Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 14/185/09. The contractual start date was in June 2016. The final report began editorial review in December 2018 and was accepted for publication in September 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Alison Avenell was chief investigator of the National Institute for Health Research (NIHR) Health Technology Assessment (HTA)-funded REBALANCE project [Avenell A, Robertson C, Skea Z, Jacobsen E, Boyers D, Cooper D, et al. Bariatric surgery, lifestyle interventions and orlistat for severe obesity: the REBALANCE mixed-methods systematic review and economic evaluation. Health Technol Assess 2018;22(68)]. Andrew Elders reports a grant from NIHR during the conduct of the study. Mark Grindle reports that he is managing director of Eos Digital Health Ltd (Dunblane, UK), which is sole owner of the copyright of the Digital Narrative Approach. Frank Kee is a member of the Public Health Research (PHR) programme Research Funding Board and the PHR Prioritisation Group (board member 2009–2014 and chairperson 2014–2019). Pat Hoddinott was a member of the HTA Commissioning Board from March 2014 to March 2019.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Dombrowski et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK. Parts of this report have been reproduced with permission from Dombrowski et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
2020 2020 Queen’s Printer and Controller of HMSO Dombrowski et al.
Chapter 1 Introduction
Parts of this report have been reproduced with permission from Dombrowski et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter introduces general background literature relevant to the study. Some of this evidence was published subsequent to the conduct of the study. Information on the specific intervention components and the evidence and approaches that underpin these are presented in the relevant chapters.
Obesity in men
In 2016, an estimated 26% of UK men were classified as obese. In the UK, men are less likely to be a healthy weight than women. 2,3 Obesity results in an increased risk of serious health conditions, such as cardiovascular disease, cancer and diabetes, and is a major public health priority. 4
Despite the growing problem of being overweight and obesity, men are a population underserved by current evidence-based weight management programmes. 5 Most interventions are designed for mixed-sex populations, but systematic review evidence5 suggests that men often require different interventions from women. Research on the most effective strategies for recruiting men to, and retaining men in, effective weight management programmes is required.
Innovative formats for delivering obesity interventions to men are needed, particularly to men in more disadvantaged circumstances. 5 Although some evidence of effective lifestyle interventions for obesity exists,6–8 little research to date has systematically consulted men on how to optimise engagement and make interventions acceptable and feasible. Rigorous feasibility studies and piloting with service user input at all stages is recommended. 5 Moreover, the evidence on the cost-effectiveness of interventions for men is limited. 5
Maintenance of initial weight loss is generally poor, even in interventions that focus specifically on maintenance. 9 Evidence suggests that ongoing and long-term support for weight loss maintenance is required,9,10 yet few weight management programmes are designed with maintenance in mind. 5 Gender-sensitised interventions that target weight loss as well as weight loss maintenance are required to support men in their weight management efforts. 11
The National Institute for Health Research (NIHR) Public Health Research programme (call number 14/185) called for research into men’s weight loss services to answer the following research question: what are the effective interventions for weight management for men and how are men best engaged with effective weight management interventions?
This feasibility study examines two components of an intervention to support men to lose weight and maintain weight loss: (1) a narrative short message service (SMS) component and (2) a financial incentive component. The study builds on the evidence from NIHR-funded systematic reviews: the ROMEO (Review Of MEn and Obesity) systematic reviews5 of interventions to address obesity in men; the Benefits of Incentives for Breastfeeding and Smoking cessation in pregnancy (BIBS) study,12 which investigated the mechanisms of action of financial incentives aimed at changing behaviour in a different population (women around the time of childbirth); and SMS interventions aimed at supporting a reduction in alcohol intake. 13–15 The study sets out to deliver an intervention over a 12-month period to support self-directed initial weight loss, followed by a period of weight loss maintenance to sustain the clinical benefits of weight change.
To ensure that the intervention components were based on the latest evidence, the searches of three systematic reviews were updated to identify new evidence relevant to the feasibility study design. This update included a systematic review of the evidence for weight maintenance,9 a systematic review of incentives for weight loss,16 and the NIHR Health Technology Assessment systematic review of the evidence for the management of obesity in men. 5 Details of the updated searches and identified evidence can be found in Appendix 1. The findings of the updated reviews underlined the original review conclusions and did not provide further evidence that would require an amendment to or an extension of the planned protocol. The evidence underpinning the intervention design and approach we implemented is presented in the following two sections.
SMS interventions
Systematic reviews5,17–19 report no SMS-focused trials that target weight loss and weight loss maintenance in men with obesity. Mobile phone technologies are available anytime and anywhere, and are accessed by all sections of the population, including those from disadvantaged backgrounds. 20 The evidence for SMS interventions for all lifestyle behaviours, including weight loss, is promising. 17–19 Moreover, recent evidence that has emerged since this study was conducted suggests that narrative SMS delivery forms can engage hard-to-reach men in behaviour change interventions, for example moderating alcohol consumption, which could also help with weight loss. 13–15
Narrative SMS
Narrative SMS can be broadly defined as interactive life stories based around a group of characters with whom recipients can identify. In this study, the narrative format follows the characters’ attempts to achieve and maintain weight loss. This medium may provide an engaging vehicle through which to deliver theory- and evidence-based behaviour change techniques (BCTs). 21 The content, embedded in imaginable real-world scenarios and enabled by characters that are similar to participants, draws on established principles of engagement from the film and games industries. 22 For details of the specific approach used to develop the narrative SMS in the current study and how it used theory and evidence-based BCTs and storytelling elements, see Chapter 3.
Group-based weight management interventions are most promising for men. Although few men engage in weight loss groups compared with women, those who do so tend to have good outcomes. 5,7 SMS-delivered interventions using theory- and evidence-based BCTs and storytelling elements may overcome the limitations of real groups, such as low uptake, logistical challenges, dropouts and costs. 5 Narrative SMS in general have the potential to tap into some men’s weight management preferences by using humour, being fact based and flexible, and providing information that is simple to understand. 5
Narrative SMS have shown high levels of intervention engagement in recent trials. 14,15 The recently published TRAM (Texting to Reduce Alcohol Misuse) trial, which examined a narrative SMS intervention to reduce binge drinking in disadvantaged men, showed that almost all (92%) of the 411 men randomised to the narrative SMS condition replied to messages, with 67% replying more than 10 times. 15
SMS-based intervention delivery is scalable and can reach men across the socioeconomic spectrum. Tailored interventions and innovative means of delivering services, especially for men that are less likely to engage, are recommended. 5,23,24 Mobile technologies, using standard mobile phones, allow evidence-based strategies to be delivered anywhere and anytime, including information on reducing food intake and increasing physical activity, using BCTs and humour, tailoring to preference and providing other scientific facts. 5
Financial incentives interventions
A recent systematic review25 of financial incentives for habitual behaviour change highlighted the potential for incentives to change behaviours and help reduce health inequalities. The evidence for financial incentives for weight loss is growing26–29 and deposit contracts are effective while the incentives are in place. 5,30 Systematic reviews identified only one incentive trial targeting men with obesity. 5,31 This old US trial compared individual contracts with group monetary contracts, whereby men deposited US$30, US$150 or US$300 of their own money, and reported significantly greater weight loss with group contracts than with individual contracts at 1 and 2 years. 31 However, the impact on health inequalities and longer-term effectiveness is uncertain. 25 Workplace incentives were recommended in a Health Select Committee report;32 however, these will not reach unemployed people, self-employed people or students. A discrete choice experiment (DCE) found that paying people (£10–30 per week, varying by age and weight) to take part in diet and physical activity interventions is likely to improve the uptake of, adherence to and maintenance of behaviour change. 33
Endowment incentive contracts
Endowment incentive contracts are financial incentives whereby participants receive a hypothetical endowment, for example £400, at the start of a trial. They can ‘keep’ the money at certain time points if they achieve a weight loss target [e.g. 10% weight loss from baseline, the top-level target suggested by the National Institute for Health and Care Excellence (NICE)6] but will ‘lose’ money if targets are unmet. This is in line with the evidence for deposit contracts5,30 and insights from behavioural economics, including loss aversion and endowment effects. 34,35 Deposit contracts are not used in this study as they are likely to have a negative impact on the engagement of men from disadvantaged backgrounds. 5 However, an endowment incentive contract can mimic the effects of a deposit contract in terms of loss aversion: people are more motivated to avoid losses than they are to achieve similarly sized gains. 34 A randomised controlled trial (RCT) examining framing financial incentives as losses compared with framing them as gains among overweight and obese adults found that incentives framed as losses were more effective for achieving physical activity goals. 36
The endowment design used in this study draws on insights that people ascribe more value to something because it belongs to them. 34 A DCE12 combining incentives and SMS attributes showed promise for smoking cessation in women. Owing to the different active ingredients and mechanisms of action, the effects of SMS and incentive components could be synergistic.
Refined logic model of the intervention
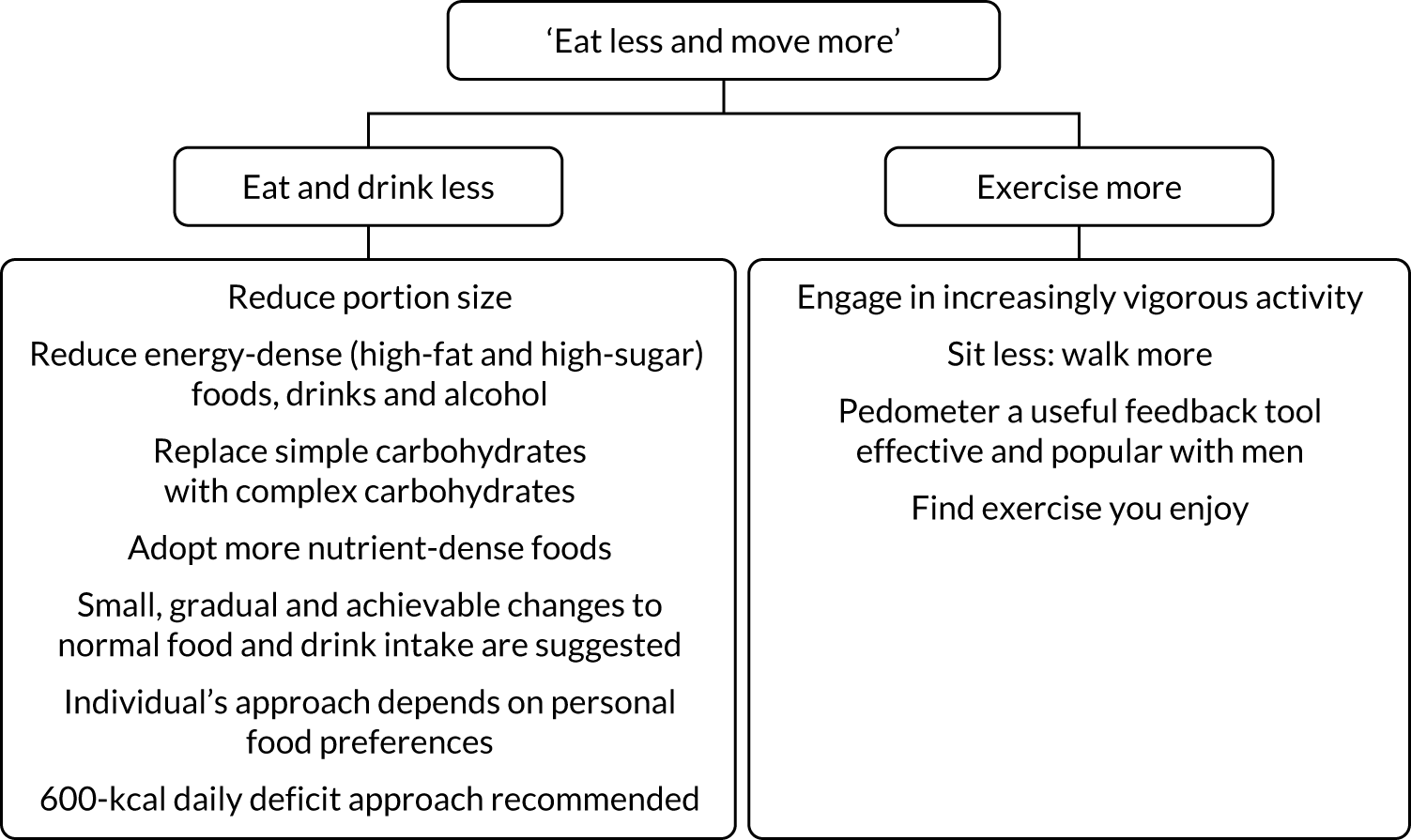
Figure 1 outlines the refined logic model based on the theory and evidence on which the behaviour change intervention components were based. (For details of how the logic model informed the development of the narrative SMS, see Chapter 3.) No single behavioural theory that fully explains the behaviour change process currently exists, and multiple theoretical approaches can inform complex behaviour change intervention design. The behavioural approach used in the current study draws on several psychological theories covering the three phases of behaviour change: (1) motivation, (2) action and (3) maintenance. The specific theories used are self-determination theory37 (motivation), health action process approach38 (motivation, action and maintenance) and Rothman’s maintenance theory39 (maintenance). These theories outline different complementary aspects across the change process and informed the study logic model. In addition, the logic model was updated to include the latest emerging evidence on theoretical maintenance of behaviour change. 40
FIGURE 1.
Refined logic model of the Game of Stones intervention.
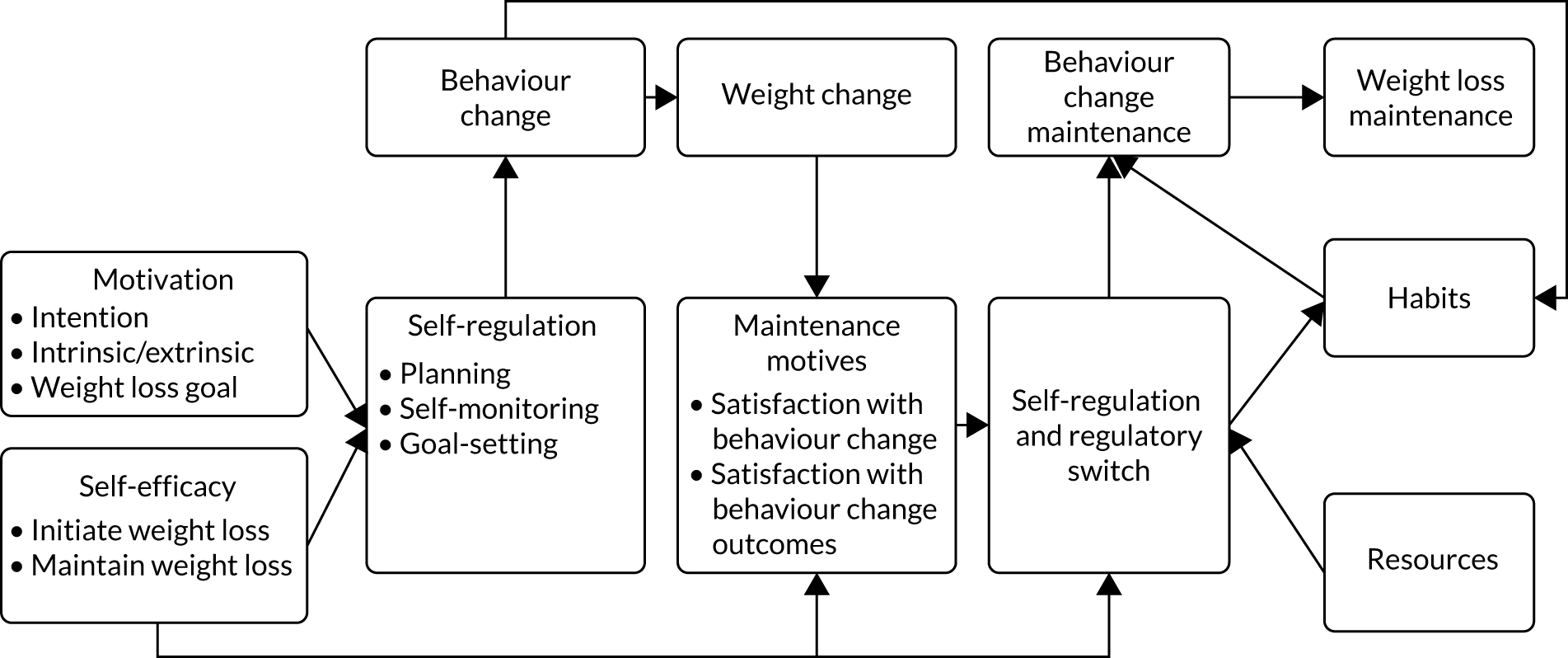
The logic model combines the interactive psychological, behavioural and physiological processes that are hypothesised to underlie successful weight management interventions. The psychological processes include both motivational (e.g. intrinsic and extrinsic motivations) and action-related factors (e.g. self-regulation), as suggested by the underpinning theoretical frameworks. These processes cover both reflective (e.g. self-efficacy) and automatic (e.g. habits) factors, in line with Rothman’s maintenance theory. 39 The logic model further distinguished the initiation and maintenance of both behaviour change and weight change. The model specifies behaviour change influencing weight change, which in turn influences the psychological factors and processes theorised to facilitate long-term change. 40 The initiation of behaviour change and the resulting weight change influence maintenance motives. These in turn promote ongoing self-regulation of behaviour change, which is moderated through the formation of habits and availability of resources (i.e. the psychological and physical assets that can be drawn on during the process of behavioural regulation).
A key element of the logic model is the regulatory switch from a change and loss mindset to a maintenance mindset, whereby the maintenance of both behaviour change and weight change is perceived to be a successful outcome worthy of pursuit. The regulatory switch to a maintenance mindset, whereby weight maintenance rather than further weight loss is considered to be the goal of self-regulation, is hypothesised to be the main driver of ongoing maintenance.
Game of Stones: a UK feasibility study
The current study aimed to test the acceptability and feasibility of engaging men with obesity with narrative SMS with or without incentives for weight loss in order to inform a future effectiveness and cost-effectiveness trial. The target population was obese adult men from disadvantaged areas who were recruited through either general practice obesity registers or community outreach. The study was divided into two phases; phase 1 focused on the adaptation and development of the intervention components and trial procedures and phase 2 focused on the feasibility trial to refine the approach, recruitment, randomisation, intervention delivery, engagement, retention and follow-up processes. A general overview of the study is shown in Figure 2.
FIGURE 2.
Schematic representation of the Game of Stones study.
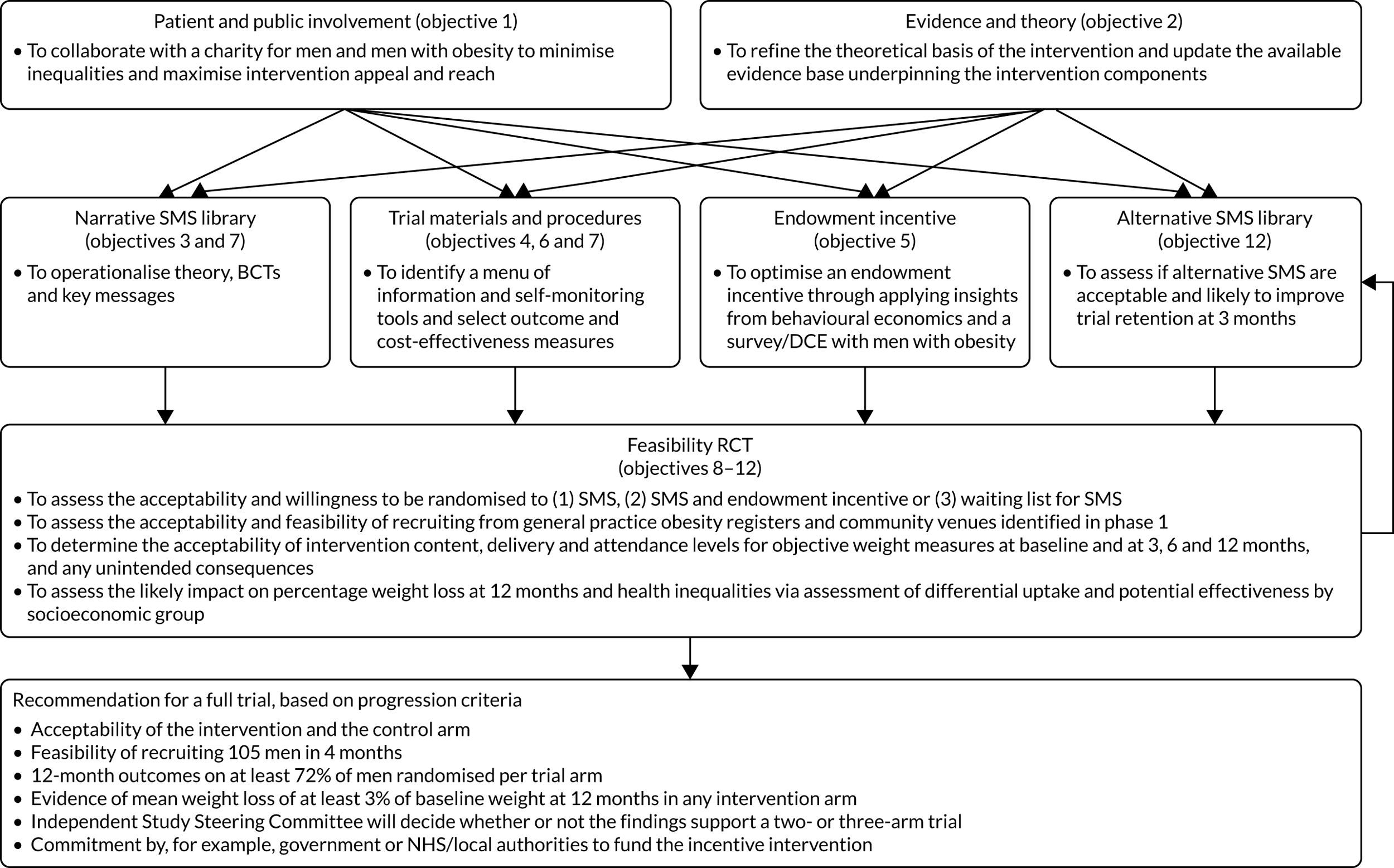
Below are the aims and objectives as detailed in the study protocol.
Aim
To co-produce with patient and public involvement (PPI) an acceptable and feasible RCT design with broad reach to test a narrative, theory-based SMS intervention with embedded BCTs, with and without an endowment incentive, compared with waiting list control, to inform a future full trial.
Objectives
Phase 1: trial design
-
To collaborate with a charity for men and men with obesity to minimise inequalities and maximise intervention appeal and reach.
-
To refine the theoretical basis of the intervention by integrating systematic review findings and NICE evidence for reducing diets, physical activity, BCTs and theory to refine a logic model.
-
To operationalise acceptable and effective BCTs to embed in a novel narrative SMS delivery form, which builds on existing NIHR-funded narrative SMS alcohol interventions.
-
To identify acceptable ways to provide a menu of information resources on, for example, diet, physical activity, visual feedback of self-reported weight and waist circumference, and pedometer readings using our own or another available open-source website.
-
To optimise an endowment incentive to motivate behaviour change. This was to be achieved by applying insights from behavioural economics and a survey/DCE with men with obesity to define the frequency, constant or varying values and contingency of incentives on targets met for (1) initial weight loss and (2) weight loss maintenance.
-
To select acceptable and valid outcome and cost-effectiveness measures that have the potential for future long-term data linkage.
-
To produce a library of SMS content, recruitment materials and a phase 2 protocol.
Phase 2: feasibility trial to refine approach, recruitment, randomisation, intervention delivery, engagement, retention and follow-up processes
-
To assess the acceptability and willingness to be randomised to (1) SMS, (2) SMS and an endowment incentive or (3) a waiting list for SMS.
-
To assess the acceptability and feasibility of recruiting from general practice obesity registers and community venues, as identified in phase 1.
-
To determine the acceptability of intervention content and delivery and the attendance levels for objective weight measures at baseline and at 3, 6 and 12 months, and any unintended consequences.
-
To assess the likely impact on percentage weight loss at 12 months and health inequalities using an assessment of differential uptake and potential effectiveness by socioeconomic group.
-
To assess if alternative SMS based on mixed-methods data analysis are acceptable and more likely to improve trial retention at 3 months than the narrative SMS intervention. This objective was added to the protocol following an approved study extension request.
Progression criteria for a full trial
Progression criteria are based on systematic review evidence5 and NIHR studies. 13–15 These may or may not support a full trial with either two or three arms.
-
Acceptability of the intervention and the control arm (by the majority of the target group): willingness to be randomised. Evidenced by quantitative and qualitative data on satisfaction, recruitment and intervention engagement.
-
Feasibility of recruiting 105 men in 4 months.
-
Twelve-month outcomes on at least 72% of men randomised per arm, consistent with a recent UK weight management trial in men7 and systematic reviews of the literature on obesity in men. 5
-
Evidence of mean weight loss of at least 3% of baseline weight at 12 months in any intervention arm; NICE defines 3% as clinically significant. 6
-
An independent Study Steering Committee will decide whether or not the findings support a two- or three-arm trial.
-
Commitment by, for example, government or NHS/local authorities to fund the incentive intervention, if it shows positive indicative effects, to ensure translation and sustainability.
Main research question for a future full trial
Is a SMS intervention with embedded BCTs, with or without an endowment incentive, effective and cost-effective in supporting weight loss and weight loss maintenance at 12 months in men with obesity compared with a waiting list control?
Changes to original protocol
Two substantial changes were made to the original protocol: changes to the phase 1 qualitative interviews and the writing of alternative text messages.
Phase 1 qualitative interviews to inform narrative SMS
It was originally planned to carry out 20–30 qualitative interviews with men with obesity during phase 1 (months 0–7) to inform the intervention development. During phase 1, 10 qualitative interviews were carried out to inform the design of the incentive DCE and survey (see Chapter 4) and one focus group with the target population was held to inform the recruitment strategies (see Chapter 5). In addition, four audio-recorded small-group discussions took place about the narrative SMS, incentive intervention and recruitment strategies at a stakeholder workshop with 27 attendees (see Chapter 2). PPI to inform the narrative SMS text library is described in Chapter 3. The project management team considered that it would be more appropriate to assess the acceptability of the narrative SMS after men had received SMS for 3 months, rather than doing this hypothetically in phase 1 or waiting until the final 12-month assessments. This allowed the possibility of amending the SMS content and frequency based on participant experience and feedback. Men were keen to share their experiences at the assessments. The overall aim of the interviews was to seek overall feedback from men on their experiences of participating in the study, the acceptability of recruitment and the intervention components.
Writing of alternative SMS
The waiting list control participants were scheduled to receive SMS for 3 months after the 12-month final assessment. It was originally planned to use the first 3 months of the current 12-month narrative SMS intervention for this purpose. No assessment at 15 months was planned. Although many men found the narrative SMS acceptable, with some showing engagement in their content at that time, this view was not universal. A few expressed strong negative reactions that led to them withdrawing from the study or stopping or blocking the SMS. The aim of examining the acceptability and feasibility of an alternative style of SMS was to explore the potential for reducing strong negative reactions and dropout as a result of the SMS. (For details on how the alternative SMS were developed, see Chapter 5.) The waiting list control arm presented a unique opportunity to test the alternative SMS. Participants were followed up after 3 months and a further 12 qualitative interviews were undertaken to assess the acceptability of the alternative SMS. (For details on the analysis that informed the writing of alternative SMS, see Chapters 5 and 6.)
Report outline
This report has the following outline:
-
Chapter 1 has introduced the general background, study aims and objectives and has provided an overview of the study.
-
Chapter 2 outlines the PPI activities conducted throughout the study.
-
Chapter 3 provides details of the development of the narrative SMS.
-
Chapter 4 presents the results of the survey/DCE of 1045 men with obesity that was carried out to inform the development of the endowment incentive component.
-
Chapter 5 describes the methods of the feasibility RCT.
-
Chapter 6 presents the results of the feasibility RCT.
-
Chapter 7 discusses the findings.
Chapter 2 Patient and public involvement
Background
Systematic reviews of weight loss interventions for men with obesity have concluded that the target population is seldom involved in intervention development, study design or conduct. 5 In this feasibility study, PPI was integrated from study conception until study dissemination. PPI was informed using co-production approaches,41 the principles and practices recommended by INVOLVE42 and an overview of how PPI and mixed-methods research with the target population can complement each other and be synergistic. 43 The PPI undertaken is reported below using the GRIPP2-SF (Guidance for Reporting Involvement of Patients and the Public short form) guidance. 44
Aims
The aim was to involve members of the public and men with obesity from study inception to dissemination to (1) ensure that the interventions, study processes and community venues were acceptable and feasible, and (2) optimise recruitment, uptake, engagement and follow-up of men, particularly those from disadvantaged areas.
Methods
A continuous and responsive approach to PPI was adopted to prepare the grant application and throughout the study, as described by Gamble et al. 45 A summary is provided in Table 1.
| PPI | Number of individuals | Phase(s) of study | Type of PPI | PPI contributors | Description of PPI activities |
|---|---|---|---|---|---|
| Study name feedback | 75 | 1 | Responsive | Men from a range of backgrounds | Feedback detailing study name preferences and key considerations for name selection |
| Information material discussions | 6 | 1 | Responsive | Target group men | Individual face-to-face discussions with a researcher |
| Stakeholder workshop | 6 (and 2 PPI co-investigators) | 1 | Continuous and responsive | Target group men, and community engagement experts | Feedback on the narrative SMS, incentive strategy and study design |
| Narrative SMS | 20 | 1 and 2 | Continuous and responsive | Target group men | Story and narrative workshops, individual consultations with scriptwriter and researcher using drafts of the narrative SMS and script conferences |
| Alternative SMS | 10 | 2 | Responsive | Target group men | Individual consultations with researcher and e-mail feedback on a sample of the alternative SMS |
| Study team | 2 | 1 and 2 | Continuous |
Men’s Health Forum GB co-investigator Men’s Health Forum in Ireland co-investigator |
Team meetings, workshop, qualitative interpretation, SMS interventions, study materials and report writing |
| Study oversight | 2 | 1 and 2 | Continuous |
ManvFat director Alliance Scotland director |
Three Study Steering Committee meetings |
Continuous PPI was provided by a co-investigator partnership with the charities Men’s Health Forum GB and Men’s Health Forum in Ireland. The partnership commenced in 2011 with the ROMEO evidence syntheses5 of weight loss interventions for men with obesity. Men’s Health Forum GB, along with Public Health England, produced a guide, How to Make Weight-Loss Services Work for Men,46 to disseminate the ROMEO systematic review findings. These quantitative and qualitative reviews and the user guide informed this study protocol. Men’s Health Forum in Ireland contributed information from a physical activity study47 and website expertise for engaging men in lifestyle behaviours relevant to obesity.
During this study, co-investigators from each of the Men’s Health Forum charities attended trial management meetings to discuss decisions, data analysis, interpretation of findings and reporting. They provided feedback on the grant application, protocol, SMS libraries and information materials and engaged the wider involvement of men from their organisations to assist with appropriate language. 48 The Men’s Health Forum GB PPI co-investigator attended narrative SMS writing sessions and two qualitative data interpretation meetings.
Continuous PPI at the study oversight level was provided by two independent lay members of the Study Steering Committee which met on three occasions. The director of the ManvFat website (www.manvfat.com; last accessed 25 June 2019) and author of the ManvFat self-help book (https://shop.manvfat.com/collections/tools; last accessed 25 June 2019) provided input both from the perspective of men accessing his organisation’s services and from his personal experiences of weight management. The director of The Health and Social Care Alliance (www.alliance-scotland.org.uk/; last accessed 25 June 2019), who has experience of promoting self-help interventions and addressing health inequalities, provided contact details of link workers (access to health and social care services) at ‘deep end’ general practices in disadvantaged areas to assist with study recruitment.
Responsive PPI occurred at the study funding application stage. Co-investigator Cindy Gray engaged men who had provided PPI input to the successful Football Fans in Training (FFIT) trial. 7 These men participated in two discussion groups. These groups disbanded before this study commenced, but two members continued to be involved and provided feedback as individuals.
During the study, members of the public from the target population or who had an interest in PPI and research activities relevant to men’s health were identified from several sources, including Men’s Health Forum GB, Men’s Health Forum in Ireland, Scottish Community Health Councils, Men’s Sheds, University of Stirling PPI group, Alliance Scotland and other co-investigator contacts. Effort was made to engage men living in more disadvantaged areas to be involved.
A total of 121 PPI contributors were involved during phase 1 and/or phase 2 of the study in a range of one-off or continuing activities (see Table 1).
Key PPI activities during the study included the following.
Study naming competition
The study name was selected by PPI during phase 1. A £20 voucher was offered for suggesting the winning name in the competition. An initial longlist of 91 potential study names was collated from suggestions by target group men, men’s health charities, co-investigators and University of Stirling staff. PPI partners, the Men’s Health Forum in Ireland, contacted individual men and asked partner organisations to request feedback on the longlist of names from their members by e-mail. This yielded feedback from 75 men from a range of ages and backgrounds, including members of Men’s Sheds; a young men’s project; a lesbian, gay, bisexual and transgender support group; a rural farmers’ project; a separated fathers’ support group; sporting clubs; and users of the Men’s Health Forum in Ireland’s online resources. Key considerations for selecting the study name were suggested and the five most popular titles were nominated.
Based on the PPI feedback and in collaboration with the Men’s Health Forum in Ireland, the three most popular study name suggestions were anonymously voted on at the stakeholder workshop towards the end of phase 1.
Stakeholder workshop
A stakeholder workshop with 27 attendees was held to finalise study procedures, intervention components and the study name, and to make final decisions on the study protocol. Workshop attendees included a senior public health manager, co-investigators and study researchers (n = 10), dietitians (n = 3) and independent academics (n = 5) with a range of expertise in weight management, public health and financial incentives. PPI included Men’s Health Forum co-investigators (n = 2), men from the target group (n = 4) and individuals with expertise in the community engagement of men in areas of deprivation (n = 2).
Four structured small-group discussions were conducted about tabled documents that provided a sample of the narrative SMS, options for the incentive structure linked to different weight loss targets met and recruitment strategies. These discussions were audio-recorded to summarise the views expressed and to ensure accuracy. They were not transcribed verbatim, as this would introduce ethical implications for the PPI. 43 Stakeholder workshop attendees voted on the final three most acceptable and popular study names identified by PPI.
One-to-one patient and public involvement feedback on study materials
Researchers met men (n = 6) on a one-to-one basis to discuss the study materials (e.g. information leaflets and questionnaires) to ensure that these were appropriate and understandable. These individuals were Men’s Sheds group members (n = 2), former participants of the Football Fans in Training weight management programme (n = 2), a target group member and former weight management service participant (n = 1) and a community worker experienced in working with men from areas of disadvantage (n = 1). The researchers took notes during these meetings to capture the feedback gained, and, where appropriate, changes were made to the study materials.
Narrative SMS patient and public involvement
Responsive PPI consultations involved feedback from individual men from the target group (n = 20) who were identified through co-investigator connections and research networks. The methods and results of having responsive and continuous PPI in the development of the narrative SMS are described in Chapter 3.
Alternative SMS patient and public involvement
Responsive PPI consultations involved feedback from individual men (n = 10) recruited through three channels: the University of Stirling PPI group, PPI co-investigator connections and researcher networks.
The men involved agreed to provide feedback by e-mail (n = 9) or in person (n = 1) on the 12-week drafts of the alternative SMS. E-mail invitations were as follows:
These texts have been written to help men lose weight, based on men’s experience of weight loss and evidence of what helps people change their behaviour. Any comments on how these texts can be improved based on your experience would be very welcome!
These comments can be about anything: words used, individual texts, strategies suggested, overall themes, general style.
Thank you for your help.
Incentive strategy patient and public involvement
To inform the design of the novel endowment incentive strategy that aimed to invoke loss aversion theory, the PPI co-investigators were involved in the design and the interpretation of the findings from the DCE, which was completed by 1045 men with obesity, and think-aloud qualitative interviews. Men’s preferences for the incentive strategy were then presented at the stakeholder workshop to guide the final decisions about the feasibility trial protocol. Those attending the workshop were asked to discuss what should happen when men were found to fall short of their weight loss targets at appointments.
Results
Study naming competition
The five most popular study names from the feedback gained from 75 men in collaboration with the Men’s Health Forum in Ireland were ‘Game of Stones’, ‘Guts 2 Lose’, ‘Lean Mean Texting Machine’, ‘Lose It or Lose Out (LILO)’ and ‘tXt Men’. These men also put forward key considerations for the selection of the study name:
-
Avoid a name that uses the word ‘fat’ or similar (e.g. CHUBS) as this terminology carries too much baggage and reminders of personal circumstances.
-
Avoid a name with the word ‘fairies’ in it. This term was disliked regardless of sexual orientation.
-
Titles with ‘slim’ or ‘slimmer’ were seen as being aimed more at women.
-
Be cautious about being too smart; for example, younger men liked the name suggestion ‘W8M8’, but this name was poorly understood by older men.
-
Do not choose anything that seems to blame men for their situation, as many men feel that they are already blamed for all the ills of the world.
Based on the key considerations highlighted by PPI, of the five nominated names, the research team removed two (‘Lean Mean Texting Machine’ and ‘Lose It or Lose Out’) because of the words ‘lean’ and ‘lose’, which could be misinterpreted. The stakeholder workshop vote found that the most popular of the final three names, and therefore the one selected, was ‘Game of Stones’.
Stakeholder workshop
Appendix 2 provides a detailed summary of the discussions held between academics, clinicians and PPI members at the stakeholder workshop. The key issue unanimously raised by workshop attendees was recruitment. Two suggestions made by PPI members were to use workplaces and gyms as settings for community recruitment. Based on this feedback, researchers recruited men from two council work premises and the foyer of a gym. As recruitment had been raised as a key issue, a focus group was conducted at the end of phase 1 with men from the target population in a very disadvantaged urban area. This focus group is described in Chapter 5.
Summaries of feedback, suggestions and decisions made by PPI at the stakeholder workshop in relation to both recruitment and study procedures and the incentive strategy were documented (see Appendices 3 and 4).
One-to-one patient and public involvement feedback on study materials
A full summary of one-to-one PPI feedback and decisions or changes made to the information materials as a result can be found in Appendix 5. One example is a sentence in the initial draft of the post-randomisation leaflets that aimed to minimise contamination and disappointment bias between trial arms. The original sentence stated that we ‘ask that you are confidential about your participation in this study’. This was included as two newspaper articles about the study were published after the lay summary became publicly available on the NIHR website. The co-investigators wanted to avoid such media publicity, which could bias the study findings. However, PPI participants suggested that after losing weight they would want to share this success with friends and family, and that this confidentiality section should make clear that this would be OK. The section was then amended to state that ‘you can talk to close friends and family’ about the study.
Narrative SMS feedback
Chapter 3 provides details of the 20 PPI men who commented on the narrative SMS. All 20 men self-identified as belonging to the target group of those carrying excess weight.
Alternative SMS feedback
Appendix 6 provides details of the 10 PPI men who provided comments on the alternative SMS. The majority of men (n = 9) self-identified as belonging to the target group of those carrying excess weight. The group included the editorial and creative consultant at Men’s Health Forum GB, who has written award-winning health guides and online material for men on weight and other health issues. 46,48
Feedback received on the alternative SMS was both general (n = 7) and specific (n = 3). The volume of comments ranged from a few sentences (65 words) to a multipage reflective letter (2152 words). The face-to-face discussion on the alternative SMS lasted for 1.5 hours. Specific comments were provided as in-text comments in the circulated electronic document, and these ranged from 15 to 35 comments.
Substantial changes were made to the draft alternative SMS in response to feedback. Examples of specific PPI feedback and decisions about or changes made to the alternative SMS can be found in Appendix 7.
Incentive strategy feedback
Options for the incentive strategy based on the findings of the DCE were discussed at the stakeholder workshop. Key PPI issues that influenced decision-making are described in Chapter 4.
Discussion
The results demonstrate the considerable influence and impact that PPI had on the study name, the development and refinement of the interventions, the study materials, the approaches to recruitment and the overall design of the feasibility RCT. This is likely to have contributed to the overall acceptability and feasibility of the Game of Stones study and facilitated meeting the progression criteria for a full RCT.
Different views about the interventions, their delivery and the study processes became evident early on. This may reflect the diversity and the number of men providing PPI to the study, the pervasive health issue the study aimed to tackle and the novelty of the intervention components used. All viewpoints, together with evidence and theory, were considered by the research team. Final decisions were made by identifying options for the study protocol and materials and weighing up the pros and cons for each in relation to the study objectives. These options were triangulated with appraisal of the published evidence, behaviour change theory and study goals relating to the testing of incentive-based and SMS-delivered interventions that would have wide reach, address health inequalities, be scalable, be logistically and practically feasible and be sustainable in the future.
Humour was a key finding of the ROMEO qualitative synthesis of men’s experiences of weight loss. 49 Feedback from the diverse PPI in this study demonstrated how easy it is to use language that is disliked by men with obesity.
Reflections
The study team was fortunate to have excellent and continuing involvement with the Men’s Health Forum charities in Great Britain and Ireland; this involvement commenced in 2011 and these charities will continue to help with the dissemination of the findings and preparations for future research. The involvement and networking with key local community and charity stakeholder groups helped to involve men in the target population and men with an interest in PPI and research.
Feedback from PPI on the alternative SMS had to be collected swiftly following official approval of the study extension. E-mail consultations on the draft alternative SMS were efficient and allowed PPI input at various levels, including comments on individual SMS and at a more general and conceptual level. The written format ensured that all feedback was captured without information being lost or misinterpreted. However, e-mail necessitates internet or smartphone access, and less literate men might not have had the confidence to take up the offer of providing input. This potentially excluded some men from being able to contribute. Electronic PPI is efficient, precise and suitable when operating on a tight timeline, but would ideally be supplemented with substantial face-to-face input, as was done for the development of the narrative SMS.
For complex multicomponent interventions such as Game of Stones, the final decisions on the study protocol are crucial. Several plausible options for the development of the incentive (see Chapter 4) or narrative SMS intervention (see Chapter 5) components could have resulted in a different feasibility trial. Engaging and hearing the views of a large number of men with obesity through individual and group PPI and a workshop worked synergistically with data collection using phase 1 surveys and a recruitment focus group with men living in disadvantaged areas. The diversity of expertise, collaborative work and values of the co-investigator team that make the final decisions is therefore critical to intervention and trial design.
Chapter 3 The writing and development of a narrative SMS intervention component to help adult men with obesity lose weight and be more active
This chapter was written by the scriptwriter who developed the narrative SMS component. It is written based on his opinions, work and approaches.
Introduction
This chapter outlines the creative practice and process by which the narrative SMS intervention component was designed and written. It reports how published behavioural theory, evidence-based BCTs, input from behaviour change experts and co-production with the target demographic informed the narrative development process. A timeline represents how the narrative intervention component changed in content and format from the start of the intervention development process, how key stakeholders influenced the process, and the guiding principles, people and factors that were prioritised when making decisions. It outlines the behaviour change theory, the BCTs and the messages that were incorporated into the narrative, and how and when, during intervention development.
This chapter aims to provide a direct analytical link between the intervention aim to help adult men with obesity, particularly those from more disadvantaged areas to lose weight by eating fewer high calorific foods and moving more. It also outlines the narrative SMS approach used to achieve this. Overall, this chapter presents a theory- and evidence-based methodology that may be replicated in further behaviour change interventions and studies across health outcomes: a ‘how-to’ guide to developing an evidence- and theory-based narrative text intervention.
What is a narrative SMS intervention?
Narrative SMS are story-based text messages sent from a computer and received by study participants on their mobile phones. Published studies suggest that ‘narrative’ can simulate the processes that make group-based interventions successful: humour, banter, peer support, facts about diet and physical activity, personal tailoring and evidence-based BCTs. 5 By creating an empathic bond with the characters, users pay more attention to and become engaged with and immersed50,51 in the story. This leads to optimal learning and conceptualisation of the target information. Narrative SMS are defined as interactive life stories based around a range of characters that can simulate the processes that make group-based interventions successful, and are used to embed how-to-do-it, diet and physical activity tips, friendly humour and support. 13–15
Narrative was defined in this intervention as the audio-visual and digital representation of how a character (or characters) interacts with the environment, objects and others and how he or she feels about it and changes over time. 22 Narrative texts in this study represented how a character reflected and acted on his need to lose weight, the familial, social, economic and environmental pressures acting against him, and how he felt about changing his established lifestyle incrementally over 12 months and overcoming his low self-esteem as a result. This specific population, the nature of the SMS channel and the term (12 months) of engagement required a coherent theory- and evidence-based, practical approach to health behaviour change, an approach designed to engage men in long-term behaviour change.
The digital narrative approach to health behaviour change (formerly the digital narrative transformation framework22) is a theory- and evidence-based practical approach to designing, writing and evaluating digital narrative health behaviour change interventions. It represents an approach to enhancing user engagement for health behaviour change in the short and longer term. The approach is interdisciplinary and draws from diverse fields: neuroscience, evolutionary psychology, human–computer interaction, philosophy, history, politics, commercial marketing and social marketing. 22 Digital narrative approach was developed in broadcasting, film and computer games by a professional scriptwriter, developer and executive producer who was engaged in this study as scriptwriter and co-investigator.
Digital narrative approach has been deployed in a number of health behaviour change studies and interventions, and has shifted the focus of health behaviour change research from ‘top down’, cognitive approaches to an emphasis on the need to engage emotionally. It adopts the theoretical stance that, by relying less on information exchange and engaging non-consciously and emotionally, digital narrative enables characters represented digitally – avatars – to convey and model the key messages and behaviours of an intervention and facilitate the viewer’s empathy. Digital narrative approach has, therefore, the potential for participants to internalise key messages and BCTs through their emotional involvement with the development of the narrative, the characters and their stories.
Digital narrative approach blends five core components at the level of the narrative: behaviour change theories, BCTs, key messages relevant to the desired outcomes, commercial digital narrative strategies and evidence from previous studies using digital narrative approach. It also incorporates PPI (see Chapter 2 and below) and input from health behaviour change experts. These core principles and structures have been used across a range of health outcomes. Examples include promoting smoking cessation among pregnant young women,52 reducing binge drinking among adult men,13,15 improving response times to symptoms of acute coronary syndrome53 and improving adherence to physiotherapy among parents of children with cystic fibrosis. 54 Levels of engagement have been encouraging, particularly the extent to which participants engage emotionally as well as rationally and behaviourally. The core narrative principles and structures apply equally to fiction and to documentary styles. They can be delivered over many digital media platforms and are applicable to a range of health outcomes. Digital narrative approach was deployed in the current study to enhance this particular intervention to have an impact on the quality of participants’ motivation (intrinsic and/or extrinsic), and to impart key messages and behaviours around the intention to lose weight and become more active in a specific demographic group (Figure 3).
FIGURE 3.
The digital narrative approach to health behaviour change.

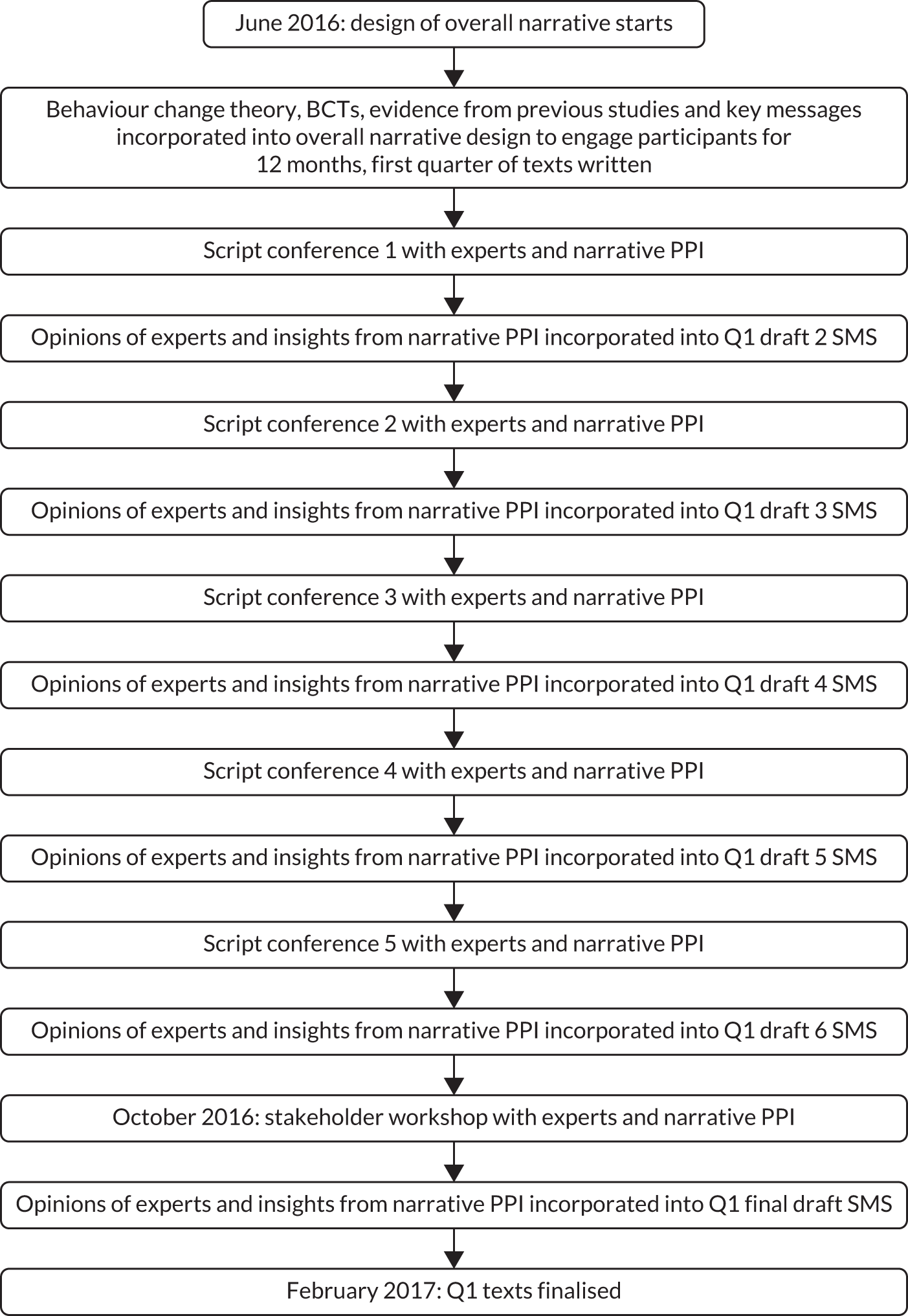
The narrative SMS design
The narrative SMS library was designed and written systematically and iteratively using professional writing and development practices as well as co-production with the target demographic. This process was broken down into two key phases: phase 1, the narrative text intervention design using PPI with the target demographic, and phase 2, the narrative text writing and intervention using live feedback from the study participants as they responded by text to the main character of the story. Figure 4 depicts phase 1. For details on the PPI participants and how PPI influenced the narrative component, see Appendices 8 and 9.
FIGURE 4.
Phase 1: narrative SMS intervention development timeline and key influences on narrative texts.
The overall narrative
The overall narrative and the first 3 months of texts were designed and written during the narrative SMS intervention design phase 1. The narrative was designed to be intimate, taking advantage of the one-to-one conversational style of the texts. It was written from the point of view of Jimmy Nesbit, a character who reports, in the first person, his experience of trying to lose weight, maintain his weight loss and overcome the threat of type 2 diabetes over a period of 12 months. The narrative draws on fictional and real-world (documentary) characters’ experiences of overcoming low self-esteem and losing weight. It characterises how Jimmy’s obesogenic environment, his home, family and social context, and the corporate determinants of obesity can influence his eating and exercise behaviours negatively, thereby throwing into relief the behaviours, lifestyle changes, attitude and beliefs he needs to adopt, and the barriers that he must overcome, if he is to lose weight, exercise more and be healthier.
The characters
Seven characters (Table 2) and their stories were written by the scriptwriter/researcher who wove together their individual storylines using commercial narrative strategies, humour, behaviour change theories, BCTs and key messages. The characters and their backgrounds were designed to reflect the lives and circumstances of, and to appeal and be credible to, the target audience. This involved extensive fieldwork and PPI with the target group in their environment.
| Character | Description |
|---|---|
| Jimmy Nesbit | Aged 39 years. Jimmy weighs 19.5 stones and is clinically obese. His friends call him ‘Slim’. Jimmy suffers from low self-esteem |
| Wilma Nesbit, Slim’s wife | Aged 35 years. Wilma wishes Slim would get a job. She enjoys the food they eat and going out to drink. But she misses their physical relationship |
| Budge, Slim’s best friend | Budge also weighs 19.5 stones. But for Budge, fat is the new black and life is for living |
| Mikey | Aged 32 years. Maintenance Mikey maintains his weight at a steady 76.2 kg. He provides Slim with help, support and guidance. He teaches him to ‘surf the urge’ when faced by triggers in the environment and helps him improve his lifestyle over 12 months |
| Dr Sharpe | Aged 56 years. Although she means for the best, Slim’s general practitioner is somewhat condescending. She tells Slim to ‘just choose a diet and stick to it’. She sees Slim as ‘hard to reach’ – rather than as a whole human who suffers from low self-esteem and is vulnerable to comfort eating |
| Claire, district nurse | Claire is 27 years old and genuinely cares for Slim’s welfare. She helps him improve his self-esteem over 12 months |
| Colin | Colin is owner of The Head, the local pub. At 24 years old he has inherited money made from importing sugar. Colin’s new ‘Power Up Super Juice’ range proves irresistible to Slim |
The scriptwriter further developed and wrote the characters by working closely with a graphic artist. This process helped to define the characters, their relationships and their stories and provided visual prompts in character and story workshops with the target demographic to assess the characters’ likeability and credibility, their stories and the real-world barriers to and facilitators of behaviour and lifestyle change. The biographies and images of the characters were published on the study website to allow participants to visualise the characters, including the main character, Slim, from whom they would receive the texts regularly.
The overall narrative synopsis
Jimmy Nesbit is 39 years old and unemployed and suffers from low self-esteem. He weighs 19.5 stones and his friends call him ‘Slim’. Dr Sharpe, Slim’s general practitioner (GP), warns him that he is at risk of developing type 2 diabetes, various forms of cancer and coronary heart disease, including the risk of having a stroke. She recommends that he needs to keep a food and exercise diary. She tells him that he must ‘choose a diet and stick to it’.
Slim reflects on his poor health and monitors his food intake and physical activity using a diary, but he is confused by the range of diets and conflicting advice available to him and remains unmotivated. His cycles of low mood leave him vulnerable to comfort eating in response to triggers in his environment (i.e. the marketing of high-fat, high-salt and high-sugar foods). Slim’s closest friend and drinking buddy is Budge, who also weighs 19.5 stones. He advises Slim that ‘fat is the new black’ and ‘life is for living’. Unlike Slim, Budge is in complete denial about the threats to his own health from poor diet and lack of physical activity.
A stranger appears in the community, Mikey, who has has embraced weight loss and maintenance for his own personal reasons. He sets up a weight loss competition between Slim and Budge. He introduces Slim to a method of ‘surfing the urge’. This is a way to control responses to the triggers in the environment that usually result in comfort eating. Slim makes an effort to take control at home. Unfortunately, the poor eating habits and the sedentary lifestyle that he has established over the past 10 years all prove to be barriers to the changes that he needs to make. Frustrated at his apparent inability to change, Wilma leaves Slim. Slim remains hopeful that Wilma will come back, even if it means building her that summer house that she has always wanted in the back garden. Claire, the district nurse, sees clearly that Slim needs not just an improved diet and exercise, but also a better sense of his own worth.
When Slim discovers that Wilma is pregnant he takes to the weight loss competition with a vengeance. He wants to be able to play football and be a good father to his son. He finds that by drinking a new brand of energy drink, ‘Power Up Super Juice’, he can eat less and exercise more, but, as Claire points out, Slim is gaining weight because of the sugar content of the drinks. The news that Wilma has given birth to a child possibly fathered by another man sends Slim back into cycles of comfort eating. He vows to be a good father regardless. Motivated, he renews his weight loss and maintenance routine. During all of this, his estranged friend and competitor Budge has a stroke.
The news that Budge is in a coma helps Slim finally see himself and his unhealthy lifestyle fully ‘in the mirror’. He manages to lose weight and maintain that loss through action. He wins the weight loss competition as well as reducing his risk of type 2 diabetes, bowel cancer, heart disease and stroke. Slim finds he has confidence in his strategies to lose weight and maintain weight loss. Most importantly, he discovers improved self-esteem, motivation and resilience.
The approach to the design of the narrative
When Slim first texts participants, he is unemployed, his marriage is on the rocks and he is suffering from low self-esteem. It was critical that Slim have significant and credible setbacks so that the narrative could be sustained in a long-term intervention.
Slim’s thoughts, perceptions, emotions and imagination, the influence of significant others and the impact of stimuli in the environment were plotted to ensure that his levels of motivation and ability to self-regulate were plausible and realistic over 12 months and also that Slim took control of his lifestyle in an engaging manner. Dramatically, this necessitated that Slim suffer relapses and setbacks along the way.
In the second quarter (months 4–6), Slim attempts to change his home environment, for instance so that he can resist the triggers of eating foods high in fats and calories. His attempts are thwarted by his wife, Wilma, as, although she wants him to be physically fit again, ironically she is unable to respect his needs and to change the habits and routines of their marriage and home life. Mikey teaches Slim how to ‘surf the urge’ to control the stimuli in his home and the external environment. In story terms, Slim’s desire to eat when he is down is continually triggered by marketing promotions for high-fat, high-salt and high-sugar foods in the supermarket and on advertising billboards. Slim is continually able to deal with relapses and plan ahead to avoid temptation when he is socialising and eating out. In the third quarter, Slim uses his new knowledge to fight against all odds to lose weight. In the final quarter, Slim develops the habits that will begin to sustain his weight loss. He learns to reflect on and enjoy his achievements and the physical, social and psychological benefits of being healthier.
The setting
The setting for the narrative overall was a secret location in Scotland with the same socioeconomic status as the target demographic. The emphasis was placed on blending comedic and dramatic storylines to maximise emotional engagement throughout. This is a potential limitation as using a real location might lead people to identify more or less with the story depending on where they come from. It is also a potential limitation if during recruitment the target group changes and represents a different demographic from that originally intended and for which the narrative was originally designed.
The theories of change embedded in the narrative intervention
Three key phases of behaviour change – motivation, action and maintenance – were merged at the core of the overall narrative according to the principles and structures of digital narrative approach: Ryan and Deci’s self-determination theory,37 which focuses on the quality of participant motivation; Schwarzer’s health action process approach, which emphasises the need for motivation, action and maintenance of behaviours;38 and Rothman et al. ’s maintenance theory,39 which focuses on the need for maintaining weight loss maintenance over time. These theories are described in detail in Chapter 2. What concerns us here is how these theories, BCTs and key messages were operationalised at the level of the narrative and in the individual texts transmitted to participants over 12 months.
Ryan and Deci’s self-determination theory37 was incorporated into the overall narrative, which sees the quality of Slim’s motivation increase incrementally over the 12-month period as his self-esteem improves. Slim’s health improves as he develops the intrinsic motivation to engage in more vigorous activity tailored to his preferences, for example his goal to walk longer and longer distances without his stick and his increased sense of control over his diet, alcohol consumption and portion sizes. Slim secures intrinsic motivation through the feedback he receives around the success in his hobby, which is writing a computer game he calls Game of Stones. It is through this game that the desired behaviours and key messages are repeated and reinforced. As he learns from Mikey the need for regular goals, rules, feedback, rewards and self-regulation, so Slim develops his game to help people like him lose weight online. This helps Slim, with Claire’s support, to overcome his low self-esteem and take full control of his marriage and lifestyle, not just his diet and physical activity regimens. By taking control over his own destiny Slim enjoys acceptance back into the local community.
The intervention overall was designed to encourage participants to lose 10% of their body weight over 12 months. It was decided that the main character, Slim, would also set this goal and achieve 10% reduction in his body weight over 12 months. If Slim had learned to lose and maintain 10% of his weight over 3 months, the story would have been resolved and it would not have been possible to sustain the intervention over 12 months in a credible and engaging manner. This meant that the actions Slim took to achieve that weight loss had to be introduced incrementally and credibly, and this progression had to be consistent with the key concepts taken from the underlying theories, such as the need for motivation, action and maintenance.
