Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 15/53/04. The contractual start date was in November 2016. The final report began editorial review in November 2018 and was accepted for publication in May 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Kate Jolly reports grants from the National Institute for Health Research (NIHR), local authority funding for the intervention and part-funding by NIHR Collaborative Leadership for Applied Health Research and Care West Midlands during the conduct of the study. Alongside her Cardiff University role, Heather Trickey worked part time as a senior researcher for NCT (London, UK) during the period in which the research was conducted. NCT provides breastfeeding peer support services. NCT volunteers were not included in this study. Pat Hoddinott is a member of the Health Technology Assessment Commissioning Board (March 2014 to present). She is working on a funding application to take forward the FEeding Support Team (FEST) feasibility trial that she led and that is cited in this report. The FEST feasibility trial informed parts of the design of the Assets-based feeding help Before and After birth study. Alice Sitch is supported by the NIHR Birmingham Biomedical Research Centre, University Hospitals Birmingham NHS Foundation Trust and University of Birmingham, UK.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Clarke et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
The benefits of breastfeeding for health and well-being
Breastfeeding (defined as the baby being put to the breast or receiving breast milk on at least one occasion) is associated with short- and long-term benefits to both the breastfed infant1–10 and the mother. 11 Internationally, the largest health gains are seen in low-income countries, as breastfeeding protects against infant mortality by reducing acute infections in infants. 1 However, considerable health gains from breastfeeding are also possible in high-income countries. Currently, only around 12% of babies in the UK are exclusively breastfed at 4 months. If this figure increased to 45% of women in the UK breastfeeding exclusively for 4 months, then at least £17M could be saved annually in NHS treatment costs for common acute illnesses in infants, with additional longer-term gains for mothers and children. 12,13
The benefits of breastfeeding are considerable. The evidence has been collated in systematic reviews1,9 and is consistent across cohort studies in a range of settings and from a randomised controlled trial (RCT) of a breastfeeding support intervention with long-term follow-up of the children. 14 For the infant and child, any breastfeeding is associated with reduced risk of gastrointestinal infection by 63% [95% confidence interval (CI) 50% to 94%],10 sudden infant death syndrome by 36% (95% CI 10% to 49%),15 otitis media by 33% (95% CI 28% to 38%),2 asthma when aged 5–18 years by 12% (95% CI 5% to 18%),3 being overweight in the future or obese by 26% (95% CI 22% to 30%),7 type 2 diabetes mellitus by 35% (95% CI 14% to 51%)7 and malocclusions by 68% (95% CI 60% to 75%). 5 Exclusive breastfeeding for > 4 months reduces the risk of hospital admission for lower respiratory tract infections in the first year by 72% [risk ratio (RR) 0.28, 95% CI 14 to 54]10 and for 3–4 months reduces the risk of eczema by 26% in children at < 2 years. 3 Exclusive breastfeeding for > 3 months is associated with a reduced risk of type 1 diabetes mellitus of up to 30%. 15 Meta-analyses show that being fed breast milk is associated with a 58% (95% CI 4% to 82%) reduced risk of necrotising enterocolitis in pre-term infants16 and with reduced mortality. It is also associated with improved performance in intelligence tests. 8 Mothers have a reduced risk of breast (26%, 95% CI 21% to 31%) and ovarian (37%, 95% CI 29% to 44%) cancers if they breastfeed for > 12 months11 and lower post-menopausal body mass index if they have ever breastfed. 17
Breastfeeding rates and duration in the UK
Breastfeeding duration in the UK is among the lowest worldwide, with routinely collected data and 5-yearly infant feeding surveys18–20 showing relatively small improvements over the past two decades, particularly for rates of exclusive breastfeeding. Although breastfeeding initiation increased from 76% in 2005 to 81% in 2010, exclusive breastfeeding at 6 weeks increased only from 21% to 23% during the same period. There are considerable health inequalities, despite government initiatives; breastfeeding initiation and duration rates are lowest in teenagers (58% initiated breastfeeding in 2010), women living in socioeconomically disadvantaged circumstances, women with lower educational outcomes and white women. 18 In 2010, 90% of UK mothers in managerial and professional occupations breastfed, compared with 74% of those in routine and manual occupations and 71% among those who had never worked. 18
The World Health Organization21 recommends exclusive breastfeeding for 6 months to optimise infant and maternal health, a recommendation endorsed by UK governments;22 however, < 1% of infants in the UK receive this. 18 Data from the Infant Feeding Survey 201018 show that the steepest decline in breastfeeding occurs soon after birth: 81% of women who give birth initiate breastfeeding but only 69% of babies are breastfed at 1 week, 66% at 2 weeks, 55% at 6 weeks and 34% at 6 months. Rates of exclusive breastfeeding are even lower: 46% at 1 week and 23% at 6 weeks. 18 More recent data collected from local authorities in England show that 44.4% of babies receive breast milk at 6–8 weeks, with the range being 19.3% to 75.6%. 23 Mothers express dissatisfaction with breastfeeding care,24,25 and 30% report feeding problems in the early weeks. 18 A 2017 survey by the National Federation of Women’s Institutes and the NCT (formerly known as the National Childbirth Trust) identified baby feeding as the greatest area of unmet need for support. 26 Women who reported that they did not receive support for breastfeeding difficulties in hospital or at home were more likely to discontinue breastfeeding within the first 2 weeks. 18
Effectiveness of peer support for breastfeeding initiation and continuation
In the UK, breastfeeding peer support has been widely recommended as a means of increasing breastfeeding initiation and continuation rates among women from disadvantaged communities. 27,28
Breastfeeding peer support has been defined as ‘support offered by women who have received appropriate training and either have themselves breastfed or have the same socio-economic background, ethnicity or locality as the women they are supporting’. 29 From a theoretical perspective, Dennis30 defines peer support as the provision of ‘emotional, appraisal and motivational assistance by a created social network member who possesses experiential knowledge of a specific behaviour or stressor, and has similar characteristics to the target population’. In comparison with health-care professionals, peer supporters may be considered more approachable and operate as positive role models to whom women can relate because of their direct experience of the challenges of breastfeeding, and in contexts where breastfeeding may not be the social norm. 31
A systematic review32 of breastfeeding peer support interventions reported a significant increase in breastfeeding initiation in three trials that targeted this support at pregnant women who had decided to breastfeed (relative risk for not initiating breastfeeding 0.64, 95% CI 0.41 to 0.99), but no difference in the three trials that offered universal peer support to all pregnant women (relative risk for not initiating breastfeeding 0.96, 95% CI 0.76 to 1.22). Heterogeneity in the meta-analysis of targeted breastfeeding peer support was high, which might be because of differences in the settings and context where the peer support was offered and the intensity of the interventions. 32
A systematic review29 to assess the impact of breastfeeding peer support on breastfeeding continuation rates reported significant effects on any breastfeeding rates and exclusive breastfeeding rates at the last study follow-up (relative risk of not breastfeeding at last follow-up 0.85, 95% CI 0.77 to 0.94, and 0.82, 95% CI 0.76 to 0.88, respectively). Heterogeneity was high and was explored using subgroup analyses and meta-regression. Peer support interventions were found to have a significantly greater effect on any breastfeeding and exclusive breastfeeding in low- or middle-income countries than in high-income countries. However, in high-income countries, peer support reduced the risk of not breastfeeding by 7% (0.93, 95% CI 0.87 to 1.00). The risk of non-exclusive breastfeeding decreased significantly, by 10% (0.90, 95% CI 0.85 to 0.97). No significant effect on any breastfeeding or exclusive breastfeeding was observed in the three UK-based studies. Peer support had a greater effect on any breastfeeding rates when given at higher intensity (five or more planned contacts; p = 0.02).
A 2017 Cochrane review33 of support for breastfeeding mothers found strong evidence that providing extra professional, lay or peer support for women who wish to breastfeed increases the duration of exclusive breastfeeding (cessation of exclusive breastfeeding at 6 months, average RR 0.88, 95% CI 0.85 to 0.92) and of babies receiving breast milk alongside other liquids or solids (cessation of any breastfeeding at 6 months, average RR 0.91, 95% CI 0.88 to 0.95). The review found that the effects of lay support were broadly similar to those of professional support. 33 Lay support is broader than peer support and does not require that the supporter and mother share experience or characteristics. Nine trials of lay support compared with usual care reported a RR of stopping breastfeeding before the last study assessment up to 6 months of 0.85 (95% CI 0.77 to 0.93), but with considerable heterogeneity, and 13 trials reported a reduced risk of stopping exclusive breastfeeding before the last study assessment (RR 0.76, 95% CI 0.65 to 0.87). However, the generalisability of these findings to the UK context is uncertain. Nine UK trials since 2000 providing additional support using a range of models, including peer, lay and professional support, have failed to improve breastfeeding outcomes significantly. 34
Similar systematic review results to those for peer support29 were reported by Renfrew et al. 35 in relation to frequency of planned contact for lay support. Interventions with four to eight contacts had a larger effect size than combined interventions with fewer than four planned contacts in trials with a usual care control group.
There is evidence that, to be effective, peer support should be offered proactively. In Canada, peer supporters with 2.5 hours’ training proactively telephoned women (n = 256) using a woman-centred format;36 the relative risk for any breastfeeding at 4 weeks was 1.10 (95% CI 1.01 to 2.72).
Preliminary research suggests that early proactive telephone support might suit a UK context. 37 In a pilot trial (69 women),37 intensive early proactive telephone support (not peer support) for women who initiated breastfeeding, delivered by a postnatal ward feeding team with personal breastfeeding experience, increased any breastfeeding by 22% (RR 1.49, 95% CI 0.92 to 2.40) at 6–8 weeks compared with the opportunity to access reactive telephone support from the team. A Cochrane review38 of telephone support for women during pregnancy and up to 6 weeks after the birth showed that women who had received a telephone support intervention were more likely to be exclusively breastfeeding (RR 1.51, 95% CI 1.19 to 1.93) at 3–6 months postpartum than those in the comparator group, but this included only three trials, and no difference was observed in the four trials that reported breastfeeding at 4–8 weeks postpartum. 38
A UK study39 applying a theory of constraints model to investigate the barriers to effective lay feeding help recommended that (1) to gain wider acceptability, interventions should be mother-centred (rather than breastfeeding-centred), both enabling breastfeeding and giving help with formula milk, (2) there should be a greater focus on the early weeks after the birth, as establishing breastfeeding can be difficult and mothers frequently stop feeding before they had planned, and (3) support should be offered proactively to improve the take-up of breastfeeding.
A recent realist review40 of breastfeeding peer support interventions in high-income countries found that breastfeeding peer support appears to rely on a chain of mechanisms firing in sequence. The realist review found that intervention design should take account of needs as perceived by the target population; integration with health professional care can be critical, and so ensuring mutual respect and overcoming local barriers to integrated working practices, collaboration and feedback are important. Peers need to be accessible when mothers most need support; support around the time of the birth can help mothers who are unsure to firm up decisions to breastfeed. Peer support also needs to be proactive, as reactive support tends to be used by mothers who are motivated or confident, and is unlikely to be effective in improving rates overall. Mothers value friendly, competent and proactive peers, and these qualities may outweigh social similarity. Mothers who experience a warm and affirming relationship with their peer supporter often feel helped to overcome challenges and to meet their feeding goals. The review also found that peer supporters are motivated when they feel valued and are demotivated when their offers of help are rejected. As a result, peers tend to focus their energy on mothers who seek support and seem to be appreciative.
These findings from the realist review are in line with a meta-synthesis41 of women’s perceptions and experiences of breastfeeding support that recommended person-centred approaches and qualitative studies24,42 of women’s experiences of infant feeding support that found that structured approaches to support-giving are unpopular24 but flexible support is acceptable. 42 How breastfeeding interventions are delivered and the intervention-context fit are important determinants of outcomes. 43 The timing of support in the very early postnatal period may be an important feature of effective breastfeeding support. 40,44,45 Continuity of targeted peer support by having an antenatal visit and postnatal support from the same local supporter is associated with psychosocial benefits for mothers, health professionals and peer supporters. 42
Existing provision of breastfeeding support in the UK
In hospital, midwives deliver breastfeeding support, with breastfeeding counsellors and hospital peer supporters also available in some areas. However, length of stay following a singleton vaginal delivery in the UK is one of the shortest internationally (1.5 days). 46 Many women, including first-time mothers, go home 6 hours after giving birth; 19.8% of women in 2016/17 were discharged on the same day as the birth. 47 This gives insufficient time to establish breastfeeding. Reduced hospital stay following birth provides a suboptimal context to support establishing breastfeeding for many new mothers. Care is transferred from midwives to health visitors between 10 and 30 days postnatally. Much community breastfeeding support is provided by lay workers in children’s centres and by peer supporters. Breastfeeding peer support is offered by a range of organisations, including voluntary and charitable organisations, local authorities and the NHS. Peers may be paid or voluntary, and training and supervision are offered by a range of providers. The UNICEF UK (United Nations Children’s Fund, London, UK) Baby Friendly Initiative stage 1 accreditation48 requires a meaningful discussion about infant feeding in the antenatal period and identifies that this might be delivered by a peer supporter. Additionally, for accreditation, local maternity services are required to have mechanisms in place to enable mothers to access support for breastfeeding with basic problem-solving via their local maternity service or other local routes, for example breastfeeding support groups or peer support, and to ensure that mothers know about these services.
The characteristics of peer support provided for pregnant and breastfeeding women across the UK are not routinely collected. A survey in 2014 of all known infant feeding co-ordinators in the UK had a 19.5% response rate, and covered of 58% of NHS trust/health board areas. 49 This study identified wide availability of breastfeeding support across the UK, with peer support available in 78% of areas and breastfeeding support groups available in 90% of areas. However, these may not be representative of all areas and the support may be provided only in selected localities within trust/health board areas. The survey identified a lack of standardisation of the provision of breastfeeding peer support across the UK and the challenging context of limited financial support. Services were reduced and increased in line with funding availability. 49 The most common providers were third-sector organisations, such as the NCT and the Breastfeeding Network, and most peer supporters were volunteers. 49 In the 2010 Infant Feeding Survey,18 69% of women reported being given the details of a voluntary organisation or community group that helped new mothers to breastfeed, and 64% were aware of the National Breastfeeding Helpline. A report of breastfeeding support in London50 found that the proportion of new mothers receiving breastfeeding support from a peer supporter varied from < 5% to 52% in London boroughs.
Research into the role of UK fathers in supporting breastfeeding reported that they wanted to be able to support their partners, but they were often excluded from antenatal breastfeeding education or were considered unimportant in postnatal support. 51 Many fathers feel ignored throughout the whole journey of pregnancy and postnatal care. 52 Men want more information about how they can practically support their partner,51 and a survey of women with young children suggested that engaging the fathers in breastfeeding education was as a way of increasing breastfeeding support. 53
Apart from the father of the child, many other ‘significant others’ influence a woman’s decisions about breastfeeding,54 and the composition of a woman’s social network changes over time. 55 Women’s support needs can be mapped in an infant feeding genogram55 that records the feeding history of family and friends and the strength of relationships with these social network members. This genogram can be used as a tool to support discussion around breastfeeding and to identify support needs.
Information needs of and risks for mothers who feed their babies formula milk
Previous UK studies to promote breastfeeding have focused solely on breastfeeding, excluding any discussion of formula feeding with mothers. The evidence shows that, for infant-feeding interventions to be acceptable to women, it is important to address issues related to mixed feeding and formula feeding. 40,56 This need is now explicitly recognised by several UK key providers of peer support; for example, NCT (the UK’s largest charity for expectant and new parents) policy is to provide support to all women with their infant feeding decisions, regardless of how they are feeding their babies. 57 The 2010 Infant Feeding Survey showed that 54% of babies had received formula milk by the age of 1 week, 88% had received it by 6 months and 95% had received it by 9 months. 18 Furthermore, the survey highlighted that half of mothers who prepared powdered infant formula did not follow all three key NHS recommendations (making only one feed at a time, making feeds within 30 minutes of the water boiling and adding the water to the bottle before the powder), which are intended to reduce the risk of infection and overconcentration of feeds. Other studies have also highlighted a high frequency of errors in formula feed preparation. 58,59 Current guidance for mothers is available on the NHS website60 and includes a 13-point set of instructions for making up a bottle of formula. The evidence indicates that an intervention to increase breastfeeding rates that fails to address mothers’ needs in relation to formula feeding (particularly in a culture where mixed feeding is common) risks alienating potential beneficiaries, limiting intervention reach and retention, and decreasing the likelihood of achieving breastfeeding-related outcomes. 40,61 Improving the preparation of formula feeds will incur additional infant health benefits from reduced gastrointestinal infections. 59 Moreover, by focusing on the mothers’ needs, there may be less guilt associated with feeding decisions. 62
Assets-based approaches in public health
The use of peer support and encouragement to access community support for breastfeeding and social opportunities for new mothers is an exemplar of an assets-based approach to public health. An assets-based approach focuses on the positive capabilities of individuals and communities, rather than solely on their needs, deficits and problems. This approach is linked to the theory of salutogenesis (health origin),63,64 which conceptualises health as a continuum and focuses on what helps individuals retain positive health and well-being rather than on factors that cause disease. 63–65 It also has parallels with economic theories of capability and well-being, from a broad physical, psychological, social and community perspective. 66
Assets-based approaches are about recognising and making the most of people’s strengths to change the balance between meeting the needs of people and communities and nurturing their strengths and resources. 67 This is accompanied by a corresponding shift in focus from the determinants of ill health to the determinants of health and well-being. Although assets can include material resources,68,69 in public health more typically, the primary focus is on valuing individual and collective psychosocial attributes. These include confidence, optimism, self-esteem, knowledge and skills, as well as features of social capital such as social networks and reciprocity. 70–73
Longitudinal qualitative research with families living in disadvantaged areas suggests that family well-being rather than potential future health benefits is the outcome that matters most and that drives decisions to stop breastfeeding. 56 In the context of breastfeeding, assets may include intrinsic personal resources such as willingness to ask for and accept help, self-efficacy in relation to infant feeding,74 and motivation and drive to maintain feeding. 74–77 These assets also include extrinsic resources such as availability of social support from partner,78–80 family and friends, wider social networks of new mothers and women who have breastfed, and community assets such as children’s centres, mother-and-baby groups, breastfeeding groups or baby cafes. Local breastfeeding peer supporters are also community assets for breastfeeding. Hopkins and Rippon’s73 theory of change approach to assets-based working focuses on recognising and mobilising assets. An assets-based approach, by focusing on a woman’s priorities, is woman-centred.
Rationale for the ABA study
In 2015, the National Institute for Health Research Public Health Research programme called for studies to determine the effectiveness of community-based interventions that promote the uptake and maintenance of breastfeeding. Our study aimed to assess the feasibility of delivering a new Assets-based feeding help Before and After birth (ABA) infant feeding helper (IFH) intervention within a RCT. The ABA intervention was built on systematic review evidence,29,32,33,41 behaviour change theory,81 extensive qualitative research41,42,56,82 and learning from the FEST (FEeding Support Team) pilot trial about woman-centred feeding support after birth. 37,83
The study took place in geographical areas of socioeconomic disadvantage, as the largest potential public health gain is obtained from improving health outcomes for disadvantaged infants. 84
The ABA intervention used an assets-based approach, drawing on the community, social network, family and personal assets of each woman. This enabled the extent of support to be tailored to the assets a woman has available for infant feeding. This assets-based approach was enhanced with behavioural change theory. In addition, we developed a new feeding helper approach that is woman-centred, aims to establish a strong supportive relationship with continuity of care from pregnancy until after birth, respects a woman’s choices, is non-judgemental and discusses both breastfeeding and formula feeding issues, should a mother wish to. 56,62,82,83 This is because trials of breastfeeding peer support in the UK have had unexpected null results contrary to the worldwide systematic review evidence. 29 One hypothesis is that women who engage with breastfeeding-centred intervention research are those who are highly motivated to breastfeed. In taking a broader feeding approach, we were compliant with current UNICEF guidance,85 and at the same time aimed not to alienate women who were considering mixed or formula feeding43,56,62 by using the term ‘infant feeding’ in ABA information materials.
Peer support is a behaviour change technique found to be effective in increasing breastfeeding initiation and continuation. 29,33,35,86 Peer support is recommended by the National Institute for Health and Care Excellence (NICE);87 many programmes are in existence in the NHS and are suggested by UNICEF as a potential mechanism for achieving effective onward community support. 85
This assets-based feeding intervention is a new approach to peer support that seeks to overcome some of the pitfalls identified in previous studies, while building in methods to enable women to identify and activate assets within their family and friendship networks and in the wider community.
Chapter 2 Methods
Aim and objectives
Aim
The overall aim of the ABA study was to investigate the feasibility of delivering the ABA intervention within a RCT.
Objectives
-
To adapt existing peer support services to provide a new IFH intervention underpinned by theory and evidence, and with service user and provider input.
-
To undertake a feasibility RCT of the new feeding helper role compared with usual care (control group) for women living in areas of low breastfeeding prevalence.
-
To determine levels of uptake of and engagement with the intervention and to describe socioeconomic/demographic profiles to ascertain intervention reach and explore health inequalities.
-
To describe care those in the usual care group received regardless of feeding method.
-
To assess fidelity of intervention delivery and any contamination, and to use feedback from feeding helpers to improve fidelity, if necessary.
-
To assess whether or not women are willing to be recruited and randomised, assess whether or not the expected recruitment rate for a subsequent full-scale effectiveness RCT is feasible and identify successful recruitment strategies.
-
To explore mothers’ and feeding helpers’ perceptions of the intervention, trial participation and processes.
-
To explore acceptability and fidelity of the intervention when it is delivered by paid and volunteer feeding helpers.
-
To assess the acceptability and integration of the intervention to other providers of maternity, postnatal care and social care.
-
To explore the relative value of the individual feeding support versus the community integration elements to inform the design of a future trial.
-
To provide estimates of the variability in the primary outcome to enable sample size calculation for a definitive trial.
-
To measure the features of the feeding helper provision and service use that would underpin the cost-effectiveness of the intervention and determine the feasibility of data collection.
-
To test components of the proposed RCT to determine its feasibility as outlined in the protocol.
Setting
The study was undertaken in two distinct geographical areas in England (site A and site B). Both areas had existing programmes of peer support, but these were provided reactively through, for example, midwife referral or self-referral. In site A paid peer supporters employed by a social enterprise organisation delivered the programme, whereas in site B peer supporters were volunteers managed by a national charity. The sites were selected from five that were initially identified as interested in participating in the study. Sites were chosen (1) to reflect the diversity of existing peer support services, but those with no proactive peer support offered antenatally, (2) as they had relatively high levels of socioeconomic disadvantage and low rates of breastfeeding initiation and continuation, and (3) because they were reasonably local to the investigators to enable oversight of the study.
Study design
We undertook a feasibility individually randomised controlled trial (1 : 1) in two UK sites with a mixed-methods process evaluation.
Study management
The ABA study was overseen by a Trial Steering Committee (TSC) made up of two subject experts, a statistician and a public representative. A study management group, comprising the principal investigator, the trial co-ordinator and the 10 co-investigators, met regularly to guide study conduct.
Ethics approval and study registration
Ethics approval was obtained on 28 November 2016 from South West – Cornwall and Plymouth Research Ethics Committee (16/SW/0336). The study was registered with the International Standard Randomised Controlled Trial Register Number ISRCTN14760978. During the course of the study, some minor revisions were made to the protocol (see Appendix 1). The final protocol was published as a journal article. 88
Participant identification
We aimed to recruit 100 women to the study (at least 50 from each site), with half randomly allocated either to the intervention group or to the usual care group. We hoped to recruit sufficient numbers of teenagers, women of low socioeconomic status and women with limited social network breastfeeding exposure to allow us to investigate their experiences of the intervention. The two study sites were selected to reflect our target population.
Community midwives in the study areas were asked to hand out a summary participant information leaflet (PIL) to women who were pregnant with their first child at their 25-week antenatal appointment. At their 28-week antenatal appointment, women were approached in clinic by a researcher. The researcher provided the woman with further information about the study, including a full PIL (see Appendix 2), and gave her an opportunity to ask any questions. The woman was then asked if she would like to take part in the study. Women were given the option of signing up to the study there and then, or having time to think about it and/or discussing with others before contacting the researcher to arrange a time and place to sign up. Women were able to enrol in the study only up until 32 weeks’ gestation; this was to allow sufficient time for intervention participants to meet with their IFH before the birth. Researchers completed screening logs to record the number of women who were approached. At recruitment, women were told that if they completed and returned follow-up questionnaires at both 8 weeks and 6 months, they would receive a £25 shopping voucher at the end of the study to thank them for their time.
Recruitment ran from 28 February 2017 until 23 May 2017 in site A and from 21 April 2017 until 31 August 2017 in site B. Follow-up took place between 24 April 2017 and 12 March 2018 in site A and between 21 June 2017 and 23 May 2018 in site B. Recruitment ended when at least 50 participants had been recruited from each site.
Inclusion and exclusion criteria
Women were eligible to take part in the study if they were:
-
pregnant with their first child (excluding previous stillbirth)
-
aged ≥ 16 years.
Women were excluded if they had had a previous live birth or were aged < 16 years.
We decided to include only first-time mothers as they would have had no experience of infant feeding and might have been more likely to be influenced by the intervention. This is because mothers often repeat the infant feeding method they used for their first baby with their second baby. 89
Consent-taking process
The researcher checked the woman’s eligibility to participate in the study before asking her to complete, sign and date three copies of the consent form (see Appendix 3). The consent form was also signed and dated by the researcher. One copy of the consent form was given to the participant, one was kept by the research team and the third was stapled into the woman’s maternity notes. Details of the discussion about informed consent were recorded in the woman’s maternity notes (including date, name of study, discussion summary, PIL and consent form version numbers). Participants’ contact details were recorded and a baseline questionnaire was completed at the time of recruitment. Women were given a fridge magnet with the ABA study team contact number and were asked to notify the team as soon as their baby was born.
Randomisation
Women were randomised to intervention or usual care in a 1 : 1 ratio. The randomisation process differed by site.
In site A, a randomisation list was developed by the clinical trials unit, minimised by age group (< 25 years and ≥ 25 years). The list was stored securely and was not available to the researcher enrolling participants. After the participant had signed the consent form, the researcher telephoned the randomisation service who checked the participant’s eligibility and assigned her to the intervention or usual care. The researcher informed the participant there and then of her allocation. If the telephone randomisation service was unavailable, the researcher contacted the woman later, by letter, to inform her of her allocation.
In site B, a different method of randomisation was required to be able to match the number of IFHs available in the different areas of the study site (in site A, all IFHs were available to cover the whole study site). Therefore, block randomisation was used to randomise multiple women from each area of the site. Each block of women was randomised simultaneously by a researcher who was not undertaking recruitment; the recruiting researcher was then informed of allocation and notified women in writing.
Intervention design
Intervention design was informed by the Medical Research Council Complex Interventions and RE-AIM (Reach, Efficacy, Adoption, Implementation, Maintenance) frameworks. 90,91 We also used information from systematic reviews, surveys and qualitative studies and discussions with our patient and public involvement (PPI) group to ascertain barriers to both breastfeeding initiation and breastfeeding continuation. We used the behaviour change wheel framework [in which behaviour is analysed in context with respect to capability, opportunity, motivation and behaviour (COM-B)] alongside the theoretical domains framework to identify a number of behaviour change functions and behaviour change techniques (BCTs) from the behaviour change taxonomy. 81,92 Following this, we considered possible BCTs using the APEASE (Affordability, Practicality, Effectiveness and cost-effectiveness, Acceptability, Side-effects/safety, Equity) criteria. Components of the intervention were identified that were simple, low cost, practical and acceptable. A review of multicomponent incentive interventions to support breastfeeding had mapped BCTs and discovered social support to be predominant. 93 Social support is fundamental to peer support. 30
The chosen BCTs, with definitions and prespecified examples based on the ABA intervention, are shown in Table 1. Core and non-core BCTs for the antenatal part of the ABA intervention were agreed by the research team (core BCTs were social support and restructuring the social environment; non-core BCTs were emotional social support and instruction of how to perform behaviour). Some of these BCTs overlapped with the social support and use of social networks within the assets-based approach.
| BCT number | Label | Definition | Examples |
|---|---|---|---|
| 1: goals and planning | |||
| 1.2 | Problem-solving | Analyse, or prompt the person to analyse, factors influencing the behaviour and generate or select strategies that include overcoming barriers and/or increasing facilitators | Prompt the woman to consider what may encourage or prevent her from successful breastfeeding. Help the woman to identify strategies, solutions and support she can access to help overcome any difficulties |
| 1.3 | Goal-setting (outcome) | Set or agree on a goal defined in terms of a positive outcome of wanted behaviour | To discuss the woman’s (postnatal only) goals for breastfeeding |
| 1.7 | Review outcome goal(s) | Review outcome goal(s) jointly with the person and consider modifying goal(s) in light of achievement. This may lead to resetting the same goal, a small change in that goal or setting a new goal instead of or in addition to the first | To have ongoing discussions about the woman’s breastfeeding achievements, and to provide support for alternatives (i.e. mixed feeding, breastfeeding cessation) as appropriate |
| 2: feedback and monitoring | |||
| 2.7 | Feedback on outcome(s) of behaviour | Monitor and provide feedback on the outcome of performance of the behaviour | Inform the woman about ongoing health benefits of breastfeeding at different stages |
| 3: social support | |||
| 3.1 | Social support (unspecified) | Advise on, arrange or provide social support (e.g. from friends, relatives, colleagues, ’buddies’ or staff) or non-contingent praise or reward for performance of the behaviour. It includes encouragement and counselling, but only when it is directed at the behaviour |
Suggest that the woman calls a ‘buddy’ if she feels that she is struggling with feeding or needs some support Provide positive feedback on the woman’s progress with breastfeeding Arrange for a family member or friend to encourage continuation with breastfeeding |
| 3.2 | Social support (practical) | Advise on, arrange or provide practical help (e.g. from friends, relatives, colleagues, ‘buddies’ or staff) for performance of the behaviour |
Suggest that the woman call an IFH, health professional, helpline or ‘buddy’ if she feels that she is struggling with feeding or needs some support Ask the partner/family members of the woman to bring her the baby when the baby is ready to feed, bring a drink for the mother Ask the partner/family members to help with other activities in the home while the mother is feeding the baby (meal preparation, washing) Encourage the woman to access a breastfeeding support group or to call a helpline during times when other people are not available to help |
| 3.3 | Social support (emotional) | Advise on, arrange or provide emotional social support (e.g. from friends, relatives, colleagues, ‘buddies’ or staff) for performance of the behaviour | Ask the woman to take a friend to the breastfeeding group, or ask the feeding helper to meet her there |
| 4: shaping knowledge | |||
| 4.1 | Instruction on how to perform a behaviour | Advise or agree how to perform the behaviour (includes ‘skills training’) |
Provide information (visual images, DVD) and model demonstrations to show the woman how to position her baby to facilitate good latching on Show a woman how to prepare a bottle of formula correctly |
| 5: natural consequences | |||
| 5.1 | Information about health consequences | Provide information (e.g. written, verbal, visual) about health consequences of performing the behaviour | Explain the health benefits of breastfeeding for both the woman and the baby |
| 6: comparison of behaviour | |||
| 6.1 | Demonstration of the behaviour | Provide an observable sample of the performance of the behaviour, directly in person or indirectly (e.g. via film or pictures) for the person to aspire to or imitate |
Demonstrate breastfeeding in a film clip or via the use of aids (e.g. breastfeeding doll). Pictures of ‘good’ positioning and attachment to be shared with women Encourage attendance at breastfeeding group to observe other women breastfeeding |
| 8: repetition and substitution | |||
| 8.1 | Behavioural practice/rehearsal | Prompt practice or rehearsal of the performance of the behaviour one or more times in a context or at a time when the performance may not be necessary to increase habit or skill | Show and ask women to practice behaviours (i.e. hand expressing or breastfeeding) using aids such as a breastfeeding doll or knitted breast |
| 12: antecedents | |||
| 12.2 | Restructuring the social environment | Change or advise to change the social environment to facilitate performance of the wanted behaviour | Encourage the woman to attend social gatherings where other mothers are breastfeeding |
| 13: identity | |||
| 13.1 | Identification of self as role model | Inform that one’s own behaviour may be an example to others | Inform the woman that if she breastfeeds she will be a role model within her community and to her child, who will be influenced by her feeding choice |
| 15: self-belief | |||
| 15.1 | Verbal persuasion about capability | Tell the person that they can successfully perform the wanted behaviour, arguing against self-doubts and asserting that they can and will succeed |
Inform the woman that she can successfully breastfeed despite initial difficulties Encourage women to talk to friends/family members as well other mothers at breastfeeding groups to hear stories of how others have managed to breastfeed successfully |
| 15.2 | Mental rehearsal of successful performance | Advise to practice imagining performing the behaviour successfully in relevant contexts | Ask and encourage women to imagine breastfeeding in public locations and plan how this can be undertaken discreetly |
Table 2 provides details of the rationale for including the intervention components drawing on behaviour change theory and assets-based approaches.
| Behaviour change item | COM-B component | BCT | Assets-based approach | Mode of delivery | Intervention function |
|---|---|---|---|---|---|
| Discuss benefits of breastfeeding | Motivation |
Information about health consequences (individual) Goal-setting (outcome) |
– | Face to face | Education |
| Video clip about breastfeeding | Motivation |
Information about health consequences (general) Mental rehearsal of behaviour Instruction on how to perform the behaviour |
– | Internet link from phone |
Education, persuasion Enablement |
| Breastfeeding support groups/social groups |
Social opportunity Capability Motivation |
Social support Rehearsal (mental or actual) of behaviour Verbal persuasion about capability Demonstration of behaviour Instruction on how to perform the behaviour Restructuring the social environment |
✓ |
Face to face Social media |
Education, persuasion Enablement |
| Written and website materials about feeding | Motivation |
Information about health consequences Instruction on how to perform the behaviour |
– |
Leaflet Study website |
Education, persuasion Enablement |
| Identification of social network, social comparison, other facilitators of and barriers to breastfeeding/support to overcome them |
Capability Social opportunity |
Social support Problem-solving |
✓ | Face to face | Enablement |
| Further telephone contact |
Capability Motivation |
Social support Feedback on outcome(s) of behaviour Verbal persuasion about capability Problem-solving Review outcome goal(s) Identification of self as role model |
✓ | Telephone |
Enablement Persuasion Education |
The ABA intervention consisted of proactive peer support underpinned by behaviour change theory and an assets-based approach. The intervention delivered person-centred care41 and used best evidence in terms of setting and frequency, duration and manner of support provision from the ABA IFH. The ABA intervention aimed to be inclusive of all feeding methods (i.e. breastfeeding, formula or mixed feeding) and to provide support to all women.
Before the intervention commenced, researchers developed an ‘assets leaflet’ at each study site that was designed by a graphic designer. This leaflet (developed with the assistance of local contacts and using internet searches) was specific to the study areas and included information on local community ‘assets’ (e.g. antenatal or postnatal groups, breastfeeding drop-in centres, details of local breastfeeding counsellors and baby groups), as well as details of national helplines and internet resources. The leaflet, entitled ‘What’s available locally for you and your baby?’, had input from two PPI groups (mothers of young babies attending children’s centre groups) that provided constructive feedback on making the leaflet more user-friendly. Quotations from previous qualitative work were included in the leaflet (e.g. concerning the usefulness of breastfeeding drop-in centres), as well as tips on what to do when feeling uncomfortable about going along to a new group. Contact details for the ABA study were included on the leaflet, along with a space for the IFH to put their name and contact details. All details were checked prior to the start of the intervention to make sure they were up to date. For an anonymised example of the leaflet, see Appendix 4.
