Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 11/3005/40. The contractual start date was in September 2017. The final report began editorial review in October 2020 and was accepted for publication in May 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2021 So et al. This work was produced by So et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 So et al.
Chapter 1 Context
The alcohol problem
Alcohol is increasingly acknowledged to be a global health problem. It is ranked as the ninth most common cause of death worldwide1 and is associated with over 200 medical conditions. Liver disease, including cirrhosis and liver cancer, is perhaps the most well-known harm, but other consequences of alcohol use include cardiovascular disease, unintended pregnancy, sexually transmitted infections, respiratory infections, some cancers, intentional and unintentional injuries, mental and behavioural disorders, diabetes mellitus and diseases of the nervous system. 2–5 The impact of alcohol use extends beyond the individual, with adverse effects on families, communities and the wider economy. As it is a major contributor to socioeconomic inequalities in health, both in the UK and elsewhere,6–9 alcohol consumption is a modifiable risk factor we can address to reduce health inequalities. 10–12
Scotland and the UK
The level of alcohol-related harm in the UK, in general, and Scotland, in particular, is high. 13,14 Scotland has a higher rate of hospital admissions due to mental and behavioural disorders caused by alcohol [International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) code F10] than any other UK country, except Northern Ireland. 15 Scotland also has a better ratio of diagnosed to treated cases (1.0 in 2017–18) for these disorders than any other UK country,15,16 suggesting that further treatment provision in Scotland is not a complete answer. Meanwhile, Scotland’s socioeconomic relative health inequalities are increasing and alcohol is a factor in this. 17,18 Relative inequalities in alcohol-related deaths in Scotland are currently higher than for other conditions monitored, but they are fluctuating and, ultimately, declining over the longer term. 19 The Scottish Government has been implementing a range of strategies to reduce alcohol consumption, alcohol-related harms and health inequalities. 20
In Scotland, in 2018, nearly two-thirds of alcohol-specific deaths were from alcohol-related liver disease. 21 The percentage of alcohol-related deaths caused by liver disease peaked in the mid-2000s and since then has been declining, but is still historically high, having doubled since 1982 (from 40% to 81%). 22 Alcohol-related deaths are highest in people aged 50–70 years and men are approximately twice as likely as women to die (or be hospitalised) because of an alcohol-attributable condition. 21 Up to 80% of alcohol-specific deaths in the UK are caused by liver disease. 23 The burden of severely ill patients admitted to hospital with liver disease in the UK continues to increase. 15
Minimum unit pricing legislation
In May 2012, Scotland became the first country to pass legislation to introduce minimum unit pricing (MUP) without reference to beverage type, a politically high-profile measure. 24–26 Introducing MUP to the Scottish Government’s agenda was challenging and resulted in valuable lessons about policy implementation27 now being applied in England, which has yet to legislate for MUP,28 although one was implemented in Wales in early March 2020. 29
The UK Government withdrew proposals to introduce MUP in England. Researchers have described how the industry used direct and indirect lobbying of politicians and policy-makers, attempted to ‘undermine’ scientific evidence, made legal challenges and sought ‘partnership’ with government agencies. 30,31 An account of the demise of one such partnership (the public health responsibility deal in England32) contrasts with the more ambitious Scottish approach,26,27,33–35 in which some parts of the alcohol industry worked closely, but not in a formal partnership, with the Scottish Government and others [e.g. the Scottish Licensed Trade Association (Edinburgh, UK) shared a platform with the Scottish Health Action on Alcohol Project (Edinburgh, UK) lobbying in the European Union for MUP]. Therefore, the Scottish Government actively sought to implement a measure to affect alcohol harm by manipulating price, despite the opposition of some elements of the alcohol industry.
This resulted in the implementation of MUP, although there was a delay of 6 years due to a legal challenge from some elements of the industry. The effectiveness and feasibility of partnerships, like the public health responsibility deal, between government agencies and the alcohol industry in reducing drinking to safe levels have come into question in a recent paper that showed that, in England, 38% of the industry’s profits are generated from people drinking more than the safe drinking guidelines of 14 units per week or less. 36 The loss of this revenue would clearly have serious and undesirable effects for the industry. As profit-led organisations, the claims of some parts of the alcohol industry freely to support safe drinking could be seen as disingenuous.
Following the legal challenges of the Scotch Whisky Association (Edinburgh, UK) and others in October 2016, a second ruling by the Scottish Court of Session ruled in favour of the legality of MUP. 37 In the final appeal, in November 2017, the UK Supreme Court ruled in favour of the Scottish Government. 38 Secondary legislation set the level at £0.50 per unit and MUP was implemented on 1 May 2018. To continue after April 2024, the Scottish Parliament must vote in its favour. The evaluation of the impact of MUP, including this study, will inform that vote.
Chapter 2 Research objectives
Text in this chapter is reproduced with permission from Katikireddi et al. 39 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Minimum unit pricing of alcohol represents a high-profile public health policy that has the potential to bring about myriad impacts. As the policy was implemented in a manner that was outside the control of the research team and introduced across the whole of Scotland on a single date, we consider the policy to be a natural experiment. 40,41 As randomisation is not possible under such circumstances, our study design involves making comparisons between our intervention area (i.e. Scotland) and a control area (i.e. the north of England).
For our quantitative analyses, we estimated the impact of the policy on health outcomes of interest by conducting a difference-in-difference (DiD) analysis, in which we compared trends in health outcomes in intervention areas with comparable control areas. 42 In doing so, we sought to identify comparable cities that had not been subject to MUP and could, therefore, provide an indication of what would have happened if the policy had not been introduced (i.e. the counterfactual for the trend in health outcomes). For this reason, we specifically selected cities in the north of England (rather than the whole of England) that are more comparable to Scottish cities in socioeconomic characteristics and drinking patterns. As the study design compares changes in health outcomes within intervention areas with changes in health outcomes in control areas, the study design does not assume similar levels of alcohol-related outcomes. However, we assume that trends in health outcomes would have been parallel in intervention and control areas if the policy had not been implemented.
For qualitative analyses, our primary interest was in understanding the perceptions, lived experiences and behavioural responses of those affected by MUP, both stakeholders and higher-risk drinkers. As our interest is in exploring potential mechanisms through which health outcomes may arise, rather than establishing causal effects, we did not collect equivalent data from control areas. Instead, we focused on achieving diversity in relation to socioeconomic position for higher-risk drinkers and professional background for stakeholders. For both sets of interviews, we were also interested in better understanding the potential role of geography (particularly urban–rural and socioeconomic differences) and, therefore, ensured that recruitment captured variation across these characteristics.
Reproduced from the published protocol (in accordance with the CC-BY license),39 this project focuses on both intended and possible unintended consequences of the intervention. 43 Although intended consequences included reduced alcohol consumption and harm, a number of potential risks arising from the introduction of MUP have been identified by policy-makers, the alcohol industry and public health professionals:27
1. Consumers may switch to alternative sources of alcohol not subject to MUP so that the price paid does not increase. Such sources include both legal (internet sales from outside Scotland, legitimate cross-border purchase for own use,44 and home fermentation) and illegal sources (counterfeit, or stolen alcohol). 45,46
2. Increased alcohol-related harm could occur through substitution (e.g. to counterfeit or industrial alcohol associated with greater toxicity) or changed drinking patterns (e.g. moving from regular drinking to binge drinking). People at higher intensities of dependence on alcohol are likely to be at risk in these ways owing to more severe withdrawal symptoms if they cannot obtain sufficient alcohol to meet their level of physical dependence. 47,48
3. Displacement effects with reductions in alcohol-related harms being accompanied by increases in harms related to other substance use could be observed,49–51 and
4. MUP could unfairly penalise deprived populations less able to absorb the additional financial cost52 and this may adversely affect access to other essentials such as food.
5. There may be adverse economic impacts on the Scottish alcohol industry retailers and/or manufacturers.
As per our published protocol,39 a broad programme of research is being co-ordinated by Public Health Scotland (previously NHS Health Scotland) that:
. . . will report to Scottish Ministers and the Scottish Parliament between five and six years after the start of the policy. This programme includes analyses of administrative data and alcohol sales data. 53 The [report] described here complements the NHS-led work and has been funded by the National Institute for Health Research Public Health Research programme to collect primary data in three associated studies.
The studies described in this report will address the first four of these potential risks, although analysis of existing data sets will further address the potential impact on access to essential goods. A study has been commissioned from the University of Sheffield (Sheffield, UK) by NHS Health Scotland to assess the effects on those drinking at harmful levels. The economic impact on the Scottish alcohol industry will not be addressed by our project, but is the subject of a study funded through the Monitoring and Evaluating Scotland’s Alcohol Strategy (MESAS) studies managed by Public Health Scotland.
The overall aim of our study is to investigate the impacts of MUP on health harms (including by deprivation, sex and age subgroups). This includes assessing the extent to which specific unintended consequences occur.
Our more specific research objectives (ROs) and how they are addressed by specific study components (C1–C3) are summarised below:
RO1: To determine the impact of MUP on alcohol-related harms and drinking patterns for the overall population and by subgroups of interest (age, sex and socioeconomic position).
Emergency Department (ED) survey of alcohol-related attendances (C1);
Survey of alcohol-related behaviours (consumption patterns, alcohol spend, source of alcohol, move to other substances) in SHCs (C2).
RO2: To determine the impact of MUP on non-alcohol substance use, and other unintended impacts, for the overall population and by subgroups of interest (age, sex and socioeconomic position).
Survey of alcohol-related behaviours in Sexual Health Clinics (SHCs) (C2);
Qualitative focus group study and stakeholders (C3).
RO3: To describe changes in experiences and norms towards MUP and alcohol use following the introduction of MUP by subgroups of interest (age, sex and socioeconomic position).
Qualitative focus groups with young people/heavy drinkers and interviews with stakeholders from public services (C3).
Chapter 3 Literature review
Minimum unit pricing
Minimum unit pricing of alcohol is a novel public health policy that aims to reduce alcohol-related harms across the population. In May 2012, Scotland became the first country to pass legislation to introduce MUP without reference to beverage type, a politically high-profile measure. 24–26 There is an inverse link between alcohol price and consumption and harm, although the strength of the association varies between studies. 10,54–60 The World Health Organization recommends pricing policies as an important method for reducing alcohol-associated health issues. 61–63 Alcohol MUP is an ‘upstream’ public health policy that aims to reduce alcohol-related harms across the population by setting a floor price for alcoholic drinks based on the amount of pure alcohol that they contain. Unlike tax increases, MUP must be passed on to the customer, reducing the opportunity for retailers to sell cheap alcohol as a ‘loss-leader’ to draw in custom. Under MUP, there are no cheaper ways of obtaining retail alcohol. As a structural intervention,64 MUP is an example of primary prevention and more likely than more ‘downstream’ approaches, such as policing, drink-driving legislation and treatment, to reduce health inequalities in alcohol-related harm. We know from recently improved estimates that there is higher consumption among the most deprived working age males in Scotland,65 which suggests that MUP is likely to reduce inequalities in alcohol consumption, as well as ameliorating inequalities in the health problems alcohol brings.
Evidence for minimum unit pricing
Reviews of alcohol control policies, in general,66 and evaluating the strategy of MUP,67 in particular,60 were limited before our study was started. Minimum pricing policies, in general, aim to set price levels below which alcohol should not be sold, but most previous policies of this type have implemented minimum prices that vary across different types of products (or apply to only certain products), rather than on the basis of alcohol content. Recently, a report from the Northern Territory in Australia studied a minimum unit price (which applies across all alcohol drinks) of AU$1.30 per 10 g of pure ethanol implemented on 1 October 2018 and found declines in alcohol-related harm across a range of key areas after its introduction. These include a 23% fall in alcohol-related assaults; a 17.3% reduction in alcohol-related emergency department (ED) presentations; reduced child protection notifications, protection orders and out-of-home care cases; fewer alcohol-related road traffic injuries and fatalities; and fewer alcohol-related ambulance attendances. 68 The evaluation reviewed routine data for varying numbers of years (i.e. before and for the year or part year after the intervention) on wholesale alcohol supply, police data, ambulance attendances, ED attendances and hospital admissions, sobering up shelter use, treatment centre sessions, road traffic crashes, child protection price monitoring, licensing, sales of substitution commodities, school attendances and tourism. The study used time series analyses. A year before implementing this MUP, a banned-drinker register was implemented in the Northern Territory (1 October 2017) and police auxiliary liquor inspectors were introduced from June 2018. Two additional interventions ran in parallel to the Northern Territory MUP intervention, making it impossible to determine effects attributable solely to MUP, and meaning that we cannot directly compare MUP in Australia and MUP in Scotland.
A version of minimum pricing referred to as ‘reference pricing’, which is not based purely on alcohol content, has been implemented in varying ways across Canadian provinces, with the minimum cost of alcoholic drinks determined by beverage type and strength. Evaluations in some Canadian provinces have found reference pricing to be effective, resulting in reductions in alcohol consumption, alcohol-attributable hospital admissions and crime. 69–77 Scotland implemented MUP in a competitive alcohol market at a national level, in contrast to the locally applied but government-owned monopolies where Canadian provinces introduced reference pricing. A more recent Canadian study showed that alcohol-related deaths increased when the price level for the reference pricing was allowed to effectively decrease because of price inflation. 78 Therefore, it may be important to link the MUP level to inflation. The evidence from Canada is not fully conclusive. One of the Canadian studies, which focused on ED visits, found no reduction in overall visits for alcohol-related injuries, although alcohol-related motor vehicle injuries did fall. 69 The introduction of minimum pricing for spirits (but not other alcoholic drinks) within The Russian Federation was associated with reductions in alcohol-related mortality, but this was, of course, beverage specific. 79
In 2018, the cost of alcohol had not risen in line with the rise in disposable income in the UK and alcohol was 61% more affordable than it was in 1987. 80 According to the Bank of England, the consumer price inflation-adjusted price would be £0.58 per unit in 2018 (from a £0.50 level in 2012). Modelling suggested that MUP would be more effective than a similar rise in UK taxation in reducing alcohol consumption, especially among the most vulnerable (i.e. heavy drinkers in poverty). 10,11,55,63,81–84 Currently, the UK tax on alcohol is beverage specific and much lower for cider than for other beverages of the same strength. 85 Early Scottish evidence from other studies has shown that alcohol sales (as a proxy for consumption) reduced post MUP86–90 and confirmed that there was good compliance with the policy. 91 As we wrote this report, the Lancet Commission into liver disease in the UK15 mentioned the fall in the volume of pure alcohol sold80,88,89 and good compliance91 in Scotland following MUP implementation. Putting pressure on the UK Government, the Lancet Commission criticised a lack of action in implementing MUP and other effective policies (e.g. alcohol duty escalator and extension of the sugar levy to alcoholic drinks) in England.
Minimum unit pricing is a logical way to prioritise public health in alcohol pricing policy because harm relates more to the amount of alcohol consumed than to beverage type. However, beverages do not contain alcohol alone and there have been suggestions that ‘white’ drinks (e.g. white cider, vodka) that contain low levels of antioxidants may be particularly damaging to the liver. 92 Emerging evidence suggests that beer or cider and spirits are associated with greater all-cause mortality and more cardiovascular events than wine and champagne, using Cox’s proportional hazards and a large population sample of 446,439 current drinkers from the UK Biobank, with adjustment for various confounders, including deprivation. 93 Angus et al. 94 reviewed taxation policies by beverage type in European Union countries and concluded that they do not primarily aim to improve public health.
Minimum unit pricing has widespread support within the public health community, which may be accused of taking a too narrowly health-focused perspective and ignoring wider social issues, such as effects on employment, the economy and crime. 2,61,95 A wider evaluation programme, MESAS, led by NHS Health Scotland (now Public Health Scotland) addresses this point. Scottish public opinion on MUP, assessed through Twitter (URL: www.twitter.com, Twitter, Inc., San Francisco, CA, USA), was divided, but more positive than negative,47 especially in tweets from Scottish public health and alcohol policy organisations. There is international interest in MUP and the results from the Scottish evaluation are likely to inform change in many countries. A small study96 showed that a minimum unit price at the Scottish level would increase prices in over half of alcohol sold from an off-license in the USA. Australia is planning a modelling study that includes the effects of MUP among other pricing policies. 97
Need for a wide real-world evaluation at the system level
Modelling alone is not always sufficient proof to implement government health policy. In a democracy, laws setting social policy must be justifiable through stronger evidence, as feasible, of a net benefit to the public or at least preventing net harm. 98 Therefore, the MUP policy needed to be evaluated once implemented. NHS Health Scotland (now Public Health Scotland) is leading the Scottish Government’s wider evaluation of Scotland’s alcohol strategy through the MESAS programme. 80 MESAS originally focused on evaluating licensing reforms, delivery of alcohol brief interventions and specialist treatment services. Public Health Scotland is building on MESAS to comprehensively evaluate MUP by using routinely collected data to assess changes in price, consumption and alcohol-related harms at a population level that occur as a result. In addition, Public Health Scotland has commissioned a number of studies to evaluate MUP,99 some of which have already reported,90,91,100–103 with others reporting later (including in 2023). These studies will cover effects on the alcohol industry, crime and those drinking at harmful levels, among a number of other topics.
Owing to the lack of real-world MUP evaluation studies covering areas inaccessible through these routine data, other studies, including our own,39 were independently funded to work alongside MESAS in an integrated programme of evaluation. We gathered primary data to measure changes in drinking and acute health harms, the possible unintended consequences of MUP and the hypothetical differential impact on young people who, in Scotland and across the world’s affluent countries, are reducing their alcohol consumption. 104,105 On average, for people living in deprived areas, there is evidence of higher levels of alcohol consumption and larger numbers of people drinking above the safe drinking guidelines; however, there is also a larger number of non-drinkers in the most deprived groups65 and so there are also likely to be different effects in deprived areas.
Scotland is the first country to implement a national MUP based on only alcohol content and so the evaluation programme will provide the first real-world evidence about the effectiveness of MUP at £0.50 per unit (one UK unit is circa 8 g or 10 cc of pure alcohol). Early evaluation work has reported reductions in the volume of pure alcohol purchased88 and sold90,103 since the introduction of MUP in Scotland.
Policy variation between England and Scotland and the natural experiment opportunity
We used the policy variation between England and Scotland to design our cross-sectional natural experiment using a DiD analysis for our two quantitative components. There was a pre-MUP baseline and two post-MUP follow-up waves in EDs at two Scottish and two northern English comparator hospitals, and at three Scottish and three comparator northern English sexual health clinics (SHCs). Natural experiments have been successful in other health research settings and there is now good knowledge about their design and validity. 40,41 Our evaluation of the natural experiment is based on a similar framework to the portfolio of studies investigating smoke-free legislation in Scotland. 106,107
Our third component was qualitative and set in Scottish communities only.
Effects on health (intended impacts)
Changes in ED attendances attributable to alcohol are likely to indicate some short- to medium-term effects of MUP, but are not available from routine data.
Estimates of the exact proportion of ED admissions attributable to alcohol range from 2% to 40% and may rise to 70% at peak times. 108 A recent paper covering England puts the mean alcohol-related attendances at 11.7% and admissions at 9.2%. 109 However, the data were for 2009–10. Alcohol-related attendances to EDs that do not result in admission are not routinely collected and so will not be included in MESAS. There was, therefore, a need for robust, prospective evaluation evidence to measure the effectiveness of MUP in preventing alcohol-related harm seen in ED attendees, and to monitor possible differential impacts and potential adverse consequences.
Our primary data collection methods and tools were based on previous studies used to quantify the national prevalence of alcohol-related attendances in EDs in England. 110 Our study was informed by the experience of the Scottish Emergency Department Alcohol Audit, which was carried out across 15–20 hospitals throughout mainland Scotland between October 2005 and June 2007. 111 We used the Fast Alcohol Screening Test (FAST), which is a reliable and validated tool that is a shortened form of the Alcohol use Disorders Identification Test Consumption (AUDIT-C) questionnaire designed for use in EDs. 112 Although the Single Alcohol Screening Questionnaire is quicker,113,114 the FAST tool was better for our purpose because it not only quantifies levels of harmful alcohol use, but also allows detection of changes in drinking patterns. 115 Such information is currently not adequately collected within routine health surveys, particularly for deprived populations that are most likely to be affected by the intervention. 116 Assessment of drinking patterns is crucial, as different patterns of consumption (e.g. binge drinking compared with chronic levels of use) are associated with different patterns of health, burden on EDs109 and other social harms. 3,117
Unintended consequences
Sexual health clinics are potentially a good setting to see both the unintended and the hoped-for effects of MUP, as attendees are younger118 and may be more open to experimentation with substances. 119,120 People at more risk of sexually transmitted infections are also more likely to have higher alcohol consumption levels, take greater sexual risks,121 drink in on-licensed (clubbing) premises122 and have more diverse sexual orientation. 120 They were, therefore, a relevant population potentially at risk of displacement effects.
Some possible unintended consequences from MUP are indicated from research and some can be theorised from other knowledge, as indicated in Chapter 2.
Communities
As stated in our protocol:39
. . . qualitative research has investigated the policy process through which MUP developed in Scotland, including assessing the role of commercial interests, and seeking to identify transferable lessons for public health advocacy. 26,27,35,123–127 The influence of econometric modelling has been specifically investigated. 128,129 The dominant media discourses and the roles of different policy stakeholders in articulating arguments to the public have been explored using content analysis of newspaper reporting and trends in newspaper coverage have been tracked over time. 33,130–132 The views of the public and heavy drinkers around MUP as planned have also been investigated. 63,133–135 There remained a need to investigate the views, experiences and norms of local service delivery stakeholders, the public, and heavy drinkers about the MUP [policy and its consequences] as implemented.
The focus of this component was on non-alcohol substance use and other unintended impacts in addition to alcohol use.
Chapter 4 Emergency department component
Component-specific research objectives
Emergency department attendances are likely to be sensitive to changes in alcohol-related harms, as they reflect both acute and chronic health problems in the target population. Therefore, we assessed the impact of MUP on alcohol-related ED attendances and drinking patterns among the ED attendees, and across age group, sex and different socioeconomic groups. Currently, alcohol-related attendances to EDs that do not result in admission are not routinely collected. Information collected through routine health surveys, meanwhile, is not adequate to understand the drinking patterns among young people and deprived populations who are most likely to be affected by MUP. 65,136 Therefore, we collected primary data to examine the changes in alcohol-related attendance and diagnosis and the trend in patterns of alcohol consumption that occur as a result of MUP. The component addresses RO1, that is to determine the impact of MUP on alcohol-related harms and drinking patterns for the overall population and by subgroups of interest (age, sex and socioeconomic position).
Methodology
Component design
We employed a repeated cross-sectional natural experiment design to study the impact of introducing MUP in Scotland. The natural experiment was the introduction of MUP in Scotland and we used the north of England as the comparison group. The component involved an audit of all alcohol-related attendances at ED, anonymised administrative data provided from hospitals and a face-to-face interviewer-administrated survey to ED patients. The component methods and tools were based on previous studies of alcohol-related attendances in EDs in England110 and experiences from the Scottish Emergency Department Alcohol Audit. 111
Setting
We recruited EDs from two hospitals in Scotland (Edinburgh and Glasgow) and two in the north of England (Liverpool and Sheffield). Table 1 shows the 2019 population137 across four cities that were chosen for this component. These cities had comparable population size and population composition. Table 1 also presents the proportion of data zone (Scotland)138/lower-layer super output areas (LSOAs) (England)139 in the most deprived 10% in Scotland/England. Edinburgh and Sheffield are the less deprived areas, whereas Glasgow and Liverpool are the more deprived areas. Northern England was chosen as the comparison group because it had the most similar drinking patterns to Scotland in terms of higher levels of hazardous drinking and binge drinking, economics and culture. 140–142
| Profile | City | |||
|---|---|---|---|---|
| Edinburgh | Glasgow | Liverpool | Sheffield | |
| Total population (n) | 524,930 | 633,120 | 498,042 | 584,853 |
| Sex (%) | ||||
| Female | 51.2 | 51.0 | 50.1 | 50.2 |
| Male | 48.8 | 49.0 | 49.9 | 49.8 |
| Age group (years) (%) | ||||
| < 16 | 15.1 | 15.9 | 17.5 | 18.1 |
| 16–25 | 14.2 | 14.5 | 17.4 | 17.4 |
| 26–45 | 33.7 | 33.4 | 28.8 | 26.7 |
| 46–65 | 22.7 | 23.7 | 22.5 | 22.6 |
| ≥ 66 | 14.2 | 12.6 | 13.8 | 15.3 |
| Median age (years) | 36.5 | 35.6 | 34.8 | 35.4 |
| Deprivation | ||||
| Proportion (%) of data zone/LSOAs in the most deprived 10% nationally | 6.6 | 46.2 | 48.7 | 23.8 |
Data collection took place over three 3-week waves. The baseline wave was conducted in February 2018 before the implementation of MUP on 1 May 2018. There were two post-implementation follow-ups in September/October 2018 and February 2019. In each wave, data collection took place from 20.00 until 03.30 the following day from Thursday to Sunday, and from 09.00 to 16.30 on Monday to Wednesday.
We also requested anonymised information (i.e. sex, age group and diagnoses) collected routinely on all attendees over the 3-week collection periods for each wave.
Participant selection
The target population was all patients aged ≥ 16 years who attended an ED to receive acute treatment for a health condition. Trained research nurse interviewers considered all patients aged ≥ 16 years for approach and decided whether or not to approach them based on the following exclusion criteria:
-
patient too unwell
-
too distressed
-
grossly intoxicated (alcohol)
-
grossly intoxicated (drugs)
-
cognitive impairment
-
police in attendance
-
clear language barrier and no interpreter available
-
patient already participating
-
routine follow-up that has been instigated by ED staff
-
patient left department
-
patient admitted
-
staff safety issue
-
end of shift
-
dead on arrival
-
other.
Research nurse interviewers recorded reasons for not approaching, as well as the sex and age group of the patients who were not approached.
Potential interviewees were then given written information about the component and had up to 40 minutes to decide whether or not to take part. Face-to-face structured interviews were carried out by interviewers using iPads (Apple Inc., Cupertino, CA, USA). There was a formal screening where the potential interviewees were asked eligibility questions before consent was taken. The eligibility criteria were:
-
aged ≥ 16 years
-
able to speak English or interpreter available
-
a new ED presentation during the shift
-
conscious
-
physically and mentally well enough
-
sober enough (alcohol)
-
sober enough (drug)
-
still in the department (i.e. had not left or been admitted)
-
safe for staff to approach.
Eligible interviewees were asked to sign their consent on an iPad and whether or not they further consented to linkage of their hospital notes to the interview data. For interviewees who consented to data linkage, we requested demographic characteristics (i.e. date of birth, sex and postcode), attendance details, discharge status and diagnoses for attendances. More details about reasons for not being approached, interviews being terminated and failing the inclusion criteria can be found in Appendix 2, Tables 14–16.
Variables
Outcomes
The primary outcome of interest was the proportion of alcohol-related attendances among all ED patients we recorded through either observation or interview. We used a dichotomised score, where 1 indicated that the attendance was alcohol related and 0 indicated that the attendance was not alcohol related. Attendance was considered alcohol related if the attendee was not approached because of alcohol intoxication, if the potential interviewee was ineligible because of being not sober enough due to alcohol, if the interviewee had binged (≥ 6/8 units for women/men) in the last 24 hours or if the attendee self-reported that the attendance was alcohol related because of their own or another’s drinking.
We also analysed a range of secondary outcomes that were related to alcohol-related diagnosis, alcohol use and drinking patterns. Table 2 lists all the secondary outcomes and the corresponding analytic samples. Most of the secondary outcomes were binary, unless specify otherwise.
| Type of outcome | Sample | Outcome |
|---|---|---|
| Primary | All recorded attendees | Alcohol-related attendance |
| Secondary | All attendees | Alcohol-related diagnosis |
| All respondents | Current alcohol use | |
| Binge drinking in the past week | ||
| Binge drinking in the past 24 hours | ||
| Respondents who were current drinkers | FAST score | |
| Alcohol misuse (FAST score ≥ 3) | ||
| Increased alcohol use in the past year | ||
| Place of last drink (private location) | ||
| Place of last drink (on-licensed premise) |
Alcohol-related diagnosis
A diagnosis was alcohol related if attributable to alcohol consumption according to the definition used previously in a burden of disease study by NHS Health Scotland. 5 Appendix 2, Table 17, lists the alcohol-related conditions that are based on ICD-10 codes. 143 Conditions where alcohol is the sole clinical cause are considered as wholly alcohol-attributable conditions, whereas conditions where alcohol may be one of the causative factors are considered as partially attributable. 144 Based on this definition, we further categorised the alcohol-related conditions as wholly chronic, wholly acute, partially chronic and partially acute. A number of diagnoses are recorded in hospital data for attendees. We carried out analyses for both all diagnoses and for the primary (first in order) diagnosis only.
Current alcohol use
All respondents were asked whether or not they had ever had a drink of alcohol that was more than a sip in the past year. Those who answered ‘yes’ were classified as ‘current drinker’, whereas those who answered ‘no’ were considered as ‘not a current drinker’.
Binge drinking in the past week
Current drinkers were asked what was the largest number of drinks they had consumed on any 1 day in the last week. Those who answered > 6 or 8 units (for women or men) were classified as ‘binge drinker in the past week’, whereas those who had < 6 or 8 units (for women or men) were classified as ‘non-binge drinker in the past week’. As non-current drinkers did not have any drinks in the past week, they were also classified as ‘non-binge drinker in the past week’.
Binge drinking in the past 24 hours
Current drinkers were also asked how many drinks they had over the past 24 hours. Again, those who had > 6 or 8 units (for women or men) were classified as ‘binge drinker in the past 24 hours’, whereas those who had < 6 or 8 units (for women or men) and those who indicated that they were not current drinkers were classified as ‘non-binge drinker in the past 24 hours’.
Fast Alcohol Screening Test score
A reliable validated tool, the FAST, which is a shortened form of the AUDIT-C questionnaire designed for use in ED, was used to quantify levels of harmful alcohol use. 112,115 Current drinkers were asked to answer four questions related to their current drinking habits. The FAST score was the overall score created by summing up the answers of these questions. The score ranged from 0 to 16, with a higher score indicating more problematic drinking behaviours. We analysed FAST score as a continuous measure.
Alcohol misuse
Current drinkers who scored ≥ 3 on the FAST were classified as ‘alcohol misuse’, whereas those who scored < 3 were classified as ‘not alcohol misuse’.
Increased alcohol use in the past year
Current drinkers were asked if their alcohol consumption changed over the last 12 months. Those who answered ‘more than 12 months ago’ were classified as ‘increased alcohol use’, whereas those who answered ‘less than 12 months ago’ or ‘about the same’ were classified as ‘did not increase alcohol use’.
Place of last drink (private location)
Current drinkers were asked where they had their last drink. For those who answered ‘home’, ‘work’ or ‘friend/family home’ were classified as ‘private drinking’, and ‘no’ otherwise.
Place of last drink (on-licensed premise)
Current drinks who answered ‘pub’ or ‘club’ as their last drinking location were classified as ‘on-licensed premise’, and ‘no’ otherwise.
Covariates
Our primary outcome focuses on all ED attendees who were recorded by research nurse interviewers. Information about attendees who were not interviewed was limited to reasons for not approaching/interviewing, as well as whether or not they were too intoxicated to participate. Interviewers also recorded sex and age group for unapproached attendees based on triage data or their observation. This information allowed us to adjust for sex and age group in the analysis of the primary outcome.
The anonymised data from the hospitals contained information about sex and age group of all attendees. Therefore, we adjusted for sex and age group in the analysis of alcohol-related diagnosis.
The questionnaire covered a range of sociodemographic data, including sex, age, ethnicity, first four digits of postcodes, employment status, marital status and housing ownership. Area-based deprivation scores were assigned to each respondent based on their postcodes. We used the 2011 Carstairs area deprivation scores calculated for wards in England and postcode sectors in Scotland. 145,146 This gave geographies with similarly sized populations and so a measure of deprivation comparable across all four cities and the two countries. In Scotland, postcode sectors were sometimes split between two Carstairs deciles when a postcode sector covered two councils. We used a population weighting method to assign a Carstairs score to the whole postcode dependent on the population split between the councils. These variables were used as covariates when we analysed the secondary outcomes.
Statistical considerations
Sample size
As stated in our published protocol:39
. . . based on the experience of the 24 hour survey of EDs in England,111 and the assumption that at least 50% of eligible ED attendees would be recruited, we anticipated that the four sites would result in 940 recruits per week. Recruiting over three three-week data collection – giving a total sample size of 5640 – would mean that we would be highly powered (> 80%) to detect an effect size of ± 5% in the proportion of alcohol-related attendances from an estimated 30% with 95% significance. We used a base rate of 30% informed by the 24 hours audit of EDs in England,111 and assumed a 5% decrease would be of public health importance and may be expected based on current evidence. For subgroup analyses, we would have good power (> 80%) to detect an effect size of 0.23 on the FAST score among those from the most deprived quintile (estimated to be 25% of attendances), and an effect size of 0.27 among those aged 18–24 (estimated to be 15% of attendances).
Statistical analysis
We evaluated the impact of the introduction of MUP by fitting fixed-effects multivariate regression models. For our main analysis, we fitted the following models:
in which y is the outcome variable, country is a dummy variable where 0 = England and 1 = Scotland, time is another dummy variable where 0 = before the introduction of MUP and 1 = after the introduction of MUP, hospital is a series of dummy variables (0 = Edinburgh, 1 = Glasgow, 2 = Liverpool and 3 = Sheffield), wave is a series of dummy variables (0 = wave 1, 1 = wave 2 and 3 = wave 3), MUP is the interaction term between country and time (i.e. a dichotomous indicator with the value 1 for patients who attended Scottish EDs after the implementation of MUP and 0 otherwise) and ε is the residuals. Our coefficient of interest is β1, the DiD estimate, which is defined as the difference in outcome between Scotland and England before and after the MUP was introduced in Scotland. We used logistic regression for binary outcomes and linear regression for continuous outcome.
Model 1 is the unadjusted model with the DiD estimate and fixed effects for country and time. The country fixed effects control for all unobserved country-specific factors that are time invariant, whereas the time fixed effects account for all seasonal effects over time. In model 2, we further adjusted for hospital and wave fixed effects. As the country and time fixed effects in the unadjusted model were confounded with the newly included hospital and wave fixed effects, we omitted them from model 2. In the final model, model 3, we further included a set of covariates (i.e. sex, age group, ethnicity, employment status, marital status, housing ownership and Carstairs deprivation score). We also performed stratified analysis to examine the primary and secondary outcomes by sex, age group, ethnicity, employment status, marital status and housing ownership.
Appendix 2 provides the percentage of missing data of each demographic (see Appendix 2, Tables 18–20) and outcome variable (see Appendix 2, Tables 21–25) by country and wave. We imputed all variables in the data set (except the anonymised data set requested from hospitals) using multiple imputation. A total of 20 imputed data sets were created and subsequently analysed in R using the MICE (multivariate imputation via chained equations) package (version 3.70) (The R Foundation for Statistical Computing, Vienna, Austria). 147 The parameters from the models were estimated in each imputed data set separately and combined using Rubin’s rules.
We included non-response weights in the imputation process and analysis regression models. Using the anonymised information for all attendees from the hospitals, we were able to calculate inverse probability weights to adjust for the differences in distribution of sex and age group between attendees and interviewees.
We undertook various sensitivity analyses to investigate whether or not our results were sensitive to the model specification and the selection bias of the sample. To examine whether or not our findings were sensitive to the FAST cut-off score, we analysed the effect of MUP against FAST cut-off points of ≥ 2 (hazardous drinker), ≥ 4 (harmful drinker) and ≥ 6 (dependent drinker). These cut-off points were validated using data from the Adult Psychiatric Morbidity Survey 2007. 148 We replicated the analyses on alcohol-related attendance (primary outcome) and alcohol-related diagnosis (secondary outcome) using the sample based on interviewees and by including ethnicity, employment status, marital status, housing ownership and Carstairs deprivation score as covariates. Finally, we performed the weighted and unweighted analyses on the complete cases, which included only cases with no missing data on both outcome variables and covariates.
Challenges for data collection
The inherent challenges for the ED data collection are consistent with challenges faced in other natural experiments, notably in minimising selection bias between waves. 149
Training
A single-site first pilot was carried out and each individual site had a further pilot. Each study site underwent a similar training session before each wave, and data collection times sites and methods were confirmed at baseline and reiterated in the training for subsequent waves. At the EDs, there was a 3- to 4-hour face-to-face training session. The nurses who had been recruited to conduct the data collection underwent the training. It was occasionally challenging to have all staff present for the training because of absence or if staff were required to keep the service running while the training was delivered. Where staff could not attend the face-to-face training, the lead nurse was given the training presentation to cascade to any staff who were unable to attend. Training was very interactive, consisting of a 15- to 20-minute presentation, outlining the aims of the research and an overview of the research tools, followed by a hands-on opportunity to use the iPads/paper questionnaires, followed by role play completion of the questionnaire, with certain scenarios presented by the trainers.
During the run up to baseline data collection, we held informal ‘huddles’ with ED sites by telephone conference to allow for the discussion of informal queries. These were useful both in resolving queries and keeping relationships with sites healthy.
Data collection times
The component protocol stipulated that all sites should collect data at the same time. ED data collection was from 09.00 to 16.30 Monday to Wednesday and from 20.00 until 03.30 from Thursday to Sunday over three 3-week periods. We could not go outside these times, but a 30-minute period after each shift was allowed for the completion of already started cases.
Research tools
Each site was given the same mechanism for data capture. This involved purchasing iPads for each ED site, making sure that all iPads were updated with the same version of iOS, that they were connected to the King’s College London (London, UK) server and that they had the same version of the data collection application (app) and all were able to access the internet through Wi-Fi within the site or through 4G mobile data. It was also imperative that each site updated the data collection software at the start of each wave of data collection to ensure that any data collection app updates were implemented and that all sites were working from the same version of the app. Sites were asked to manage the use of their iPads, ensuring that they were charged and data synchronised at the end of each shift. Although this was complex to administer across sites, we were able to synchronise the iPads successfully and this challenge was overcome.
Maintaining similar and adequate staffing levels
Given the busy nature of EDs, and we always seemed choose busy periods, it was difficult for the lead nurse at each site to schedule nurse shifts for the duration of the data collection. It was recommended that each shift had three members of staff allocated. Two research nurses would interview participants and one team member would provide administrative support. There were slightly differing models of utilising the staff, depending on the requirements of each ED. For example, in Edinburgh, one administrator was dedicated to monitoring which patients were eligible for interview, with two nurses conducting the interviews. In other sites, three nurses were used to conduct interviews. It was appropriate that each site was able to manage this individually, as the physical space and triage systems were different in each ED and it was felt that local sites were best placed to decide how to manage this aspect of data collection. However, consistency across waves was achieved by using a similar delivery model at each wave and regular weekly catch-ups with sites during each wave.
Confidentiality
The physical space in each ED was different, but a common issue reported by nurses was maintaining confidentiality during the interviews. Where possible, the interview was conducted in a private room; however, this was not always possible. Nurses were advised to respect patient confidentiality at all times, in line with their standard practice. This meant not conducting interviews within earshot of other patients or family members. This not only avoided breaches of confidentiality, but also encouraged interviewees to answer freely and honestly without fear of judgement from others.
Missing participants
On particularly busy shifts, there was potential to ‘miss’ patients who were in the ED for a short period of time. Nurses minimised this by monitoring patient flow on the ED computer system and approaching them at the earliest appropriate time.
Language barriers
It was difficult to ensure that there were always interpretation services available. Staff were trained to make use of interpretation services (i.e. a face-to-face or telephone-based interpreter) where possible; however, nurses informed the research team that this was often not possible as it could take time to connect with an interpreter, which would lead to missing other participants. Nurses were instructed not to make use of participants’ family members to translate, so as not to breach the participants’ confidentiality. There were very few cases recorded as not being able to participate because of language issues.
Avoiding disruption to regular workings of the emergency departments
Throughout the data collection process, it was essential to avoid disruption to the work of the ED for participants and other patients who were in attendance at the ED. Nurses reported that they were occasionally asked to contribute to non-research-related tasks and the principal investigator for each site was encouraged to instruct ED colleagues that the research nurses were not to be asked to complete non-research-related work unless it was completely necessary.
Obtaining sufficient recruitment numbers
Eligibility criteria meant that a number of staff could not be interviewed, but we collected observational data to measure our primary outcome. It was often a chaotic data collection environment; however, as a condition of ethics approval, we did not want to disrupt normal care for patients and so interviews were terminated while in process if a patient was to be urgently admitted.
Contextual issues
The ‘Beast from the East’ snowstorm closed data collection at most sites on 28 February 2018 and that day was excluded for all sites. There were also some staffing issues with, for example, staff off sick. Generally, the timeline for preparation for collecting data was short because of late announcement of the legality and then the relatively swift implementation date.
Ethics approval
Ethics approval had been obtained from the NHS through the Scotland A Research Ethics Committee, ED Research Ethics Committee (reference 12/SS/0120) and SHC Research Ethics Committee (reference 12/SS/0121). The Stirling Management School at the University of Stirling approved the qualitative studies for in-depth interviews with local stakeholders (application number 32) and focus group research with drinkers (application number 33). The paper meets the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist criteria for cross-sectional studies and the TREND (Transparent Reporting of Evaluations with Nonrandomized Designs) criteria for reporting evaluations with non-randomised designs. The trial registration number is ISRCTN16039407.
Changes to protocols
Changes to protocols were notified to the Ethics Committee. Version 1 was the original protocol from 1 June 2012.
The next version (v2.1, dated 13 February 2017) separated the protocols for the ED component and the sexual health component and entered this information into the new standard SPHSU (MRC/CSO Social and Public Health Sciences Unit, University of Glasgow) template. The mechanism of data collection was altered from paper and pen data collection to the use of iPads.
The following version (v2.2, dated 1 July 2017) added reviewer comments to v2.1, but there were no substantive changes.
The next change (v2.3, dated 1 August 2017) was as a result of the delay to the implementation of MUP. The chief investigator moved to Australia and a new chief investigator was appointed, and there were changes to the sponsor, local lead investigators, sites and timescales, and iPads were introduced for data collection. Our letter to the National Institute for Health Research (NIHR) (dated 21 August 2017) gives further details (see Report Supplementary Material 1).
Protocol v2.4 (dated 20 August 2017) further updated the timescales.
The next change (v2.5, submitted in December 2017), covered the following points and included questionnaire changes arising from the pre pilot:
-
apply for the introduction of a fully electronic consent process
-
change the principal investigator name for Liverpool – should now be Dr Lynn Owens
-
ask if we can collect full postcode data rather than first four digits
-
reasons for did not complete
-
change in shift times
-
update posters to be more eye catching
-
update paper copy of MUP questionnaire to be more user friendly (see Appendix 4)
-
changes to questionnaire and new consent form (see Appendix 4)
-
include data linkage information on iPad
-
changes to information sheet (see Report Supplementary Material 2).
The next change (v2.6) was submitted to the Ethics Committee on 19 January 2018. In that submission, we introduced signed electronic consent (as this was considered more ethically acceptable than a tick box), an amendment to the poster to remove any mention of MUP and a new high-awareness banner poster.
The change in February 2018 was to the information sheet for Scotland (and consent form, by simply using the version number rather than date to cross-reference). The change provided a clearer explanation of the Community Health Index number and confidentiality, and did not require a change to the protocol:
This is a unique 10-digit number that includes your date of birth and a code for gender. We take confidentiality very seriously, and all records are de-identified and held on encrypted technology. Only trained staff have access to your information, and all information is stored securely.
Emergency department study patient information sheet (Scotland) v2 5 3
The final change (v2.7, in May 2018), was minor and concerned a change to a website address and a new member of the investigative team.
Results
Descriptive of sample
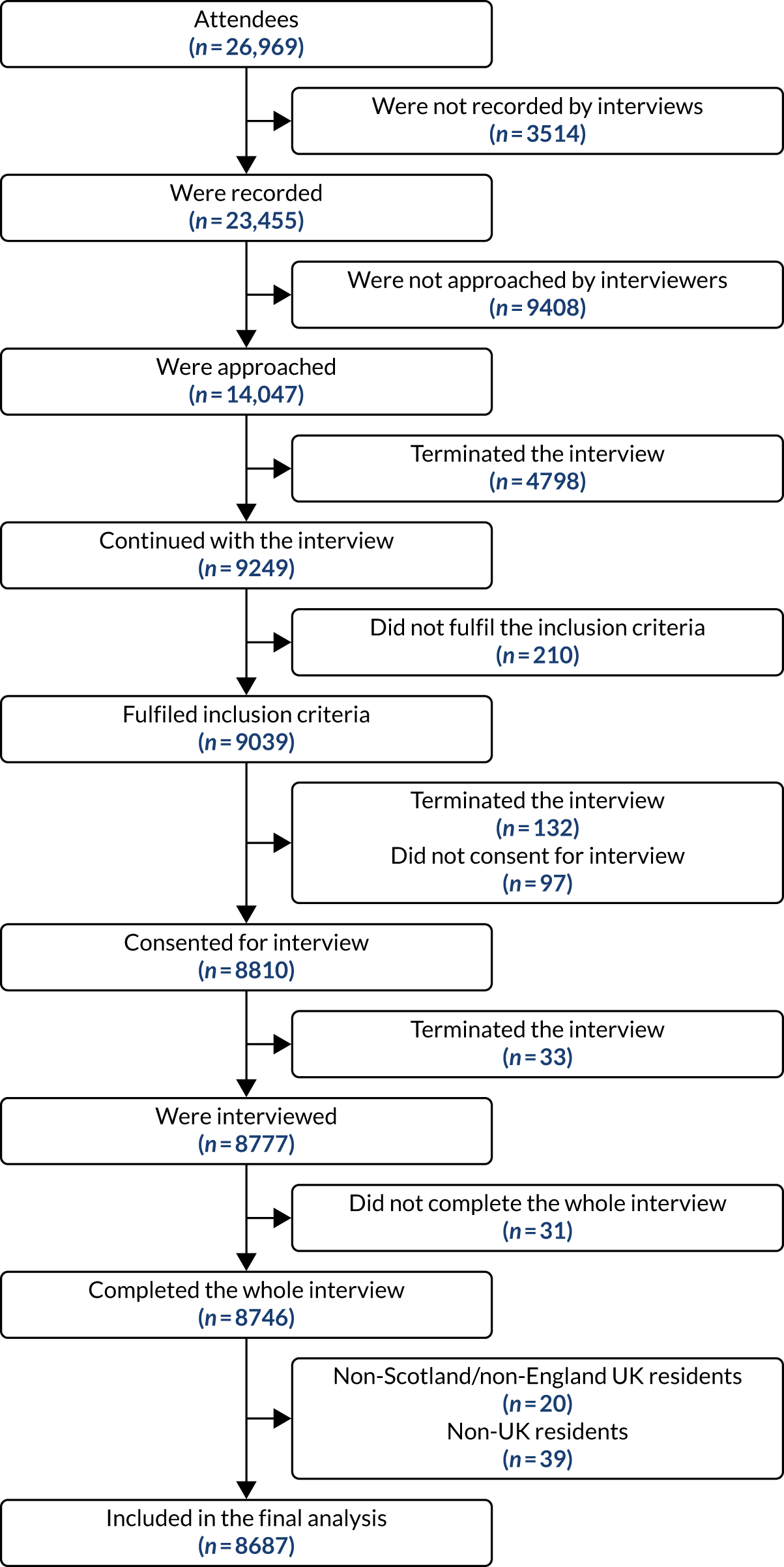
A total of 26,969 patients aged at least 16 years visited the EDs during the three study periods, and 23,455 (87.0%) of them were recorded for assessment of our primary outcome (not all interviewed) by research nurses. Among those who were recorded, 14,047 (59.9%) of them were approached and 12,249 were identified to be eligible to participate in the component, of whom 8746 (71.4%) completed the interview (Table 3). Figure 1 illustrates the flow chart that summarises the component participants in all four EDs and three waves.
| Site | Attendees | Wave 1 | Wave 2 | Wave 3 | Overall |
|---|---|---|---|---|---|
| Edinburgh | Number of attendees | 2195 | 2381 | 2446 | 7022 |
| Number of recorded attendees | 2109 | 2357 | 2428 | 6894 | |
| Number of approached attendees | 1322 | 1662 | 1657 | 4641 | |
| Number of eligible attendees | 1149 | 1428 | 1496 | 4073 | |
| Number of completed interviews | 932 | 1041 | 1105 | 3078 | |
| Glasgow | Number of attendees | 2151 | 2351 | 2527 | 7029 |
| Number of recorded attendees | 1566 | 1787 | 1960 | 5313 | |
| Number of approached attendees | 874 | 1034 | 1049 | 2957 | |
| Number of eligible attendees | 776 | 879 | 910 | 2565 | |
| Number of completed interviews | 631 | 681 | 707 | 2019 | |
| Liverpool | Number of attendees | 1744 | 2023 | 1956 | 5723 |
| Number of recorded attendees | 1096 | 1575 | 1545 | 4216 | |
| Number of approached attendees | 640 | 1278 | 1257 | 3175 | |
| Number of eligible attendees | 556 | 1061 | 1152 | 2769 | |
| Number of completed interviews | 402 | 671 | 611 | 1684 | |
| Sheffield | Number of attendees | 2213 | 2465 | 2517 | 7195 |
| Number of recorded attendees | 2156 | 2394 | 2482 | 7032 | |
| Number of approached attendees | 903 | 1160 | 1211 | 3274 | |
| Number of eligible attendees | 805 | 984 | 1053 | 2842 | |
| Number of completed interviews | 599 | 724 | 642 | 1965 | |
| Overall | Number of attendees | 8303 | 9220 | 9446 | 26,969 |
| Number of recorded attendees | 6927 | 8113 | 8415 | 23,455 | |
| Number of approached attendees | 3739 | 5134 | 5174 | 14,047 | |
| Number of eligible attendees | 3286 | 4352 | 4611 | 12,249 | |
| Number of completed interviews | 2564 | 3117 | 3065 | 8746 |
FIGURE 1.
Flow chart of study participants. As described in Participant selection, people who were too drunk to be interviewed were classified as not approached or terminated and recorded as too drunk for inclusion as alcohol related.
We calculated two response rates: (1) the realistic response rate uses a denominator of all eligible attendees and (2) the absolute response rate uses all recorded attendees as the denominator. Table 4 presents both response rates by wave and hospital. The response rates in Scotland were generally higher than those in England. The overall realistic response rates decreased over the three waves from 78.0% in wave 1 to 71.6% in wave 2 and to 66.5% in wave 3. Across the three waves, Liverpool had the lowest realistic response rate (60.8%) among four hospitals. Meanwhile, Sheffield had the lowest absolute response rate (27.9%).
| Site | Response rate | Wave 1 (%) | Wave 2 (%) | Wave 3 (%) | Overall (%) |
|---|---|---|---|---|---|
| Edinburgh | Realistic | 81.1 | 72.9 | 73.9 | 75.6 |
| Absolute | 44.2 | 44.2 | 45.5 | 44.6 | |
| Glasgow | Realistic | 81.3 | 77.5 | 77.7 | 78.7 |
| Absolute | 40.3 | 38.1 | 36.1 | 38.0 | |
| Liverpool | Realistic | 72.3 | 63.2 | 53.0 | 60.8 |
| Absolute | 36.7 | 42.6 | 39.5 | 39.9 | |
| Sheffield | Realistic | 74.4 | 73.6 | 61.0 | 69.1 |
| Absolute | 27.8 | 30.2 | 25.9 | 27.9 | |
| Overall | Realistic | 78.0 | 71.6 | 66.5 | 71.4 |
| Absolute | 37.0 | 38.4 | 36.4 | 37.3 |
We performed Pearson’s chi-squared tests to compare the sex and age differences between respondents (those who completed the interview) and the sampling frame (Table 5). In wave 1, there were no significant differences on sex (except in Glasgow, which had fewer females than expected) and no differences on age group (except in Edinburgh and Glasgow, where respondents were younger than expected in both sites). In wave 2, ED respondents differed from the sampling frame on sex in Glasgow (fewer females than expected) and on age group in all sites (respondents were generally younger in all sites). For wave 3, we did not see any significant difference by sex in any of the sites. However, there were significant differences on age group in Edinburgh, Liverpool and Sheffield (respondents were younger than the sampling frame). The differences between waves were small for sex, but there were larger differences for age groups. Despite these differences, inverse probability weights were applied in all analysis models.
| Site | Difference | Wave 1 | Wave 2 | Wave 3 | Overall | ||||
|---|---|---|---|---|---|---|---|---|---|
| χ2 | p-value | χ2 | p-value | χ2 | p-value | χ2 | p-value | ||
| Edinburgh | Sex | 4.8 | 0.028 | 6.6 | 0.010 | 1.0 | 0.315 | 11.0 | 0.001 |
| Age | 13.1 | 0.005 | 27.9 | 0.000 | 7.6 | 0.054 | 43.7 | 0.000 | |
| Glasgow | Sex | 1.2 | 0.267 | 0.0 | 0.992 | 0.7 | 0.419 | 1.3 | 0.251 |
| Age | 69.1 | 0.000 | 43.5 | 0.000 | 29.3 | 0.000 | 132.5 | 0.000 | |
| Liverpool | Sex | 1.1 | 0.295 | 1.1 | 0.298 | 0.0 | 0.945 | 1.2 | 0.267 |
| Age | 3.7 | 0.295 | 23.1 | 0.000 | 10.2 | 0.017 | 29.8 | 0.000 | |
| Sheffield | Sex | 0.7 | 0.390 | 1.2 | 0.277 | 1.9 | 0.168 | 0.1 | 0.724 |
| Age | 7.7 | 0.052 | 15.7 | 0.001 | 21.8 | 0.000 | 37.2 | 0.000 | |
| Overall | Sex | 3.5 | 0.060 | 2.1 | 0.143 | 0.0 | 0.847 | 4.2 | 0.041 |
| Age | 53.9 | 0.000 | 82.9 | 0.000 | 55.6 | 0.000 | 189.1 | 0.000 | |
Descriptive statistics
The demographic characteristics of all attendees, attendees who were recorded by nurse interviewers and those who completed the interview are shown in Tables 6 and 7. The analysis for the primary outcome focused on the sample of recorded attendees (n = 23,455). Meanwhile, the analytic sample for alcohol-related diagnosis was based on all attendees. As the diagnostic data from the Liverpool ED did not comply with ICD-10 codes, 5723 cases from Liverpool were excluded from the analysis and, hence, the total number of attendees in the analytic sample became 21,246.
| Characteristic | All attendees, n (%) | Attendees recorded by interviewers, n (%) | ||
|---|---|---|---|---|
| Scotland (N = 14,051) | England (N = 12,918) | Scotland (N = 12,207) | England (N = 11,248) | |
| Sex | ||||
| Female | 7212 (51.3) | 6552 (50.7) | 6131 (50.2) | 5634 (50.1) |
| Male | 6837 (48.7) | 6366 (49.3) | 6015 (49.3) | 5499 (48.9) |
| Non-binary | 2 (0.0) | 0 (0.0) | 2 (0.0) | 0 (0.0) |
| Missing | 0 (0.0) | 0 (0.0) | 59 (0.5) | 115 (1.0) |
| Age (years) | ||||
| 16–25 | 2509 (17.9) | 2725 (21.1) | 2450 (20.1) | 2210 (19.6) |
| 26–45 | 4211 (30.0) | 3830 (29.6) | 3769 (30.9) | 3119 (27.7) |
| 46–65 | 3832 (27.3) | 3081 (23.9) | 3155 (25.8) | 2571 (22.9) |
| ≥ 66 | 3499 (24.9) | 3251 (25.2) | 2762 (22.6) | 2846 (25.3) |
| Missing | 0 (0.0) | 31 (0.2) | 71 (0.6) | 502 (4.5) |
| Characteristic | Scotland (N = 5059) | England (N = 3628) |
|---|---|---|
| Sex, n (%) | ||
| Female | 2483 (49.1) | 1854 (51.1) |
| Male | 2574 (50.9) | 1774 (48.9) |
| Non-binary | 2 (0.0) | 0 (0.0) |
| Age (years), n (%) | ||
| 16–25 | 1137 (22.5) | 861 (23.7) |
| 26–45 | 1613 (31.9) | 1146 (31.6) |
| 46–65 | 1352 (26.7) | 901 (24.8) |
| ≥ 66 | 957 (18.9) | 720 (19.8) |
| Ethnicity, n (%) | ||
| White | 4717 (93.2) | 3172 (87.4) |
| Non-white | 325 (6.4) | 438 (12.1) |
| Missing | 17 (0.3) | 18 (0.5) |
| Employment status, n (%) | ||
| Employed | 2590 (51.2) | 1690 (46.6) |
| Economically inactive | 1938 (38.3) | 1479 (40.8) |
| Unemployed | 498 (9.8) | 431 (11.9) |
| Missing | 33 (0.7) | 28 (0.8) |
| Marital status, n (%) | ||
| Married/co-habiting | 2116 (41.8) | 1453 (40.0) |
| Separated/divorced/widowed | 770 (15.2) | 547 (15.1) |
| Single | 2097 (41.5) | 1588 (43.8) |
| Missing | 76 (1.5) | 40 (1.1) |
| Housing ownership, n (%) | ||
| Owner occupied | 1917 (37.9) | 1285 (35.4) |
| Rented | 1306 (25.8) | 1207 (33.3) |
| Housing association/council | 888 (17.6) | 446 (12.3) |
| Other | 881 (17.4) | 627 (17.3) |
| Missing | 67 (1.3) | 63 (1.7) |
| Carstairs deprivation score | ||
| Mean (SD) | 7.06 (2.60) | 7.37 (2.54) |
| Median (minimum, maximum) | 8.00 (1.00, 10.0) | 8.00 (1.00, 10.0) |
| Missing, n (%) | 54 (1.1) | 166 (4.6) |
A total of 8746 attendees completed the interview (see Table 3). We excluded those who lived outside Scotland and England (n = 20) and non-UK residents (n = 39). As a result, 8687 respondents were included in the analytic sample for the following secondary outcomes: current alcohol use, binge drinking in the past week and binge drinking in the past 24 hours. The remaining six secondary outcomes [FAST score, alcohol misuse, binge drinking (at least) weekly, increased alcohol use in the past year, private location as place of last drink and on-licensed premise as place of last drink] were based on respondents who were current drinkers (n = 6991). Although there are some slight differences in the demographic distribution between the Scottish and English samples, we accounted for these in our DiD analysis.
Main analysis
Primary outcome
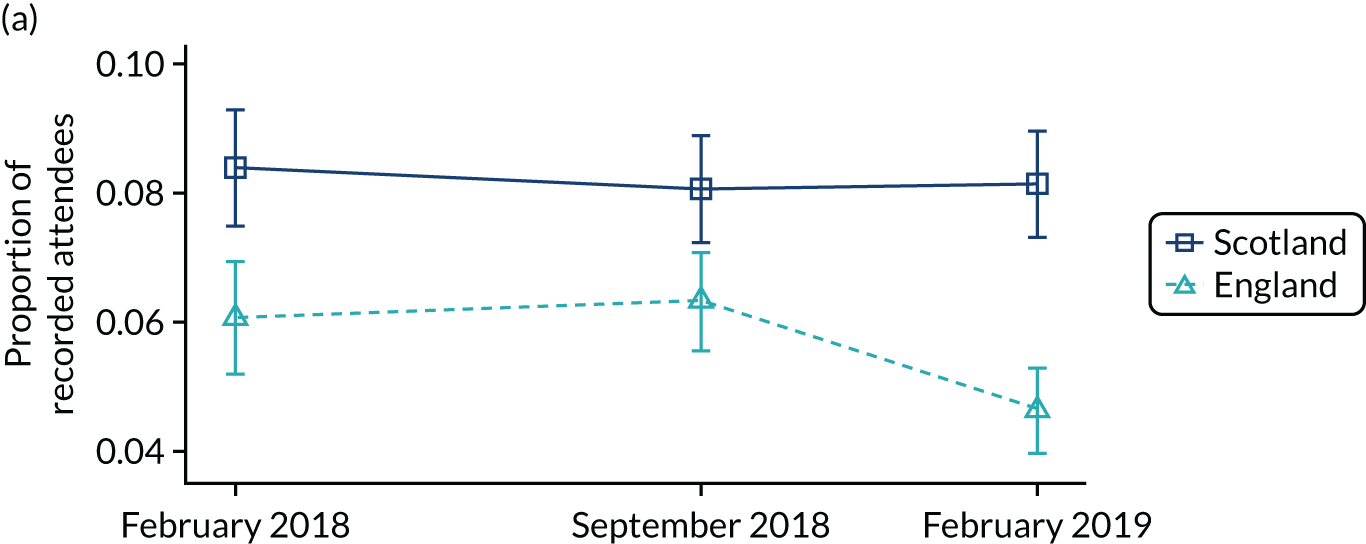
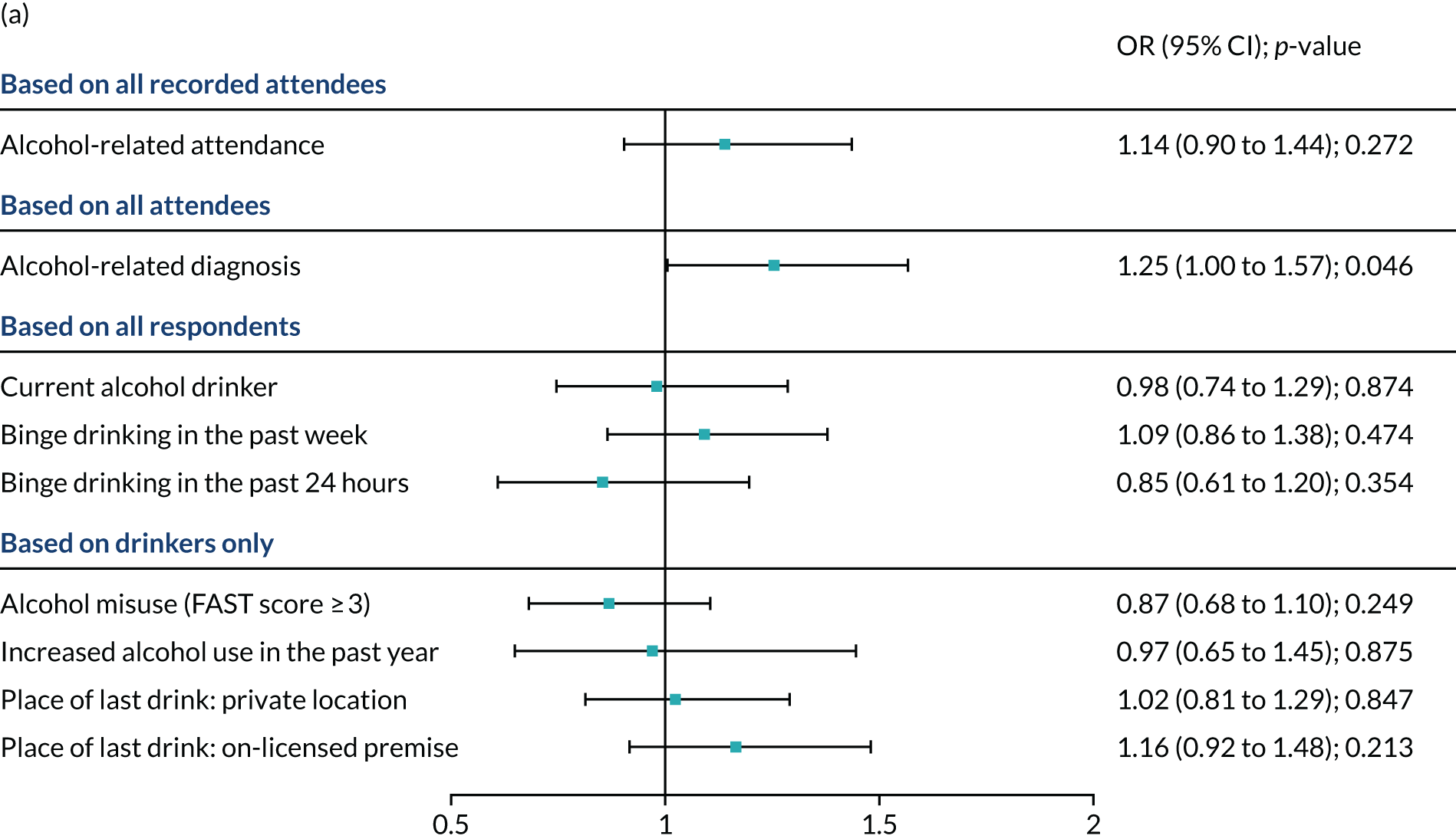
Figure 2a shows the changes in the proportion of recorded attendees with alcohol-related attendance in Scotland and England before and after the introduction of the MUP. On average, Scotland had a higher proportion of attendances that were alcohol related than England. Scotland had a stable trend, whereas there was a decreasing trend in England. There was no evidence of statistically significant differences in the primary outcome after the introduction of MUP in Scotland. The odds ratio (OR) of having an alcohol-related attendance before and after implementation of the MUP was 1.14 [95% confidence interval (CI) 0.90 to 1.44; p = 0.272] in Scotland compared with England (see Figure 4 and Appendix 2, Table 26, for the summary of DiD estimates from full regression models).
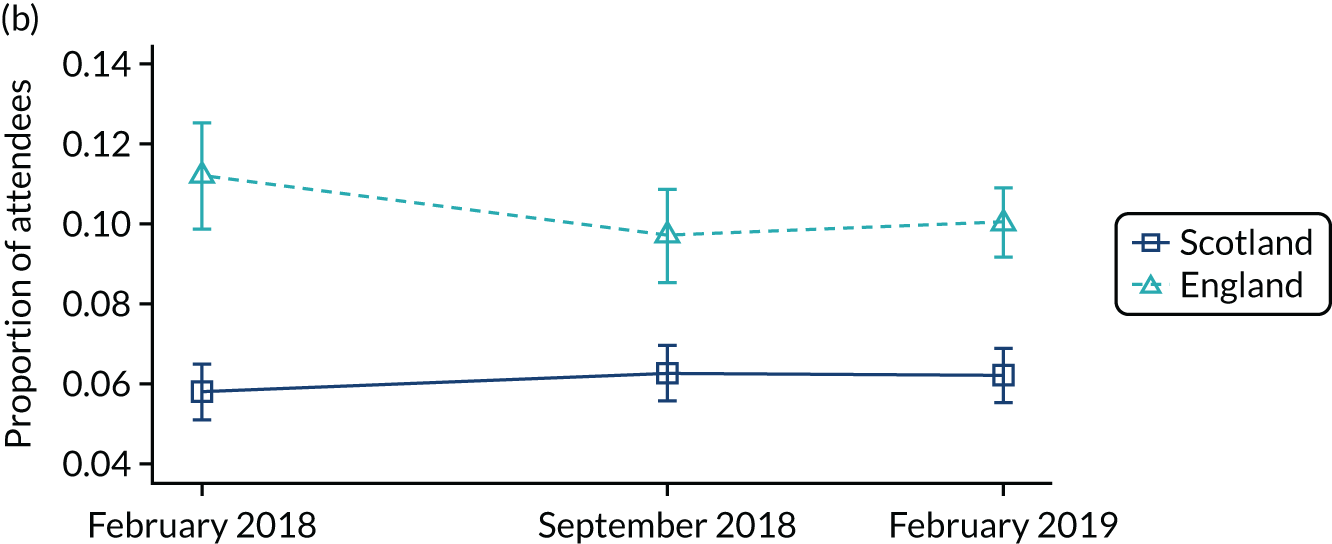
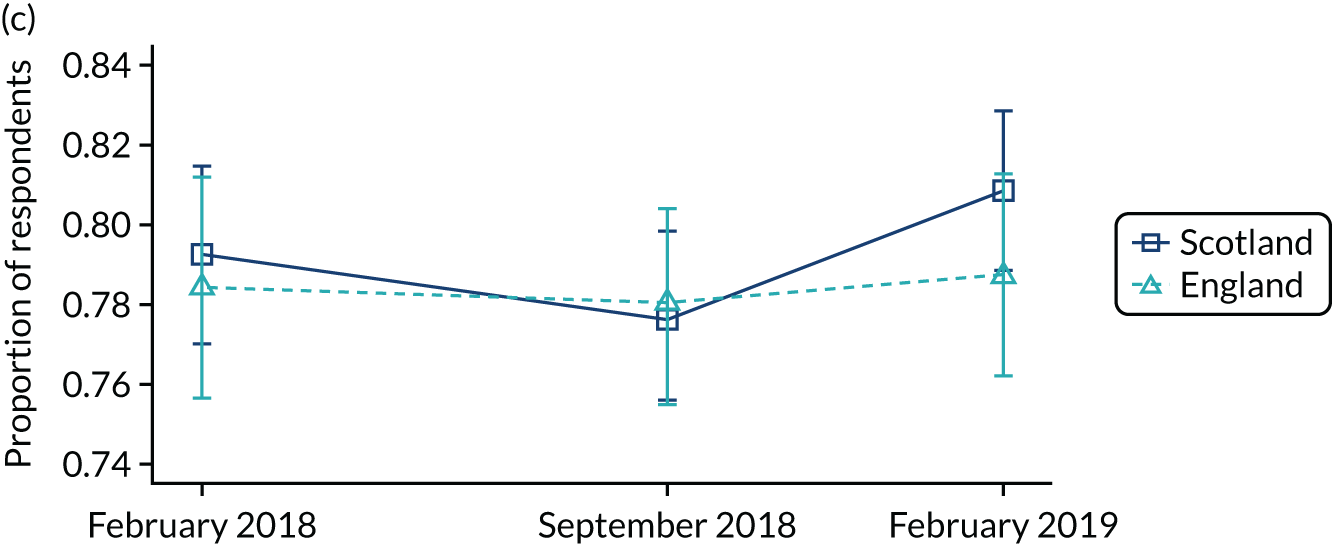
FIGURE 2.
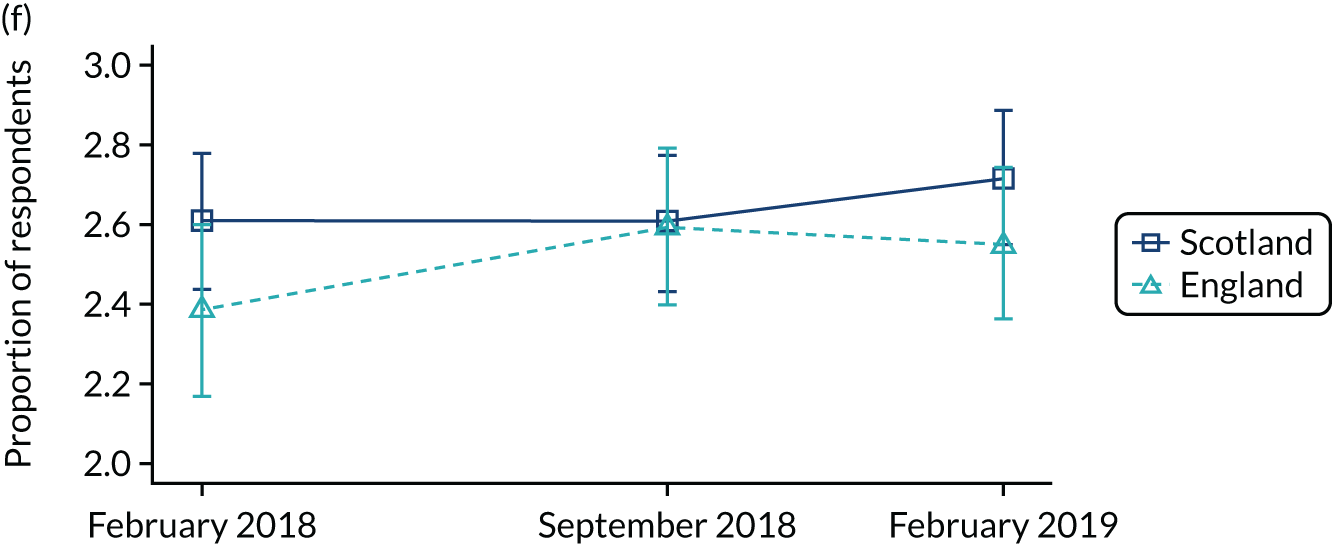
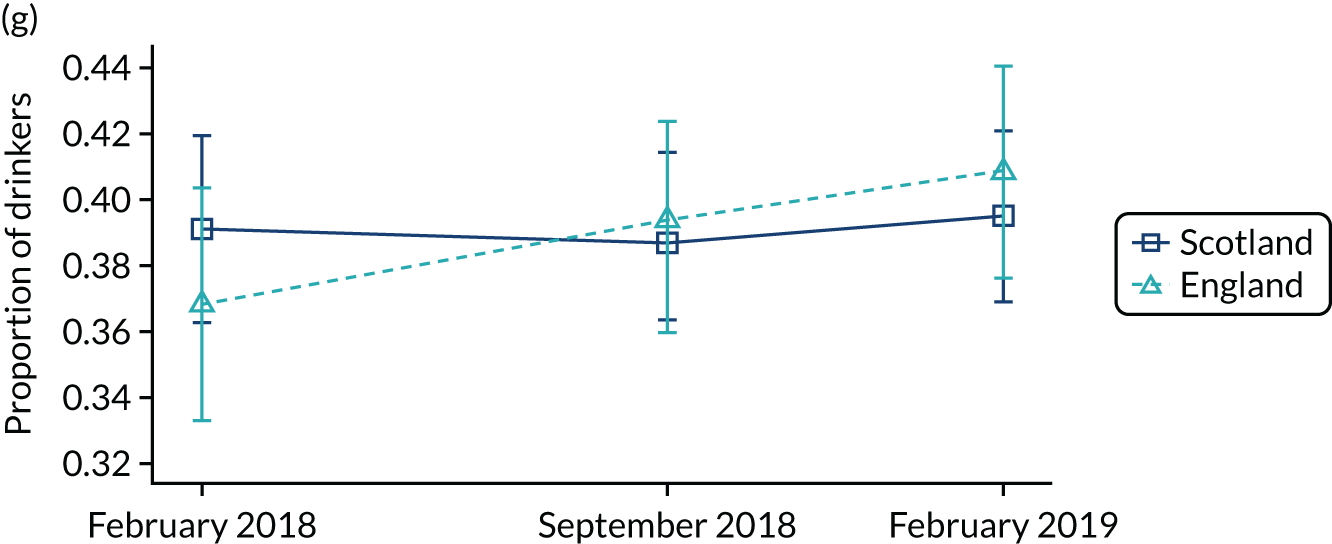
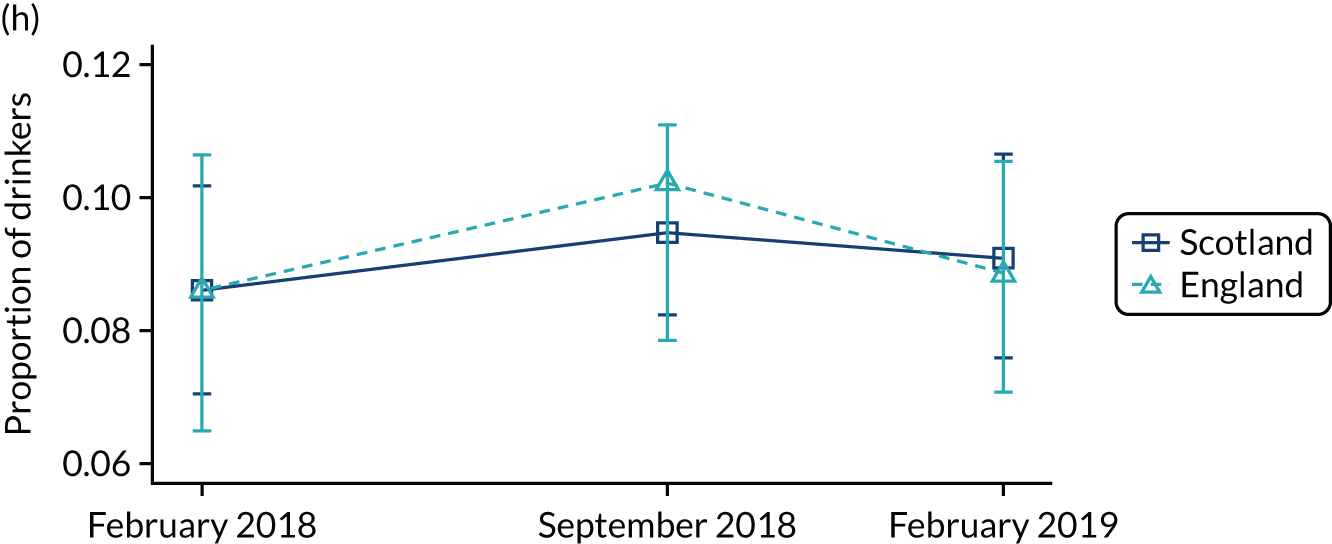
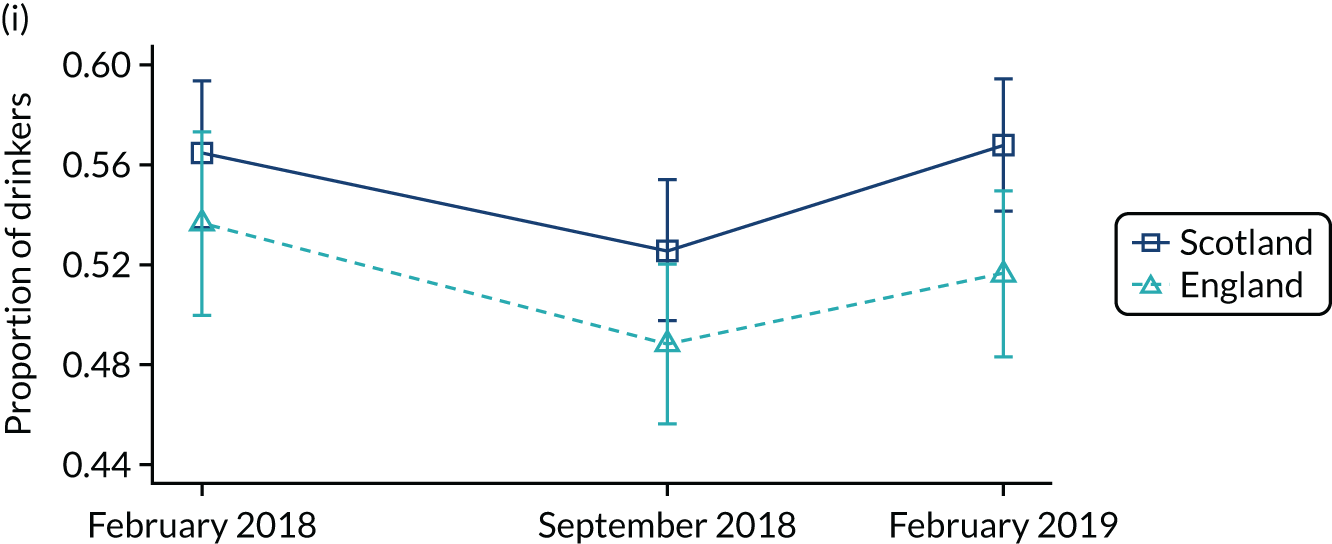
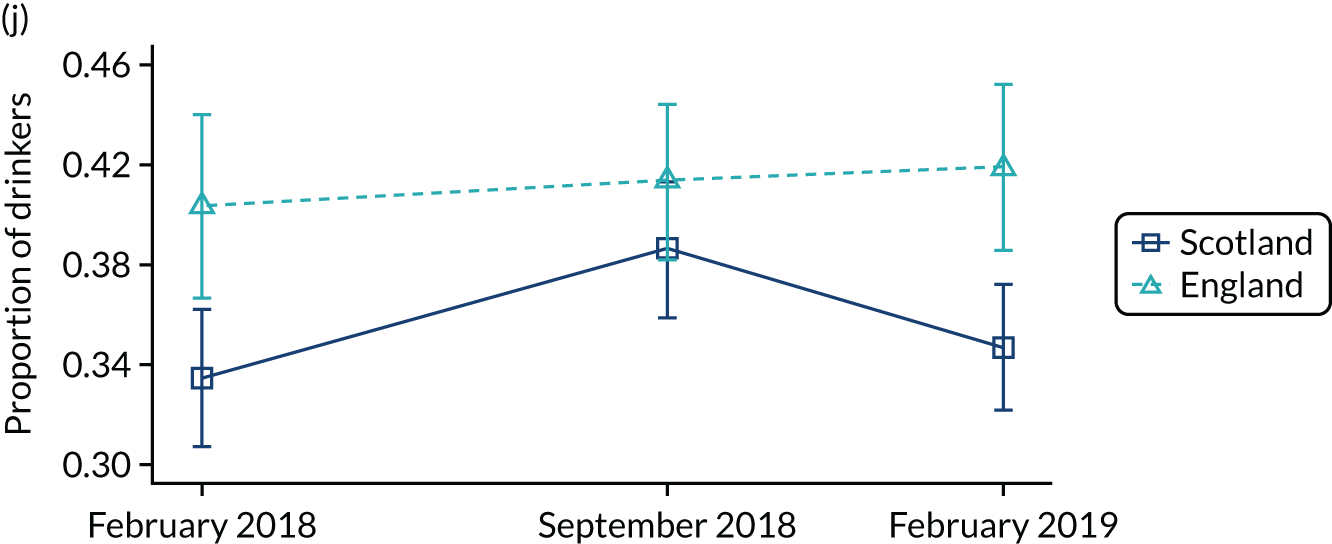
Outcome trend across three waves compared between Scotland and England. (a) Alcohol-related attendance; (b) alcohol-related diagnosis; (c) current alcohol drinker; (d) binge drinking in past week; (e) binge drinking in past 24 hours; (f) FAST score; (g) alcohol misuse (FAST score ≥ 3); (h) increased alcohol use in past year; (i) place of last drink (private location); and (j) place of last drink (on-licensed premise).


