Notes
Article history
The contractual start date for this research was in April 2018. This article began editorial review in September 2022 and was accepted for publication in July 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Nava-Ruelas et al. This work was produced by Nava-Ruelas et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Nava-Ruelas et al.
Background
Depression is a common comorbidity in people with tuberculosis (TB) and it is significantly associated with poorer health outcomes. 1,2 Depression in TB can be treated, and it can potentially improve TB outcomes,3–5 as well as the mental health of people with TB. 6,7 This study is part of a larger grant that explores the comorbidities between mental health and physical health conditions.
There is strong support within global guidelines for patient-centred approaches to TB care,8–10 including addressing the psychosocial aspects of TB. Providing depression care in TB services would be an opportunity to deliver a more patient-centred approach to TB care and address the psychosocial and mental health needs of people with TB.
However, depression is not routinely diagnosed or treated as part of TB services in low- and middle-income countries (LMICs). Despite global policy support for patient-centred approaches, there is little guidance on how to implement them into current practice. Understanding how to improve the management of comorbid depression as part of routine TB services is important, particularly for LMICs, where the provision of mental health services is already under significant constraints. 11 There have been some attempts in some LMICs to provide depression care for people with TB, but these have not been systematically documented or analysed.
Aims and objectives
In this review, we aimed to explore the approaches that had been used in LMICs to deliver depression care as part of TB services, and to understand the barriers and facilitators to implementation.
Review methods
We registered the protocol of this review with PROSPERO under registration number CRD42020201095.
Eligibility criteria
The inclusion criteria are described in Table 1. We included studies conducted in LMICs, according to the World Bank classification at the time of the searches, in primary, secondary or tertiary care, with the characteristics listed in Table 1.
| Population | We included studies addressing anxiety and depression (anxiety is a common comorbidity for depressive disorders and anxiety symptoms are commonly part of the presentation in depressive disorders) in people with TB, or attending TB services, in LMICs. Studies aimed at people attending TB services in a LMIC with pulmonary (latent, drug-susceptible or drug-resistant) TB and symptoms (or a diagnosis) of depressive disorder were included. For the purpose of this review, TB was defined as symptoms or signs suggestive of TB or a confirmed laboratory or clinical diagnosis of TB. |
| Intervention | We included studies describing approaches or arrangements for delivering services for depression as part of, alongside or co-ordinated or integrated with services (public and/or private) for pulmonary TB that have been implemented in LMICs. For the purpose of this review, these approaches can be defined as a process that brings together one or more of the funding, administrative, organisational, service delivery and clinical sectors to deliver benefits to people;12 or any management or operational changes implemented in health systems that bring together or co-ordinate the inputs, delivery, management or organisation of services and functions, with the goal of improving the quality, access, coverage, acceptability or cost-effectiveness of care.13 |
| Comparator | No studies were excluded based on the type, or absence, of comparator. |
| Outcome | No studies were excluded based on the type of outcome they measured. |
| Study design | We included any type of study that described or evaluated an attempt to implement or experience of implementing an approach to deliver depression care as part of existing TB services in LMICs. Studies consisting of primary research, secondary data analysis or reviews were eligible for inclusion. |
Search strategy
We designed and carried out the searches with advice from the librarian of the Health Sciences Department at the University of York. One reviewer (RNR) carried out the searches during June–July 2020 and covered all databases from inception. We searched 10 electronic databases for peer-reviewed and grey literature: MEDLINE, Scopus, PsycINFO, Web of Science, PubMed, EMBASE, Cochrane Library, SciELO, LILACS and Health Management Information Consortium. We searched the websites of relevant organisations (World Bank, Global Fund to Fight AIDS, Tuberculosis and Malaria and World Health Organization) using the Google Advanced Search feature. We considered these organisations important as they are major stakeholders in the delivery and funding of TB services in LMICs. 14 We also hand-searched the reference lists of the included studies to identify other relevant studies. An example of the search strategy used across databases is included in Appendix 1.
Quality assessment
We used the Mixed-Methods Appraisal Tool (MMAT) to appraise the quality of eligible studies. 15 We used this tool anticipating that the included studies would either be qualitative, quantitative or mixed methods studies. The advantage of the MMAT tool is that it provides a framework to assess qualitative, quantitative and mixed methods studies, following a minimum set of quality criteria for the methodological design. 16 This tool was developed in response to the inclusion of different types of evidence into systematic reviews for health services research. 17 This facilitates their integration into systematic reviews as it allows a comparison of overall quality between different methodological stances according to the quality criteria they have met.
Data extraction
Two reviewers (RNR, OT) participated in the screening and data extraction process. We used Rayyan software for the title and abstract screening phases. 18 We resolved disagreements through consensus and discussion before proceeding to the next stage. Two reviewers (RNR, OT) independently performed the full-text screening. One reviewer (RNR) extracted the data of the included studies, and a second reviewer (OT) cross-checked the data extracted against the original study to ensure consistency and reliability for two studies.
Data were extracted from the results and discussion sections of the included studies (see Appendix 2). We extracted the description of the study design, the type of intervention and the implementation process from the background and methods sections of the included studies (see Table 2; further descriptive information on the interventions and their implementation is described in Appendix 5).
| Study (author and numeric reference) | Year of study | Country | Intervention category | Type and no. of participants | Study design | Outcomes measured in the study | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| TB-related outcomes | Mental health outcomes | Process outcomes | Other outcomes | |||||||
| Acha et al.25 | 1999–2004 | Peru | Psychological only | Multidrug-resistant TB | 285 | Qualitative | TB treatment success (treatment completion and cure) | None reported | Adherence to TB treatment | Participants’ experiences during implementation, all-cause mortality, quality of life for people with TB |
| Contreras et al.26 | 2015–6 | Peru | Combined, with socioeconomic support | Unspecified type of TB | 192 | Quantitative (cohort study) | None reported | None reported | Number of depression screenings, mental health treatment attendance, completed socioeconomic support evaluations for people with TB | None reported |
| Das et al.27 | 2012–4 | India | Combined | Multidrug-resistant TB comorbid with HIV | 45 | Quantitative (cohort study) | None reported | Changes in depression symptoms’ severity | Number of eligible patients screened for depression; number of referrals (to hospital care for TB) | None reported |
| Diez-Canseco et al.32 | 2015 | Peru | Screening only | Unspecified type of TB | 85 | Mixed methods | None reported | None reported | Number of depression screenings, number of referrals to mental health specialist services, appointment attendance after referral | Participants’ experiences pre, during and post implementation |
| Kaukab et al.29 | 2014 | Pakistan | Combined, with socioeconomic support | Multidrug-resistant TB | 70 | Quantitative (controlled-cohort study) | None reported | Changes in depression symptoms’ severity | None reported | None reported |
| Khachadourian et al.30a | 2014 | Armenia | Psychological only | Drug-susceptible TB | 385 | Quantitative (cluster randomised trial) | TB treatment success, loss to follow-up, treatment failure | Changes in depression symptoms’ severity | None reported | Changes in stigma score, changes in quality of life, all-cause mortality, changes in perceived social support |
| Li et al.31 | 2015–6 | China | Psychological only | Unspecified type of TB | 183 | Quantitative (cluster randomised trial) | None reported | Changes in depression symptoms’ severity | None reported | None reported |
| Lovero et al.33 | 2016–7 | South Africa | Combined | Unspecified type of TB | N/A | Mixed methods | None reported | None reported | Healthcare workers’ knowledge and adherence to mental health diagnosis, treatment and referral guidelines for people with TB | Non-patient participants’ experiences of the mental health intervention |
| Vega et al.28 | 1996–9 | Peru | Combined | Multidrug-resistant TB | 75 | Quantitative (cohort study) | None reported | Changes in depression symptoms’ severity | None reported | None reported |
| Walker et al.34 | 2015 | Nepal | Psychological only | Multidrug-resistant TB | 135 | Mixed methods | None reported | Changes in depression symptoms’ severity | Fidelity, feasibility, acceptability of the intervention | Participants’ experiences during implementation |
To describe the interventions implemented, we used the description as it was stated in the included studies. After this, we classified the studies according to the main categories of interventions used for depression, according to the NICE guidelines19 and based on the descriptions provided in the studies. We created four intervention categories based on the descriptions provided: (1) psychological-only, (2) combined, (3) combined, with socioeconomic support and (4) screening-only. We defined psychological-only interventions as any type of group or individual therapy used to treat mental health conditions, such as depression, anxiety or psychosis (e.g. behavioural therapy, interpersonal therapy, cognitive–behavioural therapy, psychodynamic therapies, family therapy). We defined combined interventions as psychological and pharmacological interventions delivered simultaneously to the patient. We defined combined interventions with socioeconomic support as combined interventions provided alongside any form of support that aimed to address socioeconomic needs in people with TB. We defined screening-only interventions as screening for mental health conditions, followed by referral to mental health services outside of TB services, if needed.
In addition to the descriptive characteristics of the studies, we extracted qualitative and quantitative data, as appropriate, from the studies that described the interventions implemented for data analysis and synthesis. From the qualitative studies, or studies with qualitative components, we extracted the narrative descriptions of the intervention, such as the number and type of study participants, therapeutic strategies, the thematic content of sessions, narrative descriptions of participants’ responses to the interventions, interview responses and other excerpts verbatim from the articles. From the quantitative studies, or studies with quantitative components, we extracted narrative descriptions of the intervention and participants’ experiences (if available); numerical data on the type and number of participants, number of participants who received (or not) the intervention, number of participants who received training (if applicable), number of participants who adhered (or not) to the intervention, depression scores at baseline, depressions scores at the end of the intervention, number of death and descriptive statistics about the characteristics of participants, process outcomes (e.g. the number and type of interventions delivered, enrolment rate) and clinical outcomes (e.g. depression scores, TB treatment outcomes, lost-to-follow-up rates). From the mixed methods studies, we extracted both quantitative and qualitative data. A detailed description on the qualitative and quantitative data we extracted from each study is given in Appendix 2, where the qualitative data are described in Appendix 2, Table 5 and the quantitative data are described in Appendix 2, Table 6.
Data synthesis
We coded the quantitative and qualitative data from all studies according to the Consolidated Framework for Implementation Research (CFIR). This framework was chosen for analysis given its appropriateness to explore the facilitators and barriers to implementing diverse types of interventions. 20 This framework encompasses five main constructs (intervention characteristics, inner setting, outer setting, characteristics of individuals involved and process), divided into 26 subconstructs.
After extracting data from the eligible studies, we converted quantitative data [e.g. frequency tables, forest plots, ratios, number of participants who received (or not) the intervention] to qualitative data by creating narrative descriptions of the quantitative data and results. This process of qualitising data is used in mixed methods literature reviews to synthesise diverse types of evidence. 16 We coded the narrative descriptions of quantitative data along with the qualitative data. We used an analytical approach that was based on the framework method:21 we treated all data as primary qualitative data and coded this information in each study as barriers or facilitators. To create framework matrices, we used the CFIR constructs and subconstructs as an a priori coding framework, organised in columns while the different intervention categories were organised in rows. The data in each cell were verbatim extracts of qualitative data or narrative descriptions of quantitative results from the included studies. We defined the inner setting as the TB national services and/or where healthcare delivery for TB was routinely provided. We defined the outer setting as other governmental or private healthcare services provided within the country, or any other national and international institutions collaborating with TB national services.
The CFIR rating rules state that the coding process should consider the positive or negative influence that coded data have on implementation, and how weak or strong that influence is on implementation. 22 To determine valence, a rating of ‘X, ‘0’, ‘+’ or ‘− is assigned to the coded data. These symbols mean that the coded data had a mixed (positive and negative), null, positive or negative influence on implementation, respectively. To determine strength, a rating of ‘1’ or ‘2’ is assigned to the coded data. A notation of ‘1’ means that the coded data have a weak influence on implementation while ‘2’ means its influence is stronger. To determine the valence of the influence, we considered how many times the narrative data were mentioned in the study, the adjectives used to describe the influence of a construct (e.g. ‘very strong’, ‘very important’, ‘not strong’, ‘not important’), and whether the influence it had on implementation was negative, positive or mixed.
We adapted the CFIR construct definitions to the research objectives of the study. We used the definitions provided in the handbook and the website, and then re-interpreted them according to their relevance to TB services and mental health interventions (see Appendix 4).
