Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 16/57/01. The contractual start date was in February 2017. The final report began editorial review in December 2021 and was accepted for publication in June 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Moore et al. This work was produced by Moore et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Moore et al.
Chapter 1 Background
According to the most recent Office for National Statistics data, around one in six adults in Great Britain smoke tobacco. 1 Much has been achieved in reducing smoking rates, with almost half of adults reporting being smokers in 1974, when Office for National Statistics data began. Nevertheless, smoking remains a major driver of ill health and health inequalities, and continues to be a major national and global cause of preventable death. 2 Many adult smokers first took up smoking in adolescence,3 and earlier initiation is associated with greater endurance into adulthood. 4 Hence, as well as effective intervention to support smokers to quit, reducing the prevalence of smoking requires prevention of new generations from taking up smoking.
Young people’s smoking peaked in UK nations in the mid to late 1990s, coinciding with publication of the government’s Smoking Kills: A White Paper on Tobacco. 5 Subsequent decades have seen increasing regulation of the marketing of tobacco,6 as well as regulation on age of sales and legislation prohibiting smoking in public places. 7 Declines seen for smoking uptake are mirrored internationally across other outcomes, such alcohol use,8 perhaps indicating that broader social trends beyond tobacco policy have contributed to wider changes in adolescent risk behaviour. Nevertheless, as a whole, tobacco regulation has likely contributed significantly to the prolonged downwards trajectory in young people’s smoking since the 1990s. Regular smoking among secondary school-aged young people is now estimated at around 2–4%,9 while experimentation with tobacco has become a minority behaviour of which most young people disapprove. 10 Nevertheless, a substantial number of young people, particularly young people from poorer backgrounds, still leave school as smokers. 9 As UK nations move towards ambitions to become smoke free by 2030,11,12 further action is needed to support cessation among smokers, while preventing the next generation from taking up smoking.
Recent years have seen increasing attention to potential (positive and negative) effects of e-cigarettes on smoking and smoking-related morbidity and mortality. Many people argue that e-cigarettes have potential to improve public health by offering smokers a less harmful alternative, or even make smoking obsolete. 13 However, concerns have centred around whether or not the appeal of e-cigarettes goes beyond smokers, creating new generations of young people addicted to nicotine. 14 In particular, there are concerns that e-cigarettes may lead to a reversal of successes in reducing the appeal of tobacco to young people.
The emergence of e-cigarettes in the UK
E-cigarettes and smoking cessation
Invented in China in 2003, e-cigarettes entered European Union (EU) markets around 200715 and began to gain significant traction as smoking-cessation aids around 2011, with rapid growth over the next couple of years. 16 The devices themselves are rapidly changing, with early products looking very much like cigarettes. More recent changes in product design have moved away from resemblance to cigarettes, with increased popularity of tank-based devices. Many people argue that public health communities should endorse e-cigarettes as a means of helping smokers to quit the more harmful behaviour of smoking. 17,18 Although long-term health effects are unlikely to be known for some time, some studies show important acute health benefits of switching to e-cigarettes. 19 Hence, e-cigarettes, where effective as cessation aids, may play an important role in reducing mortality and morbidity. 20
UK trials have found that e-cigarettes, accompanied with behavioural support, can be more effective than nicotine replacement therapy (NRT) in supporting cessation. 21 Nevertheless, in early 2020, the World Health Organization still described evidence for the effectiveness of e-cigarettes in cessation as inconclusive. 22 More recently, a Cochrane review concluded that there was moderate-certainty evidence that e-cigarettes are effective in helping smokers to quit and, indeed, appear to be more effective than NRT. 23 Public Health England’s recent evidence update argues that evidence is now increasingly strong that e-cigarettes make a significant positive contribution to public health via supporting cessation. 24 Indeed, reflecting this rapidly advancing evidence base, in 2021, regulators set out new guidance on how e-cigarettes might be offered on prescription as a smoking-cessation aid in England. 25
Although there is emerging consensus that e-cigarettes have a role to play in harm-reduction strategies,26 there is also consensus that e-cigarettes are not harmless. 27 Many people in the public health community continue to argue for caution until more is known about the potential harms of e-cigarettes. 28,29 However, although much has been written about a binary divide between ‘enthusiasts’ who wish to harness the potential of e-cigarettes for cessation and ‘opponents’ who see e-cigarettes as a threat to young people,30 in reality, positions are often more nuanced. Many people are both enthusiastic about the role of e-cigarettes in cessation, while taking seriously the need to prevent use by children and young people. 31 For people accepting a position that e-cigarettes have a role in supporting cessation, it remains important that use is restricted to smokers or ex-smokers as a means of quitting and preventing relapse back to smoking. 32
Young people’s use of e-cigarettes
Today’s young people have grown up in an environment of falling prevalence of tobacco use, among adults and peers. However, today’s young people are also the first generation to have grown up in a time when e-cigarettes have become a major presence in UK society. 33 The growing presence of e-cigarettes has led to some concerns that e-cigarettes might lead to a new generation of tobacco-naive young people addicted to nicotine. Some concerns were expressed early in the emergence of e-cigarettes that marketing for e-cigarettes used approaches that mirror those used by the tobacco industry, targeting young people as potential new consumers. 34 Indeed, as tobacco companies have bought e-cigarette companies or developed their own products, there is increasing overlap between actors responsible for these markets. 35 E-cigarettes commonly have features that many people argue might appeal to young people, such as their colourful and often sweetly flavoured nature. 36,37
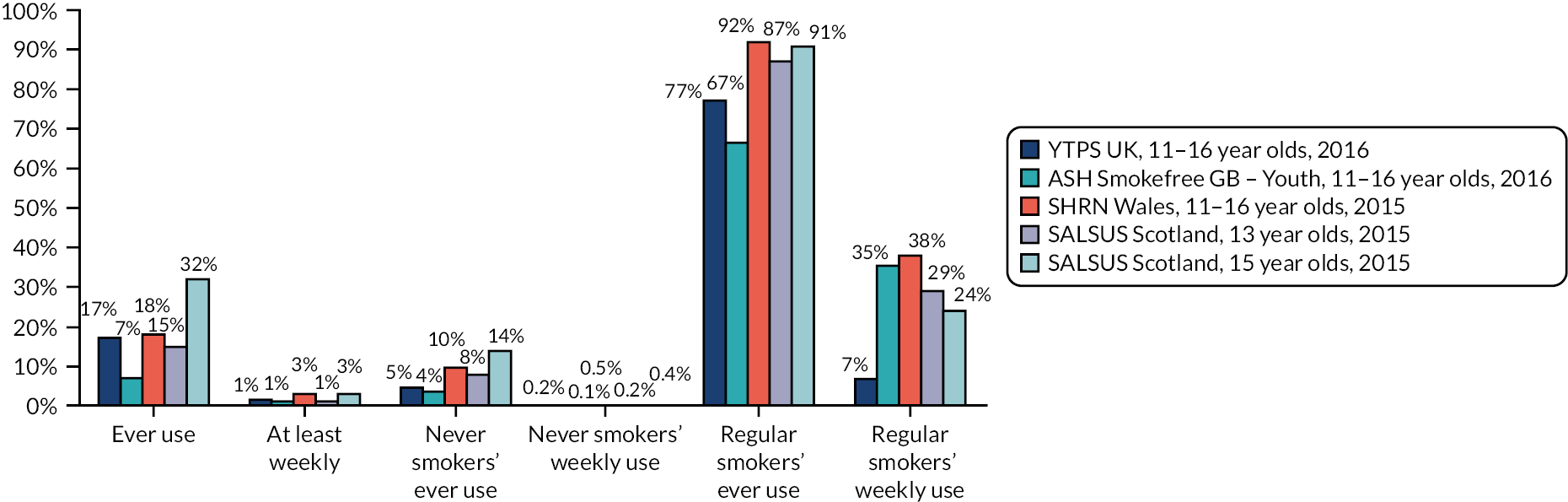
Young people’s use of e-cigarettes did not begin to be measured in UK social surveys until around 2013. Early estimates from Wales indicated that ever use of e-cigarettes was approximately equal to ever use of tobacco cigarettes, as 12% of young people had tried vaping and 12% had also tried smoking. 38 However, the proportion of young people reporting more regular use was small. Over the next 2–3 years, data accumulated from surveys across UK nations (see Figure 1), reinforcing this picture of sharp increase in experimentation with e-cigarette use, but with regular use remaining low and concentrated among smokers. 24,39
FIGURE 1.
Percentages of young people who have ever used an e-cigarette or who use an e-cigarette at least weekly, by smoking status. Reproduced with permission from Bauld et al. 39 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.
Nevertheless, rapid growth of experimentation in the early years of the emergence of e-cigarettes in the UK signalled a need for careful ongoing monitoring. Concerns that e-cigarettes may become harmful for young people centred both on potential indirect harms, via their perceived potential role in reversing successes in reducing smoking uptake, but also direct harms of use by young people who would not otherwise be smoking.
Effects of e-cigarettes on young people’s smoking uptake
There are two major hypothesis surrounding potential mechanisms through which e-cigarettes may lead to increases in young people’s smoking uptake: (1) the gateway hypothesis and (2) the renormalisation hypothesis.
The gateway hypothesis
The gateway hypothesis has a long history in drug research. The gateway hypothesis has long been debated, for example whether or not cannabis acts as a gateway into harder drug use. 40 Applying the gateway hypothesis to e-cigarette use, it is assumed that e-cigarettes might appeal to young people who would not have otherwise smoked. Therefore, these young people may then become addicted to nicotine via use of e-cigarettes, increasing vulnerability to subsequent tobacco use. 41 There is, indeed, now a very large and consistent body of systematic review-level evidence, much of which is from the UK, which finds that young people who try an e-cigarette are more likely to go onto smoke than young people who do not. 42,43 The evidence is limited by issues such as publication bias, high sample attrition and inadequate adjustment for potential confounders. Hence, it remains unclear if using e-cigarettes causally increases risk of future smoking or if this association is explained by common liability, or if both offer a partial explanation. Recent studies find that although unadjusted associations of ever e-cigarette use with subsequent smoking are large, the associations become smaller or non-significant the more common causes are adjusted for. 44 One large study in France found that among 17- to 19-year-olds, having tried an e-cigarette was associated with reduced likelihood of daily smoking, but this was moderated by age of first use, and very early experimenters who had used an e-cigarette by age 9 were more likely to become smokers. 45 Given that few non-smokers were becoming regular users of e-cigarettes while experimentation was becoming widespread, it is likely that any gateway effects which are occurring may have to date occurred on a small scale, unlikely to reverse population trends in tobacco use.
The renormalisation hypothesis
The renormalisation hypothesis, although often conflated with the gateway hypothesis, differs from the gateway hypothesis in its focuses on sociological processes around norms for tobacco use. Several decades ago, smoking was a highly normalised behaviour. 1 Smoking was a social practice adopted widely across socioeconomic groups, with non-smokers tolerant and accepting of others’ smoking. Although controversial in creation of stigma for those who continue to smoke, with this stigma falling mostly on already marginalised groups,46 much success in reducing population-level uptake of tobacco has been achieved via denormalising smoking. This denormalising has increasingly been achieved through excluding smoking from the rhythms and activities of daily life, restricting when and where smoking can take place to make tobacco an unattractive and unappealing product for non-smokers. Actions have included mandating health warnings on cigarette packs, with international evidence suggesting that these warnings can have important impacts on both cessation and uptake. 47 Smoking in enclosed workplaces was prohibited in Scotland in 2006, and elsewhere in the UK in 2007. Although implemented largely to protect hospitality workers,48 impacts on children received much attention. Plans were met with arguments that this would harm children by displacing smoking into the home, but UK and international evidence found that this was not the case, as second-hand smoke exposure and smoking in the home declined following legislation. 49,50 This legislation, recently selected by the Royal Society for Public Health (London, UK) as the greatest achievement of the twenty-first century,51 played a major role in communicating that smoking in front of non-smokers, including children, was unacceptable. It was followed by other moves, including increases in age of sales to 18 years and point of sale restrictions. Laws prohibiting proxy purchasing of tobacco sought to further restrict young people’s access to tobacco, with current arguments for increasing age of sales further to 21 years centred partly around further inhibiting the ability of young people to obtain cigarettes via older friends. 52 From 2015, bans on smoking in cars carrying children were introduced. 11
The hypothesis that e-cigarettes renormalise smoking is based around assumptions that because e-cigarettes mimic the act of smoking, their growing presence will reverse successes in denormalising smoking. 53 In support of this notion, one recent USA-based study found that greater exposure to second-hand e-cigarette aerosol in public places was associated with increased tolerance of, and susceptibility to, future smoking. 54 However, an increasing number of studies focused on whether or not smoking rates among young people increase in parallel with growing population prevalence of e-cigarettes have offered limited support for this notion. Recent international studies from Taiwan55 and New Zealand56 find that smoking rates fell as fast, or faster, during the emergence of e-cigarettes than in the preceding years. Analysis of data from the National Youth Tobacco Survey (NYTS) in the USA also indicate continuing decline in tobacco use during this period, with ever smoking declining at a faster rate post 2011, although the rate of decline in current smoking began to plateau in 2014. 57 Also using NYTS data, Foxon and Selya58 found that a counterfactual trend projected from data up to 2009 overestimated observed smoking rates from 2010 to 2018. Sokol and Feldman59 similarly found that projections of smoking rates for US 12th graders (i.e. aged 17/18 years) from Monitoring the Futures data prior to 2014 overestimated prevalence to 2018, concluding that many adolescent e-cigarette users would likely otherwise have become smokers. 59
Notions that e-cigarettes renormalise the different, but related, behaviour of tobacco smoking centre around the assumption that the behaviours are viewed by young people as sufficiently related that growth in one will renormalise the other. The extent to which this assumption is upheld may vary across contexts and may be influenced, in part, by how products are positioned in public policy and discourse. In the USA, the Food and Drug Administration include e-cigarettes as ‘tobacco products’. 60 However, given that e-cigarettes do not use tobacco, this labelling has been described as a particularly US phenomenon. 61 There is some evidence from the UK that finds that children see tobacco and e-cigarettes as distinct products. 62,63 In one study, for example, young people whose parents used e-cigarettes were most likely to perceive them as things adults use to stop smoking, with this perception of e-cigarettes as cessation aids associated with lower smoking susceptibility. 64 Hence, where perceived as stop smoking aids, others’ use of e-cigarettes might be interpreted by young people as a social display of efforts to give up smoking, rather than as an endorsement of a smoking-like behaviour.
Use of e-cigarettes among young people as an emerging public health risk in its own right
Although links between e-cigarettes and smoking have dominated debates regarding potential harms of e-cigarettes to young people, e-cigarettes themselves are unlikely to be harmless. Hence, although switching from tobacco to e-cigarettes is likely to reduce harm, taking up e-cigarette use without prior smoking introduces new potential for, as yet, unknown harms. In one recent study,65 estimates of the extent to which risk-adjusted nicotine product days decreased over time as tobacco use fell but e-cigarette use grew were described as highly dependent on assumptions regarding risks of e-cigarettes relative to tobacco. Although commonly based on animal models and, therefore, with questionable transferability, common arguments for regulating e-cigarettes to prevent young people from using them have included potential impacts of nicotine on brain development among young people. 66
As described, few young people in the UK have historically used e-cigarettes regularly, unless they are also smokers. However, in the USA, the 2018 NYTS indicated that in the space of a year the percentage of high school students reporting past 30-day use of e-cigarettes doubled to almost one in five, with more than one in four young people reporting past 30-day vaping in 2019. 67 This growth was framed widely as an epidemic of young people’s vaping,68 triggering international calls for regulation. In 2019, Hammond et al. published an influential analysis of change in young people’s smoking and e-cigarette use from 2017 to 2018, finding increases in vaping in the USA and Canada, although no growth in England. In Canada, analyses indicated that this increase in vaping was accompanied by growth in smoking. 69 In 2020, the authors published an update in which data were calibrated with external data sources, with the consequence that the previously reported increase in smoking in Canada was attenuated. Hence, although revised analysis weakened common interpretations that e-cigarettes were acting as a pathway into smoking, the analysis did signal rapid growth in young people’s use of e-cigarettes as a potential problem in its own right. Newer data from the 2020 and 2021 NYTSs indicate that rapid growth in vaping from 2017 to 2019 did quickly begin to subside. 70,71
In the context of these rising international concerns about the growth of young people’s use of e-cigarettes, concerns regarding the safety of e-cigarettes, particularly for young people, were further raised by the EVALI (e-cigarette or vaping use-associated lung injury) outbreak. 67 This was an outbreak of vaping-related lung injury, which led to a number of deaths, predominantly in the USA in 2019, attributed to the specific chemicals tetrahydrocannabinol and vitamin E acetate,72 in unregulated devices. The outbreak received intense media coverage, and one study73 found the outbreak to be associated with increased risk perceptions for e-cigarettes among English adult smokers. Following this outbreak, debate regarding potential for an epidemic of young people’s smoking in the UK intensified. 74 One group of paediatric health-care professionals, for example, wrote that with 30% of high school children in America using e-cigarettes, most of whom had never smoked tobacco, similar rates were inevitable in the UK. 75 The claim that most use was occurring among tobacco-naive young people is not borne out by reanalysis of the NYTS data, which finds that most use, particularly regular use, occurred among young people who had smoked. 76 However, this reflected growing concerns that the US epidemic would cross the Atlantic and that e-cigarette use in itself might become a commonly adopted risk behaviour among young people who would not otherwise be smokers.
E-cigarette regulation in the UK
Divergence in positions on e-cigarettes among the public health community is reflected in international approaches to regulation,77 which have ranged from highly restrictive regulation in countries such as Australia78 to more liberal approaches in countries such as the UK, where no specific regulation existed prior to 2015. Age of sales regulations for e-cigarettes were implemented in England and Wales in late 2015 and in Scotland in early 2017. In Wales, the Welsh Government’s 2015 Public Health Bill attempted to introduce legislation that would have prohibited the use of e-cigarettes in any place where tobacco cigarettes are currently prohibited. 79 This failed to pass into law after a last-minute loss of cross-party support led to a minority Labour government losing at the final stage of the legislative process. The bill returned in 2017, re-introduced by a minority Labour Government, with provisions relating to e-cigarettes removed. 80 Key arguments against including e-cigarettes alongside bans on smoking in public places have included that this may undermine quit attempts by reducing relative advantage of e-cigarettes over tobacco. 81
In the meantime, in May 2016, Tobacco Products Directive (TPD) regulations were introduced in EU member states. The TPD regulations included a broad suite of regulations for tobacco, many of which reflected tobacco control actions already implemented in the UK, with exceptions including a ban on sales of smaller packs of tobacco cigarettes and (later) bans on sale of menthol-flavoured cigarettes. 82 Article 20 was specific to e-cigarettes, and represented the first major supra-national regulation of e-cigarettes. TPD regulations prohibited cross-border advertising of e-cigarettes, with immediate effect from May 2016. Recent market liberalisation in Canada has been associated with increased marketing exposure and use of e-cigarettes among young people, with comprehensive provincial restrictions associated with lower exposure and use. 83 Hence, it is plausible that marketing restriction within TPD may act to reduce young people’s exposure and use. TPD also included a suite of regulations on the products themselves, which were to be more gradually introduced, with full implementation to be achieved by May 2017. These regulations included a mandatory warning across 30% of the packet indicating that the products contain nicotine, which is a highly addictive substance. Manufacturers are mandated to notify the Medicines and Healthcare products Regulatory Agency of intention to launch new products 6 months in advance, including notification of all product ingredients. e-cigarettes and liquids are to be sold in tamper-proof containers to include an information leaflet listing all ingredients, with nicotine strength limited to 20 mg/ml. Device refills were restricted in size. TPD regulations aligned e-cigarettes with tobacco in so far as they involve regulation under the banner of a ‘Tobacco Products Directive’, but e-cigarettes themselves are not referred to as tobacco products. There is some limited evidence that first use of flavoured e-cigarettes is associated with more persistent use among young people. 84 Hence, some EU member states went beyond mandatory requirements of TPD regulations, through introduction of flavour regulations left within TPD for individual member states to determine,77 although the UK has not to date.
The regulations were a cause of concern for the vaping community and some scientists who argued, in particular, that a reduction in nicotine strength might inhibit the usefulness of e-cigarettes as cessation devices or cause users to relapse to smoking, as the lower strength may not satisfy cravings. 85 The warning focused on the addictiveness of nicotine was found in one study86 to likely put smokers off using e-cigarettes as cessation devices. However, surveys of adult smokers, ex-smokers and vapers indicate that, after implementation, the regulations went largely unnoticed by many, with most using compliant devices while unaware that these had changed. 87 E-cigarettes remain the most popular smoking-cessation devices used by smokers and recent ex-smokers in the UK. 16 Part of the rationale for introduction of these regulations include assumptions that e-cigarettes can develop into a gateway to nicotine addiction and tobacco consumption, and that e-cigarettes mimic and normalise the act of smoking. 82 To date, however, there has been limited evaluation in the UK of (1) the role of e-cigarettes in renormalising smoking and (2) the impacts of this regulation on children and young people’s use of e-cigarettes (and tobacco).
Objectives
This report describes findings from a mixed-method natural experimental evaluation of the impacts of TPD regulations in the UK. Theoretically, we view e-cigarette regulation as an ‘event’ within a complex system88,89 that has the potential to bring about (intended and unintended) change through altering the behaviours and interactions of a diverse range of actors, including regulators, retailers, consumers and, ultimately, young people. Hence, the research first explores system history and starting points prior to regulations through examining trends in young people’s tobacco use in the lead up to regulation, addressing questions of whether or not e-cigarettes were re-normalising smoking in the lead up to implementation of TPD and exploring normative perceptions for e-cigarettes as a product in their own right. The study does this through combining quantitative analyses of trends in secondary school-based survey data in the lead up to regulation with qualitative pupil interviews, exploring perceived norms in relation to tobacco and e-cigarettes. Subsequently, interviews with policy stakeholders, trading standards officers (TSOs) and retailers are used to understand implementation processes, whereas retailer audits examine implementation fidelity. Mechanisms through which TPD regulations might achieve impact on young people’s use of e-cigarettes, and smoking, are investigated using repeated qualitative pupil interviews prior to use of before-and-after survey data to evaluate change in trend for e-cigarette use, and smoking, following TPD implementation.
Chapter 2 Methods
Material throughout the report has been adapted from the study protocol [see NIHR Journals Library www.fundingawards.nihr.ac.uk/award/16/57/01 (accessed 19 December 2022)].
Research questions
Our primary aim was to investigate the role of e-cigarette regulation, via the TPD, in influencing trajectories in young people’s use of e-cigarettes. We address the following research questions in relation to this aim:
-
Did increased regulation of e-cigarettes interrupt prior growth of young people’s e-cigarette use?
-
How did young people perceive risks and social norms surrounding e-cigarettes (and how did perceptions change over time as products become TPD compliant):
-
as a product in their own right?
-
relative to tobacco?
-
-
How did young people interpret and respond to the presence or absence of health warnings on e-cigarette packets?
-
To what extent, and in what ways, did young people continue to interact with e-cigarette marketing after the prohibition of cross-border advertising?
As a secondary aim, we also examine trends in young people’s smoking behaviour over time. This allows us to test the theoretical basis for much e-cigarette regulation, including that via the TPD, which centres on assumptions that e-cigarettes renormalise smoking. In addition, it enables us to estimate if the suite of regulation introduced in 2016 has maintained or increased the downwards trend in young people’s smoking uptake. We will address the following questions:
-
Have trajectories in young people’s ever and current smoking been significantly interrupted (positively or negatively) by growing prevalence of e-cigarettes?
-
Did the rate of decline in young people’s smoking change after additional regulation of tobacco and e-cigarettes in May 2016 (including TPD and plain packaging)?
Finally, as additional secondary aims, we explore the implementation and context of TPD regulation, including:
-
To what extent was compliance with TPD in product sales achieved, and what are the barriers to and facilitators and unintended consequences of implementation?
-
To what extent, and in what ways, did variations between UK countries in e-cigarette policy emerge during the study period?
-
What other changes to the regulatory context of tobacco and e-cigarettes occur during the study period in the UK and across individual UK countries?
Study design
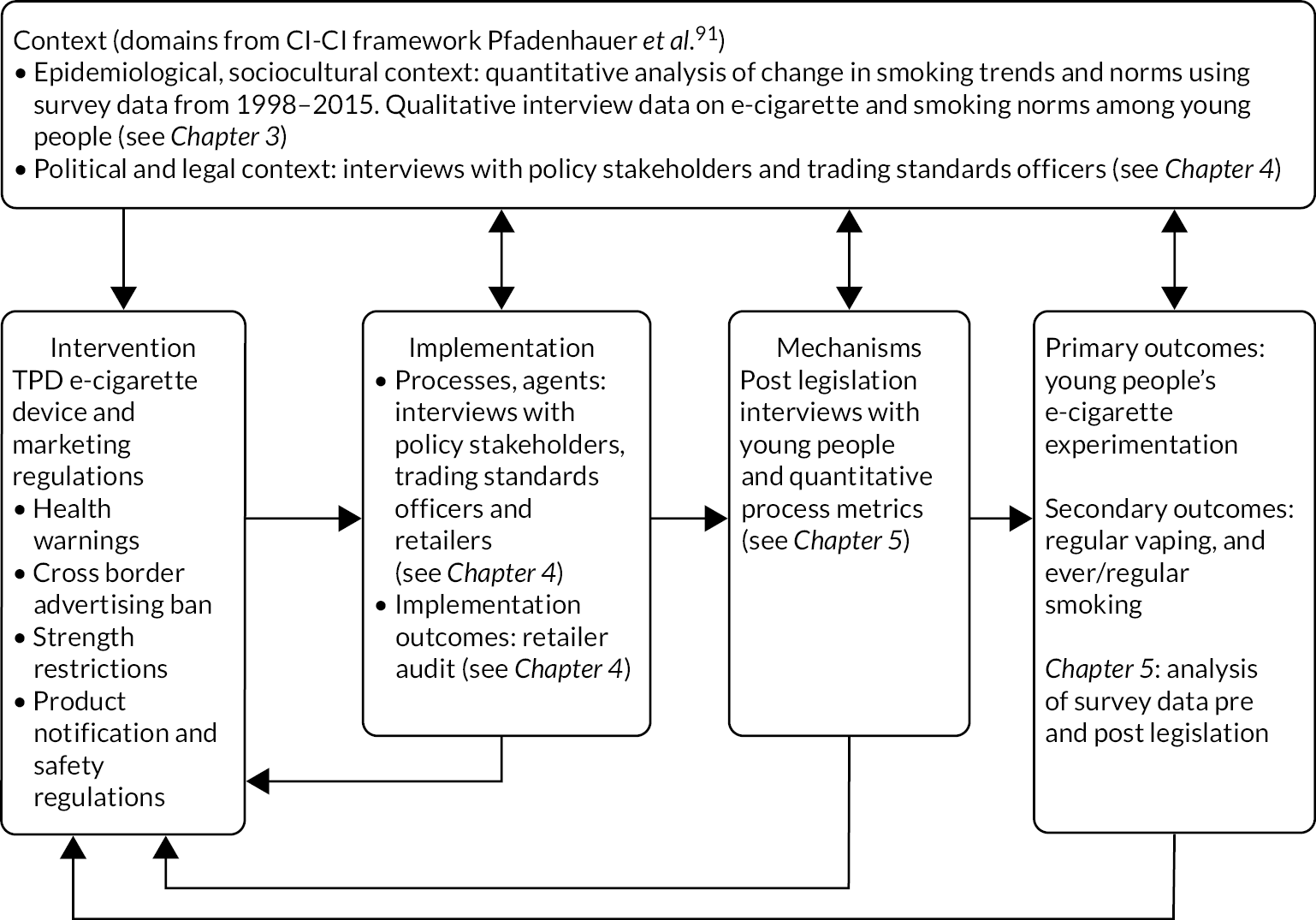
This study used a mixed-method natural experimental evaluation design to address the above research questions. The quantitative study elements drew on repeated cross-sectional secondary data from routinely undertaken surveys in Wales, Scotland and England. Study populations were nationally representative samples of secondary school-aged young people aged 13/15 years (or equivalent school years, i.e. years 9 and 11 in Wales and England and S2 and S4 in Scotland). These data were analysed alongside qualitative data from young people, policy representatives, TSOs and retailers of e-cigarettes, and retailer audits. Our overall evaluation and integration framework is presented in Figure 2, which provides an overview of how data sources are mapped onto subsequent findings chapters. Our evaluation and integration framework draws on the Medical Research Council (MRC) guidance for process evaluation90 and on the more recent context and implementation of complex interventions framework91 in framing context and implementation processes.
FIGURE 2.
Evaluation and integration framework for TPD evaluation. CI-CI, content and implementation of complex interventions. Adapted with permission from Moore et al. 90 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.
Secondary data analysis
Data sources, collection and handling
We obtained data from routinely collected school-based surveys in each UK nation. Although some of these surveys go back to the 1980s, we made an a priori decision to restrict our analyses to data sets from 1998 to 2019 because published estimates indicate that smoking rates climbed up to this point, but have followed a prolonged period of decline ever since.
Data from Wales were obtained from the Welsh Health Behaviour in School-aged Children (HBSC) survey, conducted as part of an international World Health Organization collaboration every 2–4 years,92 and the biennial School Health Research Network (SHRN) survey. 93 The SHRN survey was introduced in 2015 and was modelled on the HBSC survey, and from 2017 the SHRN survey incorporated the smaller HBSC survey as a component of it. Hence, HBSC survey data were obtained from 1998 to 2013, with SHRN survey data from 2015 to 2019. Data for Wales before 2013 were provided by the Welsh Government. SHRN and HBSC data from 2013 onwards are held by the principal investigator’s research group.
Although HBSC surveys are also conducted in England and Scotland, neither country included measures of e-cigarette use prior to TPD implementation, and these surveys are conducted only once every 4 years. Hence, in Scotland and England, we used the larger and more frequent Scottish Schools Adolescent Lifestyle and Substance Use Survey (SALSUS)94 and Smoking, Drinking and Drug Use (SDDU) survey in England. 95 In Scotland, the SALSUS is a bi-ennial, school-based survey undertaken in local authority and independent schools. E-cigarette use questions were first incorporated into the SALSUS in 2013. The UK data service includes a time series data set that provides ready-pooled data through to 2013. Our original intention was to use the SALSUS planned for 2017 and 2019 as post-TPD data sets in Scotland; however, SALSUS 2017 was postponed to 2018,and no data were collected in 2019. Hence, we integrated measures from the 2015 and 2018 data sets into the time series data set, providing only one post-TPD survey for Scotland. In England, the SDDU survey was conducted annually until 2014, but then moved to a bi-ennial cycle. Measures of e-cigarette use were included in the SDDU survey from 2014. The SDDU survey shares substantial overlap with the SALSUS, including use of similar measures of smoking and e-cigarette use. Data sets from 1998 to 2018 were obtained via the UK data service. Data files were combined into a single data set and stored on a secured network at Cardiff University. The Cardiff University-owned Welsh data will be retained, and models updated with newer data following completion of this study. Terms of use for the third party-owned data sets require these data to be deleted following completion of the use period, currently the end of 2022.
Sample sizes and response rates
Table 1 provides sample sizes by country and survey year, overall and for the target age group. Survey response rates, where available, are presented in Appendix 1, Table 19. These data indicate a gradual decline in response rates over time in Scotland (from 70% in 1998 to 52% in 2018), and a much larger decline in England (from 70% to 22%). However, there was recent growth in response rates in Wales, with the 2019 SHRN survey achieving a response rate of 77%.
| Years | Wales: HBSC/SHRN | Scotland: SALSUS | England: SDDU | |
|---|---|---|---|---|
| Target year groups sample (school year) | Target age groups sample (age) | |||
| 1998 | 2716 | 1737 | 1975 | 2174 |
| 1999 | 3629 | 3856 | ||
| 2000 | 2321 | 2376 | 2764 | 3003 |
| 2001 | 3600 | 3917 | ||
| 2002 | 2641 | 23,090 | 3758 | 4162 |
| 2003 | 4040 | 4443 | ||
| 2004 | 2755 | 7062 | 3701 | 4102 |
| 2005 | 3592 | 3916 | ||
| 2006 | 2882 | 23,180 | 3193 | 3587 |
| 2007 | 3079 | 3458 | ||
| 2008 | 10,063 | 3019 | 3381 | |
| 2009 | 3558 | 3010 | 3365 | |
| 2010 | 37,307 | 2877 | 3172 | |
| 2011 | 2549 | 2869 | ||
| 2012 | 3029 | 3364 | ||
| 2013 | 3505 | 33,685 | 2067 | 2282 |
| 2014 | 2443 | 2782 | ||
| 2015 | 11,817 | 25,304 | ||
| 2016 | 5523 | |||
| 2017 | 39,212 | |||
| 2018 | 23,365 | 5942 | ||
| 2019 | 43,404 | |||
Study measures
E-cigarette use
In Wales, young people were asked if they had ever tried e-cigarettes, with options of never, once or more than once. Young people who selected ‘more than once’ were asked how often they currently use e-cigarettes (with options of, I don’t, less than weekly, at least weekly or daily). In Scotland and England, young people were asked to select a single option from a list of statements, which included they had never tried e-cigarettes, had used e-cigarettes once or twice, have used them in the past but don’t now, use e-cigarettes now but less than once a week, or use e-cigarettes now at least once a week. In all cases, a binary variable of ever use was created, which compared ‘never’ responses with all others. A regular (at least weekly) use measure was derived by classing all young people who selected options of weekly or more as regular users.
Smoking
In Wales, young people were asked at what age they first engaged in a range of risk behaviours (including smoke a cigarette) and were instructed to select the never option if there was something they had never done. Options included ‘never’ and ages from 11 to 16 years. A second question asked young people how often they currently smoked (with options of I don’t, less than weekly, at least weekly or daily). In Scotland and England, young people were asked to select a single option from a list of statements, which included they had never tried smoking, had tried smoking only once, used to smoke but don’t now, smoke but less than once a week, smoke between one and six cigarettes a week or smoke more than six cigarettes a week. In all cases, a binary variable of ever use compared ‘never’ responses with all others. A regular (at least weekly) use measure was derived by classing all young people who selected options of at least weekly or more as regular users.
Smoking attitudes
The acceptability of smoking is measured in both the SALSUS and SDDU survey via a question asking young people whether or not they think it is OK for someone their age to try smoking a cigarette to see what it is like. In the SDDU survey, young people were also asked whether or not it was OK for someone their age to smoke cigarettes once a week. Response options for both questions were: ‘it’s OK’, ‘it’s not OK’ and ‘I don’t know’. Responses of ‘I don’t know’ were combined with ‘it’s not OK’ to create a binary variable (sensitivity analyses combining ‘don’t know’ with ‘it’s OK’ showed similar trends over time). This item was used as an indicator of the plausibility of change in trend for smoking being caused by the mechanism of smoking renormalisation (see Statistical analysis of survey data).
Cannabis use
In SALSUS, young people were presented with a grid listing a range of drugs, including cannabis, and were asked which, if any, they have ever used. In the HBSC survey, young people were asked how many times they have used cannabis in their lifetime (response options: never, once or twice, three to five times, six to nine times, 10–19 times, 20–39 times and ≥40 times). In the SDDU survey, young people were asked if they had ever tried cannabis, with response options of yes or no. A binary variable indicating whether or not young people had tried cannabis was derived, with any response other than never (or no) classed as ever use. This item is used to examine whether or not any change in trend observed for tobacco use is specific to tobacco use (see Statistical analysis of survey data).
Alcohol use
Both the SALSUS and SDDU survey asked young people whether or not they had ever had a proper alcoholic drink. Since 2002, the HBSC/SHRN surveys asked young people at what age they first did a list of things, including drinking alcohol, with response options of never, and ages from 11 to 16 years. All responses other than never were classed as indicative of ever drinking. A binary variable was derived to distinguish between ever and never use of alcohol. This item is used to examine whether or not any change in trend observed for tobacco use is specific to tobacco use (see Statistical analysis of survey data).
Energy drinks
From 2013, in the HBSC survey, students in Wales were asked how often they drank energy drinks (response options: ‘never’, ‘less once a week’, ‘once a week’, ‘2–4 days a week’, ‘5–6 days a week’, ‘once daily’ or ‘more than once daily’). A binary variable was created to distinguish students who ever used energy drinks from students who never used energy drinks. This item is used to examine whether or not any change in trend observed for e-cigarette use is specific to e-cigarette use (see Statistical analysis of survey data).