Secondary outcome
In contrast to alcohol-related attendance, which was lower in England, England had a higher prevalence of alcohol-related diagnosis than Scotland (see Figure 2b). Note that our comparison was with hospitals in the north of England. The proportion of attendees with at least one alcohol-related condition rose slightly in Scotland, but fell in England. Figure 3 shows the changes in proportion of different alcohol-related diagnosis across waves. There were more attendees diagnosed with partially chronic alcohol-related diagnoses among all alcohol-related diagnoses, followed by wholly acute, partially acute and wholly chronic alcohol-related diagnoses. As the prevalence of partially acute and wholly chronic conditions was very low, we combined all alcohol-related diagnoses as one outcome in the analysis.
FIGURE 3.
Trend for alcohol-related diagnosis by conditions across three waves. (a) Wholly chronic alcohol-related diagnosis; (b) partially chronic alcohol-related diagnosis; (c) wholly acute alcohol-related diagnosis; and (d) partially acute alcohol-related diagnosis.
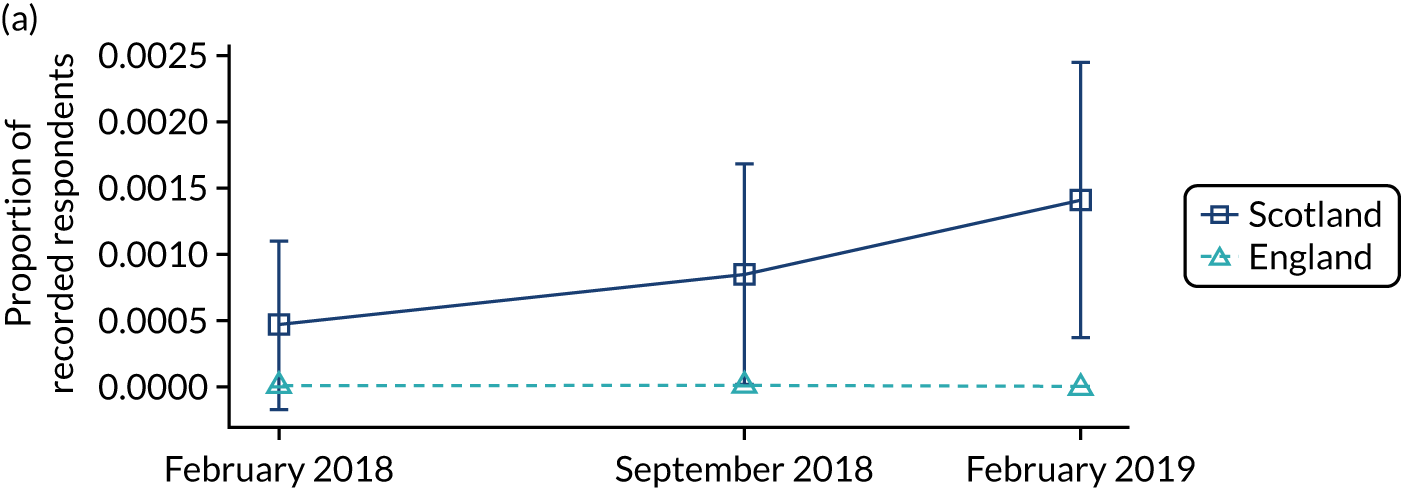
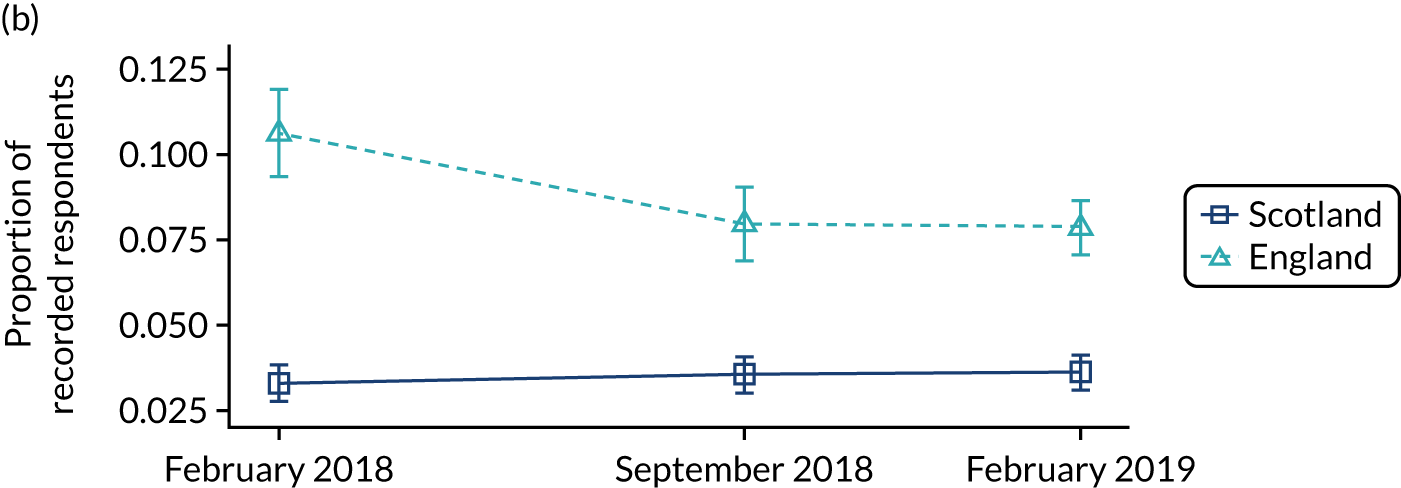
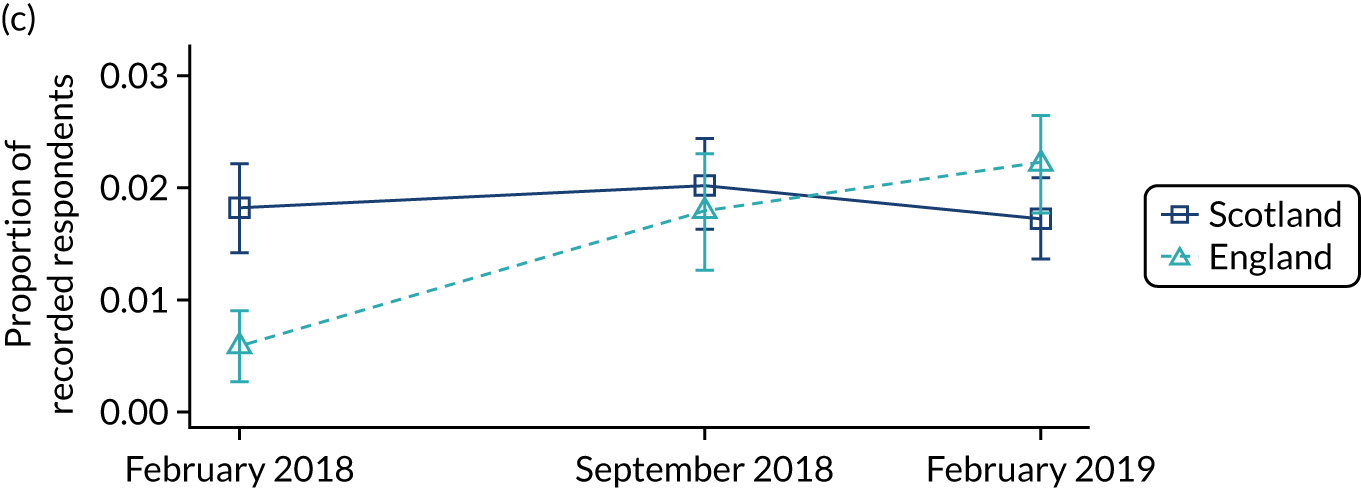

Across waves, there was a slightly increased trend in being a current alcohol drinker in both countries (see Figure 2c). Binge drinking in the past week among all respondents increased slightly in Scotland, but decreased in England (see Figure 2d). However, both countries showed a slight increase in binge drinking in the past 24 hours across waves (see Figure 2e). The mean FAST score among drinkers increased in both Scotland and England (see Figure 2f). The proportion of alcohol misuse (i.e. a FAST score ≥ 3) increased in England, whereas Scotland had a relatively stable trend (see Figure 2g). Meanwhile, the proportion of drinkers who reported an increase in alcohol use in the past 12 months also had a stable trend in both countries (see Figure 2h). Figures 2i and 2j show that the proportion of drinkers who had their last drink in a private location was higher than those in on-licensed premise. However, the trends were stable for both private location and on-licensed premise across waves.
Figure 4 shows the DiD estimates from the final regression models for our secondary outcomes (see Appendix 2, Table 26, for the summary of DiD estimates from full regression models). There was no evidence of significant differences in most outcomes after the introduction of MUP in Scotland. The DiD estimates show that among all attendees the odds for an attendee having at least one alcohol-related diagnosis increased by 25% relative to change observed in England after MUP (OR 1.25, 95% CI 1.00 to 1.57; p = 0.046). Nevertheless, there was no effect on other secondary outcomes, suggesting that the introduction of MUP in Scotland did not substantially alter these outcomes in the population studied.
FIGURE 4.
Difference-in-difference estimates of the overall effects of MUP (a) based on all recorded attendees; and (b) based on drinkers only.
Stratified analysis
We further investigated the outcomes by sex, age group, ethnicity, employment status, marital status and housing ownership. A Bonferroni correction was used to adjust the p-values for multiple comparison. The p-values reported in Figures 5–14 were uncorrected. We indicated where the corrected p-values remain significant after adjustment.
Primary outcome
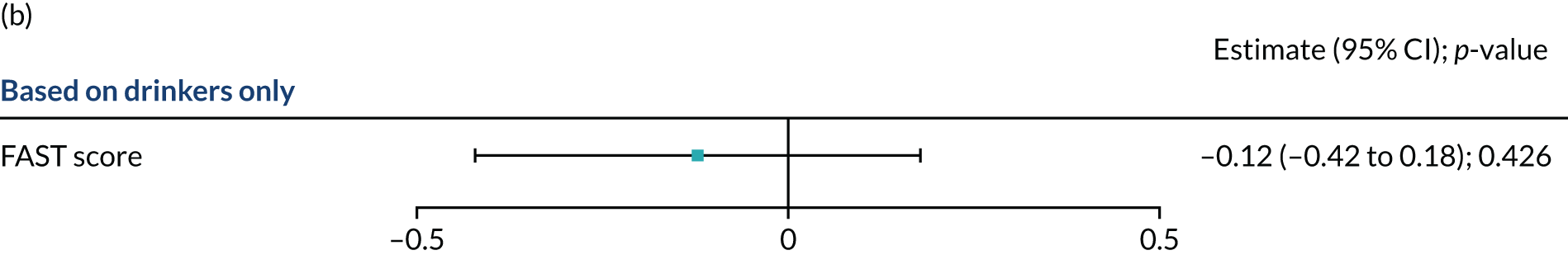
Figure 5 shows the stratified results for the primary outcome. There was no evidence to show that MUP had any differential effect across sex and age group. The summary of DiD estimates from the full regression models were presented in Appendix 2, Tables 27–39).
FIGURE 5.
Stratified analysis for primary outcome: alcohol-related attendance. Note that the p-values in the forest plot were uncorrected.
Secondary outcome
Alcohol-related diagnosis
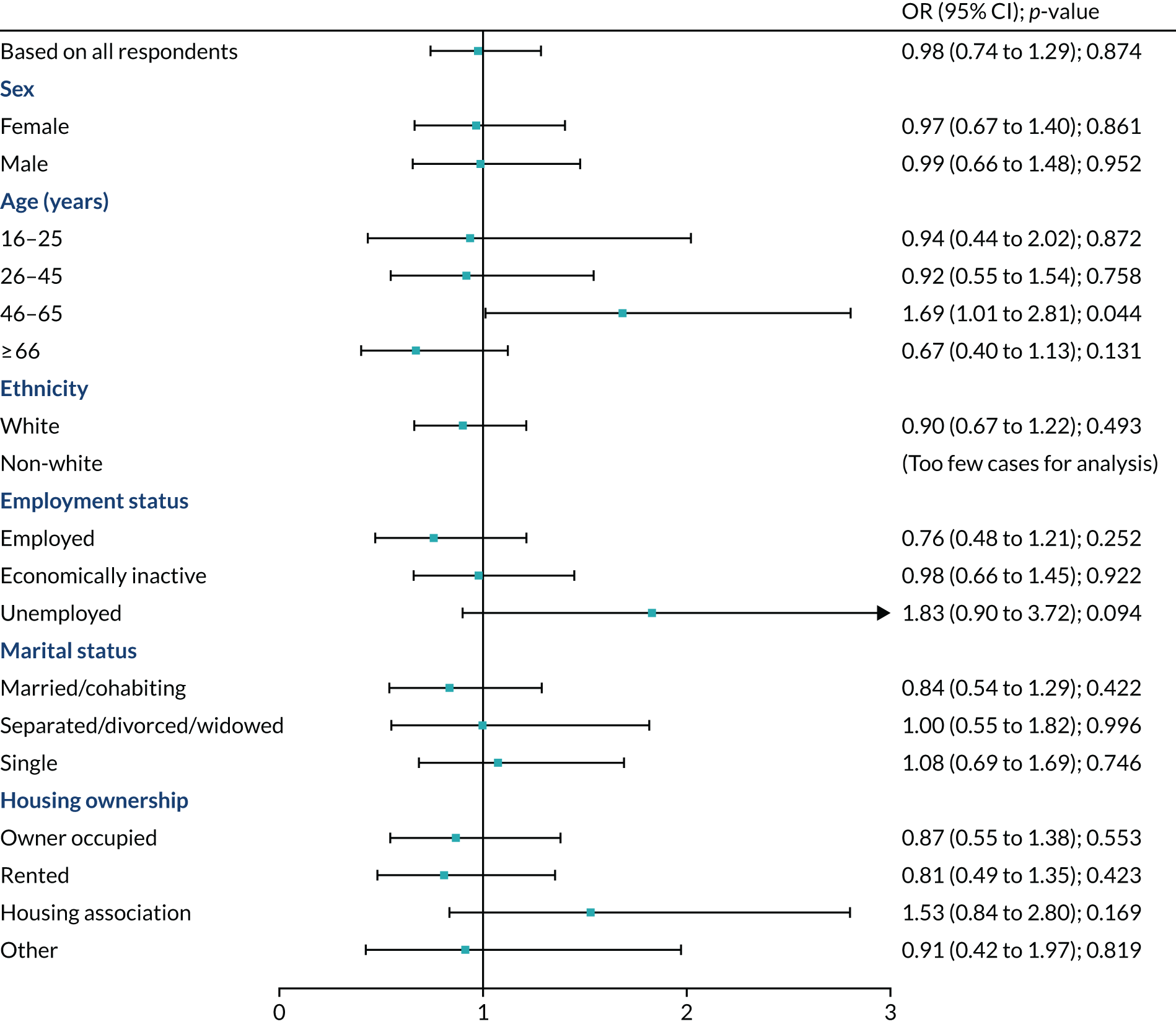
The stratified analysis in Figure 6 shows that the introduction of MUP in Scotland was associated with increased odds of alcohol-related diagnosis among men who attended the EDs (OR 1.56, 95% CI 1.16 to 2.11; p = 0.004). Meanwhile, MUP was associated with significantly reduced odds of alcohol-related diagnosis for those aged 16–25 years (OR 0.47, 95% CI 0.23 to 0.95; p = 0.035), but increased for those aged ≥ 66 years (OR 1.65, 95% CI 1.11 to 2.44; p = 0.013). After adjusting for multiple comparison, the impacts remained significant for men (corrected p = 0.022), but became non-significant for those aged 16–25 years (corrected p = 0.212) and ≥ 66 years (corrected p = 0.076).
FIGURE 6.
Stratified analysis for secondary outcome: alcohol-related diagnosis. Note that the p-values in the forest plot were uncorrected. a, Corrected p < 0.05 after Bonferroni correction for multiple comparisons.

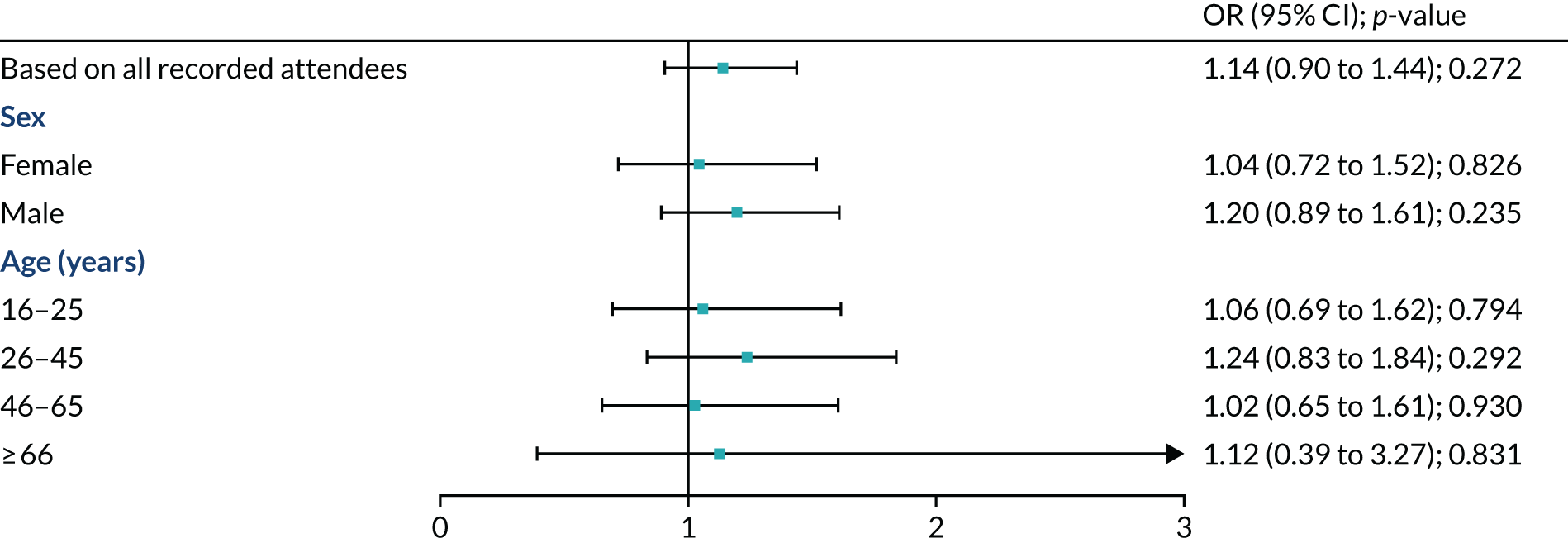
Current alcohol drinker
Results from the stratified analysis suggested that only those who were aged between 46 and 65 years were more likely to become an alcohol drinker in Scotland after the implementation of MUP (OR 1.69, 95% CI 1.69 to 2.81; p = 0.044) (Figure 7). However, after corrected for multiple comparison using Bonferroni correction, the impact of MUP on this group of population became insignificant (corrected p = 0.799).
FIGURE 7.
Stratified analysis for secondary outcome: current alcohol drinker. Note that the p-values in the forest plot were uncorrected.
Binge drinking in the past week
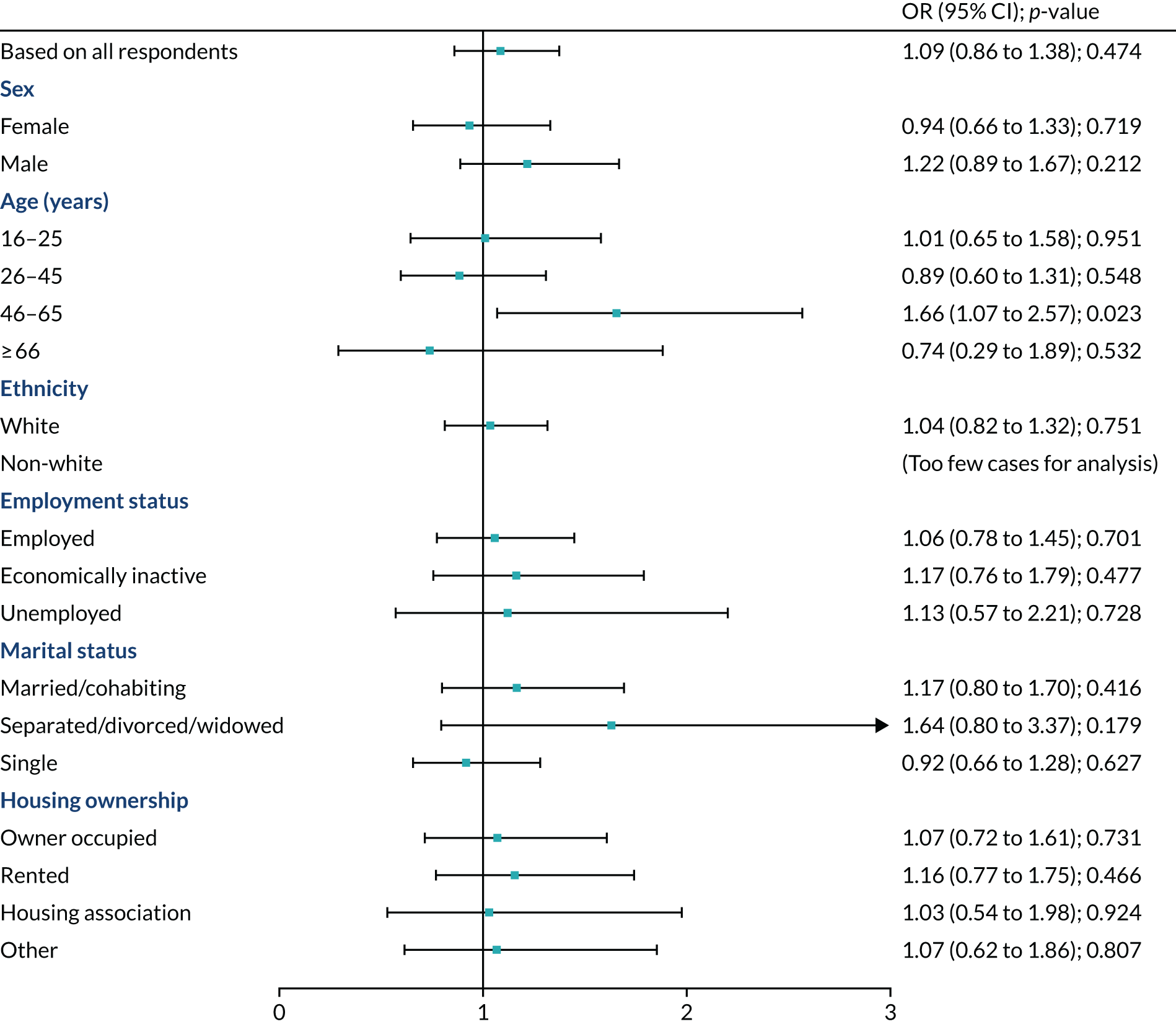
Figure 8 suggests possible increases in binge drinking in the past week in those aged 46–65 years in Scotland, relative to the comparison group (OR 1.66, 95% CI 1.07 to 2.57; p = 0.023). After adjusting for multiple comparison, the effect became insignificant (corrected p = 0.417).
FIGURE 8.
Stratified analysis for secondary outcome: binge drinking in the past week. Note that the p-values in the forest plot were uncorrected.
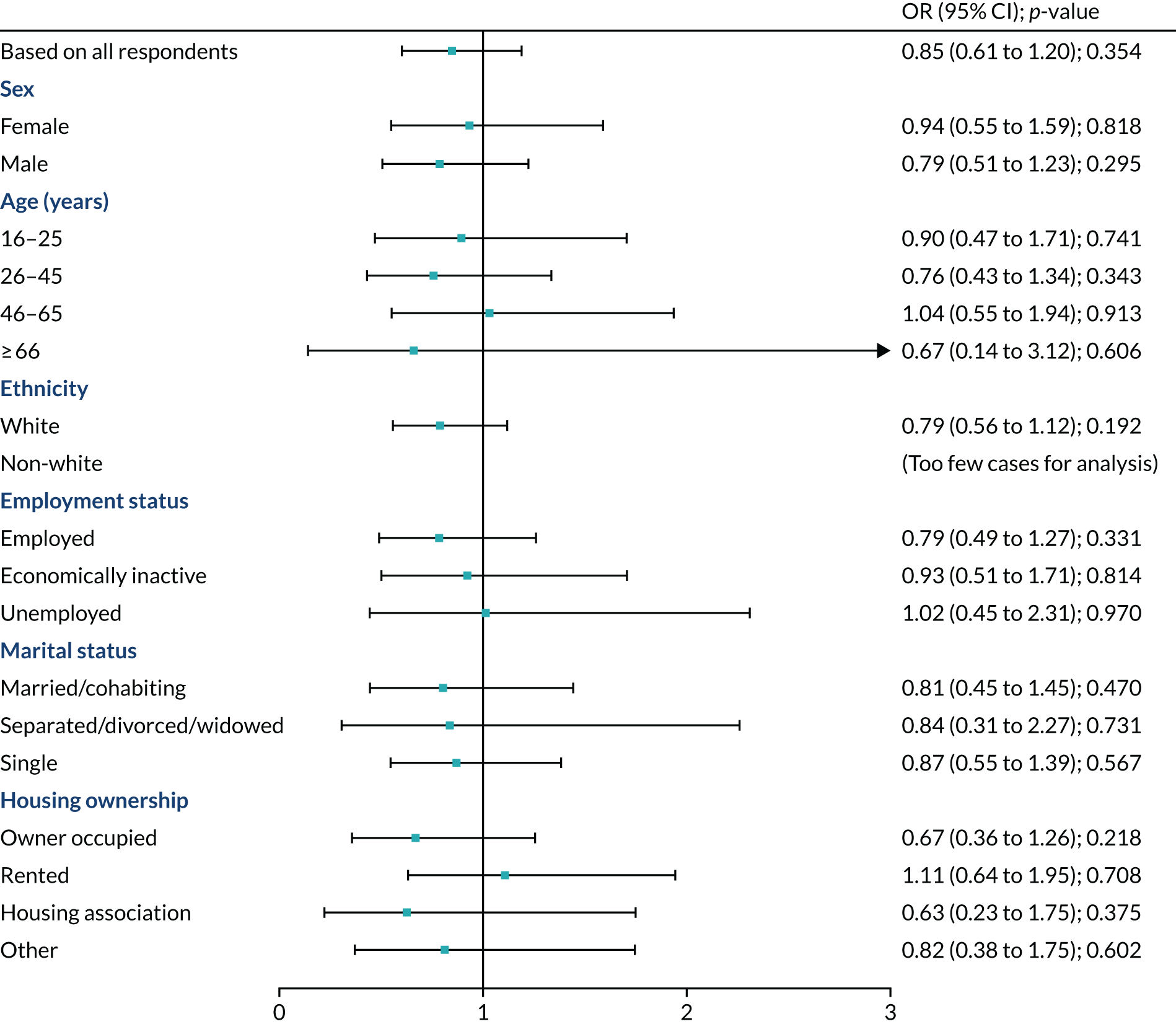
Binge drinking in the past 24 hours
The introduction of MUP did not have any differential effect on any of the subgroup for binge drinking in the past 24 hours (Figure 9).
FIGURE 9.
Stratified analysis for secondary outcome: binge drinking in the past 24 hours. Note that the p-values in the forest plot were uncorrected.
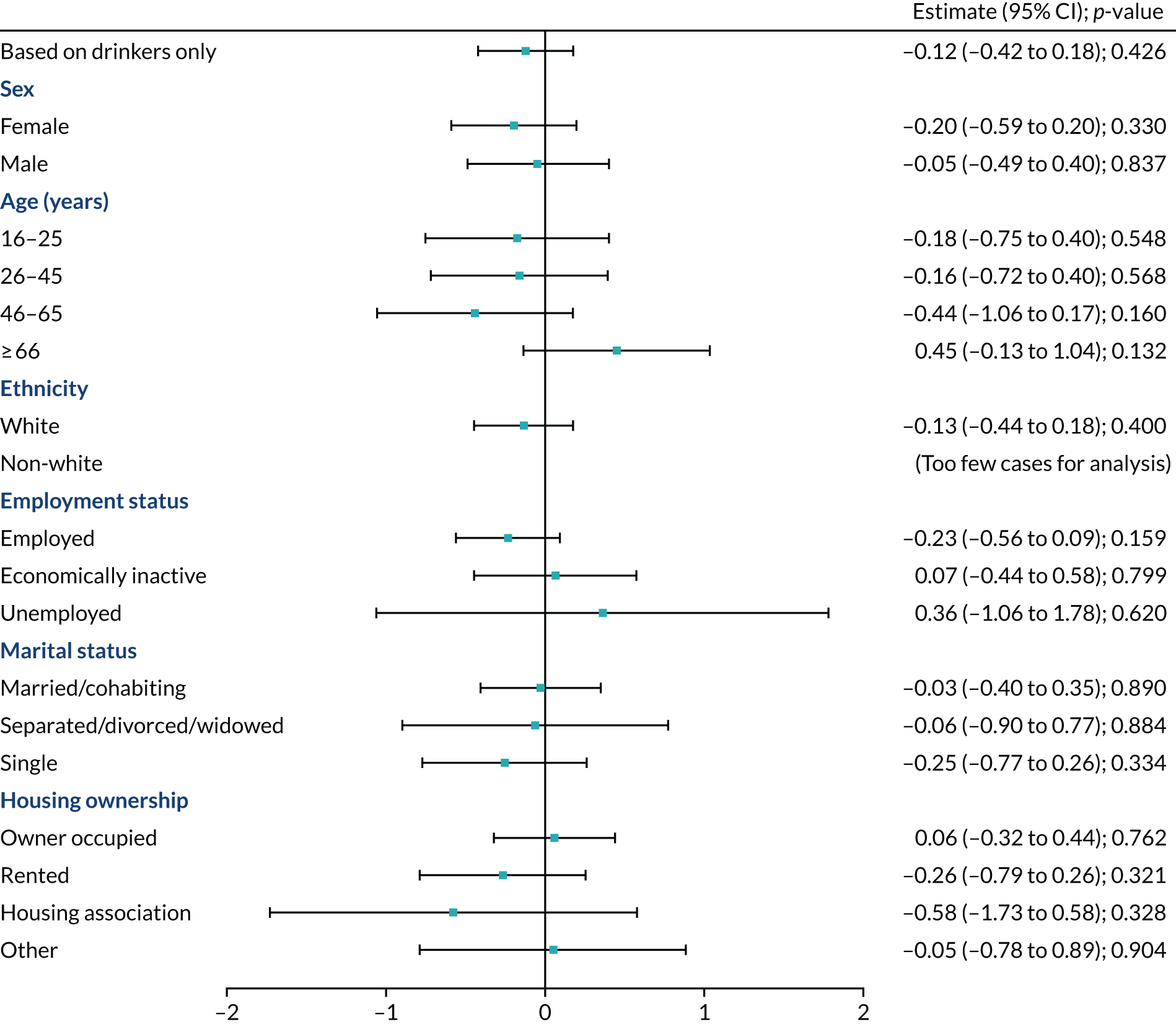
Fast Alcohol Screening Test score
Again, there was no evidence that MUP had any effect across sex, age, ethnicity, employment status, marital status and housing ownership for overall FAST score (Figure 10).
FIGURE 10.
Stratified analysis for secondary outcome: FAST score. Note that the p-values in the forest plot were uncorrected.
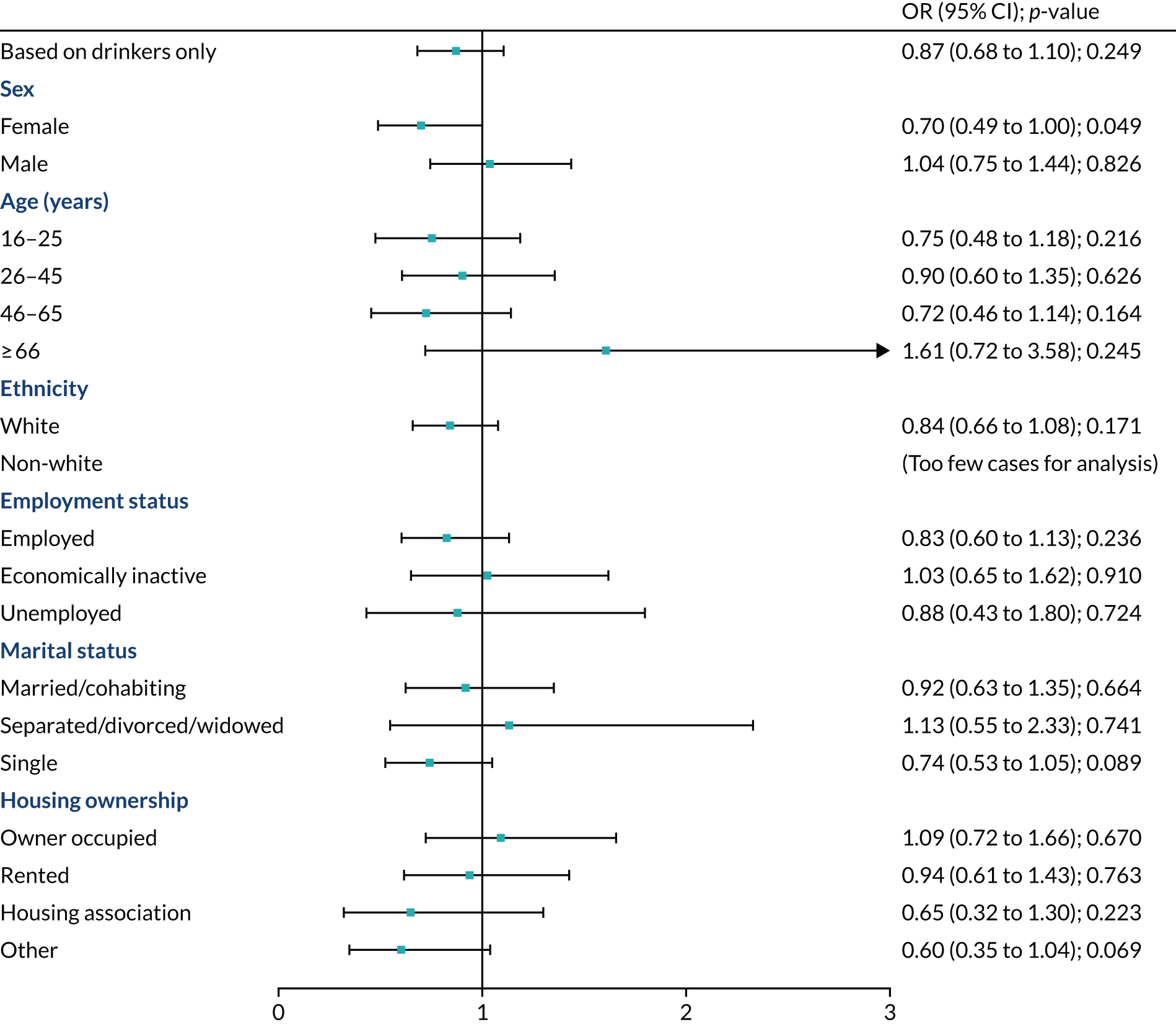
Alcohol misuse
Women’s odds for alcohol misuse decreased in Scotland after MUP was implemented (OR 0.70, 95% CI 0.49 to 1.00; p = 0.049) (Figure 11). The effect diminished after corrected for multiple testing using Bonferroni correction (corrected p = 0.884).
FIGURE 11.
Stratified analysis for secondary outcome: alcohol misuse (FAST score ≥ 3). Note that the p-values in the forest plot were uncorrected.
Increased alcohol use in the past year
Figure 12 shows that there was no evidence that the proportion of drinkers who increased their alcohol use in the past year had changed in Scotland relative to England since the MUP was introduced.
FIGURE 12.
Stratified analysis for secondary outcome: increased alcohol use in the past year. Note that the p-values in the forest plot were uncorrected.
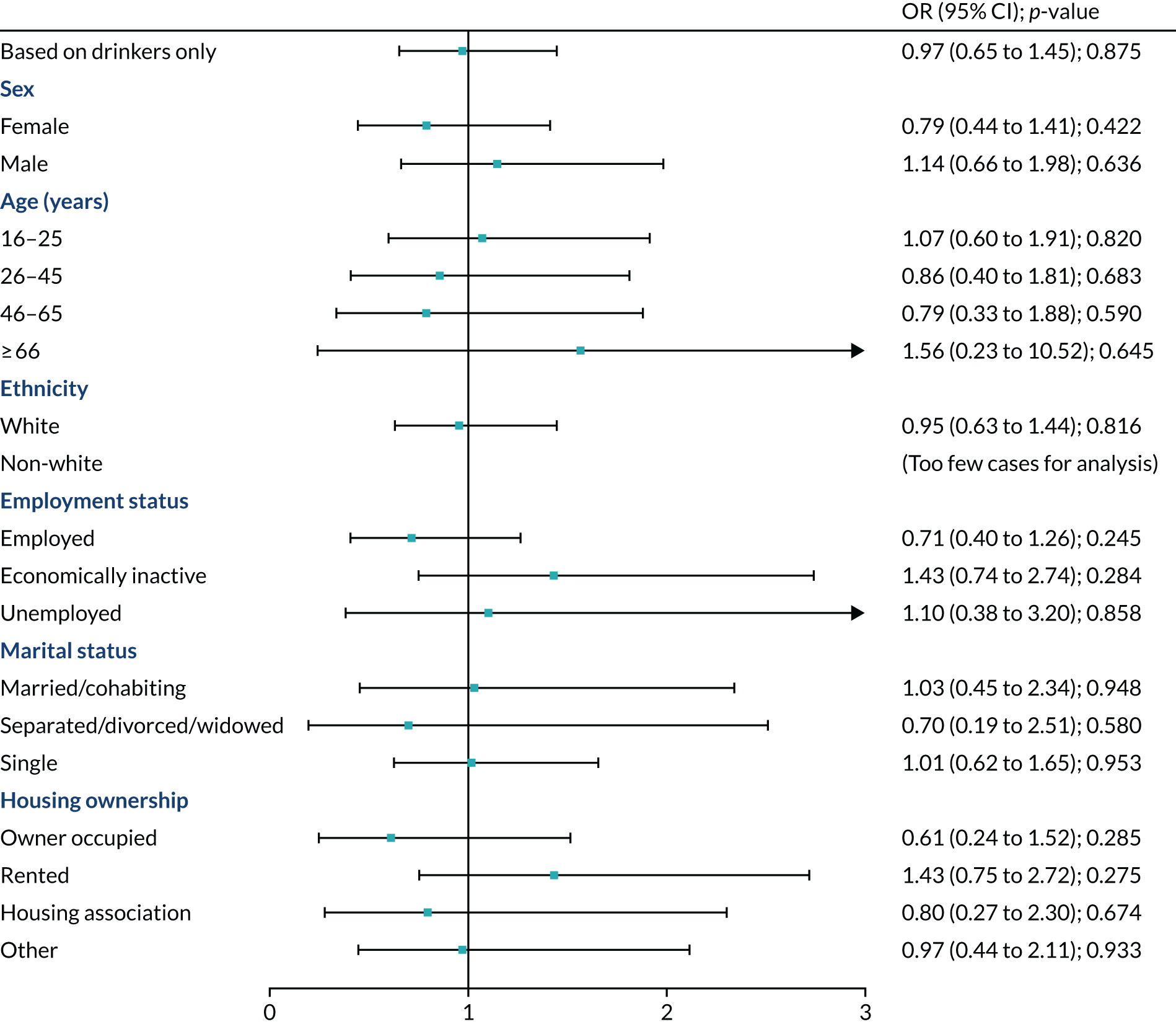
Place of last drink: private location
Those who were unemployed were more likely to have their last drink in a private location in Scotland (OR 2.26, 95% CI 1.09 to 4.65; p = 0.028) (Figure 13). After adjusting for multiple comparison using Bonferroni correction, the impact became insignificant (corrected p = 0.501).
FIGURE 13.
Stratified analysis for secondary outcome: private location as place of last drink. Note that the p-values in the forest plot were uncorrected.
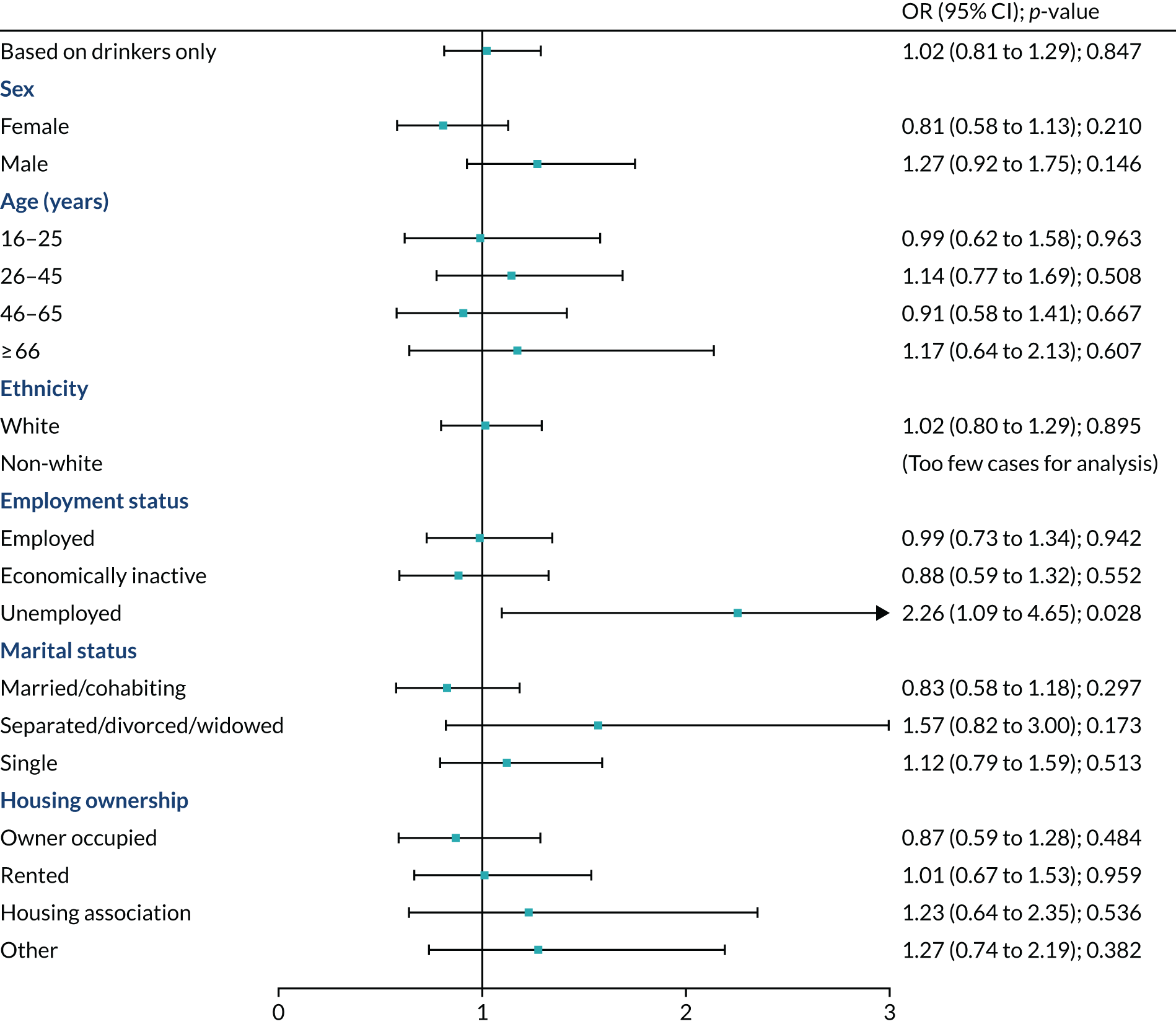
The stratified analysis shows that women (OR 1.56, 95% CI 1.10 to 2.21; p = 0.014) and those who were married (OR 1.53, 95% CI 1.05 to 2.23; p = 0.028) were more likely to have their last drink in on-licensed premises (Figure 14). However, the unemployed in Scotland had smaller odds to have their last drink in on-licensed premise (OR 0.46, 95% CI 0.21 to 0.99; p = 0.048). However, after adjusting for multiple comparison, these differential effects became insignificant (corrected p-value for females = 0.245, corrected p-value for those married = 0.505 and corrected p-value for those who were unemployed = 0.863).
FIGURE 14.
Stratified analysis for secondary outcome: on-licensed premise as place of last drink. Note that the p-values in the forest plot were uncorrected.

Sensitivity analysis
Testing the robustness of our analysis, we analysed the effect of MUP against FAST cut-off points of ≥ 2, ≥ 4 and ≥ 6, repeated the analysis on primary outcome using the sample based on survey respondents and replicated the analysis using unweighted and weighted complete cases. All these analyses produced similar results (see Appendix 2, Tables 40–43). We also performed a sensitivity analysis on alcohol-related diagnosis based on survey respondents who consented to data linkage. Results from the sensitivity analysis showed that the DiD estimate was not significant at a 5% level, whereas the main analysis showed a significant difference. As the sensitivity analysis was based on respondents who consented to data linkage, which may be subject to selection bias, we were more confident that results from the main analysis were more robust.
Discussion
We examined the impact of MUP on alcohol-related ED visits and alcohol-related diagnosis among attendees. We also studied patterns of alcohol use among those who participated in the survey interview. Our results showed that MUP was only marginally associated with prevalence of alcohol-related diagnosis and there was no evidence that MUP had any effect on primary and other secondary outcomes. Similarly, we found no evidence of MUP having differential effects across socioeconomic groups, except for alcohol-related diagnosis. After correcting for multiple comparison using Bonferroni correction, we found that MUP was associated with increased odds in alcohol-related diagnosis among male attendees only.
Our analyses have several important strengths. To our knowledge, this is the first study to examine the association between MUP and alcohol-related attendances and alcohol-related diagnosis within the ED setting in Scotland. Diagnostic data on alcohol-related attendances that do not result in admissions are not routinely captured in administrative health data in both Scotland and England. In contrast to research that relies on hospitalisations data, our study is more sensitive in detecting alcohol-related harms that result in ED attendance. Although we found a weak immediate association between MUP and alcohol-related diagnoses, the result echoes another study that examined alcohol-related injury ED visits in Canada. 69 The study provides more evidence that the MUP may be less likely to have an impact on harms that present to EDs, including those related to acute consumption among young people. However, the consequences on the broader range of alcohol-related harms remain unknown and it is, therefore, important to monitor how alcohol-related diagnoses would change in the longer term.
This component has some limitations. First, the definition of alcohol-related attendances for unapproached or ineligible attendees was based on nurse interviewers’ observations only, although this applied to approximately 2% of all attendees. Attendances were considered as alcohol related if the interviewers recorded them as alcohol intoxicated on the basis of the interview or, for non-participants, from interviewers’ observation. As a result, we may have misclassified some survey non-participants who attended the ED because of another’s drinking or underlying alcohol-related conditions that were not observable to interviewers. Therefore, our analysis is unlikely to fully capture the association between alcohol-related attendances and the introduction of MUP. This could imply that MUP may have increased ED attendances unless observation bias differed across waves and between countries (and we took measures to minimise that, as described). Second, we were unable to test the parallel trend assumption when DiD analysis was used. The Scottish Government announced, on 21 November 2017, that MUP would be implemented on 1 May 2018. It gave us limited time for data collection and, therefore, only one pre-MUP data time point was possible. However, other data suggest that the prior trends in alcohol-specific deaths23 and alcohol-related hospital admissions150,151 in Scotland and England since 2012 were broadly similar. These data provide some proxy information on alcohol-related ED attendances and alcohol drinking patterns in both countries to validate the parallel trend assumption. Third, we excluded one hospital from England when we analysed alcohol-related diagnosis among respondents who consented for data linkage. The data provided from this hospital did not allow us to convert to the ICD-10 diagnostic coding system, which the alcohol-attributable diagnoses were based on. Therefore, we lost 5723 cases (around 21.2% of total sample size) when we performed this analysis. This may have affected the statistical power and may explain why we found higher alcohol-related attendances in England, but a higher prevalence of alcohol-related diagnoses in Scotland. Finally, it should be noted that the weather in February 2018 was very different from that in February 2019. The average temperature in February 2018 and 2019 was 1.6 °C and 5.1 °C, respectively, in Scotland and 2.1 °C and 6.1 °C, respectively, in the north of England. 152 The weather disruptions may have had some impact on ED attendances and drinking patterns despite controlling for wave as a fixed effect.
The study protocol identified a number of potential risks arising from MUP:39 (1) displacement effects where reductions in alcohol-related harms may be accompanied by increases in other drug-related harms; (2) increased alcohol-related harm through substitution or changed drinking patterns; (3) consumers may switch to alternative sources of alcohol not subject to MUP, such that the price paid does not increase; and (4) MUP could unfairly penalise poorer drinkers who may be less able to absorb the additional costs and may also forgo other essentials, such as food. Our results show that, except for male attendees, there was no evidence that alcohol-related harms increased within the ED setting as a result of the implementation of MUP, which echoes the results from a previous Canadian study. 69 There was a 6-year period between the legislation being passed and implementation. The level of MUP (£0.50 per unit) was the same on introduction as that that first modelled in 2012, and by the time it was introduced the magnitude of price changes was smaller. It might also explain why we were unable to detect any significant effects of MUP on alcohol-related harms and drinking patterns, as it may not have been implemented at an adequate level. MUP might have also increased public awareness of health harms relating to alcohol, and much of that could have happened around the time of legislation and during the legal challenges from the alcohol industry. The Scottish Government has also been implementing a comprehensive alcohol policy since 2009. Our study would not pick up such effects because of the research design.
In summary, we did not find evidence of the introduction of MUP in Scotland having an impact on alcohol-related harms within the ED setting. However, the broader evidence base on the relationship between the price of alcohol and the amount consumed is more consistent with an effect of MUP on both alcohol consumption and harms. Therefore, we should interpret the results with caution and should not draw conclusions regarding the wider societal impact of MUP on alcohol harm purely based on this study.
Chapter 5 Sexual health clinic component
Aims for the sexual health clinics component
The other components in our study include a comparison of English and Scottish EDs on a primary outcome of alcohol-related attendance and a qualitative component assessing key players’ views about implementation and young people’s and heavy drinkers’ views about the MUP policy. It is in this context that the SHC setting was chosen for the current component, as it captures a younger population at particular risk of unintended consequences (see Methods).
A number of potential risks arising from MUP were identified in the protocol:39
-
Displacement effects where reductions in alcohol-related harms may be accompanied by increases in other illicit drug related harms.
-
Increased alcohol-related harm through substitution (e.g. to illicitly produced or industrial alcohol associated with greater toxicity)
-
Consumers may switch to alternative sources of alcohol not subject to MUP such that the price paid does not increase.
-
MUP could unfairly penalise poorer drinkers, who may be less able to absorb the additional costs and may also forgo other essentials such as food.
There is an absence of evidence internationally and, to the best of our knowledge, no other studies have investigated these potential adverse impacts in a robust way. Investigation of these potential impacts is important to the overall assessment of health benefits compared with harms, as well as to the distribution of those harms.
We aimed to assess unintended effects on drug and alcohol consumption in SHC attendees as a result of MUP. This covered research aim 2 in the protocol:
RA2 [research aim 2]: To determine the impact on non-alcohol substance use for the overall population and by subgroups of interest (age, sex and deprivation).
Our results are not intended to be generalisable to the general population. Approximately 5% of the general population have attended a SHC in the last year. 118 However, such alcohol-related information suffers from response and reporting bias within routine health surveys. Drugs data collected through non-health surveys have the same issues, particularly for young people and for the deprived populations most likely to be affected by the intervention. 65,136,153 Therefore, we collected primary data to assess drinking patterns, as different patterns of consumption are associated with different health and social harms. We also stratified our outcomes for different groups, but we did not assume a direction of effect for either intended or unintended outcomes in any specific subgroup. This component addresses RO2, that is to determine the impact of MUP on non-alcohol substance use, and other unintended impacts, for the overall population and by subgroups of interest (age, sex and socioeconomic position).
Objectives
Our primary outcome was the change in the proportion of all respondents using any illicit psychoactive drug other than alcohol in the last month. Any increase in such drug use would be an unintended outcome from MUP, although there may be unknown confounders, such as possible reduction in the price of illicit drugs. We asked whether or not 17 different types of illicit drugs had been used in the last month, last 6 months or more than 6 months ago. The list included one fake drug as a test of the validity of responses. Those reporting that they had used the fake drug were excluded from the final analysis.
Secondary outcomes were changes in:
-
sources of any alcohol purchase in the last month (grouped into on-licensed premises and off-licence)
-
use of individual illicit psychoactive drugs other than alcohol within the last month
-
rates of alcohol misuse (FAST score ≥ 3 on a scale of 0–16)
-
mean FAST score
-
binge drinking at least weekly in the last year
-
differential displacement in all outcomes by age group, sex, highest educational level and employment status.
Methods
Data sources
The background to this natural experiment is described in the introduction to the whole study. Our comparison was with the north of England where culture and alcohol consumption patterns were more similar to Scotland than is the rest of England. 154,155 For this component, we collected primary data using anonymous attendee-completed paper surveys. The questionnaire items covered demographics and alcohol consumption.
Variables were binge drinking in the past week, the mean FAST score and alcohol misuse (i.e. a score ≥ 3 on the FAST, as for the ED component, using the FAST112,156 modified version157), sources of alcohol, change in alcohol and drug use over the past 6 months and 1 year, and changes in illicit drug use in the last month by individual drug. The alcohol-related outcomes were for drinkers only. A sample questionnaire for the third wave is included in Report Supplementary Material 1. We recruited one SHC in each of six cities of approximately matched populations and size, three exposed to MUP in Scotland (Edinburgh, Dundee and Glasgow) and three unexposed in the north of England (Manchester, Sheffield and Leeds).
Cities in the north of England were chosen because, of all English regions, the north of England had the most similar drinking patterns to Scotland in terms of the higher levels of hazardous drinking. 23,141
The populations
The UK mid-year estimates for 2018137 (and proportion of LSOAs) (England) in the most deprived 10% of all England158 for the three English cities in 2018 were as follows.
-
Sheffield: 582,506 (proportion of LSOAs in the most deprived 10% nationally = 30%).
-
Manchester: 547,627 (proportion of LSOAs in the most deprived 10% nationally = 5%).
-
Leeds: 789,194 (proportion of LSOAs in the most deprived 10% nationally = 33%).
The 2018 population estimates137 and proportion of datazones in the most deprived 20% in Scotland159 were as follows:
-
Dundee: 148,750 [Dundee city has 36.7% (69/188) datazones in the most deprived quintile for Scotland].
-
Edinburgh:
-
Midlothian – 91,340 [Midlothian has 11.3% (13/115) datazones in the most deprived quintile for Scotland]
-
East Lothian – 105,790 [East Lothian has 4.5% (6/132) datazones in the most deprived quintile for Scotland]
-
West Lothian – 182,140 [West Lothian has 15.9% (38/239) datazones in the most deprived quintile for Scotland]
-
total population – 379,270.
-
-
Glasgow: 626,410 [Glasgow city has 48.3% (360/746) datazones in the most deprived quintile for Scotland].
Therefore, in each country there are two cities with more representation for the most deprived than the average within their country, and one city in each country with less extreme deprivation. Manchester and Edinburgh are the less deprived. We adjust for deprivation levels using a UK-based measure in our analysis.
Compared with the general population, SHC attendees tended to be younger118 and more likely to use illicit drugs. 119,120 People at more risk of sexually transmitted infections are also more likely to have higher alcohol consumption levels, take greater sexual risks,121 drink in on-licensed (clubbing) premises122 and have more diverse sexual orientation. 120 Therefore, they were a relevant population potentially at risk of displacement effects. Data collection, using attendee-completed anonymous paper questionnaires, took place in 3-week waves at three time points. The baseline wave was conducted in February 2018 (which was as early as we could collect data, given the short period between the implementation date being announced and coming in to force on 1 May 2018). Follow-ups were in September/October 2018 and February 2019, providing a 6-month post-implementation wave (to capture relatively early impacts), and at 12 months post implementation. We included wave in our regression model to adjust for seasonal differences. Each wave lasted 3 weeks, with data collected in central clinics (not satellites or outreach facilities) Monday to Friday (inclusive), during clinic opening hours. Further details are given below.
Clinic inclusions and times, and research staff by site
Glasgow
-
The 20-minute integrated clinic, test only, nurse return clinic, follow-up clinic, vaccine clinic, gynaecology clinic and also menopause and contraceptive procedures.
-
Times: 09.00–17.00, Monday to Friday (as per protocol).
-
Researchers: clinic reception staff (waves 1 and 2) and research nurses from SPHSU bank (wave 3).
Edinburgh
-
All clinics.
-
Times: 09.00–17.00, Monday to Friday (as per protocol).
-
Researchers: clinic reception staff (all waves).
Dundee
-
All clinics (walk-in and booked).
-
Times: 09.00–17.00, Monday to Friday (as per protocol).
-
Researchers: clinic reception staff (all waves).
Sheffield
-
All clinics (including youth clinic to 18.00).
-
Times: working hours between 09.00 and 17.00, Monday to Friday (as per protocol). Wednesday morning only (not Wednesday afternoon). Urgent care, nurse return clinic, vaccine clinic, pregnancy clinic, and menopause and contraceptive procedures. Not for self-tests or for people making an appointment.
-
Researchers: research nurses.
Manchester
-
All clinics: human immunodeficiency virus (HIV), family planning and contraception clinics, and the general genitourinary medicine walk-in.
-
Times: the time slots were from 08.00 to 16.00 with walk-in sessions from 08.00 to 15.00.
-
Researchers: research nurses.
Leeds
-
All clinics: booked in appointments and walk-in attendances.
-
Times: 09.00–17.00, although this was changed to 11.00–17.00 for team brief days.
-
Researchers: research nurses.
These sites, times and staff were replicated across waves, apart from a change in research staff in wave 3 in Glasgow, which was essential to improve the response rate.
Contraception patients were included at all sites. If the service design was a hub-and-spoke structure, then sites were advised that there should be enough patients at the hub and so not to include spokes. Sites were told that it was acceptable to give assistance to people who need help to complete the questionnaire. We informed sites that we would be asking for a report from the clinic information system, which would be held on computer, of the numbers of patients by age and sex who attended during the data collection time periods. Only if the clinic information system was unable to provide this information would they need to keep a manual tally of refusals. Clinics were given flexibility to vary time slots by site to allocate around 7.5 hours within the normal working hours of the site for recruitment, but it was stipulated that these should be kept the same for waves 2 and 3. People who came in to the clinic but were sent away (e.g. with a chlamydia testing kit) and were not registered as attendees were not eligible to participate.
Training
We trained the data collection staff before each wave. As repeated cross-sectional samples are vulnerable to selection bias,41 we emphasised this threat and the consequent importance of offering the questionnaire to all attendees. All sites received on-site training for waves 1 and 2, Leeds and Manchester were trained by teleconference at wave 3 and the others were trained on site.
Training comprised a presentation about the background to MUP and the aims and methods of the component. This was also an opportunity to record details of local clinics and recruitment methods, and ensure safe storage of completed questionnaires, arrangements for the secure return of these to the University of Glasgow and to confirm locations for poster display. After the presentation, participants went through the questionnaire themselves and discussed it with each other and the trainers. Clarifications were made, as necessary. Staff were also given guidance on how to introduce the questionnaire. An example of the questionnaire and an information sheet for researchers to refer to when introducing the questionnaire to potential respondents is shown in Report Supplementary Material 1. After training, the data collection procedures and questionnaires were piloted in all the sites before the first wave. A single day of data collection was the minimum required.
Support
All the sites were offered funding to employ temporary staff to approach attendees and offer them the questionnaire. Some sites were reluctant to bring in external staff and opted, instead, to ask reception staff to work additional days to accommodate this work. Sites with the lowest response levels were offered support from external researchers in the final wave. One site (in Scotland) took this up. To increase the response, the use of chocolate adjacent to survey collection points, as developed by an individual site, was harmonised across sites at the final wave. Note that attendees were not obliged to complete the survey to get a chocolate, but the chocolates were positioned to draw attention to the questionnaires. We obtained aggregate data on age band and sex for all clinic attendees in the data collection period to check the potential for bias. The number of questionnaires collected was monitored weekly during each wave by e-mail or telephone call to the data collection leads on each site and response rates were calculated retrospectively using denominators provided from clinics.
Eligibility criteria
Attendees of any age in the normal clinic opening hours for included clinics were eligible. Our eligibility criteria were:
-
able to complete the questionnaire in English or using a translated version (Hindi, simplified Chinese, Polish, Slovak and Arabic) or with assistance if necessary
-
in the department long enough to be offered a questionnaire.
Informed consent
Our ethics approval confirmed that, as this study was anonymous, completing the survey implied consent.
Modes of analysis
Statistical methods
Study size
We carried out an a priori power calculation to establish our intended minimum sample size. We calculated that a total sample of 5000 participants for each wave would detect a change of ± 4% in our primary outcome (therefore, from 30% to 34%, where 30% of people are using drugs), with 95% significance at 80% power. Our main results compare the pre-MUP baseline with all post-MUP waves, but we also compare each follow-up wave with the baseline separately to check trend.
Demographic variables: predictors, potential confounders and effect modifiers
We measured several predictors and potential effect modifiers, including age group, sex, highest educational level and employment status. The DiD design accounts for time-invariant confounders.
Comparisons
We used DiD OR for outcomes based on proportions and an estimate of the mean for the FAST score, and tested for potential effect modifiers. We present results with 95% CIs and associated p-values. We combined the two post-MUP waves in the time variable in the model by coding the baseline as time = 0 and waves 2 and 3 as time = 1.
Description of statistical methods, including those used to control for confounding
We used a fixed-effects regression model, with individuals nested within SHCs, before and after adjustment for relevant covariates. All outcomes except the FAST score are binary. We use logistic regression for binary outcomes and linear regression for the FAST score. Model 1 is unadjusted. Model 2 is adjusted for clinic site and wave. Model 3 is adjusted for clinic site, wave, age, sex, education, employment status, the interaction between age and wave, and the interaction between sex.
where y is the outcome, β1 is the interaction term between country (0 = England; 1 = Scotland) and time (0 = before MUP; 1 = after MUP, waves 2 and 3 combined), and ε is the error term. β1 is the DiD estimate and the reference category is ‘England before MUP’. It is defined as the differences in outcome between Scotland and England before and after the implementation of MUP. The inclusion of wave (with values of 1, 2 or 3) in the model controls for seasonal differences. The clinic variable is a series of five dummy variables and wave is a series of two dummy variables.
Description of statistical methods used to examine subgroups and interactions
We tested for statistical interactions of intervention and covariates on a multiplicative scale (including age, sex, highest educational category and employment status) to investigate the possibility of differential intervention effects, and subsequently stratified the analyses. In our regression model, we compare pre MUP and post MUP to allow for seasonal effects or if the effect of MUP is not immediate.
Missingness for demographic variables was between 0% and 13% when assessed for waves within countries. Missing data for both demographic and outcome variables were addressed through 20 rounds of multiple imputation using Rubin’s method and chained equations using the MICE package147 in R. We applied weights in our regression analysis according to age group within each clinic to ensure that our sample was representative of age for all clinic attendees.
Our sensitivity analysis compared outcomes using complete-case analysis and using multiple imputation. We found only minimal differences (see Appendix 3, Tables 64 and 65). We compared weighted with unweighted samples, finding minimal difference. Figures showing these analyses are included in Appendix 3, Figures 29–38. We also carried out an analysis of outcomes excluding the clinic for which we introduced extra support at the final wave (see Appendix 3, Table 66). The findings were not affected. Our final results are for model 3 after imputation and weighting.
Challenges for data collection
The inherent challenges in collecting data for this component are consistent with challenges faced in other natural experiments. 149 The primary challenge is in keeping the data collection methods consistent within each of the study sites across each wave to avoid selection bias affecting the outcome measures, as outcomes are based on comparisons between waves. The DiD design means that variations between sites will not affect the outcome, provided that these variations are consistent across waves. This section aims to outline the various challenges faced while collecting data. As indicated in Methods, the importance of maintaining consistent data collection methods across the waves and sites was paramount. We ensured that collection was as consistent as possible through training and appropriate research tools, as described below.
Training
Each study site underwent a similar training session before each wave. Data collection times, sites and methods were confirmed with each site at baseline and reiterated in the training for subsequent waves to support the replication of these as faithfully as possible. For the SHCs, this took the form of a 2-hour face-to-face training session. In the SHCs, any staff likely to welcome anyone to the clinic or register a patient’s arrival at the clinic were encouraged to undertake the training. It was occasionally challenging to have all staff present for the training because of absence or if staff were required to keep the service running while the training was delivered. Where staff could not attend the face-to-face training, the lead nurse or SHC manager was given the training presentation to cascade to any staff who were unable to attend.
During the run-up to baseline data collection, we held informal ‘huddles’ with SHC and ED sites by telephone conference to allow for the discussion of informal queries. These were useful both in resolving queries and keeping relationships with sites healthy.
Data collection took place within normal clinic working hours for three periods of 3 weeks. The baseline was in February 2018 and follow-ups were in late September/October 2018 and February 2019.
The study protocol advised that all sites should collect data at the same time. This was not always possible in the SHCs, as certain specialist services (e.g. HIV clinics, vasectomy clinics, fertility clinics) were scheduled at different times across the sites, meaning that the standard SHC hours were not exactly the same across sites.
Research tools
Each site was given the same mechanism for data capture. This involved providing paper questionnaires for each SHC. In SHCs, it was not possible to detect people who did not complete a questionnaire because of language barriers, as reasons for non-completion could not be collected because of self-completion.
We strove to avoid disruption to the regular workings of the SHCs. This meant that in SHCs staff were encouraged to treat attendees as normal. Moreover, to avoid disruption of normal care for patients, we used reception staff to introduce the questionnaire where this fitted the service preferences. This decreased the chance of a chaotic data collection environment.
To maximise our chances of obtaining sufficient recruitment numbers, we made eligibility criteria as inclusive as possible. We were also able to ensure data accuracy and reducing missing data, where possible, by excluding questionnaires that were clearly invalid because most would be left blank by most respondents.
There were seasonal issues (affecting particular waves) and contextual issues (affecting particular sites) that had to be overcome during data collection. First, the ‘Beast from the East’ (i.e. snow in late February 2018) had the potential to affect the ability of staff or patients to reach SHCs but in the end did not affect data collection. Second, there were staffing issues; in one SHC the principal investigator was on sick leave for an extended time, and there were staff shortages at another site. Third, the timeline for training and organising data collection was short because of the short period of time between the final legal challenge to MUP and its subsequent introduction. Finally, the offer of chocolates as an encouragement to return a paper questionnaire was extended to all SHCs at the third wave only.
Changes to protocol
Changes to protocols were notified to the Ethics Committee. The first change (to v2.3) was as a result of the delay to the implementation of MUP, during which the chief investigator moved to Australia and a new chief investigator was appointed. In addition, there were changes to the sponsor and local lead investigators. Our letter to NIHR, dated 23 October 2017, gives further details (see Report Supplementary Material 1). There were also updates to the list of drugs mentioned in the questionnaire and new questions as per the version provided. There was a further update (v2.5) to change the principal investigator in Tayside and to allow receptionists to be involved in providing questionnaires to attendees. This notice of amendment was signed by the principal investigator and submitted to the Ethics Committee on 5 January 2018.
There was also a violation of the protocol. A protocol deviation form was completed and sent to the Ethics Committee (see Report Supplementary Material 2). The deviation was that an earlier draft version of the questionnaire was used in error. Adjustments were made to the coding of educational categories in the analysis stage to ensure that they were mapped to the revised categories used at waves 2 and 3.
Results
Description of sample and response
Summarised response levels are shown in Table 8 for all waves and for each site using numbers of attendees by age and sex, as provided by the sites. See Appendix 3, Table 44, for complete response levels by wave and site, and Appendix 3, Table 45, for response levels by country and wave.
| Clinic site | Total number of completed surveys | Total number of eligible attendees | Total response (%) |
|---|---|---|---|
| Glasgow | 1159 | 2075 | 56 |
| Lothian | 3600 | 7425 | 48 |
| Tayside | 1114 | 2184 | 51 |
| Sheffield | 3245 | 5440 | 60 |
| Leeds | 3141 | 4171 | 75 |
| Manchester | 2959 | 5776 | 51 |
| Total | 15,218 | 27,071 | 56 |
Total responses decreased over the three waves, from 60% in wave 1, to 55% in wave 2 and to 54% in wave 3. The response for the three English sites combined was 61% and the response for the three Scottish sites combined was 50%. The minimum response level in a site for a single wave was 31%, whereas the maximum was 82%. There was variability in the site response levels by age and sex across waves. We carried out Pearson’s chi-squared tests to assess these age and sex differences between waves and also to test for age and sex differences between responders and the sampling frame of all attendees at each site (see the chi-squared results in Appendix 3, Table 46).
A summary of subgroup differences in Appendix 3, Table 46, between the responders and sampling frame follows.
In wave 1, SHC responders differed from the sampling frame on age group in Edinburgh, Glasgow and Leeds (i.e. there were more people aged 20–24 years in Edinburgh than expected, there were more people aged 20–29 years in Glasgow than expected and there were more people aged 16–19 years in Leeds than expected). Regarding sex (males/females), there were no differences, except in Glasgow (which had more males than expected) and in Leeds (which had fewer males than expected).
In wave 2, responders were different on age everywhere except in Sheffield. Edinburgh had fewer younger people aged 20–24 years, but more aged 16–19 years than expected. Glasgow and Dundee had more people aged 20–29 years than expected. Leeds had more people aged 16–19 years and fewer people aged 25–29 years than expected. Manchester had more people aged 20–24 years than expected. Regarding sex, there were differences in Glasgow (more males than expected), Sheffield (more females than expected) and Manchester (more females than expected).
In wave 3, SHC responders differed on age group from the sample, except in Glasgow and Sheffield. In Edinburgh, Dundee and Leeds there were more younger people, especially those aged 16–19 years, than expected. In Manchester, there were more people aged 20–24 years. Regarding sex, there were no significant differences, except in Edinburgh, Glasgow, Leeds and Manchester. Edinburgh, Leeds and Manchester had more females than expected and Glasgow had more males than expected.
The sex differences between waves were small, but they were somewhat greater for age group. Appendix 3, Table 47, shows these differences. We adjusted for both of these variables, and for employment status and highest educational level, in our third regression model.
Descriptive data
Table 9 shows responders’ demographics by country. As expected, the sample is younger, has more females and a higher proportion of students, compared with the general population. 137,160
| Variable | Scotland (N = 5873), n (%) | England (N = 9345), n (%) |
|---|---|---|
| Age (years) | ||
| ≤ 19 | 1016 (17.3) | 1825 (19.5) |
| 20–24 | 1816 (30.9) | 3322 (35.5) |
| 25–29 | 1011 (17.2) | 1550 (16.6) |
| 30–34 | 573 (9.8) | 974 (10.4) |
| 35–39 | 474 (8.1) | 613 (6.6) |
| 40–45 | 343 (5.8) | 430 (4.6) |
| > 45 | 638 (10.9) | 628 (6.7) |
| Missing | 2 (0.0) | 3 (0.0) |
| Sex | ||
| Male | 2389 (40.7) | 3384 (36.2) |
| Female | 3354 (57.1) | 5897 (63.1) |
| Non-binary | 123 (2.1) | 49 (0.5) |
| Missing | 7 (0.1) | 15 (0.2) |
| Employment status | ||
| Employed | 3212 (54.7) | 4426 (47.4) |
| Economically inactivea | 2285 (38.9) | 4227 (45.2) |
| Unemployed | 273 (4.6) | 564 (6.0) |
| Missing | 103 (1.8) | 128 (1.4) |
| Highest education level | ||
| Higher education | 3905 (66.5) | 5794 (62.0) |
| Further education | 374 (6.4) | 872 (9.3) |
| Upper secondary school | 799 (13.6) | 1101 (11.8) |
| Lower secondary school | 527 (9.0) | 907 (9.7) |
| No formal qualifications | 185 (3.2) | 441 (4.7) |
| Missing | 83 (1.4) | 230 (2.5) |
Although there was variability in site response levels by age and sex across waves (see Appendix 3, Tables 46 and 47), the DiD fixed-effects regression model included age, sex, occupation and education as covariates to reduce bias. Missing data for demographic variables were as shown in Table 9. The demographic data are shown by site and wave in Appendix 3, Table 48. For each outcome variable, missing data before imputation are shown in Appendix 3, Table 49.
Outcome measures
Figure 15 shows the DiD estimates for the fully adjusted model for the primary and secondary outcomes. The comparison is between baseline and waves 2 and 3 combined based on the multiply imputed data sets. The inclusion of wave in the regression models controlled for seasonality. The results reported below are for both follow-ups combined to give more statistical power. In addition, we compared baseline with each follow-up wave separately. The results for separate wave 2 and wave 3 follow-ups are given in Appendix 3, Table 51, and are also signposted below.
FIGURE 15.
Difference-in-difference estimates of the overall effects of MUP (a) based on all respondents; and (b) based on drinkers only.


Illicit drugs results
General trends
Figure 16 shows the proportion of respondents at each of the three time points, for the primary and secondary outcomes, with 95% CIs. A full set of trends with 95% CIs is also shown in Appendix 3, Figures 39–48 and Table 52.
FIGURE 16.
Outcome trend across three waves compared between Scotland and England. (a) Consumption of any illicit drugs in the last month; (b) current alcohol drinker; (c) binge drinking at least weekly; (d) alcohol misuse (FAST score ≥ 3); (e) mean FAST score; (f) alcohol purchased from on-licensed premises; and (g) alcohol purchased from off-licensed premises.

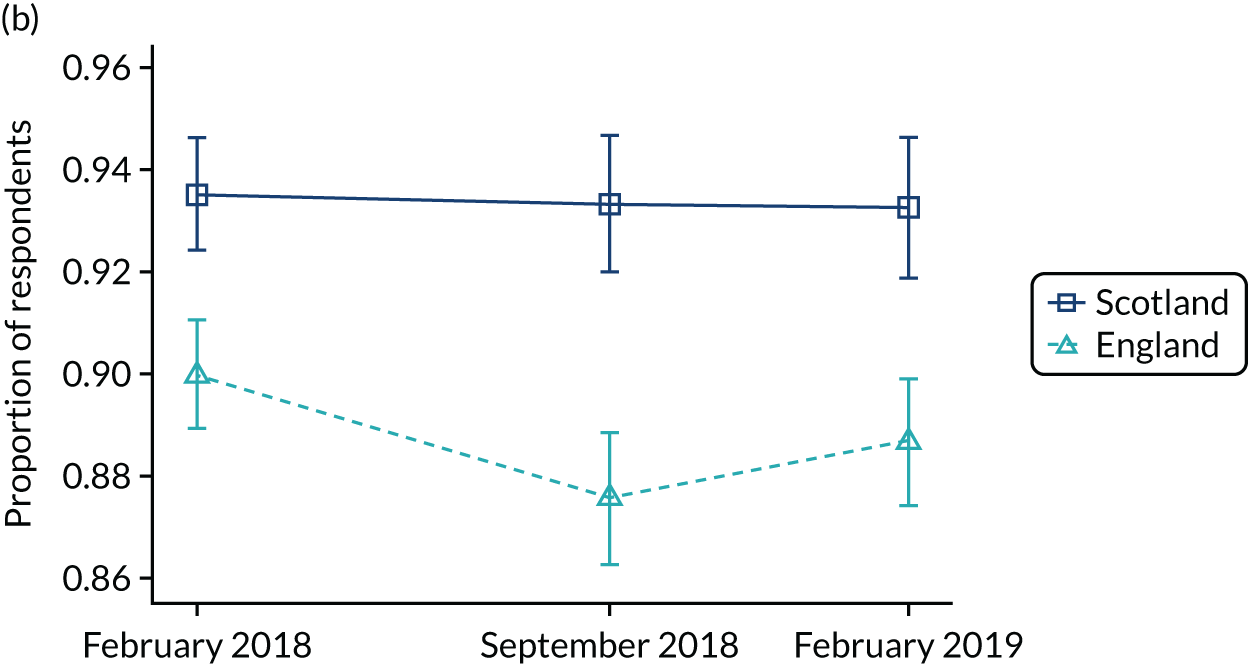
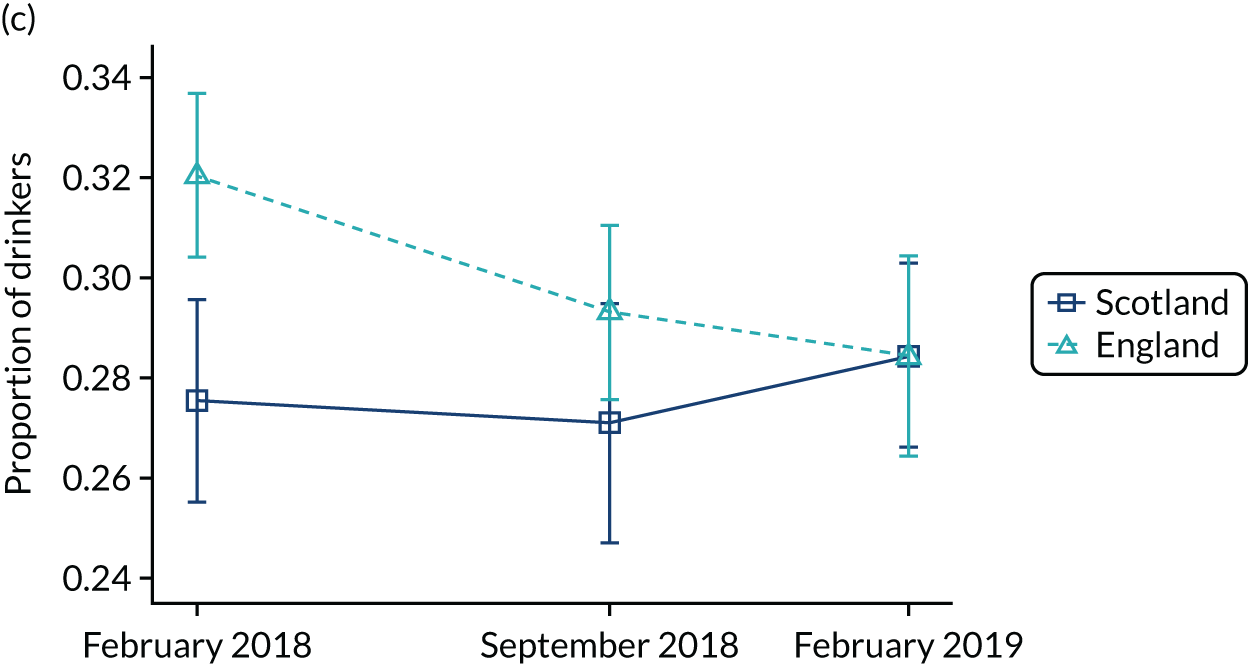
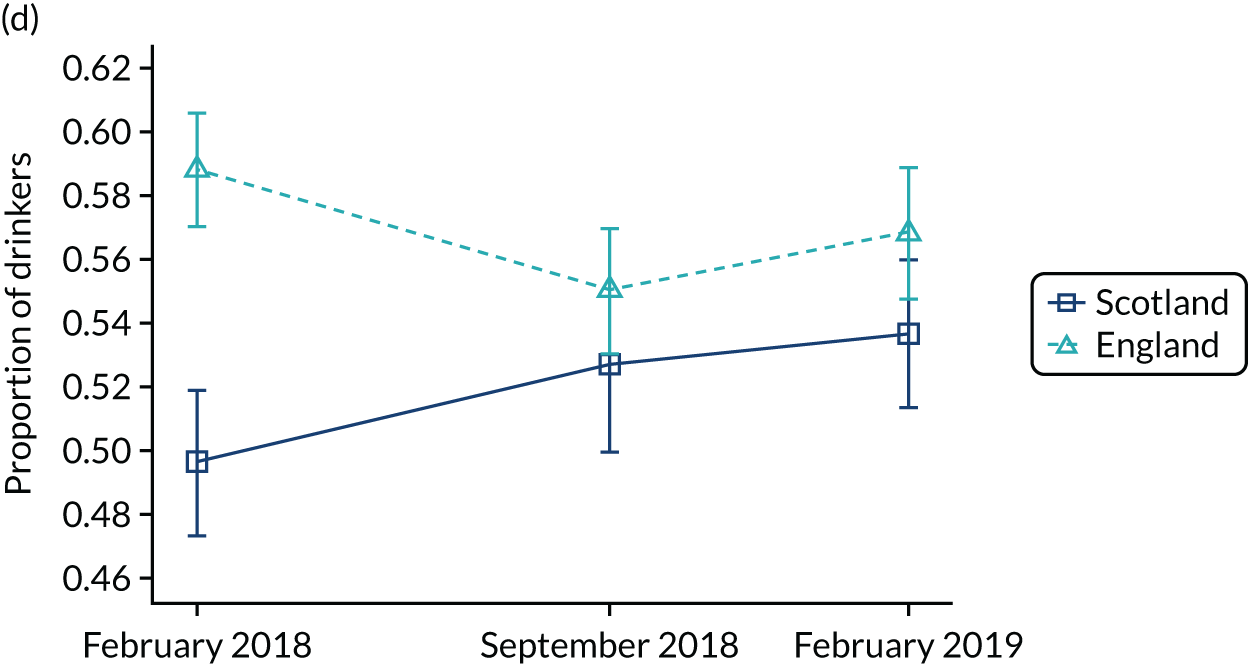

