Notes
Article history
The contractual start date for this research was in April 2018. This article began editorial review in June 2022 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Taalaibekova et al. This work was produced by Taalaibekova et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Taalaibekova et al.
Material throughout the report has been reproduced from Taalaibekova et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/.
Introduction
The greatest health service disruptions caused by the coronavirus infection 2019 (COVID-19) pandemic were experienced by low- and middle-income countries (LMICs). 2 In Kyrgyzstan, the pandemic has caused considerable disruption and burden to individuals, society and the economy. According to the Ministry of Health of Kyrgyzstan, as of 9 October 2021, there were more than 127,000 cases and more than 2600 deaths. 3 In clinical practice, doctors often encounter post-COVID syndrome and patients report long-lasting symptoms that reduce their quality of life (QoL). 4 In particular, some survivors cannot go to work and others find it difficult to carry out their daily activities. Recent data from the UK suggests that more than 70% of individuals are not fully recovered 1 year post infection, with those discharged from the hospital often experiencing one or more persistent symptoms (for at least 4 months). 5–7 In Kyrgyzstan, as with other Central Asia countries, little is known about individuals with post-COVID syndrome and this has been acknowledged as a research priority by the Ministry of Health.
For many LMICs, there is no existing infrastructure or services to support the rehabilitation of COVID-19 survivors, as has been suggested in other parts of the world. 8,9 For example, most high-income countries have adapted existing rehabilitation services, which already support a wide range of health conditions, through multidisciplinary teams. 10,11 This has been particularly apparent for symptomatic patients who share similar symptoms (e.g. breathlessness, cough and fatigue) to people attending pulmonary rehabilitation (PR). 12–14 Early evidence for COVID rehabilitation is promising in improving breathlessness, exercise tolerance and other post-COVID symptoms. 15,16
In contrast, PR is not widely available in LMICs, including Kyrgyzstan. 17,18 Additional post-COVID symptoms, such as post-traumatic stress disorder (PTSD) and coping with social isolation, must also be considered, but the extent to which individuals in Kyrgyzstan are burdened by the wide range of symptoms documented in other parts of the world is unclear. 19–22 Efforts to develop rehabilitation for COVID-19 survivors have been successful in some low-resource settings, but there is a clear need to develop interventions specific to the context in which they will be delivered. 22,23
With the lack of existing rehabilitation infrastructure in Kyrgyzstan, the development of appropriate support for the many COVID-19 survivors with post-COVID syndrome is needed. This study aimed to examine what this support might look like and specifically address persisting post-COVID symptoms, views on the optimal timing, suitable delivery methods, content of the support and obstacles to implementation. To do this, we conducted online surveys with COVID-19 survivors and clinical workers in Kyrgyzstan.
Methods
Study design
This study was conducted between 23 April and 3 September 2020 using two cross-sectional online surveys in Russian. 1 The survey was designed by the National Institute for Health and Care Research (NIHR) Global RECHARGE Group for Pulmonary Rehabilitation (17/63/20). Ethical approval was obtained from the University of Leicester (#24736). The study is reported in accordance with the Strengthening the Reporting of Observational Studies (STROBE) guidelines. 24
Community engagement and involvement
The patients and the public were not directly involved in the design of the study. When developing the research question, as well as the outcome indicators, the assessment of symptoms, barriers, priorities and patient preferences were fully taken into account. The questionnaire was tested with patients before the start of data collection. This work was carried out to study patients’ opinions to improve the quality of care they receive, ensuring appropriate support for COVID-19 survivors. The results of this study will be disseminated to participants and the general public through dedicated online and in-person events. Results will also be disseminated at national and international conferences and meetings. It is expected that the results of this study will help in the development of COVID-19 rehabilitation and rehabilitation services more broadly in Kyrgyzstan.
Participants and setting
The first group included a convenience sample of clinical workers of various specialities (including pulmonologists, infectious disease specialists and nurses) from various medical institutions [National Center for Cardiology and Internal Medicine (NCCIM), National Hospital, City Clinical Hospital #6, Family Medicine Center #7, National Center for Maternity and Childhood Protection, Republican Infectious Clinical Hospital] who worked in the places of treatment for patients with COVID-19.
The second group consisted of a convenience sample of patients aged ≥ 18 years who had recovered from COVID-19 [with or without confirmation of polymerase chain reaction (PCR), with varying degrees of severity], who were recruited from family medicine centres using a database of COVID-19 survivors. Patients had received an online consultation from a pulmonologist, visited an outpatient clinic, or were hospitalised at the NCCIM in Bishkek, Kyrgyzstan. Surveys were either conducted at the NCCIM or sent to patients with internet access in the database.
Variables and data sources
The survey consisted of 16 questions and was conducted anonymously and voluntarily with consent confirmed by completion and submission of the survey responses (see Report Supplementary Material 1). The survey for clinical workers included questions on the most important considerations when developing post-COVID-19 support, the best timing and location of support and barriers to referring patients for support. The patient survey included questions on the problems they faced due to severe-acute-respiratory-syndrome-related coronavirus (SARS-CoV-2) infection, the best way to receive support, what time commitment they would give to support their recovery and barriers to participating in post-COVID-19 support. The respondents were provided with a link to the survey and the questions were filled out on devices (tablet, phone, and computer) independently, or with the help of a researcher, if required.
Statistical methods
Data were described using frequencies and percentages, with no inferential statistics due to the descriptive nature of the surveys. Data were summarised using reports from Jisc Online Surveys® (www.onlinesurveys.ac.uk/, Bristol, UK) and Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA). Qualitative data counting was used to analyse the free-text responses, which involved identifying similar responses within the data and grouping them together. 25
Results
Survey completion and participant characteristics
One hundred and thirty-two COVID-19 survivors were invited to participate, of which 111 (84%) completed the survey (68% female, 51% aged 19–29 years). The 111 COVID-19 survivors completed all survey questions. The majority of SARS-CoV-2 survivors surveyed were in paid employment (41%), in full-time education (20%) or retired (10%). Most (77%) were diagnosed as a result of contacting medical institutions with the help of clinical workers with laboratory confirmation. Two-thirds self-isolated following diagnosis, 50% were prescribed medications, 18% were admitted to hospital and 2% were admitted to an intensive care unit.
