived positively by participants.
Reach
Participant demographics were presented in Chapter 4. As is frequently seen in weight loss studies, most participants were female (n = 76, 69.7%). 91 In terms of ethnicity, the sample was representative of people living in Scotland, with 97 (89.8%) being white British and 11 (10.2%) being of a minority ethnic or another background. The overall sample was also representative of Scotland’s relationship between obesity and socioeconomic status, with the majority of participants (n = 57, 57.6%) living in an area of high deprivation (Scottish Index of Multiple Deprivation level 1 and 2). Participants from a wide age range (25–68 years) were recruited, giving us insight into the feasibility of using an app and website intervention for different age groups. However, we had to approach (via primary care) or reach (via advertising) many people in order to recruit our sample, so it is likely to be a somewhat narrow and motivated group, which is not unexpected in a study on weight loss.
Qualitative and quantitative data were collected to measure the extent to which the intervention reached individuals other than participants, as reflected in the programme theory. Findings from participant and helper interviews demonstrated that some helpers made positive changes to their lifestyle in response to their involvement in the HelpMeDoIt! study. This included changes to physical activity and diet (see Chapter 5). Questionnaire data at follow-up also supported this finding, with 12 participants (14%) reporting their helpers making healthier food choices, 14 participants (17%) reporting their helpers increasing their physical activity, and six participants (7%) reporting that their helpers had successfully lost weight. This is an important consideration for the potential impact of this intervention in the future because if the intervention has a spillover effect, thus reaching a broader group of people, the potential impact could be positive even if only some of the individuals use the intervention as intended.
Programme theory and logic model
Chapter 2 previously described how the HelpMeDoIt! intervention was guided by a programme theory and logic model. Findings from stage 1 helped inform the second iteration of the logic model from version 1.0 to version 2.0 (see Chapter 2). In stage 2 we further explored the programme theory and the version 2.0 logic model using use statistics and qualitative data from participant and helper interviews. In addition to feedback from participants and helpers, observations by the study team and the software company helped refine a comprehensive programme theory for the HelpMeDoIt! intervention. The aim of this section is to summarise new contextual factors for consideration, how elements from the key qualitative themes influenced each other, and how they mapped onto the proposed programme theory and logic model.
Contextual factors identified within the HelpMeDoIt! programme theory
Contextual factors influenced whether or not the key mechanisms of change were successfully implemented. Various categories were identified in which contextual factors could negatively or positively influence the impact of the intervention. Categories included issues related to (1) available technology (i.e. make and model of smartphone), (2) participants themselves, (3) their helpers, (4) the environment and (5) broader contextual issues (previously described in Chapter 5). Many factors had already been considered in the early stages of development, such as aiming to develop an app/website that was easy to use and engaging, and being aware that participants would have varied access to physical activity opportunities. As the study progressed, we gained greater insight into additional contextual issues. Many of these focused on the participant–helper relationship and require consideration for a future trial. These included:
-
participants feeling uncomfortable asking helpers for support or feeling that their weight goals were a burden to their helpers
-
some participants feeling socially isolated and not having access to many helpers
-
participants feeling embarrassed to share their weight and eating habits with their helper or to start using the app again after a long period of non-use
-
invited helpers’ motivation to provide support being poorly understood (ethical constraints meant the study team could not contact helpers directly for feedback; helpers who were interviewed were contacted via the participant)
-
participants’ ability to effectively and confidently ask for support, which influenced the clarity, or lack of clarity, that helpers felt towards their role.
Mapping qualitative themes to the HelpMeDoIt! programme theory and logic model
Table 38 summarises the ‘mechanisms of change’ and ‘intermediate outcomes’ from the version 2.0 logic model (see Figure 4) and identifies which of them were strongly supported by qualitative findings (i.e. discussed by the majority of participants). Theme numbers in bold strongly supported the identified mediator as a mechanism of change (e.g. increased/improved social support is strongly supported by qualitative theme number 3.3, ‘social support’). Theme numbers in italics suggest that the identified mediator is a potential mechanism of change (i.e. it was discussed by some participants but less often). However, further exploration in a future trial is needed (e.g. increased problem-solving is identified as a potential mediator by qualitative themes number 3.1 ‘goal-setting and self-monitoring’ and number 4.1 ‘change in behaviour’).
| Participant themesa | Helper themesa | |
|---|---|---|
| Logic model mechanism of change | ||
| Increased social support | 3.3 | 9 |
| Increased engagement with helpers via the app | 2, 3.3 | 6, 7, 9 |
| Increased interaction with helpers not via the app | 2, 3.3 | 9 |
| Reflect and set ongoing goals | 3.1 | 7, 9 |
| Increased action-planning | 3.1, 4.1 | 8 |
| Increased self-monitoring | 3.1 | 7, 9 |
| Increased problem-solving | 3.1, 4.1 | 8, 9 |
| Increased skills and knowledge | 3 | 9 |
| Increased motivation | 3.2, 3.4 | 8, 9 |
| Increased self-efficacy | 3 | 8 |
| Increased autonomy | 3 | 8 |
| Logic model intermediate outcomes | ||
| Improved social support | 3.3 | 7, 9 |
| Healthy habit formation | 3.1, 3.4, 4 | 8 |
| Improved self-efficacy | 3 | 8 |
| Improved self-image or self-esteem | 3, 4 | 8 |
Exploring the qualitative findings in this way demonstrated that two of the four intermediate outcomes proposed by the logic model were strongly supported by the qualitative findings: (1) improved social support and (2) healthy habit formation. Insufficient data were provided by participant/helper interviews to support the other two intermediate outcomes, namely improved self-efficacy and improved self-image or self-esteem, as integral processes in HelpMeDoIt!. Although self-esteem and self-efficacy are supported by the evidence base,22 they may not be intermediate outcomes in the HelpMeDoIt! intervention. They should, however, be included in the programme theory for further study in a future trial.
Eight out of the 11 proposed mediators of change above were found from the data to be key processes in the HelpMeDoIt! intervention. These were increased social support, increased engagement with helpers via the app, increased interaction with helpers not via the app, reflecting on and setting ongoing goals, increased action-planning, increased self-monitoring, increased skills and knowledge, and increased motivation. Four of these eight mediators emerged from the data as the strongest elements of the HelpMeDoIt! intervention: (1) increased motivation, (2) increased social support, (3) increased goal-setting and (4) self-monitoring.
Increased motivation
Participants consistently focused on the importance of motivation to their ability to successfully make lifestyle changes. A number of elements contributed to improved motivation. The template goals in the app were well liked and helped participants to set modest, achievable goals rather than more ambitious goals that had a higher risk of failure. Participants reported that small successes would increase their motivation to continue with their healthy lifestyle changes. The website was also reported to be helpful in increasing knowledge and motivation. We found that motivation, along with life contextual factors, was a precursor to engaging with and using the HelpMeDoIt! intervention. Motivation may have been generated by a participant’s life context, such as a change in their health status that made them feel that they had to get serious about improving their health and losing weight. Some participants had tried many different weight loss interventions and had maintained enough motivation to sign up for HelpMeDoIt! in the hope that this programme would work for them. Furthermore, good social support was a contributor to maintenance of motivation.
Increased social support
Qualitative interview data showed that most of those interviewed engaged with the idea of a helper even if they did not engage with the app. They said that the intervention prompted them to ask for help from people in their social networks and let these people help support them in their efforts to change their behaviour. The interviews reflected an increase and improvement in social support (emotional, instrumental and informational) for many participants.
Increased goal-setting and self-monitoring
Goal-setting and self-monitoring were promoted through the app and website. The website provided participants with guidance on setting and maintaining SMART goals related to healthy lifestyle behaviours. Some participants reported liking the template goals in the app; however, use data show that participants overwhelmingly used bespoke goals. Most participants interviewed reported that goal-setting and monitoring were important parts of changing their behaviour (especially among those participants who lost weight). In the process of monitoring goals, participants increased action-planning, increased problem-solving when goals were not working well, increased tracking of their goals and improved their healthy habit formation (e.g. by establishing daily walks or reducing sugary treats).
The revised HelpMeDoIt! programme theory and logic model
The revised version 3.0 programme theory and logic model incorporating the above findings is presented in Figure 10. Version 3.0 more clearly identifies motivation, social support, goal-setting and self-monitoring as the key mediators of change within the HelpMeDoIt! programme theory. These have been grouped together and given hierarchical priority in the logic model (illustrated by the use of solid lines and deeper colour). Improved social support and healthy habit formation were identified as the key intermediate outcomes, and have also been given hierarchical priority in the logic model (using solid lines and deeper colour). Other mediators and intermediate outcomes, which were not strongly supported by the data and require further exploration (e.g. increased self-efficacy), are illustrated by the use of dashed lines and lighter colour. Additional considerations were added to appropriate categories within the pre-conditions and contextual factors section, for example complementary use of other lifestyle apps under ‘technology’. Any future evaluation of HelpMeDoIt! will use the version 3.0 programme theory and logic model.
FIGURE 10.
Version 3.0 of the HelpMeDoIt! programme theory and logic model.
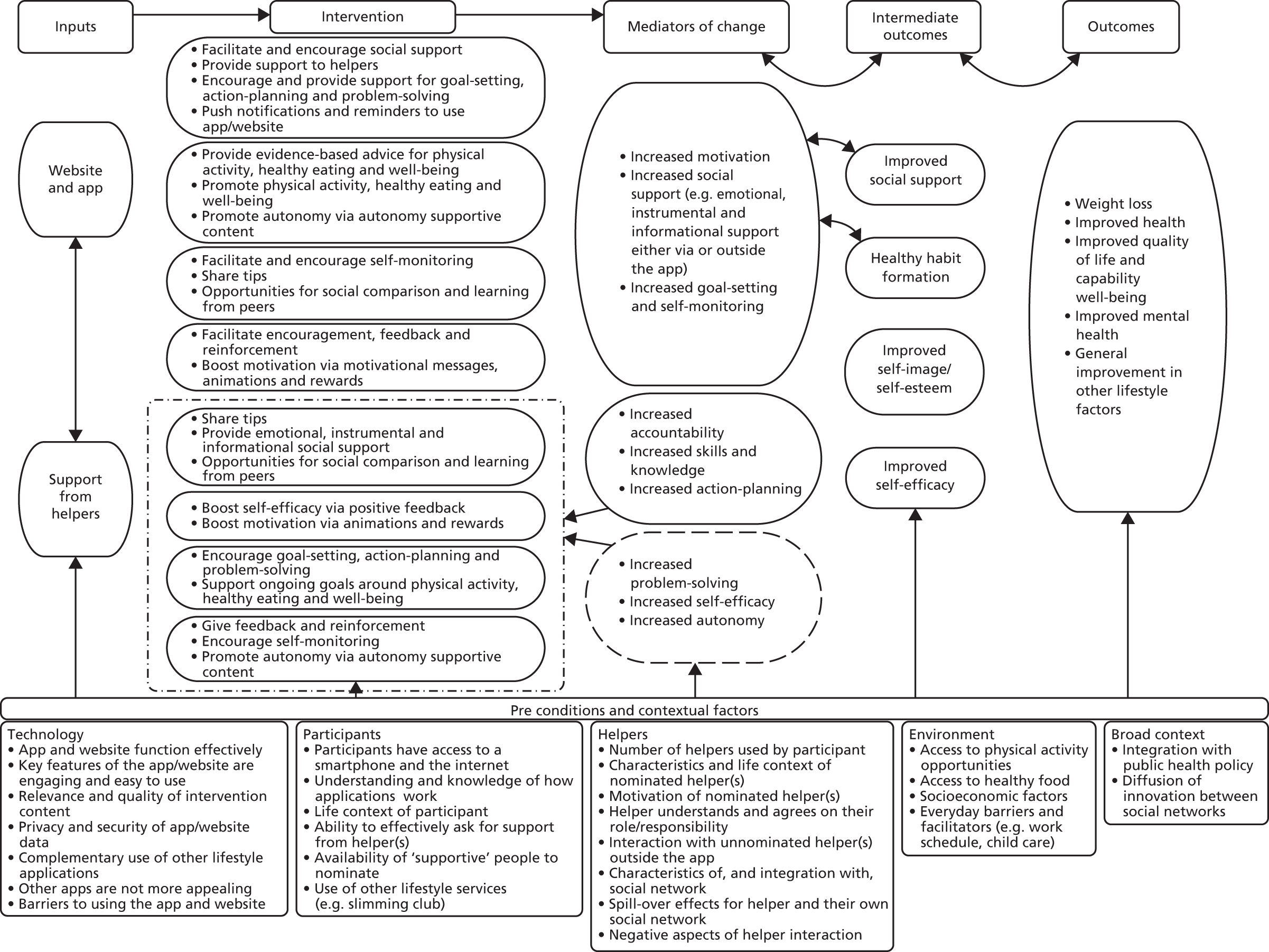
Part 2: evaluation design-related findings
Recruitment and retention
Recruitment
Overall, our multimethod strategy of recruitment was successful for recruiting a diverse sample in terms of age, gender, and socioeconomic and ethnic background. Figure 11 provides a summary of our recruitment rates by their source. The most effective methods of recruitment for HelpMeDoIt! were (1) the SPCRN, (2) newspaper advertising and (3) online Gumtree adverts. These different methods had different associated costs, which are detailed below, but all involved the research team screening people who responded. The strengths and limitations of each recruitment method are considered below.
FIGURE 11.
Recruitment sources of final sample (n = 109). SPCRN, Scottish Primary Care Research Network.
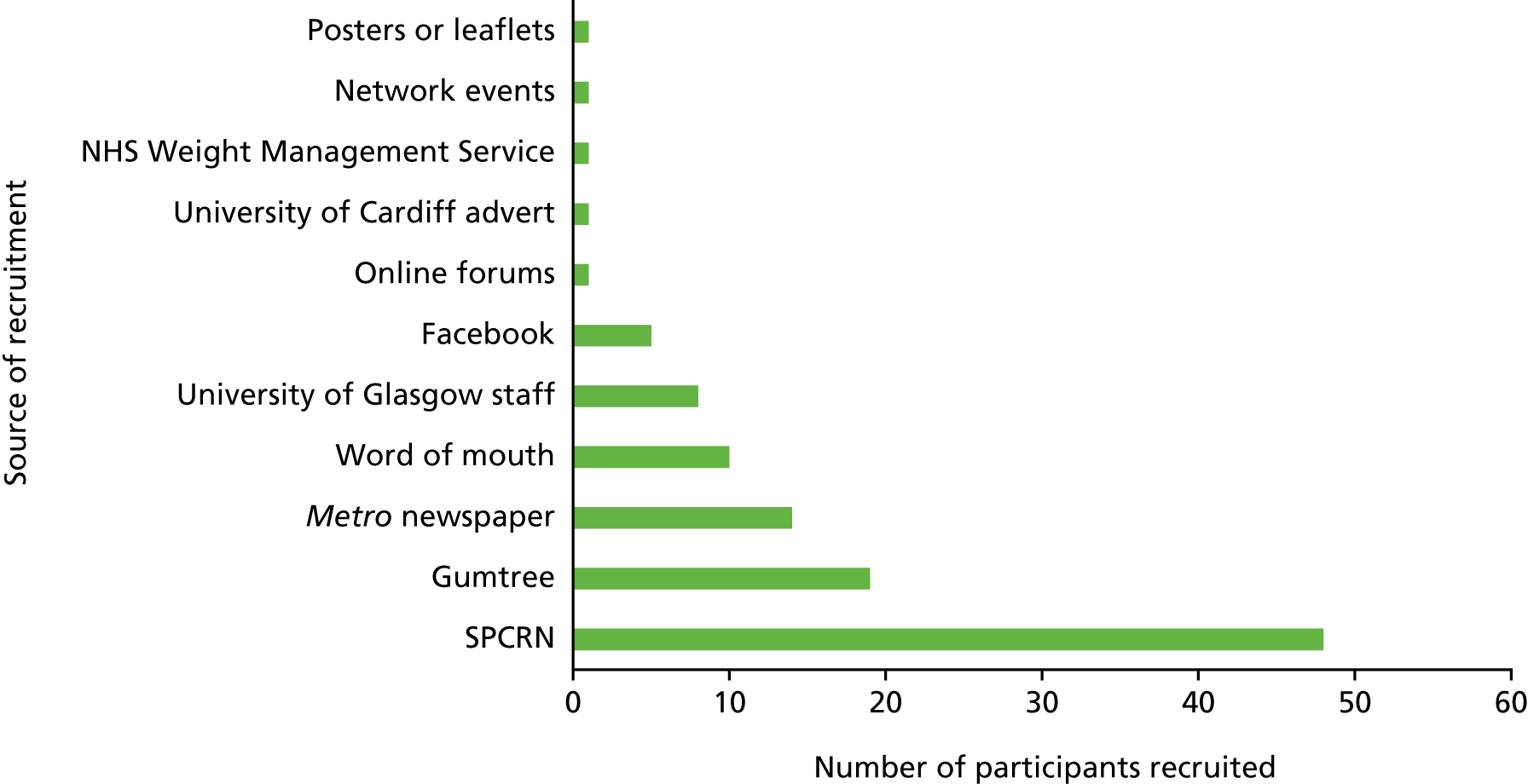
-
Scottish Primary Care Research Network: the role of this network is to support the recruitment of primary care patients to research studies. One SPCRN representative liaises with GP surgeries, searches their patient database in relation to study inclusion/exclusion criteria, and posts information to eligible participants. The positive aspect of this method was the large number of eligible individuals who were able to be informed of our study (n = 1000 from five surgeries). We anticipated a 10% response rate of expressions of interest (n = 100) and achieved an 8.8% response (n = 88); of these respondents, 55% (n = 48) proceeded to sign up to the study. The only limitation of this method was that some people misinterpreted that their GP was recommending a ‘service’ to them, rather than sharing information about our study. This resulted in the study team being contacted by many people who did not own a smartphone or have internet access, but did not want to be seen as ‘letting their GP down’. Addressing these issues was time-consuming for the study team. Emphasising the purpose of the information pack is an important point for us to consider if using recruitment from primary care in a future study. This method of recruitment required minimal time input from the research team and cost £400 (approximately £8 per participant recruited).
-
Newspaper advertising: a medium-sized newspaper advert (approximately 8 cm × 10 cm) was published in the Metro newspaper. The advert was printed 2 days per week for 2 weeks, on two separate occasions, and targeted mainly working-age commuters. Positive aspects of this method included a steady flow of expressions of interest (n = 54 in total), with approximately one in four proceeding to participate in the study (n = 14, 26% of expressions of interest). Challenges of this method included the time required for the trial manager to speak with and screen potential participants, many of whom were ineligible because they had a BMI of < 30 kg/m2. If this method were to be used again, we could provide an online eligibility screening form. Again, this method of recruitment required minimal time input from the research team and the total cost was £1000 (approximately £71 per participant recruited).
-
Online Gumtree adverts: this platform provided opportunities to upload free, ongoing adverts for the duration of the recruitment phase. The benefit of this method included that it resulted in regular expressions of interest (n = 54), mainly from people searching for ‘weight loss’ in their local area. Limitations included a fast rate of attrition of interested individuals once they were asked for further details (n = 35 non-responders). This was time intensive for the trial manager but provided a reasonable uptake of participants to the study (n = 19, 35% of the expressions of interest). An administrator to filter the initial expressions of interest would be a more effective use of resources. This method of recruitment was free other than some time from the research team to place adverts.
Other helpful methods of recruitment included promotion of the study via a ‘whole campus’ e-mail to staff and students of the University of Glasgow, and recruitment by word of mouth. Other methods of recruitment, such as using Facebook, Twitter and online forums, were less successful but were free and not resource or time intensive to deliver. We recruited one participant via the NHS Weight Management Service, which involved presenting our study methods at a staff meeting, harnessing staff’s support and leaving promotion materials for them to distribute to suitable individuals. We also recruited one participant after we were present at a local health network event. One participant reported joining the study after seeing a leaflet or poster; these were expensive (in relation to printing costs) and time intensive (in relation to sourcing appropriate leaflet/poster locations) and would not be useful for a future study.
Our multimethod recruitment strategy resulted in 253 expressions of interest. Of these, 62 (25%) were non-responders when the study team requested further details, 49 (19%) did not meet the study eligibility criteria, 18 (7%) withdrew their interest after reading the participant information sheet, 8 (3%) noted their expression of interest after the recruitment phase ended, and 7 (3%) did not attend their scheduled baseline appointment and were noted as having withdrawn their interest. This resulted in a total sample of 109 participants.
Retention
Quantitative data on trial retention were reported in Chapter 4. In brief, a total of 84 participants were retained at 12-month follow-up (77%). Of these 84 participants, 14 (17%) provided their 12-month follow-up data in the form of a ‘minimum data set’. The split between intervention (11 of 52 participants, 21%) and control (3 of 32 participants, 9%) broadly reflected the 2 : 1 recruitment ratio. The minimum data set was used when participants were reluctant to arrange face-to-face appointments for follow-up and were at high risk of withdrawing from the study. The minimum data set calculated BMI using self-reported weight.
Attrition was lower in the control group (n = 4, 11.1%) than in the intervention group (n = 21, 28.8%). This is perhaps an effect of intervention participants being frustrated with the inconsistent quality of the app or not engaging with the intervention and thus disengaging from the study. Six participants withdrew early in the study, with two participants reporting illness/injury and four participants giving no reason. At 12 months a further 19 participants were lost to follow-up. Reasons included personal or family illness (n = 3), could not use the app (n = 1), did not lose weight (n = 1), relocated (n = 1), and non-responders (n = 8). Chapter 4 has presented the characteristics of participants lost to follow-up.
Qualitative interviews explored the feasibility of outcomes measures with participants, and whether or not the choice of measures influenced their engagement with the study. All participants interviewed reported that the measures and questionnaires used were not burdensome. Qualitative feedback from four participants at 12-month follow-up also suggested that having measurements taken at baseline and follow-up was a motivating factor that kept some participants retained in the study. Although this insight was provided by intervention participants, the impact of measurement might account for the fact that the control group lost weight in the follow-up period.
When the decision was made to arrange baseline and follow-up appointments via the trial administrator rather than the field workers, a noticeable improvement on retention as well as the timeline for recruitment was observed; this approach should be used in any future trial.
Contamination and the control group
As this was a feasibility study, it was important to explore how the HelpMeDoIt! intervention would be used in everyday life. We gathered data on any other lifestyle-related activities that participants were engaged in. Of the 109 participants, 29 (26.9%) reported using another service either at the time or within the 3 months prior to the study start date (23.6% intervention vs. 33.3% control). These included Scottish Slimmers™ (Aberdeen, UK), Weight Watchers® (Maidenhead, UK) and the NHS Weight Management Service (NHS Greater Glasgow and Clyde). Some of these activities provide similar elements to the HelpMeDoIt! intervention, such as advice on how to set achievable goals for healthy eating, and tools for self-monitoring. However, the HelpMeDoIt! intervention was designed as a complementary intervention that could enhance the activities that individuals were already engaged in, primarily by harnessing greater social support. At both baseline and follow-up, three participants had taken weight loss medication in the previous 12 months compared with five in the intervention group, and a similar proportion of control and intervention participants paid for lifestyle services (e.g. gym memberships) over the duration of the study [45.0% control (n = 11); 48.8% intervention (n = 40)]. As the numbers of people accessing these services were similar between the intervention and control groups, the risk of significant contamination bias is low. Furthermore, no participants in the control reported that they had seen or had access to the intervention content. No participant in the control group acted as a helper for a participant in the intervention group, and no nominated helper was enrolled as a participant. At the end of the study, five (14%) control participants took up the offer to use the app/website.
General insights from the study team
The study team reflected on the research processes as part of the study aim to examine the feasibility of delivering a larger study. Insights were gathered from members of the study team, support staff and field workers. Several issues were identified that need consideration for any future trial. These include the following.
Insight related to recruitment and retention
-
Using a dedicated member of staff to initially screen expressions of interest and arrange baseline appointments may be a more effective strategy than communication being via the trial manager or field workers.
-
Having a dedicated member of staff (our trial administrator) contacting participants for recruitment appointments, follow-up appointments and accelerometer returns. This would improve speed of recruitment and retention and minimise loss of equipment.
-
The target sample size would probably have been achieved had media adverts not been published during a school holiday period, and if we had recruited via primary care several weeks earlier.
-
Explore methods of engaging individuals before they provide informed consent, for example including screenshots of the app/website on the information sheet/website. This may be more engaging than simply text on an information sheet.
Insight related to outcome measures
-
At baseline we collected dietary information from participants using the 24-hour multiple pass recall measure. This involved telephoning participants four times over a 10-day period and asking them to report their food intake over the previous 24 hours. This was a challenging measure to use and gathered poor-quality data. Despite obtaining a successful questionnaire completion rate of 74% (n = 81) (reflecting participant insight that questionnaires were not a burden), only 31% (n = 34) of our total sample were completed as intended, and 43% (n = 47) were completed ‘poorly’ (with the remaining 26% not completed). This measure also required significant time input (and cost) of field workers repeatedly making unsuccessful telephone calls to participants; significant time input (and cost) of research support to input poor-quality data in the dietary software system; and the disappointing quality of the dietary input software, which resulted in a lot of time spent searching the internet for comparable food macronutrients and inputting them manually. Our experience of using this measure at baseline demonstrated that it was not a feasible measure for this study. Following approval from the National Institute for Health Research (NIHR), this measure was removed from follow-up data collection. In a future study we would continue to use the other dietary measure, the DINE questionnaire, for which we received a 100% response rate.
-
Although accelerometer return by participants was high (only 15 monitors were not returned over the duration of the study), valid accelerometry data were available for fewer than half the participants. Additional incentives to use and return the accelerometers could increase response rates (e.g. postcard reminder including information on the cost of replacing the activity monitor). 128,129 We could also explore potential for the app to collect physical activity data.
Recommendations to improve the intervention
Finally, based on the findings of the process evaluation, a number of changes should be made to the app and website in anticipation of a future trial. These are summarised below.
The HelpMeDoIt! app
-
Improve the self-monitoring aspect of the app by displaying a list of all recorded weights.
-
On the helper app, display weight change instead of actual weight.
-
Provide clearer guidance on how to use the app, for example to set goals.
-
Devise strategies to encourage helper engagement via and/or outside the app.
-
Amend the scoring so that it is easier for participants and helpers to earn reward trophies.
-
Review push and e-mail notifications to ensure that they are sent with the optimal content and frequency.
-
Ensure that the ‘reminder feature’ for goals updates is enabled for all participants and helpers.
-
Encourage helpers’ engagement with participant progress charts by sending regular updates (e.g. via push notification, e-mail or text).
-
Include a link enabling participants and helpers to manage their notification settings.
-
Ensure that the app has a testing phase once it has been launched via the app stores.
-
After each software update, ensure that the app is tested in-house by the software company to identify any new software bugs caused by the update.
-
Explore the long-term potential of combining with other lifestyle apps.
-
Overall, consider whether or not the app is needed to facilitate the unique element of social support, as, based on the feasibility study results, other methods of delivering social support are also likely to be beneficial.
The HelpMeDoIt! website
-
Consider whether or not a separate website is needed and explore whether or not a future version of the intervention could provide accessible information via the app.
-
Consider revising the website so that participants have the ability to add helpers, goals and weight and view summary graphs and statistics on a bigger screen.
-
Encourage visits to the website by improved signposting to the website, clarifying the purpose of the website, and sending reminders.
-
Include guidance on the website on how to earn rewards via the app.
Chapter 7 Discussion
This study assessed the feasibility and acceptability of a theory-informed web and app intervention that sought to mobilise social support from a participant’s social network to help them with weight loss goals. In phase 1, we developed the app and website in collaboration with potential users. In phase 2, we completed a feasibility trial. The research questions primarily focus on the progression criteria and related feasibility measures. However, BMI, diet and physical activity were assessed as potential primary outcomes for a full evaluation. Other outcomes included weight, waist circumference, waist-to-hip ratio, quality of life, capability well-being, mental health, social support, motivation, self-efficacy, alcohol use and smoking. Data on resource use, participant-borne costs and cost of the intervention were collected and a process evaluation assessed both the programme theory and the evaluation methods.
The main study findings will be considered below in relation to the study objectives and the trial progression criteria. Key learning points and considerations for a future evaluation will also be discussed.
Summary of main findings in relation to the progression criteria and study objectives
The progression criteria that were agreed with the independent Trial Steering Committee have all been met, with the exception of obtaining a source of funding for the treatment costs, which will be finalised later (Table 39).
| Progression criterion | Method of assessment | Was the progression criterion achieved? |
|---|---|---|
| 1. Are appropriate and effective routes of recruitment available to achieve a powered sample size in a full trial? (Research Objective 2) |
|
Yes (see Chapter 4, Recruitment, and Chapter 6, Recruitment and retention)
|
| 2. Are participants willing to be randomised to the intervention? (Research Objective 2) |
|
Yes (see Chapter 4, Recruitment, and Chapter 6, Recruitment and retention) Both groups were recruited and randomly allocated as intended. No issues were identified with this process |
| 3. Are appropriate retention rates achieved at 12-month follow-up? (Research Objective 2) | Measured using the following scale in both the intervention and control group at 12 months: if ≥ 70% followed up, proceed; if 50–69% followed up, discuss with TSC; if ≤ 49% followed up, do not proceed |
Yes (see Chapter 4, Retention, and Chapter 6, Recruitment and retention) We achieved an overall follow-up rate of 77.1% of our baseline sample (84 of 109 participants). Although retention rates were different between the intervention group (71.2%) and the control group (88.9%), both met the progression criteria |
| 4. Is the intervention feasible to deliver and acceptable to participants and their helpers? (Research Objective 2) |
|
Yes (see Chapter 5 and Chapter 6, Exposure to the intervention)
|
| 5. Do the majority (> 50%) of participants within the intervention group visit the app at least twice or do 25% of participants randomised use it three or more times? (Research Objectives 2 and 8) |
|
Yes (see Chapter 6, Exposure to the intervention) Both criteria were met: |
| 6. Are identified barriers and challenges to implementation of the intervention planned for and surmountable? (Research Objective 4) |
|
Yes (see Chapter 6, Recommendations to improve the intervention) The process evaluation highlighted numerous strengths and challenges for delivering a future app and website-based intervention for weight loss. These include: Strengths Weaknesses Opportunities Threats Plan of action based on the findings of the feasibility trial |
| 7. Do the data collection procedures effectively collect the data required for a full trial? – successful completion of at least one data collection method (BMI, physical activity or healthy eating) at both baseline and at 12 months in those retained measured using the following scale (Research Objective 5) |
|
Yes (see Chapter 4, Exploratory primary outcomes, and Chapter 6, General insights from the study team). Strategies for improvement were discussed with the TSC:
|
| 8. Are the intervention costs of a full trial covered? |
|
Ongoing: The costs of delivering the intervention in a full trial will be low as the intervention is already developed. They will cover hosting and technical support. We are currently in the process of identifying a source of funding to cover these costs as well as to host the intervention should it be rolled out |
Objective 1: to develop an internet and web-based intervention that enables participants to set and monitor goals and facilitate effective social support
Phase 1 of the study involved designing the app and website with comprehensive consultation with potential users. In this phase we also completed initial testing of the website and app to assess their usability and acceptability. We combined four approaches to intervention development, which included an overarching intervention development framework (the 6SQuID model)74 and a review of the literature to identify relevant theories and behaviour change techniques that could be employed,16 as well as digital health-based approaches (Person-Based Approach and BIT model). 75,76 User input was at the centre of the whole development process.
Initial development of the intervention was completed in tandem with a user development panel, the study team and the software company. This was an iterative process; as different aspects were developed, they were discussed in the development panel and updated according to what was agreed. In addition, a testing group of users helped with the initial evaluation of early-stage versions of the app and website. Although users were asked to provide input and feedback from a ‘helper’ perspective, this overall phase lacked input from individuals who formally identified as a helper. This is a consideration for future work. Once the beta version of the app and website had been developed, it was tested fully by both groups, and feedback was given in focus groups or individual interviews. The majority of the feedback was positive and we updated both the app and the website in anticipation of the feasibility trial. An expert heuristic evaluation was also completed at this point, which was very positive. During this phase we also further developed the HelpMeDoIt! programme theory and logic model, which incorporated behaviour change techniques and relevant theory, and addressed multiple contextual factors.
Objectives 2 and 3: to investigate recruitment and retention; to explore the potential of the intervention to reach traditionally ‘hard to reach’ groups (e.g. lower socioeconomic groups)
The trial methods and design were acceptable and feasible to implement. Although the recruitment rate was slow at first, it then was in line with or slightly exceeded the target rate. The average number of participants recruited per month was 17 (minimum 6 and maximum 27) and we recruited and successfully randomised 109 participants in the specified time frame (progression criterion 1). This was slightly short of our original target of 120. However, the trial team and steering committee felt that this number was sufficient to answer the research questions, so recruitment was stopped at 109. Participants also found randomisation acceptable, and none refused (progression criterion 2). This study has shown that it is feasible to recruit participants and to follow them up. There was an imbalance in follow-up rates between the randomised groups, which could introduce bias in a larger study if it is not addressed. A number of key learning points related to recruitment will inform a future study, and these are discussed in Chapter 7, Limitations of the study.
The sample was broadly representative of the target population; however, as is often seen in studies of interventions for obesity, more women than men were recruited. 91 The majority of men were recruited via online Gumtree adverts. The participants in the sample were relatively well educated, with 42% having degree-level education or higher. The age range was good, although we were not successful in recruiting younger people (i.e. those aged < 25 years). Participants were relatively active at baseline, with those in the intervention arm achieving an average of 50 minutes and those in the control arm an average of 36 minutes of moderate to vigorous physical activity per day. Standard cut-off points were used for the accelerometer data. 98 Participants may have increased their physical activity in response to using the activity monitor. 130
Recruiting and engaging participants from lower socioeconomic groups131 in research remains a challenge, and many current interventions widen inequalities. 132 However, we were particularly successful in recruiting participants from across the socioeconomic spectrum, with over one-third from the highest quintile of deprivation in Scotland and a further 21% from the next most deprived quintile. There were, however, slightly higher dropout rates among those from the most deprived group.
Baseline characteristics were broadly similar between the arms, although participants in the intervention arm were more likely to have higher levels of education and physical activity. Retention rates were good, with 84 (77%) participants followed up at 12 months (progression criterion 3). This included 14 participants who provided a minimum data set over the telephone. The split between intervention (11 of 52 participants, 21%) and control (3 of 32 participants, 9%) broadly reflected the 2 : 1 recruitment ratio. The waiting list control design, and the technical issues affecting intervention participants, may have affected the engagement of some participants, leading them to opt for the minimum data set. Those in the intervention group were slightly less likely to be followed up at 12 months. This may reflect either (1) a tendency for people who had not engaged with the intervention, or had experienced technical difficulties, to be less inclined to continue participating in the trial; or (2) the motivation of control participants to remain in the trial to receive the intervention. The participants least likely to complete follow-up data were younger, male, self-employed and deprived and had a higher BMI. Those currently attending a weight loss group were more likely to be followed up, as were those who complied with the baseline physical activity assessment by wearing a physical activity monitor. Both of these factors may represent markers of increased motivation to take part in the trial.
Objectives 2 and 4: to investigate the feasibility and acceptability of the intervention; to explore the barriers to and facilitators of implementing the intervention
Although engagement with the app was moderate for participants and low for helpers, the qualitative data indicated that most of the participants and helpers interviewed engaged with the concept of the intervention around mobilising social support to help with goal achievement. Helpers engaged with participants outside the app, and some participants sought social support from informal helpers who were not signed up to the study. This is a positive finding, considering that social support was the unique aspect of the HelpMeDoIt! intervention. Apart from some technical issues with the app that are described in Chapter 6, participants found the app and website acceptable and in the main were very positive about the intervention (progression criterion 4). The USE questionnaire data were not as positive as we had hoped; however, it is likely that the technical difficulties we experienced with the app, which were ultimately resolved, will have negatively influenced these responses. Participants who used the app most frequently, and after the technical issues had been resolved, provided more positive scores for usefulness, ease of use and satisfaction. This demonstrates that when the app operated effectively, it was perceived positively by participants. Interview data were more positive, but this may reflect interviews being conducted with participants who were potentially more motivated and engaged with the intervention. The qualitative data have provided a number of suggested refinements to improve the intervention (progression criterion 6). These would be implemented before delivery in a future study and are discussed in Chapters 5 and 6.
Adherence to the intervention was superior to that seen in general app use. 94 However, commercial apps lack a recruitment phase, as in this study. Of the 54 (74%) participants who downloaded the app, 89% (n = 48) used it twice or more and 70% (n = 38) used it three times or more (progression criterion 5). In the study logic model, this level of participant engagement with the app and website was seen as necessary in order to receive a ‘dose’ of aspects of the intervention, in particular to receive key information about the importance of monitoring, setting realistic goals and social support to help with making lifestyle changes. The central aspect of the intervention was the support from the individual participant’s social network. It was not regarded as key whether this was via the app or another method, for example seeing someone face to face, sending them a text message or telephoning them. The interviews indicated that, in many cases, even though the helpers did not use the app, they gave the participants support outside the app. In the logic model, the app, and indeed the intervention as a whole, was seen as a prompt to help mobilise people’s social networks to help them in their behaviour change goals. The intervention helps start the conversation by getting the need for help ‘on the radar’. The process evaluation data indicated that this was achieved. There was also some evidence of changes in helper behaviour as a result of being nominated to help the participant. This ‘spillover’ effect could potentially be an important mechanism of impact of the intervention.
A recent expert international workshop considered the issue of engagement and concluded that engagement is complex, has many different aspects and cannot be evaluated purely on the basis of how often a person uses an app. Members of the workshop differentiated between the digital elements of the intervention and the behaviour change elements and concluded that continued engagement with the digital intervention (app/website) is not always needed for behaviour change, as delivery of the behaviour change elements via the digital intervention could kick start a process of behaviour change of developing new skills and new habits. 95 This is particularly relevant to HelpMeDoIt!, where a brief interaction with the website or app can lead to the engagement of significant and sustained social support from existing, stable and durable social resources, the effects of which on resultant behaviour are not dependent on further app use.
The key barrier to implementing the intervention was the technical issues, described in detail in Chapters 5 and 6. Participants identified a number of other barriers to changing their behaviour, including various contextual factors such as time and money issues. They also described personal barriers, including willpower, motivation and a lack of routine. Some participants also described barriers to nominating helpers. Participants made a number of suggestions to facilitate use of the app, including receiving more reminders, receiving additional guidance on use and being able to choose what information to share on diet and weight.
The data suggest that the app seems to have worked particularly well for a minority and that the engagement rates are above industry norms. An intervention such as this has the very real potential to be cost-effective even if a relatively low percentage of the initial users engage with it repeatedly.
Objective 5: to assess the feasibility and acceptability of different outcome measures for diet and physical activity in this population
One of the key objectives of the study was to inform the choice of primary outcome in a future evaluation. Three potential primary outcomes were tested: BMI, physical activity and diet. Physical activity and diet were measured in two different ways: physical activity via a self-report measure and accelerometery, and diet by two different self-report measures. One of the criteria for selection for a future study was feasibility of the measures including data completeness (progression criterion 7). The measures were generally feasible to use, and qualitative data indicated that they were acceptable to participants and not burdensome. Data completeness was good for all of the measures apart from the accelerometry data. BMI data were collected in 98% of those who were followed up. The 7-day physical activity recall (PAR) data were collected for 96% of those followed up; however, valid accelerometry data (provided at baseline and follow-up) were available for only 46% of the sample. However, when these data were obtained, they provided the most robust evidence for an intervention effect in this trial. This measure required a greater level of commitment from study participants to obtain valid data for analysis. A wrist-worn accelerometer may have had better compliance if it had been possible to collect physical activity data in a less invasive way, for example via participants’ smartphones, throughout the follow-up period; this might have reduced the burden on participants, and provided objective physical activity data for those who did not engage with follow-up data collection. In addition, in other similar studies, strategies such as giving vouchers for returning the accelerometer have led to improved adherence and return rates, so vouchers combined with other methods could significantly improve return rates. 128,133 In a future trial, accelerometry data could be collected for a subsample to validate the self-report physical activity measure, where self-report data are collected before sending out accelerometers. Alternatively, accelerometry data could be collected for the full sample but not analysed and instead used to increase the accuracy of the self-report.
For the diet measures, the collection of diet data using the 24-hour multiple pass recall was not considered feasible because, although we managed to obtain data at baseline from 74% of the participants, only 31% of the questionnaires were completed properly. In addition, this outcome also required a large amount of resources in terms of data collection and processing and, because of these issues, was not used at follow-up. The other dietary measure, the DINE questionnaire, was feasible and was completed by 96% of participants at follow-up.
Objective 6: to use outcome data (diet, physical activity, body mass index) to help decide on a primary outcome and to estimate the potential effect size of the intervention to facilitate the calculation of an appropriate sample size for a full trial
The study was not powered to assess effectiveness. Although these results should be treated with caution owing to the numbers contributing to these analyses, the objective physical activity data showed moderate to large effect size estimates across several measures, particularly the daily step count and sedentary time. These findings were amplified in per-protocol analyses, and appeared strongest in those with lower levels of physical activity at baseline. In addition, there was no evidence to suggest that self-report physical activity was different between those who did and those who did not provide valid accelerometry data, thereby increasing confidence in these results. There was also some suggestion that those who used the app more achieved better outcomes in terms of BMI, objectively measured physical activity and diet, which could potentially reflect an effect of the intervention, but would also be consistent with those who are most motivated to engage with the app or to provide follow-up data achieving better outcomes.
With regard to choice of the primary outcome for a full trial, BMI was feasible to collect and was objectively measured. Measuring diet and physical activity accurately is challenging. 134,135 Although accelerometry was objective, valid data were available for only just under half the participants. However, methods to address issues with return of the accelerometer and compliance with the data collection protocol have been used successfully in other trials and could be applied in this population. 128,133 Including interim data collection points could alleviate problems due to missing outcome data, and offering further incentives for completion of follow-up assessments could improve data collection rates. The effectiveness of these measures could be tested as part of an internal pilot within a future trial.
In terms of sample size for a future trial, there are three key parameters, namely (1) the minimum clinically important difference (MCID), in this case percentage weight loss (and its standard deviation); (2) proportion of recruited participants who engage with the intervention (among whom the MCID will apply, with zero weight loss assumed among those who do not); and (3) loss to follow-up.
If we take the MCID as 5% weight loss with a SD of 7.3% (as observed in this feasibility study; effect size 0.68), then a sample size of 47 per group would be required to achieve 90% power to detect a difference, with no loss to follow-up and 100% engagement. However, if only two-thirds of participants engaged with the intervention, as occurred in this feasibility study, then the population effect size is 0.46 (0.68 × 0.67) and 101 per group would be required. This assumes complete follow-up; allowing for 20% loss to follow-up, a study of approximately 127 per group would be required.
Recognising that it is highly risky to base sample size calculations on feasibility study data (where estimates of key parameters have wide CIs), a highly cautious set of assumptions may be to assume the SD of weight change to be 10%, 50% engagement with the intervention (giving a population effect size of 0.25) and 40% loss to follow-up, for which a sample size of 564 per group (1128 total) would be required to achieve 90% power.
