Notes
Article history
The contractual start date for this research was in April 2018. This article began editorial review in June 2022 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Fasuba et al. This work was produced by Fasuba et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Fasuba et al.
Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has caused devastation to individuals, healthcare systems and economies, with the greatest difficulties faced by low- and middle-income countries (LMICs). 1,2 As of 10 April 2021, there were 134,719,328 cases of SARS-CoV-2 and 2,915,972 deaths globally. 3 On the 27 February 2020, the first case of the novel coronavirus disease (COVID-19) was detected in Nigeria – the first reported case in sub-Saharan Africa. 4 Since then, Nigeria, the most populous country in Africa with more than 210 million people,5 has recorded 163,652 cases and 2059 deaths (as of 10 April 2021). 3 These figures likely underestimate the true burden due to limited testing and asymptomatic infections going undetected. With much of the immediate attention rightly focused on individuals in the acute and subacute phases of SARS-CoV-2 infection, the world is now starting to turn its attention to the longer-lasting impact on survivors – termed post-COVID syndrome. 6,7 Post-COVID syndrome has been defined by the National Institute for Health and Care Excellence (NICE) not as one condition, but ‘signs and symptoms that develop during or after an infection consistent with COVID-19 which continue for more than 12 weeks and are not explained by an alternative diagnosis’. 6
Growing global evidence profiles the prevalence of post-COVID syndrome and the common persistent symptoms among survivors. 8–12 A systematic review and meta-analysis of 15 studies exploring the long-term effects of SARS-CoV-2 estimated that 80% of 47,910 SARS-CoV-2 survivors developed at least one long-term symptom, most commonly fatigue (58%), headache (44%), attention disorder (27%), hair loss (25%) and dyspnoea (24%). 12 Data from the UK showed that more than 70% of people hospitalised with SARS-CoV-2 infection are not fully recovered after 1 year,11 with hospitalised patients at greater risk of experiencing long-term symptoms. 13,14 The longer-term consequences of infection are on a scale that could overwhelm healthcare systems, especially in LMICs. 15 In a cohort study following up 274 survivors from an outpatient clinic in Lagos State, Nigeria, 40% remained symptomatic for ≥ 2 weeks post discharge. 15 The most common persistent symptoms were fatigue, headache, chest pain and insomnia. 16 While the exact pathophysiology of post-COVID syndrome is not yet fully understood, there is a clear need to support people’s recovery and help them return to their usual way of life.
In high-income countries, where there are existing rehabilitation services and infrastructure, adaptations to pulmonary rehabilitation (PR) have been made to accommodate the excess demand to support people with post-COVID syndrome. 16,17 Pulmonary rehabilitation is:
[A] comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies that include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory diseases and to promote the long-term adherence to health-enhancing behaviors. 18
For many LMICs, where PR is not routinely available or widely investigated,19 dedicated interventions will need to be developed. Furthermore, examinations of the effectiveness of rehabilitation on health status, persistent symptoms and physical limitations have been viewed as international research priorities. 20 Early evidence for rehabilitation in this population is promising. 21,22 There are some rehabilitation services available in Nigeria on which to build,23 but there is also a clear need to develop interventions specific to people with post-COVID syndrome in local contexts.
Accordingly, this study aimed to examine what post-COVID syndrome support should look like in Nigeria, specifically views on the optimal timing, suitable delivery methods, content of the support and obstacles to implementation.
Methods
Study design and setting
Online surveys of healthcare workers (HCWs) were conducted. The survey was designed by the National Institute for Health and Care Research (NIHR) Global RECHARGE Group for Pulmonary Rehabilitation (17/63/20), with ethical approval obtained from the University of Leicester, UK (reference: 24736), and is reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. 24
Community engagement and involvement
The questionnaire was tested with HCWs in Nigeria and the UK prior to the start of data collection. This work was carried out to better understand the opinions of COVID-19 patients to improve the quality of their care. The results of this study may inform the development of interventions to support people post COVID in Nigeria.
Recruitment and data collection
Recruitment activities were co-ordinated from Abuja, although the online nature of the survey meant respondents could be from any state in Nigeria. The survey was distributed via social media platforms, including relevant HCW-specific WhatsApp groups (e.g. physiotherapy communities) and Twitter (e.g. tagging relevant HCW associations). Participants confirmed their willingness to engage in this research by accessing and completing the online survey. All participants completed the survey without any time constraints.
