Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 17/44/29. The contractual start date was in October 2018. The final report began editorial review in May 2020 and was accepted for publication in December 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Cox et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Smoking prevalence rates have continued to decline in the UK, with fewer young people starting to smoke and greater numbers of people quitting. 1 Smoking has also continued to decline across all socioeconomic groups. However, those from the most disadvantaged groups, such as those presenting with multiple and severe mental illness and substance use comorbidities, present smoking prevalence rates that far exceed those of other groups. 2–5
Smoking is extremely common among adults experiencing homelessness, with prevalence rates ranging from 57% to 82%;4 this is up to four times higher than the UK national average (15.1%). 1
Smoking is related to premature death and disease, and quitting can have a substantial positive impact on reducing harm and increasing life-years. 6 In smokers experiencing homelessness, tobacco-related disease has been cited as the second single cause of premature death and the single largest cause of death in those aged > 45 years. 7 Smoking is particularly fatal among this population because of a higher incidence of respiratory infection and disease. 8 These conditions are likely to be exacerbated because of a general likelihood of engaging in practices that increase the risk of developing respiratory infections, for example smoking discarded cigarettes and sharing cigarettes that act as a vessel for passing viral contaminants. 9,10 Poor respiratory health is also likely to be aggravated by smoking unfiltered and illicit tobacco, dragging harder on cigarettes and taking longer deeper puffs. 9 Beyond the health effects, smoking is also related to several social disadvantages; smokers experiencing homelessness are likely to engage in begging or ask strangers for cigarettes and are reported to spend up to one-third of their income on tobacco and cigarettes. 11
The types of lives that smokers experiencing homelessness have mean that quitting smoking is not a high priority and is also often overlooked by those who support them. 12 There is also some evidence that health and social care professionals are concerned that cessation will exacerbate mental illness and that taking something away, when many of these adults have so little, will be unfair or cruel. 13 Although these concerns are understandable, a survey we conducted in 2018 of 286 smokers accessing homeless services in England and Scotland showed that 75% of smokers have some desire to quit smoking and 75% have some history of quitting; however, quit attempts are often unsupported by behavioural support or licensed nicotine medication, and last less than 24 hours. 14
The UK has a clear goal of reducing the harms caused by tobacco smoking; central to this is the reduction in tobacco-related health inequalities by improving cessation rates. At present, however, smokers experiencing homelessness are not well represented in stop smoking services (SSSs) and cessation support is not mandatory in homeless centres. In the recent Tobacco Control Plan for England,15 the Department of Health and Social Care (DHSC) expresses its commitment to evidence-based innovations to support quitting and will seek to support smokers in adopting the use of less harmful nicotine products such as electronic cigarettes (ECs). Nevertheless, smoking cessation in the context of homelessness is underexplored in the UK. Our recent systematic review of 53 studies showed that only two cross-sectional studies had been conducted in the UK,4 of which one was conducted by our group. 14 Trial evidence from the US shows that there is potential to support cessation in this group. For example, Okuyemi et al. 16 measured the efficacy of motivational interviewing (MI) offered alongside licensed nicotine replacement therapies (NRTs) compared with NRTs alone. Using intention-to-treat (ITT) analysis, verified 7-day abstinence rates at week 26 were 9.3% for MI and NRTs, and 5.6% for NRTs alone (p = 0.15). To our knowledge, prior to the work presented here, there were no smoking cessation intervention studies in the UK. To reduce the burden of smoking among this population, more evidence of the efficacy of interventions is clearly required.
Our systematic review4 and public and patient involvement (PPI) work (conducted in 2017, with seven homeless centres, eight interviews from one major homeless charity and scoping data from 100 participants) helped to shape the design of this study. We were told that the multiple competing needs in this group meant that access to support needed to be made easy and appealing to provide the best chance of engagement. Thus, it was decided that the feasibility study should be embedded in centres that participants were already accessing. Our PPI work also suggested that ECs may be particularly appealing to smokers experiencing homelessness because (1) smokers in our scoping work were already experimenting with them, (2) they can be framed as a switch rather than a quit (which has connotations of loss), which has been highlighted as an issue of cessation, and (3) they can be offered at a location already being visited without a prescription, thus reducing the burden of making further appointments and removing a clinical approach. Taken together, the feedback was that ECs offer a pragmatic harm reduction approach to smoking cessation, and this is especially important when delivering interventions in the third sector, where substance harm reduction is already well established.
An individually randomised trial with allocation to one of two arms [ECs vs. usual care (UC)] was initially considered, but our PPI feedback (from staff and clients at homeless centres) strongly advised against this because of potential problems with compliance, contamination and issues of disharmony, for example resentment towards staff delivering the intervention in which one person had received an EC and another had not. Contamination, harmony and protection of staff were important; therefore, our decision was to opt for a feasibility cluster trial.
Here we present a pragmatic four-centre cluster feasibility study exploring the uptake and use of ECs by smokers accessing homeless support services. The overall purpose of this research was to evaluate the feasibility of supplying free EC starter kits for smoking cessation to smokers experiencing homelessness at a place that they were already accessing. The UC arm received standard existing treatment: advice to quit, an adapted NHS Choices fact sheet for smoking cessation and signposting to the local SSS, which offers weekly behavioural support and a choice of NRT or varenicline. The EC arm received a starter kit, a 4 weeks’ supply of e-liquid and a fact sheet.
Chapter 2 Objectives
To test the feasibility of future trial work, seven objectives were set. Table 1 presents the study objectives and associated outcome measures and whether the objective is specific to the cluster level or across levels.
| Objective | Outcome measure | Measured at |
|---|---|---|
| 1. Assess willingness of smokers to participate in the feasibility study to estimate recruitment rates and inform a future trial | In both arms, we will record the number of smokers asked to take part and the number of smokers who consent | Across arms |
| 2. Assess participant retention in the intervention and control arms | Record (1) how many participants complete assessment measures in each arm at each time point, and (2) how many participants still have, and are still using, ECs in the intervention arms | Across arms |
| 3. Examine the perceived value of the intervention, facilitators of and barriers to engagement, and influence of local context | Qualitative interviews with 4-week completers and non-completers, quitters and smokers (n = 24, approximately six per site) between weeks 4 and 8 across both arms | Across arms |
| 4. Assess service providers’ capacity to support the study and the type of information and training required | Qualitative interviews with keyworkers and front-line staff (n = 12, approximately three per site) across both arms | Across arms |
| 5. Assess the potential efficacy of supplying free EC starter kits | Measure breath CO levels, self-reported quit rates/cigarette consumption at each follow-up time point | Across arms |
| 6. Explore the feasibility of collecting data on contacts with health-care services among this population as an input to an economic evaluation in a full cRCT | Record participant utilisation of primary and secondary health-care services using a self-report service-use questionnaire at each time point and HRQoL using the EQ-5D-3L | Across arms |
| 7. Estimate the cost of providing the intervention and UC | Record all resources used in the delivery, including staff costs, ECs and other costs incurred. Staff will complete a pro forma to record contact time, non-contact time and other resources used in delivery | Across arms |
Chapter 3 Methods
Trial design
A four-centre cluster feasibility study with embedded qualitative process evaluation was conducted. A deviation from our protocol was made to the study design owing to the availability of centres. Centres were counterbalanced in each condition but not randomised (see Cluster allocation). However, participants joined after cluster allocation and allocation was concealed to participants until after the baseline assessment. Recruitment occurred during a discrete period starting from site initiation at each location (6 weeks).
Electronic cigarette sites offered an EC starter kit at baseline assessment. The EC arm is formed of two EC clusters.
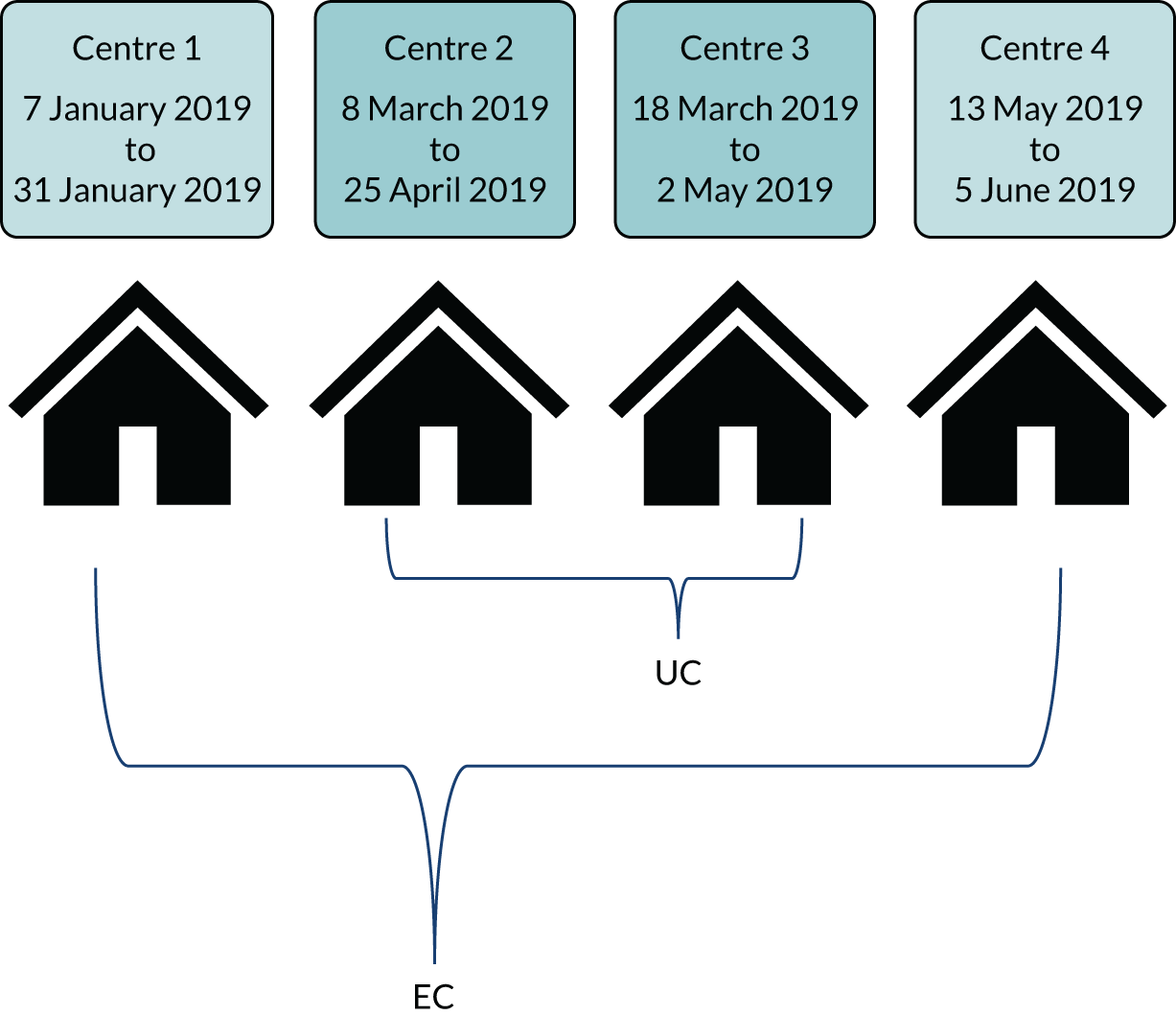
Usual care is defined as offering an adapted NHS Choices fact sheet for smoking cessation and signposting to the local SSS. The UC arm is formed of two UC clusters. The clusters are illustrated in Figure 1.
FIGURE 1.
The cluster sites. EC arm: Northampton (centre 1) and London (centre 4). UC arm: Edinburgh (centre 2) and London (centre 3).
Consent was taken at baseline by the research team. Follow-up data at 4, 12 and 24 weeks were also recorded by the research team. Keyworkers delivered the interventions (see Interventions).
Participants
Participants were selected by homeless centre staff based on the following inclusion criteria. Further eligibility checking was performed at baseline by the researcher. Eligibility criteria did not differ between clusters.
Inclusion criteria
-
Adult smokers (aged ≥ 18 years) accessing homeless support services on a regular basis and also known to staff.
-
Self-reported daily smokers only with smoking status also confirmed by support staff.
-
Smoking status also biochemically verified by exhaled carbon monoxide (CO) breath test at recruitment.
To gain wider representation, we did not exclude those who reported mental illness or substance dependence.
Exclusion criteria
-
Non-smokers or those reporting using another smoking cessation aid at the time of recruitment.
-
Anyone aged < 18 years, reporting pregnancy or unable to consent, for example they were currently intoxicated or unable to speak English.
-
All of those who were not well known to the centre staff were ineligible.
Description of settings
Centre 1 (electronic cigarette cluster)
This is a day centre (open Monday to Friday; 08.30–13.00) located within Northampton. Staff and volunteers, support workers, keyworkers, social workers and kitchen staff work to provide a range of facilities and programmes to serve the practical, physical and social needs of people experiencing or at risk of homelessness in the area. There is a breakfast and lunch service, training and employment skills programmes, and an emergency night shelter (run separately by the local council) for use during periods of inclement weather. The kitchen and day centre are open on Saturday mornings for people who are sleeping rough or in emergency accommodation.
Centre 2 (usual-care cluster)
This is a day centre (open Monday to Friday; 09.00–13.00) located within the city of Edinburgh. It offers breakfast, lunch and shower and clothing facilities, as well as spiritual support through chaplaincy and recreational facilities (TV, pool and day trips). Support staff provide crisis intervention advice and assistance with benefits, housing, accessing medical services for physical and mental health, and social and life skills emotional support.
Centre 3 (usual-care cluster)
This centre operates three linked sites of supported accommodation in London for people at risk of homelessness. Each site accommodates clients whose needs fall within the parameters of the level of care it is able to provide.
Site 1 has 21 bedsits in three adjoining three-and-a-half-storey houses with a shared garden and is staffed 24 hours for people with greater complex needs.
Site 2 has 12 bedsits for male residents who are semi-independent and benefit from the support of regular check-ins, health support, and help with advocacy and paperwork. The office staff are available Monday to Friday between 09.00 and 17.00.
Site 3 has seven units in one four-storey building. The residents are both men and women who are living mostly independently, with the support workers providing advocacy, signposting to services, and on-site management.
Centre 4 (electronic cigarette cluster)
Also located in London, centre 4 provides supported accommodation across four linked sites. Staff and volunteers include keyworkers, complex needs workers and kitchen and maintenance staff.
Site 1 is a 23-unit residential support service for men and women. Single accommodation units are set on two storeys and overlook an enclosed communal garden. There is a multipurpose meeting space in a small unit in the garden where staff run skills classes and social groups. Staff are on-site 24 hours for management and security. Residents have a range of abilities and needs, with the aim of returning to independent living. Staff aim to support people with complex needs through semi-independent living with keyworker support, advocacy and daily check-ins.
Site 2 is a 13-unit women-only supported accommodation, offering support to women who have been or are at risk of becoming homeless. The accommodation provides single-occupancy accommodation. There is a shared garden with chickens and a shared communal lounge and kitchen, but no private meeting spaces. Keyworkers provide support sessions within usual working hours: 09.00 to 17.00.
Site 3 is a short-stay house and site 4 provides first-night accommodation only (to provide emergency accommodation intended for people who are newly homeless or acutely at risk of rough sleeping).
The researchers routinely kept reflexive diaries to record observations and reflections about local contexts, as well as notes on the psychological impact of working in new and sometimes unpredictable environments where people are reacting to multiple, chronic and/or acute stressors and complex needs. These research notes formed the basis of debriefing meetings and discussions in the research team, in part to be informative of ecological differences between sites as well as to systematise the physical and psychological safety of the researchers.
Interventions
Interventions were delivered at cluster level. Appendix 1 presents the Consolidated Standards of Reporting Trials (CONSORT) flow diagram, which provides a summary of the stages of the study by intervention.
Pre-intervention staff training
The research team provided four education and training sessions to staff in each centre, 1–2 weeks before recruitment started. The educational content followed National Centre for Smoking Cessation and Training recommendations, to ensure that centre staff had a basic knowledge of the issues that surround smoking and smoking cessation and to optimise the delivery of the EC and UC interventions. The training was developed and led by Dr Deborah J Robson (King’s College London, London) with the support of the research team (LD, AT, SC, IU and AF); Table 2 presents an overview of the delivery of the staff education and training to 32 staff members across the centres. However, not all staff were able to attend the education and training sessions. In addition, new staff were employed in some centres during the intervention delivery phase of the study.
| Trial arm | Delivered by | Duration | Number of staff per training session | Materials provided |
|---|---|---|---|---|
| EC | ||||
| Centre 1 | Deborah J Robson; Allan Tyler; Lynne Dawkins | 2 hours (plus individual coaching) | 12 | EC instruction pamphlet |
| Centre 4 | Deborah J Robson; Allan Tyler; Sharon Cox; Catherine Kimber | 2 hours (plus individual coaching) | 8 | EC instruction pamphlet |
| UC | ||||
| Centre 2 | Deborah J Robson; Sharon Cox; Allison Ford; Isabelle Uny | 1.15 hours | 7 | Help-to-quit leaflet |
| Centre 3 | Deborah J Robson; Allan Tyler; Lynne Dawkins | 1.15 hours | 5 | Help-to-quit leaflet |
Education and training content for both intervention arms included the following:
-
prevalence and patterns of smoking among the wider population and people experiencing homelessness
-
health effects of smoking
-
benefit of smoking cessation
-
common misperceptions around smoking cessation in the context of other addictions and mental illness
-
why this study was important and why it was needed now
-
how to complete the baseline and follow-up forms and what was expected from staff.
Additional electronic cigarette training
Staff were expected to deliver the intervention and were therefore provided with information on the evidence base of EC use, clinical effectiveness and safety among the wider population and a rationale behind why ECs may be useful for this group. In addition, in the training session, staff were provided with information about how to deliver correct advice about ECs to participants and given a practical hands-on demonstration relating to aspects of EC assembly, how to use the device, charge it, refill the tank and replace coils, and battery safety. Including the practical hands-on demonstration meant that the EC intervention training took up to 45 minutes longer than the UC training.
The research team in the EC arm provided additional coaching in preparation for each staff member’s first two keyworker sessions at baseline, and through shadowing and feedback at ongoing sessions. Ongoing informal training was provided, in the form of question-and-answer discussions with staff between keyworker sessions and before and after participants’ arrival.
Additional usual-care training
As in the EC arm, staff were asked to deliver the UC referral information and were therefore provided with detailed information on the role of SSSs, current licensed medications available to smokers in their local SSS and evidence for their clinical effectiveness. Staff were informed that, at the time of training, licensed stop smoking medicines alongside behavioural support offered at the SSS were the most effective way of quitting smoking. Details of the centre’s local SSS and how to make a referral were also included in the training.
Electronic cigarette intervention
All participants in the EC cluster (centres 1 and 4) received the same intervention.
Participants were provided with an unboxed Aspire PockeX kit (Aspire eCig UK, Peterborough, UK) starter kit comprising a tank-style refillable EC with a spare atomiser, charger and wall adapter plug. They were offered five 10-ml bottles of e-liquid, choosing from a combination of (1) e-liquid nicotine strengths (two options: 12 or 18 mg/ml) and (2) flavours (three options: tobacco, fruit or menthol). E-liquid nicotine strengths of 12 and 18 mg/ml were chosen based on previous reports from our group and others of high nicotine dependency among smokers experiencing homelessness. 14 The EC brand and e-liquid were decided on following our PPI work and advice from vapers. Vapers known to the research team who have engaged in other research suggested four of the top-selling, easy-to-use ECs. On purchasing these, smokers from one London homeless centre tried the four different ECs and provided feedback on ease of use, nicotine hit and likeability. The Aspire PockeX was consistently rated as the easiest and most satisfying to use. The flavours were recommended by a vape retailer because they are the most popular, that is best-selling, varieties.
At this time, the keyworker showed the participant how to use the device; this included how to (re)fill the liquid in the tank, how to charge the device, how to inhale and what to expect when first using the device. Participants were also provided with the device instructions, which in response to our PPI feedback had been retyped into a larger font, and a help sheet of ‘tricks and tips’ from experienced vapers. Participants were given time to try the device and experiment with the different flavours and nicotine strengths, and were permitted to switch between flavours. (Appendix 2 presents the selection of e-liquid flavours and concentrations that were given out by keyworkers.) The keyworker recorded the participants’ choices of e-liquid and the timing of the keyworker session in case report forms (CRFs) that were kept with the study equipment.
Once per week in the 3 weeks that followed the baseline meeting, participants met centre staff to report any concerns and collect up to five 10-ml bottles of e-liquid and a new atomiser. Ideally, participants met the staff member whom they had met at the baseline session and who had attended the staff training; however, because of staff turnover and time demands this was not always feasible. Staff recorded data on e-liquid and troubleshooting in the CRFs. With a larger number of participants attending follow-up appointments at centre 1, staff adopted a drop-in ‘surgery’ in which waiting participants also received peer advice and support.
Usual care intervention
All participants in the UC cluster (centres 2 and 3) received the same assessment measures, but UC differed across the two centres in this cluster.
