Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 15/82/01. The contractual start date was in April 2017. The final report began editorial review in March 2021 and was accepted for publication in August 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Whittaker et al. This work was produced by Whittaker et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Whittaker et al.
Chapter 1 Context
The impact of parental drug use on children and families is a major public health problem. 1 In the UK, an estimated 350,000 children are affected by parental drug use. 2 Effects include the impact of in utero exposure to substances, as well as the adverse influence of the caregiving environment associated with a drug-using lifestyle. 3 Parental substance use is strongly associated with health and social inequalities,4 including intergenerational transmission of harm5,6 and child protection involvement, including repeat child removal. 7 Parental substance use is listed as a key concern in approximately one-third of serious child protection cases. 8 The estimated lifetime costs per victim of non-fatal child maltreatment in the UK is £89,390 and the cost per death from child maltreatment is £940,758. 9
In Scotland, there are between 55,800 and 58,900 problem drug users, and most (70%) are male. 10 In England, the number of opioid and crack users is estimated to be nearly 300,000, with 71% of users in treatment in any one year; of those in treatment, 79% are opioid users. 11 Most users have some parenting role and responsibility. For example, in Scotland, over 40% of new drug treatment attenders report living with dependent children. 12
Parental drug use is closely associated with compromised parenting, poor child development and increased rates of child maltreatment, particularly neglect. 3,13 As a consequence, improving outcomes for children and families affected by parental problem drug use is a key policy objective in the UK and elsewhere. 14–16
Despite policies, fathers and male carers tend to be excluded from parenting and family support services. 17 Evidence suggests that drug-using fathers have a parenting style that often involves physical and verbal aggression towards children and situational violence towards partners. 13,18 Furthermore, there have been ongoing concerns about fathers’ involvement in cases where there have been serious and catastrophic outcomes for children in families with paternal drug use. 19 This includes repeated commentary from child death inquiries20 and child protection reviews. 21,22
Literature review
Parenting programmes
Parenting programmes targeted at the general population have been successful in improving parents’ psychological functioning, including depression, anxiety, stress, anger, guilt, confidence and satisfaction with the partner relationship. 23 However, parenting studies rarely include fathers, and those that do rarely report outcomes for fathers. 24 Evidence suggests that fathers are reluctant to attend parenting programmes,25 which may relate to their perceptions regarding gendered parenting roles and mother-focused interventions. 26 Tully et al. 27 also found that lower levels of practitioner competencies, training and experience in engaging fathers in parenting programmes resulted in lower levels of father involvement. One concern is that there is some evidence that fathers benefit less from mainstream parenting programmes than mothers. 28,29 A meta-analysis of parenting intervention studies that included fathers compared with those that did not found significantly more positive changes in children’s behaviour, but fathers reported fewer desirable changes in parenting behaviours and beliefs than mothers did. 29 The authors concluded that fathers should be encouraged to engage in parenting programmes to maximise benefits for children, but that further research is needed on recruitment and retention of fathers, adjustments required to address the parenting needs of both fathers and mothers, and how mothers and fathers work together, or not, to implement the active components of the intervention.
Encouragingly, a small body of researchers have implemented and evaluated parenting programmes for marginalised fathers, such as young and low-income fathers, those engaged in intimate partner violence and those subject to child protection orders. 30–34 Findings indicate improvements in psychological functioning30,33 and father–child relationships. 31,34 However, poor engagement with fathers remains problematic. 32,35 In addition, it is not known how fathers affected by other forms of disadvantage and co-occurring problems might respond to parenting programmes, for example fathers who are drug dependent. Parents who use drugs are highly stigmatised and marginalised, and are often reluctant to engage with group-based parenting programmes. 36 Consequently, there has been growing recognition that targeted and more nuanced interventions are required for marginalised families, including fathers,23 especially when the father poses a risk of child maltreatment. 37
Parenting programmes for parents with a substance use disorder
A review of parenting programmes for those with problem drug use found that therapeutic interventions can be helpful in reducing drug use and improving parenting. 38 However, the review found that programmes commonly target parenting without taking into account the broader needs of substance-using parents. Although it is difficult to disentangle the negative impact of prenatal exposure and the postnatal environment that the child is raised in, it is clear that children need a family environment in which they feel safe and loved and are nurtured by reliable and affectionate carers. The multiple difficulties facing parents who use drugs can interfere with or lessen their ability to provide a child with this safe, loving and nurturing environment.
An innovative US intervention for fathers with problem drug use – ‘Fathers for Change’ (F4C) – was compared with ‘Dads “n” Kids’, which combines psychoeducational parenting with practical support for housing and welfare. 39 F4C addresses drug use, parenting skills and proximal psychological factors associated with intimate partner violence. Both intervention groups reduced affect dysregulation, anger and intimate partner violence. The reduction in affect dysregulation was significantly larger among participants receiving F4C, and participants were also less likely to use drugs (relapse) following the intervention. The authors suggest that F4C could be delivered in the community with fathers and their children (see also Stover40). However, the pilot randomised trial focused on fathers only, and those in abstinence-based residential drug treatment (a 12-step programme), with the majority of fathers mandated by the criminal justice system in return for reductions in their sentences.
The Parents under Pressure (PuP) programme,41 which was developed by members of the research team, is a parenting intervention that is specifically designed to address the needs of parents who use drugs. The PuP programme is underpinned by an integrated theoretical framework that draws on attachment theory,42 the concept of emotional availability,43 neurobiological models of stress and trauma44 and a socioecological developmental model of human development. 45 Each of these theoretical perspectives identifies the quality of the parent–child relationship as crucial for the healthy development of a child. Furthermore, the personal resourcefulness of parents (i.e. capacity to regulate their own emotional state, problem solve and engage social support) and the demands of the real world (e.g. housing and legal problems, financial strain and food insecurity) can have an negative impact on the parent–child relationship. Therefore, the PuP programme is based on the premise that responding to the needs of parents who use drugs requires a framework that can address problems across multiple domains of family functioning.
In the UK, the PuP programme has been subjected to a randomised controlled trial (RCT) and economic evaluation. 46 Parents were recruited from community-based drugs services in the UK and 115 primary caregivers (mostly mothers) were randomly allocated to the PuP programme or treatment as usual. The intervention was delivered by accredited PuP practitioners in the family home. Those participants receiving PuP demonstrated significantly reduced child abuse potential (primary outcome) compared with controls, and the intervention was cost-effective. 46 However, the small number of fathers in this UK study precluded an analysis of how the intervention might have affected them and their children.
Neger and Prinz38 recommended that more robust evaluations were required to assess efficacy and feasibility of these interventions. Evidence from the PuP programme and F4C studies present a compelling argument to involve fathers who use drugs in programmes that aim to improve fathering and father–child relationships within the context of family life. Greater emphasis should be given to reducing aggression towards children and partners and improving affect regulation. Given the context and target population [i.e. fathers mandated to attend residential abstinence-based drug treatment in F4C (USA) and mothers experiencing problem substance use and living in the community in PuP (UK)], difficulty with recruitment and retention46 and initial challenges embedding the intervention into existing services,39 it is efficacious to assess the feasibility of implementing an intervention for fathers into a new setting, such as the UK.
Rationale for the PuP4Dads feasibility study
We chose to focus on PuP in the current study because of our existing research collaboration with the originators of that programme. The proposed research also takes the vital next step of targeting men in parenting intervention research. It provides one of the first attempts to improve family functioning by addressing affect regulation as a key driver of parenting and couple-related behaviours among drug-dependent men receiving community-based opioid substitution therapy (OST). In addition, to the best of our knowledge, it is the first attempt to include opioid-dependent fathers, their partners/mothers, their children and their significant others in a ‘whole-family’ approach that is in line with the governmental policy priorities for this population in the UK. 14,16 In the UK, there are very few residential drug treatment units that can accommodate fathers and their children,47 and so demonstrating successful implementation within community-based settings in the UK is essential for future scale-up. As PuP has already been trialled in the UK, the research and intervention are highly relevant to the UK public health agenda, with implications for improving the quality of caregiving in families with complex needs, reducing child abuse and situational family violence, improving children’s developmental outcomes, and improving the trajectories of adults and families affected by drug use.
In addition, interventions need to include a focus on the broader ecological context of families’ lives, help families connect with a wider social environment and provide safety and some security around accommodation and financial issues. 38,48 Although relatively small in number, there is growing evidence that promotes such approaches when delivered across community settings, such as OST settings,49,50 and within the context of family drug courts. 51,52 Notably, these programmes address multiple domains in families’ lives and incorporate home visiting and a case management approach to address wider contextual factors.
Following the Medical Research Council guidance on the development and evaluation of complex interventions,53 there are five key reasons why a feasibility study was required in this instance. First, our proposed intervention is novel in that it involves an extremely high-risk group of fathers and is positioned in an area of research that is considerably under-researched. Second, given the well-known problems in engaging with parents who use drugs, we need to understand how these problems might affect the flow of participants in a research study (i.e. from recruitment to post-intervention follow-up). Third, we need to better understand the extent to which the intervention works as intended, including the facilitators of and barriers to adoption and implementation. Fourth, there is the need to establish a theoretical understanding of the mechanisms that may lead to improvement and thereby identify the most appropriate mediators, moderators and outcome variables and measures for a future evaluation. Finally, given the small number of evaluations, and drawing from guidance regarding the best use of resources,53 we need to consider the resource and methodological implications of conducting a larger evaluation, including the feasibility of an economic analysis.
Aim, research questions and objectives
Aim
Our aim was to implement and test the feasibility and acceptability of the PuP programme for opioid-dependent fathers and their families and to determine whether or not a future pilot RCT and full-scale evaluation, including an economic evaluation, could be conducted.
Research questions
For the intervention
-
How feasible is it to deliver PuP for opioid-dependent fathers in routine family-based local government and voluntary sector services?
-
How acceptable is PuP among staff and recipients, and what are the barriers to/facilitators of uptake and retention?
-
How acceptable and adequate is the training and supervision for staff?
-
To what extent can PuP be integrated into non-NHS settings across the UK?
For the study
-
What is the optimal level of recruitment, consent and retention for a future trial?
-
What are the best methods of collecting outcome data from fathers and mothers at baseline (pre-intervention), follow-up 1 (FU1), and follow-up 2 (FU2)?
-
How feasible is it to collect attendance, medical and cost data on participating families?
-
How acceptable and appropriate are the assessment methods?
-
Is the profile of change in fathers, mothers and children clinically significant?
-
What is the nature and extent of routine family support services for fathers receiving drug treatment?
-
Which study design would best suit a future evaluation, including an economic evaluation?
Objectives
-
To determine whether or not a pilot RCT and full evaluation, including an economic evaluation, could be undertaken on the PuP programme with drug-dependent fathers and their families.
-
To assess the recruitment and retention of drug-dependent fathers, as well as feasibility and acceptability of the intervention among fathers, mothers, practitioners, referrers and key services.
-
To assess the fidelity and reach of intervention delivery by PuP practitioners, including barriers to and facilitators of successful implementation.
-
To refine and test the logic model and theoretical basis of the intervention.
-
To enhance understanding of the parenting needs of drug-dependent fathers and what programme components work best with fathers.
-
To determine key trial design parameters for a possible future large-scale trial, including recruitment and retention rates and strategies, outcome measures, intracluster correlation and sample size.
-
To determine the key components of a future cost-effectiveness analysis and tested data collection methods.
-
To establish whether or not pre-set progression criteria are met and a larger-scale trial is warranted.
-
If yes, to design the protocol, including identification of required structures, resources and partnerships.
-
Structure of report
Chapter 2 includes an overview of the study methodology, providing detail of the design, setting, intervention, methods, analytic strategy, general management of the study and public engagement. The findings are then presented in two main chapters. Chapter 3 includes relevant quantitative data on recruitment, intervention delivery and engagement, retention in the study, a description of the study participants and quantitative results. Chapter 4 includes relevant qualitative and quantitative data reported for the main study research questions (RQs), and concludes with results on the progression criteria and feasibility assessment, using ADePT (A process for Decision-making after Pilot and Feasibility Trials). 54 In Chapter 5, the findings are then discussed in relation to the overall aim and objectives of the study, strengths and limitations of the study are noted, and conclusions and recommendations for a future evaluation of the PuP4Dads (Parents under Pressure programme for fathers) are provided.
Please note that our protocol (final version 5.0) for the PuP4Dads study is available via the National Institute for Health Research (NIHR) Journals Library [URL: www.journalslibrary.nihr.ac.uk/programmes/phr/158201/#/ (accessed 6 September 2021)].
Chapter 2 Methods
Study design
A mixed-methods feasibility study was designed to test the implementation and acceptability of the PuP programme for opioid-dependent fathers and their families and the parameters for a future larger evaluation, including an economic evaluation.
The study included the following:
-
staff training, supervision and accreditation in the PuP intervention, alongside implementation support
-
delivery of the PuP intervention (over a period of approximately 6 months) by two non-NHS services [i.e. CIRCLE (Edinburgh, UK), a third-sector family support service, and PREPARE (Edinburgh, UK), a local authority-led specialist multidisciplinary pregnancy support service]
-
qualitative interviews with parent participants (i.e. opioid-dependent fathers and their partners/mothers) to explore their views and experiences of usual care for fathers, the acceptability of PuP, perceived benefits of the intervention and acceptability of the study measures and procedures
-
qualitative interviews with PuP practitioners, PuP supervisors and delivery site service managers to explore their views and experiences of staff training, implementation of PuP, acceptability of PuP, perceived benefits of the intervention and ‘fit’ with existing services and models of care, and the sustainability of PuP
-
focus groups with professional/potential referrers to explore barriers to and facilitators of recruitment, uptake and engagement, acceptability and ‘fit’ with drug treatment and other services using a multiagency partnership approach
-
collection of baseline (i.e. pre-treatment), FU1 (i.e. at end of treatment/dropout or 6 months after baseline) and FU2 (i.e. post-treatment or 6 months after FU1) measures from participating parents
-
completion rates and suitability of potential outcome measures for a future evaluation and feasibility of obtaining NHS, social services and economic data
-
feasibility of conducting a future large-scale evaluation of the PuP intervention with fathers receiving OST, including recruitment, uptake, retention and completion rates
-
convening an ‘expert event’ with stakeholders involved in the treatment and care of drug-dependent parents and their families to discuss preliminary study findings and potential scalability of the intervention for a larger evaluation.
Protocol changes and project extension
Eligibility criteria and new measures
Two changes were made to the eligibility criteria for the study, one on 6 June 2017 and one on 6 July 2018. The first change was made soon after the study began because PREPARE, one of the services delivering the intervention, identifies fathers during the antenatal period and normally provides parenting support in the lead-up to the birth. Therefore, the inclusion criteria needed to include expectant fathers to enable PuP to be delivered as part of routine practice in this implementation site. Including expectant fathers also meant that we needed to introduce a new measure of attachment because the Emotional Availability Scale (EAS) (i.e. a video observation measure of parent–child interaction)55 was not suitable for first-time parents at baseline. Therefore, the Paternal Antenatal Attachment Scale56 and the Maternal Antenatal Attachment Scale56 were added to the outcome measures administered by the researcher.
A second change in the eligibility criteria was made to include the normal range of children classed as ‘early years’ (i.e. 0–8 years of age), rather than limit this to pre-school children (i.e. 0–5 years). The research team received a number of referrals for families with children aged 6–8 years who were not, at the time, eligible to take part. Given that previous studies of PuP included parents with children aged 0–8 years and expectant parents,46,49 it was considered appropriate to extend the inclusion criteria for this study to match that in previous PuP studies.
Data collection time points
During the course of the study, it became apparent that intervention delivery to a number of families was taking far longer than originally proposed in our study protocol (i.e. 4–6 months with an ‘end-of-treatment’ interview after completion). In some cases, families were taking up to 12 months to complete the programme. This was having knock-on effects on the FU1 (i.e. ‘end-of-treatment’) data collection time point and the FU2 (i.e. ‘6-month post-treatment’) data collection time point, making completion within the planned time frame impossible. With approval from NIHR and the NHS Research Ethics Committee (received on 6 August 2019), data collection time points were rescheduled for baseline and at 6 and 12 months, irrespective of intervention completion status.
Professional interviews
During the interviews with PuP practitioners, it became apparent that service/line managers would have their own opinions on the acceptability and suitability of PuP for their individual teams and staff, and would have views on the implementation of PuP from their own perspective. Therefore, we applied for an amendment so that we could invite them all into the study to take part in a qualitative interview and this was approved by the sponsor on 1 July 2019.
For a list of study protocol changes, substantial and non-substantial amendment and NHS Research Ethics Committee approvals, see Appendix 1, Table 9.
Research fellow absence
A period of research fellow (RF) sickness (approximately 6 weeks), followed shortly afterwards by a change of RF on the project, resulted in an extended period of time where recruitment into the study was curtailed, including a 3-month period when there was no RF in post (from 1 September 2018 to 30 November 2018). A no-cost extension was subsequently granted by NIHR for this 3-month time period when no RF was employed on the project (approved 25 June 2019).
Project extension
Owing to recruitment challenges and an inability to fully test the impact of additional strategies to improve recruitment, as well as prolonged intervention delivery time and associated delayed data collection, an application to extend the project for an 18-month period was submitted to NIHR. This funded extension, supported by the Study Steering Committee (SSC) and Data Monitoring and Ethics Committee (DMEC), was approved on 25 June 2019. Therefore, the project timetable was revised from a 24-month project to a 45-month project, with a start date of 1 April 2017 and an end date of 31 December 2020.
Effects of the COVID-19 pandemic
COVID-19 affected the project from March 2020 onwards. Our final data collection (home visits) with some parents was suspended, although this affected only two final follow-up interviews and our sponsor agreed that we could conduct these over the telephone. The researcher administered the questionnaires over a number of telephone calls. Interviews with one practitioner and one manager were also conducted over the telephone. One focus group was cancelled. Data collection and analysis were also affected because response times to obtain NHS and Social Work Scotland (Edinburgh, UK) data were prolonged. Lockdown meant that researchers on the team were home schooling and so final analysis and write-up were difficult to achieve as planned. Our expert event in October 2020 was convened online rather than face to face, along with our dissemination and public engagement events at the end of the study. Nevertheless, we were able to complete the project on 31 December 2020.
Research pathway diagram: PuP4Dads study
A visual representation of the research pathway is outlined in Figure 1.
FIGURE 1.
The PuP4Dads research pathway diagram. R&D, research and development.

Setting
The study was conducted in two non-NHS community-based services for adults, children and families affected by parental substance use in the Lothian region in Scotland:
-
PREPARE, which is a local-authority social work-led specialist multidisciplinary service for pregnant women, substance users and their families
-
CIRCLE, which is a Scottish charity and early years family support service for disadvantaged children and families.
The Lothian region in Scotland includes one health board (NHS Lothian) and four local authorities (The City of Edinburgh Council, East Lothian Council, Midlothian Council and West Lothian Council). This study took place in the three local authority areas in Lothian where PREPARE and CIRCLE provide services [i.e. City of Edinburgh (PREPARE and CIRCLE), East Lothian (CIRCLE) and West Lothian (CIRCLE)].
The City of Edinburgh is a largely urban area with a population of 513,210 (as of December 2020), with 11.6% of the population living in the most-deprived category [Scottish Index of Multiple Deprivation (SIMD) category 1] and 43.5% of the population living in the least-deprived category (SIMD category 5). 57 East Lothian has a population of 104,840 that is distributed fairly equally across SIMD categories 1 to 5, with approximately half of the population living in urban (21.6%) or accessible rural (23%) areas. West Lothian has a population of 181,310 that is distributed fairly equally across SIMD categories 1 to 5, with the majority (82.5%) of the population living in accessible small towns. 57 Although Edinburgh and many surrounding small towns in East Lothian and West Lothian are considered affluent, approximately 22% of all children in Edinburgh live in poverty. 58 There are several areas of extreme deprivation, comprising large social housing ‘estates’ with a high prevalence of drug use. 59
Across Scotland, health and social care is now ‘integrated’ with social care, primary and community health-care services and some acute services managed by integration joint boards. Integration joint boards are made up of representatives from councils, NHS health boards, third-sector representatives, service users and carers. These integration joint boards, through their chief officer, have responsibility for the planning, resourcing and the operational oversight of a wide range of health and social care services. The delivery of adult services are the responsibility of Health and Social Care Partnerships. Within these partnerships, there are various services for adults with drug and alcohol problems and in each local authority there is an Alcohol and Drug Partnership (ADP) that is made up of local authority, NHS, third-sector, Police Scotland and prison representatives that’s primary aim is to co-ordinate the design, delivery and evaluation of drug and alcohol services.
Although drug and alcohol services are not ‘integrated’ with children’s services, three local authority areas in Lothian commission CIRCLE (i.e. the third-sector organisation involved in this study) to provide services for families affected by parental substance use. 60 Uniquely, only the City of Edinburgh Health and Social Care Partnership provides a specialist service for pregnant women with problem substance use via PREPARE (i.e. the other service involved in this study). 61
PREPARE is a local government (City of Edinburgh Council)-led service that was established in 2006. It consists of an early intervention integrated multidisciplinary team that works with pregnant women and their partners who have significant substance use problems. The service aims to reduce substance use and related harms to mother and baby. The women and men who are allocated to PREPARE have multiple and complex needs related to poverty, substance use, poor mental health and domestic abuse. PREPARE receives approximately 50 referrals a year and normally has a caseload of up to 30 women plus their partners at any one time. Of PREPARE’s open cases, 90% will be involved in the child protection system, whereas the other 10% will be supported using the Getting It Right For Every Child (GIRFEC) model62 and Children Affected by Parental Substance Use (CAPSU) guidelines. 15 PREPARE comprises nine (full-time equivalent) staff, including a social work team leader, a senior early years officer, early years officers, community mental health (addiction) nurses, a health visitor and a midwife. The team is managed under social work children and families services and is supported by a named consultant obstetrician and consultant psychiatrist in addictions. At the start of the study, PREPARE also hosted a dedicated ‘fathers’ worker’ who was jointly funded and managed by both PREPARE and CIRCLE. The fathers’ worker is now based at CIRCLE.
CIRCLE, a Scottish charity founded in 2006, provides a range of family support services that aim to improve the lives of disadvantaged children and families. CIRCLE works in partnership with other organisations to provide whole-family support and delivers commissioned services specifically for CAPSU in the City of Edinburgh, East Lothian and West Lothian. These three services support approximately 240 families per year. In total, there are 14 (full-time equivalent) staff across the projects (Edinburgh, n = 7; West Lothian, n = 3.5; East Lothian, n = 2.5). These staff are assisted by a young person’s worker and a father’s worker in Edinburgh, and a pregnancy worker in East Lothian. Staff are qualified in social work, community development, health and social care and nursing. Funding for CIRCLE services and staff comes from a range of trusts and donations, as well as the ADPs in Edinburgh and West Lothian and a National Lottery Grant in East Lothian.
The intervention: Parents under Pressure
The PuP programme is a family support programme developed for families that may be experiencing difficult life circumstances that have an impact on family function, such as substance use, anxiety and depression, family conflict, homelessness and severe financial stress. In this study, PuP was delivered by non-NHS community-based family support services to fathers receiving OST and their families. The intervention is described here in line with TiDieR (Template for Intervention Description and Replication) reporting guidelines. 63
Parents under Pressure intervention theory of change
The PuP programme aims to enhance parents’ capacity to provide a safe and nurturing environment and sensitive and responsive caregiving for children. Sensitive and responsive caregiving, in combination with knowledge about appropriate parenting behaviours, can lead to improvement in child developmental outcome. However, to provide sensitive and responsive caregiving (including managing difficult behaviours and better limit setting), it is essential that parents are able to understand and manage their own emotions. Impulsivity and poor affect regulation are key features of substance use and can be viewed as a contributor to and a consequence of substance use. 64 Before parents, and in particular fathers/male caregivers, who have engaged in hostile and reactive behaviour patterns in the context of family life13 are able to respond sensitively to their children and partners, they need to be able to manage their own dysregulated affect.
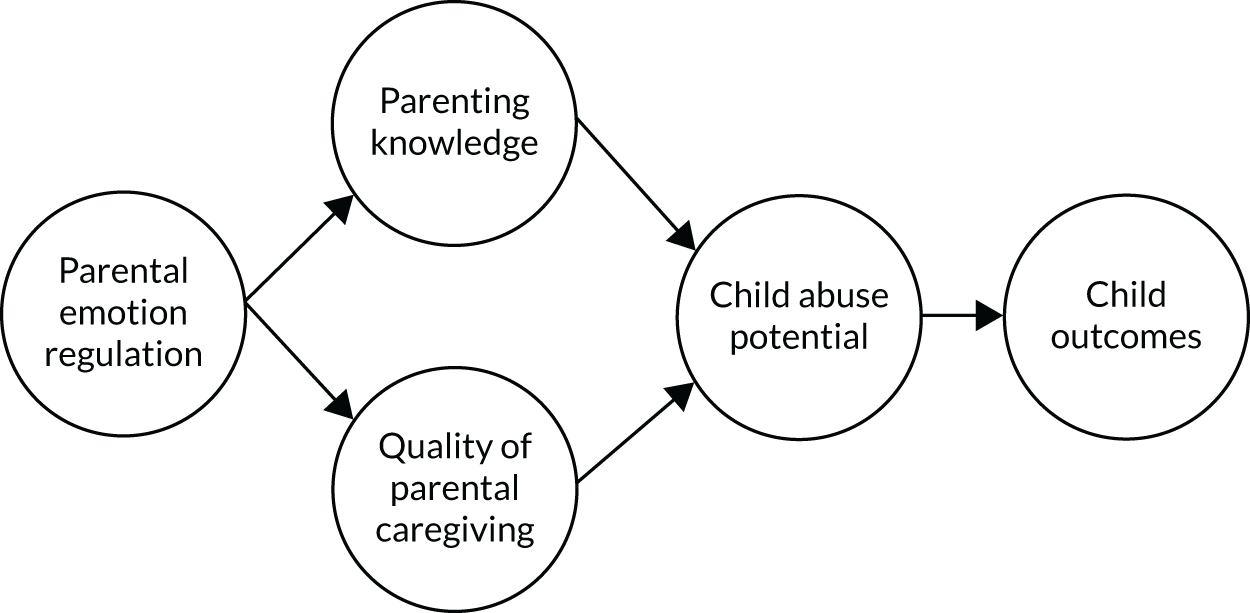
Therefore, the PuP programme extends beyond instruction in traditional behavioural parenting strategies, such as managing non-compliance, better limit setting and rewarding good behaviour, to a focus on helping to develop a calmer, less reactive family environment in which both parents and children learn how to improve emotion regulation. There is extensive evidence supporting the direct relationship between the quality of caregiving, parenting knowledge and child outcome. 19,23 However, this is also mediated by parental emotion regulation: parental emotion dysregulation is associated with poor coping skills, poorer parental sensitivity and greater likelihood of harsh and abusive parenting. These, in turn, increase child abuse potential. For the families involved in the PuP programme, parental emotion dysregulation is a significant problem and is, therefore, directly addressed during programme delivery. This can be represented as a conceptual model in which the relationship between sensitive and responsive parenting (i.e. quality of caregiving), parenting skills (i.e. knowing what to do) and child outcome is influenced by the parent’s capacity to manage their emotions, which, in turn, influences child abuse potential (Figure 2).
FIGURE 2.
Conceptual representation of the PuP integrated theoretical framework.
For the purposes of the PuP4Dads feasibility study, we proposed a logic model for the intervention that is specifically in relation to fathers with a substance use disorder (see Report Supplementary Material 1).
Parents under Pressure intervention material
To deliver the PuP programme, an individually tailored family support plan is developed in collaboration with the parent/carers. The underlying integrated theoretical framework (see Report Supplementary Material 2) for parents and practitioners provides an assessment framework in which to identify strengths and challenges across six domains of family functioning: (1) child outcome; (2) quality of the caregiving relationship; (3) parenting values, knowledge and skills; (4) parental emotion regulation; (5) connections to culture, community and family; and (6) the wider ecological context. Additional resources documenting exercises, discussion points and activities are contained in the PuP parent workbook and the PuP online toolkit, which can be used flexibly to help parents and children enhance family and child well-being. The parent workbook consists of 12 discrete modules [Table 1; see also the NIHR Journals Library URL: www.journalslibrary.nihr.ac.uk/programmes/phr/158201/#/ (accessed 6 September 2021)]. 42 The order and sequencing of the family support plan is tailored to each family. Therefore, the order and focus of the modules delivered differs across families.
| Module | Description |
|---|---|
| 1: starting the PuP journey | This module aims to assist parents to identify the strengths and challenges that they may be facing. A shared understanding of a family’s current concerns, strengths and challenges is the basis for working together to make family life better and support the development of children |
| 2: planning my PuP journey | This module provides feedback on the assessment and arrives at shared views and ways of working towards these goals. This module also helps identify involvement of partners or other carers in the PuP journey |
| 3: view of self as a parent | This module aims to help parents reflect on their view of themselves as parents |
| 4: connecting with your child to help them feel loved and safe | This module is aimed at promoting a positive parent–child relationship. This involves encouraging sensitive and responsive parenting to provide the maximum opportunity for the development of a nurturing and loving relationship |
| 5: understanding what may happen when children are exposed to trauma or loss | This module supports parents to understand the impact of children’s exposure to trauma, loss or grief. It provides information on the effects of these events to help understand children’s behaviour and strategies to support recovery |
| 6: health check your child | This module is designed to open up a discussion on health, hygiene and nutrition |
| 7: how to manage emotions when under pressure – increasing mindful awareness | The aim of this module is to teach and encourage the use of emotion regulation and self-soothing skills. There is an emphasis on mindfulness-based strategies to support both the parent and the child |
| 8: supporting your child to develop self-regulation | This module helps the parent to teach their own children how to increase self-regulation. Child-focused mindfulness activities are included, plus a range of activities that help parents support the development of overarching executive functioning |
| 9: managing substance use problems | This module aims to support parents in managing substance use problems. There is a focus on identifying potential substance use problems and/or relapse using established strategies informed by models of addiction treatment including relapse prevention |
| 10: connecting with family, community and culture | This module aims to support connection with family, community and culture. This may be around extending social supports, establishing community links (e.g. with schools) and supporting connection and/or reconnection with culture and faith |
| 11: life skills | This module addresses the day-to-day business of parenting and family life. Stressors relating to budgeting, housing and schooling can be addressed using problem-solving and supporting emotion regulation. These are considered therapeutic opportunities to test out new skills around emotion regulation |
| 12: relationships | This module addresses issues around communication skills and other problems in adult relationships. The module is used when the parent would benefit from knowing how to communicate effectively with their partner or when their relationship is experiencing difficulties (e.g. domestic violence) |
The PuP therapist manual provides the theoretical overview underpinning the programme and was provided to PuP practitioners as part of the training process. Materials are copyrighted to Griffith University (Nathan, QLD, Australia). Practitioners undergoing training and accredited practitioners in the PuP programme have access to the PuP resources, including online exercises from the parent workbook, access to standardised measures, scoring and an interpretation report. These measures (e.g. the Depression, Anxiety and Stress Scale) reflect the domains of family functioning contained in the integrated theoretical framework. Each practitioner has their own username and password used to access the PuP online toolkit.
Parents under Pressure intervention procedures
The PuP programme is individualised for each family. An assessment model allows for an individualised case plan to be developed, which is guided by a model of case conceptualisation. Immediate priority areas and goals for change are identified by the practitioner and parent, and are worked towards collaboratively. Modules are then selected and ordered according to the needs of the family and the immediate presenting issues. This approach allows for flexibility, as immediate problems may include, for example, potential homelessness and high risk of relapse to drug use, which need to be addressed to introduce both stability in the family environment and engage high-risk families. Integral to these processes is engagement of the parent(s) in the process of developing confidence in their parenting capacity, nurturance of their children and skills to identify and manage their emotions. These three ‘threads’ runs through all PuP sessions regardless of the task at hand or even the location of the session. Practitioners are encouraged to engage with the three ‘threads’ at all times (e.g. supporting a parent during a visit to the housing association provides a therapeutic opportunity to comment on and support each of the three threads).
The quality of the parent–child relationship is intrinsically linked with the capacity of parents to provide nurturing, sensitive and responsive caregiving,50 and the capacity of parents to regulate their own emotional state in the face of parenting challenges can fundamentally impact this capacity. 65,66 Therefore, many of the PuP treatment modules focus on improving parents’ emotional state and fostering a positive parent–child relationship. For example, the ‘connecting with your child to help them feel loved and safe’ and ‘supporting your child to develop self-regulation’ modules focus on helping parents to develop a range of appropriate and non-punitive child management techniques, strategies for ‘mindful play’, skills for understanding their children’s cognitive and emotional states, and mindfulness techniques to promote sensitive caregiving in stressful parenting contexts (e.g. tantrums or prolonged infant crying). Being in the ‘right state of mind’ to manage difficult parenting situations, helping parents to develop coping skills and mindfulness strategies to reduce dysregulated affect aims to reduce coercive hostile parenting behaviours, make caregiving more nurturing and child focused, and enable a reduction in situational aggression between partners. 66
With regard to parental emotion regulation, the PuP parent workbook contains several treatment modules that aim to reduce dysregulation and psychopathology through the use of mindfulness exercises (e.g. the ‘how to manage emotions when under pressure: increasing mindful awareness’ module) and urge-surfing techniques for substance use issues (e.g. the ‘managing substance use problems’ module). In addition, this study provided an opportunity for fathers and their partners to develop communication skills and to co-regulate by identifying high-risk situations for situational verbal and physical aggression, drawing from the ‘relationships’ module. This component of PuP was initially undertaken with fathers alone and then extended to couples’ sessions. Although relationship work needs to be undertaken with great sensitivity and awareness of safety issues for both partners, the work of Stover40 indicates that this approach is acceptable for both partners. PuP includes exercises on ‘communication in intimate relationships’, and these were combined with modules on managing emotions to address interpersonal aggression between partners and, potentially, towards children.
Finally, self-regulatory skills are developed with children through combined sessions with the caregivers and child/children. These self-regulatory skills, again, draw from mindfulness constructs, with a growing body of evidence supporting the relationship between mindfulness and adaptive emotion regulation,67 particularly for young children with difficulties with emotion regulation. These skills are appropriate for children aged 3–5 years. As parents become more emotionally regulated, they are able to provide more sensitive caregiving. This, in turn, is associated with the development of emotion regulation in young children. 68 Therefore, the parent workbook supports the parent by allowing for documentation of their personal journey through the programme.
Parents under Pressure intervention delivery
The PuP programme is designed to be delivered face to face by the PuP practitioner in families’ homes. When there are concerns regarding practitioner safety, it can be delivered in community-based clinical settings. It has also been delivered in residential therapeutic communities and prison settings.
The PuP programme was delivered to fathers, resident or non-resident, with or without partners/mothers. Depending on the individual needs and circumstances of the parents, some modules were delivered by the PuP practitioner to the couple, whereas other modules were delivered individually to one or both parents. If the parents were not cohabiting, then the programme was delivered individually to each parent or just to the father if the mother did not wish to participate. Participation of the partner/mother in the programme was not dependent on whether or not they enrolled in the study. One mother chose to engage in the programme with the father, but declined to enrol in the study.
The time allocated to the family support plan varied and was dependent on the family’s needs and family support remit of the agency delivering the PuP programme. Appointments were generally held on a weekly or fortnightly basis for 1–2 hours. The PuP programme has been delivered over 646,49 and 12 months. 69
Parents under Pressure intervention providers
To use the PuP programme, the intervention provider is required to have undertaken an 8-month training course, which comprised an initial 2-day training in the overall model and programme followed by implementation support provided at 2, 4 and 8 months (see Parents under Pressure training programme). (Note that COVID-19 restrictions resulted in a 2020 online adaption of the PuP training.) Completion of this training leads to accreditation as a PuP practitioner. Practitioners are not required to have a professional qualification (e.g. social work or psychology) to become an accredited PuP practitioner. However, commitment to working with complex-needs families using intensive case management and an approach that encompasses therapeutic family support is essential. The intervention in this study was delivered by accredited PuP practitioners from two organisations (CIRCLE and PREPARE) who were experienced family support workers from a variety of backgrounds, including social work, early years practice and community education.
Practitioner training and accreditation in Parents under Pressure
Underlying philosophy
A key issue with implementation of parenting and family support interventions has been the way in which training is delivered. The traditional model of training usually involves bringing together professionals for a one-time training workshop delivered across consecutive days, with the assumption that the knowledge and skills obtained will be translated into change in front-line practice. This ‘train and hope’ model has been the standard approach to delivering training and there is little to show that practice has changed as a result. 70
Training is most effective when the participants are actively involved in the training process and requires effort on the part of the participants. Training needs to include opportunities to practise the skills taught through either role playing or reviewing content via video/film to actively engage in the training process. 71 Furthermore, participants need to be provided with training aids and exercises that help them organise, apply and embed new learning knowledge across several months, with ongoing consultation and coaching to ensure uptake and quality implementation. This approach has been linked to both better training outcomes and better client outcomes. 72,73 Sustainability is enhanced by supporting or identifying champions of the programme within the organisation. PuP training has, therefore, drawn from this extensive literature and developed a training route that embeds these principles in an 8- to 12-month training process.
Parents under Pressure training programme
The PuP training programme comprises a range of training events and assessments that lead to accreditation as a PuP therapist. To achieve accreditation, practitioners are required to complete the following three tasks:
-
attendance at all PuP training events
-
assessment of three families using the PuP online toolkit
-
completion of a case study using a purpose-designed template reflecting the domains underpinning the PuP integrated theoretical framework.
Initial training comprises 2 days in which participants are provided with an overview of the PuP integrated theoretical framework (see Report Supplementary Material 3), a review of programme focus and content, and an introduction to the assessment of quality of caregiving.
In month 2, participants are invited to their first ‘case review day’, during which they revisit the PuP integrated theoretical framework and use this to develop a case conceptualisation and a family support plan. Goals are identified in discussion with the family, and practitioners are supported to develop action plans that help with goal achievement. Resources to support this are drawn from the parent workbook and the PuP online toolkit. There is an emphasis on using the PuP programme and resources as a toolkit, with the metaphor of ‘use the right tool for the right job’ embedded in the case review process.
In month 4, a second case review day provides practitioners with the opportunity to revisit the PuP integrated theoretical framework with direct application to families with whom they are working. There is an emphasis on the process of case conceptualisation. Practitioners are introduced to the case study pro forma and provided with an opportunity to begin populating the template.
In month 8, a third case review day gives practitioners the opportunity to present a case study, review cases and family support plans.
In month 12, an optional development day is offered to enhance ongoing use of the PuP programme. Specific topics are selected from a suite of topics. Example topics include (1) ‘understanding fetal alcohol spectrum disorder: a PuP programme perspective’, (2) ‘trauma-informed practice: how this is achieved within the PuP programme’ and (3) ‘enhancing the development of self-regulation and executive functioning in vulnerable children: integration with the PuP programme’.
Parents under Pressure supervision and implementation support
Expert staff supervision for practitioners in the study was provided initially by an accredited PuP supervisor and trainer. To ensure sustainability, the PuP programme training process includes the identification of senior practitioners or team managers who are able to take on additional training as an accredited PuP supervisor. Identified individuals undertake an additional 20 hours of training and support, working through a series of guided exercises and tasks. The purpose of this training programme is to provide an advanced understanding of the underlying conceptual framework of the PuP programme. A series of readings are provided and practitioners are asked to a complete set of exercises to practise the skills and demonstrate competency. This includes additional training in case conceptualisation, an understanding of the presenting issues for children with a range of developmental disorders, advanced readings and practice in mindfulness, and a comparison of the PuP programme with another parenting programme. Training is also provided in implementation support, including helping trainees to provide constructive feedback on case study requirements for accreditation as a PuP practitioner.
Project management and oversight
The chief investigator led the study and provided support to the RF employed on the study. After NHS Research Ethics Committee and research and development (R&D) approvals, the project started on 1 April 2017. With the 21-month extension, the project was 45 months in total and completed on 31 December 2020. COVID-19 affected the final phase of data collection, data analysis and write-up (from March to December 2020). However, participant recruitment had ended before the pandemic began and, therefore, most parents had completed the intervention and the final data collection and research activities could be conducted by telephone or via online video-conferencing (including the ‘expert event’ with key stakeholders), allowing the study to complete on time.