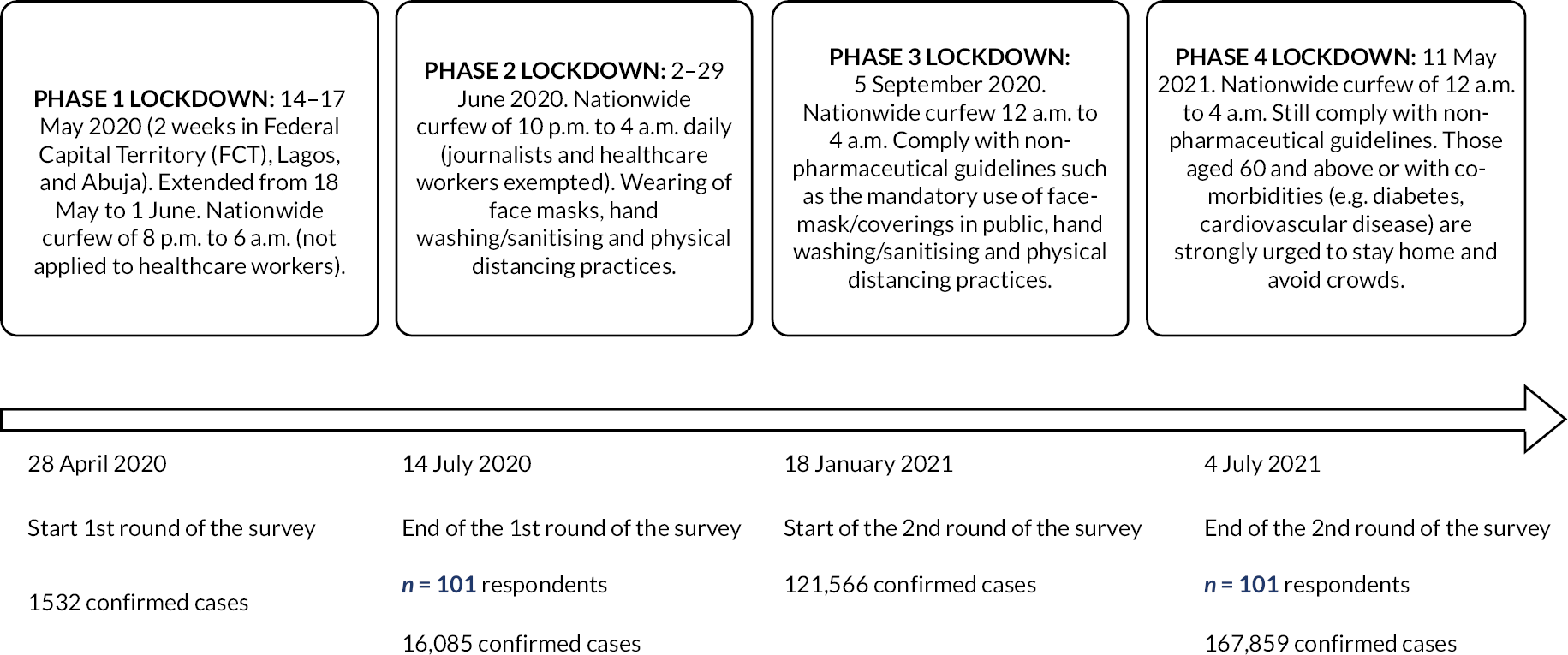
The survey was conducted in two rounds (Figure 1). The first round started on 28 April 2020 and ended on 14 July 2020, during which time there were 1532 confirmed COVID-19 cases, 255 discharged cases and 44 deaths in Nigeria. 25 The second round of survey responses commenced on 18 January 2021 and ceased on 4 July 2021, during which a total of 121,566 confirmed cases, 97,228 discharge cases and 1504 deaths were registered in the country. 25 Two rounds of survey were conducted to enable comparison of responses between early and later phases of the COVID-19 pandemic. Although similar recruitment strategies were used in both rounds, participation in the survey was voluntary and anonymous, preventing any linking of responses between the two rounds. Survey responses were only collected if respondents reported being over 18 years of age, residing in Nigeria and with a healthcare profession as their occupation.
FIGURE 1.
Timeline for rounds of data collection and lockdown phases in Nigeria.
The survey was deployed using OnlineSurveys® (Jisc, Bristol, UK) (www.onlinesurveys.ac.uk) and comprised 16 closed or open-ended questions, in English, with free text boxes for additional comments where necessary. A copy of the survey is available in Report Supplementary Material 1. The initial section of the questionnaire asked for basic demographic information from the participants, including age, gender, professional background and their responsibilities for COVID-19 patients. Remaining questions included the key components of post-COVID support; appropriate location, timing and communication strategies; barriers to HCWs referring patients; perceived barriers to patients accepting a referral and how to overcome them; and the value of supporting post-COVID-19 recovery.
Data were reported as frequencies and percentages (%) with no inferential statistics due to the descriptive nature of the study. Data were analysed using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and summary reports from OnlineSurveys®. Categorical data were descriptively compared between the two rounds of data collection by ranking the responses at each time point, then calculating the rank change (rank in Round 1 minus rank in Round 2). Data from open-ended (free-text) questions were analysed using autonomous qualitative counting,26 with responses grouped together based on their similarity, then counted.