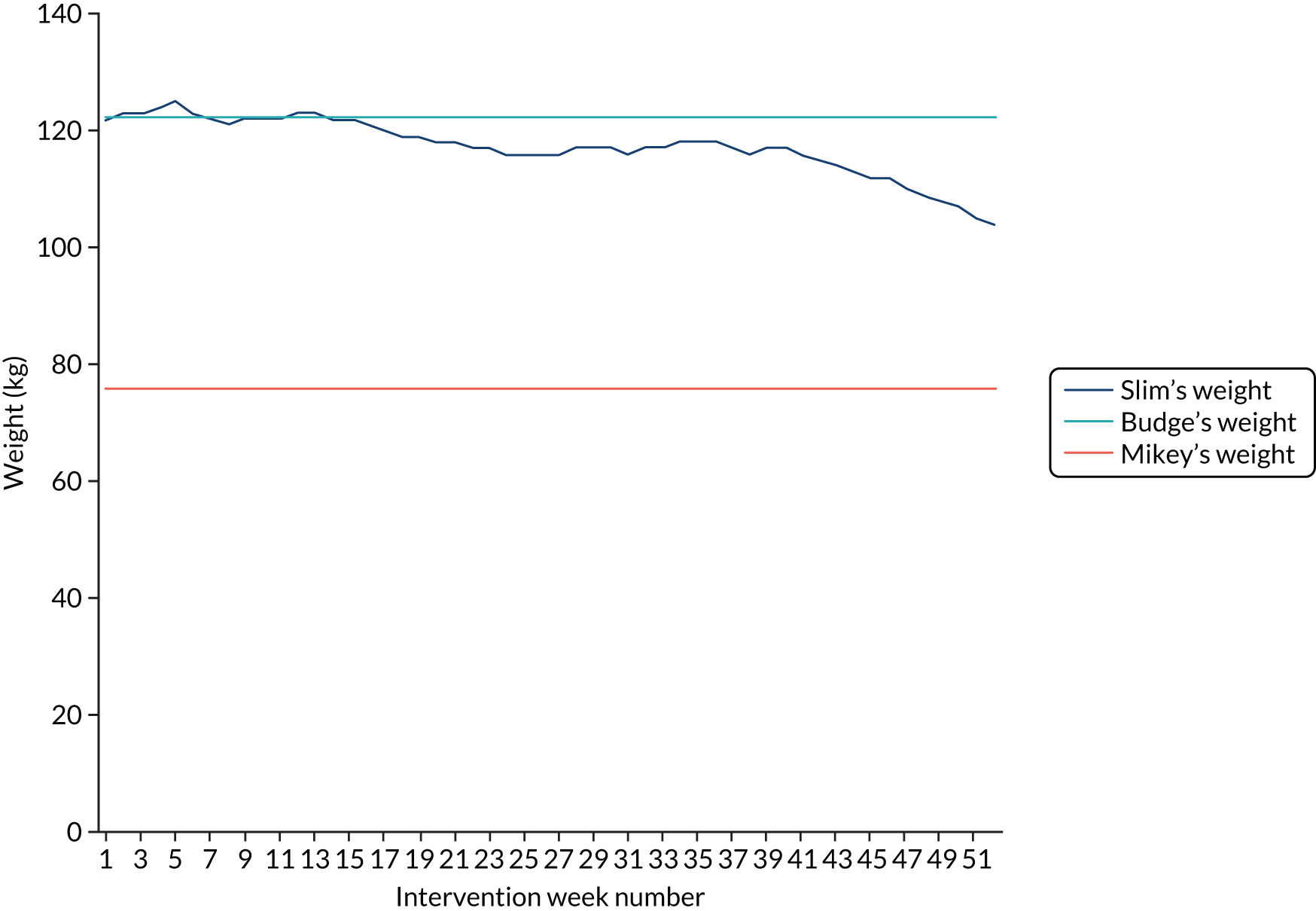
The narrative was designed to incorporate the diet component options recommended as part of the 600-calorie daily deficit approach. 6 Slim’s weight was plotted over 12 months to ensure that the cycles of weight loss, weight gain and maintenance were feasible – given his intentions, motivation, emotional state and actions – and enabled him to lose 10% of his body weight over 12 months credibly. Slim gradually started to eat more nutrient-dense foods, reduce his portion sizes of energy-dense foods and reduce his intake of snacks, sugar and alcohol over the 12-month period. How Slim put this into action depended on his initial personal food preferences, and small, gradual and achievable changes to his normal diet were incorporated in line with recommendations. 6 In narrative terms, Slim’s weight loss objective was conveyed using the story of an ongoing weight competition between Slim and his friend Budge and refereed by ‘Maintenance Mikey’, who becomes Slim’s coach. Throughout, Mikey’s advice and guidance remain consistent with his own ability to maintain a steady weight through resilience and self-regulation to control his diet and physical activity regimens. It is as a result of Mikey’s information advice, guidance and emotional support that Slim learns to recognise the environmental triggers of his eating behaviours and the barriers to changes in his lifestyle. Slim’s weight loss trajectory was then plotted against that of his friend and opponent Budge, whose attitude, intentions, levels of motivation and lack of action mean that he maintains a weight of 122.5 kg, and that of his mentor, Mikey, who maintains his weight at a mean of 76.2 kg. Figure 5 charts Slim and Budge’s weight loss trajectory, merging theory, BCTs and narrative to represent credible weight loss and behaviour change over 12 months.
FIGURE 5.
Slim’s, Budge’s and Mikey’s weight loss trajectories.
The behaviour change techniques embedded
This section shows how the main evidence-based BCTs were implemented in the narrative using digital narrative approach. The aim was to operationalise techniques at the level of the text intervention component that could be acceptable and effective in a weight loss intervention. BCTs that are most likely to be successful in sustaining behaviour change in weight loss and maintenance have been identified in systematic reviews,5 theory34,35,37–39 and NICE guidelines. 6,55 Table 3 represents the BCTs that the scriptwriter identified had been embedded in the narrative intervention.
| BCT cluster | BCT |
|---|---|
| Reward and threat | Social reward; anticipation of future rewards; incentive |
| Repetition and substitution | Behaviour substitution; habit reversal; habit formation; restructuring the social environment; avoidance of/changing exposure to cues for the behaviour |
| Antecedents | Restructuring the physical environment; restructuring the social environment; avoidance of/changing exposure to cues for the behaviour; distraction |
| Associations | Discriminative (learned) cue; prompts/cues |
| Natural consequences | Health consequences; social and environmental consequences; emotional consequences; self-assessment of affective consequences; anticipated regret |
| Feedback and monitoring | Feedback on behaviour; self-monitoring of behaviour |
| Goals and planning |
Action-planning (including implementation intentions); problem-solving/coping-planning; commitment; goal-setting (outcome); behavioural contract Discrepancy between current behaviour and goal standard; goal-setting (behaviour) Review behaviour goal(s); review of outcome goal(s) |
| Social support | Social support (practical); social support (general); social support (emotional) |
| Comparison of behaviour | Modelling the behaviour; information about others; approval; social comparison |
| Self-belief | Mental rehearsal of successful performance; focus on past success; verbal persuasion to boost self-efficacy |
| Identity | Identification of self as role model; self-affirmation; identity associated with changed behaviour; reframing; cognitive dissonance |
| Shaping knowledge | Reattribution; antecedents |
| Behavioural experiments | Instruction on how to perform a behaviour |
| Regulation | Regulate negative emotions; conserving mental resources; paradoxical instructions |
The key messages embedded
Patient and public involvement in the development of the narrative proved critical in assimilating key messages. Opinions varied; some thought that the message should be ‘just choose a diet and stick to it’, whereas others cited a wide range of diet and physical activity advice and tips available on official NHS advice websites. The PPI consultants mentioned that there was a confusing array of messages pertaining to the ideal diet and physical activity approaches ‘out there’. This issue was taken back to the narrative design team in subsequent script conferences, where it was decided that a hierarchy of key messages should be drawn up (Figure 6). This was then returned for consultation with 20 narrative patient and public participants. Through individual consultations and story and character workshops with the target demographic, it became apparent that only one message was meaningful: ‘eat less and be more active’. The rest of the messages were seen as confusing and often contradictory. ‘Eat less, move more’ then became the central key message to the thrust of the narrative and was embedded in the individual storylines.
FIGURE 6.
The hierarchy of key messages embedded in the narrative SMS.
The final key messages were consistent with current recommendations for weight management that focus on adhering to this message rather than on specific diets. 56
A total of 604 texts were sent by Slim over the 12 months. The overall narrative was first designed with enough interlinked stories to engage participants over 12 months, taking into account the number and frequency of texts used in previous studies that showed strong levels of engagement. 13,15,21,57 The number of interwoven stories was therefore increased to create an engaging narrative using no more than five texts per day over the 12 months.
Phase 2: intervention and narrative text writing
The first quarter of texts were written 12 weeks prior to the intervention start date. The scriptwriter wrote the texts and then elicited comments from health behaviour change psychologists, medics, experts in dietary control and members of the target demographic. Evidence from feedback was incorporated, as were the participants’ text responses to Slim. This feedback informed the writing and development of the texts transmitted in subsequent quarters in an iterative manner. Figure 7 represents phase 2: intervention and narrative text writing.
FIGURE 7.
Phase 2: narrative SMS intervention and key influences on final narrative texts.
Mode of narrative SMS delivery
The narrative SMS intervention was delivered using technology used in other RCTs linked to Tayside Clinical Trials Unit. 13–15 Although participants could interact by responding to the texts sent to them, there was no requirement for them to do so. This design provided the opportunity to gauge participants’ feelings about the texts. The scriptwriter received participants’ responses, which suggested how participants were feeling and acting in response to the texts sent to them in real time. The scriptwriter was then able to adjust the texts for the following quarter accordingly and in an iterative manner. For example, the scriptwriter received feedback about Slim and Wilma during character and story workshops conducted with representatives from the target demographic about the critical role a partner plays in helping to make or resisting changes in the home environment if new diet and exercise behaviours are to be adopted and triggers of old habits removed. However, Slim and Wilma’s marriage story appeared to resonate negatively with one participant during the actual intervention, who ‘had his own problems’ and felt that the story was ‘too close to home’. It was clear that the emotional power of this story was too resonant for some. The scriptwriter then reduced the number of texts featuring the marriage story. For examples of interpretations of the SMS replies and how these influenced the narrative, see Appendix 10.
Chapter 4 Phase 1 survey to inform the endowment incentive and trial processes
Background
The use of financial incentive schemes to encourage health behaviours such as smoking cessation, weight loss and physical activity has become increasingly popular. 27,29,58 However, the design of incentive schemes does not always receive sufficient attention, even though this can vary in several dimensions, including value, frequency and direction (gain or loss). Researchers argue for more thought when designing financial incentive schemes, as the evidence for the optimal configuration is currently limited. 59,60 This study optimises the design of financial incentives by drawing on insights from behavioural economics, incorporating individuals’ preferences for different incentive designs and incorporating PPI (see Chapter 2). Designing interventions in line with participants’ preferences is argued to increase uptake and engagement.
A survey of men’s preferences was conducted to inform the incentive design, as little is known about these. The survey was also used to inform all components of the intervention (including SMS) and trial processes. Preferences for the incentive design were elicited using a DCE. The usefulness of DCEs in this context was first suggested by Purnell et al. 28 Hashemi et al. 61 undertook the only study to have used a DCE to elicit preferences for three dimensions of a financial incentive scheme for weight loss: the value of the monetary incentive, the form of the incentive and the timing of the payment. The results showed that individuals preferred larger incentives, more flexible forms of incentives and more immediate payments. Our study adds to this evidence and demonstrates the usefulness of DCEs in this context.
Methods
The survey included a DCE to inform the financial incentive design, questions to inform overall intervention design and sociodemographic questions. Validated questions were used when possible. The data were collected using an online survey administered by Ipsos MORI (London, UK; www.ipsos.com/ipsos-mori-en-uk). The sample size for the survey was calculated using an estimate of the population of interest (i.e. adult men with obesity in the UK: ≈6 million), a conservative estimate of variation in answers to the question of interest of 0.25, and an assumed margin of error of 3% in line with public opinion research. The sample consisted of 1045 UK men with obesity aged 18–75 years (quotas were imposed for age and UK regions to ensure that the sample was representative of the UK population in terms of these characteristics). Men were eligible if their reported height and weight placed them in the upper body mass index (BMI) quartile (i.e. ≥ 30 kg/m2). Ethics approval was obtained from the University of Stirling Research Ethics Committee.
A discrete choice experiment to inform financial incentive design
A DCE was used to elicit men’s preferences for different configurations of the financial incentive scheme in terms of scheduling, frequency and magnitude to optimise uptake and engagement. A DCE is a survey method that presents participants with a series of choices between two configurations of services, in this case configurations of weight loss programmes. Using regression modelling, the relative importance of the different dimensions (or attributes) of the programme can be estimated. This information can be used to decide on the optimal configuration of the financial incentive scheme.
The relevant attributes of the DCE were largely predetermined. The Adams et al. 59 framework was used to identify the different domains (or attributes) of a financial incentive scheme. The attributes included direction, form, magnitude, certainty, target, frequency, immediacy, schedule and recipient. Choices for several dimensions were predetermined based on existing evidence, trial logistics, feasibility if rolled out, and perceived acceptability to the public and to service providers (Table 4). These included cash, based on evidence for the preference of cash;31 certainty, based on trial logistics; target weight as a proxy measure for behaviour (i.e. weight loss); delivery at 12 months, based on trial logistics, and individual recipients based on trial logistics. The detailed justification for the a priori £400 ceiling level of the financial incentive is provided in Appendix 11.
| Domain | Dimension | This study |
|---|---|---|
| Direction | Positive reward; avoidance of penalty | Evidence: avoidance of penalty |
| Form | Cash; vouchers for range of goods or services; specific good/service | Evidence: cash |
| Magnitude | Continuous |
Unclear Acceptability and evidence: £400 (equal to annual cost of the drug orlistat, excluding monitoring costs) |
| Certainty | Certain; certain chance; uncertain chance | Trial logistics: certain |
| Target | Process; intermediate; outcome; proxy measure of behaviour | Trial logistics and acceptability: proxy measure for behaviour – weight loss |
| Frequency | All instances incentivised; some instances incentivised |
Unclear Trial logistics: maximum number of three instances (3, 6 and 12 months) |
| Immediacy | Continuous | Trial logistics: incentive paid out at 12 months only |
| Schedule | Fixed; variable | Unclear |
| Recipient | Individual; group; significant other; clinician, parent | Trial logistics: individual |
The choice of direction of the reward was based on insights from behavioural economics. The majority of previous studies using financial incentives at part of weight loss programmes used deposit contracts,62,63 which have been shown to be effective. 58 With deposit contracts, individuals deposit their own money into an account, and the money is returned if they follow through with a predetermined goal (e.g. achieving a certain amount of weight loss). However, individuals lose the money if they do not achieve the goal. Deposit contracts focus on losses rather than gains, which in theory improves effectiveness, as individuals tend to be loss averse, that is they value losses at a higher rate than equivalent gains. 64 The preferred direction of the current financial incentive scheme was, therefore, avoidance of losses.
This study targeted men with obesity living in areas of deprivation, where men may face financial constraints likely to have a negative impact on uptake and engagement. Therefore, it was decided to use a hypothetical endowment to try to invoke loss aversion. A hypothetical endowment is pledged at the start of the scheme. Participants can then secure set values of the money at certain time points if they achieve a weight loss, but will ‘lose’ money if targets are unmet. This scheme is similar to a deposit contract, the difference being that a hypothetical amount is pledged at the start rather than participants depositing their own money. Pledging the money at the start is likely to invoke an endowment effect, with individuals ascribing a (higher) value to the money because they believe that they ‘own’ it.
Framing the incentives in term of hypothetical losses rather than gains has been shown to be effective in other settings65 and, more recently, as part of a financial incentive scheme for increasing physical activity. 36
The dimensions that were uncertain and were, therefore, the relevant attributes in the DCE were frequency, schedule and magnitude. The DCE elicited preferences for the incentives at the three time points at which weight was to be verified (3, 6 and 12 months). The value of the incentive at the different time points was determined by an overall magnitude of around £400 and a sufficient amount at 12 months to encourage weight loss maintenance. The attribute for the value of the incentive at 12 months did not include £0 (i.e. participants would always receive some amount of money if they met their target at 12 months). The attributes and the levels of the DCE were:
-
value of the incentive at 3 months: £0, £75, £100, £150
-
value of the incentive at 6 months: £0, £75, £100, £150
-
value of the incentive at 12 months: £100, £150, £200, £250.
This means that the overall magnitude of £400 falls within the range of possible overall values (this ranges from £100 to £550). The range of values means that the impact of magnitude on uptake can be examined.
To explain the incentive scheme, respondents were told that they would be pledged a hypothetical endowment at the start of a weight loss programme and they could lose or secure part of the endowment at different time points, depending on whether or not they achieved certain weight loss targets. A series of visuals were used to help explain the concept. Participants were also informed that they would receive all of the money they had secured after the 12-month study was complete, and not at individual time points.
There was uncertainty about the appropriate weight loss targets from baseline weight, and it was unclear whether or not uptake might vary across set weight loss targets. For example, if men perceived a 10% target as unrealistic, they may have been more likely to opt out. DCE participants were randomised to two different sets of targets for the DCE: 3% at 3 months, 5% at 6 months and 5% at 12 months; or 5% at 3 months, 10% at 6 months and 10% at 12 months. This is in line with guidelines suggesting that the minimum target weight loss for clinical benefit is 3% and the top target is around 10% based on existing evidence. 6 Participants were shown what the percentage weight loss targets meant for them personally in terms of stones, pounds or kilograms, based on their preference.
Participants were asked which programme, if any, they would choose. They were told that they would receive the following as part of the weight loss programme, in addition to the incentives: information on ways to lose weight, text messages and a pedometer. They were told that they could choose to receive the incentive as either cash or a donation to charity. An example of choice is presented in Figure 8.
FIGURE 8.
Screenshot of the DCE choice scenarios presented to participants.

The full factorial design consisted of 64 possible incentive configurations (three attributes with four levels each). Ngene software (ChoiceMetrics; www.choice-metrics.com) was used to produce a D-efficient design of 16 choices. The 16 choices were divided into two blocks of eight to reduce response burden. Choice 3 was repeated as choice 8 to test for consistency of responses. Respondents were therefore presented with nine choices in total.
Questions to inform overall intervention design
Several questions were included in the survey to inform the trial design. Some of these questions were also used to get respondents to think about the different components of the weight loss programme on offer in the DCE. Respondents were asked whether or not they would be interested in receiving information, a pedometer, text messages and financial incentives. The narrative text message intervention was described as follows: ‘The messages will come from fictional men who are trying to lose weight and the different ways they go about doing this, informed by research about what works’. In addition, respondents were asked whether or not competition against other men in the programme was important; where they would prefer to be weighed; how they would like to receive feedback; how often they would like to receive the texts; and the distribution of the weight loss target they preferred (i.e. lose weight gradually over 12 months; lose weight over 6 months and then maintain; lose weight over 3 months and then maintain).
Questions about the financial incentive design asked whether respondents preferred to receive a charitable donation or cash and their preferred format of the pledge (i.e. cheque, bank statement or facsimile notes). They were also asked to imagine that they would be offered up to £400 to help them achieve the 5% and 10% weight loss targets. They were then asked if they would prefer to receive all of the £400 for meeting the final weight loss target at 12 months or as three instalments at 3, 6 and 12 months. If they chose the latter option, they were asked to indicate how they would distribute the money across the three time points.
Sociodemographic characteristics
As the intervention aimed to have broad reach and include men with obesity from disadvantaged backgrounds, the study examined how preferences varied according to deprivation level. Information on a range of indicators for deprivation was elicited, namely household income, education, employment status, car ownership and home ownership. Information was also collected on age, number living in household, ethnicity, self-rated general health, smoking status and physical activity.
Further questions included views on weight and weight loss, past weight loss attempts, ideal weight and weight perception (responses being about right, too heavy, too light, don’t know). The importance to respondents of losing weight and their confidence in their ability to lose weight and maintain weight loss were measured on a 1 to 7 scale. Respondents were also asked when they had last tried to lose weight and how often they had tried to lose weight in the past.
The acceptability of financial incentives and responsibility for being overweight were elicited using a survey measure by Promberger et al. 66 Participants were asked to indicate the acceptability of NHS funding financial incentives as an add-on intervention on a scale from 1 to 7, ranging from definitely yes to definitely no. Participants were also asked how responsible overweight people are for being overweight on a scale from 1 to 7, ranging from entirely responsible to not responsible at all.
As the financial incentive design was informed by behavioural economics, the survey also collected information on behavioural parameters using standard measures. Time preferences were elicited using the multiple price list. 67 A dummy variable was created for very impatient individuals (always chose option A in the first multiple price list). The survey also measured perceived temptation. 68 Participants were asked to imagine that they had won 10 certificates for ‘dream restaurant nights’ that had to be used within the next 2 years. They were asked how many certificates they would ideally like to use in each year. They were then asked if they thought that they would be tempted to deviate from their ideal allocation. The original question then asked them to predict how they would behave (i.e. if they would give into this temptation).
Questionnaire development
Think-aloud interviews were used to test the wording and understanding of the questionnaire. Seven men were recruited from two men’s groups in Aberdeenshire, and three men were recruited using the University of Aberdeen ‘Small Ads’ system (August 2016). Participants were, on average, 57.1 years old (range 30–91 years old), had an average of 2.4 household members (range 1–4) and lived in Scottish Index of Multiple Deprivation69 (SIMD) areas 3 (n = 1), 4 (n = 4) or 5 (n = 5), and nine self-identified as having a problem with being overweight.
Participants were asked to ‘think aloud’ as they answered the questionnaire items on an iPad (Apple Inc. Cupertino, CA, USA), and open questions were used as prompts to explore their views about the proposed intervention components and trial processes. Interviews were audio-recorded and partially transcribed by the researcher. Qualitative themes that did not relate to the DCE or survey design but were relevant to the overall feasibility trial were coded independently by two researchers. The findings are summarised in Appendix 12 and were used to inform the topic guides and the analysis for the feasibility RCT (phase 2). A number of minor misunderstandings in the process were identified and corrected to clarify the instructions for the choice tasks. Appendix 13 details the changes made following the think-aloud interviews.
A pilot of the survey with 106 participants was run by Ipsos MORI prior to the full launch. This was used to check that there were no technical errors in the online link, that there were no further issues with the questions and that responses were as expected.
One minor issue was that some participants had given impossible/illogical weight, height and clothing size measurements. For example, one participant stated that his weight was 6.35 kg. In response, minimum and maximum values were set so that participants could provide answers only within a given range. The values for height were 121 to 241 cm (or 4 to 7 feet and 0 to 11 inches), the values for weight were 38 to 260 kg (or 6 to 40 stone and 0 to 13 lb) and the values for trouser waist size were 63 to 198 cm (25 to 78 inches).
The wording of two other questions was altered. It was clarified that the clothing size question referred to trouser waist size. The perceived temptation questions with the restaurant vouchers continued to be challenging to participants, with several implausible answers given (e.g. participants indicated that they would be tempted to use more vouchers in the first year, but then stated the same number as in their ideal allocation in the follow-up question). Participants were therefore reminded of their stated ideal allocation in the follow-up question.
Discrete choice experiment analysis
The analysis of the DCE responses is based on random utility theory. The utility V of weight loss programme j is a linear and additive function of the attributes and levels:
where Vj is the utility of option j and β are the parameters to be estimated indicating the relative importance of the different attributes. ‘Programme’ is the alternative specific constant that takes on the value of 1 if the option is either programme A or programme B and 0 if the option is the opt-out, and Amount3, Amount6 and Amount12 are the values of the incentive at 3, 6 and 12 months, respectively.
If individuals’ preferences are guided by their time preferences only, then the amount at 3 months will be valued highest, followed by the amounts at 6 and 12 months, respectively, although this effect may be reduced as the money is paid out at 12 months only. However, individuals may realise that maintaining weight loss is challenging and, therefore, may prefer longer-term incentives over short-term incentives. This would mean that the amount at 12 months may be valued higher than the amount at 3 months. In terms of overall amount, a rational decision-maker should prefer the programme with the highest overall amount. However, this may not be the case if the individual has ethical concerns about financial incentives and may find certain higher levels unacceptable.
A number of estimation techniques were explored, including conditional logit, random parameter logit and latent class modelling. As financial incentives can be controversial, the sample was expected to have diverging preferences for the weight loss programmes, with some participants strongly opposed to incentives and others strongly in favour. Examining this preference heterogeneity was of interest for the intervention design. Preference heterogeneity can be accounted for by using random parameter logit regression, which allows parameters to vary randomly over individuals. A disadvantage is that a distribution needs to be specified for the random parameters, which is usually either normal or log-normal. However, given the diverging views on the acceptability of financial incentives, a bimodal distribution was expected to be more appropriate. Latent class modelling was therefore used, which does not require assumptions about the distribution of the random parameters. Instead, it identifies different utility functions across unobserved subgroups or latent classes. A latent class model fits the best possible model with a predetermined number of classes. For each class, different coefficients (or discrete random effects) are estimated for the attributes. The latent class model is a better fit for the current data, confirming that the random parameters are unlikely to be normally distributed.
The optimal number of classes in the DCE was determined in an iterative process by comparing models with different numbers of classes on the basis of goodness of fit (Akaike information criterion), precision of estimates and size of class shares. As highlighted by Hole,70 there is often a trade-off between goodness of fit and the precision of the parameter estimates. A model with more than three latent classes resulted in very small class shares (< 5%) and large standard errors for some of the estimates. It was therefore decided that three latent classes were the preferred specification.
The association between observable characteristics and class membership was explored. The characteristics included socioeconomic characteristics, weight loss characteristics, acceptability of financial incentives and behavioural parameters.
The socioeconomic characteristics included age (dummy: aged 35–54 and aged 55–75 years); education (dummy: General Certificate of Secondary Education/Ordinary level/Certificate of Secondary Education/no formal qualifications), income (dummy: income < £15,000 and income £15,000–30,000), working status (dummy: unemployed/not in paid work for other reason/not in paid work because of long-term illness or disability, and retired), car ownership (dummy: no car), home ownership (dummy: owns home), single household (dummy: single household), ethnicity (dummy: non-white) and region (dummy: Scotland).
The weight loss characteristics included BMI, importance of losing weight [continuous variable on a scale from 1 (not important) to 7 (very important)]; confidence in ability to lose weight and confidence in ability to maintain weight loss [continuous variable on a scale from 1 (not confident) to 7 (very confident)], whether or not currently trying to lose weight (dummy: trying to lose weight); number of previous weight loss attempts (dummy: one to three previous weight loss attempts and four or more previous weight loss attempts); and percentage difference between current and ideal weight. Individuals who indicated that weight loss was important might have valued incentives more strongly or at more time periods. Incentives might also have been valued more strongly or at more time periods by those who indicated a low confidence in their ability to lose weight; receiving incentives at all time periods would assist with early engagement and maintenance of weight lost. Similarly, those who indicated a lack of confidence in maintaining weight loss might value more strongly long-run incentives to provide an incentive to keep off lost weight. A number of health (behaviour) characteristics including smoking status (dummy: current smoker) and physical activity (dummy: participates in vigorous physical activity) were also included.
Unacceptability of financial incentives [continuous on a scale from 1 (incentives should definitely be funded) to 7 (incentives should definitely not be funded)] and responsibility of overweight people for being overweight [continuous on a scale from 1 (people are not responsible) to 7 (people are entirely responsible)] were also included. It was hypothesised that those participants who found incentives unacceptable might opt out and not value the amounts at 3, 6 and 12 months.
The behavioural parameters include perceived temptation (dummy: tempted to consume more than their ideal allocation) and present orientation (dummy: always chose the immediate option in the first multiple price list). It was hypothesised that individuals who recognised that they might be tempted to consume more than their ideal allocation in a given year might prefer to spread the incentive payments across the year to counteract the temptation they anticipated they would feel. Finally, it was hypothesised that individuals who displayed a strong present bias would value more strongly the incentives associated with the earlier time points.
Preferences varying by weight loss target were also explored (dummy: equal to 1 if the respondent had been allocated to the hypothetical 5% target, and 0 if he had been allocated to the hypothetical 10% target).
Including a large number of characteristics in the membership part of the latent class model can lead to unstable models with large standard errors. To obtain a parsimonious model, backward stepwise regression was used and characteristics were eliminated until all remaining characteristics were statistically significant at a 5% level and there were no large standard errors.
To assess the relative ranking of different incentive designs for the latent classes, we predict uptake π of the intervention. The utility of the opt-out is set to zero. Uptake is estimated as follows, where Vj is the utility of weight loss programme j (see Equation 1):
Preferences for all intervention components
Regression analysis was carried out to determine which factors influenced preferences for different aspects of the weight loss programme: interest in receiving information/advice, a pedometer, the text messages and incentives, importance of competition in weight loss, preferred distribution of weight targets, preferred weigh-in venue, preferred frequency of weighing, preferred form of incentive (cash or donation) and timing of payment (over three time periods or all at the final weigh-in). Ordered probit regression was used to model ordinal outcomes and probit regression for binary outcomes. The same individual characteristics were included as those included in the membership part of the DCE.
Results
Sample characteristics
The sample consisted of 1045 men with an average BMI of 34.9 kg/m2 (range 30.0–125.6 kg/m2). Appendix 14 (see Table 32) reports weight and perceptions about weight loss. The percentage difference between current and ideal weight was 19.2%. Around half of the sample was currently trying to lose weight and around 95% perceived themselves as too heavy. Around 8.5% of men had never tried to lose weight. On average, men had around seven previous weight loss attempts. Losing weight was relatively important on average, but men were less confident in their ability to lose weight and to keep lost weight off.
As quotas were imposed for age and region, the sample is representative of the UK population in terms of these characteristics. Appendix 15 (see Table 33) shows the full sample characteristics. As the intervention is aimed at men living in disadvantaged areas, it is important to be able to perform subgroup analysis by socioeconomic status. About 36% (n = 665) of participants had a level of education below Advanced level; 44% (n = 461) had an income of ≤ £30,000 per annum, 17% (n = 180) had no car and 33% (n = 346) were not homeowners. These were sufficient proportions to allow subgroup analysis. Although a relatively high proportion of the sample was of white ethnicity (98%, n = 989), a sufficient number of people were of non-white ethnicity to allow subgroup analysis.
Discrete choice experiment results
The DCE responses for the two repeated choices show that 83% of participants passed the consistency check and provided the same answer in the two identical choices. This in line with findings from other studies. 71 The opt-out was chosen in only 7% of all choices. This is relatively low, but it should be noted that all weight loss programmes were associated with an incentive of at least £100.
Table 5 shows the latent class results. The average class probabilities in the sampled population were 6.0%, 29.6% and 64.4% for latent class 1, 2 and 3, respectively. For latent class 1, the coefficient for programme (alternative specific constant for programmes A and B) is negative and none of the amounts is significant, indicating that incentives are not being valued. For latent class 2, only the incentives at 6 and 12 months are significant, suggesting that this class prefers longer-term incentives. The incentive at 12 months is valued relatively more highly than the incentive at 6 months. For latent class 3, all three incentives are important, with the shorter-term incentives being relatively more important. The incentive at 6 months was valued most highly, followed by the incentives at 3 and 12 months.
| Class 1 coefficient (SE) | Class 2 coefficient (SE) | Class 3 coefficient (SE) | |
|---|---|---|---|
| Mean | |||
| Programmea | –2.939*** (0.503) | 0.708*** (0.156) | –4.255*** (1.301) |
| Amount at 3 months | –0.00131 (0.00214) | 0.000497 (0.000544) | 0.0371*** (0.00169) |
| Amount at 6 months | 0.00256 (0.00224) | 0.00377*** (0.000636) | 0.0395*** (0.00162) |
| Amount at 12 months | 0.00403* (0.00208) | 0.00458*** (0.000605) | 0.0319*** (0.00153) |
| Class probability model | |||
| Constant | –2.884*** (0.841) | –0.421 (0.437) | |
| Aged 35–54 years | 1.133* (0.588) | –0.354* (0.214) | |
| Aged 55–75 years | 1.575*** (0.590) | –0.106 (0.222) | |
| Importance of losing weight | –0.231*** (0.0719) | 0.0213 (0.0474) | |
| Tempted to consume more in year 1 | –0.317 (0.407) | –0.592** (0.239) | |
| People are responsible for being overweight | –0.153 (0.0986) | –0.172*** (0.0586) | |
| Unacceptability of financial incentives | 0.326*** (0.0794) | 0.198*** (0.0455) | |
| Class probability | |||
| Average | 0.060 | 0.296 | 0.644 |
| N | 25,080 | ||
| Log-likelihood | –5050.941 | ||
| AIC | 10,153.88 | ||
Class membership was a function of age, weight loss importance, perceived temptation, unacceptability of incentives and responsibility for being overweight. Individuals who perceived the funding of financial incentives to be unacceptable had a higher probability of belonging to class 1 (‘no incentive’ class) and class 2 (‘longer-term incentives’ class). Older age and attaching less importance to weight loss were associated with a higher probability of belonging to class 1. Perceived temptation increased the probability of belonging to class 3 (‘incentives at all time points’ class) compared with class 2, which may suggest that individuals who know that they are likely to be tempted to deviate from their optimal future choices value incentives at all three time points to deal with their temptation. Participants who thought that individuals are responsible for being overweight had a lower probability of belonging to class 2 (‘longer-term incentives’ class) than to class 3.
Table 6 shows the predicted uptake for different configurations of the financial incentive scheme (the choices offered in DCE) for latent class 2 and 3 and for the whole sample. Note that uptake is not a function of the incentives for class 1 as none of the incentive amounts was statistically significant. The same scheme with the highest overall value (£550) was ranked highest in all cases. The configuration ranked second differs between classes 2 and 3. Note that the predicted uptake is very high for latent class 3 for most configurations.
| Class 2 | Class 3 | Average | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Amount secured at 3 months (£) | Amount secured at 6 months (£) | Amount secured at 12 months (£) | Predicted uptake | Amount secured at 3 months (£) | Amount secured at 6 months (£) | Amount secured at 12 months (£) | Predicted uptake | Amount secured at 3 months (£) | Amount secured at 6 months (£) | Amount secured at 12 months (£) | Predicted uptake |
| 150 | 150 | 250 | 92.38 | 150 | 150 | 250 | 99.99 | 150 | 150 | 250 | 92.05 |
| 0 | 150 | 250 | 91.84 | 150 | 150 | 100 | 99.99 | 0 | 150 | 250 | 91.88 |
| 0 | 400 | 0 | 90.18 | 0 | 400 | 0 | 99.99 | 0 | 400 | 0 | 91.39 |
| 50 | 150 | 200 | 90.17 | 0 | 150 | 250 | 99.99 | 50 | 150 | 200 | 91.39 |
| 100 | 100 | 200 | 88.62 | 100 | 100 | 200 | 99.99 | 100 | 100 | 200 | 90.93 |
| 75 | 100 | 200 | 88.49 | 75 | 100 | 200 | 99.99 | 75 | 100 | 200 | 90.89 |
| 75 | 75 | 200 | 87.50 | 150 | 0 | 250 | 99.99 | 75 | 75 | 200 | 90.58 |
| 150 | 0 | 250 | 87.32 | 50 | 150 | 200 | 99.99 | 150 | 0 | 250 | 90.54 |
| 0 | 0 | 250 | 86.47 | 75 | 75 | 200 | 99.96 | 150 | 150 | 100 | 90.13 |
| 75 | 100 | 150 | 85.94 | 75 | 100 | 150 | 99.93 | 75 | 100 | 150 | 90.10 |
| 150 | 150 | 100 | 85.90 | 100 | 75 | 150 | 99.93 | 100 | 75 | 150 | 89.79 |
| 0 | 150 | 100 | 84.98 | 75 | 75 | 150 | 99.81 | 75 | 75 | 150 | 89.67 |
| 100 | 75 | 150 | 84.93 | 0 | 150 | 100 | 99.23 | 0 | 150 | 100 | 89.36 |
| 75 | 75 | 150 | 84.77 | 150 | 0 | 100 | 98.90 | 0 | 0 | 250 | 88.77 |
| 150 | 0 | 100 | 77.58 | 0 | 0 | 250 | 97.63 | 150 | 0 | 100 | 86.96 |
| 0 | 0 | 100 | 76.26 | 0 | 0 | 100 | 25.63 | 0 | 0 | 100 | 39.38 |
To explore the impact of the overall incentive magnitude, the uptake for a range of overall values was predicted. Figure 9 shows the predicted uptake by overall magnitude for two different distributions across the three time points: 10%, 45% and 45%, and 45%, 45% and 10%. Uptake was relatively low for class 3 at low magnitudes, but once the incentive reached a certain threshold, uptake was high and marginal increases in uptake thereafter were low. For class 2, incentives continue to increase uptake along the whole magnitude range and marginal increases remain relatively large. Although a lower magnitude could be used to encourage uptake by latent class 3, class 2 requires a larger magnitude. The £400 incentive level predicts an uptake of > 90% for class 2.
FIGURE 9.
Uptake by overall magnitude when the incentives are distributed over three time points as (a) 10%, 45%, 45%; and (b) 45%, 45%, 10%.
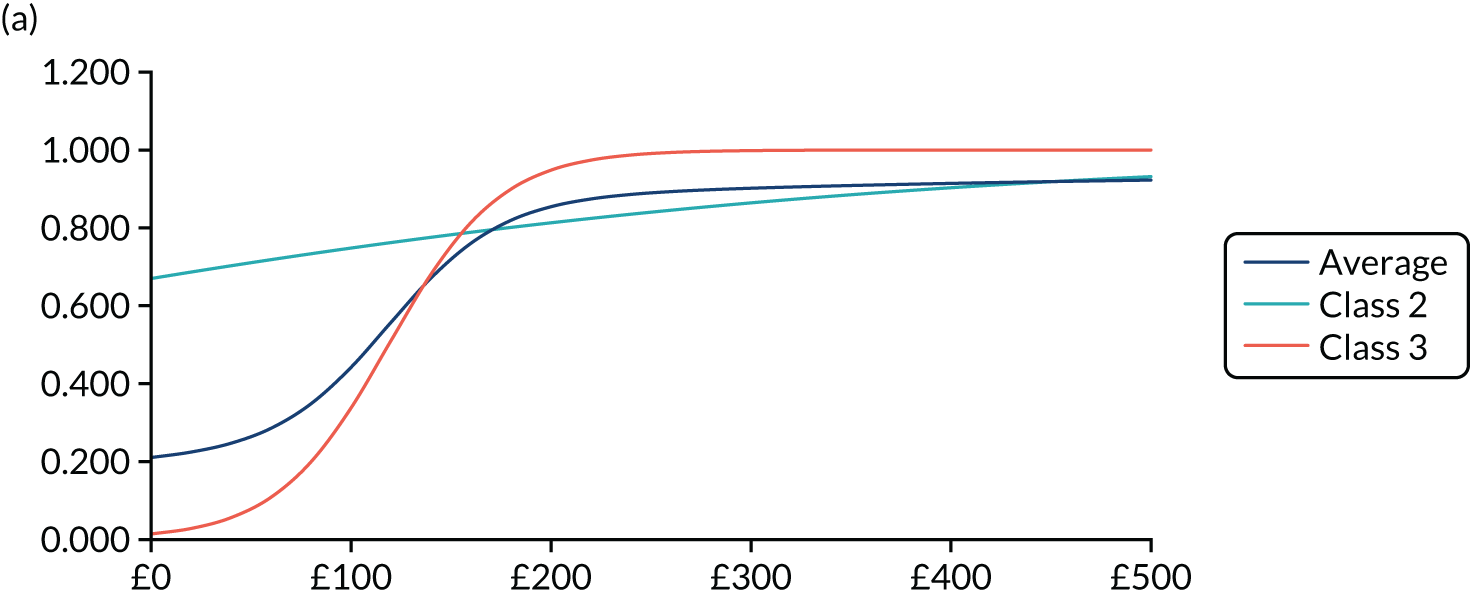
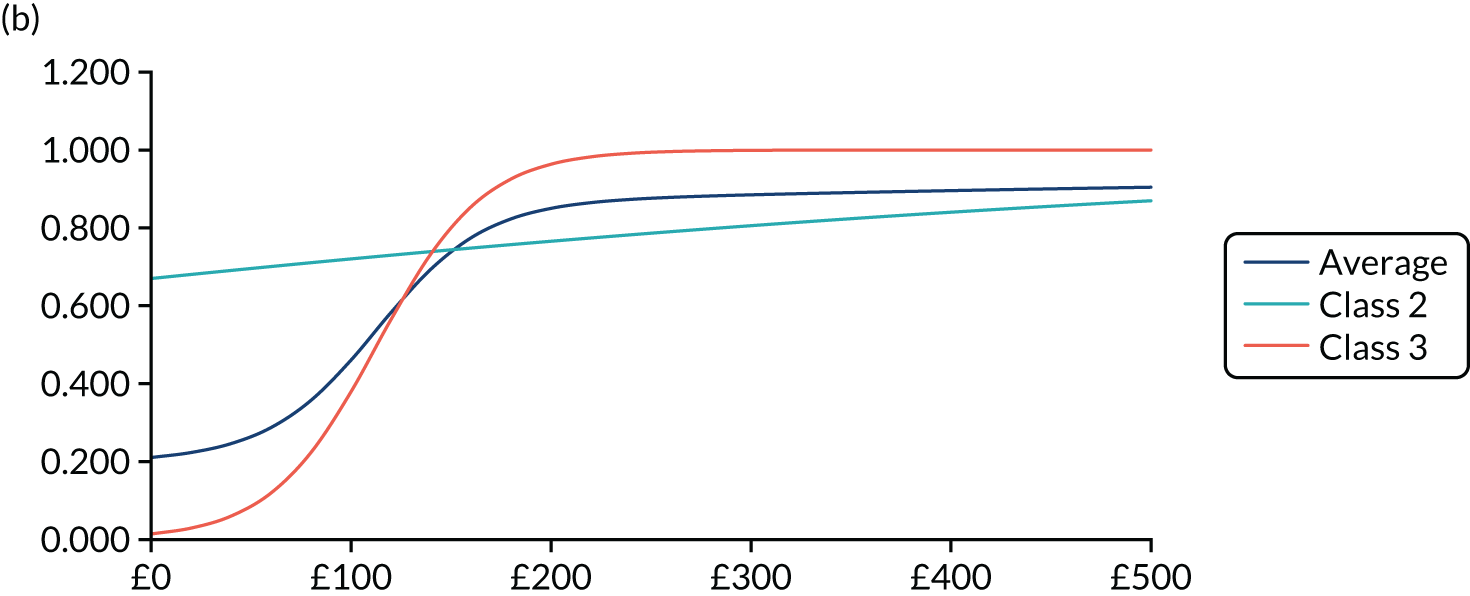
Preferences for intervention components
Table 7 shows the descriptive statistics for the questions on the different intervention components. The majority of participants were interested (yes or maybe) in all intervention components: information, pedometer, text messages and incentives. Text messages were associated with the lowest level of interest. This may be because participants were less familiar with the use of text messages for weight loss support. The preferred venue at which to be weighed was the GP surgery, followed by the pharmacy and the community hall. The most frequently mentioned venue under ‘other’ was home, with additional suggestions including a commercial weight loss class or the gym. A small number of men highlighted the importance of the weigh-in taking place in private. The most preferred frequency for weigh-ins was at the start, 3, 6 and 12 months. It should be noted that the responses to this question are likely to have been framed by the timing of the weigh-ins in the DCE. There was preference heterogeneity in terms of preferred frequency and timing of text messages.
| Programme component | Participants, n (%) |
|---|---|
| Information | |
| Yes | 621 (59.43) |
| Maybe | 307 (29.38) |
| No | 117 (11.20) |
| Pedometer | |
| Yes | 578 (55.31) |
| Maybe | 250 (23.92) |
| No | 217 (20.77) |
| Text messages (SMS) | |
| Yes | 348 (33.30) |
| Maybe | 297 (28.42) |
| No | 400 (38.28) |
| Financial incentives | |
| Yes | 609 (58.28) |
| Maybe | 292 (27.94) |
| No | 144 (13.78) |
| Competition as motivator | |
| Average; range | 3.20; 1–7 |
| Preferred frequency of SMS | |
| As much as possible | 62 (5.93) |
| Daily | 134 (12.82) |
| A few times per week | 214 (20.48) |
| Once a week | 235 (22.49) |
| Every 2 weeks | 33 (3.16) |
| Every month | 56 (5.36) |
| Never | 276 (26.41) |
| I don’t have a mobile phone | 30 (2.87) |
| Other | 5 (0.48) |
| Which days | |
| Any day | 355 (58.68) |
| Weekdays only | 87 (14.38) |
| Weekends only | 81 (13.39) |
| Only on specific days I can select | 82 (13.55) |
| Which time | |
| Any time | 254 (34.37) |
| Morning | 211 (28.55) |
| Midday | 104 (14.07) |
| Afternoon | 81 (10.96) |
| Evenings | 89 (10.96) |
| Preferred venue for weighing | |
| Community hall | 152 (14.55) |
| School | 17 (1.63) |
| Pharmacy | 175 (16.75) |
| Hospital | 36 (3.44) |
| GP surgery | 497 (47.56) |
| Supermarket | 52 (4.98) |
| Fire station | 11 (1.05) |
| Other | 105 (10.05) |
| Preferred method of receiving feedback | |
| By e-mail | 705 (67.46) |
| Through a web page | 92 (8.80) |
| By text | 168 (16.08) |
| By post | 80 (7.66) |
| Endowment options | |
| Bank statement | 395 (37.80) |
| Cheque | 566 (54.16) |
| Facsimile banknotes | 84 (8.04) |
| Preferred frequency of weighing | |
| Start, 3, 6 and 12 months | 869 (83.16) |
| Start, 3 and 12 months | 56 (5.36) |
| Start, 6 and 12 months | 59 (5.65) |
| Start and 12 months only | 33 (3.16) |
| Other | 28 (2.68) |
| Cash distribution | |
| All at 12 months | 489 (46.79) |
| In three instalments | 556 (53.21) |
| Average at 3 months (£) | 92.22 |
| Average at 6 months (£) | 100.52 |
| Average at 12 months (£) | 174.13 |
| Form | |
| Cash | 921 (88.13) |
| Donation to chosen charity | 124 (11.87) |
| Likelihood of achieving weight loss target | |
| Average; range | 7.00; 1–10 |
| Preferred distribution of target | |
| 5% target | |
| Gradually over 12 months | 177 (34.50) |
| Gradually over 6 months then maintain | 202 (39.38) |
| Lose weight over 3 months then maintain | 134 (26.12) |
| 10% target | |
| Gradually over 12 months | 226 (42.48) |
| Gradually over 6 months then maintain | 187 (35.15) |
| Lose weight over 3 months then maintain | 119 (22.37) |
The preferred method of feedback (about how much money was secured based on achieving weight loss targets) was e-mail, followed by text message. The use of hypothetical cheques was perceived as the best way to make the pledge at the start of the intervention most realistic. The majority of men preferred cash, with 11.6% preferring charity donations.
Just over half of the sample preferred to spread the incentive over the time points. The highest amount was allocated to 12 months, followed by 6 months. In total, 60 out of 556 allocated < £400 across the time points. In respect of all participants who allocated £400 (also those who allocated the full amount to 12 months), the average amounts allocated across the time points were £51 at 3 months, £55 at 6 months and £294 at 12 months. This suggests a higher importance attached to 12 months than was seen in the DCE results. However, it should be noted that the results are not directly comparable, as the open-ended questions were framed in terms of reward incentives, whereas the DCE was framed in terms of endowment incentives. In addition, evidence suggested that open-ended questions and closed-ended methods such as DCEs can produce different results. 72
The preferred distribution of the weight loss target over the 12 months varied according to the weight loss target. More participants preferred a gradual weight loss for the 10% target than for the 5% target. This may reflect that losing 10% over 6 months is perceived to be much harder than losing 5% over 6 months. The difference is statistically significant (χ2 = 7.08; p = 0.03).
Appendix 16 (see Table 34) shows how preferences for the different intervention components differ by individual characteristics. The regression techniques allow for the ordinal nature of the dependent variables. The coefficients do not allow inference of the magnitude of the impact, allowing only interpretation of the sign and significance of the estimated coefficients. For example, a positive estimated coefficient in the first model is interpreted as increasing the likelihood of being interested in information, while negative estimated coefficients are interpreted as decreasing the likelihood of being interested in information.
The results show that preferences did not seem to vary systematically by deprivation. The indicators were statistically significant in only a few models. Men with lower levels of education only (no qualifications or General Certificates of Secondary Education) were less likely than men with higher levels of education to be interested in receiving financial incentives. However, men who did not own a car were more likely to be interested in financial incentives than men who owned one or more cars. Men with household incomes of < £15,000 were less likely to be interested in receiving information than men with incomes of ≥ £30,000, and men with household incomes of between £15,000 and £30,000 were less likely to prefer a donation to charity than cash than men with incomes of ≥ £30,000.
Older men and men living in single households were less interested in text messages, pedometers and financial incentives, and men of non-white ethnicity and retired men were more interested in information. Importance of weight loss increased interest in receiving information, pedometers, text messages and financial incentives. Men with four or more previous weight loss attempts were more likely to be interested in information and text messages than men with fewer than four previous weight loss attempts. Men with a larger difference between their current and ideal weight were more likely to be interested in financial incentives and men who participated in vigorous physical activity were more likely to be interested in pedometers and text messages. Men with a higher BMI and men who viewed funding of incentives for weight loss as less acceptable were less likely to be interested in financial incentives, whereas men who had tried to lose weight four or more times and men who thought that overweight people are responsible for being overweight were more likely to be interested in financial incentives.
Older men and men in single households attached less importance to competition as a motivator to weight loss, whereas men who attached more importance to weight loss were more confident in their ability to lose weight. Smokers and men who were physically active attached more importance to competition as a motivator.
Men who were currently trying to lose weight were less likely to prefer to lose weight quickly (lose the target weight loss over the first 3 months), whereas men who had tried to lose weight four or more times were more likely to prefer to lose weight quickly.
Older men and men who were more confident in their ability to lose weight were more likely to prefer to receive all of the incentive at 12 months, whereas men who thought that they would be more tempted to use more of the restaurant vouchers in the first year than would be ideal were less likely to prefer to receive all of the incentive at 12 months. It could be argued that those who knew that they might be tempted preferred to spread the incentives to help them control their temptations.
Older men, men of non-white ethnicity, men with a household income of between £15,000 and £30,000, men with lower levels of health and men who were more present oriented were more likely to prefer the GP surgery as the location for being weighed. It may be that older men and men with lower levels of health visit their GP more often and so a GP surgery may be more convenient.
Implications for feasibility study
Final decisions for the incentive strategy were based on the DCE results, expert advice by co-investigators, and a stakeholder workshop (see Chapter 2). At the stakeholder workshop, PPI men described a common problem of successfully losing weight and then subsequently putting the weight back on. Ensuring that the incentive strategy supported behaviour change and weight loss maintenance in the long term was highlighted as very important. As a result, the target linked to the incentives to lose 10% of baseline weight remained the same at both the 6- and the 12-month appointments to encourage participants to lose weight during the initial few months of the study and to maintain weight lost during the last months. In addition, more money was allocated to the 12-month appointment target (£200) with a view to supporting long-term weight loss maintenance. Views about the incentive strategy at 3 months were more mixed, with some suggesting an incentive for turning up. Others preferred the incentive to be given only for clinically significant weight loss of ≥ 3%.
The following distribution was selected to be tested in the phase 2 feasibility RCT: £50 at 3 months, £150 at 6 months and £200 at 12 months. The predicted uptake for this configuration is 0.913. Although the configuration of £0 at 3 months, £150 at 6 months and £250 at 12 months was associated with a slightly higher average uptake, experts considered that having an incentive at 3 months was important in terms of early engagement. Based on the survey results, it was decided that a choice between donation and cash should be given. A hypothetical cheque was found to be the preferred option for making the endowment most realistic. As a result, participants randomised to the SMS + I arm were given a hypothetical cheque for £400 at the start of the study.
The results of the survey showed that the majority of men were interested in all intervention components (information, pedometer, SMS and financial incentives) and these were therefore retained. There was no strong preference for competition and this dimension was therefore not added to the intervention. The analysis showed that preferences did not seem to vary systematically as a function of indicators of deprivation. The intervention should therefore be suitable across all levels of deprivation.
The size of the weight loss target (5% or 10%) did not seem to reduce uptake in the DCE or have an impact on preferences for the financial incentive scheme. The only difference found was with regard to the preferred distribution of weight loss over the 12 months. Participants who were allocated to the 10% weight loss target were more likely to prefer to lose weight gradually than were those allocated to the 5% target. The selected weight loss target in the feasibility study was 10%. The distribution of this target was losing 10% gradually over 6 months and then maintaining weight loss, as evidence suggests that this is more effective in terms of sustained weight loss. However, this is recognised to be challenging, which is most likely to be why men allocated to the 10% weight loss target preferred the more gradual distribution. The incentive scheme was modified by allowing individuals to secure part of the money if they met part of their target at 6 and 12 months. For a full description of the final incentive scheme, see Chapter 5.
Chapter 5 Feasibility randomised controlled trial methods
Trial design
This study was a three-arm individually randomised parallel-arm controlled feasibility trial with a mixed-methods process evaluation that ran in parallel with the trial. Participants were randomised to receive narrative SMS and an endowment inventive (SMS + I) or narrative SMS only (SMS only) or be placed on a waiting list for SMS (control).
The study protocol is available on the project web page (URL: www.journalslibrary.nihr.ac.uk/programmes/phr/1418509/#/; accessed 25 June 2019).
Setting
The study was undertaken in two distinct sociodemographically diverse health boards in Scotland. Localities were selected on the basis that they included urban, suburban, town and rural populations.
Study management
The study was overseen by an independent Study Steering Committee consisting of a statistician as chairperson, two subject experts (one academic and one NHS clinical) and two PPI members (see Chapter 2). The study management group consisted of the two co-principal investigators, 11 co-investigators, the Tayside Clinical Trials Unit co-director, the Tayside Clinical Trials Unit statistician, the study research assistants and a study PhD (Doctor of Philosophy) student.
Ethics approval and study registration
Ethics approval was obtained for phase 1 (trial design) from the University of Stirling Psychology Ethics Committee on 8 January 2016.
Ethics approval was obtained for phase 2 (feasibility RCT) from the North of Scotland Research Ethics Service on 7 December 2016 (reference 16/NS/0120). Research and development approval for phase 2 was obtained on 13 February 2017 (reference FV974). Research ethics approval for a substantial protocol amendment was obtained on 2 March 2018 to deliver alternative SMS to men in the control arm and to new men volunteering to take part.
The study was registered on ClinicalTrials.gov (identifier NCT03040518) on 31 January 2017 (URL: https://clinicaltrials.gov/ct2/show/NCT03040518; accessed 7 February 2020).
Population eligibility criteria
-
Men aged > 18 years.
-
Having a BMI of ≥ 30 kg/m2 and/or a waist circumference of ≥ 40 inches (102 cm).
-
Owning a mobile phone capable of receiving SMS.
-
Being able to understand English-language SMS.
-
Not taking part in another weight loss research study.
-
Not on the waiting list for or planning to have bariatric surgery.
-
Having a home postcode within the two localities covered by NHS research and development approvals and not planning to move within the next 12 months.
-
Not having a severe medical, terminal or psychiatric illness (patient or close family member).
-
Not having significantly impaired cognitive function (general practice recruitment only).
-
Being considered by practice clinical staff as suitable for participation (general practice recruitment only).
Sample size
This study aimed to randomise 105 men, 35 to each arm, in line with recent recommendations for pilot trials that this is sufficient to estimate key parameters for a full trial. 73 A sample size of 35 participants per arm is sufficient to allow the population variance to be estimated [i.e. the standard deviation (SD) in weight loss] with enough precision to deliver at least 80% power and 90% confidence in a full trial (we would expect in most cases to have more power in a full trial but this would be the worst-case scenario if the pilot study underestimates the true variance). Furthermore, this was an efficiently designed pilot, based on evidence73 showing that when more participants are added to a pilot study, the additional precision in estimating variance becomes marginal beyond about 35 participants per arm.
Participant recruitment and procedures
Focus group to inform recruitment
At the phase 1 stakeholder workshop (see Chapter 2), recruitment was raised as central to the success of the study. Therefore, prior to recruitment commencing, an audio-recorded focus group with men (n = 5) living in a disadvantaged urban area was conducted to explore the acceptability of the planned recruitment strategies and to inform the research team’s approach to recruitment. Focus group participants were, on average, 52 years old (range 32–58 years), had an average of 1.8 household members (range 1–3 members) and lived in an SIMD 1 area (n = 5), and four were classified as overweight or obese. The researcher used a topic guide and focus group plan (see Appendix 17) to guide the discussion and used recruitment materials (e.g. the draft GP participant invitation letter) to support the questions asked. A summary of the themes and findings of the focus group can be found in Appendix 18. Learning from this focus group helped to inform and finalise the recruitment strategies for the feasibility RCT.
Participant recruitment was undertaken through two channels: (1) community outreach recruitment and (2) general practice obesity register recruitment.
Community outreach
Study information stands, usually consisting of a table displaying information leaflets and two small table banners with the study logo, were hosted in community venues such as supermarkets, fitness centres, hospital foyers, health centres, council workplaces and community centres (Figures 10 and 11). Researchers were in attendance to provide information, answer questions and discuss the study with men who showed interest. Interested men were given a brief information leaflet and asked to provide their contact details (i.e. a telephone number or alternative contact information) to arrange a face-to-face appointment. Recruitment took place in some of the most disadvantaged areas of the sites and often in the evenings and weekends to ensure that working men had an opportunity to be recruited. To ensure researcher safety, a researcher assistant pool of 10 master’s or PhD students was established to ensure that recruiting researchers could always work in pairs.
FIGURE 10.
Community outreach recruitment activity in a supermarket.

FIGURE 11.
Community outreach activity in a community venue.

Men in the community were also recruited by word of mouth, usually as a result of researchers’ discussions with friends, family, voluntary-sector staff and sports workers who passed on study information to eligible men they knew. Brief information leaflets were distributed across localities in local shops, libraries, barbers and community centres. Those interested in participating contacted researchers by telephone, SMS or e-mail to arrange a face-to-face appointment. The eligibility of those men recruited from community settings was assessed either during an initial contact (e-mail, telephone, face to face) with the researcher or during the baseline appointment.
General practice obesity register letters
The NHS Research Scotland Primary Care Network (NRSPCN) provided a list of general practices with patient list size in areas of high deprivation in the two study sites. The research team selected practices in more deprived areas (i.e. SIMD 1 and 2) and NRSPCN invited these practices to participate in the study. Overall, 33 practices were identified as suitable from deprivation and logistical perspectives (n = 13 in site A and n = 20 in site B). Five practices (n = 4 in site A and n = 1 in site B) agreed to participate. Two further general practices (n = 2 in site B) expressed an interest in participating after the study was full.
The NRSPCN ran searches on practice databases to identify men who met the inclusion criterion, namely having a documented BMI of ≥ 30 kg/m2, and these lists were then screened by clinical practice staff, who removed anyone considered to be unsuitable to take part. These lists, which included names, addresses and contact information, were transferred to The Health Informatics Centre (HIC) at the University of Dundee to be stored securely. The HIC then sent GP-headed study invitation letters and brief information leaflets to men from the five practices across both localities. Men who were interested in the study either contacted the research team directly or returned a freepost ‘opt-in’ reply card to the HIC. The contact information of those opting in was uploaded to the HIC online ‘participant tracker’ system for the researchers to access. When it was not possible to contact men to arrange a face-to-face appointment, a reminder letter was posted from the research team asking them to get in touch if they were still interested in participating.
Face-to-face follow-up appointments
Men attended face-to-face appointments with the two research assistants. At the appointment, the researcher provided men with a copy of the full study information leaflet, discussed the study in detail and answered any questions. If men wanted to proceed with the study, written informed consent was gained. Men who did not meet the BMI, waist circumference or other eligibility criteria were thanked for attending and advised that they would not be able to take part in the study. No further information was provided.
While the participant completed the baseline questionnaire, the researcher created a website login and requested randomisation (see below for details) to one of the three arms. At the end of the baseline assessment, the researcher informed the participant of his allocation, provided a trial-arm-specific post-randomisation information sheet, talked through the allocation and answered any questions. The researcher calculated weight loss targets for men randomised to the intervention arms. These targets were to lose 5% of baseline weight by 3 months, to lose 10% of baseline weight at 6 months and to keep 10% off at 12 months. The targets were calculated according to men’s measurement preferences (stones and pounds or kilograms) and were linked to the incentives for the SMS + I arm.
All participants received a pedometer, a weight loss fact sheet (British Dietetic Association Weight Loss Food Fact Sheet: www.bda.uk.com/uploads/assets/c5761f35-ec82-4449-9fed3bcfe1fd08a5/Weight-loss-food-fact-sheet.pdf; accessed 6 February 2020), a personalised participant card and access to the study website.
The participant card included reminders of the dates for future appointments, website login details and a space for appointment visit weight and waist circumference measurements to be recorded. The weight loss targets for those in the intervention arms were recorded on the card.
All participants were given login details for the study website (www.gameofstonesresearch.com; accessed 25 June 2019), described further below, the content of which varied depending on the arm allocation.
All participants received a £20 voucher as recompense for their time when attending the 12-month appointment.
Randomisation
The researcher requested independent randomisation by Tayside Clinical Trials Unit using a secure remote web-based system with telephone back-up, stratifying by recruitment method (GP and community) and recruitment site (site A and site B). For practical reasons, the two researchers who conducted the outcome assessments were not blinded to the arm allocations, with the exception of a brief trial period of blind outcome assessment. The feasibility of blinding researchers conducting intervention arm outcome assessments was tested for 11 of the 6-month appointments. This involved one of the researchers conducting 11 out of 44 6-month appointments while unaware of the arm allocation. The researcher noted if the participant disclosed their intervention arm. None of the 11 participants mentioned their allocation arm, illustrating that blinding could be feasible in a full trial. All other members of the study team were blinded to participant arm allocations.
Intervention components
Table 8 provides an overview of study components by arm. For a description of the interventions using the Template for Intervention Description and Replication (TIDieR), see the study protocol on the project web page (URL: www.journalslibrary.nihr.ac.uk/programmes/phr/1418509/#/; accessed 25 June 2019).
| Trial arm | Interventions | Website content | Additional study components | Assessment time point | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Narrative SMS | Incentive | Weight loss information | Narrative SMS character biographies | Self-monitoring | Incentive breakdown | Weight loss targets | Pedometer | Weight loss fact sheet | £20 voucher at 12 months | Baseline | 3 monthsa | 6 months | 12 monthsa | |
| SMS + I | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| SMS only | ✓ | ✗ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| WLC | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ |
Narrative SMS
For a full description of the development of the narrative SMS, including the underlying approach and narrative PPI, see Chapter 3. In summary, the narrative SMS component included a library of 604 SMS that were sent to participants over 12 months. All participants received SMS automatically according to a predetermined schedule. SMS were sent between 08.00 and 22.00 and ranged from 0 to 5 SMS per day. The SMS were delivered by the HIC using existing automated technology linked to Tayside Clinical Trials Unit. Participants could respond to the SMS but would not receive a reply. The same narrative SMS were sent to the SMS + I and SMS-only arms. Participants could request that the SMS be stopped at assessment time points, or by contacting the research assistants either by telephone or by replying to the SMS.
Endowment incentive
For a full description of the background to the incentive component, see Chapters 2 and 4. In summary, all SMS + I participants were ‘endowed’ with a £400 incentive at the start of the trial. The incentive was placed into a hypothetical personal account at the University of Stirling (no interim withdrawals were possible). For the endowment effect (perceiving the money as their own and ascribing value to it), men received a hypothetical cheque at randomisation. The full £400 could be secured by meeting weight loss targets, based on assessments at the face-to-face outcome assessment appointments: 5% of body weight lost since baseline at 3 months (£50 secured/lost), 10% at 6 months (£150 secured/lost) and 10% at 12 months (£200 secured/lost).