Results
Search results
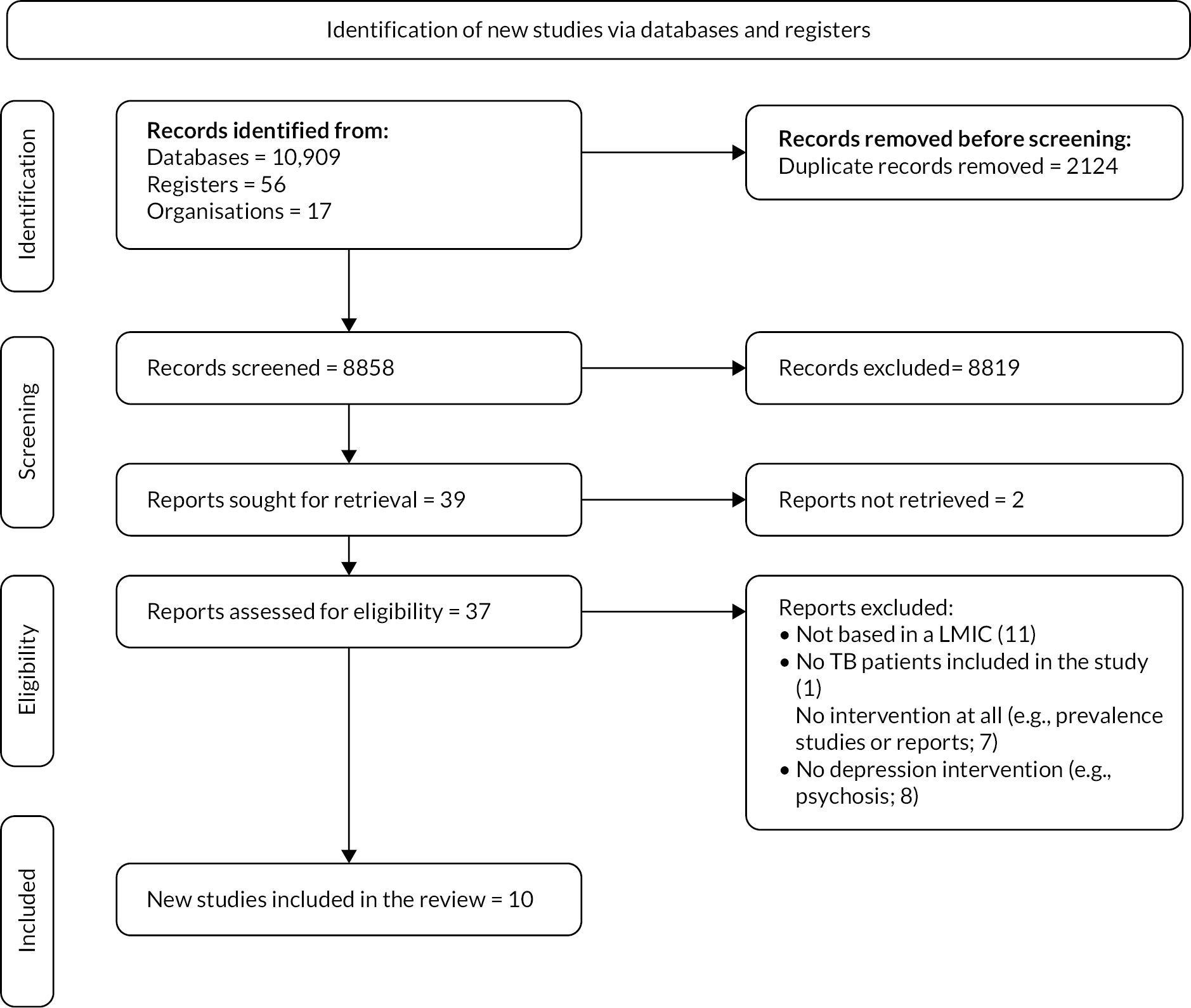
The total number of records retrieved from electronic databases was 10,982. After deduplication,23 two reviewers (RNR, OT) independently screened the titles and abstracts for 8858 records. We recorded our screening process using PRISMA guidelines (see Figure 1). 24
Thirty-nine articles were included in the full-text screening phase. At this stage, 11 articles were excluded because they were based in high-income countries, mostly the USA. One study was excluded because it did not include people with pulmonary TB. Two studies were excluded because they were prevalence studies. Five studies were excluded because they were discussion papers or reports. Eight studies were excluded because they did not describe interventions to treat depression – they focused on adherence or psychosis without depression as a comorbidity. Two articles were excluded because it was not possible to establish contact with the authors or national libraries in Brazil and Bolivia to access the full text. We give the full list of references for the excluded studies in Appendix 6.
Characteristics of the included studies
Ten articles met the inclusion criteria and were included in the analysis. They varied in terms of study design. One was a qualitative study, three were retrospective cohort studies, one was a controlled-cohort study, two were cluster randomised trials and three were mixed methods studies. 25–34 More details of the included studies are given in Table 2.
Four studies described a psychological intervention. 25,30,31,34 Three studies described interventions that combined psychological and pharmacological approaches. 27,28,33 Two studies described a pharmacological and psychological intervention that also included socioeconomic support (combined, with socioeconomic support). 26,29 One intervention consisted of screening only followed by referral to mental health services, when needed. 32
Quality assessment
Table 3 describes the results of a quality assessment using the MMAT tool. We assessed the included studies against the appropriate methodological quality criteria according to the study design. Given the research objectives of this review, we did not exclude any of the studies based on their methodological quality. The purpose of the quality assessment was to explore whether the findings from the included studies were of sufficient methodological quality. All the studies had appropriate study designs for their stated research questions, except for one. 29 In this study, we considered that the study design (quantitative non-randomised) was not appropriate for the research questions that the authors described in the study, which were to examine the effectiveness of a combined intervention, with socioeconomic support, delivered by pharmacists. 29
| Category of study designs | Methodological quality criteria | Studies | (25) | (26) | (27) | (32) | (29) | (30) | (31) | (33) | (28) | (34) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screening questions (for all types) | Are there clear research questions? | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||
| Do the collected data allow the research questions to be addressed? | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | |||
| Qualitative | Is the qualitative approach appropriate to answer the research question? | Y | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||
| Are the qualitative data collection methods adequate to address the research question? | Y | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Are the findings adequately derived from the data? | Y | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Is the interpretation of results sufficiently substantiated by the data? | Y | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Is there coherence between qualitative data sources, collection, analysis and interpretation? | Y | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Quantitative randomised controlled trials | Is randomisation appropriately performed? | N/A | N/A | N/A | N/A | N/A | Y | Y | N/A | N/A | N/A | ||
| Are the groups comparable at baseline? | N/A | N/A | N/A | N/A | N/A | Y | Y | N/A | N/A | N/A | |||
| Are there complete outcome data? | N/A | N/A | N/A | N/A | N/A | Y | N | N/A | N/A | N/A | |||
| Are outcome assessors blinded to the intervention provided? | N/A | N/A | N/A | N/A | N/A | Y | N | N/A | N/A | N/A | |||
| Did the participants adhere to the assigned intervention? | N/A | N/A | N/A | N/A | N/A | Y | Y | N/A | N/A | N/A | |||
| Quantitative non-randomised | Are the participants representative of the target population? | N/A | N | N | N/A | N | N/A | N/A | N/A | Y | N/A | ||
| Are measurements appropriate regarding both the outcome and intervention (or exposure)? | N/A | Y | Y | N/A | Y | N/A | N/A | N/A | Y | N/A | |||
| Are there complete outcome data? | N/A | Y | N | N/A | Y | N/A | N/A | N/A | Y | N/A | |||
| Are the confounders accounted for in the design and analysis? | N/A | N | N | N/A | N | N/A | N/A | N/A | Y | N/A | |||
| During the study period, is the intervention administered (or did exposure occur) as intended? | N/A | Y | N | N/A | Y | N/A | N/A | N/A | Y | N/A | |||
| Quantitative descriptive | Is the sampling strategy relevant to address the research question? | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||
| Is the sample representative of the target population? | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Are the measurements appropriate? | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Is the risk of nonresponse bias low? | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Is the statistical analysis appropriate to answer the research question? | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Mixed methods | Is there an adequate rationale for using a mixed methods design to address the research question? | N/A | N/A | N/A | Y | N/A | N/A | N/A | Y | N/A | Y | ||
| Are the different components of the study effectively integrated to answer the research question? | N/A | N/A | N/A | Y | N/A | N/A | N/A | Y | N/A | Y | |||
| Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | N/A | N/A | N/A | Y | N/A | N/A | N/A | Y | N/A | Y | |||
| Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | N/A | N/A | N/A | Y | N/A | N/A | N/A | Y | N/A | Y | |||
| Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | N/A | N/A | N/A | Y | N/A | N/A | N/A | Y | N/A | Y | |||
| Total quality criteria met | 6/7 | 5/7 | 3/7 | 7/7 | 4/7 | 7/7 | 5/7 | 7/7 | 7/7 | 7/7 | |||
Description of approaches to deliver depression care as part of TB services
The 10 studies included in this analysis describe four main types of interventions that aim to provide depression diagnosis and/or treatment or referral to mental health services to people with TB in LMICs at the point of care for TB services. The four major approaches used to deliver depression care for people with TB in LMICs were psychological interventions, combined (pharmacological and psychological) interventions, combined interventions with socioeconomic support and screening-only interventions. See Appendix 5 for a detailed description of the interventions, components and resources required for implementation.
The most commonly implemented intervention was psychological. Nine out of 10 studies included in this review described the implementation of psychological interventions, or interventions with a psychological component, alone or in combination with other approaches; one study did not describe the implementation of a psychological intervention. 32 Psychological interventions were described as counselling or psychotherapy. The most common intervention for depression was counselling. 26–30,33,34 Counselling was delivered in interventions that implemented psychological interventions only, combined interventions or combined interventions with socioeconomic support. Counselling was defined as motivational and emotional counselling, patient counselling or psychological counselling. 27,30,34 It was also defined as TB counselling. 30 Most counselling sessions were individual, except when also conducted with family members and/or patient groups. 30,34 The content of counselling sessions was not described in most interventions. Only one study described the content of the counselling sessions as based on behavioural activation. 34
None of the interventions used pharmacological treatment alone; all pharmacological interventions were part of a combined strategy, incorporating psychological and socioeconomic support components.
Two interventions included socioeconomic support components combined with psychological and pharmacological interventions. 26,29 Socioeconomic support consisted of transport subsidies, food, fees for medical tests, school fees for family members and covered diagnostic tests’ fees for other comorbidities. Both studies justified the inclusion of socioeconomic support given the socioeconomic needs of people with TB. Both studies mentioned that the socioeconomic support was provided by non-governmental organisations (NGOs). 26,29
The interventions were described inconsistently. Information on treatments’ length, dose and end points was often missing from the published data in all the included studies. The studies that reported on psychological interventions, combined interventions and combined interventions with socioeconomic support did not report on treatment length or the number of psychological sessions received by participants. The frequency of psychological treatment sessions was mentioned in four studies. 25,29–31 Of the three combined interventions, one study provided detail about the combination of pharmacological therapy with psychotherapy given to patients, which were selective serotonin reuptake inhibitor, tricyclic antidepressants or benzodiazepines;28 the dosages were not reported.
There was also variability in the instruments used to measure and diagnose depression; some studies described the use of more than one tool. 26,34 All studies reported measurements of depression scores at baseline. Baseline referred to the beginning of the intervention for depression in some studies, while in others it referred to the beginning of TB treatment. We found the same patterns in end point measurements. End-point measurements could refer to the end of the depression intervention or the end of the TB treatment. We extracted these data as reported in the studies (see Appendix 2). The follow-up measurements of depression scores were taken at different points in all the interventions; one study had no follow-up measurement. 32
All the interventions were implemented as part of routine public TB services and were often given at the same location and time as TB-service delivery, except in two interventions where patients received mental health services elsewhere. 32,33 Where applicable, the interventions used routine TB care as a control or comparator. 29–31 All the interventions relied on existing TB care pathways to incorporate screening and treatment for depression. All the interventions were provided free of charge for participants at the point of service delivery.
All the interventions relied on multidisciplinary teams to deliver the depression intervention. The teams comprised TB healthcare workers, primary healthcare workers with training in mental health or mental health specialists (i.e. psychologists or psychiatrists). In the studies that described the number and type of providers involved, there was a higher number of community or lay healthcare workers in comparison to the mental health specialists within the team. 25–27,33,34 When community or lay healthcare workers were involved in the intervention delivery, this was due to their role in the existing TB service-delivery structure, as they were often responsible for diagnosis and follow-up for people with TB and were often their first and only contact with TB services.
Most studies described how they required additional human or physical resources to those routinely used or available in the existing TB services. For example, most interventions described the requirement of additional human resources to deliver the intervention; the exceptions to this were combined and screening-only interventions where they used routinely available human resources. 27,28,32,33 Studies describing psychological interventions described the need for mental health specialists (psychologists, psychiatrists or both), social workers or additional community healthcare workers to deliver the intervention, working alongside routinely available TB healthcare workers. 25,30,31,34
All the interventions required community or lay healthcare workers to receive training for screening for depression and delivering the described intervention. The training components were described unevenly in all the studies. In some studies, it was not specified whether the training that the healthcare workers underwent was delivered as part of the intervention or before its implementation. 26–28,30 In some studies, training was only provided for the use of diagnostic tools. 31 In two studies, the training content or length was not described at all. 25,29 In the studies that described the training components, these usually covered the use of diagnostic tools and the provision of mental healthcare and were targeted to TB healthcare workers. 28,33,34 One study mentioned training the TB healthcare workers for a total period of 6 days. 34
All the interventions required the use of additional physical spaces to those routinely available in TB services in which to deliver the diagnosis or follow-up sessions for the intervention, for groups or individuals. Other requirements that were specific to the types of intervention were the use of IT infrastructure or mobile data plans to facilitate communication between patients and healthcare workers or between healthcare workers and the implementation team. 30,32 In the case of interventions that delivered antidepressants as part of the treatment, these were offered to patients at no cost. 27,28 Only one study provided in-kind incentives for community healthcare workers to participate in the intervention delivery. 32
Barriers and facilitators to delivering depression care as part of routine TB services
There was a lot of variability in terms of what represented barriers or facilitators to implementation across the intervention types and CFIR domains.
