Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 15/01/19. The contractual start date was in September 2016. The final report began editorial review in May 2020 and was accepted for publication in December 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by van Sluijs et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Benefits of physical activity
Regular physical activity in children is positively associated with a wide range of health benefits. 1,2 This includes favourable associations with cardiovascular and metabolic,3–6 skeletal7 and mental8,9 health. Improved cognitive and academic performance has also been shown to be associated with regular physical activity engagement. 10 Furthermore, harmful effects have been reported of excessive or uninterrupted sedentary behaviour, especially screen time. 11,12 Given that children and adolescents have been reported to engage in sedentary behaviours for between 6–913,14 and 5–8 hours per day,15,16 respectively, this is a particularly concerning issue. Inactivity in childhood tracks into adulthood,17 increasing the risk of diabetes, cancer and mortality. 4 The development of interventions to promote and maintain children’s physical activity levels is, therefore, a public health priority.
Children’s levels of physical activity and interventions
The UK’s Chief Medical Officers recommend that children and adolescents engage in an average of 60 minutes of moderate to vigorous physical activity (MVPA) per day. 18 The number of children meeting this guideline dropped between 2008 and 2012,19 and the most recent reports suggest that that around one-fifth of English children and youth aged 5–17 years met the recommended physical activity guidelines. 20 Using device-measured physical activity, Steene-Johansen et al. 21 reported that, across Europe, only 29% of children and adolescents were sufficiently active. Observational data show that children are less active after school and at weekends than during school time,22–24 and that as children enter adolescence their levels of MVPA decline steeply,25 particularly at weekends. 24 Last, physical activity levels vary by children’s home location, with indications not only that rural 9- to 10-year-old children are less active than their suburban counterparts,26 but also that their 4-year decline in minutes per week spent in MVPA is higher than that among children living in suburban or urban environments. 24
The issue of declining levels of physical activity is even more concerning when young people’s physical activity levels are examined separately by sex. Girls are less active than boys throughout childhood21 and their participation in physical activity declines more precipitously than that of boys during the transition to adolescence. 27 Therefore, it is critical for young people to develop positive physical activity habits, as an active childhood can track into adulthood. 17,28
An effort to, at a minimum, maintain sufficient physical activity levels should be considered a public health priority. Therefore, intervening in children’s physical activity before they reach adolescence may be an important strategy. 29,30 To date, the majority of research on young people’s physical activity promotion has focused in and around school time. For instance, a considerable amount of attention has been given to general school-based interventions,31–34 active transport to and from school,35 activity at recess,36 physical activity during physical education lessons37,38 and activity generated through after-school programs. 39 Focusing in and around the school setting is understandable because of near-universal attendance rates and the large portion of young people’s waking hours that are spent at school, which makes school an ideal place to target physical activity interventions. However, the effectiveness of school-based physical activity promotion has been limited,31–34 and out-of-school approaches should be explored.
Parents, the family environment and children’s physical activity
The socioecological model (SEM) of health40 posits that individual behaviour is influenced by factors operating at different levels of influence, including individual, intrapersonal and institutional. Beyond individual-level variables, these include those related to the school, neighbourhood and family environment. For example, children’s activity is influenced by the encouragement they receive from their parents, and modelled on their parents’ own behaviour, which is in turn affected by, for example, the time that parents have available for such pursuits, and access to recreational facilities. 41 Indeed, family factors consistently exhibit positive associations with children’s physical activity, particularly parental support and parental modelling. 42,43
The importance of positive parental role-modelling and direct parental involvement in/support (e.g. transport, co-participation and encouragement) of young people’s physical activity is well known. 29,43–47 A recent cohort study by Abbott et al. 48 reinforced the importance of parental role modelling for both physical activity and sedentary behaviour, demonstrating significant associations between preschool children’s behaviours and their parents’ behaviours. In addition, the authors observed a potentially important role of same- and mixed-sex parent–child relationships. 48 Furthermore, family support has been shown to be associated with physical activity at weekends,23,46 when young people are known to be less physically active than on weekdays. 49,50
Parents may also influence their children’s health behaviours through a variety of other mechanisms, including their general parenting style, their parenting practices (e.g. rule-setting, behavioural consequences, establishing behavioural expectations) and their control of the home environment. 51,52 Interventions that target both the child and the family are particularly effective,29,53,54 and without the involvement of family members it is unlikely that a change in children’s physical activity levels will be maintained long term. 44,55,56 Thus, targeting whole families may create a more supportive, synergistic environment for the promotion of healthy behaviours,29,57 from which wider family members may also be able to benefit. 42
Together, this evidence highlights the need for the promotion of young people’s physical activity to target the family, where wider family members may also be able to benefit. 42 That said, little is known about how best to engage families. 29,44,52 This is highlighted by Tremblay et al. ,58 who state that ‘the role of peers and parents in creating supportive environments for physical activity is unequivocal’ but conceded that they could not draw any firm conclusions from their 38-country comparison.
Previous evidence on family-based physical activity promotion
Family-based physical activity promotion has received less attention than the promotion of young people’s physical activity in other settings. In 2016, investigators on the current project published a systematic review, including a meta-analysis and a realist synthesis, in which we included 40 family-based physical activity studies. 29 The meta-analysis showed moderate efficacy in changing children’s activity levels, but only one high-quality trial was identified. Using a realist synthesis approach, it showed the value of using combined goal-setting with reinforcement in the context of family constraints; focusing on changing the family psychosocial environment, for example through the child as agent of change; and drawing attention to additional (non-health) benefits of spending time, such as family time. In addition, this review highlighted the generally low quality of the evidence base (including self-reported physical activity, small sample sizes and limited blinding), lack of post-intervention follow-up, issues with selection bias, recruitment and retention, and the lack of knowledge on how and why interventions may or may not work.
The review also highlighted that most studies focus only on promoting child physical activity, rather than considering the family as a unit that may work as a team to change behaviour. 59 Intergenerational, family-based programmes targeting, for example, early literacy or prosocial development have shown positive effects, and highlight the potential benefit of including multiple family members in an intervention to improve child health outcomes. 60
Theoretical background
In conceptualising an intervention to improve physical activity in children and families, the investigator team used a socioecological approach. 40 Specifically, the SEM provided a framework for the intervention components. Within this framework, behaviour change strategies were guided by self-determination theory (SDT). 61 Brief descriptions of the theories guiding intervention development and evaluation are provided in the following sections.
Socioecological model
The SEM of health40 posits that individual behaviour is influenced by factors operating at different levels of influence, including individual, intrapersonal and institutional. Reviews of determinants corroborate this assertion,62 showing that a multitude of factors are associated with children’s physical activity levels. Family factors, in particular, consistently exhibit positive associations with children’s physical activity. 42,43,46 The family environment is most certainly an important influence on children’s physical activity;63 thus, efforts to increase children’s physical activity should target the whole family. 64 In fact, the involvement of family members may be crucial for long-term physical activity change. 55,56
Self-determination theory
Self-determination theory is a motivational theory that has received significant empirical support in the context of health behaviour change61,65 and in the physical activity context specifically. 66–68 SDT makes a distinction between intrinsic and extrinsic forms of motivation. Intrinsically motivated individuals engage in a behaviour for its own sake (i.e. for the challenge or enjoyment). On the other hand, those motivated by extrinsic regulations engage in an activity to satisfy external demands that can be experienced as controlling or autonomous to varying degrees. 69 SDT posits that individuals move along a continuum as their extrinsic motives or reasons become more internalised they become more autonomous (or self-determined) to engage in behaviours over time (Figure 1).
FIGURE 1.
The self-determination continuum, showing the motivational, self-regulatory and perceived locus of causality from Deci and Ryan. 70 From ‘The “what” and “why” of goal pursuits: human needs and the self-determination of behavior’, Deci EL, Ryan RM, Psychological Inquiry, 1 October 2000, Taylor & Francis, reprinted by permission of the publisher (Taylor & Francis Ltd, http://www.tandfonline.com).
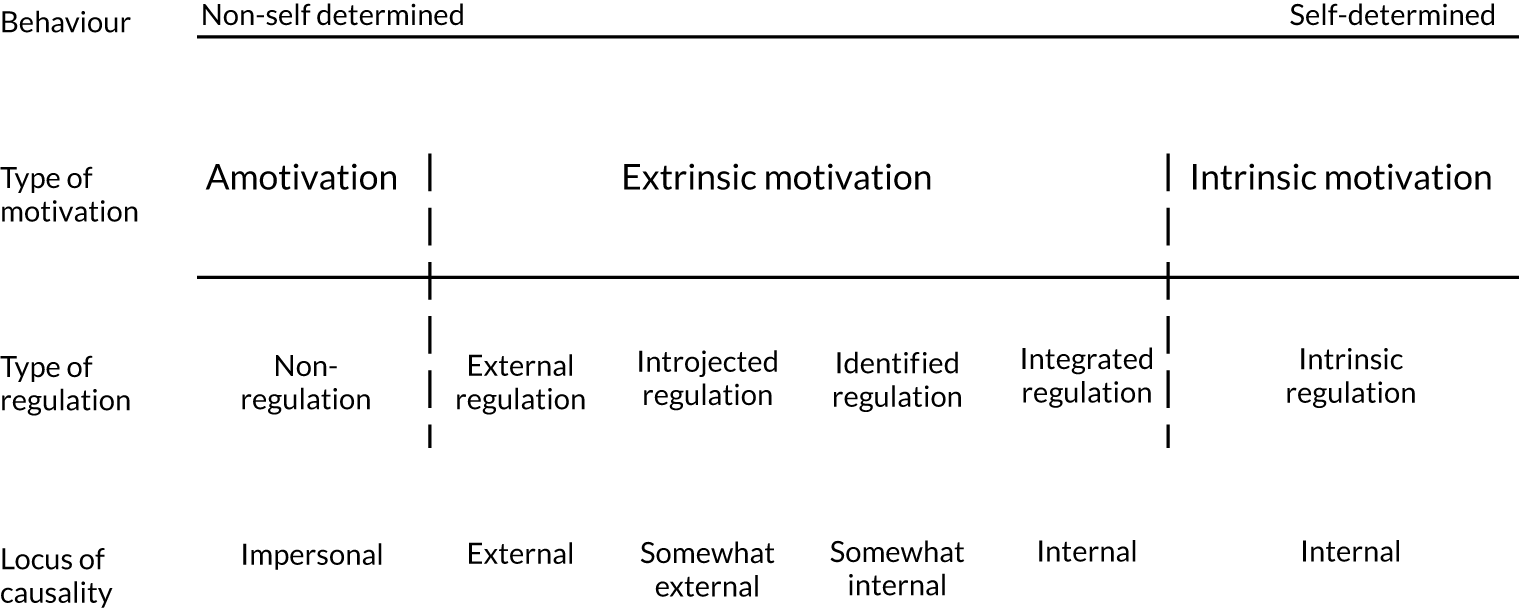
According to SDT, social environments that support individuals’ basic psychological needs (i.e. autonomy, relatedness and competence) are assumed to foster more autonomous motivational patterns. 71 When individuals are more autonomously motivated or self-determined, ‘they experience volition, or a self-endorsement of their actions’. 69 The highest level of self-determination is intrinsic motivation, whereby behaviours, such as physical activity, are performed for their own inherent rewards, such as enjoyment or challenge. 70
Specifically, SDT argues that there are basic psychological needs for autonomy, competence and relatedness, all of which are critical and universal among individuals for psychological health and to move towards autonomous motivation. 70 Satisfaction of these basic needs results in increased feelings of vitality and well-being. 72 Thus, Deci and Ryan’s concept of need support is what is thought to explain individual differences in the development of motivation across the lifespan. 70 Consequently, behaviour change interventions, including those in the area of physical activity, that enhance the satisfaction of participants’ basic needs may be particularly effective. 73,74
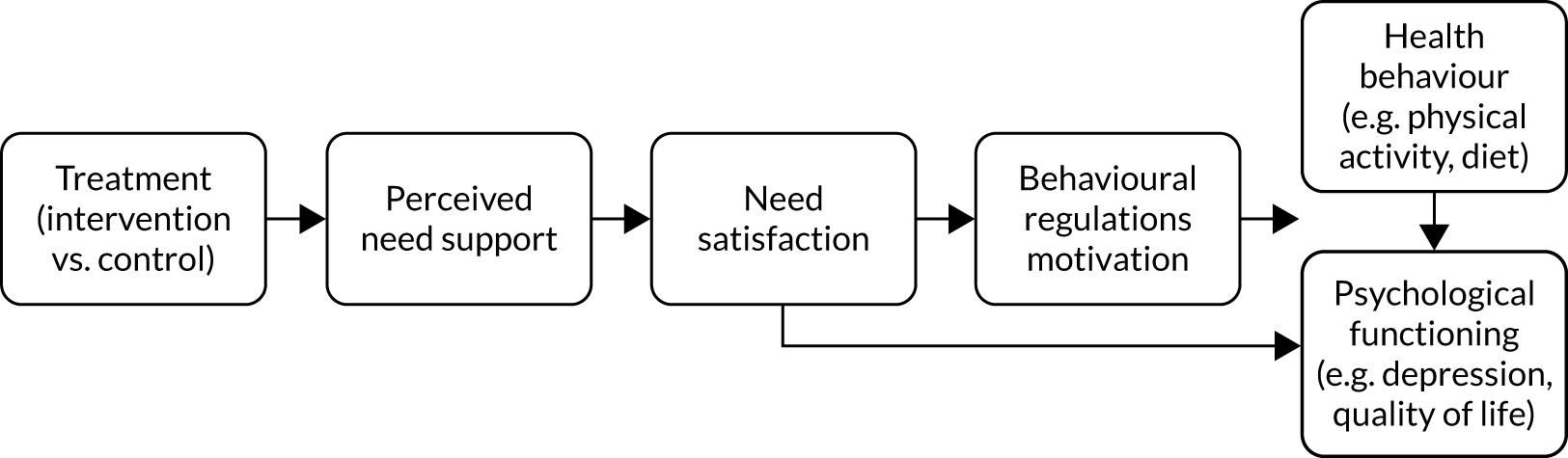
In summary, the broad purpose of SDT interventions is to assist individuals’ progress on the continuum towards more autonomous forms of motivation. Overall, when the complete SDT causal sequence (Figure 2) is used, it creates an intervention outline that has the potential to be quite powerful. 71
FIGURE 2.
The SDT process model for health behaviour change in intervention research from Fortier et al. 71 Reproduced with permission. This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Summary and rationale for the FRESH project
The above literature highlights the importance of physical activity promotion in young people. This was echoed by an international expert panel, who concluded that developing effective and sustainable interventions to increase physical activity among young people is a key research priority in children’s physical activity. 75 In addition, the National Institute for Health and Care Excellence76 in the UK has identified ‘The effect of community and family interventions on young people’s physical activity levels’ (p. 28) as an evidence uncertainty requiring further primary research.
Much of youth physical activity promotion has been predominantly targeted in and around the school setting; however, this project focuses on the important intrapersonal domain of the SEM. Moreover, most studies focus only on promoting child physical activity, instead of considering the family as a unit that may work together to change behaviour,59 despite the known potential benefit of including multiple family members in an intervention to improve child health outcomes. 60 The Families Reporting Every Step to Health (FRESH) intervention, based on extensive prior work, including input from families themselves, will target the whole family and will be able to investigate whether or not this approach is more effective than solely targeting the child. The project was proposed to show whether this approach is feasible and acceptable and potentially effective in changing whole-day physical activity levels of the child and their family members, informing a potential definitive evaluation.
The FRESH project received funding from the National Institute for Health Research (NIHR) Public Health Research programme in 2015 and commenced in late 2016. FRESH consisted of two phases: (1) intervention optimisation and feasibility testing, and (2) pilot testing. Both phases are described in this report, as is an additional project aimed at optimising family recruitment. As per NIHR definitions,77 ‘a feasibility study asks whether something can be done, should we proceed with it, and if so, how’. Feasibility studies are used to estimate important parameters that are needed to design the main study, but do not evaluate the outcome of interest. ‘A pilot study asks the same questions but also has a specific design feature: in a pilot study a future study, or part of a future study, is conducted on a smaller scale’. 77
Study aims and objectives of FRESH feasibility and pilot project
The investigator team identified several strategic and practical uncertainties that needed to be dealt with before a definitive evaluation of the FRESH intervention could commence. The project reported on here consisted of the feasibility and pilot phases of the FRESH trial to reduce these uncertainties. The results of this project were to inform the decision whether or not to proceed with a definitive trial. As stated in the original funding application, the overall aim of a future definitive trial would be ‘to establish the long-term effectiveness and cost-effectiveness of the family-based FRESH interventions to promote MVPA in 8-10 year-old children and their families living in rural Norfolk’.
The aim of the FRESH feasibility and pilot project was to assess the feasibility of delivering the FRESH intervention and its accompanying evaluation. The specific objectives are listed in Box 1.
-
To further develop and optimise the content and delivery of the FRESH interventions (child-only, family) in collaboration with families and stakeholders.
-
To demonstrate feasibility and acceptability of delivery of the FRESH interventions in a short-term feasibility study.
-
To examine the feasibility and relative efficacy of different recruitment strategies and to identify optimal recruitment strategies.
-
To describe the characteristics of families and individual participants recruited in the context of the eligible population.
-
To examine intervention uptake, adherence and maintenance in both intervention groups.
-
To estimate the recruitment and retention rate in a long-term pilot evaluation.
-
To demonstrate the feasibility and acceptability of measurement procedures.
-
To assess the effect size and 95% confidence interval for the proposed primary outcome measure.
-
To test methods of assessing family physical activity and establish an intraclass correlation coefficient.
-
To examine participants’ experience of the intervention and trial participation through questionnaires and interviews.
-
To develop and pilot a family physical activity-related expenditure questionnaire.
-
To model the long-term intervention costs and outcomes to inform discussions with potential funders of the intervention, and to inform the likely efficiency of a future definitive trial.
-
To decide on the feasibility of a definitive FRESH trial and prepare a grant application, if relevant.
The four main research questions addressed were:
-
In what ways does the FRESH intervention(s) need to be optimised prior to a definitive trial?
-
What is the feasibility and acceptability of the FRESH family-based physical activity promotion intervention and accompanying evaluation?
-
Which methods are valid and acceptable for measuring family physical activity?
-
What are the most effective and resource-efficient methods for recruiting families into obesity prevention programmes?
Progression criteria
The FRESH progression criteria were pre-defined at the grant application stage. The following parameters were to be used to inform progression to a definitive trial, taking into account qualitative findings on the acceptability of trial procedures:
-
intervention adherence (> 75% of families uploading steps at least six times in the first 3 months of the pilot study)
-
demonstrable feasibility of recruiting 20 families per month (based on pilot and accounting for increased staffing in a future definitive trial) and retaining 75% of index children at 1 year
-
intervention optimisation feasible (identified adaptations are practical, affordable and acceptable)
-
evidence to suggest that an adequately powered trial would require a feasible number of participants (n = 250 is considered logistically feasible and to provide sufficient power)
-
discontinuation of trial arm based on evidence of harm or limited acceptability/feasibility
-
positive expected net gain of sampling from definitive trial.
FRESH project study management
The overall FRESH project was managed by the FRESH project group, which was chaired by the principal investigator and consisted of all applicants, research associates working on the project, the study co-ordinator and a local stakeholder. Depending on the project phase, the project group met once every 1–3 months. Operational management was led by the FRESH operational group, consisting of the principal investigator, the study co-ordinator and the main research associate appointed on the grant.
At the start of the project, the FRESH Study Steering Committee (SSC) was established, consisting of seven independent members and the principal investigator. The independent members represented various scientific disciplines (young people’s physical activity promotion, public health, family-based interventions, health economics, physical activity measurement, feasibility and pilot trials) and included stakeholders (public health) and members of the public (including with expertise in web-design). The FRESH SSC met once or twice each year. Its stated role was to:
-
oversee the development and co-ordination of research activities
-
act as a sounding board and provide advice on research matters to ensure the long-term health, development and scientific value of the project
-
advise on the continuation of the project after the completion of a pilot study.
At its first meeting, the SSC agreed that, in addition to the pre-established progression criteria, it would consider ‘changes in MVPA’ as ‘evidence of promise’ to inform progression to a full trial.
Chapter 2 The development, trial design and methods of the FRESH feasibility trial
Parts of this chapter are reproduced with permission from Guagliano et al. 78 © The Author(s). 2019 Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
Introduction
Previous evidence indicates that home-based physical activity interventions are potentially more effective than those that require the family to travel to community or other intervention locations. 63,79 Furthermore, it is unlikely that any change in children’s physical activity levels will be sustained long term without the active involvement of wider family members. 44,55,56 Many previous studies, however, focus only on promoting children’s physical activity instead of considering the family as a unit that may work together to change behaviour. 59 Calls for physical activity research in young people and families highlight the dearth of research in this area76 and the need to develop and evaluate innovative interventions targeting children and families.
Responding to this challenge, we sought to identify and develop a family-based physical activity intervention and evaluation. In this chapter, we describe the development of the FRESH intervention and recruitment strategy, and the protocol of the FRESH feasibility study. The aims of this study were to (1) assess the feasibility and acceptability of the FRESH recruitment strategy, intervention (including intervention fidelity) and accompanying outcome evaluation; and (2) explore how FRESH could be optimised through a mixed-methods process evaluation.
Methods
Overview of study design
The reporting of this study was guided by the Consolidated Standards of Reporting Trials (CONSORT) extension to randomised pilot and feasibility trials guidelines80 and the Template for Intervention Description and Replication (TIDieR). 81 This feasibility study received ethics approval from the Ethics Committee for the School of the Humanities and Social Sciences at the University of Cambridge and was prospectively registered (ISRCTN12789422).
We conducted a 6-week, two-arm, parallel-group, randomised feasibility study, using a 1 : 1 allocation ratio, aiming to recruit 20 families with an ‘index child’ aged 8–10 years. The study focused on this age group, as these are the ages when physical activity starts to decline more steeply,25 and it was anticipated that children of in this age group could be engaged effectively with intervention implementation. After measurements were completed at baseline, families were randomly assigned to one of two intervention arms. In the ‘child-only’ arm, the index child was the focus of the intervention, with family members simply providing support. By contrast, in the ‘family’ arm, all participating family members received the FRESH intervention (described in Description of the FRESH feasibility study intervention).
An independent statistician performed the randomisation procedure in Stata® (version 14; Stata Corp LP, College Station, TX, USA) using a computer-generated algorithm and a randomised block design (blocks of four) to ensure equal numbers in each condition and enrolment in both conditions at similar time points and rates.
Eligible participants
Families were eligible to participate when at least one child aged 8–10 years (hereafter referred to as index children) and at least one adult responsible for their care and living in their main household provided consent. Participants also needed to be able to take part in light-intensity physical activity (e.g. walking), have access to the internet and have a sufficient understanding of the English language. No restrictions were placed on family type (e.g. single parent, inclusion of grandparents, siblings). All other family members living in the index child’s main household were invited to participate, but their participation was not required. In addition, intervention and evaluation participation were separate; family members could take part in the intervention irrespective of whether they participated in the accompanying evaluation, and vice versa. Specific exclusion criteria applied only to the evaluation of this study, and these are outlined below.
Study setting
Families were recruited from rural Norfolk, a county in East Anglia, UK (Figure 3). Norfolk has an area of 2074 square miles and an estimated population of 898,400. 82 About half of the population live rurally;83 rural–urban disparities in physical activity have been reported. 24,26 In accordance with the Office for National Statistics84 classification, ‘rural’ was defined as having a postcode falling in a small town, village, hamlet or dispersed settlement.
FIGURE 3.
Map of England showing study location of FRESH feasibility and pilot studies (note that the feasibility study was conducted in Norfolk only).

Recruitment method
Formative work informing the development of the FRESH recruitment strategy
The recruitment of families is known to be particularly challenging and there is little evidence to suggest how best to engage families in physical activity research. 44,52 To inform recruitment and retention, prior to the start of the FRESH project, we conducted focus groups with 17 families (82 participants, consisting of 2–6 family members). 30 The findings of these led to the following recommendations for effective recruitment: (1) using a multifaceted recruitment strategy (i.e. through different setting and different methods) and (2) highlighting the wide range of benefits of research and physical activity participation (particularly social, health and educational outcomes). The findings explicitly contributed to the planned recruitment strategies for the current study, where we planned school- and community-based (e.g. Brownies/Cubs, community centres, general practitioner clinics) recruitment, and highlighted the benefits of spending time together as a family in our recruitment material.
Recruitment protocol
To recruit schools and community-based organisations, we first contacted lead personnel (e.g. head teachers, physical education co-ordinators and heads of community-based organisations) by sending an information pack that included information sheets and a leaflet describing the purpose of the study and what it would involve for schools, parents and children. We followed this up with a telephone call if no response was received. Verbal or written approval was sought from the gatekeeper (e.g. Brownies leader, head teacher) prior to family recruitment. Gatekeepers were asked to send home study leaflets with children, circulate our leaflet to parents online (i.e. via Parentmail or an equivalent system) and send an online reminder to parents approximately 2 weeks later. From schools, we also sought permission to present the study to Year 3–5 students at a scheduled assembly.
Interested parents were asked to contact the study team by e-mail or Freephone, after which their eligibility was assessed and they were e-mailed the study information. Following this, a baseline assessment appointment was made with those families still interested in participating. At the start of the visit, written informed consent was obtained for participating adults, and written parental consent and child assent for each participating child.
Intervention selection and development
Building on previous evidence
As described in Chapter 1, we previously conducted a systematic review and meta-analysis to study the effectiveness of family-based physical activity promotion on children’s levels of physical activity. 29 The meta-analysis showed a small, but significant, effect favouring the experimental groups of family-based interventions compared with controls [Cohen’s d = 0.41, 95% confidence interval (CI) 0.15 to 0.67]. However, it also highlighted the scarcity of family-based intervention studies that (1) clearly indicated intended behaviour change mechanisms, (2) employed objective measures of physical activity, (3) engaged with/assessed intervention effects on wider family members and (4) were theory-based. The development of the FRESH intervention was informed by a programme theory for family-based physical activity interventions, developed as part of this review. 29 This programme theory highlighted the value of (1) using goal-setting combined with reinforcement in the context of family constraints (e.g. lack of time or scheduling difficulties), (2) focusing on changing the family psychosocial environment (e.g. using the child as agent/instigator of change) and (3) focusing on something other than the health benefits of physical activity (e.g. spending time together as a family). These collective findings were considered in the development of the FRESH intervention.
Intervention selection through public involvement
The research team developed four potential intervention concepts based on their previous work. 29,30 The four concepts were:
-
Buddy scheme – families would be paired or grouped to facilitate peer support for physical activity.
-
Small changes – providing a resources toolkit to each family, containing information on making small changes to increase physical activity (e.g. active travel suggestions, such as getting off the bus a stop early).
-
Sports equipment library – a ‘travelling library’ of a large range of sporting equipment would move through a community once per week, allowing families to borrow equipment.
-
Family challenge – families would be framed as a ‘team’ working towards a common goal (e.g. an overall step count to ‘walk around the world’).
These four concepts were then brought to families during a university-run community engagement event. At this event, children acted as researchers to identify which intervention concept their family would enjoy most. Based on the feedback, the most popular concepts were further refined during meetings with stakeholders (i.e. parents, teachers, family health practitioner). This led to the selection of an intervention that allowed families to work as a ‘team’, tracking their efforts towards a common goal and receiving small rewards for progress (the family challenge described above). This initial input from families and stakeholders was used as a starting point from which develop FRESH in its current form.
Description of the FRESH feasibility study intervention
In brief, FRESH was primarily a goal-setting and self-monitoring intervention aimed at increasing physical activity in whole families. The SEM (individual and interpersonal levels)40 and family systems theory85 provided a framework for the intervention components. Within this framework, behaviour change strategies were guided by SDT. 61 A detailed description of the FRESH intervention components and associated behaviour change techniques,86 targeted SDT constructs and hypothesised mediators is provided in Table 1. In addition, the FRESH feasibility study logic model can be found in Figure 4.
| Intervention components | Dose | Description | Behaviour change techniques | Targeted SDT constructs | Hypothesised mediators |
|---|---|---|---|---|---|
| 1. ‘Family time’ | Minimum once per week, 10–20 minutes | ‘Family time’ provided an opportunity for index childrena and family members to plan PA, monitor their week’s steps, discuss any potential PA barriers and strategies to overcome them by logging in their family action planners.27 Regular ‘family time’ was hypothesised to provide index children with:
|
Goal-setting Self-monitoring Positive feedback on progress Social support Praise Positive reinforcement |
Perceived competence Perceived relatedness Perceived autonomy |
Family social norms for PA PA awareness Basic needs satisfaction PA motivation |
| 2. FRESH website | Minimum once per week, 5–20 minutes | The FRESH website facilitated self-monitoring of step counts, and goal-setting through selecting challenges. Specifically, the FRESH website allowed families to choose one of three target cities to ‘walk to’ weekly, with the aim to eventually ‘walk’ around the world. Each week, families chose an easy, moderate or difficult challenge, which represented a 0%, 5% or 10% increase, respectively, relative to the average steps they had taken in preceding weeks. Increases were adjusted to 0%, 2.5% and 5% once adults and children accumulated an average of 10,000 and 12,000 steps per day, respectively. Families also had access to a general resources area that provided suggestions of activities that families could do together and a map to give a visual representation of the locations families had travelled to |
Goal-setting Self-monitoring Positive feedback on progress Rewards |
Perceived competence Perceived relatedness Perceived autonomy |
Social support Family social norms for PA PA awareness Basic needs satisfaction PA motivation |
| 3. Pedometry | Throughout intervention (6 weeks) | Participants were provided with pedometers for self-monitoring and immediate feedback. Pedometers are simple to use and convenient and are associated with effective interventions for increasing parent–child physical activity.35 Index children logged their steps (and their family members’ steps) into the FRESH website and/or onto the family action planners, which allowed participants to view their progress towards their proximal and distal step goals |
Self-monitoring Immediate feedback |
Perceived competence Perceived autonomy |
Social support Family social norms for PA PA awareness Basic needs satisfaction PA motivation |
| 4. Virtual rewards/competence reinforcement | Approximately once per week (6 weeks) | To praise effort (i.e. competence reinforcement), participants received supportive messages, virtual passport stamps (i.e. virtual rewards) and access reinforcement materials (i.e. interactive multimedia information about the cities they have visited) on the FRESH website as they completed challenges to various cities around the world. Participants received 2–4 passport stamps for completed challenges (i.e. as difficulty increased, more stamps were awarded) and one passport stamp for an incomplete challenge |
Feedback on progress Rewards |
Perceived competence |
Basic needs satisfaction PA awareness |
FIGURE 4.
The FRESH feasibility study logic model.
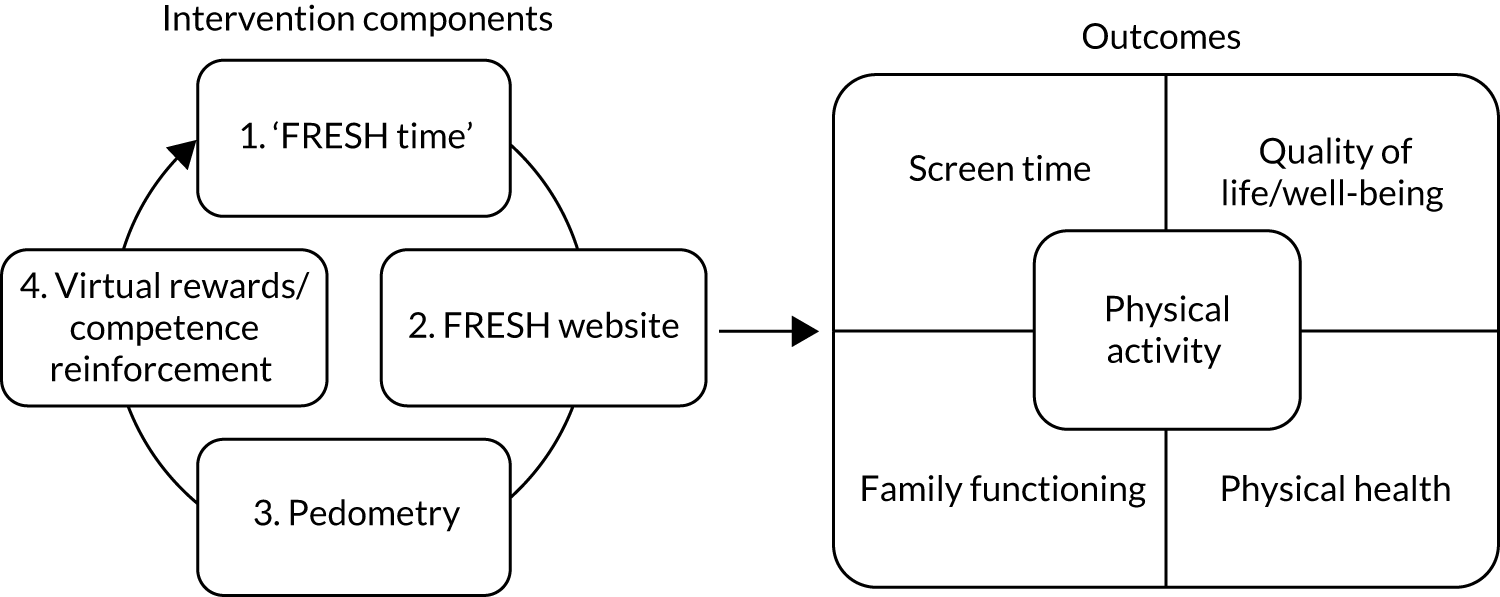
To initiate intervention participation, a facilitator visited all families a week after baseline assessments for a ‘kick-off’ meeting to introduce the families to the intervention components and accompanying materials (e.g. family action planner). The main purpose of this meeting was to familiarise families with the website and prompt them to schedule regular ‘family time’ meetings (a suggested minimum of one per week) during which they would review and update their family action planner. All meetings occurred in participating families’ homes and lasted approximately 1 hour. Participant-initiated distant support was available for the duration of the intervention.
A detailed description of the FRESH intervention components can be found in Table 1. At the start of each new weekly challenge, families had ‘family time’, during which they selected a challenge on the FRESH website and filled in their action planners. The FRESH website allowed families to choose one of three target cities to ‘walk to’ each week, with the aim of eventually ‘walking’ around the world. The FRESH website primarily facilitated the self-monitoring of step counts and goal-setting through selecting challenges of varying difficulty. In both study conditions, children were allocated the role of ‘team captain’, leading on destination selection and uploading steps online. Families were to wear their pedometers for as long as possible daily to capture their steps and were asked to upload their step counts at least once weekly. After completing a challenge, families received effort-praising messages and virtual rewards (i.e. virtual passport stamps) and were able to track their progress around the world and access reinforcement materials on the FRESH website (i.e. interactive information about the cities they had walked past and reached during their challenge). If a family did not complete a challenge, to praise their effort, they progressed to a hidden city along their challenge route and still received a supportive message, a virtual passport stamp and access to reinforcement materials. Completing a challenge (or the week coming to an end) initiated the next ‘family time’ meeting, when the above cycle was repeated (see the cycle in Figure 4).
FRESH child-only condition
The child-only condition was essentially the same as described above, but in this condition only the index child received a pedometer and was able to record their steps on the FRESH website. All other components were kept the same.
Refining the prototype FRESH intervention
The initial FRESH intervention was developed further through public involvement activities. We sought input from children (n = 7) through a talk-aloud session regarding the layout and design of the FRESH website and also from families (n = 2) who pilot-tested the intervention protocol described above. Overall, the FRESH intervention was well received, children found the website easy to navigate, and no changes were made to the protocol. However, based on participants’ suggestions, minor changes were made to the intervention website. For example, participants found it discouraging when they participated in activities that could not be captured by their pedometers (e.g. swimming). Therefore, we added a ‘step calculator’ to the website that enabled participants to estimate the number of steps that various activities, such as swimming, would give them, using data from a readily available online activity-to-step converter. 87
Outcome evaluation measures
As part of this feasibility study, we aimed to assess the feasibility and acceptability (i.e. not the effectiveness) of the planned outcome evaluation. Therefore, here we briefly describe the measures included to provide an overview of what the outcome evaluation entailed. Table 2 outlines the measures taken, including the order of assessments and the estimated duration of each. Data collection was carried out by two trained research staff in participating families’ homes. Outcomes were assessed at baseline (prior to randomisation) and at follow-up (at 6 weeks) for all participating family members (excluding children aged ≤ 2 years). All consenting family members took part in measurements, irrespective of their intervention allocation and participation.
| Measure | Duration |
|---|---|
| 1. Anthropometric measures (height, weight, waist circumference) | 5 minutes per person |
| 2. Questionnairesb | 20 minutes per family |
| 3. Blood pressure | 10 minutes per person |
| 4. Step test (aerobic fitness) | Preparation: 5 minutes per person |
| Test: 8 minutes per family | |
| 5. Accelerometer and GPS explanation | 5 minutes per family |
| 6. Fictional Family Holiday (family functioning) | 10 minutes per family |
| Total duration of measurements | Minimum of 73 minutes |
| Total duration of visit (including consent process) | Minimum of 88 minutes |
Physical activity assessment
To assess individual physical activity, and family co-participation in physical activity, participants were asked to simultaneously wear an ActiGraph GT3X+ triaxial accelerometer (ActiGraph LLC; Pensacola, FL, USA) and QStarz Travel Recorder BT1000X Global Positioning System (GPS) monitor (QStarz; Taipei, Taiwan). Participants wore the monitors affixed at each hip on an elastic belt during waking hours for 7 consecutive days. The monitors where then picked up by a member of the study team, or participants were asked to return the monitors to the study office in a prepaid enveloped. Accelerometer data were downloaded and processed. A valid week was defined as ≥ 600 minutes per day from 3 weekdays and 1 weekend day during the 7-day measurement period. 88 Non-wear was defined as ≥ 90 minutes’ consecutive zeros using vector magnitude. ActiGraph accelerometers have been shown to be valid and reliable devices for the measurement of physical activity levels in children and adults;89–91 the GPS monitor used has been shown to have high static and dynamic validity in a variety of settings. 92
Combined GPS and accelerometer data were collected to enable the assessment of family co-participation in physical activity (i.e. family members being active in proximity to each other). Accelerometer and GPS data were matched using Java; after this, data points that had a time difference of ≤ 30 seconds between the accelerometer timestamp and that of its matched GPS location were considered valid for inclusion. Matched data points with a time difference greater than this, for example when the GPS had been switched off or had lost signal, were considered as missing location information because the participant might have moved to a new, unrecorded, location. From the matched data, we computed the minutes per day for which the GPS had maintained a signal, and had therefore recorded the participants’ location, as an indicator of data completeness. Only wear time data will be presented as part of the feasibility study; therefore, we have only provided information relevant to estimating wear time using both monitors.