Time and intervention variables
Time and intervention variables differed across analyses because of differences in data availability and granularity. In each case, time was coded as a continuous variable, starting at 0 at the start of the time series and increasing by 1 point per unit of time (using ‘month’ as unit of time in our primary statistical analysis of e-cigarette use in Wales, and ‘year’ as unit of time in three country analyses of smoking trends over time). Quadratic terms were generated by squaring time variables. For analyses of change in smoking outcomes following the emergence of e-cigarettes, we use a ‘level’ variable coded 0 for the baseline period 1998–2010, and 1 within the period from 2011 to 2015. Although not an ‘intervention’, the analytical approach of examining change in level and trend following the emergence of e-cigarettes follows a similar format to the evaluation of our intervention of interest (i.e. TPD). The period of 2011–15 was chosen because survey measures in the UK began to identify e-cigarette use among adult smokers from 2011, which grew rapidly from 2011 onward. 16 We used a ‘post-slope’ variable coded 0 through the baseline period and sequentially from 1 to 5 through the period 2011–15. For our analysis of e-cigarette use, using Welsh data that were broken down by month, we used a ‘level’ term coded 0 prior to May 2016, coded 1 from May 2016 onwards and a ‘post-slope’ term coded 0 prior to May 2016, increasing by 1 point per month from the intervention point onwards. For analyses of post-TPD changes in tobacco smoking, level and post-slope variables were coded 0 prior to 2016 and 1 thereafter, and sequentially coded 1 onwards from 2016 to 2019. In simpler analyses of data for which few time points were available, time is analysed as a categorical variable (see Statistical analysis of survey data).
Sociodemographic information
In all surveys, young people were asked to indicate their gender. Historically, this question has been asked as a binary variable, which asks young people to indicate whether they consider themselves to be a boy or a girl. In SHRN in 2019, following consultations with policy and practice stakeholders and young people, a response option of ‘neither option describes me’ was provided. However, as data on young people identifying as neither male nor female are available only at one time point, our analysis of change over time is limited to young people identifying as a boy or girl. The percentage of students selecting ‘I do not want to answer’ to the question on gender was reduced (relative to 2017) by an amount equivalent to the percentage of young people selecting the new ‘neither option describes me’, suggesting that young people selecting this option were more likely to previously have declined to answer. 96
School year was used as a proxy for age, with years 9 and 11 in England and Wales and S2 and S4 in Scotland used to represent young people aged 13 and 15 years, respectively. However, from 2016, the SDDU data set removed pupil year group because of concerns regarding potential deductive identification of individual children outside the expected school year for their age. Pre-legislation analyses were complete prior to this data set being obtained. Hence, in analyses using data from 2016 onward only, a variable for age rather than school year is used throughout the time series in England (i.e. ages 13 and 15 years).
For Wales, socioeconomic status (SES) was measured using the Family Affluence Scale (FAS),97 which, from 2013, comprised six items measuring car, computer and dishwasher ownership, bedroom occupancy, number of household bathrooms and prevalence of family holidays. An overall measure of family affluence is computed via summation of individual item scores (with higher scores reflecting greater material affluence). However, although consistent from 2013 to 2019 (i.e. the time period for our primary statistical analysis of change in e-cigarette use), this scale has changed over time as material products lose their ability to differentiate between socioeconomic groups and is problematic as an indicator of affluence over time for the period 1998–2019. To help assess inequality over time with HBSC/SHRN data in analyses beginning prior to 2013, a relative measure of SES was used, whereby the sample was divided into ‘high’ and ‘low’ affluence, regardless of the content of the FAS in any given year. SES was measured by free school meals entitlement in England from 1999 to 2014 (the SDDU survey also switched to use of FAS from 2016 onward) and in Scotland from 2006 to 2013. For Scotland, a measure of SES indicated by the Scottish Index of Multiple Deprivation (reported in quintiles) was available between 2006 and 2018. Items on ethnicity were introduced into HBSC from 2009/10. The SDDU survey provided data on ethnicity for most survey years, although no measures of ethnicity were included in most SALSUS data sets.
Statistical analysis of survey data
Analyses were based on a statistical analysis plan agreed with our Study Steering Committee in advance of data sets being combined for analysis. Analyses completed at each stage of the study were presented to the committee prior to submission for publication. Although our primary aim was to evaluate impacts of TPD, analyses are described (and presented) in the order in which they were undertaken, in line with our overall evaluation and integration framework (see Figure 2), including analyses of:
-
trajectories in young people’s smoking before and after the emergence of e-cigarettes (but prior to TPD)
-
change in young people’s e-cigarette use following the implementation of TPD
-
change in trend for young people’s smoking following the 2016 suite of tobacco control legislation.
As described in our evaluation and integration framework in Figure 2, our analysis of trends in young people’s smoking prior to TPD is conceived as an element of our process evaluation, in that this provides an understanding of the epidemiological context into which intervention was introduced. This analysis is, however, described in this section to limit repetition due to methodological similarity with our primary statistical analysis.
Young people’s tobacco cigarette smoking before and after the emergence of e-cigarettes
Percentages and confidence intervals (CIs) of ever and regular smoking are presented for each outcome by year, country, age and sex. Binary logistic segmented regression analyses98 were then used to estimate change in smoking level and trends (post slope) during the emergence of e-cigarettes, relative to secular baseline trends, using the time, level and post-slope terms described in Study measures. The analysis was modelled on a similar approach used by Katikireddi et al. 99 to examine change in trend for young people’s smoking following smoke-free legislation (using many of the same data sets), with two main differences. Although Katikireddi et al. 99 conducted linear regression analyses of aggregated estimates, we had access to, and hence analysed, individual participant survey data. Furthermore, although Katikireddi et al. 99 used estimates dating back to the 1980s (see Katikireddi et al. 99 for a full list of historical data sets earlier than the cut-off point selected for this study), including a quadratic term to account for non-linearity, given that smoking rose until the mid-1990s, we limited our analyses to 1998 onward because of the continued decline in young people’s smoking from this date. Individual survey data on smoking from 1998 to 2015 for each of the three countries were used, with 2010 treated as the end of the baseline period and compared with the period 2011–15 (see Study measures). Country was included as a covariate, modelled as a set of dummy variables, and analyses were adjusted for gender and age. These analyses were conducted, presented to our Study Steering Committee and submitted for publication10 prior to obtaining post-legislation data sets.
Models were repeated for a secondary outcome of attitudes towards smoking (available from Scotland and England only). According to theories of renormalisation, e-cigarettes drive re-growth in young people’s smoking by increasing the extent to which young people see smoking as a normative behaviour. Analyses of attitudes towards smoking (i.e. the extent to which young people thought it was ‘OK’ for young people to smoke) provided evidence on plausibility of any change in trend (post slope) for smoking being causally driven by this hypothesised mechanism. For our primary statistical analysis, we were asked by the Public Health Research (PHR) Funding Committee to include falsifiability analyses, in line with the Bradford Hill criterion for causal inference of ‘specificity’. 100 The falsifiability analyses involve modelling the same time series for related variables, which would not be expected to be altered by the exposure. Hence, following discussions with our Study Steering Committee prior to undertaking analyses, changes in trend for ever alcohol and cannabis use were also modelled to test whether any break in trend observed for tobacco use was unique to smoking or reflective of wider trends in young people’s substance use behaviours.
Although our a priori analysis plans for trends in smoking assumed linearity in the relationship between time and smoking behaviours, visual inspection indicated some evidence of a quadratic trend. Hence, consistent with similar analyses on change in young people’s smoking following smoke-free legislation,99 a quadratic time variable was included to account for non-linearity in the data. Both linear and quadratic models are presented, and models including the term treated as the final model. We also handled non-linearity through a post-hoc sensitivity analysis, which limited the baseline period to 2001–10, a period during which there was no statistical evidence of departure from a linear trend for smoking outcomes, for our main models. As additional sensitivity analyses, we ran our pre-legislation models (1) for England only (the country with the largest number of data points for pre-legislation analysis) and (2) excluding SALSUS rounds conducted at a different time of year to the rest of the data series (i.e. 2002–6). Given that later analyses also switched to use of age rather than year group for England, as described, we also re-ran our main pre-legislation models using this new age classification.
To estimate change in young people’s e-cigarette use following Tobacco Products Directive regulations
Percentages and 95% CIs for ever and regular e-cigarette use are presented by year, school year/age, gender and country. Trends are presented graphically, with estimates for each country plotted on a single graph to enable comparison of trends over time by nation. Segmented regression analyses were then used to formally test changes in the prevalence of ever e-cigarette following TPD implementation, using monthly measures of time, level and post slope (see Study measures). Models were adjusted for age and gender. Quadratic terms were not significant in models for e-cigarette use and so were not included. As TPD regulations were brought in gradually with a 1-year transitional phase, we anticipated that change in trend is more likely than immediate change in level. Indeed, for a public health problem with a rising baseline trajectory, whether or not an intervention is able to reverse, or at least slow, growth in young people’s e-cigarette use is of greater interest than whether or not an intervention causes a stepped disruption followed by a return to growth. Hence, we present changes in level and trend (post slope), focusing primarily on the latter.
In segmented regression analyses, there are trade-offs between long- and short-term analyses, in that longer-term analyses will have more power, but passage of time also increases the likelihood of changes being caused by other events. 98 Hence, we model both short- (to 2017) and long-term (to 2019) changes in level and trend, and attend to similarities and differences between short- and long-term models. Models were implemented for the short-term post-implementation data (2013–17), presented to our Study Steering Committee in June 2019 and were submitted for publication before long-term data were available. Following peer review and publication of short-term effect models,101 these models were replicated and extended using the same syntax once longer-term data were available, and were presented to our Study Steering Committee in November 2020. Short-term models were constructed by a second analyst who covered a period of maternity leave for the study’s lead analyst and, hence, the lead analyst fully reproduced short-term models prior to extending them.
This analytical procedure was replicated for energy drink use in Wales to evaluate whether or not any change in level or trend was specific to e-cigarettes or replicated on an unrelated outcome. Energy drink use was selected as an example of another psychoactive substance that, like e-cigarette use, was relatively new and not following the secular decline observed among other substances, such as tobacco and alcohol use.
Although data sets in Scotland and England provided insufficient data points for more fine-grained segmented regression analyses, we use the data sets to evaluate whether trends observed within our primary statistical analyses are specific to the Welsh data or are mirrored in the data from other nations. Data from England provided one pre-TPD time point (2014) and two post-implementation time points (2016 and 2018), whereas Scottish data provided two pre-implementation time points (2013 and 2015) and one post-implementation time point (2018). Binary logistic regression models were constructed in each nation examining change over time in ever use of e-cigarettes, using the time point closest to TPD implementation as the reference category. These analyses were also conducted for our secondary outcome of regular e-cigarette use (including in Wales, where regular use was not measured until 2015).
Models using only Welsh data were adjusted for school-level clustering, but this was not possible in other data sets, as most data sets did not include school identifiers.
For our primary statistical analyses of ever e-cigarette use in Wales, we observed that in models stratified by ever smoking status, changes in trend were both of greater magnitude than for the whole group models (i.e. models including all eligible participants). We hypothesised that this may have been because ever smoking acted as a time-varying confounder. Hence, as an additional data-led post-hoc analysis, we included a term for ever smoking in whole group models, which increased the estimate of change in trend. As this was an unplanned post-hoc analysis, we refer to models without this term as our primary statistical analyses, but report the model with additional adjustment. Although our analyses were limited to 13- and 15-year-olds for comparability with nations where only these year groups are surveyed, we also ran our analysis of ever e-cigarette use for the whole Welsh sample (i.e. for 11- to 16-year-olds) as a sensitivity analysis.
To estimate post-intervention change in young people’s smoking uptake
Given the longer time series available for the secondary outcomes of ever and regular tobacco smoking, analyses involved repeating and extending models constructed to estimate pre-legislation changes in trend, with additional level and post-slope terms with 2016 as the intervention point (see Study measures). Although we aimed to analyse the same outcomes as included in pre-legislation analysis, changes in data collection schedules for some surveys and changes to question wording for some outcomes meant that fewer data were available for this analysis than had been hoped. Analyses are, therefore, limited to outcomes present in all five post-legislation data sets.
Additional analyses
Whole sample models were visually represented to aid interpretation, using plots of predicted probabilities over time, estimated following model execution in Stata® (see Report Supplementary Material 1, Figures 1 and 2). For each objective where data were available across data sets, subgroup effects were examined for gender, age/school year, SES, ethnicity and smoking status. The subgroup effects differ between analyses because of data availability. An additional data source held by the research team was the Youth Tobacco Policy Survey (YTPS) (principal investigator: AMM). These data were not integrated into our main analyses because of small numbers in the target age groups and the limited number of data points. However, the YTPS data provide an additional source of external data for triangulation of our findings. Time trends in the prevalence of our main study outcomes in the YTPS from 2002 to 2016 are presented in Appendix 2, Figures 10 and 11.
Procedure for dealing with missing data
The main outcomes for each of our objectives were available for ≥95% of respondents. For our overall primary outcome (i.e. ever e-cigarette use), data were available for 95% of young people, whereas 97–98% of young people were included in the final analytical samples for tobacco use. Hence, no imputation was undertaken, and analyses are based on complete cases.
Weighting
There is inconsistency within surveys over time in whether or not weighting is used to ensure national representativeness. Weights were included in data sets from 2006 in Scotland, 2009 in Wales and 2010 in England. In Wales, following movement from a sample to a whole population survey, weights were no longer used after 2013. Weights are calculated on the basis of the composition of the samples as a whole; however, in England and Wales, our analyses focuses on subsets of available data to harmonise age groups across countries. In plots of smoking prevalence trends over time using weighted (where available) and unweighted data, differences between these were barely discernible. Hence, for tobacco use models, we ran analyses using unweighted data, re-running whole group models with weights applied where available, as a sensitivity analyses. Survey weights were available in Scotland and England (but not Wales) for all surveys since first measurement of e-cigarette use. Hence, whole group and subgroup analyses for e-cigarette use in England and Scotland are presented with and without weights.
Software
All statistical analyses were undertaken in Stata/SE 15.0.
Process evaluation
Drawing on MRC guidance for process evaluation,90 we conducted an in-depth process evaluation focused on key uncertainties in causal logic for the TPD regulations, in relation to implementation, mechanisms and context. The evaluation included (1) qualitative interviews with young people aged 14–15 years, during the transitional phase and after full implementation of TPD regulations; (2) observation of compliance with TPD regulations in e-cigarette retailers, conducted at the same time as pupil interviews; and (3) interviews with policy stakeholders, TSOs and retailers on the context, implementation and perceived unintended consequences of the TPD regulations. In consultation with our patient and public involvement group Advice Leading to Public Health Action (ALPHA), a small number of items on potential mechanisms through which TPD might impact young people’s e-cigarette use were developed for inclusion in 2017 and 2019 SHRN surveys to enable triangulation of qualitative data on post-legislation change in these mechanisms. Process evaluation data collection materials are provided in Appendix 3.
Qualitative interviews with young people
School sampling
Although it was not possible to interview young people prior to legislation, which came into force before the study began, we aimed to interview young people as early as possible before the date of full compliance and then again 1 year later. Collecting data both during the transitional period and after full implementation of the TPD regulations enabled us to understand perceptions in relation to a context where unregulated e-cigarettes were, or were not, legally available for sale on the UK market. Our aim was to recruit 12 schools overall to provide representation of (1) schools in each of the three countries, (2) high, low and medium SES schools (as indicated by free school meal entitlement) and (3) urban and rural locations (which was a larger number than the six we had originally proposed, but followed a request from the PHR Funding Committee to expand this). However, contracting and ethics approval were not in place until March 2017, limiting time for recruitment. Hence, nine schools agreed to participate and data collection was completed within seven schools, including a total of 76 young people. The risk of low recruitment was anticipated in our protocol, given the time frame in which these were undertaken, and we indicated that should our intended level of recruitment not be achieved in the first round of data collection, then further schools would be recruited for post-legislation interviews in 2018 to provide a broader set of perspectives. Hence, in 2018, we returned to schools that participated in the first round and recruited a number of additional schools for post-implementation interviews only to provide a broader range of perspectives. We conducted post-implementation interviews in 11 schools. One original school was unable to take part in phase 2, with 62 of the same young people within six of these schools completing follow-up interviews in 2018. A further 86 young people participated in interviews at phase 2 only. Our intention was to complete follow-up interviews by Easter 2018 to reduce conflict with exams, but our planned data collection period coincided with university strikes and a period of extreme weather, including closures of schools (and in some cases universities) due to snow occurring in all three sites simultaneously, leading to challenges rescheduling school visits. Hence, data were collected between February and May 2018. Schools received a payment of £100 per data collection as compensation for administrative time supporting data collection.
Pupil sampling
We aimed to conduct four group interviews in each participating school, with three to five young people (aged 14–15 years when recruited, corresponding to Year 10 in England and Wales, and S3 in Scotland) in each group. To maximise rapport and interaction between young people within groups, we worked with school staff to identify groups of friends for interviews. Although smoking rates have historically been higher among girls, with convergence in genders in recent years, the opposite was true of e-cigarettes, which were becoming more popular among boys. Hence, we conducted single-gender group interviews, and sampled young people from higher- and lower-ability classes within secondary schools. Given that normalisation processes are driven as much by the reactions and behaviours of the majority who do not engage in a given behaviour as by the minority who do, we did not explicitly attempt to recruit young people who did smoke, or who were at high risk of smoking, or used e-cigarettes. We advised teachers of this in advance so that they did not use pupil smoking and vaping behaviours as criteria for selection.
Interview schedules
Semistructured interview schedules explored young people’s perceptions of e-cigarettes, tobacco and the inter-relationship between the two, with an emphasis on normalisation and elements of TPD theorised as likely to influence young people’s perceptions, including marketing and product-labelling. Interviews focused primarily on perceptions of tobacco and e-cigarettes among their peer group, rather than young people’s own use of e-cigarette and tobacco use. Topics included perceptions of social norms for e-cigarettes and tobacco use, including norms among their peer group and perceived parental reactions to tobacco and e-cigarettes, exposure to and perceived responses to advertising for e-cigarettes, and risk perceptions for tobacco and e-cigarettes, including views on elements of the TPD regulations, such as warnings about nicotine.
Data collection
Interviews were held on school premises during school time. Data collection was undertaken by research staff with prior experience of data collection with young people in education contexts. Researchers without this prior experience were accompanied by experienced staff in initial data collections. Interviews were recorded on a handheld digital recorder and uploaded to a secure university server at the earliest opportunity before being deleted from the recorder.
Retailer audits and interviews with professional groups
Retailer audits
We audited approximately 10 e-cigarette retailers in each country on two occasions to assess the availability of TPD-compliant/non-compliant products during and after the transitional phase. Audits were conducted at times coinciding with qualitative pupil interviews to put in context the extent to which unregulated products remain available during initial interviews conducted during the transitional phase, where non-compliant products could still legally be sold, and the extent to which fuller compliance was achieved by follow-up interviews after full compliance is expected. Our intention was that two observers independently estimate the proportion of e-cigarettes on sale in each location that have compliant labelling at each time point to enable assessment of interobserver agreement; however, because of a miscommunication in one nation, only one observer undertook each observation. Hence, estimates of interobserver agreement are based on the remaining two nations. Locations were sampled purposively to include large and small mixed retailers (e.g. supermarkets and newsagents), specialist e-cigarette shops and street vendors. Retailers sampled included any near the schools in which qualitative interviews were undertaken, and included supermarkets, specialist e-cigarette vendors, convenience store/newsagents and garages. Observations were ‘covert’ in so far as researchers did not voluntarily identify themselves as researchers to the store staff. However, researchers carried an information sheet with contact details for the study team, which was made available to any staff who asked the researchers what they were doing. Researchers were to leave the store if asked to do so.
Interviews with retailers, policy stakeholders and trading standards officers
We conducted interviews with 27 e-cigarette retailers after the final date for full compliance. Although audits included an approximately even split of retailer types, we anticipated that specialist e-cigarette retailers would provide more rich information on the implementation of TPD and regulation of e-cigarettes. Hence, two-thirds of interviewees were specialist retailers and one-third were non-specialist retailers. Interviews were conducted either by telephone or at the interviewee’s place of work. Interviews were conducted between June and November 2018, approximately 2 years after the initial implementation date for the TPD regulations (and 1 year after the date for full compliance).
We conducted interviews with 12 policy representatives and 13 TSOs across the three nations to explore perspectives on e-cigarettes, as well as barriers to and facilitators of implementing the legislation. Policy representatives were recruited through the team’s existing links with UK governments, public health agencies, non-governmental organisations and other organisations involved in the policy-making process. Interviews focused on perceived roles of e-cigarettes in movement into and out of smoking, policy implementation and compliance, local contextual factors and variations in e-cigarette policy, and theorised mechanisms of the TPD legislation in relation to e-cigarettes. Topic guides allowed flexibility in response to the roles of interviewees, for example with less emphasis on policy development and more emphasis on enforcement activity when speaking with TSOs. Interviews were conducted between June and November 2018. Interviews with policy representatives included a focus on perspectives regarding the renormalisation of smoking and were completed before our own findings relating to this were in the public domain.
Quantitative process indicators
For the 2017 SHRN survey, a number of questions were added in consultation with our patient and public involvement group to provide a snapshot of the prevalence of potential mechanisms through which TPD may impact pupil’s use of e-cigarettes, and were linked to research questions on young people’s perceptions of risks and norms for e-cigarette use and tobacco (see Table 2). In our protocol, in response to PHR programme feedback, we indicated that we would request to add questions on where young people obtained e-cigarettes from and whether or not e-cigarettes used by young people contained nicotine. In addition, we included measures of risk perceptions for e-cigarettes compare with tobacco, exposure to marketing and perceived parental attitudes, mapping onto themes arising from our qualitative analysis. Most items were repeated in 2019, allowing examination of post-legislation change over time. In both cases, owing to pressures on the survey, items were asked of a random subsample of participants, rather than all survey participants.
| Process indicator | Asked of | Question | Response options |
|---|---|---|---|
| Risk perceptions | All participants | Which of the following statements do you agree with the most? | Tobacco cigarettes are worse for your health than e-cigarettes E-cigarettes are worse for your health than tobacco cigarettes Tobacco and e-cigarettes are equally bad for you I don’t know |
| Nicotine content of last device used | Ever users of e-cigarettes | The last time you used an e-cigarette, what was in the vapour you inhaled? | Nicotine Just flavouring/water vapour (no nicotine) Cannabis or cannabis oil Something else I don’t know |
| Exposure to advertising | All participants | In the past month, have you seen advertising for e-cigarettes in any of the following places? | In bus shelters On the sides of buses On billboards In supermarkets, petrol stations, newsagents, vape shops On the internet On phone boxes Other I haven’t seen any advertising |
| Perceived parental reactions | Non-smokers/non-vapers | If you were to start smoking/using e-cigarettes, what do you think your parents/carers would do? | Try to stop me Try to persuade me to stop Do nothing They would encourage me to smoke/use e-cigarettes |
| Where e-cigarettes obtained from | Current users only | Where do you often get your e-cigarettes and/or e-liquids from? | I buy them myself I get someone else to buy them for me Someone gives them to me I take them without asking I get them in some other way I do not want to answer |
Analysis of process evaluation data
All qualitative interviews were recorded and transcribed verbatim, with identifiable details (e.g. names of individuals and organisations) removed during and following transcription. The transcribed data were subjected to thematic analyses using Braun and Clarke’s102 six-step approach, which included (1) data familiarisation, (2) generating initial codes, (3) searching for themes, (4) reviewing themes, (5) defining themes and (6) writing up the account. Data analysis and data collection were conducted in parallel. Philosophically, the analyses were conducted through an abductive critical realist lens, beginning with exploration of predefined themes derived from the intervention logic model, and pursuing themes that emerged inductively from earlier interviews in later ones. A first researcher developed draft coding frames, with a sample of interviews second coded by a second researcher. Inconsistencies and disagreements were resolved through discussion with other members of the process evaluation subteam where necessary. For pupil interviews, which included a longitudinal cohort of young people and a cross-sectional sample of pupils recruited at follow-up only, the longitudinal and cross-sectional data were analysed as separate data sets prior to synthesis of themes across data sets. For structured observations, percentage interobserver agreement is presented for each item. One observer was a priori assigned as the primary observer, with percentages of retailers selling TPD-compliant products at each wave presented by retailer type, according to the primary coder. For quantitative process indicators, simple descriptive statistics are presented graphically by year the questions were asked (i.e. 2017 and 2019). These statistics are presented alongside the themes from the qualitative analyses of pupil data to examine the extent to which views expressed in qualitative interviews concur with, or contradict, views expressed in the national surveys.
Triangulation and integration
Combining data sources
Our sampling methods for qualitative process evaluation components were directed towards obtaining views from a diverse range of participants, rather than representativeness. By contrast, quantitative surveys aimed for representative of participants’ respective countries. This combination enables us to advance nuanced explanations for quantitative trends, and examine the extent to which views expressed within our qualitative interviews concur with, contradict or build on survey fundings. At each phase, quantitative and qualitative data analyses were conducted in parallel, but converged following analysis. Qualitative and quantitative analyses were undertaken by different subgroups, with integration of quantitative and qualitative data subsequently focused on areas in which data sources aligned, challenged one another’s conclusions or added further nuance and explanation. Study components were synthesised into a whole using an evaluation and integration framework based on MRC guidance for process evaluation90 (see Figure 2), with data sources organised and presented chronologically rather than by method. Although we considered a more traditional presentation by method, with effects data followed by process evaluation data, this would involve a potentially confusing rotation between a range of different time frames. Hence, the most coherent means of narrating the current study as a whole was to position the impact of TPD as the ending of the story. Hence, Chapter 3 presents data on the context into which TPD was introduced (i.e. pre-implementation trends in smoking and young people’s perceptions of vaping), Chapter 4 presents data from policy stakeholders, TSOs and retailers on implementation of legislation, before Chapter 5 presents data on mechanisms of change and post-legislation vaping and smoking outcomes.
Owing to significant policy interest in findings and the fast-moving nature of this evidence base, we chose to conduct analyses in a sequential manner and publish these as they were completed, rather than waiting for the final report. Our analyses of smoking trends during the emergence of e-cigarettes was, for example, one of the first of its type (and formed part of an evidence review on e-cigarettes and smoking uptake within National Institute for Health and Care Excellence guideline development immediately after publication);103 however, a number of similar analyses have since been published internationally, as described in Chapter 1. All findings have been published under Creative Commons Attribution licenses that allow adaptation and re-use of material for any purpose so long as the original work is properly cited. The original contribution of this report relates to the synthesis of previously published components, and additional unpublished data, to tell the story of the study as a whole. We indicate at the beginning of each chapter which elements draw on previously published sources, and which are new.
Cross-country integration
The quantitative elements of the study involve pooling of data sets collected at differing time points, using slightly different questions in each nation. The most robust analysis available to test the impact of TPD on vaping rates is the Welsh data, which (1) is available in a monthly format, therefore, providing multiple time points within the same survey year, and (2) includes data on ever e-cigarette use since 2013, enabling a segmented regression approach. However, this is supplemented by more crude before-and-after analyses of e-cigarette and tobacco use rates across all three countries, using an integrated three-country data set to examine the transferability or context specificity of findings relating to change in trend in our primary statistical analysis in Wales to other nations in Great Britain. Analyses of tobacco use draw on an integrated three-country data set, with adjustment for country. The process evaluation is conducted using harmonised methods across countries and was analysed as a single data set.
Management and governance
Ethics and consent
Ethics approval was provided by the Cardiff University School of Social Sciences Research Ethics Committee (reference SREC/2188). Surveys included in secondary analyses used opt-out parental consent approaches, in which parents are informed about the study and provided the opportunity to opt their child out of the research. Opt-out approaches are preferred in low-risk school-based research with adolescents, as requiring active parental consent tends to lead to exclusion of the voices of higher-risk groups from research. 104 The consent process for pupil interviews comprised the following three stages: (1) school-level consent for the young people to be invited, (2) letters for parents describing the study and (3) consent from selected young people. School staff identified groups of young people who were interested in taking part and gave students information and consent materials to discuss with their parents 2 weeks prior to interviews. A summary of the study information was provided to young people on the day of interviews and a consent form completed. At phase 2, schools were asked to remind parents of the study and young people were reminded that they were under no obligation to take part again if they did not wish to, and consent repeated. Our original intention, as reflected within the proposal approved by the PHR Funding Committee, was to use a more typical opt-out consent process for interviews, which has been used in other similar parallel interview research about e-cigarettes with children as young as 7 years. 62 However, our ethics committee initially asked us to use an opt-in method for our first round of interviews. Prior to 2018 interviews, this decision was appealed and reversed with the support of our Study Steering Committee and the National Institute for Health and Care Research (NIHR) Research Manager. Opt-out consent methods were, therefore, used for follow-up interviews, with the exception of one school within a local authority in Scotland, which required that parents provide written consent for their child to take part. For adult interviewees, information sheets were provided in advance of an interview taking place, and a consent form completed prior to the interview.
Patient and public involvement
DECIPHer’s (the Centre for Development, Evaluation, Complexity and Implementation in Public Health Improvement’s) young people’s advisory group ALPHA were consulted in the development of the original grant application. Subsequently, ALPHA advised on study materials for qualitative interviews, and the selection of quantitative process indicators included in the 2017 and 2019 SHRN surveys. ALPHA also contributed to the drafting of the lay summary for this report via group discussion of a draft and provision of comments. Via the SHRN, we also discussed the study with school staff and education stakeholders in several webinars. Research user perspectives at the level of policy and third-sector representation were included via our Study Steering Committee.
Study management
The outcomes and process evaluations were managed by separate individuals, with integration of study components led by the principal investigator. Rachel Brown managed the process evaluation and oversaw collection and analysis of primary data throughout the study. Britt Hallingberg managed the quantitative outcomes evaluation, including the development and implementation of the statistical analysis plan, with oversight and guidance from senior statistician Linsay Gray. Nicholas Page covered Britt Hallingberg’s role during a period of maternity leave in late 2018/early 2019, and implemented short-term effect analyses during this time. Britt Hallingberg moved from Cardiff University to Cardiff Metropolitan University in 2019, but was appointed on an Honorary contract with Cardiff University and continued to manage the secondary data analysis. Marcus Munafò led the Bristol subcontract and was responsible for delegation of responsibilities to research staff in the Bristol study arm, with Linda Bauld fulfilling this role in Stirling. Linda Bauld left the University of Stirling for a post in University of Edinburgh on completion of the primary research in late 2018, and responsibility for the Stirling arm was assumed by Jennifer McKell, supported by Anne-Marie Mackintosh. Monthly or bi-monthly Study Management Group meetings, including co-investigators and employed staff, were held throughout the study and were chaired by the principal investigator. Additional small group operational meetings were held during periods of data collection. The study had a planned pause period from April 2019 to October 2020 while longer-term data were awaited for quantitative analyses and during which no process data were collected. The Study Management Team met every 4–6 months during this break period.
The study had an independent Study Steering Committee whose members included Amanda Amos (University of Edinburgh), Matt Egan (London School of Hygiene & Tropical Medicine), Chris Roberts (Welsh Government), David Humphreys (Oxford University), Sheila Duffy (ASH Scotland) and Ashley Gould (Public Health Wales). Amanda Amos chaired the group initially. All members declared no conflicts of interest at the first meeting, and were asked to declare any new conflicts at the start of each meeting. As Linda Bauld moved to University of Edinburgh in 2018 and remained a co-investigator on the study, this meant that a co-investigator was now in the same department as the chairperson. This new conflict of interest was declared to NIHR, which advised that Amanda Amos no longer met the criteria for independence and was, hence, no longer eligible to chair the committee. Matt Egan took over as chairperson. Sharon Cox (University College London) joined the committee at this stage as an additional independent member. The committee met approximately 6-monthly during the live study periods. Analyses reported in each journal article were presented to the group prior to submission. Our primary statistical analyses of long-term change in e-cigarette use were presented to the Study Steering Committee at a final meeting in November 2020.
Deviations from protocol
Our original protocol included an examination of social media mentions of e-cigarettes, including sites such as Facebook (URL: www.facebook.com; Meta Platforms, Inc., Menlo Park, CA, USA) and Twitter (URL: www.twitter.com; Twitter, Inc., San Francisco, CA, USA). However, our qualitative data indicated that the kinds of media covered by our proposed methods were less relevant to young people than other forms of media, particularly video-sharing websites, such as YouTube (URL: www.youtube.com; YouTube, LLC, San Bruno, CA, USA), which would not be captured by our proposed methods. Following discussion with our Study Steering Committee, this small element of the process evaluation was removed from our protocol. Owing to a miscommunication within the process evaluation subteam, in one nation, two observers each observed different premises rather than two observers per premises. Hence, inter-rater reliability assessments are based on two rather than three countries. Remaining variations from protocol largely related to data availability changes. We originally aimed to use SALSUS data from 2017 and 2019, assuming a typical 2-year cycle. However, the 2017 survey was postponed to 2018 and the 2019 survey did not take place. Our updated protocol indicated that we would seek to use data from the Scottish Health and Wellbeing census planned for 2019 if access could be negotiated; however, this also did not take place, with its launch postponed to 2021. In England, at the time of writing the protocol, funding was confirmed for the 2016 and 2018 SDDU surveys; however, with SDDU moving from an annual cycle to a biennial cycle, funding was being sought for 2017 and 2019 surveys. This funding was not obtained and, hence, the additional surveys we said that we would use if they were conducted were not. There were significant delays in the 2018 SDDU data reaching the UK data service. We sought to present all analyses to our Study Steering Committee prior to submitting for publication. At our final meeting in November 2020, we presented all analyses other than those requiring this data set, and were advised to submit the report without these analyses. However, the editorial team at NIHR asked us to wait until these were analyses available. As this final data set became available in only November 2021, the analyses using these data were finalised immediately before report submission in December 2021. Some intended subgroup analyses could not be conducted because of changes in survey methods. In England, for example, SES was measured by asking young people if they were entitled to free school meals until 2014; however, from 2016, SES was measured via the FAS.
Chapter 3 Results: the role of e-cigarettes in the renormalisation of smoking prior to full implementation of the Tobacco Products Directive regulations
Some text in this chapter has been reproduced from Hallingberg et al. 10 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
In addition, some text in this chapter has been reproduced from Brown et al. 105 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter aims to provide an understanding of the context into which TPD regulations were implemented, by addressing the following research questions:
-
Have trajectories in young people’s ever and current tobacco smoking been significantly interrupted (positively or negatively) by growing prevalence of e-cigarettes?
-
How do young people perceive risks and social norms surrounding e-cigarettes?
The chapter does so by bringing together quantitative analyses of trends in young people’s tobacco use before and after the emergence of e-cigarettes in the UK, with qualitative interview data from young people in seven schools exploring young people’s perceptions of e-cigarettes and smoking. For change in secular trends, to strengthen or challenge conclusions regarding causal inference, we examine plausibility and specificity. Specificity is assessed by examining whether change in trend is specific to tobacco or occurs for other substance use behaviours whose trajectories would not plausibly be affected by growth in e-cigarette use (e.g. alcohol and cannabis use). Plausibility is assessed (1) by testing whether or not trends in young people’s attitudes towards smoking as an acceptable thing for young people their age to do changed during emergence of e-cigarettes and (2) through qualitative interviews with young people regarding processes through which e-cigarettes might renormalise smoking.
