Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 13/164/10. The contractual start date was in June 2015. The final report began editorial review in June 2021 and was accepted for publication in May 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Dundas et al. This work was produced by Dundas et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Dundas et al.
Chapter 1 Introduction
Sections of this report have been reproduced from this study’s protocol document, available at the National Institute for Health and Care Research (NIHR) Funding and Awards website.
Background
Intervention in the early years is one of the most effective ways to prevent poor health and reduce inequalities. Health improvements during pregnancy, infancy and early childhood, and social patterning of any improvements, can track through life into adulthood and old age. Any health improvements that are made during pregnancy and the early years can reduce the prevalence of poor health and disease, and therefore increase life chances. For example, poor nutrition, tobacco exposure and pollution in pregnancy and infancy affect growth and lung development, in turn leading to respiratory illness in childhood and eventually lung disease in adulthood. 1 Poor nutrition in pregnancy and the early years of life have impacts on health. The developmental model of the origins of chronic disease proposes the causal influence of undernutrition in utero on coronary heart disease and stroke in adult life. 2 Maternal nutrition strongly influences child nutrition, which in turn tracks to adult eating patterns. 3–5 As poor nutrition is associated with lower socioeconomic status,6 these impacts may also perpetuate health inequalities. An intervention that modifies both maternal and infant diets thus has the potential to improve the health of the infant, and for these health gains to track into childhood and adulthood, thus reducing health inequalities.
The First 1000 Days7 initiative started at an international conference on global child undernutrition and has now influenced health policy in some high-income countries, including the United Kingdom (UK). 8 The premise is that the first 1000 days from conception to age 2 years is a period of rapid growth, and therefore what occurs during this time lays the foundations for future development. In 2010, the Fair Society, Healthy Lives report9 recommended giving every child the best start in life as a key policy intervention for a healthier society.
The principle of early life intervention has influenced government policy across the UK, ranging from high-level strategy documents such as Getting it Right for Every Child,10 Every Child Matters11 and Healthy Child Wales,12 through universal policies and interventions such as the Health in Pregnancy Grant13 and universal maternal and child health services to targeted interventions including the Family Nurse Partnership14 and Flying Start Wales. 15 Although these are in place across the UK countries, implementation and structure may differ. Therefore, there is a need to understand what strategies and policies improve health that so policy-makers can make better decisions about policies in the early years.
There have been some evaluations of early years policies. The Healthy Baby Program in Manitoba, Canada, was a programme for low-income pregnant women and then for their children. 16 This programme was associated with an increase in breastfeeding initiation (BI). In Sweden, the Salut Programme is a suite of interventions that combines health promotion and universal prevention interventions with the aim of improving health and well-being in children and families. 17 A positive impact on child and maternal health outcomes was found. However, there are other policies that have been introduced that have not been evaluated in terms of outcomes. In the UK these include enhanced provision of early years childcare,12,18,19 Healthy Start vouchers20 (HSVs) and the Baby Box in Scotland. 21 There have been process evaluations of some of these policies to understand acceptability and how they work in practice, but there is a need to evaluate interventions in pregnancy and childhood to determine which have an impact on health outcomes22 and which are cost-effective.
Intervention: Healthy Start vouchers
Healthy Start vouchers have the potential to improve the health of low-income families, who are likely to have poorer diets than more affluent families, and thereby reduce health inequalities. It is estimated that around 33,745 children and 10,551 women per annum across Scotland23 are entitled to HSVs and over 423,000 households in the UK claim HSVs. 24
Healthy Start vouchers, a means-tested voucher scheme, was introduced UK wide in 2006 as a replacement to the Welfare Food Scheme (WFS). The WFS started in 1940 as a universal benefit to ensure expectant and new mothers had a healthy diet during rationing. It subsequently became targeted to lower-income mothers and families. It provided tokens that could be exchanged for liquid and formula milk and vitamins to expectant and nursing mothers, and to children under the age of 4 years. The HSV scheme expands what the vouchers can be used for. The HSVs can be spent on milk, infant formula milk, fruit and vegetables. Between 2006 and 2021, vouchers worth £3.10 per week were given to eligible women; mothers with a child aged under 1 year received £6.20. The amounts were reviewed annually and have not changed since 2006. There are four main aims of the HSV scheme: to improve the nutrition of pregnant women, to increase fruit and vegetable intake, to initiate and maintain breastfeeding, and to introduce foods in addition to milk as part of a progressively varied diet when infants are 6 months old. 20
In 2002 it was estimated that it would cost the Exchequer £147M per annum to fund the HSV scheme. 25 In 2013/14, £93M was paid to retailers as reimbursement for vouchers. 24 This represented a substantial investment at a time when the UK government was trying to reduce the welfare bill.
Rationale
The effectiveness and cost-effectiveness of the HSV scheme on a range of maternal and child health outcomes have not yet been demonstrated. A previous small (n = 336) comparison of the HSV scheme to the WFS found that mothers eligible for HSV had higher daily intakes of iron, calcium, folate and vitamin C than mothers eligible for WFS. 26 Three months postpartum, the HSV scheme mothers again reported higher iron, calcium, folate, and vitamin C intakes, as well as a higher consumption of fruit and vegetables than mothers eligible for the WFS. 27 A mixed-methods study28 of practitioners and low-income mothers found that recipients valued the vouchers but that there were substantial barriers to access, including low levels of awareness of the HSV scheme among both mothers and practitioners and uncertainty about the eligibility criteria among health professionals. A repeated cross-sectional analysis of the Health Survey for England29 found that fruit and vegetable intake in households eligible for the HSV scheme was similar to that of households in control groups.
A report on the operational aspects of the HSV scheme30 concluded that a comparative study is needed to assess the effectiveness and cost-effectiveness of the scheme. To determine the effectiveness and cost-effectiveness of population-based feeding programmes including the HSV, such interventions need to be evaluated in larger studies using a wider range of outcomes with longer-term follow-up and methods appropriate for deriving causal inferences from observational data.
The evaluation of the effect of a means-tested voucher scheme can inform policies aiming to change behaviour, improve health outcomes and reduce health inequalities. It can inform public health decision-makers as to the benefits of vouchers for milk, fruit and vegetable intake during pregnancy and the postnatal/infancy period. Information on the characteristics of participants and non-participants and the reasons why women do and do not participate can also inform policy, so that if the vouchers are shown to be effective in improving vitamin use and breastfeeding rates, in addition to other health outcomes, take-up can be improved.
One criticism of the WFS was the potential to disincentivise breastfeeding because it offered tokens for formula milk. 31 The HSV scheme widened the scope of the vouchers to include fruit and vegetables and offered free vitamins to pregnant women. Therefore, the hypotheses for this study were that the HSV scheme would increase the use of vitamins in pregnancy, but that through the provision of vouchers for formula milk, it has the potential to decrease BI and duration (BD).
Aim and objectives
The overall aim is to evaluate the HSV scheme in relation to the extent to which HSV improves the nutrition of pregnant women and the health outcomes of their infants.
There are five objectives to investigate:
-
the effectiveness of the HSV scheme in relation to vitamin use in pregnancy, and BI and BD
-
the effectiveness of the HSV scheme in relation to infant and child weight and body size, child morbidity, infant and child feeding, and maternal health
-
how findings differ between different populations (Scotland and UK)
-
to establish actual voucher usage and determine the reasons for uptake and non-uptake of the HSV
-
to establish the cost-effectiveness of the HSV.
Chapter 2 Methods
Research design
The evaluation took a mixed-methods, natural experiment approach to investigate the effectiveness of the HSV scheme. The analysis used existing survey data and was enhanced with an embedded qualitative study, and the methods to conduct a health economic analysis alongside a natural experiment evaluation were established. Thus, there were three parts to this evaluation:
-
Secondary analysis of two existing data sets, including linking one to routinely collected health data (objectives 1, 2, 3).
-
Qualitative interview study of mothers, including a descriptive analysis of voucher usage (objective 4)
-
Establishing methods for a cost-effectiveness analysis (CEA), and conducting a preliminary analysis (objective 5).
As the intervention was not controlled by the researchers, we used multiple exposed and unexposed groups to assess the effectiveness of the HSV scheme. This follows Medical Research Council (MRC) guidelines for the evaluation of NEs. 32 The HSV ‘intervention’ is not randomly allocated to participants so it was difficult to have complete control for confounding; there were factors associated with both receiving HSV and the outcomes that needed to be taken into account. The use of multiple comparison/unexposed groups helped with the assessment of bias of the evaluation method.
Healthy Start voucher policy
The intervention being evaluated was the HSV scheme. There are four main aims of the scheme: to improve the nutrition of pregnant women, to increase fruit and vegetable intake, to initiate and maintain breastfeeding and to introduce foods in addition to milk as part of a progressively varied diet when infants are 6 months old. 20
It is a means-tested voucher scheme for pregnant women and families with children under the age of 4 years. If these women are in receipt of certain means-tested benefits then they are eligible for vouchers to be spent on milk, infant formula milk, fruit and vegetables. They also receive free vitamins. All mothers under the age of 18 years are eligible for the scheme. Between 2006 and 2021, vouchers worth £3.10 per week were given to eligible women; mothers with a child aged under 1 year receive £6.20. The amounts were reviewed annually and have not changed since 2006. As from April 2021, the monetary value of the voucher increased to £4.25 per week. These can be spent in neighbourhood shops and pharmacies. A health professional signs the application form confirming the pregnancy (or child under the age of 4 years) and that the applicants have received health advice. The voucher scheme was rolled out across the UK in 2006 as a replacement to the WFS.
The requirement for a health professional to countersign the application means that there is an opportunity for health promotion. The health professional who countersigns the application will have offered appropriate health, nutrition and lifestyle information to the mother.
Intervention and control groups
An issue identified from a scoping study of evaluating the HSV scheme in terms of outcomes was the lack of obvious control group. 33 There are different ways to assess the effectiveness of the HSV scheme on maternal and child outcomes. One would be to compare the WFS with the HSV scheme, but there are weaknesses in this comparison. It relies on a control group who is living at a different time period to the current HSV scheme and it would be difficult to identify and then subsequently obtain the necessary data on outcomes, exposures and confounders from existing data sets. This evaluation used contemporaneous control groups that can be identified in current existing data sources.
Guidance for the evaluation of a natural experiment advises the use of multiple comparison/unexposed groups to give multiple perspectives about sources of bias and therefore allow an assessment of these biases. 32 This evaluation used two unexposed groups.
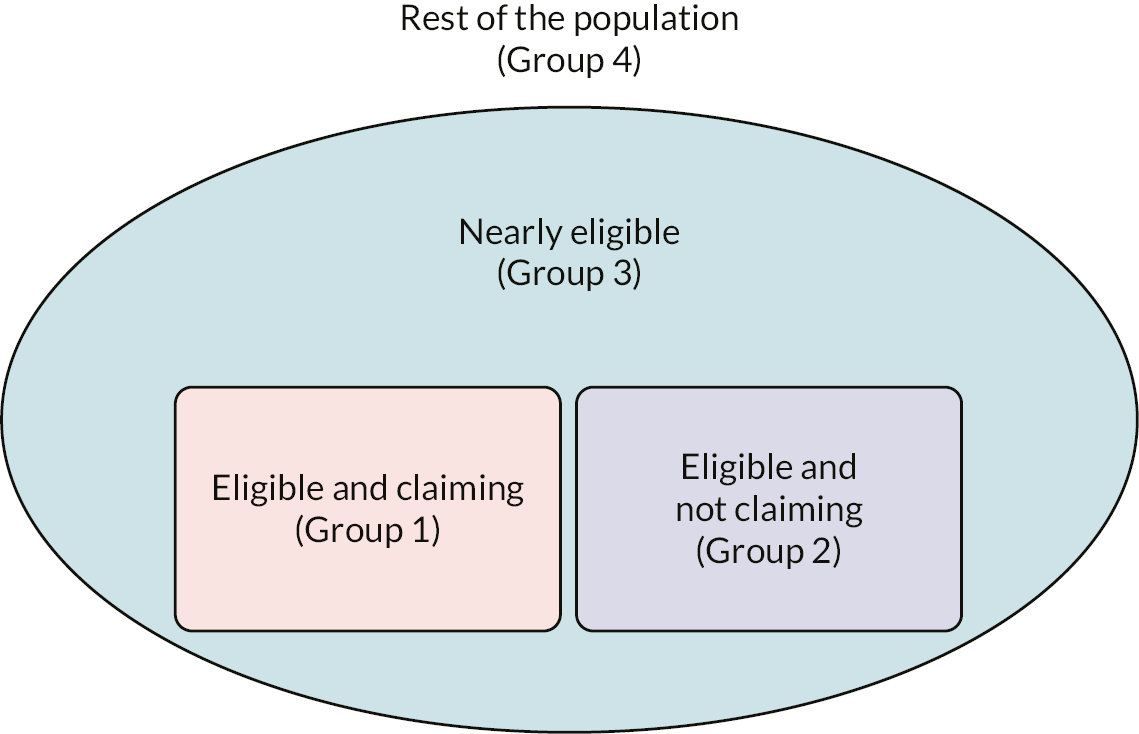
The population of mothers and their children can be divided into four mutually exclusive groups (Figure 1) according to their exposure to the intervention (HSV scheme). Group 1 is the exposed group, and they are eligible for HSV and claim the vouchers. Group 2 is the eligible but not exposed group: they are eligible for HSV but do not claim the vouchers. Group 3 is the nearly eligible group: they are those who just miss out on the eligibility criteria for HSV. Group 4 is the rest of the population: they are those who would never qualify for HSVs.
FIGURE 1.
Population of mothers and their children split by eligibility for the HSV scheme, identifying exposed and unexposed groups.
Comparison groups
With these exposure and control groups, there were three ways to compare these groups:
-
recipients versus eligible but not claiming (group 1 vs. group 2)
-
recipients versus nearly eligible (group 1 vs. group 3)
-
all eligible versus nearly eligible (group 1 and 2 combined vs. group 3).
The comparison groups represent different aspects of HSV effectiveness. Comparison groups 1 and 2 are analogous to evaluating the effectiveness of the ‘dose’ of HSV. Recipients of HSV (group 1) were compared with those who may be similar in many characteristics (group 2), especially in the eligibility criteria, but for whatever reason, they do not claim the HSV; recipients (group 1) were also compared with those who are close to the eligibility criteria but their income is just a bit too high to be eligible for HSV (group 3). Comparison 3 was effectively an intention-to-treat (ITT) analysis; this is how the HSV policy is working in practice.
Assessing effectiveness
This evaluation used a multiple analytical approach, using both propensity score matching (PSM) and regression discontinuity (RD). Using this combination of methods allowed control for both observed and unobserved confounders. In addition, the combination of methods allowed comparison of each method with their associated biases and therefore increased the robustness of the results. PSM is a technique used to limit the bias due to confounding in an observational study. The matching accounts for variables that are associated with receiving the intervention or control and therefore allows the estimation of the effect of the intervention. In RD designs, participants are assigned to an intervention or control based on a cut-off value of an assignment variable. Despite there being no random assignment, the RD design has comparable internal validity to randomised controlled trial (RCT) designs. 34
Table 1 details the method of evaluation for each of the comparison groups and notes, which method can be used for each of the data sets. The Infant Feeding Survey (IFS) does not have a suitable forcing variable for the RD method and so all comparisons were done using PSM.
| Comparison group | Data set | Evaluation method |
|---|---|---|
| 1: recipients vs. eligible but not claiming (group 1 vs. group 2) | GUS | Propensity score RD |
| 1: recipients vs. eligible but not claiming (group 1 vs. group 2) | IFS | Propensity score |
| 2: recipients vs. nearly eligible (group 1 vs. group 3) | GUS | Propensity score RD |
| 2: recipients vs. nearly eligible (group 1 vs. group 3) | IFS | Propensity score |
| 3: all eligible vs. nearly eligible (groups 1 and 2 combined vs. group 3) | GUS | Propensity score RD |
| 3: all eligible vs. nearly eligible (group 1 and 2 combined vs. group 3) | IFS | Propensity score |
All comparisons were important, but the main comparison of interest was between exposed (group 1) versus eligible but not exposed (group 2). This was a direct comparison of similar groups intended to be recipients of this targeted intervention and was the basis for the power calculation. The other two comparisons would determine the confidence in the results. The directions, sizes and significance of the effects would be indicative of the confidence in the effect of the HSV scheme. If the other two comparisons were in the same direction, significant and of the same magnitude then that would give us the most confidence that there is an effect of the HSV scheme. There would be reduced confidence if they were in the same direction but varied in size and/or significance and least confidence if the effects were in different directions, and significantly different from one another. Again, comparing effect sizes across the data sets and evaluation methods would also determine the confidence in the effect of HSVs.
Quantitative study: study population
The population was all women eligible for HSVs, that is, pregnant women and families with children under 4 years of age with low incomes or in receipt of certain means-tested benefits, all pregnant women aged < 18 years and all mothers aged < 18 years.
The Growing Up in Scotland (GUS) study was a stratified cluster random sample of the whole of Scotland and is available from the UK Data Archive. 35 Children were recruited to the second Birth Cohort in 2011 when they were about 10 months old; it had a sample size of 6127. Pre-project and preliminary inspections of the data determined that 1350 (22%) were from families that were identified as claiming HSVs and that 413 (7%) were from families that were identified as eligible but not claiming (Table 2).
| Data source | Group 1: recipients | Group 2: eligible not claiming | Group 3: nearly eligible (based on income between £15,600 and £20,799) |
|---|---|---|---|
| GUS – sweep 1 | 1320 | 413 | 507 |
The IFS23 is a random sample of births in the UK from August to October 2010. There were three stages of data collection; we used data from stage 3, when the infant is 8–10 months old. The sample size was 10,768 with 1906 (18%) were from families that were identified as claiming HSVs and 1535 (14%) were from families that were identified as eligible but not claiming (Table 3).
| Data source | Group 1 (recipients) | Group 2 (eligible not claiming) | Group 3 (nearly eligible) (IMD quintiles 1 and 2) |
|---|---|---|---|
| IFS | 1906 | 1535 | 4497 |
The IFS is available from the UK Data Archive and provides UK-wide data. It collected a wide range of detailed infant feeding patterns but does not have the range of other secondary outcomes available from the linked GUS data. The use of both complementary data sets would show the likely generalisability of the findings from GUS to the whole of the UK.
Quantitative: confounding variables
To enable greater comparability between the studies, identical/harmonised variables from IFS and GUS were used. The variables are described below.
The following groups have been identified as having more adverse birth outcomes and therefore were confounders for the analysis: those living in the most deprived areas, those in the lowest social classes, lone mothers, primiparous women, teen mothers and those in the lowest education group. The ethnic group of the mother was also an important factor for the outcomes. 36 We planned to include ethnicity as a covariate in the analyses. However, ethnicity in GUS reflects the ethnic composition of Scotland and is 95% white and 5% non-white; owing to the small sample sizes of non-white groups, it was not possible to break the non-white group into more refined ethnic groups. The ethnicity in IFS reflects the ethnic composition of Great Britain (England, Scotland and Wales) and is 82% white. Ethnicity was not asked in the Northern Irish sample.
Confounders in GUS were:
-
social class – national statistics socioeconomic classification (NS-SEC) of the mother, father and household
-
household income
-
educational status – education attainment of mother
-
family type – single mother/lone parent, couple family
-
primiparous – first born, other children
-
age of mother at birth of child – age < 20, 20–4, 25–9, 30–4, 35–9, ≥ 40 years
-
ethnic group – white, other ethnic background
-
urban/rural classification – large urban; other urban; small, accessible towns; small, remote towns; accessible rural; remote rural.
Confounders in IFS were:
-
social class – NS-SEC of the mother: 1, managerial and professional; 2, intermediate occupations; 3, routine and manual occupations; 4, never worked; 5, not classified
-
educational status – age mother left full-time education – ≤ 16, 17–8, > 18 years
-
single mother
-
primiparous – first birth, second or later birth
-
age of mother – age < 20, 20–4, 25–9, 30–4, ≥ 35 years.
When analysing GUS data and GUS/linked data, the Scottish Index of Multiple Deprivation (SIMD)37 was used. The SIMD combines information across six domains: income, employment, health, education, housing and geographical access. It provides a comprehensive picture of material deprivation in small areas within Scotland. The index ranks 6505 areas from the most deprived to the least deprived and measures the degree of deprivation of an area relative to that of other areas. The areas employed by the SIMD are data zones and are small: the 6505 data zones have a mean population of 780 people (approximately half the size of a lower super output area in England). The reason for employing small area geography at this scale is to permit identification of relatively small pockets of deprivation and minimise misclassification. Area-based deprivation was available for the IFS. It used an area deprivation measure appropriate for each country of the UK: the Index of Multiple Deprivation (IMD) for England,38 the Welsh IMD for Wales,39 the SIMD for Scotland37 and the Northern Ireland Multiple Deprivation Measure for Northern Ireland. 40
Sample size calculation
This was an analysis of existing data based on children in the GUS sample: as such the sample size was fixed. This calculation gave an indicative effect size that could be detected given the sample size. GUS has a sample size of 6127, with 1350 (22%) who were identified as being from families that were claiming HSVs and 2336 (38%) that were identified as being from families that were eligible but not claiming. GUS is a clustered sample of 199 data zones with approximately 30 respondents per cluster. Assuming an intraclass correlation coefficient of 0.01 and 63% BI, 80% power and 95% significance levels, the sample size of GUS would be able to detect a 5% difference (i.e. 68% BI).
Outcomes
Primary outcomes
There were two primary outcome measures: one relating to the mother during pregnancy and one relating to the child in early infancy. These are important periods of risk that measure different but important aspects of public health.
The aim of vitamin use during pregnancy is to create a healthy uterine environment, which is important for birth outcomes. An increase in vitamin use is one of the aims of the HSV scheme. In early infancy, breastfeeding is beneficial for many aspects of child health and morbidity. 41 An increase in breastfeeding rates and BD is one of the aims of the HSV scheme. Women from low-income families and low social class and teenage mothers have lower rates of breastfeeding and vitamin use in pregnancy than other women in the population. Providing health advice along with vouchers to use for a healthy diet (including milk and fruit and vegetables) should increase knowledge of the benefits of good maternal nutrition, reduce financial barriers to a more nutritious diet and, therefore, increase vitamin use.
The HSV scheme replaced the WFS, which provided only milk tokens for liquid and infant formula milk. There was therefore no incentive to breastfeed: if the mother was breastfeeding she could spend the vouchers on liquid milk only. The HSV scheme has broadened the scope of the vouchers to be used for fruit and vegetables as well as liquid and infant formula milk, so that mothers who choose to breastfeed are able to spend the vouchers on something other than milk. However, there is still a risk that the option of free formula milk will disincentivise breastfeeding. Conversely, the exposure to health advice associated with the HSVs could encourage higher rates of breastfeeding. Thus, comparing breastfeeding rates between those who do and those do not take up the vouchers is vital, mainly to exclude the possibility that the HSVs actually discourage breastfeeding.
Secondary outcomes
The secondary outcomes were in four categories: child weight and body size, child morbidity, infant and child feeding, and maternal health. Each secondary outcome related to at least one of the aims of the HSV and was available from up to three different data sources (Table 4).
| Outcome | HSV scheme aima | Data set |
|---|---|---|
| Primary outcome | ||
| Maternal: vitamin use in pregnancy | 1 | GUS, IFS |
| Child: BI and BD | 3 | GUS, IFS |
| Secondary outcomes | ||
| Child weight and body size | ||
| Birthweight | 1 | GUS, GUS-LK, IFS |
| Low birthweight | 1 | GUS, GUS-LK, IFS |
| Height at 3 years | 2 | GUS |
| Weight at 3 years | 2 | GUS |
| Mother’s perception of child weight at 3 years | 2 | GUS |
| Mother’s concerns about child weight at 3 years | 2 | GUS |
| Child morbidity | ||
| Pre-term birth | 1 | GUS-LK, IFS |
| Gestational age | 1 | GUS-LK, IFS |
| Morbidity in first year | 2, 3 | GUS, GUS-LK, IFS |
| Morbidity up to 3 years | 2, 3 | GUS, GUS-LK, IFS |
| Infant and child feeding | ||
| Use of formula milk | 3 | GUS, IFS |
| Use of cow’s milk before 1 year | 4 | IFS |
| Age at introduction of solids | 4 | GUS, IFS |
| Fruit intake at 3 years | 2 | GUS |
| Vegetable intake at 3 years | 2 | GUS |
| Mother’s perception of fruit/vegetable intake at 3 years | 2 | GUS |
| Vitamin intake at 3 years | 2 | GUS |
| Maternal health | ||
| Vitamin use during pregnancy | 1 | GUS, IFS |
| Current health | 2 | GUS |
| Smoking | 1 | GUS |
| Alcohol use | 1 | GUS |
| Financial strain | 1, 2 | GUS |
Data sources and numbers available for analysis
As part of the data collection process for GUS, the participants were asked if they consented to data linkage, which would allow for the individuals in GUS to have their survey data linked with routinely collected NHS data. Figure 2 displays the data sets to which we linked the GUS data. We linked the GUS data only for those participants who had consented to have their survey data linked to routinely collected NHS data. To do this, we applied to the NHS Information Services Division eDRIS service. An application was made to the Public Benefit and Privacy Panel for Health and Social Care. We provided information about the project, including why it was important and the methods and analysis, and noting the benefits it would bring to the public. We detailed the variables we required from each data set with justifications for them and also provided the variables we used from GUS. This was to ensure confidentiality. ScotCen (Edinburgh, UK) are the data owners of GUS and they provided the GUS data to eDRIS along with notices of consent. Note that this process has been superseded by a different, but similar, process since the Information Services Division became part of Public Health Scotland.
FIGURE 2.
Diagrammatic representation of the data linkage between GUS sweeps of data collection and routinely collected NHS data. Purple indicates data already collected and available; orange indicates future data collection. A&E, accident and emergency; CHSP, child health systems programme; MIDAS, Management Information and Dental Accounting System; SIRS, Scottish Immunisation and Recall System; SMR01, Scottish Morbidity Records general/acute inpatient and day case; SMR02, Scottish Morbidity Records maternity inpatient and day case.
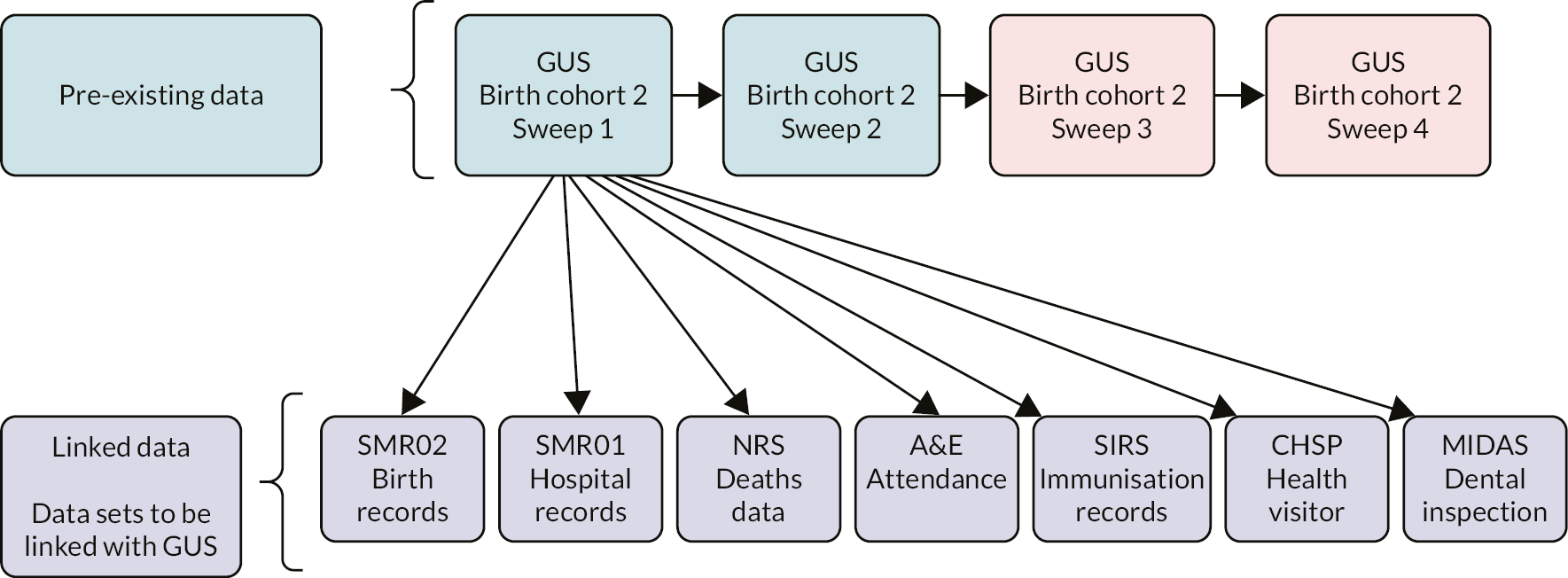
There was consent from 91% of GUS participants to link their survey responses with the routinely collected NHS data. Sample sizes available in GUS and the routinely linked NHS data are shown in Table 6, with comparisons of demographic information. We also used the GUS birth cohort 2, sweep 2. The sweep 2 follow-up visits were conducted in 2013/2014, which made the children around 3 years of age. The number of GUS participants matched to the GUS birth cohort 2, sweep 1, are shown in Table 5. There were differences between the comparison groups in terms of follow-up, with higher follow-up among group 3 (nearly eligible) than among groups 1 (recipients) and 2 (eligible, not claiming). By the time of sweep 2, some of the group 2 and group 3 mothers were claiming HSVs. This could have been due to changes in financial or family circumstances that meant they now qualified for HSVs. We kept participants in the original groups.
| Data source | Group, n (%) | ||
|---|---|---|---|
| 1 (recipients) | 2 (eligible, not claiming) | 3 (nearly eligible) | |
| GUS birth cohort 2, sweep 1 | 1320 | 413 | 507 |
| GUS children 3 years of age (sweep 2) | 939 (71) | 307 (74) | 413 (81) |
| Receiving HSVs (sweep 2) | 441 (47) | 40 (13) | 17 (4) |
| Data source | Group, n | ||
|---|---|---|---|
| 1 (recipients) | 2 (eligible, not claiming) | 3 (nearly eligible) | |
| GUS birth cohort 2, sweep 1 | 1320 | 413 | 507 |
| Linked GUS, matched by mothers | 1235 | 394 | 460 |
| Linked GUS, matched by child | 1279 | 410 | 475 |
The number of GUS participants linked with routinely collected NHS health data is shown in Table 6. There were high rates of linkage across the three groups.
Statistical analysis
The socioeconomic data from GUS are more detailed than the IFS socioeconomic data and contain information to identify all three comparison groups, allowing a fuller evaluation. The data from IFS are from a larger sample and cover the whole of the UK. Both GUS and IFS allow for multiple comparison groups. Both PSM and RD can be used with the GUS data and comparison groups, but only PSM can be used for the IFS data.
The group of women who are eligible for HSVs are also those who are less likely to breastfeed and be at risk of more adverse outcomes; even within this eligible group, there will be variation in breastfeeding rates. One difficulty is how to control for these confounding characteristics and also be able to detect an effect of HSV given all these other influences on breastfeeding. There are many background characteristics that are related to both adverse outcomes and the likelihood of being low income and therefore eligible for HSV. In both GUS and IFS these can be adjusted for these influences in the analyses. The PSM gives the probability that an eligible person will have received HSV given the characteristics associated with uptake of HSV, and probabilities for the control group. Therefore the two comparison groups should be balanced in terms of the factors associated with uptake of HSV, and any effect of HSV should be unbiased.
