Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR130576. The contractual start date was in May 2021. The final report began editorial review in November 2022 and was accepted for publication in February 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Kinsey et al. This work was produced by Kinsey et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Kinsey et al.
Chapter 1 Background
Pressure on hospitals and bed capacity
Prior to the COVID-19 pandemic, NHS hospitals were under pressure to maintain or improve their provision of care and ensure the cost-effective delivery of services. Between 2005/6 and 2015/16, there was a steady increase in the number and age of patients admitted to hospitals in England, with the number of combined elective and emergency admissions of 60–65-year-olds increasing by 57%. 1 The Office for National Statistics predicts that in England the proportion of people aged 65 years and over will increase further from 18.2% to 20.7% of the total population between mid-2018 and mid-2028. 2 In addition to the pressures of an ageing population, the COVID-19 pandemic has also had a considerable impact on waiting lists for elective procedures. The number of people waiting for elective treatment in the UK has increased from 4.24 million in March 2020 to 6.84 million in July 2022,3 and the number of patients facing delays in leaving hospital increased by 30% between December 2021 and August 2022, further contributing to increased waiting lists. 4
Compared to younger patients, older adults admitted to hospital for elective procedures face disrupted discharge trajectories out of hospital due to transport difficulties,5 are in poor physical health or living with frailty,6 are socially isolated7 or have living arrangements requiring additional support following discharge. 8 Older adult inpatients are also at increased risk of peri- or postoperative complications (e.g. delirium, falls, hospital-acquired infection, pressure sores and cognitive decline). 9–16 Such complications can impede patient recovery, increase length of stay (LOS) and influence discharge destination. 16
While hospitals are under increased pressure to speed recovery and manage capacity following elective procedures, particularly in the face of overwhelming urgent and emergency admissions, care is needed that this is not detrimental for older patients with more complex needs.
Existing literature
A recent systematic review examining the effectiveness and cost-effectiveness of multicomponent interventions to enhance recovery and/or reduce LOS in older adults undergoing elective surgery found that across 73 studies containing data for 26,365 patients, such interventions were associated with either improved clinical outcomes (e.g. LOS, readmissions, complications, mortality, morbidity, clinical markers of recovery), or performed as well as standard care. 17 These findings confirmed the significant progress made in reducing hospital LOS for older adults after planned surgery in the last 20 years. Improvements in care inevitably now lead to diminishing returns on LOS, with patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs) becoming increasingly valuable measures of service quality and thus improvement. 18,19
Recent research indicates that the transition home following discharge can be challenging and potentially unsafe for older adults, who may rely heavily on informal caregivers, emphasising the importance of examining and understanding patient outcomes and experience following this transition. 20 While there has been a drive to achieve earlier discharge from hospital, the subsequent impact on patient outcomes, such as quality of life, participation in meaningful occupations and engagement with health and social care services, is largely unknown. Given the ongoing crisis in hospital capacity in the UK, there is an urgent need to identify, appraise and synthesise the findings from studies that have considered the influence of multicomponent interventions to enhance recovery on longer-term patient recovery, PROMS and PREMS.
Our previous recent systematic review identified 208 studies evaluating the effectiveness of multi-component interventions aiming to enhance the recovery of older adult inpatients receiving planned surgery. 17 The review highlighted positive findings at the hospital level, but a striking lack of PROMS, PREMS or mid- to long-term outcomes. A narrative review of important markers of recovery following the use of enhanced recovery after surgery (ERAS) protocols further emphasised the need for studies to report such outcomes as part of their intervention evaluations. 21
Scoping searches were performed using MEDLINE in September 2019, looking for recent relevant primary qualitative evidence and systematic reviews regarding experiences of interventions to reduce LOS. 22 No systematic reviews were identified examining the experiences of patients, their carers and staff, across different types of multicomponent intervention aiming to enhance the recovery of older adults following any planned procedure, with existing reviews focusing on a narrow range of procedures, interventions and views. Jones et al. systematically reviewed evidence examining both quantitative and qualitative literature on PROMs and experiences of enhanced recovery but specific to orthopaedic surgery,23 while Sibbern et al. explored qualitative evidence about the views of adults receiving ERAS protocols specifically. 24 The latter review did not focus on older adults and excluded the views of carers, relatives and healthcare professionals. 24 Searches of the PROSPERO database for systematic reviews in February 2020 identified one systematic review examining staff experiences of implementing ERAS interventions. 25 However, this review focused on only one type of intervention and, because of this narrower focus, does not capture primary studies which we know through our scoping would be relevant for inclusion in our proposed review.
In summary, there is a dearth of systematic review evidence to inform decisions about the influence of multicomponent interventions to enhance recovery after surgery on mid- to long-term patient-reported outcomes, and to understand patient experiences of such interventions.
Why is this research important?
There is a strong evidence base supporting the effectiveness of multicomponent interventions in reducing LOS without detriment to hospital-recorded data and short-term outcomes. 17 However, it is increasingly important to look beyond what happens in the hospital. The NHS Long-Term Plan sets out a strategy that combines the desire to reduce time spent in hospital with better community care systems. 26 There is also planned investment to reduce waiting times for elective surgery, meaning that the turnover of patients undergoing such procedures will increase. Simultaneously, interventions such as ERP will become more widely implemented in hospitals, effectively minimising LOS. The utilisation of early community-led discharge pathways is also on the rise. This includes discharge to assess (or D2A) and HomeFirst initiatives, which were not included in our previous review. There will therefore be an increasing volume of older adults discharged back into the community or long-term care facilities a day or two after major surgery. After hospital discharge, older adults may require additional support from their family, carers and/or community services, including nurses, general practitioners (GPs), occupational therapists (OTs) and social workers. It is important to understand whether these demands are increased with enhanced recovery approaches or earlier discharge from hospital, particularly given the expected increase in patients meeting this profile in the coming years.
To understand the impact of multicomponent interventions intended to improve recovery of older adults, it is vital to seek the views of the patients themselves, their family/carers and professionals delivering the interventions, to identify aspects of care which can influence the quality and success of transition from hospital. This is best achieved through a combination of quantitative (e.g. PREMS, PROMS) and qualitative data.
Overall aims and objectives
To establish what is known about the impact of multicomponent interventions to enhance recovery after surgery on mid- to long-term patient outcomes and understand patient experiences of such interventions, we conducted a mixed-methods evidence synthesis which aims to:
-
understand the effect of multicomponent interventions which aim to enhance recovery and/or reduce length of stay on mid- to-long term patient-reported outcomes and health and social care utilisation
-
understand how different aspects of the content and delivery of interventions may influence patient outcomes.
This linked-evidence synthesis addressed the following research questions:
-
What is the impact of multicomponent interventions to enhance recovery and/or reduce LOS for older adults admitted for planned procedures on PROMs and service utilisation?
-
What are the experiences of patients receiving multicomponent interventions to enhance recovery and/or reduce LOS, their family and carers and staff involved with delivering care within these interventions?
-
Which aspects of multicomponent interventions to enhance recovery and/or reduce LOS are associated with better outcomes for older adults admitted to hospital for planned procedures?