Quantitative analysis
Trajectories of young people’s smoking prevalence from 1998 to 2015
The analytical sample for smoking prevalence from 1998 to 2015 included 242,855 and 243,111 young people for ever and regular smoking, respectively. Table 3 presents percentages (and 95% CIs) for each outcome from 1998 to 2015, overall and for each country. In all countries, there was a consistent downwards trend over time in both outcomes. In 1998, most young people (around three in five) aged 13–15 years had tried smoking. Over the course of the time series, this declined to become a minority behaviour, with approximately one in five young people reporting having tried smoking in 2015. In 1998, approximately one in five young people reported being regular smokers across countries. Regular smoking fell to between 4% and 6% in each country by the last measurement point. For both ever and regular smoking, there was some evidence of decline beyond the ‘intervention’ point (i.e. from 2011 to 2015 when e-cigarette use was becoming more prevalent in the UK).
| Year | Ever smoked, prevalence (95% CI) | Regular smoker, prevalence (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
| All nations | England | Scotland | Wales | All nations | England | Scotland | Wales | |
| 1998 | 59.8 (58.5 to 61.0) | 60.2 (58.0 to 62.4) | 61.9 (59.6 to 64.2) | 58.0 (56.1 to 59.9) | 19.0 (18.1 to 20.0) | 19.5 (17.7 to 21.3) | 18.7 (16.9 to 20.6) | 18.9 (17.4 to 20.4) |
| 1999 | 54.2 (52.6 to 55.9) | 54.2 (52.6 to 55.9) | 14.7 (13.6 to 15.9) | 14.7 (13.6 to 15.9) | ||||
| 2000 | 52.8 (51.6 to 53.9) | 52.2 (50.4 to 54.1) | 50.1 (48.1 to 52.2) | 56.1 (54.1 to 58.2) | 15.4 (14.6 to 16.3) | 16.0 (14.7 to 17.4) | 13.1 (11.7 to 14.5) | 17.2 (15.6 to 18.8) |
| 2001 | 53.1 (51.5 to 54.8) | 53.1 (51.5 to 54.8) | 14.7 (13.6 to 16.0) | 14.7 (13.6 to 16.0) | ||||
| 2002 | 50.0 (49.4 to 50.6) | 50.1 (48.5 to 51.7) | 50.1 (49.5 to 50.8) | 48.4 (46.4 to 50.4) | 13.9 (13.5 to 14.3) | 16.0 (14.8 to 17.2) | 13.2 (12.8 to 13.7) | 16.2 (14.8 to 17.7) |
| 2003 | 52.4 (50.8 to 54.0) | 52.4 (50.8 to 54.0) | 14.3 (13.2 to 15.4) | 14.3 (13.2 to 15.4) | ||||
| 2004 | 47.3 (46.4 to 48.1) | 48.2 (46.6 to 49.9) | 47.4 (46.2 to 48.6) | 45.6 (43.7 to 47.5) | 13.5 (12.9 to 14.1) | 13.6 (12.6 to 14.8) | 12.4 (11.6 to 13.2) | 16.1 (14.7 to 17.5) |
| 2005 | 50.7 (49.0 to 52.4) | 50.7 (49.0 to 52.4) | 13.3 (12.2 to 14.5) | 13.3 (12.2 to 14.5) | ||||
| 2006 | 39.8 (39.2 to 40.4) | 47.7 (45.9 to 49.5) | 38.6 (37.9 to 39.2) | 40.6 (38.8 to 42.4) | 10.2 (9.9 to 10.6) | 13.3 (12.2 to 14.6) | 9.4 (9.0 to 9.8) | 13.1 (11.9 to 14.4) |
| 2007 | 43.1 (41.3 to 44.9) | 43.1 (41.3 to 44.9) | 10.0 (9.0 to 11.1) | 10.0 (9.0 to 11.1) | ||||
| 2008 | 37.3 (36.5 to 38.2) | 40.9 (39.2 to 42.7) | 36.2 (35.3 to 37.2) | 9.2 (8.7 to 9.7) | 9.9 (8.9 to 11.0) | 9.0 (8.4 to 9.5) | ||
| 2009 | 32.7 (31.5 to 33.8) | 37.8 (36.1 to 39.6) | 28.2 (26.8 to 29.8) | 8.9 (8.2 to 9.6) | 9.4 (8.4 to 10.5) | 8.4 (7.5 to 9.4) | ||
| 2010 | 32.4 (31.9 to 32.8) | 35.5 (33.7 to 37.2) | 32.1 (31.7 to 32.6) | 7.9 (7.6 to 8.1) | 8.6 (7.6 to 9.7) | 7.8 (7.5 to 8.1) | ||
| 2011 | 32.9 (31.1 to 34.8) | 32.9 (31.1 to 34.8) | 6.7 (5.7 to 7.7) | 6.7 (5.7 to 7.7) | ||||
| 2012 | 31.6 (30.0 to 33.3) | 31.6 (30.0 to 33.3) | 6.6 (5.8 to 7.6) | 6.6 (5.8 to 7.6) | ||||
| 2013 | 22.6 (22.2 to 23.1) | 27.3 (25.3 to 29.2) | 22.5 (22.1 to 23.0) | 21.1 (19.7 to 22.5) | 5.1 (4.9 to 5.3) | 5.0 (4.1 to 6.1) | 5.1 (4.8 to 5.3) | 5.4 (4.7 to 6.2) |
| 2014 | 24.8 (23.1 to 26.6) | 24.8 (23.1 to 26.6) | 5.5 (4.7 to 6.5) | 5.5 (4.7 to 6.5) | ||||
| 2015 | 19.1 (18.7 to 19.5) | 20.0 (19.5 to 20.5) | 17.1 (16.4 to 17.8) | 4.5 (4.3 to 4.7) | 4.1 (3.8 to 4.3) | 5.5 (5.1 to 6.0) | ||
Table 4 shows odds ratios (ORs) and 95% CIs from segmented regression analyses for ever and regular smoking (for the whole sample and for gender and year group subgroups). In our a priori-specified models, which assumed a linear decline in smoking from 1998 to 2010, there was evidence of negative change in both level and post-slope terms after the intervention point for ever smoking. This change was consistent with a conclusion that ever smoking declined faster during the period when e-cigarettes were increasing in prevalence in the UK than it had been up to that point. However, visual inspection provided some evidence of non-linearity during the baseline period. Addition of a quadratic term confirmed that non-linearity was significant. Accounting for non-linearity led to a changed conclusion of no significant change in trend for ever smoking. For regular smoking, there was no evidence of change in trend in linear models, which is consistent with a conclusion of continued decline at the same rate as the secular trend. However, after adjusting for non-linearity of the baseline trend, a marginally significant (p = 0.03) slowing in rate of decline for regular smoking after the ‘intervention’ point was found. In both cases, significant reduction in level at the intervention point is evident. In a range of sensitivity analyses, ORs for change in trend for ever tobacco smoking ranged from 0.98 to 1.04, and were mostly non-significant, hence, providing little evidence of change in trend for ever use. ORs for change in trend for ever smoking post 2010 ranged from 0.99 to 1.11, with most ORs supporting a conclusion of a significant positive change in trend (see Report Supplementary Material 1, Table 1).
| Sample | Ever smoked | Regular smoking | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Linear | p-value | Quadratic | p-value | Linear | p-value | Quadratic | p-value | ||
| Whole sample (n = 242,855; 243,111) | Year | 0.91 (0.91 to 0.91) | <0.001 | 0.95 (0.93 to 0.96) | <0.001 | 0.93 (0.93 to 0.94) | <0.001 | 0.98 (0.96 to 1.00) | 0.025 |
| Year2 | 1.00 (1.00 to 1.00) | <0.001 | 1.00 (1.00 to 1.00) | <0.001 | |||||
| Level | 0.89 (0.84 to 0.95) | <0.001 | 0.89 (0.84 to 0.95) | <0.001 | 0.79 (0.71 to 0.88) | <0.001 | 0.80 (0.72 to 0.90) | <0.001 | |
| Post slope | 0.97 (0.96 to 0.99) | <0.001 | 1.01 (0.99 to 1.03) | 0.231 | 0.98 (0.96 to 1.01) | 0.231 | 1.04 (1.00 to 1.08) | 0.028 | |
| Boys subgroup (n = 121,879; 122,042) | Year | 0.92 (0.92 to 0.93) | <0.001 | 0.93 (0.91 to 0.95) | <0.001 | 0.94 (0.94 to 0.95) | <0.001 | 0.95 (0.92 to 0.98) | <0.001 |
| Year2 | 1.00 (1.00 to 1.00) | 0.621 | 1.00 (1.00 to 1.00) | 0.583 | |||||
| Level | 0.88 (0.81 to 0.96) | 0.005 | 0.88 (0.81 to 0.96) | 0.005 | 0.83 (0.70 to 0.97) | 0.022 | 0.83 (0.70 to 0.97) | 0.023 | |
| Post slope | 0.98 (0.95 to 1.00) | 0.034 | 0.98 (0.95 to 1.01) | 0.212 | 1.00 (0.96 to 1.04) | 0.921 | 1.01 (0.96 to 1.06) | 0.794 | |
| Girls subgroup (n = 120,976; 121,069) | Year | 0.90 (0.89 to 0.90) | <0.001 | 0.96 (0.94 to 0.98) | <0.001 | 0.92 (0.92 to 0.93) | <0.001 | 1.00 (0.98 to 1.03) | 0.922 |
| Year2 | 1.00 (0.99 to 1.00) | <0.001 | 0.99 (0.99 to 1.00) | <0.001 | |||||
| Level | 0.90 (0.83 to 0.98) | 0.014 | 0.90 (0.83 to 0.98) | 0.018 | 0.76 (0.65 to 0.89) | <0.001 | 0.78 (0.67 to 0.91) | 0.002 | |
| Post slope | 0.97 (0.95 to 0.99) | 0.009 | 1.05 (1.01 to 1.08) | 0.003 | 0.97 (0.93 to 1.01) | 0.139 | 1.07 (1.02 to 1.12) | 0.009 | |
| 13-year-olds only (n = 126,960; 127,100) | Year | 0.89 (0.89 to 0.90) | <0.001 | 0.96 (0.94 to 0.98) | <0.001 | 0.91 (0.90 to 0.92) | <0.001 | 1.02 (0.98 to 1.05) | 0.378 |
| Year2 | 1.00 (0.99 to 1.00) | <0.001 | 0.99 (0.99 to 1.00) | <0.001 | |||||
| Level | 0.82 (0.74 to 0.91) | <0.001 | 0.83 (0.75 to 0.92) | <0.001 | 0.73 (0.57 to 0.92) | 0.009 | 0.76 (0.60 to 0.97) | 0.027 | |
| Post slope | 0.99 (0.96 to 1.01) | 0.304 | 1.07 (1.03 to 1.10) | <0.001 | 1.00 (0.95 to 1.07) | 0.902 | 1.14 (1.06 to 1.23) | <0.001 | |
| 15-year-olds only (n = 115,895; 116,011) | Year | 0.93 (0.93 to 0.93) | <0.001 | 0.94 (0.92 to 0.95) | <0.001 | 0.94 (0.93 to 0.94) | <0.001 | 0.97 (0.95 to 0.99) | 0.003 |
| Year2 | 1.00 (1.00 to 1.00) | 0.390 | 1.00 (1.00 to 1.00) | 0.009 | |||||
| Level | 0.92 (0.85 to 0.99) | 0.035 | 0.92 (0.85 to 0.99) | 0.036 | 0.79 (0.70 to 0.90) | <0.001 | 0.80 (0.70 to 0.90) | <0.001 | |
| Post slope | 0.96 (0.94 to 0.98) | <0.001 | 0.96 (0.94 to 0.99) | 0.012 | 0.98 (0.95 to 1.01) | 0.240 | 1.01 (0.97 to 1.06) | 0.497 | |
In subgroup analyses, the slowing of decline for regular smoking was limited to groups for whom rates had declined most rapidly up to 2010 (i.e. girls and 13-year-olds). Additional subgroup analyses by free school meal entitlement (limited to Scotland and England) indicated a marginally significant increase in rate of decline of ever smoking for young people with a higher SES (high SES: OR 0.95, 95% CI 0.91 to 1.00, p = 0.043; low SES: OR 1.01, 95% CI 0.91 to 1.12, p = 0.919). For both groups, change in trend for regular smoking was similar to the whole sample, falling short of significance in both instances (high SES: OR 1.03, 95% CI 0.88 to 1.21, p = 0.0.561; low SES: OR 1.03, 95% CI 0.94 to 1.11, p = 0.734). Country-specific analyses according to differing measures of SES are presented in Report Supplementary Material 1 data, but should be treated with caution given the small number of data points available for individual countries other than England (for additional subgroup analyses see Report Supplementary Material 1, Tables 2–6).
Specificity of change in trend: trajectories in ever alcohol and cannabis
To evaluate whether or not changes in trend were specific to smoking, we examined time, level and post-slope terms for the same period for ever alcohol and cannabis use. Table 5 presents percentages (and 95% CIs) of young people who reported having tried alcohol and cannabis by year and country. At first measurement in 1998, most young people reported that they had tried alcohol, declining in each country to approximately half by the end of the time series. Approximately one-quarter of young people in Scotland and England, and one-third of young people in Wales, reported having tried cannabis in 1998, declining to around 1 in 10 by the end of the time series.
| Year | Ever drunk alcohol, % (95% CI) | Ever tried cannabis, % (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
| All | England | Scotland | Wales | All | England | Scotland | Wales | |
| 1998 | 78.9 (77.5 to 80.2) | 81.3 (79.4 to 83.0) | 76.2 (74.1 to 78.2) | 28.5 (27.2 to 29.7) | 24.7 (22.8 to 26.6) | 27 (24.9 to 29.2) | 36.4a (33.7 to 39.1) | |
| 1999 | 77.3 (75.9 to 78.6) | 77.3 (75.9 to 78.6) | 21.4 (20.1 to 22.8) | 21.4 (20.1 to 22.8) | ||||
| 2000 | 73.5 (72.2 to 74.7) | 75.3 (73.7 to 76.9) | 71.3 (69.4 to 73.1) | 21.0 (20.0 to 21.9) | 19.8 (18.3 to 21.3) | 19.8 (18.3 to 21.5) | 23.5 (21.8 to 25.3) | |
| 2001 | 77.9 (76.5 to 79.3) | 77.9 (76.5 to 79.3) | 25.0 (23.6 to 26.5) | 25.0 (23.6 to 26.5) | ||||
| 2002 | 79.5 (79.1 to 80.0) | 77.3 (75.9 to 78.6) | 78.5 (77.9 to 79.0) | 93.2 (92.1 to 94.2) | 23.6 (23.1 to 24.1) | 24.6 (23.3 to 26.1) | 22.9 (22.3 to 23.4) | 34.2* (31.5 to 37.0) |
| 2003 | 77.3 (75.9 to 78.5) | 77.3 (75.9 to 78.5) | 25.9 (24.5 to 27.3) | 25.9 (24.5 to 27.3) | ||||
| 2004 | 78.7 (78.0 to 79.4) | 75.5 (74.1 to 76.9) | 77.7 (76.7 to 78.7) | 85.3 (83.9 to 86.6) | 23.6 (22.9 to 24.3) | 23.1 (21.7 to 24.5) | 22.9 (21.9 to 23.9) | 26 (24.4 to 27.7) |
| 2005 | 73.8 (72.3 to 75.2) | 73.8 (72.3 to 75.2) | 22.3 (20.9 to 23.6) | 22.3 (20.9 to 23.6) | ||||
| 2006 | 72.2 (71.7 to 72.7) | 70.7 (69.1 to 72.3) | 71.2 (70.6 to 71.8) | 81.9 (80.4 to 83.3) | 15.3 (14.9 to 15.7) | 19.5 (18.2 to 21.0) | 13.9 (13.4 to 14.3) | 21.9 (20.4 to 23.5) |
| 2007 | 69.8 (68.1 to 71.4) | 69.8 (68.1 to 71.4) | 18.1 (16.8 to 19.5) | 18.1 (16.8 to 19.5) | ||||
| 2008 | 66.9 (66.1 to 67.7) | 69.3 (67.6 to 70.9) | 66.2 (65.3 to 67.1) | 13.7 (13.2 to 14.3) | 17.1 (15.7 to 18.5) | 12.7 (12.1 to 13.4) | ||
| 2009 | 70.6 (69.4 to 71.7) | 67.8 (66.1 to 69.5) | 72.9 (71.4 to 74.3) | 15.1 (14.2 to 15.9) | 16.9 (15.5 to 18.3) | 13.5 (12.3 to 14.0) | ||
| 2010 | 60.1 (59.6 to 60.5) | 61.5 (59.7 to 63.3) | 60.0 (59.5 to 60.5) | 11.3 (11.0 to 11.6) | 15.2 (13.9 to 16.6) | 11.0 (10.7 to 11.3) | ||
| 2011 | 61.0 (59.0 to 62.9) | 61.0 (59.0 to 62.9) | 13.6 (12.3 to 15.0) | 13.6 (12.3 to 15.0) | ||||
| 2012 | 58.6 (56.9 to 60.4) | 58.6 (56.9 to 60.4) | 14.3 (13.1 to 15.6) | 14.3 (13.1 to 15.6) | ||||
| 2013 | 50.5 (50.0 to 51.0) | 54.1 (52.0 to 56.3) | 49.5 (49.0 to 50.1) | 57.8 (56.1 to 59.5) | 9.8 (9.5 to 10.1) | 12.9 (11.5 to 14.4) | 9.5 (9.2 to 9.8) | 10.4 (9.2 to 11.5) |
| 2014 | 51.7 (49.7 to 53.8) | 51.7 (49.7 to 53.8) | 11.5 (10.3 to 12.9) | 11.5 (10.3 to 12.9) | ||||
| 2015 | 47.7 (47.1 to 48.2) | 44.7 (44.0 to 45.3) | 54.3 (53.3 to 55.2) | 8.7 (8.4 to 9.0) | 8.9 (8.5 to 9.0) | 8.4 (7.8 to 8.9) | ||
As indicated in Table 6, in models assuming a linear baseline trend, there was evidence of a slight acceleration of the decline in alcohol use and no change in trend for cannabis use. However, as for tobacco use, adjusting for non-linearity of the secular trend altered trend estimates. For both alcohol and cannabis use, there was a significant positive change in trend, with the decline in both slowing after the ‘intervention’ point. This was consistent across subgroups. Hence, the slight disruption in trend for regular smoking was reflected, to a larger extent, in other substances for which e-cigarettes would not be expected to cause a change in trend. Both were measures of ‘ever’ use, whose counterpart measure for tobacco did not show evidence of change in trend, hence, suggesting that any slowing in decline for smoking was lagging behind change in trend for other substances. In a range of sensitivity analyses, ORs for change in trend for alcohol ranged from 1.05 to 1.16 and for cannabis ORs ranged from 1.05 to 1.24. The ORs were significant in all analyses, consistently indicating a significant positive change in trend (i.e. slowing in decline) for ever alcohol and cannabis use (see Report Supplementary Material, Table 1).
| Sample | Ever drunk alcohol, OR (95% CI) | Ever used cannabis, OR (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Linear | p-value | Quadratic | p-value | Linear | p-value | Quadratic | p-value | ||
| Whole sample (n = 239,190; 239,457) | Year | 0.91 (0.90 to 0.91) | <0.001 | 1.10 (1.08 to 1.12) | <0.001 | 0.92 (0.92 to 0.92) | <0.001 | 1.08 (1.07 to 1.10) | <0.001 |
| Year2 | 0.99 (0.99 to 0.99) | <0.001 | 0.99 (0.99 to 0.99) | <0.001 | |||||
| Level | 0.90 (0.85 to 0.95) | <0.001 | 0.85 (0.81 to 0.90) | <0.001 | 0.98 (0.90 to 1.07) | 0.661 | 1.01 (0.93 to 1.10) | 0.761 | |
| Post slope | 0.96 (0.94 to 0.97) | <0.001 | 1.17 (1.14 to 1.19) | <0.001 | 1.00 (0.98 to 1.03) | 0.667 | 1.21 (1.18 to 1.25) | <0.001 | |
| Boys subgroup (n = 119,989; 120,025) | Year | 0.91 (0.90 to 0.91) | <0.001 | 1.06 (1.03 to 1.09) | <0.001 | 0.93 (0.92 to 0.93) | <0.001 | 1.06 (1.04 to 1.09) | <0.001 |
| Year2 | 0.99 (0.99 to 0.99) | <0.001 | 0.99 (0.99 to 0.99) | <0.001 | |||||
| Level | 0.89 (0.82 to 0.96) | 0.004 | 0.85 (0.79 to 0.92) | <0.001 | 0.92 (0.82 to 1.04) | 0.185 | 0.94 (0.84 to 1.06) | 0.337 | |
| Post slope | 0.96 (0.94 to 0.98) | <0.001 | 1.12 (1.09 to 1.16) | <0.001 | 1.02 (0.99 to 1.05) | 0.175 | 1.20 (1.15 to 1.24) | <0.001 | |
| Girls subgroup (n = 119,201; 119,432) | Year | 0.90 (0.90 to 0.91) | <0.001 | 1.15 (1.12 to 1.18) | <0.001 | 0.92 (0.91 to 0.92) | <0.001 | 1.11 (1.08 to 1.14) | <0.001 |
| Year2 | 0.99 (0.98 to 0.99) | <0.001 | 0.99 (0.99 to 0.99) | <0.001 | |||||
| Level | 0.91 (0.84 to 0.98) | 0.016 | 0.85 (0.79 to 0.92) | <0.001 | 1.06 (0.93 to 1.20) | 0.396 | 1.11 (0.98 to 1.26) | 0.110 | |
| Post slope | 0.96 (0.94 to 0.97) | <0.001 | 1.22 (1.18 to 1.26) | <0.001 | 0.99 (0.95 to 1.02) | 0.359 | 1.23 (1.17 to 1.28) | <0.001 | |
| 13-year-olds only (n = 124,842; 123,608) | Year | 0.90 (0.90 to 0.90) | <0.001 | 1.11 (1.08 to 1.13) | <0.001 | 0.90 (0.89 to 0.90) | <0.001 | 1.16 (1.12 to 1.21) | <0.001 |
| Year2 | 0.99 (0.99 to 0.99) | <0.001 | 0.98 (0.98 to 0.99) | <0.001 | |||||
| Level | 0.88 (0.82 to 0.95) | 0.001 | 0.84 (0.78 to 0.91) | <0.001 | 1.07 (0.89 to 1.28) | 0.480 | 1.14 (0.95 to 1.37) | 0.165 | |
| Post slope | 0.95 (0.93 to 0.97) | <0.001 | 1.17 (1.14 to 1.21) | <0.001 | 0.99 (0.95 to 1.04) | 0.746 | 1.34 (1.26 to 1.42) | <0.001 | |
| 15-year-olds only (n = 114,348; 115,849) | Year | 0.92 (0.91 to 0.92) | <0.001 | 1.08 (1.05 to 1.11) | <0.001 | 0.93 (0.92 to 0.93) | <0.001 | 1.06 (1.04 to 1.08) | <0.001 |
| Year2 | 0.99 (0.99 to 0.99) | <0.001 | 0.99 (0.99 to 0.99) | <0.001 | |||||
| Level | 0.92 (0.84 to 1.00) | 0.049 | 0.87 (0.80 to 0.95) | 0.002 | 0.96 (0.87 to 1.06) | 0.432 | 0.99 (0.90 to 1.09) | 0.776 | |
| Post slope | 0.96 (0.94 to 0.98) | <0.001 | 1.13 (1.09 to 1.17) | <0.001 | 1.01 (0.98 to 1.03) | 0.645 | 1.17 (1.13 to 1.20) | <0.001 | |
Plausibility of change occurring via renormalisation
Trajectories of young people’s smoking attitudes from 1999 to 2015
Table 7 presents percentages (and 95% CIs) of young people reporting that trying smoking or smoking weekly is OK for someone their age, by year and country. When first asked in England in 1999, a large majority (70%) of young people reported that it was OK for someone their age to try smoking. However, by the end of the time series in England in 2014, this percentage had approximately halved. This question was first included in Scotland in 2006, at which point slightly more than a half of young people reported that it was OK to try smoking, falling to one-quarter by 2015. The percentage of young people reporting that it was OK to try smoking appeared to continue to decline beyond 2010. In England only, from 2003, young people were also asked whether or not it was OK for someone their age to smoke weekly, with approval of regular smoking substantially lower than for experimentation (36% vs. 64%). Approval of regular smoking declined across the time series, with approximately one in seven young people reporting that it is OK for someone their age to smoke weekly by 2014. As for approval of trying smoking, this decline continued beyond the ‘intervention’ point.
| Year | Trying smoking is OK (England and Scotland), % (95% CI) | Smoking regularly is OK (England only), % (95% CI) | ||
|---|---|---|---|---|
| All | England | Scotland | ||
| 1999 | 70.0 (68.4 to 71.5) | 70.0 (68.4 to 71.5) | ||
| 2001 | 70.0 (68.4 to 71.5) | 70.0 (68.4 to 71.5) | ||
| 2003 | 63.8 (62.3 to 65.3) | 63.8 (62.3 to 65.3) | 36.2 (34.7 to 37.7) | |
| 2004 | 55.8 (54.2 to 57.5) | 55.8 (54.2 to 57.5) | 28.3 (26.9 to 29.8) | |
| 2005 | 59.1 (57.4 to 60.7) | 59.1 (57.4 to 60.7) | 30.8 (29.3 to 32.4) | |
| 2006 | 53.4 (52.8 to 54.0) | 51.1 (49.3 – 52.9 | 53.8 (53.1 to 54.4) | 25.7 (24.1 to 27.2) |
| 2007 | 52.9 (51.1 to 54.7) | 52.9 (51.1 to 54.7) | 27.3 (25.7 to 28.9) | |
| 2008 | 47.9 (47.0 to 48.8) | 48.9 (47.1 to 50.7) | 47.6 (46.6 to 48.6) | 21.2 (19.7 to 22.7) |
| 2009 | 52.4 (50.6 to 54.3) | 52.4 (50.6 to 54.3) | 25.0 (23.5 to 26.6) | |
| 2010 | 45.5 (45.0 to 46.0) | 48.6 (46.7 to 50.4) | 45.2 (44.7 to 45.7) | 22.3 (20.8 to 23.9) |
| 2011 | 48.0 (46.0 to 50.0) | 48.0 (46.0 to 50.0) | 20.4 (18.8 to 22.0) | |
| 2012 | 43.1 (41.3 to 44.9) | 43.1 (41.3 to 44.9) | 19.6 (18.2 to 21.1) | |
| 2013 | 33.6 (33.1 to 34.1) | 42.7 (40.5 to 44.9) | 33.1 (32.5 to 33.6) | 17.5 (15.9 to 19.2) |
| 2014 | 35.1 (33.2 to 37.1) | 35.1 (33.2 to 37.1) | 13.9 (12.6 to 15.4) | |
| 2015 | 27.0 (26.5 to 27.6) | 27.0 (26.5 to 27.6) | ||
Table 8 presents findings from segmented regression analyses of change in level and trend for smoking attitudes following emergence of e-cigarettes. In all models, there was a significant decline over time in the percentage of young people reporting that smoking was OK. There was some inconsistency in size and direction of change in level across models and subgroups, with these changes mostly non-significant. However, across both linear and quadratic models, and most subgroups, the rate of decline in the percentage of young people saying that trying smoking is OK and weekly smoking is OK increased post 2010. Hence, data are consistent with a conclusion that during the period of growing prevalence of e-cigarettes the percentage of young people considering smoking to be OK continued to decline and, indeed, declined at a faster rate than the baseline trend. In a range of sensitivity analyses, ORs for change in trend for attitudes towards smoking post 2010 ranged from 0.83 to 0.88, indicating a significant acceleration in decline in all cases (see Report Supplementary Material, Table 1).
| Sample | Trying smoking is OKa (don’t know = not OK) | Smoking weekly is OKb (don’t know = not OK) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Linear | p-value | Quadratic | p-value | Linear | p-value | Quadratic | p-value | ||
| Whole sample (n = 165,199; 35,890) | Year | 0.91 (0.91 to 0.92) | <0.001 | 0.87 (0.85 to 0.89) | <0.001 | 0.91 (0.90 to 0.92) | <0.001 | 0.72 (0.65 to 0.81) | <0.001 |
| Year2 | 1.00 (1.00 to 1.00) | <0.001 | 1.01 (1.01 to 1.02) | <0.001 | |||||
| Level | 1.03 (0.97 to 1.10) | 0.330 | 1.05 (0.98 to 1.12) | 0.143 | 1.15 (1.00 to 1.32) | 0.045 | 1.10 (0.96 to 1.27) | 0.152 | |
| Post slope | 0.92 (0.90 to 0.93) | <0.001 | 0.88 (0.86 to 0.90) | <0.001 | 0.95 (0.90 to 1.00) | 0.032 | 0.82 (0.75 to 0.89) | <0.001 | |
| Boys subgroup (n = 82,270; 18,042) | Year | 0.92 (0.91 to 0.93) | <0.001 | 0.84 (0.81 to 0.87) | <0.001 | 0.92 (0.91 to 0.94) | <0.001 | 0.67 (0.57 to 0.79) | <0.001 |
| Year2 | 1.01 (1.00 to 1.01) | <0.001 | 1.02 (1.01 to 1.03) | <0.001 | |||||
| Level | 1.08 (0.99 to 1.18) | 0.090 | 1.11 (1.01 to 1.22) | 0.024 | 1.33 (1.10 to 1.62) | 0.004 | 1.27 (1.04 to 1.54) | 0.020 | |
| Post slope | 0.91 (0.89 to 0.93) | <0.001 | 0.84 (0.81 to 0.88) | <0.001 | 0.88 (0.82 to 0.94) | <0.001 | 0.71 (0.62 to 0.81) | <0.001 | |
| Girls subgroup (n = 82,929; 17,848) | Year | 0.90 (0.90 to 0.91) | <0.001 | 0.89 (0.86 to 0.93) | <0.001 | 0.90 (0.88 to 0.91) | <0.001 | 0.77 (0.66 to 0.91) | 0.001 |
| Year2 | 1.00 (1.00 to 1.00) | 0.492 | 1.01 (1.00 to 1.02) | 0.067 | |||||
| Level | 0.98 (0.90 to 1.07) | 0.718 | 0.99 (0.90 to 1.08) | 0.789 | 1.02 (0.84 to 1.22) | 0.866 | 0.99 (0.82 to 1.19) | 0.917 | |
| Post slope | 0.93 (0.91 to 0.95) | <0.001 | 0.92 (0.88 to 0.95) | <0.001 | 1.01 (0.95 to 1.08) | 0.720 | 0.92 (0.81 to 1.04) | 0.180 | |
| 13-year-olds only (n = 85,713; 18,721) | Year | 0.90 (0.89 to 0.91) | <0.001 | 0.89 (0.86 to 0.92) | <0.001 | 0.90 (0.89 to 0.92) | <0.001 | 0.78 (0.65 to 0.94) | 0.007 |
| Year2 | 1.00 (1.00 to 1.00) | 0.459 | 1.01 (1.00 to 1.02) | 0.107 | |||||
| Level | 0.95 (0.86 to 1.05) | 0.321 | 0.95 (0.87 to 1.05) | 0.349 | 1.22 (0.97 to 1.53) | 0.086 | 1.19 (0.94 to 1.49) | 0.145 | |
| Post slope | 0.94 (0.92 to 0.97) | <0.001 | 0.93 (0.90 to 0.97) | <0.001 | 0.93 (0.85 to 1.01) | 0.092 | 0.84 (0.73 to 0.98) | 0.022 | |
| 15-year-olds only (n = 79,486; 17,169) | Year | 0.93 (0.92 to 0.94) | <0.001 | 0.86 (0.83 to 0.89) | <0.001 | 0.91 (0.90 to 0.93) | <0.001 | 0.70 (0.60 to 0.80) | <0.001 |
| Year2 | 1.00 (1.00 to 1.01) | <0.001 | 1.01 (1.01 to 1.02) | <0.001 | |||||
| Level | 1.09 (1.01 to 1.19) | 0.034 | 1.13 (1.04 to 1.23) | 0.006 | 1.11 (0.94 to 1.32) | 0.218 | 1.06 (0.90 to 1.26) | 0.473 | |
| Post slope | 0.89 (0.87 to 0.91) | <0.001 | 0.83 (0.80 to 0.86) | <0.001 | 0.96 (0.90 to 1.02) | 0.144 | 0.80 (0.71 to 0.89) | <0.001 | |
Further subgroup analyses by free school meal entitlement indicated that change in trend for both higher and lower SES groups was of similar magnitude for saying that trying smoking is OK (OR 0.84, 95% CI 0.81 to 0.88, p < 0.001 for high SES; OR 0.85, 95% CI 0.77 to 0.95, p = 0.003). The increase in rate of decline for smoking attitudes for saying that weekly smoking is OK was significant for young people not entitled to free school meals only (OR 0.80, 95% CI 0.72 to 0.88; p < 0.001), with a smaller and non-significant increase in decline for young people entitled to free school meals (OR 0.96, 95% CI 0.76 to 1.21; p = 0.742).
Views of young people on smoking and vaping norms
To further explore the plausibility of observed changes in trend for smoking occurring due to renormalisation, this section presents qualitative analyses from interviews with 76 young people (boys, n = 37; girls, n = 39) within seven schools in England (n = 2) Scotland (n = 2) and Wales (n = 3), collected from March to June 2017, around the end of the transitional period in the implementation of TPD regulations. Data presented here have been previously published in Brown et al. 105 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text. Data are discussed under the following four themes:
-
Perceived similarities and differences between e-cigarettes and tobacco.
-
Perceived prevalence of vaping and impacts on smoking norms.
-
Supply, device characteristics and vape marketing.
-
Attitudes towards nicotine in vapes.
Country [i.e. Wales (W), Scotland (S) and England (E)] and school code, group number and gender are indicated in brackets.
Perceived similarities and differences between e-cigarettes and tobacco cigarettes
The term ‘e-cigarette’ was widely rejected by participants, with ‘vapes’ and ‘vaping’ generally preferred. Participants most commonly described ‘tank’- or ‘pen’-style devices as used by their age group, rather than ‘cig-a-like’ models. There was general awareness of how vapes functioned, including the need to charge them and the production of vapour rather than smoke. When asked why young people vaped, reasons included for fun with peer group, for flavours, and to show off to peers both in real life and online through posting tricks on social media. These, predominantly social, reasons contrasted with perceived reasons for adult use, described primarily as to stop smoking:
Like, you don’t see people our age going round with the ones that look like cigarettes ... Maybe adults would, the ones trying to get off smoking.
W2, 1, F
Several commonalities between vapes and tobacco cigarettes were described, such as potential addictiveness, nicotine content and potential to be harmful. Stated differences were more extensive, with non-nicotine e-liquid options and range of flavours most commonly referenced and vaping defined as different from smoking. Developments in technology, including styles of device and range of flavours, appeared to enhance differentiation from tobacco cigarettes.
In discussing perceived risks of vaping, there was much variation in responses within groups, with peers often disagreeing over risks or stating something that others were unfamiliar with leading to discussion over the validity of claims. Although smoking harms are taught in school from an early age, this was not the case for vaping, with no young people reporting that their school had covered e-cigarettes and frequent reference to getting information from social media. There was also notable variation in awareness of the legal age for vaping in the UK. Types of risks identified also often differed from risks of smoking, with health risks, such as cancers and respiratory conditions, less likely to be mentioned than for smoking. For vaping, risks commonly focused on anecdotes of operating or charging problems, such as devices ‘blowing up’, with young people frequently citing stories from social media and unknown toxicity of the chemicals in liquids. Although clearly viewed as less harmful than smoking by most young people, notions of ‘harming differently’ were evident:
Some people say they have even more ... they claim to be less harmful but actually they’re more harmful in fact, apparently.
W1, 4, F
Many young people expressed caution that harms may yet be discovered in the future, as had happened with smoking:
It’s just with e-cigarettes, you are not sure what’s bad about them. Like, you know some of them are nicotine. So it’s just, what health impacts? Smoking, you know that you can get lung cancer, but e-cigarettes there isn’t the same health issues.
S1, 2, F
Perceptions of the prevalence of vaping and norms for smoking and vaping
Although advised that they did not have to discuss their own experiences with e-cigarettes, many young people did discuss trying vaping. This discussion often occurred at group level, with all young people in a group having tried e-cigarettes or none having done so, reflecting shared norms and behaviours within groups of friends. Being a regular vaper was rarely discussed but emerged in two male groups, where members reported regularly vaping non-nicotine liquids to do tricks. This patterning by group was not as evident for smoking, with fewer young people stating that they had tried smoking and just a few individuals stating that they were regular smokers. Most participants agreed that young people’s vaping had increased in the last few years, and most indicated that they saw more young people vaping than using tobacco cigarettes now. Vaping was largely described by participants as casual, or occasional, and strongly socially motivated, for example occurring with peers at parties where a device is brought by one person and shared. However, many participants also suggested that vaping was a fad that may have peaked:
Not too long ago there was like a whole new craze about it because everybody was thinking it would be a safer alternative to smoking and ever since then the boom of it has started to die down and we haven’t really seen much of anymore.