Propensity score matching
Propensity score matching is a technique used in case-control studies that enables direct comparison methods for assessing differences between groups to work more effectively through the selection of well-matched subsets of the original treated and control groups. 42–44 Theoretically, the function that produces the propensity score can be the logit, discriminate function or other functions that group treated and control units such that direct comparison becomes meaningful. 42 In PSM the number of controls has to be considerably more than the cases so that there can be a close match for each case. In current software for PSM, missing values are not allowed, and the definition of the groups is arbitrary, depending on number of subjects in each group. If the number of controls is fewer than the number of cases, as was the situation here, for a one-to-one matching for each control, a matching case would be chosen. Otherwise, there is the option of matching with a replacement, meaning that some individuals within the control group are replicated; however, there is still only one control group but in this situation the variances associated with measures would be considerably lower. The program MatchIt (version 4.5.2) package in R (version 3.0.3. The R Foundation for Statistical Computing, Vienna, Austria)43 provides sampling with replacements, but the number of matched controls does not exceed that of cases. 43,45 MatchIt also provides a weight measure when there is sampling with replacement; this weight measure can be used in subsequent regressions but is not applicable for direct comparisons, as is the case here. In situations in which the number of controls is fewer than the number of cases, there would be inevitable loss of power. For the present analyses one-to-one matching was deployed, as a direct comparison of primary and secondary outcome measures was used. It is also noted that the number of cases was more than controls for the GUS database. The following confounding variables, which define the characteristics associated with the uptake of HSVs, were used for the propensity matching process:
-
mother’s NS-SEC
-
mother’s education
-
family type
-
whether first-born child
-
mother’s age category
-
SIMD
-
urban–rural classification.
There are generally many matching methods that can be used. In general, it is recommended to use different matching methods and choose the one that works well with the data by giving the lowest mean differences between groups. For the current analyses the ‘nearest neighbour’ method was used, and three different matched groups were created. The first matched group consisted of subjects in group 2 (eligible group) to those of group 1 (receiving HSVs). The second matched group was subjects in group 3 (nearly eligible) matched to subjects in group 1 and the third matched group was subjects in groups 2 plus 3 matched to those in group 1. Therefore, a subject in group 1 could have been matched to a subject in groups 2 or 3 but as far as the group comparison was concerned the subjects in groups were unique.
Having matched the subjects according to their propensity scores, the proportions of outcome variables (one proportion for the binary and all for the categorical variables) were compared between groups using two independent proportions or chi-squared tests. 46 The continuous variables were compared using a paired t-test. The comparison groups were 1 with 2, 1 with 3, and a combination of 1 and 2 with 3. The distributions of the scoring for the matched groups together with the distribution of confounder variables are shown in Appendix 1.
Regression discontinuity
For the RD analysis, we followed the approach outlined by Imbens and Lemieux. 34 Linear regression was used when the outcome was continuous and logistic regression was used when the outcome was dichotomous. All analyses were adjusted for appropriate confounders including maternal and family social status measures and area deprivation. Regressions with polynomials were used to assess the non-linearity of the relationship between outcomes and HSVs. Local regressions, therefore, were estimated for both the intervention and comparison groups and the difference between the two estimates is the effect of HSV.
The RD is a research design in natural experimental studies for the evaluation of an intervention in a population. 34 For each unit (i) in a RD design, a quadruple (Yi, Wi, Xi, Zi) is observed, in which Yi is the outcome measure, Wi is the assignment variable (0 or 1), and Xi and Zi are covariates with Xi as a scalar and Zi a vector. Both Xi and Zi are not known to be influenced by the outcome Yi and they may influence Yi. In this design the units (generally subjects) are either completely or at least partly (fuzzy design) assigned to treatment or in the current setting the probability of belonging to the HSV-receiving group for each outcome variable after correcting for the covariate vector (Zi). The function relating the outcome variable (Yi) and income level (Xi) remains unknown but the assumption is that there is a smooth relationship. In the GUS database there are nine income categories and in the IFS income is not ascertained. Because the predictor, Xi, is associated with the outcome variable, Yi, any discontinuity of the conditional distribution (or conditional expectation) of outcome with respect to Xi at cut-off may be interpreted as a causal effect of the treatment. 34 Because the HSV scheme is a means-tested benefit the income category or equalised income would not necessarily be primary criteria for entitlement. For example, entitlement is age dependent (< 18 years) or it can be triggered during or following unemployment, or it is assessed if employed but on certain state benefits such as child tax or working tax credits, which are tied to household income. In addition, in the GUS database the stated household income is not in any way verified. The HSV scheme agency uses the Department of Work and Pension systems for verification of entitlement but the actual income level remains confidential. 17
In RD design the choice of the forcing variable (x axis) is such that for a value above or below a cut-off point (depending on the context) the unit (individual) is assigned to the intervention. The household income could be regarded as a forcing variable and the cut-off point could be set as the HSV eligibility criteria, which is a family income of ≤ £16,190 per year. The use of equivalised income as forcing variable was in keeping with RD design in that this predictor may itself be associated with potential outcome (the probability of being in the HSV group). The use of household income would entail the use of fuzzy RD design, in which the probability of exposure increases sharply at the cut-off point, but not from 0 to 1.
There were 447 out of 1320 (34%) subjects in the HSV cohort with a family income of more than the third category (£15,600–20,799). The outcome variable in RD is generally a measure with a ratio scale of measurement, such as a test score, or it can be a probability for binary outcomes, for example the odds ratio of taking vitamin D or folic acid before or during pregnancy. The odds ratios of taking vitamin D or folic acid for the HSV group were computed using logistic regression. In this logistic regression the outcome was taking vitamin D or folic acid before pregnancy, with the group assignment and optimum confounders as explanatory variables. In such a setting it was possible to obtain discontinuity at the income threshold using the ‘rdrobust’ package in R. 47
Missing data
The missing values for the confounder variables were imputed using multiple imputation with chain equations48 implemented in R. 49 The imputations were carried out for each comparison group separately. For example, for the GUS database, group 1 (recipients of HSV) with group 2 (eligible but not claiming group), similarly for group 1 with group 3 and groups 1 and 2 with 3. For each grouping 20 imputations were generated. The Stata® (Stata SE 14, StataCorp LP, College Station, TX, USA) software using Rubin’s Rule was used to estimate the coefficients of logistic regressions for comparison groups. The results were almost identical to those without imputation of the missing values. The imputations were not repeated for the IFS database because of the very low level of missing values.
Generalisability
The data used for this project came from different existing sources using different methods for collection and different questions. IFS is a questionnaire that subjects complete. Mothers are invited to take part via a letter and can complete the questionnaire either online or on paper and then post it back. GUS is a face-to-face interview with a researcher. Mothers are invited to take part via a letter and an interview time is agreed. The questionnaire is completed using computer-assisted personal interviewing; some parts of the questionnaire may be self-completed during the interview process. These different methods of data collection and differences in questions may cause bias in the results. To make statements about the generalisability of the broader range of outcomes available in GUS, we compared the propensity score-matched results from GUS and IFS for all comparison groups, for the primary outcomes of vitamin use in mothers and breastfeeding for infants.
Reporting of the quantitative results
We have reported the results of all pre-specified primary and secondary outcomes, and not just those that reached statistical significance. The analysis involved conducting many tests, which were not independent of each other. Rather than adjusting confidence intervals or p-values to account for this we have presented the results of all analyses and caution the reader regarding the interpretation of the results.
Qualitative interview study
To inform the understanding of the results of the quantitative study, and to understand the process of claiming and using the vouchers, we gathered qualitative data on the lived experiences of women, ascertaining reasons for uptake and non-uptake of HSVs and what the vouchers are spent on.
We carried out 40 in-depth interviews, spread across each of the following groups, mirroring the comparison groups identified in Figure 1:
-
GUS mothers who received HSVs
-
GUS mothers eligible for HSVs but who did not claim
-
mothers who were receiving HSVs
-
mothers who were eligible for HSVs but who did not claim
-
mothers who were nearly eligible for HSV, but did not meet the criteria.
This study started in 2015, when children in GUS were 5 years old. The HSV scheme is in place until the children are 4 years old. Mothers from GUS may have had difficulty recalling their thought processes from up to 5 years previously. We therefore complemented interviews with GUS mothers with interviews with mothers who were current claimers of HSVs and also those currently eligible for HSVs but who did not claim. We identified them from community groups that support families on low incomes. Those mothers nearly eligible for HSVs were also identified by this method. The mothers were selected to ensure that the sample contained women with a range of characteristics including age, number of children, ethnicity and education level.
The interviews were semistructured, face to face, approximately 1 hour in length and covered a range of topics, including what mothers knew about the scheme; how they found out about it; reservations about using it; and, if relevant, main reasons for not using it. If they were currently using the scheme or had used it previously, we asked about when they started using it, who knew they were using it, perceived extra monetary benefits, how conscious they were of extra money and how they used this extra money.
The interviews were recorded on an encrypted recorder, anonymised and transcribed verbatim. Recordings were anonymised before transferring to the transcribing service. The transcribing agency involved was subject to MRC/Chief Scientist Office (CSO) Social and Public Health Sciences Unit data confidentiality policies. Data were transferred and held in a secure environment subject to MRC/CSO Social and Public Health Sciences Unit data-sharing policies.
The transcripts were checked against the original recording before analysis started. They were coded according to prior and emergent themes using NVivo (QSR International, Warrington, UK) and summarised systematically by charting according to key themes, and emerging hypotheses were tested according to all the relevant data. Particular foci were the processes involved in the take-up, non-take-up or discontinuation of the HSV scheme, the experience of using HSVs and how the vouchers were used. Responses were compared between the five groups of women.
The 20 women sampled from GUS were sent an information leaflet and letter inviting them to take part in the semistructured interviews. A follow-up telephone call was made to get their response. For those who declined, they were replaced by other GUS participants with similar characteristics. The 20 women currently claiming/not claiming HSV were sampled from parent groups in deprived areas of Glasgow. Information leaflets were given to these groups inviting them to take part in the semistructured interviews. The participants were fully informed of the study before agreeing to participate. Once the women agreed to participate, an appointment for interview was made, with a reminder telephone call made in the week prior to the interview. The participating women were offered a £20 voucher in recognition of their time spent being interviewed.
Full details of the design, methods, analysis and results are in Chapter 5.
Health economics and assessment of the cost-effectiveness
Conducting health economic evaluations alongside NEs is relatively new. Therefore, the methodology for doing this is not well established. As part of this project, we developed and proposed methods and guidance for conducting such economic evaluations in population health using observation data from NEs. Such evaluations are subject to the inherent biases that affect analyses using observational data.
Our methodology drew on economic methods guidance50–53 and on evidence from economic evaluations carried out in similar early years contexts. 54,55 In addition, methods from previous studies incorporating economics into NEs in education and microeconomics,56–58 including a recent review on health economic evaluations and observational data,59 were used. Current guidance for economic evaluation focusses on RCT designs and therefore does not address the specific challenges for natural experiment designs. Using such guidance can lead to suboptimal design, data collection and analysis for NEs, leading to bias in the estimated effectiveness and cost-effectiveness of the intervention or policy. Fuller descriptions of the methods to develop the guidance and the health economics plan are reported in Chapter 6. The full economic evaluation is out with the scope of this report; it is subject to ongoing work and will be reported separately.
Patient and public involvement
When conducting patient and public involvement (PPI) for this project, we first defined our ‘population’ group. We identified low-income women as our PPI target group; their experiences reflected the population with the potential to be affected by the HSV scheme and the results of this project. The aim of PPI was to inform the qualitative interview schedule and refine and reflect initial analysis. As part of the PPI work, we undertook a focus group with 11 women to share our initial findings from the qualitative study and quantitative analysis. These women were recruited from third-sector organisations that support low-income families. During this process the women suggested adding the financial strain and challenges to the list of secondary outcomes, as they felt that, although HSVs represent a relatively small cash amount of £3.10, they do contribute some money to the family budget.
As part of the application process to link the GUS data to the routinely collected NHS data, lay members were part of the Public Benefit and Privacy Panel. Their opinions were fed into the decision to allow permission to use routine data for research and offer comment as to the public benefit of the research.
Ethics statement
Secondary analysis of existing data
Ethics approval was not required as there was no primary data collection. The data for both the IFS and GUS had already been collected and were available for use for research purposes. The linkage and release of the GUS data with the routinely collected NHS data for research purposes were subject to agreement from the Privacy Advisory Committee (and superseded by the Public Benefit and Privacy Panel) at NHS National Services Scotland. The data collection, storage and release for research purposes are subject to strict protocols governing privacy, confidentiality and disclosure of data. The project was approved subject to Public Benefit and Privacy Panel for Health and Social Care project number 1516-0614.
We used the GUS and IFS data from the UK Data Archive, subject to their end-user licence agreement. Note current arrangements for accessing GUS data may differ.
Qualitative interview study
Participants in GUS had already given consent to be contacted for research purposes. Only those who agreed to further contact for research purposes were approached to be interviewed. This qualitative study was reviewed and fully approved by the University of Glasgow, College of Social Science Ethics Committee in October 2015 (reference number 400150028). This Committee complies with the Economic and Social Research Council’s research ethics framework.
Chapter 3 Effect of Healthy Start vouchers on infant and child health
This chapter reports the results of the quantitative analysis of GUS and IFS linked to routinely collected health data sets for child outcomes. The range of outcomes covers aspects that are important for infant and child health, and they could be expected to be influenced by HSV. There are 1320 in group 1 (recipients of HSVs), 413 in group 2 (eligible but not claiming HSVs) and 507 in group 3 (those women who are nearly eligible for HSVs but their income means that they do not qualify for the HSV scheme).
Descriptive statistics for Growing Up in Scotland
Tables 7 and 8 show the descriptive statistics for the confounders contained in the GUS data set for each of the exposed and control groups. Group 2 had more mothers under the age of 20 years at the birth of their child than those in group 1, but fewer aged 20–4 years old. Apart from these differences the age groups were fairly similar for these two groups. Group 1 mothers were younger at the birth of their child than those in group 3 (see Table 7). For maternal social class, group 1 had more mothers who had never worked. Across all groups, the biggest proportion of mothers was in semi-routine or routine occupations. There was a large proportion (21%) of group 3 mothers in the intermediate occupation group. For group 1, the proportions for household social class were similar as for maternal social class, but groups 2 and 3 had different social class proportions for household and maternal social class. Group 3 had a large proportion (26.8%) in the managerial category. Groups 2 and 3 had similar profiles for mother’s education, but group 1 had more women in lower education categories than groups 2 and 3 (see Table 8). There was a gradient across the groups for lone parent families, with the highest proportion of lone parents in group 1 and the lowest in group 3. There were more women classified as living in the most deprived areas using both Carstairs Index and SIMD in group 1 than in groups 2 and 3. In terms of urban–rural, most women lived in urban areas across all three groups, but fewer group 1 mothers lived in accessible rural areas and more lived in small remote towns than those in groups 2 and 3.
| Confounder | Group 1 (recipients) (N = 1320), n (%) | Group 2 (eligible, not claiming) (N = 413), n (%) | Group 3 (nearly eligible) (N = 507), n (%) |
|---|---|---|---|
| Mother’s age at birth (years) | |||
| < 20 | 235 (17.8) | 45 (10.9) | 41 (8.1) |
| 20–4 | 358 (27.1) | 140 (33.9) | 113 (22.3) |
| 25–9 | 309 (23.4) | 115 (27.8) | 154 (30.4) |
| 30–4 | 254 (19.2) | 67 (16.2) | 123 (24.3) |
| 35–9 | 137 (10.4) | 37 (9.0) | 58 (11.4) |
| ≥ 40 | 27 (2.1) | 9 (2.2) | 18 (3.6) |
| Missing | 0 | 0 | 0 |
| Family type | |||
| Not lone parent | 679 (51.4) | 254 (61.5) | 378 (74.6) |
| Lone parent | 607 (46.0) | 152 (36.8) | 119 (23.5) |
| Missing | 34 (2.6) | 7 (1.7) | 10 (2.0) |
| Index child mother’s first born | |||
| Yes | 698 (52.9) | 175 (42.4) | 239 (47.1) |
| No | 622 (47.1) | 238 (57.6) | 268 (52.9) |
| Missing | 0 | 0 | 0 |
| Ethnicity of respondent | |||
| White | 1257 (95.2) | 395 (95.6) | 469 (92.5) |
| Non-white | 58 (4.4) | 18 (4.4) | 37 (7.3) |
| Missing | 5 (0.4) | 0 (0.0) | 1 (0.2) |
| Confounder | Group 1 (recipients) (N = 1320), n (%) | Group 2 (eligible, not claiming) (N = 413), n (%) | Group 3 (nearly eligible) (N = 507), n (%) |
|---|---|---|---|
| Maternal social class (NS-SEC) | |||
| Intermediate occupation | 147 (11.1) | 69 (16.7) | 106 (20.9) |
| Lower supervisory | 63 (4.8) | 34 (8.2) | 46 (9.1) |
| Managerial | 175 (13.3) | 54 (13.1) | 90 (17.8) |
| Never worked | 233 (17.7) | 27 (6.5) | 24 (4.7) |
| Semi-routine and routine occupation | 663 (50.2) | 206 (49.9) | 212 (41.8) |
| Small employers and own account workers | 36 (2.7) | 22 (5.3) | 28 (5.5) |
| Missing | 3 (0.2) | 1 (0.2) | 1 (0.2) |
| Household social class (NS-SEC) | |||
| Intermediate occupation | 148 (11.2) | 70 (16.9) | 102 (20.1) |
| Lower supervisory | 114 (8.6) | 44 (10.7) | 71 (14.0) |
| Managerial | 223 (16.9) | 70 (16.9) | 136 (26.8) |
| Never worked | 169 (12.8) | 16 (3.9) | 5 (1.0) |
| Semi-routine and routine occupation | 597 (45.2) | 173 (41.9) | 142 (28.0) |
| Small employers and own account workers | 66 (5.0) | 39 (9.4) | 50 (9.9) |
| Missing | 3 (0.2) | 1 (0.2) | 1 (0.2) |
| Mother’s highest education level (SCQF) | |||
| No qualification | 216 (16.4) | 26 (6.3) | 31 (6.1) |
| Lower level standard grades | 187 (14.2) | 40 (9.7) | 28 (5.5) |
| Upper level standard grades | 433 (32.8) | 133 (32.2) | 131 (25.8) |
| Higher grades and upper level vocational | 287 (21.7) | 146 (35.4) | 180 (35.5) |
| Degree level | 162 (12.3) | 55 (13.3) | 109 (21.5) |
| Other | 29 (2.2) | 13 (3.1) | 27 (5.3) |
| Missing | 6 (0.5) | 0 (0.0) | 1 (0.2) |
| SIMD 2009 quintiles | |||
| 1 (least deprived) | 95 (7.2) | 37 (9.0) | 45 (8.9) |
| 2 | 143 (10.8) | 54 (13.1) | 85 (16.8) |
| 3 | 232 (17.6) | 98 (23.7) | 93 (18.3) |
| 4 | 327 (24.8) | 101 (24.5) | 145 (28.6) |
| 5 (most deprived) | 522 (39.5) | 123 (29.8) | 139 (27.4) |
| Carstairs deciles | |||
| 1 (least deprived) | 43 (3.3) | 19 (4.6) | 23 (4.5) |
| 2 | 67 (5.1) | 28 (6.8) | 36 (7.1) |
| 3 | 92 (7.0) | 39 (9.4) | 48 (9.5) |
| 4 | 73 (5.5) | 31 (7.5) | 48 (9.5) |
| 5 | 116 (8.8) | 31 (7.5) | 47 (9.3) |
| 6 | 164 (12.4) | 46 (11.1) | 53 (10.5) |
| 7 | 140 (10.6) | 57 (13.8) | 66 (13.0) |
| 8 | 188 (14.2) | 42 (10.2) | 59 (11.6) |
| 9 | 192 (14.5) | 55 (13.3) | 53 (10.5) |
| 10 (most deprived) | 245 (18.6) | 65 (15.7) | 74 (14.6) |
| Urban–rural classification | |||
| Remote rural | 71 (5.4) | 18 (4.4) | 28 (5.5) |
| Accessible rural | 127 (9.6) | 56 (13.6) | 70 (13.8) |
| Large urban | 546 (41.3) | 162 (39.2) | 189 (37.3) |
| Other urban | 416 (31.5) | 128 (31.0) | 153 (30.2) |
| Small remote towns | 70 (5.3) | 10 (2.4) | 22 (4.3) |
| Accessible towns | 90 (6.8) | 39 (9.4) | 45 (8.9) |
Tables 9 and 10 show the descriptive statistics for the exposed (group 1) and control (groups 2 and 3) for the outcomes at age 10 months (see Table 9) and 3 years (see Table 10). There is a breastfeeding gradient, with the lowest proportion breastfeeding in group 1 and highest in group 3. There is also a gradient with BD: those in group 1 breastfed for a shorter time period than those in groups 2 and 3. Other outcomes in GUS sweep 1 are similar across the groups. For sweep 2, when the children were about 3 years of age, the outcomes were similar across the groups. There was a lower proportion of children who received vitamins at 3 years of age in group 1 than in groups 2 and 3.
| Outcome | Group 1 (recipients) (N = 1320) | Group 2 (eligible, not claiming) (N = 413) | Group 3 (nearly eligible) (N = 507) |
|---|---|---|---|
| Primary outcome | |||
| Child ever breastfed: yes, n (percentages) | 549 (0.45) | 219 (0.53) | 314 (0.62) |
| Duration of breastfeeding (months), mean (SD) | 1.18 (1.99) | 1.46 (2.16) | 1.88 (2.34) |
| Child weight and body size | |||
| Birthweight (g), mean (SD) | 3295 (629) | 3376 (625) | 3418 (507) |
| Low birthweight (< 2500 g), n (proportion) | 121 (0.092) | 27 (0.065) | 28 (0.055) |
| Child morbidity, n (percentages) | |||
| Birth timing: early | 568 (0.43) | 161 (0.39) | 233 (0.46) |
| Birth timing: on time | 145 (0.11) | 62 (0.15) | 71 (0.14) |
| Birth timing: late | 594 (0.45) | 190 (0.46) | 198 (0.39) |
| Premature birth: yes | 94 (0.071) | 28 (0.067) | 25 (0.05) |
| Infant and child feeding | |||
| Age at introduction of solid food (weeks), mean (SD) | 18.7 (5.9) | 19.4 (5.7) | 19.4 (5.5) |
| Outcome | Group 1 (recipients) (N = 939) | Group 2 (eligible, not claiming) (N = 307) | Group 3 (nearly eligible) (N = 413) |
|---|---|---|---|
| Child weight and body size, mean (SD) | |||
| Child weight (kg) | 11.71 (1.96) | 11.80 (2.23) | 11.64 (1.99) |
| Child height (cm) | 93.8 (4.6) | 94.4 (4.6) | 94.5 (3.9) |
| Mother’s perceptions of child’s weight age 3 years, n (percentages) | |||
| Normal weight | 883 (0.94) | 286 (0.93) | 384 (0.93) |
| Underweight | 38 (0.04) | 18 (0.06) | 21 (0.05) |
| Somewhat and very overweight | 19 (0.02) | 6 (0.02) | 8 (0.02) |
| Mother’s concerns about child’s weight age 3 years, n (percentages) | |||
| A little concerned | 85 (0.09) | 28 (0.09) | 41 (0.1) |
| Not concerned | 845 (0.9) | 273 (0.89) | 363 (0.88) |
| Quite and very concerned | 9 (0.01) | 6 (0.02) | 8 (0.02) |
| Infant and child feeding, n (percentages) | |||
| Daily fruit consumption | |||
| None | 85 (0.09) | 6 (0.02) | 8 (0.02) |
| 1 | 103 (0.11) | 9 (0.03) | 17 (0.04) |
| 2 or 3 | 282 (0.3) | 31 (0.1) | 66 (0.16) |
| 4 or 5 | 56 (0.06) | 9 (0.03) | 12 (0.03) |
| > 5 | 9 (0.01) | 0 (0) | 0 (0) |
| Mother’s perception of fruit consumption | |||
| Less than usual | 150 (0.16) | 12 (0.04) | 21 (0.05) |
| Same as usual | 357 (0.38) | 43 (0.14) | 78 (0.19) |
| More than usual | 19 (0.02) | 0 (0) | 4 (0.01) |
| HSV vitamin use, n (percentages) | |||
| Yes | 178 (0.19) | 95 (0.31) | 182 (0.44) |
| No | 761 (0.81) | 212 (0.69) | 231 (0.56) |
Descriptive statistics for Growing Up in Scotland data linked to routinely collected NHS data
Descriptive statistics for outcomes available in the GUS data linked to NHS routinely collected NHS data are shown in Table 11. In groups 1 and 2 the descriptive statistics were similar across all outcomes. There were differences between groups 1 and 2 and group 3, with group 3 tending to have slightly better outcomes across the range of outcomes. There were gradients for both the number of hospital stays and the average length of stay in hospital, with group 1 subjects having more stays with longer lengths of stay and group 3 subjects having fewer stays and shorter durations of stay. The exception was the proportion of children registered with a dentist. For all groups there was an increase across all years in the proportion of children registered with a dentist. By 2016, 90% of all children were registered with a dentist.
| Outcome | Database | Group 1 (recipients) | Group 2 (eligible, not claiming) | Group 3 (nearly eligible) | |
|---|---|---|---|---|---|
| Birthweight (g) from birth records | SMR02 | N = 1204 | N = 382 | N = 454 | |
| Mean (SD) | 3365 (594) | 3389 (625) | 3486 (542) | ||
| Feeding status at health visitor first visit | Health visiting | N = 1190 | N = 388 | N = 461 | |
| Breast, n (percentages) | 274 (0.23) | 97 (0.25) | 180 (0.39) | ||
| Formula, n (percentages) | 821 (0.69) | 252 (0.65) | 235 (0.51) | ||
| Mixed, n (percentages) | 71 (0.06) | 35 (0.09) | 41 (0.09) | ||
| Unknown, n (percentages) | 24 (0.02) | 4 (0.01) | 5 (0.01) | ||
| Morbidity | |||||
| Hospital stays in 5 years (number of children with event), n (percentages) | SMR01 | 675 (0.53) | 191 (0.47) | 212 (0.44) | |
| Length of hospital stays in 5 years (days), mean (SD) | 1.15 (2.98) | 1.06 (1.92) | 0.85 (1.3) | ||
| Number of visits to A&E (number of children with event), n (percentages) | A&E | 293 (0.23) | 78 (0.20) | 64 (0.14) | |
| Number of visits to A&E (number of occasions), n (SD) | 1.5 (1.1) | 1.3 (0.7) | 1.2 (0.6) | ||
| Proportion registered with dentist, by year, n (percentages) | Dental records | N = 1246 | N = 405 | N = 417 | |
| 2010 | 78 (0.06) | 25 (0.06) | 32 (0.07) | ||
| 2011 | 465 (0.37) | 140 (0.35) | 184 (0.39) | ||
| 2012 | 759 (0.61) | 248 (0.61) | 302 (0.63) | ||
| 2013 | 942 (0.76) | 299 (0.74) | 378 (0.79) | ||
| 2014 | 1035 (0.83) | 326 (0.81) | 409 (0.86) | ||
| 2015 | 1088 (0.87) | 346 (0.85) | 434 (0.91) | ||
| 2016 | 1120 (0.90) | 361 (0.89) | 439 (0.92) | ||
| Vision test, na | Vision | 1007 | 338 | 409 | |
| Hearing test, nb | Hearing | 1132 | 366 | 441 | |
| Immunisations, nc | SIRS | 1246 | 405 | 477 | |
Mothers were seen to be engaging with health services for routine tests and immunisations. This was demonstrated by 98% of children in each exposure and control group having a vision test, 100% of children in each exposure and control group having a hearing test, and 100% of children in each exposure and control group having the specified immunisations.
Descriptive statistics for the Infant Feeding Survey
Tables 12 and 13 show the descriptive statistics of confounders and outcomes across the exposure and control groups for IFS. Group 3 had consistently better levels of all confounders than groups 1 and 2. This was different from the GUS sample. There was a higher proportion of mothers in managerial and professional NS-SEC (34.4%) in group 3 than in groups 1 (6.6%) and 2 (15.8%). Group 3 had a much lower proportion of women who were aged ≤ 16 years old when they left full-time education (16.8%) than groups 1 (40.0%) and 2 (25.7%).
| Confounder | Group, n % | ||
|---|---|---|---|
| Group 1 (recipients), N = 1906 | Group 2 (eligible, not claiming), N = 1535 | Group 3 (nearly eligible), N = 4624 | |
| Mother’s age at birth (years) | |||
| < 20 | 319 (16.7) | 153 (10.0) | 127 (2.7) |
| 20–4 | 587 (30.8) | 442 (28.8) | 717 (15.5) |
| 25–9 | 478 (25.1) | 421 (27.4) | 1521 (32.9) |
| 30–4 | 305 (16.0) | 310 (20.2) | 1408 (30.4) |
| ≥ 35 | 202 (10.6) | 198 (12.9) | 830 (17.9) |
| Missing | 15 (0.8) | 11 (0.7) | 21 (0.5) |
| Maternal social class (NS-SEC) | |||
| Never worked | 564 (29.6) | 194 (12.6) | 309 (6.7) |
| Not classified | 205 (10.8) | 130 (8.5) | 356 (7.7) |
| Routine and manual occupation | 801 (42.0) | 655 (42.7) | 1344 (29.1) |
| Intermediate | 211 (11.1) | 314 (20.5) | 1025 (22.2) |
| Managerial and professional | 125 (6.6) | 242 (15.8) | 1590 (34.4) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Mother’s age when finished full-time education (years) | |||
| ≤ 16 | 763 (40.0) | 395 (25.7) | 775 (16.8) |
| 17 | 351 (18.4) | 245 (16.0) | 552 (11.9) |
| 18 | 304 (15.9) | 332 (21.6) | 775 (16.8) |
| ≥ 19 | 454 (23.8) | 546 (35.6) | 2457 (53.1) |
| Missing | 34 (1.8) | 17 (1.1) | 65 (1.4) |
| Marital status | |||
| Partnership | 441 (23.1) | 568 (37.0) | 2696 (58.3) |
| Living together | 453 (23.8) | 435 (28.3) | 1378 (29.8) |
| Widow/separated | 60 (3.1) | 41 (2.7) | 40 (0.9) |
| Single | 916 (48.1) | 472 (30.7) | 445 (9.6) |
| Missing | 36 (1.9) | 19 (1.2) | 65 (1.4) |
| Mother’s first baby | |||
| Yes | 719 (37.7) | 848 (55.2) | 2425 (52.4) |
| No | 1187 (62.3) | 687 (44.8) | 2199 (47.6) |
| Missing | 0 | 0 | 0 |
| IMD quintilesa | |||
| 1 (most deprived) | 898 (47.1) | 516 (33.6) | 2240 (48.4) |
| 2 | 476 (25.0) | 353 (23.0) | 2327 (50.3) |
| 3 | 286 (15.0) | 293 (19.1) | 27 (0.6) |
| 4 | 163 (8.6) | 230 (15.0) | 21 (0.5) |
| 5 (least deprived) | 83 (4.4) | 143 (9.3) | 9 (0.2) |
| Outcome | Group 1 (recipients), N = 1906 | Group 2 (eligible, not claiming), N = 1535 | Group 3 (nearly eligible), N = 4624 |
|---|---|---|---|
| Primary outcome | |||
| Child ever breastfed: yes, n (percentages) | 1011 (0.53) | 1059 (0.69) | 3560 (0.77) |
| Duration of breastfeeding (months), mean (SD) | 1.24 (2.47) | 1.94 (2.96) | 2.97 (3.50) |
| Child weight and body size | |||
| Birthweight (g), mean (SD) | 3334 (589) | 3383 (621) | 3424 (566) |
| Low birthweight (< 2500 g), n (percentages) | 134 (0.07) | 106 (0.069) | 222 (0.048) |
| Child morbidity, n (percentages) | |||
| Full term | 1726 (0.9) | 1397 (0.91) | 4300 (0.93) |
| Premature | 128 (0.067) | 107 (0.072) | 254 (0.054) |
| Missing | 52 (0.03) | 31 (0.02) | 70 (0.014) |
| Infant and child feeding, mean (SD) | |||
| Age at introduction of solid food (months) | 4.78 (1.54) | 4.89 (1.47) | 5.06 (1.32) |
| Baby given cow’s milk (months) | 7.39 (1.61) | 7.00 (1.76) | 6.87 (1.44) |
For the outcomes (see Table 13), there were gradients across the groups for BI and BD with group 1 having the lowest proportion and shortest duration, then group 2 and group 3 having the highest proportion breastfeeding and the longest duration. For child body weight and size outcomes, groups 1 and 2 were similar to each other. In terms of infant feeding, group 1 infants were introduced to solid food earlier than those in groups 2 and 3, but this was only by a couple of weeks.