Results
Participant characteristics
For this survey, there were two rounds of data collection with an equal number of 101 respondents per round, with all respondents answering all questions. Characteristics of the samples are presented in Table 1. The proportion of males and females in each of the rounds was similar (e.g. 57% male in Round 1 vs. 47% male in Round 2). The majority of HCWs were aged between 18 and 29 years in both rounds (54% and 49%, respectively) and were predominantly physiotherapists (55% and 50%, respectively), general practitioners (GPs) of modern medicine (12% and 10%, respectively) or nurses (8% and 10%, respectively). For both rounds of data collection, around 40% of HCWs were not involved in COVID-19 patient care; 30% of the respondents were involved in inpatient mobility assessments, and 26% were carrying out inpatient treatment.
| Variables | Round 1 | Round 2 |
|---|---|---|
| Participants (n) | 101 | 101 |
| Females, n (%) | 43 (43) | 54 (53) |
| Age, n (%) | ||
| 18–29 | 55 (54) | 49 (49) |
| 30–39 | 37 (37) | 44 (44) |
| 40–49 | 6 (6) | 4 (4) |
| 50–59 | 2 (2) | 3 (3) |
| 60–69 | 1 (1) | 1 (1) |
| Occupation, n (%) | ||
| Physiotherapist | 56 (55) | 50 (50) |
| General practitioner of Modern Medicine | 12 (12) | 9 (9) |
| Nurse | 8 (8) | 10 (10) |
| Occupational therapist | 6 (6) | 6 (6) |
| Surgeon | 4 (4) | 3 (3) |
| Pharmacist | 4 (4) | 4 (4) |
| Primary care practitioner | 2 (2) | 2 (2) |
| Public health practitioner | 2 (2) | 2 (2) |
| Other | 7 (7) | 14 (14) |
| Responsibilities for COVID-19 patients, n (%) | ||
| Not involved in COVID-19 care | 42 (42) | 37 (37) |
| Mobility assessment and exercises | 35 (35) | 25 (25) |
| Inpatient treatment | 27 (27) | 24 (24) |
| Outpatient clinics | 19 (19) | 23 (23) |
| Primary care and regular follow-up | 17 (17) | 9 (9) |
| Non-urgent care | 8 (8) | 7 (7) |
| Ongoing management | 6 (6) | 13 (13) |
| Diagnosis | 6 (6) | 4 (4) |
| Management of quarantine centres | 6 (6) | 2 (2) |
| Household/community sentinel surveillance | 5 (5) | 1 (1) |
| Oxygen therapy | 5 (5) | 4 (4) |
| Urgent assessments | 5 (5) | 6 (6) |
| Other | 13 (13) | 28 (28) |
Priority topics for post-COVID-19 support
Survey respondents in Round 1 reported coping with stigma (72%), followed by aerobic exercise/regaining fitness levels (71%), integrating back into the community (66%), support for post-traumatic stress disorder (PTSD) (64%), and advice on nutrition (64%) as most important areas for post-COVID-19 patient support (Table 2). A similar response was observed for aerobic exercise/regaining fitness levels in Round 2 (67%). However, respondents in Round 2 reported advice on nutrition (71%) and coping with social isolation (68%) as the main focuses for support.
| Round 1 data, % | Round 2 data, % | Change, % | Rank change | |
|---|---|---|---|---|
| Coping with stigma of COVID-19 infection | 72 | 63 | –9 | –3 |
| Aerobic exercise/regaining fitness levels | 71 | 67 | –4 | –1 |
| Integrating back into the community | 66 | 60 | –6 | –2 |
| Support for PTSD | 64 | 56 | –8 | –4 |
| Advice on nutrition | 64 | 71 | +7 | +3 |
| Support for anxiety or depression | 62 | 54 | –8 | –4 |
| Coping with social isolation | 59 | 68 | +9 | +5 |
| Behaviour change relating to hygiene practice | 58 | 53 | –5 | –3 |
| Advice on medications | 56 | 60 | +4 | +4 |
| Advice on returning to work | 56 | 60 | +4 | +4 |
| Resistance exercise/strength training | 56 | 53 | –3 | –2 |
| Advice on managing fatigue | 53 | 55 | +2 | +3 |
| Advice on managing breathlessness | 53 | 60 | +7 | +7 |
| Infection control relating to COVID-19 | 51 | 52 | +1 | +1 |
| Monitoring symptoms | 50 | 51 | +1 | +1 |
| Lung function testing | 50 | 46 | –4 | –1 |
| Dealing with comorbidities | 50 | 51 | +1 | +1 |
| Advice on managing cough | 50 | 50 | 0 | 0 |
| Learning how to find trustworthy information | 44 | 37 | –7 | 0 |
| Dealing with grief | 43 | 35 | –8 | 0 |
| Financial advice | 38 | 31 | –7 | 0 |
| Other | 1 | 3 | +2 | 0 |
Structure of post-COVID-19 support
In both rounds, 88% of the HCWs reported the need to support COVID-19 patients who had not been previously hospitalised. Additionally, over 63% of HCWs reported the individual’s home as the most appropriate location to deliver the support. The majority of HCWs reported the ideal timing for post-COVID-19 support to be while managing symptoms at home or in the community (57% in Round 1 and 70% in Round 2), immediately after returning home from hospital (57% and 58%, respectively) and while in hospital (56% and 58%, respectively) (see Report Supplementary Material 2, Table 1).