E2, 1, M
Regular use (i.e. daily or weekly) of e-cigarettes by young people was described as rare, adopted as either a means to perform tricks or as something primarily done by smokers. Habitual users were described as more likely to either be dual users of tobacco and vapes or as members of smoking peer groups. It was also frequently stated that this group of users was more likely to be engaged in alcohol and cannabis use, with regular vaping perceived as a component of a broader clustering of risk behaviours. Regular smokers were described in negative terms as the ‘kind of disruptive ones’ (E1, 3, F) or as the ‘people who think they’re hard’ (S1, 2, F), and were seen to be less academically engaged:
I don’t think it’s the more intelligent people that smoke.
W2, 4, M
Some participants also suggested that regular smokers they were likely to use cannabis as part of their identity as smokers:
... a lot of them will just smoke anything they can get their hands on.
W3, 1, M
Increased prevalence of casual vaping, including popularisation of tricks among peer groups and on social media, was described as making experimental use acceptable, as well as reducing concerns over associated risks. ‘Having a go’ on a vape as a social activity was met with little disapproval, with reasons for experimental use cited as (1) because peers were doing so, (2) for flavours (including swapping flavours) and (3) for doing ‘tricks’. However, many participants differentiated between acceptance of casual vaping and disapproval of regular use unless as an aid to stop smoking. Regular use was otherwise pointless and, in some cases, ‘not cool’:
If you’re just doing it to be sociable and pretend, and say, ‘Yeah I’m vaping’, and just blowing out, you’re just going to be bullied, not like bullied constantly, but you’re going to be taken the mick out of you.
E1, 2, F
An exception was regular vaping to perform tricks:
I think most people if you’re going to vape you’ve got to do tricks with it in our year because if you’re not doing tricks you’re not cool.
E1, 2, F
Throughout the data, there was little variation by gender for most themes; however, an area where variation occurred was consensus in most groups that boys were more likely to be involved in trick performance. A small number of non-smoking boys discussed this and its sharing through social media, with those who did so confident of little censure from peers:
You see some people sharing videos on Facebook and they’re having a big puff of this e-cigarette and they’re making rings with it and it looks cool, it’s almost like a new kind of trend.
W2, 4, M
Perceived peer and family disapproval of regular smoking or vaping was strong. When discussing expected peer reactions to people becoming smokers, responses included the expectation of respect for their choice [e.g. ‘... if you want to do them just do them’ (E1, 4, B)] and the, more common, expectation of negative responses, usually from concern over addiction:
I know my friendship group would say like, what are you doing? Just stop it now while you’ve got the chance.
W3, 1, F
Reactions of disgust were also mentioned:
I think with my friends it would repel them.
W1, 4, M
Potential risk of social loss due to exclusion from peer groups was often described as a consequence of becoming a smoker, but less evident for vaping. Shared norms within groups of friends were evident and tended to manifest in relative acceptance of vaping across all in the group or shared rejection, with some groups keen to identify themselves as not the ‘types’ to do that. Most group discussions suggested that smoking by young people was driven by addiction or a deliberate adoption of risk:
... because they think it [tobacco] makes them look cooler because it can harm you.
W2, 2, F
In several groups, it was suggested that, rather than making smoking acceptable, the increased availability of vaping actually made smoking seem more socially unacceptable by comparison, as there is now a less harmful alternative:
I think with the introduction of e-cigarettes, I mean tobacco was already considered pretty dangerous but I feel like people are being more sceptical about tobacco use and stuff, and e-cigarettes ... I think it kind of makes us think that tobacco is more dangerous than it was before.
E2, 1, M
All groups stated that parents would have a stronger negative reaction to smoking than vaping, although parents reacting badly to the latter was also reported by many and, again, tended to be consistent in groups. Some groups suggested, however, that parents may be less anxious about vaping than tobacco smoking:
I think they would prefer vaping to smoking, I would say, if it had to be one.
W1, 2, F
Reasons for strong parental disapproval of smoking included risks being so well established that ignorance of harm could not be a defence, and decreased peer influence to smoke due to lower prevalence and acceptability in young people:
I don’t think they’d see any excuse for tobacco cigarettes because there’s no pressure to have them, there’s no influence.
W1, 1, M
Some participants, particularly participants in groups that were keen to identify themselves as not being the type to vape, further expressed concern that parents perceived a greater alignment of drug use and tobacco and, therefore, were more likely to fear that their child was involved in other drug use, such as cannabis, if their child was smoking tobacco than if they were vaping:
I think that after that they will just think worse of us, like they think we’d be doing drugs and stuff like that because of that one thing [tobacco].
W2, 2, F
Device characteristics, supply and marketing
There was general agreement within and across groups that vapes were easily obtained, and more accessible than tobacco cigarettes. Young people predominantly discussed availability through online sales or informal school supply chains. Within-group discussion was common, with participants sharing stories of who in or around school may be the one selling supplies. Although some participants cited young people in school selling tobacco cigarettes, this was less common, with tobacco largely expected to come from older people supplying it, including peers/siblings and proxy purchasing. The dominance of this informal supply line meant that most young people had seen tobacco cigarettes outside the packaging only, with brand awareness low. Although most participants were aware of specialist shops in their area or the nearest larger town, few participants knew these shops by name or saw them as a likely source of supply, with informal and online routes seen as less restricted. Several participants cited that vaping had come into school first through the ‘populars’ and had spread as a casual and socially driven practice, including sharing flavours and performing tricks. This contrasted with the more deviant status of smoking – and smokers. Flavours were highly significant, both for taste and social gains of swapping, and lively within-group discussion was common with regard to who had tried which flavours and which were preferred:
I just liked the different flavours. ’Cos my friend had jam donut, another friend had gummy bear flavour and Heisenberg which is a minty flavour which is quite nice.
S1, 1, M
Flavours further differentiated younger, casual users from both adult vapers and from tobacco smokers:
Because they’re always shown with all the flavours and I think if you were trying to quit smoking you wouldn’t be bothered by all the flavours.
W1, 1, M
It was common for participants to discuss vaping devices as accessories, with appeal associated with the style and cost of equipment:
I think what makes it more appealing, there are some designs on them. So people are just like, ‘Oh that’s a cool design’. And different flavours and they’re comparing with their friends. Oh look at yours, yours is red and mines like camouflage.
W2, 4, M
For the few participants who reported vaping for tricks, device type was also important, including use of ‘bigger boxes’:
I think our age group normally go for them because you can make a fat cloud out of them.
W1, 1, M
This sense of vaping showing off financial status and being started by more popular young people contrasted with comments on the typology of tobacco users, commonly defined negatively, including as being the ‘scruffy’/‘naughty’/‘disruptive’ young people who were already likely to reject school rules and behavioural norms.
Attitudes towards nicotine in vapes
In initial discussions about similarities and differences between vapes and tobacco cigarettes, there was widely varying understanding of the presence or absence of nicotine in e-cigarette liquids. Some participants were unsure or unaware that nicotine could be present and were surprised when others highlighted this, stating that they had thoughts liquids were just:
... syrupy stuff in different flavours.
E1, 3, F
When asked to describe reasons why young people smoke, addiction was frequently cited, but this was not the case in relation to vaping, where social reasons, such as fitting in and showing off where dominant. However, when asked to identify potential risks of vaping, addiction was cited by at least one participant in most groups. Although some participants stated that they would avoid nicotine-based liquids because of fear of addiction, for many participants who described experimental use, nicotine content was either an unknown or less important than flavour:
I don’t know. It’s not really something you ask if its nicotine or no nicotine. You more just ask them what kind of flavour is it
S1, 2, F
This perhaps reflects the context of use, where vapes used by young people commonly belonged to someone else and were passed around for people to try rather than being something actively sought. Where vapes were tried once with little intention of using again, concerns over nicotine were secondary to social factors driving experimentation:
Int: Yeah, so just once?
E1, 3, F, P: Yeah.
Int: And do you know if that had nicotine or no nicotine in it?
E1, 3, F, P: I have no idea [laughs]
Chapter summary
Ever use of tobacco continued to decline in the period during which e-cigarette use was growing, with little evidence of change in rate of decline. There was a marginal slowing in decline for regular use. However, this was reflected to a greater extent across other substances, for which slowing in declines in ever use were occurring, by contrast to counterpart measures of ever tobacco use. Our analysis of quantitative and qualitative data did not identify plausible mechanisms via which e-cigarettes might have caused slowing in decline of regular smoking. Young people’s attitudes towards whether or not its OK for young people to smoke continued to harden against smoking during this time. In qualitative interviews, e-cigarettes were viewed by young people as distinct from tobacco use, with widespread rejection of the term ‘e-cigarette’ in favour of terms such as ‘vapes’. Growing experimentation with e-cigarettes was widely approved of, with young people discussing use of e-cigarettes in particular social contexts, such as at parties and imitating tricks, but regular use outside this context was not. Although findings provide limited support for the notion that e-cigarettes renormalise smoking, the findings highlight some concerns with potential normalisation of some forms of e-cigarette use and potentially nicotine, with many young people reportedly unaware of whether or not devices they had used contained nicotine. Young people emphasised informal supply chains and a perception that e-cigarettes were obtained via peers or the internet rather than through retailers, with social media channels also seen as a key source of marketing exposure. Hence, although data prior to implementation of the TPD regulations indicated that regular use remained limited and concentrated primarily among smokers, preventing young people’s use of e-cigarettes remains a priority.
Chapter 4 Results: political and legal context and implementation of Tobacco Products Directive regulations
Some text in this chapter has been reproduced from Brown et al. 106 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, including for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The chapter addresses the following research questions:
-
To what extent, and in what ways, do variations between UK countries in e-cigarette policy emerge during the study period?
-
What other changes to the regulatory context of tobacco and e-cigarettes occur during the study period in the UK and across individual UK countries?
-
To what extent is compliance with TPD regulations in product sales achieved, and what are the barriers to and facilitators and unintended consequences of implementation?
The chapter explores the political and legal context and implementation of the TPD regulations, from the perspectives of policy stakeholders, TSOs and both specialist vaping and non-specialist retailers. Building on findings from Chapter 3, the chapter also includes stakeholders reflections on young people’s use of e-cigarettes and perceived risks of e-cigarettes to young people. Interviews were conducted between June and October 2018.
Perspectives of policy stakeholders and trading standards officers
Policy stakeholder interviews included 12 individuals in England, Scotland and Wales whose professional roles included a significant emphasis on tobacco control policy. 106 Stakeholders included four interviewees within government roles, three interviewees with roles such as tobacco control within government agencies and five policy advocates within the voluntary sector. Trading standards representatives were interviewed from 13 local authority areas in England, Scotland and Wales. Codes next to quotations indicate country and unique participant number.
Stakeholders’ views on tobacco control and the pros and cons of e-cigarettes
Interviews commenced with a discussion of tobacco control and direction of travel within the UK over recent decades, including drivers for sustained reductions in smoking and the emergence of e-cigarettes. There was consensus that success in reducing smoking was attributable to a wide-ranging package of measures, spanning pricing, advertising constraints and restrictions on locations where smoking is permitted. Many participants felt that these measures had facilitated a shift in cultural norms, with reduced exposure and access to tobacco among young people leading to stronger disapproval than in previous generations:
There’s been a shift in culture with regards to the acceptance of people who smoke and the acceptance of passive, being exposed to passive smoking. So we’ve had a huge shift in culture, which has led to the decrease, coupled with price increases, tax increases around cigarettes as well.
W2
However, impacts were frequently described as inequitable, and this led several stakeholders to suggest that future actions in smoking harms require more effective targeting of disadvantaged groups alongside general population measures:
We want to bring the rates down across the board, but we know we need to do more targeted action, where those rates are higher.
W1
In relation to the positioning of e-cigarettes, views were highly variable in terms of whether e-cigarettes constitute a positive or negative development for public health. All participants acknowledged limitations in the evidence on potential harms at the time of interview, with some participants suggesting that this impeded ability to provide clear guidance and communication to the public. Views of what this meant for practice, and the extent to which e-cigarettes should be accepted within public health, varied significantly. Many participants saw e-cigarettes as having a positive role in providing another smoking-cessation option with less harms than those known of for tobacco. It was suggested by some participants that the market-led provision of e-cigarettes was helpful in ease of access for smokers, for whom some current smoking-cessation options could be more difficult (e.g. where there was a requirement to engage with medical professionals). Concerns were expressed, however, that profit-driven provision meant that customers may not be getting clear and consistent advice on product use from retailers. Hence, some participants argued that it would be preferable for cessation advisors in statutory services to be trained to offer advice to those accessing their service. According to some participants, this would ensure positioning of e-cigarettes as a tool to transition away from nicotine rather than a long-term maintenance option:
Let’s get the right e cigarette with the right level of nicotine for the smoker. So that would mean training those vaping advisors, to make sure that people who are giving that, who are distributing this product, are aware of, if they smoke this, then they need to have this much nicotine, because getting the right amount of nicotine is so important in that smoking-cessation journey.
W2
There was greater caution observed from respondents in Wales in particular on whether or not e-cigarettes should be actively recommended by cessation services, perhaps reflecting wider national debates across the UK nations and historical caution in Wales at policy level. Many stakeholders noted this difference, with some stakeholders suggesting that Scotland and England were both more supportive of e-cigarettes within cessation services than Wales:
Int: How would you see that actually working in practise, should vaping be recommended [in smoking-cessation services]?
E5, res: So I think it’s a done deal in England I don’t think anybody would seriously doubt it and in Scotland as well. In Wales there’s a debate.
All interviewees expressed concerns over the potential harms of e-cigarettes for young people, with consensus that monitoring uptake by young people was a priority, although interviewees were aware that evidence at the time of interviews suggested that regular use by young people was rare. The concept of tobacco renormalisation was discussed as a potential result of the growth of e-cigarette use, and the views of interviewees were highly variable on how to address this. Although many interviewees suggested that there was little evidence of renormalisation to date, this was interpreted differently as either ‘evidence of absence’ or ‘absence of evidence’. Some interviewees argued that the evidence had shown that shifting norms of tobacco use among young people were unlikely to be reversed, whereas other interviewees stated that it may be too soon to know the full impacts of e-cigarette emergence on smoking norms. Despite these variations, policy measures aimed at restricting young people’s exposure to e-cigarettes, while facilitating availability to smokers, were widely supported:
I’m generally in favour of the regulatory approach that we’ve taken in the UK which does feel like a good attempt of getting that balance right between keeping them away from kids and having information around that they are not harmless but, making them available to try and have them deliver the potential they have.
S3
Perceptions of e-cigarette regulations within the Tobacco Products Directive
All interviewees were asked to consider the main e-cigarette measures within the TPD, with discussions of marketing restrictions, the introduction of warning labels, restrictions on sizes of e-liquids available and changes to devices, such as tank sizes and tamper-proof packaging. There was consensus that the TPD regulations represented a positive step in introducing regulation to the e-cigarette market, with concerns that legislation may have been slow to catch up with rapid growth of the market and range of available products. Requirements for product notification and restrictions on ingredients were particularly supported, along with marketing restrictions, with some interviewees suggesting that such measures could prevent a growing public perception of e-cigarettes as being as dangerous as tobacco, therefore, potentially undermining smoking-cessation efforts:
It’s helpful in so much as it addresses the issue of the product as not regulated, so it means that when people say well the product’s not regulated, that you can actually say there is a regulation in place. It gives from our perspective, it means that we’re no longer dealing with a maverick product.
W2
There was also discussion of the content of the message introduced through the TPD (i.e. ‘This product contains nicotine which is a highly addictive substance’). Although the option of introducing a product warning label onto packaging and aligning this with practice in tobacco was generally well-received, there were mixed views on the content of this warning message. Many interviewees felt that the message was simplistic and could potentially alienate smokers, as well as seemingly conflicting with approaches to nicotine provision observed in other smoking-cessation products:
I find this slightly confusing, I’ve heard people suddenly talking about nicotine in a way which I don’t remember anyone talking about nicotine before ... so we’ve had NRT for what, I don’t know, about 20 years? I don’t think there is a warning on NRT saying this contains nicotine which is really highly addictive ... so why don’t we have warnings on NRT?
S1
It was argued that further research was necessary into the perceptions of the message among different population subgroups, with future revision an option. The evidence base for other key measures was also discussed in relation to the cap on the level of nicotine available in e-liquids and on restrictions on tank sizes that limit the volume of e-liquid held. Several respondents suggested that these measures were not evidence led and may result in unintended harms. Concerns over potential risks of these measures included fears that, by making use of e-cigarettes more difficult through requiring more frequent purchase and refill of liquids, smokers who had switched to e-cigarettes may be deterred from continuing:
The tank size is not based on any evidence and it is annoying for people to have to continually fill up and leak and it’s an expensive way of doing things. There will probably be people who will have gone back to smoking because they can’t take the cuffuffle of it.
S1
Among TSOs, in particular, there was discussion of restrictions as drivers for market innovations, as producers look for ‘loopholes’ to circumvent constraints. Several TSOs discussed observations of growth in sales of ‘short-fills’, where retailers stock bottles partially filled with non-nicotine e-liquids, leaving capacity for consumers to later add their own liquid nicotine, which can be purchased separately:
There are people making up fluid in their own houses, which is just absolutely mental to me.
TS1, S
Some TSOs also reported observing new products on the market that modify the existing tank on a vaping device to hold more e-liquid, meaning that the consumer is able to refill less often and the retailer is still compliant with current legislation:
The regulations say you can’t have anything more than two mil on a tank. A squonk is a bottom feeder with a little squidgy bottle and it goes in the device ... it completely circumvents the Regulations ... So yeah the squonks, the bubble glass on the tanks, expand the mil from 2 to 3 to 5.
TS1, E
Barriers to and facilitators of implementation of the Tobacco Products Directive
The process of policy implementation was discussed, including the lead-in period to full compliance and the immediate communication and enforcement activities undertaken. Initial understanding of the new legislation and the changing requirements among retailers was described as limited in comparison with tobacco because of significantly more experience of tobacco as a restricted product. Several reasons were cited for this, including limited resourcing within public health bodies and local authorities to publicise the new regulations to all those selling e-cigarettes in their area. All TSOs discussed the impacts of funding cuts on their work, with some areas losing as many as 50% of their staff in recent years:
I’m the only officer in [this area]. I’ve got 700 premises to deal with approximately ... I think it is generally down to local authority budgets, more than anything. It unfortunately comes to money.
TS1, S
This was coupled with new and emerging threats, including illicit tobacco, modern slavery and criminal gang activity. For many respondents, the choice was between acting on these issues and the perceived lower risk activity of e-cigarette use. Despite funding constraints across all nations, TSOs were reported to have increased visits to retail premises in the period leading up to the implementation of TPD regulations and during the transitional phase. In Scotland, TSOs reported that ring-fenced funding had been made available from the Scottish Government to fund and increase visits to retail premises to observe and enforce the roll-out of TPD regulations; however, this differed in England and Wales, where money had been made available in some local authorities, but had been provided on a bespoke basis from local authority budgets. As TPD regulations came shortly after introduction of age of sale restrictions in England and Wales, pre-implementation checks often involved use of young people aged 18–20 years to check on retailer requests for proof of age (with this practice more common in recent years because of restrictions on the legal basis for test purchasing by under-age young people). Many TSOs favoured this approach as conducive to good relationships with retailers and were keen to stress that they did not see their role as ‘catching out’ those who may not yet have been fully aware of TPD requirements.
Across the nations, there was consensus that the funding provided during implementation was not sufficient for direct communication with the majority of retail outlets, partly because of the rapid growth of settings selling e-cigarettes in recent years. This meant that, where limited funding and staffing were a factor, what resources were available were used to communicate more with those involved in e-cigarette manufacturing and wholesale, as opposed to attempting to communicate with direct retailers. Views varied as to the effectiveness of this approach, with some respondents observing that under-resourcing of messaging and communication left many retailers reliant on trade bodies and suppliers to inform them of the changes they were required to make:
Unless there’s more detailed funding provided then we’re unlikely to do it really and I suppose you could say that work should be done by the manufacturers, because the responsibility is there anyhow isn’t it?
TS1, W
After the expiration of the 12-month implementation period, it was reported that e-cigarette sales compliance monitoring was incorporated into normal practice for TSOs, meaning that site inspections were generally initiated only in response to intelligence being received from the public on illicit activity. However, the rate of reported incidents for e-cigarettes was described as minimal in comparison with illicit sales of tobacco and alcohol, which were much more frequently reported by concerned parents, schools and other stakeholders:
... we do get under age sales for alcohol, there is more complaints about them. And in relation to e-cigarettes we have only had three complaints since 2016.
TS1, W
However, despite limited capacity to communicate and enforce the e-cigarette regulations, including TPD regulations, there was a general perception of retailer compliance as relatively high.
When discussing perceptions and reported incidents of non-compliance with regulations among retailers, in both policy and TSO stakeholder interviews, the nature of the retailers themselves was raised as a factor. Specialist e-cigarette retailers were felt to be more likely to be fully compliant because of the desire to maintain their businesses, better links with trade bodies and often larger scale of their parent companies. More issues were cited as associated with non-specialist, often smaller, retailers who may have had limited experience of selling age-restricted products. The absence of constraints on the types of retailers able to sell e-cigarettes, coupled with the speed of market growth, meant that some businesses with little or no experience of staff training on age restrictions or legal frameworks for sales were active in the e-cigarette market. In these premises, many interviewees felt that non-compliance was more frequent than among retailers who traditionally sold tobacco or alcohol:
You can get it in a shoe shop or you can get it in a boutique or a chemist. So they never had to bother about age restricted products before. A watch repairer, mobile phone shops. People who have never had to deal with age-restricted products are selling NVPs [nicotine vaping products] and it’s like, ‘I don’t ask anybody anything’.
TS2, S
Future policy direction and potential review
The departure of the UK from the EU means that the TPD regulations can be reviewed by the UK Government, with initial commitment to do so in 2021 at the time of interview. Respondents were asked to consider what this may mean for future work in tobacco and e-cigarette regulations and most respondents felt that the direction of UK policy would remain largely unchanged, with little expectation of divergence in major areas, from either the EU or within the UK. Several respondents suggested that the UK had often been the leader in driving regulatory changes on tobacco and that this was unlikely to be reversed in the future:
We’ve gone further than the EU on most things so our advertising, tobacco advertising directive we go further than that in what we prohibit in terms of advertising, promotion and sponsorship. So we don’t just prohibit cross border advertising, promotional sponsorship we prohibit all advertising promotions and sponsorship. So there’s no reason why leaving the EU would change because that’s all translated into UK regulation.
E2
It was noted, however, that the opportunity to review those elements of the TPD regulations with less supporting evidence could be a positive outcome, specifically in relation to restrictions on e-liquid sizes, message content on warning labels and tank sizes:
And actually we’ve got our doubts about whether or not implementation of [tank size restrictions] that is generally a good idea. So you know, going forward, that’s the kind of thing where we might say actually is it good evidence around that. And if not, then that might be something that we want to change.
E4
Furthermore, the capacity to develop and adapt legislation quickly in response to new and emerging products adaptations, such as additions to tanks and ‘short-fills’, was also cited as a potential option for the UK operating outside the EU. Overall, there was little concern about the direction of policy after Brexit and little indication that major divergence across the UK nations was occurring, or was likely to occur in the future.
Retailer perspectives
Interviews with retailers were undertaken in parallel to policy stakeholders and TSOs, exploring retailer perspectives on perceptions of TPD regulations, implementation and compliance. Interviews included 27 retailers, including 18 specialist retailers and nine non-specialist retailers. Interviewee codes indicate country [Wales (W), Scotland (S), England (E)], retailer type [vaping specialist (VS), non-specialist (NVS)] and a unique identifier.
Perceptions of the role of e-cigarette retailers
Many vaping specialists argued strongly that their role was to provide advice and guidance on vaping to help the public quit smoking. Many vaping specialists identified as former smokers who wanted to help others quit like they had. Some specialists argued that all retailers selling vaping products should have knowledge of the area and should be able to give advice regarding use and cessation, with some vaping specialists arguing that vapes should be sold only by specialists with knowledge and training:
I don’t agree that e-cigarettes should be sold in petrol stations, they shouldn’t be sold in supermarkets, obviously we’re dealing with lithium ion batteries, we are dealing with a toxic substance ... I do believe that they should only be sold somewhere where the person selling it has some sort of idea what they’re selling, some sort of training for the staff.
EVS4
Alongside emphasising their role in helping smokers to quit, retailers also emphasised a perceived responsibility to discourage non-smokers from taking up vaping:
... we will get the occasional, especially among younger people we’ll get people come in looking to vape and they don’t necessarily smoke. I mean we try to recommend that they don’t, it’s pointless taking up a habit if they haven’t got an addiction to nicotine already.
EVS4
In discussions of attitudes and policies towards under-age sales, all respondents stated that they would not sell vaping products to individuals aged <18 years. Retailers described being accustomed to asking for identification to verify age if they suspected that a customer was aged <18 years. Many retailers specified that they followed the challenge 25 policy, where if a customer looks under 25 years of age then they will be asked to prove they are aged >18 years:
You get the occasional ones that come in and go I’m eighteen, and I’ll be like well I’m sorry but you have to prove it to me, oh well, and away to storm out the shop, so you are not 18 then, and you are not getting back in, and they don’t come back because they know that they are not going to get served you know.
SVS4
Retailers reported mixed experience of minors showing interest in vaping products or attempting to buy from their stores. For some retailers it was a regular occurrence, but for others it was unusual or rare. Specialist retailers were more likely than non-specialists to mention interest in vaping products from minors:
Obviously you have to ID them first of all anyway, young people are not interested in vaping products, not at the moment.
SNVS4
Yes, we often get kids coming in just asking about the products and you know that they’re not old enough so we basically just have to kick them out and ask them to leave ... I mean sometimes there’s no point even asking for ID because you know they’re about 12 so we just ask them to leave.
EVS7
Some retailers described incidents of parents attempting to buy vaping products for their (underage) child and described it as their role to regulate this:
It’s more common we’ll get the parents come in with their child and try to buy it themselves for the child but even then if someone comes in with someone who we believe it’s being bought just for we’ll still ID them and if they can’t provide ID we don’t serve the parent even if one of them is of age.
EVS4
Several Scottish and Welsh retailers said that they used a refusals log to record attempts to buy products by those suspected to be aged <18 years. For one retailer, this included recording when a customer had been asked for ID and were able to verify that they were aged ≥18 years:
Yeah we, in both our shops we keep a log book, anybody which actually tries to purchase anything under 18, we give them the benefit of the doubt, ask for ID, if they haven’t got ID and the ones which are 18 and three-quarters, look 16, they’ve got their ID, yes that’s fine, but we write it in the book. So we keep a log of all the refusals and acceptance on that there.
WVS3
Views on the Tobacco Products Directive and the principle of regulating e-cigarettes
Views on the TPD varied extensively between specialist and non-specialist retailers. Non-specialist retailers were often broadly supportive or simply unaware of its existence. Specialist retailers were often critical of the TPD and its regulations on vaping, although many recognised the importance of certain regulations, and identified aspects they saw as important:
You know we reach our peak and then they knocked us back down again. So I don’t agree with any of it, I would like to keep hold of ... like I said child lock and stuff like that. I don’t think we should eradicate small bottles completely, because some people do want the small bottles you know. I just want the TPD to go away.
WVS2
Many specialist retailers acknowledged the importance of vaping being regulated, but called for vaping to have bespoke regulations, rather than regulation being aligned with tobacco:
They should be regulated one hundred per cent, all for that there, but it’s not a tobacco product, there’s actually not tobacco in it, so it’s not tobacco product, so they can’t be related to it. A hundred per cent got to be regulated, the Laws ... some are good and some are absolutely ridiculous.
WVS3
Many retailers challenged the logic of e-cigarettes being included within the TPD, as although the process of vaping mimicked the process of smoking, e-cigarettes were seen as different products with completely different purposes, with some retailers highlighting a popular movement away from the use of the word ‘cigarette’ within their description:
They should be dealt with as a separate entity. They should be, they are completely different. A lot of people are moving away from using the word electronic cigarette as well.
EVS2
Many retailers also expressed concern about a perceived risk that if regulated in similar ways, then vaping would be seen within public perceptions as the same as smoking, rather than as a less harmful tool for smoking cessation. Specialist retailers were often keen to avoid being labelled as tobacconists, describing their role as operating in opposition to tobacco, and distancing themselves from the stigma of smoking:
I think there needs to be separate regulations for it because I think it sort of almost wants to steamroller into it that it’s like smoking. It’s like we had directory services call us up and say would you be happy for us to put you down as a tobacconist and I was like well I’m not really comfortable with that because we don’t sell tobacco you know we don’t have the use of cigarettes or smoking and that so we don’t what that sort of stigma to be attached because that’s not what we’re about. We want people to be healthier by quitting smoking and using this as a replacement for the nicotine.
EVS5
However, some non-vaping specialist retailers thought that vaping and smoking should be regulated together, with one retailer commenting that smoking and vaping were essentially the same thing:
At the end of the day you are talking, some of the lines have got nicotine in them and you are weaning yourself down on it, we all know that. But it’s exactly the same thing, it is basically six and one, and half a dozen of the other isn’t it?
WNVS3
Specialist retailers expressed concern that future changes in the regulations on vaping may lead to significant negative impacts, with some anxieties appearing not to be about the TPD specifically, but whether or not the TPD would act as a beginning of an escalation of regulations:
I don’t know they haven’t thought it through, I think there’s going to be more regulations soon and it’s going to mess everything up.
EVS7
Say the TPD decided to change their minds tomorrow and say well double battery mods are now banned. I’m automatically breaking the law just by having this. I’ll have to get rid of loads of stock, the suppliers will have to take a massive hit. So changing rules willy nilly like that is kind of annoying ... Keep it away from kids and get people off cigarettes, it’s as simple as that.
WVS4
Some specialists, although initially unhappy with the TPD, were keen to see no further changes to juices, tanks or bottles now that the regulations had been implemented. Achieving compliance was described as causing a financial burden, which would be wasted if this was reversed, particularly for smaller companies that were described as having struggled to bear additional costs of complying with regulations:
The annoying thing about it is, this regulation came from the EU, we are coming out of the EU but are they going to back track? No, and I hope they don’t because the industry has spent millions of pounds regulating all of these because each flavour has to be put through a process, so say one supplier, one brand has 10 flavours right, each flavour has to get put through this TPD process, minimum of 3000 pounds per flavour, so a lot of wee guys were wiped out.
SVS4
Specialist retailers commonly expressed strong suspicion regarding the motivations that drove the inclusion of vaping in TPD. Some specialist retailers argued that there was a perception among the vaping industry that tobacco companies had a prominent role in influencing the legislation regarding vaping and that it was an attempt to sabotage the industry:
I think it’s, it seems like a lot of people thought it was like big tobacco companies influencing government to stop, well at least cutting the amount of, because in the first year, I hit like a brick and managed to get loads of people onboard, and I noticed everyone was vaping where I was living, no one was smoking anymore, and then the second all these regulations came in and made it a lot harder for people to do stuff, it died out a little bit and people went back to smoking. Now I thought it was to do with the tobacco, the reason why the rules came in...
EVS1
Specialist retailers also described how, initially, tobacco companies had been opposed to vaping and influenced negative media campaigns and lobbied governments. However, this was believed to have altered over time, with tobacco companies investing in vaping products:
Tobacco companies were very against vaping to begin with. There was a lot of scaremongering that was released in the press about vaping and that was mainly from tobacco companies and stuff like that. But now some of them are on board because they realise there’s a market for them.
WVS2
Some specialist retailers were also suspicious of UK and European governments and regulators and what was described by some retailers as attempts to derail the vaping industry:
In terms of regulators, I suspect there was a misunderstanding of the science, possibly some deliberate. I’m sure there’s some influence from pharmaceutical industry. I think there were some memos released which talked about the need to put regulation on a product which is a competitor to nicotine ... and really not giving many of the scientists involved in the EU who will be researching electronic cigarettes the opportunity to speak up I think. Derail the vaping industry.
WVS5
Obtaining information and support for implementation of the new regulations
Knowledge of the new regulations around e-cigarettes and vaping devices in the TPD was variable between specialist and non-specialist retailers. Specialist retailers generally possessed a more comprehensive knowledge of the regulations, whereas non-specialist retailers demonstrated a much more limited understanding. In some cases, this was highlighted by the lack of distinction retailers made between regulations around tobacco control and regulations relating to vaping devices:
I appreciate that writing the TPD at the time was probably quite a tough task because, you know, they were ... they were trying to write a set of rules on an industry that was moving so quickly. By the time that it actually came to fruition, came to become statute, it ... it was so outdated it was quite hard to sort of perceive.
WVS6
Int: In terms of the warnings displayed on the e-cigarette packaging, what do you think about that?
WNVS2: It’s good because it lets people know that you are still buying a tobacco product. So that takes that, it’s trendy away, there is not pictures of dragons and stuff, there are pictures of people that are ill because of tobacco.
Despite absence of a detailed knowledge, most non-specialist retailers described access to support from other knowledgeable sources where advice was needed. Retailers who worked for companies involving multiple stores described relying on guidance from within their wider organisation, whereas other retailers described having been advised about regulations by sales representatives, sometimes described as linked to tobacco companies:
There are so many regulations ... I just depend on the advice that comes in from the reps and that’s it really.
SNVS4
Specialist vaping retailers generally reported that they had received no official advice or support to help them implement the TPD regulations, but that they or others they worked with had actively sought information on the regulations, with a variety of sources mentioned. Some retailers said that they had obtained information from discussions within the vaping community, via online forums or events, or had spoken with other vaping retailers or suppliers:
We just knew it was coming in and the reason why we were updated was because we would attend [event] which obviously, vapers from all over the world and stuff like that and that is the only way we got informed. Because the next show was going to be TPD, so everyone was freaking out and we didn’t know what was what so we went around and got a source and we found out from other people what they had been told.
WVS2
Other retailers noted that their main source of information was from within their company, with guidance handed down to stores that operated as a part of a chain. In some cases, knowledge of the regulations had been gathered from company owners who reported participating in processes related to the development of the regulations:
We’ve been involved in consultations, we’ve been to some of the parliamentary groups, we’ve read through the regulations, we discuss it in the industry and in institute groups, so it’s a multiple, gathering from multiple sources.
WVS5
Some retailers mentioned that they sought information and support from government sources, including official information online and local trading standards teams. Views on the value of these information sources, where provided, were generally negative. One specialist retailer suggested that some of the language used on government websites was confusing, and had increased anxieties by making changes within the TPD regulations appear more challenging than they were in reality:
I think everybody saw it coming in as this big black cloud and little bits off the government website, reviewers and stuff like that, they were talking about it, where until it came into play, it sounded bad, it sounded like you could potentially kill the industry off completely. And then the further and further we got into it, it sort of, you go, well it wasn’t, it’s not that bad, or as you were reading something on the government website, you think about it, and you go, it didn’t actually mean what it looks like it means ... they word it so awkwardly that it confuses you after six letters into a word, it’s yeah, it was, it was panic stations...
WVS7
Specialist retailers who sought information from local trading standards departments perceived that officials sometimes lacked the necessary knowledge themselves to be able to provide advice:
I thought someone would come around and tell us about it but actually the cigarettes [e-cigarettes] themselves, they were constantly changing so you just had to learn about it yourself ... they [trading standards officials] were asking us questions, ... originally I phoned trading standards in [Scottish local authority], she came out and obviously she wasn’t sure.
SVS2
Perhaps as a consequence of these limited communications, retailers argued that a great deal of uncertainty remained in the period before TPD implementation:
When the TPD first came round I was going through legislation and finding things that we were never told, like the sort of things we could sell and couldn’t sell which we had on the shelves like 2 days prior that we intended to keep selling so. No one ever really came round and went look this is what you’ve got to adhere to and so it was a bit of a mess to be honest.
EVS4
Uncertainties also appeared to persist for some specialist retailers in relation to what advertising and marketing of vaping products was permissible under the TPD:
Yeah, this is what you can do, so like there’s so many different rules and regulations like I can’t, it used to be but I’m not sure now, but I couldn’t display prices outside the store or on products on the shelf. I can display it on a separate sheet. I’d have to triple check that but it used to be something like that, that I couldn’t display prices outside that’s with stuff that contains nicotine. Now I think that possibly might have changed again.
