Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 16/122/57. The contractual start date was in July 2018. The final report began editorial review in September 2020 and was accepted for publication in May 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2021 Ali et al. This work was produced by Ali et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Ali et al.
Chapter 1 Introduction
Background
Intellectual disability and health and social inequalities
Intellectual disability (ID) is a life-long condition characterised by an intelligence quotient (IQ) < 70 and impaired adaptive functioning arising before the age of 18 years. 1 The UK prevalence of ID is 1–2%. 2 People with ID have complex health needs, but experience substantial inequalities in health, including poorer access to health services, higher rates of physical heath disorders3,4 and higher mortality rates, and, on average, they die 20–25 years earlier than people in the general population. 3–5 They have higher rates of mental illness, with a point prevalence of 41%. 6,7 The prevalence of depression is the same as that in the general population, but people with an ID are more likely to experience chronic depression. 8,9 People with ID have greater exposure to adverse life events and social disadvantage,10 experience social exclusion because of stigma,11 have markedly smaller social networks12,13 and have a higher prevalence of loneliness than other people. 14 These factors may increase their vulnerability to depression. 14–18
People with ID may experience behavioural side effects from antidepressant treatment (e.g. aggression and agitation)19 and encounter inequalities in accessing psychological therapies. 20 There is a need to consider alternative, accessible interventions in the management of depression. One such intervention that has shown some promise is befriending. 21
Characteristics of befriending
Befriending is a one-to-one friendship-like relationship that is initiated, supported and monitored by an agency, usually a voluntary organisation in the community. 22 There are differences in the practice and implementation of befriending, which lies on a spectrum from being very similar to a friendship, whereby the relationship is reciprocal and equal, and is delivered by lay volunteers, to being a professional and therapeutic relationship with an emphasis on goal attainment, which resembles mentoring. 23 Most types of befriending relationships lie mid-way on this spectrum and may involve listening and providing emotional support, but may be prescriptive in terms of the length and duration of meetings. Those involved usually have a discussion about the boundaries of sharing personal information,23 from not sharing any personal details to introducing the befriendee to the befriender’s family or friends. Most schemes also offer training, supervision and ongoing support to volunteers.
Motivation and experience of befriending volunteers
Volunteers are important factors in the successful delivery of befriending and, therefore, it is important to understand the motivations of volunteers. Little is known about the motivations of volunteers who work with people with ID, although they are likely to be similar to those of volunteers who befriend people with other disabilities. Motivations can be categorised into ‘giving’, whereby volunteers have a desire to help others and contribute to society, and ‘getting’, where there is an expectation that they will gain valuable work experience or new skills. 24–26 Several studies that have explored the experiences of volunteers befriending individuals with mental illness have reported that volunteers feel empowered and rewarded by their efforts to support the befriendee’s recovery, and that befriending provides volunteers with a different perspective on how they view people with mental health problems, including improving attitudes towards such individuals. 25,27,28 Some volunteers with a history of mental illness also report gaining confidence and an increased sense of acceptance. 27 Negative experiences have also been described, for example, when there has been confusion about the role of volunteers and they have been regarded as counsellors or carers, or even as a ‘cab driver’, instead of as a friend. 25,29 Volunteers also report challenges in being non-judgemental towards their befriendee and difficulties with communication. 28,29 Other concerns included dissatisfaction in the recruitment process and limited reimbursement of expenses incurred during activities. 30
Experiences of people with intellectual disability
Only one published study has explored the experiences of befriending for people with ID. 30 Lack of service user empowerment and involvement was highlighted as a barrier. Befriendees commented that they had little choice over the selection of their befriender and little influence over how often pairs met and what activities they engaged in. Many described difficulties coping with the relationship coming to an end, including feelings of disappointment, anger and despair, and that they were provided with little information from the befriending service about the link ending. This highlighted the importance of managing endings and being clear about the time-limited nature of the intervention at the outset.
Mechanism of action of befriending
The causal mechanisms of befriending have not been fully elucidated, although social support is thought to be relevant. Social support has structural characteristics, such as the number and connectedness of social ties, and functional characteristics, such as providing instrumental or emotional support, information and advice. Social support may improve well-being by acting as a buffer to stress. There is evidence to suggest that it may mediate genetic and environmental vulnerabilities to depression through its effects on neurobiological factors and other psychosocial factors (e.g. coping strategies). 31 Perceived social support rather than received social support appears to be related to psychological well-being and, therefore, providing support where it is not needed can be unhelpful. 32 The main underlying assumption in befriending interventions is that providing an individual who is lonely and lacking in social networks with additional, enacted support through a befriender will lead to an increase in the individual’s level of perceived support, resulting in improved psychological well-being. Befriending may enhance social support by providing direct emotional and instrumental support, but the befriender can also help to link the befriendee to social activities, which may be sustainable outside and beyond the end of the befriending relationship; therefore, befriending may have longer-term benefits. Befriending may also improve health outcomes thorough its effects on social networks. 33
Effectiveness of befriending
Befriending (as an active control delivered by professionals) has been found to have similar effects to cognitive–behavioural therapy34 and acceptance and commitment therapy in schizophrenia. 35 There is evidence from a comprehensive systematic review21 that befriending in the general population may have a significant but modest effect on reducing symptoms of depression when compared with no treatment or treatment as usual in both the short term [standardised mean difference –0.27 depressive symptoms, 95% confidence interval (CI) –0.48 to –0.06 depressive symptoms] and the long term (standardised mean difference –0.18 depressive symptoms, 95% CI –0.32 to –0.05 depressive symptoms). The review included studies of paid and unpaid volunteers and befriending delivered in various ways, including face-to-face and telephone contact. A more recent review and meta-analysis36 of befriending by unpaid volunteers examined the effects of befriending on participants with physical and mental health disorders across a range of social and psychological outcome measures. Befriending was associated with better patient-reported outcomes across all primary outcomes, but the effect size was small (standardised mean difference 0.18, 95% CI –0.002 to 0.36). There was limited evidence for the effectiveness of befriending on individual outcomes, such as depression, loneliness or quality of life, when the studies were combined. 36 A randomised controlled trial (RCT) of befriending of people with psychosis by lay volunteers provides further evidence for the potential beneficial effects of befriending. 37 Participants in the intervention group had significantly more social contacts at the end of the 12-month intervention (adjusted difference 0.52 social contacts, 95% CI 0.04 to 0.99 social contacts) and at 6 months’ follow-up (adjusted difference 0.73 social contacts, 95% CI 0.05 to 1.40 social contacts; p = 0.04), suggesting that befriending may help to reduce social isolation in this group.
Benefits for volunteers and wider society
A systematic review and meta-analysis38 found that volunteering in general had beneficial effects on depression, psychological well-being and life satisfaction, and was associated with a lower risk of mortality in volunteers, although the causal mechanisms for these associations are unclear. The benefits to wider society include economic impacts, such as reduced burden on government spending and improved employability of volunteers; strengthening of social connections between different sectors and organisations within the community; and safer, stronger and more cohesive communities (e.g. inverse relationship between levels of volunteering and crime). 39
Rationale for proposed research
Although the benefits of befriending have been explored in a range of disorders, its effectiveness in people with ID has not been evaluated in a randomised trial. A single-arm feasibility study of one-to-one befriending by volunteers that was conducted by a voluntary organisation40 recruited 24 volunteers, of whom 15 were matched with an individual with ID. Overall, 60% of befriendees reported a positive change: 53% reported a decrease in isolation and 40% reported an increase in confidence. The study was limited by the lack of validated outcome measures, the lack of a control group and the lack of follow-up data. The study has not been published in a scientific journal.
One Australian study examined the feasibility of using active mentoring to improve the participation of older adults with ID in mainstream community groups. 41 The intervention comprised 29 individuals receiving the intervention and a matched comparison group. The participants in the intervention group reported better social satisfaction than those in the comparison group (effect size 0.78; p = 0.02). Symptoms of depression on the carer-reported version of the Glasgow Depression Scale for people with a Learning Disability (GDS-LD) were also reduced, but not significantly. The study found that the intervention was feasible and acceptable. However, this was a non-randomised study, the sample comprised older adults living in Australia and the intervention is not directly comparable to one-to-one befriending.
Given the dearth of studies examining befriending in people with ID and an insufficient number of data on feasibility, there is a clear rationale for conducting a pilot study prior to a full RCT.
Aims and objectives
The main aim of the study was to determine the feasibility and acceptability of a full-scale RCT to estimate the effectiveness of one-to-one befriending by volunteers for people with ID, compared with an active control group.
The objectives were to:
-
examine the recruitment and retention of individuals with ID and volunteers in the trial, and number of successfully matched pairs within the 6-month study recruitment period
-
record any negative consequences/adverse effects of befriending
-
measure the extent to which the intervention is delivered as intended by the volunteers and befriending schemes
-
examine the acceptability of the intervention and study procedures by exploring the views of individuals, volunteers, carers and befriending services
-
examine changes in health and social outcomes by carrying out exploratory analyses of the impact of befriending on depressive symptoms measured by the GDS-LD42 at 12 months and other outcomes (e.g. self-esteem, loneliness, quality of life and social participation) at 6 and 12 months post randomisation
-
carry out exploratory analyses of the impact of befriending on volunteers’ well-being, self-esteem, loneliness and attitudes towards people with ID at 6 and 12 months
-
estimate the sample size required and determine the final trial design for a full-scale RCT
-
assess the feasibility of collecting data that would inform a future analysis of cost-effectiveness.
Chapter 2 Methodology
The trial protocol was developed with input from the research team, collaborating partner organisations and the Priment Clinical Trials Unit (University College London, London, UK). A summary of the protocol has been published. 43
Design
The study design was a two-arm, parallel-group, researcher-blind pilot RCT with 1 : 1 allocation. Participants were randomly allocated to either the intervention group, where they received one-to-one befriending by a volunteer, or an active control group. Both groups had access to usual care and a booklet of local resources. A process evaluation, based on mixed methods, was conducted to examine the delivery and adherence to the intervention, and to explore stakeholder views on the acceptability of the intervention.
Eligibility criteria
To be enrolled to the study, participants with ID had to:
-
be aged ≥ 18 years
-
have mild or moderate ID (i.e. an IQ of 35–69) assessed using the Wechsler Abbreviated Scale of Intelligence™ (Second Edition) (WASI-II™)44
-
not be attending college/education or a day service for ≥ 3 days per week
-
have obtained a score of ≥ 5 on the GDS-LD,42 indicating the presence of depressive symptoms, but did not need to have a clinical diagnosis of depression
-
be able to speak English
-
be able to provide informed consent.
To take part in the study, volunteers had to be:
-
aged ≥ 18 years
-
available once per week for at least 1 hour, over a period of 6 months.
Volunteers did not need to have any prior experience of supporting people with ID.
Exclusion criteria
Individuals with ID were excluded if they:
-
had limited communication and comprehension that would prevent completion of the questionnaires.
Volunteers were excluded if they:
-
had a criminal record (any documented offence, owing to the vulnerability of the befriendee population) recorded on their Disclosure and Barring Service (DBS) check
-
were unable to provide two references or had unsuitable references.
Sample size
We did not have any estimates of the number of people with ID who were likely to be eligible and consent to taking part in the trial. If we approached 50 participants who were eligible to take part, this would allow us to estimate an expected recruitment rate of 80% (40 people), with a 95% CI of 68.9% to 91.1%. A sample size of 40 recruited people with ID would allow us to estimate a 30% dropout rate in the trial, with a 95% CI of 25.7% to 54.3%. The recruitment period was 6 months. There were two participating befriending services and, therefore, we needed to recruit 3.3 participants with ID per month at each site.
Recruitment
The recruitment period for the trial was from mid-April 2019 to mid-September 2019 (5 months). Recruitment issues are discussed in Chapter 3.
Two befriending services agreed to take part in the study. One was based in east London (Outward, based in Hackney) and the other was based in Suffolk (The Befriending Scheme). They were responsible for recruiting and training volunteers, matching volunteers to participants with ID, the provision of supervision to volunteers and monitoring of the befriending relationship. Both services had previous experience of supporting befriending relationships with people with ID.
Participants with intellectual disability
Participants with ID were recruited from existing and new referrals to the participating befriending services or were recruited from the caseload of clinicians working in four community ID services within the North East London NHS Foundation Trust (NELFT). Volunteer co-ordinators and clinicians screened referrals and caseloads for participants who were potentially eligible for the study and approached individuals to discuss the study. If the individual was interested in the study, they were given an information sheet and permission was sought for their details to be passed on to the research team. A referral form was then completed by the clinician or staff at the befriending service and e-mailed to the research team. The trial research assistant reviewed the information, contacted the potential participant to discuss the study and carried out the eligibility assessment, which comprised an assessment of IQ using the WASI-II (the two subset version was used). 44 The WASI-II was selected because it is a brief and reliable measure of cognitive ability and can be used to estimate the full-scale IQ across all population groups, including people with ID, which is useful in the context of research. The two-subset version consists of vocabulary and matrix reasoning and takes approximately 15 minutes to complete. The eligibility assessment also comprised an assessment of the presence of symptoms of depression using the GDS-LD. 42 If the individual was eligible, they were required to sign the consent form before completing the baseline assessment. If the research assistant was uncertain about whether or not a participant had met the eligibility criteria, the case was discussed with the chief investigator before the baseline assessment was carried out.
Volunteers
Volunteers were recruited by the befriending services through newspaper advertisements, befriending and job websites, social media, and recruitment events at colleges and universities. Information about the study was also available on the study website hosted by University College London, Division of Psychiatry (https://www.ucl.ac.uk/psychiatry/research/epidemiology-and-applied-clinical-research-department/bid-project), and study posters were circulated to psychology undergraduate students. Interested volunteers completed an application form and were invited to an informal interview to assess their suitability and motivation for becoming a volunteer. A DBS check was completed to ensure that they had no prior criminal record, and references were obtained. After completing training (see Training and supervision of volunteers), successful candidates were invited to take part in the study. They received an information sheet and were asked to sign a consent form before completing the baseline assessment.
Randomisation
Following the baseline assessment, details of the participant with ID were entered into a web-based randomisation system hosted by sealed envelope™ (Sealed Envelope Ltd, London, UK) by a non-blinded member of the research team. The randomisation procedure used randomly varying block sizes, stratified by befriending service. The randomisation protocol was created by the trial statistician and the set-up of the service was overseen by the Priment Clinical Trials Unit.
Participants were randomly allocated by the system to either the intervention group or the control group. The unblinded researcher informed the befriending service and participants with ID of the group to which they had been allocated. Owing to the nature of the intervention, it was not possible to blind participants to their assigned allocation group. However, outcome assessments were carried out by a research assistant who was blind to the participants’ allocation group.
Intervention group
Participants who were allocated to the intervention group were contacted by the volunteer co-ordinator, who arranged to meet them to discuss their hobbies, interests and activities that they would like support to participate in. Based on this information, participants were matched to a volunteer who could accommodate the person’s interests and availability.
The befriending intervention
Frequency and types of activities
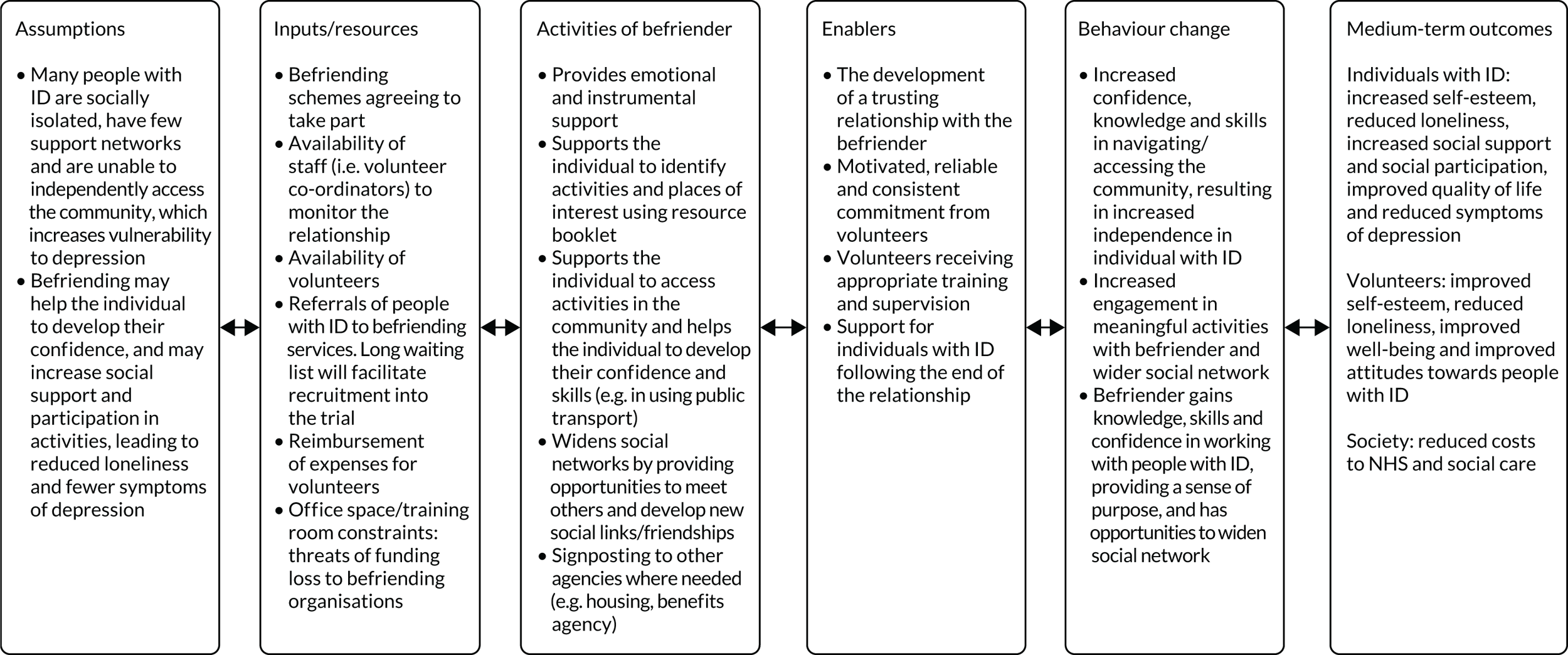
The befriending intervention was adapted from the existing models used by the two participating befriending services and from other studies of befriending. 37,40 The purpose of the befriending relationship was to provide friendship and emotional support, to facilitate community access, and to help the individual gain skills and confidence that would allow them to access activities in the community on their own (i.e. to promote sustained social activities beyond the befriending relationship). Figure 1 is a logic model of the intervention and describes the proposed mechanisms of action.
FIGURE 1.
Logic model of befriending in people with IDs.
The volunteer (befriender) and person with ID were expected to meet once per week for at least 1 hour, over a period of 6 months. However, it was anticipated that there may be breaks due to holidays or illness. The pair received a booklet with information about local activities and amenities, which was to be used as an aid to plan activities. The emphasis was on assisting the individual to make choices about the activities that they wished to pursue. The volunteer was not expected to carry out personal care, administer medication or accompany the individual to medical appointments. Contacts by telephone/social media were permitted in addition to face-to-face contact, and the pair were expected to spend at least 50% of the total number of meetings in the community. Meetings could take place during evenings/weekends, depending on the pair’s availability. Volunteers were asked to keep a record of their activities in a structured log, detailing whether or not they attended, reasons for cancellation, what they did at each visit, the duration of the activity and types of contact other than face to face. Volunteers’ travel expenses were reimbursed, but other expenses had to be agreed with the befriending service. Participants with ID were expected to pay for their travel and the other costs they incurred during outings.
Introduction and monitoring of the befriending relationship
A face-to-face meeting was arranged by the volunteer co-ordinator at the participant’s home to introduce the volunteer to the participant. If both parties were satisfied with the matching process, the pair then arranged to meet on their own. If the volunteer or individual with ID dropped out of the relationship once it had become established, they were offered the option of rematching. Volunteers were permitted to be matched to more than one participant with ID, although this did not occur in the trial.
Six weeks after matching, the volunteer co-ordinator contacted each person by telephone/face to face and then maintained contact every 4 weeks to monitor the progress of the relationship. A further meeting was held with the pair towards the end of the 6-month period to obtain general feedback about the befriending intervention, to discuss ending the relationship and to support the individual with ID in coming to terms with the ending. The pair could continue their relationship if they wished after the 6-month period was over, but arrangements for monitoring the relationship were outside the remit of the trial and varied according to the befriending service. Information was collected on any relationships that had continued beyond 6 months.
Training and supervision of volunteers
Volunteers completed face-to-face training and electronic learning prior to being matched. The training covered the following topics: benefits of befriending and issues related to confidentiality and lone working; advice on how to plan meetings effectively; health and safety; safeguarding; intellectual (learning) disability awareness, and professional boundaries, such as dealing with sensitive issues, ending relationships and expectations of the role of the volunteer. Volunteers received PowerPoint (Microsoft Corporation, Redmond, WA, USA) slides and a manual developed by the research team, with information about the study and additional information relevant to working with people with ID, such as maximising communication, understanding the reasons for challenging behaviour, common mental health problems and what volunteers should do in an emergency.
Volunteers had access to individual supervision with the volunteer co-ordinator, which was delivered face to face or over the telephone once per month. The supervision sessions addressed issues related to the training needs of the volunteer and how to overcome issues that had arisen from the befriending relationship.
Training and support for befriending services
The two befriending services completed good clinical practice training and received training on the trial research processes and procedures as part of the site initiation visit. Volunteer co-ordinators received support from the research team through regular e-mail and telephone contact, and were members of the Trial Management Group.
Control group
To control for the effects of participants in the treatment group receiving more information about local activities than those in the control group, participants in the control group were also given a copy of the activities booklet, and met with a member of the research team who discussed the booklet with them (and their carer, if present) and encouraged them to engage with activities.
Both the control group and the intervention group had access to ‘usual care’. This included access to multidisciplinary input from community ID services, including appointments with their psychiatrist, psychologist and other members of the team. Participants continued to take their usual medication, which included antidepressants and antipsychotics. They had access to primary care and other community and hospital-based health services, as well as day services (e.g. day centres and colleges). Where it was possible, participants in the control group were asked if they wished to be matched with a volunteer after they completed their follow-up assessment.
Outcomes
Feasibility outcomes
Recruitment and retention of participants
We assessed the number of participants with ID recruited from those who were eligible; the number of volunteers who were recruited over a 6-month period; the number of participants who were successfully matched with a volunteer; the number of participants and volunteers who dropped out of the intervention; and the number of participants and volunteers who completed the follow-up assessment.
Adverse events
Adverse events were collected at each follow-up assessment using open-ended questions and were also reported directly to the chief investigator by the befriending services, including concerns about safeguarding. Adverse events were recorded in the medical records and case report forms (CRFs).