For clinical workers, 87 were invited to take part in the survey, of which 85 (98%) completed the survey (84% female, 53% aged 19–29 years). The 85 clinical workers completed all survey questions. The main group of surveyed clinical workers consisted of pulmonologists (25%), nurses (12%), infectious disease specialists (9%), general practitioners of modern medicine (9%) and others comprising single professions (55%). The majority of clinical workers were actively involved in working with COVID-19 survivors: 42% of respondents were engaged in their treatment in a hospital, 21% were engaged in making a diagnosis, 20% worked on an outpatient basis, 12% delivered oxygen therapy and 28% had not worked directly with COVID-19 patients.
Responses of clinical workers
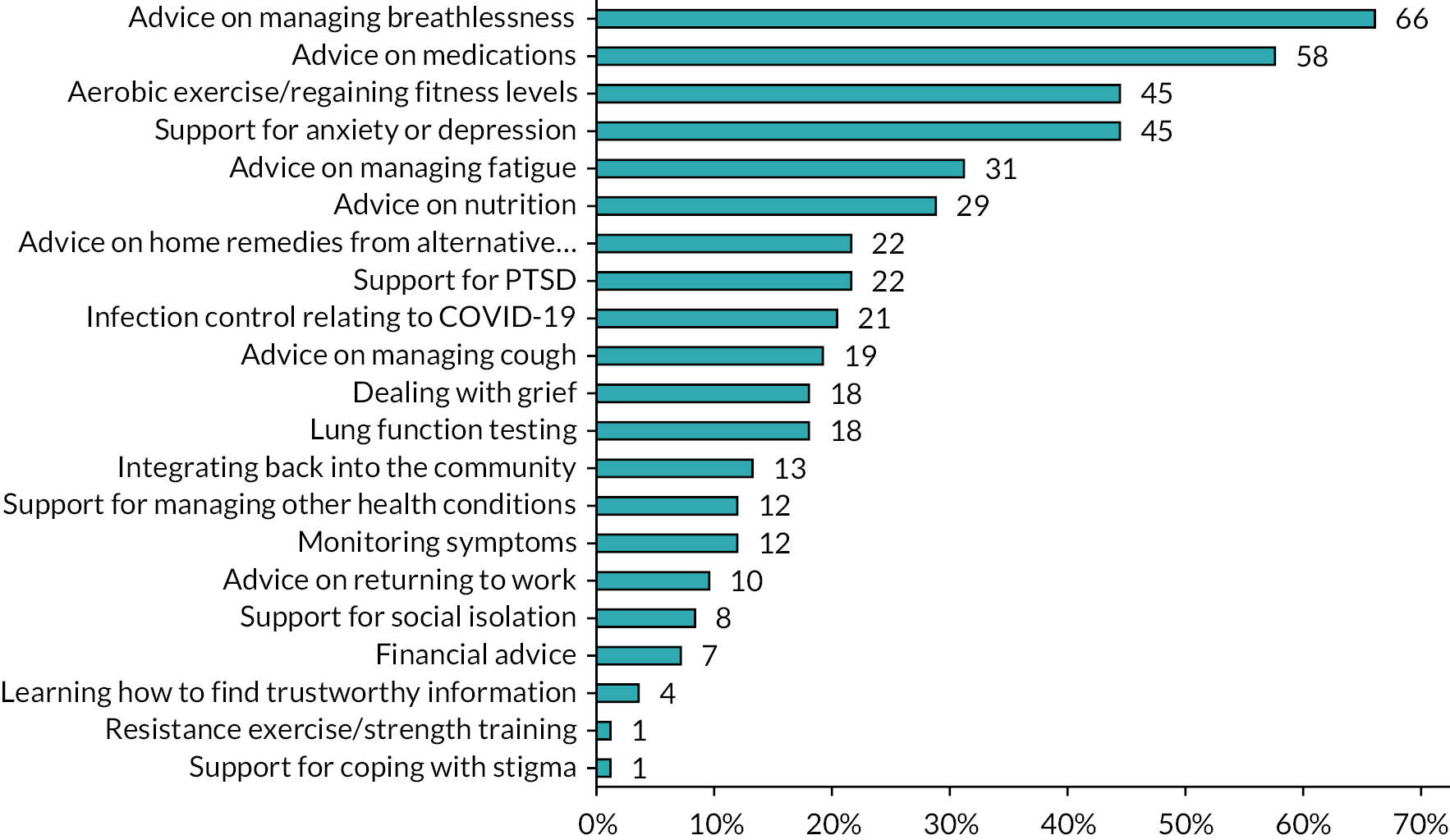
The survey asked clinical workers to list their five most important topics to support COVID-19 survivors. The top five selected topics were ‘advice on managing breathlessness’ (66%), ‘advice on medications’ (58%), ‘aerobic exercise/regaining fitness levels’ (45%), ‘support for anxiety or depression’ (45%) and ‘advice on managing fatigue’ (31%) (Figure 1). The five least selected items were ‘support for social isolation’ (8%), ‘financial advice’ (7%), ‘learning how to find trustworthy information’ (4%), ‘resistance exercise/strength training’ (1%) and ‘support for coping with stigma’ (1%).
FIGURE 1.
Which of the following potential considerations should be part of post-COVID-19 support?
When asked whether support should be provided to patients who were not hospitalised with SARS-CoV-2, 92% of clinical workers agreed. When asked where support should be delivered, most clinical workers selected community settings (55%) or at home (55%), with 37% suggesting hospitals. The majority of clinical workers were confident that patients would be receptive to support with their post-COVID recovery (88%). Some (9%) were unsure how patients would respond to the offer of support.