Appropriate methods of communication
In both rounds, 74% of HCWs selected the telephone as the most suitable means of communication with COVID-19 survivors (Table 3). A dedicated smartphone application was chosen as an appropriate communication tool by more respondents in Round 2 than Round 1 (47% in Round 1 vs. 57% in Round 2). Home visits (53% vs. 37%) and face-to-face communication (47% vs. 35%) were selected as appropriate communication strategies by fewer respondents in Round 2.
| Round 1 data, % | Round 2 data, % | Change, % | Rank change | |
|---|---|---|---|---|
| Telephone calls | 74 | 74 | 0 | 0 |
| Video consultations | 61 | 53 | –8 | –1 |
| Home visits | 53 | 37 | –16 | –5 |
| Face-to-face | 47 | 35 | –12 | –5 |
| Dedicated smartphone app | 47 | 57 | +10 | +2 |
| Website/online platform | 46 | 41 | –5 | +1 |
| Text messaging | 44 | 42 | –2 | +3 |
| 40 | 40 | 0 | +1 | |
| Messaging app | 39 | 41 | +2 | +4 |
| Television | 39 | 32 | –7 | –1 |
| Radio | 37 | 28 | –9 | 0 |
| Newspaper | 26 | 21 | –5 | 0 |
| Paper-based instructions | 24 | 21 | –3 | +1 |
Barriers to referring patients for post-COVID-19 support
Barriers to HCWs referring patients for post-COVID-19 support are presented in Table 4. In both rounds, inadequate supply of personal protective equipment (PPE) kits was reported as the greatest barrier (68% and 58%, respectively). In Round 1, stigma experienced by the patient was the second most reported barrier to patient referral (51%). Conversely, in Round 2, the cost of treatment was the second most selected barrier to post-COVID-19 referral (57%). The risk of patients being re-infected was the third-ranked barrier in both rounds (50% and 47%, respectively).
| Round 1 data, % | Round 2 data, % | Change, % | Rank change | |
|---|---|---|---|---|
| Inadequate supply of PPE kits for healthcare professionals | 68 | 58 | –10 | 0 |
| Stigma experienced by patients | 51 | 44 | –7 | –2 |
| Risk of patient being re-infected | 50 | 47 | –3 | 0 |
| Lack of social support for the patient | 49 | 37 | –12 | –3 |
| Cost of treatment | 49 | 57 | +8 | +2 |
| No perceived need for support | 44 | 32 | –12 | –2 |
| Risk of patients infecting healthcare staff | 43 | 32 | –11 | –1 |
| Risk of patient spreading infection in the community | 42 | 41 | –1 | +3 |
| Patient employment/financial concerns | 34 | 41 | +7 | +4 |
| Belief in the value of non-medical treatments | 26 | 31 | +5 | 0 |
| Time commitment for healthcare professionals | 25 | 29 | +4 | 0 |
| Transport needs of patient | 24 | 22 | –2 | –3 |
| Uncertainty of non-medical treatments | 23 | 19 | –4 | –3 |
| Time commitment for patient | 19 | 23 | +4 | +1 |
| Patient’s condition too poor to participate | 18 | 26 | +8 | +3 |
| Patient’s condition too good to participate | 15 | 18 | +3 | –1 |
| Lack of time to make referrals | 15 | 14 | –1 | –2 |
| Patient living alone | 10 | 23 | +13 | +4 |
| Risks faced by patients when exercising | 9 | 10 | +1 | 0 |
Healthcare worker-perceived patient barriers to accepting post-COVID-19 support
According to the HCWs, stigma experienced by patients (65% in Round 1 and 60% in Round 2, respectively), cost of treatment (59% and 69%, respectively) and risk of patients being re-infected (56% and 49%, respectively) were the top three perceived barriers to patients accepting post-COVID-19 support in both rounds of the survey (see Report Supplementary Material 2, Table 2).
Factors that could encourage patients to take up post-COVID-19 support
To mitigate the perceived patient barriers, HCWs advised awareness and health education programmes, availability of support systems and groups, and access to financial aid/incentives would be instrumental in encouraging patients to take up post-COVID-19 support.