Propensity score matching results for Growing Up in Scotland and Infant Feeding Survey
Tables 14–16 show the results for the propensity score analysis. Children were not randomly assigned to the comparison groups. Therefore, to ensure we were making fair comparisons across the groups in evaluating the effectiveness of HSVs, we used PSM. PSM is the probability of being assigned to a treatment being conditional on the observed baseline characteristics. This method tries to mimic the characteristics of a RCT when a RCT is not possible (or desirable) but there are other observational data that can be used. The propensity score is a balancing score, which means that if you condition on the propensity score, the distribution of observed baseline covariates will be similar between exposed and control subjects. In other words, this matching on key characteristics can allow for the groups to be more balanced on covariates. It is a technique that can minimise selection bias and is better at getting to the causal effect than simple covariate adjustment in models. Children were matched using propensity scores to balance the groups according to confounders (see Chapter 2, Methods). The distribution of propensity scores for matching for both the GUS and the IFS databases are shown in Appendix 1, Figures 5–10. These figures show the distributions for matching group 2 to group 1 (see Appendix 1, Figures 5 and 8), group 3 to group 1 (see Appendix 1, Figures 6 and 9), and groups 1 and 2 to group 3 (see Appendix 1, Figures 7 and 10).
| Outcome | Group 1 (recipients), N = 412 | Group 2 (eligible, not claiming), N = 412 | p-value | Group 1, N = 505 | Group 3 (nearly eligible), N = 505 | p-value | Groups 1 and 2, N = 505 | Group 3 | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Primary outcome | |||||||||
| Child ever breastfed: yes, percentages | 0.49 | 0.53 | 0.255 | 0.58 | 0.62 | 0.189 | 0.58 | 0.62 | 0.168 |
| Duration of breastfeeding (months), mean (SD) | 1.32 (2.1) | 1.46 (2.2) | 0.374 | 1.73 (2.3) | 1.88 (2.3) | 0.315 | 1.84 (2.4) | 1.88 (2.3) | 0.803 |
| Child weight and body size | |||||||||
| Birthweight (g), mean (SD) | 3313 (614) | 3377 (626) | 0.162 | 3357 (616) | 318 (628) | 0.117 | 3345 (620) | 3418 (628) | 0.062 |
| Low birthweight (< 2500 g), percentages | 0.085 | 0.066 | 0.358 | 0.083 | 0.056 | 0.08 | 0.081 | 0.055 | 0.13 |
| Child morbidity | |||||||||
| Premature birth: yes, percentages | 0.061 | 0.067 | 0.779 | 0.075 | 0.049 | 0.118 | 0.059 | 0.049 | 0.579 |
| Infant and child feeding | |||||||||
| Age at introduction of solid food (weeks), mean (SD) | 18.7 (6.0) | 19.4 (5.7) | 0.11 | 19.4 (5.7) | 19.4 (5.5) | 0.91 | 19.5 (5.6) | 19.4 (5.5) | 0.726 |
| Outcome | Group 1 (recipients) | Group 2 (eligible, not claiming) | p-value | Group 1 | Group 3 (nearly eligible) | p-value | Groups 1 and 2 | Group 3 | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Birthweight (g) from birth records, n | 262 | 305 | 305 | ||||||
| Mean (SD) | 3394 (627) | 3414 (560) | 0.768 | 3376 (605) | 3395 (570) | 0.683 | 3427 (618) | 3395 (570) | 0.654 |
| Morbidity | |||||||||
| Hospital stays in 5 years (number of children with event), n | 182 | 205 | 205 | ||||||
| Length of hospital stays in 5 years (days), mean (SD) | 3.6 (8.1) | 3.4 (5.4) | 0.086 | 4.4 (13.7) | 4.1 (9.5) | 0.11 | 4.3 (9.8) | 4.1 (9.5) | 0.11 |
| Number of visits to A&E (number of children with event), n | 74 | 60 | 60 | ||||||
| Number of visits to A&E (number of occasions), mean (SD) | 1.4 (0.9) | 1.3 (0.7) | 0.777 | 1.5 (1.3) | 1.2 (0.6) | 0.343 | 1.4 (0.8) | 1.2 (0.6) | 0.112 |
For outcomes in GUS sweep 1, across all comparison groups (group 1 vs. group 2, group 1 vs. group 3, and groups 1 and 2 vs. group 3), the outcomes did not differ. There was a slight difference in birthweight for the comparison groups 1 and 2 versus group 3 (p = 0.062), but the difference was only 73 g.
For outcomes in GUS linked to routinely collected NHS health data, across all comparison groups (group 1 vs. group 2, group 1 vs. group 3, and groups 1 and 2 vs. group 3), the outcomes did not differ. There was a slight difference in average length of hospital stay for the comparison group versus group 2 (p = 0.086), but the difference was only 0.2 days.
For outcomes in IFS, outcomes differed across the different comparison groups. For group 1 versus group 2, the children in group 1 were less likely to have been breastfed than those in group 2: 57% ever breastfed in group 1 compared with 69% in group 2. Those in group 1 were also breastfed for a shorter duration than those in group 2. There was a difference in ever breastfeeding and duration of breastfeeding across all the comparison groups. Birthweight differed between groups 1 and 3, and groups 1 and 2 and group 3. All outcomes differed between groups 1 and 2 and group 3 (see Table 16).
| Outcome | Group 1, (recipients), N = 1513 | Group 2 (eligible, not claiming), N = 1513 | p-value | Group 1, N = 1862 | Group 3 (nearly eligible), N = 1862 | p-value | Groups 1 and 2, N = 3375 | Group 3 N = 3375 | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Primary outcome | |||||||||
| Child ever breastfed: yes, percentages | 0.57 | 0.69 | < 0.0001 | 0.53 | 0.7 | < 0.0001 | 0.6 | 0.74 | < 0.0001 |
| Duration of breastfeeding (months), mean (SD) | 1.37 (2.58) | 1.94 (2.96) | < 0.0001 | 1.23 (2.45) | 2.09 (3.11) | < 0.0001 | 1.53 (2.70) | 2.51 (3.30) | < 0.0001 |
| Child weight and body size | |||||||||
| Birthweight (g), mean (SD) | 3350 (584) | 3381 (622) | 0.156 | 3334 (589) | 3398 (569) | 0.0007 | 3355 (604) | 3421 (560) | < 0.0001 |
| Low birthweight (< 2500 g), percentages | 0.065 | 0.071 | 0.607 | 0.071 | 0.052 | 0.025 | 0.071 | 0.048 | < 0.0001 |
| Child morbidity, percentages | |||||||||
| Full term | 0.91 | 0.9 | 0.341 | 0.9 | 0.92 | 0.186 | 0.93 | 0.91 | 0.0047 |
| Premature | 0.065 | 0.073 | 0.066 | 0.06 | 0.05 | 0.07 | |||
| Missing | 0.024 | 0.021 | 0.025 | 0.02 | 0.01 | 0.02 | |||
| Infant and child feeding, mean (SD) | |||||||||
| Age at introduction of solid food (months) | 4.78 (1.52) | 4.89 (1.47) | 0.161 | 4.78 (1.52) | 4.89 (1.50) | 0.108 | 4.83 (1.5) | 4.97 (1.37) | 0.0037 |
| Baby given cow’s milk (months) | 7.39 (1.58) |
7.00 (1.76) |
0.02 | 7.38 (1.59) |
6.96 (1.58) |
0.003 | 7.2 (1.68) |
6.93 (1.47) |
0.0069 |
Regression discontinuity results for Growing Up in Scotland
The forcing variable for the regression discontinuity method was household income. Categorical income was transformed into equivalised household income to make the forcing variable (see Chapter 2, Methods). It was not possible to use RD methods for most of the outcome variables as assumptions were not met. We present the results for the primary outcome of BI and BD, and the secondary outcomes of birthweight and low birthweight.
Table 17 gives the coefficients and 95% confidence intervals (CIs) for the RD analyses. There were no differences in the outcomes between those in group 1 (recipients) and those in group 2 (eligible). For group 1 versus group 3 (nearly eligible), children in the recipient group were less likely to be breastfed than those in the nearly eligible group. If they were breastfed, it was for a shorter duration (0.45 months shorter on average). Those in group 1 had a lower birthweight and were more likely to be in the low birthweight category than those in group 3. Those in groups 1 and 2 were breastfed for a shorter duration (0.33 months shorter on average) and had lower birthweight (0.018 g lighter on average) than those in group 3.
| Outcome | Group 1 (recipients) vs. group 2 (eligible, not claiming), coefficient of RD (95% CI) | p-value | Group 1 vs. group 3 (nearly eligible), coefficient of RD (95% CI) | p-value | Groups 1 and 2 vs. group 3, coefficient of RD (95% CI) | p-value |
|---|---|---|---|---|---|---|
| Primary outcome | ||||||
| Child ever breastfed: yes | 0.036 (–0.047 to 0.121) | 0.394 | –0.068 (–0.138 to 0.0010) | 0.053 | –0.062 (–0.135 to 0.018) | 0.135 |
| Duration of breastfeeding (months) | 0.457 (–0.179 to 0.963) | 0.179 | –0.45 (–0.7938 to –0.109) |
0.0097 | –0.332 (–0.626 to 0.011) | 0.058 |
| Child weight and body size | ||||||
| Birthweight (g) | –26.75 (–109 to 40.71) | 0.368 | –49.50 (–84.0 to –17.0) | 0.0025 | 0.018 (0.005 to 0.035) | 0.0073 |
| Low birthweight (< 2500 g) | –0.0028 (–0.0183 to 0.0120) | 0.674 | 0.024 (0.011 to 0.040) | 0.0117 | –3.22 (–30.5 to 60.05) | 0.523 |
Table 18 summarises the comparisons across the two methods (propensity score with RD) and the two data sets (GUS and IFS) for outcomes available in both data sets. The main comparison group is group 1 versus group 2. For nearly all the outcomes, apart from ever BI and BD in IFS, the results indicated that there is no effect of HSV on the outcomes. For ever breastfed and duration of breastfeeding, there are differences between propensity score results from GUS and IFS, with the IFS indicating a negative effect of HSV on breastfeeding.
| Outcome | Group 1 (recipients) vs. group 2 (eligible, not claiming) | Group 1 vs. group 3 (nearly eligible) | Groups 1 and 2 vs. group 3 |
|---|---|---|---|
| Child ever breastfed: yes | |||
| GUS (RD) | R > E | R < NE | AE < NE |
| GUS (PS) | R < E | R < NE | AE < NE |
| IFS (PS) | R < E | R < NE | AE < NE |
| Duration of breastfeeding (months) | |||
| GUS (RD) | R > E | R < NE | AE < NE |
| GUS (PS) | R < E | R < NE | AE < NE |
| IFS (PS) | R < E | R < NE | AE < NE |
| Birthweight (g) | |||
| GUS (RD) | R < E | R < NE | AE > NE |
| GUS (PS) | R < E | R < NE | AE < NE |
| IFS (PS) | R < E | R < NE | AE < NE |
| Low birthweight (< 2500 g) | |||
| GUS (RD) | R < E | R > NE | AE < NE |
| GUS (PS) | R < E | R < NE | AE < NE |
| IFS (PS) | R < E | R < NE | AE < NE |
| Premature | |||
| GUS | R < E | R > NE | AE > NE |
| IFS | R < E | R – NE | AE < NE |
| Age at introduction of solid food (months) | |||
| GUS | R < E | R – NE | AE – NE |
| IFS | R < E | R < NE | AE < NE |
For birthweight and low birthweight, the effect sizes and significance vary across the data sets and methods, indicating less confidence in the results of the HSV on birthweight. For premature births and age at introduction of solid foods, there is more consistency across the data sets and evaluation methods, indicating some confidence in the results.
Chapter 4 Effect of Healthy Start vouchers on maternal health and behaviours
This chapter reports the results of the quantitative analysis of GUS and the IFS and GUS linked with routinely collected health data sets for maternal outcomes. The range of outcomes covered aspects that are important for maternal health, and that could be expected to be influenced by HSV. There were 1320 mothers in group 1, 413 mothers in group 2 and 507 mothers in group 3. The primary outcomes were vitamin use before pregnancy and vitamin use during pregnancy.
Tables 19 and 20 show the univariable comparisons for the primary and secondary outcomes available in the GUS sweep 1 data set. Across the three comparison groups, there was a low proportion of women using vitamin C or folic acid before pregnancy: 29% in group 1, 30% in group 2 and 42% in group 3. There was a higher proportion of women in group 3 taking vitamins pre-pregnancy than in groups 1 and 2. In contrast, there was a high proportion of mothers taking vitamin C or folic acid during pregnancy: 82% in group 1, 86% in group 2 and 88% in group 3. There was a higher proportion of women in group 3 taking vitamins during pregnancy than in group 1.
| Outcome | Group 1 (recipients) (N = 1320) | Group 2 (eligible, not claiming) (N = 413) | Group 3 (nearly eligible) (N = 507) |
|---|---|---|---|
| Primary outcome, n (proportion) | |||
| Vitamin C or folic acid before pregnancy | 383 (0.29) | 124 (0.30) | 213 (0.42) |
| Vitamin C or folic acid during pregnancy | 1082 (0.82) | 355 (0.86) | 446 (0.88) |
| Mother’s health during pregnancy, n (proportion) | |||
| Very well | 515 (0.39) | 173 (0.42) | 228 (0.45) |
| Fairly well | 488 (0.37) | 157 (0.38) | 177 (0.35) |
| Not very well | 198 (0.15) | 62 (0.15) | 66 (0.13) |
| Not at all well | 119 (0.09) | 21 (0.05) | 35 (0.07) |
| Mother’s current general health, n (proportion) | |||
| Excellent/very good/good | 1056 (0.80) | 351 (0.85) | 451 (0.81) |
| Fair/poor | 264 (0.20) | 62 (0.15) | 56 (0.19) |
| SF-12, mean (SD) | |||
| Physical health | 51.41 (8.20) | 52.44 (6.83) | 53.07 (6.86) |
| Mental health | 50.17 (9.92) | 51.38 (8.74) | 52.28 (8.35) |
| SD, standard deviation | |||
| Outcome | Group 1 (recipients) (N = 1320) | Group 2 (eligible, not claiming) (N = 413) | Group 3 (nearly eligible) (N = 507) |
|---|---|---|---|
| Current smoker, n (proportion) | 620 (0.47) | 153 (0.37) | 122 (0.24) |
| Number of cigarettes smoked per day, mean (SD) | 11.42 (6.0) | 11.13 (9.56) | 8.57 (4.68) |
| Alcohol use | |||
| 2–4 occasions per week | 79 (0.06) | 23 (0.06) | 41 (0.08) |
| 2–4 occasions per month | 264 (0.2) | 103 (0.25) | 112 (0.22) |
| Monthly or less | 620 (0.47) | 198 (0.48) | 223 (0.44) |
| Never | 356 (0.27) | 87 (0.21) | 127 (0.25) |
| How household manages financially | |||
| Manage very well | 106 (0.08) | 25 (0.06) | 35 (0.07) |
| Manage quite well | 356 (0.27) | 103 (0.25) | 137 (0.27) |
| Get by alright | 634 (0.48) | 211 (0.51) | 254 (0.5) |
| Not manage very well | 92 (0.07) | 25 (0.06) | 30 (0.06) |
| Some financial difficulties | 106 (0.08) | 41 (0.1) | 51 (0.1) |
| Deep financial trouble | 106 (0.01) | 25 (0.01) | 35 (0.01) |
| Financial situation changed in past year | |||
| Improved | 224 (0.17) | 66 (0.16) | 66 (0.13) |
| Worsened | 370 (0.28) | 153 (0.37) | 198 (0.39) |
| Stayed the same | 713 (0.54) | 194 (0.47) | 243 (0.48) |
For maternal health measures (health during pregnancy and current health) a high proportion of mothers reported good/excellent health and this was similar across the three groups. Using the Short Form questionnaire-12 items (SF-12) scales, we found a gradient across the groups, with poorest physical and mental health scores for those in group 1, with those in group 2 in the middle and those in group 3 having the highest scores for physical and mental health.
For maternal health behaviours, there were differences across the groups for smoking and number of cigarettes smoked. The smoking rate was 47% in group 1, compared with 37% in group 2 and 24% in group 3. Those in groups 1 and 2 smoked more cigarettes per day than those in group 3. In contrast, alcohol use did not differ across the three groups, and most women drank on less than one occasion per week.
A further outcome topic available in GUS was the financial situation for the families. For both financial measures (how the household manages financially and if the financial situation changed over the past year) there was little difference across the groups. Despite most of the women across the groups stating that they had good financial management, there was a proportion of women who stated that they did not manage their finances well, and some had financial difficulties: 16% in group 1, 17% in group 2 and 17% in group 3.
We were able to use GUS linked to routinely collected NHS health data and assess outcomes for number of visits to accident and emergency (A&E) and number of dental treatments. For both measures there was a gradient across the three groups with most visits to A&E and most dental treatments in group 1 and fewest in group 3 (Table 21).
| Outcome | Database | Group 1 (recipients) | Group 2 (eligible) | Group 3 (nearly eligible) |
|---|---|---|---|---|
| Number of visits to A&E (number of mothers with event) | A&E | 309 | 65 | 65 |
| Number of visits to A&E, number of occasions, mean (SD) | 2.1 (3.0) | 1.6 (2.0) | 1.3 (0.7) | |
| Number of visits to dentist for treatment (number of mothers with event) | Dental records | 1129 | 360 | 412 |
| Number of visits to dentist for treatment, number of occasions, mean (SD) | 16.1 (8.9) | 15.0 (8.1) | 14.4 (7.4) |
In the IFS, the primary outcomes of vitamin C or folic acid before pregnancy and vitamin C or folic acid during pregnancy were assessed (Table 22). Similarly to GUS, across the three comparison groups, there was a low proportion of women using vitamin C or folic acid before pregnancy: 16% in group 1, 24% in group 2 and 19% in group 3. These proportions are slightly different to GUS; lower proportions took vitamin C or folic acid before pregnancy in groups 1 and 3 in IFS than in GUS.
| Primary outcome | Group 1 (recipients) (N = 1908), n (proportion) | Group 2 (eligible, not claiming) (N = 1535), n (proportion) | Group 3 (nearly eligible) (N = 4624), n (proportion) |
|---|---|---|---|
| Vitamin C or folic acid before pregnancy | 305 (0.16) | 368 (0.24) | 1711 (0.19) |
| Vitamin C or folic acid during pregnancy | 1698 (0.89) | 1320 (0.86) | 3930 (0.88) |
Again, there was a high proportion of mothers taking vitamin C or folic acid during pregnancy: 89% in group 1, 85% in group 2 and 88% in group 3. These proportions are similar to the proportions seen in the same comparison groups in GUS.
Propensity score matching results for Growing Up in Scotland and Infant Feeding Survey
Tables 23 and 24 show the results for the propensity score analysis. Mothers were not randomly assigned to the comparison groups. Therefore, to ensure that we were making fair comparisons across the groups in evaluating the effectiveness of HSVs, we used PSM. PSM is the probability of being assigned to a treatment being conditional on the observed baseline characteristics. This method tries to mimic the characteristics of a RCT when a RCT is not possible (or desirable) but there are other observational data that can be used. Matching on key characteristics can allow for the groups to be more balanced on covariates. It is a technique that can minimise selection bias and is better at getting to the causal effect than simple covariate adjustment in models. Mothers were matched using propensity scores to balance the groups according to confounders (see Chapter 2, Methods).
| Outcome | Group 1 (recipients) | Group 2 (eligible, not claiming) | p-value | Group 1 | Group 3 (nearly eligible) | p-value | Groups 1 and 2 | Group 3 | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Primary outcomes (percentages) | |||||||||
| Vitamin C or folic acid before pregnancy | 0.3 | 0.31 | 0.684 | 0.38 | 0.42 | 0.258 | 0.4 | 0.42 | 0.539 |
| Vitamin C or folic acid during pregnancy | 0.82 | 0.86 | 0.103 | 0.87 | 0.88 | 0.434 | 0.87 | 0.88 | 0.435 |
| Mother’s health during pregnancy (percentages) | |||||||||
| Very well | 0.43 | 0.41 | 0.403 | 0.39 | 0.45 | 0.136 | 0.41 | 0.45 | 0.631 |
| Fairly well | 0.35 | 0.38 | 0.35 | 0.35 | 0.36 | 0.35 | |||
| Not very well | 0.13 | 0.16 | 0.16 | 0.13 | 0.15 | 0.13 | |||
| Not at all well | 0.08 | 0.05 | 0.09 | 0.07 | 0.07 | 0.07 | |||
| Mother’s current general health (percentages) | |||||||||
| Excellent/very good/good | 0.83 | 0.85 | 0.404 | 0.81 | 0.88 | 0.0036 | 0.81 | 0.88 | 0.105 |
| Fair/poor | 0.17 | 0.15 | 0.18 | 0.12 | 0.18 | 0.11 | |||
| SF-12 scores (percentages), mean (SD) | |||||||||
| Physical health | 52.26 (7.45) | 52.43 (6.84) | 0.734 | 51.28 (8.36) | 53.09 (6.87) | 0.00021 | 51.52 (8.13) | 53.09 (6.87) | 0.001 |
| Mental health | 51.11 (9.12) | 51.36 (8.74) | 0.693 | 50.69 (9.23) | 52.28 (8.36) | 0.0045 | 50.81 (9.19) | 52.28 (8.3) | 0.0083 |
| Outcome | Group 1 (recipients) | Group 2 (eligible, not claiming) | p-value | Group 1 | Group 3 (nearly eligible) | p-value | Groups 1 and 2 | Group 3 | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Current smoker | 0.43 | 0.37 | 0.419 | 0.37 | 0.24 | < 0.0001 | 0.35 | 0.24 | < 0.0001 |
| Number of cigarettes smoked per day (SD) | 10.65 (5.2) | 11.14 (9.6) | 0.581 | 10.92 (5.7) | 8.59 (4.69) | 0.00014 | 10.92 (5.36) | 8.59 (4.69) | 0.0001 |
| Alcohol use (percentages) | |||||||||
| 2–3 occasions per week | 0.05 | 0.04 | 0.727 | 0.072 | 0.081 | 0.311 | 0.05 | 0.081 | 0.426 |
| ≥ 4 occasions per week | 0.01 | 0.01 | 0.018 | 0.004 | 0.01 | 0.004 | |||
| 2–4 occasions per month | 0.26 | 0.25 | 0.22 | 0.218 | 0.22 | 0.218 | |||
| Monthly or less | 0.44 | 0.48 | 0.428 | 0.44 | 0.45 | 0.442 | |||
| Never | 0.23 | 0.22 | 0.26 | 0.256 | 0.26 | 0.254 | |||
| How household manages financially (percentages) | |||||||||
| Manage very well | 0.089 | 0.064 | 0.206 | 0.09 | 0.07 | 0.691 | 0.085 | 0.067 | 0.486 |
| Manage quite well | 0.264 | 0.247 | 0.28 | 0.26 | 0.3 | 0.265 | |||
| Get by alright | 0.5 | 0.512 | 0.45 | 0.5 | 0.443 | 0.504 | |||
| Not manage very well | 0.07 | 0.058 | 0.06 | 0.06 | 0.063 | 0.057 | |||
| Some financial difficulties | 0.067 | 0.102 | 0.1 | 0.1 | 0.097 | 0.097 | |||
| Deep financial trouble | 0.007 | 0.014 | 0.01 | 0.01 | 0.009 | 0.008 | |||
| Financial situation changed in past year (percentages) | |||||||||
| Got better | 0.19 | 0.16 | 0.165 | 0.19 | 0.13 | 0.011 | 0.203 | 0.134 | 0.0061 |
| Got worse | 0.29 | 0.36 | 0.32 | 0.39 | 0.324 | 0.39 | |||
| Stayed the same | 0.51 | 0.48 | 0.49 | 0.48 | 0.471 | 0.475 | |||
Propensity score matching shows there was no difference in vitamin use during pregnancy for any comparison (82%, group 1 vs. 86%, group 2, p = 0.103; 87%, group 1 vs. 88%, group 3, p = 0.434; and 87%, groups 1 and 2 vs. 88%, group 3, p = 0.435). In addition, there was no difference in vitamin use pre-pregnancy for any comparison (see Table 23).
There were no differences between groups 1 and 2 for any of the secondary outcomes. However, there were differences between groups 1 and 3 for mother’s current general health, current smoking and number of cigarettes, and change in financial status. There were differences between groups 1 and 2 and group 3 for current smoking and number of cigarettes, and change in financial status (see Table 24).
PSM showed that there was no difference in the number of visits to A&E or number of dental treatments across the three comparison groups (Table 25).
| Outcome | Group 1 (recipients), n | Group 2 (eligible, not claiming), n | p-value | Group 1 | Group 3 (nearly eligible), n | p-value | Groups 1 and 2 | Group 3 | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Number of visits to A&E (number of mothers with event) | 65 | 65 | 65 | 65 | 65 | 65 | |||
| Number of visits to A&E, number of occasions, mean (SD) | 2.7 (5.7) | 1.6 (1.9) | 0.063 | 1.5 (1.4) | 1.3 (0.7) | 0.776 | 2.2 (5.3) | 1.3 (0.7) | 0.418 |
| Number of visits to dentist for treatment (number of mothers with event) | 359 | 359 | 410 | 410 | 410 | 410 | |||
| Number of visits to dentist for treatment, number of occasions, mean (SD) | 15.8 (8.4) | 15.0 (8.1) | 0.442 | 15.2 (8.6) | 14.3 (7.4) | 0.229 | 15.4 (8.3) | 14.3 (7.4) | 0.032 |
PSM was also used for the primary outcomes in IFS. In contrast to the GUS analysis, the results from the IFS showed differences across the comparison groups for vitamin use both before and during pregnancy (Table 26). Vitamin use pre pregnancy was lower for those in group 1 and groups 1 and 2 combined than those in groups 2 and 3 (17%, group 1 vs. 23%, group 2, p < 0.0001; 16%, group 1 vs. 26%, group 3, p < 0.0001; and 19%, groups 1 and 2 vs. 32%, group 3, p < 0.0001). However, for vitamin use during pregnancy, those in group 1 and groups 1 and 2 had higher proportions taking vitamins during pregnancy [89%, group 1 vs. 86%, group 2, p = 0.015; 89%, group 1 vs. 87%, group 3, p = 0.012; and 88%, groups 1 and 2 vs. 86%, group 3, p = 0.0023 (see Table 26)].
| Primary outcome | Group 1 (recipients) (N = 1513) | Group 2 (eligible, not claiming) (N = 1513) | p-value | Group 1 (N = 1862) | Group 3 (nearly eligible) (N = 1862) | p-value | Groups 1 and 2 (N = 3375) | Group 3 (N = 3375) | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Vitamin C or folic acid before pregnancy (percentages) | 0.17 | 0.23 | < 0.0001 | 0.16 | 0.26 | < 0.0001 | 0.19 | 0.32 | < 0.0001 |
| Vitamin C or folic acid during pregnancy (percentages) | 0.89 | 0.86 | 0.015 | 0.89 | 0.87 | 0.012 | 0.88 | 0.86 | 0.0023 |
Regression discontinuity results for Growing Up in Scotland
The forcing variable for the RD method was household income. Categorical income was transformed into equivalised household income to make the forcing variable (see Chapter 2, Methods). It was not possible to use RD methods for most of the outcome variables as assumptions were not met. Figures 3 and 4 show that the pre and post discontinuity trends are not stable. We present the results for the primary outcome of vitamin use before and during pregnancy; and the secondary outcomes regarding financial management.
FIGURE 3.
Regression discontinuity plot with outcome as probability of taking vitamin D or folic acid before pregnancy against log10 of household income as index variable. The coefficient estimate was 0.077 (z = 3.92, p = 0.0001).
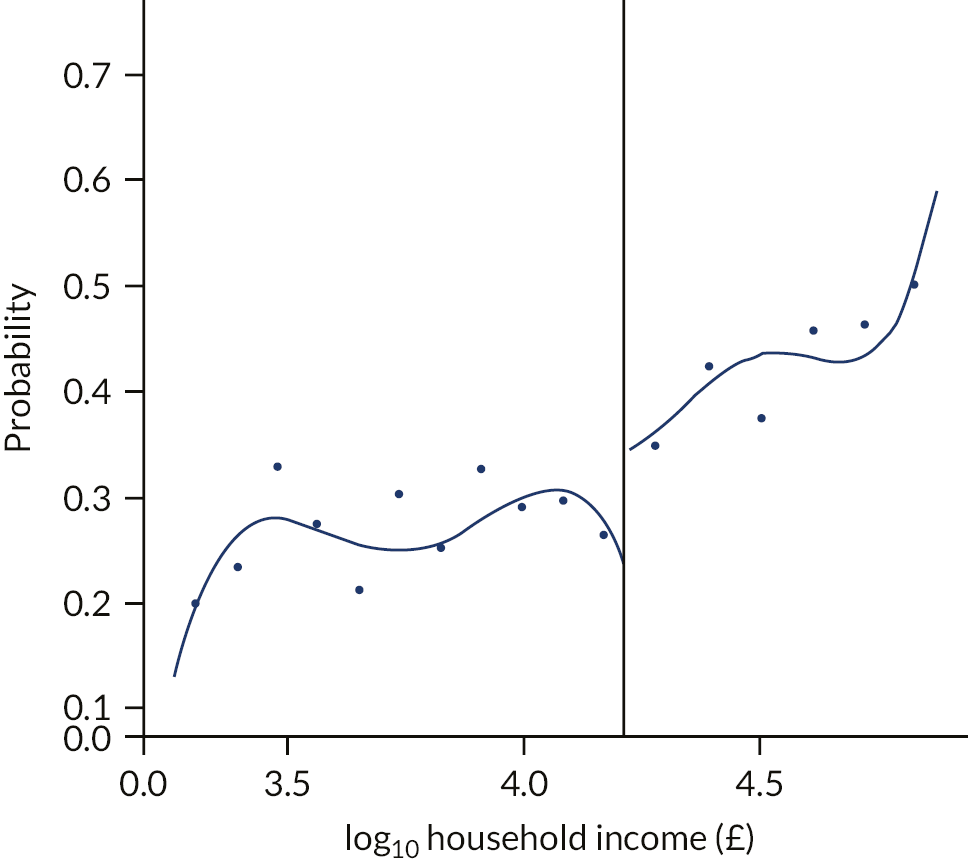
FIGURE 4.