Chapter 2 Impact of multicomponent interventions to enhance recovery and/or reduce hospital LOS for older adults admitted for planned procedures on patient-reported outcome measures and service utilisation
This chapter details the methods and findings from the systematic review of quantitative research, intended to answer research question 1: What is the impact of multicomponent interventions to enhance recovery and/or reduce LOS for older adults admitted for planned procedures on patient-reported outcome measures and service utilisation? The methods used to identify, appraise and synthesise evidence followed best-practice guidance. 27
Methods
Identification of evidence
Search strategy
For the systematic review of quantitative studies, the searches for our previous review were re-run with adaptations. 17 Search terms included terms for older people or interventions commonly undergone by older people, combined using the AND Boolean operator with terms for multicomponent interventions or terms that describe reducing length of stay, for example, ‘length’ adjacent to ‘stay’ adjacent to ‘reducing’. The full search strategy for MEDLINE ALL is included in Appendix 1. We adapted the search to include search terms for multicomponent interventions which were not relevant for our previous review, including supported discharge, and home or community rehabilitation. We also applied an adapted version of the study type filter used for our previous review, with an expanded set of search terms for non-randomised trials and controlled before-and-after (CBA) studies. 17 These terms were derived from the Cochrane EPOC study design filter (Paul Miller, EPOC, 23 August 2017, personal communication) and from inspecting the titles and abstracts of non-randomised and BA studies that were identified via supplementary searches for our previous review but which the bibliographic database searches failed to retrieve, thus ensuring that the bibliographic database searches had improved sensitivity. 17 In addition, we added search terms for quality-of-life studies.
The adapted search was developed by SB in conjunction with the review team and stakeholders in MEDLINE (via Ovid) and adapted for use in other databases. The full set of bibliographic databases searched included: MEDLINE ALL, Embase and the Health Management Information Consortium (HMIC) (all via Ovid), CENTRAL (via the Cochrane Library), and Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Allied and Complementary Medicine Database (AMED) (both via EBSCO). Searches were run in May 2021 and updated in April 2022. For the update searches, to improve the efficiency of the searching and screening process we used a Search Summary Table to identify the minimum set of bibliographic databases required to retrieve all included studies identified by the initial set of searches, and limited the search to these databases. 28 Thus, we ran the update searches in MEDLINE (via Ovid) and CENTRAL only.
Search results for both initial and update searches were exported to EndNote 20 (Clarivate Analytics, Philadelphia, PA, USA) and de-duplicated using manual checking and the EndNote de-duplication tool. To expedite the study selection process, the 218 articles included in our previous review and 282 articles we previously excluded due to population, country or language (and thus failing to meet inclusion for this review) were removed from the search results prior to screening.
We checked reference lists of all included studies and carried out forward citation searching of included studies from the initial search using the Science Citation Index (Web of Science, Clarivate Analytics) and Scopus (Elsevier) (DC). No citation searches were carried out on included studies identified by the updated searches. The results of forward citation searches were exported to EndNote 20, and reference-list checking was conducted using Microsoft Excel spreadsheets to document potentially useful studies thus identified.
Inclusion criteria
We sought studies of multicomponent interventions to improve and/or accelerate the recovery of older adults undergoing elective surgical procedures requiring an overnight stay in hospital. Additionally, studies had to assess at least one PROM relating to patient recovery. Specific inclusion/exclusion criteria were as follows.
Population
Studies were included if patients:
-
had a mean or median age of ≥ 60 years, as in our previous review, and based on the cut-off point agreed by the United Nations29
-
were undergoing planned hospital admission for surgical procedures, for example:
-
hip/knee replacement
-
cardiac surgery
-
colorectal surgery
-
-
were admitted to hospital for an overnight stay.
Studies were excluded if patients:
-
were undergoing an unplanned (i.e. non-elective or emergency) admission, as a result of an emergency or acute incident, for example following:
-
hip fracture
-
stroke
-
heart attack
-
acute injury
-
-
were receiving hospital treatment that did not require an overnight stay (e.g. day surgery)
-
had been admitted to psychiatric hospitals
-
had been admitted to hospital for a medical investigation that resulted in an unplanned inpatient stay.
Intervention
The intervention was any multicomponent hospital-based intervention or strategy for patients receiving planned care as an inpatient, which either explicitly aimed to reduce LOS or aimed to improve recovery.
Studies were included if:
-
the intervention had multiple components
-
the intervention aimed to enhance recovery such that patients were able to be discharged from hospital sooner
-
the intervention influenced the hospital stay, even if it was not strictly hospital-led.
Examples of potentially includable interventions were:
-
Enhanced recovery after surgery protocol, as described by the ERAS Society,30 which typically consist of elements delivered prior to, during and immediately after surgery. Depending on the type of surgery, this may include components such as: carbohydrate loading and no mechanical bowel preparation before surgery; goal-directed fluid management, catheter and drain protocols, modified anaesthesia and warming protocol during surgery; early mobilisation and early oral nutrition following surgery.
-
‘Fast-track’ recovery protocols. These usually feature elements seen in ERAS protocols, but are broader in nature as ‘fast track’ can have a variety of meanings.
-
The use of a comprehensive geriatric assessment (CGA) to inform a care pathway. This involves a multi-faceted and comprehensive assessment prior to surgery, and should lead to an adapted surgical pathway which involves measures to account for any identified vulnerability.
-
Prehabilitation programme consisting of a variety of exercises designed to prepare the patient physically and/or mentally for surgery. This might involve strength/fitness programmes or healthy lifestyle choices such as quitting smoking.
-
Early supported discharge interventions aim to put post-discharge measures in place to ease the transition from hospital to home and thus facilitate early discharge. Measures may include an assessment of the home environment and steps to make adaptations to negate mobility issues, home visits, provision of a healthcare contact, or education about how to change wound dressings.
Studies were excluded if:
-
the intervention focus was surgical technique
-
the intervention did not aim to enhance recovery from surgery
-
the intervention was not hospital-led or did not influence the hospital stay (e.g. a community care programme or an intervention based in a nursing home)
-
the intervention had only a single component, that is, it featured the administration of only a single dose or bout of an intervention, or it was delivered at a single time point and modality.
Examples of excludable interventions were:
-
early mobilisation in isolation
-
comprehensive geriatric assessment to identify odds of adverse events, without informing a care plan
-
minimally invasive surgery
-
an enhanced anaesthesia protocol
-
goal-directed fluid monitoring
-
home-based rehabilitation that did not influence duration of hospital stay.
Comparator(s)
The comparator was any type of control group or comparator, for example ‘treatment as usual’, ‘usual hospital care’, ‘pre-pathway implementation’ or ‘usual best clinical practice’.
Outcomes
-
Studies need to include any metric of LOS, and any PROM, PREM or service utilisation measure.
-
Examples of PROMs/PREMs of interest include:
-
patient satisfaction survey
-
patient-reported physical assessments
-
quality of life measure
-
self-reported pain.
-
-
Examples of service utilisation measures include:
-
follow-up appointments
-
use of community services to support recovery/rehabilitation
-
home visits by nursing staff.
-
Other key outcomes that were of interest, but did not influence a study’s eligibility for inclusion, were:
-
readmission rates
-
complications
-
mortality.
Study design
Any of the following comparative study designs were included:
-
randomised controlled trials
-
non-randomised controlled clinical trials
-
controlled before-and-after studies
-
interrupted time series (ITS)
-
uncontrolled before-and-after (UBA) studies.