The incentive strategy is detailed in Table 9 and was available on the SMS + I web pages. At all appointments, if not achieving a weight loss of at least 5% of their starting weight, men lost all the money allocated to that time point. At 6 and 12 months, men lost some of the money for each percentage weight loss not attained between 5% and 10%. To secure money, participants’ weight at appointment visits had to be measured on the study scales within 2 weeks either side of their target date (exactly 3, 6 or 12 months after their baseline appointment). This information was entered onto their personalised credit-card-sized card. Men received the money after the 12-month assessment based on the targets they met. Weight at 12 months had to be less than at baseline to receive any money, regardless of whether or not interim weight loss targets had been met. If men did not attend the 12-month assessment, they received no money.
| Money secured (£) | Money lost (£) | |
|---|---|---|
| 3 months: £50 – target 5% weight loss | ||
| < 5% | 0 | 50 |
| ≥ 5% | 50 | 0 |
| 6 months: £150 – target 10% | ||
| < 5% | 0 | 150 |
| 5% | 75 | 75 |
| 6% | 90 | 60 |
| 7% | 105 | 45 |
| 8% | 120 | 30 |
| 9% | 135 | 15 |
| ≥ 10% | 150 | 0 |
| 12 months: £200 – target 10% | ||
| < 5% | 0 | 200 |
| 5% | 100 | 100 |
| 6% | 120 | 80 |
| 7% | 140 | 60 |
| 8% | 160 | 40 |
| 9% | 180 | 20 |
| ≥ 10% | 200 | 0 |
Feedback to men on meeting incentive targets was sent by automated SMS 1 hour after the researcher completed the weight assessment data entry and was available on the participant’s SMS + I web page. Secure options for delivering the incentive to men were offered that minimised any risk to researcher safety: Bacs (Bacs Payment Schemes Limited, London, UK) direct transfer or cheque by post.
Web pages
Each participant was provided with a unique login ID for web pages after randomisation according to his trial arm allocation.
The front page was accessible to all participants and included essential information about the trial and links to existing online resources offering a choice of evidence-based diets, physical activity approaches, hints and tips. The web pages included:
-
the NHS choices website: www.nhs.uk/LiveWell/Loseweight/Pages/Loseweighthome.aspx (accessed 25 June 2019)
-
ManvFat website: https://manvfat.com (accessed 25 June 2019)
-
the British Dietetic Association website: www.bda.uk.com/uploads/assets/c5761f35-ec82-4449-9fed3bcfe1fd08a5/Weight-loss-food-fact-sheet.pdf (accessed 25 June 2019)
-
Men’s Health Forum GB website: www.menshealthforum.org.uk (accessed 25 June 2019).
Both the SMS + I and the SMS-only web pages had a brief biography and images of the characters featured in the narrative SMS, as well as information specific to the trial arm. There was also a link for self-monitoring weight, pedometer steps, waist circumference and belt notches that produced visual progress charts.
The SMS + I arm had access to additional pages describing the financial incentives and a visual progress chart of money secured/lost in relation to weight loss targets. The progress chart was automatically populated by the HIC database using an algorithm after weight assessment appointments.
Pedometer
The study pedometer was the 3DFitBud, A420S, manufactured by 3Dactive (Goldhat Ltd, London, UK; https://3dactive.com).
Comparator arm
The waiting list arm (control arm) received the pedometer, weight loss information links on the study website and a weight loss fact sheet (British Dietetic Association, Weight Loss Food Fact Sheet). Control arm participants attended only the baseline and 12-month appointments. The rationale was to keep the control arm as close to life as usual as possible. From a participant perspective, any assessments prior to the primary trial outcome assessment in a trial are an intervention, as meeting a researcher, being weighed and completing questionnaires would not happen outside the research context. Following 12-month data collection, participants were offered alternative SMS for 3 months and, similar to the original intervention arms, received a 5% weight loss target for their subsequent appointment along with access to the online self-monitoring tools. The study PhD student initiated contact with all study men 24 months after randomisation.
Alternative SMS
This section describes the content and development of the alternative SMS only, which occurred after all 3-month trial assessments were complete. Examining alternative SMS was an extension to the original protocol (see Chapter 1).
The waiting list control arm participants who attended the 12-month appointment (n = 30) and 10 additional (new) men who had opted in to the study after it was full were invited to receive 3 months of alternative SMS. The alternative SMS were developed combining six sources of information: (1) phase 1 findings; (2) qualitative, field note and engagement data collected at 3-month and some 6-month assessments; (3) the intervention logic model (see Chapter 1); (4) evidence-based BCTs; (5) a systematic review of SMS interventions for weight loss undertaken by the PhD student; and (6) PPI.
The alternative SMS were drafted by Stephan Dombrowski and comments were received from co-investigators (AA, CG, EC, MMcK, MMcD, PH, RS) and PPI (see Chapter 2). The following feedback received by men was incorporated: include concrete tips and facts, focus on weight management, include a range of perspectives and approaches, introduce engagement elements such as questions and prompting reflections, and reduce the number of SMS.
The content of the alternative SMS was clustered around weekly weight management themes, which were explicitly communicated to participants for coherence. Individual SMS were non-consecutive and standalone, and did not necessitate having paid attention to or engaged with previous content. The alternative SMS library consisted of 84 SMS sent over 12 weeks. SMS were sent at a rate of one message per day between 09.25 and 19.30 SMS were sent automatically through the same system as the narrative SMS. Half of the alternative SMS (n = 42) had fewer than 160 characters, and the remaining half had more than 160 characters (n = 42). All were sent as a single SMS to limit frequency of contact. Participants could request that the alternative SMS be stopped by contacting the research team or replying to the SMS.
Appendix 19 (see Table 35) provides details of how the alternative SMS map against the 93 BCTs specified in the v1 BCT taxonomy,74 theoretical functions in bringing about behaviour change in line with coding of a previous SMS-delivered intervention,75 and the refined Game of Stones logic model specified in Chapter 1. All alternative SMS focused on weight management, with 33 including examples from qualitative interviews or PPI of weight management perceptions or applications of BCTs. The alternative SMS included 20 different BCTs that targeted both motivation and self-regulation processes. Engagement was encouraged by asking direct and rhetorical questions on weight management and employing general communication techniques such as agenda-setting or use of humour. Seven alternative SMS contained web links to additional information. A minority of SMS covered maintenance processes; however, these were minimal, given the relatively short duration of the pilot (3 months). The top five BCTs used were demonstration of the behaviour (n = 18), instruction on how to perform the behaviour (n = 14), problem-solving (n = 9), goal-setting for behaviour (n = 7) and goal-setting for outcome (n = 6). For a comparison between a week 1 message in the original narrative style and the alternative SMS, see Appendix 20.
In addition to the alternative SMS, the 10 new men participating received a pedometer, website access and the weight loss fact sheet as received by the control arm at the start of the study.
Outcome assessment
Men could attend baseline appointments and follow-up assessments by themselves or with a friend or relative at a convenient time, day and venue. Previous research team experience found that participants with more disadvantaged circumstances can feel anxious attending unfamiliar appointments on their own. After an appointment was scheduled, the researcher sent a SMS to confirm the appointment details and a reminder SMS the day before.
No appointments were held at weekends. The majority of appointments were held during working hours, mainly for retirees, students and shift workers, but often men were seen at other times to accommodate work schedules; for example, many appointments were held later in the day (e.g. 17.00–19.00), some were held during lunch breaks and others were held early in the morning, for example 08.30 before work.
Appointment venues were community centres, universities, NHS clinical research facilities and voluntary-sector organisations. Most assessments for those recruited via GP letter were undertaken in rooms at their practices. A workplace or home visit was offered if necessary. Two outcome assessments took place in a participant’s home.
All outcome assessments were completed by two researchers who had completed Good Clinical Practice training and had been awarded NHS Research Passports and letters of access for the two study sites by the relevant NHS research and development offices.
At baseline and at the 3-, 6- and 12-month assessments, participants’ height (baseline only), weight and waist circumference were measured. If eligible, and at subsequent assessments, measurements were noted on the case report form. Participants initialled each measurement to confirm its accuracy. The researchers had experience of delivering weight management interventions and taking anthropometric measurements and had undergone additional training in the use of the study equipment prior to the assessments. Men completed a hard copy of the baseline questionnaire, with the researcher present to answer any questions. Online data collection was attempted at the start, but this was abandoned because of variable internet connections at assessment venues. Once completed, the questionnaire was checked for missing data.
Feasibility and acceptability outcomes
Primary feasibility outcome for this feasibility randomised controlled trial
The primary outcome was a decision about whether or not to proceed to a full effectiveness and cost-effectiveness RCT for the SMS intervention, with or without an incentive, compared with a waiting list control, based on the prespecified progression criteria. The progression criteria are detailed in Chapter 1 and assessment of whether or not they are met is based on both quantitative and qualitative data analysis and the views of the Study Steering Committee.
Secondary feasibility outcomes
-
Recruitment rate.
-
Overall withdrawal rate:
-
withdrawal because of SMS
-
withdrawal because of incentives
-
withdrawal for other reasons.
-
-
Number of appointments attended/missed.
-
Number of SMS responses made by participants.
-
Number requesting that SMS be stopped.
-
Uptake of interactive web page usage by entering self-monitoring information.
-
Process data (differential recruitment strategy, i.e. general practice or community, differential retention by socioeconomic status).
-
Feasibility of collecting primary outcomes for a potential full trial
-
weight change from baseline (percentage) at 12 months
-
weight change from baseline (absolute) at 12 months, measured in kg
-
waist circumference at 12 months, measured in cm.
-
-
Measures of quality of life [EuroQol-5 Dimensions (EQ-5D)] and mental well-being (Warwick–Edinburgh Mental Well-being Scale).
-
Theory-based mediators including confidence in weight loss and weight loss maintenance, importance of weight loss, self-regulation, self-monitoring (weight), maintenance processes (satisfaction with outcomes, satisfaction with experience, goal conflict, social support, environmental barriers), weight loss techniques, weight loss mindset (loss vs. maintenance mindset), quality of motivation (intrinsic and extrinsic), automaticity (eating fruit and vegetables, physical activity).
-
Weight loss strategy use: owning step counter, step counter use, self-weighing, weight management strategy use.
-
Health behaviours: moderate physical activity, vigorous physical activity, sedentary behaviour, alcohol consumption, smoking, fruit and vegetables consumption.
-
Intervention experience: satisfaction with intervention, satisfaction with materials, helpfulness of materials.
-
Weight change from baseline and waist circumference at 3 and 6 months (in intervention arms only).
Assessment of trial feasibility and acceptability outcomes
Data collection included baseline and follow-up assessments with mixed-methods approaches to explore the acceptability and feasibility of venues, recruitment strategies, randomisation, intervention components, retention and outcome collection.
Several data sources informed the assessment of acceptability and feasibility outcomes. Appendix 21, Table 37, outlines the assessment schedule of outcomes assessed throughout the study. The following assessments were taken throughout the study.
Recruitment activity
The NRSPCN and study researchers systematically recorded all GP and community recruitment activities, respectively, such as venue details, time spent at the venue, number of information sheets distributed and number of contact details obtained.
Anthropometry measures
Weight and waist circumference were measured by researchers at all face-to-face assessment appointments following standard operating procedures and device instruction manuals. At baseline, height was measured using a portable standing stadiometer (Seca 217, Seca, Birmingham, UK) to the nearest 0.1 cm. Prior to weight measurements, participants were asked to take off their shoes and remove any bulky clothing or items from their pockets. At all assessments, weight was recorded using portable electronic scales (Marsden M-420, Marsden Weighing Group, Rotherham, UK) to the nearest 0.01 kg. The scales were new and calibrated prior to the first outcome assessments. Waist circumference was recorded using a tape measure (Seca 203, Seca, Birmingham, UK) to the nearest 0.1 cm.
Questionnaire measures
Self-report questionnaires measured the following variables:
-
sociodemographics, comorbidities, disability, ethnicity
-
perceptions of intervention acceptability
-
lifestyle behaviours (physical activity, sedentary behaviour, smoking, alcohol consumption)
-
well-being and quality of life
-
theory-based mediators of behaviour change
-
health-related quality of life [EuroQol-5 Dimensions, five-level version (EQ-5D-5L)] and resource use.
SMS responses
Responses received to the SMS were recorded, including the content, timing, frequency and original SMS that was responded to.
Website engagement data
Engagement with self-monitoring tools (i.e. weight, steps, waist circumference, belt notches) on the website was captured.
Incentive payments
The money secured by and the payments made to participants were recorded.
For the alternative SMS arm, the same variables were collected after 3 months, as was done in the SMS-only and SMS + I arms after 3 months.
Table 10 provides an overview of the feasibility and acceptability targets, their descriptors and information on where these are presented in this report.
| Target | Descriptor | Assessment | Reported |
|---|---|---|---|
| Randomisation | Willingness to be randomised to SMS + I, SMS only and waiting list for SMS |
|
CONSORT flow diagram (see Figure 12) |
| Recruitment | Acceptability and feasibility of recruiting from general practice obesity registers and community venues within 4 months |
|
See Chapter 6, Recruitment and retention CONSORT flow diagram (see Figure 12) |
| Intervention | Acceptability and feasibility of intervention content and delivery |
|
See Chapter 6, Acceptability and feasibility of intervention components |
| Retention | Attendance levels for objective weight measures at baseline and 3, 6 and 12 months |
|
See Chapter 6, Recruitment and retention CONSORT flow diagram (see Figure 12) |
| Unintended consequences | Unintended consequences of the intervention components or study procedures |
|
See Chapter 6, Harms and unintended consequences |
| Indicative effects | Indications of weight loss (%) at 12 months |
|
See Chapter 6, Weight outcomes See Table 18 |
| Health inequalities | Examining potential differential uptake and indications of effectiveness by socioeconomic group |
|
See Chapter 6, Acceptability and feasibility of intervention components See Appendix 23, Table 39 See Appendix 25, Table 41 See Appendix 26, Table 42 |
| Alternative intervention componenta | Examine if modified SMS based on mixed-methods data analysis are acceptable and likely to improve trial retention at 3 months |
|
See Chapter 6, Alternative SMS outcomes See Appendix 35, Table 51 See Appendix 36, Table 52 |
The integration of the qualitative with the quantitative data occurred at three key stages in the mixed-methods analysis. First, owing to early concerns about men withdrawing from the study or stopping the SMS, the analysis of the 3-month qualitative interview data was conducted iteratively primarily in relation to the acceptability of the interventions and study procedures. This was to inform any early changes that might be required to the trial processes and the intervention delivery that could improve participant intervention acceptability or trial feasibility. This took place while the 3- and 6-month assessments were in progress and before the questionnaire and weight outcome data were available. Second, all study qualitative data were analysed in parallel with the analysis of the full outcome data set once the 12-month trial was complete. The research team met regularly to triangulate findings and to search for confirming or disconfirming data relating to research questions. Finally, the alternative SMS interview, baseline and outcome data were integrated into the analysis. Relationships between participant deprivation scores, 12-month intervention acceptability and weight loss outcomes were explored by developing matrix coding in QSR NVivo12 (QSR International, Warrington, UK), thus applying another technique of integrating the quantitative and qualitative analysis. 76
Assessment of adverse events
Information on possible adverse events was collected at assessment visits via open questions asking men how they had got on with the study since the last visit and probing questions seeking further information to clarify any concerns raised. Moreover, intervention participants could reply to the SMS to inform the research team of potential adverse events. All SMS replies were forwarded to the research team by e-mail. The SMS system used in this study automatically screened incoming SMS words such as ‘suicide’, ‘die’ and ‘death’ based on participant safety assessments in previous SMS intervention trials13,15,21 for alcohol reduction, and e-mail alerts to researchers from these messages were highlighted with a red flag. Researchers then followed the ethics approved protocol for following up participants.
Health economic research
The aims of the economic analysis were to (1) explore the feasibility of measuring costs and outcomes for the cost-effectiveness analysis in the full trial and (2) examine the mean and variation in costs and outcomes. Effectiveness was measured using quality-adjusted life-years (QALYs). Health-related quality of life was measured using the EQ-5D-5L. The EQ-5D-5L classifies individuals into one of 3125 health states (five dimensions, each with five levels). The five dimensions are mobility, self-care, usual activities, pain/discomfort and anxiety/depression. NICE’s current recommendation is to map the EQ-5D-5L back to the EuroQol-5 Dimensions, three-level version using the mapping function from van Hout et al. 77 The EQ-5D data were translated into ‘utility scores’ using the UK population tariff. The scores represent an index score, where 0 represents death and 1 represents full health. The EQ-5D scores were measured as part of the participant questionnaire at baseline and 6 and 12 months for the intervention arms and at baseline and 12 months for the control arm. QALYs were estimated from the area under the curve that links the utility scores obtained at baseline and 12 months. For the intervention arms, QALYs were also estimated by linking the utility scores obtained at baseline and at 6 and 12 months.
The perspective of the cost analysis is the NHS perspective favoured by NICE. The cost categories included were the costs of the interventions (SMS and financial incentives) and the cost of primary and secondary care. The intervention costs were estimated using study-specific estimates. NHS resource use (GP visits, nurse visits, accident and emergency attendances, outpatient appointments and inpatient stays) was measured as part of the participant questionnaire at baseline and at 3, 6 and 12 months for the intervention arms and at baseline and 12 months for the control arm. The questions were based on those used in the NIHR FFIT trial. 7 Each question asks whether or not the participant had used a particular service and, if so, how many times. The questions are about health service use in the last 3 months, as it is argued that asking about periods of time longer than this does not provide reliable responses because of recall bias. 78 For the control arm, resource use was available for 3 months prior to baseline and for 9–12 months only. For the intervention arms, it was assumed that resource use during months 6–9 was the same as resource use during months 9–12; for the control months, it was assumed that the average monthly resource use during months 0–9 was the same as the average monthly resource use during months 9–12.
The quantity of resource use, unit cost and average cost per participant are reported. The unit costs for NHS resource use are taken from standard sources. 79–81 The intervention costs are based on study-specific estimates for the financial year 2016/17 in order to adjust for the effects of inflation.
Qualitative research
Prior to randomisation, all participants were asked to consent to being asked about their experiences of being in the study. At the 3- and 12-month assessments, researchers stated the purpose and the confidentiality of the audio-recorded questions, offered shorter feedback or longer semistructured interviews and regained participants’ verbal consent to proceed. Shorter feedback sessions were conducted with men whose views might otherwise not be heard, for example men who were short of time or who did not like the study and those less confident about speaking to a researcher. Interviews were conducted face-to-face at general practices, university premises, community venues, a hospital clinical research facility and health centres. Two researchers (one female and one male) conducted equal numbers of interviews. The researchers completed a reflexive diary of contact with participants throughout the trial, which were used to inform qualitative interview sampling, topic guides, analysis and interpretation of the mixed-methods data.
Purposive sampling and iterative revisions of the topic guides were discussed with the Stirling qualitative research team (MMcD, RS, FH and PH) as the analysis progressed in order to maximise diversity (e.g. for ethnicity and SIMD); ensure adequate representation from each trial arm; and use researcher knowledge about participants who were information rich or contributed a different perspective from other men relevant to the study aims. Men continued to be interviewed at 12-month outcome assessments until sufficient information power82 from the mixed-methods data analysis was achieved and no new data/themes were identified.
Interviews took place during 3- and 12-month assessments, and after the 3 months of alternative SMS (i.e. 15 months post study start).
At 3 months, interviews were conducted with 50 of the 58 men from the two intervention arms who returned for follow-up assessment (7–61 minutes, median 23 minutes) to ensure that any issues with feasibility and acceptability were captured from as many men as possible to allow ongoing intervention refinement, inform the alternative SMS and optimise trial processes.
At 12 months, interviews were conducted with 33 purposively selected men. Sampling was informed by the analysis of the 3-month interviews and researcher field notes and to gain information power82 for the key uncertainties pertaining to the study objectives and the potential for a full trial. Interviews were conducted with participants from the SMS + I (n = 14; 13–65 minutes, median 33 minutes), SMS-only (n = 13; 10–59 minutes, median 28 minutes) and control (n = 6; 7–18 minutes, median 11 minutes) trial arms.
At 15 months, 14 purposively selected men who received the alternative SMS were interviewed (6–48 minutes, median 25 minutes). Eleven of these interviews were with men in the waiting list control arm (8–43 minutes, median 23 minutes) and three were with the new participants receiving the alternative texts only (6–48 minutes, median 31 minutes).
Audio-recorded interviews were transcribed by professional transcribers approved by the University of Stirling. Transcripts were anonymised by the researchers who conducted the interviews, removing any information that could potentially identify the participant.
Quantitative analysis
The trial statistician was blinded to allocation during the analysis. In effect, however, the blinding was partial, as blinding could be maintained only between the active intervention arms, but not for the control arm because it had a different response schedule (control participants were not assessed at 3 or 6 months).
All weight measurements included in the analyses were researcher verified. The primary analysis of weight outcomes is based on observed cases (i.e. participants with observed data for a specific time point). For sensitivity analyses, missing weight data were examined using baseline observation carried forward and last observation carried forward in addition to examining observed outcome data only to allow comparability with the published trial literature.
All continuous variables were summarised and tabulated using the following descriptive statistics: number of valid non-missing responses, mean and SD. Likert-scale variables were treated as continuous measures. The frequency and percentages (based on the non-missing sample size) of observed levels are reported for all categorical measures.
The proportion of individuals contacted who were recruited and the proportions retained and withdrawn at each stage of the study (i.e. 3, 6 and 12 months) by arm was determined (see Figure 12). The proportion receiving the intervention (defined as not requesting SMS to be stopped) was determined in the active intervention arms.
The Consolidated Standards of Reporting Trials (CONSORT) guidance for reporting randomised pilot and feasibility studies was followed. 83 Predetermined exploratory analyses were carried out to describe the primary outcome data (percentage weight change) between randomised arms for each of the following subgroups:
-
socioeconomic status measured as SIMD quintile (1/2 vs. 3/4/5)
-
recruitment method (GP/community).
Qualitative and mixed-methods data analysis
Anonymised transcripts of interviews, recruitment and attrition data, trial arm, participant characteristics and outcomes were entered into NVivo software for analysis guided by a framework approach. 84 Reference to researcher field notes contributed to data interpretation. Analysis was driven by the key feasibility and acceptability research questions and objectives. A coding frame was developed by three researchers independently reading a diverse sample of six interviews, followed by a team discussion to finalise the coding frame and identify key themes. Independent coding was conducted by four researchers (EC, NG, MM and RS) and checked for consistency by Fiona Harris. Emergent themes and interpretive analysis were discussed at weekly researcher meetings and at two co-investigator qualitative interpretation meetings. This group included Stephan Dombrowski (co-chief investigator), Pat Hoddinott (co-chief investigator), Cindy Gray (co-investigator), Mark Grindle (co-investigator), Martin Tod (co-investigator from Men’s Health Forum GB), Fiona Harris (co-investigator), the research assistants (MMcD, EC and NG) and PhD student (RS), which enabled the analysis to be informed by a wide range of perspectives and expertise. Rebecca Skinner generated and applied the coding index relating to her PhD work and conducted the data analysis, overseen by her PhD supervisors (PH and SD). The PhD analysis relating to the acceptability of outcome measures to men and the feasibility of future data linkage for a future full trial is briefly reported. Full reports will become available when the PhD is complete.
The analysis was informed by the framework approach84 that consists of a series of steps:
-
familiarisation
-
identifying a thematic framework
-
indexing
-
charting
-
mapping and interpretation.
At the final stage of mixed-methods data interpretation, wider quantitative data on recruitment, attrition and participant characteristics were drawn on to inform the qualitative analysis and suggest further avenues for interrogation. Based on the emerging analysis of study data, we hypothesised that disadvantage/affluence might be linked to how the narrative-based SMS and alternative SMS were received; similarly, that financial incentives might motivate men differently according to level of deprivation; and, finally, that actual weight loss at 12 months might be linked to either positive or negative views of the SMS or that views might change to become more positive over time among those men who lost weight. For the mixed-methods analysis, interview transcripts were assigned attributes for trial arm: participant SIMD and weight loss outcome at 12 months. Matrix coding queries in NVivo were generated to cross-reference these attributes, with nodes coded for views of incentives and SMS, respectively. This facilitated a more sophisticated interrogation of the data by participant characteristics, outcomes and trial participation. The NVivo memo and annotation functions were also used to document interpretive notes and link these firmly to the data, ensuring transparency for the interpretation. Credibility and reliability of the analysis were maintained by having two independent researchers (EC and NG) who were not involved in any other aspect of the study assisting with coding and analysis, ensuring that interpretation was firmly linked to data and researcher field notes, and continuing discussion within the multidisciplinary team of researchers.
Health economics analysis
The analysis was conducted by intention to treat. Feasibility was assessed by examining completion rates and validity of the responses. Completion rates assess the number of participants for whom all items were missing and the number of participants for whom some items were missing. The frequency and percentage of complete responses is reported for NHS resource use and EQ-5D questions at all available time points and across the trial period. Validity of the responses was assessed by checking for inconsistent responses, such as ticking ‘no’ to using services but recording a positive number of visits.
Patterns of missingness were examined to explore the effect of missing data. Observed completion rates (of cost and EQ-5D measure outcomes) between subgroups were compared using chi-squared tests. The same subgroups as for the statistical analysis were used.
The mean and variation in the health state values and QALYs were assessed. The mean and SD of the health state values at the different time points and QALYs over the trial period were assessed. These estimates were based on observed cases at all time points. No imputation was performed. The mean and variation in NHS resource use were assessed. The mean and SD of resource use at the different time points and over the trial period are reported. These estimates were based on observed cases.
The mean difference in QALYs and costs between the three arms are reported. Both the unadjusted differences and the adjusted differences are reported. The adjusted differences are estimated using generalised linear modelling, controlling for the relevant baseline measures (costs or EQ-5D scores). Bootstrapping was used to estimate a 95% confidence interval (CI) surrounding the cost and QALY differences.
Chapter 6 Results of the feasibility randomised controlled trial
This chapter includes the mixed-methods evidence collected and analysed to answer the aims and objectives outlined in Chapter 1. The different sections contain both quantitative and qualitative findings. All quantitative data are reported in line with CONSORT recommendations for randomised feasibility trials. 83 The results of recruitment and retention are presented first because these relate to the key feasibility objectives of the study. Baseline characteristics are then considered, followed by intervention fidelity, acceptability of interventions, control arm and outcome measures. The feasibility of measuring the weight outcomes, the secondary outcomes and the health economic outcomes is then presented. Finally, harms and unintended consequences of the study are considered, together with the outcomes for the 3-month alternative SMS intervention and a summary of whether or not the progression criteria for a future definitive trial have been sufficiently met.
Recruitment and retention
The CONSORT flow diagram shows recruitment and retention by trial arm (Figure 12) and the key results are briefly summarised below. Recruitment commenced on 1 March 2017 and was successfully completed in less than the prespecified 4 months on 16 June 2017, with the target number of 105 men randomised. Overall, 177 men expressed an interest in participating in the study by either returning an opt-in reply to a GP invitation letter (n = 90) or providing the research team with their contact information during community recruitment outreach activities (n = 87). Of the 177 men expressing an interest in the study, 111 (63%) attended a baseline appointment. Six participants (5%) attended a baseline appointment but were ineligible because they did not meet the BMI/waist measurement criteria (n = 4) or had no mobile phone (n = 1), or their postcode was outside the NHS board areas (n = 1). All 105 men gave written informed consent and were willing to be randomised to the SMS + I (n = 36), SMS-only (n = 33) or control (n = 36) arm.
FIGURE 12.
The CONSORT flow diagram of the Game of Stones study. Reproduced with permission from Dombrowski et al. 1 This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original.
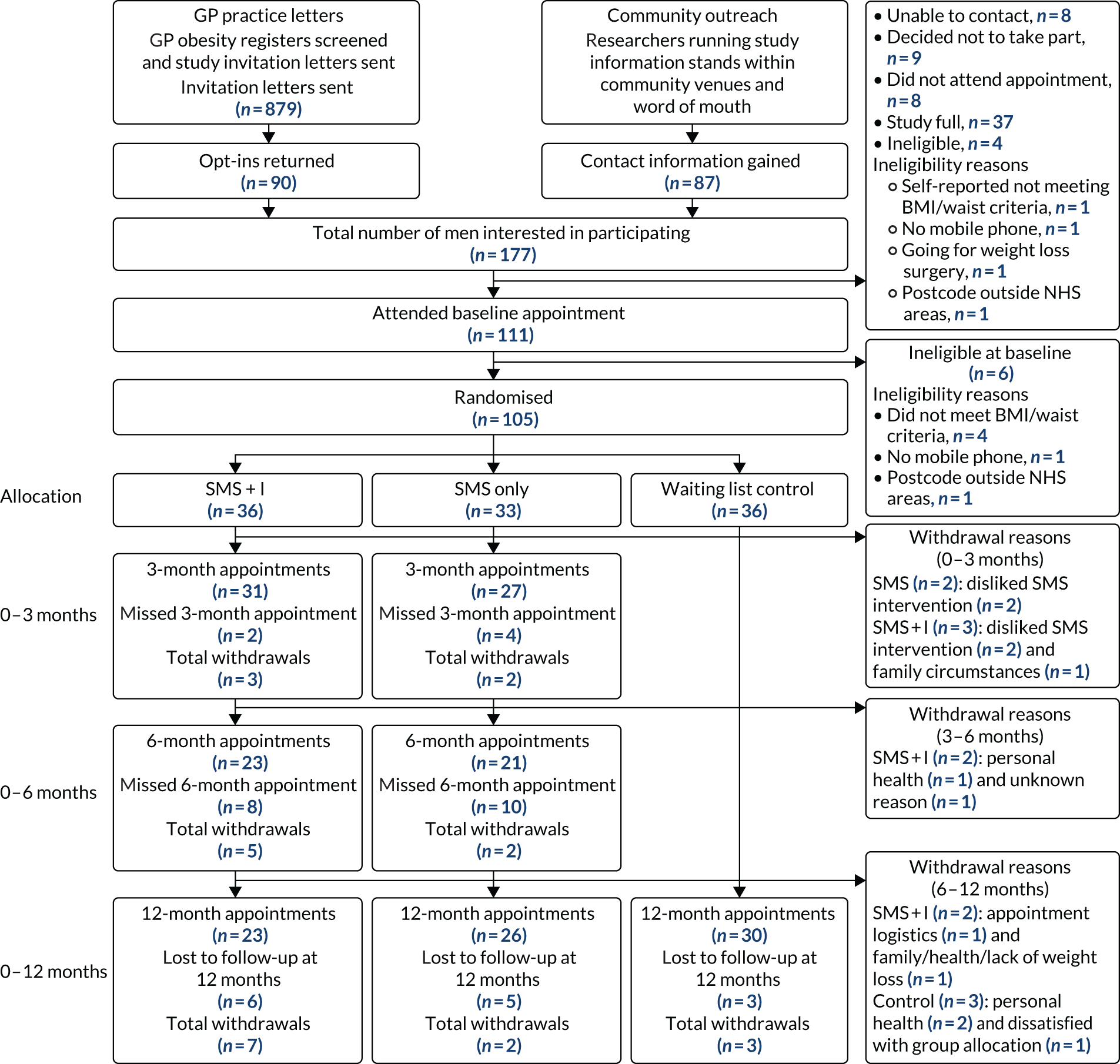
The 3-month assessment was completed by 58 out of 69 participants (84%) randomised to one of the two intervention arms (SMS + I, 31/36, 86%; SMS only, 27/33, 81%), with six participants (9%) missing the appointment and five participants (7%) withdrawing from the study. One of the 58 participants (in the SMS-only arm) provided self-report information as he was abroad for the summer and unable to attend in person within the 2-week time window.
The 6-month appointment was attended by 44 out of 69 participants (64%) randomised to one of the two intervention arms (SMS + I, 23/36, 64%; SMS only, 21/33, 64%), with 18 participants (26%) missing the appointment and seven participants (10% of intervention arms) having withdrawn from the study since the start.
The 12-month assessment overall retention rate was 75% (95% CI 66% to 83%; 79/105). Retention differed by arm and was 64% (95% CI 46% to 79%; 23/36) for SMS + I, 79% (95% CI 61% to 91%; 26/33) for SMS only and 83% (95% CI 67% to 94%; 30/36) for control. One of the 79 participants (control arm) could not attend and provided self-report information because he was out of the region because of work commitments. As verified weight is important, particularly for incentive interventions, this participant was not included in the assessment of retention to meet the progression criteria for a full trial. Fourteen participants (13%) were lost to follow-up, and 12 participants (11% overall) withdrew from the study.
The progression criterion of 72% retention at 12 months was met overall, with 78 out of 105 participants (74%) randomised to three trial arms attending the 12-month appointment in person.
General practice recruitment
General practice recruitment was undertaken in five practices (site A, n = 4; site B, n = 1). Overall, 45 men were recruited and randomised from general practices. Fewer men were recruited this way than from community outreach because of delays in practices confirming their interest in taking part and returning the screened practice lists. A total of 879 invitation letters were sent out, with 90 men (10%) opting in to receive further information about the study (see Figure 12). Owing to delays in obtaining access to screen the practice obesity registers, some men opted in after the study was full (n = 37). Of those opting in before the study was full, 45 out of 53 (85%) were randomised.
The details of individual general practice characteristics, as well as recruitment and retention rates, are given in Table 11. Practices varied in the number of patients who were eligible to participate. Practices in site A were classified as in ‘large urban areas’ and the practice in site B was classified as in ‘other urban area’. 87 All practices were in areas of deprivation (i.e. SIMD category 1 or 2) and an average of 37% of the patients in these practices were classified as living in the 15% most deprived data zones. Opt-in rates varied between practices from 17 out of 347 (5%) to 33 out of 228 (15%).
| Site/general practice | Total | |||||
|---|---|---|---|---|---|---|
| SA1 | SA2 | SA3 | SA4 | SB1 | ||
| Urban/rural classificationa | 1 | 1 | 1 | 1 | 2 | n/a |
| Practice size (n) | *** | *** | *** | *** | *** | 38,600 |
| SIMD of practiceb | 2 | 1 | 1 | 2 | 1 | n/a |
| Practice patients in the 15% most deprived data zones (%) | *** | *** | *** | *** | *** | 37 |
| Letters sent out (n) | 57 | 347 | 187 | 62 | 226 | 879 |
| Replied opting in, n (%) | 4 (7.0) | 17 (4.9) | 27 (14.4) | 9 (14.5) | 33 (14.6) | 90 (10.2) |
| Decided not to take part when contacted (n) | 0 | 1 | 0 | 0 | 4 | 5 |
| Ineligible pre baseline (n) | 0 | 1 | 0 | 0 | 0 | 1 |
| Unable to be contacted (n) | 1 | 0 | 0 | 0 | 0 | 1 |
| Not allocated: study full (n) | 0 | 3 | 23 | 9 | 2 | 37 |
| Attended baseline (n) | 3 | 12 | 4 | 0 | 27 | 46 |
| Ineligible at baseline (n) | 0 | 1 | 0 | 0 | 0 | 1 |
| Randomised (n) | 3 | 11 | 4 | 0 | 27 | 45 |
| Withdrawn (n) | 0 | 0 | 0 | 0 | 6 | 6 |
| Lost to follow-up at 12 months (n) | 0 | 2 | 0 | 0 | 1 | 3 |
| Attended at 12 months (n) | 3 | 9 | 4 | 0 | 20 | 36 |
Qualitative data suggested that some men felt that study recruitment from health settings or via health professionals was more appropriate than from non-health venues. Participants who received a study invitation letter from their GP found the letter easy to understand and felt that the invitation coming from their GP validated or legitimised the study:
Knowing that you have the support of the doctors’ practices and the health service, it gives it that legitimacy rather than it’s just one of these programmes that you pick up on the television, there’s always somebody who’s tried this programme, try that weight loss, or . . . that doesn’t do anything because the market’s full of these programmes.
110003, text only, 3 months
However, this may have been an artefact of recruitment source and wanting to please the researcher, as other participants recruited from the community felt that they would dismiss any letter from their GP as ‘junk mail’. Some general practices at site A engaged frequently in research. Some participants were already familiar with receiving research study invitations sent by a GP, and were happy to participate in research. By contrast, the single practice in site B had had no recent research activity and provided the required number of participants.
Community outreach recruitment
Overall, 60 men were recruited and randomised through community outreach. Table 12 outlines details of recruitment, retention and venue characteristics for community outreach activities. The majority of participants were recruited by researchers through active community outreach at information stands in community venues (42/60, 70%). Researchers attended 14 venues, on 23 occasions, for a total of 97.5 hours across both study sites. On average, for every man randomised, a team of two researchers spent around 2 hours running an information stand. Recruitment rates were unpredictable, varying between sites, days and times; for example, over a 2-hour period at a supermarket, five men were recruited and subsequently randomised, whereas no men were recruited or randomised the following day at the same venue and time.
| Site A | Site B | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Community/health centres | Retail outlets | On street | Hospital foyer | Word of mouth | Total | Sports centre | Retail outlets | On street | Council sites | Word of mouth | Total | |||||||
| SA1 | SA2 | SA3 | SA4 | SA5 | SA6 | SA7 | SA8 | SA9 | SB1 | SB2 | SB3 | SB4 | SB5 | SB6 | SB7 | |||
| Days | 2 | 1 | 1 | 1 | 3 | 1 | 1 | 5 | n/a | 15 | 2 | 2 | 1 | 1 | 1 | 1 | n/a | 8 |
| Researcher hours | 8 | 4 | 3.5 | 3 | 7 | 2 | 2 | 25.5 | n/a | 55 | 12 | 13.5 | 6 | 1 | 5 | 5 | n/a | 42.5 |
| Urban/rural classification85 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | n/a | n/a | 2 | 2 | 2 | 2 | 2 | 2 | n/a | n/a |
| SIMD of venue(s)86 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 2 | n/a | n/a | 5 | 4 | 2 | 2 | 2 | 2 | n/a | n/a |
| Given leaflet(s) (n) | 27 | 21 | 8 | 7 | 17 | 1 | 3 | 43 | n/a | 127 | 19 | 32 | 8 | 3 | 15 | 14 | n/a | 91 |
| Contact information provided (n) | 6 | 5 | 0 | 2 | 8 | 1 | 0 | 24 | 8 | 54 | 7 | 8 | 0 | 0 | 3 | 3 | 12 | 33 |
| Did not attend (n) | 1 | 2 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 7 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Unable to be contacted (n) | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 4 | 0 | 6 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| Ineligible pre baseline (n) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 2 |
| Decided not to take part (n) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 3 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Attended baseline (n) | 5 | 3 | 0 | 1 | 6 | 1 | 0 | 13 | 8 | 37 | 6 | 6 | 0 | 0 | 2 | 3 | 11 | 28 |
| Ineligible at baseline (n) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 2 |
| Randomised (n) | 4 | 2 | 0 | 1 | 6 | 1 | 0 | 13 | 7 | 34 | 6 | 4 | 0 | 0 | 2 | 3 | 11 | 26 |
| Withdrawn (n) | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Lost to follow-up at 12 months (n) | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 3 | 2 | 8 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 3 |
| Attended for 12 months (n) | 3 | 0 | 0 | 1 | 4 | 0 | 0 | 9 | 4 | 21 | 5 | 4 | 0 | 0 | 1 | 2 | 10 | 22 |
Some men (18/60, 30%) were recruited from the community by word of mouth, which included leaflets, friends, family, voluntary sector organisation staff and other researcher contacts. One health worker picked up study leaflets for their patients from researchers at a recruitment site (n = 3 recruited). Others picked up leaflets from local venues (e.g. barbers, shops and libraries) where these had been distributed (n = 3 recruited). Community recruitment by word of mouth differed somewhat between site A (7/34, 21%) and site B (11/26, 42%). Appendix 22 provides a breakdown of community recruitment by word of mouth.
Qualitative views on community recruitment were positive. The Game of Stones study name was popular, and some participants commented that the ‘catchy’ name was one of the reasons that they had decided to participate. Some felt that it had particular appeal to men, while others had felt encouraged to approach the researchers by the factual language used at the information stands:
Yeah, that tagline, it works because I’m a man and you want to lose weight, that was just it, factual.
120017, incentive, 3 months
Retention
Differential dropout rates between the study arms were observed, with fewer SMS + I participants completing the study (64%) than SMS-only (79%) or control arm participants (83%). A total of 12 men withdrew from the study and gave the following reasons: dislike of the narrative SMS intervention component (n = 4), health (n = 3), family (n = 1), unknown (n = 1), dissatisfaction with trial arm allocation (n = 1), appointment logistics (n = 1) and multiple reasons (n = 1). Retention differed slightly by recruitment channel; of the 45 participants recruited from general practices, 36 (80%) completed the 12-month follow-up assessment, 6 (13%) withdrew from the study and 3 (7%) were lost to follow-up. Of the 60 participants recruited from the community, 43 participants (71%) completed the 12-month follow-up assessment, 6 (10%) withdrew and 11 (18%) were lost to follow up.
Retention rates of participants from more deprived areas in the SMS + I (14/19, 74% vs. 8/16, 50%) and control (10/14, 95% vs. 20/22, 71%) arms were higher than those of participants from less deprived areas, but no difference was observed in SMS-only participants (16/21, 84% vs. 10/12, 83%). The small number of men who dropped out from or disengaged with the intervention because they disliked the SMS was similar between more and less disadvantaged areas (SIMD 1 and 2, 9/15; SIMD 3, 4 and 5, 6/15).
The qualitative analysis suggested that men had a range of motivations for attending study appointments. They reported being particularly encouraged to attend if they had managed to lose weight, as this meant that their efforts would be noted by the researchers rather than by friends and family. For many participants, the interaction with the researcher was central to their participation and continued involvement in Game of Stones, with one participant saying how highly he valued having an opportunity to discuss his weight and receive support:
To discuss my progress is what encouraged me to come along. [. . .] I’ve spoke to other people about the programme, like, friends and relatives, but there’s no one that I can really discuss my issues with, if you know what I mean, not even my wife, she’ll say ‘yeah, yeah, yeah you’re doing well, keep on going’ but coming here and discussing it with you I felt gave me the motivation to continue.
210010, SMS only, 12 months
Others felt a sense of social responsibility and altruism that was bound up with their motivations to remain in the study, perceiving the wider importance of the study to society and understanding the need to attend appointments to provide researchers with complete data. For some, this was also a matter of pride, and one man reported that he was going to come back because he was ‘a committed person’. The notion of reciprocal benefit and social contract played a role for some who remained in the study:
Yeah, absolutely because there’s a contract when you sign up for something like this, you know, how binding that contract is varies from the individual but I think because you’re providing resources to help me to achieve something I want to achieve anyway, then it seems only fair to follow through with everything that you commit to at the start.
220040, SMS + I, 12 months
Often, participants speculated that those not attending may have felt embarrassed about not achieving weight loss targets and, therefore, had decided not to attend. One participant who attended all of the study appointments and did not lose weight commented that he must have a ‘high embarrassment toleration’ in comparison with others.
Participants were positive about the strategies used in the study to maximise retention. These included appointments being offered after working hours and at convenient locations; the £20 voucher; and the appointment reminder SMS or telephone calls. Suggestions to improve retention included sending out more appointment letters and ensuring that during the baseline appointments researchers emphasised the importance of subsequent attendance, even if participants had not lost weight:
So maybe reiterating then that we need you to come back even if it doesn’t work out [. . .], which I don’t remember being told.
120030, SMS only, 12 months
Baseline characteristics
The baseline characteristics of the 105 recruited participants are in Table 13, alongside a breakdown of characteristics by recruitment channel. On average, participants were aged 52.2 years (SD 13.1 years), had a BMI of 35.7 kg/m2 (SD 5.9 kg/m2) and had a waist circumference of 116.8 cm (SD 11.8 cm). Participants’ BMI ranged from < 30 kg/m2 to ≥ 50 kg/m2, with many participants (49/105, 47%) having a BMI between 30 and 35 kg/m2. Participants intended to lose an average of 17.4 kg (SD 11.0 kg) through participating in the study, which equates to an average of around 16% of their overall average body weight. Participants had previously attempted to lose weight by changing their behaviours an average of 6.6 times (SD 11.4 times).
| Baseline characteristic | Community recruitment (N = 60) | GP recruitment (N = 45) | Total |
|---|---|---|---|
| Age (years), n, mean, SD | 57, 48.3, 13.6 | 45, 57.1, 10.8 | 102, 52.2, 13.1 |
| Weight (kg), n, mean, SD | 60, 112.7, 20.9 | 45, 104.3, 13.3 | 105, 109.1, 18.4 |
| Height (cm), n, mean, SD | 60, 176.6, 6.6 | 45, 172.8, 5.4 | 105, 175.0, 6.4 |
| BMI (kg/m2), n, mean, SD | 60, 36.2, 6.9 | 45, 35.0, 4.3 | 105, 35.7, 5.9 |
| < 30, N, n, % | 60, 6, 10.0 | 45, 5, 11.1 | 105, 11, 10.5 |
| ≥ 30 to < 35, N, n, % | 60, 26, 43.3 | 45, 23, 51.1 | 105, 49, 46.7 |
| ≥ 35 to < 40, N, n, % | 60, 14, 23.3 | 45, 9, 20.0 | 105, 23, 21.8 |
| ≥ 40 to < 45, N, n, % | 60, 10, 16.6 | 45, 6, 13.3 | 105, 16, 15.2 |
| ≥ 45 to < 50, N, n, % | 60, 1, 1.7 | 45, 2, 4.4 | 105, 3, 2.9 |
| ≥ 50, N, n, % | 60, 3, 5.0 | 45, 0, 0.0 | 105, 3, 2.9 |
| Waist circumference (cm), N, mean, SD | 60, 118.6, 13.0 | 45, 114.4, 9.4 | 105, 116.8, 11.8 |
| Highest weight (kg), N, mean, SD | 59, 119.4, 24.7 | 45, 109.8, 14.4 | 104, 115.3, 21.4 |
| Lowest weight (kg), N, mean, SD | 59, 87.4, 23.7 | 44, 82.3, 15.5 | 103, 85.2, 20.7 |
| Ideal weight (kg), N, mean, SD | 58, 94.4, 53.7 | 45, 83.8, 11.3 | 103, 89.8, 41.2 |
| Intended weight loss in study (kg), N, mean, SD | 56, 18.7, 12.6 | 45, 15.9, 8.4 | 101, 17.4, 11.0 |
| Weight loss attempts, N, mean, SD | 58, 7.4, 14.0 | 40, 5.3, 5.7 | 98, 6.6, 11.4 |
| SIMD category, N, n, % | |||
| 1 (most deprived) | 59, 23, 39.0 | 45, 15, 33.3 | 104, 38, 36.5 |
| 2 | 59, 10, 16.9 | 45, 14, 31.1 | 104, 24, 23.1 |
| 3 | 59, 8, 13.6 | 45, 4, 9.0 | 104, 12, 11.5 |
| 4 | 59, 8, 13.6 | 45, 6, 13.3 | 104, 14, 13.5 |
| 5 (least deprived) | 59, 10, 16.9 | 45, 6, 13.3 | 104, 16, 15.4 |
| Marital status, N, n, % | |||
| Cohabiting | 59, 4, 6.8 | 45, 7, 15.6 | 104, 11, 10.6 |
| Divorced | 59, 1, 1.7 | 45, 3, 6.7 | 104, 4, 3.9 |
| Married | 59, 32, 54.2 | 45, 28, 62.2 | 104, 60, 57.7 |
| Prefer not to say | 59, 1, 1.7 | 45, 0, 0.00 | 104, 1, 1.0 |
| Separated | 59, 4, 6.8 | 45, 2, 4.4 | 104, 6, 5.8 |
| Single | 59, 16, 27.12 | 45, 4, 8.9 | 104, 20, 19.2 |
| Widowed | 59, 1, 1.7 | 45, 1, 2.2 | 104, 2, 19.2 |
| Comorbidity, N, n, % | |||
| Arthritis | 59, 9, 15.0 | 45, 13, 28.9 | 104, 22, 21.2 |
| Cancer | 59, 1, 1.7 | 45, 2, 0.0 | 104, 3, 2.9 |
| Diabetes | 59, 9, 15.3 | 45, 10, 22.2 | 104, 19, 18.3 |
| Heart attack | 59, 4, 6.8 | 45, 5, 11.1 | 104, 9, 8.6 |
| High blood pressure | 59, 18, 30.5 | 45, 30, 66.7 | 104, 48, 46.1 |
| Stroke | 59, 3, 5.1 | 45, 3, 6.7 | 104, 6, 5.8 |
| At least one comorbidity | 59, 26, 44.1 | 45, 39, 86.7 | 104, 65, 62.5 |
| Ethnic group, N, n, % | |||
| Asian | 59, 1, 1.7 | 45, 3, 6.7 | 104, 4, 3.8 |
| Black | 59, 4, 6.8 | 45, 0, 0.0 | 104, 4, 3.8 |
| Prefer not to say | 59, 1, 1.7 | 45, 0, 0.0 | 104, 1, 1.0 |
| White | 59, 53, 89.8 | 45, 42, 93.3 | 104, 95, 91.4 |
| Owns a pedometer, N, n, % | |||
| Yes | 58, 19, 32.8 | 44, 5, 11.4 | 102, 24, 23.5 |
| No | 58, 39, 67.2 | 44, 39, 88.6 | 102, 78, 76.5 |
| Children, N, n, % | |||
| No | 58, 18, 31.0 | 45, 7, 15.6 | 103, 25, 24.3 |
| Yes | 58, 40, 69.0 | 45, 38, 84.4 | 103, 78, 75.7 |
| Highest educational qualification, N, n, % | |||
| Bachelor’s degree (= SVQ 5) | 59, 20, 33.9 | 44, 4, 9.1 | 103, 24, 23.3 |
| HNC/HND (= SVQ 4) | 59, 7, 11.8 | 44, 5, 11.4 | 103, 12, 11.6 |
| Advanced Higher/A level (= SVQ 3) | 59, 6, 10.2 | 44, 3, 6.8 | 103, 9, 8.7 |
| Master’s/PhD or equivalent | 59, 4, 6.8 | 44, 1, 2.3 | 103, 5, 4.8 |
| No formal qualifications | 59, 6, 10.2 | 44, 14, 31.8 | 103, 20, 19.4 |
| Other | 59, 0, 0.0 | 44, 1, 2.3 | 103, 1, 1.0 |
| Prefer not to say | 59, 0, 0.0 | 44, 4, 9.1 | 103, 4, 3.9 |
| Standard Grade/GCSE/Intermediate 1 or 2 | 59, 9, 15.3 | 44, 8, 18.2 | 103, 17, 16.5 |
| Still studying | 59, 4, 6.8 | 44, 2, 4.5 | 103, 6, 5.8 |
| Vocational qualifications (= SVQ 1 + 2) | 59, 3, 5.1 | 44, 2, 4.5 | 103, 5, 4.8 |
| Employment status, N, n, % | |||
| Full-time student | 59, 6, 10.2 | 45, 1, 2.2 | 104, 7, 6.7 |
| Have paid job – full time (≥ 30 hours per week) | 59, 29, 49.2 | 45, 21, 46.7 | 104, 50, 48.1 |
| Have paid job – part time (8–29 hours per week) | 59, 3, 5.1 | 45, 3, 6.7 | 104, 6, 5.8 |
| Not in paid work because of long-term illness or disability | 59, 4, 6.8 | 45, 7, 15.6 | 104, 11, 10.6 |
| Not in paid work for another reason | 59, 1, 1.7 | 45, 0, 0.0 | 104, 1, 1.0 |
| Not working – house husband | 59, 1, 1.7 | 45, 0, 0.0 | 104, 1, 1.0 |
| Retired | 59, 8, 13.6 | 45, 10, 22.2 | 104, 18, 17.3 |
| Self-employed | 59, 4, 6.8 | 45, 3, 6.7 | 104, 7, 6.7 |
| Unemployed and seeking work | 59, 3, 5.1 | 45, 0, 0.0 | 104, 3, 2.9 |
| Household size, N, mean, SD | 59, 2.7, 1.3 | 45, 2.3, 1.2 | 104, 2.5, 1.3 |
The majority of men lived in areas of disadvantage, with 62 out of 104 (60%) living in SIMD category 1 or 2 areas. Most participants were married (58%), reported at least one comorbidity (63%), were of white ethnicity (91%), reported that they had children (76%) and were in full-time employment (48%).
Participants recruited through the community were, on average, younger (mean age: community, 48.3 years; GP, 57.1 years) and heavier (mean BMI: community, 36.2 kg/m2; GP, 35.0 kg/m2) and had attempted to lose weight more often in the past (mean weight loss attempts: community, 7.4 times; GP, 5.3 times). Participants recruited through the GP were more likely to live in SIMD category 1 or 2 areas (community, 56%; GP, 64%) and to have an obesity-related comorbidity (community, 44%; GP, 87%). This was due to purposive sampling of practices with higher proportions of patients living in SIMD category 1 and 2 areas.
Visual inspection of the baseline characteristics by study arm showed a few minor imbalances, which are to be expected given the small sample size and the large number of characteristics measured (Table 14). Participants in the control arm had a higher BMI (SMS + I, 35.1 kg/m2; SMS only, 35.1 kg/m2; control, 36.7 kg/m2) and fewer were married (SMS + I, 61%; SMS only, 66%; control, 47%). Fewer participants in the SMS + I arm reported living in a SIMD category 1 or 2 area (SMS + I, 54%; SMS only, 64%; control, 61%).
| Baseline characteristic | Trial arm | ||
|---|---|---|---|
| SMS + I | SMS only | Control | |
| Age (years), N, mean, SD | 35, 50.9, 14.2 | 31, 52.5, 15.1 | 36, 53.1, 10.1 |
| Weight (kg), N, mean, SD | 36, 108.6, 16.4 | 33, 107.8, 20.2 | 36, 110.7, 19.0 |
| Height (cm), N, mean, SD | 36, 175.9, 6.6 | 33, 175.2, 6.7 | 36, 173.8, 5.9 |
| BMI (kg/m2), N, mean, SD | 36, 35.1, 5.3 | 33, 35.1, 5.9 | 36, 36.7, 6.5 |
| < 30, N, n, % | 36, 5, 13.9 | 33, 3, 9.1 | 36, 3, 8.3 |
| ≥ 30 to < 35, N, n, % | 36, 16, 44.4 | 33, 19, 57.6 | 36, 14, 38.9 |
| ≥ 35 to < 40, N, n, % | 36, 10, 27.8 | 33, 6, 18.2 | 36, 7, 19.4 |
| ≥ 40 to < 45, N, n, % | 36, 4, 11.1 | 33, 2, 6.1 | 36, 10, 27.8 |
| ≥ 45 to < 50, N, n, % | 36, 0, 0.0 | 33, 2, 6.1 | 36, 1, 2.8 |
| ≥ 50, N, n, % | 36, 1, 2.8 | 33, 1, 3.0 | 36, 1, 2.8 |
| Waist circumference (cm), N, mean, SD | 36, 115.8, 10.0 | 33, 114.9, 12.7 | 36, 119.5, 12.2 |
| Highest weight (kg), N, mean, SD | 36, 114.1, 19.9 | 33, 111.1, 20.7 | 36, 120.3, 22.9 |
| Lowest weight (kg), N, mean, SD | 36, 84.7, 25.2 | 33, 84.6, 17.0 | 36, 86.4, 19.2 |
| Ideal weight (kg), N, mean, SD | 36, 85.6, 20.2 | 33, 97.7, 68.9 | 36, 86.6, 10.5 |
| Intended weight loss in study (kg), N, mean, SD | 36, 16.2, 8.6 | 33, 18.1, 14.6 | 36, 18.1, 8.9 |
| Weight loss attempts, N, mean, SD | 36, 5.0, 6.5 | 33, 7.0, 17.2 | 36, 7.7, 8.1 |
| SIMD category, N, n, % | |||
| 1 (most deprived) | 35, 11, 31.4 | 33, 12, 36.4 | 36, 15, 41.7 |
| 2 | 35, 8, 22.9 | 33, 9, 27.3 | 36, 7, 19.4 |
| 3 | 35, 6, 17.1 | 33, 3, 9.1 | 36, 3, 8.3 |
| 4 | 35, 4, 11.4 | 33, 4, 12.1 | 36, 6, 16.7 |
| 5 (least deprived) | 35, 6, 17.5 | 33, 5, 15.2 | 36, 5, 13.9 |
| Marital status, N, n, % | |||
| Cohabiting | 36, 4, 11.1 | 32, 2, 6.3 | 36, 5, 13.8 |
| Divorced | 36, 2, 5.6 | 32, 0, 0.0 | 36, 2, 5.6 |
| Married | 36, 22, 61.1 | 32, 21, 65.6 | 36, 17, 47.2 |
| Prefer not to say | 36, 0, 0.0 | 32, 0, 0.0 | 36, 1, 2.8 |
| Separated | 36, 1, 2.8 | 32, 3, 9.4 | 36, 2, 5.6 |
| Single | 36, 7, 19.4 | 32, 5, 15.6 | 36, 8, 22.2 |
| Widowed | 36, 0, 0 | 32, 1, 3.1 | 36, 1, 2.8 |
| Comorbidity, N, n, % | |||
| Arthritis | 36, 11, 30.6 | 32, 3, 9.1 | 36, 8, 22.2 |
| Cancer | 36, 1, 2.8 | 32, 1, 3.1 | 36, 1, 2.8 |
| Diabetes | 36, 6, 16.6 | 32, 5, 15.6 | 36, 8, 22.2 |
| Heart attack | 36, 3, 8.3 | 32, 3, 9.4 | 36, 3, 8.3 |
| High blood pressure | 36, 17, 47.2 | 32, 14, 43.7 | 36, 17, 47.2 |
| Stroke (including TIA) | 36, 3, 8.3 | 32, 2, 6.3 | 36, 1, 2.8 |
| At least one comorbidity | 36, 25, 69.4 | 32, 18, 56.2 | 36, 22, 61.1 |
| Ethnic group, N, n, % | |||
| Asian | 36, 2, 5.6 | 32, 1, 3.1 | 36, 1, 2.8 |
| Black | 36, 2, 5.6 | 32, 1, 3.1 | 36, 1, 2.8 |
| Prefer not to say | 36, 0, 0.0 | 32, 1, 3.1 | 36, 0, 0.0 |
| White | 36, 32, 88.8 | 32, 29, 90.7 | 36, 34, 94.4 |
| Owns a pedometer, N, n, % | |||
| Yes | 35, 29, 82.9 | 33, 28, 75.8 | 34, 24, 70.6 |
| No | 35, 6, 17.1 | 33, 8, 24.2 | 34, 10, 29.4 |
| Children, N, n, % | |||
| No | 36, 10, 27.8 | 32, 7, 21.9 | 35, 8, 22.9 |
| Yes | 36, 26, 72.2 | 32, 25, 78.3 | 35, 27, 77.1 |
| Education, N, n, % | |||
| Bachelor’s degree (= SVQ 5) | 36, 7, 19.4 | 31, 6, 19.5 | 36, 11, 30.6 |
| HNC/HND (= SVQ 4) | 36, 4, 11.1 | 31, 6, 19.5 | 36, 2, 5.6 |
| Higher Grade/Advanced Higher/A level or equivalent (= SVQ 3) | 36, 3, 8.3 | 31, 5, 16.1 | 36, 1, 2.8 |
| Master’s/PhD or equivalent | 36, 1, 2.8 | 31, 1, 3.2 | 36, 3, 8.3 |
| No formal qualifications | 36, 7, 19.4 | 31, 3, 9.7 | 36, 10, 27.8 |
| Other | 36, 0, 0.0 | 31, 1, 3.2 | 36, 0, 0.0 |
| Prefer not to say | 36, 2, 5.6 | 31, 0, 0.0 | 36, 2, 5.6 |
| Standard Grade/GCSE/Intermediate 1 or 2 | 36, 6, 16.7 | 31, 7, 22.6 | 36, 4, 11.1 |
| Still studying | 36, 2, 5.6 | 31, 1, 3.2 | 36, 3, 8.3 |
| Vocational qualifications (= SVQ 1 + 2) | 36, 4, 11.1 | 31, 1, 3.2 | 36, 0, 0.0 |
| Working status, N, n, % | |||
| Full-time student | 36, 4, 11.1 | 32, 2, 6.25 | 36, 1, 2.8 |
| Have paid job – full time (≥ 30 hours per week) | 36, 16, 44.4 | 32, 16, 50.00 | 36, 18, 50.0 |
| Have paid job – part time (8–29 hours per week) | 36, 3, 8.33 | 32, 3, 9.38 | 36, 0, 0.0 |
| Not in paid work because of long-term illness or disability | 36, 2, 5.6 | 32, 1, 3.13 | 36, 8, 22.2 |
| Not in paid work for other reason | 36, 0, 0.0 | 32, 1, 3.1 | 36, 0, 0.0 |
| Not working – house husband | 36, 0, 0.0 | 32, 0, 0.0 | 36, 1, 2.8 |
| Retired | 36, 8, 22.2 | 32, 6, 18.7 | 36, 4, 11.1 |
| Self-employed | 36, 3, 8.3 | 32, 3, 9.4 | 36, 1, 2.8 |
| Unemployed and seeking work | 36, 0, 0.0 | 32, 0, 0.0 | 36, 3, 8.3 |
| Household size, N, mean, SD | 36, 2.6, 1.3 | 33, 2.6, 1.0 | 36, 2.4, 1.4 |
Table 15 compares completers (i.e. participants who remained in the study and completed 12-month assessments) with non-completers (i.e. participants who withdrew during the study or were lost to follow-up at 12 months). Completers were similar to non-completers in age, past weight loss attempts, reporting a comorbidity, and household size. Completers had a lower average BMI (non-completers, 37.5 kg/m2; completers, 35.1 kg/m2) and waist circumference (non-completers, 119.7 cm; completers, 115.8 cm) and reported wanting to lose less weight through the programme (non-completers, 19.2 kg; completers, 16.9 kg).
| Baseline characteristic | Completersa (N = 79) | Non-completersb (N = 26) |
|---|---|---|
| Age (years), mean (SD) | 52.3 (13.6) | 51.8 (11.6) |
| Weight (kg), mean (SD) | 107.3 (17.2) | 114.5 (21.1) |
| Height (cm), mean (SD) | 175.1 (6.8) | 174.7 (5.1) |
| BMI (kg/m2), mean (SD) | 35.1 (5.7) | 37.5 (6.4) |
| < 30, n (%) | 11 (13.9) | 0 (0.0) |
| ≥ 30 to < 35, n (%) | 38, (48.1) | 11 (42.3) |
| ≥ 35 to < 40, n (%) | 14 (17.7) | 9 (34.6) |
| ≥ 40 to < 45, n (%) | 12 (15.2) | 4 (15.4) |
| ≥ 45 to < 50, n (%) | 3 (3.8) | 0 (0.0) |
| ≥ 50, n (%) | 1 (1.3) | 2 (7.7) |
| Waist circumference (cm), mean (SD) | 115.8 (11.2) | 119.7 (13.1) |
| Highest weight (kg), mean (SD) | 113.5 (20.0) | 120.8 (24.7) |
| Lowest weight (kg), mean (SD) | 84.9 (20.4) | 86.1 (22.1) |
| Ideal weight (kg), mean (SD) | 90.2 (46.7) | 88.6 (13.9) |
| Intended weight loss in study (kg), mean (SD) | 16.9 (9.4) | 19.2 (14.8) |
| Weight loss attempts, mean (SD) | 6.5 (12.6) | 6.8 (6.1) |
| SIMD category, n (%) | ||
| 1 (most deprived) | 31 (39.2) | 7 (26.9) |
| 2 | 19 (24.1) | 5 (19.2) |
| 3 | 7 (8.9) | 5 (19.2) |
| 4 | 11 (13.9) | 3 (11.5) |
| 5 (least deprived) | 10 (12.7) | 6 (23.1) |
| Marital status, n (%) | ||
| Cohabiting | 7 (8.9) | 4 (15.4) |
| Divorced | 3 (3.8) | 1 (3.8) |
| Married | 44 (55.7) | 16 (61.5) |
| Prefer not to say | 0 (0.0) | 1 (3.8) |
| Separated | 4 (5.1) | 2 (7.7) |
| Single | 18 (22.8) | 2 (7.7) |
| Widowed | 2 (2.5) | 0 (0.0) |
| Comorbidities, n (%) | ||
| Arthritis | 16 (20.3) | 6 (23.1) |
| Cancer | 3 (3.8) | 0 (0.0) |
| Diabetes | 14 (17.7) | 5 (19.2) |
| Heart attack | 8 (10.1) | 1 (3.8) |
| High blood pressure | 35 (44.3) | 13 (50.0) |
| Stroke (including transient ischemic attack) | 5 (6.3) | 1 (3.8) |
| At least one comorbidity | 49 (62.0) | 16 (61.5) |
| Ethnic group, n (%) | ||
| Asian | 4 (5.1) | 0 (0.0) |
| Black | 1 (1.3) | 3 (11.5) |
| Prefer not to say | 0 (0.0) | 1 (3.8) |
| White | 73 (92.4) | 22 (84.6) |
| Owns a pedometer, n (%) | ||
| Yes | 20 (25.3) | 4 (15.4) |
| No | 57 (72.2) | 21 (80.8) |
| Children, n (%) | ||
| No | 21 (26.6) | 4 (15.4) |
| Yes | 56 (70.9) | 22 (84.6) |
| Education, n (%) | ||
| Bachelor’s degree (= SVQ 5) | 18 (22.8) | 6 (23.1) |
| HNC/HND (= SVQ 4) | 10 (12.7) | 2 (7.7) |
| Higher Grade/Advanced Higher/A level or equivalent (= SVQ 3) | 7 (8.9) | 2 (7.7) |
| Master’s degree/PhD or equivalent | 3 (3.8) | 2 (7.7) |
| No formal qualifications | 17 (21.5) | 3 (11.5) |
| Other | 1 (1.3) | 0 (0.0) |
| Prefer not to say | 3 (3.8) | 1 (3.8) |
| Standard Grade/GCSE/Intermediate 1 or 2 | 10 (12.7) | 7 (26.9) |
| Still studying | 5 (6.3) | 1 (3.8) |
| Vocational qualifications (= SVQ 1 + 2) | 3 (3.8) | 2 (7.7) |
| Working status, n (%) | ||
| Full-time student | 6 (7.6) | 1 (3.8) |
| Have paid job – full time (≥ 30 hours per week) | 34 (43.0) | 16 (61.5) |
| Have paid job – part time (8–29 hours per week) | 6 (7.6) | 0 (0.0) |
| Not in paid work because of long-term illness or disability | 10 (12.7) | 1 (3.8) |
| Not in paid work for another reason | 0 (0.0) | 1 (3.8) |
| Not working – house husband | 1 (1.3) | 0 (0.0) |
| Retired | 14 (17.7) | 4 (15.4) |
| Self-employed | 5 (6.3) | 2 (7.7) |
| Unemployed and seeking work | 2 (2.5) | 1 (3.8) |
| Household size, mean (SD) | 2.5 (1.3) | 2.7 (1.1) |
A higher proportion of participants from more disadvantaged areas completed the study, with 12 out of 62 participants from SIMD category 1 or 2 areas not completing the study (19%) compared with 14 out of 42 participants from SIMD category 3, 4 or 5 areas (33%) not completing.