In Table 4, we describe an overview of the barriers and facilitators to the implementation of the interventions according to the CFIR framework, along with information on the constructs where there were no data available. The table includes a definition of the CFIR subconstructs and a summary of their role as barriers or facilitators to the implementation of each type of intervention for depression.
| Construct | Subconstruct | Definition of the CFIR subconstructs for the purposes of this review and in line with the CFIR handbooka | Psychological-only | Combined | Combined, with socioeconomic support | Screening-only |
|---|---|---|---|---|---|---|
| Intervention characteristics | Intervention source | Defined as the perception of healthcare workers or people with TB about whether the depression intervention is developed by local or national TB services or not | ND | ND | ND | ND |
| Evidence strength and quality | Defined as the authors’, healthcare workers’ or other participants’ perceptions on the evidence supporting the belief that the depression intervention will have the desired outcomes described in the study | 2 | 2 | 2 | 0 | |
| Relative advantage | Defined as the healthcare workers’ and/or people with TB’s perception about the advantage of delivering the depression intervention over the status quo or not delivering the intervention | 2 | 1 | 2 | 2 | |
| Adaptability | Defined as the degree to which a depression intervention was or can be adapted to meet local needs | 1 | X | 1 | −1 | |
| Trialability | Defined as the ability or possibility to test the depression intervention on a small scale in existing TB services. Previous experiences of piloting the depression intervention or one of its components was also considered in this subconstruct | X | ND | ND | 2 | |
| Complexity | Defined as healthcare workers’ and/or people with TB’s perception about the difficulty of implementing or delivering the depression intervention, which could also be reflected by the intricacy and number of steps required to deliver the depression intervention | −2 | −1 | X | X | |
| Design quality and package | Defined as the perceptions of the intervention participants about the presentation and quality of the materials needed for delivering the depression intervention | 2 | ND | ND | 2 | |
| Cost of intervention and or implementation | Defined as the costs of the depression intervention and costs associated with its implementation, including opportunity costs | −2 | −2 | −1 | −1 | |
| Outer setting | Needs of those served by the organisation | Defined as the extent to which the needs of people with TB are identified or met by the depression intervention | 2 | 1 | 1 | −1 |
| Cosmopolitanism | Defined as the degree to which TB services are linked with other organisations and its influence on the implementation of the depression intervention | 2 | 2 | 2 | ND | |
| Peer pressure | Defined as the perceived competitive pressure to implement the depression intervention in TB services | ND | ND | ND | ND | |
| External policy and incentives | Defined as the local, regional or national public policies that support the implementation and delivery of depression care in TB services or for people with TB. Also defined as non-governmental organisations’ mandates and guidelines that support the implementation and delivery of the intervention | 1 | 2 | 2 | ND | |
| Inner setting | Structural characteristics of an organisation | Defined as the architecture, size and other organisational characteristics of TB services | ND | X | 1 | ND |
| Networks and communications | Defined as the quality of formal and informal social networks and communications within TB services | ND | −2 | 1 | ND | |
| Culture | Defined as the norms, values and basic assumptions of patients, communities and the healthcare workers employed by TB services or the organisation delivering the depression intervention | −1 | −2 | ND | −1 | |
| Implementation climate: | Defined as the general receptivity to change within TB services shown by healthcare workers or other participants which cannot be coded to any of the subconstructs below: | − | − | − | − | |
| a. Tension for change | Defined as the authors’, healthcare workers’ or other participants’ perceptions about the need for change in the current service provided to people with TB | 2 | ND | ND | ND | |
| b. Compatibility | Defined as the authors’, healthcare workers’ or other participants’ perceptions about the compatibility or fit of the depression intervention with their current practices, values and/or systems | 1 | 1 | 1 | 1 | |
| c. Relative priority | Defined as the authors’, healthcare workers’ or other participants’ perceptions about the importance of the implementation and delivery of depression care in existing TB services | ND | −2 | ND | ND | |
| d. Organisational incentives and rewards | Defined as the incentives and rewards provided by study leads, TB services or other organisations involved in the implementation of the intervention that have a goal to increase or improve the uptake of the depression intervention | ND | ND | ND | ND | |
| e. Goals and feedback | Defined as the communication of goals and feedback to health-care workers delivering the depression intervention | ND | −1 | ND | 2 | |
| f. Learning climate | Defined as the presence or absence of a learning climate in TB services. A learning climate is defined as a climate in which leaders express their own fallibility and need for team members’ assistance and input; team members feel that they are essential, valued and knowledgeable partners in the change process; individuals feel psychologically safe to try new methods and there is sufficient time and space for reflective thinking and evaluation (CFIR, 2021) | ND | ND | ND | ND | |
| Readiness for implementation: | Defined as the tangible indicators of a TB service’s commitment to the implementation of depression in its routine services, and which cannot be coded in the subconstructs below: | − | − | − | − | |
| a. Leadership engagement | Defined as the involvement of TB services or other relevant organisational leaders in the implementation and delivery of the depression intervention | ND | 1 | ND | ND | |
| b. Available resources | Defined as the availability of resources (i.e. physical, human, financial) dedicated to the implementation and delivery of the depression intervention | −2 | −2 | 1 | X | |
| c. Access to knowledge and information | Defined as the provision of knowledge and information to healthcare workers (e.g. training) and people with TB (e.g. educational materials or sessions) about the depression intervention and/or TB | 2 | 2 | ND | 2 | |
| Characteristics of individuals | Knowledge and beliefs about the intervention | Defined as the authors’, healthcare workers’ or other participants’ (i.e. patients) attitudes and beliefs about the depression intervention | 1 | X | ND | 2 |
| Self-efficacy | Defined as the healthcare worker’s belief in their capacity to implement and deliver the depression intervention | 2 | −2 | ND | 2 | |
| Individual stage of change | Defined as the individual stages through which healthcare workers move towards the sustained and skilled delivery of the depression intervention | 1 | 2 | ND | 2 | |
| Individual identification with organisation | Defined as healthcare workers’ and people with TB’s perceptions of TB services and their commitment to them | ND | ND | ND | ND | |
| Other individual characteristics | Defined as healthcare workers’ personality traits, such as their tolerance of ambiguity, intellectual ability, motivation, values, competence, capacity and learning style (CFIR, 2021) | 2 | ND | ND | ND | |
| Process | Planning | Defined as the development of plans and strategies for the implementation and delivery of depression care before its implementation | X | ND | ND | 2 |
| Engaging: | Defined as the strategies and outcomes of activities to engage different individuals in the implementation and use of the depression intervention, and which cannot be coded in the subconstructs below: | − | − | − | − | |
| a. Opinion leaders | Defined as individuals or groups of individuals (e.g. family, community members) that have a formal or informal influence on the attitudes or beliefs of others towards the intervention and its implementation | 2 | ND | ND | 2 | |
| b. Formally appointed internal implementation leaders | Defined as healthcare workers or individuals from within TB services who have been formally appointed as implementers, co-ordinators, project managers, team leaders or other similar roles. | ND | 0 | ND | ND | |
| c. Champions | Defined as individuals who help overcome indifference or resistance to the depression intervention within TB services or by other participants | 2 | ND | ND | ND | |
| d. External change agents | Defined as individuals affiliated with other organisations outside TB services that facilitate the implementation of the intervention | 1 | 1 | 1 | ND | |
| e. Key stakeholders | Defined as the healthcare workers within TB services or organisations involved in delivering the intervention | 2 | 2 | X | 2 | |
| f. Innovation participants | Defined as people with TB, their families and/or caregivers | 2 | 1 | 1 | 2 | |
| Executing | Defined as the implementation of the depression intervention according to what was planned (i.e. fidelity) | −1 | −2 | ND | 2 | |
| Reflection and evaluation | Defined as the feedback about the process of implementation and/or the intervention from healthcare workers and people with TB towards study leads or implementation leaders | 2 | 0 | ND | 2 |
Barriers
The construct, cost of intervention and/or implementation, is contained within the intervention characteristics domain in the CFIR framework. Most studies discussed the spill-over effects of this barrier in the context of implementation. This was a major barrier to implementation for all intervention types. There were different types of costs referenced in the studies, associated with additional human resources, lack of physical spaces and lack of funding for the mental health intervention.
All the interventions required the use of additional physical and/or human resources to those routinely available and required additional resources for training activities. Examples of additional human resources were the recruitment of specialist mental health workers (i.e. psychiatrists or psychologists) and additional community health workers. 25,34
The lack of physical spaces to deliver the interventions for depression was also a recurring barrier in most studies. Only the screening-only intervention did not mention lack of physical space as a barrier, since patients were referred to spaces outside the TB clinic to receive mental health care. 32
One study describing a combined intervention mentions the lack of funding as a worsening factor that negatively impacts on implementing mental healthcare interventions in routine primary care services: ‘the problem is human resources, material resources, and funding all combined … ’ (p. 7). 33
Other barriers across interventions
Complexity is part of the intervention characteristics construct. This was a barrier for psychological and combined interventions, but it had a mixed impact on interventions combined with socioeconomic support and screening-only interventions. For a detailed description of the role of this construct as a barrier, see Appendix 3.
Culture was referred to as a barrier when the organisational or patients’ culture clashed with the goals of the intervention. Culture was a barrier for all types of interventions, except for combined interventions with socioeconomic support, where there were no data available. For a detailed description of the role of this construct as a barrier, see Appendix 3.
Facilitators across intervention types
Relative advantage
Participants perceived that it was advantageous to implement the depression intervention since it improved the TB care provided at the time of implementation. All the studies reported statements referring to the participants’ belief in the advantage and benefit of delivering mental health care to people with TB as opposed to routine care or no mental health intervention at all. In most studies it was recognised that people with TB have complex care needs that cannot be addressed by focusing on TB treatment alone. One study explicitly stated that the intervention improved and complemented the current services provided for TB patients and improved their access to integrated care.
[The intervention] offered additional evaluations to supplement those covered by the TB services at the health facilities … [the intervention’s] strategy of having a field team who function as case managers and patient advocates is one method for offering co-ordinated care in a system where care is not integrated at the provider level. (p. 509)26
The favourable opinion about the relative advantage of the intervention was shared by patients, TB healthcare workers and policy-makers. ‘Some [patients] also stated that the intervention should be available in all multi-drug-resistant (MDR)-TB centres’ (p. 9). 34 Healthcare workers felt that the intervention helped them to provide better care to their patients.
They [the healthcare workers] believed the training made them more aware of the importance of caring for people’s mental health, provided them with knowledge and skills in mental health – an understudied topic in their professional education – taught them how to use a screening tool to assess their patients’ mental health, and offered them necessary skills to help their patients. (p. 14)32
TB programme leaders at district level mentioned that mental health delivery programmes had achieved some improvements on routinely provided TB care. 33
Compatibility of the intervention
This construct is part of the inner setting. The studies reported positive statements about the compatibility of the intervention components (i.e. screening, treatment) with the values of the TB services and current practices. In two studies, describing a psychological and a screening-only intervention, components were designed with the input from the healthcare workers delivering the intervention and adapted according to their feedback as the implementation progressed. 32,34 The studies describing combined interventions for depression also described how the screening and treatment components were compatible with their programmes and were included in their operational manuals or supported by national TB policies. 26–28,33
Innovation participants
The people who received the intervention, that is people with TB (and, in some psychological interventions, their families), were facilitators for implementation. In all the interventions, there were comprehensive measures taken to involve the people with TB and their families in the implementation of the intervention. In some interventions, this included providing home visits to people with TB. 25,26,28,31 In some interventions, family members and friends were included in the psychological component of the intervention. 25,30,31,34 In one intervention, patients were given an option of where to receive care, depending on their situation at home. 26,33 In all the interventions, the active participation of the people with TB, their families or their communities was a facilitator for the implementation of the intervention for depression, regardless of the type of intervention.
Other facilitators across intervention types
There were other facilitators across most, but not all, intervention types.
Evidence strength and quality was defined as the belief, sustained by evidence, that the intervention would have the desired outcome. This was a facilitator in psychological, combined and combined with socioeconomic support interventions. For a detailed description of the role of this construct, see Appendix 3.
Cosmopolitanism, part of the outer setting, seemed to be a facilitator for all types of interventions, except for screening-only, where there were no data to assess this. Cosmopolitanism was defined as the linkages between TB services and other public or private services. For a detailed description of the role of this construct, see Appendix 3.
External policy and incentives, part of the outer setting, seemed to be facilitators for all types of interventions, except for screening-only, for which there were no data to assess this. For a detailed description of the role of this construct, see Appendix 3.
Access to knowledge and information, part of the inner setting, acted as a facilitator for all types of interventions, except for combined interventions with socioeconomic support, where there were no data available to assess this. More details of the role of this construct are included in Appendix 3.
Individual stage of change, part of the characteristics of individuals domain, seemed to be a facilitator for all types of interventions, except for combined interventions with socioeconomic support, where there were no data to assess this. This construct refers to the stages that healthcare workers go through towards the sustained and skilled delivery of the intervention, in terms of the change in their confidence and knowledge to implement the intervention. See Appendix 3 for a detailed description of the role of this construct.
The influence of external change agents as facilitators of implementation was present in all interventions, except for the screening-only intervention, where there were no data available to assess this. External change agents were defined as individuals affiliated to other organisations that are not governmental or public TB services. See Appendix 3 for a detailed description of the role of this construct.
Discrepancies in barriers and facilitators across intervention types
There were some discrepancies in the roles that some constructs had across interventions. This section describes the constructs that were facilitators for some interventions and barriers to implementation in others, based on the data available in the included studies.