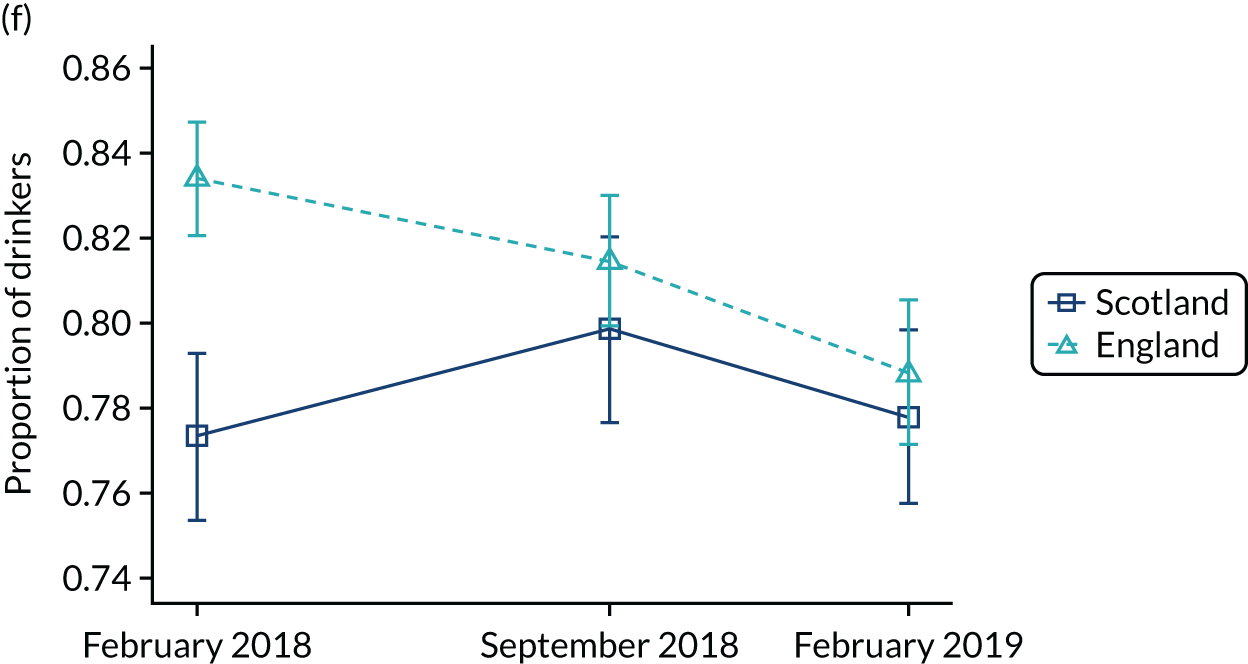

Summary of trend for illicit drugs consumption
The proportion of respondents consuming illicit drugs in the last month went up across the three waves in both countries. The countries converged. At baseline, 95% CIs did not overlap and Scotland was lower, but by wave 3 the 95% CIs overlapped (see Figure 16a).
Therefore, for the primary outcome, the general trend across waves was for an increase in the probability of consuming drugs in the last month. As Figure 16a shows, there was a steeper increase across waves in Scotland compared with England.
Difference-in-difference estimates
The DiD estimates comparing pre MUP with post MUP for model 3 (see Figure 15) showed no evidence that illicit drug consumption changed as a result of MUP in our sample (see also Appendix 3, Table 52, for all three models and general trends results for all outcomes measures). As a trend analysis, we compared each follow-up wave individually with baseline (see Appendix 3, Table 51). The DiD analysis found no evidence of a trend, as there was no difference between baseline and wave 2 or between baseline and wave 3 for the consumption of any illicit drugs in the last month (see Appendix 3, Table 51).
We investigated changes (Figure 17) in the consumption of individual drugs in the last month to see if any of these had changed with the introduction of MUP (model 3 is shown in Figure 17 and all three models for each drug with general trends added in Appendix 3, Table 53). There was little evidence of substantive differences, with the risk of mephedrone being reduced and the risk of heroin and crack increased, although both were imprecisely estimated, and, as shown in Figure 17, based on small proportions of respondents. Diazepam (Valium®; Hoffmann-La Roche, Inc., Basel, Switzerland) is not mentioned in the table, but was included by explanatory questionnaire text in the category ‘tranquillisers’.
FIGURE 17.
Difference-in-difference estimates of the effects of MUP for individual drugs. LSD, lysergic acid diethylamide.
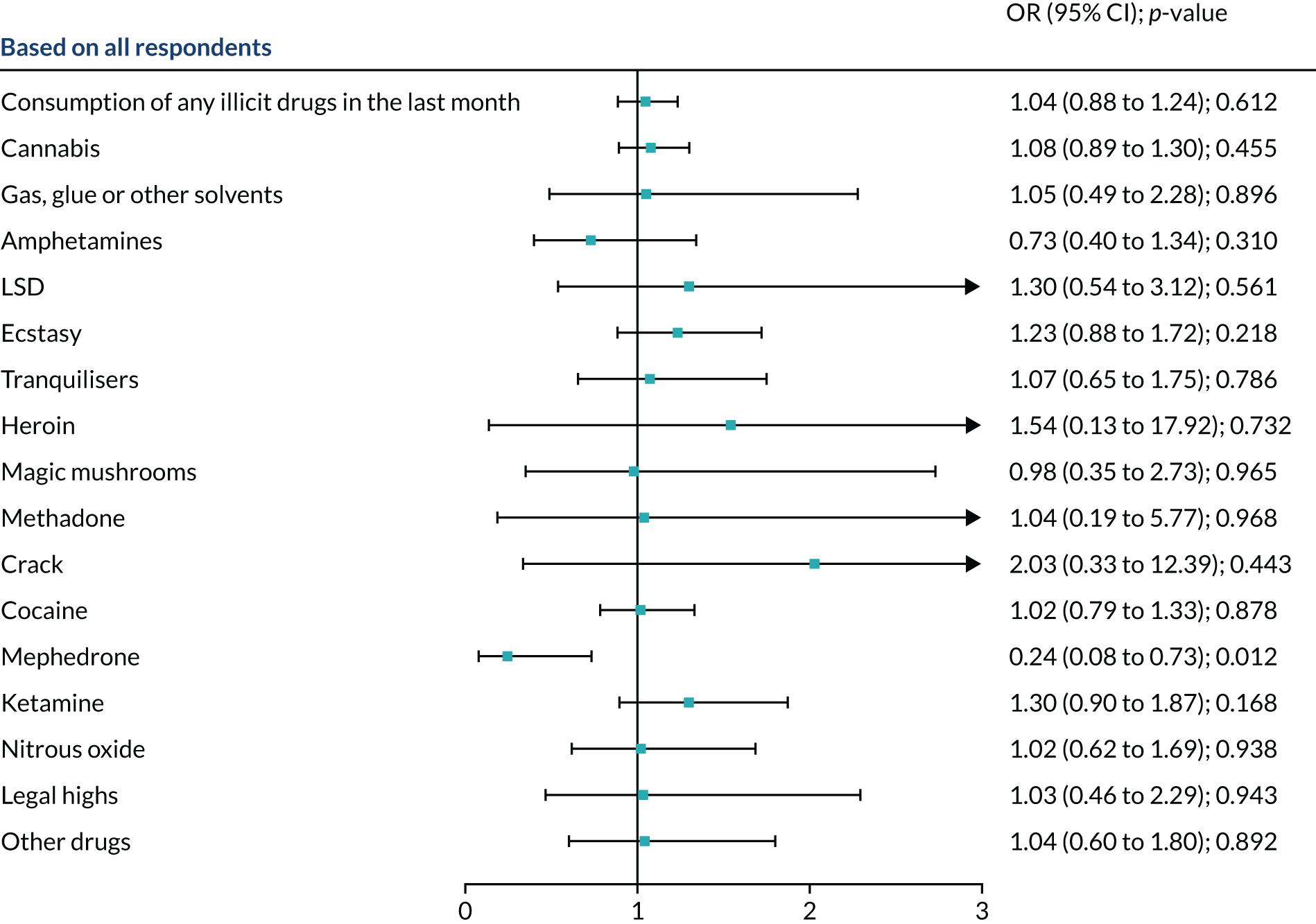
Trends by individual drug are shown in Table 10.
| Drug use | Scotland (%) | England (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | |
| Consumption of any illicit drugs in the last month | 24.2 | 25.8 | 29.3 | 29.3 | 30.1 | 31.6 |
| Cannabis | 16.8 | 19.2 | 20.8 | 20.2 | 21.7 | 21.5 |
| Gas, glue or other solvents | 0.8 | 1.2 | 1.1 | 0.9 | 0.9 | 1.3 |
| Amphetamines | 1.6 | 1.3 | 1.3 | 1.4 | 1.3 | 1.6 |
| LSD | 0.5 | 0.6 | 0.9 | 0.8 | 1.0 | 0.7 |
| Ecstasy | 4.4 | 4.4 | 5.1 | 6.4 | 5.3 | 5.3 |
| Tranquillisers | 2.0 | 1.7 | 2.4 | 2.5 | 2.3 | 2.1 |
| Heroin | 0.1 | 0.1 | 0.3 | 0.1 | 0.1 | 0.2 |
| Magic mushrooms | 0.5 | 0.9 | 0.6 | 0.4 | 0.5 | 0.6 |
| Methadone | 0.2 | 0.3 | 0.5 | 0.2 | 0.1 | 0.4 |
| Crack | 0.1 | 0.2 | 0.2 | 0.4 | 0.2 | 0.4 |
| Cocaine | 7.6 | 7.0 | 9.4 | 10.7 | 10.0 | 10.6 |
| Mephedrone | 0.7 | 0.1 | 0.3 | 0.7 | 0.9 | 0.9 |
| Ketamine | 2.7 | 3.3 | 4.5 | 6.3 | 6.2 | 6.5 |
| Nitrous oxide | 1.4 | 2.2 | 1.4 | 5.7 | 6.0 | 6.1 |
| Legal highs | 0.8 | 0.8 | 0.7 | 1.2 | 0.9 | 1.0 |
| Other drugs not given by a doctor or chemist | 1.8 | 1.2 | 2.3 | 2.1 | 1.5 | 2.5 |
From Table 10, there appeared to be a suggestion of a trend for an increase in cannabis, ecstasy and ketamine use in Scotland compared with England. However, although cannabis was the most widely used illicit drug among respondents, the DiD analysis in Figure 17 did not show a difference for any of these, as the 95% CI included 1.
Alcohol outcomes
General trend
The proportion of ‘current alcohol drinkers’ was higher in Scotland, with non-overlapping 95% CIs across all three waves. The proportion of ‘current alcohol drinkers’ in Scotland dropped at wave 2, but increased again at wave 3 (see Figure 16a). The probability of being a current drinker for all respondents declined slightly across waves in both England and Scotland. At wave 3, 93.2% of respondents in Scotland and 88.7% of respondents in England were current drinkers.
In Figure 16, we also compare four alcohol-related outcomes for drinkers only. For ‘binge drinking at least weekly’, England trended down to 28.5%, but Scotland trended slightly up to 28.4% (see Figure 16c). The proportion of respondents binge drinking in the last year was higher in England at baseline, then dropped from baseline to wave 2, dropping more in England than in Scotland, but Scotland then rebounded at wave 3 while the English decline in binge drinking continued, meaning that there were overlapping 95% CIs at waves 2 and 3.
The proportion of respondents reporting ‘alcohol misuse’ (i.e. a FAST score ≥ 3) in our samples rose in Scotland to 53.6%, but fell in England to 56.8% (see Figure 16d). The proportion of respondents reporting alcohol misuse in the last year was higher in England and lower in Scotland at baseline and there were overlapping 95% CIs at waves 2 and 3.
The mean ‘FAST score’ showed a similar pattern to alcohol misuse (i.e. a FAST score ≥ 3), rising to 3.36 in Scotland and falling to 3.50 in England (see Figure 16e). The mean FAST score in the last year was higher in England and lower in Scotland at baseline, but there were overlapping 95% CIs at waves 2 and 3.
The proportion of respondents buying alcohol from licensed premises rose slightly in Scotland to 77.8%, but fell in England to 78.8% (see Figure 16f). Note that this does not necessarily mean that people in Scotland bought a higher proportion of their alcohol from on-licensed premises than they did before, but there was a change relative to England. The proportion of respondents buying alcohol from licensed premises in the last month was higher in England and lower in Scotland at baseline, with overlapping 95% CIs at waves 2 and 3.
The proportion of respondents buying alcohol from off-licensed premises in the last month was similar in England and Scotland at all waves, with a small decline to wave 3 (see Figure 16g).
Difference-in-difference estimates
The DiD estimates for all respondents (see Figure 15 and Appendix 3, Table 52) showed no evidence that the probability of being a current drinker changed as a result of MUP in the SHC attendees we sampled. For drinkers, in model 3, there were slight increases for only two outcomes and no evidence of change for other outcomes following MUP:
-
Among current drinkers attending the SHC, the odds of alcohol misuse (i.e. a FAST score ≥ 3) increased by 22% relative to the change seen in England following MUP (OR 1.22, 95% CI 1.04 to 1.42; p = 0.012).
-
The odds for binge drinking did not change after adjustment (OR 1.13, 95% CI 0.96 to 1.34; p = 0.139).
-
The odds of purchasing alcohol from on-licensed premises increased by 24% (OR 1.27, 95% CI 1.05 to 1.55; p = 0.031) relative to the change seen in England. There was no evidence that MUP affected the probability of alcohol purchase from off-licensed premises.
We compared the baseline with each follow-up wave separately to see whether or not there was any difference in the short- and long-term outcomes using DiD analysis. There were no changes for drug misuse. This analysis showed a change in alcohol misuse (i.e. a FAST score ≥ 3 at wave 2, OR 1.25, 95% CI 1.04 to 1.51), but not at wave 3 (OR 1.19, 95% CI 1.00 to 1.42). For the increase in alcohol purchase from the on-trade, this analysis showed a change at wave 3 (OR 1.32, 95% CI 1.05 to 1.65), but not at wave 2 (OR 1.26, 95% CI 0.99 to 1.60) (see Appendix 3, Table 51).
An analysis was carried out for the drinkers’ outcomes against FAST cut-off points of ≥ 2 , ≥ 5 and ≥ 7 (see Figures 25–27 and Appendix 3, Tables 58–60). These cut-off points were validated using a re-analysis of the relationship of AUDIT-C subscales using the Adult Psychiatric Morbidity Survey. 148 There were similar patterns across waves at these cut-off points.
As a further sensitivity analysis, we compared a key outcome, from complete-case analysis, the FAST score, with the FAST score using multiple imputation for the outcome. There was very little difference in the results. Appendix 3, Figures 29–38, show all the outcomes calculated in three ways: (1) using imputed data and weighted estimates, (2) using data before imputation and unweighted estimates and (3) using data before imputation and weighted estimates.
We further investigated our outcomes by age, sex, education and occupation through stratified analysis. Full results are given in the online appendix tables (see Appendix 3, Tables 54–63). The fully adjusted DiD stratified analyses are shown in Figure 18 for the primary outcome and all other outcomes are shown in Figures 19–27.
FIGURE 18.
Stratified DiD analysis for primary outcome (illicit psychoactive drug use in the last month). Note that the p-values in the forest plot were uncorrected.
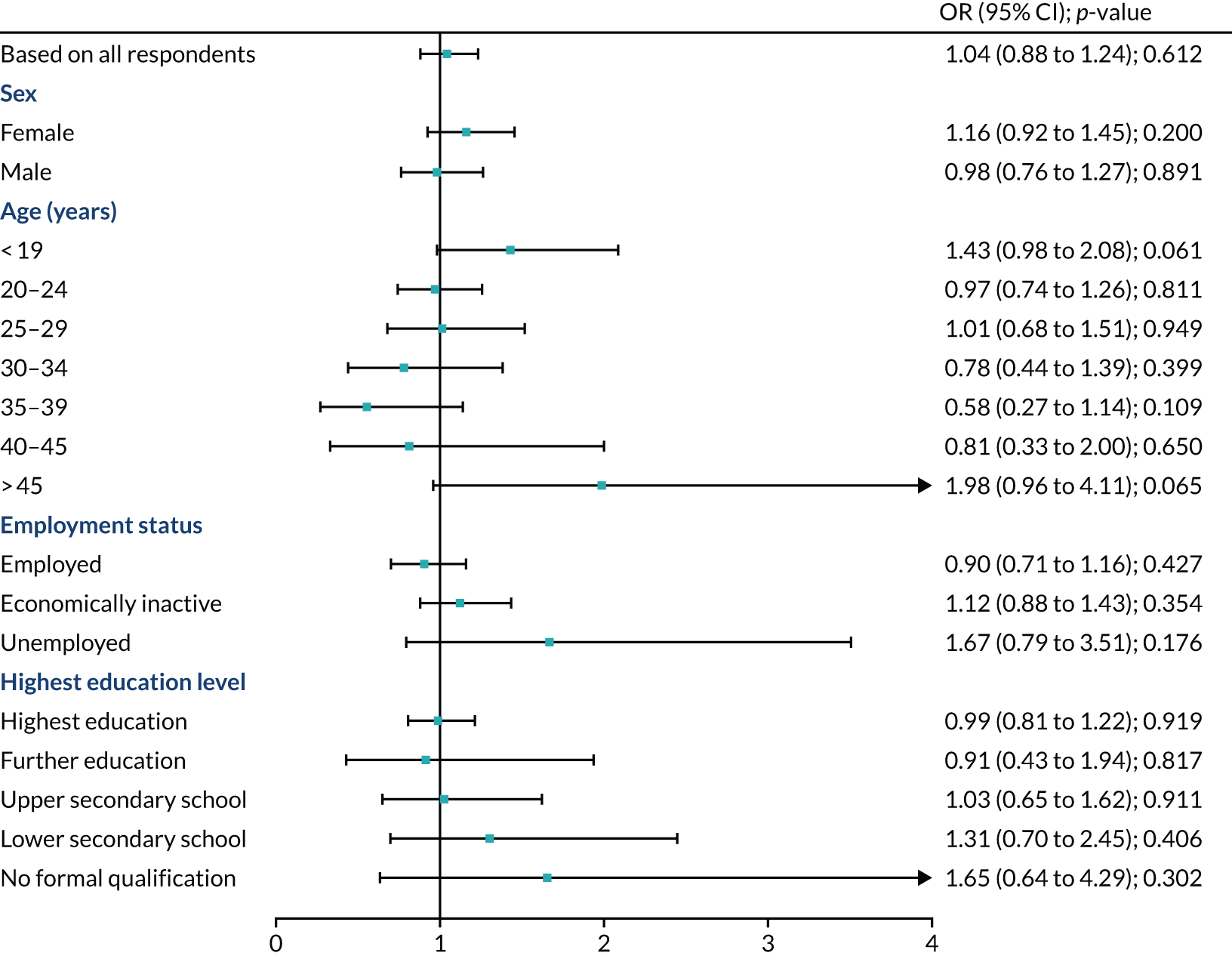
FIGURE 19.
Stratified analysis: current alcohol drinker. Note that the p-values in the forest plot were uncorrected.
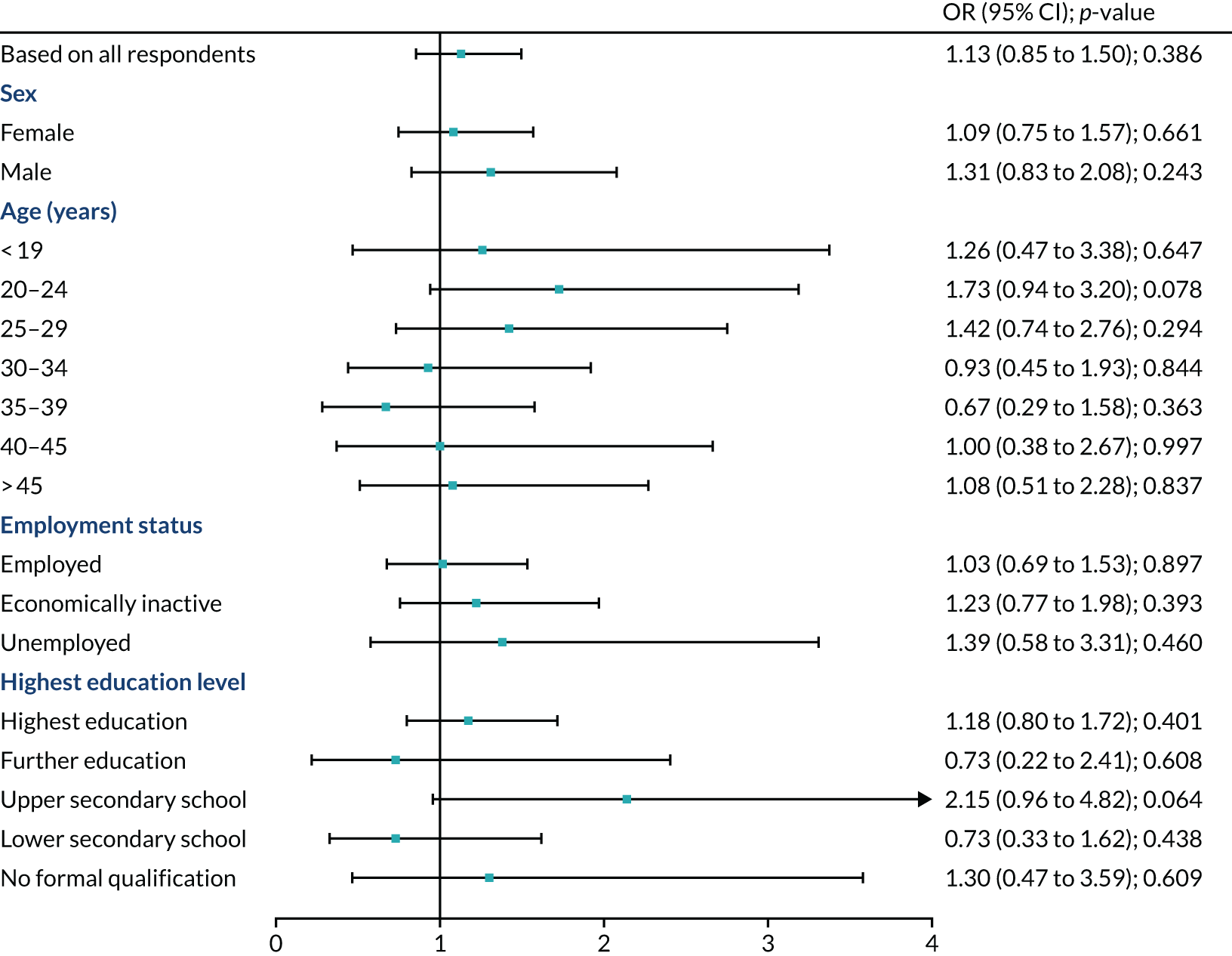
FIGURE 20.
Stratified analysis: binge drinking at least weekly. Note that the p-values in the forest plot were uncorrected.
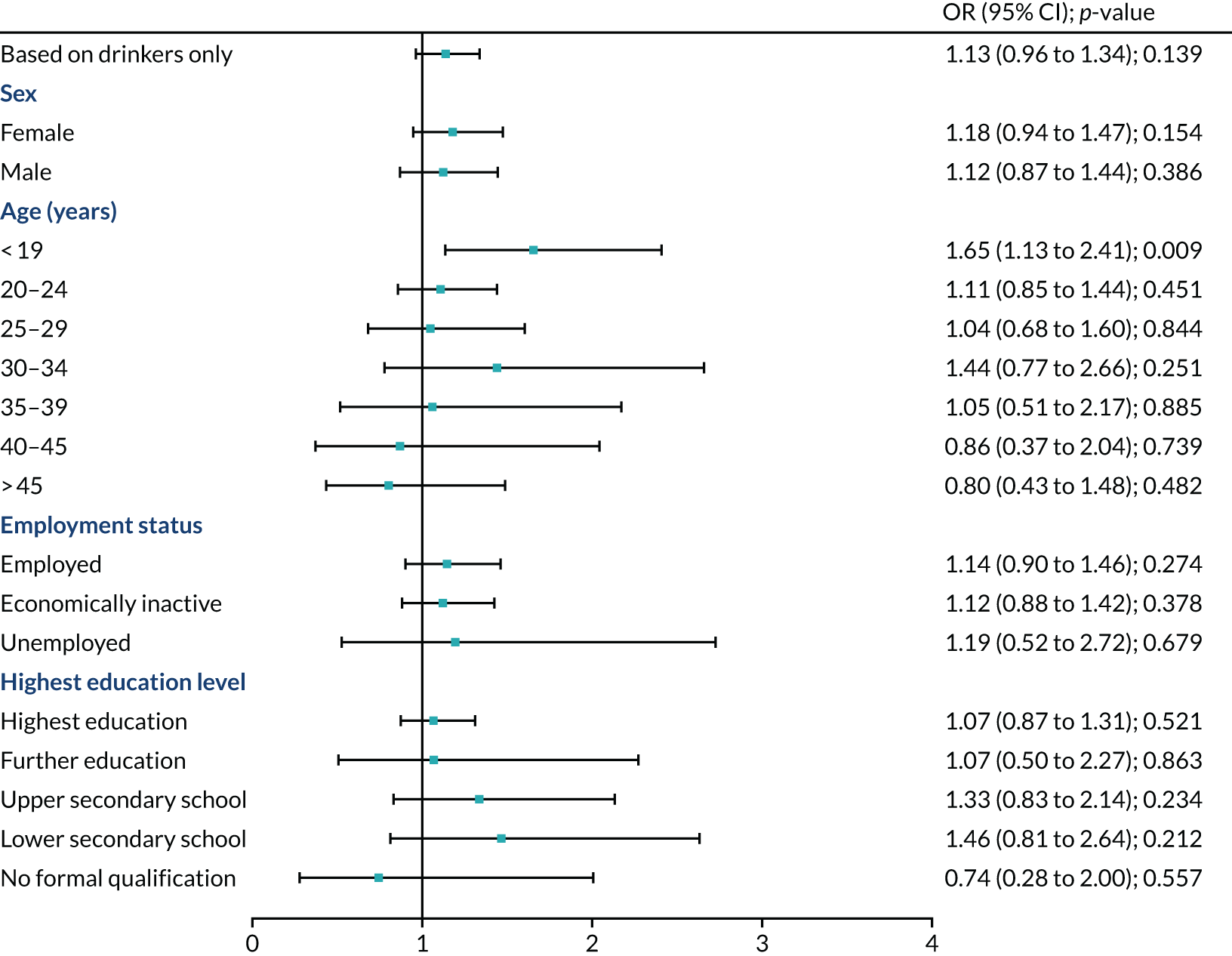
FIGURE 21.
Stratified analysis: alcohol misuse (FAST score ≥ 3 ). Note that the p-values in the forest plot were uncorrected.
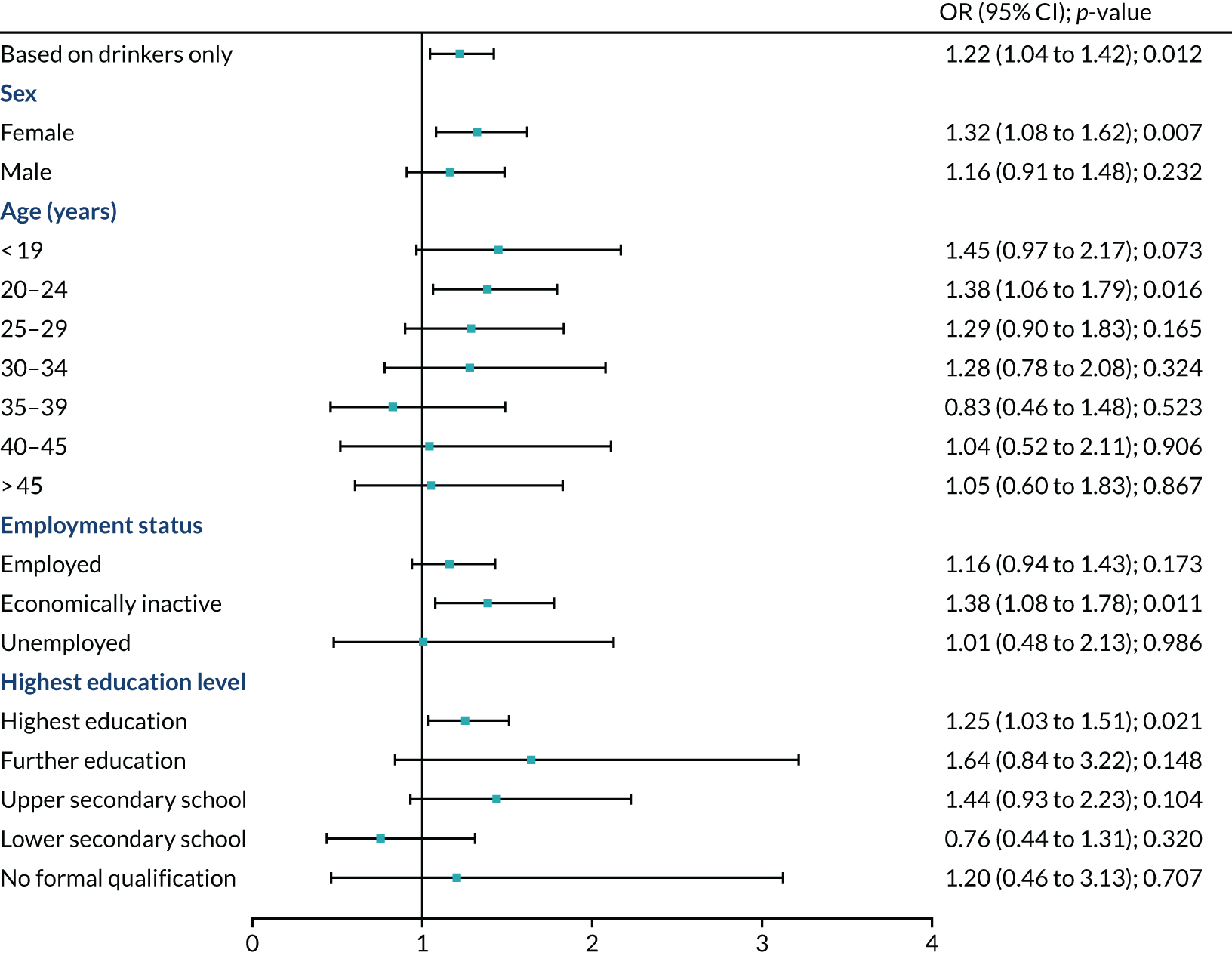
FIGURE 22.
Stratified analysis: alcohol bought from on-licensed premises. Note that the p-values in the forest plot were uncorrected. a, Corrected p < 0.01 after Bonferroni correction for multiple comparisons.
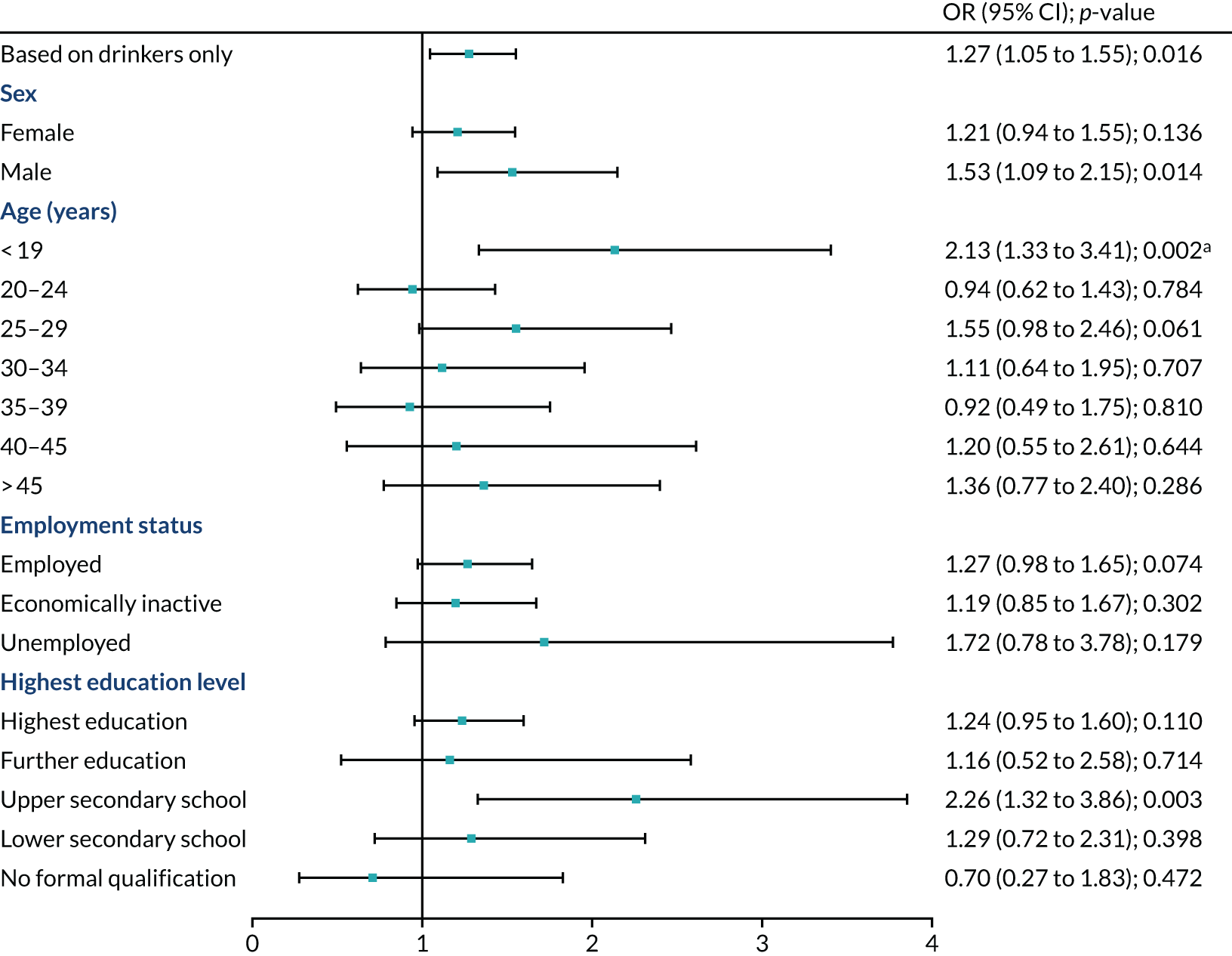
FIGURE 23.
Stratified analysis: alcohol bought from off-licensed premises. Note that the p-values in the forest plot were uncorrected. a, Corrected p < 0.01 after Bonferroni correction for multiple comparisons.

FIGURE 24.
Stratified analysis: mean FAST score. Note that the p-values in the forest plot were uncorrected.
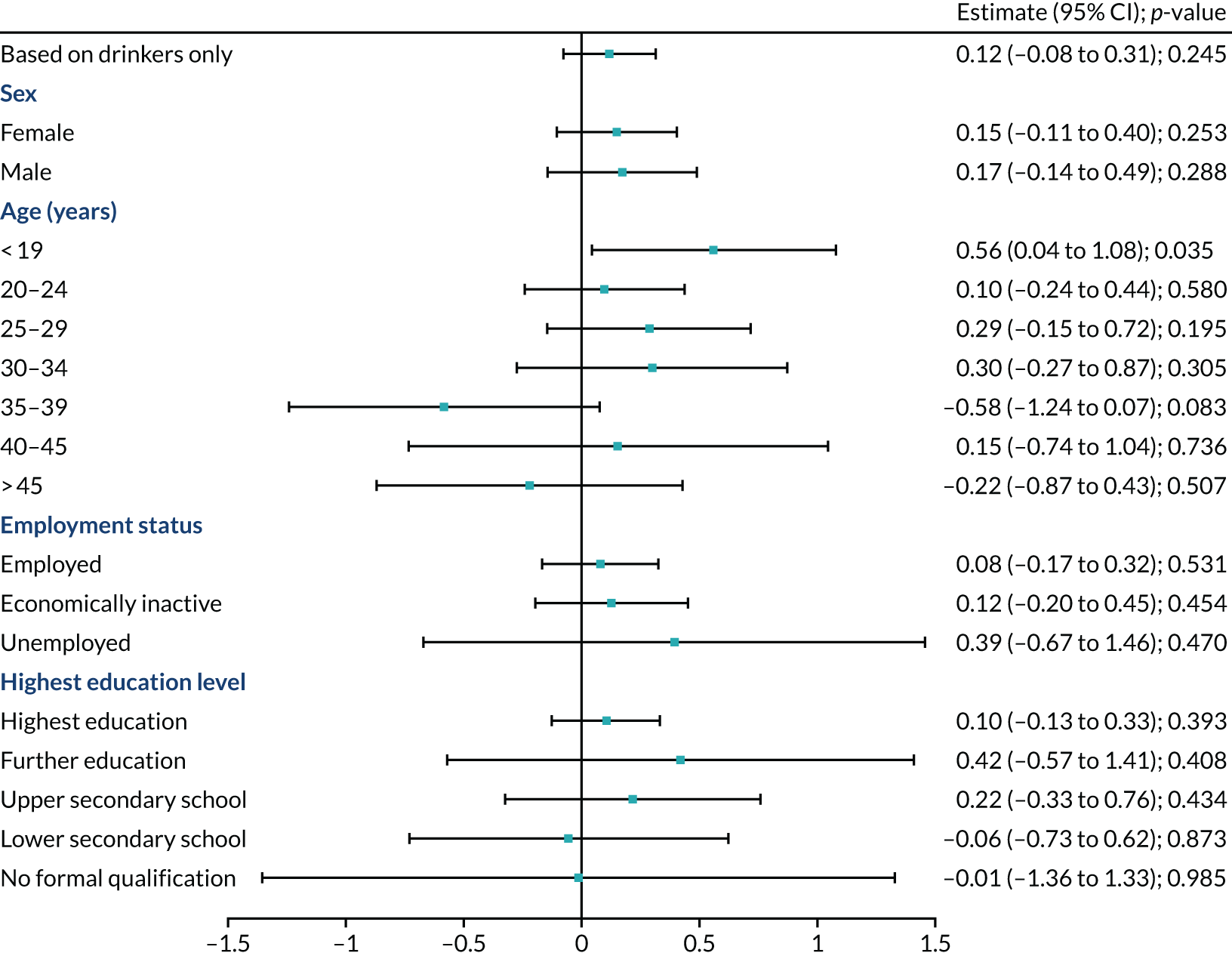
FIGURE 25.
Stratified analysis: drinkers with at least a hazardous drinking level. Note that the p-values in the forest plot were uncorrected.
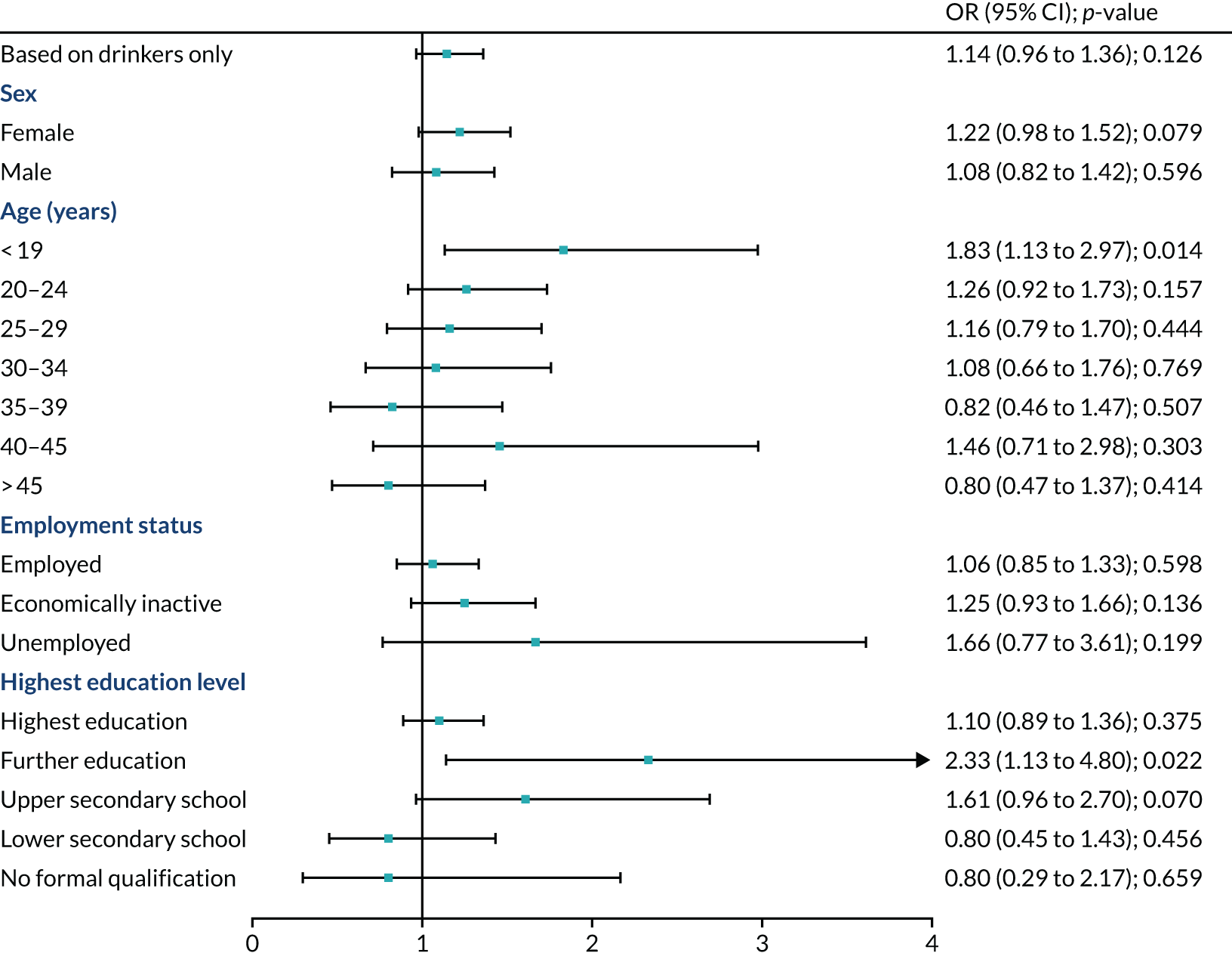
FIGURE 26.
Stratified analysis: drinkers with at least a harmful drinking level. Note that the p-values in the forest plot were uncorrected.
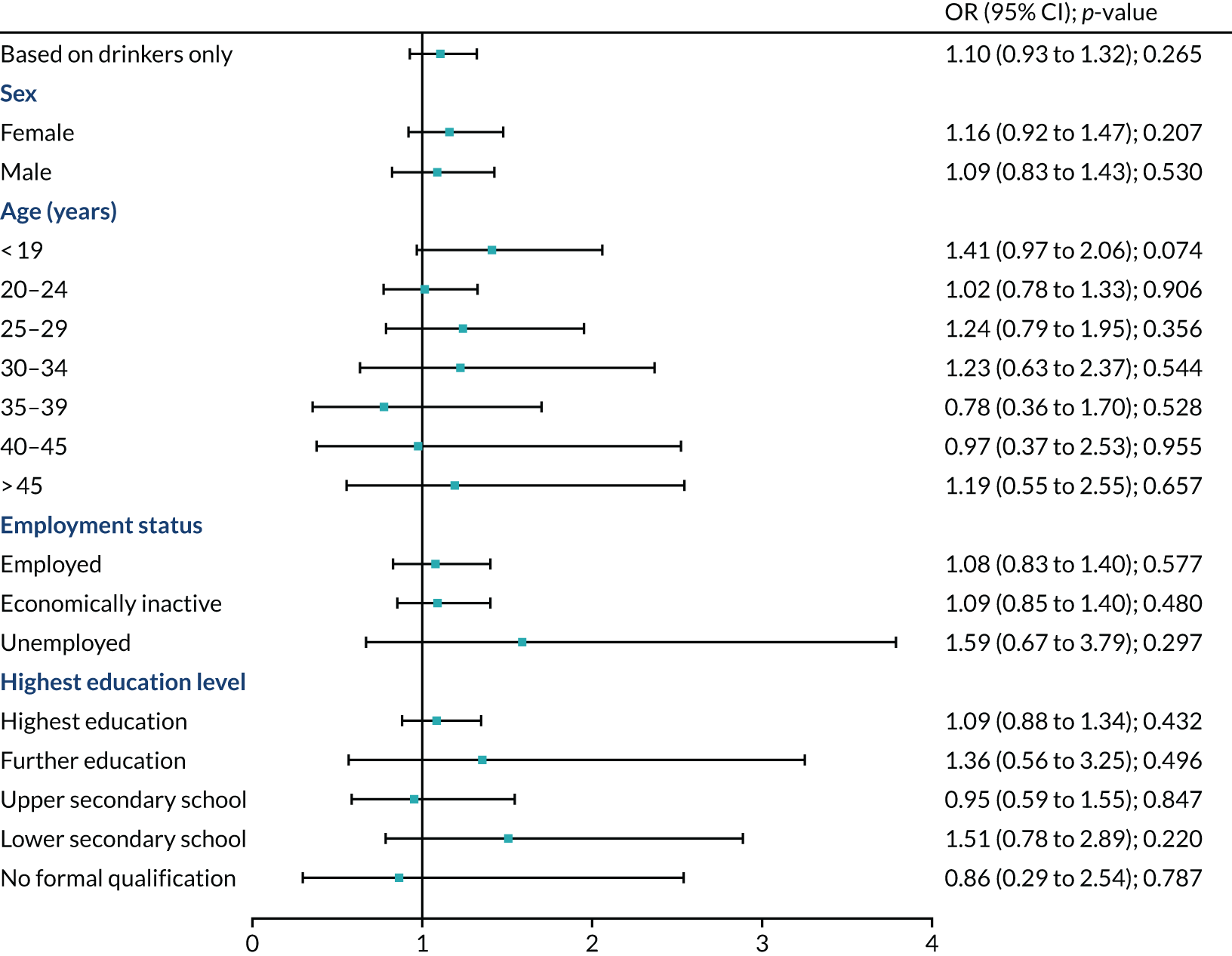
FIGURE 27.
Stratified analysis: drinkers with at least a dependent drinking level. Note that the p-values in the forest plot were uncorrected.