The two PPI groups were also asked for their opinions on a library of text messages produced by the research team, intended to be used by IFHs to engage with and support women in the intervention group. These texts aimed to take a woman-centred approach, to be infant feeding rather than breastfeeding centred and to draw on BCTs and an assets-based approach. The PPI groups were given cards with the various text messages and were asked to put them into one of three piles (yes, no or maybe). A group discussion was then facilitated by a researcher, and feedback on and suggestions about the various messages were noted. The PPI feedback was then used to finalise the library of suggested text messages available for use by the IFHs (see Appendix 5).
The ABA intervention outline is shown in Table 3. The intervention started at around 30 weeks’ gestation and could continue up until 5 months postnatally. At around 30 weeks’ gestation, the IFHs contacted women by telephone to arrange a face-to-face meeting, either at home (site A only) or at a suitable location, such as a café or children’s centre. The IFHs in site B (volunteer peer supporters) were not able to offer home visits because of local policies, unlike the paid peer supporters working in site A. Women were welcome to include partners or family members in this and subsequent meetings. The purpose of this face-to-face meeting was to talk about infant feeding and investigate the woman’s personal, family and social network assets for infant feeding. An approach of ‘narrative storytelling’ was used to produce a simple family tree diagram (‘genogram’) of experiences with infant feeding,55 incorporating the woman’s social network, to allow her to reflect on future feeding relationships and sources of support. 54 [See Appendix 6 for an example genogram from the training session (real names are not used).] At the antenatal visit, IFHs gave the woman the assets leaflets and explained the range of support available for infant feeding. In addition, contact details were swapped and a ‘Let us know when you’ve had your baby’ fridge magnet was given to the woman to encourage her to include the IFH on the list of people she would notify of the birth of the baby.
| Timing | Objectives and tasks |
|---|---|
| Antenatal face-to-face meeting (plus partner/family if woman would like this) at 30–32 weeks (duration 1 hour) |
|
| Telephone call after 2 weeks (text if no response) (approximately 32–34 weeks) |
|
| Text after 4 weeks (approximately 36–38 weeks) |
|
| Postnatal first contact | To commence contact via text or telephone calls within 24 hours of the woman’s discharge from hospital, and to offer face-to-face contact (site A only) |
| Postnatal visit/Skype™ (Microsoft Corporation, Redmond, WA, USA) (site A only) |
Practical feeding issues: observe feed if possible, advise about any difficulties experienced, encourage to take it a day at a time Find out whether or not the mother feels that she is receiving sufficient help from others Discuss practical help that the mother could ask for |
| Daily telephone calls or texts for 2 weeks |
Focus: person centred, well-being and feeding Arranged to suit mother/frequency determined by mother Encourage mother to start thinking about attending local feeding group |
| 2–8 weeks: contact and support as needed |
Encouragement to continue breastfeeding – taking it a day or a week at a time Troubleshoot any problems Advise mother of option to pull in people who will help and develop a strategy for those who do not help Encouragement to attend mother and baby groups/breastfeeding groups Planning for getting out and about Advise mother to call IFH if considering changing how she feeds her baby If formula feeding established, negotiate end of support |
| 3, 4 and 5 months – standard texts | For those still breastfeeding:
|
Following the face-to-face antenatal visit, the IFHs were asked to call and/or text the women fortnightly during the pregnancy. The aim was to encourage a strong rapport between the IFHs and the women that would facilitate successful immediate engagement after birth. In addition, IFHs were encouraged to facilitate a visit (antenatally) by the woman to a local breastfeeding group. The aim of this was so that the woman would know how and where to access support for infant feeding once her baby was born.
Postnatally, support from IFHs in both sites was by telephone calls or text messages every day until the baby was 2 weeks old. Additionally, at site A, IFHs were asked to arrange a postnatal home visit/Skype call as soon as possible after the mother and baby were discharged home.
From 2 to 8 weeks, frequency of contact was reduced based on the preferences of the mother. Text messages were sent to those still breastfeeding (or mixed feeding) at 3, 4 and 5 months. Women were able to ask for telephone calls or text messages to stop at any point. At site A, IFHs were unable to support women from 8 weeks postnatally because of their working practices. Therefore, in site A, a researcher sent out the 3-, 4- and 5-month texts and provided signposting support for women if required.
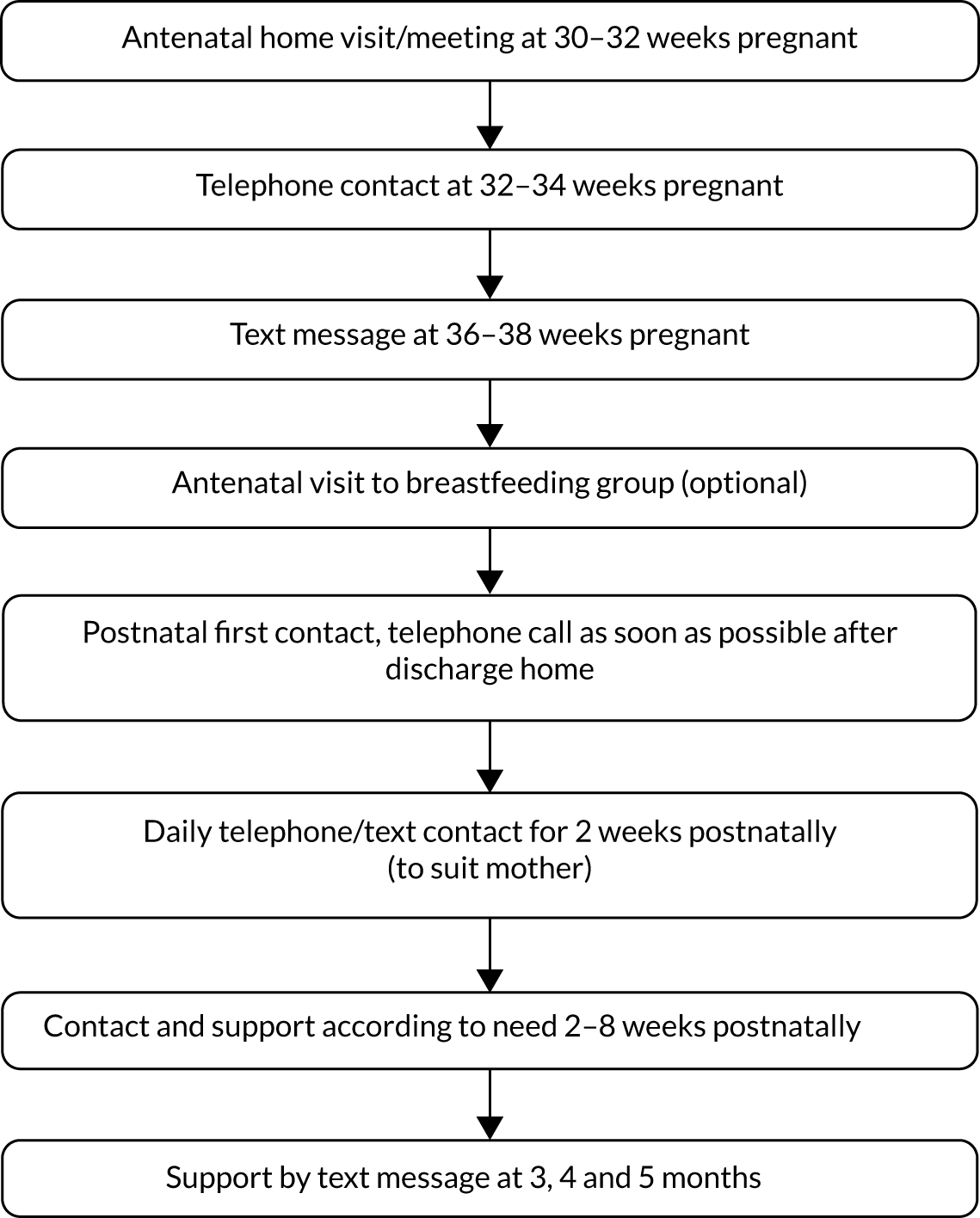
The intervention timeline is presented in Figure 1.
FIGURE 1.
The ABA intervention timeline.
Recruitment of ABA infant-feeding helpers
At site A, a paid peer support service providing reactive postnatal support (and no antenatal support) already existed. Although the service was available across the entire local authority area, peer supporters had traditionally worked within certain inner-city areas. Within the local authority, community midwives were split into three teams, each serving a distinct geographical area. For the ABA study, site A was selected as it was the area with the lowest rate of breastfeeding and highest rate of teenage pregnancy within the local authority. This area had traditionally not been served by the peer support service. The peer support service manager was willing to support the ABA study following discussions with the research team.
In site A, researchers attended part of the peer supporters’ regular team meeting on two occasions prior to the ABA training day. The purpose of these meetings was to introduce the ABA study, to encourage the peer supporters to take part in the study and to provide background information that would facilitate the smooth running of the ABA training day. Researchers also attended a team meeting after the training day to answer any questions arising from the session.
At site B, a volunteer peer support service was already in existence, which was overseen by a national charity. Again, this service provided reactive postnatal support, based around breastfeeding support groups, and no antenatal support. The geographical areas chosen within site B were those with the lowest breastfeeding rates within the local authority and with active peer supporters. Researchers met the charity manager and the peer supporter co-ordinator to discuss details of the study and recruitment of peer supporters.
Within the two sites, existing peer supporters were asked if they would like to support the ABA study. At site A, six of the seven existing peer supporters agreed to participate. At site B, seven of 11 peer supporters volunteered to be involved.
Training for ABA infant-feeding helpers
Infant feeding helpers were provided with 6 hours of training plus a study folder. The folder included details of all aspects covered in the training day. The intervention training was delivered face to face on 1 day in site A and over 2 half-days in site B. Heather Trickey led on the development of the training materials and led the training days, with input from Dr Kirsty Darwent (Programme Director, Family Therapy Training Network Ltd).
The aims of the training were (1) to promote competence and confidence in delivering the ABA intervention and (2) to facilitate understanding of the ABA study (to enhance fidelity to the intervention delivery). The training was designed to enable IFHs to learn about how to deliver the ABA intervention and to practise the skills required to deliver the intervention effectively. The training was interactive and involved simulations and role-play of contact with women as well as group-based learning activities.
Although the training did not explicitly present the BCTs to IFHs, it specifically focused on the delivery of the prespecified core BCTs (social support and restructuring the social environment) via the genogram and assets leaflet.
The training included the following.
-
Study information
Kate Jolly gave an overview of the study. She explained that the aim of the ABA study was to compare two ways of delivering feeding help to first-time mothers in areas where breastfeeding rates were low. Half of the mothers recruited to the study would have the usual feeding support from midwives, health visitors and any voluntary agencies or peer support that they choose to access; the other half would, in addition, receive the new ABA intervention.
-
Overview of the intervention
The ‘assets-based’ approach was outlined as an approach that encourages women to draw on support and help from their family, social and community networks. It was explained that the intervention was more intensive than usual peer support, and that is was peer supporter initiated rather than mother initiated. Every woman in the intervention would be offered antenatal contact, and continuity of care would be given wherever possible by women having the same IFH throughout the intervention. Trainees were informed that the intervention would end when the baby was 5 months old (if still being breastfed), or at a time when formula feeding had been established. Key principles of the ABA intervention were presented: the importance of a woman-centred approach and building a strong rapport, the use of open questions and active listening, seeing the woman (not the IFH) as the solution and viewing relationships as assets. The intervention timeline (see Figure 1) was presented to the IFHs, with opportunities given for discussion and clarification of any uncertainties.
-
Antenatal contact
In this part of the training, expectations for the antenatal visit were detailed. The trainers simulated the visit to facilitate good practice. Role-play techniques were then used to allow the IFHs to try out the approach. This session included:
-
Introducing themselves as an ABA IFH and explaining the purpose of the antenatal visit.
-
Learning how to explain the ABA timeline so the woman knows what to expect.
-
Learning how to open a conversation on infant feeding, and being led by the woman. The importance of good listening skills and using open questions was emphasised.
-
Discussing support from family and friends, including completion of a simple genogram.
-
Discussing support available in the community, and introducing the ‘assets leaflet’.
-
Offering to accompany the woman on an antenatal visit to a local breastfeeding support group and encouraging the use of the group after the baby is born.
-
Swapping telephone numbers, encouraging the women to let the IFH know when they have given birth, and discussing plans for keeping in touch.
-
The role plays were also used as an opportunity for IFHs to practise person-centred listening skills, with IFHs working in groups of three to give feedback to each other on the use of verbal and non-verbal active listening techniques.
-
Supporting mothers who use formula milk
The importance of being inclusive of all feeding types was stressed. A group discussion on supporting mothers who formula feed was facilitated, with the aid of a ‘myths and truths about formula feeding’ exercise. Key information about different kinds of formula milk and preparation of feeds, and up-to-date advice on formula feeding in response to the baby’s cues was delivered to IFHs during the session and supplemented with a key messages information leaflet and links to further information.
-
Postnatal contact
In this session, scenarios and group work were used to facilitate understanding. Groups worked together to decide how they would support women in the different scenarios. The ‘assets-based approach’ was underlined in the support provided, for example by encouraging women to use their personal and community-level assets for infant feeding.
Comparator group
Women allocated to the comparator (or ‘usual care’) group received usual care for infant feeding available in the study areas; this included routine support from midwives and health visitors. We describe the support for infant feeding that was available and accessed by women, which included local services, such as breastfeeding support groups and peer support, and national breastfeeding helplines. This usual care was available only reactively to women (i.e. the woman had to ask for support or the midwife asked for support on behalf of the woman).
In site A, peer supporters who did not volunteer to participate in the study were available to cover any requests for support received from the usual care women (as per usual care). In site B, breastfeeding support was available at any of the breastfeeding groups in the area.
Outcome assessment
All women were asked to notify the ABA study team about their baby’s birth by text message, e-mail or telephone call. To ensure that we found out about as many births as soon as possible, researchers from the ABA study team in site A also maintained daily telephone contact with the community midwives to find out if any of the women had given birth. On notification of an intervention participant giving birth, researchers contacted the IFHs to let them know. In site B, we relied on women notifying the research team or their IFH directly. Details of those who did not use either method in site B were obtained from midwives.
Feasibility outcomes
The feasibility of intervention delivery and the research methods were determined by:
-
Reach of recruitment of women to reflect required sociodemographic profile.
-
Ability to recruit, train and engage current peer supporters to the new ABA IFH role.
-
Ability to deliver planned number of contacts at a time and location convenient to participants.
-
Acceptability to women.
-
Fidelity of delivery and whether or not woman-centred care was provided.
-
Unintended consequences of the intervention.
-
The feasibility of a future definitive trial assessed by recruitment rates, willingness to be randomised, follow-up rates at 3 days, 8 weeks and 6 months and level of completion of assessments by text94 (see Criteria for progression to main trial).
-
Potential cases of intervention contamination in the usual care group; at 8 weeks’ follow-up, all women were asked if they had used national breastfeeding helplines or any breastfeeding support, whether or not there was a home visit or one-to-one meeting at a children’s centre and number of contacts by the IFHs. They were asked in interviews whether or not they had met other women taking part in the study and whether or not they had discussed the study.
Assessment of feasibility outcomes
A number of methods were used to assess feasibility outcomes. Table 4 summarises these.
| Feasibility outcome | Method of assessment |
|---|---|
| Reach of recruitment of women to reflect required sociodemographic profile |
|
| Ability to recruit, train and engage current peer supporters to the new ABA IFH role |
|
| Ability to deliver planned number of contacts at a time and location convenient to participants |
|
| Acceptability to women |
|
| Fidelity of delivery and whether or not woman-centred care was provided |
|
| Unintended consequences of the intervention |
|
| The feasibility of a future definitive trial assessed by recruitment rates, willingness to be randomised, follow-up rates at 3 days, 8 weeks and 6 months, and level of completion of assessments |
|
| Potential cases of intervention contamination in the usual care group |
|
| Presence of social desirability bias |
|
Researcher notes of meetings with peer supporters, including training sessions
Researchers kept reflective notes of all meetings with peer supporters and their organisations, including the training sessions. These notes included documentation and reflections on the number of peer supporters recruited, the ease of recruiting peer supporters to the role, and the engagement of peer supporters with the new ABA intervention.
ABA infant feeding helper electronic database (site A only)
At site A, there was an existing electronic database in place to capture details of peer supporter contact with women, including date of contact, mode of contact and notes of discussions. We secured agreement for this data set to be shared with the study.
ABA infant feeding helper case notes
At site A, case notes were already used by peer supporters to record details of home visits and ongoing support. At site A, these case notes were amended for the purposes of the ABA intervention to include the ABA logo and approach, the intervention timeline and space for notes from the antenatal visit (including whether or not the genogram was completed, the assets leaflet was handed out and telephone numbers were exchanged).
At site B, logs were developed to include similar items to the amended site A case notes to record text messages, telephone calls and other contacts, such as visits to breastfeeding groups.
Recordings of antenatal visits
The IFHs were asked to audio-record their discussions with women during the antenatal visit. IFHs were provided with encrypted voice recorders and asked to seek permission from women to record the discussion. Researchers devised a fidelity checklist (see Appendix 7) for use when listening to recordings to record:
-
the feeding intention of the mother (based on categorisation by spontaneous statements developed by Hoddinott and Pill95)
-
whether or not the IFH described the intervention as intended, including the purpose of the visit, the support she would provide as an IFH, the timeline of the intervention, and the requirement for the mother to contact the IFH once the baby was born
-
whether or not the IFH introduced local assets, including taking the mother through the local community assets leaflet and introducing specific local assets to the mother
-
whether or not the IFH used the genogram as intended, including whether or not the genogram was used to stimulate a conversation about feeding and whether or not a photograph of the genogram was taken
-
whether or not the IFH used BCTs as part of the conversation, including the use of specified core techniques – ‘social support’ and ‘restructuring the environment’ – as well as non-core techniques such as ‘emotional support’, ‘instruction to perform a behaviour’, ‘information about health consequences’, ‘verbal persuasion about capability’ and ‘mental rehearsal for successful performance’
-
whether or not the IFH achieved fidelity in terms of the overall intended tone of the encounter, including achieving rapport, demonstrating inclusivity (about intended feeding method), using active listening skills and delivering a mother-centred rather than breastfeeding-centred conversation.
All recordings were analysed by Heather Trickey using the checklist. The task of double-assessing the recordings was shared among seven other members of the research team (GT, JI, JLC, DJ, SD, KD and KJ) to ensure inter-rater reliability in fidelity testing.
Qualitative study
Semistructured interviews were undertaken with women, and focus groups (FGs)/interviews were undertaken with IFHs and midwives and other health-care providers. Further details are provided in Qualitative research.
Qualitative research
Semistructured interviews with women were carried out in the woman’s own home or in another convenient location. Sampling was purposive, aiming for a diverse range of experiences, and included teenagers, unemployed women (as indicated on the baseline questionnaire), women in socioeconomically disadvantaged areas, women with disparate feeding methods, women with different levels of contact with the IFH and women in the usual care group where intervention contamination was suspected (based on responses to the 8-week questionnaire).
With the exception of the first four, interviews took place after return of the 8-week questionnaire. After the first four interviews (all at site A), we decided to wait until after the 8-week questionnaire had been completed to avoid any possible interference with the primary outcome of a future definitive trial (any breastfeeding at 8 weeks). We aimed to interview around 15 women at each site (10 intervention, 5 usual care). Women were able to have a person of their choice present for the interview (research team experience has been that this can boost participation among socioeconomically disadvantaged groups). Interviews with women were conducted by Joanne L Clarke (site A) or Debbie Johnson (site B), both experienced qualitative researchers.
Interviews with women allocated to the intervention group explored the acceptability of the ABA intervention, as well as investigating the interaction of the intervention with other sources of support that are available, particularly with respect to existing community assets (e.g. breastfeeding support groups and baby groups). Interviews with women in the usual care group looked at their experiences of ‘usual care’ for infant feeding, and investigated possible cases of contamination. In addition, all women were asked about their experiences of being part of the ABA study, including the acceptability of the recruitment and randomisation process and follow-up methods.
We conducted FGs or interviews with all IFHs (n = 13), with the IFH manager at site B and with health-care providers (midwives and other providers of infant feeding support) working in the study areas (n = 17). FGs and interviews with IFHs investigated intervention acceptability, satisfaction with the ABA training, experiences of delivering the intervention and any barriers to or facilitators of intervention implementation. We also explored any additional training or supervision requirements.
Focus groups and interviews with health-care providers investigated how the ABA intervention fitted with existing support and whether or not the intervention had in any way changed ‘usual care’, as well as issues concerning referral or delivery. Possible cases of contamination were investigated with both IFHs and health-care providers.
Focus groups took place in a convenient location, and interviews with those unable to attend the FGs were conducted over the telephone. At the FGs with the IFHs, there was a lead facilitator (GT) who had no prior interactions with the IFHs, and at least one other member of the project team (JLC, DJ or JI) to record notes, interpersonal issues and ask follow-up questions, as appropriate. The FGs with health-care providers were conducted by Joanne L Clarke at site A and by Debbie Johnson and Jenny Ingram at site B. At the start of the FGs, all participants were asked to be mindful of confidentiality issues, whereby they should refrain from providing personal information about individual cases, and not to share what was discussed outside the FG. During the FGs, the lead facilitator encouraged all individuals to share their views, such as through seeking confirmatory or disconfirming views, and questions were directed to different individuals. At the end of the FGs, a summary of all key issues discussed was provided, with participants invited to offer any final comments.
Semistructured interview schedules were developed (see Appendix 8) based on research literature, team discussions, our logic model, PPI input and the ‘stages of breastfeeding peer support intervention design model’ constructed from a realist review of peer support intervention studies. 40
All interviews and FGs were audio-recorded. An external transcription company was employed to transcribe the recordings verbatim, including pauses and laughter, and anonymise them (by removing names of people and places). Transcriptions were checked for accuracy by researchers and reflective notes were made after every interview.
Qualitative analysis
For the qualitative analysis, we undertook thematic analysis using Braun and Clarke’s96 thematic approach supported by NVivo version 11 (QSR International, Warrington, UK). First, in line with the adopted approach, three researchers (JLC, DJ and GT) listened to the recordings and read and reread the transcripts of four participant interviews (one usual care and one intervention from each study site) before independently performing line-by-line inductive coding. Codes were discussed and developed into an initial and tentative coding framework of themes and subthemes. The remaining transcripts from all participant groups were then coded by Joanne L Clarke and Debbie Johnson using the coding framework that was iteratively refined (i.e. new codes added and/or refined), as appropriate. A number of external checks were undertaken to ensure that all data were represented within the coding framework. This involved the coding framework and NVivo files being reviewed by Gill Thomson, followed by discussions with Joanne L Clarke and Debbie Johnson, and amendments made as appropriate. The final coding framework was agreed by all researchers. In this report, we describe the qualitative results relevant to the feasibility outcomes. The full qualitative findings will be published in Health Expectations.
For each of the participant interviews, BCTs delivered by IFHs were coded as standalone themes. Coding of BCTs was based on reports of the behaviour of the IFH, regardless of the participant’s response. BCTs delivered by people other than the IFHs (e.g. midwives) were not coded for the purpose of this analysis.
Outcome measures for a future trial
The primary outcome for a future trial was any breastfeeding at 8 weeks.
Secondary outcomes for a future trial were:
-
breastfeeding initiation (at 2–3 days, as defined by the UK Infant Feeding Survey 2010,18 even if on one occasion only; includes giving expressed breastmilk)
-
exclusive breastfeeding at 6–8 weeks (exclusive breastfeeding defined in accordance with the WHO definition of infants who received only breastmilk during the previous 24 hours)97
-
any/exclusive breastfeeding at 6 months
-
duration of any and exclusive breastfeeding, if ceased breastfeeding
-
maternal well-being [Warwick–Edinburgh Mental Well-being Scale (WEMWBS)]98
-
maternal satisfaction with feeding experience and support provided at 8 weeks and 6 months (using a single-item question used in a previous trial37 and coproduced with PPI).
Outcomes for a future economic evaluation included in the feasibility trial were:
-
self-reported use of health and feeding support services
-
overall feeding support activity during the intervention
-
use of child care.
Assessment of outcomes
Table 5 presents a summary of the data items collected. At baseline (around 28 weeks’ gestation), women were asked to complete a baseline questionnaire. This included questions on demographic characteristics, feeding intentions, how they were fed as a baby, whether or not they knew anyone who had breastfed a baby, maternal well-being (WEMWBS) and use of health services. A researcher was present during questionnaire completion to answer any queries or clarify any points on the questionnaire.
| Type of data | Time point | |||
|---|---|---|---|---|
| Baseline (antenatal) | 2–3 days postnatally | 8 weeks postnatally | 6 months postnatally | |
| Demographics [date of birth, ethnicity, highest level of qualification, relationship status, postcode (for calculation of Index of Multiple Deprivation quintile), work status] | ✓ | |||
| Feeding intentions | ✓ | |||
| How participant was fed as a baby | ✓ | |||
| Knowledge of contacts who have breastfed | ✓ | |||
| Receipt of benefits | ✓ | ✓ | ✓ | |
| WEMWBS98 (score ranges from 14 to 70; 70 indicates highest level of well-being; minimum clinically important difference varies between 3 and 8 points)100 | ✓ | ✓ | ✓ | |
| Use of health services | ✓ | |||
| Feeding status | ✓ | ✓ | ✓ | |
| Delivery details and length of hospital stay | ✓ | |||
| Feeding history | ✓ | ✓ | ||
| Satisfaction with feeding support (hospital and community) | ✓ | |||
| Requests for support (frequency and location) | ✓ | |||
| Feeding experiences | ✓ | |||
| Adverse events | ✓ | |||
| Medical Outcomes Study Social Support Survey99 (score ranges from 0 to 40; 40 indicates highest level of social support) | ✓ | ✓ | ||
| Use of child care | ✓ | ✓ | ||
| Work status | ✓ | ✓ | ||
| Weaning status | ✓ | |||
At 2–3 days postnatally, women were sent a text message by the study team asking them how they had fed their baby since the birth. They were asked to text back a response: 1 for formula milk, 2 for breastmilk or 3 for formula milk and breastmilk (see Appendix 9).
At 8 weeks and at 6 months postnatally, women were sent a brief questionnaire in the post (with a prepaid return envelope). These included questions on the delivery of their baby, the length of hospital stay, feeding methods, feeding support received and satisfaction with feeding support, maternal well-being (WEMWBS) and social support. 99 Women who did not return their questionnaire within 2 weeks received a text-message reminder followed by a telephone call giving them the option of completing the questionnaire over the telephone. If women were reluctant to complete a questionnaire, attempts were made to secure the primary outcome (feeding status at 8 weeks) over the telephone.
See Putz et al. 100 for copies of the questionnaires.
For women who did not return their 8-week questionnaire, and who could not be contacted by telephone to secure data on the primary outcome of a definitive trial (feeding status at 8 weeks), local health visiting teams were contacted to request this information.
Assessment of adverse events
Information on possible adverse events was collected at 8 weeks using an open question asking about any difficulties experienced in feeding their baby and any hospital admissions related to infant feeding for mother or baby. The research team contacted the woman for more information, as required. The chief investigator reviewed adverse events to define their severity and causality. Only serious adverse events that could be related to the intervention were to be reported to the Research Ethics Committee.
Sample size
The selected sample size (n = 100) allowed us to estimate feasibility outcomes with reasonable precision, allowing us to estimate recruitment, follow-up and questionnaire completion rates to within ± 15% with 95% confidence. This was based on a worst-case (in terms of precision) estimate of 50% for each outcome, the targets being 75% for recruitment, 75% for follow-up and 70% for questionnaire completion.
To enable us to calculate the necessary sample size for a future definitive trial, we determined the percentages of participants initiating breastfeeding and breastfeeding at 6–8 weeks for both groups; 95% CIs were given for the estimates acquired.
Statistical analysis
The study statistician was blinded to allocation group. We calculated recruitment and follow-up rates (with 95% binomial exact CIs) as a measure of trial feasibility.
To determine intervention implementation and contamination levels in the usual care group, we report the frequency and method of IFH and peer support contacts for both the intervention and the usual care groups.
Although the feasibility trial was not powered to detect a difference between the groups, we calculated the percentages of women breastfeeding and exclusively breastfeeding at 6–8 weeks by allocation, with 95% CIs presented. We also determined the dropout rate and the completeness of data, which will inform the sample size calculation and feasible outcome selection for a future definitive trial.
Women’s characteristics were described by allocation group, with simple summaries presented for each outcome measure. The primary analysis was by modified intention to treat, which included all randomly assigned patients for whom data on the primary end point were available.
The variability between IFHs in the primary outcome of a future trial was assessed by calculating the intracluster correlation coefficient (ICC) using a null linear model with a random effect for IFH. These data will inform the sample size calculation for a future definitive trial.
Feasibility of data collection for a future economic evaluation
This feasibility study explored whether or not it would be possible to collect the data required for a future economic evaluation. In a future definitive trial, we would want to be able to estimate the health service costs associated with the intervention (e.g. the costs of training the IFHs, telephone calls, text messaging service, one-to-one meetings with women, staff time to respond to women’s requests and any payments to IFHs).
In a future economic evaluation, we would calculate the extra cost for each additional case of breastfeeding in the intervention group compared with the usual care group. We may also consider how appropriate it is to link the increase in the uptake of breastfeeding to longer-term health benefits using a model-based economic evaluation.
Criteria for progression to a main trial
For the Phase III trial to be considered, the following criteria (predetermined by the TSC) needed to be met:
-
The process evaluation suggests that the intervention is acceptable to a majority of mothers, their partners, ABA infant feeding team members and local services.
-
At least 75 women need to be recruited in 5 months.
-
The study must be able to recruit women of low socioeconomic status, teenagers and ethnic minorities.
-
Intervention needs to be implemented with fidelity in 75% of mothers (this will be defined as contacts made in both the antenatal period and the postnatal period).
-
75% of participants should receive the assets-based antenatal face-to-face contact.
-
> 70% follow-up should be achieved at 8 weeks and 6 months, with additional missing data able to be obtained from routine sources.
The criteria agreed by the ABA study TSC are presented in Table 6.
| Criterion | Progress – green | For TSC and funders to advise – amber | Not progress – red |
|---|---|---|---|
| Acceptable intervention | Generally positive views of women, IFHs and health service staff towards the intervention | Some concerns raised about acceptability and/or feasibility of delivery | Considerable negativity about the intervention from women |
| Recruitment | ≥ 75 women in 5 months | 50–74 women in 5 months | < 50 women in 5 months |
| Recruitment of women with socioeconomic disadvantage, teenagers, etc. | At least 5% of recruits are teenagers | > 0% to < 5% teenagers | No teenagers recruited |
| Fidelity of intervention delivery | ≥ 75% receive contact in antenatal and postnatal perioda | 50–74% receive contact in antenatal and postnatal perioda | < 50% receive contact in antenatal and postnatal perioda |
| Receipt of assets-based face-to-face contact | ≥ 75% | 50–74% | < 50% |
| Follow-up at 8 weeks and 6 months | > 70% plus ability to obtain routine data to achieve 80% of primary outcome | 70–79% of primary outcome data obtained | < 70% of primary outcome data obtained |
Chapter 3 Results
Feasibility of recruitment
In total, 135 women expecting their first child were approached at an antenatal clinic. Of these, 103 women (76.3%) agreed to participate in the study. Recruitment ran from 28 February 2017 until 23 May 2017 in site A and from 21 April 2017 until 31 August 2017 in site B.
Figure 2 shows the recruitment flow diagram for the ABA study. (See Appendix 10 for the recruitment flow diagrams for sites A and B.) The total number of births to primiparous women during the 3–4 month period was not routinely available. The researchers attended only some of the antenatal clinics during the period, so the 135 women who were approached were a sample of all of the eligible women.
FIGURE 2.