Regression discontinuity plot with outcome as probability of taking vitamin D or folic acid during pregnancy against log10 of household income as index variable. The coefficient estimate was 0.11 (z = –6.255, p = 0.0001).

Figure 3 shows the mean probability of taking vitamin D or folic acid before pregnancy for groups 1 and 2. Figure 4 shows the RD for taking vitamin D or folic acid before pregnancy with the log10 of household income as assignment variable. The log10 of the income was used to normalise the distribution. In this analysis the estimate for the coefficient was 0.077 (0.030–0.124), showing a change in probability of taking vitamin D or folic acid at the income threshold (£16,190) of 7.7%, which was also termed as average RD treatment effect. 22 It should be noted that for the logistic regression the odds ratio of taking vitamin D or folic acid before pregnancy for group 1 was 0.953 (0.737–1.235) (Table 27). For the RD there was a statistically significant increase in the use of vitamin D or folic acid of approximately 8% to the right of the threshold. The estimates of RD coefficients are reported in Table 27 for group 1 versus group 2, group 1 versus group 3, and groups 1 and 2 versus group 3. A negative estimate at the discontinuity means a drop just to the right of the threshold and a positive value an increase. A change at discontinuity should be interpreted in the context of the probability estimate for the y axis. For example, as shown in Table 27 there is a significant decrease (7.7%) at the discontinuity for the subjects with income just below the threshold. On the other hand, there is a negative significant drop of 11% for taking vitamin D or folic acid during pregnancy for the subjects with income just above the threshold, meaning that subjects with lower income at the threshold are benefiting (see Figures 3 and 4).
| Outcome | Group 1 (recipients) vs. group 2 (eligible, not claiming), RD coefficient (95% CI) | p-value | Group 1 vs. group 3 (nearly eligible), RD coefficient (95% CI) | p-value | Groups 1 and 2 vs. group 3 | p-value |
|---|---|---|---|---|---|---|
| Primary outcome | ||||||
| Taking vitamin D or folic acid before pregnancy | 0.077 (0.030 to 0.124) | 0.0012 | –0.283 (–0.35 to –0.200) |
< 0.0001 | –0.30 (–0.38 to –0.22) |
< 0.0001 |
| Probability of taking vitamin D or folic acid during pregnancy | –0.111 (–0.1577 to –0.083) |
< 0.0001 | –0.094 (–0.158 to –0.042) |
0.0007 | –0.024 (–0.104 to 0.036) | 0.350 |
| Household finances | ||||||
| Financial situation | 0.076 (0.014 to 0.156) | 0.0194 | 0.0081 (–0.0612 to 0.090) |
0.706 | 0.075 (0.037 to 0.113) | 0.0001 |
| Change in financial situation | –0.001 (–0.025 to 0.008) |
0.236 | –0.0042 (–0.0215 to 0.0150) | 0.726 | 0.010 (–0.027 to 0.004) |
0.150 |
Table 27 gives the coefficients and 95% CIs for the RD analyses.
Table 28 summarises the comparisons across the two methods (PSM with RD) and the two data sets (GUS and IFS) for outcomes available in both data sets. The main comparison group is for group 1 versus group 2. For both outcomes, vitamin use pre and during pregnancy, the results indicated that there is no effect of HSVs on the outcomes. There are differences between propensity score results from GUS and IFS, with the IFS indicating a positive effect of HSVs on vitamin use. There are differences between PSM and RD results from GUS, with the RD results indicating a negative effect of HSVs on vitamin use.
| Outcome | Group 1 (recipients) vs. group 2 (eligible, not claiming) | Group 1 vs. group 3 (nearly eligible) | Groups 1 and 2 vs. group 3 |
|---|---|---|---|
| Vitamin C or folic acid before pregnancy | |||
| GUS (RD) | R > E | R < NE | AE < NE |
| GUS (PS) | R – E | R < NE | AE < NE |
| IFS (PS) | R < E | R < NE | AE < NE |
| Vitamin C or folic acid during pregnancy | |||
| GUS (RD) | R < E | R < NE | AE < NE |
| GUS (PS) | R < E | R < NE | AE < NE |
| IFS (PS) | R > E | R > NE | AE > NE |
Chapter 5 Understanding women’s experiences of the Healthy Start voucher scheme
Introduction
The qualitative component of the HSV scheme evaluation aimed to gain an understanding of the lived experiences of those intended to benefit from the scheme. This complements the quantitative component by providing insight into some of those findings. Qualitative interviews explored the processes involved in the take-up or non-take-up of HSVs, and how the vouchers were used and perceived by women.
Methods
Recruitment and sampling
Semistructured face-to-face interviews were conducted with 40 mothers aged between 22 and 47 years who each had between one and six children. A summary of the participant characteristics is shown in Table 29, and a fuller description of the sample is in Appendix 2, Table 31.
| Characteristic | Participants (N = 40), n |
|---|---|
| Claimed HSVs | |
| Yes | 22 |
| No | 18 |
| Ethnicity (participants’ own description) | |
| White Scottish | 24 |
| White British | 6 |
| Black African | 3 |
| British Pakistani | 2 |
| Pakistani | 1 |
| Nepalese | 1 |
| White Australian | 1 |
| White Irish | 1 |
| White Polish | 1 |
| Recruitment source | |
| GUS | 17 |
| Community groups | 23 |
| Age (years) | |
| 20–9 | 15 |
| 30–9 | 16 |
| ≥ 40 | 9 |
| Highest level of qualification | |
| No qualifications | 16 |
| High school qualifications | 8 |
| College qualifications | 6 |
| Degree/studying for degree | 9 |
| Postgraduate qualification | 1 |
| Number of children | |
| 1 | 9 |
| 2 or 3 | 23 |
| ≥ 4 | 8 |
Mothers were sampled from those GUS participants who had consented to participate in follow-up research projects (n = 17) and from community groups that supported low-income families (n = 23). The GUS study allowed for fairly representative sampling of eligible mothers, but these mothers had first used the vouchers at least 5 years before the interviews. We therefore also recruited mothers from community groups as they were able to give a contemporaneous account of the HSV scheme.
Mothers were sampled to include those who had claimed the HSVs (n = 22) and those who had not (n = 18). The group who had not claimed HSV includes those who according to GUS data had fulfilled eligibility criteria when surveyed and those from the community groups who were living on a low income but were ineligible for the scheme. Mothers could be ineligible if their income was not low enough for them to be claiming the means-tested benefits, or if they were unable to claim the benefits for another reason. The sample was also recruited to give a range across a number of characteristics including age, number of children, ethnicity and education level (see Appendix 2, Table 31).
Data collection
Interviews were semistructured and, in most cases, face to face. Mothers who lived in more rural and remote areas were interviewed by telephone. The interview schedule reflected the aims of the HSV scheme evaluation and contained questions about what mothers knew about the scheme, how they found out about it, reservations about using it, reasons for not using it, when they started using it, who knew they were using it, perceived extra monetary benefits, how conscious they were of extra money and how they used this extra money.
Ethics and informed consent
Each woman was provided with an information sheet describing the purpose of the research, explaining their right to withdraw, noting that their confidentiality would be protected and providing contact information for the principal investigator. Written, informed consent was obtained from all women who took part in the interviews. All interviews were audio-recorded on an encrypted recorder and stored securely. This qualitative study was reviewed and fully approved by the University of Glasgow, College of Social Science Ethics Committee in October 2015.
Analysis
Interviews were transcribed verbatim. These transcripts were read early in the data collection process to produce an initial coding frame. The study team refined and finalised the coding frame towards the end of data collection. Analysis was ongoing throughout fieldwork and additional themes were identified and explored further in subsequent interviews. The data for each code from the complete set of interviews were summarised descriptively. Emergent themes were developed, modified or rejected in reference to these summaries. We selected quotations as illustrative examples of the findings.
Results
Main findings
In analysing the transcripts of the women’s experience of the HSV scheme, four prominent themes emerged:
-
knowledge, awareness, take up and use of the HSV scheme
-
opinions of the HSV scheme
-
the effect of the HSV scheme on diet and feeding choices for their babies and children
-
the broader lives of low-income women.
Knowledge, awareness, take up and use of the Healthy Start voucher scheme
Mothers’ accounts showed a good knowledge of the HSV scheme’s aims and what the vouchers can be used for. In general, there was a broad understanding of the eligibility criteria but confusion about the details. Awareness and take-up of the HSV scheme varied, with participants finding out about the HSV scheme from various sources and applying in different ways, both of which affected uptake.
Knowledge of the aims of the Healthy Start voucher scheme and understanding what vouchers can be used for
Those who were claiming or had claimed HSV had a clear idea that the scheme was intended to support low-income women and their children to eat healthier diets. Some interviewees focused on the idea of a ‘good start’, indicating an understanding that targeting young children’s health may track through to improved health in later life. Some participants believed that the vouchers were intended to support nutrition in pregnancy, others mentioned nutrition for breastfeeding mothers and some thought that they were intended to provide financial assistance – a ‘helping hand’ for mothers on low incomes.
The HSV scheme was designed to replace the WFS and some mothers referred to HSVs as ‘milk tokens’. This suggests that they had not recognised the wider remit of HSVs, which can be used for fruit and vegetables as well as milk:
She’s like, ‘There’s another form for milk tokens tae get your milk ‘cause you’re eligible for, like, your baby milk an’ stuff like that.’
HSV07, claimant, community group
Those who had not claimed (including those with poor understanding of the details of the scheme) thought that the scheme targeted the nutrition of low-income families, but their understanding was not as wide as that of those who claimed HSVs.
Everyone who claimed HSVs was aware that they could use the vouchers for fresh or formula milk and for fresh vegetables. Most claimants also mentioned fruit. Some who had experience of using the WFS with older children noted that now, with the HSV scheme, they could use vouchers for fruit and vegetables. There was poorer knowledge that the vouchers could be used for frozen fruit and vegetables:
Milk, baby milk, fruit, veg.
HSV29, claimant, GUS
But the good thing aboot it nooadays is like you can buy fruit an’ veg an’ a’ that. You couldnae dae that a’ they years ago.
HSV27, claimant, community group
Perhaps unsurprisingly, in the accounts of participants without experience of claiming there was lower awareness of what the vouchers could be used for. One woman thought that the vouchers were solely for vitamins, another thought that they could be used for milk and vitamins, and another thought that the vouchers could just be used for formula milk:
Well, I think the Healthy Start Vouchers only entitle you to a wee vitamin, is that right?
HSV35, no claim, community group
You get Healthy Start Vouchers for formula, is that right?
HSV38, no claim, community group
Understanding eligibility for the Healthy Start voucher scheme
Although participants understood that eligibility for the scheme was dependent on being in receipt of certain benefits there was confusion about the detail of eligibility, particularly regarding the eligibility of working families. Those who did not claim did not know whether families who were working but on a low income and receiving some benefits were eligible:
I don’t think I even looked at it, or got given any information because we were two families that, well two, pair of people that worked at the time, do you know what I mean? So I was on maternity but I’ve only ever done 16 hours.
HSV21, no claim, GUS
Participants were aware that HSV eligibility depended on having a child under a certain age, but some believed that eligibility continued until the child was 5 years old or started school. Some participants were aware and had experience of eligibility during pregnancy but others talked about eligibility beginning at the child’s birth. Only one participant mentioned that being under 18 years of age (and pregnant or a mother) was a qualifying criterion regardless of benefit entitlement or income, and that participant had received HSVs on that basis herself. One breastfeeding mother understood that the HSV scheme was to provide vouchers for formula milk and that she would therefore be ineligible:
The only people that are entitled to this, you have to have a child from birth to 4 and you have to be on a certain amount of benefit.
HSV11, claimant, community group
I’d assume when they were born, up until about 5 I think?
HSV24, claimant, GUS
Awareness and take up of the Healthy Start voucher scheme
Take up of HSV relies on the awareness of the scheme. Mothers were made aware of HSV either through contact with a health professional (midwife, health visitor or general practitioner) or through a healthcare setting (information packs at antenatal clinics). Non-health service providers were also sometimes important in making mothers aware of the scheme, for instance benefits maximisation advisers or homeless support workers. Other mothers discussed more accidental encounters, such as seeing a poster in a shop or through conversations with friends and family. A key non-health source of information was conversations among women at family centres or parent groups:
It was at a midwife appointment and the midwife had helped me wae it.
HSV10, claimant, community group
My support worker she helped me quite a lot so it was quite good that way.
HSV01, claimant, community group
It was a mum in here that actually happened to mention Healthy Start Vouchers and I kinda thought, ‘What are they?’.
HSV40, claimant, community group
A few girls about the centre do talk about it. And they say, like... You do hear people saying, like, ‘Oh, my vouchers were useful,’ ‘I got my Healthy Start vouchers yesterday,’ ‘Oh, I’m glad I got my Healthy Start Vouchers yesterday ‘cause I’m going to do this.’ So everybody does know, and I think they all appreciate them, ‘cause everybody seems to apply for them, like, again when they get another child or whatever.
HSV02, claimant, community group
In contrast, mothers who had been eligible for the HSV scheme but had not claimed had, for the most part, not claimed because they had not been aware of the scheme’s existence. These mothers were clear that health visitors or midwives had not mentioned the scheme to them. A woman from a rural location felt ‘out of the loop’ and described minimal contact with health professionals. Other participants wondered if the health professionals had made assumptions because they were not obviously eligible. Such assumptions may have been made because they had been working previously, because both parents were present or because the mother was living in a more affluent area:
When you live in a small place like this, you’re really out of the loop with a lot of things. You know, you very infrequently see anyone official.
HSV23, no claim, GUS
I think people just presume. Yeah, like, if they come and see and they know that you’re working, or you have been working.
HSV17, no claim, GUS
Often participants were not made aware of the HSV scheme until their baby was born, meaning that they missed out on months of claiming. Participants felt that more should be done to let pregnant women know they are eligible:
Since I was eligible to, when my son was born.
HSV02, claimant, community group
I think just make people aware quite earlier. Just, yeah, maybe even at their breastfeeding classes?
HSV28, claimant, community group
Accessing and using the Healthy Start voucher scheme
For those who had made successful claims the process of applying for HSVs had largely been straightforward, with either their midwife or health visitor alerting them to the scheme and co-signing the application form. These health professionals were often viewed as very supportive. Some participants accessed information and filled in the application form online. Successful claims were usually processed without issues or delay:
I was pretty l... pretty low at that time. And again, kind of my emotions and moods an’ all that was all over the place. So I think she just wanted tae make sure that I was gonnae get it.
HSV05, claimant, community group
When there were problems with claims, participants described that they had not received any information or explanation as to why the claim was unsuccessful. These participants had been encouraged and supported to apply by health professionals who believed them to be eligible, yet had had their claim rejected without explanation:
I tried to get vouchers and they just wouldn’t give me any at all... I tried phoning them and they said they’d send letters out and I never received any letters from them... I kept trying phoning them and phoning them, letting them know that I still hadn’t received any letters and could they find out what’s happening wi’ the vouchers and kinda thing but they never, ever got back to me. So I just, I gave up.
HSV01 (Claimant, Community Group)
Mothers are required to telephone the HSV helpline after their baby is born and confirm the baby’s birth. Some participants were prompted to do so by a health professional but others were not aware of this requirement, resulting in a suspension of the claim:
I got them and then they just like stopped suddenly, just kinda like with, round about like when she was due... then I mentioned it to the health visitors like about what to do and she said that sometimes they just kinda like stop and then I have to kinda apply for it again. So she gave me another form, because they have to, a professional needs to sign it as well, so she signed it, gave it to me, but before I could like post that out, they just came through the post, started back up again.
HSV30 (Claimant, Community Group)
For the most part, those who did not claim HSVs in spite of being eligible did not do so because they were unaware of the scheme. However, there were instances in which people were aware of the scheme and chose not to claim. When participants’ circumstances changed frequently, for example moving in and out of employment, the effort required in making the claim was not always viewed as worth it. One interviewee had an ethical dilemma about claiming. She agreed that she was on a low income but did not see herself as struggling and wondered who would lose out if she was to claim:
See my husband sometimes is unemployed like for like a month or two. But we don’t bother applying for them because it’s just too much hassle for what like a month? Do you know what I mean?
HSV12, claimant, community group
Once the HSV claim was made vouchers usually arrived every 4 weeks without issue. When vouchers did stop it was usually suddenly, and mothers learnt that they were no longer eligible only when they had telephoned the helpline to ask why their vouchers had stopped. Problems with benefit claims would in turn result in HSVs stopping. These problems with benefit claims were often associated with changes in address or relationship status, and mothers would prioritise sorting out issues with their main benefits. They did not always understand why their vouchers had been stopped and when they were reinstated they were not backdated. Those who had used the HSV telephone helpline reported positive experiences; however, one mother was put off telephoning the helpline to discuss issues by the cost of the call:
Once I started getting them it’s all been smooth, yeah.
HSV12, claimant, community group
I phoned up and the woman explained to me on the phone why they’d been stopped, and that I was no longer eligible for them.
HSV32, claimant, GUS
I was just mair focused on my Income Support money being paid tae me an’ having that for my two boys. Do you know what I mean? I wasnae thinking ‘Milk tokens is gonnae save me a pound or two for milk or veg or whatever.’ I was just thinking, ‘I need money every two weeks for my weans, my hoose, whatever.’
HSV07, claimant, community group
It was actually, they’re actually quite good on the phone. It’s easy, you’re no’ sitting waiting see like for the job centre you’re on the phone for forty-five minutes trying tae get through. They were actually quite quick an’ got you through.
HSV09, claimant, community group
The majority of participants used their vouchers in supermarkets rather than smaller corner shops and incorporated them in a regular weekly or fortnightly shop. Supermarkets were preferred because they offered better value and a better range and quality of fresh fruit and vegetables, they were already part of a regular shopping routine, and mothers knew that vouchers were accepted there and that they would be processed more discreetly. Most of the participants identified and shopped in supermarkets where they felt shop staff made less of an issue of checking their shopping. There were instances in which participants felt that shop staff could have processed the voucher more discreetly:
I wouldnae buy veg or fruit, wee shops like that. They’re never fresh. That’s how I feel. I don’t think they’re fresh in wee shops like that.
HSV07, claimant, community group
My wee shop’s at my bit’s rubbish.
HSV09, claimant, community group
That’s saving me a good 12 pound odds a time, do you know what I mean? I don’t get embarrassed wi’ them.
HSV07, claimant, community group
And I remember handing over two vouchers when all my shopping was packed, so she waited for my receipt to come out. And she waited, and she highlighted all down my receipt what exactly. And I felt pure mortified in the queue, and I’m like ‘Why do you need to do this to me? You can see I’ve got enough, like, to even look at it, you don’t need to count it all up.’ So I did feel quite embarrassed at that point, uh-huh. So now I just take the one voucher and just get the two milks and a packet o’ bananas and apples, and I know that that will just kinda cover it.
HSV02, claimant, community group
Opinions of the Healthy Start voucher scheme
Participants had strong opinions about the HSV scheme, in terms of its aims, eligibility and scope. These accounts were overwhelmingly supportive of HSVs and demonstrated the value of this early years intervention. There were criticisms about the amount of money the vouchers covered and what additional benefits of the scheme formula-feeding mothers could access. There was a good understanding of the eligibility criteria, but participants thought that eligibility should be extended to other groups. In terms of the scope of the HSVs, there was scepticism about the potential of HSVs to make a difference to lives of children.
Opinion of the aims of the Healthy Start voucher scheme
Those who claimed HSVs valued the vouchers because they focused on children’s well-being and because they offered a small amount of financial assistance. Participants who had not claimed were also very positive about the scheme:
I can’t speak highly enough about it, know how. I feel it’s gave us, know how, or gave [child] know how a great start in life.
HSV05, claimant, community group
It makes a lot of sense, I would have probably found that quite useful. I think every penny counts when you’ve young children.
HSV26, no claim, community group
The main criticism of the scheme was the value of the vouchers, with participants pointing out that £3.10 did not buy a lot of fruit and vegetables. Those using formula milk would have liked a greater contribution towards the milk:
When you’ve got your electric bill, your gas bill, your food shopping and this baby that’s constantly growing and you’re always having to buy clothes for. That’s [£3.10] nothing, and it disappears.
HSV32, claimant, GUS
Maybe if the milk tokens could maybe cover while your baby’s on the formula milk, to take a milk token an’ get a tub for it.
HSV27, claimant, community group
Some mothers who were not breastfeeding thought that they were discriminated against because they had to spend the vouchers on formula milk. This left them nothing for fruit and vegetables, which breastfeeding mothers could spend the vouchers on. Mothers who were not breastfeeding had very often tried to breastfeed and felt that they were losing out in spite of having done their best to follow advice to breastfeed:
It would be nice if it was more than that, especially if you’re not breastfeeding.
HSV11, claimant, community group
Opinion of eligibility of the Healthy Start voucher scheme
Participants thought that eligibility should be extended until the child was 5 years old or at school. They thought that more effort should be made to let pregnant women know that they are eligible. Participants were clear that low-income working families needed help accessing healthy food:
I think that’s pretty early because, obviously, some kids are still at nursery when they’re 4. So I think they should know how at least go on to when they’re in primary, maybe one? They should go on that wee bit longer.
HSV05, claimant, community group
Participants described circumstances in which low-income mothers were ineligible for HSVs that they thought were unfair, especially for women who worked. One woman on a very low income gave an account of her ineligibility due to living in Scotland on a student visa. Another woman described sharing her vouchers with an asylum seeker friend who could not claim:
I am on the threshold, I do work, but I do, you know, I do claim benefits also, and I do have two young children, so it would, it would have helped.
HSV22, no claim, GUS
You have to have papers – basically, you have to be a resident. If you’re an illegal immigrant they don’t get it. If you’re an asylum seeker, they don’t really get it, which is really sad because everybody should be able to eat fruit and veg, so that’s really, really sad.
HSV11, claimant, community group
One participant suggested that the HSV scheme should be widened to include all pregnant women and young children because it would give a message about the importance of nutrition for children:
I think it should be for every mum and kids... when they do get something like that then they realise, ‘Oh, okay. So it is important, that’s why government is giving you this. So you must actually do something like that to keep your kids healthy.’
HSV18, no claim, community group
Opinion of the scope of the Healthy Start voucher scheme
Although there was overwhelming support for the HSV scheme and its focus on children’s health and well-being, there was also scepticism about its impact. Several women thought that the amount of money (£3.10 per week) would be unlikely to make a difference to health in the early years:
If it’s hitting that mark, I would be surprised. Three pound ten a week to me? No. I don’t think so. I don’t think that touches this. And I think the people who genuinely need it most, and who need that education about health and nutrition and everything else, I don’t think that three pound ten... scratch the surface if I’m honest.
HSV25, no claim, GUS
The effect of the Healthy Start voucher scheme on diet and feeding choices for their babies and children
Participants described their children’s diets, including vitamin use, and decisions around feeding their babies and children. Accounts included the importance of a healthy diet: although there was an understanding of what this entailed, there was evidence of poor diets and limited knowledge. Women were open to advice about diet from health visitors and also gave accounts of other influences on diet. The vitamin part of the HSV scheme was less well used than the vouchers, despite knowledge that vitamins are recommended in infants and children. There were several motivations to breastfeed and the HSV scheme did not have an impact on the decision to breastfeed or use formula milk.
Healthy diet
Although appropriate nutrition for children is important to most mothers, and mothers did strive to give their children healthy diets, there was evidence that some children still had poor diets. This section contrasts participants who reported striving for healthy diets, those providing poor diets and some mothers who are not at these extremes, and offers some reasons for these accounts.
Mothers offered a range of reasons for believing that diet is important, including their children’s teeth and weight, and their risk of diabetes. They believed that a nutritious diet is required for a child to grow. Ensuring a healthy diet was tied to notions of giving children the best start in life and being integral to an overall healthy lifestyle, for the child and for the family as a whole. A healthy diet was also understood to facilitate an active lifestyle whereas poorer nutrition was linked to lethargy in children. The accounts indicated that for some women there was a good understanding of what a healthy diet looked like, but that others fed their children unhealthy diets. Mothers offered descriptions of what they believed were the basic principles of nutrition; for example, most were aware of the ‘5 a Day’ recommendation for fruit and vegetables, and that plenty of fruit and vegetables was desirable. The need to limit salt and sugar intake was also mentioned frequently:
Making sure she’s got her five portions of fresh food during the day.
HSV25, no claim, GUS
Not too much sugar, not too much salt, not too much fat. Try and lay off white bread.
HSV23, no claim, GUS
Interviewees had varied assessments of the healthiness of their own child’s diet: some made confident assertions about their child’s exclusively healthy diet, some admitted poor eating habits, and a number said that they tried to provide a healthy diet but were not always successful. Participants mentioned a range of influences on diet, including themselves, siblings and nurseries. Participants recognised that their eating habits had been influenced by their own parents and were cognisant that they in turn held sway over their children. Those who cooked had often learned from their own parents and they continued to cook the same recipes they had been taught:
Saturday or a Friday night – making my big pot o’ soup. My ma’s just taught me that. Following suit.
HSV07, claimant, community group
Mothers were aware that their poor eating habits influenced their children. Those who were ‘fussy eaters’ hoped that their children would not be fussy. One woman knew that her son wanted a biscuit for breakfast because that is what she has. Mothers were also aware that they could influence positively: one women described how her own diet had improved since joining Slimming World© (Slimming World, Alfreton, UK) and that in turn her children’s diet had improved. Children were also influenced by their siblings:
It’s like my son will get up in the morning and he’ll want a biscuit, know what I mean? An’ it’s kind o’ like... probably ‘cause I dae it.
HSV06, claimant, community group
She’ll eat baked beans, he won’t eat baked beans. And then she sees – if I go, ‘Do you want this?’ And she goes, ‘Yeah.’ If I say that to him, ‘Do you want this?’ He’ll go, ‘No.’ And then I say, ‘Do you want this?’ And she’ll say, ‘Yeah.’ Then he’ll want it.
HSV38, no claim, community group
Children’s nurseries were mentioned as sources of positive influence with regard to food; children were introduced to new foods there that they were then keen to have at home:
So I think the mixture of being introduced at that way, and nursery introducing fruit platters and picky foods and things that the children will try them.
HSV37, no claim, community group
Some participants had become motivated to achieve a healthy diet for their children because of a diagnosis or a specific health concern. One woman, along with her husband, had made significant changes to the family’s eating habits after her husband received a diagnosis of high blood pressure. A young mother stopped using processed foods when it became evident that her son’s digestive system could not tolerate them:
[Husband’s name] had quite a bit of a scare, his high, his blood pressure went really high. So he – that, I think that’s when we changed our lifestyle.
HSV31, claimant, GUS
Participants’ accounts contained evidence of healthy diets and they also discussed factors that facilitated healthy diets. Many elements of a healthy diet were present in accounts of cooking and eating. Some mothers said that they cooked from scratch, with some claiming always to cook and others cooking when they had time. Participants talked about teaching children to cook and about eating together as a family. A couple of mothers grew their own vegetables: one lived in a rural location but the other used pots in a small urban garden. Participants talked about encouraging children to try new tastes, giving children access to a range of tastes while young and access to foods considered unusual for children. They talked about children who were very keen on fruit and having fruit freely accessible to children. To a lesser extent they described children who were very keen on vegetables:
I don’t like the processed food, no. We eat cooked food every day.
HSV11, claimant, community group
A few times and it helps if I’m eating it, or if he’s with his dad and his dad’s eating it. He will sort of come over and be like, ‘Can I have a bit of that?’ I think that does help from him when was younger, as I did try to introduce as much different stuff as possible.
HSV32, claimant, GUS
Much effort is given to planning and preparing healthy diets, with some mothers recognising that healthy eating requires time and work. They take time to learn new ways to cook. Mothers are resourceful in their efforts by hiding and disguising fruit and vegetables to get their children to eat them. They made smoothies to increase fruit intake or soups to increase vegetable intake. They mash turnip with potato mash and cut vegetables up in ways that are fun for children. They avoid food waste by making soup or freezing vegetables that may soon ‘go off’:
What I used to with the wee yins, is mash and mash the turnip and that in the mash so that they didnae know it was in it.
HSV13, claimant, GUS
Cutting them up into different bits and pieces, and things, so that it’s fun for him.
HSV02, claimant, community group
Those who reported being successful in getting their children to eat healthily appeared confident and determined. One woman was confident that she could persuade friends’ children to eat vegetables when her friends were unable to. Another was clear that her son benefited from her saying no to his requests for treats. And another described her strategy of insisting that her daughter ate dinner if she was to get a treat afterwards. The same mother said that her approach was hard work for her when she was tired and busy:
I just give her what we’re having an’ I just don’t give in. She’s gottae eat it. If she doesn’t eat it then she doesn’t get anything. She doesn’t get a treat... It’s quite hard work not giving in when you’re tired and you’re busy.
HSV40, claimant, community group
Mothers also talked about having to persevere with efforts to get children to eat vegetables by repeatedly offering them until they were accepted. Mothers who were providing healthier diets did not appear to share any particular wider attributes other than confidence and the ability to persevere:
He didn’t like broccoli, he didn’t like it, because he didn’t like the look of it. But I tried and I tried and I tried, and he eats broccoli now.
HSV37, no claim, community group
Although there was much evidence of healthy diets there was also evidence of poor diets. Mothers described diets high in sugar, for example eating Rice Krispie (Kellogg’s, Battle Creek, MI, USA) bars for breakfast (which contain 13 g of sugar when the recommended daily intake for children aged 4–6 years is 19 g). Mothers talked about unhealthy habits such as ‘constant snacking’ and say they opted for processed and convenience food particularly on busy days. One participant was happy for her children to ask for a Pot Noodle (Unilever UK, London, UK) as it meant less cooking for her. They talked about diets that do not include vegetables or fruit. These mothers accepted that their children do not like healthier options and preferred to give their children the food they ask for, suggesting that the control of the children’s diet lies largely with the children:
I’m quite happy. See if they come in and go, ‘Is there any Pot Noodles?’ I love that. Do you know what I mean? That’s quite a... ‘cause you’re like, ‘Yes, I’m no’ having to dae all different things,’ kinda thing, you know?
HSV19, claimant, GUS
I wouldnae say I was cooking the same kinda things, like ‘cause obviously we gie wur kids what they ask for really, tae be honest.
HSV36, no claim, community group
A host of issues make providing a healthy diet difficult for low-income mothers. Most commonly mothers described children who will eat only a very limited range of (usually unhealthy) foods. Mothers talked about making different meals for different family members, according to their tastes. There were cases of children’s diets that were so limited that they included just a handful of accepted foods. Sometimes mothers hint that their actions have played a part in their children’s limited diet. The mothers of children who ate a very limited range of foods did not appreciate the long-term effects of poor diet; rather, they were reassured that their children’s diet must be adequate because the children were energetic and rarely ill:
He’s a fussy eater. He’ll only eat noodles.
HSV12, claimant, community group
I mean, he’s never no’ well an’ he obviously takes enough in tae keep him healthy enough.