Adherence to the intervention
Adherence was assessed as part of the process evaluation (see Treatment adherence).
Acceptability of the intervention
This was informed by data on retention/dropout of volunteers and participants; the data from the process evaluation (see Process evaluation) that examined the extent of engagement with the intervention by participants and volunteers (based on number of sessions attended); and qualitative data obtained from volunteers, participants with ID, carers of people with ID and staff from the befriending service.
Outcome measures in participants with intellectual disability
Health and social outcome measures were assessed with the participant at baseline and at 6 months post randomisation. All the measures that were selected for use in the study have been validated and used in people with ID. A follow-up assessment at 12 months was planned as part of the original protocol but could not be conducted because of delays in setting up the study and poor recruitment (see Chapter 3). Face-to-face assessments were conducted by the research assistant, who was blind to group allocation, and these were carried out at the participants’ homes; where this was not possible, a telephone assessment was carried out. Participants were supported by the research assistant to complete the measures, which included reading out the questions and responses, and explaining and rephrasing items that were difficult to understand. The following health and social outcomes were assessed:
-
Depressive symptoms (main outcome of interest) were measured using the GDS-LD. 42 This 20-item scale has been developed and validated in people with ID and has been used in recent trials. 45 Participants were asked to rate their symptoms over the last week using a three-point response format scored 0 (‘no’), 1 (‘sometimes’) and 2 (‘a lot’). Scores on the scale range from 0 to 40, with higher scores indicating more symptoms. The scale is reported to have good test–retest reliability (r = 0.97) and internal consistency (with an alpha of 0.90).
-
Self-esteem was measured using the adapted Rosenberg self-esteem scale for people with intellectual disabilities. 46 This is a self-report scale with six items measured on a five-point response scale ranging from ‘never true’ to ‘always true’. Scores range from 6 to 30, with higher scores indicting greater self-esteem. The scale is reported to have an adequate internal consistency (with an alpha of 0.62).
-
Quality of life was measured using the 19-item Maslow Assessment of Needs Scale – Learning Disability (MANS-LD),47 and nine items from the adapted World Health Organization Quality of Life measure (WHOQOL-8). 48 Both measures are rated using a five-point response format (1–5), where higher scores indicate better quality of life.
-
Loneliness and social satisfaction were measured using the Modified Worker Loneliness Questionnaire (MWLQ),49 which has 12 items and two subscales (aloneness and social dissatisfaction). Items are rated on a three-point scale (0–2), with a maximum score of 24. Higher scores indicate more loneliness. The test–retest reliability of the scale is reported to be between 0.76 and 0.89, and inter-rater reliability was 0.87 for aloneness and 0.85 for social dissatisfaction. The internal consistency (Cronbach’s alpha) was 0.65 for aloneness and 0.80 for social dissatisfaction.
-
Social support was measured using the Social Support Self Report for intellectually disabled adults (SSSR). 50 Participants are asked to rate support from family, staff, friends and their partner based on five items rated on a three-point scale (0–2) for each group. The maximum score is 40, with higher scores indicating receipt of more support. The scale has good internal consistency (with an alpha of 0.85).
-
Social participation was measured using the Guernsey Community Participation and Leisure Assessment (GCPLA). 51 Participants are asked to rate the frequency of their participation in five types of activities (i.e. services, vocational activities, leisure, social, and facilities and amenities) on a five-point scale ranging from never (0) to daily or more frequently (5). Higher scores indicate more social participation. It has good test–retest reliability (r = 0.87) and internal consistency (with an alpha of 0.93).
Outcome measures in volunteers
The following outcomes were assessed in volunteers at baseline (prior to matching) and 6 months after the baseline assessment:
-
Self-esteem was measured using the 10-item Rosenberg self-esteem scale. 52 Items are scored on a four-point Likert scale ranging from strongly disagree (1) to strongly agree (4). The maximum score is 40. Higher scores indicate better self-esteem. Reported test–retest reliability ranges from 0.82 to 0.88 and internal consistency (Cronbach’s alpha) ranges from 0.77 to 0.88.
-
Psychological well-being and quality of life was measured using the widely used Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS). 53 This is a 14-item scale that uses a five-point response format (1 = none of the time; 5 = all of the time). The maximum score is 70 , with higher scores indicating better well-being. It has a high internal consistency (with an alpha of 0.89) and a test–retest reliability value of 0.83.
-
Loneliness was measured using the revised University of California, Los Angeles (UCLA) Loneliness Scale. 54 This is a 20-item scale that measures feelings of loneliness and isolation. Items are rated on a four-point scale (1 = never; 4 = often). The maximum score is 80 and higher scores indicate more loneliness. The measure has a high internal consistency (with an alpha of 0.96) and a test–retest reliability value of 0.73.
-
Attitudes of volunteers was assessed using the 67-item Attitudes Towards Intellectual Disability Questionnaire (ATTID). 55 This measure has five subscales (knowledge of causes of ID, knowledge of capacity and rights, discomfort, interaction, and sensibility or tenderness). Higher scores indicate more negative attitudes. Test–retest reliability ranges from 0.44 to 0.88, with an overall internal consistency of 0.92 and a subscale reliability ranging from 0.59 to 0.89.
Feasibility of carrying out a cost-effectiveness analysis
A preliminary health economic analysis was conducted to inform planning of future economic analyses, sources of data required and how best to collect these data. The following were recorded:
-
Health-related quality of life was measured using the EuroQol-5 Dimensions – Youth (EQ-5D-Y). 56,57 There are currently no EuroQol measures that have been developed specifically for adults with ID. The EQ-5D-Y was selected because it uses simple language and has been used in other studies of people with ID. 45 The EQ-5D-Y comprises the descriptive system (five dimensions relating to mobility; looking after myself; doing usual activities; having pain or discomfort; and feeling sad, worried or unhappy) that is rated by selecting the most appropriate statement that reflects the individual’s health state (‘no’, ‘some’ or ‘a lot’) for each dimension, and the EuroQol visual analogue scale (EQ VAS), where self-rated health is recorded on a vertical visual analogue scale between two end points labelled ‘the best health you can imagine’ and the ‘the worst health you can imagine’. The EQ VAS represents the participant’s own subjective view about their health, which may not be captured by the five dimensions, and is therefore considered to provide additional information in its own right. We assessed whether or not it would be feasible to collect self-reported data from individuals with ID on both the descriptive system and the EQ VAS. This was recorded at baseline and 6 months post randomisation.
-
The Client Services Receipt Inventory (CSRI)58 was used to assess the feasibility of collecting data on participant-reported health-care service use. Based on a review of the literature and input from the wider study team, we adapted the CSRI to people with ID. The adapted CSRI was completed with participants’ carers, where possible, or health professionals who knew the person well. If they did not have a carer, then information was collected from the participant. They were asked to recall health and social care service use during the last 6 months. This included contacts with primary care, community services, community ID services and hospitals, including outpatient and inpatient care. This was recorded at baseline and at 6 months post randomisation.
-
Concomitant medication was recorded on a CRF developed for the study. This information was obtained from carers and, where this was not possible, participants were asked to show medication boxes or blister packs to the research assistant. Information was recorded at baseline and at 6 months post randomisation for the previous 6 months.
-
For the befriending intervention, we recorded the resources used by befriending services. Volunteer co-ordinators at the befriending services kept a record of all their contacts with volunteers and participants and the duration of contacts (e.g. monitoring visits and supervision) and other expenses incurred during the intervention.
Process evaluation
A process evaluation using mixed methods59 was conducted to examine:
-
Adherence (fidelity) to the intervention: whether or not the different components of the intervention were consistently followed and the extent to which volunteers delivered the intervention as intended
-
Acceptability of the intervention and trial procedures. The aim was to understand the perceived value, benefits and unintended consequences of the intervention; to understand the contextual factors influencing how the intervention was delivered; and to develop an understanding of the likely mechanisms of action of the intervention and what modifications that would need to be made to the trial procedures and processes in a future randomised trial.
Treatment adherence
Data were collected on the uptake of volunteer training, supervision and the frequency of monitoring checks carried out by volunteer co-ordinators from routine records at each site to assess fidelity to the intervention by the befriending services. To understand how the befriending intervention was delivered, the location and content of the meetings and the range of activities undertaken were described based on an analysis of structured logbooks completed by volunteers. A framework was developed to categorise different types of activity to enable different types of befriending support to be distinguished and quantified.
We examined (1) how many sessions each volunteer attended and the average number of sessions attended by the volunteers, (2) how many pairs attended at least 10 meetings during the 6-month intervention period, (3) the average duration of sessions and (4) for how many participants the minimum threshold of at least 50% of meetings being outside the participant’s home was achieved.
Acceptability of the intervention
We invited all the participants with ID in both groups of the study, the volunteers who had been matched with a participant with ID, the volunteer co-ordinators at the two befriending services and carers of participants who had received the befriending (after seeking permission from the participant) to take part in semistructured interviews. A topic guide comprising questions and prompts was developed for each of the four groups (see Appendix 1, Boxes 1–4, for a list of questions). Interviews were conducted face to face, but during the COVID-19 pandemic modifications needed to be made to accommodate the lockdown restrictions. Interviews were therefore held by telephone or videoconferencing.
All the participants were asked about their views of the intervention (e.g. training, matching, supervision, support), what they perceived to be helpful and what aspects could be improved or required modification, as well as views about trial procedures (e.g. randomisation and completion of questionnaires). The interviews were audio-taped and transcribed.
Study expenses
Following completion of the baseline assessment and, again, after the 6-month follow-up assessment, all the participants and volunteers received a £15 gift voucher for their time and effort. Participants taking part in the qualitative interviews also received a £15 gift voucher.
Data management
Quantitative data were collected using the study CRFs, which were stored at the study sites. Data were entered into the secure and General Data Protection Regulation-compliant60 Red Pill (web-based) database hosted by Sealed Envelope Ltd and managed by Priment Clinical Trials Unit. A subsample of 5% of the CRFs was checked to ensure consistency in data entry. After completion of relevant data management processes, the data were exported from the database and analysed by the trial statistician.
Statistical analysis
Demographic and clinical characteristics of participants with ID and their mental health, quality of life and social outcomes were summarised by randomised group using mean [standard deviation (SD)] or count (percentage) for continuous and categorical data, respectively, at baseline and at the 6-month follow-up.
Demographic characteristics of befriending volunteers and their mental health and attitudinal outcomes were similarly summarised at baseline and at the 6-month follow-up.
The primary mental health outcome was depressive symptoms, measured using the GDS-LD. All participants were analysed in the groups to which they had been randomised. The effect of the befriending intervention was estimated using a linear regression model, with depressive symptoms at 6 months’ follow-up as the outcome and study group as the main explanatory variable, adjusting for depressive symptoms at baseline.
Owing to the small number of participants recruited to the study, we decided that it was inappropriate to explore the effect of the intervention on the secondary outcomes and further regression analyses were not conducted
Analysis of cost-effectiveness
The main aim of the economic evaluation was to determine the costs of delivering the intervention, and test the feasibility of collecting health-care resource use and health-related quality-of-life data to calculate the incremental mean cost per quality-adjusted life-year (QALY) gained from the intervention, compared with the control (i.e. the cost-effectiveness), in people with ID for a full RCT. The detailed health economic analysis is described in Appendix 2.
We assessed the response rates from the CSRI, EQ-5D-Y and EQ VAS; and collected information on whether the CSRI was completed by carers, professionals or participants with ID. We noted any difficulties reported by participants in completing these measures.
The costs of the intervention were provided by the volunteer co-ordinators at the befriending services. They provided a breakdown of costs related to the intervention, such as costs of recruitment, DBS checks, and staff time in relation to training and supervision of volunteers and monitoring visits. Staffing costs were calculated using an hourly rate.
To calculate the costs of using health and social care services, we adopted the perspectives of the NHS and Personal Social Services. The horizon of the study was 6 months; therefore, discounting was not performed.
The mean (SD) health and social care resource use and costs of medication were calculated and costed using nationally recognised, published unit costs61–63 to estimate the mean (95% CI) costs per participant. Costs were in Great British pounds at 2019 values or adjusted for inflation if costs for 2019 were not available (see Appendix 2, Tables 10 and 11, for unit costs and prescription costs).
Responses from the EQ-5D-Y were converted into a single value (index number). The collection of index values for possible EQ-5D states is referred to as the value set. Research is currently ongoing to produce EQ-5D-Y value sets and, therefore, although not recommended, the regular EuroQol-5 Dimensions, three-level version (EQ-5D-3L), value sets were used to obtain utility values. Utility values range from 0 to 1, with scores close to 1 indicating ‘full health’ (with a score of 0 indicating ‘death’). The EQ VAS was used as a quantitative measure of health outcome that reflects the participant’s own judgement about their health status. We examined whether or not scores on the EQ VAS were consistent with the EQ-5D-Y utility values, as this would help us to determine if the EQ-5D-Y is a suitable measure of health status in people with ID.
Incremental cost per change in the primary health outcome (depression scores on the GDS-LD) between the intervention group and the control group was estimated. The incremental cost-effectiveness ratio (ICER) was calculated by dividing the difference in total costs (incremental cost) by the difference in the health outcome (incremental effect) to provide a ratio of ‘extra cost per extra unit of health effect’ for the more expensive intervention compared with the alternative. ICERs reported by economic evaluations are compared with a predetermined threshold to decide whether or not choosing the new intervention is an efficient use of resources.
Analyses followed the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) Good Reporting Practices. 64
Qualitative data analysis
Transcripts from the interviews with participants with ID, staff at befriending services, volunteers and carers were transcribed and analysed using thematic analysis65 supported by computer software (NVivo 9; QSR International, Warrington, UK). Thematic analysis aims to identify themes or patterns in the data set through a rigorous process of data familiarisation, coding of data, and the development and refinement of themes. It was selected because of its flexibility in incorporating a range of different approaches and its use in a wide range of contexts. Data were coded by two members of the research team, using both deductive (i.e. coding guided by existing concepts and ideas) and deductive (i.e. coding guided by the content of the data) approaches. The codes and initial themes were discussed with the research team, followed by further revision of themes. The analytic strategy aimed to identify themes related to the barriers and facilitators affecting the implementation of the intervention, potential benefits to participants and volunteers, and possible mechanisms of action. Analysis also allowed for the consideration of themes that arose more inductively from the data. The reliability of the coding frame was not assessed.
Progression criteria
The following criteria were used to evaluate whether or not the pilot trial had been successful:
-
At least 70% (35) of participants are recruited from the 50 potentially eligible individuals who are approached.
-
At least 70% of participants with ID in the intervention group are successfully matched to a volunteer (befriender) and they meet on a minimum of 10 occasions.
-
The dropout rate of participants with ID in both groups, post randomisation, is < 30% at 6 months’ follow-up.
-
The intervention and trial procedures are considered to be acceptable by volunteers and individuals with ID.
-
If the target recruitment rate and number of matched pairs is between 50% and 69%, or the dropout rate is between 31% and 50%, we would consider if these could be rectified by modifying the protocol. If this was the case, a full study could still be considered. If the recruitment rates were < 50% and the dropout rates were > 50%, then a full trial would not be considered feasible.
Management of the study
The study was sponsored by University College London. The study research assistant was supervised by the chief investigator and they met weekly. The Trial Management Group, comprising the research team, co-applicants, and staff from the two befriending schemes and Priment Clinical Trials Unit, met every 3 months. An independent Trial Steering Committee, comprising five members [an academic clinician, clinician in ID, statistician, health economist and patient and public involvement (PPI) representative] was appointed and approved by the funders. Meetings were held annually and minutes were made available to the funders.
Patient and public involvement
Proposal development
In developing the proposal, three befriending services for people with ID were consulted. They agreed that it was important to carry out a trial on befriending that captured a range of outcomes for individuals with ID and volunteers. Two of these services subsequently agreed to take part in the study and contributed to the design of the study. In addition, a consultation group meeting was held in July 2017 with volunteers, befriendees and volunteer co-ordinators at the Suffolk service. We discussed the nature of the befriending intervention, its impact on both befriendees and volunteers and the best choice of outcomes for the study. Feedback was obtained from an advisory group of carers and service users linked One Westminster (London, UK) befriending service who thought that the study was very important. They highlighted areas that they felt should be addressed carefully, such as ensuring participants with ID were safeguarded, that they had opportunities to voice concerns if they were dissatisfied, and that adequate training and supervision were available for volunteers. These suggestions were incorporated into the proposal.
Patient and public involvement during the trial
We advertised for people with ID who had experience of befriending to become members of an advisory group. Unfortunately, despite some initial interest, we were unable to recruit enough members during the initial stages of the trial. Following the closure of recruitment and to understand the reasons for the poor recruitment, we consulted with three people with ID and a volunteer co-ordinator who were members of Gig Buddies, a befriending service provided by My Life My Choice (Oxford, UK), a voluntary organisation. These individuals had experience of befriending as a peer befriender, which meant that they were befrienders to other people with ID. They had a unique perspective on the befriending experience. They suggested some reasons for the poor recruitment, but were largely positive about the study. These suggestions are discussed in Chapter 5.
Ethics issues
The study received ethics approval from the London – City and East Research Ethics Committee (reference 18/LO/2188) and from the Health Research Authority (HRA) on 8 January 2019. All substantial amendments to the study were approved by the sponsor and were submitted for ethics approval. Participants with ID were provided with an accessible information sheet and were required to provide written consent prior to taking part in the study. Volunteers, volunteer co-ordinators and carers were also provided with an information sheet and were required to give written consent. Data confidentiality was maintained by assigning participants study identification numbers. One of the main concerns about the study was the potentially negative impact on the participant with ID of relationships ending, particularly if they had limited access to other forms of support. Unfortunately, it was not possible to explore these issues in detail as we were unable to complete the 12-month follow-up (reasons for which are explained in Chapter 3).
Several ethics issues arose during the study. First, the Suffolk befriending service raised concerns about the randomisation of participants and expressed the view that it was unacceptable to assign participants to the control group. To manage this issue, it was agreed that individuals referred to the service would have the option of taking part in the study or remaining on the waiting list. This had significant consequences for recruitment (discussed further in Chapter 3). Second, carers were occasionally found to obstruct relationships and, on two occasions, appeared to be responsible for the breakdown of the befriending relationships. This situation was distressing for the volunteers. In both cases, the participant with ID did not express dissatisfaction with the relationship. This raises questions about the lack of autonomy that some people with ID may have in making decisions. Finally, one safeguarding alert was raised by a volunteer when their befriendee reported being bullied by a paid carer (discussed further in Chapter 3).
Chapter 3 Results
In this chapter, we report on the following feasibility outcomes:
-
recruitment of participants with ID and volunteers
-
the number of participants with ID who were successfully matched
-
the number of participants who completed the follow-up assessment at 6 months and withdrew from the trial
-
exploratory analysis of the health and social outcomes
-
exploratory data on the analysis of cost-effectiveness.
Overview of issues encountered in recruitment
The study began in July 2018 and was funded for a 2-year period. In the original study Gantt chart, we had aimed to obtain all the necessary approvals (i.e. approval of the protocol by Priment Clinical Trials Unit, sponsorship and ethics approval, exchange of site contracts and approval of the study database) and start recruitment within 4 months of the trial start date. This target proved to be unrealistic and, as a result of delays in obtaining the necessary approvals, recruitment did not begin until April 2019, 6 months later than intended. Recruitment was slow, and the number of participants with ID who were eligible or willing to take part was smaller than anticipated, as was the number of volunteers expressing an interest in taking part in the study. One issue that we encountered with recruitment through the Suffolk scheme was that it was not considered to be appropriate (or acceptable) by the scheme to change the current standard of practice, because of concerns over randomisation and the potential allocation of participants to the control group. This issue was raised after the protocol was approved and sponsorship approval had been given. It was agreed that the scheme could offer individuals the option of entering the study or remaining on the waiting list for a befriender. Owing to the uncertainty of whether service users would be allocated a befriender or be in the control group, those who were approached chose to remain on the waiting list until a volunteer was allocated through the usual route, even if it meant waiting for a longer period. Staff at the service also expressed their discomfort at the possibility of participants being left in the control group without a befriender for a year. To manage this situation, we agreed to make changes to the protocol to permit participants in the control group to be allocated a befriender after they completed their 6-month follow-up. It was not possible to change the design of the study (e.g. to a waiting list control group) because of the time frame and delays to the study, as this would have required significant changes to the protocol and approval from the funders.
A number of changes to the protocol were made to improve recruitment (see Protocol changes and amendments), such as recruiting student and staff volunteers directly through University College London and the study website, and recruiting participants through advertising on posters, but these strategies did not contribute to an overall improvement in recruitment. Further changes to the study protocol were also considered, such as expanding the number of befriending services taking part in the study and introducing patient identification sites, but these changes were not implemented as the study funders did not approve extending the recruitment period, which would have also required a costed extension to the trial duration and study end date. In September 2019, the funders communicated to the chief investigator that recruitment should close and that preparations should be made to end the study in June 2020, which was the expected end date. The chairperson of the Trial Steering Committee was consulted for advice. With this time frame, it was not possible to complete the 12-month post-randomisation follow-up outcome assessments, and the protocol was updated to reflect this change. Owing to the COVID-19 pandemic, there were some delays in conducting the qualitative interviews and, therefore, a no-cost extension of 2 months was granted.