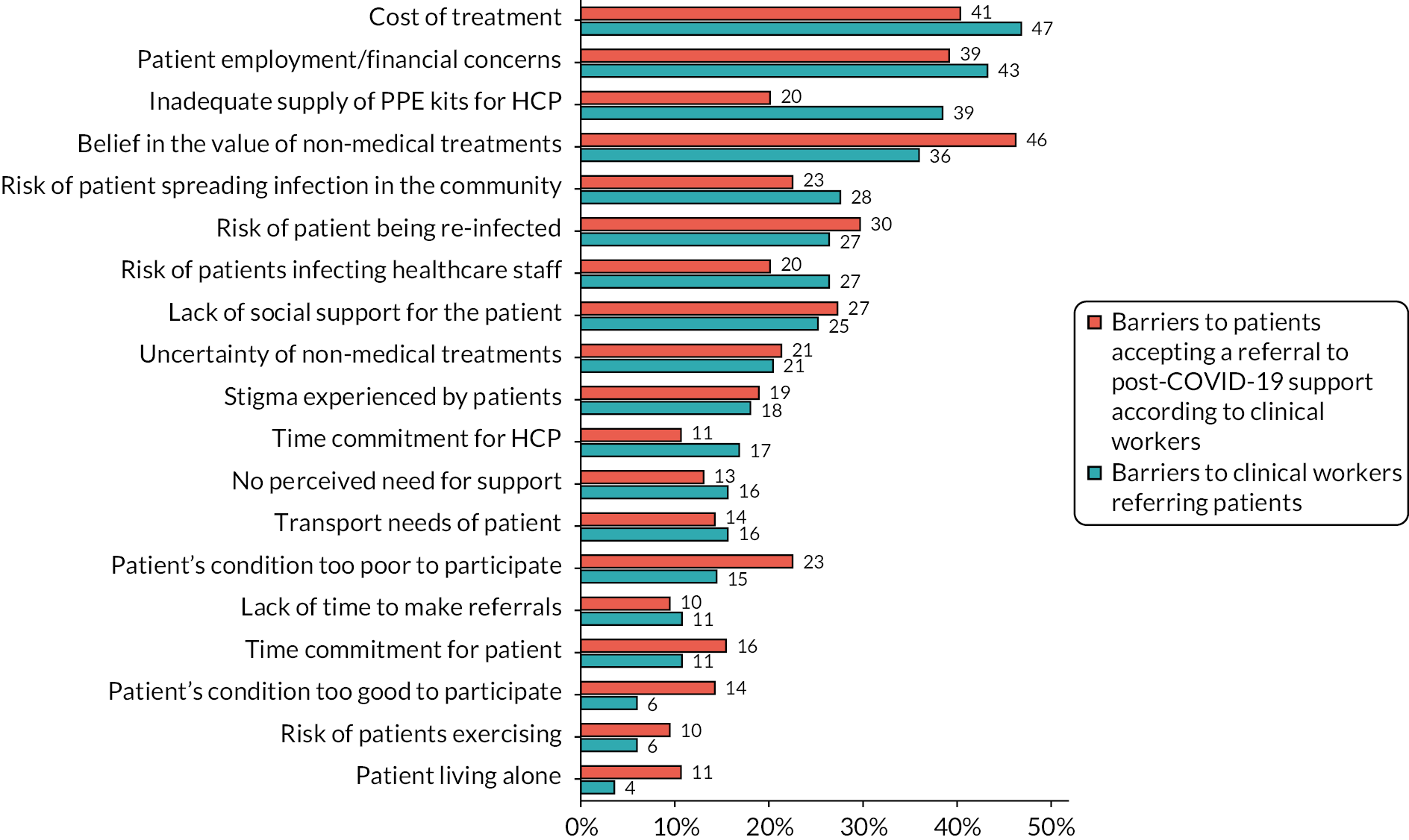
Barriers to the provision and acceptance of support according to clinical workers can be seen in Figure 2. According to clinical workers, the main barriers to providing support to patients were the cost of treatment (47%) and patient employment/financial concerns (43%). An inadequate supply of personal protective equipment (PPE) kits for healthcare professionals (HCPs) (39%) was also of great importance. Factors clinical workers believed would hinder patient acceptance of support were belief in the value of non-medical treatments (46%), cost of treatment (41%) and patient employment/financial concerns (39%).
FIGURE 2.
Which of the following may be barriers to clinical workers referring patients to post-COVID-19 support and what may be barriers to patients accepting a referral to post-COVID-19 support according to clinical workers?
Most clinical workers reported that support should be provided to COVID-19 survivors either during treatment (65%) or immediately after returning home from the hospital (59%). Clinical workers selected video consultation as the most suitable method of communication to deliver support (65%), followed by telephone calls (47%), dedicated smartphone applications (45%) and the use of television (45%). Almost a third of clinical workers (31%) selected face-to-face communications or home visits. Overall, clinical workers were positive about supporting the recovery of COVID-19 survivors, with 73% reporting they think it would be beneficial for patients.