Discussion
This study presented the views of HCWs in Nigeria on ways to support individuals’ recovery following SARS-CoV-2 infection. The findings suggest a provisional intervention to support people post COVID, in keeping with internationally recognised PR. 18,27,28 The intervention should be home-based, for hospitalised and non-hospitalised patients, with a combination of video and telephone support and dedicated smartphone application. It should focus on coping with the stigma of SARS-CoV-2 infection, aerobic exercise, integrating back into the community, support for PTSD and advice on nutrition. There is a need to address HCW-perceived patient barriers to accepting support, which include stigma, cost of treatment and risk of re-infection. Barriers to HCWs referring patients for such support included inadequate supplies of PPE.
The HCWs varied slightly in their top-ranked components for post-COVID-19 support between the two rounds of responses. Respondents in the first round selected aerobic exercise/regaining fitness levels, advice on returning to work and integrating back into the community as necessary considerations for interventions. The lockdowns and resulting movement restrictions at the time likely contributed to these preferences. In Round 2, advice on nutrition became the top-ranked consideration for post-COVID-19 support. The priority of nutrition was most likely derived from the need to strengthen the immune system,29,30 in combination with strictly observing public health preventive methods to combat the virus as vaccination programmes in Nigeria lagged behind those in other parts of the world. 31 Of course, some individuals required minimal input (e.g. only online resources) to return to their daily routines. 32
Healthcare workers perceived an urgent need to support COVID-19 survivors regardless of whether they were admitted to hospital, as the number of confirmed cases steadily increased beyond the capacity of the COVID-19 treatment centres across Nigeria. Hence, individuals who tested positive for the virus with few or no symptoms were advised to stay at home and not be transferred to designated facilities for effective care delivery. Although people hospitalised with COVID-19 would likely require rehabilitation, it is now clear that many non-hospitalised individuals also needed rehabilitation, supporting the views of HCWs in the present study. 33 Findings from this study are similar to those from an early survey conducted in the UK. 16 In both surveys (UK and Nigeria), exercise participation was viewed as being the main component of interventions, as well as a focus on supporting people to return to work.
The HCWs identified home or the community as the most ideal location for post-COVID-19 support while managing symptoms, supporting the notion of a flexible approach to delivering post-COVID support and highlighting a potential shift in location preferences in the pandemic context. 34 The culture and value system in a typical Nigerian setting is to show love, care, compassion and support, which may reduce the possible stigmatisation that patients were expected to experience. Given the stigma experienced by people with other infectious diseases, it is vital that efforts to tackle stigma associated with COVID-19 are at the forefront of interventions set up to support these individuals. 35,36 HCWs’ preference for telephone communication with COVID-19 survivors seems feasible because smartphone devices are simple and easy to use, and readily available in Nigeria.
The proposed structure and priority topics for a post-COVID intervention align well with PR, as defined by international guidelines,18,28 and are supported by studies of centre-based22 and telerehabilitation trials37 in the UK and China, respectively. However, PR is not readily available in LMICs generally,19 and current guidelines are unlikely to be wholly applicable to low-resource settings,38 including Nigeria, where a checklist for PR implementation has recently been developed. 39 This checklist may offer a suitable foundation, along with findings from the present study, to drive an increase in rehabilitation capacity in the country. For now, the additional challenge remains to develop such an intervention from the ground up. Efforts to develop PR in Africa are progressing,34 with promising early evidence for the feasibility and effectiveness of PR in chronic respiratory disease (CRD) populations. 40
Based on data from the UK, there may be an increase in demand for PR services by up to 25% due to those hospitalised with COVID-19. 41 The scale of the rehabilitation needed for the existing CRD burden, combined with the addition of COVID-19, places a great burden on developing new services, especially in low-resource settings.