Flow diagram of participant flow through the ABA study. Reproduced from Clarke et al. 101 © 2019 The Authors. Maternal & Child Nutrition published by John Wiley & Sons, Ltd. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
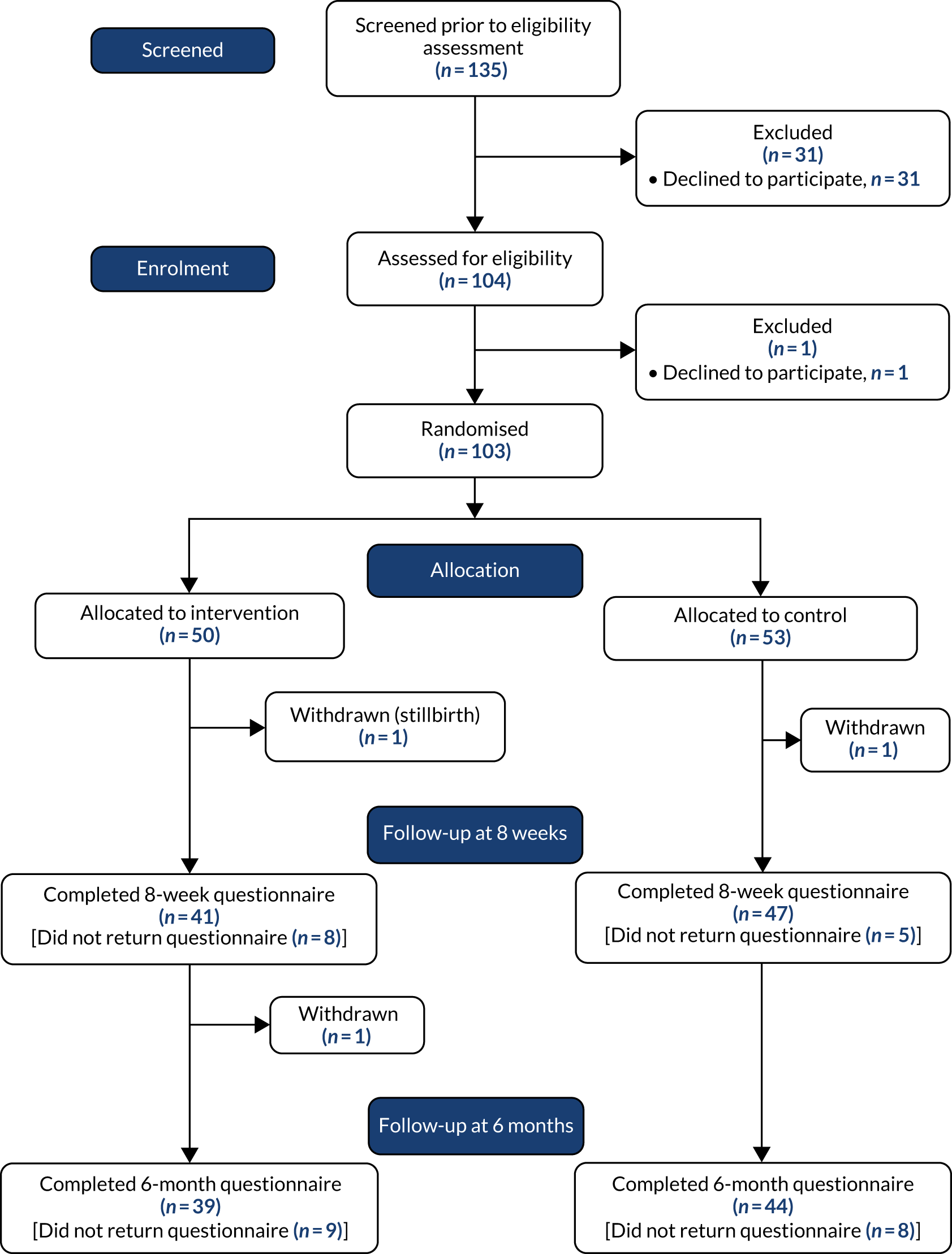
Reach of recruitment of women to reflect the required sociodemographic profile
The demographic and delivery characteristics of women who took part are presented in Table 7. (See Appendix 11 for additional details and characteristics by site.) The mean age of participants was 28.5 years. At both sites, the proportion of teenagers recruited was higher than the overall proportion for the area. Overall, nine of the study participants (8.7%) were teenagers, indicating successful reach of recruitment and acceptability of the recruitment process to this age group. The majority of women (n = 88, 86.3%) described their ethnicity as white British, a proportion that is reflected in local census data for the two sites. Most of the women were in paid employment (n = 90, 88.2%), and two (2.0%) were in full-time education or training. Nine participants (8.8%) were unemployed. Forty-six participants (45.1%) were educated to degree level or higher, 33 (32.4%) were educated to Advanced/Advanced Subsidiary (A/AS) level or equivalent, 22 (21.6%) were educated to General Certificate of Secondary Education (GCSE) or equivalent, and one participant (1%) had no formal qualifications. The majority of women were either married or in a civil partnership (n = 48, 47.5%) or living with their partner (n = 38, 37.6%). Fifteen participants (14.9%) were single. Overall, 38 participants (37.3%) resided in areas of the most deprived two Index of Multiple Deprivation quintiles, although this differed by site [33 participants (63.5%) in site A and five participants (10%) in site B]. The mean baseline score for mental well-being (WEMWBS) was 54.1 (the maximum possible score was 70).
| Characteristic | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) |
|---|---|---|---|
| Age at baseline (years), mean (SD) | 28.6 (5.2) | 28.5 (5.8) | 28.5 (5.5) |
| Age range (years), minimum–maximum | 17.7–43.0 | 17.9–42.9 | 17.7–43.0 |
| Missing, n (%) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Ethnicity, n (%) | N = 54 | ||
| White British | 43 (86.0) | 45 (86.5) | 88 (86.3) |
| Other | 7 (6.0) | 8 (7.7) | 14 (6.9) |
| Missing | 0 (0) | 1 (1.9) | 1 (1.0) |
| Employment status, n (%) | N = 49 | N = 102 | |
| In paid work | 40 (80.0) | 50 (96.2) | 90 (88.2) |
| Unemployed | 8 (16.0) | 1 (1.9) | 9 (8.8) |
| In full-time education or training | 1 (2.0) | 1 (2.0) | 2 (2.0) |
| Missing | 0 (0) | 1 (1.9) | 1 (1.0) |
| Highest level of qualification, n (%) | |||
| No formal qualification | 1 (2.0) | 0 (0) | 1 (1.0) |
| GCSE or equivalent | 12 (24.0) | 10 (19.2) | 22 (21.6) |
| A/AS level or equivalent | 20 (40.0) | 13 (25.0) | 33 (32.4) |
| Degree level or higher | 17 (34.0) | 29 (55.8) | 46 (45.1) |
| Missing | 0 (0) | 1 (1.9) | 1 (1.0) |
| Relationship status, n (%) | |||
| Married/registered civil partnership | 22 (44.0) | 26 (51.0) | 48 (47.5) |
| Living together | 18 (36.0) | 20 (39.2) | 38 (37.6) |
| Single | 10 (20.0) | 5 (9.8) | 15 (14.9) |
| Widowed, divorced or separated | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 2 (3.8) | 2 (1.9) |
| Index of Multiple Deprivation quintile, n (%) | N = 52 | N = 102 | |
| 1 (most deprived) | 14 (28.0) | 11 (21.2) | 25 (24.5) |
| 2 | 5 (10.0) | 8 (15.4) | 13 (12.8) |
| 3 | 9 (18.0) | 10 (19.2) | 19 (18.6) |
| 4 | 13 (26.0) | 14 (26.9) | 27 (26.5) |
| 5 (least deprived) | 9 (18.0) | 9 (17.3) | 18 (17.7) |
| Maternal well-being (WEMWBS), mean (SD) | 53.7 (8.1) | 54.4 (8.7) | 54.1 (8.4) |
| Missing, n (%) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Intention to feed, n (%) | |||
| Breastmilk only | 17 (34.0) | 18 (35.3) | 35 (34.7) |
| Mainly breastmilk | 17 (34.0) | 13 (25.5) | 30 (29.7) |
| Half and half | 10 (20.0) | 12 (23.5) | 22 (21.8) |
| Mainly formula | 3 (6.0) | 2 (3.9) | 5 (5.0) |
| Formula milk only | 3 (6.0) | 6 (11.8) | 9 (8.9) |
| Missing | 0 (0) | 2 (3.8) | 2 (1.9) |
| Gestational age at birth (weeks), mean (SD) | 39.4 (2.0) | 39.7 (1.6) | 39.5 (1.8) |
| Missing | 1 (2.0) | 1 (1.9) | 2 (1.9) |
| Premature baby, n (%) | 7 (14.3) | 2 (3.9) | 9 (8.9) |
| Missing | 1 (2.0) | 1 (1.9) | 2 (1.9) |
| Mode of delivery, n (%) | |||
| Vaginal birth | 15 (37.5) | 22 (50.0) | 37 (44.1) |
| C-section | 11 (27.5) | 13 (24.5) | 24 (23.3) |
| Forceps, ventouse, vacuum delivery | 14 (35.0) | 9 (20.5) | 23 (27.4) |
| Missing | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Duration of mother’s hospital stay, n (%) | |||
| < 24 hours | 8 (20.0) | 10 (22.7) | 18 (21.4) |
| 24–48 hours | 18 (45.0) | 12 (27.3) | 30 (35.7) |
| > 48 hours | 14 (35.0) | 21 (47.7) | 35 (41.7) |
| Home birth | 0 (0) | 1 (2.3) | 1 (1.2) |
| Missing | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Baby admitted to neonatal unit, n (%) | 7 (17.5) | 4 (9.1) | 11 (13.1) |
| Missing | 10 (20.0) | 9 (17.0) | 19 (18.4) |
The majority of women planned to feed their baby either breastmilk only (n = 35, 34.7%) or mainly breastmilk (n = 30, 29.7%). Twenty-two participants (21.8%) intended to feed their baby half breastmilk and half formula milk. Nine participants (8.9%) intended to feed their baby only formula milk, and a further five (5.0%) intended to feed mainly formula milk. More participants had been breastfed entirely as a baby (n = 36, 35.3%) than formula fed entirely (n = 29, 28.4%). Most of the women (n = 93, 91.2%) knew someone who had breastfed her baby.
Mean gestational age at birth was 39.5 weeks. Thirty-seven babies (44.1%) were delivered by normal vaginal birth, and 23 (27.4%) were delivered by forceps, ventouse or vacuum delivery. There were 18 births (21.4%) by emergency caesarean section and six (7.1%) by planned caesarean section. The proportion of women reporting staying in hospital for more than 48 hours after the birth was high (41.7%).
Baseline imbalances
A visual inspection of the baseline participant demographic and delivery characteristics (see Table 7) revealed some imbalances. Those in the intervention group were more likely to be unemployed, less likely to be educated to degree level and more likely to be single. In addition, there were more premature deliveries and more admissions to the neonatal unit in the intervention group than in the usual care group.
Birth notifications
The median age of babies at the time the study team found out about the birth was 3 days (interquartile range 0–30 days) (Table 8). Overall, 50.5% of births were reported to the study team when the baby was ≤ 3 days old. The source of birth notification to the study team was the community midwife in the majority of cases (57.4%), followed by the participant (35.6%) and the IFH (6.9%). However, the proportions for this differed by site. At site A, the primary source of birth notifications was the community midwife (78.4%), followed by the participant (17.1%) and the IFH (3.9%). At site B, 54.0% of birth notifications were from the participant, 36.0% were from the community midwives and 10.0% were from the IFHs.
| Age of baby and source of birth notification | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Usual care | All | Intervention | Usual care | All | Intervention | Usual care | All | |
| Baby’s age (in days) when study team notified of birth | |||||||||
| n | 24 | 27 | 51 | 25 | 25 | 50 | 49 | 52 | 101 |
| Median interquartile range | 4 (2–7.5) | 4 (2–5) | 4 (2–6) | 2 (0–4) | 6 (2–14) | 2.5 (1–8) | 3 (0–20) | 5 (2–7.5) | 3 (0–30) |
| Source of birth notification to study team, n | 24 | 27 | 51 | 25 | 25 | 50 | 49 | 52 | 101 |
| Participant, n (%) | 5 (20.8) | 4 (14.8) | 9 (17.7) | 14 (56.0) | 13 (52.0) | 27 (54.0) | 19 (38.8) | 17 (32.7) | 36 (35.6) |
| Community midwives, n (%) | 17 (70.8) | 23 (85.2) | 40 (78.4) | 6 (24.0) | 12 (48.0) | 18 (36.0) | 23 (46.9) | 35 (67.3) | 58 (57.4) |
| IFH, n (%) | 2 (8.3) | – | 2 (3.9) | 5 (20.0) | – | 5 (10.0) | 7 (14.3) | – | 7 (6.9) |
Those women who notified the study or the IFH about the birth were more likely to be breastfeeding at 8 weeks and less likely to have had a long hospital stay (Table 9).
| Feeding method and hospital stay | Participant notified study and/or IFH of birth | Participant did not notify study or IFH of birth |
|---|---|---|
| Feeding method at 8 weeks (including health visitor data), n (%) | N = 43 | N = 58 |
| Only breastmilk | 23 (53.5) | 12 (21.8) |
| Only formula | 14 (32.6) | 37 (67.3) |
| Breastmilk and formula | 3 (14.0) | 6 (10.9) |
| Length of hospital stay, n (%) | N = 41 | N = 43 |
| < 24 hours | 9 (22.0) | 9 (20.9) |
| 24–48 hours | 16 (39.0) | 14 (32.6) |
| > 48 hours | 15 (36.6) | 20 (46.5) |
| Home birth, n (%) | 1 (2.4) | 0 (0) |
Feasibility of postnatal text at 3 days
The research team sent postnatal texts (asking women how they were feeding their baby) to 81.6% of women before their baby was 10 days old (Table 10). Postnatal text responses were received from 68% of participants overall.
| Postnatal texts sent and response rate | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Usual care | All | Intervention | Usual care | All | Intervention | Usual care | All | |
| 3-day text sent (up to 10 days postnatally), n/N (%) | 20/25 (80.0) | 25/28 (89.3) | 45/53 (84.9) | 21/25 (84.0) | 18/25 (72.0) | 39/50 (78.0) | 41/50 (82.0) | 43/53 (81.1) | 84/103 (81.6) |
| Response to 3-day text (up to 14 days postnatally), n/N (%) | 14/25 (56.0) | 17/28 (68.0) | 35/53 (66.0) | 21/25 (75.0) | 18/25 (72.0) | 35/50 (70.0) | 31/50 (62.0) | 39/53 (73.6) | 70/103 (68.0) |
Follow-up rates
Follow-up data were obtained from 68% of women at 3 days postnatally. The 8-week questionnaire was completed by 85.4% of participants (including three women who provided primary outcome data only over the telephone). Primary outcome data were available from 95.1% of participants (local health visiting teams provided 6- to 8-week feeding data for 10 participants who had not returned the 8-week questionnaire). At 6-month follow-up, 80.6% of participants returned a completed questionnaire. Follow-up rates were higher at all three time points at site B than at site A (Table 11).
| Recruitment and follow-up | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | |
| Recruitment rate: eligible women who were approached by researcher and who were recruited | 53/68 | 77.9 | 66.2 to 87.1 | 50/67 | 74.6 | 62.5 to 84.5 | 103/135 | 76.3 | 68.2 to 83.2 |
| 3-day texta | 35/53 | 66.0 | 51.7 to 78.5 | 35/50 | 70.0 | 51.7 to 78.5 | 70/103 | 68.0 | 58.0 to 76.8 |
| 8-week questionnaireb | 42/53 | 79.2 | 65.9 to 89.1 | 46/50 | 92.0 | 80.8 to 97.8 | 88/103 | 85.4 | 77.1 to 91.6 |
| 6-month questionnaire | 37/53 | 69.8 | 55.7 to 81.7 | 46/50 | 92.0 | 80.8 to 97.8 | 83/103 | 80.6 | 71.6 to 87.7 |
| 8-week feeding status obtainedc | 49/53 | 92.3 | 81.8 to 97.9 | 49/50 | 98.0 | 89.4 to 99.9 | 98/103 | 95.1 | 89.0 to 98.4 |
See Appendix 12 for tables showing data completeness.
Table 12 shows follow-up rates by site and group. Follow-up rates were consistently higher in the usual care group than in the intervention group.
| Follow-up rates | Site A | Site B | Overall | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Usual care | Intervention | Usual care | Intervention | Usual care | |||||||||||||
| n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | |
| Response to 3-day text (baby aged < 14 days) | 14/25 | 56.0 | 34.9 to 75.6 | 21/28 | 75.0 | 55.1 to 89.3 | 17/25 | 68.0 | 46.5 to 85.1 | 18/25 | 72.0 | 50.6 to 87.9 | 31/50 | 62.0 | 47.2 to 75.3 | 39/53 | 73.6 | 59.7 to 84.7 |
| Response to 8-week questionnaire | 19/25 | 76.0 | 54.9 to 90.6 | 23/28 | 82.0 | 63.1 to 93.9 | 22/25 | 88.0 | 68.8 to 97.5 | 24/25 | 96.0 | 79.6 to 99.9 | 41/50 | 82.0 | 38.6 to 91.4 | 47/53 | 88.7 | 77.0 to 95.7 |
| Response to 6-month questionnaire | 17/25 | 68.0 | 46.5 to 85.1 | 20/28 | 71.4 | 51.3 to 86.8 | 22/25 | 88.0 | 68.8 to 97.5 | 24/25 | 96.0 | 79.6 to 99.9 | 39/50 | 78.0 | 64.0 to 88.5 | 44/53 | 83.0 | 70.2 to 91.9 |
Study withdrawals
In site A, there were three withdrawals from the study. One participant withdrew immediately after recruitment (no reason given; she requested that her data be destroyed), and another withdrew between the 8-week and 6-month follow-up points (she no longer wanted to be part of the study). One participant was withdrawn by the study team after midwives reported that she had experienced a stillbirth. There were no study withdrawals at site B.
Characteristics of participants who were followed up compared with characteristics of those who were lost to follow-up or withdrew
Demographic characteristics of responders (i.e. those who responded to the postnatal text and the 8-week questionnaire) were compared with those of non-responders (Table 13). At both time points, when compared with responders, non-responders were younger, more likely to be of white British ethnicity, less likely to be in paid work, less likely to be educated to degree level or higher, less likely to be married or in a civil partnership or living with their partner, less likely to be intending to breastfeed at baseline and less likely to be breastfeeding at 8 weeks.
| Participant characteristic | Returned postnatal text (baby aged < 14 days) | Did not return postnatal text (baby aged < 14 days)a | Followed up at 8 weeks (returned 8-week questionnaire) | Lost to follow-up at 8 weeksa |
|---|---|---|---|---|
| Age (years), mean (SD) | 29.8 (4.9) | 25.7 (5.7) | 28.7 (5.5) | 27.1 (5.3) |
| Ethnicity white British, n/N (%) | 59/70 (84.3) | 29/33 (90.6) | 75/88 (85.2) | 13/14 (92.9) |
| In paid work, n/N (%) | 67/70 (95.7) | 23/33 (71.9) | 79/88 (89.8) | 11/14 (78.6) |
| Educated to degree level or higher, n/N (%) | 39/70 (55.7) | 7/33 (21.9) | 42/88 (47.7) | 4/14 (28.6) |
| Married/in civil partnership/living together, n/N (%) | 62/70 (88.6) | 24/33 (77.4) | 75/88 (86.2) | 11/14 (78.6) |
| Feeding intentions (first 6 months), n/N (%) | ||||
| Breastmilk only | 28/70 (40.0) | 7/33 (22.6) | 33/88 (37.9) | 2/14 (14.3) |
| Mainly breastmilk | 23/70 (32.9) | 7/33 (22.6) | 25/88 (28.7) | 5/14 (35.7) |
| Half and half | 12/70 (17.1) | 10/33 (32.3) | 19/88 (21.8) | 3/14 (21.4) |
| Mainly formula | 2/70 (2.9) | 3/33 (9.7) | 2/88 (2.3) | 3/14 (21.4) |
| Formula only | 5/70 (7.1) | 4/33 (12.9) | 8/88 (9.2) | 1/14 (7.1) |
| Gestational age (weeks), mean (SD) | 39.8 (1.4) | 39.0 (2.5)b | 39.5 | 40.0b |
| Any breastfeeding at 8 weeks (including health visitor data), n/N (%)c | 41/69 (59.4) | 5/29 (17.2) | 45/88 (51.1) | 1/10 (10.0) |
Qualitative study participants
Thirty of the study participants were purposively sampled to take part in a qualitative interview, 15 from each site. Twenty-one interviewees were from the intervention group and nine were from the usual care group. The sample included three teenagers (site A) and two from the 35–39 years age group (site A), with the remaining spread between 20–34 years (25–29 years, n = 10; 30–34 years, n = 11). The majority were white British (n = 26, 86.6%) and in paid work (n = 25, 83.3%); all those who were unemployed (n = 4) or students (n = 1) came from site A. Over half the sample were still breastfeeding at 8 weeks (n = 17, 56.6%); the majority of these (11 out of 17, 64.7%) were from site B. One woman at site A was interviewed together with her partner.
All IFHs took part in either a FG (n = 9) or a one-to-one interview (n = 4). At site B, the IFH manager also participated in the FG. Seventeen maternity service providers (including midwives and infant-feeding staff) also participated in either a FG (n = 14) or an interview (n = 3).
Quotations in this report are labelled by type of interviewee [P (woman participant), IFH or maternity services], by number (for women participants and IFHs), by intervention or usual care (for women participants), by site (site A or site B) and by whether the data were collected during an interview or a FG (for IFHs and health-care providers). For example, ‘P1 – intervention, site A’ would be woman participant number 1 from the intervention group in site A.
Women’s and maternity services providers’ views on recruitment and randomisation process
Women’s views on recruitment
All of the women interviewed found the recruitment process acceptable, with one woman referring to how it had strengthened and affirmed her decision to breastfeed:
It was nice to be able to talk to somebody and confirm how adamant I was about doing it really . . . because it was about breastfeeding obviously my ears pricked up straight away and I was like breastfeeding yes that’s what I want to do . . . what help can I get?
P1 – intervention, site A
Women considered the timing of recruitment to be appropriate. It was felt that recruiting women at a later gestational stage and after the anomaly scan was important, as this is when women’s attention turns towards the birth and postnatal period:
I didn’t really want to acknowledge until the 20-week scan just because my brain wasn’t . . . I was still on my medical everything is going to wrong path, so I don’t know if I would have at that point, 12 weeks . . . I don’t think I was even thinking about post birth.
P16 – intervention, site B
Although there were variations in when women received the study leaflet – some pregnant women received the leaflet early, others received it on the day of recruitment – this did not affect women’s willingness to be involved:
I guess if the midwife of the previous appointment said there’s a feeding study going on, this is the leaflet about what they are doing, they’re going to be here next time and they might want to have a chat with you, then I suppose that could have given me a bit more time to have a think about it. But I wasn’t really thinking I wish I had more time to think about it or anything like that.
P17 – usual care, site B
Although one mother stated she would have preferred having more notice to consider her involvement, this still would not have affected her decision to participate:
Maybe looking back, yeah, I didn’t feel pressurised but maybe yeah, a little bit rushed . . . it wouldn’t have changed my mind, I probably still would have gone along with it, but yeah just a little bit more notice.
P18 – intervention, site A
Women found the PIL to be straightforward; however, there were mixed responses about whether or not the information conveyed a breastfeeding rather than an inclusive ‘infant-feeding’ approach. One mother recognised that her reading of the leaflet as being breastfeeding-centred could have been associated with her feeding preference and the cultural pressure to breastfeed, rather than with the information per se:
I think because I was wanting to breastfeed that’s how I read it rather than just help generally around feeding . . . I think there was so much pressure, I felt, from NCT and midwives that breastfeeding is what you should be doing so I think that’s probably why I saw it more as a breastfeeding research.
P16 – intervention, site B
Women provided diverse responses regarding the involvement of midwifery staff in study recruitment. Some were less concerned about midwifery involvement and felt that it was more important to discuss the purpose and practicalities of the study with the researcher. Others felt that midwifery endorsement helped to authenticate the study:
I probably wouldn’t have done anything if it was just you [researcher] if I was honest, it was because my midwife said . . . this is a research would you want to take part? . . . it was nice to have that confirmation that it is an actually [sic] study going on.
P28 – usual care, site B
Women’s views on the randomisation process
Overall, women in both study groups found the randomisation process to be acceptable. Women wanted to be part of a study, which may or may not have direct personal benefits, but might make a difference to others:
I think it’s interesting and it’s good to participate in this kind of research because then other people can get help afterwards, so it was OK.
P27 – intervention, site B
A few women assigned to the intervention group reported ambivalence about participating in the study (e.g. ‘I’ll go with the flow with anything really’) or about the need for additional support. More women expressed how they were hoping to have the additional help and had been ‘really pleased’ when they were told of their allocation, and for some it had provided ‘reassurance’ because they had been undecided about breastfeeding:
That felt fine because I knew I would have fell in one or the other. But when I found out I was in the enhanced I was quite happy about it, because I was so on the fence about it [breastfeeding] to have that extra support felt very reassuring.
P19 – intervention, site B
Women assigned to the usual care group generally expressed disappointment; for example, one woman referred to feeling ‘sad’ as breastfeeding was important to her and she knew that additional support would be required:
When you said I was going to be in the control group I said then that’s a real shame. I did feel sad about that because I knew I wanted to breastfeed and I knew I was going to need an awful lot of support, because everybody needs support.
P3 – usual care, site A
However, the prevailing opinion from women in the usual care group was that they understood why randomisation was important and held altruistic desires to help inform future care provision.
Maternity services providers’ views on recruitment
Some health professionals felt that issuing leaflets and informing women about the study at a later point in pregnancy (i.e. ≥ 16 weeks’ gestation) was appropriate. This was considered important to avoid recruiting women who experienced a pregnancy loss, or reduce the chances that women would not remember the information:
If you ask too early or discuss something with them too early, often people forget all about it.
Maternity services – site B, interview
A recurring issue was how introductions/discussing the study during ‘easier appointments’, such as the one at 24 weeks that involved basic antenatal checks, was more acceptable as there was ‘less going on’.
The midwives did not experience any particular difficulties or issues in giving the leaflets or introducing women to the study. They valued the researcher’s presence as she had the knowledge and time to explain the study more thoroughly:
It’s good having you there rather than us having to . . . You explain it better . . . You could spend as much time then going through it with the woman and it didn’t hold our clinic up or anything like that . . . It flowed quite well really, it didn’t cause us any problems at all.
Maternity services – site A, FG
Although some of the midwives at site B referred to how they occasionally forgot to issue the information to women, the fact that the researcher would notify/remind them about who met the eligibility criteria was helpful:
There was a couple of occasions I did forget to give it . . . but I found it all right giving out leaflets . . . It was good that she saw them when they were coming here for their clinic so it wasn’t a special visit that they had to make.
Maternity services – site B, FG
None of the midwives interviewed experienced any problems with women not wanting to participate. This, they believed, could be attributed in part to their personal introductions to the study, such as saying ‘we’ve got a study’ as opposed to ‘it’s a study’, thereby demonstrating their endorsement. Some professionals also considered that women were willing to take part as a result of the study’s general approach being ‘infant feeding rather than just breastfeeding’.
The process of identifying women who met the inclusion criteria at site B was more problematic because of the way information was stored on various hospital recording systems and because midwifery teams had different procedures: ‘each team does things differently, it’s not all standardised’. One staff member involved in helping to identify eligible women (via hospital systems) found the process to be acceptable but ‘quite time consuming’. There were also additional complications caused by staff rotation when new midwives were unaware of the study in advance of the researcher attending the clinic, despite their managers being aware of it.
Recruitment at site B was also more challenging as it needed to be staggered to prevent overburdening the IFHs. Midwives discussed the importance of making women aware that even if they expressed an interest in the study, not all women would be approached by the researcher, and participation might not be possible.
A further suggestion to improve the recruitment processes was to provide midwives with a ‘crib sheet’ that provided an overview of the study and the procedures involved.
One issue raised at site A related to privacy. Some of the midwives felt that a more private location than the waiting area of the clinic would have been more appropriate for discussing the study:
The only thing I would say is maybe having somewhere a bit more private to talk to them rather than getting all their details in the waiting room.
Maternity services – site A, FG
Social desirability bias
Self-reported ‘breastfeeding initiation’ from the 8-week questionnaire data and self-reported ‘any breastfeeding at 8 weeks’ data from the 8-week questionnaire plus health visitor data were cross-checked with IFH logs and qualitative evidence. We were able to triangulate data for 44 out of 49 intervention (90%) participants. There was no evidence of social desirability bias.
Feasibility and process outcomes for the intervention
Ability to recruit, train and engage current peer supporters to the new ABA infant-feeding helper role
In site A, researchers visited the peer support team to discuss the ABA intervention and recruit them to the new IFH role. All seven members of the peer support team agreed to attend the ABA intervention training day. Following the training day, the peer support team raised a number of uncertainties about taking part in the study. These mostly concerned additions to their existing workload and travel to a different part of the local authority where they did not usually work to undertake visits. Researchers attended a meeting with the peer supporters to discuss their concerns. Peer supporters were reassured that, although the IFH role was new, it had similarities to their existing role, and that ABA study participants would count as part of the targets that peer supporters work towards. Travel routes to the new area were also discussed. Following discussions, six out of the seven existing peer supporters volunteered to take on the new role as part of their job (leaving one peer supporter available if any of the usual care women approached the service for support).
At site B, areas were identified that met the demographics required by the ABA study, and peer supporters working in or close to these areas were asked to volunteer for the IFH role. Advertising was via a closed social media platform and was posted by the team’s supervisor. All peer supporters interested in taking part contacted the researcher directly, who then explained the study in more detail. The peer supporter supervisor supported the study and was also able to answer questions. All those who responded went on to complete the training and become IFHs (n = 7). One peer supporter who wanted to participate was pregnant at the time, and due to have her baby during the study. She was very keen to undertake the ABA training so that she would be ready to see women as soon as she felt able to after the birth of her baby.
All IFHs attended a full day’s ABA intervention training session (delivered over 2 half-days at site B) and continued with their role until the end of the intervention period. At site A, one IFH went on maternity leave towards the end of the intervention, and her participant were reallocated to another IFH. At site B, the IFH who was pregnant during the training period started to take ABA referrals when her baby was a few weeks old, and she completed four interventions. Another IFH had a baby during the intervention period, but planned and completed four interventions before giving birth; a further IFH with three young children took on a part-time job and had to stop taking participants as she became too busy, and one of her participants was transferred to another IFH before the antenatal meeting took place.
Infant-feeding helper views on ABA training
The IFHs across the two sites held varied views about the ABA training. IFHs at site A used terms such as ‘fine’, ‘good’ and ‘OK’ as general reflections, although several failed to see any differences between the ABA approach and the one they already used for supporting women: ‘because it’s what I do anyway, so couldn’t see any difference’. One described the training on ‘how to have a conversation’ as ‘patronising’. Some of the IFHs in site A reflected that the only distinctions between their previous role and that of an ABA helper were how they introduced themselves (as infant-feeding rather that breastfeeding helpers) and that they provided an antenatal contact. Although the genogram and leaflets were considered to be useful tools, the IFHs felt that the focus on identifying and raising awareness of available assets was already standard practice.
Some of the IFHs at site B reported how they had initially felt apprehensive about attending the training programme. As their usual practice was to offer support in an informal group setting, with other peer supporters on hand as needed, the idea of providing one-to-one support was daunting. However, following the training, the IFHs expressed positive views about the new approaches to engage and support mothers. The ABA intervention (and associated training), with its focus on individual, proactive mother-centred help, and relationship building, was notably different and valued:
It was all good, like [name] said the role playing, because the discussion around the mum-centred bit rather than being breastfeeding-centred, just trying to shift gear a little bit and have different mind-set about that and the importance of building . . . it was useful to have the handout about it and all the different pointers for things to go through, but I think the emphasis just being on building a relationship was useful.
IFH11 – site B, FG
Although IFHs at both sites referred to how the ABA intervention training had provided them with new knowledge about formula feeding, the perceived value of this new learning differed. For example, some considered the information to be an additional, useful skill to provide evidence-based care and to avoid being viewed as the ‘breastfeeding police’ and described how a more balanced ‘infant feeding’ approach could open up discussions about alternative feeding options (i.e. breastfeeding). From a counter perspective, other IFHs mentioned how the training had polarised opinions about the acceptability of mixed feeding, with some IFHs from both sites expressing discomfort about the principle of offering help for formula feeding:
I’ve never bottle fed my own son, so for me I learnt something when we did the training. I wouldn’t even know how to make up a bottle . . . because we are breastfeeding support so then to go in and offer the formula as well that was strange.
IFH1 – site A, interview
A few of the IFHs at site A also complained about the prescriptive nature of the training and how a focus on following a specific topic guide when engaging with women did not reflect the reality of everyday encounters. One trainee reported how this structured approach had undermined her confidence:
When we were doing that training it was that piece of paper that was given to you and you’ve got to . . . did you include this part in? Did you include that part in? Even though it was an ABA training but how important is it? . . . Because when you go and see a mum what’s important is discussing about feeding . . . using those words I couldn’t do it.
IFH5 – site A, FG
There were varied opinions about the use of role-play techniques, particularly at site B. Although observation of model interactions (provided by the facilitators) was helpful as a practice to aspire to, several IFHs expressed how they had been ‘dreading it [role-play]’. The threat of being observed and ‘tested’ in a public forum caused anxiety, and some did not consider it necessarily useful for skill development.
Others, despite their initial trepidations, considered the role-play exercises to have been a valuable technique for practising and modelling behaviours and responses. The opportunities to practise typical scenarios was reported to have helped the IFHs develop confidence in their redefined role. Some at site B had continued to use role-play post training with other peer supporters and family members:
Everyone hates role-playing and it is one of those things that you’ve just got to get on with, but it really did help being in those situations, and then we talked about it afterwards and it makes you realise actually that you can do it . . . once you’re put on the spot, but I think if you talk about them too much then you overthink it. I’m not very confident normally in doing one-on-one things so the role-play was definitely something that helped me with the interviews as well, that whole situation really.
IFH8 – site B, FG
Ability to deliver planned number of contacts at a time and location convenient for participants
Figure 3 shows the flow of participants through the intervention, and Table 14 reports IFHs’ ability to deliver the planned number of contacts.
FIGURE 3.
Participant engagement flow diagrams: (a) site A and (b) site B.
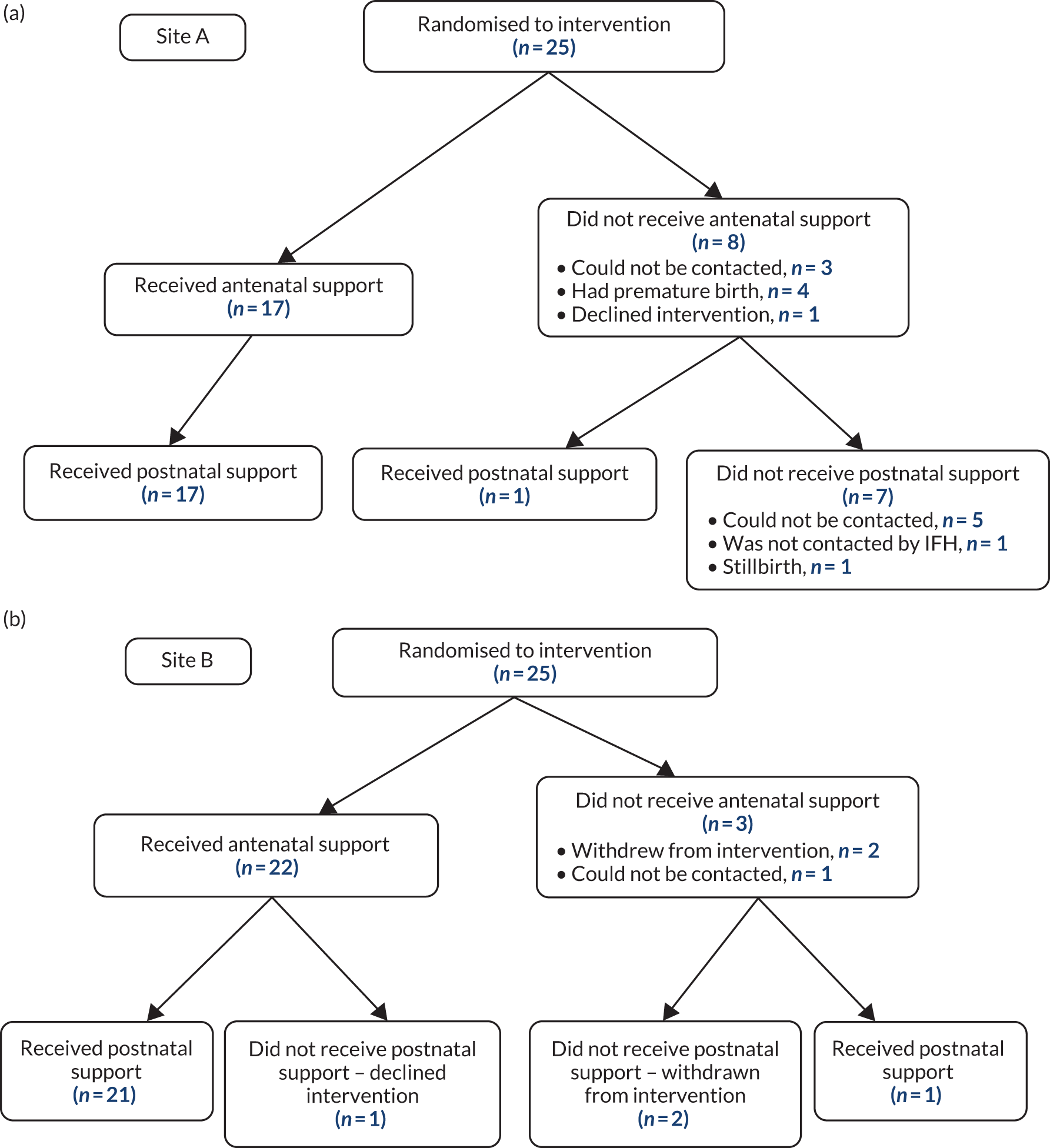
| Contact | Site A | Site B | Overall |
|---|---|---|---|
| Antenatal contact attempted, n/N (%) | 25/25 (100) | 25/25 (100) | 50/50 (100) |
| Antenatal visit completed, n/N (%) | 17/25a (68) | 22/25 (88) | 39/50 (78) |
| Postnatal contact attempted, n/N (%) | 24/25b (96) | 22/25 (88) | 46/50 (92) |
| Postnatal support provided, n/N (%) | 18/25 (72) | 22/25 (88) | 40/50 (80) |
| Contact attempted by IFH within 48 hours of birth, n/N (%) | 6/25 (24) | 18/25 (72) | 24/50 (48) |
| Number of days contact made/attempted by IFH in 2 weeks postnatally, mean (N) | 2.5 (23)c | 8.6 (25) | 5.7 (48) |
| Number of days two-way contact established in 2 weeks postnatally, mean (N) | 1.2 (23)c | 6.9 (25) | 4.1 (48) |
At site A, 17 of the 25 women randomised to the intervention group received an antenatal visit. Of these visits, 14 took place at the woman’s home, two took place in a coffee shop and two were conducted over the telephone at the woman’s request.