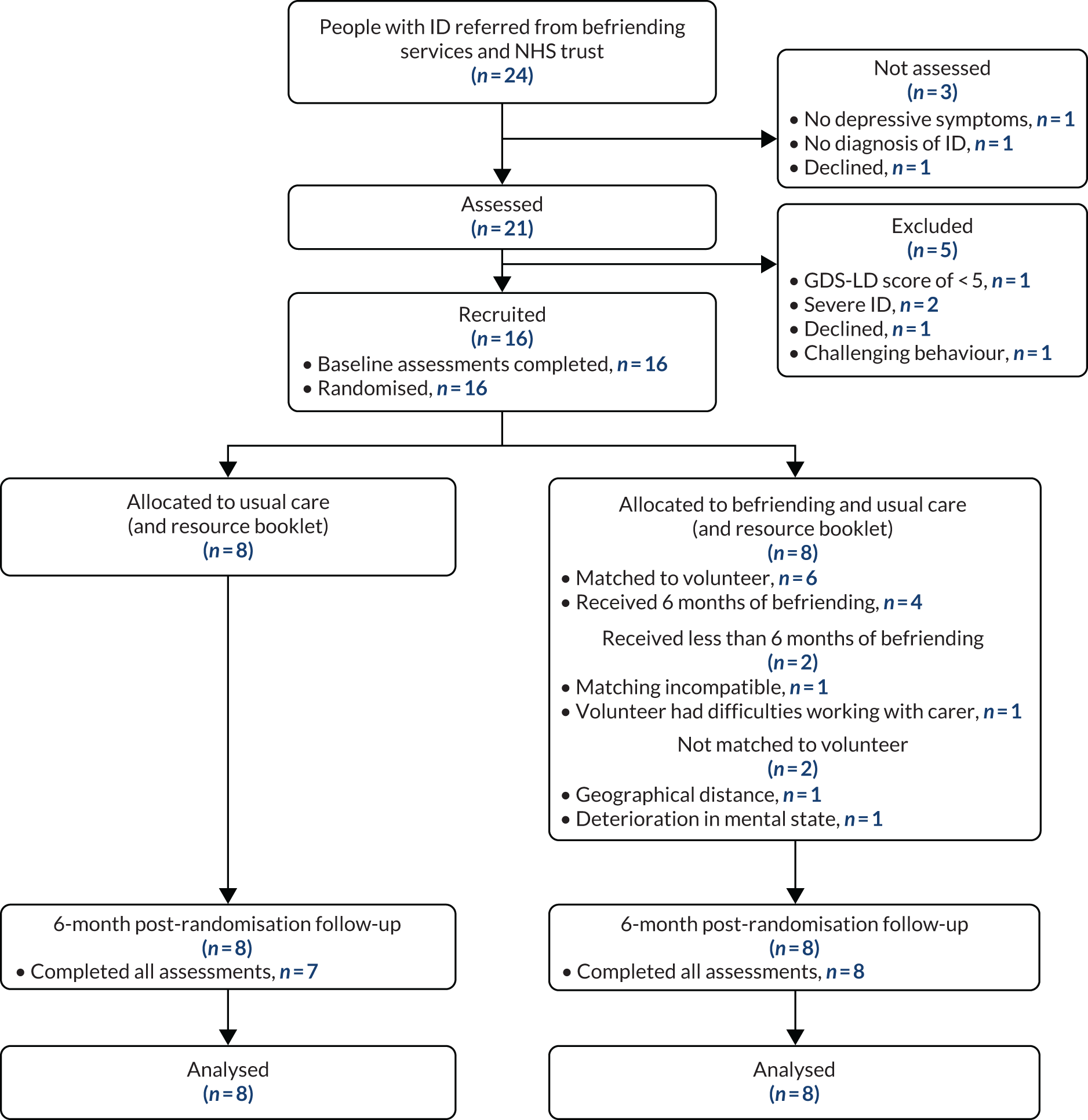
Recruitment and retention of participants
The flow of participants with ID in the pilot trial is shown in the Consolidated Standards of Reporting Trials (CONSORT) flow diagram (Figure 2). Twenty-four potential participants were referred to the study team. Fifteen referrals were from NELFT clinicians, six were from Outward (Hackney) and three were from The Befriending Scheme (Suffolk) (Table 1). The number of participants with ID and volunteers who were recruited each month is shown in Table 2. On average, just under three participants (2.7) and two (1.7) volunteers were recruited each month into the study. Of the 24 participants with ID referred to the study, 21 were assessed and five were excluded (1) because they did not meet the inclusion criteria (n = 3), (2) because they declined to take part (n = 1) or (3) because of challenging behaviour that may have put the safety of volunteers at risk (n = 1). Sixteen participants agreed to take part in the trial and were randomised to either the intervention group (befriending, resource booklet and usual care; n = 8) or the control group (resource booklet and usual care; n = 8).
FIGURE 2.
The CONSORT flow diagram for participants with ID.
| Referral | Referral source | ||
|---|---|---|---|
| NELFT | Hackney scheme (Outward) | Suffolk scheme (The Befriending Scheme) | |
| Participants with ID | |||
| Total number of referrals | 15 | 6 | 3 |
| Number eligible | 14 | 3 | 1 |
| Number randomised | 13 | 2 | 1 |
| Volunteers | |||
| Total number of referrals | N/A | 9 | 3 |
| Total number enrolled into study | N/A | 8 | 2 |
| Month | Number of participants recruited | |
|---|---|---|
| People with ID | Volunteers | |
| April | 2 | 3 |
| May | 2 | 2 |
| June | 2 | 1 |
| July | 6 | 0 |
| August | 1 | 1 |
| September | 3 | 1 |
| October | 0 | 2a |
Of the eight participants who were randomised to the intervention group, six received the befriending intervention. It was not possible to match two of the participants with a volunteer; the reasons for this were geographical distance (no local volunteer could be identified) and, in one case, deterioration in the mental state of the participant prior to matching.
Of the six participants who were matched, only four had a volunteer for the whole 6-month period. One participant was matched with another volunteer after the first volunteer dropped out because of work commitments. Of the two participants who did not have a volunteer for the 6-month period, in one case the family carer was not satisfied with the match, as they felt that the interests of the participant and the volunteer were not compatible, and in the other case the volunteer experienced difficulties working with the participant because of interference from the participant’s paid carers, who were based in the participant’s supported living accommodation.
All 16 trial participants completed the 6-month follow-up, but one participant in the control group only partially completed the outcome measures owing to a deterioration in their mental state and refusal to continue the assessment.
The flow of volunteers recruited to the study is shown in Figure 3. Twelve volunteers expressed an interest in taking part in the study (nine from the Hackney site and three from the Suffolk site). Two dropped out before being enrolled in the study (one did not complete the training and one could not be contacted for their baseline assessment). Ten volunteers completed the baseline assessment, but one dropped out shortly afterwards (no reason given). Of the nine remaining volunteers, seven were matched with a participant with ID; however, one volunteer who had been matched dropped out of the study because of work commitments. Two volunteers in Suffolk were not matched, as no participants with ID were allocated to the intervention group (the only participant to be randomised was allocated to the control group). All eight remaining volunteers completed the 6-month follow-up assessments.
FIGURE 3.
Volunteer flow chart.

Baseline characteristics of participants
The average age of the 16 participants who took part in the trial was 41.6 (SD 16.7) years; nine were female (56%), eight were of white ethnicity (50%) and nine (56%) were living in supported living accommodation. The majority of the participants had a mild ID (81%), and the average IQ was 55.3 (SD 7.6). Ten participants (63%) had a clinical diagnosis of depression and five (31%) had a diagnosis of anxiety disorder. Nine participants (56%) were taking an antidepressant.
Table 3 displays the participants’ demographic characteristics according to allocated group. The participants in the intervention group were older than those in the control group [average age 48.9 (SD 17.2) years, compared with 34.3 (SD 13.4) years, respectively], were mainly female [6 (75%) compared with 3 (38%), respectively], were less likely to have a diagnosis of depression [4 (50%) compared with 6 (75%), respectively] and there were fewer multiple mental health diagnoses [2 (25%) compared with 5 (62.5%), respectively].
| Demographic | Group | |
|---|---|---|
| Control (N = 8) | Intervention (N = 8) | |
| Age at randomisation (years), mean (SD) | 34.4 (13.4) | 48.9 (17.2) |
| Gender, n (%) | ||
| Male | 5 (63) | 2 (25) |
| Female | 3 (38) | 6 (75) |
| Ethnicity, n (%) | ||
| White | 4 (50) | 4 (50) |
| Asian | 1 (13) | 3 (38) |
| Black | 0 (0) | 1 (13) |
| Mixed | 3 (38) | 0 (0) |
| Living arrangements, n (%) | ||
| Alone | 1 (13) | 3 (38) |
| With family | 1 (13) | 1 (13) |
| Supported living (< 24 hours) | 0 (0) | 1 (13) |
| Supported living (24 hours) | 5 (63) | 3 (38) |
| Residential care | 1 (13) | 0 (0) |
| IQ score: mean (SD) | 55.6 (10.3) | 54.9 (4.1) |
| Degree of ID, n (%) | ||
| Mild | 6 (75) | 7 (88) |
| Moderate | 2 (25) | 1 (13) |
| Mental health diagnoses, n (%) | ||
| Depression | 6 (75) | 4 (50) |
| Psychosis/schizophrenia | 1 (13) | 2 (25) |
| Bipolar affective disorder | 1 (13) | 0 (0) |
| Anxiety disorder | 3 (38) | 2 (25) |
| Autism | 2 (25) | 0 (0) |
| ADHD | 2 (25) | 0 (0) |
| Other | 1 (13) | 1 (13) |
| Two or more mental health diagnoses, n (%) | 5 (62.5) | 2 (25.0) |
| Taking antidepressants: yes, n (%) | 5 (63) | 6 (75) |
| Concomitant epilepsy: yes, n (%) | 1 (13) | 0 (0) |
| Mobility, n (%) | ||
| Mobilises independently | 8 (100) | 5 (63) |
| Mobilises with walking stick or frame | 0 (0) | 3 (38) |
| Travels independently: yes, n (%) | 8 (100) | 6 (75) |
Table 4 summarises the outcome measures at baseline according to group allocation. Depressive symptoms at baseline were lower in the intervention group than in the control group, with mean GDS-LD scores of 18.6 (SD 5.7) and 21.4 (SD 9.8), respectively.
| Outcome | Group | |
|---|---|---|
| Control (N = 8) | Intervention (N = 8) | |
| Depressive symptoms (GDS-LD), mean (SD) | 21.4 (9.8) | 18.6 (5.7) |
| Self-esteem (adapted Rosenberg self-esteem scale), mean (SD) | 20.8 (4.5) | 22.4 (4.1) |
| Quality of life, mean (SD) | ||
| MANS-LD | 64.1 (10.3) | 73.0 (9.4) |
| WHOQOL-8 | 23.8 (4.7) | 30.0 (4.4) |
| Loneliness and social satisfaction (MWLQ), mean (SD) | ||
| Aloneness | 7.6 (2.8) | 8.4 (2.3) |
| Social dissatisfaction | 6.8 (3.4) | 7.9 (3.5) |
| Social support (SSSR), median (IQR) | ||
| Family | 5.0 (0.5–6.5) | 5.5 (2.5–6.5) |
| Staff | 5.5 (5.0–7.0) | 5.5 (3.5–7.5) |
| Friends | 5.5 (3.5–7.5) | 3.5 (1.5–6.0) |
| Partner | 0 (0–7.5) | 0 (0–3.5) |
| Social participation (GCPLA), mean (SD) | 73.9 (25.9) | 57.5 (23.4) |
Self-esteem, as measured by the adapted Rosenberg scale, was higher in the intervention group (mean 22.4; SD 4.1) than in the control group (mean 20.8; SD 4.5), as was quality of life, as measured by the MANS-LD [mean 73.0 (SD 9.4) and mean 64.1 (SD 10.3), respectively] and the WHOQOL-8 [mean 30.0 (SD 4.4) and mean 23.8 (SD 4.7), respectively]. Social support, as measured by the SSSR, was similar across both groups, although the control group reported more contacts with friends [median 5.5 contacts, interquartile range (IQR) 3.5–7.5 contacts] than the intervention group (median 3.5 contacts, IQR 1.5–6.0 contacts). Social participation, as measured by the GCPLA, was 16.4 units higher in the control group (mean 73.9 units, SD 25.9 units) than in the intervention group (mean 57.5 units, SD 23.4 units).
The baseline characteristics of the volunteers are summarised in Table 5. The average age of volunteers was 33.2 (SD 11.2) years. Seven (70%) volunteers were female and seven (70%) volunteers were of white ethnicity. Six (60%) volunteers were single, seven (70%) were employed and the majority had A Level (Advanced Level) qualifications or a higher level of educational qualification (n = 7; 70%). Four (30%) volunteers had prior experience of working with someone with ID and three (30%) had experience of working with someone with mental health problems. The baseline scores on the outcome measures of self-esteem, psychological well-being, loneliness and attitudes towards people with ID are shown in Table 6.
| Demographic | Befriending volunteers (N = 10) |
|---|---|
| Age at entry (years), mean (SD) | 33.2 (11.2) |
| Gender, n (%) | |
| Male | 3 (30) |
| Female | 7 (70) |
| Ethnicity, n (%) | |
| White | 7 (70) |
| Asian | 2 (20) |
| Other | 1 (10) |
| Marital status, n (%) | |
| Married or cohabiting | 4 (40) |
| Single | 6 (60) |
| Highest completed level of education, n (%) | |
| No qualification | 1 (10) |
| GCSE or equivalent | 1 (10) |
| NVQ or equivalent | 1 (10) |
| A Level or equivalent | 2 (20) |
| Degree or higher degree | 5 (50) |
| Employment status, n (%) | |
| Employed | 7 (70) |
| Unemployed, not seeking work | 1 (10) |
| Student | 2 (20) |
| Previous experience of working with, n (%) | |
| People with ID | 4 (40) |
| People with mental health problems | 3 (30) |
| Outcome | Time point, mean (SD) score | |
|---|---|---|
| Baseline (n = 10) | Follow-up (n = 8) | |
| Self-esteem (Rosenberg self-esteem scale) | 28.3 (2.3) | 32.0 (4.6) |
| Psychological well-being (WEMWBS) | 50.6 (6.9) | 53.0 (6.0) |
| Loneliness (UCLA Loneliness Scale) | 55.5 (3.9) | 56.0 (4.0) |
| Attitudes (ATTID) | ||
| Discomfort | 30.5 (10.6) | 29.9 (9.3) |
| Knowledge of capacity and rights | 46.6 (6.6) | 42.9 (6.9) |
| Interaction | 26.6 (8.7) | 24.4 (8.6) |
| Sensibility or tenderness | 16.5 (2.9) | 16.6 (3.5) |
| Knowledge of causes of ID | 18.8 (6.4) | 19.4 (7.0) |
Adverse events
There were no serious adverse events associated with the intervention for participants with ID. In the case of volunteers, there was one incident involving a disagreement between a paid carer at a supported living placement and a volunteer. The volunteer was unfairly accused of buying the participant an unhealthy meal and disregarding his care plan. This disagreement led to a breakdown in the befriending relationship and was upsetting for the volunteer. The volunteer reported this incident to the volunteer co-ordinator, who raised the issue with the manager of the placement. The manager acknowledged that there was a misunderstanding between the paid carer and volunteer.
Other incidents
A volunteer raised a safeguarding alert after their befriendee reported feeling bullied by a member of staff at their supported living placement. The volunteer supported the individual to report the incident. The incident was investigated by the local authority and the situation was satisfactorily resolved.
Outcome assessments at 6 months’ follow-up
Table 7 shows the scores on the outcome measures for participants with ID at 6 months’ follow-up. Depressive symptoms at 6 months’ follow-up were lower in the intervention group than in the control group, with mean GDS-LD scores of 12.9 (SD 6.7) and 17.5 (SD 6.5), respectively. Compared with baseline scores, there was a reduction in the GDS-LD score in both groups (3.9 units in the control group and 5.7 units in the intervention group). There was a slight increase in mean self-esteem scores in both groups: an increase of 0.6 units in the control group, to 21.4 units (SD 3.5 units), and an increase of 1.5 units in the intervention group, to 23.9 units (SD 3.4 units). Mean quality-of-life scores on the MANS-LD also increased in both groups: an increase of 7.9 units in the control group, to 72 (SD 5.5) units, and an increase of 7.0 units for the intervention group, to 80.0 (SD 9.9) units. The mean WHOQOL-8 scores in the control group increased by 4.6 units, to 28.4 (SD 3.5) units, but the scores in the intervention group decreased by 0.6 units, to 29.4 (SD 5.3) units. There were only small changes in the scores for loneliness and social dissatisfaction on the MWLQ. The median social support scores increased slightly in the control group in relation to family (an increase of 2 units, to 7.0 units, IQR 4.0–9.0 units), compared with no change in the intervention group, and in relation to friends (an increase of 1.5 units to 7.0 units, IQR 4.0–9.0 units), compared with an increase of 0.5 units in the intervention group (4.0 units, IQR 3–6.5 units). Between baseline and follow-up, the social participation score increased by 3.8 units in the intervention group (to a mean of 61.8; SD 22.5) and by 0.5 units in the control group (to a mean of 74.4; SD 20.4).
| Outcome | Group | |
|---|---|---|
| Control (n = 8) | Intervention (n = 8) | |
| Depressive symptoms (GDS-LD), mean (SD) | 17.5 (6.5) | 12.9 (6.7) |
| Self-esteem (adapted Rosenberg self-esteem scale), mean (SD) | 21.4 (3.5) | 23.9 (3.4) |
| Quality of life, mean (SD) | ||
| MANS-LD | 72.0 (5.5) | 80.0 (9.9) |
| WHOQOL-8 | 28.4 (3.5) | 29.4 (5.3) |
| Loneliness and social satisfaction (MWLQ), mean (SD) | ||
| Aloneness | 7.0 (3.7) | 8.6 (3.5) |
| Social dissatisfaction | 8.3 (2.7) | 7.6 (2.1) |
| Social support (SSSR), median (IQR) | ||
| Family | 7.0 (4.0–9.0) | 5.5 (1.5–7.0) |
| Staff | 6.0 (5.0–8.0) | 6.0 (2.5–7.5) |
| Friends | 7.0 (4.0–9.0) | 4.0 (3.0–6.5) |
| Partner | 0 (0–0) | 0 (0–5.0) |
| Social participation (GCPLA), mean (SD) | 74.4 (20.4) | 61.3 (22.5) |
Regression analysis of main outcome (depression)
After adjustment for depressive symptoms at baseline, depressive symptoms were lower in the intervention group. We estimated a four-point difference in the GDS-LD depressive symptoms score in the intervention group compared with the control group (adjusted mean difference –4.0, 95% CI –11.2 to 3.2). This difference was equivalent to a standardised effect size of 0.5 SDs.
Outcome assessments in volunteers
At 6 months’ follow-up, there was an increase in the mean scores for self-esteem (an increase of 3.7 units to 32.0 units; SD 4.6 units) and psychological well-being for volunteers (an increase of 2.4 units to 53.0 units; SD 6.0 units; see Table 6) from baseline. There was a slight increase in mean loneliness scores at 6 months’ follow-up (a 0.5-unit increase to 56.0 units; SD 4.0 units). Scores on the measure of attitudes towards ID changed very little, apart from a slight improvement in the mean scores for knowledge of capacity and rights (a decrease in score of 3.7 units to 42.9 units; SD 6.9 units).
Health economic data
The total cost of intervention implementation was £5647.38 (see Appendix 2, Table 12), which includes the cost of recruitment (staff time); DBS and reference checks; the cost of staff time and resources to deliver training, supervision, monitoring calls and visits; and volunteer expenses. The mean cost per participant was £701.00.
It was possible to obtain NHS resource data from carers or from health professionals in the majority of cases, but three participants (who lived independently and had minimal support) provided self-report data. Data were available for all 16 participants at baseline and follow-up. No significant difficulties were reported by carers or participants with ID, although participants with ID may have had difficulty recalling the number of contacts with health services over the previous 6 months. Participants were encouraged to use their diaries to record this information.
The costs of NHS resource use and EQ-5D-Y health state values at baseline and at 6 months post randomisation are provided in Appendix 2, Tables 13 and 14. Health-care resource use costs at baseline were substantially lower in the intervention group (mean £1387; 95% CI £359 to £2415) than in the control group (mean £4949; 95% CI £351 to £9548). In both groups, resource use costs at 6 months’ follow-up were lower than those at baseline (mean £855 in the intervention group and mean £4014 in the control group). The mean difference in resource use costs between the two groups was –£3159 (95% CI –£6250 to –£73), but this difference does not take into account baseline cost differences. After including the intervention cost, the mean difference was –£2458 (95% CI –£5549 to £628), but was not statistically significant.
The EQ-5D-Y and EQ VAS were completed by individuals with ID. The EQ-5D-Y was completed by all participants at baseline, but data were missing for one participant at 6-month follow-up. The EQ VAS was completed by almost all of the participants (data were missing for one participant at baseline and follow-up). No issues were reported in the completion of the EQ-5D-Y descriptive system, but some participants found the instructions for the EQ VAS difficult to understand, which may explain the discrepancies in the scores between the EQ-5D-Y and EQ VAS (see below).
At baseline, the EQ-5D-Y utility value was slightly higher in the intervention group (0.90; SD 0.10) than in the control group (0.88; SD 0.08). At 6 months, it was slightly higher in the control group (0.90; SD 0.13) than in the intervention group (0.88; SD 0.11). At baseline, the EQ VAS score was substantially higher in the intervention group (75.0; SD 23.2) than in the control group (45,6; SD 31.5), but, at 6 months’ follow-up, the EQ VAS score appeared to decrease in the intervention group (62.3; SD 40.8) and increased slightly in the control group (50.7; SD 27.6). The CIs for the EQ VAS were large, and the scores did not appear to correspond well to the EQ-5D-Y utility values, suggesting that the EQ VAS may be difficult for people with ID to complete.
We have explored further the responses to the EQ-5D-Y questionnaires that are displayed in Appendix 2, Tables 15 and 16, splitting the EQ-5D-Y levels into ‘no problem’ (level 1) and ‘any problems’ (levels 2 and 3), changing the profile into frequencies of reported problems. This is helpful, as it describes the changes in health over time. Although an overall summary is preferred, this approach shows that there were improvements in usual activities; pain and discomfort; and feeling worried, sad or unhappy in the control group; and improvements in participants looking after themselves in the intervention group.
Owing to the small sample size and discrepancies in the scores, QALYs were not calculated. Therefore, the incremental cost per change in the primary health outcome (depression scores on the GDS-LD) between the intervention group and control group was estimated. After adjustment for baseline values, the ICER was –£1810 per 1-point change in GDS-LD score.
The befriending intervention has a 35% probability of being cost-effective at a willingness to pay of £20,000 (see Appendix 5, Figure 5). These results are illustrative only and should be interpreted with caution because of the small sample size.
Protocol changes and amendments
Protocol changes and amendments were approved by the Public Health Research programme manager and submitted for sponsorship and ethics approval. The main changes were as follows:
-
Amendment 1 (approved on 21 June 2019): changes to recruitment to include recruitment of volunteers via the trial website, recruitment of undergraduate students at University College London and use of posters to recruit participants with ID from ID services in NELFT. Changes to the matching process were also introduced, following recommendations from the Trial Steering Committee, enabling participants to be rematched if a volunteer dropped out, and for more than one volunteer to be matched to a participant.
-
Amendment 2 (approved on 25 March 2020): the 12-month follow-up was removed because of significant delays to the study. Focus groups with volunteers, carers and volunteer co-ordinators were changed to interviews to assist data collection.
Chapter 4 Process evaluation results
In this chapter we will discuss:
-
adherence to the intervention by volunteers and the befriending services
-
acceptability of the intervention and trial procedures and processes.