These study designs were chosen as the typical method of evaluating interventions in hospital settings. Patients are usually allocated to intervention and control groups prospectively, or the impact of interventions is judged by looking at outcomes before and since implementation.
Geographical context
Studies were included from any high-income country as defined by the World Bank list of economies. 31
Date of publication
The search was restricted to studies published since 2000. This date was selected in consultation with stakeholders in order to capture the most relevant types of intervention.
Study selection
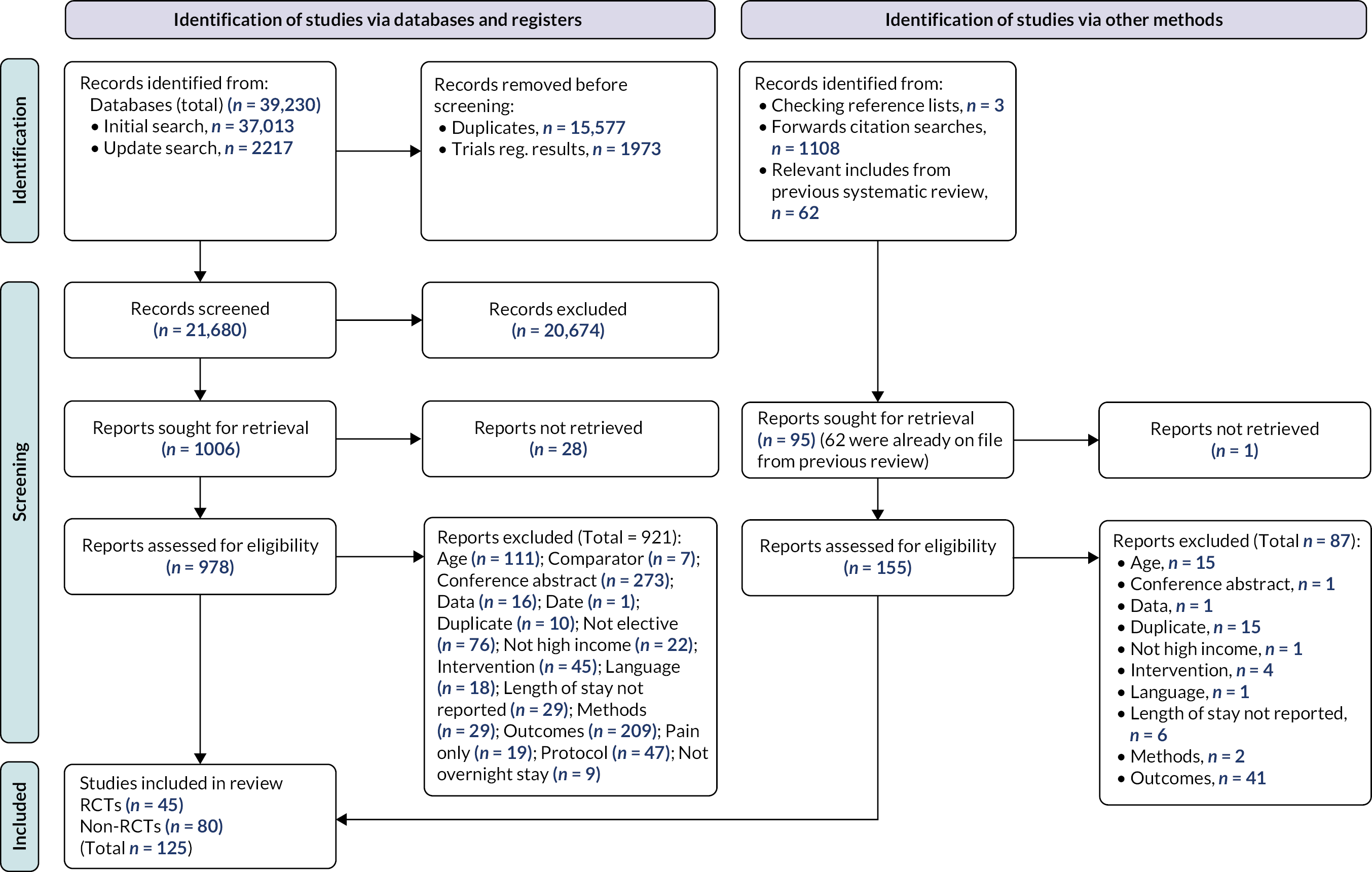
The inclusion and exclusion criteria were piloted on a sample of 100 records identified by the database searches by six reviewers (SF, DKi, DC, MN, LS, SB) independently. Following discussion, the criteria were refined and this process was repeated. After final refinement, the inclusion criteria, as detailed above, were applied to the title and abstract of each identified citation independently by two reviewers (SF, DKi, DC, MN, LS) with disagreements resolved through discussion. The full text of each potentially relevant paper was then obtained and assessed independently for inclusion by two reviewers (SF, DKi, DC, MN, LS) using the same approach. When necessary, the opinion of a third reviewer was sought. EndNote 20 software was used to support study selection. A Preferred Reporting Items for Systematic reviews and Meta Analyses (PRISMA)-style flow chart was produced, detailing the study selection process.
In line with our approach in our previous work,17 upon identifying a potentially unmanageable number of studies, we opted to prioritise randomised controlled trials (RCTs) from any high-income country and UK-based non-RCTs. Studies which did not fall into this category (non-RCTs from high-income countries other than the UK) were subject to minimal data extraction (study details, design and location; sample size, age and reason for admission; intervention type and key features; comparator type; setting; stages of care affected by the intervention, outcomes of interest), tabulated and described separately. The prioritised studies were subject to full data extraction, quality appraisal and synthesis.
Data extraction
Through piloting and refinement, we developed a data-extraction template in Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) to be used for all prioritised studies. Data extraction was performed by one reviewer and checked by another (SF, MN, DC). The following information was extracted from each prioritised study:
-
study details (author, date, title, study design, country)
-
sample details (data collection period, number invited to participate, number commencing study, dropouts and details, data lost to follow-up, adverse events, age, sex, ethnicity, socioeconomic status, sampling method, place admitted to/from, discharge destination, inclusion criteria, reason for admission, coexisting conditions, ongoing treatment)
-
intervention details: name of intervention, category of intervention, aims, full description from paper, components which differed from the comparator condition, who delivered, training provided, who received, setting, target discharge day, discharge criteria, other treatments received during inpatient stay, adaptations made in response to patients’ needs, any modifications made during the study, whether fidelity or adherence were assessed
-
control details: as for intervention details
-
outcomes: for all relevant outcomes, describe the data collection method, construct being assessed, specific scores reported, the rater, whether blinded, any description of psychometric properties
-
outcome data: for all relevant outcomes, at post-intervention and longest follow-up, report the number completing the measure (n), the mean/median, standard deviation (SD)/range/interquartile range/standard error, assessment time. Repeat for intervention and control groups.
Quality appraisal
Quality appraisal was conducted for prioritised studies during the data-extraction phase, by one reviewer and checked by a second (SF, DC, MN). The Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Quantitative Studies was used, which is suitable for randomised and non-randomised studies. 32 We added an additional item, ‘Is it clear how LOS/PROM/PREM is defined/calculated?’, which did not affect the overall rating of the paper. After rating sections A–H a global rating was allocated based on sections A–F (selection bias, study design, confounders, blinding, data collection methods, withdrawals and dropouts) as follows:
-
strong (no weak ratings)
-
moderate (one weak rating)
-
weak (two or more weak ratings).