Adaptability, part of the domain of the intervention characteristics, had a different role in the implementation of different types of intervention. It acted as a facilitator in the implementation of psychological-only and combined interventions with socioeconomic support; it was a barrier to the implementation of the screening-only intervention and it had a mixed impact in the implementation of combined interventions (without socioeconomic support). As a facilitator, the construct of availability included statements from the included studies that referred to how screening and treatment components were adapted to meet the local cultural needs. In one psychological intervention, this involved a change of screening tool from the less compatible PHQ-9 to the more compatible PHQ-2 with healthcare workers’ routine activities. 34 In another psychological intervention, this involved the use of culturally adapted treatments for depression according to patients’ needs. 31 However, in the implementation of combined interventions, one of the studies described how the adaptability of the intervention led to its uneven implementation in different primary care settings. 33 The characteristics of the screening-only intervention meant that it was not possible to fully adapt the intervention to local practices and workflows, even if it was designed to be compatible. 32
The construct, needs of those served by the organisation (i.e. people with TB needs), part of the outer setting domain, was a facilitator in psychological, combined and combined interventions with socioeconomic support. However, it was a barrier in the screening-only intervention. For a detailed description of the role of this construct as a barrier and facilitator, see Appendix 3.
The role of the available resources construct, part of the inner setting domain, was a facilitator for implementation in combined interventions with socioeconomic support. However, this construct was described in the context of barriers to implementation in psychological and combined interventions. Additionally, this construct was one of the few to have a mixed impact, as a barrier and facilitator, in the implementation of screening-only interventions. For a detailed description of the role of this construct as a barrier and facilitator, see Appendix 3.
Self-efficacy, part of the characteristics of individuals domain, was a facilitator for the implementation of psychological-only and screening-only interventions, but it was a barrier to implementation for combined interventions. For a detailed description of the role of this construct as a barrier and facilitator, see Appendix 3.
In psychological, combined and screening-only interventions, the role of key stakeholders was as a facilitator for implementation. However, the same construct had a mixed impact in the implementation of combined interventions with socioeconomic support. Key stakeholders were defined as healthcare workers who were part of TB services and involved in TB service delivery. Key stakeholders were multidisciplinary: the teams involved in the implementation of screening and treatment interventions were social workers, counsellors and psychologists or psychiatrists, nurses with mental health training, community healthcare workers or TB healthcare workers. In interventions that involved mental health specialists, such as psychologists or psychiatrists, these would often be involved in the training and supervision of community health workers or data collectors implementing the screening and treatment. 25,27,32 In these interventions, the role of specialists was also to provide ongoing support and sometimes feedback to the community health workers providing the intervention. However, in one combined intervention with socioeconomic support, the role of psychologists or mental health specialists was unclear in terms of their role in providing support or training to the healthcare workers delivering the intervention. 29 In this intervention, the role of TB healthcare workers was also unclear, as it was stated that pharmacists delivered the intervention, and their affiliation was unclear at the time of implementation.
Executing, part of the process domain, was a facilitator for the implementation of the screening-only intervention, while it was a barrier to implementation in psychological and combined interventions. In the screening-only intervention, its technological characteristics (i.e. being app-based) allowed for the consistent implementation of the intervention, and the intervention implementation process was designed so that researchers could provide support to healthcare workers quickly if they noticed that the intervention was not being implemented adequately. 32 However, for the implementation of psychological interventions, the studies described issues with the adequate execution of the intervention. These were attributed in part to the insufficient resources or the unsustainability of the interventions when healthcare workers aimed to include it in their day-to-day practice. ‘Although it only took 5–10 minutes to go through, this seemed to become a barrier to them using the flipbook. They stated that they gave the same messages but more briefly’ (p. 9). 34 In combined interventions, two studies described issues with uneven implementation. They described deficiencies associated with the adequate, sustained and consistent implementation of the intervention across settings. 33 One study mentioned that the mental health intervention components (i.e. routine screening, the use of the designated screening tool, referral and treatment) were unevenly implemented according to healthcare workers’ self-reported performance. 27
Constructs with no data
For the rest of the interventions implemented, there were some constructs that had no data available across all intervention types. Most of the data coded in the studies were attributed to the subconstructs included in the larger intervention characteristics and characteristics of individuals constructs. However, there were evident gaps in information in other domains. The most evident gap in evidence was in the inner setting construct. In this construct, few studies described data that could be used to reveal patterns about the influence of the constructs in this domain as barriers or facilitators. The lack of data was evident also in the process construct of the framework, where there was little information available on the role of planning and engaging different actors in the implementation of the intervention. See Table 4 for more details.
Discussion
In this systematic review, we aimed to explore the approaches that have been used to deliver depression care as part of TB services in LMICs. This review also aimed to describe the barriers and facilitators to their implementation using the CFIR framework as an analytical framework. While the goal of this review was not to assess effectiveness, two studies that used cluster randomised controlled trial design reported improved TB and/or mental health outcomes compared to baseline assessments. This is consistent with findings about the efficacy of delivering pharmacological and non-pharmacological interventions for common mental disorders in people with TB. 35 This potential effectiveness makes it important to identify how to best deliver mental healthcare interventions for people with TB and implement them within routine TB services.
Most studies met the criteria for quality of reporting according to their study design. However, the studies described the implemented interventions inconsistently, and some of them did not report dosage, length of treatment or follow-up information about the interventions, which are factors that can mediate the efficacy of the interventions. This is consistent with other reviews carried out to evaluate the effectiveness of pharmacological and non-pharmacological interventions for common mental disorders in people with TB where meta-analyses were not possible due to the sparse data reported in studies and the methodological variation in study designs. 35
Approaches to deliver depression care as part of TB services
There were different approaches to deliver depression care for people with TB in LMICs. The most common approach was the implementation of psychological components, alone or in combination with pharmacological components and with socioeconomic support. This is consistent with the findings of other systematic reviews for interventions that integrate mental health into primary care in LMICs. 36 Psychological and pharmacological interventions for depression have the potential to be delivered in resource-constrained settings by providing training to non-specialist mental healthcare providers and using task-shifting approaches, achieving highly effective results when delivered by non-specialists alone or supervised by mental health specialists. 37 However, the implementation process will inevitably require additional physical and training-related resources.
Barriers and facilitators to implementation
The provision of mental health training to lay or community healthcare workers was an important facilitator for implementation. This finding is in line with the results of other systematic reviews: it is essential to provide training to lay healthcare workers or community healthcare workers to provide mental health care. 38 The type of training and the number of sessions required will vary according to the healthcare workers’ baseline characteristics and their previous knowledge of mental health and mental health interventions. There is some preliminary research on the activities within training that are necessary to implement sustained change, such as the formal appointment of supervisors and self-reflection or evaluation of fidelity to the intervention, to name a few. 39 Training content should cover basic information about mental health conditions, interventions, terminology and diagnostic and referral criteria. Also, the provision of mental health and TB knowledge to patients, families and communities facilitates implementation. Other studies have similar findings: when mental health interventions facilitate interaction between providers, beneficiaries and their families, in culturally appropriate ways, it facilitates the implementation process and creates a positive experience for those involved. 40 When healthcare workers felt they lacked the skills to address mental health in their patients, they regarded this as a barrier to integrating mental health assessments or related activities in their practice. 41
All interventions and their implementation processes incurred costs, mainly related to the use of human resources, training and physical spaces. This finding is consistent with the results of a systematic review that analysed the effectiveness and cost-effectiveness of integrating mental health care in LMICs, where the findings of the study show that all intervention arms increased the effectiveness of depression treatment and costs. 36 The cost of the intervention and its implementation can be attributed to the legacy of insufficient funds allocated to mental health care. 11 ‘Given the low levels of spending on mental healthcare … the finding that increasing the availability of mental health services increases direct costs should not surprise’ (p. 48). 36 Based on evidence from 42 studies, the integration of mental health services for depression in primary care can result in an immediate increase in health costs at a service level, mainly due to the increased use of human resources and the cost of treatment but is cost-effective from a healthcare perspective or reduces costs from a societal perspective. 36
To date, there is not a systematic review that analyses the costs of implementation of depression interventions in LMICs, which makes it hard to assess what resources are needed for implementation. In all the included studies, it was mentioned that there were not enough resources available for TB services, which will impact the feasibility of the implementation of mental health interventions in routine TB services. This tension overlaps with the availability of human resources for the delivery of mental health services. It is often not enough to train existing healthcare workers to deliver mental health care in the context of a poorly resourced workforce. 40 Further resources should be created and earmarked to facilitate the training of healthcare professionals in mental health care, add dedicated healthcare workers to provide mental health care, add specific mental healthcare tasks to existing care pathways or use a care co-ordinator. 36 The findings of this review suggest that the additional workload related to mental health care for existing healthcare workers is likely to be unfeasible and unsustainable within existing TB programmes. TB services in LMICs are well-established and have dedicated resources apart from wider health systems’ structures. 42 Thus, in this context, it would be more effective to earmark existing resources to train TB healthcare workers on mental health care delivery or use care co-ordinators to integrate mental health care into people with TB’s care. Mental health interventions in LMICs can be more effectively implemented if they adhere to existing care pathways and service delivery networks. 40
The provision of training alone is not sufficient if this is not accompanied by earmarked resources that create the space to deliver these interventions in existing service delivery structures, including considerations to increase the number of providers. TB services, as part of their aim to provide patient-centred care,10 could frame that as a window of opportunity to create said space and use existing resources to deliver mental health interventions for people with TB as part of their routine care.
Greater understanding and information on the organisational characteristics of TB services, such as internal incentives and rewards, the role of peer pressure, the learning climate or individuals’ identification with the organisation, can help to inform how to integrate care for mental health into TB services so that they can be feasibly and sustainably delivered. Understanding organisational characteristics can help with planning adequate interventions and implementation strategies. For example, interventions for depression that include financial incentives can help to alleviate the economic vulnerability of people with TB in LMICs. 43,44 This is important to explore because of the way that TB care is financed and provided in LMICs, including a range of organisations and collaborations. 14 Published peer-reviewed systematic reviews hint that health system characteristics, such as funding structures and available human resources, can become important barriers to implementation if they are not addressed before implementation stages, or if there are not discrete resources allocated to the integration of mental health care in existing health services. 41
Future research
This review includes studies that were published or carried out before the COVID-19 pandemic. Thus, the results presented here are likely to not be reflective of the current status of mental health and TB services in the countries reflected in the studies included in this review. A feasible way to improve this review would be to include an analysis of how the TB and mental health services of the countries represented have been affected by the pandemic.
Lessons learnt
The availability and reliability of the information on implementation efforts depend more on the study design (e.g. feasibility and acceptability) rather than on the intervention type being implemented (e.g. psychological, combined). Because the nature of the majority of the studies was not focused on implementation, that meant that a lot of cells within the framework matrix were empty (no data) for most intervention types and studies, except for two which had implementation-focused study designs. 32,45 This is consistent with other implementation reviews that focus on depression interventions in LMICs. 46,47 Future studies should be based on implementation-based questions such as the feasibility, acceptability and sustainability of the intervention. Future research should focus on assessing the interventions’ effectiveness and their implementation in resource-constrained settings, which would focus on the later implementation stages’ outcomes, such as cost, penetration and sustainability. 46
Community engagement involvement
There was no patient and public involvement in this study. We considered this to be inappropriate given the objective of the study, which was to synthesise the available evidence.
Limitations
The CFIR framework may not be able to capture the full complexity of TB services and their impact on mental healthcare delivery in LMICs. Although this framework was useful in identifying barriers and facilitators, there were characteristics from local health systems that could not be coded to the existing constructs in the framework. For example, national and international donors for TB and mental health programmes can influence the interventions that are implemented, based on their preferences and agendas. 40 Adaptations that make the CFIR framework more relevant to LMICs’ contexts are possible and should be explored as they can help assess barriers and facilitators that are prevalent in resource-constrained settings. 47 In line with the findings from other reviews,46,47 the next research priorities should move away from trying to test the effectiveness of interventions and rather focus on the implementation strategies and outcomes that can lead to successful implementation efforts for depression interventions in LMICs.
Due to the objectives of this study, the information analysed corresponds only to that reported in the published studies and is, therefore, subjected to reporting bias in the individual studies. Although a quality assessment was made according to each study type, this did not influence the weighting of how findings were represented in this review, as this study was concerned with providing a narrative synthesis of the approaches to depression care in TB services. Thus, this study should not be interpreted as evaluating the effectiveness of the interventions included in the analysis. Nonetheless, we are confident that we were able to identify and describe the various approaches that have been implemented to provide depression care in TB services in LMIC.
Conclusion
In this review, we aimed to identify the approaches used in LMICs to provide depression care for people with TB. We also aimed to explore the barriers and facilitators to their implementation.
What this study adds
We identified psychological interventions as the most common approach used to deliver depression care for people with TB in LMICs. The findings from this review suggest that the implementation of interventions for depression is facilitated by the belief that the intervention is advantageous to the status quo (i.e. no provision of mental health care) (relative advantage), the compatibility of the intervention with existing workflows and the positive attitude that patients, families and communities display towards the intervention (innovation participants). All the interventions faced barriers to implementation related to the costs of the intervention and/or its implementation, which were expressed in terms of costs associated with insufficient human resources, lack of physical resources and lack of financial resources altogether for the provision of mental health care to people with TB. The choice of the best intervention to implement will depend on the available resources and the attitude of stakeholders to the intervention. From the evidence reported in the included evidence in this study, it appears that psychological interventions with some form of community engagement are the most compatible with local attitudes towards mental health interventions and can be delivered with existing or few additional resources, if training is provided. These are important factors that will facilitate the implementation of these types of interventions.
Key learning points
-
There are barriers and facilitators faced by all types of interventions for depression implemented into existing TB services. However, different barriers and facilitators can arise according to the types of intervention implemented.