HSV24, claimant, GUS
Healthy eating was often understood as prohibitively expensive. Participants knew the prices of most items they bought and were able to make direct comparisons between healthy and unhealthy foods. They noted that many fruits were more expensive than unhealthy snacks and that fizzy drinks could be cheaper than bottled water. However, some mothers disagreed, believing instead that it was cheaper to cook meals from scratch. People were sometimes put off buying fresh fruit and vegetables on a very limited budget as they risked waste when food went off and did not get eaten. The time required to prepare and cook healthy meals could be in short supply in the context of busy lives. There was recognition from one mother that a healthier diet required more work:
It’s two fifty for a wee tub a’ strawberries. You go up the crisps aisle, there’s a big bag, of like, that size, huge, for two fifty. Like that, ‘oh, I’ll just get the crisps, then.’
HSV10, claimant, community group
I can get him oranges an’ he can go a coupla days eating them an’ then he can see them going off.
HSV09, claimant, community group
Time really, more than anything, it’s just time, if I’m kinda kept late at work, by the time I pick them up from nursery and after school it can sometimes be kinda quarter past six by the time we’re in the house and they’re starving.
HSV14, no claim, GUS
There was acknowledgment in the accounts of external barriers to providing a healthy diet. There were a couple of particularly health-conscious mothers who believed that school lunches got in the way of their efforts to provide healthy diets for their children. They felt that the Scottish Government’s policy of offering free school meals to children in primaries one, two and three was not something they could afford to reject, but they had misgivings about the nutritional value of the food provided. Some mothers felt that efforts to provide healthy diets were thwarted by the marketing of unhealthy food and drinks being targeted at children. The opinions and habits of other family members could get in the way of efforts to improve diets:
[Son’s name] gone to school and all I’m thinking is ‘I don’t want him to have them school dinners’, but those school dinners are free.
HSV29, claimant, GUS
I think there’s a lot more like, advertisements and things of eating like junk food and like all of that. Like, so it’s more sways the kids to, ‘I want sweeties’.
HSV34, claimant, community group
But I dae try, I try kinda maintain their teeth an’ stuff an’ cut their sugary kinda sweets an’ stuff doon. But it is hard, I mean they’ve got aunties an’ uncles an’ that gie’in them things an’ you’re thinking, ‘Whit’s the point?’
HSV36, no claim, community group
There is definite scope of health professionals to provide advice on healthy diets and women are open to receiving this advice. The need for advice about diet and nutrition, especially during weaning, was evident from some of the descriptions mothers gave about the challenges they faced in trying to provide a healthy diet. Mothers were sometimes aware that they lacked knowledge and mentioned in particular not knowing how to make a bottle or lacking knowledge about weaning. However, most mothers had not talked to health professionals about their children’s diet. Some participants mentioned that contact with a health visitor had taken place when their babies were exclusively drinking milk and therefore conversations about diet may have seemed irrelevant. There were examples of health visitors asking about children’s diet and their advice had been well received:
No’ really, no. Talk aboot healthy eating? Aye. No’ really, no.
HSV06, claimant, community group
So it was just straightforward like that wi’ my health visitor. There wasnae any food talk ‘cause it was when they were babies she got this form sorted an’ that for me an’ got my milk tokens sorted.
HSV07, claimant, community group
She asks what I’m eating, what I’m providing for [daughter’s name], what foods she eats. And if I tell her what she eats sometimes she can advise me, ‘Try this, try that.’ So they’re very supportive as well.
HSV11, claimant, community group
There were quite a number of cases in which participants had received advice about nutrition as a result of non-routine contact with health professionals:
I took part in a study when I was pregnant as well because I was overweight and I was pregnant, I took part in a separate study and I can remember them talking about the healthy eating and stuff.
HSV08, claimant, community group
We’re different because my daughter had the dairy allergy, we had the visits with the nutritionist in Edinburgh two or three times a year for the first couple of years when she was young, so, we got a lot of information there.
HSV15, no claim, GUS
Advice on nutrition was also received from professionals outside the health service:
I think it might have been last year, round at the local church they had like a eating well cooking group that was on for like 6 weeks. An’ like you were making your basic things, like quite a few of them I knew, but it was quite good ‘cause there was people that went that like had like no idea about making anything from scratch, everything came from a jar and things like that. So that was quite good, they were making different things from scratch. And making a spaghetti bolognaise and putting vegetables and things in it rather than mince and sauce and things like that. So stuff like that was quite good.
HSV37, no claim, community group
The HSVs are another way to provide a healthy diet. Mothers gave accounts of what they bought with the vouchers. Mothers who had babies and were not breastfeeding invariably used their vouchers to pay part of the cost of formula milk. Participants who did not need to buy formula milk were able to use their vouchers for fresh milk, fruit and vegetables. Fresh milk was viewed as an essential for most households and the vouchers were often used for milk, sometimes exclusively so. The majority of participants also used the vouchers for fruit and vegetables, and often specified that the fruit and vegetables were intended for their children rather than the mother or the family in general. Mothers also noted that they had scope to buy more expensive fruit, such as strawberries, which their children were keen on:
Now I’d get the milk for his cereal, ‘cause cereal he has in the morning, and at night-time before he goes to his bed. And I get bananas and apples and grapes.
HSV02, claimant, community group
Just basic fruits like apples can be really, really dear, you know? And you don’t want to live on bananas forever, it’s too much. It’s too much. And strawberries can be really expensive and, you know, kids love things like that.
HSV29, claimant, GUS
Vitamin use
Healthy Start voucher claimants receive a voucher, which they can swap for Healthy Start women’s vitamin tablets when they are pregnant or Healthy Start children’s drops, which can be added to drinks. The Department of Health recommends that all children aged 6 months to 5 years are given vitamin supplements containing vitamins A, C and D every day.
The vitamin component of the scheme is used less than the vouchers for milk, fruit and vegetables. The majority of HSV claimants did not redeem the vitamin voucher. In some instances mothers had exchanged the voucher for vitamins but had not used the vitamins:
I get it but I don’t even use them.
HSV10, claimant, community group
The interviews suggested that mothers were unconvinced about the need for vitamins, believing that children should get vitamins from their diet. Some had concerns about vitamins: one women believed that people who started using vitamins and then stopped using them may be more susceptible to illnesses, and another was against ‘pill-popping’. Another woman had not used the vitamin vouchers with her young child because she had not given her older children vitamins:
I never, ever got the free vitamins. I think it’s just because I never done it wi’ any of the older kids, you know?
HSV19, claimant, GUS
Mothers were confused about how the vitamin part of the scheme works; in particular, they were unclear about where they could redeem the vouchers. One mother had been told her local pharmacy no longer stocked HSV vitamins and another described feeling embarrassed when she tried to redeem her voucher for vitamins at her local chemist.
Overall understanding of how the vitamin component of the scheme works was poor, especially when compared with understanding of how the milk, fruit and vegetable component of the scheme works. One women thought that she had to choose between whether she used the vouchers for milk, fruit and vegetables, or for vitamins. One mother, who had been receiving HSVs for some time, had no awareness of the vitamin component of the scheme:
It’s the vitamins bit I don’t get. Know how at the top o’ them it says you could also collect your free vitamins? I don’t know where tae take that tae get the free vitamins.
HSV07, claimant, community group
I just thought I had to choose, basically, between whether I used it for my fruit, veg, and bread and milk, or... the vitamins.
HSV05, claimant, community group
Mothers who did use vitamins were convinced of the benefit to their children. Mothers who felt that their children were not getting an adequate intake or adequate quality of fruit and vegetables or calcium felt that vitamin supplements offered a back-up in terms of nutrition. There was recognition that vitamin intake would ideally be through diet but that this was not always achieved. The idea of taking vitamins specifically to support the immune system arose on a number of occasions. Children were given vitamin supplements to reduce their chances of becoming ill. Vitamin D was singled out as important because of its benefits to bone health and because of the likelihood of being vitamin D deficient living in Scotland:
I think that’s important ‘cause even if they don’t have access to fruit an’ veg or the children won’t eat anything that, things like that’s a good idea because, and especially like in Scotland, like there’s a one that I remember the health visitor saying to me, ‘Look, vitamin D, like because there’s like no sunshine.’
HSV37, no claim, community group
He does look quite pale and lethargic, and things like that. And I think if you’re not getting every other intake that I think you should be getting, then you’ll get the vitamins.
HSV02, claimant, community group
In spite of the amount of confusion about the need for vitamins and about how the vitamin component part of the scheme works, it was unusual for mothers to have discussed vitamin supplements with health professionals. The only instance of a health professional discussing vitamins was when a midwife flagged up the HSV vitamin voucher to a mother whose son was developing a bow leg:
One day when the midwives were coming to visit when I had my baby, they were like... ‘cause he was developing a bow leg, and then the health visitor, now she noticed that, she was like, ‘Oh, are you not giving him some vitamin supplements?’ And I’m like, ‘No, I’m not. I’m not.’ She was like, ‘Yeah, they should come with your coupons for Healthy Start vouchers.’ And I’m like, ‘I don’t know about those. That’s when she told me about it and everything.
HSV12, claimant, community group
Some of the mothers who gave their children vitamin supplements were motivated to do so as they took vitamins themselves or had taken them while pregnant:
I had already bought vitamins when I was pregnant. I had stocked up on them from when I first found out. It’s like one of the first things I done. ‘Cause I knew, it’s quite a long story, but when I used to live with my mum, our next door neighbour, her little boy had spina bifida and so I had awareness of that and knew that you need to take like the folic acid and stuff like that. So it was the first thing I done when I fell pregnant. Apart from go to the doctors, I went to Boots [The Boots Company Plc, Nottingham, UK] and stocked up.
HSV32, claimant, GUS
There was evidence that mothers who did not claim HSVs bought vitamins for their children, and cases in which mothers had continued to provide their children with vitamins after eligibility for HSV had ceased:
They got them for the first 2 years, I think. And I, back when I’m away, I’ll go into Tesco’s [Welwyn Garden City, UK] or Boots or something and get their own cheap brand vitamin, just wee chewy things.
HSV23, no claim, GUS
Motivations to feed babies
Mothers receive two vouchers a week (value £6.20) from the birth of their child until the child’s first birthday. Mothers who breastfeed can spend the vouchers on fresh milk, fruit and vegetables for themselves during this time. The interviews sought to explore mothers’ motivation for breastfeeding to understand whether the prospect of vouchers being freed up for use on fresh milk, fruit and vegetables, or the cost of formula milk more generally, would have any influence on motivation to breastfeed. No one mentioned the HSVs as influencing their decision to breastfeed.
That breastfeeding is free was mentioned as a primary motivating factor for a few women. More often it was mentioned as one of a number of factors. Mothers became very aware of the cost of formula feeding later on when they moved to formula feeding. Mothers tended to describe their baby’s health as the main motivating factor to breastfeed. They also mentioned bonding and convenience:
This sounds such a cliché – but I wanted to give him the best start and, obviously, all the things you hear, read, and are advised, is to breastfeed, so, I thought, ‘It’s my body. I can do it. Why can’t I? Why wouldn’t I?’ It’s also free.
HSV29, claimant, GUS
Mothers were clear that breastfeeding was hard, harder than they had expected. Some mothers decided to switch to formula feeding because of the difficulties they experienced breastfeeding. Some participants thought that they would have been able to deal better with the challenges of breastfeeding if they’d been aware of how difficult it could be:
Tears are coming to your face like, I’ll just give up, this is too hard. But if you knew somebody else felt like that, you would feel a bit better.
HSV38, no claim, community group
The majority of mothers were very open to the idea of breastfeeding. Some felt that they were not given the opportunity in hospital because it was assumed that they would formula feed. Others opted for formula because they were too tired or sore after the birth to attempt breastfeeding. One woman saw formula feeding as an opportunity for her partner to contribute. Some women had health problems that prevented them from breastfeeding, either because of the health problem itself or because of the medication they took. Mothers believed that support to initiate and maintain breastfeeding would lead to better breastfeeding outcomes. One mother thought that her attempt to breastfeed may have been successful if she had had more support, and another mother attributed her success at breastfeeding her second child to the support she received on that occasion:
I really had, really wanting to breastfeed and then, it kinda just got to a point, where it was like, the whole world’s against you and you’re like, ‘I’m not gonna be able to—’
HSV32, claimant, GUS
I tried. Aye, didnae really work, aye. Probably lasted aboot 3 days an’ then I was just too tired.
HSV06, claimant, community group
I do think it was a latching problem and that he just, he didn’t know how. So I think if I’d had someone explain that to me at the time, and show me properly how to do it. ‘Cause I didn’t really get shown in the hospital either. They were absolutely stowed out. I remember them just being so busy and so over worked and so I was kinda sorta left to my own devices.
HSV32, claimant, GUS
Although no one reported being motivated to breastfeed by the prospect of being able to spend HSVs on fresh milk, fruit and vegetables, those who did not breastfeed felt aggrieved at what they perceived to be an unfairness. This was particularly the case for those who were unable to breastfeed because of medical reasons because they felt that they did not have any choice:
I think it would’ve been fair if mothers had problems, health problems that’s stopping them from breastfeeding, to get more help. Because it’s not by choice. Like, with me, it wasn’t my choice to say, ‘I don’t want to breastfeed.’ It’s because I couldn’t breastfeed because of my health conditions. So it would be nice if they did that. It would be very helpful, very supportive, because tinned milk is very expensive.
HSV11, claimant, community group
The broader lives of low-income women
This aspect of the women’s lives is crucial to understand the constraints operating on the possibilities to offer a healthy diet. The accounts were a rich source of information on the context of how women on low incomes live. Living on a low income posed a range of challenges to mothers and was a source of significant worry for many. Mothers were perplexed about how they could pay their bills on their limited income and confused about how others appeared to be managing on benefits when they could not cover outgoings. There was limited knowledge of the use of services and support available to them. Women rarely mentioned seeking financial or benefit maximisation advice. Instead, resentment was expressed towards people receiving benefits and accounts given of problems with claiming benefits. Although they discussed their strategies of managing food budgets, again there was limited awareness and knowledge of foodbanks. Some aspects of their lives that were difficult to manage were not related directly to finances but were usually related to relationship issues. The women gave accounts of support networks they used, which tended to be family and friends rather than health professionals. The HSVs were included in these accounts as strategies for supporting their income.
Financial challenges were described as worsening because income remained fixed but the cost of living was rising. Food in particular was described as expensive. Those with babies commented on the price of formula milk and said that even though babies received two HSVs per week the cost of formula was still not covered. Those living in more remote areas talked about the premium they paid for food there:
Fruit and vegetables are awfully expensive here [Scottish island]. And milk.
HSV23, no claim, GUS
Low-income mothers described spending one third to one half of their income (after rent) on food, but despite this they still shopped frugally, often describing a weekly food budget of ≤ £50 for a family of three or four. They described economies made elsewhere to be able to allocate a large proportion of income on food:
I basically get £116 every Friday, and I maybe allocate about £60 of that for food.
HSV05, claimant, community group
In spite of the financial challenges described, very few mothers mentioned seeking financial or benefits maximisation advice from formal services. Those that did had benefited financially from the advice. Those who were not working and were in receipt of benefits talked about their discomfort claiming benefits and difficulties managing financially. Those who were working (or had a partner who was working) talked about feeling resentful towards people receiving HSVs and other benefits. They questioned whether or not they were better off:
Well, they seem better aff, if that makes sense (laughs)... And I’m oot at half seven in the morning till near enough half five at night, and they’re sitting cosy in their wee hoose.
HSV33, no claim, community group
Problems with benefits were usually related to changing circumstances such as a house move or a change in relationship status. In some cases this required a new claim to be made and the form filling involved was described as daunting. These changes in circumstances could lead to mothers being without any money for protracted periods of time:
It was domestic violence and that’s why, like, he’d got arrested and stuff. And I phoned them 2 days later to go on benefits ‘cause obviously he wasn’t coming back and I’d to go through all of that and explain all that... It took, say, about 3 or 4 weeks for my claim to be processed.
HSV08, claimant, community group
Strategies for economising on food bills included shopping in cheaper shops, setting food budgets, buying cheaper foods and meal planning. To provide nutritious food on a limited budget, participants bought food that was on offer or reduced because it was going ‘out of date’. To get the most from the food they had bought mothers employed a further range of strategies including cooking enough for multiple meals at one time, or making sauces rather than buying ready-made jars:
I’m like a calculator when I’m in my messages.
HSV07, claimant, community group
The jar sauces, you know, I don’t buy them because they’re really expensive and there’s no need when I can get a 50p carton of passata and a 30p tin of tomatoes and that, like I say, I can get a beautiful – I can make a beautiful sauce and that lasts four meals, four dinners.
HSV29, claimant, GUS
When asked about foodbanks most women were unaware of where their nearest foodbank was or how they could access foodbanks. The women who were recruited from the family centre talked about appreciating fresh produce that was donated there by supermarkets:
I don’t know an awful lot about the process, I think most families have to be referred by some kind of health professional.
HSV26, no claim, community group
Mothers were resourceful and strategic in their management of income to get by. They described budgeting, economising by stopping some outgoings or by seeking out the lowest prices and using coupons:
The bills, pay the bills first, and what I’ve got left, I’ve got left (laugh). It’s as simple as that, and I do my food shop off that. If I’ve got anything left over from that, good. If I’ve not, fine.
HSV10, claimant, community group
But I think you do have tae shop around for deals.
HSV40, claimant, community group
Healthy Start vouchers are incorporated into budgeting strategies with a range of approaches employed. Mothers who were buying formula milk invariably used their vouchers towards the significant cost of the milk. Those who were not buying formula most usually factored vouchers into weekly shopping. A few mothers kept vouchers at the ‘back of the purse’ for when they had no money, thereby also offering some peace of mind:
Nine times out o’ ten I just try an’ keep them until I run out my baby food, an’ just buy like fruit an’ veg an’ milk out my own money. ‘Cause that’s the dearest.
HSV01, claimant, community group
I do try to kinda keep them, keep a hold of them and use maybe two at a time, would be my max because obviously they are a great help when obviously you see the kinda total of your food bill being reduced at the end of the sale.
HSV05, claimant, community group
In addition to the challenges inherent in existing on a low income, participants faced many other significant challenges. Some had found themselves in more precarious financial situations after relationships had ended. Difficult break ups were described, with some mothers experiencing domestic violence. Participants talked about significant mental and physical health issues and struggling with children’s behavioural problems. In some cases mothers lacked support or assistance and their issues were magnified by the isolation they felt:
The father had left me so it was pretty... an’ I had two ones at primary school, so it was a pretty rough, intense time.
HSV24, claimant, GUS
Some participants talked about being supported by their families, who offered help with childcare and sometimes finances. Mothers who accessed the family centre that assisted with study recruitment were likely to describe being well supported by it. They often described being referred to the family centre in the first instance as a result of having faced particular challenges such as post-natal depression, problems with children’s behaviour or being unable to find affordable childcare. Other participants lacked support because they did not have a local family or friendship network:
I came in in my pyjamas, and he was in his pyjamas, and I just couldn’t see, like, a light at the end of this tunnel. And ever since I went into the post-natal group, I did think, like, I wasn’t post-natal at the start, but I did become depressed... Well, it’s just like I live here, I’m in here every day.
HSV02, claimant, community group
As mothers of young children, participants necessarily had contact with health professionals; however these relationships could be deficient. Although there were some descriptions of supportive relationships with health professionals, mothers often described feeling let down or ignored. Health visitors in particular were described as fleeting presences who were hard to access:
I go to the GP [general practitioner] first because it’s not really easy to get hold of the health visitors.
HSV03, no claim, community group
The first one was not good. I only saw her twice and that was it. She never came back again. That was like, ‘Oh, your baby’s doing fine. We only come when you need us.’
HSV12, claimant, community group
Summary
This qualitative research was designed to both complement the quantitative analysis and elicit women’s lived experiences and understanding of the HSV scheme. In doing so, the findings from the quantitative analysis can be situated through the experiences of women who use and do not use the HSV scheme. We sampled women in the same comparison groups used in the quantitative analysis (eligible and claiming, eligible and not claiming, and nearly eligible) and from two different time frames (those who currently use the scheme and those who used the scheme up to 5 years previously).
The rich accounts given by the participants gave rise to four key themes: knowledge, awareness, take up and use of the HSV scheme; opinions of the HSV scheme; the effect of HSVs on diet and feeding choices for their babies and children; and the broader lives of low-income women.
The HSV scheme’s aims were well understood and the scheme was valued by participants. They thought that the eligibility criteria should be widened because they had positive experiences and appreciated the scheme and the impact the vouchers had on their lives. For some mothers, it supported them to provide a healthy diet and the opportunity to give their children a range of fruit and vegetables. The HSVs were not mentioned in their decision-making around breastfeeding. Women’s choice to breast or formula feed was based on a range of other factors, such as support to breastfeed and assumptions and expectations of health professionals. The HSVs were incorporated into budgeting strategies and were seen as a good support in the context of the lives of low-income women.
The results of this qualitative analysis support some of the findings from the quantitative analysis.
Chapter 6 Health economics: the economic evaluation of Healthy Start vouchers as a natural experiment
Background and objective
The economic case for evaluating Healthy Start vouchers
Promoting a healthy lifestyle for pregnant women and children is a key public policy priority. 60 Poor maternal nutrition during pregnancy is associated with adverse birth outcomes61 and with the onset of chronic diseases such as heart and cardiovascular diseases,3,62,63 causing significant burdens to the healthcare sector and society. Also, maternal nutrition ultimately influences child nutrition, as bad eating habits developed during childhood might perpetuate in the adulthood.
In this regard, preventive public health interventions (PHIs) implemented on a large scale such as the HSV scheme have the potential to have a significant impact on maternal and neonatal outcomes and societal costs by promoting the healthy lifestyle of pregnant women and of children who are at risk of unhealthy lifestyles either during pregnancy or in early childhood. 64
Using a relatively small sample size (n = 336) a comparison of the HSV scheme and the WFS has shown the effectiveness of the HSV scheme on vitamin intake (VI). 26,27 However, a wider-scale evaluation of the cost-effectiveness of the HSV scheme is lacking. Providing a £3.10 per week voucher to > 173,000 children each year, the HSV scheme costs > £150M, thus representing a substantial cost for the UK health system. In this regard, a comprehensive assessment of the role of the HSV scheme could provide the decision-maker with robust evidence regarding cost-effectiveness of the HSV intervention.
The economic evaluation of the HSV scheme could contribute evidence regarding the incremental cost-effectiveness associated with an intervention directed towards improving the nutrition of pregnant women and of children by evaluating the benefits of the programme against potential costs and cost savings occurred. The research question addressed by the economic evaluation of the HSV scheme was ‘does the HSV programme generate benefits in terms of improved maternal and children health outcomes (vitamin intake; breastfeeding initiation and duration) and cost savings?’.
The economic evidence generated with the economic evaluation of the HSV scheme could contribute evidence regarding the value for money provided by the HSV scheme against alternative programmes, providing evidence on whether or not this intervention is able to change behaviour, ultimately generating improved health outcomes and cost savings.
Economic evaluation alongside the Healthy Start voucher scheme natural experiment
As the efficacy analysis, the economic evaluation of the HSV scheme was designed alongside a natural experiment. The non-randomised nature of the HSV study implied a threat for internal validity, thus posing several challenges to the design of the economic evaluation of the HSV scheme (e.g. the need to integrate the statistical designs and methodologies to deal with the selection bias arising from the absence of randomisation within an economic evaluation framework). However, existing guidance65–67 for designing, conducting and reporting economic evaluations is specific to the more commonly used RCT framework, and does not account for the challenges associated with non-randomisation and the identification of the true causal effect that are typical of the natural experiment design.
In addition, the HSV scheme is a preventive PHI encompassing multiple elements of complexity, such as a high degree of user involvement, multiple components, heterogeneous recipients, and multiple and complex goals and outcomes,68 which needed to be considered in the economic evaluation.
Failing to account for the specific challenges of designing and conducting the economic evaluation of a PHI alongside a natural experiment could lead to a biased estimation of the causal effect of the HSV scheme on costs and outcomes, thus lowering the quality of evidence on cost-effectiveness.
Considering this, the design of the economic evaluation of the HSV scheme required investigation of the specific challenges inherent to the design and conduct of economic evaluations of PHIs alongside NEs, as well as an assessment of the suitability of existing economic evaluation frameworks69 and methods66 for the economic evaluation of NEs. This ultimately led to the development of a novel comprehensive framework, tailored to address the specificities of PHI evaluations alongside NEs, as a key step for the design of the economic evaluation of the HSV scheme. Full details of the methodological framework have been published. 70
As described by Deidda et al.,72 the development of such a framework has been led by a targeted scoping review on evaluations and economic evaluations of NEs and PHIs71–75 alongside critical reviews of Consolidated Health Economic Evaluation Reporting Standards (CHEERS),65 Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)76 and Transparent Reporting of Evaluation with Nonrandomized Designs (TREND)77 reporting guidelines. These guidelines summarise a set of well-established best practices in economic evaluations alongside RCTs, evaluation of non-randomised PHIs and in observational studies, respectively.
Every item listed in the three guidelines was critically appraised in relation to its relevance to the economic evaluation of PHIs alongside NEs, also considering the methodological literature on NEs and PHIs identified through the scoping review71–75,78–80 and applied case studies of economic evaluation of PHIs in a non-randomised context. 81,82 Relevant items were selected and then grouped into 10 categories pertinent to the design and conduct of economic evaluations alongside NEs. As shown in Table 30, RCTs and NEs differed for most items, thus highlighting the need for the development of specific methodological guidance for conducting economic evaluations alongside NEs. Building on these 10 categories, a critical appraisal checklist was developed addressing specific requirements for designing and conducting economic evaluations alongside NEs.
| Item | Item differs between RCTs and NEs | Item is reported in the guideline | ||
|---|---|---|---|---|
| CHEERS | TREND | STROBE | ||
| Background/objectives | Yes | Yes | Yes | Yes |
| Target population | Yes | Yes | Yes | Yes |
| Sample size | Yes | No | Yes | Yes |
| Subgroup definition and analysis | Yes | Yes | Yes | Yes |
| Setting and location | Yes | Yes | Yes | Yes |
| Study perspective | Yes | Yes | No | No |
| Comparators | Yes | Yes | Yes | No |
| Time horizon/length of follow-up | Yes | Yes | Yes | Yes |
| Data sources/measurement | Yes | No | No | Yes |
| Choice of health outcomes | Yes | Yes | Yes | Yes |
| Measurement and valuation of preference-based outcomes | Yes | Yes | No | No |
| Estimating resources and costs | Yes | Yes | No | No |
| Currency, price, date and conversion | No | Yes | No | No |
| Analytical methods | Yes | Yes | Yes | Yes |
| Methods to address confounding | Yes | No | Yes | Yes |
| Variables (outcomes, exposure, predictors, potential confounders, effect modifiers) | Yes | No | No | Yes |
| Bias and methodology to correct bias | Yes | No | Yes | Yes |
| Missing data imputation methods | No | Yes | Yes | Yes |
| Study parameters | No | Yes | No | No |
| Incremental costs and outcomes | No | Yes | No | No |
| Characterising uncertainty | No | Yes | No | Yes |
| Characterising heterogeneity | No | Yes | Yes | Yes |
| Discount rate | No | Yes | No | No |
The framework has been used as a guidance to design the economic evaluation of the HSV scheme, as described in the following sections, and the checklist has been used as a critical appraisal tool (Appendix 3).
Methods
Data sources and measurement
In the HSV scheme study the GUS database, a representative sample of Scottish births, was linked with six administrative databases, allowing the identification of a wide range of health and social care resource uses and improvement in the number of cost items collected as well as the quality of collected data. GUS contains information on HSV scheme eligibility and uptake, age, income and a wide range of socioeconomic variables, spanning from the beginning of pregnancy to when the child was 10 months old. Furthermore, GUS data allowed for the implementation of the chosen statistical design to deal with the selection bias inherent to a non-randomised design, as well as the consideration of multiple comparison groups (as described in Chapter 2, Comparison Groups). Linking GUS data with the Child Health Systems Programme (CHSP), Scottish Morbidity Records General/Acute Inpatient and Day Case (SMR01) and Scottish Morbidity Records Maternity Inpatient and Day Case (SMR02), Management Information & Dental Accounting System (MIDAS), A&E and Scottish Immunisation & Recall System (SIRS) records also enabled us to recover detailed information on a wide range of additional healthcare resources used by the mother and the child, thus providing detailed information on the costs sustained during pregnancy and early childhood.
Comparators
In line with the efficacy analysis and following best practice to evaluate effectiveness73,83 and cost-effectiveness70 alongside NEs, several treatment–control groups were identified. The following comparisons were thus considered:
-
recipients versus eligible but not claiming (group 1 vs. group 2)
-
recipients versus eligible but not claiming (group 1 vs. group 2)
-
all eligible versus nearly eligible (group 1 and 2 combined vs. group 3).
In the remaining sections, group 1 (comparisons 1 and 2) and groups 1 and 2 (comparison 3) will be referred as ‘exposure groups’ whereas group 2 (comparison 1) and groups 3a and 3b (comparisons 2 and 3) will be referred as ‘control groups’.
Economic evaluation frameworks
The main economic evaluation framework was a CEA, combining costs to the NHS and social care with primary outcomes: BI, BD and VI. Results are reported in terms of the incremental cost per additional incremental outcome (unit of increase in BI, BD and VI) associated with the exposure versus control groups.
A secondary analysis combined the costs and cost savings associated with the exposure versus control groups with a broad set of effectiveness outcomes (e.g. height and weight, overweight/obese, fruit and vegetable intake) within a cost-consequence analysis (CCA) framework, considering a 3-year time horizon.
An additional cost analysis examined whether or not any significant differences between exposure versus control groups in terms of longer-term costs existed, considering a 6-year time horizon.
Study perspective
The base-case analysis was undertaken from the perspective of the NHS and Personal Social Services (PSS), meaning that the costs relevant to the economic analysis are those incurred by the national health and social services authority (e.g. hospitalisation costs related to pregnancy, delivery and the newborn; healthcare services utilisation related to the child). In the sensitivity analysis, the societal perspective was also incorporated, adding a broader set of costs, including breastfeeding support groups, parentcraft classes and child care.
Time horizon
The time horizon for the economic evaluation was determined by the main outcome, as well as the availability of secondary data, as the GUS survey took place when children were 10 months (sweep 1) and 3 years old (sweep 2). The primary economic evaluation, in the form of a CEA, assessed the cost per primary outcome (BI, BD and VI) using a time horizon spanning from the beginning of pregnancy until the child was 10 months old. Given the absence of any short-term effects of the HSV scheme on the main outcomes, a long-term model extrapolating short-term results into longer-term costs and outcomes will not be developed. However, a secondary CCA considering costs and outcomes arising over a 3-year time horizon assessed any differences between comparison groups in terms of longer-term outcomes (e.g. height and weight; overweight/obese; fruit and vegetable intake) and costs. Furthermore, a cost-analysis considering a 6-year time horizon was performed.
Outcome measures
Outcomes used in the cost-effectiveness analysis
In line with the efficacy analysis, and considering the main aim of the HSV scheme (i.e. improving nutrition for mothers and children), the main primary outcome measures used in the economic evaluation were BI, BD and VI. Incremental mean outcomes between treatment groups were estimated for all the three comparison groups, with adjustment for baseline covariates, using non-linear models to account for the non-normality of outcomes.
Outcomes used for the cost–consequences analysis
In consideration of the array of health and non-health benefits associated with the HSV scheme, a CCA was also performed. CCAs are recommended frameworks for complex PHIs, in which all the benefits of the intervention might not be captured by a single outcome measure. 84–86 The CCA shows in a descriptive table the costs and cost savings alongside primary (BI, BD and VI) and GUS secondary outcomes (birthweight, morbidity) listed in Table 4 associated with intervention and comparison groups, for the three comparisons described in Chapter 2, Comparison Groups, considering a 3-year time horizon.