The stratified analyses in Figure 18 show that many of the stratified results were imprecisely estimated, and there was no evidence of change. Further tables showing the both the trends across waves and stratified analyses of secondary outcomes are given in Appendix 3, Tables 54–63.
Stratified analysis for the alcohol outcomes is reported in Figures 19–27. For the proportion of current drinkers, there was no evidence of relative differences between countries after MUP by sex, age group, employment status or educational level (see Figure 19).
Figures 20 and 21, again, show no evidence of change, as no effect was substantive (p < 0.05) after Bonferroni adjustment.
Figure 22 suggests that only those aged < 19 years may have been more likely to buy from on-licensed premises after MUP, as after Bonferroni adjustment this remained significant (p < 0.031). This increase is relative to any change in the probability of buying from on-licensed premises seen in the north of England.
Figure 23 suggests that respondents aged < 19 years were also more likely to buy from off-licensed premises after MUP. This effect remained at p < 0.014 after Bonferroni adjustment. There was no other evidence of change.
Figure 24 shows some imprecise estimates and no evidence of change, as no effect was substantive at p < 0.05 after Bonferroni adjustment.
Figure 25 includes some imprecise estimates and no effect had p < 0.05 after Bonferroni adjustment.
As shown in both Figures 26 and 27, there was no evidence of an increase in harmful or dependent drinking in any subgroup.
Discussion
We found no evidence of illicit drug use substituting for alcohol use after MUP. Therefore, there is no evidence of an unintended effect of MUP on illicit drug use.
There was no evidence of changes in any of the subgroups for the primary outcome. Although numbers for individual drugs were small, they were enough for us to be able to rule out a large effect.
We found that the proportion of alcohol drinkers reporting ‘alcohol misuse’ (i.e. a FAST score ≥ 3) in our samples rose in Scotland to 53.6%, but fell in England to 56.8%. In comparison, the Scottish Health Survey 2018 (revised 2020) reported that 32% of males, 16% of females and 24% of all adults were hazardous or harmful drinkers in 2018. 141 The final model (see Figure 21) suggested greater odds among drinkers of alcohol misuse (i.e. a FAST score ≥ 3) after MUP (OR 1.22, 95% CI 1.04 to 1.42; p = 0.012). We detected no effect on binge drinking. There were greater odds of sourcing alcohol from on-licensed premises after MUP (OR 1.27, 95% CI 1.05 to 1.55; p = 0.016), which could reflect the reduced price differential between the on- and off-trade and, in turn, increase the comparable attractiveness of the on-trade. This does not tell us if people bought a higher proportion of their alcohol from on-licensed premises than they did before. Other evidence showed off-license sales reduced in Scotland by 3.6%, while increasing in England by 3.2%, in the year following MUP. 90,103
The stratified analyses for alcohol showed a pattern of imprecisely estimated negative outcomes, especially among younger drinkers. The only stratified effects remaining at p < 0.05 after Bonferroni adjustment were the increase (relative to England) in odds of those aged < 19 years buying from off-licenses (OR 2.12, 95% CI 1.37 to 3.28; p < 0.014 after Bonferroni adjustment). This went down overall in both Scotland and England (see Figure 16g). Similarly, there was an increase in odds of those aged < 19 years buying from on-licenses (OR 2.13, 95% CI 1.33 to 3.41; p < 0.031 after Bonferroni adjustment).
Limitations
The varying response across waves gives a potential for selection bias, but the direction of any possible bias is unclear. Age and sex differences between interviewees and attendees and between waves are shown in Appendix 3, Tables 46 and 47. One clinic had excluded attendees with a previously expressed wish not to be involved in research projects. To increase the response, we changed the approach by agreement at wave 3 to using dedicated researchers available from our unit researcher bank rather than reception staff. These staff approached all attendees. The changed approach may be a cause of selection bias, as it may have caused a differential response, affecting comparisons between sites. As the surveys were self-completed without the presence of the researcher and returned to a collection box by the responder, social desirability bias should not have been affected by this change.
Our study faced time constraints driven by uncertainty about if and then when MUP would be implemented, a not uncommon issue for policy evaluation studies. 161 Although MUP legislation was passed in 2012, implementation did not happen until after the conclusion of the legal challenge by the Scotch Whisky Association and others, when the UK Supreme Court ruled in favour of the Scottish Government on 15 November 2017. The Scottish Government announced on 21 November 2017 that the implementation date would be 1 May 2018. Our evaluation required the establishment of a baseline early in February 2018 to reduce the effect of pre-intervention price changes. This left little time for all approval processes, budgeting and training, and meant that we had only one baseline. For our analysis, two baselines would have been preferable so that the trends in drug and alcohol consumption before the implementation of MUP could be assessed in each country. In particular, we needed to know whether pre-existing trends in the outcomes assessed were parallel, as required for the effective use of a DiD design. 162
The potential for collider bias163 was higher than originally anticipated when the study was designed in 2012. At the time of study design, we thought participation effects would be constant over time across countries. However, following the design of the study, the onset of austerity coupled with moving sexual health services into local authority provision within England but not Scotland could have introduced collider bias by changing the patient mix in the clinics in England, although we believe this unlikely. Figure 28 illustrates that MUP could have had an effect on sexual health attendance and drug use could have been influenced by MUP, but drug use could also have an effect, although smaller than alcohol, on sexual health attendances.
FIGURE 28.
Directed acyclic graph to show potential collider bias (dashed arrow) from changing patient mix.
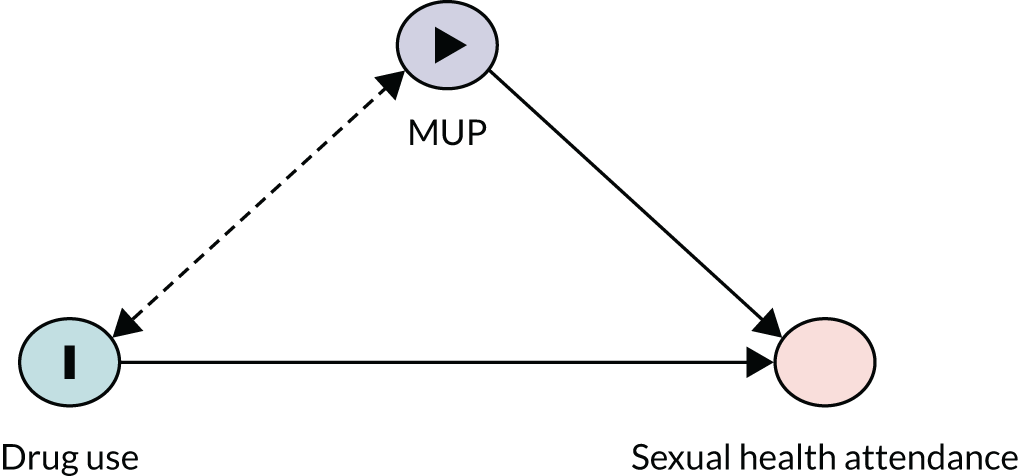
Collider bias is more likely in relation to alcohol consumption than drugs (see Figure 28). As alcohol consumption is more common than consumption of illicit drugs, attendance at SHCs and, therefore, participation in the study is more likely to be affected by alcohol than it is by illicit drugs. This is the reason why our focus in this component was on drug, rather than alcohol, consumption.
Strengths
Our early baseline reduced the chance of behaviour changes in anticipation of implementation affecting our baseline measures. For example, retailers may have gradually increased prices to prevent too sudden a price increase. Other reports now show that there was a clear step change in the alcohol price following MUP. 164 Consumers may have over purchased to stockpile cheap alcohol, and there is evidence from the focus groups in the separate qualitative component of the study, which will be reported below, that older heavy drinkers ‘stockpiled’ referring to seeing a bargain and buying a bit more than normal, but not stockpiling in anticipation of MUP. We minimised seasonal effects by timing our final wave 1 year after the February 2018 baseline (although, in the UK, February was colder than usual in 2018 and warmer in 2019).
We recorded the clinics and times used at wave 1 and reminded each site of these at training for subsequent waves to encourage as complete replication of data collection methods as possible. One clinic had in-service training in a subsequent wave, but we allowed them to substitute the same clinic in a later week to maximise numbers. We ensured that denominator data reflected that change. We also acted as a learning channel, encouraging the replication of successful response rate maximisation across sites.
We successfully co-ordinated all the sites to gather their data on the same dates for each wave. As described in Methods, we checked for selection bias by running the DiD analysis, excluding all the data from one site (site A) (see Appendix 3, Table 66). The findings were unchanged. The overall response rates were not changed for wave 1, increased by 1% for wave 2 and decreased by 2% for wave 3.
Chapter 6 Interviews with professional stakeholders to explore their anticipated and observed experiences of minimum unit pricing
Aim and research questions
This study component aimed to explore and compare key stakeholders’ anticipated outcomes of the policy with their observations and experiences of MUP post implementation. In this component, we focused on stakeholders’ perceptions of the social, health and economic impacts of MUP on the communities they serve.
This component of the research contributed to ROs 2 and 3.
Research objective 2
What are the adverse consequences of MUP in terms of displacement (i.e. change of source of alcohol to avoid MUP) and substitution to non-alcohol substance use for the overall population and by subgroups of interest (age, sex and deprivation).
Research objective 3
How do understandings, experiences, attitudes and norms towards alcohol use change following the introduction of MUP among the general population, young people and deprived communities.
Methods
Component design and sample
This part of the project took an exploratory qualitative approach using semistructured interviews. The main reason for selecting semistructured interviews was to allow stakeholders to address specific areas while giving them the opportunity to explore and reflect on their experiences of MUP.
We used purposive sampling to ensure that the perspectives of a broad range of identified stakeholder groups were represented. Recruitment was conducted through various health and social care agencies. Investigating the perspectives of different key stakeholders at different stages in its implementation helped to ensure that the MUP evaluation was explored not just through one lens, but rather a variety of lenses. The study sample included professional stakeholders from categories comprising addiction services, youth workers, primary care, police and licensing authorities. The frequencies of different categories of stakeholder interviewed at each stage of the research are illustrated in Table 11. A total of 30 professional stakeholders participated in the research, taking part in either individual (n = 23), paired (n = 2) or small group interviews (n = 5). The researchers anticipated requiring up to 30 interviews at each stage to reach data saturation (i.e. the point at which new data do not give a better understanding of the studied phenomenon, but rather repeat what was previously expressed). The baseline sample comprised 25 participants. The follow-up sample comprised 21 participants, 16 of whom had participated in baseline interviews and five of whom joined during the follow-up phase. Table 11 illustrates the characteristics of the baseline and follow-up samples by stakeholder category and area of operation.
| Stakeholder | Area 1 (affluent West) | Area 2 (deprived West) | Area 3 (deprived East) | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Pre MUP | Post MUP | Pre MUP | Post MUP | Pre MUP | Post MUP | Pre MUP | Post MUP | |
| Addiction services | 1 | 1 | 2a | 2a | 4a | 4a | 7 | 7 |
| Youth work | 1 | 1 | 1 | 1 | 2 | 2 | ||
| Primary care | 1 | 1 | 1 | 1 | 2 | 2 | 4 | 4 |
| Police | 1 | 1 + 3a | 1 | 1 | 1 | 6 | 2 | |
| Licensing authorities | 1 | 1 | 1 | 1 | 4a | 4a | 6 | 6 |
| Total | 5 | 4 | 9 | 6 | 11 | 11 | 25 | 21 |
Procedure
These interviews were conducted face to face during two distinct time periods: prior to the implementation of the MUP legislation (January–April 2018) and 6 months after the MUP implementation date (October 2018). This approach provided in-depth insights into key stakeholders’ expectations, experiences and observations of the social, health and economic impacts of MUP.
The initial interview schedule was developed with information from the scoping review and informed by preliminary data from the focus group component involving young people and heavy drinkers in disadvantaged circumstances (see Chapter 7). In addition to the topics covered in the focus group component, additional questions were added in from data emerging from the professional stakeholder interviews. The initial coding frame comprised codes capturing details of the participants’ professional role(s), descriptions of the alcohol problem, understandings and perceptions of MUP and positive and negative impacts of MUP. The interview schedule was piloted before data collection and adapted to key stakeholder groups to ensure that it was meaningful to their background and to gather more relevant information based on their experiences and knowledge. The interviews were recorded using a digital recorder and were fully transcribed.
Analysis
Initial coding was discussed and checked by the qualitative team and data organised using NVivo V.12 (QSR International, Warrington, UK). Coding was re-examined and some descriptions of codes were revised during the coding process to ensure consistency of interpretation and application. A thematic analysis approach was employed using analytical categories to describe and explain definitions, experiences and observations reported among the stakeholder participants. Our approach is based on the thematic analysis outlined by Braun and Clarke. 165 The steps included (1) transcription and checking transcripts with recordings for accuracy, (2) open coding from interview responses performed by two researchers independently (CP and RF), (3) agreement of initial codes discussed among the researchers and an initial codebook developed, (4) the code structure used for analysing the remaining responses with openness to including new codes and refining existing ones and (5) themes and subthemes identified from the final code structure and their relationships presented. Trustworthiness during thematic data analysis was ensured by the team reviewing the coding and the detailed notes about the codes and themes to establish team consensus.
Results
Results are organised by area of potential impact and by differentiating between anticipated and observed outcomes. Observed outcomes are predominantly from follow-up interviews, with some exceptions, such as licensing authority stakeholders’ observations of retailers’ compliance ahead of the introduction of MUP.
Availability, purchasing and consumption
Anticipated outcomes
Professional stakeholders representing each study region and a diverse range of categories expressed expectations that MUP would reduce purchasing and consumption of alcohol. One youth worker explained how rising prices, in the context of finite household budgets, would reduce purchasing:
Yes, because they’ll know how much money they’ve got and when you add it onto your shopping list that takes you over. You’ve still got gas and electricity. So, I do think, I do think in that respect it’s quite a good thing.
Baseline, affluent West, youth worker
However, the same participant went on to suggest that these positive effects may unfold gradually because of price increases being ‘not massive’. Despite participants identifying limited budgets as a factor in the mechanism of MUP, there was limited overt discussion of MUP affecting purchasing and consumption among low-socioeconomic-status groups.
Stakeholders predicted reductions in alcohol consumption for specific social groups, most notably young people (implicitly teenagers), constructed as constrained by limited budgets and able to make rational decisions based on budgetary pressures. A youth worker explained that:
If it’s not accessible and cheap enough there will be a realisation that they’ll manage it. [. . .] Because they do have limited resources.
Baseline, deprived West, youth worker
A general practitioner (GP) described how the measure could have an impact on young people:
I mean the other group I think it may have an impact on, which isn’t specifically in a deprived population, is younger people who’ve got a relatively limited disposable income.
Baseline, deprived East, GP
A stakeholder working in addiction services suggested that young people will be driven to opt out of some episodes of drinking:
A lot of these young people will maybe be able to afford it sometimes, you know, depending on what they’re drinking, but it probably will have, they will probably need to look at well if we’re going to do that something else will need to suffer this week or this month or whatever.
Baseline, deprived West, stakeholder
In addition to young drinkers, some stakeholders identified different age groups as likely to be affected by MUP. One youth worker (baseline, affluent West) suggested that MUP would mean that older people ‘won’t drink as much alone in the house’, whereas another youth worker suggested that middle-aged people might question and change their own drinking behaviours:
There will be an impact and it’s how they manage that impact and sometimes for the middle aged person that’s working it’s the catalyst that makes them think a wee bit.
Baseline, deprived West, youth worker
This participant went on to suggest that middle-aged people may, instead of drinking, ‘go and talk to my pal over a cup of tea, know what I mean?’, and suggested that such people’s ability to make that rational choice was because of their lifestyles not being ‘chaotic’. This participant identifies a social group who may engage in harmful drinking, but not to a chaotic degree, and whose behaviour may, therefore, be moderated by price increases. Similarly, a licensing authority stakeholder described:
Sensible-type families who work to a tight budget will lose a bottle of wine at the weekend.
Baseline, affluent West, licensing authority
Some participants expressed doubt about the impact of MUP on consumption, particularly for more affluent groups. An addiction services stakeholder in an affluent area explained that:
The more affluent someone is, it’s difficult to get them to make changes because it’s not affecting them financially.
Baseline, affluent West, addiction services stakeholder
Similarly, a GP in the same area explained that:
I don’t think it is going to make much difference locally because I don’t think people are buying the £0.20 cans of lager to drink here.
Baseline, affluent West, GP
The same GP went on to suggest that health and family pressure, not price, motivate behaviour change in their patients:
I’ve not had anyone where the driver for help was, I can’t afford this anymore. It’s that they are becoming aware of the damage it has done. Usually not the damage it’s doing to themselves, physical health wise, it’s the damage in the family.
Baseline, affluent West, GP
Some stakeholders suggested that people in more challenging social circumstances were unlikely to limit their consumption. A police stakeholder explained that:
There’s quite a majority of them who are not that poor so it’s not like they’re all unemployed, a lot of them are older and their partner’s died and they’ve had mental health issues but they’ve got some sort of income, a pension or something. So, I don’t see them stopping because it’s going to cost them an extra pound to buy a bottle of vodka or whatever.
Baseline, deprived East, police stakeholder
One GP suggested that:
It’s going to make people drink better quality alcohol, you know, they won’t drink the really cheap stuff . . .
Baseline, deprived East, GP
They also explained that:
There isn’t really any evidence that it’s better quality, it’s just marketing.
Baseline, deprived East, GP
A range of participants covering each stakeholder category and study area predicted that people simply would not let price increases affect their alcohol use. Typifying this, a police stakeholder stated:
Folks are still going to drink no matter what your price is, by hook or crook they’ll drink.
Baseline, deprived West, police stakeholder
Although this assumption was predominantly applied to dependent drinkers, a youth worker suggested the same of young people:
If they’re drinking a £2 bottle of cider or they’re drinking a £15 bottle of vodka they’ll drink, know what I mean, so they’ll adapt their budget to whatever it goes.
Baseline, deprived West, youth worker
Some expressed related concerns that prices of certain categories of alcoholic beverage would not change substantially. A GP identified wine and associated it with women’s excessive drinking:
So certainly a lot of women are drinking wine to excess. Not to excess on a particular day to the extent of getting drunk but drinking wine regularly that tots up. So those consumers may not be affected because the individual units of bottles may not go up that much.
Baseline, deprived East, GP
A police stakeholder discussing underage drinkers stated that:
If you’re telling me that [the price of] Mad Dog [Mogen David Wine Co., Westfield, NY, USA], Dragon Soop [Corinthian Brands Ltd, Knaresborough, UK] and Buckfast [J Chandler & Co (Buckfast) Ltd, Andover, UK] won’t be affected no. [MUP will have no effect] at all.
Baseline, deprived West, police stakeholder
This police stakeholder went on to suggest that ‘hardened drinkers’ may also move to those categories of drinks.
Regarding retailer compliance, a group of licensing authority stakeholders (baseline, deprived East) observed that, although price marking can be monitored, informal discounts given by shopkeepers to regular customers cannot and, therefore, some shops may not comply wholly with the minimum price.
Observed outcomes
Licensing authority stakeholders described predominantly positive observations of retailer compliance, both before and after implementation. Prior to implementation, one stakeholder reported that a supermarket had already adjusted their pricing and suggested that compliance was likely to be widespread:
I’d taken a stroll down to Asda [Asda Stores Ltd, Leeds, UK], our supermarket here, and the likes of the one in [nearby affluent area], they’re probably already roughly compliant.
Baseline, affluent West, licensing authority
Subsequent to implementation, one licensing authority stakeholder reported that compliance was:
Up at 90-odd per cent, at least, of full compliance.
Follow-up, deprived West, licensing authority
Whereas another reported that:
I’ve had no issues at all with any of the shopkeepers I’ve dealt with.
Follow-up, deprived East, licensing authority
Although licensing stakeholders’ observations were broadly positive, there were some anecdotal exceptions. One such stakeholder described observing a situation in which the manager of a branch of a chain based in England was put under pressure by having to comply with MUP when selling stock from suppliers in England:
The likes of her, for the first couple of weeks, you are talking 60% of her stock . . . she was having to calculate it and relabel it all. So, for the first month or so, maybe up to 2 months it was quite horrendous. But then, I don’t know, it seemed to calm down.
Follow-up, affluent West, licensing authority
This observation characterises MUP as a substantial operational inconvenience for some retailers, but a temporary one to which they can adjust. Another, licensing authority stakeholder perceived MUP as having increased small retailers’ competitiveness with supermarkets, but identified the potential – but not yet observed – unintended consequence of causing the re-emergence of an overprovision problem that had previously ceased to be relevant. The participants explained that:
People are using their local shops more often, or they certainly appear to be because there’s no price difference, it’s made it more relevant again because part of the thing before was most people wouldn’t go to their local shop and pay £3 or £4 extra for a bottle of vodka, whereas now because they are right across the board, if anything it’s made overprovision more relevant again because you know the prices are uniform.
Follow-up, deprived East, licensing authority
A limited number of anecdotal observations from stakeholders suggested that purchasing and consumption of alcohol had reduced. An addiction services stakeholder described a perceived reduction in consumption of white ciders, reporting that ‘I’ve not seen anybody down as drinking the cheap stuff’ and going on to say ‘It does get people thinking, “oh right”, maybe on a tighter budget’.
The same stakeholder described one woman who replaced vermouth with mulled wine. A youth worker identified a reduction in young people’s consumption of spirits, observing that:
The cheaper options are [now] more expensive options and I think the spirit thing – it’s been great cos it’s not been as easy to access. Even though you club together, you still cannae really get good value, especially if there are six or seven of you with one bottle.
Follow-up, deprived West, youth worker
A youth worker described young people’s self-reported adaptations to changing affordability:
It’s really interesting conversations about how they self-manage, to still have alcohol as part of their routine, which is really interesting, because of the good weather, they were drinking every night but they were still able to self-manage. Likely they had the same alcohol intake over the 5 days, but they wouldn’t finish drink because they were sharing it every day. I was saying that is a wee bit sensible. They were kind of taking their units in a more sensible way, rather than binge drinking.
Follow-up, deprived West, youth worker
This account also highlights how contextual factors, such as an increased drive to consume alcohol in warm weather, may moderate the impact of MUP.
A substantial set of participants described having observed no evidence that MUP affected purchasing or consumption of alcohol, and many participants characterised drinkers as resilient and resistant to change. Describing shopkeepers’ experiences, a licensing authority stakeholder explained that:
Nobody’s really said they’ve noticed a change in trends. That they could come out and say, oh [name], I’m now selling much more of – everybody that was drinking high strength cider has now moved on to vodka kind of thing. People are just saying they are selling about the same.
Follow-up, affluent West, licensing authority
The same licensing authority stakeholder as above explained that:
If you are a Frosty Jack [Aston Manor, Birmingham, UK] drinker, you are still a Frosty Jack drinker. You are just paying more for less.
Follow-up, affluent West, licensing authority
Some youth workers perceived MUP as having had little effect on young people’s consumption. One youth worker observed that:
[MUP] doesn’t seem to impact on [young people’s] ability to purchase it and consume it and they use it as part of their everyday life.
Follow-up, deprived West, youth worker
Another youth worker described MUP as not deterring young people because:
Some of them were drinking underage as well, so their ability to get alcohol cheap and illegally – they could do that anyway. It hasn’t stopped any of the older ones buying alcohol or using it.
Follow-up, affluent West, licensing authority
The same youth worker suggested that wine drinkers may not have been deterred either, because:
They can still go to Aldi [ALDI Einkauf GmbH & Co. oHG, Essen, Germany] and get a bottle for £4.98.
Follow-up, affluent West, licensing authority
Health
Anticipated outcomes
Participants from each study region, and a diverse range of stakeholder categories, expected MUP to produce improvements on population health over the long term. An addiction services worker typified this, stating:
Longer term, if the population as a whole was drinking slightly less, it’s bound to be more beneficial, physically and mentally.
Baseline, affluent West, addiction services worker
Some stakeholders indicated that improvements in health would be expressed in fewer presentations at EDs with alcohol-related illness, whereas others identified a risk of a short-term increase in presentations due to withdrawal. One GP (baseline, affluent West) characterised these as ‘short-term potential health risks’ that ‘won’t be able to go on indefinitely once people get used to the new pricing’. Similarly, an addiction services stakeholder explained that:
It’s only going to do good, but until we get to the good there’s going to be harm and other things on the way.
Baseline, deprived West, addiction services stakeholder
Some participants anticipated that health improvements would not be distributed equitably across the population. A GP (baseline, affluent West) identified that benefits will be experienced by ‘a very particular group of people with a certain income bracket, a certain amount of intake’, going on to specifically identify heavy drinkers in deprived areas. The same participant also predicted that some drinkers would manage to reduce consumption without experiencing withdrawals, such that they receive health benefits that will not be detected by health services. Some participants envisaged potential reductions in alcohol-related injury. A youth worker (baseline, affluent West) identified ‘people in their 30s and 40s who just routinely drink more than they should’ as a group that may be less likely to report at accident and emergency with injuries. Although participants from each stakeholder category expressed positive expectations for purchasing, consumption or health, only one of the six police stakeholders expressed such expectations, and did so reservedly:
Well obviously the policy is there to try and improve the health and lessen the intake of alcohol. So, I mean I’m hopeful, hopefully it will.
Baseline, deprived West, inspector police licensing
Some participants identified the magnitude of the reduction in intake they perceived necessary for some drinkers to conform with safe drinking guidelines. An addictions services worker explained that:
From 200 to 150 [weekly units] is 25%. So that is a big reduction. Yes, if you did have someone present to services and was able to – if you could get that sort of reduction, you would see some health benefits.
Baseline, affluent West, addiction services worker
One GP explained that:
Even if they reduce [consumption] by 20%, they are still going to be well over the recommended limit . . . I can’t see it making enough difference. To get someone from 50 units a day to 2 units a day, I don’t know how the minimum pricing is going to affect that.
Baseline, affluent West, GP
Although some participants characterised increased presentation at health and support services as a short-term cost for long-term benefits, others expressed more concern. An addiction services stakeholder anticipated increased presentation by deprived, alcohol-dependent groups:
You need to be prepared for the vulnerable group who are on very low incomes and who require to buy alcohol on a daily basis to maintain . . . there’s a huge population out there that don’t engage in services and that for me is maybe that hidden population that we have to be prepared for.
Baseline, deprived West, addiction services stakeholder
Similarly, a GP explained that:
All of a sudden they can only afford half the amount of alcohol they were drinking, so they there might be an abrupt presentation.
Baseline, affluent West, GP
Some participants characterised dependent drinkers as unable to sufficiently moderate their daily intake to ensure uninterrupted supply. An addiction services stakeholder explained that:
If you are used to say 150 – if you are drinking about 20 units a day, you’ll still drink 20 units a day. But if you can only afford for 5 days instead of the 7.
Baseline, affluent West, addiction services stakeholder
The same stakeholder predicted the re-emergence of a problematic pattern of behaviour:
When I first started working with problem drinkers, people would run out of money and for a good number of years now, that doesn’t seem to happen the same, where people would go into unplanned withdrawals, quite serious withdrawals, because of a shortage of money. I can see where that situation would come back into play.
Baseline, affluent West, addiction services stakeholder
In addition to withdrawals, a minority of stakeholders anticipated other health harms. An addiction services stakeholder identified risks to mental well-being among professionals:
Quite often I would relate it to your professional group and [alcohol] is their de-stressor. So, stress and anxiety levels could possibly increase if someone doesn’t find alternatives to using alcohol.
Baseline, affluent West, addiction services stakeholder
Observed outcomes
A small number of participants described observing anecdotal indications of improvements in health that may have been precipitated by the intervention. An addiction services worker reported that:
I’m no seeing just as much assessments coming in where it’s somebody who’s a bottle of wine a night. Speculating that: I would imagine it is that they are buying less but still sufficient to avoid unintentional withdrawals.
Follow-up, affluent West, addiction services stakeholder
The same stakeholder reported that ‘there has only been a handful I have heard from the team, so and so was admitted to hospital with withdrawals’, suggesting that withdrawals had not increased substantially subsequent to the intervention.
Although stakeholders predominantly reported no negative impact on health, one primary care stakeholder (follow-up, deprived East) expressed concern that their patients who ‘have had problematic issues with spirits and feel that part of their recovery was moving away from that’ have begun to consume spirits and ‘feel forced into doing so’ by the government.
Many stakeholders, covering each stakeholder category and study region, reported having observed neither a positive nor a negative impact on health. Some participants in primary care roles described noticing no changes in health or help-seeking. Typifying this, an addiction services stakeholder stated:
We haven’t sort of seen a massive increase, a crisis, any more than there has certainly been in my time in the team.
Follow-up, affluent West, addiction services stakeholder
Similarly, a GP stated:
I can’t say I’ve noticed any great difference (aside from) a couple of people [who] came in saying that this would make difference to them.
Follow-up, deprived West, GP
However, the same GP identified that changes may be evident only in admissions data:
It hasn’t made a major impact, but maybe on an individual practice level it is hard to see. You’ll be able to look at A&E [accident and emergency] admissions. When we are doing our day to day work, we are too busy seeing patients to almost even collate what we’re seeing.
Follow-up, deprived West, GP
Crime, conflict and social issues
Anticipated outcomes
Stakeholders from the primary care, addiction services and licensing authority categories identified potential social benefits of MUP related to crime, antisocial behaviour and domestic issues. Like discussion of impacts on consumption and health, police stakeholders did speculate about benefits in crime and social problems. An addiction services worker identified a broad range of benefits:
Well I suppose impact on children, that whole poverty thing and families, children affected by alcohol use. Criminality, crime, violence, intoxication, young people fighting, stabbing . . .
Baseline, deprived West, addiction services worker
Taking a broader view, a youth worker (baseline, affluent West) suggested that ‘Part of the policy is about trying to get the industry to be a bit more responsible’ and going on to suggest that the alcohol industry may play a role in improving labelling and public understandings of the content of alcoholic drinks.
Regarding families and domestic violence, a licencing authority stakeholder expressed cautious optimism:
If it works it will have a massive positive effect on that, but time will tell I think.
Baseline, affluent West, licencing authority stakeholder
Outside the domestic context, a GP talked about how people going out to drink less on weekends:
Maybe reduces the alcohol-fuelled crime if there is fewer people out on those nights of the week.
Baseline, affluent West, GP
They suggested that:
[MUP] might reduce how much alcohol someone can afford to buy in one day and therefore reduce drink related crimes.
Baseline, affluent West, GP
A GP foresaw potential reductions in unintended sexual encounters in young people:
They’re getting into fights or, you know, unintended sexual encounters that leave them with infections or pregnancy or what have you. So, it would be good if it had a positive impact on those groups because they tend to go out with a finite amount of money on a night out and once it’s gone it’s gone.
Baseline, deprived East, GP
The same participant suggested that young people may stay in education more effectively because of reduced alcohol intake:
We come across things like [young people have] had a college place and they’ve lost a college place because they’ve not been getting there on time after the weekends and things. So, they lose their place and they’re back on benefits, all that sort of thing. So that group it might have an impact on.
Baseline, deprived East, GP
Similarly, an addiction services worker (baseline, affluent West) predicted that reduced intake would ‘improve individuals . . . performance at work’.
Many stakeholders from the primary care, licensing authority and policy categories, and covering each of the three study areas, predicted increases in crime. Notably, stakeholders predicted that dependent drinkers might commit theft to fund their alcohol consumption. A police stakeholder explained that ‘If they’ve only got £5 and they can’t get a bottle of Frosty Jack any more they’re going to have to either go and threaten somebody or steal something to get enough money because they need that Frosty Jack’, going on to suggest that ‘they’re going to have to use violence whilst they’re alcohol fuelled to steal money or property from whoever’s house they happen to be drinking in that day’. One licensing authority stakeholder suggested that this behaviour was already taking place, but that MUP would exacerbate it:
I think they probably do run out of money on day 5. But [after MUP] they’ll run out of money on day 3. That’s not for everyone, that’s for some of them. They’ll sell or buy or steal or whatever to get alcohol.
Baseline, affluent West, licensing authority stakeholder
Some stakeholders suggested that shopkeepers would bear the brunt of customers’ anger at increased prices. Licensing authorities from both the affluent West and deprived East regions expressed this concern, with the former explaining that:
. . . a lot of my shops have contacted me and what they’re saying is they’re worried about conflict at the till. And they think there’s not been enough publicity, you know, a dependent drinker or somebody with a drink problem is going in and, you know, he’s wanting to pay £4 for his four cans of cider that he’s going to get told no that’s £9. That’s going to lead to conflict, and I don’t think these posters are going to diffuse that situation.
Baseline, affluent West, licensing authority stakeholder
A police stakeholder (baseline, deprived West) echoed these concerns, anticipating that:
Racial crimes will go through the roof because . . . the shopkeepers will get absolutely dogs abuse because it will be [seen as being] their fault.
Baseline, deprived West, police stakeholder
Displacement, whereby individuals forego food or other essentials to afford alcohol, was identified as a risk by stakeholders from addiction services, police, youth workers and, particularly, primary care, and covering each study region. One police stakeholder explained that:
All the other things in [dependent drinkers’] life are ancillary to their alcohol so they won’t eat, they won’t go and visit their family, there’s lots of things they’ll put out of the way because all they can do is this addiction they’ve got, they’ve got to fuel it.
Baseline, deprived West, police stakeholder
One GP identified that dependent drinkers’ diets are already often poor:
Some of these people barely eat. They get a lot of their calories from alcohol and they are already in a terrible situation.
Baseline, deprived East, GP
Another GP (baseline, deprived West) asked:
If you put the price up will their diet suffer even more?
Baseline, deprived West, GP
An addiction services stakeholder (baseline, deprived East) characterised the risk of displacement MUP within a context in which ‘the price of food in the supermarket has already gone up’. In addition to displacement, some identified the risk of accruing debt. An addiction services stakeholder (baseline, affluent West) suggested that ‘we’ll maybe see more people getting into rent arrears’.
An addiction services stakeholder typified concerns that displacement would also affect families:
If you think of a family on a low income and there’s a couple of kids to feed as well but somebody’s got to maintain a chronic alcohol problem and don’t at that point want to engage in services it’s going to affect the whole family.
Baseline, deprived West, addiction services stakeholder
In addition to families being neglected through displacement, a pair of addiction services stakeholders discussed the threat of domestic violence. One suggested that MUP ‘will have a massive impact [on domestic violence]’, explaining that:
We’re working with really vulnerable folk who have experienced high levels of trauma in their lives and their coping strategies maybe aren’t as healthy as, you know, others and they will react in a variety of ways that will have an impact on who else lives in that house. There’s a higher level of violence and aggression just through alcohol never mind if somebody’s under pressure.
Baseline, deprived West, addiction services stakeholder
The pair went on to identify situations where the affordability of alcohol may benefit the families of aggressive, dependent drinkers, discussing how ‘Loads of families feel safer when somebody is lying on the couch . . . Drunk, rather than when they start to resurface so in terms of aggression levels’. These accounts highlight how the risks of financial pressure and domestic violence are inter-related.
Stakeholders’ focus on how MUP would affect low-income, dependent drinkers implicitly positioned the measure as one that might exacerbate inequalities. Some stakeholders highlighted that issue more explicitly, using terms such as ‘poor’ (baseline, affluent West, GP), ‘on the breadline’ (baseline, deprived East, addiction services) and ‘at the lower end of the economic scale’ (baseline, deprived East, addiction services). Some stakeholders overtly characterised MUP as unfairly punitive of deprived groups. A police stakeholder (baseline, deprived West) described MUP as ‘a tax on the poor’, suggesting ‘That thing that makes their life a wee bit better in their eyes has now been put out of reach for them’. A GP highlighted the risk of exacerbating financial problems, explaining that:
These people are often very poor anyway and you sometimes even, without the pricing wonder where they get the money from. So, I don’t know by putting the price up will that mean people are just in more debt . . . ?
Baseline, deprived West, GP
Observed outcomes
Stakeholders predominantly did not report observing outcomes related to crime and social issues. Typifying this, an addiction services stakeholder whose work covered several deprived areas suggested that:
I don’t think there has been any increase [in financial hardship], because generally it would be myself that would sign off on a foodbank voucher.
Follow-up, affluent West, addiction services stakeholder
In contrast, a primary care stakeholder (follow-up, deprived East) perceived that, since the implementation of MUP, ‘I think my patients are accessing food banks more – these patients. I have heard – it is obviously sensitive – but they are resorting back to crime’. A youth worker had observed improvements in some people’s lives since the implementation of MUP, but pointed out the difficulty of identifying causal links:
What I will say, a couple of the people I spoke about last time, that were experiencing problematic use of alcohol. Their use has gone down and their circumstances have improved dramatically . . . I don’t think it’s been pricing that’s stopped it. But it’s hard to see.
Follow-up, affluent West, youth worker
Alternative substances and sources of alcohol
Anticipated outcomes
Some stakeholders discussed how increased alcohol prices might drive demand for alternative substances and sources of alcohol. In one group interview, three police stakeholders discussed alternative sources of alcohol at length, cautioning that:
People who were drinking branded vodka will go to cheap vodka. People who were on cheap vodka will go to counterfeit vodka and there’s no quality control over that, they could be drinking paint thinner for all we know. So there will be unintended consequences, people will die because they’re taking uncontrolled products.
Baseline, deprived West, police stakeholders
Although these police stakeholders identified ‘black market’ alcohol as formerly associated with older drinkers, they suggested that ‘if [young people] see older people drinking this illicit alcohol at much greatly reduced prices on the black market they’ll have to look at that’.
Stakeholders identified different categories of drug abuse that may increase because of MUP. A licensing authority stakeholder posited that:
It might be cheaper to buy cannabis for example. In fact I know kids do that just now because it’s cheaper and easier to get than it is to buy alcohol.
Baseline, affluent West, licensing authority stakeholder
A youth worker (baseline, affluent West) concurred that MUP ‘will really impact on . . . increased cannabis use’, going on to explain that ‘if they don’t have their usual alcohol on a Friday down the park then, you know, there’s probably more risk of them taking other things’. One GP (baseline, affluent West) suggested that the use of ‘so-called legal highs’ may increase as a result of MUP. A GP (baseline, deprived East) suggested that dependent drinkers would not substitute alcohol for drugs, but ‘younger people’ engaged in ‘the party culture’ may do.
In addition to recreational drugs, some stakeholders discussed prescription drug abuse. One addiction services stakeholder (baseline, affluent West) suggested that professionals who use alcohol as a ‘de-stressor’ may turn to ‘something prescribed’, with GPs being ‘put under more pressure to prescribe something’ by patients reporting stress. An addiction services stakeholder (baseline, deprived East), stated that ‘you could see an increase in things like XANAX® [a benzodiazepine used recreationally] [alprazolam; Xanax, Upjohn UK Ltd, Kent, UK]’. One GP (baseline, deprived East) described alcohol and drugs use as ‘quite fluid already’, explaining that ‘I’ve worked here for over 20 years and to me, in the last 5 years there has been much more fluidity around drug use than previously’ and highlighting the risk of prescription drugs, such as the antiepileptic medications gabapentin (Pfizer, New York, NY, USA) and pregabalin (Pfizer), interacting with alcohol. In addition to identifying a risk of increased benzodiazepine abuse, an addiction services stakeholder (baseline, deprived West) identified methylated spirits as a potential substitute.
Some participants were dismissive of the risk of MUP increasing drug abuse. A police stakeholder typified this:
No I don’t think there will be a shift of substances. If you’d asked me that two years ago, I might have said yes absolutely because legal highs was a massive problem for us but that’s kind of died off to a certain degree and I don’t see anybody switching from alcohol to legal highs or other drugs. Even in terms of the youth drinking scene.
Baseline, deprived East, police stakeholder
A GP expressed doubt that MUP would increase the relative affordability of explicit substances sufficiently to affect drug abuse:
Drugs have always been expensive compared to what people are looking at with alcohol. I’m not sure with the minimum pricing legislation it’s going to become sufficiently expensive.
Baseline, affluent West, GP
The same participant later stated that ‘I can’t imagine that someone decides to go from alcohol to heroin, just ’cause the alcohol gets a bit more expensive. It’s too big a leap’. Similarly, an addiction services stakeholder (baseline, affluent West) suggested that cannabis is ‘quite expensive’ and, therefore, unlikely to be used as a substitute for alcohol.
Observed outcomes
Despite some stakeholders expressing concerns that MUP would drive use of alternative sources of alcohol and alternative substances, no stakeholders reported observing such outcomes. One youth worker suggested that local, potentially unlicensed alcohol trade may be in decline:
Dial-a Booze [www.dialaboozeglasgow.co.uk/; Glasgow, UK] I don’t think is as popular, because I think the cost, they can get it for – it’s expensive enough. I think they’ll get what they’ve got now and once it’s done it’s done.
Follow-up, deprived West, youth worker
Similarly, a licensing authority stakeholder explained that:
There was a persistent rumour that there was [a white van] going around [area], selling cider cheap. But myself and the police have looked in to it, we’ve no seen [anything].
Follow-up, affluent West, licensing authority stakeholder
Regarding cross-border sales, a police stakeholder stated:
We haven’t heard of anything at all, which is kind of surprising.
Follow-up, deprived West, police stakeholder
This participant went on to explain that ‘We said maybe [people] would be going to England and filling up a van and selling it, but we have no knowledge of that’. Similarly, an addictions services stakeholder (follow-up, affluence West) reported having heard nothing about cross-border sales.
When asked if they had observed an increase in drug abuse, a primary care stakeholder replied:
Interestingly not actually. That is a very interesting point there, because you could argue that a bag of heroin at £10 is still £10, which is actually cheaper than a bottle of Frosty Jacks now. So yeah, I haven’t, but that could well happen. I see people on 4 to 8 weeks, it’s only now that I’m beginning to hear about changes in addiction behaviour.
Follow-up, deprived East, primary care stakeholder
Similarly, a GP had observed no change, but acknowledged the limitations of their personal observations:
I can’t say I’ve noticed any difference, but as I say I’ve not measured anything.
Follow-up, deprived West, GP
Economic impacts
Anticipated outcomes
A minority of participants discussed different potential economic impacts of MUP. An addiction services stakeholder expressed concern that large retailers, and not the government, stand to profit from the measure:
It’s not duty that they are putting on. So, if Asda, for talking sake, are charging across the board for all the alcohol, then that is a massive increase in price for some drinks. so, does that make Asda richer?
Baseline, affluent West, addiction services stakeholder
Later, the same participant framed that perceived injustice in terms of ‘the unplanned care costs that people with alcohol problems cause the NHS’, suggesting that additional customer expenditure on alcohol should fund alcohol services instead of adding to retailers’ revenue. One GP (baseline, deprived East) expressed concern that ‘little shops . . . that people depend on, that are perhaps already under pressure cos of Tesco’s [Tesco plc, Welwyn Garden City, UK] and Lidl’s [Lidl Stiftung & Co. KG, Neckarsulm, Germany] . . . will go under if quite a few of the sales are due to alcohol’, whereas another GP (baseline, deprived West) suggested that MUP might ‘have an effect on, you know, for example, the Scottish whisky industry or off license sales’.
Licensing authority stakeholders from both the East and the West expressed concerns about independent shopkeepers being unprepared for MUP. One such stakeholder explained that these retailers ‘won’t have an idea of what’s coming’ and are ‘worried that they’re going to get caught out’. This stakeholder presented three examples of the pressures on underprepared shopkeepers. In the first example, a shopkeeper was distressed by being pressured by Trading Standards to adjust her price marking, in a manner that the stakeholder regarded as ‘undiplomatic’ and unlikely to ‘create good relations’. In the second example, the same stakeholder described shopkeepers needing to sell stock at discounted prices to clear it prior to the implementation of MUP:
It’s not enough time for them to get rid of their stock so they’re now sitting with stock that they’re having to try and sell off at a discount just now before the 1 May or come after the 1 May they’re not going to be able to get rid of it.
Baseline, affluent West, licensing authority stakeholder
In the third example, the stakeholder described retailers mistakenly buying discounted alcohol unaware that impending price rises may render the products unable to be sold:
We’ve had at least one retailer in this area hoovering up Frosty Jack cider because they’re all selling it off cheap without realising I can’t sell this after the 1 May. If I don’t get shot of it by the 1 May.
Baseline, affluent West, licensing authority stakeholder
Observed outcomes
A small number of participants perceived MUP as having been economically beneficial to independent retailers. An addictions services stakeholder reported having read that:
Your corner shop saw an increase in their alcohol sales because the supermarkets couldn’t do the big deals. So, they were actually – in terms of economically, they were benefiting. It didn’t pay people to go to the supermarket because they could almost offer the same price.
Follow-up, affluent West, addiction services stakeholder
This was reinforced by licensing authority stakeholders. One such stakeholder (follow-up, deprived East) described how ‘a shopkeeper said his sales have actually gone up because a four pack of whatever it was is now the same in his shop as it is in Asda’. Another licensing authority stakeholder (follow-up, deprived West) echoed this, explaining that ‘My understanding is it has slightly evened out the market. It’s slightly more favourable for the small retailers than the bigger retailers’.
Licensing authority stakeholders identified some temporary problems for independent retailers related to the implementation of MUP. One participant (follow-up, affluent West) reinforced concerns from the baseline interviews about unprepared shopkeepers suffering economically because of finding themselves with stock they are unable to sell:
So there was at least four or five of my premises had that problem and that’s what I had to tell them. I said, you will need to get rid of it before the 1st otherwise you are going to be stuck with it. You are going to have to try and sell it for £12 a bottle.
Follow-up, affluent West, licensing authority stakeholder
Similarly, a stakeholder in the deprived East study area experienced resistance from shopkeepers around the pricing of white ciders:
That was a problem that I came across a lot. A lot of resistance from the trade because they felt I was going to put them out of business. Well not me personally but I was the one dealing with it, because they had high sellers, the strong ciders and a bottle that was price marked £3.99 was suddenly going up to £11.25 and I had a lot of people shouting at me saying you’re putting me out of business.
Follow-up, deprived East, licensing authority
The same stakeholder identified that, although bottles may be correctly price marked, tills may be set to sell them more cheaply:
There is another dimension to this that no one has even thought about, is that whilst a bottle of vodka might be displayed at £13.13 it’s what gets rung through the till. I mean that’s the unknown. So, they may have a till pre-set because its maybe not quite kosher, so rather than £13.13 they’re getting it for a fiver. They’re drinking that and then there have been instances of people going blind.
Follow-up, deprived East, licensing authority
Summary of key points
This study component aimed to explore and compare professional stakeholders’ anticipated and observed outcomes of MUP, focusing on the social, health and economic impacts of MUP on the communities that they serve. Although the participants were professionals working in fields that interact with the sale and consumption of alcohol, it should be noted that these participants’ understandings of MUP did not appear to be based substantially in evidence and were likely to be comparable to those of the lay public. Prior to implementation of MUP, stakeholders anticipated a range of negative unintended outcomes, with participants showing concern for dependent and low-income drinkers. These negative outcomes can largely be characterised as potential short-term costs that may precede long-term benefits. Importantly, the negative outcomes anticipated by stakeholders ahead of implementation were predominantly not reported as having been observed subsequent to implementation of MUP. Here, we present the key conclusions to come out of the findings in relation to (1) compliance with MUP, (2) consumption and impact on health, (3) crime and social issues and (4) economic issues.
Compliance with minimum unit pricing
Licensing authority and police participants reported that retailers’ compliance with MUP had predominantly been good, suggesting that initial concerns about poor comprehension and compliance may have been unfounded.
Consumption and impact on health
Expectations of the impact of a minimum price on people’s consumption of alcohol were mixed. Some stakeholders anticipated long-term reductions in people’s consumption of alcohol, although a few expressed concerns that a minimum unit price would not be high enough to reduce consumption among wealthier individuals or among those with ‘chaotic’ lives. Stakeholders, including youth workers and addiction services workers, observed reductions in individuals’ consumption subsequent to implementation of the measure, but these isolated observations do not constitute evidence of widespread patterns of change. There was good agreement across stakeholders that MUP was about reducing consumption to improve the long-term health benefits in the population over time. These benefits were considered as likely to be greatest if consumption of alcohol was reduced in deprived groups, heavy drinkers and people aged 30–50 years who drink excessively. A few stakeholders expressed concern about the short-term health impacts on heavy drinkers, particularly related to alcohol withdrawal. However, subsequent to the implementation of MUP, stakeholders had observed little evidence of heavy drinkers reporting withdrawal symptoms. Some stakeholders also warned ahead of implementation that MUP might reduce alcohol consumption, but drive people to seek out illicit alcohol and other illicit substances. However, no stakeholders reported such changes in people’s actual consumption behaviours subsequent to implementation.
Crime and social issues
Prior to implementation of MUP, these stakeholders raised concerns about the potential for crime and social issues to increase following implementation. However, in follow-up interviews, stakeholders largely reported no evidence of shoplifting or crime directly linked to increased alcohol prices, and evidence of food displacement or substitution of alcohol with illicit substances was limited. Similarly, stakeholders largely did not report negative economic impacts. Instead, observing that the measure had created a more ‘level playing field’ between large and independent retailers. A few stakeholders expressed disappointment that increases in retailers’ revenue were not redistributed for social good, as with Scotland’s carrier bag charge. Although stakeholders’ experiences of MUP were largely positive compared with any of their initial concerns, they identified some potential negative unintended consequences. In relation to crime and social issues, participants warned that the levelling of the ‘playing field’ between large and independent retailers may cause the re-emergence of overprovision of alcohol within communities. Within small independent shops, one participant questioned whether or not racial crime may rise because of customers’ aggression in reaction to increased prices, and another suggested that shopkeepers may give regular customers informal discounts to subvert minimum prices.
Economic issues
Although stakeholders’ experiences of MUP were largely positive compared with any of their initial concerns, they identified some potential negative unintended consequences. For example, one concern was whether MUP causes increased financial pressures on heavy drinkers resulting in them spending more on alcohol to drink the same as before MUP and then risking not have enough left-over money to cover their rent, utilities and food bills. However, these unintended consequences were generally not observed, but do require continued exploration.
The evidence presented here is characterised by various strengths. The range of stakeholder categories captured a wide range of experience related to different aspects of the sale, consumption and impacts of alcohol. The longitudinal design avoided limitations of asking participants to recall their perceptions and experiences from a year prior. However, the findings are subject to certain limitations. Although the data constitutes stakeholders’ first-hand observations and experiences, it is inherently very challenging for individuals to observe the impact of MUP on other individuals and impossible to recognise wider trends from the individual level.
The findings presented here on all the themes suggest that professional stakeholders’ concerns about MUP largely did not come to pass; however, this evidence is limited to the two time periods within which data were collected. Indeed, participants considered that many of the impacts of MUP may emerge only over time. Furthermore, many outcomes are inherently difficult to measure in such a small sample, as contextual factors may vary. With these limiting factors in mind, this exploratory study of the experiences of a diverse range of professional stakeholders provides early evidence that many concerns that some held about MUP did not come to pass after implementation.
Chapter 7 Focus groups with at-risk heavy drinkers exposed to the intervention
Aims and objectives
This qualitative study of at-risk drinkers aimed to provide an in-depth understanding of how MUP affected key subgroups within the Scottish population, namely young people and heavy drinkers living in disadvantaged circumstances, compared with similar groups in an affluent area. The study sought to explore shifts in norms and attitudes towards the legislation and drinking more generally, and contributes to ROs 2 and 3 of the main study.
Research objective 2
What are the adverse consequences of MUP in terms of displacement (i.e. change of source of alcohol to avoid MUP) and substitution to non-alcohol substance use, and what is the impact on food purchasing, for the overall population and by subgroups of interest (age, sex and deprivation)?
Research objective 3
What changes in public attitudes, experiences and norms towards MUP and alcohol use follow the introduction of MUP in the overall population and by subgroups of interest (age, sex and deprivation)?
Methods
Design and sample
Twenty-four focus group discussions were conducted with young binge drinkers aged 18–24 years and older heavy drinkers aged 30–55 years who were identified as at-risk heavy drinkers and living in contrasting communities in Central Scotland. These drinkers were selected to represent key subgroups of the Scottish population who may be differentially affected by MUP policy. Qualitative focus groups were chosen as an appropriate methodology, as they provided an opportunity for participants to express and compare their views and understanding in an open and free flowing discussion, generating data through participant interaction and group dynamics. Therefore, the focus group study design allowed exploration of specific issues related to MUP policy within participants’ cultural and social context. 166 Groups were conducted over two waves. Twelve initial groups were conducted 1–3 months pre implementation and 12 follow-up groups were conducted 5–6 months post implementation of MUP policy.
Participants were recruited from three communities in Central Scotland: (1) an affluent West Scotland urban community and two deprived urban communities, one in West Scotland and one in East Scotland. These communities were within the catchment areas served by the two Scottish hospitals participating in the ED study. Postcode deprivation (Carstairs) scores were used to identify study communities that matched socioeconomic comparators of interest (deprived Scottish Index of Multiple Deprivation quintile 1 and affluent Scottish Index of Multiple Deprivation quintile 5). Groups were segmented according to community, age and drinking type, sex and social grade (Table 12). Drinking type was categorised using the AUDIT-C tool, which is a brief three-item alcohol screening tool designed to identify those at risk of hazardous and harmful drinking. 167 At-risk drinkers were identified by scoring a total of ≥ 6 across the three items. Additionally, older heavy drinkers were identified as those who drank ≥ 7 units on a typical day when they were drinking. Young binge drinkers were identified as those who drank at least weekly, consuming ≥ 6 units if female or ≥ 8 units if male on a single occasion. Prospective participants were also asked if they had ever received or been advised by a health professional to have treatment or counselling support for alcohol use. Those who answered affirmatively or opted not to answer were excluded from the study. Social grade was assessed by occupation of the chief income earner in the participant’s household [i.e. managerial, professional and administrative occupations (ABC1) or semi-skilled and unskilled manual workers, casual and lowest grade workers, and those unemployed (DE)]. Those unemployed were identified through receipt of UK benefits, such as Jobseeker’s Allowance, Income Support, Universal Credit and Child/Working Tax Credit.
| Group number | Community | Age (years) | Drinking type | Sex | Social gradea |
|---|---|---|---|---|---|
| 1 | 1: urban affluent West Central Scotland | 18–24 | Binge drinker | Female | ABC1 |
| 2 | 1 | 18–24 | Binge drinker | Male | ABC1 |
| 3 | 1 | 30–55 | Heavy drinker | Female | ABC1 |
| 4 | 1 | 30–55 | Heavy drinker | Male | ABC1 |
| 5 | 2: urban deprived West Central Scotland | 18–24 | Binge drinker | Female | DE |
| 6 | 2 | 18–24 | Binge drinker | Male | DE |
| 7 | 2 | 30–55 | Heavy drinker | Female | DE |
| 8 | 2 | 30–55 | Heavy drinker | Male | DE |
| 9 | 3: urban deprived East Central Scotland | 18–24 | Binge drinker | Female | DE |
| 10 | 3 | 18–24 | Binge drinker | Male | DE |
| 11 | 3 | 30–55 | Heavy drinker | Female | DE |
| 12 | 3 | 30–55 | Heavy drinker | Male | DE |
Participants were purposively recruited by independent market research recruiters using door-to-door or street intercept techniques and were not previously known to researchers. Eligibility was assessed by the use of a structured recruitment questionnaire that incorporated the AUDIT-C screening questions and questions on indicators of alcohol dependency, demographics, occupation and receipt of benefits. Participants who met the recruitment criteria were invited to participate and provided with a participant information sheet that outlined the research, what participation would involve, that participation was voluntary and the right to withdraw at any time. They were then followed up 2 or 3 days later to give participants the opportunity to ask questions and to seek written consent to participate. Participants received a small cash sum as a thank you for taking part and to cover any associated costs, such as travel or child care. The study received ethics approval from the University of Stirling Departmental Ethics Committee.
The achieved sample is outlined in Table 13. Eighty-four participants took part in the pre-MUP implementation focus groups. All participants from this first wave of groups were invited to attend the relevant follow-up group. Forty-seven of these participants took part in a follow-up group. To support a minimum target sample size of five participants per discussion group, the follow-up sample was replenished by recruiting 21 new participants using the same procedures and eligibility criteria. The total sample was evenly split in terms of sex and age group. We purposively sampled a greater proportion of participants from a lower social grade, as these were the group more likely to be affected by the policy. 168,169
| Recruitment | Total | Sex | Social grade | Age (years) | |||
|---|---|---|---|---|---|---|---|
| Women | Men | ABC1 | DE | 18–24 | 30–55 | ||
| Wave 1: pre-MUP policy implementation groups, n | 84 | 41 | 43 | 30 | 54 | 44 | 40 |
| Wave 2: follow-up groups, n (na) | 68 (21) | 34 (12) | 34 (9) | 26 (7) | 42 (14) | 35 (11) | 33 (10) |
| Total,b n (%) | 105 | 53 (50) | 52 (50) | 37 (35) | 68 (65) | 55 (52) | 50 (48) |
Procedure
The first wave of focus groups was conducted in March/April 2018 (1–2 months pre implementation of MUP). Each group was attended by five to eight participants and took place in a local informal community venue. Groups lasted up to 90 minutes and were moderated by two members of a mixed-sex research team (DE, AF and MS) with extensive experience of qualitative methods. A semistructured topic guide was used flexibly to ensure that all topics were explored while giving participants freedom to discuss their thoughts and experiences. As a warm-up exercise, groups were asked about local alcohol provision. The discussion then moved on to participants’ purchasing habits, including place, types of drinks and brands, and views on price, typical weekly consumption patterns, attitudes towards alcohol, including affordability, and harm perceptions of different drinks. The final part of the discussion group focused on MUP to explore participants’ awareness and understanding of the policy, and beliefs about and response to the impact of the policy on the price of alcohol and on drinkers.
Groups were repeated over a second follow-up wave in October/November 2018 (6–7 months post implementation of MUP). Each follow-up group was attended by four to seven participants. The topic guide was revised to focus on any recent changes in purchasing habits (e.g. place, type of drinks/brands and price) and typical weekly consumption patterns. Follow-up groups included more in-depth discussion around alcohol affordability and discussion around MUP, while exploring awareness, understanding and attitudes post implementation, and any perceived impact on alcohol consumption. All discussions were digitally recorded on voice-file with participants’ consent.
Analysis
All discussions were transcribed verbatim and checked for accuracy. Data were imported into NVivo to facilitate coding and thematic analysis through an inductive and deductive approach. 165 An initial set of themes based on the research aims and topic guide was agreed among the research team. Two members of the team (DE and AF) coded the data while assessing the reliability and labelling of these themes. Coding decisions were discussed with other members of the team, enabling identification of further emerging themes and resolution of interpretive differences. Themes were compared and contrasted between groups held pre implementation (i.e. wave 1) and at post-implementation follow-up (i.e. wave 2), and between different groups of participants, for example by social grade, sex and age and drinking status (e.g. young binge drinker/older heavy drinker). The analysis focused on the sample’s drinking patterns and purchasing behaviour, community awareness, understanding and expectations of the legislation and any short-term impact. All members of the team were involved in interpreting emerging findings.
Results
The results cover four main areas. First, the results provide an overview of participants drinking patterns and purchasing behaviour. Second, a section that explores participants awareness, knowledge and understanding of MUP. Third, a section that describes levels of support for, and attitudes towards, MUP. The final section outlines views and experiences of the perceived impact of MUP.
Sample characteristics: drinking patterns and purchasing behaviour
This section examines participants’ drinking patterns and purchasing behaviour. Any subgroup differences are highlighted in the text. Differences in behaviour were most evident according to age. There were fewer differences according to sex or social grade. The data reported here relates to the participant sample at wave 1. Any perceived changes in purchasing and drinking behaviour post implementation are addressed in Perceived impact of the policy.
Across the sample, participants reported greater alcohol consumption at weekends, with occasional mid-week drinking. Weekend drinking was usually described as heavier, although there were exceptions among those who worked weekends and among younger drinkers who took advantage of mid-week student deals. Although consumption of alcohol from both on- and off-trade purchase was evident, there was a greater mix of on- and off-trade weekly drinking among younger groups:
I’d maybe go to like the pub or around someone’s house once a week and have a few drinks and then another night a week have a big night out with a lot of drinking in it.
Wave 1, FG09 – women, 18–24 years, DE, East
For many of our older drinkers, drinking on-trade was an occasional occurrence, for example several times a year rather than weekly. These older drinkers acknowledged that their drinking patterns had shifted over time:
I’m too old now to be hitting [local area with pubs] so if I go out it’s with my partner or girlfriends and dinner and a drink.
Wave 1, FG03 – women, 30–55 years, ABC1, West
I’ve still got quite a young family so we don’t get out that often . . . it’s a big deal when we go out. So it tends to be in the house.
Wave 1, FG04 – men, 30–55 years, ABC1, West
Older participants who described drinking on-trade more regularly spoke of how this tended to accompany dining out, attending a concert or social events at local clubs. Older age groups typically described their drinking as a way of socialising (males) or coping with busy family lives (females):
It’s [drinking] to be social, really, because usually it’s just when you are out with friends or your pals or whatever.
Wave 1, FG04 – men, 30–55 years, ABC1, West
See all week, I look after my mum and stuff like that and my partner is ill and I’ve got two boys, so you are running about after everybody all week, for me it’s just a down time, it’s something for me.
Wave 1, FG07 – women, 30–55 years, DE, East
These narratives were different from those reported in the younger age groups, where the norm was to describe drinking to get drunk:
I don’t have wee drinks if I am drinking then I’m drinking, . . . I don’t ever just have a couple, . . . Nor do I, I drink to get drunk, . . . I get so drunk that like I end up on Facebook [URL: www.facebook.com; Facebook, Inc., Menlo Park, CA, USA] and stuff and I’m like ‘shit!’
Wave 1, FG05 – women, 18–24 years, DE, West
Overall, and in addition to on-trade consumption, the sample was characterised by a great deal of at-home drinking, either in individuals’ own or someone else’s home. At-home drinking could take many different forms, for example a relaxed night in with friends, pre-loading before a night out, a house party or a place to continue drinking after a night out. Drinking at home was popular because of the perceived expense of on-trade alcohol purchase, something highlighted by all groups:
People canny afford to go to the pubs now . . . It’s expensive . . . A lot of people stopped going into town over the years.
Wave 1, FG06 – men, 18–24 years, DE, West
It’s expensive going out all the time.
Wave 1, FG03 – women, 30–55 years, ABC1, West
Participants spoke of spending large sums of money when purchasing alcohol on-trade. It was acknowledged that it was more difficult to control spending on a night out and there was often a sense of regret the next day at how much they had spent on alcohol. Some participants described having to budget for nights out and the strategies employed to manage spending, such as visiting only premises where the drinks were known to be cheaper, taking a set amount of cash out, avoiding buying rounds of drinks and buying drinks perceived as better value for money (e.g. double measures or shots). Therefore, purchasing alcohol off-trade was often viewed as balancing the expense of on-trade drinking.
There were some notable differences in purchasing behaviour for at-home drinking across the sample according to age. Young binge drinkers tended to purchase off-trade alcohol for specific drinking occasions, often on the same day as purchase and only the amount they intended to consume. Younger participants described pooling money to buy multipacks of beer or bottles of spirits, particularly when this was to be consumed at a house party. Although some younger participants also purchased alcohol from supermarkets; purchases from small independent local shops were more of a feature among this age group, with smaller shops described as convenient and sometimes (although not always) offering good deals. Additionally, certain drinks could be purchased in only small independent stores (e.g. Buckfast and Dragon Soop). Younger age groups were particularly price sensitive when purchasing off-trade. Participants would describe comparing prices and offers between different stores and brands to get the best deal, saving themselves small amounts of money. Budget and how drunk they intended to be often had an impact on purchasing decisions:
At the end of the day I am going to get as drunk on cheap wine as on expensive wine so it saves the money.
Wave 1, FG09 – women, 18–24 years, DE, East
Although our older heavy drinkers were similarly price conscious when buying off-trade, there were some differences in their purchasing behaviour compared with the younger age groups. Older participants described watching for offers, when they would then take the opportunity to stockpile:
I think you probably buy more because it’s on sale, the offer is going to end like the end of February, so right ‘we better stock up’.
Wave 1, FG07 – women, 30–55 years, DE, West
Although price offers influenced where they purchased alcohol from, and also how much, older participants tended to purchase alcohol from supermarkets. For some, this was while doing their weekly food shop. There was greater acknowledgement among older groups that other features of alcohol, aside from price, were important to purchasing decisions, such as volume, taste and quality.
Although our findings suggest that most of our sample were price sensitive to alcohol, either on a night out or when purchasing off-trade alcohol, affordability was further highlighted by some DE participants as an issue. These participants noted that, given their employment or family circumstances, there was a requirement to prioritise essential needs over alcohol:
If you really want it you will . . . but if it came to a choice of well I need to feed my daughter or have a drink then obviously . . .
Wave 1, FG07 – women, 30–35 years, DE, West
Well, I am not working now so it makes a big difference . . . (I) I just do without it . . .
Wave 1, FG07 – women, 30–35 years, DE, West
Awareness, knowledge and understanding of the policy
This section examines participants’ awareness, knowledge and understanding of MUP in conjunction with any subgroup differences and changes between study waves.
The majority of participants reported having heard about alcohol MUP, typically through a combination of word of mouth, news reports and social media, although some confused it with another alcohol policy in Scotland that restricted multideals:
I knew that they were changing the law, but I thought it was for special offers.
Wave 2, FG11 – women, 30–55 years, DE, East
It was widely understood to be a public health policy designed to restrict demand for alcohol by affecting the prices of cheap alcohol products:
Move on now to minimum unit pricing, what have you heard about it, what do you know about it?
I’ve just heard that it’s getting, that it’s going to go up that’s what I’ve heard, . . . It’s more the cheaper brands which are going to be not so . . .
Wave 1, FG11 – women, 30–55 years, DE, East
Participants’ narratives suggest that much of the media attention relating to the policy appeared to have focused on cheap high-strength ciders, which is the product category thought to be most affected by the policy, with frequent mention of the market’s leading brand, Frosty Jacks:
Say your ciders like your 3 litres and things like that that is really strong, is it not? Because I seen it on the news and it was something like it would go up to like £13 a bottle or something like that . . . for cheap cider.
Wave 1, FG03 – women, 30–55 years, ABC1, West
Some participants also mentioned hearing that the policy may also affect cheap wines, large beer multipacks and cheap spirits, as well as other products associated with the problem drinking, such as alcopops and the popular tonic wine Buckfast. These products were mentioned less frequently and were often accompanied by a degree of uncertainty, with some suggesting that they may be inadvertently affected.
Findings suggest that the focus on cheap high-strength ciders reinforced a widely held belief among participants that the policy was designed to target alcoholism and alcohol abuse, and groups associated with these problems with underage street drinkers and older disadvantaged or homeless dependent drinkers. Few in our sample reported drinking these products, although a few had done so when younger:
I think it’s to cut down alcohol abuse . . . It’s targeting the white cider right, your ****, aye a pound a bottle and all this eh . . .
Wave 1, FG12 – men, 30–55 years, DE, East
I think it’s more for the alcoholics, they are buying all the cheap drinks so they are putting that up to try and prevent all of that from happening.
Wave 1, FG05 – women, 18–24 years, DE, West
I think it’s the people that are trying to get as much drink as they can, like as much units as they can but at the lowest price. So underage people that don’t really have a job and don’t earn anything, they just get pocket money, obviously they’re going to try and get the cheapest thing, so that’s why they would have gone for Frosty Jacks.
Wave 2, FG01 – women, 18–24 years, ABC1, West
As well as health . . . I think it’s maybe to target the homeless because they would go and get a bottle of whatever [cheap cider] for a couple of pounds in the corner shops which are now not a couple of pounds because of how much [alcohol] is in it.
Wave 2, FG09 – women, 18–24 years, DE, East
Despite relatively wide awareness of the policy, many found it difficult to understand or to grasp how it would affect the prices of specific products and product categories:
Aren’t they meant to make it 50 pence a unit or something it was on the News tonight, . . . I think it’s all a certain proof, . . . that’s what they said something to do with it’s going to be a certain proofage before it goes up to 50 pence.
But the cider is a lot of proof isn’t it?
Wave 1, FG07 – women, 30–55 years, DE, West
When that minimum unit pricing thing came out I worked it out as a bottle of wine is 12% so that’s 12 units, so that’s what that means, so it will be at least £6. And then I realised it wasn’t that . . .
Wave 2, FG04 – men, 30–55 years, ABC1, West
This inability to fully grasp the idea of a minimum floor price for alcohol and how this was intended to limit unit consumption was responsible for many questioning the efficacy of the policy and whether or not it would be able to influence people’s drinking behaviour:
. . . like younger people most of the time are drinking to get drunk so they will just swap to a drink that is cheaper . . . say a lot of my friends are drinking Frosty Jacks then they just won’t drink that anymore they will just switch to vodka.
Wave 1, FG01 – women, 18–24 years, ABC1, West
Similarly, many misunderstood that the policy was a form of alcohol tax and that any financial benefits would accrue to central government:
I think they are looking there at a tax revenue thing if you ask me it’s a fly way of taxing the poor. You know yourself everyone knows the tax it generates on alcohol, think of the money they are going to make on this.
Wave 1, FG06 – men, 18–24 years, DE, West
There were few apparent subgroup differences relating to knowledge and understanding of the policy, nor were there any notable shifts in knowledge and understanding between waves. At the second wave, many participants continued under the misinterpretation that MUP was an alcohol tax where the policy could be circumvented by switching to cheaper products. Many also continued to struggle to grasp how to calculate minimum prices using the £0.50 floor price and to believe the policy was intended to target underage and marginalised problem drinkers.
One noteworthy subgroup difference related to the role of the media in informing participants’ understanding of the policy. In this respect, younger participants demonstrated greater reliance on and engagement with social media.
Level of support and attitudes towards the policy
This section examines those factors that helped shape attitudes and how these moderated support for the policy. In addition, the section reports subgroup differences and changes that emerged between study waves. Support for the policy was mediated by two main factors: (1) its perceived effectiveness at curbing excessive drinking and (2) the extent to which it was seen to affect the prices of those products that participants regularly consumed.
Perceived effectiveness
Many participants expressed doubts about the policy’s ability to tackle alcohol dependency, with many fearing that it may have potential adverse consequences for drinkers with dependency issues living in deprived circumstances. These narratives were dominated by predictions of the policy’s impact on crime and, in particular, on shop lifting:
They will just go to bigger lengths to get it, because if people have an addiction people rely on something they will always find a way to get it. So whether that’s stealing money or stealing the item or whatever it is, they will do it.
Wave 1, FG01 – women, 18–24 years, ABC1, West
If you’ve not got the money then you will need to find the money and what will that cause, will that not cause more crime because people will need to shop lift, they will need to do this, because people aren’t going to go, ‘Oh it’s that price I will need to stop then!’ . . . there will be a lot of desperate people running about.
Wave 1, FG08 – men, 30–55 years, DE, West
More minor themes included increases in street begging, sacrificing food purchases, consuming other products that contained alcohol [e.g. Brasso (Reckitt, Slough, UK), methylated spirits, hairspray] and getting into debt (e.g. spending the rent money). There were few mentions of violent crime (e.g. customers being abusive towards shopkeepers) or narratives describing wider social impacts on the likes of families or communities:
I do know that even families which are, which have alcohol problems will still want to subsidise it, . . . they may well already have social work care or not yet have social work care, [but] social work intervention will end up coming in because the money has got to come from somewhere. If you are an alcoholic you are going to get the money for that drink . . .
Wave 1, FG11 – women, 30–55 years, DE, East
It’s like we were saying, the people who drink that [white cider], want to drink it, they will find a way to spend £11 whether they miss food for a week, or they’re maybe stealing, or selling stuff, like if they really really want to buy it and drink it, they will find a way.
Wave 2, FG09 – women 18–24 years, DE, East
If you’ve got someone who’s homeless and they’ve got £5 there instead of spending £2 on that and then having £3 to get something to eat they then will sacrifice the food and just get what . . . that comes first, the alcohol comes first for them and then the food. So effectively in trying to help people it’s actually backfired a little bit on certain people.
Wave 2, FG09 – women, 18–24 years, DE, East
Substituting alcohol with drugs also emerged as a minor theme, but was mainly raised in connection with youth drinking, where drinking and drug-taking was reported to be relatively common:
The price of drugs aren’t changing so they [students] might end up doing that a bit more . . .
Wave 1, FG02 – men 18–24 years, ABC1, West
[When] you take cocaine the drink doesn’t hit you, whisky tastes like water, you’re guzzling it.
Wave 1, FG06 – men, 18–24 years, DE, West
The potential for cross-border shopping also emerged as a common theme, although there were few reports of this actually occurring post implementation, with distance thought to be a governing factor:
I’ve not heard of anybody doing the beer run yet, but I thought that would have materialised . . .
Wave 2, FG04 – men, 30–55 years, ABC1, West
I dare say it’s happening closer to the border I don’t know if people would justify driving all the way down there and back for the difference in the price.
Wave 2, FG08 – men, 30–55 years, DE, West
Participants from the two deprived study communities tended to take more extreme or emotive positions on the policy, in some cases rejecting it outright when considering possible adverse consequences for disadvantaged dependent drinkers:
How do you feel about this policy, this unit price thing?
It’s ridiculous . . . Especially for that Frosty Jack, that’s . . . That is just ridiculous . . . It’s outrageous . . . I actually feel sorry for the alcoholics that normally drink that because that would make them want to drink like!
Wave 2, FG11 – women, 30–55 years, DE, East
In contrast, those from the affluent study community were more likely to assume more nuanced positions, for example characterising the policy as something that was worth trying or that they’d want to see evidence of effectiveness before making any judgments:
It’s kind of targeted at poorer drinkers who are more likely to be problem drinkers. So I can understand why they’re doing it, to stop them falling into that trap of buying cheap drink. But the ones who can only afford cheap drink I worry for what . . . they can get black market stuff or try.
Wave 2, FG04 – men, 30–55 years, ABC1, West
I think they would have to justify it, you’d have to show me some statistic and prove that it’s making this a great deal. And I think people would be more inclined to get behind it . . .
Wave 2, FG04 – men, 30–55 years, ABC1, West
Participants from deprived study communities also tended to demonstrate greater empathy and identification with dependent drinkers living in deprived circumstances. In some instances, participants described what they saw as striking inequities in the way in which the policy targeted these vulnerable groups:
They are just trying to rip the poor off again aren’t they, guaranteed because we are not able to fight against it.
Wave 1, FG12 – men, 30–55 years, DE, East
See the people that is on the bread line they are going to be punished and all so they are when this comes out, because that’s their only outlet, they might just have put the wains to bed, single parent, wee bottle of wine, take that away, where is that guy going to get [his drink].
Wave 1, FG08 – men, 30–55 years, DE, West
Participants from all socioeconomic groups tended to believe that the policy was more likely to have a positive impact on underage drinking and were more likely to support it on these grounds:
I think it’s a good thing for like underagers, like to try and stop it, because of the Frosty Jacks, I think it’s good in that sense.
Wave 2, FG01 – women, 18–24 years, ABC1, West
However, as previously indicated, some highlighted the potential for youth drinkers to switch from alcohol to other mood-altering substances for recreational purposes:
See the likes of the younger ones, I think that they are going to get out of their face somehow or other, and . . . if they are not drinking it could be something else that they are doing that might be even worse. If they can’t afford the bottle of cider anymore then some drug dealer . . .
Wave 1, FG08 – men, 30–55 years, DE, West
In contrast, it was often believed that drinkers with alcohol dependency were more likely to adopt other strategies and measures, such as theft or sacrificing food purchases, to fund their alcohol habit, rather than switch to other less expensive substances. However, this view was not necessarily supported by those who had more direct experience of addiction:
That’s what happened to me . . . the likes of, you just move from one to the next, so if you canny afford that . . . I went away from alcohol to drugs and drugs to alcohol again eh . . . It’s the cheapest addiction you go for, what you can afford do you know what I mean?
Wave 1, FG12 – men, 30–55 years, DE, East
Perceived impact on prices
Support for the policy was also mediated by concerns and anxieties about how it would impact the price of those drinks they typically consumed and the amount they spent on alcohol:
So what does it do to a vodka in a bar, how much is that going to cost me? I don’t know what would it cost me!
Wave 1, FG03 – women, 30–55 years, ABC1, West
They are trying to stop alcoholism which it probably would to be fair . . . But as long as Kopparberg’s [Kopparberg Breweries, Kopparberg, Sweden] and vodka are all right [the products I drink are unaffected].
Wave 1, FG10 – men, 18–24 years, DE, East
For our age group if we are not drinking on a regular basis then I wouldn’t, if it’s going to go up then I don’t mind paying it for one night during the week I don’t mind paying a bit more for a bottle of vodka because I know it’s only for that 1 day.
Wave 1, FG01 – women, 18–24 years, ABC1, West
However, some participants from deprived study communities appeared to find the prospect of MUP more financially challenging:
I am not an alcoholic but . . . I’m still going to buy it, whether it’s a certain price or not . . . It’s not going to stop me from getting what I like at the weekend.
Wave 1, FG05 – women, 18–24 years, DE, West
We will keep drinking some way or another we will find a way around about it or we will have the cash maybe to pay a wee bit extra or whatever . . .
Wave 1, FG08 – men, 30–55 years, DE, West
At the post-implementation follow-up discussions, most reports of any changes to the prices they were paying for alcohol were relatively small. However, many continued to voice concerns about potential unintended consequences for more vulnerable drinkers. These are examined further in the next section, perceived impact of the policy.
Perceived impact of the policy
This section examines awareness and experiences of the policy’s impact on alcohol prices, any perceived changes in purchasing and drinking behaviour and any changes in attitudes towards the policy following implementation, including any subgroup differences. Participants’ recognition of price changes was low. Some noted marginal price increases on products they regularly purchased or on alcohol products more generally, but these changes were not always directly attributed to MUP. In most instances, any price changes that were noted were generally accepted and were not perceived to have had any discernible impact on participants’ purchasing or drinking behaviour:
It’s not been as bad as I thought it would be, . . . No apart from your white cider, and I don’t care about that, ken, likes a can of lager has not went up that much and the vodka has not went up that much do you know what I mean?
Wave 2, FG12 – men, 30–55 years, DE, East
I mean I think that the prices have gone up but it’s not affected me. I don’t know about other people, but it hasn’t changed the way I’ve drank. I’ve noticed the prices going up and the sizes of things changing like the Tennent’s [C&C Group plc, Wellpark Brewery Glasgow, UK] earlier, but I would say my drinking habits haven’t changed in the slightest.
Wave 2, FG02 – men, 18–24 years, ABC1, West
There was some concern expressed by participants from the disadvantaged study communities about the potential impact of the policy on how much they would have to pay for alcohol. These concerns were also echoed post implementation, most notably with regard to the impact on the price of beer multipacks:
We won’t be able to go into Tesco and get a big cheap £20 [deal] . . . how much is it going to cost to buy 24 cans or 24 bottles, do you know what I mean?
Wave 1, FG08 – men, 30–55 years, DE, West
You could go and buy a case of Becks [Beck’s Brewery, Bremen, Germany] for around about the £10 mark, and see once that new law came along here with the units, it went from about £10 to about £13.
Wave 2, FG08 – men, 30–55 years, DE, West
Others’ experience of the policy served to correct some misapprehensions about its impact on prices, most significantly allaying concerns that it would have an impact on-trade prices:
I was pure looking out for like, you know how Fire Water [Glasgow, UK], I think we spoke about that last time [wave 1 discussion group], it was 89p for a vodka mix. It’s still the exact same . . . It’s like a measure of vodka with mixer . . . it’s a club on Sauchiehall Street that sells it and it’s 89p for a vodka.
Wave 2, FG01 – women, 18–24 years, ABC1, West
In one or two exceptional cases these changes had prompted participants to adjust their consumption. However, as previously highlighted, for the vast majority, no discernible impact on drinking patterns or consumption were noted:
They don’t do 20 slabs of Tennents anymore, you only get 15 now . . . so we bought something else . . . they stopped doing them because of the pricing.
Wave 2, FG02 – men, 18–24 years, ABC1, West
What did you switch to instead of a 20 slab?
Instead we got a 10 crate of Coors [Coors Brewing Company, Golden, CO, USA] and a 10 crate of Bud [Budweiser, Anheuser-Busch, St. Louis, MO, USA] which is less because it was bottles . . .
Wave 2, FG02 – men, 18–24 years, ABC1, West
Some participants also reported up-grading from a cheap product to a better brand because the policy had the effect of narrowing the price differential:
My wine is still 11%. Its just 80p more expensive! . . . All it means is instead of getting that one I now buy Echo Falls [Accolade Wines, Reynella, SA, Australia] which is £4.50 and I’m like I’ll spend the extra 30p and get the branded wine . . . It means that my treat at the end of the month is now a more expensive wine . . .
Wave 2, FG09 – women, 18–24 years, DE, East
Although most participants found their drinking patterns and behaviour to be largely unaffected, many continued to believe that the policy would effect more vulnerable drinkers, typically poor or disadvantaged dependent drinkers who it was anticipated may turn to petty crime or limit the amount they spend on food to fund their habit:
It will affect people that do like a drink every night . . . But for somebody like me that might be 1 night 1 week, 3 nights and then the next night none, do you know what I mean? But somebody that drinks every day it will affect them . . . Me personally, no it hasn’t . . . Because I am not drinking anywhere near as much as I used to now, I’ve not noticed it at all . . .
Wave 2, FG11 – women, 30–55 years, DE, East
I think people, especially alcoholics will find the money somewhere to pay for it. It’s the same as a junkie, a drug addict, a chain smoker . . . They don’t care about what they drink as long as they get a kick from it.
Wave 2, FG07 – women, 30–55 years, DE, West
Despite these beliefs, there was little evidence of any adverse consequences reported at the follow-up discussion groups, which were conducted some 5–6 months post implementation. Any evidence that was reported tended to be anecdotal:
I’ve seen homeless people sitting outside Scotmid [Scottish Midland Co-operative Society, Edinburgh, UK], Tesco’s having enough to go in and get something, and you see them come out with like the four can of Tennents, and maybe like a sandwich. Now they don’t come out with a sandwich because they don’t have the money to afford both . . .
Follow-up, FG09 – women, 18–24 years, DE, East
You’ll see folk in the street, they’ll tap [ask] you for money and say they want £2, they’ll tap you the £2 now [rather than £1] . . .
Follow-up, FG05 – Women, 18–24 years, DE, West
Some participants living in deprived communities who worked in licensed grocers were able to provide vivid descriptions of regular customers who were dependent drinkers switching products. However, these descriptions were not accompanied by any accounts of these same customers experiencing particular hardship as a consequence of the policy, or of challenging retailers:
[One customer] was buying two [3-l bottles of Frosty Jacks] a day right, before it was going up it was only costing 6 or 7 quid, right so when it went up . . . she said the next day **** that I canny afford it, go and get me a bottle of vodka, the next day she came down she went back to the Frosty Jack . . . she felt bad on the vodka, Frosty Jacks is her drink, do you know what I mean?
Wave 2, FG08 – men, 30–55 years, DE, West
Although there was little evidence of our sample being adversely affected by the policy, there was some evidence of it having a wider impact on peoples attitudes towards alcohol, most significantly by reinforcing the belief that alcohol harm is confined to a marginalised minority of so-called problem drinkers or street drinkers. This was illustrated in the reaction of some participants, particularly drinkers from the disadvantaged study communities who challenged the policy on the grounds that they would be inadvertently punished by having to pay more for alcohol:
Minimum unit pricing, what does that mean to you, what do you know about it?
The Government is trying to cut out the cheap ciders and all that drink . . . It comes in in May doesn’t it; the law comes in in May, . . . It’s the boy that drinks the ciders . . . but everybody else has got to pay for it . . . Aye, . . . What I’d read in the paper it looked like it would actually affect guys that were buying like your Tesco shopping, your 24 pack of Tennents . . .
Wave 1, FG08 – men, 30–55 years, DE, West
Similarly, some participants expressed surprise on learning that the policy would not affect the prices of some drinks that they commonly associated with problem drinking, most notably the popular tonic wine Buckfast:
I just cannae believe what I’m seeing . . . you begin to think what’s the point in doing this, I thought it was to get rid of alcoholism and binge drinking, and poverty drinking or whatever you want to call it, and that [Buckfast] is one of the biggest adherents of that!
Wave 1, FG04 – men, 30–55 years, ABC1, West
Discussion and conclusion
Minimum unit pricing was broadly understood to affect the prices of cheap alcohol, in particular cheap high-strength ciders, and the groups of drinkers who typically consumed these products (i.e. underage street drinkers and dependent drinkers living in disadvantaged circumstances). Few in our sample regularly consumed these products. Some participants, mainly those from deprived study areas, knew of drinkers in their local communities who were alcohol dependent and who regularly drank high-strength white ciders to maintain their habit. Some also reported drinking these products when younger.
Although many held clear beliefs about who the policy was designed to target, most struggled to grasp how the policy operated to increase the price of cheap high strength alcohol products while leaving other products unaffected. In some instances, this deficit in understanding led to questions regarding the efficacy of the policy, with many suggesting that people would simply switch to buying something cheaper.
Support for the policy was mediated by two main factors: (1) the extent to which it was seen to affect the prices of those products participants regularly consumed and (2) its perceived effectiveness at reaching what were regarded as its target groups. There was fairly broad support for the policy’s potential to reduce underage drinking. However, many feared that it may have adverse unintended consequences for disadvantaged dependent drinkers who it was believed may be forced to find alternative ways to fund their addiction (e.g. through theft, begging or reducing the amount of money spent on necessities, such as food). These fears were more strongly held by participants from our deprived study communities who often demonstrated greater empathy and identification with the vulnerabilities experienced by dependent drinkers living in deprived circumstances.
Many participants reported not noticing any differences in the prices they were paying for alcohol post implementation and most differences that were noticed were relatively small and generally accepted without challenge. In most cases, changes in price were not seen to have had any discernible impact on drinking behaviours, although there were a small number of instances where the policy had encouraged participants to make slight adjustments, most notably cutting back on off-trade beer purchases as a result of less attractively priced multipacks.
Many continued to voice concerns about potential unintended consequences for more vulnerable drinkers post implementation. However, evidence of adverse consequences for these groups was largely absent in people’s accounts of the policy, including those in more deprived study communities. The only notable negative consequence to emerge with our sample was a tendency for the policy to position alcohol and public health as an issue that relates to ‘other people’ or, more specifically, to the health and social harms caused to (and by) a narrowly defined number of problem groups and products.
Therefore, to conclude, although awareness of MUP appears to have been relatively high, understanding of how the policy works and how it differentiates between alcohol products on the basis of unit price is limited. This deficit means that people’s understanding of which products were affected and how was largely driven by word of mouth communication and coverage of the policy in the media, much of which appears to have focused on the dramatic rise in prices for high strength ciders. These narratives and the brand reputations that participants associated with the products highlighted was instrumental in shaping understanding of who the policy was most likely to affect and the policy’s intended aims, namely reducing alcohol consumption among underage drinkers and older marginalised problem drinkers drinking at harmful levels. There was little appreciation that the policy had the potential to affect consumption more widely, albeit at low levels.
People’s inability to properly grasp how the policy worked (i.e. that it is based on a minimum unit price rather than absolute product price) highlights some important knowledge deficits relating to the scope and reach of the policy. It is suggested that correcting these misunderstandings and gaps in knowledge may be relevant to addressing questions of perceived discrimination by the policy against vulnerable dependent drinkers and to the negative effects of ‘othering’ or the tendency to associate health risks of alcohol consumption with others rather than with personal drinking behaviour.
Finally, our study indicates that for people whose normative drinking behaviour is at hazardous levels, the implementation of MUP has been minimally invasive. Many were not conscious of significant price increases for any products they consumed, and any changes in drinking behaviour that were noted were relatively small and widely accepted. These findings were consistent, irrespective of socioeconomic context. This raises some important questions about the efficacy of the policy for this particular study group. For example, is it simply the case that MUP has not had a significant impact on their consumption and drinking behaviour, or is it operating at a level below which its behavioural effects are discernible? Clearly, our study methods were not designed to answer these kinds of questions. However, any failure to bring about significant changes in consumption and drinking behaviour raises important questions about the floor price set for the policy and/or how this is promoted to bring about change. Alternatively, should the policy prove effective at placing positive downwards pressure on consumption then this might be regarded as an optimal outcome for targeting this group of drinkers as part of a minimally invasive strategy. These questions need to be explored in the context of other data and evidence to emerge from the evaluation of MUP in Scotland. 102,103
Chapter 8 Discussion
In general, we found no evidence for large impacts of MUP on alcohol-related harms within ED settings, but also found no evidence of unintended harmful consequences (assessed within SHCs) either. Qualitative research suggested that there was limited understanding of the policy among higher-risk drinkers, with limited awareness of any behavioural responses occurring. It should be noted that this study reports on only limited aspects of an overarching evaluation, with other studies suggesting a more positive public health impact on consumption. 88 Progress against meeting each of the three objectives is reported in turn, followed by recommendations for future research, implications for policy and strengths and weaknesses of the study.
Key findings against study objectives
Research objective 1: to determine the impact of minimum unit pricing on alcohol-related harms and drinking patterns for the overall population and by subgroups of interest (age, sex and socioeconomic position)
We met this objective primarily by examining the impact of MUP on alcohol-related harms presenting to EDs within two Scottish cities and comparing changes in these outcomes with those occurring in two cities in the north of England. Data were collected by trained research nurses who attempted to conduct a census of adult attendees (defined as aged ≥ 16 years) during selected time periods over a 4-week period on three occasions: February 2018 (shortly before the implementation date of 1 May 2018), September/October 2018 (approximately 6 months post implementation) and February 2019 (1 year after baseline). Study participants were asked to complete a short questionnaire about their reasons for attendance and their alcohol drinking patterns. Alcohol-related outcomes were studied in a variety of ways within this setting, including alcohol-related visits (i.e. being too intoxicated to approach, having binge drank within the last 24 hours and self-reporting that their attendance was due to alcohol consumption) among those consenting to completing the survey, patterns of self-reported alcohol use among those consenting and alcohol-related diagnoses among all ED attendees.
A total of 26,969 adult patients attended the EDs during the three study periods and 23,455 (87.0%) were recorded by research nurses. Among those patients recorded, 14,047 (59.9%) were approached and 12,249 were eligible to participate. Out of this group, 8746 (71.4%) patients completed the survey. The two sites in England had slightly lower response rates than Scotland. At baseline, we found a large prevalence of alcohol-related visits among participating EDs, comprising 8.4% and 6.1% in the Scottish and English sites, respectively.
We compared changes in alcohol-related visits in the two Scottish sites against the two sites in the north of England using a DiD analysis, finding limited evidence for any change in the primary outcome of interest. The introduction of MUP was not related to alcohol-related visits (OR 1.14, 95% CI 0.90 to 1.44). In absolute terms, we estimated that MUP led to 258 more alcohol-related visits (95% CI –191 to 707) across Scotland, therefore, suggesting that this effect estimate is reasonably precise. As there is potential for substantial bias arising from non-participation, we investigated the potential for an impact on alcohol-related diagnoses by analysing administrative health records from the four EDs. Again, we found no evidence of a substantial impact of MUP on alcohol-related diagnosis (OR 1.25, 95% CI 1.00 to 1.57; absolute risk 325 attendances per year, 95% CI 21 to 628 attendances per year). As per our prespecified protocol, we investigated whether or not any differential effects occurred across age, sex and socioeconomic position. After correcting for multiple comparisons, we found that MUP was associated with increased odds in alcohol-related diagnosis among male attendees only (OR 1.56, 95% 1.16 to 2.11). However, in the absence of an overall effect being observed, it is likely that this association is spurious. The availability of two follow-up time points also allowed an assessment of whether or not any differential impact was seen by length of time post implementation (i.e. 6 months vs. 12 months after the policy was introduced). No evidence of an impact was seen with either follow-up period.
In addition to this work’s primary focus on the ED setting, we also assessed harmful alcohol consumption among SHC attendees (see methodological details in Research objective 2). Using a similar comparative approach between Scotland and the north of England over time, we, again, found no evidence of substantial changes in alcohol misuse (OR 1.22, 95% 1.04 to 1.42). Assessment of differential effects by age, sex and socioeconomic position found little convincing evidence for any impacts.
Research objective 2: to determine the impact of minimum unit pricing on non-alcohol substance use, and other unintended impacts, for the overall population and by subgroups of interest (age, sex and socioeconomic position)
We mainly met this objective by examining the impact of MUP on substance use among attendees of SHCs (three clinics in Scotland and three in the north of England). The study used a similar design to the ED study described above, by comparing changes in self-reported outcomes over time. All attendees were asked to participate by self-completing an anonymous short questionnaire. The choice of SHCs was informed by an attempt to recruit a large number of participants who were likely to be at higher risk ofr substance use (given the relatively low prevalence of use in the general population) from a setting where confidentiality was perceived to be high. Data collection occurred over similar 4-week periods to the ED component and, again, over three occasions: February 2018, September/October 2018 and February 2019. The primary outcome of interest was non-alcohol substance use (defined as illicit drugs). Secondary outcomes included use of specific drugs, patterns of alcohol consumption and sources of alcohol purchasing.
We collected data from 15,218 attendees of SHCs, with 5873 attendees from Scottish clinics and 9345 attendees from English clinics. This reflected an estimated response rate of 50.3% in Scotland and 60.8% in England. At baseline, we observed a prevalence of 24.2% use of any non-alcohol substance in Scotland and 29.3% in England.
When comparing changes in substance use between Scotland and England in the DiD analysis, we found no meaningful change in use of non-alcohol substances (OR 1.04, 95% CI 0.88 to 1.24). Similarly, assessments of specific substances found no clear evidence of any increase linked to MUP, providing reassurance that drug use had not increased as a result of a substitution effect from alcohol. As expected, we observed evidence for a shift in purchasing from off-licenses (OR 1.08, 95% CI 0.91 to 1.29) to licensed premises (OR 1.27, 95% CI 1.05 to 1.55).
Investigation of potential differential effects was conducted as per the prespecified protocol. Again, we found no clear evidence that any population subgroups had experienced an increase in substance use following MUP. There was similarly no clear evidence for the shift in sources of alcohol purchasing to have been differential across population subgroups. Analyses by length of time post implementation found similar patterns of findings. It is worth noting that the consistency in the pattern of findings helps reduce potential concerns about the response level in Glasgow at wave 2.
Research objective 3: to describe changes in experiences and norms towards minimum unit pricing and alcohol use following the introduction of minimum unit pricing by subgroups of interest (age, sex and socioeconomic position)
We studied changes in experiences and norms towards MUP primarily through mixed-qualitative methods, collecting data before and after the policy was implemented. Interviews with professional stakeholders provided an understanding of experiences related to implementation, as well as professional responses to the policy. Focus groups provided insights relating to alcohol-related behaviours among young people and high-risk drinkers from the same catchment areas in Scotland as the ED component (see Chapter 4). As we were interested in reporting lived experiences and norms related to MUP specifically, and were not trying to pursue causal inference in relation to these, we did not include a control group when addressing this RO. We now report findings from the professional stakeholder interviews, followed by the focus groups with young people and high-risk drinkers.
Stakeholder interviews
We recruited a baseline sample of 25 participants pre-policy implementation (in February 2018) and re-interviewed 16 of these participants after MUP had been implemented (in October 2018). We recruited five additional interviewees at follow-up to ensure that our sample included the diversity sought, meaning that a total of 30 professional stakeholders participated in our study. Most interviews were individual one-to-one interviews (n = 23), but a minority preferred paired or small group interviews. Our sample achieved diversity in relation to professional role, including addiction services, youth workers, primary care, police and licensing authorities. We achieved geographic coverage across our three areas of interest (two deprived areas and one affluent).
Overall, our qualitative interviews (which reported professional ‘intelligence’ from across Scotland, as well as local perspectives) suggested high compliance with the policy and that the policy was implemented as intended. Licensing authority and police participants concerns reported that retailers’ compliance with MUP had predominantly been good, with any issues of non-adherence to the policy being very temporary. Prior to the policy’s implementation, expectations of the impact on consumption were mixed, with some stakeholders anticipating long-term reductions in consumption, but others expressing concern that consumption by wealthy individuals and those with ‘chaotic lifestyles’ would not change. Prior to the policy, stakeholders expressed concern about the potential for a range of negative predominantly short-term outcomes, particularly in relation to the potential for alcohol withdrawal among dependent, low-income drinkers. However, these anticipated negative outcomes were predominantly not evident in stakeholders’ experiences subsequent to implementation. Similarly, prior to the policy’s introduction, there had been concerns of increases in criminality (e.g. smuggling) and adverse economic impacts. However, interviewees felt that these did not materialise and, indeed, felt that economic impacts were often positive, with the policy helping to create a level playing field for small shops struggling to compete against large supermarkets. Although experiences of MUP were largely positive, some potential negative unintended consequences were identified. For example, there were concerns that the increased profitability of selling alcohol could cause the re-emergence of a problem of overprovision of alcohol within some communities. However, most of these concerns had not been observed to have occurred, but were rather issues that may emerge in the future.
Young people and high-risk drinkers’ experiences
To develop an understanding of the experiences of high-risk drinkers, we collected data from qualitative focus groups because they provide an opportunity for participants to explore their views in free-flowing discussions, generating data through participant interaction and group dynamics. A total of 24 focus groups were conducted with young binge drinkers (aged 18–24 years) and older heavy drinkers (aged 30–55 years) living in three different communities in Central Scotland (two deprived areas and one affluent area). These drinkers were selected to represent key subgroups of the Scottish population who may be particularly affected by MUP policy and are of substantial policy interest. A total of 105 people took part, with 68 taking part in both sets of focus groups (i.e. pre and post implementation in March/April and October/November 2018, respectively). Eighty-four people took part at baseline, of whom 47 took part in repeated focus groups, with an additional 21 recruited to maintain diversity in participant characteristics at follow-up focus groups.
In general, participants reported that they did not notice any differences in prices before and after the policy was introduced. Our results suggest that MUP was understood to be particularly targeted at the prices of cheap alcohol, especially high-strength ciders and the groups of drinkers typically associated with these products, such as underage street drinkers and poor dependent drinkers. It was generally perceived that the policy was not targeted at the focus group participants. However, their appeared to be a disconnect between this view and understanding of the practicalities of how the policy operates, with many people believing that drinkers would simply switch to buying something cheaper (which is prevented by MUP). In general, support for the policy was facilitated by the belief that it was targeted, especially at underage drinking, although there were concerns that dependent drinkers would maintain their consumption through criminality or reducing other essentials (e.g. food). Following implementation, evidence of such adverse consequences was largely absent, including in the more deprived study communities that had expressed greater concerns previously.
Interpretation
Emergency departments
There is limited research on the association between hospital admissions and the introduction of MUP. Existing studies have suggested that MUP led to a reduction in alcohol-attributable hospital admissions and alcohol-related deaths,73,77,170 but there was no immediate effect on ED attendances for alcohol-related injury in Canada. 69 These studies focus on alcohol-related admissions and attendances based on patients’ diagnosed diseases and injuries. Our study, on the other hand, examined alcohol-related attendances based on the nurse interviewers’ observations and attendees’ self-reported behaviours and reasons for attendance. Our study also examined alcohol-attributable diagnosis among all ED attendees. We combined all chronic and acute alcohol-related conditions as a whole, rather than acute injuries covered elsewhere. 69 Our data show that only < 1% of all attendees in Scotland and 0% in England were diagnosed with partially acute injuries. The zero figure indicates that some codes are just not used in England or a coding error. Therefore, it was not possible to analyse partially acute alcohol-related diagnosis individually. However, our research provides evidence that there was no immediate association between MUP and changes in the prevalence of alcohol-related diagnosis or consumption among ED attendees.
Sexual health clinics
Primary outcome: drug consumption
We have shown that there is no evidence that, overall, illicit drug consumption changed in this population as a result of MUP. In this component, the general trend was for no overall increases in illicit drug use, although there was an increase in cannabis use. Routine data shows that cannabis use in the last 30 days had fallen for 15-year-olds from 13% in 2006 to 8% in early 2018 in Scotland,171 whereas in England the proportion of young people who reported having ever used cannabis in their lifetime decreased from 41% in 2002 to 21% in 2018, although since 2014 the proportion among boys increased slightly. 172 Therefore, the pre-MUP trend was opposite to the trend we found with MUP, indicating a stronger effect of increasing cannabis use from MUP than if cannabis use had been increasing anyway.
Secondary outcomes: alcohol consumption
The greater odds of any alcohol purchase in the last month from on-licensed premises were not unexpected by the authors, as MUP almost exclusively affected off-license sales of cheap high-strength alcoholic beverages, and not the more expensive on-license trade. The Sheffield alcohol policy model82 predicted a fall in tax revenue of £15M, with £12M attributable to the off-trade and £4M to the on-trade (rounded figures). Although this was not a move to on-license purchase, it does predict a smaller effect on the on-trade.
The possible effects in substrata have implications for health inequality, but the only substantive change was the greater odds of those aged < 19 years purchasing alcohol from both on- and off-license sources. MUP is likely to have an impact on this group, as the price increase was not seen by them as a barrier to purchase and, furthermore, most products preferred by under 18s, who were part of our sample, were not affected by MUP. 100
O’Donnell et al. 88 recently reported an interrupted time series analysis of alcohol off-trade purchases data, comparing England and Scotland before and 8 months after MUP implementation. The study showed a clear immediate reduction in alcohol purchases in Scotland, compared with England, after MUP, but some uncertainty as to whether or not the effect was sustained. Purchase and sales data also give no indication of consumption stratified by social group. Owing to the different study populations, ours being younger and better educated and with more females, our results do not contradict those of O’Donnell et al. 88
As MUP is likely to have a disproportionate effect in reducing consumption of the low-cost, high-strength alcoholic drinks favoured by high-risk alcohol consumers,82 the policy is focused on those most at risk. Public health evidence about the most effective ways of reducing health inequalities64 intimated that, as a structural approach that does not require individuals to take up an intervention, MUP would also be an effective way to reduce health inequalities.
In conclusion, overall, we found no drug substitution effect arising from MUP, although there was a greater likelihood of alcohol misuse. There were some effects within substrata by age and a greater likelihood overall to have purchased alcohol from an on-licensed premises in the past month. There may be implications for young people’s health. Our evaluation,39 which itself contains multiple components, is part of a wider programme co-ordinated by Public Health Scotland and should be understood in the context of those results. 173
Stakeholder interviews
Separate interpretation is not applicable as the key points from analysis are already interpretive.
Focus groups with young people and heavy drinkers
Although awareness of MUP appears to have been relatively high, understanding of how the policy works and how it differentiates between alcohol products on the basis of unit price is limited. This deficit means that people’s understanding of which products were affected and how was largely driven by word of mouth communication and coverage of the policy in the media, much of which appears to have focused on the dramatic rise in prices for high-strength ciders. These narratives and the brand reputations that participants associated with the products highlighted were instrumental in shaping understanding of whom the policy was most likely to affect and the policy’s intended aims, namely reducing alcohol consumption among underage drinkers and older marginalised problem drinkers drinking at harmful levels. There was little appreciation that the policy had the potential to effect consumption more widely, albeit at low levels.
People’s inability to properly grasp how the policy worked (i.e. that it is based on a minimum unit price rather than absolute product price) highlights some important knowledge deficits relating to the scope and reach of the policy. It is suggested that correcting these misunderstandings and gaps in knowledge may be relevant to addressing questions of perceived discrimination by the policy against vulnerable dependent drinkers and to the negative effects of ‘othering’ or the tendency to associate health risks of alcohol consumption with others rather than with personal drinking behaviour.
Finally, our study indicates that for people whose normative drinking behaviour is at hazardous levels, implementation of MUP has been minimally invasive. Many were not conscious of significant price increases for any products that they consumed and any changes in drinking behaviour that were noted were relatively small and widely accepted. These findings were consistent irrespective of socioeconomic context. This raises some important questions about the efficacy of the policy for this particular study group. For example, is it simply the case that MUP has not had a significant impact on their consumption and drinking behaviour, or is it operating at a level below which its behavioural effects are discernible? Clearly, our study methods were not designed to answer these kinds of questions. However, any failure to bring about significant changes in consumption and drinking behaviour raises important questions about the floor price set for the policy and/or how this is promoted to bring about change. Alternatively, should the policy prove effective at placing positive downwards pressure on consumption then this might be regarded as an optimal outcome for targeting this group of drinkers as part of a minimally invasive strategy. These questions need be explored in the context of other data and evidence to emerge from the evaluation of MUP in Scotland. 102,103
Strengths and limitations
Our study has a number of strengths. We have focused on investigating both the potential positive and negative impacts of MUP using a variety of methods to help provide a more holistic picture than any individual approach could have provided. By theorising the policy as a natural experiment, we have sought to estimate the real-world impact of a major public health policy. The component design for the quantitative components, a DiD analysis, can potentially address unmeasured confounding that is time-invariant. Therefore, the main threats to making causal inference from our quantitative analyses arise from time-varying factors. We used data collection approaches that had been previously applied to study other research topics within the ED and SHC settings and piloted our methods to help standardise the processes used. Our survey instruments and questionnaires used previously validated scales, which helped minimise the chances of study participants interpreting the questions in different ways. Our quantitative components included three waves of data collection, thereby allowing shorter- and longer-term impacts to be investigated, as well as allowing for the known strong effects of seasonality to be reduced. Furthermore, each wave of data collected information from a large sample size, providing statistical power for reasonably precise effect estimates, as well as allowing for differences in impacts on population subgroups to be investigated. In the qualitative research, we collected data on both professional stakeholders and high-risk drinkers, allowing multiple perspectives to be compared. Finally, we were able to undertake some public engagement activities, which, although limited in scope due to the impacts of COVID-19, provided important feedback regarding patient and public concerns surrounding the policy.
However, there are a number of weaknesses that should also be noted. First, response rates varied over time and across study sites, thereby introducing the potential for substantial selection bias. We carried out a range of sensitivity analyses, for example by excluding sites with lower response rates, and found that our substantive findings did not change. Furthermore, for the ED study component, we were able to analyse administrative data that were not subject to this bias and found a similar pattern of findings. Second, there is the potential that trends were diverging between Scotland and the north of England even before the policy was introduced. This could arise if a cohort effect was occurring in Scotland, which was not occurring in England. However, auxiliary evidence from survey data suggests that trends in the regions were broadly comparable before the policy. Another related source of bias is history bias, where another event may have occurred at the same time as MUP, which could have masked the policy’s impact. For example, economic trends in Scotland could lead to increased harmful consumption, or the introduction of an effective alcohol measure within the study areas in England could both mask the effect of MUP. No evidence of such measures was found. Our study in the ED setting was unlikely to reveal long-term effects (e.g. changes in liver cirrhosis) and possibly our follow through was too short. The introduction of MUP was ultimately fairly rapid. This necessitated hurried data collection to ensure the collection of pre-intervention data, but it is possible that changes in alcohol sales had already started prior to this, thereby not capturing the full impact of MUP. Although our qualitative research captured people’s lived experiences of the policy to some extent, in many cases participants reported their views on other people’s experiences. Indeed, this was explicitly sought in the professional stakeholder interviews (which included people working within alcohol and drug services). Therefore, there is a risk that these reports do not reflect people’s real experiences. Last, this research provides a partial picture of the impact of MUP, with other complementary studies assessing the impacts on specific population subgroups (e.g. dependent drinkers) and other outcomes (e.g. alcohol-related hospitalisations).
Summary of key research recommendations
Although our study provides an important contribution to the limited empirical literature on the effectiveness of MUP, there remain several important limitations that should be addressed in future research.
This report focuses on several research areas that were anticipated to be difficult to study using administrative data. In particular, this work has provided reassurance that many of the unintended consequences do not appear to have occurred. The study also suggests that within the ED setting, there does not appear to have been a large impact on health harms and so there was no evidence for the existence of the intended effect of MUP. However, there is a need to study a broader range of health harms in a more varied range of settings, with administrative data playing an important role. In particular, our study was at risk of bias due to the possibility of different trends occurring in our intervention and control groups (i.e. violations of the parallel trends assumption). Further research that uses interrupted time series approaches (or similar) comparing Scotland and the north of England will be less susceptible to this bias. This approach will also be at less risk from selection bias, which is a threat in our primary quantitative data collection research. In addition to the need to better quantify any potential overall health benefits, further research is needed on specific populations that may be particularly positively or negatively affected by the policy. As noted by our professional stakeholder interviews, drinkers who have physiological dependence on alcohol are potentially at specific risk of withdrawal, forgoing essentials (e.g. food or housing) or engaging in behaviours that may be deemed undesirable for broader society (e.g. theft or begging). Although our qualitative research did not find any supportive evidence for this, our data were not collected from this group directly. Furthermore, there is a need for quantitative research better to establish causal evidence.
Most of the planned evaluations that are part of Public Health Scotland’s MUP portfolio, including this NIHR-funded work, rely on comparing trends in Scotland with trends in England (usually the north of England). However, there is a risk that all such evaluations relying on a comparison with the north of England may be biased if the control area does not provide a suitable counterfactual. This could occur, for example, if effective interventions had been implemented in the control area at around the same time as MUP was introduced in Scotland. Broader evaluation approaches that rely on multiple control areas, such as synthetic control methods, may be worth considering. 40,174
Although our research attempted to investigate the equity implications of MUP, several dimensions of health inequalities remain unanswered. Although we attempted to be proactive in being inclusive of ethnic minority communities within our research, Scotland has less ethnic diversity than other parts of the UK and the impact of MUP on ethnic inequalities remains unknown. Last, the inclusion of diverse gender identities within quantitative research remains a challenge. Although our research allowed self-identification of some gender identities, the options allowed remained limited and inclusion of very small categories can preclude meaningful quantitative analysis and reduce confidentiality.
Implications for policy
It is important that this study is seen within the context of the wider MESAS programme and its ongoing work on the evaluation of MUP. We did not find any evidence of an impact of MUP on alcohol-related attendance at EDs, suggesting that such attendees were unaffected by the policy as introduced. Similarly, in the sample drawn from SHC attendees, we found no evidence of a change in illicit drug use. Various professional stakeholders had foreseen problems with the implementation of MUP, particularly around the impact on dependent, low-income drinkers and the potential for disruption to public services, including policing and health care. Post implementation, they noted that such negative impacts had not occurred and saw the introduction of MUP as having been relatively trouble free with high compliance. The younger binge drinkers and at-risk heavy drinkers showed misconceptions about the policy, due in part to a lack of understanding as to what constituted a unit of alcohol and a belief that few drinkers would be affected by MUP apart from those drinking white cider. We were only able to evaluate MUP as it was introduced and, although some stakeholders felt that a £0.50 MUP was too low to have an impact on groups such as dependent drinkers, we are clearly unable to determine how price influenced impacts from this study. When this policy is reviewed, or if similar policies are introduced elsewhere, careful consideration needs to be given to the appropriate price. Subsequent evaluation of the impact of different prices as further policies are introduced or altered has considerable potential to form a body of evidence around the relationship between the price and impacts.
Consent was also obtained from participants in the ED component for data linkage. Therefore, data from our study provide the opportunity to investigate the longer-term sequelae of alcohol-related attendances within that setting. Given ongoing efforts to use attendance at an ED setting as a ‘teachable moment’, an improved understanding of this population may help in future intervention development and inform health economics modelling.
Patient and public involvement in this study
The aim of patient and public involvement
Our project was planned in 2012 and then implemented in a short time frame that did not allow time for patient and public involvement (PPI). PPI was not a required part of projects in 2012. The PPI element has been put in place following the completion of data gathering, which took priority. Our aim at this stage of the project was to get some feedback on if people agreed that these results were meaningful and worthwhile, and how the findings for the intervention itself should be implemented:
-
What issues need action?
-
Who do these issues most affect?
-
What can be done to address these issues?
Methods used for patient and public involvement
We have held a series of meetings that aimed to (1) engage with both patients and the public as far as we could at that stage of the project and (2) lay some foundations for further PPI work for the SPHSU for the next quinquennial period:
-
We met with the PPI representative from our Study Steering Committee who was able to recommend several local groups for PPI engagement.
-
We met with Glasgow University’s PPI co-ordinator who gave us advice on recognised means of developing PPI work in the university.
-
We conducted a question and answer (Q&A) session at the Poverty Leadership Panel in Glasgow. This session allowed us to give an overview of our research and engage in a discussion around the main messages of MUP. The audience provided valuable feedback on their opinions of the MUP policy. The group were generally welcoming of the policy and our research, but were concerned about the potential for shops/alcohol industry making additional income because of the policy.
-
We held an initial meeting with the Caring Over People’s Emotions (COPE) group, which is a mental health and well-being support group. A second Q&A session with the COPE group had to be cancelled when it proved impossible to move it online.
-
We held an online session about the interpretation of our findings with a group from Drink Wise, Age Well (Glasgow, UK).
-
We are also investigating engagement through the University of Stirling’s Public Panel on Prevention Work in Alcohol.
Key points arising from activities, impact and usefulness
Questions and answers with the Poverty Leadership Panel
We held a Q&A meeting with the Poverty Leadership Panel. It went well and the convener said that everyone seemed to really engage. The convener agreed to have us back when we had more results. We learned that we need to explain:
-
the selection of research sites and how they represented deprived populations
-
the population effect compared with lived experience and some effects can be detected only statistically
-
that the policy was separate from the evaluation, but evaluation findings will feed in to the government review, which could result in changed legislation (e.g. what happens to any extra revenue)
-
the effects on harmful drinkers, their families and people in poverty
-
that normal drinkers are mostly unaffected
-
what the situation is for increased risk of dual substance use (alcohol and drugs), which may be more harmful than either using exclusively drugs or alcohol.
Further questions and answers meeting during the Caring Over People’s Emotions strategy day
This meeting was cancelled because of COVID-19 control.
Session with the University of Stirling’s Public Panel on Prevention Work in Alcohol
This session was cancelled because of COVID-19 control.
Questions and answers session with Drink Wise, Age Well (online, August 2020)
Group composition
A presentation of our results provided the basis for an interactive discussion of the validity of our findings for each study component. There were five participants who were recovered alcohol users, three females and two males, aged between 20 and 70 years, and one worked for a non-statutory addiction support service. Participants appeared not to be from an affluent area. The session was in depth, lasting nearly 2 hours. The point was made that longer-term chronic effects such as liver cirrhosis would not be captured in our study and we cannot report anything about long-term results.
The key points arising were under three large themes: (1) the lack of effects, especially on dependent drinkers, (2) suggestions for adjustments to the approach and (3) views about whether or not the MUP should be increased.
Lack of effects
Participants were not surprised that there was little evidence of any effect from MUP, although there were anecdotes of changing beverage from white cider to spirits and people buying maybe one can less per week (which was still a reduction). As a positive, one participant suggested that people might be more likely to ask for help if they could not afford to drink as much as they needed. There was some surprise about the increased use of pubs and other on-licensed sources of alcohol. There was no surprise about the lack of effect on illicit drug consumption also, although it was agreed that this could be seen as positive. One participant cited the relative cheapness of a bag of heroin compared with a bottle of vodka, and participants agreed that more was drunk when combining drugs and spirits.
Two respondents (both females) who did not drink white cider saw no effects on their personal consumption from MUP.
There was a consensus that price would not be a deterrent for people who were chronically dependent on alcohol. Long-term drinkers would keep up their consumption and cut spending on food and fuel. However, it was thought unlikely that increased food bank use was due to MUP. It was also felt that small increases in price would also fail to deter weekend drinkers.
Adjustments to minimum unit pricing
It was suggested that beer and cider containing > 5.5% of alcohol should be banned. This would complement strength caps that already exist for wines and spirits, and would affect some of the beverages (e.g. alcopops) favoured more by young people, which participants agreed should be harder to buy.
More education about the dangers of alcohol was suggested for school children.
Alcohol was thought to be overpromoted and glamourised and to be ingrained in the Scottish culture, and this needed to be countered and promotion more restricted.
Supermarket sales of alcohol should not be allowed and licensing should be more restricted [Queensland (Australia) and Canada were mentioned as examples of alcohol being sold only from designated outlets, and pharmacies and garages mentioned as inappropriate places to sell alcohol].
The minimum unit pricing level
When asked if the minimum price should be raised from £0.50 per unit, the consensus was that people did not know, but probably not.
There was a generally high level of concern about what happened to the extra revenue. The view was that this should go not to retailers, but to services and support for dependent drinkers.
Finally, although MUP or some form of price intervention was seen as good for young people, it was thought to be only a small part of the solution to the alcohol problem.
Impact of patient and public involvement work on our minimum unit pricing research and learning opportunities
The impact has yet to be seen for informing any future phases of MUP implementation. However, for this report, which will feed into that, we note the importance of patient and public concerns from the Poverty Leadership Panel, as above. Our attempts at PPI, although small because of circumstances, will inform the future development of PPI at our unit. For example, we have learned the essentials of how to form a PPI group/panel, both as a standing body and as a project-specific group, using recruitment via study contacts and that we need to ask participants for permission to use their details when recruiting for the study. We have also learned about the Glasgow Research Involvement Newsletter and its potential for recruiting PPI panel members and publicising our results.
Therefore, our attempts to carry out some PPI have been useful learning for our unit in future projects about the PPI process itself and the importance of planning it into the project from the start. We have also realised the need to be clear about the aims of PPI before undertaking it and that these aims will vary according to project stage, including involvement in formulating aims, as well as methods to creating the most effective and relevant dissemination methods. Some projects, possibly such as the present one, being evaluations of policy interventions, may not require as much dissemination to the public, as no-one has to be persuaded to opt in as a member of the public. The most relevant persuasion in that regard is probably directed to policy-makers in other administrations who will, however, be influenced by evidence of the public acceptability of, and support for, the evaluation of MUP.
Conclusion
Within the ED setting, there was no evidence of a beneficial impact of MUP. Implementation appeared to have been successful and there was no evidence of substitution from alcohol consumption to other drugs. Drinkers reported not noticing any change in price. Given the lack of effect observed in the short term and problem-free implementation, this suggests that the price per unit that MUP was set at may be too low. Other studies have shown reduced alcohol sales in Scotland and our study may have suffered from selection biases to exclude those most affected. Furthermore, greater public awareness accompanying the policy could have enhanced the effect.
Our evaluation, which itself contains multiple components, is part of a wider programme co-ordinated by Public Health Scotland and should be understood in the context of those results.
Acknowledgements
The authors would like to thank NHS colleagues at all the research sites for their assistance with this work. The authors also wish to thank Julie Breslin and Kenneth Crawford of Addaction (London, UK) (a non-statutory addiction support body) who contributed a non-statutory and service user perspective to the Study Steering Committee. We also thank Clare Beeston of Public Health Scotland for her contribution to the original study design, guidance on contextual issues and theoretical input. In addition, we are particularly grateful to the Population Health Research Facility, and its predecessor, the Social and Public Health Sciences Surveys Unit at the University of Glasgow, for its help with non-salary project costing, study training set up, study documents design, study operations set up, data entry and data management.
The Social and Public Health Sciences Unit is funded by the Medical Research Council (MC_UU_12017/13, MC_UU_12017/15 and MC_UU_00022/2) and Scottish Government Chief Scientist Office (SPHSU13, SPHSU15 and SPHSU17). S Vittal Katikireddi acknowledges funding from a NRS Senior Clinical Fellowship (SCAF/15/02).
Contributions of authors
Vivian So (https://orcid.org/0000-0001-5839-862X) (Research Fellow) provided statistical expertise; carried out statistical analysis, led Chapter 4, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Andrew D Millard (https://orcid.org/0000-0003-3824-7458) (Research Fellow) led the study day to day, contributed to parts of the methodology used, helped acquire and analyse the data, led Chapter 5, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
S Vittal Katikireddi (https://orcid.org/0000-0001-6593-9092) (Professor of Public Health and Health Inequalities and Honorary Consultant in Public Health) conceived the study, contributed to the overall study design and grant application, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Ross Forsyth (https://orcid.org/0000-0002-0414-5640) (Project Manager) led the study day to day, contributed to parts of the methodology used, helped acquire and analyse the data, led Chapter 6, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Sarah Allstaff (https://orcid.org/0000-0002-8752-2236) [Consultant Physician (Genitourinary Medicine), Lead Clinician for Sexual Health] provided local context for Chapter 5, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Paolo Deluca (https://orcid.org/0000-0002-9511-7230) (Reader in Addiction Research) contributed to the overall study design and grant application, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Colin Drummond (https://orcid.org/0000-0001-9379-5452) (Professor of Addiction Psychiatry) contributed to the overall study design and grant application, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Allison Ford (https://orcid.org/0000-0002-3624-6673) (Research Fellow) contributed to the overall study design and grant application, led Chapter 7, collected data for Chapter 6, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Douglas Eadie (https://orcid.org/0000-0001-9969-9162) (Research Fellow) contributed to the overall study design and grant application, led Chapter 7, collected data for Chapter 6, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Niamh Fitzgerald (https://orcid.org/0000-0002-3643-8165) (Professor, Institute for Social Marketing) led Chapter 7, collected data for Chapter 6, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Lesley Graham (https://orcid.org/0000-0002-5654-2330) (Associate Specialist, Public Health at NHS National Services Scotland) contributed to the overall study design and grant application, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Shona Hilton (https://orcid.org/0000-0003-0633-8152) (Professor of Public Health Policy) contributed to the overall study design and grant application, led Chapter 6, provided information about the local context for Chapter 4, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Anne Ludbrook (https://orcid.org/0000-0003-2558-7728) (Chairperson in Health Economics) contributed to the overall study design and grant application, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Gerry McCartney (https://orcid.org/0000-0001-6341-3521) (Head of Public Health Observatory Division, Public Health Scotland) contributed to the overall study design and grant application, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Oarabile Molaodi (https://orcid.org/0000-0003-3613-0213) (Research Fellow) provided statistical expertise, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Michele Open (https://orcid.org/0000-0002-1174-5812) (Consultant in Emergency Medicine) provided information about the local context for Chapter 4, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Chris Patterson (https://orcid.org/0000-0002-5914-8718) (Research Associate) led Chapter 6, provided information about the local context for Chapter 4, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Samantha Perry (https://orcid.org/0000-0002-0655-4894) (Consultant in Emergency Medicine) provided information about the local context for Chapter 4, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Thomas Phillips (https://orcid.org/0000-0001-8020-4510) (Professor of Nursing, Addictions) contributed to the overall study design and grant application, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Gabriel Schembri (Consultant in Sexual Health and HIV Medicine/Research Lead) provided local context for Chapter 5, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Martine Stead (https://orcid.org/0000-0002-3066-4604) (Deputy Director of Institute for Social Marketing) contributed to the overall study design and grant application, led Chapter 7, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Janet Wilson (https://orcid.org/0000-0001-9865-0834) (Consultant in Genito-Urinary Medicine) provided local context for Chapter 5, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Chris Yap (Consultant in Emergency Medicine) provided information about the local context for Chapter 4, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Lyndal Bond (https://orcid.org/0000-0003-1693-5508) (Professor of Population Health and Evaluation) conceived the study, contributed to the overall study design and grant application, provided initial strategic leadership for the study, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Alastair H Leyland (https://orcid.org/0000-0003-3741-7099) (Professor of Population Health Statistics) contributed to the overall study design and grant application, provided strategic leadership for the study, provided statistical expertise, and made substantial contributions to study development, critically revised the paper and approved the final manuscript.
Publication
So V, Millard AD, Katikireddi SV, Deluca P, Drummond C, Eadie D, et al. Impact of minimum unit pricing on alcohol-related emergency department attendances in Scotland: a natural experiment study. Abstract preprint with The Lancet. http://dx.doi.org/10.2139/ssrn.3697993
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1659-724. https://doi.org/10.1016/s0140-6736(16)31679-8.
- Casswell S, Thamarangsi T. Reducing harm from alcohol: call to action. Lancet 2009;373:2247-57. https://doi.org/10.1016/S0140-6736(09)60745-5.
- Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al. Alcohol: No Ordinary Commodity: Research and Public Policy. Oxford: Oxford University Press; 2010.
- Room R, Babor T, Rehm J. Alcohol and public health. Lancet 2005;365:519-30. https://doi.org/10.1016/S0140-6736(05)17870-2.
- Tod E, Grant I, Wyper G, . Hospital Admissions, Deaths and Overall Burden of Disease Attributable to Alcohol Consumption in Scotland. Glasgow: Scottish Public Health Observatory, NHS Health Scotland; 2018.
- Herttua K, Mäkelä P, Martikainen P. Differential trends in alcohol-related mortality: a register-based follow-up study in Finland in 1987–2003. Alcohol Alcohol 2007;42:456-64. https://doi.org/10.1093/alcalc/agl099.
- Mäkelä P, Valkonen T, Martelin T. Contribution of deaths related to alcohol use to socioeconomic variation in mortality: register based follow up study. BMJ 1997;315:211-16. https://doi.org/10.1136/bmj.315.7102.211.
- Leyland AH, Dundas R, McLoone P, Boddy FA. Cause-specific inequalities in mortality in Scotland: two decades of change. A population-based study. BMC Public Health 2007;7. https://doi.org/10.1186/1471-2458-7-172.
- Mackenbach JP, Kulhánová I, Bopp M, Borrell C, Deboosere P, Kovács K, et al. Inequalities in alcohol-related mortality in 17 European countries: a retrospective analysis of mortality registers. PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001909.
- Meier PS, Holmes J, Angus C, Ally AK, Meng Y, Brennan A. Estimated effects of different alcohol taxation and price policies on health inequalities: a mathematical modelling study. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1001963.
- Holmes J, Meng Y, Meier PS, Brennan A, Angus C, Campbell-Burton A, et al. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: a modelling study. Lancet 2014;383:1655-64. https://doi.org/10.1016/S0140-6736(13)62417-4.
- Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health 2017;2:e267-e276. https://doi.org/10.1016/S2468-2667(17)30078-6.
- Jones L, Bellis MA, Dedman D, Tocque K. Alcohol-Attributable Fractions for England: Alcohol Attributable Mortality and Hospital Admissions. Liverpool: Liverpool John Moores University; 2008.
- Leon DA, McCambridge J. Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysis of routine data. Lancet 2006;367:52-6. https://doi.org/10.1016/S0140-6736(06)67924-5.
- Williams R, Aithal G, Alexander GJ, Allison M, Armstrong I, Aspinall R, et al. Unacceptable failures: the final report of the Lancet Commission into liver disease in the UK. Lancet 2020;395:226-39. https://doi.org/10.1016/S0140-6736(19)32908-3.
- Williams R, Alexander G, Aspinall R, Batterham R, Bhala N, Bosanquet N, et al. Gathering momentum for the way ahead: fifth report of the Lancet Standing Commission on Liver Disease in the UK. Lancet 2018;392:2398-412. https://doi.org/10.1016/S0140-6736(18)32561-3.
- Nimmo S, Anderson H, Duffy J. Early Mortality Gap ‘Unfair and Preventable’ 2020. https://healthandcare.scot/default.asp?page=story%26story=1346 (accessed 2 July 2021).
- Jones L, Bates G, McCoy E, Bellis MA. Relationship between alcohol-attributable disease and socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1720-7.
- Scottish Government . Long-Term Monitoring of Health Inequalities 2020.
- Scottish Government . Alcohol Framework 2018: Preventing Harm – Next Steps on Changing Our Relationship With Alcohol 2018.
- Scottish Public Health Observatory . Alcohol: Health Harm 2019. www.scotpho.org.uk/behaviour/alcohol/data/health-harm/ (accessed 4 February 2020).
- Scottish Public Health Observatory . Chronic Liver Disease: Deaths. 2019. www.scotpho.org.uk/health-wellbeing-and-disease/chronic-liver-disease/data/mortality/ (accessed 4 February 2020).
- Office for National Statistics . Alcohol-Specific Deaths in the UK: Registered in 2018. Deaths Caused by Diseases Known to Be a Direct Consequence of Alcohol Misuse by Sex, Age and Region 2019.
- Burgess L. Alcohol (Minimum Pricing) (Scotland) Bill: Passage of the Bill. Edinburgh: Scottish Parliament Information Centre; 2012.
- Scottish Parliament . Alcohol (Minimum Pricing) (Scotland) Act 2012 2012.
- Katikireddi SV, Hilton S, Bonell C, Bond L. Understanding the development of minimum unit pricing of alcohol in Scotland: a qualitative study of the policy process. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0091185.
- Katikireddi SV, Bond L, Hilton S. Changing policy framing as a deliberate strategy for public health advocacy: a qualitative policy case study of minimum unit pricing of alcohol. Milbank Q 2014;92:250-83. https://doi.org/10.1111/1468-0009.12057.
- Hawkins B, McCambridge J. Policy windows and multiple streams: an analysis of alcohol pricing policy in England. Policy Polit 2019;48:315-33. https://doi.org/10.1332/030557319X15724461566370.
- Welsh Government . Minimum Unit Pricing of Alcohol 2020. https://gov.wales/minimum-unit-pricing-alcohol (accessed 19 January 2021).
- Lee A, Campbell F. Public Health and the NHS at 70: fit enough for the challenge of new enemies in a new landscape? An example of public health measures to address alcohol consumption. Rev Fr Civil Br 2019;24. https://doi.org/10.4000/rfcb.4282.
- Gornall J. Under the influence: Scotland’s battle over alcohol pricing. BMJ 2014;348. https://doi.org/10.1136/bmj.g1274.
- Hawkins B, McCambridge J. Public-private partnerships and the politics of alcohol policy in England: the Coalition Government’s Public Health ‘Responsibility Deal’. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-7787-9.
- Katikireddi SV, Hilton S. How did policy actors use mass media to influence the Scottish alcohol minimum unit pricing debate? Comparative analysis of newspapers, evidence submissions and interviews. Drugs 2015;22:125-34. https://doi.org/10.3109/09687637.2014.977228.
- Katikireddi SV, McLean JA. Introducing a minimum unit price for alcohol in Scotland: considerations under European Law and the implications for European public health. Eur J Public Health 2012;22:457-8. https://doi.org/10.1093/eurpub/cks091.
- Katikireddi SV, Rice P, Holmes J, Meier P, Giesbrecht N, Bosma LM. Preventing Alcohol-Related Problems: Evidence and Community-Based Initiatives. Washington, DC: American Public Health Association; 2017.
- Bhattacharya A, Angus C, Pryce R, Holmes J, Brennan A, Meier P. How dependent is the alcohol industry on heavy drinking in England?. Addiction 2018;113:2225-32. https://doi.org/10.1111/add.14386.
- Scottish Courts and Tribunals . The Scotch Whisky Association and Others Against the Lord Advocate and the Advocate General 2016. www.scotcourts.gov.uk/search-judgments/judgment?id=9a1821a7-8980-69d2-b500-ff0000d74aa7 (accessed 12 July 2021).
- Scotch Whisky Association . The SWA on Its Decision to Appeal Minimum Unit Pricing (MUP) Ruling 2016 [updated 18 November 2016] n.d. www.scotch-whisky.org.uk/news-publications/news/the-swa-on-its-decision-to-appeal-minimum-unit-pricing-(mup)-ruling/#.WEQyTlyzCZc (accessed 1 January 2020).
- Katikireddi SV, Beeston C, Millard A, Forsyth R, Deluca P, Drummond C, et al. Evaluating possible intended and unintended consequences of the implementation of alcohol minimum unit pricing (MUP) in Scotland: a natural experiment protocol. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-028482.
- Craig P, Katikireddi SV, Leyland AH, Popham F. Natural experiments: an overview of methods, approaches and contribution to public health intervention research. Ann Rev Public Health 2017;38:39-56. https://doi.org/10.1146/annurev-publhealth-031816-044327.
- Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health 2012;66:1182-6. https://doi.org/10.1136/jech-2011-200375.
- Basu S, Meghani A, Siddiqi A. Evaluating the health impact of large-scale public policy changes: classical and novel approaches. Annu Rev Public Health 2017;38:351-70. https://doi.org/10.1146/annurev-publhealth-031816-044208.
- Bonell C, Jamal F, Melendez-Torres GJ, Cummins S. ‘Dark logic’: theorising the harmful consequences of public health interventions. J Epidemiol Community Health 2015;69:95-8. https://doi.org/10.1136/jech-2014-204671.
- Asplund M, Friberg R, Wilander F. Demand and distance: evidence on cross-border shopping. J Public Econ 2007;91:141-57. https://doi.org/10.1016/j.jpubeco.2006.05.006.
- Lachenmeier DW, Rehm J. Unrecorded alcohol: a threat to public health?. Addiction 2009;104:87-5. https://doi.org/10.1111/j.1360-0443.2009.02587.x.
- Paasma R, Hovda KE, Jacobsen D. Methanol poisoning and long term sequelae – a six years follow-up after a large methanol outbreak. BMC Clin Pharmacol 2009;9. https://doi.org/10.1186/1472-6904-9-5.
- Astill Wright L, Golder S, Balkham A, McCambridge J. Understanding public opinion to the introduction of minimum unit pricing in Scotland: a qualitative study using Twitter. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-029690.
- Li TK, Hewitt BG, Grant BF. The Alcohol Dependence Syndrome, 30 years later: a commentary. the 2006 H. David Archibald lecture. Addiction 2007;102:1522-30. https://doi.org/10.1111/j.1360-0443.2007.01911.x.
- Lucas P, Reiman A, Earleywine M, McGowan SK, Oleson M, Coward MP, et al. Cannabis as a substitute for alcohol and other drugs: a dispensary-based survey of substitution effect in Canadian medical cannabis patients. Addict Res Theory 2013;21:435-42. https://doi.org/10.3109/16066359.2012.733465.
- Subbaraman MS. Substitution and complementarity of alcohol and cannabis: a review of the literature. Subst Use Misuse 2016;51:1399-414. https://doi.org/10.3109/10826084.2016.1170145.
- Moore SC. Substitution and complementarity in the face of alcohol-specific policy interventions. Alcohol Alcohol 2010;45:403-8. https://doi.org/10.1093/alcalc/agq048.
- Decoster A. How progressive are indirect taxes in Russia. Econ Transit 2005;13:705-29. https://doi.org/10.1111/j.0967-0750.2005.00238.x.
- NHS Health Scotland . Monitoring and Evaluating Scotland’s Alcohol Strategy (MESAS): Briefing Paper 2009.
- Babor T, Holder H, Caetano R, Homel R, Casswell S, Livingston M, et al. Alcohol: No Ordinary Commodity: Research and Public Policy. Oxford: Oxford University Press; 2010.
- Purshouse RC, Meier PS, Brennan A, Taylor KB, Rafia R. Estimated effect of alcohol pricing policies on health and health economic outcomes in England: an epidemiological model. Lancet 2010;375:1355-64. https://doi.org/10.1016/S0140-6736(10)60058-X.
- Wagenaar AC, Salois MJ, Komro KA. Effects of beverage alcohol price and tax levels on drinking: a meta-analysis of 1003 estimates from 112 studies. Addiction 2009;104:179-90. https://doi.org/10.1111/j.1360-0443.2008.02438.x.
- Elder RW, Lawrence B, Ferguson A, Naimi TS, Brewer RD, Chattopadhyay SK, et al. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am J Prev Med 2010;38:217-29. https://doi.org/10.1016/j.amepre.2009.11.005.
- Huang C-D. Econometric Models of Alcohol Demand in the United Kingdom. London: Government Economic Service; 2003.
- Wagenaar AC, Tobler AL, Komro KA. Effects of alcohol tax and price policies on morbidity and mortality: a systematic review. Am J Public Health 2010;100:2270-8. https://doi.org/10.2105/AJPH.2009.186007.
- Jackson R, Johnson M, Campbell F, Messina J, Guillaume L, Meier P, et al. Interventions on Control of Alcohol Price, Promotion and Availability for Prevention of Alcohol Use Disorders in Adults and Young People. Sheffield: ScHARR, University of Sheffield; 2010.
- World Health Organization . Global Strategy to Reduce the Harmful Use of Alcohol 2010.
- Chisholm D, Moro D, Bertram M, Pretorius C, Gmel G, Shield K, et al. Are the ‘best buys’ for alcohol control still valid? An update on the comparative cost-effectiveness of alcohol control strategies at the global level. J Stud Alcohol Drugs 2018;79:514-22. https://doi.org/10.15288/jsad.2018.79.514.
- Burton R, Henn C, Lavoie D, O’Connor R, Perkins C, Sweeney K, et al. A rapid evidence review of the effectiveness and cost-effectiveness of alcohol control policies: an English perspective. Lancet 2017;389:1558-80. https://doi.org/10.1016/S0140-6736(16)32420-5.
- Macintyre S. Inequalities in Health in Scotland: What Are They and What Can We Do About Them? MRC Social and Public Health Sciences Unit Occasional Papers No 17. Glasgow: MRC Social and Public Health Sciences Unit; 2007.
- Gorman E, Leyland AH, McCartney G, Katikireddi SV, Rutherford L, Graham L, et al. Adjustment for survey non-representativeness using record-linkage: refined estimates of alcohol consumption by deprivation in Scotland. Addiction 2017;112:1270-80. https://doi.org/10.1111/add.13797.
- Siegfried N, Parry C. Do alcohol control policies work? An umbrella review and quality assessment of systematic reviews of alcohol control interventions (2006–2017). PLOS ONE 2019;14. https://doi.org/10.1371/journal.pone.0214865.
- Scottish Health Action on Alcohol Problems . 14th Research and Policy Briefing 2018. www.shaap.org.uk/images/web_version5_MUP_issue_14_2018.pdf (accessed 2 July 2021).
- Coomber K, Miller P, Taylor N, Livingston M, Smith J, Buykx P, et al. Investigating the Introduction of Alcohol Minimum Unit Price in the Northern Territory. Final Report (February 2020) 2020.
- Sherk A, Stockwell T, Callaghan RC. The effect on emergency department visits of raised alcohol minimum prices in Saskatchewan, Canada. Drug Alcohol Rev 2018;37:357-65. https://doi.org/10.1111/dar.12670.
- Stockwell T, Auld MC, Zhao J, Martin G. Does minimum pricing reduce alcohol consumption? The experience of a Canadian province. Addiction 2012;107:912-20. https://doi.org/10.1111/j.1360-0443.2011.03763.x.
- Stockwell T, Leng J, Sturge J. Alcohol Pricing and Public Health in Canada: Issues and Opportunities. Victoria, BC: Canadian Institute for Substance Use Research; 2006.
- Stockwell T, Zhao J, Giesbrecht N, Macdonald S, Thomas G, Wettlaufer A. The raising of minimum alcohol prices in Saskatchewan, Canada: impacts on consumption and implications for public health. Am J Public Health 2012;102:e103-10. https://doi.org/10.2105/AJPH.2012.301094.
- Stockwell T, Zhao J, Martin G, Macdonald S, Vallance K, Treno A, et al. Minimum alcohol prices and outlet densities in British Columbia, Canada: estimated impacts on alcohol-attributable hospital admissions. Am J Public Health 2013;103:2014-20. https://doi.org/10.2105/AJPH.2013.301289.
- Stockwell T, Zhao J, Marzell M, Gruenewald PJ, Macdonald S, Ponicki WR, et al. Relationships between minimum alcohol pricing and crime during the partial privatization of a Canadian Government alcohol monopoly. J Stud Alcohol Drugs 2015;76:628-34. https://doi.org/10.15288/jsad.2015.76.628.
- Stockwell T, Zhao J, Sherk A, Callaghan RC, Macdonald S, Gatley J. Assessing the impacts of Saskatchewan’s minimum alcohol pricing regulations on alcohol-related crime. Drug Alcohol Rev 2017;36:492-501. https://doi.org/10.1111/dar.12471.
- Thompson K, Stockwell T, Wettlaufer A, Giesbrecht N, Thomas G. Minimum alcohol pricing policies in practice: a critical examination of implementation in Canada. J Public Health Policy 2017;38:39-57. https://doi.org/10.1057/s41271-016-0051-y.
- Zhao J, Stockwell T. The impacts of minimum alcohol pricing on alcohol attributable morbidity in regions of British Colombia, Canada with low, medium and high mean family income. Addiction 2017;112:1942-51. https://doi.org/10.1111/add.13902.
- Shield KD, Probst C, Rehm J. A ‘buck a beer,’ but at what cost to public health?. Can J Public Health 2019;110:512-15. https://doi.org/10.17269/s41997-019-00184-6.
- McKee M. Alcohol in Russia. Alcohol Alcohol 1999;34:824-9. https://doi.org/10.1093/alcalc/34.6.824.
- Giles L, Robinson M. Monitoring and Evaluating Scotland’s Alcohol Strategy: Monitoring Report 2019 2019.
- National Institute for Health and Care Excellence (NICE) . Alcohol-Use Disorders – Preventing the Development of Hazardous and Harmful Drinking. Public Health Intervention Guidance 24 2010.
- Angus C, Holmes J, Pryce R, Meier P, Brennan A. Model-Based Appraisal of the Comparative Impact of Minimum Unit Pricing and Taxation Policies in Scotland. Sheffield: University of Sheffield; 2016.
- Meng Y, Purshouse R, Brennan A, Meier P. Model-Based Appraisal of Alcohol Minimum Pricing and Off-Licensed Trade Discount Bans in Scotland Using the Sheffield Alcohol Policy Model (v 2): An Update Based on Newly Available Data. Sheffield: ScHARR, University of Sheffield; 2010.
- Burton R, Henn C, Lavoie D, O’Conner R, Perkins C, Sweeney K, et al. The Public Health Burden of Alcohol and the Effectiveness and Cost-Effectiveness of Alcohol Control Policies – An Evidence Review. London: Public Health England; 2016.
- UK Government . Tax on Shopping and Services 2018. www.gov.uk/tax-on-shopping/alcohol-tobacco (accessed 15 November 2018).
- Christie B. Alcohol sales fall in Scotland a year after minimum pricing took effect. BMJ 2019;365. https://doi.org/10.1136/bmj.l4296.
- Mooney JD, Carlin E. Minimum unit pricing for alcohol in Scotland. BMJ 2019;366. https://doi.org/10.1136/bmj.l5603.
- O’Donnell A, Anderson P, Jané-Llopis E, Manthey J, Kaner E, Rehm J. Immediate impact of minimum unit pricing on alcohol purchases in Scotland: controlled interrupted time series analysis for 2015–18. BMJ 2019;366. https://doi.org/10.1136/bmj.l5274.
- Giles L, Robinson M, Beeston C. Minimum Unit Pricing (MUP) Evaluation. Sales-Based Consumption: A Descriptive Analysis of one Year Post-MUP Off-Trade Alcohol Sales Data. Edinburgh: NHS Health Scotland; 2019.
- Giles L, Robinson M, Beeston C. Minimum Unit Pricing (MUP) for Alcohol Evaluation. Sales-Based Consumption: A Descriptive Analysis of One Year Post-MUP Off-Trade Alcohol Sales Data. Glasgow: NHS Health Scotland; 2020.
- Dickie E, Mellor R, Myers F, Beeston C. Minimum Unit Pricing (MUP) Evaluation: Compliance (Licensing) Study. Edinburgh: NHS Health Scotland; 2019.
- Gill J, Tsang C, Black H, Chick J. Can part of the health damage linked to alcohol misuse in Scotland be attributable to the type of drink and its low price (by permitting a rapid rate of consumption)? A point of view. Alcohol Alcohol 2010;45:398-400. https://doi.org/10.1093/alcalc/agq023.
- Schutte R, Papageorgiou M, Najlah M, Huisman HW, Ricci C, Zhang J, et al. Drink types unmask the health risks associated with alcohol intake – prospective evidence from the general population. Clin Nutr 2020;39:3168-74. https://doi.org/10.1016/j.clnu.2020.02.009.
- Angus C, Holmes J, Meier PS. Comparing alcohol taxation throughout the European Union. Addiction 2019;114:1489-94. https://doi.org/10.1111/add.14631.
- Coltart CEM, Gilmore IT. Minimum alcohol pricing in England. BMJ 2011;342. https://doi.org/10.1136/bmj.d1063.
- Noel JK. Potential Impact of Minimum Unit Pricing on Advertised Alcoholic Beverage Prices. 2019. https://osf.io/preprints/socarxiv/cbgja/ (accessed 2 July 2021).
- Jiang H, Room R, Livingston M, Callinan S, Brennan A, Doran C, et al. The effects of alcohol pricing policies on consumption, health, social and economic outcomes, and health inequality in Australia: a protocol of an epidemiological modelling study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-029918.
- Oliver TR. The Politics of Public Health Policy 2006. www.annualreviews.org/doi/10.1146/annurev.publhealth.25.101802.123126 (accessed 2 July 2021).
- Beeston C, Robinson M, Craig N, Giles L. MESAS Project Team . Multi-component evaluation of minimum unit pricing in Scotland. BMJ 2019;367. https://doi.org/10.1136/bmj.l6172.
- Iconic Consulting . Minimum Unit Pricing in Scotland: A Qualitative Study of Children and Young People’s Own Drinking and Related Behaviour. Final Report 2019.
- Ford J, Myers F, Burns J, Beeston C. Minimum Unit Price for Alcohol Evaluation Research Protocol: The Impact of MUP on Protecting Children and Young People From Parents’ and Carers’ Harmful Alcohol Consumption: A Study of Practitioners’ Views. Edinburgh: Public Health Scotland; 2020.
- Stead M, Critchlow N, Eadie D, Fitzgerald N, Angus K, Purves R, et al. Evaluating the Impact of Alcohol Minimum Unit Pricing (MUP) in Scotland: Observational Study of Small Retailers. Edinburgh: Public Health Scotland; 2020.
- Robinson M, Mackay D, Giles L. Evaluating the Impact of Minimum Unit Pricing (MUP) on Sales-Based Alcohol Consumption in Scotland: Controlled Interrupted Time Series Analyses. Edinburgh: Public Health Scotland; 2020.
- Kraus L, Room R, Livingston M, Pennay A, Holmes J, Torronen J. Long waves of consumption or a unique social generation? Exploring recent declines in youth drinking. Addict Res Theory 2019;28:183-93. https://doi.org/10.1080/16066359.2019.1629426.
- Vashishtha R, Livingston M, Pennay A, Dietze P, MacLean S, Holmes J, et al. Why is adolescent drinking declining? A systematic review and narrative synthesis. Addict Res Theory 2019:1-14. https://doi.org/10.1080/16066359.2019.1663831.
- Mackay D, Haw S, Ayres JG, Fischbacher C, Pell JP. Smoke-free legislation and hospitalizations for childhood asthma. N Engl J Med 2010;363:1139-45. https://doi.org/10.1056/NEJMoa1002861.
- Pell JP, Haw S, Cobbe S, Newby DE, Pell AC, Fischbacher C, et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med 2008;359:482-91. https://doi.org/10.1056/NEJMsa0706740.
- Institute of Alcohol Studies . Alcohol’s Impact on Emergency Services 2015.
- Phillips T, Coulton S, Drummond C. Burden of alcohol disorders on emergency department attendances and hospital admissions in England. Alcohol Alcohol 2019;54:516-24. https://doi.org/10.1093/alcalc/agz055.
- Drummond C, Phillips T, Coulton S, Barnaby B, Keating S, Sabri R, et al. Saturday Night and Sunday Morning: The 2003 Twenty-Four Hour National Prevalence Survey of Alcohol-Related Attendances at Accident and Emergency Departments in England. Final Report to the Cabinet Office 2003.
- NHS Quality Improvement Scotland . NHS Quality Improvement Scotland. Scottish Emergency Department Alcohol Audit: Understanding Alcohol Misuse in Scotland – Final Report 2008.
- Hodgson R, Alwyn T, John B, Thom B, Smith A. The FAST alcohol screening test. Alcohol Alcohol 2002;37:61-6. https://doi.org/10.1093/alcalc/37.1.61.
- Deluca P, Drummond C, Coulton S, Kaner E, Newbury-Birch D, Philips T, et al. A randomized controlled trial of different methods of alcohol screening and brief intervention in routine accident and emergency department care: 12-month outcomes. Addict Sci Clin Pract 2012;7. https://doi.org/10.1186/1940-0640-7-S1-A80.
- Coulton S, Drummond C, Deluca P, Kaner E. The utility of different screening methods to detect hazardous drinking and alcohol use disorders in the Screening and Intervention Program for Sensible Drinking (SIPS) program. Addict Sci Clin Pract 2012;7. https://doi.org/10.1186/1940-0640-7-S1-A83.
- Hodgson R, Alwyn T, John B, Smith A, Newcome R, Morgan C. Manual for the Fast Alcohol Screening Test (FAST): Fast Screening for Alcohol Problems. London: Health Development Agency; 2002.
- Catto S. How Much are People in Scotland Really Drinking?: A Review of Data from Scotland’s Routine National Survey. Edinburgh: Scottish Public Health Observatory; 2008.
- Bobak M, Room R, Pikhart H, Kubinova R, Malyutina S, Pajak A, et al. Contribution of drinking patterns to differences in rates of alcohol related problems between three urban populations. J Epidemiol Community Health 2004;58:238-42. https://doi.org/10.1136/jech.2003.011825.
- Tanton C, Geary RS, Clifton S, Field N, Heap KL, Mapp F, et al. Sexual health clinic attendance and non-attendance in Britain: findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Sex Transm Infect 2018;94:268-76. https://doi.org/10.1136/sextrans-2017-053193.
- Scottish Public Health Observatory . Drug Misuse: Availability and Prevalence 2019. www.scotpho.org.uk/behaviour/drugs/data/availability-and-prevalence (accessed 10 February 2020).
- Scottish Public Health Observatory . High Risk Groups. 2019. www.scotpho.org.uk/behaviour/sexual-health/data/high-risk-groups/ (accessed 10 February 2020).
- Connor JL, Kydd RM, Dickson NP. Alcohol involvement in sexual behaviour and adverse sexual health outcomes from 26 to 38 years of age. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0135660.
- Booth R, Halliday J. UK’s nightclubs suffer as young people seek less hedonistic pursuits. The Guardian 2018.
- Holden C, Hawkins B. ‘Whisky gloss’: The alcohol industry, devolution and policy communities in Scotland. Public Policy Adm 2012;28:253-73. https://doi.org/10.1177/0952076712452290.
- Katikireddi SV, Smith KE, Hill M. Studying Public Policy: An International Approach. Bristol: Policy Press; 2014.
- Hawkins B, Holden C. Framing the alcohol policy debate: industry actors and the regulation of the UK beverage alcohol market. Crit Policy Stud 2013;7:53-71. https://doi.org/10.1080/19460171.2013.766023.
- McCambridge J, Hawkins B, Holden C. Industry use of evidence to influence alcohol policy: a case study of submissions to the 2008 Scottish government consultation. PLOS Med 2013;10. https://doi.org/10.1371/journal.pmed.1001431.
- Hawkins B, Holden C. ‘Water dripping on stone’? Industry lobbying and UK alcohol policy. Policy Polit 2014;42:55-70. https://doi.org/10.1332/030557312x655468.
- Katikireddi SV, Bond L, Hilton S. Perspectives on econometric modelling to inform policy: a UK qualitative case study of minimum unit pricing of alcohol. Eur J Public Health 2014;24:490-5. https://doi.org/10.1093/eurpub/ckt206.
- Katikireddi SV, Hilton S, Bond L. The role of the Sheffield model on the minimum unit pricing of alcohol debate: the importance of a rhetorical perspective. Evid Policy 2016;12:521-39. https://doi.org/10.1332/174426415X14430986392944.
- Wood K, Patterson C, Katikireddi SV, Hildton S. Harms to ‘others’ from alcohol consumption in the minimum unit pricing policy debate: a qualitative content analysis of UK newspapers (2005–12). Addiction 2014;109:578-84. https://doi.org/10.1111/add.12427.
- Patterson C, Katikireddi SV, Wood K, Hilton S. Representations of minimum unit pricing for alcohol in UK newspapers: a case study of a public health policy debate. J Public Health 2015;37:40-9. https://doi.org/10.1093/pubmed/fdu078.
- Hilton S, Wood K, Patterson C, Katikireddi SV. Implications for alcohol minimum unit pricing advocacy: what can we learn for public health from UK newsprint coverage of key claim-makers in the policy debate?. Soc Sci Med 2014;102:157-64. https://doi.org/10.1016/j.socscimed.2013.11.041.
- Lonsdale AJ, Hardcastle SJ, Hagger MS. A minimum price per unit of alcohol: a focus group study to investigate public opinion concerning UK government proposals to introduce new price controls to curb alcohol consumption. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-1023.
- Pechey R, Burge P, Mentzakis E, Suhrcke M, Marteau TM. Public acceptability of population-level interventions to reduce alcohol consumption: a discrete choice experiment. Soc Sci Med 2014;113:104-9. https://doi.org/10.1016/j.socscimed.2014.05.010.
- O’May F, Gill J, Black H, Rees C, Chick J, McPake B. Heavy drinkers’ perspectives on minimum unit pricing for alcohol in Scotland: a qualitative interview study. SAGE Open 2016;6. https://doi.org/10.1177/2158244016657141.
- Gorman E, Leyland AH, McCartney G, White IR, Katikireddi SV, Rutherford L, et al. Assessing the representativeness of population-sampled health surveys through linkage to administrative data on alcohol-related outcomes. Am J Epidemiol 2014;180:941-8. https://doi.org/10.1093/aje/kwu207.
- Office for National Statistics . Estimates of the Population for the UK, England and Wales, Scotland and Northern Ireland 2019. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed 10 February 2020).
- Scottish Government . Scottish Index of Multiple Deprivation 2020 – Scottish Index of Multiple Deprivation 2020v2 Local and National Share Calculator 2020. www.gov.scot/publications/scottish-index-of-multiple-deprivation-2020v2-local-and-national-share-calculator-2/ (accessed 16 June 2020).
- Ministry of Housing Communities and Local Government . English Indices of Deprivation 2019 – Local Authority District Summaries 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/833995/File_10_-_IoD2019_Local_Authority_District_Summaries__lower-tier__.xlsx (accessed 16 June 2020).
- Office for National Statistics . Adult Drinking Habits in Great Britain 2018.
- Cheong C-K, Dean L, Dougall I, Hinchliffe S, Mirani K, Vosnaki K, et al. The Scottish Health Survey 2018: Main Report – Revised 2020 2020.
- Population Health Team, NHS Digital . Health Survey for England 2018 2019.
- World Health Organization . International Classification of Diseases for Mortality and Morbidity Statistics (10th Revision) 2019. https://icd.who.int/browse10/2019/en (accessed 19 January 2021).
- Webster L, Angus C, Holmes J, Brennan A, Gillespie D. Alcohol Attributable Fractions for England. Sheffield: ScHARR, University of Sheffield; 2019.
- Brown D, Allik M, Dundas R, Layland AH. Carstairs Scores for Scottish Postcode Sectors, Datazones and Output Areas From the 2011 Census. Glasgow: MRC/CSO Social and Public Health Sciences Unit, University of Glasgow; 2014.
- Yates MA. Inequalities in Mortality Amenable to Healthcare Intervention in Scotland. Glasgow: University of Glasgow; 2018.
- van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw 2011;45:1-67. https://doi.org/10.18637/jss.v045.i03.
- Phillips T, Coulton S, Drummond C. Receiver Operating Characteristics full AUDIT with AUDIT-C, FAST (Original), Modified-FAST and Modified-SASQ subscales. Analysis to Support MUP in Scotland Study. Hull: Institute for Clinical and Applied Health Research, University of Hull; 2020.
- Leatherdale ST. Natural experiment methodology for research: a review of how different methods can support real-world research. Int J Soc Res Methodol 2019;22:19-35. https://doi.org/10.1080/13645579.2018.1488449.
- Public Health Scotland . Alcohol-Related Hospital Statistics Scotland 2019. www.opendata.nhs.scot/dataset/alcohol-related-hospital-statistics-scotland (accessed 2 June 2020).
- Public Health England . Local Alcohol Profiles for England 2020. https://fingertips.phe.org.uk/profile/local-alcohol-profiles (accessed 2 June 2020).
- Met Office . UK and Regional Series 2020. www.metoffice.gov.uk/research/climate/maps-and-data/uk-and-regional-series (accessed 5 July 2021).
- Gray L, Gorman E, White IR, Katikireddi SV, McCartney G, Rutherford L, et al. Correcting for non-participation bias in health surveys using record-linkage, synthetic observations and pattern mixture modelling. Stat Methods Med Res 2020;29:1212-26. https://doi.org/10.1177/0962280219854482.
- Public Health England . Local Alcohol Profiles for England 2019. https://fingertips.phe.org.uk/profile/local-alcohol-profiles/data#page/0/gid/1938132984/pat/6/par/E12000002/ati/101/are/E07000026/iid/91409/age/1/sex/4 (accessed 19 January 2021).
- Scottish Public Health Observatory . ScotPHO Profiles 2019. https://scotland.shinyapps.io/ScotPHO_profiles_tool/ (accessed 14 February 2020).
- Hodgson R, John B, Abbasi T, Hodgson R, Waller S, Thom B, et al. Fast screening for alcohol misuse. Addict Behav 2003;28:1453-63. https://doi.org/10.1016/s0306-4603(02)00246-0.
- Public Health England . Guidance: Alcohol Use Screening Tests 2017. www.gov.uk/government/publications/alcohol-use-screening-tests (accessed March 2019).
- Ministry of Housing Communities & Local Government . IoD2019 Interactive Dashboard – Local Authority Focus 2019. https://app.powerbi.com/view?r=eyJrIjoiOTdjYzIyNTMtMTcxNi00YmQ2LWI1YzgtMTUyYzMxOWQ3NzQ2IiwidCI6ImJmMzQ2ODEwLTljN2QtNDNkZS1hODcyLTI0YTJlZjM5OTVhOCJ9 (accessed 8 May 2020).
- Scottish Government . Scottish Index of Multiple Deprivation 2020 2020. www2.gov.scot/Topics/Statistics/SIMD/analysis/councils (accessed 8 May 2020).
- Scottish Government . Scottish Census 2011: Results at a Glance 2016. www.scotlandscensus.gov.uk/results-glance (accessed 10 February 2020).
- Kypri K. Governments as Partners in Knowledge Generation: Observations on alcohol Policy and Research in Australia and New Zealand 1999–2019. The Institute of Health and Wellbeing Maurice Bloch Annual Lecture Series 2019/20. Glasgow: MRC/CSO Social and Public Health Sciences Unit, Institute of Health and Well Being, University of Glasgow; 2019.
- Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health 2018;39:453-69. https://doi.org/10.1146/annurev-publhealth-040617-013507.
- Cole SR, Platt RW, Schisterman EF, Chu H, Westreich D, Richardson D, et al. Illustrating bias due to conditioning on a collider. Int J Epidemiol 2010;39:417-20. https://doi.org/10.1093/ije/dyp334.
- Giles L, Robinson M, Beeston C. Minimum Unit Pricing (MUP) for Alcohol Evaluation. Sales-Based Consumption: A Descriptive Analysis of One Year Post-MUP Off-Trade Alcohol Sales Data. Glasgow: NHS Health Scotland; 2020.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Kitzinger J. The methodology of focus groups: the importance of interaction between research participants. Sociol Health Illn 1994;16:103-21. https://doi.org/10.1111/1467-9566.ep11347023.
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT Alcohol Consumption Questions (AUDIT-C): an effective brief screening test for problem drinking. JAMA 1998;158:1789-95. https://doi.org/10.1001/archinte.158.16.1789.
- Meng Y, Brennan A, Holmes J. Modelled Income Group-Specific Impacts of Alcohol Minimum Unit Pricing in England 2014 15: Policy Appraisal Using New Developments to the Sheffield Alcohol Policy Model 2013. www.sheffield.ac.uk/polopoly_fs/1.291621!/file/julyreport.pdf (accessed 19 January 2021).
- Forsyth AJM, Ellaway A, Davidson N. How might the alcohol minimum unit pricing (MUP) impact upon local off-sales shops and the communities which they serve?. Alcohol Alcohol 2014;49:96-102. https://doi.org/10.1093/alcalc/agt175.
- Zhao J, Stockwell T, Martin G, Macdonald S, Vallance K, Treno A, et al. The relationship between minimum alcohol prices, outlet densities and alcohol-attributable deaths in British Columbia, 2002–09. Addiction 2013;108:1059-69. https://doi.org/10.1111/add.12139.
- Inchley J, Mokogwu D, Mabelis J, Currie D. Health Behaviour in School-Aged Children (HBSC) 2018 Survey in Scotland: National Report 2020.
- Brooks F, Klemera E, Chester K, Magnusson J, Spencer N. Health Behaviour in School-aged Children (HBSC): World Health Organization Collaborative Cross National Study Findings from the 2018 HBSC study for England. Hatfield: University of Hertfordshire; 2020.
- NHS Health Scotland . Overview of Evaluation of MUP 2019.
- Abadie A, Diamond A, Hainmueller J. Synthetic control methods for comparative case studies: estimating the effect of California’s tobacco control program. J Am Stat Assoc 2010;105:493-505. https://doi.org/10.1198/jasa.2009.ap08746.
Appendix 1 Search strategy
Review methods
We carried out a narrative literature review in 2012 to assess the relevance of alcohol MUP for tackling alcohol harms when this was first being considered in Scotland. This was updated in 2020 after legal challenges and delays. We searched MEDLINE, PsycINFO and Google Scholar (Google Inc., Mountain View, CA, USA) in early 2020 for papers on alcohol and MUP. We found 12 new references. We used the search strategy given below.
Search strategy for literature review update
Ovid MEDLINE® all
Date range searched: 1946 to 31 January 2020.
Search date: 3 February 2020.
Search strategy
-
(Alcohol and minimum and unit and price).mp. [mp = ti, ab, ot, nm, hw, fx, kf, ox, px, rx, ui, an, sy, tc, id, tm, mh] (88)
-
limit 1 to abstracts (76)
-
limit 2 to full text (15)
-
limit 3 to yr = “2012 -Current” (14)
-
remove duplicates from 4 (12)
PsycInfo
Date range searched: 2002 to January week 4 2020.
Search date: 3 February 2020.
Search strategy
-
(Alcohol and minimum and unit and price).mp. [mp = ti, ab, ot, nm, hw, fx, kf, ox, px, rx, ui, an, sy, tc, id, tm, mh] (88)
-
limit 1 to abstracts (76)
-
limit 2 to full text (15)
-
limit 3 to yr = “2012 -Current” (14)
-
remove duplicates from 4 (12)
Appendix 2 Supplementary tables for the emergency department study
| Reason | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 1479) | Wave 2 (N = 1448) | Wave 3 (N = 1682) | Wave 1 (N = 1709) | Wave 2 (N = 1531) | Wave 3 (N = 1559) | |
| Too unwell | 204 (13.8) | 188 (13.0) | 182 (10.8) | 310 (18.1) | 204 (13.8) | 188 (13.0) |
| Distressed | 83 (5.6) | 48 (3.3) | 51 (3.0) | 76 (4.4) | 83 (5.6) | 48 (3.3) |
| Gross intoxication | ||||||
| Alcohol | 74 (5.0) | 73 (5.0) | 52 (3.1) | 65 (3.8) | 74 (5.0) | 73 (5.0) |
| Drugs | 46 (3.1) | 29 (2.0) | 36 (2.1) | 28 (1.6) | 46 (3.1) | 29 (2.0) |
| Cognitive impairment | 109 (7.4) | 63 (4.4) | 71 (4.2) | 138 (8.1) | 109 (7.4) | 63 (4.4) |
| Police in attendance | 47 (3.2) | 61 (4.2) | 51 (3.0) | 11 (0.6) | 47 (3.2) | 61 (4.2) |
| Language issue | 24 (1.6) | 14 (1.0) | 27 (1.6) | 42 (2.5) | 24 (1.6) | 14 (1.0) |
| Already participated | 20 (1.4) | 3 (0.2) | 3 (0.2) | 6 (0.4) | 20 (1.4) | 3 (0.2) |
| Routine follow-up | 5 (0.3) | 5 (0.3) | 7 (0.4) | 20 (1.2) | 5 (0.3) | 5 (0.3) |
| Left ED | 292 (19.7) | 261 (18.0) | 213 (12.7) | 243 (14.2) | 292 (19.7) | 261 (18.0) |
| Admitted | 31 (2.1) | 21 (1.5) | 21 (1.2) | 8 (0.5) | 31 (2.1) | 21 (1.5) |
| Staff safety issue | 20 (1.4) | 13 (0.9) | 13 (0.8) | 32 (1.9) | 20 (1.4) | 13 (0.9) |
| End of shift | 325 (22.0) | 349 (24.1) | 410 (24.4) | 359 (21.0) | 325 (22.0) | 349 (24.1) |
| Dead on arrival | 1 (0.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.1) | 0 (0.0) |
| Other | ||||||
| Mental health | 7 (0.5) | 7 (0.5) | 6 (0.4) | 8 (0.5) | 7 (0.5) | 7 (0.5) |
| Barrier nursed/infectious | 1 (0.1) | 0 (0.0) | 0 (0.0) | 15 (0.9) | 1 (0.1) | 0 (0.0) |
| Other study | 9 (0.6) | 0 (0.0) | 0 (0.0) | 5 (0.3) | 9 (0.6) | 0 (0.0) |
| Sight/reading problem | 5 (0.3) | 1 (0.1) | 0 (0.0) | 5 (0.3) | 5 (0.3) | 1 (0.1) |
| Not clinically appropriate | 9 (0.6) | 2 (0.1) | 3 (0.2) | 7 (0.4) | 9 (0.6) | 2 (0.1) |
| Not triaged | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) |
| Asleep | 1 (0.1) | 0 (0.0) | 1 (0.1) | 7 (0.4) | 1 (0.1) | 0 (0.0) |
| Confused | 1 (0.1) | 1 (0.1) | 3 (0.2) | 5 (0.3) | 1 (0.1) | 1 (0.1) |
| Pain | 0 (0.0) | 1 (0.1) | 2 (0.1) | 2 (0.1) | 0 (0.0) | 1 (0.1) |
| Unlocatable | 0 (0.0) | 0 (0.0) | 1 (0.1) | 4 (0.2) | 0 (0.0) | 0 (0.0) |
| Unspecified | 24 (1.6) | 8 (0.6) | 61 (3.6) | 13 (0.8) | 24 (1.6) | 8 (0.6) |
| Reason | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 517) | Wave 2 (N = 889) | Wave 3 (N = 841) | Wave 1 (N = 493) | Wave 2 (N = 1022) | Wave 3 (N = 1201) | |
| Initial disinterest | 263 (50.9) | 299 (33.6) | 222 (26.4) | 162 (32.9) | 200 (19.6) | 130 (10.8) |
| Patient left without completing | 25 (4.8) | 42 (4.7) | 29 (3.4) | 31 (6.3) | 25 (2.4) | 17 (1.4) |
| Routine follow-up | 3 (0.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (0.2) | 1 (0.1) |
| Withdrew consent | 15 (2.9) | 12 (1.3) | 9 (1.1) | 6 (1.2) | 11 (1.1) | 4 (0.3) |
| Patient admitted | 2 (0.4) | 3 (0.3) | 3 (0.4) | 7 (1.4) | 3 (0.3) | 0 (0.0) |
| Already participated/refused | 7 (1.4) | 7 (0.8) | 9 (1.1) | 1 (0.2) | 7 (0.7) | 9 (0.7) |
| Barrier nursed/infectious | 1 (0.2) | 0 (0.0) | 2 (0.2) | 1 (0.2) | 0 (0.0) | 0 (0.0) |
| Cognitive problem/confused/learning disability/Alzheimer’s disease | 17 (3.3) | 37 (4.2) | 34 (4.0) | 9 (1.8) | 34 (3.3) | 29 (2.4) |
| End of shift | 4 (0.8) | 11 (1.2) | 7 (0.8) | 2 (0.4) | 5 (0.5) | 5 (0.4) |
| Sight/reading problems | 18 (3.5) | 28 (3.1) | 17 (2.0) | 10 (2.0) | 47 (4.6) | 30 (2.5) |
| Hearing problems | 2 (0.4) | 1 (0.1) | 2 (0.2) | 2 (0.4) | 5 (0.5) | 4 (0.3) |
| Refused | 13 (2.5) | 9 (1.0) | 13 (1.5) | 7 (1.4) | 9 (0.9) | 41 (3.4) |
| Language problem | 14 (2.7) | 26 (2.9) | 24 (2.9) | 21 (4.3) | 44 (4.3) | 29 (2.4) |
| Too unwell | 42 (8.1) | 123 (13.8) | 90 (10.7) | 70 (14.2) | 168 (16.4) | 105 (8.7) |
| Too intoxicated | ||||||
| Alcohol | 4 (0.8) | 18 (2.0) | 19 (2.3) | 4 (0.8) | 28 (2.7) | 6 (0.5) |
| Drugs | 2 (0.4) | 11 (1.2) | 11 (1.3) | 4 (0.8) | 5 (0.5) | 6 (0.5) |
| Incapable of consent requirement | 9 (1.7) | 6 (0.7) | 1 (0.1) | 4 (0.8) | 12 (1.2) | 1 (0.1) |
| Too much pain | 7 (1.4) | 9 (1.0) | 10 (1.2) | 6 (1.2) | 15 (1.5) | 9 (0.7) |
| Too distressed | 10 (1.9) | 35 (3.9) | 35 (4.2) | 4 (0.8) | 12 (1.2) | 15 (1.2) |
| Other: unspecified | 10 (1.9) | 36 (4.0) | 13 (1.5) | 7 (1.4) | 27 (2.6) | 14 (1.2) |
| Reason | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 106) | Wave 2 (N = 55) | Wave 3 (N = 23) | Wave 1 (N = 21) | Wave 2 (N = 3) | Wave 3 (N = 2) | |
| Aged < 16 years | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Clinically inappropriate | 23 (21.7) | 17 (30.9) | 3 (13.0) | 1 (4.8) | 0 (0.0) | 0 (0.0) |
| Did not speak English/without translators | 13 (12.3) | 4 (7.3) | 2 (8.7) | 5 (23.8) | 0 (0.0) | 0 (0.0) |
| Old ED presentation | 0 (0.0) | 1 (1.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) |
| Unconscious | 1 (0.9) | 3 (5.5) | 1 (4.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not well enough | ||||||
| Physically | 48 (45.3) | 17 (30.9) | 12 (52.2) | 8 (38.1) | 2 (66.7) | 1 (50.0) |
| Mentally | 24 (22.6) | 21 (38.2) | 4 (17.4) | 7 (33.3) | 2 (66.7) | 0 (0.0) |
| Not sober enough | ||||||
| Alcohol | 13 (12.3) | 17 (30.9) | 3 (13.0) | 4 (19.0) | 1 (33.3) | 0 (0.0) |
| Drug | 4 (3.8) | 6 (10.9) | 2 (8.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Left ED | 1 (0.9) | 11 (20.0) | 2 (8.7) | 1 (4.8) | 0 (0.0) | 0 (0.0) |
| Threatening | 0 (0.0) | 5 (9.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Description of condition | ICD-10 code | Type |
|---|---|---|
| Alcohol-induced pseudo-Cushing syndrome | E24.4 | Wholly chronic |
| Degeneration of nervous system due to use of alcohol | G31.2 | Wholly chronic |
| Alcoholic polyneuropathy | G62.1 | Wholly chronic |
| Alcoholic myopathy | G72.1 | Wholly chronic |
| Alcoholic cardiomyopathy | I42.6 | Wholly chronic |
| Alcoholic gastritis | K29.2 | Wholly chronic |
| Alcoholic liver disease | K70 | Wholly chronic |
| Alcohol-induced acute pancreatitis | K85.2 | Wholly chronic |
| Alcohol-induced chronic pancreatitis | K86.0 | Wholly chronic |
| Fetal alcohol syndrome (dysmorphic) | Q86.0 | Wholly chronic |
| Mental and behavioural disorders due to use of alcohol | F10 | Wholly acute |
| Excess alcohol blood levels | R78.0 | Wholly acute |
| Ethanol poisoning | T51.0 | Wholly acute |
| Methanol poisoning | T51.1 | Wholly acute |
| Toxic effect of alcohol, unspecified | T51.9 | Wholly acute |
| Accidental poisoning by and exposure to alcohol | X45 | Wholly acute |
| Intentional self-poisoning by and exposure to alcohol | X65 | Wholly acute |
| Poisoning by and exposure to alcohol, undetermined intent | Y15 | Wholly acute |
| Evidence of alcohol involvement determined by blood alcohol level | Y90 | Wholly acute |
| Evidence of alcohol involvement determined by level of intoxication | Y91 | Wholly acute |
| Tuberculosis | A15–A19 | Partially chronic |
| Lip, oral cavity and pharynx | C00–C14 | Partially chronic |
| Oesophagus | C15 | Partially chronic |
| Colorectal | C18–C20 | Partially chronic |
| Liver and intrahepatic bile ducts | C22 | Partially chronic |
| Larynx | C32 | Partially chronic |
| Breast | C50 | Partially chronic |
| Diabetes mellitus (type 2) | E11 | Partially chronic |
| Epilepsy and status epilepticus | G40–G41 | Partially chronic |
| Hypertensive diseases | I10–I15 | Partially chronic |
| Ischaemic heart disease | I20–I25 | Partially chronic |
| Cardiac arrhythmias | I47–I48 | Partially chronic |
| Haemorrhagic stroke | I60–I62 | Partially chronic |
| Ischaemic stroke | I63–I66, I69.3–I69.4 | Partially chronic |
| Pneumonia | J10.0–J11.0, J12–J15, J18 | Partially chronic |
| Unspecified liver disease | K73, K74 | Partially chronic |
| Cholelithiasis (gall stones) | K80 | Partially chronic |
| Acute and chronic pancreatitis | K85, K86.1 | Partially chronic |
| Oesophageal varices | I85 | Partially chronic |
| Spontaneous abortion | O03 | Partially chronic |
| Road/pedestrian traffic accidents | V021–V029, V031–V039, V041–V049, V092, V093, V123–V129, V133–V139, V143–V149, V194–V196, V203–V209, V213–V219, V223–V229, V233–V239, V243–V249, V253–V259, V263–V269, V273–V279, V283–V289, V294–V299, V304–V309, V314–V319, V324–V329, V334–V339, V344–V349, V354–V359, V364–V369, V374–V379, V384–V389, V394–V399, V404–V409, V414–V419, V424–V429, V434–V439, V444–V449, V454–V459, V464–V469, V474–V479, V484–V489, V494–V499, V504–V509, V514–V519, V524–V529, V534–V539, V544–V549, V554–V559, V564–V569, V574–V579, V584–V589, V594–V599, V604–V609, V614–V619, V624–V629, V634–V639, V644–V649, V654–V659, V664–V669, V674–V679, V684–V689, V694–V699, V704–V709, V714–V719, V724–V729, V734–V739, V744–V749, V754–V759, V764–V769, V774–V779, V784–V789, V794–V799, V803–V805, V811, V821, V830–V833, V840–V843, V850–V853, V860–V863, V870–V878, V892 | Partially acute |
| Poisoning | X40–X49 (excluding X45) | Partially acute |
| Fall injuries | W00–W19 | Partially acute |
| Fire injuries | X00–X09 | Partially acute |
| Drowning | W65–W74 | Partially acute |
| Other unintentional injuries | V01, V090, V091, V099, V100–V109, V110–V119, V120–122, V130–132, V140–V142, V150–V159, V160–V169, V170–V179, V180–V189, V191–V193, V20–V28: 0.1–0.2;V290–V293, V30–V38: 0.1–0.2; V390–V393, V40–V48: 0.1–0.2; V490–V493, V50–V58: 0.1–0.2; V590–V593, V60–V68: 0.1–0.2; V690–V693, V70–V78: 0.1–0.2; V790–V793, V800, V801, V806–V809, V810, V812–V819, V820, V822–V829, V834–V839, V844–V849, V854–V859, V864–V869, V879, V88, V890, V891, V893–V899, V90–V94,V95–V97, V98–V99, W20–W52, W75–W84, W85–W99, X10–X19, X20–X29, X30–X33, X50–X57, X58, X59, Y40–Y84 Y85, Y86, Y88, Y89 | Partially acute |
| Event of undetermined intent | Y10–Y34, Y78.2 (excluding Y15) | Partially acute |
| Intentional self-harm | X60–X84, Y87.0 | Partially acute |
| Assault | X85–Y09, Y87.1 | Partially acute |
| Demographic | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 4346) | Wave 2 (N = 4732) | Wave 3 (N = 4973) | Wave 1 (N = 3957) | Wave 2 (N = 4488) | Wave 3 (N = 4473) | |
| Sex | ||||||
| Female | 2233 (51.4) | 2384 (50.4) | 2595 (52.2) | 2008 (50.7) | 2262 (50.4) | 2282 (51.0) |
| Male | 2113 (48.6) | 2347 (49.6) | 2377 (47.8) | 1949 (49.3) | 2226 (49.6) | 2191 (49.0) |
| Non-binary | 0 (0) | 1 (0.0) | 1 (0.0) | 0 (0) | 0 (0) | 0 (0) |
| Age (years) | ||||||
| 16–25 | 744 (17.1) | 869 (18.4) | 896 (18.0) | 807 (20.4) | 982 (21.9) | 936 (20.9) |
| 26–45 | 1286 (29.6) | 1414 (29.9) | 1511 (30.4) | 1172 (29.6) | 1363 (30.4) | 1295 (29.0) |
| 46–65 | 1194 (27.5) | 1265 (26.7) | 1373 (27.6) | 917 (23.2) | 1072 (23.9) | 1092 (24.4) |
| ≥ 66 | 1122 (25.8) | 1184 (25.0) | 1193 (24.0) | 1053 (26.6) | 1058 (23.6) | 1140 (25.5) |
| Missing | 0 (0) | 0 (0) | 0 (0) | 8 (0.2) | 13 (0.3) | 10 (0.2) |
| Demographic | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 3675) | Wave 2 (N = 4144) | Wave 3 (N = 4388) | Wave 1 (N = 3252) | Wave 2 (N = 3969) | Wave 3 (N = 4027) | |
| Sex | ||||||
| Female | 1849 (50.3) | 2053 (49.5) | 2229 (50.8) | 1647 (50.6) | 1982 (49.9) | 2005 (49.8) |
| Male | 1814 (49.4) | 2073 (50.0) | 2128 (48.5) | 1571 (48.3) | 1943 (49.0) | 1985 (49.3) |
| Non-binary | 0 (0) | 1 (0.0) | 1 (0.0) | 0 (0) | 0 (0) | 0 (0) |
| Missing | 12 (0.3) | 17 (0.4) | 30 (0.7) | 34 (1.0) | 44 (1.1) | 37 (0.9) |
| Age (years) | ||||||
| 16–25 | 733 (19.9) | 847 (20.4) | 870 (19.8) | 555 (17.1) | 839 (21.1) | 816 (20.3) |
| 26–45 | 1110 (30.2) | 1271 (30.7) | 1388 (31.6) | 858 (26.4) | 1138 (28.7) | 1123 (27.9) |
| 46–65 | 969 (26.4) | 1051 (25.4) | 1135 (25.9) | 715 (22.0) | 907 (22.9) | 949 (23.6) |
| ≥ 66 | 850 (23.1) | 949 (22.9) | 963 (21.9) | 933 (28.7) | 923 (23.3) | 990 (24.6) |
| Missing | 13 (0.4) | 26 (0.6) | 32 (0.7) | 191 (5.9) | 162 (4.1) | 149 (3.7) |
| Demographic | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 1551) | Wave 2 (N = 1706) | Wave 3 (N = 1802) | Wave 1 (N = 998) | Wave 2 (N = 1385) | Wave 3 (N = 1245) | |
| Sex, n (%) | ||||||
| Female | 747 (48.2) | 820 (48.1) | 916 (50.8) | 507 (50.8) | 696 (50.3) | 651 (52.3) |
| Male | 804 (51.8) | 885 (51.9) | 885 (49.1) | 491 (49.2) | 689 (49.7) | 594 (47.7) |
| Non-binary | 0 (0) | 1 (0.1) | 1 (0.1) | 0 (0) | 0 (0) | 0 (0) |
| Age (years), n (%) | ||||||
| 16–25 | 364 (23.5) | 385 (22.6) | 388 (21.5) | 202 (20.2) | 345 (24.9) | 314 (25.2) |
| 26–45 | 468 (30.2) | 570 (33.4) | 575 (31.9) | 319 (32.0) | 434 (31.3) | 393 (31.6) |
| 46–65 | 424 (27.3) | 451 (26.4) | 477 (26.5) | 252 (25.3) | 354 (25.6) | 295 (23.7) |
| ≥ 66 | 295 (19.0) | 300 (17.6) | 362 (20.1) | 225 (22.5) | 252 (18.2) | 243 (19.5) |
| Ethnicity, n (%) | ||||||
| White | 1456 (93.9) | 1577 (92.4) | 1684 (93.5) | 886 (88.8) | 1199 (86.6) | 1087 (87.3) |
| Non-white | 94 (6.1) | 120 (7.0) | 111 (6.2) | 107 (10.7) | 181 (13.1) | 150 (12.0) |
| Missing | 1 (0.1) | 9 (0.5) | 7 (0.4) | 5 (0.5) | 5 (0.4) | 8 (0.6) |
| Employment status, n (%) | ||||||
| Employed | 785 (50.6) | 898 (52.6) | 907 (50.3) | 458 (45.9) | 671 (48.4) | 561 (45.1) |
| Economically inactive | 593 (38.2) | 630 (36.9) | 715 (39.7) | 409 (41.0) | 564 (40.7) | 506 (40.6) |
| Unemployed | 164 (10.6) | 166 (9.7) | 168 (9.3) | 126 (12.6) | 141 (10.2) | 164 (13.2) |
| Missing | 9 (0.6) | 12 (0.7) | 12 (0.7) | 5 (0.5) | 9 (0.6) | 14 (1.1) |
| Marital status, n (%) | ||||||
| Married/co-habiting | 638 (41.1) | 724 (42.4) | 754 (41.8) | 439 (44.0) | 546 (39.4) | 468 (37.6) |
| Separated/divorced/widowed | 249 (16.1) | 245 (14.4) | 276 (15.3) | 163 (16.3) | 188 (13.6) | 196 (15.7) |
| Single | 651 (42.0) | 705 (41.3) | 741 (41.1) | 387 (38.8) | 633 (45.7) | 568 (45.6) |
| Missing | 13 (0.8) | 32 (1.9) | 31 (1.7) | 9 (0.9) | 18 (1.3) | 13 (1.0) |
| Housing ownership, n (%) | ||||||
| Owner occupied | 574 (37.0) | 642 (37.6) | 701 (38.9) | 376 (37.7) | 479 (34.6) | 430 (34.5) |
| Rented | 418 (27.0) | 441 (25.8) | 447 (24.8) | 317 (31.8) | 496 (35.8) | 394 (31.6) |
| Housing association/council | 268 (17.3) | 302 (17.7) | 318 (17.6) | 125 (12.5) | 160 (11.6) | 161 (12.9) |
| Other | 277 (17.9) | 295 (17.3) | 309 (17.1) | 166 (16.6) | 233 (16.8) | 228 (18.3) |
| Missing | 14 (0.9) | 26 (1.5) | 27 (1.5) | 14 (1.4) | 17 (1.2) | 32 (2.6) |
| Carstairs deprivation score | ||||||
| Mean score (SD) | 7.06 (2.65) | 6.97 (2.64) | 7.15 (2.53) | 7.15 (2.61) | 7.46 (2.50) | 7.46 (2.53) |
| Median score (minimum, maximum) | 8.00 (1.00, 10.0) | 7.00 (1.00, 10.0) | 8.00 (1.00, 10.0) | 8.00 (1.00, 10.0) | 8.00 (1.00, 10.0) | 8.00 (1.00, 10.0) |
| Missing, n (%) | 11 (0.7) | 20 (1.2) | 23 (1.3) | 51 (5.1) | 75 (5.4) | 40 (3.2) |
| Alcohol-related attendance | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 3675) | Wave 2 (N = 4144) | Wave 3 (N = 4388) | Wave 1 (N = 3252) | Wave 2 (N = 3969) | Wave 3 (N = 4027) | |
| Alcohol related | 321 (8.7) | 335 (8.1) | 353 (8.0) | 179 (5.5) | 245 (6.2) | 180 (4.5) |
| Non-alcohol related | 3319 (90.3) | 3755 (90.6) | 3973 (90.5) | 3038 (93.4) | 3668 (92.4) | 3782 (93.9) |
| Missing | 35 (1.0) | 54 (1.3) | 62 (1.4) | 35 (1.1) | 56 (1.4) | 65 (1.6) |
| Alcohol-related diagnosisa | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 4346) | Wave 2 (N = 4732) | Wave 3 (N = 4973) | Wave 1 (N = 2213) | Wave 2 (N = 2465) | Wave 3 (N = 2517) | |
| Alcohol-related diagnosis | 252 (5.8) | 296 (6.3) | 309 (6.2) | 248 (11.2) | 239 (9.7) | 255 (10.1) |
| Non-alcohol-related diagnosis | 4094 (94.2) | 4436 (93.7) | 4664 (93.8) | 1965 (88.8) | 2226 (90.3) | 2262 (89.9) |
| Alcohol-related diagnosisa | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 1481) | Wave 2 (N = 1607) | Wave 3 (N = 1730) | Wave 1 (N = 504) | Wave 2 (N = 602) | Wave 3 (N = 542) | |
| Alcohol-related diagnosis | 67 (4.5) | 80 (5.0) | 94 (5.4) | 51 (10.1) | 55 (9.1) | 43 (7.9) |
| Non-alcohol-related diagnosis | 1414 (95.5) | 1527 (95.0) | 1636 (94.6) | 453 (89.9) | 547 (90.9) | 499 (92.1) |
| Variable | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 1551) | Wave 2 (N = 1706) | Wave 3 (N = 1802) | Wave 1 (N = 998) | Wave 2 (N = 1385) | Wave 3 (N = 1245) | |
| Alcohol-related attendance | ||||||
| Alcohol related | 228 (14.7) | 225 (13.2) | 279 (15.5) | 104 (10.4) | 174 (12.6) | 149 (12.0) |
| Non-alcohol related | 1290 (83.2) | 1428 (83.7) | 1461 (81.1) | 859 (86.1) | 1155 (83.4) | 1031 (82.8) |
| Missing | 33 (2.1) | 53 (3.1) | 62 (3.4) | 35 (3.5) | 56 (4.0) | 65 (5.2) |
| Current alcohol drinker | ||||||
| Drinker | 1263 (81.4) | 1358 (79.6) | 1481 (82.2) | 796 (79.8) | 1099 (79.4) | 994 (79.8) |
| Non-drinker | 288 (18.6) | 347 (20.3) | 319 (17.7) | 202 (20.2) | 284 (20.5) | 244 (19.6) |
| Missing | 0 (0) | 1 (0.1) | 2 (0.1) | 0 (0) | 2 (0.1) | 7 (0.6) |
| Binge drinking in the past week | ||||||
| Binger | 436 (28.1) | 458 (26.8) | 472 (26.2) | 244 (24.4) | 328 (23.7) | 290 (23.3) |
| Non-binger | 1080 (69.6) | 1193 (69.9) | 1270 (70.5) | 716 (71.7) | 997 (72.0) | 888 (71.3) |
| Missing | 35 (2.3) | 55 (3.2) | 60 (3.3) | 38 (3.8) | 60 (4.3) | 67 (5.4) |
| Binge drinking in the past 24 hours | ||||||
| Binger | 187 (12.1) | 157 (9.2) | 210 (11.7) | 84 (8.4) | 126 (9.1) | 107 (8.6) |
| Non-binger | 1334 (86.0) | 1499 (87.9) | 1539 (85.4) | 881 (88.3) | 1214 (87.7) | 1082 (86.9) |
| Missing | 30 (1.9) | 50 (2.9) | 53 (2.9) | 33 (3.3) | 45 (3.2) | 56 (4.5) |
| Variable | Scotland | England | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 1263) | Wave 2 (N = 1358) | Wave 3 (N = 1481) | Wave 1 (N = 796) | Wave 2 (N = 1099) | Wave 3 (N = 994) | |
| FAST score | ||||||
| Mean (SD) | 2.79 (2.95) | 2.70 (3.00) | 2.79 (3.16) | 2.36 (2.77) | 2.61 (2.93) | 2.64 (2.87) |
| Median (minimum, maximum) | 2.00 (0, 16.0) | 2.00 (0, 16.0) | 2.00 (0, 16.0) | 2.00 (0, 16.0) | 2.00 (0, 16.0) | 2.00 (0, 16.0) |
| Missing, n (%) | 43 (3.4) | 58 (4.3) | 59 (4.0) | 31 (3.9) | 38 (3.5) | 42 (4.2) |
| Alcohol misuse (FAST score ≥ 3), n (%) | ||||||
| Hazardous drinker (≥ 3) | 514 (40.7) | 518 (38.1) | 581 (39.2) | 277 (34.8) | 431 (39.2) | 403 (40.5) |
| Non-hazardous drinker (< 3) | 706 (55.9) | 782 (57.6) | 841 (56.8) | 488 (61.3) | 630 (57.3) | 549 (55.2) |
| Missing | 43 (3.4) | 58 (4.3) | 59 (4.0) | 31 (3.9) | 38 (3.5) | 42 (4.2) |
| Change in alcohol use in the past year, n (%) | ||||||
| Increased | 118 (9.3) | 134 (9.9) | 139 (9.4) | 65 (8.2) | 109 (9.9) | 91 (9.2) |
| Decreased/unchanged | 1116 (88.4) | 1184 (87.2) | 1294 (87.4) | 703 (88.3) | 960 (87.4) | 863 (86.8) |
| Missing | 29 (2.3) | 40 (2.9) | 48 (3.2) | 28 (3.5) | 30 (2.7) | 40 (4.0) |
| Place of last drink: private location, n (%) | ||||||
| Private location | 668 (52.9) | 676 (49.8) | 788 (53.2) | 408 (51.3) | 490 (44.6) | 465 (46.8) |
| Others | 547 (43.3) | 647 (47.6) | 632 (42.7) | 354 (44.5) | 551 (50.1) | 463 (46.6) |
| Missing | 48 (3.8) | 35 (2.6) | 61 (4.1) | 34 (4.3) | 58 (5.3) | 66 (6.6) |
| Place of last drink: on-licensed premise, n (%) | ||||||
| On-licensed premise | 435 (34.4) | 538 (39.6) | 513 (34.6) | 307 (38.6) | 448 (40.8) | 404 (40.6) |
| Others | 780 (61.8) | 785 (57.8) | 907 (61.2) | 455 (57.2) | 593 (54.0) | 524 (52.7) |
| Missing | 48 (3.8) | 35 (2.6) | 61 (4.1) | 34 (4.3) | 58 (5.3) | 66 (6.6) |
| Hazardous drinking level, n (%) | ||||||
| At least hazardous (≥ 2) | 701 (55.5) | 731 (53.8) | 781 (52.7) | 388 (48.7) | 596 (54.2) | 550 (55.3) |
| Not hazardous (< 2) | 519 (41.1) | 569 (41.9) | 641 (43.3) | 377 (47.4) | 465 (42.3) | 402 (40.4) |
| Missing | 43 (3.4) | 58 (4.3) | 59 (4.0) | 31 (3.9) | 38 (3.5) | 42 (4.2) |
| Harmful drinking level, n (%) | ||||||
| At least harmful (≥ 4) | 329 (26.0) | 309 (22.8) | 365 (24.6) | 176 (22.1) | 255 (23.2) | 229 (23.0) |
| Not harmful (< 4) | 891 (70.5) | 991 (73.0) | 1057 (71.4) | 589 (74.0) | 806 (73.3) | 723 (72.7) |
| Missing | 43 (3.4) | 58 (4.3) | 59 (4.0) | 31 (3.9) | 38 (3.5) | 42 (4.2) |
| Dependent drinking level, n (%) | ||||||
| At least dependent (≥ 6) | 182 (14.4) | 172 (12.7) | 204 (13.8) | 79 (9.9) | 127 (11.6) | 110 (11.1) |
| Not dependent (< 6) | 1038 (82.2) | 1128 (83.1) | 1218 (82.2) | 686 (86.2) | 934 (85.0) | 842 (84.7) |
| Missing | 43 (3.4) | 58 (4.3) | 59 (4.0) | 31 (3.9) | 38 (3.5) | 42 (4.2) |
| Estimate | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all recorded respondents | ||||||||||||
| Alcohol-related attendance | 8.4 | 8.1 | 8.1 | 6.1 | 6.3 | 4.6 | 1.07 (0.85 to 1.35) | 0.547 | 1.12 (0.89 to 1.41) | 0.328 | 1.14 (0.90 to 1.44) | 0.272 |
| Based on all attendees | ||||||||||||
| Alcohol-related diagnosis | 5.8 | 6.3 | 6.2 | 11.2 | 9.7 | 10.0 | 1.24 (0.99 to 1.55) | 0.058 | 1.24 (0.99 to 1.55) | 0.055 | 1.25 (1.00 to 1.57) | 0.046 |
| Based on all respondents | ||||||||||||
| Alcohol-related attendance | 13.7 | 12.7 | 15.3 | 10.5 | 12.6 | 12.2 | 0.85 (0.63 to 1.14) | 0.280 | 0.86 (0.64 to 1.16) | 0.335 | 0.87 (0.64 to 1.18) | 0.377 |
| Current alcohol drinker | 79.3 | 77.7 | 80.8 | 78.4 | 78.0 | 78.7 | 1.01 (0.78 to 1.30) | 0.957 | 1.00 (0.78 to 1.29) | 0.990 | 0.98 (0.74 to 1.29) | 0.874 |
| Binge drinking in the past 24 hours | 11.3 | 9.0 | 11.6 | 8.5 | 9.3 | 8.8 | 0.84 (0.60 to 1.17) | 0.296 | 0.85 (0.61 to 1.18) | 0.328 | 0.85 (0.61 to 1.20) | 0.354 |
| Binge drinking in the past week | 26.1 | 26.1 | 26.2 | 25.2 | 24.5 | 23.7 | 1.06 (0.85 to 1.33) | 0.609 | 1.07 (0.86 to 1.34) | 0.550 | 1.09 (0.86 to 1.38) | 0.474 |
| Based on drinkers only | ||||||||||||
| Alcohol misuse (FAST score ≥ 3) | 39.1 | 38.7 | 39.5 | 36.8 | 39.4 | 40.8 | 0.87 (0.70 to 1.10) | 0.239 | 0.89 (0.71 to 1.12) | 0.323 | 0.87 (0.68 to 1.10) | 0.249 |
| Increased alcohol use in the past year | 8.6 | 9.5 | 9.1 | 8.6 | 10.2 | 8.9 | 0.96 (0.65 to 1.41) | 0.834 | 0.98 (0.67 to 1.44) | 0.925 | 0.97 (0.65 to 1.45) | 0.875 |
| Place of last drink: private location | 56.5 | 52.6 | 56.8 | 53.6 | 48.8 | 51.6 | 1.07 (0.86 to 1.35) | 0.538 | 1.04 (0.83 to 1.31) | 0.704 | 1.02 (0.81 to 1.29) | 0.847 |
| Place of last drink: licensed premise | 33.5 | 38.6 | 34.7 | 40.4 | 41.4 | 41.9 | 1.09 (0.86 to 1.37) | 0.476 | 1.12 (0.89 to 1.41) | 0.337 | 1.16 (0.92 to 1.48) | 0.213 |
| FAST score | 2.61 | 2.60 | 2.72 | 2.38 | 2.59 | 2.55 | –0.13 (–0.46 to 0.20)a | 0.425 | –0.08 (–0.40 to 0.25)a | 0.650 | –0.12 (–0.42 to 0.18)a | 0.426 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all recorded respondents | 8.4 | 8.1 | 8.1 | 6.1 | 6.3 | 4.6 | 1.07 (0.85 to 1.35) | 0.547 | 1.12 (0.89 to 1.41) | 0.328 | 1.14 (0.90 to 1.44) | 0.272 |
| Sex | ||||||||||||
| Female | 5.8 | 5.3 | 5.2 | 4.7 | 5.1 | 3.5 | 0.99 (0.69 to 1.44) | 0.976 | 1.05 (0.72 to 1.52) | 0.816 | 1.04 (0.72 to 1.52) | 0.826 |
| Male | 11.1 | 10.9 | 11.4 | 7.4 | 7.6 | 5.8 | 1.13 (0.84 to 1.51) | 0.427 | 1.17 (0.87 to 1.57) | 0.288 | 1.20 (0.89 to 1.61) | 0.235 |
| Age (years) | ||||||||||||
| 16–25 | 14.5 | 11.0 | 12.4 | 10.4 | 9.7 | 7.1 | 0.99 (0.65 to 1.51) | 0.971 | 1.04 (0.68 to 1.59) | 0.854 | 1.06 (0.69 to 1.62) | 0.794 |
| 26–45 | 9.7 | 9.3 | 9.1 | 7.7 | 7.1 | 5.6 | 1.16 (0.79 to 1.72) | 0.452 | 1.24 (0.84 to 1.84) | 0.283 | 1.24 (0.83 to 1.84) | 0.292 |
| 46–65 | 8.8 | 9.2 | 8.0 | 6.4 | 7.3 | 5.4 | 0.98 (0.62 to 1.53) | 0.920 | 1.01 (0.64 to 1.58) | 0.975 | 1.02 (0.65 to 1.61) | 0.930 |
| ≥ 66 | 2.4 | 3.2 | 3.9 | 0.8 | 1.3 | 0.8 | 1.10 (0.38 to 3.18) | 0.859 | 1.13 (0.39 to 3.28) | 0.826 | 1.12 (0.39 to 3.27) | 0.831 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all attendees | 5.8 | 6.3 | 6.2 | 11.2 | 9.7 | 10.0 | 1.24 (0.99 to 1.55) | 0.058 | 1.24 (0.99 to 1.55) | 0.055 | 1.25 (1.00 to 1.57) | 0.046 |
| Sex | ||||||||||||
| Female | 5.0 | 4.7 | 4.8 | 9.8 | 9.7 | 9.7 | 0.96 (0.69 to 1.33) | 0.791 | 0.95 (0.68 to 1.33) | 0.773 | 0.96 (0.69 to 1.33) | 0.789 |
| Male | 6.7 | 7.9 | 7.7 | 12.7 | 9.7 | 10.4 | 1.53 (1.14 to 2.07) | 0.005 | 1.55 (1.14 to 2.09) | 0.004 | 1.56 (1.16 to 2.11) | 0.004 |
| Age (years) | ||||||||||||
| 16–25 | 6.3 | 5.3 | 4.9 | 3.3 | 5.9 | 5.6 | 0.48 (0.24 to 0.97) | 0.041 | 0.47 (0.23 to 0.95) | 0.035 | 0.47 (0.23 to 0.95) | 0.035 |
| 26–45 | 5.5 | 5.7 | 6.0 | 5.2 | 5.0 | 7.3 | 0.90 (0.55 to 1.48) | 0.674 | 0.90 (0.54 to 1.47) | 0.663 | 0.88 (0.54 to 1.45) | 0.622 |
| 46–65 | 6.0 | 8.0 | 6.8 | 14.3 | 12.9 | 12.6 | 1.44 (0.96 to 2.18) | 0.080 | 1.44 (0.95 to 2.18) | 0.083 | 1.46 (0.96 to 2.20) | 0.075 |
| ≥ 66 | 5.5 | 5.8 | 6.9 | 20.2 | 14.9 | 14.4 | 1.67 (1.13 to 2.46) | 0.010 | 1.65 (1.12 to 2.44) | 0.012 | 1.65 (1.11 to 2.44) | 0.013 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | 79.3 | 77.7 | 80.8 | 78.4 | 78.0 | 78.7 | 1.01 (0.78 to 1.30) | 0.957 | 1.00 (0.78 to 1.29) | 0.990 | 0.98 (0.74 to 1.29) | 0.874 |
| Sex | ||||||||||||
| Female | 76.0 | 73.6 | 75.8 | 76.1 | 74.5 | 75.4 | 1.00 (0.71 to 1.41) | 0.993 | 0.99 (0.71 to 1.40) | 0.972 | 0.97 (0.67 to 1.40) | 0.861 |
| Male | 82.7 | 81.7 | 86.4 | 80.8 | 81.6 | 82.2 | 1.03 (0.71 to 1.49) | 0.885 | 1.03 (0.70 to 1.50) | 0.893 | 0.99 (0.66 to 1.48) | 0.952 |
| Age (years) | ||||||||||||
| 16–25 | 92.8 | 90.0 | 89.4 | 87.4 | 84.1 | 87.8 | 0.77 (0.39 to 1.51) | 0.447 | 0.81 (0.41 to 1.59) | 0.533 | 0.94 (0.44 to 2.02) | 0.872 |
| 26–45 | 84.3 | 81.8 | 83.7 | 83.5 | 82.3 | 82.2 | 0.98 (0.62 to 1.55) | 0.932 | 0.99 (0.62 to 1.59) | 0.983 | 0.92 (0.55 to 1.54) | 0.758 |
| 46–65 | 75.4 | 77.0 | 83.8 | 82.7 | 78.5 | 77.1 | 1.84 (1.14 to 2.98) | 0.013 | 1.79 (1.10 to 2.90) | 0.018 | 1.69 (1.01 to 2.81) | 0.044 |
| ≥ 66 | 68.2 | 64.0 | 67.4 | 61.8 | 65.8 | 68.6 | 0.71 (0.43 to 1.14) | 0.158 | 0.68 (0.42 to 1.11) | 0.121 | 0.67 (0.40 to 1.13) | 0.131 |
| Ethnicity | ||||||||||||
| White | 80.8 | 79.9 | 82.6 | 81.4 | 82.8 | 82.5 | 0.94 (0.71 to 1.26) | 0.696 | 0.93 (0.70 to 1.23) | 0.603 | 0.90 (0.67 to 1.22) | 0.493 |
| Non-white | 52.8 | 45.7 | 51.1 | 53.6 | 44.9 | 49.5 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 89.3 | 87.1 | 88.3 | 86.9 | 85.7 | 88.4 | 0.85 (0.55 to 1.30) | 0.452 | 0.85 (0.56 to 1.31) | 0.473 | 0.76 (0.48 to 1.21) | 0.252 |
| Economically inactive | 69.5 | 67.9 | 72.5 | 70.2 | 71.2 | 71.6 | 0.98 (0.68 to 1.40) | 0.906 | 0.97 (0.67 to 1.39) | 0.857 | 0.98 (0.66 to 1.45) | 0.922 |
| Unemployed | 73.2 | 72.8 | 80.8 | 76.7 | 72.1 | 71.1 | 1.60 (0.82 to 3.12) | 0.171 | 1.65 (0.84 to 3.25) | 0.145 | 1.83 (0.90 to 3.72) | 0.094 |
| Marital status | ||||||||||||
| Married/co-habiting | 80.4 | 77.8 | 81.5 | 78.2 | 80.0 | 76.8 | 0.94 (0.64 to 1.38) | 0.752 | 0.94 (0.64 to 1.39) | 0.760 | 0.84 (0.54 to 1.29) | 0.422 |
| Separated/divorced/widowed | 69.3 | 66.9 | 68.8 | 65.3 | 61.1 | 67.5 | 0.97 (0.56 to 1.69) | 0.915 | 0.95 (0.54 to 1.65) | 0.844 | 1.00 (0.55 to 1.82) | 0.996 |
| Single | 83.3 | 82.9 | 85.9 | 84.8 | 82.2 | 85.7 | 1.17 (0.77 to 1.78) | 0.467 | 1.15 (0.75 to 1.76) | 0.521 | 1.08 (0.69 to 1.69) | 0.746 |
| Housing ownership | ||||||||||||
| Owner occupied | 81.3 | 80.2 | 82.3 | 79.4 | 79.5 | 79.1 | 1.00 (0.65 to 1.54) | 0.983 | 0.97 (0.63 to 1.50) | 0.908 | 0.87 (0.55 to 1.38) | 0.553 |
| Rented | 80.4 | 78.9 | 81.3 | 79.2 | 81.7 | 81.5 | 0.84 (0.52 to 1.35) | 0.466 | 0.84 (0.52 to 1.36) | 0.486 | 0.81 (0.49 to 1.35) | 0.423 |
| Housing association/council | 66.4 | 70.5 | 72.6 | 72.5 | 68.8 | 68.5 | 1.54 (0.86 to 2.76) | 0.148 | 1.52 (0.85 to 2.72) | 0.160 | 1.53 (0.84 to 2.80) | 0.169 |
| Other | 87.6 | 77.2 | 85.7 | 79.3 | 73.3 | 81.0 | 0.72 (0.37 to 1.38) | 0.316 | 0.72 (0.37 to 1.40) | 0.334 | 0.91 (0.42 to 1.97) | 0.819 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | 26.1 | 26.1 | 26.2 | 25.2 | 24.5 | 23.7 | 1.06 (0.85 to 1.33) | 0.609 | 1.07 (0.86 to 1.34) | 0.550 | 1.09 (0.86 to 1.38) | 0.474 |
| Sex | ||||||||||||
| Female | 20.6 | 19.1 | 18.8 | 19.6 | 20.2 | 18.1 | 0.93 (0.66 to 1.30) | 0.661 | 0.95 (0.67 to 1.34) | 0.753 | 0.94 (0.66 to 1.33) | 0.719 |
| Male | 31.9 | 33.1 | 34.3 | 31.0 | 28.9 | 29.6 | 1.18 (0.87 to 1.60) | 0.281 | 1.18 (0.87 to 1.60) | 0.282 | 1.22 (0.89 to 1.67) | 0.212 |
| Age (years) | ||||||||||||
| 16–25 | 42.4 | 37.1 | 38.5 | 35.6 | 33.9 | 31.5 | 0.94 (0.61 to 1.44) | 0.767 | 0.95 (0.62 to 1.45) | 0.801 | 1.01 (0.65 to 1.58) | 0.951 |
| 26–45 | 30.1 | 30.6 | 28.0 | 29.4 | 28.3 | 31.9 | 0.94 (0.64 to 1.37) | 0.741 | 0.93 (0.64 to 1.36) | 0.720 | 0.89 (0.60 to 1.31) | 0.548 |
| 46–65 | 25.7 | 28.0 | 28.6 | 33.1 | 28.1 | 24.6 | 1.57 (1.03 to 2.41) | 0.036 | 1.59 (1.04 to 2.43) | 0.032 | 1.66 (1.07 to 2.57) | 0.023 |
| ≥ 66 | 10.6 | 10.1 | 11.7 | 5.0 | 6.7 | 6.7 | 0.75 (0.31 to 1.86) | 0.542 | 0.75 (0.30 to 1.86) | 0.539 | 0.74 (0.29 to 1.89) | 0.532 |
| Ethnicity | ||||||||||||
| White | 27.0 | 26.8 | 26.9 | 26.3 | 26.7 | 25.2 | 1.01 (0.80 to 1.28) | 0.927 | 1.02 (0.81 to 1.29) | 0.864 | 1.04 (0.82 to 1.32) | 0.751 |
| Non-white | 10.4 | 14.6 | 14.3 | 15.5 | 9.3 | 12.1 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 31.9 | 31.6 | 29.7 | 32.4 | 29.7 | 30.3 | 1.05 (0.78 to 1.42) | 0.736 | 1.05 (0.78 to 1.43) | 0.736 | 1.06 (0.78 to 1.45) | 0.701 |
| Economically inactive | 17.9 | 18.8 | 20.0 | 16.6 | 18.0 | 15.5 | 1.09 (0.73 to 1.64) | 0.679 | 1.12 (0.74 to 1.68) | 0.590 | 1.17 (0.76 to 1.79) | 0.477 |
| Unemployed | 33.9 | 30.3 | 36.7 | 29.1 | 29.3 | 29.7 | 0.96 (0.51 to 1.81) | 0.911 | 1.02 (0.54 to 1.92) | 0.950 | 1.13 (0.57 to 2.21) | 0.728 |
| Marital status | ||||||||||||
| Married/co-habiting | 20.7 | 22.0 | 21.9 | 22.7 | 21.6 | 19.8 | 1.20 (0.84 to 1.73) | 0.316 | 1.21 (0.84 to 1.74) | 0.310 | 1.17 (0.80 to 1.70) | 0.416 |
| Separated/divorced/widowed | 15.9 | 16.2 | 15.1 | 16.2 | 12.3 | 11.9 | 1.37 (0.69 to 2.71) | 0.374 | 1.38 (0.69 to 2.73) | 0.361 | 1.64 (0.80 to 3.37) | 0.179 |
| Single | 37.7 | 35.6 | 36.4 | 32.2 | 31.5 | 32.7 | 0.94 (0.68 to 1.30) | 0.700 | 0.94 (0.68 to 1.29) | 0.693 | 0.92 (0.66 to 1.28) | 0.627 |
| Housing ownership | ||||||||||||
| Owner occupied | 20.3 | 22.8 | 19.4 | 21.4 | 21.3 | 19.5 | 1.11 (0.75 to 1.63) | 0.611 | 1.11 (0.75 to 1.64) | 0.605 | 1.07 (0.72 to 1.61) | 0.731 |
| Rented | 30.4 | 29.3 | 30.7 | 30.6 | 29.6 | 27.7 | 1.07 (0.72 to 1.57) | 0.738 | 1.08 (0.73 to 1.59) | 0.711 | 1.16 (0.77 to 1.75) | 0.466 |
| Housing association/council | 24.9 | 22.8 | 26.4 | 22.1 | 18.4 | 23.5 | 1.05 (0.56 to 1.96) | 0.889 | 1.06 (0.56 to 1.98) | 0.861 | 1.03 (0.54 to 1.98) | 0.924 |
| Other | 36.2 | 32.8 | 37.0 | 26.0 | 25.3 | 26.1 | 0.96 (0.57 to 1.63) | 0.882 | 0.96 (0.57 to 1.63) | 0.886 | 1.07 (0.62 to 1.86) | 0.807 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | 11.3 | 9.0 | 11.6 | 8.5 | 9.3 | 8.8 | 0.84 (0.60 to 1.17) | 0.296 | 0.85 (0.61 to 1.18) | 0.328 | 0.85 (0.61 to 1.20) | 0.354 |
| Sex | ||||||||||||
| Female | 8.7 | 5.9 | 7.5 | 7.3 | 6.6 | 5.7 | 0.91 (0.54 to 1.53) | 0.716 | 0.94 (0.55 to 1.58) | 0.803 | 0.94 (0.55 to 1.59) | 0.818 |
| Male | 14.1 | 12.1 | 16.2 | 9.7 | 12.1 | 11.9 | 0.79 (0.51 to 1.21) | 0.273 | 0.79 (0.51 to 1.20) | 0.270 | 0.79 (0.51 to 1.23) | 0.295 |
| Age (years) | ||||||||||||
| 16–25 | 17.2 | 11.8 | 17.9 | 10.9 | 10.9 | 9.4 | 0.90 (0.48 to 1.70) | 0.755 | 0.89 (0.48 to 1.67) | 0.718 | 0.90 (0.47 to 1.71) | 0.741 |
| 26–45 | 12.6 | 10.9 | 11.8 | 10.3 | 12.1 | 12.0 | 0.75 (0.43 to 1.29) | 0.296 | 0.77 (0.44 to 1.32) | 0.338 | 0.76 (0.43 to 1.34) | 0.343 |
| 46–65 | 12.8 | 10.1 | 12.5 | 11.7 | 11.1 | 10.7 | 0.95 (0.52 to 1.73) | 0.859 | 0.97 (0.53 to 1.77) | 0.914 | 1.04 (0.55 to 1.94) | 0.913 |
| ≥ 66 | 4.3 | 3.4 | 5.6 | 1.6 | 2.3 | 2.6 | 0.67 (0.14 to 3.08) | 0.602 | 0.65 (0.14 to 3.02) | 0.582 | 0.67 (0.14 to 3.12) | 0.606 |
| Ethnicity | ||||||||||||
| White | 11.9 | 9.3 | 11.9 | 8.8 | 10.5 | 9.2 | 0.77 (0.55 to 1.08) | 0.135 | 0.79 (0.56 to 1.10) | 0.162 | 0.79 (0.56 to 1.12) | 0.192 |
| Non-white | 1.2 | 4.8 | 6.1 | 6.1 | 1.4 | 5.2 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 11.8 | 9.2 | 10.8 | 9.5 | 9.9 | 10.2 | 0.78 (0.49 to 1.25) | 0.306 | 0.79 (0.49 to 1.25) | 0.314 | 0.79 (0.49 to 1.27) | 0.331 |
| Economically inactive | 9.0 | 7.2 | 9.9 | 6.0 | 7.3 | 5.2 | 0.91 (0.50 to 1.64) | 0.746 | 0.92 (0.51 to 1.65) | 0.773 | 0.93 (0.51 to 1.71) | 0.814 |
| Unemployed | 19.2 | 16.2 | 24.5 | 13.5 | 16.4 | 16.5 | 0.85 (0.39 to 1.87) | 0.693 | 0.93 (0.42 to 2.04) | 0.849 | 1.02 (0.45 to 2.31) | 0.970 |
| Marital status | ||||||||||||
| Married/co-habiting | 8.8 | 6.3 | 8.4 | 6.7 | 7.3 | 5.5 | 0.87 (0.48 to 1.55) | 0.624 | 0.86 (0.48 to 1.55) | 0.624 | 0.81 (0.45 to 1.45) | 0.470 |
| Separated/divorced/widowed | 8.3 | 5.3 | 7.0 | 6.3 | 6.5 | 6.1 | 0.72 (0.28 to 1.88) | 0.507 | 0.74 (0.28 to 1.91) | 0.531 | 0.84 (0.31 to 2.27) | 0.731 |
| Single | 15.9 | 13.9 | 17.5 | 11.5 | 12.2 | 13.0 | 0.90 (0.57 to 1.41) | 0.638 | 0.90 (0.57 to 1.40) | 0.630 | 0.87 (0.55 to 1.39) | 0.567 |
| Housing ownership | ||||||||||||
| Owner occupied | 8.1 | 6.7 | 6.8 | 6.4 | 7.7 | 7.0 | 0.72 (0.39 to 1.32) | 0.287 | 0.72 (0.39 to 1.32) | 0.287 | 0.67 (0.36 to 1.26) | 0.218 |
| Rented | 13.6 | 8.7 | 13.3 | 11.8 | 10.7 | 7.9 | 1.01 (0.58 to 1.75) | 0.972 | 1.01 (0.58 to 1.75) | 0.972 | 1.11 (0.64 to 1.95) | 0.708 |
| Housing association/council | 12.5 | 10.7 | 13.4 | 6.4 | 8.5 | 10.1 | 0.63 (0.24 to 1.70) | 0.362 | 0.64 (0.24 to 1.73) | 0.379 | 0.63 (0.23 to 1.75) | 0.375 |
| Other | 15.1 | 13.1 | 19.8 | 8.4 | 10.8 | 13.0 | 0.75 (0.36 to 1.59) | 0.459 | 0.76 (0.36 to 1.60) | 0.472 | 0.82 (0.38 to 1.75) | 0.602 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on drinkers only | 2.61 | 2.60 | 2.72 | 2.38 | 2.59 | 2.55 | –0.13 (–0.46 to 0.20) | 0.425 | –0.08 (–0.40 to 0.25) | 0.650 | –0.12 (–0.42 to 0.18) | 0.426 |
| Sex | ||||||||||||
| Female | 2.14 | 1.98 | 2.11 | 2.00 | 2.09 | 2.07 | –0.18 (–0.60 to 0.25) | 0.417 | –0.15 (–0.57 to 0.28) | 0.504 | –0.20 (–0.59 to 0.20) | 0.330 |
| Male | 3.06 | 3.17 | 3.31 | 2.76 | 3.06 | 3.01 | –0.09 (–0.57 to 0.39) | 0.705 | –0.01 (–0.49 to 0.47) | 0.959 | –0.05 (–0.49 to 0.40) | 0.837 |
| Age (years) | ||||||||||||
| 16–25 | 3.56 | 3.33 | 3.51 | 2.99 | 3.08 | 3.03 | –0.20 (–0.78 to 0.38) | 0.490 | –0.18 (–0.76 to 0.39) | 0.536 | –0.18 (–0.75 to 0.40) | 0.548 |
| 26–45 | 2.82 | 2.79 | 2.89 | 2.95 | 3.18 | 3.22 | –0.23 (–0.83 to 0.36) | 0.446 | –0.14 (–0.74 to 0.45) | 0.637 | –0.16 (–0.72 to 0.40) | 0.568 |
| 46–65 | 2.82 | 2.61 | 2.88 | 2.36 | 2.84 | 2.74 | –0.48 (–1.15 to 0.18) | 0.153 | –0.48 (–1.14 to 0.18) | 0.156 | –0.44 (–1.06 to 0.17) | 0.160 |
| ≥ 66 | 1.16 | 1.53 | 1.42 | 0.87 | 0.70 | 0.91 | 0.37 (–0.22 to 0.97) | 0.221 | 0.40 (–0.20 to 1.00) | 0.191 | 0.45 (–0.13 to 1.04) | 0.132 |
| Ethnicity | ||||||||||||
| White | 2.63 | 2.60 | 2.71 | 2.38 | 2.64 | 2.52 | –0.17 (–0.51 to 0.17) | 0.334 | –0.11 (–0.45 to 0.23) | 0.525 | –0.13 (–0.44 to 0.18) | 0.400 |
| Non-white | 2.13 | 2.66 | 2.90 | 2.41 | 1.98 | 2.98 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 2.56 | 2.38 | 2.48 | 2.41 | 2.64 | 2.46 | –0.28 (–0.62 to 0.06) | 0.108 | –0.26 (–0.59 to 0.08) | 0.136 | –0.23 (–0.56 to 0.09) | 0.159 |
| Economically inactive | 2.19 | 2.45 | 2.42 | 1.86 | 2.12 | 2.00 | 0.04 (–0.52 to 0.60) | 0.887 | 0.12 (–0.44 to 0.67) | 0.680 | 0.07 (–0.44 to 0.58) | 0.799 |
| Unemployed | 4.65 | 4.67 | 5.40 | 3.99 | 4.48 | 4.86 | –0.28 (–1.80 to 1.24) | 0.715 | 0.02 (–1.49 to 1.52) | 0.982 | 0.36 (–1.06 to 1.78) | 0.620 |
| Marital status | ||||||||||||
| Married/co-habiting | 2.00 | 2.01 | 2.08 | 1.90 | 1.86 | 1.93 | 0.06 (–0.34 to 0.47) | 0.752 | 0.07 (–0.33 to 0.47) | 0.721 | –0.03 (–0.40 to 0.35) | 0.890 |
| Separated/divorced/widowed | 2.00 | 2.07 | 2.24 | 1.67 | 1.92 | 1.70 | 0.02 (–0.90 to 0.95) | 0.960 | 0.04 (–0.88 to 0.97) | 0.928 | –0.06 (–0.90 to 0.77) | 0.884 |
| Single | 3.56 | 3.46 | 3.59 | 3.15 | 3.42 | 3.38 | –0.28 (–0.82 to 0.26) | 0.316 | –0.19 (–0.73 to 0.35) | 0.491 | –0.25 (–0.77 to 0.26) | 0.334 |
| Housing ownership | ||||||||||||
| Owner occupied | 1.69 | 1.84 | 1.70 | 1.76 | 1.73 | 1.76 | 0.10 (–0.32 to 0.51) | 0.642 | 0.12 (–0.29 to 0.53) | 0.574 | 0.06 (–0.32 to 0.44) | 0.762 |
| Rented | 2.95 | 2.78 | 3.28 | 2.61 | 3.12 | 2.99 | –0.37 (–0.93 to 0.19) | 0.193 | –0.35 (–0.90 to 0.21) | 0.219 | –0.26 (–0.79 to 0.26) | 0.321 |
| Housing association/council | 3.67 | 3.49 | 3.56 | 2.99 | 2.74 | 3.06 | –0.06 (–1.26 to 1.14) | 0.925 | –0.09 (–1.29 to 1.11) | 0.882 | –0.58 (–1.73 to 0.58) | 0.328 |
| Other | 3.47 | 3.39 | 3.71 | 2.96 | 3.33 | 3.17 | –0.20 (–1.09 to 0.70) | 0.668 | –0.06 (–0.95 to 0.83) | 0.897 | 0.05 (–0.78 to 0.89) | 0.904 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on drinkers only | 39.1 | 38.7 | 39.5 | 36.8 | 39.4 | 40.8 | 0.87 (0.70 to 1.10) | 0.239 | 0.89 (0.71 to 1.12) | 0.323 | 0.87 (0.68 to 1.10) | 0.249 |
| Sex | ||||||||||||
| Female | 31.2 | 29.1 | 31.5 | 27.9 | 33.4 | 33.6 | 0.74 (0.52 to 1.04) | 0.083 | 0.75 (0.53 to 1.06) | 0.102 | 0.70 (0.49 to 1.00) | 0.049 |
| Male | 46.7 | 47.6 | 47.2 | 45.6 | 44.9 | 47.8 | 1.00 (0.73 to 1.36) | 0.985 | 1.02 (0.75 to 1.39) | 0.916 | 1.04 (0.75 to 1.44) | 0.826 |
| Age (years) | ||||||||||||
| 16–25 | 59.0 | 52.4 | 57.0 | 47.4 | 51.7 | 52.5 | 0.69 (0.45 to 1.08) | 0.103 | 0.70 (0.45 to 1.10) | 0.120 | 0.75 (0.48 to 1.18) | 0.216 |
| 26–45 | 38.9 | 39.2 | 39.3 | 42.7 | 44.9 | 46.5 | 0.90 (0.61 to 1.32) | 0.599 | 0.94 (0.64 to 1.39) | 0.761 | 0.90 (0.60 to 1.35) | 0.626 |
| 46–65 | 41.4 | 36.9 | 39.8 | 37.9 | 41.7 | 43.8 | 0.73 (0.47 to 1.13) | 0.157 | 0.72 (0.46 to 1.12) | 0.147 | 0.72 (0.46 to 1.14) | 0.164 |
| ≥ 66 | 18.0 | 25.8 | 21.7 | 14.9 | 12.2 | 17.2 | 1.42 (0.66 to 3.07) | 0.369 | 1.45 (0.67 to 3.17) | 0.346 | 1.61 (0.72 to 3.58) | 0.245 |
| Ethnicity | ||||||||||||
| White | 39.3 | 38.9 | 39.6 | 36.8 | 40.9 | 41.0 | 0.84 (0.66 to 1.06) | 0.136 | 0.86 (0.68 to 1.08) | 0.195 | 0.84 (0.66 to 1.08) | 0.171 |
| Non-white | 33.1 | 33.6 | 37.5 | 37.3 | 19.7 | 38.8 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 41.0 | 37.4 | 39.4 | 41.0 | 44.0 | 42.8 | 0.81 (0.60 to 1.10) | 0.180 | 0.82 (0.61 to 1.11) | 0.198 | 0.83 (0.60 to 1.13) | 0.236 |
| Economically inactive | 32.6 | 37.1 | 35.5 | 28.5 | 31.1 | 32.9 | 1.00 (0.66 to 1.51) | 0.999 | 1.04 (0.69 to 1.58) | 0.838 | 1.03 (0.65 to 1.62) | 0.910 |
| Unemployed | 55.4 | 54.2 | 57.4 | 46.6 | 50.6 | 60.7 | 0.69 (0.35 to 1.36) | 0.288 | 0.77 (0.39 to 1.52) | 0.444 | 0.88 (0.43 to 1.80) | 0.724 |
| Marital status | ||||||||||||
| Married/co-habiting | 29.3 | 31.7 | 31.0 | 30.6 | 31.9 | 34.1 | 0.99 (0.68 to 1.43) | 0.954 | 0.99 (0.68 to 1.44) | 0.966 | 0.92 (0.63 to 1.35) | 0.664 |
| Separated/divorced/widowed | 26.0 | 31.1 | 28.3 | 25.9 | 28.5 | 27.0 | 1.09 (0.55 to 2.16) | 0.796 | 1.10 (0.56 to 2.16) | 0.789 | 1.13 (0.55 to 2.33) | 0.741 |
| Single | 55.8 | 49.4 | 52.9 | 47.3 | 48.8 | 51.4 | 0.75 (0.54 to 1.04) | 0.083 | 0.77 (0.55 to 1.07) | 0.115 | 0.74 (0.53 to 1.05) | 0.089 |
| Housing ownership | ||||||||||||
| Owner occupied | 24.2 | 29.7 | 26.8 | 29.4 | 28.6 | 33.1 | 1.15 (0.77 to 1.71) | 0.509 | 1.15 (0.77 to 1.72) | 0.507 | 1.09 (0.72 to 1.66) | 0.670 |
| Rented | 47.0 | 43.6 | 49.7 | 45.3 | 49.3 | 46.8 | 0.88 (0.59 to 1.31) | 0.539 | 0.89 (0.60 to 1.33) | 0.566 | 0.94 (0.61 to 1.43) | 0.763 |
| Housing association/council | 47.5 | 44.9 | 43.2 | 40.0 | 35.6 | 45.7 | 0.84 (0.44 to 1.58) | 0.587 | 0.83 (0.44 to 1.57) | 0.568 | 0.65 (0.32 to 1.30) | 0.223 |
| Other | 57.8 | 48.3 | 53.8 | 35.8 | 44.6 | 43.8 | 0.54 (0.31 to 0.92) | 0.024 | 0.57 (0.33 to 0.98) | 0.042 | 0.60 (0.35 to 1.04) | 0.069 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on drinkers only | 8.6 | 9.5 | 9.1 | 8.6 | 10.2 | 8.9 | 0.96 (0.65 to 1.41) | 0.834 | 0.98 (0.67 to 1.44) | 0.925 | 0.97 (0.65 to 1.45) | 0.875 |
| Sex | ||||||||||||
| Female | 8.5 | 7.5 | 7.6 | 8.1 | 8.3 | 9.3 | 0.80 (0.45 to 1.41) | 0.442 | 0.82 (0.46 to 1.44) | 0.486 | 0.79 (0.44 to 1.41) | 0.422 |
| Male | 8.7 | 11.3 | 10.5 | 9.0 | 12.0 | 8.4 | 1.11 (0.66 to 1.87) | 0.704 | 1.13 (0.67 to 1.91) | 0.652 | 1.14 (0.66 to 1.98) | 0.636 |
| Age (years) | ||||||||||||
| 16–25 | 18.4 | 20.7 | 19.4 | 18.9 | 20.1 | 18.1 | 1.10 (0.62 to 1.93) | 0.751 | 1.07 (0.61 to 1.89) | 0.816 | 1.07 (0.60 to 1.91) | 0.820 |
| 26–45 | 7.3 | 8.1 | 7.8 | 6.7 | 8.6 | 8.5 | 0.84 (0.41 to 1.73) | 0.634 | 0.88 (0.43 to 1.82) | 0.736 | 0.86 (0.40 to 1.81) | 0.683 |
| 46–65 | 8.2 | 7.3 | 7.4 | 6.3 | 7.7 | 6.6 | 0.78 (0.33 to 1.82) | 0.564 | 0.79 (0.34 to 1.84) | 0.581 | 0.79 (0.33 to 1.88) | 0.590 |
| ≥ 66 | 1.9 | 2.6 | 3.1 | 2.8 | 3.8 | 1.9 | 1.52 (0.22 to 10.40) | 0.670 | 1.50 (0.22 to 10.46) | 0.682 | 1.56 (0.23 to 10.42) | 0.645 |
| Ethnicity | ||||||||||||
| White | 8.8 | 9.2 | 8.9 | 8.5 | 10.2 | 8.7 | 0.92 (0.62 to 1.37) | 0.679 | 0.94 (0.63 to 1.40) | 0.763 | 0.95 (0.63 to 1.44) | 0.816 |
| Non-white | 4.8 | 16.3 | 15.0 | 9.3 | 10.8 | 10.7 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 8.6 | 7.1 | 6.0 | 7.0 | 7.8 | 7.0 | 0.70 (0.40 to 1.23) | 0.216 | 0.70 (0.40 to 1.23) | 0.211 | 0.71 (0.40 to 1.26) | 0.245 |
| Economically inactive | 7.3 | 9.9 | 10.1 | 10.5 | 11.9 | 9.4 | 1.38 (0.75 to 2.55) | 0.307 | 1.42 (0.77 to 2.64) | 0.263 | 1.43 (0.74 to 2.74) | 0.284 |
| Unemployed | 14.4 | 22.8 | 22.8 | 9.0 | 16.9 | 14.7 | 0.93 (0.33 to 2.60) | 0.892 | 1.05 (0.37 to 2.96) | 0.928 | 1.10 (0.38 to 3.20) | 0.858 |
| Marital status | ||||||||||||
| Married/co-habiting | 5.0 | 4.3 | 5.2 | 4.1 | 3.6 | 3.7 | 1.07 (0.47 to 2.41) | 0.871 | 1.09 (0.48 to 2.46) | 0.832 | 1.03 (0.45 to 2.34) | 0.948 |
| Separated/divorced/widowed | 6.4 | 6.9 | 4.8 | 6.8 | 10.4 | 6.0 | 0.76 (0.21 to 2.68) | 0.664 | 0.73 (0.20 to 2.61) | 0.628 | 0.70 (0.19 to 2.51) | 0.580 |
| Single | 13.7 | 16.1 | 14.9 | 14.0 | 16.0 | 14.2 | 1.06 (0.66 to 1.70) | 0.811 | 1.06 (0.66 to 1.71) | 0.801 | 1.01 (0.62 to 1.65) | 0.953 |
| Housing ownership | ||||||||||||
| Owner occupied | 4.5 | 3.7 | 3.5 | 4.0 | 6.1 | 4.5 | 0.59 (0.24 to 1.46) | 0.256 | 0.61 (0.25 to 1.51) | 0.286 | 0.61 (0.24 to 1.52) | 0.285 |
| Rented | 11.3 | 12.4 | 12.1 | 11.6 | 11.8 | 7.9 | 1.27 (0.68 to 2.36) | 0.446 | 1.32 (0.71 to 2.45) | 0.384 | 1.43 (0.75 to 2.72) | 0.275 |
| Housing association/council | 10.8 | 10.9 | 10.7 | 9.9 | 9.4 | 10.2 | 1.01 (0.37 to 2.77) | 0.988 | 1.00 (0.36 to 2.74) | 0.993 | 0.80 (0.27 to 2.30) | 0.674 |
| Other | 13.1 | 18.4 | 17.4 | 12.4 | 16.8 | 19.2 | 0.93 (0.44 to 1.98) | 0.849 | 0.89 (0.42 to 1.91) | 0.774 | 0.97 (0.44 to 2.11) | 0.933 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on drinkers only | 56.5 | 52.6 | 56.8 | 53.6 | 48.8 | 51.6 | 1.07 (0.86 to 1.35) | 0.538 | 1.04 (0.83 to 1.31) | 0.704 | 1.02 (0.81 to 1.29) | 0.847 |
| Sex | ||||||||||||
| Female | 61.1 | 52.6 | 57.6 | 53.9 | 49.4 | 54.8 | 0.85 (0.61 to 1.18) | 0.327 | 0.82 (0.59 to 1.14) | 0.243 | 0.81 (0.58 to 1.13) | 0.210 |
| Male | 52.0 | 52.6 | 56.0 | 53.3 | 48.3 | 48.6 | 1.34 (0.98 to 1.83) | 0.066 | 1.30 (0.95 to 1.78) | 0.099 | 1.27 (0.92 to 1.75) | 0.146 |
| Age (years) | ||||||||||||
| 16–25 | 43.7 | 42.7 | 40.0 | 39.6 | 35.7 | 35.9 | 1.06 (0.68 to 1.68) | 0.786 | 1.05 (0.66 to 1.66) | 0.834 | 0.99 (0.62 to 1.58) | 0.963 |
| 26–45 | 56.3 | 51.4 | 56.1 | 55.5 | 49.6 | 50.8 | 1.12 (0.76 to 1.64) | 0.571 | 1.11 (0.75 to 1.64) | 0.588 | 1.14 (0.77 to 1.69) | 0.508 |
| 46–65 | 59.6 | 54.8 | 61.3 | 53.8 | 51.3 | 57.4 | 0.94 (0.60 to 1.45) | 0.765 | 0.92 (0.59 to 1.42) | 0.696 | 0.91 (0.58 to 1.41) | 0.667 |
| ≥ 66 | 64.9 | 62.0 | 68.2 | 66.0 | 60.6 | 63.4 | 1.21 (0.66 to 2.22) | 0.537 | 1.16 (0.63 to 2.11) | 0.635 | 1.17 (0.64 to 2.13) | 0.607 |
| Ethnicity | ||||||||||||
| White | 56.4 | 52.1 | 56.8 | 53.4 | 48.2 | 51.2 | 1.08 (0.85 to 1.36) | 0.524 | 1.05 (0.83 to 1.32) | 0.711 | 1.02 (0.80 to 1.29) | 0.895 |
| Non-white | 57.9 | 65.0 | 56.9 | 56.1 | 56.3 | 56.8 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 52.7 | 48.5 | 54.6 | 48.0 | 45.4 | 47.5 | 1.02 (0.76 to 1.38) | 0.873 | 1.01 (0.75 to 1.37) | 0.938 | 0.99 (0.73 to 1.34) | 0.942 |
| Economically inactive | 60.4 | 56.0 | 58.0 | 55.9 | 51.9 | 57.2 | 0.92 (0.62 to 1.37) | 0.696 | 0.88 (0.59 to 1.31) | 0.529 | 0.88 (0.59 to 1.32) | 0.552 |
| Unemployed | 62.6 | 63.7 | 64.7 | 69.6 | 54.4 | 49.4 | 2.29 (1.12 to 4.70) | 0.024 | 2.25 (1.09 to 4.62) | 0.028 | 2.26 (1.09 to 4.65) | 0.028 |
| Marital status | ||||||||||||
| Married/co-habiting | 63.6 | 56.1 | 62.3 | 56.0 | 53.6 | 59.0 | 0.83 (0.58 to 1.19) | 0.321 | 0.82 (0.58 to 1.18) | 0.287 | 0.83 (0.58 to 1.18) | 0.297 |
| Separated/divorced/widowed | 60.5 | 60.9 | 65.4 | 66.6 | 56.4 | 60.7 | 1.57 (0.83 to 2.98) | 0.169 | 1.56 (0.82 to 2.96) | 0.175 | 1.57 (0.82 to 3.00) | 0.173 |
| Single | 46.7 | 45.4 | 47.5 | 46.5 | 42.7 | 42.3 | 1.17 (0.83 to 1.64) | 0.372 | 1.14 (0.81 to 1.60) | 0.450 | 1.12 (0.79 to 1.59) | 0.516 |
| Housing ownership | ||||||||||||
| Owner occupied | 63.7 | 57.0 | 62.8 | 57.9 | 54.2 | 60.6 | 0.88 (0.60 to 1.29) | 0.503 | 0.86 (0.58 to 1.26) | 0.430 | 0.87 (0.59 to 1.28) | 0.484 |
| Rented | 52.2 | 49.0 | 50.6 | 48.1 | 42.8 | 45.2 | 1.08 (0.72 to 1.62) | 0.716 | 1.06 (0.71 to 1.60) | 0.763 | 1.01 (0.67 to 1.53) | 0.959 |
| Housing association/council | 59.5 | 56.5 | 60.9 | 62.6 | 63.1 | 50.9 | 1.24 (0.65 to 2.35) | 0.509 | 1.23 (0.65 to 2.33) | 0.530 | 1.23 (0.64 to 2.35) | 0.536 |
| Other | 41.3 | 42.8 | 46.2 | 48.5 | 40.9 | 44.1 | 1.45 (0.85 to 2.47) | 0.170 | 1.38 (0.81 to 2.34) | 0.241 | 1.27 (0.74 to 2.19) | 0.382 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on drinkers only | 33.5 | 38.6 | 34.7 | 40.4 | 41.4 | 41.9 | 1.09 (0.86 to 1.37) | 0.476 | 1.12 (0.89 to 1.41) | 0.337 | 1.16 (0.92 to 1.48) | 0.213 |
| Sex | ||||||||||||
| Female | 26.6 | 37.1 | 33.4 | 38.1 | 39.1 | 38.3 | 1.45 (1.04 to 2.03) | 0.030 | 1.49 (1.07 to 2.09) | 0.020 | 1.56 (1.10 to 2.21) | 0.014 |
| Male | 40.1 | 39.9 | 36.0 | 42.6 | 43.4 | 45.4 | 0.85 (0.62 to 1.17) | 0.311 | 0.88 (0.64 to 1.21) | 0.422 | 0.92 (0.66 to 1.28) | 0.607 |
| Age (years) | ||||||||||||
| 16–25 | 50.0 | 52.7 | 54.0 | 58.5 | 60.3 | 60.3 | 1.06 (0.68 to 1.66) | 0.797 | 1.08 (0.68 to 1.69) | 0.754 | 1.14 (0.72 to 1.80) | 0.586 |
| 26–45 | 33.8 | 39.8 | 36.2 | 38.0 | 39.0 | 40.8 | 1.11 (0.75 to 1.65) | 0.610 | 1.11 (0.75 to 1.66) | 0.597 | 1.09 (0.73 to 1.63) | 0.680 |
| 46–65 | 28.9 | 36.7 | 28.8 | 36.0 | 37.9 | 35.1 | 1.15 (0.72 to 1.82) | 0.557 | 1.17 (0.74 to 1.87) | 0.497 | 1.19 (0.74 to 1.90) | 0.481 |
| ≥ 66 | 23.0 | 24.2 | 21.5 | 29.5 | 26.2 | 31.0 | 1.03 (0.54 to 1.96) | 0.928 | 1.09 (0.57 to 2.07) | 0.791 | 1.10 (0.58 to 2.10) | 0.766 |
| Ethnicity | ||||||||||||
| White | 33.7 | 39.1 | 34.6 | 40.7 | 41.8 | 42.5 | 1.07 (0.85 to 1.36) | 0.554 | 1.11 (0.88 to 1.41) | 0.387 | 1.16 (0.91 to 1.49) | 0.228 |
| Non-white | 27.1 | 26.4 | 37.4 | 36.5 | 35.5 | 34.5 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 38.0 | 43.4 | 36.8 | 46.0 | 44.9 | 45.8 | 1.12 (0.83 to 1.51) | 0.466 | 1.14 (0.84 to 1.54) | 0.396 | 1.19 (0.87 to 1.63) | 0.266 |
| Economically inactive | 28.2 | 33.4 | 33.5 | 38.2 | 38.8 | 36.4 | 1.32 (0.88 to 1.97) | 0.183 | 1.38 (0.92 to 2.08) | 0.116 | 1.42 (0.93 to 2.18) | 0.105 |
| Unemployed | 29.0 | 30.4 | 27.4 | 24.1 | 32.8 | 44.8 | 0.48 (0.23 to 1.04) | 0.064 | 0.48 (0.22 to 1.04) | 0.063 | 0.46 (0.21 to 0.99) | 0.048 |
| Marital status | ||||||||||||
| Married/co-habiting | 25.7 | 32.9 | 28.8 | 38.0 | 34.6 | 34.1 | 1.50 (1.04 to 2.18) | 0.032 | 1.53 (1.05 to 2.23) | 0.025 | 1.53 (1.05 to 2.23) | 0.028 |
| Separated/divorced/widowed | 28.7 | 29.9 | 23.1 | 22.9 | 32.7 | 31.9 | 0.55 (0.28 to 1.10) | 0.090 | 0.56 (0.28 to 1.11) | 0.095 | 0.55 (0.27 to 1.10) | 0.093 |
| Single | 44.2 | 48.3 | 45.6 | 49.1 | 49.6 | 51.9 | 1.04 (0.75 to 1.46) | 0.807 | 1.06 (0.75 to 1.48) | 0.754 | 1.08 (0.77 to 1.54) | 0.648 |
| Housing ownership | ||||||||||||
| Owner occupied | 24.8 | 32.9 | 25.7 | 34.7 | 31.5 | 32.2 | 1.42 (0.95 to 2.11) | 0.088 | 1.47 (0.98 to 2.19) | 0.061 | 1.44 (0.96 to 2.16) | 0.078 |
| Rented | 38.5 | 42.7 | 43.7 | 48.1 | 50.5 | 49.8 | 1.12 (0.75 to 1.67) | 0.588 | 1.12 (0.75 to 1.67) | 0.592 | 1.18 (0.78 to 1.79) | 0.424 |
| Housing association/council | 33.5 | 37.3 | 34.6 | 30.7 | 30.0 | 44.2 | 0.83 (0.42 to 1.61) | 0.578 | 0.84 (0.43 to 1.63) | 0.602 | 0.82 (0.42 to 1.61) | 0.558 |
| Other | 48.3 | 48.1 | 45.1 | 45.2 | 50.8 | 47.5 | 0.80 (0.47 to 1.36) | 0.408 | 0.83 (0.49 to 1.42) | 0.495 | 0.92 (0.53 to 1.60) | 0.776 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on drinkers only | 53.6 | 53.8 | 53.3 | 50.6 | 53.8 | 55.4 | 0.85 (0.68 to 1.07) | 0.165 | 0.87 (0.69 to 1.09) | 0.217 | 0.83 (0.65 to 1.05) | 0.127 |
| Sex | ||||||||||||
| Female | 45.3 | 43.1 | 46.9 | 43.2 | 51.0 | 49.9 | 0.74 (0.54 to 1.02) | 0.070 | 0.75 (0.54 to 1.04) | 0.084 | 0.69 (0.49 to 0.96) | 0.030 |
| Male | 61.6 | 63.6 | 59.4 | 57.9 | 56.3 | 60.6 | 0.97 (0.71 to 1.34) | 0.867 | 0.99 (0.72 to 1.36) | 0.939 | 1.00 (0.71 to 1.41) | 0.982 |
| Age (years) | ||||||||||||
| 16–25 | 76.2 | 72.5 | 73.3 | 66.0 | 73.7 | 72.1 | 0.60 (0.37 to 0.97) | 0.039 | 0.62 (0.38 to 1.01) | 0.053 | 0.66 (0.40 to 1.08) | 0.097 |
| 26–45 | 59.6 | 59.4 | 56.8 | 59.8 | 62.0 | 67.2 | 0.77 (0.53 to 1.14) | 0.195 | 0.78 (0.53 to 1.15) | 0.214 | 0.74 (0.50 to 1.11) | 0.147 |
| 46–65 | 54.2 | 50.2 | 52.7 | 51.5 | 54.3 | 55.1 | 0.79 (0.51 to 1.22) | 0.284 | 0.78 (0.51 to 1.21) | 0.269 | 0.77 (0.50 to 1.20) | 0.256 |
| ≥ 66 | 22.9 | 30.0 | 28.7 | 18.4 | 15.0 | 21.3 | 1.41 (0.70 to 2.83) | 0.331 | 1.46 (0.72 to 2.94) | 0.294 | 1.62 (0.79 to 3.33) | 0.191 |
| Ethnicity | ||||||||||||
| White | 54.0 | 53.9 | 53.2 | 50.4 | 54.9 | 55.0 | 0.82 (0.65 to 1.03) | 0.091 | 0.83 (0.66 to 1.05) | 0.127 | 0.80 (0.63 to 1.03) | 0.085 |
| Non-white | 41.7 | 52.9 | 54.1 | 52.9 | 39.9 | 60.4 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 60.1 | 57.9 | 56.6 | 59.6 | 60.8 | 61.9 | 0.83 (0.61 to 1.12) | 0.225 | 0.83 (0.61 to 1.13) | 0.234 | 0.82 (0.60 to 1.13) | 0.221 |
| Economically inactive | 40.8 | 45.7 | 45.2 | 36.5 | 43.4 | 43.2 | 0.91 (0.62 to 1.34) | 0.630 | 0.94 (0.64 to 1.39) | 0.759 | 0.90 (0.58 to 1.39) | 0.628 |
| Unemployed | 68.2 | 62.9 | 68.4 | 59.0 | 61.1 | 70.6 | 0.66 (0.33 to 1.33) | 0.245 | 0.72 (0.35 to 1.46) | 0.358 | 0.77 (0.37 to 1.60) | 0.483 |
| Marital status | ||||||||||||
| Married/co-habiting | 45.5 | 46.9 | 45.3 | 45.8 | 44.4 | 47.4 | 1.02 (0.73 to 1.44) | 0.907 | 1.02 (0.72 to 1.43) | 0.926 | 0.96 (0.67 to 1.38) | 0.837 |
| Separated/divorced/widowed | 34.8 | 42.1 | 36.0 | 33.4 | 35.2 | 36.0 | 1.08 (0.57 to 2.05) | 0.802 | 1.08 (0.57 to 2.05) | 0.805 | 1.06 (0.54 to 2.12) | 0.858 |
| Single | 71.0 | 66.1 | 68.5 | 61.9 | 66.9 | 68.9 | 0.65 (0.46 to 0.93) | 0.017 | 0.66 (0.46 to 0.94) | 0.023 | 0.62 (0.43 to 0.89) | 0.010 |
| Housing ownership | ||||||||||||
| Owner occupied | 39.0 | 44.6 | 40.5 | 42.5 | 40.8 | 42.0 | 1.21 (0.84 to 1.74) | 0.316 | 1.21 (0.84 to 1.74) | 0.309 | 1.16 (0.79 to 1.70) | 0.455 |
| Rented | 60.3 | 61.6 | 62.3 | 58.2 | 65.3 | 66.7 | 0.77 (0.51 to 1.16) | 0.213 | 0.77 (0.51 to 1.17) | 0.228 | 0.79 (0.51 to 1.23) | 0.298 |
| Housing association/council | 60.0 | 52.5 | 57.1 | 50.6 | 48.0 | 60.6 | 0.69 (0.37 to 1.31) | 0.261 | 0.69 (0.37 to 1.31) | 0.262 | 0.55 (0.28 to 1.09) | 0.087 |
| Other | 74.9 | 66.8 | 69.4 | 54.8 | 61.9 | 60.6 | 0.55 (0.31 to 0.96) | 0.037 | 0.57 (0.32 to 1.01) | 0.052 | 0.65 (0.37 to 1.13) | 0.129 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on drinkers only | 24.8 | 23.0 | 24.7 | 23.3 | 23.8 | 23.1 | 0.94 (0.73 to 1.22) | 0.656 | 0.97 (0.75 to 1.26) | 0.816 | 0.96 (0.73 to 1.27) | 0.797 |
| Sex | ||||||||||||
| Female | 18.2 | 15.0 | 15.9 | 17.8 | 18.2 | 16.9 | 0.83 (0.55 to 1.26) | 0.394 | 0.85 (0.56 to 1.29) | 0.455 | 0.81 (0.53 to 1.25) | 0.346 |
| Male | 31.2 | 30.4 | 33.2 | 28.7 | 29.0 | 29.0 | 1.01 (0.73 to 1.41) | 0.942 | 1.04 (0.75 to 1.46) | 0.799 | 1.08 (0.75 to 1.54) | 0.685 |
| Age (years) | ||||||||||||
| 16–25 | 39.7 | 34.0 | 38.7 | 35.0 | 33.7 | 32.1 | 0.95 (0.60 to 1.50) | 0.828 | 0.96 (0.60 to 1.51) | 0.847 | 1.01 (0.63 to 1.62) | 0.955 |
| 26–45 | 24.8 | 22.9 | 25.3 | 26.8 | 28.3 | 27.5 | 0.91 (0.59 to 1.41) | 0.675 | 0.95 (0.62 to 1.48) | 0.829 | 0.91 (0.57 to 1.45) | 0.678 |
| 46–65 | 23.7 | 19.2 | 22.9 | 23.3 | 22.8 | 23.9 | 0.86 (0.52 to 1.44) | 0.571 | 0.86 (0.51 to 1.43) | 0.557 | 0.91 (0.52 to 1.60) | 0.743 |
| ≥ 66 | 12.2 | 16.4 | 12.3 | 5.1 | 5.3 | 6.4 | 1.01 (0.32 to 3.25) | 0.984 | 1.02 (0.32 to 3.29) | 0.975 | 1.08 (0.32 to 3.60) | 0.902 |
| Ethnicity | ||||||||||||
| White | 25.1 | 23.0 | 24.6 | 23.0 | 24.6 | 22.7 | 0.90 (0.69 to 1.17) | 0.422 | 0.92 (0.71 to 1.21) | 0.563 | 0.93 (0.70 to 1.24) | 0.642 |
| Non-white | 16.8 | 23.4 | 27.7 | 27.5 | 13.9 | 27.7 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 22.8 | 19.0 | 21.7 | 22.9 | 24.2 | 20.8 | 0.88 (0.62 to 1.26) | 0.488 | 0.90 (0.63 to 1.28) | 0.552 | 0.92 (0.63 to 1.34) | 0.674 |
| Economically inactive | 22.6 | 24.3 | 23.2 | 19.6 | 19.8 | 19.0 | 1.08 (0.68 to 1.69) | 0.752 | 1.13 (0.71 to 1.77) | 0.608 | 1.11 (0.68 to 1.80) | 0.683 |
| Unemployed | 46.2 | 42.7 | 48.5 | 37.1 | 39.8 | 46.7 | 0.75 (0.38 to 1.50) | 0.419 | 0.82 (0.41 to 1.65) | 0.581 | 0.96 (0.46 to 2.03) | 0.923 |
| Marital status | ||||||||||||
| Married/co-habiting | 15.5 | 14.4 | 15.4 | 16.1 | 13.0 | 14.9 | 1.14 (0.72 to 1.82) | 0.575 | 1.15 (0.72 to 1.84) | 0.557 | 1.06 (0.66 to 1.72) | 0.803 |
| Separated/divorced/widowed | 19.3 | 19.3 | 18.8 | 15.0 | 18.5 | 12.8 | 0.96 (0.42 to 2.18) | 0.918 | 0.95 (0.42 to 2.17) | 0.903 | 1.01 (0.42 to 2.42) | 0.986 |
| Single | 37.6 | 33.8 | 36.9 | 33.9 | 34.7 | 33.5 | 0.90 (0.64 to 1.27) | 0.551 | 0.92 (0.65 to 1.31) | 0.660 | 0.90 (0.63 to 1.30) | 0.582 |
| Housing ownership | ||||||||||||
| Owner occupied | 12.3 | 14.0 | 12.5 | 15.5 | 13.0 | 14.1 | 1.28 (0.77 to 2.14) | 0.345 | 1.30 (0.78 to 2.17) | 0.315 | 1.27 (0.75 to 2.15) | 0.379 |
| Rented | 32.0 | 26.9 | 33.2 | 27.7 | 32.5 | 29.5 | 0.78 (0.50 to 1.20) | 0.250 | 0.77 (0.50 to 1.18) | 0.229 | 0.82 (0.52 to 1.29) | 0.384 |
| Housing association/council | 36.1 | 30.6 | 29.7 | 30.4 | 21.9 | 29.6 | 0.95 (0.48 to 1.89) | 0.893 | 0.94 (0.47 to 1.86) | 0.854 | 0.73 (0.34 to 1.60) | 0.434 |
| Other | 35.7 | 32.5 | 39.0 | 27.9 | 30.6 | 26.9 | 0.97 (0.55 to 1.71) | 0.908 | 1.02 (0.57 to 1.81) | 0.949 | 1.08 (0.60 to 1.95) | 0.799 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on drinkers only | 13.8 | 12.6 | 13.9 | 10.6 | 12.3 | 11.3 | 0.84 (0.60 to 1.19) | 0.333 | 0.88 (0.62 to 1.25) | 0.476 | 0.85 (0.59 to 1.23) | 0.385 |
| Sex | ||||||||||||
| Female | 9.5 | 7.0 | 7.6 | 8.6 | 7.1 | 7.3 | 0.91 (0.52 to 1.61) | 0.754 | 0.94 (0.53 to 1.67) | 0.844 | 0.87 (0.49 to 1.57) | 0.650 |
| Male | 18.0 | 17.7 | 20.0 | 12.5 | 17.1 | 15.2 | 0.79 (0.51 to 1.21) | 0.274 | 0.83 (0.54 to 1.28) | 0.391 | 0.80 (0.51 to 1.27) | 0.351 |
| Age (years) | ||||||||||||
| 16–25 | 19.3 | 17.1 | 19.2 | 15.5 | 13.7 | 12.6 | 1.12 (0.62 to 2.03) | 0.715 | 1.15 (0.63 to 2.09) | 0.647 | 1.14 (0.62 to 2.11) | 0.672 |
| 26–45 | 13.3 | 12.4 | 14.3 | 12.9 | 16.3 | 16.4 | 0.76 (0.44 to 1.34) | 0.347 | 0.82 (0.47 to 1.44) | 0.496 | 0.77 (0.42 to 1.41) | 0.399 |
| 46–65 | 16.1 | 13.0 | 14.5 | 9.8 | 13.3 | 11.5 | 0.64 (0.33 to 1.25) | 0.188 | 0.64 (0.33 to 1.25) | 0.194 | 0.64 (0.30 to 1.35) | 0.241 |
| ≥ 66 | 6.5 | 7.6 | 7.1 | 2.5 | 2.6 | 2.8 | 0.95 (0.17 to 5.43) | 0.954 | 0.96 (0.17 to 5.54) | 0.968 | 0.97 (0.16 to 5.83) | 0.969 |
| Ethnicity | ||||||||||||
| White | 13.8 | 12.5 | 13.8 | 10.5 | 12.7 | 11.0 | 0.82 (0.57 to 1.18) | 0.285 | 0.86 (0.60 to 1.23) | 0.404 | 0.84 (0.57 to 1.24) | 0.389 |
| Non-white | 12.8 | 15.9 | 17.7 | 11.3 | 7.3 | 15.6 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 10.2 | 8.6 | 9.8 | 7.5 | 11.2 | 8.1 | 0.67 (0.39 to 1.13) | 0.133 | 0.69 (0.41 to 1.17) | 0.169 | 0.72 (0.42 to 1.23) | 0.227 |
| Economically inactive | 14.0 | 13.8 | 13.6 | 9.2 | 9.8 | 8.9 | 0.96 (0.52 to 1.75) | 0.887 | 1.01 (0.55 to 1.84) | 0.978 | 0.93 (0.49 to 1.77) | 0.832 |
| Unemployed | 34.1 | 33.0 | 39.8 | 27.5 | 30.3 | 33.1 | 0.91 (0.44 to 1.89) | 0.798 | 1.00 (0.48 to 2.09) | 0.995 | 1.18 (0.53 to 2.61) | 0.691 |
| Marital status | ||||||||||||
| Married/co-habiting | 7.7 | 7.5 | 7.9 | 6.1 | 6.5 | 5.2 | 1.03 (0.52 to 2.04) | 0.932 | 1.06 (0.53 to 2.09) | 0.873 | 0.89 (0.44 to 1.81) | 0.745 |
| Separated/divorced/widowed | 13.7 | 10.6 | 13.0 | 6.6 | 8.8 | 7.4 | 0.67 (0.21 to 2.12) | 0.499 | 0.68 (0.22 to 2.14) | 0.509 | 0.67 (0.19 to 2.35) | 0.527 |
| Single | 20.6 | 18.9 | 20.8 | 16.7 | 18.3 | 17.8 | 0.87 (0.57 to 1.34) | 0.540 | 0.92 (0.60 to 1.42) | 0.707 | 0.88 (0.55 to 1.38) | 0.570 |
| Housing ownership | ||||||||||||
| Owner occupied | 5.9 | 6.0 | 5.6 | 5.0 | 5.1 | 5.1 | 0.96 (0.43 to 2.14) | 0.912 | 0.98 (0.44 to 2.20) | 0.963 | 0.96 (0.42 to 2.18) | 0.913 |
| Rented | 16.2 | 13.5 | 18.6 | 11.0 | 15.8 | 13.0 | 0.72 (0.40 to 1.29) | 0.269 | 0.74 (0.41 to 1.32) | 0.307 | 0.80 (0.43 to 1.48) | 0.469 |
| Housing association/council | 26.3 | 23.1 | 22.4 | 19.6 | 16.4 | 18.7 | 0.93 (0.42 to 2.08) | 0.863 | 0.92 (0.41 to 2.06) | 0.831 | 0.70 (0.28 to 1.78) | 0.458 |
| Other | 18.9 | 17.9 | 20.5 | 16.3 | 18.7 | 17.0 | 0.92 (0.46 to 1.83) | 0.811 | 0.99 (0.50 to 1.99) | 0.986 | 1.02 (0.49 to 2.11) | 0.957 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all attendees | 13.7 | 12.7 | 15.3 | 10.5 | 12.6 | 12.2 | 0.85 (0.63 to 1.14) | 0.280 | 0.86 (0.64 to 1.16) | 0.335 | 0.87 (0.64 to 1.18) | 0.377 |
| Sex | ||||||||||||
| Female | 10.6 | 8.7 | 9.7 | 8.1 | 9.2 | 8.4 | 0.78 (0.49 to 1.26) | 0.316 | 0.81 (0.50 to 1.31) | 0.401 | 0.82 (0.50 to 1.33) | 0.422 |
| Male | 17.0 | 16.7 | 21.4 | 13.1 | 16.2 | 16.2 | 0.89 (0.61 to 1.31) | 0.563 | 0.90 (0.61 to 1.31) | 0.575 | 0.91 (0.62 to 1.35) | 0.655 |
| Age (years) | ||||||||||||
| 16–25 | 22.6 | 16.2 | 23.7 | 14.2 | 17.1 | 14.8 | 0.74 (0.43 to 1.29) | 0.288 | 0.74 (0.43 to 1.28) | 0.283 | 0.74 (0.42 to 1.31) | 0.303 |
| 26–45 | 15.5 | 15.3 | 17.2 | 13.7 | 15.3 | 15.5 | 0.92 (0.57 to 1.51) | 0.748 | 0.94 (0.57 to 1.54) | 0.803 | 0.93 (0.56 to 1.54) | 0.776 |
| 46–65 | 14.4 | 14.0 | 15.4 | 13.2 | 14.6 | 15.5 | 0.88 (0.50 to 1.55) | 0.661 | 0.90 (0.51 to 1.59) | 0.727 | 0.97 (0.54 to 1.74) | 0.916 |
| ≥ 66 | 4.7 | 5.4 | 6.3 | 1.6 | 2.8 | 3.0 | 0.67 (0.15 to 2.99) | 0.604 | 0.66 (0.15 to 2.96) | 0.588 | 0.68 (0.15 to 3.07) | 0.616 |
| Ethnicity | ||||||||||||
| White | 14.4 | 12.9 | 15.6 | 10.8 | 13.9 | 12.9 | 0.77 (0.57 to 1.05) | 0.101 | 0.79 (0.58 to 1.07) | 0.131 | 0.80 (0.58 to 1.10) | 0.162 |
| Non-white | 2.3 | 9.9 | 10.0 | 8.4 | 4.3 | 6.6 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 14.0 | 12.3 | 15.2 | 11.5 | 13.5 | 13.4 | 0.82 (0.54 to 1.25) | 0.355 | 0.82 (0.54 to 1.25) | 0.350 | 0.82 (0.54 to 1.27) | 0.379 |
| Economically inactive | 10.7 | 10.9 | 12.4 | 7.4 | 10.3 | 7.2 | 0.90 (0.53 to 1.53) | 0.701 | 0.93 (0.54 to 1.57) | 0.776 | 0.95 (0.55 to 1.65) | 0.862 |
| Unemployed | 25.3 | 23.2 | 29.4 | 18.1 | 19.6 | 25.5 | 0.79 (0.39 to 1.61) | 0.516 | 0.87 (0.42 to 1.77) | 0.695 | 0.96 (0.45 to 2.02) | 0.911 |
| Marital status | ||||||||||||
| Married/co-habiting | 10.2 | 8.7 | 11.0 | 7.5 | 9.4 | 8.3 | 0.80 (0.47 to 1.38) | 0.425 | 0.80 (0.47 to 1.37) | 0.419 | 0.74 (0.43 to 1.28) | 0.281 |
| Separated/divorced/widowed | 8.7 | 7.4 | 8.6 | 6.4 | 8.2 | 8.1 | 0.70 (0.28 to 1.78) | 0.459 | 0.71 (0.28 to 1.80) | 0.475 | 0.82 (0.31 to 2.14) | 0.682 |
| Single | 20.5 | 19.8 | 23.3 | 15.9 | 17.2 | 17.7 | 0.96 (0.65 to 1.43) | 0.855 | 0.98 (0.66 to 1.46) | 0.910 | 0.96 (0.64 to 1.44) | 0.835 |
| Housing ownership | ||||||||||||
| Owner occupied | 9.4 | 8.5 | 8.2 | 7.2 | 10.1 | 9.8 | 0.61 (0.35 to 1.09) | 0.095 | 0.61 (0.35 to 1.09) | 0.094 | 0.58 (0.32 to 1.04) | 0.065 |
| Rented | 16.1 | 14.8 | 20.2 | 13.7 | 15.4 | 11.5 | 1.11 (0.67 to 1.83) | 0.693 | 1.12 (0.68 to 1.86) | 0.649 | 1.24 (0.74 to 2.07) | 0.411 |
| Housing association/council | 16.5 | 16.0 | 16.5 | 9.2 | 10.7 | 14.7 | 0.68 (0.30 to 1.56) | 0.366 | 0.69 (0.30 to 1.58) | 0.383 | 0.66 (0.28 to 1.55) | 0.346 |
| Other | 18.2 | 16.1 | 25.1 | 13.1 | 14.0 | 16.6 | 0.98 (0.51 to 1.86) | 0.946 | 0.99 (0.52 to 1.89) | 0.976 | 1.08 (0.56 to 2.11) | 0.810 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all attendees | 4.5 | 5.4 | 5.7 | 10.9 | 9.3 | 8.3 | 1.56 (0.96 to 2.53) | 0.075 | 1.56 (0.96 to 2.54) | 0.072 | 1.57 (0.96 to 2.58) | 0.072 |
| Sex | ||||||||||||
| Female | 4.1 | 4.8 | 5.0 | 9.4 | 8.9 | 7.8 | 1.36 (0.63 to 2.94) | 0.434 | 1.36 (0.63 to 2.94) | 0.433 | 1.45 (0.66 to 3.17) | 0.351 |
| Male | 4.9 | 5.9 | 6.4 | 12.5 | 9.7 | 8.9 | 1.75 (0.94 to 3.26) | 0.076 | 1.77 (0.95 to 3.29) | 0.073 | 1.70 (0.90 to 3.19) | 0.100 |
| Age (years) | ||||||||||||
| 16–25 | 2.2 | 2.8 | 3.7 | 2.8 | 1.8 | 3.6 | 1.57 (0.31 to 8.00) | 0.585 | 1.53 (0.30 to 7.82) | 0.607 | 1.38 (0.27 to 7.13) | 0.701 |
| 26–45 | 4.3 | 1.7 | 3.5 | 5.2 | 3.7 | 5.7 | 0.69 (0.23 to 2.00) | 0.489 | 0.66 (0.23 to 1.92) | 0.445 | 0.64 (0.22 to 1.91) | 0.427 |
| 46–65 | 4.2 | 7.9 | 5.6 | 13.0 | 13.1 | 11.6 | 1.73 (0.74 to 4.07) | 0.209 | 1.76 (0.75 to 4.15) | 0.196 | 1.69 (0.71 to 4.04) | 0.235 |
| ≥ 66 | 6.8 | 9.2 | 9.8 | 20.5 | 17.6 | 11.0 | 2.25 (0.99 to 5.08) | 0.052 | 2.20 (0.97 to 4.98) | 0.058 | 2.30 (1.01 to 5.21) | 0.047 |
| Ethnicity | ||||||||||||
| White | 4.8 | 5.7 | 5.8 | 11.0 | 9.6 | 8.2 | 1.53 (0.92 to 2.55) | 0.098 | 1.55 (0.93 to 2.57) | 0.092 | 1.56 (0.93 to 2.60) | 0.090 |
| Non-white | 0.6 | 0.8 | 3.8 | 10.2 | 7.2 | 9.2 | (Too few cases for analysis) | |||||
| Employment status | ||||||||||||
| Employed | 3.3 | 3.6 | 4.1 | 4.6 | 5.4 | 5.5 | 1.00 (0.42 to 2.34) | 0.991 | 1.00 (0.42 to 2.35) | 0.999 | 1.09 (0.46 to 2.58) | 0.844 |
| Economically inactive | 5.6 | 7.1 | 7.3 | 16.5 | 12.5 | 9.2 | 2.11 (1.07 to 4.19) | 0.032 | 2.12 (1.07 to 4.19) | 0.031 | 2.12 (1.06 to 4.23) | 0.034 |
| Unemployed | 6.1 | 6.4 | 6.2 | 14.8 | 15.3 | 17.5 | 0.90 (0.26 to 3.13) | 0.870 | 0.86 (0.25 to 3.01) | 0.818 | 0.81 (0.23 to 2.90) | 0.749 |
| Marital status | ||||||||||||
| Married/co-habiting | 4.8 | 5.7 | 5.5 | 13.3 | 12.3 | 9.0 | 1.52 (0.78 to 2.99) | 0.221 | 1.60 (0.82 to 3.15) | 0.170 | 1.51 (0.76 to 3.01) | 0.238 |
| Separated/divorced/widowed | 5.2 | 6.6 | 7.5 | 13.7 | 12.1 | 9.2 | 1.85 (0.62 to 5.55) | 0.272 | 1.81 (0.60 to 5.44) | 0.289 | 1.76 (0.58 to 5.34) | 0.321 |
| Single | 3.9 | 4.4 | 4.9 | 6.1 | 4.5 | 6.9 | 1.32 (0.52 to 3.34) | 0.561 | 1.30 (0.51 to 3.29) | 0.584 | 1.49 (0.58 to 3.81) | 0.406 |
| Housing ownership | ||||||||||||
| Owner occupied | 5.8 | 7.2 | 7.4 | 14.7 | 10.9 | 10.2 | 1.85 (0.93 to 3.68) | 0.077 | 1.86 (0.94 to 3.69) | 0.076 | 1.93 (0.96 to 3.85) | 0.064 |
| Rented | 2.6 | 3.5 | 3.8 | 5.3 | 8.5 | 3.8 | 1.14 (0.36 to 3.56) | 0.828 | 1.18 (0.38 to 3.69) | 0.771 | 1.28 (0.40 to 4.07) | 0.681 |
| Housing association/council | 5.6 | 5.5 | 4.6 | 14.7 | 8.9 | 8.1 | 1.68 (0.55 to 5.11) | 0.361 | 1.65 (0.54 to 5.02) | 0.382 | 1.63 (0.51 to 5.20) | 0.411 |
| Other | 2.9 | 3.5 | 4.9 | 6.5 | 6.7 | 9.5 | 1.17 (0.29 to 4.75) | 0.824 | 1.18 (0.29 to 4.79) | 0.819 | 0.97 (0.23 to 4.00) | 0.962 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all recorded respondents | ||||||||||||
| Alcohol-related attendance | 8.4 | 8.0 | 8.1 | 6.0 | 6.2 | 4.5 | 1.08 (0.86 to 1.36) | 0.506 | 1.13 (0.90 to 1.42) | 0.301 | 1.17 (0.92 to 1.48) | 0.194 |
| Based on all respondents | ||||||||||||
| Alcohol-related attendance | 13.7 | 12.5 | 15.4 | 10.6 | 12.6 | 11.9 | 0.87 (0.64 to 1.17) | 0.351 | 0.88 (0.66 to 1.19) | 0.414 | 0.90 (0.66 to 1.24) | 0.533 |
| Current alcohol drinker | 79.3 | 77.7 | 80.8 | 78.4 | 78.0 | 78.7 | 1.01 (0.78 to 1.30) | 0.958 | 1.00 (0.78 to 1.29) | 0.992 | 0.99 (0.74 to 1.31) | 0.928 |
| Binge drinking in the past 24 hours | 11.3 | 8.7 | 11.5 | 8.5 | 9.2 | 8.3 | 0.85 (0.61 to 1.19) | 0.344 | 0.86 (0.62 to 1.20) | 0.375 | 0.89 (0.63 to 1.27) | 0.525 |
| Binge drinking in the past week | 25.9 | 25.6 | 25.9 | 24.8 | 23.6 | 22.9 | 1.08 (0.86 to 1.35) | 0.519 | 1.09 (0.87 to 1.36) | 0.470 | 1.12 (0.88 to 1.42) | 0.367 |
| Based on drinkers only | ||||||||||||
| Alcohol misuse (FAST score ≥ 3) | 39.3 | 38.4 | 39.4 | 36.7 | 39.0 | 40.5 | 0.87 (0.69 to 1.09) | 0.215 | 0.88 (0.70 to 1.11) | 0.288 | 0.88 (0.69 to 1.13) | 0.312 |
| Increased alcohol use in the past year | 8.6 | 9.4 | 9.1 | 8.5 | 10.2 | 8.7 | 0.96 (0.66 to 1.41) | 0.849 | 0.99 (0.67 to 1.45) | 0.946 | 1.00 (0.66 to 1.51) | 1.000 |
| Place of last drink: private location | 56.3 | 52.4 | 56.7 | 53.4 | 48.4 | 51.7 | 1.07 (0.86 to 1.34) | 0.544 | 1.05 (0.84 to 1.31) | 0.690 | 1.02 (0.81 to 1.29) | 0.852 |
| Place of last drink: licensed premise | 33.6 | 38.9 | 34.9 | 40.7 | 42.0 | 42.1 | 1.09 (0.87 to 1.37) | 0.459 | 1.12 (0.89 to 1.41) | 0.339 | 1.15 (0.90 to 1.47) | 0.259 |
| FAST score | 2.62 | 2.58 | 2.71 | 2.36 | 2.54 | 2.52 | –0.13 (–0.45 to 0.19)a | 0.411 | –0.08 (–0.40 to 0.24)a | 0.626 | –0.12 (–0.42 to 0.17)a | 0.406 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all recorded respondents | ||||||||||||
| Alcohol-related attendance | 8.8 | 8.2 | 8.2 | 5.6 | 6.3 | 4.5 | 0.95 (0.76 to 1.19) | 0.663 | 0.99 (0.79 to 1.24) | 0.915 | 1.09 (0.87 to 1.38) | 0.454 |
| Based on all respondents | ||||||||||||
| Alcohol-related attendance | 15.0 | 13.6 | 16.0 | 10.8 | 13.1 | 12.6 | 0.81 (0.61 to 1.08) | 0.151 | 0.82 (0.62 to 1.10) | 0.191 | 0.89 (0.65 to 1.21) | 0.450 |
| Current alcohol drinker | 81.4 | 79.6 | 82.3 | 79.8 | 79.5 | 80.3 | 0.97 (0.76 to 1.23) | 0.777 | 0.96 (0.76 to 1.22) | 0.755 | 1.00 (0.77 to 1.31) | 0.988 |
| Binge drinking in the past 24 hours | 12.3 | 9.5 | 12.0 | 8.7 | 9.4 | 9.0 | 0.81 (0.59 to 1.12) | 0.198 | 0.82 (0.59 to 1.13) | 0.224 | 0.89 (0.63 to 1.25) | 0.503 |
| Binge drinking in the past week | 28.8 | 27.7 | 27.1 | 25.4 | 24.8 | 24.6 | 0.97 (0.78 to 1.21) | 0.800 | 0.98 (0.79 to 1.22) | 0.869 | 1.06 (0.84 to 1.35) | 0.612 |
| Based on drinkers only | ||||||||||||
| Alcohol misuse (FAST score ≥ 3) | 42.1 | 39.8 | 40.9 | 36.2 | 40.6 | 42.3 | 0.87 (0.69 to 1.09) | 0.215 | 0.88 (0.70 to 1.11) | 0.288 | 0.88 (0.69 to 1.13) | 0.312 |
| Increased alcohol use in the past year | 9.6 | 10.2 | 9.7 | 8.5 | 10.2 | 9.5 | 0.96 (0.66 to 1.41) | 0.849 | 0.99 (0.67 to 1.45) | 0.946 | 1.00 (0.66 to 1.51) | 1.000 |
| Place of last drink: private location | 55.0 | 51.1 | 55.5 | 53.5 | 47.1 | 50.1 | 1.07 (0.86 to 1.34) | 0.544 | 1.05 (0.84 to 1.31) | 0.690 | 1.02 (0.81 to 1.29) | 0.852 |
| Place of last drink: licensed premise | 35.8 | 40.7 | 36.1 | 40.3 | 43.0 | 43.5 | 1.09 (0.87 to 1.37) | 0.459 | 1.12 (0.89 to 1.41) | 0.339 | 1.15 (0.90 to 1.47) | 0.259 |
| FAST score | 2.79 | 2.70 | 2.79 | 2.36 | 2.61 | 2.64 | –0.13 (–0.45 to 0.19)a | 0.411 | –0.08 (–0.40 to 0.24)a | 0.626 | –0.12 (–0.42 to 0.17)a | 0.406 |
Appendix 3 Supplementary tables for the sexual health clinic study
| Site | Response level | Wave 1 | Wave 2 | Wave 3 | Overall |
|---|---|---|---|---|---|
| Glasgow | Returned completed surveys (n) | 353 | 149 | 657 | 1159 |
| Total attendees in time slots (na) | 630 | 483 | 962 | 2075 | |
| Inclusion rate (%) | 56.0 | 30.8 | 68.3 | 55.9 | |
| Lothian | Returned completed surveys (n) | 1319 | 1125 | 1156 | 3600 |
| Total attendees in time slots (n) | 2625 | 2018 | 2782 | 7425 | |
| Inclusion rate (%) | 50.2 | 55.7 | 41.6 | 48.5 | |
| Tayside | Returned completed surveys (n) | 415 | 270 | 429 | 1114 |
| Total attendees in time slots (n) | 875 | 563 | 746 | 2184 | |
| Inclusion rate (%) | 47.4 | 48.0 | 57.5 | 51.0 | |
| Sheffield | Returned completed surveys (n) | 1125 | 1020 | 1100 | 3245 |
| Total attendees in time slots (n) | 1687 | 2048 | 1705 | 5440 | |
| Inclusion rate (%) | 66.7 | 49.8 | 64.5 | 59.7 | |
| Leeds | Returned completed surveys (n) | 1187 | 986 | 968 | 3141 |
| Total attendees in time slots (n) | 1450 | 1308 | 1413 | 4171 | |
| Inclusion rate (%) | 81.9 | 75.4 | 68.5 | 75.3 | |
| Manchester | Returned completed surveys (n) | 1208 | 1116 | 635 | 2959 |
| Total attendees in time slots (n) | 2075 | 2070 | 1631 | 5776 | |
| Inclusion rate (%) | 58.2 | 53.9 | 38.9b | 51.2 | |
| Overall | Returned completed surveys (n) | 5607 | 4666 | 4945 | 15,218 |
| Total attendees in time slots (n) | 9342 | 8490 | 9239 | 27,071 | |
| Inclusion rate (%) | 60.0 | 55.0 | 53.5 | 56.2 |
| Site | Response rate | Wave 1 | Wave 2 | Wave 3 | Overall |
|---|---|---|---|---|---|
| Scotland | Number of attendees | 4130 | 3064 | 4490 | 11,684 |
| Number of respondents | 2087 | 1544 | 2242 | 5873 | |
| Response rate (%) | 50.5 | 50.4 | 49.9 | 50.3 | |
| England | Number of attendees | 5212 | 5426 | 4749 | 15,387 |
| Number of respondents | 3520 | 3122 | 2703 | 9345 | |
| Response rate (%) | 67.5 | 57.5 | 56.9 | 60.7 | |
| Overall | Number of attendees | 9342 | 8490 | 9239 | 27,071 |
| Number of respondents | 5607 | 4666 | 4945 | 15,218 | |
| Response rate (%) | 60.0 | 55.0 | 53.5 | 56.2 |
| Site | Variable | Wave 1 | Wave 2 | Wave 3 | |||
|---|---|---|---|---|---|---|---|
| χ2 | p-value | χ2 | p-value | χ2 | p-value | ||
| Glasgow | Sex | 13.4 | 0.000 | 9.4 | 0.002 | 20.8 | 0.000 |
| Age | 9.9 | 0.128 | 26.6 | 0.000 | 8.7 | 0.276 | |
| Lothian | Sex | 2.2 | 0.138 | 2.5 | 0.114 | 7.6 | 0.006 |
| Age | 30.1 | 0.000 | 113.5 | 0.000 | 196.4 | 0.000 | |
| Tayside | Sex | 0.4 | 0.530 | 0.8 | 0.362 | 0 | 0.985 |
| Age | 10.7 | 0.154 | 19.6 | 0.007 | 37.1 | 0.000 | |
| Sheffield | Sex | 0.1 | 0.721 | 3.9 | 0.048 | 0 | 0.963 |
| Age | 6.2 | 0.522 | 11.5 | 0.118 | 6.6 | 0.474 | |
| Leeds | Sex | 21.2 | 0.000 | 0.8 | 0.385 | 14.7 | 0.000 |
| Age | 38.5 | 0.000 | 27.1 | 0.000 | 38.4 | 0.000 | |
| Manchester | Sex | 0.1 | 0.707 | 28.8 | 0.000 | 5.3 | 0.022 |
| Age | 1.1 | 0.980 | 109.5 | 0.000 | 35.9 | 0.000 | |
| Site | Sex | Age | ||
|---|---|---|---|---|
| χ2 | p-value | χ2 | p-value | |
| Glasgow | 4.00 | 0.134 | 36.00 | 0.001 |
| Lothian | 6.20 | 0.044 | 72.00 | 0.000 |
| Tayside | 5.90 | 0.052 | 24.00 | 0.500 |
| Sheffield | 1.90 | 0.391 | 27.00 | 0.021 |
| Leeds | 4.70 | 0.093 | 18.00 | 0.186 |
| Manchester | 7.70 | 0.021 | 52.00 | 0.000 |
| Demographic | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 2087) | Wave 2 (N = 1544) | Wave 3 (N = 2242) | Wave 1 (N = 3520) | Wave 2 (N = 3122) | Wave 3 (N = 2703) | |
| Age (years) | ||||||
| < 19 | 287 (13.8) | 307 (19.9) | 422 (18.8) | 707 (20.1) | 597 (19.1) | 521 (19.3) |
| 20–24 | 673 (32.2) | 481 (31.2) | 662 (29.5) | 1234 (35.1) | 1127 (36.1) | 961 (35.6) |
| 25–29 | 385 (18.4) | 270 (17.5) | 356 (15.9) | 616 (17.5) | 507 (16.2) | 427 (15.8) |
| 30–34 | 209 (10.0) | 139 (9.0) | 225 (10.0) | 361 (10.3) | 347 (11.1) | 266 (9.8) |
| 35–39 | 155 (7.4) | 130 (8.4) | 189 (8.4) | 228 (6.5) | 198 (6.3) | 187 (6.9) |
| 40–45 | 143 (6.9) | 70 (4.5) | 130 (5.8) | 155 (4.4) | 148 (4.7) | 127 (4.7) |
| > 45 | 234 (11.2) | 147 (9.5) | 257 (11.5) | 217 (6.2) | 198 (6.3) | 213 (7.9) |
| Missing | 1 (0.0) | 0 (0) | 1 (0.0) | 2 (0.1) | 0 (0) | 1 (0.0) |
| Sex | ||||||
| Male | 847 (40.6) | 584 (37.8) | 958 (42.7) | 1272 (36.1) | 1125 (36.0) | 987 (36.5) |
| Female | 1194 (57.2) | 920 (59.6) | 1240 (55.3) | 2233 (63.4) | 1977 (63.3) | 1687 (62.4) |
| Non-binary | 45 (2.2) | 34 (2.2) | 44 (2.0) | 10 (0.3) | 13 (0.4) | 26 (1.0) |
| Missing | 1 (0.0) | 6 (0.4) | 0 (0) | 5 (0.1) | 7 (0.2) | 3 (0.1) |
| Employment status | ||||||
| Employed | 1152 (55.2) | 824 (53.4) | 1236 (55.1) | 1627 (46.2) | 1477 (47.3) | 1322 (48.9) |
| Economically inactive | 795 (38.1) | 591 (38.3) | 899 (40.1) | 1655 (47.0) | 1349 (43.2) | 1223 (45.2) |
| Unemployed | 115 (5.5) | 51 (3.3) | 107 (4.8) | 218 (6.2) | 192 (6.1) | 154 (5.7) |
| Missing | 25 (1.2) | 78 (5.1) | 0 (0) | 20 (0.6) | 104 (3.3) | 4 (0.1) |
| Highest education level | ||||||
| Higher education | 1462 (70.1) | 1019 (66.0) | 1424 (63.5) | 2171 (61.7) | 1942 (62.2) | 1681 (62.2) |
| Further education | 77 (3.7) | 119 (7.7) | 178 (7.9) | 226 (6.4) | 345 (11.1) | 301 (11.1) |
| Upper secondary school | 261 (12.5) | 213 (13.8) | 325 (14.5) | 432 (12.3) | 391 (12.5) | 278 (10.3) |
| Lower secondary school | 176 (8.4) | 127 (8.2) | 224 (10.0) | 370 (10.5) | 252 (8.1) | 285 (10.5) |
| No formal qualifications | 68 (3.3) | 49 (3.2) | 68 (3.0) | 198 (5.6) | 131 (4.2) | 112 (4.1) |
| Missing | 43 (2.1) | 17 (1.1) | 23 (1.0) | 123 (3.5) | 61 (2.0) | 46 (1.7) |
| Missing data | Scotland, n (%) | England, n (%) | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 2087) | Wave 2 (N = 1544) | Wave 3 (N = 2242) | Wave 1 (N = 3520) | Wave 2 (N = 3122) | Wave 3 (N = 2703) | |
| Current alcohol drinker | ||||||
| Drinkers | 1950 (93.4) | 1447 (93.7) | 2098 (93.6) | 3100 (88.1) | 2758 (88.3) | 2400 (88.8) |
| Non-drinkers | 128 (6.1) | 97 (6.3) | 144 (6.4) | 317 (9.0) | 351 (11.2) | 291 (10.8) |
| Missing | 9 (0.4) | 0 (0) | 0 (0) | 103 (2.9) | 13 (0.4) | 12 (0.4) |
| Consumption of any illicit drugs in the last month | ||||||
| In the last month | 477 (22.9) | 389 (25.2) | 646 (28.8) | 951 (27.0) | 906 (29.0) | 792 (29.3) |
| More than 1 month ago | 1562 (74.8) | 1105 (71.6) | 1526 (68.1) | 2372 (67.4) | 2074 (66.4) | 1744 (64.5) |
| Missing | 48 (2.3) | 50 (3.2) | 70 (3.1) | 197 (5.6) | 142 (4.5) | 167 (6.2) |
| Missing data | Scotland | England | ||||
|---|---|---|---|---|---|---|
| Wave 1 (N = 1950) | Wave 2 (N = 1447) | Wave 3 (N = 2098) | Wave 1 (N = 3100) | Wave 2 (N = 2758) | Wave 3 (N = 2400) | |
| Binge drinking at least weekly, n (%) | ||||||
| At least weekly | 538 (27.6) | 409 (28.3) | 622 (29.6) | 1000 (32.3) | 806 (29.2) | 684 (28.5) |
| Less than weekly | 1399 (71.7) | 1016 (70.2) | 1452 (69.2) | 2074 (66.9) | 1898 (68.8) | 1681 (70.0) |
| Missing | 13 (0.7) | 22 (1.5) | 24 (1.1) | 26 (0.8) | 54 (2.0) | 35 (1.5) |
| Alcohol misuse with a FAST score ≥ 3, n (%) | ||||||
| Abstinent/low-risk drinker (< 3) | 937 (48.1) | 627 (43.3) | 901 (42.9) | 1238 (39.9) | 1164 (42.2) | 976 (40.7) |
| Alcohol misuse (≥ 3) | 947 (48.6) | 751 (51.9) | 1099 (52.4) | 1788 (57.7) | 1465 (53.1) | 1298 (54.1) |
| Missing | 66 (3.4) | 69 (4.8) | 98 (4.7) | 74 (2.4) | 129 (4.7) | 126 (5.2) |
| Drinker types based on modified FAST scale, n (%) | ||||||
| Abstinent/low-risk drinker (< 2) | 588 (30.2) | 398 (27.5) | 559 (26.6) | 727 (23.5) | 690 (25.0) | 574 (23.9) |
| Hazardous drinker (≥ 2) | 854 (43.8) | 654 (45.2) | 882 (42.0) | 1421 (45.8) | 1287 (46.7) | 1061 (44.2) |
| Harmful drinker (≥ 5) | 226 (11.6) | 166 (11.5) | 296 (14.1) | 456 (14.7) | 347 (12.6) | 337 (14.0) |
| Dependent drinker (≥ 7) | 216 (11.1) | 160 (11.1) | 263 (12.5) | 422 (13.6) | 305 (11.1) | 302 (12.6) |
| Missing | 66 (3.4) | 69 (4.8) | 98 (4.7) | 74 (2.4) | 129 (4.7) | 126 (5.2) |
| Alcohol purchased from on-licensed premises, n (%) | ||||||
| In the last month | 1400 (71.8) | 1063 (73.5) | 1547 (73.7) | 2442 (78.8) | 2150 (78.0) | 1751 (73.0) |
| More than 1 month ago | 395 (20.3) | 301 (20.8) | 442 (21.1) | 500 (16.1) | 473 (17.2) | 477 (19.9) |
| Missing | 155 (7.9) | 83 (5.7) | 109 (5.2) | 158 (5.1) | 135 (4.9) | 172 (7.2) |
| Alcohol purchased from off-licensed premises, n (%) | ||||||
| In the last month | 1219 (62.5) | 960 (66.3) | 1387 (66.1) | 2135 (68.9) | 1881 (68.2) | 1482 (61.8) |
| More than 1 month ago | 470 (24.1) | 342 (23.6) | 540 (25.7) | 770 (24.8) | 687 (24.9) | 662 (27.6) |
| Missing | 261 (13.4) | 145 (10.0) | 171 (8.2) | 195 (6.3) | 190 (6.9) | 256 (10.7) |
| FAST score | ||||||
| Mean (SD) | 3.22 (2.75) | 3.30 (2.61) | 3.46 (2.83) | 3.63 (2.84) | 3.38 (2.71) | 3.54 (2.82) |
| Median (minimum, maximum) | 3.00 (0, 16.0) | 3.00 (0, 15.0) | 3.00 (0, 16.0) | 3.00 (0, 16.0) | 3.00 (0, 16.0) | 3.00 (0, 16.0) |
| Missing, n (%) | 66 (3.4) | 69 (4.8) | 98 (4.7) | 74 (2.4) | 129 (4.7) | 126 (5.2) |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | ||||||||||||
| Consumption of any illicit drugs in the last months | 24.2 | 25.8 | 29.3 | 29.3 | 30.1 | 31.6 | 1.14 (0.98 to 1.34) | 0.097 | 1.10 (0.94 to 1.29) | 0.233 | 1.04 (0.88 to 1.24) | 0.612 |
| Wave 1 + wave 2 | 1.06 (0.87 to 1.28) | 0.578 | 1.07 (0.88 to 1.30) | 0.488 | 1.03 (0.85 to 1.27) | 0.742 | ||||||
| Wave 1 + wave 3 | 1.19 (0.99 to 1.43) | 0.058 | 1.12 (0.93 to 1.34) | 0.234 | 1.05 (0.86 to 1.27) | 0.640 | ||||||
| Current alcohol drinker | 93.5 | 93.3 | 93.2 | 90.0 | 87.5 | 88.7 | 1.17 (0.89 to 1.55) | 0.268 | 1.19 (0.90 to 1.57) | 0.220 | 1.13 (0.85 to 1.50) | 0.386 |
| Wave 1 + wave 2 | 1.24 (0.89 to 1.71) | 0.199 | 1.25 (0.91 to 1.73) | 0.173 | 1.13 (0.81 to 1.58) | 0.478 | ||||||
| Wave 1 + wave 3 | 1.10 (0.79 to 1.53) | 0.572 | 1.20 (0.87 to 1.66) | 0.262 | 1.22 (0.88 to 1.68) | 0.231 | ||||||
| Based on drinkers only | ||||||||||||
| Binge drinking at least weekly | 27.5 | 27.1 | 28.4 | 32.1 | 29.3 | 28.5 | 1.18 (1.01 to 1.38) | 0.043 | 1.17 (1.00 to 1.38) | 0.049 | 1.13 (0.96 to 1.34) | 0.139 |
| Wave 1 + wave 2 | 1.11 (0.92 to 1.35) | 0.285 | 1.12 (0.92 to 1.36) | 0.254 | 1.08 (0.88 to 1.32) | 0.449 | ||||||
| Wave 1 + wave 3 | 1.24 (1.03 to 1.49) | 0.023 | 1.22 (1.02 to 1.47) | 0.033 | 1.18 (0.97 to 1.43) | 0.092 | ||||||
| Alcohol misuse | 49.6 | 52.7 | 53.6 | 58.8 | 55.0 | 56.8 | 1.30 (1.13 to 1.51) | 0.000 | 1.29 (1.12 to 1.50) | 0.001 | 1.22 (1.04 to 1.42) | 0.012 |
| Wave 1 + wave 2 | 1.32 (1.10 to 1.58) | 0.002 | 1.32 (1.10 to 1.58) | 0.002 | 1.25 (1.04 to 1.51) | 0.019 | ||||||
| Wave 1 + wave 3 | 1.27 (1.08 to 1.51) | 0.005 | 1.27 (1.07 to 1.50) | 0.007 | 1.19 (1.00 to 1.42) | 0.055 | ||||||
| Drinkers with at least a hazardous drinking level | 67.8 | 69.6 | 71.0 | 75.8 | 73.2 | 74.3 | 1.26 (1.07 to 1.48) | 0.006 | 1.24 (1.05 to 1.47) | 0.010 | 1.14 (0.96 to 1.36) | 0.126 |
| Wave 1 + wave 2 | 1.24 (1.02 to 1.51) | 0.030 | 1.25 (1.02 to 1.53) | 0.028 | 1.15 (0.94 to 1.42) | 0.177 | ||||||
| Wave 1 + wave 3 | 1.26 (1.04 to 1.52) | 0.020 | 1.24 (1.02 to 1.50) | 0.030 | 1.14 (0.93 to 1.39) | 0.196 | ||||||
| Drinkers with at least a harmful drinking level | 23.2 | 21.7 | 26.5 | 28.2 | 24.6 | 27.3 | 1.22 (1.03 to 1.44) | 0.022 | 1.19 (1.00 to 1.41) | 0.047 | 1.10 (0.93 to 1.32) | 0.265 |
| Wave 1 + wave 2 | 1.11 (0.90 to 1.36) | 0.327 | 1.10 (0.89 to 1.35) | 0.371 | 1.02 (0.82 to 1.26) | 0.863 | ||||||
| Wave 1 + wave 3 | 1.25 (1.03 to 1.52) | 0.021 | 1.24 (1.02 to 1.50) | 0.028 | 1.16 (0.95 to 1.42) | 0.143 | ||||||
| Drinkers with at least a dependent drinking level | 11.4 | 10.6 | 12.2 | 13.5 | 11.5 | 13.0 | 1.14 (0.91 to 1.42) | 0.249 | 1.12 (0.90 to 1.40) | 0.309 | 1.06 (0.85 to 1.34) | 0.601 |
| Wave 1 + wave 2 | 1.10 (0.84 to 1.45) | 0.483 | 1.10 (0.84 to 1.46) | 0.484 | 1.05 (0.79 to 1.40) | 0.745 | ||||||
| Wave 1 + wave 3 | 1.13 (0.88 to 1.46) | 0.335 | 1.14 (0.88 to 1.47) | 0.311 | 1.07 (0.83 to 1.40) | 0.595 | ||||||
| Alcohol bought from licensed premises | 77.3 | 79.8 | 77.8 | 83.4 | 81.4 | 78.8 | 1.33 (1.10 to 1.61) | 0.003 | 1.33 (1.10 to 1.61) | 0.003 | 1.27 (1.05 to 1.55) | 0.016 |
| Wave 1 + wave 2 | 1.33 (1.06 to 1.66) | 0.015 | 1.39 (1.11 to 1.74) | 0.005 | 1.26 (0.99 to 1.60) | 0.058 | ||||||
| Wave 1 + wave 3 | 1.38 (1.11 to 1.71) | 0.003 | 1.33 (1.07 to 1.65) | 0.009 | 1.32 (1.05 to 1.65) | 0.017 | ||||||
| Alcohol bought from off-licensed premises | 74.2 | 75.2 | 72.6 | 74.6 | 73.7 | 71.2 | 1.08 (0.91 to 1.29) | 0.352 | 1.10 (0.92 to 1.30) | 0.294 | 1.08 (0.91 to 1.29) | 0.389 |
| Wave 1 + wave 2 | 1.11 (0.90 to 1.36) | 0.326 | 1.12 (0.91 to 1.38) | 0.269 | 1.08 (0.88 to 1.34) | 0.466 | ||||||
| Wave 1 + wave 3 | 1.10 (0.90 to 1.33) | 0.351 | 1.09 (0.90 to 1.33) | 0.382 | 1.08 (0.89 to 1.32) | 0.443 | ||||||
| FAST score | 3.19 | 3.17 | 3.36 | 3.59 | 3.35 | 3.50 | 0.26 (0.06 to 0.46)a | 0.012 | 0.24 (0.04 to 0.44)a | 0.020 | 0.12 (–0.08 to 0.31)a | 0.245 |
| Wave 1 + wave 2 | 0.21 (–0.02 to 0.45)a | 0.077 | 0.21 (–0.03 to 0.45)a | 0.080 | 0.10 (–0.13 to 0.33)a | 0.404 | ||||||
| Wave 1 + wave 3 | 0.26 (0.02 to 0.49)a | 0.030 | 0.26 (0.02 to 0.49)a | 0.031 | 0.13 (–0.09 to 0.36)a | 0.249 | ||||||
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | ||||||||||||
| Consumption of any illicit drugs in the last months | 24.2 | 25.8 | 29.3 | 29.3 | 30.1 | 31.6 | 1.14 (0.98 to 1.34) | 0.097 | 1.10 (0.94 to 1.29) | 0.233 | 1.04 (0.88 to 1.24) | 0.612 |
| Current alcohol drinker | 93.5 | 93.3 | 93.2 | 90.0 | 87.5 | 88.7 | 1.17 (0.89 to 1.55) | 0.268 | 1.19 (0.90 to 1.57) | 0.220 | 1.13 (0.85 to 1.50) | 0.386 |
| Based on drinkers only | ||||||||||||
| Binge drinking at least weekly | 27.5 | 27.1 | 28.4 | 32.1 | 29.3 | 28.5 | 1.18 (1.01 to 1.38) | 0.043 | 1.17 (1.00 to 1.38) | 0.049 | 1.13 (0.96 to 1.34) | 0.139 |
| Alcohol misuse | 49.6 | 52.7 | 53.6 | 58.8 | 55.0 | 56.8 | 1.30 (1.13 to 1.51) | 0.000 | 1.29 (1.12 to 1.50) | 0.001 | 1.22 (1.04 to 1.42) | 0.012 |
| Drinkers with at least a hazardous drinking level | 67.8 | 69.6 | 71.0 | 75.8 | 73.2 | 74.3 | 1.26 (1.07 to 1.48) | 0.006 | 1.24 (1.05 to 1.47) | 0.010 | 1.14 (0.96 to 1.36) | 0.126 |
| Drinkers with at least a harmful drinking level | 23.2 | 21.7 | 26.5 | 28.2 | 24.6 | 27.3 | 1.22 (1.03 to 1.44) | 0.022 | 1.19 (1.00 to 1.41) | 0.047 | 1.10 (0.93 to 1.32) | 0.265 |
| Drinkers with at least a dependent drinking level | 11.4 | 10.6 | 12.2 | 13.5 | 11.5 | 13.0 | 1.14 (0.91 to 1.42) | 0.249 | 1.12 (0.90 to 1.40) | 0.309 | 1.06 (0.85 to 1.34) | 0.601 |
| Alcohol bought from on-licensed premises | 77.3 | 79.8 | 77.8 | 83.4 | 81.4 | 78.8 | 1.33 (1.10 to 1.61) | 0.003 | 1.33 (1.10 to 1.61) | 0.003 | 1.27 (1.05 to 1.55) | 0.016 |
| Alcohol bought from off-licensed premises | 74.2 | 75.2 | 72.6 | 74.6 | 73.7 | 71.2 | 1.08 (0.91 to 1.29) | 0.352 | 1.10 (0.92 to 1.30) | 0.294 | 1.08 (0.91 to 1.29) | 0.389 |
| FAST score | 3.19 | 3.17 | 3.36 | 3.59 | 3.35 | 3.50 | 0.26 (0.06 to 0.46)a | 0.012 | 0.24 (0.04 to 0.44)a | 0.020 | 0.12 (–0.08 to 0.31)a | 0.245 |
| Drug | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Consumption of any illicit drugs in the last months | 24.2 | 25.8 | 29.3 | 29.3 | 30.1 | 31.6 | 1.14 (0.98 to 1.34) | 0.097 | 1.10 (0.94 to 1.29) | 0.233 | 1.04 (0.88 to 1.24) | 0.612 |
| Cannabis | 16.8 | 19.2 | 20.8 | 20.2 | 21.7 | 21.5 | 1.15 (0.96 to 1.37) | 0.136 | 1.13 (0.94 to 1.35) | 0.199 | 1.08 (0.89 to 1.30) | 0.455 |
| Gas, glue or other solvents | 0.8 | 1.2 | 1.1 | 0.9 | 0.9 | 1.3 | 1.14 (0.53 to 2.43) | 0.740 | 1.08 (0.50 to 2.31) | 0.844 | 1.05 (0.49 to 2.28) | 0.896 |
| Amphetamines | 1.6 | 1.3 | 1.3 | 1.4 | 1.3 | 1.6 | 0.81 (0.45 to 1.44) | 0.470 | 0.77 (0.43 to 1.39) | 0.384 | 0.73 (0.40 to 1.34) | 0.310 |
| LSD | 0.5 | 0.6 | 0.9 | 0.8 | 1.0 | 0.7 | 1.31 (0.54 to 3.17) | 0.549 | 1.31 (0.55 to 3.15) | 0.541 | 1.30 (0.54 to 3.12) | 0.561 |
| Ecstasy | 4.4 | 4.4 | 5.1 | 6.4 | 5.3 | 5.3 | 1.37 (0.99 to 1.88) | 0.057 | 1.33 (0.96 to 1.84) | 0.083 | 1.23 (0.88 to 1.72) | 0.218 |
| Tranquillisers | 2.0 | 1.7 | 2.4 | 2.5 | 2.3 | 2.1 | 1.15 (0.71 to 1.87) | 0.567 | 1.09 (0.67 to 1.77) | 0.735 | 1.07 (0.65 to 1.75) | 0.786 |
| Heroin | 0.1 | 0.1 | 0.3 | 0.1 | 0.1 | 0.2 | 1.87 (0.15 to 23.77) | 0.631 | 1.70 (0.13 to 22.36) | 0.686 | 1.54 (0.13 to 17.92) | 0.732 |
| Magic mushrooms | 0.5 | 0.9 | 0.6 | 0.4 | 0.5 | 0.6 | 1.12 (0.41 to 3.05) | 0.819 | 1.11 (0.41 to 3.03) | 0.834 | 0.98 (0.35 to 2.73) | 0.965 |
| Methadone | 0.2 | 0.3 | 0.5 | 0.2 | 0.1 | 0.4 | 1.28 (0.26 to 6.37) | 0.760 | 1.14 (0.22 to 5.83) | 0.876 | 1.04 (0.19 to 5.77) | 0.968 |
| Crack | 0.1 | 0.2 | 0.2 | 0.4 | 0.2 | 0.4 | 1.77 (0.29 to 10.85) | 0.536 | 1.74 (0.28 to 10.60) | 0.550 | 2.03 (0.33 to 12.39) | 0.443 |
| Cocaine | 7.6 | 7.0 | 9.4 | 10.7 | 10.0 | 10.6 | 1.17 (0.91 to 1.51) | 0.222 | 1.10 (0.85 to 1.42) | 0.467 | 1.02 (0.79 to 1.33) | 0.878 |
| Mephedrone | 0.7 | 0.1 | 0.3 | 0.7 | 0.9 | 0.9 | 0.27 (0.09 to 0.78) | 0.016 | 0.24 (0.08 to 0.71) | 0.010 | 0.24 (0.08 to 0.73) | 0.012 |
| Ketamine | 2.7 | 3.3 | 4.5 | 6.3 | 6.2 | 6.5 | 1.50 (1.05 to 2.15) | 0.026 | 1.42 (0.99 to 2.03) | 0.057 | 1.30 (0.90 to 1.87) | 0.168 |
| Nitrous oxide | 1.4 | 2.2 | 1.4 | 5.7 | 6.0 | 6.1 | 1.15 (0.70 to 1.90) | 0.577 | 1.14 (0.69 to 1.88) | 0.605 | 1.02 (0.62 to 1.69) | 0.938 |
| Legal highs | 0.8 | 0.8 | 0.7 | 1.2 | 0.9 | 1.0 | 1.02 (0.48 to 2.16) | 0.962 | 0.99 (0.46 to 2.11) | 0.978 | 1.03 (0.46 to 2.29) | 0.943 |
| Other drugs not given by a doctor or chemist | 1.8 | 1.2 | 2.3 | 2.1 | 1.5 | 2.5 | 1.12 (0.66 to 1.92) | 0.671 | 1.04 (0.60 to 1.78) | 0.895 | 1.04 (0.60 to 1.80) | 0.892 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | 24.2 | 25.8 | 29.3 | 29.3 | 30.1 | 31.6 | 1.14 (0.98 to 1.34) | 0.097 | 1.10 (0.94 to 1.29) | 0.233 | 1.04 (0.88 to 1.24) | 0.612 |
| Sex | ||||||||||||
| Female | 19.9 | 21.9 | 25.9 | 26.7 | 27.8 | 27.8 | 1.24 (1.00 to 1.54) | 0.049 | 1.21 (0.97 to 1.51) | 0.084 | 1.16 (0.92 to 1.45) | 0.200 |
| Male | 30.4 | 31.4 | 34.1 | 33.9 | 33.7 | 36.7 | 1.07 (0.84 to 1.36) | 0.592 | 1.03 (0.81 to 1.31) | 0.815 | 0.98 (0.76 to 1.27) | 0.891 |
| Non-binary | 22.5 | 26.9 | 19.2 | 29.1 | 49.2 | 76.9 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 32.2 | 38.4 | 43.1 | 40.4 | 38.1 | 42.8 | 1.51 (1.03 to 2.20) | 0.033 | 1.41 (0.98 to 2.04) | 0.063 | 1.43 (0.98 to 2.08) | 0.061 |
| 20–24 | 30.9 | 32.6 | 37.4 | 35.6 | 40.0 | 40.9 | 1.00 (0.77 to 1.29) | 0.998 | 0.98 (0.76 to 1.27) | 0.900 | 0.97 (0.74 to 1.26) | 0.811 |
| 25–29 | 24.5 | 24.4 | 32.2 | 23.1 | 27.5 | 24.8 | 1.08 (0.73 to 1.59) | 0.716 | 1.01 (0.68 to 1.49) | 0.969 | 1.01 (0.68 to 1.51) | 0.949 |
| 30–34 | 20.2 | 21.4 | 23.0 | 19.3 | 22.8 | 25.9 | 0.89 (0.52 to 1.55) | 0.688 | 0.84 (0.48 to 1.47) | 0.551 | 0.78 (0.44 to 1.39) | 0.399 |
| 35–39 | 23.1 | 12.9 | 19.0 | 17.9 | 17.9 | 19.6 | 0.65 (0.32 to 1.30) | 0.221 | 0.61 (0.31 to 1.23) | 0.169 | 0.55 (0.27 to 1.14) | 0.109 |
| 40–45 | 14.3 | 24.1 | 13.4 | 15.8 | 17.4 | 20.7 | 1.05 (0.46 to 2.43) | 0.908 | 1.02 (0.43 to 2.43) | 0.963 | 0.81 (0.33 to 2.00) | 0.650 |
| > 45 | 11.1 | 11.1 | 13.2 | 21.9 | 12.9 | 15.1 | 2.03 (1.00 to 4.12) | 0.051 | 2.02 (1.00 to 4.11) | 0.052 | 1.98 (0.96 to 4.11) | 0.065 |
| Employment | ||||||||||||
| Employed | 20.7 | 22.3 | 24.5 | 21.9 | 24.7 | 25.0 | 1.02 (0.81 to 1.29) | 0.877 | 0.99 (0.78 to 1.25) | 0.925 | 0.90 (0.71 to 1.16) | 0.427 |
| Economically inactive | 28.7 | 30.3 | 35.1 | 36.7 | 36.0 | 39.6 | 1.20 (0.95 to 1.53) | 0.123 | 1.17 (0.92 to 1.48) | 0.203 | 1.12 (0.88 to 1.43) | 0.354 |
| Unemployed | 29.9 | 40.8 | 42.4 | 32.8 | 33.7 | 33.0 | 1.61 (0.83 to 3.14) | 0.158 | 1.67 (0.85 to 3.31) | 0.140 | 1.67 (0.79 to 3.51) | 0.176 |
| Education | 0.000 | |||||||||||
| Higher | 24.2 | 24.4 | 27.9 | 28.8 | 29.5 | 31.5 | 1.07 (0.88 to 1.29) | 0.521 | 1.03 (0.85 to 1.25) | 0.788 | 0.99 (0.81 to 1.22) | 0.919 |
| Further | 28.2 | 32.9 | 33.3 | 28.4 | 33.1 | 28.7 | 1.09 (0.55 to 2.16) | 0.814 | 1.09 (0.53 to 2.20) | 0.820 | 0.91 (0.43 to 1.94) | 0.817 |
| Upper | 27.0 | 27.8 | 37.0 | 35.5 | 33.9 | 42.1 | 1.25 (0.82 to 1.92) | 0.305 | 1.10 (0.71 to 1.70) | 0.663 | 1.03 (0.65 to 1.62) | 0.911 |
| Lower | 20.7 | 29.2 | 25.7 | 27.8 | 25.2 | 26.9 | 1.53 (0.86 to 2.71) | 0.149 | 1.56 (0.88 to 2.77) | 0.128 | 1.31 (0.70 to 2.45) | 0.406 |
| No formal education | 20.0 | 21.8 | 27.1 | 26.6 | 31.1 | 28.2 | 1.18 (0.48 to 2.90) | 0.725 | 1.21 (0.48 to 3.03) | 0.690 | 1.65 (0.64 to 4.29) | 0.302 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | 93.5 | 93.3 | 93.2 | 90.0 | 87.5 | 88.7 | 1.17 (0.89 to 1.55) | 0.268 | 1.19 (0.90 to 1.57) | 0.220 | 1.13 (0.85 to 1.50) | 0.386 |
| Sex | ||||||||||||
| Female | 93.2 | 92.4 | 93.1 | 89.4 | 86.5 | 88.9 | 1.13 (0.80 to 1.59) | 0.499 | 1.14 (0.81 to 1.61) | 0.465 | 1.09 (0.75 to 1.57) | 0.661 |
| Male | 94.3 | 95.1 | 94.3 | 90.8 | 89.2 | 88.4 | 1.34 (0.85 to 2.11) | 0.207 | 1.36 (0.86 to 2.15) | 0.183 | 1.31 (0.83 to 2.08) | 0.243 |
| Non-binary | 86.8 | 83.8 | 80.1 | 98.0 | 100.0 | 87.3 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 96.6 | 97.6 | 92.3 | 93.0 | 88.4 | 90.2 | 0.93 (0.31 to 2.79) | 0.901 | 1.25 (0.50 to 3.11) | 0.631 | 1.26 (0.47 to 3.38) | 0.647 |
| 20–24 | 95.4 | 96.0 | 97.0 | 94.9 | 93.7 | 94.4 | 1.61 (0.90 to 2.89) | 0.112 | 1.69 (0.94 to 3.05) | 0.082 | 1.73 (0.94 to 3.20) | 0.078 |
| 25–29 | 94.0 | 94.8 | 93.2 | 90.6 | 89.4 | 86.5 | 1.28 (0.67 to 2.45) | 0.453 | 1.34 (0.70 to 2.56) | 0.377 | 1.42 (0.74 to 2.76) | 0.294 |
| 30–34 | 89.8 | 90.0 | 90.0 | 83.8 | 84.3 | 84.3 | 0.99 (0.50 to 1.94) | 0.968 | 1.01 (0.51 to 2.01) | 0.968 | 0.93 (0.45 to 1.93) | 0.844 |
| 35–39 | 93.4 | 88.3 | 92.4 | 78.3 | 77.2 | 81.8 | 0.64 (0.27 to 1.50) | 0.307 | 0.60 (0.26 to 1.43) | 0.251 | 0.67 (0.29 to 1.58) | 0.363 |
| 40–45 | 90.3 | 90.4 | 92.3 | 77.1 | 79.6 | 82.8 | 0.92 (0.37 to 2.25) | 0.851 | 0.94 (0.37 to 2.38) | 0.903 | 1.00 (0.38 to 2.67) | 0.997 |
| > 45 | 90.3 | 87.8 | 90.0 | 85.9 | 79.7 | 84.5 | 1.20 (0.59 to 2.45) | 0.620 | 1.10 (0.54 to 2.25) | 0.799 | 1.08 (0.51 to 2.28) | 0.837 |
| Employment | ||||||||||||
| Employed | 94.5 | 93.3 | 94.4 | 91.0 | 89.0 | 89.7 | 1.10 (0.75 to 1.62) | 0.630 | 1.09 (0.74 to 1.61) | 0.656 | 1.03 (0.69 to 1.53) | 0.897 |
| Economically inactive | 93.4 | 94.6 | 92.1 | 90.8 | 87.6 | 89.9 | 1.19 (0.74 to 1.93) | 0.469 | 1.27 (0.81 to 2.00) | 0.303 | 1.23 (0.77 to 1.98) | 0.393 |
| Unemployed | 84.3 | 80.2 | 87.4 | 76.2 | 76.0 | 70.1 | 1.21 (0.54 to 2.71) | 0.636 | 1.24 (0.54 to 2.86) | 0.614 | 1.39 (0.58 to 3.31) | 0.460 |
| Education | ||||||||||||
| Higher | 94.3 | 94.1 | 95.2 | 92.5 | 91.1 | 91.4 | 1.28 (0.89 to 1.84) | 0.186 | 1.30 (0.90 to 1.87) | 0.167 | 1.18 (0.80 to 1.72) | 0.401 |
| Further | 93.1 | 94.3 | 90.0 | 87.9 | 85.1 | 88.4 | 0.93 (0.32 to 2.69) | 0.892 | 0.99 (0.34 to 2.86) | 0.991 | 0.73 (0.22 to 2.41) | 0.608 |
| Upper | 93.3 | 93.7 | 93.7 | 91.9 | 86.2 | 86.2 | 1.94 (0.90 to 4.19) | 0.092 | 1.93 (0.88 to 4.25) | 0.102 | 2.15 (0.96 to 4.82) | 0.064 |
| Lower | 92.3 | 91.1 | 83.6 | 85.1 | 80.8 | 81.7 | 0.67 (0.28 to 1.62) | 0.378 | 0.70 (0.31 to 1.56) | 0.385 | 0.73 (0.33 to 1.62) | 0.438 |
| No formal education | 81.9 | 75.4 | 89.3 | 70.0 | 63.4 | 72.7 | 1.29 (0.51 to 3.24) | 0.593 | 1.13 (0.44 to 2.92) | 0.795 | 1.30 (0.47 to 3.59) | 0.609 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Binge drinking at least weekly | 27.5 | 27.1 | 28.4 | 32.1 | 29.3 | 28.5 | 1.18 (1.01 to 1.38) | 0.043 | 1.17 (1.00 to 1.38) | 0.049 | 1.13 (0.96 to 1.34) | 0.139 |
| Sex | ||||||||||||
| Female | 25.0 | 25.6 | 26.2 | 29.6 | 26.8 | 26.6 | 1.21 (0.98 to 1.50) | 0.079 | 1.21 (0.98 to 1.50) | 0.080 | 1.18 (0.94 to 1.47) | 0.154 |
| Male | 31.7 | 29.3 | 32.2 | 36.3 | 33.6 | 31.3 | 1.15 (0.90 to 1.46) | 0.280 | 1.14 (0.89 to 1.46) | 0.304 | 1.12 (0.87 to 1.44) | 0.386 |
| Non-binary | 14.7 | 27.0 | 10.0 | 12.3 | 8.6 | 37.8 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 41.4 | 43.1 | 45.8 | 41.6 | 30.6 | 38.4 | 1.58 (1.10 to 2.29) | 0.015 | 1.50 (1.05 to 2.15) | 0.027 | 1.65 (1.13 to 2.41) | 0.009 |
| 20–24 | 34.9 | 33.9 | 35.2 | 37.3 | 39.0 | 31.1 | 1.08 (0.84 to 1.40) | 0.544 | 1.13 (0.87 to 1.46) | 0.357 | 1.11 (0.85 to 1.44) | 0.451 |
| 25–29 | 20.7 | 21.6 | 19.8 | 22.4 | 21.1 | 21.2 | 1.07 (0.70 to 1.62) | 0.760 | 1.05 (0.69 to 1.60) | 0.819 | 1.04 (0.68 to 1.60) | 0.844 |
| 30–34 | 15.6 | 20.4 | 17.1 | 23.3 | 19.4 | 18.9 | 1.55 (0.85 to 2.82) | 0.151 | 1.53 (0.83 to 2.82) | 0.169 | 1.44 (0.77 to 2.66) | 0.251 |
| 35–39 | 16.1 | 14.5 | 22.6 | 22.1 | 24.5 | 25.5 | 1.05 (0.52 to 2.14) | 0.883 | 1.00 (0.49 to 2.03) | 0.995 | 1.05 (0.51 to 2.17) | 0.885 |
| 40–45 | 22.2 | 19.2 | 16.7 | 26.6 | 27.7 | 20.4 | 0.86 (0.39 to 1.89) | 0.702 | 0.95 (0.42 to 2.17) | 0.903 | 0.86 (0.37 to 2.04) | 0.739 |
| > 45 | 23.7 | 17.1 | 25.6 | 28.9 | 22.3 | 31.8 | 1.02 (0.57 to 1.83) | 0.951 | 0.91 (0.50 to 1.64) | 0.750 | 0.80 (0.43 to 1.48) | 0.482 |
| Employment | ||||||||||||
| Employed | 21.8 | 22.7 | 23.6 | 26.1 | 25.3 | 23.3 | 1.19 (0.94 to 1.51) | 0.148 | 1.18 (0.93 to 1.50) | 0.162 | 1.14 (0.90 to 1.46) | 0.274 |
| Economically inactive | 36.3 | 34.6 | 35.8 | 38.7 | 34.4 | 35.0 | 1.13 (0.90 to 1.43) | 0.293 | 1.14 (0.90 to 1.44) | 0.272 | 1.12 (0.88 to 1.42) | 0.378 |
| Unemployed | 27.3 | 26.2 | 30.6 | 29.1 | 28.0 | 26.1 | 1.19 (0.56 to 2.55) | 0.652 | 1.11 (0.51 to 2.42) | 0.799 | 1.19 (0.52 to 2.72) | 0.679 |
| Education | ||||||||||||
| Higher | 27.7 | 26.9 | 27.6 | 32.7 | 31.1 | 29.1 | 1.10 (0.91 to 1.34) | 0.319 | 1.11 (0.92 to 1.35) | 0.277 | 1.07 (0.87 to 1.31) | 0.521 |
| Further | 27.9 | 25.8 | 26.5 | 28.7 | 24.9 | 20.7 | 1.24 (0.60 to 2.57) | 0.564 | 1.21 (0.58 to 2.52) | 0.611 | 1.07 (0.50 to 2.27) | 0.863 |
| Upper | 25.5 | 27.0 | 32.1 | 34.2 | 27.0 | 34.7 | 1.51 (0.96 to 2.38) | 0.074 | 1.41 (0.89 to 2.24) | 0.146 | 1.33 (0.83 to 2.14) | 0.234 |
| Lower | 28.5 | 29.6 | 29.2 | 30.0 | 23.7 | 22.5 | 1.50 (0.86 to 2.61) | 0.158 | 1.44 (0.82 to 2.53) | 0.211 | 1.46 (0.81 to 2.64) | 0.212 |
| No formal education | 29.6 | 31.1 | 34.5 | 26.6 | 32.7 | 40.7 | 0.75 (0.30 to 1.85) | 0.531 | 0.70 (0.28 to 1.77) | 0.454 | 0.74 (0.28 to 2.00) | 0.557 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Alcohol misuse (FAST score ≥ 3) | 49.6 | 52.7 | 53.6 | 58.8 | 55.0 | 56.8 | 1.30 (1.13 to 1.51) | 0.000 | 1.29 (1.12 to 1.50) | 0.001 | 1.22 (1.04 to 1.42) | 0.012 |
| Sex | ||||||||||||
| Female | 47.1 | 50.3 | 52.7 | 57.6 | 52.9 | 55.3 | 1.39 (1.15 to 1.68) | 0.001 | 1.38 (1.14 to 1.67) | 0.001 | 1.32 (1.08 to 1.62) | 0.007 |
| Male | 53.6 | 56.1 | 56.1 | 60.9 | 58.5 | 59.1 | 1.21 (0.96 to 1.54) | 0.111 | 1.21 (0.95 to 1.53) | 0.125 | 1.16 (0.91 to 1.48) | 0.232 |
| Non-binary | 40.4 | 50.2 | 29.7 | 47.5 | 54.5 | 63.2 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 69.7 | 69.7 | 71.0 | 70.0 | 63.0 | 66.6 | 1.33 (0.88 to 2.02) | 0.178 | 1.31 (0.89 to 1.94) | 0.173 | 1.45 (0.97 to 2.17) | 0.073 |
| 20–24 | 60.0 | 66.5 | 65.0 | 67.1 | 67.4 | 64.8 | 1.33 (1.03 to 1.71) | 0.030 | 1.39 (1.08 to 1.80) | 0.012 | 1.38 (1.06 to 1.79) | 0.016 |
| 25–29 | 44.8 | 50.9 | 48.4 | 49.7 | 47.3 | 50.2 | 1.26 (0.89 to 1.78) | 0.193 | 1.24 (0.88 to 1.76) | 0.221 | 1.29 (0.90 to 1.83) | 0.165 |
| 30–34 | 38.5 | 41.3 | 43.9 | 48.8 | 42.0 | 47.6 | 1.43 (0.89 to 2.29) | 0.137 | 1.34 (0.83 to 2.17) | 0.226 | 1.28 (0.78 to 2.08) | 0.324 |
| 35–39 | 38.0 | 32.6 | 41.9 | 44.0 | 46.9 | 48.8 | 0.86 (0.48 to 1.52) | 0.599 | 0.82 (0.46 to 1.45) | 0.492 | 0.83 (0.46 to 1.48) | 0.523 |
| 40–45 | 42.1 | 37.9 | 40.0 | 46.4 | 41.1 | 36.3 | 1.22 (0.63 to 2.36) | 0.562 | 1.17 (0.59 to 2.30) | 0.657 | 1.04 (0.52 to 2.11) | 0.906 |
| > 45 | 30.8 | 29.8 | 37.9 | 42.6 | 35.8 | 49.8 | 1.20 (0.71 to 2.04) | 0.497 | 1.12 (0.65 to 1.90) | 0.689 | 1.05 (0.60 to 1.83) | 0.867 |
| Employment | ||||||||||||
| Employed | 43.2 | 44.5 | 47.5 | 52.3 | 49.3 | 50.2 | 1.26 (1.03 to 1.54) | 0.026 | 1.24 (1.01 to 1.52) | 0.040 | 1.16 (0.94 to 1.43) | 0.173 |
| Economically inactive | 59.9 | 66.4 | 63.7 | 66.7 | 62.5 | 65.2 | 1.40 (1.10 to 1.79) | 0.007 | 1.43 (1.12 to 1.82) | 0.004 | 1.38 (1.08 to 1.78) | 0.011 |
| Unemployed | 46.4 | 51.8 | 51.0 | 49.4 | 51.8 | 54.1 | 1.06 (0.54 to 2.11) | 0.857 | 1.02 (0.50 to 2.07) | 0.953 | 1.01 (0.48 to 2.13) | 0.986 |
| Education | ||||||||||||
| Higher | 50.3 | 54.0 | 51.9 | 60.7 | 56.4 | 57.3 | 1.30 (1.09 to 1.55) | 0.004 | 1.32 (1.10 to 1.58) | 0.003 | 1.25 (1.03 to 1.51) | 0.021 |
| Further | 42.4 | 46.4 | 59.4 | 54.3 | 50.6 | 51.5 | 1.81 (0.95 to 3.44) | 0.070 | 1.75 (0.92 to 3.33) | 0.086 | 1.64 (0.84 to 3.22) | 0.148 |
| Upper | 51.6 | 54.9 | 61.7 | 62.3 | 56.0 | 61.7 | 1.59 (1.05 to 2.41) | 0.030 | 1.47 (0.97 to 2.24) | 0.073 | 1.44 (0.93 to 2.23) | 0.104 |
| Lower | 48.2 | 44.1 | 51.0 | 50.9 | 49.3 | 54.3 | 0.98 (0.58 to 1.65) | 0.935 | 0.91 (0.54 to 1.53) | 0.710 | 0.76 (0.44 to 1.31) | 0.320 |
| No formal education | 40.0 | 50.1 | 50.1 | 45.9 | 53.8 | 57.9 | 1.02 (0.43 to 2.40) | 0.973 | 0.95 (0.40 to 2.28) | 0.913 | 1.20 (0.46 to 3.13) | 0.707 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Drinkers with at least a hazardous drinking level | 67.8 | 69.6 | 71.0 | 75.8 | 73.2 | 74.3 | 1.26 (1.07 to 1.48) | 0.006 | 1.24 (1.05 to 1.47) | 0.010 | 1.14 (0.96 to 1.36) | 0.126 |
| Sex | ||||||||||||
| Female | 65.5 | 67.8 | 69.7 | 75.4 | 72.5 | 73.7 | 1.32 (1.07 to 1.63) | 0.009 | 1.31 (1.06 to 1.62) | 0.012 | 1.22 (0.98 to 1.52) | 0.079 |
| Male | 71.9 | 72.1 | 74.0 | 76.3 | 74.3 | 75.2 | 1.17 (0.89 to 1.52) | 0.262 | 1.14 (0.87 to 1.50) | 0.325 | 1.08 (0.82 to 1.42) | 0.596 |
| Non-binary | 50.7 | 68.2 | 46.7 | 83.6 | 69.6 | 81.5 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 79.1 | 84.4 | 83.9 | 84.8 | 83.1 | 82.3 | 1.63 (0.96 to 2.79) | 0.073 | 1.63 (1.01 to 2.63) | 0.044 | 1.83 (1.13 to 2.97) | 0.014 |
| 20–24 | 78.9 | 81.9 | 80.1 | 83.2 | 82.0 | 82.1 | 1.23 (0.90 to 1.69) | 0.197 | 1.28 (0.94 to 1.76) | 0.122 | 1.26 (0.92 to 1.73) | 0.157 |
| 25–29 | 67.9 | 69.2 | 70.4 | 70.8 | 67.4 | 71.7 | 1.17 (0.81 to 1.70) | 0.408 | 1.14 (0.78 to 1.66) | 0.494 | 1.16 (0.79 to 1.70) | 0.444 |
| 30–34 | 57.9 | 61.9 | 60.1 | 65.8 | 64.8 | 65.6 | 1.16 (0.72 to 1.87) | 0.533 | 1.15 (0.71 to 1.85) | 0.581 | 1.08 (0.66 to 1.76) | 0.769 |
| 35–39 | 58.0 | 53.0 | 60.9 | 60.6 | 64.7 | 64.9 | 0.82 (0.47 to 1.45) | 0.500 | 0.80 (0.45 to 1.41) | 0.444 | 0.82 (0.46 to 1.47) | 0.507 |
| 40–45 | 60.8 | 58.6 | 63.1 | 68.2 | 55.1 | 55.0 | 1.81 (0.92 to 3.55) | 0.086 | 1.63 (0.82 to 3.25) | 0.164 | 1.46 (0.71 to 2.98) | 0.303 |
| > 45 | 48.8 | 43.2 | 56.2 | 56.0 | 56.6 | 64.4 | 0.91 (0.55 to 1.52) | 0.729 | 0.87 (0.52 to 1.46) | 0.600 | 0.80 (0.47 to 1.37) | 0.414 |
| Employment | ||||||||||||
| Employed | 64.1 | 63.0 | 68.0 | 71.7 | 69.2 | 69.5 | 1.22 (0.98 to 1.51) | 0.077 | 1.18 (0.95 to 1.47) | 0.128 | 1.06 (0.85 to 1.33) | 0.598 |
| Economically inactive | 74.9 | 80.3 | 76.6 | 80.8 | 78.4 | 80.9 | 1.29 (0.97 to 1.72) | 0.081 | 1.31 (0.99 to 1.74) | 0.059 | 1.25 (0.93 to 1.66) | 0.136 |
| Unemployed | 57.5 | 73.6 | 65.1 | 69.1 | 71.1 | 69.1 | 1.48 (0.72 to 3.01) | 0.284 | 1.61 (0.78 to 3.34) | 0.199 | 1.66 (0.77 to 3.61) | 0.199 |
| Education | ||||||||||||
| Higher | 68.7 | 70.4 | 69.3 | 77.0 | 73.7 | 75.2 | 1.21 (0.99 to 1.48) | 0.064 | 1.22 (1.00 to 1.49) | 0.055 | 1.10 (0.89 to 1.36) | 0.375 |
| Further | 54.4 | 66.4 | 75.5 | 73.2 | 68.8 | 73.1 | 2.38 (1.22 to 4.66) | 0.011 | 2.32 (1.19 to 4.55) | 0.014 | 2.33 (1.13 to 4.80) | 0.022 |
| Upper | 72.1 | 71.4 | 80.0 | 81.2 | 74.6 | 75.5 | 1.82 (1.12 to 2.96) | 0.016 | 1.66 (1.02 to 2.73) | 0.043 | 1.61 (0.96 to 2.70) | 0.070 |
| Lower | 63.1 | 63.7 | 68.2 | 68.5 | 73.4 | 69.7 | 1.02 (0.57 to 1.80) | 0.957 | 0.96 (0.55 to 1.67) | 0.874 | 0.80 (0.45 to 1.43) | 0.456 |
| No formal education | 61.3 | 64.2 | 67.8 | 63.3 | 72.0 | 72.9 | 0.82 (0.34 to 2.00) | 0.667 | 0.77 (0.31 to 1.89) | 0.564 | 0.80 (0.29 to 2.17) | 0.659 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Drinkers with at least a harmful drinking level | 23.2 | 21.7 | 26.5 | 28.2 | 24.6 | 27.3 | 1.22 (1.03 to 1.44) | 0.022 | 1.19 (1.00 to 1.41) | 0.047 | 1.10 (0.93 to 1.32) | 0.265 |
| Sex | ||||||||||||
| Female | 21.9 | 19.2 | 25.0 | 27.4 | 22.7 | 25.4 | 1.24 (0.99 to 1.55) | 0.057 | 1.22 (0.97 to 1.53) | 0.083 | 1.16 (0.92 to 1.47) | 0.207 |
| Male | 25.4 | 24.9 | 28.9 | 29.8 | 27.9 | 29.6 | 1.17 (0.90 to 1.52) | 0.234 | 1.14 (0.87 to 1.48) | 0.333 | 1.09 (0.83 to 1.43) | 0.530 |
| Non-binary | 15.4 | 27.3 | 17.5 | 13.8 | 14.9 | 62.4 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 37.9 | 37.0 | 42.6 | 38.1 | 28.0 | 37.2 | 1.46 (1.00 to 2.12) | 0.048 | 1.37 (0.95 to 1.97) | 0.094 | 1.41 (0.97 to 2.06) | 0.074 |
| 20–24 | 32.1 | 28.1 | 34.6 | 34.3 | 33.1 | 34.8 | 1.00 (0.77 to 1.31) | 0.974 | 1.04 (0.80 to 1.36) | 0.763 | 1.02 (0.78 to 1.33) | 0.906 |
| 25–29 | 16.5 | 17.6 | 21.5 | 20.1 | 19.1 | 20.5 | 1.28 (0.82 to 2.00) | 0.278 | 1.25 (0.80 to 1.96) | 0.330 | 1.24 (0.79 to 1.95) | 0.356 |
| 30–34 | 14.8 | 14.0 | 17.0 | 19.9 | 14.8 | 16.6 | 1.46 (0.78 to 2.74) | 0.237 | 1.36 (0.71 to 2.58) | 0.352 | 1.23 (0.63 to 2.37) | 0.544 |
| 35–39 | 14.5 | 13.2 | 17.1 | 16.8 | 20.8 | 22.0 | 0.80 (0.37 to 1.71) | 0.564 | 0.77 (0.36 to 1.65) | 0.498 | 0.78 (0.36 to 1.70) | 0.528 |
| 40–45 | 15.5 | 10.4 | 15.0 | 20.7 | 16.5 | 15.1 | 1.17 (0.47 to 2.88) | 0.740 | 1.15 (0.45 to 2.90) | 0.771 | 0.97 (0.37 to 2.53) | 0.955 |
| > 45 | 11.9 | 11.4 | 17.1 | 17.3 | 15.7 | 16.6 | 1.41 (0.68 to 2.92) | 0.362 | 1.36 (0.66 to 2.81) | 0.403 | 1.19 (0.55 to 2.55) | 0.657 |
| Employment | ||||||||||||
| Employed | 17.5 | 17.6 | 20.7 | 20.5 | 19.6 | 20.7 | 1.16 (0.90 to 1.49) | 0.253 | 1.13 (0.88 to 1.46) | 0.347 | 1.08 (0.83 to 1.40) | 0.577 |
| Economically inactive | 31.9 | 28.9 | 35.2 | 36.4 | 30.4 | 36.4 | 1.20 (0.94 to 1.52) | 0.147 | 1.17 (0.92 to 1.50) | 0.195 | 1.09 (0.85 to 1.40) | 0.480 |
| Unemployed | 23.2 | 18.4 | 31.0 | 28.6 | 26.7 | 18.9 | 1.57 (0.71 to 3.48) | 0.264 | 1.49 (0.67 to 3.36) | 0.331 | 1.59 (0.67 to 3.79) | 0.297 |
| Education | ||||||||||||
| Higher | 24.2 | 21.4 | 26.3 | 29.3 | 24.7 | 28.0 | 1.17 (0.96 to 1.43) | 0.129 | 1.16 (0.95 to 1.42) | 0.143 | 1.09 (0.88 to 1.34) | 0.432 |
| Further | 17.8 | 24.3 | 26.9 | 21.7 | 20.3 | 23.4 | 1.60 (0.68 to 3.79) | 0.282 | 1.54 (0.64 to 3.68) | 0.336 | 1.36 (0.56 to 3.25) | 0.496 |
| Upper | 23.3 | 22.5 | 27.7 | 30.4 | 27.3 | 33.2 | 1.17 (0.74 to 1.85) | 0.509 | 1.06 (0.67 to 1.68) | 0.813 | 0.95 (0.59 to 1.55) | 0.847 |
| Lower | 17.3 | 18.3 | 26.0 | 25.9 | 22.4 | 21.1 | 1.84 (1.00 to 3.36) | 0.049 | 1.75 (0.95 to 3.21) | 0.073 | 1.51 (0.78 to 2.89) | 0.220 |
| No formal education | 22.8 | 27.0 | 27.1 | 20.8 | 32.1 | 27.4 | 0.77 (0.29 to 2.10) | 0.615 | 0.72 (0.26 to 2.00) | 0.526 | 0.86 (0.29 to 2.54) | 0.787 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Drinkers with at least a dependent drinking level | 11.4 | 10.6 | 12.2 | 13.5 | 11.5 | 13.0 | 1.14 (0.91 to 1.42) | 0.249 | 1.12 (0.90 to 1.40) | 0.309 | 1.06 (0.85 to 1.34) | 0.601 |
| Sex | ||||||||||||
| Female | 11.0 | 9.2 | 11.4 | 12.4 | 10.5 | 12.2 | 1.05 (0.78 to 1.42) | 0.738 | 1.05 (0.77 to 1.41) | 0.766 | 1.02 (0.75 to 1.38) | 0.915 |
| Male | 12.2 | 12.6 | 13.5 | 15.4 | 13.2 | 13.7 | 1.28 (0.91 to 1.80) | 0.158 | 1.25 (0.89 to 1.77) | 0.201 | 1.21 (0.85 to 1.72) | 0.290 |
| Non-binary | 4.1 | 9.3 | 5.7 | 1.4 | 14.3 | 38.9 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 17.7 | 19.4 | 19.0 | 18.6 | 12.0 | 18.1 | 1.47 (0.92 to 2.35) | 0.107 | 1.45 (0.90 to 2.32) | 0.124 | 1.44 (0.89 to 2.31) | 0.139 |
| 20–24 | 14.5 | 12.4 | 15.9 | 15.1 | 15.5 | 16.2 | 0.94 (0.66 to 1.33) | 0.718 | 0.98 (0.69 to 1.38) | 0.892 | 0.96 (0.67 to 1.36) | 0.814 |
| 25–29 | 8.1 | 10.0 | 8.5 | 10.0 | 8.8 | 6.5 | 1.50 (0.81 to 2.78) | 0.193 | 1.54 (0.83 to 2.86) | 0.171 | 1.47 (0.79 to 2.75) | 0.222 |
| 30–34 | 7.7 | 6.3 | 7.5 | 11.2 | 8.2 | 8.4 | 1.27 (0.55 to 2.92) | 0.582 | 1.18 (0.50 to 2.79) | 0.698 | 1.14 (0.47 to 2.73) | 0.773 |
| 35–39 | 7.9 | 6.1 | 8.5 | 6.9 | 8.6 | 10.5 | 0.68 (0.24 to 1.92) | 0.461 | 0.64 (0.22 to 1.83) | 0.405 | 0.70 (0.23 to 2.07) | 0.515 |
| 40–45 | 10.4 | 6.6 | 9.5 | 10.6 | 8.8 | 10.7 | 0.88 (0.30 to 2.62) | 0.817 | 0.89 (0.30 to 2.69) | 0.840 | 0.74 (0.23 to 2.33) | 0.604 |
| > 45 | 7.3 | 5.6 | 8.5 | 11.0 | 8.8 | 11.3 | 1.11 (0.44 to 2.82) | 0.821 | 1.05 (0.41 to 2.67) | 0.916 | 0.88 (0.33 to 2.30) | 0.788 |
| Employment | ||||||||||||
| Employed | 8.5 | 9.6 | 9.7 | 10.0 | 9.2 | 9.0 | 1.27 (0.90 to 1.80) | 0.176 | 1.26 (0.89 to 1.78) | 0.195 | 1.22 (0.86 to 1.73) | 0.271 |
| Economically inactive | 15.1 | 12.2 | 15.5 | 16.9 | 14.4 | 18.4 | 0.97 (0.71 to 1.33) | 0.872 | 0.97 (0.71 to 1.32) | 0.839 | 0.91 (0.66 to 1.26) | 0.575 |
| Unemployed | 15.8 | 11.6 | 18.4 | 15.5 | 11.9 | 8.4 | 1.61 (0.62 to 4.14) | 0.328 | 1.48 (0.56 to 3.91) | 0.429 | 1.49 (0.52 to 4.22) | 0.456 |
| Education | ||||||||||||
| Higher | 11.7 | 10.3 | 11.5 | 13.3 | 11.5 | 13.0 | 1.02 (0.78 to 1.34) | 0.869 | 1.03 (0.78 to 1.35) | 0.843 | 0.98 (0.75 to 1.30) | 0.904 |
| Further | 13.1 | 14.9 | 12.6 | 11.2 | 10.6 | 11.3 | 1.07 (0.37 to 3.07) | 0.906 | 1.05 (0.37 to 3.01) | 0.924 | 1.05 (0.38 to 2.87) | 0.931 |
| Upper | 10.1 | 8.5 | 13.1 | 15.5 | 11.6 | 17.2 | 1.28 (0.69 to 2.36) | 0.437 | 1.11 (0.60 to 2.07) | 0.740 | 0.98 (0.51 to 1.86) | 0.941 |
| Lower | 9.7 | 10.5 | 13.0 | 14.3 | 10.5 | 9.6 | 1.93 (0.90 to 4.15) | 0.093 | 1.85 (0.85 to 4.03) | 0.123 | 1.58 (0.69 to 3.62) | 0.284 |
| No formal education | 11.3 | 17.5 | 20.6 | 12.6 | 18.0 | 14.8 | 1.38 (0.42 to 4.60) | 0.598 | 1.31 (0.39 to 4.36) | 0.659 | 1.40 (0.42 to 4.71) | 0.584 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Alcohol purchased from on-licensed premises | 77.3 | 79.8 | 77.8 | 83.4 | 81.4 | 78.8 | 1.33 (1.10 to 1.61) | 0.003 | 1.33 (1.10 to 1.61) | 0.003 | 1.27 (1.05 to 1.55) | 0.016 |
| Sex | ||||||||||||
| Female | 75.4 | 76.7 | 75.2 | 81.7 | 80.6 | 77.2 | 1.21 (0.96 to 1.53) | 0.105 | 1.22 (0.97 to 1.54) | 0.094 | 1.21 (0.94 to 1.55) | 0.136 |
| Male | 80.9 | 84.7 | 83.3 | 86.1 | 82.8 | 81.9 | 1.63 (1.18 to 2.26) | 0.003 | 1.62 (1.17 to 2.25) | 0.004 | 1.53 (1.09 to 2.15) | 0.014 |
| Non-binary | 60.5 | 71.8 | 35.2 | 89.3 | 76.9 | 60.2 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 72.1 | 71.2 | 81.0 | 82.1 | 82.5 | 72.9 | 1.65 (1.04 to 2.62) | 0.033 | 1.58 (1.02 to 2.42) | 0.038 | 2.13 (1.33 to 3.41) | 0.002 |
| 20–24 | 89.4 | 89.0 | 87.3 | 90.8 | 90.1 | 89.1 | 0.99 (0.66 to 1.47) | 0.942 | 1.00 (0.67 to 1.49) | 0.982 | 0.94 (0.62 to 1.43) | 0.784 |
| 25–29 | 81.2 | 85.4 | 81.1 | 84.0 | 80.3 | 79.7 | 1.47 (0.94 to 2.31) | 0.092 | 1.46 (0.93 to 2.30) | 0.099 | 1.55 (0.98 to 2.46) | 0.061 |
| 30–34 | 73.4 | 72.2 | 73.6 | 76.8 | 74.7 | 70.7 | 1.21 (0.71 to 2.05) | 0.485 | 1.19 (0.69 to 2.03) | 0.534 | 1.11 (0.64 to 1.95) | 0.707 |
| 35–39 | 68.8 | 69.9 | 69.1 | 71.3 | 73.7 | 78.2 | 0.81 (0.44 to 1.51) | 0.515 | 0.80 (0.43 to 1.49) | 0.477 | 0.92 (0.49 to 1.75) | 0.810 |
| 40–45 | 65.9 | 69.0 | 63.7 | 75.1 | 75.0 | 63.9 | 1.31 (0.63 to 2.74) | 0.468 | 1.28 (0.60 to 2.71) | 0.522 | 1.20 (0.55 to 2.61) | 0.644 |
| > 45 | 66.3 | 75.7 | 64.4 | 70.7 | 66.6 | 67.6 | 1.34 (0.77 to 2.33) | 0.307 | 1.34 (0.77 to 2.32) | 0.302 | 1.36 (0.77 to 2.40) | 0.286 |
| Employment | ||||||||||||
| Employed | 76.1 | 79.6 | 76.1 | 82.4 | 79.4 | 77.9 | 1.38 (1.07 to 1.77) | 0.013 | 1.38 (1.07 to 1.77) | 0.012 | 1.27 (0.98 to 1.65) | 0.074 |
| Economically inactive | 81.2 | 81.7 | 81.2 | 86.0 | 85.5 | 81.3 | 1.23 (0.89 to 1.69) | 0.206 | 1.23 (0.90 to 1.69) | 0.197 | 1.19 (0.85 to 1.67) | 0.302 |
| Unemployed | 62.6 | 63.2 | 71.8 | 69.0 | 70.0 | 66.1 | 1.36 (0.66 to 2.81) | 0.408 | 1.34 (0.63 to 2.84) | 0.443 | 1.72 (0.78 to 3.78) | 0.179 |
| Education | ||||||||||||
| Higher | 81.6 | 84.8 | 80.6 | 87.7 | 86.4 | 83.5 | 1.32 (1.03 to 1.69) | 0.027 | 1.35 (1.05 to 1.73) | 0.018 | 1.24 (0.95 to 1.60) | 0.110 |
| Further | 69.2 | 70.0 | 74.0 | 76.4 | 72.8 | 71.9 | 1.44 (0.70 to 2.94) | 0.324 | 1.41 (0.68 to 2.90) | 0.357 | 1.16 (0.52 to 2.58) | 0.714 |
| Upper | 70.6 | 74.3 | 78.5 | 84.7 | 76.2 | 78.1 | 2.29 (1.39 to 3.78) | 0.001 | 2.22 (1.34 to 3.69) | 0.002 | 2.26 (1.32 to 3.86) | 0.003 |
| Lower | 62.4 | 59.3 | 66.1 | 69.5 | 68.4 | 64.0 | 1.23 (0.71 to 2.16) | 0.461 | 1.28 (0.73 to 2.22) | 0.389 | 1.29 (0.72 to 2.31) | 0.398 |
| No formal education | 62.4 | 61.1 | 54.7 | 57.6 | 67.5 | 59.3 | 0.62 (0.26 to 1.49) | 0.287 | 0.65 (0.27 to 1.56) | 0.334 | 0.70 (0.27 to 1.83) | 0.472 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Alcohol purchased from off-licensed premises | 74.2 | 75.2 | 72.6 | 74.6 | 73.7 | 71.2 | 1.08 (0.91 to 1.29) | 0.352 | 1.10 (0.92 to 1.30) | 0.294 | 1.08 (0.91 to 1.29) | 0.389 |
| Sex | ||||||||||||
| Female | 73.7 | 75.0 | 71.8 | 72.8 | 71.8 | 71.0 | 1.05 (0.84 to 1.30) | 0.688 | 1.05 (0.84 to 1.31) | 0.661 | 1.03 (0.82 to 1.30) | 0.783 |
| Male | 75.5 | 76.1 | 75.3 | 77.7 | 76.6 | 71.7 | 1.21 (0.92 to 1.59) | 0.179 | 1.24 (0.94 to 1.64) | 0.132 | 1.21 (0.91 to 1.61) | 0.180 |
| Non-binary | 63.4 | 62.1 | 42.1 | 77.4 | 84.0 | 64.2 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 72.8 | 77.4 | 76.2 | 77.6 | 73.6 | 65.8 | 1.81 (1.15 to 2.83) | 0.010 | 1.89 (1.24 to 2.86) | 0.003 | 2.12 (1.37 to 3.28) | 0.001 |
| 20–24 | 80.5 | 82.3 | 79.3 | 80.0 | 78.5 | 76.7 | 1.15 (0.85 to 1.57) | 0.362 | 1.14 (0.84 to 1.56) | 0.401 | 1.12 (0.82 to 1.54) | 0.477 |
| 25–29 | 72.2 | 75.6 | 71.3 | 69.2 | 71.9 | 68.1 | 1.00 (0.68 to 1.47) | 0.997 | 1.02 (0.69 to 1.50) | 0.927 | 1.05 (0.71 to 1.56) | 0.792 |
| 30–34 | 68.1 | 65.2 | 65.1 | 67.1 | 72.1 | 67.6 | 0.76 (0.46 to 1.25) | 0.276 | 0.76 (0.46 to 1.26) | 0.285 | 0.71 (0.42 to 1.18) | 0.188 |
| 35–39 | 70.7 | 65.9 | 70.2 | 70.3 | 68.9 | 72.2 | 0.89 (0.48 to 1.64) | 0.701 | 0.87 (0.47 to 1.62) | 0.666 | 0.91 (0.49 to 1.71) | 0.773 |
| 40–45 | 73.6 | 71.7 | 66.4 | 74.9 | 72.3 | 71.1 | 0.91 (0.43 to 1.93) | 0.813 | 0.88 (0.41 to 1.90) | 0.749 | 0.90 (0.41 to 1.97) | 0.795 |
| > 45 | 72.1 | 69.9 | 66.5 | 67.3 | 65.6 | 68.6 | 0.83 (0.47 to 1.44) | 0.505 | 0.78 (0.45 to 1.36) | 0.387 | 0.79 (0.44 to 1.40) | 0.414 |
| Employment | ||||||||||||
| Employed | 71.9 | 72.2 | 70.5 | 71.4 | 72.2 | 68.2 | 1.02 (0.81 to 1.27) | 0.879 | 1.02 (0.82 to 1.28) | 0.834 | 1.02 (0.81 to 1.28) | 0.871 |
| Economically inactive | 78.9 | 81.0 | 76.6 | 79.2 | 76.5 | 75.6 | 1.16 (0.87 to 1.56) | 0.305 | 1.19 (0.90 to 1.59) | 0.228 | 1.15 (0.86 to 1.55) | 0.347 |
| Unemployed | 66.0 | 68.0 | 66.7 | 64.7 | 67.3 | 63.2 | 1.01 (0.50 to 2.05) | 0.982 | 1.10 (0.53 to 2.28) | 0.801 | 1.32 (0.61 to 2.88) | 0.483 |
| Education | ||||||||||||
| Higher | 76.6 | 78.4 | 74.5 | 76.8 | 76.4 | 74.8 | 1.04 (0.84 to 1.28) | 0.732 | 1.06 (0.86 to 1.31) | 0.574 | 1.01 (0.81 to 1.26) | 0.913 |
| Further | 60.2 | 67.9 | 69.7 | 71.8 | 68.7 | 61.2 | 2.00 (1.03 to 3.90) | 0.042 | 2.00 (1.02 to 3.91) | 0.043 | 1.91 (0.92 to 3.97) | 0.081 |
| Upper | 70.5 | 71.3 | 74.8 | 74.7 | 70.4 | 71.2 | 1.42 (0.89 to 2.25) | 0.140 | 1.38 (0.87 to 2.21) | 0.173 | 1.36 (0.84 to 2.21) | 0.210 |
| Lower | 70.5 | 63.5 | 61.8 | 67.1 | 67.0 | 62.3 | 0.77 (0.44 to 1.37) | 0.380 | 0.76 (0.44 to 1.34) | 0.346 | 0.79 (0.44 to 1.43) | 0.436 |
| No formal education | 64.3 | 64.1 | 58.9 | 64.2 | 67.5 | 61.2 | 0.85 (0.35 to 2.06) | 0.714 | 0.88 (0.36 to 2.16) | 0.786 | 0.87 (0.34 to 2.21) | 0.772 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| FAST score | 3.19 | 3.17 | 3.36 | 3.59 | 3.35 | 3.50 | 0.26 (0.06 to 0.46) | 0.012 | 0.24 (0.04 to 0.44) | 0.020 | 0.12 (–0.08 to 0.31) | 0.245 |
| Sex | ||||||||||||
| Female | 3.09 | 3.01 | 3.30 | 3.50 | 3.25 | 3.39 | 0.27 (0.01 to 0.52) | 0.042 | 0.26 (0.00 to 0.51) | 0.050 | 0.15 (–0.11 to 0.40) | 0.253 |
| Male | 3.36 | 3.39 | 3.50 | 3.74 | 3.52 | 3.61 | 0.28 (–0.05 to 0.60) | 0.093 | 0.25 (–0.08 to 0.58) | 0.132 | 0.17 (–0.14 to 0.49) | 0.288 |
| Non-binary | 2.41 | 3.17 | 2.12 | 2.95 | 3.33 | 6.38 | (Too few cases for analysis) | |||||
| Age (years) | ||||||||||||
| < 19 | 4.17 | 4.26 | 4.39 | 4.30 | 3.66 | 4.20 | 0.57 (0.01 to 1.13) | 0.045 | 0.52 (–0.01 to 1.04) | 0.053 | 0.56 (0.04 to 1.08) | 0.035 |
| 20–24 | 3.80 | 3.74 | 3.94 | 4.00 | 4.01 | 3.98 | 0.06 (–0.28 to 0.40) | 0.735 | 0.13 (–0.21 to 0.47) | 0.464 | 0.10 (–0.24 to 0.44) | 0.580 |
| 25–29 | 2.88 | 2.98 | 3.06 | 3.14 | 2.96 | 3.01 | 0.31 (–0.12 to 0.74) | 0.161 | 0.29 (–0.14 to 0.72) | 0.187 | 0.29 (–0.15 to 0.72) | 0.195 |
| 30–34 | 2.60 | 2.63 | 2.70 | 3.07 | 2.68 | 2.81 | 0.41 (–0.16 to 0.98) | 0.156 | 0.36 (–0.21 to 0.93) | 0.212 | 0.30 (–0.27 to 0.87) | 0.305 |
| 35–39 | 2.61 | 2.26 | 2.70 | 2.58 | 3.05 | 3.07 | –0.58 (–1.24 to 0.09) | 0.091 | –0.64 (–1.30 to 0.03) | 0.061 | –0.58 (–1.24 to 0.07) | 0.083 |
| 40–45 | 2.79 | 2.56 | 2.77 | 3.03 | 2.61 | 2.56 | 0.34 (–0.53 to 1.21) | 0.442 | 0.32 (–0.58 to 1.21) | 0.488 | 0.15 (–0.74 to 1.04) | 0.736 |
| > 45 | 2.19 | 2.03 | 2.56 | 2.56 | 2.45 | 3.00 | 0.01 (–0.64 to 0.67) | 0.966 | –0.06 (–0.70 to 0.59) | 0.867 | –0.22 (–0.87 to 0.43) | 0.507 |
| Employment | ||||||||||||
| Employed | 2.82 | 2.85 | 3.01 | 3.12 | 3.03 | 3.05 | 0.20 (–0.05 to 0.45) | 0.111 | 0.18 (–0.07 to 0.43) | 0.157 | 0.08 (–0.17 to 0.32) | 0.531 |
| Economically inactive | 3.73 | 3.69 | 3.88 | 4.09 | 3.76 | 4.12 | 0.24 (–0.10 to 0.58) | 0.166 | 0.24 (–0.09 to 0.57) | 0.157 | 0.12 (–0.20 to 0.45) | 0.454 |
| Unemployed | 3.27 | 3.18 | 3.67 | 3.51 | 3.30 | 3.04 | 0.55 (–0.54 to 1.64) | 0.323 | 0.46 (–0.63 to 1.54) | 0.409 | 0.39 (–0.67 to 1.46) | 0.470 |
| Education | ||||||||||||
| Higher | 3.21 | 3.17 | 3.27 | 3.63 | 3.35 | 3.51 | 0.21 (–0.03 to 0.45) | 0.080 | 0.22 (–0.02 to 0.46) | 0.070 | 0.10 (–0.13 to 0.33) | 0.393 |
| Further | 2.97 | 3.32 | 3.54 | 3.31 | 3.10 | 3.29 | 0.60 (–0.45 to 1.65) | 0.261 | 0.57 (–0.48 to 1.61) | 0.288 | 0.42 (–0.57 to 1.41) | 0.408 |
| Upper | 3.23 | 3.15 | 3.61 | 3.91 | 3.52 | 3.86 | 0.45 (–0.10 to 1.00) | 0.110 | 0.33 (–0.22 to 0.88) | 0.239 | 0.22 (–0.33 to 0.76) | 0.434 |
| Lower | 3.04 | 2.96 | 3.33 | 3.34 | 3.28 | 3.23 | 0.25 (–0.47 to 0.96) | 0.497 | 0.15 (–0.55 to 0.86) | 0.671 | –0.06 (–0.73 to 0.62) | 0.873 |
| No formal education | 3.05 | 3.12 | 3.96 | 3.05 | 3.80 | 3.72 | –0.11 (–1.44 to 1.22) | 0.875 | –0.28 (–1.58 to 1.01) | 0.668 | –0.01 (–1.36 to 1.33) | 0.985 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | ||||||||||||
| Consumption of any illicit drugs in the last months | 23.4 | 26.0 | 29.7 | 28.6 | 30.4 | 31.2 | 1.16 (0.99 to 1.36) | 0.062 | 1.12 (0.95 to 1.31) | 0.175 | 1.04 (0.88 to 1.23) | 0.648 |
| Current alcohol drinker | 93.8 | 93.7 | 93.6 | 90.7 | 88.7 | 89.2 | 1.18 (0.90 to 1.53) | 0.229 | 1.19 (0.91 to 1.55) | 0.195 | 1.18 (0.89 to 1.57) | 0.260 |
| Based on drinkers only | ||||||||||||
| Binge drinking at least weekly | 27.8 | 28.7 | 30.0 | 32.5 | 29.8 | 28.9 | 1.26 (1.08 to 1.47) | 0.004 | 1.25 (1.07 to 1.47) | 0.005 | 1.18 (1.00 to 1.39) | 0.053 |
| Alcohol misuse | 50.3 | 54.5 | 55.0 | 59.1 | 55.7 | 57.1 | 1.34 (1.16 to 1.55) | 0.000 | 1.33 (1.15 to 1.53) | 0.000 | 1.24 (1.06 to 1.44) | 0.007 |
| Drinkers with at least a hazardous drinking level | 68.8 | 71.1 | 72.1 | 76.0 | 73.8 | 74.8 | 1.26 (1.07 to 1.48) | 0.005 | 1.24 (1.05 to 1.46) | 0.010 | 1.13 (0.96 to 1.35) | 0.149 |
| Drinkers with at least a harmful drinking level | 23.5 | 23.7 | 28.0 | 29.0 | 24.8 | 28.1 | 1.32 (1.12 to 1.56) | 0.001 | 1.28 (1.09 to 1.51) | 0.003 | 1.18 (0.99 to 1.41) | 0.058 |
| Drinkers with at least a dependent drinking level | 11.5 | 11.6 | 13.2 | 13.9 | 11.6 | 13.3 | 1.27 (1.02 to 1.58) | 0.034 | 1.24 (0.99 to 1.55) | 0.056 | 1.17 (0.93 to 1.47) | 0.178 |
| Alcohol bought from on-licensed premises | 78.0 | 77.9 | 77.8 | 83.0 | 82.0 | 78.6 | 1.18 (0.98 to 1.42) | 0.078 | 1.18 (0.98 to 1.42) | 0.076 | 1.25 (1.02 to 1.53) | 0.029 |
| Alcohol bought from off-licensed premises | 72.2 | 73.7 | 72.0 | 73.5 | 73.2 | 69.1 | 1.14 (0.97 to 1.35) | 0.123 | 1.16 (0.98 to 1.37) | 0.081 | 1.18 (0.99 to 1.41) | 0.061 |
| FAST score | 3.22 | 3.30 | 3.46 | 3.63 | 3.38 | 3.54 | 0.35 (0.15 to 0.55)a | 0.001 | 0.32 (0.12 to 0.52)a | 0.002 | 0.18 (–0.01 to 0.38)a | 0.068 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | ||||||||||||
| Consumption of any illicit drugs in the last months | 22.9 | 24.6 | 28.0 | 28.0 | 29.2 | 29.9 | 1.14 (0.97 to 1.33) | 0.122 | 1.09 (0.93 to 1.28) | 0.286 | 1.01 (0.85 to 1.20) | 0.942 |
| Current alcohol drinker | 93.6 | 93.3 | 93.3 | 90.5 | 87.6 | 88.8 | 1.21 (0.92 to 1.61) | 0.173 | 1.23 (0.93 to 1.62) | 0.148 | 1.14 (0.85 to 1.53) | 0.371 |
| Based on drinkers only | ||||||||||||
| Binge drinking at least weekly | 27.5 | 27.1 | 28.4 | 32.0 | 29.3 | 28.4 | 1.18 (1.01 to 1.39) | 0.042 | 1.17 (1.00 to 1.38) | 0.050 | 1.12 (0.94 to 1.32) | 0.200 |
| Alcohol misuse | 49.2 | 52.0 | 52.7 | 58.5 | 54.5 | 56.1 | 1.30 (1.12 to 1.51) | 0.001 | 1.28 (1.11 to 1.49) | 0.001 | 1.19 (1.01 to 1.39) | 0.034 |
| Drinkers with at least a hazardous drinking level | 67.5 | 68.9 | 70.4 | 75.5 | 72.7 | 73.7 | 1.25 (1.06 to 1.48) | 0.008 | 1.23 (1.04 to 1.46) | 0.014 | 1.11 (0.93 to 1.32) | 0.255 |
| Drinkers with at least a harmful drinking level | 22.9 | 21.4 | 26.1 | 28.4 | 24.4 | 27.2 | 1.23 (1.04 to 1.46) | 0.017 | 1.19 (1.00 to 1.41) | 0.046 | 1.10 (0.92 to 1.31) | 0.315 |
| Drinkers with at least a dependent drinking level | 11.4 | 10.6 | 12.0 | 13.7 | 11.6 | 12.9 | 1.15 (0.92 to 1.44) | 0.228 | 1.13 (0.90 to 1.41) | 0.305 | 1.06 (0.84 to 1.34) | 0.615 |
| Alcohol bought from on-licensed premises | 76.3 | 79.3 | 77.2 | 82.9 | 81.0 | 77.9 | 1.37 (1.13 to 1.65) | 0.001 | 1.37 (1.14 to 1.66) | 0.001 | 1.34 (1.09 to 1.64) | 0.005 |
| Alcohol bought from off-licensed premises | 71.6 | 73.5 | 71.1 | 73.4 | 72.5 | 68.8 | 1.16 (0.98 to 1.38) | 0.091 | 1.18 (0.99 to 1.40) | 0.060 | 1.17 (0.97 to 1.40) | 0.093 |
| FAST score | 3.17 | 3.15 | 3.33 | 3.59 | 3.34 | 3.48 | 0.27 (0.06 to 0.47)a | 0.011 | 0.24 (0.03 to 0.44)a | 0.022 | 0.09 (–0.11 to 0.29)a | 0.366 |
| Analysis | Scotland (%) | England (%) | Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 1 | Wave 2 | Wave 3 | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Based on all respondents | ||||||||||||
| Consumption of any illicit drugs in the last months | 23.5 | 25.3 | 27.9 | 29.3 | 30.1 | 31.6 | 1.12 (0.94 to 1.33) | 0.203 | 1.10 (0.92 to 1.30) | 0.299 | 1.05 (0.87 to 1.25) | 0.616 |
| Current alcohol drinker | 93.7 | 92.9 | 94.6 | 90.0 | 87.5 | 88.7 | 1.24 (0.93 to 1.66) | 0.148 | 1.24 (0.93 to 1.67) | 0.145 | 1.15 (0.85 to 1.56) | 0.379 |
| Based on drinkers only | ||||||||||||
| Binge drinking at least weekly | 27.3 | 26.4 | 27.4 | 32.1 | 29.3 | 28.5 | 1.14 (0.96 to 1.35) | 0.132 | 1.14 (0.96 to 1.36) | 0.125 | 1.10 (0.92 to 1.31) | 0.290 |
| Alcohol misuse | 48.9 | 52.3 | 52.8 | 58.8 | 55.0 | 56.8 | 1.31 (1.12 to 1.53) | 0.001 | 1.30 (1.12 to 1.53) | 0.001 | 1.23 (1.05 to 1.45) | 0.012 |
| Drinkers with at least a hazardous drinking level | 66.7 | 69.1 | 70.2 | 75.8 | 73.2 | 74.3 | 1.28 (1.08 to 1.52) | 0.005 | 1.28 (1.07 to 1.52) | 0.006 | 1.18 (0.98 to 1.41) | 0.075 |
| Drinkers with at least a harmful drinking level | 23.2 | 20.9 | 24.4 | 28.2 | 24.6 | 27.3 | 1.10 (0.92 to 1.32) | 0.294 | 1.10 (0.92 to 1.32) | 0.309 | 1.03 (0.85 to 1.24) | 0.755 |
| Drinkers with at least a dependent drinking level | 11.1 | 10.0 | 11.8 | 13.5 | 11.5 | 13.0 | 1.11 (0.88 to 1.42) | 0.377 | 1.11 (0.88 to 1.41) | 0.383 | 1.07 (0.83 to 1.36) | 0.614 |
| Alcohol bought from on-licensed premises | 76.0 | 78.5 | 78.0 | 83.4 | 81.4 | 78.8 | 1.40 (1.15 to 1.71) | 0.001 | 1.40 (1.15 to 1.71) | 0.001 | 1.31 (1.06 to 1.61) | 0.011 |
| Alcohol bought from off-licensed premises | 73.5 | 74.8 | 73.5 | 74.6 | 73.7 | 71.2 | 1.15 (0.96 to 1.37) | 0.130 | 1.15 (0.96 to 1.38) | 0.125 | 1.11 (0.92 to 1.34) | 0.267 |
| FAST score | 3.15 | 3.11 | 3.29 | 3.59 | 3.35 | 3.50 | 0.22 (0.01 to 0.43)a | 0.040 | 0.22 (0.01 to 0.43)a | 0.042 | 0.11 (–0.10 to 0.32)a | 0.303 |
FIGURE 29.
Consumption of any illicit drugs in the last month: pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
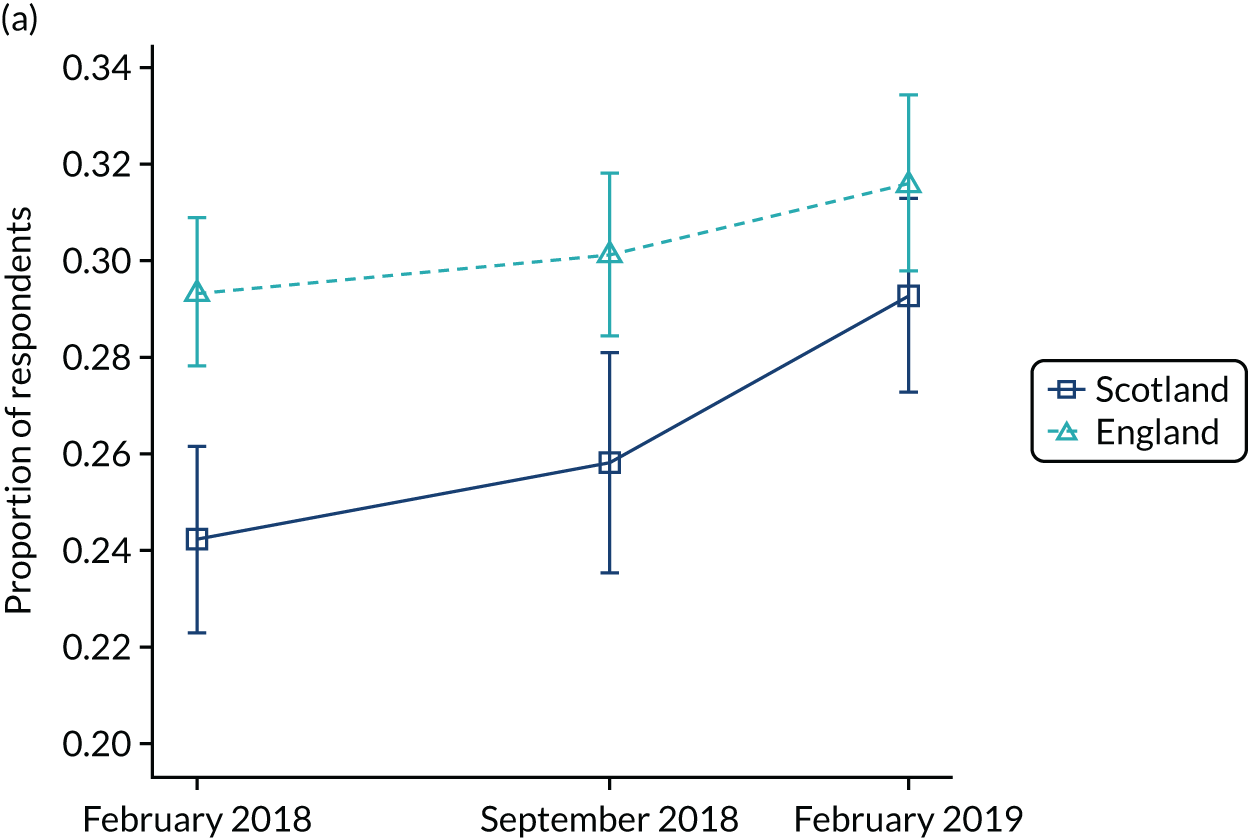
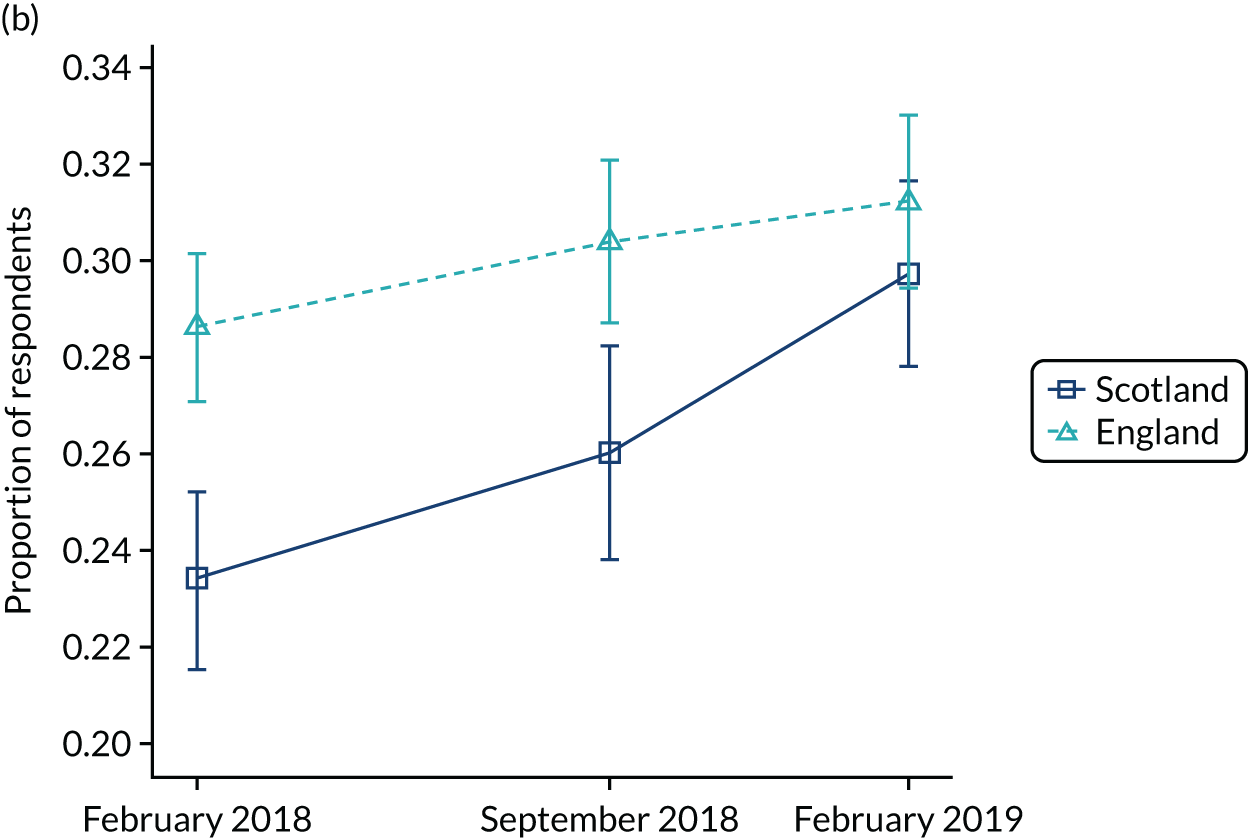
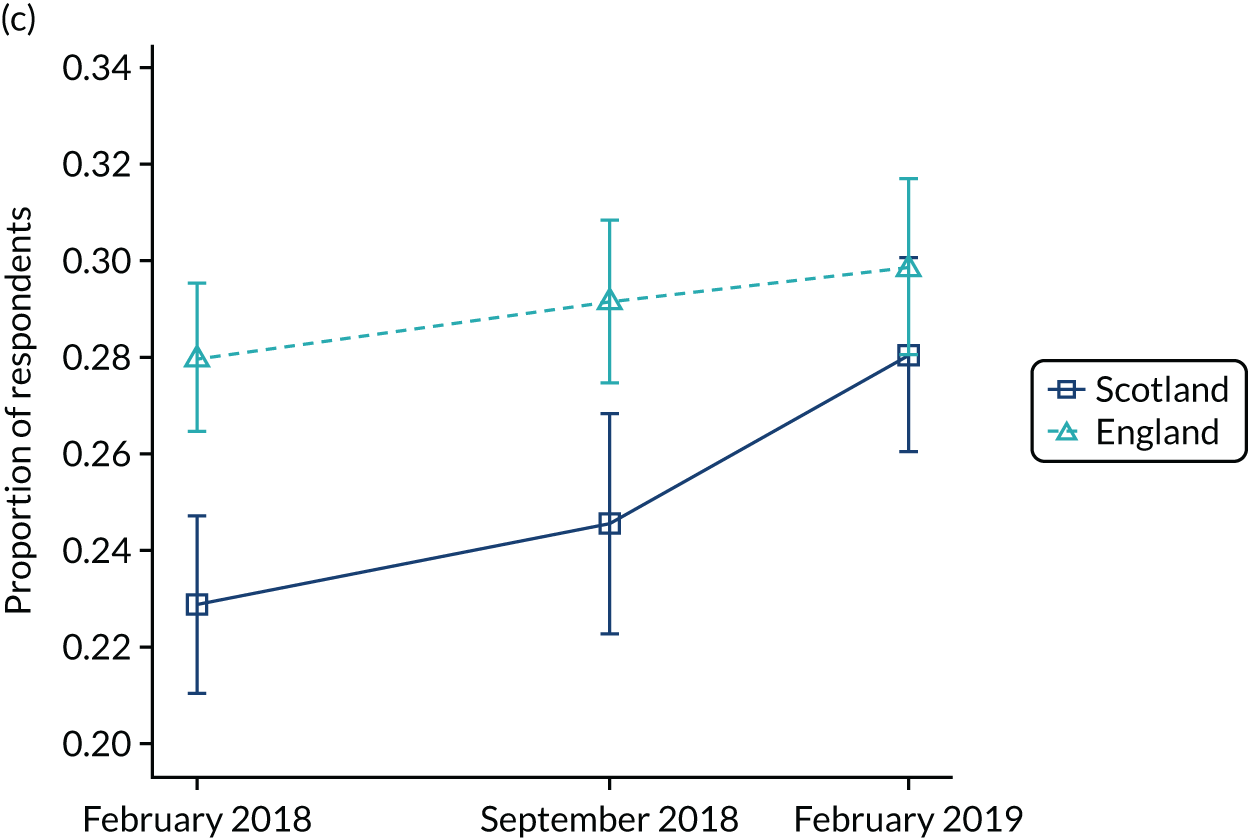
FIGURE 30.
Current alcohol drinker: pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
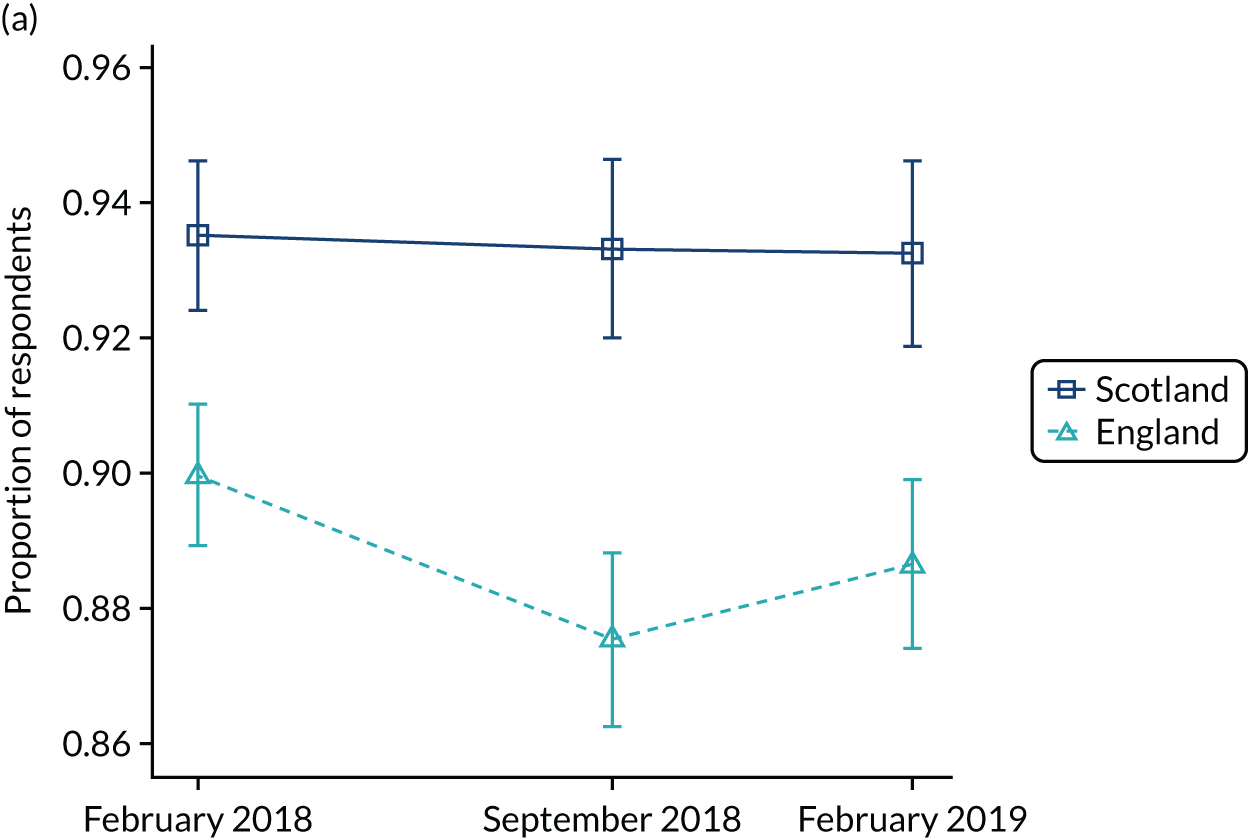
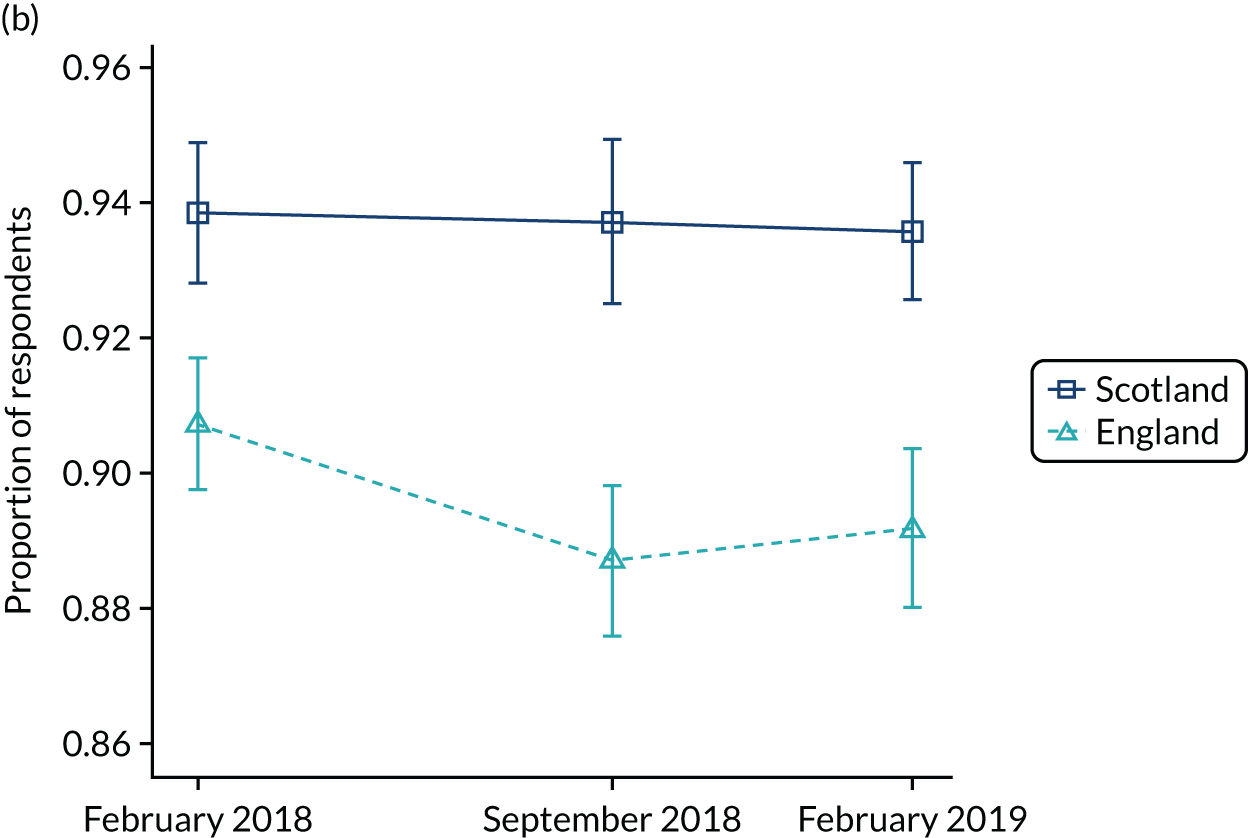
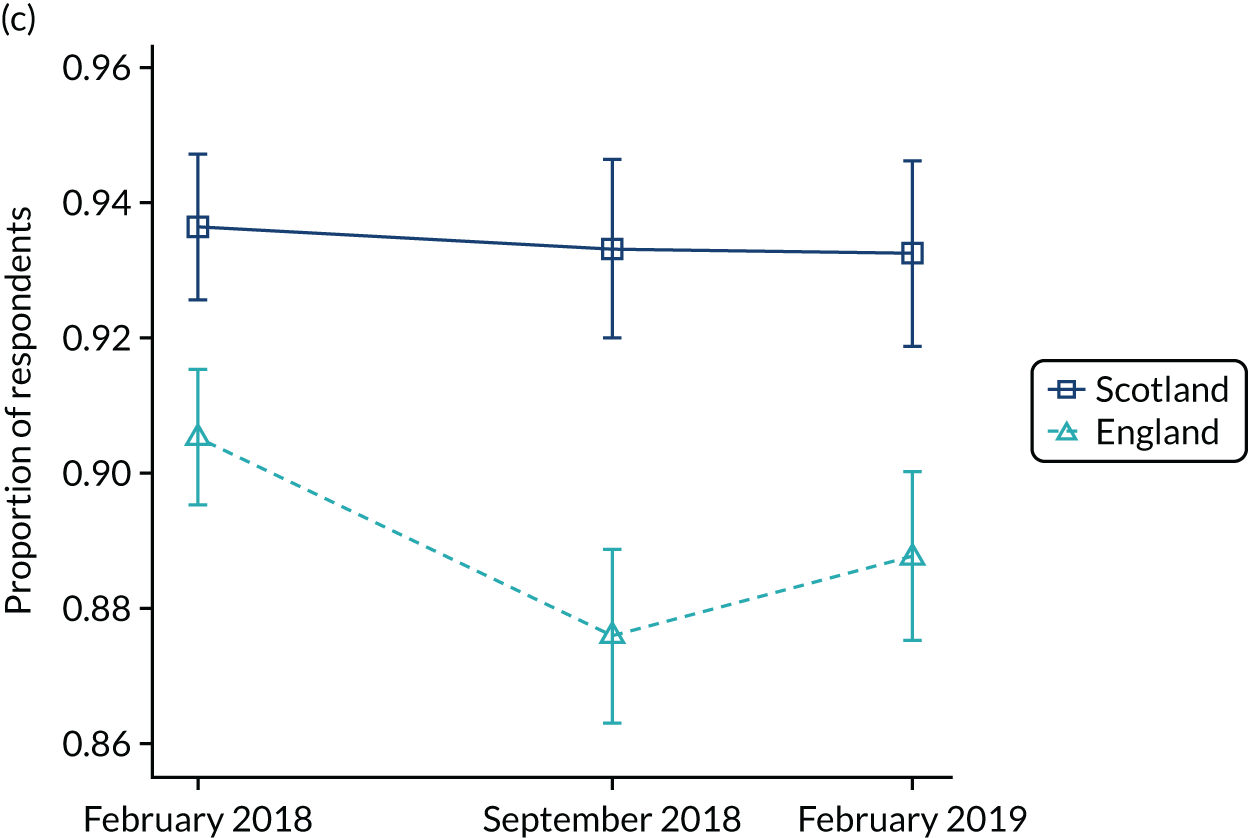
FIGURE 31.
Binge drinking at least weekly: pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
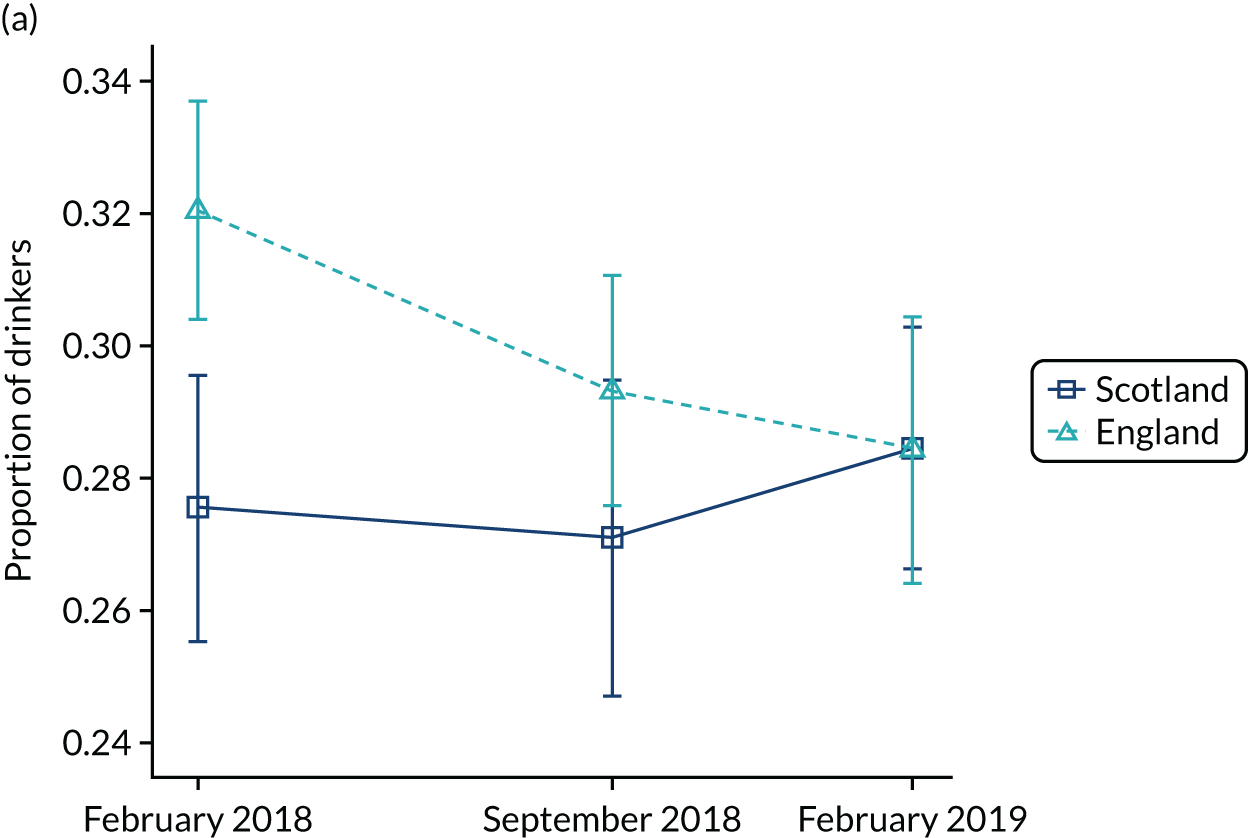
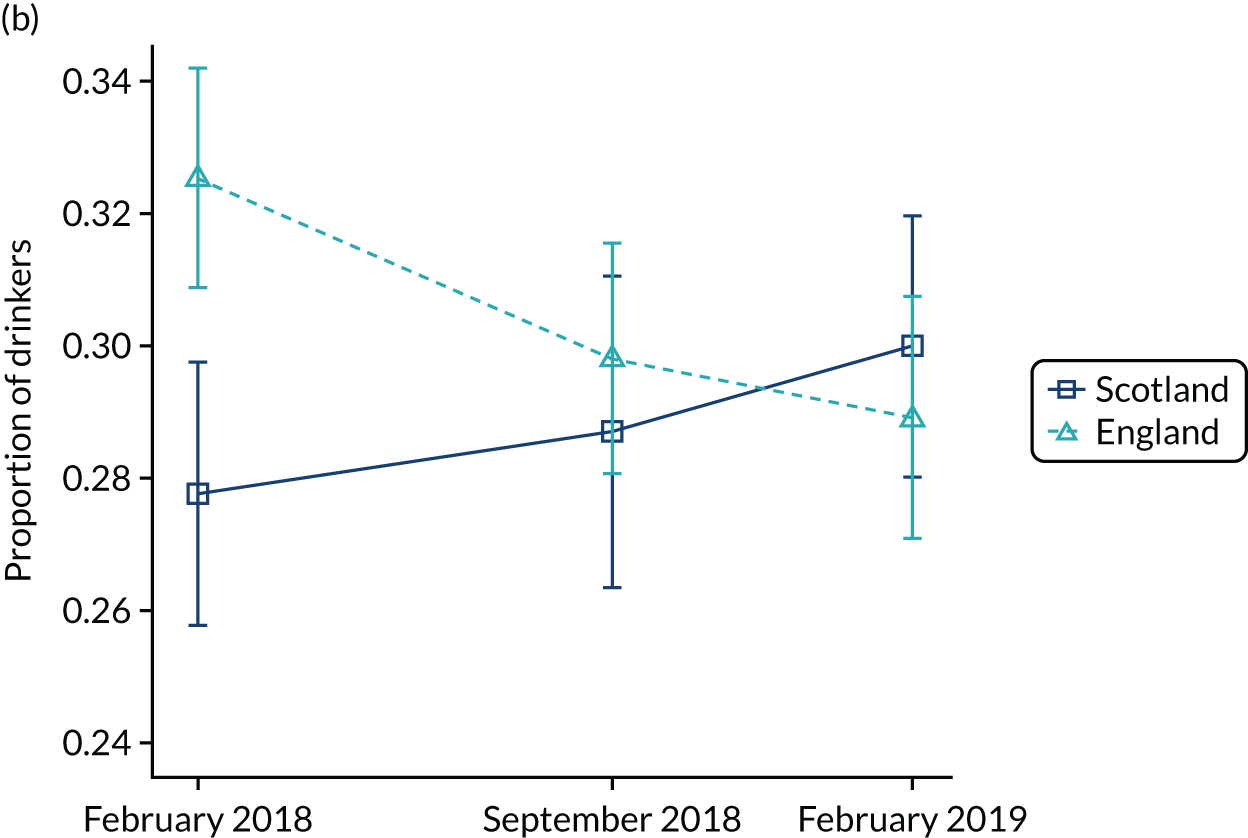
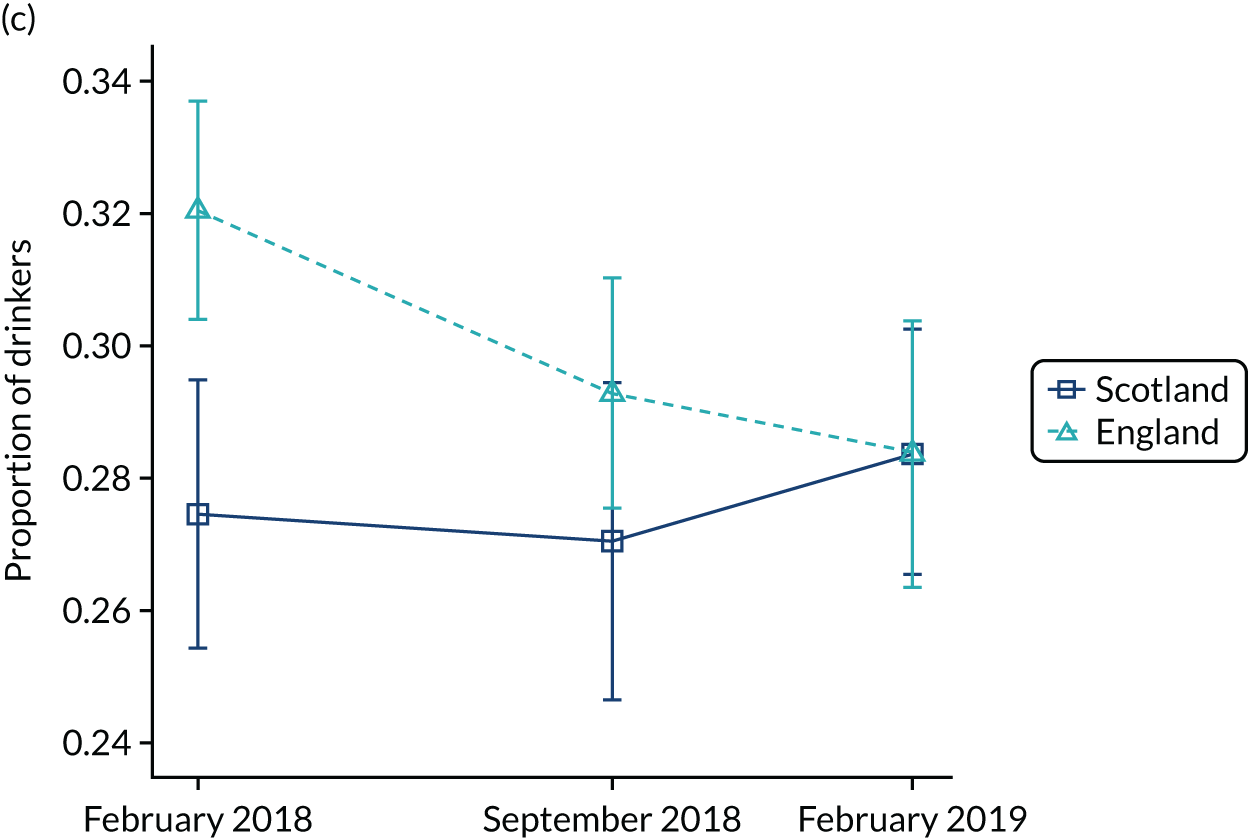
FIGURE 32.
Alcohol misuse (FAST score ≥ 3): pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
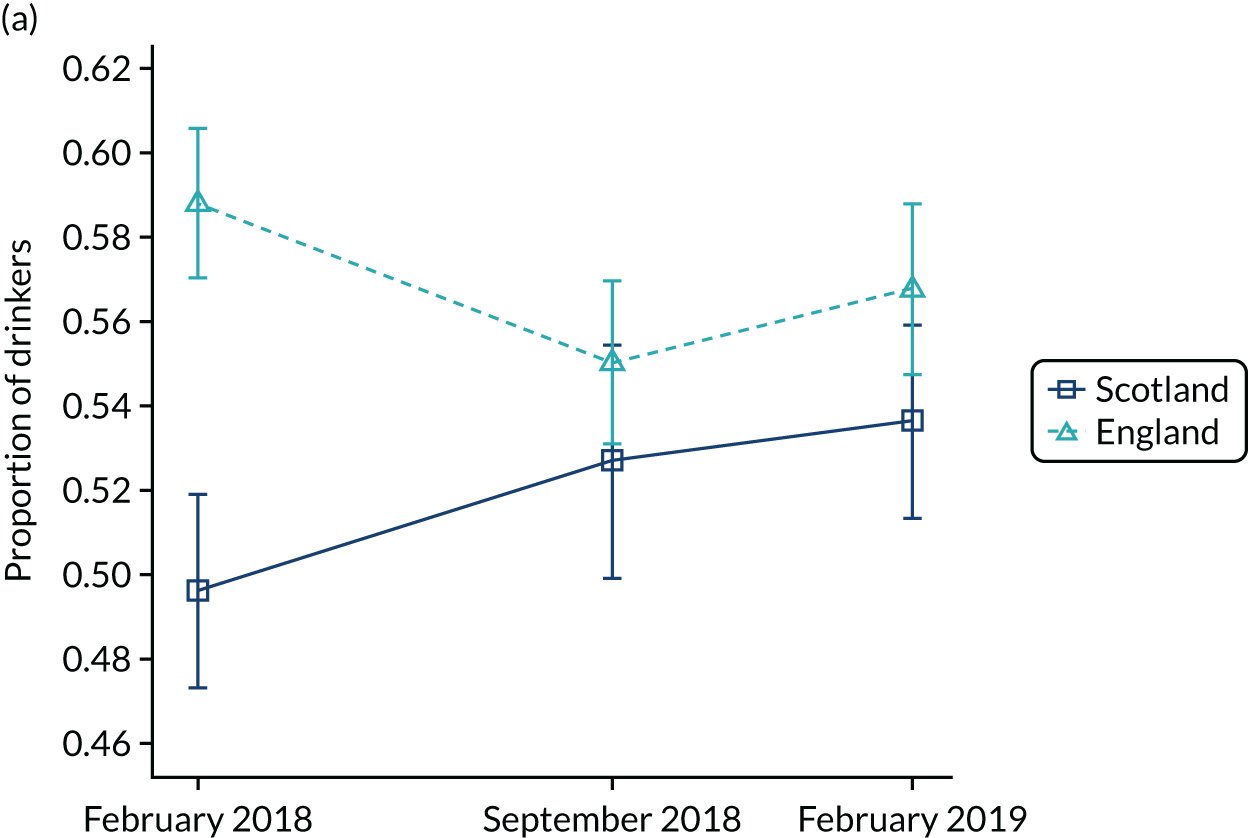