-
Interventions to treat depression among TB patients are unlikely to be feasible without investment in human resources to deliver care.
-
The implementation of any mental health intervention in TB services will require some degree of training. However, for the sustainable delivery of the intervention, mental health tasks and activities could be included in routine TB care or there could be a designated workforce for the delivery of this intervention.
Deviations from protocol
Outcomes of interest as stated in the protocol were defined as
those described in eligible studies, which could be process or clinical outcomes, for example: process outcomes (e.g. number of diagnostic tests performed, number of patients with access to the intervention to treat depression) or clinical outcomes (e.g. patients with negative sputum smear test, mortality, patients with reduced depression severity).
In practice, none of these data were extracted as they were not consistently reported across studies, and they were not required for the main analysis of barriers and facilit
Additional information
Contributions of authors
Rocio Nava-Ruelas (https://orcid.org/0000-0001-5890-7519) (PhD Candidate, Health Sciences, University of York) contributed to the design of the study and conducted the literature searches, screening, analysis and writing of the report.
Olamide Todowede (https://orcid.org/0000-0002-5785-1426) (Research Fellow, Health Sciences, University of Nottingham) conducted the screening and collaborated with writing the report.
Najma Siddiqi (https://orcid.org/0000-0003-1794-2152) (Professor of Psychiatry, Health Sciences, University of York) contributed to the design of the study and the writing of the report.
Helen Elsey (https://orcid.org/0000-0003-4724-0581) (Senior Lecturer in Global Health, Health Sciences, University of York) contributed to the design of the study and the writing of the report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/GRWH1425.
Primary conflicts of interest: Rocio Nava-Ruelas received grant support from Consejo Nacional de Ciencia y Tecnologia for her doctoral studies. Olamide Todowede declares no competing interest. Najma Siddiqi was part of Grant 17/63/130 NIHR Global Health Research Group: Improving Outcomes in Mental and Physical Multimorbidity and Developing Research Capacity (IMPACT) in South Asia at the University of York. Helen Elsey declares no competing interest.
Data-sharing statement
Data can be obtained from the corresponding author upon request.
Ethics statement
This study did not require ethical approval as it did not involve human participants as data subjects.
Equality, diversity and inclusion
We designed our study to be of relevance to the population of interest (people with TB), regardless of their socioeconomic status, gender, ethnicity, religion or age. We believe that the study population from the included studies is reflective of the population of interest. We believe we have addressed EDI concerns pertaining to the study design, which is an evidence synthesis, in that we did not exclude any study based on the type of population as long as they met the principal inclusion criteria.
Department of Health and Social Care disclaimer
This report presents independent research commissioned by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, CCF, NETSCC, the GHR programme or the Department of Health and Social Care.
Study registration
The protocol of this review is registered with PROSPERO under registration number CRD42020201095.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme as award number 17/63/130 using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government. Research is published in the NIHR Global Health Research Journal. See the NIHR Funding and Awards website for further award information.
About this article
The contractual start date for this research was in April 2018. This article began editorial review in September 2022 and was accepted for publication in July 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Copyright
Copyright © 2024 Nava-Ruelas et al. This work was produced by Nava-Ruelas et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
This article reports on one component of the research award Approaches used to deliver depression care in TB services in LMICs and barriers and facilitators to implementation: a systematic review. For more information about this research please view the award page (https://www.fundingawards.nihr.ac.uk/award/17/63/130)
List of abbreviations
- CFIR
- Consolidated Framework for Implementation Research
- LMICs
- low- and middle-income countries
- MMAT
- Mixed Methods Appraisal Tool
- NGO
- non-governmental organisation or not-for-profit organisations
- TB
- tuberculosis; for the purposes of this article, this encompasses only pulmonary TB, in drug-resistant and drug-susceptible variants
References
- Alene KA, Clements ACA, McBryde ES, Jaramillo E, Lonnroth K, Shaweno D, et al. Mental health disorders, social stressors, and health-related quality of life in patients with multidrug-resistant tuberculosis: a systematic review and meta-analysis. J Infect 2018;77:357-67.
- Koyanagi A, Vancampfort D, Carvalho AF, DeVylder JE, Haro JM, Pizzol D, et al. Depression comorbid with tuberculosis and its impact on health status: cross-sectional analysis of community-based data from 48 low- and middle-income countries. BMC Med 2017;15.
- Janmeja AK, Das SK, Bhargava R, Chavan BS. Psychotherapy improves compliance with tuberculosis treatment. Respiration 2005;72:375-80.
- Morisky DE, Malotte CK, Choi P, Davidson P, Rigler S, Sugland B, et al. A patient education program to improve adherence rates with antituberculosis drug regimens. Health Educ Q 1990;17:253-67.
- M’Imunya JM, Kredo T, Volmink J. Patient education and counselling for promoting adherence to treatment for tuberculosis. Cochrane Database Syst Rev 2012;2012.
- Baral SC, Aryal Y, Bhattrai R, King R, Newell JN. The importance of providing counselling and financial support to patients receiving treatment for multi-drug resistant TB: mixed method qualitative and pilot intervention studies. BMC Public Health 2014;14.
- Zarova C, Chiwaridzo M, Tadyanemhandu C, Machando D, Dambi JM. The impact of social support on the health-related quality of life of adult patients with tuberculosis in Harare, Zimbabwe: a cross-sectional survey. BMC Res Notes 2018;11.
- WHO . International Standards for Tuberculosis Care 2014.
- WHO . Global Tuberculosis Report 2021.
- Global Fund . Modula Framework Handbook 2019.
- Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low-and middle-income Countries. Health Serv Insights 2017;10. https://doi.org./1178632917694350.
- Kodner DL, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications – a discussion paper. Int J Integr Care 2002;2.
- Chuah FLH, Haldane VE, Cervero-Liceras F, Ong SE, Sigfrid LA, Murphy G, et al. Interventions and approaches to integrating HIV and mental health services: a systematic review. Health Policy Plan 2017;32:iv27-47.
- Bowser D, Sparkes SP, Mitchell A, Bossert TJ, Bärnighausen T, Gedik G, et al. Global Fund investments in human resources for health: innovation and missed opportunities for health systems strengthening. Health Policy Plan 2014;29:986-97.
- Hong QN, Pluye P, Fabregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT). Gatineau, QC: Canadian Intellectual Property Office; 2018.
- Heyvaert M, Hannes K, Onghena P. Using Mixed Methods Research Synthesis for Literature Reviews. Thousand Oaks, CA: SAGE Publications, Inc; 2017.
- Pluye P, Gagnon MP, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. Int J Nurs Stud 2009;46:529-46.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan – a web and mobile app for systematic reviews. Syst Rev 2016;5.
- NICE . Depression in Adults: Treatment and Management 2022.
- Damschroder L, Reardon C, Lowery J. Handbook on Implementation Science. Cheltenham: Edward Elgar Publishing Limited; 2020.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13.
- CFIR . Consolidated Framework for Implementation Research: CFIR Research Team – Center for Clinical Management Research 2021. https://cfirguide.org/ (accessed 1 September 2022).
- Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 2016;104:240-3.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372.
- Acha J, Sweetland A, Guerra D, Chalco K, Castillo H, Palacios E. Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health 2007;2:404-17.
- Contreras CC, Millones AK, Santa Cruz J, Aguilar M, Clendenes M, Toranzo M, et al. Addressing tuberculosis patients’ medical and socio-economic needs: a comprehensive programmatic approach. Trop Med Int Health 2017;22:505-11.
- Das M, Isaakidis P, Van den Bergh R, Kumar AM, Nagaraja SB, Valikayath A, et al. HIV, multidrug-resistant TB and depressive symptoms: when three conditions collide. Glob Health Action 2014;7.
- Vega P, Sweetland A, Acha J, Castillo H, Guerra D, Smith Fawzi MC, et al. Psychiatric issues in the management of patients with multidrug-resistant tuberculosis. Int J Tuberc Lung Dis 2004;8:749-59.
- Kaukab INB, Abrar M, Muneer S, Kanwal N, Shah N, Aahmad S, et al. Effect of pharmacist-led patient education on management of depression in drug resistance tuberculosis patients using cycloserine. A prospective study. Lat Am J Pharm 2015;34:1403-10.
- Khachadourian V, Truzyan N, Harutyunyan A, Petrosyan V, Davtyan H, Davtyan K, et al. People-centred care versus clinic-based DOT for continuation phase TB treatment in Armenia: a cluster randomized trial. BMC Pulm Med 2020;20.
- Li X, Wang B, Tan D, Li M, Zhang D, Tang C, et al. Effectiveness of comprehensive social support interventions among elderly patients with tuberculosis in communities in China: a community-based trial. J Epidemiol Community Health 2018;72:369-75.
- Diez-Canseco F, Toyama M, Ipince A, Perez-Leon S, Cavero V, Araya R, et al. Integration of a technology-based mental health screening program into routine practices of primary health care services in Peru (The Allillanchu Project): development and implementation. J Med Internet Res 2018;20.
- Lovero KL, Lammie SL, van Zyl A, Paul SN, Ngwepe P, Mootz JJ, et al. Mixed-methods evaluation of mental healthcare integration into tuberculosis and maternal-child healthcare services of four South African districts. BMC Health Serv Res 2019;19.
- Walker IF, Khanal S, Hicks JP, Lamichhane B, Thapa A, Elsey H, et al. Implementation of a psychosocial support package for people receiving treatment for multidrug-resistant tuberculosis in Nepal: a feasibility and acceptability study. PLOS ONE 2018;13.
- Farooq S, Tunmore J, Comber R. Pharmacological or non-pharmacological interventions for treatment of common mental disorders associated with Tuberculosis: a systematic review. Chron Respir Dis 2021;18.
- Cubillos L, Bartels SM, Torrey WC, Naslund J, Uribe-Restrepo JM, Gaviola C, et al. The effectiveness and cost-effectiveness of integrating mental health services in primary care in low- and middle-income countries: systematic review. BJPsych Bull 2021;45:40-52.
- Barbui C, Purgato M, Abdulmalik J, Acarturk C, Eaton J, Gastaldon C, et al. Efficacy of psychosocial interventions for mental health outcomes in low-income and middle-income countries: an umbrella review. Lancet Psychiat 2020;7:162-72.
- Connolly SM, Vanchu-Orosco M, Warner J, Seidi PA, Edwards J, Boath E, et al. Mental health interventions by lay counsellors: a systematic review and meta-analysis. Bull World Health Organ 2021;99:572-82.
- Murray LK, Dorsey S, Bolton P, Jordans MJ, Rahman A, Bass J, et al. Building capacity in mental health interventions in low resource countries: an apprenticeship model for training local providers. Int J Ment Health Syst 2011;5.
- Qureshi O, Endale T, Ryan G, Miguel-Esponda G, Iyer SN, Eaton J, et al. Barriers and drivers to service delivery in global mental health projects. Int J Ment Health Syst 2021;15.
- Wakida EK, Talib ZM, Akena D, Okello ES, Kinengyere A, Mindra A, et al. Barriers and facilitators to the integration of mental health services into primary health care: a systematic review. Syst Rev 2018;7.
- Lei X, Liu Q, Escobar E, Philogene J, Zhu H, Wang Y, et al. Public–private mix for tuberculosis care and control: a systematic review. Int J Infect Dis 2015;34:20-32.
- Richterman A, Steer-Massaro J, Jarolimova J, Luong Nguyen LB, Werdenberg J, Ivers LC. Cash interventions to improve clinical outcomes for pulmonary tuberculosis: systematic review and meta-analysis. Bull World Health Organ 2018;96:471-83.
- Boccia D, Hargreaves J, Lönnroth K, Jaramillo E, Weiss J, Uplekar M, et al. Cash transfer and microfinance interventions for tuberculosis control: review of the impact evidence and policy implications. Int J Tuberc Lung Dis 2011;15:37-49.
- Walker IF, Baral SC, Wei X, Huque R, Khan A, Walley J, et al. Multidrug-resistant tuberculosis treatment programmes insufficiently consider comorbid mental disorders. Int J Tuberc Lung Dis 2017;21:603-9.
- Wagenaar BH, Hammett WH, Jackson C, Atkins DL, Belus JM, Kemp CG. Implementation outcomes and strategies for depression interventions in low- and middle-income countries: a systematic review. Glob Ment Health (Camb) 2020;7.
- Means AR, Kemp CG, Gwayi-Chore M-C, Gimbel S, Soi C, Sherr K, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implement Sci 2020;15.