Given that the intervention is very low cost and has the potential to reach large numbers, it would feasibly be cost-effective at a population level if the achieved MCID was 3% among those who engaged, and/or if engagement levels were < 50%. This would equate to population effect sizes of ≤ 0.15, and thus sample sizes at 90% power > 2000. Appendix 10 includes a range of potential sample sizes across different assumptions for the three key parameters.
Objective 7: to assess data collection tools and obtain estimates of key cost drivers to inform the design of a future cost-effectiveness analysis
The health economics feasibility component assessed procedures, validity and reliability of resource use data collection, quality of life and capability well-being tools in addition to prior estimation of parameters such as the variance of the outcome variable. Without conducting formal between-group statistical comparisons, it can be seen that health and social care resource use, food and drink and lifestyle activity spend patterns were broadly similar between the groups. The HelpMeDoIt! mean EQ-5D-3L values across groups were slightly lower than published population norms; however, values exhibited typical variance around mean values. The ICECAP-A instrument identified and measured responses across all levels of capability well-being across the control and intervention arms. The results reveal that the ICECAP-A was able to distinguish between different levels of self-reported capability well-being in this population group.
Overall, the results of the health economics feasibility study showed that the questionnaires designed for measuring health and social care resource use, food, drink and lifestyle activity spend, quality of life (EQ-5D-3L) and capability well-being (ICECAP-A) would be suitable for inclusion in a full study with some slight changes to the resource use questions. The costs of developing the app and website were mostly upfront, which meant that the cost per participant for the intervention was relatively high in this study. In a future trial, the delivery of the intervention would be a low per-participant cost, which would mainly cover the technical support and ongoing hosting. The low expected cost per participant would permit even modest reductions in BMI, equivalent to the low population effect sizes discussed in the previous section, to attain cost-effectiveness in a future trial.
Objectives 8, 9 and 10: to investigate how participants and helpers engage with goal-setting, monitoring and social support using new technologies and how these elements interact within a behaviour change intervention; to develop a conceptual model of how the key mechanisms of goal-setting, monitoring by self and others, social support and behaviour change are facilitated by the intervention; to test the logic model and theoretical basis of the intervention in stages 1 and 2
The above objectives broadly relate to the intervention theory and logic model. These objectives were addressed in both Chapters 5 and 6. Overall, participants and helpers engaged with the intervention concept but not necessarily via the app. Data from the interviews led to support for the hypothesised intervention logic model and programme theory and has led to further refinements (see Figure 10). Key changes relate to the importance of some of the hypothesised mediators and intermediate outcomes. Eight of the 11 proposed mediators of change were identified as being central to the HelpMeDoIt! intervention. These were increased social support; increased engagement with helpers via the app; increased interaction with helpers not via the app; reflecting and setting on-going goals; increased action planning; increased self-monitoring; increased skills and knowledge; and increased motivation. Increased motivation, increased social support and increased goal-setting and self-monitoring were identified as key mediators. Two out of four intermediate outcomes were also supported by the findings, namely improved social support and healthy habit formation. Although supported by the evidence base, improved self-efficacy136 and improved self-esteem137 do not appear to be integral processes. Indications in the qualitative data were that those with the strongest social support lost the most weight; they also reported more rigorous goal-setting and monitoring and had more successful workarounds for their identified barriers. This provides further support for the logic model. A number of key contextual factors were also identified that were incorporated into the revised logic model (see Figure 10).
Objective 11: to explore the characteristics of participants’ social networks and the influence social networks have on participant experiences and outcomes of the intervention
As noted at the beginning of this report, objective 11 was not part of the original funding application. Although some aspects of this objective were briefly mentioned within the qualitative findings, data for this additional objective will be analysed and published at a later date.
Objective 12: to assess whether an effectiveness trial is warranted
The results of the study indicate that an effectiveness trial is feasible and warranted. All of the progression criteria have been met, apart from obtaining intervention costs (progression criterion 8). We are in the process of negotiating with relevant bodies to cover the treatment costs associated with the intervention and to host the website and app in any future roll-out.
Strengths of the study
The intervention was developed with significant user involvement from the outset and using recommended frameworks for developing complex interventions and digital interventions. The extended development and early stage testing in stage 1, which incorporated the views of users throughout the process, led to the development of a high-quality app and website that were acceptable to users. The intervention was theory based and the programme theory and logic model was refined and tested in the feasibility trial. We used a mixed-methods approach to assessing the feasibility and acceptability as well as the potential impact of the intervention. We were able to triangulate these data to strengthen the internal and external validity of the findings.
The feasibility trial used rigorous methods for data collection and analyses. Objective measures were used to assess weight, BMI and physical activity, and self-report measures were chosen based on previous evidence of validity and reliability. The study also included measures of quality of life and capability well-being and collected cost data to inform a future cost-effectiveness analysis. A key strength is that we were able to successfully recruit a large number of participants from lower socioeconomic groups. The process evaluation allowed us to address the progression criteria, in particular to explore the feasibility and acceptability of the intervention and trial methods as well as to obtain feedback on and suggestions for improving the intervention and enhancing engagement. The qualitative methods were robust and the large number of interviews gave extensive, in-depth accounts of the experiences of both the study participants and their helpers. These data will be used to further refine the intervention ready for further evaluation. Further strengths of the trial were that all key progression criteria were achieved, recruitment rates were adequate, retention was good and engagement with the intervention was acceptable. The results are reported in line with CONSORT (Consolidated Standards of Reporting Trials) guidelines.
Limitations of the study
A key limitation of the study was the low engagement of helpers via the app. Although this was disappointing, the qualitative data indicated that the programme theory of the intervention was delivered, as the app facilitated engagement with helpers that then occurred outside the app. Technical issues with the app during the early stages of the trial led to a number of users disengaging with the intervention and perhaps also with the trial. Some participants and helpers chose to interact outside the app for this reason. The study could have benefited from greater helper input during the development stage. Although we did cover the ‘helper aspect’ of the intervention with users in stage 1, as well as gather ‘think aloud’ feedback from individuals tasked with giving feedback on the ‘helper’ aspects of the app and website, individuals who formally identified as helpers were not included in the development process. In addition, during the stage 2 follow-up, ethical constraints meant that we were unable to contact helpers directly to ask if they would be willing to be interviewed, which meant that the number of helper interviews was smaller than anticipated.
Potential sources of bias include that it is likely that more motivated individuals enrolled in the study, skewing the engagement data, although it is likely that similarly motivated individuals would engage with any future study or roll-out of the intervention. It is also likely that the more motivated and engaged individuals took part in the interviews, so they may have given more positive views of the intervention. We recruited only four participants for interview at 12 months, which meant that we obtained only limited insights into longer-term weight maintenance behaviours.
Another limitation relates to the geography, as people were recruited only from Greater Glasgow and Clyde. This is a large area including rural and urban areas and a range of demographics. However, it has poorer health than other areas of the UK with similar levels of deprivation and this could have an impact on the generalisability of the study approach.
Attrition was higher in the intervention group than in the control group. Attrition is typically higher in control groups for weight loss studies. The higher attrition in the intervention group for our study could be attributed to technical issues with the app, although this could also be explained by keen participants remaining in the control group in order to receive the intervention. The retention rate in the intervention arm may be more likely to be what would be seen in a full trial. One final limitation of the study is that 12 participants self-reported BMI, meaning that, overall, when considering obtaining an objective measure of BMI, our retention rate was 63% (69/109), so methods for improving this will need to be explored.
Key learning points
There are a number of key learnings from the feasibility trial that would be incorporated into the design of any future study. The focus of this feasibility trial has been to explore parameters for a full trial and, although our findings are mostly positive, a full trial may not be the only option for further evaluating the HelpMeDoIt! intervention. Other options include further refinement of the intervention with users, particularly focusing on the helper element and additional feasibility testing, which we plan to do in advance of applying for funding for a full trial.
Other key learnings have been presented in Chapter 6. With regard to evaluation design, we would include an online eligibility form to screen expressions of interest and additional administrative support to arrange recruitment and follow-up appointments. In terms of methods of recruitment, we would use the same methods, but focus more on primary care from the start, as this was the most effective recruitment method (after slight modifications to paperwork).
With regard to the intervention, a number of findings will inform the refinement of the app and website (see Chapter 6, Recommendations to improve the intervention). The option of accessing guidance via the app without the need for a website will be explored with users. Following refinement, we would ensure that there was a testing phase once the app was launched in the app store before allowing participants access, in order to smooth out any technical issues. A number of insights from the qualitative data will help to enhance both helper and participant engagement with the intervention. One key suggestion is to download the app when the field worker is present so that participants can be shown what to do and any issues can be ironed out at that point. We will also look to give further guidance on the participant–helper interactions, for example how to approach helpers and how to most effectively give and receive help. The helper nomination process could be streamlined and we would look to improve this. We could also provide guidance on how to pick a good helper based on our process evaluation findings. Another suggestion was to allow participants in the intervention arm to be peer supporters for other participants. This could potentially address the issue whereby a small minority of participants did not have anyone to nominate or they found it difficult to ask for help. It could also mean that the intervention effect could be enhanced by adding further opportunities for social support.
Planned dissemination of findings
Various routes of dissemination are planned for the findings of this study. First, in addition to the published protocol,73 we will publish the main outcomes in an open-access peer-reviewed journal. We have presented our methods and findings at numerous conferences, covering expertise in both behavioural medicine and social network analysis. We will continue to present findings at future conferences. Additional routes of dissemination have included five public engagement events with children and adults, and discussion of our study with other stakeholders at government events and other networking events.
Conclusions
This study has shown that the HelpMeDoIt! intervention is acceptable and feasible to deliver, although further work is needed to explore the helper role. It is also feasible to recruit participants, and to follow them up and collect outcomes at 12 months, suggesting that a large-scale study would be possible. We found evidence of promise for the intervention in both the qualitative and quantitative data. Some further refinement of both the trial methods and the intervention is needed, based on the results of the feasibility trial. The intervention refinements suggested are not fundamental changes to the content or mechanisms of the intervention. Based on the findings from the process evaluation, some changes are needed to the programme theory, the logic model and the intervention content, as well as functionality of the app and website to enhance engagement and improve the intervention. In particular, refinement is needed to improve helper engagement. These changes do not affect the key elements of the intervention: social support, goal-setting and self-monitoring. The results from the feasibility trial support the case for further evaluation of the HelpMeDoIt! Intervention.
A key challenge of working in digital health is that apps can rapidly become obsolete. However, although technology is continually advancing and the platform may change, the key issue is what the platform is delivering (i.e. the behaviour change approaches including mobilising people’s close social networks to assist with behaviour change). These are the key elements of this intervention, which could be delivered by an updated refined app or via a new platform. It is also possible to continue to improve the app during any evaluation as long as the key functions of the intervention are retained and delivered. 138 As Hawe et al. 138 have argued, the form of the intervention can be flexible as long as the key functions of the programme theory are delivered.
While the aim of this research was to develop an intervention that maximised effect size and participation rate, an intervention such as this has a potentially high reach and can therefore tolerate small effects and low use while still remaining cost-effective. It will also be important to consider the contribution of such digital health approaches within the wider ecological public health context for weight management and sustained weight reduction.
Implications for health care
This was a feasibility study. However, if effectiveness was demonstrated in a full trial there are several implications, including the following.
-
HelpMeDoIt! may have the potential to deliver a low-cost, potentially high-reach intervention for adults with obesity.
-
HelpMeDoIt! could be used as a complementary intervention used alongside other health-care or lifestyle services, including other apps.
-
HelpMeDoIt! may have potential to positively influence the lifestyle of individuals in a participant’s broader social network.
-
This approach to mobilising social support could be used in other areas of health behaviour change.
Recommendations for research
-
To further understand the motivation and engagement of helpers in relation to providing social support to participants.
-
To assess the effectiveness and cost-effectiveness of the HelpMeDoIt! intervention after further refinement of the intervention.
-
To further explore the key mechanisms of change identified by the HelpMeDoIt! feasibility findings.
Acknowledgements
The HelpMeDoIt! team would like to thank:
-
Selin Campbell for her valuable contribution as PPI member to our Trial Management Group
-
our software collaborators at JamHot (Glasgow, UK) for their development and hosting of the app and website
-
Dr Jean McQueen for conducting and analysing a sample of the 6-month interviews, and also for supporting the trial management of the study
-
Dr Sarah Barry and Dr Mohsen Rezaeihemami for their work on the quantitative and health economic analysis
-
PhD researchers, Bernardette Bonello, Ian MacNeill and Simon Barrett, for their support with interview transcription
-
the Scottish Primary Care Network for their help with recruitment
-
and our NIHR liaisons (Lewis Bradley, Margarida Resende and Dawn Kean) for their advice throughout the study.
We would also like to thank all members of our Trial Steering Committee for their valuable input during the study: Professor Colin Greaves (chairperson), Dr Marilyn Lennon, Dr Haroon Ahmed, Dr Ruth Jepson and Mr Kenneth Wallace (PPI).
Additional time on the study was supported by UK MRC and Chief Scientist Office (CSO) core funding as part of the MRC/CSO Social and Public Health Sciences Unit ‘Complexity in Health Improvement’ programme (MC_UU_12017/14 and SPHSU14) and ‘Social Relationships and Health Improvement’ programme (MC_UU_12017/11 and SPHSU11). Sharon Anne Simpson was further supported by MRC Strategic Award MC_PC_13027.
Contributions of authors
Sharon Anne Simpson (Professor, Behavioural Medicine) was principal investigator of the study, and led the design, implementation and interpretation of study findings, as well as contributing to the drafting, revision and approval of the final report.
Lynsay Matthews (Research Fellow, Social and Public Health) was trial manager of the study, conducted the process evaluation and prepared the overall findings for publication in the report.
Juliana Pugmire (Research Associate, Social and Public Health) was primary researcher for the qualitative component of the study. She led the data collection, analysis and prepared the qualitative results for publication in the report.
Alex McConnachie (Assistant Director of Biostatistics, Statistics) conducted the quantitative statistical analysis and prepared the quantitative results for publication in the report.
Emma McIntosh (Professor, Health Economics) conducted the health economic analysis and prepared these results for publication in the report.
Elinor Coulman (Research Associate, Trial Management) contributed to the study’s design, implementation and interpretation, and was involved in drafting and revising the final report.
Kathryn Hughes (Clinical Lecturer, Primary Care) contributed to the study’s design, implementation and interpretation, and was involved in drafting and revising the final report.
Mark Kelson (Senior Lecturer, Statistics) contributed to the study’s design, implementation and interpretation, and was involved in drafting and revising the final report.
Sarah Morgan-Trimmer (Research Fellow, Process Evaluation) contributed to the study’s design, implementation and interpretation, and was involved in drafting and revising the final report.
Simon Murphy (Professor, Social Interventions and Health) contributed to the study’s design, implementation and interpretation, and was involved in drafting and revising the final report.
Olga Utkina-Macaskill (Trial Administrator) contributed to the development of the HelpMeDoIt! intervention, was involved in drafting and revising the final report and reviewing the plain English summary.
Laurence Moore (Professor, Social and Public Health) contributed to the study’s design, implementation and interpretation, was involved in drafting and revising the final report.
Publication
Matthews L, Pugmire J, Moore L, Kelson M, McConnachie A, McIntosh E, et al. Study protocol for the ‘HelpMeDoIt!’ randomised controlled feasibility trial: an app, web and social support-based weight loss intervention for adults with obesity. BMJ Open 2017;7:e017159.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- World Health Organization . Obesity: Preventing and Managing the Global Epidemic 2000.
- World Health Organization . Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks 2009.
- Raine KD, Nykiforuk CI, Vu-Nguyen K, Nieuwendyk LM, VanSpronsen E, Reed S, et al. Understanding key influencers’ attitudes and beliefs about healthy public policy change for obesity prevention. Obesity 2014;22:2426-33. https://doi.org/10.1002/oby.20860.
- Organisation for Economic Co-operation and Development (OECD) . Obesity Update 2017.
- Scottish Public Health Observatory (ScotPHO) . Obesity 2017.
- Nørtoft E, Chubb B, Borglykke A. Obesity and healthcare resource utilization: comparative results from the UK and the USA. Obes Sci Pract 2018;4:41-5. https://doi.org/10.1002/osp4.148.
- Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med 2001;161:1581-6. https://doi.org/10.1001/archinte.161.13.1581.
- House of Lords Science and Technology Select Committee . Behaviour Change 2011.
- Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J, et al. Foresight. Tackling Obesities: Future Choices – Project Report. London: Government Office for Science; 2007.
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q 1988;15:351-77. https://doi.org/10.1177/109019818801500401.
- Simpson SA, Shaw C, McNamara R. What is the most effective way to maintain weight loss in adults?. BMJ 2011;343. https://doi.org/10.1136/bmj.d8042.
- Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1376.
- Greaves CJ, Sheppard KE, Abraham C, Hardeman W, Roden M, Evans PH, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-119.
- Shaw K, O’Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev 2005;2. https://doi.org/10.1002/14651858.CD003818.pub2.
- National Institute for Health and Care Excellence . Behaviour Change: Individual Approaches. 2014.
- Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011;26:1479-98. https://doi.org/10.1080/08870446.2010.540664.
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. https://doi.org/10.1037/a0016136.
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health 1998;13:623-49. https://doi.org/10.1080/08870449808407422.
- Carver CS, Scheier MF. Control theory: a useful conceptual framework for personality-social, clinical, and health psychology. Psychol Bull 1982;92:111-35. https://doi.org/10.1037/0033-2909.92.1.111.
- Pearson ES. Goal setting as a health behavior change strategy in overweight and obese adults: a systematic literature review examining intervention components. Patient Educ Couns 2012;87:32-4. https://doi.org/10.1016/j.pec.2011.07.018.
- Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966–017–0494-y.
- Williams S, French D. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour – and are they the same?. Health Educ Res 2011;26:308-22. https://doi.org/10.1093/her/cyr005.
- Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol 2006;38:69-119. https://doi.org/10.1016/S0065-2601(06)38002-1.
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357:370-9. https://doi.org/10.1056/NEJMsa066082.
- Scheffler RM, Brown TT. Social capital, economics, and health: new evidence. Health Econ Policy Law 2008;3:321-31. https://doi.org/10.1017/S1744133108004593.
- Stewart DW, Gabriele JM, Fisher EB. Directive support, nondirective support, and health behaviors in a community sample. J Behav Med 2012;35:492-9. https://doi.org/10.1007/s10865–011–9377-x.
- Heaney CA, Israel BA, Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: John Wiley & Sons; 2008.
- Ballantine PW, Stephenson RJ. Help me, I’m fat! Social support in online weight loss networks. J Consum Behav 2011;10:332-7. https://doi.org/10.1002/cb.374.
- Smith KP, Christakis NA. Social networks and health. Annu Rev Sociol 2008;34:405-29. https://doi.org/10.1146/annurev.soc.34.040507.134601.
- Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exercise among older Mexican Americans with type 2 diabetes. Diabetes Educ 2004;30:980-93. https://doi.org/10.1177/014572170403000619.
- Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol 1999;67:132-8. https://doi.org/10.1037/0022-006X.67.1.132.
- Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, et al. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. Community HIV Prevention Research Collaborative. Lancet 1997;350:1500-5. https://doi.org/10.1016/S0140-6736(97)07439-4.
- Maton KI. Social support, organizational characteristics, psychological well-being, and group appraisal in three self-help group populations. Am J Community Psychol 1988;16:53-77. https://doi.org/10.1007/BF00906072.
- Lemstra M, Fox J, Klassen R, Dodge D. The Healthy Weights Initiative: the first 1,000 participants. Patient Prefer Adherence 2017;11:283-9. https://doi.org/10.2147/PPA.S123914.
- Dailey R, Romo L, Myer S, Thomas C, Aggarwal S, Nordby K, et al. The buddy benefit: increasing the effectiveness of an employee-targeted weight-loss program. J Health Commun 2018;23:272-80. https://doi.org/10.1080/10810730.2018.1436622.
- Hogan BE, Linden W, Najarian B. Social support interventions: do they work?. Clin Psychol Rev 2002;22:383-442. https://doi.org/10.1016/S0272-7358(01)00102-7.
- Sherwood NE, Jeffery RW. The behavioral determinants of exercise: implications for physical activity interventions. Annu Rev Nutr 2000;20:21-44. https://doi.org/10.1146/annurev.nutr.20.1.21.
- O’Connell KA. Theories used in nursing research on smoking cessation. Annu Rev Nurs Res 2009;27:33-62. https://doi.org/10.1891/0739-6686.27.33.
- Lim YM, Sung MH, Joo KS. Factors affecting health-promoting behaviors of community-dwelling Korean older women. J Gerontol Nurs 2010;36:42-50. https://doi.org/10.3928/00989134-20100504-05.
- Molloy GJ, Dixon D, Hamer M, Sniehotta FF. Social support and regular physical activity: Does planning mediate this link?. Br J Health Psychol 2010;15:859-70. https://doi.org/10.1348/135910710X490406.
- Priebe CS, Spink KS. When in Rome: descriptive norms and physical activity. Psychol Sport Ex 2011;12:93-8. https://doi.org/10.1016/j.psychsport.2010.09.001.
- Ferranti EP, Dunbar SB, Higgins M, Dai J, Ziegler TR, Frediani JK, et al. Psychosocial factors associated with diet quality in a working adult population. Res Nurs Health 2013;36:242-56. https://doi.org/10.1002/nur.21532.
- Aggarwal B, Liao M, Mosca L. Predictors of physical activity at 1 year in a randomized controlled trial of family members of patients with cardiovascular disease. J Cardiovasc Nurs 2010;25:444-9. https://doi.org/10.1097/JCN.0b013e3181defd3e.
- Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among US community-dwelling adults. J Comm Health 2008;33:40-5. https://doi.org/10.1007/s10900-007-9066-4.
- Anderson-Bill ES, Winett RA, Wojcik JR. Social cognitive determinants of nutrition and physical activity among web-health users enrolling in an online intervention: the influence of social support, self-efficacy, outcome expectations, and self-regulation. J Med Internet Res 2011;13. https://doi.org/10.2196/jmir.1551.
- Neuhauser L, Kreps GL. Rethinking Communication in the E-health Era. J Health Psychol 2003;8:7-23. https://doi.org/10.1177/1359105303008001426.
- Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet 2011;378:49-55. https://doi.org/10.1016/S0140-6736(11)60701-0.
- Broekhuizen K, Mireille van Poppel NM, Lj LK, Brug J, van Mechelen W. Is the process of delivery of an individually tailored lifestyle intervention associated with improvements in LDL cholesterol and multiple lifestyle behaviours in people with familial hypercholesterolemia?. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-348.
- Carter MC, Burley VJ, Nykjaer C, Cade JE. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J Med Internet Res 2013;15. https://doi.org/10.2196/jmir.2283.
- Aalbers T, Baars MA, Rikkert MG. Characteristics of effective Internet-mediated interventions to change lifestyle in people aged 50 and older: a systematic review. Ageing Res Rev 2011;10:487-97. https://doi.org/10.1016/j.arr.2011.05.001.
- Militello LK, Kelly SA, Melnyk BM. Systematic review of text-messaging interventions to promote healthy behaviors in pediatric and adolescent populations: implications for clinical practice and research. Worldviews Evid Based Nurs 2012;9:66-77. https://doi.org/10.1111/j.1741-6787.2011.00239.x.
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56-69. https://doi.org/10.1093/epirev/mxq004.
- McNamee P, Murray E, Kelly MP, Bojke L, Chilcott J, Fischer A, et al. Designing and undertaking a health economics study of digital health interventions. Am J Prev Med 2016;51:852-60. https://doi.org/10.1016/j.amepre.2016.05.007.
- Wildman J, McMeekin P, Grieve E, Briggs A. Economic evaluation of integrated new technologies for health and social care: suggestions for policy makers, users and evaluators. Soc Sci Med 2016;169:141-8. https://doi.org/10.1016/j.socscimed.2016.09.033.
- National institute for Health and Care Excellence . Minutes of Public Board Meeting on 16th November 2016 2016. www.nice.org.uk/Media/Default/Get-involved/Meetings-In-Public/Public-board-meetings/agenda-and-papers-nov-16.pdf (accessed 21 April 2018).
- Elbert NJ, van Os-Medendorp H, van Renselaar W, Ekeland AG, Hakkaart-van Roijen L, Raat H, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.2790.
- Bacigalupo R, Cudd P, Littlewood C, Bissell P, Hawley M, Buckley Woods H. Interventions employing mobile technology for overweight and obesity: an early systematic review of randomized controlled trials. Obes Rev 2013;14:279-91. https://doi.org/10.1111/obr.12006.
- Wei J, Hollin I, Kachnowski S. A review of the use of mobile phone text messaging in clinical and healthy behaviour interventions. J Telemed Telecare 2011;17:41-8. https://doi.org/10.1258/jtt.2010.100322.
- Ofcom . Communications Market Report 2017.
- Deloitte . Global Mobile Consumer Survey 2017: The UK Cut, ‘State of the Smart’ 2017. www2.deloitte.com/uk/en/pages/technology-media-and-telecommunications/articles/mobile-consumer-survey.html (accessed 30 January 2019).
- Scottish Government . Scottish Household Survey 2016: Annual Report 2017.
- StickK . StickK 2016. www.stickk.com (accessed 1 June 2016).
- MyFitnessPal 2016. www.myfitnesspal.com (accessed 1 June 2016).
- Chen J, Cade JE, Allman-Farinelli M. The most popular smartphone apps for weight loss: a quality assessment. JMIR Mhealth Uhealth 2015;3. https://doi.org/10.2196/mhealth.4334.
- Ritterband LM, Thorndike FP, Cox DJ, Kovatchev BP, Gonder-Frederick LA. A behavior change model for internet interventions. Ann Behav Med 2009;38:18-27. https://doi.org/10.1007/s12160-009-9133-4.
- Khaylis A, Yiaslas T, Bergstrom J, Gore-Felton C. A review of efficacious technology-based weight-loss interventions: five key components. Telemed J E Health 2010;16:931-8. https://doi.org/10.1089/tmj.2010.0065.
- Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions. BMJ 2004;328. https://doi.org/10.1136/bmj.328.7449.1166.
- Maher CA, Lewis LK, Ferrar K, Marshall S, De Bourdeaudhuij I, Vandelanotte C. Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.2952.
- Nieminen T, Prättälä R, Martelin T, Härkänen T, Hyyppä MT, Alanen E, et al. Social capital, health behaviours and health: a population-based associational study. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-613.
- National Health Service (NHS) . Understanding the Costs of Digital Delivery of Healthcare; And Potential Savings 2016.
- Carr LJ, Dunsiger SI, Lewis B, Ciccolo JT, Hartman S, Bock B, et al. Randomized controlled trial testing an internet physical activity intervention for sedentary adults. Health Psychol 2013;32:328-36. https://doi.org/10.1037/a0028962.
- Brindal E, Freyne J, Saunders I, Berkovsky S, Smith G, Noakes M. Features predicting weight loss in overweight or obese participants in a web-based intervention: randomized trial. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.2156.
- Matthews L, Pugmire J, Moore L, Kelson M, McConnachie A, McIntosh E, et al. Study protocol for the ‘HelpMeDoIt!’ randomised controlled feasibility trial: an app, web and social support-based weight loss intervention for adults with obesity. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017–017159.
- Wight D, Wimbush E, Jepson R, Doi L. Six steps in quality intervention development (6SQuID). J Epidemiol Community Health 2016;70:520-5. https://doi.org/10.1136/jech-2015-205952.
- Yardley L, Morrison L, Bradbury K, Muller I. The Person-Based Approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4055.
- Mohr DC, Schueller SM, Montague E, Burns MN, Rashidi P. The Behavioral Intervention Technology Model: an integrated conceptual and technological framework for eHealth and mHealth Interventions. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3077.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Prestwich A, Webb TL, Conner M. Using theory to develop and test interventions to promote changes in health behaviour: evidence, issues, and recommendations. Curr Opinion Psychol 2015;5:1-5. https://doi.org/10.1016/j.copsyc.2015.02.011.
- Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev 2015;9:323-44. https://doi.org/10.1080/17437199.2014.941722.
- Michie S, Prestwich A. Are interventions theory-based? Development of a theory coding scheme. Health Psychol 2010;29:1-8. https://doi.org/10.1037/a0016939.
- Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ 2014;348. https://doi.org/10.1136/bmj.g2646.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. https://doi.org/10.1037/0278-6133.27.3.379.
- Michie S. Designing and implementing behaviour change interventions to improve population health. J Health Serv Res Policy 2008;13:64-9. https://doi.org/10.1258/jhsrp.2008.008014.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68-7. https://doi.org/10.1037/0003-066X.55.1.68.
- Cohen S, Underwood LG, Gottlieb BH. Social Support Measurement and Intervention: A Guide for Health and Social Scientists. Oxford: Oxford University Press; 2000.
- Lund AM. Measuring Usability with the USE Questionnaire. STC Usability SIG Newsletter 2001;8.
- Charters E. The use of Think-aloud methods in qualitative research. Brock Educ 2003;12:68-82. https://doi.org/10.26522/brocked.v12i2.38.
- Nielsen J, Mack RL, Nielsen J. Usability Inspection Methods. New York: NY: John Wiley & Sons Inc; 1994.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Warburton DER, Jamnik VK, Bredin SSD. Collaboration. GNobotP-Q . The Physical Activity Readiness Questionnaire for Everyone (PAR-Q+) and Electronic Physical Activity Readiness Medical Examination (ePARmed-X+). Health Fit J Can 2011;4:3-23.
- Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity 2012;20:1234-9. https://doi.org/10.1038/oby.2011.140.
- National Institute for Health Research . Good Clinical Practice (GCP) n.d. www.nihr.ac.uk/our-research-community/clinical-research-staff/learning-and-development/national-directory/good-clinical-practice/ (accessed 30 January 2019).
- Rogers E. Diffusion of Innovations. New York: NY: Simon and Schuster; 1962.
- Localytics . 21% of Users Abandon an App After First Use 2018. http://info.localytics.com/blog/21-percent-of-users-abandon-apps-after-one-use (accessed 1 May 2018).
- Michie S, Yardley L, West R, Patrick K, Greaves F. Developing and evaluating digital interventions to promote behavior change in health and health care: recommendations resulting from an international workshop. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.7126.
- Roe L, Strong C, Whiteside C, Neil A, Mant D. Dietary intervention in primary care: validity of the DINE method for diet assessment. Fam Pract 1994;11:375-81. https://doi.org/10.1093/fampra/11.4.375.
- Holmes B, Dick K, Nelson M. A comparison of four dietary assessment methods in materially deprived households in England. Public Health Nutr 2008;11:444-56. https://doi.org/10.1017/S1368980007000559.
- Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc 1998;30:777-81. https://doi.org/10.1097/00005768-199805000-00021.
- Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-day PAR. Med Sci Sports Exerc 2003;35:801-9. https://doi.org/10.1249/01.MSS.0000064941.43869.4E.
- EuroQol Group . EuroQol – a new facility for the measurement of health related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res 2012;21:167-76. https://doi.org/10.1007/s11136-011-9927-2.
- Goldberg DP, Williams P. A user’s guide to the General Health Questionnaire. Basingstoke: NFER Nelson; 1988.
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med 1987;16:825-36. https://doi.org/10.1016/0091-7435(87)90022-3.
- Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol 1991;59:739-44. https://doi.org/10.1037/0022-006X.59.5.739.
- Rodgers WM, Wilson PM, Hall CR, Fraser SN, Murray TC. Evidence for a multidimensional self-efficacy for exercise scale. Res Q Exerc Sport 2008;79:222-34. https://doi.org/10.1080/02701367.2008.10599485.
- Rodgers WM, Sullivan MJL. Task, coping, and scheduling self-efficacy in relation to frequency of physical activity. J App Social Psychol 2001;31:741-53. https://doi.org/10.1111/j.1559-1816.2001.tb01411.x.
- Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ. Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health Educ Res 2007;22:691-702. https://doi.org/10.1093/her/cyl148.
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict 1989;84:791-9. https://doi.org/10.1111/j.1360-0443.1989.tb03059.x.
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 2007;31:1208-17. https://doi.org/10.1111/j.1530-0277.2007.00403.x.
- Bingham SA. Limitations of the various methods for collecting dietary intake data. Ann Nutr Metab 1991;35:117-27. https://doi.org/10.1159/000177635.
- Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act 2008;5. https://doi.org/10.1186/1479-5868-5-56.
- Rueda-Clausen CF, Ogunleye AA, Sharma AM. Health benefits of long-term weight-loss maintenance. Annu Rev Nutr 2015;35:475-516. https://doi.org/10.1146/annurev-nutr-071714-034434.
- Actigraph Corp . Actilife 6 Software 2017. http://actigraphcorp.com/ (accessed 1 May 2018).
- Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol 1985;121:91-106. https://doi.org/10.1093/oxfordjournals.aje.a113987.
- Tinuviel Software . WISP Version 4.0 2015. www.tinuvielsoftware.co.uk/wisp4.htm (accessed 1 May 2018).
- Medical Research Council (MRC) . Process Evaluation of Complex Interventions 2015.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- Longworth L, Rowen D. Mapping to obtain EQ-5D utility values for use in NICE health technology assessments. Value Health 2013;16:202-10. https://doi.org/10.1016/j.jval.2012.10.010.
- Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in Health and Medicine. New York: Oxford University Press; 1996.
- Methods for the Development of NICE Public Health Guidance. London: National Institute for Health and Care Excellence; 2012.
- R Core Team . R: A Language and Environment for Statistical Computing 2017.
- van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw 2011;45:1-67. https://doi.org/10.18637/jss.v045.i03.
- Solt F, Hu Y. interplot: Plot the Effects of Variables in Interaction Terms. The Comprehensive R Archive Network (CRAN); 2015.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. PAFS consensus group . CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- V BVaC . Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Szende AJ, Janssen B, Cabases J. Self-Reported Population Health: An International Perspective Based on EQ-5D. London: Springer Open; 2014.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10. https://doi.org/10.1186/1471-2288-10-67.
- Audrey S, Bell S, Hughes R, Campbell R. Adolescent perspectives on wearing accelerometers to measure physical activity in population-based trials. Eur J Public Health 2012;23:475-80. https://doi.org/10.1093/eurpub/cks081.
- Tudor-Locke C, Barreira TV, Schuna JM, Mire EF, Chaput JP, Fogelholm M, et al. Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE). Int J Behav Nutr Phys Act 2015;12. https://doi.org/10.1186/s12966-015-0172-x.
- Baumann S, Groß S, Voigt L, Ullrich A, Weymar F, Schwaneberg T, et al. Pitfalls in accelerometer-based measurement of physical activity: the presence of reactivity in an adult population. Scand J Med Sci Sports 2018;28:1056-63. https://doi.org/10.1111/sms.12977.
- Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer 2008;112:228-42. https://doi.org/10.1002/cncr.23157.
- White M, Adams J, Heywood P, Babones SJ. Social Inequality and Public Health. Bristol: Policy Press; 2009.
- Sharpe PA, Wilcox S, Rooney LJ, Strong D, Hopkins-Campbell R, Butel J, et al. Adherence to accelerometer protocols among women from economically disadvantaged neighborhoods. J Phys Act Health 2011;8:699-706. https://doi.org/10.1123/jpah.8.5.699.
- Sylvia LG, Bernstein EE, Hubbard JL, Keating L, Anderson EJ. Practical guide to measuring physical activity. J Acad Nutr Diet 2014;114:199-208. https://doi.org/10.1016/j.jand.2013.09.018.
- Illner A-K, Freisling H, Boeing H, Huybrechts I, Crispim SP, Slimani N. Review and evaluation of innovative technologies for measuring diet in nutritional epidemiology. Int J Epidiomol 2012;41:1187-203. https://doi.org/10.1093/ije/dys105.
- Byrne S, Barry D, Petry NM. Predictors of weight loss success. Exercise vs. dietary self-efficacy and treatment attendance. Appetite 2012;58:695-8. https://doi.org/10.1016/j.appet.2012.01.005.
- Lasikiewicz N, Myrissa K, Hoyland A, Lawton CL. Psychological benefits of weight loss following behavioural and/or dietary weight loss interventions. A systematic research review. Appetite 2014;72:123-37. https://doi.org/10.1016/j.appet.2013.09.017.
- Hawe P, Shiell A, Riley T. Complex interventions: how ‘out of control’ can a randomised controlled trial be?. BMJ 2004;328:1561-3. https://doi.org/10.1136/bmj.328.7455.1561.