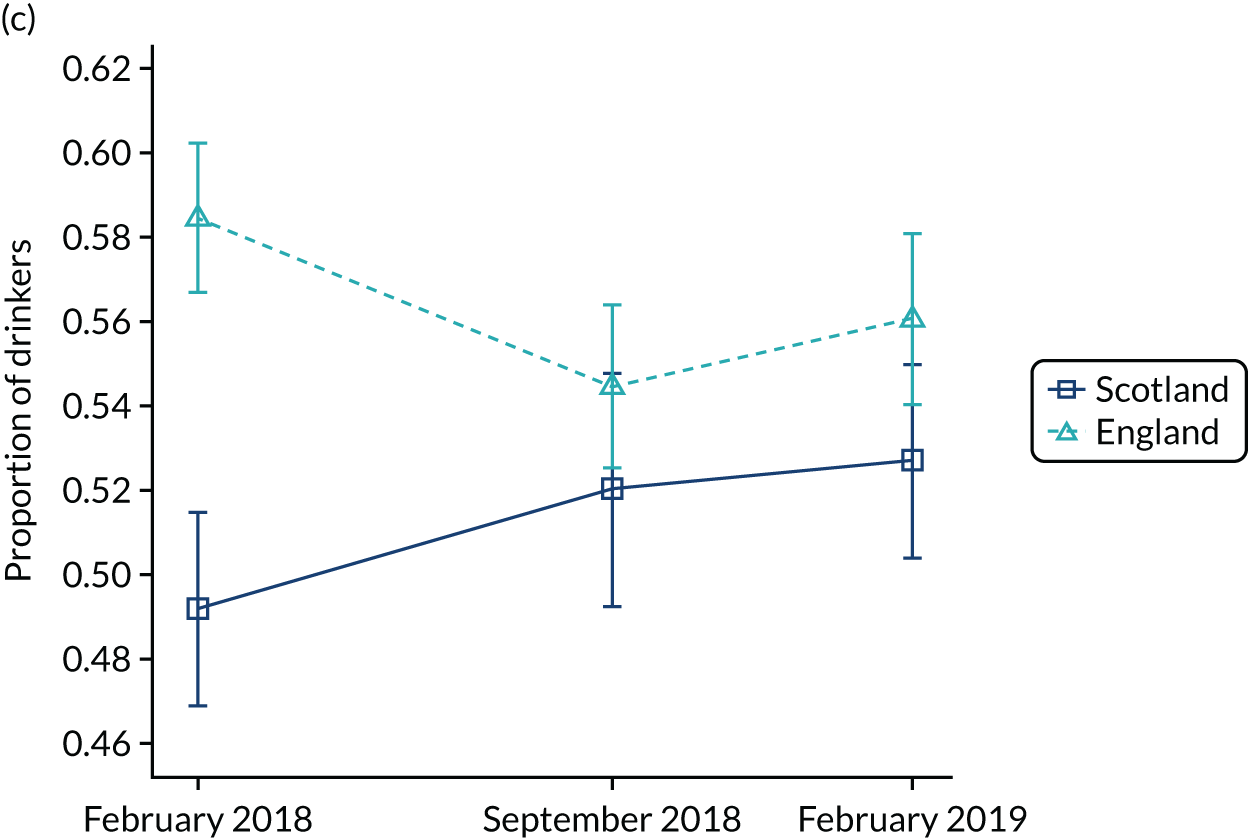
FIGURE 33.
Drinker with at least a hazardous drinking level (FAST score ≥ 2): pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
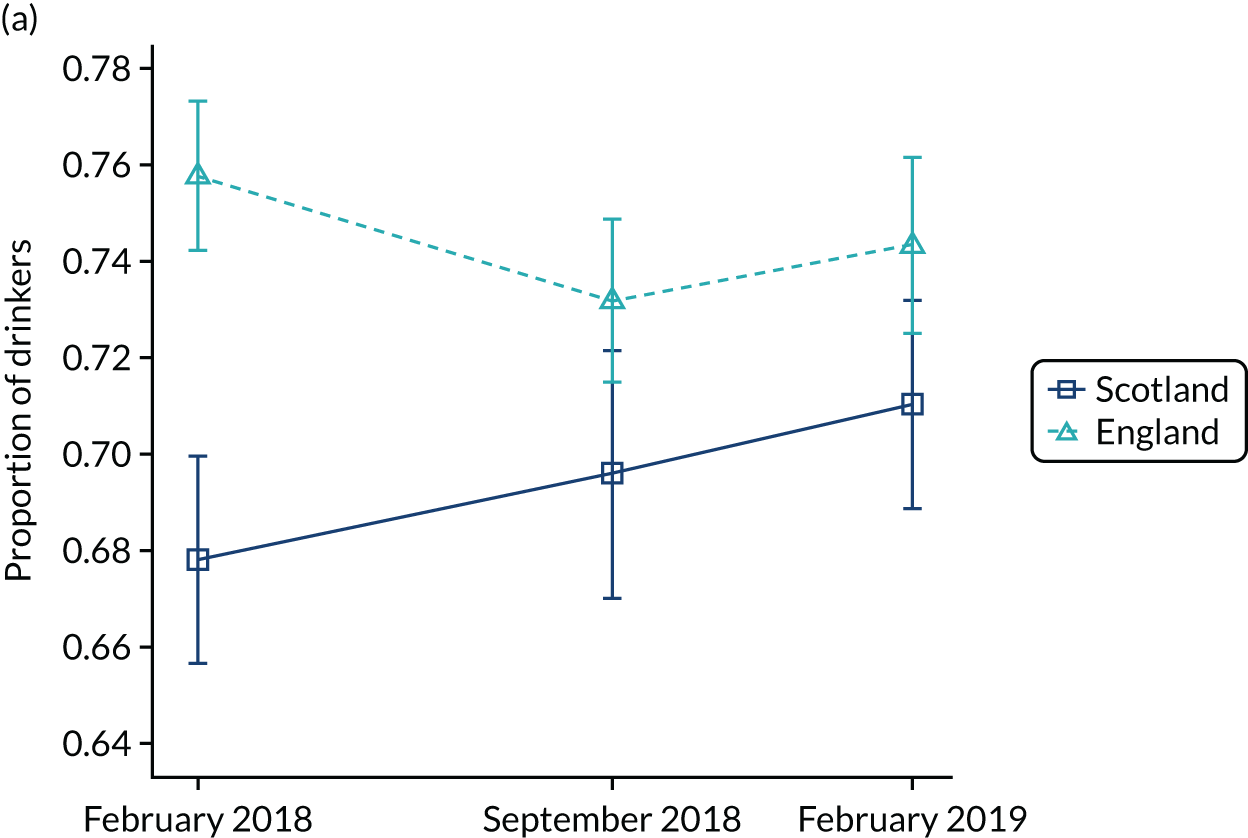
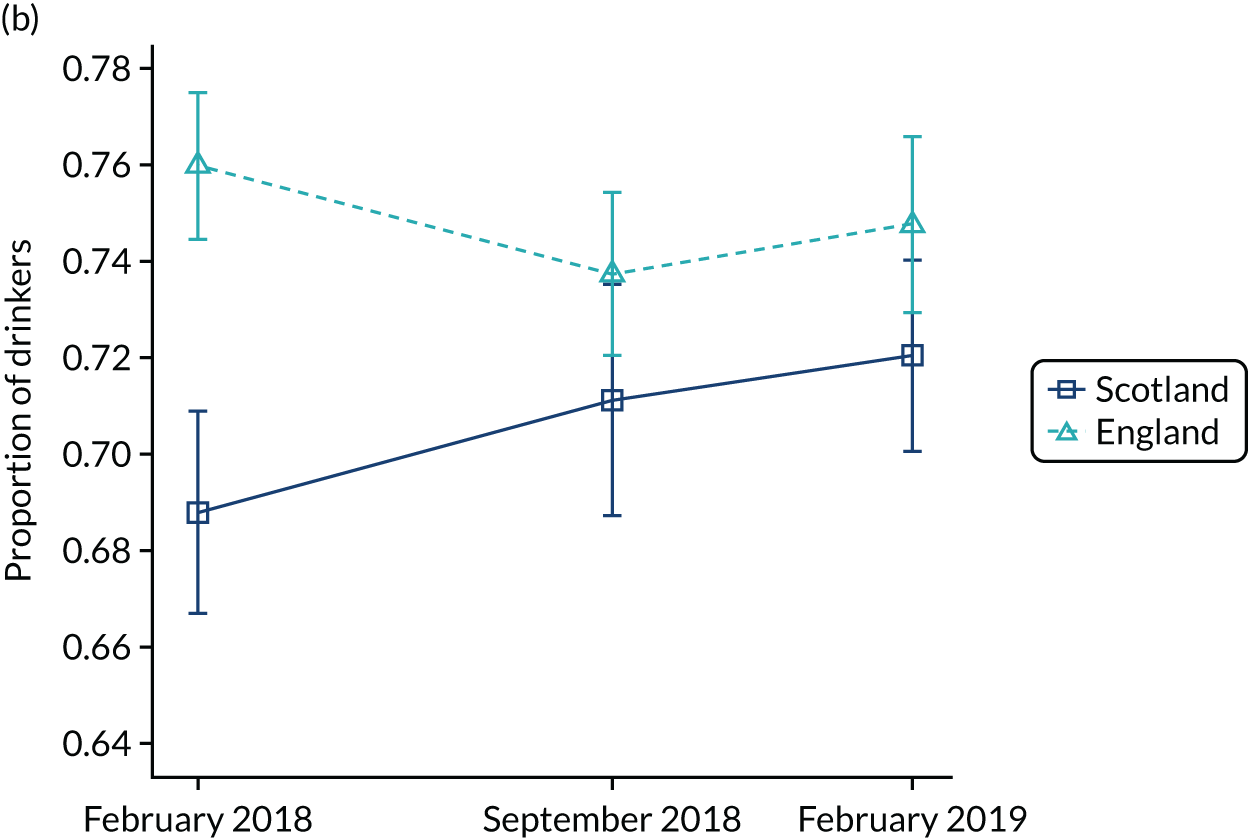