All three teenagers at site A allocated to the intervention group received an antenatal visit. Of the eight women who did not receive an antenatal visit, four gave birth prematurely before contact could be established, three could not be contacted by the IFHs and did not respond to messages, and one arranged to receive a home visit and then refused entry to the IFH. One woman who did not receive an antenatal visit at site A intended to feed her baby formula milk only, and the others wanted to breastfeed at least partially. Eighteen women at site A received some postnatal support from their IFH (counted as at least one two-way communication via text, telephone or face-to-face contact). Five women could not be contacted postnatally, and one woman was not contacted because of safety concerns. One woman experienced a stillbirth and was withdrawn from the study by the research team.
Beyond 2 weeks postnatally, 14 women at site A received some support from their IFH. Six women received text support at 3–5 months.
At site B, 22 of the 25 women randomised to the intervention group received an antenatal visit. Of these visits, 10 took place in a children’s centre, nine were in a coffee shop and three were at the woman’s home. Of the three women who did not receive a visit, one woman intended to feed her baby formula milk only and the other two wanted to breastfeed at least partially. Two women withdrew from the intervention (but not from the study) without meeting their IFH antenatally. Despite having telephone conversations with her IFH antenatally, the third woman did not meet antenatally with her IFH, and had one postnatal conversation in which she said that she had opted to formula feed her baby. The IFH continued to offer ongoing support postnatally with no response, so contact was discontinued. This participant is counted as receiving the offer of some postnatal support. One woman met with her IFH antenatally, but sent a text after her baby was born to say she had initiated formula feeding and no IFH help was required.
Twenty-two women at site B received some postnatal support in the first 2 weeks. IFHs contacted 17 women on the day of the birth or the following day. IFHs continued to contact 15 women beyond 2 weeks postnatally. At least 10 of these women were attending breastfeeding groups run by their IFHs. Many of these postnatal contacts took the form of text conversations of varying length; in some up to 20 texts were exchanged. Most of these conversations were initiated by the IFHs; there were very few occasions when women made unsolicited contact.
Views and experiences of organising antenatal contacts
The IFHs in site A were used to visiting women in their own homes, so they generally tried to arrange the antenatal meeting at this location. However, as they were working in an unfamiliar area this created travel difficulties, with comments such as it being ‘too far’ and ‘a nightmare’ to get to, and ‘you spend half your time travelling’. The geographical distance was also reported by one woman and her partner to have had an impact on how comfortable they felt about asking for visits postnatally, leading to conflicting feelings about the ABA intervention:
It’s meant to be like a service that you can call out and that you can have support, and if you think oh no I won’t call her because she’s going to need an hour on the bus then that’s really not fair on her, it’s not that bad and we’ll wait . . . it didn’t directly put us off, but you could see that it would.
Partner of P2 – intervention, site A
In site B, travel was not an issue as the IFHs were all seeing women from their local area. These IFHs did not normally visit women in their homes and were encouraged to hold the ABA antenatal meeting at their local children’s centres whenever possible. This had the advantage of familiarising women with the location of the breastfeeding group(s) and other services offered in the children’s centres. Several women commented on the convenience of this location:
Yeah, she dropped me a text and then we met up . . . at the [place] children’s centre. But we met up in another room down there and had a coffee and a chat and that was really good.
P20 – intervention, site B
Occasionally, antenatal meetings took place in coffee shops as these offered a mutually convenient location (site A) or time, for example at the weekend (site B). Being able to sit down and have a drink together helped create a relaxed atmosphere in a familiar and comfortable environment:
All of my meetings actually on the weekend, so we did have to meet in a café which that wasn’t a children’s centre or anywhere . . . I had four ladies altogether and I think three of them were still at work when we did the meeting, they hadn’t yet gone on maternity leave, so actually that suited them fine to do it on the weekend.
IFH8 – site B, interview
The organisational differences between IFHs at both sites meant that they had different approaches to arranging antenatal meetings with women. Site B IFHs worked locally to their own homes and were able to arrange visits flexibly to suit both themselves and the women (e.g. evenings or weekends when child care was available at home). Site A IFHs were restricted to providing support during working hours. Although this could create difficulties in co-ordinating meetings for mothers who were working full time, one woman was willing to take annual leave to meet her IFH:
She called me to say ‘I’m going to be part of the study, can I arrange to meet you?’, I was still working at the time so I had to arrange the day off.
P1 – site A, intervention
Making these arrangements was achieved through discussion between IFHs and women, with agreement on a time and place to suit both parties. However, the meeting often took place later than at the intended time of 32 weeks of pregnancy. This was sometimes because women were still at work, or had not been recruited until this stage of pregnancy:
We didn’t get the details in time for the 32 weeks, so I think a lot of ours were after that weren’t they from the [place] group? We didn’t know if that mattered or not in terms of the research timeline.
IFH11 – site B, FG
Despite numerous attempts, a few women were uncontactable during the antenatal period, causing frustration for IFHs:
It was sad that the women didn’t actually respond back, so it was very difficult to get hold of them, especially with the making the antenatal appointments and getting to know them as a person before they actually have the baby, that was quite difficult, they didn’t really engage.
IFH4 – site A, FG
Infant-feeding helpers’ and women’s experiences of maintaining contact throughout the intervention
Maintaining contact, and women’s willingness to engage in ongoing communication, was unproblematic for some IFHs who negotiated the frequency and mode (i.e. text, telephone) of contact with each woman. This could involve reducing contact as a result of knowing, for example, ‘she is doing really well’ (at breastfeeding) or providing additional help as it was felt to be ‘the best thing to do’:
My first lady, the one that went into hospital . . . we did text for quite a long time not necessarily about baby stuff but about her being ill and that, probably longer than the 2 or 3 weeks just because I thought we were getting on quite well . . . I probably messaged her more than I was supposed to but I just felt like that was the best thing to do really, I didn’t want to just abandon her when she was mid treatment, so I followed it through.
IFH8 – site B, interview
The IFHs also encouraged women to contact them and seek out help as needed:
I made it clear that they could text me whenever they wanted and I would get back to them as soon as I could.
IFH7 – site B, FG
Positive comments were made about having the schedule of planned contacts as, for example, ‘you could see what you had to do’. The smaller caseloads at site B meant that providing the agreed number of contacts was manageable, although one IFH reported difficulties associated with managing a work–life balance:
When you’ve got your own children it’s trying to fit it all in, and I think there might have been a few times where I missed by a few days.
IFH12 – site B, interview
The IFHs in site A found fitting ABA postnatal contacts around their busy working schedules more difficult. Home visits, which they would normally offer, were often not possible, and calls and texts might have to be done at weekends instead:
Yeah, it was time, so if you couldn’t manage to always get the ABA mums in the week that you had that weekend time to just focus on them.
IFH4 – site A, FG
Some IFHs in both sites expressed concerns that the frequency of proactive contacts could be construed as ‘hassling’, particularly when there was a lack of response, and they could be unsure how to proceed:
Yeah, a couple of times I did feel I was [hassling] . . . do I keep texting her or am I bothering her?
IFH8 – site B, FG
One IFH reported that although one mother had been engaged and responsive during the antenatal period, this had tapered off to ‘one-word answers’ in the postnatal period, leaving the helper with the feeling that the woman was ‘getting annoyed with me’. There were also challenges when women replied saying that they would recontact the IFH at a convenient time and then no further contact was received. A lack of response could result in the IFH reducing the number of contacts to give the mother ‘a bit of space’, suggestive of a sensitive, woman-based approach.
On the other hand, mothers seemed grateful for a proactive approach to contact, finding it reassuring that help was there if they needed it. Failure to respond to messages on their part was often as a result of the demands of caring for their new baby and not needing to ask for advice rather than because they did not want to be contacted. One woman articulated that receiving texts gave her ‘permission’ to continue seeking advice for longer than if she had had to instigate the contact:
If they hadn’t offered their help I’m not sure how good I would have been about asking for help . . . I suppose I kept feeling like I should be beyond the stage of needing their help . . . but with them asking how I was it gave me permission.
P4 – intervention, site A
The IFHs used various methods (telephone, text, e-mail) to maintain contact with women, with texts proving women’s most preferred and the most effective method of contact. This was mainly because it was ‘easy’ and women could respond in their own time and ‘have time to process it’:
I preferred that. I didn’t really have much energy to form proper sentences at that point . . . so texting was much better.
P27 – intervention, site B
The value of having met their IFH antenatally was also apparent in enabling women to feel confident about the postnatal contacts:
Once I had met her and I can put a face to the name, just gives you that reassurance again really that there’s somebody there . . . so then didn’t have a problem . . . if I need to text her then I would.
P22 – intervention, site B
One IFH recommended that further guidance should be given about frequency of contact and how to manage when women do not reply.
Fidelity of delivery and whether or not woman-centred care was provided
Fidelity of delivery from analysis of antenatal recordings
Overall, 22 antenatal meetings were recorded for fidelity purposes (site A, n = 3; site B, n = 19). Non-recording in both sites related to a recording device not being available or IFHs feeling uncomfortable about using one.
Infant-feeding helpers in site A gave added reasons for not recording such as deeming it inappropriate for women who were experiencing ‘too many social issues’ and that recording the conversation would be ‘intrusive’ as it could inhibit ‘natural’ conversations and women making sensitive disclosures:
I wouldn’t do it. Sometimes they tell you something personal . . .
IFH6 – site A, interview
Infant-feeding helpers in site B reported no problems with women consenting to their conversation being recorded, whereas there appeared to be more uncertainty about the process in site A:
Some of them weren’t happy about doing it, because they said that they didn’t know that there was recording involved.
IFH3 – site A, FG
Attitudes towards recording were very different between the two sites, with IFHs at site B being much more willing. Despite feeling ‘a bit nervous’ about the process to begin with, they agreed that as they gained in confidence it became easier:
As time goes by that you forget it’s on.
IFH7 – site B, FG
When asked about their experiences of recording the antenatal discussion, one IFH felt that it was too ‘clinical’, and for others it was a distraction, with one IFH reporting that she would have been more comfortable to have been ‘shadowed’ instead. Others expressed no difficulties, as long as the mother was happy to be recorded:
I didn’t have a problem at all, as long as the mums were aware of it and they were happy with me recording the conversation.
IFH2 – site A, interview
Description of the fidelity check sample
The scale developed by Hoddinott and Pill95 for assessing feeding intention based on spontaneous statements in the recordings indicated that the majority (13/18) of recorded antenatal visits included in the fidelity-check subsample were with ‘probable breast feeders’; the subsample also included two recordings of antenatal conversations with ‘committed breast feeders’ and three with ‘possible breast feeders’. None of the recordings used in this fidelity testing was with ‘probable formula feeders’ or ‘committed formula feeders’.
Delivery of staged components of the antenatal visit
Description of the intervention
The IFHs tended to include the intended description of the intervention to the mothers. In a minority of cases, the IFH did not make it clear that the ABA intervention support was inclusive of mothers who formula fed. Timeline descriptions were sometimes unclear and in two cases it was unclear whether or not the timeline had been shown to the mother.
Use of the genogram
Genograms were used in all the encounters; however, the extent to which the genogram was used to ‘facilitate a conversation about feeding’ varied. In some cases, the genogram was used as intended to stimulate a conversation about sources of help. It was also sometimes used effectively to sum up a long introductory conversation about family members and friends that had already occurred. The genogram was used in different ways that were at variance with the intended approach; in one of the site A recordings, it appeared to be used as a data collection tool, with the IFH asking questions and collecting information to take away for her own records.
Introduction to community-level assets
IFHs described using the assets leaflets in all their encounters. In two instances it was not clear that the leaflet had been given to the mother for her own use. IFHs varied considerably in the extent to which they offered to facilitate access to existing services or to which the conversation could be said to address mothers’ emotional and practical barriers to accessing services.
Delivery of core and non-core behaviour change techniques
The intervention was intended to deliver core and non-core BCTs, as set out in Table 1.
Core behaviour change techniques
The conversations tended to include instances of IFHs delivering social support (BCT 3.1) and restructuring the social environment (BCT 12.2). The extent to which these BCTs were used varied from helper to helper. For example, some helpers contributed to ‘restructuring the social environment’ by giving the mother the assets leaflet; this restructuring might be considered minimal. Others proactively arranged to accompany a mother to a group, a development that might be considered significant restructuring.
Non-core behaviour change techniques
Infant-feeding helpers did not tend to pursue conversations about the health benefits of breastfeeding or the risks of formula feeding (BCT 5.1). This approach was consistent with the intended inclusive tone. Some helpers did affirm mothers’ own offered understanding that breastfeeding was beneficial. The two antenatal recordings sampled from the site A encounters included an IFH-led health benefits conversation, including unsolicited information about the role of breastmilk in protecting the baby’s gut lining; although these conversations did address the non-core BCT 5.1, they were out of keeping with the intended woman-centred tone of the intervention. Some, but not all, conversations incorporated instructions about how to perform breastfeeding (BCT 4.1); often these were initiated by an enquiry from the mother. However, sometimes (and especially in one site A encounter) they included detailed unsought information about how to breastfeed. A few of the recordings included instances of IFHs delivering the ‘emotional support’ BCT (BCT 3.3); for example, the conversation covered helping the mother to think through how she would overcome emotional barriers to a decision to breastfeed. However, emotional support was not a consistent feature of the conversations. Verbal persuasion about the mother’s capability to breastfeed (BCT 15.1) was a less common feature of the conversations, although affirmational support tended to be given, affirming mothers’ own statements about the likelihood that they would manage. Mental rehearsal (BCT 15.2) was common and tended to cover a wide range of issues relating to early parenting rather than simply how the baby would be fed. There were examples of IFHs encouraging mothers to imagine or talk through how they would deal with breastfeeding outside the home, difficult conversations with relatives, lack of sleep, breastfeeding pain, frequent feeding, and feeling anxious and tired.
Delivery of a woman-centred tone
The site B IFHs tended to achieve a strong rapport with the mothers they supported. Especially strong rapport was associated with long conversations in which the IFH used the script loosely, covering the bases but jumping around. These encounters often included a long introductory conversation starting with ‘How is the pregnancy so far . . .’ and talking about work, illness, pregnancy tiredness and the mother’s wider family. There was often a lengthy period of chat before the conversation about infant feeding began; in some cases, this meant that many points had already been covered so that the focused conversation was used to recap the earlier discussion. These conversations were marked by mutual sharing of stories and experiences. By contrast, ‘rapport’ achieved by the two site A IFHs was notably less strong. There seemed to be a professional distance between the helper and the mother and the IFH seemed to be following a script and offering a service.
In all except one of the recordings, inclusivity of mothers who were formula feeding was indicated. However, this inclusivity should be considered in relation to the fact that all mothers intended to at least try to breastfeed. Active listening skills varied and were generally good among site B IFHs. However, even when there was good rapport, there were missed opportunities to pick up on women’s concerns. A woman-centred rather than breastfeeding-centred approach was apparent in the majority of the recordings. There were overlaps between good rapport, inclusivity, active listening and taking a woman-centred approach.
Fidelity of delivery: analysis of behaviour change techniques discussed in qualitative interviews
All qualitative interviews with intervention participants (n = 21) were checked for evidence of BCTs. A summary of the BCTs reported in qualitative interviews with women is presented in Table 15. The core BCTs were those most frequently used, with 20 out of 21 participants demonstrating evidence of ‘restructuring the social environment’ (BCT 12.2); many of these were related to the use of the genogram in the antenatal meeting:
They did the . . . diagram of support to show you and who you’ve got, so your parents, people that are around you, friends, and then the groups you can go to, and the stuff like that.
P2 – intervention, site A
It helped me think about the pathways in my head a little bit better in terms of ‘Oh yeah I forgot about that person’. Just by going through the process of drawing it . . . that process of seeing it laid out, my network of support as it were.
P20 – intervention, site B
Some talked about the IFH inviting them to breastfeeding groups:
Yeah, different groups, yeah. She said if I wanted to she would meet me at them and to come with me, yeah she went through all the different groups and stuff.
P21 – intervention, site B
| BCT number | BCT | Number of women reporting this BCT (n = 21) |
|---|---|---|
| 1 | Goals and planning | |
| 1.2 | Problem-solving | 8 |
| 1.3 | Goal-setting (outcome) | 0 |
| 1.7 | Review outcome goal(s) | 0 |
| 2 | Feedback and monitoring | |
| 2.7 | Feedback on outcome(s) of behaviour | 1 |
| 3 | Social support | |
| 3.1 | Social support (unspecified) | 18 |
| 3.2 | Social support (practical) | 12 |
| 3.3 | Social support (emotional) | 6 |
| 4 | Shaping knowledge | |
| 4.1 | Instruction on how to perform a behaviour | 3 |
| 5 | Natural consequences | |
| 5.1 | Information about health consequences | 2 |
| 6 | Comparison of behaviour | |
| 6.1 | Demonstration of the behaviour | 1 |
| 8 | Repetition and substitution | |
| 8.1 | Behavioural practice/rehearsal | 0 |
| 12 | Antecedents | |
| 12.2 | Restructuring the social environment | 20 |
| 13 | Identity | |
| 13.1 | Identification of self as role model | 0 |
| 15 | Self-belief | |
| 15.1 | Verbal persuasion about capability | 7 |
| 15.2 | Mental rehearsal of successful performance | 0 |
Evidence of core BCT social support (unspecified) (BCT 3.1) was also widespread, with 18 participants demonstrating that they felt reassured by knowing where to go for appropriate advice and support:
There was always the opportunity for somebody to come and visit me if I wanted them to, or a phone or a text whenever I needed or wanted.
P6 – intervention, site A
I had someone to ask what this cluster feeding was and had the reassurance that you don’t run out of milk.
P19 – intervention, site B
Social support was also demonstrated by women reporting positive feedback and encouragement from their IFH:
I would say fed him X amount of times and it’s tiring, I was so tired or something like that, and [she] would be going you’re doing a great job, and keep going, just support in just telling me I’m doing really well and keep going.
P22 – intervention, site B
The other non-core social support-related BCTs were also well represented, with 12 women demonstrating social support (practical) (BCT 3.2) and six having examples of social support (emotional) (BCT 3.3). Most examples of practical social support (BCT 3.2) concerned receiving appropriate advice from IFHs during telephone calls or in text messages, which women found particularly helpful for specific problems such as mastitis or the frequency of breastfeeding. Examples of emotional social support demonstrated the value of the IFHs, with women saying that they found them ‘reassuring’, ‘kind’ and ‘supportive’:
They helped me a lot, they give me a lot of positive energy really. Whenever she come she makes me really happy, she makes me really good.
P7 – intervention, site A
Seven participants had examples of verbal persuasion about capability (BCT 15.1) and eight had examples of problem-solving (BCT 1.2).
Acceptability of the ABA intervention to women, infant-feeding helpers and maternity services
Overall experience
The majority of women from the intervention group spoke positively about their experience of the ABA intervention, saying that their involvement had been a ‘nice experience’ and that they had been ‘happy to take part’. Many women reported that the intervention had helped them and, for some, their IFH had been key to them enabling and maintaining breastfeeding:
I genuinely do believe if it wasn’t for the study and for [helper] and even if it was just introducing me to the breast friends group I don’t think I would have got this far and certainly not breastfeeding exclusively this far, and now we’ve got this far I don’t want to stop.
P19 – intervention, site B
I would just really say thank you to ABA study about their really great help and support. It was really nice experience for me, I’ve learnt a lot of things from ABA about breastfeeding, and I would recommend it anyone.
P7 – intervention, site A
This positive feeling was reflected by the IFHs in site B, who were generally very excited about the study and eager to get involved. After training, they set up a group for themselves on a social media platform so that they could share their experiences. The following observation sums up their experiences:
So the big elation when [we] first started meeting antenatally, you’re all really excited about it, and you’re all planning where [we’re] going to meet, and meeting these women, and [we] were so amazed by the diversity of the women we were meeting, and that was really powerful, and how different they were to women we were meeting in our ordinary groups and those sort of things, they were really different, and you found that interesting. And then when the first ones were born that’s really exciting and there’s all this wonderful excitement bubble about babies coming, ‘our babies are being born’, and then if some of them carried on breastfeeding that was properly amazing, and then they came to groups and that was amazing. But then when the women found it was difficult or if anybody became mixed feeding or went to formula there was definitely disappointment, some . . . found it really hard.
IFH manager – site B, FG
On the other hand, the IFHs at site A were less enthusiastic. They found ABA more restrictive than their usual practice as they saw women less often postnatally and found it difficult to rely on telephone calls and texts instead. Despite this, they saw the antenatal meeting with women as a positive addition:
The way it works at the moment the support is when they need it, so it was knowing that it was there beforehand I think which I think does make a difference.
IFH1 – site A, interview
Infant-feeding helpers in both sites agreed that the ABA intervention would be good to adopt in practice and could see its value as a ‘good service’, especially for women in more socially deprived areas:
I definitely think it is something that should be made the norm . . . I think it’s all good in terms of the breastfeeding, if the mum is getting the information it can’t be a bad thing, so no I don’t think there’s anything I disagreed with, no.
IFH1 – site A, interview
Women similarly reported seeing the worth of the ABA intervention even when they had not needed much support from their IFH (e.g. because they had ceased breastfeeding early or had not had any feeding issues):
I didn’t make use of it as well as I could have, but no there was always the opportunity for somebody to come and visit me if I wanted them to, or a phone or a text whenever I needed or wanted.
P6 – intervention, site A
Women typically recalled their antenatal meetings with their IFHs as a relaxed discussion and they welcomed the opportunity to have a ‘chat’ about infant feeding. The ‘face-to-face’ element of the antenatal meeting was considered important for women meet and develop a relationship with the IFH, and to encourage them to continue contact with the IFH after their baby was born:
But just relieved once I had met her and I can put a face to the name, just gives you that reassurance again really that there’s somebody there, you know who they are and she was really friendly and approachable as well, so it’s nice, then I wouldn’t feel like I’m texting her thinking what’s she going to be like? She was really friendly, really approachable, so then didn’t have a problem going away and thinking if I need to text her then I would.
P22 – intervention, site B
Most women found the antenatal meeting useful, and a positive experience when it worked well – ‘it was really a good experience at that time’ – and found that it could stimulate an interesting conversation:
Yeah it was good. I didn’t think I had so many thoughts around breastfeeding as I did when she was starting asking questions around it, I didn’t think I had really thought about it as much as I obviously had, which was quite good.
P16 – intervention, site B
Although the meeting with their IFH resulted in some women ‘feeling a lot more positive’ about breastfeeding, one woman (who had been intending to formula feed) referred to how it had helped her to reconsider her feeding decision:
It made me rethink about breastfeeding . . . but having that chat with her it did rejog my memory there is another option sort of thing, yeah it did, it definitely.
P6 – intervention, site A
The antenatal meeting was less interesting to women when it seemed a fact-giving exercise, or when women knew how they wanted to feed their baby and already felt well informed:
Yeah, so I think it was helpful, and it was nice to meet her, and nice to have the discussions and things, but yeah I’m not . . . I think I already knew that, I already knew what help I could have.
P1 – intervention, site A
Overall, providers of maternity services were positive about the ABA intervention. However, there was little evidence that staff understood the differences between the usual peer support and that provided by the IFHs during the study. Despite this, they agreed that such support was universally needed and should be available to all mothers, especially as staff recognised that their service was ‘beleaguered’ and that the amount of time for postnatal visiting was limited. As a result it was helpful for them to know that women were being supported:
I think it would help us as well knowing that actually they are being supported that if we haven’t got that time necessarily that they are still being supported.
Maternity services – site A, FG
Use of and views on the assets leaflet
The majority of women provided positive comments about the acceptability of the assets leaflet.
Women often referred to how they were aware of some, but not all, of the resources listed, and how the leaflet had offered new insights into the range of available support networks. One woman reflected that although she had already been contemplating accessing local groups, the assets leaflet helped raise her awareness about where and when these activities were provided, and she particularly valued the offer from the IFH to accompany her:
She said if I wanted to she would meet me at them and to come with me. She went through all the different groups and stuff . . . so that was helpful.
P21 – intervention, site B
The only negative comment was about the abundance of printed information that pregnant women/new mothers receive, with the assets leaflet being just one more document to keep track of:
Not really, no, haven’t really used it [assets leaflet]. Just because you get given that many different things, different sheets of paper, you’re like if I see another piece of paper again . . .
P8 – intervention, site A
Several women reported that they used the resources detailed in the assets leaflet (during the antenatal and/or postnatal period), such as attending breastfeeding groups, accessing websites or joining Facebook (Facebook, Inc., Menlo Park, CA, USA) groups.
One woman stated that she kept the leaflet ‘to hand’ for ease of access, and explained how it had provided an invaluable means to seek out information and answers:
Yes I have, it’s somewhere, I think it’s in the changing bag actually, I try to keep it to hand, and yeah just spent probably many a late night at first going through it looking on websites, is this normal?
P22 – intervention, site B
The IFHs also confirmed women’s use of the asset leaflet, including accessing antenatal group sessions, or attendance at the breastfeeding groups:
When I rang her . . . she says that she’s been to [a group] ‘It’s local to me and I’ve been to that one and it’s quite good and I’ll go again every week.’
IFH2 –site A, interview
Although some of the women did not use any of the resources provided, this was often because they did not require additional help, rather than because of the quality or availability of support.
Some women referred to the value of having this information available ‘should they need it’:
I knew that if I needed help I could access it, so I suppose that was in the back of my mind, it was like well at least it’s there.
P1 – intervention, site A
Views on the genogram
Women provided mixed views on the acceptability of the genogram. From a positive perspective, some found the genogram to be a useful exercise as it led them to recognise how much support was available to them:
It helped to see all the names as well, all the lots of people, I didn’t think I had lots of people and I was like oh I do.
P24 – intervention, site B
Some mothers described the process of completing the genogram as ‘reassuring’ and said that it reminded them how fortunate they were to have available support. It could also enable new mothers to feel ‘not so alone’. Women referred to how the genogram had stimulated positive reflections by encouraging them to appreciate the quality of support available to them:
She did a really useful thing actually, which was we did a map of people in my life that I could ask any help for feeding advice and things like that . . . and just it just made me rethink and evaluate how much I appreciate having some family closer by.
P23 – intervention, site B
One mother divulged that, although family bereavements and relocations had left her feeling isolated, the genogram had helped her to realise the extent of her networks:
I saw all those names around me I thought I haven’t got no one, they may not be my family, but I’ve actually got people, and I wouldn’t have really thought of that before.
P25 – intervention, site B
The genogram prompted some women to consider how their family and friends had influenced their infant-feeding decisions, as well as how it could stimulate conversations and ‘interesting’ insights into different breastfeeding experiences:
I found it interesting that the majority of my friends of a similar age have found breastfeeding really very difficult in terms of either pain or other people have had milk supply issues, but the majority of people of my mum’s generation seem to have found it really very easy.
P4 – intervention, site A
Some mothers felt that the genogram was redundant as they were already aware of available support: ‘we knew what we had already’.
Critical comments about the genogram were particularly evident in site A, where IFHs felt that whereas they normally covered this sort of information with women, doing an exercise on paper could be a ‘barrier’ to forming a relationship with them:
Some way down the line she will say I was breastfed or partner was breastfed, it will just automatically come in anyway . . . So it wasn’t anything new that we were doing, but it’s just this time we had to put it on a piece of paper.
IFH5 – site A, FG
Another IFH felt concerned about the tool’s utility, saying that it might be appropriate for ‘certain’ women only, as it could emphasise the lack of available social support for those from specific demographic populations, such as a ’17-year-old girl with very little support’. IFHs could see the value of using their judgement about when to use the genogram with individual woman rather than using it with everyone.
Some mothers stated that completing the genogram had not been particularly helpful, perhaps because they did not have ‘anyone close to me that had breastfed’, or that the conversations they had gone on to have with others might not have been particularly useful had those others had divergent experiences of breastfeeding:
She [sister] said from the beginning it would be about half an hour to breastfeed him, and then they would be fed within 10/15 minutes, and I thought great, this is brilliant, but obviously that didn’t happen with me.
P5 – intervention, site A
Although most IFHs completed a genogram with women, one IFH considered that it had taken her some time to appreciate its purpose and value (‘took a while to get my head around it’) and had used it more successfully with women she had supported latterly:
I found that I did sort of refer back to it in my head a little bit like you said . . . and then I think for them again especially the second, third and fourth ladies it just reaffirmed the support that they had.
IFH9 – site B, FG
Site A IFHs reported that the completed genogram did not specifically feature during subsequent helper–mother interactions:
No, we didn’t refer back to it, but it may have come up in a conversation, but we would never actually have gone with the physical genogram.
IFH3 – site A, FG
Additionally, some women did not want to keep their completed diagram:
I did use it but I found that I didn’t actually leave it with them, they were like, ‘It’s alright you can keep it,’ they were like, ‘We don’t want to keep a copy of it,’ which I knew we were supposed to leave it with them but they didn’t actually want to keep it for the reflection, they were quite happy for me to take it with me.
IFH1 – site A, interview
The lack of awareness about how the continued use of the genogram could have facilitated women’s access to wider support may well reflect a training need, rather than the utility of this tool per se:
I never thought of that [using the genogram in subsequent interactions to prompt women’s use of personal assets] to be honest, but I suppose I would think they would have come to you after they had been to those support points.
IFH1 – site A, interview
However, although women confirmed that they did not subsequently use the physical copy of the genogram, it is important to highlight that they often found the initial process of identifying available support networks to have been sufficient, and many referred to having retained the information mentally following the exercise:
I haven’t really [referred back to the genogram]. I think it’s put it in my mind once I seen it, but I don’t need to look back on the paper, obviously knew who I had and just having contact with [helper] and my sister-in-law, and obviously my partner has been here all along.
P26 – intervention, site B
Some of the IFHs (site B only) stated that although they had not used the physical copy of the genogram, they still used the information contained as prompts during helper–mother contacts. One IFH reported how she had regularly referred to the named individuals in a woman’s genogram during their communications. She considered that this helped to demonstrate her personal interest and to feel more involved in a woman’s life:
I would refer back to them and say is your sister [name] still popping round? . . . It certainly helped me feel like I was a little bit more involved in their actual lives rather than just them just being numbers on a page really.
IFH8 – site B, FG
Potential cases of intervention contamination in the usual care group
Overall, there was no clear evidence of contamination in the study. Although there were some indications of women sharing resources and learning with others (either those in the usual care group or other expectant/postnatal women), this is inevitable and to be expected within a community of mothers. However, as the key components of the ABA intervention were an antenatal contact and targeted, intensive one-to-one tailored support in the early postnatal period, these were non-transferable elements:
When I was pregnant as well I mentioned it [ABA study] to a few people, and . . . they just want to know what I’m doing sort of thing, yeah, and offer some support, and a lot of people said that’s really well needed after pregnancy . . . and I thought it was a really good idea actually.
P6 – intervention, site A
A few mothers (and, on one occasion, the woman’s partner) referred to how they had passed on information (e.g. about the breastfeeding groups), shared the assets leaflet and discussed the value of the genogram, but with no clear evidence of take-up. Others referred to how discussions with friends who were either pregnant or new mothers highlighted the value of and need for this supplementary support, rather than sharing specific details that would facilitate breastfeeding:
I know I suggested it [breastfeeding group(s)] to quite a few of the girls in the NCT group because I knew about it and they didn’t know about it, especially one that was having quite a few troubles.
P16 – intervention, site B
On discharge from hospital, women at site A received information on local breastfeeding groups in a leaflet included in the discharge packs. Women at site B were signposted to the local council website to find out about local breastfeeding groups, and as a result some of the IFHs at site B considered that mothers ‘may well have come anyway’. However, this was not supported by women at site B, many of whom said that they would not have known about the group had it not been for their IFH telling them about it.
Some women referred to ‘mentioning’ or discussing their participation in the ABA study with health professionals who either were aware or were not aware of their involvement: ‘I’ve told them about it and they were very interested, but they didn’t seem to know about it before’. During interviews, health professionals gave mixed responses, either being unaware that women were involved in the study or being vague about women’s involvement.
Outcomes for a definitive trial
Outcome data for any breastfeeding at 8 weeks and 6 months are presented in Table 16. For data by site, see Appendix 13.
| Breastfeeding outcome | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |||
|---|---|---|---|---|---|---|
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Any breastfeeding at 8 weeks | 23/41 | 56.1 (39.7 to 71.5) | 22/47 | 46.8 (32.1 to 61.9) | 45/88 | 51.1 (40.2 to 61.9) |
| Any breastfeeding at 8 weeks (including health visitor data) | 24/48 | 50.0 (35.2 to 64.8) | 22/50 | 44.0 (30.0 to 58.7) | 46/98 | 46.9 (36.8 to 57.3) |
| Any breastfeeding at 6 months | 18/39 | 46.2 (30.1 to 62.8) | 16/44 | 36.4 (22.4 to 52.2) | 34/83 | 41.0 (30.3 to 52.3) |
Primary outcome: any breastfeeding at 8 weeks
For the primary outcome of any compared with no breastfeeding at 8 weeks, questionnaire data were collected from 88 out of the 103 participants (85.4%, 95% CI 77.1% to 91.6%). Additional data from health visitors brought the completeness of data on the primary outcome to 95.1% (95% CI 89.0% to 98.4%).
Any breastfeeding at 8 weeks was self-reported by 51.1% of women overall (95% CI 40.2% to 61.9%), with a higher percentage in the intervention group than in the usual care group both overall [56.1% (95% CI 39.7% to 71.5%) vs. 46.8% (95% CI 32.1% to 61.9%)] and by site [site A intervention 42.1% (95% CI 20.3% to 66.5%) vs. usual care 39.1% (95% CI 19.7% to 61.5%); site B intervention 68.2% (95% CI 45.1% to 86.1%) vs. usual care 54.2% (95% CI 32.8 to 74.4%)].
Including the additional data from health visitors, rates of any breastfeeding at 8 weeks were lower, indicating a higher rate of questionnaire completion at 8 weeks among women who were breastfeeding. Overall, 46.9% of women were breastfeeding at 8 weeks (95% CI 36.8% to 57.3%). Rates of any breastfeeding still favoured the intervention group both overall [50.0% (95% CI 35.2% to 64.8%) vs. 44.0% (95% CI 30.0% to 58.7%)] and by site [site A, 39.1% (95% CI 19.7% to 61.5%) vs. 34.6% (95% CI 17.2% to 55.7%); site B, 60.0% (95% CI 38.7% to 78.9%) vs. 54.2% (95% CI 32.8% to 74.4%)]. The ICC for any breastfeeding at 8 weeks was 0.039 (95% CI 0.00 to 0.97), indicating considerable clustering by IFH.
Secondary outcomes
Any breastfeeding at 6 months
The ‘any breastfeeding at 6 months’ outcome was obtained from 83 out of 103 participants (80.6%). Overall, 41% of women (95% CI 30.3% to 52.3%) self-reported any breastfeeding on the 6-month questionnaire, with higher rates in the intervention group than in the usual care group [46.2% (95% CI 30.1% to 62.8%) compared with 36.4% (95% CI 22.4% to 52.2%)]. By site, any breastfeeding at 6 months was lower in the intervention group than in the usual care group at site A [29.4% (95% CI 10.35% to 56.0%) compared with 40.0% (95% CI 19.1% to 63.9%)], but higher in the intervention group than in the usual care group at site B [59.1% (95% CI 36.4% to 79.3%) compared with 33.3% (95% CI 15.6% to 55.3%)]. In the control group at site A, the percentage of responders reporting breastfeeding at 6 months appears higher than at 8 weeks. This is probably because of the difference in response rate, with data obtained for 26 participants at 8 weeks and only 20 at 6 months; the number of women reporting breastfeeding decreased from nine to eight from 8 weeks to 6 months.