Intervention adherence
Intervention adherence by volunteers
Volunteers were asked to meet their befriendee once per week for 1 hour, over a period of 6 months (24 visits). Volunteers were required to document their activities with their befriendee in a structured logbook following each session. They were required to record whether or not they had had a meeting and reasons for cancellation, what activities they did with their befriendee, where they spent their time together (e.g. at the person’s home or in the community), the duration of the meetings and their reflections on the visit in terms of aspects that did or did not go well.
Six volunteers returned their structured logbooks. The total number of meetings between the volunteer and participant with ID ranged from 1 to 21. Two pairs met only once or twice (in one case because of dissatisfaction with the matching process, which was raised by a family carer, and in the other case because conflict with carers led to the breakdown of the pair’s relationship ). Two pairs completed 20 and 21 meetings. The total number of meetings by all the pairs was 71, and the average number of meetings was 11.8. Four out of the six pairs met on more than 10 occasions, which was the minimum number of stipulated meetings that was considered to be acceptable. Only six recorded contacts were not face to face (i.e. were by telephone or video call). The average duration of meetings for each pair ranged from 67 to 210 minutes, with an average duration of 118 minutes, which was well above the minimum of 60 minutes that was required for each meeting. Most volunteers met their befriendee approximately every 2 weeks, and this may be the reason why they spent a longer period of time together when they did meet. Reasons for pairs not being able to meet up included volunteers being unwell, going on leave or holiday or having university commitments. Four of the pairs have continued their relationship beyond the 6-month period and remained in contact.
Tables 8 and 9 show the types of activities that the pairs engaged in, categorised into activities that took place outside the home and inside the home. The majority of activities were outside the home (59/91 activities; 68.8%). Apart from one participant with ID who refused to leave their home, all the other participants spent over 50% of their time in the community. The most common types of activities outside the home involved going to cafes (18 meetings; 19.8%), going for a walk (12 meetings; 13.2%) and going to a restaurant (10 visits; 11.0%). The most common indoor activity was having a conversation (16 meetings; 17.6%), followed by playing games (six meetings; 6.6%) and arts and crafts activities (four meetings; 4.4%). According to the logbook entries, the majority of activities (> 90%) were described as being pleasant or enjoyable by the volunteers.
| Type/location of activity | Number of pairs that engaged in the activity | Total number of meetings | Percentage of outdoor activities (n = 45) | Percentage of all activities (n = 71) |
|---|---|---|---|---|
| Cafe | 2 | 18 | 30.5 | 19.8 |
| Restaurant | 4 | 10 | 16.9 | 11.0 |
| Walking | 3 | 12 | 20.3 | 13.2 |
| Shopping | 3 | 8 | 13.6 | 8.8 |
| Gallery/museum | 1 | 2 | 3.4 | 2.2 |
| Pub | 1 | 2 | 3.4 | 2.2 |
| Library | 1 | 1 | 1.7 | 1.1 |
| Cinema | 1 | 1 | 1.7 | 1.1 |
| Social club | 1 | 1 | 1.7 | 1.1 |
| Park | 1 | 1 | 1.7 | 1.1 |
| Place of worship | 1 | 1 | 1.7 | 1.1 |
| Political activity (voting) | 1 | 1 | 1.7 | 1.1 |
| Theme park | 1 | 1 | 1.7 | 1.1 |
| Type of activity | Number of pairs that engaged with activity | Total number of meetings | Percentage of total number of indoor activities (n = 26) | Percentage of total number of all activities (n = 71) |
|---|---|---|---|---|
| Conversation | 1 | 16 | 50.0 | 17.6 |
| Playing games | 1 | 6 | 18.8 | 6.6 |
| Arts and crafts | 1 | 4 | 12.5 | 4.4 |
| Cooking | 1 | 2 | 6.3 | 2.2 |
| Reading books/magazines | 1 | 1 | 3.1 | 1.1 |
| Listening to music | 1 | 1 | 3.1 | 1.1 |
| Creating shopping list | 1 | 1 | 3.1 | 1.1 |
| Cleaning home | 1 | 1 | 3.1 | 1.1 |
Intervention adherence by befriending services
All the volunteers who were matched were recruited by the Outward befriending scheme in Hackney. Training was completed by all the volunteers prior to matching, which included training modules on confidentiality, depression, diversity and equality, health and safety, and safeguarding of vulnerable adults. These modules were delivered through an online social care provider (Social Care TV, Hingham, UK). The volunteers also completed a 2-hour classroom-based session on volunteer induction training.
Supervision of volunteers was intended to occur on a monthly basis over the 6-month intervention and was provided face to face or by telephone. Five volunteers participated in supervision. A total of 21 supervision sessions were completed by the volunteers. The average number of sessions completed was 4.2 (range 3–6 sessions). The majority of the sessions were face to face (16; 76.2%). A supervision form was used to record discussions, which was developed by the befriending service. Volunteers were asked about their general well-being, their ability to manage their role and commitments, what they felt has gone well or they had enjoyed, if they had any concerns about their befriendee or their relationship, issues around maintaining boundaries, activities that the befriendee had requested and any support or training needs. Work or family commitments were the main reasons for volunteers not being able to attend supervision. Topics/issues that were discussed at supervision are presented in Appendix 3, Table 17. Managing the balance between work and personal commitments with the befriending role was mentioned by four volunteers [discussed in five (23.8%) sessions]. The issues that were most commonly raised in supervision were concerns about the participant’s physical health [discussed in seven (33.3%) sessions by three volunteers]; concerns about the befriendee’s finances, such as the befriendee not having enough money to participate in activities [discussed in seven sessions (33.3%) by two volunteers]; reasons for missed sessions [discussed in five sessions (23.8%) by two volunteers]; managing repetitive questioning [discussed in four sessions (19.0%) by three volunteers]; concerns about the befriendee’s mental health [discussed in four sessions (19.0%) by two volunteers]; time management [discussed in three sessions (14.1%) by three volunteers]; and dealing with carers [discussed in three sessions (14.1%) by three volunteers]. Safeguarding issues were discussed by two volunteers (in two sessions; 9.5%) and managing the ending of the relationship was raised by one volunteer (in two sessions; 9.5%).
Monitoring sessions were also held with participants with ID who were receiving the befriending intervention. The volunteer co-ordinator was able to make contact (face-to-face meetings or telephone contact) with five out of the six participants who were matched. There were 12 monitoring contacts in total. The number of monitoring sessions for each participant ranged from 1 to 4 (average 2.4 sessions). The reasons for monitoring contacts not taking place included participants not being contactable, declining to meet up or being unable to meet up because they were busy with other commitments. The befriending service developed their own monitoring forms. Nine monitoring forms were completed with four participants. During these sessions, participants were asked about any issues that they had and to rate their satisfaction with the intervention on a three-point scale (yes, no, sometimes). They were asked questions about whether or not the volunteer visited when they expected them to (rated ‘yes’ on all nine forms), about satisfaction with the matching process (rated ‘yes’ on all the forms), about feeling comfortable talking to the volunteer (rated ‘yes’ on all the forms except one, which was rated as ‘sometimes’) and if the volunteer had helped them to do something new or to go out (rated as ‘yes’ on seven forms and ‘no’ on two forms). No major concerns were raised by participants.
Acceptability of the intervention and study processes
Twenty-five participants (12 participants with ID, five volunteers, five carers and three volunteer co-ordinators) were approached and 21 agreed to take part in interviews. Four declined participation or were unavailable to take part (three participants and one family carer). There was a total of 20 interviews (one interview was carried out with two volunteer co-ordinators at the Suffolk service owing to time constraints, as one staff member was leaving her job). There were nine interviews with participants with ID (involving five participants in the control group and four participants in the intervention group); six participants were female and three were male. There were five interviews with volunteers who had been matched (four females and one male). The three volunteer co-ordinators and four carers who were interviewed were all female (three were paid carers and one was a family member). The duration of the interviews ranged from 7.3 to 31.2 (mean 18.1) minutes for participants with ID, from 19.3 to 40.4 (mean 32.6) minutes for volunteers, from 59.1 to 89.5 (mean 74.3) minutes for staff at befriending services and from 11.2 to 44.5 (mean 31.5) minutes for carers.
Results
We discuss the findings in relation to the three broad areas of acceptability of trial processes, acceptability of the befriending intervention (including perceived benefits) and suggestions for improvements to the intervention and study processes.
Acceptability of trial processes (information about the study and randomisation)
There were some concerns that participants had not understood the process of randomisation or what the study entailed:
They understood it in the fact that they would either get a befriender or not but I don’t think there was a huge understanding about the randomisation processes, control and that sort of thing.
Befriending service 1
The customer said she didn’t understand what it was all about because she didn’t understand it was a study. Although the staff understood what they were doing, but the customers didn’t have a lot of information about it. To them they were getting somebody for them to go out and do activities and for them that was the main focus.
Participant 16, carer
Participants had mixed feelings about the randomisation process. Two participants with ID reported feeling worried about which group they would be allocated to and one participant reported being unhappy about being in the control group:
When you found out that you were – when you were phoned and you found out you were in the control group, usual-care group, how did you feel about that?
A bit annoyed.
Other participants stated that they thought that the randomisation process was fair, even if they were disappointed at not being allocated a befriender:
Yeah that’s the only thing you know, that did disappoint me a little bit because, you know, I think we should have the choice to choose which group we are in. But if that’s what the rules are then that’s the rules.
Participant 2
Acceptability of the intervention
Recruitment process
During the trial, volunteers and participants were recruited concurrently. The volunteer co-ordinator at the Outward scheme commented that it would have been helpful if participants with ID had been recruited first before recruiting volunteers, as volunteers lost interest or dropped out while they were waiting for a suitable match:
I suppose one of the – we had a lot of interest at the beginning – one of the problems that we did have was that we recruited quite early and then we lost people because people weren’t ready to be matched.
Befriending service 2
Matching process
The limited pool of volunteers and participants meant that there was limited choice in relation to finding matches based on interests and hobbies. One of the matches was rejected by a carer who did not feel that the volunteer’s interests were aligned to those of the participant. It was felt that carers could act as a barrier or hindrance to the matching process. This left the volunteer feeling dismayed by the process and the person with ID without a suitable alternative match:
But I suppose one of the difficulties really was just having the support and care team on board with befriending – the reasons for it and how it could benefit somebody and how they are not a member of staff . . . But I think she felt a little bit disheartened by the experience, so, which is understandable, but it was just a big learning curve, I think, with that matching.
Befriending service 2
Intervention: training for volunteers
Volunteers found the face-to-face training helpful, but also appreciated being able to complete the online training in their own time:
I think the one . . . online was really helpful because I kind of just got to look at that in my own time. But then I also thought that the training with [name of person] was really, really helpful, just because it was a nice informal setting where she explain to me how the study would work, what befriending would entail and questions that I did have she was able to answer really well, so I thought that was a really, really helpful experience, just because it kind of cleared up any questions and any concerns and any preferences that I may have had in terms of the befriending; it was really, really helpful.
Participant 12, volunteer
Volunteers also commented that the training did not prepare them for some situations in which they had to make rapid decisions and when it involved going against the advice they were given:
There were certain situations where the training said I am not allowed to, let’s say, handle money for the person, but we came into a situation where I had to do it if that makes sense. So maybe those kind of details where you have to have a quick decision-making skills, I think that was a bit tricky.
Participant 13, volunteer
Intervention duration
Some interviewees thought that the duration of the intervention, 6 months, may have deterred some potential volunteers from taking part, as they were unable to commit this amount of time:
Potentially, at the beginning, when we said it was 6 months that may have put some people off, but I mean, obviously, that was the whole point of the study. I think when people come in to volunteering, sometimes they only want to dip their toe in the water and just see whether they like it rather than having to commit to something.
Befriending service 2
Volunteers and participants generally commented that the 6-month time frame was appropriate:
I think the 6-month period, I think it went quite quickly to be honest, it did go quite quickly so I think the 6 months is a good amount what time.
Participant 12, volunteer
Only one participant commented that the duration was too long. One participant with ID and two carers commented that they thought that the duration of the intervention should be longer. One carer commented that they were worried about the visits ending and the impact on the participant as she was fond of the volunteer’s dog and they spent many sessions walking the dog (they are continuing to meet):
I think it should be ongoing rather than 6 months. She looks forward to seeing the dog every week even though it’s not her dog, it’s kind of like she’s a dog keeper, you know going with [person’s name] to take dog for a walk and back not far from here. I think that’s where they normally go to and then she looks forward to that. If that stops in 6 months, I think that will dishearten and you know she’s not going to be – it will be devastating for her.
Participant 10, carer
Intervention: frequency of visits
Volunteers reported that weekly visits were difficult to maintain, with visits often being scheduled every 2 weeks. They felt that it was important to have flexibility over the frequency of visits because of other commitments:
So yeah, I found it better if it wasn’t weekly, if it was every other week. I think because, for me, it had to be after work, so it just made it a bit tricky in terms of meeting up in the evening. I suppose sometimes I was a bit tired from work and that kind of thing. Because we met up on weekends as well – but that wasn’t as much, tended to be on the sort of mid-week in the evening, which was bit better for me.
Participant 9, volunteer
We didn’t meet every week, so we met every second week, this was something that was kind of decided between myself and his mum. She felt that every second week would be best and it worked for me as well, so that was that.
Participant 13, volunteer
One volunteer reported that it was difficult scheduling meetings during the week as the participant was busy with other activities:
Yeah, it was difficult because [name of person] – well I work during the week but I could – sort of met [name of person] early evening and sort of in the morning and stuff. But [name of person] is quite busy Monday to Friday – she goes out to her activities, so we only had the opportunity to meet on a Saturday or Sunday, which was difficult for me to do every week. So we kind of got into a pattern of meeting for a whole afternoon every 2 or 3 weeks and just sort of putting the time together really to go out and drive somewhere, go for lunch, go for a walk.
Participant 18, volunteer
Intervention: duration of sessions
Sessions often went on longer than planned because of the nature and type of activities that the pair had decided to embark on. Activities involving long-distance travelling, such as visits to the museum, took longer. One volunteer reported that he had difficulty managing his time and balancing other commitments, but this improved over time:
So in the first 1 to 2 months I actually found it quite demanding because of the time management and the things that we done together have changed quite a lot throughout the programme. The first few times – not few times, I mean six to seven times – what we usually did was we travel around London, and sometimes I found it quite hard to really manage the time because of queuing up and stuff, so I found it really demanding in terms of balancing between school and travelling round. Luckily in later times, because of the weather and things, my befriendee asked if we could do things indoors more . . . I got more hold of how to manage time better and I actually felt more comfortable after that, yeah.
Participant 11, volunteer
Use of resource booklet
None of the volunteers and participants reported that they used the resource booklet of activities to plan activities. Volunteers used their own knowledge or asked the participant what they wanted to do:
. . . because I live anyway in [name of area] and I know the area where [name of person] really well so we just chatted about what we knew was around and yeah, what [name of person] wanted to do.
Participant 18, volunteer
One volunteer co-ordinator commented that the activities in the booklet were not all appropriate and recommended some changes:
I think it’s useful to have so, but maybe suggestion of activities rather than specific ones so could you find bowling in your local area or could you do this.
Befriending service 1
Intervention: types of activities
One volunteer commented that they were able to engage their befriendee in a range of activities at home and outside:
We have done quite a lot of things actually, we have done origami . . . we have done some drawings before, and then actually more recently we did cooking, yeah we have done actually two or three times, cooking and bakery, that was really good . . . traveling around London a bit . . . and also Bible study, I forgot.
Participant 11, volunteer
One participant with ID commented that he was pleased with the activities:
It was great, it was absolutely great, having a befriender that communicates, that can take me out. We would be going to cinema, we were going to bowling . . . erm . . . museums, we were going to the bookstore. It’s been absolutely great.
Participant 8, befriendee
A couple of volunteers reported having difficulties deciding on and planning activities with their befriendee and feeling uncertain about what they should be doing:
But I think I expected to kind of, to have more of a clear understanding of the kind of activities we were supposed to be doing and I think everyone involved had this idea that someone else would figure out what activities we would be doing with this person to integrate them back into the society kind of . . . But I think there was just no clear effort on anyone’s side to kind of say ‘this is what you could do with the person each weekend or every second weekend’.
Participant 13, volunteer
One volunteer commented that there were not many options in the person’s local area, which was not helped by the weather at the time:
We basically just went into the cafe near his house and we had some food and just a chat. But the weather wasn’t great back then, I think it was November, December, so it was quite grim honestly. There wasn’t a lot to do, if this was now it would be a lot different.
Participant 13, volunteer
Intervention: supervision and support
All the volunteers reported that they had felt supported throughout the study:
Yeah definitely. Every session I was asked if there is anything wrong or anything that I have any concerns about. So yeah, I definitely felt comfortable to, you know, mention any concerns or if I needed any support.
Participant 12, volunteer
However, one volunteer reported that they did not feel supported:
Just before I was about to go to my first session, the first aid kit I got sent in the post, I received too late. I know that [volunteer co-ordinator] didn’t always respond on time and things like that.
Participant 13, volunteer
Volunteers commented that they were satisfied with the supervision sessions and that they felt supported by the volunteer co-ordinators. They felt that the frequency was adequate:
I think it was really nice to have just a monthly meeting catch-up and just talk about how the experience was going. And I think just overall it was nice to have that kind of support and especially it being monthly, I thought it was a good balance.
Participant 12, volunteer
One volunteer commented that she would have preferred to have had the supervision sessions when she needed them, as she did not have much to report:
So I don’t know – like, I didn’t find it that beneficial for me because things hadn’t changed that much month to month. So maybe it would be more – I would probably find it more useful if I could say to them when would be good for me to sort of have a check-in, it didn’t necessarily need to be every month, maybe it could have been every other month or something like that.
Participant 9, volunteer
Ending of the relationship
Four pairs were continuing to meet after the 6-month period and, therefore, no significant issues were identified in relation to the ending. Carers reported some concerns about how participants may react. Two participants with ID did express that they may feel unhappy when the befriending came to an end:
It would be a pity when it does, because I will be . . . I might [not] be alright, you know what I mean.
Participant 3
Other themes
There were a number of other themes that were related to the intervention. These included ‘motivations for taking part’, ‘managing expectations’ and ‘communication is crucial’.
Motivations for taking part
Most of the volunteers cited gaining experience for career progression as their main motivation for becoming a befriender:
I was thinking of doing something related to psychology, which is my university course, and I guess it aligns with my career prospects because I want to work in future in jobs that interact with people.
Participant 11, volunteer
Some volunteers noted that they enjoyed befriending as it allowed them to meet new people or that they wished to do something useful with their free time:
Have done some befriending before doing this befriending and I sort of really enjoyed meeting that individual.
Participant 9, volunteer
I wanted to do something to sort of interact with people a bit more and use a bit more of my free time.
Participant 18, volunteer
Most of the participants with ID mentioned that getting a befriender was their main motivation for taking part in the study as this option was not readily available:
Having the befriender.
Participant 7
One participant stated that they wanted to experience something new:
The reason I wanted to take part is because I think it would be useful for me to find out different things and learn different things.
Participant 8
Managing expectations
Participants, volunteers and carers had misconceptions about befriending. Some participants with ID had unrealistic expectations about their befrienders. One participant mistook the role of the befriender for a romantic partner:
She was expecting a male because I think just the word befriender some kind of, you know, erm, made out to feel like it was going to maybe pair her up with a male figure . . . she wants a boyfriend, she’s interested in having a boyfriend.
Participant 14, carer
When discussing the role of the befriender, some volunteers reported that they were unsure of what was expected of them:
I mean, if we could know more about how we – like as befriender[s] – it may be better in some ways. Because like the programme has fixed meeting times, like as a normal friend we wouldn’t have like fixed meeting times right, so I guess in a sense my expectation of befriending wasn’t really that clear at first.
Participant 11, volunteer
It was also apparent that carers also misunderstood the role of the befriender. Some carers believed that volunteers were like support workers, and they expected them to take responsibility for many things that did not concern them. The lack of understanding of the befriender’s role resulted in a conflict whereby a volunteer dropped out of the study:
They also went to Pizza Express [Uxbridge, UK] together and as a result of them going to Pizza Express together the staff threatened to raise a safeguarding against [befriender] for putting [befriendee]’s health in danger [. . .] there is only so much that a volunteer can stop somebody from doing without policing them; there has to be that understanding.
Befriending services 2
Communication is crucial
This theme encompasses the importance of communication. Participants with ID valued the communication they had with their befrienders, as they were often socially isolated; thus, befriending gave them the opportunity to talk to someone. Almost all participants spoke about having a positive experience in terms of communication with their befrienders:
The good thing is about having a befriender is someone who’s there for you, someone who understands you, someone who will communicate with you, someone who will always be beside you.
Participant 8, befriendee
A carer spoke about the importance of having someone independent of the care staff for the befrienders to talk to:
Because of the nature of the clients that I work with, they don’t have families, so it gives them somebody to talk to, somebody to trust, somebody to vent out. Like sometimes you don’t want to talk to staff and you don’t want to talk to your housemate, so that’s [an] extra person you can talk to, someone independent who’s not connected to the staff.
Participant 16, carer
On the other hand, there were occasions when there had been a lack of communication between the befriending services, carers and volunteers. Carers complained that there was little or no communication between them and the volunteers, and this caused some tension. This manifested as concerns about the health and safety of the participant and also led to conflict.
Several carers mentioned that they did not get the chance to meet the befrienders and they were concerned about the befriendee’s safety:
Because they would meet up outside the service, because [befriendee] is independent, he goes out in the community by himself, but then it’s also a risk because we don’t know who [befriendee] is meeting out there. At least we should have a picture of who [befriendee] is meeting in case, you know.
Participant 14, carer
One carer felt that conflicts could have been avoided if there had been early communication, but recognised that this was a learning experience:
If it, the communication, was open, if it was discussed openly from the beginning maybe things would have worked better . . . I see it as a learning curve, because befriender to us, the service was new, it was new to the customers, it was new to the staff and I think now that we know more about what is expected and what can go wrong, so risks would be looked at in the future.
Participant 16, carer
Benefits of the intervention
All the participants in the study reported that they had gained something positive out of the experience. It was reported that participants with ID were ‘happier’ and that befriending contributed to their well-being:
I feel like every time I see her she seems – like it seems like it boosts her morale a bit when we meet up. And it feels like she has – either it may be the similar sort of stuff that we chat about, she always is very, very chatty. So it seems like she really does benefit from having someone to sort of chat about things with.
Volunteer 9
It is a positive thing for them, it lifted their moods up.
Participant 10, carer
Befriending was perceived to have increased the participants’ confidence and their willingness to seek help:
He has built my confidence, he has made me feel [I want to] improve myself, to come forward, ask him anything that I wanted.
Participant 8, befriendee
I think it kind of just brought out the confidence in him for him to be able to show me around, you know, places he is comfortable with, he knows the route of which train to take, so I think definitely, it benefited him, yeah.