FIGURE 34.
Drinker with at least a harmful drinking level: pre and post imputation (FAST score ≥ 5). (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
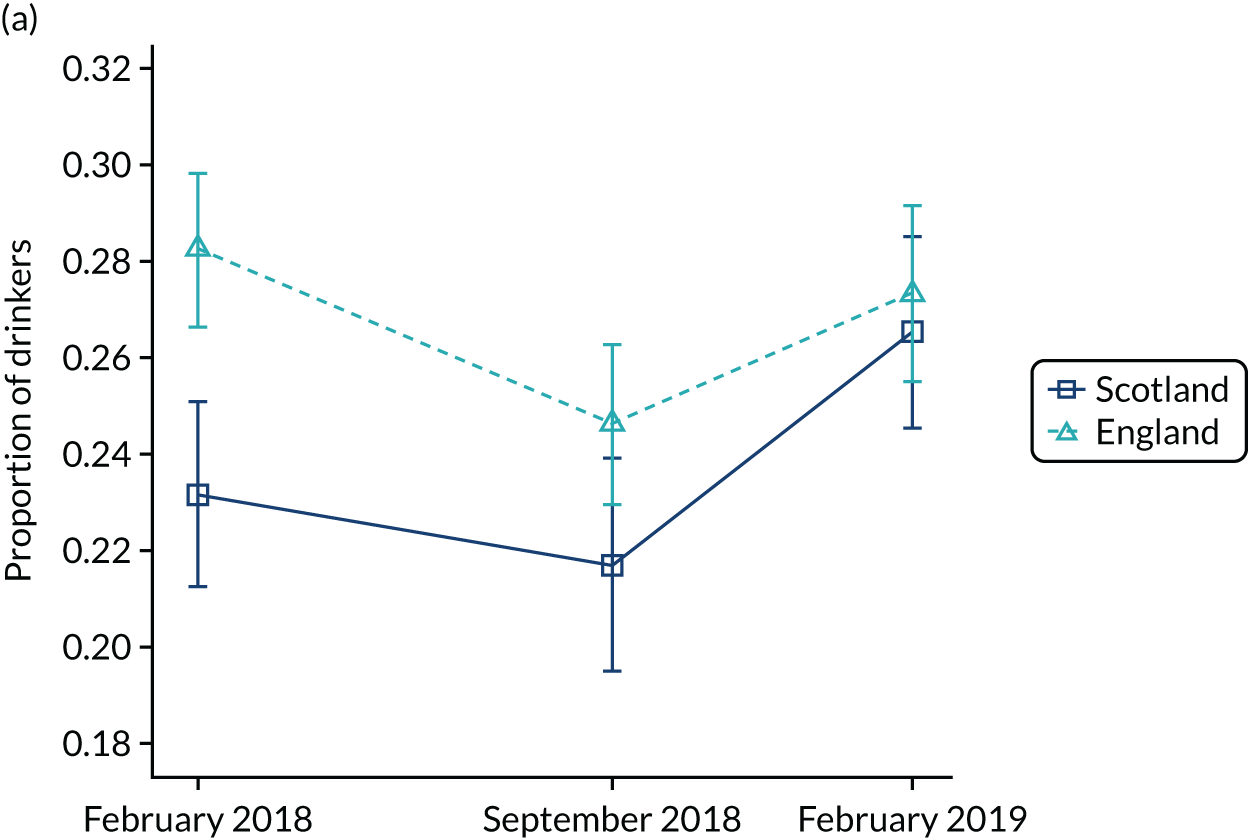
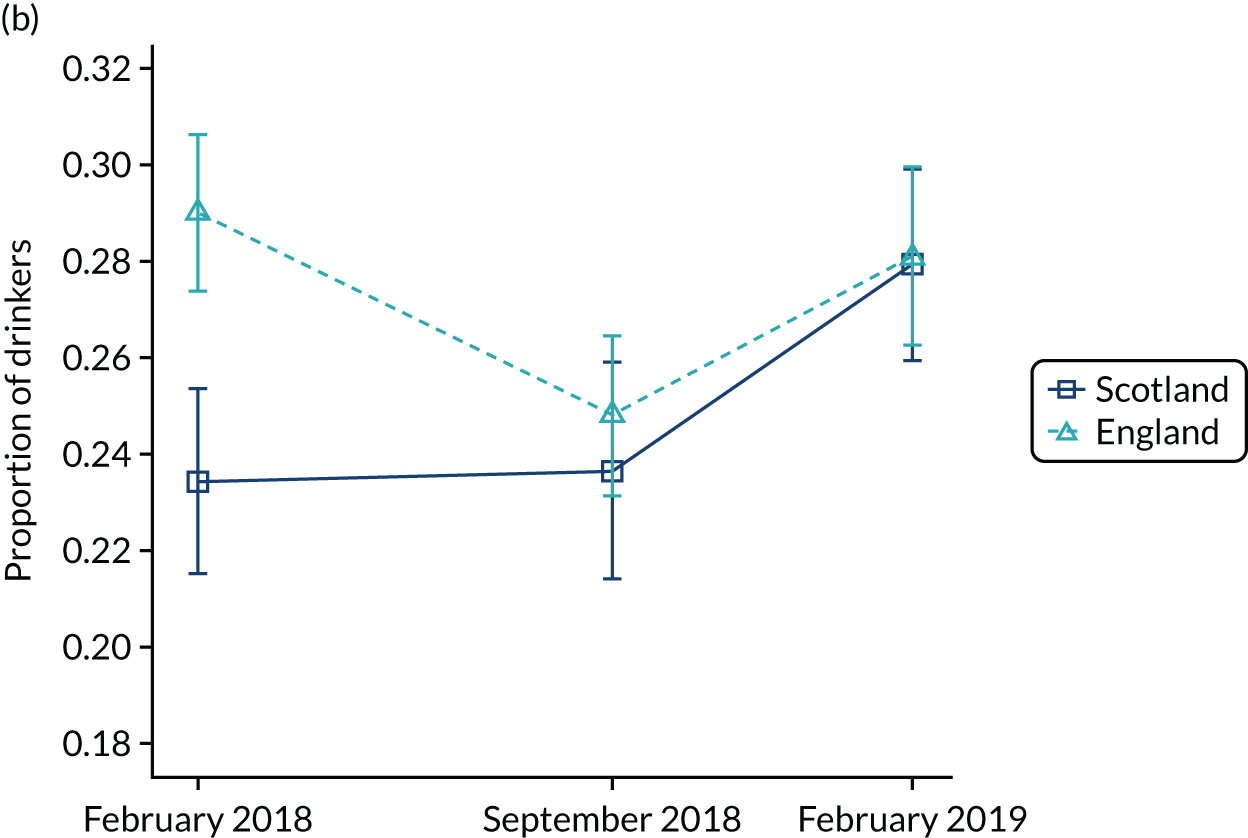