Quality appraisal was used to inform the interpretation of results, and not to inform inclusion in either the review or aspects of the synthesis.
Synthesis
We planned to perform three stages of synthesis for prioritised studies: first, a mix of meta-analyses and narrative synthesis to summarise the findings of all included effectiveness studies, second, a network meta-analysis and third a qualitative comparative analysis (QCA). As part of the process for assessing the feasibility of network meta-analyses, we considered evidence networks by outcome and type of surgery. All evidence networks included too few studies to generate meaningful comparisons, especially given the risk of imbalance of effect modifiers across sparse networks that could not be addressed through meta-regression. Evidence of the feasibility assessment is provided in Appendix 2, Tables 14 and 15. Therefore, this section describes the conduct of meta-analysis and narrative synthesis. The QCA is described in its entirety (methods, results and interpretation) in Chapter 4.
All studies were initially grouped by procedure and intervention category, as described previously. 17 Categories were informed by discussion with clinical stakeholders (JM, CL, AH). Briefly, interventions fell into the following categories:
-
enhanced recovery protocol – a broad category capturing interventions with components at multiple stages of the pathway
-
Prehab – focused on preparing the patient for surgery
-
Rehab – focused on postoperative exercise for recovery, whether in hospital or at home
-
discharge planning – an intervention focusing specifically on planning and supporting discharge from hospital (usually early discharge)
-
preoperative assessment with care plan (PACP) – an assessment prior to hospital admission, with a subsequent care plan for the patient.
Procedure categories were defined based on surgical specialty, in consultation with clinical stakeholders (JM, CL, AH), as follows: colorectal, lower-limb arthroplasty (LLA), cardiac, pelvic, upper abdominal, abdominal, removal of tumours at various sites. Outcomes were then categorised as follows: LOS, readmissions, complications, mortality, quality of life, mental health, physical function, physical activity, patient satisfaction, pain, fatigue, social function, service utilisation. After categorisation, effectiveness findings were tabulated and summarised.
Data processing
Between-group differences were evaluated at post-intervention and longest follow-up. For dichotomous outcomes (e.g. readmissions, complications) odds ratios (ORs) were calculated in Microsoft Excel using standard equations described in section 9.2.2 of the Cochrane Handbook for Systematic Reviews of Interventions, version 6.3. 27 In addition, the statistical significance of the OR was assessed by calculating a p-value from the z-score for the difference and ascertaining 95% confidence intervals (CIs). 33
For continuous outcomes (e.g. scores on PROMs) Cohen’s d was calculated using the metan command in Stata (version 14.2, StataCorp, College Station, TX, USA). Effect sizes were interpreted in line with Cohen’s guidance (i.e. where d = 0.2 to 0.49, class as ‘small’; where d = 0.5 to 0.79, class as ‘medium’; and where d = 0.8 or above, class as ‘large’). 34 In addition, 95% CIs for the effect were calculated using the metan command in Stata. The p-value for the difference was obtained using the ttesti command in Stata, using data from the two-tailed analysis.
Where mean and standard deviation (SD) for an outcome were not provided, we used standard approaches to impute the required values27 (Cochrane ref section 7.7.3). Our approach to imputation is described elsewhere. 17 We did not impute data where studies only provided median and range for an outcome, due to high risk of skewness in the data.
Where similar procedure, intervention, comparator and outcome categories were present for two or more RCTs, random-effects meta-analysis was conducted. Forest plots were produced as part of the metan command in Stata. Pooled effects with 95% CIs and p-values were reported. Statistical heterogeneity was assessed using the I2-statistic, with greater a percentage indicating a greater proportion of total variance due to between-study variance as opposed to sampling error. 35 Meta-analysis of ORs was performed using log-transformed data.
When multiple measures of LOS or complications were presented within the same outcome category for a study included in the meta-analysis, one measure was chosen as the ‘best representative’. In the case of LOS, this meant the outcome that most closely accounted for the longest portion of the hospital stay, without consideration of readmissions. For example, ‘total LOS’ would be chosen ahead of ‘postoperative LOS’. For complication data, summary or composite outcomes were preferred, rather than incidences of specific complications. When only incidences of individual complications were presented, they were summed and the total number was used in meta-analysis.
Where multiple PROMs were available within the same outcome category, for example multiple mental health measures, we sought to calculate a composite score using standard approaches. 36
Studies that were not eligible for meta-analysis were described narratively. This included a description of the main characteristics and findings of each study.
Results
This section is structured as follows:
-
Description of study selection process and characteristics of included studies.
-
Description of study outcomes and meta-analysis, arranged by procedural category.
Study selection
The PRISMA flow diagram in Figure 1 summarises the study selection process. Database searches identified 37,013 records initially, and a further 2217 through the update search, which reduced to 21,680 following de-duplication. After excluding 20,674 records at the title and abstract screening stage, 978 full texts were reviewed. We excluded 921 papers for reasons listed in Figure 1. The most common reasons for exclusion were being conference abstracts only (n = 273), no relevant outcomes (n = 209) and the mean/median sample age being below 60 (n = 111). Supplementary search methods yielded a further 1111 studies to review at title and abstract, of which 155 were reviewed at full text. The most common reason for exclusion at this stage was outcomes (n = 41). Reasons for exclusion for each paper excluded at full text are provided in Report Supplementary Material 1, Table 1. Following full text screening, 125 papers were included in the review, of which 45 were reports on 42 RCTs, eight were reports on 7 UK-based non-RCTs, and 72 were reports of non-UK-based non-RCTs. The eight papers reporting on seven UK-based non-RCTs and the 45 papers reporting on 42 RCTs were prioritised for full extraction and synthesis. The remaining 72 non-RCTs are described in Report Supplementary Material 2, Tables 1 and 2.
FIGURE 1.
PRISMA diagram – review of quantitative evidence.