At the end of the baseline assessment, and during the same session, participants were informed of their centre allocation. Participants were then referred to their keyworkers/other centre staff who advised them to consider quitting and provided them with the fact sheet and an adapted NHS Choices ‘help-to-quit’ leaflet; this included information about the location and opening hours of SSSs local to the centre. Paper copies of the help-to-quit leaflet (with SSSs’ contact details) were available as posters/flyers at homeless centres in the UC condition/cluster. Centre staff were asked to follow up with participants once per week for 4 weeks to record whether or not they had made contact with the SSS and to remind them to do so.
Process evaluation
All participants were asked after baseline CRF completion if they would be interested in taking part in the qualitative process evaluation. Individual interviews were conducted in a quiet, private space on homeless centre premises, between weeks 4 and 8 of the trial. A semistructured topic guide was used to ensure that all relevant topics were covered, and interviews were digitally recorded with participants’ consent.
The participants’ guide covered smoking history; awareness of local SSSs; experiences of trial processes; expectations and experiences of vaping (EC arm); and experiences of signposting to SSSs (UC arm).
The staff topic guide covered staff role and trial involvement; existing cessation support for clients; and views and experiences of the trial, processes, and the EC or UC interventions. Both guides covered unintended consequences and recommendations for improvements.
Incentives for retention
The wider literature on smoking and homelessness has shown that it is common practice to offer a financial incentive to participants and that this improves retention. 4 Regardless of cluster, all participants were compensated with a £15 high-street gift card (Love2Shop, Birkenhead, UK) for completing assessments at baseline and follow-up and the qualitative interview (totalling £75). Staff did not receive a gift card for taking part in the interviews. Participant payment was not contingent on quitting or cutting down and this was stressed to the individuals taking part.
Outcome measures
Some parts of the following text have been reproduced with permission from Dawkins et al. 17 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Table 1 presents the outcomes and associated measures, including the relationship to each intervention arm.
Baseline measures (across clusters)
-
Demographic information and homeless status/history.
-
Cigarettes smoked per day, smoking history (e.g. length of smoking, previous number of quit attempts, support used) and past and current EC use.
-
Severity of tobacco dependence, measured by the Fagerström Test of Cigarette Dependence (FTCD) (Fagerström18) and expired CO.
-
Motivation to stop smoking (MTSS), measured by the Motivation to Stop Scale, a seven-level single-item instrument that incorporates intention, desire and belief in quitting smoking. 19
-
Mental health status, measured using the Patient Health Questionnaire-9 items (PHQ-9)20,21 for depression (total score ranging from 0 to 27, with a higher score indicating greater severity of depression) and Generalised Anxiety Disorder-7 (GAD-7) questionnaire (total score ranging from 0 to 21, with a higher score indicating greater severity of anxiety). 22
-
Alcohol use, measured using the Alcohol Use Disorders Identification Test (AUDIT), a 10-item screening instrument developed by the World Health Organization to screen for alcohol problems. Scores range from 0 to 40, with a score of > 8 indicating harmful or hazardous drinking and > 13 (females) or > 15 (males) indicating alcohol dependence. 23
-
Drug use measured using the Severity of Dependence Scale (SDS), a five-item screening measure of psychological aspects of dependence yielding a total possible score ranging from 0 (no/low dependence) to 15 (high dependence). 24
-
General health-care and service use measured using an adapted health-care and social service utilisation questionnaire relating to services accessed in the last 4 weeks.
-
Health-related quality of life (HRQoL) measured using the EuroQol-5 Dimensions, three-level version (EQ-5D-3L), a widely used measure that provides a single value for health status that can be used in the clinical and economic evaluation of an intervention. 25,26
All questionnaires and measures have good psychometric properties and have been used in previous research with vulnerable populations.
Follow-up data collection
Usual care
At weeks 4, 12 and 24, the following information was collected:
-
smoking information: self-reported smoking abstinence; number of cigarettes smoked in the past 7 days (to measure 7-day point prevalence abstinence); number smoked per day (to calculate smoking reduction from baseline)
-
exhaled CO breath test
-
engagement with the local SSS (appointments made and attended)
-
use of EC and other tobacco/nicotine-containing products
-
general health-care and service use; HRQoL; mental health status (GAD-7, PHQ-9)
-
other drug use/dependence (AUDIT, SDS)
-
direct and indirect staff contact time.
Electronic cigarettes
At weeks 4, 12 and 24, in addition to the aforementioned information, the following was collected:
-
Self-report information about 12 positive effects (e.g. throat hit, satisfaction, pleasant, craving reduction) and 21 negative effects (e.g. mouth/throat irritation, nausea, headache, heartburn) of EC use. This was reported using a visual analogue scale (VAS) and summed to create a percentage score (higher score = higher positive or negative effect) as used in our previous studies. 27
-
Information to further monitor risk and adverse effects (e.g. EC theft, exchanges, use for other substances), an unintended consequences checklist was developed specifically for this trial.
The research team collected all of the baseline and consent data and the 4-, 12- and 24-week follow-up data.
Feasibility study outcome measures
-
To assess willingness to take part in the study, we recorded (1) the number of people who were asked, (2) the number eligible to take part and (3) the number who consented to take part.
-
Retention and engagement were measured by recording (1) the proportion of participants who completed assessment measures in each arm at each time point, and (2) the proportion of participants still using ECs in the intervention arm and who had visited the SSS in the UC arm.
-
To estimate the parameters for future trial at each follow-up point, we recorded (1) CO-validated sustained abstinence (from 2 weeks post quit date allowing up to five slips); (2) CO-validated 7-day point prevalence abstinence (i.e. no smoking at all in the past 7 days); and (3) the proportion achieving 50% smoking reduction [calculated by subtracting cigarettes per day (CPD) at follow-up from baseline].
-
To explore the feasibility of collecting data on contacts with health-care services, we recorded participant utilisation of primary and secondary health-care services using a self-report questionnaire.
-
Data on staff contact time, non-contact time and other resources used in EC and UC delivery, including staff costs, ECs and other costs incurred, were collected to provide an indicative cost of the intervention.
The research team collected all of the baseline and consent data and the 4-, 12- and 24-week follow-up data.
Sample size
As this was a feasibility study for a main trial, no formal power calculation based on detecting evidence for efficacy was conducted; the outcomes of the study allowed us to calculate the required sample size [and an intracluster correlation coefficient (ICC)] for a possible future definitive cluster randomised controlled trial (cRCT).
As per our published protocol,28 a pragmatically chosen sample size (N = 120; n = 30 per centre, n = 60 per cluster) was based on our pre-feasibility PPI work and also taking information from published works in similar samples. This information allowed us to identify evidence of feasibility, recruitment rates and any problems with the intervention or research methods. Our pre-feasibility scoping work suggested that the centres had daily contact with between 25 and 120 individuals, of whom 70–90% were likely to be smokers. Other studies on homeless populations have reported follow-up rates ranging between 24% and 88% (depending on the location of visits, provision of incentives and use of prompts). 29 Therefore, we estimated that 50% of those who agree would drop out in the period between consenting to participate and the final follow-up at 24 weeks, leaving an estimated sample size at the final follow-up of 60.
In relation to the qualitative process evaluation, we planned to interview a subgroup of 24 homeless smokers (approximately six per centre) and 12 staff members (approximately three per centre). We also aimed to include continuing participants and those who did not complete their 4-week follow-up, and those in the EC and UC arms. This sample size is adequate for collection of qualitative data necessary to assess objectives 3 and 4.
Although there was no formal interim analysis or stopping guidelines, we did specify in our ‘project timetable and milestones’ that we would assess recruitment and 4-week retention at centre 1 after 2 months to determine whether or not to proceed with recruitment at centres 2, 3 and 4.
Cluster allocation
The centres in Northampton (centre 1) and Edinburgh (centre 2) are both day centres, whereas the two London centres (centres 3 and 4) are residential units. We planned to pair and match centres on accommodation provision; that is, each one of the residential centres would be paired with one of the day centres. We would then randomly allocate the two London centres, that is, one to the EC arm and the other to the control (UC) arm, with their accompanying pair (day centre) allocated to the other arm.
However, when we were ready to begin recruitment, the centres in London had not confirmed their availability for training and study start date. Thus, centre allocation could not be randomised and therefore deviated from protocol: we started with the centre that was ready to start training and recruitment, which was the centre in Northampton. We allocated this first centre to the EC condition so that we could explore recruitment, 4-week retention and any unintended consequences associated with the intervention to determine whether or not to proceed with recruitment at centres 2, 3 and 4. Centre 2 (Edinburgh) as the other day centre was therefore allocated to the UC condition. Centres 3 and 4 (London) were allocated to the UC and EC arms, respectively. Centre 3 was allocated to UC, as it was geographically closer to the researcher who was still collecting follow-up data from centre 1 and we expected lower uptake in the UC condition.
Thus, the actual allocation of centres to each arm was non-random; it was a pragmatic decision based on centre readiness and staff/researcher availability, though we balanced potential confounders and differences in environment by ensuring each cluster (EC and UC) contained one day centre and one residential unit.
Allocation concealment mechanism
As this represents feasibility work, a pragmatic approach to the concealment of the intervention was taken. Participants were told of the condition that they had been allocated to only after consent and baseline assessment; this was the same across the clusters. However, because of the nature of the conditions, namely that those in the EC clusters were provided with a starter pack and the social dynamics in the centres (particularly the day centres) were close-knit and interactive, the centre allocation was quickly revealed between participants and also to new participants.
Contamination
Contamination in the context of this design was defined as a participant receiving the intervention delivered by another participating centre, for example a participant in UC receiving a free EC starter pack from one of the EC clusters.
Implementation
This section is not applicable to this work.
Analytical method
This is a feasibility study for a trial in preparation for a future cRCT, and analyses of effect are not appropriate. Analyses were conducted to evaluate the feasibility study outcomes (see Table 1). Similarly, because this is a feasibility study for a trial, subgroup analyses are not appropriate.
Table 1 presents the objectives and associated outcome measure for each objective. Objectives 1, 2, 5, 6 and 7 were measured quantitatively, and objectives 3 and 4 were measured through the qualitative process evaluation. Each objective was measured across the whole sample, with the exception of objectives 5 and 7, which relate to efficacy and cost-effectiveness of the interventions. Chapter 4 (see Table 3) presents the descriptive data for participant characteristics for the trial. Appendix 3 also presents the data for the subset of participants in the process evaluation.
Baseline demographic data were summarised using frequencies and descriptive statistics, and the arms (EC vs. UC) were compared using a t-test/Mann–Whitney U-test or Fisher’s exact test for continuous and categorical variables, respectively. EC effects are summarised descriptively. Changes in mental health status and substance use were explored over time and between arms using repeated-measures analysis of variance (ANOVA).
-
Objectives 1 and 2: participant willingness to take part and retention
Frequency information regarding the number of smokers who (1) were invited to take part, (2) were eligible to take part, (3) consented/completed the baseline assessment and (4) attended and completed each follow-up.
-
Objectives 3 and 4: to examine the perceived value of the intervention, facilitators of and barriers to engagement, and influence of local context, and to assess service providers’ capacity to support the study and the type of information and training required
Interviews lasted between 16 and 65 minutes, were transcribed verbatim by professional transcribers, were checked for accuracy and were entered into NVivo 12 software (QSR International, Doncaster, UK) to facilitate coding and analysis. Data were analysed using thematic analysis. 30 Separate coding frameworks for both participants and staff, with themes initially formed deductively, were developed using the main objectives and interview topics. The qualitative team (AF, IU and AT) conducted a first round of coding with AF, checking all coding for consistency. Through discussion, inductive themes were identified and agreed, leading to a second round of coding. Using an iterative approach, coded themes were then used as the categories for analysis. Data were carefully examined to identify the range and diversity of responses and themes, and subthemes were created and/or refined as appropriate. Findings were interpreted and discussed among the wider team. Quotations were selected to illustrate findings. The study arm for each participant [EC or UC, centre code (01–04)] and whether or not the quotation was from a trial participant or a staff member are indicated alongside the quotations.
-
Objective 5: assess the potential efficacy of supplying free EC starter kits
The proportion of participants reporting sustained smoking abstinence, 7-day point prevalence abstinence (both CO verified) and a 50% reduction in smoking in each arm at each follow-up time point were recorded. These variables are presented with the denominator being the number of people who attended follow-up. Sustained abstinence is also presented and analysed using ITT analysis; that is, all those allocated are included in the analysis as belonging to the group to which they were originally allocated and those with missing outcome data were treated as smokers. The ICC was calculated by the Fleiss–Cuzick method. 31
-
Objectives 6 and 7: to explore the feasibility of collecting data on contacts with health-care services among this sample as an input to an economic evaluation in a full cRCT and to estimate the cost of providing the intervention and UC
The completeness of EQ-5D-3L and service use questionnaires was examined. We used the UK population tariff32 to convert the results of EQ-5D-3L to utility value. Quality-adjusted life-years (QALYs) were then calculated in each arm using the area under the curve plotted from baseline and follow-up points. 33 A set of national weighted average unit costs were extracted from secondary or published sources (see Appendix 4 and Appendix 5). The quantities of services reported by participants were multiplied by the respective unit costs to present a preliminary cost profile. We also present the costs of the programme, including training and delivery, the details of which were recorded by the research team. Results from the health economics component will be used to refine the instruments for a full randomised controlled trial (RCT).
Recruitment
Recruitment and 4-week follow-ups ran sequentially across the three sites in England, with 12- and 24-week follow-ups overlapping. Recruitment and data collection in Edinburgh ran in parallel with the second centre in England.
The feasibility study was completed within the planned time frame. However, although we planned to recruit for 4 weeks at each centre, recruitment was extended to 6 weeks in the UC arm. This was a pragmatic decision taken with assistance from the Trial Steering Group, the research team and centre staff. Centre 1 saw high levels of interest in the study and extending the recruitment period to 6 weeks was not required. We did extend capacity in the 4-week window to recruit more participants who were interested in taking part, anticipating potentially lower uptake in smaller centres. Conversely, centre 2 proved to be particularly challenging for recruitment because of staff time and competing needs and resources. The research team had to adapt to the conditions of the centre, appointments had to be rescheduled, and staff were not always available to assist. Centre 3 was quieter and overlapped with data follow-up at centre 1. Residents also had daytime commitments that clashed with recruitment, so again the research team needed to be flexible and therefore recruitment was continued over 6 weeks until we reached saturation.
Sampling and recruitment for the qualitative process evaluation
All those enrolled in the trial were asked at baseline about their willingness to take part in the process evaluation interviews and whether or not they were willing to be contacted at a later date to arrange an interview. After the intervention phase, those who had consented to be contacted were approached by a researcher by telephone, or in person at the homeless centre, and invited to take part. At centre 1, staff identified participants whom they felt would be most willing to take part. Throughout the centres, staff who were supporting the participants and the project were also eligible to take part in an interview. Potential interviewees were provided with a participant information sheet and re-contacted several days later. An interview date and time were arranged for interested participants. Written consent was obtained at the start of the interview.
Purposive sampling was utilised with a pre-determined target to recruit approximately six trial participants and three staff members at each of the four homeless centres. Trial participants were also to be sampled according to (1) smoking status at week 4 of the trial and (2) whether or not they completed the week 4 follow-up.
Centre 1: electronic cigarettes
Recruitment/baseline: 7 January to 31 January 2019.
4-week follow-up: 4 February to 28 February 2019.
12-week follow-up: 1 April to 25 April 2019.
24-week follow-up: 24 June to 17 July 2019.
Centre 2: usual care
Recruitment/baseline: 8 March to 25 April 2019.
4-week follow-up: 8 April to 17 May 2019.
12-week follow-up: 4 June to 25 July 2019.
24-week follow-up: 23 August to 10 October 2019.
Centre 3: usual care
Recruitment/baseline: 18 March to 2 May 2019.
4-week follow-up: 18 April to 18 May 2019.
12-week follow-up: 18 June to 18 July 2019.
24-week follow-up: 10 September to 25 September 2019.
Centre 4: electronic cigarettes
Recruitment/baseline: 13 May to 5 June 2019.
4-week follow-up: 10 June to 4 July 2019.
12-week follow-up: 7 August to 28 August 2019.
24-week follow-up: 28 October to 20 November 2019.
Process evaluation
Interviews were conducted between February and July 2019 by one of a mixed-sex team of three full-time qualitative researchers experienced in interviewing vulnerable groups (AF, AT and IU).
Chapter 4 Results
Baseline data
Baseline data are presented in Table 3.
| Characteristic | Trial arm | Total (N = 80) | p-value | |
|---|---|---|---|---|
| EC | UC | |||
| Age (years), mean (SD) | 42.75 (10.90) | 42.53 (10.78) | 42.66 (10.79) | 0.93 |
| Sex, n (%) | 0.34 | |||
| Female | 19 (40) | 9 (28.13) | 28 (35) | |
| Male | 29 (60) | 23 (71.88) | 52 (65) | |
| Employment status, n (%) | 0.11 | |||
| Full-time school or college | 0 (0) | 0 (0) | 0 (0) | |
| Paid employment/self-employed | 2 (4.16) | 0 (0) | 2 (2.50) | |
| Government training scheme | 1 (2.08) | 1 (3.13) | 2 (2.50) | |
| Unpaid or voluntary work | 9 (18.75) | 0 (0) | 9 (11.30) | |
| Waiting to work, already obtained | 1 (2.08) | 0 (0) | 1 (1.30) | |
| Looking for work/training scheme | 7 (14.58) | 5 (15.63) | 12 (15.00) | |
| Prevented by temporary sickness/injury | 2 (4.16) | 3 (9.38) | 5 (6.30) | |
| Permanently unable to work | 21 (43.75) | 17 (53.13) | 38 (47.50) | |
| Unemployed and not looking for work | 3 (6.25) | 2 (6.25) | 5 (6.30) | |
| Other | 2 (4.16) | 4 (12.5) | 6 (7.50) | |
| Current sleeping situation (past 7 days), n (%)a | ||||
| Sleeping rough on streets/in parks | 3 (6.25) | 4 (12.5) | 7 (8.80) | 0.42 |
| Hostel or supported accommodation | 31 (64.58) | 17 (53.13) | 48 (60) | 0.36 |
| Sleeping on somebody’s floor/sofa | 1 (2.08) | 2 (6.25) | 3 (3.80) | 0.56 |
| Emergency accommodation (refuge, shelter) | 8 (16.66) | 1 (3.13) | 9 (11.30) | 0.08 |
| B&B or temporary accommodation | 1 (2.08) | 1 (3.13) | 2 (2.50) | 1.00 |
| Housed: own tenancy | 8 (16.66) | 10 (31.25) | 18 (22.50) | 0.17 |
| Other | 2 (4.16) | 0 (0) | 2 (2.50) | 0.51 |
| Background, n (%)a | ||||
| Spent time in prison | 19 (40) | 21 (65.63) | 40 (50) | 0.04 |
| Spent time in secure/young offender unit | 9 (18.75) | 9 (28.13) | 18 (22.50) | 0.41 |
| Spent time in local authority care | 7 (14.58) | 10 (31.25) | 17 (21.30) | 0.10 |
| Spent time in the armed forces | 3 (6.25) | 4 (12.50) | 7 (8.80) | 0.43 |
| Admitted to hospital because of mental illness | 18 (37.50) | 13 (40.63) | 31 (38.80) | 1.00 |
| Been a victim of domestic violence | 18 (37.50) | 13 (40.63) | 31 (38.80) | 1.00 |
| Highest level of education, n (%) | 0.40 | |||
| School: stopped prior to GCSE/Standard Grade | 17 (35.42) | 7 (21.88) | 24 (30) | |
| School: GCSE/Standard Grade | 13 (27.08) | 13 (40.63) | 26 (32.50) | |
| College: A level/FE/Highers | 15 (31.25) | 10 (31.25) | 25 (31.30) | |
| University: degree level | 3 (6.25) | 1 (3.13) | 4 (5) | |
| University: postgraduate or higher level | 0 (0) | 1 (3.13) | 1 (1.30) | |
| Ethnicity, n (%) | 0.64 | |||
| White | 35 (72.92) | 26 (81.25) | 61 (76.30) | |
| Asian/Asian British | 6 (12.50) | 2 (6.25) | 2 (2.60) | |
| Black/black British | 2 (4.17) | 0 (0) | 9 (11.40) | |
| Mixed race/multiple ethnic groups | 5 (10.42) | 4 (12.50) | 8 (10.20) | |
| Sexual orientation, n (%) | 0.81 | |||
| Heterosexual or straight | 40 (83.33) | 28 (87.50) | 68 (85) | |
| Gay or lesbian | 1 (2.08) | 0 (0) | 1 (1.30) | |
| Bisexual | 2 (4.16) | 1 (3.13) | 3 (3.80) | |
| Prefer to self-define | 2 (4.16) | 1 (3.13) | 3 (3.80) | |
| Prefer not to say | 3 (6.25) | 0 (0) | 3 (3.80) | |
| Missing | 0 (0) | 2 (6.25) | 2 (2.50) | |
| Immigration status, n (%) | 0.68 | |||
| UK national | 45 (93.75) | 29 (90.63) | 74 (92.50) | |
| EEA national | 3 (6.25) | 3 (9.38) | 6 (7.50) | |
| Receiving public funds (benefits), n (%) | 0.16 | |||
| Yes | 48 (100) | 30 (93.75) | 78 (97.50) | |
| No | 0 (0) | 2 (6.25) | 2 (2.50) | |
| Long-standing illness, disability or infirmity, n (%) | 0.02 | |||
| Yes | 30 (62.50) | 29 (90.63) | 59 (73.80) | |
| No | 13 (27.08) | 3 (9.38) | 16 (20) | |
| Prefer to self-define | 4 (8.33) | 0 (0) | 4 (5) | |
| Prefer not to say | 1 (2.08) | 0 (0) | 1 (1.30) | |
| Number of CPD, mean (SD) | 20.5 (16.78) | 19.41 (13.07) | 20.07 (15.33) | 0.86 |
| Expired CO, mean (SD) | 19.60 (9.58) | 21.31 (10.77) | 20.29 (10.04) | 0.46 |
| Number of joints per day, mean (SD) | 0.29 (1.13) | 1.73 (2.69) | 0.7 (1.69) | 0.02 |
| FTCD, mean score (SD) | 5.24 (2.53) | 6.13 (2.35) | 5.51 (2.47) | 0.12 |
| Age (years) started smoking, mean (SD) | 16.02 (6.30) | 13.92 (3.72) | 15.17 (5.47) | 0.09 |
| Sharing cigarettes, n (%) | 0.10 | |||
| Not at all | 25 (52.08) | 9 (28.13) | 35 (43.80) | |
| Occasionally | 10 (20.83) | 7 (21.88) | 18 (22.50) | |
| Regularly | 3 (6.25) | 5 (15.63) | 7 (8.80) | |
| Daily | 9 (18.75) | 11 (34.38) | 19 (23.80) | |
| Smoking discarded cigarettes, n (%) | 0.43 | |||
| Not at all | 30 (62.50) | 15 (46.88) | 45 (56.30) | |
| Occasionally | 12 (25) | 10 (31.25) | 22 (27.50) | |
| Regularly | 3 (6.25) | 4 (12.50) | 7 (8.80) | |
| Daily | 2 (4.16) | 3 (9.38) | 5 (6.30) | |
| Asking strangers for cigarettes, n (%) | 0.35 | |||
| Not at all | 31 (64.58) | 16 (50) | 47 (58.80) | |
| Occasionally | 12 (25) | 9 (28.13) | 21 (26.30) | |
| Regularly | 2 (4.16) | 3 (9.38) | 5 (6.30) | |
| Daily | 2 (4.16) | 4 (12.50) | 6 (7.50) | |
| MTSS, n (%) | 0.04 | |||
| I do not want to stop smoking | 1 (2.08) | 4 (12.50) | 5 (6.30) | |
| I think I should stop but do not really want to | 4 (8.33) | 4 (12.50) | 8 (10) | |
| I want to stop but have not thought about when | 6 (12.50) | 4 (12.50) | 14 (17.50) | |
| I really want to stop but I do not know when I will | 3 (6.25) | 8 (25) | 11 (13.80) | |
| I want to stop smoking and hope to soon | 16 (33.33) | 5 (15.63) | 18 (22.50) | |
| I really want to stop and intend to within 3 months | 5 (10.42) | 3 (9.38) | 7 (8.80) | |
| I really want to stop and intend to within 1 month | 11 (22.92) | 3 (9.38) | 14 (17.50) | |
| Missing | 2 (4.16) | 1 (3.13) | 3 (3.80) | |
| Importance of quitting at this attempt, n (%) | 0.25 | |||
| Desperately important | 10 (20.83) | 3 (9.38) | 13 (16.30) | |
| Very important | 25 (52.08) | 15 (46.88) | 38 (47.50) | |
| Quite important | 7 (14.58) | 10 (31.25) | 19 (23.80) | |
| Not at all important | 5 (10.42) | 3 (9.38) | 8 (10) | |
| Determination to quit at this attempt, n (%) | 0.52 | |||
| Extremely determined | 13 (27.08) | 6 (18.75) | 19 (23.80) | |
| Very determined | 16 (33.33) | 10 (31.25) | 26 (32.50) | |
| Quite determined | 14 (29.16) | 10 (31.25) | 24 (30.50) | |
| Not at all determined | 3 (6.25) | 5 (15.63) | 8 (10.00) | |
| Missing | 3 (3.80) | |||
| Self-rated chance of quitting (1 = very low; 6 = extremely high), mean (SD) | 4.09 (1.21) | 3.81 (1.35) | 3.74 (1.53) | 0.34 |
| GAD-7, mean score (SD) | 9.87 (6.86) | 13.33 (7.04) | 11.22 (7.09) | 0.04 |
| PHQ-9, mean score (SD) | 12.46 (7.97) | 13.67 (8.50) | 12.93 (8.15) | 0.53 |
| AUDIT, mean score (SD) | 9.50 (10.46) | 8.80 (9.93) | 9.22 (10.20) | 0.77 |
| SDS, mean score (SD) | 3.49 (4.13) | 7.44 (4.90) | 5 (4.81) | < 0.01 |
The mean age of the sample was 42.66 years, and 65% of the participants were male. Participants were primarily white (76.3%) and heterosexual (85%).