Health outcomes
Aerobic fitness was measured using an 8-minute submaximal step test. 93 Children aged < 8 years were excluded from the aerobic fitness test because of the height of the step. Older children and adults were all asked to complete the step test. Height, weight, waist circumference and blood pressure [using an OMRON 705IT digital blood pressure monitor (OMRON Healthcare UK Ltd, Milton Keynes, UK)] were measured in accordance with standardised operating procedures. Body mass index (BMI) was calculated and was converted into age- and sex-specific percentiles using standard growth charts for children using LMSgrowth Program version 2.77 (Child Growth Foundation, London, UK). 94
Behavioural and psychosocial measures
Questionnaires assessed behavioural and psychosocial measures: adult and child screen-use time;95–98 quality of life;99–102 family co-participation in physical activity;98 physical activity awareness;103,104 family social norms for physical activity;105,106 family support;105 children’s and adult’s motivation for physical activity;107,108 and children’s perceived autonomy, competence, and relatednesss. 108 Table 3 provides an overview of the measures used with children and adults. Children aged ≤ 4 years did not complete this questionnaire. Research assistants were available to answer questions during completion.
| Measure | Assessment method§ |
|---|---|
| Screen time | Adult: two items from the Recent Physical Activity Questionnaire95 |
| Child: parent proxy using one item from the Children’s Physical Activity Questionnaire96 | |
| Family co-participation in screen time | Four items derived from the SPEEDY study questionnaire |
| Screen-based restriction | Restricting access to screen-based activities was measured with two versions (parent-report and child-report versions) of the Activity Support Scale for Multiple Groups97 |
| Quality of life | Adult: EQ-5D-5L99,100 The EQ-5D-5L asks respondents to describe their health today using five dimensions, each at five levels. The dimensions are mobility, self-care usual activities, pain/discomfort and anxiety/depression |
| Child: CHU-9D.101,102 The CHU-9D asks respondents to rate their health today using nine dimensions, for example pain and usual activities, school work/homework, tired and sleep. Algorithms exist based on population preferences for both scales to be converted into a ‘health state utility’, an index relative to two anchor points of 0 (dead) and 1 (perfect health). Integrating these over time allows the calculation of QALYs | |
| Physical activity awareness | Adult: self-report whether or not they achieve enough MVPA to meet national guidelines, as used previously104 |
| Child: one item on the child and parent questionnaire from Corder et al.103 | |
| Family social norms for PA | Adult: single item using previously used question105 |
| Child: four items from previously used questionnaires106 | |
| Family support | Adult and child: six items using previously used questionnaires105 |
| Motivation for PA | Adult: BREQ-2, developed by Markland and Tobin107 |
| Child: questionnaire developed by Sebire et al.108 | |
| Basic psychological needs satisfaction | Children’s perceived autonomy, competence, and relatedness will be assessed in child participants only, using a questionnaire developed by Sebire et al.108 |
Fictional Family Holiday
The Fictional Family Holiday paradigm, a 10-minute video-recorded activity where families were asked write out a week-long holiday itinerary with unlimited budget, was used to assess family functioning via family relationships109 and connectedness. 110 This is because the activity requires ‘power sharing’ (i.e. taking turns) and prompts the viewpoints of all family members on the topic, eliciting both individuality (through suggestions for destinations/activities or disagreements) and connectedness (through agreements, questions, or initiating compromise), contributing to the family’s final plan. 109
Family out-of-pocket expenditure for physical activity
Information on family expenditure related to physical activity was collected using a questionnaire that was developed and tested for the current study. This was completed by one adult for their whole family. The questionnaire consisted of two questions about expenditure related to membership fees and subscriptions (e.g. for sports clubs, fitness centres) and sports equipment (e.g. sportswear, gadgets).
Process evaluation
A mixed-methods process evaluation was conducted at the end of the 6-week intervention. In questionnaires, adults self-reported their overall opinion of FRESH, their opinion of the intervention components and measurements, and suggestions for improvement using open-ended and 5-point Likert-scale questions (1 = strongly disagree, 5 = strongly agree). Children also self-reported on the above topics, responding to dichotomous ‘yes/no’ questions. In addition, we conducted semistructured focus groups with 11 out of 12 families (one family declined to participate), focusing on families’ perceived acceptability of the individual FRESH intervention components, intervention fidelity, challenges/barriers to engaging with FRESH, and suggested improvements. The mean duration of focus groups was 34 minutes [standard deviation (SD) 10 minutes; range 17–50 minutes]. All focus groups were audio-recorded and transcribed verbatim.
Data analysis
Quantitative data
Frequencies, percentages, means and SDs were calculated to describe the data related to recruitment, retention, fidelity, intervention optimisation, website engagement and outcome measures.
Qualitative data
Using a long-table approach, a content analysis was conducted using existing guidelines. 111 Specifically, the analysis was conducted in two separate phases. During the data organisation phase, text from each transcript was divided into segments (i.e. meaning units) to produce a set of concepts that reflected meaningful pieces of information. 111 Tags were then assigned to each meaning unit. Tagging was performed by one researcher, with a second double-tagging approximately 25% of the transcripts. In the data interpretation phase, the inventory of tags from all transcripts was examined by two researchers, which led to the emergence of themes and subthemes within each overarching category.
Chapter 3 FRESH feasibility trial findings
Parts of this chapter are reproduced with permission from Guagliano et al. 78 © The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
The FRESH feasibility study was conducted in May–August 2017, in accordance with the protocol described in Chapter 2. This chapter describes the findings of this study, which had the following aims: (1) to assess the feasibility and acceptability of the FRESH recruitment strategy, intervention (including intervention fidelity) and accompanying outcome evaluation; and (2) to explore how FRESH could be optimised through a mixed-methods process evaluation.
Recruitment and retention
Owing to intervention development delays, we were only able to deploy school recruitment strategies. Of 11 schools approached, three declined (too busy, n = 2; doing enough physical activity promotion already, n = 1), and three did not respond. Five schools with an estimated 437 eligible students in Years 3–5 agreed to disseminate the FRESH recruitment material (reach).
Figure 5 shows the flow of participants from the number of families assessed for eligibility through to the number analysed. Of those families reached, 6.4% (i.e. 28 families) expressed interest; initial interest came from 23 mothers and 5 fathers. Expressions of interest occurred at a rate of three or four families per week or five or six families per school assembly conducted. Fewer than half of the families expressing interest in participation subsequently signed up to participate in FRESH (n = 12 families), and these were enrolled at a rate of one or two families per week. All families were retained at the 6-week follow-up.
FIGURE 5.
Flow of participants in the FRESH feasibility study.
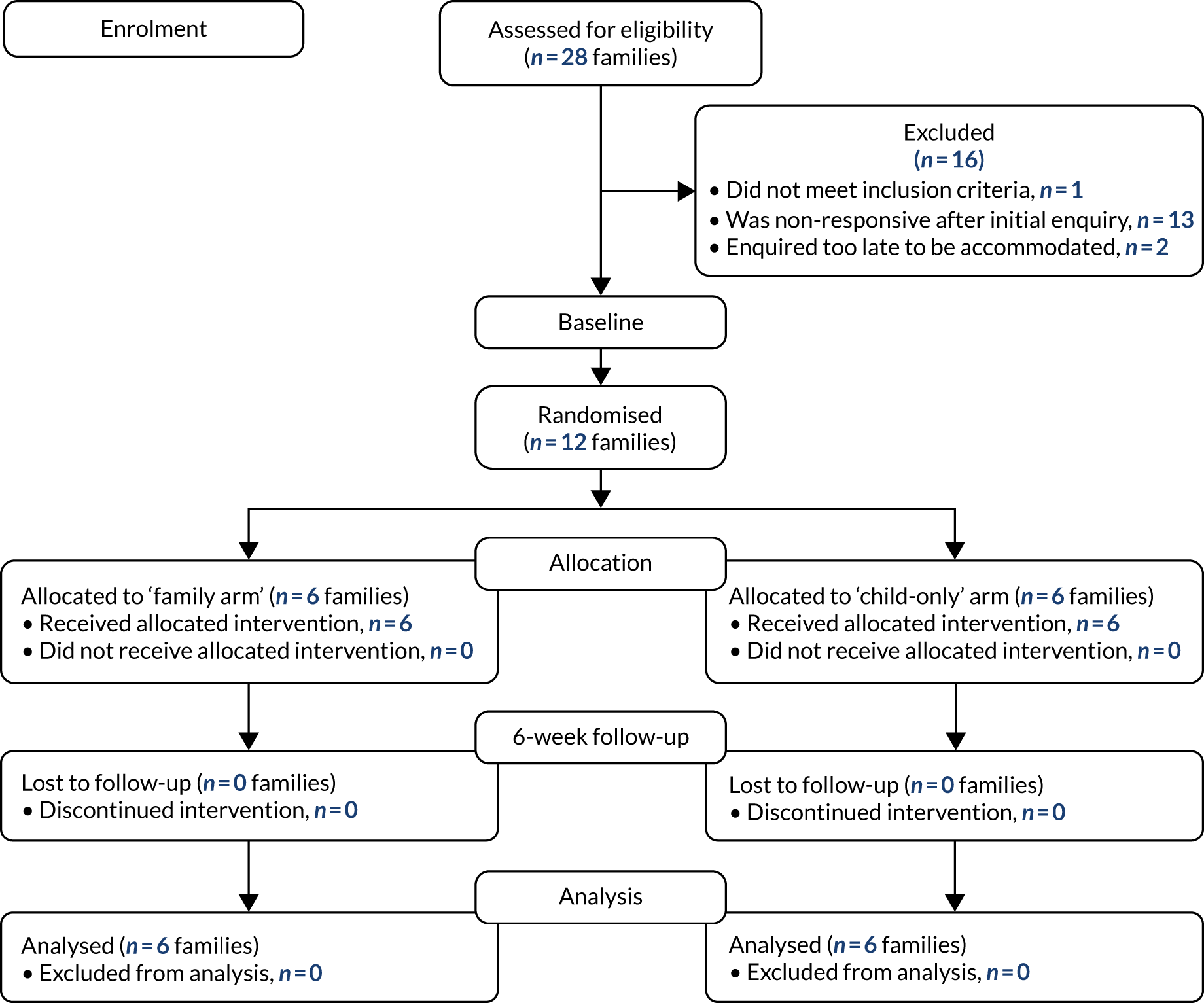
Of the 12 families enrolled, four were whole families and six were dyads (i.e. one parent and one index child); 32 family members participated overall. About two or three family members took part per family (range 2–4 family members); four families had an additional eligible adult, three families had an additional eligible child and one family had both. Table 4 describes the participant characteristics.
| Variable | Adults (n = 18) | Children (n = 14) |
|---|---|---|
| Sex (% male) | 38.9 | 50.0 |
| Age (years), mean (SD) | 39.8 (8.2) | 8.3 (1.7) |
| Height (cm), mean (SD) | 168.6 (8.6) | 133.6 (12.7) |
| Weight (kg), mean (SD) | 74.7 (15.9) | 32.5 (10.8) |
| BMI (kg/m2), mean (SD) | 26.3 (5.8) | N/A |
| BMI z-score, mean (SD) | N/A | 0.5 (1.1) |
| Waist circumference (cm), mean (SD) | 92.0 (12.7) | 66.6 (12.3) |
| Blood pressure (mmHg), mean (SD) | ||
| Systolic | 127.8 (16.2) | 110.0 (105) |
| Diastolic | 72.6 (9.1) | 64.6 (7.2) |
| Pulse rate | 68.3 (7.1) | 81.0 (7.8) |
In focus groups, families were asked about the perceived challenges to recruitment, which revealed four challenges to be considered for optimising future recruitment. A brief description of the challenges is provided below, with supporting quotations in the first part of Table 5.
| Subheading | Supporting quotations |
|---|---|
| Findings related to recruitment and retention | |
| Children trying to convey what FRESH was to parents | I guess because you did it in assemblies, I wasn’t sure what he was going on about. It wasn’t till [a mother of a participating family] had obviously been in touch with you that we found out more. But going back to the whole thing of trying to then explain [FRESH], if the kids can’t do it, it becomes sort of Chinese whispers between the parents, doesn’t it?Mother 7, family arm |
| Participation would be time-consuming | I think people have misconceptions . . . I think they just heard the words research project and thought, ‘oh no, we’re going to have to do a load of stuff’ ’. . . but you don’t have to do anything, just wearing this [pedometer] and going about what I do normally and log on the website every night or a couple of times a week and have a look at how we’re doing. I didn’t think it was a hassle at allFather 5, child-only arm |
| Lack of confidence for physical activity | Exercise is a funny thing, you know . . . Like if they’re overweight or they don’t eat healthy . . . they may think they’re being judged by it and actually they’re not being judged by it at all. That’s not what this was about . . . but there’s a fear factor when it comes to exercise for some people . . . And given that I think obesity levels are pretty high around here for the national average, I think West Norfolk’s one of the fatter areas, people may be a bit . . . I don’t know, possibly there was lack of confidence about signing up to something like thisMother 5, child-only arm |
| Reluctance to be measured | It was the measurements, I would’ve done the other stuff . . . I think with some people that just puts you off straightaway. I think it did for me . . . I was like ‘no, I don’t want to do that’ and I’m sure others felt the same. Luckily [father] didn’t mind because she really wanted to do thisMother 12, family arm |
| Findings related to intervention feasibility, acceptability, fidelity and optimisation | |
| Feasibility and acceptability of FRESH | Definitely more aware, I underlined that [on the process evaluation questionnaire] because I think in terms of our awareness, it has made us a lot more aware of the steps that we are doing. I really, really liked that, for me that has been the best thingFather 6, family arm |
| . . . you [speaking about index child] wanted to walk more didn’t you, like if we were going to nursery you were like, ‘can I walk because I want to get more steps’. I noticed that on a few things, whereas before she would have been like, ‘oh, can we go in the car?’Mother 12, family arm | |
| I do think if you’d given step counters to everyone in the family it gives us more onus to do it. Once you’d gone, it was all about him and no one else in the family, I felt like I’d done my bit and it was all down to just him and his step counter; whereas, if I’d have had a step counter . . . for the 6 weeks I probably would have been more aware about how active I was, and not necessarily competed with you, but just the fact that I had my own one to keep an eye on how active I’d been, then I’d have probably felt more involvedFather 8, child-only arm | |
| ‘Family time’ | We would actually compare on a daily basis . . . we’d be like ‘who’s done the most steps today?’ and you know, ‘oh, you’ve done more than you normally do, [index child]’ or ‘you have done less then you normally do’. So, we were able gauge, ‘oh, it’s been a slow day, why has been it slow day? What have you been doing at school today?’Father 6, family arm |
| We had the planner out the whole time in the kitchen, so it was easier to fill in. [Index child] was involved with it because, at the end of the day, I would say,’ have you written your log?’ And before bed she would have a look and she would write her number down and [father] and I would shout our numbers to her and say, ‘oh this is mine, put mine in’Mother 6, family arm | |
| FRESH website | We pretty much just went on [the website] to log [steps] . . . I think we found that hardest thing, we would fall out over whose going to log [on the website] . . . so that wasn’t that helpful for the family dynamic [laughs]Father 6, family arm |
| Well I’d like to have a leaderboard, that shows everyone doing it and it says, ‘you’ve got to beat this person and their name’, like it says on my football gameBoy 5, child-only armYeah, a family one would be good. That would spur us all on wouldn’t it! It would spur us all on massively, yeahFather 5, child-only arm | |
| Rewards | He enjoyed that [virtual badges], but . . . maybe do a certificate or stickers or something, you know, even if you posted one to them, so they receive the post and we could be like ‘oh yeah, look what you’ve done!’ and . . . especially if you named it to them personally, so they actually got the physical post . . . ‘I’ve got a letter, I get to open that, wow, got my certificate in it!Mother 3, family arm |
Children trying to convey what FRESH was to parents
Delivering school assemblies emerged as an effective strategy for captivating children’s interest in FRESH. The children’s interest in FRESH following assemblies appeared to be the main reason parents expressed interested in participating. However, children struggled, or were unable, to explain to their parents what FRESH involved, which is likely to have had an impact on the likelihood of recruiting the family unit.
Participation would be time-consuming
Parents suggested that one of the main barriers was the perception that participation in FRESH would be burdensome and time-consuming. However, participating parents reported that FRESH participation did not impede their normal daily activities.
Lack of confidence about physical activity
One family said that a major challenge in recruiting families in their county might be a high prevalence of obesity, and they suggested that families would be reluctant to register for a physical activity intervention owing to a lack of confidence.
Reluctance to be measured
It was also confirmed that some family members chose not to participate in FRESH at all because they did want to participate in measurement sessions.
Family focus groups also revealed suggested strategies for improved recruitment. This included a return visit to schools to give parents an opportunity to hear about FRESH and ask questions; exploring recruitment strategies that targeted adults through formal (e.g. employers) or informal settings (e.g. clubs, local fetes, shopping centres); using social media, such as Facebook or Twitter; and providing endorsements from previous participants or familiar organisations.
Intervention feasibility, acceptability, fidelity and optimisation
Feasibility and acceptability of FRESH
All children reported that they liked taking part in FRESH and thought that it was fun. Table 6 shows adults’ overall perceptions of FRESH. Scores were generally positive. In particular, adults agreed that FRESH was fun, encouraged their family to do more physical activity, and made their family more aware of the amount of physical activity they did, which was confirmed in focus groups (see Table 5). Goal-setting also emerged as a major theme, particularly in those randomised to the ‘family’ arm. Participants (adults and children) were aware of the daily step counts required to complete their weekly challenge and were able to identify ways to accumulate additional steps to meet the daily targets (e.g. active travel; see Table 5). Participants also reported receiving socioemotional (e.g. feeling ‘closer’ as a family) and perceived cognitive benefits (e.g. to the index child’s maths ability) as a result of their participation. Last, all six families allocated to the child-only arm demonstrated a clear preference for the whole family to be involved in FRESH. This finding was particularly evident among fathers (see Table 5).
| Overall | Family arm (n = 8 adults) | Child-only arm (n = 6 adults) | |
|---|---|---|---|
| The FRESH study . . . | |||
| . . . was fun for my family and me | 4.2 (0.8) | 4.3 (0.7) | 4.2 (1.0) |
| . . . encouraged my family and me to do more physical activity | 3.9 (0.8) | 4.0 (0.6) | 3.8 (1.0) |
| . . . has led my family and me to do more physical activity than we did before FRESH | 3.5 (1.0) | 3.6 (0.7) | 3.2 (1.3) |
| . . . has led my family and me to do more activities (other than physical activity) together than we did before FRESH | 3.4 (0.7) | 3.3 (0.7) | 3.5 (0.8) |
| . . . has made my family and me more aware of the amount of physical activity we do | 4.6 (0.5) | 4.7 (0.5) | 4.6 (0.5) |
| . . . is something my family and I would like to continue to be part of | 3.8 (1.3) | 4.3 (0.8) | 3.4 (1.5) |
| Regarding ‘family time’, to what extent do you agree or disagree with the following? | |||
| It was easy to schedule ‘family time’ | 3.1 (1.1) | 3.1 (1.4) | 3.1 (0.8) |
| My family consistently scheduled ‘family time’ | 3.1 (1.2) | 3.1 (1.4) | 3.2 (1.0) |
| My child reminded us about ‘family time’ | 2.9 (1.6) | 3.0 (1.7) | 2.7 (1.5) |
| My child led/initiated ‘family time’ | 2.6 (1.4) | 2.7 (1.5) | 3.0 (1.5) |
| Regarding the FRESH website, to what extent do you agree or disagree with the following? | |||
| It was easy to use | 3.6 (1.3) | 3.6 (1.4) | 3.5 (1.4) |
| I enjoyed using it | 3.6 (0.9) | 3.6 (1.1) | 3.7 (0.8) |
| My child/children enjoyed using it | 4.0 (1.2) | 3.9 (1.3) | 4.2 (1.0) |
| I thought the website was appealing | 3.7 (0.9) | 3.6 (0.8) | 3.8 (1.0) |
| I liked that there were varying degrees of difficulty with the challenges | 4.3 (0.9) | 4.3 (1.1) | 4.3 (0.8) |
| I enjoyed the information about the cities | 3.9 (1.1) | 3.6 (1.3) | 4.3 (0.8) |
| My child/children enjoyed the information about the cities | 3.8 (1.1) | 3.4 (1.3) | 4.3 (0.8) |
| The step converter was useful (e.g. converting swimming to steps) | 3.3 (1.3) | 2.8 (1.2) | 4.0 (1.2) |
| The resources page was useful | 3.2 (1.1) | 3.0 (1.2) | 3.5 (1.0) |
| I enjoyed the recipes | 3.3 (0.9) | 3.1 (1.1) | 3.5 (0.8) |
| My child/children enjoyed the recipes | 3.4 (1.0) | 3.1 (1.1) | 3.7 (1.0) |
| Logging our steps was easy | 3.7 (1.5) | 3.9 (1.7) | 3.5 (1.4) |
| Regarding the step counter we gave out to log your steps, to what extent do you agree or disagree with the following? | |||
| I didn’t mind wearing it | 4.0 (1.2) | 4.0 (1.2) | N/A |
| My child/children didn’t mind wearing it | 3.9 (0.9) | 3.9 (1.1) | 4.0 (0.6) |
| It was easy to use | 4.5 (0.7) | 4.6 (0.5) | 4.3 (0.8) |
| I thought it was reasonably reliable at counting steps | 4.3 (0.7) | 4.6 (0.5) | 3.8 (0.8) |
| I used the memory feature to go back and look at the number steps my family and/or I took | 4.6 (0.5) | 4.6 (0.5) | 4.5 (0.5) |
Intervention acceptability and fidelity
Kick-off meeting
Using a five-point Likert-scale (1 = strongly disagree, 5 = strongly agree), all families felt that the ‘kick-off’ meeting was useful (family vs. child only: mean 4.4, SD 0.8, vs. mean 4.5, SD 0.8) and appreciated the fact that it was a face-to-face meeting as opposed to a telephone or video meeting. Most families felt that they had enough technical support (mean 3.9, SD 1.5; mean 4.2, SD 1.0), and the majority of families stated that a single meeting was enough for them to understand the protocol and how to use the intervention website and materials. However, two families would have liked a follow-up meeting the following week.
‘Family time’
Overall, adults disagreed that children led or reminded them of ‘family time’ (see Table 6). In line with the adult data, the majority of children did not view themselves as their family’s team captain to lead on ‘family time’. Several children said that they forgot they were team captain or they could not be bothered to be the team captain. There was also evidence to suggest that some parents took over the team captain role.
Overall, adults reported that it was not particularly easy for their family to schedule ‘family time’ or to have it consistently. Most families claimed they either rarely or never had ‘family time’. A lack of time was the most commonly cited challenge to having ‘family time’. In addition, some parents’ work schedules (i.e. shift work) made it difficult to organise ‘family time’ with all family members present. However, focus group evidence shows that some families were discussing physical activity in a manner that would have been unlikely prior to FRESH (see Table 5).
Generally, families used their action planners only to log daily step counts and not to plan weekly activities or anticipate barriers to meeting step goals. Most families preferred to write their step counts out on their paper-based action planners and transfer them to the FRESH website once, near the end of their weekly challenge (see Table 5).
FRESH website
Compared with the child-only arm, the family arm exhibited greater website engagement, as they travelled to more cities (mean 36, SD 11, vs. mean 13, SD 8) and failed fewer challenges (mean 1.5, SD 1, vs. mean 3, SD 1). All children in the family arm and most (≈ 80%) children in the child-only arm wanted to continue using the FRESH website. Children in the family arm also found it easier to use the website than those in the child-only arm (83% vs. 60%). Overall, adults’ mean scores were generally positive in relation to the FRESH website (see Table 6), although more critical opinions were voiced during the focus groups. For the majority of families, the extent of their website engagement entailed selecting challenges and logging steps, which was normally a task performed reluctantly by parents (see Table 5). Many adults and children were unaware of or had not used several of the website elements (e.g. step calculator, parent resources, virtual rewards). Others stated that children had been interested in the website (e.g. information about cities) but that their interest wore off and only an interest in accumulating steps remained.
Technical issues arose with the website, particularly with the algorithm that calculated the number of steps that families needed to accumulate to complete their challenge. This might have negatively affected some participants’ experiences. Aside from technical bugs that needed resolving, families provided input on other potential improvements that could be made to the website. Almost unanimously, families wanted an element of competition on the website. It was evident from numerous focus groups that within-family competition occurred throughout the intervention period. However, the ability to compete against other families was also suggested in several focus groups (see Table 5). Other suggested website improvements included (1) adding a step history page to enable families to view progression over the intervention period; (2) providing more feedback/praise from the research team; (3) providing more flexibility in challenge destinations; (4) sending a text or e-mail reminder to log steps, and (5) improving the website design.
Pedometers
Overall acceptability of the pedometers was high among adults in both arms (see Table 6). Generally, adults stated that it became ‘routine’ or ‘second nature’ to wear pedometers, although some would have preferred wrist-worn pedometers. The most frequently cited reason children gave for wanting to participate in FRESH was to receive a pedometer. Families reported that there were few settings where children were not allowed to wear their pedometers, with the most cited setting being during physical education. Wearing the pedometer was more acceptable to children in the family arm than to those in the child-only arm (≈ 80% vs. 60%).
Rewards
Overall, parents moderately agreed that their child enjoyed receiving virtual rewards (mean 3.5, SD 1.2), with slightly higher scores in the child-only arm than in the family arm (mean 3.8, SD 1.0 vs. mean 3.1, SD 1.3). Children’s responses in the focus group generally supported parents’ perceptions that the virtual rewards were not particularly of long-term interest to them. Most parents suggested that a small, tangible reward, such as a posted certificate or stickers, would appeal to their child more than a virtual reward. Other suggestions included vouchers, clothing or equipment that encouraged physical activity (see Table 5).
Risk of contamination
Focus groups revealed that children were aware of other FRESH participants in their school and that some families did indeed communicate among each other about FRESH, with some even revealing their allocated condition. One family allocated to the child-only arm disclosed that they had purchased a set of pedometers.
Findings related to feasibility of outcome evaluation
Data collection took a mean of 91.1 (SD 27.7) minutes per family at baseline and 77.1 (SD 24.5) minutes per family at follow-up. Overall, adults disagreed that there were too many measures and that data collection took too long. All children self-reported that they ‘liked’ being measured. With the exception of accelerometer/GPS and step test assessment (one refusal each), all participants completed all measures at baseline. At follow-up, 91% of participants accepted an accelerometer/GPS and completed the step test; 94% of participants completed all other measures.
At baseline, mean valid accelerometer wear time was 851.5 (SD 54.1) minutes for adults and 755.7 (SD 29.7) minutes for children. At follow-up, mean wear time was 843.1 (SD 78.6) for adults and 742.3 (SD 56.4) for children. The GPS provided a location for a mean of 750.6 (SD 191.4) (adults) and 646.2 (SD 189.0) (children) minutes at baseline and for a mean of 720.0 (SD 237.6) (adults) and 586.8 (SD 262.8) (children) at follow-up. Valid data (600 minutes) on ≥ 4 days (including one weekend day) was available for 83% of adults at both baseline and follow-up; this was slightly lower for children, at 75% and 67%, respectively. A visual inspection of wear-time data revealed a tendency for children to remove their devices at around dinner time, for parents to remove their devices after their child had gone to bed, and for families to put on their devices much later in the day at the weekend than on weekdays.
An initial assessment of family functioning via the video-recorded Fictional Family Holiday activity showed poor to moderate data quality, as discussions were limited and cursory. Three factors may have affected data quality: (1) most families enrolled were dyads, limiting opportunities for whole-family discussion; (2) providing families with a planner to write out their itinerary may have shifted the emphasis away from open-ended discussion; and (3) the activity was completed at the end of the visit, when participants may have been fatigued from data collection.
The physical activity-related expenditure questionnaire developed for this study appeared to have appropriate face validity and was capable of providing rich data related to membership fees and subscriptions (e.g. for sports clubs, fitness centres, after-school clubs) and sports equipment (e.g. sportswear, gadgets).
Chapter 4 Lessons learned from the FRESH feasibility study
Parts of this chapter are reproduced with permission from Guagliano et al. 78 © The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The text below includes minor additions and formatting changes to the original text.
The FRESH feasibility study described in Chapters 2 and 3 provides a response to calls for the need for innovative interventions targeting young people and families. 76 To our knowledge, FRESH is among the first physical activity interventions to specifically target whole family engagement, helping to create supportive, synergistic environments for the promotion of healthy behaviours and long-term change. 29,57,59 We assessed the feasibility and acceptability of the FRESH intervention and accompanying evaluation to inform future research. Our findings showed that it was feasible and acceptable to deliver and evaluate a family-targeted physical activity promotion intervention with generally high acceptability from participating families. This feasibility study, however, also revealed areas for improvement.
Optimising recruitment
Previous literature has identified family-based recruitment as being particularly difficult. 44,112 Our formative work30 and other studies (see a review by Morgan et al. 52) recommend a multifaceted recruitment strategy in family-based research. Owing to unforeseen delays, we were unable to employ our planned multifaceted recruitment strategy, which likely contributed to our under-recruitment of families (60% of targeted 20). Of the families enrolled, only one-third included all family members. There was some suggestion that this may have been because of either a lack of confidence in physical activity or a reluctance to be measured. Improved messaging is, therefore, required early in the recruitment process to reassure low-active families, and individual family members, that FRESH is tailored to their activity levels and to highlight that they have the option of opting out of (parts of) the measurements. Allowing family members to be involved in the intervention, regardless of their participation in the evaluation, as was done in FRESH, may improve effectiveness and long-term behaviour change. 44,55,56,59
Interestingly, our findings showed that fathers appeared to be interested in participating in FRESH, but only 5 out of 28 expressions of interest were initiated by fathers. This may be because, among heterosexual parents, tasks such as making telephone calls (e.g. to express interest) or family event preparation (e.g. study participation) are more likely to be performed by mothers than fathers. 113 Therefore, recruiting whole families, whereby any parent can initiate an expression of interest, may be an important catalyst for the inclusion of more fathers in family-based research.
Other key areas of improvement to recruitment include optimising the conversion from children reached to families expressing an interest (e.g. extending the age range of index children to cover the whole of UK Key Stage 2 (Years 3–6, covering ages 7–11 years); reducing the burden on children to explain FRESH to their parents (e.g. by directing parents to a video); targeting adults directly via community- and employer-based recruitment or social media; and obtaining recruitment support from local organisations.
Optimising the FRESH intervention
FRESH was designed as a goal-setting and self-monitoring intervention, aimed at increasing family physical activity. Encouragingly, these behaviour change techniques resonated with most families and align with recommendations to increase family physical activity. 29 Participants reported being aware of what their daily step goals needed to be in order to complete their weekly challenges. Interestingly, the challenge context did not seem to be important to participating families (i.e. choosing challenge cities to walk to virtually). Instead, focus group interviews revealed that meeting daily step goals, completing weekly challenges and intrafamily competition appeared to be the key drivers motivating families throughout the intervention period.
We found that families did not implement all of the intervention components as intended, and strategies may be needed to improve intervention delivery and families’ fidelity to the intervention protocol. For instance, most families did not select new challenges on the FRESH website together during ‘family time’, and families used their action planners only to log their steps and not to also identify family activities or upcoming challenges for the week ahead. This may be resolved by the facilitator placing a greater emphasis on ‘family time’ and helping the family to schedule this at the ‘kick-off’. Facilitators are critical to the delivery of interventions, and a recent review found that facilitators have an important moderating influence on the effectiveness of any programme. 114 Ongoing follow-up with the facilitator would also support this. Other strategies to improve intervention fidelity include sending e-mail reminders to log steps, adding competition elements to the website (e.g. a leaderboard), providing more regular feedback/praise from the research team, and including small, tangible rewards.
Although the FRESH intervention was well received overall, in our focus groups it was evident that families, and in particular fathers in the child-only arm, would have preferred to have their whole family involved in FRESH. Consideration, therefore, should be given to discontinuing the child-only arm. Furthermore, the finding that fathers were particularly interested in having their whole family participate in FRESH is noteworthy. Fathers have an independent influence on their children’s health and development115 and are an important influence on children’s physical activity,116–118 but they are very under-represented in family-based interventions. 119 Fathers’ engagement with FRESH is consistent with recent evidence that fathers are more willing to participate in family-based interventions when the focus is on their children,120 and as a result reported newfound enjoyment for family-based physical activity and a desire to be a positive role model. 121 The online delivery of FRESH may have also appealed to some fathers. 120
Optimising measurement
The duration of data collection at both time points was in line with our estimates, and acceptability of the duration and number of measures was high among both adults and children. Nevertheless, the duration of the data collection process may have acted as a barrier to participation. Minor adjustments are needed to improve the quality of data from the Fictional Family Holiday, and monitor wear time. For example, for the Fictional Family Holiday paradigm, a greater emphasis on recruiting whole families, removal of the written aspect of the activity and shifting the order of measures, so that the assessment occurs earlier during data collection, might improve the quality of the family functioning data. To improve monitor wear time, emphasis should be placed on participants wearing the monitors for as long as possible from the time that they wake up until the time that they go to sleep, as opposed to going by their children’s bedtime. In addition, reminders (e.g. e-mail, telephone) could improve wear time,122 particularly at the end of the week to improve weekend wear.
Study strengths and limitations
This study is among the first physical activity interventions that aim to target and measure whole families, providing novel evidence in an area where more primary research is needed. 76 The phased approach of assessing feasibility and acceptability to inform refinement for pilot study is in accordance with established guidelines. 86 Public involvement was used extensively to inform development and refinement of FRESH, as suggested previously. 123,124 Furthermore, our use of a mixed-methods design provides unique insight and context for our quantitative findings, assisting in identifying strategies to further optimise FRESH. Limitations include that we were unable to fully employ our recruitment strategy and did not have the opportunity to test the efficacy of recruiting families through community-based recruitment. In addition, only one-third of families enrolled in FRESH included all family members.
Conclusions FRESH feasibility study
This study demonstrates feasibility and acceptability of the family-targeted FRESH intervention and provides valuable suggestions for further optimisation. This work informs a future pilot trial testing the impact of these adaptations and the preliminary effectiveness of FRESH on family physical activity. The findings of our upcoming pilot trial will inform sample size/power calculations for a future definitive trial, should the pilot study findings suggest that a definitive trial is warranted.
Chapter 5 Trial design and methods for the FRESH pilot trial
Parts of this chapter are reproduced with permission from Guagliano et al. 125 © Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY. Published by BMJ. This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter are reproduced with permission from Guagliano et al. 126 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Introduction
The feasibility study described in Chapters 3 and 4 was among the first physical activity interventions to specifically target whole family engagement. The findings showed that it was feasible and acceptable to deliver and evaluate a family-targeted physical activity promotion intervention with high acceptability from participating families. However, as described in Chapter 4, multiple areas for further improvement of the intervention and its evaluation procedures were identified. This chapter describes the protocol of revised FRESH interventions and evaluation, evaluated in a pilot randomised controlled trial (RCT).
The primary aim of the FRESH pilot trial was to assess the feasibility and acceptability of the revised recruitment strategy, intervention and outcome evaluation. The secondary aims were (1) to explore the preliminary effectiveness of the intervention on potential outcomes of interest and (2) to assess whether or not prespecified criteria were sufficiently met to warrant progression to a full-scale definitive trial.
Trial design
The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT)80 was used to guide the reporting of this study. We also used TIDieR81 to guide our description of the intervention. All protocol amendments from the FRESH feasibility study described below were made following consultation with the FRESH SSC and the funder (the NIHR Public Health Research programme).
The FRESH pilot study was a three-arm, parallel-group, randomised controlled pilot trial using a 1 : 1 : 1 allocation ratio with follow-up assessments at 8 and 52 weeks post baseline (Figure 6). Following baseline assessment, families were randomly allocated to one of three arms: (1) FRESH arm, (2) pedometer-only arm or (3) no-treatment control arm. All family members in the pedometer and FRESH arms received pedometers and generic family physical activity promotion information. The FRESH arm additionally received access to the intervention website. Those in the control arm were asked to carry on as normal.
FIGURE 6.