Sample characteristics
Table 1 displays information about the prioritised studies, and the patients sampled within. Of the 49 prioritised studies (53 articles), 14 (15 articles) were conducted in the UK,37–51 7 of which were RCTs, 3 were uncontrolled before-and-after UBA trials,41,46,47 2 ITS studies,39,40 1 controlled trial42,43 and 1 CBA study. 48
| Study, country | Study design | Sample size | % female | Mean age (SD) (range) | Place of admission | Comorbidities (intervention vs. comparator) | Inclusion criteria |
|---|---|---|---|---|---|---|---|
| Broad procedural category: abdominal surgery | |||||||
| Kapritsou 2020,81 GRE | RCT | 85 | 62.6% | 62.6 (11.8) (NR) | Oncology hospital | NR | Pancreatoduodenectomy, age 30–82 years, ASA I–III, normal level of consciousness, ability to communicate verbally. Excluded if: chronic pain (long-term use of analgesics), kidney disease, neuropathy, and systemic/chronic treatment with analgesics |
| Takagi 2019,87 JAP | RCT | 80 | 45.9% | 67.3 (9.5) (NR) | Hospital | ASA 1: 8% vs. 16%, 2: 62% vs. 70%, 3: 30% vs. 14%, HTN: 49% vs. 38%, diabetes: 38% vs. 41% | Pancreatoduodenectomy, 20–80 years. Excluded if: unable to obtain consent; severe respiratory dysfunction (arterial PaO2 < 70 mmHg), severe cardiac dysfunction (New York Heart Association 3), severe hepatic dysfunction (Child Pugh classification C), severe renal dysfunction (hemodialysis), pregnancy, preoperative chemotherapy and/or radiation therapy, acute bacterial infection, severe psychiatric disorder, advanced malignancy, palliative surgery, emergency surgery |
| Broad procedural category: cardiac surgery | |||||||
| Arthur 2000,52 CAN | RCT | 249 | 15.0%a | 62.8 (8.15) (NR) | General hospital | Previous myocardial infarction: 52.6% vs. 52.1%, diabetes: 16.4% vs. 25.6%, current smoker: 20.3% vs. 13%, aortocoronary bypasses (mean/median): 2.6/3 vs. 2.6/3 | First CABG, low risk, surgery date > 10 weeks away. Excluded if combined CABG and valve surgery, if ejection fractions < 0.40, if could not attend exercise classes, unable to participate because of physical limitations |
| Bennett 2020,37 | RCT | 182 | 24.0% | N = 38 aged 60 or below; n = 104 aged 61 to 75; n = 40 aged 76 or over | Hospital | Diabetes: 33.3% vs. 66.7%, HTN: 49.6% vs. 50.4%, Neurological history: 50% vs. 50%, Arrhythmias: 50% vs. 50% | Elective and stable-urgent, inpatients undergoing cardiac surgery with cardiopulmonary bypass who were capable and willing to complete the pre-operative neurocognitive tests |
| King 2008,76 USA | RCT | 146 | 47.9% | 73.5 (9.67) (47–79) | Hospital | NR | Short-stay cardiac implant placement over 18 years, suitable for elective resection and no pre-operative radiological or clinical evidence of metastases. Patients with transverse colon cancers or who had had a malignancy within the last five years were included |
| Rief 2017,72 Auer 2017,71 GER | RCT | 83 (SMC and EXPECT) | 12.8% | 66.5 (8.3) (NR) | University hospital | Smoker: 16.2 vs. 14.6%, EuroSCORE II [median (SD)] 1.25 (0.8) vs. 1.53 (0.8); NYHA I: 0% vs. 2.4%, II: 32.4% vs. 22.0%, III: 45.9% vs. 68.3%, IV 8.1% vs. 2.4%, LVEF ≥ 50: 78.4% vs. 48.8%, LVEF 49-30: 10.8% vs. 31.7%, LVEF < 30: 0% vs. 4.9%, Previous myocardial infarction: 16.7% vs. 23.1%, Current mental disorder: 21.6% vs. 9.8% | Elective on pump CABG or CABG combined with valve surgery over 18 years, able to give informed consent, sufficient fluency in German. Excluded if presence of a serious non-cardiac medical condition or psychiatric condition that substantially affected disability |
| Sadlonova 2022,73 GER | RCT | 64 (SMC and IB) | 20.7% | 64.87 (11.22) (NR) | University hospital | Angina pectoris: 27.6% vs. 27.6%, chest pain: 24.1% vs. 27.6%, dyspnoea: 34.5% vs. 69%, syncope: 6.9% vs. 6.9%, NYHA I:13.8% vs. 10.7, II: 48.3% vs. 60.7%, III or IV: 37.9% vs. 28.6%, hypertension: 89.7% vs. 86.2%, Dyslipidaemia: 62.1% vs. 48.3%, Diabetes: 34.5% vs. 37.9%, Smoker: 13.8% vs. 17.2% | Elective CABG surgery, German fluency, able to provide informed consent. Excluded if: previous open-heart surgery, unable to complete self-assessment questionnaires or study procedures, serious comorbid psychiatric condition (i.e., psychotic disorder, substance use disorder other than tobacco use disorder, dementia, severe depressive disorder, recent suicidal ideation), malignant tumour (except curative with treatment or relapse free), inability to use VR glasses or headphones (i.e. blindness or disease of the eye or ears) |
| van der Peijl 2004,64 NED | RCT | 309 | 21.1% | 62.65 (10.2) (NR) | University medical centre | Diabetes mellitus: 19% vs. 19%, COPD 12% vs. 6%, peripheral or CVD: 9% vs. 5%, HTN: 47% vs. 33%, main stem lesion (> 50%): 20% vs. 21% |
Excluded if: concomitant surgical procedures, severe comorbidity interfering with daily life, insufficient Dutch language, mental disorders, PO complications jeopardising standardised exercise programme |
| Broad procedural category: colorectal surgery | |||||||
| Bousquet-Dion 2018,54 CAN | RCT | 80 | 27.0% | Prehab median 74 (67.5–78), Rehab median 71 (54.5–74.5) | Hospital | ASA status 1: 3% vs. 12%, 2: 62% vs. 42%, 3+: 35% vs. 46%, diabetes: 27% vs. 15%, COPD: 5% vs. 15%, CAD: 5% vs. 15%, HTN 62% vs. 42%, PVD: 5% vs. 4%, AF: 11% vs. 4%, tumour stage 0: 11% vs. 15%, 1 and 2: 59% vs. 42%, 3 and 4: 30% vs. 42% | Non-metastatic colon cancer resection, excluded if: presence of metastatic cancer, did not speak English or French or had concurrent medical conditions that contraindicated exercise |
| Carli 2010,56 CAN | RCT | 133 | 42.0% | 60.5 (15.5) (NR) | University health centre | NR | Resection of benign or malignant colorectal lesions, or for colonic reconstruction of non-active inflammatory bowel disease, ≥ 18 years old, receiving pre-op chemo/radiotherapy. Excluded if: health conditions prohibiting participation in exercise programmes/testing procedures |
| Carli 2020,55 CAN | RCT | 110 | 28.2% | 78 (7) (NR) | 2 × hospitals | Prehab: Rehab; DM2: 35% vs. 38%, hypertension: 53% vs. 76%, CVD: 27% vs. 35%, AF: 16% vs. 9%, OSA: 9% vs. 9%, COPD: 15% vs. 5%, arthritis/connective tissue disease: 27% vs. 43%, Dyslipidaemia: 49% vs. 48%, hypothyroidism: 22% vs. 20%, Asthma: 13% vs. 2%, Frailty scores (2, 3, 4, 5): score 2: 45% vs. 31%, score 3: 29% vs. 40%, score 4: 13% vs. 18%, score 5: 13% vs. 11% | Surgical treatment of non-metastatic colorectal cancer, > 65 years, scheduled for surgical treatment of non-metastatic colorectal cancer. Excluded if: Fried Frailty Index of 1, did not speak English or French, presence of metastatic cancer or premorbid conditions (i.e. cardiorespiratory, musculoskeletal, and/or neurological) that contraindicated exercise and fitness assessments |