Mental illness, health and substance use comorbidities
Seventy-four per cent of the sample self-reported a long-standing illness, 38.8% had been previously admitted to hospital owing to mental illness, 55% scored 10 or over on the GAD-7 indicating the presence of generalised anxiety disorder, and 60% of participants scored 10 or over on the PHQ-9 indicating the presence of major depression.
In relation to alcohol use, 33.8% of participants had an AUDIT score over 8, suggesting that they were drinking at harmful or hazardous levels. SDS scores were also high, indicating a high prevalence of substance dependence.
Half the participants reported having previously spent time in prison. A significant proportion (38.8%) of the participants, women and men, reported being a victim of domestic violence.
The arms also differed significantly on a number of baseline variables, namely GAD-7, SDS, cannabis joints per day, time spent in prison, physical illness and motivation to quit, with the UC arm scoring higher in all cases but having lower motivation to quit (see Table 3).
Education, employment and housing status
Overall, 37.6% were educated to A level/Highers (or equivalent) or above. Employment status varied: 2.5% reported being in current paid employment and 97.5% reported recourse to benefits (social security/benefits). Just over half of the sample (60%) were currently housed in supported accommodation or in a hostel, and 8.8% reported sleeping rough.
Cigarette dependence and smoking behaviour
The mean number of cigarettes smoked per day (including roll-ups) was 20 [standard deviation (SD) 15.33 cigarettes]; this is equal to a pack of cigarettes per day in the UK. The mean expired CO breath level was 20.29 parts per million (p.p.m.) (SD 10.04 p.p.m). The FTCD score was 5.51 (SD 2.47). In relation to smoking practices that increase the risk of respiratory infection, 55% reported that they shared cigarettes (24% reported doing this daily), and 43% reported that they had smoked discarded cigarettes (6% reported doing this daily).
Furthermore, MTSS varied considerably; although only 6% reported that they did not want to stop smoking, the large majority expressed a desire to quit smoking in the near future.
Differences between the intervention arms
The proportion of participants who had previously spent time in prison or who had a long-standing illness, disability or infirmity was significantly higher in the UC arm than in the EC arm. UC arm participants also scored higher on anxiety and substance dependence, smoked more cannabis joints per day and were less motivated to quit smoking. Given these differences and the differences between centres (see Description of settings), we conducted sensitivity analyses (one-way ANOVA with post hoc tests for continuous variables and Fisher’s exact tests for categorical variables; not per protocol) to explore differences between the four centres regarding variables in which there was a significant difference between arms. Cannabis smoking and substance dependence scores were significantly higher at the day centre in Edinburgh (centre 2; UC) than at all other centres (all p-values for cannabis smoking were < 0.01 and all p-values for SDS were < 0.05), which did not differ from each other. Similarly, anxiety (GAD-7) scores were also highest at centre 2, and these differed significantly from centre 1 (day centre, Northampton, EC) and centre 4 (residential centre, London; EC) (p < 0.05) but not from centre 3 (residential centre, London, UC). In addition, MTSS was significantly higher at centre 1 than at all other centres (p < 0.01), which did not differ from each other. A higher proportion of participants from centre 2 had spent time in prison (73% compared with 36%, 50% and 56% in centres 1, 3 and 4, respectively). The difference between centre 1 and centre 2 was statistically significant (p < 0.01). A higher proportion of participants from centres 2 (91%) and 3 (90%) (both UC) reported a long-standing illness than participants from centres 1 (67%) and 4 (44%). Significant differences were observed between centres 2 and 4 and 3 and 4 (p < 0.05).
Numbers analysed
Appendix 1 presents the CONSORT flow diagram showing the numbers for each intervention arm.
Objective 1: assess willingness of smokers to participate in the feasibility study to estimate recruitment rates and inform a future trial
Outcome: record the number of smokers asked to take part and the number of smokers who consent
Across the four centres, 177 participants were initially invited to take part. Of these, 24 were not eligible (16 in the EC arm and eight in the UC arm). Of the remaining 153 eligible individuals (90 in the EC arm and 63 in the UC arm), 80 consented to take part in the study: 48 (56%) in the EC arm and 32 (50.5%) in the UC arm. Although we did not reach the recruitment goal of 120 that we set ourselves (based on our preliminary scoping work), we did recruit these 80 participants during the originally specified 5-month period. Recruitment also differed between centres; the two day centres were most successful in terms of recruitment (39 consented at centre 1 and 22 at centre 2), together accounting for 77.5% of the total sample, and there was a waiting list of participants who could not be recruited at centre 1 as the researcher had to move on to the next centre. The residential units had fewer eligible individuals, including fewer smokers, and potential participants were less available because of work or other appointments and less interested in the study. Furthermore, there was less opportunity to recruit in the residential centres because of centre space and room availability, and issues around disturbing residents (see Discussion for more information).
Summary of learning points for a future trial
Ensure sufficient researchers are employed on the project to deal with recruitment and limit sites to day centres only.
Objective 2: assess participant retention in the intervention and control arms
Outcome: record (1) how many participants complete assessment measures in each arm at each time point, and (2) how many participants are still using electronic cigarettes in the intervention arm
The CONSORT flow diagram presents the participant numbers at recruitment, and follow-up data by intervention (Appendix 1). In the EC cluster, retention rates were 81%, 69% and 73% at 4, 12 and 24 weeks, respectively. In the UC cluster, retention rates were 66%, 53% and 38% at 4, 12 and 24 weeks, respectively.
There was a lower rate of attendance in the UC intervention at the 12- and 24-week follow-ups. The most common reason for not following up was that participants were no longer attending the services; although exact reasons were not formally documented by the research team, these reasons were highlighted informally by conversations with centre staff.
This difference in retention between arms did not appear to be due to the UC condition per se but, rather, due to baseline differences that might influence the ability to attend follow-ups. The UC arm was associated with a higher incidence of criminal background, illness, disability, substance abuse, anxiety and lower motivation to quit (see Table 3). This was particularly the case for centre 2 (day centre in Edinburgh; see Differences between the intervention arms), which was also associated with a far lower 24-week retention rate (26%) than centre 3 (residential centre in London; 67%).
We asked all participants in the EC intervention if they were still in possession of the EC that we had provided (although they did not have to present it at the appointment), and whether or not they were still using the EC. Assuming that all those who did not attend follow-up sessions did not still have, or were not still using, the EC, at 24 weeks 46% (22/48) still had the EC that we had provided and 56% (27/48) were still using it. Table 4 presents the data based on the number of participants who attended and answered the question at each follow-up. The greatest fall in use was between the 12-week and the 24-week follow-ups; however, 63% of those asked self-reported that they were still in possession of the device. Similarly, in relation to still using an EC, the greatest fall was between the 12-week and the 24-week follow-ups; however, of those in attendance at 24 weeks, 79% reported that they were still using an EC, either the device that was provided at baseline or a different one.
| EC intervention | Time point, n (%) | ||
|---|---|---|---|
| 4-week follow-up | 12-week follow-up | 24-week follow-up | |
| Still have the EC? | |||
| Yes | 33 (85) | 28 (82) | 22 (63) |
| No | 6 (15) | 6 (18) | 13 (37) |
| Still using an EC? | |||
| Yes | 37 (95) | 30 (91) | 27 (79) |
| No | 2 (5) | 3 (9) | 7 (21) |
Summary of learning points for a future trial
Larger numbers, more clusters and official randomisation should reduce baseline differences between arms. Randomisation with stratification by region should also ensure that variables that predict dropout are equally distributed between arms, thus reducing the difference in retention across arms. In the event of a future trial, it would be important to consider ways in which retention could be maximised, including other ways of maintaining more regular contact with participants, for example increasing text and verbal contact between appointments. 29
Objective 3: examine the perceived value of the intervention, facilitators of and barriers to engagement, and influence of local context
Outcome: qualitative interviews with 4-week completers and non-completers, quitters and smokers (N = 24, approximately six per site) between weeks 4 and 8 across both arms
This section presents the findings of 22 in-depth qualitative interviews with a subsample of study participants. Given the difficulty in contacting most of those participants who had not completed their 4-week follow-up, and with the majority of study participants smoking at week 4, it was not possible to conduct interviews with a good range of completers and non-completers, quitters and smokers as intended. However, there is a good spread of qualitative participants across the four homeless centres and both study arms (see Appendix 3 for the qualitative sample characteristics). Nineteen interviewees (86.4%) had completed their 4-week follow-up and three (13.6%) had not completed this follow-up. At the 4-week follow-up, 18 of the 22 interview participants (81.8%) were smoking, one was abstinent and three did not provide smoking information.
We explored participants’ experiences of the study in line with research objective 3. The findings present six topic summary themes: barriers to and facilitators of the study and intervention engagement; experiences of the EC intervention; experiences of UC; perceptions of study processes; unintended consequences; and perceived value. Local differences, if they exist, are highlighted in the text. The section ends with a summary of key learning points for a future trial.
Barriers to study and intervention engagement
Participants’ personal barriers
Interview narratives highlighted the psychological and emotional vulnerability of many of our participants. Some explained that their mental state, attention difficulties, anxiety around social interaction and difficulties with appointments made engaging in treatment programmes challenging:
It is partly my mental health . . . I do panic about talking to people . . . It’s very hard sometimes, just to sit and explain yourself.
Participant 16, C03, UC
Several displayed mistrust in authorities and research:
I thought ‘oh this definitely a government initiative. They’re going to run a test on the homeless . . . maybe they’ve got a dodgy batch of [e-liquid] and they just want to see if it takes anyone out before they put them up for sale.
Participant 02, C01, EC
Although some reported being comfortable providing personal data as part of the study, this was a major concern for others, with particular anxiety around whether or not data would be shared:
. . . if I thought my information was being shared, then I wouldn’t take part.
Participant 11, C02, UC
Participants also lacked confidence in their ability to stop smoking, and many reported that their ideal outcome would be to cut down first, rather than stop straight away: ‘if you can cut down, then you can go that further field’ (Participant 09 C02, UC). This was due to their reported reliance on smoking to deal with stress, isolation or boredom. Traditional stop smoking approaches, particularly NRT, which was reported to have interacted unpleasantly with substance use or mental health in previous quit attempts, were unappealing to participants. This presented a significant barrier to engagement with local SSSs for those in the UC arm.
Cannabis smoking
For participants regularly smoking cannabis mixed with tobacco, most reported wanting to reduce or stop their cannabis consumption, although this presented concerns and was highlighted as especially difficult given the associated pleasure: ‘I feel relaxed [smoking cannabis when] I’ve been wound up all day’ (Participant 11, C02, UC). Some noted how cannabis use had drawn them back to smoking in previous quit attempts:
I’ve quit smoking a couple of times and the thing that always brought me back was smoking weed with the tobacco.
Participant 04, C01, EC
Two participants, previously dependent on heroin, described reliance on cannabis as a protective factor in abstaining from other substances:
I’m an ex-addict, I used to inject heroin etcetera, now I stopped all that and started smoking cannabis and that stopped me taking any other drug.
Participant 13, C02, UC
Participants experiencing mental health distress explained that cannabis helped them to cope and were anxious that stopping cannabis use would exacerbate their symptoms:
I suffer from a lot of anxiety and depression, so it’s just heightened it. It made it worse, trying to stop.
Participant 11, C02, UC
Facilitators of the study and intervention engagement
Opportunity: right time and place
All our interviewees reported a desire to stop or reduce their smoking, expressing concerns about finances or health. Although most had tried to quit previously, negative experiences with NRT and mainstream routes of support [e.g. general practitioner (GP) appointments] meant that these approaches were unattractive. This made opting in to an incentivised, on-site smoking treatment programme appealing. Many illustrated their receptivity to engaging with support at a place they already attended. Bringing smoking cessation aids and services to participants in their own environments was therefore a key facilitator of engagement:
I just thought if you were coming here and Tuesday is my day off, I’d definitely benefit by taking part . . . So why not?
Participant 15, C03, UC
So I’m glad that this has come along because I don’t think, if this hadn’t have happened, I would have bothered to give up. I had no plans of giving up, until that day, none.
Participant 19, C04, EC
Free electronic cigarette starter kit and gift cards
The incentive of receiving a free EC starter kit and/or Love2Shop follow-up gift cards played an important role in study engagement. Although the gift cards received for attending follow-up appointments were valued by all participants, they were especially important for facilitating study recruitment for the UC arm:
My main incentive – I can’t tell lies – is the £15 voucher aye. Why not? If you can come to the centre and make £15 pounds, well then that is fine. Happy days.
Participant 11, C02, UC
In the EC arm, the offer of a starter kit capitalised on participants’ desire to quit and perceived lack of existing cessation options. Despite some participants’ lack of initial enthusiasm for vaping, participants said it prevailed as worth trying, given the availability and offer of the device and e-liquid, especially at a time of financial hardship:
[I] didn’t have to go out and buy it you see, you know, ‘here it is, just try it’.
Participant 07, C01, EC
. . . the thought of maybe it might work and there’s nothing to be lost, there’s only something to be gained, you don’t have to pay for the device . . .
Participant 02, C01, EC
Providing free starter kits also overcame start-up cost barriers for those who had expressed previous interest in vaping:
I have wanted to do it before but thought it was going to be really costly to start up. I haven’t got a spare 30 quid to lay down, ever.
Participant 19, C04, EC
Social context
Social dynamics facilitated EC intervention engagement. Some participants described becoming strong study and vaping advocates. EC intervention buy-in, particularly from individuals with social status among peers, helped raise awareness and interest. Word-of-mouth communication quickly relayed vaping benefits to potential participants:
Everyone I see who smokes I tell them you’ve got to try it, and I really try and talk them into it. But I’m worried I’m becoming one of those [laughs] people that gives up smoking and just like is a pest. But I want to pester them because it’s – I know it’s good.
Particioant 19, C04, EC
. . . now four or five key people have done it and no one, there was no ‘oh are you vaping?’
Participant 02, C01, EC
Positive peer influence was especially prevalent at the day drop-in centre (centre 1), with high demand for the intervention and the creation of a vaping community, characterised by peer advice on equipment and technique, and social vaping norms:
I’ll go out, still socially . . . six or seven of us are vaping away . . . there’s no stigma attached to it anymore. You can just vape happily.
Participant 02, C01, EC
. . . they encourage you to stop smoking, you encourage them. So it’s a bit of like support in a way. Moral support to try and cut down.
Participant 03, C1, EC
A vaping community was not as evident in the residential centre (centre 4). Generally, in these residential units, the service users we met tended not to mix as much and reported more solitary activity, often staying in their rooms:
I don’t [notice others vaping] . . . I don’t pay any attention to them. I just come in and go out.
Participant 21, C04, EC
Participants’ experiences of the electronic cigarette intervention
Participants in the EC arm provided detailed descriptions of their initial expectations, the information and instructions they received, the EC and e-liquids, and their experiences with vaping.
Initial expectations
Most participants had not tried vaping before, reporting little knowledge of ECs. Many described their initial scepticism and low expectation that ECs would help them to reduce or stop smoking. It was common for participants to think the intervention would not be suited to them. For others, engagement in the study meant going against their negative view on vaping:
I was anti-vape.
Participant 02, C01, EC
I did not think for a minute it would fit for me, and work with me at all. I had no hope . . . hugely low expectations . . . I didn’t give myself a hope in hell.
Participant 05, C01, EC
Electronic cigarette information and instructions
Most participants reported satisfaction with the information provided. Instructions were considered thorough and participants particularly valued the practical demonstration, which included advice on device set-up, maintenance and use. Some said the practical help leaflets were useful to refer back to:
They basically showed me how to use the vape and how to change the liquid . . . how to charge it . . . change my coil . . . what to do when I need to clean the vape out. So it was just a really big help because I didn’t really understand anything about vaping and vape pens before.
Participant 03, C01, EC
Electronic cigarette device
Perceptions of the device were mixed. Some found it easy to use and liked its compact size, light weight and long-lasting battery. Although there were several reports of batteries overheating, this issue was a suspected manufacturer fault. Others reported problems with durability, reporting that the device broke easily when dropped (a common occurrence), resulting in cracks and leak of e-liquid:
I mean I’ve dropped mine several times . . . I’ve sort of repaired it . . . it’s still leaking juice.
Participant 02, C01, EC
With no money readily available to replace devices or replacement parts, some had used tape to repair their devices. One highlighted the importance of accessible and affordable replacement parts:
If you are going to use a vape on a study with vulnerable and homeless people, I would suggest you pick a vape that the parts are more accessible. Because, most of these things you have to go online to get them. And most of these people don’t have a bank account, let alone be able to go online.