FIGURE 35.
Drinker with at least a dependent drinking level (FAST score ≥ 7): pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
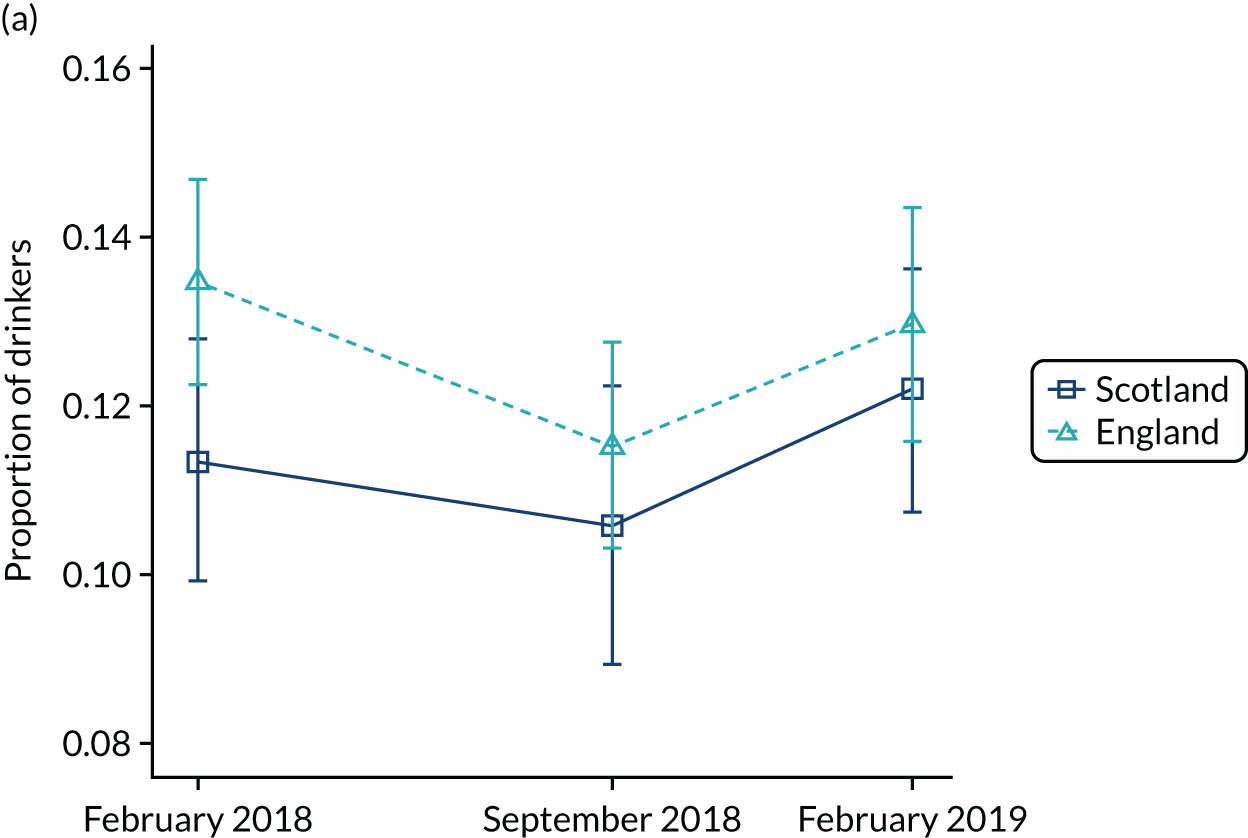
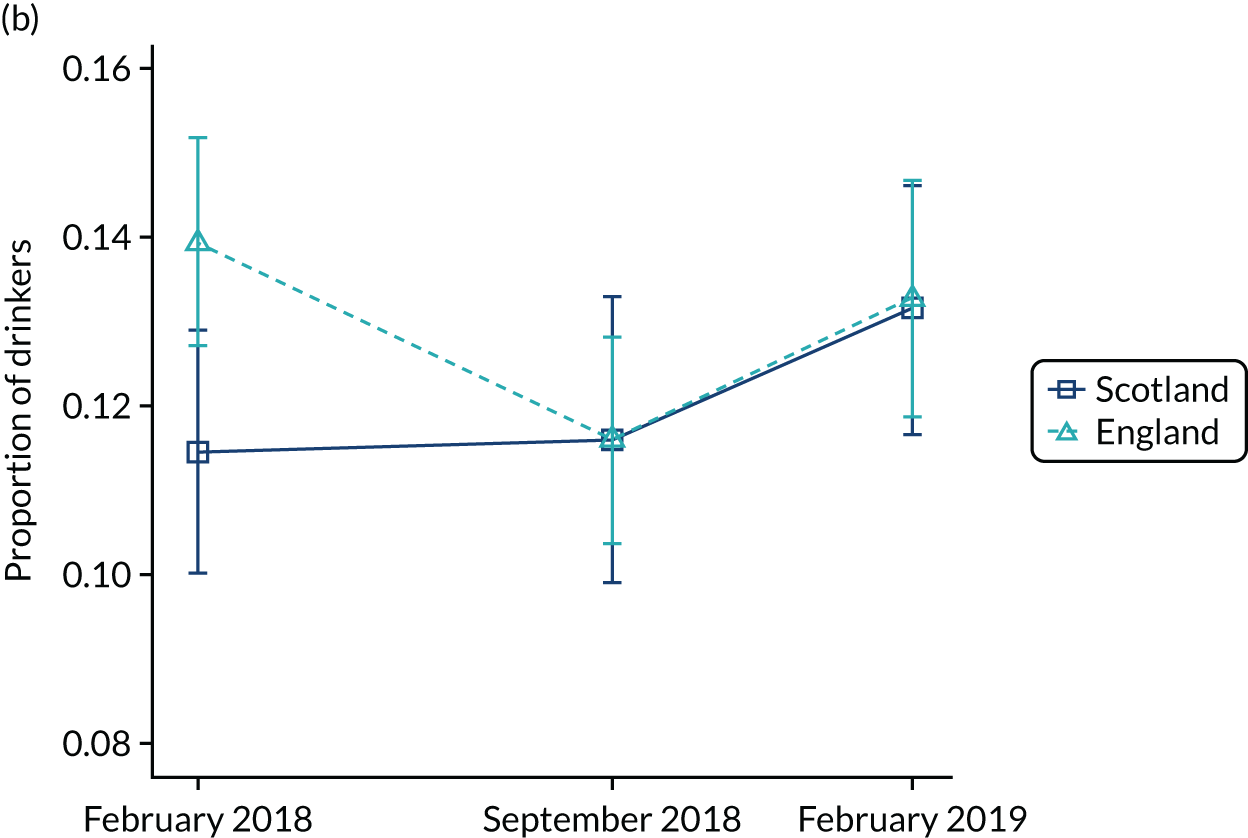
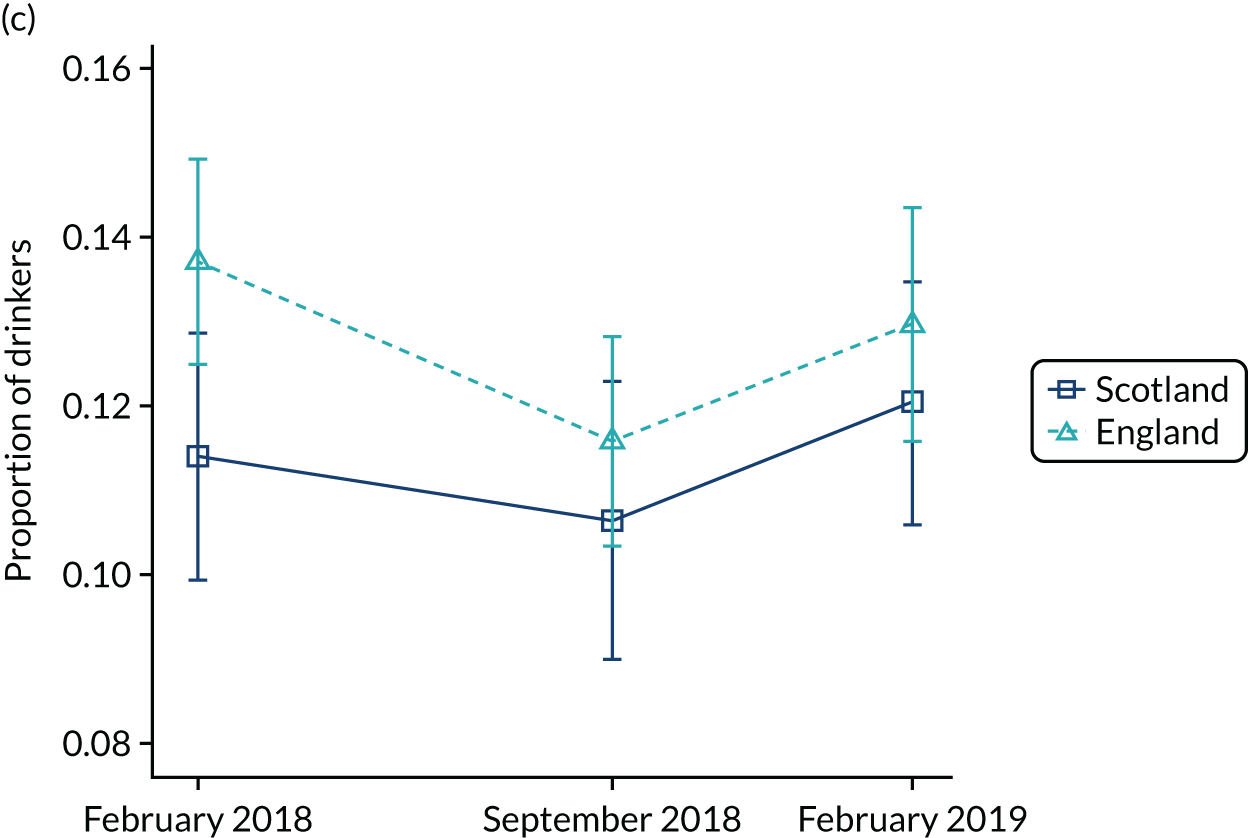
FIGURE 36.
Alcohol purchased from on-licensed premises: pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
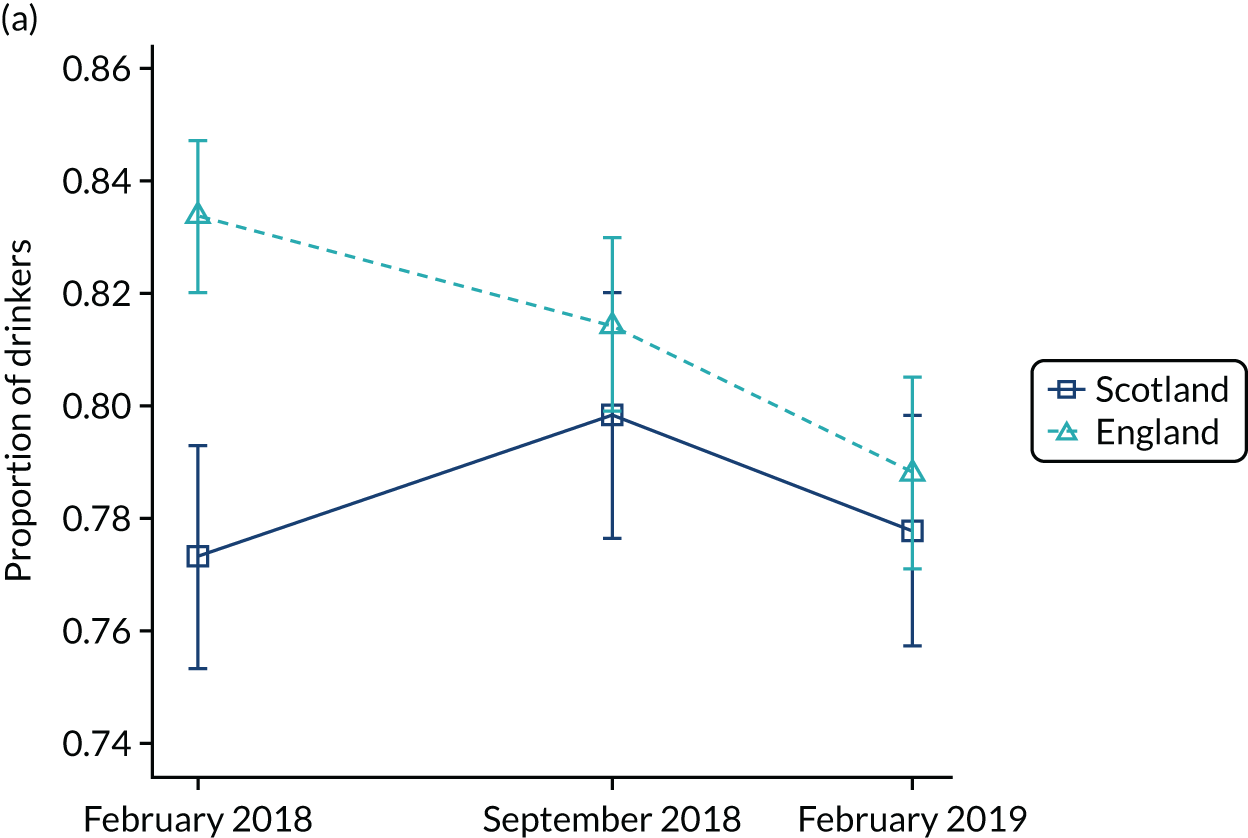
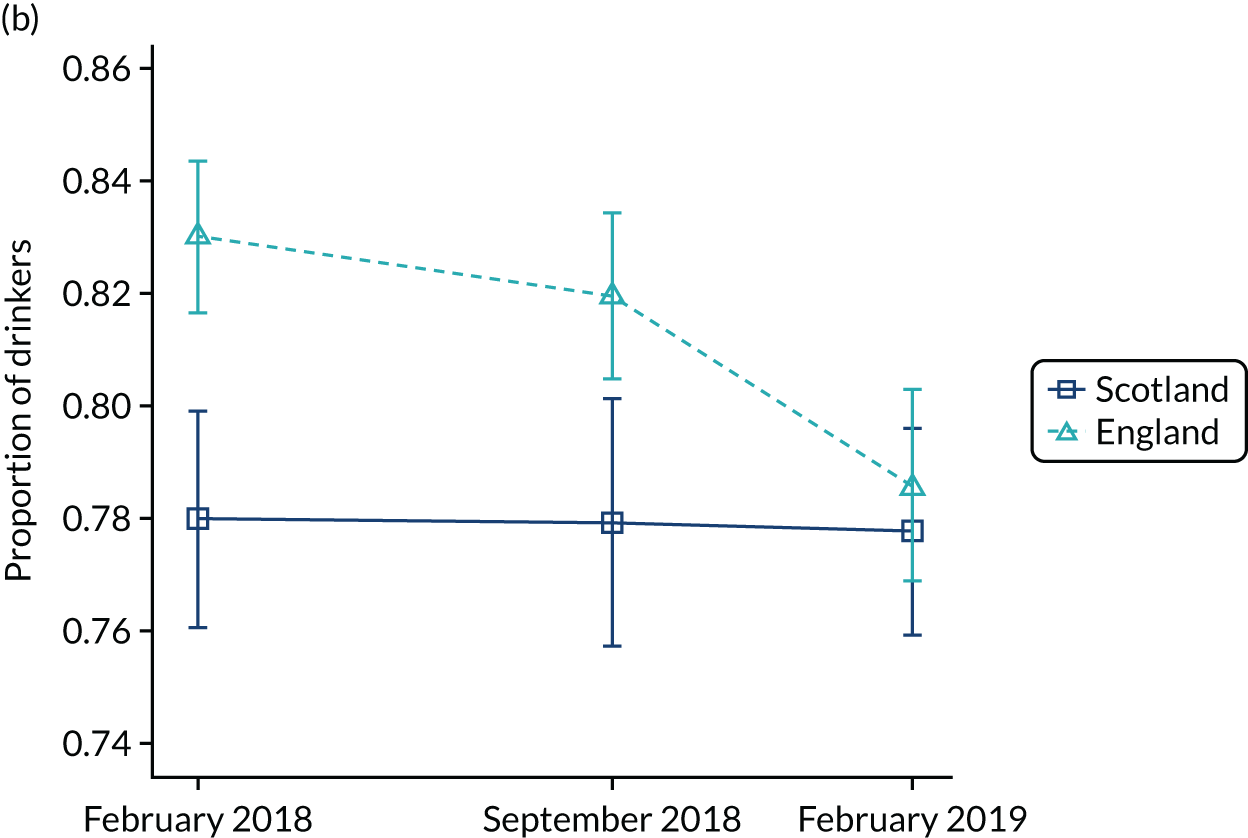