Oversight and management of the PuP4Dads study was undertaken by the following groups and committees: the Study Research Group, including service delivery collaborators, the SSC and the DMEC. The membership, role and remit of each group, as well as meeting dates, are detailed in the appendices (see Appendices 2–4).
Patient and public involvement and engagement
Our public engagement strategy at the beginning of the study included:
-
involving fathers and mothers with lived experience of opioid dependence as advisors on the study
-
including clinicians with experience of working with this population on the SSC
-
conducting an expert event towards the end of the study to present and discuss the preliminary findings with a wider stakeholder group
-
involving study participants in dissemination events.
A father and mother with a history of drug use [identified via the Scottish Drugs Forum’s Addiction Worker Training Project (Glasgow, UK)] were invited to join the SSC before the start of the study and their appointment was approved by NIHR. The first RF (KK) met with the parents individually and then together at the beginning of the study to pilot the participant information sheet, consent form and interview schedules designed for parents. The parents also commented on the ‘participant details sheet’, planned questionnaires (e.g. in what order they should be administered) and the qualitative interview schedules. The parents’ input helped to ensure that these materials were suitable and understandable for participants and could be sensitively administered to parents to maximise completion rates. The parent representatives declined our invitation to attend SSC meetings, citing difficulty in taking time off work [i.e. they would have needed to take a whole day off to travel to the University of Stirling (Stirling, UK) from Glasgow and both parent representatives were new into employment]. The research team also felt that the parents were more relaxed and comfortable in one-to-one meetings and could contribute more meaningfully this way.
Around the time of the next SSC meeting, the researcher contacted the parents by telephone to discuss recruitment strategies and then again 6 months later to discuss plans for a project extension. Parents provided input into the decision-making process, including the time frame for extending the recruitment period and intervention delivery times. In addition, parents were of the opinion that intervention timelines should be tailored to individual families (according to what the parents and family needed) and they supported the idea of changing the data collection time points to fixed time points (i.e. baseline and at 6 and 12 months) to enable the study to complete on time. Therefore, parents were against the idea that families should be pressurised into completing the programme within a certain time frame.
The research team were unable to contact the two parents towards the end of the study, as both were in full-time employment and did not respond to messages. We contacted the Scottish Drugs Forum to see if we could re-establish contact, but were unsuccessful. In preparation for the expert event in October 2020, the research team decided to invite a number of fathers who had taken part in the study to attend the event. Two fathers (FA22 and FA23) who had participated in the PuP programme and study agreed to attend. Both fathers joined the online sessions on the day [via Microsoft Teams video-conferencing (Microsoft Corporation, Redmond, WA, USA)] and contributed well to the discussion. Feedback from other participants at the event confirmed the value of the fathers’ input as recipients of the programme and participants of the study. FA22 and FA23 also provided assistance with the Plain English summary for this report and both engaged in discussions on the study design for a future evaluation of PuP4Dads. This input helped confirm the fathers’ support for research on the effectiveness of the programme and their views on maintaining an ‘inclusive’ approach to the eligibility criteria for a main study (they were both keen that non-resident fathers should be included and that all fathers should ‘be given the chance’ to receive the programme).
For a full description of the expert event and results from this public engagement activity, see Chapter 4, Expert event (public engagement).
Reflections on our experience of patient and public involvement and engagement for this study
Engaging parents who are drug dependent in patient and public involvement and engagement (PPIE) presents a number of challenges, as they are a stigmatised and marginalised group of parents who often lack the confidence to participate in groups or committee meetings, and the families have child care responsibilities, but often do not have child care or the spare time to engage in PPIE activities. Engagement often needs to be on a one-to-one basis and in settings that are comfortable and non-threatening (e.g. home visits, coffee shops or over the telephone). Families are often engaged with multiple services and can be working in jobs with irregular hours, and so achieving contact within usual ‘office hours’ can be challenging. Therefore, extreme flexibility is required by the RFs. In addition, parents need to be reasonably ‘stable’ drug users (not intoxicated) to be able to contribute to discussions and to maintain contact with the study team. Even when they are stable and motivated to be involved in research, this population often lack the resources to contribute (e.g. time, effort, equipment and money, including sufficient credit to return missed calls and enough data to attend video-conferencing meetings). Therefore, considerable research resource is needed to engage this population in the research process in a meaningful and consistent way. Despite these difficulties, the involvement of parents in this study who were active drug users (prescribed OST and involved in drug treatment services) was really valuable, as they were able to provide up-to-date accounts of some of the challenges that fathers who use drugs face.
Study procedures
This section of the report describes the study procedures, including data collection methods, for each participant sample that took part in the study, beginning with the fathers and their families and followed by PuP practitioners, supervisors, service managers and referring professionals.
Participants: fathers and families
The target population for this study were families living in Lothian with children (aged 0–8 years) affected by paternal drug use, namely families with fathers/male caregivers diagnosed with opioid dependence and currently prescribed OST. We anticipated that most fathers who enrolled in the study would reflect the population of men normally engaged in OST (i.e. the majority were aged between 18 and 55 years, on a low income or unemployed and in receipt of welfare benefits, living in social housing in areas of deprivation and had a history of polydrug use and criminal justice involvement, including imprisonment).
Sample size
The target was to recruit 24 families with a father/male caregiver receiving OST. This number was expected to be sufficient to allow the qualitative and quantitative progression criteria to be assessed and to provide information on key parameters for the design of a future evaluation, allowing for expected attrition of one-third [see sample size justification in study protocol v5.0, NIHR Journals Library URL: www.journalslibrary.nihr.ac.uk/programmes/phr/158201/#/ (accessed 6 September 2021)].
The sampling strategy aimed to include a diverse range of fathers and families who broadly reflect the diversity of family constellations that are commonplace among this population, for example:
-
biological and non-biological (‘social’ or ‘step’) fathers
-
resident and non-resident fathers (living with or apart from the children)
-
concordant couples (where both the father and the mother are drug dependent)
-
discordant couples (where only one adult – the father – is drug dependent).
Inclusion and exclusion criteria
Inclusion criteria
-
Fathers with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision,74 diagnostic criterion for opioid dependence and prescribed OST {e.g. methadone [methadone hydrochloride, Alliance Healthcare (Distribution) Ltd] or buprenorphine [subutex, Indivios UK Ltd]}.
-
Mothers/partners of fathers recruited into the study (regardless of whether or not they had a diagnosis of substance dependence themselves).
-
Families that have at least one ‘index’ child aged 0–8 years or are expectant parents (revised in June 2017 from pre-school children only).
-
Biological or non-biological fathers.
-
Fathers/male carers involved in the day-to-day care of the index child.
-
Fathers in a relationship with the mother/partner for at least 6 months.
Exclusion criteria
-
Either parent had a serious mental illness (e.g. active psychosis) that prevented them from fully participating in the programme.
-
Families in which domestic abuse or child abuse resulted in the father being prohibited from contact with the target child or family.
-
Families in which the father was facing an imminent prison sentence of > 6 months or a criminal justice order of > 6 months that would prohibit their active involvement in the programme.
-
Either parent was aged < 16 years.
-
Either parent was not officially resident in the Lothian region.
Recruitment process
Treating clinicians were contacted, informed about the study and encouraged to invite eligible fathers to take part. Recruitment sites included NHS Lothian substance misuse directorate and partner drug agencies (third sector), selected primary care teams in areas of deprivation in Edinburgh [with general practitioners (GPs) who prescribed OST to drug users], health visiting teams throughout Lothian and the two implementation site services (PREPARE and CIRCLE). A study invitation letter was sent to all recruitment sites, which included information on the study, participant eligibility criteria and clear instructions on how to refer into the study. Meetings were arranged with potential referrers working in community-based teams across Lothian (n = 8) to answer questions about the study and the intervention. Staff were asked to approach eligible fathers when they attended for routine appointments. If fathers showed an interest in taking part in the study, the clinician passed the contact details of the father (i.e. name, address and telephone number) onto the research team. Potential participants were then contacted by the research team by telephone to discuss the study. If the father was interested, arrangements were made to meet the father and family in their home to discuss participation in full and to provide a participant information sheet. Informed written consent was obtained if the father agreed to take part [see NIHR Journals Library URL: www.journalslibrary.nihr.ac.uk/programmes/phr/158201/#/ (accessed 7 September 2021)].
The consent process involved agreement regarding confidentiality (including the limits of confidentiality in respect of child and adult protection and legal issues), permissions regarding data collection (including audio- and video-recording and follow-up), data management and anonymity, GP notification, payment of expenses, consent to access NHS prescribing data and social work child protection data, and freedom to withdraw from the study. When the father had an eligible partner, mother or co-parent, they were invited to take part in the study. Children in the family who were deemed to have the capacity to consent and who wished to participate in the intervention were eligible to take part. Similarly, kinship carers or other family members (e.g. grandparents) who wished to take part in the programme were invited to enrol in the study. However, neither young people nor kinship carers were enrolled in this study.
For safety reasons, and in accordance with lone-worker and home-visiting policies, two researchers attended the first home visit with participants or, where appropriate, the researcher arranged a joint visit with the practitioner from PREPARE or CIRCLE. When it was assessed as safe to do so, subsequent appointments were conducted by a lone researcher, unless the EAS (video observational measure) was administered, in which case the principal investigator (AW) attended the visit to administer this measure using an NHS laptop (a requirement to ensure security of personal identifiable video data).
Strategies to promote retention
The following strategies were used to enhance engagement and retention of fathers in the study:
-
On enrolment, seeking permission from the parents to document the name, address and mobile telephone number of significant others who may know the whereabouts of the family if the study team could not contact or locate them. This involved completing an ‘alternative contacts form’ with a list of professionals, family members and others who the parents agreed could be contacted if required. This allowed the research team to locate several fathers and families, for example, after they had moved address, changed their telephone number or had separated from their partners.
-
Mobile telephone text messaging was used to arrange appointments, send appointment reminders and to generally communicate and ‘check-in’ with families. A lot of families had very limited finances and so would not make audio calls or listen to voicemail, as these cost more. However, mobile telephone communications could be unreliable, as many parents ‘ran out of credit’ and their telephones were switched off, so appointment letters were also posted to participants.
-
Researcher interview appointments were also arranged at a convenient time to suit participants, and appointments were flexible and could be rearranged at short notice to accommodate the changing availability of the parents.
-
When participants failed to attend research appointments or cancelled appointments, repeat offers were made and there was no limit placed on the number of appointments missed or cancelled (which were numerous).
-
Parents who had children in out-of-home placements were also interviewed with their children where this was possible to arrange. This often involved seeking permission from the ‘corporate parent’ (i.e. via the allocated social worker) to accompany the parent to a supervised contact visit. Assent from the child was then sought and the researcher attended the contact visit site with the parent.
-
Maintaining contact with the parents was also undertaken by sending Christmas, birthday and Father’s Day/Mother’s Day cards to participants.
-
The researcher maintained contact with the PuP practitioner to ensure that any parents who dropped out of the intervention could be approached for a follow-up interview.
-
Participants were offered gift vouchers for taking part in each research interviews as a thank you and to cover any out-of-pocket expenses (e.g. child care costs, travel costs and subsistence costs). The voucher payment schedule was escalated so that follow-up interviews were worth more for the participants (i.e. £15 at baseline, £20 at FU1 and £25 at FU2).
Data collection
Data were collected at three time points with parents:
-
baseline (pre-treatment interview)
-
FU1 (end of treatment/dropout or 6 months after baseline)
-
FU2 (post treatment or 12 months after baseline).
Once consent was given, arrangements were made to collect baseline data at a time convenient for the father (and mother). The researcher administered the questionnaires separately to fathers and mothers, often on different days over two, sometimes three, visits. The researcher also then referred the family to a PuP practitioner in one of the implementation sites (if the referral was not from an implementation site practitioner).
Measures
The measures taken at each time point are listed in Table 2 and described in more detailed below.
| Measure | Time point | |||
|---|---|---|---|---|
| Baseline | FU1 | FU2 | After FU2 | |
| Sociodemographic data | ✓ | ✓ | ✓ | |
| BCAPI | ✓ | ✓ | ✓ | |
| PSCS | ✓ | ✓ | ✓ | |
| DERS | ✓ | ✓ | ✓ | |
| CTS2 | ✓ | ✓ | ✓ | |
| TOP | ✓ | ✓ | ✓ | |
| EQ-5D-5L (quality-of-life measure) | ✓ | ✓ | ✓ | |
| EAS | ✓ | ✓ | ✓ | |
| PAAS/MAAS | ✓ | |||
| BITSEA or SDQ (dependent on age of child) | ✓ | ✓ | ✓ | |
| PuP fidelity bespoke questionnaire (on one occasion only, when the PuP programme is completed) | ✓ | ✓ | ||
| Short qualitative interview exploring previous experience of parenting and family support services | ✓ | |||
| Longer qualitative interview exploring experiences of PuP and study measures and procedures | ✓ | |||
| PuP session attendance data from PuP practitioners (requested at the end of treatment) | ✓ | ✓ | ||
| Service use survey (health economics) | Participants requested to complete this after each PuP session throughout the intervention period | |||
| OST prescription data requested from NHS (health service) prescriber | ✓ | |||
| Details of child protection status requested from Social Work Scotland records | ✓ | |||
Baseline
At the pre-treatment assessment (i.e. baseline interview), sociodemographic data were collected on a ‘participant details sheet’ and both fathers and mothers were asked to take part in a brief semistructured qualitative interview to explore their views on ‘usual’ parenting/family support services for fathers and previous experiences of parenting interventions [see NIHR Journals Library URL: www.journalslibrary.nihr.ac.uk/programmes/phr/158201/#/ (accessed 7 September 2021)]. Interviews were audio-recorded and transcribed verbatim. In addition, the following measures were administered, as appropriate, to both fathers and mothers.
-
The Brief Infant Toddler Social and Emotional Assessment (BITSEA)75 has 42 items, is widely used, is sensitive to change and is used for infants aged 12–36 months.
-
The Strengths and Difficulties Questionnaire (SDQ)76 has 25 items (including subscales of attention and concentration, conduct problems and emotional problems) and is used for children aged 2–16 years. The SDQ is widely used across diverse groups and showed sensitivity to change in the PuP RCT. 46
-
The EAS55 assesses emotional availability using a 10-minute video-recording of a parent and a child engaging in an age-appropriate game or activity. The EAS55 draws from attachment theory and emotional availability constructs and has good convergent validity with attachment style as assessed by the Strange Situation procedure. 78 The EAS is suitable from infancy to late childhood.
-
The Maternal Antenatal Attachment Scale (MAAS) or Paternal Antenatal Attachment Scale (PAAS)56 were used when parents were expecting a baby and were not caring for another child. The PAAS56 is the corresponding measure to the MAAS and is a 16-item self-report scale used to measure paternal antenatal attachment. It is an accurate predictor of post-birth father–child attachment. The PAAS was conducted at baseline and before the estimated date of delivery. The MAAS56 is a 19-item self-report scale used to measure antenatal maternal attachment and is widely used. The MAAS is suitable for first-time parents or those without current child care responsibilities during the antenatal period. The MAAS was conducted once at baseline and before the estimated date of delivery.
-
The Parenting Sense of Competence Scale (PSCS)79 is a 17-item self-report scale used to measure satisfaction/comfort with being a parent, parental self-efficacy (i.e. perception of knowledge and skills) and interest in parenting. The PSCS is widely used in parenting literature and is sensitive to change.
-
The Difficulties in Emotion Regulation Scale (DERS)80 is a 36-item scale that measures six dimensions of emotion dysregulation (e.g. lack of awareness of emotional responses, limited access to emotion regulation strategies and difficulties controlling impulses when experiencing negative emotions). The DERS is well validated psychometrically and widely used in intervention studies that focus on mindfulness.
-
The Revised Conflict Tactics Scale (CTS2)81 is a 39-item scale that is used to assess the presence and severity of intimate partner violence, including psychological and physical abuse subscales, and is sensitive to change. The CTS2 has been used by Stover et al. 18 in studies of intimate partner violence prevention in substance-using men.
-
The Treatment Outcomes Profile (TOP)82,83 has 20 items measuring domains of drug-related harm, including daily illicit drug use and alcohol use in last 28 days (drug type and amount), and is based on the Timeline Followback questionnaire. 84 The TOP also includes items on injecting risk behaviour, crime, physical and psychological health, and quality of life. The TOP is widely used in clinical practice in the UK to measure change and progress during drug treatment.
-
The EuroQol-5 Dimensions, five-level version (EQ-5D-5L),85 is a five-item health-related quality-of-life survey that is used in the generation of quality-adjusted life-years.
-
At baseline, parents were provided with the ‘service use survey’ and were shown how to self-complete the forms. Parents were asked to complete one survey form each after every PuP session (assumed to be weekly or fortnightly). This form included a simple record of their health, social care and criminal justice service use since the last PuP session. Completed forms were collected by the researcher at the FU2 interview.
Follow-up 1
At 6 months after baseline or at end of treatment/dropout, a follow-up interview was arranged. A longer qualitative interview was conducted with all participants, exploring the acceptability of the PuP programme, perceived benefits of engaging in the PuP programme and acceptability of the study measures and procedures [see NIHR Journals Library URL: www.journalslibrary.nihr.ac.uk/programmes/phr/158201/#/ (accessed 7 September 2021)]. Interviews were audio-recorded and transcribed verbatim.
Once the interview was complete, all the measures taken at baseline were repeated, except for the MAAS and PAAS,56 which were not applicable because all participants’ babies had been born by FU1.
The PuP fidelity measure (a bespoke 20-item scale used to assess which components of the PuP programme were received, according to each parent) was administered if the participant had finished undertaking the programme.
On completion of the programme or dropout/discharge from the service, PuP session attendance data for fathers and mothers were recorded by the PuP practitioner on an attendance sheet provided by the researcher. This recording sheet included the participant’s unique identification code, dates of appointments ‘attended’ and dates of appointments ‘not attended’ (fathers and mothers recorded separately) so that the length of programme delivery could be calculated along with attendance rates.
Follow-up 2
Follow-up 2 (i.e. the third interview with parent participants) was scheduled for 12 months after baseline (or 6 months post completion of treatment /dropout). At FU2, all questionnaire measures completed in FU1 were administered by the researcher.
After follow-up 2
The following data were collected retrospectively for all consenting participants for the study period.
-
Data about child protection registrations and de-registrations and out-of-home placements were obtained from Social Work Scotland records (with participants’ permission) for the period from enrolment to FU2. The research team wrote to the chief social work officer in each local authority area to request these data.
-
Data about medications prescribed for the treatment of opioid dependence (i.e. OST) were obtained from prescribers (i.e. GPs) or from the addiction service prescription database (with participants’ permission) to show changes in drug type and daily dosage for the period from enrolment to FU2. The research team wrote to GP prescribers and contacted the NHS addiction team to request these data and a payment was provided to reimburse clinicians for the time required to obtain and report these data.
Participants: Parents under Pressure practitioners, supervisors and service managers
Sample
Parents under Pressure practitioners (n = 8) who delivered the intervention to study participants were invited to join the study and take part in a qualitative interview. Two PuP practitioners (one in PREPARE and one in CIRCLE who later trained to become an accredited PuP supervisor) were also invited to take part in a second interview after they qualified. In addition, all line managers and senior managers in PREPARE and CIRCLE (n = 7) were invited to join the study and take part in a qualitative interview towards the end of the intervention delivery phase.
Recruitment
Parents under Pressure practitioners were approached to take part in the study after they had delivered the PuP programme with one study family. The researcher sent an invitation e-mail, which included a participant information sheet and consent form. PuP supervisors were invited to a second interview after they qualified and were providing regular supervision to other PuP practitioners delivering the programme. Practitioners and supervisors were asked to reply to the researcher by e-mail if they were interested. The researcher followed up with a telephone call to answer any questions and to consent them into the study. Likewise, managers were sent an invitation e-mail, which included a participant information sheet and consent form. If they agreed to take part, they were also consented into the study.
Procedures
Once staff enrolled into the study, an appointment was arranged to conduct the interview at a convenient time and place. Interviews with practitioners and supervisors explored their views and experiences of staff training and supervision; recruiting fathers; delivering the PuP programme; the benefits and drawbacks of the programme for fathers, mothers and families, as well as for themselves; and their service and multiagency working. Interviews with managers explored their views and experiences of implementing the programme; staff training and supervision; recruitment and retention of families in the programme; the benefits and drawbacks of the programme for families, practitioners and the service as a whole; and how well the programme model fitted with organisational objectives and priorities. All interviews were audio-recorded and transcribed. Owing to the COVID-19 pandemic, one final practitioner interview and a manager interview were conducted by telephone.
Participants: referrers
Sample
Health and social care professionals working in agencies involved in the care of parents who use drugs were asked to identify and refer eligible fathers into the study and were invited to take part in a focus group. Five focus groups were planned (Edinburgh, n = 3; East Lothian, n = 1; West Lothian n = 1). Agencies included addiction services (in Health and Social Care Partnerships), third-sector drug agencies, primary care staff treating drug users in their practice, health visitors in areas of deprivation and PREPARE and CIRCLE staff who were not involved in the delivery of the PuP programme.
Recruitment
Senior managers and local team managers in eligible agencies (approximately n =10) were sent an e-mail by the research team to ask if they would be willing to circulate an invitation letter to front-line practitioners to invite them to take part in the study. All managers agreed and a participant information sheet and consent form were sent to managers to cascade, along with suggested dates and times for the focus groups. Staff were asked to e-mail the research team directly if they were interested and could attend on the dates and times suggested. The researcher followed up staff who responded and consented them into the study.
Study procedures
Focus groups were convened in local community-based health centres over the lunchtime period (from 12.00 to 14.00) to minimise disruption to clinical practice. Participants who attended the focus groups were provided with a selection of sandwiches and beverages. On arrival at the focus group, participants were asked to complete a simple form to provide some details about themselves to describe the characteristics of participants who took part. These details included job title, department and organisation, age range, gender, qualifications and level of training and experience in working with parental drug use, fathers and families. Two researchers facilitated each focus group and started with some ground rules on the purpose and conduct of the focus group, confidentiality, anonymisation and reporting of data. A focus group topic guide was used to guide the discussion. Participants were encouraged to talk among themselves with open questions posed by the researchers. Topics included the recruitment of drug-using fathers, their understanding of the PuP programme, engaging fathers in parenting and family support services, potential benefits and drawbacks of involving fathers (including non-resident and non-biological fathers) in family work, the extent to which the PuP model was suitable for the population and whether or not it was a good fit for the kind of multiagency working required for families affected by parental drug use.
Randomisation
As this study did not include the randomisation of families, acceptability of randomisation in a future PuP trial was explored in qualitative interviews with parents and services. We asked a selection of parents (hypothetically) whether or not they’d be willing to be randomised in an evaluation of this intervention. This question was accompanied by a brief description of what the randomised process and comparison would be (e.g. randomisation to early vs. delayed receipt of the PuP or randomisation to PuP vs. ‘usual’ care). To explore the feasibility of cluster randomisation, we asked senior service managers if they’d be willing, in principle, for their service to be randomised to implementing PuP or standard care. Randomisation was also explored in our public engagement events with key stakeholders by discussing study design options for a larger evaluation and if randomisation by individual family, service, or area (e.g. by health board or local authority) would be acceptable and feasible.
Analytic framework
Feasibility for a main study was assessed in a number of ways. Quantitative and qualitative data, as well as project monitoring data, were used to assess pre-set progression criteria (see Appendix 5, Table 10) and all the study RQs and objectives outlined in the study protocol (see Chapter 4). In addition, we used the ADePT framework,54 a tool used to systematically identify and appraise issues and solutions in feasibility studies, to inform our decision-making on whether or not a future main study was feasible and justified.
To assess the degree to which our progression criteria were met, and to answer the specific feasibility RQs, the following quantitative and qualitative analyses were undertaken.
Quantitative analysis
All quantitative data obtained were entered into SPSS, version 25 (IBM SPSS Statistics, Armonk, NY, USA), and cleaned and checked for errors. An SPSS syntax file was written (available on request) and the analysis run on the cleaned data file. Participants’ sociodemographic data and time intervals within the study (e.g. time from enrolment to commencement of intervention) were summarised using descriptive statistics. Data were not normally distributed and so medians and interquartile ranges (IQRs) are reported.
Intervention fidelity was assessed using a five-point rating as to how strongly parent participants agreed they had received each core component of the PuP programme. This was converted to a binary variable (i.e. agree/disagree that the component was delivered) and summarised.
EuroQol-5 Dimensions, five-level version
Participants responded to five items on the EQ-5D-5L on a five-point scale for each item. This provided a five-digit code for each participant that was used to calculate an index score at each time point (i.e. baseline, FU1 and FU2) using the crosswalk index value calculator recommended by EuroQol. 86 Medians and IQRs for each time point were reported.
Brief Child Abuse Potential Inventory
Participants responded ‘agree’ or ‘disagree’ to 34 items in the BCAPI (scored 1 or 0) and a total score was calculated, as per the instructions of the authors of the scale. 87 The BCAPI contains items designed to detect participants simply agreeing/disagreeing with most items, answering randomly or ‘faking good’, and suggests removing these responses from the analysis. However, research suggests that these scales may not necessarily reflect validity issues and so we elected to include all responses. Higher scores indicate greater child abuse potential. 77 Medians and IQRs for each time point were reported.
Difficulties in Emotion Regulation Scale
Participants responded to 36 statements in the DERS, indicating how often each statement applied to them [from 1 (almost never) to 5 (almost always)]. To calculate a total score, reverse-scored items (1, 2, 6, 7, 8, 10, 17, 20, 22, 24 and 34) had a negative sign placed before the value and then all values were summed. Higher scores suggest greater problems with emotion regulation. Medians and IQRs for each time point were reported.
Revised Conflict Tactics Scale
Participants responded to 39 items describing various relationship behaviours, indicating how often they had undertaken each behaviour (1) in the previous 12 months and (2) prior to that. Participants also reported how often their partner engaged in each behaviour towards them in the same period. Subscales of behaviour were calculated and a total of the non-positive behaviours (i.e. psychological aggression, physical assault, injury and sexual coercion) performed in last 12 months was calculated for each participant. Medians and IQRs for each time point were reported.
Treatment Outcomes Profile
Participants responded to four domains describing drug-related harm: (1) substance use, (2) injecting risk behaviour, (3) crime and (4) health and social functioning. Substance use was assessed using the Timeline Followback method to establish the ‘number of days using in each of the past 4 weeks’ (28 days) for alcohol, illicit opiates/opioids, crack, cocaine, amphetamine, cannabis and other substances. This allowed the number of days abstinent (out of 28) from illicit drugs and alcohol to be calculated and reported. The number of days abstinent from illicit drugs but not alcohol and cannabis in the past 28 days was also calculated and reported. Medians and IQRs were used to summarise data for fathers and mothers at each time point.
Child well-being
Different measures were used to assess child well-being, depending on the age of the child at the point of assessment. The BITSEA was used for children aged 12–23 months and the SDQ was used for children aged 24 months to 8 years. Owing to the small numbers of participants completing each item, scores were not summarised, but, instead, scores for each child were reported for each time point.
The 43 child behaviours of the BITSEA are scored zero (not true/rarely), 1 (somewhat true/sometimes) or 2 (very true/often). These behaviours were scored, as per author instructions to create ‘competence’ and ‘problem’ scores for each participant for each of their eligible children (aged 12–35 months).
There are 25 child behaviours on the SDQ that are scored zero (not true), 1 (somewhat true) or 2 (certainly true), followed by a further eight items. These were scored, as per author instructions, to create a ‘difficulties’ score for each eligible child (aged 2–8 years).
Quality of parent–child relationship
Different measures were used, depending on the age of the child at the point of assessment. The PAAS and MAAS56 were used at baseline for expectant parents. The EAS, which is a video observational measure, was used for parents who could be video-recorded with their child.
The 16 items of the PAAS and the 19 items of the MAAS are scored on a five-point Likert scale. These were scored, as per author instructions, to create a total score for global attachment.
The EAS consists of six subscales. Four subscales measure caregiver behaviour (e.g. sensitivity, structuring, non-intrusiveness and non-hostility) and two subscales measure the child’s behaviour during parent–child interactions (e.g. child involvement and child responsiveness). Ratings of parent–child interactions (via video-recordings) are made by trained observers who rate each subscale on a scale of 1 to 7, where higher scores reflects higher levels of emotional availability. 78
Reliable Change Index
Clinically significant change is calculated using the Reliable Change Index (RCI). Reliable change is defined as a change in scores on a measure that is unlikely to be due to measurement error. The RCI was used to analyse change over time for the outcome measures of emotion regulation (DERS) and child abuse potential (BCAPI). The standard deviation of scores at baseline and the internal reliability from larger cohorts (0.93 and 0.9 for the DERS80 and BCAPI,87 respectively) were used to estimate whether or not reliable change (improvement or deterioration) had occurred for individual participants.
Attendance data (obtained from Parents under Pressure practitioners)
The length of engagement (i.e. number of weeks) and the number of sessions attended (and not attended) were calculated for each participant. Length of engagement was calculated as the length of time between first and last session attended (except for those who attended only one session, for whom 1 week was reported as better reflecting engagement than ‘zero’).
Prescription data (obtained from NHS)
At baseline, OST drug type (i.e. methadone or buprenorphine) and daily dose were recorded. At FU1 and FU2, drug type and change in daily dose (i.e. increased, decreased or stayed the same) were recorded. Parent-reported OST prescription data were compared with NHS prescription records.
Child protection data (obtained from Social Work Scotland records)
Child protection registration, de-registration, out-of-home placement and de-registrations at enrolment were recorded. Change in status from enrolment to FU1 and FU2 was reported.
Qualitative analysis
Framework analysis was used for the management and analysis of the qualitative data. 88 It was chosen because it provides a rigorous and systematic approach to analysing multiple perspectives of complex interventions and has been used extensively in health-care research. 89
Our framework analysis included the following seven stages.
Stage 1: transcription
Data from interviews with parents, PuP practitioners, PuP supervisors, service managers and the focus groups with referrers were audio-recorded and transcribed verbatim. Transcripts were checked against the recordings for accuracy, then pseudonymised and anonymised to ensure that no personal identifiable information or the identity of participants could be revealed. Anonymised transcripts were then uploaded to NVivo, version 12 (QSR International, Warrington, UK).
Stage 2: familiarisation with the interviews and focus groups
The two main researchers (BF and HS) involved in the analysis of the data familiarised themselves with the interview and focus group transcriptions. One of these researchers (HS) was an experienced qualitative researcher with previous experience of using framework analysis in health-related research. Heather Strachan was employed for the final 6 months of the project specifically to assist with the qualitative data analysis and had no prior knowledge or involvement in the study. The other researcher (BF) had conducted most of the interviews with parent and practitioner participants and had attended all the focus groups with referrers. The third researcher involved in the analysis (AW) had also conducted a small number of parent, practitioner and manager interviews and had facilitated all the focus groups with referrers. Anne Whittaker is an experienced qualitative researcher, formulated the semistructured interview schedules and was familiar with all the transcripts. The three researchers met to devise and agree the analytic plan.
Stage 3: coding
Each transcript was initially coded line by line by Barbara Farquharson and Heather Strachan, and the two researchers independently double coded 20% of the entire data set, using a mixture of deductive coding (based on the feasibility RQs and topic guides) and an inductive open-coding approach. Data sets were grouped together on NVivo to easily review coding for each of the different participant samples (i.e. fathers, mothers, practitioners, managers and referrers) and data sets were designated as potential ‘cases’ for answering each of the study RQs. For instance, some RQs (e.g. fathers’ previous experiences of engaging with parenting and family support services) could be answered by examining the first interview transcripts of fathers and mothers only, whereas the RQ about the perceived impact of the programme could be answered by practitioner interview transcripts and second interview transcripts of fathers and mothers.
Stage 4: developing a working analytical framework
The two researchers (BF and HS) who coded all the data met, compared the codes and agreed a set of codes to apply to all subsequent transcripts, which were grouped into categories that followed the key feasibility RQs. Initial broad codes (for each category) included, for example, barriers to and facilitators of recruitment of fathers, acceptability and suitability of the PuP programme for the population, impact of the programme on fathers, implementation and deliverability of the programme, staff training/supervision issues, professionals’ understanding of the programme and participants views on how the programme and its implementation could be improved. The two researchers (BF and HS) met with the principal investigator (AW) to discuss initial impressions from the coding, emergent themes and how to apply and refine the analytic framework across the available cases and data sets (see Appendix 6).
Stage 5: applying the analytical framework
The developed analytic framework was applied to the remaining transcripts using the categories and codes. The researchers (BF and HS) met with the principal investigator (AW) to discuss analytic summaries and emerging themes, and to compare and contrast the findings across the data sets (e.g. father vs. mother, parent vs. practitioner, practitioner vs. manager accounts). Additional codes were added as new themes emerged.
Stage 6: charting the data into the framework matrix
A framework matrix plan was developed that listed the codes and cases that would answer each RQ. Data were then charted into the matrix using automatically generated framework matrices in NVivo. The data from each framework was then extracted onto a spreadsheet. Charting of the data was undertaken, which involved further summarising the data and extracting references and illustrative quotations. Further meetings between the researchers (BF and HS) and the principal investigator (AW) were held to discuss and review the analytic summaries.
Stage 7: interpreting the data
Characteristics of and differences between the data were identified and mapped to explore relationships and linking themes, including gendered practice as a barrier to recruitment; engagement, retention and implementation; views on key components of the programme (e.g. mode of delivery and therapeutic approach); programme model; and broader themes related to implementation issues (e.g. adoption of the model, sustainability and training/supervision) and multiagency working (e.g. fit with other services, agency ‘ethos’ and policy agenda). These data were discussed between researchers involved in the coding (BF and HS), the principal investigator (AW) and the study team, and interpretations were written up to address each RQ. Finally, an appendix of illustrative quotations was prepared for the final report, aligning excerpts with categories (key RQs) and themes.
Reflections on the analytic process, researcher positionality and trustworthiness of the findings
The three researchers (BF, HS and AW) who jointly conducted the qualitative analysis had different levels of knowledge and experience of the study population/clinical field, differing levels of experience undertaking qualitative data analysis and were involved in the data collection to differing degrees. The researcher who was employed in the last 6 months of the project to assist with the data analysis (HS) was able to provide a ‘fresh set of eyes’ on the data, identified dominant and recurring themes and asked questions that were then contextualised by the two researchers (BF and AW) who were more familiar with the study, the intervention and the participants. These discussions led to further testing of the themes and a clearer understanding and interpretation of how the data could inform answers to the RQs. Using this method of analysis was challenging because views of participants shifted over time (e.g. in relation to professionals’ opinions of PuP training, supervision, implementation, deliverability and sustainability from the start of the project to the end). Interpretations also needed to be ‘sense-checked’ with the co-investigators and developers of the programme who understood and had knowledge of this work (e.g. training/supervision of staff and implementation support for the two agencies who delivered the programme). Therefore, it took some time to tease out and capture the developmental aspects of the study, which proved to be important data. This iterative analytic process was extremely time-consuming, but it did enable the two researchers (HS and BF) to systematically chart and summarise the findings. This then allowed the principal investigator (AW) to write up the findings as a narrative report (see Chapter 4), combining the qualitative and quantitative data analysis where required.
Chapter 3 Findings
Recruitment and retention
The recruitment and flow of participants is summarised in the CONSORT (Consolidated Standards of Reporting Trials) flow diagram (Figure 3).
FIGURE 3.
The CONSORT flow diagram. DNA, did not attend.

During the recruitment period (from July 2017 to July 2019), a total of 44 fathers and their families were referred to the study. Six referrals in the early stages of recruitment were not eligible (three because the father’s children were not ‘preschool-aged’ children, as per inclusion criteria at the start of the study, and three because the fathers were from a geographic location that did not yet have an accredited PuP practitioner).
Of the 38 eligible referrals, 25 (66%) were enrolled in the study (and consented to take part). Reasons for non-enrolment were that the family declined to take part because they were not interested (n = 6) or felt that it was not an appropriate time for them (n = 4), or that the family could not be contacted (n = 3).
Referrals were most commonly received from the agencies delivering PuP (PREPARE, n = 14; CIRCLE, n = 7), the Substance Misuse Directorate and NHS drug services (n = 12), primary care teams providing the National Enhanced Service for Drug Misuse (n = 7) and self-referrals (n = 3). One referral was received from a health visitor (child health). The proportion of referrals converted to enrolments was highest for PREPARE and CIRCLE referrals (71%) and drug service referrals (58%), and lowest for primary care (29%) and child health referrals (0%) (Figure 4).
FIGURE 4.
Source of referrals and enrolments. SMD, Substance Misuse Directorate.

Time from referral to first contact with potential participants ranged from 0 to 133 days (i.e. 0–19 weeks), with a median of 19 (IQR 46.2) days. Time from referral to enrolment ranged from 0 to 165 days (i.e. 0–24 weeks), with a median 22.5 (IQR 33.7) days. Time from enrolment to the PuP programme starting ranged from 1 to 69 days (i.e. 1 day–10 weeks), with a median of 19.5 (IQR 42.25) days.
Median time from enrolment to FU1 was 37 weeks (range 22–70 weeks, IQR 14 weeks). Median time from enrolment to FU2 was 63 weeks (range 43–94 weeks, IQR 19 weeks). The first referral was received on 19 July 2017 and the last follow-up was completed on 30 September 2020; therefore, the total time to recruit and follow the whole cohort was 3 years, 2 months and 11 days.
Follow-up 1 was initially conducted following completion of the PuP programme (or after dropout from the programme for any reason) and FU2 was conducted 6 months after FU1. However, owing to programme completion variability among the sample, with some participants taking far longer than anticipated (around 12 months), from August 2019 onwards, follow-ups were conducted at 6 and 12 months after baseline, irrespective of programme completion status. The times taken to complete each component of the study are summarised in Figure 5.
FIGURE 5.
Study timelines per participant. Participant 16 completed PuP at day 421. Participant 18 completed PuP at day 285.