Participant 01, C01, EC
E-liquid
Finding a preferred e-liquid was important for continued use and participants had differing preferences. Perceptions of the e-liquid provided were generally positive. Many interviewees said that they were satisfied with the variety of flavours and amount and nicotine content of the e-liquid. Experimentation was important for participants to find what suited them best. The flavour options were not liked by all, however, and several suggested the study should provide a greater variety. Some described mixing flavours, exchanging flavours with others and purchasing different flavours:
I think [the variety] covered all bases . . . I was telling everyone three quarters blueberry or half blueberry and half polar bear and seems to have gone down rather well.
Participant 02, C01, EC
Some also commented that the available strengths were too high, leading to initial adverse effects such as coughing and feeling sick, which could put them off continued use:
I shouldn’t have started on 18 [mg] straight away . . . I think I went full out too strong . . . I didn’t give myself a chance.
Participant 06, C01, EC
. . . the 12 [mg]s and 18 [mg]s are very high. A lot of people get head rushes and things . . . I can hit it about twice before nearly passing out. I have to mix mine down.
Participant 04, C01, EC
Vaping experience
Many interviewees noted that their vaping frequency increased over time, with the reported realisation that vaping was helping with smoking reduction and was more useful than NRT. Many were pleasantly surprised with these changes and intended to continue:
It surprised me . . . I know 65% [smoking reduction] isn’t massive but I’ve been smoking 30 years. It’s a dramatic amount in the short space of time . . .
Participant 01, C01, EC
Well at first . . . I thought maybe it’s just going to be a couple of days thing and then just put it on the side but no I use it every single day . . . it’s helped.
Participant 18, C04, EC
For some, vaping easily fitted in with existing routines and habits; it was easy to vape and more convenient than rolling a cigarette, especially when outdoors. One noted that vaping helped them to relax. Others found it more difficult to replace certain cigarettes with vaping, for example the first one in the morning or after dinner, and some described quickly choosing to smoke if their EC was unavailable or they were experiencing stress:
I probably smoke about 35% cigarettes and 65% vape . . . It changed for a little bit where I was doing about 50/50, but I was having a well stressful time . . . if I have a stressful day like I know I’m going to have today, I will have about five [cigarettes].
Participant 01, C01, EC
Participants’ usual-care experiences
There was little evidence of engagement with UC among our interviewees. Although some said that they appreciated the information provided in the help-quit leaflet, many acknowledged that they had not looked at it since the baseline appointment: ‘I’m sorry to say that I didn’t actually read through it’ (Participant 12, C02, UC).
Only three of our interviewees made contact with local cessation support. When accessing support, participants emphasised that making contact with, or contact being facilitated by, someone they trust was important. At centre 2, participants with a methadone prescription reported good relationships with the local pharmacist. Although one participant obtained a nicotine inhalator this way, another did not obtain support as he was reluctant to speak with anyone else:
Have you managed to go to the pharmacy to get some advice on reducing your smoking?
No because every time I go [pharmacist] is not there.
OK. But they must have someone else who can do it?
Aye but I get on well with [pharmacist] so I would rather talk to people that I know.
Participant 13, C02, UC
At centre 3, two of our interviewees attended the local SSS accompanied by their keyworker. Without this keyworker support, one participant noted: ‘I wouldn’t have gone on my own’ (Participant 15, C03, UC). Participants who had tried the UC approach were ambivalent about their experiences. The participant who used an inhalator complained of a sore head and nausea, had not found the nicotine delivery satisfying, and had not returned for further advice or support. At centre 3, participants received a combination of patches and lozenges; however, they were critical of the advice provided and lack of availability of appropriate products:
. . . they didn’t have the appropriate strength to my taste and they gave me a weaker one. But I’ve tried it maybe 4 or 5 days . . . I didn’t quit smoking completely, but I reduced it like notably.
Participant 15, C03, UC
One UC interviewee reported greater success by combining NRT with an EC. It was common for UC participants to be interested in ECs or to have purchased and used one during the study. Cross-contamination was a feature of the study, as one participant explained:
[Vaping] is helping me – buying my own one . . . [Researcher] told me that the other places were doing that. I thought ‘well, I’ll try my own one’.
Participant 10, C02, UC
Perceptions of study processes
Understanding of the study
Most of our interviewees reported awareness of which study arm they were allocated to prior to the baseline meeting. Some also noted a lack of detailed initial information about the study and its aims. This ties in with staff reports of how they communicated the study (see objective 4). There were two notable exceptions whereby EC arm participants likened the baseline assessment to a test, as they perceived that the offer of an EC would be ‘based on the answers’ (Participant 03, C01, EC).
Pragmatic cluster design
Participants’ accounts gave some indication of the appropriateness of the pragmatic cluster study design. In centre 1, some participants perceived resentment from those not able to be recruited because the sample target had been reached as they observed others receiving a free EC. This, combined with interviewees saying they would have felt ‘scorned’ (Participant 02, C01, EC) or ‘like I’d just wasted my time’ (Participant 21, C04, EC) if they had not been allocated an EC after completing the baseline questionnaires, suggests disharmony should both study arms have operated in one centre.
Case report form
Some of our interviewees reported issues with the length of the baseline CRF, describing how sitting through a long appointment was difficult: ‘it’s not as easy for me to just sit, I fidget a lot’ (Participant 03, C01, EC). Others observed that questions alluding to substance use and mental health appeared to be misplaced in a smoking study: ‘why do you want to know about drug history or drinking?’ (Participant 18, C04, EC). Some noted emotional difficulty in responding to more sensitive questions:
It was difficult . . . it just brings back memories of things that – I tried to commit suicide three times . . . it did stress me a bit, but [researcher] was a nice man and he got me through it and we sat and sorted it out.
Participant 16, C03, UC
Follow-up appointments
Although some interviewees reported no difficulty in attending weekly or the 4-week follow-up appointment, this was problematic for some, who attributed missed appointments to issues such as other commitments, difficulty with remembering, hospital admission and being distracted by other life events, such as those requiring police involvement. Having no credit on their mobile phone to rearrange, having their phone stolen and sleep patterns were reasons given for non-completion by our small number of interviewees who had not completed their 4-week follow-up.
Unintended consequences
Use of electronic cigarettes to vape other substances
There was minimal evidence from our interview participants that the EC provided through the study was used to consume other substances. Only one interviewee said that they had vaped cannabis e-liquid, which they had made, though they reported using this in a device previously purchased, not obtained through the study.
It was, however, common for interviewees across both arms to report anecdotes of other people, not connected to the study, vaping cannabis e-liquid [‘. . . yeah, people smoke weed in it . . .’ (Participant 01, C01, EC)], cannabidiol (CBD) oil or tetrahydrocannabinol (THC) [‘. . . of course I’ve heard about it because I’m in [that] lifestyle . . .’ (Participant 09, C02, UC)]. In addition, one participant at a UC centre, where no EC had been provided as part of the study, reported to have heard of somebody who had ‘cooked up heroin and put it in’ (Participant 11, C02, UC). In response to interviewers’ enquiries, some participants with a history of drug use speculated about the possibility of using EC to vape other substances:
[I] suppose you could put heroin in an e-cigarette and it would do something. Not so with crack or coke. Don’t think there are many drugs you can put in there. Liquid ones, yes.
Participant 05, C01, EC
There’s a definite similarity to smoking crack in its method and the sucking in . . . Yes the thought did pop into my head . . .
Participant 19, C04, EC
Love2Shop gift cards
None of our participant interviews provided evidence that the gift cards received for attending follow-up appointments had been traded for other substances or cash (although there were a small number of informal reports of this occurring from trial participants who did not take part in a qualitative interview). Rather, the qualitative data highlighted that, in most cases, participants had used their gift card to buy essentials, most commonly food: ‘I really need[ed] some food in. I had nothing. I was probably eating about twice a week at that point’ (Participant 05, C01, EC). Some described the gift card as an opportunity to save up or buy something for a family member: ‘I can get my child school shoes now’ (Participant 10, C02, UC). One interviewee said that they had purchased alcohol with the gift card.
Perceived value of the study and intervention
All participants in the EC arm placed great value on the intervention and the opportunity to try vaping. Although most had not made a complete switch from smoking to vaping, they described a strong belief in the EC as a quitting aid, and valued their increased vaping and tobacco harm reduction knowledge. Many described feeling healthier and better about themselves since starting vaping:
I look in the mirror sometimes and see that I’m progressing, I feel a bit healthier. I’m not always having a cigarette.
Participant 03, C01, EC
I feel very proud of myself for the first time in ages . . . and I’m glad that it’s had a healthy impact on my life . . .
Participant 19, C04, EC
It does give you confidence . . . it’s made me think, ‘I can do something’. Cos my confidence has been knocked a lot. It’s good.
Participant 05, C01, EC
Some believed that the EC intervention could be wide-reaching in its ability to help disadvantaged smokers, saying that it could ‘help a lot of people’ (Participant 04, C01, EC) and ‘potentially save lives’ (Participant 02, C01, EC):
You’re giving people a chance because you’re giving them the equipment so, you know, they’re halfway there and then it’s up to you . . . that’s a good thing. People, like myself, that would have never thought of buying one.
Participant 05, C01, EC
Among the UC arm, some participants said that they valued how the study made them consider their smoking and appreciated the information on where to access support: ‘. . . even just participating, just even the thought that there is help out there to stop smoking is good enough’ (Participant 08, C02, UC). Most, however, believed that the EC would have been a more useful and effective approach:
It could have been useful to have been in the half of the study that had electronic cigarettes given to them.
Participant 14, C03, UC
Overall, however, UC participants said that they were pleased to have taken part. Across both arms, participants valued how the study had enabled them to have their ‘voice heard’ (Participant 17, C03, UC) in relation to smoking. Some said that they liked the thought that the study findings may help other homeless smokers in the future:
I’ve enjoyed it. It makes me feel important to be part of something that is important.
Participant 19, C04, EC
Summary of learning points for a future trial
Participants’ anxieties presented a significant barrier to study engagement. A sensitive and flexible research approach, characterised by participant/researcher trust, can help to engage participants.
Although cannabis smoking is a barrier to smoking cessation more generally, a future trial would need to consider how best to manage and monitor cannabis use so that study objectives are not undermined.
Bringing smoking cessation aids and services to participants in their own environments was a key facilitator of engagement. Gift cards also incentivised participants to engage.
Despite low expectations, participants were willing to engage with the EC intervention. Clear, practical instructions, a durable device with easily accessible parts, and the option of a lower e-liquid nicotine strength may help facilitate use.
UC support was less attractive for participants. Previous negative experiences with NRT and anxieties about engaging with others were barriers to engagement.
Participants’ accounts suggest that a cluster design is appropriate in homeless settings. Participants may have benefited from clearer information on the study at the recruitment stage and a shorter CRF. A future study should carefully consider the questions included in the CRF to minimise the burden on participants and reduce potential areas of sensitivity.
There was minimal evidence of unintended consequences, namely use of the EC provided to vape other substances and trading of gift cards; however, a future study should continue to monitor this closely. Nevertheless, device breakages were reported (see Harms).
Perceived value of the study and intervention was high among all participants. Participants’ desire to change their smoking behaviour and willingness to engage in the study presents a significant opportunity to engage homeless smokers in smoking discussions and treatment programmes.
Local context had implications for the study on two issues. First, social dynamics at the busy drop-in centre facilitated intervention engagement and vaping social norms. Future EC interventions might therefore benefit from capitalising on peer influence to create a supportive vaping community. Second, centre links and relationships, that is with keyworkers and the local pharmacy, were a key feature of whether or not participants in the UC arm engaged with support. Studies should consider the impact of these relationships on UC uptake.
Objective 4: assess service providers’ capacity to support the study and the type of information and training required
Outcome measure: qualitative interviews with keyworkers and front-line staff (n = 12, approximately three per site) across both arms
This section presents the findings of 12 in-depth qualitative interviews with keyworker and support staff involved in facilitating and supporting the study. This included assisting with recruitment and appointments, setting EC arm participants up with the device, for example showing them how to use the device and helping them choose an e-liquid, providing EC arm participants with weekly EC support and further e-liquid, and providing UC arm participants with brief advice on quitting and information about and signposting to the local SSS. The sample is spread across the four centres (see Appendix 3). We explored their experiences of the study in line with research objective 4. The findings present five key issues: staff assumptions; staff training; communicating the study; staff capacity to support the study; and perceived value of the study. The section ends with a summary of key learning points for a future trial.
Staff assumptions about smokers experiencing homelessness
Most staff, across centres and study arms, perceived that stopping smoking was not a concern or priority for clients given other issues, including mental health, substance use and chaotic lifestyles: ‘[smoking is] the less of all the evils’ (Staff 01, C01, EC). Other support needs were prioritised, as staff believed that smoking provided clients with comfort and enjoyment. These assumptions underpinned the lack of discussion about smoking between staff and clients: ‘it’s not something I would really discuss with them’ (Staff 07, C02, UC). Staff had few links to the local SSSs, little knowledge of smoking cessation and few established processes to support clients:
They have bigger things on their plates to deal with. I’m not going to try take away the one thing that they might enjoy. I’m already working with bigger challenges than that.
Staff 12, C04, EC
Prior assumptions meant that some staff made judgements about which clients, if any, would engage in the study: ‘I thought no one would be interested’ (Staff 09, C03, UC). Other staff expected EC arm participants to sell their devices. These assumptions, however, were not borne out by their study experiences:
I’m amazed that [devices] have not been sold as far as I know . . . It was not at all how I expected it to go. It was nice as well because it taught me something – so you don’t know everything about these guys. There are still things you can learn.
Staff 12, C04, EC
Staff training
Prior to study commencement, the research team delivered staff training on smoking prevalence and harm, ECs, local SSSs and supporting the study. The training was well received by those who participated in the session and was described as a key facilitator of their engagement with, and belief in, the study; staff felt ‘better equipped’ (Staff 10, C03, EC) to have more confident discussions with clients on smoking, local SSSs and vaping. For many, the training facilitated a change in attitude regarding the importance of stopping smoking for their clients, as well as greater motivation to discuss smoking. Some also noted a new understanding of tobacco harm reduction, making a comparison with drug harm reduction:
Doing that training . . . it made sense because we work with a lot of people with COPD [chronic obstructive pulmonary disease] and actually smoking wasn’t a priority at all. So the whole study actually has made me rethink . . . it’s the same discussion, part of harm reduction as we have about safer injecting techniques.
Staff 06, C02, UC
Our staff sample described having limited prior EC experience and initial ambivalence towards ECs. Post training, all reported increased knowledge of and interest in ECs as a harm reduction and smoking cessation aid. Staff in the EC arms appreciated the practical, ‘hands-on’ EC training, researcher support, and clear, simple handouts. Some said that this training assisted them in intervention delivery and also helped alleviate initial nervousness at providing the starter kit and instructions:
The handout sheets, I think those were the best things. It actually showed you – if you forget, this is what [to do].
Staff 02, C01, EC
The timing of the training was important. Some staff expressed concerns about remembering information if there was a gap between training delivery and study commencement. Some suggested that additional advice on local vape shops and vaping policies would be useful. Aware of some participants’ anxiety around providing data, some suggested that a better overview of the CRF be given, to give staff greater understanding of the types of questions and measures used in the study. Some staff noted that more training around facilitating recruitment, approaching participants and what information should be given to potential participants would be useful in communicating the study (see the following section):
Going back to the information stage, the recruitment stage. Just having a bit more information available for the staff to be able to use as a bit of a prompt. Or as a consistent communication style for all of them. I think that would be useful.
Staff 04, C01, UC
Communicating the study
How staff communicated the study to participants was one of two deviations from the feasibility study protocol. As per the protocol, all participants were to receive the same study information at recruitment and complete baseline assessments before being told about their allocation to the EC arm or UC. For practical reasons, staff knew whether their centre was allocated to the EC arm or the UC arm. When facilitating recruitment, our sample of staff in the EC arm reported routinely introducing the study as an EC or ‘vape study’, in which participants would receive a free EC if they signed up:
I just basically told them, ‘hey listen, I know you are smoking, are you interested in vaping, they are doing a smoking study, they are probably giving you free vapes if you are wanting to do that’.
Staff 12, C04, 12
I did hear some conversations where it was really quite low level, where it was a vape [study] and you are going to get the vape.
Staff 04, C01, EC
Conversely, our sample of staff in the UC arm said that they focused their description of the study on smoking, quitting and local support, and did not suggest that participants would receive an EC:
I’m not sure actually I introduced it really well . . . Just first asking them if they were a smoker . . . if they ever think of stopping and if so, that they could meet with [researcher] . . . you could help them and give them advice on how to stop . . . I don’t think I even mentioned the e-cigarette. I completely forgot about the e-cigarette, because we don’t get it.
Staff 07, C02, UC
Staff capacity to support the study
Electronic cigarette condition
Few staff capacity issues to support the intervention were described by EC arm staff. There was some initial trial and error with setting up efficient processes, but once resolved facilitating the intervention was described as straightforward. High demand for the intervention at centre 1 led the manager to take control of managing referrals and baseline appointments, by organising an appointment diary consisting of a main and ‘backup’ list: ‘[Manager] was able to manage it really well from there . . . just one central point’ (Staff 03, C01, EC). This same model was less successful at the smaller, residential units in centre 4, where there were fewer alternative candidates and less motivation to be disrupted from their ordinary activity.
Staff across centres highlighted that weekly follow-ups, during which staff provided participants with e-liquid and vaping support, could be challenging as some participants lost their appointment cards, did not show up at agreed times or could not be contacted: ‘it did happen quite a bit – people missing appointments, turning up late, turning up early’ (Staff 03, C01, EC). In centre 1, implementing a daily vaping ‘surgery’ overcame some of these difficulties; however, staff said that it could still be challenging if several participants came at once or did not attend on their set day. Some noted the importance of flexibility if participants approached keyworkers at different times: ‘if someone came in the afternoon and I’m free I would issue them the liquids then’ (Staff 01, C01, EC). One staff member also noted the importance of maintaining consistency for the follow-up sessions:
So what we did was set up a smoking surgery between 10 and 11 every day. So people could come along, talk to other people that were vaping, and also get help if they needed it . . . also get their liquids and coils if it was their day to get them.
Staff 03, C01, EC
Mainly, staff reported responding to participant queries relating to coils: ‘it was just about changing the coil . . . that was the main thing’ (Staff 11, C04, EC). Some noted requests to help with broken devices and suggested that staff having access to spare parts would be useful. Some also noted that they had been asked to open e-liquid bottles because some participants had poor dexterity. Most staff reported receiving few problems with batteries or charging devices. For managing participants’ e-liquid supply, some noted that the variety on offer through the study was a good amount, any more may have overwhelmed participants and staff:
If you give people too much choice, it just becomes a nightmare. So having that restricted number I think was absolutely fine.
Staff 02, C01, EC
Usual care condition
There were some challenges for staff supporting the UC arm around recruitment and weekly follow-ups. Although some described facilitating recruitment as straightforward, others found this challenging. At centre 2, the day drop-in centre, staff reported that, once the small number of regular clients had agreed to take part, they had difficulty engaging those who were more transient. Although the Love2Shop follow-up gift cards had been especially important for facilitating UC recruitment, some expressed discomfort in their reliance on the gift cards as an incentive:
It was almost like we were encouraging people to do it because they would get a voucher out of it. But it just felt a bit uncomfortable if I’m honest . . .
Staff 06, C02, UC
In addition, some reported negative feedback from participants about the length of the baseline CRF and the types of questions, and expressed concern about recruiting some clients to the study: ‘knowing that actually . . . it was going to be a challenge for them to answer all those questions’ (Staff 06, C02, UC).
Staff signposting UC services and maintaining weekly follow-up contact was the second main deviation from the study protocol. At centre 3, keyworker staff reported that this process worked well. Two staff members had escorted their participating clients to local SSSs and had attempted to quit alongside their clients:
I escort clients to the stop smoking van, where they can get nicotine patches, all sorts of paraphernalia to help them stop smoking . . . [I’m] still going with them to the van. Every Tuesday . . . we all go for a coffee afterwards as well. So we’ve turned it into a real social event actually.
Staff 08, C03, UC
In contrast, at centre 2 our interviewees reported some capacity issues to complete these tasks because of lack of staff, busy workloads and client demands. Some described dealing with challenges requiring immediate attention, rather than resources to focus on stronger client relationships as a factor. Finding private space for researchers to conduct baseline or follow-up appointments could also be a challenge, with rooms often purposed for other support services:
I have found it, personally, really difficult to do the follow-up . . . You are always on the go and basically I forget . . . It seems feasible . . . and then the reality is it hasn’t been . . . maybe because here we don’t keywork as such.
Staff 07, C01, UC
Staff’s perceived value of the study
Similar to our participants, staff also placed high value on the study. Across arms, staff appreciated the opportunity to become involved in supporting clients’ quit attempts: ‘it’s really important that we are involved in stuff like this’ (Staff 06, C02, UC). Many highlighted that the study had resulted in positive shifts in practice, increasing smoking-related discussions:
I can’t think of any other time we had a conversation about smoking with any other client.
Staff 12, C04, EC
It’s an excellent thing, just being part of this study that is potentially going to inform practice and policies and how we deal with smoking amongst the homeless, it’s just immense. The study is going to change the way we do things.