Appendix 1 Intervention development approaches for the HelpMeDoIt! study
| Approach | Purpose of the approach | Key components | Why this approach was beneficial for HelpMeDoIt! |
|---|---|---|---|
| 6SQuID model69 | General intervention development: To provide a step-by-step framework for the development of complex interventions |
|
|
| Person-Based Approach70 | Digital health focus: To guide the co-development of digital health interventions via user input |
|
|
| Behaviour Intervention Technology model71 | Digital health focus: To precisely map technological components to behaviour change features identified by the other methods | Integration of five key elements:
|
|
| Mapping behaviour change theory and techniques15 | Robust intervention development founded on tested theories of behaviour change: To identify the most appropriate behaviour change theories and behaviour change techniques |
|
|
Appendix 2 Guiding principles of the HelpMeDoIt! intervention
| Intervention design objective | Key features |
|---|---|
| To support individuals to safely and effectively lose weight |
Encouraging engagement with self-selected social network for help and encouragement Providing engaging evidence-based information to support relevant lifestyle change Promoting user competence by building self-regulatory skills (e.g. goal-setting and self-monitoring) |
| To support positive interaction between participants and nominated helpers |
Promoting autonomous ‘helper relationships’ via the provision of engaging evidence based guidance on social support Helping study participants to set mutually agreed on expectations Provision of easy access routes of communication Encouraging participant and helper interaction via the delivery of notifications and motivational messaging (i.e. thumbs up, animated positive messages, etc.) Providing information for helpers on how to support their friend (e.g. non-judgemental language, being positive, helping their friend to identify what might not be working if they are not meeting their goals) |
| To encourage individuals with previous unsuccessful weight loss attempts that this method can be successful |
Promoting the uniqueness (and benefit) of the helper aspect of the intervention Promoting the use of ‘tiny habits’ and SMART goals to increase chances of goal completion and success Promoting self-monitoring through use of feedback given by the app, which helpers can also see |
| To promote ongoing use of the apps |
Providing information and content that is helpful, enjoyable, fun, interactive, reliable and relevant Enhancing elements of gamification to make using the app fun and interactive for helpers and participants |
Appendix 3 Heuristic evaluation: criteria and findings
| Criteria | Mean score | Example of comments from heuristic reviewer | Example solutions provided by heuristic reviewer |
|---|---|---|---|
| Evaluation of the website | |||
| 1. Appearance and aesthetics | |||
| Pleasing colour scheme | 4/5 – good | The colours were very carefully chosen and were very relaxing and pleasing | N/A |
| Appropriate use of space | 4/5 – good | Yes, the spacing was good and the website was responding perfectly in the changes of resolution | N/A |
| Consistent design | 4 – good | The visual and navigational design is clear and consistent | N/A |
| Text and colours are consistent | 3/4 – good with some improvements | Could reduce the amount of bold text | Reduce the amount of bold text |
| Images are meaningful and serve a purpose | 4/5 – good | Really good use of images and icons | N/A |
| 2. Content | |||
| Purpose of page/headings are easy to understand | 4 – good | No issues noted | N/A |
| Easy to scan | 3/4 – good with some improvements needed | Quite a lot to read in helper section | Advise helpers that they should/can read a bit at a time and come back for extra support and material in stages |
| Minimal text/information presented | 3 – some improvements needed | Even though the overall design is minimal, the text presentation is not | N/A |
| Clear terminology, no jargon | 5 – excellent | The tone of the material is really accessible and pitched just right to be supportive but not patronising | N/A |
| 3. Navigation | |||
| Clear method of returning to main navigation menu | 4 – good | No issues noted | N/A |
| Clear method of returning to main dashboard | 4 – good | The icon on the top left was clear and always taking me to the home page | N/A |
| Easy to identify your location on the app | 4 – good | No issues noted | N/A |
| Appropriate number of buttons and links | 4 – good | Even though the number of buttons was good, the same navigation buttons were not present in all the pages | N/A |
| Organisation of information makes sense | 4 – good | No issues noted | N/A |
| Links to all app screens work | Checked all links – all worked for me | N/A | |
| Criteria | Mean score | Example of comments from heuristic reviewer | Example solutions provided by heuristic reviewer |
|---|---|---|---|
| Evaluation of the app | |||
| 1. Appearance and aesthetics | |||
| Primary purpose is clear | 4 – good | Have given lots of example in section 4 on how to make purpose clearer (e.g. Helpers, and messages and smiles – the purpose of them is not entirely clear on first use) | Have pop-up or about boxes for (1) helpers, (2) smiles and (3) awards |
| Clean and simple design | 4/5 – good | I found the visual design and layout very simple, clean and effective – professional looking but friendly – not overly clinical which I see as a good thing for this type of app and what would make me buy in and sustain use | N/A |
| Pleasing colour scheme | 4/5 – good | Clean and simple, friendly yet professional – right balance – I found the colour scheme calming and somewhat motivational actually | N/A |
| Appropriate use of space | 4/5 – good | Really good use of white space | N/A |
| Consistent design | 3/4 – could be improved | Visual design good – but I have given some examples below of some improvements for example use of arrows for both navigation and visual layout (record your steps) and also some headings are visual only (static) and some and clickable and this is not always obvious from visuals alone | Avoid use of arrows for both navigation and visual layout (record your steps). Make it clearer (colour/outline/style of text or button) when something is and is not clickable |
| Texts and colours are consistent | 4/5 – good | I found no issues with colours and actually found they helped me orient which feature I was in within the app | N/A |
| Images are meaningful and serve a purpose | 4 – good | Yes – actually I found that the icon design was pretty much spot on – I might have liked some more images but I think that might be personal choice and I wouldn’t go overboard on that at this stage with this version in case you decrease simplicity and design by adding in more images | Introduce more images as people progress through the app, or even allow people to add their own motivational images |
| 2. Content | |||
| Purpose of page/headings are easy to understand | 3 – could be improved | I have indicated in my notes in section 4 several occasions where the section or page headings did not help me orient in the app or tell me what I should be doing, This was only true for a few screens and I have detailed them below | Add your first goal – needs to be ‘Add a new goal’ after ‘I have a goal that exists’ |
| Minimal text/information presented | 4 – good | The amount and typesetting and layout of content was very good – just the right amount of text and content | N/A |
| Clear terminology, no jargon | 4 good | Really clear text this has been really well thought out – and ready sensible menu item naming which really helped me navigate around and discover features naturally | Explain more what a helper is and what a smile is as on first use |
| 3. Navigation | |||
| Clear method of returning to main navigation menu | 3 – could be improved | This was one of my only real complaints that I would say needs fixing – I found it difficult to find my way back naturally (from some places) to the main dashboard/main screen | Have a button on the main screen that takes you back to dashboard – or allow use of phones back button to allow user to naturally navigate back pages to where they came from |
| Clear method of returning to main dashboard | 3 – could be improved | Same as above | Same as above |
| Easy to identify your location on the app | 3 – could be improved | Not always – after not long (an hour) I could figure it out but I was confused at times | Have the main navigation menu – match what you can do and see on the main screen/dashboard so that there is no doubt what the main ‘home’ page is and there is no doubt that you can get to every page you need to either from the menu or the dashboard |
| Appropriate number of buttons and links | 4 – good | Just the right amount of buttons and links in my opinion – although I would liked to have been able to click on my medals and also on my progress so that they took me somewhere or let me interrogate those features more | Allow clicking on these features – clicking on weight might take you to change my weight – clicking on awards might take you to images |
| Organisation of information makes sense | 4 – good | Mostly I found the information to be well organised – only bit out of place for me was finding where to edit my weight – it seemed really out of place and hard to find in the main navigation menu | Add the change my weight to the start of the menu before add a new goal – or then end before (or even inside) ‘Your Details’ |
| Links to all app screens work | 2/3 – could be improved | See notes in section 4 – update goal – takes you to a well done message – is this correct? Also – change my details – save took me nowhere | Create a site map and make sure that everywhere does in fact lead you to where you want it to lead to and check from broken paths or wrong paths |
Appendix 4 Feedback from the stage 1 testing group
| Component of the app | Feedback |
|---|---|
| Look, colour, layout, functionality |
Overall, interviewees liked the colour scheme, swipe motion, illustration style and font style. Some suggested the colour was too ‘pastel’. Some users found the font a bit too small Users initially missed intro slides as they went by too quickly The first three intro slides had the same text even though icons were different Screens did not always load properly: screens sometimes appeared blank and other times the text would be stacked or jumbled together User hits back arrow on upper left hand corner of screen but screen sweeps in from the ‘wrong direction’ – the right. Intuitively this could be from the left |
| Guidance and reminders | Consider short tutorial or tip box at beginning in relation to goal-setting and earning medals and trophies |
| Inputting data |
The ‘send invite to helper’ did not seem to do anything, i.e. there was no indication anything had been sent. It was unclear what to do next Days ticked during goal-setting did not consistently stick Unclear where to enter weight as text box is not prominent Suggestion to input height (on weight page) so BMI is reflected Be able to input weight using unit of choice (e.g. stone and lb, kg, and include half lb and half kg) |
| Goal-setting |
Overall, interviewees were happy with the amount of information they would need to input and liked the initial set-up steps for goal-setting Might not need page with ‘Choose a goal’ or ‘Create goal’ but feed directly into template goals with the ‘None suit? Create your own’ tab Loved being able to change the details in goals (numbers, activities) A few interviewees commented that goal screen looked too busy/wording looked too small. One user said they would prefer more screens and less text and suggested even one goal per screen would be good Put number of goals set bubble next to category (e.g. physical activity 2, healthy eating 1) Rather than having a list of all goals on the screen there could be two buttons: one which shows ‘today’s goals’ and the other which shows ‘more goals’ Include guidance and/or prompts to increase goals as time goes on Reminders from the app of the goals set that day/week Prompts to ‘consider adding a healthy eating goal’ if they have not Advice or a prompt on a goal limit so that people were not setting too many Reminders from the app of the goals set that day/week Title and longer goal are not looking very intuitive. Some confusion with goal title versus goal detail. Not sure SMART goal is really coming across in examples Not very clear you can create your own goal – text box is relatively nondescript at the bottom of other colourful categories After setting one goal, jumps right to dashboard – felt jarring Got stuck trying to make more than one goal. We had to log out and in to set any subsequent goals and had to enter weight every time Change wording of ‘work out when tired goal’ to clarify its meaning Bin button should give feedback that you have deleted and a message that asks ‘Are you sure you want to delete your goal?’ |
| Self-monitoring |
Ability to view data different ways (i.e. pie charts, graphs, bar charts, etc.) App could compare current status with historic status (e.g. met X goals more than last month, walked X fewer miles than last month, etc.) Ability to upload data into Excel and use it as they want – most apps use data and present it one way with no ability to access those data and do anything with them Regarding progress, a suggestion was that the screen colour could change as you improved Occasionally goal completion is not reflected in progress graphs |
| Difficult to visualise progress graphs with so few data. Playing around with one goal does not give a clear picture of how useful they’ll be | |
| No indication you could swipe between goals on the dashboard | |
| Helpers | On ‘Add Helpers’ could have guidance to fill the blank space. Only two Add Helper icons |
| Overall | Felt that the app was intuitive and friendly but had some bugs to work out |
| Component of the website | Feedback |
| Look, colour, layout, functionality |
Overall positive feedback for layout and design Easy to navigate with suggestions to improve navigation of the ‘Info and Tips’ content Embed all hyperlinks within the text for improved readability Consider amending font size on several pages for consistency |
| Content |
Overall a lot of content but the website design presents the information in a manageable format Update several hyperlinks that no longer work on ‘helpful links’ page The ‘Top Ten Tips’ feature was highly praised Numerous helpful suggestions for grammar changes e.g. ‘If you slip up’ rather than ‘When you slip up’ Update the inconsistent use of ‘participant’ versus ‘friend’ |
| Helpers |
Consider adding a ‘helper quiz’ to engage and increase knowledge of helpers Content was well received, in particular the example conversations Consider use of bullet points to help with readability of helper content |
Appendix 5 Stage 1 results of the USE questionnaire
| Question number | Question text | Mean score | Range |
|---|---|---|---|
| Q1 | It helps me be more effective | 4.3 | 3–6 |
| Q2 | It helps me be more productive | 4.4 | 3–6 |
| Q3 | It is useful | 5.4 | 4–7 |
| Q4 | It gives me more control over the activities in my life | 4.9 | 3–7 |
| Q5 | It makes the things I want to accomplish easier to get done | 4.4 | 3–6 |
| Q6 | It saves me time when I use it | 4.3 | 3–6 |
| Q7 | It meets my needs | 4.6 | 4–6 |
| Q8 | It does everything I would expect it to do | 3.7 | 3–5 |
| Q9 | It is easy to use | 5.0 | 4–6 |
| Q10 | It is simple to use | 4.8 | 4–6 |
| Q11 | It is user friendly | 4.5 | 3–6 |
| Q12 | It requires the fewest steps possible to accomplish what I want to do with it | 4.2 | 2–5 |
| Q13 | It is flexible | 4.2 | 3–6 |
| Q14 | Using it is effortless | 4.2 | 3–5 |
| Q15 | I can use it without written instructions | 6.2 | 5–7 |
| Q16 | I don’t notice any inconsistencies as I use it | 4.0 | 3–6 |
| Q17 | Both occasional and regular users would like it | 5.0 | 3–6 |
| Q18 | I can recover from mistakes quickly and easily | 4.6 | 3–7 |
| Q19 | I can use it successfully every time | 4.0 | 3–7 |
| Q20 | I learned to use it quickly | 5.6 | 3–7 |
| Q21 | I easily remember how to use it | 5.4 | 3–6 |
| Q22 | It is easy to learn to use it | 5.0 | 3–6 |
| Q23 | I quickly became skilful with it | 4.9 | 3–7 |
| Q24 | I am satisfied with it | 4.5 | 3–6 |
| Q25 | I would recommend it to a friend | 5.2 | 3–6 |
| Q26 | It is fun to use | 4.7 | 3–6 |
| Q27 | It works the way I want it to work | 4.0 | 3–5 |
| Q28 | It is wonderful | 4.2 | 3–6 |
| Q29 | I feel I need to have it | 3.8 | 2–5 |
| Q30 | It is pleasant to use | 4.8 | 3–6 |
Appendix 6 Mapping of software elements to the HelpMeDoIt! logic model
| Logic model component | Associated software components | |
|---|---|---|
| Participant | Helper | |
| Facilitate and encourage social support |
‘Nominate your helper’ feature on app Two methods of interaction via app Guidance on website |
‘Nominate your helper’ feature on app Two methods of interaction via app Guidance on website |
| Provide support to helpers | Animated smile feature on app | Guidance on website |
| Encourage and provide support for goal-setting, action-planning and problem-solving |
Guidance on website Goal categories and templates on app Encouragement and advice via daily app messages/tips |
Guidance on website View participant’s goals via app Encouragement and advice via daily app messages/tips |
| Facilitate and encourage self-monitoring |
Self-monitoring and progress graphs feature on app Self-monitoring guidance on website |
View participants progress on app Self-monitoring guidance on website Helper guidance on website |
| Share tips |
Top Ten Tips feature on website Encouragement and advice via daily app messages/tips |
Top Ten Tips feature on website Encouragement and advice via daily app messages/tips |
| Boost self-efficacy via positive feedback |
Self-monitoring and progress graphs feature on app Encouraging messages received via app for goal progress Weekly e-mail summary report Motivational messages from helpers Receiving animated smiles |
Helper guidance via website Instant method of interaction via app with animated smiles |
| Boost motivation |
Self-monitoring and progress graphs In-app reward of medals/trophies for regular login and progress Encouragement via animated smiles from helper Encouragement and advice via daily app messages/tips Guidance on website |
In-app reward of medals/trophies for frequent login and input Encouragement via animated smiles from participants Helper guidance via website Encouragement and advice via daily app messages/tips |
| Provide evidence-based advice for physical activity, healthy eating and well-being |
Guidance on website Encouragement and advice via daily app messages/tips |
Guidance on website Encouragement and advice via daily app messages/tips |
| Facilitate encouragement, feedback and reinforcement |
Animated smiles feature on app Encouragement and advice via daily app messages/tips Messages from helpers |
Guidance on website Animated smiles feature on app Encouragement and advice via daily app messages/tips |
| Promote physical activity, healthy eating and well-being |
Physical activity, healthy eating and well-being goal categories and templates Guidance on website Top Ten Tips feature on website Encouragement and advice via daily app messages/tips |
Guidance on website Top Ten Tips feature on website Encouragement and advice via daily app messages/tips |
| Opportunities for social comparison and learning from peers |
Case stories feature on website (to be added after stage 2 commences) Helper interaction |
Case stories feature on website (to be added after stage 2 commences) |
| Promote autonomy via autonomy supportive content |
Encourage customisation of goals Ability to add own goals Encouragement and advice via daily app messages/tips Website and app designed in an autonomy supportive way Personalisation of settings |
Guidance on website to support participant to set own goals in an autonomy supportive way Encouragement and advice via daily app messages/tips |
| Provide social support (instrumental and emotional) |
Guidance on website Encouragement and advice via daily app messages/tips |
Guidance on website Encouragement and advice via daily app messages/tips |
| Support ongoing goals around physical activity, diet and well-being |
Guidance on website Encouragement and advice via daily app messages/tips |
Guidance on website Encouragement and advice via daily app messages/tips |
Appendix 7 Amendments to the HelpMeDoIt! study protocol
| Amendment number | Version number | Date issued | Author(s) of changes | Details of changes made |
|---|---|---|---|---|
| 1 | 2.0 | 22 July 2015 | SS |
Section 2: ‘think aloud’ methods added to study schema and main text Section 3: (i) some terminology reworded and missing aim added; (ii) primary outcome terminology reworded; (iii) BP and cholesterol measures removed from the protocol Section 4: ‘social support’ amended to ‘managing social influences’ Section 5: (i) objective 8 reworded to include ‘stage 1 and stage 2’; (ii) objective 10 reworded to include ‘modelling’ Section 8: (i) example of slimming club added; (ii) ‘In stage 2 only’ added to clarify recruitment sources Section 10: (i) ‘think-aloud methods and the USE questionnaire’ added to outcome measures; (ii) clarification of timing of smoking and alcohol questionnaires added; (iii) ICECAP-A measure added to complement EuroQol-5 Dimensions quality-of-life measure; (iv) text and table updated to reflect decision to collect smoking and alcohol use at 12 months only Section 11: (i) ‘we will have’ reworded to ‘we propose’ throughout section 11; (ii) reference to ‘forum’ removed from experimental group; (iii) ‘access via Facebook account’ added; (iv) information added regarding ‘participant-specific’ area of app and website Section 12: (i) progression criteria updated; (ii) incorrect reference to Trial Steering Committee meeting at 6 months removed; (iii) two questions added to assess researcher bias; (iii) ‘consent bias’ amended and reworded; (iv) secondary analyses section updated; (v) sentence added regarding exploration of goal-setting and self-monitoring Section 13: (i) reporting of SAEs to funder and ethics included; (ii) trial manager contact details added Section 14: (i) economic analyses section updated; (ii) process analyses and logic model testing added to analyses; (iii) thematic analysis replaces framework method Section 17: information related to Data Protection Agreement with software company added |
| 2 | 3.0 | 8 March 2016 | SS |
Page 7: randomisation telephone number added Section 3: ‘social network’ added to outcome measures Section 5: social network analysis added to the overall study objectives Section 10: social network analysis added to outcome measures/mediators Section 12.2.1: revised version of the logic model added |
| 3 | 4.0 | 27 September 2016 | SS | Section 12.3: progression criteria added for stage 2 to full RCT |
| 4 | 5.0 | 28 February 2017 | SS |
Job title of principal investigator amended from Dr to Professor Section 3: study summary study duration amended from 30 months to 34 months due to delayed start Section 7: participant sampling amended to ensure we select based on high, low or no use of the app Section 8.2: recruitment process removed the need for an additional consent form for participant stage 2 interviews in its place verbal consent will be obtained prior to interview |
Appendix 8 Full statistical outputs
HelpMeDoIt
Final analysis of HelpMeDoIt
External collaborator: Professor Sharon Anne Simpson.
Report description: Final.
Prepared by: Sarah Barry.
Last run on: Tuesday 20 March 2018 at 15:16:10 by Sarah Barry.
Created by program: \\Rcb-storage\filestore\Studies\HelpMeDoIt\statistics\programs\HelpMeDoIt_Analysis_v1_0.R.
Created using software: R version 3.4.1 (2017-06-30) for windows with additional packages mice interplot.
Source data file: \\Rcb-storage\filestore\Studies\HelpMeDoIt\statistics\data\\v1_0.
Protocol version: v5.0 (28 February 2017).
SAP version: v1.0 (17 January 2018).
Assumptions document: \\Rcb-storage\filestore\Studies\HelpMeDoIt\statistics\programs\Assumptions\HelpMeDoIt_Analysis_Report_v1_0_Assumptions.doc.
| Variable | n per month | Cumulative n |
|---|---|---|
| April 2016 | 4 | 4 |
| May 2016 | 7 | 11 |
| June 2016 | 9 | 20 |
| July 2016 | 27 | 47 |
| August 2016 | 12 | 59 |
| September 2016 | 26 | 85 |
| October 2016 | 24 | 109 |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Age (years) | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 47.3 (10.7) | 46.2 (10.6) | 49.4 (10.7) | |
| Median (IQR) | 48.0 (40.0–56.0) | 47.0 (39.0–55.0) | 50.5 (41.0–57.0) | |
| Range | (25.0–68.0) | (25.0–62.0) | (27.0–68.0) | |
| Gender | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Male | n (%) | 33 (30.3%) | 24 (32.9%) | 9 (25.0%) |
| Female | n (%) | 76 (69.7%) | 49 (67.1%) | 27 (75.0%) |
| SIMD quintile | Nobs (Nmiss) | 99 (10) | 66 (7) | 33 (3) |
| Most deprived | n (%) | 36 (36.4%) | 25 (37.9%) | 11 (33.3%) |
| 2 | n (%) | 21 (21.2%) | 15 (22.7%) | 6 (18.2%) |
| 3 | n (%) | 13 (13.1%) | 7 (10.6%) | 6 (18.2%) |
| 4 | n (%) | 16 (16.2%) | 10 (15.2%) | 6 (18.2%) |
| Least deprived | n (%) | 13 (13.1%) | 9 (13.6%) | 4 (12.1%) |
| Source of hearing about HelpMeDoIt! | Nobs (Nmiss) | 104 (5) | 70 (3) | 34 (2) |
| Letter from GP | n (%) | 46 (44.2%) | 28 (40.0%) | 18 (52.9%) |
| Exercise Referral Scheme | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| n (%) | 9 (8.7%) | 5 (7.1%) | 4 (11.8%) | |
| n (%) | 1 (1.0%) | 1 (1.4%) | 0 (0.0%) | |
| Gumtree | n (%) | 19 (18.3%) | 14 (20.0%) | 5 (14.7%) |
| Word of mouth | n (%) | 6 (5.8%) | 4 (5.7%) | 2 (5.9%) |
| Saw a poster/leaflet advert | n (%) | 23 (22.1%) | 18 (25.7%) | 5 (14.7%) |
| Marital status | Nobs (Nmiss) | 103 (6) | 68 (5) | 35 (1) |
| Married | n (%) | 45 (43.7%) | 29 (42.6%) | 16 (45.7%) |
| Civil partnership | n (%) | 1 (1.0%) | 1 (1.5%) | 0 (0.0%) |
| Cohabiting | n (%) | 15 (14.6%) | 11 (16.2%) | 4 (11.4%) |
| Single | n (%) | 25 (24.3%) | 18 (26.5%) | 7 (20.0%) |
| Widowed | n (%) | 2 (1.9%) | 1 (1.5%) | 1 (2.9%) |
| Divorced | n (%) | 15 (14.6%) | 8 (11.8%) | 7 (20.0%) |
| Ethnicity | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| White – British | n (%) | 87 (80.6%) | 55 (76.4%) | 32 (88.9%) |
| White – Irish | n (%) | 4 (3.7%) | 2 (2.8%) | 2 (5.6%) |
| Any other white background | n (%) | 6 (5.6%) | 5 (6.9%) | 1 (2.8%) |
| Mixed – white and black Caribbean | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Mixed – white and black African | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Mixed – white and Asian | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Any other mixed background | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Asian/Asian British – Indian | n (%) | 2 (1.9%) | 1 (1.4%) | 1 (2.8%) |
| Asian/Asian British – Pakistani | n (%) | 2 (1.9%) | 2 (2.8%) | 0 (0.0%) |
| Asian/Asian British – Bangladeshi | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Any other Asian background | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Black/black British – Caribbean | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Black/black British – African | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Any other black background | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Chinese | n (%) | 1 (0.9%) | 1 (1.4%) | 0 (0.0%) |
| Other | n (%) | 6 (5.6%) | 6 (8.3%) | 0 (0.0%) |
| Education | Nobs (Nmiss) | 104 (5) | 70 (3) | 34 (2) |
| Higher degree | n (%) | 18 (17.3%) | 14 (20.0%) | 4 (11.8%) |
| First degree | n (%) | 26 (25.0%) | 18 (25.7%) | 8 (23.5%) |
| Certificate/diploma | n (%) | 20 (19.2%) | 15 (21.4%) | 5 (14.7%) |
| A or AS levels | n (%) | 4 (3.8%) | 2 (2.9%) | 2 (5.9%) |
| O levels | n (%) | 28 (26.9%) | 16 (22.9%) | 12 (35.3%) |
| Other | n (%) | 8 (7.7%) | 5 (7.1%) | 3 (8.8%) |
| Employment | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Employee | n (%) | 86 (78.9%) | 57 (78.1%) | 29 (80.6%) |
| Self-employed with employees | n (%) | 3 (2.8%) | 1 (1.4%) | 2 (5.6%) |
| Self-employed/freelance without employees | n (%) | 13 (11.9%) | 11 (15.1%) | 2 (5.6%) |
| Unemployed | n (%) | 7 (6.4%) | 4 (5.5%) | 3 (8.3%) |
| Employment type | Nobs (Nmiss) | 105 (4) | 70 (3) | 35 (1) |
| Modern professional occupations | n (%) | 43 (41.0%) | 27 (38.6%) | 16 (45.7%) |
| Clerical and intermediate occupations | n (%) | 12 (11.4%) | 9 (12.9%) | 3 (8.6%) |
| Senior manager or administrators – finance manager, chief executive, project manager | n (%) | 15 (14.3%) | 12 (17.1%) | 3 (8.6%) |
| Technical and craft occupations | n (%) | 7 (6.7%) | 7 (10.0%) | 0 (0.0%) |
| Semi-routine manual and service occupations | n (%) | 14 (13.3%) | 8 (11.4%) | 6 (17.1%) |
| Routine manual and service occupations | n (%) | 6 (5.7%) | 3 (4.3%) | 3 (8.6%) |
| Middle or junior managers | n (%) | 3 (2.9%) | 1 (1.4%) | 2 (5.7%) |
| Traditional professional occupations | n (%) | 5 (4.8%) | 3 (4.3%) | 2 (5.7%) |
| Annual household income | Nobs (Nmiss) | 95 (14) | 64 (9) | 31 (5) |
| < £14,999 | n (%) | 21 (22.1%) | 13 (20.3%) | 8 (25.8%) |
| £15,000–29,000 | n (%) | 21 (22.1%) | 15 (23.4%) | 6 (19.4%) |
| £30,000–49,999 | n (%) | 30 (31.6%) | 19 (29.7%) | 11 (35.5%) |
| ≥ £50,000 | n (%) | 23 (24.2%) | 17 (26.6%) | 6 (19.4%) |
| Computer at home | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| No | n (%) | 5 (4.6%) | 4 (5.6%) | 1 (2.8%) |
| Yes | n (%) | 103 (95.4%) | 68 (94.4%) | 35 (97.2%) |
| How often do you use the internet? | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Every day | n (%) | 105 (97.2%) | 69 (95.8%) | 36 (100.0%) |
| Once a week or more | n (%) | 2 (1.9%) | 2 (2.8%) | 0 (0.0%) |
| Once a month | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Less than once a month | n (%) | 1 (0.9%) | 1 (1.4%) | 0 (0.0%) |
| Internet used for | ||||
| Education | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 31 (28.4%) | 19 (26.0%) | 12 (33.3%) |
| Yes | n (%) | 78 (71.6%) | 54 (74.0%) | 24 (66.7%) |
| Work | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 38 (34.9%) | 26 (35.6%) | 12 (33.3%) |
| Yes | n (%) | 71 (65.1%) | 47 (64.4%) | 24 (66.7%) |
| Shopping | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 18 (16.5%) | 13 (17.8%) | 5 (13.9%) |
| Yes | n (%) | 91 (83.5%) | 60 (82.2%) | 31 (86.1%) |
| Social networking | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 17 (15.6%) | 11 (15.1%) | 6 (16.7%) |
| Yes | n (%) | 92 (84.4%) | 62 (84.9%) | 30 (83.3%) |
| Chat room | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 91 (83.5%) | 60 (82.2%) | 31 (86.1%) |
| Yes | n (%) | 18 (16.5%) | 13 (17.8%) | 5 (13.9%) |
| Gaming | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 85 (78.0%) | 58 (79.5%) | 27 (75.0%) |
| Yes | n (%) | 24 (22.0%) | 15 (20.5%) | 9 (25.0%) |
| Music | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 42 (38.5%) | 31 (42.5%) | 11 (30.6%) |
| Yes | n (%) | 67 (61.5%) | 42 (57.5%) | 25 (69.4%) |
| Blogs | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 89 (81.7%) | 58 (79.5%) | 31 (86.1%) |
| Yes | n (%) | 20 (18.3%) | 15 (20.5%) | 5 (13.9%) |
| TV | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 60 (55.0%) | 38 (52.1%) | 22 (61.1%) |
| Yes | n (%) | 49 (45.0%) | 35 (47.9%) | 14 (38.9%) |
| Other | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 60 (55.0%) | 38 (52.1%) | 22 (61.1%) |
| Yes | n (%) | 49 (45.0%) | 35 (47.9%) | 14 (38.9%) |
| Phone used for | ||||
| Phone calls | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 1 (0.9%) | 1 (1.4%) | 0 (0.0%) |
| Yes | n (%) | 108 (99.1%) | 72 (98.6%) | 36 (100.0%) |
| Texting | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 2 (1.8%) | 2 (2.7%) | 0 (0.0%) |
| Yes | n (%) | 107 (98.2%) | 71 (97.3%) | 36 (100.0%) |
| Internet | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 11 (10.1%) | 6 (8.2%) | 5 (13.9%) |
| Yes | n (%) | 98 (89.9%) | 67 (91.8%) | 31 (86.1%) |
| Apps | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 13 (11.9%) | 9 (12.3%) | 4 (11.1%) |
| Yes | n (%) | 96 (88.1%) | 64 (87.7%) | 32 (88.9%) |
| Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) | |
| No | n (%) | 14 (12.8%) | 11 (15.1%) | 3 (8.3%) |
| Yes | n (%) | 95 (87.2%) | 62 (84.9%) | 33 (91.7%) |
| Instant messaging | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 37 (33.9%) | 25 (34.2%) | 12 (33.3%) |
| Yes | n (%) | 72 (66.1%) | 48 (65.8%) | 24 (66.7%) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Height (cm) | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 166.5 (9.4) | 166.9 (8.9) | 165.8 (10.2) | |