EVS2
Compliance and enforcement
Ensuring stock compliance with the Tobacco Products Directive
Retailers’ experiences of preparing for compliance with the new TPD regulations were mixed. Non-specialist retailers reported no issues with the process and indicated that it simply involved the removal of non-compliant stock or selling-off non-compliant stock prior to the compliance date. Several non-specialist retailers also reported receiving practical help from sales representatives, including representatives with links to tobacco companies, who visited the store and replaced non-compliant stock with compliant stock:
We had to have the new regulations on it and the company were very good about that. They actually sent their reps in to collect it and replace it before. So they just replaced it and we were never out of pocket.
SNVS5
One representative who reported receiving help from sales representatives noted that they had no problems selling off their non-compliant stock prior to the regulations coming into force:
Int: OK right, so were you able to sell-off that stock before the change over date?
SNVS6: Oh aye it was quite easy we just ran it down a wee bit.
Int: I was wondering if maybe the reps [representatives] were willing to take it away if you couldn’t sell it?
SNVS6: No we definitely, I am sure we got rid of it all you know.
Experience and perceptions of enforcement
In terms of enforcement of the new regulations, retailers’ experiences were, again, varied. Some retailers had received a visit from TSOs to inspect their compliance with regard to vaping products and these visits generally revealed few issues:
We’ve seen Trading Standards once or twice ... we saw them a couple of times in the first 6 months [after the cut-off date] but they were perfectly happy with what we were doing so I don’t think they bothered since.
EVS4
Some non-specialist retailers and one vaping specialist who also sold other age-restricted items noted that their stores had been inspected by TSOs, but that officials had paid no special attention to the vaping products. When asked whether or not TSOs took much interest in the e-cigarettes that they were selling, the manager of a one non-specialist retailer said:
No, never, as long as we’ve got out signs up for the tobacco, I don’t think there is a lot of regulation over the e-cigs [e-cigarettes] at the moment that they have any say...
SNVS5
Some retailers said that they had no awareness of their store undergoing inspection. However, a few suspected that this may have happened without their knowledge. Some retailers indicated that they would prefer to have more of a supportive and open relationship with local TSOs:
The problem we have got is environmental health [sic: trading standards] don’t tell us when they have been in and gone if everything is OK ... If we pass, they don’t tell us we don’t know. So it’s only if we fail we will know. So we have had them in, we have definitely had them in because they work quite close county halls round the corner. So we know they have been in, and they haven’t bought nothing, they have been in, they have observed and gone. So I think it should be less secret service and more supportive.
WNVS2
Retailers stated that they were complying with the new regulations, but there was a perception among some that other retailers were operating without complying:
We welcome Trading Standards coming in, we’ve got no issues with them coming in, they can check our paperwork and what we’re selling, it’s all above board. When it comes to smaller stores that pop up and think that they can make a quick buck and they still sell thirty mil bottles under the counter and stuff like that...
WVS7
Retailers also perceived that others were not complying with the new regulations in relation to advertising. For example, despite television advertising of vaping products being prohibited by the regulations, retailers perceived that e-cigarette brands, particularly those owned by tobacco companies, had found ways to advertise on television. Again, suspicion of the motives and interests of government actors was intertwined with suspicion of the role of the tobacco industry:
Yeah because a lot of the time, people think well if they’re that good, then why aren’t they advertised more, when you watch, I think X have adverts on the telly and that’s only because they’re run by I think X, so they have the money behind them, and obviously tobacco companies have the government, or whatever you want to say on their side, they always have. So they’re able to advertise their products, which every product of X that’s come through these doors, because people think that we sell it, is diabolical, it’s terrible, but again, it’s owned by a tobacco company, so they’re allowed to advertise, we’re not.
WVS2
It was suggested that a lack of other retailers’ compliance resulted from a lack of enforcement, which some retailers blamed on official authorities being under-resourced and overstretched:
A lot of these shops feel like they can get away with murder. Because where’s the presence, it doesn’t feel like it’s being enforced in any way. I’m following it because I know that it’s the only way to keep the business healthy. When you start bending the rules here and there and stuff, and start, you end up on this slippery slope and before you know it you’ll be shut down because you’ve broken a huge rule here or something like that.
WVS4
Perceived unintended consequences of the Tobacco Products Directive
Perceived impacts on businesses
Specialist retailers’ experiences of compliance with the new regulations focused on the sale or disposal of non-compliant stock before the implementation date. For some retails, the experience of implementation seemed largely straightforward:
We were in a good position to deal with it, like I say, we did very well, we were offering sales beforehand but since then we’re doing as well as we used to beforehand.
EVS4
For other retailers, however, implementation of the new regulations was described as having had a substantial impact on stores and businesses. Several specialist retailers described selling-off non-compliant stock at a discounted price in the final weeks before the regulations came into force, with some retailers noting that this had a negative impact on their profit levels:
The last couple of weeks, up until the TPD we were running sales and they [customers] were wondering why their £10 bottle of juice was now £2.50, because we needed to get rid of it, because we can no longer sell it.
WVS7
Some retailers noted that at the point of TPD implementation, they still had large amounts of stock they had been unable to sell, causing, in some cases, substantial financial loss.
One retailer also discussed a financial impact from implementing the regulations from the point of view of being a manufacturer of e-liquids. The retailer noted that they had invested a lot of money in regulating each of the liquids they sold:
I do think it should definitely be regulated of course. Which is something that maybe shops like, that don’t make their own juice they don’t have to do that, it’s more for the juice side of it. We really felt it because now we have to pay to regulate every flavour which again makes sense of course.
SVS3
Specialist retailers who discussed the impact of new regulations around advertising demonstrated mixed perceptions. For some specialist retailers, the new restrictions around advertising appeared to have had very little impact on their stores or businesses because, for instance, they had previously relied on ‘word of mouth’ for promotion:
We don’t really market too much to be honest, I mean we’ve never really advertised outside the stores we’ve always gone down the route of word of mouth we do far better. So we didn’t really change anything we’ve never really advertised much.
EVS4
Other retailers perceived the new regulations around advertising and marketing to have a negative impact:
Advertising is really important ... we are severely limited in advertising, which is, kind of, sucked because we want to let people know. Look you can save your health, save your money, and obviously as a business we want to grow and we want to advertise ourselves, but we just simply can’t.
WVS4
Perceived impacts on smokers and young people
The TPD regulations and the possibility of future tighter restrictions were considered by many specialist retailers to reduce cessation opportunities and were likely to lead to people going back to smoking:
Well if they can make it really awkward and inconvenient for vapers to vape, we will go back to smoking cigarettes again, so if they take away all the flavours which they wanted to originally, taking away the bigger tanks that they keep talking about, they’ve taken away the stronger nicotine...
WVS3
There was a perception among some retailers that there was a particular problem with compliance on the internet. The regulation of traditional sales and young people’s growing reliance on social media were seen as potentially interacting to displace sales of vaping products to minors onto the internet, where devices were likely to be cheaper but unregulated:
Young people generally access most things through social media, so as soon as they’re part of these groups it’s bang, it’s in their face all the time ... So, the availability of products through social media ... that are (a) unregulated products, and (b) become even cheaper through that is an issue, definitely. The problem that that has is there are certain parts of the ... certain parts of the market, the products could be quite dangerous if they’re not used properly.
WVS6
Retailer observations
Overall, 34 retailers were observed in 2017 and 32 retailers were observed in 2018. Inter-rater reliability of 100% was observed for the presence of health warnings and tamper-proof packaging, and inter-rater reliability of 85% was observed for the presence of oversized refills at wave 1 (but this increased to 100% at wave 2). Most retailers (n = 26, 76.5%) were displaying devices with the health warning included at first observation, prior to full implementation. Observers noted that, in most cases, older non-compliant stock continued to be sold alongside devices with the health warnings. In 2017, older non-compliant stock, with no stock with the health warnings, was present in eight retail outlets, including four (19%) non-specialist shops and four (31%) specialist shops. However, by wave 2, 100% of observed retailers displayed compliant devices, and in only two cases did observers note that a minority of stock appeared to be still non-compliant. Almost half of the retailers (n = 16, 47.0%) displayed oversized refills available for sale in 2017, including nearly all (n = 12) specialist retailers and a smaller number of non-specialist retailers (n = 4). After the date of full compliance, these oversized refills were no longer observed on sale in any retailer. Most stores at both time points for whom observation was completed sold devices in tamper-proof packs, although many observers noted that it was not possible to clearly observe whether or not this was the case.
Chapter summary
Views on the role of e-cigarettes in public health were mixed, with policy stakeholders emphasising benefits for cessation, and risks for young people, varying in the relative emphasis placed on risks and benefits in deciding their position on e-cigarettes. There were few differences between nations in formal policy surrounding e-cigarettes, but nations differed in the extent to which e-cigarettes were accepted as a means for cessation that the public health community should advocate. Non-specialist retailers often had limited knowledge of e-cigarettes, or their regulation, and were sometimes unaware of the TPD. Vaping specialists, however, positioned themselves as advocates and supporters of smoking cessation, and all groups emphasised a responsibility to prevent use of e-cigarettes by young people. E-cigarette retailers emphasised that although some regulation for e-cigarettes was justified, regulating e-cigarettes as if they are tobacco products may lead to their being perceived as similar products in terms of their health risks. In common with a positioning as separate from tobacco, specialist retailers expressed antipathy towards the tobacco industry, with some specialist retailers describing suspicions that regulation of e-cigarettes had been lobbied for by the tobacco industry to harm this emerging market. However, with limited perceived communications on the requirements of the TPD, some non-specialist retailers, in particular, emphasised that their primary source of information on how to comply with the TPD came via industry actors. A perceived unintended consequence emphasised by retailers, and consistent with young people’s perceptions, was that the internet was a more common source of e-cigarette purchase than retailers, with growing sales in online black markets. Nevertheless, a high degree of compliance with TPD regulations was apparent within observations.
Chapter 5 Results: post-legislation changes in young people’s e-cigarette perceptions and use and smoking behaviours
Some text in this chapter has been reproduced from Moore et al. 101 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, including for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text. Short-term analyses, as published in Moore et al.,101 are reported alongside the long-term models that include data for 2019 to enable side-by-side comparison of estimated change using shorter- and longer-term data.
This chapter addresses the following research questions:
-
Has regulation of e-cigarettes via the TPD interrupted growth in young people’s e-cigarette use?
-
How do young people perceive risks and social norms surrounding e-cigarettes (and how do these change over time as products become TPD compliant)?
-
How do young people interpret and respond to the presence or absence of health warnings on e-cigarette packets?
-
To what extent, and in what ways, do young people continue to interact with e-cigarette marketing (e.g. via online marketing) after the prohibition of cross-border advertising?
-
Did the rate of decline in young people’s smoking change after additional regulations of tobacco and e-cigarettes were introduced May 2016?
The chapter begins with analysis of qualitative interviews with young people in England, Scotland and Wales in 2017 and 2018, focussing on change over time in perceptions of e-cigarettes. The qualitative interviews are augmented with quantitative data on processes discussed by young people, using items added to the SHRN survey in Wales in 2017 and 2019. Data sources are compared to corroborate or challenge one another. We then present analyses of change over time in e-cigarette use before and after the introduction of TPD regulations. Finally, analysis of long-term trends in tobacco smoking, and change at the point of intervention, extends the quantitative analyses presented in Chapter 3.
Sample description
As indicated in Table 9, in 2017, more participants took part in Wales, with an approximately equal division of boys and girls in each country and an average group size of three or four young people. In 2018, participants were more equally distributed across the three nations, with additional schools recruited in England and Scotland. Although in Scotland and Wales there remained an even split of girls and boys taking part in group interviews, in England there was a tendency for more participation among girls than among boys.
| 2017 | 2018 | |||||
|---|---|---|---|---|---|---|
| England | Scotland | Wales | England | Scotland | Wales | |
| Number of schools | 2 | 2 | 3 | 3 | 4 | 4 |
| Number of interviews | 7 | 4 | 10 | 15 | 14 | 12 |
| Number of participants | 27 | 12 | 37 | 47 | 48 | 53 |
| Percentage male/female | 52/48 | 50/50 | 46/54 | 33/67 | 48/52 | 49/51 |
Young people’s perceptions of e-cigarettes following implementation of the Tobacco Products Directive
Changes in perceived prevalence and norms for e-cigarette use
In 2017, a large majority of young people across all groups had stated that e-cigarette use had recently risen rapidly among their age group and was now perceived as more common than tobacco smoking. Experimental use of e-cigarettes was widely viewed as unproblematic. Trying an e-cigarette was driven by various factors, including sharing with peers, fun and the appeal of flavours:
Yeah and you can get them like scented and stuff like that and so it entices young people.
W1(2)F
I just liked the different flavours. ’Cos my friend had jam donut, another friend had gummy bear flavour and Heisenberg which is a minty flavour which is quite nice.
S1(1)M
However, regular e-cigarette use was judged negatively. When asked to consider who regular users were among their school cohort, some young people felt that regular users came from the same groups as smokers, characterised as ‘outsiders’ or disengaged young people. Although experimentation with e-cigarettes was very evident, it was also a discussion point in many groups that this behaviour was a trend that seemed to have peaked and was likely to decrease among their cohort going forward:
Like the fidget spinners, and then I think as soon as fidget spinners die it’s going to be the same kind of, ‘Oh why are you still using them?’ kind of approach, the same as vaping.
E1(1)M
To explore this perceived peak in use, perceptions of prevalence were discussed in repeat interviews with young people in 2018. The repeat interviews appeared to confirm initial indications of e-cigarettes as a ‘fad’ that had peaked, with young people losing interest over time:
... you’ll see things of it occasionally but I don’t see anyone doing it just to show off now, any more.
W1(2)M
E-cigarettes were now described as being more commonly used by young adults who were using them to quit smoking. However, some interviewees argued that young people younger than themselves were still attracted by flavours and features that had drawn interviewees to try them previously. In 2018, approval of e-cigarette use was more variable than in 2017, with increased likelihood of peer censure associated with e-cigarettes being seen as an outdated fad:
They just go – [mocking tone] I’ve got a vape, I’m sick, look at me!
E4(3)F
I know some of the kids in our year they’re like, oh they just made jokes about it, oh you’re vaping, and think it’s a bit chavvy, and some, they think it’s cool.
W4(1)F
When initially discussing reasons for e-cigarette use in 2017, very few interviewees cited quitting smoking as a driver for young people’s e-cigarette use. However, in the 2018 follow-up interviews, cessation was often cited as a reason for young people using e-cigarettes. Regular use of e-cigarettes as a cessation aid was largely approved of, as opposed to regular use of e-cigarettes in non-smokers:
I think that if it’s used to actually try and give up smoking then I see a huge advantage to it, but obviously if you’re videoing yourself doing tricks and stuff that’s not trying to give it up [smoking], is it?
W3(2)F
Perceived family and peer reactions to e-cigarette use
At both time points, most participants reported that their parents would strongly disapprove of them using e-cigarettes or tobacco, with almost all participants suggesting that they would anticipate a worse parental reaction to tobacco. Some interpreted this as parental fear of tobacco being more clearly associated with moving on to other substances such as cannabis, while others suggested it being due to harms of smoking being better known than for vaping:
My parents would not be happy. Because they know the damage it does to your body ... My mum’s a nurse and she knows all about it, and it wouldn’t be very approved of in my family.
W3(2)F
In 2017, young people described some expectation of negative peer reaction to both smoking and e-cigarette use, but at lower levels than that expected from parents. Most young people suggested that peers would be more likely to censure smoking than use of e-cigarettes. In 2018, some young people expressed a general decrease in disapproval of ‘social’ smoking relative to their previous year in school, associated with maturation, although disapproval of regular smoking remained strong:
I think it is more socially accepted like, now, like in our year to smoke than it was last year. Like you see a lot more people smoking than before especially at parties.
E1(1)M
Survey data from Wales in 2017 and 2019 concurred with perceptions of high perceived parental disapproval of tobacco and e-cigarettes, with stronger disapproval of tobacco than e-cigarettes. Among young people who did not report current use of tobacco or e-cigarettes, a clear majority said that if they were to start, then their parents would try to stop them. At both time points, young people were more likely to report that their parents would try to stop them smoking than try to stop them using e-cigarettes, with a larger proportion of young people saying that their parents would try and persuade them to stop using e-cigarettes (see Figure 3).
FIGURE 3.
Percentage of non-smoking/non-vaping 13- to 15-year-olds reporting that were they to take up smoking/vaping then their parents would try to stop them or persuade them to stop. The question was asked of a random subsample of young people in the 2017/19 SHRN surveys (2017, n = 11,442; 2019, n = 11,197; smoking, n = 8535; vaping, n = 8329).

Among young people who reported current use of tobacco or e-cigarettes, half reported that their parents did not know. Among young people whose parents did know about their smoking or vaping, most reported that their parents’ either tried to stop them or tried to persuade them to stop (see Figure 4).
FIGURE 4.
Percentage of current users of e-cigarettes and tobacco reporting parental responses to their use. The question was asked of of a random subsample of current users in the 2017/19 SHRN surveys (2017, n = 989/993; 2019, n = 744/706, repectively).
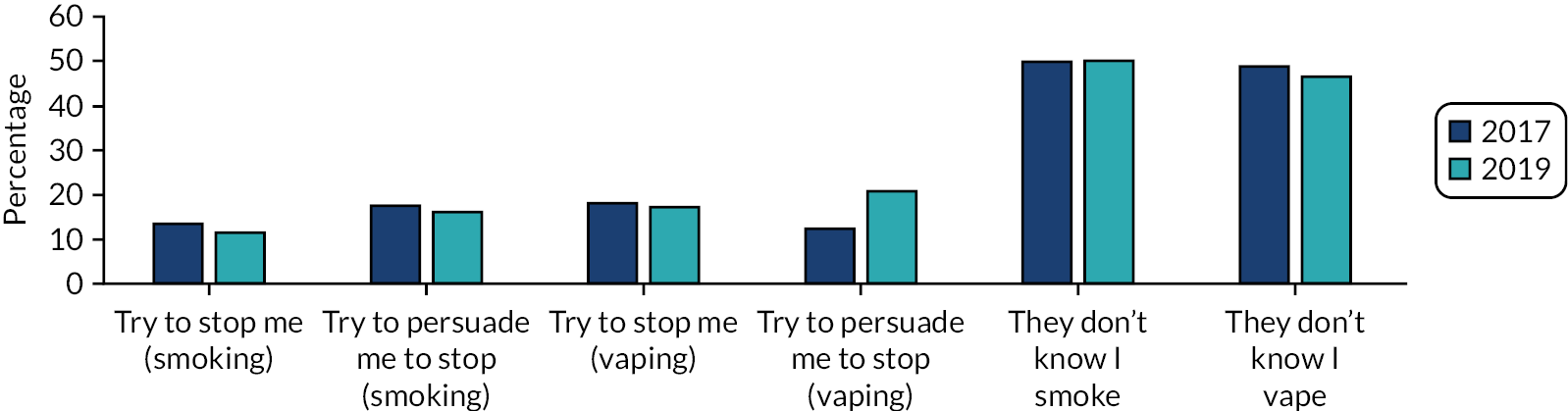
Risk perception
In 2017, increased visibility of e-cigarettes in recent years had been widely cited as instrumental in increasing acceptability of e-cigarettes and reducing risk perceptions. Nevertheless, young people frequently cited mechanical risks (e.g. malfunctioning devices), potentially dangerous ingredients in liquids and, most commonly, as-yet unidentified harms:
Because they know what’s in the cigarette, like in tobacco cigarettes but they don’t know what’s fully in the e-cigarettes or the vapes.
W2(3)M
In both rounds of qualitative interviews, mechanical risks and unknown harms were commonly referenced. In 2017, addiction to nicotine was also mentioned in around two-thirds of groups as a risk of e-cigarette use. However, in 2018, addiction was less frequently mentioned. Many young people who had used e-cigarettes said that they were unsure if it had contained nicotine or not, with use driven by flavour rather than nicotine.
The SHRN survey data indicated that in both 2017 and 2019 a minority of young people who had tried e-cigarettes reported that the last e-cigarettes they used contained nicotine (see Figure 5). At both time points, around one in seven young reported not knowing what was in the last e-cigarette they used (14% in 2017 vs. 13% in 2019). Survey data also indicated changing views on relative harms of tobacco and e-cigarettes during this time. In 2017, approximately one in three young people reported that e-cigarettes were as harmful to health as tobacco, whereas almost half reported that tobacco cigarettes were worse (of the remaining young people, 3% reported that e-cigarettes were worse and 14% said that they did not know). In 2019, almost half of young people reported that e-cigarettes were as harmful to health as tobacco cigarettes, whereas approximately one-third reported that tobacco cigarettes were worse (of the remaining young people, 5% reported that e-cigarettes were worse and 13% said that they did not know).
FIGURE 5.
Percentage of current e-cigarette users’ (n = 8887/2880) reporting whether or not their last e-cigarette contained nicotine, and all young people’s (n = 12,824/9481) perceived relative harmfulness of tobacco and e-cigarettes in Wales in 2017 and 2019, respectively.
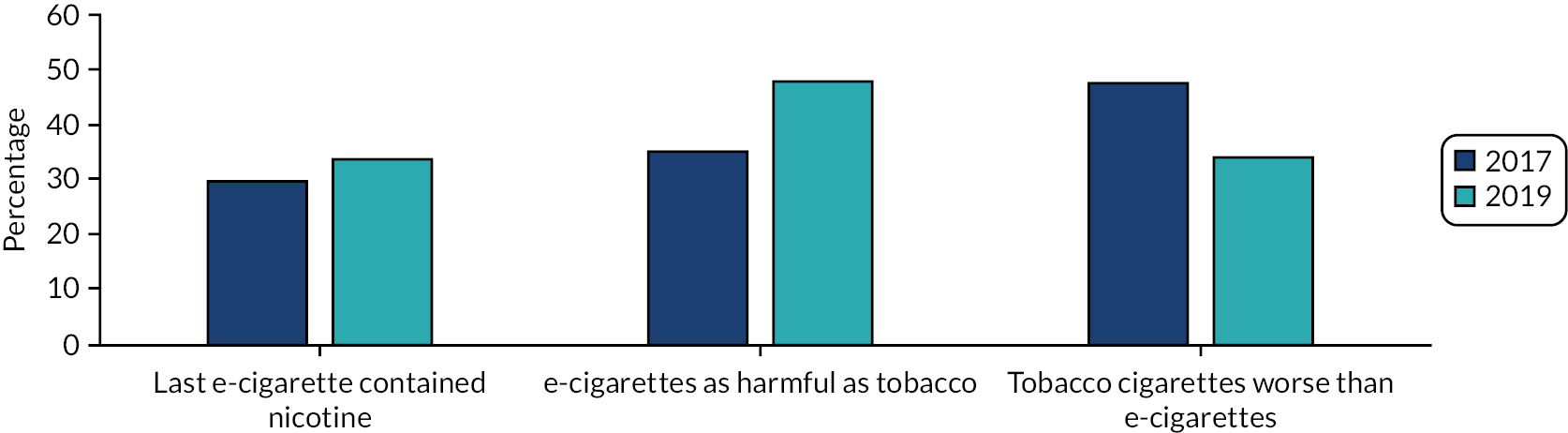
Availability of e-cigarettes
In 2017, most young people agreed that they would find it easier to obtain e-cigarettes than tobacco cigarettes, with few young people suggesting that both were equally obtainable:
But, like, e-cigarettes, it seems to be that you can get hold of one quite easily. But cigarettes – you have to like, know somebody who’s old enough to go buy you some.
S1(2)F
For most interviewees who had tried an e-cigarette, this had been through an informal supply route (e.g. a friend at a social event), although some interviewees reported awareness of someone at school who had bulk bought online with the intention to sell them on:
I was also one of the people who were making profit from them, people would ask me could you order one for me, and I was like OK well I’ll order them. I’d order 10 at once.
E1(1)M
Few interviewees stated that e-cigarettes were available through retailers. Qualitative data indicated that when purchased face to face, this was through shops known locally to be willing to sell illicit products, rather than via specialist vape shops:
Like I’ve seen down in X market, they sell to someone who was 9.
W2(3)M
Discussions a year later suggested that the landscape of obtaining e-cigarettes had changed. Many young people still felt that they could obtain e-cigarettes if desired, mostly through older peers or online purchase, but it was seen as more challenging to buy through school supply chains. This was associated with a perception of decreased use, which meant that fewer people were now selling e-cigarettes:
Int: Do you think it’s got easier or harder to get hold of vapes?
W1(1)M: I think it’s a bit harder because you don’t really see that many people do it anymore.
Int: ... people selling them, would that go on in school or after school?
W1(1)M: I don’t think it’s much in school. I know some people used to do it [sell vapes], but I don’t know anyone now who does it.
In 2018, tobacco was viewed as being as easy to obtain as e-cigarettes. This was attributed to factors such as increased age, which meant greater likelihood of having older peers or appearing old enough to self-purchase in shops, and also to increased smoking prevalence in the year group and, hence, a larger number of people to obtain tobacco from if desired. A significant number of young people were aware of someone at school who sold individual cigarettes, making cigarettes an affordable option:
I know in school obviously a lot of people do it in the corner, but some people sell them individually for 50 pence or maybe a £1 or something, and people do pay that money for them individually.
W3(2)F
Quantitative data from Wales (items included in only the 2017 survey) concurred with the view that most young people who used e-cigarettes obtained the e-cigarettes via means other than a retailer, with the most commonly reported supply route used being peers (see Figure 6). Approximately one-third of young people reported buying e-cigarettes from, or being given e-cigarettes by, peers. The next most commonly selected option was ‘some other way’, not captured by our response options, followed by obtaining e-cigarettes via adults. Fewer than one in six young people reported purchasing e-cigarettes from shops, with approximately 7% reporting buying e-cigarettes via the internet. Among young people who reported online purchase, approximately one in three (n = 29, 35.0%) reported that they had changed where they purchased e-cigarettes from in the past 6 months.
FIGURE 6.
The percentage of current e-cigarette-using young people reporting obtaining e-cigarettes via each supply route. The question was asked of a random sample of young people who reported having used an e-cigarette more than once: 2017 SHRN survey only (n = 3313).
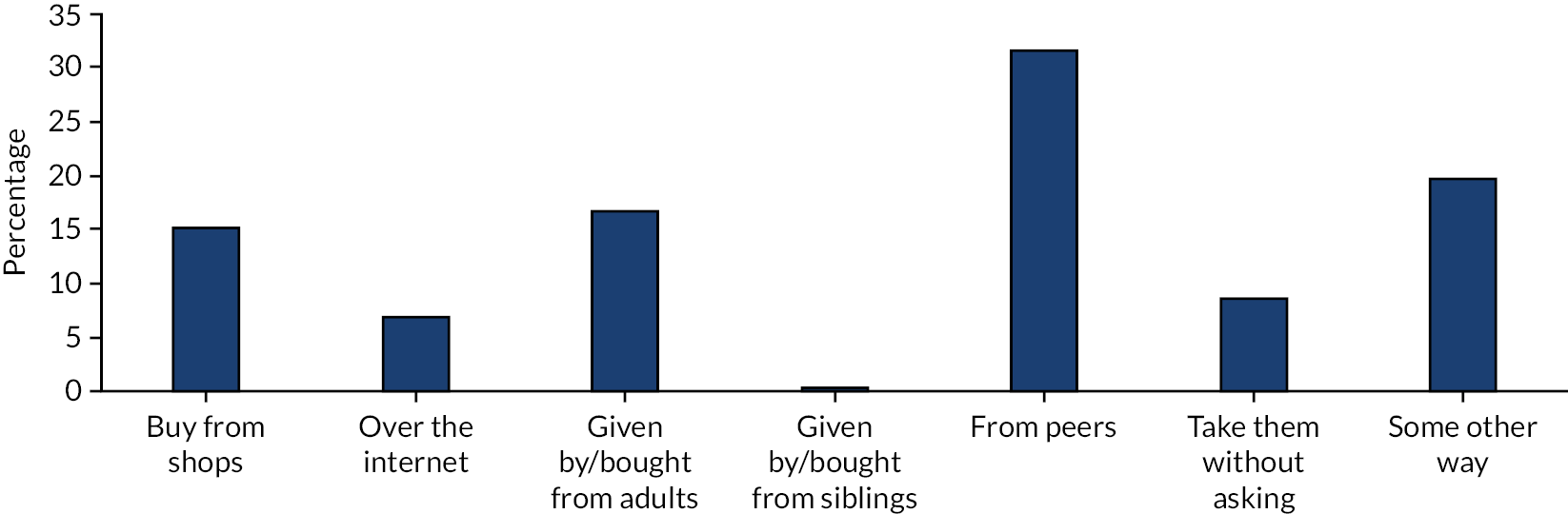
Exposure to warning information and e-cigarette marketing
The TPD introduced a mandated warning, stating ‘this product contains nicotine, which is a highly addictive substance’. In 2017, recognition of this warning among interviewees was low. In 2018, recognition slightly increased, although remained limited, with young people continuing to indicate limited exposure to e-cigarettes within their packaging:
Int: Have you seen any warnings on vape packets?
E4(1)F: No. Can you even get vape packets?
When asked to discuss the current warning, a large majority of young people suggested that it would likely be ineffective at discouraging e-cigarette use among their age group. Young people commonly assessed the warning in relation to more graphic and more well-known visuals present on tobacco packaging, deeming e-cigarette warnings mild by comparison:
Like if I was vaping and like I was like ‘oh it’s fine because look at how bad cigarettes were, like I’m fine’, because there’s no health warnings on any of the [e-cigarette] packets.
S2(2)F
Brand awareness among young people was very low across both rounds of interviews. The most commonly reported avenue for seeing adverts in 2017 was vape shops, followed by online sources (i.e. streamed videos of e-cigarette users performing tricks). Exposure to advertising in public spaces, such as billboards, was seen as relatively common. In the 2018 interviews, however, few young people reported seeing any e-cigarette advertising.
Contrasting with these reports, approximately two-thirds of young people in SHRN surveys in Wales in both 2017 and 2019 reported exposure to at least one form of e-cigarette advertising in the past month. The most common location in which young people reported seeing advertising for e-cigarettes was in shops, followed by exposure to advertising on the internet. However, consistent with qualitative data on of reduced online engagement with e-cigarette-related material, the percentage of young people reporting internet-based advertising exposure declined from 39% to 34% by 2019. There were small increases in exposure to advertising on buses or in bus shelters (see Figure 7).
FIGURE 7.
Percentage of young people reporting having seen adverts in each location in the past month in 2017 and 2019. The question was asked of a random sample of participants in the SHRN surveys (n = 13,503/10,109).
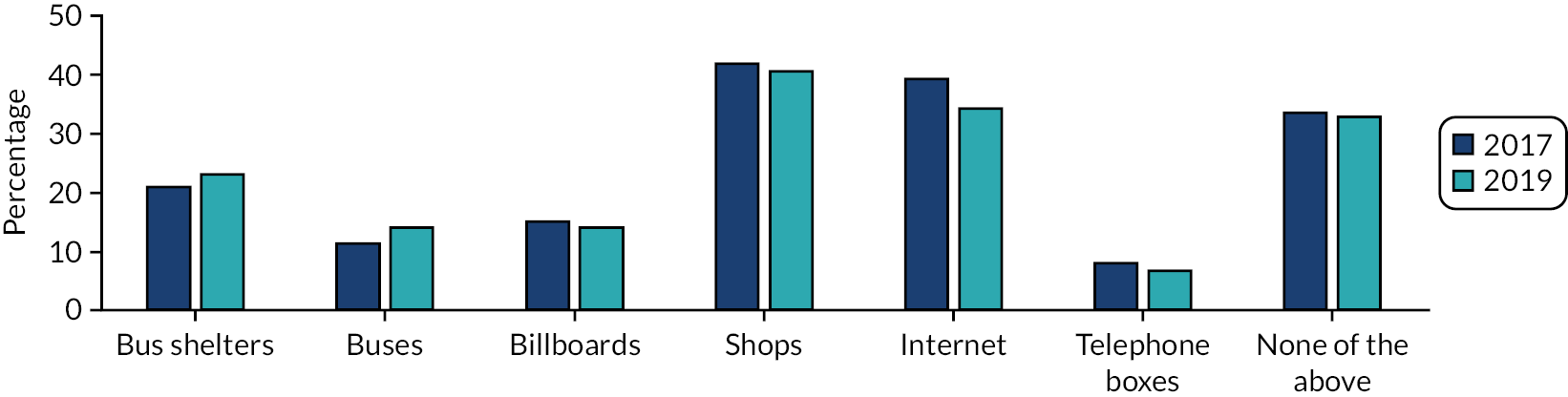
Change in young people’s e-cigarette use after the Tobacco Products Directive
This section analyses change over time in young people’s e-cigarette use before and after the implementation of the TPD. The section begins with our primary segmented regression analysis of data from Wales, and is followed by analyses of yearly data from England and Scotland to examine the transferability of findings from our primary statistical analysis in Wales to other countries in the UK.
Descriptive cross country comparison of changes in young people’s use of e-cigarettes
Figure 8 provides a descriptive overview of the percentage of ever and regular users of e-cigarettes over time, by country, between 2013 and 2019. The black line indicates the beginning of the intervention period (i.e. TPD implementation).
FIGURE 8.
Percentage of 13- to 15-year-olds reporting ever and regular use of e-cigarettes by year and country from 1998 to 2019. The black bars represent the beginning of one ‘intervention’ period (i.e. the introduction of TPD).
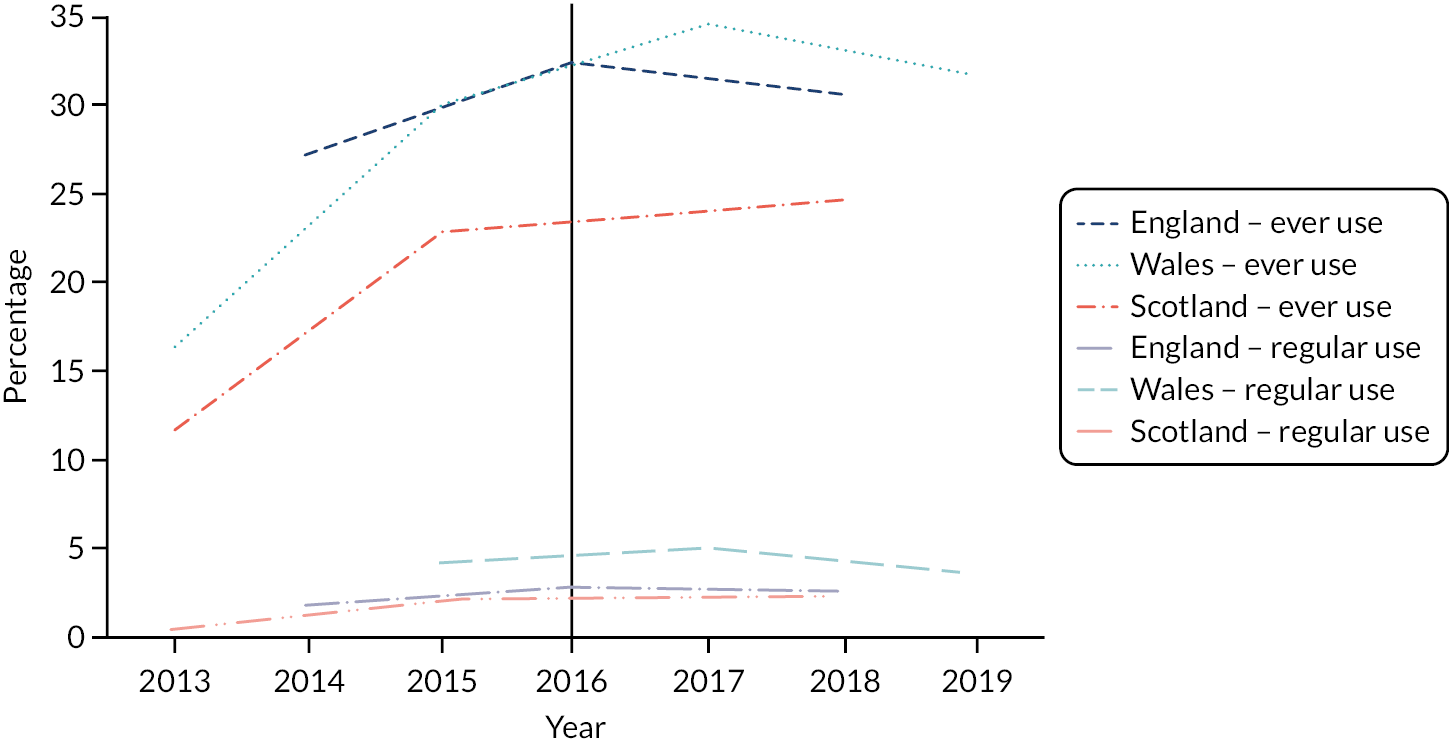
In Wales and Scotland, a near doubling in prevalence of ever use of e-cigarettes is evident in pre-TPD surveys from 2013 to 2015, with growth from 16% to 30% in Wales and from 12% to 23% in Scotland. In Wales, where post-TPD data are available from both the 2017 and 2019 surveys, a smaller continued growth was observed from 2015 to 2017, with ever use reaching 35% by 2017, followed by a marginal decline from 2017 to 2019 to 32%. In Scotland, where only one post-TPD survey was available, a slight increase in prevalence of ever use of e-cigarettes was observed in 2018 (25%) relative to 2015. In England, the first measurement was in 2014, at which point 27% of young people reported having tried an e-cigarette, and this rose to 33% by the 2016 survey (conducted marginally after the implementation of TPD), with no further growth after this time point. Hence, in all nations, there was evidence of rapid growth in ever use in the years leading up to the TPD regulations, with plateauing or marginal decline after the intervention point. Similarly, for the percentage of young people reporting regular use (i.e. at least weekly use) of e-cigarettes, all data sets provided evidence of some growth in the period prior to the TPD regulations, but with plateauing or marginal decline between the two most recent survey periods.