Appendix 1 General search strategy
The general search strategy consists of using relevant terms for tuberculosis, depression and approaches to integration listed in bold in at least one of three modes: as MeSH terms, as subject headings or as keywords in the title or abstract. Their usage will depend on the indexing rules of each database.
| (Relevant terms for pulmonary tuberculosis): |
| tuberculosis as MeSH OR tuberculosis as subject heading (i.e. exp) OR tuberculosis as keyword in title or abstract (i.e..mp.kw.ti..ab) |
| AND (relevant terms for depression): |
| depression as MeSh OR depression as subject heading (i.e. exp) OR depressive disorder as MeSh OR depressive disorder as subject heading (i.e. exp) OR depress* as keyword in title or abstract (i.e..mp.kw.ti.ab) OR ((psych* OR emotion* OR mental* OR socio* OR behavio#r*) next/adj1 (disease* OR health* OR problem* OR state* OR aspect* OR ill* OR disord* OR disturb* OR condition*)) as keyword in title or abstract (i.e..mp.kw.ti..ab) OR (‘mental health*’ OR ‘mental illness*’ OR ‘mental disorder*’) as subject heading (i.e. exp) OR (‘mental health*’ OR ‘mental illness*’ OR ‘mental disorder*’) as MeSh OR (‘mental health*’ OR ‘mental illness*’ OR ‘mental disorder*’) as keyword in title or abstract (i.e..mp.kw.ti..ab) |
| AND (relevant terms for approaches to integration): |
| ((patient* OR person* OR people*) adj1 cent*) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR (outpatient* adj/3 (care* OR service* OR clinic*)) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR (team* adj2 (care* OR treat* OR assess* OR consult*)) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR (care adj2 (coordinat* OR co-ordinat* OR program* OR continu*)) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR continuity of care as MeSH OR continuity of care as subject heading OR ‘continuity of care’ as keyword in title or abstract (i.e..mp.kw.ti.ab) OR integrated care as MeSH OR integrated care as subject heading OR ‘integrated care’ as keyword in title or abstract (i.e..mp.kw.ti.ab) OR integrated healthcare system as MeSH OR integrated healthcare system as subject heading OR ‘integrated health*’ as keyword in title or abstract (i.e..mp.kw.ti.ab) OR integrated services as MeSH OR integrated services as subject heading OR integrated services as keyword in title or abstract (i.e..mp.kw.ti.ab) OR referral and consultation as MeSH OR referral and consultation as subject heading OR refer* as keyword in title or abstract (i.e..mp.kw.ti.ab) OR consult* as keyword in title or abstract (i.e..mp.kw.ti.ab) OR comprehensive care as MeSH OR comprehensive care as subject heading OR (integrat* adj3 (care* OR service* OR deliver* OR strateg* OR program OR manage*)) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR (deliver* adj3 (with OR within OR together)) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR (multi* adj2 (care* OR service* OR clinic* OR disciplin*)) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR (multicare OR multiservice* OR multiclinic* OR multidisciplin*) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR ((collaborat* OR manage* OR integrat* OR link* OR join* OR co#rdinat* OR comprehensive OR contin*) adj3 (health* OR care* OR therap* OR intervent* OR treat* OR program* OR service* OR strateg* OR deliver*)) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR case management as MeSH OR case management as subject heading OR (case adj1 manag*) as keyword in title or abstract (i.e..mp.kw.ti.ab) OR ((psych* OR emotion* OR mental* OR socio* OR behavio#r*) adj3 (educat* OR therap* OR support* OR program* OR intervent* OR service* OR train* OR consult* OR refer* OR treat*)) as keyword in title or abstract (i.e..mp.kw.ti.ab) |
Appendix 2 Description of quantitative and qualitative data extracted from the included studies
| Study | Populationa | Intervention | Results | Qualitative method |
|---|---|---|---|---|
| Acha et al.25 | n = 285 | Psychological only | Narrative description of attendance patterns and participants; description of therapeutic strategies; description of thematic content of the sessions; description of workshops for recreation and family members | Participant observation, focus groups, documentation (session summaries and transcripts) |
| bDiez-Canseco et al.32 | n = 127/143 patients n = 21/22 primary healthcare practitioners |
Screening only | Narrative description of study participants, description of the implementation of the screening, description of positive cases detection and referrals; help-seeking and access to mental health care; primary healthcare practitioners’ assessment of the project, delivery of results and referral, feasibility of integrating mental health screening | Documentation (routinely collected data); interviews with patients; interviews with primary healthcare practitioners |
| bLovero et al.33 | n = 5 | Combined | Participants’ description of integrated mental health service provision, challenges to implementation of integrated mental health services in primary care | Interviews with TB programme managers |
| bWalker et al.34 | n = 11 | Psychological only | Feasibility and acceptability of the psychosocial package (the screening process, the counselling, the group support, other challenges and benefits), narrative description of depression symptom outcomes for patients | Documentation (counsellors’ diary); interviews with patients; interviews with TB health workers; observations |
| Study | Population description | Intervention | Comparator | Quantitative outcomes | |
|---|---|---|---|---|---|
| Process outcomes | Clinical outcomes | ||||
| Contreras et al.26 | n = 192 | Combined, with socioeconomic support Cut-off scores for mental health scales: SRQ18 ≥ 1 (on the psychotic and alcoholism section) PHQ9 ≥ 10 |
None; not applicable | Number of people screened for comorbidities (including mental health) = 135/192 Number of people referred to mental health services (including those at risk for all mental health conditions including depression) = 47/62 Number of people who refused mental health screening = 57/192 Number of people who attended the mental health appointment = 41/47 Number of people screened for socioeconomic assistance = 126/192 Number of people who declined or did not complete socioeconomic assistance assessment = 66/192 Number of people that required follow-up to initial assessment = 192 (100%) Number of people receiving socioeconomic assistance = 76/192 |
Number of people with poor adherence to TB treatment = 192/192a No measurement of mental health outcomes at the end of the intervention, only measured attendance to psychological services Number of people at risk of depression = 36/192 Number of people without mental health condition identified at screening point = 80/192 |
| Das et al.27 | n = 61 | Combined Cut-off scores for mental health scales: PHQ-9 ≥ 4 |
None; not applicable | Number of eligible patients screened for depression 45/61 | Number of people with depressive symptoms at baseline = 7/45 Number of people without depressive symptoms = 38 at baseline Number of people without depressive symptoms at follow-up (3 months) = 41/44 Number of people with depressive symptoms at follow-up (3 months) = 3/44 Number of deaths = 1 |
| bDiez-Canseco et al.32 | Patients n = 85 Primary healthcare providers (all female) n = 22 |
Screening only Screening tool and cut-off scores not reported |
None; not applicable | Number of patients screened = 733 Number of screenings in TB services = 85/733 Number of positive cases of mental health illness and suicide risk in TB patients = 13/85 Number of cases of detected mental health illness and suicide risk in all types of patients = 159/733 Number of referrals to psychologist (includes number of patients with conditions other than TB) = 143/159 Number of patients who sought help after positive diagnosis of mental health illness or suicide risk = 92/127 Number of patients who had access to specialised care = 70/92 |
None reported |
| Kaukab et al.29 | n = 70 | Combined, with socioeconomic support Cut-off scores for mental health scales: BDI ≥ 9 |
Intervention n = 35 Control n = 35 |
None reported | Number of participants with depression at baseline, intervention = 35/35 Number of participants with depression at baseline, control = 35/35 Number of participants with depression at end of intervention = 20/35 Number of participants with depression at end of intervention = 35/35 |
| cKhachadourian et al.30 | n = 385 | Psychological only Cut-off scores for mental health scales: CES-D; no cut-off point; higher scores indicate higher levels of depression symptoms |
Intervention n = 187 Control n = 198 |
TB knowledge score intervention M (SD) = 23.9 (3.1) TB knowledge score control M (SD) = 23.1 (3.5) Support score intervention M (SD) = 43.2 (5.3) Support score control M (SD) = 41.8 (7.5) |
TB treatment success intervention = 172/187 TB treatment success control = 184/198 Lost to follow-up intervention = 12/187 Lost to follow-up control = 10/198 Failure intervention = 0/187 Failure control = 0/198 Death intervention = 3/187 Death control = 3/198 Not evaluated intervention = 0/187 Not evaluated control = 1/198 Depression score intervention M (SD) = 4.3 (7.5) Depression score control M (SD) = 4.7 (7.6) |
| Li et al.31 | n = 201 | Psychological only Cut-off scores for mental health scales: SDS; no cut-off point; higher scores indicate higher levels of depression symptoms |
Intervention n = 69 Control = 132 |
None reported | Number of deaths intervention = 1/69 Number of deaths control = 2/132 Depression score baseline intervention M (SD) = 59 (7.49) Depression score baseline control M (SD) = 57 (9.66) Depression score end of intervention M (SD) = 43 (8.53) Depression score end of intervention control M (SD) = 48 (9.13) |
| bLovero et al.33 | Nurses n = 59 Mental health practitioners n = 17 |
Combined Cut-off scores for mental health scales: PC101 (cut-off score not reported or rated) |
None; not applicable | Number of nurses that received mental health training = 46/59 Number of nurses that received training in primary care guidelines, including mental health-care guidelines = 37/59 Number of nurses that consider the primary care guidelines easy or very easy to use = 53/59 Number of nurses that feel comfortable or very comfortable managing mental illness = 35/59 Number of mental health screenings done by nurses in the past 3 months = 51/59 Number of nurses that screen patients at every visit = 43/59 Number of nurses that use a tool to assess mental illness in patients = 26/59 Number of nurses that manage positive mental illness cases at clinic = 2/59 Number of nurses that refer patients to treatment elsewhere inside clinic = 34/59 Number of nurses that refer patients to mental health practitioners = 30/59 Number of nurses that refer patients to other clinic = 21/59 Number of mental health practitioners that assess mental illness = 14/17 Number of mental health practitioners that use a tool to assess mental illness = 5/14 Number of mental health practitioners that offer treatment to positive cases of mental illness = 14/17 Number of mental health practitioners that offer psychiatric medications = 7/14 Number of mental health practitioners that offer individual therapy = 4/14 Number of mental health practitioners that offer group therapy = 1/14 |
None reported |
| Vega et al.28 | n = 75 | Combined Based on DSM-IV criteria |
None; not applicable | None reported | Number of depression cases at baseline (n = 69) = 36 Number of incident cases of depression during anti-TB therapy = 10/75 Number of hospitalisations due to depression during anti-TB treatment = 0/75 Persistent psychiatric symptoms throughout MDR-TB treatment requiring psychiatric medications (new depression) = 8/10 Persistent psychiatric symptoms throughout MDR-TB treatment requiring psychiatric medications (baseline depression) = 2/12 |
| bWalker et al.34 | n = 135 | Psychological Cut-off scores for mental health scales: HSCL (anxiety) ≥ 17 HSCL (depression) ≥ 24 MSPSS ≤ 3 PHQ-9 ≥ 10 |
None; not applicable | Fidelity, feasibility, acceptability of the intervention. Number of eligible patients referred to counselling = 29/30 Number of assessments made by counsellor after referral = 29/29 Number of patients referred to psychiatric care due to severity of symptoms = 6/29 Number of people with low PHQ-9 scores (PHQ-9 ≤ 10) not eligible for counselling = 11/29 Number of patients that received information leaflet = 115/135 Number of patients that received one information and education session = 80/135 Number of patients that completed counselling sessions = 9/18d |
Number of patients with positive anxiety and depression scores at baseline (HSCL and MSPSS) = 30/135 Number of patients with severe depression score at baseline (PHQ-9 ≥ 19) = 6/29 |
Appendix 3 Other barriers and facilitators across interventions
Other barriers across interventions
Complexity is part of the intervention characteristics construct. This was a barrier for psychological and combined interventions, but it had a mixed impact in interventions combined with socioeconomic support and screening-only interventions. In psychological and combined interventions, the participants’ perspective was that the initial screening component of the intervention was complicated to implement due to the additional time and paperwork required, or the number of steps required to implement some components of the intervention. 34 In one intervention, the feedback from healthcare workers made the implementing team change the original screening tool for one more acceptable to TB healthcare workers and their practices. TB healthcare workers also found it challenging to deliver the psychological treatment component of the intervention. 25 In interventions where complexity had a mixed impact, the studies report that participants expressed positive and negative opinions regarding the implementation of the intervention. In the screening-only intervention there was some flexibility to allow healthcare workers to implement the intervention as they saw fit but they still considered that the intervention was hard to implement, even though the technological elements of the intervention facilitated their paperwork activities. 32 In some interventions, the processes of delivering the intervention components had been designed with the input of the healthcare workers, and were adapted during implementation according to their feedback. 32,34
Culture, part of the inner setting, was referred to as a barrier when organisational or patient culture clashed with the goals of the intervention. Culture as a barrier is best exemplified in the quote by Lovero et al. ,33 where they compare the goals of the intervention with the goals of patients and the organisation (i.e. public TB services):
The goals of the intervention did not align with wider organizational goals, as these often conflicted with each other, causing the clinic staff to feel stressed by the competing directives and interests … most DPMs [district programme managers] highlighted a need for increased mental health literacy and awareness among district-level administrators to better facilitate mental healthcare integration.
In the screening-only intervention, the cultural attitude towards mental health was reflected in patients’ and healthcare workers’ discomfort when asking diagnostic questions regarding patients’ mental health. 32 This challenge was echoed in the implementation of two psychological interventions, which affected the screening and treatment components of the intervention. 25,34 Culture was a barrier for all types of interventions, except for combined interventions with socioeconomic support, where there were no data available.
Other facilitators across interventions
Evidence strength and quality was defined as the belief, sustained by evidence, that the intervention would have the desired outcome. This was a facilitator in psychological, combined and combined with socioeconomic support interventions. In studies that described these types of interventions, the interventions were justified based on previous empirical research. In studies that reported quantitative outcome assessments, the interventions improved depression symptoms, decreased stigma scores and improved TB knowledge in patients and family members,30,31 which were the interventions’ desired outcomes. In qualitative studies, patients and participants expressed their belief in the beneficial impact of the intervention, particularly in interventions where current and cured patients interacted. 25,34
Cosmopolitanism, part of the outer setting, seemed to be a facilitator for all types of interventions, except for the screening-only intervention where there were no data to assess this. Cosmopolitanism, defined as the linkages between TB services and other public or private services, was an obvious facilitator in interventions that were implemented as part of collaborations between public TB services and private NGOs. 26–29 In three combined interventions, NGOs were the main point of delivery of TB services, which acted as the main point of delivery of the intervention for depression. 26–28 The role of NGOs as the main community healthcare service delivery and their role as facilitators of the implementation for the depression intervention were more prominent in the studies that described interventions implemented in Peru. 25,26,28
External policy and incentives, part of the outer setting, seemed to be facilitators for all types of interventions, except for the screening-only intervention for which there were no data to assess this. We considered the influence of local, national and international policies. In the implementation of psychological interventions, the existence of policies that supported the provision of mental health care to people with TB, or supported patient-centred care, acted as a facilitator for implementation. For example, the description of one psychological intervention mentioned that the provision of mental health care to people with TB was ‘… a strategy that is well aligned with and supported by the people-centred model of care advocated by the WHO’ (Khachadourian et al. ). 30 In one combined intervention, the implementation of training, diagnosis, treatment and referral components was enshrined in a national mental health policy which supported the integration of mental health services into primary care services.