This survey study identified barriers to referring patients from the perspective of HCWs and the perceived barriers of patients accepting post-COVID-19 support. The analysis of these barriers showed inadequate supply of PPE, cost of treatment, risk of patient re-infection and patient stigmatisation were of primary concern. Prior to the pandemic, PPE was readily available, with a balance in its demand and supply chain in Nigeria. However, the pandemic placed a great demand on its availability, which led to severe PPE shortages. 42 Thus, it is understandable that concerns about PPE were noted. Regarding cost of treatment, not all patients infected with COVID-19 were admitted to the designated centres where they could access free care. These individuals paid for services, food and medication, often at great expense. Although the international community, private sector and individuals helped provide medical and food supplies,43 the HCW respondents noted that the support was insufficient to cover the most populous nation in Africa. The risk of patient re-infection was also expressed as a barrier to post-COVID-19 support, aligned with previous work44 and likely exacerbated by low vaccine availability. 45,46
HCWs identified the need to encourage survivors to take up post-COVID-19 support with education and information provision, health promotion/public health and the need for financial support as the main suggestions. In practice, post-COVID-19 support is unlikely to have a high uptake in Nigeria unless it is available for free, is convenient and engages the local communities to provide additional support for those impacted by the virus. While there is early evidence that COVID rehabilitation (adapted from PR33) improves symptoms,22 with larger definitive trials ongoing,47 it is the ability of existing services to maintain this delivery when people with CRDs resume participation in PR that is a cause for concern. 22,48 Results from this survey support the need to develop rehabilitation systems in settings such as Nigeria, as well as LMICs more broadly, where PR is not readily available. 19,49
Limitations
This survey study was exploratory, with a convenience sample of HCWs recruited via online methods only. Therefore, selection biases related to social media use and internet access are likely to be present. The influence of the timing of responses in the context of COVID-19 was minimised by having two separate rounds of data collection (April–July 2020 and January–July 2021). The longer time frame needed for Round 2 highlights challenges with recruitment, driven mainly by experiences deeper into the pandemic. However, the different duration of the time frames should have a minimal impact on comparability. Recruitment of people living with post-COVID-19 symptoms was not possible due to staffing, resource and COVID restrictions, further exacerbated by limited access to the internet. Respondents were predominantly aged 18–34 years, which likely reflects social media usage. A third of participants were not directly involved in COVID-19 care, which may have limited their drawing on direct experiences, but nonetheless contributes to capturing a broad range of HCW perspectives. Further in-depth qualitative insights are needed to inform the development of suitable post-COVID rehabilitation, building on the present study findings.
In summary, the study provided information on ways to support people’s recovery following SARS-CoV-2 infection in Nigeria from the perspective of HCWs. Based on two rounds of responses, it is recommended to address challenges for hospitalised and non-hospitalised patients with home or community-based interventions combining video and telephone support. Internationally recognised PR18,27,28 is an appropriate intervention to modify for this population, and efforts should be made to increase its availability as a clinical service in Nigeria. The focus of future interventions should be on coping with the stigma of SARS-CoV-2 infection, aerobic exercise, integrating back into the community, support for PTSD and advice on nutrition. HCW-perceived patient barriers to taking up support interventions were inadequate supply of PPE, cost of treatment, risk of patient re-infection and stigmatisation, while HCW barriers to referring patients for such support focused mainly on inadequate PPE supplies. Survivors’ education and information provision, targeting public health messages and financial support were noted as important factors to encourage survivors to engage in post-COVID-19 services. The findings of this study can be used to inform future work developing post-COVID rehabilitation in Nigeria.
Additional information
Acknowledgements
The authors would like to thank all participants who volunteered for this project.
CRediT contribution statement
Ayobami Fasuba (https://orcid.org/0000-0002-2221-542X): Data curation (lead), Formal analysis (lead), Investigation (lead), Methodology (equal), Project administration (equal), Visualisation (lead), Writing – original draft (lead). Ilaria Pina (https://orcid.org/0000-0002-6294-5398): Formal analysis (supporting), Methodology (supporting), Supervision (supporting), Validation (supporting), Visualisation (supporting), Writing – original draft (supporting), Writing – editing and reviewing (supporting). Zainab K Yusuf (https://orcid.org/0000-0001-7859-5102): Formal analysis (supporting), Methodology (equal), Validation (equal), Writing – editing and reviewing (supporting). Laura Wilde (https://orcid.org/0000-0002-1404-6304): Formal analysis (supporting), Methodology (supporting), Validation (supporting), Writing – editing and reviewing (supporting). Sally J Singh (https://orcid.org/0000-0002-9834-0366): Conceptualisation (equal), Funding acquisition (lead), Methodology (equal), Project administration (equal), Writing – editing and reviewing (supporting). Mark W Orme (https://orcid.org/0000-0003-4678-6574): Conceptualisation (equal), Formal analysis (supporting), Funding acquisition (supporting), Methodology (equal), Project administration (equal), Supervision (lead), Validation (lead), Writing – original draft (supporting), Writing – editing and reviewing (lead).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/UTNT4760.
Primary conflicts of interest: Sally J Singh is a National Institute for Health and Care Research (NIHR) Senior Investigator and declares the following: NIHR Programme Grant (NIHR: 202020), HTA Project Grant (NIHR: 131015), NIHR DHSC/UKRI COVID-19 Rapid Response Initiative (HTA 13/146/02), NIHR Global Research Group (NIHR 17/63/20) and NICE Expert Adviser Panel – Long COVID.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethical approval was obtained from the University of Leicester (reference: 24736) on 21 April 2020.
Information governance statement
The University of Leicester is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Leicester is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here (https://le.ac.uk/ias/data-protection).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the GHR programme or the Department of Health and Social Care.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme as award number 17/63/20 using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK government. Research is published in the NIHR Global Health Research Journal. See the NIHR Funding and Awards website for further award information.