Change in e-cigarette use by country
Primary statistical analysis: ever e-cigarette use in Wales
As indicated in Table 10, the trend displayed in Figure 8, that is of large growth in ever use of e-cigarettes from 2013 to 2015, followed by much smaller growth from 2015 to 2017 (which incorporates the beginning of TPD implementation), and small decline thereafter was observed across subgroups. Ever use was slightly higher among boys, older young people and young people from lower SES families throughout, and substantially higher among ever smokers.
| Subgroup | Ever e-cigarette use, % (95% CI) | |||
|---|---|---|---|---|
| 2013 | 2015 | 2017 | 2019 | |
| All | 16.4 (14.3 to 18.7) | 30.1 (27.6 to 32.8) | 34.6 (33.2 to 36.0) | 31.7 (30.4 to 33.0) |
| Boys | 17.0 (14.2 to 20.2) | 30.5 (27.7 to 33.5) | 37.0 (35.5 to 38.5) | 32.8 (31.5 to 34.2) |
| Girls | 15.7 (13.1 to 18.6) | 29.7 (26.9 to 32.7) | 32.2 (30.6 to 33.8) | 30.5 (29.0 to 32.1) |
| 13-year-olds | 11.5 (9.4 to 14.0) | 22.0 (19.4 to 24.8) | 26.0 (24.7 to 27.4) | 22.6 (21.3 to 24.0) |
| 15-year-olds | 22.1 (19.1 to 25.4) | 39.8 (37.0 to 42.7) | 45.5 (43.7 to 47.3) | 42.5 (40.8 to 44.2) |
| High SES family | 14.5 (12.1 to 17.2) | 26.9 (24.1 30.0) | 33.4 (31.9 to 35.0) | 30.4 (28.9 to 31.9) |
| Low SES family | 17.7 (15.3 to 20.3) | 31.8 (29.3 to 34.5) | 35.8 (34.3 to 37.3) | 32.4 (31.0 to 33.9) |
| White | 16.3 (14.2 to 18.7) | 30.2 (27.6 to 32.9) | 34.9 (33.5 to 36.3) | 32.2 (30.9 to 33.4) |
| Ethnic minority | 16.9 (12.5 to 22.5) | 30.0 (24.2 to 36.5) | 33.2 (30.2 to 36.5) | 28.6 (25.1 to 32.3) |
| Ever smoker | 53.3 (48.9 to 57.7) | 83.9 (80.7 to 86.7) | 88.5 (87.5 to 89.5) | 88.5 (87.4 to 89.5) |
| Never smoker | 6.4 (5.1 to 8.1) | 18.4 (16.5 to 20.5) | 22.3 (21.2 to 23.4) | 19.9 (18.9 to 21.0) |
For short-term post-implementation segmented regression analysis, which disaggregated data sets by survey month, data were available for 12 time points between November 2013 and December 2017, representing 51,056 young people in Wales. Our longer-term analysis through to December 2019 included four further data points, with a total analytical sample of 91,687 young people included in primary statistical analysis. There was no evidence of a non-linear trend (quadratic term OR 1.00, 95% CI 0.999 to 1.001; p = 0.91) and, hence, a quadratic term was not included in our models. As indicated in Table 11, ever use of e-cigarettes increased significantly prior to TPD implementation, with an approximately 4% (i.e. an OR of 1.04) increase in odds of ever use of e-cigarettes with each month passed prior to legislation. The whole sample regression model is presented visually in a predicted probability plot in Report Supplementary Material 1, Figure 1. In both our short- and long-term models, there was no clear evidence of a step change in prevalence at the intervention point (indicated by the variable ‘level’), with direction and size of ORs varying between subgroups, and CIs wide. However, for the whole sample, and among all subgroups (with the exception of young people from ethnic minority backgrounds in short-term analyses), ORs for change in trend were in the direction of a negative change in trend, indicating that growth in e-cigarette use beyond implementation was significantly lower than predicted from the secular trend. ORs in both short- and long-term models indicated an approximately 4% reduction (i.e. an OR of 0.96) in odds of ever e-cigarette use each month beyond the TPD implementation date of May 2016, relative to baseline trend. In the short-term analysis, this was not statistically significant; however, in models including longer-term data, the point estimate remained unchanged but CIs narrowed and reached statistical significance. Hence, overall, data are consistent with a hypothesis of negative change in trend (i.e. significant disruption to secular growth) at the point of TPD implementation. A sensitivity analysis including all young people in the Welsh surveys (i.e. aged 11–16 years) was highly consistent with our primary statistical analysis.
| Sample | Short-term analysis (2013–17) | Long-term analysis (2013–19) | |||
|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| All (n = 51,056a;91,687b) | Time | 1.04 (1.03 to 1.05) | <0.001 | 1.04 (1.03 to 1.05) | <0.001 |
| Level | 1.09 (0.41 to 2.89) | 0.860 | 1.10 (0.93 to 1.29) | 0.252 | |
| Post slope | 0.96 (0.91 to 1.01) | 0.125 | 0.96 (0.95 to 0.97) | <0.001 | |
| Boys (n = 24,993; 45,008) | Time | 1.04 (1.03 to 1.05) | <0.001 | 1.04 (1.03 to 1.05) | <0.001 |
| Level | 1.88 (0.70 to 5.06) | 0.213 | 1.27 (1.05 to 1.53) | 0.013 | |
| Post slope | 0.94 (0.89 to 0.99) | 0.020 | 0.96 (0.95 to 0.97) | <0.001 | |
| Girls (n = 26,063; 46,679) | Time | 1.04 (1.03 to 1.05) | <0.001 | 1.04 (1.03 to 1.05) | <0.001 |
| Level | 0.64 (0.19 to 2.22) | 0.485 | 0.96 (0.80 to 1.16) | 0.664 | |
| Post slope | 0.98 (0.91 to 1.05) | 0.587 | 0.96 (0.95 to 0.97) | <0.001 | |
| 13-year-olds (n = 28,471; 50,619) | Time | 1.04 (1.02 to 1.05) | <0.001 | 1.04 (1.03 to 1.05) | <0.001 |
| Level | 1.49 (0.39 to 5.68) | 0.563 | 1.13 (0.91 to 1.40) | 0.257 | |
| Post slope | 0.94 (0.88 to 1.02) | 0.124 | 0.96 (0.95 to 0.97) | <0.001 | |
| 15-year-olds (n = 22,585; 41,068) | Time | 1.04 (1.03 to 1.05) | <0.001 | 1.04 (1.03 to 1.05) | <0.001 |
| Level | 0.85 (0.26 to 2.78) | 0.789 | 1.08 (0.89 to 1.31) | 0.459 | |
| Post slope | 0.97 (0.91 to 1.04) | 0.375 | 0.96 (0.95 to 0.97) | <0.001 | |
| White (n = 45,727; 81,810) | Time | 1.04 (1.03 to 1.05) | <0.001 | 1.04 (1.03 to 1.05) | <0.001 |
| Level | 1.19 (0.45 to 3.15) | 0.726 | 1.10 (0.94 to 1.29) | 0.223 | |
| Post slope | 0.95 (0.90 to 1.01) | 0.089 | 0.96 (0.95 to 0.97) | <0.001 | |
| Ethnic minority (n = 4528; 8536) | Time | 1.03 (1.01 to 1.05) | 0.001 | 1.03 (1.01 to 1.05) | 0.001 |
| Level | 0.56 (0.04 to 7.35) | 0.662 | 1.12 (0.66 to 1.90) | 0.685 | |
| Post slope | 1.00 (0.86 to 1.15) | 0.963 | 0.96 (0.94 to 0.98) | <0.001 | |
| High SES (n = 25,002; 38,898) | Time | 1.04 (1.03 to 1.05) | <0.001 | 1.04 (1.03 to 1.05) | <0.001 |
| Level | 1.76 (0.62 to 4.97) | 0.285 | 1.24 (1.02 to 1.51) | 0.029 | |
| Post slope | 0.94 (0.88 to 1.00) | 0.037 | 0.96 (0.95 to 0.97) | <0.001 | |
| Low SES (n = 25,167; 50,374) | Time | 1.04 (1.03 to 1.05) | <0.001 | 1.04 (1.03 to 1.05) | <0.001 |
| Level | 0.73 (0.23 to 2.28) | 0.592 | 1.07 (0.90 to 1.28) | 0.453 | |
| Post slope | 0.98 (0.92 to 1.04) | 0.500 | 0.96 (0.95 to 0.97) | <0.001 | |
| Never smoker (n = 40,703; 73,952) | Time | 1.06 (1.04 to 1.07) | <0.001 | 1.06 (1.04 to 1.07) | <0.001 |
| Level | 1.05 (0.39 to 2.83) | 0.917 | 1.01 (0.84 to 1.21) | 0.950 | |
| Post slope | 0.94 (0.89 to 0.99) | 0.022 | 0.94 (0.93 to 0.95) | <0.001 | |
| Ever smoker (n = 8746; 15,327) | Time | 1.07 (1.06 to 1.08) | <0.001 | 1.07 (1.06 to 1.08) | <0.001 |
| Level | 2.34 (0.36 to 15.38) | 0.376 | 0.95 (0.68 to 1.34) | 0.777 | |
| Post slope | 0.89 (0.80 to 0.98) | 0.024 | 0.93 (0.92 to 0.95) | <0.001 | |
Overall, estimates of change in trend were more consistent between subgroups in the long-term analysis than in the short term analysis. Reductions in the secular growth of ever use were greater for boys than for girls in the short-term analysis, with an estimated 6% reduction in odds per month for boys and a 2% reduction in odds per month for girls. In the short-term analysis, subgroup analyses by ethnicity and SES indicated no change in trend in ethnic minority groups; however, a significant change in trend was observed for children from higher SES families, although this trend did not persist in the long-term analysis.
At both time points, for both never smokers and ever smokers, the ORs suggested larger changes in trend for both groups than for the whole sample. In short-term analysis, odds declined by 6% per month post implementation for never smokers and by 11% per month post implementation for ever smokers. In long-term analysis, odds declined by 6% per month post implementation for never smokers and by 7% per month post implementation for ever smokers (see Table 11). As a post hoc investigation to understand these differences, a binary term for ever smoking was added to the whole group model. In short-term analysis, the negative change in trend post intervention increased in magnitude, and was statistically significant (OR 0.93, 95% CI 0.88 to 0.98). This same estimate was repeated at long-term follow-up, with CIs narrowed because of the larger sample size (OR 0.93, 95% CI 0.92 to 0.94). This is consistent with a conclusion that ever smoking operated as a time-variant confounder, and that in a priori models change in trend was underestimated because of changes in ever smoking occurring in the opposing direction across the time series.
Regular e-cigarette use in Wales
Data on regular e-cigarette use were not collected in Wales until 2015 (i.e. pre TPD), and were collected again in 2017 (i.e. short-term analysis post TPD) and in 2019 (i.e. long-term analysis post TPD) (n = 87,704). A small increase in prevalence of regular use to 2017, followed by a small decline to 2019, was consistent across all subgroups, with 2019 estimates marginally lower than 2015 estimates in all cases (see Table 12). ORs from logistic regression analyses of data for each of the 3 years indicate an estimated 15% increase in odds of regular e-cigarette use between 2015 and 2017, falling short of statistical significance (OR 1.15, 95% CI 0.97 to 1.36; p = 0.11). The odds of e-cigarette use in 2019 declined by approximately 16% relative to 2015 (OR 0.84, 95% CI 0.70 to 1.02; p = 0.09). Only for high SES groups did increase in regular e-cigarette use from 2015 to 2017 reach significance, whereas contrasts between 2015 and 2019 were significant for boys and Year 11 students, indicating significantly reduced use in these groups. Regular use of e-cigarettes among never smokers remained low throughout, at approximately 1% across the time series.
| Sample | Percentage (95% CI) | OR (95% CI); p-value | |||
|---|---|---|---|---|---|
| 2015 | 2017 | 2019 | 2017 vs. 2015 | 2019 vs. 2015 | |
| All (n = 87,704) | 4.2 (3.9 to 4.6) | 4.8 (4.6 to 5.1) | 3.6 (3.5 to 3.8) | 1.15 (0.97 to 1.36); 0.111 | 0.84 (0.70 to 1.02); 0.085 |
| Boys (n = 42,989) | 5.1 (4.5 to 5.7) | 6.1 (5.8 to 6.5) | 4.1 (3.8 to 4.4) | 1.23 (0.99 to 1.53); 0.056 | 0.79 (0.64 to 0.98); 0.035 |
| Girls (n = 44,715) | 3.5 (3.0 to 4.0) | 3.6 (3.3 to 3.9) | 3.2 (3.0 to 3.5) | 1.04 (0.82 to 1.31); 0.767 | 0.92 (0.71- to 1.19); 0.528 |
| 13-year-olds (n = 48,384) | 2.8 (2.4 to 3.2) | 3.6 (3.3 to 3.9) | 2.7 (2.5 to 2.9) | 1.29 (1.01 to 1.65); 0.041 | 0.95 (0.72 to 1.25); 0.709 |
| 15-year-olds (n = 39,320) | 6.0 (5.3 to 6.7) | 6.4 (6.0 to 6.8) | 4.8 (4.5 to 5.1) | 1.07 (0.87 to 1.31); 0.543 | 0.78 (0.63 to 0.98); 0.033 |
| High SES (n = 37,080) | 3.6 (3.1 to 4.1) | 4.6 (4.3 to 4.9) | 3.2 (2.9 to 3.5) | 1.28 (1.04 to 1.57); 0.019 | 0.88 (0.70 to 1.11); 0.276 |
| Low SES (n = 48,312) | 4.4 (3.9 to 5.0) | 5.1 (4.8 to 5.4) | 3.7 (3.5 to 4.0) | 1.16 (0.93 to 1.46); 0.193 | 0.83 (0.65 to 1.06); 0.138 |
| White (n = 78,113) | 4.0 (3.6 to 4.4) | 4.8 (4.5 to 5.0) | 3.5 (3.4 to 3.7) | 1.20 (1.01 to 1.44); 0.043 | 0.87 (0.71 to 1.07); 0.199 |
| Ethnic minority (n = 8277) | 5.9 (4.6 to 7.4) | 6.0 (5.2 to 6.9) | 4.6 (4.0 to 5.3) | 1.02 (0.67 to 1.58); 0.912 | 0.77 (0.54 to 1.09); 0.141 |
| Ever smoker (n = 14,375) | 19.7 (17.9 to 21.6) | 21.1 (20.1 to 22.2) | 17.5 (16.6 to 18.4) | 1.06 (0.89 to 1.27); 0.502 | 0.85 (0.69 to 1.03); 0.104 |
| Never smoker (n = 71,195) | 0.9 (0.7 to 1.1) | 1.2 (1.0 to 1.3) | 0.8 (0.8 to 1.0) | 1.29 (0.97 to 1.73); 0.081 | 0.93 (0.66 to 1.31); 0.664 |
E-cigarette use in Scotland and England
As indicated in Table 13, ever use of e-cigarettes in Scotland approximately doubled from 2013 to 2015 among all subgroups, with more modest increase thereafter. Odds of ever e-cigarette use were 2.5 times lower in 2013 than in 2015. Odds of ever e-cigarette use increased more marginally from 2015 to 2018, despite a longer gap between data points. Despite some variation in magnitude across subgroups, this pattern of substantially larger growth from 2013 to 2015 than from 2015 to 2018 is observed across all subgroup analyses. There was an almost threefold increase in ever use of e-cigarettes among never smokers from 2013 to 2015, although with marginal increase thereafter. Regular use, although remaining low at approximately 2%, grew substantially in relative terms from 2013 to 2015, with little further growth from 2015 to 2018. This pattern was observed across all subgroups, with significant growth between 2013 and 2015 in all subgroups, but no significant growth from 2015 to 2018 in any group. The only group for whom near significant growth in regular use was observed from 2015 to 2018 was never smokers, although, notably, a 45% increase in relative odds of regular use from 2015 to 2018 reflects an absolute growth from 0.2% to 0.3%, with regular use remaining very low in absolute terms. It was not possible to analyse differential change by ethnicity in Scotland, as the 2015 and 2018 SALSUS data sets did not include a variable on ethnicity. In England (see Table 14), although there was evidence of growing prevalence of ever use from 2014 until 2016, there was no further growth and, indeed, a marginal reduction in ever use to 31% in the whole sample in the 2 years following the TPD (i.e. from 2016 to 2018). A similar pattern was observed across subgroups defined by age and gender, although decline from 2016 to 2018 was significant for only ethnic minority participants. Regular use increased between 2014 and 2016, but fell between 2016 and 2018, with significant declines among the whole sample, and among boys and younger children. In both Scotland and England, regular e-cigarette use among never smokers remained below 1% throughout the time series. Hence, data from England and Scotland concur with findings from Wales that e-cigarette use grew in the period prior to the TPD regulations, but limited or no further increase occurred in the years beyond the TPD regulations. Results from weighted models were largely consistent with unweighted models (see Report Supplementary Material 1, Tables 7 and 8), although marginally significant declines in ever and regular use in England from 2016 to 2018 were reduced and no longer significant following application of weights.
| E-cigarette use | Sample | Percentage (95% CI) | OR (95% CI); p-value | |||
|---|---|---|---|---|---|---|
| 2013 | 2015 | 2018 | 2013 vs. 2015 | 2018 vs. 2015 | ||
| Ever e-cigarette use | All (n = 78,422) | 11.8 (11.5 to 12.2) | 22.8 (22.3 to 23.4) | 24.7 (24.1 to 25.3) | 0.43 (0.41 to 0.45); <0.001 | 1.11 (1.07 to 1.16); <0.001 |
| Boys (n = 38,934) | 12.2 (11.7 to 12.7) | 25.0 (24.2 to 25.7) | 27.7 (26.9 to 28.6) | 0.40 (0.38 to 0.43); <0.001 | 1.17 (1.11 to 1.25); <0.001 | |
| Girls (n = 39,488) | 11.4 (10.9 to 11.9) | 20.8 (20.1 to 21.5) | 21.6 (20.9 to 22.4) | 0.47 (0.44 to 0.50); <0.001 | 1.05 (0.98 to 1.12); 0.152 | |
| 13-year-olds (n = 41,422) | 7.3 (6.9 to 7.7) | 15.2 (14.6 to 15.9) | 16.6 (15.9 to 17.3) | 0.44 (0.40 to 0.47); <0.001 | 1.10 (1.03 to 1.18); 0.006 | |
| 15-year-olds (n = 37,000) | 16.6 (16.0 to 17.2) | 31.6 (30.8 to 32.5) | 34.2 (33.2 to 35.1) | 0.43 (0.41 to 0.46); <0.001 | 1.12 (1.06 to 1.19); <0.001 | |
| High SES (n = 36,525) | 10.4 (9.9 to 10.9) | 21.1 (20.3 to 21.9) | 23.2 (22.4 to 24.0) | 0.41 (0.38 to 0.44); <0.001 | 1.14 (1.07 to 1.22); <0.001 | |
| Low SES (n = 41,823) | 13.0 (12.5 to 13.5) | 24.1 (23.4 to 24.9) | 26.2 (25.4 to 27.0) | 0.45 (0.42 to 0.48); <0.001 | 1.12 (1.06 to 1.19); <0.001 | |
| Ever smoker (n = 16,295) | 39.5 (38.4 to 40.6) | 71.6 (70.3 to 72.9) | 74.6 (73.2 to 75.9) | 0.26 (0.24 to 0.28); <0.001 | 1.16 (1.06 to 1.28); 0.001 | |
| Never smoker (n = 61,182) | 3.8 (3.5 to 4.0) | 10.5 (10.1 to 10.9) | 11.5 (11.0 to 12.0) | 0.33 (0.30 to 0.36); <0.001 | 1.11 (1.04 to 1.19); 0.002 | |
| Regular e-cigarette use | All (n = 78,422) | 0.5 (0.4 to 0.6) | 2.1 (2.0 to 2.3) | 2.2 (2.0 to 2.4) | 0.23 (0.20 to 0.28); <0.001 | 1.06 (0.93 to 1.20); 0.400 |
| Boys (n = 38,934) | 0.7 (0.6 to 0.8) | 3.0 (2.7 to 3.3) | 3.0 (2.7 to 3.4) | 0.22 (0.18 to 0.27); <0.001 | 1.03 (0.89 to 1.20); 0.691 | |
| Girls (n = 39,488) | 0.4 (0.3 to 0.5) | 1.3 (1.1 to 1.5) | 1.5 (1.2 to 1.7) | 0.27 (0.20 to 0.36); <0.001 | 1.11 (0.89 to 1.38); 0.356 | |
| 13-year-olds (n = 41,422) | 0.3 (0.2- to 0.4) | 1.3 (1.1 to 1.5) | 1.3 (1.1 to 1.5) | 0.25 (0.18 to 0.33); <0.001 | 1.03 (0.83 to 1.28); 0.792 | |
| 15-year-olds (n = 37,000) | 0.7 (0.6 to 0.9) | 3.1 (2.8 to 3.5) | 3.3 (3.0 to 3.7) | 0.23 (0.18 to 0.28); <0.001 | 1.07 (0.92 to 1.25); 0.392 | |
| High SES (n = 36,525) | 0.5 (0.4 to 0.6) | 1.9 (1.7 to 2.2) | 2.1 (1.8 to 2.4) | 0.23 (0.18 to 0.31); <0.001 | 1.11 (0.91 to 1.34); 0.300 | |
| Low SES (n = 41,823) | 0.6 (0.5 to 0.7) | 2.3 (2.0 to 2.6) | 2.4 (2.1 to 2.7) | 0.24 (0.19 to 0.30); <0001 | 1.03 (0.87 to 1.22); 0.702 | |
| Ever smoker (n = 16,295) | 2.1 (1.7 to 2.4) | 9.7 (8.9 to 10.6) | 9.4 (8.6 to 10.3) | 0.20 (0.16 to 0.24); <0.001 | 0.96 (0.83 to 1.11); 0.582 | |
| Never smoker (n = 61,182) | 0.1 (0.0 to 0.1) | 0.2 (0.2 to 0.3) | 0.3 (0.2 to 0.4) | 0.31 (0.18 to 0.54); <0.001 | 1.45 (0.97 to 2.15); 0.067 | |
| E-cigarette use | Sample | Percentage (95% CI) | OR (95% CI); p-value | |||
|---|---|---|---|---|---|---|
| 2014 | 2016 | 2018 | 2014 vs. 2016 | 2018 vs. 2016 | ||
| Ever e-cigarette use | All (n = 14,010) | 27.3 (25.7 to 29.0) | 32.5 (31.3 to 33.8) | 30.7 (29.5 to 31.9) | 0.75 (0.68 to 0.83); <0.001 | 0.92 (0.85 to 0.99); 0.036 |
| Boys (n = 6881) | 29.0 (26.6 to 31.4) | 35.2 (33.4 to 37.1) | 34.1 (32.4 to 35.8) | 0.72 (0.62 to 0.83); <0.001 | 0.93 (0.83 to 1.05); 0.239 | |
| Girls (n = 7129) | 25.6 (23.3 to 28.0) | 30.1 (28.4 to 31.8) | 27.3 (25.7 to 29.0) | 0.79 (0.68 to 0.92); 0.002 | 0.90 (0.80 to 1.01); 0.085 | |
| 13-year-olds (n = 6940) | 19.4 (17.3 to 21.6) | 23.8 (22.2 to 25.4) | 21.9 (20.4 to 23.5) | 0.77 (0.65 to 0.90); 0.002 | 0.90 (0.80 to 1.03); 0.116 | |
| 15-year-olds (n = 7070) | 34.4 (31.9 to 36.9) | 41.2 (39.3 to 43.0) | 39.6 (37.8 to 41.4) | 0.74 (0.65 to 0.85); <0.001 | 0.93 (0.84 to 1.04); 0.184 | |
| White (n = 10,825) | 27.6 (25.8 to 29.5) | 32.9 (31.5 to 34.3) | 32.7 (31.3 to 34.2) | 0.77 (0.69 to 0.86); <0.001 | 0.98 (0.90 to 1.08); 0.736 | |
| Ethnic minority (n = 2623) | 25.3 (21.3 to 29.5) | 30.3 (27.1 to 33.5) | 24.8 (22.5 to 27.2) | 0.78 (0.60 to 1.02); 0.065 | 0.78 (0.64 to 0.94); 0.011 | |
| Ever smoker (n = 3051) | 69.0 (65.3 to 72.6) | 79.0 (76.7 to 81.2) | 80.9 (78.5 to 83.1) | 0.58 (0.46 to 0.71); <0.001 | 1.10 (0.90 to 1.35); 0.341 | |
| Never smoker (n = 10,775) | 14.3 (12.8 to 15.9) | 18.0 (16.8 to 19.2) | 18.2 (17.1 to 19.3) | 0.75 (0.64 to 0.86); <0.001 | 1.01 (0.90 to 1.13); 0.888 | |
| Regular e-cigarette use | All (n = 14,010) | 1.7 (1.2 to 2.2) | 3.4 (2.9 to 3.9) | 2.6 (2.2 to 3.1) | 0.46 (0.33 to 0.64); <0.001 | 0.76 (0.61 to 0.95); 0.015 |
| Boys (n = 6881) | 1.9 (1.3 to 2.8) | 4.9 (4.1 to 5.8) | 3.6 (2.9 to 4.3) | 0.37 (0.24 to 0.56); <0.001 | 0.71 (0.54 to 0.92); 0.011 | |
| Girls (n = 7129) | 1.4 (0.9 to 2.2) | 2.0 (1.5 to 2.6) | 1.7 (1.3 to 2.2) | 0.71 (0.42 to 1.20); 0.204 | 0.89 (0.61 to 1.31); 0.562 | |
| 13-year-olds (n = 6940) | 1.0 (0.5 to 1.7) | 2.4 (1.8 to 3.0) | 1.4 (1.0 to 1.8) | 0.41 (0.23 to 0.75); 0.004 | 0.57 (0.38 to 0.85); 0.006 | |
| 15-year-olds (n = 7070) | 2.3 (1.6 to 3.2) | 4.3 (3.6 to 5.2) | 3.9 (3.2 to 4.7) | 0.49 (0.33 to 0.73); <0.001 | 0.87 (0.67 to 1.14); 0.316 | |
| White (n = 10,825) | 1.7 (1.2 to 2.3) | 3.3 (2.8 to 3.9) | 2.9 (2.4 to 3.5) | 0.48 (0.33 to 0.69); <0.001 | 0.85 (66.8 to 1.09); 0.202 | |
| Ethnic minority (n = 2623) | 1.5 (0.6 to 3.1) | 2.9 (1.9 to 4.3) | 1.6 (1.0 to 2.5) | 0.53 (0.22 to 1.23); 0.139 | 0.59 (0.33 to 1.05); 0.074 | |
| Ever smoker (n = 3051) | 6.1 (4.4 to 8.2) | 12.3 (10.5 to 14.2) | 11.1 (9.4 to 13.1) | 0.44 (0.30 to 0.63); <0.001 | 0.86 (0.67 to 1.10); 0.231 | |
| Never smoker (n = 10,775) | 0.2 (0.1 to 0.6) | 0.6 (0.4 to 0.8) | 0.5 (0.3 to 0.7) | 0.41 (0.16 to 1.08); 0.071 | 0.88 (0.49 to 1.56); 0.652 | |
Specificity of change in trend: energy drink use in Wales
Energy drink use in Wales was analysed to examine whether changes in trend were specific to e-cigarettes or were also observed for another psychoactive substance (i.e. energy drinks) for which change could not be attributed to the TPD regulations. Descriptive data indicated a somewhat different pattern than for e-cigarette use, with little change in energy drink use from 2013 (53.5%) to 2015 (53.4%), a substantial drop between 2015 and 2017 (43.1%) and a more modest continued decrease from 2017 to 2019 (39.3%). In segmented regression analyses (see Table 15), although not significant, changes in trend of similar magnitude to those for e-cigarettes were also observed for energy drinks in short-term analyses, with a 4% reduction in the odds of energy drink use per month, relative to the baseline trend. However, the high degree of consistency from short- to long-term analyses observed with our e-cigarette models was not replicated for energy drink use, which, in long-term analyses, indicated a significant negative step change at the intervention point and a reduced, although marginally significant, change in trend. Hence, particularly in longer-term analyses, change in trend for energy drink consumption did not mirror change for use of e-cigarettes.
| Sample | Short-term analysis (2013–17) | Long-term analysis (2013–19) | |||
|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| All (n = 52,794a; 94,935b) | Time | 1.00 (1.00 to 1.01) | 0.856 | 1.00 (1.00 to 1.01) | 0.871 |
| Level | 1.38 (0.60 to 3.18) | 0.453 | 0.76 (0.68 to 0.85) | <0.001 | |
| Post slope | 0.96 (0.92 to 1.01) | 0.089 | 0.99 (0.99 to 1.00) | 0.014 | |
| Boys (n = 25,888; 46,682) | Time | 1.00 (0.99 to 1.00) | 0.285 | 1.00 (0.99 to 1.00) | 0.286 |
| Level | 1.32 (0.55 to 3.14) | 0.534 | 0.89 (0.78 to 1.02) | 0.092 | |
| Post slope | 0.97 (0.93 to 1.02) | 0.272 | 0.99 (0.99 to 1.00) | 0.167 | |
| Girls (n = 26,906; 48,253) | Time | 1.00 (1.00 to 1.01) | 0.183 | 1.00 (1.00 to 1.01) | 0.182 |
| Level | 1.46 (0.51 to 4.14) | 0.477 | 0.65 (0.57 to 0.74) | <0.001 | |
| Post slope | 0.95 (0.89 to 1.01) | 0.075 | 0.99 (0.98 to 1.00) | 0.012 | |
| 13-year-olds (n = 29,545; 52,561) | Time | 1.00 (1.00 to 1.01) | 0.261 | 1.00 (1.00 to 1.01) | 0.271 |
| Level | 1.25 (0.44 to 3.57) | 0.673 | 0.69 (0.61 to 0.78) | <0.001 | |
| Post slope | 0.96 (0.90 to 1.02) | 0.150 | 0.99 (0.98 to 1.00) | 0.008 | |
| 15-year-olds (n = 23,249; 42,374) | Time | 1.00 (0.99 to 1.00) | 0.352 | 1.00 (0.99 to 1.00) | 0.350 |
| Level | 1.53 (0.55 to 4.24) | 0.415 | 0.86 (0.75 to 0.99) | 0.037 | |
| Post slope | 0.96 (0.91 to 1.02) | 0.199 | 1.00 (0.99 to 1.00) | 0.219 | |
| White (n = 47,137; 84,455) | Time | 1.00 (0.99 to 1.01) | 0.936 | 1.00 (1.00 to 1.01) | 0.918 |
| Level | 1.38 (0.60 to 3.21) | 0.449 | 0.80 (0.71 to 0.89) | <0.001 | |
| Post slope | 0.96 (0.92 to 1.01) | 0.112 | 0.99 (0.99 to 1.00) | 0.022 | |
| Ethnic minority (n = 4787; 9009) | Time | 1.00 (0.99 to 1.01) | 0.807 | 1.00 (0.99 to 1.01) | 0.831 |
| Level | 2.54 (0.48 to 13.39) | 0.273 | 0.60 (0.48 to 0.76) | <0.001 | |
| Post slope | 0.92 (0.84 to 1.01) | 0.067 | 0.99 (0.98 to 1.01) | 0.409 | |
| High SES (n = 25,644; 40,018) | Time | 1.00 (0.99 to 1.01) | 0.993 | 1.00 (0.99 to 1.01) | 0.989 |
| Level | 1.53 (0.56 to 4.17) | 0.401 | 0.79 (0.69 to 0.90) | <0.001 | |
| Post slope | 0.96 (0.90 to 1.01) | 0.116 | 0.99 (0.99 to 1.00) | 0.032 | |
| Low SES (n = 25,836; 51,951) | Time | 1.00 (0.99 to 1.01) | 0.772 | 1.00 (0.99 to 1.01) | 0.754 |
| Level | 1.31 (0.54 to 3.16) | 0.550 | 0.82 (0.72 to 0.93) | 0.003 | |
| Post slope | 0.97 (0.92 to 1.01) | 0.172 | 0.99 (0.99 to 1.00) | 0.026 | |
| Never smoker (n = 41,457; 75,345) | Time | 1.00 (1.00 to 1.01) | 0.422 | 1.00 (1.00 to 1.01) | 0.433 |
| Level | 1.40 (0.60 to 3.30) | 0.437 | 0.71 (0.64 to 0.80) | <0.001 | |
| Post slope | 0.95 (0.91 to 1.00) | 0.054 | 0.99 (0.99 to 1.00) | 0.004 | |
| Ever smoker (n = 8805; 15,516) | Time | 1.00 (0.99 to 1.01) | 0.794 | 1.00 (1.00 to 1.01) | 0.795 |
| Level | 2.26 (0.63 to 8.07) | 0.210 | 0.79 (0.63 to 0.99) | 0.045 | |
| Post slope | 0.94 (0.87 to 1.00) | 0.065 | 0.99 (0.99 to 1.00) | 0.239 | |
Change in young people’s tobacco use following the Tobacco Products Directive regulations and the 2016 suite of tobacco regulation
Given the longer time series available for tobacco use, secondary analyses of change in trend for young people’s tobacco use drew on the integrated three-country data set used in Chapter 3, with additional data sets from 2016 onward. The analytical samples for smoking prevalence from 1998 to 2019 included 358,713 and 359,111 students for ever and regular smoking, respectively (i.e. 97% of all students within the target year groups).
As indicated in Figure 9, although decline continued during the period when e-cigarettes were growing in popularity (see Chapter 3) there is some evidence of a plateauing in the most recent data points. In Scotland and Wales, ever smoking falls until 2015, with little evidence of decline in subsequent years. However, there was tentative evidence of a continued decline in smoking in England from 2016 to 2018, having remained unchanged from 2014 to 2016. Similarly, although rates of regular smoking flattened in Scotland and Wales in the most recent data sets, there was some continued decline in England. In England, year group data were removed from data sets beyond 2014 and post-TPD analyses used age rather than year group. Differences between estimates for England where using year group (pre-legislation only) or age data are negligible.
FIGURE 9.
Percentage of young people reporting ever or regular (weekly or more) smoking by country and year from 1998 to 2019. The black bars represent the beginning of two ‘intervention’ periods (i.e. emergence of e-cigarettes and then their regulation via the TPD).