| Dronkers 2010,67 NED | RCT | 42 | 25.0%b | 70 (6.73) (NR) | General hospital | COPD: 3/21 vs. 3/17, coughing: 2/20 vs. 2/18, diabetes: 8/14 vs. 1/19c | First elective colon surgery for gastric cancer, minimum waiting period of 2 weeks, age 60 years, adequate cognitive functioning (good understanding and accurate execution of instructions). Excluded if: heart disease/orthopaedic conditions which impede exercise, severe systemic illness, recent embolism, thrombophlebitis, uncontrolled diabetes,d wheelchair dependent |
| Forsmo 2016,88 NOR | RCT | 324 | 46.3% | Median: 65.5 (NR) (19–93) | University hospital | NR | Elective open or laparoscopic colorectal surgery, (including patients with rectal cancer previously treated with pelvic radiation) for malignant or benign disease, older than 18 years. Excluded if: multivisceral resection planned/ASA grade IV, pregnant, emergency operations, difficulty providing informed consent due to impaired mental capacity, inability to adapt to ERAS criteria. Randomised patients excluded if intended colonic or rectal surgery not performed |
| Frontera 2014,82 ITA | RCT | 74 | 30.0% | 72 (NR) (40–95) | Rural hospital | ASA I: 26.3% vs. 30.6%, II: 65.8% vs. 52,8%, III: 7.9% vs. 16.7% | Elective surgical colon-rectal resection for benign or malignant disease, over 18 years. Excluded if: unable to consent, ASA IV, patients with serious cardiovascular dysfunction (NYHA class > 3), respiratory dysfunction (arterial pO2 value < 70 mmHg) or hepatic dysfunction (Child C), extensive metastases, other pathologies requiring relevant surgery treatment, neoplasm of the lower rectum |
| Gillis 2014,59 CAN | RCT | 89 | 37.7% | 65.9 (11.3) (NR) | University-affiliated tertiary centre | Ischaemic heart disease: n = 3 (7.5%) vs. 2 (5%), HTN: n = 8 (21%) vs. 12 (31%), Diabetes: n = 3 (7.5%) vs. 5 (13%) | Curative resection of non-metastatic colorectal cancer, excluded if: did not speak English/French, premorbid conditions that contraindicated exercise |
| Khoo 2007,45 UK | RCT | 81 | 61.0% | Median: intervention: 69.3, comparator: 73.0 (overall range = 46.3–87.7) | Hospital | NR | Colorectal resection for cancer, no upper age limit. Excluded if: unable to mobilise independently over 100 m at pre-op assessment, contraindications to thoracic epidurals, pre-existing clinical depression, palliative care only, undergoing joint operation involving another surgical specialty |
| Lee 2011,85 KOR | RCT | 100 | 44.0% | 61.2 (7.62) (NR) | University hospital | NR | Laparoscopic resection for colonic tumour, suitable for laparoscopic colonic resection, between 20 and 80 years old. Excluded if: synchronous distant metastasis, intestinal obstruction/perforation, previous MAS, severe pulmonary disease/cardiovascular disease |
| Lee 2013,84 KOR | RCT | 98 | 34.7% | 61.4 (10.8) (NR) | Hospital | NR | Laparoscopic resection for colonic tumour, suitable for laparoscopic colonic resection, between 20 and 80 years old. Excluded if: synchronous distant metastasis, intestinal, obstruction/perforation, previous MAS, severe pulmonary disease/cardiovascular |
| Pappalardo 2016,83 ITA | RCT | 50 | 48.0% | 66.65 (NR) (45–83) | NR | Pulmonary: 48% vs. 56%, cardiovascular/hypertension: 64% vs. 60%, diabetes: 24% vs. 20% | Open extra-peritoneal rectal cancer surgery, without a primary derivative stoma (DS) with or without a secondary DS, extra-peritoneal tumour location,e cT2–T4 tumours, with or without positive lymph nodes, use of modified FTP, neoadjuvant therapy where indicated (T3–T4 or N+). Excluded if: tumours located over 12 cm above the anal verge, cT1 or M1, urgent procedures; patients ASA > 3, operated on with abdominoperineal resection or Hartmann’s procedure, refusing neoadjuvant therapy, refusing or unable to follow FTP, coagulation disorders contraindicating epidural catheter insertion |
| Vlug 2011,65 2011 NED | RCT | 427 | 41.5% | 66.5 (8.68) (NR) | Three university hospitals and 6 general hospitals | % with comorbidities per group: Lap+FT = 71%; Open+FT = 59%; Lap+standard = 68%; Open+standard = 68% | Elective segmental colectomy for histologically confirmed adenocarcinoma or adenoma, and without evidence of metastatic disease, between 40 and 80 years of age, had an American Society of Anesthesiologists (ASA) grade of I, II or III. Excluded if: previous midline laparotomy, unavailability of a laparoscopic surgeon, emergency surgery, or a planned stoma |
| Broad procedural category: lower-limb arthroplasty | |||||||
| Beaupre 2004,53 CAN | RCT | 131 | 55.0% | 67 (6.5) (NR) | University hospital | % with no morbid condition: 70% vs. 55% | TKA, between 40 and 75 years with diagnosis of non-inflammatory arthritis, were able to understand and comprehend verbal and written English or have a translator |
| Borgwardt 2009,66 DEN | RCT | 50 | 55.0%f | 65.6 (NR) (44–86) | University hospital | NR | UKR, resident in the county of Copenhagen, ASA I or II, no medical history of GI bleeding, someone to look after following discharge. Excluded if: major psychiatric disease, incapable of managing own affairs, inflammatory joint disease, neurological/other disease(s) affecting lower limbs, previous major surgery of the knee |
| Cavill 2016,79 AUS | RCT | 64 | 52.0% | 66.15 (9.5) (NR) | Hospital | NR | Hip or knee arthroplasty, Risk Assessment and Prediction Tool (RAPT) score ≥ 6. Excluded if: lived outside the catchment areas; having surgery < 4 weeks from surgical review; unable to follow commands; having revision surgery; unable to mobilise without a wheelchair; corticosteroid injection within last 6 months |
| den Hertog 2012,75 GER | RCT | 160 | 70.8% | 67.41 (8.11) (40–85) | Non-academic hospital specializing in orthopaedic surgery | Diagnoses (n): degenerative arthritis: 72 vs. 72, posttraumatic arthritis: 0 vs. 1, Ahlback’s disease: 2 vs. 0, arthritis in knee without surgical procedure: 38 vs. 34, secondary disorders/concomitant diseases (n): cardiac: 50 vs. 39 gastrointestinal: 16 vs. 14, allergies: 4 vs. 5, kidney/urinary tract: 2 vs. 4 | TKA, male and female (age range 40–85 years). Excluded if: missing informed consent, lack of cooperation capability, ASA score > 3, RA, cancer, substance abuse, previous major surgery on affected joint, neurological or psychiatric disease, pregnant, participation in other clinical studies |