Estimating resources and costs
Cost of the Healthy Start voucher
The HSVs are transfer payments with no net cost to society incurred through transferring the grant from government to individuals, apart from administrative costs. 87 Therefore, this was not included in the economic evaluation. However, a sensitivity analysis including the overall costs of £3.10 per week of HSV transfer payments is recommended. Also, as the administrative cost of running the programme was not available, the resulting downward bias needs to be taken into account in the interpretation of results.
Resource-use data collection
The base-case analysis was undertaken from the perspective of the NHS and PSS, meaning that the costs relevant to the economic analysis were those incurred by the national health and social services authority. In a sensitivity analysis, the societal perspective was also incorporated, adding a broader set of costs including breastfeeding support groups, parentcraft and child care. A further sensitivity analysis included the HSV transfer payment in the total cost.
Resource-use data were derived from secondary data sources, including GUS and several sources of administrative data. Further details of these are presented in Appendix 4:
-
Hospital records (SMR01) providing information on child admission and discharge dates, specialty/discipline of admission, patient category, admission type and reason, and whether or not it was an emergency/acute admission.
-
Birth records (SMR02) providing information on patient maternity admission and discharge dates, specialty/discipline (obstetrics, midwifery), patient category, admission type and reason, and whether or not it was an emergency/acute admission.
-
Accident and emergency attendance providing information on A&E admission and discharge dates, arrival mode, diagnoses, investigation type, procedure and triage category.
-
Immunisation records (SIRS) providing dates and type of vaccines.
-
Health visitor reports (CHSP) providing information about child health visitor first visits and reviews, and hearing and orthoptist screenings.
-
Dental inspection (MIDAS), providing details on the type and number of dental treatment.
Linking GUS with the above sources of administrative data enabled the identification of a wide range of health and social care resource-use data related to the mother’s pregnancy and to the child:
-
Hospitalisation costs during pregnancy and delivery (CHM) such as antenatal check-ups, number of days spent by the mother in the hospital, costs directly related to delivery (e.g. type of delivery, usage of methods to relieve the pain).
-
Hospitalisation costs related to the newborn (CHNB) (e.g. admission to special care).
-
Healthcare services utilisation related to the child (CHC). This included contacts with general practitioners and nurses, and health-related appointments (e.g. immunisation, dental inspection) and overnight hospital stays.
-
Costs related to the usage of social services (CSoc), such as parentcraft classes that were provided to new mothers to help with infant feeding/breastfeeding (e.g. surestart, start4life, advice provided by nurses or midwives), antenatal classes, helping services (e.g. link website/telephone line, parentline scotland, childsmile).
-
Personal cost (CP) (e.g. child care).
Equation 1 illustrates the two main resource categories of total cost in the reference base-case analysis from an NHS/PSS perspective: (CTot); hospitalisation costs during pregnancy and delivery (CHM); hospitalisation costs related to the new born (CHNB); costs related to the usage of social services (CSoc):
Societal total cost (SCTot) (Equation 2) adds the personal costs to CTot:
Equation 3 illustrates the components of total cost in the sensitivity analysis when the cost of the intervention is added to CTot:
In some instances, usage of certain resources was reported as a yes/no response (e.g. participation to antenatal classes). In this case, a decision rule was applied consistently in the exposure and control groups (e.g. women reporting participation to ‘some’ antenatal classes have been considered as participating to half of the classes).
A list of resources used, alongside with unit costs and decision rules has been provided in Appendix 4.
The estimated cost of resources used was derived through a bottom-up exercise.
Valuation of resource use: unit costs
The cost for each individual (child or mother) was calculated by multiplying their use of health care and social care resources by the associated unit costs. When unit cost data associated to specific resource use were not available, the decision rule of using the most frequently used service was applied (e.g. the generic cost of parentcraft has been used to cost the Triple P Positive Parenting Program and parenting classes organised by the charity Mellow Parenting).
Cost information was collected from UK routine sources such as NHS Reference Costs,88 the British National Formulary89 and Unit Costs of Health and Social Care. 90
Appendix 4 outlines the unit cost for all resources identified in the study.
Economic evaluation analysis methods
In a non-randomised design, the effect of the treatment on outcomes and costs may be confounded with systematic differences in individual characteristics between treated and untreated subjects. 80 For this reason, it was necessary to adjust for the observed confounding arising from non-randomisation. In line with the efficacy analysis, we used PSM. The idea behind PSM is to match treated and non-treated individuals on the basis of some observable characteristics. If this is done correctly, the true effect of the treatment is identified, so that any difference between treated and non-treated individuals can be attributable to the intervention. PSM was incorporated in a cost-effectiveness framework, following available literature guidance. 80,91
Designing and conducting economic evaluations alongside NEs encompasses challenges related to non-randomisation, including identifying a control group that best approximates an ideal randomised experiment and using multiple statistical designs and control groups to examine the sensitivity of the economic evaluations to multiple sources of bias. In addition to these challenges, common to the efficacy analysis, the complex data structure inherent to the CEA implies additional challenges, such as skewed outcomes, cost data and correlated outcomes.
In the economic evaluation of the HSV scheme two PSM methods were used to adjust for the bias arising from observed confounding. These were integrated into the CEA framework and applied to all comparison groups:
-
Regression adjusted matching, in which the CEA is performed on a sample matched with propensity score. 80 In the first step, PSM was performed. In line with the efficacy analysis, matching with replacement is used in order to account for the fact that the number of controls was lower than the number of treated individuals. After matching, a parametric regression approach was applied to the matched sample, using frequency weights generated from the matching as frequency weights in the regression. Compared with PSM alone, this method has been demonstrated to be more efficient, reducing the sensitivity of the estimated average treatment effect (ATE) to the outcome and cost model. 91
-
Weighted regression, in which cost and outcome regression models are weighted by inverse probability treatment (IPT) weights. This method combines the advantages of inverse probability of treatment weighting (IPTW) (e.g. keeping the sample size while guaranteeing balancing), with those of regression adjustment (i.e. controlling for residual imbalance by covariate adjustment). Extreme weights, which can potentially hinder the reliability of IPTW, were explored.
These methods accounted for the non-linear relationships between covariates and end points, as well as skewness and heavy tails associated with cost data. The joint uncertainty in the estimates of incremental cost-effectiveness was recognised with a non-parametric bootstrap.
As these methods relied on the assumption of no unobserved confounding, Rosembaum bounds could be used to check the sensitivity of the estimated results to the bias that might arise as a consequence of unobserved variables affecting assignment into treatment, outcomes and cost variables. 92,93
Outcomes were analysed using non-linear parametric models, specifically logit (BI and VI) and survival models (BD). Considering that cost data are typically right skewed with a long heavy tail, costs were analysed using generalised linear models. 94 The modified Park test was conducted to choose the best family, whereas a battery of tests (Pearson correlation tests, Pregibon Link test and Modified Hosmer and Lemeshow test) was used to guide the choice of the best link function. All analyses were performed using Stata® (StataCorp LP, College Station, TX, USA) version 16.
Comparisons
As described in Chapter 6, Methods, Comparators, three incremental comparisons were conducted: (1) exposed (group 1) versus eligible but not exposed (group 2), (2) exposed (group 1) versus nearly eligible (groups 3a and 3b) and (3) eligible (groups 1 and 2) versus nearly eligible (groups 3a and 3b).
In the CEA analysis the cost-effectiveness of group 1 versus group 2, group 1 versus groups 3a and 3b, and groups 1 and 2 versus groups 3a and 3b was evaluated by comparing the costs and outcomes (BI, BD and VI) incurred in group 1 versus those incurred in group 2, group 1 versus those incurred in groups 3a and 3b, and groups 1 and 2 versus those incurred in groups 3a and 3b, considering a 10-month time horizon. The incremental cost-effectiveness ratio (ICER), defined as the ratio between the incremental cost and the incremental outcome, was calculated for the comparisons (1), (2) and (3), providing an estimate of the additional cost per additional unit of outcome (BI, BD and VI) generated by the HSV scheme. ICERs calculated for the three comparison groups are plotted in the cost-effectiveness plane.
Handling missing cost and outcome data
Following best practice,95 a thorough analysis was performed to assess the extent of missingness, as well as the missing data mechanism. The 5% threshold rule of thumb suggested that complete-case analysis results were reliable only if the percentage of missing data was below the 5% threshold. 96
In addition to missing data quantity, the mechanism of missing data97 (i.e. missing completely at random, covariate-dependent missing at random, missing at random and missing not at random) will be explored thoroughly. Multiple imputation procedures using chained equations were used to impute missing follow-up data separately for intervention and control groups for all the three comparisons. 98 Predictive mean matching was used to deal with non-normality of cost and outcome data. 95 Multiple imputations were performed in Stata 16 using the programme ‘mi impute chained’.
Adjustment of timing of costs and benefits
Allowance for differential timing of costs was made using the recommended discount rate for economic evaluation of PHIs, namely 1.5% (National Institute for Health and Care Excellence Methods Guidance99). All costs were estimated for the baseline year 2010.
Each type of resource use relative to the mother and the child was valued using relevant unit costs. Mothers’ and children’s costs were thus aggregated, providing an estimate of the total cost per participant. All partial costs sustained within the 10-month period (i.e. pregnancy-related costs; children’s hospitalisation costs) were aggregated to estimate total cost per participant within each group, and the mean cost per participant per group. The difference in average costs (and significance) between the three comparison groups was estimated using regression techniques (section 2.7).
Resource-use quantities and mean participant cost values are reported separately to increase transparency, as per standard economic evaluation guidance. 100
Reporting and presenting of within-trial economic evaluation results
Study parameters
Key study parameters (e.g. unit costs) as well as summary statistics for the primary economic evaluation outcomes (BI, BD and VI) scores and resource use at baseline and follow-ups are planned.
Incremental cost and outcomes
Results are presented in terms of mean outcome, mean cost and ICER for the three comparison groups. The 1000 incremental cost-outcome pairs generated by the probabilistic sensitivity analysis are then represented graphically in a cost-effectiveness plane and translated into cost-effectiveness acceptability curves indicating the likelihood that results fall below any given cost-effectiveness ceiling ratio.
Characterising uncertainty
A sensitivity analysis (including probabilistic sensitivity analysis) was used to explore and quantify uncertainty in the cost-effectiveness results. A probabilistic sensitivity analysis was performed to quantify the joint effect of uncertainty around the costs and outcomes. 101 Bootstrapping was used to estimate the probability that each intervention was cost-effective for a range of cost-effectiveness threshold values. In bootstrapping, the trial data were sampled with replacements 1000 times, thus generating 1000 incremental costs, incremental outcomes and ICERs, which provided an empirical estimate of the CIs around mean incremental costs and outcomes. In addition to a probabilistic sensitivity analysis, several scenarios were explored in the deterministic sensitivity analysis, including the inclusion of a broader range of costs, considering a societal perspective, and an inclusion of the cost of HSV (transfer payment).
Chapter 7 Discussion
Having a good start in life during pregnancy and infancy has been shown to be important for living both a healthy life and a longer life. 1,9,62 The First 1000 days initiative started in 2010 and focused on global child undernutrition. 7 It has now influenced health policy in high-income countries including the UK. 8 The idea is that the first 1000 days from conception to age 2 years is a period of rapid growth and what happens during this time lays the foundations for future health and development. There is a willingness to invest in policies with the aim of improving early-years experiences,10–12 but as there have been few outcome evaluations of such policies, evidence of their effectiveness is limited. We used a mixed-methods design and evaluated the HSV scheme as a natural experiment to understand the impact of the vouchers on maternal and child health. A qualitative interview study was embedded in the design and we established methods to undertake a health economic evaluation alongside a natural experiment, using observational data.
In this chapter we discuss the main findings of the evaluation and their implications for future research in five sections: (1) impact on child health, (2) impact on maternal health, (3) understanding women’s experiences of the HSV scheme, (4) integration of the qualitative and quantitative findings, and (5) applying and developing methods. We also present the strengths and limitations of the study. The health economic evaluation is currently ongoing and will result in a further submission to a peer reviewed journal.
It is important to examine the health outcomes of a policy and not just examine the implementation or conduct a process evaluation. 22 We used a range of health outcomes to examine the effects of the HSV scheme on both maternal and child health. We reported all results, regardless of significance. This provided a comprehensive evaluation of the HSV scheme across the range of outcomes. Previous evaluations of the HSV scheme were partial evaluations of the implementation,28,30 its acceptability for women28 and how the voucher system worked for retailers,30 and a qualitative evaluation to understand the perspectives and experiences of women who use the HSV scheme. 30 Previous studies to determine the effect of the HSV on outcomes have been limited by small sample size26,27 or limited to a few outcomes. 29
As there were two control groups, giving rise to three comparisons, pre-analysis, we specified that the primary analysis would be the PSM analysis comparing recipients with those who were eligible but not claiming. The other comparisons provided strength of evidence for the effect of HSV on the outcomes. The comparison of all eligible with nearly eligible provided an ITT analysis and gave information about how the policy was working in practice. This evaluation of HSV as currently implemented demonstrated good external validity and generalisability of the results. Previous studies have shown that take-up of the HSV scheme is not optimal and have recommended strategies to improve take-up of the HSV scheme for all eligible women. 102 This means our ITT results provided an underestimation of the possible effect of the HSV scheme if take-up was maximised.
The next sections summarise the results against the study objectives and are structured according to (1) child health, which concerned the effectiveness of the HSV on breastfeeding (objective 1) and other child health outcomes (objective 2) and how these compare in the two study populations (objective 3); (2) maternal health, which concerned the effectiveness of the HSV scheme on vitamin use (objective 1) and other maternal health outcomes (objective 2) and how these compare in the two study populations (objective 3); and (3) understanding women’s experiences of the HSV scheme, which establishes voucher usage and determines the reasons for uptake and non-uptake of the HSV scheme (objective 4).
Impact on child health
Most of the child outcomes were available in both GUS and IFS. For the main comparison group (group 1 vs. group 2) for the primary outcome of ever breastfed and duration of breastfeeding, there were differences between the propensity score results from GUS and IFS, with the IFS indicating a negative effect of the HSV scheme on breastfeeding. For all the secondary outcomes, birthweight, low birthweight, prematurity and age starting solid foods, the results indicated that there was no effect of the HSV scheme on the outcomes.
When using the other comparison groups, for birthweight and low birthweight the effect sizes and significance varied across the data sets and methods, indicating less confidence in the results of the HSV scheme on birthweight. For premature births and age at introduction of solid foods, there was more consistency across the data sets and evaluation methods, indicating some confidence in the results.
Previous studies that examined outcomes of the HSV scheme did not examine the range of birth and child outcomes, but instead compared fruit and vegetable intake and found that fruit and vegetable intake did not differ between HSV recipients and non-recipients. 29 Another programme that provides universal multisectoral health promotion interventions during pregnancy and early childhood was found to produce positive effects and was cost effective for birth outcomes. 17
Impact on maternal health
There were high rates of vitamin use during pregnancy across all groups in both data sets (group 1, 82%; group 2, 86%; and group 3, 88% in GUS, and group 1, 89%; group 2, 85%; group 3, 88% in IFS). For the main comparison of group 1 versus group 2, only the primary outcomes of vitamin use pre and during pregnancy were available in both GUS and IFS. The results indicated that there was no effect of HSVs on the outcomes. There were differences between propensity score results from GUS and IFS, with the IFS indicating a positive effect of HSVs on vitamin use. There were differences between propensity score and RD results from GUS, with the RD results indicating a negative effect of HSVs on vitamin use.
Previous studies that examined outcomes for the HSV scheme were smaller than this evaluation. They compared HSV recipients to WFS recipients and found higher daily intakes of iron, calcium, folate and vitamin C for HSV recipients than for WFS recipients. 26 Three months postpartum, the HSV mothers again reported higher iron, calcium, folate and vitamin C intake than WFS recipients, as well as a higher consumption of fruit and vegetables. 27
Further details on health outcomes, health behaviours and financial difficulties of the mothers were available in the GUS data set. For health during pregnancy, alcohol use and household managing financially, there was no effect of HSVs across all the comparison groups. There were slight differences in the mother’s current health as assessed by the SF-12 (physical and mental health domains) when group 2 was used as the control group. For smoking there were no differences for the primary comparison comparing group 1 with group 2, but there were large differences when group 2 was used as the control group. This finding is concerning as it could represent an unintended consequence of HSVs. The HSV scheme provides an opportunity to intervene for mothers with low incomes. The HSV scheme is a nutritional programme but is meant to encompass other aspects of health promotion. A report on the status of the HSV scheme 10 years after its implementation recommended that a package of health promotion measures should be incorporated into the scheme to provide this additional support for mothers and their children. 102
Understanding women’s experiences of the Healthy Start voucher scheme
The rich accounts given by the participants gave rise to four key themes: knowledge, awareness, take-up and use of HSVs; opinions of HSVs; the effect of HSVs on diet and feeding choices for babies and children; and the lives of low-income women.
The HSV scheme aims were well understood and the scheme was valued by participants. Participants had some opinions about the eligibility criteria (mainly to widen access) as they had positive experiences and appreciated the scheme and the impact that the vouchers had on their lives, supporting them to provide a healthy diet and the opportunity to give their children a range of fruit and vegetables. The HSVs were not mentioned in the decision-making around breastfeeding. Women’s choice to breast or formula feed was based on a range of other factors, such as support to breastfeed and assumptions and expectations of health professionals. The HSVs were incorporated into budgeting strategies and were seen as a good support in the context of the lives of low-income women.
A recent report on the development and planned purpose of the HSV scheme undertook a review of how the policy works in practice. 102 Their findings were similar to our study in that uptake could be low during pregnancy; the beneficiaries were not provided with consistent information on how to use the food vouchers or the importance of taking vitamins pre pregnancy, or with support to breastfeed. The report recommended including a package of information to be sent with the vouchers.
Integration of the qualitative and quantitative findings
A key feature of the mixed-methods approach is the ability to integrate the findings between the quantitative and qualitative studies. The accounts of the women in the qualitative study can be used to inform the findings from the quantitative study. There are a number of reasons that the quantitative analysis was inconclusive, and the qualitative study offered rich data on five themes that could help explain this:
1. Women were not using the vouchers during pregnancy
Often participants were not made aware of HSVs until their baby was born, meaning they had missed out on months of claiming (‘Since I was eligible to, when my son was born’, HSV02). Mothers were not routinely learning about HSVs from their midwives during pregnancy. Some were told about the scheme by midwives but others were informed about the scheme by general practitioners or health visitors (after the baby was born). And others learn about HSVs through a variety of ad hoc routes: information packs in the waiting room at antenatal clinics, a homelessness support worker, conversations with friends or family, a benefits maximisation service, online while investigating benefit entitlement or a poster in a shop. The lack of voucher use during pregnancy may explain the inconclusive impact of HSVs on birth outcomes (birthweight, low birthweight and prematurity).
2. The opportunity for health professionals to discuss nutrition was not utilised
There was little evidence of discussions with health professionals about nutrition. (‘No’ really, no. Talk aboot healthy eating? Aye. No’ really, no,’ HSV06). When there was discussion, it came at the wrong point in the child’s life. Mothers mentioned that contact with a health visitor had taken place when their babies were exclusively drinking milk and therefore conversations about diet may have seemed irrelevant (‘There wasnae any food talk ‘cause it was when they were babies she got this form sorted an’ that for me an’ got my milk tokens sorted,’ HSV07). However, the few examples of health visitors asking about children’s diet and the advice they had given were well received (She asks what I’m eating, what I’m providing for Hayley, what foods she eats. And if I tell her what she eats sometimes she can advise me, ‘Try this, try that’. So they’re very supportive as well’, HSV11). This may explain the finding that there were no differences across the comparisons for age at introduction of solid food.
3. The vitamin component of the scheme was not used
The vitamin component of the scheme was used less than the vouchers for milk fruit and vegetables. There is evidence that people were confused about the need for vitamins (‘I think, to be honest, I think unless you have a really, really poor diet, I think it’s a bit of a con’, HSV25). There was also confusion about how the voucher part of the scheme works (‘I just thought I had to choose, basically, between whether I used it for my fruit, veg, and bread and milk, or... the vitamins’, HSV05). In particular, there was confusion regarding where vitamin vouchers could be redeemed (‘It’s the vitamins bit I don’t get. Know how at the top o’ them it says you could also collect your free vitamins? I don’t know where tae take that tae get the free vitamins’, HSV07). This confusion around vitamins contrasts with a clear sense, for claimants, of how the milk and fruit and veg voucher operated. This may explain the lack of differences between exposed and control groups on vitamin use in pregnancy, in which we expected vitamin use to be higher for those using the HSVs than those not using them.
4. The broader lives of low-income women
Living on a low income poses a range of challenges to mothers. Mothers were perplexed about how they could pay their bills on their limited income (‘It’s very hard (small laugh). It’s very expensive for everything, electricity or gas bill and food’, HSV39). Women rarely referred to seeking financial or benefit maximisation advice, indicating that they had limited knowledge of the use of services and support available to them. One mother who had used the service said, ‘[t]hey effectively just took some information, said, “We’d need to check online,” and send me out some information and they just sent me out screeds of stuff that I didn’t understand’ (HSV35). This aspect of lives of low-income women is crucial to understand the constraints operating on the possibilities of offering a healthy diet, and therefore mitigates any potential impact of the HSV on child and maternal health outcomes.
5. The monetary value of the voucher is low, yet it is also hugely valued
The monetary value of HSVs (during this study) was £3.10 per week. Participants described this as being too low to make a difference:
If it’s hitting that mark, I would be surprised. Three pound ten a week to me? No. I don’t think so. I don’t think that touches this. And I think the people who genuinely need it most, and who need that education about health and nutrition and everything else, I don’t think that three pound ten... scratch the surface if I’m honest.
HSV25
In addition, food was often considered expensive, particularly in rural areas (‘Fruit and vegetables are awfully expensive here. And milk’, HSV23). However, vouchers were hugely valued (‘They’re precious tae me’, HSV01). This theme of low monetary value is likely to be the main reason for inconclusive results of the quantitative data analysis. It is costly to provide a healthy diet and the monetary value of the HSVs did little to support access to such a diet. It is unrealistic to expect such a small sum of £3.10 per week (£6.20 in the first year of infant life) to make a difference in the child and maternal health outcomes we had available in our data.
There is scope for the HSV scheme to be improved if each of the above themes was addressed. Previous research also noted that the vouchers were not used optimally in pregnancy and that uptake of the vitamin component could be improved. 30 The monetary value has recently been increased from £3.10 per week (£6.20 in the first year of life) to £4.25 (£8.50 in the first year of life) per week. 103 But this increase was the first increase since 2006; it still represents a small increase and the impact on maternal and child health outcomes could remain limited. There could be real value in increasing the support offered by health professionals through the HSV scheme. In the US, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides a range of additional services and benefits for low-income mothers and their infants. These services comprise: supplemental foods, healthcare referrals, and nutrition education for low-income pregnant, breastfeeding, and non-breastfeeding postpartum women. 104 Although similar to the HSV scheme, it offers much more in terms of health professional support and has been shown to improve a range of birth outcomes, including an increase in birthweight and length of gestation and a decrease in the probability of low birthweight, prematurity and admission to a neonatal intensive care unit. 105 It should be noted that the context of WIC in the US will be different to the UK context and therefore research should be undertaken to understand how the transferability of such a programme to the UK may lead to improved outcomes for UK infants and children.
Applying and developing methods
Policy evaluation using existing data
This study represents an example of a policy evaluation taking a natural experiment approach. The evaluation used existing data at the individual level, not aggregations, to understand the impact of the HSV scheme on health outcomes. An advantage of using existing data means that policy that is already implemented can be evaluated. Once a policy is in place it is not possible to undertake baseline primary data collection. It is not possible to undertake a randomised study in which women would be randomly allocated to receive HSVs or not, as this policy is currently in place and it would be unethical to withhold HSVs from a potential control group.
Developing a framework to undertake economic evaluation alongside a natural experiment
As part of this study, we outlined the need for guidance for conducting an economic evaluation alongside a natural experiment. The framework70 identified best practice in the context of the challenges of NEs over RCT designs; for example, selection bias inherent to the design and reliance on existing data sources means that the economist is unable to design the data collection to include utility-based outcomes. The framework proposed new reporting guidelines as CHEERS69 did not incorporate all necessary items. This framework is available for other researchers to use when conducting economic evaluations alongside natural experiment evaluations of many different policies.
Challenges, limitations and strengths of the study
This study used a mixed-methods approach to understand the effectiveness of the HSV scheme: a quantitative analysis of existing data sets, a qualitative study of mothers’ experiences of the HSV and the development of methods to undertake a health economic evaluation to assess cost-effectiveness. The results should be read in the context of the challenges, limitations and strengths of the study.
Challenges
The guidelines for conducting NEs32 state that multiple sources of data and multiple design or analysis methods should be used. The use of these multiple methods and data sources means that any bias inherent in one can be addressed by using a different method or data source. When a policy is already in place, it is not possible to undertake baseline data collection. When that policy is national, therefore covering the whole population, it is not possible to use a control group that is not subject to the policy. This poses a challenge as any control group will necessarily be different from the exposed group. This lack of an obvious control group was recognised in previous process evaluations of the HSV scheme. 33
We were able to find two existing data sets that identified the exposed group of claiming HSVs: GUS, birth cohort 2, and the IFS. Both of these data sources had questions on eligibility for the HSVs and we were able to use the group of women who were eligible but not claiming HSVs as one control group. The other control group was women who were nearly eligible for HSVs but just missed out owing to having a higher income. A further challenge of using existing data sets was that the data not only had to identify exposed and control groups, but also collect measures relating to nutrition for mothers and children. We had to rely on the measures collected in these existing data sets. Although the study addressed nutrition outcomes we were not able to measure dietary intake for mothers and their children.
Limitations
There are several limitations of this study, mainly related to the quantitative study. The scope of the study was to understand and measure the effectiveness of the aims of the HSVs. One of the aims was to improve the nutrition of the pregnant women. As we used existing data sets we were unable to measure dietary intake of mothers and their children. Instead, we had to use the measures that were available in the data: vitamin use and breastfeeding rates. These measures were chosen as they related to wider aims of the HSV scheme (to initiate and maintain breastfeeding). For vitamin use the questions asked did not include the dose of vitamin D, only if the mother took vitamin D.
We used PSM to account for the fact that mothers were not randomly assigned to these exposed or control groups. However, PSM is a strong method as it can mimic a RCT by ensuring that the groups will be similar on the observed baseline characteristics. PSM is a technique that can therefore minimise selection bias and is better at approximating the causal effect of the policy than simple covariate adjustment in regression models. The limitation of propensity scores is that although PSM improves balance on the measured confounders, it does not necessarily guarantee balance on the unmeasured confounders. It can only balance on the unmeasured confounders in as far as the these are related to the covariates used in the propensity score model. 106,107 We used a range of confounders in the PSM and while these did offer good balance (see Appendix 1), the extent of unmeasured confounding in the analysis remains unknown. While we strived to make the groups comparable, the comparison group of group 3 obviously differed in respect of income compared with those in group 1.
Regression discontinuity is a population-based method for detecting the effects of policy change or intervention on measures considered as the primary or secondary outcomes. For this analysis, some of the assumptions were not met. The choice of forcing variable is important for a RD analysis. The income variable in GUS was not continuous but categorical. Therefore, we transformed it to make it more like a continuous variable. As the entitlement of HSVs does not depend on a single measure, equivalised household income was used as the forcing variable. It was noted that the income categories, not the equivalised household incomes, had been used for the group selections, thus avoiding the situation in which the same variable had been used on both axes. The magnitudes of discontinuity at the income threshold of £16,190 [log10(16,190) = 4.21] were used as population measures for the treatment effects. In the plots (see Figures 3 and 4), the discontinuity is seen but the trends either side of the cut-off are not smooth. Over-fitting a trend line to such data can lead to a ‘false’ discontinuity. We therefore downgraded the evidence from the RD analysis.
The identification of those belonging to group 3 was not straightforward in either GUS or IFS. In GUS, the income variable was used to determine those women who were nearly eligible for HSVs, but missed out owing to their income being out of the criteria for HSV eligibility. The criterion (in 2010) was an annual income < £16,160 per year. We identified those mothers in GUS who were not claiming HSVs, were not claiming the other means-tested benefits and had an income between £15,600 and £20,799 per year owing to the income bandings available in GUS. In IFS, there was no income variable and therefore we used an area deprivation measure to determine those in group 3. Women who were not claiming HSVs and living in one of the 40% most deprived areas (IMD, SIMD, WIMD quintiles 1 and 2) were categorised as being in group 3 in IFS. This was problematic as not all people of low income live in areas of high deprivation: they could be living in areas of lower deprivation. In addition, not all people who live in areas of high deprivation have low incomes. 108 Therefore, there was misclassification in group 3. We used PSM to overcome some of this confounding. Despite this limitation, from the plots (see Appendix 1), the matching of the groups seems to have been of high quality.
Strengths
Despite the challenges of identifying multiple data sources and multiple control groups and of using multiple methods, we were able to do all three in this evaluation. The use of multiple control groups gave rise to multiple comparisons of the exposed and control groups. This allowed for a detailed examination of the effect of the HSV scheme on maternal and child health outcomes, which gives added strength to the findings. If we had found strong effects, in the same direction and of similar magnitude across all comparison groups and in both data sets, we would have had greater confidence in the results. As effects were not always in the same direction, of the same magnitude or of similar statistical significance across all comparison groups and data sets, the effect of HSV on outcomes was inconclusive.
We were able to undertake complex data linkages between GUS cohort 2 and routine NHS data in Scotland. We linked GUS to seven routinely collected data sources. These include hospitalisations (SMR01) for both mother and child, birth records (SMR02), A&E attendance, immunisation records (SIR), dental inspections (MIDAS), health visiting records (CHSP) and the National Records Scotland vital statistics register. This can now be used by other researchers subject to them going through the approval process for GUS and Public Benefit and Privacy Panel (PBPP).
A further strength of this evaluation was the use of mixed methods. The analysis of the qualitative study was designed both to complement the quantitative analysis and to elicit the lived experiences and women’s understanding of the HSV scheme. In doing so, the findings from the quantitative analysis can be situated through the experience of women who use the HSV scheme and those who do not use the scheme. We sampled women in the same comparison groups used in the quantitative analysis and from two different time frames – those who currently use the scheme and those who used the scheme up to 5 years previously. The qualitative findings provided understanding and some explanation of the findings of the quantitative analysis. Without this part of the study, it would have been difficult to understand why the findings were inconclusive.
Implications for future research
There is a need for future research to replicate some of the findings in different comparison groups and different data sets, especially with data that can assess dietary measures. Any replication study should address and overcome some of the challenges and limitations noted in this study. The GUS data linked to routinely collected NHS data provide an opportunity to assess longer-term outcomes for children and mothers in a cost-effective and non-burdensome way on participants. Further research is needed to understand the barriers to providing a healthy diet. Mothers stressed the importance of providing a good diet but were not always able to provide this. One of the reasons could be that the information and discussions come too early in the child’s life, so there is a need to understand the optimal timing for provision of this advice and support. The HSV scheme provides a good intervention point for women who are pregnant or mothers of young children. This could be used as an opportunity to undertake research to understand more about lifestyles of women of childbearing age, and what extra support could be offered alongside the HSVs.