Flow chart of process of the FRESH pilot study.

Participants
Families were deemed eligible to participate in this study if there was consent from at least one child in school years 3–6 (aged 7–11 years, hereafter referred to as the index child) and at least one adult responsible for the index child. The adult had to live with the index child in the main household (i.e. the index child’s primary residence as indicated by the parent). No restrictions were placed on family type (e.g. single parent, shared parenting, inclusion of extended family living in the main household) and there was no maximum number of participants per family. If requested, we also enabled the inclusion of parents or siblings who lived outside the main household, or extended family members (e.g. grandparents) living in or outside the index child’s main household. All participants needed to be able to perform light-intensity physical activity (e.g. walking), have access to the internet and understand the English language sufficiently well to provide informed consent. Family members were able to take part in the intervention irrespective of their participation in the accompanying evaluation and vice versa. Exclusion criteria related to participation in specific assessments are outlined below.
The eligible age range of the index child was expanded to reflect the age range of children attending Key Stage 2 in UK primary schools, which meant that all children attending assemblies about the FRESH project were eligible to take part.
Setting
Families were initially recruited from rural Norfolk and Suffolk, counties in East Anglia, UK (see Figure 3). Norfolk is 2074 square miles in size and had a total estimated population of 898,400 in 2017 (most recent estimate)82 and Suffolk is 1466 square miles and had a total estimated population of 756,978 in 2017 (most recent estimate). 127 According to Norfolk and Suffolk County Councils,128,129 approximately 53% and 42% of the Norfolk and Suffolk populations, respectively, are classified as living in a rural area. Based on the Office for National Statistics84 classification, ‘rural’ will be defined as having a postcode falling in a small town, village, hamlet or dispersed settlement. In both counties, existing inequalities have been identified, including physical activity, obesity and other indicators of child ill health, school readiness and attainment. 24,26,130 Following recruitment challenges, the requirement for participating families to live in a rural location was dropped after consultation with, and approval from, the FRESH SSC and the funder.
Recruitment
To overcome the challenges encountered in the FRESH feasibility study, in the pilot study we used a multifaceted recruitment strategy, including targeting adults (parents) directly, and messaging that focused on the wider benefits of research participation (e.g. spending more time together as a family) as opposed to solely focusing on increasing physical activity or obesity prevention. 30 Recruitment was scheduled to be undertaken over an estimated 3 months (with a recruitment rate of ≈ 20 families per month), using two main strategies that target adults and children, as summarised in Figure 7. The first strategy involved recruitment in the school setting and the second in employer-based and community-based settings (e.g. Brownies/Cubs, community centres, GP surgeries). Alternative recruitment settings were also explored (e.g. online/traditional media) as needed, following the same procedure as in the second strategy. For logistical purposes, we aimed to find recruitment settings located roughly within an hour’s drive of Cambridge, UK.
FIGURE 7.
Overview of recruitment methods in the FRESH pilot RCT.
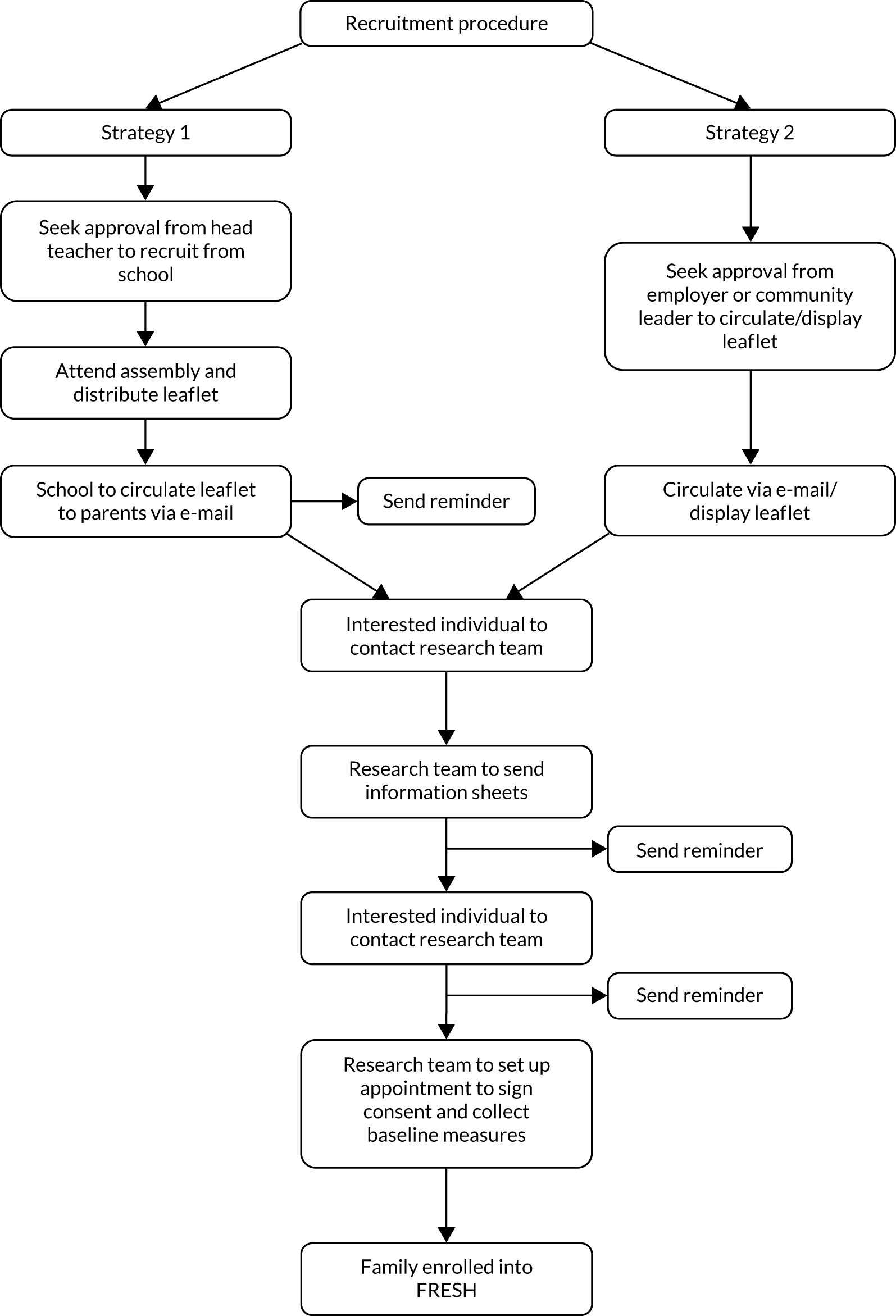
Recruitment protocol
To recruit schools, employers and community-based organisations, we first contacted those in leadership positions (e.g. head teachers, human resources, health and well-being leaders, heads of community-based organisations). An information pack detailing the purpose of the study and all procedures was included in our correspondence with the individual identified. This included a link to a recruitment video, which was developed with families following the suggestion of participants in the FRESH feasibility study (URL: www.youtube.com/watch?v=UxUHN1JsjUM; accessed 19 July 2021, also see below). For school-based recruitment, verbal or written approval was sought from the school to send home study leaflets with children, to circulate our leaflet to parents online, and to send an online reminder to parents approximately 2 weeks later. We also sought permission to present the study to Key Stage 2 students (Years 3–6; aged 7–11 years) at a scheduled school assembly. Similarly, for employer- and community-based recruitment, we sought approval to circulate our study information to employees or members either online or as a hard copy. In all cases, similar to the feasibility study, interested parents were asked to express their interest by contacting the study team by e-mail or a free-to-call telephone number, after which eligibility was assessed and further detailed study information was e-mailed. A baseline assessment appointment was made with families who were still interested in participating. Written informed consent was obtained for all participating adults and written parental consent and child assent was obtained for each participating child during this appointment, prior to the baseline assessments.
To inform the assessment of the progression criteria (see Chapter 1, Progression criteria), recruitment success and rate were monitored closely by the study team. Information was tracked regarding source of recruitment, conversion from expressing interest to participation, the family member expressing interest, and the number and type of family members participating.
Retention
To encourage retention, we remained in regular contact with all participating families (through the intervention website, newsletter/holiday cards), and offered measurement incentives and study feedback. Each individual participant (adults and children) received a £5 voucher on return of the accelerometer and GPS monitors at each measurement time point (maximum £15 per participant over 1-year follow-up). To inform assessment of the progression criteria (see Chapter 1, Progression criteria), retention was monitored closely by study group and demographic characteristics to observe whether or not differences in retention occurred.
Randomisation
Randomisation occurred after the baseline assessments were completed; the unit of randomisation was at the family level (i.e. the index child and all participating family members). Families were randomised in blocks of six by an independent statistician using a computer-generated algorithm produced with Stata version 14 and stratified by county (i.e. Norfolk or Suffolk). This strategy ensured that families were randomised to the three different groups at an equal rate, and that similar numbers of families were allocated to each arm within the two counties. The random allocation sequence was implemented via a database created in-house on Microsoft Access by independent data management staff. A study co-ordinator used the database after baseline to determine which study arm a family was allocated to. No one directly involved in the evaluation had access to the allocation code or complete sequence.
Interventions
FRESH arm
As in the FRESH feasibility study, the intervention the FRESH arm received is primarily a goal-setting and self-monitoring intervention, delivered online, aimed at increasing physical activity in whole families. The intervention used concepts from the SEM40 and family systems theory85 and operationalised constructs from SDT61 to inform behaviour change strategies. The full FRESH logic model can be found in Figure 8.
As in the feasibility study, 1 week after baseline measures, each family allocated to the FRESH arm had an hour-long kick-off meeting, which took place in the family home with a facilitator (who was a member of the study team). The facilitator introduced families to the intervention components and the accompanying materials (e.g. family action planner) and distributed pedometers. In the pilot study, families also received their first of four pieces of generic walking information, similar to the pedometer-only arm (described in Protocol for pedometer and control families). The main goals of this meeting were to familiarise families with the intervention website and their pedometers and to prompt weekly ‘FRESH time’ meetings (described in Table 1; rebranded from ‘family’ time, following feasibility evaluation) during which they were to complete their action planners and select a new challenge city to ‘walk to’ on the FRESH intervention website. All families received a follow-up telephone call 1 week after their kick-off meeting so that they could discuss any issues and ask any clarifying questions. Participant-initiated distant support continued to be available, whereby participants could contact the research team with questions or to report issues (e.g. website bugs, pedometer issues).
Table 7 provides a detailed description of the FRESH pilot intervention components and highlights where changes were made from our feasibility study. In each family, the index child (or children, if multiple) were designated ‘team captain(s)’, which involved taking the lead in selecting challenges and uploading steps online. Evidence suggests that children may act as change agents to elicit changes to the psychosocial environment;29 therefore, promoting the index children to the role of family ‘team captain(s)’ may strengthen child buy-in and perceived autonomy, and improve intervention fidelity. All family members were given pedometers with instructions to wear them for as long as possible daily so that their steps would be captured during challenges. The team captain(s) led weekly ‘family time’ meetings. During these meetings, families completed family action planners and accessed the FRESH website, which enabled them to choose weekly step challenges. Family action planners prompted families to plan weekly family physical activities to help them meet their step challenge for a given week. It was intended that families would plan activities they would do together; however, participants had the flexibility to also set individual goals. The action planners also prompted families to monitor weekly step counts, and discuss any potential upcoming barriers for physical activity and strategies to overcome them. Pedometers are simple to use, convenient and associated with effective interventions for increasing parent–child physical activity. 131
| Intervention components | Dose | Description | Behaviour change techniques | Targeted SDT constructs | Hypothesised mediators |
|---|---|---|---|---|---|
| 1. ‘FRESH time’ | Minimum once per week, 10–21 minutes | ‘FRESH time’ was expected to provide a weekly (at minimum) opportunity for index childrena and family members to review, revise, and update their family action planners. Family action planners prompt families to plan PA, monitor weekly steps, discuss any potential upcoming PA barriers and strategies to overcome them. Index children will be allocated as their family’s ‘team captain’ leading in challenge selection and uploading steps on the FRESH website |
Goal-setting Self-monitoring Positive feedback on progress Social support Praise Positive reinforcement |
Perceived competence Perceived relatedness Perceived autonomy |
Social support Family social norms for PA PA awareness Basic needs satisfaction PA motivation |
| 2. FRESH website | Minimum once per week, 5–20 minutes |
The FRESH website provided a place for families to self-monitor their step counts and set goals by selecting challenges of varying difficulty. Specifically, the website allowed families to ‘walk’ around the world by choosing one of three target cities to ‘walk to’ weekly. The challenges were framed as easy, moderate or hard, which represented a 0%, 5% or 10% increase, respectively, relative to the average steps they took in preceding weeks. Once adults and children accumulated an average of 10,000 and 12,000 steps per day, the step challenge increases were reduced to 0%, 2.5% and 5%, respectively Families also had access to:Families with an ongoing challenge received e-mail reminders to log steps 3 days and 1 day before an impending challenge ends |
Goal-setting Self-monitoring Positive feedback on progress Rewards |
Perceived competence Perceived relatedness Perceived autonomy |
Social support Family social norms for PA PA awareness Basic needs satisfaction PA motivation |
| 3. Pedometry | Throughout intervention (8 weeks) | All family members received pedometers to enable self-monitoring and provide immediate feedback. To allow families to view their progress towards their proximal and distal step goals, they were encouraged to log their steps on the FRESH website and/or in the family action planners |
Self-monitoring Immediate feedback |
Perceived competence Perceived autonomy |
Social support Family social norms for PA PA awareness Basic needs satisfaction PA motivation |
| 4. Competence reinforcement/rewards | Approximately once per week (8 weeks) |
After completing a challenge or if the challenge week ended, to praise effort (i.e. competence reinforcement) children received personalised supportive letters in the post and messages on the FRESH website They also received small online and tangible rewardsChildren received two to four passport stamps/cards for completed challenges (i.e. as difficulty increased, more stamps were awarded) and one passport stamp/card for an incomplete challenge |
Feedback on progress Rewards |
Perceived competence |
Basic needs satisfaction PA awareness |
After a challenge week was over, whether or not a family had completed their challenge, they received personalised competence reinforcement messages praising their effort online. In response to the feedback from the feasibility study, reinforcement messages were also sent in hard-copy letters (addressed and mailed to all participating children in the family). In addition, both online and tangible rewards were given to participating children after a challenge week. The tangible rewards were sent to each participating child in the family and consisted of playing cards representing the cities the families had visited, which could also be used to play rock, paper, scissors. If a family did not complete a challenge, they still progressed to a hidden city along their challenge route, as opposed to the city they had chosen, and received the accompanying reinforcement message and reward, as described above. In the pilot study, we also implemented reminders as requested by some families in the feasibility study: families with an ongoing challenge would receive e-mail reminders to log steps 3 days and 1 day before a challenge ended. After every challenge week, the above cycle would be repeated, starting with the next ‘FRESH time’ meeting. Following the assessments at 8 weeks post baseline, families retained access to the website and their pedometers, and were able to continue using these for as long as they liked. There was also continued support in terms of website updates (e.g. leaderboard and parental resource updates) and participants continued to receive competence reinforcement letters and rewards.
Protocol for pedometer and control families
Following less positive feedback during the FRESH feasibility study, the study team decided to drop the child-only arm (see Chapter 4). In consultation with the FRESH SSC, the study team decided to replace this with a pedometer arm to assess whether or not access to the FRESH website provided additional benefits over and above family pedometer-wear. Families allocated to the pedometer arm were mailed pedometers and the same generic family physical activity promotion information as FRESH families received. This information was produced by Walk4Life, a sub-brand of Change4Life (www.nhs.uk/change4life). Information continued to be e-mailed to families (in the pedometer and FRESH arms) fortnightly on four occasions. The information provided families with tips to get walking daily and games that can be played while walking.
Control families were asked to carry on as normal and did not receive access to the intervention website, pedometers or any generic information.
Outcome evaluation measures
Table 8 outlines a summary of the measures taken as part of the FRESH pilot study, including the order of assessments and the estimated duration of each prior to data collection. Data collection was carried out by two trained research staff and occurred in participating families’ homes. Outcomes were assessed at baseline (prior to randomisation; April–August 2018), at 8 weeks post baseline (June–November 2018) and at follow-up (52 weeks post baseline; May–October 2019) for all consenting family members.
| Measure | Duration |
|---|---|
| Anthropometric measures (height, weight, waist circumference) | 5 minutes per person |
| Questionnaire | 20 minutes per family |
| Blood pressureb | 10 minutes per person |
| Step test (aerobic fitness) | Preparation: 5 minutes per person |
| Test: 10 minutes per family | |
| Accelerometer and GPS explanation | 5 minutes per family |
| Fictional Family Holiday (family functioning) | 10 minutes per family |
| Total duration of baseline measurement session (includes consent/assent process) | 120 minutes |
| Total duration of subsequent measurement sessions | 105 minutes |
Accelerometer and global positioning system assessment protocol
To assess physical activity, a similar protocol to that applied in the feasibility study was used. All participants were asked to simultaneously wear an ActiGraph GT3X+ triaxial accelerometer (ActiGraph LLC; Pensacola, FL, USA) and a QStarz Travel Recorder BT1000X GPS monitor [QStarz; Taipei, Taiwan (Province of China)]. The accelerometer was initialised to record data at a sampling rate of 50 Hz, and the GPS was set to record a location every 10 seconds. Participants were instructed to wear the devices on each hip during waking hours for 7 consecutive days. Following evaluation of the feasibility study data, participants were clearly instructed to wear the monitor during their waking day to maximise wear. All monitors were picked up by a member of the study team or mailed back in a prepaid envelope.
Defining participant physical activity
For accelerometer data, a valid week was defined as a minimum of 420 minutes per day from 3 days (including 1 weekend day) over the 7-day measurement period. Non-wear was defined as ≥ 90 minutes consecutive zeros using the vector magnitude. Raw accelerometer counts were downloaded and integrated into 5-second epochs to enable application of prespecified cut-off points. Evenson et al. 132 cut-off points have been recommended for estimating physical activity intensity in youth90,133 and Troiano et al. 134 cut-off points have been recommended for this in adults; these cut-off points were used in this study.
Defining family co-participants in physical activity
A novel methodology was developed to establish times when family members were physically active in each other’s proximity. Data from the accelerometers were downloaded and interpolated to a 10-second epoch using the ActiLife software. Data from the GPS devices were downloaded and entered into the ArcGIS v10.3 (Esri Inc., Redlands, CA, USA) Geographical Information System, and then longitude and latitude values were converted to easting and northing values, respectively, in accordance with the British National Grid co-ordinate reference system. 135
The accelerometer and GPS data were then integrated based on their date and time stamps using bespoke software written in Java. After the accelerometer and GPS data had been matched, data points that had a time difference of ≤ 30 seconds between the accelerometer time stamp and that of its matched GPS location were considered valid for inclusion in the study. Matched data points with a time difference greater than this, for example where the GPS had been switched off or had lost signal, were considered as missing location information because the participant might have moved to a new unrecorded location since the last locational data were available. The data were also cleaned to remove GPS locations with low location confidence, in accordance with the protocol of Schipperijn et al. 136 This resulted in the removal of just 0.8% of data points.
All accelerometer-derived measures of physical activity were calculated for valid days (i.e. those on which there were at least 10 hours’ wear time). To maximise the available data, participants with at least 1 day of valid wear time for the accelerometer were included for analysis. As it was not possible to differentiate times when the GPS had no signal because it was indoors from times when it had no signal because it had been switched off, no minimum wear-time requirements were set for the GPS.
Periods when the accelerometer was continuously recording zero acceleration for ≥ 90 minutes were excluded from analysis, as these were considered to be times when the accelerometer was not worn. 137 The remaining data points were then classified into four physical activity intensity categories (sedentary, light, moderate or vigorous activity), using the widely adopted Evenson et al. 132 cut-off points for children and the Troiano et al. 134 cut-off points for adults. These categories were then used to generate a binary variable for every child and adult that indicated whether or not they were undertaking light, moderate or vigorous physical activity (LMVPA) during any given 10-second interval. We focused on LMVPA rather than solely higher-intensity activity to ensure that we captured a range of activities from walking to more vigorous ones such as running.
To compute individual measures of time spent with and without other family members present, a script was written in Stata (version 16; StataCorp LLC, College Station, TX, USA) that calculated the straight-line distance between each participant and every member of their family for all 10-second intervals, based on each participant’s easting and northing locations. This produced a matrix that depicted the straight-line distance in metres between all possible family dyad combinations. This matrix was then used to compute a binary variable for every child and adult that indicated whether or not they were located within ≤ 50 m (which was taken as indicative of being at the same location) of other members of their family during any given 10-second interval. A distance of ≤ 50 m was selected because this is approximately equivalent to a ball court (e.g. tennis, basketball) or a large residential garden. 138
Finally, we generated measures for each participant of the time they spent undertaking LMVPA in the same location as other members of their family. This was computed for all possible family dyad combinations by summing the binary variables for LMVPA for each pair of family members along with the binary variable indicating whether the pair were within the target distance of ≤ 50 m, with the resulting variable indicating for any given 10-second interval whether or not the family was were being physically active in the same location. For each participant, all times spent doing dyad-based LMVPA were summed to obtain the outcome measures used.
Health outcomes
Aerobic fitness was measured using an 8-minute submaximal step test (with 2-minute rest), which provides an individual calibration of heart rate to work rate (energy expenditure per unit time) to predict a fitness estimate of a participants’ heart rate recovery index. 93,139 Children outside the age range for eligible index children (i.e. aged < 8 years) were excluded from the aerobic fitness test. To improve measurement efficiency, the study team conducted the step test with up to four family members simultaneously, using a maximum of two steps.
Height and weight were measured once with a Leicester portable stadiometer and a Seca 877 digital scale, respectively. Waist circumference was measured at least twice, using a non-elastic tape measure. A third measure was taken if the first two measures differed by ≥ 3 cm, and the mean of these measures was used in analyses. BMI was calculated [(height in cm)/(weight in kg)2], and converted into age- and sex-specific percentiles using standard growth charts for participants aged < 18 years using LMSgrowth Program.
Behavioural and psychosocial measures
Behavioural and psychosocial measures were assessed using questionnaires distributed to adults and children (participants aged ≤ 4 years did not complete questionnaires). The questionnaires were largely unaltered from the feasibility study (see Table 3). These measures included adult and child screen-use time;95–98 quality of life;99–102 family co-participation in physical activity;98 physical activity awareness;103,104 family social norms for physical activity;105,106 family support;105 children’s and adult’s motivation for physical activity;107,108 and children’s perceived autonomy, competence and relatedness. 108
Family functioning
The Fictional Family Holiday Paradigm was used to assess family functioning via family relationships109 and connectedness. 110 In this observational paradigm, each family was asked to spend 10 minutes planning and discussing a week-long holiday itinerary with unlimited budget. The video-recorded activity was then transcribed and coded by two to four trained research assistants per time point for ‘power sharing’ (i.e. taking turns); positive talk (e.g. expressions of amity, elicitation of family members’ viewpoints, agreement, compromise)110 and discussions that revolve around physical activity.
Family out-of-pocket expenditure for physical activity
Physical activity-related expenditure for each family member was collected using a questionnaire that was developed and refined following our feasibility study. 78 Refinement focused on amending the layout of the questionnaire to improve ease of completion. The questionnaire comprised two questions about expenditure related to membership fees and subscriptions (e.g. for sports clubs, fitness centres) and sports equipment (e.g. sportswear, gadgets) and was completed by the same adult at each time point for their whole family. Baseline expenditure covered the 3 months prior to study participation. At the follow-ups, participants were asked to record their expenditure during the first 8 weeks of the study and then until 1 year after randomisation.
Process evaluation
A mixed-methods process evaluation was conducted after assessments 8 weeks post baseline. Using open-ended and four-point Likert-scale questions (with 1 = strongly disagree and 4 = strongly agree), adults self-reported their overall opinion of FRESH, the intervention components (FRESH arm only; Pedometer arm adults responded to pedometer-related questions only) and the measurements and suggestions for improvement. Children also self-reported on the above topics, responding to dichotomous ‘yes/no’ questions. In addition, semistructured focus groups were planned to be conducted online with 10 out of 20 FRESH arm families and 5 out of 20 families from each of the other two arms (i.e. pedometer and control). Focus groups focused on families’ experiences of taking part in the trial, perceived acceptability of individual intervention components, intervention fidelity, challenges/barriers encountered and suggested improvements, as appropriate based on study arm allocation. All focus groups were transcribed verbatim. We also explored families’ engagement with the intervention website (e.g. page views, challenges accepted/completed) and aspects of the recruitment process (e.g. recruitment duration, resources used, comparisons of recruitment strategies).
Patient and public involvement
FRESH was developed with substantial input from children and families from the public, as detailed in Chapter 2. Since the completion of the FRESH feasibility study, families from the public have been further involved with the optimisation of FRESH in a number of ways. As mentioned earlier, we sought the involvement of families from the public to develop a recruitment video; these families helped develop the script and acted in the video, which can be viewed at www.youtube.com/watch?v=UxUHN1JsjUM. We also asked two families to engage with the FRESH website and provide feedback to inform modifications that could be made.
Sample size considerations
As this was a pilot study, a sample size calculation was not performed. We planned to recruit a sample of 60 families, with a sample size of ≈ 180–240 participants, based on three or four members per family. Our estimated sample size is based on previous study experience30 and on sample sizes of previous pilot studies. 140,141
Progression criteria assessment
The prespecified criteria used to inform progression to a definitive trial have been outlined in Chapter 1, Progression criteria. Where applicable, quantitative and qualitative findings were taken into account to assess whether or not a criterion had been met. As detailed in Chapter 1, FRESH project study management, on the recommendation of the SSC, ‘changes in MVPA’ as ‘evidence of promise’ was to be considered in addition to the pre-established progression criteria to inform progression to a full trial.
Data analysis
A prespecified data analysis plan was approved by the FRESH SSC before the start of the analyses.
Quantitative data
Descriptive statistics are provided for all process evaluation and outcome measures at all relevant time points. Statistical analyses of the physical activity variables were conducted using analysis of covariance (adjusting for baseline values) in Stata (version 15; StataCorp LP, College Station, TX, USA), stratified by age group (adults and children). Participants with missing values at baseline were included in the analysis using the missing indicator method. 142 An estimate of effect and 95% CI were calculated for primary and selected secondary outcomes; no p-values were calculated.
To inform one of the progression criteria, post hoc sample size calculations were carried out to provide 80% power to detect a difference of 10 minutes in MVPA in index children (p < 0.05), using a SD of 16.3 minutes of MVPA and a pre–post correlation of 0.63 (values obtained from the 52-week follow-up).
To estimate the intraclass correlation coefficient of MVPA within families, a base model was created, with participants nested within families. Intraclass correlation coefficients were calculated for each time point. As different accelerometer cut-off points were applied to children’s and adults’ data, intraclass correlation coefficients were calculated using both (whereby all participants had their level of MVPA estimated using the same cut-off point).
Economic analyses
In a change to the published protocol, agreed with the funder, the aim of the health economic analysis was to investigate the incremental cost of the FRESH intervention, focusing on the intervention cost per family and family expenditures on physical activities. A full economic evaluation was not warranted, given the findings from the main study in terms of the lack of a treatment effect and recruitment difficulties. The following approach was applied.
Intervention and follow-up cost
The intervention costs were calculated by deploying a micro-costing approach. The cost components associated with the interventions were retrieved from the published protocol. 125 The unit costs used in the micro-costing process were obtained from either publicly available resources or personal communications for market prices. Table 9 reports the resources used per family, and the monetary value of these resources, alongside the subsequent cost per item. All families, irrespective of trial arm, were assumed to incur the same intervention cost, except the pedometers. The cost of pedometers was calculated considering the number of participants in each family. The reported family physical activity expenditure was summed to produce the mean cost per family at each time point.
| Item | Resource use | Unit cost (£) | Cost per item (£) | Source |
|---|---|---|---|---|
| FRESH intervention | ||||
| Kick-off meeting | 75 minutesa | 0.33 | 25 | Protocol,125 personal communication |
| Accompanying booklet | 12 pages | 0.20 | 2.40 | Protocol,125 personal communication143 |
| Pedometers | 1 pedometer per study participant | 4.00 | 4 | Protocol,125 personal communication |
| Personalised messages | 118 minutesb | 0.33 | 39.30 | Protocol,125 personal communication |
| Online and tangible rewards | 5 cards | 0.20 | 1 | Protocol,125 personal communication143 |
| FRESH intervention total cost | – | – | 71.70 | |
| Pedometer-only intervention | ||||
| Pedometers | 1 pedometer per study participant | 4.00 | 4 | Protocol,125 personal communication |
| Accompanying booklet | 12 pages | 0.20 | 2.40 | Protocol,125 personal communication143 |
| Pedometer-only total cost | – | – | 6.40 | |
Descriptive statistics for resource consumption were calculated for all available families at each time point as counts and proportions. The mean cost per family and the 95% CI around the mean were estimated at each time point. The average costs of the intervention components, such as the pedometers and other activities costs, were also estimated.
We conducted a comparative analysis based on the complete-case data set at 1 year. A linear regression was used to estimate the between-group differences in mean costs per family; unadjusted and adjusted differences were estimated. The adjusted estimates accounted for the cost at baseline. 144 The 95% CIs of both the adjusted and the unadjusted estimates were constructed by resampling the data set 5000 times, performing a non-parametric bootstrap with replacement.
Qualitative data
A content analysis was conducted using existing guidelines111 to explore the feasibility and acceptability of the revised FRESH intervention, the outcome evaluation and suggestions for further intervention optimisation using family focus groups. The approach to data-analysis was the same as that taken in the FRESH feasibility study. Specifically, the analysis was conducted in two separate phases. During the data organisation phase, text from each transcript was divided into segments (meaning units) to produce a set of concepts that reflected meaningful pieces of information. 111 Tags were then assigned to each meaning unit. Tagging was performed by one researcher, with a second researcher double-tagging ≈ 25% of transcripts. For the data interpretation phase, the inventory of tags from all transcripts were examined by two researchers, which led to the emergence of themes and subthemes within each overarching category.
Chapter 6 FRESH pilot trial findings
Parts of this chapter are reproduced with permission from Guagliano et al. 126 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Recruitment and retention
Table 10 provides a summary of the recruitment sources used in this study and Figure 9 shows the recruitment flow. Owing to under-recruitment, the recruitment period was extended from 12 to 24 weeks. Expressions of interest occurred at a rate of four or five families per week over the 24-week recruitment period. Approximately 77% of families expressing interest were eligible for participation and 48% of eligible families were enrolled with an enrolment rate of one or two families per week.
| Recruitment stage | Schools | Employers | Communitya | Traditional mediab | Social mediac | Referral | Unknown | Total |
|---|---|---|---|---|---|---|---|---|
| Approached | 87 | 102 | 56 | N/A | 12 | N/A | N/A | 257 |
| Agreed | 16 | 10 | 7 | N/A | 5 | N/A | N/A | 38 |
| Families reached | ≈ 1641 | ≈ 8761 | ≈ 1740 | ≈ 2371 | 24,333 | N/A | N/A | ≈ 38,846 |
| Expressions of interest | 42 | 11 | 26 | 22 | 1 | 4 | 6 | 112 |
| Eligible | 41 | 9 | 22 | 7 | 1 | 4 | 2 | 86 |
| Families enrolled | 23 | 7 | 4 | 4 | 0 | 3 | 0 | 41 |
| Enrolment (%) | 56 | 17 | 10 | 10 | – | 7 | – | 100 |
FIGURE 9.
Flow chart of recruitment and retention in the FRESH pilot study.
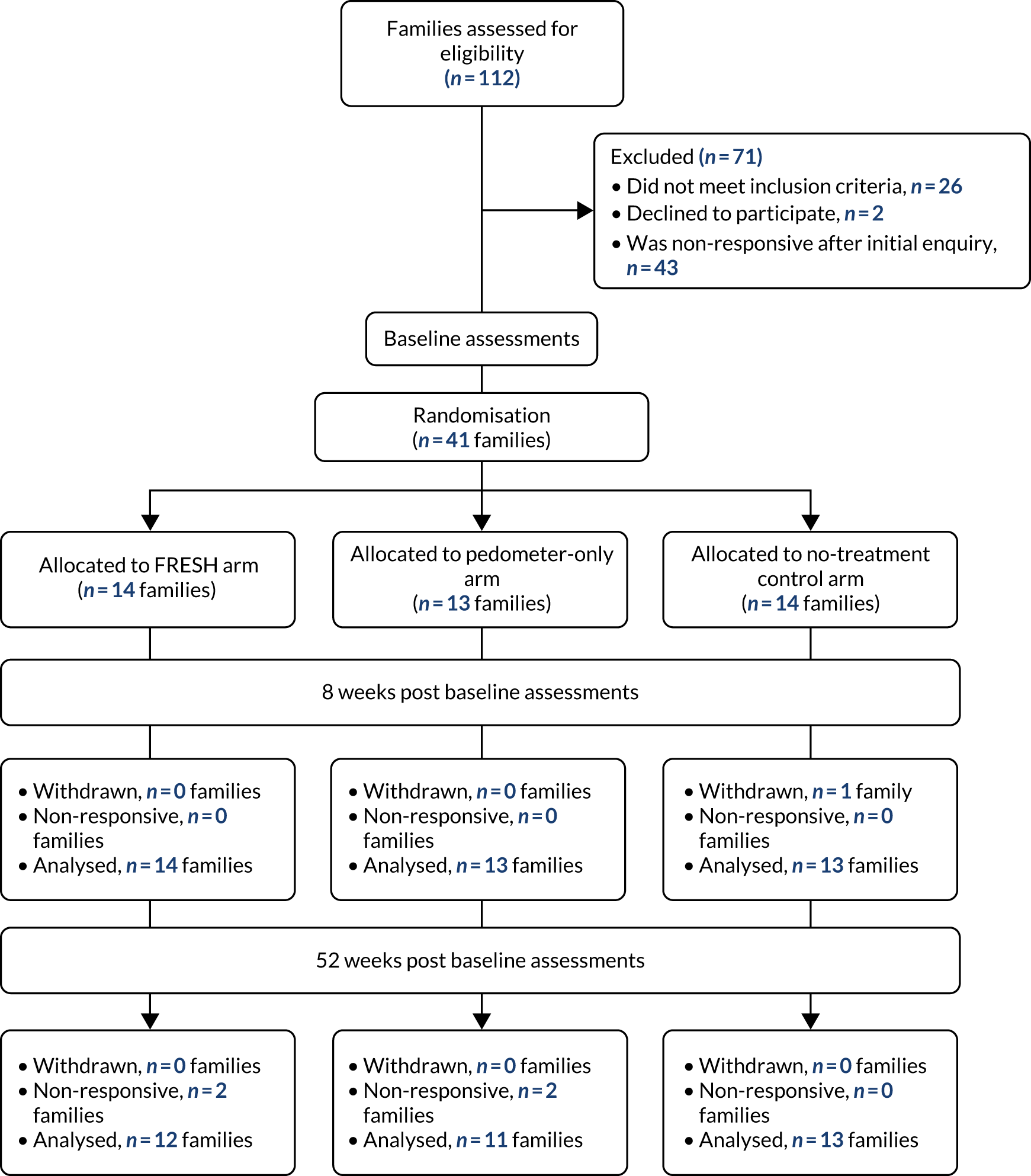
Of the 41 families enrolled, 73% were whole families (n = 30 families) and ≈10% (n = 4 families) were dyads of one parent and one index child. The remaining families either only included index parent–child dyads (n = 4 families) or the index parent, index child, and an additional parent and/or children (n = 7 families); however, in all cases there were additional adults and/or children living with the index child that chose not to participate in the study. We did not recruit any extended family members or any family members that lived outside the index child’s main household. Consent was obtained for 149 participants, averaging four members per family (range 2–6 family members) and included 39 mothers (95%), 31 fathers (76%) and 41 siblings (from 32 families with an eligible sibling; 78%). Eleven siblings were younger than the index child (i.e. aged < 7 years), 15 were in the same age category as the index child (aged 7–11 years) and 15 were older than the index child (aged > 11 years). Table 11 describes the participant characteristics at baseline. Notably, children in the family arm were older than children in the other two arms (FRESH, mean 10.1 years, SD 2.8 years; pedometer only, mean 8.6 years, SD 1.9 years; control, mean 8.9 years, SD 2.7 years) and fewer girls were allocated to the pedometer arm (FRESH, 50.0%; pedometer only, 17.4%; control, 48.3). Approximately 92% of adults reported being married or living as married, 94% of adults reported their ethnicity as white, and the mean age at which adults had finished full-time education was 20.5 (SD 3.5) years.
| Variable | Overall | FRESH | Pedometer | Control | ||||
|---|---|---|---|---|---|---|---|---|
| Adults (n = 67) | Children (n = 82) | Adults (n = 21) | Children (n = 30) | Adults (n = 24) | Children (n = 23) | Adults (n = 22) | Children (n = 29) | |
| Sex (% female) | 56.7 | 40.2 | 54.2 | 50.0 | 50.3 | 17.4 | 57.1 | 48.3 |
| Age (years) | 41.3 (5.8) | 9.3 (2.6) | 42.7 (5.3) | 10.1 (2.8) | 39.0 (6.2) | 8.6 (1.9) | 42.2 (5.7) | 8.9 (2.7) |
| Height (cm) | 171.8 (9.1) | 136.3 (15.6) | 172.4 (8.8) | 140.4 (14.8) | 172.8 (9.6) | 135.1 (11.7) | 170.0 (9.0) | 132.9 (18.4) |
| Weight (kg) | 78.1 (14.2) | 32.5 (9.6) | 81.3 (13.8) | 35.2 (9.1) | 76.5 (13.0) | 31.4 (7.8) | 76.3 (15.7) | 30.7 (10.9) |
| BMI (kg/m2) | 26.5 (4.6) | 17.1 (2.4) | 27.5 (5.0) | 17.6 (2.4) | 25.6 (3.4) | 16.9 (2.3) | 26.3 (5.3) | 16.8 (2.5) |
| BMI z-score | N/A | 0.1 (1.1) | N/A | 0.2 (1.1) | N/A | 0.3 (1.1) | N/A | 0.0 (1.1) |
| Waist circumference (cm) | 89.1 (12.2) | 61.0 (8.0) | 93.4 (12.0) | 62.4 (9.1) | 86.6 (12.5) | 62.0 (5.8) | 86.9 (11.3) | 59.0 (8.2) |
At the 8- and 52-week assessments, 98% and 88% of families were retained (family dropout: FRESH, n = 2; pedometer only, n = 2; control, n = 1). Participant loss to follow-up at 52 weeks comprised nine adults (FRESH, n = 4; pedometer only, n = 3; control, n = 2) and 11 children (FRESH, n = 4; pedometer only, n = 3; control, n = 4).