This article reports on one component of the research award Views of healthcare workers to help develop support for people with post-COVID syndrome in Nigeria: a survey study. For more information about this research please view the award page (www.fundingawards.nihr.ac.uk/award/17/63/20)
About this article
The contractual start date for this research was in April 2018. This article began editorial review in June 2022 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Copyright
Copyright © 2024 Fasuba et al. This work was produced by Fasuba et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- COVID
- coronavirus disease
- GP
- general practitioner
- HCWs
- healthcare workers
- LMICs
- low- and middle-income countries
- NIHR
- National Institute for Health and Care Research
- PPE
- personal protective equipment
- PR
- pulmonary rehabilitation
- PTSD
- post-traumatic stress disorder
- SARS-CoV-2
- severe acute respiratory syndrome coronavirus-2
- STROBE
- Strengthening the Reporting of Observational Studies in Epidemiology
Notes
The following supporting information can be downloaded on the NIHR Journals Library webpage (https://doi.org/10.3310/UTNT4760).
References
- Bong CL, Brasher C, Chikumba E, McDougall R, Mellin-Olsen J, Enright A. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg 2020;131:e174-5.
- Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents 2020;55.
- Coronavirus Resource Centre . COVID-19 Dashboard n.d. https://coronavirus.jhu.edu/map.html (accessed 10 April 2021).
- Oduwole O. One Year of COVID-19 Response in Nigeria. Nigeria Centre for Disease Control; 2021.
- Worldometer . Nigeria Population n.d. www.worldometers.info/world-population/nigeria-population/#:~:text=The%20current%20population%20of%20Nigeria,the%20latest%20United%20Nations%20data (accessed 10 April 2021).
- National Institute for Health and Care Excellence (NICE) . COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19 n.d. www.nice.org.uk/guidance/NG188 (accessed 10 April 2021).
- WHO Headquarters . A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus 2021. www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (accessed 23 October 2021).
- Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA 2020;324:603-5.
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-62.
- Davido B, Seang S, Tubiana R, de Truchis P. Post–COVID-19 chronic symptoms: a postinfectious entity?. Clin Microbiol Infect 2020;26:1448-9.
- Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med 2021;9:1275-87.
- Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep 2021;11.
- Cortinovis M, Perico N, Remuzzi G. Long-term follow-up of recovered patients with COVID-19. Lancet 2021;397:173-5.
- Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med 2022;10:863-76.
- Osikomaiya B, Erinoso O, Wright KO, Odusola AO, Thomas B, Adeyemi O, et al. ‘Long COVID’: persistent COVID-19 symptoms in survivors managed in Lagos State, Nigeria. BMC Infect Dis 2021;21.
- Singh SJ, Barradell AC, Greening NJ, Bolton C, Jenkins G, Preston L, et al. British Thoracic Society survey of rehabilitation to support recovery of the post-COVID-19 population. BMJ Open 2020;10.
- Grigoletto I, Cavalheri V, Lima FF, Ramos EMC. Recovery after COVID-19: the potential role of pulmonary rehabilitation. Braz J Phys Ther 2020;24:463-4.
- Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013;188:e13-64.
- Habib GMM, Rabinovich R, Divgi K, Ahmed S, Saha SK, Singh S, et al. Systematic review of clinical effectiveness, components, and delivery of pulmonary rehabilitation in low-resource settings. NPJ Prim Care Respir Med 2020;30.
- Adeloye D, Elneima O, Daines L, Poinasamy K, Quint JK, Walker S, et al. International COVID-19 Airways Diseases Group . The long-term sequelae of COVID-19: an international consensus on research priorities for patients with pre-existing and new-onset airways disease. Lancet Respir Med 2021;9:1467-78.
- Fugazzaro S, Contri A, Esseroukh O, Kaleci S, Croci S, Massari M, et al. Rehabilitation interventions for post-acute COVID-19 syndrome: a systematic review. Int J Environ Res Publ Health 2022;19.
- Daynes E, Gerlis C, Chaplin E, Gardiner N, Singh SJ. Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition: a cohort study. Chron Respir Dis 2021;18.
- Ige OM, Olarewaju RK, Lasebikan VO, Adeniyi YO. Outpatient pulmonary rehabilitation in severe chronic obstructive pulmonary disease. Ind J Chest Dis Allied Sci 2010;52:197-201.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ 2007;85:867-72.
- n.d. https://ncdc.gov.ng/news/237/update-on-covid-19-in-nigeriacovid19.ncdc.gov.ng (accessed 7 February 2024).
- Hannah DR, Lautsch BA. Counting in qualitative research: why to conduct it, when to avoid it, and when to closet it. J Manag Inq 2011;20:14-22.
- Rochester CL, Alison JA, Carlin B, Jenkins AR, Cox NS, Bauldoff G, et al. Pulmonary rehabilitation for adults with chronic respiratory disease: an official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med 2023;208:e7-26.