| Fransen 2018,60 NED | RCT | 49 | 59.0% | 62.5 (8) (NR) | Teaching hospital | NR | TKA, ASA status I or II and were willing and able with the rehabilitation programme. Excluded if: other lower-limb problems, insulin-dependent diabetes, severe osteoporosis, rheumatoid arthritis, or a different inflammatory cause for osteoarthritis |
| Garriga 2019,40 UK | ITS | 486,579 | 57.0% | 70 (9) (NR) | Hospitals | NR | TKA, between 1 April 2008, and 31 December 2016. Excluded if: without a concordant date of surgery between the UK National Joint Registry (NJR) and Hospital Episode Statistics (HES) databases. Further exclusions were made specific to the outcome being analysed. Excluded patients with a hospital stay beyond 15 days |
| Garriga 2019,39 UK | ITS | 438,921 | 60.0% | 69 (11) (NR) | Hospitals | NR | THA, between 1 April 2008, and 31 December 2016. Excluded if: without a concordant date of surgery between the UK National Joint Registry (NJR) and Hospital Episode Statistics (HES) databases. Further exclusions were made specific to the outcome being analysed. Excluded patients with a hospital stay beyond 15 days |
| Higgins 2020,41 UK | UBA | 1256 | 58.0% | 68.8 (9.8) (NR) | University teaching hospital | Adjusted Charlson Comorbidity Index, class 0: 115 (33.6) vs. 277 (35.4), class 1: 131 (38.3) vs. 293 (37.4), class 2: 50 (14.6) vs. 141 (18.0), class 3: 29 (8.5) vs. 54 (6.8), class 4+: 17 (5) vs. 19 (2.4); ASA classification, class 0 8 (1.7) vs. 0 (0), class 1: 24 (5.1) vs. 31 (4.0), class 2: 352 (75) vs. 592 (76), class 3: 17.2 (7.8) vs. 18.4 (7.7) | TKA, The Pre-PES cohort was made up of TKA patients from 1 April 2014 to 31 March 2015. All data were assessed retrospectively from within the institutional databases. The PES cohort included all patients planned for TKA surgery from 1 April 2015 to 1 December 2015 with each patient being invited to participate in the study and providing informed consent. All patients experiencing PES were assessed prospectively |
| Hoogeboom 2010,63 NED | RCT | 21 | 67.0% | 76 (4.1) (69–90) | Hospital | Mean n = 1.5 and 1 in Experimental and Comparator groups, range 0–4 | Primary THA, 70+ years, OA of the hip, minimum waiting time of 3 weeks, score of ≥ 2 on Clinical Frailty Scale. Excluded if: unable to communicate, severe heart disease |
| Hunt 2009,42 2009, Salmon 2013,43 UK | CT | 579; 599 | 54.3%; 58.4% | 67.4 (NR) (23–93);g 67.8 (10.5) (NR) | One of three sites: General Hospital. South-West London Elective Orthopaedic Centre (SWLEOC), University Hospital | Comorbidities (%) in Intervention vs. Comparator 1 vs. Comparator 2: hypertension: 47 vs. 45 vs. 51, CAD: 14 vs. 12 vs. 5, COPD: 16 vs. 12 vs. 20, diabetes: 9 vs. 10 vs. 13, thyroid disorders: 10 vs. 4 vs. 3, CVD: 7 vs. 3 vs. 2, GI disease: 14 vs. 14 vs. 10, psychiatric disorders: 6 vs. 3 vs. 7 | Unilateral primary hip arthroplasty |
| Larsen 2008,69 Larsen 2008 (Thesis),68 DEN | RCT | 90 | 50.6% | 65 (10) (NR) | Regional hospital | NR | Primary THA, TKA or UKA. Excluded if: mental disability or (2) severe neurological disease |
| Maempel 2015,47 UK | UBA | 165 | 52.1% | 69.9 (9.7) (NR) | Hospital | NR | Prosthetic total knee replacement. Excluded if: unicompartmental knee replacements, patellofemoral replacements and revision TKRs |
| Maempel 2016,46 UK | UBA | 1161 | 60.9% | Median age: 65 (NR) (IQR 25–94) | General hospital | NR | Primary THA. Excluded if: patients undergoing THA between April and December 2010, simultaneous bilateral THA, transferred from a medical ward for planned semi urgent THA and returned to the medical ward PO, sustained a per prosthetic femoral fracture, requiring further surgery and prolonged rehabilitation |
| McDonald 2012,48 UK | CBA | 1816 | 68.9% | 69.4 (11.8) (NR) | Hospital | NR | UKA. Excluded if: revision knee surgery, unicompartmental knee replacement, bilateral knee replacement or patients requiring general anaesthesia, planned postoperative epidural analgesia or peripheral nerve blockade |
| McDonnall 2019,89 UK | RCT | 241 | 55.1% | 66.5 (9.2) (NR) | Private (not-for-profit) teaching hospital | NR | TKR, aged > 18 years, elective admission for primary, unilateral, TKR surgery. Excluded if: cognitively impaired or difficulties with informed consent or ability to complete questionnaires |
| McGregor 2004,49 UK | RCT | 39 | 71.4% | 71.9 (9.3) (51–92)h | Hospital | NR | THA. Excluded if: revision or bilateral arthroplasty, previous hip arthroplasty, coexisting morbidity, e.g. history of severe cardiovascular, respiratory, neuromuscular disease, RA, mentally confused, inadequate comprehension of English |
| Pour 2007,78 USA | RCT | 100 | 46.9%i | 60.8 (8.9) (NR)j |
University hospital | NR | Unilateral THA, 18–75 years, any gender/race, underlying diagnosis of OA, consent to participate in the study. Excluded if: BMI > 30 kg/m2, cognitive impairment/severe psychiatric illness precluding participation in the protocol procedures |
| Reilly 2005,50 UK | RCT | 41 | 41.5% | 63 (NR) | Nuffield Orthopaedic Centre | NR | UKA, diagnosed with anteromedial OA,k good understanding of procedure, tolerance of large doses of NSAIDs, suitable home situation within 25 mile radius, upper age limit of 75 years. Excluded if: diagnosis of diabetes/severe respiratory disease/DVT, previous heart surgery, diagnosed with tri-compartmental arthritis at Pre Admission Clinic |
| Siggeirsdottir 2005,86 ICE | RCT | 50 | 52.0% | Overall mean: 68 (NR) (28–86) | University hospital or general hospital | Diagnosis: 24 patients had osteoarthrosis: 24 vs. 21, RA: 1 vs. 1, previous fractures: 2 vs. 0, deformity after Perthes disease: 0 vs. 1 | Primary hip replacement, diagnosed with OA of the hip, RA, primary segmental collapse of femoral head, and sequelae after developmental diseases and hip trauma, living in their own home. Excluded if: primary hip fracture, metastastatic tumours, dementia |
| Soeters 2018,77 USA | RCT | 126 | 63.5% | 61 (9) (37–85) | Hospital | NR | TJA, 18–85 years old, ambulate independently half a block or more and perform nonreciprocal stairs with/without an assistive device, planned to be discharged home after surgery |
| Vesterby 2017,70 DEN | RCT | 73 | 46.6% | Medians: Intervention: 63 (NR) (43–80), Comparator: 64 (NR) (45–84) | Urban teaching hospital | NR | Primary fast-track elective THR. Excluded if: distance to hospital > 60 km, previous hip surgery, mental disability, inability to communicate in Danish, no support person, no internet connection |