Intervention feasibility, acceptability, fidelity and optimisation
Most children reported that they liked taking part in the study (> 90%) and thought that it was fun (> 80%). Compared with the pedometer (45%) and control (39%) arms, a higher percentage of children in the FRESH arm (81%) reported doing more activities with their family at the 8-week follow-up. Table 12 shows adults’ overall perceptions of FRESH. Scores were generally positive and favoured the FRESH arm over the pedometer arm. In particular, adults agreed that FRESH encouraged their family to do more physical activity and made their family more aware of the amount of physical activity that they did. Themes related to family physical activity, physical activity awareness and parental modelling also emerged in our focus groups:
It was really fun, it pushed us to get our steps in and do more activities and sports together, you know. I never really thought about how many steps or exercise I’ve done to be honest, so since these [step] counters, I just look and go ‘3000 [steps] only? I have to do something’. So sometimes they [her three sons] come home and they see me . . . dancing, doing something, or skipping, they say, ‘what are you doing, Mum?’ [laughs] and I say, ‘I’m just putting effort in to get my steps’ and then they join me, you know. It just made your more aware . . . I even started walking for small shopping instead of driving just to get my steps up [laughs] . . . small things, you know, it just made you aware.
Mother 127, FRESH arm
| Questionnaire item | FRESH arm (n = 25 adults) | Pedometer-only arm (n = 21 adults) |
|---|---|---|
| (a) The FRESH study . . . | ||
| . . . was fun for my family and I | 3.2 (0.7) | 3.1 (0.5) |
| . . . encouraged my family and I to do more physical activity | 3.2 (0.7) | 2.7 (0.8) |
| . . . has led my family and I to do more physical activity than we did before FRESH | 3.0 (0.8) | 2.4 (0.8) |
| . . . has led my family and I to do more activities (other than physical activity) together than we did before FRESH | 2.6 (0.8) | 2.2 (0.5) |
| . . . has made my family and I more aware of the amount of physical activity we do | 3.6 (0.6) | 3.2 (0.7) |
| . . . is something my family and I would like to continue to be part of | 3.3 (0.9) | 3.2 (0.6) |
| (b) Regarding the step counter we gave out to log your steps, to what extent do you agree or disagree with the following? | ||
| I didn’t mind wearing it | 3.4 (1.0) | 3.1 (1.1) |
| My child/children didn’t mind wearing it | 3.2 (1.0) | 3.2 (0.9) |
| It was easy to use | 3.1 (0.9) | 3.6 (0.5) |
| I thought it was reasonably reliable at counting steps | 2.8 (1.0) | 3.0 (0.6) |
| I used the memory feature to go back and look at the number steps my family and/or I took | 3.0 (1.1) | 2.0 (1.1) |
| (c) Regarding ‘family time’, to what extent do you agree or disagree with the following? | ||
| It was easy to schedule ‘family time’ | 3.0 (1.0) | N/A |
| My family consistently scheduled ‘family time’ | 2.4 (1.0) | N/A |
| My child reminded us about ‘family time’ | 3.0 (0.9) | N/A |
| My child led/initiated ‘family time’ | 3.1 (0.8) | N/A |
| (d) Regarding the FRESH website, to what extent do you agree or disagree with the following? | ||
| It was easy to use | 3.8 (0.7) | N/A |
| I enjoyed using it | 3.4 (0.8) | N/A |
| My child/children enjoyed using it | 3.4 (0.8) | N/A |
| I thought the website was appealing | 3.5 (0.7) | N/A |
| I liked that there were varying degrees of difficulty with the challenges | 3.5 (0.8) | N/A |
| I enjoyed the information about the cities | 3.5 (0.8) | N/A |
| My child/children enjoyed the information about the cities | 3.4 (0.8) | N/A |
| The step converter was useful (e.g. converting swimming to steps) | 3.6 (0.8) | N/A |
| The resources page was useful | 3.5 (1.0) | N/A |
| I enjoyed the recipes | 3.6 (1.4) | N/A |
| My child/children enjoyed the recipes | 3.6 (1.4) | N/A |
| Logging our steps was easy | 3.5 (0.9) | N/A |
The overall acceptability of the pedometers was fairly high among adults in both the FRESH and the pedometer arms (see Table 12). Families in both groups reported that wearing the pedometers had become habitual. One parent stated:
I think it’s become quite habitual now, we pick them up first thing in the morning and take them off last thing at night and they [her children] were quite happy to do that, so that was good from a parent point of view.
Mother 125, FRESH arm
A greater percentage of pedometer-only children than FRESH children self-reported that they liked wearing their pedometer (86% vs. 62%, respectively). In addition, compared with our previous feasibility study, we replaced a greater number of malfunctioning pedometers (despite using the same make and model of pedometers in both studies) and families’ preference for wearing wrist-worn pedometers was emphasised more strongly during focus group discussions.
Adults in the FRESH arm found the kick-off meeting useful (3.6 ± 1.0) to help them get started, felt that they had enough technical support if needed (3.9 ± 0.6) and found it feasible to schedule ‘family time’, albeit not consistently (see Table 12). The focus groups revealed that families rarely used their action planners. One parent said, ‘we probably didn’t fill that [action planner] in as much as we should’ve . . . we use that [action planner] more to actually record our steps’ (father 146, FRESH arm).
The majority of children in the FRESH arm found the website easy to use (93%), wanted to keep using the website (81%), enjoyed being their family’s team captain (70%) and did not find it too difficult to reach their step goals (65%). Overall, adults’ mean scores in relation to the intervention website were generally positive (see Table 12). In particular, adults strongly agreed that the website was easy to use and found various website elements useful (e.g. the step converter). Parents agreed that their child enjoyed receiving rewards and competence reinforcement after each challenge week (3.5 ± 1.2). When asked in focus groups about suggestions for improvement, families in the pedometer-only arm suggested elements that were delivered to the FRESH arm. For example:
I think if you can walk so many steps and it gets you to a place, like a country or something like that. So maybe there could be mini challenges like you walk to London or walk to Paris, you know, or something. Yeah, something like that would be probably quite good for you guys [referring to her children]. [. . .] We haven’t been around the world, but we’d like to go around the world. [. . .] I think that’s something you can add to this [study].
Mother 114, pedometer-only arm
Google Analytics data indicated that 59 users accessed the website (≈ 4 users/family), with a median of 2 [interquartile range (IQR) 1–5] sessions per user viewing about 5 (IQR 2–11) pages per session for approximately 7 (IQR 3–12) minutes per session. The most common behaviour flow was to log on, access the challenge page (to select a new challenge) and then access the steps page (to add steps to complete the challenge). Families selected an average of 11 challenges and completed nine of those. During a challenge, families uploaded steps at least once 86% of the time.
Findings related to the feasibility and acceptability of the outcome evaluation
Data collection took an average of 119.5 (SD 26.4) minutes per family at baseline and 95.0 (SD 16.7) and 82.3 (SD 35.8) minutes per family at the 8- and 52-week follow-ups, respectively. Overall, adults disagreed that there were too many measures [mean values of answers on a 4-point Likert scale, 1.5 (SD 0.7)] and that data collection took too long [mean values of answers on a 4-point Likert scale, 1.7 (SD 0.8)]. In the focus groups, families mentioned the convenience of home-based data collection and, in some cases, said that this had been essential to their participation. One parent said:
. . . it was a lot more convenient you coming to us and you guys being quite flexible in offering us multiple dates and times you could come . . . if you hadn’t come to us, we probably wouldn’t have participated.
Father 125, FRESH arm
In addition, > 80% of children reported that they ‘liked’ the measurement sessions. At each time point, > 90% of eligible adults and children completed all measures, except for the submaximal step test (86%) and the video-recorded activity assessing family functioning (89%).
Mean valid accelerometer wear time was 835.6 (SD 76.5) and 734.9.4 (SD 62.7) minutes for adults and children across time points, respectively. Valid accelerometer data on ≥ 3 days (including 1 weekend day) were available for 82% of adults and 77% of children at all three assessment points. On average, across time points, the GPS provided a location for 757.0 (SD 126.3) minutes and 541.6 (SD 200.3) minutes for adults and children, respectively.
Preliminary effectiveness
Children’s and adults’ levels of MVPA and sedentary behaviour at all time points are presented in Table 13. Subgroup analyses are given in Tables 14 and 15 and the data on family co-participation in physical activity are available in Table 16 and Figure 10. Children and adults either met or were close to meeting the recommended levels of MVPA at baseline, with the exception of children in the FRESH arm, who accumulated notably less MVPA than children in the pedometer and control arms. Within-family intraclass correlation coefficients ranged from 0.42 to 0.52 and were largely similar at the two cut-off points applied.
| Outcome variable | FRESH | Pedometer | Control | Adjusted difference between arms,a mean (95% CI) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FRESH vs. control | FRESH vs. pedometer | Pedometer vs. control | |||||||||||||
| T1 | Change T1 to T2 | Change T1 to T3 | T1 | Change T1 to T2 | Change T1 to T3 | T1 | Change T1 to T2 | Change T1 to T3 | Mean change T1 to T2 | Mean change T1 to T3 | Mean change T1 to T2 | Mean change T1 to T3 | Mean change T1 to T2 | Mean change T1 to T3 | |
| Children | |||||||||||||||
| n | 24 | 15 | 15 | 24 | 18 | 15 | 25 | 23 | 22 | ||||||
| MVPA | 48.4 (15.8) | –8.0 (13.1) | –14.8 (17.4) | 60.5 (22.5) | –7.3 (14.2) | –6.4 (16.4) | 54.2 (20.4) | –4.7 (10.3) | –8.4 (14.6) | –3.1 (–9.9 to 3.8) | –3.9 (–13.7 to 5.9) | 0.0 (–8.2 to 8.1) | –3.1 (–9.2 to 15.4) | –3.0 (–10.1 to 4.1) | –0.8 (–10.8 to 9.3) |
| SED | 552.3 (59.1) | –2.6 (62.9) | –28.6 (59.2) | 469.1 (56.5) | –1.6 (78.1) | 46.5 (52.5) | 524.6 (70.1) | –4.2 (56.1) | 2.4 (62.3) | 7.1 (–18.0 to 32.2) | 12.3 (–12.3 to 36.8) | 8.5 (–21.2 to 38.3) | 10.1 (–21.0 to 41.2) | –1.5 (–27.5 to 24.5) | 2.2 (–23.3 to 27.6) |
| Adults | |||||||||||||||
| n | 21 | 16 | 15 | 21 | 17 | 13 | 17 | 19 | 18 | ||||||
| MVPA | 52.0 (17.7) | 2.1 (14.8) | –4.6 (16.3) | 52.0 (19.2) | –12.9 (17.7) | –0.9 (10.5) | 47.8 (16.3) | –7.1 (11.3) | 0.7 (17.6) | 9.4 (0.4 to 18.4) | –5.7 (–16.7 to 5.3) | 15.3 (6.0 to 24.5) | 1.2 (–11.7 to 14.2) | –5.8 (–15.1 to 3.3) | –6.9 (–19.3 to 5.5) |
| SED | 647.3 (92.6) | –17.3 (86.5) | –49.2 (45.9) | 604.3 (70.9) | 6.8 (65.7) | 19.9 (55.1) | 648.1 (55.4) | 18.4 (50.1) | –39.5 (68.4) | –17.2 (–41.3 to 7.0) | 7.5 (–17.2 to 32.3) | –8.6 (–33.9 to 16.7) | –6.3 (–23.2 to 35.8) | –8.6 (–33.0 to 15.9) | 13.8 (–14.1 to 41.7) |
| Outcome variable | FRESH | Pedometer | Control | ||||||
|---|---|---|---|---|---|---|---|---|---|
| T1 | Change T1 to T2a | Change T1 to T3a | T1 | Change T1 to T2a | Change T1 to T3a | T1 | Change T1 to T2a | Change T1 to T3a | |
| Boys | |||||||||
| n | 11 | 5 | 9 | 17 | 15 | 12 | 14 | 12 | 13 |
| MVPA | 50.3 (18.2) | –0.7 (11.1) | –12.5 (18.3) | 62.8 (23.9) | –9.2 (14.5) | –7.3 (16.9) | 60.2 (22.6) | –2.3 (10.3) | –6.8 (15.6) |
| SED | 569.9 (70.0) | –47.5 (38.8) | –41.5 (67.7) | 469.5 (61.5) | –1.6 (83.8) | 48.3 (53.9) | 520.2 (68.8) | –12.5 (71.4) | 3.7 (67.3) |
| Girls | |||||||||
| n | 13 | 10 | 6 | 4 | 3 | 3 | 11 | 11 | 9 |
| MVPA | 46.8 (18.2) | –11.7 (13.0) | –18.4 (17.1) | 50.9 (12.8) | 2.2 (9.8) | –2.8 (16.9) | 46.5 (17.8) | –7.3 (10.0) | –10.8 (13.5) |
| SED | 537.5 (45.2) | 19.9 (61.7) | –9.1 (41.4) | 467.4 (32.6) | –1.3 (51.8) | 39.4 (56.6) | 530.2 (74.7) | 4.9 (33.6) | 0.6 (63.6) |
| Index child | |||||||||
| n | 11 | 7 | 8 | 12 | 11 | 8 | 14 | 13 | 13 |
| MVPA | 51.6 (9.7) | –9.8 (11.7) | –13.5 (17.4) | 63.0 (23.0) | –10.0 (14.5) | –8.9 (16.3) | 56.2 (23.9) | –2.5 (10.9) | –5.6 (16.0) |
| SED | 537.0 (64.9) | –17.4 (54.4) | –32.5 (54.8) | 470.9 (62.0) | 2.1 (89.2) | 52.3 (43.2) | 532.9 (72.3) | –12.5 (65.0) | 3.0 (43.7) |
| Additional child | |||||||||
| n | 12 | 7 | 6 | 9 | 7 | 7 | 11 | 10 | 9 |
| MVPA | 45.9 (20.5) | –4.1 (14.3) | –16.2 (20.5) | 57.3 (22.7) | –3.2 (17.3) | –3.6 (17.3) | 51.6 (15.4) | –7.5 (9.2) | –12.4 (11.9) |
| SED | 565.9 (54.9) | –0.6 (68.4) | –24.8 (74.4) | 466.6 (51.6) | –7.4 (63.0) | 39.9 (64.5) | 514.0 (67.8) | 6.7 (42.7) | 1.6 (89.4) |
| Less deprived | |||||||||
| n | 10 | 7 | 3 | 15 | 14 | 12 | 14 | 14 | 13 |
| MVPA | 41.6 (9.0) | –12.0 (14.2) | –11.4 (5.3) | 56.2 (23.5) | –5.9 (13.4) | –1.9 (14.3) | 50.5 (17.3) | –5.5 (9.8) | –5.5 (9.8) |
| SED | 533.7 (49.6) | 36.6 (51.2) | 19.4 (64.4) | 477.2 (41.8) | 6.8 (61.4) | 43.9 (46.8) | 517.5 (74.8) | –8.1 (63.2) | 3.5 (78.4) |
| More deprived | |||||||||
| n | 14 | 8 | 12 | 6 | 4 | 3 | 11 | 9 | 9 |
| MVPA | 53.4 (18.0) | –4.5 (11.9) | –15.7 (19.4) | 71.5 (16.6) | –12.5 (18.0) | –24.4 (12.2) | 58.8 (23.8) | –3.4 (11.5) | –8.9 (18.0) |
| SED | 565.6 (63.4) | –36.9 (52.8) | –40.6 (54.0) | 448.6 (84.6) | –30.9 (129.4) | 57.0 (83.8) | 533.5 (66.1) | 2.1 (45.6) | 0.8 (40.2) |
| Outcome variable | FRESH | Pedometer | Control | ||||||
|---|---|---|---|---|---|---|---|---|---|
| T1 | Change T1 to T2a | Change T1 to T3a | T1 | Change T1 to T2a | Change T1 to T3a | T1 | Change T1 to T2a | Change T1 to T3a | |
| Men | |||||||||
| n | 10 | 7 | 7 | 9 | 7 | 5 | 6 | 8 | 7 |
| MVPA | 55.0 (23.1) | 2.3 (21.3) | 0.4 (11.3) | 61.3 (18.5) | –23.5 (19.4) | 3.7 (11.1) | 42.9 (18.4) | –11.8 (7.7) | 7.3 (17.1) |
| SED | 642.8 (108.4) | 2.8 (88.61) | –23.4 (30.0) | 612.9 (60.5) | 1.9 (82.1) | –16.1 (55.1) | 661.7 (44.4) | 14.6 (68.6) | –54.7 (62.5) |
| Women | |||||||||
| n | 11 | 9 | 8 | 12 | 10 | 8 | 11 | 11 | 11 |
| MVPA | 49.3 (11.5) | 2.0 (8.4) | –9.0 (19.4) | 45.0 (17.2) | –5.5 (12.5) | –3.8 (9.8) | 50.5 (15.2) | –3.8 (12.6) | –3.5 (17.4) |
| SED | 651.3 (81.0) | –33.0 (86.6) | –71.8 (46.9) | 597.8 (79.9) | 10.3 (56.2) | 42.4 (44.5) | 640.7 (61.3) | 21.1 (34.7) | –29.9 (73.0) |
| Index parent | |||||||||
| n | 12 | 10 | 8 | 13 | 11 | 8 | 13 | 13 | 13 |
| MVPA | 47.7 (11.8) | 0.8 (14.9) | –6.4 (18.3) | 46.0 (16.8) | –8.7 (15.9) | –3.8 (9.8) | 46.2 (17.6) | –4.1 (11.7) | 1.1 (19.5) |
| SED | 653.0 (99.6) | –13.5 (92.1) | –56.6 (44.8) | 591.8 (79.8) | 19.1 (60.8) | 42.4 (44.5) | 640.4 (61.2) | 11.8 (51.6) | –34.3 (67.5) |
| Additional parent | |||||||||
| n | 9 | 6 | 7 | 8 | 6 | 5 | 4 | 6 | 5 |
| MVPA | 57.8 (23.1) | 4.4 (15.7) | –2.5 (14.9) | 61.9 (19.7) | –20.7 (19.6) | 3.7 (11.1) | 52.9 (11.1) | –13.8 (7.0) | –0.3 (13.3) |
| SED | 639.6 (87.7) | –23.7 (84.0) | –40.7 (49.2) | 624.4 (52.1) | –15.6 (74.1) | –16.1 (55.1) | 673.3 (16.6) | 33.6 (47.7) | –53.2 (76.5) |
| Less deprived | |||||||||
| n | 6 | 4 | 2 | 13 | 12 | 9 | 10 | 10 | 10 |
| MVPA | 50.4 (4.4) | –4.0 (14.7) | –7.0 (7.4) | 52.4 (19.8) | –12.2 (13.2) | –3.0 (10.2) | 47.3 (16.8) | –4.9 (12.6) | 3.9 (0.1) |
| SED | 547.8 (69.5) | 97.5 (40.2) | 11.0 (2.8) | 616.6 (80.6) | 6.5 (61.1) | 3.5 (53.5) | 622.1 (55.9) | 5.3 (55.9) | –46.8 (86.6) |
| More deprived | |||||||||
| n | 15 | 12 | 13 | 8 | 5 | 4 | 7 | 9 | 8 |
| MVPA | 48.5 (16.7) | 4.2 (14.9) | –4.2 (17.4) | 51.5 (19.4) | –14.6 (27.8) | 3.8 (11.1) | 48.5 (16.7) | –9.7 (9.7) | –3.3 (14.3) |
| SED | 687.0 (67.8) | –55.6 (58.0) | –58.5 (42.0) | 584.2 (50.1) | 7.5 (83.8) | 56.9 (43.5) | 685.2 (27.9) | 32.9 (41.0) | –30.5 (39.2) |
| Outcome variable | FRESH | Pedometer | Control | ||||||
|---|---|---|---|---|---|---|---|---|---|
| T1 | Change T1 to T2 | Change T1 to T3 | T1 | Change T1 to T2 | Change T1 to T3 | T1 | Change T1 to T2 | Change T1 to T3 | |
| Children | |||||||||
| n | 22 | 13 | 16 | 14 | 13 | 12 | 22 | 19 | 20 |
| Child–child LMVPA | 90.4 (59.0) | –58.5 (67.4) | –38.9 (77.0) | 117.1 (69.6) | –55.0 (110.0) | –75.4 (68.0) | 80.2 (49.3) | –31.5 (68.0) | –28.4 (54.3) |
| n | 22 | 19 | 18 | 18 | 19 | 17 | 23 | 23 | 22 |
| Adult–child LMVPA | 46.0 (35.7) | –27.5 (46.3) | –9.1 (39.4) | 40.0 (22.5) | –3.4 (33.8) | –10.0 (36.4) | 55.0 (42.4) | –28.2 (49.0) | –18.6 (53.5) |
| Adults | |||||||||
| n | 14 | 12 | 16 | 16 | 16 | 14 | 8 | 12 | 12 |
| Adult–adult LMVPA | 19.4 (14.0) | –1.1 (6.1) | –6.7 (22.1) | 13.7 (10.6) | –1.3 (17.6) | –0.7 (13.5) | 25.0 (19.0) | –10.4 (11.5) | –7.8 (9.7) |
| n | 21 | 18 | 16 | 18 | 18 | 15 | 19 | 19 | 18 |
| Adult–child LMVPA | 53.4 (62.0) | –37.0 (77.1) | –29.8 (22.8) | 54.9 (28.6) | –12.3 (30.4) | –29.8 (22.8) | 58.6 (47.0) | –22.2 (57.6) | –14.6 (61.9) |
FIGURE 10.
Mean minutes of family co-participation in LMVPA (T1, baseline; T2, 8 weeks post baseline; T3, 52 weeks post baseline). (a) Child with sibling; (b) child with parent; (c) parent with other parent; and (d) parent with child.
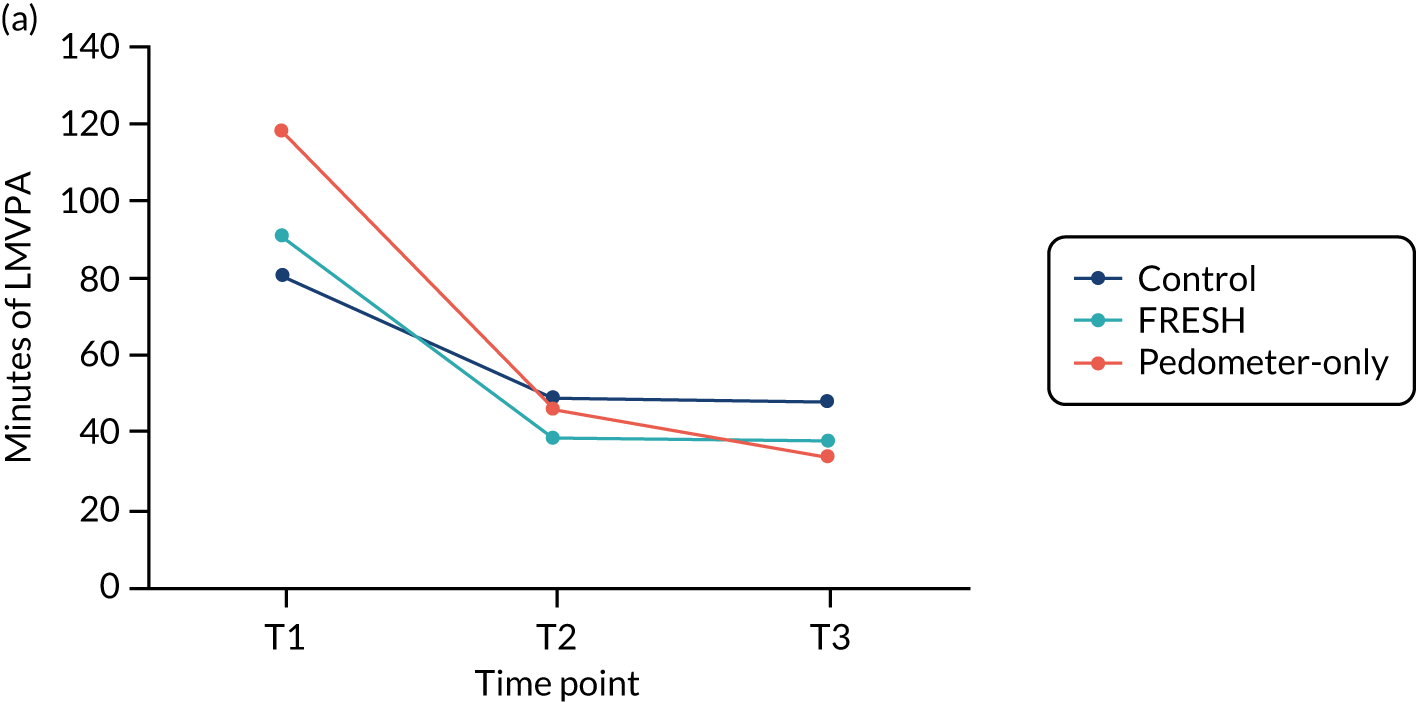
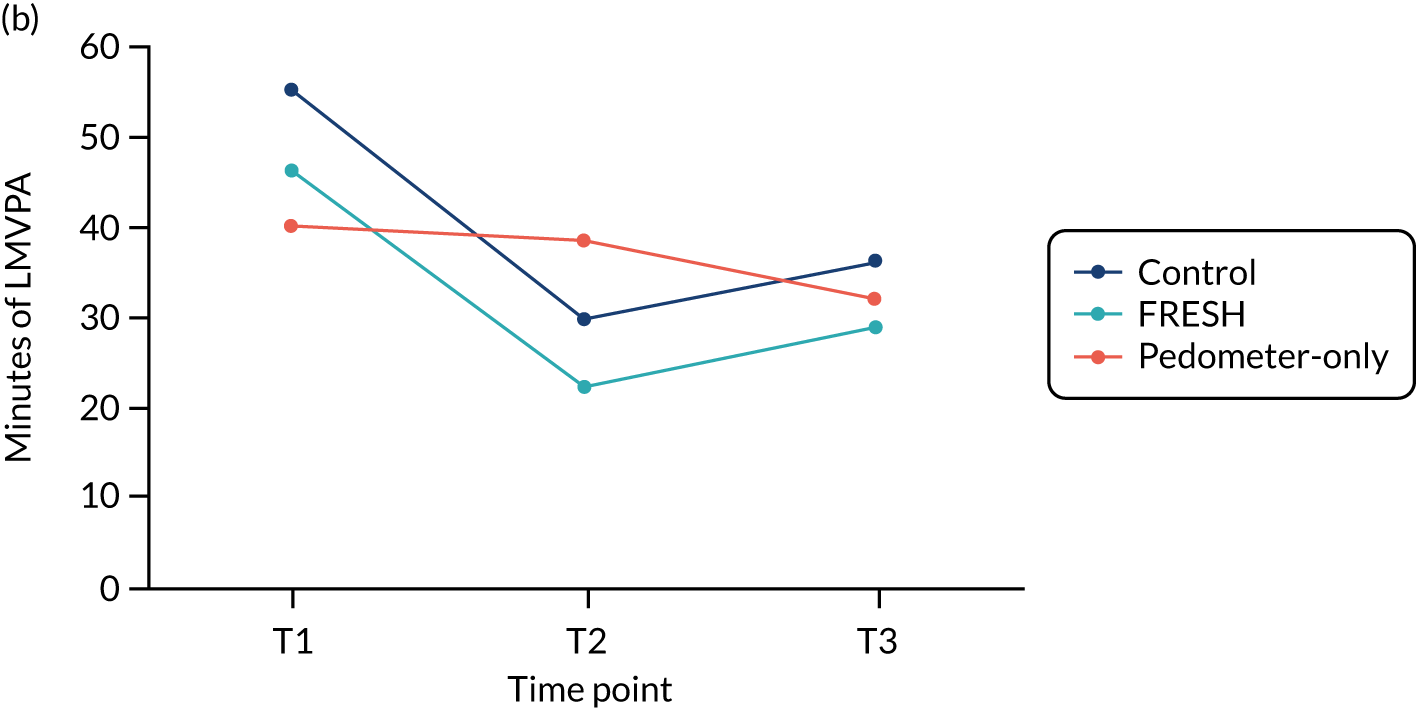
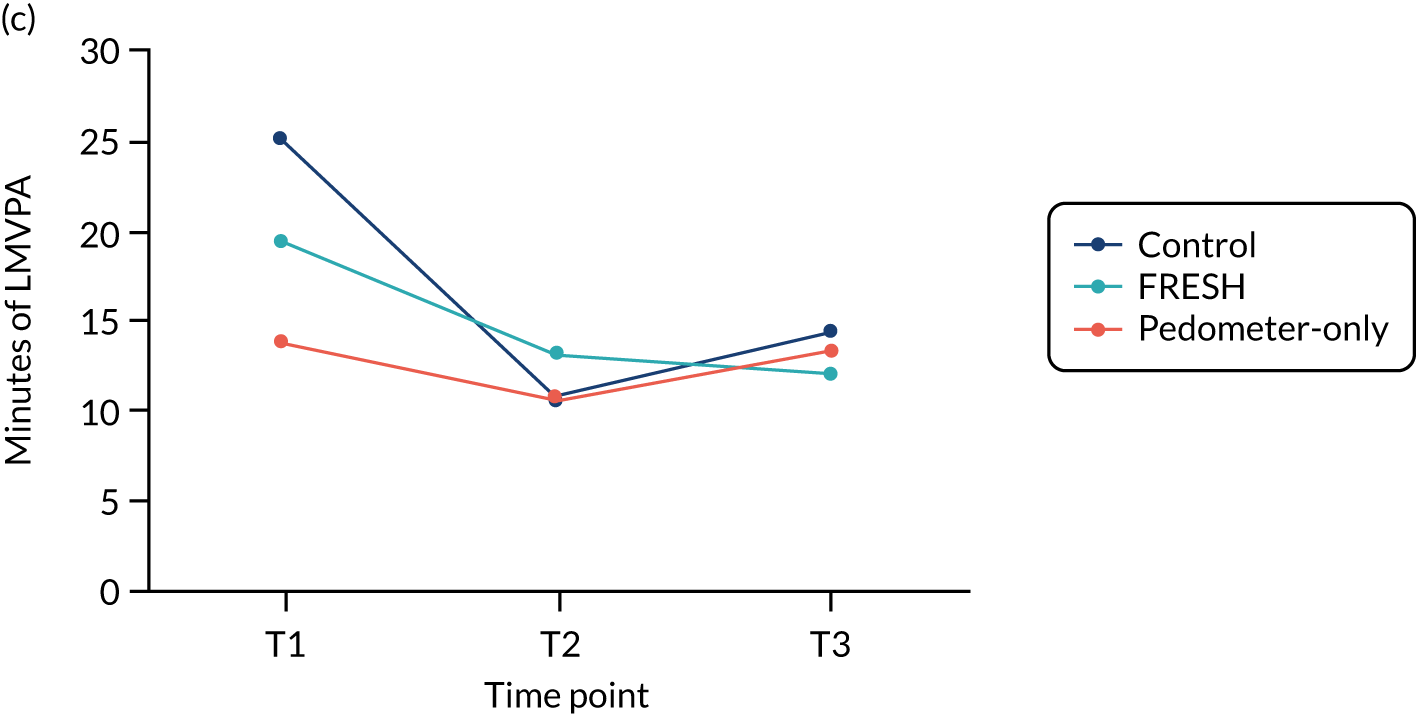
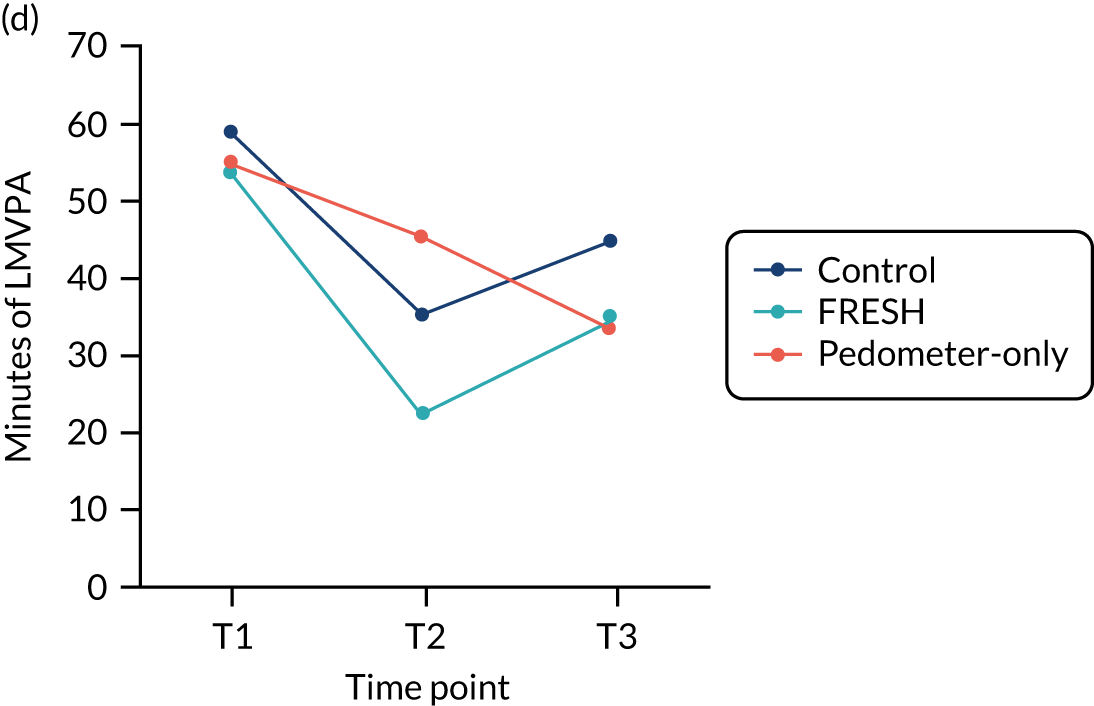
Among children, no notable between-group differences were found in minutes of MVPA, time spent sedentary or co-participation in physical activity with family members at either of the follow-up time points. However, at 12 weeks a sizeable difference in change of 9.4 (95% CI 0.4 to 18.4) and 15.3 (95% CI 6.0 to 24.5) minutes in MVPA was found for adults in the FRESH arm compared with those in the pedometer or control arm, respectively. Adults in the FRESH arm also increased their activity with other family members (co-participation) more than those in the control and pedometer arms (10.0, 95% CI 2.9 to 17.1 minutes, and 10.6, 95% CI –3.6 to 17.6 minutes, respectively). No between-group group differences were found for time spent sedentary among adults.
Exploratory subgroup analyses (see Tables 13 and 14) showed a greater decline in MVPA among FRESH girls and FRESH children from less deprived areas than among their counterparts. The latter group also showed a greater increase in sedentary behaviour than those in the other groups. By contrast, FRESH adults, in particular men, showed a greater increase in MVPA at 8 weeks than the other groups.