Staff 02, C01, EC
Although staff at the UC centres were positive about the study and pleased to have taken part [‘I feel privileged that we were included in this’ (Staff 03, C03, UC)], some expressed less enthusiasm for UC cessation support and disappointment that they had been unable to provide clients with ECs: ‘I think getting the e-cigs . . . I think that would be very helpful for people’ (Staff 05, C02, UC).
Staff in the EC arm were particularly enthusiastic about the intervention. Many noted positive impacts on their clients’ well-being. They valued being able to offer clients a tangible, practical tool, rather than just offering them stop smoking information. Many reported that the intervention had facilitated client trust and interactions and boosted staff morale:
It has brought them to the centre every day, which is good. Building a bit of trust, which is always a winner.
Staff 03, C01 EC
I think this is a lot more immediate [than other cessation support]. With the attention deficit some of our clients have got, to be given something tangible – to be given something, not just information, something practical they can use.
Staff 01, C01, EC
Summary of learning points for a future trial
Staff training was key to changing staff misperceptions about smokers experiencing homelessness and engaging staff in the study. Recommendations to further improve staff training include consideration of the timing of training in relation to study commencement; advice on local vape shops and policies; a more comprehensive overview of the CRF measures and questions; and greater training on facilitating recruitment.
For a cluster study design, consideration should be given to how best to communicate the study to participants, and whether or not it is practically feasible for participants across arms to be provided with the same information at recruitment.
Staff capacity to support the intervention was good at the EC centres and in one UC centre, suggesting that service providers are well placed to offer stop smoking interventions.
Local differences made some study processes more challenging. In one UC centre, lack of adequate staffing numbers, a busy environment, and staff having to support people with acute challenges requiring immediate attention, outside their allocated one-to-one keyworker hours, highlighted capacity issues in signposting to UC and following up participants. Service providers could be further supported by suggesting systems for managing referrals, appointments, signposting and follow-ups, taking into account differences at each site.
Objective 5: assess the potential efficacy of supplying free electronic cigarette starter kits
Outcome measure: measure breath carbon monoxide levels, self-reported quit rates/cigarette consumption at each follow-up time point
Table 5 presents the cessation and smoking reduction outcomes. The CO-validated sustained abstinence rate at 24 weeks was 3 out of 35 (8.57%) for the EC arm and 0 out of 12 (0%) for the UC arm. Assuming that all those with missing follow-up data were smoking, the 24-week sustained abstinence rate was 6.25% (3/48) in the EC arm and 0% (0/32) in the UC arm.
Seven-day point prevalence rates at 24 weeks were the same as sustained abstinence rates.
Of those who returned for 24-week follow-up (not ITT), the percentage of participants who reported > 50% reduction in CPD from baseline was 43% in the EC arm and 25% in the UC arm. The percentage of those participants with > 50% reduction in expired CO was a little lower and similar between arms (EC = 20%; UC = 25%).
| Outcome and time point | Trial arm, n/N (%) | |
|---|---|---|
| EC | UC | |
| Sustained abstinence | ||
| 4 weeks | 8/39 (21) | 0/21 (0) |
| 12 weeks | 2/34 (6) | 0/18 (0) |
| 24 weeks | 3/35 (9) | 0/12 (0) |
| 7-day point prevalence | ||
| 4 weeks | 7/39 (18) | 0/21 (0) |
| 12 weeks | 5/34 (15) | 0/18 (0) |
| 24 weeks | 3/35 (9) | 0/12 (0) |
| 50% reduction in CPD | ||
| 4 weeks | 21/39 (54) | 4/21 (19) |
| 12 weeks | 20/34 (59) | 4/18 (22) |
| 24 weeks | 15/35 (43) | 3/12 (25) |
| 50% reduction in expired CO | ||
| 4 weeks | 10/39 (26) | 2/21 (10) |
| 12 weeks | 7/34 (21) | 1/18 (6) |
| 24 weeks | 7/35 (20) | 3/12 (25) |
Intracluster correlation coefficient
The ICC was calculated by the Fleiss–Cuzick method31 and was estimated to be 0.0157. The ICC is the ‘proportion of the total variance in the outcome attributable to variance between clusters’. 31 Although the estimated ICC is relatively small, neglecting to factor this into the sample size calculation for a full cRCT would result in reduced statistical power.
Summary of learning points for a future trial
Based on the feasibility average recruitment of 16 participants per month, it would take 24 months to recruit 384 participants. A main trial would therefore need more (at least double the number of) researchers recruiting and collecting data simultaneously.
The estimation of the ICC used the Fleiss–Cuzick method and was not adjusted for individual-level baseline measures. In the full trial, the analysis is likely to be carried out by mixed-effects models, in which adjustment for prognostic covariates (e.g. baseline nicotine dependence, number of years smoking) is possible. This adjustment for covariates is likely to reduce cluster-level correlation in outcomes; therefore, an estimated ICC of 0.01 is used for the sample size calculation for the full trial.
Objective 6: explore the feasibility of collecting data on contacts with health-care services among this population as an input to an economic evaluation in a full cluster randomised controlled trial
Outcome measure: record participant scoring on EQ-5D-3L and utilisation of primary and secondary health-care services using a self-report service-use questionnaire at each time point
The missing information on EQ-5D-3L was mostly due to absence at follow-up visits. Most of those who attended completed the measure. At baseline, 46 out of 48 participants in the EC arm and 31 out of 32 participants in the UC arm completed EQ-5D-3L. At 4 weeks, all participants in both arms who were followed up completed it. At 12 weeks, 33 out of 34 attending participants in the EC arm and all 18 attending participants in the UC arm completed it. At 24 weeks, 34 out of 35 attending participants in the EC arm and all 12 in the UC arm completed EQ-5D-3L.
Among the observed cases, no one in either arm reported severe problems with mobility at any time point. The domain with the highest percentage of severe problems was anxiety/depression at baseline, 4 weeks and 12 weeks in both arms, followed by pain/discomfort. At 24 weeks, the percentage was similar in the two domains in each arm. The proportion of participants who reported no problem was consistently higher in the EC arm than in the UC arm across all domains and all time points. This led to a consistently higher mean utility score in the EC arm among those who completed the measure (Table 6). Among those participants who completed EQ-5D-3L at all time points, the mean QALY gain was 0.195 (SD 0.097) in the UC arm (n = 11) and 0.315 (SD 0.120) in the EC arm (n = 26), over 24 weeks.
| Time point | Trial arm | |||||
|---|---|---|---|---|---|---|
| UC (N = 32) | EC (N = 48) | |||||
| n | Mean (SD) | n | Mean (SD) | |||
| Utility | VASa | Utility | VASa | |||
| Baseline | 31 | 0.394 (0.362) | 57.0 (21.7) | 46 | 0.548 (0.341) | 52.7 (20.7) |
| 4 weeks | 21 | 0.330 (0.308) | 48.6 (24.7) | 39 | 0.602 (0.346) | 61.4 (21.5) |
| 12 weeks | 18 | 0.350 (0.351) | 59.3 (22.7) | 33 | 0.683 (0.309) | 65.6 (21.3) |
| 24 weeks | 12 | 0.619 (0.238) | 61.0 (22.5) | 34 | 0.653 (0.363) | 61.8 (21.6) |
There were three sections concerning services use: SSS use at follow-ups, smoking cessation help from primary/community health-care professionals, and general health-care services. Overall, most of those participants who attended the follow-up visits completed these sections, with only individual participants having an item missing in a few questions.
Attendance at SSS sessions was very low in the UC arm. At 4 weeks, four participants out of 21 contacted a SSS. One attended two sessions, three attended one and one did not answer. At 12 weeks, two participants out of 18 contacted a SSS; one attended one session and the other attended two. At 24 weeks, 2 out of 12 participants contacted a SSS; one attended one session and the other attended two. Using the resource impact template for smoking cessation service,34 the unit cost per session was estimated at £12.82. In the UC arm, the mean cost of SSS sessions was £3.21 (SD £9.18) at 4 weeks (n = 20), £2.14 (SD £6.60) at 12 weeks (n = 18) and £3.21 (SD £7.97) at 24 weeks (n = 12). In the EC arm, there was no SSS session cost incurred as none of the participants reported attending any session.
At 4 weeks, 3 out of 21 participants in the UC arm used other medications supplied by a SSS, including inhaler, patches and lozenges, with a mean cost of £5.68 (SD £14.30). At 12 weeks, 2 out of 18 used patches and lozenges in the UC arm, with a mean cost of £5.43 (SD £16.01). At 24 weeks, 1 out of 12 in the UC arm used gums and patches, with a mean cost of £3.38 (SD £11.71). None of the attending participants in the EC arm reported using cessation aids supplied by a SSS. The majority of them reported using their EC device only. Among those in the EC arm who claimed that they were not using any aids supplied by a SSS or the research team, two reported using another EC device.
No one reported using varenicline or bupropion. No one purchased any NRT product. The purchase of an EC device or e-liquid was reported by a small group of participants in both arms (Table 7). Although the number of participants who reported purchasing an EC device or e-liquid remained low in the UC arm at all times, spending was higher than that in the EC arm. In the EC arm, an increasing number of participants reported purchasing an EC device/e-liquid, after the initial 4 weeks of the study.
| Time point and type of e-cigarette-related purchase | Trial arm | |||||
|---|---|---|---|---|---|---|
| UC (N = 32) | EC (N = 48) | |||||
| n of null use | n (range) (£) when use > 0 | Missing (n) | n of null use | n (range) (£) when use > 0 | Missing (n) | |
| 4 weeks | n = 21 | n = 39 | ||||
| EC device | 17 | 3 (10–75) | 1 | 36 | 3 (1–40) | 0 |
| EC e-liquid | 15 | 5 (5–168) | 1 | 32 | 6 (1–12) | 1 |
| 12 weeks | n = 18 | n = 34 | ||||
| EC device | 17 | 1 (10) | 0 | 30 | 4 (5–19) | 0 |
| EC e-liquid | 15 | 3 (39–448) | 0 | 17 | 17 (1–50) | 0 |
| 24 weeks | n = 12 | n = 35 | ||||
| EC device | 10 | 2 (40–100) | 0 | 24 | 11 (3–52) | 0 |
| EC e-liquid | 10 | 1 (288) | 2 | 17 | 18 (3–240) | 0 |
There were very few participants receiving smoking cessation help from primary/community care professionals (GP, practice nurse, pharmacist, NHS helpline), and those who did did not access them frequently. Owing to the rare and low frequency of use, the costs of smoking cessation help from primary health-care professionals were low and, in some cases, null. Especially for the UC arm, from 12 weeks onwards, no one reported any use. The mean costs in the UC arm were £1.45 (SD £6.75) among 31 participants at baseline, and £5.81 (SD £11.83) among 21 participants at 4 weeks. In the EC arm, the mean costs were £3.66 (SD £14.41) among 47 participants at baseline, null cost among 39 participants at 4 weeks, £1.56 (SD £9.09) among 34 participants at 12 weeks, and £2.11 (SD £12.51) among 35 participants at 24 weeks. Overall, the majority of the costs were contributed to by GP advice on smoking cessation.
Very few participants reported getting NRT products, mostly on prescription or from a SSS. The participants who had got NRT products all came from the UC arm, with only one exception: two participants in the EC arm at 24 weeks also received NRT. In the UC arm, only one or two participants at each follow-up point reported getting NRT on prescription or from a SSS. At 12 weeks, one of those reported four packs of patches and four packs of lozenges in total, but five packs of each were on prescription or from a SSS, causing a discrepancy in quantity. The only participant who received NRT that was not on prescription or from a SSS was in the EC arm at 24 weeks. Overall, the costs of NRT on prescription or from a SSS were £1.72 (SD £9.59) at baseline (n = 31), £4.13 (SD £18.73) at 4 weeks (n = 21), £16.30 (SD £51.81) at 12 weeks (n = 18) and £11.46 (SD £39.69) at 24 weeks, in the UC arm. In the EC arm, no costs of NRT on prescription or from a SSS were incurred until 24 weeks (n = 35), when it was £0.89 (SD £5.26).
Among the general health-care and social services asked, some services were used by none or close to none. Among all participants who answered in this section, no one received any visit from a GP at any point in the study. In the UC arm, only one participant received one visit from a practice nurse. In the EC arm, at both 4 weeks and 12 weeks, one participant received one visit from a practice nurse, whereas at 24 weeks one participant received two. These were probably due to the homeless situation of the participants. No participant accessed a maternity service during the study period. Sex health clinic was not visited at all at baseline (i.e. the 4 weeks prior to the baseline appointment) or at 12 weeks. At 4 weeks, one participant in the UC arm reported having visited a sex health clinic twice, whereas two participants in the EC arm had done so, one once and one four times. At 24 weeks, one participant in each arm reported having visited a sex health clinic once. Except for one participant in the EC arm at 12 weeks and one in the UC arm at 24 weeks, no participants had visited an early intervention team. Both participants visited the team only once. No participant in the UC arm stayed in a detox or rehab unit. One participant in the EC arm reported both at baseline and at 4 weeks having stayed in a detox or rehab unit, and another participant reported having done so twice at the 12-week follow-up.
There was a low but constant use of emergency and hospital services in both arms. Although the majority of the responding participants did not report any use, a small group of participants visited accident and emergency (A&E) frequently or had hospital admissions (see Appendix 6). In the UC arm, 4–7 participants reported having visited A&E at different time points. The number of visits per participant ranged from one to nine. In the EC arm, 5–7 participants reported having visited A&E at different time points. The number of visits per participant ranged from one to six. Owing to the design of the questions, we were unable to tell the number of visits that led to admission. However, in the UC arm, at least five participants at baseline, two at 4 weeks, one at 12 weeks and one at 24 weeks were admitted following the A&E visit. In the EC arm, at least two participants at baseline, three at 4 weeks and one at 12 weeks were admitted following the A&E visit. The highest number of hospital outpatient appointments reported at baseline, for over the 4 weeks before baseline, was 10 in the EC arm. The longest hospital stay was 14 days, reported in the UC arm at baseline and 4 weeks, and in the EC arm at 24 weeks.
Most of the participants in both arms received prescriptions. Other more frequently used services included GP, practice nurse and adult mental health team. Overall, 10 participants in the UC arm and 14 in the EC arm accessed a drug and alcohol service at baseline. This number dropped to almost none afterwards in the UC arm, whereas it remained more or less stable in the EC arm. Similarly, a housing team was visited by nine participants in the UC arm and 12 in the EC arm at baseline. The number of participants in the UC arm who used this service then dropped to one at 4, 12 and 24 weeks, whereas in the EC arm service use ranged from 7 to 10 participants at different time points (see Appendix 7).
Owing to the ambiguous phrasing of the question regarding detox/rehab unit, the meaning of ‘visit’ was unclear, namely whether or not it indicates a period of stay. Consequently, two possible unit costs to quantify the number of use were identified: by day or by week. We could not estimate the unit cost of a simple visit to the facility. Despite this, the overall mean costs of the health-care service did not differ much because the use of a detox/rehab unit was very rare. We therefore reported the higher one of the two (by week) to present a conservative number.
The mean costs among observed cases were consistently higher in the UC arm than in the EC arm (Table 8). The large difference between arms at baseline and 4 weeks was mostly due to the much longer hospital stay in the UC arm. At 12 weeks, although the mean cost of hospital stay was still higher in the UC arm, the mean cost of drug/alcohol service and early intervention team in the EC arm offset part of the difference. At 24 weeks, the mean cost of hospital stay and drug/alcohol service in the EC arm was much higher, whereas the mean cost of A&E, early intervention team and adult mental health team in the UC arm was much higher. However, this comparison has to be taken with caution, as around 30–60% of the participants in the UC arm were lost to follow-up during the study.
| Time point | Trial arm | |||
|---|---|---|---|---|
| UC (£) (N = 32) | EC (£) (N = 48) | |||
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 31 | 1480 (3188) | 47 | 518 (754) |
| 4 weeks | 21 | 1559 (4489) | 39 | 539 (987) |
| 12 weeks | 18 | 957 (1849) | 34 | 682 (885) |
| 24 weeks | 12 | 1207 (1494) | 35 | 1172 (1952) |
Recommendation for future revision of the questionnaire
The structure and wording of the health-utilisation questionnaire would need to be considered carefully if a full trial were to go ahead. Some of the questions about health-care utilisation were confusing for participants, repetitive or not applicable to everyone in the sample. Others (such as A&E admissions) were useful and endorsed by all participants, suggesting that a more granular follow-up question was needed.
Objective 7: estimate the cost of providing the intervention and usual care
Outcome measure: record all resources used in the delivery including staff costs, electronic cigarettes and other costs incurred. Staff will complete a pro forma to record contact time, non-contact time and other resources used in delivery
The training for the centre staff to deliver standard support in the UC arm and EC guidance in the EC arm was provided by the research team. For the convenience of costing, we divided the training into three components: core component, auxiliary component and extra component.
The core component of the training was the group training programme, which was delivered by the centre: two for the UC arm and two for the EC arm. For the UC arm, it was a 1.15-hour programme delivered by four trainers to one centre (seven staff) and three to the other (five staff). The help-to-quit leaflet used was printed in-house at a cost of £0.20 per leaflet. For the EC arm, the training was slightly longer, taking 3 hours (including individual coaching). Each member of staff who attended the training was provided with an EC device instruction pamphlet and an EC helpful tips pamphlet, which were both printed in-house at a cost of £0.20 per pamphlet. The training was similarly delivered by four trainers to one centre (12 staff) and three to the other (eight staff). The demonstration models of the EC were shown to the staff at the ratio of one unit per two trainees during the training, and six bottles of e-liquid (three flavours with two strengths each) were also shown. The EC starter kit was costed at £20 per kit and the e-liquid was £3 per bottle. One of the research team members who delivered the training was grade 9, three were grade 7 and three were grade 6. Their hourly costs, including superannuation and national insurance, were calculated based on the financial records of the project. The staff who received the training held various roles, resulting in varied pay grades. We used the costs information collected from centre 1 as an estimate for all those involved. The time cost of staff was £13.38 per hour, including superannuation and national insurance. The cost of staff time in delivering the EC training was £1040.93 in total and the cost in delivering the UC training was £246.65 in total. Overall, 20 staff attended EC training and 12 attended UC training. Their staff time costs were therefore £802.80 in the EC arm and £184.64 in the UC arm. The demonstration EC kit and e-liquid were reused for each training. The maximum number of staff for one training was 12. Therefore, the number of demonstration models was estimated to be six. Combining this with six bottles of e-liquid, the total costs of the EC and e-liquid were £138.00. The two pamphlets were printed for all 20 staff attending the EC training, costing £8.00 in total. The pamphlets for the UC training were printed for 12 staff, costing £2.40 in total. The costs of core component of the training were £433.70 in the UC arm and £1989.73 in the EC arm.
The auxiliary component of the training included travel, accommodation and meals for those delivering and receiving the training. These costs would vary depending on the arrangement of the training programme. In this study, we included the costs of these items if they were claimed in expenses. For travelling, only train journeys were included. Travelling within a city was not taken into account. For the train journeys, the journey duration was estimated using the National Rail website. 35 It was then multiplied by the hourly costs of the personnel who took that journey. Centres 3 and 4 were located in the same city as most of the research team and, therefore, they did not require train travel; as a result, the travelling expense and time were not costed. The return train journey to centre 1 cost £29.30 in terms of ticket and 2 hours in terms of time. To centre 2, the return journey cost £118 (one-way £59) in terms of ticket and 9 hours in terms of time (4.5 hours one-way). Three team members took a return journey to centre 1, costing £205.83 in terms of travelling time and £87.90 in terms of train tickets. Two team members went to centre 2 and stayed in a hotel. Owing to personal arrangements, only one return ticket to centre 2 was claimed and the other was a one-way ticket. This led to £425.97 in terms of travelling time and £177.00 in terms of train tickets. Their stay cost £500 for accommodation and £40 for meals. The costs of the auxiliary component of the training were £293.73 in the EC arm and £1142.97 in the UC arm.
The extra component of the training was ECs given to staff who were smokers so that they themselves could become familiar with the device. This was not applicable to all staff trained; only four EC devices were given to the staff in one centre and two to the staff in the other centre during EC training. In total, six EC devices cost £120.
In total, the cost of the training for the UC arm was £1576.66 and the cost of the training for the EC arm was £2403.46. Allocating the costs evenly to participants in each arm, they amounted to £49.27 per participant in the UC arm and £50.07 per participant in the EC arm (Table 9).
| Costs | Trial arm | |
|---|---|---|
| UC (£) (n = 32) | EC (£) (n = 48) | |
| Core component: delivery of training programme | 433.70 | 1989.73 |
| Auxiliary component: travelling, accommodation, meals in relation to training programme | 1142.97 | 293.73 |
| Extra component: EC devices given to staff who smoke | – | 120.00 |
| Total costs of training | 1576.66 | 2403.46 |
| Mean costs of training per participant | 49.27 | 50.07 |
The delivery of intervention in both arms was recorded in the keyworkers’ form at baseline (visit 0), 1 week post baseline (visit 1), 2 weeks post baseline (visit 2) and 3 weeks post baseline (visit 3). Contact time was costed by multiplying the staff hourly cost by the duration of the contact. The printing cost of the help-to-quit pamphlets for the UC arm and the EC device instruction pamphlets and the EC helpful tips pamphlets for the EC arm was recorded by the research team at £0.20 per pamphlet.