| Median [IQR] | 165.5 [161.0, 172.5] | 165.5 [161.3, 173.4] | 164.6 [158.0, 171.4] | |
| Range | (146.0, 192.5) | (146.0, 186.0) | (149.4, 192.5) | |
| Weight (kg) | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 104.6 (20.7) | 105.7 (21.4) | 102.2 (19.4) | |
| Median [IQR] | 100.4 [86.8, 119.0] | 101.1 [88.1, 119.0] | 98.2 [85.6, 118.6] | |
| Range | (72.4, 165.0) | (72.8, 165.0) | (72.4, 157.1) | |
| BMI (kg/m2) | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 37.6 (5.9) | 37.8 (6.0) | 37.1 (5.7) | |
| Median [IQR] | 36.0 [32.9, 39.7] | 36.7 [33.1, 39.7] | 35.6 [31.9, 39.5] | |
| Range | (30.4, 52.9) | (30.7, 52.9) | (30.4, 50.8) | |
| Waist circumference (cm) | Nobs (Nmiss) | 108 (1) | 73 (0) | 35 (1) |
| Mean (SD) | 114.1 (14.7) | 113.9 (15.4) | 114.6 (13.2) | |
| Median [IQR] | 112.3 [103.2, 123.3] | 111.5 [103.2, 123.7] | 114.7 [105.3, 123.3] | |
| Range | (87.7, 160.0) | (89.9, 160.0) | (87.7, 154.0) | |
| Hip circumference (cm) | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 124.3 (13.4) | 125.0 (14.2) | 122.7 (11.7) | |
| Median [IQR] | 122.3 [113.7, 130.1] | 122.3 [114.0, 132.6] | 122.0 [113.4, 128.0] | |
| Range | (104.7, 171.8) | (104.7, 171.8) | (106.5, 154.0) | |
| Weight change in last 3 months | Nobs (Nmiss) | 107 (2) | 71 (2) | 36 (0) |
| No | n (%) | 41 (38.3%) | 31 (43.7%) | 10 (27.8%) |
| Yes | n (%) | 66 (61.7%) | 40 (56.3%) | 26 (72.2%) |
| If so, by how much | Nobs (Nmiss) | 66 (0) | 40 (0) | 26 (0) |
| Mean (SD) | 1.8 (7.2) | 1.7 (7.0) | 2.0 (7.7) | |
| Median [IQR] | 3.2 [–3.2, 5.0] | 3.2 [–3.2, 4.5] | 3.2 [–3.2, 5.0] | |
| Range | (–19.1, 27.2) | (–19.1, 27.2) | (–15.9, 20.0) | |
| Currently attending weight loss group | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| No | n (%) | 79 (73.1%) | 55 (76.4%) | 24 (66.7%) |
| Yes | n (%) | 29 (26.9%) | 17 (23.6%) | 12 (33.3%) |
| If so, how often | Nobs (Nmiss) | 29 (0) | 17 (0) | 12 (0) |
| More than once a week | n (%) | 12 (41.4%) | 8 (47.1%) | 4 (33.3%) |
| Once a week | n (%) | 15 (51.7%) | 8 (47.1%) | 7 (58.3%) |
| Every other week | n (%) | 1 (3.4%) | 1 (5.9%) | 0 (0.0%) |
| Once a month | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Other (please specify) | n (%) | 1 (3.4%) | 0 (0.0%) | 1 (8.3%) |
| How often you weigh yourself | Nobs (Nmiss) | 102 (7) | 70 (3) | 32 (4) |
| Daily | n (%) | 12 (11.8%) | 7 (10.0%) | 5 (15.6%) |
| Once a week | n (%) | 26 (25.5%) | 15 (21.4%) | 11 (34.4%) |
| Every other week | n (%) | 12 (11.8%) | 7 (10.0%) | 5 (15.6%) |
| Once a month | n (%) | 16 (15.7%) | 14 (20.0%) | 2 (6.2%) |
| Other (please specify) | n (%) | 36 (35.3%) | 27 (38.6%) | 9 (28.1%) |
| Motivated to lose weight | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Not at all motivated | n (%) | 3 (2.8%) | 3 (4.1%) | 0 (0.0%) |
| 2 | n (%) | 4 (3.7%) | 1 (1.4%) | 3 (8.3%) |
| 3 | n (%) | 16 (14.7%) | 11 (15.1%) | 5 (13.9%) |
| 4 | n (%) | 38 (34.9%) | 28 (38.4%) | 10 (27.8%) |
| Very motivated | n (%) | 48 (44.0%) | 30 (41.1%) | 18 (50.0%) |
| Confident can lose weight | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Not at all confident | n (%) | 4 (3.7%) | 3 (4.1%) | 1 (2.8%) |
| 2 | n (%) | 9 (8.3%) | 7 (9.6%) | 2 (5.6%) |
| 3 | n (%) | 36 (33.0%) | 24 (32.9%) | 12 (33.3%) |
| 4 | n (%) | 32 (29.4%) | 22 (30.1%) | 10 (27.8%) |
| 5 Very confident | n (%) | 28 (25.7%) | 17 (23.3%) | 11 (30.6%) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Taken weight loss medication in last 12 months | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| No | n (%) | 100 (92.6%) | 67 (93.1%) | 33 (91.7%) |
| Yes | n (%) | 8 (7.4%) | 5 (6.9%) | 3 (8.3%) |
| Weight loss medication type (last 12 months) | Nobs (Nmiss) | 8 (0) | 5 (0) | 3 (0) |
| Conjugated linoleic acid | n (%) | 1 (12.5%) | 1 (20.0%) | 0 (0.0%) |
| Glucomannan Supplement K weight loss [brand name] | n (%) | 1 (12.5%) | 1 (20.0%) | 0 (0.0%) |
| Raspberry Ketones Herbal | n (%) | 1 (12.5%) | 0 (0.0%) | 1 (33.3%) |
| Glucomannan 50 mg | n (%) | 1 (12.5%) | 1 (20.0%) | 0 (0.0%) |
| Garcinia Cambogia, Trim FX (Zenutrix Anaheim, CA, USA) (herbal supplement) | n (%) | 1 (12.5%) | 0 (0.0%) | 1 (33.3%) |
| Orlistat (Xenical, Roche Holding AG, Basel, Switzerland) | n (%) | 3 (37.5%) | 2 (40.0%) | 1 (33.3%) |
| Still taking weight loss medication | Nobs (Nmiss) | 7 (1) | 5 (0) | 2 (1) |
| No | n (%) | 6 (85.7%) | 4 (80.0%) | 2 (100.0%) |
| Yes | n (%) | 1 (14.3%) | 1 (20.0%) | 0 (0.0%) |
| Weight loss medication type (still taking) | Nobs (Nmiss) | 1 (0) | 1 (0) | 0 (0) |
| Conjugated linoleic acid | n (%) | 1 (100.0%) | 1 (100.0%) | 0 (–) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Heart disease | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 107 (98.2%) | 72 (98.6%) | 35 (97.2%) |
| Yes | n (%) | 2 (1.8%) | 1 (1.4%) | 1 (2.8%) |
| Diabetes | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 103 (94.5%) | 69 (94.5%) | 34 (94.4%) |
| Yes | n (%) | 6 (5.5%) | 4 (5.5%) | 2 (5.6%) |
| Depression | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 92 (84.4%) | 62 (84.9%) | 30 (83.3%) |
| Yes | n (%) | 17 (15.6%) | 11 (15.1%) | 6 (16.7%) |
| Stroke | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 108 (99.1%) | 72 (98.6%) | 36 (100.0%) |
| Yes | n (%) | 1 (0.9%) | 1 (1.4%) | 0 (0.0%) |
| Arthritis | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 97 (89.0%) | 66 (90.4%) | 31 (86.1%) |
| Yes | n (%) | 12 (11.0%) | 7 (9.6%) | 5 (13.9%) |
| Hypertension | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 97 (89.0%) | 64 (87.7%) | 33 (91.7%) |
| Yes | n (%) | 12 (11.0%) | 9 (12.3%) | 3 (8.3%) |
| High cholesterol | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 102 (93.6%) | 68 (93.2%) | 34 (94.4%) |
| Yes | n (%) | 7 (6.4%) | 5 (6.8%) | 2 (5.6%) |
| Asthma | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 100 (91.7%) | 67 (91.8%) | 33 (91.7%) |
| Yes | n (%) | 9 (8.3%) | 6 (8.2%) | 3 (8.3%) |
| COPD | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 107 (98.2%) | 71 (97.3%) | 36 (100.0%) |
| Yes | n (%) | 2 (1.8%) | 2 (2.7%) | 0 (0.0%) |
| Back pain | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 91 (83.5%) | 65 (89.0%) | 26 (72.2%) |
| Yes | n (%) | 18 (16.5%) | 8 (11.0%) | 10 (27.8%) |
| Other | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 97 (89.0%) | 63 (86.3%) | 34 (94.4%) |
| Yes | n (%) | 12 (11.0%) | 10 (13.7%) | 2 (5.6%) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| At GP surgery | ||||
| Any health professional at GP surgery | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 34 (31.2%) | 23 (31.5%) | 11 (30.6%) |
| Yes | n (%) | 75 (68.8%) | 50 (68.5%) | 25 (69.4%) |
| GP: how many times | Nobs (Nmiss) | 60 (0) | 43 (0) | 17 (0) |
| Mean (SD) | 2.4 (2.8) | 2.4 (3.2) | 2.2 (1.5) | |
| Median [IQR] | 2.0 [1.0, 2.0] | 2.0 [1.0, 2.0] | 2.0 [1.0, 3.0] | |
| Range | (1.0, 16.0) | (1.0, 16.0) | (1.0, 6.0) | |
| Nurse: how many times | Nobs (Nmiss) | 33 (0) | 22 (0) | 11 (0) |
| Mean (SD) | 1.4 (0.9) | 1.5 (1.0) | 1.1 (0.3) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.0 [1.0, 2.0] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 5.0) | (1.0, 5.0) | (1.0, 2.0) | |
| Other health professional: how many times | Nobs (Nmiss) | 22 (0) | 10 (0) | 12 (0) |
| Mean (SD) | 1.9 (1.5) | 1.5 (1.1) | 2.2 (1.7) | |
| Median [IQR] | 1.0 [1.0, 3.0] | 1.0 [1.0, 1.0] | 1.0 [1.0, 3.0] | |
| Range | (1.0, 6.0) | (1.0, 4.0) | (1.0, 6.0) | |
| At home | ||||
| Any health professional at home | Nobs (Nmiss) | 105 (4) | 70 (3) | 35 (1) |
| No | n (%) | 103 (98.1%) | 70 (100.0%) | 33 (94.3%) |
| Yes | n (%) | 2 (1.9%) | 0 (0.0%) | 2 (5.7%) |
| GP: how many times | Nobs (Nmiss) | 4 (0) | 2 (0) | 2 (0) |
| Mean (SD) | 1.2 (0.5) | 1.5 (0.7) | 1.0 (0.0) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.5 [1.0, 2.0] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 2.0) | (1.0, 2.0) | (1.0, 1.0) | |
| Nurse: how many times | Nobs (Nmiss) | 3 (0) | 2 (0) | 1 (0) |
| Mean (SD) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 1.0) | (1.0, 1.0) | (1.0, 1.0) | |
| Other health professional: how many times | Nobs (Nmiss) | 4 (0) | 2 (0) | 2 (0) |
| Mean (SD) | 1.5 (1.0) | 1.0 (0.0) | 2.0 (1.4) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 2.0 [1.0, 3.0] | |
| Range | (1.0, 3.0) | (1.0, 1.0) | (1.0, 3.0) | |
| Hospital | ||||
| A&E visits | Nobs (Nmiss) | 105 (4) | 71 (2) | 34 (2) |
| No | n (%) | 93 (88.6%) | 67 (94.4%) | 26 (76.5%) |
| Yes | n (%) | 12 (11.4%) | 4 (5.6%) | 8 (23.5%) |
| A&E visits: how many times | Nobs (Nmiss) | 11 (1) | 3 (1) | 8 (0) |
| 1 | n (%) | 9 (81.8%) | 3 (100.0%) | 6 (75.0%) |
| 2 | n (%) | 1 (9.1%) | 0 (0.0%) | 1 (12.5%) |
| 3 | n (%) | 1 (9.1%) | 0 (0.0%) | 1 (12.5%) |
| Hospital visits | Nobs (Nmiss) | 90 (19) | 60 (13) | 30 (6) |
| No | n (%) | 87 (96.7%) | 60 (100.0%) | 27 (90.0%) |
| Yes | n (%) | 3 (3.3%) | 0 (0.0%) | 3 (10.0%) |
| Hospital visits: how many times | Nobs (Nmiss) | 3 (0) | 0 (0) | 3 (0) |
| 1 | n (%) | 2 (66.7%) | 0 (0.0%) | 2 (66.7%) |
| 2 | n (%) | 1 (33.3%) | 0 (0.0%) | 1 (33.3%) |
| Hospital visits: how many nights | Nobs (Nmiss) | 3 (0) | 0 (0) | 3 (0) |
| 1 | n (%) | 1 (33.3%) | 0 (0.0%) | 1 (33.3%) |
| 4 | n (%) | 1 (33.3%) | 0 (0.0%) | 1 (33.3%) |
| 7 | n (%) | 1 (33.3%) | 0 (0.0%) | 1 (33.3%) |
| Prescriptions | ||||
| Any prescriptions received | Nobs (Nmiss) | 91 (18) | 63 (10) | 28 (8) |
| No | n (%) | 17 (18.7%) | 14 (22.2%) | 3 (10.7%) |
| Yes | n (%) | 74 (81.3%) | 49 (77.8%) | 25 (89.3%) |
| Pay for lifestyle services (e.g. slimming/health clubs) | Nobs (Nmiss) | 106 (3) | 71 (2) | 35 (1) |
| No | n (%) | 55 (51.9%) | 40 (56.3%) | 15 (42.9%) |
| Yes | n (%) | 51 (48.1%) | 31 (43.7%) | 20 (57.1%) |
| Pay how much for lifestyle services | Nobs (Nmiss) | 51 (0) | 31 (0) | 20 (0) |
| Mean (SD) | 73.6 (67.7) | 70.8 (63.5) | 77.9 (75.3) | |
| Median [IQR] | 60.0 [45.0, 70.5] | 60.0 [45.0, 69.0] | 60.0 [30.0, 75.0] | |
| Range | (10.0, 360.0) | (10.0, 350.0) | (12.0, 360.0) | |
| Referral to exercise referral service | Nobs (Nmiss) | 105 (4) | 70 (3) | 35 (1) |
| No | n (%) | 100 (95.2%) | 66 (94.3%) | 34 (97.1%) |
| Yes | n (%) | 5 (4.8%) | 4 (5.7%) | 1 (2.9%) |
| Referred how often | Nobs (Nmiss) | 5 (0) | 4 (0) | 1 (0) |
| Mean (SD) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (0.0%) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 1.0) | (1.0, 1.0) | (1.0, 1.0) | |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Monitor worn | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| No | n (%) | 28 (25.7%) | 18 (24.7%) | 10 (27.8%) |
| Yes | n (%) | 81 (74.3%) | 55 (75.3%) | 26 (72.2%) |
| Minimum wear time achieved | Nobs (Nmiss) | 81 (0) | 55 (0) | 26 (0) |
| No | n (%) | 7 (8.6%) | 4 (7.3%) | 3 (11.5%) |
| Yes | n (%) | 74 (91.4%) | 51 (92.7%) | 23 (88.5%) |
| % in MVPA | Nobs (Nmiss) | 74 (0) | 51 (0) | 23 (0) |
| Mean (SD) | 5.2 (3.0) | 5.6 (3.3) | 4.1 (2.1) | |
| Median [IQR] | 5.1 [2.9, 6.6] | 5.6 [3.2, 7.0] | 4.1 [2.2, 5.6] | |
| Range | (0.9, 19.9) | (0.9, 19.9) | (1.2, 8.2) | |
| Average MVPA per day (minutes per day) | Nobs (Nmiss) | 74 (0) | 51 (0) | 23 (0) |
| Mean (SD) | 43.3 (25.9) | 46.7 (28.4) | 35.6 (17.5) | |
| Median [IQR] | 40.4 [26.2, 59.3] | 44.4 [26.2, 61.3] | 34.5 [23.3, 44.7] | |
| Range | (5.9, 172.4) | (5.9, 172.4) | (7.6, 65.9) | |
| Average sedentary minutes per day | Nobs (Nmiss) | 74 (0) | 51 (0) | 23 (0) |
| Mean (SD) | 649.3 (102.0) | 641.2 (92.3) | 667.3 (121.0) | |
| Median [IQR] | 635.0 [583.6, 723.4] | 653.2 [578.2, 719.2] | 632.3 [592.2, 724.6] | |
| Range | (407.9, 1054.1) | (407.9, 858.1) | (529.4, 1054.1) | |
| Average steps per day | Nobs (Nmiss) | 74 (0) | 51 (0) | 23 (0) |
| Mean (SD) | 6226.3 (2708.8) | 6519.2 (3088.7) | 5577.0 (1423.4) | |
| Median [IQR] | 5926.1 [4473.0, 7594.1] | 6108.3 [4361.7, 8274.2] | 5454.1 [4473.0, 6693.6] | |
| Range | (1114.6, 20,315.3) | (1114.6, 20,315.3) | (3302.2, 8667.5) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Total weekly expenditure by kg (kcal/kg/week) | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 259.9 (37.3) | 257.1 (30.9) | 265.7 (47.5) | |
| Median [IQR] | 251.3 [236.9, 270.2] | 252.9 [236.1, 268.0] | 248.4 [239.5, 270.2] | |
| Range | (218.0, 445.0) | (218.0, 408.5) | (227.0, 445.0) | |
| Total daily expenditure by kg (kcal/kg/day) | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 37.1 (5.3) | 36.7 (4.4) | 38.0 (6.8) | |
| Median [IQR] | 35.9 [33.8, 38.6] | 36.1 [33.7, 38.3] | 35.5 [34.2, 38.6] | |
| Range | (31.1, 63.6) | (31.1, 58.4) | (32.4, 63.6) | |
| Total daily expenditure (kcal/day) | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 3867.4 (870.9) | 3857.4 (752.3) | 3887.3 (1081.8) | |
| Median [IQR] | 3802.1 [3234.5, 4251.6] | 3834.3 [3234.5, 4235.4] | 3679.3 [3109.0, 4315.5] | |
| Range | (2512.2, 8086.3) | (2569.3, 6131.7) | (2512.2, 8086.3) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| DINE primary analysis | ||||
| DINE fibre score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 19.7 (11.2) | 20.3 (11.4) | 18.6 (10.8) | |
| Median [IQR] | 18.5 [10.0, 26.0] | 19.5 [10.0, 25.0] | 18.0 [9.0, 27.0] | |
| Range | (2.0, 67.0) | (4.0, 67.0) | (2.0, 40.0) | |
| DINE fibre rating | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Low fibre intake | n (%) | 90 (83.3%) | 59 (81.9%) | 31 (86.1%) |
| Medium fibre intake | n (%) | 13 (12.0%) | 8 (11.1%) | 5 (13.9%) |
| High fibre intake | n (%) | 5 (4.6%) | 5 (6.9%) | 0 (0.0%) |
| DINE fat score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 28.7 (12.3) | 29.5 (12.4) | 27.0 (12.2) | |
| Median [IQR] | 25.0 [19.0, 37.0] | 28.0 [20.0, 37.0] | 24.0 [18.0, 36.0] | |
| Range | (9.0, 58.0) | (9.0, 58.0) | (10.0, 57.0) | |
| DINE fat rating | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Low fat intake | n (%) | 63 (58.3%) | 39 (54.2%) | 24 (66.7%) |
| Medium fat intake | n (%) | 27 (25.0%) | 19 (26.4%) | 8 (22.2%) |
| High fat intake | n (%) | 18 (16.7%) | 14 (19.4%) | 4 (11.1%) |
| DINE healthy eating score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | –9.0 (15.4) | –9.2 (15.6) | –8.4 (15.3) | |
| Median [IQR] | –7.5 [–19.0, 1.0] | –7.5 [–19.0, 0.0] | –7.5 [–15.0, 2.0] | |
| Range | (–54.0, 37.0) | (–48.0, 37.0) | (–54.0, 15.0) | |
| DINE unsaturated fat score | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 9.2 (2.1) | 9.2 (2.2) | 9.3 (1.8) | |
| Median [IQR] | 10.0 [8.0, 11.0] | 10.0 [8.0, 11.0] | 10.0 [8.0, 11.0] | |
| Range | (0.0, 12.0) | (0.0, 12.0) | (5.0, 12.0) | |
| DINE unsaturated fat rating | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Low unsaturated fat intake | n (%) | 5 (4.6%) | 4 (5.5%) | 1 (2.8%) |
| Medium unsaturated fat intake | n (%) | 47 (43.1%) | 31 (42.5%) | 16 (44.4%) |
| High unsaturated fat intake | n (%) | 57 (52.3%) | 38 (52.1%) | 19 (52.8%) |
| DINE fruit and vegetable score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 4.8 (2.9) | 4.5 (2.5) | 5.3 (3.6) | |
| Median [IQR] | 4.0 [3.0, 6.0] | 4.0 [3.0, 5.0] | 4.5 [3.0, 6.0] | |
| Range | (0.0, 16.0) | (0.0, 13.0) | (0.0, 16.0) | |
| DINE fruit and vegetable rating | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Poor fruit and vegetable consumption | n (%) | 58 (53.7%) | 40 (55.6%) | 18 (50.0%) |
| Good fruit and vegetable consumption | n (%) | 50 (46.3%) | 32 (44.4%) | 18 (50.0%) |
| DINE fizzy drink score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 0.3 (0.8) | 0.3 (0.9) | 0.2 (0.7) | |
| Median [IQR] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 5.0) | (0.0, 5.0) | (0.0, 3.0) | |
| DINE sugar score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 0.7 (3.1) | 0.6 (1.5) | 1.0 (5.0) | |
| Median [IQR] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 30.0) | (0.0, 9.0) | (0.0, 30.0) | |
| DINE secondary analysis | ||||
| DINE unsaturated fat score | Nobs (Nmiss) | 104 (5) | 68 (5) | 36 (0) |
| Mean (SD) | 9.5 (1.7) | 9.5 (1.7) | 9.3 (1.8) | |
| Median [IQR] | 10.0 [8.0, 11.0] | 10.0 [8.0, 11.0] | 10.0 [8.0, 11.0] | |
| Range | (5.0, 12.0) | (6.0, 12.0) | (5.0, 12.0) | |
| DINE unsaturated fat rating | Nobs (Nmiss) | 104 (5) | 68 (5) | 36 (0) |
| Low unsaturated fat intake | n (%) | 1 (1.0%) | 0 (0.0%) | 1 (2.8%) |
| Medium unsaturated fat intake | n (%) | 46 (44.2%) | 30 (44.1%) | 16 (44.4%) |
| High unsaturated fat intake | n (%) | 57 (54.8%) | 38 (55.9%) | 19 (52.8%) |
| DINE fruit and vegetable score | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 4.7 (3.0) | 4.4 (2.5) | 5.3 (3.6) | |
| Median [IQR] | 4.0 [3.0, 6.0] | 4.0 [3.0, 5.0] | 4.5 [3.0, 6.0] | |
| Range | (0.0, 16.0) | (0.0, 13.0) | (0.0, 16.0) | |
| DINE fruit and vegetable rating | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Poor fruit and vegetable consumption | n (%) | 59 (54.1%) | 41 (56.2%) | 18 (50.0%) |
| Good fruit and vegetable consumption | n (%) | 50 (45.9%) | 32 (43.8%) | 18 (50.0%) |
| DINE fizzy drink score | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 0.3 (0.8) | 0.3 (0.9) | 0.2 (0.7) | |
| Median [IQR] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 5.0) | (0.0, 5.0) | (0.0, 3.0) | |
| DINE sugar score | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Mean (SD) | 0.7 (3.1) | 0.6 (1.5) | 1.0 (5.0) | |
| Median [IQR] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 30.0) | (0.0, 9.0) | (0.0, 30.0) | |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Family encouragement score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 13.3 (6.1) | 13.0 (6.0) | 14.0 (6.3) | |
| Median [IQR] | 12.5 [8.0, 18.0] | 12.0 [7.0, 17.0] | 14.0 [9.0, 19.0] | |
| Range | (5.0, 25.0) | (5.0, 25.0) | (5.0, 25.0) | |
| Family sabotage score | Nobs (Nmiss) | 107 (2) | 71 (2) | 36 (0) |
| Mean (SD) | 11.6 (3.9) | 11.3 (3.7) | 12.1 (4.2) | |
| Median [IQR] | 11.0 [9.0, 15.0] | 11.0 [9.0, 14.0] | 12.5 [9.0, 16.0] | |
| Range | (5.0, 22.0) | (5.0, 22.0) | (5.0, 20.0) | |
| Friends encouragement score | Nobs (Nmiss) | 107 (2) | 72 (1) | 35 (1) |
| Mean (SD) | 9.0 (4.1) | 8.5 (3.9) | 10.0 (4.5) | |
| Median [IQR] | 8.0 [5.0, 12.0] | 8.0 [5.0, 11.0] | 9.0 [7.0, 13.0] | |
| Range | (5.0, 21.0) | (5.0, 21.0) | (5.0, 20.0) | |
| Friends sabotage score | Nobs (Nmiss) | 105 (4) | 69 (4) | 36 (0) |
| Mean (SD) | 10.4 (4.5) | 10.4 (4.3) | 10.3 (4.7) | |
| Median [IQR] | 9.0 [7.0, 13.0] | 10.0 [7.0, 13.0] | 9.0 [6.0, 13.0] | |
| Range | (5.0, 21.0) | (5.0, 21.0) | (5.0, 21.0) | |
| Combined encouragement score | Nobs (Nmiss) | 107 (2) | 72 (1) | 35 (1) |
| Mean (SD) | 22.4 (8.7) | 21.5 (8.4) | 24.2 (8.9) | |
| Median [IQR] | 22.0 [15.0, 27.0] | 21.0 [15.0, 26.0] | 25.0 [16.0, 30.0] | |
| Range | (10.0, 45.0) | (10.0, 45.0) | (10.0, 44.0) | |
| Combined sabotage score | Nobs (Nmiss) | 105 (4) | 69 (4) | 36 (0) |
| Mean (SD) | 22.0 (7.2) | 21.8 (6.8) | 22.4 (8.0) | |
| Median [IQR] | 22.0 [16.0, 26.0] | 22.0 [16.0, 26.0] | 21.5 [16.0, 27.0] | |
| Range | (10.0, 38.0) | (10.0, 37.0) | (10.0, 38.0) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Family participation score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 20.6 (8.9) | 20.2 (8.1) | 21.2 (10.5) | |
| Median [IQR] | 19.0 [12.0, 28.0] | 19.0 [13.0, 27.0] | 19.5 [11.0, 31.0] | |
| Range | (9.0, 39.0) | (9.0, 39.0) | (9.0, 39.0) | |
| Family punishment score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 3.7 (1.2) | 3.6 (1.2) | 3.8 (1.3) | |
| Median [IQR] | 3.0 [3.0, 4.0] | 3.0 [3.0, 4.0] | 3.0 [3.0, 5.0] | |
| Range | (3.0, 9.0) | (3.0, 9.0) | (3.0, 7.0) | |
| Friends participation score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 16.1 (7.8) | 16.2 (7.9) | 16.0 (7.8) | |
| Median [IQR] | 14.0 [9.0, 20.0] | 14.0 [9.0, 19.0] | 13.5 [9.0, 20.0] | |
| Range | (9.0, 42.0) | (9.0, 42.0) | (9.0, 36.0) | |
| Friends punishment score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 3.4 (1.4) | 3.5 (1.6) | 3.3 (0.7) | |
| Median [IQR] | 3.0 [3.0, 3.0] | 3.0 [3.0, 3.0] | 3.0 [3.0, 3.0] | |
| Range | (3.0, 15.0) | (3.0, 15.0) | (3.0, 6.0) | |
| Combined participation score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 36.7 (13.4) | 36.4 (12.9) | 37.2 (14.6) | |
| Median [IQR] | 33.5 [25.0, 47.0] | 33.5 [25.0, 48.0] | 35.0 [24.0, 47.0] | |
| Range | (18.0, 74.0) | (18.0, 67.0) | (18.0, 74.0) | |
| Combined punishment score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 7.1 (2.3) | 7.1 (2.5) | 7.1 (1.8) | |
| Median [IQR] | 6.0 [6.0, 7.0] | 6.0 [6.0, 7.0] | 6.0 [6.0, 8.0] | |
| Range | (6.0, 21.0) | (6.0, 21.0) | (6.0, 13.0) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Availability score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 15.8 (9.5) | 15.0 (10.1) | 17.3 (7.9) | |
| Median [IQR] | 15.0 [9.0, 23.0] | 14.0 [7.0, 23.0] | 17.5 [10.0, 23.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (4.0, 33.0) | |
| Negative emotions score | Nobs (Nmiss) | 107 (2) | 71 (2) | 36 (0) |
| Mean (SD) | 14.6 (10.3) | 13.7 (11.0) | 16.2 (8.7) | |
| Median [IQR] | 14.0 [5.0, 21.0] | 12.0 [5.0, 21.0] | 17.0 [9.0, 21.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (0.0, 32.0) | |
| Social pressure score | Nobs (Nmiss) | 107 (2) | 71 (2) | 36 (0) |
| Mean (SD) | 21.1 (9.3) | 20.9 (9.8) | 21.4 (8.2) | |
| Median [IQR] | 22.0 [15.0, 28.0] | 21.0 [15.0, 28.0] | 22.5 [15.0, 27.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (2.0, 34.0) | |
| Physical discomfort score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 20.0 (8.7) | 19.2 (9.1) | 21.7 (7.8) | |
| Median [IQR] | 20.5 [13.0, 27.0] | 19.5 [12.0, 26.0] | 23.0 [15.0, 27.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (3.0, 36.0) | |
| Positive activities score | Nobs (Nmiss) | 107 (2) | 71 (2) | 36 (0) |
| Mean (SD) | 21.0 (8.5) | 20.3 (9.1) | 22.4 (7.2) | |
| Median [IQR] | 22.0 [15.0, 26.0] | 21.0 [14.0, 26.0] | 22.0 [18.0, 26.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (4.0, 36.0) | |
| Total score | Nobs (Nmiss) | 106 (3) | 70 (3) | 36 (0) |
| Mean (SD) | 92.6 (39.0) | 89.3 (42.2) | 99.1 (31.4) | |
| Median [IQR] | 98.0 [69.0, 118.0] | 89.0 [65.0, 117.0] | 100.5 [73.0, 118.0] | |
| Range | (0.0, 180.0) | (0.0, 180.0) | (31.0, 165.0) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Task score | Nobs (Nmiss) | 107 (2) | 72 (1) | 35 (1) |
| Mean (SD) | 4.4 (2.4) | 4.3 (2.5) | 4.6 (2.4) | |
| Median [IQR] | 4.0 [2.7, 6.0] | 4.2 [2.0, 6.0] | 4.0 [3.0, 5.7] | |
| Range | (1.0, 10.0) | (1.0, 10.0) | (1.0, 10.0) | |
| Coping score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 7.5 (2.0) | 7.6 (2.0) | 7.2 (2.1) | |
| Median [IQR] | 7.8 [6.8, 9.0] | 7.8 [6.8, 9.0] | 7.8 [5.8, 8.8] | |
| Range | (2.0, 10.0) | (2.0, 10.0) | (3.0, 10.0) | |
| Scheduling score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 5.8 (2.7) | 6.0 (2.7) | 5.5 (2.5) | |
| Median [IQR] | 5.7 [3.7, 8.0] | 6.0 [3.7, 8.3] | 5.2 [3.7, 7.0] | |
| Range | (1.0, 10.0) | (1.0, 10.0) | (1.0, 10.0) | |
| Total score | Nobs (Nmiss) | 107 (2) | 72 (1) | 35 (1) |
| Mean (SD) | 5.9 (1.9) | 6.0 (2.0) | 5.8 (1.7) | |
| Median [IQR] | 5.8 [4.6, 7.3] | 5.9 [4.6, 7.4] | 5.6 [4.5, 7.3] | |
| Range | (1.5, 10.0) | (1.5, 10.0) | (2.7, 9.8) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Autonomous regulation score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 6.2 (0.8) | 6.1 (0.9) | 6.5 (0.6) | |
| Median [IQR] | 6.5 [5.8, 6.8] | 6.2 [5.7, 6.7] | 6.7 [6.2, 7.0] | |
| Range | (3.0, 7.0) | (3.0, 7.0) | (5.0, 7.0) | |
| Controlled regulation score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 3.5 (1.3) | 3.6 (1.3) | 3.2 (1.2) | |
| Median [IQR] | 3.5 [2.5, 4.5] | 3.7 [2.7, 4.7] | 3.2 [2.3, 4.0] | |
| Range | (1.0, 6.0) | (1.0, 6.0) | (1.0, 5.8) | |
| Amotivational score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 1.8 (0.9) | 1.9 (0.9) | 1.7 (0.9) | |
| Median [IQR] | 1.4 [1.0, 2.5] | 1.7 [1.0, 2.7] | 1.0 [1.0, 2.0] | |
| Range | (1.0, 4.7) | (1.0, 4.7) | (1.0, 3.7) | |
| Relative autonomy index | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 2.7 (1.3) | 2.5 (1.3) | 3.2 (1.3) | |
| Median [IQR] | 2.7 [1.8, 3.6] | 2.5 [1.3, 3.4] | 3.3 [2.3, 4.2] | |
| Range | (0.0, 6.0) | (0.0, 5.5) | (0.8, 6.0) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Autonomous regulation score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 6.3 (0.9) | 6.2 (1.0) | 6.5 (0.6) | |
| Median [IQR] | 6.5 [5.8, 7.0] | 6.5 [5.8, 7.0] | 6.7 [6.0, 7.0] | |
| Range | (1.0, 7.0) | (1.0, 7.0) | (5.2, 7.0) | |
| Controlled regulation score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 3.2 (1.3) | 3.3 (1.3) | 3.0 (1.1) | |
| Median [IQR] | 3.2 [2.2, 4.0] | 3.2 [2.3, 4.2] | 3.1 [2.0, 3.7] | |
| Range | (1.0, 7.0) | (1.0, 7.0) | (1.0, 4.8) | |
| Amotivational score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 1.9 (1.0) | 1.9 (1.0) | 1.9 (0.9) | |
| Median [IQR] | 1.5 [1.0, 2.7] | 1.3 [1.0, 2.3] | 1.7 [1.0, 2.7] | |
| Range | (1.0, 5.0) | (1.0, 5.0) | (1.0, 4.0) | |
| Relative autonomy index | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 3.1 (1.4) | 2.9 (1.5) | 3.5 (1.2) | |
| Median [IQR] | 3.2 [2.2, 4.0] | 3.2 [1.8, 4.0] | 3.5 [2.7, 4.3] | |
| Range | (–0.3, 6.0) | (–0.3, 6.0) | (0.7, 6.0) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| GHQ score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 3.0 (3.2) | 3.1 (3.5) | 2.8 (2.6) | |
| Median [IQR] | 2.0 [0.0, 5.0] | 2.0 [0.0, 5.0] | 2.0 [0.0, 4.0] | |
| Range | (0.0, 12.0) | (0.0, 12.0) | (0.0, 8.0) | |
| GHQ score (Likert scoring) | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 13.6 (5.3) | 13.8 (5.6) | 13.1 (4.7) | |
| Median [IQR] | 12.0 [10.0, 17.0] | 12.0 [10.0, 17.0] | 13.0 [10.0, 14.0] | |
| Range | (5.0, 30.0) | (5.0, 30.0) | (6.0, 26.0) | |
| GHQ case (Likert score of ≥ 12) | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| No | N (%) | 47 (43.5%) | 33 (45.8%) | 14 (38.9%) |
| Yes | N (%) | 61 (56.5%) | 39 (54.2%) | 22 (61.1%) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Settled | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I am able to feel settled and secure in all areas of my life | n (%) | 8 (7.4%) | 5 (6.9%) | 3 (8.3%) |
| I am able to feel settled and secure in many areas of my life | n (%) | 63 (58.3%) | 45 (62.5%) | 18 (50.0%) |
| I am able to feel settled and secure in a few areas of my life | n (%) | 34 (31.5%) | 19 (26.4%) | 15 (41.7%) |
| I am unable to feel settled and secure in any areas of my life | n (%) | 3 (2.8%) | 3 (4.2%) | 0 (0.0%) |
| Independence | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I am able to be completely independent | n (%) | 43 (39.8%) | 31 (43.1%) | 12 (33.3%) |
| I am able to be independent in many things | n (%) | 51 (47.2%) | 31 (43.1%) | 20 (55.6%) |
| I am able to be independent in a few things | n (%) | 13 (12.0%) | 9 (12.5%) | 4 (11.1%) |
| I am unable to be at all independent | n (%) | 1 (0.9%) | 1 (1.4%) | 0 (0.0%) |
| Achievements | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I can achieve and progress in all aspects of my life | n (%) | 23 (21.3%) | 19 (26.4%) | 4 (11.1%) |
| I can achieve and progress in many aspects of my life | n (%) | 58 (53.7%) | 36 (50.0%) | 22 (61.1%) |
| I can achieve and progress in a few aspects of my life | n (%) | 26 (24.1%) | 16 (22.2%) | 10 (27.8%) |
| I cannot achieve and progress in any aspects of my life | n (%) | 1 (0.9%) | 1 (1.4%) | 0 (0.0%) |
| Pleasure | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I can have a lot of enjoyment and pleasure | n (%) | 39 (36.1%) | 32 (44.4%) | 7 (19.4%) |
| I can have a quite a lot of enjoyment and pleasure | n (%) | 49 (45.4%) | 27 (37.5%) | 22 (61.1%) |
| I can have a little enjoyment and pleasure | n (%) | 20 (18.5%) | 13 (18.1%) | 7 (19.4%) |
| I cannot have any enjoyment and pleasure | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Total ICECAP-A score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 12.1 (2.1) | 12.3 (2.2) | 11.7 (1.9) | |
| Median [IQR] | 12.0 [11.0, 13.0] | 13.0 [11.0, 14.0] | 12.0 [11.0, 13.0] | |
| Range | (6.0, 16.0) | (6.0, 16.0) | (8.0, 16.0) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Mobility | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I have no problems in walking about | n (%) | 78 (72.2%) | 54 (75.0%) | 24 (66.7%) |
| I have some problems in walking about | n (%) | 30 (27.8%) | 18 (25.0%) | 12 (33.3%) |
| I am confined to bed | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Self-care | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I have no problem with self-care | n (%) | 99 (91.7%) | 66 (91.7%) | 33 (91.7%) |
| I have some problems washing or dressing myself | n (%) | 9 (8.3%) | 6 (8.3%) | 3 (8.3%) |
| I am unable to wash or dress myself | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Usual activities | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I have no problems with performing my usual activities | n (%) | 81 (75.0%) | 56 (77.8%) | 25 (69.4%) |
| I have some problems with performing my usual activities | n (%) | 27 (25.0%) | 16 (22.2%) | 11 (30.6%) |
| I am unable to perform my usual activities | n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Pain | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I have no pain or discomfort | n (%) | 47 (43.5%) | 37 (51.4%) | 10 (27.8%) |
| I have moderate pain or discomfort | n (%) | 55 (50.9%) | 33 (45.8%) | 22 (61.1%) |
| I have extreme pain or discomfort | n (%) | 6 (5.6%) | 2 (2.8%) | 4 (11.1%) |
| Anxiety | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| I am not anxious or depressed | n (%) | 59 (54.6%) | 38 (52.8%) | 21 (58.3%) |
| I am moderately anxious or depressed | n (%) | 45 (41.7%) | 31 (43.1%) | 14 (38.9%) |
| I am extremely anxious or depressed | n (%) | 4 (3.7%) | 3 (4.2%) | 1 (2.8%) |
| EQ-5D score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 0.900 (0.090) | 0.906 (0.089) | 0.888 (0.092) | |
| Median [IQR] | 0.913 [0.850, 1.000] | 0.924 [0.866, 1.000] | 0.886 [0.816, 0.942] | |
| Range | (0.697, 1.000) | (0.697, 1.000) | (0.697, 1.000) | |
| EQ-VAS score | Nobs (Nmiss) | 108 (1) | 72 (1) | 36 (0) |
| Mean (SD) | 64.5 (18.8) | 65.3 (18.0) | 62.9 (20.5) | |
| Median [IQR] | 65.0 [60.0, 75.0] | 65.0 [60.0, 75.0] | 65.0 [55.0, 75.0] | |
| Range | (10.0, 100.0) | (10.0, 100.0) | (10.0, 95.0) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Follow-up status | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| Followed up | n (%) | 84 (77.1%) | 52 (71.2%) | 32 (88.9%) |
| Not followed up | n (%) | 25 (22.9%) | 21 (28.8%) | 4 (11.1%) |
| 95% CI for follow-up rate | (68.0% to 84.6%) | (59.4% to 81.2%) | (73.9% to 96.9%) | |
| Withdrawal reason | Nobs (Nmiss) | 109 (0) | 73 (0) | 36 (0) |
| n (%) | 84 (77.1%) | 52 (71.2%) | 32 (88.9%) | |
| None given | n (%) | 23 (21.1%) | 19 (26.0%) | 4 (11.1%) |
| Injury | n (%) | 1 (0.9%) | 1 (1.4%) | 0 (0.0%) |
| Moved away from the Glasgow area | n (%) | 1 (0.9%) | 1 (1.4%) | 0 (0.0%) |
| Variable | Statistic | All (N = 109) | Intervention (N = 73) | Control (N = 36) |
|---|---|---|---|---|
| Usefulness | Nobs (Nmiss) | 23 (86) | 22 (51) | 1 (35) |
| Mean (SD) | 41.3 (14.3) | 41.9 (14.3) | 28.0 (–) | |
| Median [IQR] | 43.0 [28.0, 56.0] | 45.5 [35.0, 56.0] | 28.0 [28.0, 28.0] | |
| Range | (8.0, 56.0) | (8.0, 56.0) | (28.0, 28.0) | |
| Ease of use | Nobs (Nmiss) | 22 (87) | 21 (52) | 1 (35) |
| Mean (SD) | 51.4 (19.7) | 52.1 (19.9) | 36.0 (–) | |
| Median [IQR] | 51.5 [37.0, 71.0] | 52.0 [38.0, 71.0] | 36.0 [36.0, 36.0] | |
| Range | (14.0, 77.0) | (14.0, 77.0) | (36.0, 36.0) | |
| Ease of learning | Nobs (Nmiss) | 25 (84) | 24 (49) | 1 (35) |
| Mean (SD) | 15.3 (8.6) | 15.2 (8.8) | 17.0 (–) | |
| Median [IQR] | 14.0 [9.0, 24.0] | 13.0 [8.0, 24.0] | 17.0 [17.0, 17.0] | |
| Range | (4.0, 28.0) | (4.0, 28.0) | (17.0, 17.0) | |
| Satisfaction | Nobs (Nmiss) | 25 (84) | 24 (49) | 1 (35) |
| Mean (SD) | 36.4 (13.4) | 36.8 (13.6) | 27.0 (–) | |
| Median [IQR] | 40.0 [29.0, 49.0] | 41.0 [29.0, 49.0] | 27.0 [27.0, 27.0] | |
| Range | (7.0, 49.0) | (7.0, 49.0) | (27.0, 27.0) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Study group | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Control | n (%) | 36 | 32 (88.9%) | 4 (11.1%) |
| Intervention | n (%) | 73 | 52 (71.2%) | 21 (28.8%) |
| Age (years) | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 47.3 (10.7) | 48.3 (10.4) | 43.9 (11.2) | |
| Median [IQR] | 48.0 [40.0, 56.0] | 50.0 [41.0, 56.0] | 43.0 [34.0, 55.0] | |
| Range | (25.0, 68.0) | (25.0, 68.0) | (27.0, 60.0) | |
| Gender | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Male | n (%) | 33 | 22 (66.7%) | 11 (33.3%) |
| Female | n (%) | 76 | 62 (81.6%) | 14 (18.4%) |
| SIMD quintile | Nobs (Nmiss) | 99 (10) | 76 (8) | 23 (2) |
| Most deprived | n (%) | 36 | 24 (66.7%) | 12 (33.3%) |
| 2 | n (%) | 21 | 17 (81.0%) | 4 (19.0%) |
| 3 | n (%) | 13 | 11 (84.6%) | 2 (15.4%) |
| 4 | n (%) | 16 | 14 (87.5%) | 2 (12.5%) |
| Least deprived | n (%) | 13 | 10 (76.9%) | 3 (23.1%) |
| Source of hearing about HelpMeDoIt! | Nobs (Nmiss) | 104 (5) | 79 (5) | 25 (0) |