Tables 17–19 display the findings for children and adults for all other outcomes. No notable or consistent between-group or subgroup differences were found for any other outcome measured at 8 or 52 weeks for children or for adults.
| Outcome variable | FRESH | Pedometer | Control | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | T1 | Change T1 to T2 | Change T1 to T3 | n | T1 | Change T1 to T2 | Change T1 to T3 | n | T1 | Change T1 to T2 | Change T1 to T3 | |
| Weight (z-score) | 30 | 0.27 (0.85) | 0.04 (0.18) | 0.11 (0.22) | 22 | 0.64 (0.86) | 0.00 (0.14) | –0.06 (0.28) | 29 | 0.01 (1.0) | 0.06 (0.11) | 0.04 (0.27) |
| WC (z-score) | 30 | 0.57 (1.33) | 0.14 (0.64) | 0.04 (0.66) | 22 | 1.17 (0.94) | –0.21 (0.61) | –0.41 (0.57) | 29 | 0.37 (1.21) | 0.13 (0.71) | –0.01 (0.59) |
| BMI (z-score) | 30 | 0.16 (1.09) | 0.01 (0.26) | 0.08 (0.25) | 22 | 0.29 (1.07) | –0.06 (0.27) | –0.14 (0.36) | 29 | –0.02 (1.12) | 0.03 (0.15) | –0.01 (0.34) |
| Predicted VO2max | 25 | 41.3 (4.1) | –1.0 (3.3) | 1.2 (4.7) | 17 | 43.8 (5.6) | 0.3 (4.0) | 1.9 (3.1) | 18 | 42.4 (5.2) | –0.7 (3.5) | 0.4 (3.5) |
| Quality of life | 26 | 0.93 (0.03) | –0.02 (0.08) | –0.07 (0.12) | 19 | 0.89 (0.11) | 0.01 (0.08) | 0.04 (0.17) | 22 | 0.92 (0.06) | –0.03 (0.05) | 0.02 (0.08) |
| TV viewing (minutes/week) | 23 | 609.1 (309.2) | –200.9 (281.5) | –221.1 (423.1) | 22 | 525.0 (380.0) | –26.8 (290.7) | –130.6 (453.2) | 18 | 406.7 (212.4) | 63.5 (292.0) | –35.3 (303.8) |
| Video games (minutes/week) | 21 | 217.1 (347.5) | –91.4 (264.0) | –112.9 (408.4) | 22 | 278.2 (434.8) | –48.6 (308.2) | –15.9 (273.7) | 18 | 91.2 (255.9) | –18.5 (158.3) | 87.6 (226.8) |
| Computer use (minutes/week) | 23 | 469.6 (420.9) | –103.0 (273.7) | –187.9 (363.3) | 22 | 288.2 (292.3) | 26.4 (265.9) | 32.4 (357.6) | 18 | 257.5 (316.5) | 12.5 (195.7) | 30.8 (194.7) |
| Phone use (minutes/week) | 23 | 133.0 (280.2) | –93.6 (269.9) | –48.3 (125.7) | 22 | 78.2 (145.9) | 5.0 (139.1 | 10.6 (166.0) | 19 | 0.5 (2.3) | 26.3 (47.2) | 24.7 (61.3) |
| Outcome variable | FRESH | Pedometer | Control | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | T1 | Change T1 to T2 | Change T1 to T3 | n | T1 | Change T1 to T2 | Change T1 to T3 | n | T1 | Change T1 to T2 | Change T1 to T3 | |
| Weight (kg) | 23 | 81.3 (13.8) | –0.1 (1.3) | –1.4 (2.8) | 21 | 76.5 (13.0) | 0.3 (1.3) | 0.3 (2.3) | 21 | 76.3 (15.7) | 0.3 (1.1) | 1.4 (2.2) |
| WC (cm) | 23 | 93.4 (12.0) | –1.3 (5.3) | –2.2 (5.5) | 21 | 86.6 (12.5) | –1.3 (4.4) | –8.4 (30.8) | 21 | 86.9 (11.3) | 1.4 (3.9) | 2.4 (4.4) |
| BMI | 23 | 27.5 (5.0) | 0.1 (0.7) | –0.5 (1.0) | 21 | 25.6 (3.4) | 0.1 (0.6) | –2.1 (8.7) | 20 | 26.3 (5.3) | 0.0 (0.4) | 0.5 (0.7) |
| Predicted VO2max | 22 | 33.2 (4.7) | 1.2 (3.0) | 1.4 (1.7) | 21 | 37.0 (4.8) | 0.9 (3.5) | 1.3 (2.8) | 20 | 35.8 (6.1) | –0.2 (2.8) | 0.3 (5.3) |
| Quality of life | 23 | 75.4 (14.0) | 2.0 (10.3) | 6.5 (11.4) | 22 | 82.7 (11.1) | –0.2 (12.8) | 1.3 (7.9) | 19 | 86.5 (8.3) | –2.2 (11.8) | –2.8 (10.0) |
| Time | FRESH | Pedometer | Control | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | T1 | Change T1 to T2 | Change T1 to T3 | n | T1 | Change T1 to T2 | Change T1 to T3 | n | T1 | Change T1 to T2 | Change T1 to T3 | |
| Mean turns | 6 | 82.5 (21.3) | 10.6 (6.3) | 13.4 (8.7) | 5 | 76.6 (9.9) | –12.6 (20.9) | 2.4 (25.2) | 5 | 82.8 (20.7) | 1.5 (14.8) | 29.0 (22.4) |
| Positive talk/turn | 14 | 0.06 (0.06) | –0.01 (0.05) | 0 (0.03) | 12 | 0.09 (0.05) | –0.03 (0.03) | –0.03 (0.04) | 13 | 0.07 (0.04) | –0.01 (0.03) | –0.02 (0.03) |
| Activity talk/turn | 14 | 0.10 (0.08) | –0.02 (0.07) | 0.01 (0.04) | 12 | 0.06 (0.05) | 0.02 (0.05) | 0.02 (0.06) | 13 | 0.11 (0.12) | –0.01 (0.03) | –0.06 (0.11) |
Evaluation of costs
The proportion of families who bought any sports items was materially unaltered throughout the study. Table 20 reports the costs incurred by families and the intervention cost (incurred by local authority budgets). There was no difference across groups in the cost observed at baseline. The summation of the costs from randomisation until 1 year showed that for families enrolled in the FRESH arm expenditure was on average £157.92 (95% CI –£154.76 to £484.79) more than the no treatment group. The majority of this cost difference is accounted for by cost of the intervention. Conversely, the cost incurred by the families receiving only the pedometers tended to be smaller than that incurred by the families randomised to the control arm (B: –£90.50, 95% CI –£301.30 to £104.45). Adjusting these differences by the cost at baseline did not qualitatively change the findings.
| Cost/time | No treatment, average cost (£) (95% CI) [n (%)] | FRESH intervention, average cost (£) (95% CI) [n (%)] | Pedometer-only intervention, average cost (£) (95% CI) [n (%)] |
|---|---|---|---|
| Baseline | 200.86 (130.96 to 270.76) [13 (100%)] | 195.05 (110.22 to 279.88) [14 (100%)] | 183.09 (118.08 to 248.10) [13 (100%)] |
| Intervention | 0 (–) [13 (100%)] | 89.97 (84.54 to 95.40) [14 (100%)] | 24.55 (19.03 to 30.07) [13 (100%)] |
| Other components | 0 (–) [13 (100%)] | 67.69 (–) [14 (100%)] | 2.40 (–) [13 (100%)] |
| Pedometers | 0 (–) [13 (100%)] | 22.29 (16.86 to 27.72) [14 (100%)] | 22.15 (16.63 to 27.67) [13 (100%)] |
| 8 weeks | 115.56 (65.27 to 165.85) [13 (100%)] | 89.79 (33.90 to 145.68) [14 (100%)] | 104.92 (39.90 to 169.94) [13 (100%)] |
| 52 weeks | 322.22 (171.43 to 473.01) [13 (100%)] | 409.76 (137.58 to 681.94) [12 (85.71%)] | 239.52 (112.03 to 367.01) [11 (84.62%)] |
| Total cost – 1 year | 437.78 (275.89 to 599.67) [13 (100%)] | 595.7 (307.5 to 883.90) [12 (85.71%)] | 347.29 (216.31 to 478.27) [11 (84.62%)] |
| Unadjusted differencesa | Reference | 157.92 (–154.76 to 484.79) | –90.5 (–301.3 to 104.45) |
| Adjusted differencesb | Reference | 191.45 (–62.5 to 506.32) | –55.65 (–250.07 to 143.61) |
Assessment against progression criteria
Table 21 outlines the prespecified progression criteria, whether or not the study team considers that the specific criterion was met, and the evidence to support that assessment.
| Description | Criterion met? | Assessment |
|---|---|---|
| 1. > 75% of families upload steps at least six times in the first 3 months of pilot study | Yes |
|
| 2. Demonstrable feasibility of recruiting 20 families per month (accounting for increased staffing in future definitive trial) and retaining 75% of index children at 52-week follow-up | Partially |
|
| 3. Intervention optimisation feasible (identified adaptations are practical, affordable, acceptable) | Yes |
|
| 4. Evidence to suggest an adequately powered trial would require a feasible number of participants (n = 250 is considered to be logistically feasible and provide sufficient power) | Yes |
|
| 5. Discontinuation of trial arm based on evidence of harm or limited acceptability/feasibility | Yes |
|
| 6. Preliminary effectiveness on MVPAa | No |
|
Discussion of the FRESH pilot study results
Our findings show that it was feasible to deliver and evaluate a family-targeted physical activity promotion intervention with generally high acceptability from participating families. In addition, each of the prespecified progression criteria was met at least partially (see Table 21). However, we found a favourable indication of effectiveness only for adults and not for children, that is, a sizeable positive change in MVPA for adults in the FRESH arm compared with the other arms. The between-group difference found for adults’ time spent in MVPA was not maintained at the 52-week follow-up, and we also found no notable between-group differences for any other outcome measured at either time point.
Family recruitment posed a substantial challenge, and this progression criterion was not entirely met (i.e. recruiting 20 families/month). Our average recruitment rate was ≈ 7 families/month (range 2–15 families/month), despite using a multifaceted recruitment strategy that targeted adults and children, included a wide range of settings, and used direct and indirect recruitment strategies. A review of 73 publicly funded trials in the UK (through the NIHR) found that only 55% recruited 100% of their target sample size within their pre-agreed timescale and nearly 45% received an extension of some kind. 145 There is little evidence of major improvement in recruitment into experimental research over time. 146 Several studies have reported that the recruitment of families is particularly challenging,44,52 and we have described specific recruitment challenges that we have encountered previously. 78 Little methodological research is currently available to support the optimisation of family recruitment methods. Therefore, further research into how to recruit families to family-based research is needed.
In terms of recruitment, 94% of adults reported their ethnicity as white. Although this figure is reflective of the population of the counties where recruitment occurred,82 the potential effectiveness of this intervention on minority families is unclear. Several studies have acknowledged the under-representation of minority groups in trials. 147,148 Therefore, further research to better establish how to recruit families in family-based research is needed, and in particular, greater consideration should be given to recruiting families from ethnic minority groups. Targeting specific recruitment settings and tailoring messaging on recruitment materials are strategies that could be used. 148,149
An extensive measurement protocol was applied in the FRESH studies, and it is not possible to disentangle whether the challenges of recruiting families were because families lacked interest in increasing their physical activity or in FRESH in particular, or that the commitment to three rounds of home-based assessment of all family members was a barrier. Families in both the FRESH feasibility and the pilot studies indicated that the level of measurement was acceptable to them, but this is likely to have been a biased perception of a group of families that had made the commitment to take part in the FRESH study. Further research is needed to identify whether families may not be interested in physical activity promotion per se, or whether the research commitment required poses a barrier. With this in mind, researchers and funders should carefully balance the scientific need for detailed data collection (driven, for example, by questions around how interventions work, and impacts on important physical health outcomes beyond the target behaviour) with the burden on participants and the impact that it has on the recruitment of a representative sample of participants.
Encouragingly, we found evidence of preliminary short-term effectiveness for adults and, in particular, for fathers in the FRESH arm. Similar interventions with mothers have resulted in positive physical activity promotion. 150 However, the effect on fathers may be noteworthy as evidence indicates that fathers have an independent influence on their children’s health and development115 and an important influence on children’s physical activity. 116–118
We did not find evidence of preliminary effectiveness for children or for co-participation in physical activity between parents and their children in this study. This may be for a number of reasons. First, our process evaluation and focus groups revealed that family planning time was not being implemented as intended. In a family-based physical activity intervention that included a similar planning component, the authors found that children’s MVPA significantly increased in the short term compared with a condition that received education only. 151 Therefore, without implementing the planning component in our study, the step challenges alone may have not been enough to change children’s MVPA. There were also group differences in children’s sex and age, with fewer girls in the pedometer-only arm and more older children in the FRESH arm. Observational data reveal that children’s physical activity declines with age,22–24 girls accumulate less physical activity than boys throughout childhood,134,152 and girls’ physical activity declines more precipitously than boys’ with age. 49,153,154 These differences may have affected preliminary intervention effectiveness on MVPA, but this issue would likely be resolved through randomisation in an adequately powered trial. Last, there may have been a healthy volunteer bias, as participants across groups were generally already meeting the physical activity recommendations at baseline. In future, excluding families that are sufficiently active could be considered.
Delivery of the FRESH intervention was estimated to cost £90 per family (≈ £15 per participant), including pedometers for all family members, the face-to-face kick-off meeting and personalised follow-up support. The last of these accounted for ≈ 55% of the costs. These costs could be reduced in future, as this part of the intervention delivery had not been automated but was processed manually by research staff. The automation of these processes will help reduce delivery costs, and make it more attractive to funding agencies to consider delivering FRESH as part of their portfolio of physical activity interventions, if it is proven effective. Previous work has estimated the cost of delivering a multicomponent school-based physical activity intervention at ≈ £190 per participant,155 and an after-school intervention at £51 per participant,156 suggesting that cost of delivering the FRESH intervention is low in comparison. However, the definitions, scope and perspectives of the costs considered across studies were quite different, making comparison difficult. Moreover, little is known about how much local authorities or other delivery agents are willing to pay, and future research should explore this.
Strengths and limitations of the FRESH pilot trial
This study has several noteworthy strengths, which include its randomised design, high retention rates, device-measured physical activity, a measure of family functioning, and a long-term follow-up assessment (i.e. 52 weeks post baseline). There were also some limitations. Despite bolstering our recruitment strategy after our feasibility study, we were still unable to recruit the desired number of families into this study; therefore, further optimisation regarding recruitment in family-based research appears prudent. In addition, the children and adults who participated in this pilot study were generally sufficiently physically active at baseline, which may have affected the potential of the intervention. The populations of Norfolk and Suffolk are not representative of the wider UK population, and the potential feasibility of FRESH in other locations should be tested. The assessment of cost was focused on intervention implementation as these would be the costs directly incurred by local providers such as local authority. Costs of longer-term maintenance and implementation (including website updates) were not included. The analyses presented do not account for the clustering of participants within families. Within-family intraclass correlation coefficients for MVPA ranged between 0.42 and 0.52, and this level of clustering should be taken into account in the design and analyses of future family-based physical activity studies. Last, randomisation did not lead to balanced groups as there were large differences in sex and age among children across groups, with noticeably fewer girls in the pedometer group and fewer older children in the FRESH arm. This may have affected our findings for preliminary intervention effectiveness. The randomisation procedure is likely to have been affected by small sample size and the use of a stratified randomisation procedure by county owing to funding. There is no indication that this issue would also affect an adequately powered trial; however, stratifying randomisation by child sex and/or age could also be considered.
Conclusion
In conclusion, this study demonstrates feasibility and acceptability of the family-targeted FRESH intervention, as well as satisfying all progression criteria, at least partially. However, we failed to recruit the target sample size and did not find a signal of effectiveness on MVPA particularly long term or in children. Therefore, further refinements around intervention delivery and recruitment may be required prior to progressing to a full-scale trial.
Chapter 7 A systematic review with expert opinion assessing effective and resource-efficient strategies for recruiting families to physical (in)activity, nutrition and obesity prevention research
Parts of this chapter are reproduced with permission from Guagliano et al. 157 © 2020 The Authors. Obesity Reviews published by John Wiley & Sons Ltd on behalf of World Obesity Federation. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
Introduction
As described before, physical activity promotion interventions targeting families may be a valuable way to increase physical activity among children. 158,159 However, the study team’s experience in the FRESH feasibility and pilot studies demonstrated that effective strategies are needed to overcome barriers to recruitment.
As noted earlier in this report, recruitment of participants into intervention research is notoriously difficult. 160,161 Two reviews of publicly funded trials in the UK (through the NIHR) found that only about half of the included trials recruited 100% of their target sample size within their pre-agreed timescale. 146,162 The overall start to recruitment was delayed in 41% of trials, early recruitment problems occurred in 63% of trials,146 and just over one-third of trials received an extension of some kind. 146,162 There is little evidence that recruitment into experimental research is improving over time. 146,160 The recruitment of multiple family members to research projects is particularly challenging. 29,30,44,52 We have described specific recruitment challenges that we have encountered previously,78,125,126 but there has not been a comprehensive assessment of how to recruit families to family-based health promotion research.
The aim of this study was, therefore, to systematically identify effective and resource-efficient strategies for recruiting families into intervention research aimed at improving physical activity or nutrition or reducing levels of sedentary behaviour (including screen time) and overweight/obesity. Our objectives were to (1) describe procedures used and outcomes related to recruitment (e.g. recruitment duration, strategies used, recruitment settings, reach, expressions of interest, enrolment rates); and (2) determine the most optimal family-based recruitment strategies.
Methods
This study was conducted in two phases:
-
a systematic review of family recruitment methods
-
a Delphi consensus study.
Both phases examined the settings (i.e. where recruitment occurred) and the strategies (i.e. how recruitment was implemented) used by researchers conducting family-based intervention research with outcomes related to physical activity, sedentary behaviour (including screen time), nutrition, and obesity prevention. Details of the protocol for this study were registered on PROSPERO (CRD42019140042) and can be accessed at www.crd.york.ac.uk/prospero/display_record.php?RecordID=140042.
Phase 1: systematic review
Search strategy overview
Reporting of the systematic review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). 163 In short, we identified relevant intervention studies through a systematic search of published reviews on the relevant topic. Intervention studies were then extracted from those included reviews. Subsequently, a forward search of the included intervention studies identified more recently published studies that had not been captured in the included reviews.
Eligibility criteria
Systematic reviews
All types of reviews describing the results of family-based experimental studies with outcomes related to physical activity, sedentary behaviour, nutrition or obesity prevention were eligible for inclusion.
Intervention studies
Intervention studies were eligible for inclusion if they met the following inclusion criteria:
-
Participants. Generally healthy school-aged children and young people and at least one adult primarily responsible for their care. Studies focused on preschool or post-secondary-aged youth samples were excluded, as were those with clinical populations (e.g. populations with any illness, disorder or disability) or those exclusively targeting overweight/obese children and youth.
-
Interventions. Interventions that deliberately attempted to implement a change in physical activity, sedentary behaviour, screen time use or diet or prevent overweight/obesity were included. No restriction was placed on the type of comparison. Treatment interventions (e.g. weight management interventions) were excluded.
-
Study type. All experimental (e.g. RCTs, crossover designs) and quasi-experimental designs were included. Cross-sectional and cohort studies were excluded. No limitations were set on the duration of the intervention or the follow-up period.
-
Types of outcome measures. Studies could be included if they had employed any outcome measure related to physical activity, sedentary behaviour, screen-use time, diet, or overweight/obesity prevention. However, outcomes must have been measured in at least one child and at least one adult primarily responsible for their care.
For both reviews and intervention studies, we set no limits on the earliest publication date. We included English-language, peer-reviewed full-text articles that reported primary data or protocols and had been published by February 2019. Forward searching was conducted in August 2019.
Search strategy
We conducted a systematic search for review articles in Cochrane Library, PubMed, PsycInfo and Scopus. The search included keywords related to the population (‘children/young people’ and ‘parents’), interventions (‘physical activity’, ‘diet’, etc.) and study type (e.g. ‘review’), Box 2 provides an example of the full search strategy. Identified references were imported into EndNote reference manager and duplicates were removed. Titles and abstracts were screened by a single reviewer, with a second reviewer double-screening a random 10% as a check. Full-text papers were screened by two reviewers independently, with any discrepancies resolved by discussion. Reasons for exclusion were identified at this full-text screening stage. Reference lists of included reviews were reviewed in duplicate, and references of potentially relevant studies were extracted into EndNote. Following deduplication, two reviewers independently screened the titles/abstracts and then the full-text versions of additional interventions studies identified. Any disagreements were discussed by the two reviewers until a consensus was reached.
((TITLE-ABS-KEY (child* OR boy* OR girl* OR teen* OR adolesc* OR youth OR young* OR dyad*)) AND (TITLE-ABS-KEY (parent* OR mom* OR mum* OR dad* OR mother* OR father* OR famil* OR dyad*))) AND (TITLE-ABS-KEY (trial* OR intervention* OR experiment*)) AND (TITLE (review OR “meta-analys*”)) AND (((TITLE-ABS-KEY (“physical activit*” OR exercis* OR sport* OR fitness OR “activity intens*” OR “activity level*” OR movement)) OR (TITLE-ABS-KEY (overweight OR obesity OR adipos* OR “body mass” OR “body weight” OR “waist circumference” OR “weight loss”)) OR (TITLE-ABS-KEY (“healthy eat*” OR “healthy snack*” OR beverage* OR diet* OR nutrition OR vegetable* OR fruit* OR “energy intake” OR “energy balanc*” OR “soft drink*” OR soda OR sugar*))) OR (TITLE-ABS-KEY (sedentar* OR screen* OR game* OR computer* OR television OR tv OR tablet*))) AND (LIMIT-TO (DOCTYPE, “re”) OR LIMIT-TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “ip”)) AND (LIMIT-TO (LANGUAGE, “English”)).
The same key words were used in our searches of the other three databases (Cochrane Library, PubMed and PsycInfo).
Data extraction
The following data were extracted from each intervention study: characteristics of study design and sampling, recruitment duration and strategies used, recruitment settings, and information about reach, expressions of interest and enrolment. We sent the extracted data to the first and last authors of studies published within the last 5 years (i.e. since 2014), inviting them to check the extracted data for accuracy and to add any missing information, if possible. We only contacted authors of articles published within the last 5 years as we believed that this was a reasonable time period for which their records would be available and they were likely to have adequate recall of the study.
Risk of bias in individual studies and across studies
We were only interested in examining the strategies used for recruiting families into family-based intervention research, which does not inherently affect the internal validity (risk of bias) of a study. Therefore, we decided not to include a risk-of-bias (quality) assessment.
Summary measures and synthesis of results
As indicated above, only family-based recruitment strategies were of interest in this study and not the main outcome findings of an included study; thus, we present findings descriptively only.
Phase 2: Delphi consensus study
Study design
The Delphi procedure or technique is a group process involving the interaction between the researcher and a group of identified experts on a specified topic. 164 This procedure is appropriate for research questions which cannot be answered with complete certainty, but rather by the subjective opinion of a collective group of informed experts. 165 Here, we used a Delphi procedure to determine, through the consensus of experts, the most effective and resource efficient strategies for recruiting families into intervention studies. Our protocol was guided by a similar published study. 75 Ethics approval for the study was obtained in July 2019 through a Medical Research Council (MRC) Epidemiology Unit departmental ethics review.
Study procedures
Two groups of experts were invited by e-mail: (1) all first and senior authors of the intervention studies identified in phase 1, and (2) known experts in the field identified by the study team. Participants were also permitted to suggest other experts for invitation. All participants were asked to complete an informed consent online prior to the start of the study.
The Delphi study included three rounds using an online questionnaire created in Qualtrics (Provo, UT, USA), a web-based survey tool. To start each round, participants were sent an e-mail containing a direct link to the online questionnaire, which they were given 1–2 weeks to complete. One reminder was sent 3 days before the deadline. After each round, a summary of the findings was fed back to the participants.
In round 1, participants responded to questions related to the most recent family-based study they had conducted (e.g. about recruitment strategies, recruitment duration, sample size), and to provide their top two strategies for recruiting families in intervention studies (Box 3 lists the questions asked). Following the deadline, the study team reviewed the panel’s responses to their top strategies. We then collated responses into overarching themes based on the setting in which recruitment occurred (e.g. schools) and then organised similar recruitment strategies used under each overarching theme.
-
Was the most recent family-based experimental study that you conducted a pilot/feasibility trial or full-scale trial?
-
How many families did you aim to recruit in the study?
-
How many families were enrolled in the study?
-
How much time (in weeks) was allotted for recruitment?
-
Was this enough time to recruit the number of families you aimed to recruit?
-
Was the recruitment period extended?
-
How much additional time (in weeks) was allotted for recruitment?
-
In your opinion, what are the top two recruitment strategies that you have used in the family-based experimental research that you have conducted?
-
Please provide a detailed description of the recruitment strategies.
-
Whom did you find to be the best contact person when initiating the recruitment strategies?
-
How effective were the recruitment strategies the most recent time you used them?
-
What resources were required with the recruitment strategies the most recent time you used it?
-
Are there any recruitment strategies that you have used in previous studies that you have stopped or plan to stop using?
-
Are there any recruitment strategies that you would like to try but have not yet used?
In round 2, participants reviewed the recruitment strategies put forward in round 1 and rated how effective and resource-efficient they believed each strategy to be separately on two different four-point Likert scales (4 = very effective/resource-efficient, 1 = not effective/resource-efficient). To rank strategies, summary scores were created in which scores for effectiveness were weighted by a factor of 2. Therefore, the weighted scores for effectiveness ranged between 2 and 8 and the scores for resource efficiency ranged between 1 and 4. Effectiveness was weighted more than resource efficiency as we believed that effectiveness was a more important factor related to recruitment strategies. The top 10 recruitment strategies were then taken forward to round 3.
In the final round (round 3), participants were asked to rank the top 10 recruitment strategies into their individual top 10. Following completion, all rankings were summed to determine the overall rank of each strategy (i.e. a lower score indicated a higher rank).
Results
Findings of phase 1: systematic review
Phase 1: systematic review findings
Figure 11 shows the study selection process. Fifty-five relevant reviews met the inclusion criteria; from these, 360 references to potentially relevant intervention studies were extracted and 50 were included. An additional 14 intervention studies were identified through forward searching, and, therefore, a total of 64 articles, describing 49 intervention studies, met the inclusion criteria. The study characteristics are detailed in Table 22. Of the 49 separate studies, the majority were undertaken in the USA (57%), were pilot or feasibility studies (43%), aimed to improve physical activity only (37%) and recruited parent–child dyads (53%). Publication dates ranged from 1983 to 2019, with 27% of the included articles published in the last 5 years (i.e. since 2014; 17 of 64 articles). After attempting to contact the authors of the 17 studies published in the last 5 years, we received responses for seven of the 17 studies. Modifications were made or additional information was provided for five out of these seven studies.
FIGURE 11.
Flow chart of identification of family-based intervention studies for systematic review.
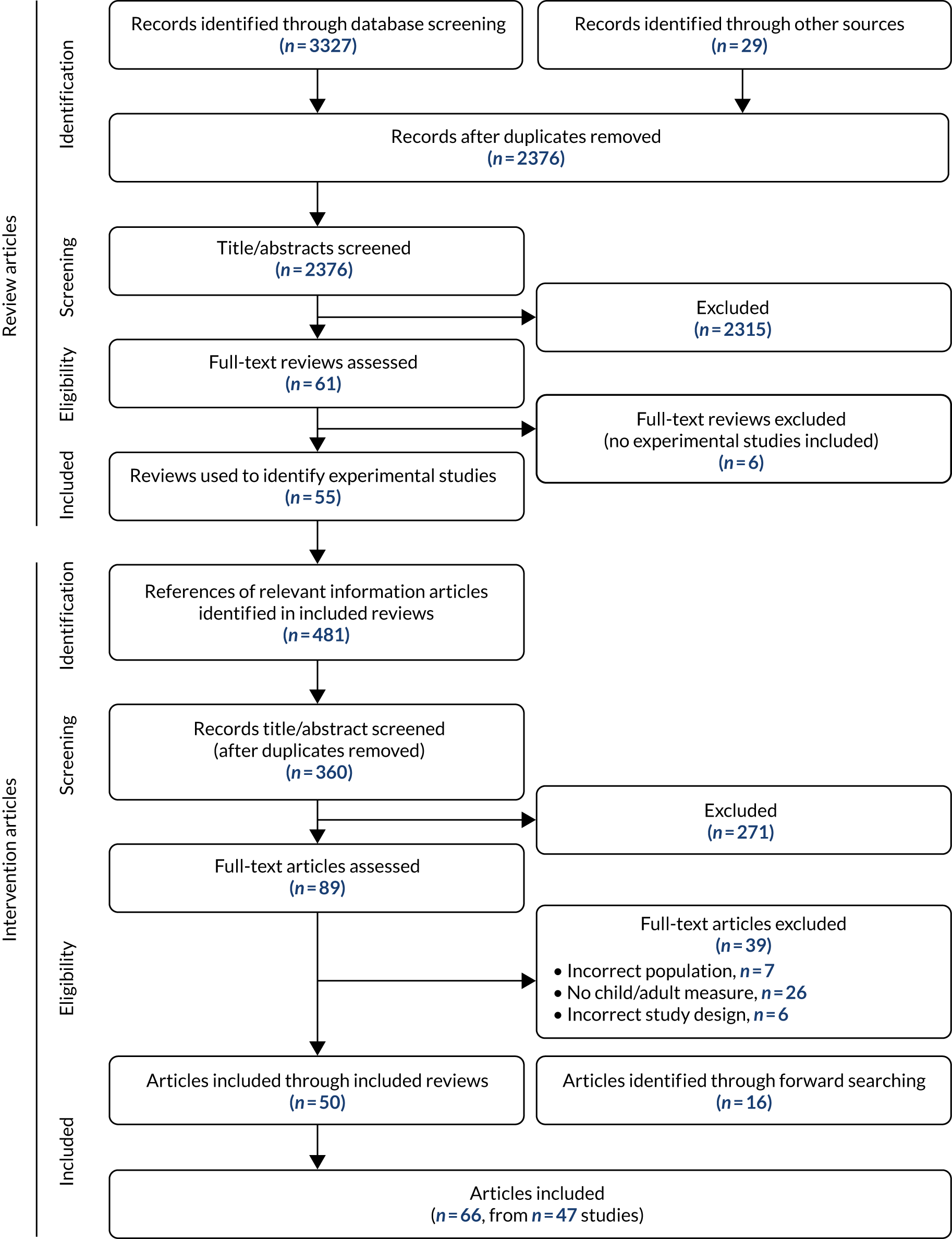
| Intervention name, study (first author, year of publication, country) | Study design (assessments), study arms, aims/objectives | Families/participants [recruitment target; target and actual sample size; mean (SD) years of age at baseline; % female] | Recruitment (duration; settings; strategies used) | Reach, expressions of interest and enrolment |
|---|---|---|---|---|
| No intervention name, Alhassan, 2018, USA166 |
Pilot RCT (pre and 2 post measures) Study arms: child–mother, child alone or control Aims/objective: to examine the feasibility and efficacy of a mother–daughter intervention on African American girls’ physical activity |
Recruitment target: African American mother–daughter dyads Target sample size: 60 dyads (20 dyads/group) Actual sample size: 76 dyads (child–mother, n = 28; child alone, n = 25; or control, n = 23) Family characteristics: children: 8.3 (1.3) years (100%); adults: 37.4 (7.7) years (100%) |
Duration: not reported Setting: not reported Strategies: not reported |
Reach: not reported Expressions of interest: 125 dyads Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| SHARE-AP ACTION, Anand, 2007, Canada167 |
RCT (pre and 2 post measures) Study arms: experimental or usual care control Aims/objective: to determine if a household-based lifestyle intervention was effective at reducing energy intake and increasing energy expenditure |
Recruitment target: families on a Six Nations Reserve (minimum parent–child dyad required) Target sample size: not reported Actual sample size: 57 families (intervention, n = 29; control, n = 28) Family characteristics: children: experimental – 10.9 (2.9) years (62.5%), control – 9.9 (3.2) years (60.5%); adults: experimental – 41.3 (9.0) years (not reported), control – 37.2 (8.8) years (not reported) 57 families (participants: intervention, n = 88; control, n = 86); average three participants/family |
Duration: 48 weeks Setting: not reported Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Arredondo, 2014, USA168 |
Pilot trial (pre and post measures) Study arms: experimental arm only Aims/objective: to examine the acceptability, feasibility and preliminary efficacy of an intervention on physical activity and correlates of physical activity of Latina preadolescents and their mothers |
Recruitment target: Latina mother–daughter dyads Target sample size: 11 dyads Actual sample size: 11 dyads Family characteristics: children: 9.6 (1.1) years (100%); adults: 36.7 (6.2) years (100%) |
Duration: 8 weeks Setting: church (approached, n = 1; agreed, n = 1) Strategies: Announcements in Spanish from the pulpit; flyers distributed by study staff and church leaders |
Reach: ≈ 864 parishioners (the church had 1800 enrolled parishioners and 48% were Latino) Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Baranowski, 1990, USA;169 Baranowski, 1990, USA170 |
Randomised controlled feasibility study (pre and post measures) Study arms: experimental or no treatment control Aims/objective: to reduce sodium, saturated fat and total fat, and to increase aerobic activity |
Recruitment target: families who self-identified as Black American (minimum parent–child dyad required) Target sample size: not reported Actual sample size: 96 families (intervention, n = 50; control, n = 46) Family characteristics: children: experimental – 10.6 years (51.6%), control – 10.0 years (66.1%); adults: experimental – 31.8 years (79.4%), control – 32.9 years (88.2%) 96 families (participants: n = 63 adults and 64 children intervention; n = 51 adults and 56 children intervention) |
Duration: not reported Setting: schools only (number not reported) Strategies: mail, telephone calls and home visits (up to five visits) of all Black-American students identified in listings in the public or private school systems |
Reach: 728 Black-American families identified Expressions of interest: N/A. This was not a sample of self-presenting volunteers Initiated expression of interest: N/A Expressions of interest rate: N/A Enrolment rate: not reported |
| Mothers and Daughters Exercising for Life (MADE4LIFE), Barnes, 2015, Australia171 |
Pilot RCT (pre and 2 post measures) Study arms: experimental or 6-month wait-list control Aims/objective: to evaluate the feasibility and preliminary efficacy of a mother–daughter programme to improve physical activity |
Recruitment target: mother–daughter dyads Target sample size: 40 dyads Actual sample size: 40 dyads (mothers, n = 40; daughters, n = 48) Family characteristics: children: 8.5 (1.7) years (100%); adults: 39.1 (4.8) years (100%) |
Duration: ≈ 3 weeks Setting: schools (n = not reported) Strategies: media releases, school newsletter advertisements, school presentations to students and parents, local newspapers and local television news |
Reach: not reported Expressions of interest: 122 families Initiated expression of interest: not reported Expressions of interest rate: ≈ 40–41 families/week Enrolment rate: ≈ 13 families/week |
| Family Affair, Barr-Anderson, 2014, USA172 |
Pilot trial (pre and post measures) Study arms: experimental arm only Aims/objective: to test the feasibility and acceptability of an intervention designed to impact obesity-related behaviours (physical activity, healthy eating and sedentary behaviour) among African American adolescent girls and their mothers |
Recruitment target: African American mother-daughter dyads Target sample size: not reported Actual sample size: 18 dyads Family characteristics: children: 12.4 ± 1.3 years (100%); adults: 36.9 ± 5.7 years (100%) |
Duration: not reported Setting: not reported Strategies: radio advertisements, flyers and recruitment letters sent to or posted at youth- and family-serving organisations, health-related businesses, churches, social and professional organisations; e-mail distribution lists; Facebook posts; word-of-mouth |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Healthy Kids & Families study, Borg, 2019, USA173 |
Quasi-experimental protocol (pre and 4 post measures) Study arms: experimental or attention-control Aims/objective: to test the effectiveness of an intervention to promote a healthier lifestyle and to prevent childhood obesity among low-income and minority families |
Recruitment target: parent–child dyads Target sample size: 240 dyads Actual sample size: 247 dyads (intervention, n = 121; attention-control, n = 126) Family characteristics: children: 7.8 (2.1) years (49%); adults: 36.2 (7.4) years (92%) |
Duration: not reported Setting: schools only (n = 9 schools) Strategies: letter from the school principal placed in child’s backpack by school staff; automated telephone messages from principals; research staff presented study at school events (e.g. parent nights, family events, parent–teacher organisation meetings); interactions with parents at school drop-off/pick-up and after-school programmes |
Reach: not reported Expressions of interest: 605 parents Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Back-to-Basics Healthy Lifestyle program, Burrows, 2013, Australia174 |
Pilot trial (pre and post measure) Study arm: experimental arm only Aims/objective: to assess the feasibility and acceptability of an after-school obesity prevention strategy for families |
Recruitment target: parent–child dyads Target sample size: 10 dyads Actual sample size: 10 dyads Family characteristics: children: 7.3 (3.8) years (80%); adults: 31.0 (7.2) years (100%) |
Duration: 2 weeks Setting: schools only (n = 1) Strategies: study flyers; word-of-mouth by school staff |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: 5 dyads/week |
| No intervention name, De Bourdeaudhuij, 2002, Belgium175 |
Quasi-experimental (pre and post measure) Study arms: family arm, individual arm (adolescents) or individual arm (parents) Aims/objective: to explore the differences between a family- and an individual-based tailored nutrition education programme on fat reduction |
Recruitment target: parent–child dyads Target sample size: not reported Actual sample size: family condition: n = 55 dyads (n = 110 participants); individual condition (adolescents): n = 71 adolescents; individual condition (parents): n = 47 parents Family characteristics: children: range 15–18 years (not reported); adults: not reported |
Duration: not reported Setting: schools only (n = 52 classes from two secondary schools) Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| MOVE/me Muevo Project, Elder, 2014, USA176 |
RCT (pre and 2 post measures) Study arms: experimental or control Hypotheses: (1) children in the experimental arm would have lower BMI z-scores than control children after 2 years; (2) children in the experimental arm spend more time in MVPA and less time sedentary, eat fewer high-fat foods and sugary beverages, and have more fruits, vegetables and water vs. control children |
Recruitment target: families Target sample size: not reported Actual sample size: 541 families Family characteristics: children: 6.6 (0.7) years (55%); adults: not reported |
Duration: not reported Setting: schools, libraries, street fairs, recreation centres (n = not reported) Strategies: targeted telephone calls using telephone numbers obtained from a research marketing company (n = 8600); families contacted via school- and community-based recruitment efforts (n = 1000) |
Reach: 9607 families Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Epstein, 2001, USA177 |
Randomised trial (pre and post measures) Study arms: increase fruit and vegetable (FV) intake treatment condition or decrease high-fat/high-sugar intake (FS) treatment condition Aims/objective: to evaluate the effect of a parent-focused intervention on parent and child eating changes and on the percentage of overweight changes in families |
Recruitment target: families (minimum parent–child dyad required) Target sample size: not reported Actual sample size: 30 families (FV: n = 13 parents and n = 13 children; FS: n = 12 parents and n = 13 children) Family characteristics: children: FV – 8.8 (1.8) years (54%), FS – 8.6 (1.9) years (77%); adults: FV – 39.1 (4.1) years (92%), FS – 42.2 (4.8) years (92%) |
Duration: not reported Setting: physician practices (n = not reported) Strategies: physician referrals, posters, newspapers, and television advertisements |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Fitzgibbon, 1995, USA178 |
Pilot trial (pre and post measures) Study arms: experimental or control Aims/objective: to examine the effects of an obesity prevention programme on eating-related knowledge and behaviour of low income, Black American girls and their mothers |
Recruitment target: Black American mother–daughter dyads Target sample size: not reported Actual sample size: 20 dyads (10 dyads/group) Family characteristics: children: experimental – 11.0 (1.0) years (100%), control – 11.0 (1.0) years (100%); adults: experimental – 31.0 (10.0) years (100%), control – 33.0 (5.0) years (100%) |
Duration: not reported Setting: tutoring programme (n = 1) Strategies: advertisements in tutoring newsletter |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Children First Study, Fornari, 2013, Brazil179 |
RCT (pre and post measures) Study arms: experimental or control Aims/objective: to evaluate whether or not an educational programme for children could improve cardiovascular risk in parents |