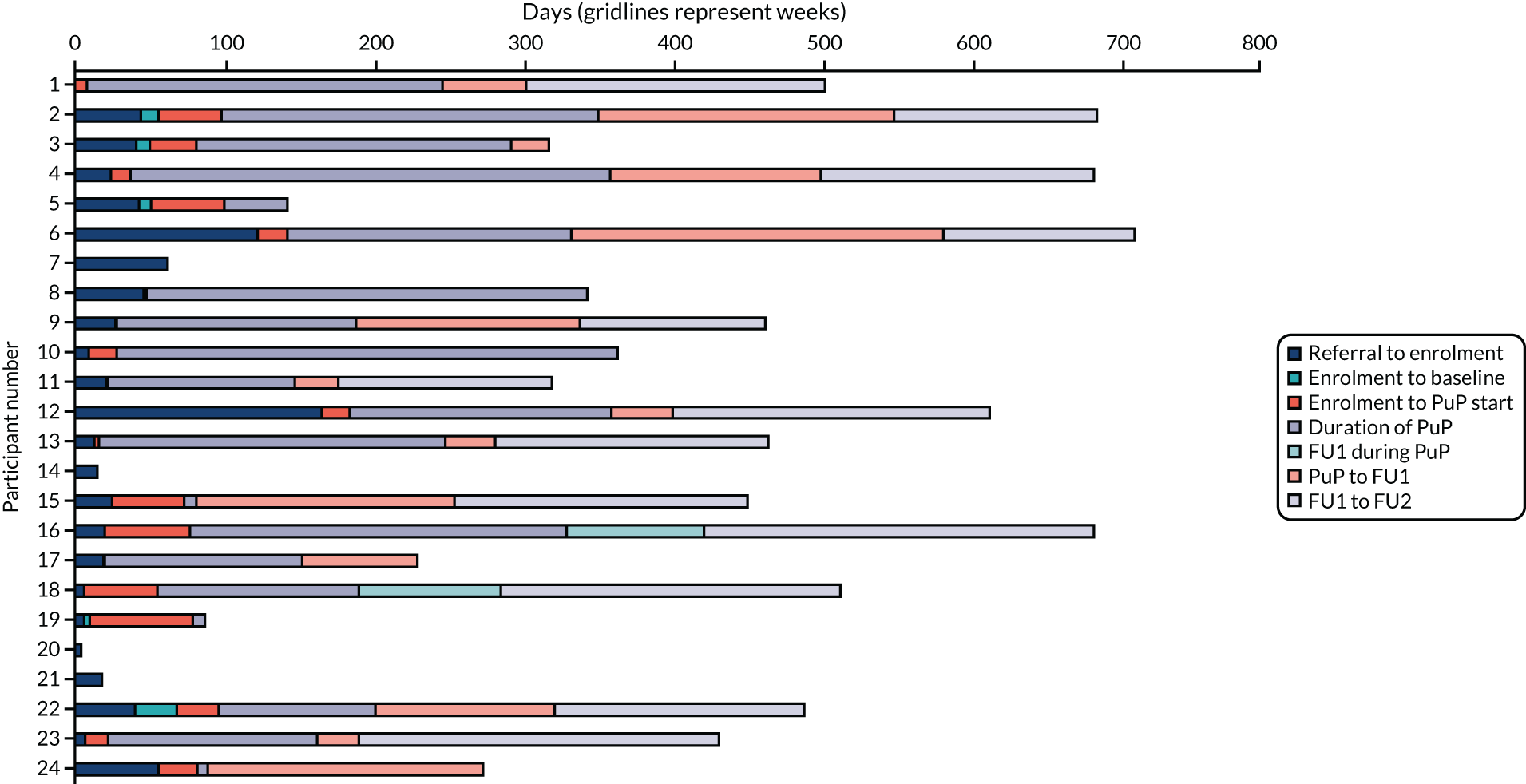
Of the 25 fathers who enrolled into the study, baseline measures were completed by 23 fathers. Reasons for non-completion were impending criminal court proceedings (FA07) and permanency proceedings beginning for the family (FA25). These two fathers were deemed no longer eligible for the intervention. Another father (FA14) withdrew from the study following collection of baseline measures, as he found the RQs too ‘intrusive’.
Twenty-two families were referred to the participating organisations to receive the PuP intervention. Two families referred to the study were assessed as eligible for the intervention by the research team, but were assessed by the service as not suitable for their service (owing to violence and no reunification plan) and so did not receive the intervention. Therefore, a total of 20 fathers (out of 25 consented into the study) were accepted for the PuP intervention by the two PuP delivery sites. PREPARE delivered the intervention to nine families and CIRCLE delivered the intervention to 11 families.
Partners/mothers enrolled in the study with father participants
Of the 25 fathers who were consented into the study, 19 were identified as living, or co-parenting with partners/mothers. Of these partners/mothers, 17 (89%) agreed to take part and were consented into the study. One mother did not take part because the father wanted to undertake the programme alone and the other mother did not want to take part in the study, but did want to engage with the PuP programme.
Description of participants
Participants who consented to take part in the study included fathers (n = 25), mothers (n = 17), PuP practitioners (n = 8), practitioners who became PuP supervisors (n = 2), service managers (n = 7) and professional referrers (n = 28). Each group of participants is described in detail below.
Fathers
Of the 25 fathers enrolled into the study, baseline measures were obtained for 23 (92%). The characteristics of the fathers who provided baseline data are summarised in Table 3. Fathers were aged between 27 and 52 years (mean age 39 years), the majority were white British and all were prescribed OST, as this was an inclusion criterion for the study. Fathers were prescribed methadone (n = 18) or buprenorphine (n = 5) and five fathers were also prescribed diazepam for benzodiazepine dependence. Fathers reported a history of problematic drug use for 4–30 years (mean 21 years). Most fathers had a current (female) partner (n = 17), but four were single (one because the mother of his child had died of a drug overdose) and two were co-parenting with the mothers of their children, but living apart. Most fathers were living in social housing or rented accommodation in areas of deprivation. Six fathers were homeless and living in temporary accommodation.
| Characteristic | Parent participant | |
|---|---|---|
| Fathers (N = 23) | Mothers (N = 17) | |
| Age (years), mean (SD) | 39 (5) | 34 (5) |
| Length of problem drug use in years, mean (SD) | 21 (6) | 14 (5) |
| Marital status, n (%) | ||
| Married/cohabiting | 17 (74) | 16 (94) |
| Co-parenting but living apart | 2 (9) | 0 (0) |
| Divorced | 1 (4) | 1 (6) |
| Single | 3 (13) | 0 (0) |
| Highest education level, n (%) | ||
| No qualifications | 6 (26) | 4 (24) |
| Nat 5/O Level | 10 (42) | 7 (41) |
| Higher | 1 (4) | 0 (0) |
| Diploma/vocational | 4 (17) | 4 (23) |
| Missing | 2 (9) | 2 (12) |
| Main income, n (%) | ||
| Paid employment | 1 (4) | 1 (6) |
| Benefits | 21 (84) | 13 (76) |
| Missing | 1 (4) | 3 (18) |
| Housing, n (%) | ||
| Tenancy | 16 (70) | 11 (65) |
| Homeless/temporary accommodation | 6 (26) | 4 (24) |
| Owned | 1 (4) | 1 (6) |
| Missing | 0 (0) | 1 (6) |
| Criminal record, n (%) | ||
| Yes, ever | 17 (74) | 6 (35) |
| Yes, within last 12 months | 5 (22) | 6 (35) |
| Missing | 1 (4) | 5 (29) |
| Opioid replacement therapy, n (%) | ||
| Methadone | 18 (78) | 14 (82) |
| Buprenorphine | 5 (22) | 0 (0) |
| Dihydrocodeine (dihydrocodeine tartrate, AAH Pharmaceuticals Ltd) | 0 (0) | 1 (6) |
| Non-drug user | 0 (0) | 2 (12) |
Fathers left school aged between 11 and 17 years (mean age 15 years). Data gathered on educational attainment indicated that 21 (84%) fathers had < 10 years of formal education, with six leaving school with no qualifications. Most fathers (n = 17) had a history of incarceration, and five reported current legal issues at baseline (for a range of criminal offences). Twenty-one fathers (84%) reported government benefits as their main source of income, one reported full-time employment and data on income were missing for one. Ten (43%) fathers reported current financial debts.
Mothers
Of the 17 mothers who were consented into the study, 17 provided sociodemographic data. Participating mothers were aged between 22 and 41 years (mean age 34 years). Of the 17 mothers who provided baseline sociodemographics, 14 (82%) were prescribed methadone, one was prescribed dihydrocodeine and two were non-drug users (discordant couples). The mothers receiving OST reported a history of problematic drug use for 9–20 years (mean 14 years). Mothers reported having left school aged between 12 and 17 years (mean age 15 years), with 13 mothers leaving when they were aged ≤ 16 years and four mothers leaving with no qualifications. Six mothers reported current criminal justice issues and six had previously spent time in prison. Thirteen (76%) mothers reported government benefits as their main source of income, one reported full-time employment and data on income were missing for two. Two (12%) mothers reported current financial debts.
Length of relationship between fathers and the mothers in the study ranged from 8 months to 16 years (median 7 years, IQR 7.0 years). The majority of fathers and their partners reported physical and/or mental health comorbidities (commonly pain, anxiety, depression, trauma/history of childhood abuse, domestic abuse, etc.) and low levels of wider family and social support (see Appendix 7, Table 14).
Children
Based on data reported at baseline, the 25 fathers who enrolled had a total of 51 children (aged 0–16 years). Fathers had between zero and eight children each (median 2 children, IQR 2.0 children; note that three fathers were expecting their first child). Fathers reported living with very few of their biological children [11/51 (22%)]: fifteen fathers had no children at home, six fathers had one child, one father had two children and one father had three children.
At baseline, the families reported a total of 47 children in the formal state care system (including children of both fathers and mothers). Thirty-eight children were living with kinship carers, four were in foster care and three were in residential care, and two had been adopted. Five fathers also reported having grown-up (adult) children living away from home. All fathers recruited to the study had regular contact with at least one child aged 0–8 years (referred to as the ‘index child’ in the remainder of the report).
The varied, complex and evolving nature of the circumstances of families in this study is illustrated in infographics of the families from baseline to FU2 (see Report Supplementary Material 3). Complex blended family structures, movement of children between places of care, formation and break-up of relationships, homelessness, unplanned house moves and incarceration were all observed in this sample of families in their time in the study.
Practitioners
Eight staff from PREPARE and CIRCLE were trained in 2016 in preparation for delivering the intervention as part of the study. However, only four practitioners were accredited at the start of the study in April 2017 (reasons for this included staff being on maternity leave or long-term sick leave, staff moving agencies, staff being promoted to managerial post and accreditation was derailed because of commissioning cycle). Both agencies committed to a further cohort of staff training in the PuP programme in 2017 and the intervention was eventually delivered by eight accredited PuP practitioners across the two organisations. To support implementation, both agencies opted to train one experienced PuP practitioner to PuP supervisor level, and this development helped to further embed the model in routine practice. Implementation support was provided to practitioners during formally organised sessions ran by the independent trainer/supervisor initially and then collaboratively with the PuP-trained ‘in-house’ supervisors. The formal PuP development training sessions were conducted approximately every 2 months across the study period. Of the eight practitioners who delivered the programme to participants, six were female and two were male.
Service managers
All service and team managers (n = 7) in CIRCLE and PREPARE were invited to take part in a qualitative interview during the research study and all agreed to take part. Interviews took place between 1 October 2019 and 28 April 2020. Managers came from a range of backgrounds, including social work, community education and management, and had been in their roles for between 3 months and 12 years (one senior manager who was instrumental in the study set-up was interviewed 3 months after leaving the organisation). Five managers were female and two were male.
Referrers
Referrers were contacted via their managers or directly by e-mail and telephone and so data on the total numbers invited and the proportion who took part are not available. However, none of the organisations or managers refused to assist with recruitment. A total of 28 professionals took part in four focus groups held between 12 March and 26 June 2019. Professionals based in East Lothian and all areas of the City of Edinburgh took part. A final focus group was planned for West Lothian, but was cancelled because it coincided with the start of the COVID-19 pandemic and, therefore, no data from referrers from West Lothian are available. However, key stakeholders from West Lothian were invited to attend the online expert event in October 2020.
Participation of a range of referrers was achieved, including community mental health nurses (n = 13), social workers (n = 4), family support workers (n = 3), health visitors (n = 3), third-sector drug recovery co-ordinators (n = 2), GPs (n = 1), clinical psychologists (n = 1) and midwives (n = 1). The age ranges of participants were 25–34 years (n = 8), 35–44 years (n = 7), 45–54 years (n = 9) and 55–64 years (n = 2). The mean length of experience working with drug-using parents was 9 years (range 1–20 years).
Intervention delivery and engagement
Fathers
The 20 fathers who were accepted into the PuP programme had a median engagement with their PuP practitioner of 182 days (i.e. 26 weeks) [range 7–344 days (i.e. 1–49 weeks)]. The median number of sessions was 13 (range 1–34 sessions, IQR 13.25 sessions). Seventy per cent (14/20) of fathers attended six or more sessions and were classed as ‘engagers’ (in line with classification in UK PuP RCT46). Non-attendance at scheduled sessions ranged from zero to 17 sessions (median 4 sessions, IQR 5.0 sessions). As a proportion of the total number of sessions offered, fathers’ attendance ranged from 11% to 100%, with a mean of 71%.
Mothers
Fourteen mothers accepted for the PuP programme had a median engagement with their PuP practitioner of 211 days (i.e. 30 weeks) [range 0–386 days (i.e. 1–55 weeks)]. The median number of sessions was 14.5 (range 1–29 sessions, IQR 19.5 sessions). Seventy-one per cent (10/14) of mothers attended six or more sessions and were classed as ‘engagers’. Non-attendance at scheduled sessions ranged from zero to 17 sessions (median 4.5 sessions, IQR 6.25 sessions). As a proportion of the total number of sessions offered, mothers’ attendance ranged from 0% to 100%, with a mean of 71%. As can be seen in Figure 6, within families, rates of attendance at sessions were similar for fathers and mothers.
FIGURE 6.
Fathers’ and mothers’ attendance as a proportion of PuP sessions scheduled.

Delivery of the Parents under Pressure programme to couples enrolled in the study
Fourteen mothers were concurrently enrolled in the study alongside the father. The number of PuP sessions delivered by practitioners ranged from 2 to 43 per couple (median 15.5, IQR 26.7). Practitioners (n = 8) delivered 248 sessions to couples [140 (56%) sessions were joint sessions, with the remaining 108 (44%) sessions being individual sessions for the father (n = 52) or for the mother (n = 56)].
For individual families, the frequency of joint sessions (with both parents present) varied from 0% to 100% (mean 60%). For sessions with fathers, the frequency of sessions that were joint ranged from 0% to 100% (median 76%). For sessions with mothers, the frequency of sessions that were joint ranged from 0% to 100% (median 85%).
Overall, there were no differences in the level of engagement in the programme between fathers and mothers.
Non-engagers and dropouts
Six fathers (and four mothers) attended five or fewer PuP sessions (classed as ‘non-engagers’). The following reasons were provided for non-attendance:
-
One father was working shift work and was too tired (father and mother completed five sessions each).
-
One family stopped engaging because of problems with their older child (father completed one session and mother completed none).
-
One family stopped engaging when they experienced urgent housing issues (father and mother completed two sessions each).
-
Two fathers stopped attending without giving particular reasons (one father attended one session but the mother did not attend and the other father, who did not have a partner, attended one session).
-
One father did not attend as he felt that he and his family were doing well and did not need the PuP programme (the father completed one session and his partner attended three sessions, although she was not enrolled in the study).
Fidelity
The PuP programme is individually tailored to each family and so there is variability in the delivery of components (i.e. not all families needed all 12 modules). The following data illustrate parent reports of the PuP programme components that they received. Excluding the six non-engaging families (i.e. those who received five or fewer sessions of the PuP programme), fathers reported receiving a range of 9–20 components (median 15 components) of the PuP fidelity measure and partners reported receiving a range of 5–19 components (median 15 components) of the PuP fidelity measure (with a maximum possible score of 20). As shown in Figure 7, the PuP programme components most frequently endorsed by fathers as having been received were setting targets for change, having shared goals and discussing their child’s best qualities, whereas using relaxation techniques, using mindfulness and using wise mind were reported less frequently. For partners (mothers), setting targets for change, discussing their child’s best qualities and having a good understanding of child’s developmental stage were the components most frequently endorsed as having been received, and using wise mind was reported less frequently (Figure 8). For both fathers and mothers, formal components of mindfulness were less frequently reported, but, notably, one of the key elements of mindful parenting – ‘being in the moment with your child’ –was one of the most frequently reported. This suggests that, although formal mindfulness exercises, such as mindful eating and mindful walking, were endorsed less, the key to engaging with children by being fully present was endorsed by both fathers and mothers.
FIGURE 7.
Father-reported intervention components received.
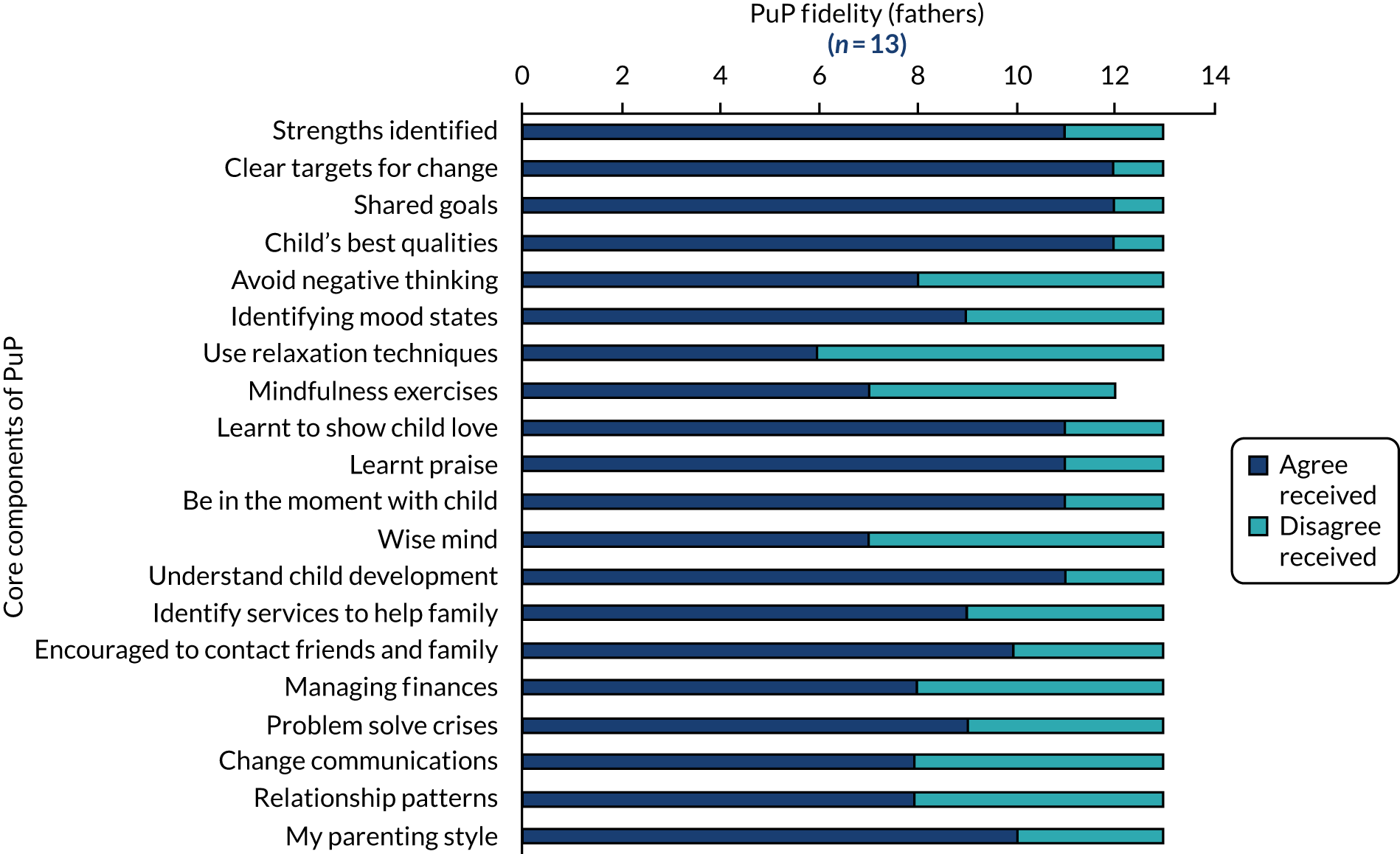
FIGURE 8.
Partner (mother)-reported intervention components received.

Retention in the study
Fathers
Retention is summarised in Figure 3. Of the 21 fathers remaining in the study at FU1 [i.e. after completion of the PuP programme (pre August 2019) or 6 months after enrolment (post August 2019)], 16 (76%) completed follow-up measures and participated in an in-depth qualitative interview [i.e. 16 of the total 25 (64%) fathers consented into the study]. Reasons fathers did not complete FU1 were:
-
incarceration (n = 1, FA10)
-
unreachable (n = 3, FA08, FA19 and FA20)
-
declined and withdrew from study (n = 1, FA21, a family who were not offered the PuP programme by the agency).
Of the 20 fathers remaining in the study at FU2 [i.e. 6 months after FU1 (pre August 2019) or at 12 months after FU1 (post August 2019)], 13 (65%) completed follow-up measures [i.e. 13 of the total 25 (52%) fathers who were consented into the study]. Reasons fathers did not complete FU2 were:
-
incarceration (n = 1, FA10)
-
unreachable (n = 6, FA03, FA08, FA17, FA19, FA20 and FA24).
Mothers
Of the 17 mothers who consented to be part of the study and provided baseline data, 13 (76%) mothers remained in the study at FU1 and 11 (65%) completed follow-up measures and participated in a qualitative interview [i.e. 11 of the total 14 (79%) mothers enrolled in the PuP programme]. Reasons mothers did not complete FU1 were being:
-
unreachable (n = 1, MO08)
-
separated from father, restraining order preventing contact and unreachable (n = 1, MO19).
Of the 13 mothers remaining in the study at FU2, nine (69%) completed FU2 [i.e. 9 of total 14 (64%) mothers enrolled in the PuP programme]. The reason mothers did not complete FU2 was:
-
unreachable (n = 4, MO03, MO08, MO15 and MO19).
In four cases (families 3, 8, 19 and 20), the father and mother participants were lost to follow-up together. In two cases, the father was lost to follow-up but the mother completed (FA10 and FA17) and in one case the mother was lost to follow-up but the father completed (FA15).
Quantitative results
Completion rates for validated questionnaires for fathers/mothers enrolled in the study and for PuP ‘engagers’ at baseline, FU1 and FU2 are presented in Chapter 4 (see Table 6). Individual questionnaire results are presented below and in Appendices 8–14.
Treatment Outcomes Profile
Fathers
All fathers who participated at baseline (23/23), FU1 (16/16) and FU2 (13/13) completed the TOP with no missing data. Median reported number of days abstinent from illicit drugs and alcohol increased from baseline (median 18 days, IQR 10.06 days) to FU1 (median 24 days, IQR 7.0 days) and to FU2 (median 26 days, IQR 9.0 days).
Mothers
Fourteen of the 16 mothers who completed baseline measures were receiving OST (and prescribed methadone). The TOP was administered to these 14 mothers. At baseline, 20 of the 23 (87%) TOP items were completed by all 14 mothers. At FU1, 20 of the 23 (87%) TOP items were completed by all 10 mothers. At FU2, all 23 items (100%) were completed by all eight mothers. No particular patterns in missing items were noted. Mothers reported being highly abstinent from illicit drugs and alcohol throughout [baseline, days abstinent median 26.5 (IQR 13.0); FU1, days abstinent median 27.5 (IQR 1.0); FU2, days abstinent median 26.5 (IQR 4.0)] (see Appendix 8, Table 15).
EuroQol-5 Dimensions, five-level version
Fathers
All but one father completed the EQ-5D-5L at baseline (22/23). The reason for non-completion was not recorded. The questionnaire was completed by all those it was administered to at baseline (22/22, 100%), FU1 (16/16, 100%) and FU2 (13/13, 100%) and all items were completed.
Mothers
All mothers who participated at baseline (17/17), all but one (MO15) at FU1 (10/11) and all mothers at FU2 (9/9) completed the EQ-5D-5L with no missing data (see Appendix 7, Table 14).
Brief Child Abuse Potential Inventory
Fathers
Twenty fathers participated in completing the BCAPI at baseline (20/23, 87%). One measure was incomplete because of time constraints. The reasons for other non-completions were not recorded. Three first-time fathers were interviewed at baseline and so it is possible that the researcher thought that this measure was not applicable and did not administer it. All fathers who participated in FU1 (16/16, 100%) and FU2 (13/13, 100%) completed the BCAPI. There were few missing items and no systematic patterns of missed items noted (see Appendix 9, Table 16). At FU2, one participant (FA11) was unable to complete 16 of the 34 items because of drowsiness and so a total score could not be calculated.
Mothers
The BCAPI was administered to 14 of the 17 (82%) mothers who completed baseline. Reasons for non-completions were not recorded (although three mothers were first-time mothers and so this may have been a researcher error). The BCAPI was administered to all mothers who participated in FU1 (11/11) and FU2 (9/9), with few missing items. Item 7 (i.e. ‘everything in the home should always be’) was missed by three mothers (MO02, MO6 and MO08) (see Appendix 9, Table 16).
Parenting Sense of Competence Scale
Fathers
Sixteen fathers participated in completing the PSCS at baseline (16/23). Six fathers did not complete any items on this questionnaire at this time, as they were expectant fathers with no parenting experience. At FU1, 15 of 16 (94%) fathers completed the PSCS. One father (FA17) did not complete, as he did not feel that he had enough contact with his child to be able to respond to the items. At FU2, 11 of 13 fathers participated in completing the PSCS. One father (FA11) was unable to complete (because of feeling drowsy) and one PSCS was not administered in error (FA09). At baseline, 11 of 16 (69%) items were completed by all fathers. There were six missing responses to item 16. This was the last item of the scale and printed on a separate sheet and, therefore, it is likely that this was overlooked by the researcher. At FU1, 13 of 16 (81%) items were completed by 15 fathers. At FU2, 12 of 16 (75%) items were completed by all 11 fathers (see Appendix 10, Table 17).
Mothers
The PSCS was administered to 9 of the 17 mothers enrolled in the study at baseline (eight mothers did not complete it as they were expecting their first child). At FU1, 9 of 11 mothers responded to the PSCS [questionnaires were not administered to two mothers (MO10 and MO15) in error]. At FU2, one mother (MO02) did not want to complete the PSCS, as she found it upsetting. The PSCS was largely completed fully; however, as with the fathers at baseline, item 16 was not completed by five mothers, as it was probably overlooked by the researcher. At FU1, eight items were not completed by one mother (MO15) who felt that she did not have enough contact with her child to respond to those. At FU2, 15 of 16 (94%) items were completed by all seven (100%) mothers (see Appendix 10, Table 17).
Difficulties in Emotion Regulation Scale
Fathers
The DERS was administered to 21 of the 23 fathers enrolled at baseline. One father did not complete because of lack of time and one was a recording error. All 16 (100%) fathers at FU1 and 13 (100%) at FU2 completed the DERS, with very few missing items (see Appendix 11, Table 18). At FU2, one father (FA11) did not complete items 13–34 because of drowsiness.
Mothers
At baseline, 33 of 36 (92%) items were completed by all 17 (100%) mothers. At FU1, all 36 (100%) items were completed by all 11 (100%) mothers. At FU2, 35 of 36 (97%) items were completed by all nine mothers (see Appendix 11, Table 18).
Revised Conflict Tactics Scale
Fathers
The CTS2 was administered to 18 fathers at baseline. One father did not complete the CTS2 because of time and four fathers were not in relationships. At FU1, the CTS2 was administered to all 12 of the 16 fathers who were in a relationship (four fathers were not in a relationship at this time). At FU2, the CTS2 was administered to 6 of 13 fathers (seven fathers were not in a relationship at this time). At baseline, 72 of 78 (92%) items were completed by all fathers. At FU1, 77 of 78 (99%) items were completed by all 12 (100%) fathers. At FU2, all 78 (100%) items were completed by all six (100%) fathers (see Appendix 12, Table 19).
Mothers
The CTS2 was administered to 16 of the 17 mothers who participated at baseline. One mother (MO03) did not complete any items on this questionnaire at baseline, but the reason for non-completion was not recorded. At FU1, the CTS2 was administered to 10 of 11 mothers who completed FU1 [one mother (MO10) did not complete, as she was no longer in a relationship]. At FU2, the CTS2 was administered to five of the nine mothers who completed FU2 [four mothers (MO02, MO10, MO16 and MO17) were no longer in relationships]. At baseline, 69 of the 78 items were completed by all mothers, with very few missing data. At FU1, 76 of the 78 (97%) items were completed by all 10 mothers. At FU2, all items (78/78) were completed by all five mothers (see Appendix 12, Table 19).
Child well-being measures (Brief Infant Toddler Social and Emotional Assessment and Strengths and Difficulties Questionnaire)
Fathers
Nine fathers at baseline, seven fathers at FU1 and 10 fathers at FU2 completed a measure of child well-being (see Appendix 13, Table 20).
Mothers
Four mothers at baseline, three mothers at FU1 and eight mothers at FU2 completed a measure of child well-being (see Appendix 13, Table 20).
Reasons for non-completion of child well-being questionnaires included a measure appropriate for the age of the child not being available (i.e. between birth and 1 year) and the parent not having sufficient contact to be able to comment on child attributes. One father was unable to complete a child well-being questionnaire because of fatigue. The same measure was used across two or more study time points for only seven children, limiting our ability to measure change over time. The main reason was that different measures of child well-being or no measure of child well-being were appropriate at each study time point. Some fathers completed the BITSEA and the SDQ for more than one child (see Appendix 13, Table 20).
Parent–child relationship (Paternal Antenatal Attachment Scale, Maternal Antenatal Attachment Scale and Emotional Availability Scale)
Fathers: Paternal Antenatal Attachment Scale
Five of eight (63%) fathers completed a measure of attachment (i.e. the PAAS) at baseline (see Appendix 14, Table 21).
Mothers: Maternal Antenatal Attachment Scale
Four of eight (50%) mothers completed a measure of attachment (i.e. the MAAS) at baseline (see Appendix 14, Table 21).
Emotional Availability Scales
At baseline, EAS video-recordings were conducted with no fathers and no mothers. At FU1, video-recordings were conducted with three fathers and one mother. At FU2, video-recordings were conducted with three fathers and no mothers. One couple did not consent to the observational measure, voicing concerns over confidentiality. One mother was willing to be recorded at FU2, but her baby was asleep when the researcher visited the home. The EAS data collected were not analysed, as COVID-19 travel restrictions prevented coding by an independent coder trained in the method (the coder was required to travel to Edinburgh to access the data). The feasibility of administering the EAS video-observation measure and the reasons why this was not a suitable measure for this study and population are described in more detail in Chapter 4, Suitability of measures.
Chapter 4 Answers to the study research questions
In this chapter, we draw on our analysis of the qualitative and quantitative data to answer the main feasibility questions and objectives for the study. The findings are presented in order of the original study protocol RQs, up to and including RQ10.
Where the answer to a RQ has been informed by our analysis of qualitative data, we include selected excerpts to illustrate key points. Excerpts from qualitative interviews and focus groups by RQ are also presented in Appendix 15, Table 22, for ease of reference.
The answer to RQ11 on the feasibility of a main study and design of a future evaluation of PuP4Dads includes progression criteria results, a summary of our expert event with key stakeholders, an assessment of feasibility, using ADePT,54 and a proposed main study design and rationale.
Research question 1: how feasible is it to deliver the Parents under Pressure programme for opioid-dependent fathers in routine family-based local government and voluntary sector services?
Generally speaking, the mothers have been very supportive of the dad’s involvement. They’ve really wanted the dad to be given appropriate support. It’s been very interesting.
Manager 6
The programme was delivered successfully in the two agencies that took part in this study, despite there being substantive differences in their role and remit, organisational and managerial structures, staffing mix and qualifications, and criteria for entry into the service. PREPARE delivered the intervention to nine study families and CIRCLE delivered the intervention to 11 study families. Both organisations have continued to deliver PuP to opioid-dependent fathers beyond the implementation phase of this study and both agencies have committed to further staff training in the PuP programme to ensure sustainability of the programme. Although ‘deliverability’ of the programme for opioid-dependent fathers was achieved within both agencies, the adoption and implementation process was different and unique to each service.
PREPARE, a local authority and social work-led service, has a specific remit to undertake parenting capacity assessments and deliver parenting interventions for families involved in the child protection system. Qualitative data showed that the PuP model was a good fit for this service in which many of the families have infants who are at significant risk of harm and who require intensive home-visiting parenting support. The PREPARE team is a multidisciplinary and multiagency service (i.e. social work and health), but all team members are co-located in the one community-based centre. Although PREPARE is a specialist service for pregnant women with substance use problems, it adopts a ‘whole-family’ approach and routinely includes fathers in the parenting assessments and parenting interventions that it delivers. A small number of ‘early years’ officers’ undertake most of this work in the team and it was these practitioners (and a ‘fathers’ worker’ at the beginning of the study) who delivered the PuP intervention to study participants. Adoption of the PuP model in the service and embedding it in routine practice with fathers who are opioid dependent appeared to be relatively straightforward for the PREPARE team. A senior early years officer also trained to become an accredited PuP supervisor and this development helped to embed the PuP model in the team. The service made a decision by the end of the first year of the study to deliver the PuP programme to all families referred to the service, irrespective of whether or not they agreed to join the study. This then made the recruitment and delivery of the programme to fathers in the study more achievable. Despite this, the population of families normally referred to PREPARE during the antenatal period are ‘hard-to-engage’ parents and are often very fearful of their infants being taken into care after birth. It can sometimes take many months before parents develop a good working alliance with practitioners and, for various reasons, some never do. One or two of these families accounted for some of our study dropouts.
CIRCLE, is a third-sector service that provides family support services across three different Health and Social Care Partnerships and local authorities in Lothian. The organisation includes independent teams in each area for families affected by parental substance use, each with its own team manager and staff complement, and each with its own specific commissioned role and remit for the area it serves and the funding it receives. CIRCLE engage with families on a voluntary basis and are often an integral part of the ‘team around the child’. CIRCLE contribute to family support plans for families who have children involved in the child protection system, as well as those who are not involved with social services. Referrals to CIRCLE for ‘family support’ can originate from social services and a variety of other agencies. PREPARE refers to CIRCLE when families are discharged from the service (at around 6–24 months postnatal). CIRCLE also works in partnership with substance misuse services across Lothian and some staff are co-located in community-based ‘recovery hubs’. Selected staff from across the three CIRCLE teams in Lothian were trained in the PuP programme and it was these staff who delivered the intervention to study families. Qualitative data from practitioners and managers across the three CIRCLE teams suggested that the PuP programme was a good fit for the overall role and remit of the organisation, as practitioners would normally provide a home-visiting service to support very disadvantaged and marginalised families, including those affected by parental substance use. PuP4Dads was appealing as a model because it fitted well with the national practice model for children in Scotland (i.e. GIRFEC) and strategic priorities for improving the care of children and families affected by substance use, including the provision for ‘whole-family’ support. In addition, PuP4Dads fitted well with CIRCLE’s commitment to providing a specific support service for dads through their funded ‘father’s worker’ appointments:
We’ve now got a father’s worker as part of the team. Any of our [staff] could have worked with dads, and, for some reason, there’s obviously some kind of mental block where people don’t seem to refer dads, even though they could work with them. But as soon as you put a father’s worker [in the service] they were like ‘we can refer dads to you’ and you’re like, ‘really?!’
Manager 3
Some, but not all, staff interviewed in the first year of the study suggested that embedding the PuP programme in CIRCLE was challenging to begin with, perhaps understandably because CIRCLE staff who were trained in the PuP programme in 2016 were spread thinly over the three teams, and, therefore, adoption of the programme as part of ‘routine’ practice was not universal. In addition, at the start of the study, PuP-trained practitioners were at different stages in their accreditation process. However, a second cohort of staff in CIRCLE started PuP training in 2017 and these staff began delivering the programme with families (who were not part of the study). In addition, one of the PuP practitioners in CIRCLE trained to become an accredited PuP supervisor. These developments seemed to build ‘momentum’ within the service. Likewise, accounts from practitioners and managers in years 2 and 3 of the study suggested that having a ‘critical mass’ of staff trained in the PuP programme, or at least knowledgeable about the programme, had helped to embed the programme and, over time, a ‘community of practice’ started to emerge:
If everybody has [PuP programme] knowledge within teams, you can get a lot more back as well and a lot more involvement within team meeting discussions, if that makes sense. Whereas, if you’ve got a team that’s half trained in PuP and half not, you know, you kind of isolate half the team if you’re having discussions.
Manager 1
These larger kind of pieces of work [referring to PuP], training, accreditation . . . [you need] a more kind of collective approach within a team so I think you get a kind of, you get a momentum.
Manager 7
With regard to whether or not the PuP programme itself was ‘deliverable’ to opioid-dependent fathers as part of routine practice, most practitioners in the two agencies reported that it was, with some providing examples of how they applied the programme model and content in their practice, and with fathers, couples and families more broadly:
We would still maybe draw on some of the emotional regulation work or mindful child management type [modules]. That really compliments what we were already doing, so PuP [has] given us a nice framework to do that with. So, yeah formally and informally PuP is used in most of our cases [now].
Practitioner 3
The strengths-based approach too, getting a sense of what it is that they want and need, and starting from that position rather than, you know, us telling them all about their problems, kind of thing, focusing on their problems all the time.
Practitioner 4
In terms of engaging [fathers], I mean, certainly the ones I’ve had, it’s been very much . . . although the partner’s around, it’s been very much focused on him and she’s always been happy for him to have that time, ’cause she’s thinking ‘oh it’ll help him be a better dad’.
Practitioner 5
In addition, the PuP programme was seen to enhance good partnership working and enabled practitioners to make their work with fathers more visible (e.g. practitioners indicated that the programme had enabled them to make the voices of fathers ‘heard’ and their needs better understood). Practitioners also commented on the PuP model as a coherent ‘framework’ that provided them with ‘tools’ to work with fathers in a more ‘structured’ and therapeutic way. The PuP model was portrayed as something that could ‘complement’ or enhance routine practice with families affected by parental substance use. That is, it was not spoken of as an entirely new intervention that needed to supplant current good practice:
I think [PuP] does help, maybe when you’re articulating something at a meeting, or they’re saying ‘oh, there’s an issue with this’ and I’ll say ‘well, we’ve worked through this’ and I can then talk of what we’ve worked through at the moment.
Practitioner 2
The [PuP] framework is a good kind of guide for us, for probably most of the families that we work with.
Practitioner 4
I think PuP complements GIRFEC nicely in the way that we work.
Practitioner 3
Because [PuP is] very similar to our practice anyway. We work very closely with all the services. Not on all families, but the majority of families have addictions or social work involved as well. So, yeah, it all ties in.
Practitioner 7
Deliverability of the PuP programme to opioid-dependent fathers, according to those interviewed, was enhanced by a combination of factors, including having external PuP supervision and external implementation support, having internal support from senior managers and line managers who ‘understood’ the model and could encouraged staff to implement it with families, having ‘in-house’ PuP supervisors so that supervision was more available and ‘on hand’ when required, having a ‘critical mass’ of PuP-trained and PuP-accredited staff in each team to deliver the programme, and having staff and teams who were willing to adopt the programme and integrate it into their practice with fathers.
In summary, our findings demonstrate that it is feasible to deliver the PuP programme for opioid-dependent fathers and their families in routine practice in local authority and third-sector organisations. A fundamental starting point for a main study would be to involve services, like PREPARE and CIRCLE, that are committed to working with opioid-dependent fathers and have staff who are already skilled in working with this hard-to-engage population of families. Importantly, the delivery of the programme is likely to be more straightforward and successful, with a well thought through adoption and implementation support plan that is tailored to the needs of each service/team in charge of recruitment and delivery in sites in a main study.
Research question 2: how acceptable is the Parents under Pressure programme among staff and recipients and what are the barriers to/facilitators of uptake and retention?
The acceptability and suitability of the programme for opioid-dependent fathers and families was rated highly by practitioners, managers and the parents themselves, and was primarily expressed in terms of how ‘useful’ or ‘helpful’ the programme had been for fathers and families, professional practice or multidisciplinary working:
I was going along to case conferences, reviews and things, and they were saying ‘how’s dad?’ . . . Really good, you know, we’re meeting regularly, de, de, de. But there was no structure . . . since I’ve introduced PuP and doing, even the questionnaires, it’s steering towards, a direction. So I’m now going along to meetings and saying, you know, ‘we’ve undertaken the questionnaires and these are the areas that we’re now focusing on . . . I’m meeting dad on a weekly basis. This is the work we’re doing.’ So there’s a real structure. So I can really see the benefit.
Practitioner 5
Fathers who were interviewed (n = 16) gave a lot of positive feedback on the programme and all said that they would recommend the programme to other parents who use drugs. Likewise, PuP4dads also seemed to win the support of most mothers. For practitioners, this seemed important too, with several remarking on the acceptability of the programme for mothers and the benefits of involving the father for her. According to most practitioners, the programme provided a unique therapeutic focus on fathers, father–child relationships and co-parenting for fathers who previously lacked parenting support:
[PuP] helped me to set small goals, and go out and get, you know, taking the bairn [child] to school and things like that. [PuP] helped [me] to know I’m not a bad dad. I know I’m doing all the right things, but I’m doing more things now, and I’m enjoying it.
Father 4
It helped our workers see our strengths and our goals, what we wanted to happen, and it gave us a starting point on what to work for, areas that we wanted.
Mother 9
[PuP] causes you to look at how you’re parenting . . . You never do that because you just dawdle along when you’re a parent and you do what’s needed, whereas, until you look at yourself, then you can’t change nothing, until you look at it.