One of the main objectives of the Strategic Plan is to scale up decentralized integrated primary mental health services, with the goal of including universal, routine screening and a stepped approach to management of mental disorders in primary care clinics.
Lovero et al. 33
In another combined intervention, implemented as part of NGO-provided TB services, the availability of external policies and incentives supported implementation and facilitated the delivery of screening and treatment.
Patients were also eligible for services provided by the municipality such as quarterly food baskets for patients with TB … In Lima, Peru, all these interventions are available and supported by local or national policy. Thus, it is feasible to implement a comprehensive approach to managing the health issues …
Contreras et al. 26
National and international policies acted as facilitators for implementation. International policies and guidelines, like those of the WHO, acted as facilitators at the local level.
Access to knowledge and information, part of the inner setting, acted as a facilitator for all types of interventions, except for combined interventions with socioeconomic support, where there were no data available to assess this. In all studies that described psychological, combined or screening-only information, the access to knowledge and information (e.g. training, provision of educational materials) for healthcare workers was a facilitator for implementation. This was particularly relevant for the implementation of the interventions’ screening components, as it was reported that some interventions provided training to healthcare workers to use mental health screening tools in their day-to-day practice in TB services. Only one study described the number of training sessions, along with the content of the training. 34 One combined intervention recognised the importance of providing training to healthcare workers but also acknowledged that training was provided unevenly and it was hard to assess its impact as there were no indicators to measure its effect. 33 In the screening-only intervention, it was stated that healthcare workers valued the mental health training they received to implement the intervention. ‘[Healthcare workers] believed the training made them more aware of the importance of caring for people’s mental health … and offered them necessary skills to help their patients’ (Diez-Canseco et al.). 32
Individual stage of change, part of the characteristics of individuals domain, seemed to be a facilitator for all types of interventions, except for combined interventions with socioeconomic support, where there were no data to assess this. This construct refers to the stages that healthcare workers go through towards the sustained and skilled delivery of the intervention, in terms of the change in their confidence and knowledge to implement the intervention. In one psychological intervention, the progression of healthcare workers in their mental health treatment skills was considered a facilitator. ‘Primary healthcare workers showed willingness to learn to deliver the intervention either as co-facilitators alongside a mental health specialist or in the absence of one’ (Acha et al. ). 25 In combined interventions, healthcare workers felt more comfortable providing screening and treatment components of the intervention after receiving training in mental health. ‘though the majority [of healthcare workers] … responded they felt “very comfortable” or “comfortable” with the management of mental illness in patients’ (Lovero et al. ). 33 A similar opinion was echoed in the screening-only intervention, in which healthcare workers felt more confident in their mental health screening abilities and decisions after receiving training (Diez-Canseco et al.). 32
The influence of external change agents as facilitators of implementation was present in all interventions, except for the screening-only intervention where there were no data available to assess this. External change agents were defined as individuals affiliated to other organisations that are not governmental or public TB services. The role of external change agents as a facilitator was more evident in the studies describing interventions implemented in partnership with NGOs, as these had collaborations with local public health authorities. For example, in one combined intervention with socioeconomic support that was implemented in the context of a pre-existing collaboration between NGOs and governmental health services, external change agents influenced the recruitment of participants for the intervention and its delivery, including the delivery of psychological treatment components and training for healthcare workers. 26 This was also the case in two combined interventions (without socioeconomic support) where the role of external change agents was also to provide training to healthcare workers and provide psychological and pharmacological treatment to participants in the intervention. 27,28,31 In interventions that were implemented solely by governmental services, the influence of external change agents in the implementation of the intervention was less clear or not mentioned at all. 30,32,33
Discrepancies in barriers and facilitators across intervention types
The construct, needs of those served by the organisation (i.e. people with TB needs), part of the outer setting domain, was a facilitator in psychological, combined and combined interventions with socioeconomic support. However, it was a barrier in the screening-only intervention. In the studies that described interventions where this construct was a facilitator, it was mentioned that the interventions were based on the care needs expressed or manifested by people with TB and their families. In one psychological intervention where depression treatment was delivered in a group setting, the intervention addressed the non-clinical needs of patients, like emotional support and the reduction of stigma. ‘… for many patients the support groups appeared to be one of the only places in which patients could speak freely about their experiences and feelings and receive empathetic support from others’ (Acha et al. ). 25 Two studies mentioned how the delivery of combined interventions was rooted in the mental health needs of people with TB that had been observed in pre-implementation years. 33 Combined interventions with socioeconomic support were underpinned by the economic needs often expressed by people with TB and their families. One study described how socioeconomic support for the person with TB often involved helping them to provide for their families, which the intervention supported by means of covering school fees and transport and food costs or linking them to existing social assistance services. 26 However, in screening-only interventions, this construct was defined as a barrier to the implementation as the patients’ needs were only partially met or not met at all. The study describing this intervention mentioned that, after screening, not all patients were referred to mental health services even if they needed to be and screening was not done consistently for all patients; this was possibly because the depression-screening activities were not included in performance assessments at the time the intervention was implemented. 32
The role of available resources, a construct part of the inner setting domain, was a facilitator for implementation in combined interventions with socioeconomic support. However, this construct was described in the context of barriers to implementation in psychological and combined interventions. Additionally, this construct was one of the few to have a mixed impact, as a barrier and facilitator, in the implementation of screening-only interventions. In combined interventions with socioeconomic support, the role of NGOs was a facilitator to improving the available resources for the implementation of screening, treatment and socioeconomic support components of the intervention. In these interventions, NGOs would provide the socioeconomic support, provide mental health training to TB healthcare workers and offer support to link patients with socioeconomic assistance available in their communities. 26 This finding seems to overlap with the role of costs of intervention and implementation: in the case of combined interventions with socioeconomic support, it was stated that the increased costs were mainly absorbed by the NGOs working locally, as they supplied sufficient human resources, training, socioeconomic support components and other relevant components for the delivery of the intervention. In terms of psychological interventions, one of the studies reported how physical and human resources were constantly hard to obtain during the 5 years that the intervention lasted. 25 For combined interventions, the negative impact of the lack of available resources was echoed and it conflated the reasons behind the lack of human and physical resources as a general lack of funding for mental health and primary care services. ‘Most [district programme managers] cited shortages in personnel and training opportunities, both of which often corresponded with a lack of funding’ (Lovero et al. ). 33
Self-efficacy, part of the characteristics of individuals domain, was a facilitator for the implementation of psychological-only and screening-only interventions, but it was a barrier to implementation for combined interventions. One study describing the implementation of a psychological-only intervention mentioned that the self-efficacy of the healthcare workers delivering the intervention was a facilitator. Healthcare workers were able to implement the intervention by themselves, with initial guidance from psychiatrists. 25 This was described as a progressive process in the study, meaning that the healthcare workers were more confident in implementing the intervention with time. This echoes the findings described in the screening-only intervention study, where the study discussed how healthcare workers were able to overcome challenges during the delivery of the intervention by applying their learning from the training provided to them. ‘Furthermore, some PHCPs reported referring patients who, despite having negative screening results, showed symptoms that they deemed relevant’ (Diez-Canseco et al. ). 32
Appendix 4 Adaptation of CFIR domain definitions for the purposes of this study
| Construct | Subconstruct | Definition of the CFIR subconstructs for the purposes of this review and in line with the CFIR handbooka |
|---|---|---|
| Intervention characteristics | Intervention source | Defined as the perception of healthcare workers or people with TB about whether or not the depression intervention is developed by their own local or national TB services |
| Evidence strength and quality | Defined as the authors’, healthcare workers’ or other participants’ perceptions on the evidence supporting the belief that the depression intervention will have the desired outcomes described in the study | |
| Relative advantage | Defined as the healthcare workers’ and/or people with TB’s perception about the advantage of delivering the depression intervention over the status quo or not delivering the intervention | |
| Adaptability | Defined as the degree to which a depression intervention was or can be adapted to meet local needs | |
| Trialability | Defined as the ability or possibility to test the depression intervention on a small scale in existing TB services. Previous experiences of piloting the depression intervention or one of its components were also considered in this subconstruct | |
| Complexity | Defined as healthcare workers’ and/or people with TB’s perception about the difficulty of implementing or delivering the depression intervention, which could also be reflected in the intricacy and number of steps required to deliver the depression intervention | |
| Design quality and package | Defined as the perceptions of the intervention participants about the presentation and quality of the materials needed for delivering the depression intervention | |
| Cost of intervention and or implementation | Defined as the costs of the depression intervention and costs associated with its implementation, including opportunity costs | |
| Outer setting (defined as the wider health system, NGOs and private healthcare institutions, at national and international level) | Needs of those served by the organisation | Defined as the extent to which the needs of people with TB are identified or met by the depression intervention |
| Cosmopolitanism | Defined as the degree to which TB services are linked with other organisations and their influence on the implementation of the depression intervention | |
| Peer pressure | Defined as the perceived competitive pressure to implement the depression intervention in TB services | |
| External policy and incentives | Defined as the local, regional or national public policies that support the implementation and delivery of depression care in TB services or for people with TB. Also defined as NGOs’ mandates and guidelines that support the implementation and delivery of the intervention | |
| Inner setting (national TB services) | Structural characteristics of an organisation | Defined as the architecture, size and other organisational characteristics of TB services |
| Networks and communications | Defined as the quality of formal and informal social networks and communications within TB services | |
| Culture | Defined as the norms, values and basic assumptions of patients, communities or the healthcare workers employed by TB services or the organisation delivering the depression intervention | |
| Implementation climate: | Defined as the general receptivity to change within TB services and shown by healthcare workers or other participants, and which cannot be coded to any of the subconstructs below | |
| a. Tension for change | Defined as the authors’, healthcare workers’ or other participants’ perceptions about the need for change in the current service provided to people with TB | |
| b. Compatibility | Defined as the authors’, healthcare workers’ or other participants’ perceptions about the compatibility or fit of the depression intervention with their current practices, values and/or systems | |
| c. Relative priority | Defined as the authors’, healthcare workers’ or other participants’ perceptions about the importance of the implementation and delivery of depression care in existing TB services | |
| d. Organisational incentives and rewards | Defined as the incentives and rewards provided by study leads, TB services or other organisations involved in the implementation of the intervention that have a goal to increase or improve the uptake of the depression intervention | |
| e. Goals and feedback | Defined as the communication of goals and feedback to healthcare workers delivering the depression intervention | |
| f. Learning climate | Defined as the presence or absence of a learning climate in TB services. A learning climate is defined as a climate in which leaders express their own fallibility and need for team members’ assistance and input; team members feel that they are essential, valued and knowledgeable partners in the change process; individuals feel psychologically safe to try new methods and there is sufficient time and space for reflective thinking and evaluation (CFIR, 2021)22 | |
| Readiness for implementation: | Defined as the tangible indicators of TB services’ commitment to the implementation of depression interventions in their routine services, and which cannot be coded in the subconstructs below | |
| a. Leadership engagement | Defined as the involvement of TB services or other relevant organisational leaders in the implementation and delivery of the depression intervention | |
| b. Available resources | Defined as the availability of resources (i.e. physical, human, financial) dedicated to the implementation and delivery of the depression intervention | |