Recruitment target: children and their parents Target sample size: 150 parents per group Actual sample size: 197 children and 323 parents (intervention: n = 105 children, n = 162 parents; control: n = 92 children, n = 161 parents) Family characteristics: children: experimental – 8.2 (1.5) years (50%), control – 9.0 (1.5) years (51%); adults: experimental – 38.3 (6.0) years (55%), control – 39.3 (6.7) years (53%) |
Duration: not reported Setting: schools only (n = 1) Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Active Families in the Great Outdoors, Flynn, 2017, USA180 |
Feasibility trial (pre and post measures) Study arms: experimental arm only Aims/objective: to determine whether changes could be observed in duration, frequency and type of outdoor physical activities performed by families; parent social cognitive outcomes and physical activity support behaviours |
Recruitment target: families (minimum parent–child dyad required) Target sample size: not reported Actual sample size: 16 families (N = 52 participants: parents, n = 25; children, n = 27) Family characteristics: children: 10.7 (3.3) years (52%); adults: 41.5 (7.9) years (60%) |
Duration: not reported Setting: not reported Strategies: flyers, e-mail, word-of-mouth |
Reach: not reported Expressions of interest: 38 families Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Take Action, French, 2011, USA181 |
CRCT (pre and post measures) Study arms: experimental or control Hypothesis: the experimental group would gain less weight and increase healthful behaviours related to energy balance over 1 year compared with the control group |
Recruitment target: families Target sample size: not reported Actual sample size: 90 households (n = 45 households/group) Family characteristics: children, not reported; adults, 41.0 years (93%) ≈ 4 members per family (≈ 2 adults and ≈ 2 children/family) |
Duration: 32 weeks Setting: libraries, worksites, schools, day-care centres, health clinics, religious institutions, park and recreation centres, grocery stores, and food co-ops (number not reported) Strategies: not reported |
Reach: not reported Expressions of interest: 723 households Initiated expression of interest: not reported Expressions of interest rate: 22 or 23 households per week Enrolment rate: 2 or 3 households per week |
| Families Reporting Every Step to Health (FRESH), Guagliano, 2019, UK |
Feasibility trial (pre and post measures) Study arms: ‘child-only’ or ‘family’ Aims/objectives: to describe intervention and recruitment strategy; assess the feasibility and acceptability of the FRESH recruitment strategy, intervention and outcome evaluation; explore options for optimisation |
Recruitment target: families (minimum parent–child dyad required) Target sample size: 20 families Actual sample size: 12 families (children, n = 14; adults, n = 18) Family characteristics: children: 8.3 (1.7) years (50%); adults: 39.8 (8.2) years (61%) Whole families 4, parent–child dyads 6, families with an additional adult or child 2; 2 or 3 members per family (range 2–4 members per family) |
Duration: 8 weeks Setting: schools only. N = 11 schools approached, n = 5 agreed, n = 3 declined, n = 3 no response. Recruitment from community-based organisations planned, but not implemented Strategies: assembly delivered to students; study leaflets given to students to bring home and emailed to parents from schools; reminder e-mail sent from schools to parents 2 weeks after assembly |
Reach: ≈ 437 students Expressions of interest: 28 families Initiated expression of interest: 23 mothers, 5 fathers Expressions of interest rate: 3 or 4 families per week, 5 or 6 families per school assembly Enrolment rate: 1 or 2 families per week |
| Scouting Nutrition and Activity Program+ (SNAP+), Guagliano, 2012, USA182 |
Quasi-experimental (pre and post measures) Study arms: experimental arm only Aims/objectives: to evaluate a physical activity promotion intervention with a channel of communication to parents |
Recruitment target: Girl Scouts troops and their parents Target sample size: not reported Actual sample size: three troops (children, n = 32; adults, n = 26) Family characteristics: children: 9.5 (1.4) years (100%); adults: 37.1 (5.4) years (92%) |
Duration: not reported Setting: Girl Scouts troops (n = 3 troops invited and agreed) Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Active 1 + FUN, Ha, 2019, Hong Kong183 |
RCT protocol (pre and 2 post measures) Study arms: experimental or control Aims/objective: to evaluate the effectiveness of a family-based intervention on parents and their children’s physical activity |
Recruitment target: students and their parents (minimum parent–child dyad required) Target sample size: 204 children Actual sample size: 187 children Family characteristics: children: 9.8 (1.2) years (41%); adults: unknown (78%) |
Duration: ≈ 4–6 weeks Setting: Schools only (n = 100 invited; n = 9 responded and agreed; n = 1 dropped out) Strategies: written information was circulated to parents; face-to-face parent–researcher sessions |
Reach: unknown Expressions of interest: ≈ 229 Initiated expression of interest: unknown (not collected) Expressions of interest rate: unknown (researchers only received a confirmed list from schools) Enrolment rate: unknown (researchers only received a confirmed list from schools) |
| Abriendo Caminos, Hammons, 2013, USA184 |
Pilot trial (pre and post measures) Study arms: experimental arm only Aims/objective: to test the effectiveness of a family-based healthy eating programme aimed to reduce obesogenic behaviours among Latino parents and children |
Recruitment target: Latino families; only 1 target child (5–13 years) and 1 parent measured Target sample size: not reported Actual sample size: 73 families Family characteristics: children: 8.5 years (49%); adults: 34.4 years (100%) ≈ 4 family members per family (range 2–9) |
Duration: 104 weeks Setting: trailer park (n = 1) and elementary school (n = 1) with known Latino population Strategies: flyers, announcements, and word-of-mouth. Project co-ordinators were Latino and fluent Spanish speakers |
Reach: unknown Expressions of interest: unknown Initiated expression of interest: unknown Expressions of interest rate: unknown Enrolment rate: < 1 family per week |
| Fit ‘n’ Fun Dudes Programme, Hardman, 2009, UK185 |
CRCT (pre and 2 post measures) Study arms: experimental or control Aims/objective: to increase daily step counts of girls with the support of their parents to maintain increases over time |
Recruitment target: parent–daughter dyads Target sample size: not reported Actual sample size: n = 32 children (intervention, n = 14 children; control, n = 18 children) Family characteristics: children: 10.6 (0.7) years (100%); adults: 41.0 (4.7) years (83%) |
Duration: not reported Setting: not reported Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Hopper, 1992, USA186 |
CRCT (pre and 2 post measures) Study arms: school-and-home treatment condition, school-only treatment condition, and standard treatment control condition Aims/objective: to compare the effect of including versus not including a family participation component in a school-based programme to develop children’s heart-healthy exercise and nutrition habits |
Recruitment target: parents and children or children only Target sample size: not reported Actual sample size: school-and-home condition, n = 45 children and 42 parents; school-only condition, n = 43 children; control condition, n = 44 children Family characteristics: children: 11.6 (0.7) years (not reported); adults: 37.8 (6.8) years (74%) |
Duration: not reported Setting: not reported Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Teamplay, Jago, 2013, UK187 |
Randomised controlled feasibility trial (pre and 2 post measures) Study arms: experimental or no treatment control Aims/objectives: six specific aims related to feasibility of recruitment, retention and data collection; intervention development and optimisation; estimating effect sizes of outcomes of interest (e.g. physical activity, screen viewing) and sample size for definitive trial |
Recruitment target: parents of children aged 6–8 years Target sample size: between 80 and 340 participants Actual sample size: 48 participants (intervention, n = 25; control, n = 23) Family characteristics: children: experimental – 6–8 years (62%), control – 6–8 years (69%); adults: experimental – age not reported (100%), control – age not reported (96%) |
Duration: not reported Setting: schools, coffee shops, children’s centres, play groups, school playgrounds (number not reported) Strategies: leaflets, advertisements, face-to-face recruitment |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Motivating Families with Interactive Technology (mFIT), Jake-Schoffman, 2018, USA188 |
Pilot trial (pre and post measures) Study arms: tech or tech+ Aims/objective: to test the feasibility, acceptability and preliminary effectiveness of two family-based programs targeting improvements in parent–child dyad’s physical activity and healthy eating and delivered remotely |
Recruitment target: parent–child dyads Target sample size: not reported Actual sample size: 33 dyads (tech+, n = 17; tech, n = 16) Family characteristics: children: 11.0 (0.9) years (64%); adults: 43.0 (5.8) years (88%) |
Duration: not reported Setting: not reported Strategies: e-mail announcements, flyers posted in community settings, paid newspaper ads, direct mail postcards |
Reach: not reported Expressions of interest: 98 Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Childhood and Adolescence Surveillance and Prevention of Adult Non communicable disease (CASPIAN) Study, Kargarfard, 2012, Iran;189 Kelishadi, 2010, Iran190 |
Non-RCT (pre and 2 post measures) Study arms: mother/daughter arm or student-only arm Aims/objective: to examine the effect of a physical activity programme for high-school girls and their mothers |
Recruitment target: mother–daughter dyads or students only Target sample size: not reported Actual sample size: mother/daughter group (n = 206 girls and n = 204 mothers); student-only group (n = 60 girls) Family characteristics: children: 15.8 (1.0) years (100%) in mother/daughter group; 15.9 (1.3) years (100%) in student-only group; adults: age not reported (100%) in either group |
Duration: not reported Setting: schools (number not reported) Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| 4-Health, Lynch, 2012, USA191 |
Pilot RCT protocol (pre and 2 post measures) Study arms: experimental or ‘best practices’ control Aims/objective: to develop, implement and evaluate a parent-centred obesity prevention programme for rural families |
Recruitment target: children and their parents Target sample size: 75 participants per group Actual sample size: unknown Family characteristics: unknown |
Duration: not reported Setting: 4-H (n = 25 4-H extension agents) Strategies: announcements and information at county fairs, announcements in 4-H newsletters, electronic and/or printed announcements to 4-H clubs, e-mails to 4-H listservs, and telephone calls to 4-H leaders |
Reach: unknown Expressions of interest: unknown Initiated expression of interest: unknown Expressions of interest rate: unknown Enrolment rate: unknown |
| No intervention name, Mark, 2013, Canada192 |
Pilot RCT (pre and post measure) Study arms: GameBike (experimental) or traditional stationary bike (control) Aims/objective: primarily, to compare usage of a GameBike with that of a traditional stationary bike placed in front of the television among parents and children |
Recruitment target: families Target sample size: not reported Actual sample size: 30 families (adults, n = 59; children, n = 38) Family characteristics: children: experimental – 6.0 (2.1) years (42%); control – 5.4 (1.7) years (42%); adults: experimental – 37.1 (6.6) years (52%), control – 36.6 (6.1) years (50%) |
Duration: not reported Setting: health-care centres, recreation centres, day cares, preschools and shopping malls (number not reported) Strategies: not reported |
Reach: not reported Expressions of interest: 58 families Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Kick Start Your Day, Mohammad, 2012, USA193 |
Pilot trial (pre and post measure) Study arms: experimental or control Aims/objective: to evaluate a family-based nutrition and physical activity programme targeting low-income Latino families |
Recruitment target: Latino families Target sample size: not reported Actual sample size: 56 parents (intervention, n = 25; control, n = 31) and their children (n = not reported) Family characteristics: children: range 6–12 years (not reported); adults: 37.0 (7.0) years (not reported) |
Duration: not reported Setting: community centre (n = 1) and clinic (n = 1) Strategies: flyers and brochures written in English and Spanish, presentation delivered at a parent–teacher association meeting and community leader forum |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Children, parents and pets exercising together (CPET), Morrison, 2013, UK;194 Yam, 2012, UK195 |
Randomised controlled feasibility trial (pre and post measure) Study arms: experimental or no treatment control Aims/objectives: to assess the feasibility and acceptability of the CPET intervention and trial, preliminary evidence of its potential efficacy, planning and powering a future intervention, and to improve understanding of the frequency, intensity and duration of dog walking among dog-owning families in Scotland |
Recruitment target: families with dogs Target sample size: 40 families Actual sample size: 28 families (experimental, n = 16 families; control, n = 12 families) Family characteristics: children: 10.9 years (76%), adults: 44.8 years (82%) |
Duration: not reported Setting: primary schools (approached, n = 37; agreed, n = 35) Strategies: invitation letters sent to dog-owning parents with children attending primary schools in one local authority area |
Reach: 350 letters sent Expressions of interest: 127 families Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Dads and Daughters Exercising and Empowered (DADEE), Morgan, 2019, Australia131 |
RCT (pre and 2 post measures) Study arms: experimental or wait-list control Aims/objective: to evaluate a programme designed to improve father–daughter physical activity and daughters’ fundamental movement skill competency; fathers’, daughters’ screen-time; fathers’ physical activity parenting practices |
Recruitment target: fathers and their daughters Target sample size: 86 fathers and 134 daughters Actual sample size: 115 fathers and 153 daughters (DADEE: fathers, n = 57; daughters, n = 74; wait-list control: fathers, n = 58; daughters, n = 79) Family characteristics: children: 7.7 (1.8) years (100%); adults: 41.0 (4.6) years (0%) |
Duration: 11 weeks Setting: not reported Strategies: university media release picked up by local television, radio, newspaper news outlets |
Reach: not reported Expressions of interest: 160 Initiated expression of interest: not reported Expressions of interest rate: 14 or 15 families per week Enrolment rate: ≈ 10 families per week |
| Healthy Dads, Healthy Kids, Morgan, 2014, Australia;196 Morgan, 2011, Australia197,198 Williams, 2018, Australia199 |
Community RCT (pre and post measures) Study arms: experimental or a wait-list control Aims/objective: to evaluate the Healthy Dads, Healthy Kids intervention when delivered by trained local facilitators in the community |
Recruitment target: fathers and their children Target sample size: 50 fathers and their children Actual sample size: 93 fathers and 132 children Family characteristics: children: 8.1 (2.1) years (45%); adults: 40.3 (5.3) years (0%) |
Duration: ≈ 8 weeks Setting: schools (n not reported) Strategies: school newsletters, school presentations, interactions with parents at school pick-up, local media, and flyers distributed through local communities |
Reach: not reported Expressions of interest: 116 Initiated expression of interest: not reported Expressions of interest rate: ≈ 14–15 families per week Enrolment rate: ≈ 11–12 families per week |
| Healthy Dads, Healthy Kids, Morgan, 2011, Australia197,198 Lubans, 2012, Australia;117 Burrows, 2012, Australia200 |
RCT (pre and 2 post measures) Study arms: experimental or a wait-list control Aims/objective: to evaluate the feasibility and efficacy of Healthy Dads, Healthy Kids to help fathers lose weight and model positive health behaviours to their children |
Recruitment target: fathers and their children Target sample size: 44 fathers and their children Actual sample size: 53 fathers and 71 children Family characteristics: children: 8.1 (2.1) years (45%); adults: 40.3 (5.3) years (0%) |
Duration: ≈ 8 weeks Setting: schools (n not reported) Strategies: school newsletters, local media |
Reach: not reported Expressions of interest: 107 Initiated expression of interest: not reported Expressions of interest rate: ≈ 13 families per week Enrolment rate: ≈ 6 or 7 families per week |
| The San Diego Family Health Project, Nader, 1989, USA;201 Nader, 1992, USA;202 Nader, 1983, USA;203 Patterson, 1988, USA204 |
CRCT (pre and 3 post measures) Study arms: Mexican American experimental, Anglo-American experimental, Mexican American control, or Anglo-American control Aims/objective: to decrease consumption of high-salt, high-fat foods; and increase frequency and intensity of physical activity |
Recruitment target: families (only up to two children and two adults measured) Target sample size: not reported Actual sample size: 206 families Family characteristics: Mexican American experimental: children: 12.1 (1.7) years (55%); adults: 37.1 (6.8) years (88%) Anglo-American experimental: children: 12.1 (1.9) years (38%); adults: 39.4 (7.1) years (62%) Mexican American control: children: 12.0 (1.7) years (49%); adults: 35.6 (6.9) years (75%) Anglo-American control: children: 11.8 (1.4) years (48%); adults: 36.9 (5.1) years (58%) |
Duration: not reported Setting: primary schools (n not reported) Strategies: newspaper articles, Parent–Teacher Association meetings, community groups and a family fun night (covered by a local TV station) |
Reach: ≈ 6000 children Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Behavior Opportunities Uniting Nutrition, Counseling, and Exercise (BOUNCE), Olvera, 2010, USA;205 Olvera, 2008, USA206 |
CRCT (pre and post measures) Study arms: experimental or control Aims/objective: primarily, to assess the efficacy of the BOUNCE intervention for improving physical fitness and activity in Latino mother–daughter pairs |
Recruitment target: Latino mother–daughter dyads Target sample size: 50 dyads Actual sample size: 46 dyads (experimental, n = 26; control, n = 20) Family characteristics: children: experimental – 9.9 (1.1) years (100%), control – 10.4 (1.1) years (100%); adults: experimental – 33.3 (4.6) years (100%), control – 38.2 (10.6) years (100%) |
Duration: not reported Setting: not reported Strategies: flyers mailed to homes of Latino families |
Reach: not reported Expressions of interest: 57 parents Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Owens, 2011, USA207 |
Quasi-experimental (pre and post measures) Study arms: experimental or control Aims/objective: to examine changes in physical activity and fitness in families after 3 months of home use of the Wii Fit |
Recruitment target: families Target sample size: not reported Actual sample size: 8 families (n = 21 participants) Family characteristics: children: 10.0 (1.6) years (50%); adults: 37.8 (4.9) years (78%) |
Duration: not reported Setting: not reported Strategies: local newspaper advertisement |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Etude Longitudinale Prospective Alimentation et Santé (ELPAS) study, Paineau, 2008, France208 |
RCT (pre and post measures) Study arms: group A (experimental), group B (experimental) and group C (no-treatment control) Hypothesis: family dietary coaching would improve nutritional intakes and weight control in free-living children and parents |
Recruitment target: families (parent–child dyad minimum) Target sample size: 295 families per experimental group and 420 families in the control group Actual sample size: 1013 families (Group A, n = 297 families; Group B, n = 298 families; Group C, n = 418 families) Family characteristics: children, 7.7. years (52%); adults, 40.5 (82%) |
Duration: 16 weeks Setting: schools only (n = 54) Strategies: mailed study information |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Y Living, Parra-Medina, 2015, USA209 |
Quasi-experimental (pre and post measures) Study arms: experimental arm only Aims/objective: to examine the impact of the Y Living Program on the weight status of adult and child participants |
Recruitment target: families Target sample size: not reported Actual sample size: 242 adults, 106 children Family characteristics: children, 12 (interquartile range 10–14) years (49%); adults, 41 (interquartile range 33–53) (81%) |
Duration: not reported Setting: churches, schools (number not reported) Strategies: organisational newsletters, neighbourhood newspapers, word-of-mouth |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Choosing 5 Fruits and Veg Every Day, Pearson, 2010, UK210 |
Pilot trial (pre and 2 post measures) Study arms: experimental or no treatment control Aims/objective: to evaluate the feasibility and effectiveness of a family-based newsletter intervention to increase fruit and vegetable consumption among adolescents |
Recruitment target: parent–adolescent dyads Target sample size: not reported Actual sample size: 49 dyads Family characteristics: children: experimental – 12.6 (1.0) years (44%), control – 12.3 (0.7) years (42%); adults: experimental – 44.4 (5.3) years (71%), control – 43.9 (3.6) years (75%) |
Duration: 16 weeks Setting: schools, universities, factories, warehouses, clubs/societies (number not reported) Strategies: newspaper and website advertisements, posters in workplaces (universities, factories, warehouses), and letters through schools and activity clubs/societies |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Daughters and Mothers Exercising Together (DAMET), Ransdell, 2004, USA;211 Ransdell, 2003, USA;212 Ransdell, 2001, USA213 |
Pilot trial (pre and post measures) Study arms: community-based or home-based experimental arms Aims/objective: to assess the effectiveness of home- and community-based physical activity interventions that target mothers and daughters to increase physical activity and improve health-related fitness |
Recruitment target: mother–daughter dyads Target sample size: not reported Actual sample size: 20 dyads Family characteristics: children: community-based – 15.2 (1.2) years (100%), home-based – 15.7 (1.5) years (100%); adults: community-based – 46.0 (8.5) years (100%), home-based – 44.0 (6.1) years (100%) |
Duration: not reported Setting: not reported Strategies: newspaper articles, local Girl Scout troop announcements, referral |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Generations Exercising Together to Improve Fitness (GET FIT), Ransdell, 2004, USA;214 Ornes, 2005, USA215 |
Pilot trial (pre and post measure) Study arms: experimental or no treatment control Aims/objective: to compare a 6-month home-based physical activity intervention with a control condition for physical activity and health-related fitness in three generations of women |
Recruitment target: grandmother–mother–daughter triads Target sample size: not reported Actual sample size: 17 triads Family characteristics: children: experimental – 10.8 (1.4) years (100%), control – 9.4 (1.5) years (100%); mothers: experimental – 37.8 (4.2) years (100%), control – 36.6 (4.2) years (100%); grandmothers: experimental – 60.7 (4.3) years (100%), control – 62.9 (4.5) years (100%) |
Duration: not reported Setting: not reported Strategies: newspaper, e-mail and flyer advertisements, word-of-mouth |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Rhodes, 2019, Canada;151 Quinlan, 2015, Canada216 |
RCT (pre and 3 post measures) Study arms: physical activity education + planning (experimental) or physical activity education (control) Aims/objective: to evaluate whether or not a planning condition improves regular physical activity compared with an education-only control condition among families |
Recruitment target: families (minimum parent–child dyad required) Target sample size: 160 families Actual sample size: 102 families Family characteristics: children: intervention – 8.8 (2.3) years (50%), control – 9.1 (1.9) years (54%); adults: intervention – 42.2 (5.7) years (76%) intervention, control – 43.0 (5.7) years (83%) Dual-parent families, 52%; single families, 44%; families with siblings, 29% |
Duration: not reported Setting: schools, recreation centres, health-care centres, children’s recreation classes, shopping malls and outdoor markets (number not reported) Strategies: newspaper advertisements. Snowball recruitment was also used, whereby families received a CA$25 grocery store gift card if they referred another family Recruitment was conducted by stratifying the city into regions to ensure diversity of families |
Reach: not reported Expressions of interest: 188 parents Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Rhodes, 2010, Canada141 |
Pilot RCT (pre and post measures) Study arms: standard intervention or standard intervention + planning Aims/objective: to examine the effect of a planning intervention compared with a standard condition on intergenerational physical activity in families |
Recruitment target: families Target sample size: not reported Actual sample size: 85 families Family characteristics: children: standard – range 4–10 years (not reported) standard+ – range 4–10 years (not reported); adults: standard – 38.6 (5.30 years (79%), standard+ – 39.0 (5.2) years (90%) |
Duration: 52 weeks Setting: day cares, recreation centres, preschools, primary schools (number not reported) Strategies: flyers, poster advertisements |
Reach: not reported Expressions of interest: 107 families Initiated expression of interest: not reported Expressions of interest rate: ≈ 2 families per week Enrolment rate: ≈ 1 or 2 families per week |
| Scouting Nutrition & Activity Program, Rosenkranz, 2010, USA;217 Rosenkranz, 2009, USA218 |
CRCT (pre and post measure) Study arms: experimental or standard-care control Aims/objective: to evaluate an intervention designed to prevent obesity by modifying Girl Scout troop meeting environments, and by empowering girls to improve the quantity and/or quality of family meals in their home environments |
Recruitment target: Girl Scout troops and their parents Target sample size: 8 troops with 20 girls per troop Actual sample size: 7 troops (mean 11 girls per troop) Family characteristics: children: experimental – 10.6 (1.1) years (100%), control – 10.5 (1.3) years (100%); adults: experimental – age and % female not reported, adults: control – age and % female not reported |
Duration: not reported Setting: Girl Scouts troops (n = 7 troops) Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Salimzadeh, 2010, Iran219 |
Quasi-experimental (pre and post measures) Study arms: experimental arm only Aims/objective: to evaluate the effectiveness of an exercise programme on the body composition and physical fitness of mothers and daughters |
Recruitment target: mother–daughter dyads Target sample size: not reported Actual sample size: 35 dyads Family characteristics: children: 15.0 (1.6) years (100%); adults: 40.0 (3.8) years (100%) |
Duration: not reported Setting: schools only (n = 5) Strategies: not reported |
Reach: 300 students Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Schwinn, 2014, USA220 |
Pilot trial (pre and 2 post measures) Study arms: experimental or control Aims/objective: to improve the well-being of girls living in public housing by improving dietary intake, increasing physical activity and reducing drug use risks |
Recruitment target: mother–daughter dyads Target sample size: not reported Actual sample size: 67 dyads (intervention, n = 36; control, n = 31) Family characteristics: children: 11.9 (0.9) years (100%); adults: 36.2 (6.2) years (100%) |
Duration: 4 weeks Setting: public housing development (n = 1) Strategies: Google AdWords, public housing development newspapers, Facebook and Craigslist advertisements |
Reach: not reported Expressions of interest: 86 Initiated expression of interest: not reported Expressions of interest rate: 21 or 22 families per week Enrolment rate: 16 or 17 families per week |
| Brighter Bites, Sharma, 2016, USA221 |
Quasi-experimental (pre and post measures) Study arms: Brighter Bites (experimental) or school health programme (control) Aims/objective: to evaluate the effectiveness of a school-based food co-op programme to increase fruit and vegetable intake, and home nutrition environment among low-income children and their parents |
Recruitment target: parent–child dyads Target sample size: not reported Actual sample size: 717 dyads (intervention, n = 407; control, n = 310) Family characteristics: children: 6.2 (0.4) years (52%); adults: 34.3 (7.4) years (90%) |
Duration: 2 school years Setting: schools only (n = 12) Strategies: not reported |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: 358 or 359 dyads per school year |
| No intervention name, Stolley, 1997, USA222 |
Pilot trial (pre and post measures) Study arms: experimental or control Aims/objective: to assess the effectiveness of an obesity prevention programme on pre-adolescent girls and their mothers |
Recruitment target: mother–daughter dyads Target sample size: not reported Actual sample size: 65 dyads Family characteristics: children: intervention – 9.9 (1.3) years (100%), control – 10.0 (1.5) years (100%); adults: intervention – 31.5 (3.4) years (100%), control – 33.7 (6.8) years (100%) |
Duration: not reported Setting: tutoring programme (n = 1) Strategies: advertisement in tutoring newsletter, letters sent to mothers of children registered in tutoring programme, presentation delivered to parents at tutoring programme orientation |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| One Body, One Life, Towey, 2011, UK223 |
Quasi-experimental (pre and post measures) Study arms: experimental arm only Aims/objective: to evaluate a family-based programme designed to prevent obesity |
Recruitment target: families Target sample size: not reported Actual sample size: 272 children and 182 parents. Family characteristics: children: 8.0 years (50%); adults: age not reported (87%) |
Duration: not reported Setting: neighbourhood groups, local fetes, community groups, general practitioner surgeries, libraries, children’s centres, print media, schools (number not reported) Strategies: flyers, posters, newsletters, word-of-mouth, referrals from health-care professionals and local newspapers, and making team members visible in the community (e.g. attending events, delivering ‘taster sessions’) |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| Family Eats, Cullen, 2017, USA224 |
RCT (pre and 2 post measures) Study arms: experimental or control Aims/objective: to improve parent and child fruit and vegetable intake |
Recruitment target: families Target sample size: not reported Actual sample size: 126 families (n = 92 intervention; n = 34 control) Family characteristics: children: age not reported (55%); adults: 59% aged < 40 years (98%) |
Duration: not reported Setting: schools, churches, health fairs, community centres (number not reported) Strategies: flyers, radio advertisements |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
| No intervention name, Ziebarth, 2012, USA225 |
Quasi-experimental (pre and post measures) Study arms: experimental arm only Aims/objective: to evaluate a family intervention programme designed to decrease overweight and obesity in Hispanic families |
Recruitment target: Hispanic families Target sample size: not reported Actual sample size: 47 families (adults, n = 57; children, n = 54) Family characteristics: children: age and % female not reported, adults: age 32 years (not reported) |
Duration: not reported Setting: local churches, medical clinics, schools, self-service laundries and community programmes (number not reported) Strategies: posters, announcements, word-of-mouth |
Reach: not reported Expressions of interest: not reported Initiated expression of interest: not reported Expressions of interest rate: not reported Enrolment rate: not reported |
Table 23 provides the details of all relevant recruitment data. Overall, a target sample size was presented a priori in 33% of studies, with a median target sample size of 120 (IQR 65–182) participants. Actual sample size was reported in 98% of studies and included a median of 100 (IQR 53–304) participants. Of the 16 studies in which target and actual sample sizes were provided, 56% recruited a sufficient number of participants. The duration of recruitment was reported in 33% of studies, and this was a median of 10 (IQR 8–36) weeks. Few studies reported figures on reach (18%), expressions of interest (33%), expressions of interest rate (16%), who initiated an expression of interest (< 1%) and enrolment rate (22%). Where reported, the median estimated reach was 437 (IQR 350–864) families, of whom 122 (IQR 92–174) expressed interest. The single study describing who expressed initial interest showed that in 82% (23/28) of the cases these were mothers. The median weekly expression of interest rate was 14 (IQR 11–21) families per week, with median enrolment rate at about 5 (IQR 2–11) families/dyads per week.
| Overall | Number of studies with relevant data (n = 49 studies) | |
|---|---|---|
| Target sample size (participants) | 120 (65–182) | 16 |
| Actual sample size (participants) | 100 (53–304) | 48 |
| Recruitment duration (weeks) | 10 (8–36) | 16 |
| Reach | 437 (350–864) | 9 |
| Expressions of interest | 119 (95–167) | 16 |
| Initiated expression of interest | 82% mothers | 1 |
| Expressions of interest rate (per week) | 14 (11–21) | 8 |
| Enrolment rate (families per week) | 5 (2–11) | 11 |
| Percentage of studies with under-recruitment | 44% | N/A |
Details on family recruitment settings and strategies were reported in 84% and 73% of studies, respectively. On average, researchers recruited from 2.2 ± 1.9 different settings and used 2.7 ± 1.2 recruitment strategies per study; there was no difference between full-scale trials, pilot/feasibility or quasi-experimental trials in the number of recruitment settings or strategies used. School-based recruitment was the most common recruitment setting, with community-based recruitment second. Community-based recruitment settings included churches, recreation centres, play groups, libraries, fairs/fetes, sports clubs, 4-H, day cares, preschools, tutoring programs, malls, grocery stores, farmers’ markets, cafes, trailer parks and laundromats. Recruitment also occurred through employers, primary care (e.g. general practitioners, health centres, other health-related businesses), and print/electronic media.
Across settings, the most commonly used recruitment strategies included disseminating study information through leaflets, posters or newsletters. School-based recruitment had the most recruitment strategies specific to the setting and included leaflets, posters, newsletters, letters from the head teacher (principal), research teams presenting study information to students and parents at assemblies, research teams presenting study information at other school events (e.g. parent–teacher association meetings), and research teams approaching parents during pick-up/drop-off times. Local newspapers and referral-based recruitment (e.g. word-of-mouth) were also popular recruitment strategies. Less commonly reported recruitment strategies included using: electronic/digital media (e.g. television, radio, social media, Google AdWords, Craigslist), face-to-face recruitment (e.g. home visits, community demonstrations), mail, telephone calls and distribution lists (e.g. via marketing companies).
Phase 2: Delphi study
We invited 107 experts, representing all inhabited continents, to participate in the Delphi study. Twenty-three experts actively declined as they were no longer conducting family-based research (n = 3) or did not have the time (n = 2), or gave no reason (n = 18). Six e-mail invitations bounced back and no other e-mail addresses were identified for these experts. Thirty-five experts participated in at least one round of the study; only 13 completed all rounds. Most participants were experienced researchers (full/associate/assistant professors, lecturers/senior lecturers; 82.8%), and most were from North America (71.4%), followed by Europe (11.4%), Australia/Oceania (8.6%), Asia (5.7%) and South America (2.9%).
Round 1: overview of experience with recruitment settings and strategies
Twenty-one participants provided information in round 1. Table 24 summarises the median (IQR) duration of recruitment and the sample sizes of the participants’ family-based studies. The participants recommended 36 different recruitment strategies, which fell into six overarching themes: school-based strategies (n = 14 Delphi participants recruited in schools), print and electronic media strategies (n = 8), community settings-based strategies (n = 7), primary care-based recruitment strategies (n = 4), employer-based strategies (n = 3) and referral-based recruitment (n = 3). Table 25 provides an overview of the 36 recruitment strategies described.
| Overall | Feasibility/pilot trials | Full-scale trials | |
|---|---|---|---|
| Studies (n) | 21 | 11 | 10 |
| Target sample size | 80 (60–210) | 60 (45–70) | 225 (170–486) |
| Actual sample size | 79 (41–180) | 41 (37–65) | 190 (131–375) |
| Initial recruitment duration (weeks) | 12 (7.5–52) | 8.5 (6–12) | 52 (10–68) |
| Percentage of studies in which recruitment was extended | 33 | 36 | 30 |
| Recruitment extension duration (weeks) | 20 (8–37.5) | 8 (8–11) | 48 (37.5–50) |
| Enrolment rate (families per week) | 4 (2–9) | 3 (2–6) | 8 (2–18) |
| Percentage of studies with under-recruitment | 62 | 55 | 70 |
| Category | Strategy | n | Mean | SD |
|---|---|---|---|---|
| Referral | Word-of-mouth | 23 | 4.8 | 1.8 |
| Schools | Letter about the study from head teacher to parents on behalf of research team | 25 | 4.4 | 1.7 |
| Media (print and electronic) | Social media posts (e.g. Facebook, Twitter) | 22 | 4.3 | 1.7 |
| Employers | Study information emailed to employees from within organisation on behalf of the research team (e.g. an e-mail sent from HR to employees within an organisation) | 24 | 4.2 | 1.4 |
| Schools | Assembly delivered to parents by research team | 25 | 4.2 | 2.0 |
| Primary care | Letters sent from GPs or health-care providers on behalf of research team | 23 | 4.2 | 1.8 |
| Community | Research team speaking to parents while waiting for their children (e.g. during their child’s swimming lesson) | 24 | 4.1 | 2.0 |
| Primary care | Letters from research team directly to potential participants | 23 | 4.0 | 1.8 |
| Schools | Research team attending parent meetings (e.g. orientation meetings, Parent Teacher Association meetings) | 25 | 4.0 | 1.9 |
| Media (print and electronic) | Television (local news story promoting study) | 22 | 4.0 | 2.0 |
| Media (print and electronic) | E-blasts (e.g. university news, third-party media groups, corporate mailing lists) | 22 | 4.0 | 1.6 |
| Media (print and electronic) | Electronic newsletter mailing list | 22 | 3.9 | 1.4 |
| Schools | Leaflets via e-mail (e.g. ParentMail) or other third-party companies (e.g. Peachjar) | 25 | 3.9 | 1.5 |
| Community | Research team speaking to parents during pick-up time (e.g. at the end of an after-school programme or a summer camp day) | 24 | 3.9 | 2.0 |
| Schools | Research team attending school events (e.g. sports day) | 25 | 3.8 | 1.9 |
| Media (print & electronic) | Radio (ads or story promoting study) | 23 | 3.8 | 1.9 |
| Schools | Study information in school newsletter (hard copy) | 25 | 3.8 | 1.4 |
| Community | Hard-copy leaflets to parents | 24 | 3.7 | 1.6 |
| Primary care | Telephone calls from research team directly to potential participants | 23 | 3.7 | 2.1 |
| Schools | Assembly delivered to students by research team | 25 | 3.7 | 1.5 |
| Media (print and electronic) | Print – newspaper (advertisements or story promoting study) | 23 | 3.6 | 1.6 |
| Primary care | Pull-tab poster displays in GP clinic | 22 | 3.6 | 1.1 |
| Schools | Hard-copy leaflets to parents via children | 25 | 3.6 | 1.7 |
| Schools | Study information written in students’ diary/agenda | 25 | 3.6 | 1.5 |
| Primary care | Hard-copy leaflets displayed in GP clinic | 23 | 3.5 | 1.1 |
| Employers | Hard-copy leaflets displayed in employee common areas (e.g. kitchen) | 24 | 3.5 | 1.3 |
| Media (print and electronic) | Print – other local publications (advertisements or story promoting study) | 23 | 3.4 | 1.3 |
| Community | Electronic neighbourhood bulletin boards | 23 | 3.4 | 1.1 |
| Community | Pull-tab poster displays | 23 | 3.4 | 1.1 |
| Schools | Research team hosting parent/researcher night to discuss study | 25 | 3.4 | 1.7 |
| Community | Pop-up stands disseminating study information directly (e.g. at local market) | 24 | 3.4 | 1.7 |
| Media (print and electronic) | Craigslist (an American classified advertisement website) | 20 | 3.4 | 1.5 |
| Media (print and electronic) | Print – magazines (advertisements or story promoting study) | 23 | 3.4 | 1.3 |
| Schools | Research team speaking to parents during ‘pick-up’ time | 25 | 3.3 | 2.0 |
| Schools | Research team hosting after school ‘drop-in’ sessions for parents | 25 | 3.1 | 1.6 |
School-based recruitment
School-based recruitment strategies included study information distributed by: hard copy leaflets to parents via children, school newsletters, letters from head teachers on behalf of research team, leaflets by e-mail (e.g. ParentMail) or via other third-party companies (e.g. Peachjar), assemblies with students and/or parents, students’ diary/agenda, research team attending parent meetings (e.g. orientation meetings, Parent–Teacher Association meetings) or other school events (e.g. sports day), hosting parent/researcher nights or after school ‘drop in’ sessions, speaking to parents during pick up time.