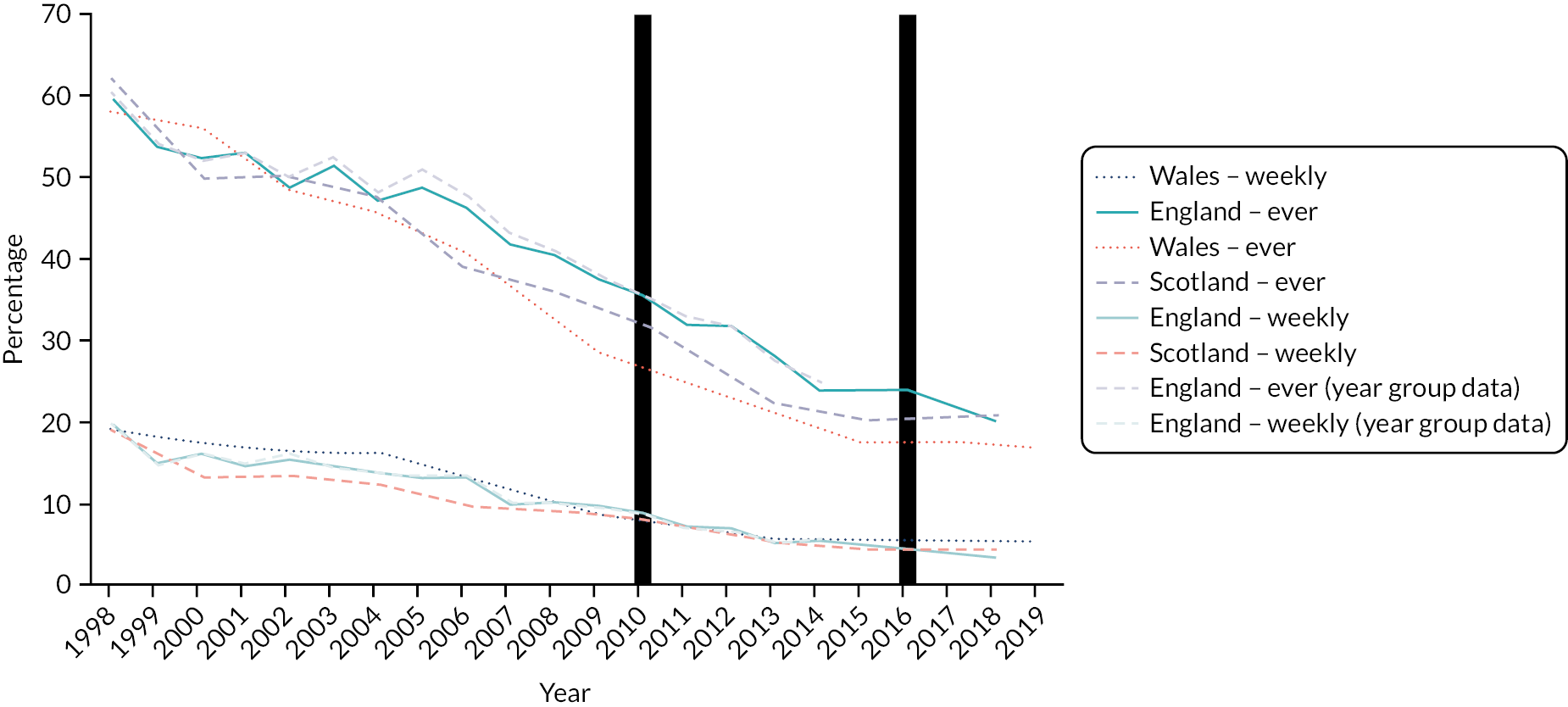
Odds ratios from segmented regression analyses in Table 16 indicate that for the sample as a whole, and among subgroups defined by gender and year group, there was a positive change in trend in both linear and quadratic models for ever and regular smoking. Hence, these models provide consistent evidence that the decline in young people’s smoking was slower in the years following the intervention point than it had been previously. Findings are consistent with a conclusion that the suite of tobacco regulation introduced in 2016 did not maintain or accelerate the downwards trend in young people’s smoking, and that this had begun to plateau. These conclusions were robust to a range of sensitivity analyses (see Report Supplementary Material 1, Table 1). Predicted probability plots for quadratic models of ever and regular smoking (see Report Supplementary Material 1, Figure 2) illustrate that trends for tobacco followed the opposite pattern to those observed for e-cigarette use, falling from 2011 to 2015 (as e-cigarette use was rising) but plateauing thereafter (as e-cigarette use was plateauing or falling).
| Sample | Ever smoked | Regular smoking | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Linear | p-value | Quadratic | p-value | Linear | p-value | Quadratic | p-value | ||
| Whole sample (n = 358,713/359,111) | Year | 0.91 (0.91 to 0.91) | <0.001 | 0.94 (0.93 to 0.95) | <0.001 | 0.93 (0.93 to 0.93) | <0.001 | 0.97 (0.96 to 0.99) | 0.005 |
| Year2 | 1.00 (1.00 to 1.00) | <0.001 | 1.00 (1.00 to 1.00) | <0.001 | |||||
| Level | 1.16 (1.10 to 1.23) | <0.001 | 1.15 (1.08 to 1.22) | <0.001 | 0.96 (0.87 to 1.07) | 0.471 | 0.94 (0.85 to 1.05) | 0.269 | |
| Post slope | 1.07 (1.05 to 1.09) | <0.001 | 1.09 (1.06 to 1.11) | <0.001 | 1.10 (1.06 to 1.15) | <0.001 | 1.13 (1.09 to 1.18) | <0.001 | |
| Boys subgroup (n = 179,174/179,494) | Year | 0.92 (0.92 to 0.93) | <0.001 | 0.92 (0.90 to 0.94) | <0.001 | 0.94 (0.93 to 0.95) | <0.001 | 0.95 (0.92 to 0.97) | <0.001 |
| Year2 | 1.00 (1.00 to 1.00) | 0.819 | 1.00 (1.00 to 1.00) | 0.696 | |||||
| Level | 1.17 (1.07 to 1.27) | <0.001 | 1.17 (1.07 to 1.27) | <0.001 | 0.98 (0.85 to 1.14) | 0.833 | 0.98 (0.84 to 1.14) | 0.808 | |
| Post slope | 1.05 (1.01 to 1.08) | 0.005 | 1.05 (1.01 to 1.08) | 0.009 | 1.09 (1.03 to 1.15) | 0.005 | 1.09 (1.03 to 1.16) | 0.005 | |
| Girls subgroup (n = 179,539/179,617) | Year | 0.90 (0.89 to 0.90) | <0.001 | 0.95 (0.94 to 0.97) | <0.001 | 0.92 (0.92 to 0.93) | <0.001 | 1.00 (0.97 to 1.02) | 0.698 |
| Year2 | 1.00 (0.99 to 1.00) | <0.001 | 1.00 (0.99 to 1.00) | <0.001 | |||||
| Level | 1.16 (1.07 to 1.26) | <0.001 | 1.13 (1.05 to 1.22) | 0.002 | 0.95 (0.82 to 1.09) | 0.454 | 0.92 (0.79 to 1.06) | 0.227 | |
| Post slope | 1.09 (1.06 to 1.13) | <0.001 | 1.13 (1.09 to 1.16) | <0.001 | 1.12 (1.06 to 1.18) | <0.001 | 1.17 (1.10 to 1.23) | <0.001 | |
| 13-year-olds only (n = 187,347/187,534) | Year | 0.89 (0.89 to 0.89) | <0.001 | 0.94 (0.92 to 0.96) | <0.001 | 0.91 (0.90 to 0.92) | <0.001 | 1.00 (0.97 to 1.04) | 0.908 |
| Year2 | 1.00 (0.99 to 1.00) | <0.001 | 0.99 (0.99 to 1.00) | <0.001 | |||||
| Level | 1.21 (1.10 to 1.33) | <0.001 | 1.18 (1.07 to 1.30) | 0.001 | 0.98 (0.80 to 1.19) | 0.821 | 0.93 (0.76 to 1.14) | 0.472 | |
| Post slope | 1.08 (1.04 to 1.12) | <0.001 | 1.11 (1.07 to 1.16) | <0.001 | 1.11 (1.03 to 1.21) | 0.009 | 1.18 (1.08 to 1.28) | <0.001 | |
| 15-year-olds only (n = 171,366/171,577) | Year | 0.93 (0.93 to 0.93) | <0.001 | 0.94 (0.92 to 0.95) | <0.001 | 0.94 (0.93 to 0.94) | <0.001 | 0.97 (0.95 to 1.00) | 0.003 |
| Year2 | 1.00 (1.00 to 1.00) | 0.406 | 1.00 (1.00 to 1.00) | 0.005 | |||||
| Level | 1.12 (1.05 to 1.21) | 0.002 | 1.12 (1.04 to 1.21) | 0.002 | 0.95 (0.84 to 1.08) | 0.443 | 0.94 (0.83 to 1.06) | 0.330 | |
| Post slope | 1.06 (1.04 to 1.09) | <0.001 | 1.07 (1.04 to 1.10) | <0.001 | 1.09 (1.04 to 1.14) | <0.001 | 1.11 (1.06 to 1.16) | <0.001 | |
To examine whether change in trend was specific to tobacco or were observed across other substances, we provide estimates over time for cannabis use (see Table 17). Descriptive data (see Report Supplementary Material 1, Table 16) indicate plateauing or slight increase in ever use of cannabis, with segmented regression analyses showing a similar disruption to secular decline in ever cannabis use to that observed for smoking. Consistent with descriptive data, which provide some suggestion of growth in cannabis use, as opposed to flattening in tobacco use, changes in trend are consistently somewhat larger for cannabis use than for tobacco. We did not formally model whether or not this change in trend was also observed for alcohol use because of changes in how this question was asked from 2016 in England (which gave rise to an artificial stepped increase in estimates of alcohol use in England, and mean the English data cannot be treated as a single time series pre and post 2016). However, in Wales, there was only marginal further decline in ever drinking (from 54.3% in 2015 to 53.2% in 2019) and in Scotland there was an increase in ever drinking (from 44.5% in 2015 to 52.5% in 2018). Hence, plateauing in tobacco use observed in the most recent surveys appears not to be unique to tobacco, but is reflected in other substance use behaviours. In line with between-country differences in observed smoking trends, for smoking attitudes, although not formally modelled as only available in three post-legislation data sets, there were small declines beyond legislation in England in the percentage of young people reporting that it is OK for someone their age to try smoking (with 34.1% of young people saying that it is OK to try smoking in 2014 vs. 30.1% of young people in 2018), whereas in Scotland there was a small increase in the percentage of young people reporting that it is OK for someone their age to try smoking (from 27.0% of young people in 2015 to 30.5% of young people in 2018).
| Sample | Cannabis use | ||||
|---|---|---|---|---|---|
| Linear | p-value | Quadratic | p-value | ||
| Whole sample (n = 355,422) | Year | 0.92 (0.92 to 0.93) | <0.001 | 1.08 (1.06 to 1.10) | <0.001 |
| Year2 | 0.99 (0.99 to 0.99) | <0.001 | |||
| Level | 1.37 (1.27 to 1.47) | <0.001 | 1.28 (1.18 to 1.37) | <0.001 | |
| Post slope | 1.07 (1.04 to 1.11) | <0.001 | 1.17 (1.14 to 1.21) | <0.001 | |
| Boys (n = 177,463) | Year | 0.93 (0.92 to 0.93) | <0.001 | 1.06 (1.04 to 1.08) | <0.001 |
| Year2 | 0.99 (0.99 to 0.99) | <0.001 | |||
| Level | 1.35 (1.35 to 1.22) | <0.001 | 1.27 (1.15 to 1.40) | <0.001 | |
| Post slope | 1.06 (1.02 to 1.10) | 0.005 | 1.14 (1.09 to 1.19) | <0.001 | |
| Girls (n = 177,959) | Year | 0.92 (0.91 to 0.92) | <0.001 | 1.10 (1.07 to 1.13) | <0.001 |
| Year2 | 0.99 (0.99 to 0.99) | <0.001 | |||
| Level | 1.40 (1.26 to 1.56) | <0.001 | 1.29 (1.16 to 1.44) | <0.001 | |
| Post slope | 1.10 (1.05 to 1.14) | <0.001 | 1.21 (1.16 to 1.27) | <0.001 | |
| 13-year-olds (n = 184,231) | Year | 0.89 (0.89 to 0.90) | <0.001 | 1.13 (1.09 to 1.17) | <0.001 |
| Year2 | 0.98 (0.98 to 0.99) | <0.001 | |||
| Level | 1.41 (1.22 to 1.63) | <0.001 | 1.26 (1.09 to 1.46) | 0.002 | |
| Post slope | 1.11 (1.04 to 1.17) | <0.001 | 1.26 (1.18 to 1.34) | <0.001 | |
| 15-year-olds (n = 171,191) | Year | 0.93 (0.93 to 0.93) | <0.001 | 1.06 (1.04 to 1.08) | <0.001 |
| Year2 | 0.99 (0.99 to 0.99) | <0.001 | |||
| Level | 1.36 (1.25 to 1.47) | <0.001 | 1.28 (1.18 to 1.39) | <0.001 | |
| Post slope | 1.06 (1.03 to 1.10) | <0.001 | 1.14 (1.10 to 1.18) | <0.001 | |
For descriptive information for all variables overall and by subgroup, from 1998 to 2019, see Report Supplementary Material 1, Tables 9–19.
Chapter summary
Following the TPD regulations, e-cigarettes were increasingly described as something young people had tried, but were now losing interest in. Interactions with elements of the TPD regulations, such as device labelling, were described as limited, although risk perceptions for e-cigarettes relative to tobacco were increasing. Although some stakeholders in Chapters 3 and 4 emphasised emergence of e-cigarette markets on the internet as an unintended consequence of TPD, few young people described online purchase or having switched to purchasing e-cigarettes via the internet. In qualitative interviews, young people described little exposure to marketing, although, by contrast, surveys indicated that most young people continued to see some form of advertising in the years after implementation, with point of sale the most common source of exposure followed by the internet. Our analyses of survey data consistently indicated that young people’s experimentation with e-cigarettes, and regular use of e-cigarettes, had grown prior to TPD regulations, but did not continue to do so afterward, which is consistent with a hypothesised effect of the TPD regulations. However, secondary analyses of changes in trend for young people’s use of tobacco indicate that the suite of tobacco and e-cigarette regulation in May 2016 may not have been sufficient to maintain downwards pressure on young people’s smoking, with smoking rates beginning to plateau. Tobacco use exhibited the inverse trend to that observed for e-cigarettes, declining when e-cigarette use increased, but now plateauing as e-cigarette use begins to decline.
Chapter 6 Discussion
In this chapter, we provide an overview of our key findings, and locate these findings within the rapidly developing literature on young people’s e-cigarette and tobacco use. The primary aim of our study was to evaluate impacts of TPD on young people’s e-cigarette use. However, in line with our evaluation and integration framework (see Chapter 2, Figure 2), we present findings chronologically, beginning with understanding the context and role of e-cigarettes before the TPD regulations, moving into implementation, before focusing on mechanisms of change and impacts. This frames impacts of the legislation as the end of the story the integration of our multiple data sources enables us to tell. For consistency with the presentation of our results chapters (see Chapters 3–5), we follow the same ordering in discussing our findings in this chapter.
The role of e-cigarettes in renormalising smoking prior to the implementation of the Tobacco Products Directive regulations
In our study, we found little evidence of change in decline for ever use of tobacco during the period when e-cigarettes were gaining popularity as cessation devices16 and young people’s experimental e-cigarette use was increasing. 39 There was a slight slowing in the decline in regular smoking post 2010; however, this was mirrored in other substances, reflecting a broader slowing of decline in adolescent substance use behaviours, rather than being specific to tobacco. Measures of ever use for cannabis and alcohol indicated a slowing in decline while equivalent measures of tobacco did not, suggesting that disruptions to declines in tobacco lagged behind other substance use behaviours. We also found that young people’s attitudes had hardened against smoking, during the time that e-cigarette use was gaining traction in the UK.
Although at the time of initial publication our analyses was one of the first of its kind, numerous studies have since concurred with these findings across varying international contexts. Studies from Taiwan55 and New Zealand56 find that young people’s smoking rates fell as fast, or faster, during the emergence of e-cigarettes. An analysis of NYTS data in the USA found continuing decline in tobacco use following the emergence of e-cigarettes,57 with ever use declining at a faster rate post 2011. In Italy, where tobacco smoking remains high compared with other European countries,107 data from the Global Youth Tobacco Survey in 2010, 2014 and 2018 showed a decline in ever smoking among young people aged 13–15 years (from 46% to 41%) and smoking in the past 30 days (from 8% to 5%). From the UK, data from the YTPS (see Appendix 2, Figures 10 and 11) also finds a continued decline in tobacco use and perceived norms during the emergence of e-cigarettes.
FIGURE 10.
Changes in tobacco use and perceived smoking prevalence within YTPSs.
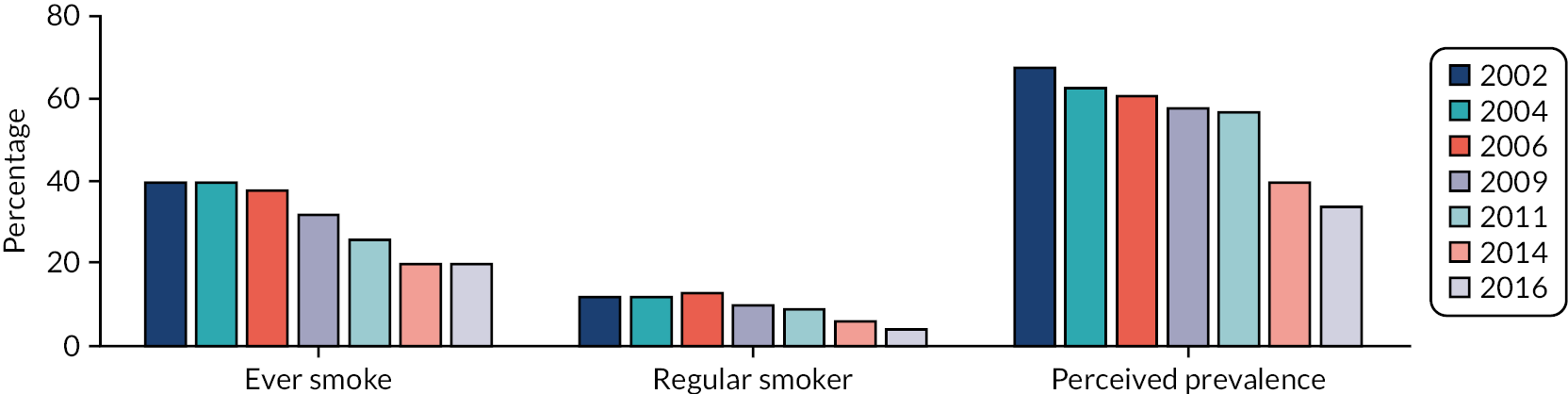
FIGURE 11.
Percentage of ever and regular e-cigarette users in 2014 and 2016 within YTPSs.
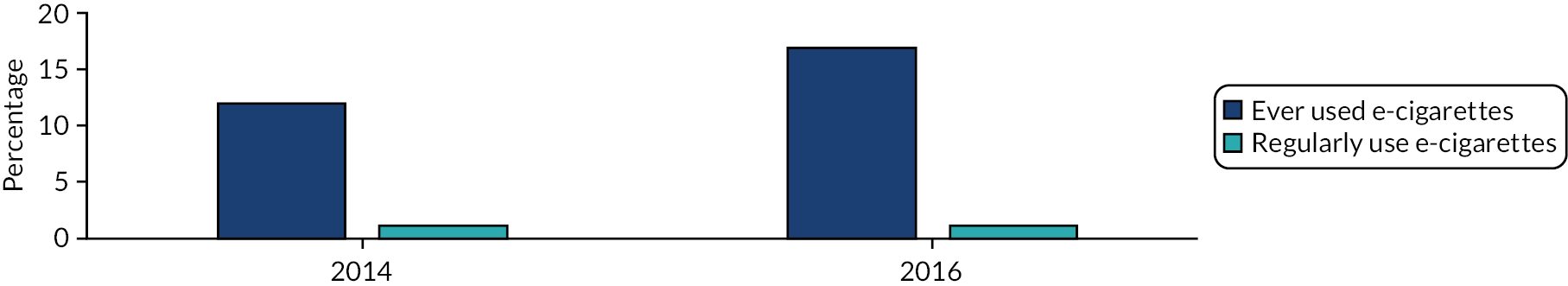
Young people’s perceptions of e-cigarettes and the normalisation of vaping
In group interviews prior to the full implementation of the TPD regulations, young people tended to differentiate between e-cigarettes and tobacco, preferring the word ‘vapes’ to ‘e-cigarettes’. Consistent with similar qualitative research with younger children,62,63 young people tended to interpret adult use of e-cigarettes as an attempt to quit smoking, rather than as an endorsement of smoking behaviour. Disapproval of smoking remained strong, although approval of e-cigarette use by young people was more nuanced. Experimental and social use in contexts such as performing tricks at parties were largely approved of, but regular use outside these social contexts was largely disapproved of, and was seen as ‘something the smokers do’. Our qualitative findings of dual acceptance of experimental vaping but disapproval of regular use have been observed in international qualitative studies. 108 Similar to a number of previous qualitative studies,36,37 young people in our sample emphasised flavours as key drivers of e-cigarette use. The internet was described as playing an important role in young people’s exposure to e-cigarettes both in terms of perceived access to devices and media exposure to use, as many young people perceived that peers bought devices online and described online trick culture as forming a key driver of social use of e-cigarettes, particularly among boys. 108 Hence, although there was no evidence of the renormalisation of smoking, initial qualitative data provided evidence that some forms of e-cigarette use itself were becoming normalised.
Stakeholders views on the regulation of tobacco and e-cigarettes
Long-standing declines in young people’s smoking were largely attributed by policy stakeholders to increasingly strong regulation of tobacco. Although views on e-cigarettes are often characterised into binary pro and anticamps,31 policy stakeholders perceptions of likely impact on public health were nuanced. Stakeholders described simultaneously positive views about the potential role of e-cigarettes in smoking cessation, alongside anxieties about potential harms of e-cigarettes for young people, differing to some extent in the emphasis placed on risks and benefits, rather than occupying binary positions. Within the TPD, marketing restrictions and moves to notification of new products were largely seen as proportionate in achieving goals, such as limiting appeal to non-smokers. However, device regulations were seen as potentially needing some refinement going forward, with some concerns about the evidence base behind elements such as the nicotine warning86 and refill size restrictions. Stakeholders argued that reviews following exit from the EU might offer opportunities to refine elements of the TPD regulations, but that departure from the EU was unlikely to substantially impact the TPD regulations or the trajectory of UK tobacco control action more broadly. Although elements of e-cigarette marketing were regulated via the TPD, concerns have continued to be expressed that e-cigarettes continue to be marketed to young people via their packaging, and that loopholes enable companies to give free samples of e-cigarettes to those underage, so long as these are not being sold. 109 Hence, there are a number of key areas in which research into the refinement of existing regulations may be warranted.
Interviews with specialist and non-specialist e-cigarette retailers highlighted differences in awareness and perceptions of TPD legislation. Non-specialist retailers were less aware of regulations and were more ambivalent about e-cigarettes. Many specialist retailers acknowledged the importance of some regulation to limit appeal of e-cigarettes by young people, but voiced anxieties about the direction of travel for regulation. In particular, there were concerns that TPD signalled a movement towards regulating e-cigarettes as if they were ‘the same as tobacco’. Although EU regulations do not go so far as Food and Drug Administration communications in classing e-cigarettes themselves as tobacco products,60 they are, nevertheless, regulated under a broader banner of a ‘tobacco products’ directive. There was a common view that moving further towards regulating e-cigarettes as if they are tobacco might undermine their relative advantage over tobacco, leading to public perception of e-cigarettes and tobacco as the same. Retailers expressed suspicion that tobacco companies had a role in shaping e-cigarette regulation to reduce the relative advantage of a competing product. Retailers commonly positioned themselves as advocates of cessation110 and, hence, potential allies of public health,111 often expressing opposition to the tobacco industry and its associated interests. Nevertheless, a small number of retailers described reliance on tobacco industry actors for knowledge about the TPD because of a perceived lack of communication from authorities. Involvement of tobacco representatives in supporting retailers’ compliance with regulations resonates with findings from Scotland on implementation of plain packaging regulations. 112 TSOs in our study also indicated that a lack of resource to support or enforce TPD regulations, and limited consistent communication for retailers on what was TPD compliance, meant that trade bodies stepped in to fill this gap. The relationship between the tobacco and e-cigarette industry has become increasingly complex, as tobacco companies have invested in e-cigarette companies or developed their own products. 113 In some cases, it is possible that limited official communication on expectations of the TPD created a vacuum that enabled industry actors to further alliances with elements of the e-cigarette industry.
In line with findings from a post-implementation review in England,114 compliance with TPD regulations was largely seen as having been good by most stakeholders, and in our audits. However, consistent with young people’s perceptions that e-cigarettes were commonly accessed by peers via online purchase, additional perceived unintended consequences with particular implications for young people included displacement of sales of unregulated products onto the internet.
Young people’s interactions with elements of Tobacco Products Directive regulations and change in vaping perceptions
Following full implementation of the TPD regulations, young people reported limited interaction with e-cigarettes within their packaging and, hence, little exposure to nicotine warnings. Although an increased proportion of young people perceived e-cigarettes and tobacco as equally harmful in the years following the TPD regulations, given the apparently limited exposure to warning labels, the EVALI outbreak may offer a more plausible explanation for this sudden change in risk perceptions among young people. 73 In 2018 interviews, e-cigarettes were seen by many young people as a fad that was beginning to lose its appeal, a finding that has been observed in international contexts independent of the TPD. Drawing on data from Norway, Tokle115 highlighted the similarity of e-cigarettes and ‘fidget spinners’, which was also cited by young people in our interviews. In qualitative interviews, most young people recalled little exposure to marketing, and it is plausible that marketing restrictions played a role in reducing the ability of industry to maintain young people’s interest in e-cigarettes. 83 However, by contrast to interviews, survey data indicated that most young people reported that they had seen some form of advertising in the past month, with point of sale the most common source. One recent study, which compared exposure to e-cigarette marketing among 16- to 19-year-olds in England, Canada and the USA from 2017 to 2019, found that exposure remained common and increased in all countries. 116 However, this occurred to a far smaller extent in England, perhaps indicating partial displacement of marketing to unregulated channels, although not to a sufficient extent to overcome effects of restrictions relative to less regulated environments.
Across interviews, the internet featured strongly as a perceived source of exposure to e-cigarettes. Notably, however, according to survey data, the internet was the only source in which young people’s exposure decreased in the years following TPD regulations, and this perhaps reflected diminishing interest in e-cigarettes, with fewer young people actively seeking e-cigarette-related material on the internet. Despite concerns expressed by both young people and retailers, quantitative data from Wales after the implementation of TPD regulations indicated that few young people reported online purchase, with quantitative data providing little support for the hypothesis that young people had switched to online purchase following new regulations. The most common routes of supply included via peers and other informal supply chains, with a minority of young people obtaining e-cigarettes directly from retailers. This contrasts with findings from the International Tobacco Control four-country study, in which young people were equally likely to report obtaining e-cigarettes via informal or commercial supply routes, although, notably, the study focused on 16- to 19-year-olds and, hence, included a significant number of young people who could legally buy e-cigarettes themselves. 117
Change in young people’s use of e-cigarettes following Tobacco Products Directive regulations
As reported in the years prior to the TPD regulations,39 and consistent with qualitative reports of widespread approval of experimentation with e-cigarettes, experimentation with e-cigarettes had been growing rapidly, including among never smokers. However, our primary statistical analyses of data from Wales found that, at both short- and long-term follow-up, the odds of ever e-cigarette use decreased by 4% per month following the TPD regulations, relative to the baseline trend. Although there was some evidence of emerging inequality in short-term analysis, with smaller changes in minority ethnic groups, for example, these differences did not follow through to long-term analysis, where very similar estimates were observed for all subgroups. Analyses of data from England and Scotland were consistent with the pattern observed in Wales of growth in e-cigarette use prior to TPD regulations and, subsequently, plateauing or declining thereafter. Regular e-cigarette use also followed a pattern of pre-regulation increase followed by post-regulation plateauing or decline. Consistent with qualitative reports of less widespread approval of regular use, regular use remained rare among never smokers, at 1% or lower in all countries and years. Hence, concerns regarding regular use of e-cigarettes acting as a gateway to nicotine addiction for a new generation of tobacco-naive young people are not reflected in data from Great Britain,39 pre or post regulation.
Some international divergence has emerged in relation to young people’s use of e-cigarettes, and it is likely that this reflects differences in regulatory landscapes. 77 In particular, our findings contrast with a large growth in e-cigarette use by young people around the same time in the USA. 67,76 This was largely attributed to high-strength devices whose entry to UK markets was delayed by the TPD and, because of the TPD, were limited to lower levels of nicotine strength than US versions. Our findings on the plateauing of e-cigarette use are, however, largely consistent with other UK national surveys monitoring trends in e-cigarette use and smoking overtime. Hammond et al. 69 found no change in vaping in England in the post-TPD period from 2017 and 2018 among slightly older adolescents, despite substantial growth in the same period in both the USA and Canada. In ASH smoke-free Great Britain surveys118,119 of 11- to 18-year-olds, the percentage of young people having used e-cigarettes had increased over time from 4% in 2013 to around 10% by 2015, but the percentage remained relatively stable thereafter. Although young people’s accounts indicated that interest in e-cigarettes was waning, and interaction with many elements of the TPD regulations was limited, it is plausible that marketing restrictions coupled with new reporting requirements and product regulations inhibited the ability for new products to be introduced rapidly and promoted in ways that appeal to young people. 116 More recent data from the USA indicate that although young people’s e-cigarette use did initially grow rapidly, it is now declining. 70
Changes in young people’s use of tobacco after the implementation of Tobacco Products Directive regulations
Tobacco use continued to decline during the emergence of e-cigarettes up to 2015, which, as our data confirms, was also the period of most rapid growth in young people’s experimentation with e-cigarettes. However, the most recent data sets indicate some plateauing in rates of both ever and regular smoking across nations, during a period beyond regulation and in which young people’s experimentation with e-cigarettes was no longer growing. The only nation in which there was some indication of continued decline in smoking was England. As noted elsewhere,26 however, the English survey is smaller and has seen more substantial drop-offs in its response rates than have the Welsh or Scottish surveys and, hence, it is unclear whether this represents divergence between nations or an artefact of methodological differences.
The plateauing observed for tobacco use was also reflected in other substances, as has been reported elsewhere. 120 Indeed, disruption to long-standing declines in tobacco use appears to have lagged somewhat behind those for other substances, with ever use of tobacco beginning to plateau more recently than equivalent measures of both alcohol or cannabis, which had already begun to plateau from 2011 to 2015. Recent data from the USA indicate that growing cannabis use may act as a driver of nicotine dependence and sustained tobacco use among young people, with growing co-occurrence of tobacco and cannabis use, and dependence strongest among combined users. 121 Although there were insufficient data points to model continued change in attitudes towards smoking in post-legislation models, data from SALSUS and the SDDU survey indicate that the proportion of young people who report that it is OK to try smoking rose from 2015 to 2018 in Scotland and remained flat from 2016 to 2018 in England. Data published by the SDDU and SALSUS teams indicate that this change is also mirrored in recent increases in the acceptability of drug use and alcohol consumption,94,95 again indicating broad social trends in terms of attitudes towards substance use, rather than being specific to tobacco. Nevertheless, this supports a conclusion that the suite of tobacco regulation implemented in 2016, including the TPD regulations and plain packaging for tobacco cigarettes, may not have been sufficient to maintain or increase the downwards trajectory in young people’s use of tobacco. Further action will be needed to reach young people who continue to take up smoking if UK nations are to achieve goals of becoming smoke free by 2030. 122 Given the clustered nature of adolescent risk behaviours, and their often shared trajectories over time, it is perhaps unlikely that the goal of becoming smoke free by 2030 will be achieved through tobacco-specific intervention alone and, instead, it may require an increased emphasis on engaging with the broader context of adolescent risk behaviour and identifying and modifying common determinants. 123 One possible interpretation might be that there is an interaction between regulation of e-cigarettes and tobacco, with regulation of e-cigarettes leading young people who might have used e-cigarettes towards tobacco instead. Although such a conclusion is highly tentative, future research could usefully explore the effects of tobacco regulation on e-cigarette uptake, and vice versa. For example, following completion of this study, flavoured tobacco was banned in the EU as a final stage of the TPD; however, flavoured e-cigarettes remain available in many countries, including the UK. Conversely, flavoured e-cigarettes were regulated in the USA, although flavoured tobacco cigarettes remain available. Whether or not these respective legislative decisions lead young people to switch from flavoured tobacco or e-cigarettes to the alternative deserves attention.
Recommendations for future research
Recommendations for research, not ordered in terms of priority, include the following:
-
Continued population-level monitoring of trends over time in young people’s tobacco cigarette and e-cigarette use and perceptions remains vital.
-
Harmonised international data sets may be particularly valuable in enabling changes following new policies to be compared with an external comparator.
-
As regulatory divergences have emerged between nations, international comparisons of recent trends in e-cigarette use and smoking may provide insight into impacts of different regulatory environments on young people’s smoking and e-cigarette use.
-
There are high levels of confusion on the harms of e-cigarettes relative to tobacco among young people. Future research should seek to understand how to reinforce the role of e-cigarettes as cessation devices for smokers, while discouraging use by non-smokers and acknowledging ambiguity and unknown long-term harms.
-
Although young people’s e-cigarette use is no longer continuing to grow, a substantial proportion of young people continue to use e-cigarettes. Hence, research into how exposure can be further reduced, without reducing the effectiveness of e-cigarettes as cessation aids for smokers, remains important.
-
Given the prominent role of the internet and video-sharing platforms in young people’s exposure to e-cigarettes, further understanding of how young people interact with these platforms is an important area for future research.
-
Although much has been achieved in reducing young people’s use of tobacco, there is now tentative evidence from our secondary analysis that this decline may be stalling, particularly in the devolved nations, and this is reflected in other substances and is not unique to tobacco. Hence, it is vital to understand how tobacco-specific interventions, and interventions that address common causes of multiple adolescent risk behaviours, can enable further reduction in the prevalence of tobacco use among young people.
Our study demonstrates the value of complex mixed-method designs in understanding the implementation, mechanisms, context and effects of policies within complex and ever-changing contexts. Engagement with rapid developments in theory-driven and complexity-informed evaluation approaches might be valuable in future similar studies.
Strengths and limitations
This study represents, one of the first robust evaluations of the introduction of e-cigarette regulations, as well as being one of the first studies to robustly examine the renormalisation hypothesis. The quantitative elements of the study benefited from use of large historical data sets across all three UK nations. Quantitative findings are contextualised and explanations for estimated trends generated through qualitative work with a diverse range of stakeholders.
Nevertheless, there were some important limitations. Although there are few viable alternatives for measuring substance use behaviour at scale, outcome measures rely on self-report. The outcome measures are, therefore, subject to social desirability bias, which may change in magnitude over time as behaviours become more or less socially unacceptable. There were differences in timing of surveys across nations, and in questions used. Although a limitation insofar as these differences make direct comparisons across countries challenging, the fact that similar changes in trend are observed across nations despite these differences enhances confidences that these are real social changes. The infrequent nature of some data collections and the rapid escalation of tobacco control measures through the study period meant that adjusting models for all potential interventions as confounders was not feasible. Although our primary statistical analysis of Welsh data was adjusted for school-level clustering, for many secondary analyses this was not possible because of the removal of school identifiers from archived data sets. Hence, the statistical significance of some changes in trend may be overstated because of inability to inflate standard errors to account for non-independence of young people within schools. Given that the TPD regulations were supranational legislation and no ‘similar’ country without regulations but comparable historical data was identified, we had no external control group. Hence, we cannot rule out the possibility that plateauing would have occurred without legislation. The limited pre-legislation data points for our primary analysis is another limitation, which is unavoidable where evaluating emerging public health issues for which measurement has been only recently integrated into surveys. Capturing and assessing trends in e-cigarette use over a longer time period provides more power in statistical analyses, but also risks weakening causal inference by increasing the likelihood of events external to the legislation occurring and causing change in trends. 99 Notably, as the study approached the long-term data collection, the EVALI outbreak occurred in the USA, which might offer an alternative explanation for changes in trend for e-cigarette use. The consistency of change in trend in short- and long-term analysis, however, provides some confidence that change occurred prior to EVALI and continued thereafter, rather than occurring after or being further catalysed by EVALI. This conclusion is reinforced by comparison against simpler analyses of data from England and Scotland, which in both instances extended to only 2018 (i.e. prior to the EVALI outbreak), yet showed clear evidence of slowed growth in e-cigarette use in the years beyond TPD regulations. Recent research has indicated that young people’s tobacco use increased during the first COVID-19 lockdown in the UK,124 likely as a means of dealing with stresses of the pandemic. Although future rounds of data will enable us to monitor trends in the longer term, our ability to attribute these trends to the TPD regulations, rather than to more recent events, such as the COVID-19 pandemic, will diminish with time.