Volunteer 13
She is more active in asking for help, rather than keeping all the difficulties to herself.
Participant 11, volunteer
The befriending intervention was beneficial not only to participants, but also to volunteers and carers.
One volunteer reported an increase in their own confidence as a result of the befriending experience, and also felt that she had benefited from attending a social group where she met other people with IDs:
I definitely felt like my confidence probably grew a bit more from meeting [name of befriendee]. And because I actually went to one – she has a social meet-up every month as part of the [name of charity] charity where it is different people in the area with learning disability sort of come together and they just meet up and play music and that kind of thing . . . I think that was quite a good one to push myself into sort of doing something slightly out of my comfort zone.
Participant 9, volunteer
Two volunteers expressed their appreciation of the reciprocal emotional support that they had received from the befriendee during challenges they had encountered in their own lives:
I had encountered a person and he had upset my faith and then I just briefly told her what happened and she just told me that that guy doesn’t really understand me and I should be encouraged that I, because I have friends and church and stuff that shouldn’t be really that upset. I think yeah, emotional support was definitely a very unexpected thing to happen for us.
Participant 11, volunteer
Because my mum had been very ill during the period of time and actually [name of befriendee] was a lovely support for me as well during that period.
Participant 18, volunteer
Another volunteer reported that the experience had provided them with a different perspective of how to view life experiences:
I think I saw the world through [name of person]’s eyes, which obviously is, I think I would like to see how people experience things, how they see them. It just made me grateful as well about things that we take for granted. Especially because it is volunteering, if you are not paid for something, I think you find more meaning in what you do.
Participant 13, volunteer
One carer commented that the presence of a befriender was beneficial to her and other staff as it enabled them to focus on other tasks or provide support to other residents:
I think for the befriender to come over, it has really helped us a lot . . . it gives me the opportunity to carry on with the paperwork, gives me the opportunity to, you know, spend time with people that live here . . . so of course, yeah, I benefit from it.
Participant 10, carer
Suggestions for improvements to the study or intervention
Changes to recruitment
Volunteer co-ordinators from the Suffolk scheme suggested that events for volunteers organised by the study team could have attracted more interest in the study:
More of physical presence from the study team going out to see volunteers to try and organise events or something like that.
Befriending service 1
They also expressed some confusion about the timing of recruitment and suggested arranging events prior to recruitment to raise awareness:
We weren’t quite sure when the recruitment had started when it hadn’t so it was a bit back and forth. I think maybe the study could’ve done a few open days or a few contact days beforehand, maybe sort of raising interest before the study began so we had a bit of a buffer, sort of, that we could take some people forward at the very beginning and that way we had looked at more to work with.
Befriending service 1
Changes to study information and processes
Participants with ID reported wanting more time to decide whether or not to take part in the study and wanted shorter questionnaires. One participant also thought that the information about the study was difficult to understand and should be presented in an easier, more accessible format:
Easier read document . . . explain a bit more.
Participant 7
One volunteer commented that it would have been helpful if they had known not to discuss who they had been matched with, during meetings with the research assistant, as doing so would lead to unblinding:
. . . just kind of like knowing up front not to sort of mention that I had and who it was.
Participant 9, volunteer
Changes to the intervention
Volunteers commented on the need to make training more practical as they felt unprepared to deal with certain aspects of their role.
One volunteer mentioned that the training should cover what participants with ID struggle with on a daily basis to prepare the befriender:
I guess my point here would be like, it is like the gap between how you deal with daily things and how they deal with daily things, [. . .] I guess like, in terms of decision-making, it would be better if we could know more about the difficulties, they face like decision-making.
Participant 11, volunteer
Another volunteer commented that they would have valued the opportunity to have kept in touch with their befriendee on social media and that this should be encouraged, although they acknowledged the need for guidance:
I think I wasn’t encouraged to keep in contact with my befriendee on social media actually. So I think in the sense, in terms of intervention, I was thinking – like as a normal friend, like sometimes people exchange contacts and keep in touch on social media, and I think I am not sure whether the intervention really captures that aspect of it. And I do think that actually social media could really help these people a lot . . . if they are capable of managing it.
Participant 11, volunteer
Summary of the main themes and findings
Overall, the interviewees reported being satisfied with the trial processes, although some participants with ID reported not understanding relevant information about the study, including randomisation. Participants, volunteers and carers reported positive experiences of the intervention and of feeling supported, and there were benefits to all three groups. However, the intervention was perceived to be too rigid and prescriptive in terms of frequency of visits (i.e. once per week was too frequent) and the nature of contacts (other types of contacts should be encouraged, e.g. via social media), and the recruitment process for volunteers could be improved through the hosting of events.
A case study (Jane’s story) illustrates how one participant and their volunteer experienced the befriending intervention and describes some of the challenges they encountered (see Appendix 4).
Chapter 5 Discussion
This study was conducted as part of a commissioned call by the National Institute for Health Research Public Health Research funding stream to evaluate interventions in community organisations to improve health and well-being and reduce health inequalities. We were funded to undertake a pilot study owing to the uncertainties of conducting a randomised trial in people with ID. This chapter will review each of the study objectives against the progression criteria. We will discuss the barriers that we encountered and make suggestions about how these barriers could be overcome. We will also discuss the strengths and limitations of our study, and implications for future research.
Progression criteria
We listed a number of criteria that would be considered in evaluating whether or not the trial had been successful:
-
At least 70% (35) of participants are recruited from the 50 potentially eligible individuals who are approached.
-
At least 70% of participants with ID in the intervention group are successfully matched to a volunteer (befriender) and they meet for a minimum of 10 meetings.
-
The dropout rate of participants with ID in both groups, post randomisation, is < 30% at 6 months’ follow-up.
-
The intervention and trial procedures are considered to be acceptable by volunteers and individuals with ID.
-
If the target recruitment rate and number of matched pairs is between 50% and 69%, or the dropout rate is between 31% and 50%, we would consider if these could be rectified by modifying the protocol. If this was the case, a full study could still be considered. If the recruitment rates were < 50% and the dropout rates were > 50%, then a full trial would not be considered feasible.
Recruitment
Participants with intellectual disability
Recruitment of participants with ID and volunteers was the most important feasibility objective and the most challenging. Our recruitment period was 6 months. We recruited 16 participants with ID (our target was at least 40 participants, based on 50 participants being approached). We therefore recruited 40% of our target in relation to people with ID. In our progression criteria, we stated that a recruitment target below 50% would indicate that our trial was not feasible.
Challenges in recruiting to RCTs have been demonstrated across a range of different populations and settings. Only 56% of studies funded by the Health Technology Assessment programme have achieved their target sample size, which demonstrates the importance of conducting feasibility studies first. 67 Recruitment of participants with ID to clinical trials is considered to be particularly challenging, with a number of RCTs failing to recruit. 68,69 Reasons for this include communication difficulties, the need to access participants through gatekeepers, issues related to consent and capacity, and limited knowledge of the value of RCTs among carers. 70–72 However, there is also evidence for the increasing acceptability of RCTs. 73
One of the reasons for the lower than expected success in recruitment to our study was that we significantly overestimated recruitment of participants via the befriending schemes. Initial consultation with the schemes (particularly the Suffolk scheme) appeared to indicate that there were a large number of people who were waiting to be matched (figures suggested that there were 100 people waiting to be matched). However, the Suffolk scheme thought that it was unethical to randomise participants as it would undermine their relationship with their service users, and offered individuals the option of entering the study or befriending through their usual route. As a consequence, most people decided not to enrol in the study. This severely affected the recruitment of participants to the study.
Conducting research outside the NHS had several challenges. During the study, the Suffolk befriending scheme experienced funding cuts, which led to the two volunteer co-ordinators involved in the study being employed on a part-time basis when they were formerly full time. They had responsibility for managing existing befriending relationships that were not part of the study as well as assisting the research team with recruitment. These changes undoubtedly had an impact on the effectiveness of recruitment to the study, as intervention costs (e.g. staff costs) were not covered by the grant funding. We also did not have access to support from clinical studies officers from the Clinical Research Network to assist with recruitment from the befriending schemes, as they were not NHS services.
A review of barriers and facilitators in the evaluation of evidence-based interventions in third-sector organisations found that lack of financial resources and knowledge of appropriate research methodology and outcome indicators were the main barriers preventing service evaluation. Facilitators included getting appropriate support, an organisational culture that supported research and the motivation to be accountable to stakeholders. 74 In our study, we worked collaboratively with the befriending services to provide the expertise in research methods, and the services were motivated to engage in research and to demonstrate an evidence base for their service. However, we were not able to provide financial support. In a recent national survey of befriending services for people with ID in the UK, carried out by the research team, staff reported that funding and the recruitment of volunteers were the major challenges encountered by their services. 75
Priebe et al. 37 were able to recruit participants with psychosis into their study, possibly because they received research funding to deliver the intervention, which gave them more control over the recruitment of volunteers and the intervention itself. However, there are clearly financial and implementation implications of using this approach as, should the befriending intervention be effective, it would not be sustainable without continued funding.
Another issue that may have affected recruitment was the eligibility criteria. This was fed back to us at a PPI meeting with individuals with ID. They felt that the study should have been open to all people with ID and commented that some people who are depressed may not want to admit that they are depressed, or may find it more difficult to take part in this type of study because of their depression. When participants were approached by clinicians to take part in the study from ID services in NELFT, we received feedback that many were reluctant to take part because they were afraid of meeting someone new, or that they had anxieties about going out. It appears that those people who most needed the intervention (e.g. those who were socially isolated and had few opportunities to access the community) were often the people who were less willing to take part. Of the 24 referrals, only 16 met the eligibility criteria (66.7%), and it is likely that more referrals could have been received if the eligibility criteria were less rigid, for example in relation to meeting a threshold score on the GDS-LD. In addition, depression and depressive symptoms may be under-recognised in people with ID, as many people may have low-grade, chronic symptoms. Although we set an inclusion criterion of a GDS-LD score of 5, which is below the threshold for a diagnosis of depression (score of 12), the mean score at baseline in both groups was well above the cut-off value for depression (18.6 in the intervention group and 21.4 in the control group), suggesting that the majority of participants were experiencing episodes of moderate depression and were more impaired than expected. If individuals with significant depressive symptoms were being approached to take part in the study, it is not surprising that there was a reluctance to take part, and that the number of individuals being approached was smaller than anticipated. This indicates that there was possible confusion about the eligibility criteria, which may have contributed to the low recruitment rate.
The 6-month study recruitment period was possibly overambitious. A volunteer co-ordinator who was part of the PPI group and runs ‘the Gig Buddy Scheme’ in Oxford thought that a 12-month recruitment period would have been more realistic based on their own experiences.
Suggestions for improving recruitment
The PPI group made suggestions that recruitment via peers may have helped by reducing anxieties that people with ID may have about talking to professionals. They also made suggestions to broaden the eligibility criteria and to remove the need for individuals to have depressive symptoms. Another approach to improving recruitment that we considered but were not able to implement was an extension to the recruitment period, which was not granted, including approaching additional befriending services to take part, increasing the number of NHS sites from which referrals were received (including Patient Identification Sites) and involving the Clinical Research Network in recruiting participants from NHS sites. Another source of recruitment that we considered was voluntary services, such as advocacy organisations.
Recruitment of volunteers
Over the 6-month period, we recruited 10 volunteers (our target was to match all participants randomised to the intervention group with a volunteer, and we were therefore aiming to recruit at least 20 volunteers).
The participating befriending schemes were responsible for recruiting volunteers; they recruited through their websites and other volunteering sites, local newspapers, and colleges and universities. We were aware that recruitment of volunteers was potentially going to be challenging, particularly in the Suffolk area, which is a more rural location and has fewer transportation links than London. Therefore, access to transportation (e.g. a car) may have had an impact on the willingness of volunteers to take up this role.
Attempts were made to bolster recruitment through the research team advertising the study and benefits of volunteering to undergraduate psychology students at University College London. There was a lot of initial interest from students, but many were deterred by the duration of the intervention and the location of the befriendees who lived on the outskirts of London, with students preferring to work with people living in central London. We had limited control over the recruitment of volunteers as this process was managed by the befriending services. However, feedback from the befriending services in the qualitative interviews suggests that more support could have been provided by the research team in advertising the study at volunteer recruitment event days.
Suggestions for improving recruitment of volunteers
Understanding the motivation of volunteers may enable targeted recruitment based on clear messages and incentives. The volunteers who participated in the study cited career progression, enjoyment and good use of spare time as motivations for taking part. Students in health-related professions may volunteer because it gives them work experience that may help them to progress in their career. 26 The recruitment of students from colleges and institutions nearer to the location of befriendees could help to overcome recruitment issues. The PPI group also suggested that volunteers may be apprehensive about working with people with IDs if they have not had prior contact. Inviting volunteers to a social activity group with people with ID beforehand may help to alleviate their anxieties and provide an opportunity to meet new people.
Retention of participants and volunteers
The retention of participants with ID who had been randomised was excellent. No participant dropped out of the study, and they all agreed to complete the outcome assessments at baseline and follow-up, apart from one participant who completed only a few measures at follow-up.
Retention of volunteers was fairly good. Of the 10 volunteers who participated in the study, only two dropped out (retention of 80%). The remaining eight volunteers completed the baseline and follow-up assessments. We therefore met our minimum criterion of < 30% dropout rate from the study.
Matching of participants and volunteers
We matched six out of eight participants in the intervention group with a volunteer (75%), which met our minimum criterion of 70%. One participant could not be matched because of geographical distance and another because of a deterioration in their mental health. One participant had to be rematched with another volunteer after the first volunteer dropped out of the study. No volunteers were matched with more than one participant. Four pairs continued their relationship beyond the 6-month period.
Adverse effects and unintended consequences
Befriending was not associated with any serious adverse events for people with ID. However, we were unable to complete the 12-month assessment and, therefore, it was not possible to monitor the impact of relationships ending on the well-being of individuals beyond the 6-month period. Four out of the six matched pairs had decided to continue their relationship beyond 6 months and the other two pairs met on only a few occasions. There was a positive outcome for one participant, who was supported to report an incident of mistreatment by a paid carer at their supported living placement. The participant may not have reported this incident without the support they received from the volunteer.
However, there were unintended consequences for volunteers. One volunteer experienced conflict with members of staff at their befriendee’s supported living placement, which arose because of a misunderstanding about the volunteer’s role. This consequently led to the volunteer becoming distressed and deciding to drop out of the study. Another volunteer was unable to continue with their relationship with the befriendee because the befriendee’s mother was not satisfied with the match. The volunteer was disappointed with this situation, particularly as the befriendee was not involved in making the decision. In both situations, the volunteer co-ordinator attempted to resolve the dispute and provided emotional support to the volunteers. Similar conflicts with staff and carers were reported in our survey of befriending services and volunteers in the UK,75 suggesting that this is not an uncommon issue encountered by volunteers. More support should be provided to volunteers to negotiate such challenging situations to prevent relationships breaking down unnecessarily, and service users with ID should be empowered to make decisions about whether or not they wish to continue with relationships, rather than these decisions being made by carers.
Adherence to the intervention
There was good adherence to the training by volunteers, and most volunteers engaged with the supervision process. The pairs were expected to meet for a minimum of 60 minutes per meeting, but this was exceeded (with an average meeting duration of 118 minutes). We set a minimum target of 10 meetings between the befriender and the participant. The average number of meetings was almost 12 (11.8) and, based on this, the minimum target was met. However, only four of the six pairs (66.7%) actually met ≥ 10 times. In Priebe et al. ’s37 RCT of befriending in people with psychosis, only half the participants met their predefined threshold of at least 13 meetings over 1 year, suggesting that implementation may be an issue in befriending trials. In our survey of befriending services for people with ID, we found that there was a large variation in the frequency of meetings, with the majority of pairs meeting for a period ranging from every 2 weeks to every other month. 75 In our study, we also stipulated that the majority of the sessions should be in the community, which did occur, but the range of activities was limited and mainly consisted of visiting cafes and restaurants, and going for walks. Trips to museums/galleries and to the cinema occurred on only a few occasions and there were no activities involving recreational activities, such as swimming or going to the gym. These findings are consistent with our survey of befriending services, which found that the most frequently reported activities involved going to cafes and restaurants, followed by visits to parks and outdoor spaces. 75 One possible explanation is that individuals with ID did not always have sufficient funds to cover activities (this was raised by several volunteers), which might have prevented pairs from engaging in more novel activities, or it may be related to difficulties in motivating individuals who have depressive symptoms. Spending time indoors and having ‘a conversation’ was also frequently reported, highlighting the role of volunteers in providing emotional support. No particular types of activities were regarded as being more pleasurable, indicating that spending time together may be more important than the nature of the activity.
Acceptability of study procedures
Volunteers were satisfied with the trial processes and procedures and thought that the questionnaires were relevant and of the right length. Some participants with ID expressed their frustration at being allocated to the control group. They thought that some of the information was difficult to understand and that the questionnaires were too long.
Acceptability of the intervention
Based on the qualitative interviews, overall, the participants and volunteers valued the opportunity to have a befriender and to take part in the study. This, alongside the very high retention rates of participants in the study and the fact that four out of the six matched pairs had plans to continue their relationship beyond 6 months, suggests that the intervention may have been acceptable, at least to those who took part in the study. We did not conduct interviews with individuals who did not want to take part in the study, and their views about the intervention may have been different. The low recruitment rate may also indicate that the intervention was not widely acceptable to people with ID who had symptoms of depression because they were anxious about meeting someone they were not familiar with or were not motivated to engage in new activities.
There were some issues with the intervention. Volunteers commented on the need for more flexibility in relation to the frequency of visits, with a preference for visits every 2 weeks rather than weekly because of other commitments. Flexibility in supervision arrangements and the nature of contacts (e.g. permitting contact via social media) was also suggested. A recent qualitative study of the experiences of befriendees and befrienders who had participated in a RCT of befriending76 highlighted the importance of having a flexible approach in relation to the role of the befriender and the nature of the intervention, and that befriending was an authentic relationship that developed over a period of time. 77 Burn et al. 77 also discovered that befriending was a considerable commitment for volunteers and necessitated balancing a number of competing commitments, which was also reported in our study. The mutual benefits of befriending was a positive finding in our trial, which indicated that we should not assume that only participants with ID will benefit from the intervention.
Another highlighted issue, which may affect the acceptability of the intervention, was the expectations of carers, who had a strong influence on aspects of the intervention, such as whether or not a match should continue (this led to one participant being left unmatched after one session) and conflict with another volunteer over their selection of activities. As discussed above, this led to two volunteers dropping out. Carers misunderstood the role of volunteers and thought that they should assume the same responsibilities as a support worker. Guidelines on how to work with carers, and clear discussions with carers about the roles and responsibilities of volunteers need to be considered. Financial issues were raised by a number of volunteers, particularly during supervision. On occasions, volunteers had to pay for the participants’ expenses during visits, as carers did not realise that these expenses were not covered. Good communication between carers, volunteers and the befriending service was considered to be essential.
Measurement of outcomes
The lower than expected recruitment rate resulted in a small sample size and unbalanced groups, despite randomisation. However, our exploratory analysis of outcome revealed a mean four-point reduction in the GDS-LD score in the intervention group, after adjusting for the baseline score, which equates to a standardised effect size of 0.5 SDs. The 95% CIs around this difference in GDS-LD score (95% CI –11.2 to 3.2 SDs) suggest that, although this is a non-significant result, an important clinical difference could be found in a main trial. However, there were baseline differences in the characteristics between the two groups and, given the small sample size and that only six participants in the intervention group actually received the intervention (a further two received one or two sessions), it may well be a chance finding. Nevertheless, the findings are similar to that of a feasibility study of mentoring in 29 people with ID and a matched comparison group. They found a reduction in GDS-LD (proxy) scores in the intervention group, with an effect size of 0.51, and this approached significance (p = 0.10). 41 This suggests that befriending may reduce depressive symptoms, but that our results should be treated with considerable caution because of the small sample size.
Previous studies of befriending in other populations have found small effect sizes in reducing depressive symptoms. 21 However, one trial of a ‘visiting service’ for elderly widows found that participants who had high levels of social isolation, two or more physical illnesses or low levels of education (no education or primary school only) responded better to the intervention, with statistically significant effect sizes of between 0.54 and 0.63 for a reduction in depressive symptoms. 76 This group shares characteristics with people with ID, suggesting that the benefits of befriending may be greater for more disadvantaged groups.
Health economic evaluation
Data collection methods for a future economic evaluation were developed, and their feasibility was tested during this study. There was a good return of the resource use questionnaire from carers. Data on intervention costs were obtained from befriending services. Participants completed the EQ-5D-Y descriptive system and the EQ VAS, but there were important discrepancies between the scores, which could make calculation of QALYs for a cost–utility analysis less reliable. The differences may have been due to a number of reasons, such as poor understanding of instructions on how to complete the EQ VAS or because the EQ-5D-Y is not an appropriate measure for adults with ID (it has not been validated for use in this group) and may not capture relevant aspects of health that are perceived to be important. In the absence of a validated measure of health-related quality of life in this population, perhaps the EQ-5D-Y should not be used in isolation to assess health-related quality-of-life outcomes in trials involving adults with ID, and should be used in conjunction with a proxy measure.
The results of our study show that the intervention has a probability of 35% of being cost-effective. These results are conservative and should be interpreted with caution because of the small sample size and other issues that affected the study.
Strengths of the study
-
To the best of our knowledge, this is the first pilot study to investigate the feasibility and acceptability of conducting a RCT of one-to-one befriending by volunteers for people with ID and symptoms of depression. Other studies used a non-randomised design or did not have a control group. 40,41
-
The befriending intervention was delivered by community befriending schemes. This reflected actual practice, as the majority of befriending services are not funded by the NHS and may receive only partial or no funding from local authorities.
-
Although some attempt was made to standardise the intervention through the recommendation of weekly visits (each lasting at least 60 minutes, over a period of 6 months), there was room for flexibility in terms of how the matched pair spent their time and, therefore, the trial was pragmatic in its approach.
-
The mixed-methods process evaluation provided useful insights into the perspectives of the participants and data on adherence, which could potentially inform changes to the intervention in a future study.
-
The trial included an economic evaluation to assess the feasibility of data collection methods and some preliminary data on resource use.
Limitations of the study
-
The study recruited only 40% of the target sample of people with ID, which suggests that recruitment is not feasible without changes to our approach.
-
Some of the recruitment issues identified could be rectified through better planning in a full trial; for example, there were clearly issues relating to poor communication between the study team and the befriending services. We could have been more proactive in our engagement with the befriending services and made more sustained efforts to ensure that they understood and were in full agreement with the study design and randomisation process, rather than assuming that they were on board. They provided feedback indicating that they would have appreciated support with the recruitment of volunteers through events hosted by the study team, and this is another aspect that could be improved.