| c. Access to knowledge and information | Defined as the provision of knowledge and information to healthcare workers (e.g. training) and people with TB (e.g. educational materials or sessions) about the depression intervention and/or TB | |
| Characteristics of individuals (participants delivering or receiving the intervention) | Knowledge and beliefs about the intervention | Defined as the authors’, healthcare workers’ or other participants’ (i.e. patients) attitudes and beliefs about the depression intervention |
| Self-efficacy | Defined as the healthcare worker’s belief in their capacity to implement and deliver the depression intervention | |
| Individual stage of change | Defined as the individual stages through which healthcare workers move towards the sustained and skilled delivery of the depression intervention | |
| Individual identification with organisation | Defined as healthcare workers’ and people with TB’s perceptions of TB services and their commitment to them. | |
| Other individual characteristics | Defined as healthcare workers’ personality traits, such as tolerance of ambiguity, intellectual ability, motivation, values, competence, capacity and learning style (CFIR, 2021)22 | |
| Process (implementation process) | Planning | Defined as the development of plans and strategies for the implementation and delivery of depression care before its implementation |
| Engaging: | Defined as the strategies and outcomes of activities to engage different individuals in the implementation and use of the depression intervention, and which cannot be coded in the subconstructs below | |
| a. Opinion leaders | Defined as individuals or groups of individuals (e.g. family, community members) that have a formal or informal influence on the attitudes or beliefs of others towards the intervention and its implementation | |
| b. Formally appointed internal implementation leaders | Defined as healthcare workers or individuals from within TB services who have been formally appointed as implementers, co-ordinators, project managers, team leaders or other similar roles | |
| c. Champions | Defined as individuals who help overcome indifference or resistance to the depression intervention within TB services or by other participants | |
| d. External change agents | Defined as individuals affiliated with other organisations outside of TB services that facilitate the implementation of the intervention | |
| e. Key stakeholders | Defined as the healthcare workers within TB services or organisations involved in delivering the intervention | |
| f. Innovation participants | Defined as people with TB, their families and/or caregivers | |
| Executing | Defined as the implementation of the depression intervention according to what was planned (i.e. fidelity) | |
| Reflection and evaluation | Defined as the feedback about the process of implementation and/or the intervention from healthcare workers and people with TB given to study leads or implementation leaders |
Appendix 5 Approaches to delivering depression care as part of routine TB services
| Intervention type | Psychological only | Psychological and pharmacological (combined) | Psychological and pharmacological, with socioeconomic support | Screening only | |
|---|---|---|---|---|---|
| Definition | Defined as any type of group or individual therapy used to treat mental health conditions, such as depression, anxiety or psychosis. Examples of psychological interventions for depression are behavioural therapy (e.g. behavioural activation), interpersonal therapy, cognitive–behavioural therapy (including third-wave cognitive–behavioural therapies, such as behavioural activation), psychodynamic therapies (e.g. group therapy or psychoanalytic therapy) and other types of psychological therapies (e.g. family therapy) | Defined as psychological and pharmacological interventions delivered simultaneously (e.g. combined treatment) | Defined as psychological and pharmacological treatment with provision of socioeconomic support for people with TB | Defined as screening for mental health conditions, followed by referral to mental health services outside TB services, if needed | |
| Studies included in this review that described this type of intervention | Acha et al.25 Khachadourian et al.30 Li et al.31 Walker et al.34 |
Das et al.27 Lovero et al.33 Vega et al.28 |
Contreras et al.26 Kaukab et al.29 |
Diez-Canseco et al.32 | |
| Intervention description | Content | Defined in the included studies as screening for depression, followed by psychological interventions for depression, such as counselling (Khachadourian et al.),25 psychotherapy (Li et al.),31 or behavioural activation (Walker et al.)34 Other: Educational session (Khachadourian et al.);30 daily SMS and phone calls to patients and supporters (Khachadourian et al.);30 peer support and psychoeducational workshops (Li et al.);31 bonding activities, such as excursions and celebrations (Acha et al.)25 |
Screening for depression, followed by psychological and pharmacological treatment for depression when needed Psychological component: individual counselling (Das et al.),27 individual psychotherapy (Vega et al.)28 or unspecified (Lovero et al.)33 Pharmacological component: Antidepressants and anxiolytics in one intervention (Vega et al.);28 unspecified for two interventions (Das et al.; Lovero et al.)27,33 |
Screening for depression, followed by psychological and pharmacological treatment, with socioeconomic support when needed, for all interventions Psychological component: counselling, for all interventions Pharmacological component: unspecified, for all interventions Other: socioeconomic support, for all interventions |
Screening followed by referral to mental health services, if needed. The type of treatment that was received is unspecified |
| Dose, frequency, number of sessions and length | Bi-weekly group sessions (Acha et al.);25 one group session and daily individual reminders (Khachadourian et al.);30 individual bi-weekly, 30-minute sessions, home visits (Li et al.);31 30–45-minute individual or group sessions, with frequency unspecified (Walker et al.)34 | No data for all interventions | Unspecified (Contreras et al.)26 or individual, monthly (Kaukab et al.)29 | Unspecified | |
| Screening tool | Unspecified (Acha et al.),25 CES-D (Khachadourian et al.),30 Zung self-rating depression scale (Li et al.)31 or HCSL, PHQ-9 and PHQ-2 (Walker et al.)34 | PHQ-9 (Das et al.),27 PC101 (Lovero et al.)33 or DSM-IV (Vega et al.)28 | SRQ-18 (Contreras et al.),26 PHQ-9 (Contreras et al.)26 or BDI (Kaukab et al.)29 | Unspecified | |
| Points of screening | At baseline for all interventions. At follow-up of TB appointments (monthly or tri-monthly) for three interventions (Li et al.; Khachadourian et al.; Walker et al.)30,31,34 | At baseline for all interventions and at 3 months for one intervention (Das et al.)27 | At beginning of intervention for one intervention (Kaukab et al.);29 at first visit to TB health centre for one intervention (Contreras et al.)26 and at end of treatment for one intervention (Kaukab et al.)29 | At baseline | |
| Individuals or groups delivering the intervention | Multidisciplinary teams for three interventions (e.g. community health workers, trained therapists, community administrators, psychologists, nurses) (Khachadourian et al.; Li et al.);30,31 community healthcare workers for one intervention (Walker et al.)34 | Multidisciplinary teams, for all interventions (e.g. nurses, mental health primary healthcare workers, psychologists or psychiatrist) | Multidisciplinary team (Contrera et al.)26 or pharmacists (Kaukab et al.)29 | Primary healthcare workers | |
| Setting of intervention delivery | At outside facilities and/or at TB treatment centres for two interventions. At TB treatment centre and at home for one intervention (Khachadourian et al.).30 Not specified for one intervention, at home (Li et al.)31 | At TB treatment centre for all interventions and at participants’ homes for one intervention (Vega et al.)28 | At TB treatment site for all interventions | Screening at TB treatment site. Unspecified for treatment | |
| Training for delivery | Yes, for diagnosis screening and for delivering the intervention, for all interventions | Yes, for screening, in two interventions (Das et al.; Lovero et al.)27,33 | Unspecified for all interventions | Yes, training for screening | |
| Physical resources | Defined as those necessary to deliver the intervention (i.e. facilities) or additional to those routinely used (i.e. training materials, educational materials, equipment) | Subsidies for transport, physical space to deliver the sessions, training sessions, financing group activities outside intervention sessions (Acha et al.).25 Mobile data to communicate with patients (Khachadourian et al.).30 For conducting home visits, training materials (Li et al.).31 Educational materials, training materials, physical space to deliver the sessions (Walker et al.)34 | Antidepressants for one intervention (Vega et al.),28 unspecified for other interventions (Das et al.; Lovero et al.)27,33 | In-kind support (i.e. food vouchers, transport, coverage of other medical fees, healthcare supplies, rent and utilities), for all interventions | Yes, educational vouchers for HCWs, IT equipment, mobile data plan. Yes, educational material used by pharmacists, free antidepressants, food basket, transport, coverage of other medical fees |
| Human resources | Defined as additional human resources needed to deliver the intervention and that are not routinely available in existing TB services (i.e. psychologists, psychiatrists, translators and other personnel not routinely available in existing TB services) | Psychiatrists and/or psychologists for three interventions (Acha et al.; Khachadourian et al.; Li et al.).25,30,31 Mental health nurses for one intervention (Khachadourian et al.).30 Community healthcare workers for one intervention (Walker et al.)34 | None other than routinely used, for all interventions | Additional psychologists, nurses and social workers in one intervention (Contreras et al.),26 unknown for the other intervention (Kaukab et al.)29 | None other than those routinely available |
Appendix 6 List of excluded studies
Eleven articles were excluded because they were based in high-income countries, mostly the USA.
-
Crane GE. Further studies on iproniazid phosphate; isonicotinil-isopropyl-hydrazine phosphate marsilid. J Nerv Ment Dis 1956;124:322–31. https://doi.org/10.1097/00005053-195609000-00014. PMID: 13429360.
-
Jentoft B. Convulsive treatment in 56 tuberculous mental patients. J Ment Sci 1949;95:651–4. https://doi.org/10.1192/bjp.95.400.651
-
Choi YH. An experimental study of the effects of supportive nursing intervention on family support behavior and sick role behavior. Taehan kanho. The Korean Nurse 1985;24:10–20.
-
Dockhorn JM. The influence of social and emotional factors in the treatment of tuberculosis. Am Rev Respir Dis 1960;82:223–31.
-
Grabener J. Psychological care of tuberculotics from the viewpoint of the public health physician. Der Öffentliche Gesundheitsdienst 1963;25:606–12.
-
Kienast HW, Fisher RA, Rodriguez G. Psychiatric treatment of tuberculous patients in a state hospital setting. Dis Nerv Syst 1965;26:284–7.
-
Nagata Y, Urakawa M, Kobayashi N, Kato S. [Analysis on workload for hospital DOTS service]. Kekkaku. 2014;89:495–502. Japanese. PMID: 24908810.
-
Pleasure H. 233 patients with mental illness treated with electroconvulsive therapy in the presence of tuberculosis. Am J Psychiatry 1954;111:177–83.
-
Roncati C. Treatment of tuberculosis in psychiatric hospitals. Rassegna di neuropsichiatria e scienze affini 1952;6:214–8.
-
Silverman M. Electrical convulsive therapy in psychiatric patients with pulmonary tuberculosis. Br J Tuberc Dis Chest 1953;47:172–8.
-
Crouzatier A. Psychoanalysis and psychotherapy of recent pulmonary tuberculosis patients. In Cumulated Index Medicus. National Institutes of Health; 1969.
One study was excluded because it did not include patients with pulmonary TB in its cohort.
-
Forsythe AM, Venter C. Behavioral economics, motivating psycho-education improvements: a mobile technology initiative in South Africa. Front Psychol 2019;10:1560. https://doi.org/10.3389/fpsyg.2019.01560. PMID: 31354576; PMCID: PMC6635590.
Two studies were excluded because they measured the prevalence of depression in TB patients.
-
Aydin IO, Uluşahin A. Depression, anxiety comorbidity, and disability in tuberculosis and chronic obstructive pulmonary disease patients: applicability of GHQ-12. Gen Hosp Psychiatry 2001;23:77–83. https://doi.org/10.1016/s0163-8343(01)00116-5. PMID: 11313075.
-
Ambaw F, Mayston R, Hanlon C, Alem A. Depression among patients with tuberculosis: determinants, course and impact on pathways to care and treatment outcomes in a primary care setting in southern Ethiopia – a study protocol. BMJ Open 2015;5:e007653. https://doi.org/10.1136/bmjopen-2015-007653. PMID: 26155818; PMCID: PMC4499723.
Five studies were excluded because they were discussion papers or reports.
-
Borzenko AS, Zubova EI, Iaitskii IA. [Evaluation of the efficiency of a hospital stage of treatment in delivering antituberculous care to mental patients with active pulmonary tuberculosis]. Problemy tuberkuleza i boleznei legkikh 2007:37–40.
-
Kostnapfel J. Mental hygiene services in tuberculosis hospitals. Tuberkuloza 1964;16:454–6.
-
Mohan Reddy M. An alternative model to combat mental illness: a collaborative approach. Indian J Psychiatry 2019;61:S452.
-
Streltsov VV, Siresina NN, Zolotova NV, Baranova GV, Stolbun IV, Dolgova IV, et al. Psychoemotional changes in patients with pulmonary tuberculosis during therapy using psychological and neuropsychological methods. Problemy tuberkuleza i bolezneǐ legkikh 2009:31–7.
-
WHO. The World Health Report 2001: Mental Health: New Understanding, New Hope. Geneva: WHO; 2001.
Eight studies were excluded because they did not describe interventions to treat depression – they focused on adherence or psychosis.
-
Egwaga S, Mkopi A, Range N, Haag-Arbenz V, Baraka A, Grewal P, et al. Patient-centred tuberculosis treatment delivery under programmatic conditions in Tanzania: a cohort study. BMC Med. 2009;7:80. https://doi.org/10.1186/1741-7015-7-80. PMID: 20025724; PMCID: PMC2801503.
-
Yan-Yan L, Hong-Mei Z, Zhao-Xia Z. Effects of comprehensive nursing intervention on the quality of life and prognosis of patients with smear-positive tuberculosis. Biomed Res 2017;28.
-
Janmeja AK, Das SK, Bhargava R, Chavan BS. Psychotherapy improves compliance with tuberculosis treatment. Respiration 2005;72:375–80.
-
Maas G. Psychotherapy in a tuberculosis sanatorium with special reference to autogenous training. Der Tuberkulosearzt 1957;11:633–9.
-
Poleksic J, Vuckovic S, Bogicevic D, Joanovic T, Lalevic P. 1963. Modern active psychiatric therapy of tuberculous mental patients. Neuropsihijatrija 1963;11:97–101.
-
Streltsov VV, Zolotova NV, Streltsov VV, Zolotova NV. [Psychological Support for the patient with pulmonary tuberculosis: a case report]. Couns Psychology and Psychotherapy 2019;27:102–18. https://doi.org/10.17759/cpp.2019270107
-
Tadesse Y, Yesuf M, Williams V. Evaluating the output of transformational patient-centred nurse training in Ethiopia. Int J Tuberc Lung Dis 2013;17(10; Suppl. 1):9-14. https://doi.org/10.5588/ijtld.13.0386. PMID: 24020595.
-
Pleasure H. Tuberculosis in a State Hospital: A Practical Program with Five-year Follow-up. New York: New York State Department of Mental Hygiene, Central Islip State Hospital; 1948.
Two articles were excluded because it was not possible to establish contact with the authors or national libraries in Brazil and Bolivia to access the full text.
-
Sun S, Zhang L. Effect of drug combined with psychological intervention therapy on mental status of MDR-TB patients. Boletin de Malariologia y Salud Ambiental 2020;60:431–6.
-
Vieira EA, Chevitarese MF. Investigacao diagnostica das caracteristicas psicossocias dos pacientes no hospital de tuberculose. HE Rev 1981;8:227–46.