| Letter from GP | n (%) | 46 | 35 (76.1%) | 11 (23.9%) |
| Exercise Referral Scheme | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| n (%) | 9 | 9 (100.0%) | 0 (0.0%) | |
| n (%) | 1 | 0 (0.0%) | 1 (100.0%) | |
| Gumtree | n (%) | 19 | 13 (68.4%) | 6 (31.6%) |
| Word of mouth | n (%) | 6 | 5 (83.3%) | 1 (16.7%) |
| Saw a poster/leaflet advert | n (%) | 23 | 17 (73.9%) | 6 (26.1%) |
| Marital status | Nobs (Nmiss) | 103 (6) | 79 (5) | 24 (1) |
| Married | n (%) | 45 | 34 (75.6%) | 11 (24.4%) |
| Civil partnership | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Cohabiting | n (%) | 15 | 9 (60.0%) | 6 (40.0%) |
| Single | n (%) | 25 | 20 (80.0%) | 5 (20.0%) |
| Widowed | n (%) | 2 | 1 (50.0%) | 1 (50.0%) |
| Divorced | n (%) | 15 | 14 (93.3%) | 1 (6.7%) |
| Ethnicity | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| White – British | n (%) | 87 | 67 (77.0%) | 20 (23.0%) |
| White – Irish | n (%) | 4 | 2 (50.0%) | 2 (50.0%) |
| Any other white background | n (%) | 6 | 6 (100.0%) | 0 (0.0%) |
| Mixed – white and black caribbean | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Mixed – white and black African | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Mixed – white and Asian | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Any other mixed background | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Asian/Asian British – Indian | n (%) | 2 | 2 (100.0%) | 0 (0.0%) |
| Asian/Asian British – Pakistani | n (%) | 2 | 0 (0.0%) | 2 (100.0%) |
| Asian/Asian British – Bangladeshi | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Any other Asian background | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Black/black British – Caribbean | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Black/black British – African | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Any other black background | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Chinese | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Other | n (%) | 6 | 5 (83.3%) | 1 (16.7%) |
| Education | Nobs (Nmiss) | 104 (5) | 81 (3) | 23 (2) |
| Higher degree | n (%) | 18 | 17 (94.4%) | 1 (5.6%) |
| First degree | n (%) | 26 | 21 (80.8%) | 5 (19.2%) |
| Certificate/diploma | n (%) | 20 | 14 (70.0%) | 6 (30.0%) |
| A or AS levels | n (%) | 4 | 4 (100.0%) | 0 (0.0%) |
| O levels | n (%) | 28 | 18 (64.3%) | 10 (35.7%) |
| Other | n (%) | 8 | 7 (87.5%) | 1 (12.5%) |
| Employed | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Employee | n (%) | 86 | 71 (82.6%) | 15 (17.4%) |
| Self-employed | n (%) | 16 | 8 (50.0%) | 8 (50.0%) |
| Unemployed | n (%) | 7 | 5 (71.4%) | 2 (28.6%) |
| Employment type | Nobs (Nmiss) | 105 (4) | 82 (2) | 23 (2) |
| Modern professional occupations | n (%) | 43 | 37 (86.0%) | 6 (14.0%) |
| Clerical and intermediate occupations | n (%) | 12 | 9 (75.0%) | 3 (25.0%) |
| Senior manager or administrators – finance manager, chief executive, project manager | n (%) | 15 | 13 (86.7%) | 2 (13.3%) |
| Technical and craft occupations | n (%) | 7 | 2 (28.6%) | 5 (71.4%) |
| Semi-routine manual and service occupations | n (%) | 14 | 9 (64.3%) | 5 (35.7%) |
| Routine manual and service occupations | n (%) | 6 | 5 (83.3%) | 1 (16.7%) |
| Middle or junior managers | n (%) | 3 | 3 (100.0%) | 0 (0.0%) |
| Traditional professional occupations | n (%) | 5 | 4 (80.0%) | 1 (20.0%) |
| Annual household income | Nobs (Nmiss) | 95 (14) | 75 (9) | 20 (5) |
| < £14,999 | n (%) | 21 | 15 (71.4%) | 6 (28.6%) |
| £15,000–29,000 | n (%) | 21 | 16 (76.2%) | 5 (23.8%) |
| £30,000–49,999 | n (%) | 30 | 25 (83.3%) | 5 (16.7%) |
| ≥ £50,000 | n (%) | 23 | 19 (82.6%) | 4 (17.4%) |
| Computer at home | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| No | n (%) | 5 | 4 (80.0%) | 1 (20.0%) |
| Yes | n (%) | 103 | 79 (76.7%) | 24 (23.3%) |
| How often do you use the internet? | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Every day | n (%) | 105 | 82 (78.1%) | 23 (21.9%) |
| Once a week or more | n (%) | 2 | 1 (50.0%) | 1 (50.0%) |
| Once a month | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Less than once a month | n (%) | 1 | 0 (0.0%) | 1 (100.0%) |
| Internet used for | ||||
| Education | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 31 | 22 (71.0%) | 9 (29.0%) |
| Yes | n (%) | 78 | 62 (79.5%) | 16 (20.5%) |
| Work | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 38 | 29 (76.3%) | 9 (23.7%) |
| Yes | n (%) | 71 | 55 (77.5%) | 16 (22.5%) |
| Shopping | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 18 | 13 (72.2%) | 5 (27.8%) |
| Yes | n (%) | 91 | 71 (78.0%) | 20 (22.0%) |
| Social networking | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 17 | 15 (88.2%) | 2 (11.8%) |
| Yes | n (%) | 92 | 69 (75.0%) | 23 (25.0%) |
| Chat room | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 91 | 70 (76.9%) | 21 (23.1%) |
| Yes | n (%) | 18 | 14 (77.8%) | 4 (22.2%) |
| Gaming | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 85 | 66 (77.6%) | 19 (22.4%) |
| Yes | n (%) | 24 | 18 (75.0%) | 6 (25.0%) |
| Music | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 42 | 30 (71.4%) | 12 (28.6%) |
| Yes | n (%) | 67 | 54 (80.6%) | 13 (19.4%) |
| Blogs | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 89 | 69 (77.5%) | 20 (22.5%) |
| Yes | n (%) | 20 | 15 (75.0%) | 5 (25.0%) |
| TV | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 60 | 46 (76.7%) | 14 (23.3%) |
| Yes | n (%) | 49 | 38 (77.6%) | 11 (22.4%) |
| Other | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 60 | 46 (76.7%) | 14 (23.3%) |
| Yes | n (%) | 49 | 38 (77.6%) | 11 (22.4%) |
| Phone used for | ||||
| Phone calls | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Yes | n (%) | 108 | 83 (76.9%) | 25 (23.1%) |
| Texting | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 2 | 2 (100.0%) | 0 (0.0%) |
| Yes | n (%) | 107 | 82 (76.6%) | 25 (23.4%) |
| Internet | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 11 | 9 (81.8%) | 2 (18.2%) |
| Yes | n (%) | 98 | 75 (76.5%) | 23 (23.5%) |
| Apps | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 13 | 9 (69.2%) | 4 (30.8%) |
| Yes | n (%) | 96 | 75 (78.1%) | 21 (21.9%) |
| Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) | |
| No | n (%) | 14 | 11 (78.6%) | 3 (21.4%) |
| Yes | n (%) | 95 | 73 (76.8%) | 22 (23.2%) |
| Instant messaging | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 37 | 29 (78.4%) | 8 (21.6%) |
| Yes | n (%) | 72 | 55 (76.4%) | 17 (23.6%) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Height (cm) | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 166.5 (9.4) | 165.6 (9.3) | 169.6 (8.9) | |
| Median [IQR] | 165.5 [161.0, 172.5] | 164.8 [159.8, 171.8] | 168.0 [162.7, 176.6] | |
| Range | (146.0, 192.5) | (146.0, 192.5) | (155.5, 186.0) | |
| Weight (kg) | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 104.6 (20.7) | 101.9 (19.7) | 113.7 (21.8) | |
| Median [IQR] | 100.4 [86.8, 119.0] | 97.7 [85.5, 115.2] | 111.7 [97.5, 124.5] | |
| Range | (72.4, 165.0) | (72.4, 165.0) | (82.0, 164.9) | |
| BMI (kg/m2) | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 37.6 (5.9) | 37.0 (5.4) | 39.5 (7.0) | |
| Median [IQR] | 36.0 [32.9, 39.7] | 35.6 [32.5, 39.0] | 37.8 [34.0, 45.7] | |
| Range | (30.4, 52.9) | (30.4, 52.6) | (30.8, 52.9) | |
| Waist circumference (cm) | Nobs (Nmiss) | 108 (1) | 84 (0) | 24 (1) |
| Mean (SD) | 114.1 (14.7) | 112.2 (13.8) | 120.7 (16.0) | |
| Median [IQR] | 112.3 [103.2, 123.3] | 111.2 [102.0, 118.5] | 119.1 [108.6, 132.2] | |
| Range | (87.7, 160.0) | (87.7, 158.6) | (95.0, 160.0) | |
| Hip circumference (cm) | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 124.3 (13.4) | 123.2 (12.5) | 128.1 (15.7) | |
| Median [IQR] | 122.3 [113.7, 130.1] | 122.3 [113.6, 128.0] | 123.2 [113.7, 145.8] | |
| Range | (104.7, 171.8) | (104.7, 171.8) | (109.0, 160.0) | |
| Weight change in last 3 months | Nobs (Nmiss) | 107 (2) | 82 (2) | 25 (0) |
| No | N (%) | 41 | 29 (70.7%) | 12 (29.3%) |
| Yes | N (%) | 66 | 53 (80.3%) | 13 (19.7%) |
| If so, by how much | Nobs (Nmiss) | 66 (0) | 53 (0) | 13 (0) |
| Mean (SD) | 1.8 (7.2) | 1.8 (6.3) | 2.0 (10.5) | |
| Median [IQR] | 3.2 [–3.2, 5.0] | 3.2 [–3.2, 4.5] | 3.2 [–3.2, 6.4] | |
| Range | (–19.1, 27.2) | (–15.9, 20.0) | (–19.1, 27.2) | |
| Currently attending weight loss group | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| No | n (%) | 79 | 57 (72.2%) | 22 (27.8%) |
| Yes | n (%) | 29 | 26 (89.7%) | 3 (10.3%) |
| If so, how often | Nobs (Nmiss) | 29 (80) | 26 (58) | 3 (22) |
| More than once a week | n (%) | 12 | 11 (91.7%) | 1 (8.3%) |
| Once a week | n (%) | 15 | 14 (93.3%) | 1 (6.7%) |
| Every other week | n (%) | 1 | 0 (0.0%) | 1 (100.0%) |
| Once a month | n (%) | 0 | 0 (–) | 0 (–) |
| Other (please specify) | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| How often you weigh yourself | Nobs (Nmiss) | 102 (7) | 80 (4) | 22 (3) |
| Daily | n (%) | 12 | 9 (75.0%) | 3 (25.0%) |
| Once a week | n (%) | 26 | 21 (80.8%) | 5 (19.2%) |
| Every other week | n (%) | 12 | 11 (91.7%) | 1 (8.3%) |
| Once a month | n (%) | 16 | 11 (68.8%) | 5 (31.2%) |
| Other (please specify) | n (%) | 36 | 28 (77.8%) | 8 (22.2%) |
| Motivated to lose weight | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Not at all motivated | n (%) | 3 | 3 (100.0%) | 0 (0.0%) |
| 2 | n (%) | 4 | 4 (100.0%) | 0 (0.0%) |
| 3 | n (%) | 16 | 10 (62.5%) | 6 (37.5%) |
| 4 | n (%) | 38 | 33 (86.8%) | 5 (13.2%) |
| Very motivated | n (%) | 48 | 34 (70.8%) | 14 (29.2%) |
| Confident can lose weight | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Not at all confident | n (%) | 4 | 3 (75.0%) | 1 (25.0%) |
| 2 | n (%) | 9 | 7 (77.8%) | 2 (22.2%) |
| 3 | n (%) | 36 | 29 (80.6%) | 7 (19.4%) |
| 4 | n (%) | 32 | 25 (78.1%) | 7 (21.9%) |
| Very confident | n (%) | 28 | 20 (71.4%) | 8 (28.6%) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Taken weight loss medication in last 12 months | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| No | n (%) | 100 | 78 (78.0%) | 22 (22.0%) |
| Yes | n (%) | 8 | 5 (62.5%) | 3 (37.5%) |
| Still taking weight loss medication | Nobs (Nmiss) | 7 (1) | 4 (1) | 3 (0) |
| No | n (%) | 6 | 3 (50.0%) | 3 (50.0%) |
| Yes | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Heart disease | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 107 | 82 (76.6%) | 25 (23.4%) |
| Yes | n (%) | 2 | 2 (100.0%) | 0 (0.0%) |
| Diabetes | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 103 | 80 (77.7%) | 23 (22.3%) |
| Yes | n (%) | 6 | 4 (66.7%) | 2 (33.3%) |
| Depression | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 92 | 73 (79.3%) | 19 (20.7%) |
| Yes | n (%) | 17 | 11 (64.7%) | 6 (35.3%) |
| Stroke | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 108 | 83 (76.9%) | 25 (23.1%) |
| Yes | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Arthritis | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 97 | 74 (76.3%) | 23 (23.7%) |
| Yes | n (%) | 12 | 10 (83.3%) | 2 (16.7%) |
| Hypertension | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 97 | 74 (76.3%) | 23 (23.7%) |
| Yes | n (%) | 12 | 10 (83.3%) | 2 (16.7%) |
| High cholesterol | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 102 | 77 (75.5%) | 25 (24.5%) |
| Yes | n (%) | 7 | 7 (100.0%) | 0 (0.0%) |
| Asthma | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 100 | 76 (76.0%) | 24 (24.0%) |
| Yes | n (%) | 9 | 8 (88.9%) | 1 (11.1%) |
| COPD | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 107 | 83 (77.6%) | 24 (22.4%) |
| Yes | n (%) | 2 | 1 (50.0%) | 1 (50.0%) |
| Back pain | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 91 | 72 (79.1%) | 19 (20.9%) |
| Yes | n (%) | 18 | 12 (66.7%) | 6 (33.3%) |
| Other | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 97 | 73 (75.3%) | 24 (24.7%) |
| Yes | n (%) | 12 | 11 (91.7%) | 1 (8.3%) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| At GP surgery | ||||
| Any health professional at GP surgery | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 34 | 27 (79.4%) | 7 (20.6%) |
| Yes | n (%) | 75 | 57 (76.0%) | 18 (24.0%) |
| GP: how many times | Nobs (Nmiss) | 60 (0) | 44 (0) | 16 (0) |
| Mean (SD) | 2.4 (2.8) | 2.1 (2.4) | 3.1 (3.8) | |
| Median [IQR] | 2.0 [1.0, 2.0] | 2.0 [1.0, 2.0] | 2.0 [1.0, 3.0] | |
| Range | (1.0, 16.0) | (1.0, 16.0) | (1.0, 16.0) | |
| Nurse: how many times | Nobs (Nmiss) | 33 (0) | 25 (0) | 8 (0) |
| Mean (SD) | 1.4 (0.9) | 1.2 (0.5) | 1.9 (1.5) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 1.0 [1.0, 2.0] | |
| Range | (1.0, 5.0) | (1.0, 3.0) | (1.0, 5.0) | |
| Other health professional: how many times | Nobs (Nmiss) | 22 (0) | 18 (0) | 4 (0) |
| Mean (SD) | 1.9 (1.5) | 1.5 (1.0) | 3.5 (2.1) | |
| Median [IQR] | 1.0 [1.0, 3.0] | 1.0 [1.0, 1.0] | 3.5 [1.0, 4.0] | |
| Range | (1.0, 6.0) | (1.0, 4.0) | (1.0, 6.0) | |
| At home | ||||
| Any health professional at home | Nobs (Nmiss) | 105 (4) | 81 (3) | 24 (1) |
| No | n (%) | 103 | 80 (77.7%) | 23 (22.3%) |
| Yes | n (%) | 2 | 1 (50.0%) | 1 (50.0%) |
| GP: how many times | Nobs (Nmiss) | 4 (0) | 3 (0) | 1 (0) |
| Mean (SD) | 1.2 (0.5) | 1.3 (0.6) | 1.0 (–) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.0 [1.0, 2.0] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 2.0) | (1.0, 2.0) | (1.0, 1.0) | |
| Nurse: how many times | Nobs (Nmiss) | 3 (0) | 2 (0) | 1 (0) |
| Mean (SD) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (–) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 1.0) | (1.0, 1.0) | (1.0, 1.0) | |
| Other health professional: how many times | Nobs (Nmiss) | 4 (0) | 2 (0) | 2 (0) |
| Mean (SD) | 1.5 (1.0) | 2.0 (1.4) | 1.0 (0.0) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 2.0 [1.0, 3.0] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 3.0) | (1.0, 3.0) | (1.0, 1.0) | |
| Hospital | ||||
| A&E visits | Nobs (Nmiss) | 105 (4) | 80 (4) | 25 (0) |
| No | n (%) | 93 | 70 (75.3%) | 23 (24.7%) |
| Yes | n (%) | 12 | 10 (83.3%) | 2 (16.7%) |
| A&E visits: how many times | Nobs (Nmiss) | 11 (1) | 9 (1) | 2 (0) |
| 1 | n (%) | 9 | 7 (77.8%) | 2 (22.2%) |
| 2 | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| 3 | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Hospital visits | Nobs (Nmiss) | 90 (19) | 71 (13) | 19 (6) |
| No | n (%) | 87 | 69 (79.3%) | 18 (20.7%) |
| Yes | n (%) | 3 | 2 (66.7%) | 1 (33.3%) |
| Hospital visits: how many times | Nobs (Nmiss) | 3 (0) | 2 (0) | 1 (0) |
| 1 | n (%) | 2 | 1 (50.0%) | 1 (50.0%) |
| 2 | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Hospital visits: how many nights | Nobs (Nmiss) | 3 (0) | 2 (0) | 1 (0) |
| 1 | n (%) | 1 | 0 (0.0%) | 1 (100.0%) |
| 4 | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| 7 | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Prescriptions | ||||
| Any prescriptions received | Nobs (Nmiss) | 91 (18) | 69 (15) | 22 (3) |
| No | n (%) | 17 | 12 (70.6%) | 5 (29.4%) |
| Yes | n (%) | 74 | 57 (77.0%) | 17 (23.0%) |
| Pay for lifestyle services (eg. slimming/health clubs) | Nobs (Nmiss) | 106 (3) | 82 (2) | 24 (1) |
| No | n (%) | 55 | 42 (76.4%) | 13 (23.6%) |
| Yes | n (%) | 51 | 40 (78.4%) | 11 (21.6%) |
| Pay how much for lifestyle services | Nobs (Nmiss) | 51 (0) | 40 (0) | 11 (0) |
| Mean (SD) | 73.6 (67.7) | 81.5 (73.8) | 44.9 (23.0) | |
| Median [IQR] | 60.0 [45.0, 70.5] | 60.0 [45.0, 75.0] | 50.0 [20.0, 68.0] | |
| Range | (10.0, 360.0) | (12.0, 360.0) | (10.0, 70.5) | |
| Referral to exercise referral service | Nobs (Nmiss) | 105 (4) | 80 (4) | 25 (0) |
| No | n (%) | 100 | 76 (76.0%) | 24 (24.0%) |
| Yes | n (%) | 5 | 4 (80.0%) | 1 (20.0%) |
| Referred how often | Nobs (Nmiss) | 5 (0) | 4 (0) | 1 (0) |
| Mean (SD) | 1.0 (0.0) | 1.0 (0.0) | 1.0 (–) | |
| Median [IQR] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 1.0) | (1.0, 1.0) | (1.0, 1.0) | |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Monitor worn | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| No | n (%) | 28 | 18 (64.3%) | 10 (35.7%) |
| Yes | n (%) | 81 | 66 (81.5%) | 15 (18.5%) |
| Minimum wear time achieved | Nobs (Nmiss) | 81 (0) | 66 (0) | 15 (0) |
| No | n (%) | 7 | 7 (100.0%) | 0 (0.0%) |
| Yes | n (%) | 74 | 59 (79.7%) | 15 (20.3%) |
| % in MVPA | Nobs (Nmiss) | 74 (0) | 59 (0) | 15 (0) |
| Mean (SD) | 5.2 (3.0) | 5.3 (3.2) | 4.4 (2.1) | |
| Median [IQR] | 5.1 [2.9, 6.6] | 5.3 [3.0, 6.8] | 4.9 [2.1, 6.5] | |
| Range | (0.9, 19.9) | (0.9, 19.9) | (1.5, 7.7) | |
| Average MVPA per day(minutes per day) | Nobs (Nmiss) | 74 (0) | 59 (0) | 15 (0) |
| Mean (SD) | 43.3 (25.9) | 45.1 (27.3) | 36.1 (18.6) | |
| Median [IQR] | 40.4 [26.2, 59.3] | 42.8 [26.5, 60.1] | 36.7 [18.6, 51.6] | |
| Range | (5.9, 172.4) | (5.9, 172.4) | (12.0, 66.2) | |
| Average sedentary minutes per day | Nobs (Nmiss) | 74 (0) | 59 (0) | 15 (0) |
| Mean (SD) | 649.3 (102.0) | 650.0 (106.1) | 646.6 (86.9) | |
| Median [IQR] | 635.0 [583.6, 723.4] | 631.2 [578.2, 724.6] | 665.5 [604.0, 692.2] | |
| Range | (407.9, 1054.1) | (407.9, 1054.1) | (462.9, 767.3) | |
| Average steps per day | Nobs (Nmiss) | 74 (0) | 59 (0) | 15 (0) |
| Mean (SD) | 6226.3 (2708.8) | 6539.8 (2776.0) | 4993.6 (2071.9) | |
| Median [IQR] | 5926.1 [4473.0, 7594.1] | 6108.3 [4849.1, 7772.0] | 5187.5 [3302.2, 6088.5] | |
| Range | (1114.6, 20,315.3) | (1114.6, 20,315.3) | (2100.3, 9217.0) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Total weekly expenditure by kg (kcal/kg/week) | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 259.9 (37.3) | 263.2 (40.7) | 249.0 (19.0) | |
| Median [IQR] | 251.3 [236.9, 270.2] | 253.5 [237.8, 275.5] | 243.9 [235.4, 260.3] | |
| Range | (218.0, 445.0) | (218.0, 445.0) | (219.0, 286.2) | |
| Total daily expenditure by kg (kcal/kg/day) | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 37.1 (5.3) | 37.6 (5.8) | 35.6 (2.7) | |
| Median [IQR] | 35.9 [33.8, 38.6] | 36.2 [34.0, 39.4] | 34.8 [33.6, 37.2] | |
| Range | (31.1, 63.6) | (31.1, 63.6) | (31.3, 40.9) | |
| Total daily expenditure (kcal/day) | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 3867.4 (870.9) | 3818.8 (902.8) | 4028.5 (749.7) | |
| Median [IQR] | 3802.1 [3234.5, 4251.6] | 3649.8 [3189.8, 4215.8] | 3998.3 [3629.8, 4344.7] | |
| Range | (2512.2, 8086.3) | (2512.2, 8086.3) | (2803.5, 6131.7) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| DINE primary analysis | ||||
| DINE fibre score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 19.7 (11.2) | 19.3 (9.9) | 21.2 (14.6) | |
| Median [IQR] | 18.5 [10.0, 26.0] | 20.0 [11.0, 26.0] | 18.0 [10.0, 29.0] | |
| Range | (2.0, 67.0) | (2.0, 47.0) | (5.0, 67.0) | |
| DINE fibre rating | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Low fibre intake | n (%) | 90 | 71 (78.9%) | 19 (21.1%) |
| Medium fibre intake | n (%) | 13 | 10 (76.9%) | 3 (23.1%) |
| High fibre intake | n (%) | 5 | 2 (40.0%) | 3 (60.0%) |
| DINE fat score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 28.7 (12.3) | 28.1 (12.3) | 30.5 (12.5) | |
| Median [IQR] | 25.0 [19.0, 37.0] | 24.0 [19.0, 36.0] | 30.0 [22.0, 37.0] | |
| Range | (9.0, 58.0) | (9.0, 58.0) | (9.0, 58.0) | |
| DINE fat rating | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Low fat intake | n (%) | 63 | 52 (82.5%) | 11 (17.5%) |
| Medium fat intake | n (%) | 27 | 17 (63.0%) | 10 (37.0%) |
| High fat intake | n (%) | 18 | 14 (77.8%) | 4 (22.2%) |
| DINE healthy eating score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | –9.0 (15.4) | –8.8 (14.8) | –9.3 (17.8) | |
| Median [IQR] | –7.5 [–19.0, 1.0] | –7.0 [–18.0, 1.0] | –10.0 [–22.0, –1.0] | |
| Range | (–54.0, 37.0) | (–54.0, 17.0) | (–39.0, 37.0) | |
| DINE unsaturated fat score | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 9.2 (2.1) | 9.1 (2.1) | 9.5 (2.1) | |
| Median [IQR] | 10.0 [8.0, 11.0] | 9.5 [8.0, 11.0] | 10.0 [8.0, 11.0] | |
| Range | (0.0, 12.0) | (0.0, 12.0) | (4.0, 12.0) | |
| DINE unsaturated fat rating | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Low unsaturated fat intake | n (%) | 5 | 4 (80.0%) | 1 (20.0%) |
| Medium unsaturated fat intake | n (%) | 47 | 38 (80.9%) | 9 (19.1%) |
| High unsaturated fat intake | n (%) | 57 | 42 (73.7%) | 15 (26.3%) |
| DINE fruit and vegetable score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 4.8 (2.9) | 4.8 (2.9) | 4.5 (3.2) | |
| Median [IQR] | 4.0 [3.0, 6.0] | 4.0 [3.0, 6.0] | 4.0 [3.0, 6.0] | |
| Range | (0.0, 16.0) | (0.0, 16.0) | (0.0, 15.0) | |
| DINE fruit and vegetable rating | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Poor fruit and vegetable consumption | n (%) | 58 | 43 (74.1%) | 15 (25.9%) |
| Good fruit and vegetable consumption | n (%) | 50 | 40 (80.0%) | 10 (20.0%) |
| DINE fizzy drink score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 0.3 (0.8) | 0.1 (0.4) | 0.9 (1.4) | |
| Median [IQR] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 5.0) | (0.0, 3.0) | (0.0, 5.0) | |
| DINE sugar score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 0.7 (3.1) | 0.6 (3.4) | 1.0 (2.1) | |
| Median [IQR] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 30.0) | (0.0, 30.0) | (0.0, 9.0) | |
| DINE secondary analysis | ||||
| DINE unsaturated fat score | Nobs (Nmiss) | 104 (5) | 80 (4) | 24 (1) |
| Mean (SD) | 9.5 (1.7) | 9.4 (1.6) | 9.7 (1.8) | |
| Median [IQR] | 10.0 [8.0, 11.0] | 10.0 [8.0, 11.0] | 10.0 [8.0, 11.0] | |
| Range | (5.0, 12.0) | (5.0, 12.0) | (6.0, 12.0) | |
| DINE unsaturated fat rating | Nobs (Nmiss) | 104 (5) | 80 (4) | 24 (1) |
| Low unsaturated fat intake | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Medium unsaturated fat intake | n (%) | 46 | 37 (80.4%) | 9 (19.6%) |
| High unsaturated fat intake | n (%) | 57 | 42 (73.7%) | 15 (26.3%) |
| DINE fruit and vegetable score | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 4.7 (3.0) | 4.8 (2.9) | 4.5 (3.2) | |
| Median [IQR] | 4.0 [3.0, 6.0] | 4.0 [3.0, 6.0] | 4.0 [3.0, 6.0] | |
| Range | (0.0, 16.0) | (0.0, 16.0) | (0.0, 15.0) | |
| DINE fruit and vegetable rating | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Poor fruit and vegetable consumption | n (%) | 59 | 44 (74.6%) | 15 (25.4%) |
| Good fruit and vegetable consumption | n (%) | 50 | 40 (80.0%) | 10 (20.0%) |
| DINE fizzy drink score | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 0.3 (0.8) | 0.1 (0.4) | 0.9 (1.4) | |
| Median [IQR] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 5.0) | (0.0, 3.0) | (0.0, 5.0) | |
| DINE sugar score | Nobs (Nmiss) | 109 (0) | 84 (0) | 25 (0) |
| Mean (SD) | 0.7 (3.1) | 0.6 (3.4) | 1.0 (2.1) | |
| Median [IQR] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 30.0) | (0.0, 30.0) | (0.0, 9.0) | |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Family encouragement score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 13.3 (6.1) | 13.6 (6.4) | 12.4 (5.0) | |
| Median [IQR] | 12.5 [8.0, 18.0] | 13.0 [7.0, 19.0] | 11.0 [9.0, 15.0] | |
| Range | (5.0, 25.0) | (5.0, 25.0) | (5.0, 24.0) | |
| Family sabotage score | Nobs (Nmiss) | 107 (2) | 82 (2) | 25 (0) |
| Mean (SD) | 11.6 (3.9) | 11.7 (3.9) | 11.3 (3.8) | |
| Median [IQR] | 11.0 [9.0, 15.0] | 12.0 [9.0, 15.0] | 10.0 [9.0, 13.0] | |
| Range | (5.0, 22.0) | (5.0, 20.0) | (6.0, 22.0) | |
| Friends encouragement score | Nobs (Nmiss) | 107 (2) | 82 (2) | 25 (0) |
| Mean (SD) | 9.0 (4.1) | 8.9 (4.3) | 9.2 (3.6) | |
| Median [IQR] | 8.0 [5.0, 12.0] | 8.0 [5.0, 12.0] | 9.0 [5.0, 13.0] | |
| Range | (5.0, 21.0) | (5.0, 21.0) | (5.0, 15.0) | |
| Friends sabotage score | Nobs (Nmiss) | 105 (4) | 80 (4) | 25 (0) |
| Mean (SD) | 10.4 (4.5) | 10.7 (4.7) | 9.4 (3.5) | |
| Median [IQR] | 9.0 [7.0, 13.0] | 10.0 [6.0, 14.0] | 9.0 [7.0, 11.0] | |
| Range | (5.0, 21.0) | (5.0, 21.0) | (5.0, 21.0) | |
| Combined encouragement score | Nobs (Nmiss) | 107 (2) | 82 (2) | 25 (0) |
| Mean (SD) | 22.4 (8.7) | 22.6 (9.2) | 21.6 (6.9) | |
| Median [IQR] | 22.0 [15.0, 27.0] | 23.0 [14.0, 27.0] | 20.0 [17.0, 26.0] | |
| Range | (10.0, 45.0) | (10.0, 45.0) | (10.0, 39.0) | |
| Combined sabotage score | Nobs (Nmiss) | 105 (4) | 80 (4) | 25 (0) |
| Mean (SD) | 22.0 (7.2) | 22.4 (7.5) | 20.7 (5.9) | |
| Median [IQR] | 22.0 [16.0, 26.0] | 22.0 [16.0, 27.0] | 20.0 [17.0, 23.0] | |
| Range | (10.0, 38.0) | (10.0, 38.0) | (11.0, 35.0) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Family participation score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 20.6 (8.9) | 20.7 (9.2) | 20.0 (8.2) | |
| Median [IQR] | 19.0 [12.0, 28.0] | 19.0 [12.0, 28.0] | 19.0 [13.0, 29.0] | |
| Range | (9.0, 39.0) | (9.0, 39.0) | (9.0, 33.0) | |
| Family punishment score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 3.7 (1.2) | 3.7 (1.3) | 3.5 (1.0) | |
| Median [IQR] | 3.0 [3.0, 4.0] | 3.0 [3.0, 4.0] | 3.0 [3.0, 4.0] | |
| Range | (3.0, 9.0) | (3.0, 9.0) | (3.0, 6.0) | |
| Friends participation score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 16.1 (7.8) | 16.4 (8.3) | 15.0 (6.0) | |
| Median [IQR] | 14.0 [9.0, 20.0] | 14.0 [9.0, 20.0] | 13.0 [9.0, 19.0] | |
| Range | (9.0, 42.0) | (9.0, 42.0) | (9.0, 27.0) | |
| Friends punishment score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 3.4 (1.4) | 3.4 (0.9) | 3.6 (2.4) | |
| Median [IQR] | 3.0 [3.0, 3.0] | 3.0 [3.0, 3.0] | 3.0 [3.0, 3.0] | |
| Range | (3.0, 15.0) | (3.0, 7.0) | (3.0, 15.0) | |
| Combined participation score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 36.7 (13.4) | 37.1 (13.8) | 35.0 (12.4) | |
| Median [IQR] | 33.5 [25.0, 47.0] | 34.0 [25.0, 48.0] | 33.0 [25.0, 46.0] | |
| Range | (18.0, 74.0) | (18.0, 74.0) | (18.0, 59.0) | |
| Combined punishment score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 7.1 (2.3) | 7.1 (2.0) | 7.1 (3.1) | |
| Median [IQR] | 6.0 [6.0, 7.0] | 6.0 [6.0, 8.0] | 6.0 [6.0, 7.0] | |
| Range | (6.0, 21.0) | (6.0, 16.0) | (6.0, 21.0) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Availability score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 15.8 (9.5) | 16.0 (9.8) | 14.9 (8.6) | |
| Median [IQR] | 15.0 [9.0, 23.0] | 15.0 [8.0, 23.0] | 14.0 [10.0, 21.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (0.0, 32.0) | |
| Negative emotions score | Nobs (Nmiss) | 107 (2) | 82 (2) | 25 (0) |
| Mean (SD) | 14.6 (10.3) | 14.5 (10.0) | 14.9 (11.6) | |
| Median [IQR] | 14.0 [5.0, 21.0] | 14.5 [6.0, 21.0] | 14.0 [5.0, 21.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (0.0, 36.0) | |
| Social pressure score | Nobs (Nmiss) | 107 (2) | 82 (2) | 25 (0) |
| Mean (SD) | 21.1 (9.3) | 20.6 (9.5) | 22.6 (8.5) | |
| Median [IQR] | 22.0 [15.0, 28.0] | 21.5 [15.0, 27.0] | 22.0 [17.0, 28.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (0.0, 36.0) | |
| Physical discomfort score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 20.0 (8.7) | 20.2 (8.4) | 19.4 (9.9) | |
| Median [IQR] | 20.5 [13.0, 27.0] | 21.0 [14.0, 26.0] | 20.0 [11.0, 29.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (0.0, 34.0) | |
| Positive activities score | Nobs (Nmiss) | 107 (2) | 83 (1) | 24 (1) |
| Mean (SD) | 21.0 (8.5) | 21.4 (8.2) | 19.8 (9.7) | |
| Median [IQR] | 22.0 [15.0, 26.0] | 21.0 [17.0, 26.0] | 23.5 [12.0, 27.0] | |
| Range | (0.0, 36.0) | (0.0, 36.0) | (0.0, 34.0) | |
| Total score | Nobs (Nmiss) | 106 (3) | 82 (2) | 24 (1) |
| Mean (SD) | 92.6 (39.0) | 92.9 (38.5) | 91.6 (41.5) | |
| Median [IQR] | 98.0 [69.0, 118.0] | 96.5 [71.0, 117.0] | 101.5 [58.0, 118.0] | |
| Range | (0.0, 180.0) | (11.0, 180.0) | (0.0, 166.0) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Task score | Nobs (Nmiss) | 107 (2) | 82 (2) | 25 (0) |
| Mean (SD) | 4.4 (2.4) | 4.7 (2.5) | 3.7 (2.0) | |
| Median [IQR] | 4.0 [2.7, 6.0] | 4.3 [2.7, 6.3] | 3.7 [1.7, 5.0] | |
| Range | (1.0, 10.0) | (1.0, 10.0) | (1.0, 7.0) | |
| Coping score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 7.5 (2.0) | 7.5 (2.0) | 7.2 (2.1) | |
| Median [IQR] | 7.8 [6.8, 9.0] | 7.8 [6.8, 9.0] | 7.8 [6.5, 8.8] | |
| Range | (2.0, 10.0) | (2.0, 10.0) | (2.0, 10.0) | |
| Scheduling score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 5.8 (2.7) | 6.0 (2.7) | 5.2 (2.6) | |
| Median [IQR] | 5.7 [3.7, 8.0] | 6.0 [3.7, 8.0] | 5.0 [3.3, 7.0] | |
| Range | (1.0, 10.0) | (1.0, 10.0) | (1.0, 10.0) | |
| Total score | Nobs (Nmiss) | 107 (2) | 82 (2) | 25 (0) |
| Mean (SD) | 5.9 (1.9) | 6.1 (1.9) | 5.4 (1.8) | |
| Median [IQR] | 5.8 [4.6, 7.3] | 5.9 [4.9, 7.4] | 5.8 [4.3, 6.4] | |
| Range | (1.5, 10.0) | (2.2, 10.0) | (1.5, 8.2) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Autonomous regulation score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 6.2 (0.8) | 6.3 (0.8) | 6.1 (0.9) | |
| Median [IQR] | 6.5 [5.8, 6.8] | 6.5 [5.8, 6.8] | 6.3 [5.7, 7.0] | |
| Range | (3.0, 7.0) | (3.0, 7.0) | (3.7, 7.0) | |
| Controlled regulation score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 3.5 (1.3) | 3.4 (1.3) | 3.8 (1.3) | |
| Median [IQR] | 3.5 [2.5, 4.5] | 3.5 [2.3, 4.3] | 3.8 [2.7, 4.8] | |
| Range | (1.0, 6.0) | (1.0, 6.0) | (1.3, 5.8) | |
| Amotivational score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 1.8 (0.9) | 1.8 (0.8) | 2.1 (1.2) | |
| Median [IQR] | 1.4 [1.0, 2.5] | 1.3 [1.0, 2.3] | 1.7 [1.0, 2.7] | |
| Range | (1.0, 4.7) | (1.0, 4.3) | (1.0, 4.7) | |
| Relative autonomy index (diet) | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 2.7 (1.3) | 2.8 (1.3) | 2.3 (1.3) | |
| Median [IQR] | 2.7 [1.8, 3.6] | 2.8 [1.8, 3.8] | 2.3 [1.5, 3.3] | |
| Range | (0.0, 6.0) | (0.3, 6.0) | (0.0, 4.5) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Autonomous regulation score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 6.3 (0.9) | 6.3 (0.9) | 6.3 (1.0) | |
| Median [IQR] | 6.5 [5.8, 7.0] | 6.5 [5.8, 7.0] | 6.7 [5.8, 7.0] | |
| Range | (1.0, 7.0) | (1.0, 7.0) | (3.8, 7.0) | |
| Controlled regulation score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 3.2 (1.3) | 3.1 (1.2) | 3.5 (1.4) | |
| Median [IQR] | 3.2 [2.2, 4.0] | 3.0 [2.2, 4.0] | 3.7 [2.5, 4.2] | |
| Range | (1.0, 7.0) | (1.0, 6.5) | (1.3, 7.0) | |
| Amotivational score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 1.9 (1.0) | 1.8 (0.9) | 2.1 (1.3) | |
| Median [IQR] | 1.5 [1.0, 2.7] | 1.7 [1.0, 2.7] | 1.3 [1.0, 3.3] | |
| Range | (1.0, 5.0) | (1.0, 4.3) | (1.0, 5.0) | |
| Relative autonomy index (exercise) | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 3.1 (1.4) | 3.2 (1.4) | 2.7 (1.6) | |
| Median [IQR] | 3.2 [2.2, 4.0] | 3.2 [2.3, 4.2] | 3.0 [1.8, 3.5] | |
| Range | (–0.3, 6.0) | (0.0, 6.0) | (–0.3, 5.2) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| GHQ score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 3.0 (3.2) | 2.7 (3.1) | 4.0 (3.5) | |
| Median [IQR] | 2.0 [0.0, 5.0] | 2.0 [0.0, 4.0] | 2.0 [2.0, 7.0] | |
| Range | (0.0, 12.0) | (0.0, 12.0) | (0.0, 11.0) | |
| GHQ score (Likert scoring) | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 13.6 (5.3) | 13.1 (5.0) | 15.2 (6.0) | |
| Median [IQR] | 12.0 [10.0, 17.0] | 12.0 [10.0, 16.0] | 12.0 [11.0, 20.0] | |
| Range | (5.0, 30.0) | (5.0, 26.0) | (9.0, 30.0) | |
| GHQ case (Likert score of ≥ 12) | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| No | n (%) | 47 | 37 (78.7%) | 10 (21.3%) |
| Yes | n (%) | 61 | 46 (75.4%) | 15 (24.6%) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Settled | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I am able to feel settled and secure in all areas of my life | n (%) | 8 | 5 (62.5%) | 3 (37.5%) |
| I am able to feel settled and secure in many areas of my life | n (%) | 63 | 51 (81.0%) | 12 (19.0%) |
| I am able to feel settled and secure in a few areas of my life | n (%) | 34 | 24 (70.6%) | 10 (29.4%) |
| I am unable to feel settled and secure in any areas of my life | n (%) | 3 | 3 (100.0%) | 0 (0.0%) |
| Independence | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I am able to be completely independent | n (%) | 43 | 33 (76.7%) | 10 (23.3%) |
| I am able to be independent in many things | n (%) | 51 | 43 (84.3%) | 8 (15.7%) |
| I am able to be independent in a few things | n (%) | 13 | 7 (53.8%) | 6 (46.2%) |
| I am unable to be at all independent | n (%) | 1 | 0 (0.0%) | 1 (100.0%) |
| Achievements | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I can achieve and progress in all aspects of my life | n (%) | 23 | 19 (82.6%) | 4 (17.4%) |
| I can achieve and progress in many aspects of my life | n (%) | 58 | 45 (77.6%) | 13 (22.4%) |
| I can achieve and progress in a few aspects of my life | n (%) | 26 | 18 (69.2%) | 8 (30.8%) |
| I cannot achieve and progress in any aspects of my life | n (%) | 1 | 1 (100.0%) | 0 (0.0%) |
| Pleasure | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I can have a lot of enjoyment and pleasure | n (%) | 39 | 32 (82.1%) | 7 (17.9%) |
| I can have a quite a lot of enjoyment and pleasure | n (%) | 49 | 39 (79.6%) | 10 (20.4%) |
| I can have a little enjoyment and pleasure | n (%) | 20 | 12 (60.0%) | 8 (40.0%) |
| I cannot have any enjoyment and pleasure | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Total ICECAP-A score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 12.1 (2.1) | 12.2 (2.1) | 11.6 (2.2) | |