Exclusive breastfeeding at 8 weeks and 6 months
Outcome data for exclusive breastfeeding at 8 weeks and 6 months are shown in Table 17. For data by site, see Appendix 14.
| Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | ||||
|---|---|---|---|---|---|---|
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Exclusive breastfeeding at 6–8 weeks (last 24 hours) | 16/41 | 39.0 (24.2 to 55.5) | 17/47 | 36.2 (22.7 to 51.5) | 33/88 | 37.5 (27.4 to 48.5) |
| Exclusive breastfeeding at 6–8 weeks (since birth) | 11/41 | 26.8 (14.2 to 42.9) | 12/47 | 25.5 (13.9 to 40.3) | 23/88 | 26.1 (17.3 to 36.6) |
| Exclusive breastfeeding at 6 months (last 24 hours definition) | 12/39 | 30.8 (17.0 to 47.6) | 13/44 | 29.5 (16.8 to 45.2) | 25/83 | 30.1 (20.5 to 41.2) |
| Exclusive breastfeeding at 6 months (no other food/drink ever definition) | 3/39 | 7.7 (1.6 to 20.9) | 2/44 | 4.5 (0.5 to 20.9) | 5/83 | 6.0 (2.0 to 13.5) |
The exclusive breastfeeding at 6–8 weeks outcome was obtained from 88 out of 103 participants (85.4%). Two definitions of exclusive breastfeeding are presented here: ‘last 24 hours’ (WHO definition)97 and ‘since birth’.
Exclusive breastfeeding at 8 weeks (last 24 hours) was self-reported by over one-third of women (37.5%, 95% CI 27.4% to 48.5%), with a slightly higher rate in the intervention group (39.0%, 95% CI 24.2% to 55.5%) than in the usual care group (36.2%, 95% CI 22.7% to 51.5%). By site, exclusive breastfeeding at 6–8 weeks (last 24 hours) was lower in the intervention group than in the usual care group at site A [26.3% (95% CI 9.1% to 51.2%) compared with 30.4% (95% CI 13.2% to 52.9%)], but higher in the intervention group than in the usual care group at site B [50.0% (95% CI 28.2% to 71.8%) compared with 41.7% (95% CI 22.1% to 63.4%)].
Exclusive breastfeeding at 8 weeks (since birth) was self-reported by just over one-quarter of women (26.1%, 95% CI 17.3% to 36.6%), with a slightly higher rate in the intervention group (26.8%, 95% CI 14.2% to 42.9%) than in the usual care group (25.5%, 95% CI 13.9% to 40.3%). By site, exclusive breastfeeding at 6–8 weeks (since birth) was higher in the intervention group than in the usual care group at site A [21.1% (95% CI 6.1% to 45.6%) compared with 13.0% (95% CI 2.8% to 33.6%)], but lower in the intervention group than in the usual care group at site B [31.8% (95% CI 13.9% to 54.9%) compared with 37.5% (95% CI 18.8% to 59.4%)].
Data for the ‘exclusive breastfeeding at 6 months’ outcome were obtained from 83 out of 103 participants (80.6%).
Exclusive breastfeeding at 6 months (last 24 hours) was self-reported by 30.1% of women (95% CI 20.5% to 41.2%). There were only very small differences between the intervention and usual care groups both overall [30.8% (95% CI 17.0% to 47.6%) vs. 29.5% (95% CI 16.8% to 45.2%)] and by site [site A, 29.4% (95% CI 10.3% to 56.0%) vs. 30.0% (95% CI 11.9% to 54.3%); site B, 31.8% (95% CI 13.9% to 54.9%) vs. 29.2% (95% CI 12.6% to 51.1%)].
Exclusive breastfeeding at 6 months (since birth) was self-reported by 6% of women (95% CI 2.0% to 13.5%), and was higher in the intervention group (7.7%, 95% CI 1.6% to 20.9%) than in the usual care group (4.5%, 95% CI 0.5% to 20.9%). At site A, exclusive breastfeeding at 6 months (since birth) was higher in the intervention group (11.8%, 95% CI 1.5% to 36.4%) than the usual care group (zero). At site B, exclusive breastfeeding at 6 months (since birth) was lower in the intervention group (4.5%, 95% CI 0.1% to 22.8%) than in the usual care group (8.3%, 95% CI 1.0% to 27.0%).
Breastfeeding initiation and feeding status at 3 days postnatally
Outcome data for breastfeeding initiation (collected at 2–3 days and at 8 weeks) and feeding status at 3 days postnatally are shown in Table 18. For data by site, see Appendix 15.
| Breastfeeding initiation and feeding status | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |||
|---|---|---|---|---|---|---|
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Breastfeeding initiation (from 8-week questionnaire) | 35/41 | 85.4 (70.8 to 94.4) | 36/47 | 76.6 (62.0 to 87.7) | 71/88 | 80.7 (70.9 to 88.3) |
| Breastfeeding initiation (from 3-day text data) | 30/31 | 96.8 (83.3 to 99.9) | 32/39 | 82.1 (66.5 to 92.5) | 62/70 | 88.6 (78.7 to 94.9) |
| Feeding since birth at 3 days (from 3-day text data) (%) | ||||||
| Only formula milk | 1/31 | 3.2 (0.1 to 16.7) | 7/39 | 17.9 (7.5 to 33.5) | 8/70 | 11.4 (5.1 to 21.3) |
| Only breastmilk | 22/31 | 71.0 (52.0 to 85.8) | 14/39 | 35.9 (21.2 to 52.8) | 36/70 | 51.4 (39.2 to 63.6) |
| Mixed feeding | 8/31 | 25.8 (11.9 to 44.6) | 18/39 | 46.2 (30.1 to 62.8) | 26/70 | 37.1 (25.9 to 49.5) |
Breastfeeding initiation data were collected via postnatal text from 70 out of 103 participants (68%). In addition, initiation data were collected from 88 of the 103 participants (85.4%) using the 8-week questionnaire.
From postnatal text data, breastfeeding initiation (baby had received some breastmilk since birth) was reported by 88.6% of respondents overall (95% CI 78.7% to 94.9%), with a higher rate in the intervention group than in the usual care group both overall [96.8% (95% CI 83.3% to 99.9%) vs. 82.1% (95% CI 66.5% to 92.5%)] and by site [site A, 92.9% (95% CI 66.1% to 99.8%) vs. 71.4% (95% CI 47.8% to 88.7%); site B, 100% vs. 94.4% (95% CI 72.7% to 99.9%)]. Just over half of the women reported that their baby had received only breastmilk since birth (51.4%, 95% CI 39.2% to 63.6%). This was higher in the intervention group than in the usual care group, both overall [71.0% (95% CI 52.05% to 85.8%) compared with 35.9% (95% CI 21.2% to 52.8%)] and by site [site A, 57.1% (95% CI 28.9% to 82.3%) compared with 33.3% (95% CI 14.6% to 57.0%); site B, 82.4% (95% CI 56.6% to 96.2%) compared with 38.9% (95% CI 17.3% to 64.3%)]. Feeding their baby only formula milk since birth was reported by 11.4% (95% CI 5.1% to 21.3%) of women via postnatal text. This was lower in the intervention group than in the usual care group both overall [3.2% (95% CI 0.1% to 16.7%) vs. 17.9% (95% CI 7.5% to 33.5%)] and by site [site A, 7.1% (95% CI 1.8% to 33.9%) vs. 28.6% (95% CI 11.3% to 52.2%); site B, 0% vs. 5.6% (95% CI 0.1% to 27.3%)]. Mixed feeding since birth was reported by 37.1% of participants via postnatal text.
From 8-week questionnaire data, rates of breastfeeding initiation (baby had ever been given breastmilk or had been put to the breast, even if this was only once) were lower overall than rates from the postnatal text data, with 80.7% of respondents reporting initiation (95% CI 70.9% to 88.3%). Again, initiation rates favoured the intervention group both overall [85.4% (95% CI 70.8% to 94.4) vs. 76.6% (95% CI 62.0% to 87.7%)] and by site [site A, 78.9% (95% CI 54.4% to 93.9%) vs. 69.6% (95% CI 47.1% to 86.87); site B, 90.9% (95% CI 70.8% to 98.9%) vs. 83.3% (95% CI 62.6% to 95.3%)].
The lower rate of breastfeeding initiation reported at 8 weeks than that reported via the postnatal text could be related to the lower response rate to the postnatal text among formula feeders (see Table 13).
A cross-check of individual participant responses to both the postnatal text and the 8-week questionnaire revealed two women who reported solely formula feeding at 3 days postnatally, yet who indicated breastfeeding initiation on the 8-week questionnaire. This could be because of late initiation of breastfeeding, or difference in the wording of questions at the different time points.
Ceased breastfeeding at 8 weeks and 6 months (of those who had initiated breastfeeding)
For outcome data for cessation of breastfeeding at 8 weeks and at 6 months, see Appendix 16.
Over one-third of women who had self-reported breastfeeding initiation in the 8-week questionnaire had stopped by 8 weeks (36.6%, 95% CI 25.5% to 48.9%), with a lower rate in the intervention group (34.3%, 95% CI 19.1% to 52.2%) than in the usual care group (38.9%, 95% CI 23.1% to 56.5%). At site A, there was a higher rate in the intervention group (46.7%, 95% CI 21.3% to 73.4%) than in the usual care group (43.8%, 95% CI 19.8% to 70.1%). Cessation rates were lower at site B than at site A, and were lower in the intervention group (25.0%, 95% CI 8.7% to 49.1%) than in the usual care group (35.0%, 95% CI 15.4% to 59.2%).
Over half of the women who had self-reported breastfeeding initiation on questionnaire had stopped by 6 months (53.4%, 95% CI 41.4% to 65.2%), with a lower rate in the intervention group (51.4%, 95% CI 34.4% to 68.1%) than in the usual care group (55.6%, 95% CI 38.1% to 72.1%). There were higher rates of cessation at site A than at site B. At site A, there was a higher rate of cessation in the intervention group (66.7%, 95% CI 38.4% to 88.2%) than in the usual care group (50.0%, 95% CI 24.7% to 75.3%). Conversely, at site B there was a lower rate of cessation in the intervention group (40.9%, 95% CI 20.7% to 63.6%) than in the usual care group (60.0%, 95% CI 36.1% to 80.9%).
Duration of any breastfeeding (including those still breastfeeding)
Outcome data for duration of any breastfeeding are shown in Table 19.
| Duration of breastfeeding (days) including those still breastfeeding | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |
| n | 16 | 17 | 33 | 22 | 20 | 42 | 38 | 37 | 75 |
| Mean (95% CI) | 94.5 (55.0 to 134.0) | 96.4 (52.9 to 139.9) | 95.5 (67.7 to 123.3) | 122.4 (87.4 to 157.5) | 110.2 (75.9 to 144.5) | 116.6 (93.0 to 140.2) | 110.7 (85.3 to 136.1) | 103.9 (77.9 to 129.8) | 107.3 (89.6 to 125.1) |
The mean duration of any breastfeeding (including those still breastfeeding) was 107.3 days (95% CI 89.6 to 125.1 days). Overall, the mean duration was higher in the intervention [110.7 days (95% CI 85.3 to 136.1 days)] than in the usual care group [103.9 days (95% CI 77.9 to 129.8 days)]. At site B, the mean duration was also higher in the intervention [122.4 days (95% CI 87.4 to 157.5 days)] than in the usual care group [110.2 days (95% CI 75.9 to 144.5 days)]. However, at site A, the mean duration was higher in the usual care group [96.4 days (95% CI 52.9 to 139.9 days)] than in the intervention group [94.5 days (95% CI 55.0 to 134.0 days)].
Adverse events (hospital admissions for feeding-related problems)
See Appendix 17 for data on serious adverse events. Overall, five women reported hospital admissions for feeding-related problems: two in the intervention group and three in the usual care group. The two cases in the intervention group were as a result of the baby losing too much weight and becoming dehydrated because of breastfeeding problems, but in both cases the mothers had not contacted the IFH and these serious adverse events were assessed as not being related to the intervention.
Maternal well-being at 8 weeks and 6 months, social support at 8 weeks and 6 months, and satisfaction with home and hospital support for feeding
Data on maternal well-being at 8 weeks and 6 months, social support at 8 weeks and 6 months, and satisfaction with home and hospital support for feeding are shown in Table 20.
| Well-being, social support and satisfaction with support for feeding | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |
| WEMWBS | |||||||||
| Baseline | |||||||||
| n | 25 | 27 | 52 | 25 | 25 | 50 | 50 | 52 | 102 |
| Mean (SD) | 54.1 (9.8) | 55.0 (9.2) | 54.6 (9.4) | 53.4 (6.2) | 53.7 (8.4) | 53.6 (7.3) | 53.7 (8.1) | 54.4 (8.7) | 54.1 (8.4) |
| 8 weeks | |||||||||
| n | 19 | 20 | 39 | 21 | 24 | 45 | 40 | 44 | 84 |
| Mean (95% CI) | 49.8 (44.8 to 54.9) | 55.5 (50.6 to 60.5) | 52.8 (49.3 to 56.2) | 51.9 (49.2 to 54.6) | 53.5 (50.0 to 57.0) | 52.7 (50.6 to 54.9) | 50.9 (48.3 to 53.6) | 54.4 (51.6 to 57.3) | 52.8 (50.8 to 54.7) |
| Change from baseline to 8 weeks |
n = 19 –3.1 (–6.1 to –0.03) |
n = 20 0.1 (–6.3 to 6.4) |
n = 39 –1.5 (–4.9 to 2.0) |
n = 21 –2.0 (–5.0 to 1.0) |
n = 24 –0.2 (–2.8 to 2.5) |
n = 45 –1.0 (–3.0 to 0.9) |
n = 40 –2.5 (–4.6 to –0.5) |
n = 44 –0.1 (–3.1 to 3.0) |
n = 84 –1.2 (–3.1 to 0.6) |
| 6 months | |||||||||
| n | 17 | 20 | 37 | 22 | 24 | 46 | 39 | 44 | 83 |
| Mean (95% CI) | 51.2 (45.8 to 56.6) | 54.1 (49.1 to 59.0) | 52.7 (49.2 to 56.3) | 51.5 (48.3 to 54.7) | 54.8 (51.4 to 58.2) | 53.2 (50.9 to 55.5) | 51.4 (48.6 to 54.2) | 54.4 (51.6 to 57.2) | 53.0 (51.0 to 55.0) |
| Change from baseline to 6 months |
n = 17 –3.3 (–6.4 to –0.1) |
n = 20 –1.8 (–6.9 to 3.4) |
n = 37 –2.5 (–5.5 to 0.5) |
n = 22 –2.6 (–5.1 to –0.1) |
n = 24 1.1 (–1.2 to 3.4) |
n = 46 –0.7 (–2.4 to 1.0) |
n = 39 –2.9 (–4.8 to –1.0) |
n = 44 –0.2 (–2.8 to 2.4) |
n = 83 –1.5 (–3.1 to 0.1) |
| Social support | |||||||||
| 8 weeks | |||||||||
| n | 19 | 20 | 39 | 21 | 24 | 45 | 40 | 44 | 84 |
| Mean (95% CI) | 32.6 (29.3 to 36.0) | 37.4 (35.9 to 38.9) | 35.1 (33.2 to 37.0) | 34.8 (32.5 to 37.1) | 36.2 (34.3 to 38.0) | 35.5 (34.1 to 37.0) | 33.8 (31.8 to 35.7) | 36.7 (35.5 to 37.9) | 35.3 (34.2 to 36.5) |
| 6 months | |||||||||
| n | 17 | 20 | 37 | 22 | 24 | 46 | 39 | 44 | 83 |
| Mean (95% CI) | 32.6 (28.4 to 36.8) | 35.6 (32.7 to 38.5) | 34.2 (31.8 to 36.6) | 34.5 (32.4 to 36.5) | 36.1 (34.6 to 37.7) | 35.3 (34.1 to 36.6) | 33.7 (31.6 to 35.7) | 35.9 (34.4 to 37.4) | 34.8 (33.6 to 36.1) |
| Maternal satisfaction | |||||||||
| Hospital support (score out of 10) | |||||||||
| n | 19 | 18 | 37 | 21 | 24 | 45 | 40 | 42 | 82 |
| Mean (95% CI) | 7.5 (6.0 to 9.0) | 7.2 (5.8 to 8.6) | 7.3 (6.3 to 8.3) | 7.0 (5.7 to 8.3) | 7.1 (6.0 to 8.2) | 7.0 (6.2 to 7.8) | 7.2 (6.3 to 8.1) | 7.1 (6.3 to 7.9) | 7.2 (6.5 to 7.8) |
| Health service support at home (score out of 10) | |||||||||
| n | 19 | 20 | 39 | 21 | 24 | 45 | 40 | 44 | 84 |
| Mean (95% CI) | 7.2 (5.7 to 8.7) | 8.3 (7.4 to 9.2) | 7.8 (6.9 to 8.6) | 8.3 (7.4 to 9.2) | 7.2 (6.1 to 8.2) | 7.7 (7.0 to 8.4) | 7.8 (7.0 to 8.6) | 7.7 (7.0 to 8.4) | 7.7 (7.2 to 8.3) |
Maternal well-being was measured with the 8-week and 6-month questionnaires using the WEMWBS,98 with data available for 81.6% and 80.6% of participants, respectively.
Change in WEMWBS score between baseline and 8 weeks and between baseline and 6 months was calculated. At 8 weeks, the WEMWBS score was lower than at baseline both overall [–1.2 (95% CI –3.1 to 0.6)] and by site [site A, –1.5 (95% CI –4.9 to 2.0); site B, –1.0 (95% CI –3.0 to 0.9)]. The intervention group showed larger decreases in maternal well-being score between baseline and 8 weeks both overall [–2.5 (95% CI –4.6 to –0.5) in the intervention group compared with –0.1 (95% CI –3.1 to 3.0) in the usual care group] and by site [site A, –3.1 (95% CI –6.1 to –0.03) in the intervention group compared with 0.1 (95% CI –6.3 to 6.4) in the usual care group; site B, –2.0 (95% CI –5.0 to 1.0) in the intervention group compared with –0.2 (95% CI –2.8 to 2.5) in the usual care group]. The same pattern is seen in the change in WEMWBS scores from baseline to 6 months (see Table 20).
Social support
At 8 weeks, the mean social support score overall was 35.3 out of 40 (95% CI 34.2 to 36.5). The social support score was slightly lower in the intervention than in the usual care group both overall [33.8 (95% CI 31.8 to 35.7) compared with 36.7 (95% CI 35.5 to 37.9)] and by site [site A, 32.6 (95% CI 29.3 to 36.0) compared with 37.4 (95% CI 35.9 to 38.9); site B, 34.8 (95% CI 32.5 to 37.1) compared with 36.2 (95% CI 34.3 to 38.0)].
At 6 months, the mean social support score overall was 34.8 out of 40 (95% CI 33.6 to 36.1). The social support score was slightly lower in the intervention group than the usual care group both overall [33.7 (95% CI 31.6 to 35.7) compared with 35.9 (95% CI 34.4 to 37.4)] and by site [site A, 32.6 (95% CI 28.4 to 36.8) compared with 35.6 (95% CI 32.7 to 38.58); site B, 34.5 (95% CI 32.4 to 36.5) compared with 36.1 (95% CI 34.6 to 37.7)].
Maternal satisfaction (hospital and home) for feeding support
At 8 weeks, women reported a mean score of 7.2 out of 10 (95% CI 6.5 to 7.8) for satisfaction with feeding support received in hospital, and a mean score of 7.7 out of 10 (95% CI 7.2 to 8.3) for satisfaction with help received at home from the health service for feeding their baby. There were only very minor differences in scores by site and by study group.
Outcomes for a future economic evaluation
Self-reported use of health services at baseline (Table 21) was received from 96.1% of participants. The mean number of times women had consulted a midwife in the previous 3 months was greater in the intervention group (3.4 times, 95% CI 2.8 to 3.9 times) than in the usual care group (2.6 times, 95% CI 2.1 to 3.1 times). The mean number of times participants had consulted a general practitioner (GP) or a practice nurse in the previous 3 months was the same in the intervention and usual care groups.
| Health service use | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |
| Number of times consulted GP in past 3 months (baseline) | |||||||||
| n | 25 | 27 | 52 | 22 | 25 | 47 | 47 | 52 | 99 |
| Mean (95% CI) | 1.8 (0.7 to 3.0) | 1.3 (0.7 to 2.0) | 1.6 (1.0 to 2.2) | 1.1 (0.7 to 1.5) | 1.7 (1.1 to 2.3) | 1.4 (1.1 to 1.8) | 1.5 (0.9 to 2.1) | 1.5 (1.1 to 2.0) | 1.5 (1.1 to 1.9) |
| Number of times consulted practice nurse in past 3 months (baseline) | |||||||||
| n | 25 | 27 | 52 | 22 | 25 | 47 | 47 | 52 | 99 |
| Mean (95% CI) | 0.6 (0.3 to 1.0) | 0.3 (0.04 to 0.6) | 0.5 (0.3 to 0.7) | 0.4 (0.1 to 0.7) | 0.7 (0.3 to 1.2) | 0.6 (0.3 to 0.8) | 0.5 (0.3 to 0.7) | 0.5 (0.3 to 0.8) | 0.5 (0.3 to 0.7) |
| Number of times consulted midwife in past 3 months (baseline) | |||||||||
| n | 25 | 27 | 52 | 22 | 25 | 47 | 47 | 52 | 99 |
| Mean (95% CI) | 3.4 (2.5 to 4.2) | 2.1 (1.5 to 2.7) | 2.7 (2.2 to 3.2) | 3.4 (2.6 to 4.2) | 3.1 (2.4 to 3.9) | 3.3 (2.7 to 3.8) | 3.4 (2.8 to 3.9) | 2.6 (2.1 to 3.1) | 3.0 (2.6 to 3.3) |
Self-reported use of health and feeding support services for advice on infant feeding since birth (see Appendix 18) was reported on the 8-week questionnaire by 79.6% of participants. More women in the intervention group (than in the usual care group) reported no use of midwife, health visitor or GP services for feeding support (35.0% vs. 21.4%, 45.0% vs. 28.6%, and 87.5% vs. 73.8%, respectively). Conversely, more women in the intervention group reported accessing support from an infant-feeding counsellor/breastfeeding supporter (51.3%, compared with 16.7% in the usual care group). Very few women in either group accessed a national breastfeeding telephone helpline (4.9% overall). Half of the women reported accessing the internet for infant-feeding advice, with more women in the intervention group using this source of support (57.5%) than in the usual care group (42.9%).
Use of child care at 8 weeks and 6 months was reported by 80.6% of participants at both time points. Use of paid child care was very low: 1.2% (95% CI 0.01% to 8.4%) of participants reported using occasional paid child care at 8 weeks; at 6 months 2.4% of participants (95% CI 0.6% to 9.4%) reported using regular paid child care and 1.2% (95% CI 0.2% to 8.4%) reported using occasional paid child care (see Appendix 19).
Information on receipt of benefits was obtained from 91.3%, 81.6% and 80.6% of participants at baseline, 8 weeks and 6 months, respectively (see Appendix 20).
Achievement of progression criteria
Our achievement of the progression criteria approved by the TSC is shown in Table 22. The criteria have all been met, although, with the small sample size, the lower boundary of the 95% CIs for the proportion of teenagers, the fidelity of intervention delivery and the receipt of assets-based face-to-face contact do exclude the percentage for progression for these criteria.
| Progression criteria | Progress – green | Study results | Progression criterion met |
|---|---|---|---|
| Acceptable intervention | Generally positive views of women, IFHs and health service staff about the intervention | Generally positive views of women, IFHs and health service staff about the intervention. Some concerns raised by the IFHs at one site | Yes |
| Recruitment | ≥ 75 women in 5 months | 103 women in 5 months | Yes |
| Recruitment of women with socioeconomic disadvantage, teenagers, etc. | At least 5% of recruits are teenagers | 8.7% (95% CI 4.1% to 15.9%) teenagers | Yes |
| Fidelity of intervention delivery | ≥ 75% receive contact in antenatal and postnatal perioda | 77.6% (95% CI 61.8% to 86.9%)b | Yes |
| Receipt of assets-based face-to-face contact | ≥ 75% | 78% (95% CI 64.0% to 88.8%) | Yes |
| Follow-up at 8 weeks and 6 months | > 70% and ability to obtain routine data to achieve 80% of primary outcome |
Follow-up at 8-weeks: 85.4% (95% CI 77.1% to 91.6%) 6-week feeding status obtained: 95.1% (95% CI 89.0% to 98.4%) 6-month follow-up: 80.6% (95% CI 71.6% to 87.7%) |
Yes |
Chapter 4 Discussion and conclusions
In this chapter, we provide a summary and interpretation of the key findings of the study, compare our findings with those of other studies, discuss strengths and limitations, describe PPI in the study and provide recommendations for future research.
Summary of findings of the feasibility study
The main aim of the ABA study was to assess the feasibility of delivering the ABA intervention within a definitive RCT. To achieve this aim, we assessed the feasibility of recruiting peer supporters into the new ABA IFH role, the fidelity of the intervention and training needs of the peer supporters, the acceptability of the intervention to women and peer supporters, women’s engagement with the ABA service, recruitment and retention into the study and the collection of outcome measures. In addition, we explored two different models of ABA delivery: by employed, paid peer supporters and by volunteer peer supporters.
We found that it was feasible to recruit peer supporters, to train them to take on the ABA role and for them to deliver the intervention with adequate fidelity. We were able to recruit women to the study in the planned time frame and the women reported the ABA support to be acceptable. The study demonstrates that the processes for a future definitive RCT were feasible. These findings are discussed in more detail below.
Interpretation of findings of the feasibility study
Recruitment and characteristics of participants
The study proved that a RCT would be feasible with a good reach to those women who are least likely to breastfeed. 18 We were able to recruit to the study within the expected time frame; 8.7% of the recruited women were teenagers, which is higher than the average percentage of pregnancies among teenagers for England and Wales (3%),102 and 13% were from a minority ethnic group. We recruited women who had lower educational attainments than average. 103 We succeeded in recruiting women who intended to formula feed and showed that we could recruit women from socioeconomically deprived localities; in site A, almost half (46.2%) of the recruited women lived in areas in the highest quintile of deprivation, measured using the Index of Multiple Deprivation. Although we recruited from only those women who attended an antenatal clinic when one of the researchers was present, we have no evidence that there was selection bias in recruitment, and the recruitment rate was 76.3% (95% CI 68.2% to 83.2%), which suggests that this method of recruitment was acceptable. A shopping voucher as a ‘thank you’ on completion of 6-month follow-up was mentioned at recruitment, which is likely to have increased recruitment to the trial, particularly of women from the most disadvantaged groups.
Our recruitment methods were suitable for recruiting women from a small defined geographical area, given that the feasibility study aimed to recruit only 50 women per site. We therefore cannot extrapolate from the proportion of all pregnant women seen in a site to estimate the likely recruitment rates for a future RCT (objective 6); however, the proportion of women approached who took part in the study was high (76.3%). In a definitive trial with a large sample size, or in a more geographically dispersed population, our original plan to recruit from scanning clinics might be an option, whereas it was considered inefficient for the feasibility study.
Recruitment of the infant-feeding helpers
We found that it was feasible to recruit and train existing paid and volunteer peer supporters to the new ABA role. Compared with the volunteer peer supporters at site B, where recruitment was relatively easy, there were greater challenges in recruitment of the site A paid peer supporters, who were relatively ‘professionalised’, having worked as peer supporters for many years, and who had targets to meet from the local authority commissioners in terms of the number of women they supported. In consequence, the study represented a change in practice for these IFHs. To deliver the study, the site A IFHs were asked to undertake home or community venue visits in a geographical locality that, in practice, they had not historically tended to visit as paid peer supporters, even though, in theory, their existing practice area encompassed the whole local authority area, including the study site.
Training of the infant-feeding helpers
The training programme for the peer supporters lasted 1 day, with site A training occurring first and the learning from this taken forward to the site B training. Site A paid peer supporters had previously been trained to deliver a semiprofessionalised service using an established approach, whereas site B volunteer supporters had been trained by a national charity to support women in community breastfeeding groups. There were mixed responses, with the IFHs from site A disliking the prescriptive nature of the intervention and not always being able to see what was different from the delivery of antenatal support that they had offered in the past. Other peer supporters were positive about the new approach to supporting women. The IFHs understood the focus on infant feeding and supporting all women whatever their feeding choice, but not all felt comfortable about the change in emphasis from supporting breastfeeding only. The feasibility study did not provide information about frequency of refresher training that is likely to be required in a full trial or service situation. Embedding the training in the regular updates that peer supporters receive would be a way to ensure that the components of the intervention continue to be delivered as intended.
Intervention fidelity
By measuring the fidelity of delivery through listening to and analysing recordings of the antenatal face-to-face meetings, qualitative interviews with women, and FGs with the IFHs, we have shown that the intervention was delivered with acceptable fidelity. The fidelity assessment of the antenatal visit indicates that assets-based conversations, incorporating intended BCTs, can be delivered by peer supporters with additional training for the IFH role. The qualitative interviews suggest that BCTs were also incorporated during postnatal contacts, particularly social support, restructuring the social environment and problem-solving. There was some success with the assets-based approach in site B, where the IFHs provided peer support in local breastfeeding groups. We were able to identify areas that should be addressed in the training of IFHs, which are addressed in Potential improvements to the content and tone of the intervention contacts.
Acceptability
The intervention was acceptable to women and to IFHs. Women reported that they used the assets leaflet; some attended groups detailed in the leaflet or joined social media groups for new mothers. The value of this is highlighted by the fact that some women shared the content with other new mothers.
Although there was a more mixed response from the IFHs to using the genogram, women found this acceptable in the antenatal meeting, with some reporting that it had highlighted the amount of support they had in their family and social networks. The issue of the genogram highlighting to some women their lack of support was theoretical, with no instances of this occurring in the study.
There was a high contact rate between the mothers and volunteer IFHs in the 2 weeks after giving birth, with 72% of IFHs attempting contact within 48 hours of birth and an average of 6.9 contacts per woman in the first 2 weeks at site B, but a lower rate at the site with paid IFHs (site A). In neither site A nor site B was daily contact made, but the intervention was meant to be woman-centred with contact negotiated between the IFH and the woman. There were reports of breastfeeding support that was highly valued by some women in both localities.
The volunteer IFHs were generally supportive of the intervention and gained satisfaction from the different support role, in particular supporting different women from those whom they saw at the breastfeeding support groups.
Women’s engagement with the intervention service
Women in the intervention group engaged well with the service. The IFHs attempted to make contact with all the women in the intervention group, with 78% of the women receiving an antenatal contact. Rates were lower at site A, where there were several preterm births and more women living in socioeconomically disadvantaged and challenging circumstances. In the postnatal period, support was provided to 76% of women, although it generally commenced later than 48 hours after birth. Women who did not respond to offers of postnatal support had chosen to formula feed and were managing satisfactorily, had no breastfeeding issues, or were overwhelmed by new motherhood; others were not contactable or had moved from the area. This highlights an issue that needs to be addressed in the training of IFHs for a future trial as the lack of engagement was challenging for the IFHs who were used to women requesting support and being very engaged postnatally. Shopping vouchers were used as a ‘thank you’ for the inconvenience incurred during recruitment and follow-up. The vouchers are unlikely to have been an incentive to adhere to the intervention as no qualitative interviews identified that women or IFHs linked adherence to them.
Breastfeeding outcomes
We were able to obtain information about the method of feeding at 8 weeks for 95.1% (95% CI 89.0% to 98.4%) of the sample from questionnaires and data from health visitor records, and for 80.6% (95% CI 71.6% to 87.7%) of the sample at 6 months. This demonstrates that method of feeing at 8 weeks would be a feasible primary outcome measure in a future definitive trial. The women who did not respond to the 8-week questionnaire were more likely to have the characteristics associated with not breastfeeding, and most of those for whom we obtained feeding status at 8 weeks were formula feeding. This confirms the importance of the primary outcome being measured at a point when feeding method is routinely collected and our recommendation that this should be at 8 weeks, given that this is the last time that infant feeding method is collected routinely. Our response rates should be seen in the context of a ‘thank-you’ voucher for returning the 6-month follow-up questionnaire, which may have affected the response rates. Women who did not return questionnaires in our study were less likely to be educated to degree level and less likely to be in paid work. As these characteristics are associated with lower breastfeeding rates, it is likely that the actual breastfeeding rates for the full sample would be lower than those reported.
This was a feasibility trial with a small sample size and it was not powered to detect a difference between the study groups in breastfeeding outcomes; thus, no statistical testing of differences between the study groups has been carried out. Acknowledging this, we did find that the proportion of the intervention women initiating breastfeeding and breastfeeding, at least partially, at both 8 weeks and 6 months was higher than in the usual care group. Given that the intervention group had more characteristics associated with not breastfeeding, the difference between the groups may be an underestimate. The ICC for the outcome of any breastfeeding at 8 weeks was high (0.039) but based on a very small sample, as IFHs generally supported only four women each.
We found that collecting the feeding method status at 3 days postnatally was challenging, with information collected about only 68% of the women by 14 days postnatally. This low proportion was largely due to delays in the research team finding out that women had given birth; of those who received the text within 10 days of birth, 85% responded at this time. The follow-up rate at 6 months has a lower 95% CI of 71.6%, so additional measures may be required to increase follow-up at this point in a definitive trial.
Differences between sites, and barriers to and facilitators of intervention delivery
There were considerable differences between the sites in terms of setting (large urban conurbation vs. urban and suburban), type of peer supporter recruited to the IFH role (paid vs. volunteer), organisational situation (threat of loss of breastfeeding support contract vs. stable) and the embeddedness of the IFHs in their communities. At site A, the IFHs had initially been recruited as peer supporters to reflect the ethnic diversity of the area they were supporting, but, with mergers of primary care trusts into one local authority, they were now covering a wider geographical area; thus, there was a lack of concordance between the IFHs and the women in terms of ethnicity. The area selected for the ABA study had a large white British population and was socioeconomically deprived, both of which are characteristics associated with low rates of breastfeeding. 18 This meant that, in practice, site A peer supporters did not tend to have ethnically similar characteristics to the women they supported, so that this aspect of the principle of homophily did not hold.
The threat of major organisational change and potential loss of jobs in site A had an impact on the delivery of the ABA intervention and the morale of the IFHs. Providing the intervention largely during working hours at that site restricted the responsiveness of the support and the ability of IFHS to meet women in the evenings or at weekends. Additional resources were provided to enable telephone contact during weekends and this was used to try to organise the antenatal contacts and to call women after they had given birth. In contrast to these challenges, site B, which had volunteer IFHs, was able to offer more flexible support, with the IFHs meeting women in the evenings and at weekends when they themselves had child care. However, because they were volunteers, it was essential to not overload the IFHs with women to support, so the recruitment of study participants had to be carefully controlled to ensure that each IFH had only one woman to support with an expected due date in any 1 month. Even so, some of the IFHs from site B reported that it was time-consuming.
The availability of support groups and activities in the community differed between the sites. Site B had community breastfeeding groups that were attended by the peer supporters, whereas site A had breastfeeding groups led by professional breastfeeding counsellors. Both sites had a range of other groups and activities for women with babies. This heterogeneity is likely to be reflective of the situation across the UK and in planning a definitive trial this needs to be considered. Stratification of randomisation by site would ensure that differences were balanced between the intervention and usual care groups.
Harms and contamination
There were no reported harms related to the intervention; five women (two in the intervention group and three in the control group) reported hospital admissions for feeding-related problems but, from the information available, none was considered by the principal investigator to be related to the intervention.
We identified one case of contamination whereby a woman in the intervention group and a woman in the usual care group attended the same NCT group. One participant from site B reported sharing the assets leaflet with her friends, some of whom were in the usual care group. The impact of this contamination is likely to have been minimal, as the assets leaflet represents only one component of the intervention. We therefore believe that contamination was low.