Generally, most Delphi study participants were successful at gaining approval from someone at most schools that they approached to distribute study information. However, gaining approval could be time-consuming and included multiple e-mails, telephone calls and/or face-to-face meetings (e.g. with head teachers, physical education co-ordinators, parent representatives). Some reported that, in future, they planned to either stop recruiting in schools or stop using passive recruitment strategies in schools (e.g. sending hard copy leaflets home with children to give to their parents). Staff time was considered a major resource requirement for recruiting in schools (e.g. searching for schools, visiting schools, travel time, assemblies/meetings preparation). In addition, many reported having to make multiple e-mails, phone calls and/or face-to-face meetings for permission to distribute study information. Other resource requirements reported for school-based recruitment were travel costs (e.g. petrol, car hire), printing costs and postage costs.
Print and electronic media-based recruitment
Participants reported using advertisements or stories about their study printed in magazines, newspapers, or other local publications as effective print-based recruitment strategies. Regarding recruitment strategies using electronic media, Delphi participants reported the following strategies as their most effective: social media posts (e.g. Twitter, Facebook, Instagram) radio, television news, e-blasts (e.g. via university news, third party media groups, corporate mailing lists), and electronic newsletters.
Disseminating study information through social media was the strategy that the most participants planned to implement in future. They reported that print and electronic media were wide-reaching and generally inexpensive to use. However, those with experience with this recruitment strategy reported low and slow response rates. Creating regular content on social media platforms or newsletters (e.g. update posts, quarterly newsletter, blogs) was considered more beneficial than one-off posts, advertisements, or newsletters. Caution was raised that some media-driven strategies can be less targeted than others (e.g. posts in social media groups, television advertisements/stories), which can lead to a lot of interest from ineligible participants (and increased staff requirements). Staff time was considered the greatest resource requirement (e.g. searching for online groups/communities, creating content, increased eligibility checking).
Community setting-based recruitment
The strategies applied in community setting-based recruitment were hard-copy leaflets or pull-tab posters, speaking to parents during pick-up time after community clubs, using pop-up stands at local events to speak to families, and using electronic neighbourhood bulletin boards. A wide variety of recruitment settings were reported, including churches, local museums, summer camps, Scouts/Guides, YMCA/YWCA, after-school programs, swimming pools, local events, local markets, Parkrun, newsagents, shopping centres, community centres, electronic neighbourhood bulletins and local businesses.
Generally, reports indicated that recruiting from community settings was unpredictable, with high yields at some events and no interest at others. It was reported to be very time-consuming to find appropriate places to recruit and stay on top of upcoming local events (and gaining approval to be at those events to recruit). Having staff attend events (e.g. local market, shopping centre) was also time-consuming and generally occurred outside normal working hours. Some participants planned to stop recruiting in some settings, specifically newsagents, community centres, and shopping centres because of the time investment required and poor yield. However, under some circumstances, community settings-based recruitment was suggested to be particularly effective, especially if the intervention is directly or partly tied to the recruitment setting. Some suggested that having outgoing staff could be important for engaging families and it may be beneficial to target parents while they are waiting for their children to complete an activity (e.g. during swimming lessons). Again, staff time was the biggest resource requirement (finding appropriate locations to recruit and events to attend, gaining approval to attend, and attending and distributing recruitment material). Other resource requirements reported for community settings-based recruitment were costs associated with printing, postage, travel, and equipment (e.g. pop-up gazebo, banners).
Employer-based recruitment
Employer-based recruitment strategies included displaying hard-copy leaflets in employee common areas (e.g. staff kitchen) or e-mails being sent to employees from within an organisation on behalf of the research team (e.g. an e-mail sent from human resources to employees within an organisation).
Generally, most participants found employer-based recruitment very time-consuming and had low levels of success at reaching and gaining approval from someone within an organisation to distribute study information. Recruitment in this setting allows a researcher to directly expose family decision-makers (i.e. parents) to study information; however, it is quite untargeted as many will be ineligible. Staff time was considered the major resource requirement for recruiting employers as many participants reported having to make multiple e-mails and telephone calls (mostly to generic email addresses or telephone numbers) for permission to distribute study information. Costs associated with travel, printing and postage need to be considered.
Primary care-based recruitment
Recruitment strategies used during primary care-based recruitment included displaying hard-copy leaflets in general practitioners’ offices, general practitioners or health-care providers sending letters on behalf of the research team, health-care providers making telephone calls on behalf of the research team and the research team sending letters or making telephone calls directly to potential participants.
Gaining access to electronic health records was considered a very effective way of identifying potential participants, but not necessarily of reaching participants, as their contact information was sometimes not current. Approaches that were deemed minimally effective included letters about the study sent from health-care providers to potential participants. It was cautioned that primary care-based recruitment can be very expensive (e.g. to access electronic medical records, time/reimbursement of the health-care provider or general practitioners) and technically challenging.
Referral-based recruitment
Referral-based recruitment (i.e. word of mouth) was usually not a method that was explicitly used by participants, but they reported that a modest number of enrolled families in their studies had been recruited through word of mouth (≈ 10–30% of their total sample). One Delphi study participant reported that referral-based recruitment was particularly effective in studies that had multiple waves of recruitment.
Round 2: effectiveness and resource efficiency of recruitment strategies
Table 25 shows the mean ratings of 25 participants for each recruitment strategy suggested in round 1 based on its perceived effectiveness and resource efficiency.
Round 3: ranking recruitment strategies
The 10 highest scoring strategies were ranked by 17 participants in round 3. Table 26 shows participants’ rankings of the top 10 most effective and resource efficient strategies for recruiting families into intervention studies. Findings between the top-rated strategies in round 2 and the final ranking of the top 10 strategies in round 3 were largely similar, apart from ‘speaking to parents’ and ‘attending parent meetings’, which were rated higher in the final ranking, and ‘word of mouth’ and ‘social media posting’, which were rated lower.
| Rank | Recruitment source | Recruitment strategy | Totala | Top rankb |
|---|---|---|---|---|
| 1 | Community | Research team speaking to parents while they are waiting for their children (e.g. while waiting during their child’s swimming lesson) | 64 | 4 |
| 2 | School | Letter sent from head teacher to parents on behalf of research team | 77 | 1 |
| 3 | School | Research team attending parent meetings (e.g. orientation meetings) | 79 | 2 |
| 4 | Employer | Study information emailed to employees from within organisation on behalf of the research team (e.g. from human resources) | 86 | 3 |
| 5 | Primary care | Letters sent from general practitioner or health-care providers on behalf of research team | 86 | 3 |
| 6 | School | Assembly delivered to parents by research team | 96 | 2 |
| 7 | Referral | Word of mouth | 97 | 1 |
| 8 | Primary care | Letters sent directly to potential participants from research team | 98 | 0 |
| 9 | Media | Social media posts (e.g. Facebook, Twitter, Instagram) | 106 | 1 |
| 10 | Media | Television (e.g. local news story promoting study) | 146 | 0 |
Discussion
The aim of this study was to systematically identify effective and resource-efficient strategies for recruiting families into physical activity, sedentary behaviour/screen time, diet and obesity prevention intervention research. Our systematic review showed that, despite being checklist items on the Consolidated Standards of Reporting Trials,80,226 data related to recruitment strategies and their effectiveness were scarcely reported among the included studies. Moreover, most studies applied similar recruitment strategies, predominantly through schools, despite the known challenges of recruiting families through school settings. Overall, a multisetting and multistrategy approach may be most effective, and the top 10 identified strategies may help researchers allocate limited resources effectively.
The data shown here indicate that researchers conducting family-based intervention studies were unable to attract sufficient expressions of interest, let alone recruit target sample sizes. We extracted very little information from the included studies related to expressions of interest and enrolment, which was similar to another review. 193 In particular, only one study reported which parent (i.e. mother or father) initiated an expression of interest. 78 That study found that 82% of the parents who initiated an expression of interest were mothers; however, once enrolled, fathers were enthusiastic about and benefited from their family’s participation in the study. The fact that most parents who expressed interest were mothers may not come as a surprise as, historically, mothers have been more likely than fathers to be their family’s social agent and lead on tasks such as family event preparation. 113,227 It may be prudent to consider this in the recruitment of families in two ways. First, recruitment materials that target mothers and their family may be the most efficient method of attracting expressions of interest; and it may also be an important catalyst for the inclusion of more fathers in family-based research. Second, separate recruitment materials that explicitly target fathers may also be useful and should be considered; Morgan and colleagues52,119,228 have written extensively on recruiting and engaging with fathers in family-based research.
Related to target sample size, we found that only 38% and 56% of the studies included in our Delphi study and review, respectively, recruited their target sample size. Similarly, other reviews of publicly funded trials have found that only 33–50% of included trials recruited 80–100% of their target sample size within their pre-agreed timescale. 145,146,162,229 Few studies reported on reach and representativeness, but, generally, healthy and affluent families were recruited. Only one study, as far as we are aware, described formative work in which families were consulted to inform the development of the recruitment strategy. 78 Although the target sample size was not achieved in that study, public involvement should be encouraged and has been highlighted as a good method for helping with participant recruitment, engagement and retention. 230 It is also possible that the chance of being randomly allocated into a study arm that was not a family’s preferred study arm may have negatively affected recruitment;231 however, no study reported that the randomisation procedure hindered their recruitment.
Analogous to our Delphi study findings, one-third of trials received an extension of some kind because of recruitment-related issues. 146,162 Our findings showed the planned median recruitment duration to be about 10–11 weeks and when recruitment extensions were implemented recruitment was extended for an additional 20 weeks, which would have a substantial impact on a study’s timeline. A recent survey on research priorities related to the methodology of trials among directors of the Clinical Trials Units registered with the NIHR Clinical Research Network in the UK identified the recruitment of participants in trials as among the top three priorities for improvement;232 overall, our findings reinforce these concerns.
The majority of included studies reported the settings from which they recruited participants, and our findings indicate that researchers recruited in about two settings per study, on average. In both our review and our Delphi study, we found that the two most common recruitment settings were schools and the community. Other recruitment settings included primary care settings, employers and social media. Although it was positive to find that recruitment occurred in multiple settings, as recommended by others,29,30,233 usually it was not possible to discern what proportion of a study’s sample had been recruited by setting.
On average, researchers used about three recruitment strategies per study. As in other studies,233,234 the most commonly used recruitment strategies for family-based recruitment included disseminating study information through leaflets, posters or newsletters. Placing advertisements in local newspapers, using electronic media (e.g. social media platforms, radio, television) and referral-based recruitment (e.g. word-of-mouth) were also popular. Considering that school-based recruitment was the most used recruitment setting, it was unsurprising that this setting had the greatest number of recruitment strategies. Generally, recruitment strategies were only listed in study manuscripts and not described in any great detail, particularly in terms of how and by whom these strategies were actually implemented. However, among the few studies that recruited a sufficient sample size, many included strategies that targeted adults and children and often while they were together. 204,205,207,208 For example, interacting with parents and children at school drop-off/pick-up, giving study presentations at school events (e.g. parent nights) or making announcements from the pulpit are some of the strategies used in the studies that recruited their target sample size. Furthermore, based on the top 10 recommended recruitment strategies identified here, it appears that leveraging familiar, and perhaps trusted, relationships would be beneficial. For example, disseminating study information in correspondence from head teachers, general practitioners and human resources staff and by word of mouth (e.g. through family friends) are strategies that generally assume that potential participants would have at least some familiarity with the person disseminating the information. Even those Delphi participants who were most enthusiastic about recruiting through social media platforms appeared to be trying to build rapport with their followers (i.e. potential participants). Delphi participants recommended that creating regular content on social media platforms or newsletters (e.g. update posts, quarterly newsletter, blogs) would be more beneficial than one-off posts, advertisements or newsletters. The top 10 strategies also include several face-to-face recruitment strategies (e.g. delivering assemblies, attending parent–teacher meetings). Although face-to-face recruitment can be extremely time (and resource) consuming, studies that included this type of recruitment were more likely to achieve close to their target sample size. 229 In addition, face-to-face recruitment allows for quick rapport-building and gives potential participants the ability to receive responses to their questions about the study in real time, while they are still interested. 235
Strengths and limitations
As far as we are aware, this study is the first comprehensive assessment of recruitment in family-based intervention research. We conducted a systematic review of the available evidence, and the inclusion of the Delphi procedure provides additional credibility and insight to the findings of the review. In addition, our Delphi procedure had several strengths, including participant blinding, iterative data collection, controlled feedback and purposive sampling. Despite these strengths, there are some limitations that should be considered. We conducted a comprehensive literature search but cannot rule out that we may have missed some publications. The data available related to recruitment duration, reach, expressions of interest, expressions of interest rate and enrolment rate were scant, and details about the implementation of recruitment strategies were often vague. Although we made efforts to contact authors for this information (if available), few authors responded to our e-mails. In addition, we had a low and variable response rate to our Delphi study. Generally, Delphi study participants reported recruitment strategies that they perceived to be effective and resource efficient; therefore, self-report could be considered a limitation. Moreover, the majority of included studies and Delphi study participants were from North America and Europe. Optimum recruitment strategies and setting may differ by context, and we recognise the lack of a global perspective on how best to recruit families and that some recommended recruitment strategies may not be feasible or appropriate everywhere. Last, our review was limited to articles published in English and our Delphi study was also limited to researchers who were competent in English.
Concluding remarks
In conclusion, this study highlights that (1) under-recruitment is a major issue in family-based trials and (2) there is a clear need to improve reporting related to recruitment, for example by following the checklist items in the Consolidated Standards of Reporting Trials. 80,226 Improved reporting on the effectiveness of recruitment will give future researchers the ability to better budget their time and resources, as well as provide them with greater confidence that they will meet their target sample size. Our findings suggest that researchers should employ a multifaceted recruitment approach that targets adults and children and provides potential participants with repeated exposure to study information. This study also provides experts’ recommendations for recruitment strategies; future research should investigate the effectiveness of these strategies in different settings. In future, analyses should be conducted to estimate the cost of recruiting families into trials. Future research should explore more sophisticated and innovative research strategies, which may include, for example, consultation with experts in data science, marketing, graphic design or social media.
Chapter 8 Recommendations for research
Recommendations for research have been discussed in the discussion sections of the chapters included in this report. They are summarised here for ease of reference.
-
Future research should continue exploring ways of engaging whole families in physical activity. The FRESH project demonstrates that family-based physical activity promotion is feasible and acceptable, but the intervention generally had limited effectiveness. The findings and experiences reported here should be used as building blocks to help researchers identify novel avenues for intervention and evaluation. This may include, for example, capitalising on the active engagement of fathers in the FRESH intervention following sign-up by mothers.
-
Recruiting whole families, where any parent could initiate an expression of interest, may be an important catalyst for the inclusion of more fathers in family-based research. It is important that researchers consider this in the recruitment of families in two ways. First, recruitment materials that target mothers and their family may be the most efficient method of attracting expressions of interest. Second, separate recruitment materials that explicitly target fathers should be considered.
-
The FRESH study included an extensive outcome assessment protocol. The duration of data collection was broadly in line with a priori estimates, and the acceptability of the duration and number of measures was high among both adults and children. Nevertheless, the duration and number of measures may have acted as a barrier to participation. Researchers and funders should, therefore, carefully balance the scientific need for extensive data collection (driven, for example, by questions around how interventions work, and impacts on important physical health outcomes beyond the target behaviour) with the burden of data collection on participants and the impact it has on recruitment of a representative sample of participants.
-
Methodological research is required to support the optimisation of family recruitment methods. This should focus on the cost and effectiveness of diverse recruitment strategies in different settings, and should consider the impact on recruiting hard-to-reach populations.
-
Future family-based physical activity promotion research should explore the potential of compensatory effects on children’s physical activity behaviours, whereby increased physical activity with family members replaces physical activity otherwise done in other settings and with other co-participants (e.g. friends).
-
Device-based assessment of family co-participation in physical activity is feasible and provides objectively-assessed insights into the context of children’s and adults’ physical activity behaviour. Future research should continue to explore the utility of combined accelerometry and GPS data for understanding the social context of physical activity behaviour, accounting for clustering of physical activity behaviours within families.
-
Future family-based physical activity promotion research should consider conducting exploratory cost-effectiveness analyses. This could focus on the cost per quality-adjusted life-year gained and/or the cost of improving an additional unit of MVPA. Future research should also explore how much local authorities or other delivery agents are willing or able to pay for children’s physical activity interventions in general and for family-based physical activity in particular.
-
Research into family-based physical activity promotion may benefit from focusing intervention efforts on low-active families. These families may have more to gain from intervention engagement and this could represent a more targeted use of scarce resources.
-
Researchers are encouraged to provide more detail in relation to family recruitment strategies and their effectiveness in published documents, as included in relevant CONSORT statements. This should include, for example, information on who led on recruitment, the methods and materials used, the time to recruit the target population, reach, expressions of interest and the demographic characteristics of the population recruited. A more detailed account of recruitment efforts and their effectiveness will help researchers to better plan and resource future studies.
-
Researchers are encouraged to apply a multisetting and multistrategy approach targeting both adults and children to family recruitment and to test the effectiveness of the top 10 strategies identified in this project in different contexts.
-
Future research should consider more sophisticated and innovative recruitment strategies, which may include, for example, consultation with experts in data science, marketing, graphic design or social media.
Chapter 9 Conclusions
The FRESH project demonstrates the feasibility and acceptability of the family-targeted FRESH intervention, satisfying the majority of progression criteria set a priori. However, in both the feasibility and the pilot study we failed to recruit the target sample size. Moreover, in the pilot study we were unable to demonstrate a signal of effectiveness on time spent in MVPA. This was particularly the case at the long-term assessment and in children, whereas change in children's MVPA at long-term follow-up was the prespecified main outcome measure for a potential future full-scale trial. We successfully demonstrated the potential for device-based assessment of family physical activity, which we recommend for use in future studies. We also show that future family-based research would benefit from a multifaceted recruitment approach that targets adults and children and provides potential participants with repeated exposure to study information. Prior to progressing to a full-scale trial of the FRESH family-based physical activity intervention, further refinements around intervention delivery (particularly planning with families, efficient online delivery and capitalising on the involvement of fathers) and recruitment methods should be implemented.
Acknowledgements
Acknowledgement of contributions and funding
We thank Active Norfolk and Suffolk County Council for providing funding for the delivery of the FRESH programme. We are grateful to participating families their enthusiastic involvement in the study and to the schools, workplaces and community settings that enabled us to recruit families from their locations. We acknowledge FRESH, Centre for Family Research, Cambridge Research Methods Hub, and MRC Epidemiology Unit staff and students past and present for their involvement in the project. We also thank the FRESH Study Steering Committee and patient and public involvement groups who have provided valuable advice through the project. This work was supported by the National Institute for Health Research Public Health Research programme (project number 15/01/19). This work was additionally supported by the MRC [Unit Programme number MC_UU_12015/7], and undertaken under the auspices of the Centre for Diet and Activity Research (CEDAR), a UKCRC Public Health Research Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, MRC, the National Institute for Health Research, and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged (087636/Z/08/Z; ES/G007462/1; MR/K023187/1).
Contributions of authors
Esther MF van Sluijs (https://orcid.org/0000-0001-9141-9082) (MRC Programme Leader, Behavioural Epidemiology) gained funding, conceptualised the study, acted as chief investigator of the studies included in this report and drafted this report.
Helen E Brown (https://orcid.org/0000-0001-7632-1714) (Research Associate, Behavioural Epidemiology) gained funding, initially conceptualised the intervention, and advised on study conduct and the interpretation of the results.
Emma Coombes (https://orcid.org/0000-0002-7980-5850) (Research Fellow, Public Health) led on the methodological development of the family co-participation measure.
Claire Hughes (https://orcid.org/0000-0003-2545-3025) (Professor, Psychology) gained funding, conceptualised the study, led on the assessment of family functioning and provided a family perspective on the interpretation of the results.
Andrew P Jones (https://orcid.org/0000-0002-3130-9313) (Professor, Public Health) gained funding, conceptualised the study and provided a public health perspective on the interpretation of the results.
Katie L Morton (https://orcid.org/0000-0002-9961-6491) (Research Associate, Behavioural Epidemiology) gained funding, advised on conduct and analyses of qualitative data and provided a behavioural science perspective on the interpretation of the results.
Justin M Guagliano (https://orcid.org/0000-0002-4450-5700) (Research Associate, Behavioural Epidemiology) operationalised the intervention, led on recruitment and data collection, conducted statistical analyses and prepared the results for publication.
Publications
Guagliano JM, Brown HE, Coombes E, Haines ES, Hughes C, Jones AP, et al. Whole family-based physical activity promotion intervention: the Families Reporting Every Step to Health pilot randomised controlled trial protocol. BMJ Open 2019;9:e030902.
Guagliano JM, Brown HE, Coombes E, Hughes C, Jones AP, Morton KL, et al. The development and feasibility of a randomised family-based physical activity promotion intervention: the Families Reporting Every Step to Health (FRESH) study. Pilot Feasibility Stud 2019;5:21.
Guagliano JM, Armitage SM, Brown HE, Coombes E, Hughes C, Jones AP, et al. A whole family-based physical activity promotion intervention: Findings from the Families Reporting Every Step to Health (FRESH) pilot randomised controlled trial. Int J Behav Nutr Phys Act 2020;17:120.
Guagliano JM, Morton KL, Hughes C, van Sluijs EMF. Effective and resource efficient strategies for recruiting families in physical activity, sedentary behaviour, nutrition, and obesity prevention research: a systematic review with expert opinion. Obes Rev 2021;22:e13161.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following favourable review of a research proposal.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Poitras VJ, Gray CE, Borghese MM, Carson V, Chaput JP, Janssen I, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab 2016;41:197-239. https://doi.org/10.1139/apnm-2015-0663.
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010;7. https://doi.org/10.1186/1479-5868-7-40.
- Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A. International Children’s Accelerometry Database (ICAD) Collaborators . Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA 2012;307:704-12. https://doi.org/10.1001/jama.2012.156.
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Lancet Physical Activity Series Working Group . Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219-29. https://doi.org/10.1016/S0140-6736(12)61031-9.
- Hills AP, Andersen LB, Byrne NM. Physical activity and obesity in children. Br J Sports Med 2011;45:866-70. https://doi.org/10.1136/bjsports-2011-090199.
- Schmitz K, Jacobs D, Hong C, Steinberger J, Moran A, Sinaiko A. Association of physical activity with insulin sensitivity in children. Int J Obes Relat Metab Dis 2002;26:1310-16. https://doi.org/10.1038/sj.ijo.0802137.
- Gunter KB, Almstedt HC, Janz KF. Physical activity in childhood may be the key to optimizing lifespan skeletal health. Exerc Sport Sci Rev 2012;40:13-21. https://doi.org/10.1097/JES.0b013e318236e5ee.
- Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med 2011;45:886-95. https://doi.org/10.1136/bjsports-2011-090185.
- Brown HE, Pearson N, Braithwaite RE, Brown WJ, Biddle SJ. Physical activity interventions and depression in children and adolescents: a systematic review and meta-analysis. Sports Med 2013;43:195-206. https://doi.org/10.1007/s40279-012-0015-8.
- Singh A, Uijtdewilligen L, Twisk JW, van Mechelen W, Chinapaw MJ. Physical activity and performance at school: a systematic review of the literature including a methodological quality assessment. Arch Pediatr Adolesc Med 2012;166:49-55. https://doi.org/10.1001/archpediatrics.2011.716.
- Liu M, Wu L, Yao S. Dose–response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br J Sports Med 2015;6:S240-65.
- Carson V, Hunter S, Kuzik N, Gray CE, Poitras VJ, Chaput JP, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutr Metab 2016;41:240-65. https://doi.org/10.1139/apnm-2015-0630.
- Janz KF, Levy SM, Burns TL, Torner JC, Willing MC, Warren JJ. Fatness, physical activity, and television viewing in children during the adiposity rebound period: the Iowa Bone Development Study. Prev Med 2002;35:563-71. https://doi.org/10.1006/pmed.2002.1113.
- Fisher A, Reilly JJ, Montgomery C, Kelly LA, Williamson A, Jackson DM, et al. Seasonality in physical activity and sedentary behavior in young children. Pediatric Exercise Sci 2005;17:31-40. https://doi.org/10.1123/pes.17.1.31.
- Sardinha LB, Andersen LB, Anderssen SA, Quitério AL, Ornelas R, Froberg K, et al. Objectively measured time spent sedentary is associated with insulin resistance independent of overall and central body fat in 9- to 10-year-old Portuguese children. Diabetes Care 2008;31:569-75. https://doi.org/10.2337/dc07-1286.
- Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian children and youth: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep 2011;22:15-23.
- Telama R. Tracking of physical activity from childhood to adulthood: a review. Obes Facts 2009;2:187-95. https://doi.org/10.1159/000222244.
- Department of Health and Social Care . UK Chief Medical Officers’ Physical Activity Guidelines 2019.
- Townsend N, Wickramasinghe K, Williams J, Bhatnagar P, Rayner N. Physical Activity Statistics 2015. London: British Heart Foundation; 2015.
- Wilkie H, Standage M, Sherar L, Cumming S, Parnell C, Davis A, et al. Results from England’s 2016 report card on physical activity for children and youth. J Phys Act Health 2016;13:143-9. https://doi.org/10.1123/jpah.2016-0298.
- Steene-Johannessen J, Hansen BH, Dalene KE, Kolle E, Northstone K, Møller NC, et al. Variations in accelerometry measured physical activity and sedentary time across Europe – harmonized analyses of 47,497 children and adolescents. Int J Behav Nutr Phys Act 2020;17. https://doi.org/10.1186/s12966-020-00930-x.
- Brooke HL, Atkin AJ, Corder K, Ekelund U, van Sluijs EM. Changes in time-segment specific physical activity between ages 10 and 14 years: a longitudinal observational study. J Sci Med Sport 2016;19:29-34. https://doi.org/10.1016/j.jsams.2014.10.003.
- Corder K, Craggs C, Jones AP, Ekelund U, Griffin SJ, van Sluijs EM. Predictors of change differ for moderate and vigorous intensity physical activity and for weekdays and weekends: a longitudinal analysis. Int J Behav Nutr Phys Act 2013;10. https://doi.org/10.1186/1479-5868-10-69.
- Corder K, Sharp SJ, Atkin AJ, Griffin SJ, Jones AP, Ekelund U, et al. Change in objectively measured physical activity during the transition to adolescence. Br J Sports Med 2015;49:730-6. https://doi.org/10.1136/bjsports-2013-093190.
- Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Lancet Physical Activity Series Working Group . Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247-57. https://doi.org/10.1016/S0140-6736(12)60646-1.
- Craggs C, van Sluijs EM, Corder K, Panter JR, Jones AP, Griffin SJ. Do children’s individual correlates of physical activity differ by home setting?. Health Place 2011;17:1105-12. https://doi.org/10.1016/j.healthplace.2011.05.013.
- Farooq A, Martin A, Janssen X, Wilson MG, Gibson AM, Hughes A, et al. Longitudinal changes in moderate-to-vigorous-intensity physical activity in children and adolescents: a systematic review and meta-analysis. Obes Rev 2020;21. https://doi.org/10.1111/obr.12953.
- DeBate RD, Pettee Gabriel K, Zwald M, Huberty J, Zhang Y. Changes in psychosocial factors and physical activity frequency among third- to eighth-grade girls who participated in a developmentally focused youth sport program: a preliminary study. J Sch Health 2009;79:474-84. https://doi.org/10.1111/j.1746-1561.2009.00437.x.
- Brown HE, Atkin AJ, Panter J, Wong G, Chinapaw MJ, van Sluijs EM. Family-based interventions to increase physical activity in children: a systematic review, meta-analysis and realist synthesis. Obes Rev 2016;17:345-60. https://doi.org/10.1111/obr.12362.
- Brown HE, Schiff A, van Sluijs EM. Engaging families in physical activity research: a family-based focus group study. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2497-4.
- Love R, Adams J, van Sluijs EMF. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes Rev 2019;20:859-70. https://doi.org/10.1111/obr.12823.
- Jones M, Defever E, Letsinger A, Steele J, Mackintosh KA. A mixed-studies systematic review and meta-analysis of school-based interventions to promote physical activity and/or reduce sedentary time in children. J Sport Health Sci 2020;9:3-17. https://doi.org/10.1016/j.jshs.2019.06.009.
- Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ 2012;345. https://doi.org/10.1136/bmj.e5888.
- Borde R, Smith JJ, Sutherland R, Nathan N, Lubans DR. Methodological considerations and impact of school-based interventions on objectively measured physical activity in adolescents: a systematic review and meta-analysis. Obes Rev 2017;18:476-90. https://doi.org/10.1111/obr.12517.
- Larouche R, Mammen G, Rowe DA, Faulkner G. Effectiveness of active school transport interventions: a systematic review and update. BMC Public Health 2018;18. https://doi.org/10.1186/s12889-017-5005-1.
- Escalante Y, García-Hermoso A, Backx K, Saavedra JM. Playground designs to increase physical activity levels during school recess: a systematic review. Health Educ Behav 2014;41:138-44. https://doi.org/10.1177/1090198113490725.
- Lonsdale C, Rosenkranz RR, Peralta LR, Bennie A, Fahey P, Lubans DR. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical education lessons. Prev Med 2013;56:152-61. https://doi.org/10.1016/j.ypmed.2012.12.004.
- Hollis JL, Sutherland R, Williams AJ, Campbell E, Nathan N, Wolfenden L, et al. A systematic review and meta-analysis of moderate-to-vigorous physical activity levels in secondary school physical education lessons. Int J Behav Nutr Phys Act 2017;14. https://doi.org/10.1186/s12966-017-0504-0.
- Atkin AJ, Gorely T, Biddle SJ, Cavill N, Foster C. Interventions to promote physical activity in young people conducted in the hours immediately after school: a systematic review. Int J Behav Med 2011;18:176-87. https://doi.org/10.1007/s12529-010-9111-z.
- Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot 1996;10:282-98. https://doi.org/10.4278/0890-1171-10.4.282.
- Davison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obes Rev 2001;2:159-71. https://doi.org/10.1046/j.1467-789x.2001.00036.x.
- Bellows-Riecken KH, Rhodes RE. A birth of inactivity? A review of physical activity and parenthood. Prev Med 2008;46:99-110. https://doi.org/10.1016/j.ypmed.2007.08.003.
- Yao CA, Rhodes RE. Parental correlates in child and adolescent physical activity: a meta-analysis. Int J Behav Nutr Phys Act 2015;12. https://doi.org/10.1186/s12966-015-0163-y.
- O’Connor TM, Jago R, Baranowski T. Engaging parents to increase youth physical activity: a systematic review. Am J Prev Med 2009;37:141-9. https://doi.org/10.1016/j.amepre.2009.04.020.
- Fuemmeler BF, Anderson CB, Mâsse LC. Parent-child relationship of directly measured physical activity. Int J Behav Nutr Phys Act 2011;8. https://doi.org/10.1186/1479-5868-8-17.
- McMinn AM, Griffin SJ, Jones AP, van Sluijs EM. Family and home influences on children’s after-school and weekend physical activity. Eur J Public Health 2013;23:805-10. https://doi.org/10.1093/eurpub/cks160.
- Gustafson SL, Rhodes RE. Parental correlates of physical activity in children and early adolescents. Sports Med 2006;36:79-97. https://doi.org/10.2165/00007256-200636010-00006.
- Abbott G, Hnatiuk J, Timperio A, Salmon J, Best K, Hesketh KD. Cross-sectional and longitudinal associations between parents’ and preschoolers’ physical activity and television viewing: the HAPPY study. J Phys Act Health 2016;13:269-74. https://doi.org/10.1123/jpah.2015-0136.
- Nader PR, Bradley RH, Houts RM, McRitchie SL, O’Brien M. Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA 2008;300:295-30. https://doi.org/10.1001/jama.300.3.295.
- Rowlands AV, Pilgrim EL, Eston RG. Patterns of habitual activity across weekdays and weekend days in 9–11-year-old children. Prev Med 2008;46:317-24. https://doi.org/10.1016/j.ypmed.2007.11.004.
- Ventura AK, Birch LL. Does parenting affect children’s eating and weight status?. Int J Behav Nutr Phys Act 2008;5. https://doi.org/10.1186/1479-5868-5-15.
- Morgan PJ, Jones RA, Collins CE, Hesketh KD, Young MD, Burrows TL, et al. Practicalities and research considerations for conducting childhood obesity prevention interventions with families. Children 2016;3. https://doi.org/10.3390/children3040024.
- Marsh S, Foley LS, Wilks DC, Maddison R. Family-based interventions for reducing sedentary time in youth: a systematic review of randomized controlled trials. Obes Rev 2014;15:117-33. https://doi.org/10.1111/obr.12105.
- Schlechter CR, Rosenkranz RR, Guagliano JM, Dzewaltowski DA. A systematic review of children’s dietary interventions with parents as change agents: application of the RE-AIM framework. Prev Med 2016;91:233-43. https://doi.org/10.1016/j.ypmed.2016.08.030.
- van Sluijs EM, McMinn A. Preventing obesity in primary schoolchildren. BMJ 2010;340. https://doi.org/10.1136/bmj.c819.
- Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014;348. https://doi.org/10.1136/bmj.g3256.
- Gruber KJ, Haldeman LA. Using the family to combat childhood and adult obesity. Prev Chronic Dis 2009;6.
- Tremblay MS, Barnes JD, González SA, Katzmarzyk PT, Onywera VO, Reilly JJ, et al. Global Matrix 2.0: report card grades on the physical activity of children and youth comparing 38 countries. J Phys Act Health 2016;13:343-66. https://doi.org/10.1123/jpah.2016-0594.
- Shonkoff JP, Fisher PA. Rethinking evidence-based practice and two-generation programs to create the future of early childhood policy. Dev 2013;25:1635-53. https://doi.org/10.1017/S0954579413000813.
- Park A-L. The effects of intergenerational programmes on children and young people. Int J School Cognitive Psychol 2015;2. https://doi.org/10.4172/2469-9837.1000118.
- Deci EL, Ryan RM. Intrinsic Motivation and Self-determination in Human Behavior. Plenum, NY: Springer Science & Business Media; 1985.
- Uijtdewilligen L, Nauta J, Singh AS, van Mechelen W, Twisk JW, van der Horst K, et al. Determinants of physical activity and sedentary behaviour in young people: a review and quality synthesis of prospective studies. Br J Sports Med 2011;45:896-905. https://doi.org/10.1136/bjsports-2011-090197.
- van Sluijs EM, Kriemler S, McMinn AM. The effect of community and family interventions on young people’s physical activity levels: a review of reviews and updated systematic review. Br J Sports Med 2011;45:914-22. https://doi.org/10.1136/bjsports-2011-090187.
- Timperio A, Salmon J, Ball K. Evidence-based strategies to promote physical activity among children, adolescents and young adults: review and update. J Sci Med Sport 2004;7:20-9. https://doi.org/10.1016/S1440-2440(04)80274-3.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68-7. https://doi.org/10.1037/0003-066x.55.1.68.
- Biddle SJ, Nigg CR. Theories of exercise behavior. Int J Sport Psychol 2000;31:290-304.
- Fortier MS, Kowal J, Hagger M, Chatzisarantis N. Self-determination Theory in Exercise and Sport. Champaign, IL: Human Kinetics; 2007.
- Wilson PM, Mack DE, Grattan KP. Understanding motivation for exercise: a self-determination theory perspective. Can Psychol 2008;49. https://doi.org/10.1037/a0012762.
- Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Can Psychol 2008;49:182-5. https://doi.org/10.1037/a0012801.
- Deci EL, Ryan RM. The ‘what’ and ‘why’ of goal pursuits: human needs and the self-determination of behavior. Psychol Inquiry 2000;11:227-68. https://doi.org/10.1207/S15327965PLI1104_01.