| Median [IQR] | 12.0 [11.0, 13.0] | 12.0 [11.0, 14.0] | 12.0 [10.0, 13.0] | |
| Range | (6.0, 16.0) | (6.0, 16.0) | (8.0, 16.0) |
| Variable | Statistic | All (N = 109) | Followed up (N = 84) | Not followed up (N = 25) |
|---|---|---|---|---|
| Mobility | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I have no problems in walking about | n (%) | 78 | 61 (78.2%) | 17 (21.8%) |
| I have some problems in walking about | n (%) | 30 | 22 (73.3%) | 8 (26.7%) |
| I am confined to bed | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Self-care | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I have no problem with self-care | n (%) | 99 | 77 (77.8%) | 22 (22.2%) |
| I have some problems washing or dressing myself | n (%) | 9 | 6 (66.7%) | 3 (33.3%) |
| I am unable to wash or dress myself | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Usual activities | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I have no problems with performing my usual activities | n (%) | 81 | 67 (82.7%) | 14 (17.3%) |
| I have some problems with performing my usual activities | n (%) | 27 | 16 (59.3%) | 11 (40.7%) |
| I am unable to perform my usual activities | n (%) | 0 | 0 (0.0%) | 0 (0.0%) |
| Pain | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I have no pain or discomfort | n (%) | 47 | 42 (89.4%) | 5 (10.6%) |
| I have moderate pain or discomfort | n (%) | 55 | 36 (65.5%) | 19 (34.5%) |
| I have extreme pain or discomfort | n (%) | 6 | 5 (83.3%) | 1 (16.7%) |
| Anxiety | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| I am not anxious or depressed | n (%) | 59 | 49 (83.1%) | 10 (16.9%) |
| I am moderately anxious or depressed | n (%) | 45 | 32 (71.1%) | 13 (28.9%) |
| I am extremely anxious or depressed | n (%) | 4 | 2 (50.0%) | 2 (50.0%) |
| EQ-5D score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 0.900 (0.090) | 0.912 (0.090) | 0.861 (0.083) | |
| Median [IQR] | 0.913 [0.850, 1.000] | 0.924 [0.866, 1.000] | 0.866 [0.816, 0.893] | |
| Range | (0.697, 1.000) | (0.697, 1.000) | (0.697, 1.000) | |
| EQ-VAS score | Nobs (Nmiss) | 108 (1) | 83 (1) | 25 (0) |
| Mean (SD) | 64.5 (18.8) | 67.0 (17.0) | 56.1 (22.2) | |
| Median [IQR] | 65.0 [60.0, 75.0] | 65.0 [60.0, 75.0] | 60.0 [40.0, 70.0] | |
| Range | (10.0, 100.0) | (15.0, 100.0) | (10.0, 90.0) |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Study group (intervention vs. control) | 0.31 (0.10, 0.98) | 0.047 |
| Age (per 10 years) | 1.47 (0.96, 2.26) | 0.074 |
| Gender (female vs. male) | 2.21 (0.88, 5.60) | 0.093 |
| SIMD quintilea | ||
| 2 | 2.13 (0.58, 7.73) | 0.252 |
| 3 | 2.75 (0.52, 14.44) | 0.232 |
| 4 | 3.50 (0.68, 17.96) | 0.133 |
| Least deprived | 1.67 (0.39, 7.21) | 0.494 |
| SIMD quintile (2–5 vs. 1) | 2.36 (0.91, 6.11) | 0.076 |
| Married, cohabiting or CPb | 0.52 (0.20, 1.33) | 0.171 |
| White British (yes/no) | 0.99 (0.32, 3.01) | 0.979 |
| Higher education | 1.76 (0.72, 4.33) | 0.218 |
| Employedc | ||
| Self-employed | 0.21 (0.07, 0.65) | 0.007 |
| Unemployed | 0.53 (0.09, 2.98) | 0.470 |
| Annual household incomed | ||
| £15,000–29,000 | 1.28 (0.32, 5.09) | 0.726 |
| £30,000–49,999 | 2.00 (0.52, 7.70) | 0.314 |
| ≥ £50,000 | 1.90 (0.45, 7.98) | 0.381 |
| Computer at home | 0.82 (0.09, 7.72) | 0.864 |
| Use internet daily | 3.57 (0.48, 26.71) | 0.216 |
| Internet used for | ||
| Education | 1.59 (0.61, 4.10) | 0.342 |
| Work | 1.07 (0.42, 2.71) | 0.892 |
| Shopping | 1.37 (0.43, 4.29) | 0.594 |
| Social networking | 0.40 (0.08, 1.88) | 0.246 |
| Chat room | 1.05 (0.31, 3.53) | 0.937 |
| Gaming | 0.86 (0.30, 2.48) | 0.785 |
| Music | 1.66 (0.67, 4.10) | 0.270 |
| Blogs | 0.87 (0.28, 2.69) | 0.808 |
| TV | 1.05 (0.43, 2.58) | 0.913 |
| Other | 1.05 (0.43, 2.58) | 0.913 |
| Phone used for | ||
| Internet | 0.72 (0.15, 3.60) | 0.694 |
| Apps | 1.59 (0.44, 5.67) | 0.477 |
| 0.90 (0.23, 3.54) | 0.886 | |
| Instant messaging | 0.89 (0.34, 2.32) | 0.815 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Height (cm) | 0.95 (0.91 to 1.00) | 0.060 |
| Weight (kg) | 0.97 (0.95 to 1.00) | 0.016 |
| BMI (kg/m2) | 0.93 (0.87 to 1.00) | 0.063 |
| Waist circumference (cm) | 0.96 (0.93 to 0.99) | 0.016 |
| Hip circumference (cm) | 0.97 (0.94 to 1.01) | 0.110 |
| Weight change in last 3 months | 1.69 (0.68 to 4.17) | 0.258 |
| Currently attending weight loss group | 3.35 (0.92 to 12.18) | 0.067 |
| Motivated/very motivated to lose weighta | 1.24 (0.43 to 3.60) | 0.686 |
| Confident can lose weightb | ||
| 2 | 1.17 (0.07 to 18.35) | 0.913 |
| 3 | 1.38 (0.12 to 15.36) | 0.793 |
| 4 | 1.19 (0.11 to 13.30) | 0.887 |
| 5 Very confident | 0.83 (0.08 to 9.25) | 0.882 |
| Taken weight loss medication in last 12 months | 0.47 (0.10 to 2.12) | 0.326 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Diabetes | 0.58 (0.10 to 3.34) | 0.538 |
| Depression | 0.48 (0.16 to 1.46) | 0.194 |
| Arthritis | 1.55 (0.32 to 7.61) | 0.587 |
| Hypertension | 1.55 (0.32 to 7.61) | 0.587 |
| Asthma | 2.53 (0.30 to 21.24) | 0.394 |
| Back pain | 0.53 (0.18 to 1.59) | 0.256 |
| Other | 3.62 (0.44 to 29.46) | 0.230 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Any health professional at GP surgery | 0.82 (0.31 to 2.20) | 0.695 |
| Any health professional at home | 0.29 (0.02 to 4.78) | 0.385 |
| A&E visits | 1.64 (0.34 to 8.05) | 0.540 |
| Hospital visits | 0.52 (0.04 to 6.08) | 0.604 |
| Any prescriptions received | 1.40 (0.43 to 4.53) | 0.577 |
| Pay for lifestyle services (e.g. slimming/health clubs) | 1.13 (0.45 to 2.80) | 0.799 |
| Referral to exercise referral service | 1.26 (0.13 to 11.85) | 0.838 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Monitor worn | 2.44 (0.94 to 6.35) | 0.067 |
| Minimum wear time achieved | 1.57 (0.62 to 3.98) | 0.338 |
| % in MVPA | 1.14 (0.90 to 1.43) | 0.281 |
| Average MVPA per day (minutes per day) | 1.02 (0.99 to 1.05) | 0.229 |
| Average sedentary minutes per day | 1.00 (0.99 to 1.01) | 0.908 |
| Average steps per day | 1.00 (1.00 to 1.00) | 0.039 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Total weekly expenditure by kg (kcal/kg/week) | 1.02 (1.00 to 1.04) | 0.099 |
| Total daily expenditure by kg (kcal/kg/day) | 1.12 (0.98 to 1.28) | 0.099 |
| Total daily expenditure (kcal/day) | 1.00 (1.00 to 1.00) | 0.296 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| DINE primary analysis | ||
| DINE fibre score | 0.98 (0.95 to 1.02) | 0.445 |
| DINE fibre ratinga | ||
| Medium fibre intake | 0.89 (0.22 to 3.57) | 0.872 |
| High fibre intake | 0.18 (0.03 to 1.15) | 0.069 |
| DINE fat score | 0.98 (0.95 to 1.02) | 0.388 |
| DINE fat ratingb | ||
| Medium fat intake | 0.36 (0.13 to 0.99) | 0.049 |
| High fat intake | 0.74 (0.20 to 2.68) | 0.647 |
| DINE healthy eating score | 1.00 (0.97 to 1.03) | 0.892 |
| DINE unsaturated fat score | 0.91 (0.72 to 1.15) | 0.431 |
| DINE unsaturated fat ratingc | ||
| Medium unsaturated fat intake | 1.06 (0.10 to 10.62) | 0.963 |
| High unsaturated fat intake | 0.70 (0.07 to 6.77) | 0.758 |
| DINE fruit and vegetable score | 1.05 (0.89 to 1.23) | 0.588 |
| DINE fruit and vegetable ratingd | ||
| Good fruit and vegetable consumption | 1.40 (0.56 to 3.46) | 0.472 |
| DINE fizzy drink score | 0.32 (0.15 to 0.65) | 0.002 |
| DINE sugar score | 0.97 (0.86 to 1.10) | 0.649 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Family encouragement score | 1.04 (0.96 to 1.12) | 0.367 |
| Family sabotage score | 1.03 (0.91 to 1.15) | 0.658 |
| Friends encouragement score | 0.98 (0.88 to 1.09) | 0.742 |
| Friends sabotage score | 1.07 (0.96 to 1.19) | 0.218 |
| Combined encouragement score | 1.01 (0.96 to 1.07) | 0.594 |
| Combined sabotage score | 1.04 (0.97 to 1.10) | 0.286 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Family participation score | 1.01 (0.96 to 1.06) | 0.741 |
| Family punishment score | 1.17 (0.78 to 1.78) | 0.444 |
| Friends participation score | 1.03 (0.96 to 1.09) | 0.422 |
| Friends punishment score | 0.92 (0.69 to 1.22) | 0.563 |
| Combined participation score | 1.01 (0.98 to 1.05) | 0.491 |
| Combined punishment score | 1.01 (0.82 to 1.23) | 0.956 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Availability score | 1.01 (0.97 to 1.06) | 0.605 |
| Negative emotions score | 1.00 (0.95 to 1.04) | 0.863 |
| Social pressure score | 0.98 (0.93 to 1.03) | 0.342 |
| Physical discomfort score | 1.01 (0.96 to 1.06) | 0.690 |
| Positive activities score | 1.02 (0.97 to 1.08) | 0.434 |
| Total score | 1.00 (0.99 to 1.01) | 0.885 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Task score | 1.19 (0.97 to 1.46) | 0.093 |
| Coping score | 1.07 (0.86 to 1.33) | 0.525 |
| Scheduling score | 1.12 (0.94 to 1.33) | 0.198 |
| Total score | 1.23 (0.96 to 1.57) | 0.102 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Autonomous regulation score | 1.29 (0.76 to 2.18) | 0.344 |
| Controlled regulation score | 0.80 (0.55 to 1.14) | 0.216 |
| Amotivational score | 0.68 (0.43 to 1.09) | 0.106 |
| Relative autonomy index (diet) | 1.36 (0.96 to 1.94) | 0.085 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Autonomous regulation score | 1.04 (0.63 to 1.71) | 0.886 |
| Controlled regulation score | 0.75 (0.52 to 1.08) | 0.116 |
| Amotivational score | 0.74 (0.48 to 1.15) | 0.178 |
| Relative autonomy index (exercise) | 1.27 (0.92 to 1.74) | 0.141 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| GHQ score | 0.89 (0.78, 1.02) | 0.087 |
| GHQ score (Likert scoring) | 0.93 (0.86, 1.01) | 0.080 |
| GHQ case (Likert score of ≥ 12) | 0.83 (0.33, 2.06) | 0.686 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Settled (all/many areas)a | 1.38 (0.55 to 3.48) | 0.491 |
| Independence (completely/many things)a | 4.22 (1.31 to 13.56) | 0.016 |
| Achievements (all/many aspects)a | 1.59 (0.59 to 4.24) | 0.359 |
| Pleasure (a lot/quite a lot)a | 2.78 (0.98 to 7.87) | 0.053 |
| Total ICECAP-A score | 1.15 (0.93 to 1.42) | 0.185 |
| Variable | Odds ratio (95% CI) | p-value |
|---|---|---|
| Mobilitya | ||
| I have some problems in walking about | 0.77 (0.29 to 2.02) | 0.591 |
| Self-careb | ||
| I have some problems washing or dressing myself | 0.57 (0.13 to 2.47) | 0.454 |
| Usual activitiesc | ||
| I have some problems with performing my usual activities | 0.30 (0.12 to 0.79) | 0.015 |
| Paind | ||
| I have moderate pain or discomfort | 0.23 (0.08 to 0.66) | 0.007 |
| I have extreme pain or discomfort | 0.60 (0.06 to 6.17) | 0.664 |
| Anxietye | ||
| I am moderately anxious or depressed | 0.50 (0.20 to 1.28) | 0.150 |
| I am extremely anxious or depressed | 0.20 (0.03 to 1.62) | 0.133 |
| EQ-5D scoref | 1.84 (1.12 to 3.04) | 0.016 |
| EQ-VAS scoreg | 1.35 (1.06 to 1.73) | 0.015 |
| Variable | Statistic | All data (N = 73) |
|---|---|---|
| Used app | Nobs (Nmiss) | 73 (0) |
| No | n (%) | 19 (26.0%) |
| Yes | n (%) | 54 (74.0%) |
| Used app ≥ 2 times | Nobs (Nmiss) | 73 (0) |
| No | n (%) | 25 (34.2%) |
| Yes | n (%) | 48 (65.8%) |
| Used app ≥ 3 times | Nobs (Nmiss) | 73 (0) |
| No | n (%) | 35 (47.9%) |
| Yes | n (%) | 38 (52.1%) |
| Number of logins | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 17.7 (56.3) | |
| Median [IQR] | 4.5 [2.0, 11.0] | |
| Range | (1.0, 408.0) | |
| Number of views of main dashboard | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 13.2 (57.1) | |
| Median [IQR] | 1.5 [1.0, 3.0] | |
| Range | (0.0, 412.0) | |
| Number of views of progress charts | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 3.9 (13.7) | |
| Median [IQR] | 1.0 [0.0, 2.0] | |
| Range | (0.0, 96.0) | |
| Number of enter your weight updates | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 2.0 (4.2) | |
| Median [IQR] | 1.0 [0.0, 2.0] | |
| Range | (0.0, 21.0) | |
| Number of views of smiles features | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 1.4 (6.0) | |
| Median [IQR] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 43.0) | |
| Number of views of rewards features | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 1.6 (5.0) | |
| Median [IQR] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 32.0) | |
| Number of ‘view profile’ | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 1.1 (3.7) | |
| Median [IQR] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 24.0) | |
| Number of template goals created | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 1.1 (3.0) | |
| Median [IQR] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 16.0) | |
| Number of custom goals created | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 16.6 (24.9) | |
| Median [IQR] | 9.5 [4.0, 18.0] | |
| Range | (0.0, 143.0) | |
| Number of goals deleted | Nobs (Nmiss) | 42 (0) |
| Mean (SD) | 0.7 (2.3) | |
| Median [IQR] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 12.0) | |
| Number of goals completed | Nobs (Nmiss) | 42 (0) |
| Mean (SD) | 13.8 (25.5) | |
| Median [IQR] | 3.0 [0.0, 21.0] | |
| Range | (0.0, 109.0) | |
| Number of goals updated | Nobs (Nmiss) | 42 (0) |
| Mean (SD) | 5.8 (27.9) | |
| Median [IQR] | 0.0 [0.0, 2.0] | |
| Range | (0.0, 181.0) | |
| Number of helpers invited | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 1.7 (1.2) | |
| Median [IQR] | 1.0 [1.0, 2.0] | |
| Range | (1.0, 6.0) | |
| Number of helpers denominated | Nobs (Nmiss) | 19 (0) |
| Mean (SD) | 1.5 (1.2) | |
| Median [IQR] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 5.0) | |
| Number of uses of ‘contact helper feature’ | Nobs (Nmiss) | 19 (0) |
| Mean (SD) | 1.8 (1.0) | |
| Median [IQR] | 1.0 [1.0, 2.0] | |
| Range | (1.0, 4.0) | |
| Number of smiles sent to helper | Nobs (Nmiss) | 19 (0) |
| Mean (SD) | 4.4 (10.2) | |
| Median [IQR] | 0.0 [0.0, 3.0] | |
| Range | (0.0, 40.0) | |
| Read summary e-mail | Nobs (Nmiss) | 54 (0) |
| Mean (SD) | 2.8 (5.9) | |
| Median [IQR] | 1.0 [0.0, 3.0] | |
| Range | (0.0, 40.0) | |
| Unsubscribe from e-mail | Nobs (Nmiss) | 54 (0) |
| 0 | n (%) | 51 (94.4%) |
| 1 | n (%) | 2 (3.7%) |
| 2 | n (%) | 1 (1.9%) |
| Forgotten password | Nobs (Nmiss) | 54 (0) |
| 0 | n (%) | 52 (96.3%) |
| 1 | n (%) | 2 (3.7%) |
| View of notifications (new feature) | Nobs (Nmiss) | 54 (0) |
| 0 | n (%) | 52 (96.3%) |
| 3 | n (%) | 1 (1.9%) |
| 5 | n (%) | 1 (1.9%) |
| View of FAQs (new feature) | Nobs (Nmiss) | 54 (0) |
| 0 | n (%) | 53 (98.1%) |
| 7 | n (%) | 1 (1.9%) |
| Variable | Statistic | All data (N = 73) |
|---|---|---|
| Used website | Nobs (Nmiss) | 73 (0) |
| No | n (%) | 18 (24.7%) |
| Yes | n (%) | 55 (75.3%) |
| Total number of website sessions | Nobs (Nmiss) | 54 (1) |
| Mean (SD) | 3.1 (2.6) | |
| Median [IQR] | 2.0 [1.0, 4.0] | |
| Range | (1.0, 12.0) | |
| Average website duration (minutes) | Nobs (Nmiss) | 54 (1) |
| Mean (SD) | 6.8 (8.6) | |
| Median [IQR] | 3.8 [1.2, 7.5] | |
| Range | (0.0, 43.8) | |
| Total number of page views | Nobs (Nmiss) | 55 (0) |
| Mean (SD) | 12.4 (11.1) | |
| Median [IQR] | 8.0 [5.0, 18.0] | |
| Range | (1.0, 45.0) |
| Variable | Statistic | All data (N = 28) |
|---|---|---|
| Used app | Nobs (Nmiss) | 28 (0) |
| No | n (%) | 3 (10.7%) |
| Yes | n (%) | 25 (89.3%) |
| Number of logins | Nobs (Nmiss) | 25 (0) |
| Mean (SD) | 4.9 (9.5) | |
| Median [IQR] | 2.0 [1.0, 4.0] | |
| Range | (1.0, 48.0) | |
| Number of views of progress charts | Nobs (Nmiss) | 25 (0) |
| Mean (SD) | 0.0 (0.0) | |
| Median [IQR] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 0.0) | |
| Number of views of smiles features | Nobs (Nmiss) | 25 (0) |
| Mean (SD) | 0.4 (1.0) | |
| Median [IQR] | 0.0 [0.0, 0.0] | |
| Range | (0.0, 5.0) | |
| Number of views of rewards features | Nobs (Nmiss) | 25 (0) |
| Mean (SD) | 0.5 (1.0) | |
| Median [IQR] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 4.0) | |
| Number of ‘view profile’ | Nobs (Nmiss) | 25 (0) |
| Mean (SD) | 0.5 (0.7) | |
| Median [IQR] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 2.0) | |
| Number of times goals liked | Nobs (Nmiss) | 25 (0) |
| Mean (SD) | 0.8 (1.8) | |
| Median [IQR] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 8.0) | |
| Number of uses of ‘contact friend feature’ | Nobs (Nmiss) | 25 (0) |
| Mean (SD) | 0.4 (0.6) | |
| Median [IQR] | 0.0 [0.0, 1.0] | |
| Range | (0.0, 2.0) | |
| Number of smiles sent to participant | Nobs (Nmiss) | 25 (0) |
| Mean (SD) | 3.8 (8.9) | |
| Median [IQR] | 2.0 [1.0, 3.0] | |
| Range | (0.0, 46.0) | |
| Forgotten password | Nobs (Nmiss) | 25 (0) |
| 0 | n (%) | 25 (100.0%) |
| View of notifications (new feature) | Nobs (Nmiss) | 25 (0) |
| 0 | n (%) | 25 (100.0%) |
| View of FAQs (new feature) | Nobs (Nmiss) | 25 (0) |
| 0 | n (%) | 25 (100.0%) |
| Variable | Statistic | All data (N = 28) |
|---|---|---|
| Used website | Nobs (Nmiss) | 28 (0) |
| No | n (%) | 9 (32.1%) |
| Yes | n (%) | 19 (67.9%) |
| Total number of website sessions | Nobs (Nmiss) | 19 (0) |
| Mean (SD) | 1.2 (0.4) | |
| Median [IQR] | 1.0 [1.0, 1.0] | |
| Range | (1.0, 2.0) | |
| Average website duration (minutes) | Nobs (Nmiss) | 19 (0) |
| Mean (SD) | 5.9 (6.5) | |
| Median [IQR] | 3.8 [2.4, 5.6] | |
| Range | (1.6, 27.2) | |
| Total number of page views | Nobs (Nmiss) | 19 (0) |
| Mean (SD) | 2.8 (2.0) | |
| Median [IQR] | 2.0 [1.0, 4.0] | |
| Range | (1.0, 8.0) |
| Variable | All (N = 39) | Intervention (N = 24) | Control (N = 15) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| % in MVPA | |||||||||
| Baseline | 5.6 (3.6) | 6.5 (4.0) | 4.1 (2.3) | ||||||
| 12 months | 4.8 (2.6) | 5.6 (2.5) | 3.5 (2.3) | ||||||
| Change | –0.8 (3.0) | –0.9 (3.8) | –0.6 (1.0) | –0.3 (–2.2 to 1.7) | –0.08 (–0.73 to 0.56) | 0.799 | 1.3 (–0.1 to 2.7) | 0.44 (–0.02 to 0.90) | 0.068 |
| Average MVPA per day (minutes per day) | |||||||||
| Baseline | 47.4 (30.6) | 54.8 (34.3) | 35.5 (19.4) | ||||||
| 12 months | 40.5 (21.3) | 46.3 (20.2) | 31.3 (20.3) | ||||||
| Change | –6.9 (25.9) | –8.5 (32.2) | –4.3 (10.5) | –4.2 (–21.1 to 12.7) | –0.16 (–0.81 to 0.48) | 0.626 | 9.3 (–2.3 to 20.9) | 0.35 (–0.09 to 0.80) | 0.127 |
| Average sedentary minutes per day | |||||||||
| Baseline | 650.0 (111.7) | 642.7 (94.0) | 661.7 (138.2) | ||||||
| 12 months | 659.2 (125.0) | 631.5 (82.8) | 703.4 (166.6) | ||||||
| Change | 9.1 (83.0) | –11.2 (77.6) | 41.7 (83.5) | –52.9 (–104.4 to –1.4) | –0.66 (–1.31 to –0.02) | 0.051 | –60.8 (–110.5 to –11.0) | –0.76 (–1.38 to –0.14) | 0.022 |
| Average steps per day | |||||||||
| Baseline | 6623.4 (3131.4) | 7231.8 (3712.2) | 5650.0 (1525.5) | ||||||
| 12 months | 6334.9 (2426.2) | 6959.9 (2568.0) | 5334.8 (1844.4) | ||||||
| Change | –288.5 (2935.8) | –271.9 (3669.1) | –315.2 (1129.7) | 43.3 (–1876.0 to 1962.6) | 0.01 (–0.63 to 0.66) | 0.965 | 1187.4 (–180.1 to 2554.9) | 0.40 (–0.06 to 0.86) | 0.098 |
| Variable | All (N = 81) | Intervention (N = 49) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Total weekly expenditure by kg (kcal/kg/week) | |||||||||
| Baseline | 263.3 (41.0) | 260.5 (34.3) | 267.6 (49.9) | ||||||
| 12 months | 256.6 (27.0) | 256.6 (26.2) | 256.7 (28.6) | ||||||
| Change | –6.7 (40.5) | –3.9 (37.0) | –10.9 (45.6) | 7.0 (–11.1 to 25.1) | 0.17 (–0.27 to 0.62) | 0.450 | –0.2 (–11.8 to 11.4) | 0.00 (–0.29 to 0.28) | 0.974 |
| Total daily expenditure by kg (kcal/kg/day) | |||||||||
| Baseline | 37.6 (5.9) | 37.2 (4.9) | 38.2 (7.1) | ||||||
| 12 months | 36.7 (3.9) | 36.7 (3.7) | 36.7 (4.1) | ||||||
| Change | –1.0 (5.8) | –0.6 (5.3) | –1.6 (6.5) | 1.0 (–1.6 to 3.6) | 0.17 (–0.27 to 0.62) | 0.450 | 0.0 (–1.7 to 1.6) | 0.00 (–0.29 to 0.28) | 0.974 |
| Total daily expenditure (kcal/day) | |||||||||
| Baseline | 3782.1 (896.4) | 3717.4 (715.1) | 3879.2 (1120.8) | ||||||
| 12 months | 3576.5 (763.3) | 3556.9 (779.1) | 3605.8 (750.2) | ||||||
| Change | –205.6 (649.9) | –160.5 (502.2) | –273.4 (828.4) | 112.9 (–178.6 to 404.4) | 0.17 (–0.27 to 0.62) | 0.450 | 61.7 (–180.5 to 303.9) | 0.09 (–0.28 to 0.47) | 0.619 |
| Variable | All (N = 81) | Intervention (N = 49) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| DINE fibre score | |||||||||
| Baseline | 19.3 (10.0) | 19.8 (9.7) | 18.6 (10.6) | ||||||
| 12 months | 17.4 (11.7) | 16.3 (11.8) | 19.2 (11.6) | ||||||
| Change | –1.9 (11.5) | –3.6 (10.6) | 0.6 (12.6) | –4.1 (–9.2 to 0.9) | –0.36 (–0.81 to 0.08) | 0.114 | –3.3 (–8.1 to 1.5) | –0.29 (–0.71 to 0.13) | 0.182 |
| DINE fat score | |||||||||
| Baseline | 27.9 (11.9) | 28.4 (11.6) | 27.1 (12.6) | ||||||
| 12 months | 22.9 (11.5) | 22.9 (12.7) | 22.9 (9.6) | ||||||
| Change | –5.0 (11.1) | –5.5 (11.4) | –4.1 (10.8) | –1.4 (–6.4 to 3.6) | –0.13 (–0.57 to 0.32) | 0.581 | –0.4 (–4.8 to 4.0) | –0.04 (–0.43 to 0.36) | 0.862 |
| DINE healthy eating score | |||||||||
| Baseline | –8.5 (14.4) | –8.6 (13.3) | –8.5 (16.1) | ||||||
| 12 months | –5.5 (13.0) | –6.6 (12.9) | –3.8 (13.2) | ||||||
| Change | 3.1 (13.8) | 2.0 (11.7) | 4.7 (16.6) | –2.7 (–8.9 to 3.4) | –0.20 (–0.64 to 0.25) | 0.385 | –2.9 (–8.0 to 2.2) | –0.21 (–0.58 to 0.16) | 0.271 |
| DINE unsaturated fat score | |||||||||
| Baseline | 9.2 (2.1) | 9.2 (2.2) | 9.3 (1.8) | ||||||
| 12 months | 6.6 (4.7) | 5.8 (5.0) | 8.2 (3.7) | ||||||
| Change | –2.6 (5.1) | –3.3 (5.6) | –1.1 (3.5) | –2.3 (–4.3 to –0.3) | –0.45 (–0.85 to –0.06) | 0.028 | –2.2 (–4.0 to –0.4) | –0.44 (–0.80 to –0.07) | 0.021 |
| DINE fruit and vegetable score | |||||||||
| Baseline | 4.8 (2.9) | 4.7 (2.6) | 5.0 (3.4) | ||||||
| 12 months | 5.1 (2.7) | 5.2 (2.5) | 4.9 (2.9) | ||||||
| Change | 0.3 (2.8) | 0.5 (2.2) | –0.1 (3.4) | 0.7 (–0.6 to 1.9) | 0.24 (–0.21 to 0.69) | 0.305 | 0.4 (–0.6 to 1.5) | 0.16 (–0.23 to 0.55) | 0.417 |
| DINE fizzy drink scorea | |||||||||
| Baseline | 0.1 (0.4) | 0.0 (0.0) | 0.2 (0.6) | ||||||
| 12 months | 0.2 (0.7) | 0.2 (0.6) | 0.3 (0.9) | ||||||
| Change | 0.2 (0.5) | 0.2 (0.6) | 0.1 (0.4) | 0.00 (0.00 to 0.00) | – | 0.762 | |||
| DINE sugar scorea | |||||||||
| Baseline | 0.7 (3.5) | 0.5 (1.3) | 0.9 (5.3) | ||||||
| 12 months | 0.5 (2.4) | 0.3 (0.8) | 0.8 (3.5) | ||||||
| Change | –0.2 (1.4) | –0.2 (0.9) | –0.2 (1.9) | 0.00 (0.00 to 0.00) | – | 0.134 | |||
| DINE fibre ratingb | |||||||||
| Baseline | 81 (0) | 49 (0) | 32 (0) | ||||||
| Low fibre intake | 69 (85.2%) | 41 (83.7%) | 28 (87.5%) | ||||||
| Medium fibre intake | 10 (12.3%) | 6 (12.2%) | 4 (12.5%) | ||||||
| High fibre intake | 2 (2.5%) | 2 (4.1%) | 0 (0.0%) | ||||||
| 12 months | 81 (0) | 49 (0) | 32 (0) | ||||||
| Low fibre intake | 67 (82.7%) | 40 (81.6%) | 27 (84.4%) | ||||||
| Medium fibre intake | 11 (13.6%) | 8 (16.3%) | 3 (9.4%) | ||||||
| High fibre intake | 3 (3.7%) | 1 (2.0%) | 2 (6.2%) | ||||||
| Change | 81 (0) | 49 (0) | 32 (0) | ||||||
| Improvement | 8 (9.9%) | 3 (6.1%) | 5 (15.6%) | –9.5% | |||||
| Same | 68 (84.0%) | 44 (89.8%) | 24 (75.0%) | 14.8% | |||||
| Deterioration | 5 (6.2%) | 2 (4.1%) | 3 (9.4%) | –5.3% | 0.260 | ||||
| DINE fat ratingb | |||||||||
| Baseline | 81 (0) | 49 (0) | 32 (0) | ||||||
| Low fat intake | 51 (63.0%) | 30 (61.2%) | 21 (65.6%) | ||||||
| Medium fat intake | 17 (21.0%) | 10 (20.4%) | 7 (21.9%) | ||||||
| High fat intake | 13 (16.0%) | 9 (18.4%) | 4 (12.5%) | ||||||
| 12 months | 81 (0) | 49 (0) | 32 (0) | ||||||
| Low fat intake | 60 (74.1%) | 35 (71.4%) | 25 (78.1%) | ||||||
| Medium fat intake | 17 (21.0%) | 11 (22.4%) | 6 (18.8%) | ||||||
| High fat intake | 4 (4.9%) | 3 (6.1%) | 1 (3.1%) | ||||||
| Change | 81 (0) | 49 (0) | 32 (0) | ||||||
| Improvement | 19 (23.5%) | 13 (26.5%) | 6 (18.8%) | 7.8% | |||||
| Same | 57 (70.4%) | 32 (65.3%) | 25 (78.1%) | –12.8% | |||||
| Deterioration | 5 (6.2%) | 4 (8.2%) | 1 (3.1%) | 5.0% | 0.458 | ||||
| DINE unsaturated fat ratingb | |||||||||
| Baseline | 109 (0) | 73 (0) | 36 (0) | ||||||
| Low unsaturated fat intake | 5 (4.6%) | 4 (5.5%) | 1 (2.8%) | ||||||
| Medium unsaturated fat intake | 47 (43.1%) | 31 (42.5%) | 16 (44.4%) | ||||||
| High unsaturated fat intake | 57 (52.3%) | 38 (52.1%) | 19 (52.8%) | ||||||
| 12 months | 109 (0) | 73 (0) | 36 (0) | ||||||
| Low unsaturated fat intake | 39 (35.8%) | 32 (43.8%) | 7 (19.4%) | ||||||
| Medium unsaturated fat intake | 24 (22.0%) | 13 (17.8%) | 11 (30.6%) | ||||||
| High unsaturated fat intake | 46 (42.2%) | 28 (38.4%) | 18 (50.0%) | ||||||
| Change | 109 (0) | 73 (0) | 36 (0) | ||||||
| Improvement | 43 (39.4%) | 34 (46.6%) | 9 (25.0%) | 21.6% | |||||
| Same | 49 (45.0%) | 27 (37.0%) | 22 (61.1%) | –24.1% | |||||
| Deterioration | 17 (15.6%) | 12 (16.4%) | 5 (13.9%) | 2.5% | 0.049 | ||||
| DINE fruit and vegetable ratingb | |||||||||
| Baseline | 77 (0) | 45 (0) | 32 (0) | ||||||
| Poor fruit and vegetable consumption | 41 (53.2%) | 25 (55.6%) | 16 (50.0%) | ||||||
| Good fruit and vegetable consumption | 36 (46.8%) | 20 (44.4%) | 16 (50.0%) | ||||||
| 12 months | 77 (0) | 45 (0) | 32 (0) | ||||||
| Poor fruit and vegetable consumption | 37 (48.1%) | 19 (42.2%) | 18 (56.2%) | ||||||
| Good fruit and vegetable consumption | 40 (51.9%) | 26 (57.8%) | 14 (43.8%) | ||||||
| Change | 77 (0) | 45 (0) | 32 (0) | ||||||
| Improvement | 14 (18.2%) | 9 (20.0%) | 5 (15.6%) | 4.4% | |||||
| Same | 53 (68.8%) | 33 (73.3%) | 20 (62.5%) | 10.8% | |||||
| Deterioration | 10 (13.0%) | 3 (6.7%) | 7 (21.9%) | –15.2% | 0.181 | ||||
| Variable | All (N = 74) | Intervention (N = 42) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| DINE unsaturated fat score | |||||||||
| Baseline | 9.4 (1.6) | 9.4 (1.5) | 9.4 (1.7) | ||||||
| 12 months | 9.3 (2.4) | 9.3 (2.5) | 9.2 (2.3) | ||||||
| Change | –0.1 (2.6) | –0.1 (2.7) | –0.2 (2.5) | 0.1 (–1.1 to 1.3) | 0.04 (–0.42 to 0.50) | 0.881 | 0.1 (–1.0 to 1.2) | 0.05 (–0.38 to 0.47) | 0.835 |
| DINE fruit and vegetable score | |||||||||
| Baseline | 4.7 (3.0) | 4.4 (2.5) | 5.3 (3.6) | ||||||
| 12 months | 3.6 (3.2) | 3.3 (3.2) | 4.3 (3.2) | ||||||
| Change | –1.1 (3.6) | –1.2 (3.2) | –1.0 (4.3) | –0.2 (–1.6 to 1.2) | –0.05 (–0.45 to 0.35) | 0.793 | –0.7 (–1.9 to 0.5) | –0.19 (–0.53 to 0.15) | 0.278 |
| DINE fizzy drink scorea | |||||||||
| Baseline | 0.3 (0.8) | 0.3 (0.9) | 0.2 (0.7) | ||||||
| 12 months | 0.2 (0.6) | 0.1 (0.5) | 0.2 (0.8) | ||||||
| Change | –0.1 (0.9) | –0.2 (1.0) | 0.1 (0.5) | 0.00 (0.00 to 0.00) | – | 0.122 | |||
| DINE sugar scorea | |||||||||
| Baseline | 0.7 (3.1) | 0.6 (1.5) | 1.0 (5.0) | ||||||
| 12 months | 0.4 (2.2) | 0.3 (1.2) | 0.7 (3.3) | ||||||
| Change | –0.3 (1.8) | –0.3 (1.8) | –0.3 (1.9) | 0.00 (0.00 to 0.00) | – | 0.147 | |||
| DINE unsaturated fat ratingb | |||||||||
| Baseline | 74 (0) | 42 (0) | 32 (0) | ||||||
| Low unsaturated fat intake | 1 (1.4%) | 0 (0.0%) | 1 (3.1%) | ||||||
| Medium unsaturated fat intake | 34 (45.9%) | 21 (50.0%) | 13 (40.6%) | ||||||
| High unsaturated fat intake | 39 (52.7%) | 21 (50.0%) | 18 (56.2%) | ||||||
| 12 months | 74 (0) | 42 (0) | 32 (0) | ||||||
| Low unsaturated fat intake | 7 (9.5%) | 4 (9.5%) | 3 (9.4%) | ||||||
| Medium unsaturated fat intake | 24 (32.4%) | 13 (31.0%) | 11 (34.4%) | ||||||
| High unsaturated fat intake | 43 (58.1%) | 25 (59.5%) | 18 (56.2%) | ||||||
| Change | 74 (0) | 42 (0) | 32 (0) | ||||||
| Improvement | 12 (16.2%) | 7 (16.7%) | 5 (15.6%) | 1.0% | |||||
| Same | 48 (64.9%) | 26 (61.9%) | 22 (68.8%) | –6.8% | |||||
| Deterioration | 14 (18.9%) | 9 (21.4%) | 5 (15.6%) | 5.8% | 0.838 | ||||
| DINE fruit and vegetable ratingb | |||||||||
| Baseline | 109 (0) | 73 (0) | 36 (0) | ||||||
| Poor fruit and vegetable consumption | 59 (54.1%) | 41 (56.2%) | 18 (50.0%) | ||||||
| Good fruit and vegetable consumption | 50 (45.9%) | 32 (43.8%) | 18 (50.0%) | ||||||
| 12 months | 109 (0) | 73 (0) | 36 (0) | ||||||
| Poor fruit and vegetable consumption | 69 (63.3%) | 47 (64.4%) | 22 (61.1%) | ||||||
| Good fruit and vegetable consumption | 40 (36.7%) | 26 (35.6%) | 14 (38.9%) | ||||||
| Change | 109 (0) | 73 (0) | 36 (0) | ||||||
| Improvement | 14 (12.8%) | 9 (12.3%) | 5 (13.9%) | –1.6% | |||||
| Same | 71 (65.1%) | 49 (67.1%) | 22 (61.1%) | 6.0% | |||||
| Deterioration | 24 (22.0%) | 15 (20.5%) | 9 (25.0%) | –4.5% | 0.788 | ||||
| Variable | All (N = 82) | Intervention (N = 50) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | |||||||||
| Baseline | 36.9 (5.4) | 36.9 (5.3) | 36.9 (5.7) | ||||||
| 12 months | 35.8 (5.7) | 35.7 (5.4) | 36.0 (6.3) | ||||||
| Change | –1.1 (2.7) | –1.2 (2.4) | –0.9 (3.3) | –0.3 (–1.5 to 0.9) | –0.11 (–0.56 to 0.33) | 0.614 | –0.2 (–1.4 to 1.0) | –0.08 (–0.52 to 0.37) | 0.734 |
| Variable | All (N = 82) | Intervention (N = 50) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Weight (kg) | |||||||||
| Baseline | 101.3 (19.6) | 101.4 (19.8) | 101.2 (19.7) | ||||||
| 12 months | 98.3 (19.8) | 98.1 (19.7) | 98.7 (20.3) | ||||||
| Change | –3.0 (7.7) | –3.3 (6.5) | –2.5 (9.3) | –0.7 (–4.2 to 2.7) | –0.10 (–0.54 to 0.35) | 0.673 | –0.6 (–4.1 to 2.9) | –0.08 (–0.53 to 0.37) | 0.740 |
| Waist circumference (cm) | |||||||||
| Baseline | 111.7 (13.6) | 110.1 (13.3) | 114.0 (13.9) | ||||||
| 12 months | 107.9 (15.2) | 108.0 (15.5) | 107.7 (15.1) | ||||||
| Change | –3.9 (13.5) | –2.1 (8.1) | –6.4 (18.5) | 4.3 (–2.1 to 10.7) | 0.32 (–0.16 to 0.80) | 0.195 | 3.2 (–3.0 to 9.4) | 0.24 (–0.22 to 0.70) | 0.314 |
| Waist-to-hip ratio | |||||||||
| Baseline | 0.91 (0.09) | 0.90 (0.09) | 0.94 (0.09) | ||||||
| 12 months | 0.91 (0.09) | 0.90 (0.09) | 0.92 (0.08) | ||||||
| Change | 0.00 (0.05) | 0.00 (0.05) | –0.02 (0.04) | 0.02 (0.00 to 0.04) | 0.39 (–0.08 to 0.87) | 0.110 | 0.01 (–0.01 to 0.04) | 0.30 (–0.12 to 0.73) | 0.169 |
| Variable | All (N = 77) | Intervention (N = 45) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Mobilitya | |||||||||
| Baseline | 77 (0) | 45 (0) | 32 (0) | ||||||
| I have no problems in walking about | 57 (74.026%) | 35 (77.778%) | 22 (68.750%) | ||||||
| I have some problems in walking about | 20 (25.974%) | 10 (22.222%) | 10 (31.250%) | ||||||
| I am confined to bed | 0 (0.000%) | 0 (0.000%) | 0 (0.000%) | ||||||
| 12 months | 77 (0) | 45 (0) | 32 (0) | ||||||
| I have no problems in walking about | 69 (89.610%) | 44 (97.778%) | 25 (78.125%) | ||||||
| I have some problems in walking about | 8 (10.390%) | 1 (2.222%) | 7 (21.875%) | ||||||
| I am confined to bed | 0 (0.000%) | 0 (0.000%) | 0 (0.000%) | ||||||
| Change | 77 (0) | 45 (0) | 32 (0) | ||||||
| Improvement | 14 (18.182%) | 10 (22.222%) | 4 (12.500%) | 9.7% | |||||
| Same | 61 (79.221%) | 34 (75.556%) | 27 (84.375%) | –8.8% | |||||
| Deterioration | 2 (2.597%) | 1 (2.222%) | 1 (3.125%) | –0.9% | 0.612 | ||||
| Self carea | |||||||||
| Baseline | 77 (0) | 45 (0) | 32 (0) | ||||||
| I have no problem with self-care | 72 (93.506%) | 43 (95.556%) | 29 (90.625%) | ||||||
| I have some problems washing or dressing myself | 5 (6.494%) | 2 (4.444%) | 3 (9.375%) | ||||||
| I am unable to wash or dress myself | 0 (0.000%) | 0 (0.000%) | 0 (0.000%) | ||||||
| 12 months | 77 (0) | 45 (0) | 32 (0) | ||||||
| I have no problem with self-care | 39 (50.649%) | 26 (57.778%) | 13 (40.625%) | ||||||
| I have some problems washing or dressing myself | 31 (40.260%) | 17 (37.778%) | 14 (43.750%) | ||||||
| I am unable to wash or dress myself | 7 (9.091%) | 2 (4.444%) | 5 (15.625%) | ||||||
| Change | 77 (0) | 45 (0) | 32 (0) | ||||||
| Improvement | 0 (0.000%) | 0 (0.000%) | 0 (0.000%) | 0.0% | |||||
| Same | 43 (55.844%) | 28 (62.222%) | 15 (46.875%) | 15.3% | |||||
| Deterioration | 34 (44.156%) | 17 (37.778%) | 17 (53.125%) | –15.3% | 0.245 | ||||
| Usual activitiesa | |||||||||
| Baseline | 77 (0) | 45 (0) | 32 (0) | ||||||
| I have no problems with performing my usual activities | 63 (81.818%) | 40 (88.889%) | 23 (71.875%) | ||||||
| I have some problems with performing my usual activities | 14 (18.182%) | 5 (11.111%) | 9 (28.125%) | ||||||
| I am unable to perform my usual activities | 0 (0.000%) | 0 (0.000%) | 0 (0.000%) | ||||||
| 12 months | 77 (0) | 45 (0) | 32 (0) | ||||||
| I have no problems with performing my usual activities | 46 (59.740%) | 27 (60.000%) | 19 (59.375%) | ||||||
| I have some problems with performing my usual activities | 27 (35.065%) | 16 (35.556%) | 11 (34.375%) | ||||||
| I am unable to perform my usual activities | 4 (5.195%) | 2 (4.444%) | 2 (6.250%) | ||||||
| Change | 77 (0) | 45 (0) | 32 (0) | ||||||
| Improvement | 6 (7.792%) | 3 (6.667%) | 3 (9.375%) | –2.7% | |||||
| Same | 48 (62.338%) | 26 (57.778%) | 22 (68.750%) | –11.0% | |||||
| Deterioration | 23 (29.870%) | 16 (35.556%) | 7 (21.875%) | 13.7% | 0.452 | ||||
| Paina | |||||||||
| Baseline | 77 (0) | 45 (0) | 32 (0) | ||||||
| I have no pain or discomfort | 39 (50.649%) | 29 (64.444%) | 10 (31.250%) | ||||||
| I have moderate pain or discomfort | 34 (44.156%) | 16 (35.556%) | 18 (56.250%) | ||||||
| I have extreme pain or discomfort | 4 (5.195%) | 0 (0.000%) | 4 (12.500%) | ||||||
| 12 months | 77 (0) | 45 (0) | 32 (0) | ||||||
| I have no pain or discomfort | 57 (74.026%) | 35 (77.778%) | 22 (68.750%) | ||||||
| I have moderate pain or discomfort | 20 (25.974%) | 10 (22.222%) | 10 (31.250%) | ||||||
| I have extreme pain or discomfort | 0 (0.000%) | 0 (0.000%) | 0 (0.000%) | ||||||
| Change | 77 (0) | 45 (0) | 32 (0) | ||||||