Responses of COVID-19 survivors
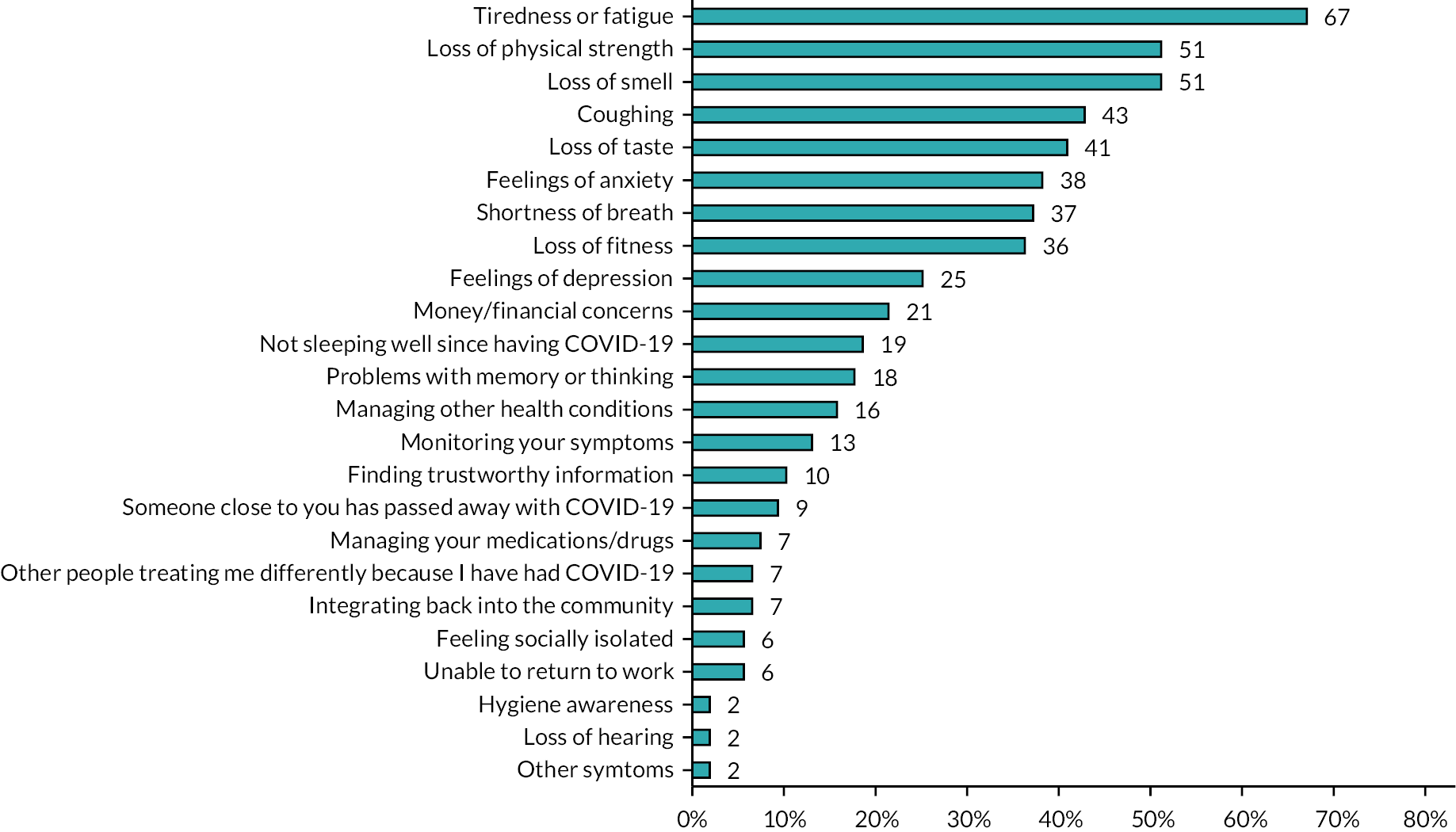
Problems faced by patients as a result of COVID-19 and the areas in which they wanted help can be seen in Figure 3. The most common were tiredness or fatigue (67%), loss of physical strength (51%), loss of smell (51%), coughing (43%) and loss of taste (41%).
FIGURE 3.
What problems are you facing as a result of COVID-19?
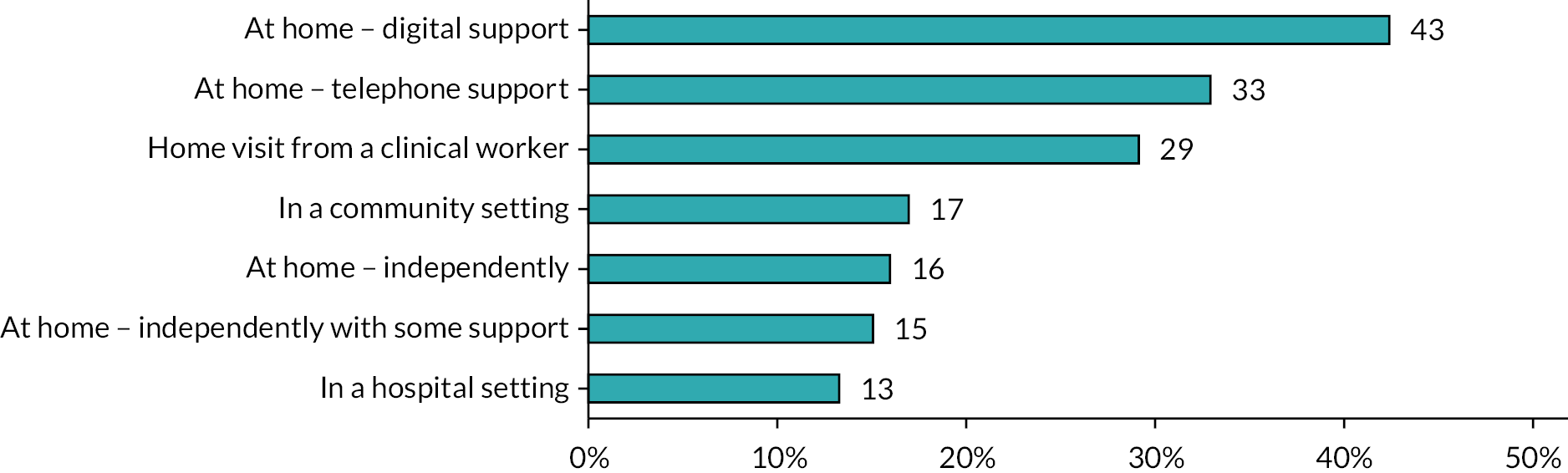
When patients were asked, ‘How would you like to receive such support?’ and ‘How would you like to receive such assistance?’, the most common approaches were receiving support at home with digital support (43%), at home with telephone support (33%) or receiving a home visit from a clinical worker (29%), as seen in Figure 4.