Father 15
Yes, and she kind of let me take control of what we were talking about, even though she would be asking me all the questions and that.
Father 11
When I look at the [parent work]book and I know if I don’t [want to open it] . . . because I’m unsure of what I’m going to come up with, I can just look at it and then just look at it, dread it . . . but then I just do it.
Father 18
Professionals considered the programme suitable for a diverse groups of families, including single and non-resident fathers through to couples who were in a relationship, living together or apart, through to parents whose children were in kinship care or other out-of-home placement. Accounts were generally positive about the underlying theory of the programme, its structure and content. Professionals seemed appreciative of, for example, the ‘themed’ modules, mindfulness exercises, information related to healthy diets and budgeting, and relapse prevention strategies. In addition, this helped practitioners to communicate with other health and social care services about the work they were doing with parents and their progress over time:
I’ve got more of an understanding about why I’m doing certain things with families, and then it helps the families to understand why we’re doing certain things, and then other professionals to understand what the point of us working alongside families are, and it’s not just a case of taking families out for a cup of tea . . . and I know a lot of families have fed back that they really like the ‘view of self as parent’ module, and it gives them an opportunity to, I guess, put into context their own experiences and then go on to have an understanding about why that’s impacting on the way that they run their own lives or the way that they parent their children, and their coping strategies.
Practitioner 3
Practitioners frequently commented that many parents have a history of trauma and that this was often disclosed in the ‘view of self as a parent’ module, where the parent’s history of being parented as a child is explored. Practitioners noted that past trauma needed to be dealt with sensitively (although there were helpful tools in the programme to do this, e.g. the ‘memory box’).
The aspects of the programme that participants valued the most were the:
-
mode of delivery (e.g. home visiting, ‘flexibility’ of how the programme could be delivered, length of delivery and the use of ‘workbooks’ and video-feedback)
-
therapeutic approach (e.g. strengths based, collaborative goal-setting, focus on parental emotion regulation, emotional availability and the needs of the child, and parental self-efficacy)
-
programme model (e.g. ‘whole-family’ approach, individually tailored, ‘holistic’, relationship based, structured ‘modular’ system, the PuP database and use of questionnaires to reassess and report progress).
The aspects of the programme that participants thought could be improved were as follows:
-
Some practitioners wanted more support and guidance around managing confidentiality and the different, sometimes competing, needs of each parent. The added complexity of working with couple relationships and co-parenting, as well as parent–child relationships, was new for some practitioners who were used to working primarily with mothers.
-
Some parents expressed concerns about their reading and writing ability (i.e. literacy) and this posed a problem for them in engaging in the parent workbook. Practitioners also reiterated this point. Both parents and practitioners suggested that other formats could be developed (e.g. audiobooks, visual methods/pictures or an interactive smartphone application).
-
Practitioners mentioned that some parents did not understand all the language, expressions, questions and instructions in the parent workbook, and suggested that these could be simplified and ‘sense-checked’ by parents to ensure that the content is more culturally appropriate.
-
Some programme content was considered less relevant for fathers/parents who had limited contact with their children or those who had newborn babies/very small infants. Some mothers who were opioid dependent also said that they would like more content on how to care for a baby with neonatal abstinence syndrome. However, practitioners gave examples of how they could adapt the delivery of the programme to include tools, exercises and activities that were more relevant to these parents.
Barriers to and facilitators of uptake and retention
Referrers and practitioners reported that fathers who use drugs can be a very challenging population to identify. Their fatherhood status is not always known, even if they are attending drug treatment services. They were portrayed as a ‘hidden’ population who could remain ‘under the radar’, especially if their partner is not a drug user. Some practitioners also portrayed opioid-dependent fathers as being largely disinterested in parenting and parenting programmes:
[Fathers] don’t really want to engage with that type of programme [parenting programmes]; they feel it’s more geared towards the mums than themselves . . . I find it quite difficult to kind of engage with the dads . . . I’m working with the mum and the children, not really the dad.
Referrer, focus group 3
Even if fathers were known about, professionals suggested that approaching opioid-dependent fathers and talking to them about parenting can be difficult to do. The ‘stigma’ of being a parent who uses drugs and their fear of social services was not conducive to talking about getting involved in parenting programmes:
I was really glad that you said that [PuP is] strengths based, because I feel that . . . and it’s not about criticising social work in any way, but I feel like the interaction between our [drug service] patients and social work can be really negative and very stigmatising.
Referrer, focus group 2
Professionals needed to feel as though they could ‘sell it’ to fathers. In addition, professionals needed to have a good rapport with fathers before they would ‘raise the subject’. It seemed important for referrers that the intervention was supportive and empowering and was not likely to result in a negative experience, as many parents who use drugs have had previous encounters with children’s services that had been unhelpful:
I suppose from the very beginning, maybe selling it to dads and getting them . . . because the focus is on them and they’re not used to that maybe, you know, why this would benefit them . . . family support has really been, just all a whole load of discussions about what drugs they take, primarily . . . so no sense that they’ve, you know, been involved in setting their own goals and being an active agent in the whole process.
Practitioner 4
The focus groups with referrers and the interviews with practitioners and parents all highlighted gendered practice as a barrier to father-inclusive practice. Parenting and family support services traditionally focused on mothers and mothering. Fathers also assumed that most services were for mothers and children, and not for them. Fathers were often perceived and treated as optional, rather than essential, to the parenting and child welfare agenda:
[Practitioners] are very comfortable working with mothers, you know, that’s the norm . . . and even if unconsciously they don’t want to exclude fathers, they would . . . they’d find themselves kind of doing that anyway.
Practitioner 4
Participants suggested that uptake and retention in the programme were more likely if there was an organisational culture that supported a ‘whole-family’ and father-inclusive approach, and where practitioners understood the intervention and could emphasise the supportive nature of the programme (as opposed to psychoeducation-type parenting programmes that ‘tell parents what to do’). To overcome practitioners’ lack of knowledge about the programme and to build confidence in ‘selling it’ to fathers, there were suggestions for programme information materials that could include direct quotes from fathers with experience of the programme (e.g. on leaflets, as a short video, as a podcast or as a blog/short story). Professionals could then use these materials to demonstrate to fathers how the programme could be helpful for them, their children and family.
Research question 3: how acceptable and adequate is the training and supervision for staff?
Accounts of the PuP training, supervision and accreditation process were integrally linked with experiences of how the intervention was adopted and implemented with each agency and, in the case of CIRCLE, within each of the three teams located in Edinburgh, East Lothian and West Lothian. In many respects, it was difficult to tease out views on the acceptability of the training and supervision from implementation processes and views on implementation support (i.e. the ability of the practitioners to apply their learning in practice with families and how well this was supported through PuP supervision, line management and their peers, etc). For example, there were some practitioners who were trained in the early cohort who reported applying the model soon afterwards with families and there were others who found this more difficult. Likewise, there were some practitioners who engaged well in PuP supervision sessions in the first year and benefited from it, and there were others who did not. Providing individual and group supervision and the development of ‘in-house’ supervisors in year 2 of the study, along with regular ‘PuP development’ training days and individual support to write-up family case studies, appeared to build confidence in applying the model and this, in turn, had a synergistic effect. To a certain extent, this fits with the PuP training model, which is based on a combination of theoretical and experiential training over a period of ≥ 8 months, alongside implementation support (see Chapter 2, Practitioner training and accreditation in Parents under Pressure, for a description of the training).
Practitioners who had a positive experience of the initial 2 training days, supervision and the implementation of PuP4Dads in their team were enthusiastic about embracing the PuP model as a parenting and family support intervention, and spoke about how the programme had enhanced their own knowledge or practice (e.g. by providing them with a ‘useful framework’, a ‘structure’ and ‘tools’ for practice). Practitioners also spoke about the benefits of applying some of the underlying theroretical approaches to the programme (e.g. emotional availability, strengths-based approach and mindfulness strategies) and how families with complex needs had responded to the programme:
Some of [the families] are up at 12 months [length of time delivering PuP], they’re complex families, and the mum has really complex problems, the dad has really complex problems, in their own right, as well as a family.
Practitioner 3
[If] they want to do it as a couple, [I’ve] tried to do it with both of them in the same session, and then maybe had separate sessions for specific things. [Gave an example of a dad with anxiety.]
Practitioner 4
It’s quite traumatic stories, you know, for a lot of the dads I’m working with . . . so they get a real understanding of, if they’ve not been [well] parented, how can they be . . . how can they parent? . . . how are they expected to be a good parent? . . . that’s been really, really powerful.
Practitioner 5
Accounts from practitioners and managers suggested that the PuP training programme and PuP supervision sessions had worked well when the following had occurred:
-
Practitioners understood that there was a good ‘fit’ between PuP and existing models of practice, as well as the service ‘ethos’ (i.e. practitioners could see the ‘added value’ of the PuP programme and the potential benefits of including fathers in the intervention).
-
Practitioners and managers had a clear sense of how they could operationalise the PuP programme as part of routine practice. For example, when both managers and practitioners understood how the model could ‘work’ for different families referred into the service.
-
Staff understood and were well prepared for the PuP training programme, supervision and accreditation process and requirements (i.e. there was ‘buy-in’).
-
Supervision was prioritised, structured and scheduled well in advance, with sufficient time allocated and there was a clear distinction between ‘PuP supervision’ and ‘line management’ supervision.
-
Supervisors had a good understanding and practical first-hand experience of using the PuP model with fathers and families affected by substance use and were able to articulate the application of the model and support practitioners to integrate the PuP programme into their work.
-
There was an opportunity for ‘shared learning’, and adequate support and supervision was offered for practical aspects of the programme (e.g. how to use the database and download/upload documents, such as the family assessments).
A key issue for managers was the sustainability of the programme and how to ensure that a ‘rolling programme’ of PuP training was available for new staff coming into the service so they could start delivering the programme in a timely manner. This was important for managers, as they needed to feel confident about having capacity to deliver the intervention consistently with families, especially if they were to start advertising the PuP intervention as a core service or if they included the delivery of the PuP programme to this population of families as part of a commissioned contract.
At the time the interviews were conducted with managers, the training was face to face and required quite a bit of planning to organise and deliver. However, during the COVID-19 pandemic in 2020, the developers of the PuP programme converted the face-to-face delivery to an online training programme, making access more feasible for services.
Research question 4: to what extent can the Parents under Pressure programme be integrated into non-NHS settings across the UK?
[PuP] is holistic, so it very much fits in with the fact that we’re holistic, strengths based, solution focused and that we’re working with all of the different kind of elements within the family in terms of resources, internal and external, and parenting strategies. So I do think it kind of fits in with [our] model really well; obviously PuP for dads fits in with our kind of ethos around positively involving dads.
Manager 5
Although the PuP programme was successfully integrated into non-NHS services in this study, there is still the question of whether or not the intervention could be delivered in other similar settings across the UK and scaled up for a main study. We considered evidence on PuP implementation elsewhere and explored scale-up explicitly in our ‘expert event’ with wider stakeholders in October 2020 [see Expert event (public engagement)] and in subsequent public engagement events in November 2020 (with Public Health England programme leads), January 2021 (with service managers and commissioners from England and Scotland) and in February 2021 (with key stakeholders from England, Scotland and Ireland).
In the PuP RCT,46 the programme was delivered successfully across multiple sites in England, Scotland and Wales, and the programme has been delivered across Ireland by third-sector agencies [see Evaluation of Parents under Pressure Programme (PuP) at Coolmine90 as an example]. The model itself is specifically designed to be adaptable to different families living in different situational contexts, including residential drug rehabilitation units, supported housing and prison environments. The model is flexibly delivered to individual families so that the only prerequisite is that there is a workforce that can provide direct family support to parents and their children. In theory, it could be delivered anywhere, so long as the parent has time to engage with the practitioner and has regular access to the children or there is a reunification plan in place. It can be delivered to single parents or couples/co-parents and it can include other carers who are significant in the child’s life, for example kinship carers, foster carers and, of course, non-resident fathers.
Evidence from our expert event with key stakeholders, and subsequent follow-up public engagement events since October 2020, provides some confidence that the PuP programme is a ‘good fit’ with current policy and practice, and could potentially be integrated into many different non-NHS settings in the future. For further details on the findings from the expert event, and stakeholder views on how this could be achieved, see Expert event (public engagement).
Research question 5: what is the optimal level of recruitment, consent and retention for a future trial?
Optimal level of recruitment and consent
There were 44 fathers referred into the study, of whom 38 (86%) met the eligibility criteria. Of these fathers, 25 (66%) consented to take part in the study (i.e. 57% of referral numbers). For this population, this is a very reasonable conversion rate. In most cases, if the research team managed to speak to the father and meet them in person, then they were willing to take part and so were the mothers. However, one father was incarcerated during the intervention phase and four other fathers had criminal court cases and/or permanency proceedings instigated on account of serious levels of violence that made them ineligible to proceed to allocation for the PuP intervention after consenting into the study. Only one father withdrew of his own volition before allocation. These situations are perhaps more likely to occur with fathers than mothers in parenting research involving substance-using parents. If one subtracts these five fathers from the total number eligible, then the percentage to allocation is 52% (or 45% of all referrals). In a recent study in Glasgow involving the recruitment of ‘hard-to-engage’ mothers into THRIVE (Trial for Healthy Relationship Initiatives in the Very Early years), MacLachlan et al. 91 reported that 50% of women referred were recruited to the trial. This suggests that a realistic rate of referral to consent in a main study would be around 50% (i.e. double the number of participants would be required to ensure that enough patients were eligible, consented and allocated to the intervention).
One way of ensuring that a larger number of eligible fathers are referred into the study is to check that the study inclusion criteria is compatible with the inclusion criteria for the service that will be delivering the intervention. In our study, these ‘thresholds’ varied somewhat between areas and across services, with some fathers and families accepted into the programme where there were permanency proceeding in place, and others not. Although the decisions regarding the inclusion or not of fathers in the intervention were made for very good reasons, these referrals were quite challenging to manage. For example, when these fathers were included in the study, supervised contact arrangements for the father and child to meet with the PuP practitioner were not always sanctioned by the corporate parents (social services) and only two researcher meetings could be arranged to conduct the EAS video-observational measure during contact visits. Therefore, the practicalities of delivering the intervention with fathers who have very little contact with their children, and where the practitioner cannot work with the parent and child together, limits the delivery of the programme as intended, although, arguably, the delivery of the programme could change the course of proceedings. With one family enrolled in the study, this is exactly what happened and their child was returned to the parents’ home. Therefore, agreeing eligibility to join the study with the service delivering the intervention may be the most pragmatic way to manage consent with a population whose circumstances are complex and difficult to predict.
Optimal level of retention
Retention in the study was also very respectable for this population. Twenty-three fathers completed baseline measures and the first qualitative interview, 16 completed FU1 and a second qualitative interview and 13 completed FU2. In terms of our pre-set progression criteria, we proposed a minimum of 10 fathers to complete FU2 measures plus one qualitative interview.
Retention of those who were allocated to the intervention (n = 20) was also reasonable. Thirteen of 20 (65%) fathers were retained in the study for a period of up to 18 months. By applying all the learning from this study about strategies that can improve retention with this population (see Chapter 5), it would be reasonable to expect that we could reach a 70% retention rate, provided all fathers who consent are allocated to the intervention and contact between the researcher and the family is frequent (e.g. monthly).
In terms of retention in the intervention, 14 of 20 (70%) fathers completed six or more sessions. The median number of sessions was 13, the median length of engagement was 26 weeks and mean attendance was 71%. Again, these are high retention and attendance rates for this population. However, there was a great deal of variation in participant’s timelines through the study, from referral to consent, to baseline, to intervention start date and to follow-up time points. Allowance for these variations and measures to mitigate them would be important considerations in a larger trial. Time from baseline to PuP intervention start dates varied from 1 day to 10 weeks. Three of the four families (FA05, FA15 and FA19) that waited longest for a PuP practitioner to be allocated subsequently had very short engagement with the intervention, suggesting that timely engagement with a practitioner may be an important factor. Capacity issues were a factor in the delays and so ensuring adequate capacity and sustainability of intervention delivery in a main study will be important issues to address.
A number of families did not complete the PuP programme and reasons for this were not always available. However, for at least four families (FA15, FA17, FA19 and FA24), life events and crises had an impact on their capacity to fully engage with the practitioner at an early stage. Repeat non-attendance at appointments led to families being discharged from the service in all these cases. When interviewed at follow-up, one family (FA17 and MO17) expressed disappointment at the speed of this and a desire to re-engage, which involved re-referral and a lengthy delay. Planning mechanisms to accommodate short-term disengagement might be worth considering if the service can manage this in terms of their waiting lists, role and remit, and commissioning targets.
Research question 6: what are the best methods of collecting outcome data from fathers and mothers at baseline and follow-up time points?
The methods employed in this study were largely very successful in collecting outcome data from fathers and mothers, resulting in very few missing data. Once contact with participants was achieved, completion rates for most measures were very high. Completion rates at each time point for administered questionnaires are reported in Appendices 8–14.
The methods employed were extremely resource intensive. Undertaking interviews in people’s homes was complex to organise and difficult to manage because of a range of issues, including participants changing address and telephone numbers frequently and, therefore, often being difficult to reach; co-ordinating availability between participants and two researchers, where needed for safety reasons, was challenging; the home environment was unpredictable and sometimes chaotic and, therefore, administration of the questionnaires was not straightforward; time was needed to build a rapport with parents before asking sensitive and intrusive questions; and mothers and fathers needed to be interviewed separately and in private, and this often took some time to achieve. However, if these issues were managed well, it did help to create trust and this, in turn, helped to facilitate successful interviews with this hard-to-engage population. With the exception of one measure (i.e. the service use survey; see Research question 8: how acceptable and appropriate are the assessment methods?) the questionnaires were researcher administered, which helped overcome any issues with literacy and numeracy. It also allowed the researcher to offer explanations, where required, to contextualise questions that were sensitive (e.g. around domestic violence) and to be alert for signs of distress.
Interviews with each parent were also very lengthy and it was important to allow lots of time, for example, to chat and establish a rapport; to engage with participants who were sometimes affected by medication or other drug use, or who were distressed because of life crises; and to accommodate the busy schedules of families with young children (e.g. nursery/school pickups or meals), who were often very busy with appointments for various services (commonly midwives, health visitors, social work, prescriber, psychologist, other drug workers, housing department and welfare benefits agencies).
Research question 7: how feasible is it to collect attendance, medical and cost data on participating families?
The feasibility of collecting research data via other sources and using other methods, other than researcher-administered questionnaires and parent self-report, was tested in this study. In this section of the report, we consider the results of collecting attendance data, NHS data on OST prescriptions, social work data on child protection interventions and parent self-completed cost data for a future economic evaluation.
Attendance data
Results show that attendance data can be reliably collected from practitioners who deliver the programme, and with relative ease. We requested attendance data from practitioners by creating an attendance sheet (one for each father and mother participant with ID codes) that asked for the date of every PuP session scheduled and whether or not it was attended. Sheets were sent and returned by e-mail and practitioners referred to their case notes and diaries to complete the sheets. This approach resulted in no missing data (assuming that case records and practitioner diaries were accurate).
Completed attendance sheets allowed for the calculation of the total number of sessions delivered to the cohort (and to fathers, mothers and couples), as well as father and mother attendance rates, the number of sessions attended and the length of engagement in the programme. Attendance sheets also provided a useful insight into variability in the way the programme was delivered to different families, with some couples attending all sessions together and some families receiving a large number of individual-based sessions (i.e. father- and mother-only sessions) as well as couple sessions. We were able to conclude from these attendance data that fathers who enrolled in this study engaged in the programme in similar ways, and to much the same extent, as mothers.
Based on these findings, it would be feasible to obtain attendance data in a main study. These data would be required to further examine ‘dose’ response. The dose parameters could potentially be extended, for example, to include not only the frequency, duration and number of PuP sessions, but also the number and type of modules completed/not completed as per individual family case formulation. These additional data could enable a more nuanced analysis of dose response in relation to identified family needs and goals, and the degree of fidelity could be evaluated across the intervention dose parameters. This could be supplemented, for example, by asking participants about their views on the acceptability, feasibility and effectiveness of a programme in which the dose is tailored to a family’s needs or delivered more uniformly to accommodate service capacity. 92
NHS prescription data
Twenty-three out of 25 (92%) fathers consented to their OST prescription data being obtained from NHS records (two fathers did not consent). Two fathers withdrew from the study and so we requested data on 21 fathers and their partners (if opioid dependent, n = 13). Data were requested from NHS Lothian drug treatment services and participants’ GP prescriber if their drug treatment was managed in primary care. Our approach for obtaining the prescription data was to request this by e-mail to the secondary care addiction service lead pharmacist and by letter to GP prescribers.
Our approach was moderately successful. Approval to obtain data from the addiction service prescription database was granted by the lead pharmacist soon after requesting it in October 2020. However, pressures on the service because of COVID-19 meant that the data were not extracted and made available to the research team until 30 December (after several prompts). There were no refusals from GPs to provide data, but returns were incomplete. It is acknowledged that not all data could be obtained from GPs, as participants frequently changed their GP if they changed address and participants also moved between GPs and the addiction service for their OST prescription (e.g. if they needed to be titrated to a higher dose, the GP would refer back to the addiction service). Owing, in part, to this movement, and to the long time period of the request, addiction service prescription data were more reliable and complete than data from GPs.
Fathers
Prescribing data were obtained for 13 of 21 (62%) fathers. Data were obtained from a GP prescriber for 6 of 13 (46%) fathers and data were obtained from addiction services for seven of eight (87.5%) fathers (although there were no addiction records for one father who, presumably, was wrongly categorised). Table 4 provides data on the opioid prescribed and daily dose at baseline and reported increases, decreases or use of the same dose at FU1 and FU2.
| Data collection time period | Dosea | |||
|---|---|---|---|---|
| Range (mg) | Mean (mg) | Number of fathers | Missing | |
| Methadone | ||||
| Baseline | 30–125 | 90 | 9 | 1 |
| FU1 | 65–120 | 87.5 | 10 | 0 |
| FU2 | 50–120 | 85.5 | 10 | 0 |
| Buprenorphine | ||||
| Baseline | 8–16 | 11.3 | 3 | 0 |
| FU1 | 8–14 | 10.7 | 3 | 0 |
| FU2 | 6–12 | 9 | 2 | Changed substitution therapy (n = 1) |
| Same dose | Increased dose | Decrease dose | ||
| Baseline to FU1, n (%) | 5 (38.5) | 2 (15.4) | 5 (38.5) | 1 at baseline |
| FU1 to FU2, n (%) | 7 (53.8) | 2 (15.4) | 3 (23.1) | Changed substitution therapy at FU2 (n = 1) |
| Baseline to FU2, n (%) | 3 (23.1) | 4 (30.7) | 4 (30.7) | Baseline (n = 1). Changed substitution therapy at FU2 (n = 1) |
Mothers
For mothers in the study, 13 of 17 consented to data about their prescriptions being obtained (two mothers withdrew from the study and two did not consent). Prescribing data were obtained from GP prescribers and addiction services for 8 of 13 (62%) mothers, from GP prescribers for three of eight (38%) mothers and from addiction services for five (100%) mothers. Table 5 provides data on the opioid prescribed and daily dose at baseline, as well as reported increases, decreases or use of the same dose at FU1 and FU2.
| Data collection time period | Dosea | |||
|---|---|---|---|---|
| Range (mg) | Mean (mg) | Number of mothers | Missing | |
| Methadone | ||||
| Baseline | 60–90 | 73.5 | 7 | 0 |
| FU1 | 60–90 | 75.8 | 6 | 1 |
| FU2 | 10–90 | 55.8 | 6 | 1 |
| Dihydrocodeine | ||||
| Baseline | 125 | 1 | 0 | |
| FU1 | 125 | 1 | 0 | |
| FU2 | 125 | 1 | 0 | |
| Same dose | Increased dose | Decreased dose | ||
| Baseline to FU1, n (%) | 5 (62.5) | 2 (25) | 0 | 1 |
| FU1 to FU2, n (%) | 4 (50) | 0 | 3 (37.5) | 1 |
| Baseline to FU2, n (%) | 3 (37.5) | 1 (12.5) | 3 (37.5) | 1 |
We compared NHS prescription data reports with parent self-reported OST data (i.e. drug type, daily dose and dose changes over time). There was high congruity between self-reported data (from both opioid-dependent fathers and mothers) and NHS administrative data records. Given the level of accuracy of self-reported OST dose, it may be a more reliable data source and more feasible to collect for a future study, and NHS prescription data can be accessed to fill in any missing data and as a random cross-check on a percentage of the sample at baseline and follow-up (assuming permissions to access the data are obtained).
Child protection data
Social Work Scotland data were requested from two local authority children and families services. We requested child protection data on two children (from two families) from East Lothian Council in early January 2020 (this request was sent to the chief social work officer, as instructed by Social Work Scotland). Our request was treated as a freedom of information request and processed as such. It was then passed to the data protection officer for the council. After some correspondence back and forth, we received approval on 17 February 2020. It was then passed back to the chief social work officer to extract the data and return to the research team. However, the COVID-19 pandemic took effect in March 2020 and we were unable to pursue the return of the requested data.
We also requested data on 10 children (from eight families) from the City of Edinburgh Council in January 2020. We were then asked to complete a research study ethics application to conduct research in the council. However, COVID-19 delayed the completion and processing of this request for many months. We decided to pursue this application again in October 2020 to test whether or not ethics approval could be obtained, in principle, as the majority of families in the study were located in this local authority. We were given approval in December 2020 and the request was then sent to a social work manager to extract the data and return to the research team. This resulted in a full data set for these children.
In summary, the feasibility of obtaining child protection data from social services records on index children in this study was successful in terms of obtaining informed consent from study participants (only two families refused) and receiving approval to access and extract the data from responsible local authorities. However, COVID-19 created unavoidable obstacles to the data being provided within the timescale of this study. In a future larger evaluation of PuP4Dads, assuming that it is not conducted within the context of a pandemic, it would be reasonable to conclude that data of this nature could be obtained, although retrieving these data may take some months.
Cost data
Only one father returned the service use survey sheets to the researcher (a full set). Parents were open to the idea of self-completing a service use questionnaire, which included questions on health care, social work, criminal justice and drug treatment utilisation, to test the feasibility of a conducting a future health economic assessment in a main study. Participants were asked to self-complete the questionnaire after each PuP session and return the questionnaire to the researcher at follow-up. Participants were given a supply of forms at baseline. Reasons for not completing the forms included ‘forgot to fill them in’, ‘had lost or misplaced the forms’ or ‘had moved house and lost them in the move’.
Practitioners in this study refused to administer the questionnaires and/or collect them, citing concerns over their responsibilities in terms of child protection if they were party to any of the information contained in the service use reports (e.g. if the parent recorded that they had taken the child to accident and emergency, but had not disclosed this information to the practitioner, then they would have to pass this information on to social services if the child was on the child protection register). After a number of parents failed to return the forms, the research team asked the practitioners if they would be willing to remind parents to complete the forms at each PuP session visit. Practitioners agreed to do this. However, this resulted in no further returns. This highlights the critical importance of researcher support for data collection with this population.
Research question 8: how acceptable and appropriate are the assessment methods?
Acceptability of the measures
The majority of fathers and mothers reported that the study measures were acceptable, with no refusals to answer the questions asked of them. One father withdrew from the study after he completed all the baseline measures because he found the interview ‘intrusive’. He specifically objected to questions contained in the sociodemographic sheet (e.g. regarding his and his family’s income). He did not voice any objections to the validated measures themselves. One family declined to take part in the video-observational measure (i.e. the EAS), voicing concerns over confidentiality, and one mother declined consent for video-recording for the EAS measure and obtaining data from social work about child protection (this mother had experienced having a child removed from her care previously). A few other parents were reluctant to consent to researcher access to NHS and social services data, but were reassured when they were told that detailed child protection reports would not be obtained and their wider health records would not be available to the research team. A few parents required reassurance about confidentiality before they were willing to disclose illicit drug use (via the TOP measure). There were no objections to requests for criminal justice/offending data (contained in sociodemographic data and received via the TOP measure and service use survey). Some parents found the CTS2 long and repetitive and the language in the CTS2 challenging because of the explicit content and non-culturally relevant references (e.g. ‘rape at gun point’), although this did not stop parents answering the questions.
Some PuP practitioners voiced initial concerns over the CTS2 after the researcher told them it was ‘intrusive’ and ‘sexually explicit’. Practitioners felt that this may negatively affect their relationship with the family and, for the first 6 months of the study, these practitioners were reluctant to refer families. The PuP practitioners were reassured after the research team indicated that the fathers/mothers themselves voiced no strong objections to the CTS2 questionnaire and that completion rates were high.
Suitability of measures
Approximately half the measures used in this study were found to be suitable for the study population at every time point and were easily understood and appropriate for the circumstances of the parent. These included the BCAPI, the DERS, the TOP and the EQ-5D-5L. Other measures were found not to be not suitable (i.e. the service use questionnaire) or only partially suitable (i.e. the EAS, the SDQ, the BITSEA, the PAAS and MAAS, the PSCS and the CTS2).
Although the EAS (i.e. the video-observational measure of parent and child interaction) was acceptable to most parents (with 22 of 23 fathers consenting to video-recording), ultimately it proved infeasible to undertake for most families at most time points. Some participants were expectant parents when enrolled in the study and so the baseline EAS measure could not be obtained. Some parents did not have custody of their index child at FU1 and some did not have custody at FU2, and so, again, the EAS measure could not be obtained. In two of these cases, the corporate parent (social services) consented to the video measure being taken during a supervised contact visit between the father and child, but this took considerable time and effort to arrange. Nevertheless, it demonstrated that administering this measure when children are accommodated is technically feasible. However, the main obstacle to collecting video-recordings in this study was obtaining and complying with NHS R&D requirements for data management and security. This included purchasing an NHS laptop and having this set up by the NHS information technology department, negotiating to use the laptop to record video files on the device (this required Caldicott Guardian approval) and negotiating permission to store the data on NHS servers. This whole process took over 12 months before the first video measure could be undertaken. In addition, the NHS laptop (and hence all the videos) could be used only by the principal investigator (AW), who was an NHS employee. This meant that the principal investigator needed to attend all home visits (at baseline and at 6 and 12 months) where it was possible to obtain a video-recording. This required considerable flexibility because of the high rates of cancellations/rearranging appointments and so the feasibility of successfully obtaining the data was extremely low (hence the limited numbers of completed EAS measures). In addition, the EAS measure requires coding by trained EAS coders (to be undertaken by Griffith University) and this was not possible because of COVID-19.
The child development/well-being measures (i.e. the SDQ and the BITSEA) were partially suitable because the age range of children in this study (i.e. 0–8 years), the longitudinal nature of data collection (over three time points and spanning a minimum of 12 months) and the age limits for the use of the measures meant that infants aged < 12 months at any time point had no measures taken, some who were aged between 12 and 36 months completed the BITSEA only, and some completed the BITSEA and then the SDQ. In addition, the BITSEA contains several questions that assumes that the parent has custody of the child, as they relate to everyday child care/contact, and so this measure was inappropriate for several participants whose children were accommodated (e.g. in kinship or foster care). Therefore, very few index children in the study had the same measure administered at all three time points. In a larger evaluation, child development and well-being could be consistently measured across multiple time points using the SDQ, but only for children who are aged > 24 months at baseline. Arguably, a measure of child development/well-being for infants aged 0–24 months who are accommodated for substantive periods of time or hospitalised as neonates on account of neonatal abstinence syndrome (both of which can affect early development) may not reflect parental care provided by the study participants. Likewise, the antenatal attachment scales (i.e. the PAAS and MAAS) were easy to administer, but were administered only once at baseline (before the baby was born), as the EAS was the preferred measure after the baby was born.
Other measures were found to be unsuitable for some study participant because of their circumstances. The CTS2 (domestic violence) questionnaire was only partially suitable, as some fathers were not in a relationship at one or more of the data collection time points and so this measure was not applicable to them. Likewise, the PSCS was suitable for only those participants who were already parents. First-time expectant parents were unable to complete this scale. However, in a larger evaluation with multiple data collection time points, this measure could be suitable for expectant parents, as only the baseline measure would be missing data.
Burden on participants
The number of questionnaires administered (i.e. nine at baseline, 10 at FU1 and nine at FU2) and their length and complexity (i.e. the large number of questions per questionnaire and time taken to explain some questions) meant that administration of the measures was burdensome for many parents, with the length of time to complete each interview being approximately 2–3 hours. Many questionnaires broached highly sensitive topics, including illicit drug use, domestic violence, child abuse, criminal justice issues, parenting attitudes and values, and so could not be administered ‘cold’. The researcher needed to build rapport with the parents before launching into the data collection and so sociodemographic data were collected beforehand. Most parents had complex social circumstances and multiple health problems to report. This meant that the researcher needed to arrange two home visits with couples for each interview time point.
Administration of measures
Data were not to be obtained by asking the parents to complete the measures unaided or over the telephone, via the internet or in a clinic setting. The reasons for this were that some parents in this population had poor literacy and numeracy skills, some questions needed to be explained to parents (or parents asked for clarity on their meaning), some parents had a limited attention span/poor concentration and need to be prompted, and most parents would not return data if requested to do so. Clinic appointments are also not suitable, as attendance is often poor and parents do not have access to reliable child care (or they have limited child care) and so attending long appointments is not feasible. Administration by telephone or via the internet was not feasible because of the duration of administration, poor mobile telephone connections or unreliable internet access (i.e. no money for data), and many parents did not have internet access in the home or were not digitally literate. Last, many of the topics are sensitive in nature and the data are not appropriate to obtain remotely, as privacy and confidentiality could not be assured (i.e. other people present in the home). It should be noted that in line with policies on lone working and home visiting, two staff must attend the first home visit for safety reasons and to undertake a fieldwork risk assessment to establish whether or not it is safe to return alone. In addition, where the study involved both the father and mother enrolled in the programme, the researcher often had to visit the home on two separate days to interview each parent individually (to maintain confidentiality and also because one parent had to look after a child while the other completed the questionnaires/recorded interviews).
Feasibility of collecting data
Overall, most measures administered in this study were well tolerated by the participants, and completeness of data within and across measures were high. However, data collection was extremely time-consuming and resource intensive. Nevertheless, the methods we employed to overcome barriers to data collection were largely successful and we identified several strategies that could be employed in a future evaluation to improve completion and retention rates. Most notably, more frequent researcher contact with participants and fewer measures administered per contact. In addition, more rigorous methods of contact tracing participants who become unobtainable could be employed, along with telephone calls to complete short questionnaires (e.g. the ED-5D-5L) or small numbers of missing data (e.g. sociodemographics). Some repeat measures in a future study may be suitable for video calls (e.g. the BCAPI) if headsets could be provided to participants to offer privacy and mobile data costs could be paid for, although, as stated previously, digital literacy is likely to remain problematic in this population.
Research question 9: is the profile of change in fathers, mothers and children clinically significant?
We assessed the profile of change in families, and the potential clinical significance of the findings, in three ways:
-
Data from measures completed at baseline, FU1 and FU2 (before and after the intervention) were examined.
-
The RCI was used to determine individual change in relation to parental child abuse risk (a potential primary outcome for a main study) and parental emotion regulation (a potential mediator to measure in a main study).
-
Qualitative data on the perceived benefits of the programme for families from a parent and practitioner perspective were examined.
The pattern of results observed before and after the intervention for those who were followed up were in a positive direction. Quality of life and parenting sense of competence increased between baseline and FU1 and, again, between FU1 and FU2, whereas parental child abuse risk, difficulties with emotion regulation and levels of violence within couple relationships decreased between the same time points. In addition, fathers reported an increase in the number of days abstinent from alcohol and illicit drug use (on the TOP measure) between baseline and FU1 and, again, between FU1 and FU2. The whole sample is presented in Table 6, along with the fathers who engaged in six or more PuP sessions (classed as ‘engagers’).
| Cohort sample and measure | Baseline | FU1 | FU2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Range | Median | IQR | n | Range | Median | IQR | n | Range | Median | IQR | |
| Fathers | ||||||||||||
| Quality of life: EQ-5D-5L | 22 | 0.23 to 1.00 | 0.69 | 0.16 | 16 | 0.48 to 1.00 | 0.75 | 0.18 | 13 | 0.6 to 1.00 | 0.84 | 0.31 |
| BCAPI | 20 | 1 to 24 | 12 | 14.5 | 16 | 2 to 19 | 9 | 8 | 12 | 1 to 18 | 6.5 | 10.75 |
| PSOC | 16 | 42 to 91 | 65.7 | 16.25 | 15 | 45 to 92 | 68 | 25.4 | 10 | 57 to 91 | 74.5 | 21.25 |
| DERS | 21 | 38 to 152 | 95 | 73.12 | 16 | 42 to 124 | 79 | 29.25 | 12 | 37 to 123 | 74 | 52.5 |
| CTS2 total violence in previous 12 months | 17 | 0 to 93 | 25 | 44 | 12 | 0 to 32 | 5.5 | 24.75 | 6 | 0 to 10 | 0 | 4 |
| TOP (days abstinent/28) | 23 | 0 to 28 | 18 | 10.06 | 16 | 0 to 28 | 24 | 7 | 13 | 0 to 28 | 26 | 9 |
| TOP [days abstinent (except cannabis and alcohol)/28 days] | 23 | 0 to 28 | 28 | 8.536 | 16 | 23 to 28 | 28 | 1 | 13 | 20 to 28 | 28 | 2 |
| Mothers | ||||||||||||
| Quality of life: EQ-5D-5L | 17 | 0.14 to 1.00 | 0.74 | 0.37 | 10 | –0.35 to 1.00 | 0.71 | 0.68 | 9 | –0.15 to 1.00 | 0.8 | 0.42 |
| BCAPI | 13 | 2 to 22 | 10 | 12.5 | 11 | 3 to 20 | 13 | 13 | 8 | 3 to 18 | 6 | 9.25 |
| PSOC | 9 | 53 to 88 | 73.6 | 9.33 | 8 | 41 to 87 | 75.5 | 22.75 | 7 | 55 to 88 | 72 | 14.2 |
| DERS | 17 | 43 to 138 | 69 | 44.69 | 11 | 42 to 129 | 65 | 45 | 9 | 51 to 136.8 | 68 | 25 |
| CTS2 total violence in previous 12 months | 14 | 4 to 94 | 33 | 36 | 9 | 3 to 69 | 23 | 42 | 5 | 5 to 33 | 20 | 23 |
| TOP (days abstinent/28) | 14 | 0 to 28 | 26.5 | 13 | 10 | 26 to 28 | 27.5 | 1 | 8 | 20 to 28 | 26.5 | 4 |
| TOP [days abstinent (except cannabis and alcohol)/28 days] | 14 | 0 to 28 | 28 | 8 | 10 | 26 to 28 | 27.5 | 1 | 8 | 26 to 28 | 28 | 2 |
| PuP engagers only | ||||||||||||
| Fathers | ||||||||||||
| Quality of life: EQ-5D-5L | 13 | 0.42 to 1.00 | 0.73 | 0.31 | 12 | 0.55 to 1.00 | 0.75 | 0.13 | 11 | 0.60 to 1.00 | 0.81 | 0.36 |
| BCAPI | 12 | 1 to 24 | 10 | 17.25 | 12 | 4 to 18 | 9 | 4.75 | 10 | 1 to 18 | 9.25 | 10.75 |
| PSOC | 7 | 42.29 to 74.00 | 65.23 | 7.27 | 12 | 44.57 to 92.00 | 68 | 20.6 | 8 | 57.00 to 85.00 | 70 | 16.9 |
| DERS | 13 | 38 to 152.23 | 81 | 72 | 12 | 42 to 124.00 | 79 | 27 | 10 | 37 to 123.00 | 74 | 64.75 |
| CTS2 total violence in previous 12 months | 10 | 0 to 93 | 10 | 57.75 | 10 | 0 to 32 | 2.5 | 12.75 | 5 | 0 to 10 | 0 | 6 |
| TOP (days abstinent/28) | 14 | 0 to 28 | 23 | 11 | 12 | 0 to 28 | 25 | 9 | 11 | 0 to 28 | 22 | 10 |
| TOP [days abstinent (except cannabis and alcohol)/28 days] | 14 | 10 to 28 | 28 | 5 | 12 | 23 to 28 | 28 | 1 | 11 | 20 to 28 | 28 | 3 |
| Mothers | ||||||||||||
| Quality of life: EQ-5D-5L | 10 | 0.21 to 1.00 | 0.78 | 0.17 | 9 | –0.35 to 1.00 | 0.75 | 0.45 | 8 | –0.15 to 1.00 | 0.86 | 0.5 |
| BCAPI | 7 | 2 to 21.5 | 10 | 13 | 9 | 3 to 20 | 13 | 13.5 | 7 | 3 to 18 | 5 | 7 |
| PSOC | 2 | 72.53 to 73.6 | 73.1 | – | 8 | 41.0 to 86.86 | 75.5 | 22.79 | 6 | 55 to 88 | 73 | 17.25 |
| DERS | 10 | 58.63 to 120 | 69 | 31.75 | 9 | 42 to 129 | 64 | 49.5 | 8 | 51 to 136.8 | 66.5 | 28 |
| CTS2 total violence in previous 12 months | 8 | 5 to 83 | 34 | 33.5 | 8 | 3 to 69 | 19 | 44 | 5 | 5 to 33 | 20 | 23 |
| TOP (days abstinent/28) | 9 | 14 to 28 | 26 | 11 | 8 | 26 to 28 | 28 | 1 | 7 | 20 to 28 | 26 | 4 |
| TOP [days abstinent (except cannabis and alcohol)/28 days] | 9 | 14 to 28 | 28 | 10 | 8 | 26 to 28 | 28 | 1 | 7 | 26 to 28 | 28 | 2 |
Parental child abuse risk
Evidence of statistically significant improvement in child abuse risk, using the BCAPI measure, was seen for 4 out of 14 (29%) fathers at FU1 and this was maintained at FU2. One of eight (12.5%) mothers at FU1 and four of six (67%) mothers at FU2 showed evidence of statistically significant improvement using the BCAPI. When the results of PuP programme ‘engagers’ were examined (i.e. those who had attended six or more PuP sessions), the pattern was similar.