More completers were single (non-completers, 8%; completers, 23%) and had no formal qualification (non-completers, 12%; completers, 22%),
In comparison with non-completers, more completers were of white ethnicity (non-completers, 88%; completers, 94%), fewer reported having children (non-completers, 88%; completers, 70%) and fewer worked in a full-time paid job (non-completers, 62%; completers, 45%).
Intervention fidelity
The majority of the 38,214 SMS sent to the SMS + I and SMS-only arms were delivered to the mobile phone, with 1782 (4.6%) having no delivery status (this includes SMS that expired as a result of lack of response from the mobile phone provider after 48 hours and invalid telephone numbers due to participants changing their phone numbers). One SMS error occurred when a SMS-only participant received a SMS that was meant for those in the SMS + I arm. One minor issue emerged (temporarily) when SMS were sent at the wrong times due to daylight saving time changes on 25 March 2017.
All participants who secured financial incentives were paid by their preferred method, which was direct bank transfer.
Acceptability and feasibility of intervention components
Overall acceptability ratings and contamination
Table 16 displays intervention satisfaction indicators over the course of the study for participants attending assessments. Overall mean satisfaction with the intervention was 81%, 77% and 87% for the SMS + I, SMS-only and control arms, respectively. Satisfaction over time was comparable between the two intervention arms, and highest in the control arm at 12 months. Participants mostly scored 4 out of 5 on average for the programme attributes ‘understandable’, ‘useful’, ‘helpful’, ‘interesting’ and ‘relevant’.
| Time point | |||||||
|---|---|---|---|---|---|---|---|
| 3 months | 6 months | 12 months | |||||
| SMS + I | SMS only | SMS + I | SMS only | SMS + I | SMS only | Control | |
| Overall satisfaction (0–100), n, mean, SD | 31, 80.3, 21.1 | 27, 75.0, 22.2 | 23, 76.2, 29.6 | 21, 79.0, 20.7 | 22, 80.9, 20.0 | 26, 77.0, 20.8 | 29, 87.3, 17.5 |
| Programme has been . . . (1 = low, 5 = high), n, mean, SD | |||||||
| Understandable | 31, 4.5, 0.9 | 26, 4.4, 0.8 | 22, 4.4, 1.2 | 21, 4.4, 1.2 | 20, 4.6, 1.1 | 25, 4.6, 1.1 | 29, 4.6, 0.9 |
| Useful | 31, 4.4, 0.9 | 27, 4.0, 1.0 | 23, 4.1, 1.3 | 20, 4.1, 1.1 | 22, 4.1, 1.2 | 26, 4.0, 1.0 | 30, 4.3, 0.9 |
| Helpful | 30, 4.3, 0.9 | 27, 3.9, 1.0 | 23, 4.1, 1.3 | 20, 4.1, 1.1 | 22, 4.1, 1.1 | 26, 4.0, 1.0 | 30, 4.3, 0.9 |
| Interesting | 31, 4.3, 1.0 | 27, 4.2, 1.1 | 23, 4.2, 1.1 | 20, 4.4, 1.3 | 22, 4.3, 0.8 | 26, 4.3, 1.2 | 30, 4.5, 1.0 |
| Relevant | 31, 4.2, 1.1 | 27, 3.9, 1.2 | 23, 4.0, 1.3 | 20, 4.3, 1.1 | 22, 4.1, 1.1 | 26, 4.2, 1.1 | 30, 4.5, 1.0 |
| Helpfulness (1 = low, 5 = high), n, mean, SD | |||||||
| Text messages | 31, 3.4, 1.5 | 27, 3.1, 1.3 | 23, 3.1, 1.3 | 21, 3.6, 1.3 | 22, 3.4, 1.3 | 26, 3.3, 1.4 | n/a |
| Website | 28, 3.3, 1.2 | 26, 3.3, 0.9 | 23, 3.3, 1.2 | 20, 3.2, 0.8 | 22, 3.6, 1.0 | 24, 3.4, 0.7 | 26, 3.5, 1.1 |
| Pedometer | 30, 4.1, 1.2 | 27, 4.1, 0.9 | 23, 3.7, 1.4 | 21, 4.0, 1.0 | 21, 3.9, 1.2 | 25, 4.0, 1.0 | 30, 3.7, 1.4 |
| Met other men in programme, N, n, % | |||||||
| Yes | 31, 0, 0.0 | 27, 0, 0.0 | 23, 1, 4.3 | 21, 0, 0.0 | 22, 1, 4.5 | 26, 0, 0.0 | 30, 1, 3.3 |
Helpfulness ratings of the narrative SMS, web page and pedometer showed that the pedometer received the highest scores over time. At 12 months, helpfulness ratings for the pedometer were 3.9 out of 5, 3.3 out of 5 and 3.7 out of 5 for the SMS + I, SMS-only and control arms, respectively. The narrative SMS (SMS + I, 3.4/5; SMS only, 3.3/5) and the web page (SMS + I, 3.6/5; SMS only, 3.4/5; control, 3.5/5) were perceived as somewhat helpful on average at 12 months. Helpfulness ratings were relatively stable throughout the measurement time points for all three intervention components.
Acceptability ratings in the two intervention arms at 12 months were comparable across deprivation status (see Appendix 23, Table 39). Comparing SIMD category 1 and 2 participants (n = 30) with those in SIMD category 3–5 (n = 17) suggested similar mean ratings for overall satisfaction (SIMD 1 and 2, 4.1/5; SIMD 3–5, 4.1/5), helpfulness of the programme (SIMD 1 and 2, 78%; SIMD 3–5, 81%) and helpfulness of the narrative SMS (SIMD 1 and 2, 3.2/5; SIMD 3–5, 3.6/5).
The potential for contamination was assessed. One participant at 6 and 12 months (SMS + I arm) and another participant at 12 months (control arm) reported meeting other men in the study. Two men who reported meeting someone else in the study out of 78 who were asked this question at 12 months gives a contamination rate of 3%. It is unknown whether these two men met each other or met men who were lost to follow up. Documentation suggests that this meeting was likely to have occurred between 3 and 6 months.
Acceptability of narrative SMS
Acceptability was assessed through questionnaire ratings (see Table 16), the qualitative interview data and engagement in narrative SMS. Engagement was measured by examining the number of replies in response to the SMS, as well as the number of participants withdrawing or disengaging from the study because they disliked narrative SMS. Table 17 details the replies to the narrative SMS, as well as the number of participants who withdrew or disengaged from the narrative SMS component.
| 0–3 months | 3–6 months | 6–12 months | ||||
|---|---|---|---|---|---|---|
| SMS + I | SMS only | SMS + I | SMS only | SMS + I | SMS only | |
| Replying to SMS, N, n, % | ||||||
| 0 replies to SMS | 36, 2, 58.3 | 33, 23, 69.7 | 36, 30, 83.3 | 33, 31, 93.9 | 36, 28, 77.8 | 33, 28, 84.8 |
| 1–5 replies to SMS | 36, 9, 25.0 | 33, 7, 22.3 | 36, 6, 16.7 | 33, 2, 6.1 | 36, 7, 19.4 | 33, 5, 15.2 |
| 6–10 replies to SMS | 36, 2, 5.6 | 33, 1, 3.0 | 36, 0, 0.0 | 33, 0, 0.0 | 36, 0, 0.0 | 33, 0, 0.0 |
| 11–15 replies to SMS | 36, 0, 0.0 | 33, 0,0.0 | 36, 0, 0.0 | 33, 0, 0.0 | 36, 0, 0.0 | 33, 0, 0.0 |
| 16–20 replies to SMS | 36, 1, 2.8 | 33, 1, 3.0 | 36, 0, 0.0 | 33, 0, 0.0 | 36, 0, 0.0 | 33, 0, 0.0 |
| > 20 replies to SMS | 36, 3, 8.3 | 33, 1, 3.0 | 36, 0, 0.0 | 33, 0, 0.0 | 36, 1, 2.8 | 33, 0, 0.0 |
| Number of replies to SMS, N, mean, SD | 289, 8.0, 24.2 | 81, 2.5, 7.9 | 10, 0.3, 0.7 | 6, 0.3, 1.0 | 28, 0.8, 3.3 | 11, 0.3, 1.0 |
| Stopping SMS, N, n, % | 36, 1, 2.8 | 33, 2, 6.1 | 36, 3, 8.3 | 33, 3, 9.1 | 36, 1, 2.8 | 33, 1, 3.0 |
| Withdrawal due to SMS (self-report), N, n, % | 36, 2, 5.6 | 33, 2, 6.1 | 36, 0, 0.0 | 33, 0, 0.0 | 36, 0, 0.0 | 33, 0, 0.0 |
| Participants using website overall, N, n, % | ||||||
| Participants recording weight | 36, 8, 22.2 | 33, 5, 15.2 | 36, 6, 16.7 | 33, 3, 9.1 | 36, 4, 11.1 | 33, 3, 9.1 |
| Participants recording steps | 36, 10, 27.8 | 33, 6, 18.2 | 36, 7, 19.4 | 33, 2, 6.1 | 36, 3, 8.3 | 33, 2, 6.1 |
| Participants recording waistline | 36, 4, 11.1 | 33, 3, 9.1 | 36, 3, 8.3 | 33, 0, 0.0 | 36, 1, 2.8 | 33, 0, 0.0 |
| Participants recording belt notches | 36, 2, 5.6 | 33, 0, 0.0 | 36, 2, 5.6 | 33, 0, 0.0 | 36, 0, 0.0 | 33, 0, 0.0 |
| Number of participants self-monitoring, N, n, % | ||||||
| Used no self-monitoring feature | 36, 24, 66.7 | 33, 26, 78.8 | 36, 28, 77.8 | 33, 30, 90.1 | 36, 31, 86.1 | 33, 29, 87.9 |
| Used one self-monitoring feature | 36, 5, 13.9 | 33, 2, 6.1 | 36, 2, 5.6 | 33, 1, 3.1 | 36, 3, 8.3 | 33, 3, 9.1 |
| Used two self-monitoring features | 36, 3, 8.3 | 33, 3, 9.1 | 36, 3, 8.3 | 33, 2, 6.1 | 36, 1, 2.8 | 33, 1, 3.0 |
| Used three self-monitoring features | 36, 3, 8.3 | 33, 2, 6.1 | 36, 2, 5.6 | 33, 0, 0.0 | 36, 1, 2.8 | 33, 0, 0.0 |
| Used four self-monitoring features | 36, 1, 2.8 | 33, 0, 0.0 | 36, 1, 2.8 | 33, 0, 0.0 | 36, 0, 0.0 | 33, 0, 0.0 |
| Number of times participants used self-monitoring feature, n, mean, SD | ||||||
| Number of times participants recorded weight | 69, 1.9, 4.3 | 115, 3.5, 11.4 | 45, 1.3, 3.2 | 23, 0.7, 2.6 | 42, 1.2, 4.8 | 46, 1.4, 5.5 |
| Number of times participants recorded steps | 419, 11.6, 26.9 | 296, 9.0, 23.0 | 350, 9.7, 27.0 | 102, 3.1, 16.7 | 397, 11.0, 41.0 | 74, 2.2, 9.1 |
| Number of times participants recorded waistline | 4, 0.1, 0.3 | 7, 0.2, 0.7 | 5, 0.1, 0.3 | 0, 0, 0.0 | 2, 0, 0.0 | 0, 0, 0.0 |
| Number of times participants recorded belt notches | 8, 0.2, 1.0 | 0, 0, 0.0 | 4, 0.1, 0.5 | 0, 0, 0.0 | 0, 0, 0.0 | 0, 0, 0.0 |
The majority of intervention participants remaining in the study (54/69, 78%) did not request for the narrative SMS to stop. However, some participants reported strong negative reactions. Eleven participants (16%) requested that the narrative SMS stop but chose to remain in the trial at the time. Of the eleven participants who requested to stop receiving the narrative SMS, one later withdrew from the study and one was lost to follow-up at 12 months. Requests to stop the narrative SMS were similar in both arms (SMS + I, 5/36, 14%; SMS only, 6/33, 18%), and occurred throughout the study, with at least one participant per arm requesting the narrative SMS to stop between 0 and 3 months, 3 and 6 months, and 6 and 12 months, respectively. Four participants (6%) asked to withdraw from the study completely because of the narrative SMS. Complete study withdrawal because of the narrative SMS was comparable between the arms (SMS + I, 2/36, 6%; SMS only, 2/33, 6%). All withdrawals because of the narrative SMS occurred between 0 and 3 months.
Some participants replied spontaneously to one or more of the narrative SMS received (0–3 months, 36%; 3–6 months, 12%; 6–12 months, 19%). Most replies were received between 0 and 3 months (n = 370 replies), with fewer replies sent at 3–6 months (n = 16 replies) and 6–12 months (n = 39 replies). The number of replies differed between the two arms, with those in the SMS + I arm sending more replies during the study (289 vs. 81 at 0–3 months, 10 vs. 6 at 3–6 months, and 28 vs. 11 at 6–12 months for SMS + I and SMS only, respectively).
Based on the qualitative interviews at 3 and 12 months, polarised views of the narrative SMS emerged. Participants’ views ranged from extremely positive to indifferent or extremely negative. Those with extremely negative views tended to subsequently request to stop receiving the narrative SMS. The qualitative analysis supports the quantitative findings reported in Table 16 that satisfaction with the narrative SMS did not appear to change over time.
A matrix coding query and analysis of the quotations generated from the NVivo qualitative and demographic data suggested no obvious relationships between participant SIMD category and the qualitative accounts of acceptability of the narrative SMS (see Appendix 24). This is in line with quantitative data showing similar acceptability ratings for overall programme satisfaction and helpfulness ratings of the narrative SMS across SIMD categories. Those who expressed positive views described the narrative SMS as well written and entertaining and as having some resonance with their own lives. The storyline was engaging, and some participants felt a certain camaraderie with the main character:
. . . it’s like having a friend who’s in the same boat, and you’re both trying to achieve the same thing. And that’s always helpful.
110024, SMS + I, 3 months
It appeared that the more participants reported identifying with the characters and empathising with their situations, the more likely they were to enjoy the stories and look forward to the next ‘episode’:
You get involved in the content and you start following the script, they’re very funny and me being a [from city name] you can see the funny side and you can see the wit in that . . . and that’s what keeps you reading them.
210010, SMS only, 12 months
Participants who were happy to receive the narrative SMS found the indirect nature of the prompts appealing, providing a ‘nudge’ towards healthy eating or more exercise through the actions of the characters. Being part of a storyline encouraged engagement and adoption of the suggested behaviours:
I’m more likely to read them and notice them because they are a story, rather than just an alert on the phone saying, eat properly or walk today or something. So that combination of a story with an objective and a character, a developing character I think is useful in just implanting it in the mind somewhere.
110021, SMS only, 3 months
The balance of entertaining narrative and weight loss messages was considered to be about right by those who liked and felt engaged by the narrative SMS.
Some participants welcomed the main character’s gradual realisation that he needed to lose weight. When he began to take heed of advice from his health-conscious mentor, participants perceived this as more of an incentive to follow suit and apply some of the hints and tips to their own lives. It was suggested that this should have happened from the beginning in order to maximise the benefits.
However, even those who enjoyed the narrative SMS were less certain about the role of the SMS in helping to support weight loss:
I found that I was doing that myself without . . . they were amusing, don’t get me wrong, the scripts were quite funny, but they didn’t really do anything for me in terms of motivating me.
210010, SMS only, 3 months
A matrix coding query suggested no obvious relationships between participant weight change and acceptability of the narrative SMS. For instance, exploring the views of those who lost the most weight (≥ 10% at 12 months) showed a range of views about the narrative SMS from very positive to negative.
Many participants expressed an indifference towards the narrative SMS or were unsure what the point of them was but continued to receive them as they regarded them as part of the programme. Others described how their interest in the narrative waned over time or that they would engage with them intermittently. Some would have appreciated interactive feedback and an opportunity to engage in a dialogue with the characters or storyline:
I’m thoughtful that others might not [respond to replies] and then just get switched off and not just by the story but from the whole thing of being interactive with their weight loss because this character’s not interacting with me.
220045, SMS + I, 3 months
However, even participants who were indifferent to the narrative SMS saw the value of receiving a regular reminder that they were taking part in a weight loss programme:
I often wonder, do they relate to myself here. And the only commonality is both trying to lose weight. So in that respect it’s just a reminder all the time, you should be reviewing your weight and watching what you’re eating, so . . . from that it’s a positive, yeah.
220017, SMS + I, 3 months
Those participants who did not enjoy the SMS and either ignored them or requested that they be stopped reported that the storyline did not resonate with their experience or that they did not empathise with the main characters. The characters were perceived to be stereotypical ‘fat guys’ who had gained weight by eating badly, drinking too much and being couch potatoes, whereas many of the participants had gained weight despite perceiving themselves to be active and have a good diet. Very few felt that they drank to a risky extent or drank excessively. They knew that they ate too much, but it was not necessarily unhealthy food:
I’m not a lover of chocolate, biscuits, cake, ice cream, I hardly ever touch them, hardly ever so hearing about somebody eating pizza or sweets means nothing to me because I don’t eat them anyway.
120002, SMS + I, 12 months
I paid attention to them for the first probably month, month and a half, but I found I had no relation to the guy, he just was a prat and he annoyed me.
110011, SMS only, 3 months
Other participants said that the frequency of SMS became a source of irritation that added to their perception that the SMS were not aiding their weight loss:
Three months I’ve had it, and I’m getting more than four a day, roughly four a day, so that’s going to be about 1500 texts in a year. And if they’re all like this, why? It’s not helping to lose weight, it’s not encouraging me one little bit.
220014, SMS + I, 3 months
Although some ‘wouldn’t change anything’ about the narrative SMS, others would have preferred the SMS to be based on more factual information and be more ‘encouraging’. A few participants felt that it took too long for the main character to start making health behaviour changes and they wanted to have more information about his approach to weight loss. Another suggestion was to draw on the stories of participants’ own weight loss experiences and write these into the SMS:
A person who is overweight or has been overweight for quite some time, it would be good for them to get the message over and say, yes, I was like that and I did this and this is how I feel, this is what I’m doing to keep the weight off, which is another important message.
110003, SMS, 3 months
The story-based style of the narrative SMS carried the risk of being too similar to participants’ real experiences and potentially raising distressing emotions. One example was the storyline about the impact of the main character’s possible divorce, a situation that had led to a participant’s relative demonstrating suicidal behaviour. The research fellows followed the study’s ethics protocol to ensure participant well-being.
Acceptability of endowment incentive
Two health boards were prepared to fund the financial incentives offered in the study, with agreement that the £400 endowment would be made by the University of Stirling, with money subsequently reimbursed.
At 3 months, 31 out of 36 SMS + I participants attended the appointment, with eight men losing ≥ 5% of their baseline weight and securing the £50. One of these participants who met the weight loss target at 3 months withdrew from the study for an unknown reason prior to the 6-month appointment and, consequently, did not receive any financial incentive. Attendance at 6 months was lower (n = 23/36), with five participants achieving the weight loss target of > 10% weight loss securing £150 each, and a further three participants losing between ≥ 5% and 10% of weight securing between £75 and £150. At the 12-month appointment, 23 out of 36 participants attended, with three achieving >10% weight loss securing £200, and a further seven losing between ≥5% and 10% of weight securing between £100 and £200.
Overall, participants received £2955 as a result of meeting or partially meeting weight loss targets. The full amount of £400 was secured by three participants who met weight loss targets at 3, 6 and 12 months.
Researchers did not noticed any instances of gaming in the SMS + I arm when the participants were asked to empty their pockets during the baseline assessments. Participants did not display any strong emotional reactions to not meeting weight loss targets at study appointments.
Qualitative interview evidence suggests that there were no negative views about the endowment incentive; however, only one person randomised to the SMS + I arm said that he was motivated by the financial incentive. Instead, participants appeared to stress their indifference to receiving financial gain regardless of their SIMD category, and implicit cultural and moral norms and values appeared to be associated with the question of incentives.
Participants often highlighted that the weight loss was reward enough and they were more likely to emphasise how important the health benefits associated with losing weight were to them rather than any financial gain. Motivations included reducing diabetes risk, reducing joint pain and improving mobility. Thus, men reported focusing more on increasing their physical capabilities rather than achieving weight loss targets:
The money’s not that much of an issue. I think the incentive for me is the health that, at the end of the day, your health improves. That’s the most important incentive. The money, it’s fine, it’s there, but it’s not the incentive.
120022, SMS + I, 3 months
Some participants made oblique references to the positive aspect of the incentives, often saying that this was a good idea and that having weight loss targets could be motivating. Contradictory views were expressed in interviews, when participants began by talking about their lack of interest in the financial incentive, but later expressed positive views about such incentives in an abstract sense. They appeared to demonstrate a desire to establish moral high ground by distancing themselves from the financial incentive. They also demonstrated a willingness to comment favourably on the intervention, potentially in an effort to please the researcher. Accountability at the appointment visits was raised as an incentive linked to weight loss targets:
The incentive was the result rather than money ‘cause I know that I always work better towards something if I’ve got an account at the end, you know, so I’ve got to either come here and be weighed and measured and either have successfully reached the target or not, whereas if it’s nothing, there’s no accountability then that for me is the bigger variant rather than the financial side.
220040, SMS + I, 12 months
A sense of moral value or self-worth appeared to be associated with the issue of financial incentives for weight loss. For instance, many men appeared to keep the incentive aspect of the study a secret from their friends and family. Reasons for this appeared to be mixed, including that others might believe that one is losing weight only for the money. This may have been an indication that the money was more important than participants admitted openly and that they wished to avoid potential family pressure to bring home the money. However, there may also have been some confusion in relation to the participant information leaflet, which asked men not to talk publicly about the incentives to minimise unwanted publicity and avoid contamination between arms. The ambivalent views on incentives were possibly linked to guilt around weight for some and a feeling that one does not deserve a reward for what is perceived as a self-inflicted problem. As one participant put it:
[T]here’s somebody at the background putting the money into it because they recognise there’s a problem with overweight men, particularly in my age group. So somebody’s trying to do something somewhere and that’s the main thing; there’s somebody somewhere saying ‘by the way our NHS can’t afford this overweight people coming in here all the time’.
210016, SMS + I, 3 months
Varied levels of understanding about the loss aversion aspect of the incentives emerged, whereby some fully understood the concept and others simply thought that a final reward was linked to their weight loss targets. Participants who fully understood the concept commented favourably on it, using the analogy of the difference between finding money and losing it. As one participant put it:
[W]e all know how much more distress it causes you to lose money than the pleasure of finding a fiver down the back of the couch, you know, so I think if you lose something it almost has a bigger impact on you than if you gain.
220040, SMS + I, 3 months
However, some men compared loss aversion with working towards payday or spoke of the money as being a reward. In another nod to the issue of morality and self-worth, one participant said ‘it’s not as if it’s money that I’ve earned’ (210016, SMS + I, 12 months).
Some suggestions were made for improving understanding about and impact of the loss aversion approach in future studies, such as using an animation to illustrate a dwindling sum of money linked to weigh-ins. Some suggested improving the link between the SMS and the endowment incentive:
If you get a message or two every week that was like ‘hey man £400 in this amount of time, put the crisps down . . .’, you know, the information’s there, but . . . there’s no reminder that this is what you can lose and there’s no reminder that this is what you can gain.
120017, SMS + I, 12 months
Participants who achieved or partially achieved their weight loss targets tended to have plans for the money. Some men had charitable intentions; for example, one participant planned to give some of the money to a friend who was ‘not doing financially well’, whereas another pledged money to a charity as he felt that he had already ‘had a benefit out it [the study]’ and that ‘somebody else can get the benefit’ from the incentive. Others either had already ‘spent it’ or planned to spend the money on new clothes, as their current clothes had become ill-fitting after their weight loss. Another participant was determined not to waste the money and had decided to ‘treat himself’ to reward his successful efforts to lose weight:
I’m certainly not going to just put it in the bank and fritter it away, I’m actually going to buy something that actually is a celebration of the study over the last 12 months. So yeah it might be a kilt, it might just be a laptop [laugh].
220045, SMS + I, 12 months
Acceptability of study web page
Table 17 displays engagement with the web page in terms of the number of participants who used the different self-monitoring features and the number of self-monitoring features that were used over time. Some participants used the self-monitoring features (0–3 months, 27%; 3–6 months, 16%; 6–12 months, 13%). Among those engaging in self-monitoring, recording of weight and of step count were the most popular web page features, with frequency of recording decreasing over time. Recording waist circumference and belt notches was uncommon.
Qualitative evidence from participants who used the web pages was that they enjoyed being able to visually track their weight on the website and found that this motivated them to keep working towards their weight loss targets:
. . . it’s like having targets, you see it starting to change ‘oh yes I’ve got to keep going’. So yes I found the website more beneficial than the text messages.
210010, SMS only, 3 months
However, others found the appeal short-lived, particularly when their weight loss progress was not reflected in the self-monitoring graph:
What I didn’t like about logging my weight on the Game of Stones website was the increments. I mean, my line looks like that and, although I’ve lost all this weight, when you look at my line on the site it looks like they’re seeing it as more of incline. [. . .] When you’ve got a visual thing and you’re putting in a loss of, say, two kilos a week or something like that, or a kilo a week, and you’ve logging it every day, you like to see the line coming down, you know.
110019, SMS only, 3 months
Others did not access the website because they had low computer literacy, did not have time to use it or found it hard to navigate. Another participant suggested that the web page would be more appealing if it had more content, such as nutrition and exercise plans. On balance, the web page is something that works well for those with computer literacy and can be a motivator. However, men clearly expressed the view that more work could be done to improve the access (e.g. speed and number of clicks required to self-monitor) and content of the website.
Acceptability of pedometer
The majority (77%) of participants did not own a pedometer at baseline and all were given a pedometer as part of the study. At 12 months, many intervention arm participants reported using a pedometer at least a few times per week (SMS + I, 59%; SMS only, 58%). Around half (47%) of control arm participants reported using a pedometer weekly.
Qualitative views suggested that many participants were very positive about the pedometer, describing it as ‘helpful’, ‘interesting’, ‘ideal’ or ‘fantastic’. This is in line with the quantitative helpfulness ratings, as the pedometer received the highest average ratings of all of the intervention components. Some participants described how they used the pedometer every day. Noticing that their step count was lower than normal gave some men ‘a wee kick in the rear’ or started to get ‘embarrassing’, prompting them to make a ‘conscious effort to go on a walk’ or to ‘try and up it the next day’:
The step counter, I carried that absolutely everywhere with me and I’ve found that a great benefit, something small and simple like that being such a great benefit.
210010, SMS only, 3 months
Conversely, some had not used the step counter or had decided that they were ‘not great with pedometers’ after trying it initially. One participant reported that the pedometer had not been taken out of its packaging (210004, researcher field notes). In some cases, participants reported that they had not used the pedometer because a family member had appropriated it for their own use. Others used a step counter on their mobile phone or an app other than the one provided. Some men noted that the pedometer was ‘not 100% accurate’ and that there was ‘quite a disparity’ between the pedometer provided and other step counters. However, regular users of the study pedometer felt that it was ‘cheap and cheerful’ and provided a ‘good indication’ of steps:
I’m pretty damn sure it’s not accurate but it doesn’t matter, it’s consistent and it’s more accurate than colleagues who swank around with their iPhones [Apple Inc., Cupertino, CA, USA].
110021, SMS only, 3 months
Acceptability of control arm
Participants in the control arm were interviewed to gain an understanding of their views about being randomised to the waiting list to receive the SMS after 12 months. Many participants were pleased to be involved in the study despite being randomised to the control arm. As the retention figures illustrate (see Figure 12), most control arm participants were willing to attend the 12-month appointment. Altruism and the desire to support the overall study was a common motivator, although other reasons included wanting to share their final weight loss results and being appreciative of the £20 voucher offered at the final assessment:
Yeah, happy to be involved and I suppose disappointed not to be more actively involved because at the time I was setting myself my own targets of weight loss for other reasons, so the two would’ve coincided. But yes happy to assist and if it’s of overall benefit to the community, the world at large or the health service then so be it, so it was good.’
220030, control, 12 months
However, some participants allocated to the control arm were unclear about why the control arm was required for the research and one participant suggested that it could have been better explained. One participant had a strongly negative reaction to being randomised into the control arm at baseline and felt that the study had wasted his time; he subsequently decided to withdraw from the study (220052, researcher field notes).
Some participants had decided that the time was right for them to lose weight, with one joining a commercial weight loss group and losing a large amount of weight during the 12-month waiting list period (220032, researcher field notes).
Acceptability of outcome measures and feasibility of future data linkage
Acceptability of data linkage was determined by examining the qualitative interviews at 3, 12 and 15 months. The detailed methodology, results and implications of the data linkage and the outcomes that matter to men will be discussed in the associated PhD of Rebecca Skinner. A brief summary of key findings is provided here.
When data linkage was explained during interviews at 3 months, participants did not understand the concept. Thus, men providing PPI to our study were asked to advise on an accessible way of describing data linkage. This resulted in selecting videos explaining data linkage, which were shown to men to seek their views. A video was identified as a clear way to explain and visualise data linkage. Vignettes were also created with PPI input to demonstrate health-based examples of data linkage that were specific to the context of linking Game of Stones participants and their NHS data. Participants were asked their opinion of the vignettes, and a general consensus on the acceptability of data linkage emerged:
Yeah, yeah I love that sort of tracking thing.
110024, SMS + I, 12 months
When asked if any areas of data linkage were off limits, participants had no concerns other than that the data be kept anonymous:
. . . again it’s all anonymous so I don’t see any reason why anything should be off limits, nobody’s being named and shamed or anything like that, you know what I mean, so I don’t see why anything should be off limits. I think it’s a very good idea actually.
110026, control, 15 months
No, no, no as long as I’m anonymous yeah, well my only concern would be that work, you know, in terms of work they all start going ‘oh well actually I see that you drink every single weekend and I see that you’re on this website and that website’ as long as it doesn’t link with your work it’s fine.
120015, control, 12 months
The outcomes that mattered to the men participating in Game of Stones were explored in the qualitative interviews. Among the outcomes participants mentioned spontaneously in interviews at 3 months, three key concepts recurred: health, well-being and body image. In addition, nine more specific outcomes emerged from the interviews: live longer, reduce hospital visits, reduce prescriptions, reduce pain, prevent diseases, feel more comfortable, mental health, confidence and feel stronger. The relevance and importance of these three key concepts and nine specific outcomes were explored in qualitative interviews and ranking activities with participants at 12 and 15 months:
[Health] I think the underlying health issues I have, my knees wouldn’t be as sore if I didn’t carry as much weight around. I think it’s that thing of my knees are always going to be sore but let’s make them less sore.
120003, control, 12 months
[Well-being] I have issues with [mental health] cause I was always depressed and things like that, I do feel a lot better now. As I say I’ve not got the palpitations.
120031, SMS + I, 12 months
[Body image] I don’t know, obviously I don’t like the way I look at the moment because I used to be reasonably fit and I had a flat stomach whereas now I don’t have a flat stomach . . . so I know if I just lost the two or three inches of fat that I can feel there I would look better and I’d feel better. But you always do, if you look better you feel better inside yourself.
110011, SMS only, 12 months
The Game of Stones feasibility trial measures health and well-being outcomes; however, consideration is required of how body image might be measured in a future trial.
Weight outcomes
The overall rate for full follow-up (i.e. attending all follow-up appointments) was 72 out of 105 (69%). Full follow-up by arm was 21 out of 36 (58%) for SMS + I, 21 out of 33 (63%) for SMS only, and 30 out of 36 (83%) for the control arm. Full follow-up included four face-to-face appointments for the intervention arms and two face-to-face appointments for the control arm.
Table 18 shows the weight change outcomes at 3, 6 and 12 months. All weight measures for all arms at all time points indicated that participants, on average, decreased their weight. Examining observed cases, the SMS + I arm displayed mean weight loss of > 3% at 12 months (–3.51%, SD 5.83%), whereas the SMS-only and control arms remained below this threshold specified in the progression criteria (SMS only, –1.51%, SD 4.65%; control, –1.00%, SD 5.31%). At 12 months, the mean percentages of weight lost for baseline observation carried forward were –2.24% (SD 4.93%), –1.19% (SD 4.16%) and –0.80% (SD 4.77%) in the SMS + I, SMS-only and control arms, respectively. In both intervention arms, weight change peaked at 6 months for all weight measures. Weight loss was highest in the SMS + I arm for all weight measures at all time points.
| 3 months | 6 months | 12 months | |||||
|---|---|---|---|---|---|---|---|
| SMS + I | SMS only | SMS + I | SMS only | SMS + I | SMS only | Control | |
| Weight change (kg), n, mean, SD | |||||||
| Observed cases only | 31, –2.79, 3.50 | 26, –1.97, 3.97 | 23, –4.59, 5.62 | 21, –3.30, 4.92 | 23, –3.93, 5.74 | 26, –1.64, 5.64 | 29, –1.06, 6.29 |
| BOCF | 36, –2.40, 3.38 | 33, –1.55, 3.60 | 36, –2.93, 4.98 | 33, –2.10, 4.21 | 36, –2.51, 4.94 | 33, –1.29, 5.03 | 36, –0.86, 5.64 |
| LOCF | 36, –2.40, 3.38 | 33, –1.86, 3.88 | 36, –3.38, 4.92 | 33, –2.21, 4.39 | 36, –2.98, 4.91 | 33, –1.33, 5.04 | 36, –0.86, 5.64 |
| Weight change (%), n, mean, SD | |||||||
| Observed cases only | 31, –2.54, 3.47 | 26, –1.95, 3.72 | 23, –4.20, 5.54 | 21, –3.02, 4.22 | 23, –3.51, 5.83 | 26, –1.51, 4.65 | 29, –1.00, 5.31 |
| BOCF | 36, –2.18, 3.33 | 33, –1.53, 3.39 | 36, –2.69, 4.84 | 33, –1.92, 3.65 | 36, –2.24, 4.93 | 33, –1.19, 4.16 | 36, –0.80, 4.77 |
| LOCF | 36, –2.18, 3.33 | 33, –1.53, 3.39 | 36, –3.11, 4.80 | 33, –2.06, 3.85 | 36, –2.68, 4.92 | 33, –1.22, 4.16 | 36, –0.80, 4.77 |
| Weight loss categories (observed cases only), N, n, % | |||||||
| Weight gain | 31, 6, 19.35 | 26, 8, 30.77 | 23, 2, 8.70 | 21, 6, 28.57 | 23, 5, 21.74 | 26, 10, 38.46 | 29, 14, 48.28 |
| 0% to < 3% weight loss | 31, 13, 41.94 | 26, 10, 38.46 | 23, 10, 43.48 | 21, 7, 33.33 | 23, 5, 21.74 | 26, 9, 34.62 | 29, 7, 24.14 |
| ≥ 3% to < 5% weight loss | 31, 4, 12.90 | 26, 4, 15.38 | 23, 3, 13.04 | 21, 2, 9.52 | 23, 3, 13.04 | 26, 4, 15.38 | 29, 0, 0.00 |
| ≥ 5% to < 10% weight loss | 31, 8, 25.81 | 26, 2, 7.69 | 23, 3, 13.04 | 21, 4, 19.05 | 23, 7, 30.43 | 26, 2,7.69 | 29, 6, 20.69 |
| ≥ 10% weight loss | 31, 0, 0.00 | 26, 2, 7.69 | 23, 5, 21.74 | 21, 2, 9.52 | 23, 3, 13.04 | 26, 1,3.85 | 29, 2, 6.90 |
| BMI change, n, mean, SD | |||||||
| Observed cases only | 31, –0.89, 1.11 | 27, –0.73, 1.32 | 23, –1.45, 1.79 | 21, –1.04, 1.49 | 23, –1.24, 1.89 | 26, –0.49, 1.68 | 30, –0.47, 2.13 |
| BOCF | 36, –0.75, 1.07 | 33, –0.59, 1.22 | 36, –0.92, 1.58 | 33, –0.66, 1.28 | 36, –0.78, 1.60 | 33, –0.37, 1.50 | 33, –0.37, 1.96 |
| LOCF | 36, –0.75, 1.07 | 33, –0.59, 1.22 | 36, –0.93, 1.56 | 33, –0.69, 1.34 | 36, –0.93, 1.59 | 33, –0.38, 1.50 | 33, –0.37, 1.96 |
| Waist circumference change (cm), n, mean, SD | |||||||
| Observed cases only | 31, –3.74, 4.62 | 26, –3.14, 4.34 | 23, –4.70, 6.29 | 21, –3.14, 4.34 | 23, –4.40, 6.08 | 26, –2.30, 4.37 | 29, –2.26, 4.97 |
| BOCF | 36, –3.22, 4.47 | 33, –2.49, 3.94 | 33, –3.00, 5.49 | 33, –2.00, 3.76 | 36, –2.81, 5.82 | 33, –1.82, 3.98 | 36, –1.82, 4.53 |
| LOCF | 36, –3.22, 4.47 | 33, –2.49, 3.94 | 33, –3.71, 5.76 | 33, –2.23, 4.03 | 36, –3.51, 4.48 | 33, –1.85, 3.97 | 36, –1.82, 4.53 |
At 12 months, both the SMS + I and the SMS-only arms lost more weight on average than the control arm, and the SMS + I arm lost more weight on average than the SMS-only arm. Furthermore, the observed difference in weight loss between the SMS + I and SMS-only arms is larger than the difference in weight loss between the SMS-only and control arms. This pattern was observed for all three measures of weight loss. The unadjusted difference in mean percentage weight loss was −2.51% (95% CI −6.03% to 1.01%) for SMS + I compared with control and −0.51% (95% CI −3.91% to 2.89%) for SMS only compared with control. Similarly, the difference in absolute weight loss was −2.87 kg (95% CI −6.82 to 1.08 kg) for SMS + I compared with control and −0.57 kg (95% CI −4.40 to 3.25 kg) for SMS only compared with control. The difference in waist circumference was −2.15 cm (95% CI −5.58 to 1.28 cm) for SMS + I compared with control and −0.05 cm (95% CI −3.37 to 3.27 cm) for SMS only compared with control.
At 3 and 6 months, more participants in the SMS + I arm achieved the 5% and 10% weight loss targets, respectively, than did SMS-only participants (SMS + I, 8/36, 22%, vs. SMS only, 4/33, 12%, at 3 months; SMS + I, 5/36, 14%, vs. SMS only, 2/33, 6%, at 6 months). At 12 months, the numbers of participants achieving 10% weight loss were 3 out of 36 (8%), 1 out of 33 (3%) and 2 out of 36 (6%) for the SMS + I, SMS-only and control arms, respectively. The SMS + I arm had the greatest number of participants achieving at least 5% weight loss (10/36, 28%), followed by the control arm (8/36, 22%) and the SMS-only arm (3/33, 9%).
Mean percentage weight loss was examined and is reported descriptively by SIMD status and recruitment channel over time for observed cases (see Appendix 25, Table 41). In the SMS + I arm, greater weight loss across measurement time points was seen in participants from less disadvantaged areas (SIMD 3, 4 and 5) than in those from more disadvantaged areas (SIMD 1 and 2). Higher weight loss in participants from less disadvantaged areas was also found among control arm participants. This pattern was reversed in the SMS-only arm, which showed greater weight loss across measurement time points among participants from more disadvantaged areas. The magnitude of weight loss for participants from more disadvantaged areas was comparable between the SMS + I and SMS-only arms and higher in both intervention arms than in the control arm at 12 months. The magnitude of weight loss for participants from less disadvantaged areas was higher in the SMS + I arm than in the SMS-only arm. In addition, weight loss among participants from less disadvantaged areas was greater in the control arm than in the SMS-only arm.
The SMS + I arm showed similar levels of weight loss among participants recruited from community outreach and among participants recruited from general practices over time. The SMS-only arm showed a higher mean percentage weight loss in the participants recruited from general practices than in those recruited in the community at 3 months (community, –0.85%; GP, –2.89%), which was reversed at 12 months (community, –1.87%; GP, –1.20%). At 12 months, control arm participants showed a difference by recruitment channel, with those recruited from the community losing more percentage weight on average than those recruited via the GP (community, –1.75%; GP, –0.08%).
Secondary outcomes
Completion rates of all secondary outcome measures were acceptable. The rates range from 88% to 100%, with all but three items having completion rates of ≥ 95% (see Appendices 26–30).
Health behaviours
Participants provided outcomes on physical activity, sedentary behaviour, fruit and vegetable consumption, alcohol consumption and smoking status (see Appendix 26, Table 42). Small changes in the intended direction over time emerged for physical activity, fruit and vegetable consumption and alcohol consumption, with little change in smoking status and sedentary behaviours.
Weight management strategies
Participants reported using a variety of weight management strategies (see Appendix 27, Table 43). Few participants reported attending a weight reduction clinic (no attendance at 12 months: SMS + I, 96%; SMS only, 92%; control, 90%) or a commercial weight loss programme (no attendance at 12 months: SMS + I, 96%; SMS only, 92%; control, 93%) in addition to the Game of Stones programme. Modest and inconsistent increases in strategy use emerged in line with the non-prescriptive approach of the intervention.
Theory-based mediators
Theory-based mediators were measured, with acceptable rates of completion (see Appendices 28–30, Tables 33–35). Small positive changes in the expected direction were noted for several variables. Autonomous regulation (i.e. performing behaviours for internal reasons) remained relatively stable throughout the study across intervention arms over time and remained comparable at 12 months (SMS + I 6.1, SD 0.9; SMS only 5.7, SD 1.1; control 5.8, SD 1.3). Controlled regulation (i.e. performing behaviours for external reasons) in the SMS + I arm did not increase substantially over time (baseline 3.6, SD 1.6; 3 months 3.9, SD 1.4; 6 months 3.6, SD 1.5; 12 months 3.7, SD 1.5). At 12 months, the three arms remained comparable on levels of controlled regulation (SMS + I 3.7, SD 1.5; SMS only 3.8, SD 1.5; control 4.0, SD 1.6).
Health economics feasibility outcomes
Completeness of measures for economic evaluation
Of the 105 participants randomised, 57 (54%) completed resource use questions at all the time points required to estimate the costs over the trial period. Note that the required time points varied by trial arm. Complete data were required at 3, 6 and 12 months for the intervention arms, but only at 12 months for the control arm. The majority of missing data resulted from participants not completing the questionnaires at all at the required time points (n = 44, 42%). Among the 71 participants who completed the questionnaires at all required time points, one or more resource use items were missing for 14 participants. For 4 of those 14 participants, resource use was missing at all of the required time points. There were no invalid answers to the resource use questions. For further details, see Appendix 31, Table 47.
Of the 105 randomised participants, 66 (63%) completed the EQ-5D-5L at all the time points required to estimate QALYs over the trial period. Note that the required time points varied by trial arm. Complete data were required at baseline and at 6 and 12 months for the intervention arms, but only at baseline and 12 months for the control arm.
The majority of missing data resulted from participants not completing the questionnaires at the required time points (n = 34, 32%). Of the 71 participants who completed the questionnaires, five were missing one or more EQ-5D-5L responses. At 6 and 12 months, all domains were completed at the same rate. There is some variation across domains at baseline, but no clear pattern. For further details, see Appendix 32, Table 48.
Completers and non-completers of resource use and EQ-5D-5L questions did not vary systematically in terms of age, SIMD category, recruitment method, ethnicity, baseline BMI, age, comorbidity, intended weight loss, importance of weight loss and previous weight loss attempts.
Costs and quality-adjusted life-years
The intervention delivery costs are reported in Table 19 and are split into fixed and variable costs. The fixed cost includes items such as hosting the network, the study website and equipment. The total fixed cost is £17,526, which equates to £254 per participant randomised to the interventions.
| Units | Unit cost (£) | Total cost (£) | |
|---|---|---|---|
| Fixed cost | |||
| Hosting the website | 16.5 months | 1000 per year | 1650 |
| Supporting the website | 16.5 months | 304 per month | 5016 |
| Programming SMS | 2 days | 607 per day | 1214 |
| Monitoring and supporting SMS system | 12 days | 607 per day | 7284 |
| Dedicated telephone number | 16.5 months | 180 per 12 months | 247.50 |
| Hosting/supporting/maintaining network | 16.5 months | 1000 per 12 months | 1650 |
| Scales | 2 | 100 | 200 |
| Height measure | 2 | 132 | 264 |
| Total fixed cost | 17,526 | ||
| Total fixed cost per participant | 254 | ||
| Variable cost (cost per person) | |||
| SMS | Up to 604 | 0.049 per text | Up to 29.60 |
| Monitoring replies | 0.48 red-flag message per participant – 10 minutes each | 0.38 per minutea | 1.84 |
| Weighing participants | |||
| Baseline | 30 minutes | 0.70 per minuteb | 21.00 |
| 3 months | 10 minutes | 0.70 per minute | 7.00 |
| 6 months | 10 minutes | 0.70 per minute | 7.00 |
| 12 months | 20 minutes | 0.70 per minute | 14.00 |
| Incentives for SMS + I arm | |||
| Incentives | Up to 400 | ||
| Administration costs (arranging bank transfer) | 5 minutes | 0.38 per minutea | 1.92 |
The costs associated with weighing the participants at baseline and at 3, 6 and 12 months are included as these are considered integral components of the interventions rather than part of the study procedures. The baseline visit is estimated to be longer to allow time to explain the interventions and the final weigh-in at 12 months also includes a debrief.
Participants in the SMS + I arm could secure up to £400. In total, 11 participants secured money and completed the study. The average amount of money received by these 11 participants was £268.84. The average cost per participant randomised to SMS + I was £81.94 (95% CI £34.59 to £129.30). In terms of narrative SMS, participants received up to 604 messages; however, some participants opted out and the average number of SMS per participant randomised to the intervention arms was 519. Among observed cases, the average total interventions costs were £333.05 for SMS and £465.87 for SMS + I.
NHS resource use
Table 20 shows the resource use by trial arm at the different time points for the participants who completed all resource use questions to allow an estimation of the NHS costs over the trial period (N = 57; control, n = 26; SMS, n = 17; SMS + I, n = 14). This illustrates the feasibility of collecting resource use data. The numbers are small but are reported for completeness and in case other researchers want to use these estimates in future. Most notable are the high-use outliers in the control arm. One participant in this arm reported 20 days of inpatient stay and another participant reported 24 days (as well as 20 outpatient appointments). Outliers in terms of high health-care users are common in trials and unlikely to be directly related to the interventions. Outliers do not pose a problem as long as they are evenly distributed across trial arms, which is more likely to be the case in large trials.
| Resource | –3 to 0 months | 0 to 3 months | 3 to 6 months | 9 to 12 months | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SMS only | SMS + I | Control | SMS only | SMS + I | SMS only | SMS + I | SMS only | SMS + I | Control | |
| GP visits | 0.93 (1.27, 0–3) | 1.77 (1.36, 0–4) | 1.95 (3.03, 0–12) | 1.12 (1.36, 0–4) | 1.36 (1.45, 0–4) | 0.88 (1.50, 0–6) | 0.93 (1.21, 0–4) | 0.94 (0.90, 0–3) | 1.07 (1.14, 0–3) | 1.35 (1.87, 0–6) |
| Nurse visits | 0.57 (1.02, 0–3) | 0.46 (0.66, 0–2) | 1.60 (5.35, 0–24) | 1.24 (2.86, 0–12) | 0.93 (1.00, 0–3) | 0.29 (0.69, 0–2) | 0.43 (0.65, 0–2) | 0.59 (0.71, 0–2) | 0.71 (0.99, 0–3) | 2.15 (9.79, 0–50) |
| A&E attendances | 0.07 (0.27, 0–1) | 0.38 (0.65, 0–2) | 0.15 (0.49, 0–2) | 0.00 (0.00, 0–0) | 0.29 (0.47, 0–1) | 0.06 (0.24, 0–1) | 0.07 (0.27, 0–1) | 0.12 (0.33, 0–1) | 0.07 (0.27, 0–1) | 0.08 (0.27, 0–1) |
| Outpatient appointments | 0.50 (0.76, 0–2) | 1.00 (1.22, 0–3) | 1.00 (2.71, 0–12) | 0.41 (0.71, 0–2) | 1.14 (1.29, 0–4) | 0.12 (0.33, 0–1) | 1.14 (1.56, 0–5) | 0.29 (0.59, 0–2) | 0.86 (1.29, 0–4) | 0.50 (1.30, 0–6) |
| Inpatient stays | 0.00 (0.00, 0–0) | 0.38 (1.39, 0–5) | 0.20 (0.62, 0–2) | 0.12 (0.49, 0–2) | 0.00 (0.00, 0–0) | 0.06 (0.24, 0–1) | 0.00 (0.00, 0–0) | 0.00 (0.00, 0–0) | 0.14 (0.53, 0–2) | 1.69 (6.01, 0–24) |
Resource use varied considerably during the trial period across all arms of the trial (see Appendix 33, Table 49). The mean total cost was highest for the control arm, which is likely to have been caused by the outliers. It should be noted that the impact of the outliers is magnified as the resource use during months 9–12 is multiplied by four to obtain an estimate of resource use during the trial period for the control arm. The mean cost in the SMS + I arm is higher than the mean cost in the SMS-only arm. This is mainly because of differences in inpatient stays and outpatient appointments.
Quality-adjusted life-years
Table 21 shows the EQ-5D utility values by trial arm at the different time points for the participants who completed all EQ-5D questions to allow an estimation of QALYs over the trial period (N = 66; control, n = 27; SMS, n = 19; SMS + I, n = 20). At baseline, the EQ-5D utility value was lower for the control arm than for the intervention arms. The QALYs estimated using two time points only are similar to those estimated using all three time points in the intervention arms.
| Baseline | 6 months | 12 months | QALYs; three time points for intervention arms and two time points for control | QALYs; two time points for all arms (N = 72) | |
|---|---|---|---|---|---|
| SMS (n = 19) | 0.79 (0.16, 0.45 to 1.00) | 0.75 (0.19, 0.32 to 1.00) | 0.76 (0.14, 0.50 to 1.00) | 0.76 (0.14, 0.42 to 1.00) | 0.75 (0.18, 0.12 to 1.00) |
| SMS + I (n = 20) | 0.74 (0.27, –0.10 to 1.00) | 0.73 (0.30, –0.10 to 1.00) | 0.76 (0.25, 0.08 to 1.00) | 0.74 (0.27, –0.05 to 1.00) | 0.73 (0.24, –0.01 to 1.00) |
| Control (n = 27) | 0.65 (0.29, –0.17 to 1.00) | – | 0.71 (0.21, 0.24 to 1.00) | 0.68 (0.23, 0.03 to 0.95) | 0.68 (0.23, 0.03 to 0.95) |
Appendix 34 (see Table 50) shows the mean difference in cost and QALYs. The numbers are small and there are outliers. Results are reported for completeness and in case other researchers want to use these estimates in future. The difference in costs are also estimated excluding the two high-use outliers in the control arm. The sample sizes are small and the estimates therefore provide only an indication of the mean and variance of the differences. When excluding the outliers, the mean cost is higher in the intervention arms. The CIs surrounding the QALY estimates are large and the means are sensitive to including baseline utility.
Harms and unintended consequences
No harms or unintended consequences were encountered as a result of the study.
Alternative SMS outcomes
Alternative SMS were offered to 41 men at the 12-month time point: 30 waiting list control arm participants and 11 men who had previously expressed an interest in joining the study after recruitment was complete. The 11 additional men who were invited to join the study just to receive the alternative SMS were not randomised. Of the 41 men who expressed an interest in receiving the alternative SMS, 39 (95%) took up the offer (waiting list control arm participants, n = 29; additional men, n = 10).
The baseline characteristics of men who received alternative SMS are outlined in Appendix 35 (see Table 51). The men were aged 54.5 years (SD 10.4 years) and had an average BMI of 36.8 kg/m2 (SD 6.6 kg/m2), and 24 out of 39 (62%) participants lived in SIMD category areas 1 or 2.
The following section presents a comparison of alternative SMS and narrative SMS only outcomes 3 months following the initiation of the SMS. These comparisons are descriptive and are limited by a variety of factors, including (1) the difference in sample recruitment (recruitment after waiting for 12 months vs. immediate recruitment); (2) the difference in the length of the overall interventions (3 vs. 12 months); (3) the heterogeneity of the alternative SMS sample (waiting list control and new participants); (4) the lack of randomisation; and (5) the fact that SMS were delivered in different years (2018 vs. 2017), with the time of the year (March–August) roughly similar between the arms.
Appendix 36 (see Table 52) provides details of engagement, weight outcomes and intervention satisfaction ratings for the alternative SMS and narrative SMS-only arms after 3 months. After 3 months, alternative and narrative SMS were broadly comparable in terms of participants responding (alternative SMS, 39%; narrative SMS only, 30%), retention (alternative SMS, 33/39, 85%; narrative SMS only, 27/33, 83%), overall satisfaction (alternative SMS 79.4, SD 21.6; narrative SMS only 75.0, SD 22.2), helpfulness ratings of SMS (alternative SMS 3.9, SD 0.8; SMS only, 3.1, SD 1.3) or weight change (baseline observation carried forward, alternative SMS –1.72%, SD 3.68%; narrative SMS only –1.53%, SD 3.39%).
None of the participants requested to stop the alternative SMS or dropped out because they disliked the alternative SMS, compared with four participants (12%) in the narrative SMS-only arm who withdrew for that reason. All 10 men who were newly recruited (i.e. those who had not been randomised to the waiting list control arm) returned for follow-up assessment at 3 months.
Similar to the results of NVivo matrix coding related to the narrative SMS, there appeared to be no clear relationship between the acceptability of the alternative SMS and participant SIMD category. There were no strongly negative views on the alternative SMS. The more indifferent or less positive views appeared to be balanced between those living in areas of high disadvantage and those from more affluent areas.
Comments on the alternative SMS suggested that these were perceived as not drawing on stereotypes of men with obesity and did not generate a polarised response:
They didn’t strike me as too stereotypical, you know, in terms of gender which is good because we’re beyond all that now and so they weren’t laddish.
210015, control, 15 months
The factual nature of the alternative SMS was received positively, although integrating this with the interaction with different and perceived ‘real’ people seems to have made this more acceptable and enjoyable:
It was like getting texts from your mates, you know, and it came through and this is what I’m doing today or I’m not doing this or I’m having a biscuit or having a glass of wine, etc., and all it did was make you think, that’s exactly what it did and that’s what I enjoyed about it, it wasn’t highbrow.
110032, control, 15 months
The alternative SMS were informed by the qualitative interviews with Game of Stones participants after they had received 3 months of narrative SMS. Overall, the balance in the alternative SMS between the factual element and the human element was acceptable and was a reason that most men seemed to have few issues with these. Furthermore, both the variety in content and the lower frequency of messages were regarded as ways to maintain interest:
I think that was a great idea ‘cause I think everybody has a different take on it and everybody had . . . there was never two the same and that was the beauty of it, you thought ‘what’s going to come tomorrow?’
110032, control, 15 months
However, others were more indifferent to the messages and engaged with them intermittently:
I read the first three or four and to be honest I didn’t pay attention to any of the rest of them [. . .] I’ve heard this kinda stuff before so I know what helps people and what doesn’t so they didn’t do anything for me to be honest.
110026, control, 15 months
Some participants felt that the alternative SMS acted as a timely reminder that they were participating in a weight loss programme and others appreciated the tone of the messages, which offered suggestions without being authoritarian:
I think it was shall we say low key, it wasn’t ramming it down my throat, etc., it was just like prodding wasn’t it, just think about this and here this is what I’m doing, etc., it might not work for you, [. . .] but it worked for me, and you think OK, let’s have a go.
110032, control, 15 months
Some participants assumed that the alternative SMS were generated from other men’s experiences on the programme and one person thought that the alternative SMS came from the researcher conducting the appointments. Some control arm participants felt that the researchers were ‘the face of Game of Stones’, and the relationship established with them over the course of the programme may well have contributed to their continued engagement with the alternative SMS.
The narrative SMS and alternative SMS compared
The timing and frequency of both the narrative SMS and the alternative SMS was a key factor and it was noted that just getting a short ‘have a nice weekend’ message was enough to jog the memory and retain the focus on the weight management aim. There was some ambivalence around whether the actual content of the SMS (whether narrative or alternative style) effected a change in behaviour or whether the messages simply served as a reminder of the intention to lose weight.
Both styles showed promise. The narrative SMS appeared to generate stronger, more polarised views because the storyline either resonated with men’s lives or did not. Men who were unable to empathise with the characters found the messages irritating and either ignored, deleted or blocked them. This suggests that storylines with wider social relevance may have wider appeal. However, no clear link between deprivation levels and preference for styles of SMS was found among the small number of men interviewed. Although it is possible to compare the two styles only on an interpretive level, it is clear that, whereas the narrative SMS attracted positive and negative reactions, the alternative SMS attracted more muted responses, with no very strong negative or positive reactions.
Progression criteria for a definitive trial
To conclude, this chapter has shown how the a priori progression criteria for a full definitive trial have been sufficiently met. The results were discussed with the Study Steering Committee, which confirmed that Game of Stones is both feasible and acceptable to the target population of men with obesity and has demonstrated broad reach, engaging men living in disadvantaged areas. As no trial group showed superior acceptability and feasibility against the progression criteria, a three-arm trial was recommended by the Study Steering Committee.
Chapter 7 Discussion
Principal findings
The Game of Stones study successfully recruited 105 men who were obese from across the socioeconomic spectrum to a three-arm RCT within the designated time period of 4 months, and retained 74% at 12-month follow-up. Men living in SIMD category 1 and 2 areas formed 59% of the sample and more of these men were followed up after 12 months than were those living in SIMD category 3–5 areas. Participants appreciated the flexibility shown by the researchers for appointments to be undertaken after working hours and at venues that were in proximity to their home or place of work. GP surgeries were among the most acceptable venues for weight assessments. It was acceptable and feasible to deliver a narrative SMS intervention with and without endowment financial incentives to participants randomised to the intervention arms.