FIGURE 4.
How would you like to receive such support?
When patients were asked ‘How much time per day and how many days per week are you willing to devote to participating in an intervention to alleviate their symptoms after COVID-19?’, they responded as ready to devote one to three sessions per week (84%) with a duration of no more than 1 hour (90%).
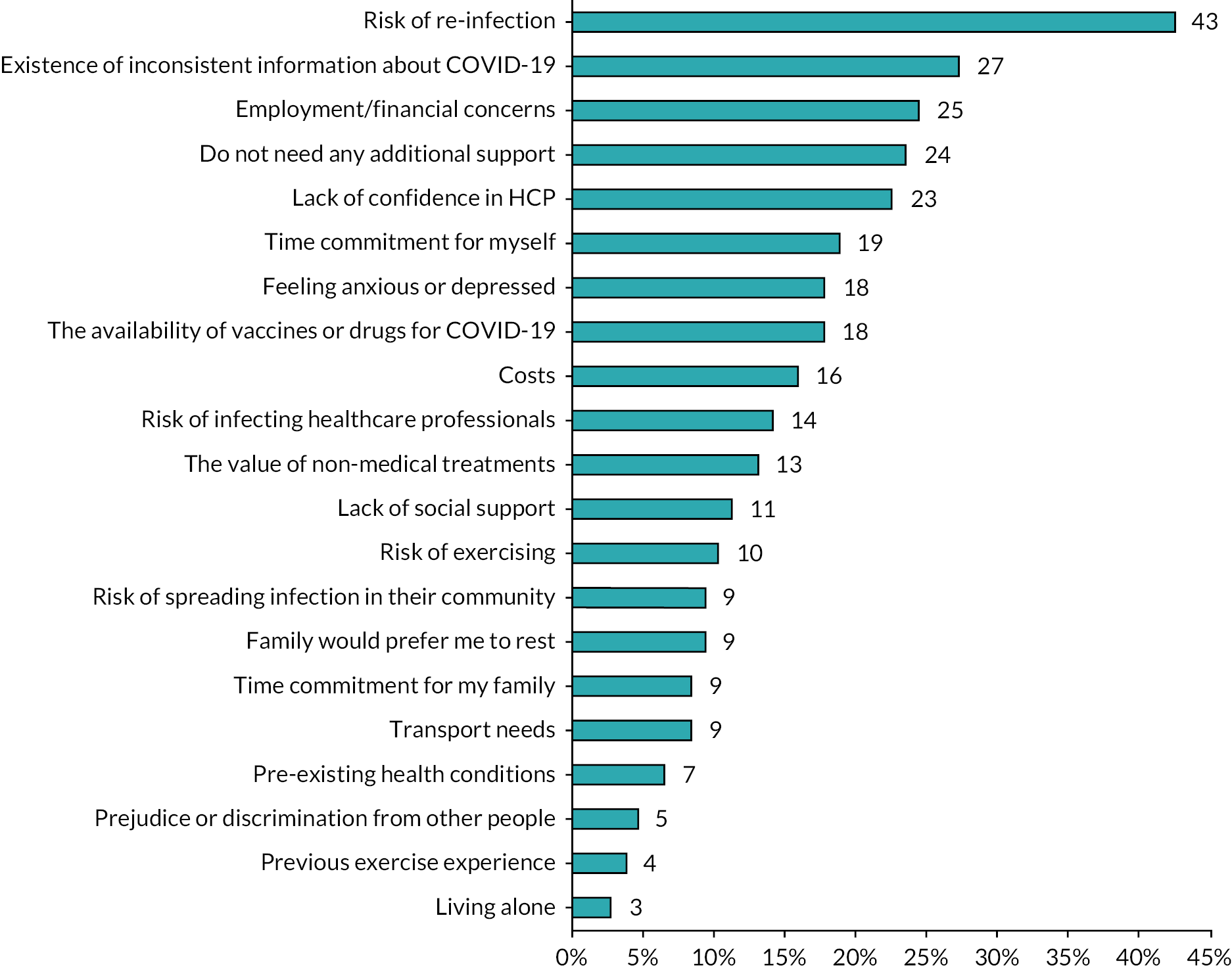
Factors that could prevent patients from accepting rehabilitation assistance after COVID-19 can be seen in Figure 5. Risk of re-infection was the main barrier for patients accepting support (43%), followed by inconsistent information about COVID-19 (27%) and a lack of confidence in HCPs (23%). Almost a quarter (24%) of patients reported not needing additional support.
FIGURE 5.
What might make it difficult for you to access support to help you recover from COVID-19?
Discussion
The data were obtained from patients who experienced COVID-19 and various clinical workers who dealt with COVID-19 survivors in Kyrgyzstan. Based on our results, a post-COVID support intervention might be more acceptable if it were home-based, for hospitalised and non-hospitalised patients, with a combination of face-to-face, video and telephone support, with a focus on strength and aerobic training, and symptom management. There is a need to address patient barriers to accepting support, which include risk of re-infection, inconsistent information about COVID, a lack of confidence in clinical workers and financial concerns. Barriers to clinical workers referring patients for such support included inadequate supplies of PPE.