Owing to staff capacity, the data on delivery sessions were not collected in the UC arm. We therefore did not know the attendance of weekly sessions (visit 0–3) and if the pamphlet was given to the participants.
For the EC arm, one participant did not attend any session and did not receive the EC starter kit or e-liquid. The remaining 47 participants attended visit 0 and received an EC starter kit and five bottles of e-liquid. Excluding one participant with a missing response, 46 participants also received the EC ‘tips and tricks’ help sheet. The mean duration of session 0 (baseline) with homeless centre staff/keyworkers was 25 minutes (SD 16 minutes, range 7–80 minutes). Overall, 30 participants attended visit 1, of whom 29 received five bottles of e-liquid and one received two bottles. Except for a missing answer for one participant, the mean session duration of visit 1 was 8 minutes (SD 4 minutes, range 1–20 minutes). Among the 22 participants who attended visit 2, 20 received five bottles of e-liquid, one received four and one received 10. Except for a missing answer for one participant, the mean session duration of visit 2 was 6 minutes (SD 3 minutes, range 1–15 minutes). The number of participants who attended visit 3 was also 22, all of whom received five bottles of e-liquid. Duration was not recorded for two participants. Among the remaining 20 participants, the mean session duration was 5 minutes (SD 2 minutes, range 2–10 minutes).
The mean cost of the EC starter kit and e-liquid was £57.46 (SD £19.91) among the 48 participants in the EC arm. The mean cost of the pamphlet was £0.39 (SD £0.06) among 47 participants in the arm. The mean cost of the sessions was £7.51 (SD £4.60) among 43 participants. The cost of intervention delivery was therefore estimated for 43 participants whose data were complete in this part; the cost was £64.35 (SD £22.89) per participant. In total, the mean cost of the EC intervention, including training and delivery, was £114.42 (SD £22.89) among 43 participants in the EC arm (Table 10).
| Costs | Trial arm | |||
|---|---|---|---|---|
| UC (N = 32) | EC (N = 48) | |||
| n | Mean (SD) | n | Mean (SD) | |
| Training | 32 | £49.27 (–) | 48 | £50.07 (–) |
| EC starter kit and e-liquid | 32 | – | 48 | £57.46 (£19.91) |
| Pamphlet | 32 | Data not available | 47 | £0.39 (£0.06) |
| Keyworker session | 32 | 43 | £7.51 (£4.60) | |
| Total | 32 | Data not available | 43 | £114.42 (£22.89) |
Summary of learning points for a future trial
Although it was feasible to collect information relating to the costs of delivery in the EC arm, collecting data from staff about contact time was not feasible in the UC arm. If staff are unable to complete this information each time they engage with a research participant, approaching them at a quieter time (e.g. at the end of the follow-up data collection period at each centre) may improve compliance.
Chapter 5 Outcomes and estimations
In respect of estimations for a future trial, based on the findings presented here, namely the proportions with sustained CO-validated abstinence in each arm (6.25% in the intervention, 0% in UC) and assuming 0.05 alpha, 90% power and an ICC of 0.01, a future cRCT would require 12 participants per cluster (the feasibility average) and 16 sites per arm, totalling 192 participants per arm and 384 participants across both conditions. This sample size estimate assumes equal cluster sizes. These estimates are not adjusted for attrition, as it is anticipated that the primary analysis will be by ITT and participants lost to follow-up will be assumed to have relapsed entailing no loss of power.
Chapter 6 Ancillary analyses
Substance use and mental illness scores were collected at each follow-up point. The mean (SD) scores for the mental health and substance use measures for those participants who were retained in the study through to the 24-week follow-up are presented in Table 11. GAD-7 anxiety and PHQ-9 depression scores significantly declined steadily from baseline to the 24-week follow-up, although no causal association can be assumed. A similar decline in alcohol use as measured by the AUDIT scores was also evident; however, substance use as measured by the SDS remained stable.
| Outcome measure | Trial arm | Total | p-value | |
|---|---|---|---|---|
| EC | UC | |||
| GAD-7 | ||||
| Participants, n | 27 | 10 | 37 | Main effect time = 0.02; main effect group < 0.01 |
| Time point, mean (SD) | ||||
| Baseline | 8.48 (6.81) | 14.40 (5.36) | 10.08 (6.91) | |
| 4 weeks | 7.15 (6.38) | 14.40 (5.02) | 9.11 (6.81) | |
| 12 weeks | 6.44 (6.54) | 13.20 (6.49) | 8.27 (7.12) | |
| 24 weeks | 5.63 (6.34) | 12.70 (4.42) | 7.54 (6.64) | |
| PHQ-9 | ||||
| Participants, n | 25 | 11 | 36 | Main effect time = 0.02 |
| Time point, mean (SD) | ||||
| Baseline | 10.76 (8.34) | 13.27 (8.17) | 11.53 (8.26) | |
| 4 weeks | 9.08 (7.76) | 13.82 (6.46) | 10.53 (7.62) | |
| 12 weeks | 8.36 (7.53) | 13.45 (8.37) | 9.92 (8.03) | |
| 24 weeks | 7.12 (7.22) | 10.82 (7.23) | 8.25 (7.38) | |
| AUDIT | ||||
| Participants, n | 24 | 11 | 35 | Main effect time = 0.03 |
| Time point, mean (SD) | ||||
| Baseline | 11.83 (12.15) | 7.91 (8.08) | 10.60 (11.07) | |
| 4 weeks | 9.08 (9.76) | 5.18 (8.48) | 7.86 (9.34) | |
| 12 weeks | 10.29 (10.37) | 4.82 (7.15) | 8.57 (9.72) | |
| 24 weeks | 8.92 (8.83) | 6.00 (7.64) | 8.00 (8.47) | |
| SDS | ||||
| Participants, n | 27 | 10 | 37 | No statistically significant effects |
| Time point, mean (SD) | ||||
| Baseline | 3.15 (4.33) | 5.50 (6.52) | 3.81 (5.05) | |
| 4 weeks | 2.81 (4.51) | 4.20 (4.49) | 3.19 (4.48) | |
| 12 weeks | 3.35 (4.05) | 4.90 (4.41) | 3.78 (4.15) | |
| 24 weeks | 3.23 (4.46) | 5.20 (3.82) | 3.78 (4.33) | |
Chapter 7 Reporting against success/progression criteria
In our application, we stated that we would continue without modifications to a full trial if the following success criteria were met:
-
at least 50% of eligible participants can be recruited within a 4-week period
-
no more than 5% of all recruited participants crossover from one arm to the other
-
at least 50% of all recruited participants complete follow-up assessments.
If we did not meet these success criteria, we planned to assess the reasons for this and consider how these could be improved in a main trial. We stated that, if less than 20% of participants complete follow-up assessments, we would consider the main trial unfeasible and would not proceed with a future larger trial application.
Success criterion 1 was met; we recruited 52% of all eligible participants. Although we extended the recruitment period slightly to 6 weeks at some centres, recruitment was completed within the originally specified 5-month period and this target was met despite some researchers working part-time. More participants could have been recruited at some centres (mainly centre 1) if we had had the resources. Success criterion 2 was not met; 67% of UC participants reported any use of an EC during the study period. Unfortunately, we did not ask about extent of use, so whether or not it was regular, sustained use remains unclear. Although some EC use was reported, none of the UC participants received the EC intervention as delivered (i.e. a free EC starter kit offered at homeless centres). Contamination across arms can be a problem for many RCTs; however, supported use of an EC is increasingly being incorporated into the ‘usual care’ offered by SSSs and should not, therefore, invalidate our findings. The pragmatic question that will be explored in a main trial (and for which this feasibility study sought to provide preliminary evidence) will be whether or not the provision of a free EC starter kit offered at a location already being accessed by homeless smokers can increase smoking cessation rates over UC. Success criterion 3 was fully met; we exceeded 50% retention at each and every follow-up point. However, we note that retention did drop below 50% in the UC arm because of poor retention at the Edinburgh site. Given that some of our success criteria were not fully met, we will include an inbuilt pilot study with clear stop–go criteria in our main cRCT.
Chapter 8 Harms
In the early phases of the study design, our funders panel and PPI work raised several concerns that EC devices provided free of charge to those presenting with substance use disorders or very little income might be sold, stolen or used for inhaling illicit street trade substances. Therefore, despite a well-intended act of offering an EC, this could invite several unintended consequences.
To systemically monitor risk and the occurrence of unintended consequences, we developed a checklist of questions that participants would be asked at each follow-up assessment. The questionnaire is based on our extensive PPI, with input from our expert and multidisciplinary team, our Trial Steering Group and those working in the third sector. These data, although recorded retrospectively, do not prevent the occurrence of these incidents. The rationale for the inclusion of this checklist was twofold: first, it was included so that we could capture the number of times these events occurred and, second, it was included to offer support if required.
The rationale for each question based on our PPI work is as follows:
-
Do you still have the electronic cigarette that we supplied?
This question was asked to ascertain whether or not the participant was still in possession of the product that had been supplied to them as part of the study. It was raised during our PPI consultation work that adults who are not securely housed or sharing residences may easily lose their EC, have it stolen or sell it.
-
(If no) Since our last meeting has your electronic cigarette been lost, stolen, sold, exchanged?
Here we are seeking to gather information as to what happened to the device. Understanding if people are retaining their EC can help with future planning for more definitive studies or service provision.
-
If yes, to any of the above, please provide details.
This allowed free-text responses so that the participant could elaborate and give the study team more information related to the event. By collecting more detailed information, study teams can try to further mitigate risks such as theft and understand the nature of the event (e.g. coercive theft) surrounding the incidents.
-
Have you added any of the following to your electronic cigarette?
A frequent concern when designing the study was that participants may use the EC for vaping substances other than e-liquid. Here we aim to capture if the EC is being used for vaping any other substances and which ones.
-
Have you used the electronic cigarette for any other purposes?
To monitor unforeseen or unpredicted use, we were advised to include this question to capture a broad range of usage.
-
For you, does the experience of using an electronic cigarette have any other similarities to drug use (for example crack)?
Although not common, in our scoping and PPI work, a small number of clients from homeless centres commented that, for them, use of a pen-like second-generation EC triggered memories of historic crack cocaine smoking owing to the device’s shape and the sensory aspect of inhalation.
The majority of the participants used the device as intended. Table 12 presents frequency and percentage data at each follow-up point.
| Unintended consequences | Time point, n (%) | 24 weeks (since 12-week follow-up) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 4 weeks | 12 weeks (since 4-week follow-up) | ||||||||
| Yes | No | N/A | Yes | No | N/A | Yes | No | N/A | |
| Still has EC? | 33 (41) | 6 (7.5) | 28 (35) | 6 (7.5) | 22 (27.5) | 13 (16.3) | |||
| EC lost | 3 (6.3) | 36 (75) | 9 (18.8) | 2 (4.2) | 30 (62.5) | 16 (33.4) | 2 (4.2) | 29 (60.4) | 17 (35.4) |
| EC stolen | 3 (6.3) | 36 (75) | 9 (18.8) | 1 (2.1) | 31 (64.6) | 16 (33.4) | 2 (4.2) | 29 (60.4) | 17 (35.4) |
| Sold | 0 | 39 (81.3) | 9 (18.8) | 0 | 32 (66.7) | 16 (33.4) | 0 | 31 (64.6) | 17 (35.4) |
| Exchanged/swapped | 1 (2.1) | 38 (79.2) | 9 (18.8) | 0 | 32 (66.7) | 16 (33.4) | 0 | 31 (64.6) | 17 (35.4) |
| Given away | 0 | 39 (81.3) | 9 (18.8) | 1 (2.1) | 31 (64.6) | 16 (33.4) | 2 (4.2) | 29 (60.4) | 17 (35.4) |
| Broken | 14 (29.3) | 25 (52.1) | 9 (18.8) | 11 (22.9) | 20 (41.7) | 17 (35.5) | 11 (22.9) | 21 (43.8) | 16 (33.3) |
| Added substance? | 0 | 39 (81.3) | 9 (18.8) | 0 | 34 (70.8) | 14 (29.2) | 2 (2.5) | 32 (40) | 12 (15) |
| EC used for any other purpose? | 1 (1.3) | 38 (47.5) | 7 (8.8) | 0 | 34 (42.5) | 18 (22.5) | 1 (1.3) | 33 (41.3) | 12 (15) |
| EC has any similarities to drug use? | 1 (1.3) | 38 (47.5) | 41 (51.2) | 2 (2.5) | 32 (40) | 46 (57.6) | 2 (2.5) | 32 (40) | 46 (57.6) |
Electronic cigarette, lost, stolen or exchanged
At the 24-week follow-up, 63% of participants still had the EC we provided. Across the follow-up period, there were only seven individual incidents of EC loss and six reported thefts, and nobody reported selling their device. However, one person reported exchanging their device at 4 weeks and three people gave their device away. Other reasons why people did not have their device was because they did not like the taste or the feel of it (n = 2) or reported accidentally leaving it elsewhere (n = 5); one person reported having it confiscated upon admission to hospital.
There was a high percentage of breakages; across the follow-up times, breakages were reported on average 25% of the time. The most common breakage reported was cracked glass tanks.
Adding other substances
There were two reports across the follow-up period of adding other substances not intended for vaping. At 24 weeks, one person reported adding THC and another CBD oil; however, these were added to other devices, not the devices that were provided in this study, suggesting that regular second-generation ECs as provided here may not be compatible with vaping other substances.
Use of the electronic cigarette for any other purpose
At all follow-up appointments, the majority of people said that they had not used their device for any other purpose. At 4 weeks, one person reported using it to mimic vaping without actually switching the device on (‘I put my lips on it’). There were no reports of unintentional use at 12 weeks. At the 24-week follow-up, one person reported using it as a back scratcher and attempted to use it to light a cigarette.
Similarities to drug use
The majority of participants reported no similarities to drug use experiences. However, two did. One participant noted at all three follow-up points that using the device was similar to crack use, and one other participant reported a similarity to smoking cannabis through a ‘bong’.
Chapter 9 Discussion
To the best of our knowledge, presented here is the first UK feasibility study with an embedded qualitative process evaluation exploring smoking cessation in the context of smokers accessing homeless centres, and the first known trial with adults experiencing homelessness on the use of ECs for cessation. This report presents data on participant recruitment, retention, engagement, service capacity, perceived value and preliminary efficacy and cost-effectiveness. The initial results are promising, and with careful consideration and future PPI and stakeholder (homeless charity) input, a future trial may be feasible with some changes to the structure and delivery of the intervention. We discuss the facilitators and barriers in more detail later in this section, including recommended changes needed to progress to a main trial.
In relation to our first objective, recruitment, of all those who were eligible, just over half of those invited agreed to take part and completed the baseline assessment. Only one person withdrew from the study. Our process evaluation has provided useful information that has helped us to understand how to increase participant trust and therefore willingness to take part in a future trial. One stand-out point relates to participant vulnerability and nervousness in taking part in research and sharing personal information. The longer we stayed at the centres – especially centres 1 and 2 – the more likely service users were to engage and to want to take part; this represents growing trust and a ‘snowball effect’, as other service users were seen to be taking part and speaking to the research team, although this also had the unintended consequence of ‘unblinding’ centre allocation. In terms of future work, this highlights the need for the research team to introduce the study to service users as well as staff before baseline assessment. Building trust and offering the opportunity to be seen and be known should, as per our qualitative interviews, reduce any concerns around confidentiality and misperceptions about the nature of the study.
In addition to this, the type of centres taking part in this trial and in a future full cRCT is important. Day centres, defined as those that offer services within usual working hours, were the more successful in terms of recruitment than residential units. Specifically, the two day centres (i.e. centres 1 and 2) accounted for 77.5% of the total sample. The research team and the participants themselves observed that, in the context of these services, a study taking place or a new service being offered was not particularly out of the ordinary. Both of these day centres already offer a range of services and support; thus, our study was within the realm of what was being offered. Furthermore, as noted by our participants when discussing the differences between centres, the day centres offered access to potential participants who, by virtue of their presence at the centres, were already engaged with the service. At the residential units, there was notably less activity and a significantly lower footfall of potential participants. Contrary to expectations, recruitment and follow-ups were not easier at residential units than at day centres. Residents who were ‘at home’ would often not respond to door-knocking or would reply that they did not want to be disturbed, whether or not they had scheduled appointments and received reminder messages. Offering the service in residential units at times felt more intrusive, and this needs to be considered for future studies. It should also be noted that there were fewer smokers in the residential units, and more people were at work. This point is important for considering targeting the most vulnerable smokers; it should not be assumed that, because these adults are facing homelessness, the levels of need will be the same across the population.
Centre 1 (EC) was the most successful in terms of recruitment and retention. There were very few limitations to this centre, but it was observed by the researcher that, although its scale was positive for recruitment, it was also often busy and there could be disturbances. Disturbances and commotion were common in both day centres. For example, at centre 2 (UC), it was common for events outside the staff/researchers’ control (e.g. arguments, drug poisoning, other urgent needs) to take over, making it difficult, or at times impossible, to recruit, collect data and elicit staff support for the study. Despite this, with flexible researchers and a good connection between the research team and the centre staff, these problems were overcome, and by extending the recruitment period to 6 weeks rather than 4 we were able to recruit 22 people. Follow-up was difficult at centre 2 not only for the aforementioned reasons but also because many of the participants were not able to come back for follow-up; many had moved on or were not visiting the centre during the follow-up period. The lower follow-up rate at centre 2 than at centre 1 may also reflect baseline differences between the groups and the fact that centre 2 was within a busy national capital city centre with a highly transient population.
The two residential units had the lowest recruitment rates, despite extending our recruitment period. Centre 3 (UC), despite being known as a ‘centre’, comprised three geographically separate sites and residents did not congregate in the communal spaces much when our researchers were present. Even during periods of good weather, very few people sat in the gardens; they often left the site or stayed in their rooms, and in some cases were active at night and slept during the day. A number of potential participants were out in the daytime, attending day centres, work, part-time education or health appointments, or volunteering. This is in comparison with the bustling environments and continual footfall of the day centres. In addition to this, with centre 3 being located at three different locations, the opportunities to ‘fill’ unattended appointments or serendipitously ‘catch’ one person while waiting for another were fewer than at centres 1 and 2, where the scale of daily interactions and activities was greater. Likewise, there were far fewer interactions between residents, so there was less effect from word of mouth, even related to the opportunity to receive an incentive gift card.
Similarly, centre 4 (EC) had four separate sites at three geographically separate locations. Generally, the residents we met who smoked at this centre had consistently complex needs (e.g. substance use and severe mental health comorbidities and side effects from prescription medications). There were few structured communal interaction events and, if these did exist, take-up by residents was low. Participation in activities such as coffee mornings was moderate, but such activities were more often attended by people who were already non-smokers. Newly hired staff already had full workloads with inductions, compulsory training and patterns of shadowing colleagues so were not able to prioritise supporting the research as much as had been anticipated at the planning stages. At the women-only accommodation (one site making up centre 4), there were no private meeting rooms for data collection or meetings, so all data collection was conducted in the multipurpose room. This was challenging at times because of the lack of privacy, as the garden and residents’ units were accessed through the multipurpose room. These are wider considerations that would need to be taken into account for a future trial by planning with the centres how the study needs to be run and what the conditions for a ‘good assessment’ look like.
However, despite some expected and unexpected challenges, the fact that we were able to recruit 80 participants across four centres in a 5-month period, despite the limited pool of participants at the residential centres, is encouraging. We are especially encouraged given that our participants presented with a high prevalence of mental illness and illicit substance use.
Retention was also assessed for a future trial. The overall 24-week total retention rate was 59%; this compares well with other studies that have recruited smokers from homeless services. 4 Indeed, here we add to the growing evidence base that, despite many competing needs, the majority of our participants were willing to come and speak to the research team. As reflected in our qualitative process evaluation, the financial incentive was instrumental in securing a sufficient number of people in the trial, and, moving forward, the incentive system should remain in place. Financial incentives have been used widely across smoking cessation studies in this environmental context and have also been shown to be a direct measure of increased participation. 4
The results show that 24-week retention rates were higher in the EC arm than in the UC arm. There are several explanations for this. Firstly, the EC arm received weekly sessions to provide e-liquid for the first 4 weeks. This differential level of contact may have encouraged retention in this arm. Nevertheless, this is unlikely to be a key factor given that 4-week retention rates did not differ dramatically between arms (81% vs. 66%). Secondly, baseline characteristics indicate that our UC arm presented with greater mental health and substance use comorbidities, in terms of both incidence and severity. This may be a consequence of our non-randomised design; however, the differences across arms appeared to be mainly due to higher levels of anxiety, and especially substance dependence and cannabis use at centre 2 in Edinburgh, which were significantly higher than at any of the other centres (which did not differ from each other). This is likely to affect attendance because of competing health and social needs, and indeed this centre was associated with far lower 24-week follow-ups than the other three. This sample (at centre 2) was also especially transient in nature, and it was difficult to keep in touch with the participants by 24 weeks (some of whom had been hospitalised or incarcerated). Nevertheless, it is encouraging that individuals with such high-level needs were willing to take part, and it provides proof of concept of the wide-reaching engagement of this study. Future research with this population would need to work closely with PPI representatives to explore how participants could be retained in research trials.