Parental emotion regulation
Evidence of statistically significant improvement in emotion regulation, using the DERS measure, was seen for 7 of 15 (47%) fathers overall at FU1 and for 4 of 11 (36%) fathers at FU2. One of 11 (9%) mothers at FU1 and two of nine (22%) mothers at FU2 showed evidence of statistically significant improvement in emotion regulation. When the results of PuP programme ‘engagers’ were examined (i.e. those who attended six or more PuP sessions), the pattern was similar, but a larger proportion of fathers who engaged in the PuP programme maintained the improvement in emotion regulation at FU2 than the overall sample (40% vs. 27%, respectively).
Profile of change outcome measures for fathers and mothers is presented in Table 7.
| Cohort sample and measure | Baseline to FU1, n (%) | Baseline to FU2, n (%) | ||||
|---|---|---|---|---|---|---|
| Deterioration | No change | Improvement | Deterioration | No change | Improvement | |
| Fathers | ||||||
| BCAPI: all | 0 (0) | 10 (71) | 4 (29) | 0 (0) | 10 (71) | 4 (29) |
| BCAPI: PuP ‘engagers’ | 0 (0) | 7 (70) | 3 (30) | 0 (0) | 6 (75) | 2 (25) |
| DERS: all | 2 (13) | 6 (40) | 7 (47) | 0 (0) | 7 (54) | 4 (27) |
| DERS: PuP ‘engagers’ | 2 (17) | 5 (42) | 5 (42) | 0 (0) | 6 (60) | 4 (40) |
| Mothers | ||||||
| BCAPI: all | 0 (0) | 7 (87.5) | 1 (12.5) | 0 (0) | 2 (33) | 4 (67) |
| BCAPI: PuP ‘engagers’ | 0 (0) | 5 (83) | 1 (17) | 0 (0) | 2 (40) | 3 (60) |
| DERS: all | 1 (9) | 9 (82) | 1 (9) | 1 (11) | 6 (67) | 2 (22) |
| DERS: PuP ‘engagers’ | 1 (11) | 7 (78) | 1 (11) | 1 (12.5) | 6 (75) | 1 (12.5) |
Qualitative data on the impact of PuP4Dads
Fathers reported multiple benefits as a result of engaging in the PuP programme, which, to a large extent, were good and accurate reflections of some of the core components of the programme and the goals of the intervention, namely improved relationships with their children, a better understanding of their children’s needs, improved parental emotion regulation, increased parental self-efficacy, better couple relationships and co-parenting, increased social support, improved goal-setting and multiagency working and a greater understanding of the effects of their substance use on their children. Woven into many of the accounts from fathers were references to the therapeutic alliance with their PuP practitioner and the importance of trust, respect and collaborative working. The selected excerpts below illustrate some of these points.
The following quotation illustrates better understanding of children’s behaviour and developmental needs:
Oh, a lot better. More, a better understanding of his way of thinking . . . I never used to, it’s like, I was brought up with my grandparents, as I said, brought up where children should be seen and not heard. So, that’s kind of the deal I had at first with my other kids, and with [my boy] . . . and everything[s] changing. I’ve kind of, you know, it’s more about him . . . I can understand where he’s coming from as a kid, and not knowing things . . . I do get why, sometimes, they react the way they react . . . and not understanding . . . and security and safety, and how important that is, to feel secure.
Father 4
The following quotation illustrates a helpful approach to goal-setting:
Yes, instead of getting muddled up, likes the drug workers telling you ‘right, they want you to do this’ . . . and social worker this, this and this. Then you’re muddled up. You don’t know what you’re doing. If you’ve just got one set of goals to do instead of three or four different sets of goals, [if] you get muddled up and you forget to do some of it . . . it goes badly against you.
Father 11
The following quotation illustrates parents connecting with their children:
Just getting me to connect more with my daughter, ’cause I felt disconnected because of my anxiety, and not going out and that, not being able to play. Like, not a lot of dad stuff, going to school, go to the park.
Father 6
The following quotation illustrates parents building parental self-efficacy:
Just being able to have one-to-one time with someone who was a professional in that field and getting feedback from them about myself was . . . I found that really, really good; most of their feedback was . . . in fact just about all of their feedback was really positive.
Father 12
The following quotation illustrates parents connecting with their family and building social support:
I’ve started talking to my own family more, you know, these are just things that I was speaking to with [the PuP practitioner], yeah . . . I’m getting on a lot better with my mother than I did. I see my dad a little bit more than I did, you know. And we’re going to be looking at getting in contact with my other two children . . . that’s something we’re going to look at in the future, you know.
Father 13
The following quotation demonstrates emotion regulation:
Just like if he’s misbehaving, just . . . what’s it called, the pause button or something, so you’re not jumping right in and shouting or giving him a row. Just like stopping and thinking is it really that bad what he had done.
Father 6
The following quotation demonstrates therapeutic alliance and trust:
Honesty and trust, like, aye, being able to approach them and if things go wrong . . . then you know, that it’s just not going to fall apart . . . and they’ll work with you, you know, and make things better if things go wrong, and I think that’s the key thing there.
Father 9
The following quotation illustrates the impact of substance use on children:
[PuP has] given me a lot more insight into how my kids were, kind of, thinking, you know. Obviously, as I’ve said to you before, it’s the kids that suffer. I can sit and I can wax lyrical all day long about, like, woe is me, and how bad I feel; but really . . . learning a lot more about how it [substance use] affected them, that was really, really super helpful.
Father 23
The following quotation demonstrates a ‘whole-family’ approach:
I think, [names PuP practitioner], I think, he works more with the whole family, whereas other services they’re just working with [names his child] or like with our drug use.
Father 6
Some fathers directly attributed their engagement in the programme to getting their child home, having more contact with their child or being ‘given a chance’ to retain custody of their children:
They’ve even said it recently, so you are . . . what’s the right word, like a rare example of a child, a baby going into care, and how quickly you managed to turn it all around, and get her back home, and get yourselves straightened up.
Father 12
I think [PuP] should be made compulsory, especially if the social worker’s thinking of removing the children, I think it might be, like, giving the parents more of a chance, and having more things in place to help parents, rather than just stepping in and taking the bairn [child] away straightaway.
Father 2
Mothers reiterated many of the same positive aspects of the programme, but also made the point that the programme had helped them as mothers and as a couple because the programme engaged with the father and involved the father in co-parenting:
We did it at the same time, so we were communicating the whole way through, but yeah, I think we both got a lot out of it.
Mother 10
We are all doing [PuP] together, it’s something you can get out of together. Because everything is kind of separate at the moment, like [my partner]’s no really been involved in anything, it’s kind of all sort of been on me, and I found that a bit frustrating, and putting me proper under pressure sometimes, because I’m thinking ‘well why is everything end at me!’ and he’s kind of like being left in the background . . . everything’s kind of changing [now], he is involved and people are involving him in things and it’s kind of like, turned round a bit . . . [and] he’s involved.
Mother 13
In summary, the profile of change in individual fathers and families in this study, analysed using quantitative and qualitative data, provides an indication of change that is clinically relevant and important, and is feasible to measure and examine in a main study. Combined with our assessment of the delivery of the intervention, we revised the logic model for the study to account for maternal factors and change in relation to intervention outcomes (see Research question 11: which study design would best suit a future evaluation, including an economic evaluation?).
Research question 10: what is the nature and extent of routine family support services for fathers in drug treatment?
I’ve not had access to, you know, any support for parents that are maybe run by like the council or the government, or anything like that. I’ve had nothing.
Father 23
Data on usual care for fathers in drug treatment emerged in a number of ways, including through interviews with parents at baseline where it was asked about directly, through end-of-treatment interviews with parents (often when they were comparing PuP4dads with previous levels of support for fatherhood) and also from practitioner and service manager interviews where they talked about ‘normal’ practice and the way fathers are conceptualised and treated within a broader parenting support framework. Referrers who took part in focus groups also spoke about ‘normal’ parenting programmes and their views on if they were suitable, accessible or helpful for opioid-dependent fathers.
Fathers who completed an interview at baseline (n = 23) were asked to talk about their prior involvement with parenting or family support services as a father. The majority reported little or no involvement with services in terms of support for fatherhood. Many said that this was the first time they had ever been invited to take part in a family support programme as a parent in their own right. As such, most fathers indicated that taking part in PuP4Dads was meeting an unmet need.
Most mothers who were interviewed (n = 17) agreed:
Back when I had my other two kids, I had never heard of fathers having support. It’s always just been mothers, not fathers, but hopefully things are getting better and there will be more for dads out there.
Mother 1
Both fathers and mothers spoke about routine care for parents who use drugs as being mainly focused on scrutiny (assessing risk), surveillance (monitoring risk) and child protection procedures (managing risk):
I’ve got my social worker, and my social worker’s asking me ‘am I injecting?’ and ken [you know], you’ve asked for help and things like that but, I just felt that I was getting punished for asking for the help, you know.
Father 4
Many fathers and mothers reported negative previous or current experiences with services, particularly social work, but also education and child health services. Accounts drew attention to preconceived negative ideas about fathers who use drugs, a lack of transparency and trust, and services working in silos, for example drug services providing individual psychological support but not parenting support:
I just felt that because I was on methadone at the time, I believe that the social workers had a pre-made view on me, you know, and they stuck to that view, and as I had no-one at the time, I felt like I wasn’t getting supported at all, and I wasn’t part of the child and family unit sort of thing.
Father 13
Fathers indicated a desire to be included in family support services, but reported feeling ignored or excluded, as services were ‘for the mums’ or for mothers and children. Some fathers described being actively excluded from children and family social services (e.g. on account of their non-resident status):
Yeah, for me as a dad . . . I was basically told that it was a child and family service and as I was no longer a member of the family, they couldn’t help me.
Father 13, non-resident father
Some specifically stated that they would have benefited from parenting support at a much earlier stage of fatherhood, for example when their children were much younger or at a difficult developmental stage.
Accounts of both parents and professionals drew attention to structural barriers to engaging fathers in the parenting and child welfare agenda. Examples of gendered practice were common, where the emphasis of professionals and services is on mothers and mothering, with fathers often being ignored or treated as peripheral or as an ‘add on’:
. . . like maternity services . . . you know, by the name, it’s maternal. It’s mum, and dad’s an add on. I think what’s really important about PuP is the way it’s . . . I suppose the way it’s sold for the want of a better expression . . . for dads not to be . . . an add on . . . ’cause that’s what I’m finding really powerful . . . I’m going along to meetings where there’s a wealth of knowledge and information about mum and nothing about dad, and that’s where I feel PuP [has] been crucial . . . I can now go along to meetings and say ‘well, actually, we’ve sat down, this is dad’s views,’ you know; if dad doesn’t want to speak or can’t speak, his views have been heard.
Practitioner 5
In summary, accounts from fathers, mothers and professionals in this study seemed to concur that ‘usual care’ for opioid-dependent fathers was often little or nothing in terms of support for parenting in their own right. This has implications for the design of a main study, which is addressed in Research question 11: which study design would best suit a future evaluation, including an economic evaluation?.
Feasibility assessment
Progression criteria results
Pre-set progression criteria were assessed using project monitoring data, quantitative data results and the analysis of qualitative data. The results are summarised in Table 8.
| Criterion | Indicator | Method of assessment | Results |
|---|---|---|---|
| Successful recruitment of families to the PuP programme intervention and study |
Trained practitioners to recruit and deliver the PuP programme to a minimum of one in five families approached or the average of two families per month Total: n = 24 |
Project monitoring data Note that the recruitment period was extended to July 2019 |
Total number of father referrals: n = 44
|
| Delivery of the PuP programme | The PuP programme delivered to required standard |
A bespoke treatment fidelity measure, rating whether or not 20 core components of the programme were received Administered by the researcher and independently rated by the father and mother |
Good adherence to the model. Median score of 15 of 20 core components of the programme received, according to parent report All practitioners (n = 8) who delivered the intervention to study participants were accredited PuP practitioners All practitioners attended the required training days and submitted a case study to qualify as a PuP practitioner |
| Acceptability of the PuP programme to practitioners | Broad satisfaction of the PuP programme among staff delivering the intervention | Qualitative interviews and regular feedback from practitioners to the Study Research Group |
High level of satisfaction and acceptability of the PuP programme reported by practitioners (n = 8) and PuP supervisors (n = 2) Service managers (n = 7) in delivery sites reported the programme to be a good ‘fit’ with service role and remit, as well as with policy and practice requirements for working with children and families affected by parental drug use |
| Engagement with PuP practitioners in research | 87.5% (7/8) of those approached agree to participate in a qualitative interview | Qualitative interview data | Eight (100%) of the practitioners approached consented to take part in the study and completed an individual qualitative interview. Two practitioners also took part in a second qualitative interview when they qualified as PuP supervisors |
| Engagement in research with staff from agencies referring to the PuP programme | 80% of those approached agree to participate in qualitative interview |
Qualitative interview data Note that referrers were invited to attend focus groups |
Service managers/team leaders cascaded invites to staff and so actual numbers approached are unknown. However, no service declined to promote staff involvement in the research Four out of five (80%) of the focus groups arranged were conducted and a total of 28 staff attended the four groups. One focus group was not convened because of COVID-19 |
| Family engagement with the PuP programme |
66% of families recruited complete the PuP intervention Total: n = 16 |
Project monitoring data Attendance data reported by practitioners |
Completion rates according to allocation, attendance and engagement rates: Four of 25 fathers were excluded from taking part in the PuP programme because they became ineligible after consenting to take part in the study (n = 2) or because the service considered the fathers ineligible for the programme (n = 2). Therefore, 21 fathers consented into the study were allocated to the intervention. One father (and mother) withdrew from the study following baseline, leaving 20 fathers who started the PuP programme Fourteen of 20 (70%) fathers allocated to the programme, or 14 of 21 (67%) fathers eligible to start the programme, completed ≥ 6 sessions (classed as ‘engagers’), and six completed ≤ 5 sessions (classed as ‘non-engagers’) The median length of engagement for fathers was 26 weeks and for mothers it was 30 weeks The median number of sessions attended by fathers was 13 and for mothers it was 14.5 Mean attendance rates for both fathers and mothers was 71% |
| Acceptability of the PuP programme to families | Broad satisfaction of the PuP programme among families receiving the intervention | Qualitative interviews with fathers and mothers | Acceptability of the programme was highly rated among fathers and mothers. All parents interviewed said that they would recommend the programme to other parents who use drugs |
| Family engagement with research component to inform the development of the logic model | Minimum of 10 fathers recruited to the research study to complete the baseline and 6-month (post-intervention FU2) quantitative interviews and at least one qualitative interview | Baseline and 6-month questionnaire data and qualitative interview data |
Twenty-three of 25 (92%) fathers completed the baseline interview and first qualitative interview Sixteen of 25 (64%) fathers completed the FU1 interview and the second qualitative interview Thirteen of 25 (52%) fathers completed the FU2 interviews |
| Adverse effects | Maintain a list of all adverse effects that might arise for each family, comprising those that may be attributed to the intervention and/or the research study | Discussion and decision regarding adverse effects at monthly management, SSC and DMEC meetings | No adverse events were reported and there were no unintended consequences observed as a result of the intervention or research study |
Expert event (public engagement)
Our study protocol included a plan to organise an expert event with a wider group of stakeholders approximately 3 months before the end of the study. In this section, we describe the event and report the findings.
Aim of event
We convened the expert event on 7 October 2020 to present and discuss the preliminary findings from the study with key stakeholders and experts working in the field of child protection, family support and drug treatment services. Owing to COVID-19, this event was delivered online and included the following.
Part 1
An hour-long audiovisual presentation, summarising the findings of the study, presented by the principal investigator (AW). The presentation link was shared with participants who signed up to attend the event. Participants were encouraged to view the presentation in the week prior to the event.
Part 2
Video-conferencing (Microsoft Teams) sessions were conducted with stakeholders to enable a live discussion of the findings and their implications for policy, practice and future research. These sessions were scheduled for 1.5 hours each throughout the day, starting at 09.15, 12.00 and 14.00. The first two sessions were divided into two groups and the last session was held with one group.
At the event, research team members were introduced and the principal investigator provided a brief overview of the study. Stakeholders were then asked to discuss three key questions:
-
What are the implications of the research findings for policy and practice (i.e. impact)?
-
Based on the research findings, what recommendations do you have for future research (i.e. next steps)?
-
What future involvement, including dissemination, would you like to have in a future research study (i.e. buy-in)?
Participants
Policy-makers, commissioners, senior service managers and front-line practitioners from children’s services, drug services, health and social care partnerships and the Government attended the event. In addition, two fathers who took part in the PuP programme as study participants joined the sessions and spoke about their experience of the programme. A total of 31 stakeholders and eight research team members attended. Two research team members facilitated each session and the two PuP developers, a PuP trainer, a PuP supervisor and implementation service managers took part and answered questions on the delivery of the programme, training and implementation issues.
Response to the preliminary findings
Participants were very interested in the study findings and commented that it was the first robust evaluation of involving this population of fathers in a parenting programme in the UK. Stakeholders thought that the ‘deliverability’ of the programme and the level of engagement of fathers was a very good sign that the programme had great potential in ‘real-world’ clinical practice. Most stakeholders acknowledged that there had been efforts to address the needs of this population of fathers (e.g. by employing ‘fathers’ workers’ in family support services for substance users), but that there was an urgent need to include more fathers in ‘whole-family’ interventions, as recommended in policy. 14–16 Stakeholders noted that although most family support services reported that they provide intensive parenting ‘support’, there was often little clarity about what this actually entailed and little evidence that the ‘support’ offered was theoretically informed and could address the complex parenting and child welfare needs of this population. Participants reflected that the PuP model did provide a solid theoretical and operational framework for delivering family support that was compatible with a multiagency ‘partnership’ approach involving NHS, social services and third-sector agencies. From this perspective, the PuP programme was a ‘good fit’ with current practice and service delivery models in both Scotland and England, and also ‘timely’ in terms of current developments, where commissioners are looking to fill the gap in the provision of ‘whole-family’ interventions that governments now promote.
Next steps
Stakeholders were enthusiastic about the prospect of a larger evaluation of the programme and there was considerable discussion on how this could work. There was a strong plea for a pragmatic study that was able to align with ‘real-world’ families and the realities of working with a very challenging population that are stigmatised and fearful of child removal. The inclusion criteria for a main study was discussed and participants felt that there should be efforts to deliver the intervention to more families before they enter the child protection system or at the point of entry to maximise opportunities for families to benefit from the programme and to retain the care of their children and/or to reduce levels of harm to children.
There was some discussion about the ecological model underpinning the programme and how this could foster a more ‘joined-up’ approach to helping this population of families. Some thought that a ‘whole-team’ or area-wide approach to adopting the model would be more strategic and could lead to ‘wider skills development’ of the workforce (e.g. implementation across a local authority or ADP area would ensure that the programme was deliverable and implemented at scale). A locality-wide approach to implementation would also help to create a ‘shared language’ and ‘shared approach’ around supporting children and families within the context of parental substance use. Some suggested that a number of ‘early adopters’ could be identified to begin scale-up of the intervention and these areas could then be involved in a future larger evaluation of the programme. It was noted, however, that most local authorities had only one agency that was providing support for these families (usually a third-sector agency).
Scale-up of the intervention
Stakeholders from both Scotland and England thought that the PuP programme had the potential to address a number of key policy agendas and local strategic planning priorities for children and family services in Scotland and England. For example, the PuP model fitted well with policy and practice initiatives, such as ‘whole-family’ support, ‘family-inclusive’ practice, GIRFEC,62 ‘The Promise’93 and Adverse Childhood Experiences practice development in Scotland. In England, the programme fit well with the ‘Troubled Families Programme’,94 Adverse Childhood Experiences, Family Drug Courts95 and efforts to transform child protection and reduce repeat child removals.
Strategic programme leads for these policy areas indicated that this was ‘good timing’ for scaling up the intervention, as there was an ‘appetite’ for evidence-based intensive home-visiting programmes for families with complex needs who do not engage with ‘standard’ group-based parenting programmes.
Some of the opportunities and challenges of scale-up were discussed and these included the following:
-
Short-term funding and the precariousness of third-sector services that deliver much of the parenting/family support to this population (‘endless commissioning and procurement cycles’). However, the ability of these services to provide an evidenced-based programme would enhance their prospects for successful funding bids and sustainability of programme delivery.
-
The cost of staff training, implementation support for services and sustainability of the model across local authority/ADP areas would need to be considered. However, most thought that the potential positive gains from families engaging in the PuP programme would offset the high costs associated with high rates of child removal (including repeat child removal) and child protection interventions in this population.
Overall, the expert event provided the research team with good evidence that there was sufficient interest in the PuP programme and broad agreement that scale-up of the intervention was feasible and a main study was clinically justified. The expert event resulted in correspondence from policy-makers and commissioners who requested further presentations. On 10 November, we presented the findings to programme leads in Public Health England, and then followed this up with correspondence and a further meeting in January with key service providers in England interested in delivering the intervention and taking part in the research. In addition, follow-up meetings were arranged with interested ADP leads in Scotland and the National Society for the Prevention of Cruelty to Children (Glasgow, UK), which is currently providing the programme, as well as agencies in Ireland that deliver the programme. This interest in the PuP4Dads study culminated in another public engagement event held on 11 February 2021 with potential service providers for a main study to consult on a main study design.
Decision-making using ADePT
The ADePT55 framework was used to guide the decision-making on the feasibility of a main study and whether or not it was justified. The ADePT framework involves the identification and appraisal of problems and solutions to a series of 14 methodological questions in feasibility studies. It allows the research team to consider problems and solutions related to the intervention, the context and the study design to be systematically appraised. Our analytic summary using the ADePT framework is presented in Appendix 16, Table 23.
When we considered problems and solutions to the main methodological issues in the study, we concluded that the results of the study indicate that a main study is feasible. The intervention itself was highly acceptable and suitable for the study population, it was delivered successfully within non-NHS settings and is a good fit for the current policy environment. Recruitment (including eligibility and consent) and retention were very challenging, although the results were more than acceptable for this study population and successful strategies were identified to improve rates. Participant engagement and attendance rates were very encouraging for this population and problems with allocation can be addressed with some revisions to eligibility criteria. Outcome measures were acceptable and well tolerated by the population and completion rates were high (using intensive data collection methods). Most measures were suitable and appropriate for most families. We identified a primary outcome measure (i.e. the BCAPI) and were able to calculate a sample size for a main trial. Interventions costs can be calculated and the feasibility of an economic evaluation for a main study was considered (see The feasibility of health economic evaluation in a main study). We considered the logistics for a multicentre study and tested these in a series of public engagement events, including scale-up in Scotland, England and Ireland. Last, all the components of the protocol, with some adjustments, worked well together, and much of the learning from the feasibility study could be incorporated in a future larger evaluation of the intervention.
In the light of our feasibility assessment and the success of involving the fathers’ partners (mothers) in the study, we revised the logic model for the intervention to include the following: mother’s affect regulation, mother’s problem-solving, couple relationship and co-parenting, increase in mother’s capacity to manage stressful situations and reduced child abuse potential as a short-term outcome (see Report Supplementary Material 4).
When we considered the question of whether or not a main study is justified, as well as being feasible, three key issues and decisions were identified: (1) whether or not the clinical need for the intervention justifies a main study, (2) whether or not there had been any significant advances in knowledge since the beginning of the study that would make a main study redundant and (3) whether or not the high costs to conduct a main study would be justifiable. The clinical need for the intervention is compelling and there is good evidence that the needs of this population are largely unmet and the adverse consequences are serious. Although the size of the study population is relatively small, the very high costs associated with not treating this population have been clearly demonstrated and there is growing evidence that targeted interventions for this population can be cost-effective. To the best of our knowledge, there has been little advancement in this field since the study began and only a handful of research teams worldwide are developing interventions specifically for this population (see Parenting programmes for parents with a substance use disorder). Therefore, a main study would be novel and innovative research. Last, the justification for funding a main study (and one that is likely to be high cost) is a decision that involves weighing up the evidence on the clinical need for the intervention and the costs of not treating this population, and deciding whether or not the investment could result in significant learning and short- and long-term benefits to the affected population of children and families who are the subject of this study. We would argue that it is, given that this population of families are among the most marginalised and disadvantaged in society.
Research question 11: which study design would best suit a future evaluation, including an economic evaluation?
A key aim of this study was to determine the most suitable study design for a future evaluation of PuP4Dads. It was envisaged that a pilot RCT and/or a large-scale RCT would be the preferred study design option. However, we considered all options for randomised trials and ruled them out one by one for the following reasons: challenges with individual randomisation, ethics considerations and difficulty of randomising fathers to ‘usual care’ or a wait-list control (because it would potentially mean leaving children in at-risk environments and clinicians would not refer into the study).
Depending on the size of the organisation and location team clusters, individual randomisation could cause contamination within locations (usually only one agency provides family support for this population per geographic area). A parallel-group cluster randomised controlled design could resolve some of the individual randomisation issues, although a large sample of extremely hard-to-engage parents would be required.
We asked some fathers if they would be prepared to be randomised in a future study. They said yes, but only if they received some kind of equivalent parenting/family support service as an alternative to the PuP programme. However, usual care for fathers is often no parenting support and, within services that could deliver a service to these fathers, there would likely be contamination effects, with practitioners not able to ‘do or not do’ the PuP programme. The following quotation illustrates this:
Because we’re a voluntary organisation and . . . we need clients to sort of buy into the service, we encourage them to identify with, what they want to do. So, if they outright said no [to PuP] . . . then we’d still work with them, but . . . covering a lot of what PuP does, but just not under the PuP banner.
Practitioner 3
In the case of expectant fathers or fathers with a newborn baby, a ‘usual-care’ option would not be acceptable on account of low-risk thresholds for the care of pregnant women and very small infants. Dose of intervention in the programme is variable and so an equivalent matching dose of an alternative intervention, if one could be found, would be difficult to attain. These are common problems reported in RCTs with complex needs families [e.g. New Orleans (Helen Minnis, Claudia-Martina Messow, Kathleen Boyd, Andrew Carter, Matte Forde, Tom Rahilly, et al. ; University of Glasgow; 2017), THRIVE trial91 and the UK trial of the PuP programme46], where the reluctance of clinicians to refer families into the trial severely affected recruitment. Similar to individual randomisation, the service managers, commissioners and policy-makers who took part in our public engagement events indicated that it would be difficult to recruit organisations or teams to not undertake an intervention. A second problem that was highlighted was that, in most areas, there is only one family support service commissioned to provide a home-visiting service to families affected by parental drug use.
A stepped-wedge randomised design could resolve the issue of organisation, team or individual unwillingness to be randomised and the ethics issue of no intervention, in addition to addressing the challenges of individual randomisation. However, this design would create a lengthy and overly complex study because of the length of the practitioner’s training/accreditation process (i.e. over an 8-month period) and length of intervention delivery (i.e. 6–12 months). Organisations would be unlikely to wait 2 or 3 years to receive the trial intervention and there would be a range of threats to internal validity (e.g. maturation, interactive effects and contamination effects).
The feasibility of health economic evaluation in a main study
Although qualitative interviews suggested no aversion to questionnaires on criminal justice and social service use among participants, only one participant completed and returned the self-report surveys (albeit almost in full) when asked to complete them in their own time. In the UK RCT of the PuP programme,46 in which similar questionnaires were administered by researchers, completion rates were much higher. Nevertheless, this suggests a willingness to provide such data, but an inability to manage the task at hand (parents forgot to complete and lost forms).
Permissions for access to routine NHS and child protection data were obtained, with few exceptions, and there were no refusals from NHS or social services to provide these data. However, the completeness and usability of these data could be only partially assessed, as the COVID-19 pandemic affected the ability to pursue missing data. Assuming that these data are, at least, partially usable, they have the potential to reduce patient burden and enable some elements of long-term follow-up, as participants were largely willing to consent, which could be taken at recruitment to study. In principle, consent would also be viable for in-person researcher access to GP and addiction service records to extract prescribing data and for other resource use, although the challenges around patients moving between GPs and addiction services, and changing address over the course of the study could make this challenging for any items where a central tracking identifier cannot be used. Therefore, it is likely that some resource use will need to be measured and/or validated by researcher-administered self-report. For example, the prescription data reported by parents in this study appeared to be reliably accurate.
On the health outcomes side of the cost-effectiveness equation, the EQ-5D-5L was acceptable and well completed by participants, and showed a small increase in index score (see Appendix 7, Table 14). Barlow et al. 46 observed a similar pattern. Although this finding is non-significant and underpowered, examination of the subscales driving this showed an improvement in the ‘anxiety and depression’ and ‘mobility’ scales (with the former being plausible and the latter arguably not). Consultation with the lead economist of the UK RCT of PuP46 (Stavros Petrou, University of Oxford, 2020, personal communication) confirmed a similar improvement in ‘anxiety and depression’, but not in mobility, implying that at least the mobility improvement may be an artefact of underpowering. Nevertheless, improvements in index scores in either study were not to scale with improvements in BCAPI or DERS (see Research question 9: is the profile of change in fathers, mothers and children clinically significant?), suggesting that the EQ-5D-5L may be underestimating improvements in health-related quality of life and potentially undervaluing the PuP programme in cost-efficiency calculations.
The matter is further complicated by outcomes, such as child abuse and parental drug use, being multifaceted and having long-term implications that are challenging to quantify. Many of these outcomes may be brought forward by successful interventions, minimising long-term cost and harm. However, for research with a limited follow-up period, a cost–consequence approach may be more appropriate for primary health economic analysis in such circumstances,96 with EQ-5D-5L being used as an opportunistic secondary measure alongside other consequences to most.
In summary, the RQ for the economic component of a main study would be:
-
What are the economic costs and consequences associated with the implementation of PuP4Dads, in terms of health care, social care, child protection and criminal justice costs and outcomes?
Proposed main study design
We propose a mixed-methods quasi-experimental single cohort pre- and post-test study design, based on a structural equation model with an embedded process evaluation, informed by a realist evaluation approach.
The main aim would be to evaluate the clinical effectiveness and cost consequences of the PuP programme for reducing child abuse potential among families with opioid-dependent fathers, and to determine how well the intervention works for different families, how and under what circumstances.
Key research objectives and questions
Implementation objective
-
To determine whether or not PuP4Dads can be successfully delivered at scale and with fidelity to non-NHS children and in family services in differing practice, commissioning and policy environments.
Outcome evaluation: research question 1
-
Does PuP4Dads reduce child abuse potential in opioid-dependent fathers and their partners (mothers), and what dose is required to obtain clinically significant effects?
Process evaluation: research question 2
-
In relation to PuP4Dads implementation and effectiveness, what works, for whom, under what circumstances and why?
Economic evaluation: research question 3
-
What are the economic costs and consequences associated with the implementation of PuP4Dads in terms of health care, social care, child protection and criminal justice costs and outcomes?
Impact objective
-
Determine what lessons can be learned and what policy, practice and service delivery responses are required to maximise any benefits, including costs, of PuP4Dads for children and families.
Setting
Study sites would ideally include agencies that are already delivering the PuP programme, or an equivalent home-visiting family support service, to families affected by parental substance use and/or to families with complex needs. Sites in England, Scotland and elsewhere in the UK or Europe, where there is a high prevalence of opioid use and well-developed OST community-based treatment programmes, would be ideally placed to take part in a main study. PuP programme staff training can now be delivered online over an 8-month period and there is built-in implementation support that accompanies new adopters of the programme, and this would be essential for agencies that collaborate in a main study as a recruitment and implementation site.
Target population
For a main study, the target population would be opioid-dependent fathers and their families, as in the feasibility study. However, revised inclusion criteria would be required to maximise successful allocation to the intervention and, subsequently, retention in the study. In addition, participants in a main study would include PuP practitioners, supervisors, agency managers and the wider multiagency team around the child and family to build a clearer assessment of how well the intervention fits with current multiagency working and the wider policy and practice environment across sites.
Methods
Given the necessity for a quasi-experimental design, it would be important to estimate intervention effects within an appropriate causal inference framework to mitigate potential bias. We will use structural equation modelling to model both observed and latent variables, while accounting for within-participant variation, effect modifiers and covariance within a single model. We will incorporate repeated outcome measures (collected quarterly over 18 months) and investigate the direct effect of the PuP programme, potential mediators (e.g. parental emotion regulation and quality of caregiving) and dose–response (e.g. attendance rates and number of PuP modules). In addition to the observed measures of the primary and secondary outcomes, the models will include observed measures of parental mental health and drug use, child behaviour, staff/organisation indicators and demographic measures. Latent variables will comprise social support, abuse risk, co-parenting, therapeutic alliance and socioeconomic status.
Measures
The primary outcome measure will be the BCAPI to measure parental child abuse risk. Using data from the feasibility study, a clinically significant difference of 9 points on the BCAPI was determined using a RCI approach. 97 The feasibility study also estimated a standard deviation of 4.7 points for the change in BCAPI score from baseline to follow-up. Given these parameter estimates, and our structural equation modelling framework with an anticipated 15 observed variables and four latent variables, a minimum sample size of 116 participants will be required. This sample will provide 90% power to detect important differences over time (assuming a two-sided significance of 5%) and to ensure propriety, given the planned model structure. 98 Allowing for an anticipated 70% retention rate gives a total sample size required of 165 participants.
Other measures will include parental psychopathology, including transdiagnostic symptoms (e.g. emotion dysregulation due to substance use, trauma, depression and personality disorder), and quality of the caregiving environment (e.g. parent–child attachment and relationships, parental stress and the home environment), although as a latent variable to account for out-of-home placement effects. This could potentially be explored using a combination of social work child protection records and qualitative data as part of the realist evaluation, which could investigate complexity of home environments through the development of kinship maps for children.
Process evaluation informed by a realist evaluation approach99
The process evaluation will explore family, as well as organisational and policy, context to explore the key questions of what works, for whom, under what circumstances and why? The study will take the innovative step of seeking to interpret measured outcomes for a subset of intervention participants within the contexts in which they are achieved to explain the mechanisms of action that impede or facilitate success. Drawing on the QuaSIC (Qualitative approach to exploring SynergistIC interactions) method,100 we will explore the synergistic and catalytic impact of the intervention through conducting in-depth case studies with participants as the unit of analysis. This will explore experiences and views of the intervention, implementation and organisation (e.g. by including interviews with the diverse mix of staff involved in family support of individual participants) to explore unanticipated outcomes. This could be undertaken with a subset of five case studies, each with a purposive sample of six services (totalling 30 case studies). The purpose sample would ensure a diverse service mix to explore variations in mechanisms of action. Context–mechanism–outcome analysis would seek to situate outcomes within their variable contexts, thereby seeking a more nuanced understanding of how best to roll out the PuP programme at scale if the outcomes data suggests positive effects. Reporting of the results would adhere to RAMESES (Realist And Meta-narrative Evidence Syntheses: Evolving Standards) II criteria for reporting the results of realist evaluations. 101
Health economics component
In the light of our feasibility scoping, a cost–consequence analysis will be conducted to profile the health/social care, addiction, criminal justice, and child protection services, alongside key participant and child outcomes, such as parental child abuse risk, parental emotion regulation, parental drug use, child out-of-home placements and quality of caregiving. A detailed activity-based costing exercise102 will be undertaken to quantify the usual per-component cost and total cost of the delivering the PuP programme, and participants will be consented to allow data on each service type to be collected by researchers with access to case notes (where feasible), topped up with researcher-administered self-report for items unavailable and to validate data in the light of changes of address. Service use will be combined with standard UK price weights,103,104 applied where available, to estimate costs. We will additionally search the literature for cost-impact estimates of less tangible or longer-term issues, such as child protection and criminal justice end points. Rates of service use and cost for health/social care, addiction, criminal justice and child protection services will be compared between baseline and follow-up.
Potential to include a matched cohort identified via administrative data
The study will also explore whether or not routinely collected administrative data could identify a ‘virtual’ control group of drug-dependent fathers for the PuP programme-exposed participants. Administrative data sets do not routinely record fatherhood/male caregiving, but the potential for record linkage between paternal data (e.g. OST prescription data) and child records would be explored. If it were possible, it could result in a biased sample of biological, resident fathers who hold legal parental rights for children, as opposed to those who do not meet these criteria. Nevertheless, the feasibility of identifying an untreated comparator group for our study would be a worthwhile exercise.
Chapter 5 Discussion
This study aimed to test the implementation and acceptability of the PuP programme for opioid-dependent fathers and their families, delivered in non-NHS community-based family support services, and to determine whether or not a future large-scale evaluation of the intervention, including an economic evaluation, could be conducted.
The PuP programme is a parenting and family support intervention specifically designed for parents who have a substance use disorder. Although a RCT of the PuP programme46 provides evidence on the implementation and effectiveness of the PuP programme in the UK, the evidence pertains mainly to mothers as ‘primary caregivers’. Our study aimed to take the next step in parenting research with this population and engage fathers in the programme. The design of our study was informed by a systematic review of the global evidence on father engagement in parenting research. 24 This review recommended three key priorities for future parenting research: (1) to engage fathers and co-parents; (2) to disaggregate process and outcome data by fathers, mothers and co-parents; and (3) to examine implementation issues, such as reach, sustainability and scale-up. Panter-Brick et al. 24 suggested that this kind of research would ‘constitute a game change in this field’.
In this study, the intervention was delivered to families with a father who had been prescribed OST and who was caring for at least one child aged 0–8 years. Partners (mothers) of consenting fathers were also encouraged to enrol in the study, and most did. Most mothers were also prescribed OST. Parents reported multiple and complex needs that were often longstanding. Their drug use history ranged from 4 to 30 years.
The intervention was implemented in two agencies in the Lothian region of Scotland: (1) PREPARE, a local authority social work-led multidisciplinary service for pregnant substance users (one team), and (2) CIRCLE, a third-sector charity that provide early years’ family support services (three separate teams in three local authorities). Most fathers were identified and referred into the study via drug treatment providers and the two services delivering the PuP programme.
The RQs for the study were divided into two parts. The first part aimed to answer key feasibility questions regarding the implementation of the PuP programme and its acceptability and deliverability within the non-NHS organisations. The second part aimed to answer key questions regarding the feasibility of conducting a main study, including recruitment, retention, study throughput, data collection, study measures, potential clinical significance of the intervention, logic model testing and the parameters and design for a future larger evaluation.