Potential improvements for future intervention delivery
In terms of future intervention delivery, we have identified the need to use a locality with stable commissioning of an IFH service (volunteer or paid) and with good management support for the IFHs to facilitate the change in mode of working (antenatal contact, one-to-one support for volunteers and supporting women who might formula feed). The IFHs need to be embedded in their communities so that their travel is reduced and they have an understanding and experience of the local ‘assets’.
A big challenge at both sites was in receiving notification of the birth. Ideally, the midwife who delivered the baby would notify the IFHs and/or the research team; however, it was clear from our discussions with the community midwives that this was very unlikely to happen. To try to ensure that the IFHs were told about the birth, a focus of the antenatal contacts was the IFH developing a relationship with the pregnant woman so that she would notify the IFH about the birth, along with family and friends. We had fridge magnets made to remind the women to call/text the IFH and encouraged the IFHs and women to swap telephone numbers to ensure that barriers to letting the IFH know were few. Other trials of peer support in the UK have struggled to achieve early contact after birth. 104,105
Potential improvements to the content and tone of the intervention contacts
We identified excellent examples of delivery of the ABA intervention, but there was variation. We have identified elements of the training that could be enhanced by providing a longer period for training, by changing the emphasis of the training or by changing how some of the training elements are delivered.
-
Describing the intervention: training could include asking participants to practise specific statements about the inclusive nature of the ABA help and reminding them to use the time line explaining what support will be offered when.
-
Linking to community assets: use of the leaflet could be enhanced by including a requirement for IFHs to help the mother to make a specific plan to connect with local services in the antenatal period.
-
Use of the genogram: IFHs may benefit from practising in using the genogram to stimulate conversation. The conversations appeared to flow better when the IFH ‘owned’ the genogram, so that the content of the genogram was either used to stimulate conversation or included naturally as part of a conversation that had already taken place. Training sessions could be adapted to include real-life recordings demonstrating good practice in building rapport and including the diagram. The training should also emphasise that the genogram can be used flexibly during the antenatal contact meeting.
-
Use of BCTs: the BCTs were a theoretical tool that we used to design the intervention and communication, but we did not explicitly cover BCTs as part of the IFH training. In future, IFHs may need more explicit guidance to ensure that they sufficiently use the core BCTs of social support and restructuring the social environment. IFHs may also benefit from greater clarity about appropriate information giving, particularly in the context of a woman-centred approach. Inclusion of mental rehearsal as a core BCT could be considered for the intervention, as IFHs reported conversations including this BCT to be helpful.
-
Tone: fidelity checking suggests that the intervention can be delivered with a good level of rapport, inclusivity and woman-centredness. Training could be adapted to ensure the development of active listening skills and a woman-centred approach. Alternatively, consideration could be given to recruiting IFHs who already have basic skills that could be developed in active listening and delivering a non-judgemental, inclusive approach.
Comparison of findings with those from other research
The ABA feasibility study was not powered to determine the difference in breastfeeding between the study groups, so conclusions about the effectiveness of the intervention cannot be drawn between ABA and other trials of breastfeeding peer support in the UK. Unlike previous RCTs of breastfeeding peer support in the UK,104–107 we offered a more intensive intervention, which included antenatal contact but had a particular focus on the key period of the 2 weeks after birth, when rates of breastfeeding fall dramatically. Other studies that aimed to support breastfeeding included daily calls in the first 2 weeks37,108 and showed promise in increasing breastfeeding rates.
A recent uncontrolled feasibility trial of breastfeeding peer support, the Mam-Kind study,31 reported that delivery of that intervention, which included motivational interviewing by paid peer supporters, was feasible and acceptable. A particular strength of the Mam-Kind report was its detailed process evaluation, which enables us to make comparisons with the ABA study’s intervention design and findings. In Mam-Kind, the invitation to the study was made by the community midwife but, unlike in ABA, the midwife passed on the woman’s details to the research team for recruitment at a later date. In ABA, we were more successful with recruitment, and recruited a higher proportion of women approached (76% vs. 24% in Mam-Kind). We recruited to target, unlike Mam-Kind, which recruited only 78% of planned participants, and we obtained a broader reach, with higher proportions of teenagers, women with lower educational attainment and women from minority ethnic groups. Our inclusion criteria were wider, with women pregnant for the first time being eligible for ABA regardless of feeding intention, whereas the Mam-Kind study recruited only women who planned to breastfeed and included women expecting their first and subsequent babies. Mam-Kind’s requirement for women to be intending to breastfeed may have excluded teenagers and women in more socioeconomically disadvantaged circumstances.
The Mam-Kind study31 had a midwife who supervised the peer supporter teams and worked to encourage the hospital midwives to notify the peer supporters about the birth. As a consequence, Mam-Kind contacted 73% of women within 48 hours of birth. In ABA, contact was attempted with 48% of women within 48 hours of birth, but with wide variation between the sites (24% and 72%, respectively). Mam-Kind recruited and employed peer supporters through the university, in contrast to our study, in which we worked within existing peer support services. All the Mam-Kind peer supporters were paid, and they experienced similar challenges to those in site A, where an existing, paid peer support service took on the trial intervention participants in addition to its usual workload.
Our early follow-up rates were similar to that of Mam-Kind. 31 We had data on feeding method within 14 days from 68% of women and Mam-Kind achieved 63% follow-up at 10 days using telephone follow-up. At 8 weeks, ABA obtained 85% follow-up and data on feeding status on an additional 10% of women from health visitor records. Rates were lower in Mam-Kind, suggesting that offering a shopping voucher at follow-up and using paper-based questionnaires may have been successful strategies.
Both ABA and Mam-Kind31 achieved reasonable intervention fidelity, while identifying aspects for improvement and additional training. Mam-Kind used a motivational interviewing approach as a key component,31 whereas in ABA we focused on an assets-based approach with behaviour change theory. Mam-Kind reported that the peer supporters found it challenging to move from information giving to a collaborative approach, something also identified by our IFHs who worked in the paid peer support service (site A).
The Mam-Kind intervention31 ceased at 14 days, with the peer supporters asked to facilitate the transition to a breastfeeding group or another community support group. Some women reported that the exit felt rather abrupt, which validates the ABA approach of withdrawing support much more gradually and maintaining contact up to 5 months postnatally for women still breastfeeding to encourage maintenance of breastfeeding.
Strengths and limitations
This feasibility study used robust methods, including a detailed process evaluation and a usual care group, unlike the Mam-Kind study. 31 The usual care comparator enabled us to characterise the breastfeeding support received in usual care and showed a low uptake of peer support. The randomised feasibility design enabled us to assess the feasibility of recruiting to and delivering the ABA study, as well as investigate the intervention’s acceptability to women, IFHs and maternity services. Furthermore, the use of two study sites that had existing peer support services enabled the comparison of processes between paid and volunteer services and an exploration of how the ABA intervention could fit into an existing service. The recruitment of trained peer supporters enabled us to reduce the duration of training required to become an IFH. Although we had sufficient interest from peer supporters in taking on the IFH role, we did not have enough interest to enable us to select peer supporters for the role based on woman-centredness or listening skills. To ensure transparency and replicability, we have reported the intervention using all the items in the TIDieR checklist. 109 The organisational disruptions and threats to the peer support service at site A, although challenging, provided an important insight into the risks associated with changing public health budgets and the short-term commissioning of services. We have used statistically robust methods; estimates of the primary outcome in the intervention and control groups have been presented with 95% binomial exact CIs to demonstrate the uncertainty of results. The ICC is also estimated with a 95% CI to indicate the variability between IFHs, which will occur only in the intervention group.
Limitations of the study include the small number of recordings of antenatal contacts at site A. The IFHs were reluctant to be recorded and also cited concerns about making recordings in noisy public places and with women living in particularly challenging social circumstances. This means that the fidelity assessment of the antenatal intervention can really be applied only to site B.
Another limitation was that our qualitative interviews were with women who had provided follow-up at 8 weeks; we did not interview women who were lost to follow-up. The sociodemographic characteristics of women who were not followed up are those associated with a lower likelihood of breastfeeding and it is likely that the responses of the women who were interviewed will have had a positive bias.
The participant recruitment process was resource intensive as it required a researcher to sit in community midwives’ antenatal clinics awaiting eligible women; nevertheless, this approach is likely to have contributed considerably to the successful recruitment. To recruit the required 103 participants, researchers spent approximately 130 hours in clinics. Despite this time commitment, we were successful in recruiting women living in areas of socioeconomic disadvantage, pregnant teenagers and women intending to formula feed. Feedback from women in the interviews indicated that the face-to-face explanation of the study was helpful in encouraging them to participate. If the ABA intervention were rolled out to usual care, we would envisage community midwives signposting women to the service during a routine appointment.
Encouraging timely notification of birth was problematic, with only half of women notifying the study team within 3 days of the birth. This resulted in delays in the collection of postnatal feeding status data and, in the case of the intervention participants, delays in the offer of postnatal support. We encouraged women to let us know of the birth by giving them a ‘let us know when you’ve had your baby’ fridge magnet recruitment and sending a reminder text at 38 weeks’ gestation. Intervention women were also encouraged to let their IFH know of their baby’s arrival as soon as possible after birth (with processes in place for the IFH to then let the study team know). In cases in which the participant did not inform the study of the birth, we relied on collecting this information from community midwifery teams. However, as community midwives receive information about only those women who have been discharged from hospital, this led to delays in receiving information about women who had a longer hospital stay. Women who notified the study or their IFH of the birth were more likely to be breastfeeding at 8 weeks than those women for whom we relied on community midwife contact, indicating some possible early disengagement of mothers who were formula feeding. From qualitative interviews and PPI discussions, women indicated that more text reminders before and around the due date would be acceptable. Going forward, processes for increasing the rate of early birth notification would need to be put in place, as would protocols for notifications of preterm births or perinatal death.
From the process data, it is clear that the ABA intervention was less successful in accommodating women who delivered prematurely, with only three in seven of these women receiving any support from the IFHs either antenatally or postnatally. Going forward, methods to include women who deliver prematurely must be considered. In the case of women who miss the antenatal assets-based component because of preterm birth (or other reasons), the process needs to ensure that the assets-based component is offered in the postnatal period. This needs to be addressed in the training of the IFHs.
Although we received follow-up questionnaires from 85.5% and 80.6% of participants at 8 weeks and 6 months, respectively, there were differences between those who were followed up and those who were lost to follow-up. In particular, non-responders were less likely to intend to breastfeed at baseline, and less likely to be breastfeeding at 8 weeks (from health visitor data), indicating possible further disengagement of formula-feeding mothers, who may have perceived the intervention to be about breastfeeding support, despite intentions for it to apply to all women.
In the future, the use of electronic questionnaires may help to boost response rates. Reliance on postal questionnaires was problematic, with a small number of women reporting that they had returned questionnaires that never arrived at the study offices. In addition, waiting for questionnaires to arrive back in the post led to delays in sending out reminders to women. On the whole, PPI input and findings from the qualitative interviews indicate that electronic questionnaires should be offered going forward.
Communication difficulties between IFHs and women sometimes caused issues. In one example, explored in a qualitative interview, a woman texted her IFH for breastfeeding advice, but phone records showed that the text message did not get through. By the time contact was re-established, the woman had moved on to formula feeding. In future, IFHs need to be aware of these possible issues; backup telephone calls should be considered when a woman does not respond to text messages. To mitigate technology failure, the FEST study37 used a combination of text and telephone.
In some cases, IFHs failed to establish any contact with women despite numerous attempts. More in-depth explanation of the intervention at randomisation may assist in increasing contact in future. It could be that, despite the woman-centred approach to recruitment and explanation that the intervention is inclusive of all feeding types, women were put off by the initial approach from IFHs. In a future trial, the content of initial text or telephone messages should be more fully considered to be the crucial first contact with women.
We have presented data by site to capture the differences in feasibility and in outcomes. Given that sites differed in more than just type of feeding helper (voluntary or paid), caution must be taken not to attribute differences to this factor alone.
Economic evaluation methods
Any future definitive trial of the ABA intervention would include a cost-effectiveness work package to assess the costs and the relative cost-effectiveness of the ABA intervention compared with the status quo from an NHS/Personal Social Services perspective. The ABA feasibility study included an objective to measure the features of the ABA infant feeding team provision and service utilisation to inform the design of a future cost-effectiveness study and specifically determine the feasibility of data collection.
We collected self-reported use of health and feeding support services using the 8-week questionnaire given to women. Although this had high rates of completion, the questionnaire would require further refinements to ensure accurate data capture. For example, we asked women about contact with peer supporters and attendance at breastfeeding support groups; in some cases, women commented on the questionnaire that they had met a breastfeeding peer supporter at a feeding support group and that there was overlap.
Overall IFH activity for each woman supported was obtained from logs kept by the IFHs and from their mobile phone records. A considerable amount of activity went into trying to contact women, particularly at site A, and this would need to be recorded and differentiated from research costs in a definitive trial.
The research proposal’s peer reviewers requested data collection on the use of child care and the uptake of benefits. It was clearly acceptable to women to ask about their use of benefits and we had good completion of the questions, although we are unable to confirm the accuracy of the responses. The interpretation of these data, however, is challenging. In particular, the relevance of the uptake of benefits and demand for child care and how that affects infant feeding decisions was not clear. We would not recommend collecting these data in a future trial.
Another challenge for a future trial that we identified is how to cost a volunteer IFH/peer supporter. Conventionally, health economic analyses cost volunteers at the national minimum wage, as there is an opportunity cost of their time. However, many peer supporters volunteer for a relatively short time prior to returning to work or having another baby, often citing that they want to give something back after receiving support themselves. 110 Additionally, the peer support role enables them to take their baby with them, which may not be possible in many other volunteer roles. A future study should explore with peer supporters whether or not they would volunteer in a different capacity if the breastfeeding peer supporter role was not available. A future cost-effectiveness analysis should undertake sensitivity analyses of a range of costs of the peer supporters’ time.
Training may have to be provided on an annual basis to ensure that, with high turnover of peer supporters, sufficient numbers are trained to deliver the intervention and this will be an important component of the overall costs.
In the Mam-Kind study31 the peer supporters were paid, as in one of our sites, and the overall cost of supporting a woman was estimated at £480, but this would have been as low as £350 had the study recruited women at the planned rate.
From the qualitative interviews, we did not identify additional costs to family or social networks in supporting a mother in her breastfeeding; therefore, the need to undertake a societal perspective in a future economic evaluation is not supported.
Patient and public involvement in the study
In this section, we describe the PPI in the ABA study, using the GRIPP2 short form111 as a guide to content.
Aim of patient and public involvement in the study
The aim of PPI within the study was to gain insight from pregnant women/new parents on their experiences of infant feeding, and to ensure that the proposed intervention, methods of communication and data collection were appropriate given their lived experiences and competing priorities.
Methods used for patient and public involvement in the study
During the study design period, the Public and Researchers Involvement in Maternity and Early Pregnancy (PRIME) group (a University of Birmingham PPI group interested in maternity services) was asked to comment on the protocol, the funding bid and the reviewer feedback on the bid. In addition, the PRIME group chairperson convened a separate group of mothers with young children to comment on aspects of the protocol.
Two members of the PRIME group were invited to join the Study Management Group and attended the first two meetings. For the TSC, a PPI representative was recruited.
During the intervention development period (January 2017), we convened two PPI sessions (involving nine new mothers in total) in children’s centres serving deprived populations. The women provided feedback on the proposed intervention (see Chapter 2).
Further PPI sessions were held in September 2017 and February 2018 at an established baby group close to study site A (attended by seven and five new mothers and fathers, respectively). At these sessions, we asked parents about issues arising within the study. These included understanding of the term ‘infant feeding’, views on paper-based versus electronic questionnaires and ideas on how to get women to tell the study team they had given birth.
In July 2018, we attended two PPI groups in areas of socioeconomic disadvantage. These were held at existing ‘research engagement sessions’ as part of a University of Birmingham Wellcome Trust-funded project in which women attend this session before participating in a free pregnancy yoga session. At these groups (attended by nine women altogether), we discussed methods of dissemination of study results as well as views on recruitment methods.
Reimbursement was provided for PPI input. Attendees at PPI sessions were provided with a £10 shopping voucher as a thank you. The PPI members of the Study Management Group and TSC were reimbursed the equivalent of £150 per day for attending a meeting.
Results of patient and public involvement in the study
During the study design period, the PPI members advised on the overall approach of the potential feeding support intervention, highlighting the importance of taking a non-judgemental approach to women who chose not to, or ceased to, breastfeed. They supported giving advice about safe formula feeding as part of the intervention and welcomed both antenatal contact between the woman and the IFH and early contact after giving birth to ensure timely support. The lay chairperson of the PRIME group contributed to the lay summary.
Patient and public involvement sessions in the period of intervention development provided positive feedback about the proposed assets leaflet. The groups liked most of the proposed text messages but thought that some were too long or pushy. As a result, some text messages were changed to be shorter, more open and less breastfeeding centred.
During discussions at subsequent PPI sessions, it became clear that the term ‘infant feeding’ meant different things to different people, with some women saying that they ‘assumed it was about breastfeeding’. There was clear guidance from PPI that, in future, electronic questionnaires should be provided as an option for women. Some suggestions were put forward to improve the number of women notifying the study of the birth, including increasing the frequency of communication before birth, involving partners, and providing a study tag for the hospital bag. These will be taken forward in designing a full trial.
When asked about the dissemination of study results, PPI representatives thought that it was important to provide women with a summary of the results in easy-to-read information sent in the post (with no research jargon), as well as by inviting them to an informal, child-friendly event.
At the TSC, the PPI representative offered a useful perspective and ensured that we remained participant-focused. For example, they highlighted the importance of involving partners, wherever possible, and suggested asking a wider PPI group about the use of paper versus electronic questionnaires.
Outcomes (the extent to which patient and public involvement influenced the study overall)
Patient and public involvement was essential to shaping the development of the ABA study and intervention, and in enabling us to discuss ongoing issues with women with current or recent experience of pregnancy and infant feeding.
The assumption among a number of our PPI representatives that ‘infant feeding’ meant breastfeeding means that in a future study we need to consider how this term might be interpreted.
Reflections on use of patient and public involvement in the study
Although PPI provided us with a vital user perspective, we found it challenging to sustain relationships with our PPI contributors (with the exception of our TSC PPI representative, who remained throughout the trial). Women are pregnant and have young children for a small period of their lives and, inevitably, move on, for example by returning to full-time work, making continuity of contributors difficult.
The recently established ‘research engagement sessions’ offered a novel way of involving women in research. Although women’s attendance is limited to the duration of their pregnancy, we were able to establish contact with a small number of women who were interested in participating further should the ABA study continue. However, successfully integrating short-term PPI input into time-limited research remains a challenge.
Recommendations for future research
We consider that the intervention was feasible to deliver with acceptable fidelity and it was acceptable to the women in the intervention group, to the IFHs who delivered it and to maternity services. This was an individually randomised trial in two sites, and we showed that it was feasible to recruit women from more disadvantaged socioeconomic areas, teenagers and women who planned to formula feed. These women were willing to be randomised and the follow-up rates were acceptable.
On the basis of the findings from this feasibility study, the ABA study’s independent TSC agreed that the criteria for progression to a definitive trial have been met. Our main recommendation for future research is that there is a need for a future definitive trial to evaluate the effectiveness and cost-effectiveness of the ABA intervention. Below we discuss the factors that need to be modified from the feasibility trial and other issues for consideration.
Study design
We recommend that the definitive trial be an individually randomised trial. Although a cluster RCT would reduce the risk of contamination, the sample size required for a cluster trial would not be cost-effective. We had one report of contamination between the intervention and the usual care group, when a woman in the intervention group shared the assets leaflet with a woman in the usual care group; however, the assets leaflet was only one part of the overall intervention, so this is unlikely to have had a major effect. We also calculated the ICC for the proposed primary outcome of any breastfeeding at 8 weeks and recommend that a definitive trial take account of clustering by IFH in the intervention group. Given the differences in delivery and in rates of outcome assessment between the sites in this feasibility study, we would recommend stratifying by site to take account of differences in the characteristics of local populations, as well as evaluating in several different sites to increase generalisability.
Given the importance of the context, we would recommend that a definitive trial include a process evaluation and consider incorporating realist principles alongside the RCT.
Settings
We were successful in recruiting women in more socioeconomically disadvantaged localities and we would recommend, given that the rates of breastfeeding are lowest among women in these localities, among white British women and among women with lower educational qualifications, that areas that reflect these characteristics be targeted. Areas would need to have a peer support service and good supervisory provision for the IFHs. In the current circumstances of limited public health budgets and the greater engagement of the volunteer peer supporters, we would recommend that the intervention be delivered by volunteer peer supporters trained in the ABA intervention. It is important to ensure that the peer supporters trained to become IFHs are managed within organisations that are willing to provide ongoing training and indemnity for the supporters.
Population
Recruitment to the ABA feasibility trial was limited to women expecting their first baby, regardless of their feeding intention. We would recommend that this be retained, given the influence of previous infant feeding method on subsequent feeding choice89,112 and the likelihood that women who have already had a child will be better linked to local assets that may support breastfeeding.
The ABA intervention
We identified some additional training needs for IFHs and would need to modify the training. This related particularly to describing the intervention, linking to the community assets, using the genogram and incorporating the core BCTs of social support and restructuring the social environment. Ensuring that peer supporters recruited to the IFH role have good woman-centred communication skills is important, as is highlighting the importance of the assets-based component and of offering this postnatally, if it is not delivered in the antenatal period due, for example, to preterm birth. A definitive trial should monitor delivery of the antenatal component as part of a process evaluation and might consider a ‘per protocol’ analysis to explore the importance of this component.
Outcome measures
Our greatest challenge was finding out when women had given birth, and this requires greater integration of care with the midwifery services. Although we had good engagement with the community midwifery teams, it is hospital midwives who are best placed to notify the research team when a woman has given birth. In a future study, we need to engage with hospital midwives to seek a solution to this.
The feasibility trial proposal considered that any breastfeeding at 8 weeks would be the likely primary outcome of a future definitive trial and we were able to collect this for 95% of the participants; thus, we would recommend that this be the primary outcome of a definitive RCT. Given the World Health Organization recommendation of exclusive breastfeeding up to 6 months, a further follow-up at 24 weeks should be maintained. The UK has very low rates of exclusive breastfeeding and any breastfeeding is proposed as the primary outcome measure, as increasing this is needed before we focus on exclusivity. Given the focus on supporting any feeding, including formula, it will also be important to measure consultations and admission of infants to hospital because of infections.
We offered a ‘thank-you’ voucher at follow-up to all women and would recommend that this be retained in a definitive trial, as it may have been an important factor in achieving the follow-up rates that we did.
Rather than ask women about their delivery details, we recommend seeking their consent to collect these data from their maternity records.
The Medical Outcomes Study Social Support Scale was not sensitive to change in this group and we recommend the use of a feeding-specific support questionnaire. Collecting data on benefits and child-care costs to inform an economic analysis is not recommended for a future trial.
Patient and public involvement
To address issues of acceptability among women least likely to choose to breastfeed, we recommend that PPI prior to a definitive trial take place in areas of low breastfeeding prevalence and high socioeconomic disadvantage.
Conclusions
This feasibility RCT has demonstrated that the ABA intervention is essentially acceptable to women and peer supporters. We have tested the feasibility of delivering the ABA intervention and have developed a training package for peer supporters. We have identified modifications that would enhance the training for intervention delivery and some of the trial processes. We were able to demonstrate the feasibility of recruiting women to, and retaining women in, the ABA study, as well as of collecting breastfeeding and health-related outcomes.
A full trial should be considered to test the effectiveness of the ABA intervention in increasing breastfeeding initiation and maintenance.
Acknowledgements
We thank all of the women, IFHs and health-care professionals who participated in the study.
We acknowledge the support and involvement of the organisations managing the peer supporters.
We thank the community midwives who supported participant recruitment.
We acknowledge the support of Helena Stopes-Roe in the development and delivery of the ABA training and the facilitation of PPI groups.
We acknowledge Dr Kirsty Darwent (Programme Director, Family Therapy Training Network Ltd), who contributed towards the design and delivery of the training of the IFHs with Heather Trickey.
We thank all of the administrative and research staff who contributed to the study: Janice Gunnell, Kiya Hurley and June Johnstone.
We acknowledge the contribution of our PPI, in particular the involvement of Jo Kidd-Chadwick and Bibiana Mas.
We acknowledge Zainab Abdali from the University of Birmingham Health Economics Unit for her contribution to the economic analysis.
We acknowledge members of the study TSC for overseeing the study: Professor Angela Harden (chairperson), University of East London; Professor Amy Brown, Swansea University; Mrs Gulnaz Iqbal, University of Warwick; and Mrs Rebecca Jennings, PPI representative.
Contributions of authors
Dr Joanne L Clarke (https://orcid.org/0000-0003-2563-5451) (Research Fellow, Public Health) was study co-ordinator for the duration of the ABA study. She undertook the recruitment and data collection at site A, led on PPI, undertook the statistical analysis, contributed substantially to the qualitative analysis and process evaluation, and co-ordinated the writing of the final report, leading on the writing of Chapters 2 and 3.
Dr Jenny Ingram (https://orcid.org/0000-0003-2366-008X) (Senior Research Fellow, Child Health) oversaw the conduct of the study at site B and contributed to the qualitative analysis. She was a co-investigator and contributed to the study design and interpretation of findings.
Mrs Debbie Johnson (https://orcid.org/0000-0001-7390-6514) (Research Associate, Child Health) undertook the recruitment and data collection at site A. She contributed substantially to the qualitative analysis and process evaluation.
Dr Gill Thomson (https://orcid.org/0000-0003-3392-8182) [Reader (Associate Professor) in Perinatal Health] oversaw the qualitative research, conducted the data collection for the IFH interviews, and contributed substantially to the qualitative analysis and process evaluation. She was a co-investigator and contributed to the study design and interpretation of findings.
Ms Heather Trickey (https://orcid.org/0000-0002-3707-456X) (Research Fellow, Public Health) led on the development and delivery of the ABA training for IFHs. She also contributed substantially to the process evaluation, leading on the development and analysis of the antenatal fidelity checking. She was a co-investigator and contributed to the study design and interpretation of findings.
Dr Stephan U Dombrowski (https://orcid.org/0000-0001-9832-2777) (Assistant Professor, Psychology) contributed to the qualitative analysis and process evaluation, in particular the use of BCTs. He was a co-investigator and contributed to the study design and interpretation of findings.
Ms Alice Sitch (https://orcid.org/0000-0001-7727-4497) (Statistician, Medical Statistics) was a co-investigator and contributed to the study design and interpretation of findings. She oversaw the statistical analysis.
Professor Fiona Dykes (https://orcid.org/0000-0002-2728-7967) (Professor of Maternal and Infant Health) was a co-investigator and contributed to the study design and interpretation of findings.
Dr Max G Feltham (https://orcid.org/0000-0002-3891-5068) (Team Lead – Women’s Health, Birmingham Clinical Trials Unit) oversaw the running of the study from a trials unit perspective, including the randomisation process and setting up the database.
Professor Christine MacArthur (https://orcid.org/0000-0003-0434-2158) (Professor of Maternal and Child Epidemiology) was a co-investigator and contributed to the study design and interpretation of findings.
Professor Tracy Roberts (https://orcid.org/0000-0002-0624-0537) (Professor in Health Economics) oversaw the economic analysis. She was a co-investigator and contributed to the study design and interpretation of findings.
Professor Pat Hoddinott (https://orcid.org/0000-0002-4372-9681) (Professor in Primary Care) was a co-investigator. She had the original idea for ABA and for combining an assets-based approach with some of the learning gained from the FEST pilot trial, which she led. She contributed to the study design and interpretation of findings.
Professor Kate Jolly (https://orcid.org/0000-0002-6224-2115) (Professor of Public Health) led the study as principal investigator, leading on the design and conduct of the study throughout. She oversaw the writing of the final report, leading on the writing of Chapters 1 and 4.
Publications
Jolly K, Ingram J, Clarke J, Johnson D, Trickey H, Thomson G, et al. Protocol for a feasibility trial for improving breast feeding initiation and continuation: assets-based infant feeding help before and after birth (ABA). BMJ Open 2018;8:e019142.
Clarke JL, Ingram J, Johnson D, Trickey H, Dombrowski SU, Sitch A, et al. The ABA intervention for improving breastfeeding initiation and continuation: feasibility study results. Matern Child Nutr 2020;16:e12907.
Ingram J, Thomson G, Johnson D, Clarke JL, Trickey H, Hoddinott P, et al. Women's and peer supporters' experiences of an assets-based peer support intervention for increasing breastfeeding initiation and continuation: a qualitative study [published online ahead of print March 21 2020]. Health Expect 2020.
Data-sharing statement
All data are available on request from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet 2016;387:475-90. https://doi.org/10.1016/S0140-6736(15)01024-7.
- Bowatte G, Tham R, Allen KJ, Tan DJ, Lau M, Dai X, et al. Breastfeeding and childhood acute otitis media: a systematic review and meta-analysis. Acta Paediatr 2015;104:85-9. https://doi.org/10.1111/apa.13151.
- Lodge CJ, Tan DJ, Lau MX, Dai X, Tham R, Lowe AJ, et al. Breastfeeding and asthma and allergies: a systematic review and meta-analysis. Acta Paediatr 2015;104:38-53. https://doi.org/10.1111/apa.13132.
- Giugliani ER, Horta BL, Loret de Mola C, Lisboa BO, Victora CG. Effect of breastfeeding promotion interventions on child growth: a systematic review and meta-analysis. Acta Paediatr 2015;104:20-9. https://doi.org/10.1111/apa.13160.
- Peres KG, Cascaes AM, Nascimento GG, Victora CG. Effect of breastfeeding on malocclusions: a systematic review and meta-analysis. Acta Paediatr 2015;104:54-61. https://doi.org/10.1111/apa.13103.
- Tham R, Bowatte G, Dharmage SC, Tan DJ, Lau MX, Dai X, et al. Breastfeeding and the risk of dental caries: a systematic review and meta-analysis. Acta Paediatr 2015;104:62-84. https://doi.org/10.1111/apa.13118.
- Horta BL, Loret de Mola C, Victora CG. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta-analysis. Acta Paediatr 2015;104:30-7. https://doi.org/10.1111/apa.13133.
- Horta BL, Loret de Mola C, Victora CG. Breastfeeding and intelligence: a systematic review and meta-analysis. Acta Paediatr 2015;104:14-9. https://doi.org/10.1111/apa.13139.
- Horta BL, Victora CG. Long-term Effects of Breastfeeding: A Systematic Review. Geneva: World Health Organization; 2013.
- Horta BL, Victora CG. Short-term Effects of Breastfeeding: A Systematic Review of the Benefits of Breastfeeding on Diarrhoea and Pneumonia Mortality. Geneva: World Health Organization; 2013.
- Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr 2015;104:96-113. https://doi.org/10.1111/apa.13102.
- Renfrew MJ, Pokhrel S, Quigley M, McCormick F, Fox-Rushby J, Dodds R, et al. Preventing Disease and Saving Resources: The Potential Contribution of Increasing Breastfeeding Rates in the UK. London: UNICEF UK; 2012.
- Scientific Advisory Committee on Nutrition . Feeding in the First Year of Life. 2018.
- Kramer MS, Chalmers B, Hodnett ED, Sevkovskaya Z, Dzikovich I, Shapiro S, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA 2001;285:413-20. https://doi.org/10.1001/jama.285.4.413.
- Eidelman AI, Schanler RJ. Breastfeeding and the use of human milk. Pediatrics 2012;129:e829-41. https://doi.org/10.1542/peds.2011-3552.
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess 2007;153:1-186.
- Bobrow KL, Quigley MA, Green J, Reeves GK, Beral V. Persistent effects of women’s parity and breastfeeding patterns on their body mass index: results from the Million Women Study. Int J Obes 2013;37:712-7. https://doi.org/10.1038/ijo.2012.76.
- McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ. Infant Feeding Survey 2010. Leeds: NHS Digital; 2012.
- Public Health England (PHE) . Breastfeeding Statistics 2016. www.gov.uk/government/collections/breastfeeding-statistics (accessed 6 November 2018).
- Information Services Division (ISN), NHS Scotland . Infant Feeding Statistics Scotland 2017.
- World Health Organization, UNICEF . Global Strategy for Infant and Young Child Feeding 2003.
- National Collaborating Centre for Primary Care . Postnatal Care: Routine Postnatal Care of Women and Their Babies 2006.
- Public Health England (PHE) . Breastfeeding Prevalence at 6–8 Weeks After Birth (Experimental Statistics): 2016 17 Annual Data Statistical Commentary (November 2017 Release). 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/666391/2016-17_Annual_-_Breastfeeding_Statistical_Commentary.pdf (accessed 6 November 2018).
- Hoddinott P, Craig L, Britten J, McInnes R. A Prospective Study Exploring the Early Infant Feeding Experiences of Parents and Their Significant Others During the First 6 Months of Life: What Would Make a Difference. Edinburgh: NHS Health Scotland; 2010.
- Bhavnani V, Newburn M. Left to Your Own Devices: The Postnatal Care Experiences of 1260 First-time Mothers. London: NCT; 2010.
- The National Federation of Women’s Institutes (NFWI), NCT . Support Overdue: Women’s Experiences of Maternity Services 2017.
- National Institute for Health and Care Excellence (NICE) . Maternal and Child Nutrition 2008.
- Department of Health and Social Care (DHSC), Department for Children, Schools and Families (DCSF) . Commissioning Local Breastfeeding Support Services 2009.
- Jolly K, Ingram L, Khan KS, Deeks JJ, Freemantle N, MacArthur C. Systematic review of peer support for breastfeeding continuation: metaregression analysis of the effect of setting, intensity, and timing. BMJ 2012;344. https://doi.org/10.1136/bmj.d8287.
- Dennis CL. Peer support within a health care context: a concept analysis. Int J Nurs Stud 2003;40:321-32. https://doi.org/10.1016/S0020-7489(02)00092-5.
- Paranjothy S, Copeland L, Merrett L, Grant A, Phillips R, Gobat N, et al. A novel peer-support intervention using motivational interviewing for breastfeeding maintenance: a UK feasibility study. Health Technol Assess 2017;21. https://doi.org/10.3310/hta21770.
- Ingram L, MacArthur C, Khan K, Deeks JJ, Jolly K. Effect of antenatal peer support on breastfeeding initiation: a systematic review. CMAJ 2010;182:1739-46. https://doi.org/10.1503/cmaj.091729.
- McFadden A, Gavine A, Renfrew MJ, Wade A, Buchanan P, Taylor JL, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev 2017;2. https://doi.org/10.1002/14651858.CD001141.pub5.
- Hoddinott P, Seyara R, Marais D. Global evidence synthesis and UK idiosyncrasy: why have recent UK trials had no significant effects on breastfeeding rates?. Matern Child Nutr 2011;7:221-7. https://doi.org/10.1111/j.1740-8709.2011.00336.x.
- Renfrew MJ, McCormick FM, Wade A, Quinn B, Dowswell T. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev 2012;5. https://doi.org/10.1002/14651858.CD001141.pub4.
- Dennis CL, Hodnett E, Gallop R, Chalmers B. The effect of peer support on breast-feeding duration among primiparous women: a randomized controlled trial. CMAJ 2002;166:21-8.
- Hoddinott P, Craig L, Maclennan G, Boyers D, Vale L. NHS Grampian and the University of Aberdeen FEST Project Team . The FEeding Support Team (FEST) randomised, controlled feasibility trial of proactive and reactive telephone support for breastfeeding women living in disadvantaged areas. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2011-000652.