Further research on modelling the monetary value of the HSVs would provide research evidence to understand if an increased value of the vouchers could have more of an impact on child and maternal health outcomes and offer a better mechanism for mothers to provide a healthy diet. In this study HSVs were £3.10 per week (with £6.20 for the first year of life). Recently, the value of HSV has been increased to £4.25 (and £8.50) per week.
One of the challenges of evaluating existing policies is it is difficult to ascertain a suitable control group. 33 Policy makers and researchers should identify evaluation criteria, methods and opportunities at an early stage in the policy life cycle. 109,110 That way, rigorous outcome evaluations can be embedded during policy development as well as during roll out and implementation. The evaluation can be designed optimally and suitable control groups and data can be identified. There is a need for more outcome evaluations, as well as process evaluations of policies to understand their effects on the population. 22
Research that can provide answers for the above implications will provide policy makers with options on how to optimise the HSV scheme to improve maternal and child health, and to therefore make real changes to the life chances of children.
Implications for policy
The results of this study identify inherent structural limitations of HSV. Some of these are noted in previous research, for example access and eligibility to the HSV scheme and accessing vitamins. These structural limitations limit the possible effectiveness of the HSVs but could be addressed by increasing awareness of the HSV scheme, increasing access to vitamins during pregnancy and consideration of the increased monetary value of HSVs.
Acknowledgements
The authors would like to thank the respondents of GUS and the IFS, and the study participants who gave their time and permission to be involved in the study. We are also grateful to the members of the community group who contributed to the PPI of the study. We would like to thank the anonymous reviewers for critically reading the report and providing comments and improvements; these reviewer comments have significantly strengthened the work.
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Contributions of authors
Ruth Dundas (https://orcid.org/0000-0002-3836-4286) led the design and execution of the study; oversaw data linkage, study analyses and integration of methods; and led the preparation of the final report.
Massoud Boroujerdi (https://orcid.org/0000-0002-5722-9645) conducted the quantitative analysis and contributed to the methods and results chapters of the report.
Susan Browne (https://orcid.org/0000-0003-1785-1429) conducted the qualitative interview study, collected and analysed the data, and contributed to the methods and results chapters of the report.
Manuela Deidda (https://orcid.org/0000-0002-0921-6970) conducted the health economics analysis, and contributed to the methods and results chapters of the report.
Paul Bradshaw (https://orcid.org/0000-0002-8590-6156) provided expertise in the use of GUS and contributed to the data linkage application process and to chapters in the report.
Peter Craig (https://orcid.org/0000-0002-7653-5832) provided expertise in the natural experiment methods and the policy evaluation, and contributed to the design of the quantitative analysis and interpretation, and to chapters in the report.
Emma McIntosh (https://orcid.org/0000-0001-6340-3083) oversaw the health economics aspects (including design, methods and analysis) and contributed to chapters in the report.
Alison Parkes (https://orcid.org/0000-0002-4177-8041) provided expertise in the use of GUS and contributed to chapters in the report.
Daniel Wight (https://orcid.org/0000-0002-1234-3110) oversaw the qualitative study aspects (including design, methods and analysis) and contributed to interpretation and to chapters in the report.
Charlotte Wright (https://orcid.org/0000-0001-6256-6315) provided expertise in child health, feeding and nutrition, and contributed to chapters in the report.
Alastair H Leyland (https://orcid.org/0000-0003-3741-7099) provided expertise in statistics, natural experiment methods and policy evaluation in maternal health, and contributed to the design, methods and interpretation, and to chapters in the report.
Data-availability statement
The quantitative analysis used third-party data made available under licence that the author does not have permission to share. Requests to access the data should be directed to the UK Data Service DOI: 10.5255/UKDA-SN-7432-4 for GUS data; DOI: 10.5255/UKDA-SN-7281-2 for IFS data. For the qualitative data, requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol 2002;31:285-93.
- Barker DJP. The Fetal and Infant Origins of Adult Disease. BMJ Books; 1992.
- Skinner JD, Carruth BR, Bounds W, Ziegler PJ. Children’s food preferences: a longitudinal analysis. J Am Diet Assoc 2002;102:1638-47.
- Skinner JD, Carruth BR, Bounds W, Ziegler P, Reidy K. Do food-related experiences in the first 2 years of life predict dietary variety in school-aged children?. J Nutr Educ Behav 2002;34:310-5.
- Mishra GD, Prynne CJ, Paul AA, Greenberg DC, Bolton-Smith C. The impact of inter-generational social and regional circumstances on dietary intake patterns of British adults: results from the 1946 British Birth Cohort. Public Health Nutr 2004;7:737-44.
- Tseng M. Social circumstances and dietary intake. Public Health Nutr 2004;7:695-6.
- FHI Solutions LLC . First 1,000 Days n.d. https://thousanddays.org/ (accessed 24 March 2023).
- House of Commons Health and Social Care Committee . First 1000 Days of Life. Thirteenth Report of Session 2017–19 2019.
- Marmot M, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, et al. Fair Society, Healthy Lives (The Marmot Review). London: Institute of Health Equity; 2010.
- Scottish Government Cabinet Secretary for Education and Skills, Minister for Children and Young People . Getting It Right for Every Child (GIRFEC) n.d. www.gov.scot/policies/girfec/ (accessed 24 March 2023).
- HM Treasury . Every Child Matters 2003.
- Welsh Government . An Overview of the Healthy Child Wales Programme 2016.
- Department of Health 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/200521/post_legislative_assessment.pdf (accessed 24 March 2023).
- Family Nurse Partnership: The Office for Health Improvement and Disparities (OHD) 2023. https://fnp.nhs.uk (accessed 24 March 2023).
- Flying Start Wales: Welsh Government 2023. www.gov.wales/flying-start-guidance (accessed 22 March 2023).
- Brownell M, Chartier M, Au W, Schultz J. Evaluation of the Health Baby Program. Winnipeg, MB: Manitoba Centre for Health Policy; 2010.
- Häggström J, Sampaio F, Eurenius E, Pulkki-Brännström AM, Ivarsson A, Lindkvist M, et al. Is the Salut Programme an effective and cost-effective universal health promotion intervention for parents and their children? A register-based retrospective observational study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016732.
- Minister for Children and Young People . Early Education and Care. ELC for Two Year Old Children n.d. www.gov.scot/policies/early-education-and-care/elc-for-two-year-old-children/ (accessed 24 March 2023).
- HM Government . Childcare Choices n.d. www.childcarechoices.gov.uk (accessed 24 March 2023).
- NHS . Get Help to Buy Food and Milk (the Healthy Start Scheme) n.d. www.healthystart.nhs.uk/ (accessed 24 March 2023).
- Scottish Government . Scotland’s Baby Box – Parents’ Views on Contents 2017.
- House of Commons Health and Social Care Committee . Health Inequalities. Third Report of Session 2008–09 2009.
- McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ. Infant Feeding Survey 2010. London: Health and Social Care Information Centre; 2012.
- Hansard HCW. 25 Jun 2014: Column 243W 2014.
- London; 2002.
- Ford FA, Mouratidou T, Wademan SE, Fraser RB. Effect of the introduction of ‘Healthy Start’ on dietary behaviour during and after pregnancy: early results from the ‘before and after’ Sheffield study. Br J Nutr 2009;101:1828-36. https://doi.org/10.1017/S0007114508135899.
- Mouratidou T, Ford FA, Wademan SE, Fraser RB. Are the benefits of the ‘Healthy Start’ food support scheme sustained at three months postpartum? Results from the Sheffield ‘before and after’ study. Matern Child Nutr 2010;6:347-57. https://doi.org/10.1111/j.1740-8709.2009.00215.x.
- McFadden A, Green JM, Williams V, McLeish J, McCormick F, Fox-Rushby J, et al. Can food vouchers improve nutrition and reduce health inequalities in low-income mothers and young children: a multi-method evaluation of the experiences of beneficiaries and practitioners of the Healthy Start programme in England. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-148.
- Scantlebury RJ, Moody A, Oyebode O, Mindell JS. Has the UK Healthy Start voucher scheme been associated with an increased fruit and vegetable intake among target families? Analysis of Health Survey for England data, 2001-2014. J Epidemiol Community Health 2018;72:623-9. https://doi.org/10.1136/jech-2017-209954.
- McFadden A, Fox-Rushby J, Green JM, Williams V, Pokhrel S, McLeish J, et al. Healthy Start: Understanding the Use of Vouchers and Vitamins. Dundee: University of Dundee; 2013.
- Department of Health and Social Care . Scientific Review of the Welfare Food Scheme 2002.
- Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health 2012;66:1182-6. https://doi.org/10.1136/jech-2011-200375.
- Dyson L, Renfrew MJ, Jenkins R, Thomas J, McCormick F, Pearce A, et al. Approaches to Evaluating Healthy Start – A Scoping Review. York: Mother and Infant Research Unit, Public Health Research Consortium; 2007.
- Imbens GW, Lemieux T. Regression discontinuity designs: a guide to practice. J Economet 2008;142:615-35.
- Bradshaw P, Corbett J. Edinburgh: Scottish Centre for Social Research (ScotCen); 2013.
- Bansal N, Chalmers JW, Fischbacher CM, Steiner MF, Bhopal RS. Scottish Health and Ethnicity Linkage Study. Ethnicity and first birth: age, smoking, delivery, gestation, weight and feeding: Scottish Health and Ethnicity Linkage Study. Eur J Public Health 2014;24:911-6. https://doi.org/10.1093/eurpub/cku059.
- Scottish Government . Scottish Index of Multiple Deprivation 2012 n.d. www.webarchive.org.uk/wayback/archive/20200207120848/https://www2.gov.scot/Topics/Statistics/SIMD/DataAnalysis (accessed 24 March 2023).
- Government . DfCaL. English Indices of Deprivation n.d. www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed 24 March 2023).
- Welsh Government . Welsh Index of Multiple Deprivation n.d. www.gov.wales/welsh-index-multiple-deprivation-full-index-update-ranks-2011 (accessed 24 March 2023).
- Northern Ireland Statistics and Research Agency . Northern Ireland Multiple Deprivation Measure 2010 n.d. www.nisra.gov.uk/publications/northern-ireland-multiple-deprivation-measure-2010 (accessed 8 September 2022).
- Hoddinott P, Tappin D, Wright C. Clinical review: breast feeding. BMJ 2008;336.
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983;70:41-55.
- Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis 2007;15:199-236.
- Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med 2008;27:2037-49. https://doi.org/10.1002/sim.3150.
- Ho D, King G, Stuart E. Matchit nonparametric preprocessing for parametric causal inference. J Sta Softw 2011;42:1-28. https://doi.org/10.18637/jss.v042.i08.
- Dalgaard P. Introductory Statistics with R. New York, NY: Springer; 2008.
- Calonico S, Cattaneo MD, Titiunik R. rdrobust: An R package for robust nonparametric inference in regression-discontinuity designs. R Journal 2015;7:38-51.
- Little R, Rubin DB. Statistical Analysis with Missing Data. Hoboken, NJ: John Wiley & Sons; 2002.
- Su YS, Gelman A, Hill J, Yajima M. Multiple imputation with diagnostics (mi) in R: opening windows into the black box. J Stat Soft 2011;45:1-31.
- Dusheiko M, Gravelle H, Jacobs R, Smith P. The Effect of Budgets on Doctor Behaviour: Evidence from a Natural Experiment. York: University of York; 2003.
- Imbens GW, Wooldridge JM. Recent developments in the econometrics of program evaluation. J Econ Lit 2009;47:5-86.
- Meyer BD. Natural and quasi-experiments in economics. J Bus Econ Stat 1995;13:151-61.
- Rosenzweig MR, Wolpin KI. Natural ‘natural experiments’ in economics. J Econ Lit 2000;38:827-74.
- Postma MJL, Veenstra M, de Walle HEK, de Jong-van den Berg LTW. Cost effectiveness of periconceptional supplementation of folic acid. Pharm World Sci 2002;24:8-11. https://doi.org/10.1023/a:1014848928212.
- Filby A, Lewis L, Taylor M. An economic evaluation of interventions to improve the uptake of vitamin D supplements in England and Wales: Economic modelling for NICE. York Health Economics Consortium; The University of York; 2014.
- Angrist JD, Keueger AB. Does compulsory school attendance affect schooling and earnings?. Quart J Econ 1991;106:979-1014.
- Angrist JD, Lavy V. Using maimonides’ rule to estimate the effect of class size on scholastic achievement. Quart J Econ 1999;114:533-75.
- Blundell R, Costa Dias M. Alternative Approaches to Evaluation in Empirical Microeconomics. Cemmap Working Paper; 2002.
- Rovithis D. Do health economic evaluations using observational data provide reliable assessment of treatment effects?. Health Econ Rev 2013;3.
- National Institute for Health and Care Excellence (NICE) . Maternal and Child Nutrition 2014.
- Abu-Saad K, Fraser D. Maternal nutrition and birth outcomes. Epidemiol Rev 2010;32:5-25. https://doi.org/10.1093/epirev/mxq001.
- Barker DJ. The fetal and infant origins of adult disease. BMJ 1990;301.
- Mishra GD, Prynne CJ, Paul AA, Greenberg DC, Bolton-Smith C. The impact of inter-generational social and regional circumstances on dietary intake patterns of British adults: results from the 1946 British Birth Cohort. Public Health Nutr 2004;7:737-44.
- Lucas PJ, Jessiman T, Cameron A. Healthy start: the use of welfare food vouchers by low-income parents in England. Soc Pol Soc 2015;14.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Int J Technol Assess Health Care 2013;29:117-22. https://doi.org/10.1017/S0266462313000160.
- Drummond M, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Glick H, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2007.
- Byford S, Sefton T. Economic evaluation of complex health and social care interventions. Nat Instit Econ Rev 2003;186:98-108.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) – explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health 2013;16:231-50. https://doi.org/10.1016/j.jval.2013.02.002.
- Deidda M, Geue C, Kreif N, Dundas R, McIntosh E. A framework for conducting economic evaluations alongside natural experiments. Soc Sci Med 2019;220:353-61.
- Craig P, Katikireddi SV, Leyland A, Popham F. Natural experiments: an overview of methods, approaches, and contributions to public health intervention research. Annu Rev Public Health 2017;38:39-56. https://doi.org/10.1146/annurev-publhealth-031816-044327.
- Petticrew M, Cummins S, Ferrell C, Findlay A, Higgins C, Hoy C, et al. Natural experiments: an underused tool for public health?. Public Health 2005;119:751-7.
- Lorgelly PK, Lawson KD, Fenwick EA, Briggs AH. Outcome measurement in economic evaluations of public health interventions: a role for the capability approach?. Int J Environ Res Public Health 2010;7:2274-89.
- Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy 2009;93:85-92. https://doi.org/10.1016/j.healthpol.2009.07.012.
- Drummond M, Weatherly H, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Assessing the Challenges of Applying Standard Methods of Economic Evaluation to Public Health Interventions. York: Public Health Research Consortium; 2007.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495-9. https://doi.org/10.1016/j.ijsu.2014.07.013.
- Des Jarlais DC, Lyles C, Crepaz N. TREND Group . Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health 2004;94:361-6.
- Smith RD, Petticrew M. Public health evaluation in the twenty-first century: time to see the wood as well as the trees. J Public Health 2010;32:2-7. https://doi.org/10.1093/pubmed/fdp122.
- Kreif N, Grieve R, Sadique MZ. Statistical methods for cost-effectiveness analyses that use observational data: a critical appraisal tool and review of current practice. Health Econ 2013;22:486-500. https://doi.org/10.1002/hec.2806.
- Manca A, Austin PC. Using Propensity Score Methods to Analyse Individual Patient Level Cost Effectiveness Data from Observational Studies. The University of York: Health Economics and Data Group Working Paper 2008;8.
- Leyland AH, Ouédraogo S, Nam J, Bond L, Briggs AH, Gray R, et al. Evaluation of health in pregnancy grants in Scotland: a natural experiment using routine data. Public Health Research 2017;5.
- Alfonso YN, Bishai D, Bua J, Mutebi A, Mayora C, Ekirapa-Kiracho E. Cost-effectiveness analysis of a voucher scheme combined with obstetrical quality improvements: quasi experimental results from Uganda. Health Policy Plan 2015;30:88-99. https://doi.org/10.1093/heapol/czt100.
- Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, et al. Using Natural Experiments to Evaluate Population Health Interventions. Glasgow, UK: Medical Research Council; 2011.
- Edwards RT, McIntosh E. Applied Health Economics for Public Health Practice and Research. Oxford: Oxford University Press; 2019.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal. Process and Methods (PMG9) 2013.
- Dundas R, Ouédraogo S, Bond L, Briggs AH, Chalmers J, Gray R, et al. Evaluation of health in pregnancy grants in Scotland: a protocol for a natural experiment. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-006547.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2011–12 2012.
- Joint Formulary Committee . British National Formulary 2011.
- Curtis L, Netten A. Unit Costs of Health and Social Care 2004. Canterbury: PSSRU, University of Kent; 2004.
- Kreif N, Grieve R, Radice R, Sekhon JS. Regression-adjusted matching and double-robust methods for estimating average treatment effects in health economic evaluation. Health Serv Outcomes Res Methodol 2013;13:174-202.
- Rosenbaum PR. Observational Studies. New York, NY: Springer; 2002.
- Becker SO, Caliendo M. Sensitivity analysis for average treatment effects. Stata J 2007;7:71-83.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2014.
- Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. PharmacoEconomics 2014;32:1157-70. https://doi.org/10.1007/s40273-014-0193-3.
- Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials - a practical guide with flowcharts. BMC Med Res Methodol 2017;17. https://doi.org/10.1186/s12874-017-0442-1.
- Little RJ, Rubin DB. Statistical Analysis with Missing Data. Hoboken, NJ: John Wiley & Sons, Inc.; 2019.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377-99. https://doi.org/10.1002/sim.4067.
- National Institute for Clinical Excellence (NICE) . Methods for the Development of NICE Public Health Guidance 2012.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Int J Technol Assess Health Care 2013;29:117-22. https://doi.org/10.1017/S0266462313000160.
- Briggs AH. Statistical approaches to handling uncertainty in health economic evaluation. Eur J Gastroenterol Hepatol 2004;16:551-61.
- Crawley H, Dodds R. The UK Healthy Start Scheme. What Happened? What Next?. London: First Steps Nutrition Trust; 2018.
- NHS Get Help to Buy Food and Milk (Healthy Start) . What You’ll Get and How to Shop n.d. www.healthystart.nhs.uk/what-youll-get-and-how-to-shop/ (accessed 24 March 2023).
- US Food and Nutrition Service . Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) n.d. www.fns.usda.gov/wic (accessed 24 March 2023).
- Sonchak L. The impact of WIC on birth outcomes: new evidence from South Carolina. Matern Child Health J 2016;20:1518-25. https://doi.org/10.1007/s10995-016-1951-y.
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46:399-424. https://doi.org/10.1080/00273171.2011.568786.
- Rubin DB. On principles for modeling propensity scores in medical research. Pharmacoepidemiol Drug Saf 2004;13:855-7. https://doi.org/10.1002/pds.968.
- Fischbacher CM. Identifying ‘Deprived Individuals’: Are There Better Alternatives to the Scottish Index of Multiple Deprivation (SIMD) for Socioeconomic Targeting In Individually Based Programmes Addressing Health Inequalities in Scotland?. Edinburgh: ISD Scotland/ScotPHO; 2014.
- Leviton LC, Khan LK, Dawkins N, Cotton D. Evaluability Assessment to Improve Public Health Policies, Programs, and Practices. Annu Rev Public Health 2020;31:213-33.
- Craig P, Campbell M. Evaluability Assessment: A Systematic Approach to Deciding Whether and How to Evaluate Programmes and Policies [Working Paper]. Edinburgh: What Works Scotland; 2015.
- Griffith R, von Hinke Kessler Scholder S, Smith S. Getting a Healthy Start?: Nudge Versus Economic Incentives. Bristol: Centre for Market and Public Organisation; 2014.
- Duijts L, Ramadhani MK, Moll HA. Breastfeeding protects against infectious diseases during infancy in industrialized countries. A systematic review. Matern Child Nutr 2009;5:199-210. https://doi.org/10.1111/j.1740-8709.2008.00176.x.
- Ajetunmobi OM, Whyte B, Chalmers J, Tappin DM, Wolfson L, Fleming M, et al. Breastfeeding is associated with reduced childhood hospitalization: evidence from a Scottish Birth Cohort (1997-2009). J Pediatr 2015;166:620-5.e4. https://doi.org/10.1016/j.jpeds.2014.11.013.
- Basu A, Manca A. Regression estimators for generic health-related quality of life and quality-adjusted life years. Med Decis Making 2012;32:56-69. https://doi.org/10.1177/0272989X11416988.
Appendix 1 Distribution of propensity scores
FIGURE 5.
The distribution of propensity scores for the GUS database, matching group 2 to group 1.

FIGURE 6.
The distribution of propensity scores for the GUS database, matching group 3 to group 1.
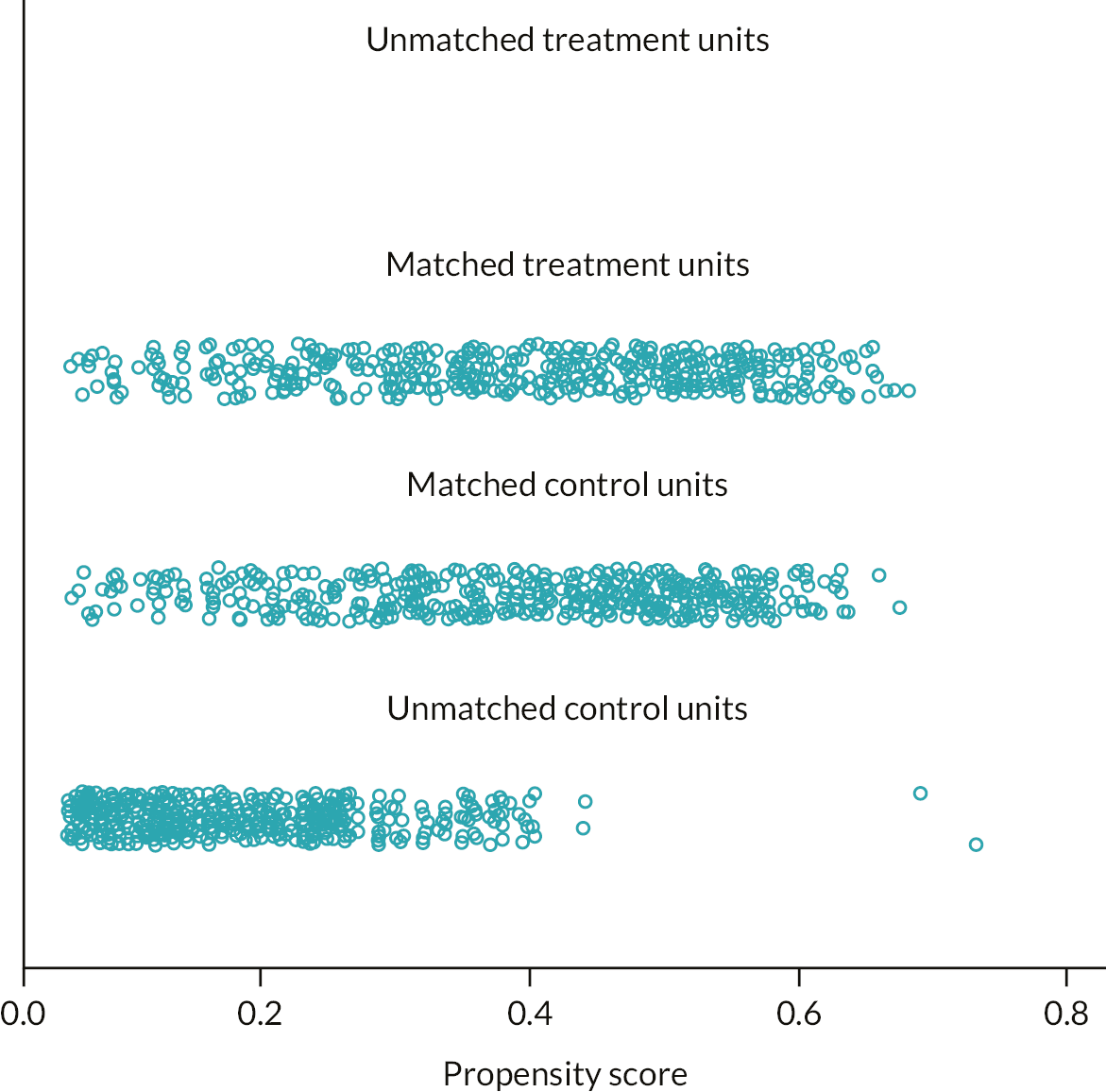
FIGURE 7.
The distribution of propensity scores for the GUS database, matching groups 1 and 2 to group 3.
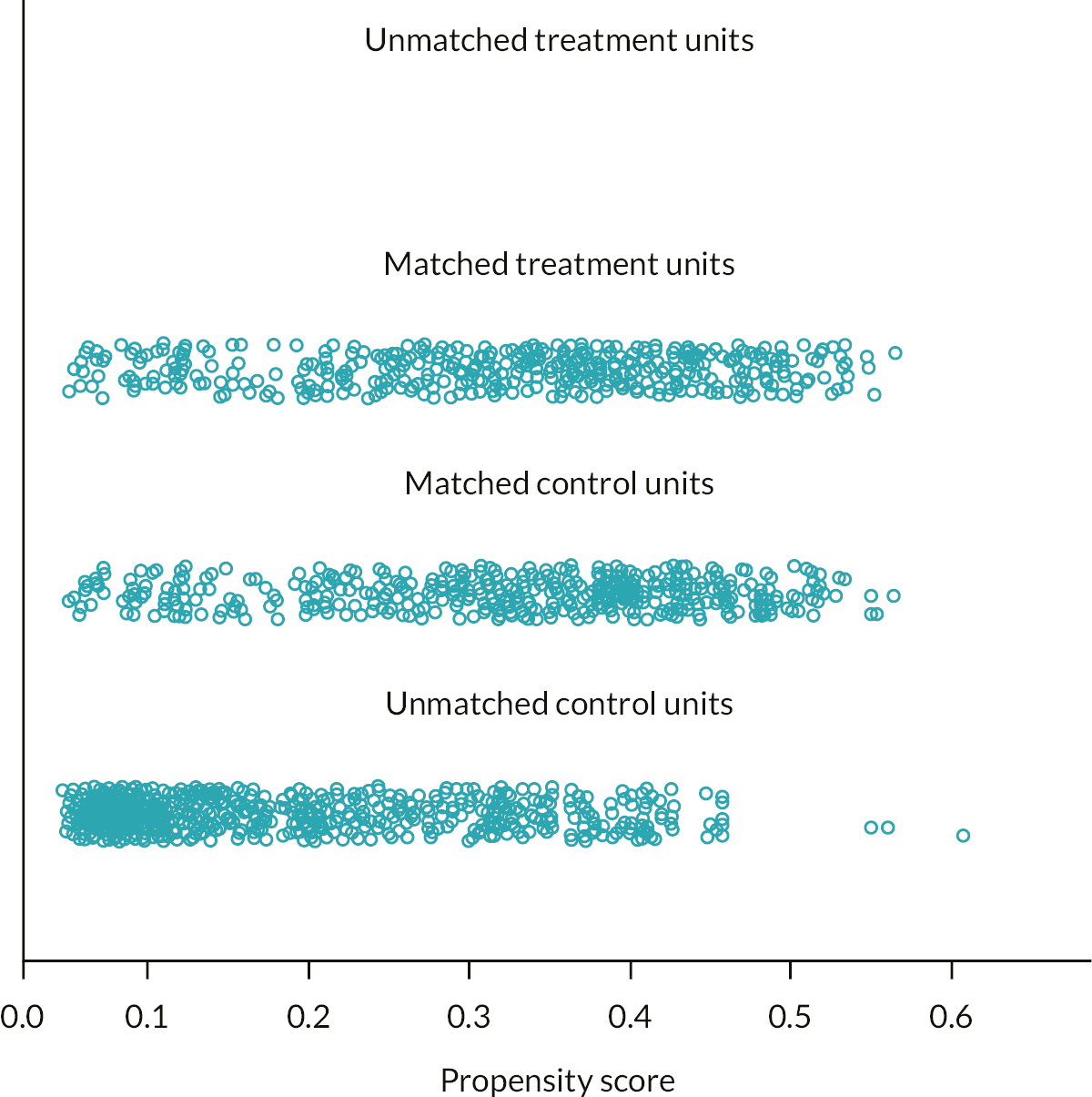
FIGURE 8.
The distribution of propensity scores for the IFS database, matching group 2 to group 1.
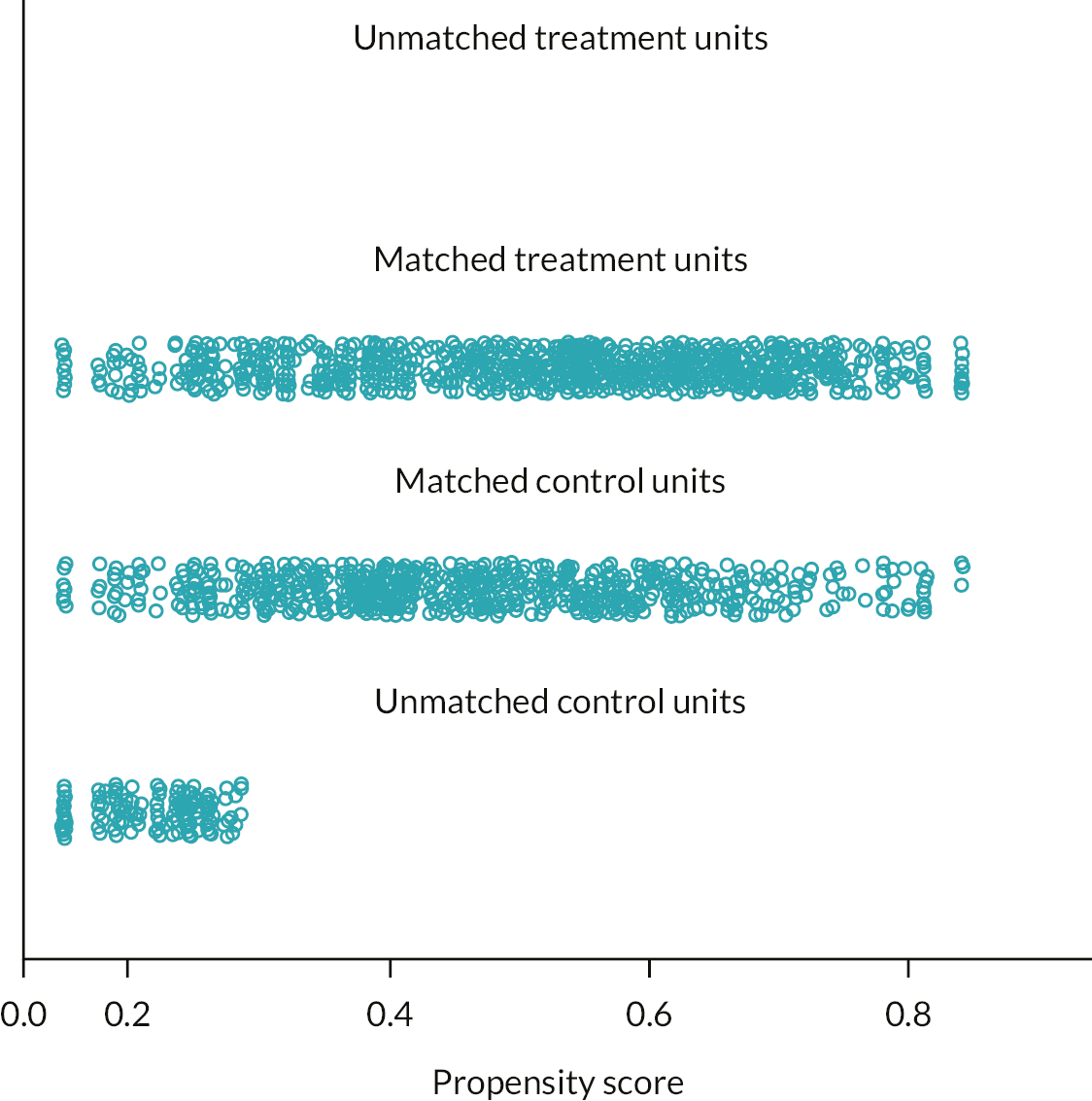
FIGURE 9.