Structure and timing of the support
The importance of rehabilitation after COVID-19 has been emphasised according to the framework of the International Classification of Functioning, Disability and Health. 26 Taking into account the opinion of the surveyed clinical workers, the developed rehabilitation programme requires an integrated approach, including exercise as a major component in supporting COVID-19 survivors. It must be noted that the majority of the respondents also stated the importance of psychological support. Isolated mental health issues or psychological issues, such as PTSD, anxiety and depression, are documented following SARS-CoV-2 infection. 27 The Respiratory Rehabilitation Committee of the Chinese Association of Rehabilitation Medicine and the Cardiopulmonary Rehabilitation Group of the Chinese Society of Physical Medicine and Rehabilitation suggest that, apart from easing respiratory distress, improving physical function and QoL, rehabilitation programmes can be useful in improving both anxiety and depression. 27 Six-week respiratory rehabilitation can improve respiratory function and anxiety in elderly patients with COVID-19. 28 Shortness of breath and fatigue have been consistently identified as some of the most common symptoms. 29 Rehabilitation assessment should be offered to all patients suffering from post-COVID-19 symptoms, not just laboratory-confirmed patients or only those who have been hospitalised. 30
Regarding the issue of the location of rehabilitation, most COVID-19 survivors and clinical workers consider community settings and their homes as the most suitable places. This may be associated with a perceived reduced risk of (re)infection and/or community transmission, compared with attending hospitals. Moreover, one should take into account the fact that most of the Kyrgyz population uses public transport for daily travel, which increases the risk of infection. Still, one-third of the respondents preferred the inpatient facility to be more suitable for rehabilitation, possibly due to the availability of professional medical care.
Coronavirus infection 2019 survivors wanted to receive home-based rehabilitation via the internet and/or telephone, suggesting that they want to avoid unnecessary contact with others and minimise the risk of re-infection. Digital methods are gaining popularity in Kyrgyzstan every year. Their advantages are availability, ease of handling and elimination of the risk of infection. With modified communications, remote rehabilitation has significant potential in a wide variety of situations in the near future, including those at high risk of infection or those that can be treated at a distance, such as at home or in more remote regions. 30 However, it should be noted that this is a very simple method and one cannot see the patient or demonstrate techniques for safe exercising. Consequently, nearly a third of clinical workers and COVID-19 survivors opted for in-person or home visits, possibly because older adults and clinical workers are reluctant to use the internet. In addition, in many remote villages of Kyrgyzstan, there is no internet or mobile communication.
When COVID-19 survivors were asked about the frequency of the sessions, the most suitable schedule would be 1–3 days a week with the duration of the session not more than 1 hour. Patients noted some barriers that would prevent them from accepting support. The risk of re-infection was the main obstacle to accepting support, in line with the preference of receiving support at home. In contrast to the opinion of clinical workers, almost a quarter of COVID-19 survivors reported that they did not need additional support.
Main issues/symptoms to address
The majority of COVID-19 survivors noted the importance of rehabilitation to eliminate persistent symptoms, restore lost or reduced functions of various organs and systems and for the subsequent improvement of QoL. In our study, the main long-term symptoms of COVID-19 survivors were tiredness or fatigue, loss of physical strength, cough, and loss of smell and taste. A systematic review has shown that symptoms of COVID-19 usually persist after the acute phase of infection, with implications for health-related functioning and QoL. 31
There is now a large amount of data on the long-term symptoms experienced by COVID-19 survivors after being discharged from the hospital. An Italian study that followed 143 patients 7 weeks after discharge found that 53% of patients reported fatigue (which is similar to our data), 43% reported shortness of breath, 27% reported joint pain and 22% reported chest pain. 18 In a similar study in the UK, fatigue associated with a new illness was the most common symptom, reported by 72% of participants in the intensive care group and 60.3% of participants in the ward group. The next common symptoms were shortness of breath (65.6% in the intensive care group and 42.6% in the ward group) and psychological stress (46.9% in the intensive care group and 23.5% in the ward group). 28
Barriers to referral and participation
Clinical workers and COVID-19 survivors highlighted common barriers in providing and receiving support for COVID-19 survivor care, such as the cost of treatment, the impact on patient employment and financial problems. Differences were also found, for example, the necessity of PPE kits for clinical workers. In addition, for COVID-19 survivors receiving rehabilitation, one of the main obstacles was the credibility of non-medical therapies. The lack of specialists and doubts about the quality of the prescribed drugs influence residents of Kyrgyzstan to use non-medical therapies. For example, methods such as bloodletting, drinking tinctures from plants and eating certain foods (e.g. garlic, soda, onions) seem to be gaining popularity, based on clinical experiences and observations.
Limitations of the study
This exploratory study recruited convenience samples of COVID-19 survivors and clinical workers, mostly from the Bishkek and Chui regions. Data collection was limited to an online survey, which may have led to selection bias. We attempted to minimise selection bias by supporting participants without their own devices to complete the survey. Due to limitations in staffing and resources, we were able to recruit a small proportion of patients hospitalised with COVID-19. Future work should consider in-depth, qualitative exploration to further develop possible interventions in this population. However, the inclusion of free-text responses was sufficient to identify barriers to setting up post-COVID-19 support interventions. The results of this study provide a valuable initial insight into how to develop and implement post-COVID support in Kyrgyzstan, but monitoring of the implementation will be required. Evidence of the benefit of interventions such as rehabilitation is growing, with larger studies in progress. 32
Conclusions
Coronavirus infection 2019 survivors and clinical workers appear receptive to the provision of support for ongoing symptoms. However, the views of clinical workers and patients did not always align. Our findings could be used to inform further development of appropriate post-COVID-19 support activities for people living in Kyrgyzstan. Based on our findings, preferences for such support included a home-based intervention, delivered primarily through video and telephone communication, and with a focus on strength and aerobic training and symptom management. Risk of re-infection, inconsistent information about COVID-19, a lack of confidence in clinical workers, financial concerns and inadequate supplies of PPE were the main barriers to implementation.
Additional information
Acknowledgements
We gratefully acknowledge all the participants for taking part in this survey.