There were also some deviations to protocol. Although we had planned to include tracking of mentions of e-cigarettes on social media, sites such as Facebook and Twitter, our qualitative data indicated that other forms of social media were more influential, such as video-sharing websites. Hence, although the internet was cited as an important source of exposure, we were not able to quantitatively track this in our study. Some external data collections in England and Scotland did not take place, meaning that some analyses are based on fewer data points than in our original protocol. In particular, for secondary analysis of smoking trends, although there was a longer baseline time series than for e-cigarettes, the reduced frequency of some surveys meant that there was fewer data available for post-implementation analyses than we had hoped, and findings regarding plateauing in young people’s smoking since 2016 should be treated with caution until further rounds of data are available.
Although we specified a number of secondary analyses to examine the specificity of changes in use of e-cigarettes and tobacco, it is perhaps possible that these variables might themselves have been impacted by external legislation brought in alongside the TPD regulations. Energy drink use, for example, might have been impacted by the recent sugar tax announced around the same time as the TPD regulations were implemented. It is possible that the observed co-occurring changes in trend for tobacco and cannabis use might have reflected increased use of e-cigarettes as devices to support use of cannabis.
Given that the study started during the transitional phase of TPD implementation, it was not possible to collect qualitative data prior to this and, hence, initial data on young people’s perceptions of the recent emergence of e-cigarettes might have already began to be influenced by new regulations. The choice to involve teachers in selection of pupils for interviews, although pragmatic when sampling from within schools, may have led to some biases in who was put forward for qualitative interviews. In 2016, when this study was designed, we made a decision to conduct single-gender group interviews because of the gendered nature of historical smoking trends. However, our own survey data have since illustrated the extent to which young people who do not identify as male or female, and who may have been excluded by this decision, are affected by tobacco use. 96 Were we to design the study again, we would not repeat this decision. We also collected somewhat limited demographic information from young people and a broader range of demographic information would have allowed us to better understand the diversity of views represented within our data.
As reflected in updated MRC guidance for development and evaluation of complex interventions125 (published between completion of this study and the submission of this report), recent years have seen rapid developments in the accommodation of theory-driven approaches to evaluation, such as realist evaluation,126,127 into mainstream evaluation practice and has increased the influence of complexity-informed approaches and systems perspectives. 88,128 Our integrated mixed-method design is a strength. However, it is possible that future similar studies may benefit from more explicit engagement with these advances, enabling fuller understandings of cause and effect within complex open systems where co-occurring interventions and epidemiological events collide.
Chapter 7 Conclusions
Our primary aim was to understand the effects of TPD regulations on young people’s use of e-cigarettes. To achieve this, we explored the context of young people’s smoking and e-cigarette use prior to TPD regulations, the implementation of the regulations, and the mechanisms and outcomes that followed from implementation. Table 18 provides an overview of the key conclusions mapped against each of the original study aims.
| Aim | Conclusion |
|---|---|
| Did increased regulation of e-cigarettes interrupt prior growth of young people’s e-cigarette use? | E-cigarette use, both ever and regular use, peaked around the time of implementation of TPD regulations. Although alternative causal explanations cannot be ruled out, this is consistent with an effect of the TPD on young people’s use of e-cigarettes |
| How did young people perceive risks and social norms surrounding e-cigarettes (and how did perceptions change over time as products become TPD compliant)? | Young people typically differentiated between e-cigarette and tobacco products and viewed both as risky, but in different ways, with e-cigarettes associated with unknown harms and potential electrical accidents. Between 2017 and 2019, perceived harms changed and young people increasingly saw e-cigarettes as being at least as harmful as tobacco |
| How did young people interpret and respond to the presence or absence of health warnings on e-cigarette packets? | Perhaps owing to informal supply chains, many young people did not report having ever seen e-cigarettes in their packets and exposure to warning labels was low. The message was seen as unlikely to influence young people when compared when more powerful health messaging on tobacco cigarettes |
| To what extent, and in what ways, did young people continue to interact with e-cigarette marketing after the prohibition of cross-border advertising? | Young people reported little exposure to marketing and little brand awareness in qualitative interviews, although much exposure centred around video-sharing websites. Quantitative data indicated that many young people could recall exposure to at least one form of marketing in the past month after cross-border advertising had been removed |
| Have trajectories in young people’s ever and current smoking been significantly interrupted (positively or negatively) by growing prevalence of e-cigarettes? | There was little evidence of change, positive or negative, in the decline in young people’s smoking during the period when e-cigarettes were gaining substantial popularity among adult smokers, but the products were largely unregulated |
| Did the rate of decline in young people’s smoking change after additional regulation of tobacco and e-cigarettes in May 2016 (including TPD and plain packaging)? | In more recent data sets, following the regulation of e-cigarettes alongside a broader suite of tobacco regulation, there was some tentative evidence that declines in young people’s use of tobacco were beginning to stall, and this was particularly evident in Scotland and Wales |
| To what extent was compliance with TPD in product sales achieved, and what are the barriers to and facilitators and unintended consequences of implementation? | Although stakeholders described challenges stemming from a lack of communication from official bodies, compliance with the legislation was perceived by stakeholders as high, which concurred with our observations. Trade bodies were seen as playing a major role in facilitating implementation by providing information on what was required to achieve compliance. A number of legal loopholes for enabling the use of high-strength e-cigarettes were identified, and some concerns remain among some stakeholders that some of the less evidence-based aspects of the regulations might deter smokers from using e-cigarettes |
| To what extent, and in what ways, did variations between UK countries in e-cigarette policy emerge during the study period? | There were no major divergences between nations identified during the study period. However, policy stakeholders cited more informal differences between UK nations in the extent to which e-cigarettes were endorsed as a smoking-cessation aid |
| What other changes to the regulatory context of tobacco and e-cigarettes occur during the study period in the UK and across individual UK countries? | There were few changes to the regulatory context, other than those anticipated at the beginning of the study. However, major events, such as the EVALI outbreak, had far reaching spill-over effects in other nations, likely acting as a key explanation for young people’s increased perception of e-cigarettes as ‘as bad as tobacco’ |
Our data provided limited support for the notion that e-cigarettes were renormalising smoking prior to their regulation via the TPD. Qualitative findings suggested that some forms of e-cigarette use itself, predominantly casual use in social contexts, such as parties, were becoming normalised. However, throughout the time series, regular use of e-cigarettes remained low, particularly among never smokers and, hence, concerns that e-cigarettes are acting as a gateway to addiction for a new generation of never smokers are not currently reflected in the data. TPD regulations were, to some extent, contested by stakeholders in terms of the extent to which the restrictions represented a move to treat e-cigarettes like tobacco, or proportionate restrictions aimed at achieving goals of limiting the appeal of e-cigarettes to non-smokers. Aspects such as marketing restrictions were generally viewed positively, although some elements relating to device characteristics were described as needing some ongoing refinement. Nevertheless, regulations were, for the most part, well implemented. Our study provides evidence that young people’s experimental use of e-cigarettes appears to have stopped growing in the nations of Great Britain around about the time of TPD regulations being implemented. A conclusion that this trend was caused by the TPD regulations is challenged by young people’s reports of limited interactions with elements of the regulations, such as device labelling, and reports that e-cigarettes were seen as a fad that had begun to run its course. However, the fact that this plateauing in e-cigarette use has occurred in the UK just as e-cigarette use was undergoing a substantial period of growth in less-regulated contexts, such as North America, perhaps strengthens a potential conclusion that regulations, such as marketing restrictions and mandatory declaration of new products, might have inhibited the ability of manufacturers to reignite young people’s interest in e-cigarettes as this began to wane. Our study took place in a context of rapidly evolving support for a role for e-cigarettes in cessation from smoking. The findings of our study are reassuring in that, during this time, young people’s interest in e-cigarettes appears to have stopped increasing. Nevertheless, continued collection of robust national data to monitor whether or not this trend continues remains important. The suite of tobacco regulation implemented in 2016, including the TPD regulations and plain packaging for tobacco cigarettes, appears, however, not to have been sufficient to maintain or increase the downwards trajectory in young people’s use of tobacco, which, particularly in Scotland and Wales, appears to have plateaued in very recent years. If UK nations are to achieve goals of becoming smoke free by 2030, then further action will likely be needed to prevent smoking uptake among the minority of young people who are likely to continue to take up smoking in contemporary society.
Acknowledgements
We are grateful to all study participants and the DECIPHer ALPHA young people’s advisory group for providing a public perspective on study methods and supporting the drafting of the Plain language summary. We also acknowledge the support of our Study Steering Committee whose members included Professor Amanda Amos (University of Edinburgh), Professor Matt Egan (London School of Hygiene & Tropical Medicine), Dr Chris Roberts (Welsh Government), Dr David Humphreys (Oxford University), Mrs Sheila Duffy (ASH Scotland), Dr Ashley Gould (Public Health Wales) and Dr Sharon Cox (University College London).
We thank Douglas Eadie and Elen deLacy for supporting collection of data in Scotland and Wales, respectively, and Lindsey Allen for providing administrative support to the study. In addition to team members who have contributed throughout the study and to its final report, the Study Management Group at various stages of the project included Professor Laurence Moore (University of Glasgow) who contributed to early publications, and Professor Simon Murphy (Cardiff University) who supported access to the SHRN survey and inclusion of bespoke measures for this study, and provided initial mentoring to the (at the time) early career principal investigator, during study set-up.
We are grateful to the Welsh Government for providing HBSC data for analysis and to the UK Data Service for provision of data sets for Scotland and England. We also thank the SHRN team, which is based in DECIPHer and funded by Welsh Government through Health and Care Research Wales, for provision of data from Wales.
Ethics approval was provided by the Cardiff University School of Social Sciences Research Ethics Committee (reference SREC/2188) in March 2017.
Contributions of authors
Graham Moore (https://orcid.org/0000-0002-0205-7436) (Professor of Social Sciences and Public Health) led the conceptualisation of the study and the integration of study components, as well as the writing of the report.
Britt Hallingberg (https://orcid.org/0000-0001-8016-5793) [Lecturer in Health and Wellbeing (Cardiff Metropolitan University) and Honorary Research Associate (Cardiff University)] managed the quantitative elements of the study, including conduct of all survey data analysis (except short-term impact analysis), and contributed to writing the first draft of the report, including sections in Chapters 2, 3 and 5.
Rachel Brown (https://orcid.org/0000-0002-4475-1733) (Research Fellow) managed the process evaluation, led qualitative analysis and wrote first drafts of sections of all results chapters.
Jennifer McKell (https://orcid.org/0000-0002-2912-0837) (Research Fellow) undertook qualitative interviews and observations in Scotland, contributed to qualitative data analysis, led the Scottish study arm (following Linda Bauld’s move to the University of Edinburgh) and wrote first drafts of sections of Chapter 4.
Jordan Van Godwin (https://orcid.org/0000-0001-5288-6614) (Research Associate) supported qualitative work in Cardiff, including fieldwork and contributions to qualitative data analysis, and wrote first drafts of sections of Chapter 4.
Linda Bauld (https://orcid.org/0000-0001-7411-4260) (Bruce and John Usher Chair of Public Health) contributed to study design and conceptualisation, contributed to qualitative data collection in Scotland, and contributed to all study elements, providing policy advice and input into publications. Led the University of Stirling team until movement to University of Edinburgh in 2018.
Linsay Gray (https://orcid.org/0000-0002-6918-5037) (Senior Investigator Scientist) was involved in study design and conceptualisation, led the design of the statistical analysis plan, advised on its implementation and contributed to reporting of quantitative study elements.
Olivia Maynard (https://orcid.org/0000-0002-9048-6627) (Senior Lecturer in Experimental Psychology) led qualitative work and observations in the English study arm, and contributed to writing up of all study components.
Anne-Marie Mackintosh (https://orcid.org/0000-0003-2998-8203) (Senior Researcher) was involved in study design and conceptualisation, and contributed to all study elements, providing comments and input into publications.
Marcus Munafò (https://orcid.org/0000-0002-4049-993X) (Professor of Biological Psychology) led the University of Bristol team, was involved in study design and conceptualisation, and contributed to reporting of quantitative study elements.
Anna Blackwell (https://orcid.org/0000-0002-4984-1818) (Senior Research Associate) supported qualitative data collection in Bristol and contributed to the write-up of qualitative study components.
Emily Lowthian (https://orcid.org/0000-0001-9362-0046) (Lecturer in Education) led the merging of quantitative data sets, undertook quality checks of analyses undertaken by Britt Hallingberg and Nicholas Page, and contributed to the write-up of quantitative study components.
Nicholas Page (https://orcid.org/0000-0002-4671-2797) (Research Associate) led the quantitative components of the study during Britt Hallingberg’s maternity leave mid-way through the study (including implementing short-term effects analysis in Chapter 4), undertook quality checks of analyses undertaken by Britt Hallingberg and contributed to the write-up of quantitative study components.
Publications
Brown R, Bauld L, de Lacy E, Hallingberg B, Maynard O, McKell J, et al. A qualitative study of e-cigarette emergence and the potential for renormalisation of smoking in UK youth. Int J Drug Policy 2020;75:102598.
Hallingberg B, Maynard OM, Bauld L, Brown R, Gray L, Lowthian E, et al. Have e-cigarettes renormalised or displaced youth smoking? Results of a segmented regression analysis of repeated cross sectional survey data in England, Scotland and Wales. Tob Control 2020;29:207–16.
Moore G, Brown R, Page N, Hallingberg B, Maynard O, McKell J, et al. Young people’s use of e-cigarettes in Wales, England and Scotland before and after introduction of EU Tobacco Products Directive regulations: a mixed-method natural experimental evaluation. Int J Drug Policy 2020;85:102795.
Brown R, Van Godwin J, Page N, Bauld L, McKell J, Hallingberg B, et al. Implementation of e-cigarette regulation through the EU Tobacco Products Directive (2016) in Wales, Scotland and England from the perspectives of stakeholders involved in policy introduction and enforcement. Tob Prev Cessat 2021;7:36.
Data-sharing statement
All requests for data held by the lead institution should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. Other data sets used in this report, but not owned or retained by the lead institution, are accessible via the UK Data Service as below:
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2000. [data collection]. UK Data Service; 2002. Available from: http://doi.org/10.5255/UKDA-SN-4485-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2001. [data collection]. UK Data Service; 2003. Available from: http://doi.org/10.5255/UKDA-SN-4648-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2002. [data collection]. 2nd edn. UK Data Service; 2004. Available from: http://doi.org/10.5255/UKDA-SN-4764-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2003. [data collection]. UK Data Service 2005. Available from: http://doi.org/10.5255/UKDA-SN-5287-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2004. [data collection]. UK Data Service; 2005. Available from: http://doi.org/10.5255/UKDA-SN-5288-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2005. [data collection]. UK Data Service 2007. Available from: http://doi.org/10.5255/UKDA-SN-5568-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2006. [data collection]. 2008. Available from: http://doi.org/10.5255/UKDA-SN-5789-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2007. [data collection]. UK Data Service; 2008. Available from: http://doi.org/10.5255/UKDA-SN-6005-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2008. [data collection]. UK Data Service; 2009. Available from: http://doi.org/10.5255/UKDA-SN-6287-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2009. [data collection]. UK Data Service.; 2010. Available from: http://doi.org/10.5255/UKDA-SN-6603-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2010. [data collection]. UK Data Service; 2011. Available from: http://doi.org/10.5255/UKDA-SN-6883-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2011. [data collection].: UK Data Service; 2012. Available from: http://doi.org/10.5255/UKDA-SN-7156-1
National Centre for Social Research, National Foundation for Educational Research. Smoking, Drinking and Drug Use Among Young People, 2012. [data collection]. UK Data Service; 2013. Available from: http://doi.org/10.5255/UKDA-SN-7393-1
National Centre for Social Research. Smoking, Drinking and Drug Use Among Young People, 2013. [data collection]. UK Data Service; 2015. Available from: http://doi.org/10.5255/UKDA-SN-7662-1
NatCen Social Research. Smoking, Drinking and Drug Use Among Young People, 2014. [data collection]. UK Data Service; 2015. Available from: http://doi.org/10.5255/UKDA-SN-7811-1
Office for National Statistics, Social Survey Division. Smoking, Drinking and Drug Use Among Young Teenagers, 1998. [data collection]. UK Data Service; 2000. Available from: http://doi.org/10.5255/UKDA-SN-4125-1
Office for National Statistics, Social Survey Division. Smoking, Drinking and Drug Use Among Young Teenagers, 1999. [data collection]. UK Data Service; 2001. Available from: http://doi.org/10.5255/UKDA-SN-4382-1
NHS Digital. Smoking, Drinking and Drug Use Among Young People, 2016. [data collection]. UK Data Service. Available from: https://doi.org/10.5255/UKDA-SN-8320-1
NHS Digital. Smoking, Drinking and Drug Use Among Young People, 2018. [data collection]. UK Data Service; 2021. Available from: http://doi.org/10.5255/UKDA-SN-8863-1
Ipsos MORI Scotland. Scottish Schools Adolescent Lifestyle and Substance Use Survey Trend Data, 1990–2013. [data collection]. UK Data Service; 2015. Available from: http://doi.org/10.5255/UKDA-SN-7849-2
Ipsos MORI Scotland. Scottish Schools Adolescent Lifestyle and Substance Use Survey, 2015. [data collection]. UK Data Service; 2017. Available from: http://doi.org/10.5255/UKDA-SN-8174-1
Ipsos MORI Scotland. Scottish Schools Adolescent Lifestyle and Substance Use Survey, 2018. [data collection]. UK Data Service. SN: 8615. Available from: http://doi.org/10.5255/UKDA-SN-8615-1
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
Appendix 1 Response rates
| Survey data | Response rate, % | ||
|---|---|---|---|
| Walesa | Scotlandb | Englandc | |
| 1998 | 70 | 70 | |
| 1999 | 76 | ||
| 2000 | 64 | 63 | |
| 2001 | 61 | ||
| 2002 | 65 | 63 | |
| 2003 | 65 | ||
| 2004 | 62 | 62 | |
| 2005 | 50 | ||
| 2006 | 57 | 55 | |
| 2007 | 53 | ||
| 2008 | 59 | 51 | |
| 2009 | 60 | 47 | |
| 2010 | 62 | 41 | |
| 2011 | 42 | ||
| 2012 | 43 | ||
| 2013 | 46 | 60 | 38 |
| 2014 | 35 | ||
| 2015 | 53 | ||
| 2016 | 26 | ||
| 2017 | 73 | ||
| 2018 | 52 | 22 | |
| 2019 | 77 | ||
Appendix 2 Youth Tobacco Policy Survey estimates over time
Data from the YTPS, led by investigator Anne-Marie Mackintosh, were not integrated with other surveys for our main analyses because of small sample sizes in the included age range. However, the YTPS provides an external data source for triangulation of our findings, completed by a total of 8593 young people in seven waves between 2002 and 2016. The 2011 and 2014 data points are within the period analysed in Chapter 3, during which e-cigarettes were emerging with limited regulation. The 2016 survey occurred within the ‘post-implementation’ period defined as the period after May 2016 (data were collected in August 2016). Consistent with findings from the much larger surveys conducted within individual nations in Great Britain, young people’s experimentation with, and regular use of, tobacco continued to decline during the period between the emergence of e-cigarettes and their regulation under the TPD. Also consistent with the much larger data sets analysed in this study, smoking rates appeared to show some plateauing between 2014 and 2016. The YTPS used different indicators of smoking attitudes and norms, including the perceived prevalence of smoking among 15-year-olds. As with perceptions of whether or not it is OK for young people to smoke in our main analyses, the percentage of young people perceiving smoking as a ‘normal’ behaviour, which half or more 15-year-olds engage in, declined across the time series, with the sharpest drop from 2011 to 2014, and continued decline from 2014 to 2016. In 2002, a large majority of young people perceived smoking as something most 15-year-olds do (see Figure 10).
E-cigarette use was first measured in the YTPS in 2014, with ever e-cigarette use having reached 12% by first measurement and growing to 17% by 2016, although regular use remained low at 1% (see Bauld et al. 39) (see Figure 11).
The survey does not include measures of alcohol and cannabis use to compare whether or not, as observed in other surveys, plateauing in smoking is mirrored in other substances.
Appendix 3 Process evaluation materials
Pupil topic guide
Section 1: group guidelines
Because this is a group discussion I’d like to go over how this can work best. You’re not expected to all have the same opinions so feel free to disagree (politely!), there are no right or wrong answers during the discussion. Don’t feel like you have to answer directly to me all the time, you can answer each other’s points as well. My role is to ask the questions and to try to make sure that everyone can join in. If you don’t want to answer a question that’s OK.
To make it a clear recording and a better discussion, I’ll ask you to speak one at a time and allow whoever is speaking to finish their point. If you want to respond to someone else’s point, either to agree, disagree or add something else, please feel free to do this once they’ve finished. I might also write notes while we’re talking to remember things that I want to follow up on.
Does anyone have any questions?
Ice breaker task?
Now, I’d like you to name all the words you use for these devices so that we can make sure we’re all clear on different language we might hear (brief group shout out of terminology). (Show images of cigarette-style and vaping devices and read out definitions. Include shisha devices.)
What word would you prefer to use to include all of these? In what ways do you think e-cigarettes (or chosen wording) are similar to tobacco cigarettes? How are they different? (Do they contain nicotine?)
Section 1: research theme – social norms of e-cigarette use in relation to tobacco and as a standalone product
-
How common is it for you to see people using e-cigarettes around the place now?
-
How many adults in your area do you think use e-cigarettes? (Prompt for estimate. ) Do you think this is more or less than the number who use tobacco cigarettes? Compared to when you started secondary school, do you think the number of adults using e-cigarettes has gone up or down? How about tobacco cigarettes?
-
How many people your age in your area do you think use e-cigarettes? (Prompt for estimate. ) Do you think this is more or less than the number who use tobacco cigarettes? Compared to when you started secondary school, do you think the number of young people using e-cigarettes is going up or down? How about tobacco cigarettes?
-
Why do you think young people might use e-cigs instead of smoking? (Prompt: using to quit, social reasons?)
-
What types of young people do you think use e-cigs? Are they the same kinds of young people that smoke tobacco? (Prompt: how are they similar? How are they different?)
-
Why do you think young people who smoke might carry on doing this rather than vaping?
-
Do you think you’ll use e-cigs when you’re older? Reasons either way.
-
What do you think your friends would say or do if you starting using e-cigs?
-
What do you think your parents would say or do if you were using e-cigs? (Prompts: be angry, try to stop you, be OK?) Why?
-
What about if you were smoking tobacco? (Prompt: as above on parents and peers views. )
Section 2: research theme – interaction with, and awareness of, e-cigarette marketing
-
Do you know the law on who can buy e-cigarettes?
-
Can you get hold of e-cigarettes if you want them? Where have you seen them on sale? (If yes, prompt on whether this means buying them or obtaining from someone else. )
-
Do you think you’d find it easier to get hold of (a) e-cigarettes or (b) tobacco?
-
Have you seen any adverts for e-cigarettes? Where? (Prompt: on public spaces, social online spaces, mainstream media, event sponsorship?) Do you remember the brands?
-
Who do you think the adverts were aimed at? (Prompt: adults, young people, current users/non-users?)
-
What do you think it is about them that would make them appeal to that group?
Section 3: research theme – perceived risk of e-cigarettes and interpretation of health warnings
-
(If positive in response to section 1, questions 1 and 3.) You said earlier that you thought more people your age were using e-cigarettes now than before. Do you think this might have any effect on the way e-cigarettes are seen by:
-
young people your age?
-
younger children?
-
-
What about the way tobacco cigarettes are seen by:
-
people your age?
-
younger children?
-
-
Are e-cigarettes safe? (Prompt here on perceived risk relative to tobacco: more or less safe?)
-
Do you think e-cigarettes have any risks to health? How and why? (Prompt here on nicotine content, ingredients, addictiveness?)
-
Have you seen any warnings on packaging for e-cigs? What do you remember?
-
(Use visual examples of types of warnings now on e-cigarette packets. ) What impact do you think health warnings like this might have on people your age? (Prompt: smokers and non-smokers?)
-
(Next show examples of warnings on tobacco packets and explore the same thing. ) Do you think e-cigarette products should have more warnings? Why or why not? What should they be about?
Closure
That’s all the questions I have. We’ve covered a lot of issues and I appreciate your patience, but is there anything else you would like to add? Do you have any questions about the interview or the research as a whole? Please feel free to contact me by e-mail if you have any queries at a later date. I’ll be in touch again in the next school year so that we can talk again.
Thanks again for your time and your contribution to the project.
Policy stakeholders topic guide
Section 1: job role
-
First, could you tell me about your job role? (Involvement in tobacco control. )
-
How long have you been in this role?
-
How would you like it defined in the research?
Section 2: approaches to tobacco control
I’d like to start by discussing tobacco control more broadly and then moving on specifically to TPD a bit later. First:
-
What do you think have been the key influences on reductions in adult smoking over recent years?
-
What about for young people? Have the same factors been important or are there differences?
-
Do you think policy actions on youth smoking have had varied impact by demographic groups? And why?
-
Tobacco control policy has been increasingly devolved across the nations: positive or negative? Why?
Section 3: e-cigarettes
E-cigarette use has grown rapidly in recent years. Overall, do you think e-cigarettes have made a positive or negative contribution to public health, or do you think it’s not made any difference?
-
Why is that?
-
We know opinions are split on whether e-cigarettes should be recommended as a stop smoking tool. What do you think? (Why?)
-
What should regulation on e-cigarettes aim to do? Any additional measures you’d like to see in place on e-cigarettes?
-
E-cigarette regulation varies a lot internationally. Do you think the balance of e-cigarette regulation overall is about right? Too liberal? Too restrictive? Why?
-
Many policy concerns centre around young people and potential for nicotine addiction. What are your views on that?
-
Other concerns are that e-cigarette use mimics smoking behaviour and so will lead young people to see smoking as ‘normal’ again. What do you think?
Section 3a: Tobacco Products Directive theory
I’d like to talk more specifically now about the Tobacco Products Directive (TPD) legislation.
-
What do you think is good or bad about the changes introduced by TPD? (Prompt on why for each point made. )
-
How do you think these fit with the wider tobacco control agendas that we discussed earlier?
-
Looking down the line, how will we know if TPD has been effective?
-
Do you think there might be any unintended harms from TPD? What?
Section 3b: Tobacco Products Directive implementation
-
How was TPD communicated to the public? Has this been effective?
-
What do you think has already changed since TPD came in?
-
What do you think of the warnings displayed on e-cigarette packaging as a result of TPD?
-
Do you think these are expressed the right way? Why?
-
Do you think these warnings might change the way people see e-cigarettes? In what ways?
-
Section 4: future directions
-
What do you think the next few years hold for e-cigarette regulation here?
-
And what about for tobacco control policy over the next few years?
-
We mentioned devolution earlier, do you expect any more policy divergence across the UK nations in the next few years?
-
TPD is EU regulation. Going forward, do you think Brexit might present any challenges (or opportunities) in relation to:
-
tobacco policy
-
e-cigarette policy.
-
Interview schedule: trading standards officers
Section 1: introduction and context
I’d like to start by explaining the aims of the project. This research looks at the impact of regulation of e-cigarettes via the Tobacco Products Directive, introduced in May 2016. We’re talking to young people and policy stakeholders about this as well. Your job role means that you can make a valuable contribution to understanding on this topic.
-
First, how long have you been in this role?
-
What are your main duties?
-
What area do you work across?
-
Do you work with any other organisations as part of your role? Who?
Section 2: approaches to tobacco control
Smoking rates have been in decline for some years now in the UK and there have been major changes to tobacco control policy over the years. I’d like to discuss your views on this.
-
What kinds of changes have you seen in people’s smoking in recent years?
-
Have you noticed any changes among adults in particular?
-
What about young people?
-
How has this impacted your role? (Prompts: changes to required enforcement, focus on different age groups or problems like illegal tobacco. )
-
-
What do you think have been the key influences on reductions in adult smoking over recent years?
-
What about influences on reductions in youth smoking?
-
-
How do you think tobacco control policies have contributed to this?
-
And how has policy change led to any changes in your role?
-
-
What other social changes do you think have contributed?
Section 3: e-cigarettes
-
Since the emergence of e-cigarettes, use has grown rapidly in recent years. What has that meant for your role, if anything?
-
To what extent do you think e-cigarettes should be regulated (a) in line with tobacco cigarettes and (b) as a distinct product? Why? What should regulation on e-cigarettes aim to do? (Prompt on: restricting availability of devices and/or liquids; providing health information; stopping youth uptake. )
-
E-cigarette regulation varies a lot internationally. Do you think the balance of e-cigarette regulation overall in Wales/Scotland/England is about right? Too liberal? Too restrictive? Why?
-
Overall, do you think e-cigarettes have made a positive or negative contribution to public health, or do you think it’s not made any difference?
-
Why is that?
Section 4: I’d like to talk more specifically now about the Tobacco Products Directive legislation
-
What do you think is good or bad about the changes introduced by TPD? (Prompt on why for each point made. )
-
TPD was introduced in May 2016 with a transitional 12-month period:
-
What actions were taken in preparation prior to May 2016? (Prompt on: communication, enforcement, planning. )
-
What type of information/support did you receive about TPD?
-
What actions were you taking during the transitional period?
-
And what happened after May 2017 (end of transitional period)? How did your actions change?
-
-
And thinking about now, are there any actions still going on that are related to TPD?
-
How has TPD been communicated to the public? Has this been effective?
-
What were your observations from visits to retailers? OR What did your staff report from visits to retailers? (Dependent on interviewee role. )
-
Did compliance vary by type of retailer?
-
What type of actions were taken/can be taken for non-compliance?
-
What do you think the challenges are for retailers in being complaint?
-
What do you think the challenges are for Trading Standards in enforcing TPD?
-
-
How do you think TPD fits with the wider tobacco control agendas that we discussed earlier?
-
How will we know if TPD has been effective? What would change? (Prompt here on both youth and adult behaviour. )
-
Do you think there might be any unintended harms from TPD? What might they be?
Interview schedule: e-cigarette retailers
Section 1: introduction and retail context
I’d like to start by explaining the aims of the project. This research looks at the impact of regulation of e-cigarettes via the Tobacco Products Directive, introduced in May 2016. We’re talking to young people and policy stakeholders about this as well. Your job role means that you can make a valuable contribution to understanding on this topic.
-
First, could you tell me about the business and your job here?
-
How long have you been in this role?
-
Is the store(s) you work in part of bigger chain or independent?
-
Customer base: who buys e-cigarettes in this store?
-
What kind of age group comes here most?
-
Do you think most people who just vape are ex-smokers?
-
Do many of your customers just vape now?
-
-
What do you think is appealing about e-cigarettes for your customers? (Prompt for function, flavours, branding, design, etc., and whether more or less appealing for younger and older customers?)
-
Do you have any experience dealing with minors trying to buy e-cigarettes in your shop?
-
-
What are the regulations on this?
-
Are there specific store policies for this?
-
Section 2: approaches to tobacco control
Smoking rates have been in decline for some years now in the UK and there have been major changes to tobacco control policy over the years. I’d like to discuss your views on this.
-
What kinds of changes have you seen in people’s smoking in recent years?
-
Have you noticed any changes among adults in particular?
-
What about young people?
-
-
What do you think have been the key influences on reductions in adult smoking over recent years?
-
What about influences on reductions in youth smoking?
-
-
How do you think tobacco control policies have contributed to this? What other social changes do you think have contributed to these?
Section 3: e-cigarettes
-
E-cigarette use has grown rapidly in recent years. Overall, do you think e-cigarettes have made a positive or negative contribution to public health, or do you think it’s not made any difference?
-
Why is that?
-
-
Some people believe that e-cigarettes should be used to help people stop smoking, for example by being recommended by health services, while others do not. What do you think? Why?
-
To what extent do you think e-cigarettes should be regulated (a) in line with tobacco cigarettes and (b) as a distinct product? Why? What should regulation on e-cigarettes aim to do? (Prompt on: restricting availability of devices and/or liquids; providing health information; stopping youth uptake. )
-
E-cigarette regulation varies a lot internationally. Do you think the balance of e-cigarette regulation overall in Wales/Scotland/England is about right? Too liberal? Too restrictive? Why?
-
What impacts do you think e-cigarettes have had for young people? Or what kind of effects might they have in the future?
-
Some people say that e-cigarettes are likely to lead to nicotine addiction in young people. What are your views on that?
-
Some people say that e-cigarette use mimics smoking behaviour and so will lead people to see smoking as ‘normal’ again. What are your views on that?
-
Section 3a: Tobacco Products Directive theory
I’d like to talk more specifically now about the TPD legislation.
-
Are you familiar with the Tobacco Products Directive? Where do/have you information about this from? What type of information/support have you received?
-
What do you think is good or bad about the changes introduced by TPD? (Prompt on why for each point made. )
-
How do you think these fit with the wider tobacco control agendas that we discussed earlier?
-
Who do you think the changes introduced by the TPD are aimed at and why? (Prompt on consumers, producers, retailers. )
-
How will we know if TPD has been effective? What would change? (Prompt here on both youth and adult behaviour.)
-
Do you think there might be any unintended harms from TPD? What?
Section 3b: now I’d like to talk more about Tobacco Products Directive implementation and impacts on your business
-
TPD was introduced in May 2016. What do you think has changed? (Prompt on users, retailers, norms. )
-
What do you think of the warnings displayed on e-cigarette packaging as a result of TPD? (Use visuals if needed. )
-
Do you think these are expressed the right way? Why?
-
Do you think these warnings might change the way people see e-cigarettes? In what ways?
-
Have any of your customers commented on/discussed the warnings with you?
-
How has TPD been communicated to the public? Has this been effective?
-
Were you aware of any local campaigns designed to raise awareness of the new regulations?
-
Has there been any local monitoring and enforcement activity? Is that ongoing?
-
-
What impact (if any) has TPD had on your business? Why? (Any changes in local competition/prevalence of retailers?)
-
Have you made any changes to the way you market your products? In store/online?
-
What impact (if any) has TPD had on your customers purchasing decisions/willingness to try e-cigs? Why?
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/WTMH3198).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
Glossary
- Change in trend
- Where interpreting regression models refers to change in the post-slope variable.
- Current smoking/e-cigarette use
- Any current smoking/e-cigarette use (including less frequent use).
- E-cigarette use
- Use of e-cigarettes is described as ‘vaping’ or ‘e-cigarette use’.
- Great Britain
- A collective term that refers to England, Scotland and Wales.
- Primary data
- Research data collected specifically for the purpose of this study.
- Primary statistical analysis
- The main prespecified analysis used to judge whether or not change in our primary outcome occurred following intervention.
- Regular smoking/e-cigarette use
- Smoking/e-cigarette use once per week or more.
- Secondary data/data analysis
- Data collected for another purpose, but used for analysis in this study.
- Significance
- Unless otherwise indicated, significance relates to statistical significance.
- Smoking
- Inhaled use of combustible tobacco.
- Social media
- Interactive web-based sites, such as Facebook (URL: www.facebook.com; Meta Platforms, Inc., Menlo Park, CA, USA), Twitter (URL: www.twitter.com; Twitter, Inc., San Francisco, CA, USA) and YouTube (URL: www.youtube.com; YouTube, LLC, San Bruno, CA, USA).
- Tobacco
- Combustible tobacco, but does not include e-cigarettes.
List of abbreviations
- CI
- confidence interval
- DECIPHer
- Centre for Development, Evaluation, Complexity and Implementation in Public Health Improvement
- EU
- European Union
- EVALI
- e-cigarette or vaping use-associated lung injury
- FAS
- Family Affluence Scale
- HBSC
- Health Behaviour in School-aged Children
- MRC
- Medical Research Council
- NIHR
- National Institute for Health and Care Research
- NRT
- nicotine replacement therapy
- NYTS
- National Youth Tobacco Survey
- OR
- odds ratio
- PHR
- Public Health Research
- SALSUS
- Schools Adolescent Lifestyle and Substance Use Survey
- SDDU
- Smoking, Drinking and Drug Use
- SES
- socioeconomic status
- SHRN
- School Health Research Network
- SPECTRUM
- Shaping Public hEalth poliCies To Reduce ineqUalities and harm
- TPD
- Tobacco Products Directive
- TSO
- trading standards officer
- YTPS
- Youth Tobacco Policy Survey