The distribution of propensity scores for the IFS database, matching group 1 to group 3.
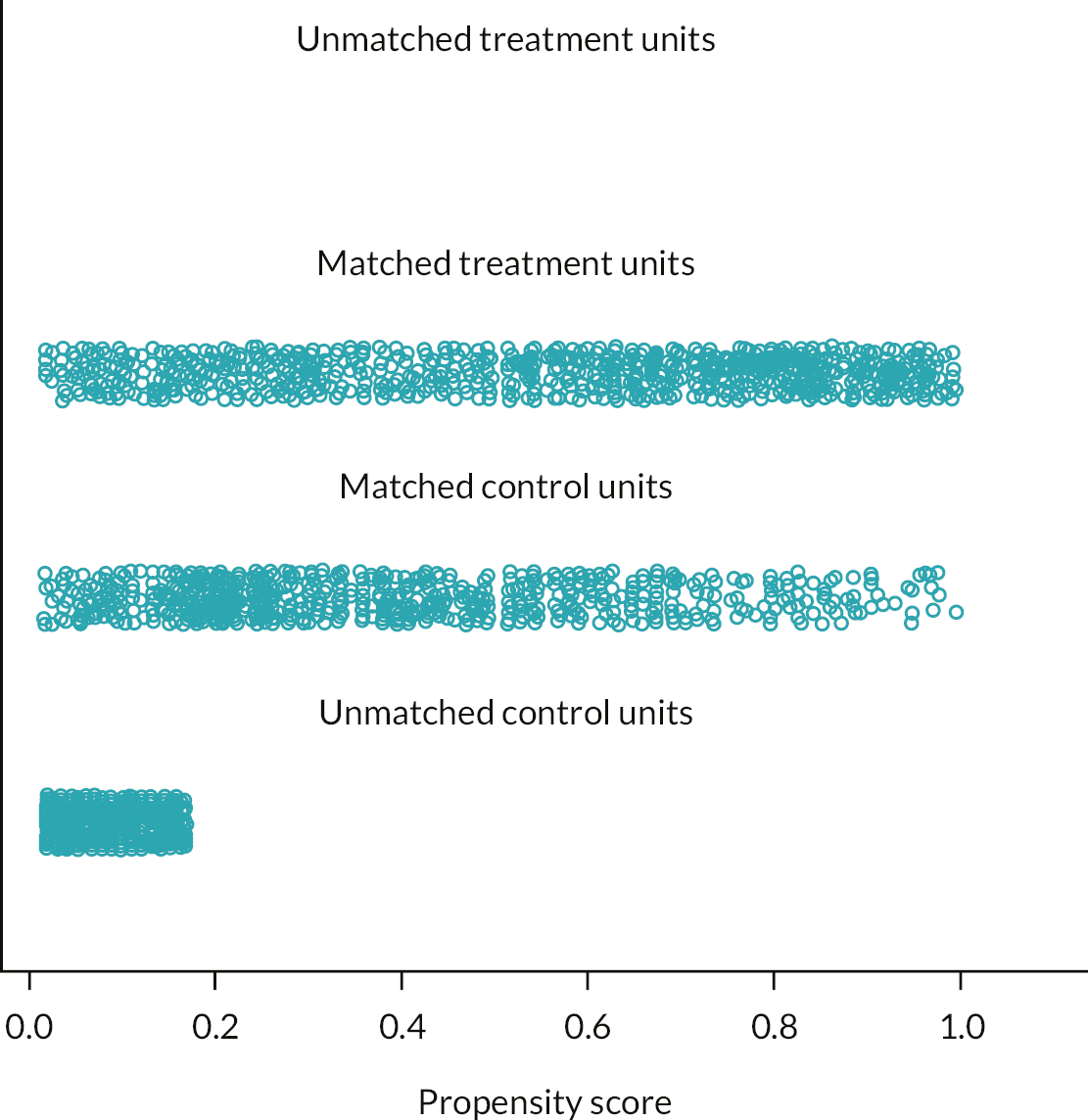
FIGURE 10.
The distribution of propensity scores for the IFS database, matching groups 1 and 2 to group 3.
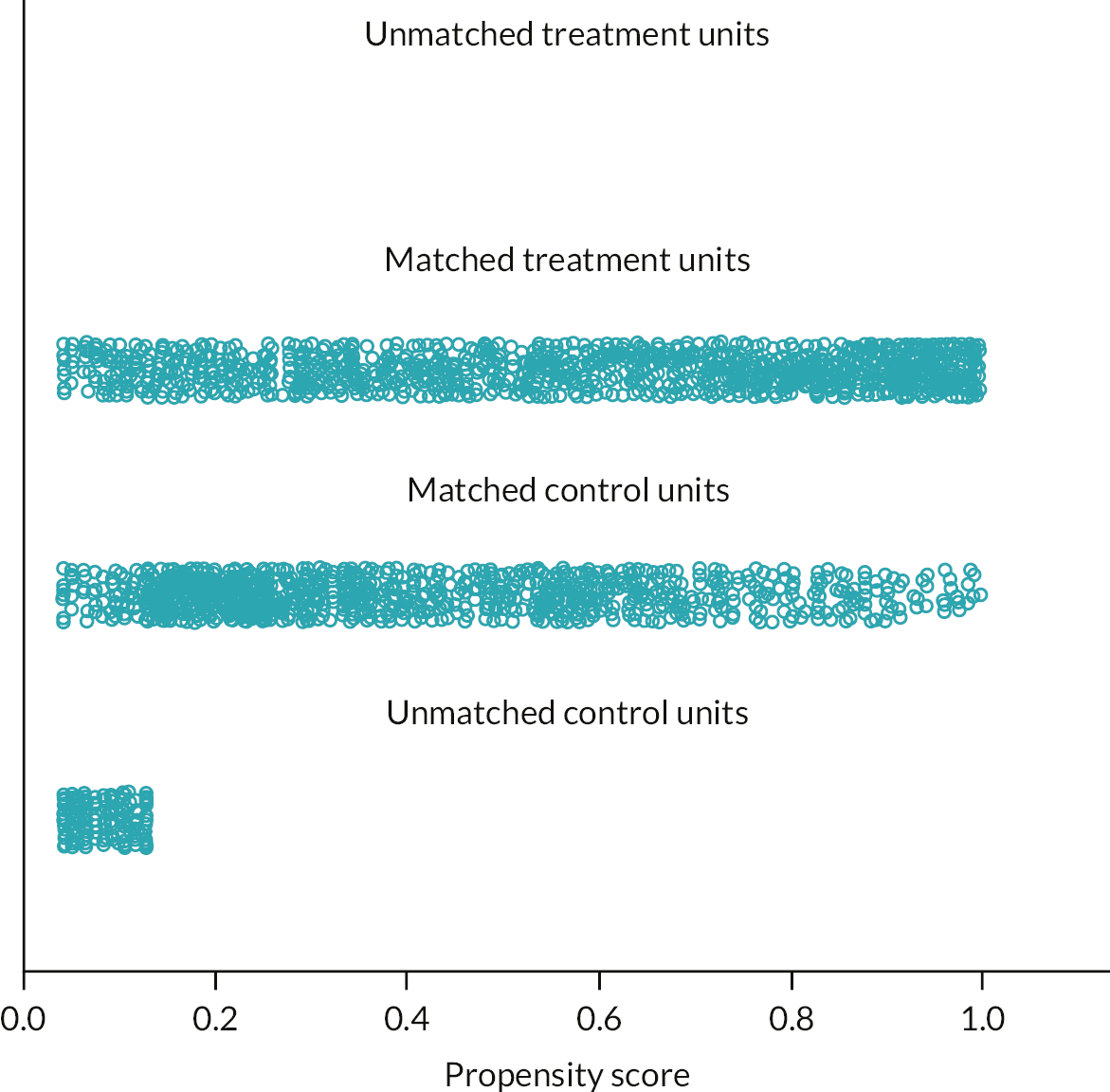
Appendix 2 Participants in the qualitative interviews
| Participant ID | Claim | Ethnicity | Age (years) | Highest-level qualification | Number of children | Partner/single | Recruitment source |
|---|---|---|---|---|---|---|---|
| HSV01 | HSV claimant | White Scottish | 23 | No qualifications | 3 | Single | Community group |
| HSV02 | HSV claimant | White Scottish | 24 | No qualifications | 1 | Partner | Community group |
| HSV03 | No HSV claim | Black African | 26 | Studying for degree | 2 | Partner | Community group |
| HSV04 | No HSV claim | Nepalese | 29 | No qualifications | 2 | Partner | Community group |
| HSV05 | HSV claimant | White Scottish | 40 | No qualifications | 3 | Single | Community group |
| HSV06 | HSV claimant | White Scottish | 24 | No qualifications | 3 | Single | Community group |
| HSV07 | HSV claimant | White Scottish | 27 | No qualifications | 2 | Single | Community group |
| HSV08 | HSV claimant | White Scottish | 32 | No qualifications | 2 | Single | Community group |
| HSV09 | HSV claimant | White Scottish | 23 | High school qualifications | 1 | Single | Community group |
| HSV10 | HSV claimant | White Scottish | 22 | No qualifications | 1 | Single | Community group |
| HSV11 | HSV claimant | Black African | 39 | No qualifications | 2 | Single | Community group |
| HSV12 | HSV claimant | Black African | 36 | Studying for degree | 2 | Partner | Community group |
| HSV13 | HSV claimant | White Scottish | 39 | No qualifications | 4 | Partner | GUS |
| HSV14 | No HSV claim | White British | 38 | Postgraduate qualification | 4 | Partner | GUS |
| HSV15 | No HSV claim | White Australian | 43 | Degree | 3 | Partner | GUS |
| HSV16 | No HSV claim | White Scottish | 40 | Degree | 4 | Partner | GUS |
| HSV17 | No HSV claim | White Scottish | 35 | College qualification | 2 | Partner | GUS |
| HSV18 | No HSV claim | Pakistani | 40 | No qualifications | 3 | Single | Community group |
| HSV19 | HSV claimant | White British | 44 | No qualifications | 6 | Partner | GUS |
| HSV20 | No HSV claim | White British | 34 | Degree | 2 | Partner | GUS |
| HSV21 | No HSV claim | White Scottish | 32 | High school qualifications | 3 | Partner | GUS |
| HSV22 | No HSV claim | White British | 29 | College qualification | 2 | Single | GUS |
| HSV23 | No HSV claim | White Scottish | 47 | Degree | 2 | Partner | GUS |
| HSV24 | HSV claimant | White Scottish | 40 | College qualification | 3 | Single | GUS |
| HSV25 | No HSV claim | White Scottish | 37 | College qualification | 2 | Partner | GUS |
| HSV26 | No HSV claim | White Scottish | 29 | Degree | 2 | Partner | Community group |
| HSV27 | HSV claimant | White Scottish | 41 | No qualifications | 5 | Partner | Community group |
| HSV28 | HSV claimant | White Polish | 33 | Degree | 1 | Single | Community group |
| HSV29 | HSV claimant | White Irish | 35 | High school qualifications | 1 | Single | GUS |
| HSV30 | HSV claimant | British Pakistani | 39 | High school qualifications | 5 | Single | Community group |
| HSV31 | HSV claimant | White British | 43 | No qualifications | 2 | Partner | GUS |
| HSV32 | HSV claimant | White Scottish | 24 | College qualification | 1 | Single | GUS |
| HSV33 | No HSV claim | White Scottish | 29 | High school qualifications | 2 | Single | Community group |
| HSV34 | HSV claimant | White Scottish | 23 | High school qualifications | 1 | Single | Community group |
| HSV35 | No HSV claim | White Scottish | 33 | Degree | 1 | Single | Community group |
| HSV36 | No HSV claim | White Scottish | 36 | High school qualifications | 6 | Partner | Community group |
| HSV37 | No HSV claim | White British | 29 | No qualifications | 4 | Partner | Community group |
| HSV38 | No HSV claim | White Scottish | 32 | College qualification | 2 | Partner | Community group |
| HSV39 | HSV claimant | Pakistani | 27 | No qualifications | 1 | Single | Community group |
| HSV40 | HSV claimant | White Scottish | 30 | High school qualifications | 3 | Single | Community group |
Appendix 3 Applying the Natural Experiment Checklist to the Healthy Start voucher evaluation
| 1. Data sources and measurement | |
|---|---|
| 1.1 The data used and the reason(s) why it has been chosen has been identified, stated and described in relation to: | |
| 1.1.1 All relevant intersectoral outcomes and costs being captured | In the HSV study the GUS database, a representative sample of Scottish births, has been linked with six administrative databases, allowing the identification of a wide range of health and social care resource use and improving the number of cost items collected as well as the quality of collected data. GUS contains information on HSV eligibility and uptake, and information about age and income, plus a wide range of socioeconomic variables, and it covers the first 10 months of the children, plus the mother’s pregnancy. Linkage to CHSP, SMR01 and SMR02, MIDAS and SIRS has allowed to recover detailed information on a wide range of healthcare resources used by the mother and the child over a longer time horizon (6 years), thus providing information on whether the envisaged change in feeding and breastfeeding habits has led to better health outcomes in the long term |
| 1.1.2 Implementation of the chosen statistical design | GUS has allowed the identification of three control groups, associated with the chosen statistical approaches: eligible, but not receiving HSV; nearly eligible (those who just miss the eligibility criteria for HSV, regarding income and age) |
| 1.2 The application to routinely collected administrative data has been done on time to avoid delays in conducting economic evaluations (e.g. due to bureaucratic procedures, anonymisation, privacy and confidentiality requirements) | Data linkage required an application to the public benefit and privacy panel to ensure the research is beneficial to the public and is carried out appropriately to avoid disclosure. Even if the application has been done on time, there have been delays in receiving the linked data as well as subsequent data amendments |
| 1.3 The study recognises and addresses attrition and missing data and its consequences for the health economics analysis (bias) | A suitable method for missing data imputation will be chosen, according to the nature of missingness. No attrition bias is expected, given that only one wave of GUS will be used |
| 1.4 The study recognises and addresses measurement errors (e.g. due to discrepancies between the timing of the intervention and period of data availability) and its consequences for the health economics analysis (bias) | The linkage of GUS with administrative sources would give rise to additional reasons for missingness, given that routine data sources and clinical databases are often incomplete. A suitable method for missing data imputation will be chosen, according to the nature of missingness |
| 2. Setting and location | |
| 2.1 Setting and location are stated and explained in relation to social and political priorities | In the HSV example, the vouchers are directed towards deprived mothers and pregnant women, given the aim to improve the mothers’ and children’s health |
| 2.2 The source of secondary data that best meets the economic evaluation needs in terms of setting and location has been stated | The economic evaluation of the HSV was mainly conducted using Scottish data (GUS), even if it has been implemented throughout UK. The GUS survey was chosen as primary source of data since it allows for the identification of multiple intervention and comparison groups |
| 2.3 Concurrent interventions have been: | |
| 2.3.1 Identified | N/A |
| 2.3.2 Tackled with appropriate statistical analysis (e.g. robustness checks; subsample analysis) | N/A |
| 2.4 Potential spillovers/externalities effects have been: | |
| 2.4.1 Identified through the usage of an economic evaluation logic model | N/A |
| 2.4.2 Addressed through appropriate sensitivity analysis | N/A |
| 3. Choice of comparators | |
| 3.1 The choice of comparators is justified in relation to reduction of selection bias due to non-randomisation, the unit of assignment (individual or aggregate) and data availability | In the HSV, two comparators are used: eligible, but not taking HSV; nearly eligible, not taking HSV |
| 3.2 The existence of potential spillovers/crossovers has been considered in the choice of comparators | N/A |
| 3.3 Multiple intervention/control groups have been used to examine sensitivity of the economic evaluation to multiple sources of bias | In the HSV study, the propensity score method has been applied on different intervention and control groups |
| 4. Subgroups | |
| 4.1 If equity concerns are included in the economic evaluation, subgroups are defined in relation to distributional concerns | The analysis of HSV will provide preliminary evidence of subgroups (defined by age or social deprivation) which are more likely to benefit from the intervention. However, given that the intervention is directed towards a relatively homogeneous population (low-income women, in receipt of means tested benefit), it’s unlikely that it is going to generate unfair health inequalities |
| 4.2 Potential behavioral responses (e.g. ‘nudge effects’), have been identified and measured | In the HSV case study ‘nudge effects’ has been not formally analysed, due to lack of data, but their existence has been accounted for. A similar case study 111 using longitudinal data on food purchase investigated whether consumption of fruit and vegetables changed after the introduction of the policy for ‘distorted’ households (i.e. those who would spend less than the value of the vouchers on fruit and vegetables if given an equivalent cash benefit) an ‘inframarginal’ households. They eventually found no difference between the two groups of households, thus not supporting the existence of a ‘nudge effect’ |
| 5. Outcome | |
| 5.1 An economic evaluation model mapping routinely collected intermediate outcomes to QALYs has been developed, using additional evidence from systematic reviews to identify utility values | In the HSV case study the primary outcomes in the evaluation are vitamin use in pregnancy and breastfeeding initiation and duration. These outcomes are intermediate, ‘proxy’ outcomes for final, longer term outcomes including quality of life, life expectancy and a range of non-health outcomes such as employment and income There is published evidence that breastfeeding duration is linked to longer-term outcomes, including reduced risk of developing conditions including infectious diseases 112 and a lower relative risk of hospitalisation for a range of individual illnesses reported in childhood. 113 Hence, for the purposes of the HSV economic evaluation, if evidence of short-term effectiveness of the intervention will be found, hazard ratios from such studies will be adapted to provide risk estimates for developing these conditions for the development of a long term economic evaluation model |
| 5.2 An economic evaluation framework such as CCA, CBA or MCDA has been chosen and justified | The cost per unit of increase in breastfeeding duration, initiation and vitamin intake will be analysed in a CEA framework. A CCA framework will be also used to provide descriptive evidence of any incremental effect or cost over 3 and 6 years’ time horizon |
| 6. Costs | |
| 6.1 Costing has been done considering a societal perspective | Costing in the HSV has been done using a societal perspective, considering costs arising from the usage of social services, such as breastfeeding support groups, parentcraft, childcare |
| 6.2 When unit cost data associated to a specific resource use are not available, a decision rule (e.g. usage of the average unit cost of the most frequently used service) is explained and justified | In the HSV case, the generic cost of ‘parentcraft’ has been attributed to a wide range of support-community programmes (PPP, mellow parenting), in the absence of a specific unit cost to be associated to each of these services |
| 6.3 When specific categories of resource use are not publicly available (e.g. HRG-specific length of stay), a decision rule (e.g. using the average cost/bed day) is explained and justified | The administrative cost of running the program is not available in the HSV, and this is going to cause a downward bias in the estimated cost of the program |
| 6.4 The opportunity cost of transfer payments (i.e. transfer of resources from the government to beneficiaries, with a null net impact on society) has been identified and measured | The HSV, as the earlier HiP grant, 87 was such a transfer payment with no net cost to society incurred through transferring the grant from government to individuals, apart from administrative costs. 87 In the economic evaluation of HSV, sensitivity analysis using the overall cost of £3.10/week HSV transfer payment has been done |
| 7. Time horizon | |
| 7.1 Linked data are adequate to capture the presence of long-term effects | Linked data covering 6 years will allow considering potential beneficial effects (e.g. reduced hospitalisations) after the end of the intervention |
| 7.2 Appropriate discount rates, in line with the most up to date guidance have been applied | A discount rate of 3.5% will be applied. Sensitivity analysis using 1.5% will be done |
| 8. Inclusion of a logic model | |
| 8.1 A logic model has been developed, and it addresses: | |
| 8.1.1 Time horizon (e.g. long term effects) | Yes |
| 8.1.2 Possible subgroups effect | N/A |
| 8.1.3 Externalities and spillovers | N/A |
| 9. Analytical methods | |
| 9.1 The researchers have justified the source of variation in the receipt of the intervention, choosing a design and a statistical approach which is appropriate in relation to that source of variation | In the HSV case, a design aiming to construct a control group which best approximates an ideal randomised experiment (propensity score matching, IPTW) has been used, using two control groups: eligible but not claiming HSV; ‘nearly eligible’ (slightly below or above 18; income close to the 15,600 threshold) |
| 9.1.1 If the study is a before-and-after design, frequent measurements of data on long pre-treatment time periods have been collected | N/A |
| 9.2 Multiple statistical designs have been employed to examine the sensitivity of economic evaluation to multiple sources of bias | The HSV evaluation protocol propensity score matching approach to create multiple comparison groups for robustness in evaluation |
| 9.3 The list of potential confounders has been presented | The HSV protocol states a list of potential confounders, including demographic (age, gender, civil status) and socioeconomic characteristics (e.g. deprivation index) |
| 9.4 Causal effects have been interpreted considering potential contaminating policies | N/A |
| 9.5 The interpretation of the estimated effectiveness and cost-effectiveness is in line with the estimated parameter | ATE estimated using the propensity score (intervention group: eligible and in receipt of HSV; control group: eligible, but not receiving HSV) measures the incremental effect (cost) of HSV if all women would take HSV (vs. not taking HSV); ITT estimated using the propensity score (intervention group: eligible; control group: not eligible) measures the incremental effect (cost) of being made eligible for HSV (regardless of uptake) |
| 9.6 The methodologies to reduce selection bias have been incorporated into an econometric framework, considering health economics-specific challenges (i.e. skewed outcome and cost data, correlated outcome and cost data) | Appropriate methodologies are used to conduct cost-effectiveness analysis using a sample matched with propensity score 114 and a double-robust approach 91 |
| 10. Uncertainty and sensitivity analysis | |
| 10.1 All sources of uncertainty have been identified using appropriate methods (e.g. probabilistic sensitivity analysis; tornado diagrams) | Yes |
| 10.2 Cost-effectiveness results according to the different analytical choices have been reported | Yes |
| 10.3 Sensitivity analysis has been done in relation to: | |
| 10.3.1 Assumptions made in relation to unit cost | Yes |
| 10.3.2 Potential spillovers | N/A |
| 10.3.3 Comparators | N/A |
| 10.3.4 Different designs | N/A |
| 10.3.5 Econometric methodology chosen | N/A |
| 10.3.6 Unobserved confounding | N/A |
| 10.3.7 Transfer payments and administrative costs | N/A |
Appendix 4 Resource use and unit costs
| Database | Resource use item description | Unit of measure | Unit cost source | Unit cost value | Assumptions |
|---|---|---|---|---|---|
| GUS | First antenatal appointment with (options provided: GP/family doctor; midwife; private consultant; hospital clinic; independent midwife) | Cost/1 visit | PSSRU 2011 | GP/family doctor £53 per clinic consultation lasting 17.2 minutes; with qualifications; midwife/independent midwife £50/average unit cost National Schedule of Reference Costs Year: 2010-11 – NHS Trusts Community Midwifery Services: Visits Private consultant £143/average unit cost National Schedule of Reference Costs Year: 2010-11 – NHS Trusts Consultant Led: First Attendance Non-Admitted Face to Face Hospital clinic: £118/average unit cost National Schedule of Reference Costs Year: 2010-11 – NHS Trusts Outpatient Attendances Data-gynaecology |
|
| GUS | Attendance of antenatal class > 1: yes – went to most or all the classes > 2: yes – only went to some of the classes > 3: no – did not attend any |
Cost/session | NHS 2010–11 | Health visiting services: all other services: parentcraft - group MaPGan01, national average unit cost = £47 |
Average duration of antenatal class is between 12 and 16 hours. Assume if ‘YES’, participation to the entire course; if ‘only went to some of the classes’ assume participation to half of the classes |
| GUS | Receive breastfeeding advice from health visitor/midwife/National Childbirth Trust etc | Cost/contact | PSSRU 2011 | Health visitor £43 (with qualifications, average face to face mean average cost) | Assume 1 contact |
| GUS | Took part in support-community programmes (PPP, mellow parenting) in the past 12 months | Cost/contact | NHS 2010–11 | Health visiting services: all other services: parentcraft - group MaPGan01, national average unit cost = £47 |
Assume 1 contact |
| GUS | Use of web-based helping services (Mumsnet, Facebook, Bebo, ivillage) | Cost/contact | NHS 2010–11 | Health visiting services: all other services: parentcraft - group MaPGan01, national average unit cost = £47 |
Assume 1 contact |
| GUS | Use of childcare (COST) | Cost/week or/month | Self-reported | ||
| GUS | Frequency grandparents help/look after the child/babysitting every day or almost every day > 2: at least once a week > 3: at least once a month > 4: at least once every 3 months > 5: less than |
Cost/month | ONS | £6.08 an hour, ONS statistics about minimum wage | Assume lower value in each category (e.g. at least one a month = once a month) |
| SMR01 | Hospital stays (child) – length of stay, detailed by specialty, HRG, facility | Count | Scottish ISD costs R040 | Cost/bed/day provided by specialty | |
| SMR02 | Abortion | Cost/intervention | NHS 2010–11 | £1327, MA20Z (medical or surgical termination of pregnancy, 20 weeks or more), average cost | The variable distinguishes between different types of abortion; assume average cost |
| SRM02 | Antenatal steroids | Cost/tot dose | BNF | £564.48 (bethamethasone) £120.94 (dexamethasone) |
The variable considers different kinds of antenatal steroids; assume the most used ones (bethamethasone and dexamethasone) |
| SMR02 | Type of delivery mode of delivery (Baby 1, 2, 3) 0 Normal, spontaneous vertex vaginal delivery, occipito-anterior 1 Cephalic vaginal delivery, with abnormal presentation of the head at delivery 2 Low forceps – no rotation, forceps NOS (including Wrigleys) A Mid-cavity forceps – no rotation (including Haig-Fergusson, Neville Barnes, etc) B Rotational forceps (including Kiellands) C Ventouse – no rotation or unspecified D Ventouse with rotation E Other forceps delivery (includes ‘high-cavity’ high forceps) 5 Breech delivery, spontaneous, assisted or unspecified partial breech extraction 6 Breech extraction, NOS. Version with breech extraction 7 Elective (planned) caesarean section 8 Emergency and unspecified caesarean section 9 Other and unspecified method of delivery |
Cost/intervention | NHS 2010–11 | 0: NZ11A normal without cc £1192 1, 5: NZ11B normal with cc £1751 2, A, B, C, D: NZ12B assisted delivery without cc £1621 7: NZ13Z planned lower uterine c-section £2623 8: NZ14Z emergency or upper uterine cs without cc £3239 |
|
| SMR02 | Resuscitation | Cost/intervention | NHS 2010–11 | £1186 neonatal care intensive | |
| SMR02 | Induction of labour 0 None 1 Artificial rupture of membranes (ARM) 2 Oxytocics 3 ARM + oxytocics 4 Prostaglandins (includes cervical priming) 5 Prostaglandins + ARM 6 Prostaglandins and oxytocics 7 Prostaglandins and ARM and oxytocics 8 Other 9 Not known |
Cost/intervention | NHS 2010–11 | To be used in combination with type of delivery if type of delivery is normal/assisted: normal with induction, with cc £2306 normal with induction, with/out cc £1594 assisted with induction, with cc £2781 assisted with induction, with/out cc £2116 |
|
| First Visit | Average cost of visit (information on medical practitioner involved in the visit) | Cost/visit | PSSRU 2011 | Mean average cost of a face-to-face visit with health visitor £43 | |
| First Visit | Vitamin K given | BNF | 4.71 | ||
| First Visit | BCG vaccine | Cost/dose | PSSRU 2011 | NHS reference costs for children’s health services, community nursing service, national average, vaccination programmes (£82) | Overlapping with SIRS database |
| 6–8 weeks | Average cost of visit (info on medical practitioner involved in the visit) | Cost/visit | PSSRU 2011 | Mean average cost of a face-to-face visit with health visitor £43 | |
| Vitamin K given | BNF | 4.71 | |||
| 27–30 weeks | Cost of visit (medical practitioner nurse, staff nurse, other) and place of visit (home, clinic, GP practice) reported | Cost/visit | PSSRU 2011 | GP £66 per patient contact lasting 17.2 minutes HV £47 with qualifications (average face-to-face mean average cost) Nurse – GP practice 40/hour for average contact lasting 15.5 minutes, qualified Nurse – other location different than GP practice, community nurse £39 mean average cost for a face-to-face contact page 183 |
|
| Recall | Cost of visit | Cost/visit | PSSRU 2011–16 | 2011: mean average cost of a face-to-face visit with health visitor £43 2012: mean average cost of a face-to-face visit with health visitor £44 2013: mean average cost of a face-to-face visit with health visitor £47 2014: mean average cost of a face-to-face visit with health visitor £51 2015: mean average cost of a face-to-face visit with health visitor £54 2016: health visitor cost not reported – use previous year value (inflated) |
|
| Hearing screening | Cost of visit | Cost/visit | NHS 2010–11 | Audiological services: neonatal screening £32 | |
| Vision screening | Cost of visit | Cost/visit | NHS 2014–15 | Paediatric ophthalmology, outpatient £121 (average) | |
| Dental visits | Cost of visit | Cost/visit | Dentist fee reported in the dental database | ||
| SIRS | Dummy (took vaccine; age in days) | Cost/dose + administration cost | BNF | Average cost vaccinations within 10 months £358.15; £601.59 (6 years). Own calculations |
List of abbreviations
- A&E
- accident and emergency
- AE
- all eligible
- BD
- breastfeeding duration
- BI
- breastfeeding initiation
- CCA
- cost-consequence analysis
- CEA
- cost-effectiveness analysis
- CHSP
- Child Health Systems Programme
- CSO
- Chief Scientist Office
- E
- eligible
- GUS
- Growing Up in Scotland
- HSV
- Healthy Start voucher
- ICER
- incremental cost-effectiveness ratio
- IFS
- Infant Feeding Survey
- IMD
- Index of Multiple Deprivation
- ITT
- intention-to-treat
- MIDAS
- Management Information & Dental Accounting System
- MRC
- Medical Research Council
- NE
- nearly eligible
- NEs
- natural experiments
- NS-SEC
- National Statistics socio-economic classification
- PHI
- public health intervention
- PPI
- patient and public involvement
- PSM
- propensity score matching
- PSS
- Personal Social Services
- R
- recipient
- RCT
- randomised controlled trial
- RD
- regression discontinuity
- SD
- standard deviation
- SF-12
- Short Form questionnaire-12 items
- SIMD
- Scottish Index of Multiple Deprivation
- SIRS
- Scottish Immunisation & Recall System
- SMR01
- Scottish Morbidity Records General/Acute Inpatient and Day Case
- SMR02
- Scottish Morbidity Records Maternity Inpatient and Day Case
- VI
- vitamin intake
- WFS
- Welfare Food Scheme