- Holland AE, Cox NS, Houchen-Wolloff L, Rochester CL, Garvey C, ZuWallack R, et al. Defining modern pulmonary rehabilitation: an official American Thoracic Society workshop report. Ann Am Thorac Soc 2021;18:e12-29.
- da Silveira MP, da Silva Fagundes KK, Bizuti MR, Starck E, Rossi RC, de Resende e Silva DT. Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature. Clin Exp Med 2021;21:15-28.
- Lee SW, Lee J, Moon SY, Jin HY, Yang JM, Ogino S, et al. Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med 2021;56:901-12.
- Nasir M. Nigeria Scales Up Its COVID-19 Vaccination with New Funding for Vaccine Purchase and Deployment. The World Bank; 2021.
- NHS . Your COVID Recovery n.d. www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/11/Your-COVID-Recovery-guidance191120.pdf (accessed 31 October 2021).
- Spruit MA, Holland AE, Singh SJ, Tonia T, Wilson KC, Troosters T. COVID-19: interim guidance on rehabilitation in the hospital and post-hospital phase from a European Respiratory Society and American Thoracic Society-coordinated International Task Force. Eur Respir J 2020;56.
- Katagira W, Jones AV, Orme MW, Yusuf ZK, Ndagire P, Nanyonga J, et al. Identifying appropriate delivery of and referral to pulmonary rehabilitation in Uganda: a survey study of people living with chronic respiratory disease and health care workers. Int J Chron Obstruct Pulmon Dis 2021;16:2291-9.
- Saeed F, Mihan R, Mousavi SZ, Reniers RL, Bateni FS, Alikhani R, et al. A narrative review of stigma related to infectious disease outbreaks: what can be learned in the face of the COVID-19 pandemic?. Front Psychiatr 2020;11.
- Yuan K, Huang XL, Yan W, Zhang Y-X, Gong Y-M, Su S-Z, et al. A systematic review and meta-analysis on the prevalence of stigma in infectious diseases, including COVID-19: a call to action. Mol Psychiatr 2021;27:19-33.
- Li J, Xia W, Zhan C, Liu S, Yin Z, Wang J, et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): a randomised controlled trial. Thorax 2021;77.
- Singh SJ, Halpin DM, Salvi S, Kirenga BJ, Mortimer K. Exercise and pulmonary rehabilitation for people with chronic lung disease in LMICs: challenges and opportunities. Lancet Respir Med 2019;7:1002-4.
- Mohammed J, Thornton J. Development, validation, and testing of a physiotherapist initiated checklist of items for implementing pulmonary rehabilitation in Nigeria. J Pan Afr Thorac Soc 2021;2:140-7.
- Bickton FM, Fombe C, Chisati E, Rylance J. Evidence for pulmonary rehabilitation in chronic respiratory diseases in sub-Saharan Africa: a systematic review. Int J Tuberc Lung Dis 2020;24:991-9.
- Daynes E, Gerlis C, Singh SJ. The demand for rehabilitation following COVID-19: a call to service providers. Physiotherapy 2021;113:A1-3.
- Amzat J, Aminu K, Kolo VI, Akinyele AA, Ogundairo JA, Danjibo MC. Coronavirus outbreak in Nigeria: burden and socio-medical response during the first 100 days. Int J Infect Dis 2020;98:218-24.
- Dixit S, Ogundeji YK, Onwujekwe O. How Well Has Nigeria Responded to COVID-19?. Brookings; 2020.
- Oluwaseyi I. Highlighting the possibility of COVID-19 reinfection after recovery: a case report from Nigeria. Figshare 2020. https://doi.org/10.6084/m9.figshare.12813212.v1.
- Choi EM. COVID-19 vaccines for low- and middle-income countries. Trans R Soc Trop Med Hyg 2021;115:447-56.
- Figueroa JP, Hotez PJ, Batista C, Amor YB, Ergonul O, Gilbert S, et al. Achieving global equity for COVID-19 vaccines: stronger international partnerships and greater advocacy and solidarity are needed. PLOS Med 2021;18.
- Daynes E, Baldwin M, Greening NJ, Yates T, Bishop NC, Mills G, et al. The effect of COVID rehabilitation for ongoing symptoms Post HOSPitalisation with COVID-19 (PHOSP-R): protocol for a randomised parallel group controlled trial on behalf of the PHOSP consortium. Trials 2023;24:1-10.
- Goodwin V, Allan L, Bethel A, Cowley A, Cross JL, Day J. Rehabilitation to enable recovery from COVID-19: a rapid systematic review. Physiotherapy 2021;111:4-22.
- Brown DA, O’Brien KK. Conceptualising Long COVID as an episodic health condition. BMJ Glob Health 2021;6.