- Lavender T, Richens Y, Milan SJ, Smyth RM, Dowswell T. Telephone support for women during pregnancy and the first six weeks postpartum. Cochrane Database Syst Rev 2013;7. https://doi.org/10.1002/14651858.CD009338.pub2.
- Trickey H, Newburn M. Goals, dilemmas and assumptions in infant feeding education and support: applying theory of constraints thinking tools to develop new priorities for action. Matern Child Nutr 2014;10:72-91. https://doi.org/10.1111/j.1740-8709.2012.00417.x.
- Trickey H, Thomson G, Grant A, Sanders J, Mann M, Murphy S, et al. A realist review of one-to-one breastfeeding peer support experiments conducted in developed country settings. Matern Child Nutr 2018;14. https://doi.org/10.1111/mcn.12559.
- Schmied V, Beake S, Sheehan A, McCourt C, Dykes F. A meta-synthesis of women’s perceptions and experiences of breastfeeding support. JBI Libr Syst Rev 2009;6:583-614. https://doi.org/10.11124/jbisrir-2009-195.
- Ingram J. A mixed methods evaluation of peer support in Bristol, UK: mothers’, midwives’ and peer supporters’ views and the effects on breastfeeding. BMC Pregnancy Childbirth 2013;13. https://doi.org/10.1186/1471-2393-13-192.
- Hoddinott P, Britten J, Pill R. Why do interventions work in some places and not others: a breastfeeding support group trial. Soc Sci Med 2010;70:769-78. https://doi.org/10.1016/j.socscimed.2009.10.067.
- Chapman DJ, Damio G, Young S, Pérez-Escamilla R. Effectiveness of breastfeeding peer counseling in a low-income, predominantly Latina population: a randomized controlled trial. Arch Pediatr Adolesc Med 2004;158:897-902. https://doi.org/10.1001/archpedi.158.9.897.
- Anderson AK, Damio G, Young S, Chapman DJ, Pérez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Arch Pediatr Adolesc Med 2005;159:836-41. https://doi.org/10.1001/archpedi.159.9.836.
- Campbell OM, Cegolon L, Macleod D, Benova L. Length of stay after childbirth in 92 countries and associated factors in 30 low- and middle-income countries: compilation of reported data and a cross-sectional analysis from nationally representative surveys. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1001972.
- NHS Digital . NHS Maternity Statistics, England 2016–17 Statistics 2017. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-maternity-statistics/2016-17#resources (accessed 6 November 2018).
- UNICEF UK . The Baby Friendly Initiative. Stage 1: A Firm Foundation. n.d. www.unicef.org.uk/babyfriendly/accreditation/maternity-neonatal-health-visiting-childrens-centres/stage-1-a-firm-foundation/ (accessed 10 January 2020).
- Grant A, McEwan K, Tedstone S, Greene G, Copeland L, Hunter B, et al. Availability of breastfeeding peer support in the United Kingdom: a cross-sectional study. Matern Child Nutr 2018;14. https://doi.org/10.1111/mcn.12476.
- Department of Health and Social Care (DHSC), Regional Public Health Group for London . Breastfeeding Peer Support in London: A Guide for Commissioners. 2012.
- Brown A, Davies R. Fathers’ experiences of supporting breastfeeding: challenges for breastfeeding promotion and education. Matern Child Nutr 2014;10:510-26. https://doi.org/10.1111/mcn.12129.
- Burgess A, Goldman R. Who’s the Bloke in the Room? Fathers During Pregnancy and at the Birth in the UK. London: Fatherhood Institute; 2018.
- Brown A. What do women really want? Lessons for breastfeeding promotion and education. Breastfeed Med 2016;11:102-10. https://doi.org/10.1089/bfm.2015.0175.
- McInnes RJ, Hoddinott P, Britten J, Darwent K, Craig LC. Significant others, situations and infant feeding behaviour change processes: a serial qualitative interview study. BMC Pregnancy Childbirth 2013;13. https://doi.org/10.1186/1471-2393-13-114.
- Darwent KL, McInnes RJ, Swanson V. The Infant Feeding Genogram: a tool for exploring family infant feeding history and identifying support needs. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-1107-5.
- Hoddinott P, Craig LC, Britten J, McInnes RM. A serial qualitative interview study of infant feeding experiences: idealism meets realism. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2011-000504.
- Trickey H, Allmark H, Dodds R, Figueras J, Neil H, Newburn M, et al. NCT Values and Approaches to Infant Feeding Support. London: NCT; 2011.
- Renfrew MJ, Ansell P, Macleod KL. Formula feed preparation: helping reduce the risks – a systematic review. Arch Dis Child 2003;88:855-8. https://doi.org/10.1136/adc.88.10.855.
- Lakshman R, Ogilvie D, Ong KK. Mothers’ experiences of bottle-feeding: a systematic review of qualitative and quantitative studies. Arch Dis Child 2009;94:596-601. https://doi.org/10.1136/adc.2008.151910.
- NHS . Bottle Feeding Advice 2018. www.nhs.uk/conditions/pregnancy-and-baby/bottle-feeding-advice/ (accessed 6 November 2018).
- McInnes RJ, Stone DH. The process of implementing a community-based peer breast-feeding support programme: the Glasgow experience. Midwifery 2001;17:65-73. https://doi.org/10.1054/midw.2000.0236.
- Thomson G, Ebisch-Burton K, Flacking R. Shame if you do – shame if you don’t: women’s experiences of infant feeding. Matern Child Nutr 2015;11:33-46. https://doi.org/10.1111/mcn.12148.
- Antonovsky A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well. San Francisco, CA: Jossey-Bass; 1987.
- Antonovsky A. The salutogenic model as a theory to guide health promotion. Health Promot Int 1996;11:11-8. https://doi.org/10.1093/heapro/11.1.11.
- NHS Health Scotland . Asset-Based Approaches to Health Improvement. 2012.
- Nussbaum M, Sen A. The Quality of Life. New York, NY: Oxford University Press; 1993.
- McLean J. Asset Based Approaches to Health Improvement: Redressing the Balance. Glasgow: Glasgow Centre for Population Health; 2011.
- Aradon G. On the Borderline: Development Trusts Tackling Poverty in the UK. London: Development Trusts Association; 2007.
- Cooke I. Trust in the community?. Concept J Comtemp Community Educ Pract Theor 2010;1:22-6.
- O’Leary T. Does Asset Based Community Development Deliver Social Justice 2006.
- Foot J, Hopkins T. A Glass Half Full: How an Asset Approach Can Improve Community Health and Well Being. London: Improvement and Development Agency for Local Government (IDeA); 2010.
- Lindström B, Eriksson M, Morgan A, Ziglio E, Davies M. Health Assets in a Global Context. New York, NY: Springer; 2010.
- Rippon S, Hopkins T. Head, Hands and Heart: Asset-based Approaches in Health Care. London: The Health Foundation; 2015.
- Lawton R, Ashley L, Dawson S, Waiblinger D, Conner M. Employing an extended Theory of Planned Behaviour to predict breastfeeding intention, initiation, and maintenance in White British and South-Asian mothers living in Bradford. Br J Health Psychol 2012;17:854-71. https://doi.org/10.1111/j.2044-8287.2012.02083.x.
- Dyson L, Green JM, Renfrew MJ, McMillan B, Woolridge M. Factors influencing the infant feeding decision for socioeconomically deprived pregnant teenagers: the moral dimension. Birth 2010;37:141-9. https://doi.org/10.1111/j.1523-536X.2010.00394.x.
- Forster DA, McLachlan HL, Lumley J. Factors associated with breastfeeding at six months postpartum in a group of Australian women. Int Breastfeed J 2006;1. https://doi.org/10.1186/1746-4358-1-18.
- Racine EF, Frick KD, Strobino D, Carpenter LM, Milligan R, Pugh LC. How motivation influences breastfeeding duration among low-income women. J Hum Lact 2009;25:173-81. https://doi.org/10.1177/0890334408328129.
- Bar-Yam NB, Darby L. Fathers and breastfeeding: a review of the literature. J Hum Lact 1997;13:45-50. https://doi.org/10.1177/089033449701300116.
- Rempel LA, Rempel JK. The breastfeeding team: the role of involved fathers in the breastfeeding family. J Hum Lact 2011;27:115-21. https://doi.org/10.1177/0890334410390045.
- Ogbo FA, Eastwood J, Page A, Arora A, McKenzie A, Jalaludin B, et al. Prevalence and determinants of cessation of exclusive breastfeeding in the early postnatal period in Sydney, Australia. Int Breastfeed J 2016;12. https://doi.org/10.1186/s13006-017-0110-4.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Thomson G, Crossland N, Dykes F. Giving me hope: women’s reflections on a breastfeeding peer support service. Matern Child Nutr 2012;8:340-53. https://doi.org/10.1111/j.1740-8709.2011.00358.x.
- Hoddinott P, Craig L, Maclennan G, Boyers D, Vale L. NHS Grampian and the University of Aberdeen FEST project team . Process evaluation for the FEeding Support Team (FEST) randomised controlled feasibility trial of proactive and reactive telephone support for breastfeeding women living in disadvantaged areas. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2012-001039.
- Marmot M, Bell R. Fair society, healthy lives. Public Health 2012;126:4-10. https://doi.org/10.1016/j.puhe.2012.05.014.
- UNICEF UK . Guide to the Unicef UK Baby Friendly Initiative Standards 2012.
- Chung M, Raman G, Trikalinos T, Lau J, Ip S. Interventions in primary care to promote breastfeeding: an evidence review for the US Preventive Services Task Force. Ann Intern Med 2008;149:565-82. https://doi.org/10.7326/0003-4819-149-8-200810210-00009.
- National Institute for Health and Care Excellence (NICE) . Behaviour Change: Individual Approaches – Public Health Guideline (PH49). 2014.
- Jolly K, Ingram J, Clarke J, Johnson D, Trickey H, Thomson G, et al. Protocol for a feasibility trial for improving breast feeding initiation and continuation: assets-based infant feeding help before and after birth (ABA). BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019142.
- Phillips G, Brett K, Mendola P. Previous breastfeeding practices and duration of exclusive breastfeeding in the United States. Matern Child Health J 2011;15:1210-16. https://doi.org/10.1007/s10995-010-0694-4.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the New Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7. https://doi.org/10.2105/AJPH.89.9.1322.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Morgan H, Hoddinott P, Thomson G, Crossland N, Farrar S, Yi D, et al. Benefits of Incentives for Breastfeeding and Smoking cessation in pregnancy (BIBS): a mixed-methods study to inform trial design. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19300.
- Whitford HM, Donnan PT, Symon AG, Kellett G, Monteith-Hodge E, Rauchhaus P, et al. Evaluating the reliability, validity, acceptability, and practicality of SMS text messaging as a tool to collect research data: results from the Feeding Your Baby project. J Am Med Inform Assoc 2012;19:744-9. https://doi.org/10.1136/amiajnl-2011-000785.
- Hoddinott P, Pill R. Qualitative study of decisions about infant feeding among women in east end of London. BMJ 1999;318:30-4. https://doi.org/10.1136/bmj.318.7175.30.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- World Health Organization . Indicators for Assessing Infant and Young Child Feeding Practices, Part 3: Country Profiles. 2010.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705-14. https://doi.org/10.1016/0277-9536(91)90150-B.
- Putz R, O’Hara K, Taggart F, Stewart-Brown S. Using WEMWBS to Measure the Impact of Your Work on Mental Wellbeing: A Practice-based User Guide. Coventry: Coventry City Council; 2012.
- Clarke JL, Ingram J, Johnson D, Trickey H, Dombrowski SU, Sitch A, et al. The ABA intervention for improving breastfeeding initiation and continuation: feasibility study results. Matern Child Nutr 2020;16.
- Office for National Statistics (ONS) . Births in England and Wales: Summary Tables. 2018.
- Department for Education . Participation Rates in Higher Education: 2006 to 2016 2017.
- Graffy J, Taylor J, Williams A, Eldridge S. Randomised controlled trial of support from volunteer counsellors for mothers considering breast feeding. BMJ 2004;328. https://doi.org/10.1136/bmj.328.7430.26.
- Jolly K, Ingram L, Freemantle N, Khan K, Chambers J, Hamburger R, et al. Effect of a peer support service on breast-feeding continuation in the UK: a randomised controlled trial. Midwifery 2012;28:740-5. https://doi.org/10.1016/j.midw.2011.08.005.
- MacArthur C, Jolly K, Ingram L, Freemantle N, Dennis CL, Hamburger R, et al. Antenatal peer support workers and initiation of breast feeding: cluster randomised controlled trial. BMJ 2009;338. https://doi.org/10.1136/bmj.b131.
- Muirhead PE, Butcher G, Rankin J, Munley A. The effect of a programme of organised and supervised peer support on the initiation and duration of breastfeeding: a randomised trial. Br J Gen Pract 2006;56:191-7.
- Forster D, McLardie-Hore F, McLachlan H, Davey M-A, Amir LH, Gold L, et al. Ringing up about breastfeeding: a random controlled trial exploring early telephone peer support for breastfeeding (RUBY) – primary outcomes. Women Birth 2017;30. https://doi.org/10.1016/j.wombi.2017.08.023.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Aiken A, Thomson G. Professionalisation of a breast-feeding peer support service: issues and experiences of peer supporters. Midwifery 2013;29:e145-51. https://doi.org/10.1016/j.midw.2012.12.014.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- Rayfield S, Oakley L, Quigley MA. Association between breastfeeding support and breastfeeding rates in the UK: a comparison of late preterm and term infants. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009144.
- Ingram J, Thomson G, Johnson D, Clarke JL, Trickey H, Hoddinott P, et al. Women‘s and peer supporters’ experiences of an assets-based peer support intervention for increasing breastfeeding initiation and continuation: a qualitative study [published online ahead of print March 21 2020]. Health Expect 2020. https://doi.org/10.1111/hex.13042.
Appendix 1 Revisions to the ABA study protocol
The funded study protocol is available on the project web page (URL: www.journalslibrary.nihr.ac.uk/programmes/phr/155304/#/; accessed 16 March 2020).
Amendment 1, 4 April 2017
-
Several minor errors were identified on the 8-week and 6-month questionnaires. These included:
-
duplicate requests to tick and cross response boxes
-
incorrect numbering in 8-week questionnaire
-
incorrect signposting to next relevant question.
-
These were amended in the questionnaires.
-
We started the study using paper randomisation, rather than the web-based programme specified in the protocol. As the recruitment period was quite short, we proposed to continue using telephone randomisation at site A. Practical challenges led to a reconsideration of the randomisation method at site B. As volunteers were to deliver the intervention, they had constraints on how many women they could support at any one time. We amended the randomisation process to blocks for each locality at site B. When the number of women required to complete a block was recruited at a site, the women would be randomised at the same time and notified of their allocation status by telephone and/or letter. Changes were made in the protocol to reflect the changes to the randomisation process.
-
We clarified the procedure for following up participants if they did not return questionnaires at 8 weeks and 6 months. This was not clearly specified in the original protocol. The amended protocol reads:
‘Follow-up questionnaires will either be posted to participants to be completed at home, or participants will be called to complete the questionnaire over the telephone (according to preference indicated at recruitment).
In the case of follow up questionnaires not being returned by participants, the following methods will be employed:
-
Sending another copy of the questionnaire in the post
-
A telephone call/text to the participant from the research team to encourage completion, or offer phone completion
-
Collection of the primary outcome only by telephone or text’
-
-
At the request of one of the organisations delivering the intervention, a sentence was inserted into the consent form:
‘The Sponsor, subject to agreement from the [ORGANISATION], may appoint a third party to access my identifiable data.’
-
In the study eligibility form, which was completed by the research fellow at recruitment, we added a question about whether the participant is aged < 25 years/≥ 25 years and a question about whether the participant is aged at least 16 years. This was to make the telephone randomisation process easier.
All amendments to the protocol were agreed on 12 June 2017 by South West – Cornwall and Plymouth Research Ethics Committee (16/SW/0336).
Appendix 2 Participant information leaflet (anonymised)
Appendix 3 Consent form (anonymised)
Appendix 4 Anonymised version of the ‘assets leaflet’ used in the ABA intervention
Appendix 5 The ABA study text library
Hi, it’s Jo, from the ABA feeding team. I tried to call you earlier, when is a good time for a catch-up?
Best wishes for the birth – don’t forget to let me know when your baby is born. If there’s anything you want to discuss send a text and I’ll call back.
Hi Abby, it’s Jo from the ABA feeding team. I tried to call you earlier. Give me a call or text a good time to get back you.
There are national breastfeeding helplines [open 9.30am to 9.30pm] you can call. Store this number in case you need it: XXXX
Hi Abby, how are you managing?
Hi Abby, how are you? How is the feeding going?
Hi Abby, how are you, how was last night?
How’s the feeding going? Here to talk if you need.
If there is anything that you would like to chat through do give me a call.
Any feeding questions or problems let me know, always happy to talk things through.
Do you have any social events coming up? Are you wondering how you will cope with feeding? If you want to talk about anything I would really like you to give me a call.
If you want to talk about anything I would really like you to give me a call.
If you’d like to chat about feeding or just to chat do give me a call... here if you need me.
Details of mother & baby and feeding groups are on the leaflet we gave you and available here [weblink or document]. You can take a friend along.
If you are thinking of mixed feeding, or even stopping breastfeeding, please give me a call, I can help with all types of feeding.
Hi Abby, It’s Jo, from the ABA feeding team. Just wondering how it’s all going.
If you have any feeding questions you can call me on [tel no.]
Hi Abby, It’s Jo, from the ABA feeding team. How are you and [baby name] getting on?
Hi Abby, I haven’t heard back from you. I won’t keep texting, but if you’d like to chat about feeding or just to chat give me a call.
It’s Jo from the feeding team. I won’t contact you again, but the ABA study team will send you a questionnaire when [baby name] is 8 weeks and 6 months old. If you complete these, they will send you a £25 voucher when [baby name] is 6 months. Best wishes for the future.
Appendix 6 Example genogram
Reproduced from Ingram et al. 113 © 2020 The Authors Health Expectations published by John Wiley & Sons Ltd. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
Appendix 7 Fidelity checklist for ABA antenatal visit recordings
Appendix 8 Semistructured interview schedules
Appendix 9 Text message sent to women 2–3 days postnatally
Hello from the ABA research team. Congratulations on the birth of your baby.
We would like to know how your baby has been fed since birth.
If your baby has had only formula milk please text 1.
If your baby has had only breast milk please text 2.
If your baby has had both breast and formula milk please text 3.
Thank you – we will next be in touch when your baby is 8 weeks old.
Appendix 10 Recruitment flow diagrams for sites A and B
Site A
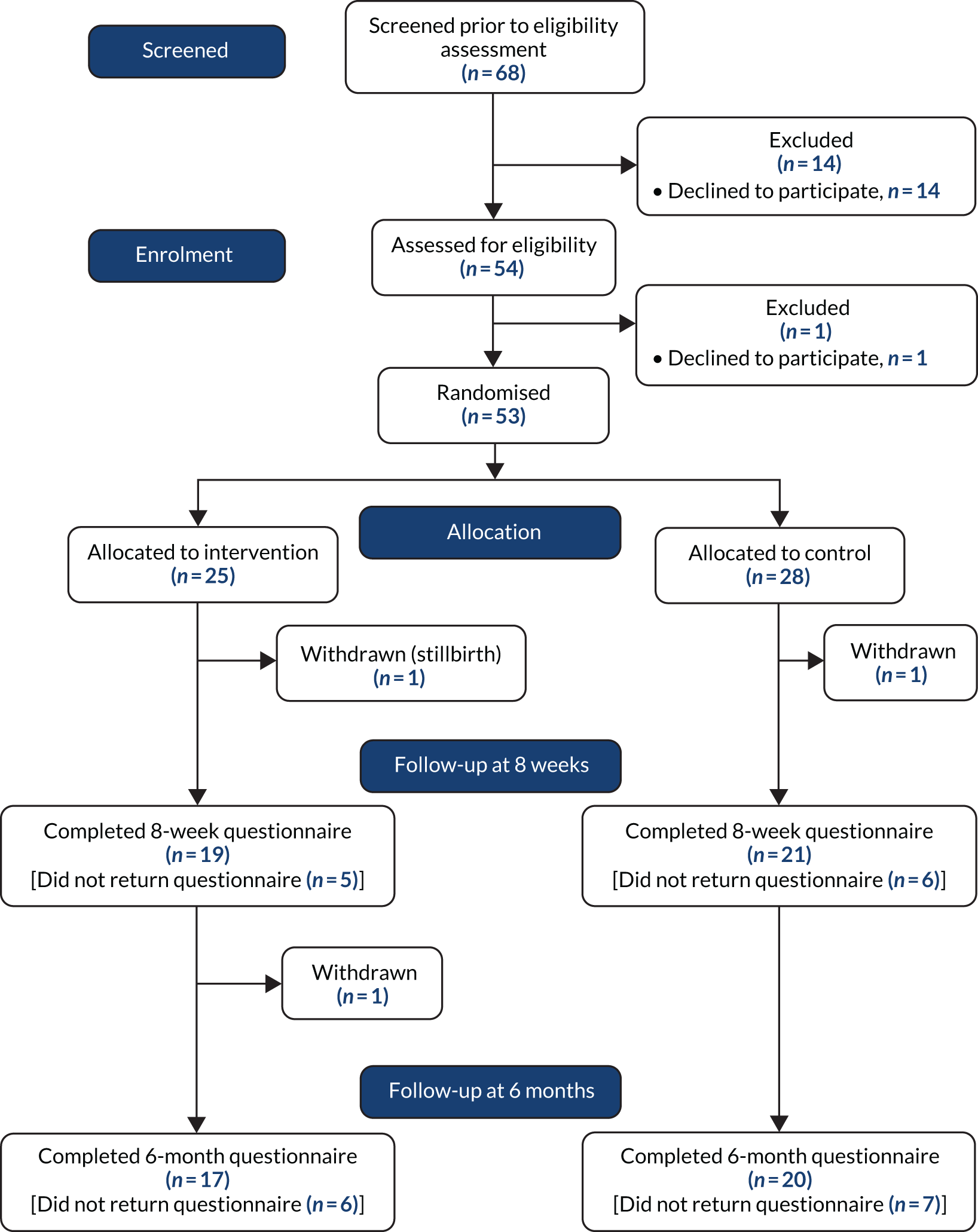
Site B
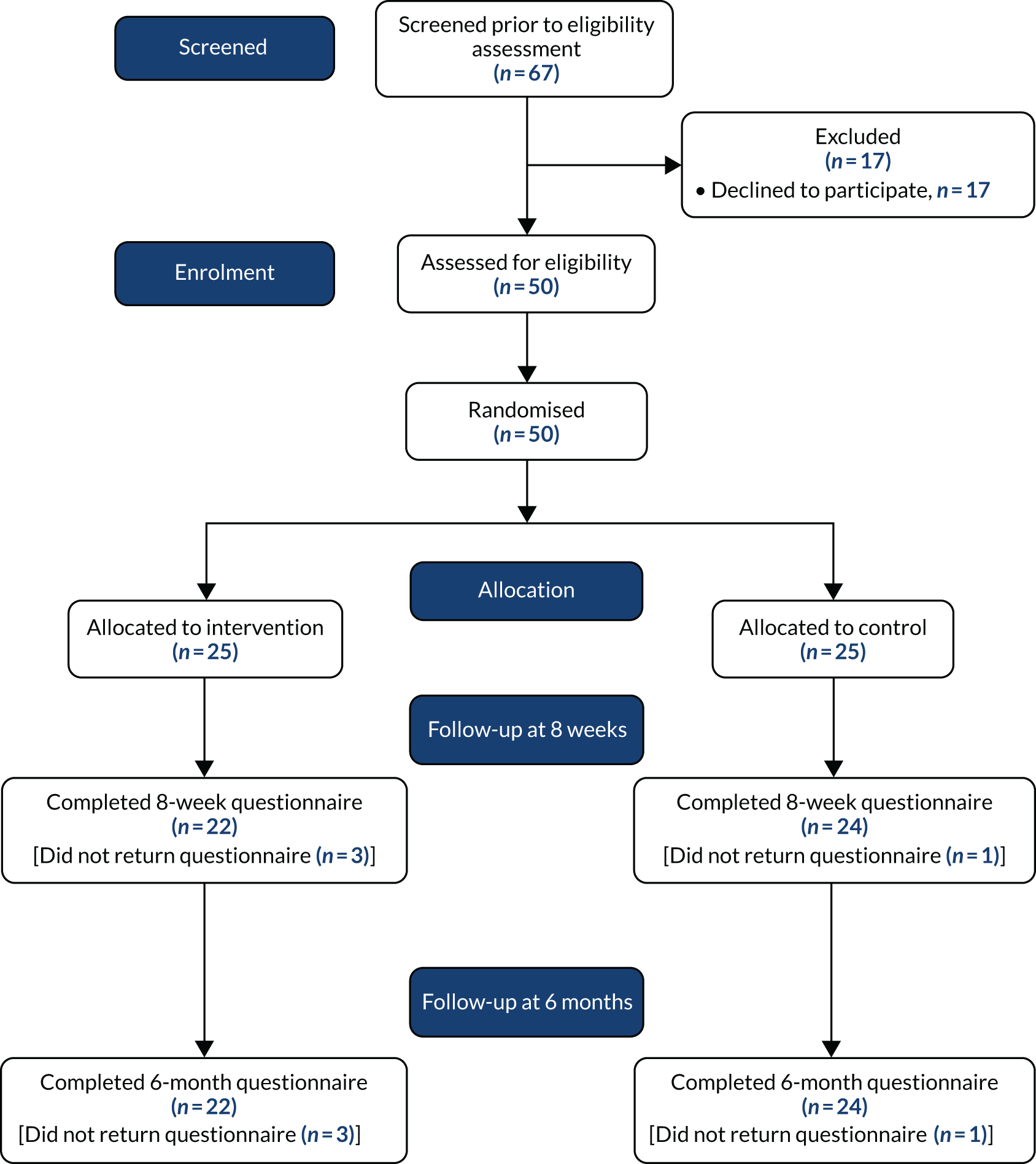
Appendix 11 Participant demographic and delivery characteristics by site
| Characteristic | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |
| Age at baseline (years), mean (SD) | 27.9 (5.2) | 27.7 (5.9) | 27.8 (5.5) | 29.2 (20.5) | 29.3 (5.6) | 29.3 (5.4) | 28.6 (5.2) | 28.5 (5.8) | 28.5 (5.5) |
| Age range (years), minimum–maximum | 17.7–37.7 | 17.9–39.0 | 17.7–39.0 | 20.5–43.0 | 17.9–42.9 | 17.9–43.0 | 17.7–43.0 | 17.9–42.9 | 17.7–43.0 |
| Missing, n (%) | 0 (0) | 1 (3.6) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Ethnicity, n (%) | N = 54 | ||||||||
| White British | 21 (84.0) | 22 (81.5) | 43 (82.7) | 22 (88.0) | 23 (92.0) | 45 (90.0) | 43 (86.0) | 45 (86.5) | 88 (86.3) |
| White other | 1 (4.0) | 3 (11.1) | 4 (7.7) | 2 (8.0) | 1 (4.0) | 3 (6.0) | 3 (6.0) | 4 (7.7) | 7 (6.9) |
| Asian | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (4.0) | 1 (2.0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Black African | 0 (0) | 1 (3.7) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Black Caribbean | 1 (4.0) | 0 (0) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 1 (2.0) | 1 (1.9) | 1 (1.0) |
| Mixed | 1 (4.0) | 1 (3.7) | 2 (3.9) | 1 (4.0) | 0 (0) | 1 (2.0) | 2 (4.0) | 1 (1.9) | 3 (2.9) |
| Other | 1 (4.0) | 0 (0) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 1 (2.0) | 0 (0) | 1 (1.0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Employment status, n (%) | N = 24 | N = 52 | N = 49 | N = 102 | |||||
| In paid work | 18 (72.0) | 25 (92.6) | 43 (82.7) | 22 (88.0) | 25 (100) | 47 (94.0) | 40 (80.0) | 50 (96.2) | 90 (88.2) |
| Unemployed | 6 (24.0) | 1 (3.7) | 7 (13.5) | 2 (8.0) | 0 (0) | 2 (4.0) | 8 (16.0) | 1 (1.9) | 9 (8.8) |
| Looking after family/home | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Unable to work (long-term health problem) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Full-time education or training | 0 (0) | 1 (3.7) | 1 (1.9) | 1 (4.0) | 0 (0) | 1 (2.0) | 1 (2.0) | 1 (2.0) | 2 (2.0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Highest level of qualification, n (%) | N = 30 | ||||||||
| No formal qualification | 1 (4.0) | 0 (0) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 1 (2.0) | 0 (0) | 1 (1.0) |
| GCSE or equivalent | 6 (24.0) | 5 (18.5) | 11 (21.2) | 6 (24.0) | 5 (20.0) | 11 (22.0) | 12 (24.0) | 10 (19.2) | 22 (21.6) |
| A/AS level or equivalent | 8 (32.0) | 6 (22.2) | 14 (26.9) | 12 (48.0) | 7 (28.0) | 19 (38.0) | 20 (40.0) | 13 (25.0) | 33 (32.4) |
| Degree level or higher | 10 (40.0) | 16 (59.3) | 26 (50.0) | 7 (28.0) | 13 (52.0) | 20 (40.0) | 17 (34.0) | 29 (55.8) | 46 (45.1) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Relationship status, n (%) | |||||||||
| Married/registered civil partnership | 9 (36.0) | 12 (46.2) | 21 (41.2) | 13 (52.0) | 14 (56.0) | 27 (54.0) | 22 (44.0) | 26 (51.0) | 48 (47.5) |
| Living together | 9 (36.0) | 11 (42.3) | 20 (39.2) | 9 (36.0) | 9 (36.0) | 18 (36.0) | 18 (36.0) | 20 (39.2) | 38 (37.6) |
| Single | 7 (28.0) | 3 (11.5) | 10 (19.6) | 3 (12.0) | 2 (8.0) | 5 (10.0) | 10 (20.0) | 5 (9.8) | 15 (14.9) |
| Widowed, divorced or separated | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 2 (7.1) | 2 (3.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (3.8) | 2 (1.9) |
| Index of Multiple Deprivation quintile, n (%) | N = 27 | N = 52 | N = 52 | N = 102 | |||||
| 1 (most deprived) | 13 (52.0) | 11 (40.7) | 24 (46.2) | 1 (4.0) | 0 (0) | 1 (2.0) | 14 (28.0) | 11 (21.2) | 25 (24.5) |
| 2 | 3 (12.0) | 6 (22.2) | 9 (17.3) | 2 (8.0) | 2 (8.0) | 4 (8.0) | 5 (10.0) | 8 (15.4) | 13 (12.8) |
| 3 | 1 (4.0) | 7 (25.9) | 8 (15.4) | 8 (32.0) | 3 (12.0) | 11 (22.0) | 9 (18.0) | 10 (19.2) | 19 (18.6) |
| 4 | 7 (28.0) | 3 (11.1) | 10 (19.2) | 6 (24.0) | 11 (44.0) | 17 (34.0) | 13 (26.0) | 14 (26.9) | 27 (26.5) |
| 5 (least deprived) | 1 (4.0) | 0 (0) | 1 (1.9) | 8 (32.0) | 9 (36.0) | 17 (34.0) | 9 (18.0) | 9 (17.3) | 18 (17.7) |
| Maternal well-being (WEMWBS), mean (SD) | 54.1 (9.8) | 55.0 (9.2) | 54.6 (9.4) | 53.4 (6.2) | 53.7 (8.4) | 53.6 (7.3) | 53.7 (8.1) | 54.4 (8.7) | 54.1 (8.4) |
| Missing, n (%) | 0 (0) | 1 (3.6) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Intention to feed, n (%) | |||||||||
| Breastmilk only | 10 (40.0) | 9 (33.3) | 19 (36.5) | 7 (28.0) | 9 (37.5) | 16 (32.7) | 17 (34.0) | 18 (35.3) | 35 (34.7) |
| Mainly breastmilk | 7 (28.0) | 7 (25.9) | 14 (26.9) | 10 (40.0) | 6 (25.0) | 16 (32.7) | 17 (34.0) | 13 (25.5) | 30 (29.7) |
| Half and half | 4 (16.0) | 6 (22.2) | 10 (19.2) | 6 (24.0) | 6 (25.0) | 12 (24.5) | 10 (20.0) | 12 (23.5) | 22 (21.8) |
| Mainly formula | 2 (8.0) | 2 (7.4) | 4 (7.7) | 1 (4.0) | 0 (0) | 1 (2.0) | 3 (6.0) | 2 (3.9) | 5 (5.0) |
| Formula milk only | 2 (8.0) | 3 (11.1) | 5 (9.6) | 1 (4.0) | 3 (12.5) | 4 (8.2) | 3 (6.0) | 6 (11.8) | 9 (8.9) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 0 (0) | 1 (4.0) | 1 (2.0) | 0 (0) | 2 (3.8) | 2 (1.9) |
| How participant was fed as a baby, n (%) | |||||||||
| Breastfed entirely | 7 (28.0) | 8 (29.6) | 15 (28.9) | 9 (36.0) | 12 (48.0) | 21 (42.0) | 16 (32.0) | 20 (38.5) | 36 (35.3) |
| Formula fed entirely | 8 (32.0) | 13 (48.2) | 21 (40.4) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 13 (26.0) | 16 (30.8) | 29 (28.4) |
| Mixed feeding | 10 (40.0) | 5 (18.5) | 15 (28.9) | 7 (28.0) | 6 (24.0) | 13 (26.0) | 17 (34.0) | 11 (21.2) | 28 (27.5) |
| Don’t know | 0 | 1 (3.7) | 1 (1.9) | 4 (16.0) | 4 (16.0) | 8 (16.0) | 4 (8.0) | 5 (9.6) | 9 (8.8) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Participant knows anyone who has breastfed their baby, n (%) | 22 (88.0) | 25 (92.6) | 47 (90.4) | 21 (84.0) | 25 (100) | 46 (92.0) | 43 (86.0) | 50 (96.2) | 93 (91.2) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.9) | 1 (1.0) |
| Baby’s gestational age at birth (weeks), mean (SD) | 39.0 (2.3) | 40.1 (1.2) | 39.6 (1.9) | 39.7 (1.7) | 39.3 (1.8) | 39.5 (1.8) | 39.4 (2.0) | 39.7 (1.6) | 39.5 (1.8) |
| Missing | 1 (2.0) | 1 (3.6) | 2 (3.8) | 0 (0) | 0 (0) | 0 (0) | 1 (2.0) | 1 (1.9) | 2 (1.9) |
| Premature baby, n (%) | 5 (20.8) | 0 (0) | 5 (9.8) | 2 (8.0) | 2 (8.0) | 4 (8.0) | 7 (14.3) | 2 (3.9) | 9 (8.9) |
| Missing | 1 (2.0) | 1 (3.6) | 2 (3.8) | 0 (0) | 0 (0) | 0 (0) | 1 (2.0) | 1 (1.9) | 2 (1.9) |