-
We were unable to implement significant changes to the recruitment strategies owing to delays in the study being set up and our request for an extension to the study not being approved.
-
We were unable to complete a 12-month follow-up because of delays in the set-up of the study. We therefore do not have data on adverse effects and unintended consequences beyond the 6-month period, including the impact of relationships ending on depressive symptoms and the well-being of participants. This information was not available at the 6-month follow-up as several of the pairs were planning to continue their relationship beyond 6 months.
-
Proxy outcome measures (e.g. for depressive symptoms) were not used, and they may have been helpful, alongside the self-report measures, in establishing whether or not the intervention had positive outcomes. Some of the measures used in the study had a limited number of data on psychometric properties.
-
We did not collect demographic data on car ownership and whether volunteers were working full time or part time, which might be helpful in understanding the characteristics of volunteers who are likely to take part in such a study.
-
We could not mobilise PPI in the study as well as we intended.
Amendments to the logic model
Based on our experiences of conducting this study, we have proposed a few changes to the logic model (see Appendix 5). These include the need for additional inputs and resources, such as clear eligibility criteria and a comprehensive recruitment strategy in relation to people with ID, and the need for individuals with ID to have access to sufficient funds to be able to access activities in the community. Additional enablers include ensuring that carers are aware of the roles and responsibilities of volunteers, and the need for good communication between the befriending services, carers and volunteers to reduce the likelihood of potential conflict.
Implications and recommendations for future research
Although our results suggest that a fully powered RCT would not be feasible, it is possible to rectify these issues through alternative recruitment strategies, including recruiting participants through multiple NHS trusts and recruiting volunteers from multiple befriending services, or the provision of adequate resources to fund the intervention outside community befriending services. A future study should explore these alternative recruitment strategies.
There are challenges in conducting research with voluntary organisations as they often lack the necessary resources to recruit participants and implement the intervention, and researchers may have limited influence over these aspects of the research. Circumstances may also change during the course of the research project, owing to financial insecurity associated with external funding sources. The importance and value of collaborating with voluntary organisations in research should be encouraged.
Conducting research involving participants with depressive symptoms (many of whom had a clinical diagnosis of depression) proved to be challenging owing to difficulties in motivating depressed individuals to engage in novel activities. It is not clear whether the low recruitment rate was because the intervention was not acceptable to individuals with depressive symptoms or because the recruitment strategy was limited. This requires further exploration. For example, individuals with ID and depressive symptoms could be surveyed about whether or not they would be willing to engage in a befriending intervention. A future study on befriending in people with ID could have broader eligibility criteria and not be restricted to participants with depressive symptoms or other symptoms of mental ill health, and have a focus on evaluating whether or not it leads to improvements in well-being and social outcomes in the short and long term.
One of the issues elucidated by this study was the need for improved communication between all parties involved in the befriending relationship. Poor communication and misunderstandings between carers and volunteers led to relationships breaking down. It is paramount that all befriending services develop guidelines on how to work more effectively with carers.
Future research studies could also explore the use of peer support, which is defined as the mutual receiving and giving of emotional, social or practical support between individuals with shared lived experience. 78 It has been shown to have positive outcomes in studies of people with mental illness. 79 Although the use of a peer support model or a ‘buddy scheme’ in relation to people with ID has been used in a number of settings, research has been limited to only a few studies. One pilot study suggests that peer support may be useful in facilitating supported employment in young people with ID80 and another suggests that having a ‘buddy’ may help young people transition to a new school or college. 81 Peer support could be used more broadly to deliver changes in social outcomes and may be more acceptable to some individuals with ID, as they may find it easier to relate to peers than lay volunteers.
Future studies should give careful consideration to the design of the study, such as the use of non-randomised study designs in evaluating befriending. 37 For example, a prospective longitudinal study that involves the collection of data from a large number of services, and takes into account key confounders, could provide data on longer-term benefits.
A further recommendation is the need for effective involvement of patients and the public in the study design and in the recruitment of participants to identify and overcome key barriers to recruitment. Recruitment approaches could involve people with ID publicising the study (through the use of film clips and social media) and directly recruiting participants by explaining the study to their peers and describing personal experiences of befriending and how it has benefited them.
Conclusion
This pilot RCT of one-to-one befriending in people with ID and depressive symptoms failed to recruit a sufficient number of participants. Therefore, a future, larger-scale RCT is unlikely to be feasible unless there are substantial changes to the recruitment of participants with ID involving multicentre recruitment from NHS and social care services.
Acknowledgements
This study would not have been possible without the support, advice and substantial contributions of the two befriending services (The Befriending Scheme and Outward) that agreed to provide the befriending intervention. We would also like to thank the volunteers and participants with ID who participated in the study, and the clinicians at the North East London NHS Foundation Trust (NELFT) who assisted with recruitment. We are grateful for the support from staff at the Priment Clinical Trials Unit who provided advice on the study protocol, developed the study database and randomisation procedure, and monitored the study, and to Ms Yazz Davies from the Oxford Gig Buddies scheme and her volunteers who provided PPI input. We would also like to thank Professor Mike Crawford (chairperson of the Trial Steering Committee) and the other members of the Trial Steering Committee for their helpful advice throughout the study.
Contributions of authors
Afia Ali (https://orcid.org/0000-0002-0104-9370) (Associate Professor in Intellectual Disability Psychiatry) was the chief investigator and led the drafting of the final report. She is accountable for the integrity and accuracy of the report.
Emma Mckenzie (https://orcid.org/0000-0002-5213-2561) (Study Research Assistant) was involved in collecting the data and analysing the qualitative data. She contributed to the writing of the final report, particularly Chapter 4.
Zara Rasoul (https://orcid.org/0000-0001-9453-7906) (Honorary Research Assistant) was involved in analysing the qualitative data. She contributed to the writing of the final report, particularly Chapter 4.
Angela Hassiotis (https://orcid.org/0000-0002-9800-3909) (Professor of Intellectual Disability Psychiatry) made substantial contributions to the conceptualisation and design of the study, and contributed to the writing of the final report.
Stefan Priebe (https://orcid.org/0000-0001-9864-3394) (Professor of Social and Community Psychiatry) made substantial contributions to the conceptualisation and design of the study, and contributed to the writing of the final report.
Brynmor Lloyd-Evans (https://orcid.org/0000-0001-9866-788X) (Associate Professor in Mental Health and Social Care) made substantial contributions to the conceptualisation and design of the study, and contributed to the writing of the final report.
Rebecca Jones (https://orcid.org/0000-0001-6924-0924) (Clinical Research Fellow) analysed the results and contributed to the writing of the final report, particularly Chapters 3 and 5.
Monica Panca (https://orcid.org/0000-0002-4031-6478) (Research Associate) analysed the health economics data and contributed to the writing of the final report, particularly Chapter 3.
Rumana Omar (https://orcid.org/0000-0003-1483-1932) (Professor of Medical Statistics) was the lead statistician and supervised the statistical analysis of the results (Chapter 3).
Sally Finning (https://orcid.org/0000-0001-9934-7669) (Manager, Outward befriending service) made substantial contributions to the conceptualisation and design of the study and had oversight of the implementation of the intervention at the study site.
Shirley Moore (https://orcid.org/0000-0002-9658-7808) (Chief Executive of The Befriending Scheme) made substantial contributions to the conceptualisation and design of the study, and had oversight of the implementation of the intervention at the study site.
Christine Roe (https://orcid.org/0000-0002-6719-3279) (Volunteer Co-ordinator, The Befriending Scheme) facilitated the implementation of the intervention at the study site.
Michael King (https://orcid.org/0000-0003-4715-7171) (Professor of Primary Care Psychiatry and Trial Methodologist for Priment Clinical Trials Unit) made substantial contributions to the conceptualisation and design of the study, and contributed to the writing of the final report, particularly Chapter 5.
Publications
Ali A, Mckenzie E, Hassiotis A, Priebe S, Lloyd-Evans B, Omar R, et al. One-to-one befriending for people with intellectual disability and symptoms of depression: protocol for a pilot randomised controlled trial. BMJ Open 2020;10:e033989.
Tse CY, Mckenzie E, Hassiotis A, Ali, A. A survey of befriending services for people with intellectual disabilities in the United Kingdom [published online ahead of print 8 July 2021]. J Policy Pract Intellect Dis 2021.
Ali A, McKenzie E, Hassiotis A, Priebe S, Lloyd-Evans B, Jones R, et al. A pilot randomised controlled trial of befriending by volunteers in people with intellectual disability and depressive symptoms [published online ahead of print 27 September 2021]. J Intellect Dis Res 2021.
Data-sharing statement
The data are available upon request. Please contact the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Public Health England . Learning Disabilities Observatory. People With Learning Disabilities in England 2015: Main Report 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/613182/PWLDIE_2015_main_report_NB090517.pdf (accessed 20 February 2021).
- Emerson E, Baines S. Health Inequalities and People with Learning Disabilities in the UK: 2010. Improving Health and Lives Learning Disability Observatory; 2010.
- van Splunder J, Stilma JS, Bernsen RM, Evenhuis HM. Prevalence of visual impairment in adults with intellectual disabilities in the Netherlands: cross-sectional study. Eye 2006;20:1004-10. https://doi.org/10.1038/sj.eye.6702059.
- Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 2014;383:889-95. https://doi.org/10.1016/S0140-6736(13)62026-7.
- Cooper SA, Smiley E, Morrison J, Williamson A, Allan L. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry 2007;190:27-35. https://doi.org/10.1192/bjp.bp.106.022483.
- Buckles J, Luckasson R, Keefe E. A systematic review of the prevalence of psychiatric disorders in adults with intellectual disability, 2003–2010. J Ment Health Res Intellect Disabil 2013;6:181-207. https://doi.org/10.1080/19315864.2011.651682.
- Cooper S-A, Smiley E, Morrison J, Williamson A, Allan L. An epidemiological investigation of affective disorders with a population-based cohort of 1023 adults with intellectual disabilities. Psychol Med 2007;37:873-82. https://doi.org/10.1017/S0033291707009968.
- Richards M, Maughan B, Hardy R, Hall I, Strydom A, Wadsworth M. Long-term affective disorder in people with mild learning disability. Br J Psychiatry 2001;179:523-7. https://doi.org/10.1192/bjp.179.6.523.
- Emerson E. Commentary: childhood exposure to environmental adversity and the wellbeing of people with intellectual disability. J Intellect Disabil Res 2013;57:589-600. https://doi.org/10.1111/j.1365-2788.2012.01577.x.
- Ali A, Hassiotis A, Strydom A, King M. Self stigma in people with intellectual disabilities and courtesy stigma in family carers: a systematic review. Res Dev Disabil 2012;33:2122-40. https://doi.org/10.1016/j.ridd.2012.06.013.
- Verdonschot MM, de Witte LP, Reichrath E, Buntinx WH, Curfs LM. Impact of environmental factors on community participation of persons with an intellectual disability: a systematic review. J Intellect Disabil Res 2009;53:54-6. https://doi.org/10.1111/j.1365-2788.2008.01128.x.
- Hill RA, Dunbar RI. Social network size in humans. Hum Nat 2003;14:53-72. https://doi.org/10.1007/s12110-003-1016-y.
- Petroutsou A, Ali A, Hassiotis A. Loneliness in people with intellectual and developmental disorders (IDD) across the life span: a systematic review of prevalence and interventions. J Appl Res Intellect Disabil 2018;31:643-58. https://doi.org/10.1111/jar.12432.
- Ali A, King M, Strydom A, Hassiotis A. Self-reported stigma and symptoms of anxiety and depression in people with intellectual disabilities: findings from a cross sectional study in England. J Affect Disord 2015;187:224-31. https://doi.org/10.1016/j.jad.2015.07.046.
- Emerson E. Self reported exposure to disablism is associated with poor self reported health and wellbeing among adults with intellectual disabilities in England: a cross sectional survey. Public Health 2010;124:682-9. https://doi.org/10.1016/j.puhe.2010.08.020.
- Ailey SH, Miller AM, Heller T, Smith EV. Evaluating an interpersonal model of depression among adults with Down syndrome. Res Theory Nurs Pract 2006;20:229-46. https://doi.org/10.1891/rtnp.20.3.229.
- Merrick J, Merrick E, Lunsky Y, Kandel I. A review of suicidality in persons with intellectual disability. Isr J Psychiatry Relat Sci 2006;43:258-64.
- Biswas AB, Bhaumik S, Branford D. Treatment-emergent behavioural side effects with selective serotonin re-uptake inhibitors in adults with learning disabilities. Hum Psychopharmacol 2001;16:133-7. https://doi.org/10.1002/hup.233.
- Leyin A. Improving access to psychological therapies for people with learning disabilities. Tizard Learn Disabil Rev 2011;16:29-37. https://doi.org/10.1108/13595471111185747.
- Mead N, Lester H, Chew-Graham C, Gask L, Bower P. Effects of befriending on depressive symptoms and distress: systematic review and meta-analysis. Br J Psychiatry 2010;196:96-101. https://doi.org/10.1192/bjp.bp.109.064089.
- Dean J, Goodlad R. Supporting Community Participation: The Role and Impact of Befriending. Brighton: Pavilion Publishing and Joseph Rowntree Foundation; 1998.
- Thompson R, Valenti E, Siette J, Priebe S. To befriend or to be a friend: a systematic review of the meaning and practice of ‘befriending’ in mental health care. J Ment Health 2016;25:71-7. https://doi.org/10.3109/09638237.2015.1021901.
- Klug G, Toner S, Fabisch K, Priebe S. Characteristics and motivations of volunteers providing one-to-one support for people with mental illness: a survey in Austria. Soc Psychiatry Psychiatr Epidemiol 2018;53:841-7. https://doi.org/10.1007/s00127-018-1514-1.
- Toner S, Hickling LM, Pinto da Costa M, Cassidy M, Priebe S. Characteristics, motivations and experiences of volunteer befrienders for people with mental illness: a systematic review and narrative synthesis. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1960-z.
- Cassidy M, Thompson R, El-Nagib R, Hickling LM, Priebe S. Motivations and experiences of volunteers and patients in mental health befriending: a thematic analysis. BMC Psychiatry 2019;19. https://doi.org/10.1186/s12888-019-2102-y.
- Barlow J. Supporting women with perinatal mental health problems: the role of the voluntary sector. Community Pract 2013;86:23-7.
- Mitchell G, Pistrang N. Befriending for mental health problems: processes of helping. Psychol Psychother Theory Res Pr 2011;84:151-69. https://doi.org/10.1348/147608310X508566.
- Hallett C, Klug G, Lauber C, Priebe S. Volunteering in the care of people with severe mental illness: a systematic review. BMC Psychiatry 2012;12. https://doi.org/10.1186/1471-244X-12-226.
- Heslop P. Good practice in befriending services for people with learning difficulties. Br J Learn Disabil 2005;33:27-33. https://doi.org/10.1111/j.1468-3156.2004.00310.x.
- Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry 2007;4:35-40.
- Melrose KL, Brown GDA, Wood AM. When is received social support related to perceived support and well-being? When it is needed. Pers Individ Dif 2015;77:97-105. https://doi.org/10.1016/j.paid.2014.12.047.
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med 2000;51:843-57. https://doi.org/10.1016/S0277-9536(00)00065-4.
- Sensky T, Turkington D, Kingdon D, Scott JL, Scott J, Siddle R, et al. A randomised controlled trial of cognitive–behavioural therapy for persistent symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry 2000;57:165-72. https://doi.org/10.1001/archpsyc.57.2.165.
- Shawyer F, Farhall J, Thomas N, Hayes SC, Gallop R, Copolov D, et al. Acceptance and commitment therapy for psychosis: randomised controlled trial. Br J Psychiatry 2017;210:140-8. https://doi.org/10.1192/bjp.bp.116.182865.
- Siette J, Cassidy M, Priebe S. Effectiveness of befriending interventions: a systematic review and meta-analysis. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014304.
- Priebe S, Chevalier A, Hamborg T, Golden E, King M, Pistrang N. Effectiveness of a volunteer befriending programme for patients with schizophrenia: randomised controlled trial. Br J Psychiatry 2020;217:477-83. https://doi.org/10.1192/bjp.2019.42.
- Jenkinson CE, Dickens AP, Jones K, Thompson-Coon J, Taylor RS, Rogers M, et al. Is volunteering a public health intervention? A systematic review and meta-analysis of the health and survival of volunteers. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-773.
- Wu H. Social Impact of Volunteerism. Atlanta, GA: Points of Light Institute; 2011.
- Florides T. Running a Befriending Project for People With Learning Disabilities. Final Project Report 2012.
- Stancliffe RJ, Bigby C, Balandin S, Wilson NJ, Craig D. Transition to retirement and participation in mainstream community groups using active mentoring: a feasibility and outcomes evaluation with a matched comparison group. J Intellect Disabil Res 2015;59:703-18. https://doi.org/10.1111/jir.12174.
- Cuthill FM, Espie CA, Cooper SA. Development and psychometric properties of the Glasgow Depression Scale for people with a learning disability. Individual and carer supplement versions. Br J Psychiatry 2003;182:347-53. https://doi.org/10.1192/bjp.182.4.347.
- Ali A, Mckenzie E, Hassiotis A, Priebe S, Lloyd-Evans B, Omar R, et al. One-to-one befriending for people with intellectual disability and symptoms of depression: protocol for a pilot randomised controlled trial. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-033989.
- Wechsler D. Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI-II). San Antonio, TX: NCS Pearson; 2011.
- Jahoda A, Hastings R, Hatton C, Cooper SA, Dagnan D, Zhang R, et al. Comparison of behavioural activation with guided self-help for treatment of depression in adults with intellectual disabilities: a randomised controlled trial. Lancet Psychiatry 2017;4:909-19. https://doi.org/10.1016/S2215-0366(17)30426-1.
- Dagnan D, Sandhu S. Social comparison, self-esteem and depression in people with intellectual disability. J Intellect Disabil Res 1999;43:372-9. https://doi.org/10.1046/j.1365-2788.1999.043005372.x.
- Skirrow P, Perry E. The Maslow Assessment of Needs Scales (MANS): an Outcome Measure and Planning Tool for People with Intellectual Disabilities. Liverpool: Mersey Care NHS Trust; 2009.
- World Health Organization Quality of Life Assessment Group . The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med 1998;46:1569-85. https://doi.org/10.1016/S0277-9536(98)00009-4.
- Stancliffe RJ, Keane S. Outcomes and costs of community living: a matched comparison of group homes and semi-independent living. J Intellect Dev Disabil 2000;25:281-305. https://doi.org/10.1080/13668250020019584.
- Lunsky Y, Benson BA. Reliability of ratings of consumers with mental retardation and their staff on multiple measures of social support. Am J Ment Retard 1997;102:280-4. https://doi.org/10.1352/0895-8017(1997)102<0280:ROROCW>2.0.CO;2.
- Baker PA. Measurement of community participation and use of leisure by service users with intellectual disabilities: the Guernsey Community Participation and Leisure Assessment (GCPLA). J Appl Res Intellect Disabil 2000;13:169-85. https://doi.org/10.1046/j.1468-3148.2000.00015.x.
- Rosenberg M. Society and the Adolescent Self-image. Princeton, NJ: Princeton University Press; 1965.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol 1980;39:472-80. https://doi.org/10.1037/0022-3514.39.3.472.
- Morin D, Crocker AG, Beaulieu-Bergeron R, Caron J. Validation of the attitudes toward intellectual disability: ATTID questionnaire. J Intellect Disabil Res 2013;57:268-78. https://doi.org/10.1111/j.1365-2788.2012.01559.x.
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. https://doi.org/10.1007/s11136-010-9648-y.
- EuroQol Research Foundation . EQ-5D-Y (Youth) About n.d. https://euroqol.org/eq-5d-instruments/eq-5d-y-about/ (accessed 20 February 2021).
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London; 2001.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Great Britain . Data Protection Act (2018) 2018.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2019. Canterbury: Personal Social Services Research Unit, University of Kent; 2019.
- Department of Health and Social Care . National Schedule of Reference Costs 2018–19 2020.
- Joint Formulary Committee . British National Formulary n.d. www.medicinescomplete.com (accessed 20 February 2021).
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health 2013;16:231-50. https://doi.org/10.1016/j.jval.2013.02.002.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Ali A, McKenzie E, Hassiotis A, Priebe S, Lloyd-Evans B, Jones R, et al. A pilot randomised controlled trial of befriending by volunteers in people with intellectual disability and depressive symptoms [published online ahead of print 27 September 2021]. J Intellect Dis Res 2021. https://doi.org/10.1111/jir.12886.
- Walters SJ, Bonacho Dos Anjos Henriques-Cadby I, Bortolami O, Flight L, Hind D, Jacques RM, et al. Recruitment and retention of participants in randomised controlled trials: a review of trials funded and published by the United Kingdom Health Technology Assessment Programme. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-015276.
- Tyrer P, Oliver-Africano PC, Ahmed Z, Bouras N, Cooray S, Deb S, et al. Risperidone, haloperidol, and placebo in the treatment of aggressive challenging behaviour in patients with intellectual disability: a randomised controlled trial. Lancet 2008;371:57-63. https://doi.org/10.1016/S0140-6736(08)60072-0.
- Kouimtsidis C, Bosco A, Scior K, Baio G, Hunter R, Pezzoni V, et al. A feasibility randomised controlled trial of extended brief intervention for alcohol misuse in adults with mild to moderate intellectual disabilities living in the community; the EBI-LD study. Trials 2017;18. https://doi.org/10.1186/s13063-017-1953-0.
- Oliver PC, Piachaud J, Done J, Regan A, Cooray S, Tyrer P. Difficulties in conducting a randomised controlled trial of health service interventions in intellectual disability: implications for evidence-based practice. J Intellect Disabil Res 2002;46:340-5. https://doi.org/10.1046/j.1365-2788.2002.00408.x.
- Lennox N, Taylor M, Rey-Conde T, Bain C, Purdie DM, Boyle F. Beating the barriers: recruitment of people with intellectual disability to participate in research. J Intellect Disabil Res 2005;49:296-305. https://doi.org/10.1111/j.1365-2788.2005.00618.x.
- Oliver-Africano P, Dickens S, Ahmed Z, Bouras N, Cooray S, Deb S, et al. Overcoming the barriers experienced in conducting a medication trial in adults with aggressive challenging behaviour and intellectual disabilities. J Intellect Disabil Res 2010;54:17-25. https://doi.org/10.1111/j.1365-2788.2009.01195.x.
- Robotham D, King M, Canagasabey A, Inchley-Mort S, Hassiotis A. Social validity of randomised controlled trials in health services research and intellectual disabilities: a qualitative exploration of stakeholder views. Trials 2011;12. https://doi.org/10.1186/1745-6215-12-144.