CRediT contribution statement
Aijan Taalaibekova (https://orcid.org/0000-0001-8439-4710): Conceptualisation (equal), Data curation (lead), Formal analysis (lead), Investigation (equal), Methodology (equal), Visualisation (lead), Writing – original draft (lead). Alena Oleinik (https://orcid.org/0009-0009-3436-5626): Conceptualisation (equal), Data curation (supporting), Formal analysis (supporting), Investigation (equal), Methodology (equal), Writing – original draft (supporting). Kamila Magdieva (https://orcid.org/0009-0002-8534-2765): Conceptualisation (equal), Data curation (supporting), Formal analysis (supporting), Investigation (equal), Methodology (equal), Writing – original draft (supporting). Gulzada Mirzalieva (https://orcid.org/0000-0002-7507-1570): Conceptualisation (equal), Data curation (supporting), Formal analysis (supporting), Investigation (equal), Methodology (equal), Writing – original draft (supporting). Zainab K Yusuf (https://orcid.org/0000-0001-7859-5102): Conceptualisation (equal), Data curation (supporting), Formal analysis (supporting), Funding acquisition (supporting), Methodology (equal), Validation (supporting). Maamed Mademilov (https://orcid.org/0000-0001-8528-3115): Conceptualisation (equal), Data curation (supporting), Formal analysis (supporting), Investigation (equal), Methodology (equal), Writing – original draft (supporting). Azamat Akylbekov (https://orcid.org/0000-0001-5761-399X): Conceptualisation (equal), Data curation (supporting), Formal analysis (supporting) Investigation (equal), Methodology (equal), Validation (supporting), Writing – original draft (supporting). Amy V Jones (https://orcid.org/0000-0001-6565-8645): Conceptualisation (equal), Funding acquisition (supporting), Methodology (equal). Ruhme B Miah (https://orcid.org/0000-0002-2412-3756): Conceptualisation (equal), Funding acquisition (supporting), Methodology (equal), Project administration (equal), Writing – reviewing and editing (supporting). Dominic Malcolm (https://orcid.org/0000-0002-5898-2911): Conceptualisation (equal) Methodology (equal), Writing – reviewing and editing (supporting). Andy Barton (https://orcid.org/0000-0003-2245-1446): Conceptualisation (equal), Funding acquisition (supporting), Writing – reviewing and editing (supporting). Talant Sooronbaev (https://orcid.org/0000-0002-5609-0944): Conceptualisation (equal), Funding acquisition (supporting), Methodology (equal), Project administration (equal), Supervision (supporting), Writing – reviewing and editing (supporting). Sally J Singh (https://orcid.org/0000-0002-9834-0366): Conceptualisation (equal), Funding acquisition (lead), Methodology (equal), Project administration (equal), Supervision (supporting), Writing – reviewing and editing (supporting). Mark W Orme (https://orcid.org/0000-0003-4678-6574): Conceptualisation (equal), Data curation (supporting), Formal analysis (supporting), Funding acquisition (supporting), Methodology (equal), Project administration (equal), Supervision (lead), Validation (lead), Writing – original draft (supporting), Writing – reviewing and editing (lead).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/DGWW4396.
Primary conflicts of interest: Sally J Singh is a National Institute for Health and Care Research (NIHR) Senior Investigator. She declares the following: NIHR Programme Grant (NIHR202020), HTA Project Grant (NIHR131015), NIHR DHSC/UKRI COVID-19 Rapid Response Initiative, HTA 13/146/02, NIHR Global Research Group (NIHR 17/63/20) and NICE Expert Adviser Panel – Long COVID.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethical approval was obtained from the University of Leicester (#24736).
Information governance statement
The University of Leicester is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Leicester is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here (https://le.ac.uk/ias/data-protection).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the NIHR. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the GHR programme or the Department of Health and Social Care.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme as award number 17/63/20 using UK aid from the UK Government to support global health research and the University of Leicester International Research Development Funding Call (M631PC27). The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government. Research is published in the NIHR Global Health Research Journal. See the NIHR Funding and Awards website for further award information.
This article reports on one component of the research award Views of healthcare workers on development of support for people with post-COVID syndrome in Kyrgyzstan: a survey study. For more information about this research please view the award page (www.fundingawards.nihr.ac.uk/award/17/63/20)
About this article
The contractual start date for this research was in April 2018. This article began editorial review in June 2022 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Copyright
Copyright © 2024 Taalaibekova et al. This work was produced by Taalaibekova et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- COVID-19
- coronavirus infection 2019
- HCP
- healthcare professional
- LMIC
- low- and middle-income countries
- NCCIM
- National Center for Cardiology and Internal Medicine
- NIHR
- National Institute for Health and Care Research
- PCR
- polymerase chain reaction
- PPE
- personal protective equipment
- PR
- pulmonary rehabilitation
- PTSD
- post-traumatic stress disorder
- QoL
- quality of life
- SARS-CoV-2
- severe-acute-respiratory-syndrome-related coronavirus
- STROBE
- Strengthening the Reporting of Observational Studies
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/DGWW4396).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
References
- Taalaibekova A, Oleinik A, Magdieva K, Mirzalieva G. The development of support for people following COVID-19 infection in Kyrgyzstan: survey study of patients and clinical workers [preprint] n.d. https://doi.org/10.21203/rs.3.rs-1010492/v1.
- World Health Organization . In WHO Global Pulse Survey, 90% of Countries Report Disruptions to Essential Health Services Since COVID-19 Pandemic 2020. www.who.int/news/item/31-08-2020-in-who-global-pulse-survey-90-of-countries-report-disruptions-to-essential-health-services-since-covid-19-pandemic (accessed 10 October 2023).
- Ministry of Health of the Kyrgyz Republic . COVID-19: Official Information n.d. https://med.kg/covid/recomendations (accessed 10 October 2023).
- NICE COVID-19 rapid guidelines. PharmacoEcon Outc News 2021;877. https://doi.org/10.1007/s40274-021-7682-3.
- Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, et al. PHOSP-COVID Collaborative Group . Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Resp Med 2021;9:1275-87. https://doi.org/10.1016/S2213-2600(21)00383-0.
- Cortinovis M, Perico N, Remuzzi G. Long-term follow-up of recovered patients with COVID-19. Lancet 2021;397:173-5. https://doi.org/10.1016/S0140-6736(21)00039-8.
- Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med 2022;10:863-76. https://doi.org/10.1016/S2213-2600(22)00126-6.
- Singh SJ, Barradell AC, Greening NJ, Bolton C, Jenkins G, Preston L, et al. British Thoracic Society survey of rehabilitation to support recovery of the post-COVID-19 population. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-040213.
- Grigoletto I, Cavalheri V, de Lima FF, Ramos EMC. Recovery after COVID-19: the potential role of pulmonary rehabilitation. Braz J Phys Therap 2020;24:463-4. https://doi.org/10.1016/j.bjpt.2020.07.002.
- Crisafulli E, Gorgone P, Vagaggini B, Pagani M, Rossi G, Costa F, et al. Efficacy of standard rehabilitation in COPD outpatients with comorbidities. Eur Respir J 2010;36:1042-8. https://doi.org/10.1183/09031936.00203809.
- Vanfleteren LEGW, Spruit MA, Groenen M, Gaffron S, van Empel VPM, Bruijnzeel PLB, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2013;187:728-35. https://doi.org/10.1164/rccm.201209-1665OC.
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute COVID-19 in primary care. BMJ 2020;370. https://doi.org/10.1136/bmj.m3026.
- Daynes E, Gerlis C, Briggs-Price S, Jones P, Singh SJ. COPD assessment test for the evaluation of COVID-19 symptoms. Thorax 2021;76:185-7. https://doi.org/10.1136/thoraxjnl-2020-215916.
- Spruit MA, Burtin C, De Boever P, Langer D, Vogiatzis I, Wouters EFM, et al. COPD and exercise: does it make a difference?. Breathe (Sheff) 2016;12:e38-49. https://doi.org/10.1183/20734735.003916.
- Daynes E, Gerlis C, Chaplin E, Gardiner N, Singh SJ. Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition – a cohort study. Chron Respir Dis 2021;18. https://doi.org/10.1177/14799731211015691.
- Fugazzaro S, Contri A, Esseroukh O, Kaleci S, Croci S, Massari M, et al. Reggio Emilia COVID-19 Working Group . Rehabilitation interventions for post-acute COVID-19 syndrome: a systematic review. Int J Environ Res Public Health 2022;19. https://doi.org/10.3390/ijerph19095185.
- Habib GMM, Rabinovich R, Divgi K, Ahmed S, Saha SK, Singh S, et al. Systematic review of clinical effectiveness, components, and delivery of pulmonary rehabilitation in low-resource settings. NPJ Prim Care Respir Med 2020;30. https://doi.org/10.1038/s41533-020-00210-y.
- Bickton FM, Fombe C, Chisati E, Rylance J. Evidence for pulmonary rehabilitation in chronic respiratory diseases in sub-Saharan Africa: a systematic review. Int J Tuberc Lung Dis 2020;24:991-9. https://doi.org/10.5588/ijtld.19.0526.
- Carfì A, Bernabei R, Landi F. Gemelli Against COVID-19 Post-Acute Care Study Group . Persistent symptoms in patients after acute COVID-19. JAMA 2020;324:603-5. https://doi.org/10.1001/jama.2020.12603.
- Ramanathan K, Antognini D, Combes A, Paden M, Zakhary B, Ogino M, et al. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med 2020;8:518-26. https://doi.org/10.1016/S2213-2600(20)30121-1.
- Davido B, Seang S, Tubiana R, De Truchis P. Post-COVID-19 chronic symptoms: a postinfectious entity?. Clin Microbiol Infect 2020;26:1448-9. https://doi.org/10.1016/j.cmi.2020.07.028.
- Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol 2021;93:1013-22. https://doi.org/10.1002/jmv.26368.
- Bickton FM, Chisati E, Rylance J, Morton B. An improvised pulmonary telerehabilitation program for postacute COVID-19 patients would be feasible and acceptable in a low-resource setting. Am J Phys Med Rehabil 2021;100:209-12. https://doi.org/10.1097/PHM.0000000000001666.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495-9. https://doi.org/10.1016/j.ijsu.2014.07.013.
- Hannah DR, Lautsch BA. Counting in qualitative research: why to conduct it, when to avoid it, and when to closet it. J Manage Inq 2011;20:14-22. https://doi.org/10.1177/1056492610375988.
- Sheehy LM. Considerations for postacute rehabilitation for survivors of COVID-19. JMIR Public Health Surveill 2020;6. https://doi.org/10.2196/19462.
- Siddiq MAB, Rathore FA, Clegg D, Rasker JJ. Pulmonary rehabilitation in COVID-19 patients: a scoping review of current practice and its application during the pandemic. Turk J Phys Med Rehabil 2020;66:480-94. https://doi.org/10.5606/tftrd.2020.6889.
- Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract 2020;39. https://doi.org/10.1016/j.ctcp.2020.101166.
- Sykes DL, Holdsworth L, Jawad N, Gunasekera P, Morice AH, Crooks MG. Post-COVID-19 symptom burden: what is long-COVID and how should we manage it?. Lung 2021;199:113-9. https://doi.org/10.1007/s00408-021-00423-z.
- O’Sullivan O, Barker-Davies RM, Thompson K, Bahadur S, Gough M, Lewis S, et al. Rehabilitation post-COVID-19: cross-sectional observations using the Stanford Hall remote assessment tool. BMJ Mil Health 2023;169:243-8. https://doi.org/10.1136/bmjmilitary-2021-001856.
- Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Netw Open 2021;4. https://doi.org/10.1001/jamanetworkopen.2021.11417.
- Daynes E, Baldwin M, Greening NJ, Yates T, Bishop NC, Mills G, et al. The effect of COVID rehabilitation for ongoing symptoms Post HOSPitalisation with COVID-19 (PHOSP-R): protocol for a randomised parallel group controlled trial on behalf of the PHOSP consortium. Trials 2023;24. https://doi.org/10.1186/s13063-023-07093-7.