| Mode of delivery, n (%) | |||||||||
| Vaginal birth | 5 (26.3) | 10 (50.0) | 15 (38.5) | 10 (47.6) | 12 (50.0) | 22 (48.9) | 15 (37.5) | 22 (50.0) | 37 (44.1) |
| C-section (planned) | 1 (5.3) | 1 (5.0) | 2 (5.1) | 2 (9.5) | 2 (8.3) | 4 (8.9) | 3 (7.5) | 3 (6.8) | 6 (7.1) |
| C-section (emergency) | 4 (21.1) | 4 (20.0) | 8 (20.5) | 4 (19.1) | 6 (25.0) | 10 (22.2) | 8 (20.0) | 10 (22.7) | 18 (21.4) |
| Forceps, ventouse, vacuum delivery | 9 (47.4) | 5 (25.0) | 14 (35.9) | 5 (23.8) | 4 (16.7) | 9 (20.0) | 14 (35.0) | 9 (20.5) | 23 (27.4) |
| Missing | 6 (24.0) | 8 (28.6) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Duration of mother’s hospital stay, n (%) | |||||||||
| < 24 hours | 3 (15.8) | 6 (30.0) | 9 (23.1) | 5 (23.8) | 4 (16.7) | 9 (20.0) | 8 (20.0) | 10 (22.7) | 18 (21.4) |
| 24–48 hours | 11 (57.9) | 6 (30.0) | 17 (43.6) | 7 (33.3) | 6 (25.0) | 13 (28.9) | 18 (45.0) | 12 (27.3) | 30 (35.7) |
| > 48 hours | 5 (26.3) | 7 (35.0) | 12 (30.8) | 9 (42.9) | 14 (58.3) | 23 (51.1) | 14 (35.0) | 21 (47.7) | 35 (41.7) |
| Home birth | 0 | 1 (5.0) | 1 (2.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (2.3) | 1 (1.2) |
| Missing | 6 (24.0) | 8 (28.6) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Baby admitted to neonatal unit, n (%) | 4 (21.1) | 2 (10.0) | 6 (15.4) | 3 (14.3) | 2 (8.3) | 5 (11.1) | 7 (17.5) | 4 (9.1) | 11 (13.1) |
| Missing | 6 (24.0) | 8 (28.6) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
Appendix 12 Data completeness
Data completeness: participant characteristics
| Data item | Intervention | Control | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Potential total | Number collected | Completed (%) | Potential total | Number collected | Completed (%) | Potential total | Number collected | Completed (%) | |
| Age | 50 | 50 | 100 | 53 | 52 | 98.1 | 103 | 102 | 99.0 |
| Ethnicity | 50 | 50 | 100 | 53 | 52 | 98.1 | 103 | 102 | 99.0 |
| Employment status | 50 | 50 | 100 | 53 | 52 | 98.1 | 103 | 102 | 99.0 |
| Qualifications | 50 | 50 | 100 | 53 | 52 | 98.1 | 103 | 102 | 99.0 |
| Relationship status | 50 | 50 | 100 | 53 | 51 | 96.2 | 103 | 101 | 98.1 |
| Index of Multiple Deprivation | 50 | 50 | 100 | 53 | 52 | 98.1 | 103 | 102 | 99.0 |
| Maternal well-being (baseline) | 50 | 50 | 100 | 53 | 52 | 98.1 | 103 | 102 | 99.0 |
| Intention to feed | 50 | 50 | 100 | 53 | 51 | 96.2 | 103 | 101 | 98.1 |
| How participant was fed as a baby | 50 | 50 | 100 | 53 | 52 | 98.1 | 103 | 102 | 99.0 |
| Participant knows anyone who has breastfed their baby | 50 | 50 | 100 | 53 | 52 | 98.1 | 103 | 102 | 99.0 |
| Baby’s gestational age at birth | 50 | 49 | 98 | 53 | 52 | 98.1 | 103 | 101 | 98.1 |
| Mode of delivery | 50 | 40 | 80 | 53 | 44 | 83.0 | 103 | 84 | 81.6 |
| Duration of mother’s hospital stay | 50 | 40 | 80 | 53 | 44 | 83.0 | 103 | 84 | 81.6 |
| Baby admitted to neonatal unit | 50 | 40 | 80 | 53 | 44 | 83.0 | 103 | 84 | 81.6 |
Data completeness: estimates from feasibility study
| Data item | Intervention | Control | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Potential total | Number collected | Completed (%) | Potential total | Number collected | Completed (%) | Potential total | Number collected | Completed (%) | |
| Any breastfeeding at 8 weeks | 50 | 41 | 82 | 53 | 47 | 88.7 | 103 | 88 | 85.4 |
| Any breastfeeding at 8 weeks (including health visitor data) | 50 | 48 | 96 | 53 | 50 | 94.3 | 103 | 98 | 95.1 |
| Any breastfeeding at 6 months | 50 | 39 | 78 | 53 | 44 | 83.0 | 103 | 83 | 80.6 |
| Exclusive breastfeeding at 6–8 weeks (last 24 hours) | 50 | 41 | 82 | 53 | 47 | 88.7 | 103 | 88 | 85.4 |
| Exclusive breastfeeding at 6–8 weeks (since birth) | 50 | 41 | 82 | 53 | 47 | 88.7 | 103 | 88 | 85.4 |
| Exclusive breastfeeding at 6 months (last 24 hours definition) | 50 | 39 | 78 | 53 | 44 | 83.0 | 103 | 83 | 80.6 |
| Exclusive breastfeeding at 6 months (no other food/drink ever definition) | 50 | 39 | 78 | 53 | 44 | 83.0 | 103 | 83 | 80.6 |
| Breastfeeding initiation (from 8-week data) | 50 | 41 | 82 | 53 | 47 | 88.7 | 103 | 88 | 85.4 |
| Breastfeeding initiation (from 3-day text data) | 50 | 31 | 62 | 53 | 39 | 73.6 | 103 | 70 | 68.0 |
| Feeding since birth at 3 days (from 3-day text data) | 50 | 31 | 62 | 53 | 39 | 73.6 | 103 | 70 | 68.0 |
| Serious adverse events (hospital admissions for feeding-related problems) | 50 | 40 | 80 | 53 | 44 | 83.0 | 103 | 84 | 81.6 |
| Maternal well-being (8 weeks) | 50 | 40 | 80 | 53 | 44 | 83.0 | 103 | 84 | 81.6 |
| Maternal well-being (6 months) | 50 | 39 | 78 | 53 | 44 | 83.0 | 103 | 83 | 80.6 |
| Social support (8 weeks) (mean) | 50 | 40 | 80 | 53 | 44 | 83.0 | 103 | 84 | 81.6 |
| Social support (6 months) (mean) | 50 | 39 | 78 | 53 | 44 | 83.0 | 103 | 83 | 80.6 |
| Maternal satisfaction (home support) (mean) | 50 | 40 | 80 | 53 | 44 | 83.0 | 103 | 84 | 81.6 |
| Maternal satisfaction (hospital support) (mean) | 50 | 40 | 80 | 53 | 42 | 79.2 | 103 | 82 | 79.6 |
Data completeness: data for economic evaluation
| Data item | Intervention | Control | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Potential total | Number collected | Completed (%) | Potential total | Number collected | Completed (%) | Potential total | Number collected | Completed (%) | |
| Number of times consulted GP in past 3 months (baseline) (mean) | 50 | 47 | 94 | 53 | 52 | 98.1 | 103 | 99 | 96.1 |
| Number of times consulted practice nurse in past 3 months (baseline) (mean) | 50 | 47 | 94 | 53 | 52 | 98.1 | 103 | 99 | 96.1 |
| Number of times consulted midwife in past 3 months (baseline) (mean) | 50 | 47 | 94 | 53 | 52 | 98.1 | 103 | 99 | 96.1 |
| Use of health and feeding support services (8 weeks) | 50 | 40 | 80 | 53 | 42 | 79.2 | 103 | 82 | 79.6 |
| Use of child care (8 weeks) | 50 | 40 | 80 | 53 | 43 | 81.1 | 103 | 83 | 80.6 |
| Use of child care (6 months) | 50 | 39 | 78 | 53 | 44 | 83.0 | 103 | 83 | 80.6 |
| Benefits (baseline) | 50 | 45 | 90 | 53 | 49 | 92.5 | 103 | 94 | 91.3 |
| Benefits (8 weeks) | 50 | 40 | 80 | 53 | 44 | 83.0 | 103 | 84 | 81.6 |
| Benefits (6 months) | 50 | 39 | 78 | 53 | 44 | 83.0 | 103 | 83 | 80.6 |
Appendix 13 Estimates from feasibility study: any breastfeeding at 8 weeks and 6 months, by site
| Data item | Site A | Site B | Overall | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | ||||||||||
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Any breastfeeding at 8 weeks | 8/19 | 42.1 (20.3 to 66.5) | 9/23 | 39.1 (19.7 to 61.5) | 17/42 | 40.5 (25.6 to 56.7) | 15/22 | 68.2 (45.1 to 86.1) | 13/24 | 54.2 (32.8 to 74.4) | 28/46 | 60.9 (45.4 to 74.9) | 23/41 | 56.1 (39.7 to 71.5) | 22/47 | 46.8 (32.1 to 61.9) | 45/88 | 51.1 (40.2 to 61.9) |
| Any breastfeeding at 8 weeks (including health visitor data) | 9/23 | 39.1 (19.7 to 61.5) | 9/26 | 34.6 (17.2 to 55.7) | 18/49 | 36.7 (23.4 to 51.7) | 15/25 | 60.0 (38.7 to 78.9) | 13/24 | 54.2 (32.8 to 74.4) | 28/49 | 57.1 (42.2 to 71.2) | 24/48 | 50.0 (35.2 to 64.8) | 22/50 | 44.0 (30.0 to 58.7) | 46/98 | 46.9 (36.8 to 57.3) |
| Any breastfeeding at 6 months | 5/17 | 29.4 (10.3 to 56.0) | 8/20 | 40.0 (19.1 to 63.9) | 13/37 | 35.1 (20.2 to 52.5) | 13/22 | 59.1 (36.4 to 79.3) | 8/24 | 33.3 (15.6 to 55.3) | 21/46 | 45.7 (30.9 to 61.0) | 18/39 | 46.2 (30.1 to 62.8) | 16/44 | 36.4 (22.4 to 52.2) | 34/83 | 41.0 (30.3 to 52.3) |
Appendix 14 Estimates from feasibility study: exclusive breastfeeding at 8 weeks and 6 months, by site
| Data item | Site A | Site B | Overall | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | ||||||||||
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Exclusive breastfeeding at 6–8 weeks | ||||||||||||||||||
| Last 24 hours | 5/19 | 26.3 (9.1 to 51.2) | 7/23 | 30.4 (13.2 to 52.9) | 12/42 | 28.6 (15.7 to 44.6) | 11/22 | 50.0 (28.2 to 71.8) | 10/24 | 41.7 (22.1 to 63.4) | 21/46 | 45.7 (30.9 to 61.0) | 16/41 | 39.0 (24.2 to 55.5) | 17/47 | 36.2 (22.7 to 51.5) | 33/88 | 37.5 (27.4 to 48.5) |
| Since birth | 4/19 | 21.1 (6.1 to 45.6) | 3/23 | 13.0 (2.8 to 33.6) | 7/42 | 16.7 (7.0 to 31.4) | 7/22 | 31.8 (13.9 to 54.9) | 9/24 | 37.5 (18.8 to 59.4) | 16/46 | 34.8 (21.4 to 50.2) | 11/41 | 26.8 (14.2 to 42.9) | 12/47 | 25.5 (13.9 to 40.3) | 23/88 | 26.1 (17.3 to 36.6) |
| Exclusive breastfeeding at 6 months | ||||||||||||||||||
| Last 24 hours | 5/17 | 29.4 (10.3 to 56.0) | 6/20 | 30.0 (11.9 to 54.3) | 11/37 | 29.7 (15.9 to 47.0) | 7/22 | 31.8 (13.9 to 54.9) | 7/24 | 29.2 (12.6 to 51.1) | 14/46 | 30.4 (17.7 to 45.8) | 12/39 | 30.8 (17.0 to 47.6) | 13/44 | 29.5 (16.8 to 45.2) | 25/83 | 30.1 (20.5 to 41.2) |
| No other food/drink ever | 2/17 | 11.8 (1.5 to 36.4) | 0/20 | 0 (0 to 16.8) | 2/37 | 5.4 (0.7 to 18.2) | 1/22 | 4.5 (0.1 to 22.8) | 2/24 | 8.3 (1.0 to 27.0) | 3/46 | 6.5 (1.4 to 17.9) | 3/39 | 7.7 (1.6 to 20.9) | 2/44 | 4.5 (0.5 to 20.9) | 5/83 | 6.0 (2.0 to 13.5) |
Appendix 15 Estimates from feasibility study: breastfeeding initiation and feeding status at 3 days postnatally, by site
| Data item | Site A | Site B | Overall | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | ||||||||||
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Breastfeeding initiation | ||||||||||||||||||
| From 8-week questionnaire | 15/19 | 78.9 (54.4 to 93.9) | 16/23 | 69.6 (47.1 to 86.8) | 31/42 | 73.8 (58.0 to 86.1) | 20/22 | 90.9 (70.8 to 98.9) | 20/24 | 83.3 (62.6 to 95.3) | 40/46 | 87.0 (73.7 to 95.1) | 35/41 | 85.4 (70.8 to 94.4) | 36/47 | 76.6 (62.0 to 87.7) | 71/88 | 80.7 (70.9 to 88.3) |
| From 3-day text data | 13/14 | 92.9 (66.1 to 99.8) | 15/21 | 71.4 (47.8 to 88.7) | 28/35 | 80.0 (63.1 to 91.6) | 17/17 | 100 (80.5 to 100) | 17/18 | 94.4 (72.7 to 99.9) | 34/35 | 97.1 (85.1 to 99.9) | 30/31 | 96.8 (83.3 to 99.9) | 32/39 | 82.1 (66.5 to 92.5) | 62/70 | 88.6 (78.7 to 94.9) |
| Feeding since birth at 3 days (from 3-day text data) | ||||||||||||||||||
| Only formula milk | 1/14 | 7.1 (1.8 to 33.9) | 6/21 | 28.6 (11.3 to 52.2) | 7/35 | 20.0 (8.4 to 36.9) | 0/17 | 0 (0 to 0.20) | 1/18 | 5.6 (0.1 to 27.3) | 1/35 | 2.9 (0.1 to 14.9) | 1/31 | 3.2 (0.1 to 16.7) | 7/39 | 17.9 (7.5 to 33.5) | 8/70 | 11.4 (5.1 to 21.3) |
| Only breastmilk | 8/14 | 57.1 (28.9 to 82.3) | 7/21 | 33.3 (14.6 to 57.0) | 15/35 | 42.9 (26.3 to 60.6) | 14/17 | 82.4 (56.6 to 96.2) | 7/18 | 38.9 (17.3 to 64.3) | 21/35 | 60.0 (42.1 to 76.1) | 22/31 | 71.0 (52.0 to 85.8) | 14/39 | 35.9 (21.2 to 52.8) | 36/70 | 51.4 (39.2 to 63.6) |
| Mixed feeding | 5/14 | 35.7 (12.8 to 64.9) | 8/21 | 38.1 (18.1 to 61.6) | 13/35 | 37.1 (21.5 to 55.1) | 3/17 | 17.7 (3.8 to 43.4) | 10/18 | 55.6 (30.8 to 78.5) | 13/35 | 37.1 (21.5 to 55.1) | 8/31 | 25.8 (11.9 to 44.6) | 18/39 | 46.2 (30.1 to 62.8) | 26/70 | 37.1 (25.9 to 49.5) |
Appendix 16 Estimates from feasibility study: ceased breastfeeding at 8 weeks and 6 months
| Data item | Site A | Site B | Overall | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | ||||||||||
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Ceased breastfeeding at 8 weeks (of those who had initiated breastfeeding) | 7/15 | 46.7 (21.3 to 73.4) | 7/16 | 43.8 (19.8 to 70.1) | 14/31 | 45.2 (27.3 to 64.0) | 5/20 | 25.0 (8.7 to 49.1) | 7/20 | 35.0 (15.4 to 59.2) | 12/40 | 30.0 (16.6 to 46.5) | 12/35 | 34.3 (19.1 to 52.2) | 14/36 | 38.9 (23.1 to 56.5) | 26/71 | 36.6 (25.5 to 48.9) |
| Ceased breastfeeding at 6 months (of those who had initiated breastfeeding) | 10/15 | 66.7 (38.4 to 88.2) | 8/16 | 50.0 (24.7 to 75.3) | 18/31 | 58.1 (39.1 to 75.4) | 9/22 | 40.9 (20.7 to 63.6) | 12/20 | 60.0 (36.1 to 80.9) | 21/42 | 50.0 (34.2 to 65.8) | 19/37 | 51.4 (34.4 to 68.1) | 20/36 | 55.6 (38.1 to 72.1) | 39/73 | 53.4 (41.4 to 65.2) |
Appendix 17 Estimates from feasibility study: serious adverse events (hospital admissions for feeding-related problems)
| Data item | Site A | Site B | Overall | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | ||||||||||
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Serious adverse events (hospital admissions for feeding-related problems) | 2/19 | 10.5 (1.3 to 33.1) | 2/20 | 10.0 (1.2 to 31.7) | 4/39 | 10.3 (2.9 to 24.2) | 0/21 | 0 (0 to 16.1) | 1/24 | 4.2 (0.1 to 21.1) | 1/45 | 2.2 (0.1 to 11.8) | 2/40 | 5.0 (0.6 to 16.9) | 3/44 | 6.8 (1.4 to 18.7) | 5/84 | 5.9 (1.9 to 18.7) |
Appendix 18 Self-reported use of health and feeding support services at 8 weeks for advice on infant feeding
| Feeding support service | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |
| Midwife, n (%) | |||||||||
| 0 times | 9 (47.4) | 6 (31.6) | 15 (39.5) | 5 (23.8) | 3 (13.0) | 8 (18.2) | 14 (35.0) | 9 (21.4) | 23 (28.1) |
| 1–2 times | 6 (31.6) | 9 (47.4) | 15 (39.5) | 10 (47.6) | 12 (52.2) | 22 (50.0) | 16 (40.0) | 21 (50.0) | 37 (45.1) |
| ≥ 3 times | 4 (21.1) | 4 (21.1) | 8 (21.1) | 6 (28.6) | 8 (34.8) | 14 (31.8) | 10 (25.0) | 12 (28.6) | 22 (26.8) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| Health visitor, n (%) | |||||||||
| 0 times | 12 (63.2) | 6 (31.6) | 18 (47.4) | 6 (28.6) | 6 (26.1) | 12 (27.3) | 18 (45.0) | 12 (28.6) | 30 (36.6) |
| 1–2 times | 7 (36.8) | 13 (68.4) | 20 (52.6) | 10 (47.6) | 16 (69.6) | 26 (59.1) | 17 (42.5) | 29 (69.1) | 46 (56.1) |
| ≥ 3 times | 0 | 0 | 0 | 5 (23.8) | 1 (4.4) | 6 (13.6) | 5 (12.5) | 1 (2.4) | 6 (7.3) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| GP, n (%) | |||||||||
| 0 times | 18 (94.7) | 12 (63.2) | 30 (79.0) | 17 (81.0) | 19 (82.6) | 36 (81.8) | 35 (87.5) | 31 (73.8) | 35 (87.5) |
| 1–2 times | 1 (5.3) | 7 (36.8) | 8 (21.1) | 4 (19.1) | 4 (17.4) | 8 (18.2) | 5 (12.5) | 11 (26.2) | 5 (12.5) |
| ≥ 3 times | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| Practice nurse, n (%) | |||||||||
| 0 times | 18 (94.7) | 18 (94.7) | 36 (94.7) | 19 (90.5) | 0 | 42 (95.5) | 37 (92.5) | 41 (97.6) | 78 (95.1) |
| 1–2 times | 1 (5.3) | 1 (5.3) | 2 (5.3) | 1 (4.8) | 0 | 1 (2.3) | 2 (5.0) | 1 (2.4) | 3 (3.7) |
| ≥ 3 times | 0 | 0 | 0 | 1 (4.8) | 0 | 1 (2.3) | 1 (2.5) | 0 | 1 (1.2) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| Infant feeding counsellor/breastfeeding supporter, n (%) | |||||||||
| 0 times | 12 (63.2) | 18 (94.7) | 30 (79.0) | 7 (35.0) | 17 (73.9) | 24 (55.8) | 19 (48.7) | 35 (83.3) | 54 (66.7) |
| 1–2 times | 5 (26.3) | 1 (5.3) | 6 (15.8) | 3 (15.0) | 5 (21.7) | 8 (18.6) | 8 (20.5) | 6 (14.3) | 14 (17.3) |
| ≥ 3 times | 2 (10.5) | 0 | 2 (5.3) | 10 (50.0) | 1 (4.4) | 11 (25.6) | 12 (30.8) | 1 (2.4) | 13 (16.1) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| Children’s centre, n (%) | |||||||||
| 0 times | 18 (94.7) | 18 (94.7) | 36 (94.7) | 20 (95.2) | 21 (91.3) | 41 (93.2) | 38 (95.0) | 39 (92.9) | 77 (93.9) |
| 1–2 times | 1 (5.3) | 1 (5.3) | 2 (5.3) | 0 | 1 (4.4) | 1 (2.3) | 1 (2.5) | 2 (4.8) | 3 (3.7) |
| ≥ 3 times | 0 | 0 | 0 | 1 (4.8) | 1 (4.4) | 2 (4.6) | 1 (2.5) | 1 (2.4) | 2 (2.4) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| National breastfeeding telephone helpline, n (%) | |||||||||
| 0 times | 18 (94.7) | 18 (94.7) | 36 (94.7) | 20 (95.2) | 22 (95.7) | 42 (95.5) | 38 (95.0) | 40 (95.2) | 78 (95.1) |
| 1–2 times | 1 (5.3) | 1 (5.3) | 2 (5.3) | 1 (4.8) | 1 (4.4) | 2 (4.6) | 2 (5.0) | 2 (4.8) | 4 (4.9) |
| ≥ 3 times | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| Breastfeeding group, n (%) | |||||||||
| 0 times | 17 (89.5) | 16 (84.2) | 33 (86.8) | 12 (57.1) | 15 (65.2) | 27 (61.4) | 29 (72.5) | 31 (73.8) | 60 (73.2) |
| 1–2 times | 1 (5.3) | 2 (10.5) | 3 (7.9) | 7 (33.3) | 7 (30.4) | 14 (31.8) | 8 (20.0) | 9 (21.4) | 17 (20.7) |
| ≥ 3 times | 1 (5.3) | 1 (5.3) | 2 (5.3) | 2 (9.5) | 1 (4.4) | 3 (6.8) | 3 (7.5) | 2 (4.8) | 5 (6.1) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| Internet/web resources, n (%) | |||||||||
| 0 times | 8 (42.1) | 13 (68.4) | 21 (55.3) | 9 (42.9) | 11 (47.8) | 20 (45.5) | 17 (42.5) | 24 (57.1) | 41 (50.0) |
| 1–2 times | 4 (21.1) | 2 (10.5) | 6 (15.8) | 2 (9.5) | 6 (26.1) | 8 (18.2) | 6 (15.0) | 8 (19.1) | 14 (17.1) |
| ≥ 3 times | 7 (36.8) | 4 (21.1) | 11 (29.0) | 10 (47.6) | 6 (26.1) | 16 (36.4) | 17 (42.5) | 10 (23.8) | 27 (32.9) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| Social media, n (%) | |||||||||
| 0 times | 17 (89.5) | 16 (84.2) | 33 (86.8) | 15 (71.4) | 20 (87.0) | 35 (79.6) | 32 (80.0) | 36 (85.7) | 68 (82.9) |
| 1–2 times | 1 (5.3) | 2 (10.5) | 3 (7.9) | 3 (14.3) | 1 (4.4) | 4 (9.1) | 4 (10.0) | 3 (7.1) | 7 (8.5) |
| ≥ 3 times | 1 (5.3) | 1 (5.3) | 2 (5.3) | 3 (14.3) | 2 (8.7) | 5 (11.4) | 4 (10.0) | 3 (7.1) | 7 (8.5) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
| Someone else, n (%) | |||||||||
| 0 times | 10 (52.6) | 13 (68.4) | 23 (60.5) | 12 (57.1) | 10 (45.5) | 23 (52.3) | 22 (55.0) | 23 (56.1) | 45 (54.9) |
| 1–2 times | 7 (36.8) | 3 (15.8) | 10 (26.3) | 5 (23.8) | 5 (22.7) | 10 (22.7) | 12 (30.0) | 8 (19.5) | 20 (24.4) |
| ≥ 3 times | 2 (10.5) | 3 (15.8) | 56 (13.2) | 4 (19.1) | 7 (31.8) | 11 (25.0) | 6 (15.0) | 10 (24.4) | 16 (19.5) |
| Missing | 6 (24.0) | 9 (32.1) | 15 (28.3) | 4 (16.0) | 2 (8.0) | 6 (12.0) | 10 (20.0) | 11 (20.8) | 21 (20.4) |
Appendix 19 Use of child care
Use of child care at 8 weeks
| Child care | Site A | Site B | Overall | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |||||||||||||||||||
| n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | |
| Regular paid child care | 0/19 | 0 | – | 0/20 | 0 | – | 0/39 | 0 | – | 0/21 | 0 | – | 0/23 | 0 | – | 0/44 | 0 | – | 0/40 | 0 | – | 0/43 | 0 | – | 0/83 | 0 | – |
| Occasional paid child care | 0/19 | 0 | – | 0/20 | 0 | – | 0/39 | 0 | – | 0/21 | 0 | – | 1/23 | 4.3 | 0.5 to 28.4 | 1/44 | 2.3 | 0.3 to 15.5 | 0/40 | 0 | – | 1/43 | 2.3 | 0.3 to 15.8 | 1/83 | 1.2 | 0.01 to 8.4 |
| Regular unpaid child care from family or friends | 2/19 | 10.5 | 2.3 to 37.1 | 0/20 | 0 | – | 2/39 | 5.1 | 1.2 to 19.3 | 0/21 | 0 | – | 1/23 | 4.3 | 0.5 to 28.4 | 1/44 | 2.3 | 0.3 to 15.5 | 2/40 | 5.0 | 1.2 to 18.9 | 1/43 | 2.3 | 0.3 to 15.8 | 3/83 | 3.6 | 1.1 to 10.8 |
| Occasional unpaid child care from family or friends | 2/19 | 10.5 | 2.3 to 37.1 | 1/20 | 5.0 | 0.5 to 32.2 | 3/39 | 7.7 | 2.3 to 22.2 | 4/21 | 19.0 | 6.7 to 43.6 | 9/23 | 39.1 | 20.6 to 61.4 | 13/55 | 29.5 | 17.6 to 45.1 | 6/40 | 15.0 | 6.7 to 30.4 | 10/43 | 23.3 | 12.7 to 38.8 | 16/83 | 19.3 | 12.0 to 29.4 |
| None of the above | 15/19 | 78.9 | 52.7 to 92.7 | 19/20 | 95.0 | 67.7 to 99.4 | 34/39 | 87.2 | 71.8 to 94.8 | 17/21 | 81.0 | 56.4 to 93.3 | 12/23 | 52.2 | 31.0 to 72.6 | 29/44 | 65.9 | 50.3 to 78.7 | 32/40 | 80.0 | 64.0 to 90.0 | 31/43 | 72.1 | 56.3 to 83.8 | 63/83 | 75.9 | 65.3 to 84.0 |
Use of child care at 6 months
| Child care | Site A | Site B | Overall | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |||||||||||||||||||
| n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | n/N | % | 95% CI | |
| Regular paid child care | 1/17 | 5.8 | 0.6 to 37.3 | 1/20 | 5.0 | 0.5 to 32.3 | 2/37 | 5.4 | 0.12 to 20.3 | 0/22 | 0 | – | 0/24 | 0 | – | 0/46 | 0 | – | 1/39 | 2.6 | 0.3 to 17.4 | 1/44 | 2.3 | 0.3 to 15.5 | 2/83 | 2.4 | 0.6 to 9.4 |
| Occasional paid child care | 0/17 | 0 | – | 1/20 | 5.0 | 0.5 to 3.2 | 1/37 | 2.7 | 0.3 to 18.3 | 0/22 | 0 | – | 0/24 | 0 | – | 0/46 | 0 | – | 0/39 | 0 | – | 1/44 | 2.3 | 0.3 to 15.5 | 1/83 | 1.2 | 0.2 to 8.4 |
| Regular unpaid child care from family or friends | 1/17 | 5.9 | 0.6 to 37.3 | 0/20 | 0 | – | 1/37 | 2.7 | 0.3 to 18.3 | 0/22 | 0 | – | 1/24 | 4.2 | 0.5 to 2.7 | 1/46 | 2.2 | 0.3 to 14.8 | 1/39 | 2.6 | 0.3 to 17.4 | 1/44 | 2.3 | 0.3 to 15.5 | 2/83 | 2.4 | 0.6 to 9.4 |
| Occasional unpaid child care from family or friends | 4/17 | 23.5 | 8.1 to 51.8 | 6/20 | 30.0 | 13.1 to 55.0 | 10/37 | 27.0 | 14.7 to 44.2 | 5/22 | 22.7 | 9.1 to 46.5 | 12/24 | 50.0 | 29.7 to 70.3 | 17/46 | 37.0 | 23.9 to 52.2 | 9/39 | 23.1 | 12.1 to 39.5 | 18/44 | 40.9 | 27.0 to 56.4 | 27/83 | 32.5 | 23.2 to 43.5 |
| None of the above | 11/17 | 64.7 | 37.7 to 84.8 | 12/20 | 60.0 | 36.0 to 80.0 | 23/37 | 62.2 | 45.0 to 76.7 | 16/22 | 72.7 | 49.0 to 88.1 | 11/24 | 45.8 | 26.3 to 66.8 | 27/46 | 59.0 | 43.6 to 72.3 | 27/39 | 69.2 | 52.5 to 82.1 | 23/44 | 52.3 | 37.2 to 67.0 | 50/83 | 60.2 | 49.2 to 70.4 |
Appendix 20 Receipt of benefits
Receipt of benefits at baseline
| Benefit | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |
| Healthy Start vouchers, n (%) | 3 (12.0) | 2 (7.4) | 5 (9.6) | 0 (0) | 0 (0) | 0 (0) | 3 (6.7) | 2 (4.1) | 5 (5.3) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Maternity allowance, n (%) | 3 (12.0) | 1 (3.7) | 4 (7.7) | 0 (0) | 1 (4.6) | 1 (2.4) | 3 (6.7) | 2 (4.1) | 5 (5.3) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Statutory maternity pay, n (%) | 1 (4.0) | 2 (7.4) | 3 (5.8) | 0 (0) | 0 (0) | 0 (0) | 1 (2.2) | 2 (4.1) | 3 (3.2) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Sure Start maternity grant, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Income support, n (%) | 3 (12.0) | 0 (0) | 3 (5.8) | 1 (5.0) | 0 (0) | 2 (4.8) | 4 (8.9) | 1 (2.0) | 5 (5.3) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Jobseeker’s allowance, n (%) | 3 (12.0) | 0 (0) | 3 (5.8) | 0 (0) | 0 (0) | 0 (0) | 3 (6.7) | 0 (0) | 3 (3.2) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Housing benefit, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Disability living allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Attendance allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Carer’s allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Income-related employment and support allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
| Tax credits, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 0 (0) | 1 (3.6) | 1 (1.9) | 5 (20.0) | 3 (12.0) | 8 (16.0) | 5 (10.0) | 4 (7.5) | 9 (17.0) |
Receipt of benefits at 8 weeks
| Benefit | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |
| Healthy Start vouchers, n (%) | 3 (15.8) | 1 (5.0) | 4 (10.3) | 0 (0) | 0 (0) | 0 (0) | 3 (7.5) | 1 (2.3) | 4 (4.8) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Maternity allowance, n (%) | 2 (10.5) | 4 (20.0) | 6 (15.4) | 4 (19.1) | 7 (29.2) | 11 (24.4) | 6 (15.0) | 11 (25.0) | 17 (20.2) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Statutory maternity pay, n (%) | 10 (52.6) | 9 (45.0) | 19 (48.7) | 11 (52.4) | 15 (62.5) | 26 (57.8) | 21 (52.5) | 24 (54.6) | 45 (53.6) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Sure Start maternity grant, n (%) | 2 (5.1) | 0 (0) | 2 (10.5) | 1 (4.8) | 0 (0) | 1 (2.2) | 3 (7.5) | 0 (0) | 3 (3.6) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Income support, n (%) | 4 (21.1) | 2 (10.0) | 6 (15.4) | 0 (0) | 1 (4.2) | 1 (2.2) | 4 (10.0) | 3 (6.8) | 7 (8.3) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Jobseeker’s allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Housing benefit, n (%) | 0 (0) | 0 (0) | 0 (0) | 1 (4.8) | 0 (0) | 1 (2.2) | 1 (2.5) | 0 (0) | 1 (1.2) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Disability living allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Attendance allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Carer’s allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Income-related employment and support allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
| Tax credits, n (%) | 1 (5.3) | 2 (10.0) | 3 (7.7) | 4 (19.1) | 0 (0) | 4 (8.9) | 5 (12.5) | 2 (4.5) | 7 (8.3) |
| Missing | 9 (36.0) | 5 (17.9) | 14 (26.4) | 4 (16.0) | 1 (4.0) | 5 (10.0) | 10 (20.0) | 9 (17.0) | 19 (18.4) |
Receipt of benefits at 6 months
| Benefit | Site A | Site B | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 25) | Usual care (N = 28) | All (N = 53) | Intervention (N = 25) | Usual care (N = 25) | All (N = 50) | Intervention (N = 50) | Usual care (N = 53) | All (N = 103) | |
| Healthy Start vouchers, n (%) | 2 (11.8) | 2 (10.0) | 4 (10.8) | 0 (0) | 0 (0) | 0 (0) | 2 (5.1) | 2 (4.6) | 4 (4.8) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Maternity allowance, n (%) | 2 (11.8) | 3 (15.0) | 5 (13.5) | 1 (4.6) | 4 (16.7) | 5 (10.9) | 3 (7.7) | 7 (15.9) | 10 (12.1) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Statutory maternity pay, n (%) | 11 (64.7) | 11 (55.0) | 22 (59.5) | 16 (72.7) | 19 (79.2) | 35 (76.1) | 27 (69.2) | 30 (68.2) | 57 (68.7) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Sure Start maternity grant, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Income support, n (%) | 2 (11.8) | 2 (10.0) | 4 (10.8) | 1 (4.6) | 0 (0) | 1 (2.2) | 3 (7.7) | 2 (4.6) | 5 (6.0) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Jobseeker’s allowance, n (%) | 1 (5.9) | 0 (0) | 1 (2.7) | 0 (0) | 0 (0) | 0 (0) | 1 (2.6) | 0 (0) | 1 (1.2) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Housing benefit, n (%) | 1 (5.9) | 0 (0) | 1 (2.7) | 1 (4.6) | 2 (8.3) | 3 (6.5) | 2 (5.1) | 2 (4.6) | 4 (4.8) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Disability living allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Attendance allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Carer’s allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Income-related employment and support allowance, n (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
| Tax credits, n (%) | 1 (5.9) | 3 (15.0) | 4 (10.8) | 3 (13.6) | 3 (12.5) | 6 (13.0) | 4 (10.3) | 6 (13.6) | 10 (12.1) |
| Missing | 8 (32.0) | 8 (28.6) | 16 (30.2) | 3 (12.0) | 1 (4.0) | 4 (8.0) | 11 (22.0) | 9 (17.0) | 20 (19.4) |
List of abbreviations
- ABA
- Assets-based infant feeding help Before and After birth
- BCT
- behaviour change technique
- CI
- confidence interval
- COM-B
- capability, opportunity, motivation and behaviour
- FEST
- FEeding Support Team
- FG
- focus group
- GP
- general practitioner
- ICC
- intracluster correlation coefficient
- IFH
- infant-feeding helper
- PIL
- participant information leaflet
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- RR
- risk ratio
- TSC
- Trial Steering Committee
- UNICEF
- United Nations Children’s Fund
- WEMWBS
- Warwick–Edinburgh Mental Well-being Scale