- Bach-Mortensen AM, Montgomery P. What are the barriers and facilitators for third sector organisations (non-profits) to evaluate their services? A systematic review. Syst Rev 2018;7. https://doi.org/10.1186/s13643-018-0681-1.
- Tse CY, Mckenzie E, Hassiotis A, Ali A. A survey of befriending services for people with intellectual disabilities in the United Kingdom [published online ahead of print 8 July 2021]. J Policy Pract Intellect Dis 2021. https://doi.org/10.1111/jppi.12387.
- Onrust S, Willemse G, Van Den Bout J, Cuijpers P. Effects of a visiting service for older widowed individuals: a randomised controlled trial. Death Stud 2010;34:777-803. https://doi.org/10.1080/07481181003761252.
- Burn E, Chevalier A, Leverton M, Priebe S. Patient and befriender experiences of participating in a befriending programme for adults with psychosis: a qualitative study. BMC Psychiatry 2020;20. https://doi.org/10.1186/s12888-020-02776-w.
- Mead S, Hilton D, Curtis L. Peer support: a theoretical perspective. Psychiatr Rehabil J 2001;25:134-41. https://doi.org/10.1037/h0095032.
- Mahlke CI, Priebe S, Heumann K, Daubmann A, Wegscheider K, Bock T. Effectiveness of one-to-one peer support for patients with severe mental illness – a randomised controlled trial. Eur Psychiatry 2017;42:103-10. https://doi.org/10.1016/j.eurpsy.2016.12.007.
- Kaehne A, Beyer S. Supported employment for young people with intellectual disabilities facilitated through peer support: a pilot study. J Intellect Disabil 2013;17:236-51. https://doi.org/10.1177/1744629513495265.
- Foundation for People with Learning Disabilities . What About Us? 2008. www.learningdisabilities.org.uk/learning-disabilities/publications/what-about-us (accessed 20 February 2021).
- National Institute for Health and Care Excellence (NICE) . Updated Guide to the Methods of Technology Appraisal 2013.
- Ross S, Fenney D, Ward D, Buck D. The Role of Volunteers in the NHS. Views From the Frontline. London: The King’s Fund; 2018.
Appendix 1 Topic guide questions
-
Why did you want to take part in the study?
-
Did you understand what the study was about?
-
Did you understand that you had a 50/50 chance of being in the group who got a befriender/volunteer?
-
The researcher asked you lots of questions about different things in your life. What did you think about the questions you were asked?
Questions for participants in the intervention group:
-
You were in the group that had a befriender. What was it like having a befriender?
-
What was your first meeting like?
-
How often did you meet up?
-
How did you decide what to do together?
-
What were the good things about having a befriender?
-
Do you think having a befriender has helped you in any way?
-
Were there any bad things about having a befriender?
-
Are you still meeting up with your befriender?
-
How did you feel when the befriending period was over?
-
How did you cope with the ending?
-
Would you recommend befriending to anyone else?
-
Is there anything you would change about befriending?
-
Is there anything else that you would like to say about how you were treated in the study that has not been covered?
-
Is there anything else that could be changed/improved?
-
What motivated you to become a befriender?
-
What were your reasons for taking part in the trial?
-
How did you feel about the way the study was explained?
-
What did you think about the questionnaires/assessments that you had to complete?
Questions about the befriending intervention:
-
What did you think about the training that you received?
-
What did you think about the matching process and the introductory meeting?
-
What was your experience of being a befriender in the study?
-
What did you think about the manual?
-
What did you think about the supervision and support you received during the study?
-
Do you think that the befriending intervention has benefited your befriendee?
-
Do you think that the befriending intervention has benefited you in any way?
-
How did you feel about the study overall?
-
Is there anything else that could be changed/improved?
-
What were your thoughts about the recruitment process of volunteers into the study?
-
What were your thoughts about the training offered to volunteers?
-
What were your thoughts about the process of randomisation?
-
What did you think about the matching process and the introductory meeting?
-
What were your thoughts about the befriending intervention?
-
What was your experience of supervising volunteers?
-
What was your experience of supporting individuals with learning disability?
-
Do you think that the befriending intervention has benefited the individuals with learning disability taking part in the study?
-
Were there any negative consequences of the befriending intervention?
-
Do you think that the befriending intervention has benefited carers?
-
How did you feel about the study overall?
-
Did you get enough support and information from the study team? Could this have been improved?
-
Would you take part in a study evaluating befriending again?
-
Is there anything else that could be changed/improved?
-
How did you feel about the way the study was explained to you and the person you care for?
-
As part of the study, you may have completed a questionnaire about how often the person has used different types of services. What were your views about this questionnaire?
Questions about the befriending intervention:
-
What did you think about the matching process and the introductory meeting?
-
What did you think about the befriending intervention?
-
What did you think about the support that the person you care for received during the study?
-
Do you think that the befriending intervention has benefited the person you care for?
-
Were there any negative consequences of the befriending intervention?
-
Do you think that the befriending intervention has benefited you in any way?
-
How did you feel about the study overall?
-
Would you recommend the befriending intervention?
-
Is there anything else that could be changed/improved?
Appendix 2 Health economic analysis
This appendix reports on the cost-effectiveness of a pilot randomised controlled trial of one-to-one befriending by volunteers, compared with usual care, in reducing symptoms of depression in people with intellectual disability.
Aim
The main aim of the economic evaluation was to determine the costs of delivering the befriending intervention and test the feasibility of collecting health-care resource use and health-related quality-of-life data to calculate the incremental mean cost per QALY gained of the befriending intervention compared with control (i.e. the cost-effectiveness) for a full RCT in people with ID.
Outcomes
-
Health-related quality of life measured using the EQ-5D-Y and the EQ VAS questionnaire at baseline and at 6 months post randomisation.
-
Health-care resource use recorded at baseline and at 6 months post randomisation.
The economic analysis was conducted from the primary perspectives of the NHS and personal social services. The horizon of the study is 6 months; therefore, discounting was not performed.
Methods
Cost of delivery of the befriending intervention
The costs of the befriending intervention were provided by the volunteer co-ordinators at the befriending services. They provided a breakdown of costs related to the intervention, such as costs of recruitment, DBS checks, staff time in relation to the training and supervision of volunteers and monitoring of visits. Staffing costs were calculated using an hourly rate. 61
Health-care resource use
An adapted CSRI58 was used to assess the feasibility of collecting data on participant-reported service use at baseline and at 6 months post randomisation. The adapted CSRI was completed with the participant’s carers, health professionals who knew the person well or the participant. This included contacts with primary care, community services, community ID services and hospitals, including outpatient and inpatient care. Concomitant medication was recorded on a CRF developed for the study.
The mean (SD) health and social care resource use was estimated, and costs were calculated using nationally recognised, published unit costs61–63 (Tables 10 and 11) to estimate the mean (95% CI) costs per participant. Costs were in Great British pounds at 2019 values, or adjusted for inflation if costs for 2019 were not available.
Utilities and quality-adjusted life-years
The EQ-5D-Y56,57 was collected at baseline and at 6 months post randomisation to calculate QALYs. There are currently no EuroQol measures that have been developed specifically for adults with ID. The EQ-5D-Y was selected because it uses simple language and has been used in other studies of people with ID. 45
Responses from the EQ-5D-Y were converted into a single value (index number) and the regular EQ-5D-3L value sets (although not recommended) were used to obtain utility values. The EQ VAS was used as a quantitative measure of health outcome that reflects the participant’s own judgement about their health status. We examined whether or not scores on the EQ VAS were consistent with the EQ-5D-Y utility values as this would help us to determine if the EQ-5D-Y is a suitable measure of health status in people with ID.
Cost-effectiveness analysis
Participants completed the EQ-5D-Y descriptive system and the EQ VAS, but there were important discrepancies between the scores, which could make calculation of QALYs for a cost–utility analysis less reliable.
Therefore, incremental cost per change in the primary health outcome (depression scores on the GDS-LD) between the intervention and control group was estimated. The ICER was calculated by dividing the difference in total costs (incremental cost) by the difference in the health outcome (incremental effect) to provide a ratio of ‘extra cost per extra unit of health effect’ for the more expensive intervention compared with the alternative. ICERs reported by economic evaluations are compared with a predetermined threshold82 to decide whether or not choosing the new intervention is an efficient use of resources.
The analyses followed CHEERS. 64
Results
Cost of delivery of the befriending intervention
The total cost of the befriending intervention implementation was £5647.38 (Table 12), which includes the cost of recruitment (staff time), DBS and reference checks; the cost of staff time and resources to deliver training, supervision, monitoring calls and visits; and volunteer expenses. The mean cost per participant was £701.
Health-care resource use costs
The costs of NHS resource use at baseline and 6 months post randomisation are displayed in Tables 4 and 5, respectively. Health-care resource use costs at baseline were substantially lower in the befriending group (£1387, 95% CI £359 to £2415) than in the control group (£4949, 95% CI £351 to £9548). Resource use at 6 months’ follow-up was lower than at baseline in both groups (£855 in the intervention group and £4014 in the control group). The mean difference in resource use in the intervention group at 6 months was –£3161 (95% CI –£6250 to –£73), but this difference does not consider baseline differences. After including the intervention cost, the mean difference was –£2460 (95% CI –£5549 to £628), but this was not statistically significant.
Utilities and quality-adjusted life-years
The EQ-5D-Y health state values at baseline and 6 months post randomisation are displayed in Tables 13 and 14, respectively. The mean EQ-5D-Y utility value was slightly higher in the befriending group at baseline (0.90; SD 0.10) than in the control group (0.88; SD 0.08). At 6 months, the mean was slightly higher in the control group (0.90; SD 0.13) than in the befriending group (0.88; SD 0.11). The mean EQ VAS score was substantially higher in the befriending group at baseline (75.0; SD 23.2) than in the control group (45.6; SD 31.5), but appeared to decrease at 6 months’ follow-up in the befriending group (62.3; SD 40.8); however, scores increased slightly in the control group (50.7; SD 27.6). EQ VAS scores did not appear to correspond well to the EQ-5D-Y utility values, suggesting that the EQ VAS may be difficult for people with ID to complete. Owing to the small sample size and discrepancies in the scores, QALYs were not calculated.
We have explored further the responses to the EQ-5D-Y questionnaires that are displayed in Tables 15 and 16, respectively, splitting the EQ-5D-Y levels into ‘no problem’ (level 1) and ‘any problems’ (levels 2 and 3), changing the profile into frequencies of reported problems. This is helpful as it describes the changes in health over time. Although an overall summary is preferred, this approach shows that there were improvements in usual activities; pain and discomfort; and feeling worried, sad or unhappy in the control group and improvements in looking after themselves in the intervention group.
Cost-effectiveness analysis
Linear regression including covariates for randomisation to befriending intervention or control, baseline costs and effects was used to calculate the mean difference in costs/effects between the befriending intervention and the control group, and 95% CIs. After adjustment for baseline values, the ICER was –£1810 per point change in GDS-LD.
The befriending intervention has a 35% probability of being cost-effective at a willingness-to-pay threshold of £20,000 (see Figure 4).
Discussion
The results of our study show that the intervention has a 35% probability of being cost-effective. These results are conservative and should be interpreted with caution because of the small sample size and other issues that affected the study.
Data collection methods for a future economic evaluation were developed, and their feasibility was tested during this study. There was a good return of the resource use questionnaire from carers. Data on intervention costs were obtained from befriending services. Participants completed the EQ-5D-Y descriptive system and the EQ VAS, but there were important discrepancies between the scores, which could make the calculation of QALYs for a cost–utility analysis less reliable. The differences may have been due to a number of reasons, such as poor understanding of instructions on how to complete the EQ VAS or because the EQ-5D-Y is not an appropriate measure for adults with ID (it has not been validated for use in this group) and may not capture relevant aspects of health that are perceived to be important. In the absence of a validated measure of health-related quality of life in this population, perhaps the EQ-5D-Y should not be used in isolation to assess health-related quality-of-life outcomes in trials involving adults with ID, and should be used in conjunction with a proxy measure.
| Resource | Unit cost (£) | Source |
|---|---|---|
| GP: at surgery | 37 | Unit Costs of Health and Social Care 2019 61 |
| Practice nurse | 36 | Unit Costs of Health and Social Care 2019 61 |
| Practice nurse: telephone | 8 | Unit Costs of Health and Social Care 2019 61 |
| Community nurse | 43 | Unit Costs of Health and Social Care 2019 61 |
| Community nurse: home visit | 62 | Unit Costs of Health and Social Care 2019 61 |
| Community nurse: telephone | 8 | Assumption |
| Psychiatric nurse: home visit | 70 | Unit Costs of Health and Social Care 2019 61 |
| ID nurse | 45 | Unit Costs of Health and Social Care 2019 61 |
| ID nurse: home visit | 70 | Unit Costs of Health and Social Care 2019 61 |
| Psychiatrist | 356 | Unit Costs of Health and Social Care 2019 61 |
| Psychiatrist: home visit | 356 | Unit Costs of Health and Social Care 2019 61 |
| Psychologist | 44 | Unit Costs of Health and Social Care 2019 61 |
| Psychologist: home visit | 44 | Unit Costs of Health and Social Care 2019 61 |
| Care manager/social worker | 40 | Unit Costs of Health and Social Care 2019 61 |
| Care manager/social worker: home visit | 40 | Unit Costs of Health and Social Care 2019 61 |
| Care manager/social worker: telephone | 8 | Assumption |
| Occupational therapist | 43 | Unit Costs of Health and Social Care 2019 61 |
| Occupational therapist: home visit | 43 | Unit Costs of Health and Social Care 2019 61 |
| Physiotherapy | 46 | Unit Costs of Health and Social Care 2019 61 |
| Dentist | 104 | Unit Costs of Health and Social Care 2019 61 |
| Speech and language therapist | 83 | Unit Costs of Health and Social Care 2019 61 |
| Optician | 33 | Unit Costs of Health and Social Care 2019 61 |
| Community support worker: at home visit | 23 | Unit Costs of Health and Social Care 2019 61 |
| Acute psychiatric ward admission | 298 | Unit Costs of Health and Social Care 2019 61 |
| General medical elective/planned inpatient admission | 4078 | National Schedule of Reference Costs 2018–19 62 |
| General medical non-elective/unplanned inpatient admission | 589 | National Schedule of Reference Costs 2018–19 62 |
| A&E physical health related: not admitted | 209 | National Schedule of Reference Costs 2018–19 62 |
| A&E physical health related: admitted | 257 | National Schedule of Reference Costs 2018–19 62 |
| A&E mental health related: admitted | 209 | National Schedule of Reference Costs 2018–19 62 |
| Prescription drug | Unit dose | Cost for 6 months (£)58 |
|---|---|---|
| Amisulpride | 100 mg | 21.54 |
| 200 mg | 32.64 | |
| Aripiprazole | 10 mg | 10.56 |
| Aspirin | 75 mg | 1.56 |
| Atorvastatin | 10 mg | 4.50 |
| 20 mg | 6.12 | |
| Calcichew-D3 chewable tablets (Takeda UK Ltd, London, UK) | 25 mg | 25.44 |
| Chlorpromazine | 50 mg | 31.32 |
| Citalopram | 10 mg | 3.96 |
| 20 mg | 4.08 | |
| 40 mg | 6.06 | |
| Clobazam | 10 mg | 33.48 |
| Clozaril® (Mylan Products Ltd, Potters Bar, UK) | 300 mg | 47.04 |
| Folic acid | 5 mg | 4.80 |
| Indapamide | 1.5 mg | 20.40 |
| Lansoprazole | 15 µg | 3.48 |
| Levothyroxine | 25 µg | 17.46 |
| 50 µg | 7.68 | |
| Losartan | 25 mg | 4.80 |
| Metformin | 500 mg | 13.20 |
| Montelukast | 10 mg | 9.66 |
| Omeprazole | 20 mg | 6.72 |
| Oxybutynin | 2.5 mg | 6.90 |
| 5 mg | 8.94 | |
| Pregabalin | 100 mg | 492.66 |
| 150 mg | 328.44 | |
| Promethazine hydrochloride | 25 mg | 8.88 |
| Propranolol | 40 mg | 5.10 |
| Quetiapine | 50 mg | 6.06 |
| 25 mg | 6.06 | |
| Ramipril | 100 mg | 7.44 |
| Risperidone | 1 mg | 9.12 |
| Sertraline | 50 mg | 6.48 |
| 100 mg | 7.56 | |
| Simvastatin | 40 mg | 4.56 |
| Sitagliptin | 100 mg | 199.56 |
| Tegretol prolonged release | 200 mg | 11.49 |
| 400 mg | 30.12 | |
| Topiramate | 25 mg | 9.96 |
| 50 mg | 11.22 | |
| Trihexyphenidyl | 2 mg | 8.55 |
| Venlafaxine | 37.5 mg | 5.76 |
| Intervention component | Unit | Cost (£) | |
|---|---|---|---|
| Unit | Total | ||
| DBS checks (n) | 11 | 18.00 | 198.00 |
| Reference checks (staff time in hours) | 22 | 16.19 | 356.18 |
| Cost of training volunteers (staff time in hours) | 85 | 16.19 | 1376.15 |
| Cost of supervision (staff time in hours) | 80 | 16.19 | 1295.20 |
| Costs relating to monitoring visits/telephone calls to volunteers/carers/individuals with LDs (staff time in hours) | 60 | 16.19 | 971.40 |
| Volunteer expenses (travel, food, other) | 210.00 | ||
| Other costs (e.g. volunteer rewards, identification cards) | 350.00 | ||
| Recruitment (staff time in hours) | 55 | 16.19 | 890.45 |
| Total | 5647.38 | ||
| Variable | Control group (N = 8) | Intervention group (N = 8) | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| EQ-5D-Y utility value | 8 | 0.880 (0.081) | 8 | 0.896 (0.103) |
| EQ VAS | 8 | 45.6 (31.5) | 7 | 75.0 (23.2) |
| Health and social care resource use | ||||
| GP: at surgery | 7 | 6.6 (8.4) | 6 | 3.7 (1.9) |
| Practice nurse | 2 | 4.0 (1.4) | 2 | 1.0 (0.0) |
| Practice nurse: telephone | 1 | 2.0 | – | – |
| Community nurse | – | – | – | – |
| Community nurse: home visit | – | – | – | – |
| Community nurse: telephone | 1 | 3.0 | – | – |
| Psychiatric nurse: home visit | – | – | – | – |
| ID nurse | – | – | 1 | 2.0 |
| ID nurse: home visit | 2 | 18.0 (8.5) | 1 | 6.0 |
| Psychiatrist | 6 | 3.5 (2.6) | 4 | 2.0 (1.4) |
| Psychiatrist: home visit | – | – | – | – |
| Psychologist | 3 | 9.0 (5.1) | 1 | 6.0 |
| Psychologist: home visit | – | – | – | – |
| Care manager/social worker | 1 | 4.0 | – | – |
| Care manager/social worker: home visit | 4 | 2.8 (2.4) | 4 | 1.3 (0.5) |
| Care manager/social worker: telephone | – | – | 1 | 4.0 |
| Occupational therapist | – | – | – | – |
| Occupational therapist: home visit | 1 | 2.0 | – | – |
| Physiotherapy | 1 | 3.0 | 1 | 3.0 |
| Dentist | 5 | 1.0 (0.0) | 3 | 2.0 (1.0) |
| Speech and language therapist | 1 | 6.0 | – | – |
| Optician | 5 | 1.0 (0.0) | 4 | 1.3 (0.5) |
| Community support worker: at home visit | 1 | 12.0 | 1 | 24.0 |
| Acute psychiatric ward admission | 1 | 1.0 | – | – |
| Acute psychiatric ward LoS (days) | 1 | 42.0 | – | – |
| General medical elective/planned inpatient admission | 1 | 1.0 | – | – |
| General medical elective/planned inpatient LoS (days) | 1 | 1.0 | – | – |
| General medical non-elective/unplanned inpatient admission | – | – | 1 | 1.0 |
| General medical non-elective/unplanned inpatient LoS (days) | – | – | 1 | 4.0 |
| A&E physical health related: not admitted | – | – | 1 | 1.0 |
| A&E physical health related: admitted | 2 | 6.5 (4.9) | 2 | 1.0 (0.0) |
| A&E mental health related: admitted | – | – | 1 | 1.0 |
| Day patient procedure/test | 2 | 1.0 (0.0) | 3 | 1.7 (1.2) |
| General medical outpatient appointment | 2 | 11.0 (12.7) | 1 | 2.0 |
| Other: number | – | – | 1 | 6.0 |
| Prescriptions | 7 | 3.7 (2.6) | 7 | 4.9 (2.9) |
| Mean health and social care resource use cost (95% CI) | 8 | £4949 (£351 to £9548) | 8 | £1387 (£359 to £2415) |
| Variable | Control group (N = 8) | Intervention group (N = 8) | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| EQ-5D-Y utility value | 7 | 0.903 (0.128) | 8 | 0.878 (0.111) |
| EQ VAS | 7 | 50.7 (27.6) | 8 | 62.3 (40.8) |
| Health and social care resource use | ||||
| GP: at surgery | 7 | 8.0 (9.7) | 7 | 4.0 (3.1) |
| Practice nurse | 4 | 3.8 (4.3) | 4 | 1.3 (0.5) |
| Practice nurse: telephone | – | – | – | – |
| Community nurse | 1 | 24.0 | – | – |
| Community nurse: home visit | 1 | 2.0 | – | – |
| Community nurse: telephone | – | – | – | – |
| Psychiatric nurse: home visit | 1 | 6.0 | 1 | 8.0 |
| ID nurse | – | – | – | – |
| ID nurse: home visit | – | – | 1 | 3.0 |
| Psychiatrist | 5 | 2.4 (2.2) | 3 | 1.7 (1.2) |
| Psychiatrist: home visit | 1 | 6.0 | – | – |
| Psychologist | 2 | 12.5 (16.3) | 1 | 1.0 |
| Psychologist: home visit | 1 | 6.0 | – | – |
| Care manager/social worker | – | – | – | – |
| Care manager/social worker: home visit | 7 | 2.3 (1.6) | 4 | 1.3 (0.5) |
| Care manager/social worker: telephone | – | – | – | – |
| Occupational therapist | 1 | 2.0 | – | – |
| Occupational therapist: home visit | 1 | 1.0 | – | – |
| Physiotherapy | 2 | 2.0 (1.4) | 1 | 3.0 |
| Dentist | 4 | 1.3 (0.5) | 4 | 2.0 (0.8) |
| Speech and language therapist | – | – | – | – |
| Optician | 4 | 1.3 (0.5) | 5 | 1.0 (0.0) |
| Community support worker: at home visit | – | – | – | – |
| Acute psychiatric ward admission | – | – | – | – |
| Acute psychiatric ward LoS (days) | – | – | – | – |
| General medical elective/planned inpatient admission | – | – | – | – |
| General medical elective/planned inpatient LoS (days) | – | – | – | – |
| General medical non-elective/unplanned inpatient admission | 1 | 1.0 | – | – |
| General medical non-elective/unplanned inpatient LoS (days) | 1 | 10.0 | – | – |
| A&E physical health related: not admitted | 3 | 10.7 (16.7) | – | – |
| A&E physical health related: admitted | 1 | 1.0 | – | – |
| A&E mental health related: admitted | – | – | – | – |
| Day patient procedure/test: number | 2 | 1.5 (0.7) | 1 | 1.0 |
| General medical outpatient appointment: number | 2 | 15.5 (20.5) | 1 | 4.0 |
| Other: number | – | – | – | – |
| Prescriptions | 7 | 3.6 (2.4) | 7 | 4.9 (2.9) |
| Mean health and social care resource use cost (95% CI) | 8 | £4014 (£666 to £7367) | 8 | £855 (£247 to £1464) |
| Level | Mobility | Looking after myself | Doing usual activities | Having pain or discomfort | Feeling worried, sad or unhappy | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| 1, n (%) | 6 (86) | 6 (86) | 6 (86) | 5 (71) | 5 (71) | 6 (86) | 2 (29) | 4 (57) | 2 (29) | 4 (57) |
| 2, n (%) | 1 (14) | 0 (0) | 0 (0) | 2 (29) | 2 (29) | 0 (0) | 4 (57) | 2 (29) | 3 (43) | 2 (29) |
| 3, n (%) | 0 (0) | 1 (14) | 1 (14) | 0 (0) | 0 (0) | 1 (14) | 1 (14) | 1 (14) | 2 (29) | 1 (14) |
| Total, n (%) | 7 (100) | 7 (100) | 7 (100) | 7 (100) | 7 (100) | 7 (100) | 7 (100) | 7 (100) | 7 (100) | 7 (100) |
| Numbers reporting some problems (level 2 and level 3) | 1 | 1 | 1 | 2 | 2 | 1 | 5 | 3 | 5 | 3 |
| Change in numbers reporting problems | 0 | 1 | –1 | –2 | –2 | |||||
| Per cent change in numbers reporting problems | 0 | 100 | –50 | –40 | –40 | |||||
| Rank of dimensions reporting problems | 3 | 4 | 1 | 2 | 2 | |||||
| Level | Mobility | Looking after myself | Doing usual activities | Having pain or discomfort | Feeling worried, sad or unhappy | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| 1, n (%) | 4 (50) | 2 (25) | 6 (75) | 7 (87.5) | 6 (75) | 6 (75) | 4 (50) | 3 (37.5) | 6 (75) | 6 (75) |
| 2, n (%) | 2 (25) | 3 (37.5) | 2 (25) | 0 (0) | 2 (25) | 2 (25) | 3 (37.5) | 3 (37.5) | 2 (25) | 2 (25) |
| 3, n (%) | 2 (25) | 3 (37.5) | 0 (0) | 1 (12.5) | 0 (0) | 0 (0) | 1 (12.5) | 2 (25) | 0 (0) | 0 (0) |
| Total, n (%) | 8 (100) | 8 (100) | 8 (100) | 8 (100) | 8 (100) | 8 (100) | 8 (100) | 8 (100) | 8 (100) | 8 (100) |
| Numbers reporting some problems (level 2 and level 3) | 4 | 6 | 2 | 1 | 2 | 2 | 4 | 5 | 2 | 2 |
| Change in numbers reporting problems | 2 | –1 | 0 | 1 | 0 | |||||
| Per cent change in numbers reporting problems | 50 | –50 | 0 | 25 | 0 | |||||
| Rank of dimensions reporting problems | 4 | 1 | 2 | 3 | 2 | |||||
FIGURE 4.