A minority of participants disengaged or withdrew from the study because they disliked the narrative SMS or for personal reasons. Alternative SMS were composed based on participant feedback and showed potential to reduce early negative reactions. The endowment incentives were acceptable, but men randomised to this arm seldom reported perceiving them as the primary motivator for weight loss. Positive indicative effects of weight loss were found in the intervention and control arms, which were highest in participants who received the narrative SMS with incentives.
Around one in three participants (12/36) randomised to the SMS + I arm secured at least part of the incentive, meaning that they achieved 5% weight loss at some point during the 12 months and their weight at 12 months was lower than at baseline. Few men chose to self-monitor their weight or waist circumference on the low-cost study website. The catchy study name, low-cost pedometer, personalised weight loss targets based on baseline weight, and weighing by a research assistant at 3, 6 and 12 months with some sharing of experiences were popular. A small feasibility test of blinding the research assistant to arm allocation during assessments found that this was possible.
No adverse events or evidence of gaming incentives were identified and contamination through information sharing across trial arms was minimal. Health, well-being and body image were identified as the key outcome domains that matter most to men. The acceptability of gaining consent for future follow-up and data linkage to health and well-being outcomes for a future cost effectiveness trial was demonstrated. The development and 3-month piloting of alternative SMS showed that incorporating participant feedback might improve retention and acceptability in a future trial. Two health boards funded the financial incentives offered in the study paid by the University of Stirling, with money subsequently reimbursed.
Strengths and weaknesses of the study
Strengths
This study was underpinned by the ROMEO systematic reviews and qualitative evidence synthesis of weight loss interventions for men with obesity, led by co-investigator Alison Avenell,49,88 which commenced a continuing PPI partnership with the Men’s Health Forum GB and Ireland charities. Pat Hoddinott led the qualitative evidence synthesis for ROMEO. The interventions incorporated key findings from these reviews, in particular the need for men in the target population to be involved in programme design, and gender-specific features to facilitate engagement such as the use of humour. The breadth and diversity of PPI, including Study Steering Committee guidance from the directors of ManvFat and The Alliance, helped to make the study a success.
Mixed-methods research combined process, quantitative and qualitative data, which, together with co-production and stakeholder involvement, provided a multilens perspective on feasibility and acceptability outcomes important to men. This resulted in intervention components that were novel, appealed to men including those living in disadvantaged areas and engaged men with a broad range of sociodemographic and health characteristics. Novel narrative SMS were developed based on the principles and practices of a professional commercial scriptwriter with research qualifications and experience. Endowment incentives were systematically developed based on behavioural economics and informed by a DCE with a survey of 1045 men with obesity representative of the UK population.
A workshop with men in the target group, clinicians, policy-makers, topic experts and the research team finalised the trial design. Recruitment of men focused on areas with high levels of disadvantage. The higher retention of men from those living in disadvantaged areas suggests that intervention components have the potential to positively affect health inequalities. The majority of men reported one or more obesity-related health conditions, suggesting that the intervention is acceptable for both primary and secondary prevention of obesity-related morbidity.
Two changes to the original protocol demonstrate the strength of the iterative approach undertaken to optimise intervention components in this feasibility study. Instead of hypothetical qualitative interviews in phase 1 to ascertain the acceptability of the narrative SMS, actual experiences from trial participants were sought in semistructured interviews at 3 months. Following some early negative feedback about the narrative SMS, the majority of men from both intervention arms, rather than a smaller sample, were interviewed so that a diversity of perspectives could be heard. The early finding that a narrative style of SMS did not suit all men, and men’s suggestions for changes, meant that new alternative SMS were written that maximised learning through analysis of data. Being open about limitations, analysing data and then refining interventions is important in intervention development studies to maximise the likelihood of broad reach and implementation in the future. 89
There is potential for centralised remote delivery of SMS linked to online information sources. One of the research assistants assessing men had worked as an NHS band 3 weight loss programme assistant prior to this study. Efficient incentive design linked to weight loss targets, with weight confirmed by the equivalent of NHS band 3 staff in health centre or community venues, shows promise for scale-up and future implementation, if shown to be effective in a full trial.
Weaknesses
Researchers were unable to interview men who withdrew from the study or were lost to follow-up at the 12-month appointment, but did find out brief withdrawal reasons for most participants through communication by SMS or over the telephone. Those providing a withdrawal reason may have provided socially desirable responses; for example, no participants from the SMS + I arm mentioned that they withdrew because they had failed to meet weight loss targets and missed out on a financial incentive.
SMS were personalised by including the participant’s name and weight change, but no further tailoring was possible owing to the technical limitations of the delivery system. The narrative SMS combined many information sources underpinned by differing principles and approaches and demanded artistic and creative freedom. Although leading to novel and imaginative intervention content, the development approach and the detailed social storyline have the potential to dilute exposure to evidence-based BCTs. The narrative SMS were developed iteratively, which was partially informed by the SMS responses from some participants. Replying to the SMS was optional, not all men replied and the views of non-replying participants were not considered. The lack of interactivity in response to participant replies to the SMS was a further limitation, as pointed out in qualitative interviews with study participants.
A comparison between alternative SMS and narrative SMS-only participants is limited because of differences in participant time since enrolment, intervention length and randomisation status. The content of SMS replies were not examined in depth by the qualitative research team.
The progression criterion of 12-month outcomes on at least 72% of men randomised per arm could be seen as overly sharp. The somewhat ambitious nature of the target was taken into consideration when the Study Steering Committee made recommendations for study progression to a full trial. Future studies should consider using progression criteria based on a prespecified range, such as proceed when > 75% retention, review procedures when between 60% and 75% retention, and stop the study when < 60% retention.
Owing to technical limitations, the proposed online recording of questionnaire responses and automatic upload of weight outcomes via Bluetooth-enabled (Bluetooth SIG, Inc., Kirkland, WA, USA) scales could not be implemented. The completion of online questionnaires was tested at baseline, but owing to unreliable internet connections at appointment venues the risk of missing data was high. Instead, participants completed paper-based questionnaires during the appointment and initialled the weight recorded by the research assistant to confirm its accuracy. Additional researcher time was then required for them to manually enter the data.
The study received some unintended attention in the national media around financial incentives (two newspaper articles) triggered by information in the lay summary and protocol published on the NIHR website. This may have had an impact on recruitment and attitudes towards the incentives. Every effort should be taken to avoid this happening in a full trial as it has the potential to bias the results.
Strengths and weaknesses in relation to other studies
The strengths and weaknesses of Game of Stones are discussed primarily in relation to four sets of studies, interspersed with other relevant systematic review, theory and primary evidence. These sets of studies examined (1) men-only SMS interventions delivered to men living in disadvantaged areas of Scotland; (2) international mixed-sex SMS interventions for weight loss that reported weight outcomes at ≥ 12 months; (3) financial incentive RCTs for weight loss or weight loss maintenance that reported weight outcomes at ≥ 12 months; and (4) definitive weight loss RCTs delivered in the UK NHS context.
The first set of studies are three SMS-based intervention studies delivered to men recruited from disadvantaged areas of Scotland. These studies informed the recruitment methods for our study and the decision to design bespoke narrative SMS. They took place in broadly the same geographical area as the current study. They included a feasibility RCT of 36 SMS delivered for 12 weeks targeted at reducing the frequency of heavy drinking among men from disadvantaged backgrounds,13 and the full TRAM trial, which compared 112 narrative SMS for 12 weeks with an attentional control group comprising 89 SMS on general health on the frequency of binge-drinking among disadvantaged men. 15 The MACRO (Modifying Alcohol Consumption to Reduce Obesity) study examined 95 narrative SMS for 12 weeks with one face-to-face session to support men with obesity from disadvantaged backgrounds, compared with an active control group, who received the face-to-face session only to reduce alcohol intake with a view to reducing weight. 14
The second set of studies are three international SMS-delivered weight management RCTs that report weight outcomes at ≥ 12 months. The studies include SMS weight management programmes in Finland,90 the USA91 and Latvia92 that were delivered to mixed-sex groups of participants who were overweight or obese.
The third set of studies includes three US-based financial incentive intervention RCTs for weight loss and weight loss maintenance reporting weight outcomes at ≥ 12 months. John et al. 93 examined the effectiveness of adding two different versions of deposit contracts and SMS feedback to an oral consultation with a dietitian in a three-group RCT. Leahey et al. 94 examined the addition of financial incentives or optional group meetings to a web-based intervention in a three-group RCT. Yancy et al. 95 examined two different financial incentive strategies in addition to daily self-weighing with SMS feedback.
The fourth set of studies includes three definitive recent UK weight management RCT studies reporting weight outcomes at 12 months. The FFIT study7 was a 12-week-long men-only weight management programme delivered by community coaching staff through group sessions held at professional football clubs. The study by Aveyard et al. 96 examined a brief primary care intervention with GP referral of patients of either sex with obesity to Slimming World compared with brief advice. The POWeR+ (Positive Online Weight Reduction) study97 was a 6-month mixed-sex web-based intervention delivered with face-to-face or remote additional support, compared with two printable web pages giving brief structured advice.
Recruitment
In Game of Stones, recruitment of 105 men with obesity within 4 months was feasible through both community outreach and general practice. The MACRO study14 examining a narrative SMS intervention recruited 69 men with obesity who drank > 21 units of alcohol per week in 3 months through community outreach and general practice list invitations. Another Scottish feasibility study13 examining a SMS intervention used community and general practice recruitment strategies and recruited 67 men who had had two or more binge drinking episodes in the preceding month. This recruitment strategy was, subsequently, employed in a multicentre RCT15 that consisted of four Scottish sites recruiting 825 men, demonstrating the generalisability across various contexts. Game of Stones adds to the evidence base demonstrating the feasibility of recruiting men for research on sensitive subjects such as obesity and alcohol consumption through a combination of community outreach and general practice lists.
Sample composition
Game of Stones included 59% of participants from more disadvantaged areas of Scotland, defined as areas in the SIMD 1 or 2 quintile. 69 In comparison, two Scottish men-only weight management studies recruited lower proportions of participants from SIMD category 1 or 2 areas. The FFIT study7 used community recruitment activities, and 35% of the participants randomised were from disadvantaged backgrounds. Irvine et al. 21 recruited 44% of participants from SIMD category 1 or 2 areas to a SMS intervention, including a face-to-face component, using similar recruitment strategies to those in Game of Stones. Two large English weight management studies delivered in primary care96,97 included a minority of men and recruited participants who were more affluent, on average, than the English population. Aveyard et al. 96 randomised 1882 participants (43% men) to an advice or a support group, with average Index of Multiple Deprivation scores of 15.7 and 16.4, respectively. Little et al. 97 randomised 818 participants (36% men) to a web-based intervention with face-to-face or remote nurse support or a control group, with average Index of Multiple Deprivation scores of 13.7, 13.3 and 14.3, respectively.
The BMI of around 35 kg/m2 and age of around 50–55 years of the Game of Stones participants is similar to those of participants in UK weight management trials recruiting in the community,7 primary care,96 or a combination of community and primary care. 14 Three international SMS-based weight management studies examining outcomes after 12 months recruited younger participants with lower BMI. 90–92 However, three mixed-sex weight management studies with financial incentives (two including SMS components) reported broadly similar participant demographics to those in Game of Stones. 93–95
The current sample reported average weight loss expectations at baseline that could be considered unrealistic. NICE recommends setting realistic targets for weight loss; for adults, the targets are usually a maximum weekly weight loss of 0.5–1 kg, with the overall aim to lose 5–10% of original weight. 6 The Game of Stones weight loss targets of losing 5% by 3 months and losing 10% by 6 months are in line with NICE recommendations. The relationship between initial weight loss expectations and weight loss outcomes is complex. 98 A previous study found that weight loss was higher in those with high weight loss expectations who also engaged in the BCTs by formulating specific plans. 99 Future studies need to balance participant ambition with the potential weight loss that can be achieved realistically using a self-management intervention.
Sample composition by recruitment channel
Differences in sample composition emerged between the two recruitment channels in Game of Stones. GP recruits were more likely to live in disadvantaged areas, were older, were more likely to report having a comorbidity and had a lower BMI than community recruits. Community recruitment may have more potential than GP recruitment for the primary prevention of obesity-related morbidity. The employment status of the two cohorts was broadly comparable, potentially reflecting the recruitment activity that took place at evenings and weekends to ensure that men in full-time employment were represented in the study.
Differences between community and GP recruits are comparable with those in other studies where these recruitment channels have been used. In the MACRO study,14 men with obesity recruited in the community also had a higher average BMI, and more individuals from disadvantaged backgrounds were recruited through GP obesity registers than were recruited from the community. GP recruitment in MACRO resulted in 19 out of 32 participants (59%) from SIMD category 1 or 2 areas being randomised to the study, compared with 8 out of 30 (27%) from community recruitment. Game of Stones found the same difference, albeit less pronounced (SIMD 1 or 2: community 56% vs. GP 64%). Thus, evidence suggests that community outreach activities attract participants across the socioeconomic spectrum, whereas GP recruitment is most suitable for the focused recruitment of participants living in areas of high disadvantage.
Retention
Retention levels in Game of Stones were acceptable, with 74% of the 105 men completing the 12 months’ follow-up. Differential dropout rates between the study arms were recorded, with fewer SMS + I participants completing the study (64%) than SMS-only (79%) or control arm participants (83%). Retention in the control arm was highest. Several factors contributed: a continuing desire to lose weight after the 12-month appointment, the wish to receive the 3 months of SMS, the follow-up visit with the researcher and the £20 voucher for attending follow-up. Most of the control arm participants who attended the 12-month appointment took up the offer of the alternative SMS (29/30). There was minimal information about the incentives (and no mention of the amount of money linked to weight loss targets) in the pre-randomisation information materials, and this aspect of the study was not emphasised during recruitment. The finding that retention in the SMS-only and control arms was higher than in the SMS + I arm suggests that participants did not volunteer for the study to receive the financial incentive and stayed in the trial when randomised to a non-incentive arm; therefore, disappointment bias was largely avoided, as intended.
The participant retention rate of 74% in Game of Stones is similar to systematic review evidence of men-only weight loss interventions, which found an average retention rate of 78%, ranging from 44% to 100%. 88 The men-only FFIT study7 that recruited Premier League Club football fans achieved a higher retention rate, with 89% of participants in the intervention group and 95% in the control group remaining in the study at 12 months. Similarly, the MACRO study,14 consisting of a 3-month SMS intervention for men with obesity, achieved 98% retention overall after 5 months. Two large UK studies recruiting participants of either sex with obesity to weight management in primary care reported 75%96 and 81%97 retention at 12 months.
Retention levels in Game of Stones are similar to those in international SMS-delivered intervention studies for weight management in men and women. Three RCTs reported retention rates after 12 months following a SMS weight management intervention. A Finnish study90 reported 68% retention of 125 participants (intervention, 73%; control, 64%), and a US study91 retained 76% of 170 participants (intervention, 71%; control, 82%). One Latvian study92 showed superior retention, with 95% of 123 participants completing the 12-month study.
Retention by recruitment channel
Retention differed slightly by recruitment channel, with more participants recruited from general practices completing the study (general practice, 80%; community, 71%). Interview data suggest that recruitment by GPs and assessments at general practices could increase participant retention because of the perceived endorsement of the study and the familiarity of the venue. The study data and the PPI and stakeholder feedback suggest that the difference in site retention might be due to multiple factors, such as population composition, number of local research activities or familiarity with those seen to be endorsing the study by providing venues for assessments.
Crombie et al. ’s TRAM study15 found that 93% of participants recruited through general practice registers were followed up at 12 months, compared with 77% of community recruits. Taken together with Game of Stones, this suggests that between 11% and 16% more participants complete a 12-month behaviour change intervention delivered by SMS when recruited from general practice registers as opposed to when recruited from the community.
Retention by baseline characteristics
Differences between participants completing the 12-month assessment and those withdrawing or not returning for assessment emerged, although caution is required as numbers were small. Non-completers were slightly heavier and intended to lose more weight through the programme. The modest levels of weight loss typically achieved through self-management interventions such as this programme8,18 may have left some men with greater weight loss expectations, or with higher levels of obesity, to feel disappointed at a perceived lack of progress. One of the participants who withdrew from the study, who had a BMI of > 50 kg/m2, reported multiple withdrawal reasons including a perceived lack of weight loss success. Social desirability may have prevented others reporting lack of weight loss as a withdrawal reason.
More participants from disadvantaged backgrounds remained in the study, suggesting potential for the intervention to make a positive impact on health inequalities. This could be random and there were no demographic patterns in relation to retention or intervention acceptability observed in the qualitative data analysis. Recruiting from disadvantaged areas can increase the likelihood of drop-out due to additional challenges involved in maintaining contact with participants such as changing contact information or the research competing with more pressing life priorities. 100
Game of Stones and a recent study by Crombie et al. 15 demonstrate that high retention of men from disadvantaged backgrounds participating in SMS-delivered intervention studies is possible. Crombie et al. 15 reported a retention rate at 12 months of 86% (intervention, 85%; control, 87%) for a 3-month narrative SMS intervention to reduce alcohol consumption delivered to a sample including 77% of participants from SIMD category 1 or 2 areas. Overall, the observed retention rates for men living in disadvantaged areas demonstrate promise for SMS interventions to engage men from across the socioeconomic spectrum.
Retention and relationship with the researcher
From a participant perspective, appointments with researchers for measurements, questionnaires or qualitative interviews constitute ‘an intervention’ as they would not happen in usual life outside the research context. 101,102 Nine out of 11 participants that requested to stop the narrative SMS remained in the study and attended a 12-month appointment. This indicates that these men valued other components and being part of research aside from the SMS. Qualitative findings from Game of Stones suggest that there is uncertainty about how the relationship with the researcher at the 3- and 6-month assessments affected trial retention and outcomes at 12 months. The direction of any impact cannot be assumed. The decision to undertake qualitative interviews at 3 months in the intervention arms to assess trial participants’ actual experience of receiving the narrative SMS affected the relationship with the researcher. The open questioning and active listening in qualitative interviewing contributed to supportive accountability,103 as researcher field notes documented that some participants were disappointed that the 6-month assessments were so brief. Some men valued the opportunity to share their experiences. This has implications for a full trial, where the 3- and 6-month assessments for incentive intervention linked to weight loss targets will be standardised and no qualitative interviews will take place.
Acceptability of narrative SMS
Narrative SMS were acceptable to most participants who were positive or indifferent to them, with a minority of men showing negative reactions. Two previous narrative SMS intervention studies in men targeting alcohol reduction reported high acceptability levels. The MACRO pilot RCT14 and TRAM RCT15 report no dropout or requests to stop SMS. Moreover, in both studies a high level of responses to narrative SMS were reported, with 92% of participants responding to at least one SMS at 3 months respectively, compared with 32% in Game of Stones. Both narrative SMS interventions differ from Game of Stones as they were 12 weeks in duration, contained fewer overall SMS (at 12 weeks, MACRO, n = 95; TRAM, n = 112; Game of Stones, n = 182), focused on alcohol consumption as the target behaviour and were developed closely in line with a single behaviour change theory. Moreover, both the SMS of the MACRO pilot14 and the TRAM full RCT15 interspersed narrative elements with factual information and questions that were outside the narrative story. One possibility is that narrative SMS may be more universally acceptable when used as an adjunct to, rather than the main vehicle for, intervention content delivery.
There were no obvious relationships between participant weight change and acceptability of the narrative SMS when analysing the mixed-methods data. Social comparison theory104 proposes that people can be motivated to change their behaviours through upwards and downwards comparisons with their peers. The qualitative findings from Game of Stones suggest that both of these comparisons were taking place for men during the narrative SMS.
Acceptability of financial incentives
The use of a financial incentive strategy for weight loss in men with obesity living in disadvantaged areas was feasible and acceptable. None of the men withdrew from the study because they disliked the incentives. The findings on financial incentives are in line with the PPI work that the research team undertook in preparation for the study, where the incentive component was seen as ‘probably not for everyone, but very important for some’.
As in Game of Stones, two previous studies have used SMS to inform participants about their achievement of weight loss targets, and found it acceptable. 93,95 These studies used daily SMS on weight loss and incentive achievements, compared with three SMS sent over 12 months following face-to-face appointments in Game of Stones. More frequent SMS reminders related to incentives might have increased the visibility of this intervention component. However, in Game of Stones, the decision was taken to keep the narrative SMS intervention component completely separate from the incentive intervention component, with no cross-referencing between the two. As incentive values remained the same between appointments and were available on the study website, and because participants already received frequent and relatively intensive narrative SMS, this was not necessary.
Game of Stones demonstrated that financial incentives could be used alongside an SMS intervention component containing no incentive-related elements. This extends the evidence base on the use of financial incentives as a complementary behaviour change intervention to the other components. 16,29
The financial incentive strategy was designed to have a low administrative burden, with one payout after 12 months and weight loss goals for participants that were set for a minimum of 3-monthly intervals. To objectively verify weight loss during the 12-month period, face-to-face appointments were scheduled for 3, 6 and 12 months. The selection of these time points were informed by the DCE/survey. Yancy et al. ,95 for example, provided the incentives that participants accrued through programme engagement and weight loss at 3 and 6 months for their 6-month incentive intervention, similar to the current study. John et al. 93 used more frequent follow-up schedules, with participants returning monthly to be weighed, for which they received US$20 per visit. Few RCTs have examined financial incentive strategies that are delivered for ≥ 12 months. 16 Two older studies96,105 providing financial incentives for ≥ 12 months integrated the provision of the financial incentives into weekly106 or monthly105 face-to-face meeting schedules, thus providing a somewhat more intensive intervention than Game of Stones.
Overall, 12 men secured money; 11 men received the money when they attended the 12-month appointment (study completers) and, of those, three secured the full £400. Two out of three men failed to reach the 5% weight loss target at any time point and, therefore, did not secure any money. A balance needs to be struck between weight loss targets that are ambitious enough to incentivise meaningful weight loss and targets that are achievable to avoid disappointment and withdrawal from the study. Previous studies typically have provided participants with weekly weight loss goals, such as 1 lb (0.45 kg) per week, on which financial incentives are contingent. 16 Although these goals are similar to the weight loss targets that participants were given in Game of Stones, there were no intermittent or weekly targets. A future option might be to reward lower levels of weight loss, particularly at 3 months, when, in Game of Stones, money was secured only if participants had met the overall 5% target. Rewarding any weight loss at 3 months might reinforce early weight loss achievements. Although retention was lowest in the SMS + I arm (64%), seven of the eight men who met their 3-month weight loss target went on to complete the study. A balance needs to be struck between encouraging engagement, rewarding progress and achieving meaningful and clinically significant weight loss targets.
The financial incentive strategy was designed to invoke loss aversion in a similar way to deposit contracts, whereby participants deposit their own money, which is refunded contingent on attaining weight loss goals. Deposit contracts are one of the most common strategies in financial incentive weight management interventions. 16,58 Game of Stones did not require participants to commit their own money; this was to avoid barriers to study participation, particularly from men who may experience financial constraints. A hypothetical cheque was provided to make the money seem ‘real’ for participants – a precondition for loss aversion effects to influence weight loss motivation and efforts. There was mixed evidence as to whether or not this was achieved. The qualitative evidence from this study suggests that whereas some men understood the endowment incentive, to others this was not clear. The use of visuals and more frequent reminders may improve this aspect of the financial incentive scheme.
Loss aversion framing has been used by a previous study examining the addition of financial benefits to a web-based behavioural programme. Leahey et al. 94 included a ‘bank’ web page that displayed financial incentive earnings in addition to loss aversion framed reminders. Patel et al. 36 applied a similar framing, which they called a loss incentive. University employees were allocated a monthly incentive of US$42 upfront, and US$1.40 was taken away each time their daily goal of 7000 steps was not met. The scheme was provided through the employer, making it likely that participants believed that the money was allocated.
Based on the DCE results, both the participant information and the researcher discussions at study enrolment mentioned that incentives could either be kept by the participant or donated to a charity of their choice. However, direct discussion with research assistants raising the option of a charity donation had the potential to place men in a moral dilemma, creating discomfort and potentially straining relations with the study and the researcher. To avoid this, researchers did not mention the option of charity donations in later appointments. Care should be taken in a future trial to make clear that participants can do anything they want with any financial incentive secured.
Previous evidence has suggested that the provision of financial incentives may undermine motivational quality. 107 This was not found in the current study. The SMS + I arm showed no increase in average levels of controlled regulation, and levels of autonomous regulation remained high and stable. Qualitative evidence suggested that participants frequently reported their internal motivation for losing weight. The endowment incentive did not appear to undermine the quality and strength of participants’ motivation to lose weight. This is in line with a systematic review that examined whether or not the provision of extrinsic incentives eroded intrinsic motivation (183 studies; 212,468 participants), which concluded that ‘incentives and intrinsic motivation are not necessarily antagonistic and are best considered simultaneously’. 108
Acceptability of other intervention components
The low-cost intervention website was acceptable and used by some to self-monitor behaviour and weight, but most did not engage with this component. Compared with web-based weight management studies,97 the Game of Stones interventions offered the web page as an adjunct to, rather than the main vehicle for, delivering intervention content, but more effective engagement109 with this study element could be promoted in the future. This could be achieved by engaging website designers to improve the usability and appeal, as some participants disengaged because they found navigating the web pages and information time-consuming.
The study pedometer was the most popular intervention component based on helpfulness ratings. The majority of participants (76%) reported that they had not owned a pedometer prior to the study, underlining the relevance of including this when recruiting men living in disadvantaged areas. Previous research has also found pedometers acceptable as a behaviour change tool,110,111 including for weight loss interventions for men. 88
Acceptability of waiting list control
The acceptability of the waiting list control and the high retention rates in this arm suggest that no change is required in a future full trial. In the light of the qualitative findings relating to social accountability arising from the participant–researcher relationship, the decision to only assess outcomes at baseline and 12 months is endorsed and provides as close to ‘life as usual’ over 12 months as is possible in a RCT.
Feasibility of study procedures
Feasibility of intervention delivery was demonstrated by high intervention fidelity. No major technical errors occurred. The majority of the sent SMS (95%) were returned with a successful delivery status, similar to previous SMS-based intervention studies. 13–15 Numbers of missing data were acceptable once the initial online questionnaire completion had been abandoned. The selected cost and outcomes measures for the cost-effectiveness analysis were also feasible, with missing data mainly resulting from questions being overlooked by participants when completing self-report questionnaires.
Of the 105 participants randomised, 57 (54%) completed resource use at all of the time points required to estimate the costs over the trial period. There are two limitations to the resource use measures used in this study. First, no data were collected on medications, which may differ across intervention arms; for example, Hunt et al. 7 found lower medication costs (antidepressants, painkillers, asthma, pain gels/creams, anti-inflammatories and sleeping tablets) among participants in the FFIT intervention than among those in the control group. Excluding medication costs may, therefore, result in more conservative estimates of the cost-effectiveness of the interventions. A full trial should consider using routine data to collect information on medication use and other resource use in the NHS for each participant. Men found routine data linkage acceptable in this study once a video explaining the rationale for anonymisation had been provided. Second, resource use in the control group was only measured for months 9–12 during the trial follow-up. Assumptions therefore had to be made to estimate the cost for the full trial period. Outliers that occur during this period are magnified and can bias results.
Two men reported that they had met other men in the programme, suggesting that the recruitment strategies used are unlikely to lead to high levels of contamination.
No adverse events were encountered in this study, similar to a previous narrative SMS study targeting obesity in disadvantaged men. 14
Indicative effects
The Game of Stones study was designed to assess the feasibility of outcome data collection and is not powered to detect effects on weight loss, so study and weight outcomes should be interpreted with caution. Favourable indicative effects of weight loss in the Game of Stones intervention arms support a fully powered RCT. The MACRO14 pilot RCT that aimed to reduce obesity by targeting alcohol consumption in men reported an increase of 0.4 kg in the intervention group, which received narrative SMS that were considered highly acceptable.
In full-scale trials, weight loss in the men-only FFIT trial delivered face-to-face at professional football grounds was 5·56 kg (95% CI 4.70 to 6.43 kg) at 12 months. 7 Another recent UK trial delivered to mixed-sex participants, examining a brief intervention delivered in primary care, reported –2.43 kg (SD 5.16 kg) in the intervention group. 96 A UK trial of a 6-month web-based weight management intervention with either face-to-face or remote nurse support found that participants receiving web support alone lost almost 3 kg at 12 months, with those receiving face-to-face nurse or remote nurse support showing an additional weight reduction of 1.5 kg (95% CI 0.6 to 2.4 kg) and 1.3 kg (0.34 to 2.2 kg). 97 International SMS intervention studies reporting weight loss outcomes following 12 months of SMS have found weight loss of –4.5,90 –1.6591 and –2.40 kg. 92
The evidence for the effectiveness of financial incentives for weight loss and weight loss maintenance when added to behaviour change interventions remains mixed. 16,29,58 A recent trial95 examining the effects of lottery or direct financial incentives found no additional benefit to daily self-weighing and SMS feedback interventions on weight loss maintenance at 12 months [lottery −1.8 (SD 10.5) kg; direct −0.7 (SD 10.7) kg; and control −0.3 (SD 9.4) kg]. Another study94 examined the addition of small financial incentives to a web-based behavioural intervention, reporting higher weight loss at 12 months [web + incentives: –3.1% (95% CI 1.8% to 4.4%); web only: –1.2% (95% CI 0.1% to 2.6%)].
Meaning of the study: implications for future research
The Game of Stones study has demonstrated the feasibility and acceptability of proceeding to a fully powered three-arm randomised trial of SMS with and without incentive interventions, compared with waiting list control, for men with obesity. An independent Study Steering Committee agreed that the prespecified progression criteria had been sufficiently met. Given that there was no strong evidence for changing to a two-arm trial, the committee recommended proceeding with a three-arm trial. There is insufficient evidence from the literature that incentives alone, without any additional support, are effective for the complex and sustained behaviour change that is required for long-term weight loss. If incentives were rolled out outside the context of a research study, men would be free to engage in a range of additional existing interventions currently offered in and outside the NHS, such as group programmes, to support them to reach their targets. By combining incentives with a low-cost scalable SMS component, a standardised support component is provided. The findings of this feasibility study support a fully powered three-arm trial. The current study design will not be able to demonstrate the effectiveness of the endowment incentive approach, compared with alternative ways of framing incentives, for example as rewards. Implications for and potential minor modifications to a fully powered trial are noted below.
SMS content and delivery
Tailoring SMS content and delivery might increase intervention engagement and improve study retention. Many men reported in phases 1 and 2 that they would have preferred fewer SMS or to receive the SMS at specific times only. A greater focus on weight management topics, including the use of factual information and links to sources of information, was suggested by several men. A future fully powered trial will require SMS that are optimally acceptable, are delivered over 12 months, and balance tailoring options important to men with the delivery of key active ingredients specified in the underlying study logic model and supported by evidence. In addition to tailoring, interactivity was an element desired by several participants, but this was not possible in the context of the underlying SMS system. Future studies should explore including interactivity and feedback elements in SMS.
Based on study findings and current evidence on SMS for weight management, SMS interventions can engage men in weight management. The mechanisms of action for the features of SMS and their relationship to acceptability and effectiveness warrant further research.
Endowment incentive strategy
In the SMS + I arm, retention was lowest and indicative effects on weight loss were highest. Findings suggest several possible reasons, although the numbers were small and the differential dropout might have been random. Disappointment at not achieving weight loss targets and losing the incentive could have been amplified for some by the loss framing of the intervention or the lack of perceived helpfulness of the narrative SMS. Social desirability, disappointment or social accountability to the researcher might be influences. Incentives were not prominent in recruitment materials, so some participants might have been indifferent to the intervention, particularly those who did not report that the incentives motivated them. PPI suggests that future iterations of the endowment incentive strategy could introduce incremental incentives for each 1% of weight loss between 3% and 5% at 3 months to improve motivation and reduce disappointment for some men. Given the controversy around financial incentives as an intervention, members of the public, service providers and policy-makers could find the provision of incentives for weight loss below the clinical significance level of 3% unacceptable. During the design of the incentive schedule for weight loss in phase 1, careful attention was paid to a variety of elements, such as the incentive size, spacing, presentation and weight loss targets, to balance the motivational potential of incentives with avoiding undue disappointment. There was no strong evidence to suggest that any of the elements that were carefully selected in the current study induced unintended consequences.
In a future trial, careful attention will be required to explore whether or not endowment incentives differentially influence weight loss and retention at 12 months according to participant level of disadvantage. Men in the SMS + I arm from more disadvantaged areas were more likely to stay in the study for 12 months than, but did not lose as much weight on average as, 12-month appointment attendees from less disadvantaged areas; however, the numbers are small. Effectiveness is known to be the key determinant of public acceptability overall,66 but this might be compromised if incentive interventions favour more advantaged individuals.
There is a case for a longer assessment window for all weight loss assessments as, particularly during the school holidays, it was problematic for researchers to schedule appointments within a 2-week window. Some flexibility and trust is required when participants miss appointments because of transport problems, admissions to hospital or other incidents96 outside their control, when financial loss is at stake.
Assessment schedules
Assessment schedules for intervention participants at 3, 6 and 12 months were feasible and acceptable, and these should be retained in a future trial. Attendance at the 6-month appointment was lowest. An option would be to provide reimbursement for engagement with study procedures at 6 and 12 months; however, this would be unlikely to be rolled out after the research and could potentially interact with the interventions, particularly with a waiting list control arm who do not receive the interim assessments. No evidence emerged to suggest that a 9-month appointment would have added value or increased retention. The assessment schedule of baseline and 12 months was feasible and acceptable to the control arm and should be retained.
Qualitative evidence suggests that intervention participants valued personal contact with researchers during the otherwise remotely delivered intervention. Given that the incentives are contingent on verified weight loss, some level of sustainable and scalable personal contact will need to be retained for the delivery of this intervention component. Data suggest that verifying weight and providing brief motivational support would be feasible for a NHS band 3 health promotion or dietetic assistant (the previous employment role of one of our research assistants) and cost £49 per participant attending all four scheduled meetings (see Table 19). The verified weight and brief motivational support intervention component has the potential to be more cost-effective than a brief intervention delivered by GPs and to release valuable GP time. 96
Refine participant information
Study information materials and researcher discussion at baseline and follow-up appointments could further emphasise that it is important for men to attend appointments regardless of what has happened to their weight. Qualitative data analysis suggests that researchers could emphasise to participants that they are there to make measurements and to listen to experiences, and will not be disappointed if weight loss has not occurred or, indeed, if weight gain has occurred. Including this in researcher recruitment and follow-up protocols would acknowledge that supportive accountability is possible, particularly when assessments are undertaken in the participant’s general practice.
Outcome measures
Two changes to assessments of key variables could be considered. First, data linkage to routinely collected data was found to be acceptable in this study and could complement self-reported health service use measures. Longer recall periods (i.e. 12 months) for health service use questions would allow comparisons between intervention and control arms. In the current study, health service use was reported for the last 3 months only, which made comparison between intervention and control participants possible for only the final 3 months of the study. Second, the current study focused primarily on weight and waist circumference as these would be the primary outcomes of a future fully powered trial. Other potentially important outcomes that matter to men could be added as relevant outcomes. This is currently being investigated by the Game of Stones PhD student.
Study website
The study website was low cost and has room for improvement; engaging with experienced website designers could improve its functionality, design and content. Some participants used the self-monitoring features offered. A future study might signpost participants to existing self-monitoring options, including links in SMS, rather than offering this on the current website, which could act as an information point rather than as an intervention tool.
Recruitment channels
Both the community and the GP recruitment channels were successful and each has advantages and disadvantages. Additional back-up strategies to improve recruitment rates, which had ethics approval, were not required. There was no evidence of gaming (e.g. deliberately increasing baseline weight by not disclosing objects in a pocket) among the financial incentive participants recruited from either channel.
There are strong arguments for keeping both recruitment strategies in a full trial, as both are feasible and acceptable, and some participant characteristics differed by recruitment channel. Beyond the full trial, we propose that men could be signposted to the intervention by GPs and other NHS and social care providers and through media promotion, as both the SMS and the incentive payment systems could be centralised and delivered remotely. Signposting through general practice, NHS and community routes would offer both primary and secondary prevention for men with obesity. General practice recruitment requires more set-up time for recruiting practices and for the clinical staff to screen lists of potentially eligible patients. Then, men opting in to the study could often be seen concurrently at general practices, making it logistically easy and efficient for researchers doing fieldwork. However, general practices are currently experiencing significant resource and time restraints that can impede recruitment to research. These issues are not unique to this study and require consideration by policy-makers and senior decision-makers.
Community recruitment of around 2 hours per participant randomised is comparable with that of many trials and returns participants from across the socioeconomic spectrum, including those without obesity-related comorbidities. It is a reliable and a steady source of participants, especially once research assistants develop community networks and gain experience. Broader community recruitment activities are an additional option, such as online social media and local media recruitment via adverts. This would be potentially less resource and time intensive and could increase participants recruited through word of mouth, but would decrease the traceability of participants and could increase the potential for contamination.
Conclusion
The men-only remotely delivered weight management interventions consisting of narrative SMS and financial incentives were broadly acceptable. Tailoring options for SMS may improve acceptability and retention. The intervention components and trials procedures require minor revisions in the light of the obtained feedback for testing in a multisite definitive RCT.
Acknowledgements
This project was funded by the NIHR Public Health Research programme. Further information is available at www.gameofstonesresearch.com (last accessed 25 June 2019).
The Nursing, Midwifery and Allied Health Professions Research Unit at the University of Stirling and Glasgow Caledonian University, the Health Services Research Unit and Health Economics Research Unit at the University of Aberdeen are core funded by the Chief Scientist Office of the Scottish Government Health and Social Care Directorate. The views and opinions expressed are those of the authors and do not necessarily reflect those of the funders.
We would like to acknowledge the following people who have contributed to this study.
All men who contributed to PPI and who participated in the study.
Colin Fowler from the Men’s Health Forum in Ireland, who was involved in the ROMEO systematic review that informed this study, and commented on the grant application, the protocol and this final report. Together with Paula Carroll, he accessed wider PPI in Ireland, as described in Chapter 2.
Fiona Hogarth, Director Tayside Clinical Trials Unit, oversaw randomisation, data management and the running of the study from a Clinical Trials Unit perspective.
Hannah Collacott was employed as a research assistant at the Health Economics Research Unit, University of Aberdeen, in 2016–17. She undertook the think-aloud interviews and PPI and assisted in the design and preliminary analysis of the DCE described in Chapter 4.
Clinical, Community and Academic Networks advised our team on many aspects of this study, including NHS Research Scotland Primary Care Network and the general practices involved, Alliance Scotland, community health councils and health centres.
The following master’s students accompanied the research assistants when recruiting men from the community (in alphabetical order): Norelle Calder-Macphee, Ines Elenin Lucy Gunatillake, Bryony Lang, Heather Renwick and Amy Spiteri.
Karen Stanton, Lorna Kerr, Karen Murray, Siobhan McDermott and Suzannah Hunter provided administrative support.
The previous work of Professor Crombie and his team at Dundee, who assisted with the grant application for this study. The following publications by Professor Crombie and his team informed this study:
-
Crombie IK, Falconer DW, Irvine L, Williams B, Ricketts IW, Humphris G, et al. Reducing alcohol-related harm in disadvantaged men: development and feasibility assessment of a brief intervention delivered by mobile telephone. Public Health Res 2013;1(3).
-
Crombie IK, Irvine L, Falconer DW, Williams B, Ricketts IW, Jones C, et al. Alcohol and disadvantaged men: a feasibility trial of an intervention delivered by mobile phone. Drug Alcohol Rev 2017;36:468–76.
-
Irvine L, Crombie IK, Cunningham KB, Williams B, Sniehotta FF, Norrie J, et al. Modifying alcohol consumption to reduce obesity: a randomized controlled feasibility study of a complex community-based intervention for men. Alcohol Alcohol 2017;52:677–84.
-
Crombie IK, Irvine L, Williams B, Sniehotta Falko F, Petrie D, Jones C, et al. Texting to Reduce Alcohol Misuse (TRAM): main findings from a randomized controlled trial of a text message intervention to reduce binge drinking among disadvantaged men. Addiction 2018;113:1609–18.
The Study Steering Committee:
-
Associate Professor Ed Juszczak Director, NPEU Clinical Trials Unit, Nuffield Department of Population Health, University of Oxford (chairperson).
-
Professor Kate Jolly, Professor of Public Health & Primary Care, University of Birmingham.
-
Mr Mark Kelvin, Programme Director (until 2018), Health and Social Care Alliance Scotland (the ALLIANCE) (PPI representative).
-
Mr Andrew Shanahan, Director of ManvFat – the weight loss website for men (PPI representative).
-
Ms Martine Stead, Institute for Social Marketing, University of Stirling (sponsor’s representative).
-
Miss Joyce Thompson, Dietetic Consultant in Public Health Nutrition and Tayside Nutrition MCN Lead Clinician, NHS Tayside.
Contributions of authors
Stephan U Dombrowski (https://orcid.org/0000-0001-9832-2777) (Assistant Professor, Health Psychology) co-led the study with Pat Hoddinott as joint chief investigator. He co-led the design and overall conduct of the study and led the writing of the report.
Matthew McDonald (https://orcid.org/0000-0002-8191-8854) (Research Assistant, Health Sciences) undertook the study set-up, recruitment and data collection, co-ordinated various PPI activities, contributed substantially to qualitative and quantitative data analysis and interpretation. He wrote the first drafts of substantial sections of the report concerning PPI (see Chapter 2), recruitment, assessment, retention and acceptability of financial incentives (see Chapters 5–7).
Marjon van der Pol (https://orcid.org/0000-0003-0636-1184) (Professor, Health Economics) was a co-investigator. She contributed to the design and the interpretation of findings. She led the DCE and health economic analysis for the feasibility trial. She wrote Chapter 4 and the health economic sections of Chapters 5 and 6.
Mark Grindle (https://orcid.org/0000-0002-3237-7369) (Senior Lecturer, Scriptwriter in Digital Health) was a co-investigator. He contributed to the design and the interpretation of findings. He led the development of the narrative SMS component, the related PPI work and wrote Chapter 3.
Alison Avenell (https://orcid.org/0000-0003-4813-5628) (Professor, Health Services Research) was a co-investigator. She contributed to the design and the interpretation of findings. She supported updates to relevant systematic reviews.
Paula Carroll (https://orcid.org/0000-0001-8465-4535) (Men’s Health Forum in Ireland) was as a co-investigator, linked to PPI networks, contributed to the design and interpretation of the findings.
Eileen Calveley (https://orcid.org/0000-0001-8731-2338) (Research Fellow, Health Sciences) contributed to the analysis and interpretation of the qualitative data.
Andrew Elders (https://orcid.org/0000-0003-4172-4702) (Senior Statistician, Trials Methodology) was a co-investigator. He contributed to the design and the interpretation of findings. He oversaw the statistical analysis.
Nicola Glennie (https://orcid.org/0000-0002-8857-4417) (Dietitian, Masters in Research, Student) contributed to the analysis and interpretation of the qualitative data.
Cindy M Gray (https://orcid.org/0000-0002-4295-6110) (Senior Lecturer, Social Sciences) was a co-investigator. She facilitated PPI from the FFIT trial to inform the study, contributed to the design and the interpretation of findings.
Fiona M Harris (https://orcid.org/0000-0003-3258-5624) (Associate Professor, Social Sciences) was a co-investigator. She oversaw the qualitative data collection and analysis and contributed to the interpretation of findings
Adrian Hapca (https://orcid.org/0000-0003-0145-0700) (Research Statistician, Statistics) undertook the statistical analysis at Tayside Clinical Trials Unit.
Claire Jones (https://orcid.org/0000-0001-6136-7111) (Senior Software Engineer, Health Informatics) was a co-investigator. She contributed to the design and the interpretation of findings. She oversaw the automated SMS delivery system, recruitment tracking, the study website and integration of data with databases at Tayside Clinical Trials Unit.
Frank Kee (https://orcid.org/0000-0002-0606-8167) (Professor, Public Health) was a co-investigator. He contributed to the design and the interpretation of findings.
Michelle C McKinley (https://orcid.org/0000-0003-3386-1504) (Reader, Public Health Nutrition) was a co-investigator. She contributed to the design and the interpretation of findings.
Rebecca Skinner (https://orcid.org/0000-0002-8399-4527) (PhD student, Psychology) contributed to recruitment, data collection and undertaking qualitative interviews and analysis focusing on her PhD questions: the acceptability of data linkage and outcomes that matter to men with obesity. Detailed methods, findings and interpretation relating to her work will be reported separately in her PhD thesis. She conducted a systematic review of SMS interventions for weight loss. She was supervised by Stephan Dombrowski, Pat Hoddinott and Dr Sinead Currie.
Martin Tod (https://orcid.org/0000-0002-4801-1978) (Men’s Health Forum GB) was a co-investigator. He linked to PPI networks, contributed to the design and the interpretation of findings.
Pat Hoddinott (https://orcid.org/0000-0002-4372-9681) (Professor, Primary Care) co-led the study with Stephan Dombrowski as joint chief investigator. She co-led the design and overall conduct of the study and oversaw the writing of the report.
Publications
Hoddinott P, Dombrowski SU, Van der Pol M, Kee F, Grindle M, Gray C, et al. , on behalf of the Study Team. Opportunities and pitfalls encountered when using the Template for Intervention Description and Replication (TIDieR) to develop a complex intervention to reduce obesity in men. Poster at 38th Society for Clinical Trials/International Clinical Trials Methodology Conference, Liverpool, UK, May 2017. Published in Trials 2017;18(Suppl. 1):P249.
McDonald M, Skinner R, Dombrowski S, Hoddinott P, on behalf of the Game of Stones team. Game of Stones: Recruitment of Obese Men from Across the Socio-economic Spectrum into a Text-message based Weight Management Study. Faculty of Public Health Scotland Annual Conference, Aviemore, UK, 2–3 November 2017.
McDonald M, Skinner R, Hoddinott P, Dombrowski S, on behalf of the Game of Stones team. Game of Stones: Recruitment of Obese Men from Across the Socio-economic Spectrum into a Text-message based Weight Management Study. UK Society of Behavioural Medicine, Liverpool Hilton Hotel, Liverpool, UK, 13–14 December 2017.
Van der Pol M, Collacott H, Hoddinott P, Dombrowski SU, Kee F, on behalf of the Game of Stones research team. Optimising the Design of a Financial Incentive Scheme for Weight Loss using Behavioural Economics and a Survey of Individuals’ Preferences. Health Economics Study Group, University of Birmingham, Birmingham, UK, January 2017.
Van der Pol M, Collacott H, Hoddinott P, Dombrowski SU, Kee F on behalf of the Game of Stones research team. Optimising the Design of a Financial Incentive Scheme for Weight Loss using Behavioural Economics and a Survey of Individuals’ Preferences. ESRC workshop: Health Behaviours and Health Information, London, UK, 15–16 March 2018.
Invited to display poster at the 2018 Mackenzie Lecture. How Can Data and Informatics Support Clinical Research? 9 May 2018, Ninewells Hospital, Dundee, UK.
Dombrowski SU, McDonald M, van der Pol M, Grindle M, Avenell A, Carroll P, et al. Game of Stones: feasibility randomised controlled trial of how to engage men with obesity in text message and incentive interventions for weight loss. BMJ Open 2020;10:e032653.
Data-sharing statement
Access to data can be arranged through the co-principal investigators of the study; contact Pat Hoddinott (University of Stirling; p.m.hoddinott@stir.ac.uk) and Stephan Dombrowski (University of New Brunswick; stephan.dombrowski@unb.ca), to discuss data sharing, data requirements and conflicts of interest, in line with any EU and other regulations, including ethics approvals.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Dombrowski SU, McDonald M, van der Pol M, Grindle M, Avenell A, Carroll P, et al. Game of Stones: feasibility randomised controlled trial of how to engage men with obesity in text message and incentive interventions for weight loss. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-032653.
- Scottish Government . The Scottish Health Survey 2016 2017.
- NHS Digital . Health Survey for England 2016 2016.
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766-81. https://doi.org/10.1016/S0140-6736(14)60460-8.
- Robertson C, Archibald D, Avenell A, Douglas F, Hoddinott P, van Teijlingen E, et al. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18350.
- National Institute for Health and Care Excellence (NICE) . Guidance on the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children 2014.
- Hunt K, Wyke S, Gray CM, Anderson AS, Brady A, Bunn C, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet 2014;383:1211-21. https://doi.org/10.1016/S0140-6736(13)62420-4.
- Dombrowski SU, Avenell A, Sniehott FF. Behavioural interventions for obese adults with additional risk factors for morbidity: systematic review of effects on behaviour, weight and disease risk factors. Obes Facts 2010;3:377-96. https://doi.org/10.1159/000323076.
- Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ 2014;348. https://doi.org/10.1136/bmj.g2646.
- Middleton KM, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obes Rev 2012;13:509-17. https://doi.org/10.1111/j.1467-789X.2011.00972.x.
- Sharp P, Bottorff JL, Hunt K, Oliffe JL, Johnson ST, Dudley L, et al. Men’s perspectives of a gender-sensitized health promotion program targeting healthy eating, active living, and social connectedness. Am J Mens Health 2018;12:2157-66. https://doi.org/10.1177/1557988318799159.
- Morgan H, Hoddinott P, Thomson G, Crossland N, Farrar S, Yi D, et al. Benefits of Incentives for Breastfeeding and Smoking cessation in pregnancy (BIBS): a mixed-methods study to inform trial design. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19300.
- Crombie IK, Irvine L, Falconer DW, Williams B, Ricketts IW, Jones C, et al. Alcohol and disadvantaged men: a feasibility trial of an intervention delivered by mobile phone. Drug Alcohol Rev 2017;36:468-76. https://doi.org/10.1111/dar.12455.
- Irvine L, Crombie IK, Cunningham KB, Williams B, Sniehotta FF, Norrie J, et al. Modifying alcohol consumption to reduce obesity: a randomized controlled feasibility study of a complex community-based intervention for men. Alcohol Alcohol 2017;52:677-84. https://doi.org/10.1093/alcalc/agx067.
- Crombie IK, Irvine L, Williams B, Sniehotta FF, Petrie D, Jones C, et al. Texting to Reduce Alcohol Misuse (TRAM): main findings from a randomized controlled trial of a text message intervention to reduce binge drinking among disadvantaged. Addiction 2018;113:1609-18. https://doi.org/10.1111/add.14229.
- Paul-Ebhohimhen V, Avenell A. Systematic review of the use of financial incentives in treatments for obesity and overweight. Obes Rev 2008;9:355-67. https://doi.org/10.1111/j.1467-789X.2007.00409.x.
- Shaw R, Bosworth H. Short message service (SMS) text messaging as an intervention medium for weight loss: a literature review. Health Informatics J 2012;18:235-50. https://doi.org/10.1177/1460458212442422.
- Hall AK, Cole-Lewis H, Bernhardt JM. Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health 2015;36:393-415. https://doi.org/10.1146/annurev-publhealth-031914-122855.
- Palmer M, Sutherland J, Barnard S, Wynne A, Rezel E, Doel A, et al. The effectiveness of smoking cessation, physical activity/diet and alcohol reduction interventions delivered by mobile phones for the prevention of non-communicable diseases: a systematic review of randomised controlled trials. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0189801.
- Ofcom . Adults’ Media Use and Attitudes Report 2018.
- Irvine L, Melson AJ, Williams B, Sniehotta FF, Humphris G, Crombie IK. Design and development of a complex narrative intervention delivered by text messages to reduce binge drinking among socially disadvantaged men. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-018-0298-0.
- Grindle M. The Power of Digital Storytelling to Influence Human Behaviour 2014.
- Bray GA, Wadden TA. Improving long-term weight loss maintenance: can we do it?. Obesity 2015;23:2-3. https://doi.org/10.1002/oby.20964.
- Bottorff JL, Seaton CL, Johnson ST, Caperchione CM, Oliffe JL, More K, et al. An updated review of interventions that include promotion of physical activity for adult men. Sports Med 2015;45:775-800. https://doi.org/10.1007/s40279-014-0286-3.
- Mantzari E, Vogt F, Shemilt I, Wei Y, Higgins JP, Marteau TM. Personal financial incentives for changing habitual health-related behaviors: a systematic review and meta-analysis. Prev Med 2015;75:75-8. https://doi.org/10.1016/j.ypmed.2015.03.001.
- Burns RJ, Donovan AS, Ackermann RT, Finch EA, Rothman AJ, Jeffery RW. A theoretically grounded systematic review of material incentives for weight loss: implications for interventions. Ann Behav Med 2012;44:375-88. https://doi.org/10.1007/s12160-012-9403-4.
- Giles EL, Robalino S, McColl E, Sniehotta FF, Adams J. The effectiveness of financial incentives for health behaviour change: systematic review and meta-analysis. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0090347.
- Purnell JQ, Gernes R, Stein R, Sherraden MS, Knoblock-Hahn A. A systematic review of financial incentives for dietary behavior change. J Acad Nutr Diet 2014;114:1023-35. https://doi.org/10.1016/j.jand.2014.03.011.
- Ananthapavan J, Peterson A, Sacks G. Paying people to lose weight: the effectiveness of financial incentives provided by health insurers for the prevention and management of overweight and obesity – a systematic review. Obes Rev 2018;19:605-13. https://doi.org/10.1111/obr.12657.
- Paloyo AR, Reichert AR, Reinermann H, Tauchmann H. The causal link between financial incentives and weight loss: an evidence-based survey of the literature. J Econ Surv 2014;28:401-20. https://doi.org/10.1111/joes.12010.
- Jeffery RW, Gerber WM, Rosenthal BS, Lindquist RA. Monetary contracts in weight control: effectiveness of group and individual contracts of varying size. J Consult Clin Psychol 1983;51:242-8. https://doi.org/10.1037//0022-006x.51.2.242.
- House of Commons Health Committee . Impact of Physical Activity and Diet on Health 2015.
- Ryan M, Yi D, Avenell A, Douglas F, Aucott L, van Teijlingen E, et al. Gaining pounds by losing pounds: preferences for lifestyle interventions to reduce obesity. Health Econ Policy Law 2015;10:161-82. https://doi.org/10.1017/S1744133114000413.
- Camerer CF, Loewenstein G, Rabin M. Advances in Behavioral Economics. Princeton, NJ: Princeton University Press; 2003.
- Cawley J, Downs JS, Loewenstein G. Behavioral Economics and Obesity. Oxford: Oxford University Press; 2012.
- Patel MS, Asch DA, Rosin R, Small DS, Bellamy SL, Heuer J, et al. Framing financial incentives to increase physical activity among overweight and obese adults: a randomized, controlled trial. Ann Intern Med 2016;164:385-94. https://doi.org/10.7326/M15-1635.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68-7. https://doi.org/10.1037/0003-066x.55.1.68.
- Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008;57:1-29. https://doi.org/10.1111/j.1464-0597.2007.00325.x.
- Rothman AJ, Sheeran P, Wood W. Reflective and automatic processes in the initiation and maintenance of dietary change. Ann Behav Med 2009;38:4-17. https://doi.org/10.1007/s12160-009-9118-3.
- Kwasnicka D, Dombrowski SU, White M, Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev 2016;10:277-96. https://doi.org/10.1080/17437199.2016.1151372.
- INVOLVE . Guidance on Co-Producing a Research Project 2018. www.invo.org.uk/wp-content/uploads/2019/04/Copro_Guidance_Feb19.pdf (accessed 13 August 2019).
- INVOLVE . Briefing Notes for Researchers: Public Involvement in NHS, Public Health and Social Care Research 2012. www.invo.org.uk/wp-content/uploads/2014/11/9938_INVOLVE_Briefing_Notes_WEB.pdf (accessed 13 August 2019).
- Hoddinott P, Pollock A, O’Cathain A, Boyer I, Taylor J, MacDonald C, et al. How to incorporate patient and public perspectives into the design and conduct of research. F1000Res 2018;7. https://doi.org/10.12688/f1000research.15162.1.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358. https://doi.org/10.1136/bmj.j3453.
- Gamble C, Dudley L, Allam A, Bell P, Buck D, Goodare H, et al. An evidence base to optimise methods for involving patient and public contributors in clinical trials: a mixed-methods study. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03390.
- Men’s Health Forum . How to Make Weight-Loss Services Work for Men 2014.
- Canavan L. Men on the Move Activity Programme – Evaluation Report 2013. www.drugsandalcohol.ie/30668/1/men-on-the-move-evaluation-report.pdf (accessed 13 August 2019).
- Men’s Health Forum . Mind Your Language: How Men Talk About Mental Health 2018.
- Archibald D, Douglas F, Hoddinott P, van Teijlingen E, Stewart F, Robertson C, et al. A qualitative evidence synthesis on the management of male obesity. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008372.
- Keen S. Fast tracks to narrative empathy: anthropomorphism and dehumanization in graphic narratives. Subst Abus 2011;40:135-55. https://doi.org/10.1353/sub.2011.0003.
- Albæk KR, Arsovski A, Baceviciute S, Chu X, Lancor TB, Zilmer L. The Influence of Interactivity on Immersion Within Digital Interactive Narratives. 2011.
- Steele M. Development of a Theory and Evidence Informed Intervention to Promote Smoking Cessation During Pregnancy Using Narrative, Text-Messages and Images As Modes of Delivery 2015.
- Farquharson B, Johnston M, Smith K, Williams B, Treweek S, Dombrowski SU, et al. Reducing patient delay in Acute Coronary Syndrome (RAPiD): research protocol for a web-based randomized controlled trial examining the effect of a behaviour change intervention. J Adv Nurs 2017;73:1220-34. https://doi.org/10.1111/jan.13191.
- France EF, Semple K, Grindle M, Rowland C, Duncan K, McGhee J. WS05.5 Developing an audio-visual intervention to support children’s adherence to home chest physiotherapy for cystic fibrosis. J Cyst Fibros 2015;14. https://doi.org/10.1016/S1569-1993(15)30031-X.
- National Institute for Health and Care Excellence (NICE) . Behaviour Change: Individual Approaches. 2014.
- Lean MEJ, Astrup A, Roberts SB. Making progress on the global crisis of obesity and weight management. BMJ 2018;361. https://doi.org/10.1136/bmj.k2538.
- Irvine L, Falconer D, Jones C, Ricketts I, Williams B, Crombie IK. Can text messages reach the parts other process measures cannot reach: an evaluation of a behavior change intervention delivered by mobile phone?. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0052621.
- Sykes-Muskett BJ, Prestwich A, Lawton RJ, Armitage CJ. The utility of monetary contingency contracts for weight loss: a systematic review and meta-analysis. Health Psychol Rev 2015;9:434-51. https://doi.org/10.1080/17437199.2015.1030685.
- Adams J, Giles EL, McColl E, Sniehotta FF. Carrots, sticks and health behaviours: a framework for documenting the complexity of financial incentive interventions to change health behaviours. Health Psychol Rev 2014;8:286-95. https://doi.org/10.1080/17437199.2013.848410.
- Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA 2008;300:2631-7. https://doi.org/10.1001/jama.2008.804.
- Hashemi A, You W, Boyle K, Parmeter C, Kanninen B, Estabrooks P. Identifying financial incentive designs to enhance participation in weight loss programs. J Obes Weight Loss Ther 2015;5.
- Jeffery RW, Thompson PD, Wing RR. Effects on weight reduction of strong monetary contracts for calorie restriction or weight loss. Behav Res Ther 1978;16:363-9. https://doi.org/10.1016/0005-7967(78)90005-0.
- Mann RA. The behavior-therapeutic use of contingency contracting to control an adult behavior problem: weight control. J Appl Behav Anal 1972;5:99-109. https://doi.org/10.1901/jaba.1972.5-99.
- Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica 1979;47:263-91. https://doi.org/10.2307/1914185.
- Hossain T, List JA. The behavioralist visits the factory: increasing productivity using simple framing manipulations. Manage Sci 2012;58:2151-67. https://doi.org/10.1287/mnsc.1120.1544.
- Promberger M, Brown RC, Ashcroft RE, Marteau TM. Acceptability of financial incentives to improve health outcomes in UK and US samples. J Med Ethics 2011;37:682-7. https://doi.org/10.1136/jme.2010.039347.
- Andersen S, Harrison GW, Lau MI, Rutström EE. Elicitation using multiple price list formats. Exp Econ 2006;9:383-405. https://doi.org/10.1007/s10683-006-7055-6.
- Ameriks J, Caplin A, Leahy J, Tyler TOM. Measuring self-control problems. Am Econ Rev 2007;97:966-72. https://doi.org/10.1257/aer.97.3.966.
- Scottish Government . Definition of SIMD Quintiles 2013.
- Hole AR. Modelling heterogeneity in patients’ preferences for the attributes of a general practitioner appointment. J Health Econ 2008;27:1078-94. https://doi.org/10.1016/j.jhealeco.2007.11.006.
- Ozdemir S, Mohamed AF, Johnson FR, Hauber AB. Who pays attention in stated-choice surveys?. Health Econ 2010;19:111-18. https://doi.org/10.1002/hec.1452.
- van der P, M., Shiell A, Au F, Johnston D, Tough S. Convergent validity between a discrete choice experiment and a direct, open-ended method: comparison of preferred attribute levels and willingness to pay estimates. Soc Sci Med 2008;67:2043-50. https://doi.org/10.1016/j.socscimed.2008.09.058.
- Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-264.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Michie S, Free C, West R. Characterising the ‘Txt2Stop’ smoking cessation text messaging intervention in terms of behaviour change techniques. J Smok Cessat 2012;7:55-60. https://doi.org/10.1017/jsc.2012.12.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. https://doi.org/10.1136/bmj.c4587.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev 2006;63:217-35. https://doi.org/10.1177/1077558705285298.
- Curtis A, Burns L. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- NHS Improvement . Reference Costs 2016 17 n.d. https://improvement.nhs.uk/resources/reference-costs/ (accessed 11 February 2020).
- Information Services Division Scotland . Scottish Health Service Costs: Year Ended 31 March 2017 2017. www.isdscotland.org/Health-Topics/Finance/Publications/2017-11-21/2017-11-21-Costs-Report.pdf (accessed 11 February 2020).