FIGURE 37.
Alcohol purchased from off-licensed premises: pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
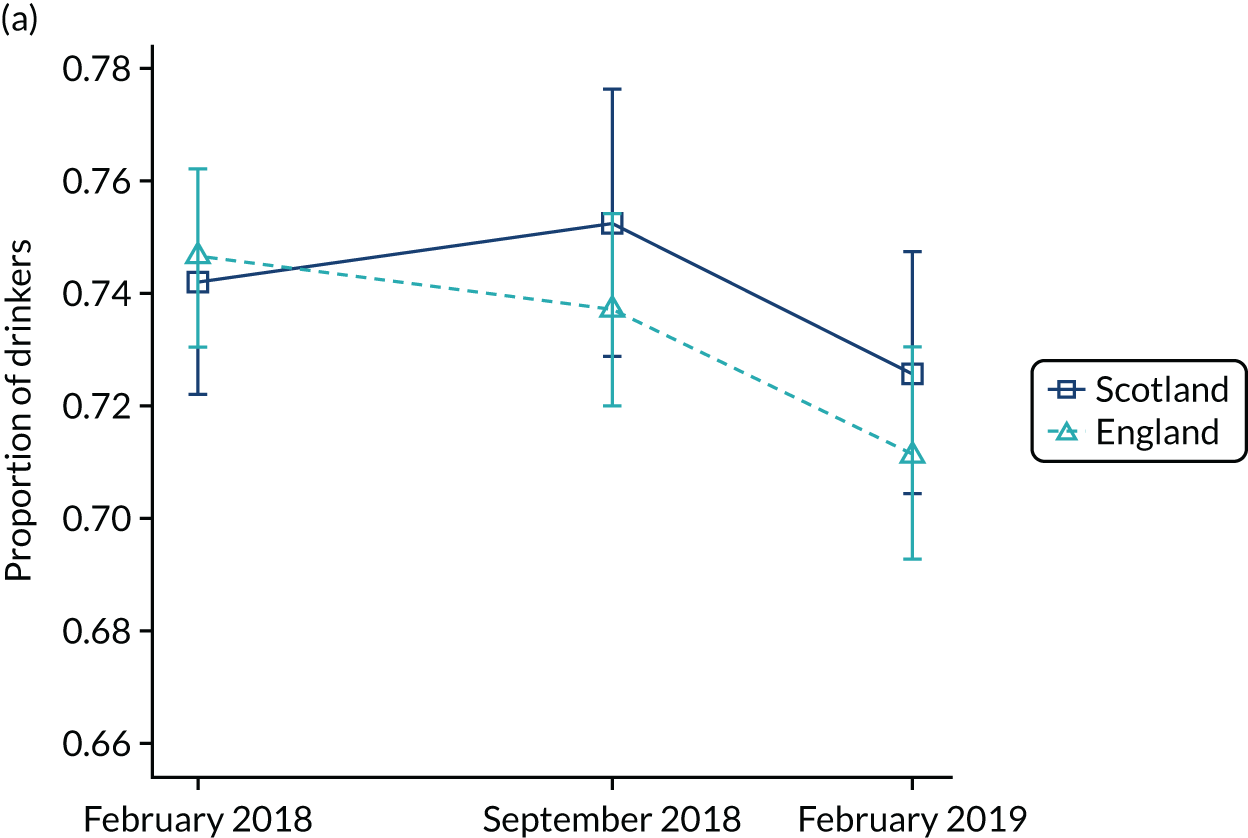
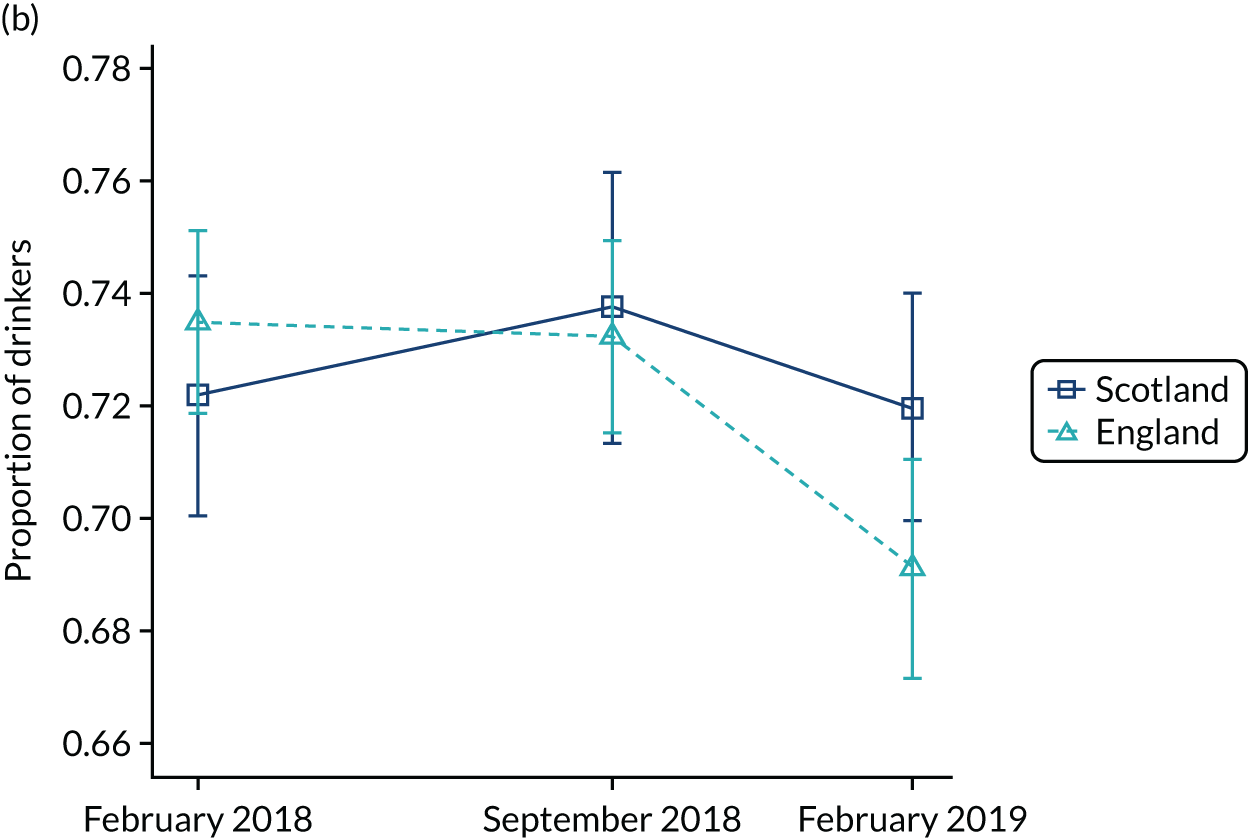
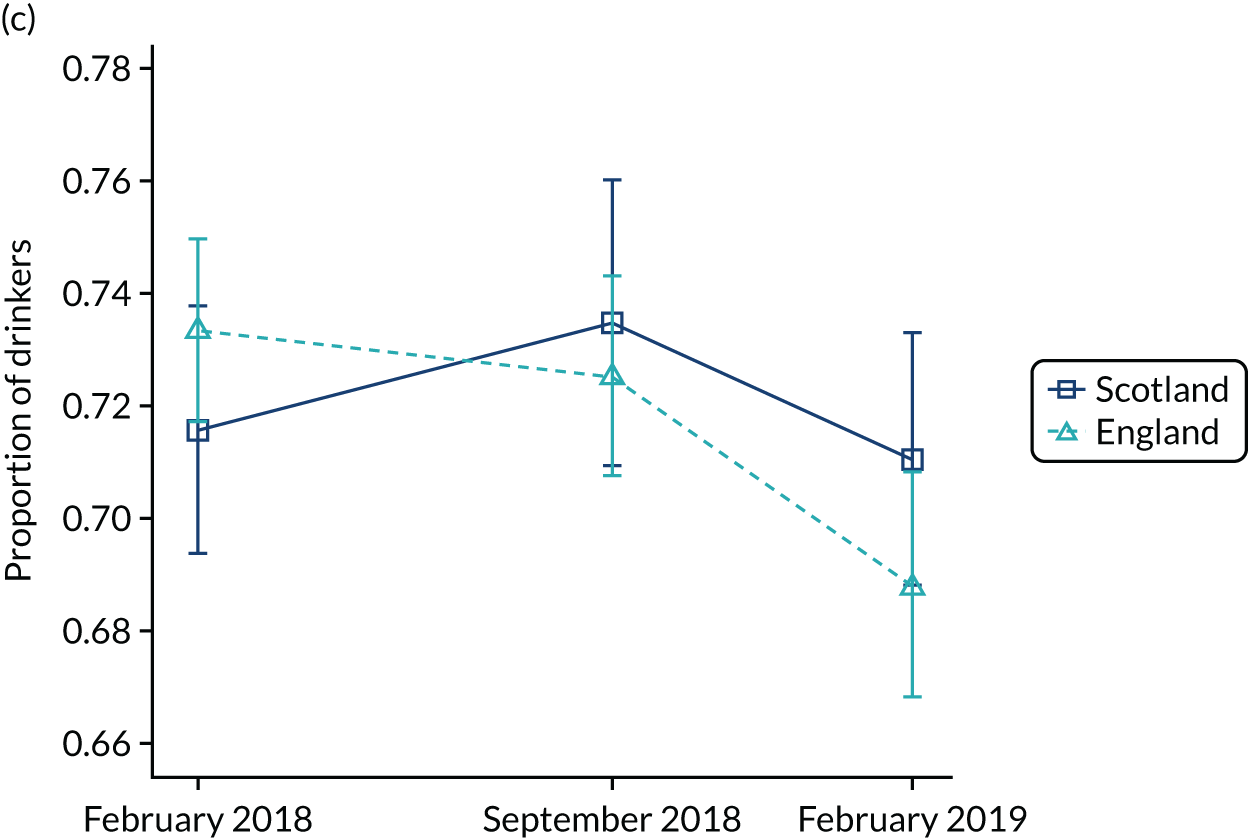
FIGURE 38.
Mean FAST score: pre and post imputation. (a) Imputed data set, weighted estimate; (b) before imputation, unweighted estimate; and (c) before imputation, weighted estimate.
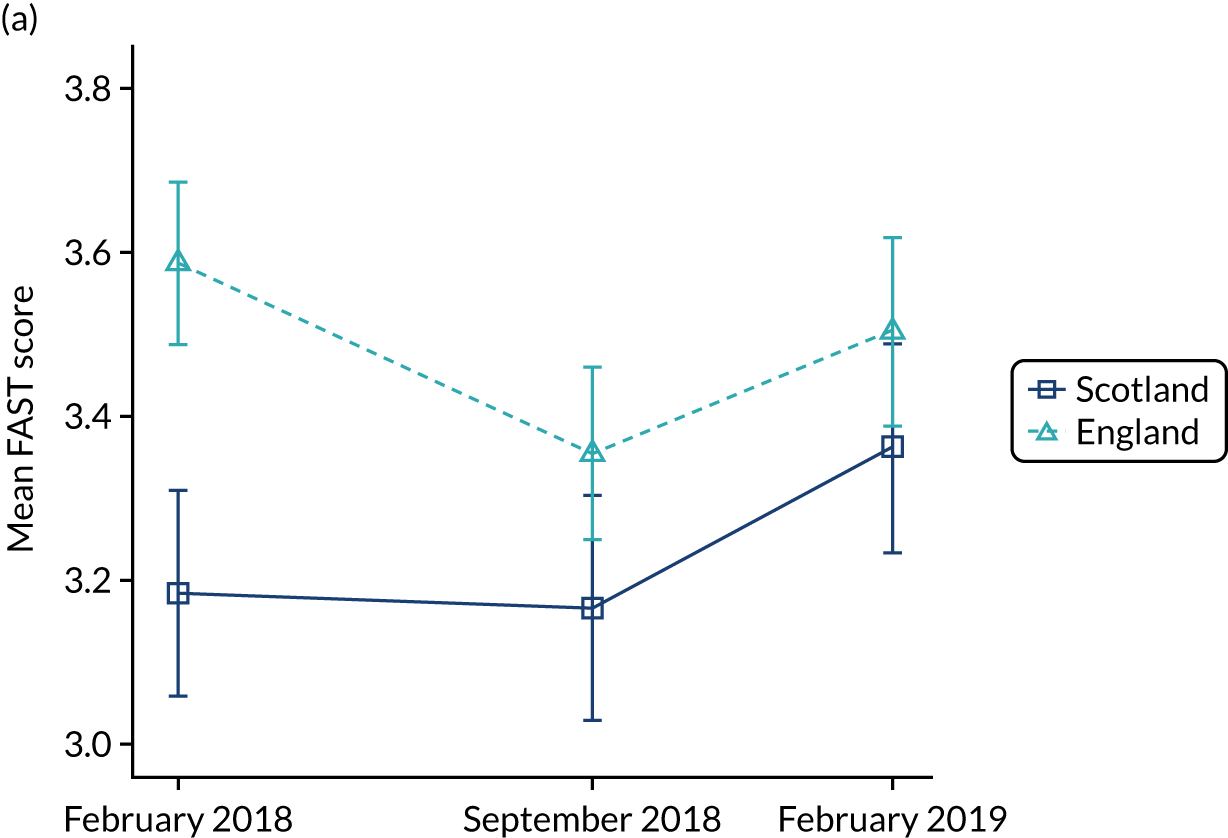
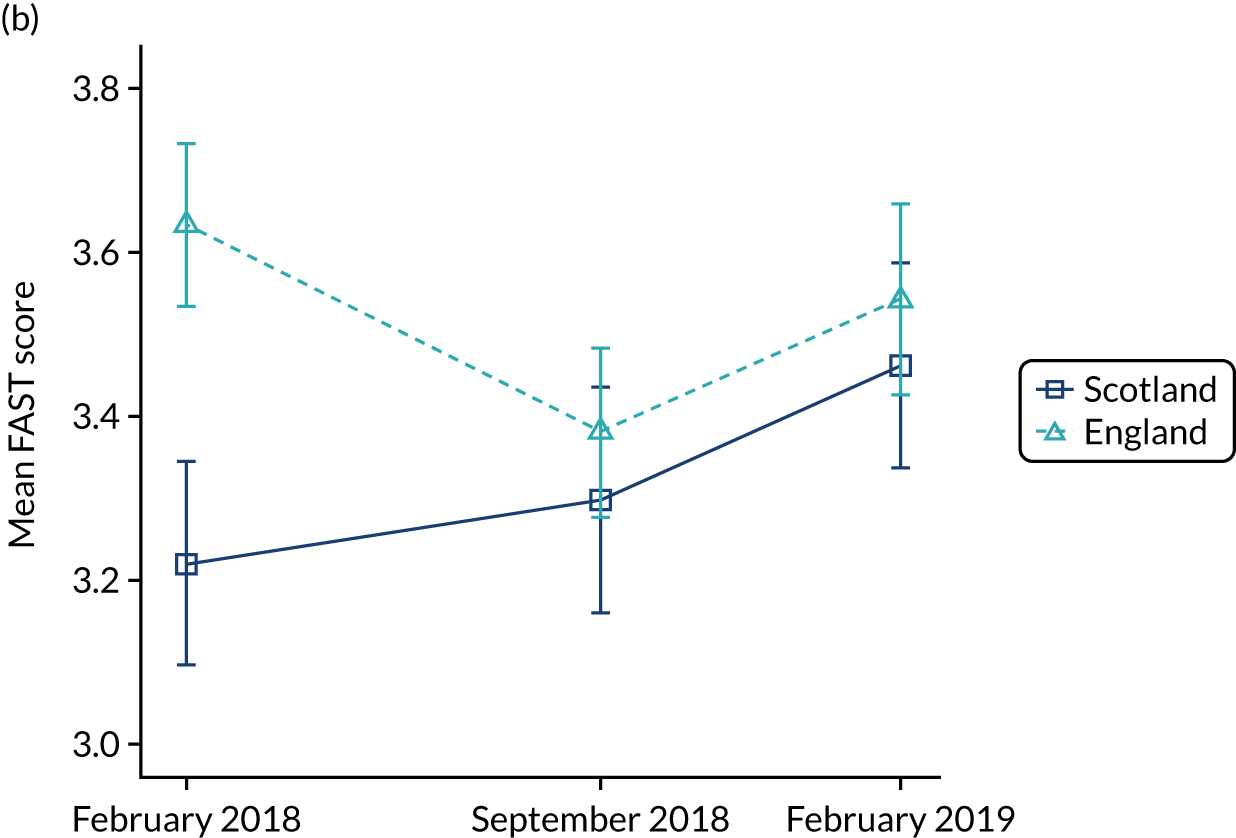
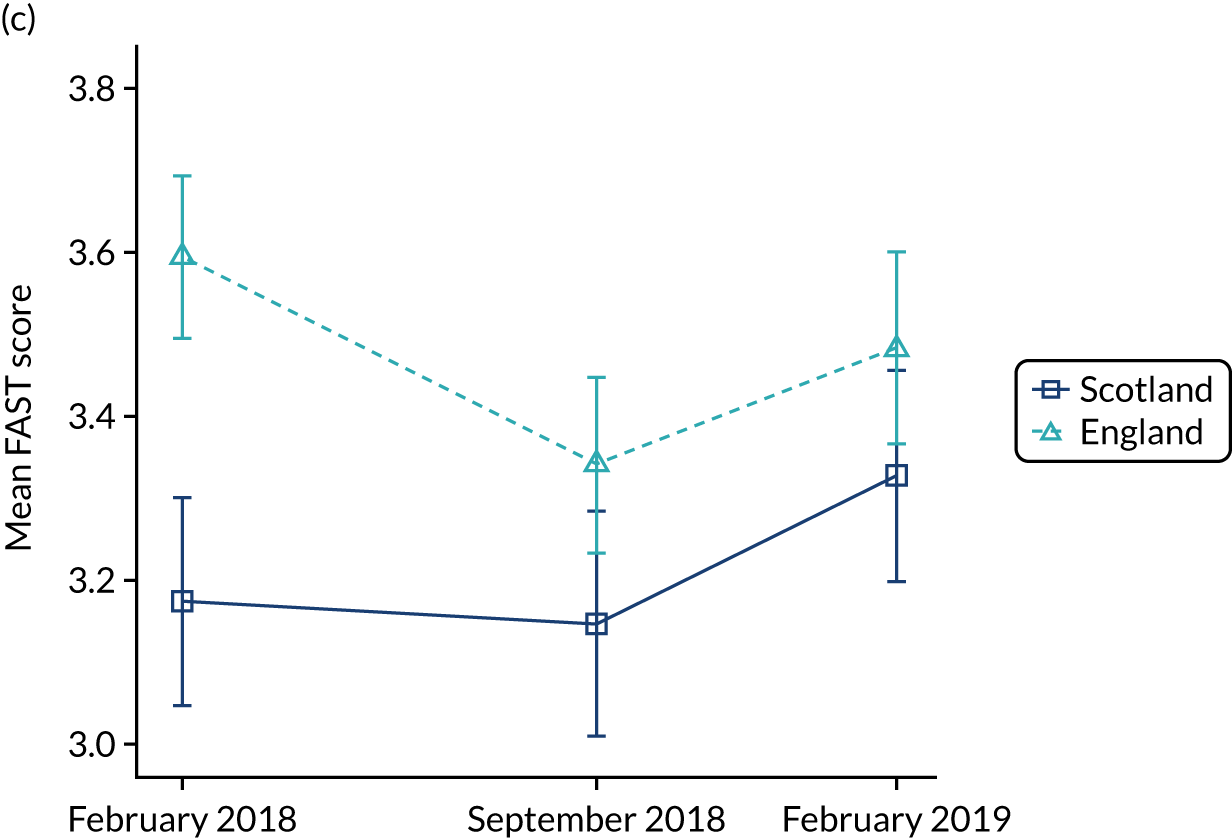
FIGURE 39.
Consumption of any illicit drugs in the last month: trend across three waves.

FIGURE 40.
Current alcohol drinker: trend across three waves.

FIGURE 41.
Binge drinking at least weekly: trend across three waves.
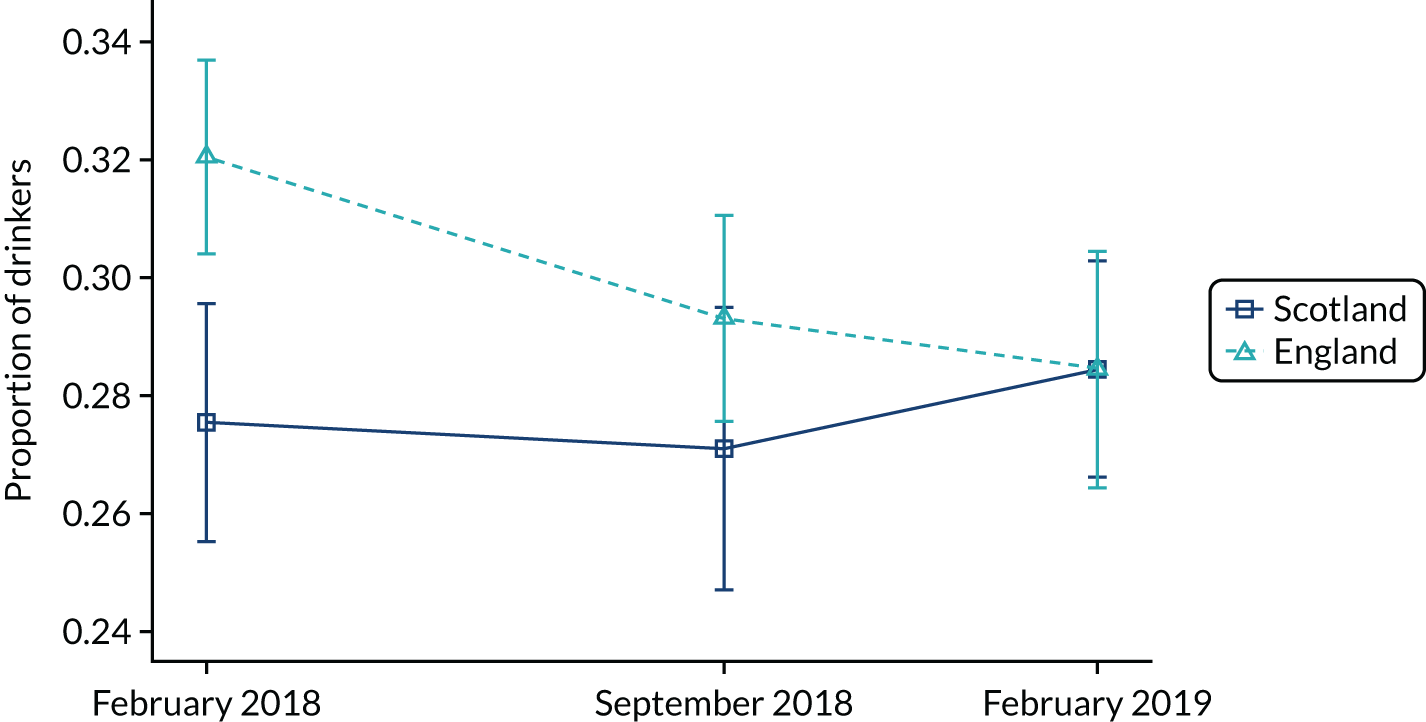
FIGURE 42.
Alcohol misuse: trend across three waves (FAST score ≥ 3).

FIGURE 43.
Drinkers with at least a hazardous drinking level: trend across three waves (FAST score ≥ 2).
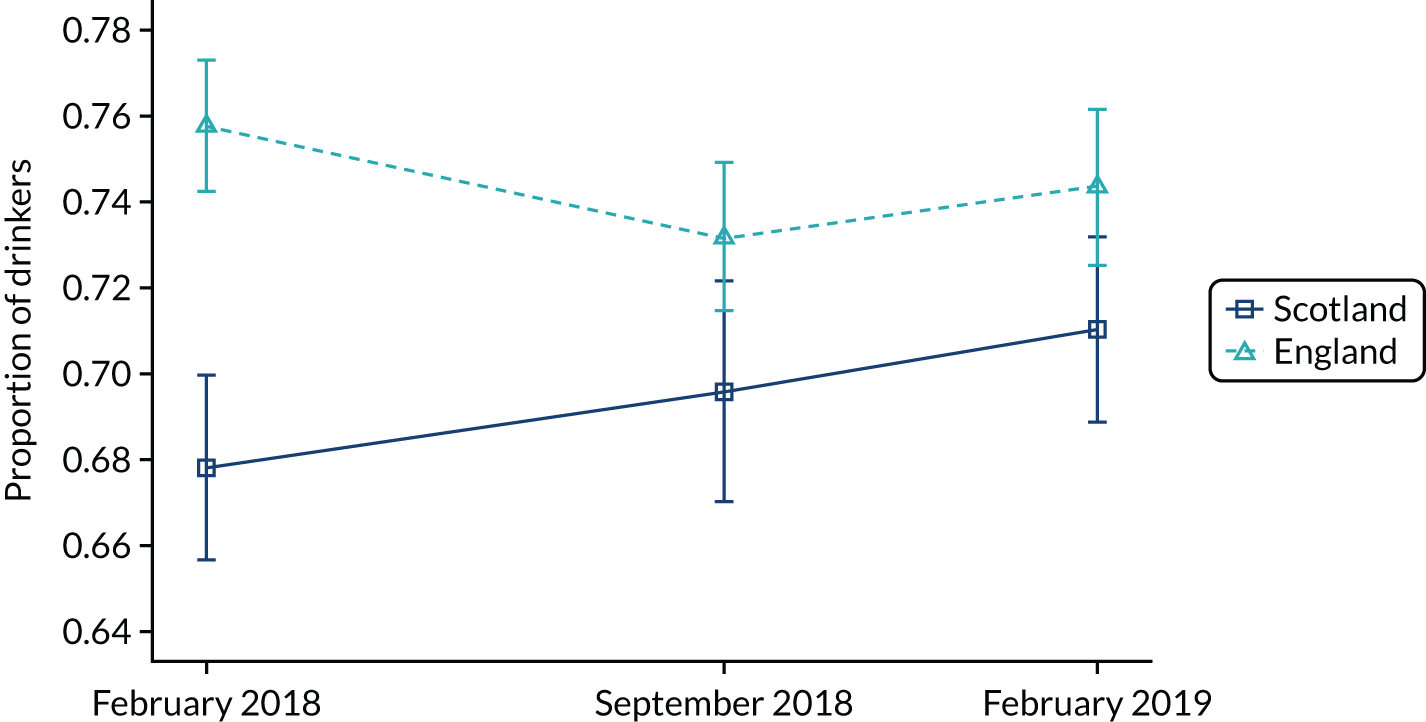
FIGURE 44.
Drinkers with at least a harmful drinking level: trend across three waves (FAST score ≥ 5).
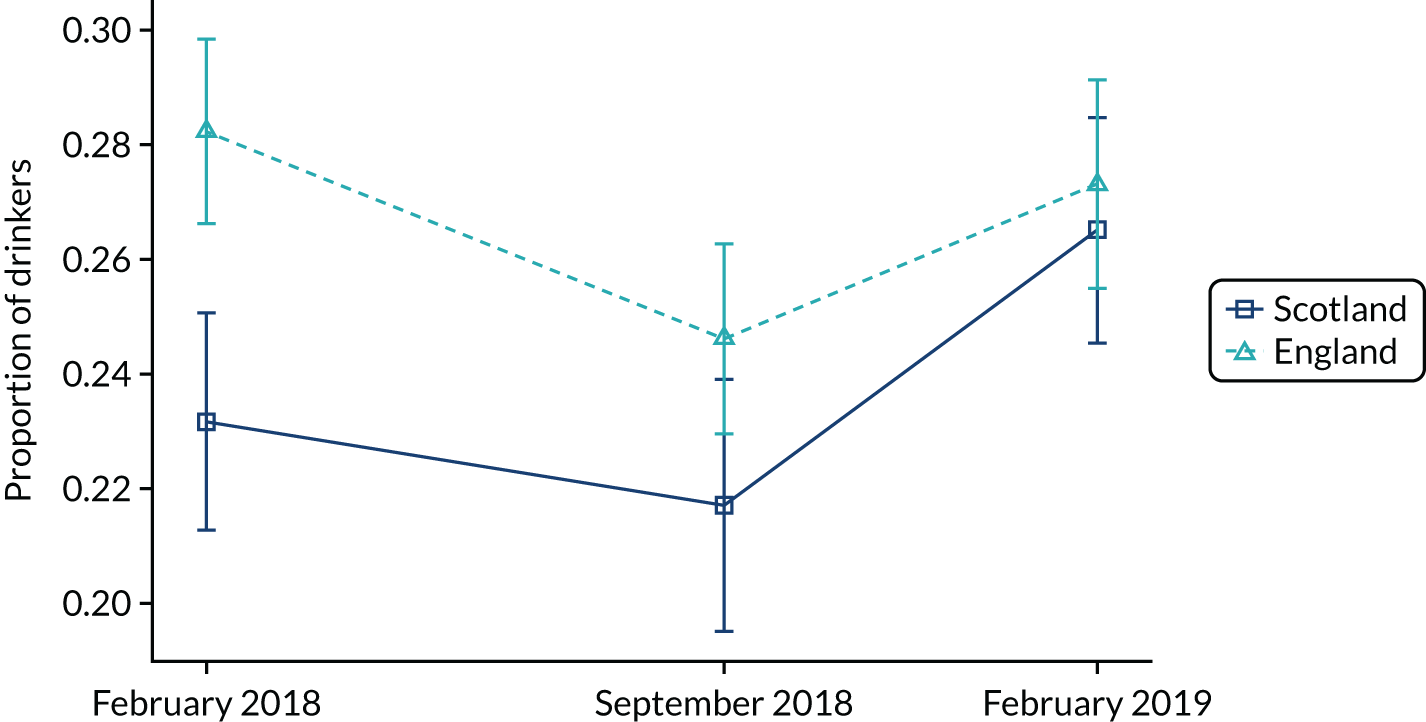
FIGURE 45.
Drinkers with at least a dependent drinking level: trend across three waves (FAST score ≥ 7).
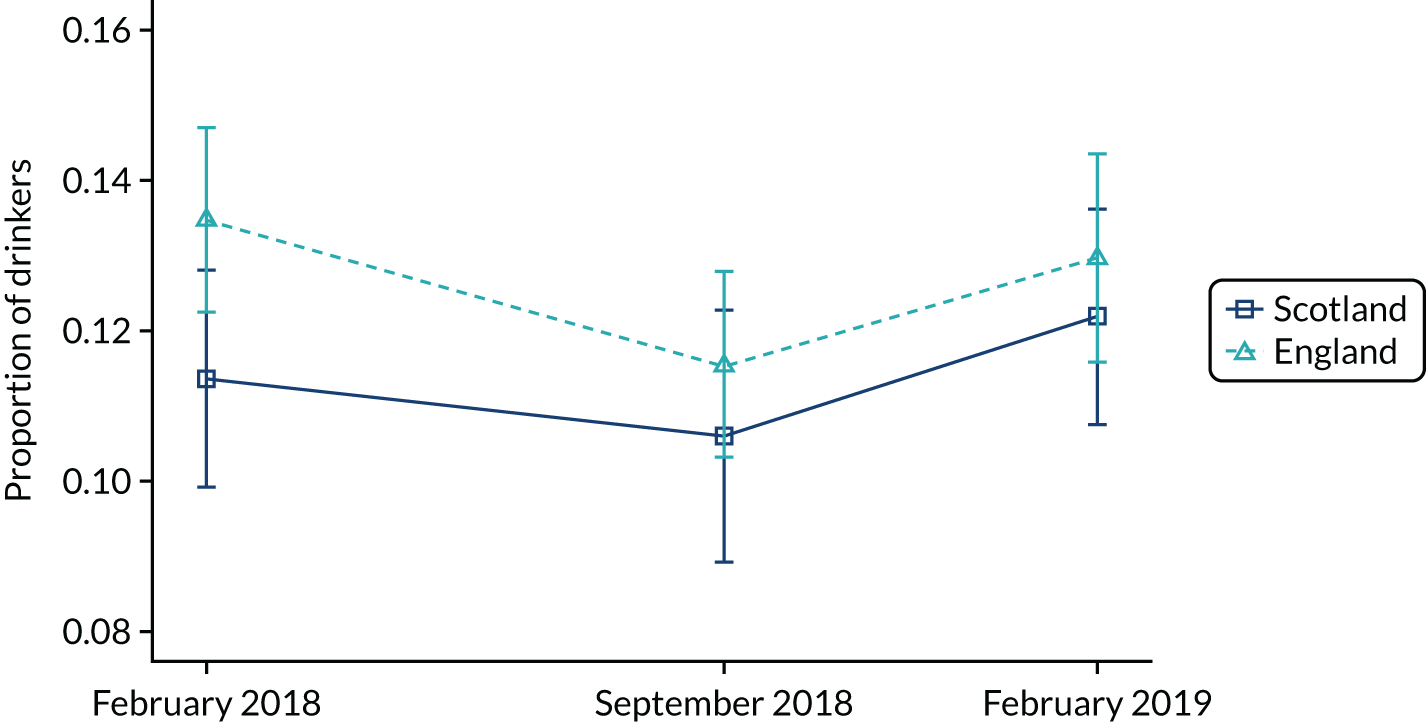
FIGURE 46.
Alcohol purchased from on-licensed premises: trend across three waves.
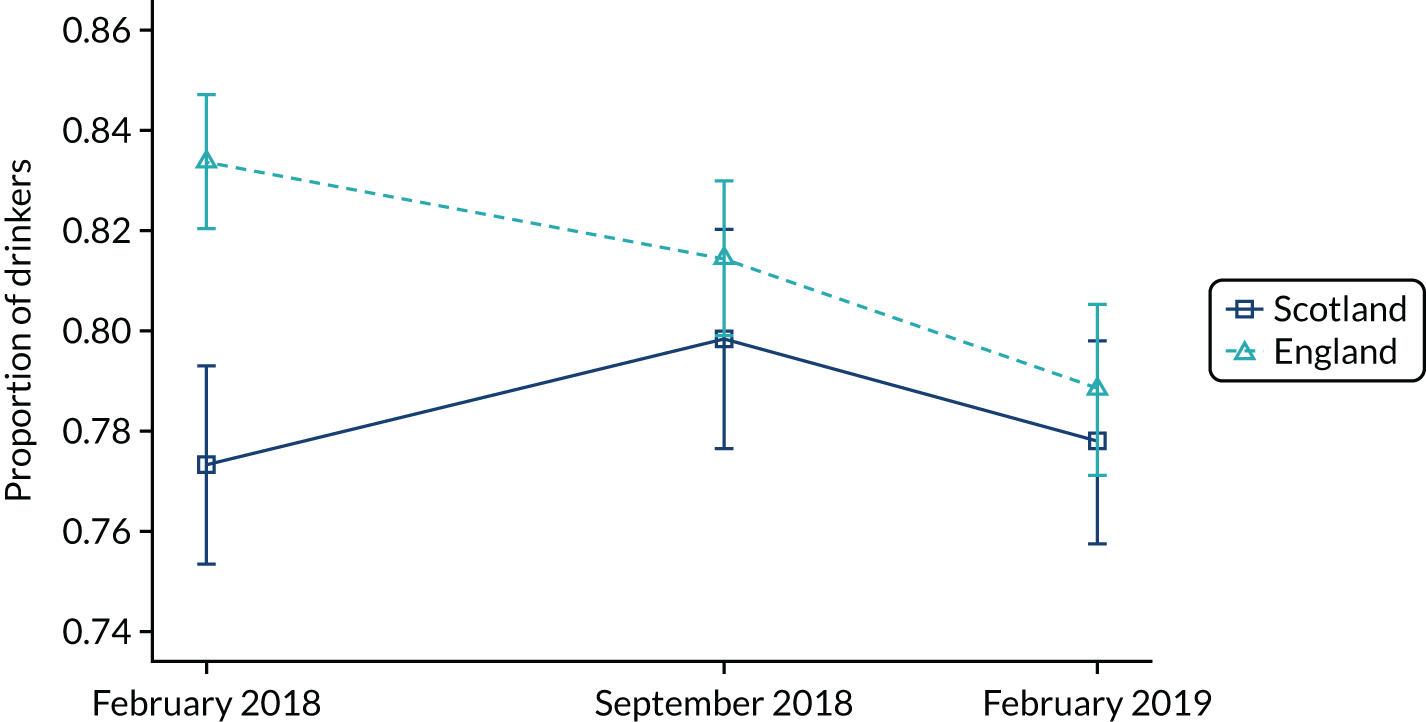
FIGURE 47.
Alcohol purchased from off-licensed premises: trend across three waves.

FIGURE 48.
Mean FAST score: trend across three waves.
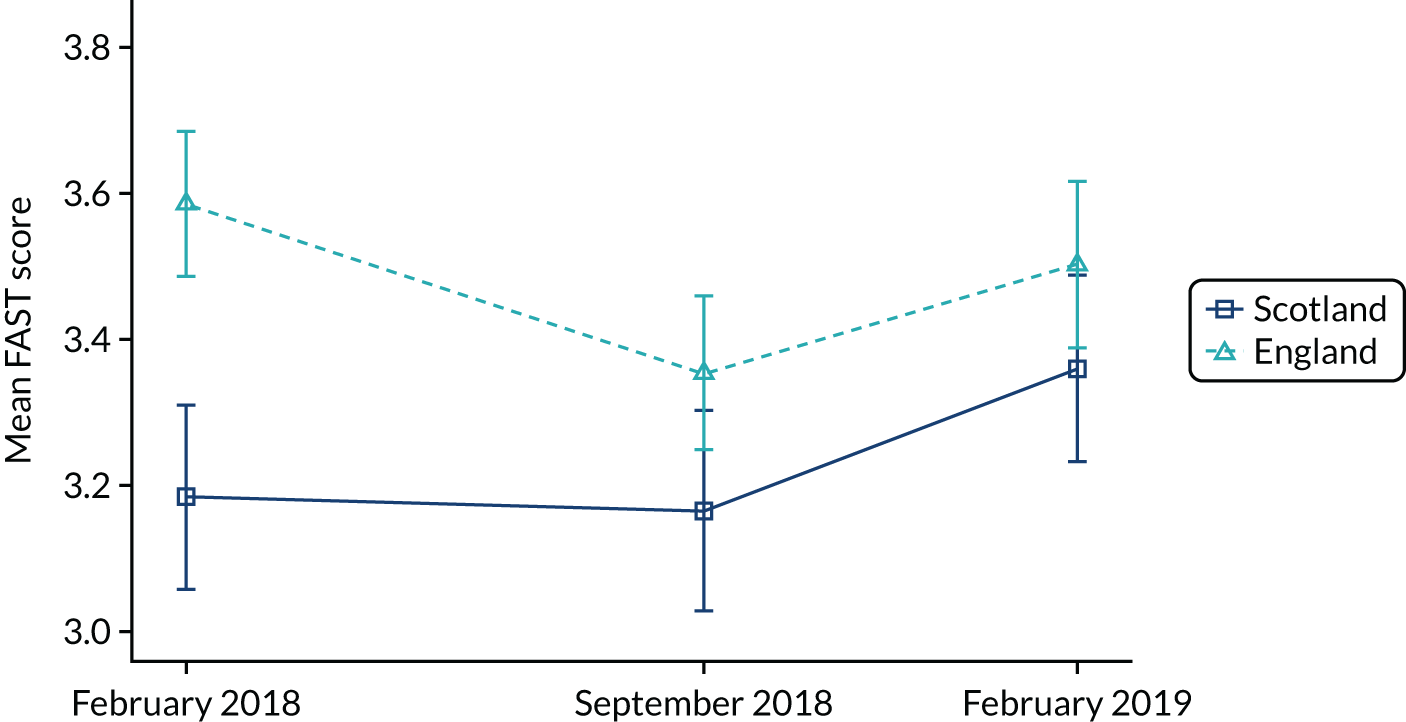
FIGURE 49.
Predicted percentage change in alcohol consumption: Sheffield alcohol policy model 2012 and 2016. SAPM, Sheffield alcohol policy model.
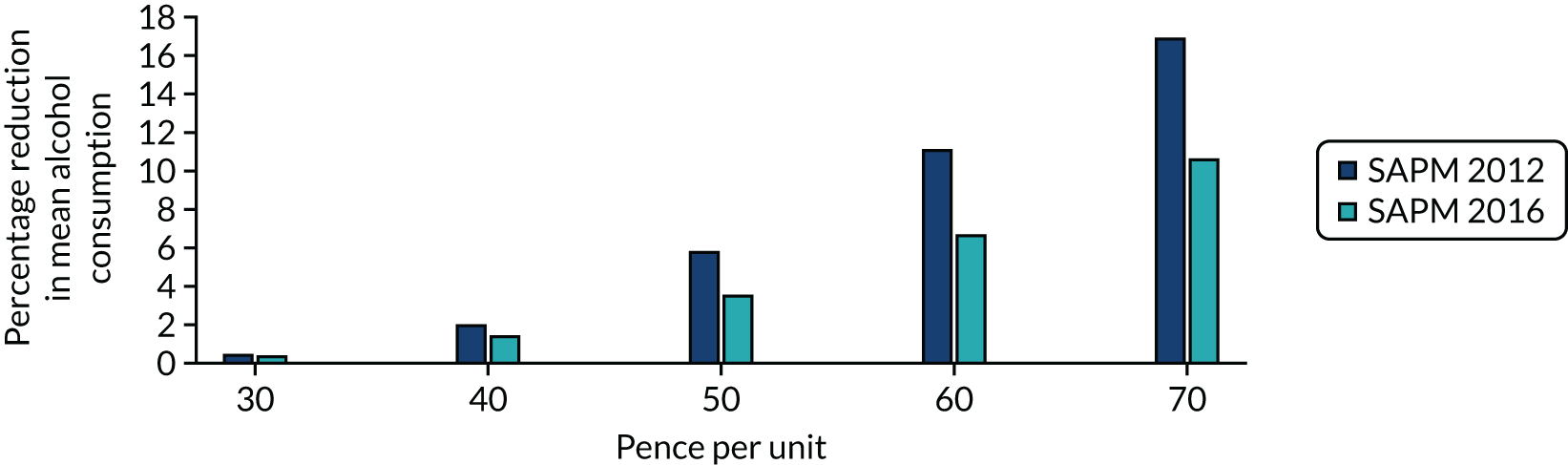
Appendix 4 Questionnaire for the emergency department study
List of abbreviations
- ABC1
- managerial, professional and administrative occupations
- app
- application
- AUDIT-C
- Alcohol use Disorders Identification Test Consumption
- CI
- confidence interval
- DE
- semi-skilled and unskilled manual workers, casual and lowest grade workers, and those unemployed
- DiD
- difference in difference
- ED
- emergency department
- FAST
- Fast Alcohol Screening Test
- GP
- general practitioner
- HIV
- human immunodeficiency virus
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- LSOA
- lower-layer super output area
- MESAS
- Monitoring and Evaluating Scotland’s Alcohol Strategy
- MICE
- multivariate imputation via chained equations
- MUP
- minimum unit pricing
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- PPI
- patient and public involvement
- Q&A
- question and answer
- RO
- research objective
- SHC
- sexual health clinic
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/phr09110).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