However, for those participants who did return, 6% achieved sustained CO-verified abstinence rate at 24 weeks (ITT) in the EC arm, compared with 0% in the UC arm. Cessation rates are low and our sample size is small but these figures are in line with those reported in other studies conducted in similar settings. 16 However, to the best of our knowledge, our study is the first study to also monitor continuous abstinence at 24 weeks’ follow-up among this population; the general trend has been to capture 24-hour or 7-day point prevalence at 6 months. 4 Given that we have measured continuous abstinence, our results compare favourably with those of two similar trials using NRT: 4% reported at 26 weeks by Segan et al. ,36 and 5.6% and 9.3% 7-day point prevalence reported at 26 weeks in a larger sample of 430 smokers receiving, respectively, NRT or motivational interviewing and NRT at a homeless centre. 16
Importantly, we were able to collect the data from our participants that would be needed for a full cRCT and include a full economic evaluation (although see later in this section regarding contact time with staff in the UC arm). Amendments can be made to the questionnaires that allow for less extensive intrusion of people’s background and lived experience but at the same time still allow the relevant data on health and demographics to be collected.
Completion rates of HRQoL and general health-care and social services questionnaires suggest that the use of these measures was feasible while indicating potential areas for the refinement of data collection. More detailed data collection will be included for services used frequently by this population, whereas services with little use can be omitted from the final data collection pro forma.
Self-reported SSS use showed that few participants in the UC arm sought SSSs for quitting and they did not ask for help from GP services after 4 weeks. In the EC arm, patients did not seek any SSSs during the study period and instead used GP services when they were no longer offered help by their keyworkers in the centre.
Overall, feedback from participants about the study was positive; as noted in Harms, there were very few unintended consequences, and as noted by the qualitative process evaluation the experience of being offered an EC and use after assistance was well received. Encouragingly, the majority of participants reported that they still had and were still using, though not exclusively, the EC at the 24-week follow-up. This is an important issue for breaking the stereotype that this may be a group of adults who will not be able to keep an EC in their possession. There were extra signs of encouragement in the form of participants purchasing their own products, which can be taken as a personal investment in vaping. Around one-third of participants reported having purchased their own EC; this may also explain why the number of participants reporting having used an EC was greater than the number of participants originally supplied with one.
The use of an EC was also commonly reported in the UC arm; around two-thirds of participants reported that they had used one, and one-third had purchased an EC at some point during the study period. However, we did not explore the extent or the frequency of this use. The use of an EC is not uncommon in smokers experiencing homelessness,14,37 and use and experimentation are common among the general population of smokers in the UK. 38 As has been reported elsewhere, cluster designs cannot fully mitigate the occurrence of EC use in UC, and, in fact, EC use is beginning to be supported or actively encouraged in SSSs under ‘usual care’. Although there was some EC use in our UC arm, no participants experienced the EC intervention ‘as delivered’ in the EC arm (i.e. a free EC starter kit and e-liquid offered at homeless centres).
Staff capacity to support the study was generally good, and staff across three of our four centres reported few issues in the process evaluation interviews. The additional responsibilities placed on staff in the EC arm, including initial device set-up, administration of e-liquid and general participant support, were met well by the staff in our study. The high value that staff and management placed on the EC intervention probably helped to better engage staff in these processes. Staff training on ECs and researcher support were also important in building staff belief in ECs as a harm reduction tool and developing their confidence for EC intervention delivery. This helped staff overcome initial nervousness at supporting participants in using their EC. As the study progressed, staff concerns surrounding ECs were alleviated; for example, they reported receiving few problems regarding batteries or charging devices and they were able to manage participants’ e-liquid supply well during the intervention phase. Although some of our participants would have welcomed a greater variety of e-liquid, staff were content with the quantity of different e-liquids on offer, which needs to strike the right balance between participant choice and staff ability to administer.
Daily challenges for service delivery, particularly those experienced at the busier drop-in centres, highlight that service providers may need further support by providing efficient and effective processes for facilitating the study alongside their usual work. Although daily challenges were similar for the drop-in centres (centres 1 and 2), centre 1 was better able to support the study by having better resources to draw on, including staffing and space. Lack of adequate staffing and space presented some challenges for the study at centre 2. Although staff at centre 1 could cope with and support the high level of interest in the study from clients, staff at centre 2 were not able to facilitate participant signposting to SSSs or follow up with participants weekly to check their engagement with SSSs, and where they were able to we could not collect data on this. Busy workloads and client demands primarily accounted for reduced capacity for staff to support the study at centre 2, and alternative ways of capturing contact time to fully cost UC would need to be considered if moving to a full trial. However, it is also possible that a lower value placed on the UC intervention may also account for lower staff engagement with these aspects of these study. Service providers could be further supported by suggesting systems for managing referrals, appointments, signposting and follow-ups, taking into account the differences at each site. Training for staff in the UC arm could also encourage them to see the benefits of UC support.
The qualitative interviews found that perceived value of the study and EC intervention was high among participants. Given participants’ reported desire to change their smoking behaviour, irrespective of whether their primary goal was cessation or harm reduction, the chance to engage in smoking-related discussions was welcomed. The fact that this opportunity could be accessed at a place where participants resided or regularly attended and was incentivised through provision of the EC starter kit and/or Love2Shop gift cards was an added bonus for participants, facilitating their engagement despite low expectations for behaviour change. Those participants in the EC arm who took part in an interview were particularly enthusiastic about the EC intervention, with strong belief in the value of ECs as a harm reduction tool. Social dynamics, especially at centre 1, where some individuals with social standing became vaping advocates, contributed greatly to this belief. This contrasted with the lower perceived value of the UC approach, which largely stemmed from previous negative experiences of NRT, and probably accounts for the poorer engagement with local SSSs. The fact that many participants in the UC arm expressed interest in ECs as a result of the study may also provide an explanation for the level of contamination across study arms.
Limitations
We did not meet the original recruitment target we set ourselves of 120. However, this was a pragmatically chosen target based on our early scoping work and there was potential for further recruitment from some sites if our schedule had permitted it. A second limitation was that we were not able to randomise clusters to condition as planned, and this may have led to the differential retention rates, retention being lower in the UC arm. Our arms also differed on some important baseline characteristics, which may have contributed to the lower retention rates at UC sites. This was particularly the case for centre 2, in Edinburgh, which differed from the English sites on many of these baseline variables. A fully powered randomised cluster design stratified by region in a main trial should mitigate baseline differences across groups. Blinding was not possible for the assessment of outcome measures, which may have led to assessment bias or reduced effort in attempting to contact some participants for follow-up. Furthermore, staff working at the centres were not blinded to the intervention arms, and this could potentially have introduced some bias, for example staff members’ beliefs regarding who would be interested and most able to take part, not least their beliefs regarding who would attend and quit. Finally, we were unable to collect information in the UC arm on staff contact time with research participants.
The qualitative process evaluation has some additional limitations. Owing to the small subsample of trial participants and sample of centre staff, the qualitative findings may not be representative of all our trial participants or staff involved in supporting the study. As in the previous paragraph, it is possible that those who agreed to take part in an interview may have held stronger views about the EC intervention or the UC intervention; however, many of our interviewees in the UC arm had not engaged with UC support, which was reflective of the wider trial sample. Given this, the qualitative process was not able to fully detect any potential bias across intervention arms. We had difficulty recruiting 4-week non-completers to take part in an interview, primarily as a result of challenges in maintaining contact rather than a reluctance to take part. Although interviewing a greater number of non-completers may have identified further barriers to engagement, interview narratives of the small number of non-completers who did take part were not substantially different from those of the majority of the sample.
Generalisability
Our data derive from three geographically distinct areas of the UK and from a variety of different centres. The demographics of our data are similar to those of the wider UK population experiencing homelessness (see www.homeless.org.uk/facts/understanding-homelessness/impact-of-homelessness; accessed 16 March 2021), although the percentage in current employment was lower and the percentage experiencing long-term physical health problems and using drugs was higher than the percentage reported among the UK homeless population by www.homeless.org. Based on these facts, and although centre staff recruited those who were known and actively engaging with the services, it does not appear that our sample was any less disadvantaged than the UK homeless population as a whole. The sample is small relative to the numbers of people engaging with the homeless sector, but we see no reason why the results and methods here cannot be generalised to other homeless service settings as a potential area for future work. Furthermore, it is important to stress that our sample included those with both current and historical substance use and mental health comorbidities, meaning that our participants presented with the complex needs that one expects in these services. It is encouraging that we are able to reach participants from a wide range of backgrounds with differing levels of needs. Central to DHSC’s vision of reducing smoking prevalence rates is directly tackling smoking where tobacco-related health inequalities are most felt by driving smoking rates down among groups with a high incidence of social disadvantage. This work provides a baseline for that vision. This feasibility study provides proof of concept that, even among adults with complex and competing needs, there is a desire to take part in cessation research and attempts to quit are good; our participants used and held on to their EC. Encouragingly, overall, the intervention was well accepted and provides a baseline for future work. Specifically, findings suggest that a fully powered cRCT to explore efficacy and cost-effectiveness may be feasible, but, to fulfil this, recruitment across multiple sites must be considered against service provision type and plans for retention need to be explored to increase follow-up rates. A larger trial is important to establish a stronger evidence base for smoking among this population and to work towards the shared vision of reducing smoking prevalence among adults experiencing homelessness.
Research recommendations
Objective 1: recruitment – assess willingness of smokers to participate
The residential units had fewer eligible individuals, and potential participants were less available and less interested in taking part in research.
Recommendation
Any future study should ensure that a sufficient number of researchers is employed on the project to deal with recruitment and explore limiting sites to day centres only. This is especially important given the transient nature of the population; staff may need to be responsive to the availability of the participants.
Objective 2: assess retention and engagement in the electronic cigarette and usual-care arms
Retention rates were moderate to good and were comparable to those seen in other studies on deprived groups; however, one site’s poor retention rates negatively skewed retention rates.
Recommendation
In designing a future trial, we advise, based on our findings, that a larger number of clusters with fewer people at each one and official randomisation should help to reduce residual confounding factors between the groups. Randomisation should also ensure that variables predicting dropout are equally distributed between groups, thus reducing the difference in retention across arms.
Objective 3: examine the perceived value of the intervention, facilitators of and barriers to engagement, and influence of local context
Perceived value of the intervention was high. Barriers were participants’ personal and psychological difficulties, especially in relation to answering the questionnaires, a sense of nervousness around research, cannabis use and staff assumptions about smoking. Facilitators were participants’ desire to change, lack of existing cessation support, a free EC and social dynamics.
Recommendation
Future studies should make time to introduce the research team to the participants and outline the project to the service users (all those who access the service, who may or may not take part in the study). Researchers should also identify opportunities to increase trust and build relationships before recruitment. We strongly recommend reconsidering questionnaire burden and intrusiveness, including shortening some questionnaires. Future work should also seek to understand what person-centred language would be most appropriate and acceptable with users of homeless services – there is currently a dearth of literature on this.
Specifically for intervention studies that include staff training, from our own experiences, we suggest adding an element to the staff training on fostering a community around the study, highlighting the benefits that this brings to motivation. Qualitative work should be designed to fully capture service user and staff views about their experiences of taking part in research studies, including not only barriers but also facilitators; this would complement our own findings and develop this evidence base.
Objective 4: assess service providers’ capacity to support the study and the type of information and training required
Overall, in the EC arm, staff were well equipped to support the intervention, with few capacity issues, although there was some evidence that staff misremembered key points from the EC training and facts around their use. Some challenges were highlighted in one UC centre, but this is reflective of the unique challenges of this centre and not the UC intervention.
Recommendation
If a full trial was successfully awarded, planning randomisation and a larger number of clusters should reduce any similar issues. Furthermore, fewer participants in each cluster will reduce the burden on recruitment and follow-up at each centre. A future trial should also explore topping up staff training with smaller, intermittent sessions, especially at EC centres.
Objective 5: assess the potential efficacy of supplying free electronic cigarette starter kits
The offer of a free EC starter kit was well accepted by staff and participants. Using ITT analysis, we found sustained 24-week abstinence rates of 0% in the UC arm and 6.25% in the EC arm, which provides preliminary evidence of potential efficacy; however, the absolute numbers were small (3/48 in the EC arm and 0/32 in the UC arm). The UC sample size was also lower than expected; the 0% abstinence rates may therefore be an underestimate of true cessation rates with UC.
Recommendation
To definitively measure efficacy, a future trial with smoking cessation rates as the primary outcome should include more clusters with a fully powered sample size, perhaps using a slightly higher abstinence rate with UC (e.g. 0.5–1%). To fully understand the mechanisms through which change occurs, we recommend an embedded process evaluation that seeks to explore fidelity of implementation and treatment context.
Objective 6: explore the feasibility of collecting data on contacts with health-care services among this population as an input to an economic evaluation in a full cluster randomised controlled trial
Almost all participants who were present at follow-up visits provided data on health-care service utilisation and HRQoL measures; however, as reflected in our interview data, some participants found this data collection intrusive or the questionnaires overly complicated.
Recommendation
Alongside experts with lived experience, any future trial should consider the structure and wording of the health utilisation questionnaire.
Objective 7: estimate the cost of providing the intervention and usual care
Although it was feasible to collect information relating to the cost of delivery in the EC arm, collecting data from staff about contact time was not always possible in the UC arm.
Recommendation
Alternative ways of capturing contact time (or supporting staff in capturing contact time) should be considered (e.g. improving reporting mechanisms and collecting data at a quieter time, such as the end of the follow-up data collection period at each centre) to fully cost UC.
Conclusion
This study focused on a group of people who are not well considered in traditional smoking cessation treatments, and, despite some issues with recruitment and retention, there is promising evidence that a full trial may be feasible with iterations to the main trial design and with further discussion with project partners. We observed early signs of acceptability and potential efficacy of offering free EC starter kits. Centre staff were a crucial element in helping people to take part in the study, training helped to support staff in regard to how to be involved in the study, and building trust between the researchers and the participants was also key. However, the study was challenging in some sites, and parts of the delivery of the study need to be optimised so that we can plan a trial that would be likely to progress fully through a clear stop–go criterion. In considering this, and planning to mitigate future issues, we will explore the findings from the process evaluation alongside the quantitative data, so as to help inform the design of a main trial.
Acknowledgements
In addition to thanking the funders for their support throughout the research process, we would also like to thank Alicja Pytlik, Dr Catherine Kimber and Emily Hussey for their support in assisting with the running of this study.
We would especially like to thank the homeless charities involved – the Northampton Hope Centre, St Mungo’s, London, and the Salvation Army, Edinburgh – and the support workers who provided exceptional levels of assistance and continual support.
We would also like to thank our Trial Steering Committee for their counsel and advice throughout the process. Members: Professor Ann McNeill, Martin Dockrell, Louise Ross, Sarah Jakes, Matthew Carlisle, Vicky Salt, Hazel Cheeseman and Melanie Getty.
Ethics consent was gained from London South Bank University School of Applied Sciences [REF: SAS 1821 (quantitative component) and SAS 1830 (qualitative component)], and also from the University of Stirling.
The electronic cigarettes were funded by the Centre for Addictive Behaviours Research, School of Applied Sciences, London South Bank University.
Contributions of authors
Sharon Cox (https://orcid.org/0000-0001-8494-5105) conceptualised the study with Lynne Dawkins, led the early stage PPI work, led the daily running of the project, led on the writing of this report and contributed to the writing of other outputs.
Allison Ford (https://orcid.org/0000-0002-3624-6673) led the qualitative process evaluation and led the Scottish site. She led the writing of the qualitative component and wrote the process evaluation outcomes for this report.
Jinshuo Li (https://orcid.org/0000-0003-1496-7450) led the economic evaluation and contributed to the writing of this report and the economic outcomes for the quantitative paper.
Catherine Best (https://orcid.org/0000-0002-3652-2498) led the statistical elements for the study and contributed to the writing of this report.
Allan Tyler (https://orcid.org/0000-0003-1210-8476) led the data collection at the London and Northampton sites, assisted with data curation and preparation, and qualitative data analysis, and has contributed to the writing of all the outputs.
Deborah J Robson (https://orcid.org/0000-0002-6447-3523) prepared and led the staff training for the study and has contributed to the writing of all the outputs.
Linda Bauld (https://orcid.org/0000-0001-7411-4260) has provided trial expertise throughout the whole study and has contributed to the writing of all the outputs.
Peter Hajek (https://orcid.org/0000-0001-9160-4296) has provided expertise in smoking cessation, EC use and trial methodology throughout the whole study and has contributed to the writing of all the outputs.
Isabelle Uny (https://orcid.org/0000-0002-9548-5332) contributed to the data collection and data preparation and curation at the Scottish site, contributed to the analysis of the qualitative data and has contributed to the writing of all the outputs.
Steve J Parrott (https://orcid.org/0000-0002-0165-1150) helped to design the economic evaluation in the early stages of the study and also oversaw the economic evaluation analysis. He has contributed to the writing of all the outputs.
Lynne Dawkins (https://orcid.org/0000-0003-1236-009X) is the principal investigator and conceptualised the study with Sharon Cox. She assisted with the daily project running, and oversaw data analysis and writing of all output.
Publication
Dawkins L, Bauld L, Ford A, Robson D, Hajek P, Parrott S, et al. A cluster feasibility trial to explore the uptake and use of e-cigarettes versus usual care offered to smokers attending homeless centres in Great Britain. PLOS ONE 2020;15:e0240968.
Data-sharing statement
The fully anonymised data have been made publicly available by the principal investigator’s institute, in the London South Bank University’s open repository (https://openresearch.lsbu.ac.uk/item/8q255).
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Cornish D, Brookman A, Horto M, Scanlon S. Adult Smoking Habits in the UK: 2018 2018. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2018 (accessed 11 May 2020).
- Guydish J, Passalacqua E, Pagano A, Martínez C, Le T, Chun J, et al. An international systematic review of smoking prevalence in addiction treatment. Addiction 2016;111:220-30. https://doi.org/10.1111/add.13099.
- Richardson S, McNeill A, Brose LS. Smoking and quitting behaviours by mental health conditions in Great Britain (1993–2014). Addict Behav 2019;90:14-9. https://doi.org/10.1016/j.addbeh.2018.10.011.
- Soar K, Dawkins L, Robson D, Cox S. Smoking amongst adults experiencing homelessness: A systematic review of prevalence rates, interventions and the barriers and facilitators to quitting and staying quit. J Smok Cessat 2020;15:94-108. www.cambridge.org/core/journals/journal-of-smoking-cessation/article/abs/smoking-amongst-adults-experiencing-homelessness-a-systematic-review-of-prevalence-rates-interventions-and-the-barriers-and-facilitators-to-quitting-and-staying-quit/5DF8012E78FCB4D86931F961AFF12F37 (accessed 16 March 2021).
- Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ 2014;348. https://doi.org/10.1136/bmj.g1151.
- Jha P, Peto R, Zatonski W, Boreham J, Jarvis MJ, Lopez AD. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 2006;368:367-70. https://doi.org/10.1016/S0140-6736(06)68975-7.
- Baggett TP, Hwang SW, O’Connell JJ, Porneala BC, Stringfellow EJ, Orav EJ, et al. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med 2013;173:189-95. https://doi.org/10.1001/jamainternmed.2013.1604.
- Lebrun-Harris LA, Baggett TP, Jenkins DM, Sripipatana A, Sharma R, Hayashi AS, et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 patient survey. Health Serv Res 2013;48:992-1017. https://doi.org/10.1111/1475-6773.12009.
- Tucker JS, Shadel WG, Golinelli D, Mullins L, Ewing B. Sniping and other high-risk smoking practices among homeless youth. Drug Alcohol Depend 2015;154:105-10. https://doi.org/10.1016/j.drugalcdep.2015.06.036.
- Cox S. Sharon Cox: Risky Smoking Practices and the Coronavirus – A Deadly Mix for Our Most Vulnerable Smokers 2020. https://blogs.bmj.com/bmj/2020/03/20/sharon-cox-risky-smoking-practices-and-the-coronavirus-a-deadly-mix-for-our-most-vulnerable-smokers/ (accessed 11 May 2020).
- Arnsten JH, Reid K, Bierer M, Rigotti N. Smoking behavior and interest in quitting among homeless smokers. Addict Behav 2004;29:1155-61. https://doi.org/10.1016/j.addbeh.2004.03.010.
- Garner L, Ratschen E. Tobacco smoking, associated risk behaviours, and experience with quitting: a qualitative study with homeless smokers addicted to drugs and alcohol. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-951.
- Porter M, Harvey J, Gavin JK, Carpenter MJ, Michael Cummings K, Pope C, et al. A qualitative study to assess factors supporting tobacco use in a homeless population. AIMS Med Sci 2017;4:83-98. https://doi.org/10.3934/medsci.2017.1.83.
- Dawkins L, Ford A, Bauld L, Balaban S, Tyler A, Cox S. A cross sectional survey of smoking characteristics and quitting behaviour from a sample of homeless adults in Great Britain. Addict Behav 2019;95:35-40. https://doi.org/10.1016/j.addbeh.2019.02.020.
- Department of Health and Social Care . Towards a Smokefree Generation A Tobacco Control Plan for England 2017. www.gov.uk/government/publications/towards-a-smoke-free-generation-tobacco-control-plan-for-england (accessed 11 May 2020).