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016;26:1753-60. https://doi.org/10.1177/1049732315617444.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. PAFS consensus group . CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- Ritchie J, Spencer L. Qualitative Data Analysis for Applied Policy Research. SAGE Publications Ltd; 2002.
- Scottish Government . Scottish Government Urban Rural Classification 2016 n.d. www.gov.scot/publications/scottish-government-urban-rural-classification-2016/pages/2/ (accessed 21 May 2020).
- Scottish Government . The Scottish Index of Multiple Deprivation n.d. https://www2.gov.scot/Topics/Statistics/SIMD (accessed 21 May 2020).
- Scottish Government . Defining Scotland by Rurality 2018. www2.gov.scot/Topics/Statistics/About/Methodology/UrbanRuralClassification (accessed 4 November 2018).
- Robertson C, Avenell A, Stewart F, Archibald D, Douglas F, Hoddinott P, et al. Clinical effectiveness of weight loss and weight maintenance interventions for men: a systematic review of men-only randomized controlled trials (The ROMEO Project). Am J Mens Health 2017;11:1096-123. https://doi.org/10.1177/1557988315587550.
- Hoddinott P. A new era for intervention development studies. Pilot Feasibility Stud 2015;1. https://doi.org/10.1186/s40814-015-0032-0.
- Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutr 2009;12:2382-91. https://doi.org/10.1017/S1368980009005230.
- Shapiro JR, Koro T, Doran N, Thompson S, Sallis JF, Calfas K, et al. Text4Diet: a randomized controlled study using text messaging for weight loss behaviors. Prev Med 2012;55:412-17. https://doi.org/10.1016/j.ypmed.2012.08.011.
- Silina V, Tessma MK, Senkane S, Krievina G, Bahs G. Text messaging (SMS) as a tool to facilitate weight loss and prevent metabolic deterioration in clinically healthy overweight and obese subjects: a randomised controlled trial. Scand J Prim Health Care 2017;35:262-70. https://doi.org/10.1080/02813432.2017.1358435.
- John LK, Loewenstein G, Troxel AB, Norton L, Fassbender JE, Volpp KG. Financial incentives for extended weight loss: a randomized, controlled trial. J Gen Intern Med 2011;26:621-6. https://doi.org/10.1007/s11606-010-1628-y.
- Leahey TM, Subak LL, Fava J, Schembri M, Thomas G, Xu X, et al. Benefits of adding small financial incentives or optional group meetings to a web-based statewide obesity initiative. Obesity 2015;23:70-6. https://doi.org/10.1002/oby.20937.
- Yancy WS, Shaw PA, Wesby L, Hilbert V, Yang L, Zhu J, et al. Financial incentive strategies for maintenance of weight loss: results from an internet-based randomized controlled trial. Nutr Diabetes 2018;8. https://doi.org/10.1038/s41387-018-0036-y.
- Aveyard P, Lewis A, Tearne S, Hood K, Christian-Brown A, Adab P, et al. Screening and brief intervention for obesity in primary care: a parallel, two-arm, randomised trial. Lancet 2016;388:2492-500. https://doi.org/10.1016/S0140-6736(16)31893-1.
- Little P, Stuart B, Hobbs FR, Kelly J, Smith ER, Bradbury KJ, et al. An internet-based intervention with brief nurse support to manage obesity in primary care (POWeR+): a pragmatic, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol 2016;4:821-8. https://doi.org/10.1016/S2213-8587(16)30099-7.
- Crawford R, Glover L. The impact of pre-treatment weight-loss expectations on weight loss, weight regain, and attrition in people who are overweight and obese: a systematic review of the literature. Br J Health Psychol 2012;17:609-30. https://doi.org/10.1111/j.2044-8287.2011.02059.x.
- Dombrowski SU, Endevelt R, Steinberg DM, Benyamini Y. Do more specific plans help you lose weight? Examining the relationship between plan specificity, weight loss goals, and plan content in the context of a weight management programme. Br J Health Psychol 2016;21:989-1005. https://doi.org/10.1111/bjhp.12212.
- Bonevski B, Randell M, Paul C, Chapman K, Twyman L, Bryant J, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-42.
- O’Cathain A, Hoddinott P, Lewin S, Thomas KJ, Young B, Adamson J, et al. Maximising the impact of qualitative research in feasibility studies for randomised controlled trials: guidance for researchers. Pilot Feasibility Stud 2015;1. https://doi.org/10.1186/s40814-015-0026-y.
- McCambridge J, Kypri K, Elbourne D. In randomization we trust? There are overlooked problems in experimenting with people in behavioral intervention trials. J Clin Epidemiol 2014;67:247-53. https://doi.org/10.1016/j.jclinepi.2013.09.004.
- Mohr DC, Cuijpers P, Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Internet Res 2011;13. https://doi.org/10.2196/jmir.1602.
- Festinger L. A theory of social comparison processes. Hum Relat 1954;7:117-40. https://doi.org/10.1177/001872675400700202.
- Kramer FM, Jeffery RW, Snell MK, Forster JL. Maintenance of successful weight loss over 1 year: effects of financial contracts for weight maintenance or participation in skills training. Behav Ther 1986;17:295-301. https://doi.org/10.1016/S0005-7894(86)80058-2.
- Jeffery RW, Wing RR, Thorson C, Burton LR, Raether C, Harvey J, et al. Strengthening behavioral interventions for weight loss: a randomized trial of food provision and monetary incentives. J Consult Clin Psychol 1993;61:1038-45. https://doi.org/10.1037/0022-006x.61.6.1038.
- Deci EL, Koestner R, Ryan RM. A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychol Bull 1999;125:627-68. https://doi.org/10.1037/0033-2909.125.6.627.
- Cerasoli CP, Nicklin JM, Ford MT. Intrinsic motivation and extrinsic incentives jointly predict performance: a 40-year meta-analysis. Psychol Bull 2014;140:980-1008. https://doi.org/10.1037/a0035661.
- Yardley L, Spring BJ, Riper H, Morrison LG, Crane DH, Curtis K, et al. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med 2016;51:833-42. https://doi.org/10.1016/j.amepre.2016.06.015.
- Harris T, Kerry S, Victor C, Iliffe S, Ussher M, Fox-Rushby J, et al. A pedometer-based walking intervention in 45- to 75-year-olds, with and without practice nurse support: the PACE-UP three-arm cluster RCT. Health Technol Assess 2018;22. https://doi.org/10.3310/hta22370.
- Harris T, Kerry SM, Victor CR, Ekelund U, Woodcock A, Iliffe S, et al. A primary care nurse-delivered walking intervention in older adults: PACE (pedometer accelerometer consultation evaluation)-Lift cluster randomised controlled trial. PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001783.
- Tsai AG, Felton S, Wadden TA, Hosokawa PW, Hill JO. A randomized clinical trial of a weight loss maintenance intervention in a primary care population. Obesity 2015;23:2015-21. https://doi.org/10.1002/oby.21224.
- Coughlin JW, Brantley PJ, Champagne CM, Vollmer WM, Stevens VJ, Funk K, et al. The impact of continued intervention on weight: five-year results from the weight loss maintenance trial. Obesity 2016;24:1046-53. https://doi.org/10.1002/oby.21454.
- Aller EE, Larsen TM, Claus H, Lindroos AK, Kafatos A, Pfeiffer A, et al. Weight loss maintenance in overweight subjects on ad libitum diets with high or low protein content and glycemic index: the DIOGENES trial 12-month results. Int J Obes 2014;38:1511-17. https://doi.org/10.1038/ijo.2014.52.
- Lowe MR, Butryn ML, Thomas JG, Coletta M. Meal replacements, reduced energy density eating, and weight loss maintenance in primary care patients: a randomized controlled trial. Obesity 2014;22:94-100. https://doi.org/10.1002/oby.20582.
- Wadden TA, Hollander P, Klein S, Niswender K, Woo V, Hale PM, et al. NN8022-1923 Investigators. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE Maintenance randomized study. Int J Obes 2013;37:1443-51. https://doi.org/10.1038/ijo.2013.120.
- Giles EL, Sniehotta FF, McColl E, Adams J. Acceptability of financial incentives and penalties for encouraging uptake of healthy behaviours: focus groups. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1409-y.
- Promberger M, Dolan P, Marteau TM. ‘Pay them if it works’: discrete choice experiments on the acceptability of financial incentives to change health related behaviour. Soc Sci Med 2012;75:2509-14. https://doi.org/10.1016/j.socscimed.2012.09.033.
- Tappin D, Bauld L, Purves D, Boyd K, Sinclair L, MacAskill S, et al. Financial incentives for smoking cessation in pregnancy: randomised controlled trial. BMJ 2015;350. https://doi.org/10.1136/bmj.h134.
Appendix 1 Overview of updated systematic review evidence
To ensure that intervention components were based on the latest evidence, the searches of three systematic reviews were updated. The aim was to identify new evidence relevant to the feasibility study design. The reviews were:
-
a systematic review of the evidence for weight maintenance9
-
a systematic review of incentives for weight loss16
-
a NIHR Health Technology Assessment systematic review of the quantitative, qualitative and health economic evidence for the management of obesity in men. 5
Incentive interventions for weight loss
Previous review findings
A systematic review3 of incentives for weight loss reviewed RCTs that reported follow-up of at least 1 year. Nine studies were included in the original review. Most of the participants were women recruited through media advertisements. No significant effect of using financial incentives on weight loss or maintenance at 12 and 18 months was found.
Update of review
An update of the original search was conducted between the end of the original search and June 2015. Out of 1816 unique records, two additional studies5,6 met the inclusion criteria.
John et al. 93 conducted a three-group RCT consisting of a 24-week weight loss phase followed by an 8-week maintenance phase, which was followed up 36 weeks after the intervention finished. Participants were 66 obese US veterans (83% male, with a BMI of ≥ 34 kg/m2) randomised to one of three conditions: (1) a weight monitoring programme (n = 22) involving an oral consultation with a dietitian, discussion of weight loss strategies, weight loss goal, provision of scale, and US$20 for attending weigh-ins; (2) a weight monitoring programme plus deposit contract (n = 22), which involved the same weight monitoring programme as in 1, as well as a handout depicting daily weight goals and describing incentive plan, self-weighing, oral reporting of weight, text message feedback on weight loss goal and incentives earned, and financial incentive for weight loss; and (3) a weight monitoring programme plus deposit contract plus maintenance framing (n = 22), which involved the same weight monitoring programme as 1 and the same deposit contract intervention as 2, as well as a distinction between weeks 1–24, framed as the ‘weight loss period’, and weeks 25–32, framed as the ‘maintenance period’.
The deposit contract had the following elements. At the beginning of each month, participants could contribute between US$0.00 and US$3.00 per day of their own funds. During the month, participants accumulated rewards for self-reporting a weight at or below the weight loss goal that was equal to their daily deposit, plus a one-to-one match from the study. Awards were paid at the end of the month if participants weighed at or below their weight loss goal at an in-person weigh-in. Participants could earn US$84 net (US$168 gross) per month.
The SMS component had the following elements. Participants were instructed to weigh themselves each morning and to report their weight by noon. Every day, participants received same-day feedback via SMS on their progress and incentives. Non-adherent participants received feedback about what they would have earned had they met their target weight.
The results indicated that participants in the financial incentive conditions showed significant weight loss over an 8-month intervention, with no difference between the two conditions (weight monitoring programme –0.54 kg; deposit contract –3.44 kg; deposit contract and maintenance –4.35 kg). However, participants regained weight post intervention, and there was no difference in weight loss after 17 months (monitoring programme –0.13 kg, deposit contract combined –0.54 kg). Retention of study participants at 17 months was 65%.
Leahey et al. 94 conducted a three-group RCT consisting of a 3-month web-based community wellness initiative followed by a no-treatment follow-up period until 12 months. Participants (n = 236) were predominantly female (82.5%), of white ethnicity (88.7%) and obese on average (BMI of 33.6 kg/m2) and were randomised to one of three conditions: (1) a team-competition-based weight loss programme with access to a behavioural weight loss programme (n = 91); (2) a team-competition-based weight loss programme with access to a behavioural weight loss programme plus financial incentive for weight loss and website use (n = 89); or (3) a team-competition-based weight loss programme plus optional group sessions with private weigh-in and group discussion (n = 88).
The financial incentive component included small financial rewards for website use. Participants submitted 5 days of weight, calorie and activity information online to earn between US$1 and US$10 per week. Larger incentives were delivered at the start (week 1, US$8; week 2, US$10) and incentive size varied thereafter (e.g. US$1, US$2, US$7). Participants could earn a maximum of US$45 overall. The website included a ‘bank’ that displayed the previous week’s and the total earnings. Weekly reminders to submit information were framed using regret aversion language (‘Don’t miss out on your money, be sure to submit your information by Sunday at midnight’). A clinically significant weight loss was incentivised, with those who lost 5–10% of their initial body weight entered into a US$50 raffle. Those who lost ≥ 10% were entered into a US$100 raffle. Participants received all payouts after their 3-month assessment.
The results indicated that the team-competition-based weight loss programme with financial incentives resulted in significantly greater weight loss at the end of the 3 months than did the programme without financial incentives (incentive 6.4% vs. control 4.2% weight loss). There was no significant difference between the financial incentive and optional group session conditions (incentive 6.4% vs. group 5.8% weight loss). At the 12-month no-treatment follow-up visit, both the financial incentives and the group-based condition showed significantly greater weight loss than the team-competition-based weight loss programme alone (incentive 3.1% vs. group 4.5% vs. control 1.2%). The financial condition was the most cost-effective approach at both 3 (incentive US$34/kg; group US$87/kg; control US$34/kg) and 12 months (incentive US$64/kg; group US$113/kg; control US$140/kg). Retention of study participants at 12 months was 91.4%.
Relevance to current study
Both studies have elements relevant to the current study.
John et al. 93 recruited predominantly male obese participants, used a deposit contract approach, sent participants text messages, used a weight loss maintenance frame and conducted in-person weigh-ins. Although the study did not find any advantage of financial incentives at 17 months, the study sample was small (n = 22 per group). The general feasibility of using these elements was encouraging. Several points of difference from the current study include that deposit contracts were not advisable for hard-to-reach men who might lack personal resources; monthly weigh-ins and customised daily SMS were too resource intensive and might affect intervention scalability; the SMS focused on financial incentive only; and the weight loss maintenance frame had already been considered.
Leahey et al. 94 used loss aversion language to communicate financial incentive outcomes, rewarded the achievement of clinically significant weight loss goals and examined cost effectiveness of the different intervention groups. The finding that adding financial incentives to existing behaviour change programmes leads to increased long-term effects on weight loss was encouraging. Several points of difference from the current study include that incentives were provided for study engagement rather than for weight loss and were based on self-report, whereas this study focused on rewarding objective weight loss; the active intervention was of 3 months’ duration, whereas this study comprised a 12-month intervention.
In summary, the two identified studies have several elements of overlap with the current study in terms of the general approach (e.g. loss framing), forms of delivery (e.g. text messages, web page) and intervention goals (e.g. incentivising clinically significant weight loss targets). Owing to the differences in context, timescale and resources, specific elements of these studies were not directly relevant.
Weight loss maintenance
Previous review findings
A systematic review of the evidence for weight maintenance2 reviewed RCTs that reported follow-up of at least 1 year. Behavioural interventions that deal with both diet and physical activity were found to have small but significant benefits on weight loss maintenance. Moreover, orlistat in combination with behavioural interventions led to significant increases in weight loss.
Update of review
An update of the original search was conducted between the time period of the end of the original search and July 2016. Out of 2802 unique records, five additional studies met the inclusion criteria. Weight loss maintenance interventions included a mix of behaviour/lifestyle interventions for diet and physical activity, behavioural/lifestyle interventions for diet including meal replacements and one pharmacotherapy and behaviour therapy with diet and physical activity.
Tsai et al. 112 examined the effects of an intensified maintenance intervention compared with a control group. The overall mean difference in weight change was 3.4 kg (95% CI 3.08 to 3.72 kg). Those in the intervention group regained 1.6 kg, compared with those in the control group who regained 5.0 kg.
Coughlin et al. 113 examined the long-term effects of a continued personal contact intervention following a 30-month maintenance intervention of personal contact. Participants who received a personal contact intervention for 30 months were re-randomised to continued contact or to no contact for a further 30 months. The difference between the personal contact group and the control group was 0.6 kg (95% CI –1.4 to 2.7 kg). Mean weight change for the original personal contact group was –3.2 kg compared with –1.6 kg in the original control condition (95% CI –3.0 to –0.1 kg).
Aller et al. 114 compared diets with high or low protein/glycaemic index, and found an average weight regain at 12 months of 3.9 kg (95% CI 3.0 to 4.8 kg). High-protein diets led to less regain than low-protein diets; the difference in weight regain was 2.0 kg (95% CI 0.4 to 3.6 kg). No consistent effects were found of glycaemic index diets on weight regain.
Lowe et al. 115 compared the absence or presence of meal replacements and/or a reduced energy density eating programme. The results suggest that at both the 24- and the 36-month follow-up the energy density group showed significantly less weight regain than the control group.
Wadden et al. 116 examined the effects of liraglutide combined with lifestyle change compared with placebo and lifestyle change. The overall mean difference was –5.9 kg (95% CI –7.3 to –4.4 kg).
Relevance to current study
The findings of the updated review underline the conclusions of the original review. Lifestyle behaviour change interventions targeting both diet and physical activity and pharmacotherapy have the potential to increase weight loss maintenance. Effects of individual dietary approaches for weight loss maintenance remain inconsistent. The current study, although not a weight loss maintenance study per se, will thus focus on targeting diet and physical activity, focusing on dietary approaches that the participants can adhere to, without being prescriptive. Pharmacotherapy, although associated with increased weight loss maintenance, is not an option in the current lifestyle behaviour change study.
Management in men with obesity
Previous review findings
A comprehensive systematic review examined the clinical effectiveness of weight loss and weight maintenance interventions for men. 5 The findings of this review directly underpinned the funding call for the current study.
Update of review
An update of the original search was conducted in the summer of 2015. As the review had been conducted recently, no new relevant studies were found.
Appendix 2 Stakeholder workshop summary
| Workshop participant | Study interest | Sex | Background/expertise/experience |
|---|---|---|---|
| 1 | Co-investigator | Female | NHS primary care and mixed methods for large public health trials |
| 2 | Co-investigator | Male | Health psychology and behaviour maintenance for weight loss |
| 3 | Co-investigator | Male | Digital narrative engagement in social marketing and behaviour change |
| 4 | Co-investigator | Male | Statistics and trial methodology |
| 5 | Co-investigator | Female | Health informatics, randomisation system development and behaviour change trials |
| 6 | Co-investigator | Female | Behaviour change and weight management |
| 7 | Co-investigator | Female | NHS clinical academic in weight management |
| 8 | Co-investigator/PPI | Male | Men’s Health Forum representative |
| 9 | Co-investigator/PPI | Female | Men’s Health Forum representative |
| 10 | Co-investigator | Female | Health economics and survey design |
| 11 | Co-investigator | Male | Nutrition, weight management and community engagement |
| 12 | Co-investigator | Female | Health psychology and behaviour change |
| 13 | Stakeholder | Female | Incentive research |
| 14 | Stakeholder | Female | NHS dietetics and weight management research |
| 15 | Stakeholder | Female | NHS dietetics, weight management and public health |
| 16 | Stakeholder | Female | NHS senior manager |
| 17 | Stakeholder | Female | Physical activity for health research |
| 18 | Stakeholder | Female | Diabetes and obesity research |
| 19 | Stakeholder | Female | Obesity research and awareness |
| 20 | Stakeholder | Female | NHS nursing and weight management research |
| 21 | Stakeholder | Female | NHS dietetics and weight management research |
| 22 | PPI | Male | Community engagement in areas of deprivation |
| 23 | PPI | Male | Weight loss and maintenance experience |
| 24 | PPI | Male | Community engagement |
| 25 | PPI | Male | Weight loss and maintenance experience |
| 26 | PPI | Male | From the target group |
| 27 | PPI | Male | From the target group |
Slides presented at the workshop

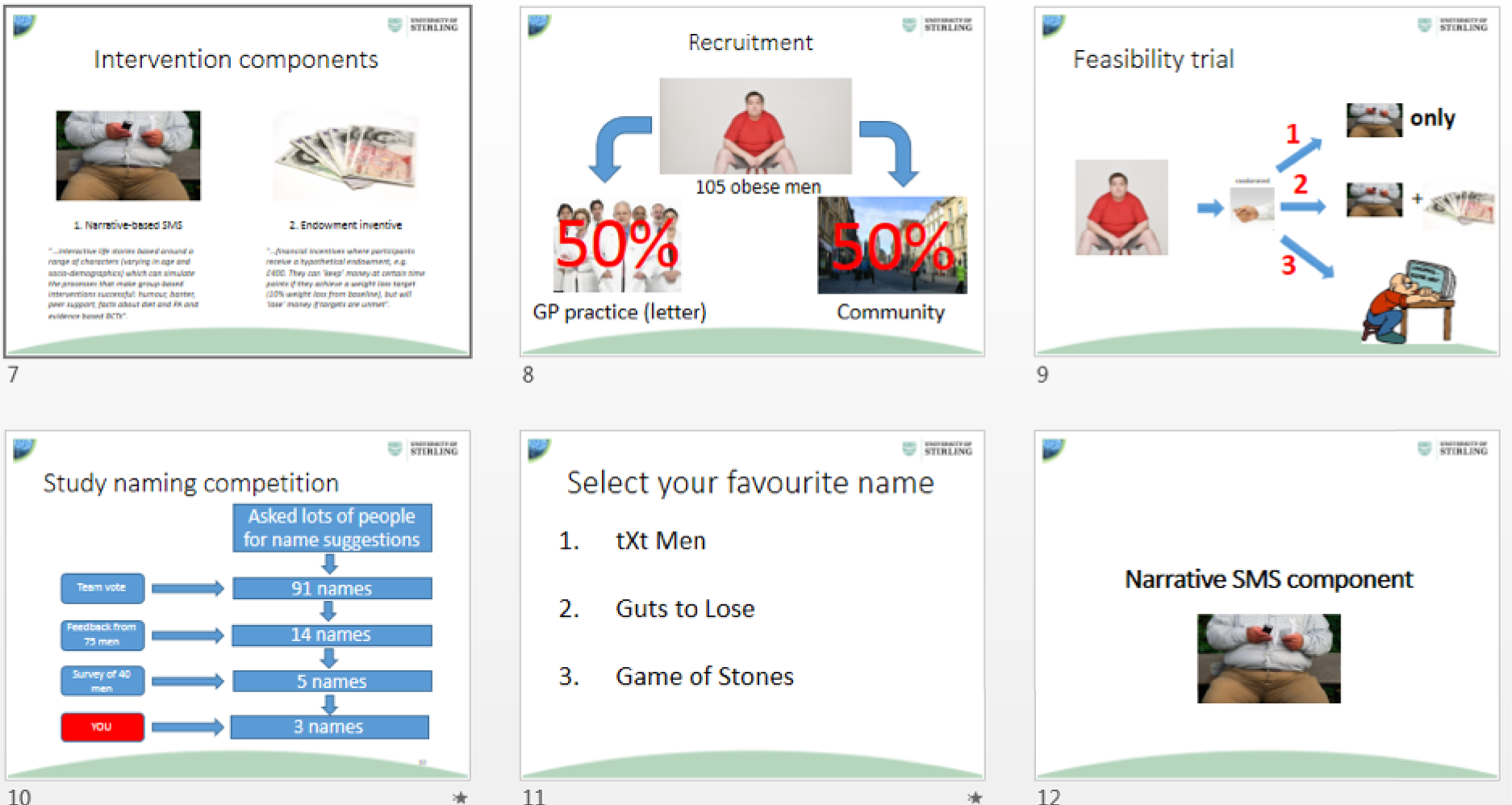
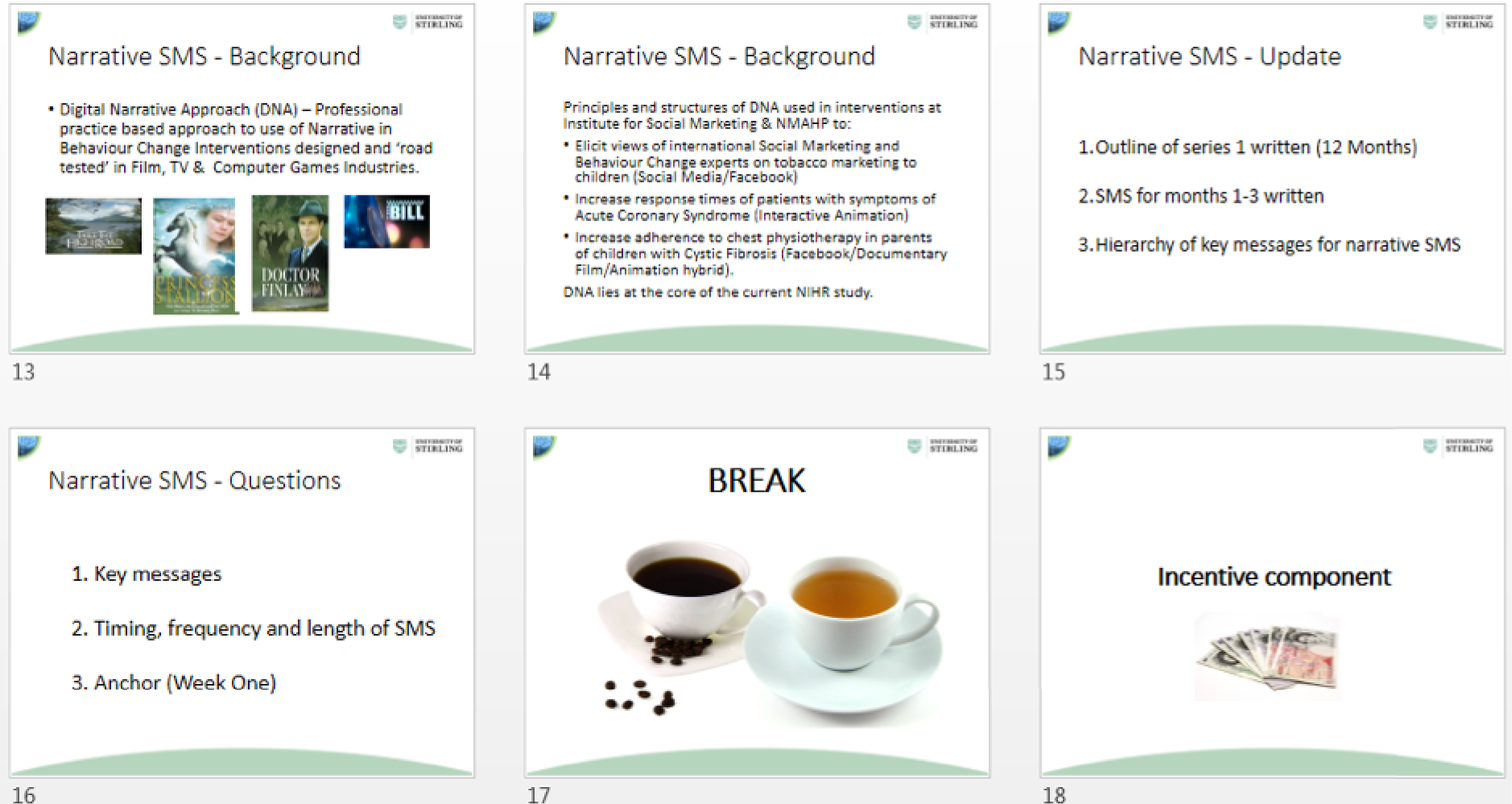
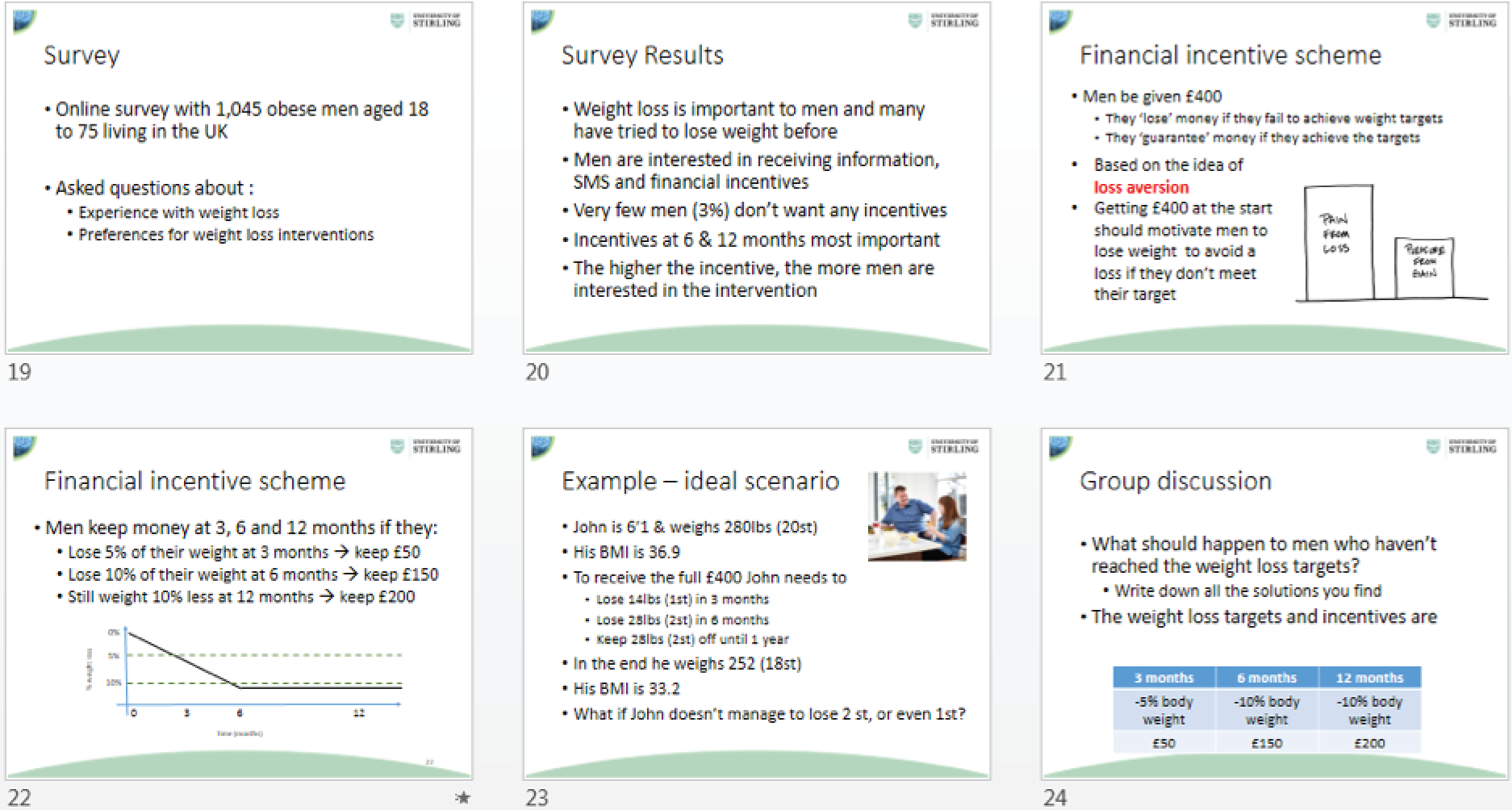
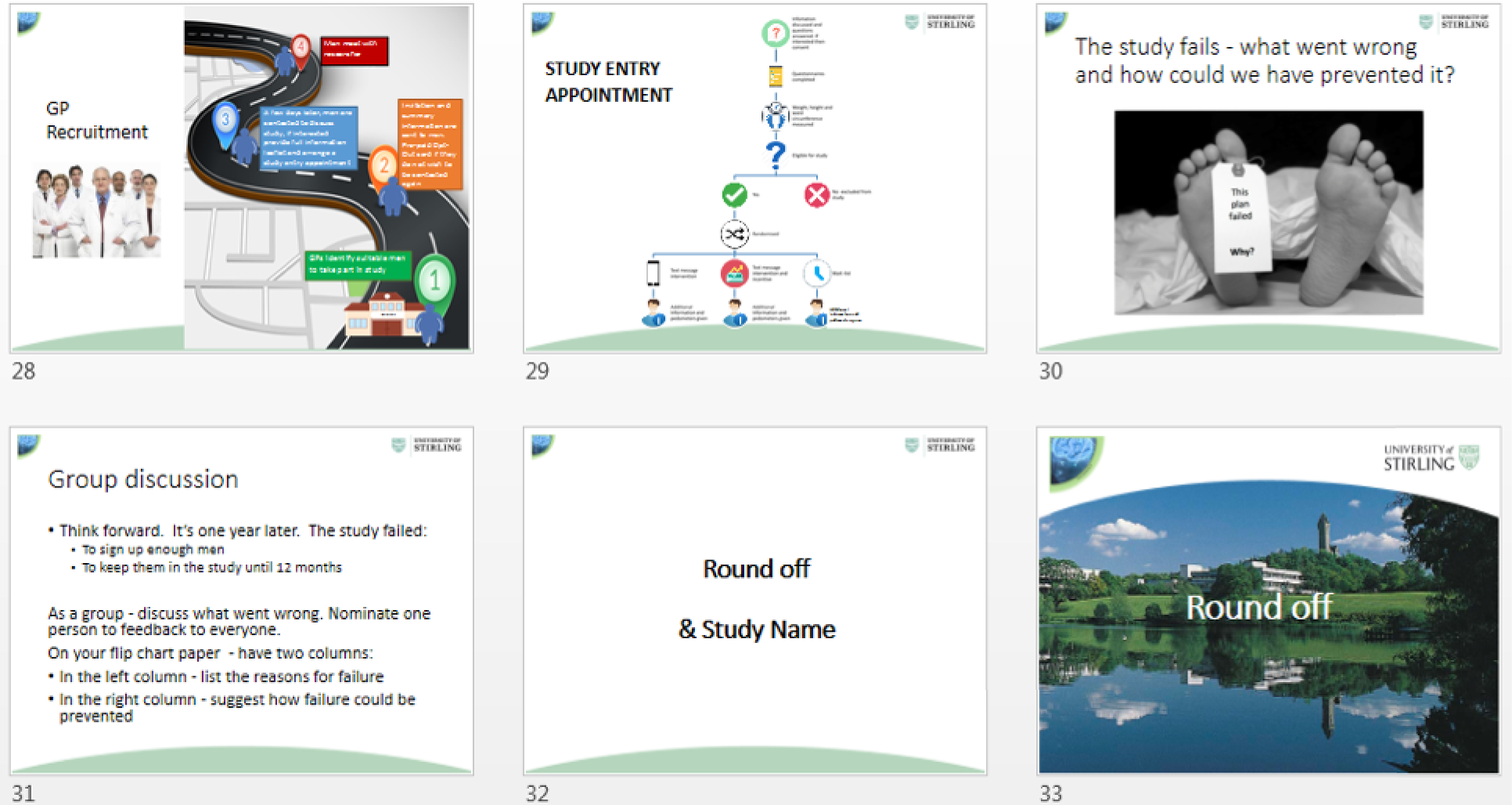
Workshop discussions and feedback
Study name
-
Participants vote on the study name: tXt Men, Guts 2 lose, Game of Stones. Result was revealed at the end of the workshop.
Narrative texts
What do you think that narrative texts can achieve over a year?
-
Create a support system for men.
-
Texts may remind participant that they are managing their weight.
-
Keeping the men on track.
-
Something with humour may be best.
-
Involvement in the study may be enough to promote change.
-
Have to be careful with the texts to try to avoid them annoying people.
What is Slim doing wrong? (Participants had viewed the first week of the texts)
-
Eating too much and not moving enough.
-
Not facing up to the problem.
-
There’s a lot going on in Slim’s life – perhaps he is not ready to make changes.
-
PPI – one concern was that men would not necessarily know what Slim was doing wrong – may need to seek guidance.
-
He’s in a routine – it’s not wrong for him.
-
He seems to have nothing to do, and isn’t busy. In this situation men may be more likely to eat more/unhealthy foods. So therefore exercise may be important to give him motivation, use his time usefully and steps to making dietary changes can follow.
-
His environment seems to be set up to make it very difficult for him to make better choices.
-
PPI – time is an important factor for men. We don’t hear an awful lot about what his schedule is.
-
PPI – should go through messages and adapt for a Scottish audience, e.g. a pack of four pizzas (I’ve never seen that), soda.
-
The initial texts have set the scene, and we do feel empathy for Slim.
-
He’s just doing what he normally does – it’s his routine.
Where would you like to see Slim in 12 months?
-
‘Alive’.
-
Could be a trigger to instigate change, e.g. a health event, something bugging him like having to use his stick or his friend’s jokes or his wife nagging him or loneliness.
What could he do differently?
-
Modify his drinking.
-
There may need to be a trigger for Slim to start to make changes.
-
Any changes may tie in with his ‘nagging’ wife.
-
PPI – or peer pressure from his friends.
-
PPI – having an ‘a-ha’ moment within the texts (could be subtle) each week could be important.
General points
-
Concern over whether this story would resonate with the participants or be relevant for them – or would they say ‘that’s not me’ and be turned off from the story.
-
Concern from one PPI that from the first week the texts should highlight what Slim’s behaviours should be, e.g. shopping habits.
-
Concern over how long he should go on struggling/not knowing what to do before he starts to implement change.
-
Key messages – ‘vigorous’ activity to come out.
-
PPI – Slim should be a weight that people can identify with – not way heavier. Perhaps around 17 stones/250 Ib. Or could Slim’s weight be the same as what each of the participants is and inserted in accordingly?
-
Perhaps put weight in stones?
-
PPI – exercise is an important starting point and can be a catalyst to help men in managing their weight. When people are exercising they aren’t eating and it’s important in itself for keeping weight off and health. It can break a cycle and increase motivation to improve diet. Eating is necessary, but it is not a past-time.
-
PPI – the concept of the 2-4-1 deals, etc., in the narrative is good and should be explored further. First-hand experience of buying things that are not needed just because it looks like a good deal. This way you also end up spending more than you would have in the first place. As it goes further there should be more information ‘debunking’ what the supermarkets want you to believe that you are saving money. The poorest people are targeted in this way, and it’s the high-fat/high-sugar foods that are on these offers.
-
PPI – the intervention may be more relevant for younger people, rather than older people. The storyline may be appropriate for older people, but the delivery method, through text, may not be the best way.
-
Slim could be given a pedometer in the storyline to reflect what participants are given.
-
PPI – unsure that the texts will work for everyone.
-
PPI – gradual changes are important.
-
PPI – for the key messages, although exercise is important, it should be clear that dietary changes are the most important factor for weight loss. Suggest an 80–20 split in emphasis towards diet.
-
It’s important that these texts emphasise that it is a fault of the obesogenic environment – not because they are lazy or not strong-willed. This could help to empower people. It could provide pointers to improve this environment like walking to the shop, not going to the shop when hungry, etc. Every week a little hint could be provided.
-
PPI – not sure that texting is the right medium for communication.
-
Important to have a question asking about other services used, e.g. ‘Have you utilised any other services?’.
Incentive strategy
What should happen to men who do not meet these weight loss targets (5%, 10%, 10%)?
-
Value in having a 10% target – something to strive for.
-
May be much harder for someone with a BMI of 30 to lose 10% than a man with a higher BMI.
-
The 3-month target could be lowered to 3% (NICE), giving the men a very achievable weight loss target at that stage.
-
PPI – ‘double the text messages’.
-
For something to work at a public health level it should be realistic.
-
Those who don’t meet targets could have their motivation ‘re-screened’ and asked what the barriers were to them losing weight.
-
One inclusion criterion at baseline should be that people are sufficiently ‘motivated’ to lose weight.
-
Would be interesting to assess body fat percentage lost.
-
Proportionate incentives were proposed. One example was £10 for each % of weight lost at 3, 6 and 12 months.
-
Could be proportionate but then a ‘bonus’ for having achieved targets.
-
Or £10 per kg or %.
-
PPI – might be demotivating if the ‘goalposts are changing’, e.g. if targets are reset to when they are not met.
-
PPI – could secure the incentive (or some of it) by losing a stone. Plays into the name ‘Game of Stones’.
-
If you are at the same stage as Slim, then it may be difficult to achieve the initial target.
-
PPI – maintenance is very important. I’ve been able to lose a lot of weight before and be at a weight I was happy with. But, unfortunately, I put this weight back on.
-
What’s happening to the men who don’t lose weight? Are they just not complying or have they not been successful for other reasons? Any support/or discussion for these men?
-
PPI – I think the 5% and 10% targets are good targets.
-
PPI – could create a 9-month appointment, giving men an extra chance to reach the 10% target if they don’t achieve it by 6 months.
-
PPI – those coming to the 12-month appointment could get an incentive just for turning up.
-
PPI – a small incentive for ‘turning up’, then a basic incentive for achieving 5%, then an increased incentive, or a ‘big win’ for those achieving 10%.
‘Pre-mortem’
What is going to go wrong with this study? And how do we prevent that from happening?
-
Approaching men in the street for recruitment. Some experience around approaching men for a type 2 diabetes study, which was difficult. Could speak to local patient groups, e.g. Diabetes UK – could advertise the study there. Scottish Health Council could link into local organisations in different areas.
-
PPI – depends on what kind of mood I was in if I would talk to someone who approached me on the street. Slightly against the idea of approaching in the street, wouldn’t say it’s a ‘no-no’ but you may not get much engagement. It may be better to link in with local all-male groups, GP practices, community centres, etc.
-
PPI – it’s important that men on the study do not talk to each other as it may distort the study results. They may start competing against each other, so any weight loss may not be due to the intervention.
-
Could be a lack of data due to problems with recruitment or men not coming back to future appointments.
-
Could access men through the Keepwell programme for men who have been for health checks.
-
Although the venue may be local and convenient, it may be important that the person whom the men see (i.e. the research assistant) has built up a relationship with them.
-
You want to get interested and motivated people along. So do you ‘weed’ some of those out who are not particularly motivated?
-
Concerns over data protection for GP-recruited participants.
-
Technology issues, changes of phone numbers.
-
It doesn’t matter if the study doesn’t work as it is a feasibility study, but what’s important is that you capture why it’s not working and early enough to change parts of the study if required.
-
Recruitment, recruitment, recruitment and dropouts.
-
Contamination could be a major problem.
-
Weight loss might not be.
-
Could be too many texts.
-
PPI – don’t think approaching men on the street is the correct way to do it.
-
PPI – workplace should/could be used as a site for participant recruitment.
-
PPI – would approach people with an information ‘postcard’ (get 1000 printed); you can say it may or may not be appropriate. But be careful with the terminology, perhaps use the phrase ‘at risk’ rather than saying it’s for obese men. Maybe give the men something which isn’t just about the study, e.g. a small calendar with some information and contact details.
-
PPI – local football ground could be a good place to recruit.
-
PPI – as long as we get the 105 participants it is a success, as then you will get a result, and be able to find out the promise of the text intervention and/or the incentives.
-
Have to be very flexible with the recruitment.
-
PPI – could go and try out venues, e.g. local community centre and find out the success rate, e.g. 1 in every 20 approached.
-
PPI – the gym could be a good place to go to recruit participants.
-
PPI – men not engaging with the narrative texts could be an issue.
-
The quality of the interviews, e.g. at 3 months, may be very important to determine what is working well and what isn’t working well.
-
Technical problems, e.g. texts sent to the wrong number.
Study name
-
‘Game of Stones’ was revealed as the winner of the study naming vote.
Appendix 3 Workshop patient and public involvement input on recruitment and study procedures
| PPI workshop feedback | Decision made on recruitment and study procedures |
|---|---|
| Some did not think approaching men on the street was the correct way to do it. Others felt that it depended on what kind of mood they were in if they would talk to someone who approached them on the street. They would not say it is a ‘no-no’ but there may not be much engagement. Suggestions made to link in with local all-men groups, general practices, community centres, etc. | On-street recruitment was briefly tested together with a variety of methods and venues for community recruitment. The test of on-street recruitment was unsuccessful (see Chapter 6) |
| Suggestion to approach people with an information ‘postcard’ and say this may or may not be appropriate. Care should be used with the terminology, perhaps the phrase ‘at risk’ rather than saying it is for obese men. Maybe give the men something that is not just about the study (e.g. a small calendar with some information and contact details) | A shorter ‘summary’ information leaflet was used during community recruitment. The word ‘obese’ was not used on the information materials and care was taken that community recruitment was undertaken in a sensitive manner. All participating men received a low-cost pedometer |
| The workplace could be used as a site for participant recruitment | Community recruitment was conducted at two council workplaces |
| Could try out venues like community centres and work out the success rate (e.g. 1 in every 20 approached became a participant) | Researchers collated information on the number of individuals given information leaflets, the number of potential participants who gave the researchers their contact information, the number of hours researchers spent at each venue and the number of men randomised (see Chapter 6) |
| The gym and football grounds were suggested as potentially good places to recruit participants | Community recruitment was conducted in a variety of venues including outside a sports centre. Football grounds were not used as there is an existing weight management programme7 that links into football clubs and specifically recruits football supporters |
| It is important that men on the study do not talk to each other as it may distort the study results. They may start competing against each other, so any weight loss may not be due to the intervention | The trial was set up as an individual RCT. Efforts were made by researchers not to recruit participants who knew each other. The post-randomisation leaflet stated:We will keep your information confidential and ask that you are confidential about your participation in this study. Please do not discuss this study with other men that are taking part. However if you wish to, you can talk to close friends and family about your participation in the study |
| Men not engaging with the narrative texts could be an issue | An option for participants to continue in the study but stop receiving the SMS was introduced for those who disliked the narrative SMS |
Appendix 4 Workshop patient and public involvement input on the incentive strategy
| PPI workshop feedback | Decision made on incentive strategy |
|---|---|
| Might be de-motivating if the ‘goalposts are changing’, for example if the targets are reset to a different amount when they are not met | The weight loss targets linked to the incentives were set at baseline and this did not change regardless of whether or not the targets were met |
| Could secure the incentive (or some of it) by losing a stone. Plays into the name Game of Stones | This change was not added to the incentive strategy as it would have overcomplicated the incentive structure. Percentage weight loss targets from baseline weight were chosen |
| Maintenance is very important. I’ve been able to lose a lot of weight before and be at a weight I was happy with but unfortunately I put this weight back on | The weight loss targets for both the 6- and the 12-month appointments were 10% of baseline weight. This was to incentivise participants to lose weight and then to maintain weight loss. More money was allocated to the 12-month appointment target (£200) with a view to supporting long-term weight loss maintenance |
| I think the 5% and 10% targets are good targets | To secure the full incentive (£400), participants in the SMS + I arm needed to lose 5% of their baseline weight at 3 months and 10% at 6 months and to keep the 10% off at 12 months |
| Those coming to the 12-month appointment could get an incentive just for turning up | A £20 voucher was offered to all participants who attended the 12-month appointment |
| A small incentive for ‘turning up’, then a basic incentive for achieving 5%, then an increased incentive, or a ‘big win’ for those achieving 10% | A £20 voucher was offered to all participants who attended the 12-month appointment. There were no ‘turning up’ incentives at 3 months and 6 months. There were no incremental incentives for weight loss of < 5% from baseline |
| Could create a 9-month appointment, giving men an extra chance to reach the 10% target if they don’t achieve it by 6 months | No 9-month appointment was added as funding had already been secured based on researcher time to conduct appointments at baseline, 3, 6 and 12 months only |
Appendix 5 One-to-one patient and public involvement input on study materials
| Documents reviewed by PPI | PPI feedback | Decisions and changes made to study materials |
|---|---|---|
| Pre-randomisation full information leaflet | The word ‘financial’ should be avoided pre randomisation as some men, particularly those from less well-off areas, may participate only for financial gain and may be likely to drop out if they are not randomised to SMS + I | Decision: the word financial was not used in any pre-randomisation materials. The incentive component was not emphasised, and, when asked about them, research assistants replied by advising that ‘you will be given more information regarding the incentives if that is the group you are randomly placed into’ |
| All post-randomisation leaflets (SMS + I, SMS only and control) | After losing a lot of weight they would want to share this success with friends and family. Therefore, the confidentiality section should be adapted to emphasise that this is OK |
Original: ‘. . . and ask that you are confidential about your participation in this study’ Adapted: ‘. . . and ask that you are confidential about your participation in this study. Please do not discuss this study with other men that are taking part. However, if you wish to, you can talk to close friends and family about your participation in the study’ |
| Post-randomisation SMS + I and SMS-only leaflets |
The narrative SMS intervention is a bit of an unknown. PPI members were unclear about the idea of narrative texts and fictional characters How regularly will texts be received? Currently it is not clear |
Decision: randomisation will occur at the end of the baseline visit. The research assistant was there to explain the narrative texts in detail, showed the participants an example of the narrative SMS on a mobile phone and answered any questions the participant had Addition: ‘How often you will receive the texts will vary, some days at the start of the study you will get up to 5 text messages and on other days you won’t get any’ |
| Post-randomisation SMS + I leaflet |
Understandable for some but may need a clearer presentation of the incentive strategy than the written description alone. Much easier to understand when shown in a table format The wording used to describe the incentive strategy could have been more positive, describing gains or what can be achieved rather than losses |
Original: a text description of the incentive strategy only Adapted: the incentive strategy was presented using a combination of text and tables Reason for no change: to ensure adherence to the theoretical concept of loss aversion, it was necessary to frame the incentive strategy in a way that described how men would lose endowed money if weight targets were not met. Words such as ‘win’ and ‘gain’ were avoided |
|
Did not like the word ‘rules’ in the title of the section explaining the incentive strategy as they felt they were being told what to do Two suggestions were ‘how to win’ and ‘how it works’ Someone would be required to be there to explain this leaflet |
Original: ‘Rules of the Game of Stones’ Adapted: ‘How will the financial incentives work?’ Reason: the word ‘win’ was avoided to adhere to loss aversion theory Decision: randomisation occurred at the end of the baseline visit. As a result, the research assistant was there to explain the incentive strategy in detail and to answer any questions the participants had. Blinding the researcher to allocated group at the baseline assessment was not possible |
|
| Post-randomisation SMS only |
Advised to add personal weight loss targets to this information sheet. Even though no financial incentive is being provided, setting weight loss targets were seen as important PPI members were unclear when their next appointment would be when reading this leaflet |
Addition: ‘At these appointments you should aim to lose 5% (xx kg) of your starting weight at 3 months, 10% (xx kg) at 6 months and maintain 10% (xx kg) weight loss at 12 months’ Addition: ‘You will be weighed by a member of the research team at 3, 6 and 12 months at a convenient venue to suit you’ |
| Baseline questionnaire | One PPI man had no concerns about the questionnaire length, whereas PPI contacts and expert opinion within the Study Steering Committee advised that the outcome measure questionnaires (especially baseline) should be reduced to reduce participant burden and to encourage trial retention |
Adapted: the length of the baseline questionnaire was reduced from 22 to 13 pages Reasoning: substantial feedback from the Study Steering Committee and the PPI contact who was happy with the questionnaire length had participated in another weight management trial and was used to completing lengthy questionnaires |
Appendix 6 Characteristics of patient and public involvement participants who received alternative SMS
| ID | Route of feedback | Overweight/obese | Level of feedback | Type of comments | Volume |
|---|---|---|---|---|---|
| AltPPI1 | Not known | Specific | Direct in text comments | 35 comments | |
| AltPPI2 | Yes | Specific | Direct in text comments | 15 comments | |
| AltPPI3 | Yes | Specific | Direct in text comments | 22 comments | |
| AltPPI4 | Yes | General | Overall reflections | 65 words | |
| AltPPI5 | Yes | General | Overall reflections | 235 words | |
| AltPPI6 | Yes | General | Reflective letter | 2152 words | |
| AltPPI7 | Yes | General | Overall reflections | 140 words | |
| AltPPI8 | Yes | General | Overall reflections | 123 words | |
| AltPPI9 | Face to face | Yes | General | Overall reflections | 1.5 hours |
| AltPPI10 | Yes | General | Overall reflections | 120 words |
Appendix 7 Example patient and public involvement feedback on alternative SMS and the changes/decisions made as a result
| ID | Example feedback | Decisions and changes made to study materials |
|---|---|---|
| AltPPI1 | General: some good stuff here. It’s not easy to come up with so many original texts. Can we mention the Men’s Health Forum website? I can provide specific links for many tips | Addition: included more links to Men’s Health Forum resourcesCheck out this helpful wee booklet full of tips from the Men’s Health Forum. www.issuu.com/menshealthforum/docs/eat_well_final_hrnon-border [last accessed 25 June 2019]AltSMS6Hi <name>. Week 2. This week we’ll talk about planning and making changes. What are your weight loss plans for this week? Here is a useful link with some great info on healthy food. www.menshealthforum.org.uk/food-faqs [last accessed 25 June 2019]AltSMS8Chris says he found it difficult to decide what the healthy options are in the supermarket. There is so much choice. Sounds familiar? Here are some great tips on how to read food labels. www.menshealthforum.org.uk/how-read-food-labels [last accessed 25 June 2019]AltSMS24Jan says you should eat things you like and don’t force yourself to eat food you don’t like, as you’ll never stick to eating them regularly. This booklet from the Men’s Health Forum has loads more tips, so worth sending you the link again. https://issuu.com/menshealthforum/docs/eat_well_final_hrnon-border [last accessed 25 June 2019]AltSMS40 |
| AltPPI1 | Don’t like ‘managed’ – men who lost weight |
Original SMS: We’ve put these texts together with the help of men who managed to lose weight. They are based on facts and experience of how to do it in real life Changed SMS: We’ve put these texts together with the help of men who successfully lost weight. They are based on facts and real life experience (AltSMS1) |
| AltPPI1 | No is the answer for a lot of men so why not give some tips for how to eat more slowly? |
Original SMS: Steve started to eat a lot more slowly now. Starting to eat more slowly works very well for some – but would you have the patience? Changed SMS: Steve started to eat a lot more slowly. Eating more slowly gives your stomach time to tell your brain when you’re full, which reduces overeating. How to do it though? Try sitting down at a table when eating, switch off any distractions, put knife and fork down between bites and count 30 chews before swallowing |
| AltPPI2 | Reducing [highlighting the word slashing] |
Original SMS: Changing your eating includes a few things: stopping, starting, swapping, slashing. Is there anything you could stop, start, swap or slash this week? Changed SMS: Changing your eating includes a few things: stopping, starting, swapping, reducing. Is there anything you could stop, start, swap or reduce this week? (AltSMS10) |
| AltPPI2 | Insert a [highlighting the word mindset] |
Original SMS: Simon says it’s mindset, if you’ve got a pattern of eating healthily, you’ve got the results, that’s when you become encouraged to keep doing that Changed SMS: Simon says it’s a mindset, if you’ve got a pattern of eating healthily, you’ve got the results, that’s when you become encouraged to keep doing that (AltSMS52) |
| AltPPI2 | Delete [highlighting ‘unless you’re lost in the woods and you see a path then please follow that path’] |
Original SMS: Follow your passion, stay true to yourself, never follow someone else’s path unless you’re lost in the woods and you see a path then please follow that path Action taken: deleted entire SMS |
| AltPPI3 | The issue here is that it will put off men with any long term condition who can only do limited physical activity like walking a short distance. Most overweight men will not go near a gym |
Original SMS: Quick fact: Losing weight is 80% about what you eat and 20% about your physical activity. Maintaining weight loss is 50% eating and 50% activity Added to next SMS: Physical activity is anything that takes a bit of effort and makes you breathe fast and feel warmer – not just going to the gym or running a marathon (AltSMS16) |
| AltPPI3 | Why is it well done? Maybe a short explanation would help? |
Original SMS: Ian used to have toast with his tea at night and has completely stopped that . . . Well done to Ian, we toast to that Changed SMS: Ian used to have toast with his tea at night and completely stopped that. Well done Ian, reducing the amount of bread you eat can be great for weight loss (AltSMS10) |
| AltPPI3 | We don’t eat junk. We eat food . . . Often too much; and often too many carbs/sugar etc |
Original SMS: Carl had his birthday and was out for dinner and drinks, eating a lot of junk, so it caused him to fall back again and he’s not got back into it yet Changed SMS: Carl was out for his birthday party, eating and drinking too much, so it caused him to fall back again and he’s not got back into it yet (AltSMS72) |
| AltPPI4 | The texts messages are funny and motivating. Would believe they would make you feel less like you’re doing it alone and that someone is looking out for you. They reinforce that this shouldn’t be counted as a diet but as a lifestyle change. That by changing all the small things in your basic diet, you can make big changes | Changed SMS: none |
| AltPPI5 | I would mention the difficulties, particularly if they are young people, about the partying at weekends and beer and wine which can undo all the new ‘lifestyle’ foods | Added SMS: One of the biggest triggers is around you, just now. Can you see it? A thing called ‘weekend’. Many men struggle a bit on weekends. Sounds familiar? Bob says he tries to balance enjoying himself without going overboard (AltSMS48) |
| AltPPI6 | I think you cover this point at number 8, but might be put not in just the shape, but the mental benefits. I say this was trying to manage a condition for years and whilst it’s nice to look lighter and fit into clothes etc, but the mental boast you get is far far more. When you think about it, lots of people overeat as they are depressed |
Original SMS: Physical activity is good for you in many ways and helps you get into shape, but on its own it probably won’t help you lose much weight Changed SMS: Here’s the thing though. Our men on Game of Stones tell us if they exercise they feel better and if they feel better they eat better. Win-win. The more active you are, the better you feel, and the better you feel, the better you eat (AltSMS19) |
| AltPPI6 |
Week 8 Yea I’m beginning to like your jokes here lol |
Changed SMS: none |
| AltPPI6 | What I would say here is it’s important about the variety of food you can take here. Many diets end here because it’s boring and stale. It’s partly covered with point 7 but it’s important to stress this | Added SMS: Kamal keeps going by mixing it up. Do a variety of activities and eat a variety of foods. The less bored you are the easier it is to stick to a new lifestyle |
| AltPPI7 | We would not recommend the use your written text message based approach. The content needs to be simplified and presented graphically as it is in all computer or video games | Changed SMS: none, as the advice given was outside the remit of the current intervention |
| AltPPI8 | Texts and scenarios are fab, very well written | Changed SMS: none |
| AltPPI8 | Some repetitive questions, like the same question every week might help reinforce routine | Added SMS: added reflective questions at the end of the week, e.g. Have you made any changes this week <name>? (AltSMS7); How has your week been? (AltSMS14); What are your weight loss plans this week <name>? (AltSMS27) |
| AltPPI8 | Also the supermarket and stimulus control could be closer to the beginning as it’s got good information to set the guys up for changing eating habits | Changed made: moved stimulus control section from week 10 to week 4 |
| AltPPI9 | PPI representative suggested: Make a plan and write it down. What fits into your life? What works, what doesn’t, then modify it | Added SMS: John says you should make a plan and write it down. What fits into your life? What works, what doesn’t, then modify it (AltSMS39) |
| AltPPI9 | PPI representative suggested ‘Eat things you like and don’t force yourself to eat food you don’t like, as you’ll never stick to eating them regularly’ | Added SMS: Jan says you should eat things you like and don’t force yourself to eat food you don’t like, as you’ll never stick to eating them regularly (AltSMS40) |
| AltPPI10 | Week 5–1. word order a bit strange maybe ‘Now we’ll let the men who lost weight on this programme speak.’ instead? |
Original SMS: Week 5. Tips and tricks week. We’ll let the men speak who lost weight on this programme. Maybe their words of wisdom might also work for you? Changed SMS: Week 6. Tips and tricks week. We share some tips from men who successfully lost weight on this programme. Maybe those also work for you? (AltSMS36) |
| AltPPI10 | Love the little jokes and colloquialisms, make it more human and engaging | Changed SMS: none |
Appendix 8 Characteristics of patient and public involvement participants receiving narrative SMS
| ID | Age (years) | Sex | SIMD | Currently overweight or obese? | Previous weight loss and maintenance | Interview, workshop group, other | SMS development stage |
|---|---|---|---|---|---|---|---|
| 1 | 52 | Male | Fourth most deprived decile 2016 | Yes | Yes | Script conference, Game of Stones workshop and direct script consultancy | Overall narrative design |
| 2 | 41 | Male | Data not available | No | Yes | Informal interview | Overall narrative design |
| 3 | 49 | Male | Ninth most deprived decile 2016 | Yes | Yes | Informal interview | Overall narrative design |
| 4 | 24 | Male | First and second most deprived decile 2016 | No | No | Character and story workshops | Overall narrative design |
| 5 | 57 | Male | First and second most deprived decile 2016 | No | Yes | Character and story workshops and direct script consultancy | Overall narrative design; Q1–Q4 |
| 6 | NA | Male | First and second most deprived decile 2016 | No | No | Character and story workshops | Overall narrative design |
| 7 | 67 | Male | First and second most deprived decile 2016 | Yes | No | Character and story workshops | Overall narrative design |
| 8 | NA | Male | First and second most deprived decile 2016 | Yes | No | Character and story workshops | Overall narrative design |
| 9 | NA | Male | First and second most deprived decile 2016 | No | No | Character and story workshops | Overall narrative design |
| 10 | NA | Male | First and second most deprived decile 2016 | Yes | No | Character and story workshops and direct script consultancy | Overall narrative design; Q1–Q4 |
| 11 | NA | Male | First and second most deprived decile 2016 | Yes | No | Character and story workshops | Overall narrative design |
| 12 | NA | Male | First and second most deprived decile 2016 | No | No | Character and story workshops | Overall narrative design |
| 13 | NA | Male | First and second most deprived decile 2016 | No | No | Character and story workshops | Overall narrative design |
| 14 | NA | Male | First and second most deprived decile 2016 | No | No | Character and story workshops | Overall narrative design |
| 15 | NA | Female | Information not available | Husband obese | Husband had not tried weight loss and maintenance | Telephone interview and direct script consultancy | Overall narrative design |
| 16 | 55 | Male | Information not available | Yes | Yes | Informal interview and direct script consultancy | Q1 |
| 17 | 64 | Male | Third most deprived decile 2016 | Yes | No | Direct script consultancy | Q1–Q4 |
| 18 | 62 | Male | Fifth most deprived decile 2016 | Yes | Yes | Direct script consultancy | Overall narrative design; Q1 and Q2 |
| 19 | 62 | Male | Ninth most deprived decile 2016 | Yes | Yes | Direct script consultancy | Q1–Q4 |
| 20 | 50 | Male | Fifth most deprived decile 2016 | Yes | No | Informal interview | Q1–Q4 |
Appendix 9 Summary of patient and public involvement feedback on narrative SMS and changes/decisions made as a result
| Interview, workshop group, other | ID | Narrative and SMS library changes | SMS development stage |
|---|---|---|---|
| Attendance at script conference, Game of Stones co-investigator workshop | 1 | Use of belt buckle as visual feedback device; Slim was too heavy and atypical; weight reduced by 30 lb | Overall narrative design |
| Informal one-to-one interviews | 2 and 3 | Importance of role of female wife/partner in male weight loss behaviour change – led to Slim and Wilma story; need for social support and extrinsic motivation – informed Mikey and Slim’s story | |
| Need to change domestic environment to remove old eating habits and resisting stimuli to eat, e.g. hiding high-fat and high-sugar food to resist temptation. Led to ‘Slim hides the triggers’ story | |||
| Character and story workshops (×3) | 4 to 14 | Guilt and shame of being overweight leading to ‘ostrich’ behaviour and denial of the severity of the problem – informed Slim’s denial as he reflects on but does not act effectively in first 3 months | |
| Recognition of positive emotional effects of even small amounts of exercise; problem of triggers and stimuli in supermarkets and public spaces; lack of community contributing to lack of social support; appreciation of humour storylines | |||
| Need for partner/wife to be on board with diet and physical activity change; problems in marriage leading to alcohol and high fat, salt and sugar consumption – informed Slim and Wilma story. Recognised and familiar with inability to resist triggers in the environment when depressed – informed Slim’s comfort eating in response to environmental stimuli and need to learn to control temptation | |||
| Friends and peers asserting plans for social interaction; not wanting to be left out when everyone else is eating and drinking too much alcohol. Informed Slim’s social habits | |||
| Domestic habits. Men can’t cook so shouldn’t cook. What the partner says goes. Leads to conflict so easier not to change and have a peaceful life | |||
| Information available on diets is really confusing; doctors don’t really seem to care, just keen to get you out of the door. Led to Slim’s initial inactivity and use of Dr Sharpe’s dismissive dietary advice to Slim. Influenced use of and genuine knowledge of how to care for someone with low self-esteem and poor diet from character of care nurse Claire | |||
| Hard to resist high-calorie food and drinks that are high in sugar when that’s all you see around you, especially when you are socialising. Led to subplot of Colin the owner of the pub marketing his own high-sugar drinks that Slim becomes addicted to | |||
| Fire station never visited. Not a good basis for a storyline as men don’t go there or have anything to do with them. Highly unlikely to go there for gym or to weigh themselves. Better to set story in local pub. Led to pub setting and Mikey’s ambition to want to train as a firefighter | |||
| Telephone interview and direct script consultancy | 15 | Husband lost weight because she changed his diet gradually. He just said he felt fitter. Led to further use of drama and comedy in Slim’s domestic life | |
| Informal interview and direct script consultancy | 16 | Character of Slim likeable; recognition of Slim’s initial denial of problem as source of humour because ‘it feels real’. Timing, frequency and length of texts acceptable | Q1 |
| Direct script consultancy | 2, 10, 17, 18 and 19 | Slim’s diet too extremely poor – ‘men like that don’t exist’ – led to reduction in Slim’s initial intake of HFSS foods; if you like something it’s worth sticking to as a reward for not eating; led to Soor plums – Slim’s preferred sweeties and his reward | Q1 and Q2 |
| Vegetables are disgusting. Culturally defined habits hard to break and a real barrier to change; language adjusted to Scots; pub names changed to be more Scottish; number, frequency and length of texts acceptable (but participant reading script not receiving texts) | Q1–4 | ||
| The need for more readily available and affordable fresh fruit and vegetables in deprived areas; the possible use of allotments and public land set aside to grow and cultivate own grown. Led to Mikey’s The Green allotment story, Slim’s increasing interest in it and its incremental impact on his change in diet | |||
| Men can’t talk about losing weight; weight loss is therefore a lonely and unlikely journey for many; resulted in further ironic use of Budge as best friend as opponent in weight loss journey | |||
| Informal interviews and direct script consultancy | 20 | Use of humour effective |
Appendix 10 The influence of participants’ responses to Slim’s texts
This appendix outlines how participants’ SMS replies to Slim informed the writing and modification of subsequent texts. This responds to the need to report accurately how the narrative engagement process was designed iteratively and with what intent if the study is to be replicated. How a sample of texts sent by participants back to Slim during the first quarter were interpreted and informed the writing of subsequent texts proves revealing.