| Improvement | 24 (31.169%) | 8 (17.778%) | 16 (50.000%) | –32.2% | |||||
| Same | 50 (64.935%) | 35 (77.778%) | 15 (46.875%) | 30.9% | |||||
| Deterioration | 3 (3.896%) | 2 (4.444%) | 1 (3.125%) | 1.3% | 0.008 | ||||
| Anxietya | |||||||||
| Baseline | 75 (0) | 44 (0) | 31 (0) | ||||||
| I am not anxious or depressed | 44 (58.667%) | 24 (54.545%) | 20 (64.516%) | ||||||
| I am moderately anxious or depressed | 29 (38.667%) | 19 (43.182%) | 10 (32.258%) | ||||||
| I am extremely anxious or depressed | 2 (2.667%) | 1 (2.273%) | 1 (3.226%) | ||||||
| 12 months | 75 (0) | 44 (0) | 31 (0) | ||||||
| I am not anxious or depressed | 40 (53.333%) | 27 (61.364%) | 13 (41.935%) | ||||||
| I am moderately anxious or depressed | 25 (33.333%) | 13 (29.545%) | 12 (38.710%) | ||||||
| I am extremely anxious or depressed | 10 (13.333%) | 4 (9.091%) | 6 (19.355%) | ||||||
| Change | 75 (0) | 44 (0) | 31 (0) | ||||||
| Improvement | 13 (17.333%) | 9 (20.455%) | 4 (12.903%) | 7.6% | |||||
| Same | 38 (50.667%) | 26 (59.091%) | 12 (38.710%) | 20.4% | |||||
| Deterioration | 24 (32.000%) | 9 (20.455%) | 15 (48.387%) | –27.9% | 0.043 | ||||
| EQ-5D total score | |||||||||
| Baseline | 0.912 (0.086) | 0.924 (0.079) | 0.894 (0.095) | ||||||
| 12 months | 0.888 (0.104) | 0.910 (0.082) | 0.858 (0.123) | ||||||
| Change | –0.024 (0.085) | –0.015 (0.071) | –0.037 (0.100) | 0.022 (–0.017 to 0.061) | 0.26 (–0.20 to 0.71) | 0.268 | 0.032 (–0.007 to 0.070) | 0.37 (–0.08 to 0.83) | 0.109 |
| EQ-VAS | |||||||||
| Baseline | 66.2 (17.0) | 67.3 (16.1) | 64.8 (18.3) | ||||||
| 12 months | 72.0 (16.7) | 74.9 (14.8) | 68.0 (18.6) | ||||||
| Change | 5.8 (17.6) | 7.6 (17.0) | 3.2 (18.3) | 4.4 (–3.6 to 12.4) | 0.25 (–0.20 to 0.70) | 0.283 | 5.3 (–1.4 to 12.0) | 0.30 (–0.08 to 0.68) | 0.123 |
| Variable | All (N = 77) | Intervention (N = 45) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Settleda | |||||||||
| Baseline | 77 (0) | 45 (0) | 32 (0) | ||||||
| I am able to feel settled and secure in all areas of my life | 4 (5.2%) | 2 (4.4%) | 2 (6.2%) | ||||||
| I am able to feel settled and secure in many areas of my life | 49 (63.6%) | 33 (73.3%) | 16 (50.0%) | ||||||
| I am able to feel settled and secure in a few areas of my life | 22 (28.6%) | 8 (17.8%) | 14 (43.8%) | ||||||
| I am unable to feel settled and secure in any areas of my life | 2 (2.6%) | 2 (4.4%) | 0 (0.0%) | ||||||
| 12 months | 77 (0) | 45 (0) | 32 (0) | ||||||
| I am able to feel settled and secure in all areas of my life | 56 (72.7%) | 35 (77.8%) | 21 (65.6%) | ||||||
| I am able to feel settled and secure in many areas of my life | 17 (22.1%) | 9 (20.0%) | 8 (25.0%) | ||||||
| I am able to feel settled and secure in a few areas of my life | 4 (5.2%) | 1 (2.2%) | 3 (9.4%) | ||||||
| I am unable to feel settled and secure in any areas of my life | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||||||
| Change | 77 (0) | 45 (0) | 32 (0) | ||||||
| Improvement | 59 (76.6%) | 37 (82.2%) | 22 (68.8%) | 13.5% | |||||
| Same | 16 (20.8%) | 7 (15.6%) | 9 (28.1%) | –12.6% | |||||
| Deterioration | 2 (2.6%) | 1 (2.2%) | 1 (3.1%) | –0.9% | 0.382 | ||||
| Independencea | |||||||||
| Baseline | 76 (0) | 44 (0) | 32 (0) | ||||||
| I am able to be completely independent | 28 (36.8%) | 18 (40.9%) | 10 (31.2%) | ||||||
| I am able to be independent in many things | 42 (55.3%) | 24 (54.5%) | 18 (56.2%) | ||||||
| I am able to be independent in a few things | 6 (7.9%) | 2 (4.5%) | 4 (12.5%) | ||||||
| I am unable to be at all independent | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||||||
| 12 months | 76 (0) | 44 (0) | 32 (0) | ||||||
| I am able to be completely independent | 16 (21.1%) | 11 (25.0%) | 5 (15.6%) | ||||||
| I am able to be independent in many things | 41 (53.9%) | 25 (56.8%) | 16 (50.0%) | ||||||
| I am able to be independent in a few things | 17 (22.4%) | 7 (15.9%) | 10 (31.2%) | ||||||
| I am unable to be at all independent | 2 (2.6%) | 1 (2.3%) | 1 (3.1%) | ||||||
| Change | 76 (0) | 44 (0) | 32 (0) | ||||||
| Improvement | 7 (9.2%) | 4 (9.1%) | 3 (9.4%) | –0.3% | |||||
| Same | 41 (53.9%) | 25 (56.8%) | 16 (50.0%) | 6.8% | |||||
| Deterioration | 28 (36.8%) | 15 (34.1%) | 13 (40.6%) | –6.5% | 0.884 | ||||
| Achievementsa | |||||||||
| Baseline | 76 (0) | 44 (0) | 32 (0) | ||||||
| I can achieve and progress in all aspects of my life | 17 (22.4%) | 14 (31.8%) | 3 (9.4%) | ||||||
| I can achieve and progress in many aspects of my life | 42 (55.3%) | 23 (52.3%) | 19 (59.4%) | ||||||
| I can achieve and progress in a few aspects of my life | 16 (21.1%) | 6 (13.6%) | 10 (31.2%) | ||||||
| I cannot achieve and progress in any aspects of my life | 1 (1.3%) | 1 (2.3%) | 0 (0.0%) | ||||||
| 12 months | 76 (0) | 44 (0) | 32 (0) | ||||||
| I can achieve and progress in all aspects of my life | 27 (35.5%) | 19 (43.2%) | 8 (25.0%) | ||||||
| I can achieve and progress in many aspects of my life | 30 (39.5%) | 16 (36.4%) | 14 (43.8%) | ||||||
| I can achieve and progress in a few aspects of my life | 18 (23.7%) | 9 (20.5%) | 9 (28.1%) | ||||||
| I cannot achieve and progress in any aspects of my life | 1 (1.3%) | 0 (0.0%) | 1 (3.1%) | ||||||
| Change | 76 (0) | 44 (0) | 32 (0) | ||||||
| Improvement | 23 (30.3%) | 13 (29.5%) | 10 (31.2%) | –1.7% | |||||
| Same | 39 (51.3%) | 23 (52.3%) | 16 (50.0%) | 2.3% | |||||
| Deterioration | 14 (18.4%) | 8 (18.2%) | 6 (18.8%) | –0.6% | 1.000 | ||||
| Pleasurea | |||||||||
| Baseline | 76 (0) | 44 (0) | 32 (0) | ||||||
| I can have a lot of enjoyment and pleasure | 30 (39.5%) | 23 (52.3%) | 7 (21.9%) | ||||||
| I can have a quite a lot of enjoyment and pleasure | 35 (46.1%) | 17 (38.6%) | 18 (56.2%) | ||||||
| I can have a little enjoyment and pleasure | 11 (14.5%) | 4 (9.1%) | 7 (21.9%) | ||||||
| I cannot have any enjoyment and pleasure | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||||||
| 12 months | 76 (0) | 44 (0) | 32 (0) | ||||||
| I can have a lot of enjoyment and pleasure | 11 (14.5%) | 6 (13.6%) | 5 (15.6%) | ||||||
| I can have a quite a lot of enjoyment and pleasure | 43 (56.6%) | 28 (63.6%) | 15 (46.9%) | ||||||
| I can have a little enjoyment and pleasure | 20 (26.3%) | 9 (20.5%) | 11 (34.4%) | ||||||
| I cannot have any enjoyment and pleasure | 2 (2.6%) | 1 (2.3%) | 1 (3.1%) | ||||||
| Change | 76 (0) | 44 (0) | 32 (0) | ||||||
| Improvement | 8 (10.5%) | 4 (9.1%) | 4 (12.5%) | –3.4% | |||||
| Same | 30 (39.5%) | 13 (29.5%) | 17 (53.1%) | –23.6% | |||||
| Deterioration | 38 (50.0%) | 27 (61.4%) | 11 (34.4%) | 27.0% | 0.060 | ||||
| Total ICECAP-A score | |||||||||
| Baseline | 12.2 (2.0) | 12.7 (1.9) | 11.6 (1.9) | ||||||
| 12 months | 12.5 (2.3) | 12.9 (2.1) | 12.0 (2.5) | ||||||
| Change | 0.3 (1.8) | 0.2 (1.5) | 0.4 (2.1) | –0.2 (–1.0 to 0.6) | –0.11 (–0.57 to 0.34) | 0.626 | 0.0 (–0.8 to 0.8) | 0.01 (–0.45 to 0.47) | 0.964 |
| Variable | All (N = 66) | Intervention (N = 38) | Control (N = 28) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| GHQ change score | |||||||||
| Baseline | 3.0 (3.1) | 2.9 (3.5) | 3.2 (2.7) | ||||||
| 12 months | 2.9 (3.6) | 2.4 (3.5) | 3.5 (3.8) | ||||||
| Change | –0.1 (4.0) | –0.4 (3.7) | 0.4 (4.4) | –0.8 (–2.8 to 1.1) | –0.20 (–0.69 to 0.29) | 0.421 | –0.8 (–2.5 to 0.9) | –0.21 (–0.63 to 0.21) | 0.339 |
| GHQ change score (Likert scoring) | |||||||||
| Baseline | 13.5 (5.2) | 13.4 (5.3) | 13.6 (5.2) | ||||||
| 12 months | 12.2 (6.6) | 11.5 (6.8) | 13.2 (6.2) | ||||||
| Change | –1.3 (6.8) | –1.9 (5.8) | –0.4 (7.9) | –1.5 (–4.8 to 1.8) | –0.22 (–0.70 to 0.27) | 0.388 | –1.4 (–4.2 to 1.5) | –0.20 (–0.63 to 0.22) | 0.345 |
| GHQ case (Likert score of ≥ 12) at 12 monthsa | |||||||||
| Baseline | 66 (0) | 38 (0) | 28 (0) | ||||||
| No | 27 (40.9%) | 17 (44.7%) | 10 (35.7%) | ||||||
| Yes | 39 (59.1%) | 21 (55.3%) | 18 (64.3%) | ||||||
| 12 months | 66 (0) | 38 (0) | 28 (0) | ||||||
| No | 33 (50.0%) | 19 (50.0%) | 14 (50.0%) | ||||||
| Yes | 33 (50.0%) | 19 (50.0%) | 14 (50.0%) | 1.00 (0.38 to 2.65) | – | 1.000 | 1.16 (0.33 to 4.02) | – | 0.814 |
| Variable | All (N = 109) | Intervention (N = 73) | Control (N = 36) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| AUDIT score | |||||||||
| 12 months | 2.6 (2.5) | 2.9 (2.8) | 2.2 (2.2) | 0.7 (–0.9 to 2.2) | 0.26 (–0.33 to 0.84) | 0.397 | 0.7 (–0.9 to 2.4) | 0.29 (–0.34 to 0.92) | 0.371 |
| AUDIT positivea | |||||||||
| 12 months | 43 (66) | 24 (49) | 19 (17) | ||||||
| No | 38 (88.4%) | 21 (87.5%) | 17 (89.5%) | ||||||
| Yes | 5 (11.6%) | 3 (12.5%) | 2 (10.5%) | 1.21 (0.18 to 8.12) | – | 0.841 | 1.27 (0.12 to 13.67) | – | 0.842 |
| Smoking (yes/no)b | |||||||||
| 12 months | 68 (41) | 39 (34) | 29 (7) | ||||||
| No | 63 (92.6%) | 37 (94.9%) | 26 (89.7%) | 5.2% | |||||
| Yes | 5 (7.4%) | 2 (5.1%) | 3 (10.3%) | –5.2% (–21.3% to 10.9%) | 0.644 | ||||
| Number of cigarettes per dayc | |||||||||
| 12 months | 13.0 (7.9) | 8.5 (9.2) | 16.0 (6.9) | 5.8 (–7.0 to 18.0) | – | 0.374 | |||
| Time from waking to first cigaretteb | |||||||||
| 12 months | 5 (0) | 2 (0) | 3 (0) | ||||||
| Within 5 minutes | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.0% | |||||
| 6 to 30 minutes | 3 (60.0%) | 1 (50.0%) | 2 (66.7%) | –16.7% | |||||
| 31 to 60 minutes | 1 (20.0%) | 0 (0.0%) | 1 (33.3%) | –33.3% | |||||
| ≥ 61 minutes | 1 (20.0%) | 1 (50.0%) | 0 (0.0%) | 50.0% | 1.000 | ||||
| Variable | All (N = 67) | Intervention (N = 38) | Control (N = 29) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Family encouragement score | |||||||||
| Baseline | 13.0 (6.1) | 12.6 (5.9) | 13.6 (6.5) | ||||||
| 12 months | 12.8 (5.3) | 12.3 (4.5) | 13.4 (6.3) | ||||||
| Change | –0.3 (5.5) | –0.3 (5.3) | –0.1 (5.8) | –0.2 (–2.9 to 2.5) | –0.04 (–0.52 to 0.45) | 0.881 | –0.5 (–2.7 to 1.8) | –0.09 (–0.50 to 0.32) | 0.679 |
| Family sabotage score | |||||||||
| Baseline | 11.5 (4.0) | 11.1 (3.7) | 12.1 (4.3) | ||||||
| 12 months | 10.8 (4.0) | 10.2 (4.0) | 11.4 (4.1) | ||||||
| Change | –0.8 (3.9) | –0.9 (3.9) | –0.6 (4.0) | –0.3 (–2.2 to 1.7) | –0.07 (–0.55 to 0.42) | 0.783 | –0.9 (–2.7 to 0.9) | –0.23 (–0.67 to 0.22) | 0.327 |
| Friends encouragement score | |||||||||
| Baseline | 8.9 (4.0) | 8.0 (3.4) | 10.1 (4.4) | ||||||
| 12 months | 8.7 (4.2) | 8.5 (3.8) | 8.9 (4.6) | ||||||
| Change | –0.2 (4.9) | 0.5 (3.3) | –1.2 (6.6) | 1.7 (–0.7 to 4.1) | 0.34 (–0.15 to 0.84) | 0.178 | 0.5 (–1.6 to 2.6) | 0.10 (–0.34 to 0.54) | 0.653 |
| Friends sabotage score | |||||||||
| Baseline | 10.8 (4.9) | 11.0 (4.9) | 10.6 (5.0) | ||||||
| 12 months | 9.7 (4.8) | 9.8 (5.1) | 9.6 (4.6) | ||||||
| Change | –1.1 (4.9) | –1.2 (4.8) | –1.0 (5.2) | –0.2 (–2.7 to 2.3) | –0.04 (–0.54 to 0.45) | 0.871 | 0.1 (–2.1 to 2.3) | 0.02 (–0.42 to 0.46) | 0.923 |
| Combined encouragement score | |||||||||
| Baseline | 21.9 (8.5) | 20.6 (8.0) | 23.7 (9.1) | ||||||
| 12 months | 21.4 (7.6) | 20.8 (6.7) | 22.4 (8.8) | ||||||
| Change | –0.5 (8.4) | 0.2 (7.6) | –1.4 (9.5) | 1.5 (–2.6 to 5.7) | 0.18 (–0.31 to 0.68) | 0.473 | 0.3 (–3.2 to 3.7) | 0.03 (–0.39 to 0.45) | 0.887 |
| Combined sabotage score | |||||||||
| Baseline | 22.4 (7.9) | 22.2 (7.4) | 22.7 (8.5) | ||||||
| 12 months | 20.5 (7.1) | 20.1 (6.6) | 21.0 (7.7) | ||||||
| Change | –1.9 (7.1) | –2.1 (6.6) | –1.6 (7.7) | –0.5 (–4.0 to 3.1) | –0.07 (–0.56 to 0.43) | 0.796 | –0.7 (–3.8 to 2.4) | –0.10 (–0.54 to 0.33) | 0.643 |
| Variable | All (N = 63) | Intervention (N = 36) | Control (N = 27) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Family participation score | |||||||||
| Baseline | 20.0 (8.8) | 20.0 (8.0) | 20.1 (9.8) | ||||||
| 12 months | 18.9 (9.6) | 18.0 (7.8) | 20.1 (11.6) | ||||||
| Change | –1.1 (8.5) | –2.0 (7.1) | 0.1 (10.0) | –2.1 (–6.3 to 2.1) | –0.25 (–0.75 to 0.25) | 0.333 | –1.3 (–5.4 to 2.8) | –0.16 (–0.64 to 0.33) | 0.528 |
| Family punishment score | |||||||||
| Baseline | 3.6 (1.1) | 3.5 (0.9) | 3.9 (1.3) | ||||||
| 12 months | 3.4 (0.8) | 3.2 (0.6) | 3.7 (1.0) | ||||||
| Change | –0.2 (1.0) | –0.2 (1.0) | –0.2 (0.9) | –0.1 (–0.5 to 0.4) | –0.07 (–0.57 to 0.43) | 0.793 | –0.3 (–0.7 to 0.1) | –0.35 (–0.75 to 0.06) | 0.097 |
| Friends participation score | |||||||||
| Baseline | 16.9 (8.1) | 17.3 (8.2) | 16.4 (8.1) | ||||||
| 12 months | 16.7 (9.1) | 17.0 (8.6) | 16.2 (10.0) | ||||||
| Change | –0.3 (9.0) | –0.3 (6.5) | –0.2 (11.8) | –0.1 (–4.7 to 4.6) | –0.01 (–0.51 to 0.50) | 0.982 | 0.4 (–3.9 to 4.6) | 0.04 (–0.42 to 0.50) | 0.865 |
| Friends punishment score | |||||||||
| Baseline | 3.4 (0.9) | 3.4 (0.9) | 3.4 (0.8) | ||||||
| 12 months | 3.1 (0.5) | 3.1 (0.4) | 3.2 (0.7) | ||||||
| Change | –0.3 (0.9) | –0.3 (1.0) | –0.2 (0.9) | –0.2 (–0.6 to 0.3) | –0.17 (–0.67 to 0.33) | 0.511 | –0.2 (–0.5 to 0.1) | –0.19 (–0.49 to 0.10) | 0.208 |
| Combined participation score | |||||||||
| Baseline | 37.0 (13.4) | 37.1 (12.8) | 36.9 (14.5) | ||||||
| 12 months | 35.1 (14.9) | 34.6 (12.8) | 35.7 (17.6) | ||||||
| Change | –1.9 (13.9) | –2.5 (10.8) | –1.2 (17.5) | –1.2 (–8.3 to 5.9) | –0.09 (–0.59 to 0.42) | 0.737 | –1.0 (–7.7 to 5.6) | –0.07 (–0.55 to 0.40) | 0.762 |
| Combined punishment score | |||||||||
| Baseline | 7.1 (1.8) | 6.9 (1.6) | 7.3 (2.0) | ||||||
| 12 months | 6.5 (1.1) | 6.3 (0.9) | 6.9 (1.3) | ||||||
| Change | –0.5 (1.7) | –0.6 (1.8) | –0.4 (1.5) | –0.3 (–1.1 to 0.6) | –0.15 (–0.66 to 0.35) | 0.550 | –0.6 (–1.2 to –0.1) | –0.37 (–0.69 to –0.05) | 0.026 |
| Variable | All (N = 65) | Intervention (N = 36) | Control (N = 29) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Availability scorea | |||||||||
| Baseline | 15.9 (9.2) | 15.6 (10.1) | 16.3 (8.0) | ||||||
| 12 months | 17.7 (10.1) | 16.8 (10.4) | 18.8 (9.9) | ||||||
| Change | 1.7 (9.1) | 1.1 (8.7) | 2.5 (9.7) | 0.6 (–4.0 to 5.0) | – | 0.802 | |||
| Negative emotions scorea | |||||||||
| Baseline | 14.2 (10.0) | 12.8 (10.8) | 15.8 (8.8) | ||||||
| 12 months | 16.3 (10.0) | 15.2 (10.5) | 17.7 (9.4) | ||||||
| Change | 2.2 (7.3) | 2.4 (7.1) | 1.9 (7.7) | –1.0 (–4.0 to 2.0) | – | 0.701 | |||
| Social pressure scorea | |||||||||
| Baseline | 20.5 (9.3) | 20.2 (10.0) | 20.9 (8.6) | ||||||
| 12 months | 21.9 (9.5) | 21.4 (9.7) | 22.4 (9.3) | ||||||
| Change | 1.3 (7.7) | 1.2 (7.2) | 1.5 (8.4) | 0.5 (–4.0 to 5.0) | – | 0.786 | |||
| Physical discomfort scorea | |||||||||
| Baseline | 20.2 (8.9) | 19.5 (9.7) | 20.9 (7.9) | ||||||
| 12 months | 21.2 (9.0) | 20.5 (9.0) | 22.2 (9.1) | ||||||
| Change | 1.1 (8.2) | 0.9 (8.6) | 1.2 (7.9) | 0.0 (–4.0 to 4.0) | – | 0.905 | |||
| Positive activities scorea | |||||||||
| Baseline | 21.7 (8.1) | 21.4 (8.8) | 22.1 (7.3) | ||||||
| 12 months | 22.6 (8.6) | 22.8 (9.2) | 22.4 (7.8) | ||||||
| Change | 0.9 (7.1) | 1.3 (6.5) | 0.3 (7.9) | –1.0 (–5.0 to 1.0) | – | 0.375 | |||
| Total score | |||||||||
| Baseline | 92.4 (38.3) | 89.3 (43.7) | 96.1 (31.2) | ||||||
| 12 months | 100.2 (40.9) | 97.4 (42.8) | 103.4 (39.0) | ||||||
| Change | 7.8 (30.3) | 8.1 (29.4) | 7.4 (31.9) | 0.7 (–14.4 to 15.9) | 0.02 (–0.47 to 0.52) | 0.927 | 0.9 (–13.8 to 15.5) | 0.03 (–0.45 to 0.51) | 0.909 |
| Variable | All (N = 63) | Intervention (N = 37) | Control (N = 26) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Task scorea | |||||||||
| Baseline | 4.7 (2.5) | 4.6 (2.7) | 4.8 (2.4) | ||||||
| 12 months | 5.0 (2.8) | 5.0 (2.8) | 5.1 (2.8) | ||||||
| Change | 0.3 (2.4) | 0.3 (2.5) | 0.3 (2.2) | 0.0 (–1.0 to 1.0) | – | 0.828 | |||
| Coping scorea | |||||||||
| Baseline | 7.4 (1.9) | 7.8 (1.6) | 7.0 (2.3) | ||||||
| 12 months | 7.4 (1.8) | 7.8 (1.5) | 7.0 (2.1) | ||||||
| Change | 0.0 (1.7) | 0.0 (1.4) | 0.0 (2.1) | 0.0 (–0.8 to 0.8) | – | 0.833 | |||
| Scheduling scorea | |||||||||
| Baseline | 5.8 (2.6) | 6.3 (2.7) | 5.0 (2.5) | ||||||
| 12 months | 5.9 (2.6) | 5.9 (2.8) | 6.0 (2.5) | ||||||
| Change | 0.2 (2.7) | –0.4 (2.4) | 1.0 (3.0) | 1.0 (0.0 to 2.3) | – | 0.065 | |||
| Total score | |||||||||
| Baseline | 6.0 (1.9) | 6.2 (2.0) | 5.7 (1.9) | ||||||
| 12 months | 6.1 (2.0) | 6.2 (2.1) | 6.0 (2.0) | ||||||
| Change | 0.1 (1.5) | 0.0 (1.6) | 0.3 (1.3) | –0.3 (–1.0 to 0.4) | –0.21 (–0.71 to 0.29) | 0.414 | –0.2 (–0.9 to 0.6) | –0.11 (–0.60 to 0.38) | 0.662 |
| Variable | All (N = 66) | Intervention (N = 37) | Control (N = 29) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Autonomous regulation score (diet)a | |||||||||
| Baseline | 6.2 (0.7) | 6.1 (0.7) | 6.4 (0.6) | ||||||
| 12 months | 5.9 (1.0) | 5.9 (1.0) | 5.9 (1.1) | ||||||
| Change | –0.3 (0.8) | –0.2 (0.7) | –0.5 (1.0) | –0.2 (–0.5 to 0.0) | – | 0.165 | |||
| Controlled regulation score (diet)a | |||||||||
| Baseline | 3.4 (1.2) | 3.5 (1.2) | 3.3 (1.2) | ||||||
| 12 months | 3.1 (1.2) | 3.1 (1.2) | 3.2 (1.2) | ||||||
| Change | –0.3 (1.1) | –0.5 (1.1) | –0.1 (1.0) | 0.3 (–0.2 to 0.8) | – | 0.292 | |||
| Amotivational score (diet)a | |||||||||
| Baseline | 1.8 (0.8) | 1.8 (0.8) | 1.7 (0.9) | ||||||
| 12 months | 1.8 (1.0) | 1.7 (1.0) | 2.0 (1.1) | ||||||
| Change | 0.1 (1.1) | –0.1 (1.2) | 0.2 (1.0) | 0.3 (0.0 to 0.8) | – | 0.081 | |||
| Relative autonomy score (diet) | |||||||||
| Baseline | 2.8 (1.3) | 2.6 (1.3) | 3.1 (1.3) | ||||||
| 12 months | 2.8 (1.5) | 2.8 (1.4) | 2.7 (1.6) | ||||||
| Change | 0.0 (1.3) | 0.3 (1.3) | –0.3 (1.3) | 0.6 (0.0 to 1.2) | 0.45 (–0.03 to 0.94) | 0.072 | 0.5 (–0.1 to 1.1) | 0.40 (–0.07 to 0.87) | 0.103 |
| Variable | All (N = 62) | Intervention (N = 35) | Control (N = 27) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Autonomous regulation score (exercise)a | |||||||||
| Baseline | 6.2 (0.9) | 6.1 (1.1) | 6.4 (0.6) | ||||||
| 12 months | 5.9 (1.1) | 6.0 (1.0) | 5.9 (1.1) | ||||||
| Change | –0.3 (1.0) | –0.1 (1.1) | –0.5 (1.0) | –0.3 (–0.7 to 0.2) | – | 0.208 | |||
| Controlled regulation score (exercise)a | |||||||||
| Baseline | 3.2 (1.2) | 3.2 (1.3) | 3.2 (1.0) | ||||||
| 12 months | 3.0 (1.2) | 3.0 (1.1) | 2.9 (1.4) | ||||||
| Change | –0.2 (1.1) | –0.2 (1.2) | –0.2 (1.0) | 0.0 (–0.5 to 0.5) | – | 1.000 | |||
| Amotivational score (exercise)a | |||||||||
| Baseline | 1.9 (0.9) | 1.9 (0.9) | 1.9 (1.0) | ||||||
| 12 months | 2.0 (1.0) | 1.9 (0.8) | 2.0 (1.2) | ||||||
| Change | 0.1 (0.9) | 0.0 (0.9) | 0.2 (1.0) | 0.0 (–0.3 to 0.7) | – | 0.678 | |||
| Relative autonomy score (exercise) | |||||||||
| Baseline | 3.0 (1.4) | 2.9 (1.5) | 3.2 (1.1) | ||||||
| 12 months | 3.0 (1.4) | 3.0 (1.2) | 3.0 (1.6) | ||||||
| Change | –0.1 (1.5) | 0.1 (1.6) | –0.3 (1.3) | 0.4 (–0.4 to 1.1) | 0.25 (–0.25 to 0.76) | 0.325 | 0.3 (–0.4 to 0.9) | 0.19 (–0.27 to 0.64) | 0.424 |
| Variable | All (N = 33) | Intervention (N = 18) | Control (N = 15) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| % in MVPA | |||||||||
| Baseline | 4.9 (2.8) | 5.5 (3.0) | 4.1 (2.3) | ||||||
| 12 months | 4.7 (2.7) | 5.6 (2.7) | 3.5 (2.3) | ||||||
| Change | –0.2 (2.1) | 0.1 (2.7) | –0.6 (1.0) | 0.8 (–0.7 to 2.2) | 0.36 (–0.33 to 1.04) | 0.312 | 1.4 (0.2 to 2.7) | 0.69 (0.09 to 1.28) | 0.032 |
| Average MVPA per day (minutes per day) | |||||||||
| Baseline | 41.6 (23.4) | 46.6 (25.7) | 35.5 (19.4) | ||||||
| 12 months | 39.6 (22.5) | 46.6 (22.4) | 31.3 (20.3) | ||||||
| Change | –2.0 (18.3) | 0.0 (23.1) | –4.3 (10.5) | 4.2 (–8.5 to 16.9) | 0.23 (–0.46 to 0.91) | 0.521 | 10.4 (0.0 to 20.8) | 0.56 (0.00 to 1.13) | 0.061 |
| Average sedentary minutes per day | |||||||||
| Baseline | 656.4 (117.0) | 652.0 (99.9) | 661.7 (138.2) | ||||||
| 12 months | 659.3 (128.4) | 622.6 (71.0) | 703.4 (166.6) | ||||||
| Change | 2.9 (83.7) | –29.5 (70.7) | 41.7 (83.5) | –71.1 (–123.7 to –18.5) | –0.93 (–1.61 to –0.24) | 0.013 | –73.2 (–126.0 to –20.5) | –0.95 (–1.64 to –0.27) | 0.011 |
| Average steps per day | |||||||||
| Baseline | 5969.0 (2140.7) | 6234.8 (2558.4) | 5650.0 (1525.5) | ||||||
| 12 months | 6291.2 (2571.7) | 7088.2 (2858.0) | 5334.8 (1844.4) | ||||||
| Change | 322.3 (2008.9) | 853.4 (2426.5) | –315.2 (1129.7) | 1168.6 (–168.1 to 2505.3) | 0.60 (–0.09 to 1.28) | 0.097 | 1397.4 (179.6 to 2615.2) | 0.72 (0.09 to 1.34) | 0.033 |
| Variable | All (N = 69) | Intervention (N = 37) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Total weekly expenditure by kg (kcal/kg/week) | |||||||||
| Baseline | 264.1 (43.4) | 261.0 (37.3) | 267.6 (49.9) | ||||||
| 12 months | 257.1 (27.0) | 257.4 (26.0) | 256.7 (28.6) | ||||||
| Change | –7.0 (41.7) | –3.5 (38.4) | –10.9 (45.6) | 7.4 (–12.4 to 27.2) | 0.18 (–0.30 to 0.65) | 0.466 | 0.6 (–11.8 to 13.1) | 0.02 (–0.28 to 0.31) | 0.919 |
| Total daily expenditure by kg (kcal/kg/day) | |||||||||
| Baseline | 37.7 (6.2) | 37.3 (5.3) | 38.2 (7.1) | ||||||
| 12 months | 36.7 (3.9) | 36.8 (3.7) | 36.7 (4.1) | ||||||
| Change | –1.0 (6.0) | –0.5 (5.5) | –1.6 (6.5) | 1.1 (–1.8 to 3.9) | 0.18 (–0.30 to 0.65) | 0.466 | 0.1 (–1.7 to 1.9) | 0.02 (–0.28 to 0.31) | 0.919 |
| Total daily expenditure (kcal/day) | |||||||||
| Baseline | 3810.4 (933.0) | 3749.3 (738.7) | 3879.2 (1120.8) | ||||||
| 12 months | 3597.3 (773.9) | 3589.7 (805.0) | 3605.8 (750.2) | ||||||
| Change | –213.1 (679.1) | –159.6 (518.4) | –273.4 (828.4) | 113.8 (–210.9 to 438.5) | 0.17 (–0.31 to 0.64) | 0.494 | 117.7 (–142.4 to 377.9) | 0.17 (–0.21 to 0.55) | 0.378 |
| Variable | All (N = 69) | Intervention (N = 37) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| DINE fibre score | |||||||||
| Baseline | 18.6 (9.9) | 18.6 (9.3) | 18.6 (10.6) | ||||||
| 12 months | 17.8 (11.7) | 16.7 (11.9) | 19.2 (11.6) | ||||||
| Change | –0.7 (11.1) | –1.9 (9.7) | 0.6 (12.6) | –2.5 (–7.7 to 2.8) | –0.22 (–0.70 to 0.25) | 0.357 | –2.2 (–7.3 to 2.9) | –0.20 (–0.65 to 0.26) | 0.399 |
| DINE fat score | |||||||||
| Baseline | 27.8 (11.8) | 28.5 (11.2) | 27.1 (12.6) | ||||||
| 12 months | 23.1 (11.4) | 23.3 (12.9) | 22.9 (9.6) | ||||||
| Change | –4.7 (10.8) | –5.2 (11.0) | –4.1 (10.8) | –1.0 (–6.2 to 4.1) | –0.10 (–0.57 to 0.38) | 0.695 | 0.0 (–4.6 to 4.6) | 0.00 (–0.42 to 0.42) | 0.997 |
| DINE healthy eating score | |||||||||
| Baseline | –9.2 (14.4) | –9.9 (12.9) | –8.5 (16.1) | ||||||
| 12 months | –5.3 (13.1) | –6.6 (13.0) | –3.8 (13.2) | ||||||
| Change | 3.9 (14.2) | 3.3 (11.9) | 4.7 (16.6) | –1.4 (–8.2 to 5.3) | –0.10 (–0.57 to 0.37) | 0.675 | –2.3 (–7.9 to 3.3) | –0.16 (–0.55 to 0.23) | 0.427 |
| DINE unsaturated fat score | |||||||||
| Baseline | 9.3 (1.8) | 9.4 (1.8) | 9.3 (1.8) | ||||||
| 12 months | 7.1 (4.4) | 6.3 (4.8) | 8.2 (3.7) | ||||||
| Change | –2.2 (4.5) | –3.1 (5.0) | –1.1 (3.5) | –2.0 (–3.9 to –0.2) | –0.47 (–0.90 to –0.04) | 0.037 | –1.8 (–3.6 to 0.1) | –0.40 (–0.83 to 0.02) | 0.066 |
| DINE fruit and vegetable score | |||||||||
| Baseline | 4.7 (2.8) | 4.4 (2.3) | 5.0 (3.4) | ||||||
| 12 months | 5.0 (2.6) | 5.1 (2.3) | 4.9 (2.9) | ||||||
| Change | 0.3 (2.9) | 0.7 (2.3) | –0.1 (3.4) | 0.8 (–0.6 to 2.2) | 0.29 (–0.20 to 0.77) | 0.249 | 0.4 (–0.8 to 1.6) | 0.14 (–0.27 to 0.55) | 0.503 |
| DINE fizzy drink scorea | |||||||||
| Baseline | 0.1 (0.4) | 0.0 (0.0) | 0.2 (0.6) | ||||||
| 12 months | 0.2 (0.7) | 0.1 (0.5) | 0.3 (0.9) | ||||||
| Change | 0.1 (0.5) | 0.1 (0.5) | 0.1 (0.4) | 0.00 (0.00 to 0.00) | – | 0.979 | |||
| DINE sugar scorea | |||||||||
| Baseline | 0.8 (3.8) | 0.6 (1.4) | 0.9 (5.3) | ||||||
| 12 months | 0.5 (2.5) | 0.3 (0.8) | 0.8 (3.5) | ||||||
| Change | –0.2 (1.5) | –0.3 (1.0) | –0.2 (1.9) | 0.00 (0.00 to 0.00) | – | 0.058 | |||
| DINE fibre ratingb | |||||||||
| Baseline | 69 (0) | 37 (0) | 32 (0) | ||||||
| Low fibre intake | 61 (88.4%) | 33 (89.2%) | 28 (87.5%) | ||||||
| Medium fibre intake | 7 (10.1%) | 3 (8.1%) | 4 (12.5%) | ||||||
| High fibre intake | 1 (1.4%) | 1 (2.7%) | 0 (0.0%) | ||||||
| 12 months | 69 (0) | 37 (0) | 32 (0) | ||||||
| Low fibre intake | 57 (82.6%) | 30 (81.1%) | 27 (84.4%) | ||||||
| Medium fibre intake | 9 (13.0%) | 6 (16.2%) | 3 (9.4%) | ||||||
| High fibre intake | 3 (4.3%) | 1 (2.7%) | 2 (6.2%) | ||||||
| Change | 69 (0) | 37 (0) | 32 (0) | ||||||
| Improvement | 8 (11.6%) | 3 (8.1%) | 5 (15.6%) | –7.5% | |||||
| Same | 58 (84.1%) | 34 (91.9%) | 24 (75.0%) | 16.9% | |||||
| Deterioration | 3 (4.3%) | 0 (0.0%) | 3 (9.4%) | –9.4% | 0.078 | ||||
| DINE fat ratingb | |||||||||
| Baseline | 69 (0) | 37 (0) | 32 (0) | ||||||
| Low fat intake | 43 (62.3%) | 22 (59.5%) | 21 (65.6%) | ||||||
| Medium fat intake | 16 (23.2%) | 9 (24.3%) | 7 (21.9%) | ||||||
| High fat intake | 10 (14.5%) | 6 (16.2%) | 4 (12.5%) | ||||||
| 12 months | 69 (0) | 37 (0) | 32 (0) | ||||||
| Low fat intake | 51 (73.9%) | 26 (70.3%) | 25 (78.1%) | ||||||
| Medium fat intake | 15 (21.7%) | 9 (24.3%) | 6 (18.8%) | ||||||
| High fat intake | 3 (4.3%) | 2 (5.4%) | 1 (3.1%) | ||||||
| Change | 69 (0) | 37 (0) | 32 (0) | ||||||
| Improvement | 16 (23.2%) | 10 (27.0%) | 6 (18.8%) | 8.3% | |||||
| Same | 49 (71.0%) | 24 (64.9%) | 25 (78.1%) | –13.3% | |||||
| Deterioration | 4 (5.8%) | 3 (8.1%) | 1 (3.1%) | 5.0% | 0.492 | ||||
| DINE unsaturated fat ratingb | |||||||||
| Baseline | 84 (0) | 48 (0) | 36 (0) | ||||||
| Low unsaturated fat intake | 2 (2.4%) | 1 (2.1%) | 1 (2.8%) | ||||||
| Medium unsaturated fat intake | 36 (42.9%) | 20 (41.7%) | 16 (44.4%) | ||||||
| High unsaturated fat intake | 46 (54.8%) | 27 (56.2%) | 19 (52.8%) | ||||||
| 12 months | 84 (0) | 48 (0) | 36 (0) | ||||||
| Low unsaturated fat intake | 26 (31.0%) | 19 (39.6%) | 7 (19.4%) | ||||||
| Medium unsaturated fat intake | 22 (26.2%) | 11 (22.9%) | 11 (30.6%) | ||||||
| High unsaturated fat intake | 36 (42.9%) | 18 (37.5%) | 18 (50.0%) | ||||||
| Change | 84 (0) | 48 (0) | 36 (0) | ||||||
| Improvement | 31 (36.9%) | 22 (45.8%) | 9 (25.0%) | 20.8% | |||||
| Same | 44 (52.4%) | 22 (45.8%) | 22 (61.1%) | –15.3% | |||||
| Deterioration | 9 (10.7%) | 4 (8.3%) | 5 (13.9%) | –5.6% | 0.147 | ||||
| DINE fruit and vegetable ratingb | |||||||||
| Baseline | 66 (0) | 34 (0) | 32 (0) | ||||||
| Poor fruit and vegetable consumption | 35 (53.0%) | 19 (55.9%) | 16 (50.0%) | ||||||
| Good fruit and vegetable consumption | 31 (47.0%) | 15 (44.1%) | 16 (50.0%) | ||||||
| 12 months | 66 (0) | 34 (0) | 32 (0) | ||||||
| Poor fruit and vegetable consumption | 32 (48.5%) | 14 (41.2%) | 18 (56.2%) | ||||||
| Good fruit and vegetable consumption | 34 (51.5%) | 20 (58.8%) | 14 (43.8%) | ||||||
| Change | 66 (0) | 34 (0) | 32 (0) | ||||||
| Improvement | 12 (18.2%) | 7 (20.6%) | 5 (15.6%) | 5.0% | |||||
| Same | 45 (68.2%) | 25 (73.5%) | 20 (62.5%) | 11.0% | |||||
| Deterioration | 9 (13.6%) | 2 (5.9%) | 7 (21.9%) | –16.0% | 0.203 | ||||
| Variable | All (N = 64) | Intervention (N = 32) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| DINE unsaturated fat score | |||||||||
| Baseline | 9.5 (1.6) | 9.6 (1.4) | 9.4 (1.7) | ||||||
| 12 months | 9.2 (2.5) | 9.1 (2.6) | 9.2 (2.3) | ||||||
| Change | –0.3 (2.6) | –0.5 (2.6) | –0.2 (2.5) | –0.3 (–1.6 to 0.9) | –0.12 (–0.61 to 0.37) | 0.628 | –0.1 (–1.4 to 1.1) | –0.06 (–0.54 to 0.43) | 0.815 |
| DINE fruit and vegetable score | |||||||||
| Baseline | 4.9 (2.9) | 4.6 (2.3) | 5.3 (3.6) | ||||||
| 12 months | 3.9 (3.1) | 3.6 (3.0) | 4.3 (3.2) | ||||||
| Change | –1.0 (3.8) | –0.9 (3.5) | –1.0 (4.3) | 0.0 (–1.6 to 1.7) | 0.01 (–0.42 to 0.44) | 0.968 | –0.5 (–1.9 to 0.9) | –0.13 (–0.48 to 0.22) | 0.472 |
| DINE fizzy drink scorea | |||||||||
| Baseline | 0.2 (0.6) | 0.2 (0.6) | 0.2 (0.7) | ||||||
| 12 months | 0.2 (0.6) | 0.1 (0.4) | 0.2 (0.8) | ||||||
| Change | 0.0 (0.7) | –0.1 (0.8) | 0.1 (0.5) | 0.00 (0.00 to 0.00) | – | 0.262 | |||
| DINE sugar scorea | |||||||||
| Baseline | 0.8 (3.4) | 0.6 (1.3) | 1.0 (5.0) | ||||||
| 12 months | 0.4 (2.2) | 0.2 (0.7) | 0.7 (3.3) | ||||||
| Change | –0.4 (1.5) | –0.4 (1.0) | –0.3 (1.9) | 0.00 (0.00 to 0.00) | – | 0.041 | |||
| DINE unsaturated fat ratingb | |||||||||
| Baseline | 64 (0) | 32 (0) | 32 (0) | ||||||
| Low unsaturated fat intake | 1 (1.6%) | 0 (0.0%) | 1 (3.1%) | ||||||
| Medium unsaturated fat intake | 26 (40.6%) | 13 (40.6%) | 13 (40.6%) | ||||||
| High unsaturated fat intake | 37 (57.8%) | 19 (59.4%) | 18 (56.2%) | ||||||
| 12 months | 64 (0) | 32 (0) | 32 (0) | ||||||
| Low unsaturated fat intake | 7 (10.9%) | 4 (12.5%) | 3 (9.4%) | ||||||
| Medium unsaturated fat intake | 22 (34.4%) | 11 (34.4%) | 11 (34.4%) | ||||||
| High unsaturated fat intake | 35 (54.7%) | 17 (53.1%) | 18 (56.2%) | ||||||
| Change | 64 (0) | 32 (0) | 32 (0) | ||||||
| Improvement | 12 (18.8%) | 7 (21.9%) | 5 (15.6%) | 6.2% | |||||
| Same | 44 (68.8%) | 22 (68.8%) | 22 (68.8%) | 0.0% | |||||
| Deterioration | 8 (12.5%) | 3 (9.4%) | 5 (15.6%) | –6.2% | 0.690 | ||||
| DINE fruit and vegetable ratingb | |||||||||
| Baseline | 84 (0) | 48 (0) | 36 (0) | ||||||
| Poor fruit and vegetable consumption | 43 (51.2%) | 25 (52.1%) | 18 (50.0%) | ||||||
| Good fruit and vegetable consumption | 41 (48.8%) | 23 (47.9%) | 18 (50.0%) | ||||||
| 12 months | 84 (0) | 48 (0) | 36 (0) | ||||||
| Poor fruit and vegetable consumption | 50 (59.5%) | 28 (58.3%) | 22 (61.1%) | ||||||
| Good fruit and vegetable consumption | 34 (40.5%) | 20 (41.7%) | 14 (38.9%) | ||||||
| Change | 84 (0) | 48 (0) | 36 (0) | ||||||
| Improvement | 12 (14.3%) | 7 (14.6%) | 5 (13.9%) | 0.7% | |||||
| Same | 53 (63.1%) | 31 (64.6%) | 22 (61.1%) | 3.5% | |||||
| Deterioration | 19 (22.6%) | 10 (20.8%) | 9 (25.0%) | –4.2% | 0.948 | ||||
| Variable | All (N = 68) | Intervention (N = 36) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | |||||||||
| Baseline | 36.8 (5.1) | 36.8 (4.7) | 36.9 (5.7) | ||||||
| 12 months | 35.7 (5.6) | 35.4 (5.0) | 36.0 (6.3) | ||||||
| Change | –1.1 (2.6) | –1.3 (2.0) | –0.9 (3.3) | –0.5 (–1.7 to 0.8) | –0.18 (–0.65 to 0.30) | 0.474 | –0.4 (–1.6 to 0.9) | –0.14 (–0.62 to 0.34) | 0.573 |
| Variable | All (N = 30) | Intervention (N = 15) | Control (N = 15) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| % in MVPA | |||||||||
| Baseline | 5.0 (2.9) | 5.9 (3.2) | 4.1 (2.3) | ||||||
| 12 months | 4.7 (2.9) | 5.8 (2.9) | 3.5 (2.3) | ||||||
| Change | –0.3 (2.2) | 0.0 (2.9) | –0.6 (1.0) | 0.6 (–0.9 to 2.2) | 0.28 (–0.43 to 1.00) | 0.445 | 1.7 (0.4 to 3.1) | 0.80 (0.19 to 1.41) | 0.017 |
| Average MVPA per day (minutes per day) | |||||||||
| Baseline | 42.6 (24.3) | 49.7 (27.2) | 35.5 (19.4) | ||||||
| 12 months | 39.8 (23.5) | 48.3 (24.1) | 31.3 (20.3) | ||||||
| Change | –2.8 (19.0) | –1.4 (25.2) | –4.3 (10.5) | 2.8 (–11.0 to 16.6) | 0.15 (–0.57 to 0.86) | 0.690 | 13.7 (3.0 to 24.5) | 0.71 (0.16 to 1.27) | 0.019 |
| Average sedentary minutes per day | |||||||||
| Baseline | 657.2 (121.0) | 652.8 (105.8) | 661.7 (138.2) | ||||||
| 12 months | 660.6 (134.5) | 617.8 (76.2) | 703.4 (166.6) | ||||||
| Change | 3.4 (86.4) | –34.9 (73.1) | 41.7 (83.5) | –76.6 (–132.7 to –20.5) | –0.98 (–1.69 to –0.26) | 0.012 | –78.4 (–134.8 to –21.9) | –1.00 (–1.72 to –0.28) | 0.012 |
| Average steps per day | |||||||||
| Baseline | 6101.0 (2170.1) | 6552.0 (2644.3) | 5650.0 (1525.5) | ||||||
| 12 months | 6294.2 (2652.7) | 7253.6 (3033.5) | 5334.8 (1844.4) | ||||||
| Change | 193.2 (2059.0) | 701.5 (2636.7) | –315.2 (1129.7) | 1016.7 (–435.0 to 2468.4) | 0.50 (–0.21 to 1.22) | 0.181 | 1663.7 (389.0 to 2938.4) | 0.82 (0.19 to 1.45) | 0.017 |
| Variable | All (N = 62) | Intervention (N = 30) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Total weekly expenditure by kg (kcal/kg/week) | |||||||||
| Baseline | 264.0 (44.1) | 260.0 (37.4) | 267.6 (49.9) | ||||||
| 12 months | 257.3 (28.1) | 257.8 (28.1) | 256.7 (28.6) | ||||||
| Change | –6.7 (42.5) | –2.2 (39.3) | –10.9 (45.6) | 8.7 (–12.5 to 30.0) | 0.20 (–0.29 to 0.70) | 0.424 | 1.5 (–12.1 to 15.1) | 0.04 (–0.28 to 0.35) | 0.830 |
| Total daily expenditure by kg (kcal/kg/day) | |||||||||
| Baseline | 37.7 (6.3) | 37.1 (5.3) | 38.2 (7.1) | ||||||
| 12 months | 36.8 (4.0) | 36.8 (4.0) | 36.7 (4.1) | ||||||
| Change | –1.0 (6.1) | –0.3 (5.6) | –1.6 (6.5) | 1.2 (–1.8 to 4.3) | 0.20 (–0.29 to 0.70) | 0.424 | 0.2 (–1.7 to 2.2) | 0.04 (–0.28 to 0.35) | 0.830 |
| Total daily expenditure (kcal/day) | |||||||||
| Baseline | 3823.6 (976.8) | 3762.2 (804.0) | 3879.2 (1120.8) | ||||||
| 12 months | 3601.8 (802.8) | 3597.5 (870.6) | 3605.8 (750.2) | ||||||
| Change | –221.7 (699.8) | –164.8 (532.3) | –273.4 (828.4) | 108.6 (–245.0 to 462.2) | 0.15 (–0.35 to 0.66) | 0.549 | 113.2 (–169.9 to 396.3) | 0.16 (–0.24 to 0.56) | 0.437 |
| Variable | All (N = 62) | Intervention (N = 30) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| DINE fibre score | |||||||||
| Baseline | 18.5 (9.9) | 18.3 (9.4) | 18.6 (10.6) | ||||||
| 12 months | 18.1 (11.3) | 17.0 (11.2) | 19.2 (11.6) | ||||||
| Change | –0.3 (10.8) | –1.3 (8.7) | 0.6 (12.6) | –1.9 (–7.3 to 3.5) | –0.17 (–0.67 to 0.32) | 0.495 | –1.2 (–6.2 to 3.9) | –0.11 (–0.58 to 0.36) | 0.649 |
| DINE fat score | |||||||||
| Baseline | 27.2 (11.9) | 27.4 (11.2) | 27.1 (12.6) | ||||||
| 12 months | 22.5 (9.7) | 22.1 (9.9) | 22.9 (9.6) | ||||||
| Change | –4.7 (9.9) | –5.3 (8.9) | –4.1 (10.8) | –1.1 (–6.1 to 3.8) | –0.11 (–0.61 to 0.38) | 0.653 | –0.4 (–4.5 to 3.6) | –0.04 (–0.45 to 0.36) | 0.830 |
| DINE healthy eating score | |||||||||
| Baseline | –8.7 (14.6) | –9.0 (13.0) | –8.5 (16.1) | ||||||
| 12 months | –4.4 (11.3) | –5.1 (9.0) | –3.8 (13.2) | ||||||