Part 1: summary of findings and recommendations for a main study
The PuP programme was successfully delivered within the two organisations. It worked equally well in the specialist pregnancy/postnatal team (i.e. PREPARE) and the third-sector family support service (i.e. CIRCLE). It also worked equally well with a diverse group of families, including concordant and discordant couples (in terms of the parents’ drug use), non-resident fathers, single dads, first-time and experienced dads, co-parenting couples (living together and apart) and families involved in the child protection system, as well as those who were not. Learning from the implementation process highlighted the importance of having a well thought through adoption plan that is developed in collaboration with the service/line managers, front-line practitioners (PuP practitioners), PuP trainers and supervisors. Ongoing implementation support was provided until practitioners reached accreditation level and the teams were able to integrate the programme into their routine practice with families. A total of eight accredited practitioners delivered the intervention to 20 fathers and their families. The number of study families allocated to each service was fairly evenly distributed between the two agencies.
Accounts from qualitative interviews suggested that adoption of the intervention across the four teams was variable, with more successful adoption when line managers understood the PuP model, when there were sufficient numbers of practitioners trained in the programme in teams and across all four teams (who could support each other to apply the model in practice), and when there was a ‘commitment’ to regular PuP programme supervision. One team made a strategic decision to adopt the programme as their overarching framework for parenting support for all families in the service and this, in turn, made engaging fathers in the study more straightforward. Both organisations identified a skilled PuP practitioner to train as a PuP supervisor. This ‘in-house’ supervision, delivered individually and in group format, offered practitioners accessible support to share knowledge and skills and to develop a ‘shared language’ around the core components of the programme.
Acceptability of the PuP programme was rated highly by the majority of study participants, including parents, practitioners and managers. The PuP model, particularly its mode of delivery and therapeutic approach, was liked by parents, including those who had their children taken into care. Acceptability of the programme among fathers and mothers was reflected in their willingness to recommend it to other parents who use drugs. Qualitative interviews with practitioners described the PuP model to be a good fit for the population of fathers and families in the study, and a good fit for the multiagency approach required for many, if not all, of the families. Practitioners frequently noted its potential value in contributing to shared assessments, goal-setting and progress reviews, particularly in the context of child protection decision-making.
Sustainability of the programme was also high. Both agencies (and all four teams) involved in the study continued to deliver the PuP programme beyond the end of the study intervention phase (including through the pandemic) and have committed to ongoing staff training and supervision to ensure sustainability. This has been made easier with the delivery of the PuP training moved online in response to the COVID-19 pandemic in 2020. Managers reported that the PuP model was a good fit with their service ‘ethos’, role and remit, and organisational goals for children and families. Notably, this varied between the two services, with one service (PREPARE) having a designated role in conducting parenting capacity and child welfare assessments for child protection cases and the other service (CIRCLE) not. In terms of fit with the wider policy and practice environment, the PuP programme was seen as very complementary to the national practice model for child well-being in Scotland (i.e. GIRFEC),62 national guidance on the care of children and families affected by parental substance use (CAPSU guidelines15) and the most recent drug strategy,14 which advocates ‘whole-family’ approaches and ‘family-inclusive’ practice.
There was much talk in the focus groups with referrers, and in interviews with parents and professionals, about what we called ‘gendered practice’, where the focus of parenting and family support is primarily focused on mothers, mothering and mother–child relationships. There were many accounts of fathers being ignored or excluded from the parenting and child welfare agenda. In addition, fathers were also portrayed as absent, uninvolved, disinterested or problematic and even dangerous (where it was perhaps wise to exclude them and/or not encourage them to take part in a parenting programme). To a certain extent, this applied to all fathers, and has been well-documented elsewhere. 17 However, professionals thought that this phenomenon was particularly pertinent to the fathers in this study, who were stigmatised and marginalised and for whom there were concerns about their vulnerability, violence and aggression, criminal activities and involvement in the illicit drug scene. Coupled with the well-known fact that parents who use drugs are very wary of involvement with services for fear of their children being removed, professionals indicated that this posed significant challenges for them in terms of their ability to identify and approach eligible fathers for the study and engage them in the PuP programme. Of course, parents’ fears of child protection services are perhaps well founded, when one considers the very high rates of child removal and repeat child removals and care proceedings in this population. 7,105
Parents views on ‘usual care’ for fathers in terms of parenting and family support echoed the views of professionals, with stories of exclusion, stigma and fear, signifying that ‘gendered practices’ were particularly problematic and perhaps deep-rooted when it came to ‘bad dads’ like fathers who take drugs. Most fathers in the study indicated that ‘usual’ parenting or family support for opioid-dependent fathers was little or nothing, and there was little recognition from services that fathers might need, or want, parenting support in their own right or at least as part of a family support programme alongside the mother or co-parent, and most mothers agreed.
The implications of these structural barriers to father recruitment and engagement in the study intervention need to be addressed with some success to ensure that a larger evaluation of the PuP programme is feasible. As part of this study, we focused on strategies that both professionals and parents told us were successful. These entailed a personalised approach to inviting and encouraging fathers to take part, providing them with reassurances about the ‘supportive’ and ‘strengths-based’ nature of the programme, and providing both professionals and parents with first-hand accounts from fathers who have had experience of the PuP programme, describing the potential benefits of engaging in the intervention. ‘Father-friendly’ leaflets on the intervention and recruiting through fathers’ workers were also suggested, along with recruitment during ‘transition periods’ (e.g. at the point of entry into the child protection system, on release from prison and during the antenatal/early postnatal period). These periods were thought to be ‘good timing’ in terms of, perhaps, higher motivation to take part in a parenting programme and could be incorporated into a recruitment strategy in a main study.
Data on rates of consent into the study (after referral) and levels of father engagement in the PuP programme (after allocation to the intervention) told a different story. These data showed that once the hurdle of being referred into the study was overcome, and they passed the eligibility test, a high percentage (66%) of the fathers did consent to take part and so did their partners (89%). Furthermore, once the fathers were allocated to the intervention, their levels of engagement were encouragingly high and comparable to the mothers. This challenges some widely held perceptions of opioid-dependent fathers (reproduced in our qualitative data), including that they are more likely to be disinterested and avoidant than mothers. Our findings offer some confidence that adequate levels of father engagement and retention in the intervention (≈ 70%) can be achieved in a larger evaluation.
Fidelity of the programme (i.e. delivery of the core components of the model) was rated highly by parents who completed a bespoke PuP programme fidelity measure. Practitioners who delivered the intervention were accredited and provided examples of applying the core components of the model in practice, although practitioners did report that fathers were not always willing to engage in every module or component of the programme. Evidence on fidelity was limited, however, by our lack of practitioner-reported quantitative data on components delivered to families (to compare with parent reports) and the reasons why some core components were not endorsed (according to both practitioners and parents). Formal instruction in mindfulness exercises seemed to be less widely used by practitioners and/or reported by participants. However, the key component of mindful parenting is being fully present with your child, and this was endorsed by both fathers and mothers. Further evaluation of this component should be considered in a larger trial, with explicit measures of mindful parenting incorporated into the evaluation.
Part 2: summary of findings and recommendations for a main study
Our feasibility assessment of the parameters for a main study provided evidence on study throughput and retention, the most appropriate methods of data collection, suitability of the measures and completion rates, and the most suitable study design for a large evaluation of the intervention.
Although we reached our recruitment target of 24 fathers, referrals into the study were far slower than originally forecast. An 18-month extension to the project allowed recruitment to continue beyond 12 months, and we were able to test various recruitment strategies to increase referral rates. In total, our recruitment period lasted 24 months. However, approximately 6 months of this time involved minimal or no recruitment efforts because of RF absences. Therefore, we estimate that, for a main study, a recruitment period of 18 months would be realistic, assuming predicted estimates of throughput are realised. In a main study, we would also recommend recruitment from social services departments (e.g. child protection teams, children’s centres, fostering teams and kinship carer groups). It was acknowledged by the research team and implementation site managers that not including social services as recruitment sites in this feasibility study was a mistake. Many of these families are referred into family support services by allocated social workers, and these professionals are also likely to identify discordant couples (i.e. opioid-dependent fathers with non-drug dependent partners), as well as fathers not in drug treatment who could be assisted to enter treatment as part of the PuP programme. In addition, the recruitment process could be further improved by specifying more clearly the inclusion and exclusion criteria for the study to avoid consenting fathers not being allocated to the intervention because the service will not accept them (e.g. because of permanency proceedings or levels of violence). Although some of these cases may be unavoidable or unpredictable, a clear pathway from referral to allocation would help to minimise dropout early on.
Study throughput, from receipt of referral through to completion of the third and final research interview, was variable and often lengthy. Families who engaged well with the PuP programme often did not finish within the originally proposed 4- to 6-month time period. We resolved this problem halfway through the study by fixing the data collection time points (to baseline and 6 and 12 months), irrespective of the length of delivery of the intervention. This allowed practitioners to deliver the intervention as intended (i.e. an individualised support plan for each family), while, at the same time, ensuring that the study could be completed on time.
Retention rates for fathers were satisfactory and better than our minimum pre-set progression criterion of 10 (of 24) fathers completing the three research interviews (validated measures) and one qualitative interview. Of the 20 fathers who were allocated to the intervention, 13 completed all three research interviews and two qualitative interviews. Learning from the study included the importance of the researcher maintaining frequent contact with the families to improve retention; using robust ‘contact-tracing’ strategies; and having flexible, but persistent, appointment tactics, including ‘joint’ appointments with practitioners. Vouchers for participation in research interviews were found to be acceptable and a useful incentive for this population, most of whom were living in poverty, although the vouchers were not enough of an incentive for some families. In a main study, we would recommend frequent repeat measures (with vouchers) during the intervention and post-intervention period, to improve retention, maximise completion rates of measures, reduce burden on participants and enable better explanation of intervention and/or study dropout.
The methods of data collection employed in this study were found to be largely acceptable. Home visits and researcher administration of validated questionnaires resulted in high completion rates and few missing data, despite some questionnaires being long, repetitive and/or involving sensitive and intrusive questions (e.g. illicit drug use, domestic violence, criminal offences, parenting practices and child welfare issues). However, data collection methods were extremely time-consuming and resource intensive, and placed a high burden on participants (especially couples who had infants/children at home). In terms of the measures tested, some measures were suitable for all families at every time point (e.g. parental child abuse potential, emotion dysregulation, substance use and quality-of-life measures). Other measures, however, were suitable for only some parents/children and/or only appropriate at certain time points, for example child well-being measures (because different measures were used over time and there were no suitable measures for infants under 12 months), the couple relationship functioning measure (as this was not applicable to parents who were not in a couple relationship) and the parenting competence measure (was unsuitable for first-time parents during the antenatal period). The feasibility of collecting the emotional availability (video-observational) measure and the economic ‘service use survey’ measure was not confirmed due to substantive missing data. Consent to access NHS and social services data was provided by most participants and organisational approvals to extract the data were obtained (although this was a lengthy process with social services). Unfortunately, COVID-19 pressures on services limited returns and our ability to fully test feasibility (e.g. locating missing data). Despite this, we obtained sufficient data from administrative records to inform the design of a future study and would recommend the inclusion of child protection orders, out-of-home placements and reunification data in a main study. Parent self-reported data on OST prescriptions was largely congruent with NHS prescription data and so NHS data requests in a main study could concentrate on missing data and selected verification. Based on the results of our feasibility testing of measures, we established that parental child abuse risk (measured by the BCAPI) would be the most applicable primary outcome measure for a larger evaluation.
Logic model testing of the programme in this study largely relied on qualitative feedback from parents, practitioners and managers, who highlighted the appropriateness of the model and mechanisms of change for fathers. This feedback highlighted the importance (and challenge) of addressing maternal psychopathology in addition to the fathers (particularly in relation to maternal affect regulation), and the need to address co-parenting (in both cohabiting and non-cohabiting parents). The feedback also stressed the importance of the therapeutic alliance between parents and practitioners in terms of levels of intervention engagement. Therefore, we revised the logic model to include both paternal and maternal psychopathology (e.g. emotion regulation, problem-solving and ability to manage stressful situations) and co-parenting. In a main study, co-parenting and ‘working alliance’ measures would make useful addition and would be applicable across the cohort (except for single fathers with an entirely absent mother who would not report on co-parenting).
The potential clinical significance of the intervention for opioid-dependent fathers and their families was assessed at an individual change level in relation to parental child abuse risk, emotion regulation and substance use. Numbers were too small to draw any firm conclusions, but sustained improvement in these measures from baseline to post intervention in some fathers classed as intervention ‘engagers’ was reassuring. Most data on the potential impact of the intervention and its clinical importance, however, relied on qualitative interviews with parents and practitioners. Again, reassuringly, both parents and practitioners reported largely positive effects on families that were congruent with the core components of the programme and its goals, for example improvements in parental self-efficacy, emotion regulation, goal-setting, quality of father–child relationships and attachment, increased understanding of their children’s developmental needs, improvements in couple relationships and co-parenting, and increased contact and involvement between fathers and children. Learning from the study highlighted the importance of taking into account contextual factors that could potentially affect family trajectories and outcomes (e.g. housing and financial problems), variables (e.g. relationship breakdown between fathers and mothers, the age of the children, child protection status at baseline and out-of-home placement after the birth of a baby) and various aspects of programme delivery (e.g. contact visit appointments and wait times). The complexity of families in this study and the context in which the programme was delivered, coupled with complex family trajectories during and after the intervention, suggests that, in a future evaluation, understanding who the intervention works best for, how, why and under what circumstances, could provide a more nuanced explanation to the overall question of whether or not the PuP programme is effective for opioid-dependent fathers in terms of the primary outcome measure.
In terms of professionals’ engagement in qualitative interviews and focus groups, and practitioners willingness to provide data (e.g. attendance data) and co-operate with the research team (e.g. arrange joint home visits to see parents), our results were very positive. No practitioners or managers declined to take part in interviews and there was a good level of engagement from referrers in focus groups. Likewise, our expert event was well attended by a wide range of stakeholders, including policy-makers, commissioners and senior managers who were interested in the study findings and their potential implications for policy and practice. We can, therefore, assume that, in a main study, professional engagement in the research will be unproblematic. Online video-conferencing calls, now routine as a result of the COVID-19 pandemic, also mean that interviews with staff could be easily conducted online, saving researcher travel time and expense. Focus groups, however, because of the nature of the desired interaction between participants, would be more difficult to conduct online, although small groups (e.g. with three or four participants) would be feasible and could increase levels of participation.
Last, scale-up of the intervention for a main study appears feasible. Stakeholders who attended our expert event, and subsequent follow-up dissemination and public engagement events, were enthusiastic about the PuP programme and were clear that it fits well with current governmental policy for child health and well-being, child protection and marginalised and complex needs families. Notably, a ‘whole-family’ approach is now explicitly included in drug strategies across the UK.
Strengths and limitations
A strength of this study is that it was designed as a mixed-methods feasibility study to fully test ‘real-world’ implementation and acceptability of a parenting programme for a highly marginalised and hard-to-engage population (i.e. opioid-dependent fathers and their families). Given the dearth of evidence on parenting programmes for opioid-dependent fathers and their children, this study provides new knowledge in this field. In addition, this study included consenting fathers’ and their partners (concordant and discordant mothers) and, therefore, the findings will inform current policy and practice on the delivery of ‘whole-family’ interventions for these families.
The study was also designed to test the parameters for a main study, including recruitment, consent and eligibility, allocation to the intervention, levels of engagement and retention, data collection methods and the suitability and acceptability of measures. This allowed the research team to determine not only the feasibility of conducting a main study, but also the most suitable design and parameters for a larger evaluation. Although, it was originally intended that a main study would be a randomised trial design, the results of this study demonstrate that a pragmatic study design would be more suitable and potentially more clinically informative in terms of providing evidence for practice on who the intervention works best for, under what circumstances and why.
Another strength of this study was the testing of multiple data sources for a future evaluation, including researcher-administered validated questionnaires, parent self-completion questionnaires, NHS and social services data, practitioner-completed data, project monitoring data, interviews and focus groups with key stakeholders, and public engagement. The testing of these multiple data sources provides important information on the acceptability and suitability of data collection methods for this population of families.
Limitations of the study include the lack of data on the service use survey for the economic component of the study. Although, this finding usefully reinforced the importance of researcher-administered measures with this population and informed the decision-making for an economic evaluation in a main study.
Similarly, there was insufficient data collected on quality of caregiving, using the EAS and video observation of parent–child interactions. This objective measure was not feasible, largely because of logistical reasons, including NHS information governance and information technology security requirements. However, even if these technical barriers could be overcome and the researcher could use a portable video-recording device and administer it opportunistically (i.e. as and when the parent and child are seen together), there were many parents in this study whose children were in out-of-home placements at one or more of the data collection time points. This would mean obtaining permissions from corporate parents and guardians to include these children in the study and arranging parent contact visits, where feasible, to obtain video data. This would be resource intensive and possibly too costly for a main study.
Lack of diversity data obtained in this study (e.g. in relation to ethnicity, gender and religion/spirituality) would be important to address in a larger UK-wide study involving areas and services with more diverse populations.
Last, a limitation of this study was that we did not include interviews with other professionals and agencies that were involved with study families and so were unable to assess views and experiences of the intervention from the perspective of ‘outsiders’, although a number of PuP practitioners did report on interprofessional practice (i.e. responses from drug workers and child protection social workers who were involved with the families). Given the importance of multidisciplinary and multiagency working with this population of families, this would be an important additional source of data in a larger evaluation.
Conclusion
Based on the results of this feasibility study, we conclude that a larger evaluation of the PuP programme involving opioid-dependent fathers and their families is feasible. Ideally, such a study would be a pragmatic, mixed-methods and multisite evaluation, delivered across a variety of non-NHS family support services to maximise real-world learning about the effectiveness of the programme, variables that affect outcomes and implementation at scale, including cost implications. Such a study would require sufficient resources for the intensive recruitment, data collection and retention strategies required for this marginalised and hard-to-engage population.
This feasibility study has demonstrated clearly that although parenting research with opioid-dependent fathers and their families is both complex and resource intensive, they are a population of families who are willing and able to take part in research. The learning from a main study could be, as Panter-Brick et al. 24 stated, a game changer, given the dearth of research in this field. Therefore, we conclude that a larger evaluation of PuP4Dads is justifiable, as well as feasible.
Acknowledgements
First, we would like to thank all the fathers, mothers and families who took part in this study. Without their willing involvement and engagement in the intervention and research, the learning from this study would not have been possible. We are also grateful to the two fathers who attended the expert event and who assisted the research team with the writing of this final report and the Plain English summary.
Likewise, we would like to thank all the staff from PREPARE (City of Edinburgh Council) and CIRCLE who took part in the study. Both agencies contributed immensely to the project as intervention delivery sites and as partners in the project. Without their interest, dedication and collaboration, this study would not have been possible.
Thanks also to all the services and professionals who helped to recruit fathers and families into the study and to those staff who took part in the focus groups. These staff included many different professionals and agencies across Edinburgh, East Lothian and West Lothian, including NHS Lothian drug treatment, child health and midwifery staff, third-sector drug agency staff, primary care teams and social work staff.
We would also like to acknowledge the contribution from Stephen Donnelly, a Master of Research student on placement with the research team, who prepared the infographics on the study families.
Last, we would like to acknowledge our SSC members, DMEC members, the NHS Lothian R&D Office, NHS Lothian substance use services and the City of Edinburgh Council for providing support for this project. In addition, Edinburgh Napier University (Edinburgh, UK) and the University of Stirling for acting as sponsors for this study and NIHR for funding this study.
Contributions of authors
Anne Whittaker (https://orcid.org/0000-0001-8960-5070) (Professor of Nursing and Clinical Academic in Applied Alcohol and Drugs Research) led and managed the study from conception to design, analysis and interpretation of data; drafted and revised the manuscript critically for important intellectual content; and approved the final version for publication.
Lawrie Elliott (https://orcid.org/0000-0001-7727-231X) (Professor of Nursing and Community Health) contributed to the study from conception to design, analysis and interpretation of data; drafted and revised the manuscript critically for important intellectual content; and approved the final version for publication.
Julie Taylor (https://orcid.org/0000-0002-7259-0906) (Professor of Child Protection) contributed to the study from conception to design, analysis and interpretation of data; drafted and revised the manuscript critically for important intellectual content; and approved the final version for publication.
Sharon Dawe (https://orcid.org/0000-0003-3533-1101) (Professor of Psychology and Child Protection) contributed to the study from conception to design, analysis and interpretation of data; advised on intervention model, training and implementation; drafted and revised the manuscript critically for important intellectual content; and approved the final version for publication.
Paul Harnett (https://orcid.org/0000-0001-6831-0978) (Associate Professor) contributed to the study from conception to design, analysis and interpretation of data; advised on intervention model, training and implementation; drafted and revised the manuscript critically for important intellectual content; and approved the final version for publication.
Andrew Stoddart (https://orcid.org/0000-0002-1958-3897) (Senior Health Economist) contributed to the study from conception to design, advised on the health economic component, provided analysis and interpretation of data, drafted and revised the manuscript critically for important intellectual content and approved the final version for publication.
Peter Littlewood (https://orcid.org/0000-0002-1805-7246) (Consultant Clinical Psychologist) contributed to the study from conception to design, advised on recruitment and data collection within drug treatment services, contributed to the interpretations of data and approved the final version for publication.
Roy Robertson (https://orcid.org/0000-0001-8237-816X) (Professor of Addiction Medicine) contributed to the study from conception to design, advised on recruitment and data collection within primary care settings, contributed to the interpretations of data and approved the final version for publication.
Barbara Farquharson (https://orcid.org/0000-0001-9295-3156) (RF) contributed to and assisted with data collection, data analysis and interpretation of data; drafted and revised the manuscript critically for important intellectual content; and approved the final version for publication.
Heather Strachan (https://orcid.org/0000-0003-2232-5634) (RF) contributed to the study through the analysis and interpretation of data, drafted and revised the manuscript critically for important intellectual content and approved the final version for publication.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patients data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- Advisory Council on the Misuse of Drugs . Hidden Harm: Responding to the Needs of Children of Problem Drug Users 2003.
- Manning V, Best DW, Faulkner N, Titherington E. New estimates of the number of children living with substance misusing parents: results from UK national household surveys. BMC Public Health 2009;9. https://doi.org/10.1186/1471-2458-9-377.
- Cleaver H, Unell I, Aldgate J. Children’s Needs – Parenting Capacity: Child Abuse, Parental Mental Illness, Learning Disability, Substance Misuse, and Domestic Violence. London: The Stationery Office; 2011.
- Bywaters P, Bunting L, Davidson G, Hanratty J, Mason W, McCartan C, et al. The Relationship Between Poverty, Child Abuse and Neglect: An Evidence Review. York: Joseph Rowntree Foundation; 2016.
- Brook JS, Whiteman M, Zheng L. Intergenerational transmission of risks for problem behavior. J Abnorm Child Psychol 2002;30:65-76. https://doi.org/10.1023/a:1014283116104.
- Velleman RD, Templeton LJ. Substance misuse by children and young people: the role of the family and implications for intervention and prevention. Paediatr Child Health 2007;17:25-30. https://doi.org/10.1016/j.paed.2006.12.002.
- Broadhurst K, Mason C. Child removal as the gateway to further adversity: birth mother accounts of the immediate and enduring collateral consequences of child removal. Qual Soc Work 2020;19:15-37. https://doi.org/10.1177/1473325019893412.
- Child Welfare Information Gateway . Parental Substance Use and the Child Welfare System 2009.
- Conti G, Morris S, Melnychuk M, Pizzo E. The Economic Costs of Child Maltreatment in the UK: A Preliminary Study. London: National Society for the Prevention of Cruelty to Children; 2017.
- Information Services Division . Prevalence of Problem Drug Use in Scotland: 2015 16 Estimates 2017.
- Public Health England . Adult Drug Statistics from the National Drug Treatment Monitoring System (NDTMS) 1 April 2013 to 31 March 2014 2014.
- Information Services Division . Scottish Drug Misuse Database – Information on Problem Drug Use in Scotland 2013 2014 2015.
- Moore BC, Easton CJ, McMahon TJ. Drug abuse and intimate partner violence: a comparative study of opioid-dependent fathers. Am J Orthopsychiatry 2011;81:218-27. https://doi.org/10.1111/j.1939-0025.2011.01091.x.
- Scottish Government . Rights, Respect and Recovery: Alcohol and Drug Treatment Strategy 2018.
- Scottish Government . Getting Our Priorities Right – Updated Good Practice Guidance for All Agencies and Practitioners Working With Children, Young People and Families Affected by Problematic Alcohol Andor Drug Use 2013.
- Home Office . Drug Strategy 2017 2017. https://www.gov.uk/government/publications/drug-strategy-2017 (accessed 1 February 2021).
- Maxwell N, Scourfield J, Featherstone B, Holland S, Tolman R. Engaging fathers in child welfare services: a narrative review of recent research evidence. Child Fam Soc Work 2012;17:160-9. https://doi.org/10.1111/j.1365-2206.2012.00827.x.
- Stover CS, Spink A. Affective awareness in parenting of fathers with co-occurring substance abuse and intimate partner violence. Adv Dual Diagn 2012;5:74-85. https://doi.org/10.1108/17570971211241903.
- Brandon M, Bailey S, Belderson P, Larsson B. Neglect and Serious Case Reviews. London: National Society for the Prevention of Cruelty to Children; 2013.
- Hammond H, McKinnon M. Report of the Caleb Ness Inquiry 2003.
- Munro E. The Munro Review of Child Protection: Part One: A Systems Analysis. Cheshire: Department for Education; 2010.
- Munro E. The Munro Review of Child Protection: Final Report, A Child-Centred System 2011.
- Barlow J, Coren E. The effectiveness of parenting programs: a review of Campbell reviews. Res Soc Work Pract 2018;28:99-102. https://doi.org/10.1177/1049731517725184.
- Panter-Brick C, Burgess A, Eggerman M, McAllister F, Pruett K, Leckman JF. Practitioner review: engaging fathers – recommendations for a game change in parenting interventions based on a systematic review of the global evidence. J Child Psychol Psychiatry 2014;55:1187-212. https://doi.org/10.1111/jcpp.12280.
- Tully LA, Piotrowska PJ, Collins DAJ, Mairet KS, Black N, Kimonis ER, et al. Optimising child outcomes from parenting interventions: fathers’ experiences, preferences and barriers to participation. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4426-1.
- Sicouri G, Tully L, Collins D, Burn M, Sargeant K, Frick P, et al. Toward father-friendly parenting interventions: a qualitative study. Aust N Z J Fam Ther 2018;39:218-31. https://doi.org/10.1002/anzf.1307.
- Tully LA, Collins DAJ, Piotrowska PJ, Mairet KS, Hawes DJ, Moul C, et al. Examining practitioner competencies, organizational support and barriers to engaging fathers in parenting interventions. Child Psychiatry Hum Dev 2018;49:109-22. https://doi.org/10.1007/s10578-017-0733-0.
- Fletcher R, Freeman E, Matthey S. The impact of behavioural parent training on fathers’ parenting: a meta-analysis of the Triple P-Positive Parenting Program. Father J Theory Res Pract Men Fathers 2011;9:291-312. https://doi.org/10.3149/fth.0903.291.
- Lundahl BW, Tollefson D, Risser H, Lovejoy MC. A meta-analysis of father involvement in parent training. Res Soc Work Pract 2008;18:97-106. https://doi.org/10.1177/1049731509828.
- Chacko A, Fabiano GA, Doctoroff GL, Fortson B. Engaging fathers in effective parenting for preschool children using shared book reading: a randomized controlled trial. J Clin Child Adolesc Psychol 2018;47:79-93. https://doi.org/10.1080/15374416.2016.1266648.
- Brown AL. Fathering Interventions for Men Who Use Intimate Partner Violence and Child Maltreatment: Perceived Benefits and Risks 2016. https://doi.org/10.15760/honors.297.
- Scourfield J, Allely C, Coffey A, Yates P. Working with fathers of at-risk children: insights from a qualitative process evaluation of an intensive group-based intervention. Child Youth Serv Rev 2016;69:259-67. https://doi.org/10.1016/j.childyouth.2016.08.021.
- McConnell N, Barnard M, Holdsworth T, Taylor J. Caring Dads: Safer Children: Evaluation Report 2014.
- Cowan PA, Cowan CP, Pruett MK, Pruett K, Wong JJ. Promoting fathers’ engagement with children: preventive interventions for low income families. J Marriage Fam 2009;71:663-79. https://doi.org/10.1111/j.1741-3737.2009.00625.x.
- Lechowicz ME, Jiang Y, Tully LA, Burn MT, Collins DA, Hawes DJ, et al. Enhancing father engagement in parenting programs: translating research into practice recommendations. Aust Psychol 2019;54:83-9. https://doi.org/10.1111/ap.12361.
- McMahon TJ, Suchman NE, Paulo M, Mayes LC. Parenting and Substance Abuse: Developmental Approaches to Intervention. London: Oxford University Press; 2013.
- Smith TK, Duggan A, Bair Merritt MH, Cox G. Systematic review of fathers’ involvement in programmes for the primary prevention of child maltreatment. Child Abuse Rev 2012;21:237-54. https://doi.org/10.1002/car.2195.
- Neger EN, Prinz RJ. Interventions to address parenting and parental substance abuse: conceptual and methodological considerations. Clin Psychol Rev 2015;39:71-82. https://doi.org/10.1016/j.cpr.2015.04.004.
- Stover CS, McMahon TJ, Moore K. A randomized pilot trial of two parenting interventions for fathers in residential substance use disorder treatment. J Subst Abuse Treat 2019;104:116-27. https://doi.org/10.1016/j.jsat.2019.07.003.
- Stover CS. Fathers for change for substance use and intimate partner violence: initial community pilot. Fam Process 2015;54:600-9. https://doi.org/10.1111/famp.12136.
- Parents Under Pressure . Program Overview 2020. www.pupprogram.net.au/program-overview.aspx (accessed 7 January 2021).
- Bowlby EJM. Attachment: Volume One of the Attachment and Loss Trilogy. New York, NY: Random House; 2008.
- Biringen Z. Raising a Secure Child: Creating an Emotional Connection Between You and Your Child. New York, NY: TarcherPerigee; 2004.
- Porges SW. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation (Norton Series on Interpersonal Neurobiology). New York, NY: W.W. Norton & Company; 2011.
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979.
- Barlow J, Sembi S, Parsons H, Kim S, Petrou S, Harnett P, et al. A randomized controlled trial and economic evaluation of the Parents Under Pressure program for parents in substance abuse treatment. Drug Alcohol Depend 2019;194:184-94. https://doi.org/10.1016/j.drugalcdep.2018.08.044.
- Mathews-King A. Residential addiction services in England cut by third amid drug overdose and funding crisis, figures show. The Independent 2019. www.independent.co.uk/news/health/addiction-drug-alcohol-treatment-austerity-cuts-government-council-a8992696.html (accessed 17 March 2021).
- Niccols A, Milligan K, Smith A, Sword W, Thabane L, Henderson J. Integrated programs for mothers with substance abuse issues and their children: a systematic review of studies reporting on child outcomes. Child Abuse Negl 2012;36:308-22. https://doi.org/10.1016/j.chiabu.2011.10.007.
- Dawe S, Harnett P. Reducing potential for child abuse among methadone-maintained parents: results from a randomized controlled trial. J Subst Abuse Treat 2007;32:381-90. https://doi.org/10.1016/j.jsat.2006.10.003.
- Suchman NE, DeCoste C, Castiglioni N, McMahon TJ, Rounsaville B, Mayes L. The mothers and toddlers program, an attachment-based parenting intervention for substance using women: post-treatment results from a randomised clinical pilot. Attach Hum Dev 2010;12:483-504. https://doi.org/10.1080/14616734.2010.501983.
- Harwin J, Alrouh B, Ryan M, Tunnard J. Changing Lifestyles, Keeping Children Safe: An Evaluation of the First Family Drug and Alcohol Court (FDAC) in Care Proceedings. London: Brunel University; 2014.
- Dakof GA, Cohen JB, Henderson CE, Duarte E, Boustani M, Blackburn A, et al. A randomized pilot study of the engaging moms program for family drug court. J Subst Abuse Treat 2010;38:263-74. https://doi.org/10.1016/j.jsat.2010.01.002.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Bugge C, Williams B, Hagen S, Logan J, Glazener C, Pringle S, et al. A process for Decision-making after Pilot and feasibility Trials (ADePT): development following a feasibility study of a complex intervention for pelvic organ prolapse. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-353.
- Biringen Z. The Emotional Availability (EA) Scales. Fort Collins, CO: Colorado State University; 2008.
- Condon JT. The assessment of antenatal emotional attachment: development of a questionnaire instrument. Br J Med Psychol 1993;66:167-83. https://doi.org/10.1111/j.2044-8341.1993.tb01739.x.
- Scottish Government . Scottish Index of Multiple Deprivation 2020 2020.
- Edinburgh Poverty Commission . Poverty in Edinburgh 2018 2018.
- The Royal College of Psychiatrists in Scotland . Written Submission to the Scottish Affairs Committee Inquiry on the Use and Misuse of Drugs in Scotland 2018. https://www.rcpsych.ac.uk/members/devolved-nations/rcpsych-in-scotland/policy-and-public-affairs/consultation-work (accessed 7 January 2021).
- CIRCLE . Supporting Families in Scotland n.d. https://circle.scot/ (accessed 17 March 2021).
- Dragic A. Children in Families With Alcohol and Drug Problems n.d. www.edinburgh.gov.uk/protect-someone-harm/children-families-alcohol-drug-problems/1 (accessed 17 March 2021).
- Scottish Government . Getting It Right for Every Child (GIRFEC) 2018. www.gov.scot/policies/girfec/ (accessed 17 March 2021).
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev 2004;28:343-51. https://doi.org/10.1016/j.neubiorev.2004.03.007.
- Barlow J, Sembi S, Gardner F, Macdonald G, Petrou S, Parsons H, et al. An evaluation of the parents under pressure programme: a study protocol for an RCT into its clinical and cost effectiveness. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-210.
- Harnett PH, Dawe S. The contribution of mindfulness-based therapies for children and families and proposed conceptual integration. Child Adolesc Ment Health 2012;17:195-208. https://doi.org/10.1111/j.1475-3588.2011.00643.x.
- Roemer L, Williston SK, Rollins LG. Mindfulness and emotion regulation. Curr Opin Psychol 2015;3:52-7. https://doi.org/10.1016/j.copsyc.2015.02.006.
- Kiel EJ, Kalomiris AE. Current themes in understanding children’s emotion regulation as developing from within the parent–child relationship. Curr Opin Psychol 2015;3:11-6. https://doi.org/10.1016/j.copsyc.2015.01.006.
- Harnett PH, Barlow J, Coe C, Newbold C, Dawe S. Assessing capacity to change in high-risk pregnant women: a pilot study. Child Abuse Rev 2018;27:72-84. https://doi.org/10.1002/car.2491.
- Henggeler SW, Schoenwald SK, Liao JG, Letourneau EJ, Edwards DL. Transporting efficacious treatments to field settings: the link between supervisory practices and therapist fidelity in MST programs. J Clin Child Adolesc Psychol 2002;31:155-67. https://doi.org/10.1207/S15374424JCCP3102_02.
- Beidas RS, Koerner K, Weingardt KR, Kendall PC. Training research: practical recommendations for maximum impact. Adm Policy Ment Health 2011;38:223-37. https://doi.org/10.1007/s10488-011-0338-z.
- Powell BJ, Beidas RS, Lewis CC, Aarons GA, McMillen JC, Proctor EK, et al. Methods to improve the selection and tailoring of implementation strategies. J Behav Health Serv Res 2017;44:177-94. https://doi.org/10.1007/s11414-015-9475-6.
- Beidas RS, Edmunds JM, Marcus SC, Kendall PC. Training and consultation to promote implementation of an empirically supported treatment: a randomized trial. Psychiatr Serv 2012;63:660-5. https://doi.org/10.1176/appi.ps.201100401.
- World Health Organization (WHO) . International Statistical Classification of Diseases and Related Health Problems, Tenth Revision 2010.
- Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The Brief Infant-Toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. J Pediatr Psychol 2004;29:143-55. https://doi.org/10.1093/jpepsy/jsh017.
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45. https://doi.org/10.1097/00004583-200111000-00015.
- Ondersma SJ, Chaffin MJ, Mullins SM, LeBreton JM. A brief form of the child abuse potential inventory: development and validation. J Clin Child Adolesc Psychol 2005;34:301-11. https://doi.org/10.1207/s15374424jccp3402_9.
- Biringen Z, Derscheid D, Vliegen N, Closson L, Easterbrooks MA. Emotional availability (EA): theoretical background, empirical research using the EA Scales, and clinical applications. Dev Rev 2014;34:114-67. https://doi.org/10.1016/j.dr.2014.01.002.
- Ohan JL, Leung DW, Johnston C. The Parenting Sense of Competence Scale: evidence of a stable factor structure and validity. Can J Behav Sci Can Sci Comport 2000;32. https://doi.org/10.1037/h0087122.
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess 2008;30. https://doi.org/10.1007/s10862-008-9102-4.
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): development and preliminary psychometric data. J Fam Issues 1996;17:283-316. https://doi.org/10.1177/019251396017003001.
- Marsden J, Farrell M, Bradbury C, Dale-Perera A, Eastwood B, Roxburgh M, et al. Development of the Treatment Outcomes Profile. Addiction 2008;103:1450-60. https://doi.org/10.1111/j.1360-0443.2008.02284.x.
- Public Health England . Treatment Outcomes Profile 2018.
- Sobell LC, Sobell MB, Buchan G, Cleland PA, Fedoroff I, Leo GI. The Reliability of the Timeline Followback Method Applied to Drug, Cigarette, and Cannabis Use n.d.
- The EuroQol Research Foundation . EQ-5D-5L: About 2020.
- The EuroQol Research Foundation . EQ-5D-5L Valuation Crosswalk Index Value Calculator 2020.
- Dawe S, Taplin S, Mattick RP. Psychometric investigation of the Brief Child Abuse Potential Inventory in mothers on opioid substitution therapy. J Fam Violence 2017;32:341-8. https://doi.org/10.1007/s10896-016-9821-3.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Ivers J, Barry J. Evaluation of Parents Under Pressure programme (PuP) at Coolmine. Dublin: Trinity College; 2018.
- MacLachlan A, Crawford K, Shinwell S, Nixon C, Henderson M. Recruiting hard-to-reach pregnant women at high psychosocial risk: strategies and costs from a randomised controlled trial. Trials 2021;22. https://doi.org/10.1186/s13063-021-05348-9.
- Voils CI, King HA, Maciejewski ML, Allen KD, Yancy WS, Shaffer JA. Approaches for informing optimal dose of behavioral interventions. Ann Behav Med 2014;48:392-401. https://doi.org/10.1007/s12160-014-9618-7.
- Independent Care Review . The Promise 2020. www.carereview.scot/wp-content/uploads/2020/02/The-Promise.pdf (accessed 14 September 2021).
- Ministry of Housing, Communities and Local Government . National Evaluation of the Troubled Families Programme 2015–2020 2019.
- Harwin J, Broadhurst K, Cooper C, Taplin S. Tensions and contradictions in family court innovation with high risk parents: the place of family drug treatment courts in contemporary family justice. Int J Drug Policy 2019;68:101-8. https://doi.org/10.1016/j.drugpo.2018.04.019.
- HM Government . Cost Consequence Analysis: Health Economic Studies 2020.
- Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991;59:12-9. https://doi.org/10.1037/0022-006X.59.1.12.
- Westland JC. Lower bounds on sample size in structural equation modeling. Electron Commer Res Appl 2010;9:476-87. https://doi.org/10.1016/j.elerap.2010.07.003.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 1997.
- Harris FM, Maxwell M, O’Connor R, Coyne JC, Arensman E, Coffey C, et al. Exploring synergistic interactions and catalysts in complex interventions: longitudinal, mixed methods case studies of an optimised multi-level suicide prevention intervention in four European countries (OSPI-Europe). BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-2942-z.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0643-1.