Participants responded to Slim emotionally as if he were a real person, in line with previous narrative SMS interventions. 13–15 They engaged with and responded to Slim’s diet and physical activity habits, his relationship with his wife and his friend Budge and the relative influence they were having on his potential to lose weight. The scriptwriter strengthened focus on these elements in subsequent quarters. The texts saw participants engaging with and responding to key messages, to embedded behaviour change strategies and to Slim’s reflection on his diet and physical activity goals, for example ‘Great advice Slim’. They offered Slim positive emotional support when it was not going so well: ‘keep trying slim’, ‘Well done and keep at it’. ‘Stick with it. It will benefit you eventually’. Participants gave Slim advice on his comfort eating ‘E.g. Stick to your diet; Just cut out the snacks and fast food and all canned soft drinks plus no beer and you will lose weight’; ‘go easy on the drink and food. Think calories’. They appeared to have internalised the dangers of too much sugar consumption through the Power Up Juice story, advising Slim: ‘drinking loads of sugar is really bad for you and your body’. Participants also appeared to have identified with Slim’s tendency to comfort eat when he was emotionally down: ‘Your [sic] just comfort eating’. They advised him to resist commercial marketing strategies used for high-fat, salt and sugar foods such as ‘buy two for one’ deals at the supermarket when he was down: ‘Don’t bogof’ (buy one get one free). The scriptwriter used this feedback to strengthen the power of the Power Up Juice story, for example, which tests Slim’s increasing resilience, self-regulation and ability to resist the triggers in his environment.
Participants also gave Slim advice on his physical exercise: ‘E.g. Go for a walk. It helps clear your head and takes your mind off food’. They responded to Slim’s early sedentary habits: ‘Why not go for a walk instead of sitting in front of a computer. I am just back from a 3 mile walk (12,354 steps). No wonder your [sic] fat. Keep it up. I loose [sic] more weight gardening than I do exercising. When you are working and have a target you forget the effort you are putting in!’
Participants appear to have internalised messages in response to the embedded BCTs in a positive manner, for example, around diet and physical activity goal-setting, ‘Good idea on the goal and sharing it. Always helps me’. They reported back on their own progress: ‘Slim I set my goal too high. I thought I could lose at least 1stone in 3 months but only managed 1’; ‘I’m down to 15 stone hope to make new target of 14,5’. The key messages around goal-setting were then further reinforced in the ‘Slim’s computer game’ subplot.
Participants also responded to Mikey’s advice to Slim and the embedded BCTs to encourage self-monitoring, self-regulation and the need for feedback. Participants empathised with the subplot of Slim’s failed attempts to buy the right scales: ‘Pity about the scales, maybe a trip to Boots once a week to use theirs until you’re on the range of your own scales?’. This evidence of participants’ empathy with Slim’s failed initial attempts to monitor his weight resulted in further use of black humour to point out Slim’s setbacks: when and where he was going wrong.
Some participants advised Slim to resist the negative influence of his close friend Budge: ‘Friends do not understand how hard it is to keep weight off’; ‘They sometimes say things like this to you because you really want to feel better about yourself and they do not want you to succeed, who needs friends like that’; ‘Keep up ignoring him and do your own thing’. The scriptwriter responded by testing Slim and Budge’s friendship further and more dramatically. This led to the story of Budge’s stroke, which motivated Slim to reverse his type 2 diabetes through self-regulation, weight loss and maintenance.
Other participants engaged with Wilma’s story and advised Slim about the impact that the dysfunctional relationship was having on his emotional state: ‘I think Wilma is selfish and is playing you, she was away for a while then comes back and shortly after she says that she’s pregnant, who is being above themselves Slim, keep the good work going and your eyes open’; ‘Emotional blackmail, who needs that, you could be driven to comfort eat’. This demonstrated that this story was proving engaging and informed the strengthening of this storyline. This has to be weighed against participants’ less favourable responses. One participant’s response during the first quarter suggested that Slim’s dysfunctional relationship with his wife paralleled that of his own: ’I have enough troubles of my own’. It appeared also that this particular participant did not like the open and frank approach to men’s emotional lives and responded to Slim, ‘Get yourselves on Jeremy Kyle’. The unforeseen consequences of emotional engagement therefore have to be taken into account. However, as this response was from only one participant and was not representative of the wider study population, it did not warrant changing the overall narrative or its approach for all participants.
One participant’s response to one text in the first quarter suggested that the number of texts was too large: ‘Too many texts today’. As the number and frequency of the texts was a function of the number of stories woven across the narrative – and this was dictated upfront to ensure that the narrative SMS built on previous studies – this could be reduced only to a degree.
Participants appeared to be internalising key messages in a positive manner: ‘I’ve put on a bit of weight, gonna have to do the same as you’ and ‘Eat less: move more’. They responded to Mikey when Slim was in hospital asking him to pass on the positive message to Slim: ‘Tell him my weight loss and maintenance is going well’. This resulted in the key and positive messaging being reinforced in subsequent texts.
Participants engaged on an emotional level to key aspects of the narrative, for example in response to Slim’s realisation that he must change: ‘It’s a horrible feeling, isn’t it? That realisation something needs to change. I feel for you’. This degree of emotional engagement with the overall narrative and specific story strands appeared to work in accordance with the intention to engage emotionally through the use of a digital narrative approach. Subsequent storylines and texts were therefore written to augment and refine this approach over 12 months where possible.
Appendix 11 A priori justification for the £400 incentive ceiling
The incentive level needs to be acceptable from both a public and an ethical point of view, as well as scalable. In addition, for a 10% weight loss at 12 months, a balance needs to be struck between having an incentive large enough to matter to participants but not seeming to be unreasonably high. The chosen ceiling level of incentive was based on several strands of evidence, including (1) the costs of other treatment options for which this population would be eligible, (2) public acceptability and (3) evidence of effectiveness. Therefore, the ceiling level of £400 is based on several pieces of evidence that, cumulatively, suggest both acceptability and effectiveness.
Cost of comparable interventions
The level of £400 is equivalent in value to a 1-year supply of the weight loss medication Orlistat (without the costs of monitoring and prescribing consultations) and equates to just over £1 per day over 12 months. The amount of £400 over 12 months is similar to the cost of weekly Weight Watchers (Weight Watchers UK, Maidenhead, UK) attendance and substantially lower than surgical treatments that NICE guidelines6 recommend as cost-effective. If the incentive intervention is found to be as effective and cost-effective as, or more effective and cost-effective than, other treatment options, then this would add an evidence-based weight management option for men not willing to take part in group-based or invasive interventions. In addition, men are less likely than women to do well on Orlistat for weight loss maintenance. 3
Public consultation work
Our PPI work prior to developing the study indicated that men found £400 over 12 months for 10% weight loss an acceptable amount of money if it helped with weight loss and weight loss maintenance. This is in line with evidence suggesting that if incentives are shown to be effective and cost-effective then they are likely to be considered acceptable by the public. 117 Promberger et al. 118 conducted a UK DCE and found that even a small change in effectiveness from 10% to 11% increased the proportion favouring incentives from 46% to 55% and that incentives for weight loss were more acceptable than for smoking cessation (60% vs. 40%). 5
Empirical work on effectiveness
Although no UK study has examined financial incentives for weight loss over 12 months, a recent UK trial found £400 to be effective in changing smoking behaviour among pregnant women. 119 Moreover, a DCE in the UK recently suggested that engagement in lifestyle interventions involving healthy eating and physical activity with around 10% weight loss required payment of £10.73 per week (i.e. £557.96 for 12 months overall). 33 The endowment incentives in this study are unique, and so generalising from a recent systematic review of US studies investigating contingency contracts for weight loss is not appropriate. With commitment contracts, the money is the participant’s own, which has implicit health inequalities, and in many studies participants choose the amount they deposit. The mean deposit in the review by Sykes-Muskett et al. 58 was £119.80 (adjusted for inflation), with a range of durations from 4 weeks to 1 year. The largest deposit was £480.24. Based on consideration of all of the above evidence, an a priori incentive ceiling value of £400 was set.
Appendix 12 Think-aloud survey interviews (n = 10): summary of responses about and appeal acceptability of financial incentives for weight loss
| Themes | Quotation |
|---|---|
| Unacceptable or no personal interest | |
| A moral issue to be paid to benefit yourself | I don’t think it’s right to get paid for doing something that’s good for yourself, to be honest . . . This is not acceptable even if benefits were to outweigh any negative effects . . . I think it’s totally wrong for the government to pay folks to lose weightP4. . . if you’re paying overweight people cash to lose weight, it makes the people who are not overweight feel ‘why are they getting money?’ The only person who’s going to benefit from somebody losing weight is the person themselves. It’s like rewarding people, I mean it depends how you get overweight in the first place but it’s usually through personal choice. So it’s rewarding you for getting overweight, so I’ll go for . . . I can imagine no benefits could ever outweigh the negative effects this hasP7- not overweight |
| 12-month programme is too short | I think it should incentivise people to maintain their weight. I think a 12-year, 12 months’ programme will not achieve that . . . it’s not a long enough time. So I think in general it’s a good programme so I think I would put this is acceptable if leads benefits over any negativesP1 |
| Other factors would be a bigger motivation | I think that the biggest incentive is gonna be what the diet is, rather than what the cash incentives are . . . Erm. I think an incentive would be some decent menus . . . And along with dietary advice, the quantity as well as the . . . Yes, how to. How to lose the weightP4 |
| No need for money | Well, it’s just the sort of person that I am. I can say that from a position of comfort . . . I’ve got two properties, I’ve got cars. You know, I don’t spend all the money that I earn, you know . . . I mean, if that’s what motivates people, then fineP6 |
| Ambivalence and views that changed during the course of the interview | I’m quite ambivalent about that. If I’m doing it, it’s for myself and my family, for my grandchildren . . . The whole thing is, I don’t think the money is any kind of incentive to me. I don’t have, say ‘right I could do this with that, or I could do that’, it’s of no consequence to me. It doesn’t mean, that I, you know, I wish I was, didn’t have money worries. Like everybody else I do. [Later] The obesity epidemic that we have must be costing us, the taxpayer, a fortune . . . So it would be lesser of the two evils, to pay them money to lose weightP8I find it interesting that it’s [the DCE] just purely based on a financial incentive, whereas I would tend to pay more attention to statistics on illness and life chances and all that sort of stuff. [Later] If you lose weight, you are personally going to benefit . . . and the country benefits, because you’ll hopefully get less illnesses. That’s the two benefits. The only negative would be if they didn’t actually lose weight but still got the cash, so if you’ve got cash, and you’ve lost weight, everybody wins. Well shit, I could use £400 I supposeP5 |
| Acceptable if donate to charity | No, no. I don’t want to get paid for anything . . . I’ll give it to the RNLI [Royal National Lifeboat Institution]P10That probably would be a bigger incentive to me, actually, than cash, because you’re doing something to help somebody else at the same timeP4Well if you received it in cash, you tend to go and treat yourself. So I think a donation to charityP7 not overweight |
| Acceptable and interested in receiving an incentive | If anyone says no to financial incentives they should be [inaudible] for lyingP2Definitely . . . to get some money. I’m not so fussed about the other stuff ‘cause I mean I know, eat less exercise more. I mean, it’s . . . [laughter]. But it’s just kinda, doing itP9 |
| Mixed views about value and distribution of incentive linked to weight loss targets. Some uncertainty, with views changing as interview progressed | £400, that’s actually quite a high incentive, more than I thought. I would try to get £400, that would be quite niceP1I think you need to do it consistently over 12 months. [Later, the interviewer gives examples such as more money at the end, or more money at the start.] That wouldn’t matter at allP5I would rather have the money at the end, as a rewardP8I’m more likely to lean towards a highest sum right at the end . . . Yeah. Whereas if you get something for doing a bit then it’s maybe not as motivating, especially if you’ve to get through the whole yearP9 |
| Competition: unimportant for most but seeing others lose weight might motivate | Competition against other men. For me personally that’s not a motivation at allP1I’m getting a bit competitive, so. I wouldn’t know that unless I was doing a weight loss programme . . . But, erm, if I was overweight, really overweight, and somebody lost a lot of weight, I would want to . . . It might motivate me, yeah. I suppose that is competitionP7 not overweight |
Appendix 13 Changes made to survey in response to think-aloud interview feedback
| ID | Issues raised | Changes made |
|---|---|---|
| F1 | Table explaining incentive scheme was unnecessary – preferred graphics and felt text description was possibly even enough | Table deleted, leaving only graphics and text |
| Unsure of what to do on example DCE choice | Now explicitly states ‘EXAMPLE CHOICE’ | |
| Unsure how to interpret the second restaurant voucher question | Wording changed to indicate that the ‘ideal’ allocation is that which they indicated in the previous question | |
| Preference for progress bar | Discussed and decided against | |
| Valued likelihood of achieving weight loss as same each time | Remove likelihood question from individual DCE choices, instead asking once at the end of the DCE choice set | |
| F2 | Unsure about text messages, felt it wasn’t clear what they would include | Additional information provided on what the texts would include |
| Felt the DCE explanation page was wordy | Spread information over two pages | |
| Felt table explaining incentive scheme was confusing | Table deleted, leaving only graphics and text | |
| Strong preference for cash – choices made on that basis | Charity/cash attribute removed from choice sets | |
| Difficulty in valuing likelihood of losing weight – without seeing other choice sets can’t make a relative judgement | Removed questions from each choice set asking only once at end | |
| Unsure of what benefits/negatives there are when judging how he feels about government paying incentives | Discussed and decided not to provide any further information | |
| Unsure how to interpret the second restaurant voucher question | Wording changed to indicate that the ‘ideal’ allocation is that which they indicated in the previous question | |
| Unclear whether to answer both weekly and annual income | Changed to annual income on advice from Ipsos | |
| Valued likelihood of achieving weight loss as same each time | Remove likelihood question from individual DCE choices, instead asking once at the end of the DCE choice set | |
| Layout of ethnicity and house questions unclear | Number group categories to clarify | |
| F3 | Unsure where/how to answer on target distribution question | Added text to clarify participants should click on a graph |
| Preference for graphics over table – found table somewhat confusing | Table deleted, leaving only graphics and text | |
| Unsure of answer choices in question about format they wish to receive information about money | Altered wording – ‘online’ now both ‘email’ and ‘web page’ | |
| Felt DCE explanation was wordy | Spread information over two pages | |
| Lottery question misunderstood | Deleted question | |
| Voucher/time preference question confusing – connecting it to previous weight loss questions | Move to end – further from weight loss questions | |
| Valued likelihood of achieving weight loss as same each time | Remove likelihood question from individual DCE choices, instead asking once at the end of the DCE choice set | |
| Strong preference for charity donation | Charity/cash attribute removed from choice sets | |
| F4 | Unsure of table explanation of incentive scheme | Table deleted, leaving only graphics and text |
| Unsure of lottery question – misunderstood | Deleted question | |
| Wording in restaurant voucher question unclear – ‘as opposed to’ – but inclusion of space to answer for both years | Altered answer choices – now answer only for year 1 | |
| Education question – uncertain which category qualification held fell into | Awaiting feedback from Ipsos | |
| Valued likelihood of achieving weight loss as same each time | Remove likelihood question from individual DCE choices, instead asking once at the end of the DCE choice set | |
| Strong preference for charity donation | Charity/cash attribute removed from choice sets | |
| F5 | Felt graphics were unnecessary, text would be enough | Left graphics as they will benefit others |
| Unsure of what to do on example DCE choice | Now clearly states ‘EXAMPLE CHOICE’ | |
| Valued likelihood of achieving weight loss as same each time | Remove likelihood question from individual DCE choices, instead asking once at the end of the DCE choice set | |
| Somewhat confused by question around opinion on government paying incentives – not clear what negatives/benefits are | Question switched for similar | |
| Time preference questions – not clear as being interpreted separately from weight loss questions | Moved to end of survey | |
| Ethnicity/house subgroups unclear | Number group categories to clarify | |
| Strong preference for charity donation | Charity/cash attribute removed from choice sets | |
| F6 | Weight target distribution question – unclear what to do/where to answer | Clarify with text that participants should click on the graph they prefer |
| Prefer graphics over table – more easily understood. Felt he didn’t need as many graphics | Table deleted leaving only graphics and text. Left all graphics as some will benefit | |
| Valued likelihood of achieving weight loss as same each time | Remove likelihood question from individual DCE choices, instead asking once at the end of the DCE choice set | |
| Uncertainty around weekly/monthly income – answer both or one? | Changed to annual income on advice from Ipsos | |
| Subgroup labels for ethnicity/home ownership somewhat unclear | Number group categories to clarify | |
| F7 | Weight target distribution question – unclear what to do/where to answer | Clarify with text that participants should click on the graph they prefer |
| Felt DCE explanation page was fairly wordy | Spread information over two pages | |
| Strong preference for charity donation | Charity/cash attribute removed from choice sets | |
| Felt graphics were tedious, didn’t require them | Left graphics as they will benefit others | |
| Objected to one of the DCE examples where don’t achieve final target but still paid from previous targets | Added text to graphic – only receive money from initial targets if they still weigh less than baseline at 12 months | |
| Example page too wordy and unclear it’s an example | Information spread over two pages and clarified in words ‘EXAMPLE CHOICE’ | |
| Opinion on government paying incentives – too wordy and too many options | Removed question and replaced with similar | |
| Time preference – unclear it’s to be interpreted separately from weight loss questions | Moved to end of survey | |
| F8 | Weight target distribution question – unclear what to do/where to answer | Clarify with text that participants should click on the graph they prefer |
| Felt that graphics were unnecessary, understood scheme with just text | Left graphics as others will benefit from them | |
| Unclear that the example choice shouldn’t be answered | Clarified in words ‘EXAMPLE CHOICE’ | |
| Time preference questions unclear – thought they should be interpreted alongside weight loss questions | Move to end of survey, further from weight loss questions | |
| FI no motivation – answered same programme each time | Not an issue – all others valued FI | |
| F9 | Felt graphics were unnecessary – quickly scrolled past | Graphics left as they will benefit others |
| Weight loss targets mentioned too many times | Left in – others didn’t raise this | |
| Valued likelihood of achieving weight loss targets as same each time | Remove likelihood question from individual DCE choices, instead asking once at the end of the DCE choice set | |
| Unsure why the voucher/time preference question is there | Nobody else raised this issue | |
| F10 | Felt 10% target was too high | Didn’t have much weight to lose. Targets in survey set using evidence from multiple sources |
| Too many graphics – tedious scrolling through them | Left graphics as they will benefit others | |
| Difficulty understanding concept of DCE – as a result repeatedly chose no weight loss programme. Felt financial incentive was no motivation | All others grasped the concept. Perhaps age-related, additionally felt financial incentive was no motivation |
Appendix 14 Data table of survey participants’ weight and weight perceptions
| Average | Range | |
|---|---|---|
| Weight | ||
| Current BMI (kg/m2) | 34.92 | 30.00–125.55 |
| Current height (cm) | 177.61 | 121.92–238.76 |
| Current weight (kg) | 110.13 | 52.62–260 |
| Size of clothing (cm) | 102.06 | 32–198.12 |
| Least weight (kg) | 87.93 | 38–254.01 |
| Ideal weight (kg) | 88.33 | 38.10–250 |
| Confident in ability to lose weight (score) | 3.51 | 1–7 |
| Confident in ability to keep lost weight off (score) | 3.38 | 1–7 |
| Importance of losing weight (score) | 5.04 | 1–7 |
| Number of times changed eating and/or activity to lose weight | 6.96 | 0–100 |
| Weight perception, n (%) | ||
| About right | 49 | 4.76 |
| Too heavy | 978 | 94.95 |
| Too light | 3 | 0.29 |
| Don’t know | 0 | 0.0 |
| Last time tried to lose weight, n (%) | ||
| Trying to lose weight at the moment | 519 | 49.67 |
| In the last 3 months | 97 | 9.28 |
| In the last 6 months | 78 | 7.46 |
| In the last 12 months | 87 | 8.33 |
| > 12 months ago | 175 | 16.75 |
| Never | 89 | 8.52 |
Appendix 15 Data table of survey and discrete choice experiment participants
| Characteristic | Number of participants | % |
|---|---|---|
| Age (years) | ||
| 18–24 | 47 | 4.50 |
| 25–34 | 156 | 14.93 |
| 35–44 | 218 | 20.86 |
| 45–54 | 262 | 25.07 |
| 55–64 | 224 | 21.44 |
| 65–75 | 138 | 13.21 |
| UK region | ||
| Scotland | 111 | 10.62 |
| Rest of the UK | 934 | 89.38 |
| Highest level of education completed | ||
| GCSE/O level/CSE | 198 | 18.95 |
| Vocational qualifications | 112 | 10.72 |
| A level or equivalent | 242 | 23.16 |
| Bachelor’s degree or equivalent | 321 | 30.72 |
| Master’s degree/PhD or equivalent | 102 | 9.76 |
| Other | 15 | 1.44 |
| No formal qualifications | 41 | 3.92 |
| Still studying | 7 | 0.67 |
| Prefer not to say | 7 | 0.67 |
| Current employment status | ||
| Working full time (≥ 30 hours per week) | 553 | 52.92 |
| Working part time (8–29 hours per week) | 57 | 5.45 |
| Working part time (< 8 hours per week) | 4 | 0.38 |
| Not working – house husband | 16 | 1.53 |
| Self-employed | 72 | 6.89 |
| Full-time student | 24 | 2.30 |
| Unemployed and seeking work | 44 | 4.21 |
| Retired | 170 | 16.27 |
| Not in paid work for other reason | 16 | 1.53 |
| Not in paid work because of long-term illness or disability | 89 | 8.52 |
| Estimate of annual household income | ||
| < £15,000 | 174 | 16.65 |
| Between £15,001 and £20,000 | 99 | 9.47 |
| Between £20,001 and £30,000 | 188 | 17.99 |
| Between £30,001 and £40,000 | 171 | 16.36 |
| Between £40,001 and £50,000 | 131 | 12.54 |
| Between £50,001 and £75,000 | 136 | 13.01 |
| Between £75,001 and £100,000 | 51 | 4.88 |
| > £100,000 | 34 | 3.25 |
| Don’t know | 9 | 0.86 |
| Prefer not to say | 52 | 4.98 |
| Ethnicity | ||
| White | 989 | 94.64 |
| Mixed/multiple ethnic groups | 6 | 0.57 |
| Asian/Asian British | 29 | 2.78 |
| Black/African/Caribbean/black British | 13 | 1.24 |
| Other | 1 | 0.10 |
| Prefer not to say | 7 | 0.67 |
| Number in household | ||
| 1 | 201 | 19.23 |
| 2 | 389 | 37.22 |
| 3 | 194 | 18.56 |
| 4 | 163 | 15.60 |
| > 4 | 94 | 9.00 |
| Prefer not to say | 4 | 0.38 |
| Car ownership | ||
| None | 180 | 17.22 |
| 1 | 529 | 50.62 |
| 2 | 264 | 25.26 |
| 3 | 58 | 5.55 |
| ≥ 4 | 14 | 1.34 |
| Accommodation | ||
| A whole house or bungalow that is | ||
| Detached | 234 | 22.39 |
| Semidetached | 339 | 32.44 |
| Terraced (including end-terrace) | 244 | 23.35 |
| A flat, maisonette or apartment that is | ||
| In a purpose-built block of flats or tenement | 180 | 17.22 |
| Part of a converted or shared house (including bedsits) | 39 | 3.73 |
| In a commercial building (e.g. in an office building, hotel or over a shop) | 6 | 0.57 |
| A mobile or temporary structure | ||
| A caravan or other mobile or temporary structure | 3 | 0.29 |
| Own or rent accommodation | ||
| Owns outright | 298 | 28.52 |
| Owns with a mortgage or loan | 389 | 37.22 |
| Part owns and part rents (shared ownership) | 12 | 1.15 |
| Rents (with or without housing benefit) | 333 | 31.87 |
| Lives here rent free | 13 | 1.24 |
| Health | ||
| Very poor | 37 | 3.54 |
| Poor | 150 | 14.35 |
| Fair | 411 | 39.33 |
| Good | 385 | 36.84 |
| Very good | 62 | 5.93 |
| Smoker | ||
| Yes | 175 | 16.75 |
| No | 643 | 61.53 |
| Used to | 227 | 21.72 |
| Vigorous activity | ||
| Days per week (average; range) | 1.65 | 0–7 |
| Moderate activity | ||
| Days per week (average; range) | 3.23 | 0–7 |
| Exercise intention | ||
| Less than intended | 439 | 42.01 |
| Slightly less than intended | 289 | 27.66 |
| As much as intended | 285 | 27.27 |
| Slightly more | 26 | 2.49 |
| Much more | 6 | 0.57 |
| Views | ||
| Add-on financial incentive should be funded (average; range) | 3.50 | 1–7 |
| Own responsibility for being overweight (average; range) | 5.17 | 1–7 |
| Time preference | ||
| Always chose A in multiple price list | 92 | 8.80 |
| Perceived temptation | ||
| Not tempted to depart from ideal allocation | 779 | 74.55 |
| Tempted to depart from ideal allocation | 266 | 25.45 |
| Use more in year 2 | 91 | |
| Use more in year 1 | 175 | |
Appendix 16 Data table of preferences for intervention components
| Characteristic | Interested in information | Interested in pedometer | Interested in SMS | Interested in incentives | Donation is preferred | Receive incentive at 12 months | Competition is a motivator | Prefer to lose weight quickly | GP surgery is preferred venue |
|---|---|---|---|---|---|---|---|---|---|
| 10% weight loss target | –0.00683 (0.111) | 0.0214 (0.0829) | –0.0716 (0.0689) | –0.220*** (0.0735) | 0.112 (0.0834) | ||||
| Aged 35–54 years | 0.0121 (0.116) | –0.0951 (0.116) | –0.270** (0.108) | –0.195 (0.122) | 0.324* (0.184) | 0.102 (0.119) | –0.177* (0.0963) | –0.126 (0.104) | 0.157 (0.120) |
| Aged 55–75 years | –0.0974 (0.139) | –0.299** (0.138) | –0.514*** (0.132) | –0.645*** (0.143) | 0.605*** (0.207) | 0.339** (0.144) | –0.457*** (0.120) | –0.233* (0.127) | 0.299** (0.145) |
| No qualifications/GCSE/O level/CSE | –0.0509 (0.0985) | 0.00675 (0.0965) | 0.0303 (0.0939) | –0.214** (0.0974) | 0.115 (0.133) | 0.0902 (0.102) | 0.0155 (0.0852) | 0.0814 (0.0902) | –0.0154 (0.103) |
| Does not own a car | 0.0813 (0.121) | 0.191 (0.119) | 0.165 (0.117) | 0.316** (0.127) | 0.117 (0.176) | –0.0351 (0.126) | 0.00546 (0.105) | 0.0683 (0.112) | 0.102 (0.126) |
| Income < £15,000 | –0.335** (0.144) | 0.0158 (0.142) | –0.242* (0.139) | –0.124 (0.144) | –0.321 (0.201) | 0.0496 (0.149) | 0.00715 (0.126) | –0.0705 (0.133) | 0.00520 (0.150) |
| Income £15,000–30,000 | –0.0972 (0.0991) | 0.00781 (0.0966) | –0.0618 (0.0933) | 0.00255 (0.0992) | –0.408*** (0.141) | 0.0280 (0.102) | 0.0300 (0.0846) | –0.153* (0.0902) | 0.234** (0.102) |
| Unemployed/not in paid work | –0.0455 (0.144) | –0.208 (0.143) | –0.0223 (0.140) | –0.136 (0.147) | 0.140 (0.214) | 0.170 (0.151) | 0.0462 (0.126) | 0.101 (0.135) | 0.119 (0.152) |
| Retired | 0.364*** (0.138) | –0.101 (0.130) | 0.0798 (0.130) | 0.0782 (0.131) | 0.346** (0.169) | –0.0427 (0.140) | 0.160 (0.120) | 0.0903 (0.126) | 0.261* (0.140) |
| Single household | –0.198* (0.113) | –0.234** (0.112) | –0.240** (0.110) | –0.238** (0.115) | –0.100 (0.164) | –0.160 (0.118) | –0.205** (0.1000) | 0.0636 (0.104) | –0.126 (0.118) |
| Owns house | –0.0598 (0.0964) | –0.0327 (0.0942) | –0.0901 (0.0914) | –0.0534 (0.0977) | –0.0120 (0.137) | 0.119 (0.0993) | 0.00453 (0.0824) | 0.0238 (0.0879) | –0.113 (0.0999) |
| Non-white ethnicity | 0.519** (0.218) | –0.0238 (0.192) | –0.0168 (0.186) | 0.0694 (0.204) | 0.0397 (0.299) | –0.242 (0.206) | 0.191 (0.165) | 0.0726 (0.180) | 0.437** (0.206) |
| Scotland | 0.0755 (0.130) | 0.0766 (0.128) | 0.139 (0.121) | –0.0394 (0.129) | 0.0536 (0.178) | 0.228* (0.133) | –0.0917 (0.113) | –0.175 (0.119) | 0.134 (0.135) |
| BMI | –0.00564 (0.00978) | –0.00359 (0.00954) | 0.00149 (0.00937) | –0.0235** (0.00992) | 0.00560 (0.0137) | 0.00810 (0.0102) | 0.000192 (0.00845) | –0.0119 (0.00906) | –0.00501 (0.0103) |
| Confidence in ability to lose weight | –0.0230 (0.0272) | –0.0129 (0.0260) | 0.0148 (0.0250) | –0.0319 (0.0271) | –0.0691* (0.0364) | 0.0605** (0.0273) | 0.0675*** (0.0227) | –0.0116 (0.0240) | –0.0205 (0.0273) |
| Importance of losing weight | 0.286*** (0.0288) | 0.242*** (0.0282) | 0.226*** (0.0279) | 0.190*** (0.0288) | 0.0544 (0.0409) | –0.0343 (0.0296) | 0.116*** (0.0251) | 0.0511* (0.0264) | –0.0303 (0.0298) |
| Currently trying to lose weight | –0.0982 (0.0963) | –0.143 (0.0936) | –0.0495 (0.0881) | –0.0411 (0.0965) | –0.198 (0.130) | 0.0146 (0.0974) | –0.116 (0.0805) | –0.180** (0.0861) | 0.0567 (0.0979) |
| 1–3 previous weight loss attempts | 0.222 (0.136) | 0.0154 (0.136) | 0.125 (0.141) | 0.117 (0.138) | –0.0170 (0.197) | 0.259* (0.148) | –0.0586 (0.126) | 0.250* (0.135) | 0.0906 (0.150) |
| ≥ 4 previous weight loss attempts | 0.403*** (0.141) | 0.113 (0.140) | 0.343** (0.143) | 0.286** (0.142) | 0.0193 (0.201) | 0.0732 (0.152) | 0.140 (0.128) | 0.361*** (0.137) | 0.131 (0.152) |
| Percentage difference between current and ideal weight | 0.00245 (0.00485) | –0.000228 (0.00467) | 0.00812* (0.00455) | 0.0156*** (0.00486) | –0.00451 (0.00670) | 0.00105 (0.00497) | 0.000878 (0.00411) | 0.00405 (0.00440) | 0.00512 (0.00499) |
| Self-reported health | 0.0238 (0.0530) | 0.0317 (0.0516) | –0.0296 (0.0498) | –0.0327 (0.0541) | 0.0352 (0.0721) | 0.0356 (0.0540) | 0.0221 (0.0452) | 0.0726 (0.0478) | –0.206*** (0.0549) |
| Participates in vigorous activity | 0.172* (0.0926) | 0.286*** (0.0892) | 0.223*** (0.0864) | 0.144 (0.0931) | 0.0698 (0.126) | 0.0193 (0.0948) | 0.405*** (0.0789) | –0.0154 (0.0841) | 0.0500 (0.0946) |
| Smoker | –0.0956 (0.108) | –0.0328 (0.106) | 0.0243 (0.104) | –0.0848 (0.108) | –0.608*** (0.196) | 0.111 (0.113) | 0.302*** (0.0926) | –0.0460 (0.0992) | –0.00973 (0.113) |
| Present oriented | 0.111 (0.147) | –0.0636 (0.142) | 0.0599 (0.139) | –0.121 (0.146) | 0.293 (0.192) | –0.0962 (0.151) | 0.0236 (0.124) | 0.0973 (0.132) | 0.326** (0.151) |
| Tempted to consume more in year 1 | 0.0986 (0.112) | 0.111 (0.108) | 0.0291 (0.102) | 0.166 (0.113) | –0.0286 (0.154) | –0.319*** (0.114) | 0.0796 (0.0928) | 0.189* (0.0991) | 0.0577 (0.112) |
| People are responsible for being overweight | –0.0150 (0.0297) | –0.0351 (0.0288) | –0.0226 (0.0280) | 0.0790*** (0.0297) | 0.00770 (0.0407) | –0.0158 (0.0304) | 0.00823 (0.0254) | –0.0154 (0.0270) | 0.0492 (0.0305) |
| Unacceptability of financial incentives | –0.123*** (0.0225) | 0.0915*** (0.0305) | |||||||
| Constant | –2.036*** (0.649) | –0.855* (0.460) | 0.159 (0.463) | ||||||
| Observations | 971 | 971 | 971 | 971 | 971 | 971 | 971 | 971 | 971 |
| Pseudo-R2 | 0.1255 | 0.0827 | 0.0936 | 0.1280 | 0.0885 | 0.0358 | 0.0447 | 0.0218 | 0.0500 |
Appendix 17 Recruitment focus group plan and topic guide
Research question
What are the perspectives of men from a disadvantaged area of Scotland on strategies for recruiting men onto a study to help support weight loss and maintenance?
Sampling strategy
Purposive sampling.
Eligibility
Men living in an area of disadvantage who:
-
are overweight or obese
-
have previously been overweight or obese
-
are experienced at working with men from deprived areas.
Recruitment
Participants will be recruited through local community contacts.
Venue
A private and quiet room, no anticipated interruptions, convenient for the participants. Drinks and food available at the end of meeting, not at the beginning.
On arrival
Welcome. Name badges. Researcher introductions. Ask participants to sign a consent form. Give demographics sheet to complete.
Introduction by group facilitator (MM)
This focus group is part of the Game of Stones trial which is funded by the National Institute for Health Research. This trial is looking at a new approach to helping men lose weight. Today you will be taking part in a focus group to help us finalise our plans for recruiting men when the study starts in the New Year.
Firstly, for the benefit of those of you who have never taken part in a focus group before, I will start by telling you a little bit about the process. A focus group is a focused discussion about a topic. The discussion is recorded, then transcribed, entered onto computer software and the discussion is then coded and analysed by the research team. All information is completely confidential. I will be leading the focus group today and Rebecca will be observing and taking notes to make the transcribing easier. Participants often enjoy focus groups, as they feel they can have a voice and an opportunity to reflect with colleagues about a topic. So I hope you will all find today both enjoyable and useful.
All information is confidential – in written reports of the study, names will be changed and the location of the group will not be revealed.
-
Explain that the focus is on getting the opinions of men on what the best way to recruit, approach and retain men in the study (there are no rights and wrongs – everyone’s view is important to us).
-
Provide an opportunity to ask any questions.
-
Introduce the audio-recorder underlining the importance of confidentiality.
Topic guide
-
We know that many women go to Weight Watchers and Slimming World to lose weight, but very few men join weight loss services. What are your views about what is available to help men to lose weight?
-
What are the barriers/what would put men off taking part?
-
Have you tried anything to lose weight before? What did you try? Did it work?
-
Do you have any male friends that have tried to lose weight before? What did they try? Did it work?
-
Are there any ways of losing weight you have thought about but haven’t tried yet? What has stopped you? What would encourage you to give it a go?
-
Short study summary
Men that participate in our study will receive text messages for up to 12 months to see if this can help them lose weight. Men will also receive a pedometer and access to website information that could help them lose weight. The study will involve meeting a researcher on up to 4 occasions over the year to be weighed and answer some questions.
-
If, as an overweight man, you were approached on the street by a researcher from the University of Stirling (with an ID badge) and offered a chance to take part in a study which could help you lose weight, what would your reaction be?
-
What might put you off in this situation? Why?
-
Would it make a difference if it were researchers from your local university? Would it make a difference if the researchers were wearing fleeces/clothes with the University of Stirling logo on?
-
What would be the best way to approach men in this way?
-
Where would be the best place to approach men? (prompt: health centre, on the street?)
-
What language would be best to use for approaching men in this way? Are there any words that should be avoided? Are there any words which it would be ok to use?
-
If someone you knew told you about a study that could help you lose weight, would your response be similar or not? Who would you be likely to listen to and why? Who would be most likely to encourage you to take part? (prompt: wife/partner, friend, local community worker, nurse?) Why would you respond in this way?
-
If the researcher offered to talk you through the leaflet (shows summary information sheet) would you take one away? Would you consider hearing about the study and agreeing there and then? How might we increase the number of men who get back to us? How do we recruit men from all walks of life?
-
-
If you were sent a letter by your GP asking if you would like to take part in a study that could help you lose weight, would you be interested? Would you return a freepost return opt-in/-out card? (shows card/show letter)
-
At this point, if you forgot to return the opt-in/-out card, how would you feel about a researcher phoning you to remind you about the study?
-
-
If you had agreed to take part in the study, what local venue would be best for you to attend 4 times over the course of a year to be weighed? (Prompt: community centre, health centre, GP practice?) Why would you choose this venue?
-
Would you mind attending a different venue at the different time points?
-
Would you mind if a venue was not in the local area, would you be likely to travel to make the appointment? Would reimbursing travel costs make a difference?
-
-
Do you have any suggestions for how best we can get men to volunteer for our study and attend the 4 appointments for weighing?
-
Would you prefer to meet the same researcher over 4 appointments or would you not mind who you saw?
-
Thanks for taking part in this group today. We have brought some lunch along today . . .
Appendix 18 Recruitment focus group results summary
Community recruitment and safety
Focus group participants warned researchers to be cautious about how they approached men in the community. Some felt that men would deliberately ‘body swerve’ researchers attempting to recruit in public spaces, often because they would assume that they were ‘wanting my debit card’ and ‘money every month off me’. They also expressed concern about researcher safety, joking that one possible outcome was to get ‘your [expletive] kicked in [laughter]’. In particular, the focus group participants advised that being approached on the street would be unwelcome because they would ‘think you were from the social’ or that ‘there’s going to be a cost here’. On-street approaches were felt to be particularly ineffective or even ‘dodgy’ in more deprived areas:
It’d probably work some place like in [less deprived] area, but in the schemes you’d just get ridiculed.
Focus group participant, SIMD 1
Relational recruitment and trust
Focus group participants felt that a lack of a relationship with the researcher could be a barrier to recruiting men from more deprived areas because of ‘issues with trust and reassurance’. They suggested that going to ‘the heart of communities’ by recruiting in local spaces and community centres, and engaging with local staff and community members, would be the most effective way to build up relationships. Moreover, masculine identity was seen as another major barrier to participation, which may be at least partially broken down if recruitment takes place in environments that men are comfortable in:
See you’ve got this [area name], everybody’s a hard man and I’m not doing that’s stuff for wimps and all that, but I think if you get them in their own environment like i.e. this place, it would be a lot better.
Focus group participant, SIMD 1
Trust, relationships, and listening to and consulting with potential participants were described in this focus group as particularly important; otherwise, sceptical community members might just ask ‘what’s the con?’. Indeed, a lack of consultation with men from the target group was seen as a major flaw in previous weight management work in deprived communities:
Aye that’s what I’m saying, but they don’t consult, they draw up that programme without asking folk. I’ve never known anybody that’s took part in a study to say ‘what kinda . . . we’re going to draw up a programme to go and deliver a weight loss, how d’you think we should do it?’ They don’t, they come in and just prescribe to us how they think we should be doing it.