- Fortier MS, Duda JL, Guerin E, Teixeira PJ. Promoting physical activity: development and testing of self-determination theory-based interventions. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-20.
- Deci EL, Ryan RM. Handbook of Self-determination Research. Rochester, NY: University of Rochester Press; 2002.
- Silva MN, Vieira PN, Coutinho SR, Minderico CS, Matos MG, Sardinha LB, et al. Using self-determination theory to promote physical activity and weight control: a randomized controlled trial in women. J Behav Med 2010;33:110-22. https://doi.org/10.1007/s10865-009-9239-y.
- Fortier MS, Sweet SN, O’Sullivan TL, Williams GC. A self-determination process model of physical activity adoption in the context of a randomized controlled trial. Psychol Sport Exercise 2007;8:741-57. https://doi.org/10.1016/j.psychsport.2006.10.006.
- Gillis L, Tomkinson G, Olds T, Moreira C, Christie C, Nigg C, et al. Research priorities for child and adolescent physical activity and sedentary behaviours: an international perspective using a twin-panel Delphi procedure. Int J Behav Nutr Phys Act 2013;10. https://doi.org/10.1186/1479-5868-10-112.
- National Institute for Health and Care Excellence . Promoting Physical Activity for Children and Young People: Evidence Update 2015.
- NIHR . Guidance on Applying for Feasibility Studies n.d. www.nihr.ac.uk/documents/guidance-on-applying-for-feasibility-studies/20474 (accessed 22 July 2021).
- Guagliano JM, Brown HE, Coombes E, Hughes C, Jones AP, Morton KL, et al. The development and feasibility of a randomised family-based physical activity promotion intervention: the Families Reporting Every Step to Health (FRESH) study. Pilot Feasibility Stud 2019;5. https://doi.org/10.1186/s40814-019-0408-7.
- Rhodes RE, Lim C. Promoting parent and child physical activity together: elicitation of potential intervention targets and preferences. Health Educ Behav 2018;45:112-23. https://doi.org/10.1177/1090198117704266.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Norfolk County Council . Data and Information About Norfolk’s Population 2015. www.norfolkinsight.org.uk/ (accessed 27 June 2018).
- Norfolk County Council . Rural-Urban Classification 2015. www.norfolkinsight.org.uk/dataviews/tabular?viewId=99%26geoId=54%26subsetId=12 (accessed 27 June 2018).
- Office for National Statistics . 2011 Rural Urban Classification 2011. www.ons.gov.uk/methodology/geography/geographicalproducts/ruralurbanclassifications/2011ruralurbanclassification (accessed 27 June 2018).
- Christensen P. The health-promoting family: a conceptual framework for future research. Soc Sci Med 2004;59:377-87. https://doi.org/10.1016/j.socscimed.2003.10.021.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- University of Worcester . Activity to Step Converter 2018. www.worcester.ac.uk/discover/moon-mission-activity-to-step-converter.html (accessed 24 December 2018).
- Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc 2011;43:357-64. https://doi.org/10.1249/MSS.0b013e3181ed61a3.
- Plasqui G, Westerterp KR. Physical activity assessment with accelerometers: an evaluation against doubly labeled water. Obesity 2007;15:2371-9. https://doi.org/10.1038/oby.2007.281.
- Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 2011;43:1360-8. https://doi.org/10.1249/MSS.0b013e318206476e.
- Aadland E, Ylvisåker E. Reliability of the Actigraph GT3X+ accelerometer in adults under free-living conditions. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0134606.
- Rodriguez DA, Shay E, Winn P. Comparative Review of Portable Global Positioning System Units. New York, NY: Nova Science Publishers; 2013.
- Collings PJ, Wijndaele K, Corder K, Westgate K, Ridgway CL, Dunn V, et al. Levels and patterns of objectively-measured physical activity volume and intensity distribution in UK adolescents: the ROOTS study. Int J Behav Nutr Phys Act 2014;11. https://doi.org/10.1186/1479-5868-11-23.
- Pan H, Cole TJ. LMSgrowth Program Version 2.77. London: Child Growth Foundation; 2012.
- Wareham NJ, Jakes RW, Rennie KL, Mitchell J, Hennings S, Day NE. Validity and repeatability of the EPIC-Norfolk Physical Activity Questionnaire. Int J Epidemiol 2002;31:168-74. https://doi.org/10.1093/ije/31.1.168.
- Corder K, van Sluijs EM, Wright A, Whincup P, Wareham NJ, Ekelund U. Is it possible to assess free-living physical activity and energy expenditure in young people by self-report?. Am J Clin Nutrition 2009;89:862-70. https://doi.org/10.3945/ajcn.2008.26739.
- Lampard AM, Nishi A, Baskin ML, Carson TL, Davison KK. The Activity Support Scale for Multiple Groups (ACTS-MG): child-reported physical activity parenting in African American and Non-Hispanic white families. Behav Med 2016;42:112-19. https://doi.org/10.1080/08964289.2014.979757.
- van Sluijs EM, Skidmore PM, Mwanza K, Jones AP, Callaghan AM, Ekelund U, et al. Physical activity and dietary behaviour in a population-based sample of British 10-year old children: the SPEEDY study (Sport, Physical activity and Eating behaviour: environmental Determinants in Young people). BMC Public Health 2008;8. https://doi.org/10.1186/1471-2458-8-388.
- The EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- Stevens KJ. Working with children to develop dimensions for a preference-based, generic, pediatric, health-related quality-of-life measure. Qual Health Res 2010;20:340-51. https://doi.org/10.1177/1049732309358328.
- Stevens K. Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy 2011;9:157-69. https://doi.org/10.2165/11587350-000000000-00000.
- Corder K, van Sluijs EM, McMinn AM, Ekelund U, Cassidy A, Griffin SJ. Perception versus reality awareness of physical activity levels of British children. Am J Prev Med 2010;38:1-8. https://doi.org/10.1016/j.amepre.2009.08.025.
- Godino JG, Watkinson C, Corder K, Sutton S, Griffin SJ, van Sluijs EM. Awareness of physical activity in healthy middle-aged adults: a cross-sectional study of associations with sociodemographic, biological, behavioural, and psychological factors. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-421.
- D’Haese S, Gheysen F, De Bourdeaudhuij I, Deforche B, Van Dyck D, Cardon G. The moderating effect of psychosocial factors in the relation between neighborhood walkability and children’s physical activity. Int J Behav Nutr Phys Act 2016;13. https://doi.org/10.1186/s12966-016-0452-0.
- Motl RW, Dishman RK, Trost SG, Saunders RP, Dowda M, Felton G, et al. Factorial validity and invariance of questionnaires measuring social-cognitive determinants of physical activity among adolescent girls. Prev Med 2000;31:584-94. https://doi.org/10.1006/pmed.2000.0735.
- Markland D, Tobin V. A modification to the behavioural regulation in exercise questionnaire to include an assessment of amotivation. J Sport Exercise Psychol 2004;26:191-6. https://doi.org/10.1123/jsep.26.2.191.
- Sebire SJ, Jago R, Fox KR, Edwards MJ, Thompson JL. Testing a self-determination theory model of children’s physical activity motivation: a cross-sectional study. Int J Behav Nutr Phys Act 2013;10. https://doi.org/10.1186/1479-5868-10-111.
- Grotevant HD, Cooper CR. Patterns of interaction in family relationships and the development of identity exploration in adolescence. Child Dev 1985;56:415-28. https://doi.org/10.2307/1129730.
- Bengston PL, Grotevant HD. The Individuality and Connectedness Q-sort: a measure for assessing individuality and connectedness in dyadic relationships. Pers Relatsh 1999;6:213-25. https://doi.org/10.1111/j.1475-6811.1999.tb00188.x.
- Côté J, Salmela JH, Baria A, Russell S. Organizing and interpreting unstructured qualitative data. Sport Psychol 1993;7:127-37. https://doi.org/10.1123/tsp.7.2.127.
- Spoth R, Redmond C. Research on family engagement in preventive interventions: Toward improved use of scientific findings in primary prevention practice. J Primary Prevent 2000;21:267-84. https://doi.org/10.1023/A:1007039421026.
- Goldberg AE, Smith JZ, Perry-Jenkins M. The division of labor in lesbian, gay, and heterosexual new adoptive parents. J Marriage Family 2012;74:812-28. https://doi.org/10.1111/j.1741-3737.2012.00992.x.
- Morgan PJ, Young MD, Smith JJ, Lubans DR. Targeted health behavior interventions promoting physical activity: a conceptual model. Exerc Sport Sci Rev 2016;44:71-80. https://doi.org/10.1249/JES.0000000000000075.
- Sarkadi A, Kristiansson R, Oberklaid F, Bremberg S. Fathers’ involvement and children’s developmental outcomes: a systematic review of longitudinal studies. Acta Paediatr 2008;97:153-8. https://doi.org/10.1111/j.1651-2227.2007.00572.x.
- Lloyd AB, Lubans DR, Plotnikoff RC, Morgan PJ. Paternal lifestyle-related parenting practices mediate changes in children’s dietary and physical activity behaviors: findings from the Healthy Dads, Healthy Kids community randomized controlled trial. J Phys Act Health 2015;12:1327-35. https://doi.org/10.1123/jpah.2014-0367.
- Lubans DR, Morgan PJ, Collins CE, Okely AD, Burrows T, Callister R. Mediators of weight loss in the ‘Healthy Dads, Healthy Kids’ pilot study for overweight fathers. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-45.
- Zahra J, Sebire SJ, Jago R. ‘He’s probably more Mr. sport than me’ – a qualitative exploration of mothers’ perceptions of fathers’ role in their children’s physical activity. BMC Pediatr 2015;15. https://doi.org/10.1186/s12887-015-0421-9.
- Morgan PJ, Young MD, Lloyd AB, Wang ML, Eather N, Miller A, et al. Involvement of fathers in pediatric obesity treatment and prevention trials: a systematic review. Pediatrics 2017;139. https://doi.org/10.1542/peds.2016-2635.
- Jansen E, Harris H, Daniels L, Thorpe K, Rossi T. Acceptability and accessibility of child nutrition interventions: fathers’ perspectives from survey and interview studies. Int J Behav Nutr Phys Act 2018;15. https://doi.org/10.1186/s12966-018-0702-4.
- Mailey EL, Huberty J, Dinkel D, McAuley E. Physical activity barriers and facilitators among working mothers and fathers. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-657.
- Tudor-Locke C, Barreira TV, Schuna JM, Mire EF, Chaput JP, Fogelholm M, et al. Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE). Int J Behav Nutr Phys Act 2015;12. https://doi.org/10.1186/s12966-015-0172-x.
- Davison KK, Jurkowski JM, Li K, Kranz S, Lawson HA. A childhood obesity intervention developed by families for families: results from a pilot study. Int J Behav Nutr Phys Act 2013;10. https://doi.org/10.1186/1479-5868-10-3.
- Jurkowski JM, Green Mills LL, Lawson HA, Bovenzi MC, Quartimon R, Davison KK. Engaging low-income parents in childhood obesity prevention from start to finish: a case study. J Community Health 2013;38:1-11. https://doi.org/10.1007/s10900-012-9573-9.
- Guagliano JM, Brown HE, Coombes E, Haines ES, Hughes C, Jones AP, et al. Whole family-based physical activity promotion intervention: the Families Reporting Every Step to Health pilot randomised controlled trial protocol. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-030902.
- Guagliano JM, Armitage S, Brown HE, Coombes E, Hughes C, Jones AP, et al. A whole family-based physical activity promotion intervention: findings from the Families Reporting Every Step to Health (FRESH) pilot randomised controlled trial. Int J Behav Nutr Phys Act 2020;17. https://doi.org/10.1186/s12966-020-01025-3.
- Suffolk Observatory . Population Estimates 2018. www.suffolkobservatory.info/population/report/view/0c18eadb6fb544c1bee07bc75618ec49/E10000029/ (accessed 27 June 2018).
- Norfolk County Council . Norfolk Rural Development Strategy 2013–2020 2013.
- Suffolk County Council . Suffolk Demographic Profile 2015.
- Norfolk County Council Public Health . Annual Report by the Director of Public Health 2009.
- Morgan PJ, Young MD, Barnes AT, Eather N, Pollock ER, Lubans DR. Engaging fathers to increase physical activity in girls: the ‘Dads And Daughters Exercising and Empowered’ (DADEE) randomized controlled trial. Ann Behav Med 2019;53:39-52. https://doi.org/10.1093/abm/kay015.
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557-65. https://doi.org/10.1080/02640410802334196.
- Crouter SE, Horton M, Bassett DR. Validity of ActiGraph child-specific equations during various physical activities. Med Sci Sports Exerc 2013;45:1403-9. https://doi.org/10.1249/MSS.0b013e318285f03b.
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40:181-8. https://doi.org/10.1249/mss.0b013e31815a51b3.
- Ordnance Survey . British National Grid 2020. https://getoutside.ordnancesurvey.co.uk/guides/beginners-guide-to-grid-references (accessed 20 April 2020).
- Schipperijn J, Kerr J, Duncan S, Madsen T, Klinker CD, Troelsen J. Dynamic accuracy of GPS receivers for use in health research: a novel method to assess GPS accuracy in real-world settings. Front Public Health 2014;2. https://doi.org/10.3389/fpubh.2014.00021.
- Choi L, Ward SC, Schnelle JF, Buchowski MS. Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med Sci Sports Exerc 2012;44:2009-16. https://doi.org/10.1249/MSS.0b013e318258cb36.
- Dunton GF, Liao Y, Almanza E, Jerrett M, Spruijt-Metz D, Pentz MA. Locations of joint physical activity in parent-child pairs based on accelerometer and GPS monitoring. Ann Behav Med 2013;45:162-72. https://doi.org/10.1007/s12160-012-9417-y.
- Brage S, Ekelund U, Brage N, Hennings MA, Froberg K, Franks PW, et al. Hierarchy of individual calibration levels for heart rate and accelerometry to measure physical activity. J Appl Physiol 2007;103:682-92. https://doi.org/10.1152/japplphysiol.00092.2006.
- Beech BM, Klesges RC, Kumanyika SK, Murray DM, Klesges L, McClanahan B, et al. Child- and parent-targeted interventions: the Memphis GEMS pilot study. Ethn Dis 2003;13:40-53.
- Rhodes RE, Naylor PJ, McKay HA. Pilot study of a family physical activity planning intervention among parents and their children. J Behav Med 2010;33:91-100. https://doi.org/10.1007/s10865-009-9237-0.
- White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:993-1007. https://doi.org/10.1002/sim.1981.
- Ryman . Printing Services n.d. www.ryman.co.uk/services/print (accessed 13 May 2020).
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- McDonald AM, Knight RC, Campbell MK, Entwistle VA, Grant AM, Cook JA, et al. What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials 2006;7. https://doi.org/10.1186/1745-6215-7-9.
- Sully BG, Julious SA, Nicholl J. A reinvestigation of recruitment to randomised, controlled, multicenter trials: a review of trials funded by two UK funding agencies. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-166.
- Robinson L, Adair P, Coffey M, Harris R, Burnside G. Identifying the participant characteristics that predict recruitment and retention of participants to randomised controlled trials involving children: a systematic review. Trials 2016;17. https://doi.org/10.1186/s13063-016-1415-0.
- Cui Z, Seburg EM, Sherwood NE, Faith MS, Ward DS. Recruitment and retention in obesity prevention and treatment trials targeting minority or low-income children: a review of the clinical trials registration database. Trials 2015;16. https://doi.org/10.1186/s13063-015-1089-z.
- Schoeppe S, Oliver M, Badland HM, Burke M, Duncan MJ. Recruitment and retention of children in behavioral health risk factor studies: REACH strategies. Int J Behav Med 2014;21:794-803. https://doi.org/10.1007/s12529-013-9347-5.
- Rhodes RE, Quinlan A, Beauchamp MR, Eys MA. Group Dynamics in Exercise and Sport Psychology. London: Routledge; 2014.
- Rhodes RE, Blanchard CM, Quinlan A, Naylor PJ, Warburton DER. Family physical activity planning and child physical activity outcomes: a randomized trial. Am J Prev Med 2019;57:135-44. https://doi.org/10.1016/j.amepre.2019.03.007.
- Hardy LL, Okely AD, Dobbins TA, Booth ML. Physical activity among adolescents in New South Wales (Australia): 1997 and 2004. Med Sci Sports Exerc 2008;40:835-41. https://doi.org/10.1249/MSS.0b013e318163f286.
- Kimm SY, Glynn NW, Kriska AM, Barton BA, Kronsberg SS, Daniels SR, et al. Decline in physical activity in black girls and white girls during adolescence. N Engl J Med 2002;347:709-15. https://doi.org/10.1056/NEJMoa003277.
- Kahn JA, Huang B, Gillman MW, Field AE, Austin SB, Colditz GA, et al. Patterns and determinants of physical activity in US adolescents. J Adolesc Health 2008;42:369-77. https://doi.org/10.1016/j.jadohealth.2007.11.143.
- Sutherland R, Reeves P, Campbell E, Lubans DR, Morgan PJ, Nathan N, et al. Cost effectiveness of a multi-component school-based physical activity intervention targeting adolescents: the ‘Physical Activity 4 Everyone’ cluster randomized trial. Int J Behav Nutr Phys Act 2016;13. https://doi.org/10.1186/s12966-016-0418-2.
- Gc VS, Suhrcke M, Atkin AJ, van Sluijs E, Turner D. Cost-Effectiveness of Physical Activity Interventions in Adolescents: Model Development and Illustration Using Two Exemplar Interventions 2019;9. https://doi.org/10.1136/bmjopen-2018-027566.
- Guagliano JM, Morton KL, Hughes C, van Sluijs EMF. Effective and resource efficient strategies for recruiting families in physical activity, sedentary behaviour, nutrition, and obesity prevention research: a systematic review with expert opinion. Obes Rev 2021;22. https://doi.org/10.1111/obr.13161.
- Kaushal N, Rhodes RE. The home physical environment and its relationship with physical activity and sedentary behavior: a systematic review. Prev Med 2014;67:221-37. https://doi.org/10.1016/j.ypmed.2014.07.026.
- Maitland C, Stratton G, Foster S, Braham R, Rosenberg M. A place for play? The influence of the home physical environment on children’s physical activity and sedentary behaviour. Int J Behav Nutr Phys Act 2013;10. https://doi.org/10.1186/1479-5868-10-99.
- Treweek S, Pitkethly M, Cook J, Fraser C, Mitchell E, Sullivan F, et al. Strategies to improve recruitment to randomised trials. Cochrane Database Syst Rev 2018;2. https://doi.org/10.1002/14651858.MR000013.pub6.
- Planner C, Bower P, Donnelly A, Gillies K, Turner K, Young B. Trials need participants but not their feedback? A scoping review of published papers on the measurement of participant experience of taking part in clinical trials. Trials 2019;20. https://doi.org/10.1186/s13063-019-3444-y.
- Walters SJ, Bonacho Dos Anjos Henriques-Cadby I, Bortolami O, Flight L, Hind D, Jacques RM, et al. Recruitment and retention of participants in randomised controlled trials: a review of trials funded and published by the United Kingdom Health Technology Assessment programme. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-015276.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264-9. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs 2000;32:1008-15. https://doi.org/10.1046/j.1365-2648.2000.t01-1-01567.x.
- Yousuf MI. Using experts’ opinions through Delphi technique. Pract Assess Res Eval 2007;12:1-8.
- Alhassan S, Nwaokelemeh O, Greever CJ, Burkart S, Ahmadi M, St Laurent CW, et al. Effect of a culturally-tailored mother-daughter physical activity intervention on pre-adolescent African-American girls’ physical activity levels. Prev Med Rep 2018;11:7-14. https://doi.org/10.1016/j.pmedr.2018.05.009.
- Anand SS, Davis AD, Ahmed R, Jacobs R, Xie C, Hill A, et al. A family-based intervention to promote healthy lifestyles in an aboriginal community in Canada. Can J Public Health 2007;98:447-52. https://doi.org/10.1007/BF03405436.
- Arredondo EM, Morello M, Holub C, Haughton J. Feasibility and preliminary findings of a church-based mother-daughter pilot study promoting physical activity among young Latinas. Fam Community Health 2014;37:6-18. https://doi.org/10.1097/FCH.0000000000000015.
- Baranowski T, Henske J, Simons-Morton B, Palmer J, Tiernan K, Hooks PC, et al. Dietary change for cardiovascular disease prevention among Black–American families. Health Educ Res 1990;5:433-43. https://doi.org/10.1093/her/5.4.433.
- Baranowski T, Simons-Morton B, Hooks P, Henske J, Tiernan K, Dunn JK, et al. A center-based program for exercise change among black–American families. Health Educ Q 1990;17:179-96. https://doi.org/10.1177/109019819001700205.
- Barnes AT, Plotnikoff RC, Collins CE, Morgan PJ. Feasibility and preliminary efficacy of the MADE4Life program: a pilot randomized controlled trial. J Phys Act Health 2015;12:1378-93. https://doi.org/10.1123/jpah.2014-0331.
- Barr-Anderson DJ, Adams-Wynn AW, Alhassan S, Whitt-Glover MC. Culturally-appropriate, family- and community-based physical activity and healthy eating intervention for African-American middle school-aged girls: a feasibility pilot. J Adolesc Family Health 2014;6.
- Borg A, Haughton CF, Sawyer M, Lemon SC, Kane K, Pbert L, et al. Design and methods of the Healthy Kids & Families study: a parent-focused community health worker-delivered childhood obesity prevention intervention. BMC Obes 2019;6. https://doi.org/10.1186/s40608-019-0240-x.
- Burrows T, Bray J, Morgan PJ, Collins C. Pilot intervention in an economically disadvantaged community: the back-to-basics after-school healthy lifestyle program. Nutr Dietetics 2013;70:270-7. https://doi.org/10.1111/1747-0080.12023.
- De Bourdeaudhuij I, Brug J, Vandelanotte C, Van Oost P. Differences in impact between a family- versus an individual-based tailored intervention to reduce fat intake. Health Educ Res 2002;17:435-49. https://doi.org/10.1093/her/17.4.435.
- Elder JP, Crespo NC, Corder K, Ayala GX, Slymen DJ, Lopez NV, et al. Childhood obesity prevention and control in city recreation centres and family homes: the MOVE/me Muevo Project. Pediatr Obes 2014;9:218-31. https://doi.org/10.1111/j.2047-6310.2013.00164.x.
- Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes Res 2001;9:171-8. https://doi.org/10.1038/oby.2001.18.
- Fitzgibbon ML, Stolley MR, Kirschenbaum DS. An obesity prevention pilot program for African–American mothers and daughters. J Nutr Educ 1995;27:93-9. https://doi.org/10.1016/S0022-3182(12)80349-9.
- Fornari LS, Giuliano I, Azevedo F, Pastana A, Vieira C, Caramelli B. Children First Study: how an educational program in cardiovascular prevention at school can improve parents’ cardiovascular risk. Eur J Prev Cardiol 2013;20:301-9. https://doi.org/10.1177/2047487312437617.
- Flynn JI, Bassett DR, Fouts HN, Thompson DL, Coe DP. Active Families in the Great Outdoors: a program to promote family outdoor physical activity. J Adventure Educ Outdoor Learn 2017;17:227-38. https://doi.org/10.1080/14729679.2017.1291355.
- French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: Take Action – a group-randomized trial. Obesity 2011;19:2082-8. https://doi.org/10.1038/oby.2010.328.
- Guagliano JM, Rosenkranz RR. Physical activity promotion and obesity prevention in Girl Scouts: Scouting Nutrition and Activity Program+. Pediatr Int 2012;54:810-15. https://doi.org/10.1111/j.1442-200X.2012.03681.x.
- Ha AS, Ng JYY, Lonsdale C, Lubans DR, Ng FF. Promoting physical activity in children through family-based intervention: protocol of the ‘Active 1 + FUN’ randomized controlled trial. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-6537-3.
- Hammons AJ, Wiley AR, Fiese BH, Teran-Garcia M. Six-week Latino family prevention pilot program effectively promotes healthy behaviors and reduces obesogenic behaviors. J Nutr Educ Behav 2013;45:745-50. https://doi.org/10.1016/j.jneb.2013.01.023.
- Hardman CA, Horne PJ, Lowe CF. A home-based intervention to increase physical activity in girls: the Fit ‘n’Fun Dudes program. J Exerc Sci Fit 2009;7:1-8. https://doi.org/10.1016/S1728-869X(09)60001-0.
- Hopper CA, Gruber MB, Munoz KD, Herb RA. Effect of including parents in a school-based exercise and nutrition program for children. Res Q Exerc Sport 1992;63:315-21. https://doi.org/10.1080/02701367.1992.10608748.
- Jago R, Sebire SJ, Turner KM, Bentley GF, Goodred JK, Fox KR, et al. Feasibility trial evaluation of a physical activity and screen-viewing course for parents of 6 to 8 year-old children: Teamplay. Int J Behav Nutr Phys Act 2013;10. https://doi.org/10.1186/1479-5868-10-31.
- Jake-Schoffman DE, Turner-McGrievy G, Wilcox S, Moore JB, Hussey JR, Kaczynski AT. The mFIT (Motivating Families with Interactive Technology) Study: a randomized pilot to promote physical activity and healthy eating through mobile technology. J Technol Behav 2018;3:179-89. https://doi.org/10.1007/s41347-018-0052-8.
- Kargarfard M, Kelishadi R, Ziaee V, Ardalan G, Halabchi F, Mazaheri R, et al. The impact of an after-school physical activity program on health-related fitness of mother/daughter pairs: CASPIAN study. Prev Med 2012;54:219-23. https://doi.org/10.1016/j.ypmed.2012.01.010.
- Kelishadi R, Ziaee V, Ardalan G, Namazi A, Noormohammadpour P, Ghayour-Mobarhan M, et al. A national experience on physical activity initiatives for adolescent girls and their mothers: CASPIAN Study. Iran J Pediatr 2010;20:420-6.
- Lynch WC, Martz J, Eldridge G, Bailey SJ, Benke C, Paul L. Childhood obesity prevention in rural settings: background, rationale, and study design of ‘4-Health,’ a parent-only intervention. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-255.
- Mark RS, Rhodes RE. Testing the effectiveness of exercise videogame bikes among families in the home-setting: a pilot study. J Phys Act Health 2013;10:211-21. https://doi.org/10.1123/jpah.10.2.211.
- Mohammad R, McMahan S, Mouttapa M, Zhang Y. Kick Start Your Day: a pilot investigation of a family based nutrition and physical activity program targeting low-income Latino families. Cali J Health Promot 2012;10:26-33. https://doi.org/10.32398/cjhp.v10iSI-Obesity.1468.
- Morrison R, Reilly JJ, Penpraze V, Westgarth C, Ward DS, Mutrie N, et al. Children, parents and pets exercising together (CPET): exploratory randomised controlled trial. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-1096.
- Yam PS, Morrison R, Penpraze V, Westgarth C, Ward DS, Mutrie N, et al. Children, parents, and pets exercising together (CPET) randomised controlled trial: study rationale, design, and methods. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-208.
- Morgan PJ, Collins CE, Plotnikoff RC, Callister R, Burrows T, Fletcher R, et al. The ‘Healthy Dads, Healthy Kids’ community randomized controlled trial: a community-based healthy lifestyle program for fathers and their children. Prev Med 2014;61:90-9. https://doi.org/10.1016/j.ypmed.2013.12.019.
- Morgan PJ, Lubans DR, Callister R, Okely AD, Burrows TL, Fletcher R, et al. The ‘Healthy Dads, Healthy Kids’ randomized controlled trial: efficacy of a healthy lifestyle program for overweight fathers and their children. Int J Obes 2011;35:436-47. https://doi.org/10.1038/ijo.2010.151.
- Morgan PJ, Lubans DR, Plotnikoff RC, Callister R, Burrows T, Fletcher R, et al. The ‘Healthy Dads, Healthy Kids’ community effectiveness trial: study protocol of a community-based healthy lifestyle program for fathers and their children. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-876.
- Williams A, de Vlieger N, Young M, Jensen ME, Burrows TL, Morgan PJ, et al. Dietary outcomes of overweight fathers and their children in the Healthy Dads, Healthy Kids community randomised controlled trial. J Hum Nutr Diet 2018;31:523-32. https://doi.org/10.1111/jhn.12543.
- Burrows T, Morgan PJ, Lubans DR, Callister R, Okely T, Bray J, et al. Dietary outcomes of the healthy dads healthy kids randomised controlled trial. J Pediatr Gastroenterol Nutr 2012;55:408-11. https://doi.org/10.1097/MPG.0b013e318259aee6.
- Nader PR, Sallis JF, Patterson TL, Abramson IS, Rupp JW, Senn KL, et al. A family approach to cardiovascular risk reduction: results from the San Diego Family Health Project. Health Educ Q 1989;16:229-44. https://doi.org/10.1177/109019818901600207.
- Nader PR, Sallis JF, Abramson IS, Broyles SL. Family-based cardiovascular risk reduction education among Mexican- and Anglo-Americans. Fam Community Health 1992;15:54-7. https://doi.org/10.1097/00003727-199204000-00007.
- Nader PR, Baranowski T, Vanderpool NA, Dunn K, Dworkin R, Ray L. The family health project: cardiovascular risk reduction education for children and parents. J Dev Behav Pediatr 1983;4:3-10. https://doi.org/10.1097/00004703-198303000-00002.
- Patterson TL, Sallis JF, Nader PR, Rupp JW, McKenzie TL, Roppe B, et al. Direct observation of physical activity and dietary behaviors in a structured environment: effects of a family-based health promotion program. J Behav Med 1988;11:447-58. https://doi.org/10.1007/BF00844838.
- Olvera N, Bush JA, Sharma SV, Knox BB, Scherer RL, Butte NF. BOUNCE: a community-based mother-daughter healthy lifestyle intervention for low-income Latino families. Obesity 2010;18:102-4. https://doi.org/10.1038/oby.2009.439.
- Olvera NN, Knox B, Scherer R, Maldonado G, Sharma SV, Alastuey L, et al. A healthy lifestyle program for Latino daughters and mothers: the BOUNCE overview and process evaluation. Am J Health Educ 2008;39:283-95. https://doi.org/10.1080/19325037.2008.10599052.
- Owens SG, Garner JC, Loftin JM, van Blerk N, Ermin K. Changes in physical activity and fitness after 3 months of home Wii Fit™ use. J Strength Cond Res 2011;25:3191-7. https://doi.org/10.1519/JSC.0b013e3182132d55.
- Paineau DL, Beaufils F, Boulier A, Cassuto DA, Chwalow J, Combris P, et al. Family dietary coaching to improve nutritional intakes and body weight control: a randomized controlled trial. Arch Pediatr Adolesc Med 2008;162:34-43. https://doi.org/10.1001/archpediatrics.2007.2.
- Parra-Medina D, Liang Y, Yin Z, Esparza L, Lopez L. Weight outcomes of Latino adults and children participating in the Y Living Program, a family-focused lifestyle intervention, San Antonio, 2012–13. Prevent Chronic Dis 2015;12. https://doi.org/10.5888/pcd12.150219.
- Pearson N, Atkin AJ, Biddle SJ, Gorely T. A family-based intervention to increase fruit and vegetable consumption in adolescents: a pilot study. Public Health Nutr 2010;13:876-85. https://doi.org/10.1017/S1368980010000121.
- Ransdell LB, Detling NJ, Taylor A, Reel J, Shultz B. Effects of home- and university-based programs on physical self-perception in mothers and daughters. Women Health 2004;39:63-81. https://doi.org/10.1300/J013v39n02_05.
- Ransdell LB, Eastep E, Taylor A, Oakland D, Schmidt J, Moyer-Mileur L, et al. Daughters and mothers exercising together (DAMET): effects of home-and university-based interventions on physical activity behavior and family relations. Am J Health Educ 2003;34:19-2. https://doi.org/10.1080/19325037.2003.10603521.
- Ransdell LB, Dratt J, Kennedy C, O’Neill S, DeVoe D. Daughters and mothers exercising together (DAMET): a 12-week pilot project designed to improve physical self-perception and increase recreational physical activity. Women Health 2001;33:101-16. https://doi.org/10.1300/J013v33n03_07.
- Ransdell LB, Robertson L, Ornes L, Moyer-Mileur L. Generations Exercising Together to Improve Fitness (GET FIT): a pilot study designed to increase physical activity and improve health-related fitness in three generations of women. Women Health 2004;40:77-94. https://doi.org/10.1300/j013v40n03_06.
- Ornes LL, Ransdell LB, Robertson L, Trunnell E, Moyer-Mileur L. A 6-month pilot study of effects of a physical activity intervention on life satisfaction with a sample of three generations of women. Percept Mot Skills 2005;100:579-91. https://doi.org/10.2466/pms.100.3.579-591.
- Quinlan A, Rhodes RE, Blanchard CM, Naylor PJ, Warburton DE. Family planning to promote physical activity: a randomized controlled trial protocol. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2309-x.
- Rosenkranz RR, Behrens TK, Dzewaltowski DA. A group-randomized controlled trial for health promotion in Girl Scouts: healthier troops in a SNAP (Scouting Nutrition & Activity Program). BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-81.
- Rosenkranz RR, Dzewaltowski DA. Promoting better family meals for girls attending summer programs. J Nutr Educ Behav 2009;41:65-7. https://doi.org/10.1016/j.jneb.2008.02.003.
- Salimzadeh H, Shojaeizadeh D, Pashaee T, Abdollahi S. School-based physical activity intervention improves the physical fitness of the adolescent girls and their mothers. Pakistan J Med Sci 2010;26.
- Schwinn TM, Schinke S, Fang L, Kandasamy S. A web-based, health promotion program for adolescent girls and their mothers who reside in public housing. Addict Behav 2014;39:757-60. https://doi.org/10.1016/j.addbeh.2013.11.029.
- Sharma SV, Markham C, Chow J, Ranjit N, Pomeroy M, Raber M. Evaluating a school-based fruit and vegetable co-op in low-income children: a quasi-experimental study. Prev Med 2016;91:8-17. https://doi.org/10.1016/j.ypmed.2016.07.022.
- Stolley MR, Fitzgibbon ML. Effects of an obesity prevention program on the eating behavior of African American mothers and daughters. Health Educ Behav 1997;24:152-64. https://doi.org/10.1177/109019819702400204.
- Towey M, Harrell R, Lee B. Evaluation of ‘one body, one life’: a community-based family intervention for the prevention of obesity in children. J Obes 2011;2011. https://doi.org/10.1155/2011/619643.
- Cullen KW, Thompson D, Chen T-A. Outcome evaluation of Family Eats: an eight-session web-based program promoting healthy home food environments and dietary behaviors for African American families. Health Educ Behav 2017;44:32-40. https://doi.org/10.1177/1090198116643917.
- Ziebarth D, Healy-Haney N, Gnadt B, Cronin L, Jones B, Jensen E, et al. A community-based family intervention program to improve obesity in Hispanic families. WMJ 2012;111:261-6.
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-18.
- Lundahl BW, Tollefson D, Risser H, Lovejoy MC. A meta-analysis of father involvement in parent training. Res Social Work Pract 2008;18:97-106. https://doi.org/10.1177/1049731507309828.
- Morgan PJ, Young MD. The influence of fathers on children’s physical activity and dietary behaviors: insights, recommendations and future directions. Curr Obes Rep 2017;6:324-33. https://doi.org/10.1007/s13679-017-0275-6.
- Denhoff ER, Milliren CE, de Ferranti SD, Steltz SK, Osganian SK. Factors associated with clinical research recruitment in a pediatric academic medical center – a web-based survey. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0140768.
- Hayes H, Buckland S, Tarpey M. Briefing Notes for Researchers: Public Involvement in NHS, Public Health and Social Care Research. London: National Institute for Health Research; 2012.
- Beasant L, Brigden A, Parslow RM, Apperley H, Keep T, Northam A, et al. Treatment preference and recruitment to pediatric RCTs: a systematic review. Contemp Clin Trials Commun 2019;14. https://doi.org/10.1016/j.conctc.2019.100335.
- Tudur Smith C, Hickey H, Clarke M, Blazeby J, Williamson P. The trials methodological research agenda: results from a priority setting exercise. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-32.
- Brown O, Quick V, Colby S, Greene G, Horacek TM, Hoerr S, et al. Recruitment lessons learned from a tailored web-based health intervention Project YEAH (Young Adults Eating and Active for Health). Health Educ 2015;115:470-9. https://doi.org/10.1108/HE-06-2014-0075.
- Anderson CA, Beresford SA, Lampe J, Knopp RH, Motulsky AG. Enhancing recruitment of healthy African American volunteers in a city with a small African American community: results from a dietary supplement crossover trial. Ethn Dis 2007;17:555-9.
- Ryan C, Dadabhoy H, Baranowski T. Participant outcomes from methods of recruitment for videogame research. Games Health J 2018;7:16-23. https://doi.org/10.1089/g4h.2017.0049.
List of abbreviations
- BMI
- body mass index
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- FRESH
- Families Reporting Every Step to Health
- GPS
- Global Positioning System
- IQR
- interquartile range
- LMVPA
- light, moderate and vigorous physical activity
- MRC
- Medical Research Council
- MVPA
- moderate to vigorous physical activity
- NIHR
- National Institute for Health Research
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
- randomised controlled trial
- SD
- standard deviation
- SDT
- self-determination theory
- SEM
- socioecological model
- SSC
- Study Steering Committee
- TIDieR
- Template for Intervention Description and Replication