- Kaplan RS, Anderson SR. Time-Driven Activity-Based Costing: A Simpler and More Powerful Path to Higher Profits. Boston, MA: Harvard Business School Publishing; 2007.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2019. Canterbury: PSSRU, University of Kent; 2019.
- HM Government . NHS Reference Costs 2014 2014.
- Philip G, Youansamouth L, Bedston S, Broadhurst K, Hu Y, Clifton J, et al. ‘I had no hope, I had no help at all’: insights from a first study of fathers and recurrent care proceedings. Societies 2020;10. https://doi.org/10.3390/soc10040089.
- NHS Health Research Authority . UK Policy Framework for Health and Social Care Research 2017.
- NHS Health Research Authority . Good Clinical Practice 2020.
- Bradley RH, Caldwell BM, Brisby J, Magee M, Whiteside L, Rock SL. The HOME Inventory: a new scale for families of pre- and early adolescent children with disabilities. Res Dev Disabil 1992;13:313-33. https://doi.org/10.1016/0891-4222(92)90009-U.
Appendix 1 Research ethics and governance
A favourable ethics opinion was obtained for the study on 14 March 2017 from South East Scotland NHS Research Ethics Committee 02 (reference 17/SS/0023) with protocol version 2.0 (dated 6 March 2017). NHS Lothian R&D Office approval was provided on 6 April 2017.
Changes to the protocol were made (Table 9). These changes were submitted to the Research Ethics Committee and approved as substantial amendments [see study protocol v5.0 via the NIHR Journals Library URL: www.journalslibrary.nihr.ac.uk/programmes/phr/158201/#/ (accessed 10 September 2021)].
| Substantial amendment | Protocol version | Date | Reason | Ethics approval received |
|---|---|---|---|---|
| 1 | 3 | 29 May 2017 | Inclusion criteria changed to include expectant parents (i.e. recruitment of fathers during antenatal period and delivery of intervention during antenatal period). Addition of PAAS and MAAS antenatal attachment questionnaires | 6 June 2017 |
| 2 | 4 | 11 June 2018 | PI changed institution and change of sponsor. Addition of further recruitment and intervention delivery sites in Midlothian and West Lothian. Further expanded inclusion criterion to include children aged up to 8 years old | 6 July 2018 |
| 3 | 5 | 31 July 2019 | Change follow-up intervals from end of treatment to 6 and 12 months after baseline measures, irrespective of intervention completion status. Incorporated non-substantial amendment to include service managers in qualitative interviews. Reverted back to original recruitment sites as the additional sites in Midlothian and West Lothian were not able to deliver the intervention | 6 August 2019 |
A non-substantial amendment to interview service managers was approved by the sponsor on 1 July 2019. This change was included in amendment number 3 (and received Research Ethics Committee approval).
Appendix 2 Study Research Group
The Study Research Group met, on average, once monthly for the duration of the study to discuss and review progress on the study and agree the project work plan as it developed over time. The Study Research Group included the co-investigators, RFs and implementation site collaborators. The chief investigator led the study and provided support to the RFs.
Dates of meetings
2017
-
12 April.
-
10 May.
-
15 June.
-
6 July.
-
3 August.
-
13 September.
-
5 October.
-
8 November.
-
7 December.
2018
-
27 February.
-
22 March.
-
19 April.
-
28 June.
-
26 July.
-
20 September.
-
29 November.
2019
-
24 January.
-
27 February.
-
11 April.
-
23 May.
-
25 June.
-
22 August.
-
10 October.
2020
-
7 January.
-
3 March.
-
23 June.
-
13 July.
-
27 July.
-
13 August.
-
9 September.
-
30 September.
-
14 October.
-
11 November.
-
3 December.
-
15 December.
Role and remit
-
To ensure the conduct of the study is compliant with the protocol and relevant regulatory requirements.
-
To review progress and update the project plan accordingly.
-
To discuss training, supervision and implementation issues related to the PuP programme.
-
To direct and monitor referral, recruitment and consent procedures.
-
To track, report and monitor adverse events.
-
To liaise with the research sponsor and funders.
-
To supervise data collection, analysis, interpretation and presentation.
-
To provide regular progress reports to the SSC and convene meetings with DMEC as required.
Membership of the Study Research Group
Chairperson of the Study Research Group
-
Professor Anne Whittaker, University of Stirling (chief investigator).
Research fellows
-
Dr Kirsty Killick, University of Stirling (RF until 31 August 2018).
-
Dr Barbara Farquharson, University of Stirling (RF from 1 December 2018).
-
Dr Heather Strachan, University of Stirling (RF from 1 January 2020).
Co-investigators
-
Professor Lawrie Elliott, Glasgow Caledonian University.
-
Professor Julie Taylor, University of Birmingham.
-
Professor Sharon Dawe, Griffith University.
-
Professor Paul Harnett, Griffith University.
-
Andrew Stoddart, University of Edinburgh.
-
Dr Peter Littlewood, NHS Lothian.
-
Professor Roy Robertson, University of Edinburgh.
Service collaborators
-
Michelle Kirkpatrick, Manager, PREPARE.
-
Natalie Duffill, PuP practitioner and PuP supervisor, PREPARE.
-
Rhona Hunter, Chief Executive Officer, CIRCLE (end date 30 March 2019).
-
Mark Kennedy, Chief Executive Officer, CIRCLE (start date 20 April 2019).
-
Lindsay Fraser, PuP practitioner and PuP supervisor, CIRCLE.
Appendix 3 Study Steering Committee
The SSC members were nominated by the Study Research Group and appointed by NIHR. The SSC comprised an independent chairperson, clinical and academic members and two service users. The chief investigator, RFs and co-applicants attended meetings as non-voting members. A SSC charter was approved by NIHR.
Dates of meetings
2017
-
13 June.
-
30 November.
2018
-
16 May.
2019
-
10 January.
-
27 June.
2020
-
9 January.
-
2 July.
-
22 November.
Note that a November 2018 meeting was deferred while the study was paused.
Role and remit
The role of the SSC was to provide overall supervision for the project on behalf of the project sponsor and project funder and to ensure that the project was conducted to the rigorous standards set out in the UK Policy Framework for Health and Social Care Research106 and the guidelines for Good Clinical Practice. 107
Membership of the Study Steering Committee
Chairperson of the Study Steering Committee
-
Mr David Liddell, Chief Executive Officer, Scottish Drugs Forum.
Members
-
Professor Christopher Weir, Professor of Medical Statistics and Clinical Trials, Edinburgh Clinical Trial Unit, University of Edinburgh.
-
Professor Thomas McMahon, Professor of Psychiatry and The Child Study Center, Yale School of Medicine.
-
Dr Tessa Parkes, Senior Lecturer, University of Stirling.
-
Ms Anne Neilson, Director of Public Protection, NHS Lothian.
-
Dr Alison Munro, Senior RF, University of Dundee.
-
Dr Claire McIntosh, Consultant Psychiatrist in Addictions, NHS Forth Valley.
-
Ms Gwynne Rayns, Senior Social Worker, City of York Council.
-
Mr Chris Cuthbert, Director of Learning and Development, A Better Start (previously National Society for the Prevention of Cruelty to Children).
-
Professor Brigid Daniels, Dean of the School of Arts, Social Sciences and Management, Queen Margaret University (start date 9 January 2020).
-
Dr Catherine Nixon, Research Officer, Scottish Children’s Reporter Administration, University of Glasgow (start date 9 January 2020).
-
Parent representatives (one mother and one father).
In attendance
-
Professor Anne Whittaker (chief investigator), University of Stirling.
-
RFs and other co-investigators.
Appendix 4 Data Monitoring and Ethics Committee
The DMEC members were nominated by the Study Research Group and appointed by NIHR. DMEC members comprised an independent chairperson and four other clinical and academic members.
Dates of meetings
-
25 July 2017.
-
14 January 2019.
Role and remit
The primary responsibility of the DMEC was to protect the ethics and safety interests of the participants recruited into the study, while safeguarding, as far as possible, the scientific validity of the study. The DMEC was available, if required, to review information on the progress of the study, including the safety and efficacy of the intervention and selected data accruing from the study, and to request additional data if considered necessary to support the assessment of relative risk and benefit within the study. The DMEC could also provide recommendations about stopping, modifying or continuing the study to the SSC. The DMEC is advisory to the SSC and, in this feasibility study, it was agreed that the DMEC would be a ‘sleeping’ committee, unless convening the committee was advisable, for example, to discuss adverse events.
Membership of Data Monitoring and Ethics Committee
Chairperson of the Data Monitoring and Ethics Committee
-
Dr Christine Jones, Lecturer, School of Social Work and Social Policy, University of Strathclyde.
Members
-
Dr Vicky Ryan, Statistician, Institute of Health and Society, Newcastle University.
-
Professor Bernie Carter, Professor of Children’s Nursing, Faculty of Health and Social Care, Edgehill University.
-
Professor Tony Long, Professor of Child and Family Health, School of Nursing, Midwifery, Social Work and Social Sciences, University of Salford.
-
Professor Graham Connelly, Senior Lecturer, School of Social Work, University of Strathclyde.
In attendance
-
Professor Anne Whittaker (chief investigator) and RFs.
Appendix 5 Pre-set progression criteria
| Criterion | Indicator | Method of assessment |
|---|---|---|
| Successful recruitment of families to the PuP intervention and study |
Trained practitioners to recruit and deliver the PuP programme to a minimum of one in five of the families approached or an average of two families per month Total: n = 24 |
Project monitoring data |
| Delivery of the PuP programme | PuP programme delivered to required standard | Bespoke treatment fidelity measure |
| Acceptability of the PuP programme to practitioners | Broad satisfaction of the programme among staff delivering the intervention | Qualitative interviews and regular feedback from practitioners to the Study Research Group |
| Engagement with the PuP programme practitioners in research | 87.5% (7/8) of those approached agree to participate in a qualitative interview | Qualitative interview data |
| Engagement in research with staff from agencies referring to the PuP programme | 80% of those approached agree to participate in qualitative interview | Qualitative interview data |
| Family engagement with the PuP programme |
66% of families recruited complete the PuP programme intervention Total: n = 16 |
Project monitoring data |
| Acceptability of the PuP programme to families | Broad satisfaction of the programme among families receiving the intervention | Qualitative interviews with fathers and mothers |
| Family engagement with research components to inform the development of the logic model | Minimum of 10 fathers recruited to the research study to complete the baseline and 6-month (post-intervention FU2) quantitative interviews and at least one qualitative interview | Baseline and FU2 questionnaire data and qualitative interview data |
| Adverse effects and events | Maintain a list of all adverse effects and events that might arise for each family, comprising those that may be attributed to the intervention and those that may be attributed to the research study | Discussion and decision regarding the adverse effects and events at monthly management, SSC and DMEC meetings |
Appendix 6 Example coding frame
Analytic plan: initial categories, codes, themes and cases
Category: feasibility/deliverability/adoption/implementation
| Code | Potential theme | Case |
|---|---|---|
| Pract.Perspec. – strategies recruitment/engagement – what worked/did not work | Practitioner | |
| Refer.Perspec. – difficulty identifying/engaging dads – reasons | Gendered practice | Focus group |
| Refer.Perspec. – feasibility of PuP | Focus group | |
| Refer.Perspec. – confidence about referring – understanding the programme, protecting patients | Focus group | |
| Pract.Perspec. – fit with other services | Good fit | Practitioners |
| Pract.Perspec. – experience of working with other agencies | Practitioners | |
| Pract.Perspec. – fit with existing model of work | Good fit | Practitioners |
| Pract.Perspec. – couples work or separate | Programme model | Practitioners |
| Pract.Perspec. – initial resistance to new intervention | Implementation support | Practitioners |
| Pract.Perspec. – be realistic about achievements | Practitioners | |
| Pract.Perspec. – length of programme | Mode of delivery | Practitioners |
| F&M.Perspec. – engagement with PuP | Father and mothers: 6 months | |
| Experience of starting/engaging with PuP | Father and mothers: 6 months | |
| Experience of engaging with PuP – time and place, home visiting | Mode of delivery | Father and mothers: 6 months |
| Experience of engaging with PuP – pract.attendance/input, fit with other services | Programme model | Father and mothers: 6 months |
| Experience of engaging with PuP – pract.attend. – what would help | Father and mothers: 6 months | |
| Experience of engaging with PuP – pract.attend. – suggested changes | Father and mothers: 6 months | |
| Experience of engaging with PuP – attending sessions | Father and mothers: 6 months | |
| Experience of engaging with PuP – completing modules | Father and mothers: 6 months |
Category: acceptability of the Parents under Pressure programme/suitability of the programme for father
| Code | Potential theme | Case |
|---|---|---|
| Pract. Perspec. – acceptability of PuP | Practitioners | |
| Pract. Perspec. – barriers (what fathers not suitable for?) | Gendered practice | Practitioners |
| Refer. Perspec – suggestions how to ‘sell it’ to dads, strengths-based approach | Programme model | Focus group |
| Refer.Perspec. – stigma, fear, dads hidden, overcome barriers | Programme model | Focus group |
| Pract. Perspec. – flexible delivery, tailored to individual families, home visiting | Mode of delivery | Practitioners |
| Pract. Perspec. – relationship with family, strengths-based approach, empowering | Therapeutic approach | Practitioners |
| Pract. Perspec. – still using it/embedding | Adoption/deliverability | Practitioners |
| Pract. Perspec. – leadership support needed | Implementation support | Practitioners |
| Managers.Perspec. – acceptability of different stakeholders important, fit with ‘ethos’ of the team approach to working with parents | Programme model and therapeutic approach | Managers |
| Managers.Perspec. – shared language, shared goals | Multiagency approach | Managers |
| Managers.Perspec. – sustainability of training/supervision | Implementation support | Managers |
| Managers.Perspec. – implementation – capacity issues, momentum | ‘Critical mass’ | Managers |
| Baseline – doing PuP with partner | Programme model | Fathers and mothers: baseline |
| Structural Issues – gendered stereotypes of drug-using fathers | Gendered practice | Fathers and mothers: baseline |
| Acceptability – aspects least liked | Fathers and mothers: baseline | |
| Acceptability – aspects most liked | Fathers and mothers: baseline | |
| Acceptability – doing PuP together | Programme model and mode of delivery | Fathers and mothers: baseline |
| Acceptability – recommend to others? | Fathers and mothers: baseline | |
| Acceptability – adjunct to other services, fit with service, join goals | Multiagency working | Fathers and mothers: baseline |
| Acceptability – difference from previous services/parenting support – inclusion of dads | Gendered practice | Fathers and mothers: baseline |
| Acceptability – suggestions for improvements to PuP | Fathers and mothers: baseline | |
| Engagement with PuP – experience of PuP – goals | Fathers and mothers: baseline | |
| Engagement with PuP – relationships with practi., therapeutic alliance, supportive nature of PuP | Therapeutic approach | Fathers and mothers: baseline |
| Pract.Perspec. – suggestions for improvement | Practitioners | |
| Managers.Perspec – suggestions for improvement | Manager |
Category: impact of the Parents under Pressure programme
| Code | Potential theme | Case |
|---|---|---|
| Pract.Perspec. – engagement with PuP – expectations of intervention, impact on practice – structure, framework for practice, tools for practice, core groups, goal setting, flexibility, home visiting | Programme model, therapeutic approach and mode of delivery | Practitioners |
| Pract.Perspec. – benefits of PuP – therapeutic, focus on dads, couple work or individual parent work | Therapeutic approach and mode of delivery | Practitioners |
| Managers.Perspec – benefits for service, competitive for bids, structured model | Programme model, implementation and sustainability | Managers |
| Managers.Perspec – benefits of PuP – therapeutic value, restorative justice | Therapeutic approach | Managers |
| Benefits or impact of PuP – child contact, child home from care | Impact and link with core components of PuP model | Fathers and mothers: 6 months |
| Benefits or impact of PuP – child development, child’s needs | Impact | Fathers and mothers: 6 months |
| Benefits or impact of PuP – patience and ‘pause button’, less ‘jumping in’ | Impact | Fathers and mothers: 6 months |
| Benefits or impact of PuP– goal setting, in charge, empowering | Impact | Fathers and mothers: 6 months |
| Benefits or impact of PuP – relationship partner improved/co-parenting, mothers happy dad is involved | Impact | Fathers and mothers: 6 months |
| Benefits or impact of PuP – relationship child, child connectedness, child activities | Impact | Fathers and mothers: 6 months |
| Benefits or impact of PuP – outcomes for family, broader benefits, housing, benefits, increased social support | Impact | Fathers and mothers: 6 months |
| Negative impact of PuP – dislikes, more of?, improvements | Improvements | Fathers and mothers: 6 months |
Appendix 7 EuroQol-5 Dimensions, five-level version, results at baseline
Summary results
Adapted from the quality-of-life measure (i.e. the EQ-5D-5L) from the EuroQol Research Foundation (Table 14). 86
| Quality-of-life domain | Score | ||||
|---|---|---|---|---|---|
| 0 (no problems) | 1 | 2 | 3 | 4 (severe problems) | |
| Fathers (N = 22), n (%) | |||||
| Mobility | 13 (59) | 4 (18) | 5 (23) | 0 (0) | 0 (0) |
| Self-care | 19 (86) | 1 (4) | 2 (9) | 0 (0) | 0 (0) |
| Usual activities | 14 (64) | 6 (27) | 1 (4) | 1 (4) | 0 (0) |
| Physical health | 7 (32) | 9 (41) | 6 (27) | 0 (0) | 0 (0) |
| Mental health | 4 (18) | 8 (36) | 6 (27) | 2 (9) | 2 (9) |
| Mothers (N = 17), n (%) | |||||
| Mobility | 7 (41) | 6 (35) | 3 (18) | 1 (6) | 0 (0) |
| Self-care | 11 (65) | 4 (24) | 2 (12) | 0 (0) | 0 (0) |
| Usual activities | 11 (65) | 2 (12) | 3 (18) | 1 (6) | 0 (0) |
| Physical health | 6 (35) | 6 (35) | 1 (6) | 3 (18) | 1 (6) |
| Mental health | 7 (41) | 6 (35) | 3 (18) | 1 (6) | 0 (0) |
Appendix 8 Treatment Outcomes Profile item response data at baseline, follow-up 1 and follow-up 2
| Item number | TOP | Fathers | Mothers | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (N = 23) | FU1 (N = 16) | FU2 (N = 13) | Baseline (N = 14) | FU1 (N = 10) | FU2 (N = 8) | ||||||||||||||
| n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | ||
| 1 | Alcohol days/28 | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 2 | Opiates days/28 | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 3 | Crack days/28 | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 4 | Cocaine days/28 | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 5 | Amphetamine days/28 | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 6 | Cannabis days/28 | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 7 | Fath_TOP_Baseline_other_specify | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 8 | Days injected/28 | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 9 | Fath_TOP_Baseline_Injectedwithsharedneedle | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 10 | Fath_TOP_Baseline_Injectedusingsharedequip | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 11 | Fath_TOP_Baseline_Shoplifting | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 12 | Fath_TOP_Baseline_Sellingdrugs | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 13 | Fath_TOP_Baseline_Theft_vehicle | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 14 | Fath_TOP_Baseline_Other_theft | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 15 | Fath_TOP_Baseline_Fraud_forge | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 16 | Fath_TOP_Baseline_Assault | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 17 | Fath_TOP_Baseline_Psychohealth | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 9 | 90 | MO01 | 8 | 100 | |||||
| 18 | Fath_TOP_Baseline_Daysinpaidwork | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 9 | 90 | MO01 | 8 | 100 | |||||
| 19 | Fath_TOP_Baseline_Daysschoolcollege | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 9 | 90 | MO01 | 8 | 100 | |||||
| 20 | Fath_TOP_Baseline_Physicalhealth | 23 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 10 | 100 | 8 | 100 | ||||||
| 21 | Fath_TOP_Baseline_Housingprob | 23 | 100 | 16 | 100 | 13 | 100 | 13 | 93 | M010 | 10 | 100 | 8 | 100 | |||||
| 22 | Fath_TOP_Baseline_Riskeviction | 23 | 100 | 16 | 100 | 13 | 100 | 13 | 93 | M010 | 10 | 100 | 8 | 100 | |||||
| 23 | Fath_TOP_Baseline_QOL | 23 | 100 | 16 | 100 | 13 | 100 | 13 | 93 | M010 | 10 | 100 | 8 | 100 | |||||
Appendix 9 Brief Child Abuse Potential Inventory item response data at baseline, follow-up 1 and follow-up 2
| BCAPI item | Fathers | Mothers | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (N = 20) | FU1 (N = 16) | FU2 (N = 13) | Baseline (N = 14) | FU1 (N = 11) | FU2 (N = 9) | |||||||||||||
| n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | |
| 1 | 20 | 100 | 16 | 100 | 13 | 100 | 13 | 93 | MO02 | 11 | 100 | 9 | 100 | |||||
| 2 | 19 | 95 | FA19 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 3 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 4 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 5 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 6 | 20 | 100 | 16 | 100 | 13 | 100 | 12 | 86 | M002; MO09 | 11 | 100 | 9 | 100 | |||||
| 7 | 20 | 100 | 16 | 100 | 13 | 100 | 11 | 79 | MO02; MO06; MO08 | 11 | 100 | 9 | 100 | |||||
| 8 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 9 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 10 | 19 | 95 | FA10 | 16 | 100 | 13 | 100 | 13 | 93 | MO09 | 11 | 100 | 9 | 100 | ||||
| 11 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 12 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 13 | 20 | 100 | 16 | 100 | 13 | 100 | 13 | 93 | MO09 | 11 | 100 | 9 | 100 | |||||
| 14 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 15 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 16 | 20 | 100 | 16 | 100 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | ||||||
| 17 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 18 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 19 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 20 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 21 | 20 | 100 | 15 | 94 | FA04 | 13 | 100 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 22 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 23 | 20 | 100 | 16 | 100 | 11 | 85 | FA16 | 13 | 93 | MO20 | 11 | 100 | 8 | 89 | MO02 | |||
| 24 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 25 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 26 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 27 | 19 | 95 | FA20 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | ||||
| 28 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 29 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 10 | 91 | MO02 | 8 | 89 | M002 | |||
| 30 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 31 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 32 | 20 | 100 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | |||||
| 33 | 19 | 95 | FA10 | 16 | 100 | 12 | 92 | FA11 | 14 | 100 | 11 | 100 | 9 | 100 | ||||
| 34 | 18 | 90 | FA10, FA19 | 15 | 94 | FA12 | 12 | 92 | FA11 | 14 | 100 | 10 | 91 | MO12 | 9 | 100 | ||
Appendix 10 Parenting Sense of Competence Scale item response data at baseline, follow-up 1 and follow-up 2
| PSCS item | Fathers | Mothers | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (N = 16) | FU1 (N = 15) | FU2 (N = 11) | Baseline (N = 9) | FU1 (N = 9) | FU2 (N = 7) | |||||||||||||
| n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | |
| 1 | 15 | 94 | FA06 | 15 | 100 | 11 | 100 | 9 | 100 | 9 | 100 | 7 | 100 | |||||
| 2 | 16 | 100 | 15 | 100 | 10 | 91 | FA18 | 9 | 100 | 9 | 100 | 6 | 86 | MO17 | ||||
| 3 | 16 | 100 | 15 | 100 | 10 | 91 | FA18 | 9 | 100 | 9 | 100 | 7 | 100 | |||||
| 4 | 16 | 100 | 15 | 100 | 10 | 91 | FA18 | 9 | 100 | 9 | 100 | 7 | 100 | |||||
| 5 | 15 | 94 | FA24 | 14 | 93 | FA24 | 11 | 100 | 9 | 100 | 9 | 100 | 7 | 100 | ||||
| 6 | 16 | 100 | 15 | 100 | 11 | 100 | 9 | 100 | 8 | 89 | MO03 | 7 | 100 | |||||
| 7 | 16 | 100 | 15 | 100 | 11 | 100 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | |||||
| 8 | 16 | 100 | 15 | 100 | 10 | 91 | FA13 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | ||||
| 9 | 16 | 100 | 15 | 100 | 11 | 100 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | |||||
| 10 | 15 | 94 | FA06 | 15 | 100 | 11 | 100 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | ||||
| 11 | 16 | 100 | 15 | 100 | 11 | 100 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | |||||
| 12 | 15 | 94 | FA04 | 15 | 100 | 11 | 100 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | ||||
| 13 | 16 | 100 | 15 | 100 | 11 | 100 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | |||||
| 14 | 16 | 100 | 15 | 100 | 11 | 100 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | |||||
| 15 | 16 | 100 | 14 | 93 | FA11 | 11 | 100 | 9 | 100 | 8 | 89 | MO15 | 7 | 100 | ||||
| 16 | 10 | 63 | FA04; FA05; FA06; FA08; FA11; FA14 | 12 | 80 | FA01; FA03; FA11 | 11 | 100 | 4 | 44 | MO05; MO06; MO07; MO12; MO14 | 8 | 89 | MO03 | 7 | 100 | ||
Appendix 11 Difficulties in Emotion Regulation Scale item response data at baseline, follow-up 1 and follow-up 2
| DERS item | Fathers | Mothers | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (N = 21) | FU1 (N = 16) | FU2 (N = 13) | Baseline (N = 17) | FU1 (N = 11) | FU2 (N = 9) | |||||||||||||
| n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | |
| 1 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 2 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 3 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 4 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 5 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 6 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 7 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 8 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 8 | 89 | MO02 | |||||
| 9 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 10 | 21 | 100 | 16 | 100 | 13 | 100 | 16 | 94 | MO02 | 11 | 100 | 9 | 100 | |||||
| 11 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 12 | 21 | 100 | 16 | 100 | 13 | 100 | 17 | 100 | 11 | 100 | 9 | 100 | ||||||
| 13 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 14 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 15 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 16 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 16 | 94 | MO02 | 11 | 100 | 9 | 100 | ||||
| 17 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 18 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 19 | 20 | 95 | FA02 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | ||||
| 20 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 21 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 22 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 15 | 88 | MO02; MO09 | 11 | 100 | 9 | 100 | ||||
| 23 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 24 | 20 | 95 | FA05 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | ||||
| 25 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 26 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 27 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 28 | 20 | 95 | FA05 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | ||||
| 29 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 30 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 31 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 32 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 33 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 34 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 35 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
| 36 | 21 | 100 | 16 | 100 | 12 | 92 | FA11 | 17 | 100 | 11 | 100 | 9 | 100 | |||||
Appendix 12 Revised Conflict Tactics Scale item response data at baseline, follow-up 1 and follow-up 2
| CTS2 item | Fathers | Mothers | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (N = 18) | FU1 (N = 12) | FU2 (N = 6) | Baseline (N = 16) | FU1 (N = 10) | FU2 (N = 5) | |||||||||||||
| n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | n | % | Missed by | |
| 1 | 18 | 100 | 12 | 100 | 6 | 100 | 14 | 88 | MO05; MO09 | 10 | 100 | 5 | 100 | |||||
| 18 | 100 | 12 | 100 | 6 | 100 | 14 | 88 | MO05; MO09 | 10 | 100 | 5 | 100 | ||||||
| 2 | 18 | 100 | 12 | 100 | 6 | 100 | 15 | 94 | MO05 | 10 | 100 | 5 | 100 | |||||
| 17 | 94 | FA03 | 12 | 100 | 6 | 100 | 15 | 94 | MO05 | 10 | 100 | 5 | 100 | |||||
| 3 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 4 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 9 | 90 | MO15 | 5 | 100 | |||||
| 18 | 100 | 12 | 100 | 6 | 100 | 15 | 94 | MO05 | 10 | 100 | 5 | 100 | ||||||
| 5 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 6 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 7 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 15 | 94 | MO05 | 10 | 100 | 5 | 100 | ||||||
| 8 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 9 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 10 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 11 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 12 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 13 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 14 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 17 | 94 | FA01 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 15 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 16 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 17 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 18 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 19 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 20 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 21 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 22 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 23 | 17 | 94 | FA01 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||
| 17 | 94 | FA01 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 24 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 25 | 17 | 94 | FA01 | 12 | 100 | 6 | 100 | 14 | 88 | MO01; MO05 | 10 | 100 | 5 | 100 | ||||
| 17 | 94 | FA01 | 12 | 100 | 6 | 100 | 15 | 94 | MO01 | 10 | 100 | 5 | 100 | |||||
| 26 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 27 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 28 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 29 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 30 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 31 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 32 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 15 | 94 | MO01 | 10 | 100 | 5 | 100 | ||||||
| 33 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 34 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 11 | 92 | FA02 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 35 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 36 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 37 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 38 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | |||||||
| 39 | 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 10 | 100 | 5 | 100 | ||||||
| 18 | 100 | 12 | 100 | 6 | 100 | 16 | 100 | 9 | 90 | MO16 | 5 | 100 | ||||||
Appendix 13 Brief Infant Toddler Social and Emotional Assessment and Strengths and Difficulties Questionnaire item response data at baseline, follow-up 1 and follow-up 2
| Parent/family | Age of child (years) | BITSEA 12–35 months | SDQ 2–4 years | SDQ 4–16 years | Same measure twice? Reason if not | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | FU1 | FU2 | Baseline | FU1 | FU2 | Baseline | FU1 | FU2 | |||
| Father 1 | Expectant | n/a | n/a | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 0; no measure appropriate for age at FU1 |
| Mother 1 | Expectant | n/a | n/a | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 0; no measure appropriate for age at FU1 |
| Father 2 | 2.5 | n/a | n/a | n/a | ✓ | ✓ | ✓ | n/a | n/a | n/a | 1 |
| Mother 2 | 2.5 | n/a | n/a | n/a | ✓ | ✓ | ✓ | n/a | n/a | n/a | 1 |
| Father 3 | Expectant | n/a | n/a | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; missing at baseline and no measure appropriate for age at FU1 |
| Mother 3 | Expectant | n/a | n/a | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; missing at baseline and no measure appropriate for age at FU1 |
| Father 4 | 3 | n/a | n/a | n/a | ✓ | n/a | n/a | n/a | ✓ | ✓ | 1 |
| Father 5 | 3 | n/a | LTFU | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; LTFU |
| Mother 5 | 3 | n/a | LTFU | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; LTFU |
| Father 6 | 0.75 | n/a | ✓ | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 1 |
| Mother 6 | 0.75 | n/a | ✓ | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 1 |
| Father 7 | 0.06 | LTFU | LTFU | LTFU | 0; LTFU | ||||||
| Father 8 | Expectant | n/a | LTFU | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; missing at baseline and LTFU at FU1 |
| Father 8 | 1 | Missinga | n/a | n/a | n/a | LTFU | LTFU | n/a | n/a | n/a | 0; LTFU |
| Father 8 | 4 | Missinga | n/a | n/a | ✓ | LTFU | LTFU | n/a | LTFU | LTFU | 0; LTFU |
| Mother 8 | Expectant | n/a | LTFU | LTFU | n/a | LTFU | LTFU | n/a | n/a | n/a | 0; missing at baseline and LTFU at FU1 |
| Mother 8 | 1 | Missinga | n/a | n/a | ✓ | LTFU | LTFU | n/a | LTFU | LTFU | 0; LTFU |
| Mother 8 | 4 | Missinga | n/a | n/a | ✓ | LTFU | LTFU | n/a | LTFU | LTFU | 0; LTFU |
| Father 9 | Expectant | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 0; no measure appropriate for age at FU2 |
| Mother 9 | Expectant | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 0; no measure appropriate for age at FU1 and FU2 |
| Father 10 | Expectant | n/a | LTFU | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; LTFU |
| Mother 10 | Expectant | n/a | n/a | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 0; different measures (antenatal and BITSEA) |
| Father 11 | 6 | n/a | n/a | n/a | n/a | n/a | n/a | ✓ | ✓ | ✓c | 1 |
| Father 12 | 0.25 | n/a | n/a | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 0; no measure appropriate at baseline or FU1 |
| Mother 12 | 0.25 | n/a | n/a | ✓ | ✓ | n/a | n/a | n/a | n/a | n/a | 0 |
| Father 13 | Expectant | n/a | n/a | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 0; different measures (antenatal and BITSEA) |
| Mother 13 | Expectant | n/a | n/a | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 0; different measures (antenatal and BITSEA) |
| Father 14 | 1.6 | Missinga | LTFU | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; LTFU |
| Mother 14 | 1.6 | Missinga | LTFU | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; LTFU |
| Father 15 | 3 | n/a | n/a | n/a | ✓ | ✓ | ✓ | n/a | n/a | n/a | 1 |
| Mother 15 | 3 | n/a | n/a | n/a | ✓ | ✓ | LTFU | n/a | n/a | n/a | 1 |
| Father 16 | Expectant | n/a | ✓ | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 0; different measures (antenatal and BITSEA) |
| Mother 16 | Expectant | n/a | n/a | ✓ | n/a | n/a | n/a | n/a | n/a | n/a | 0; different measures (antenatal and BITSEA) |
| Father 17 | 8 | n/a | n/a | n/a | n/a | n/a | n/a | Missingb | Missingb | LTFU | 0; no contact with child at baseline |
| Mother 17 | 8 | n/a | n/a | n/a | n/a | n/a | n/a | Missingb | Missingb | ✓ | 0; no contact with child at baseline |
| Father 18 | 6 | n/a | n/a | n/a | n/a | n/a | n/a | Missingb | Missingb | Missingb | 0; no contact with child at baseline |
| Father 19 | 3 | n/a | n/a | n/a | ✓ | LTFU | LTFU | n/a | n/a | n/a | 0; LTFU |
| Mother 19 | 3 | LTFU | LTFU | LTFU | 0; LTFU | ||||||
| Father 20 | 4 | ✓ | n/a | n/a | n/a | LTFU | LTFU | n/a | LTFU | LTFU | 0; LTFU |
| Mother 20 | 4 | ✓ | n/a | n/a | n/a | LTFU | LTFU | n/a | LTFU | LTFU | 0; LTFU |
| Father 21 | 0.25 | n/a | LTFU | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; no measure appropriate at baseline and then LTFU |
| Mother 21 | 0.25 | n/a | LTFU | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 0; no measure appropriate at baseline and then LTFU |
| Father 22 | Expectant | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 0; missing at baseline, no measure appropriate for age at FU1 and FU2 |
| Father 23 | 4 | n/a | n/a | n/a | n/a | n/a | n/a | ✓ | ✓ | ✓ | 1 |
| Father 23 | 6 | n/a | n/a | n/a | n/a | n/a | n/a | ✓ | ✓ | ✓ | 1 |
| Father 24 | 1 | ✓ | ✓ | LTFU | n/a | n/a | n/a | n/a | n/a | n/a | 1 |
| Father 25 | Expectant | LTFU | LTFU | LTFU | 0; LTFU | ||||||
| Total | 11 | ||||||||||
Appendix 14 Paternal Antenatal Attachment Scale and Maternal Antenatal Attachment Scale item response data at baseline, follow-up 1 and follow-up 2
| Parent/family | Age of child (years) | Maternal/paternal attachment | |||
|---|---|---|---|---|---|
| Baseline | FU1 | FU2 | |||
| Father 1 | 1 | Expectant | ✓ | n/a | n/a |
| Mother 1 | Expectant | Missinga | n/a | n/a | |
| Father 2 | 1 | 2.5 | n/a | n/a | n/a |
| Mother 2 | 2.5 | n/a | n/a | n/a | |
| Father 3 | Expectant | Missinga | n/a | n/a | |
| Mother 3 | Expectant | Missinga | n/a | n/a | |
| Father 4 | 1 | 3 | n/a | n/a | n/a |
| Father 5 | 3 | n/a | n/a | n/a | |
| Mother 5 | 3 | n/a | n/a | n/a | |
| Father 6 | 1 | 0.75 | n/a | n/a | n/a |
| Mother 6 | 0.75 | n/a | n/a | n/a | |
| Father 7 | 0.06 | LTFU | |||
| Father 8 | Expectant | Missinga | n/a | n/a | |
| Father 8 | 1 | n/a | n/a | n/a | |
| Father 8 | 1 | 4 | n/a | n/a | n/a |
| Mother 8 | Expectant | Missinga | n/a | n/a | |
| Mother 8 | 1 | n/a | n/a | n/a | |
| Mother 8 | 4 | n/a | n/a | n/a | |
| Father 9 | 1 | Expectant | ✓ | n/a | n/a |
| Mother 9 | Expectant | ✓ | n/a | n/a | |
| Father 10 | 1 | Expectant | ✓ | n/a | n/a |
| Mother 10 | Expectant | ✓ | n/a | n/a | |
| Father 11 | 1 | 6 | n/a | n/a | n/a |
| Father 12 | 1 | 0.25 | n/a | n/a | n/a |
| Mother 12 | 0.25 | n/a | n/a | n/a | |
| Father 13 | 1 | Expectant | ✓ | n/a | n/a |
| Mother 13 | 1 | Expectant | ✓ | n/a | n/a |
| Father 14 | 1.6 | n/a | n/a | n/a | |
| Mother 14 | 1.6 | n/a | n/a | n/a | |
| Father 15 | 1 | 3 | n/a | n/a | n/a |
| Mother 15 | 3 | n/a | n/a | n/a | |
| Father 16 | 1 | Expectant | ✓ | n/a | n/a |
| Mother 16 | Expectant | ✓ | n/a | n/a | |
| Father 17 | 8 | n/a | n/a | n/a | |
| Mother 17 | 1 | 8 | n/a | n/a | n/a |
| Father 18 | 6 | n/a | n/a | n/a | |
| Father 19 | 1 | 3 | n/a | n/a | n/a |
| Mother 19 | 3 | LTFU | |||
| Father 20 | 1 | 4 | n/a | n/a | n/a |
| Mother 20 | 4 | n/a | n/a | n/a | |
| Father 21 | 0.25 | n/a | n/a | n/a | |
| Mother 21 | 0.25 | n/a | n/a | n/a | |
| Father 22 | Expectant | Missingb | n/a | n/a | |
| Father 23 | 1 | 4 | n/a | n/a | n/a |
| Father 23 | 6 | n/a | n/a | n/a | |
| Father 24 | 1 | 1 | n/a | n/a | n/a |
| Father 25 | Expectant | LTFU | |||
| Total | 18 | ||||
Appendix 15 Selected excerpts from qualitative interviews and focus groups by research question
| RQ | Themes and excerpts |
|---|---|
| Parent participants | |
| RQ1: how feasible is it to deliver the PuP programme for opioid-dependent fathers in routine family-based local government and voluntary sector services? | Partnership working across services:I know that [the PuP Practitioner] goes to the meetings once a week, so I mean, it’s always been, kind of, really useful to have him there to ask his opinion about, if I’ve got anything that I want to know about, like other services.Father 23Flexibility (mode of delivery):Being flexible, I think, is key, especially when you’ve got kids, being flexible is. Because anything could happen, they could get no well, you could get no well.Father 2Early intervention/child protection:I think [PuP] should be made compulsory, especially if the social worker’s thinking of removing the children. I think it might be, like, giving the parents more of a chance, and having more things in place to help parents, rather than just stepping in and taking the bairn [child] away straightaway.Father 2Multiple agencies (barrier):It was just I’d got so much snowed under with social work and that. It’s really demanding when you’re dealing with social work when [baby] first came. It’s all the time. It’s like two, three, four times a week at the moment and I’m having meetings with school. It’s constant at the moment.Father 15I had so many people to see, like the midwife, . . . and the health visitor, and like hospital appointments and this and that, so it got like . . . and drugs worker, social work; so yeah, I think there was like a couple of occasions they [appointments with PuP practitioner] just clashed.Mother 13 |
| Practitioners | |
| RQ1: how feasible is it to deliver the PuP programme for opioid-dependent fathers in routine family-based local government and voluntary sector services? | Good fit:Again, because it’s [PuP] very similar to our practice anyway. We work very closely with all the services. Not on all families but the majority of families have addictions or social work involved as well. So, yeah, it all ties in.Practitioner 7I think PuP complements GIRFEC nicely in the way that we work.Practitioner 3The [PuP] framework is a good kind of guide for us. for probably most of the families that we work with.Practitioner 4Partnership working:So, it’s very much about the kind of relationship that you can build with the other professionals involved in the family support plan . . . and how easy the communication is, whether you’re on the same page in terms of what goals you’re working towards, etc.Practitioner 3Complex needs:Some of them are up at 12 months [length of time delivering PuP], they’re complex families, and the mum has really complex problems, the dad has really complex problems, in their own right, as well as a family.Practitioner 3Working with couples and individual parents (mode of delivery):. . . [if] they want to do it as a couple, [I] tried to do it with both of them in the same session, and then maybe had separate sessions for specific things [dad had anxiety].Practitioner 4Gendered practice/working with dads:The majority of [my] cases have been either single mums or dads being around, but he’s taken himself out of the equation; so because of that, as you say, that skill set, you become much more confident when working with mums.Practitioner 3Early intervention and child protection:I’ve found that, generally, when dads are engaging it’s because it’s part of the child protection plan that kind of, I guess, brings them in initially.Practitioner 3Multiple agencies (barrier):We’ve had that difficulty, people having so many services and professionals crawling all over them. It’s been actually difficult to get time to see them.Practitioner 4Need for implementation support:We kind of understood the model and the theory behind that, but how to actually practically start it off; I think we were all a bit in the dark. So, it was a bit trial and error.Practitioner 4Support from line managers (implementation support):. . . our manager didn’t come to the training. So I don’t feel like there was anybody that fully understood what we were supposed to be doing [in the beginning].Practitioner 3 |
| Managers | |
| RQ1: how feasible is it to deliver the PuP programme for opioid-dependent fathers in routine family-based local government and voluntary sector services? | Good fit:[PuP] is holistic, so it very much fits in with the fact that we’re holistic, strengths based, solution focused and that we’re working with all of the different kind of elements within the family in terms of resources, internal and external and parenting strategies. So I do think it kind of fits in with [our] model really well; obviously PuP4Dads fits in with our kind of ethos around positively involving dads.Manager 5Home-visiting/individualised approach (mode of delivery):I think knowing that this sort of clientele won’t access [parenting programmes] or find it very difficult to maintain that, I think the fact that we can offer it on the one-to-one basis within their family home is a real plus . . .Manager 1Flexibility:. . . [PuP is] not a rigid, it’s not so rigid that you have to go ‘today I am doing PuP and I am doing page dah, dah . . .’Manager 4Whole-team approach:I think if we keep insisting that everybody is trained, goes [to] supervision [sessions], and they find that they are benefitting from those, then I think it will, as time goes on, be more embedded.Manager 2Working with couples/including dads (acceptability and deliverability):And, generally speaking, the mothers have been very supportive of the dad’s involvement. They’ve really wanted the dad to be given appropriate support. It’s been very interesting.Manager 6Staff buy-in (implementation support):You need your practitioners to be onboard as to why you’re kind of doing that [implementing a new programme] because I think it can be interpreted potentially as a kind of criticism [of their current practice] at times.Manager 7Staff buy-in:So the staff, the disengagement among the staff teams, I think, was mostly around the fact that they didn’t really know what was going on [in the beginning] and they didn’t really feel that anyone had ever properly explained to them.Manager 2 |
| Parents | |