Focus group participant, SIMD 1
Appendix 19 Alternative SMS coding for behaviour change techniques, theoretical functions and the Game of Stones logic model
| # | SMS | BCT | Function | Logic model |
|---|---|---|---|---|
| 1 | Welcome to Game of Stones <name>! Over 12 weeks we’ll send you some texts. The bad news: reading texts won’t change your weight. The good news: they’re low calorie. We’ve put these texts together with the help of men who successfully lost weight. They are based on facts and real life experience | General communication technique | ||
| 2 | The goal is to lose 5% in 12 weeks. John said the goal gave him confidence to try changing his eating knowing that he’s got something to work towards. Losing more than 3% of your body weight has health benefits and helps to cut your chances of cancer, heart disease and diabetes |
1.3 Goal-setting (outcome) 5.1 Information about health consequences |
Motivation | Motivation (weight loss goal) |
| 3 | Ok, here’s the deal. Some texts will be useful and others maybe won’t. Just pick whatever works for you and ignore the rest. If you want to reply to any of the texts please do. We read every text but usually we won’t be able to write back. Sorry | General communication technique | ||
| 4 | How to lose weight? Here’s a simple fact: sensible eating works… but only if you stick to it. Go to our Game of Stones web page with links to web pages full of information that our men find useful. www.gameofstonesresearch.com (last accessed 25 June 2019) | 15.1 Verbal persuasion about capability | Motivation, engagement | Self-efficacy (initiate weight loss) |
| 5 | Most of our men make up their own sensible eating rules. Carl said that it’s straightforward, eat less rubbish. Everybody knows it, but hard to do. Cutting down and reducing portion sizes is the main strategy that works for our men. Losing weight is about finding what works for you and your life | 4.1 Instruction on how to perform the behaviour | Self-regulation | Self-regulation (planning) |
| 6 | You’re changing what you’re eating and drinking, you’re not dieting. Think about it as improving your lifestyle, not being on a diet. Check out this helpful wee booklet full of tips from the Men’s Health Forum. www.issuu.com/menshealthforum/docs/eat_well_final_hrnon-border (last accessed 25 June 2019) | 4.3 Re-attribution | Motivation, engagement | Motivation (intention) |
| 7 | Have you made any changes this week <name>? Cut down on something or made some sensible eating changes? Let us know. Have a nice rest of the weekend | 2.3 Self-monitoring of behaviour | Self-regulation, engagement | Self-regulation (self-monitoring) |
| 8 | Hi <name>. Week 2. This week we’ll talk about planning and making changes. What are your weight loss plans for this week? Here is a useful link with some great info on healthy food. www.menshealthforum.org.uk/food-faqs (last accessed 25 June 2019) | 1.1 Goal-setting (behaviour) | General communication technique, engagement | Self-regulation (planning) |
| 9 | To weigh or not to weigh? Our Game of Stones men are split right down the middle. Half check their weight at least once a week, others don’t. Rob told us he started weighing himself two or three times a week and he has kept that up afterwards |
2.4 Self-monitoring of outcome(s) of behaviour 6.1 Demonstration of the behaviour |
Self-regulation | Self-regulation (self-monitoring) |
| 10 | Changing your eating includes a few things: stopping, starting, swapping, reducing. Is there anything you could stop, start, swap or reduce this week? Ian used to have toast with his tea at night and completely stopped that. Well done Ian, reducing the amount of bread you eat can be great for weight loss |
1.4 Action-planning 6.1 Demonstration of the behaviour 4.1 Instruction on how to perform the behaviour |
Motivation, self-regulation, general communication technique | Motivation (intention), self-regulation (planning) |
| 11 | Steve started to eat a lot more slowly. Eating more slowly gives your stomach time to tell your brain when you’re full, which reduces overeating. How to do it though? Try sitting down at a table when eating, switch off any distractions, put knife and fork down between bites and count 30 chews before swallowing |
4.1 Instruction on how to perform the behaviour 6.1 Demonstration of the behaviour 4.1 Instruction on how to perform the behaviour |
Motivation, self-regulation | Motivation (intention), self-regulation (planning) |
| 12 | Planning what to eat and when is worth considering. Plans don’t always work, but they are better than making it up as you go along. Simon plans his mealtimes, so he’ll go to the supermarket with a wee list and gets food for the week, with one top up trip for the fresh stuff like fruit, veg, milk and bread |
4.1 Instruction on how to perform the behaviour 6.1 Demonstration of the behaviour 4.1 Instruction on how to perform the behaviour |
Motivation, self-regulation | Motivation (intention), self-regulation (planning) |
| 13 | Reducing portion size is what most Game of Stones men plan to do. John eats 3 regular size meals, no seconds, few snacks. He lost nearly 2 stones in 12 weeks. How to reduce portion sizes? Check this useful tip from the Men’s Health Forum www.menshealthforum.org.uk/only-diet-always-works (last accessed 25 June 2019) |
4.1 Instruction on how to perform the behaviour 6.1 Demonstration of the behaviour |
Motivation, self-regulation, engagement | Motivation (intention), self-regulation (planning) |
| 14 | Ok, that’s week 2 wrapped up. How has your week been? Next week we’ll chat a bit about physical activity. Enjoy your Sunday | 1.5 Review behaviour goal(s) | Communication | Self-regulation (self-monitoring) |
| 15 | Week 3 – let’s talk activity. Folk normally think weight loss is about eating less and moving more. Correct, but the balance matters. Quick fact: Losing weight is 80% about what you eat and 20% about your physical activity. Maintaining weight loss is 50% eating and 50% activity |
4.1 Instruction on how to perform the behaviour 1.1 Goal-setting (behaviour) |
Motivation | Motivation (intention) |
| 16 | Most Game of Stones men started walking more to get the step count up. Do you have any activity plans for this week? Physical activity is anything that takes a bit of effort and makes you breathe fast and feel warmer – not just going to the gym or running a marathon |
4.1 Instruction on how to perform the behaviour 1.1 Goal-setting (behaviour) |
Motivation | Motivation (intention) |
| 17 | Walter says he put on weight because he stopped being active because of a knee injury. True, but the food he ate probably paid an even bigger role | 4.3 Re-attribution | Motivation | Motivation (intention) |
| 18 | Our men told us that one of their favourite web pages on men’s weight loss is ManvFat – www.manvfat.com/ (last accessed 25 June 2019). Lots of useful advice and interesting articles | Engagement | ||
| 19 | Here’s the thing though. Our men on Game of Stones tell us if they exercise they feel better and if they feel better they eat better. Win-win. The more active you are, the better you feel, and the better you feel, the better you eat. Are you planning any activities this weekend? |
1.1 Goal-setting (behaviour) 5.1 Information about health consequences 4.3 Re-attribution |
Motivation, engagement | Motivation (intention) |
| 20 | Having a wee treat after physical activity, or chilling for the rest of the day can backfire. That little voice in your head saying. ‘You deserve it <name>‘. The next time you did some physical activity and you think ‘You deserve a treat or to chill out’, what are you going to do? | 1.2 Problem-solving | Self-regulation, engagement | Self-regulation (planning) |
| 21 | That’s all on physical activity. Hope you had an active and successful week and your weight loss is going well <name> | Engagement | ||
| 22 | Week 4. This week we talk about the world we live in, which sometimes feels like there is a temptation lurking around every corner. What are your weight loss plans this week <name>? |
1.1 Goal-setting (behaviour) 1.3 Goal-setting (outcome) |
Motivation, engagement | Motivation (intention, weight loss goal) |
| 23 | Often the easy thing to do in our environment is to eat a lot and move little. We can deal with it by making better choices, but that takes some effort. Steve thinks that the supermarkets are tricky when you’re losing weight. He makes a list before going. If it’s not on the list, it doesn’t go in the trolley |
4.1 Instruction on how to perform the behaviour 6.1 Demonstration of the behaviour |
General communication technique, adjuvant behaviours | Self-regulation (planning) |
| 24 | Chris says he found it difficult to decide what the healthy options are in the supermarket. There is so much choice. Sounds familiar? Here are some great tips on how to read food labels. www.menshealthforum.org.uk/how-read-food-labels (last accessed 25 June 2019) | Engagement, adjuvant behaviours | ||
| 25 | Jan says if you don’t buy it, you can’t eat it. So think about how to buying less of it in the first place. He used to love biscuits in the evenings. Digestives. 73 calories a biscuit and he would have half a pack minimum. Now he just doesn’t have them in the house |
5.1 Information about health consequences 6.1 Demonstration of the behaviour 12.1 Restructuring the physical environment |
Self-regulation | Self-regulation (planning) |
| 26 | Gavin has a couple of tins of soup in the house or something easy to heat up in the freezer as a plan B. That avoids going out for dinner or ordering in take-away when he feels lazy or has little time. He still eats out sometimes, but only when he plans it |
1.2 Problem-solving 6.1 Demonstration of the behaviour |
Self-regulation | Self-regulation (planning) |
| 27 | Any exciting plans for this weekend <name>? Hope you have a good one | General communication technique | ||
| 28 | The bottom line this week: prepare for the supermarket battle and try and keep the less healthy stuff as far away from you as you can. Hope you had a successful week <name> | General communication technique | ||
| 29 | Week 5 –This week we will cover keeping an eye on things. What weight loss plans do you have for this week <name>? |
1.1 Goal-setting (behaviour) 1.3 Goal-setting (outcome) |
Motivation, general communication technique | Motivation (intention, weight loss goal) |
| 30 | Our men say keeping a record of what they eat and drink is helpful. Smartphone apps are most popular, but anything goes: app, paper, photos. Why is keeping a record so useful? Jan says it kinda forces him to think about what he’s eating and drinking and keeps him more focused |
2.3 Self-monitoring of behaviour 6.1 Demonstration of the behaviour |
Self-regulation, adjuvant behaviours | Self-regulation (self-monitoring) |
| 31 | Lukasz is keeping a record which makes him watch what he eats and drinks, he tries to go for fresh stuff as much as possible and sticks mostly to water. Have you ever kept a food and drinks record? Or are you thinking about it? |
2.3 Self-monitoring of behaviour 6.1 Demonstration of the behaviour |
Self-regulation, engagement, adjuvant behaviours | Self-regulation (self-monitoring) |
| 32 | Keeping a record isn’t everyone’s cup of tea, but if you can do it even for a wee while it’s worth giving it a shot. If you can’t be bothered to write things down you could try taking pictures with your phone | 2.3 Self-monitoring of behaviour | Self-regulation, adjuvant behaviours, general communication technique | Self-regulation (self-monitoring) |
| 33 | It can be interesting to keep a record just for a bit, many of our men say they didn’t realise how much they snack in between meals. Some say it showed them how many sugary drinks they are having. Sticking mainly to water, tea or coffee can make a big difference |
4.1 Instruction on how to perform the behaviour 2.3 Self-monitoring of behaviour |
Self-regulation, adjuvant behaviours | Self-regulation (self-monitoring) |
| 34 | Alcohol is also worth keeping an eye on. Two pints of beer have 364 calories, more than a burger. Worse, many feel peckish afterwards and crave food. Double trouble |
4.2 Information about antecedents 5.1 Information about health consequences 12.3 Avoidance/reducing exposure to cues for the behaviour |
Self-regulation | Self-regulation (self-monitoring) |
| 35 | That’s week 5 done! How has this week been for you and how’s the weekend going <name>? | General communication technique | ||
| 36 | Week 6. Tips and tricks week. We share some tips from men who successfully lost weight on this programme. Maybe those also work for you? | General communication technique | ||
| 37 | Rick keeps his weight loss goal on his wall next to a couple of things that he looks at daily. It’s good to have a daily reminder of what you’re aiming for | 6.1 Demonstration of the behaviour | Motivation, adjuvant behaviours | Motivation (weight loss goal) |
| 38 | Rob says he only has a treat occasionally now, for a special occasion. Cause it’s not a treat when you have it every day, is it? | 6.1 Demonstration of the behaviour | Self-regulation | Self-regulation (planning) |
| 39 | John says you should make a plan and write it down. What fits into your life? What works, what doesn’t, then modify it |
1.4 Action-planning 6.1 Demonstration of the behaviour |
Self-regulation | Self-regulation (planning) |
| 40 | Jan says you should eat things you like and don’t force yourself to eat food you don’t like, as you’ll never stick to eating them regularly. This booklet from the Men’s Health Forum has loads more tips, so worth sending you the link again. https://issuu.com/menshealthforum/docs/eat_well_final_hrnon-border | 6.1 Demonstration of the behaviour | Self-regulation, engagement | Maintenance motives (satisfaction with behaviour change) |
| 41 | If you had to give someone a tip on how to lose weight, what would you tell them <name>? | Engagement | ||
| 42 | Were any of these tips this week useful to you? There are many ways to get to your goal, and no one tip is right or wrong. Have a nice weekend <name> | Engagement | ||
| 43 | Week 7 – past the half-way point already. This week is about triggers which can tempt us into less healthy food choices. Everyone has a weak spot when it comes to food. Your triggers can be anything like feeling stressed, time of day, the weekend or a particular place |
1.2 Problem-solving 7.1 Prompts/cues |
Self-regulation, general communication technique | Self-regulation (planning) |
| 44 | Knowing our triggers helps us deal with them. Either by avoiding them, or by working through them, knowing that they will pass. How will you deal with your triggers? |
1.2 Problem-solving 7.1 Prompts/cues |
Self-regulation, engagement | Self-regulation (planning) |
| 45 | You know what’s good and what isn’t, sort of. Men tell us about loads of unhealthy foods they eat, for example Kamal says that chocolate is his downfall. The thing is though, having chocolate once in a while is not really the problem, having loads of it all the time would be a problem | General communication technique | ||
| 46 | Andre says he often craves something sweet after dinner. The craving always passes even when he doesn’t have it. It gets easier over time. His tip is that you resist the craving for 15 minutes and after that time it’s usually gone |
4.1 Instruction on how to perform the behaviour 6.1 Demonstration of the behaviour |
Self-regulation | Self-regulation (planning) |
| 47 | What are your triggers? The wee sneaky chocolate bar when getting petrol? Couple of beers at the end of the day because you deserve it? How can you deal with them? Buy chewing gum instead? Try having only one? |
1.2 Problem-solving 7.1 Prompts/cues |
Self-regulation, engagement | Self-regulation (planning) |
| 48 | One of the biggest triggers is around you, just now. Can you see it? A thing called ‘weekend’. Many men struggle a bit on weekends. Sounds familiar? Bob says he tries to balance enjoying himself without going overboard | General communication technique | ||
| 49 | How has your week been <name>? Hope you’re having a great weekend. Next week we’ll talk about what you managed to achieve so far | General communication technique, engagement | ||
| 50 | Welcome to week 8, only 4 more to go! Time to look back. What have you changed? What things are different for you? Those kind of questions | General communication technique, engagement | ||
| 51 | Gregor says seeing the results coming through motivates even more and you think, this is achievable, I can get there, I can go further. Around week 8 men tell us they can feel a real difference from the changes: more energy, clothes not as tight, perhaps the belt went back a notch | 6.3 Information about others’ approval | Motivation | Maintenance motives (satisfaction with behavioural outcomes) |
| 52 | Simon says it’s a mindset, if you’ve got a pattern of eating healthily, you’ve got the results, that’s when you become encouraged to keep doing that. How satisfied are you with what you have achieved so far? | 8.3 Habit formation | Motivation, engagement | Maintenance motives (satisfaction with behavioural outcomes), habit |
| 53 | One thing that is quite important for long term weight loss is that you actually like doing the things that you’ve changed. If you eat broccoli every day and you don’t like broccoli, chances are that it’s not going to work for you in the long term | 5.2 Salience of consequences | Motivation | Maintenance motives (satisfaction with behaviour change) |
| 54 | Walter told us that after a few weeks he sat down for 5 minutes and thought about it. Can I keep this up? That told him what to keep and what to ditch |
1.1 Goal-setting (behaviour) 6.1 Demonstration of the behaviour |
Motivation | Maintenance motives (satisfaction with behaviour change) |
| 55 | What is your one change or achievement since you’ve started this programme that you are most proud of <name>? | 15.3 Focus on past success | Motivation, engagement | Maintenance motives (satisfaction with behaviour change) |
| 56 | Next week we’ll talk about habits and routines. Hope it was a successful week and enjoy the rest of your weekend <name>! | General communication technique | ||
| 57 | Hi <name>. How are you getting on? Week 9 already. Right, this week is about habits and routines. Routines are things you plan and do regularly and they help you build good habits which are like our mental autopilot | General communication technique | ||
| 58 | Kamal says it might sound daft, but it’s quite hard to eat sensibly, but when you’ve got your routine it’s just that little bit easier | 6.3 Information about others’ approval | Self-regulation | Self-efficacy (maintenance) |
| 59 | If you have started doing things a few times then you might get into routines. The more you make things a routine, the easier it gets as you build your habits. How to build routines and habits? You repeat things, at the same time and in the same place. Simple in theory, not quite so simple in practice | 8.3 Habit formation | Self-regulation, engagement | Habits, self-efficacy (maintenance) |
| 60 | Your old routines are in strong competition with the new ones. Routines can work for you, and work against your progress…Walter said when he gets back into the old routine, that’s when you start to slip down the slippery slope again, with eating between meals and things like that | Self-regulation | Habits | |
| 61 | Time, patience and commitment can pay off. John says he’s got to the stage where sensible eating routines have changed, the old routines are mostly gone | 6.3 Information about others’ approval | Self-regulation | Habits, self-efficacy (maintenance) |
| 62 | Any interesting plans for the weekend? We have a good one for you! Why did the tomato blush? Stay tuned for the answer tomorrow | General communication technique, engagement | ||
| 63 | Why did the tomato blush? Because it saw the salad dressing . . . J Hope you’re having a nice weekend <name>! Apologies for the dodgy sense of humour | General communication technique | ||
| 64 | Week 10, how was the weekend and what are your plans for this week? Over the next few days we’ll cover setbacks. They are a normal part of weight loss, but that doesn’t make them any easier to deal with | General communication technique, engagement | ||
| 65 | Gavin says that when you’re getting fed up and you want to go off the wagon you’ll make excuses for yourself and you’ll legitimise it. Does that sound familiar? Do you sometimes make excuses for yourself? (you wouldn’t be the only one) | Self-regulation | Self-regulation (goal setting) | |
| 66 | Two questions to ask yourself after setbacks: 1. Were my plans realistic enough?, 2. What could I do better the next time? The reality is that sometimes life will get in the way of weight loss and you take your eye off the ball. It’s the way you respond that will make the difference to your weight loss | 1.2 Problem-solving | Self-regulation, general communication technique | Self-regulation (planning) |
| 67 | Our men sometimes kick the can down the road. After today I’ll change. I’ll start next week. Next month will be different. It’s normal to think that way. What would you tell someone who avoids getting back on track? | 13.1 Identification of self as role model | General communication technique, engagement | Motivation (intention) |
| 68 | Rick says it’s about falling off the wagon and getting back on, but maintain your vision, I’m at point A and I want to get to point F. Remember your vision | 1.3 Goal-setting (outcome) | Motivation | Motivation (intention) |
| 69 | That’s enough talking about setbacks! What was your best accomplishment this week <name>? | 15.3 Focus on past success | Motivation | Motivation (intention) |
| 70 | No worries, we won’t do bad jokes this weekend like asking why the banana went to see the doctor (it was not peeling very well). Ok, ok, we’ll stop | General communication technique | ||
| 71 | Week 11. How’s it going <name>? This week will be about special occasions: birthdays, weddings, and holidays. Some men tell us that they do well with their weight loss, then a special occasion comes along and things fall down | General communication technique | ||
| 72 | Carl was out for his birthday party, eating and drinking too much, so it caused him to fall back again and he’s not got back into it yet. Rob says his holidays probably set him back a lot, he went a bit over the top. Do you have any words of wisdom for the Carls and Robs in this world? | 13.1 Identification of self as role model | Engagement | Self-regulation (planning) |
| 73 | You should continue to have a good time on birthdays, weddings and holidays. But without feeling guilty. How can you do that? | 1.2 Problem-solving | Self-regulation | Self-regulation (planning) |
| 74 | Rick says that when he’s got a special occasion coming up he prepares for it and makes sure he has a period where you are doing well before making loads of sensible eating choices – this way you will have earned it even more |
1.2 Problem-solving 6.1 Demonstration of the behaviour |
Self-regulation | Self-regulation (planning) |
| 75 | Garry’s golden rule is to make the first drink a soft one. He says it’s easy to get carried away with the drinks and they are quite calorific. He also has regular water breaks – you can enjoy an occasion without going completely overboard |
1.2 Problem-solving 6.1 Demonstration of the behaviour |
Self-regulation | Self-regulation (planning) |
| 76 | Another way to handle your special occasion after they happened is to make up for it. Have a period after your birthday or holiday when you put effort into a sensible eating and drinking routine | 4.1 Instruction on how to perform the behaviour | Self-regulation | Self-regulation (planning) |
| 77 | It’s all about balance. If your new lifestyle ruins the fun then why stick to it? If your old routines ruin your hard work, then why bother? Right, 1 more week, you’ve nearly done it. Hope the weekend is going well . . . | General communication technique | ||
| 78 | It’s the final countdown da da da da! Week 12, the last one. Any grand plans for this week <name>? | General communication technique, engagement | ||
| 79 | You’ve done great, keep it up. Just keep on going. Great advice, but doesn’t help, does it? Gavin says maintaining changes is harder than making changes in the first place. The novelty has worn off, but you still have to put in a lot of effort | Self-regulation | Resources | |
| 80 | Kamal keeps going by mixing it up. Do a variety of activities and eat a variety of foods. The less bored you are the easier it is to stick to a new lifestyle | 4.1 Instruction on how to perform the behaviour | Self-regulation | Resources, self-efficacy (maintenance) |
| 81 | Keeping your motivation high is crucial now. Why are you losing weight? What’s your vision? Keep your focus on what you want to achieve. Men tell us they lose weight for a reason: feeling better, being able to do stuff more easily and being healthy | 1.3 Goal-setting (outcome) | Motivation | Motivation (intrinsic/extrinsic) |
| 82 | Planning and preparation, keeping an eye on things, habits and routines, getting back on track, handling supermarkets and special occasions. We’ve covered a lot in 12 weeks! Making better food choices and moving more can be tricky, but you have all the tools that our successful men say worked for them | General communication technique | ||
| 83 | What are your weight loss goals for the next weeks and months and how do you know it’s working for you? | 1.3 Goal-setting (outcome) | Motivation, engagement | |
| 84 | We have sent you a couple of texts, but any changes to your eating, activity and weight were made by you! You don’t really need us. Thank you for your time and efforts on Game of Stones. We hope that it’s been useful to you. Take care <name>. If you have any feedback please get in touch | General communication technique |
Appendix 20 Week 1 sample of narrative SMS and alternative SMS
| Narrative SMS | Day | Time | Alternative SMS | Day | Time |
|---|---|---|---|---|---|
| Hi <N>, Jimmy Nesbit here. Just back 2 flat from the doctor’s. I’m <A1>. People call me Slim | Monday | 11.01 | Welcome to Game of Stones <Name>! Over 12 weeks we’ll send you some texts. The bad news: reading texts won’t change your weight. The good news: they’re low calorie. We’ve put these texts together with the help of men who successfully lost weight. They are based on facts and real life experience | Monday | 10.00 |
| Slim here. I got overweight after the building work stopped. Dr. Sharpe says I’ve 2 write what I eat and when I exercise. Can’t get far without my stick now | Monday | 16.58 | |||
| Doctor say my weight puts me at a health risk. Am starting food and exercise diary tomorrow. Will let you know how it goes, Slim | Monday | 17.02 | |||
| Slim here. Custard creams for breakfast – Just a packet. Pie, salad cream and crisps for morning snack. Not sure what 2 have for lunch yet | Tuesday | 10.48 | The goal is to lose 5% in 12 weeks. John said the goal gave him confidence to try changing his eating knowing that he’s got something to work towards. Losing more than 3% of your body weight has health benefits and helps to cut your chances of cancer, heart disease and diabetes | Tuesday | 15.30 |
| Pizza and 3 cans for lunch. Doctor said alcohol is fattening. Didn’t know there was any fat in it! Out Thursday night for a few pints with my pal, Budge | Tuesday | 13.59 | |||
| You’d like Budge. He’s heavy like me – <A1>. Reckons we should eat what we like and live life to the full ‘cause the 33 bus could hit us any day | Tuesday | 14.01 | |||
| Txted Wilma, my wife. She went 2 stay at her mum’s in Glasgow last week. We’d had a row. Heard nothing since. She’ll be back soon enough, you’ll see | Tuesday | 18.05 | |||
| Slim here. Found myself staring in the fridge. 4 pizzas on top shelf, pies, cheese and cans on the bottom and 2 big bottles of coke in the door | Wednesday | 10.13 | Ok, here’s the deal. Some texts will be useful and others maybe won’t. Just pick whatever works for you and ignore the rest. If you want to reply to any of the texts please do. We read every text but usually we won’t be able to write back. Sorry | Wednesday | 11.15 |
| We’d no biscuits or crisps so went 2 shop. Huge picture of donuts says ‘Obey the Urge! Bought 12 for price of 4. Bargain! Need to watch the pennies these days | Wednesday | 16.15 | |||
| Slim here. Waiting outside The King’s Head. Budge’s always late. Don’t like going in on my own. Budge’s better at dealing with the fat jokes than me | Thursday | 18.00 | How to lose weight? Here’s a simple fact: sensible eating works . . . but only if you stick to it. Go to our Game of Stones web page with links to web pages full of information that our men find useful. www.gameofstonesresearch.com [last accessed 25 June 2019] | Thursday | 15.00 |
| Here’s Budge now. Orange dyed hair and dressed in black. Walks like a cross between a cowboy and a rap artist. My best pal. Txt you later, Slim | Thursday | 18.02 | |||
| Absoluterly blootered! Outside Spice of Life, the Chinese. Budge’s treat. He can afford it. Made loads of money selling mobile phones. Out tomorrow night too! | Thursday | 21.59 | |||
| Colin, owns The Heid, says ‘Slim, your wife ran away. Now you need 2 seduce a woman your own size. His mate says: ‘How?’ Budge: ‘Piece of cake’. It got a laugh | Friday | 18.01 | Most of our men make up their own sensible eating rules. Carl said that it’s straightforward, eat less rubbish. Everybody knows it, but hard to do. Cutting down and reducing portion sizes is the main strategy that works for our men. Losing weight is about finding what works for you and your life | Friday | 14.00 |
| Budge is funny with a few pints in him. People like him. There’s an open mic night at the end of the month. Me and Budge are thinking of doing a turn | Friday | 18.02 | |||
| Hi, Forgot food diary. Get this, Doc. 5 pints, 3 packets crisps and about 2 chase it down with chicken, lemon sauce ‘n fried rice. Am living it large! | Friday | 21.59 | |||
| Hi <Name>, heard nothing from Wilma. Tried calling her but no answer. Just need to know when she’s coming back | Saturday | 11.45 | You’re changing what you’re eating and drinking, you’re not dieting. Think about it as improving your lifestyle, not being on a diet. Check out this helpful wee booklet full of tips from the Men’s Health Forum. www.issuu.com/menshealthforum/docs/eat_well_final_hrnon-border [last accessed 25 June 2019] | Saturday | 18.20 |
| Found myself staring into the fridge again. Microwave fish and chips for lunch. Mibbes stay in, veg and play games | Saturday | 12.31 | |||
| Will start food diary again on Monday. What else should I be doing to lose weight? | Saturday | 17.58 | |||
| No SMS | Sunday | Have you made any changes this week <Name>? Cut down on something or made some sensible eating changes? Let us know. Have a nice rest of the weekend | Sunday | 11.30 |
Appendix 21 Assessment schedule of study variables
| Variable | 0 months | 3 months | 6 months | 12 months |
|---|---|---|---|---|
| Sociodemographics, comorbidities, disability, ethnicity | ✓ | |||
| Anthropometry (weight, waist circumference) | ✓ | ✓ | ✓ | ✓ |
| Mixed-methods process/acceptability data | ✓ | ✓ | ✓ | ✓ |
| Lifestyle behaviours (diet, physical activity, smoking, alcohol) | ✓ | ✓ | ✓ | |
| Health economic outcomes: EQ-5D, NHS health-care use | ✓ | ✓ | ✓ | |
| Theory-based mediators | ✓ | ✓ | ✓ | ✓ |
| Well-being: Warwick–Edinburgh Mental Well-being Scale | ✓ | ✓ |
Appendix 22 Word-of-mouth community recruitment
| Recruitment sources/links | SA randomised (n) | SB randomised (n) | Total (N) |
|---|---|---|---|
| Leaflet distribution | 0 | 3 | 3 |
| Researcher contacts | 1 | 3 | 4 |
| Health worker | 3 | 0 | 3 |
| Voluntary sector organisations | 1 | 3 | 4 |
| Sports worker | 0 | 1 | 1 |
| Through a friend/relative/other | 2 | 1 | 3 |
| Total | 7 | 11 | 18 |
Appendix 23 Data table of satisfaction and helpfulness ratings for programme and narrative SMS at 12 months by deprivation status
| SMS + I | SMS only | Total | ||||
|---|---|---|---|---|---|---|
| SIMD 1 or 2 (n = 14) | SIMD 3–5 (n = 7) | SIMD 1 or 2 (n = 16) | SIMD 3–5 (n = 10) | SIMD 1 or 2 (n = 30) | SIMD 3–5 (n = 17) | |
| Overall satisfaction (mean, SD) | 81.8, 21.7 | 79.9, 19.2 | 74.6, 23.5 | 81.0, 16.0 | 77.9, 22.6 | 80.5, 16.8 |
| Programme has been helpful (mean, SD) | 4.2, 1.1 | 3.9, 1.1 | 3.9, 1.1 | 4.2, 1.0 | 4.1, 1.1 | 4.1, 1.0 |
| Helpfulness of SMS (mean, SD) | 3.4, 1.3 | 3.4, 1.4 | 3.0, 1.5 | 3.8, 1.2 | 3.2, 1.4 | 3.6, 1.3 |
Appendix 24 Matrix coding query on acceptability of narrative SMS by deprivation status
| SIMD | Strong dislike/blocked narrative SMS | Indifferent to narrative SMS | Likes narrative SMS |
|---|---|---|---|
| High deprivation (SIMD 1 or 2) | 6 | 10 | 13 |
| Less deprived (SIMD 3–5) | 5 | 6 | 11 |
Appendix 25 Data table weight change by deprivation status and recruitment channel
| 3 months, n, mean, SD | 6 months, n, mean, SD | 12 months, n, mean, SD | |||||
|---|---|---|---|---|---|---|---|
| SMS + I | SMS only | SMS + I | SMS only | SMS + I | SMS only | Control | |
| By deprivation status | |||||||
| Weight change (kg) | |||||||
| Less deprived (SIMD 3–5) | 14, –2.86, 2.53 | 11, –1.25,3.29 | 9, –5.16, 4.61 | 10, –2.20, 4.27 | 8, –5.04, 4.26 | 10, –0.53, 4.90 | 10, –1.90, 6.10 |
| More deprived (SIMD 1 or 2) | 17, –2.74, 4.21 | 15, –2.49, 4.44 | 13, –4.27, 6.58 | 11, –4.30, 5.46 | 14, –2.33, 6.11 | 16, –2.33, 6.11 | 19, –0.62, 6.50 |
| Weight change (%) | |||||||
| Less deprived (SIMD 3–5) | 14, –2.62, 2.36 | 11, –1.23, 3.28 | 9, –4.85, 4.63 | 10, –2.15, 4.12 | 8, –4.69, 4.21 | 10, –0.76, 4.45 | 10, –1.56, 5.51 |
| More deprived (SIMD 1 or 2) | 17, –2.47, 4.24 | 15, –2.47, 4.04 | 13, –3.83, 6.43 | 11, –3.81, 4.35 | 14, –2.58, 6.73 | 16, –1.97, 4.86 | 19, –0.70, 5.34 |
| BMI change | |||||||
| Less deprived (SIMD 3–5) | 14, –0.92, 0.80 | 11, –0.40, 1.10 | 9, –1.67, 1.51 | 10, –0.72, 1.44 | 8, –1.63, 1.39 | 10, –0.14, 1.63 | 10, –0.64, 1.92 |
| More deprived (SIMD 1 or 2) | 17, –0.87, 1.33 | 15, –0.83, 1.41 | 13, –1.67, 1.51 | 11, –1.33, 1.54 | 14, –0.94, 2.17 | 16, –0.72, 1.72 | 19, –0.20, 2.17 |
| Waist circumference change | |||||||
| Less deprived (SIMD 3–5) | 14, –4.51, 4.31 | 11, –2.00, 2.44 | 9, –3.44, 6.61 | 10, –2.25, 4.26 | 8, –3.68, 5.58 | 10, –0.55, 4.58 | 10, –4.56, 4.73 |
| More deprived (SIMD 1 or 2) | 17, –3.10, 4.90 | 15, –4.01, 5.05 | 13, –5.54, 6.44 | 11, –3.95, 4.45 | 14, –4.78, 6.74 | 16, –3.40, 3.99 | 19, –1.04, 4.76 |
| By recruitment channel | |||||||
| Weight change (kg) | |||||||
| Community | 18, –2.69, 3.82 | 12, –0.88, 2.43 | 15, –4.38, 5.79 | 10, –3.10, 5.34 | 14, –4.14, 5.15 | 12, –2.25, 6.98 | 16, –1.84, 6.99 |
| GP | 13, –2.93, 3.14 | 14, –2.90, 4.82 | 8, –4.98, 5.64 | 11, –3.49, 4.77 | 9, –3.62, 6.89 | 14, –1.11, 4.40 | 13, 0.11, 5.42 |
| Weight change (%) | |||||||
| Community | 18, –2.31, 3.85 | 12, –0.85, 2.49 | 15, –3.87, 3.85 | 10, –2.60, 4.21 | 14, –3.50, 5.43 | 12, –1.87, 5.36 | 16, –1.75, 5.49 |
| GP | 13, –2.85, 2.99 | 14, –2.89, 4.82 | 8, –4.83, 5.34 | 11, –3.39, 4.40 | 9, –3.52, 6.76 | 14, –1.20, 4.14 | 13, –0.08, 5.15 |
| Waist circumference change (cm) | |||||||
| Community | 18, –3.90, 4.86 | 12, –2.91, 3.38 | 15, –4.75, 5.29 | 10, –3.61, 3.75 | 14, –4.87, 5.19 | 12, –2.71, 4.81 | 16, –3.14, 5.42 |
| GP | 13, –3.52, 4.45 | 14, –3.37, 4.92 | 8, –4.60, 8.27 | 11, –2.71, 4.96 | 9, –3.68, 7.56 | 14, –1.96, 4.10 | 13, –1.16, 4.30 |
| BMI change (kg/m2) | |||||||
| Community | 18, –0.86, 1.21 | 12, –0.28, 0.82 | 15, –1.38, 1.87 | 10, –0.95, 1.53 | 14, –1.29, 1.73 | 12, –0.63, 1.96 | 16, –1.15, 2.21 |
| GP | 13, –0.94, 0.99 | 14, –2.89, 4.82 | 8, –1.60, 1.75 | 11, –1.13, 1.52 | 9, –1.15, 2.21 | 14, –0.38, 1.46 | 13, –0.07, 1.82 |
Appendix 26 Data table of health behaviours
| Health behaviour | Baseline | 6 months | 12 months | |||||
|---|---|---|---|---|---|---|---|---|
| SMS + I | SMS only | Control | SMS + I | SMS only | SMS + I | SMS only | Control | |
| Vigorous physical activity in past week (days), N, mean, SD | 35, 1.5, 1.8 | 33, 2.4, 2.3 | 34, 1.6, 2.1 | 23, 2.2, 2.5 | 21, 2.2, 1.6 | 21, 1.9, 1.8 | 26, 2.8, 2.2 | 29, 2.6, 2.4 |
| Moderate physical activity in past week (days), N, mean, SD | 35, 3.1, 2.1 | 33, 4.2, 2.4 | 34, 3.6, 2.3 | 23, 3.9, 2.3 | 21, 4.2, 2.0 | 22, 4.6, 2.2 | 26, 4.3, 2.0 | 30, 4.5, 2.2 |
| Sedentary behaviour in past week (hours: minutes), N, mean, SD | 35, 8:30, 5:37 | 33, 8:30, 10:17 | 34, 7:01, 3:49 | 23, 8:28, 5:02 | 21, 6:08, 6:03 | 22, 10:32, 14:01 | 26, 9:22, 8:07 | 30, 7:26, 4:56 |
| Number of daily portions of fruit and vegetables consumed, N, median, SD | 34, 3.4, 1.4 | 33, 2.8, 1.7 | 34, 2.9, 2.3 | 23, 3.1, 1.9 | 21, 3.0, 1.9 | 22, 3.4, 2.1 | 26, 3.3, 1.7 | 30, 2.9, 1.8 |
| Frequency of alcohol consumption, N, n, % | ||||||||
| Every day | 34, 1, 2.9 | 33, 2, 6.1 | 34, 0, 0.0 | 23, 1, 4.4 | 21, 0, 0.0 | 22, 0, 0.0 | 26, 1, 3.9 | 30, 1, 3.3 |
| Five or six times a week | 34, 0, 0.0 | 33, 3, 9.1 | 34, 2, 5.9 | 23, 0, 0.0 | 21, 2, 9.5 | 22, 0, 0.0 | 26, 1, 3.9 | 30, 2, 6.7 |
| Three or four times a week | 34, 8, 23.5 | 33, 3, 9.1 | 34, 4, 11.8 | 23, 3, 13.0 | 21, 3, 14.3 | 22, 5, 22.7 | 26, 5, 19.2 | 30, 3, 10.0 |
| Twice a week | 34, 8, 23.5 | 33, 11, 33.3 | 34, 5, 14.7 | 23, 3, 13.0 | 21, 5, 23.8 | 22, 3, 13.6 | 26, 7, 26.9 | 30, 3, 10.0 |
| Once a week | 34, 5, 14.7 | 33, 3, 9.1 | 34, 7, 20.1 | 23, 7, 30.4 | 21, 5, 23.8 | 22, 2, 9.1 | 26, 6, 23.1 | 30, 5, 16.7 |
| Two or three times a month | 34, 2, 5.9 | 33, 3, 9.1 | 34, 2, 5.9 | 23, 3, 13.0 | 21, 1, 4.8 | 22, 1, 4.6 | 26, 3, 11.5 | 30, 4, 13.3 |
| Once a month | 34, 5, 14.7 | 33, 5, 15.1 | 34, 5, 14.7 | 23, 3, 13.0 | 21, 3, 14.3 | 22, 5, 22.7 | 26, 1, 3.9 | 30, 3, 10.0 |
| Never | 34, 5, 14.7 | 33, 3, 9.1 | 34, 9, 26.5 | 23, 3, 13.0 | 21, 2, 9.5 | 22, 6, 27.3 | 26, 2, 7.7 | 30, 9, 30.0 |
| Smoking status, N, n, % | ||||||||
| Never smoked | 34, 19, 55.9 | 33, 18, 54.6 | 34, 15, 44.1 | 23, 12, 52.2 | 21, 11, 52.4 | 22, 12, 54.6 | 26, 15, 57.7 | 30, 14, 46.7 |
| Current smoker (irregular) | 34, 0, 0.0 | 33, 2, 6.1 | 34, 1, 2.9 | 23, 0, 0.0 | 21, 1, 4.8 | 22, 2, 9.1 | 26, 1, 3.9 | 30, 4, 13.3 |
| Current smoker (regular) | 34, 3, 8.8 | 33, 1, 3.0 | 34, 3, 8.8 | 23, 3, 13.0 | 21, 0, 0.0 | 22, 0, 0.0 | 26, 1, 3.9 | 30, 0, 0.0 |
| Ex-smoker | 34, 12, 35.3 | 33, 12, 36.1 | 34, 15, 44,1 | 23, 8, 34.8 | 21, 9, 42.9 | 22, 8, 36.4 | 26, 9, 34.6 | 30, 12, 40.0 |
Appendix 27 Data table of weight management strategies
| Strategy | Time point, N, n, % | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | |||||||
| SMS + I | SMS only | Control | SMS + I | SMS only | SMS + I | SMS only | SMS + I | SMS only | Control | |
| Current weight management strategy | ||||||||||
| Planning meals ahead of time | ||||||||||
| Never/rarely | 36, 6, 16.7 | 33, 10, 30.3 | 34, 13, 38.2 | 31, 4, 12.9 | 27, 7, 25.9 | 23, 5, 21.7 | 21, 3, 14.3 | 22, 6, 27.3 | 26, 2, 7.7 | 30, 3, 10.0 |
| Sometimes | 36, 19, 52.7 | 33, 17, 51.2 | 34, 10, 29.4 | 31, 15, 48.4 | 27, 13, 48.1 | 23, 4, 17.4 | 21, 9, 42.9 | 22, 10, 45.5 | 26, 18, 69.2 | 30, 19, 63.3 |
| Often | 36, 11, 30.6 | 33, 6, 18.2 | 34, 11, 32.3 | 31, 12, 38.7 | 27, 7, 25.9 | 23, 14, 60.9 | 21, 9, 42.9 | 22, 6, 27.3 | 26, 6, 23.1 | 30, 8, 26.7 |
| Slowing pace of eating | ||||||||||
| Never/rarely | 36, 22, 61.1 | 31, 21, 67.7 | 31, 18, 51.4 | 30, 10, 33.3 | 27, 11, 40.7 | 21, 7, 30.4 | 21, 7, 33.3 | 22, 6, 27.3 | 26, 9, 34.6 | 30, 17, 56.7 |
| Sometimes | 36, 12, 33.3 | 31, 9, 29.0 | 31, 13, 37.1 | 30, 14, 46.7 | 27, 12, 44.4 | 21, 13, 56.5 | 21, 9, 42.8 | 22, 12, 54.6 | 26, 11, 42.3 | 30, 9, 30.0 |
| Often | 36, 2, 5.6 | 31, 1, 3.2 | 31, 4, 11.4 | 30, 6, 20.0 | 27, 4, 14.8 | 21, 3, 13.0 | 21, 5, 23.8 | 22, 4, 18.2 | 26, 6, 23.1 | 30, 4, 13.3 |
| Recording food and drink consumption | ||||||||||
| Never/rarely | 35, 25, 71.4 | 31, 27, 87.1 | 35, 25, 71.4 | 30, 15, 50.0 | 27, 19, 70.4 | 23, 14, 60.9 | 21, 15, 71.4 | 22, 12, 54.6 | 26, 19, 73.1 | 30, 14, 46.7 |
| Sometimes | 35, 7, 20.0 | 31, 3, 9.7 | 35, 7, 20.0 | 30, 8, 26.7 | 27, 5, 18.5 | 23, 3, 13.0 | 21, 3, 14.39 | 22, 5, 22.7 | 26, 4, 15.4 | 30, 12, 40.0 |
| Often | 35, 3, 8.6 | 31, 1, 3.2 | 35, 3, 8.57 | 30, 7, 23.3 | 27, 3, 11.1 | 23, 6, 26.1 | 21, 3, 14.3 | 22, 5, 22.7 | 26, 3, 11.5 | 30, 4, 13.3 |
| Portion control | ||||||||||
| Never/rarely | 36, 6, 16.7 | 32, 9, 28.1 | 35, 12, 34.3 | 31, 2, 6.5 | 27, 2, 7.4 | 23, 2, 8.70 | 21, 0, 0.0 | 22, 3, 13.6 | 26, 4, 15.4 | 30, 7, 23.3 |
| Sometimes | 36, 25, 69.4 | 32, 17, 53.1 | 35, 16, 45.7 | 31, 15, 48.4 | 27, 18, 66.7 | 23, 14, 60.9 | 21, 15, 71.4 | 22, 11, 50.0 | 26, 12, 46.1 | 30, 19, 63.3 |
| Often | 36, 5, 13.9 | 32, 6, 18.8 | 35, 7, 20.0 | 31, 14, 45.2 | 27, 7, 25.9 | 23, 7, 30.4 | 21, 6, 28.6 | 22, 8, 36.4 | 26, 10, 38.5 | 30, 4, 13.3 |
| Following an exercise routine | ||||||||||
| Never/rarely | 36, 14, 38.9 | 33, 7, 21.2 | 33, 7, 20.0 | 31, 9, 29.0 | 27, 7, 26.0 | 23, 4, 17.4 | 21, 3, 14.3 | 22, 6, 27.3 | 26, 5, 19.2 | 30, 9, 30.0 |
| Sometimes | 36, 12, 33.3 | 33, 13, 39.4 | 33, 17, 48.6 | 31, 11, 35.5 | 27, 10, 37.0 | 23, 8, 34.8 | 21, 8, 38.10 | 22, 11, 50.0 | 26, 12, 46.1 | 30, 10, 33.3 |
| Often | 36, 10, 27.8 | 33, 13, 39.4 | 33, 11, 31.4 | 31, 11, 35.5 | 27, 10, 37.0 | 23, 11, 47.8 | 21, 10, 47.6 | 22, 5, 22.7 | 26, 9, 34.62 | 30, 11, 36.7 |
| Eating regularly | ||||||||||
| Never/rarely | 36, 4, 11.1 | 33, 1, 3.1 | 34, 6, 17.6 | 31, 0, 0.0 | 27, 3, 11.1 | 21, 2, 9.1 | 21, 0, 0.0 | 22, 2, 9.1 | 26, 0, 0.0 | 30, 1, 3.3 |
| Sometimes | 36, 11, 30.6 | 33, 13, 39.4 | 34, 7, 20.6 | 31, 9, 29.0 | 27, 10, 37.0 | 21, 7, 31.8 | 21, 10, 47.6 | 22, 8, 36.4 | 26, 9, 34.6 | 30, 8, 26.7 |
| Often | 36, 21, 58.3 | 33, 19, 57.6 | 34, 21, 61.8 | 31, 22, 71.0 | 27, 14, 51.9 | 21, 13, 59.1 | 21, 11, 52.4 | 22, 12, 54.5 | 26, 17, 65.4 | 30, 21, 70.0 |
| Weight loss approach used in last 3 months | ||||||||||
| Limit eating and drinking | ||||||||||
| Once or twice per month | 36, 7, 19.4 | 33, 14, 42.4 | 35, 13, 37.1 | 31, 0, 0.0 | 27, 3, 11.1 | 23, 0, 0.0 | 21, 2, 9.5 | 22, 2, 9.1 | 26, 6, 23.1 | 30, 2, 6.7 |
| About weekly | 36, 11, 30.6 | 33, 9, 27.3 | 35, 11, 31.4 | 31, 8, 25.8 | 27, 12, 44.4 | 23, 9, 39.1 | 21, 9, 42.9 | 22, 7, 31.81 | 26, 11, 42.3 | 30, 16, 53.3 |
| Every day or most days | 36, 10, 27.8 | 33, 5, 15.2 | 35, 3, 8.6 | 31, 21, 67.7 | 27, 12, 44.4 | 23, 11, 47.8 | 21, 10, 47.6 | 22, 9, 40.9 | 26, 7, 26.9 | 30, 10, 33.3 |
| Not at all | 36, 8, 22.2 | 33, 5, 15.2 | 35, 8, 22.9 | 31, 2, 6.5 | 27, 0, 0.0 | 23, 3, 13.0 | 21, 0, 0.0 | 22, 4, 18.2 | 26, 2, 7.7 | 30, 2, 6.7 |
| Exercise workout at home | ||||||||||
| Once or twice per month | 36, 4, 11.1 | 33, 6, 18.2 | 35, 6, 17.1 | 31, 3, 9.7 | 26, 1, 3.9 | 23, 3, 13.1 | 21, 2, 9.5 | 22, 2, 9.1 | 26, 4, 15.4 | 30, 7, 23.3 |
| About weekly | 36, 4, 11.1 | 33, 6, 18.2 | 35, 6, 17.1 | 31, 3, 9.7 | 26, 1, 3.9 | 23, 5, 21.7 | 21, 2, 9.5 | 22, 4, 18.1 | 26, 4, 15.4 | 30, 2, 6.7 |
| Every day or most days | 36, 3, 8.4 | 33, 0, 0.0 | 35, 2, 5.8 | 31, 9, 29.0 | 26, 5, 19.1 | 23, 5, 21.7 | 21, 3, 14.3 | 22, 6, 27.3 | 26, 2, 7.7 | 30, 5, 16.7 |
| Not at all | 36, 25, 69.4 | 33, 21, 63.6 | 35, 21, 60.0 | 31, 16, 51.6 | 26, 19, 73.1 | 23, 10, 43.5 | 21, 14, 66.7 | 22, 10, 45.5 | 26, 16, 61.5 | 30, 16, 53.3 |
| Attend commercial weight loss programme | ||||||||||
| Once or twice per month | 36, 1, 2.8 | 33, 1, 3.1 | 35, 0, 0.0 | 31, 0, 0.0 | 27, 0, 0.0 | 22, 1, 4.4 | 21, 0, 0.0 | 22, 1, 4.6 | 26, 0, 0.0 | 30, 1, 3.3 |
| About weekly | 36, 1, 2.8 | 33, 0, 0.0 | 35, 1, 2.9 | 31, 0, 0.0 | 27, 2, 7.4 | 22, 0, 0.0 | 21, 0, 0.0 | 22, 0, 0.0 | 26, 1, 3.9 | 30, 1, 3.3 |
| Every day or most days | 36, 0, 0.0 | 33, 0, 0.0 | 35, 1, 2.9 | 31, 1, 3.3 | 27, 0, 0.0 | 22, 0, 0.0 | 21, 0, 0.0 | 22, 0, 0.0 | 26, 1, 3.9 | 30, 0, 0.0 |
| Not at all | 36, 34, 94.4 | 33, 32, 96.9 | 35, 33, 94.3 | 31, 30, 96.8 | 27, 25, 92.6 | 22, 21, 95.6 | 21, 21, 100.0 | 22, 21, 95.5 | 26, 24, 92.3 | 30, 28, 93.3 |
| Attend gym, leisure centre or sports facility | ||||||||||
| Once or twice per month | 36, 3, 8.3 | 33, 3, 9.1 | 35, 8, 22.9 | 31, 2, 6.5 | 26, 2, 7.7 | 23, 1, 4.4 | 21, 0, 0.0 | 22, 3, 13.6 | 22, 3, 11.5 | 30, 5, 16.7 |
| About weekly | 36, 4, 11.1 | 33, 8, 24.2 | 35, 5, 14.3 | 31, 4, 12.9 | 26, 8, 30.8 | 23, 6, 26.1 | 21, 7, 33.3 | 22, 3, 13.6 | 22, 6, 23.1 | 30, 5, 16.7 |
| Every day or most days | 36, 5, 13.9 | 33, 3, 9.1 | 35, 3, 8.6 | 31, 5, 16.1 | 26, 4, 15.3 | 23, 4, 17.4 | 21, 3, 14.3 | 22, 3, 13.6 | 22, 5, 19.2 | 30, 5, 16.7 |
| Not at all | 36, 24, 66.7 | 33, 19, 57.6 | 35, 19, 54.3 | 31, 20, 64.5 | 26, 12, 46.2 | 23, 12, 52.1 | 21, 11, 52.4 | 22, 13, 59.2 | 22, 12, 46.2 | 30, 15, 50.0 |
| Attend weight reduction clinic | ||||||||||
| Once or twice per month | 36, 2, 5.7 | 33, 1, 3.0 | 35, 2, 5.9 | 31, 2, 6.5 | 27, 1, 3.7 | 23, 2, 8.7 | 21, 0, 0.0 | 22, 0, 0.0 | 22, 2, 7.7 | 22, 2, 6.7 |
| About weekly | 36, 1, 2.9 | 33, 0, 0.0 | 35, 1, 2.9 | 31, 1, 3.2 | 27, 0, 0.0 | 23, 0, 0.0 | 21, 1, 4.8 | 22, 1, 4.6 | 22, 0, 0.0 | 22, 1, 3.3 |
| Every day or most days | 36, 0, 0.0 | 33, 0, 0.0 | 35, 0, 0.0 | 31, 1, 3.2 | 27, 0, 0.0 | 23, 0, 0.0 | 21, 0, 0.0 | 22, 0, 0.0 | 22, 0, 0.0 | 22, 0, 0.0 |
| Not at all | 36, 32, 91.4 | 33, 32, 97.0 | 35, 31, 91.2 | 31, 27, 87.1 | 27, 26, 96.3 | 23, 21, 91.3 | 21, 20, 95.2 | 22, 21, 95.5 | 22, 24, 92.3 | 22, 27, 90.0 |
| Pedometer use | ||||||||||
| Every day | n/a | n/a | n/a | 31, 13, 41.9 | 27, 11, 40.7 | 23, 8, 34.8 | 21, 8, 38.1 | 22, 6, 27.3 | 26, 5, 19.2 | 30, 6, 20.0 |
| A few times per week | n/a | n/a | n/a | 31, 3, 9.7 | 27, 1, 3.7 | 23, 1, 4.4 | 21, 1, 4.8 | 22, 1, 4.5 | 26, 2, 7.7 | 30, 1, 3.3 |
| Once per week | n/a | n/a | n/a | 31, 5, 16.1 | 27, 4, 14.8 | 23, 6, 26.1 | 21, 2, 9.5 | 22, 6, 27.3 | 26, 8, 30.8 | 30, 7, 23.3 |
| Once per month | n/a | n/a | n/a | 31, 3, 9.7 | 27, 3, 11.1 | 23, 1, 4.4 | 21, 4, 19.1 | 22, 2, 9.1 | 26, 2, 7.7 | 30, 8, 26.7 |
| Less than once per month | n/a | n/a | n/a | 31, 0, 0.0 | 27, 1, 3.7 | 23, 0, 0.0 | 21, 1, 4.8 | 22, 1, 4.5 | 26, 2, 7.7 | 30, 1, 3.3 |
| Never | n/a | n/a | n/a | 31, 7, 22.6 | 27, 7, 25.9 | 23, 7, 30.4 | 21, 5, 23.8 | 22, 6, 27.3 | 26, 7, 26.9 | 30, 7, 23.3 |
| Self-weighing in past week (number of days), n, mean, SD | 36, 0.6, 0.8 | 33, 1.0, 1.8 | 35, 1.1, 1.8 | 31, 2.1, 2.2 | 27, 2.3, 2.6 | 23, 1.9, 1.9 | 21, 1.2, 1.2 | 22, 1.5, 2.3 | 26, 1.5, 1.8 | 30, 1.9, 2.4 |
Appendix 28 Data table of weight loss and maintenance cognitions
| Cognition | Time point, n, mean, SD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | |||||||
| SMS + I | SMS only | Control | SMS + I | SMS only | SMS + I | SMS only | SMS + I | SMS only | Control | |
| Confidence in ability to lose weight (1 = not confident, 7 = very confident) | 36, 4.5, 1.4 | 33, 4.0, 1.6 | 34, 4.2, 1.8 | 31, 5.6, 1.3 | 27, 5.0, 1.6 | 23, 4.8, 1.7 | 21, 4.9, 1.7 | 22, 5.2, 1.4 | 26, 4.8, 1.7 | 30, 4.8, 1.8 |
| Confidence in long-term ability to maintain lost weight (1 = not confident, 7 = very confident) | 36, 4.4, 1.4 | 33, 4.1, 1.4 | 34, 4.0, 1.9 | 31, 5.4, 1.2 | 27, 4.8, 1.7 | 23, 5.2, 1.3 | 21, 5.1, 1.5 | 22, 4.9, 1.5 | 26, 4.7, 1.4 | 30, 4.4, 1.7 |
| Importance of losing weight (1 = not important, 7 = very important) | 35, 6.1, 1.2 | 33, 6.1, 0.9 | 35, 6.3, 0.9 | 31, 6.5, 1.0 | 27, 6.1, 1.0 | 23, 6.2, 0.9 | 21, 5.9, 1.2 | 22, 6.2, 0.9 | 26, 6.0, 1.3 | 30, 6.0, 1.4 |
| Automaticity fruit and vegetable consumption (1 = low, 7 = high) | 34, 4.9, 2.1 | 33, 5.2, 1.5 | 32, 4.3, 2.3 | 31, 5.9, 1.4 | 27, 5.7, 1.5 | 23, 5.5, 1.5 | 21, 5.2, 1.9 | 22, 5.7, 1.6 | 26, 5.4, 1.5 | 30, 5.1, 2.0 |
| Automaticity physical activity (1 = low, 7 = high) | 34, 4.0, 2.3 | 33, 5.2, 1.7 | 33, 3.5, 2.0 | 31, 5.0, 1.8 | 27, 5.3, 1.8 | 23, 4.3, 2.0 | 21, 5.2, 1.5 | 21, 5.0, 1.4 | 26, 5.1, 1.7 | 29, 4.4, 1.9 |
| Autonomous regulation (1 = low, 7 = high) | 35, 6.1, 0.9 | 31, 5.9, 0.7 | 33, 5.9, 1.0 | 30, 6.2, 0.8 | 27, 5.8, 1.0 | 23, 5.8, 1.0 | 21, 6.1, 0.8 | 22, 6.1, 0.9 | 25, 5.7, 1.1 | 30, 5.8, 1.3 |
| Controlled regulation (1 = low, 7 = high) | 33, 3.6, 1.6 | 29, 3.5, 1.3 | 31, 3.4, 1.4 | 30, 3.9, 1.4 | 27, 4.0, 1.4 | 23, 3.6, 1.5 | 20, 4.0, 1.1 | 22, 3.7, 1.5 | 26, 3.8, 1.5 | 29, 4.0, 1.6 |
Appendix 29 Data table of self-regulation of eating behaviour
| Questionnaire item | Time point, N, n, % | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | ||||||
| SMS + I | SMS only | Control | SMS + I | SMS only | SMS + I | SMS only | Control | |
| Tempted by specific foods | ||||||||
| Chocolate | 35, 17, 48.6 | 33, 10, 30.3 | 34, 16, 47.1 | 23, 10, 43.5 | 21, 4, 19.1 | 22, 9, 10.9 | 26, 5, 19.2 | 30, 19, 63.3 |
| Crisps | 35, 21, 60.0 | 33, 13, 39.4 | 34, 18, 52.9 | 23, 8, 34.8 | 21, 10, 47.6 | 22, 10, 45.5 | 26, 9, 34.6 | 30, 17, 56.7 |
| Cakes | 35, 10, 28.6 | 33, 12, 36.4 | 34, 10, 29.4 | 23, 5, 21.7 | 21, 3, 14.3 | 22, 6, 27.3 | 26, 5, 19.2 | 30, 12, 40.0 |
| Ice cream | 35, 5, 14.3 | 33, 11, 33.3 | 34, 8, 23.5 | 23, 1, 4.4 | 21, 6, 28.6 | 22, 2, 9.1 | 26, 5, 19.2 | 30, 10, 33.3 |
| Bread/toast | 35, 23, 65.7 | 33, 19, 57.6 | 34, 19, 55.9 | 23, 13, 56.5 | 21, 11, 52.4 | 22, 15, 68.2 | 26, 13, 50.0 | 30, 15, 50.0 |
| Fizzy drinks | 35, 13, 37.1 | 33, 11, 33.3 | 34, 17, 50.0 | 23, 8, 34.8 | 21, 6, 28.6 | 22, 8, 36.4 | 26, 7, 26.9 | 30, 7, 23.3 |
| Biscuits | 35, 10, 28.6 | 33, 17, 51.5 | 34, 13, 38.2 | 23, 7, 30.4 | 21, 9, 42.9 | 22, 9, 40.9 | 26, 10, 38.5 | 30, 15, 50.0 |
| Sweets | 35, 8, 22.9 | 33, 12, 36.4 | 34, 9, 26.5 | 23, 5, 21.7 | 21, 4, 19.1 | 22, 1, 4.6 | 26, 3, 11.5 | 30, 6, 20.0 |
| Popcorn | 35, 2, 5.7 | 33, 3, 9.1 | 34, 1, 2.9 | 23, 2, 8.7 | 21, 0, 0.0 | 22, 3, 13.6 | 26, 0, 0.0 | 30, 1, 3.3 |
| Pastries | 35, 8, 22.9 | 33, 12, 36.4 | 34, 7, 20.6 | 23, 4, 17.4 | 21, 3, 14.3 | 22, 4, 18.2 | 26, 4, 15.4 | 30, 6, 20.0 |
| Pizza | 35, 11, 31.4 | 33, 11, 33.3 | 34, 14, 41.2 | 23, 6, 26.1 | 21, 6, 28.6 | 22, 8, 36.4 | 26, 9, 34.6 | 30, 13, 43.3 |
| Fried foods | 35, 11, 31.4 | 33, 11, 33.3 | 34, 13, 38.2 | 23, 7, 30.4 | 21, 4, 19.1 | 22, 5, 22.7 | 26, 7, 26.9 | 30, 6, 20.0 |
| Chips | 35, 14, 40.0 | 33, 11, 33.3 | 34, 16, 47.1 | 23, 9, 39.1 | 21, 5, 23.8 | 22, 8, 36.4 | 26, 6, 23.1 | 30, 11, 36.7 |
| No foods | 35, 1, 2.9 | 33, 1, 3.0 | 34, 1, 2.9 | 23, 3, 13.0 | 21, 3, 14.3 | 22, 2, 9.1 | 26, 1, 3.9 | 30, 1, 3.3 |
| Intention not to eat too much tempting food | ||||||||
| Yes | 34, 29, 85.3 | 33, 28, 84.6 | 34, 31, 91.2 | 23, 18, 78.3 | 20, 16, 80.0 | 22, 19, 86.4 | 26, 25, 96.1 | 29, 25, 86.2 |
| Intention to have a healthy diet | ||||||||
| Yes | 35, 34, 97.1 | 33, 32, 97.0 | 34, 33, 97.1 | 23, 21, 91.3 | 21, 21, 100.0 | 22, 21, 95.5 | 26, 26, 100.0 | 30, 29, 96.7 |
| Self-Regulation of Eating Behaviour Questionnaire score, N, mean, SD | 34, 3.2, 0.5 | 31, 3.1, 0.7 | 32, 3.0, 0.6 | 23, 3.6, 0.6 | 20, 3.3, 0.6 | 22, 3.4, 0.6 | 26, 3.2, 0.6 | 30, 3.0, 0.7 |
| High (≥ 3.6) | 34, 4, 11.8 | 31, 5, 16.1 | 32, 3, 9.4 | 23, 7, 30.4 | 20, 6, 30.0 | 22, 7, 31.8 | 26, 4, 15.4 | 30, 4, 13.3 |
| Medium (2.8 to > 3.6) | 34, 22, 64.7 | 31, 14, 45.2 | 32, 12, 37.5 | 23, 13, 56.5 | 20, 9, 45.0 | 22, 10, 45.5 | 26, 16, 61.5 | 30, 11, 36.7 |
| Low (< 2.8) | 34, 8, 23.5 | 31, 12, 38.7 | 32, 17, 53.1 | 23, 3, 13.0 | 20, 5, 25.0 | 22, 5, 22.7 | 26, 6, 23.1 | 30, 15, 50.0 |
Appendix 30 Data table of maintenance relevant cognitions
| Cognition | Time point, n, mean, SD | ||||||
|---|---|---|---|---|---|---|---|
| 3 months | 6 months | 12 months | |||||
| SMS + I | SMS only | SMS + I | SMS only | SMS + I | SMS only | Control | |
| Satisfaction with weight loss (1 = low, 7 = high) | 31, 5.0, 1.8 | 27, 4.5, 2.1 | 23, 4.1, 2.1 | 21, 4.0, 2.1 | 22, 4.4, 2.0 | 26, 4.3, 1.4 | 30, 4.0, 2.0 |
| Maintenance mindset (1 = low, 7 = high) | 31, 2.7, 1.5 | 27, 2.8, 1.5 | 23, 3.4, 1.6 | 21, 2.5, 1.2 | 22, 4.1, 1.8 | 26, 3.7, 1.7 | 30, 3.3, 1.8 |
| In the last 3 months I was . . . (1 = low, 7 = high) | |||||||
| Motivated to lose weight | 31, 3.5, 0.6 | 26, 3.2, 0.7 | 23, 3.3, 0.8 | 21, 3.2, 0.5 | 22, 3.1, 0.8 | 24, 3.0, 0.7 | 29, 3.0, 0.7 |
| Tired most of the time | 31, 2.6, 0.8 | 27, 2.6, 0.9 | 23, 2.4, 0.9 | 20, 2.3, 0.8 | 22, 2.6, 0.9 | 26, 2.7, 1.0 | 30, 2.8, 0.7 |
| Stressed most of the time | 31, 2.1, 0.9 | 27, 2.6, 1.0 | 23, 2.3, 0.9 | 21, 2.6, 0.9 | 22, 2.5, 0.9 | 26, 2.6, 1.0 | 30, 2.7, 0.8 |
| Hungry most of the time | 31, 2.0, 0.5 | 26, 2.0, 0.7 | 23, 2.1, 0.7 | 20, 2.0, 0.6 | 21, 2.0, 0.7 | 25, 2.1, 0.6 | 30, 2.3, 0.8 |
| Having to think a lot about my weight loss plan | 30, 2.6, 1.0 | 27, 2.2, 0.9 | 23, 2.5, 0.9 | 21, 2.6, 0.7 | 22, 2.5, 0.9 | 24, 2.2, 0.7 | 30, 2.5, 1.0 |
| Following my weight loss plan without having to think much about it | 31, 2.6, 0.8 | 27, 2.3, 0.8 | 22, 2.5, 0.7 | 18, 2.4, 0.6 | 16, 2.6, 0.6 | 21, 2.7, 0.7 | 24, 2.6, 0.8 |
| Satisfied with the results of my weight loss efforts | 31, 2.7, 1.0 | 27, 2.7, 1.0 | 23, 2.5, 0.9 | 21, 2.3, 0.9 | 22, 2.5, 1.1 | 26, 2.2, 0.9 | 30, 2.2, 1.1 |
| Enjoyed following my weight loss plan | 28, 3.0, 0.8 | 27, 2.7, 0.8 | 23, 2.9, 0.7 | 21, 2.7, 0.7 | 22, 3.0, 0.9 | 26, 2.7, 0.8 | 30, 2.6, 0.9 |
| Doing things which conflicted with my weight loss plan | 31, 2.6, 0.6 | 27, 2.7, 0.8 | 23, 2.7, 0.7 | 21, 2.6, 0.9 | 22, 3.2, 0.7 | 26, 2.6, 0.9 | 30, 2.7, 0.8 |
| Doing things which helped me with my weight loss plan | 30, 3.1, 0.6 | 26, 2.9, 0.6 | 23, 3.0, 0.6 | 21, 2.8, 0.7 | 22, 3.0, 0.9 | 26, 2.5, 0.9 | 30, 2.6, 0.9 |
| Supported by my friends and family to stick to my weight loss plan | 31, 3.0, 0.8 | 27, 2.5, 0.9 | 23, 2.7, 0.9 | 21, 3.0, 0.9 | 15, 2.5, 0.5 | 23, 2.1, 0.8 | 26, 2.1, 0.8 |
| In places and situations that made it difficult to follow my weight loss plan | 31, 2.8, 1.0 | 27, 3.0, 0.7 | 23, 2.9, 0.9 | 21, 3.0, 0.8 | 22, 3.0, 0.8 | 26, 2.8, 0.9 | 30, 2.7, 1.0 |
Appendix 31 Data table of participants completing resource questions
| Time point | GP, n (%) | Nurse, n (%) | A&E, n (%) | Outpatient, n (%) | Inpatient, n (%) | All items, n (%) |
|---|---|---|---|---|---|---|
| Baseline | ||||||
| SMS | 31 (93.9) | 32 (97.0) | 32 (97.0) | 31 (93.9) | 30 (90.9) | 28 (84.8) |
| SMS + I | 34 (94.4) | 33 (91.7) | 35 (97.2) | 34 (94.4) | 35 (97.2) | 33 (91.7) |
| Control | 33 (91.7) | 31 (86.1) | 33 (91.7) | 32 (88.9) | 32 (88.9) | 27 (75.0) |
| 3 months | ||||||
| SMS | 27 (81.8) | 26 (78.8) | 26 (78.8) | 26 (78.8) | 26 (78.8) | 26 (78.8) |
| SMS + I | 31 (86.1) | 29 (80.6) | 31 (86.1) | 30 (83.3) | 30 (83.3) | 28 (77.8) |
| 6 months | ||||||
| SMS | 21 (63.6) | 21 (63.6) | 21 (63.6) | 21 (63.6) | 21 (63.6) | 21 (63.6) |
| SMS + I | 23 (63.9) | 23 (63.9) | 23 (63.9) | 23 (63.9) | 23 (63.9) | 23 (63.9) |
| 12 months | ||||||
| SMS | 24 (72.7) | 23 (69.7) | 23 (69.7) | 22 (66.7) | 20 (60.6) | 20 (60.6) |
| SMS + I | 20 (55.6) | 21 (58.3) | 21 (58.3) | 21 (58.3) | 20 (55.6) | 18 (50.0) |
| Control | 27 (75.0) | 29 (80.6) | 29 (80.6) | 30 (83.3) | 29 (80.6) | 26 (72.2) |
Appendix 32 Data table of participants completing EuroQol-5 Dimensions
| Time point | EQ-5D domain, n (%) | |||||
|---|---|---|---|---|---|---|
| Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | Tariff score | |
| Baseline | ||||||
| SMS | 32 (97.0) | 32 (97.0) | 32 (97.0) | 33 (100.0) | 33 (100.0) | 31 (93.9) |
| SMS + I | 35 (97.2) | 35 (97.2) | 35 (97.2) | 35 (97.2) | 35 (97.2) | 35 (97.2) |
| Control | 34 (94.4) | 34 (94.4) | 33 (91.7) | 34 (94.4) | 34 (94.4) | 33 (91.7) |
| 6 months | ||||||
| SMS | 21 (63.6) | 21 (63.6) | 21 (63.6) | 21 (63.6) | 21 (63.6) | 21 (63.6) |
| SMS + I | 23 (63.9) | 23 (63.9) | 23 (63.9) | 23 (63.9) | 23 (63.9) | 23 (63.9) |
| 12 months | ||||||
| SMS | 26 (78.8) | 26 (78.8) | 26 (78.8) | 26 (78.8) | 26 (78.8) | 26 (78.8) |
| SMS + I | 21 (58.3) | 21 (58.3) | 21 (58.3) | 21 (58.3) | 21 (58.3) | 21 (58.3) |
| Control | 30 (83.3) | 30 (83.3) | 30 (83.3) | 30 (83.3) | 30 (83.3) | 30 (83.3) |
Appendix 33 Data table of resource use
| Resource | SMS only, mean, (SD, range) | SMS + I, mean, (SD, range) | Control, mean, (SD, range) | |||
|---|---|---|---|---|---|---|
| Resource use | Cost (£) | Resource use | Cost (£) | Resource use | Cost (£) | |
| GP visits | 2.94 (3.05, 0–11) | 143.65 (133.97, 0–444) | 3.36 (3.13, 0–10) | 163.86 (148.51, 0–444) | 1.35 (1.87, 0–6) | 199.23 (277.49, 0–888) |
| Nurse visits | 2.12 (3.00, 0–12) | 28.82 (34.19, 0–126) | 2.07 (2.23, 0–7) | 29.75 (33.38, 0–107.1) | 2.15 (9.79, 0–50) | 93.48 (425.00, 0–2170) |
| A&E attendances | 0.18 (0.39, 0–1) | 43.53 (101.53, 0–296) | 0.43 (0.65, 0–2) | 74.00 (112.41, 0–296) | 0.08 (0.27, 0–1) | 45.54 (160.87, 0–592) |
| Outpatient appointments | 0.82 (1.13, 0–4) | 134.12 (189.18, 0–600) | 3.14 (3.70, 0–10) | 480.00 (574.54, 0–1560) | 0.50 (1.30, 0–6) | 240.00 (625.84, 0–2880) |
| Inpatient stays | 0.18 (0.53, 0–2) | 500.82 (1500.15, 0–5676) | 0.14 (0.53, 0–2) | 810.86 (3033.95, 0–11,352) | 1.69 (6.01, 0–24) | 19,211.08 (68,170.19, 0–272,448) |
| Total | 6.24 (6.38, 0–21) | 850.94 (1664.91, 0–6264) | 9.14 (7.29, 0–22) | 1558.46 (3089.68, 0–11,980) | 5.77 (15.74, 0–79) | 19,789.32 (68,799.19, 0–272,448) |
Appendix 34 Data table of general linear model results
| Difference in costs (mean, 95% CI) | Difference in cost – excluding two outliers in control arm (mean, 95% CI) | Difference in QALYs (mean, 95% CI) | ||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted for baseline costs | Unadjusted | Adjusted for baseline costs | Unadjusted | Adjusted for baseline EQ-5D utility | |
| SMS vs. control | –18,605 (–48,954 to 1135) | –10,650 (–37,199 to 1594) | 805 (139 to 1803) | 1014 (133 to 2014) | 0.081 (–0.020 to 0.192) | –0.032 (–0.075 to 0.013) |
| SMS + I vs. control | –17,752 (–47,673 to 2496) | –9732 (–36,372 to 2783) | 1659 (493 to 3469) | 1777 (347 to 3835) | 0.057 (–0.095 to 0.193) | –0.013 (–0.074 to 0.049) |
| SMS + I vs. SMS | 853 (–684 to 2915) | 918 (–961 to 3435) | 853 (–684 to 2915) | 918 (–961 to 3435) | –0.024 (–0.170 to 0.106) | 0.018 (–0.039 to 0.077) |
Appendix 35 Data table of baseline characteristics for alternative SMS participants
| Baseline | Alternative SMS |
|---|---|
| Age (years), N, mean, SD | 39, 54.5, 10.4 |
| Weight (kg), N, mean, SD | 39, 110.7, 18.1 |
| Height (cm), N, mean, SD | 39, 173.9, 6.0 |
| BMI (kg/m2), N, mean, SD | 39, 36.8, 6.6 |
| < 30 | 39, 4, 10.3 |
| ≥ 30 to < 35 | 39, 14, 35.9 |
| ≥ 35 to < 40 | 39, 10, 25.6 |
| ≥ 40 to < 45 | 39, 8, 20.5 |
| ≥ 45 to < 50 | 39, 2, 5.1 |
| ≥ 50 | 39, 1, 2.6 |
| Waist circumference (cm), N, mean, SD | 39, 120.1, 12.3 |
| SIMD category, N, n, % | |
| 1 (most deprived) | 39, 16, 41.0 |
| 2 | 39, 8, 20.5 |
| 3 | 39, 5, 12.8 |
| 4 | 39, 7, 18.0 |
| 5 (least deprived) | 39, 3, 7.7 |
| Ethnic group, N, n, % | |
| Asian | 39, 1, 2.6 |
| Black | 39, 0, 0.00 |
| White | 39, 38, 97.4 |
| Prefer not to say | 39, 0, 0.0 |
| Highest educational qualification, N, n, % | |
| Bachelor’s degree or equivalent (= SVQ 5) | 39, 10, 25.6 |
| HNC/HND or equivalent (= SVQ 4) | 39, 5, 12.8 |
| Higher Grade/Advanced Higher/A level or equivalent (= SVQ 3) | 39, 2, 5.1 |
| Master’s degree/PhD or equivalent | 39, 2, 5.1 |
| No formal qualifications | 39, 10, 25.64 |
| Other | 39, 1, 2.56 |
| Prefer not to say | 39, 2, 5.13 |
| Standard Grade/GCSE/Intermediate 1 or 2 | 39, 4, 10.26 |
| Still studying | 39, 3, 7.69 |
| Vocational qualifications (=SVQ1+2) | 39, 0, 0.0 |
| Employment status, N, n, % | |
| Full-time student | 39, 1, 2.6 |
| Have paid job: full time (≥ 30 hours per week) | 39, 21, 53.8 |
| Have paid job: part time (8–29 hours per week) | 39, 0, 0.0 |
| Not in paid work because of long-term illness or disability | 39, 8, 20.5 |
| Not in paid work for other reason | 39, 0, 0.0 |
| Not working: house husband | 39, 1, 2.6 |
| Retired | 39, 6, 15.4 |
| Self-employed | 39, 0, 0.0 |
| Unemployed and seeking work | 39, 2, 5.1 |
| Household size, N, mean, SD | 39, 2.1, 1.3 |
Appendix 36 Data table comparison of alternative SMS and SMS-only arms
| Outcome | Alternative SMS | SMS only |
|---|---|---|
| Replying to SMS, N, n, % | ||
| 0 replies to SMS | 39, 24, 61.5 | 33, 23, 69.7 |
| 1–5 replies to SMS | 39, 9, 23.1 | 33, 7, 22.3 |
| 6–10 replies to SMS | 39, 3, 7.7 | 33, 1, 3.0 |
| 11–15 replies to SMS | 39, 1, 2.6 | 33, 0, 0.0 |
| 16–20 replies to SMS | 39, 0, 0.0 | 33, 1, 3.0 |
| > 20 replies to SMS | 39, 2, 5.1 | 33, 1, 3.0 |
| Number of replies to SMS (n) | 126 | 81 |
| Stopping SMS, N, n, % | 39, 0, 0 | 33, 2, 6.1 |
| Withdrawal owing to SMS (self-report), N, n, % | 39, 0, 0 | 33, 2, 6.1 |
| Overall satisfaction (0–100), n, mean, SD | 33, 79.4, 21.6 | 27, 75.0, 22.2 |
| Programme has been . . . (1 = low, 5 = high), n, mean, SD | ||
| Understandable | 32, 4.8, 0.8 | 26, 4.4, 0.8 |
| Useful | 32, 4.2, 1.1 | 27, 4.0, 1.0 |
| Helpful | 32, 4.3, 1.1 | 27, 3.9, 1.0 |
| Interesting | 31, 4.3, 0.9 | 27, 4.2, 1.1 |
| Relevant | 31, 4.5, 0.9 | 27, 3.9, 1.2 |
| Helpfulness (1 = low, 5 = high), n, mean, SD | ||
| Text messages | 33, 3.9, 0.8 | 27, 3.1, 1.3 |
| Website | 27, 3.4, 0.9 | 26, 3.3, 0.9 |
| Pedometer | 31, 3.9, 1.2 | 27, 4.1, 0.9 |
| Met other men in programme, N, n, % | ||
| Yes | 33, 0, 0.0 | 27, 0, 0.0 |
| Weight change (kg), n, mean, SD | ||
| BOCF | 39, –1.69, 4.80 | 33, –1.55, 3.60 |
| Complete cases only | 33, –1.99, 5.17 | 26, –1.97, 3.97 |
| LOCF | 39, –1.69, 4.80 | 33, –1.55, 3.60 |
| Weight change (%), n, mean, SD | ||
| BOCF | 39, –1.72, 3.68 | 33, –1.53, 3.39 |
| Complete cases only | 33, –2.03, 3.93 | 26, –1.95, 3.72 |
| LOCF | 39, –1.72, 3.68 | 33, –1.53, 3.39 |
| Weight loss targets, N, n, % | ||
| Weight gain | 33, 8, 24.2 | 26, 8, 30.77 |
| 0 to > 3% weight loss | 33, 9, 27.3 | 26, 10, 38.46 |
| ≥ 3 to > 5% weight loss | 33, 9, 27.3 | 26, 4, 15.38 |
| ≥ 5 to > 10% weight loss | 33, 7, 21.2 | 26, 2, 7.69 |
| ≥ 10% weight loss | 33, 0, 0.0 | 26, 2, 7.69 |
| BMI change, n, mean, SD | ||
| BOCF | 39, –0.54, 1.6 | 33, –0.59, 1.22 |
| Complete cases only | 33, –0.68, 1.8 | 27, –0.73, 1.32 |
| LOCF | 39, –0.54, 1.6 | 33, –0.59, 1.22 |
| Waist circumference change (cm), n, mean, SD | ||
| BOCF | 39, –2.91, 3.77 | 33, –2.49, 3.94 |
| Complete cases only | 33, –3.55, 3.88 | 26, –3.14, 4.34 |
| LOCF | 39, –2.91, 3.77 | 33, –2.49, 3.94 |
List of abbreviations
- BCT
- behaviour change technique
- BMI
- body mass index
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DCE
- discrete choice experiment
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FFIT
- Football Fans in Training
- GP
- general practitioner
- HIC
- Health Informatics Centre
- MACRO
- Modifying Alcohol Consumption to Reduce Obesity
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NRSPCN
- NHS Research Scotland Primary Care Network
- PhD
- Doctor of Philosophy
- PPI
- patient and public involvement
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- ROMEO
- Review Of MEn and Obesity
- SD
- standard deviation
- SIMD
- Scottish Index of Multiple Deprivation
- SMS
- short message service
- SMS + I
- short message service plus incentives
- TRAM
- Texting to Reduce Alcohol Misuse