| Change | 4.4 (14.1) | 4.0 (11.1) | 4.7 (16.6) | –0.8 (–7.8 to 6.3) | –0.05 (–0.55 to 0.45) | 0.836 | –0.7 (–6.0 to 4.6) | –0.05 (–0.43 to 0.32) | 0.788 |
| DINE unsaturated fat score | |||||||||
| Baseline | 9.4 (1.7) | 9.5 (1.7) | 9.3 (1.8) | ||||||
| 12 months | 7.6 (4.3) | 7.1 (4.8) | 8.2 (3.7) | ||||||
| Change | –1.8 (4.3) | –2.4 (5.0) | –1.1 (3.5) | –1.4 (–3.3 to 0.6) | –0.32 (–0.77 to 0.14) | 0.176 | –1.2 (–3.1 to 0.8) | –0.27 (–0.72 to 0.17) | 0.236 |
| DINE fruit and vegetable score | |||||||||
| Baseline | 4.8 (2.9) | 4.6 (2.4) | 5.0 (3.4) | ||||||
| 12 months | 5.1 (2.6) | 5.4 (2.3) | 4.9 (2.9) | ||||||
| Change | 0.4 (3.0) | 0.9 (2.4) | –0.1 (3.4) | 1.0 (–0.5 to 2.5) | 0.35 (–0.16 to 0.85) | 0.181 | 0.7 (–0.6 to 1.9) | 0.23 (–0.20 to 0.65) | 0.298 |
| DINE fizzy drink scorea | |||||||||
| Baseline | 0.1 (0.5) | 0.0 (0.0) | 0.2 (0.6) | ||||||
| 12 months | 0.2 (0.7) | 0.2 (0.5) | 0.3 (0.9) | ||||||
| Change | 0.1 (0.5) | 0.2 (0.5) | 0.1 (0.4) | 0.00 (0.00 to 0.00) | – | 0.878 | |||
| DINE sugar scorea | |||||||||
| Baseline | 0.8 (4.0) | 0.7 (1.5) | 0.9 (5.3) | ||||||
| 12 months | 0.6 (2.6) | 0.3 (0.8) | 0.8 (3.5) | ||||||
| Change | –0.3 (1.5) | –0.4 (1.0) | –0.2 (1.9) | 0.00 (0.00 to 0.00) | – | 0.035 | |||
| DINE fibre ratingb | |||||||||
| Baseline | 62 (0) | 30 (0) | 32 (0) | ||||||
| Low fibre intake | 55 (88.7%) | 27 (90.0%) | 28 (87.5%) | ||||||
| Medium fibre intake | 6 (9.7%) | 2 (6.7%) | 4 (12.5%) | ||||||
| High fibre intake | 1 (1.6%) | 1 (3.3%) | 0 (0.0%) | ||||||
| 12 months | 62 (0) | 30 (0) | 32 (0) | ||||||
| Low fibre intake | 52 (83.9%) | 25 (83.3%) | 27 (84.4%) | ||||||
| Medium fibre intake | 7 (11.3%) | 4 (13.3%) | 3 (9.4%) | ||||||
| High fibre intake | 3 (4.8%) | 1 (3.3%) | 2 (6.2%) | ||||||
| Change | 62 (0) | 30 (0) | 32 (0) | ||||||
| Improvement | 7 (11.3%) | 2 (6.7%) | 5 (15.6%) | –9.0% | |||||
| Same | 52 (83.9%) | 28 (93.3%) | 24 (75.0%) | 18.3% | |||||
| Deterioration | 3 (4.8%) | 0 (0.0%) | 3 (9.4%) | –9.4% | 0.115 | ||||
| DINE fat ratingb | |||||||||
| Baseline | 62 (0) | 30 (0) | 32 (0) | ||||||
| Low fat intake | 41 (66.1%) | 20 (66.7%) | 21 (65.6%) | ||||||
| Medium fat intake | 13 (21.0%) | 6 (20.0%) | 7 (21.9%) | ||||||
| High fat intake | 8 (12.9%) | 4 (13.3%) | 4 (12.5%) | ||||||
| 12 months | 62 (0) | 30 (0) | 32 (0) | ||||||
| Low fat intake | 48 (77.4%) | 23 (76.7%) | 25 (78.1%) | ||||||
| Medium fat intake | 13 (21.0%) | 7 (23.3%) | 6 (18.8%) | ||||||
| High fat intake | 1 (1.6%) | 0 (0.0%) | 1 (3.1%) | ||||||
| Change | 62 (0) | 30 (0) | 32 (0) | ||||||
| Improvement | 13 (21.0%) | 7 (23.3%) | 6 (18.8%) | 4.6% | |||||
| Same | 46 (74.2%) | 21 (70.0%) | 25 (78.1%) | –8.1% | |||||
| Deterioration | 3 (4.8%) | 2 (6.7%) | 1 (3.1%) | 3.5% | 0.726 | ||||
| DINE unsaturated fat ratingb | |||||||||
| Baseline | 74 (0) | 38 (0) | 36 (0) | ||||||
| Low unsaturated fat intake | 2 (2.7%) | 1 (2.6%) | 1 (2.8%) | ||||||
| Medium unsaturated fat intake | 31 (41.9%) | 15 (39.5%) | 16 (44.4%) | ||||||
| High unsaturated fat intake | 41 (55.4%) | 22 (57.9%) | 19 (52.8%) | ||||||
| 12 months | 74 (0) | 38 (0) | 36 (0) | ||||||
| Low unsaturated fat intake | 19 (25.7%) | 12 (31.6%) | 7 (19.4%) | ||||||
| Medium unsaturated fat intake | 20 (27.0%) | 9 (23.7%) | 11 (30.6%) | ||||||
| High unsaturated fat intake | 35 (47.3%) | 17 (44.7%) | 18 (50.0%) | ||||||
| Change | 74 (0) | 38 (0) | 36 (0) | ||||||
| Improvement | 23 (31.1%) | 14 (36.8%) | 9 (25.0%) | 11.8% | |||||
| Same | 42 (56.8%) | 20 (52.6%) | 22 (61.1%) | –8.5% | |||||
| Deterioration | 9 (12.2%) | 4 (10.5%) | 5 (13.9%) | –3.4% | 0.601 | ||||
| DINE fruit and vegetable ratingb | |||||||||
| Baseline | 61 (0) | 29 (0) | 32 (0) | ||||||
| Poor fruit and vegetable consumption | 32 (52.5%) | 16 (55.2%) | 16 (50.0%) | ||||||
| Good fruit and vegetable consumption | 29 (47.5%) | 13 (44.8%) | 16 (50.0%) | ||||||
| 12 months | 61 (0) | 29 (0) | 32 (0) | ||||||
| Poor fruit and vegetable consumption | 28 (45.9%) | 10 (34.5%) | 18 (56.2%) | ||||||
| Good fruit and vegetable consumption | 33 (54.1%) | 19 (65.5%) | 14 (43.8%) | ||||||
| Change | 61 (0) | 29 (0) | 32 (0) | ||||||
| Improvement | 11 (18.0%) | 6 (20.7%) | 5 (15.6%) | 5.1% | |||||
| Same | 43 (70.5%) | 23 (79.3%) | 20 (62.5%) | 16.8% | |||||
| Deterioration | 7 (11.5%) | 0 (0.0%) | 7 (21.9%) | –21.9% | 0.023 | ||||
| Variable | All (N = 59) | Intervention (N = 27) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| DINE unsaturated fat score | |||||||||
| Baseline | 9.5 (1.5) | 9.6 (1.3) | 9.4 (1.7) | ||||||
| 12 months | 9.4 (2.4) | 9.5 (2.5) | 9.2 (2.3) | ||||||
| Change | –0.2 (2.5) | –0.1 (2.4) | –0.2 (2.5) | 0.1 (–1.2 to 1.3) | 0.03 (–0.48 to 0.54) | 0.906 | 0.2 (–1.0 to 1.5) | 0.09 (–0.41 to 0.60) | 0.724 |
| DINE fruit and vegetable score | |||||||||
| Baseline | 5.1 (3.1) | 4.8 (2.4) | 5.3 (3.6) | ||||||
| 12 months | 4.2 (3.1) | 4.2 (3.1) | 4.3 (3.2) | ||||||
| Change | –0.8 (4.0) | –0.7 (3.7) | –1.0 (4.3) | 0.3 (–1.5 to 2.1) | 0.07 (–0.38 to 0.53) | 0.759 | –0.1 (–1.6 to 1.3) | –0.03 (–0.39 to 0.33) | 0.867 |
| DINE fizzy drink scorea | |||||||||
| Baseline | 0.1 (0.6) | 0.1 (0.5) | 0.2 (0.7) | ||||||
| 12 months | 0.2 (0.7) | 0.1 (0.5) | 0.2 (0.8) | ||||||
| Change | 0.0 (0.6) | 0.0 (0.7) | 0.1 (0.5) | 0.00 (0.00 to 0.00) | – | 0.753 | |||
| DINE sugar scorea | |||||||||
| Baseline | 0.8 (3.6) | 0.7 (1.4) | 1.0 (5.0) | ||||||
| 12 months | 0.5 (2.4) | 0.2 (0.8) | 0.7 (3.3) | ||||||
| Change | –0.4 (1.5) | –0.4 (1.0) | –0.3 (1.9) | 0.00 (0.00 to 0.00) | – | 0.045 | |||
| DINE unsaturated fat ratingb | |||||||||
| Baseline | 59 (0) | 27 (0) | 32 (0) | ||||||
| Low unsaturated fat intake | 1 (1.7%) | 0 (0.0%) | 1 (3.1%) | ||||||
| Medium unsaturated fat intake | 24 (40.7%) | 11 (40.7%) | 13 (40.6%) | ||||||
| High unsaturated fat intake | 34 (57.6%) | 16 (59.3%) | 18 (56.2%) | ||||||
| 12 months | 59 (0) | 27 (0) | 32 (0) | ||||||
| Low unsaturated fat intake | 5 (8.5%) | 2 (7.4%) | 3 (9.4%) | ||||||
| Medium unsaturated fat intake | 20 (33.9%) | 9 (33.3%) | 11 (34.4%) | ||||||
| High unsaturated fat intake | 34 (57.6%) | 16 (59.3%) | 18 (56.2%) | ||||||
| Change | 59 (0) | 27 (0) | 32 (0) | ||||||
| Improvement | 9 (15.3%) | 4 (14.8%) | 5 (15.6%) | –0.8% | |||||
| Same | 42 (71.2%) | 20 (74.1%) | 22 (68.8%) | 5.3% | |||||
| Deterioration | 8 (13.6%) | 3 (11.1%) | 5 (15.6%) | –4.5% | 0.919 | ||||
| DINE fruit and vegetable ratingb | |||||||||
| Baseline | 74 (0) | 38 (0) | 36 (0) | ||||||
| Poor fruit and vegetable consumption | 36 (48.6%) | 18 (47.4%) | 18 (50.0%) | ||||||
| Good fruit and vegetable consumption | 38 (51.4%) | 20 (52.6%) | 18 (50.0%) | ||||||
| 12 months | 74 (0) | 38 (0) | 36 (0) | ||||||
| Poor fruit and vegetable consumption | 41 (55.4%) | 19 (50.0%) | 22 (61.1%) | ||||||
| Good fruit and vegetable consumption | 33 (44.6%) | 19 (50.0%) | 14 (38.9%) | ||||||
| Change | 74 (0) | 38 (0) | 36 (0) | ||||||
| Improvement | 11 (14.9%) | 6 (15.8%) | 5 (13.9%) | 1.9% | |||||
| Same | 47 (63.5%) | 25 (65.8%) | 22 (61.1%) | 4.7% | |||||
| Deterioration | 16 (21.6%) | 7 (18.4%) | 9 (25.0%) | –6.6% | 0.791 | ||||
| Variable | All (N = 61) | Intervention (N = 29) | Control (N = 32) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | |||||||||
| Baseline | 37.0 (5.3) | 37.1 (5.0) | 36.9 (5.7) | ||||||
| 12 months | 35.8 (5.8) | 35.5 (5.3) | 36.0 (6.3) | ||||||
| Change | –1.2 (2.7) | –1.6 (2.0) | –0.9 (3.3) | –0.7 (–2.1 to 0.7) | –0.26 (–0.76 to 0.25) | 0.322 | –0.7 (–2.0 to 0.7) | –0.24 (–0.75 to 0.27) | 0.354 |
| Variable | Unadjusted intervention – control estimate | 95% CI | p-value | Adjusted intervention – control estimate | 95% CI | p-value |
|---|---|---|---|---|---|---|
| Physical activity accelerometer change from baseline | ||||||
| % in MVPA | –0.2 | –1.7 to 1.4 | 0.846 | 0.7 | –0.6 to 2.0 | 0.295 |
| Average MVPA per day (minutes per day) | –1.4 | –13.2 to 10.5 | 0.820 | 4.4 | –5.0 to 13.8 | 0.353 |
| Average sedentary minutes per day | –19.2 | –75.0 to 36.5 | 0.482 | –39.9 | –88.2 to 8.3 | 0.101 |
| Average steps per day | 141.5 | –1291.2 to 1574.3 | 0.844 | 675.7 | –578.2 to 1929.5 | 0.281 |
| Physical activity 7-day recall change from baseline | ||||||
| Total weekly expenditure by kg (kcal/kg/week) | 7.9 | –8.0 to 23.7 | 0.327 | –0.4 | –11.4 to 10.5 | 0.938 |
| Total daily expenditure by kg (kcal/kg/day) | 0.4 | –2.0 to 2.8 | 0.727 | –0.5 | –2.3 to 1.3 | 0.560 |
| Total daily expenditure (kcal/day) | 62.8 | –209.2 to 334.8 | 0.646 | 34.5 | –200.9 to 269.9 | 0.770 |
| DINE change from baseline, primary analysis | ||||||
| DINE fibre score | –3.7 | –8.8 to 1.4 | 0.152 | –2.8 | –7.7 to 2.1 | 0.251 |
| DINE fat score | –1.9 | –6.7 to 2.9 | 0.431 | –0.2 | –4.3 to 4.0 | 0.935 |
| DINE healthy eating score | –1.5 | –8.1 to 5.1 | 0.649 | –2.1 | –7.9 to 3.7 | 0.472 |
| DINE unsaturated fat score | –2.5 | –4.5 to –0.5 | 0.014 | –2.3 | –4.1 to –0.4 | 0.017 |
| DINE fruit and vegetables score | 0.7 | –0.5 to 1.9 | 0.229 | 0.3 | –0.7 to 1.3 | 0.565 |
| DINE fizzy drink score | 0.0 | –0.2 to 0.3 | 0.716 | 0.0 | –0.2 to 0.3 | 0.744 |
| DINE sugar score | 0.0 | –0.5 to 0.5 | 0.962 | –0.1 | –0.4 to 0.1 | 0.313 |
| BMI change from baseline | ||||||
| BMI (kg/m2) | –0.3 | –1.5 to 0.9 | 0.637 | –0.2 | –1.4 to 1.1 | 0.780 |
| Variable | Age | Gender | SES | Baseline |
|---|---|---|---|---|
| Average sedentary minutes per day | p = 0.208 | p = 0.736 | p = 0.891 | p = 0.021 |
| Average steps per day | p = 0.406 | p = 0.220 | p = 0.742 | p = 0.110 |
| Variable | All (N = 37) | Intervention (N = 23) | Control (N = 14) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Average sedentary minutes per day | |||||||||
| Baseline | 645.6 (83.6) | 652.9 (81.4) | 633.7 (88.8) | ||||||
| 12 months | 651.0 (111.0) | 633.6 (84.0) | 679.6 (144.1) | ||||||
| Change | 5.4 (80.5) | –19.3 (68.2) | 45.9 (84.9) | –65.2 (–114.9 to –15.5) | –0.87 (–1.54 to –0.21) | 0.015 | –68.6 (–118.2 to –19.0) | –0.92 (–1.58 to –0.25) | 0.011 |
| Average steps per day | |||||||||
| Baseline | 6263.1 (2207.0) | 6662.9 (2507.5) | 5650.0 (1525.5) | ||||||
| 12 months | 6305.7 (2451.8) | 6938.8 (2623.6) | 5334.8 (1844.4) | ||||||
| Change | 42.6 (2112.1) | 275.9 (2558.5) | –315.2 (1129.7) | 591.0 (–788.3 to 1970.4) | 0.28 (–0.37 to 0.93) | 0.407 | 1063.3 (–219.0 to 2345.5) | 0.50 (–0.10 to 1.11) | 0.114 |
| Variable | Age | Gender | SES | Baseline |
|---|---|---|---|---|
| Average sedentary minutes per day | p = 0.247 | p = 0.584 | p = 0.640 | p = 0.041 |
| Average steps per day | p = 0.317 | p = 0.391 | p = 0.622 | p = 0.282 |
| Variable | All (N = 69) | Intervention (N = 40) | Control (N = 29) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | |||||||||
| Baseline | 36.7 (5.3) | 36.4 (5.0) | 37.2 (5.9) | ||||||
| 12 months | 35.8 (5.9) | 35.5 (5.3) | 36.3 (6.6) | ||||||
| Change | –0.9 (2.7) | –0.9 (2.2) | –0.8 (3.4) | –0.1 (–1.4 to 1.2) | –0.04 (–0.51 to 0.44) | 0.880 | –0.1 (–1.4 to 1.3) | –0.02 (–0.51 to 0.46) | 0.922 |
| Weight (kg) | |||||||||
| Baseline | 100.5 (19.2) | 99.8 (19.3) | 101.5 (19.4) | ||||||
| 12 months | 98.1 (20.2) | 97.3 (20.1) | 99.1 (20.7) | ||||||
| Change | –2.5 (7.5) | –2.5 (5.9) | –2.4 (9.5) | –0.2 (–3.8 to 3.5) | –0.02 (–0.50 to 0.45) | 0.925 | –0.6 (–4.4 to 3.2) | –0.08 (–0.57 to 0.42) | 0.765 |
| Variable | All (N = 39) | Intervention (N = 24) | Control (N = 15) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Total weekly expenditure by kg (kcal/kg/week) | |||||||||
| Baseline | 258.1 (35.2) | 251.2 (21.0) | 269.0 (49.2) | ||||||
| 12 months | 258.3 (30.2) | 254.9 (29.7) | 263.7 (31.2) | ||||||
| Change | 0.3 (36.7) | 3.7 (33.7) | –5.3 (41.8) | 8.9 (–14.9 to 32.8) | 0.24 (–0.40 to 0.89) | 0.467 | –6.3 (–25.2 to 12.5) | –0.17 (–0.68 to 0.34) | 0.514 |
| Total daily expenditure by kg (kcal/kg/day) | |||||||||
| Baseline | 36.9 (5.0) | 35.9 (3.0) | 38.4 (7.0) | ||||||
| 12 months | 36.9 (4.3) | 36.4 (4.2) | 37.7 (4.5) | ||||||
| Change | 0.0 (5.2) | 0.5 (4.8) | –0.8 (6.0) | 1.3 (–2.1 to 4.7) | 0.24 (–0.40 to 0.89) | 0.467 | –0.9 (–3.6 to 1.8) | –0.17 (–0.68 to 0.34) | 0.514 |
| Total daily expenditure (kcal/day) | |||||||||
| Baseline | 3681.5 (773.0) | 3667.5 (654.8) | 3703.8 (957.3) | ||||||
| 12 months | 3571.9 (815.3) | 3616.1 (877.7) | 3501.2 (728.0) | ||||||
| Change | –109.6 (540.9) | –51.4 (492.9) | –202.6 (616.4) | 151.2 (–199.0 to 501.5) | 0.28 (–0.37 to 0.92) | 0.403 | 132.4 (–219.6 to 484.4) | 0.24 (–0.40 to 0.89) | 0.466 |
| Variable | All (N = 39) | Intervention (N = 24) | Control (N = 15) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| DINE fibre score | |||||||||
| Baseline | 20.9 (11.4) | 22.2 (12.0) | 18.7 (10.4) | ||||||
| 12 months | 19.4 (11.3) | 19.2 (11.5) | 19.5 (11.4) | ||||||
| Change | –1.5 (12.2) | –3.0 (11.2) | 0.8 (13.8) | –3.8 (–11.6 to 4.1) | –0.31 (–0.95 to 0.34) | 0.356 | –1.8 (–8.9 to 5.3) | –0.15 (–0.73 to 0.43) | 0.627 |
| DINE fat score | |||||||||
| Baseline | 26.9 (11.9) | 29.0 (11.6) | 23.7 (12.2) | ||||||
| 12 months | 23.5 (9.3) | 24.3 (10.3) | 22.2 (7.5) | ||||||
| Change | –3.4 (11.2) | –4.7 (11.9) | –1.5 (10.1) | –3.2 (–10.5 to 4.1) | –0.28 (–0.93 to 0.36) | 0.394 | 0.3 (–5.4 to 6.0) | 0.03 (–0.48 to 0.53) | 0.914 |
| DINE healthy eating score | |||||||||
| Baseline | –6.1 (14.7) | –6.8 (14.9) | –4.9 (14.7) | ||||||
| 12 months | –4.2 (12.4) | –5.1 (12.7) | –2.7 (12.2) | ||||||
| Change | 1.9 (15.4) | 1.7 (11.4) | 2.3 (20.7) | –0.6 (–10.6 to 9.5) | –0.04 (–0.68 to 0.61) | 0.914 | –2.2 (–9.8 to 5.4) | –0.14 (–0.63 to 0.35) | 0.576 |
| DINE unsaturated fat score | |||||||||
| Baseline | 9.4 (1.7) | 9.1 (1.7) | 9.8 (1.7) | ||||||
| 12 months | 9.8 (2.1) | 9.5 (2.4) | 10.2 (1.4) | ||||||
| Change | 0.4 (2.6) | 0.4 (3.0) | 0.4 (2.0) | 0.0 (–1.7 to 1.7) | 0.01 (–0.64 to 0.65) | 0.985 | –0.7 (–2.2 to 0.8) | –0.26 (–0.82 to 0.29) | 0.356 |
| DINE fruit and vegetable score | |||||||||
| Baseline | 5.1 (2.9) | 4.8 (2.9) | 5.5 (2.9) | ||||||
| 12 months | 5.3 (2.9) | 5.5 (2.5) | 5.0 (3.6) | ||||||
| Change | 0.2 (2.4) | 0.7 (1.9) | –0.5 (3.0) | 1.2 (–0.3 to 2.7) | 0.51 (–0.14 to 1.15) | 0.132 | 1.0 (–0.4 to 2.5) | 0.44 (–0.19 to 1.07) | 0.179 |
| DINE fizzy drink scorea | |||||||||
| Baseline | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | ||||||
| 12 months | 0.2 (0.5) | 0.2 (0.6) | 0.1 (0.3) | ||||||
| Change | 0.2 (0.5) | 0.2 (0.6) | 0.1 (0.3) | 0.00 (0.00 to 0.00) | – | 0.546 | |||
| DINE sugar scorea | |||||||||
| Baseline | 0.2 (0.7) | 0.2 (0.8) | 0.0 (0.0) | ||||||
| 12 months | 0.2 (0.6) | 0.1 (0.6) | 0.2 (0.6) | ||||||
| Change | 0.0 (0.8) | –0.1 (0.9) | 0.2 (0.6) | 0.00 (0.00 to 0.00) | – | 0.157 | |||
| Variable | All (N = 38) | Intervention (N = 23) | Control (N = 15) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| DINE unsaturated fat score | |||||||||
| Baseline | 9.5 (1.6) | 9.3 (1.5) | 9.8 (1.7) | ||||||
| 12 months | 9.7 (2.1) | 9.4 (2.5) | 10.2 (1.4) | ||||||
| Change | 0.3 (2.5) | 0.2 (2.8) | 0.4 (2.0) | –0.2 (–1.9 to 1.4) | –0.09 (–0.74 to 0.56) | 0.787 | –0.7 (–2.2 to 0.7) | –0.29 (–0.88 to 0.30) | 0.338 |
| DINE fruit and vegetable score | |||||||||
| Baseline | 5.1 (2.9) | 4.8 (2.9) | 5.5 (2.9) | ||||||
| 12 months | 5.3 (2.9) | 5.5 (2.5) | 5.0 (3.6) | ||||||
| Change | 0.2 (2.4) | 0.7 (1.9) | –0.5 (3.0) | 1.2 (–0.3 to 2.7) | 0.51 (–0.14 to 1.15) | 0.132 | 1.0 (–0.4 to 2.5) | 0.44 (–0.19 to 1.07) | 0.179 |
| DINE fizzy drink scorea | |||||||||
| Baseline | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | ||||||
| 12 months | 0.2 (0.5) | 0.2 (0.6) | 0.1 (0.3) | ||||||
| Change | 0.2 (0.5) | 0.2 (0.6) | 0.1 (0.3) | 0.00 (0.00 to 0.00) | – | 0.546 | |||
| DINE sugar scorea | |||||||||
| Baseline | 0.2 (0.7) | 0.2 (0.8) | 0.0 (0.0) | ||||||
| 12 months | 0.2 (0.6) | 0.1 (0.6) | 0.2 (0.6) | ||||||
| Change | 0.0 (0.8) | –0.1 (0.9) | 0.2 (0.6) | 0.00 (0.00 to 0.00) | – | 0.157 | |||
| Variable | All (N = 39) | Intervention (N = 24) | Control (N = 15) | Unadjusted intervention – control estimate (95% CI) | Unadjusted intervention – control effect estimate (95% CI) | p-value | Adjusted intervention – control estimate (95% CI) | Adjusted intervention – control effect estimate (95% CI) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | |||||||||
| Baseline | 36.3 (5.4) | 36.8 (5.5) | 35.6 (5.4) | ||||||
| 12 months | 35.2 (6.0) | 35.5 (5.5) | 34.6 (6.8) | ||||||
| Change | –1.2 (3.1) | –1.3 (2.4) | –1.0 (4.0) | –0.3 (–2.3 to 1.7) | –0.09 (–0.73 to 0.56) | 0.789 | –0.2 (–2.3 to 1.9) | –0.06 (–0.74 to 0.61) | 0.857 |
| Variable | p-value for interaction with treatment difference |
|---|---|
| Physical activity 7-day recall | |
| Total weekly expenditure by kg (kcal/kg/week) | p = 0.314 |
| Total daily expenditure by kg (kcal/kg/day) | p = 0.314 |
| Total daily expenditure (kcal/day) | p = 0.603 |
| DINE | |
| DINE fibre score | p = 0.569 |
| DINE fat score | p = 0.939 |
| DINE healthy eating score | p = 0.713 |
| DINE unsaturated fat score | p = 0.213 |
| DINE fruit and vegetables score | p = 0.514 |
| DINE fizzy drink score | p = 0.791 |
| DINE sugar score | p = 0.734 |
| BMI | |
| BMI (kg/m2) | p = 0.861 |
| Variable | Statistic | All (N = 73) | Female (N = 49) | Male (N = 24) | mannw.pval |
|---|---|---|---|---|---|
| Number of app logins (subject) | Nobs (Nmiss) | 73 (0) | 49 (0) | 24 (0) | |
| Mean (SD) | 13.1 (49.0) | 16.8 (58.8) | 5.5 (14.6) | ||
| Median [IQR] | 3.0 [0.0 to 8.0] | 4.0 [1.0 to 10.0] | 2.0 [0.0 to 3.0] | ||
| Range | (0.0 to 408.0) | (0.0 to 408.0) | (0.0 to 72.0) | 0.042 | |
| Number of goals created (subject) | Nobs (Nmiss) | 73 (0) | 49 (0) | 24 (0) | |
| Mean (SD) | 13.1 (24.0) | 17.9 (27.9) | 3.3 (5.4) | ||
| Median [IQR] | 5.0 [0.0 to 13.0] | 10.0 [0.0 to 19.0] | 0.5 [0.0 to 4.0] | ||
| Range | (0.0 to 143.0) | (0.0 to 143.0) | (0.0 to 18.0) | 0.002 | |
| Number of app logins (helper)a | Nobs (Nmiss) | 28 (0) | 24 (0) | 4 (0) | |
| Mean (SD) | 4.4 (9.1) | 4.7 (9.8) | 2.2 (1.7) | ||
| Median [IQR] | 2.0 [1.0 to 3.0] | 2.0 [1.0 to 3.0] | 2.5 [0.0 to 3.0] | ||
| Range | (0.0 to 48.0) | (0.0 to 48.0) | (0.0 to 4.0) | 0.947 |
| Variable | Statistic | All (N = 66) | SIMD1 (N = 25) | SIMD2 (N = 15) | SIMD3 (N = 7) | SIMD4 (N = 10) | SIMD5 (N = 9) | trend.pval |
|---|---|---|---|---|---|---|---|---|
| Number of app logins (subject) | Nobs (Nmiss) | 66 (0) | 25 (0) | 15 (0) | 7 (0) | 10 (0) | 9 (0) | |
| Mean (SD) | 14.0 (51.4) | 4.6 (6.0) | 35.8 (103.5) | 16.1 (29.1) | 8.1 (12.5) | 8.8 (23.8) | ||
| Median [IQR] | 3.0 [0.0 to 9.0] | 2.0 [1.0 to 7.0] | 4.0 [2.0 to 23.0] | 7.0 [0.0 to 14.0] | 3.5 [0.0 to 11.0] | 0.0 [0.0 to 2.0] | ||
| Range | (0.0 to 408.0) | (0.0 to 25.0) | (0.0 to 408.0) | (0.0 to 81.0) | (0.0 to 41.0) | (0.0 to 72.0) | 0.986 | |
| Number of app logins (subject) | Nobs (Nmiss) | 66 (0) | 25 (0) | 15 (0) | 7 (0) | 10 (0) | 9 (0) | |
| Mean (SD) | 14.1 (25.0) | 8.4 (10.1) | 25.3 (40.1) | 22.9 (37.3) | 13.9 (18.1) | 4.4 (7.0) | ||
| Median [IQR] | 6.0 [0.0 to 17.0] | 1.0 [0.0 to 17.0] | 7.0 [2.0 to 52.0] | 10.0 [0.0 to 24.0] | 10.0 [0.0 to 24.0] | 0.0 [0.0 to 10.0] | ||
| Range | (0.0 to 143.0) | (0.0 to 35.0) | (0.0 to 143.0) | (0.0 to 105.0) | (0.0 to 58.0) | (0.0 to 18.0) | 0.838 | |
| Number of app logins (helper)a | Nobs (Nmiss) | 26 (0) | 6 (0) | 11 (0) | 3 (0) | 3 (0) | 3 (0) | |
| Mean (SD) | 4.5 (9.4) | 1.8 (0.8) | 8.0 (13.9) | 1.0 (1.0) | 3.0 (3.5) | 2.3 (2.1) | ||
| Median [IQR] | 2.0 [1.0 to 4.0] | 2.0 [1.0 to 2.0] | 3.0 [1.0 to 8.0] | 1.0 [0.0 to 2.0] | 1.0 [1.0 to 7.0] | 3.0 [0.0 to 4.0] | ||
| Range | (0.0 to 48.0) | (1.0 to 3.0) | (0.0 to 48.0) | (0.0 to 2.0) | (1.0 to 7.0) | (0.0 to 4.0) | 0.711 |
| Variable | Statistic | All (N = 66) | SIMD1 (N = 25) | SIMD2to5 (N = 41) | mannw.pval |
|---|---|---|---|---|---|
| Number of app logins (subject) | Nobs (Nmiss) | 66 (0) | 25 (0) | 41 (0) | |
| Mean (SD) | 14.0 (51.4) | 4.6 (6.0) | 19.8 (64.7) | ||
| Median [IQR] | 3.0 [0.0 to 9.0] | 2.0 [1.0 to 7.0] | 4.0 [0.0 to 10.0] | ||
| Range | (0.0 to 408.0) | (0.0 to 25.0) | (0.0 to 408.0) | 0.534 | |
| Number of goals created (subject) | Nobs (Nmiss) | 66 (0) | 25 (0) | 41 (0) | |
| Mean (SD) | 14.1 (25.0) | 8.4 (10.1) | 17.5 (30.4) | ||
| Median [IQR] | 6.0 [0.0 to 17.0] | 1.0 [0.0 to 17.0] | 7.0 [0.0 to 17.0] | ||
| Range | (0.0 to 143.0) | (0.0 to 35.0) | (0.0 to 143.0) | 0.571 | |
| Number of app logins (helper)a | Nobs (Nmiss) | 26 (0) | 6 (0) | 20 (0) | |
| Mean (SD) | 4.5 (9.4) | 1.8 (0.8) | 5.3 (10.7) | ||
| Median [IQR] | 2.0 [1.0 to 4.0] | 2.0 [1.0 to 2.0] | 2.0 [1.0 to 4.0] | ||
| Range | (0.0 to 48.0) | (1.0 to 3.0) | (0.0 to 48.0) | 0.733 |
| Variable | Number of logins (subject) | Number of goals created (subject) | Number of logins (helper) |
|---|---|---|---|
| Age (years) | r = 0.014, p = 0.908 | r = –0.089, p = 0.456 | r = –0.065, p = 0.742 |
| SIMD quintile | r = –0.083, p = 0.506 | r = –0.058, p = 0.646 | r = –0.068, p = 0.741 |
| BMI (kg/m2) | r = 0.021, p = 0.862 | r = 0.043, p = 0.720 | r = 0.089, p = 0.651 |
| Average steps per day | r = 0.102, p = 0.476 | r = 0.198, p = 0.164 | r = 0.269, p = 0.215 |
| Average sedentary minutes per day | r = 0.098, p = 0.495 | r = –0.080, p = 0.578 | r = –0.166, p = 0.448 |
| DINE healthy eating score | r = –0.055, p = 0.645 | r = –0.083, p = 0.489 | r = 0.254, p = 0.193 |
| DINE unsaturated fat score | r = 0.040, p = 0.735 | r = 0.079, p = 0.507 | r = –0.157, p = 0.424 |
| DINE fruit and vegetable score | r = 0.155, p = 0.194 | r = –0.013, p = 0.915 | r = 0.212, p = 0.279 |
| Variable | Number of logins (subject) | Number of goals created (subject) | Number of logins (helper) |
|---|---|---|---|
| BMI (kg/m2) | r = –0.381, p = 0.006 | r = –0.237, p = 0.098 | r = –0.276, p = 0.182 |
| % in MVPA | r = 0.426, p = 0.038 | r = 0.337, p = 0.107 | r = –0.166, p = 0.571 |
| Average MVPA per day (minutes per day) | r = 0.353, p = 0.090 | r = 0.253, p = 0.234 | r = –0.157, p = 0.593 |
| Average steps per day | r = 0.405, p = 0.050 | r = 0.332, p = 0.113 | r = –0.134, p = 0.649 |
| Average sedentary minutes per day | r = –0.408, p = 0.048 | r = –0.223, p = 0.295 | r = 0.218, p = 0.453 |
| Total weekly expenditure by kg (kcal/kg/week) | r = 0.259, p = 0.073 | r = 0.202, p = 0.165 | r = 0.429, p = 0.029 |
| Total daily expenditure by kg (kcal/kg/day) | r = 0.259, p = 0.073 | r = 0.202, p = 0.165 | r = 0.429, p = 0.029 |
| Total daily expenditure (kcal/day) | r = 0.170, p = 0.249 | r = 0.256, p = 0.079 | r = 0.251, p = 0.226 |
| DINE fibre score | r = 0.245, p = 0.090 | r = 0.335, p = 0.019 | r = –0.151, p = 0.463 |
| DINE fat score | r = –0.007, p = 0.964 | r = 0.008, p = 0.958 | r = 0.015, p = 0.941 |
| DINE healthy eating score | r = 0.262, p = 0.069 | r = 0.276, p = 0.054 | r = –0.056, p = 0.786 |
| DINE unsaturated fat score | r = 0.273, p = 0.019 | r = 0.255, p = 0.029 | r = 0.229, p = 0.242 |
| DINE fruit and vegetable score | r = 0.091, p = 0.551 | r = 0.266, p = 0.077 | r = –0.352, p = 0.078 |
| DINE fizzy drink score | r = –0.101, p = 0.510 | r = –0.060, p = 0.695 | r = –0.163, p = 0.427 |
| DINE sugar score | r = –0.039, p = 0.799 | r = –0.088, p = 0.567 | r = 0.256, p = 0.207 |
Appendix 9 Main outputs from health economics analysis
Tables 146–150 show the main outputs from health economics analysis.
| Resource use (number of visits) | Control (N = 36) | Intervention (N = 73) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | |
| At surgery | ||||||||||||
| GP | 1.09 | 1.52 | 0 | 0 | 6 | 1.44 | 2.75 | 1 | 0 | 16 | ||
| Practice nurse | 0.33 | 0.53 | 0 | 0 | 2 | 0.45 | 0.88 | 0 | 0 | 5 | ||
| At home | ||||||||||||
| GP | 0.06 | 0.23 | 0 | 0 | 1 | 0.04 | 0.26 | 0 | 0 | 2 | ||
| Practice nurse | 0.03 | 0.17 | 0 | 0 | 1 | 0.03 | 0.16 | 0 | 0 | 1 | ||
| Physiotherapist | 0.31 | 0.89 | 0.00 | 0.00 | 4.00 | 0.11 | 0.59 | 0.00 | 0.00 | 4.00 | ||
| Dietitian | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.12 | 0.00 | 0.00 | 1.00 | ||
| Dentist | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Gastroenterologist | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Orthopaedic consultant | 0.03 | 0.17 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Ear, nose and throat consultant | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Respiratory consultant | 0.03 | 0.17 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Urologist consultant | 0.08 | 0.50 | 0.00 | 0.00 | 3.00 | 0.01 | 0.12 | 0.00 | 0.00 | 1.00 | ||
| Oncologist consultant | 0.03 | 0.17 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Endocrinologist consultant | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.12 | 0.00 | 0.00 | 1.00 | ||
| Rheumatologist consultant | 0.06 | 0.23 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Infectious disease consultant | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Psychiatrist | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.12 | 0.00 | 0.00 | 1.00 | ||
| Community psychiatric nurse | 0.25 | 1.11 | 0.00 | 0.00 | 6.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| NHS weight management | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| A&E attending | 0.31 | 0.67 | 0 | 0 | 3 | 0.04 | 0.2 | 0 | 0 | 1 | ||
| Hospitalisation | 0.33 | 1.33 | 0 | 0 | 7 | 0 | 0 | 0 | 0 | 0 | ||
| Resource use (number of visits) | Control (N = 29) | Intervention (N = 40) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | |
| At surgery | ||||||||||||
| GP | 2.07 | 4.41 | 1 | 0 | 24 | 0.98 | 1.07 | 1 | 0 | 4 | ||
| Practice nurse | 0.83 | 1.23 | 1 | 0 | 6 | 0.85 | 1.83 | 0 | 0 | 10 | ||
| At home | ||||||||||||
| GP | 0 | 0 | 0 | 0 | 0 | 0.05 | 0.32 | 0 | 0 | 2 | ||
| Practice nurse | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Physiotherapist | 0.62 | 2.29 | 0.00 | 0.00 | 12.00 | 0.28 | 1.06 | 0.00 | 0.00 | 6.00 | ||
| Dietitian | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Dentist | 0.03 | 0.19 | 0.00 | 0.00 | 1.00 | 0.03 | 0.16 | 0.00 | 0.00 | 1.00 | ||
| Gastroenterologist | 0.03 | 0.19 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Orthopaedic consultant | 0.07 | 0.26 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Ear, nose and throat consultant | 0.03 | 0.19 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Respiratory consultant | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.03 | 0.16 | 0.00 | 0.00 | 1.00 | ||
| Urologist consultant | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Oncologist consultant | 0.03 | 0.19 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Endocrinologist consultant | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.22 | 0.00 | 0.00 | 1.00 | ||
| Rheumatologist consultant | 0.10 | 0.56 | 0.00 | 0.00 | 3.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Infectious disease consultant | 0.03 | 0.19 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| Psychiatrist | 0.03 | 0.19 | 0.00 | 0.00 | 1.00 | 0.05 | 0.22 | 0.00 | 0.00 | 1.00 | ||
| Community psychiatric nurse | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| NHS weight management | 0.03 | 0.19 | 0.00 | 0.00 | 1.00 | 0.03 | 0.16 | 0.00 | 0.00 | 1.00 | ||
| A&E attending | 0.24 | 0.64 | 0 | 0 | 3 | 0.13 | 0.4 | 0 | 0 | 2 | ||
| Hospitalisation | 0.9 | 3.37 | 0 | 0 | 17 | 0.13 | 0.56 | 0 | 0 | 3 | ||
| Type of food/drink | Weekly cost (£) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | Intervention | |||||||||||
| n | Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | |
| Baseline | (N = 36) | (N = 73) | ||||||||||
| Grocery | 62.86 | 26.21 | 60 | 15 | 150 | 61.22 | 31.58 | 60 | 0 | 150 | ||
| Alcohol | 6.45 | 9.77 | 0 | 0 | 45 | 8.5 | 16.72 | 0 | 0 | 120 | ||
| Takeaway food | 8.06 | 9.48 | 6 | 0 | 30 | 13.79 | 15.61 | 10 | 0 | 80 | ||
| Meals out | 21.56 | 27.34 | 17.5 | 0 | 100 | 21.24 | 21.27 | 20 | 0 | 100 | ||
| Follow-up | (N = 29) | (N = 40) | ||||||||||
| Grocery | 52.22 | 26.18 | 47.5 | 5 | 100 | 59.02 | 25.07 | 57.5 | 0 | 140 | ||
| Alcohol | 3.81 | 6.77 | 0 | 0 | 30 | 7.46 | 9.3 | 0 | 0 | 30 | ||
| Takeaway food | 7.97 | 9.31 | 2.5 | 0 | 30 | 6.87 | 9.81 | 0 | 0 | 40 | ||
| Meals out | 13.81 | 20.63 | 6.5 | 0 | 100 | 23.76 | 25.06 | 20 | 0 | 130 | ||
| Cost | Control | Intervention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | |
| Baseline | 43.29 | 68 | 23 | 0 | 360 | 30.08 | 54.05 | 0 | 0 | 350 | ||
| Follow-up | 51.46 | 44.29 | 60 | 0 | 135 | 55.23 | 133.33 | 10.25 | 0 | 651 | ||
| ICECAP-A dimension | Baseline | Follow-up | ||
|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |
| 1. Feeling settled and secure | ||||
| Level 4 (full capability well-being) | 3 (8.33) | 5 (6.94) | 5 (15.63) | 6 (13.33) |
| Level 3 | 18 (50) | 45 (62.5) | 15 (46.88) | 28 (62.22) |
| Level 2 | 15 (41.67) | 19 (26.39) | 11 (34.38) | 9 (20) |
| Level 1 (no capability well-being) | 0 (0) | 3 (4.17) | 1 (3.13) | 2 (4.44) |
| 2. Being independent | ||||
| Level 4 (full capability well-being) | 12 (33.33) | 31 (43.06) | 13 (40.63) | 27 (60) |
| Level 3 | 20 (55.56) | 31 (43.06) | 12 (37.5) | 13 (28.89) |
| Level 2 | 4 (11.11) | 9 (12.5) | 6 (18.75) | 5 (11.11) |
| Level 1 (no capability well-being) | 0 (0) | 1 (1.39) | 1 (3.13) | 0 (0) |
| 3. Achievement and progress | ||||
| Level 4 (full capability well-being) | 4 (11.11) | 19 (26.39) | 5 (15.63) | 11 (24.44) |
| Level 3 | 22 (61.11) | 36 (50) | 16 (50) | 26 (57.78) |
| Level 2 | 10 (27.78) | 16 (22.22) | 10 (31.25) | 7 (15.56) |
| Level 1 (no capability well-being) | 0 (0) | 1 (1.39) | 1 (3.13) | 1 (2.22) |
| 4. Enjoyment and pleasure | ||||
| Level 4 (full capability well-being) | 7 (19.44) | 32 (44.44) | 8 (25) | 19 (42.22) |
| Level 3 | 22 (61.11) | 27 (37.5) | 14 (43.75) | 16 (35.56) |
| Level 2 | 7 (19.44) | 13 (18.06) | 9 (28.13) | 9 (20) |
| Level 1 (no capability well-being) | 0 (0) | 0 (0) | 1 (3.13) | 1 (2.22) |
Appendix 10 Sample size calculation for a future trial
| MCID | SD | Uptake (%) | ES | Loss to follow-up (%) | 80% power | 90% power | ||
|---|---|---|---|---|---|---|---|---|
| n/group | n (total) | n/group | n (total) | |||||
| 5 | 7.3 | 100 | 0.68 | 0 | 35 | 70 | 47 | 94 |
| 20 | 44 | 88 | 59 | 118 | ||||
| 40 | 59 | 118 | 79 | 158 | ||||
| 67 | 0.46 | 0 | 76 | 152 | 101 | 202 | ||
| 20 | 95 | 190 | 127 | 154 | ||||
| 40 | 127 | 154 | 169 | 338 | ||||
| 50 | 0.34 | 0 | 137 | 174 | 183 | 366 | ||
| 20 | 172 | 344 | 229 | 458 | ||||
| 40 | 229 | 458 | 305 | 610 | ||||
| 5 | 10 | 100 | 0.50 | 0 | 64 | 128 | 86 | 172 |
| 20 | 80 | 160 | 108 | 216 | ||||
| 40 | 107 | 214 | 144 | 288 | ||||
| 67 | 0.33 | 0 | 146 | 292 | 194 | 388 | ||
| 20 | 183 | 366 | 243 | 486 | ||||
| 40 | 244 | 488 | 324 | 648 | ||||
| 50 | 0.25 | 0 | 253 | 506 | 338 | 676 | ||
| 20 | 317 | 634 | 423 | 846 | ||||
| 40 | 422 | 844 | 564 | 1128 | ||||
| 3 | 7.3 | 100 | 0.41 | 0 | 95 | 190 | 126 | 252 |
| 20 | 119 | 238 | 158 | 316 | ||||
| 40 | 159 | 318 | 210 | 420 | ||||
| 67 | 0.28 | 0 | 202 | 404 | 270 | 540 | ||
| 20 | 253 | 506 | 338 | 676 | ||||
| 40 | 337 | 674 | 450 | 900 | ||||
| 50 | 0.21 | 0 | 357 | 714 | 478 | 956 | ||
| 20 | 447 | 894 | 598 | 1196 | ||||
| 40 | 595 | 1190 | 797 | 1594 | ||||
| 3 | 10 | 100 | 0.3 | 0 | 176 | 352 | 235 | 470 |
| 20 | 220 | 440 | 294 | 588 | ||||
| 40 | 294 | 588 | 392 | 784 | ||||
| 67 | 0.2 | 0 | 394 | 788 | 527 | 1054 | ||
| 20 | 493 | 986 | 659 | 1318 | ||||
| 40 | 657 | 1314 | 879 | 1758 | ||||
| 50 | 0.15 | 0 | 699 | 1398 | 935 | 1870 | ||
| 20 | 874 | 1748 | 1169 | 2338 | ||||
| 40 | 1165 | 2330 | 1559 | 3118 | ||||
List of abbreviations
- 6SQuID
- 6 Steps in Quality Intervention Development
- A&E
- accident and emergency
- app
- application
- AUDIT-C
- Alcohol Use Disorders Identification Test – Consumption
- BIT
- Behaviour Intervention Technology
- BMI
- body mass index
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CRF
- case report form
- CSO
- Chief Scientist Office
- DINE
- Dietary Instrument for Nutrition Education
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- GHQ
- General Health Questionnaire
- GHQ-12
- General Health Questionnaire – 12 items
- GP
- general practitioner
- HSI
- Heaviness of Smoking Index
- ICECAP-A
- ICEpop CAPability measure for Adults
- MCID
- minimum clinically important difference
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PAR
- physical activity recall
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- SD
- standard deviation
- SIMD
- Scottish Index of Multiple Deprivation
- SMART
- specific, measurable, attainable, relevant and time-bound
- SMS
- short message service
- SPCRN
- Scottish Primary Care Research Network
- TIDieR
- Template for Intervention Description and Replication
- TSRD
- Treatment Self-Regulation Questionnaire Concerning the Motivation for Eating a Healthy Diet
- TSRE
- Treatment Self-Regulation Questionnaire Concerning the Motivation for Exercising Regularly
- TV
- television
- USE
- Usefulness, Satisfaction, and Ease of Use
- VAS
- visual analogue scale
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/phr08030).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