| RQ2 (part A): how acceptable is the PuP programme among staff and recipients? | Home visiting (mode of delivery):Aye, I prefer them at home, aye, it’s easier. My own environment, I’m more safer in my own environment, especially with new things, and [mother/partner] is the exact same, sort of being at home, we sort of do everything at home.Father 2Preparation for parenthood (therapeutic approach):Well like I said, it taught me things I didn’t really know about being a parent and it just got me prepared and ready for my child coming into the world.Father 15Confidence building (therapeutic approach):. . . [the PuP practitioner] helped me, because I was in such a bad place it kind of helped, likes of just talking to someone and thinking about the positive things about parenting.Father 11Strengths-based approach (therapeutic approach and programme model):It helped our workers see our strengths and our goals, what we wanted to happen, and it gave us a starting point on what to work for, areas that we wanted.Mother 9Co-ordinated goal-setting (therapeutic approach and programme model):Yes, instead of getting muddled up, likes the drug workers telling you ‘right, they want you to do this’ . . . and social worker this, this and this. Then you’re muddled up you don’t know what you’re doing. If you’ve just got one set of goals to do instead of three or four different sets of goals. [If] you get muddled up and you forget to do some of it . . . it goes badly against you.Father 11Trust (therapeutic approach):So, through that time, I’ve really developed a great deal of respect and trust for [PuP Practitioner]. He knows what he’s talking about, you know.Father 23Supportive approach (therapeutic approach):Honesty and trust, like, aye, you know, being able to approach them and if things go wrong . . . then you know, that it’s just not going to fall apart . . . and they’ll work with you, you know, and make things better, if things go wrong, and I think that’s the key thing there.Father 9Empowerment (therapeutic approach/programme model):Yes, and she kind of let me take control of what we were talking about even though she would be asking me all the questions and that.Father 11Positive affirmation (therapeutic approach):Just having somebody to talk to, who’s there, you know, and just somebody who’s . . . who can kind of help point out where you’ve maybe went wrong in the past; and you know, eh, and positive . . . what’s that . . . positive reinforcement?Father 13Childhood trauma (therapeutic approach):Yes, saying about something about your upbringing and that it’s just . . . That stuff I wasn’t . . . I just don’t like talking about things like that.Father 3Use of workbook (programme model):. . . when I look at the book and I know if I don’t [want to open it] . . . because I’m unsure of what I’m going to come up with, I can just look at it and then just look at it, dread it, and then . . . but then I just do it.Father 18Managing poor literacy (barrier):I would find it hard when they write things down so the way [PuP practitioner] did it was just talked to me, just come up and visit me and talk to me about how I feel about with [child] and different situations.Mother 10 |
| Practitioners | |
| RQ2 (part A): how acceptable is the PuP programme among staff and recipients? | Home visiting (model of delivery):. . . it’s a comfortable environment for the parents, and sometimes if they’re reflecting on the past, or just something that’s going to make them feel a bit sad or unhappy, then the home’s probably the safest environment to do it.Practitioner 1Theory-driven practice (programme model):I’ve got more of an understanding about why I’m doing certain things with families, and then it helps the families to understand why we’re doing certain things, and then other professionals to understand what the point of us working alongside families are, and it’s not just a case of taking families out for a cup of tea.Practitioner 3Structure and therapeutic focus (programme model):I was going along to case conferences, you know, reviews and things and they were saying ‘how’s dad?’ ‘Really good, you know, we’re meeting regularly, de, de, de, de’. But there was no structure. And since I’ve introduced PuP and doing . . . even the questionnaires, it’s steering towards a direction. So I’m now going along to meetings and saying, you know, ‘we’ve undertaken the questionnaires and these are the areas that we’re now focusing on’.Practitioner 5Supporting communication (programme model):But I think it does help, maybe, when you’re articulating something at a meeting, or they’re saying ‘oh, there’s an issue with this’ and I’ll say ‘well, we’ve worked through this’ and I can then talk of what we’ve worked through at the moment.Practitioner 2Content (programme model):And I know a lot of families have fed back that they really like the ‘View of self as parent’ module, and it gives them an opportunity to, I guess, put into context their own experiences and then go on to have an understanding about why that’s impacting on the way that they run their own lives or the way that they parent their children, and their coping strategies.Practitioner 3Content (therapeutic approach):. . . it’s quite traumatic stories, you know, for a lot of the dads I’m working with . . . so they get a real understanding of, if they’ve not been [well] parented, how can they be . . . how can they parent . . . how are they expected to be a good parent? And . . . that’s been really, really powerful.Practitioner 5Strengths-based approach (programme model and therapeutic approach):. . . the strengths-based approach too . . . getting a sense of what it is that they want and need and starting from that position rather than, you know, us telling them all about their problems, kind of thing, or focusing on their problems all the time.Practitioner 4Co-ordinated goal-setting (programme model):Definitely the goals were really important as well, because his CPN [community psychiatric nurse] knew what goals I was setting for him in my appointments, so it meant that he was reinforcing that in his appointments, and it worked really, really nicely.Practitioner 3Preventing crisis (programme model):. . . instead of constantly responding to crisis after crisis and dealing with exactly what’s in front of us in terms of case management, it’s been really helpful to get a bit behind that as well and give people strategies to prevent getting into those crises in the first place.Practitioner 3 |
| Managers/referrers | |
| RQ2 (part A): how acceptable is the PuP programme among staff and recipients? | Flexibility (mode of delivery):. . . the families say our responsivity, our flexibility and our solidarity is super important to them.Manager 5Strengths based (programme model):I was really glad that you said that [PuP is] strengths-based, because I feel that . . . and it’s not about criticising social work in any way, but I feel like the interaction between our patients and social work can be really negative and very stigmatising.Referrer, FG2Supportive (therapeutic approach):. . . you’re still having to go into child protection case conference where the jargon is used and the reports are written, but if you can do it from a point where you are being supportive and you care and they know that, and you’ve got empathy, because empathy is rooted within that framework.Manager 6 |
| Parents | |
| RQ2 (part B): what are the barriers to/facilitators of uptake and retention in the PuP programme? | Whole-family approach (programme model):. . . I think, [PuP Practitioner 2], I think, he works more with the whole family whereas other services they’re just working with [your child] or like with our drug use.Father 6Father-inclusive practice (programme model):. . . we are all doing [PuP] together, it’s something you can get out of it together. Because everything is kind of separate at the moment, like [my partner]’s no really been involved in anything, it’s kind of all sort of been on me, and I found that a bit frustrating, and putting me proper under pressure sometimes, because I’m thinking, ‘well why is everything end at me!’, and he’s kind of like being left in the background . . . everything’s kind of changing [now], he is involved and people are involving him in things and it’s kind of like, turned round a bit . . . [and] he’s involved . . .Mother 13Relationship with PuP practitioner (therapeutic approach):So, through that time, I’ve really developed a great deal of respect and trust for [PuP practitioner]. He knows what he’s talking about, you know.Father 23Child protection (programme model):I think it should be made compulsory. Especially if the social worker’s thinking of removing the children, I think it might be, like, giving the parents more of a chance. And having more things in placed to help parents, rather than just stepping in and taking the bairn [child] away straightaway.Father 2Lack of trust (therapeutic approach):PuP is really good for people, but the social work involvement can just make people scared.Mother 16Gendered practice (barrier):Yeah, for me as a dad . . . I was basically told that it was a child and family service and as I was no longer a member of the family they couldn’t help me.Father 13, non-resident dad |
| Practitioners | |
| RQ2 (part B): what are the barriers to/facilitators of uptake and retention in the PuP programme? | Whole-family approach (programme model):. . . family support has really been just all a whole load of discussions about what drugs they take, you know, primarily . . . so no sense that they’ve, you know, been involved in setting their own goals and being an active agent in the whole process.Practitioner 4Practitioner’s selling the programme (barriers/facilitators):I suppose, from the very beginning, maybe selling it to dads and getting them . . . because the focus is on them and they’re not used to that maybe . . . you know, why this would benefit them.Practitioner 4Father-inclusive practice (facilitator):I think what’s really important about PuP is the way it’s . . . I suppose the way it’s sold for the want of a better expression, that . . . for dads not to be . . . not to think as an add on.Practitioner 5Knowledge of the PuP programme (barrier):But I think apart from that, people [referrers] don’t know about [PuP], and aren’t aware. I don’t think it means anything to them, to be honest.Practitioner 2Child protection incentive (facilitator):I’ve found that, generally, when dads are engaging it’s because it’s part of the child protection plan that kind of, I guess, brings them in initially.Practitioner 3Gendered practice (barrier/facilitator):I think there are some dads that have felt that they’ve not been included, or felt as important in their child’s life, which I think this study is showing that, well, what we’re trying to aim to do is about that. So, I think that gives them a bit of a purpose.Practitioner 2Gendered practice (barrier):I was again at a meeting and it was commented on that dad . . . you know, dad never stayed . . . when the midwife or the health visitor came in, dad always got up and left and things like that, and, you know, he just didn’t seem interested. And on speaking to dad, it was like, I always thought it was a mum and baby appointment and I wanted to give them their time and space.Practitioner 5. . . you know, [practitioners] are very comfortable working with mothers, you know, that’s the norm . . . and even if unconsciously they don’t want to exclude fathers, they would . . . they’d find themselves, kind of doing that anyway.Practitioner 4 |
| Managers/referrers | |
| RQ2 (part B): what are the barriers to/facilitators of uptake and retention in the PuP programme? | Whole-family approach (programme model):. . . we’ve got a practice model, well, a practice model that’s always developing in terms of an iterative way, which is around whole family approach and we’ve got the practice principles that kind of underpin that.Manager 5Knowledge of the PuP programme (barrier):I think that’s where I struggle is like what the benefits of actually doing the programme would be, because I don’t know what they actually do.Referrer, FG1Mothers encouraging fathers (facilitator):And, generally speaking, the mothers have been very supportive of the dad’s involvement. They’ve really wanted the dad to be given appropriate support. It’s been very interesting.Manager 6Father-inclusive practice (facilitator):We’ve now got a father’ worker as part of the team. Any of our people could have worked with dads and for some reasons there’s obviously some kind of mental block where people don’t seem to refer dads even though they could work with them. But as soon as you put a father’s worker [in the service] they were like ‘we can refer dads to you’ and you’re, like ‘really?’Manager 3Gendered practice (barrier):. . . we’ve just split our service into a female and a male service, and we’re a lot less involved. The workers in the women’s service are very much involved in the child care and quite often there’s a big push for working towards mothers getting care of their children or contact. The men have a tendency to be side-lined, partly because they tend to be very chaotic and in and out of prison.Referrer, FG1Fear of social services (barrier):You will find that they [parents] maybe don’t disclose things as much if they know they have got care of their children – they might not be completely honest because they’re afraid of social work involvement.Referrer, FG3Difficulties identifying fathers (barrier):A lot of the dads that we would see just don’t live with their kids. They’re often very socially isolated, they’re often living at home or homeless, they often . . . don’t have contact with anyone at all except coming to get their methadone script.Referrer, FG2Lack of trust (barrier):I feel like the interaction between our patients and social work can be really negative and very stigmatising and I feel that a lot of our patients, especially when child protection, feel that social work are there as a punitive thing, to really . . . they’re terrified of losing their kids, a lot of these families are really scared.Referrer, FG2Gendered practice (barrier):I don’t know if it’s just an assumption that it’s the mum’s job to see the health visitor rather than the dad’s, yeah. So, it definitely blurs the picture and it’s quite difficult to do a family assessment.Referrer, FG3. . . [fathers] don’t really want to engage with that type of programme [parenting programmes]; they feel it’s more geared towards the mums than themselves . . . I find it quite difficult to kind of engage with the dads . . . I’m working with the mum and the children, not really the dad.Referrer, FG3 |
| Practitioners | |
| RQ3: acceptability and adequacy of PuP programme training and supervision | Practitioners see added (therapeutic) value (programme model):We would still maybe draw on some of the emotional regulation work or mindful child management type thing. That really compliments what we were already doing, so PuP’s given us a nice framework to do that with. So, yeah formally and informally PuP is used in most of our cases.Practitioner 3Clear guidance (programme model):But there’s a bit of confusion as . . . well how do we actually . . . how do we implement it? You know, are we doing the whole thing as a set programme? Or are we using it as more of a tool? And can pick things from.Practitioner 4Experienced supervisors (implementation/sustainability):. . . understanding different services and how they can differ, and different relationships that different services have with this client group. Having an understanding of that before any training happens and certainly before any supervision. I think that’s really key.Practitioner 3Structured supervision (adoption):For me at the moment, it [supervision] works OK for me. I mean, I’m working jointly with somebody, and we’ve got supervision and I’m keeping the contacts; so that, for me, is OK, but I’m aware for the other staff, I think it needs to be more structured and more set.Practitioner 2Clear guidance for implementation (adoption):But there’s a bit of confusion as . . . well how do we actually . . . how do we implement it? You know, are we doing the whole thing as a set programme? Or are we using it as more of a tool? And can pick things from it.Practitioner 3Clear supervision division (adoption):I had, sort of, team supervision, we had obviously management supervision and peer supervision and PuP supervision. And it just seemed to be an overload.Practitioner 5 |
| Managers | |
| RQ3: acceptability and adequacy of PuP programme training and supervision | Practitioners see added value (adoption):So, they need to go through it in more of a supported way, experience the outcome and the positive benefits that that’s brought to their work and then they can maybe find it easier to adapt.Manager 2Whole-team approach (adoption):. . . if everybody has that knowledge within teams, you can get a lot more back as well and a lot more involvement within team meeting discussions, if that makes sense. Whereas, if you’ve got a team that’s half trained in PuP and half not, you know, you kind of isolate half the team if you’re having discussions.Manager 1. . . these larger kind of pieces of work training accreditation as having a more kind of collective approach within a team so I think you get a kind of more . . . you get a momentum.Manager 7Practitioners supported (adoption):So you’ve got a core team of professionals that are all wanting this to be managed. So, and that’s from the staff who are doing the training to come to it and attend it and be on board with it.Manager 6Sustainability:. . . there needs to be, obviously, continued external supervision of some sort, but also, we need to know that there’s training there for when we bring new people in.Manager 2Resources (sustainability):. . . if we were saying that PuP was a core intervention and we want practitioners to be trained in it, you know, that budget would be increased.Manager 1 |
| Parents | |
| RQ9: profile of change in fathers, mothers and children (perceived benefits of the PuP programme) | Positive affirmation from professionals (therapeutic approach):. . . just being able to have one-to-one time with someone who was a professional in that field and getting feedback from them about myself was . . . I found that really, really good. Most of their feedback was . . . in fact just about all of their feedback was really positive . . .Father 12Emotion regulation (programme model):Just like if he’s misbehaving just . . . what’s it called, the pause button or something, so you’re not jumping right in and shouting or giving him a row. Just like stopping and thinking ‘is it really that bad what he had done’.Father 6And I’ve got a lot more patience for him now. So I think PuP, to be honest, I think PuP has helped me more deal with his mum, than him.Father 2Just being able to step back and think before reacting and that’s probably one of the main things rather than just lashing out, [and] maybe shouting at him, or stuff like that.Mother 6Self as parent (programme model):. . . the course work, it’s helped me discover a wee bit more about myself: the fact that I wasn’t particularly very good at planning things out when it came to the kids, and I always thought I was, you know; but I wasn’t really as proactive as I thought I was.Father 23. . . [PuP has] given me a lot more insight into how my kids were, kind of, thinking, you know. Obviously, as I’ve said to you before, it’s the kids that suffer. I can sit and I can wax lyrical all day long about, like, woe is me, and how bad I feel; but really, you know, learning a lot more about how it [substance use] affected them, that was really, really super helpful.Father 23Parent–child relationship (programme model):Just getting me to connect more with my daughter, ’cause I felt disconnected because of my anxiety and not going out and that, not being able to play. Like, not a lot of dad stuff, going to school, go to the park.Father 4Relationships with partner (mode of delivery):And, just to talk about how we used to be. It makes us stronger as a couple to think, wow we have came a long way.Mother 15Relationships with wider family (programme model):I’ve started talking to my own family more, you know, there are just things that I was speaking to with [PuP practitioner]. Yeah, I’m getting on a lot better with my mother than I did. I see my dad a little bit more than I did, you know. And we’re going to be looking at getting in contact with my other two children . . . that’s something we’re going to look at in the future, you know.Father 13Father–child relationship (programme model):Oh, a lot better. More, a better understanding of his way of thinking . . . I never used to, it’s like, I was brought up with my grandparents, as I said, brought up where children should be seen and not heard. So, that’s kind of the deal I had at first with my other kids, and with [my boy]. And everything[s] changing, I’ve kind of, you know, it’s more about him . . . I can understand where he’s coming from as a kid, and not knowing things . . . I do get why sometimes, they react the way they react, and things like that, and not understanding . . . and security and safety, and how important that is, to feel secure.Father 4Self as parent (programme model):But it causes you to look at how you’re parenting anyway. You never do that because you just dawdle along when you’re a parent and you do what’s needed, whereas, until you look at yourself, then you can’t change nothing until you look at it.Father 15Confidence (mode of delivery/programme model):. . . just being able to have one-to-one time with someone who was a professional in that field and getting feedback from them about myself was . . . I found that really, really good, most of their feedback was . . . in fact, just about all of their feedback was really positive.Father 12Confidence (programme model):. . . [PuP] helped me to set small goals, and go out and get . . . you know, taking the bairn [child] to school and things like that. [PuP] helped . . . to know, I’m not a bad dad. I know I’m doing all the right things . . . but I’m doing more things now. And I’m enjoying it.Father 4Getting baby home (programme model):They’ve even said it recently, so you are . . . you are a . . . what’s the right word, like a rare example of a child, a baby going into care, and how quickly you managed to turn it all around and get her back home and get yourselves straightened up.Father 12 |
| Practitioners | |
| RQ9: profile of change in fathers, mothers and children (perceived benefits of the PuP programme) | A focus on fathering is good for mothers too (therapeutic approach):I think when they’ve got the end result of what they want for their child, and what they want to be like, and it’s changing their whole lives around. So I think the mums are just engaging with the dads and get just as much from it.Practitioner 2. . . in terms of engaging [fathers], I mean, certainly the ones I’ve had, it’s been very much . . . although the partner’s around, it’s been very much focused on him and she’s always been happy for him to have that time, ’cause she’s thinking ‘oh it’ll help him be a better dad’.Practitioner 5Emotional availability/attachment (programme model):. . . the emotional availability framework has been really helpful in helping, certainly me anyway, I can’t speak for everyone, but I think a lot of staff, in understanding the more complex nature of the client group that we’re working with and why parents are behaving in certain ways and where that comes back to; and I think it’s really, really helped.Practitioner 3Emotion regulation/psychological component (programme model):. . . usually, what I’ve found anyway, is, if you succeed as you wish at the practical side of things, it really gives you an in for the more sort of abstract complex kind of emotional side of working with people. And I think PuP lends itself really nicely to that as well.Practitioner 3Understanding child development (programme model/therapeutic approach):So, I think it’s given him an insight into what the issues are, or what, you know, the development stages of the child. So, it’s preparing him; so, I think that has been positive.Practitioner 2Strengths-based approach (programme model):. . . there was a lot of positives, so pointing them out to them and actually confirming that, yeah, they were actually doing things really well. I think that was often a surprise to them.Practitioner 4 |
| Parents | |
| RQ10: what is routine family support services for fathers in drug treatment? | Limited support for dads (barriers):There’s not a lot of things out there for dads so that’s why I did it as well, just anything to help. It tends to be hard for dads, doesn’t it, to get stuff.Father 15I’ve not had access to, you know, any support for parents that are maybe run by like the council or the government, or anything like that. I’ve had nothing.Father 23Focus on surveillance (barrier):I’ve got my social worker, and my social worker’s asking me ‘am I injecting’ and ‘I ken you’ve asked for help’ and things like that but I just felt that I was getting punished for asking for the help, you know.Father 4Negative previous experience (facilitator):. . . the help I’m getting now is better than what I was getting previous . . . how are you getting on and how are you feeling being a dad and how are you enjoying or how are you handling everything. Do you have any issues? It’s more detailed and it’s more . . . it’s really more helpfulFather 12Negative previous experience (gendered practice/barrier):I just felt that because I was on methadone at the time, I believe that the social workers had a pre-made view on me, you know, and they stuck to that view, and as I had no-one at the time, I felt like I wasn’t getting supported at all, and I wasn’t part of the child and family unit sort of thing.Father 13Negative previous experience (barrier):. . . she [social worker] was nasty like, she hated me from the start, she hated [Mother 19] from the start, she never, ever wanted [son] to come back to us.Father 19Focus on mothers and children (gendered practice/barrier):. . . anything to dae wie [mother]’s health or [son]’s health . . . me personally, nut, I’ve had nae help.Father 2I was [involved] at the beginning and then, when we separated, I found there was no support for me . . . I was basically told that it was a child and family service and as I was no longer a member of the family, they couldn’t help me.Father 13Mother positive about fathers’ engagement (gendered practice):Yes, and back when I had my other two kids, I had never heard of fathers having support. It’s always just been mothers, not fathers, but hopefully things are getting better and there will be more for dads out there.Mother 1Mother positive about fathers’ engagement (therapeutic approach):We did it at the same time, so we were communicating the whole way through, but yeah, I think we both got a lot out of it.Mother 10 |
Appendix 16 The ADePT for the PuP4Dads feasibility study
| Methodological issue | Findings | Evidence |
|---|---|---|
| Did the feasibility/pilot study allow a sample size calculation for the main trial? | Yes. Sample size for main trial calculated | Using data from the BCAPI (clinically significant difference and standard deviation) suggests a minimum sample size of 165 participants will be required for a future study, allowing for an anticipated 70% retention rate |
| What factors influence eligibility and what proportion of those approached were eligible? |
Numbers approached unknown. Over 150 staff across Lothian were potential referrers. Meetings with staff teams seemed to indicate small numbers of eligible fathers, although most staff could identify fathers on their caseload who would be eligible Most referrals met the inclusion criteria for the study. There were few ‘inappropriate’ referrals, although eligibility of some fathers changed after consenting into study. Future study would need to take this exclusion of eligible fathers by service providers into account in terms of retention rate The numbers of families referred to PREPARE and CIRCLE per year are only a small proportion of eligible fathers (especially those with non-drug-dependent partners) |
Thirty-eight of 44 (86%) referrals were eligible to participate in the study Three fathers did not meet criteria because of the age of the children and three were from a locality that did not have an accredited practitioner to deliver the programme. Ten fathers declined to participate and three could not be reached. Good data on reasons for exclusion were recorded Eligibility in a larger evaluation would need to take into account the eligibility criteria for individual services, as some fathers were refused the programme by the service after enrolment and/or baseline measures were completed. These parents did not have court orders preventing them from contact with the children, but there were concerns regarding violence and there were permanency proceedings in place, with no plan for reunification. Wait times for intervention to start is also a factor to consider with families whose circumstances can change rapidly |
| Was recruitment successful? |
Yes, but recruitment of fathers was very slow and it took some time for practitioners to feel comfortable referring into the study Recruitment was more successful when researcher attended home visit with practitioner who works with family Fathers’ workers in agencies were also a good source of referrals Recruitment of practitioners and service managers was straightforward and everyone approached agreed to take part Referrers’ focus groups were more challenging because of the logistics of getting busy clinicians together at the same time. Nevertheless, a good level of engagement from staff was achieved |
The target of 24 fathers recruited into study was achieved In addition to drug treatment and PuP programme delivery sites, additional referrers could include local authority children and families services (e.g. child protection teams, early years’ children’s centres, Housing First services). Clinicians need to feel knowledgeable and equipped to ‘sell’ intervention to fathers and it helped when the ‘supportive’ nature of the programme was emphasised. Plain English publicity that practitioners could give to parents would be helpful Gendered practice was a barrier, as practitioners were more experienced at working with mothers than fathers. An extended recruitment period was required to achieve the target. The most successful referrers were drug treatment clinicians, PREPARE, CIRCLE, and primary care (i.e. GP prescribers). Health visitors were a poor source of referrals All PuP practitioners (n = 8) who were approached consented to take part in the study and completed an individual qualitative interview. PuP supervisors (n = 2) also agreed to a second interview All service managers approached took part. The numbers of referrers invited was not known, but four of five focus groups were convened, with 28 staff attending. COVID-19 prevented one focus group from being arranged |
| Did eligible participants consent? | Yes. High conversion to consent for this population | There was a high conversion rate from referral to consent (25/38; 66%). Ten (26%) participants declined to participate and three (8%) could not be contacted. Good data on reasons for exclusion were recorded. Only one mother declined to take part in the study, although she wanted to do the programme with the father. One father wanted to do the programme on his own and not with his partner |
| Were participants successfully randomised and did randomisation yield equality in groups? | n/a | Fathers reported that they would be prepared to be randomised in a future trial; however, this was conditional on them getting an equivalent parenting programme. As usual care for fathers is variable, if it exists at all, this would not be possible |
| Were blinding procedures adequate? | n/a | Were not able to apply blinding to intervention or data collection, although blinding to analysis of some measures (e.g. EAS video) can be achieved |
| Did participants adhere to the intervention? |
Yes, engagement in the programme and attendance rates were adequate for this population. The majority of participants attended six sessions or more. There was good adherence to model components, although this varied between families Engagement was better when participants were allocated quickly to start the programme. Intervention delivery is individualised and so it is impossible to tell when the intervention was ‘completed’ |
Fourteen of 20 (70%) fathers and 10 of 14 mothers who started the programme completed six or more sessions Practitioners delivered a total of 248 sessions to the 20 families, including couples (n = 140), father-only (n = 52) and mother-only sessions (n = 56) The median length of engagement of fathers was 26 weeks. The median length of engagement of mothers was 30 weeks Attendance of both fathers and mothers was good (mean 71%) The median number of sessions for fathers was 13. The median number of sessions for mothers was 14.5 Participants reported receiving a median of 15 (out of a total of 20 possible) components of the programme |
| Was the intervention acceptable to the participants? | Yes, acceptability of the intervention was rated highly by the majority of fathers, mothers, PuP practitioners, PuP supervisors and service managers who completed qualitative interviews |
Fathers and mothers reported that they would recommend the programme to other parents who use drugs Aspects of the programme that were most valued included the mode of delivery (i.e. home visiting, individually tailored to the needs of each family, the ‘whole-family’ approach, use of ‘parent workbooks’ and flexible length of delivery), the therapeutic approach (i.e. it was strengths based, involved collaborative goal-setting, there was a therapeutic alliance between parents and practitioners, it focused on emotion regulation, the use of video-feedback and the therapeutic focus on parent–child relationships/fatherhood) and the programme model (i.e. structured modules that provide a therapeutic exploration of parenting knowledge and skills, and use of validated questionnaires and databases to measure and report progress) Implementation sites are continuing to deliver the PuP programme after the study intervention phase ended. Both services have invested in more staff being trained in the programme |
| Was it possible to calculate the intervention cost and duration? |
Yes, in theory, it costs £1000 per practitioner trained to accreditation level Eight practitioners delivered the programme (£8000). More (n = 4) were trained in preparation for the study, but did not deliver the programme The costs of staff salaries can be calculated; however, there were no added costs in this study, as all staff provide family support service to families irrespective of the PuP intervention Workbooks were costed as part of grant at £480 |
For the purposes of this study, most implementation support costs were provided in kind, including external supervision during the implementation phase and developer meetings with teams and managers. Eight staff were trained in 2016, but only four were accredited and able to deliver the intervention at the start of the study. Another cohort was trained in 2017 after the start of study and four of these staff then delivered the intervention to study participants. A total of eight practitioners delivered the intervention to 20 families Staff trained in the PuP programme were absent for a variety of reasons, including maternity leave, long-term sick leave, promotion, left agency and commissioning cycles interrupted training/accreditation A future evaluation would need to consider sustainability of programme delivery and include additional ongoing training and implementation support |
| Were outcome assessments completed? |
Yes (the majority). Acceptability of assessments was high, with few refusals to complete Researcher-administered questionnaires resulted in few missing data The EAS video measure was not feasible to administer in most cases because of logistical reasons and out-of-home placements The service use survey was not feasible to collect, as it required parent self-completion and was reportedly forgotten or lost |
Our minimum target of 10 fathers completing all three research interviews and at least one qualitative interview was achieved. Results show that 13 fathers completed all three interviews and 16 fathers completed both qualitative interviews Overall, researcher-administered questionnaires were successful. Completion rates and retention are likely to be higher with more frequent researcher contact with family However, there were some researcher error in administration of some measures and so more careful auditing would be required in a larger study. A checklist and immediate data entry to SPSS would ensure that missing data could be avoided in the future Although completion rates were high, burden on participants was noted. If the number of questionnaires were reduced (burden per interview) then this would likely result in even higher completion rates and better retention. More frequent and smaller quantity measures would be advisable based on the results of this feasibility study. Parent self-completion of questionnaires should be avoided, as this is likely to result in very poor returns and missing data |
| Were outcome measurers those that were the most appropriate? |
Yes, most measures that would be important for a future evaluation were suitable, acceptable and completed well (e.g. BCAPI, DERS, TOP and EQ-5D-5L) Some measures were not suitable for families because of the age of child, out-of-home placements and the father not being in a couple relationship |
Child well-being measures were difficult to replicate across age of index child (e.g. newborn to infant to pre-school age). It was difficult to get repeat measures over time, which is a common problem in research with children aged 0–8 years A co-parenting measure was not included in the feasibility study, but this would be important to include in a larger evaluation, as would quality of caregiving environment (possibly using the HOME108 measure) In addition, a therapeutic alliance measure would be useful in a future study, as this quality was highlighted by most participants |
| Was retention to the study good? |
Yes, retention exceeded the minimum required as per progression criteria Retention could be improved significantly by implementing a range of strategies to maintain contact with parents and incentivise completion of research interviews |
Twenty-three fathers completed baseline measures and the qualitative interview Sixteen fathers completed FU1 measures and the qualitative interview Thirteen fathers completed FU2 measures Fourteen of 20 fathers engaged well in the intervention and attended six or more sessions Median length of engagement for fathers was 26 weeks There was no difference between father and mother engagement and retention (taking into account incarceration and issues of violence prohibiting fathers from taking part in the intervention) |
| Were the logistic of running a multicentre trial assessed? | Yes. Findings from the expert event (October 2020) and subsequent PPIE events with Public Health England (December 2020) and service stakeholders (January and February 2021) demonstrate that scale-up of the intervention is likely and would meet the requirements (e.g. delivery sites, sample size, recruitment numbers) for a larger evaluation |
Policy-makers at the expert event and subsequent PPIE events have indicated that the PuP intervention is a very suitable intervention for this population and fits well with the ‘whole-family’ approach that is now advocated across the UK There are already three agencies and four teams in Scotland who are delivering the programme: NSPCC in Glasgow, PREPARE and CIRCLE in Edinburgh, CIRCLE in East Lothian and CIRCLE in West Lothian. In addition, in Ireland, there are several community-based agencies delivering the programme to this population. In England, several agencies and areas across the South West and East and Midlands indicated interest in delivering the programme. These agencies are now seeking funding for training. Therefore, a multicentre trial is feasible, given the level of interest However, the resource required for research-led recruitment, retention and data collection in a multicentre trial would be substantial and expensive to allow, for example, home visits and/or digital inclusion for video calling for this population |
| Did all components of the protocol work together? |
Yes, although COVID-19 did disrupt the final phase of data collection, analysis and write-up of the report Data collection time points need to be fixed, irrespective of how long families take to complete the intervention |
The protocol was revised a number of times to alter eligibility criteria (i.e. expectant fathers and children up to 8 years of age), data collection time points (to accommodate families who took > 6 months to complete the intervention) and to add interviews with service managers Owing to COVID-19, one focus group was cancelled, some participants were followed up by telephone rather than face to face and the expert event was held via video-conference rather than face to face. Write-up was also affected by prolonged lockdown More frequent data collection time points is advisable to aid retention and to maximise data collection and analysis |
Glossary
- A process for Decision-making after Pilot and Feasibility Trials
- A process that (1) encourages the systematic identification and appraisal of problems and potential solutions, (2) improves the transparency of decision-making processes and (3) reveals the tensions that exist between pragmatic and explanatory choices.
- Child maltreatment
- A behaviour towards a child that is outside the norms of conduct and entails significant risk of causing physical and/or emotional harm and/or death. Four main types of maltreatment are generally recognised: (1) physical abuse, (2) sexual abuse, (3) emotional abuse (psychologic abuse) and (4) neglect.
- Concordant couples
- Couples where the father and mother are drug dependent.
- Consolidated Standards of Reporting Trials diagram
- A simple flow diagram showing the enrolment of subjects, their allocation to treatment, disposition status and how they are analysed in the trial.
- Discordant couples
- Couples where one parent is drug dependent and the other is not. In this study, discordant couples included drug-dependent fathers and non-drug-using mothers.
- Drug dependence
- Generally understood to be a syndrome that involves a cluster of physiological, behavioural and cognitive phenomena in which the use of a substance, or a class of substances, takes on a much higher priority for a given individual than other behaviours that once had greater value. Central characteristics of dependence syndrome include increasing tolerance to the drug, withdrawal symptoms, compulsion to take substances regardless of harm and relapse to former levels of consumption after cessation.
- Emotion/affect dysregulation
- An inability to manage emotional responses or to keep them within an acceptable range of typical emotional reactions. This can refer to a wide range of emotions, including sadness, anger, irritability and frustration.
- EuroQol-5 Dimensions, five-level version
- A quality-of-life instrument that allows respondents to evaluate their overall health status. The ‘5L’ refers to five scores for each of the five health dimensions.
- Feasibility studies
- Research conducted before a main study to answer the question ‘can this study be carried out?’. The studies are used to estimate important parameters that are needed to design the main study.
- Getting It Right For Every Child
- A Scottish national framework for practice for working with children and families. The framework aims to support families by making sure children and young people can receive the right help, at the right time and from the right people. The framework aspires to help children to grow up feeling loved, safe and respected so that they can realise their full potential.
- Looked-after children
- Defined under the Children (Scotland) Act 1995 [Great Britain. Children (Scotland) Act 1995. London: The Stationery Office; 1995] as those in the care of their local authority. There are many reasons why children may become looked after, including that they face abuse or neglect at home, that they have disabilities that require special care, that they are unaccompanied minors who are seeking asylum or that they have been involved in the youth justice system.
- NVivo
- A qualitative data software program produced by QSR International (Warrington, UK). NVivo helps researchers to organise, code, sort and manage large qualitative data sets.
- Opioid substitution therapy
- A treatment for opioid dependence. Opioid drug users are prescribed a ‘substitute’ drug that is either similar or identical to the illicit drug normally consumed {e.g. prescribed methadone [methadone hydrochloride, Alliance Healthcare (Distribution) Ltd] to replace the use of street (illicit) heroin}. Also known as opioid replacement therapy, methadone maintenance therapy and medication-assisted treatment.
- Polydrug use
- The use of more than one psychoactive drug or type of psychoactive drug by an individual, consumed at the same time or sequentially. It can include the use of alcohol, illegal drugs, prescription drugs, solvents and over-the-counter medications.
- PROSPERO
- An international database of prospectively registered systematic reviews in health and social care.
- SPSS®
- A statistical software program produced by IBM SPSS Statistics (Armonk, NY, USA) that helps researchers extract actionable insights from quantitative data.
- Template for Intervention Description and Replication
- A reporting guideline for describing interventions in sufficient detail to allow their replication.
List of abbreviations
- ADePT
- A process for Decision-making after Pilot and Feasibility Trials
- ADP
- Alcohol and Drug Partnership
- BCAPI
- Brief Child Abuse Potential Inventory
- BITSEA
- Brief Infant Toddler Social and Emotional Assessment
- CAPSU
- Children Affected by Parental Substance Use
- CONSORT
- Consolidated Standards of Reporting Trials
- CTS2
- Revised Conflict Tactics Scale
- DERS
- Difficulties in Emotion Regulation Scale
- DMEC
- Data Monitoring and Ethics Committee
- EAS
- Emotional Availability Scale
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- F4C
- Fathers for Change
- FU1
- follow-up 1
- FU2
- follow-up 2
- GIRFEC
- Getting It Right For Every Child
- GP
- general practitioner
- IQR
- interquartile range
- MAAS
- Maternal Antenatal Attachment Scale
- NIHR
- National Institute for Health Research
- OST
- opioid substitution therapy
- PAAS
- Paternal Antenatal Attachment Scale
- PPIE
- patient and public involvement and engagement
- PSCS
- Parenting Sense of Competence Scale
- PuP
- Parents under Pressure
- PuP4Dads
- Parents under Pressure programme for fathers
- R&D
- research and development
- RCI
- Reliable Change Index
- RCT
- randomised controlled trial
- RF
- research fellow
- RQ
- research question
- SDQ
- Strengths and Difficulties Questionnaire
- SIMD
- Scottish Index of Multiple Deprivation
- SSC
- Study Steering Committee
- THRIVE
- Trial for Healthy Relationship Initiatives in the Very Early years
- TOP
- Treatment Outcomes Profile
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/YOWK7214).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