Cost-effectiveness acceptability curve.
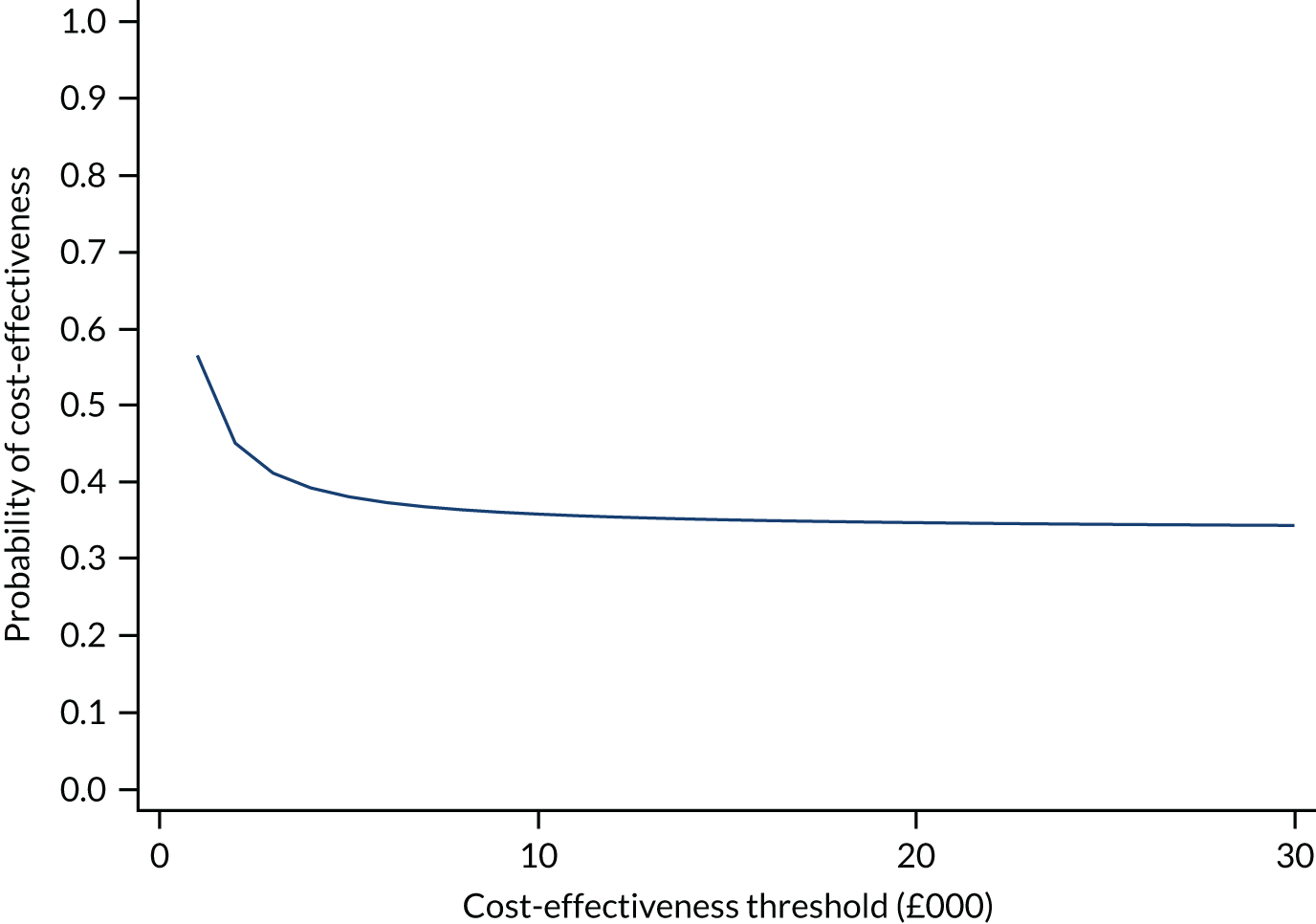
Appendix 3 Supervision topics
| Topics | Sessions, n (%) | Volunteers who raised an issue, n |
|---|---|---|
| Safeguarding concerns | 2 (9.5) | 2 |
| Concerns about mental health | 4 (19.0) | 2 |
| Concerns about health | 7 (33.3) | 3 |
| Concerns around finance | 7 (33.3) | 2 |
| Training needs | 1 (4.8) | 1 |
| Time management | 3 (14.3) | 3 |
| Help with planning sessions | 1 (4.8) | 1 |
| Issues around befriendees’ relationship with their family | 2 (9.5) | 1 |
| Concerns about carers | 3 (14.3) | 3 |
| Balancing personal life/workload and volunteering | 5 (23.8) | 4 |
| Staying safe online | 2 (9.5) | 1 |
| Repetitive activities/conversations | 4 (19.0) | 3 |
| Lateness | 2 (9.5) | 1 |
| Positive feedback from befriendee regarding volunteer | 1 (4.8) | 1 |
| Missed sessions | 5 (23.8) | 2 |
| Discussion about managing ending | 2 (9.5) | 1 |
Appendix 4 Jane’s story: a case study
This case study describes the experiences of an individual with ID who participated in the study and engaged with the befriending intervention. All personal identifiers have been removed or modified to ensure anonymity. This case study was selected as an example of an individual with a history of clinical depression who had limited opportunities for social engagement and contact, and represents a ‘typical’ example of an individual who might benefit from such an intervention. The case study uses information derived from the qualitative interviews with the volunteer, the individual and their carer, and supervision records.
Jane is a woman in her fifties with mild ID who lives in supported living accommodation, where she receives some support from paid carers (e.g. help with shopping). She has diagnoses of depression and schizophrenia. Staff at the supported living accommodation report that it is difficult to motivate Jane to engage in activities, and she spends most of her time indoors. Jane was initially apprehensive about taking part in the study.
Jane was introduced to her volunteer, Susan, who was a woman in her mid-forties. Susan had previous experience of working with individuals with ID and had formerly worked as a support worker. The relationship got off to a good start. During the first supervision session, Susan commented that things were going well. It was a challenge supporting Jane to choose activities that interested her, but they agreed to work towards a plan:
It’s going well, I’m happy to keep volunteering, we get on well . . . Jane is very compliant and it can sometimes be a problem finding what she wants to do . . . We have talked about what to do in the winter as Jane has expressed that she gets depressed with the seasons, so we have made a plan to try and go for a walk when we meet.
Susan, supervision notes
Susan and Jane were able to find common interests that helped to stimulate conversation and motivated Jane to spend more time outdoors:
Yeah, we get along really well, yeah. So my mum has got significant mental health problems and Jane has mental health problems and I think she found – well we both found it interesting to talk about how it affects your life and you know. And generally – she loves dogs and I had just got this puppy a couple of months before we first started seeing each other and we both love food.
Susan, interview transcript
Jane really enjoys seeing Fluffy (my dog), she has even stated that her dream job would be to work in a vet . . . we have been out for a few meals and to take my dog for a walk, which Jane has really enjoyed.
Susan, supervision record
Susan explored with Jane the activities that she would like to pursue:
Jane would like to go to [name] Dogs Home. We have spoken about pet rescue centres, and we’ll probably start with somewhere nearer, like [name] City Farm, or the farm in [name of place]. There may be volunteering opportunities which may interest Jane for the future.
Susan, supervision record
Susan was unable to meet Jane weekly because of work and family commitments, and there were frequent breaks of several weeks when neither Susan nor Jane was available. They met each other on 11 occasions in total. Susan and Jane spent most of their meetings going on walks (usually with Susan’s dog) and having lunch at a local cafe or restaurant:
Well, mainly, we would meet for lunch or we would go out for walks with dog. That was the main things really. We went shopping, but Jane has trouble with her legs so she can’t walk really far – and sometimes we would just spend time in her flat, you know, chatting and things like that.
Susan, interview transcript
Jane reported positive experiences about befriending during the end-of-study interview:
Tell me, what’s been good about it for you?
She listens and we talk about everything.
Do you feel that having a befriender has made you less lonely?
Yeah. . . because it’s something to look forward to.
Jane’s carer (manager of the home) stressed that the activities that the befriender provided were different from those that staff could provide, and that Jane valued the attention that she received from Susan:
Because, I mean, yeah, the difference is just for her, the person is for her. We are in the house – Jane is sharing with three other people that live in the house. When they come for that hour, it’s just about Jane, it’s not about anybody else . . . so that concentration they have to themselves, that message goes a long way, it makes a difference for her . . .
Carer, interview transcript
Jane’s carer also commented that Jane often spoke to staff about looking forward to meeting Susan:
You can see the positive, you can see she is looking forward to it because she’s coming and you understand she is happy about seeing this person and looking forward to ‘I’m walking dog with Susan on Sunday’, so she looks forward to and she is happier and it motivates her and takes her out of the house doing all those things.
Carer, interview transcript
During the course of their relationship, Susan reported that there were apparent improvements in Jane’s mood:
Jane was previously feeling down, but she seems a lot better recently.
Susan, supervision record
One of the barriers to Susan’s relationship with Jane was the poor reception that she received from paid carers at the supported living accommodation:
On occasion, staff have seemed quite unhelpful when I have visited. This could be due to agency staff being employed rather than permanent staff.
Susan, supervision record
As Susan became more familiar with Jane, she noticed subtle changes in Jane’s demeanour, which led to her enquiring about the possibility that something was wrong. Jane was able to confide in Susan that she had experienced bullying from a member of staff:
As Jane and I got to know each other better, I picked up on – there was one issue – well, I noticed that Jane wasn’t herself one time when we went out for lunch together, so I was kind of asking what was wrong and she disclosed to me that some staff at her service were not treating her very nicely . . .
Susan, interview transcript
Susan supported Jane to report the incident, thus helping her to make decisions for herself:
It was challenging in the sense that I know this isn’t correct, I am a befriender, I am not a member of staff, so I can’t go behind her back and report it without her consent because she has capacity to make that decision. So, it was quite challenging, actually, trying to talk to her and give her confidence that if we reported it together it would get fixed, and luckily it did and the staff were moved out of the service and the manager picked it up and she was great. So it all worked out well, but it was challenging.
Susan, interview transcript
Susan thought that their relationship had a positive impact on Jane because they viewed each other as friends:
I am sure it wasn’t life-changing, but hopefully she would say that she enjoyed seeing me, I think. But also you can sort of tell the impact of her sort of getting some things off her chest and talking about things. Picking up on some little nuances, you know, she might not be sleeping well and things. I think because when you get to know somebody, like a friend, you say ‘oh, you seem a bit tired’.
Susan, interview transcript
Susan reflected on her awareness that an individual could live in supported accommodation but still feel lonely and, therefore, volunteers played a crucial role:
Well, it definitely reminded me that there are lots of people out there who, even if they are living in a supported housing environment, it doesn’t mean to say that they are not lonely. I think we have this assumption that if people are getting an adult social care service – with all the cuts and the limited time they do have with staff – you know, it does sort of remind you how services are underfunded and the value of volunteers. So it was a good reminder to me really that there are lots of people out there who would benefit from some help to meet people.
Susan, interview transcript
Susan and Jane agreed to continue meeting each other after the end of the 6-month period. Jane fed back that she thought the intervention period was too short:
Is there anything you would change about the befriending?
6 months a bit too short I think . . .
So you maybe prefer it to be a bit longer?
Yeah.
Changes in outcome scores
Jane had a baseline score of 18 on the GDS-LD and this decreased to 17 at her 6-month follow-up. There was a slight improvement in her self-esteem scores, which increased by 2 units, from 16 at baseline to 18 at follow-up. There was an improvement for scores on aloneness (7) and social dissatisfaction (8) at follow-up (total score of 15) compared with baseline scores (9 and 12, respectively; total score 21), but there was a reduction in the quality-of-life scores in the MANS-LD (63 at baseline and 54 at follow-up), and scores on the social support scale (SSSR) were largely unchanged.
Reflection
Jane’s history of depression and comorbid schizophrenia culminated in Jane lacking the desire and motivation to engage in activities. Jane’s relationship with Susan was successful because they shared common interests, such as an interest in animals, and Susan’s experience of previously working with individuals with ID and manging her mother’s mental health problems enabled her to understand and empathise with Jane. Susan described Jane as a ‘friend’, which was distinct from the relationship that Jane had with paid staff at her accommodation. Although befriending may be described as a ‘friendship-like relationship’, the fact that it is monitored by an external agency implies that there are certain distinctions, including safeguards to protect individuals (such as DBS checks, training and supervision) that would not occur in natural relationships. 36 Jane remarked that she thought that a duration of 6 months was too short for the intervention. In the context of this study, where there was a clear time-limited intervention, the nature of the befriending relationship is likely to have been constrained and, therefore, may not fully reflect how befriending would occur in practice, where pairs may continue to meet for many years, and the relationship may be unmonitored after a period of time.
Susan introduced Jane to her pet dog, which suggests that their relationship had relatively loose boundaries. This highlights the importance of differentiating befriending from the support that individuals may receive from support workers or paid staff, where the emphasis may be on the provision of practical support and there are stricter boundaries between staff and the individuals they support. Thus, although individuals with ID may be supported by informal and paid carers, the nature of the relationship with a befriender is different and, therefore, the befriender has the potential to make an important contribution to the person’s life. Indeed, Jane’s carer commented that Jane looked forward to her meetings with Susan as she was given undivided attention, which staff are often not able to provide.
Susan remarked that staff were sometimes ‘unhelpful’, which might suggest a lack of understanding from staff about the role of volunteers and how the volunteers’ roles may differ from their own. Similar findings have been described in other population groups and settings, and indicate the need for improved training and more collaborative working between staff and volunteers. 83
Jane was able to benefit from befriending by engaging in activities outside the home and particularly enjoyed going on walks with Susan’s dog. Susan also provided emotional support and assisted Jane to raise concerns about a member of staff who had been mistreating her, which may not have occurred if Susan had not encouraged her to talk openly about her concerns. Although Jane’s depressive symptoms did not appear to improve substantially from the befriending intervention based on self-report, information from the other sources appears to indicate that she did benefit from the relationship, which emphasises the need for more sensitive and valid outcome measures for people with ID and the importance of obtaining feedback based on both patient- and carer-reported outcomes.
Appendix 5 Revised logic model
FIGURE 5.
Revised logic model of befriending in people with IDs.
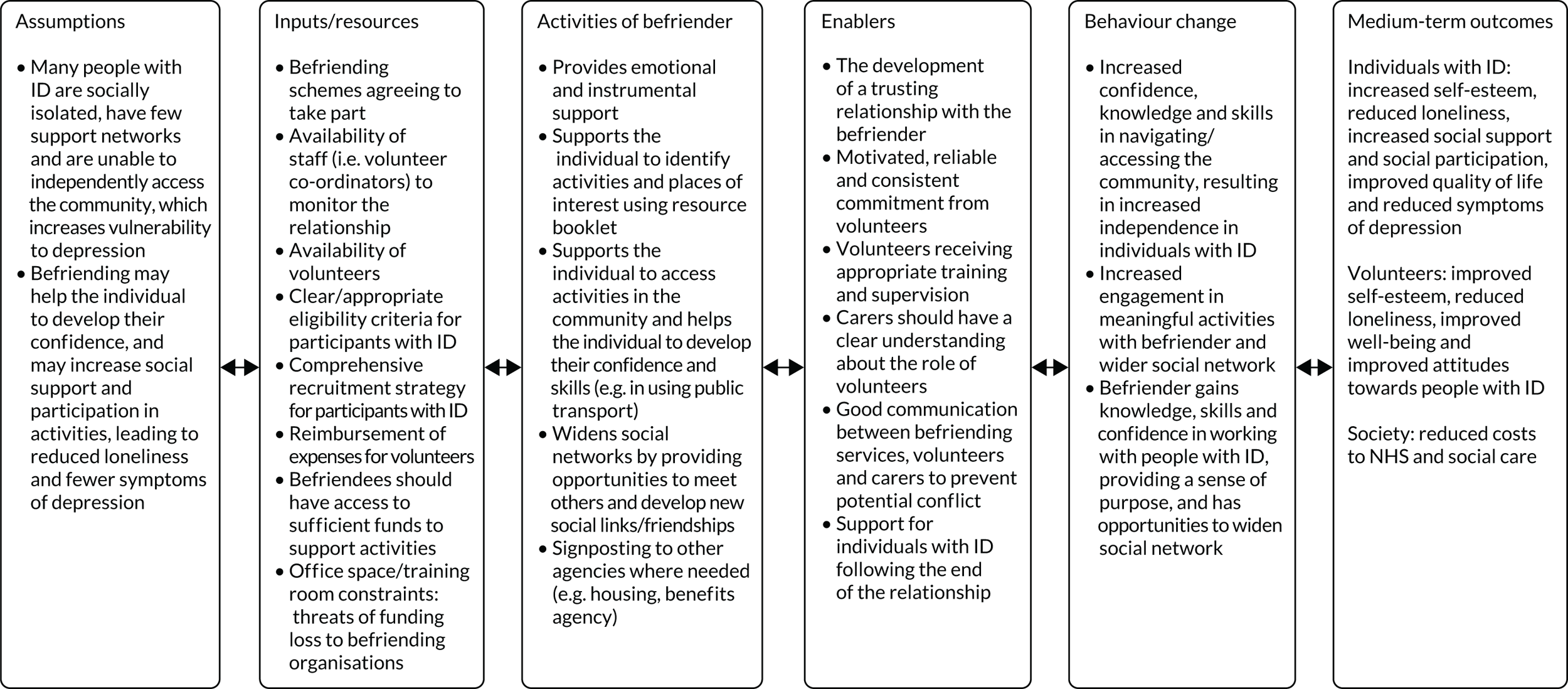
List of abbreviations
- A level
- Advanced level
- ATTID
- Attitudes Towards Intellectual Disability Questionnaire
- CHEERS
- Consolidated Health Economic Evaluation Reporting Standards
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CRF
- case report form
- CSRI
- Client Services Receipt Inventory
- DBS
- Disclosure and Barring Service
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-Y
- EuroQol-5 Dimensions – Youth
- EQ VAS
- EuroQol visual analogue scale
- GCPLA
- Guernsey Community Participation and Leisure Assessment
- GDS-LD
- Glasgow Depression Scale for people with a Learning Disability
- ICER
- incremental cost-effectiveness ratio
- ID
- intellectual disability
- IQ
- intelligence quotient
- IQR
- interquartile range
- MANS-LD
- Maslow Assessment of Needs Scale – Learning Disability
- MWLQ
- Modified Worker Loneliness Questionnaire
- NELFT
- North East London NHS Foundation Trust
- PPI
- patient and public involvement
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SD
- standard deviation
- SSSR
- Social Support Self Report for intellectually disabled adults
- UCLA
- University of California, Los Angeles
- WASI-II™
- Wechsler Abbreviated Scale of Intelligence™ (Second Edition)
- WEMWBS
- Warwick–Edinburgh Mental Wellbeing Scale
- WHOQOL-8
- adapted World Health Organization Quality of Life measure