- Okuyemi KS, Goldade K, Whembolua GL, Thomas JL, Eischen S, Sewali B, et al. Motivational interviewing to enhance nicotine patch treatment for smoking cessation among homeless smokers: a randomized controlled trial. Addiction 2013;108:1136-44. https://doi.org/10.1111/add.12140.
- Dawkins L, Bauld L, Ford A, Robson D, Hajek P, Parrott S, et al. A cluster feasibility trial to explore the uptake and use of e-cigarettes versus usual care offered to smokers attending homeless centres in Great Britain. PLOS ONE 2020;15. https://doi.org/10.1371/journal.pone.0240968.
- Fagerström K. Determinants of tobacco use and renaming the FTND to the Fagerström Test for Cigarette Dependence. Nicotine Tob Res 2012;14:75-8. https://doi.org/10.1093/ntr/ntr137.
- Kotz D, Brown J, West R. Predictive validity of the Motivation To Stop Scale (MTSS): a single-item measure of motivation to stop smoking. Drug Alcohol Depend 2013;128:15-9. https://doi.org/10.1016/j.drugalcdep.2012.07.012.
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr Ann 2002;32:509-15. https://doi.org/10.3928/0048-5713-20020901-06.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. GAD-7 Anxiety 2006. www.torbayandsouthdevon.nhs.uk/uploads/score-sheet-gad-7-anxiety-and-phq-9-depression.pdf (accessed 12 December 2018).
- Saunders JB, Aasland OG, Babor TF, Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 1993;88:791-804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x.
- Gossop M, Darke S, Griffiths P, Hando J, Powis B, Hall W, et al. The Severity of Dependence Scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction 1995;90:607-14. https://doi.org/10.1046/j.1360-0443.1995.9056072.x.
- The EuroQol Group . EQ-5D-3L: About 2017. https://euroqol.org/eq-5d-instruments/eq-5d-3l-about/ (accessed 12 December 2018).
- The EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Dawkins L, Corcoran O. Acute electronic cigarette use: nicotine delivery and subjective effects in regular users. Psychopharmacology 2014;231:401-7. https://doi.org/10.1007/s00213-013-3249-8.
- Cox S, Bauld L, Ford A, Robson D, Hajek P, Parrott S, et al. Exploring the Uptake and Use of Electronic Cigarettes Provided to Smokers Accessing Homeless Centres: A Feasibility Study 2018:1-5. https://njl-admin.nihr.ac.uk/document/download/2025909 (accessed 16 June 2020).
- Richards CM, Sharif F, Eischen S, Thomas J, Wang Q, Guo H, et al. Retention of homeless smokers in the power to quit study. Nicotine Tob Res 2015;17:1104-11. https://doi.org/10.1093/ntr/ntu210.
- QSR International.com . NVivo Qualitative Data Analysis n.d. www.qsrinternational.com/nvivo-qualitative-data-analysis-software/about/nvivo (accessed 26 April 2021).
- Wu S, Crespi CM, Wong WK. Comparison of methods for estimating the intraclass correlation coefficient for binary responses in cancer prevention cluster randomized trials. Contemp Clin Trials 2012;33:869-80. https://doi.org/10.1016/j.cct.2012.05.004.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ 2004;13:1203-10. https://doi.org/10.1002/hec.901.
- National Institute for Health and Care and Excellence . Putting NICE Guidance into Practice. Resource Impact Report: Chronic Heart Failure in Adults 2018. www.nice.org.uk/guidance/ng92/resources/resource-impact-report-pdf-4788823645 (accessed 11 May 2020).
- National Rail Enquiries . Train Times and Tickets n.d. www.nationalrail.co.uk (accessed 11 May 2020).
- Segan CJ, Maddox S, Borland R. Homeless clients benefit from smoking cessation treatment delivered by a homeless persons’ program. Nicotine Tob Res 2015;17:996-1001. https://doi.org/10.1093/ntr/ntv062.
- Collins SE, Orfaly VE, Wu T, Chang S, Hardy RV, Nash A, et al. Content analysis of homeless smokers’ perspectives on established and alternative smoking interventions. Int J Drug Policy 2018;51:10-7. https://doi.org/10.1016/j.drugpo.2017.09.007.
- Action on Smoking and Health . ASH Fact Sheet: Use of E-Cigarettes Among Adults in Great Britain 2017. http://ash.org.uk/information-and-resources/fact-sheets/use-of-e-cigarettes-among-adults-in-great-britain-2017/ (accessed 6 December 2017).
- NHS Digital . Prescription Cost Analysis – England 2018 2019. https://digital.nhs.uk/data-and-information/publications/statistical/prescription-cost-analysis/2018 (accessed 11 May 2020).
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2019. Canterbury: Personal Social Services Research Unit, University of Kent; 2019.
- NHS England and NHS Improvement . National Cost Collection Guidance 2019: For Data Being Collected in 2019 2019. https://improvement.nhs.uk/documents/4883/National_cost_collections_19.pdf (accessed 11 May 2020).
- NHS England and NHS Improvement . 2017/18/Reference/Costs/and/Guidance 2018. https://improvement.nhs.uk/resources/reference-costs/ (accessed 16 March 2021).
- NHS Business Service Authority . NHS Prescription Service. PD1 Reports 2019. www.nhsbsa.nhs.uk/prescription-data/dispensing-data/pd1-reports (accessed 24 March 2020).
Appendix 1 The Consolidated Standards of Reporting Trials flow diagram
Reproduced with permission from Dawkins et al. 17 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
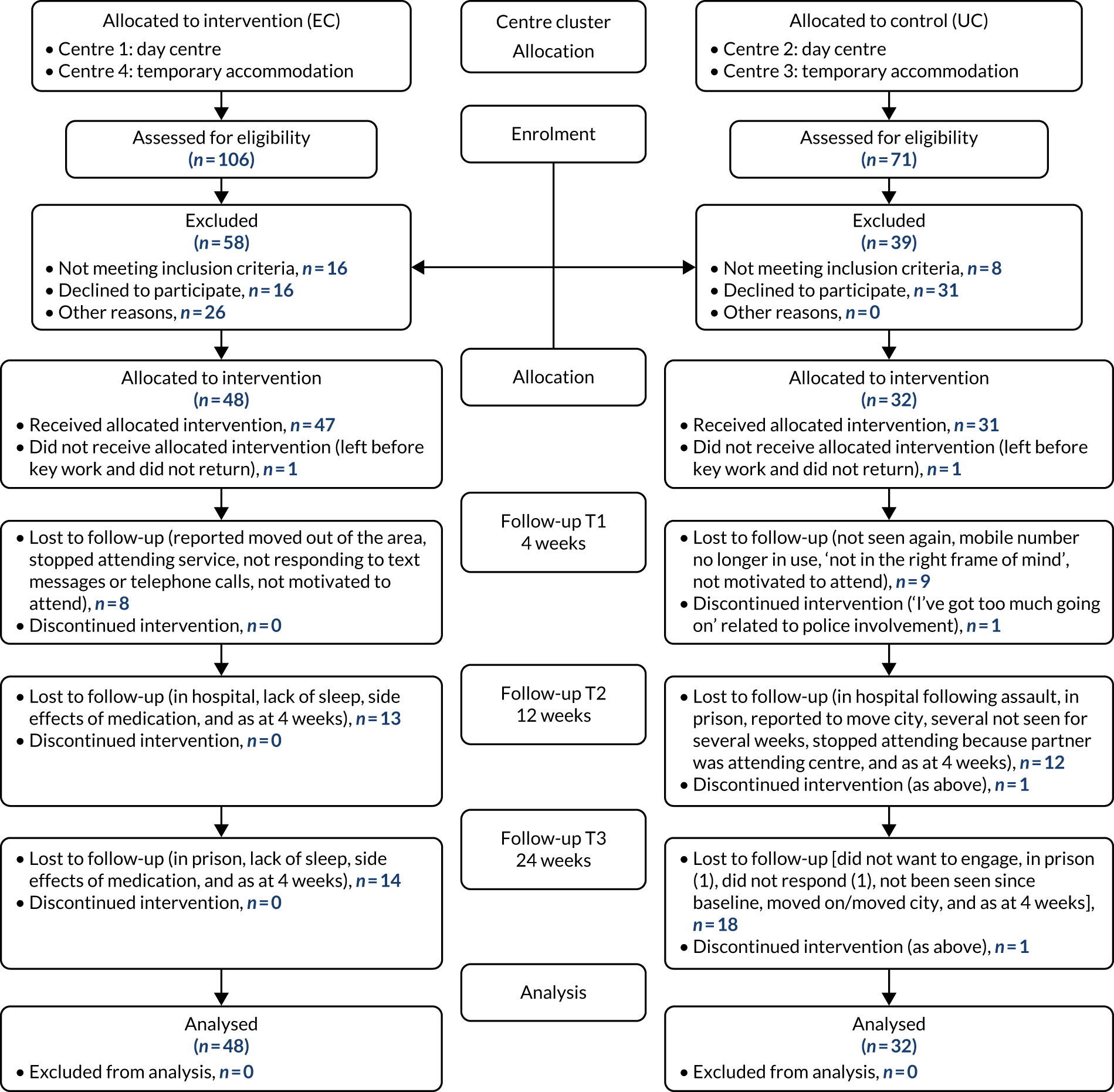
Appendix 2 Participant selection of e-liquid flavours and nicotine concentrations
| Flavour and strength | Time point (n) | Total (n) | |||
|---|---|---|---|---|---|
| Baseline | Visit 1 | Visit 2 | Visit 3 | ||
| Tobacco: 18 mg | 34 | 10 | 8 | 2 | 54 |
| Tobacco: 12 mg | 38 | 14 | 13 | 17 | 82 |
| Menthol: 18 mg | 22 | 16 | 17 | 17 | 72 |
| Menthol: 12 mg | 25 | 27 | 17 | 14 | 83 |
| Fruit: 18 mg | 59 | 29 | 17 | 16 | 121 |
| Fruit: 12 mg | 60 | 51 | 42 | 44 | 197 |
| Total | 238 | 147 | 114 | 110 | 609 |
Appendix 3 Qualitative process evaluation participant characteristics
| Characteristic | Participants (N = 22) | Staff (N = 12) |
|---|---|---|
| Centre and feasibility study arm, n (%) | ||
| Total | 4 | |
| Centre 1: EC arm | 7 (31.8) | 3 |
| Centre 2: UC arm | 6 (27.3) | 3 |
| Centre 3: UC arm | 4 (18.2) | 2 |
| Centre 4: EC arm | 5 (22.7) | |
| Completion at 4-week follow-up, n (%) | ||
| Completer | 19 (86.4) | |
| Non-completer | 3 (13.6) | |
| Smoking at 4-week follow-up | 17 | |
| Yes | 18 (81.8) | |
| No | 1 (4.5) | |
| Missing | 3 (13.6) | |
| Sex, n (%) | ||
| Male | 13 (59.1) | |
| Female | 9 (40.9) | |
| Age (years) | ||
| Mean (SD) (range) | 42 (9.4) (26–60) | |
| Ethnicity, n (%) | ||
| White UK | 13 (59.1) | |
| White other | 2 (9.1) | |
| Mixed white and Caribbean | 1 (4.5) | |
| Mixed white and African | 1 (4.5) | |
| Mixed other | 2 (9.1) | |
| Black African, black British African | 2 (9.1) | |
| Black Caribbean, black British Caribbean | 1 (4.5) | |
| Where participant slept last night, n (%) | ||
| Hostel or supported accommodation | 12 (54.5) | |
| On someone’s sofa or floor | 2 (9.1) | |
| Emergency accommodation | 2 (9.1) | |
| B&B accommodation | 1 (4.5) | |
| Housed – own tenancy | 5 (22.7) | |
| Long-standing illness or disability, n (%) | ||
| Yes | 18 (81.8) | |
| No | 4 (18.2) | |
| Previous mental health hospital admission, n (%) | ||
| Yes | 10 (45.5) | |
| No | 12 (54.5) | |
Appendix 4 Unit costs of prescribed nicotine replacement therapy products
Appendix 5 Unit costs of smoking cessation and health-care services
| Service | Unit cost (£) (2018–19) | Sources |
|---|---|---|
| Smoking cessation help from primary care professionals | ||
| GP | 37/10-minute session | Curtis and Burns40 |
| Practice nurse | 8/10-minute session | Curtis and Burns40 |
| Pharmacist | 8/10-minute session | Curtis and Burns40 |
| NHS helpline | 6/call | Curtis and Burns40 |
| Health-care and social services | ||
| A&E | 192/attendance | NHS England and NHS Improvement41 |
| Outpatient | 144/appointment | NHS England and NHS Improvement41 |
| Inpatient (nights) | 642/night | NHS England and NHS Improvement;41 NHS England and NHS Improvement42 |
| Day case | 752/case | NHS England and NHS Improvement41 |
| Ambulance (travel) | 257/journey | NHS England and NHS Improvement41 |
| GP | 34/9.22-minute consultation | Curtis and Burns40 |
| Practice nurse | 11/15.5-minute consultation | Curtis and Burns40 |
| GP (home visit) | 79/9.22-minute consultation and 12-minute travel | Curtis and Burns40 |
| Practice nurse (home visit) | 19/15.5-minute consultation and 12-minute travel | |
| Prescriptions (NIC and fees) | 20/prescription | NHS Prescription Service43 |
| Sex health clinic | 263/visit | NHS England and NHS Improvement41 |
| Drug/alcohol service | 113/visit | NHS England and NHS Improvement41 |
| Early intervention | 2721/patient-year | Curtis and Burns40 |
| Adult mental health team | 155/contact | NHS England and NHS Improvement41 |
| Crisis team | 87/contact | NHS England and NHS Improvement41 |
| Maternity service | 232/contact | NHS England and NHS Improvement41 |
| Detox/rehab unit | 1114/week, 154/day | Curtis and Burns40 |
| Housing team | 26/visit | Curtis and Burns40 |
Appendix 6 Participants’ use of emergency and hospital services, by arm
| Time point | Trial arm | |||||
|---|---|---|---|---|---|---|
| UC (N = 32) | EC (N = 48) | |||||
| n of null use | n (range) when use > 0 | Missing (n) | n of null use | n (range) when use > 0 | Missing (n) | |
| Baseline | n = 32 | n = 48 | ||||
| A&E | 24 | 7 (1–2) | 1 | 40 | 7 (1–3) | 1 |
| Of whom admitted | – | 5 yes | 2 | – | 2 yes, 5 no | 0 |
| Outpatient | 29 | 2 (1–1) | 1 | 40 | 7 (1–10) | 1 |
| Inpatient (nights) | 25 | 6 (1–14) | 1 | 46 | 1 (1) | 1 |
| Day case | 29 | 2 (1–1) | 1 | 42 | 5 (1–4) | 1 |
| Ambulance | 27 | 4 (1–2) | 1 | 43 | 4 (1–2) | 1 |
| 4 weeks | n = 21 | n = 39 | ||||
| A&E | 16 | 3 (2–9) | 2 | 34 | 5 (1–4) | 0 |
| Of whom admitted | – | 2 yes, 1 no | 0 | – | 3 yes, 2 no | 0 |
| Outpatient | 20 | 1 (6) | 0 | 34 | 5 (1–1) | 0 |
| Inpatient (nights) | 19 | 2 (9–14) | 0 | 37 | 2 (4–4) | 0 |
| Day case | 20 | 1 (6) | 0 | 35 | 4 (1–3) | 0 |
| Ambulance | 18 | 3 (3–6) | 0 | 36 | 3 (1–2) | 0 |
| 12 weeks | n = 18 | n = 34 | ||||
| A&E | 15 | 3 (3–6) | 0 | 28 | 5 (1–2) | 1 |
| Of whom admitted | – | 1 yes, 1 no | 1 | – | 1 yes, 4 no | 0 |
| Outpatient | 17 | 1 (3) | 0 | 30 | 4 (1–8) | 0 |
| Inpatient (nights) | 16 | 2 (1–8) | 0 | 34 | 0 (–) | 0 |
| Day case | 15 | 2 (1–3) | 1 | 31 | 3 (1–2) | 0 |
| Ambulance | 16 | 2 (1–1) | 0 | 34 | 0 (–) | 0 |
| 24 weeks | n = 12 | n = 35 | ||||
| A&E | 8 | 4 (1–4) | 0 | 28 | 5 (1–6) | 0 |
| Of whom admitted | – | 1 yes, 2 no | 1 | – | 5 no | 0 |
| Outpatient | 11 | 1 (1) | 0 | 33 | 2 (3–4) | 0 |
| Inpatient (nights) | 11 | 1 (1) | 0 | 34 | 1 (14) | 0 |
| Day case | 10 | 2 (1–1) | 0 | 29 | 6 (1–2) | 0 |
| Ambulance | 11 | 1 (2) | 0 | 35 | 0 (–) | 0 |
Appendix 7 Participants’ use of primary and community services, by arm
| Time point | Trial arm | |||||
|---|---|---|---|---|---|---|
| UC (N = 32) | EC (N = 48) | |||||
| n of null use | n (range) when use > 0 | Missing (n) | n of null use | n (range) when use > 0 | Missing (n) | |
| Baseline | n = 32 | n = 48 | ||||
| GP | 20 | 11 (1–4) | 1 | 30 | 17 (1–4) | 1 |
| Practice nurse | 23 | 8 (1–2) | 1 | 40 | 7 (1–2) | 1 |
| Prescriptions | 6 | 25 (1–12) | 1 | 14 | 33 (1–16) | 1 |
| Drug/alcohol service | 21 | 10 (1–30) | 1 | 33 | 14 (1–9) | 1 |
| Adult mental health team | 22 | 9 (1–30) | 1 | 39 | 8 (1–4) | 1 |
| Crisis team | 27 | 4 (1–30) | 1 | 45 | 2 (1–1) | 1 |
| Housing team | 22 | 9 (1–30) | 1 | 35 | 12 (1–4) | 1 |
| 4 weeks | n = 21 | n = 39 | ||||
| GP | 10 | 11 (1–14) | 0 | 29 | 10 (1–2) | 0 |
| Practice nurse | 15 | 6 (1–4) | 0 | 35 | 3 (1–1) | 1 |
| Prescriptions | 7 | 14 (1–34) | 0 | 13 | 25 (1–6) | 1 |
| Drug/alcohol service | 18 | 3 (2–4) | 0 | 25 | 14 (1–8) | 0 |
| Adult mental health team | 16 | 5 (1–4) | 0 | 37 | 2 (1–1) | 0 |
| Crisis team | 20 | 1 (1) | 0 | 39 | 0 (–) | 0 |
| Housing team | 20 | 1 (1) | 0 | 32 | 7 (1–4) | 0 |
| 12 weeks | n = 18 | n = 34 | ||||
| GP | 9 | 9 (1–5) | 0 | 22 | 12 (1–5) | 0 |
| Practice nurse | 13 | 5 (1–4) | 0 | 28 | 6 (1–2) | 0 |
| Prescriptions | 5 | 13 (1–12) | 0 | 14 | 20 (1–24) | 0 |
| Drug/alcohol service | 18 | 0 (–) | 0 | 24 | 10 (1–24) | 0 |
| Adult mental health team | 13 | 5 (1–8) | 0 | 29 | 5 (1–2) | 0 |
| Crisis team | 17 | 1 (5) | 0 | 33 | 1 (1) | 0 |
| Housing team | 17 | 1 (1) | 0 | 24 | 10 (1–8) | 0 |
| 24 weeks | n = 12 | n = 35 | ||||
| GP | 3 | 9 (1–3) | 0 | 22 | 13 (1–4) | 0 |
| Practice nurse | 9 | 3 (1–3) | 0 | 26 | 9 (1–3) | 0 |
| Prescriptions | 3 | 9 (1–24) | 0 | 7 | 28 (1–60) | 0 |
| Drug/alcohol service | 11 | 1 (1) | 0 | 22 | 13 (1–26) | 0 |
| Adult mental health team | 9 | 3 (1–24) | 0 | 28 | 7 (1–6) | 0 |
| Crisis team | 12 | 0 (–) | 0 | 34 | 1 (1) | 0 |
| Housing team | 11 | 1 (1) | 0 | 25 | 10 (1–12) | 0 |
List of abbreviations
- A&E
- accident and emergency
- ANOVA
- analysis of variance
- AUDIT
- Alcohol Use Disorders Identification Test
- CBD
- cannabidiol
- CO
- carbon monoxide
- CONSORT
- Consolidated Standards of Reporting Trials
- CPD
- cigarettes per day
- cRCT
- cluster randomised controlled trial
- CRF
- case report form
- DHSC
- Department of Health and Social Care
- EC
- electronic cigarette
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- FTCD
- Fagerström Test of Cigarette Dependence
- GAD-7
- Generalised Anxiety Disorder-7
- GP
- general practitioner
- HRQoL
- health-related quality of life
- ICC
- intracluster correlation coefficient
- ITT
- intention to treat
- MI
- motivational interviewing
- MTSS
- motivation to stop smoking
- NRT
- nicotine replacement therapy
- PHQ-9
- Patient Health Questionnaire-9 items
- PPI
- public and patient involvement
- p.p.m.
- parts per million
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SDS
- Severity of Dependence Scale
- SSS
- stop smoking service
- THC
- tetrahydrocannabinol
- UC
- usual care
- VAS
- visual analogue scale