| Williamson 2007,51 UK | RCT | 181 | 54.0% | 70.7 (8.8) (NR) | General hospital | NR | Knee-replacement surgery, (total, unicondylar, unilateral, bilateral). Excluded if: taking anticoagulants; within 2 months after receiving an intra-articular steroid injection: experiencing back pain associated with referred leg pain; suffering from ipsilateral OA of the hip; psoriasis or other skin disease in the region of knee; RA, received acupuncture or PT within last year |
| Broad procedural category: pelvic surgery | |||||||
| Frees 2018,58 CAN | RCT | 23 | 22.0% | 68.33 (NR) (49–86) | General hospital | ASA I: 10% vs. 0%, 2: 10% vs. 54%, 3: 10% vs. 46% | Radical cystectomy, diagnosis of BC with an indication for RC, able to complete a QoL questionnaire, study subject diary, and subject experience and satisfaction questionnaires. Excluded if: diagnosis of insulin-dependent diabetes mellitus, Parkinson’s disease, and other neurological co-morbidities |
| Broad procedural category: thoracic | |||||||
| Ferriera 2021,57 CAN | RCT | 124 | 46.0% | 67.0 (9.4) (NR) | General hospital | Prehab vs. Rehab – ASA I: 2% vs. 2%, II: 64% vs. 54%, ≥ III: 35% vs. 44%, diabetes: 14% vs. 16%, HTN: 48% vs. 26%, CVD: 10% vs. 16%, COPD: 10% vs. 16%, tumour stage 0: 19% vs. 14%, IA1: 4% vs. 5%, IA2: 19% vs. 23%, IA3: 21% vs. 14%, IB: 6% vs. 14%, IIA: 4% vs. 0%, IIB: 13% vs. vs. 5%, IIIA: 10% vs. 23%, IV: 4% vs. 2%, current smoker: 19% vs. 26% | Non-small cell lung cancer resection. Excluded if: metastatic cancer, did not speak English or French, concurrent medical conditions that contraindicated exercise |
| Broad procedural category: surgery to remove tumours (various locations) | |||||||
| Hempenius 2013,61 Hempenius 2016,62 NED | RCT | 297; 260 | 64.0%; 62.0% | 77.54 (7.21) (NR); 77.4 (7.3) (NR) | University medical centre, medical centre, community hospital | Comorbidities: 2013: ≤ 2: 39.6% vs. 40.4%, > 2: 60.4% vs. 59.6%. 2016: ≤ 40.2% vs. 41.4%, > 2: 59.8% vs. 58.6% | Surgery for solid tumour, over 65 years of age |
| Schmidt 2015,74 GER | RCT | 652 | 31.5% | 71.8 (4.85) (NR) | Two tertiary medical centres | ASA I/II: 67.2% vs. 63.2%, ASA III/IV 32.8% vs. 36.8%, ECOG 0: 99.6% vs. 95.4%. 1: 2.5% vs. 3.7%, 2/3: 0.9% vs. 0.9%, comorbidities (POSSUM) both groups 2 (2–4) (median, IQR) | Surgery for gastro-intestinal, genitourinary, gynaecological, or thoracic cancer age > 65 years, for major onco-surgery, proficient in German language, a Mini Mental Score (MMSE) of ≥ 24 points, able to consent. Excluded if: 2 or > concurrent carcinomas, emergency surgery, life expectancy of > 2 months, as well as current participation in another trial, living in a closed institution due to an official or judicial ruling |
| Broad procedural category: upper abdominal surgery | |||||||
| Dunne 2016,38 UK | RCT | 38 | 31.6% | Median: 62 (NR) (IQR 54–69) | University hospital | Comorbidity (n): cardiovascular: 10 vs. 8, respiratory: 3 vs. 4, diabetes: 2 vs. 2, renal disease: 1 vs. 0, none: 1 vs. 3, primary tumour: node-positive; 12 vs. 10, adjuvant or neoadjuvant treatment: 11 vs. 7, metastatic presentation; synchronous presentation: 8 vs. 10, extrahepatic metastatic disease: 3 vs. 4, > 3 hepatic metastases; 5 vs. 7, metastasis > 5 cm in diameter; 7 vs. 6 | Liver resection, aged > 18 years and able to: give informed consent, partake in cycle-based exercise, and complete the exercise programme before proposed surgery date, metastases deemed surgically treatable with curative intent. Excluded if: known pre-existing chronic liver disease |
| Jones 2013,44 UK | RCT | 104 | 41.0% | 65.5 (NR) (27–84) | Hospital | NR | Open liver resection, all adult patients presenting for procedure eligible. Excluded if: patients entirely laparoscopic operation, needed a second concomitant procedure, inoperable at the time of surgery, unable to consent |
| Kapritsou 2017,80 GRE | RCT | 63 | 39.7% | 60.9 (11.7) (NR) | Oncology hospital | NR | Hepatectomy or pancreatectomy, up to 2 months after cancer diagnosis, ASA classification of I–III, age > 18 years, normal level of consciousness and communication. Excluded if: presence of chronic pain, kidney disease, neuropathy, systemic or chronic treatment with analgesics |
Thirty-five (38 articles) were RCTs conducted in 1 of 12 other high-income countries, the most common of which was Canada (n = 8), studies. 52–59 Five studies were from the Netherlands,60–65 four each from Denmark66–70 and Germany,71–75 three from the USA,76–78 two each from Australia,48,79 Greece,80,81 Italy82,83 and Korea84,85 and one each from Iceland,86 Japan87 and Norway. 88
All the prioritised articles were published in peer-reviewed journals, apart from two which were PhD theses. 68,76 Most articles (83.1%) were published from 2008 onwards, with 28 published since 2014 (52.8%). 37–41,46,47,54,55,57–62,70–74,77,79–83,87–89 Data were collected from 936,859 patients across 49 studies, with a mean number of 19,119 patients per study, ranging from 21 in an RCT63 to 486,579 within an ITS40 utilising database sampling. With the large database studies by Garriga and colleagues removed,39,40 the mean number of patients per study was 242, with a median of 100 and a range of 1795. The proportion of female participants across all studies was 58.3%.
Ten studies had an upper age limit for inclusion: 75 years,50,53,78 80 years,65,84,85,87 85 years,75,77 82 years. Kapritsou and colleagues81 and Dronkers et al. 67 exclusively recruited patients aged ≥ 60 years, whilst patients in four studies:55,61,62,74 had to be > 65 years for inclusion and 70+ years in the study by Hoogeboom and colleagues. 63
Studies explicitly excluded patients who lived with cognitive impairment (n = 5)67,73,74,78,89 had ‘psychiatric illness’ (n = 6),66,69,71–73,75,78 had mental disability (n = 6),45,64,68–70,73,88 had periods of confusion (n = 3),49,80,81 or were unable to consent (n = 7). 38,44,74,78,87–89 In contrast two studies55,63 selected more frail patients.
The reasons for admission, according to our broad procedural categories, were LLA (n = 22)39–41,43,46–51,53,60,63,68–70,75,77–79,86,89,90 colorectal surgery (n = 12),45,54–56,59,65,67,82–85,88 cardiac surgery (n = 6),37,52,64,71–73,76 upper abdominal surgery (n = 3),38,44,80 abdominal surgery (n = 2),81,87 tumour removal (various locations) (n = 2),61,62,74 pelvic surgery (n = 1)58 and thoracic surgery (n = 1). 57
Intervention characteristics
Intervention characteristics are summarised in Table 2. The most common category of intervention was ERP (n = 28 studies),37,39–42,44–48,50,58,60,65,66,69,73,78,80–89 followed by Prehab (n = 16 studies),38,49,51–57,59,63,67,71,72,74,77,79 with Rehab (n = 3 studies),64,70,75 and single studies evaluating discharge planning76 and a preoperative assessment and care plan61,62 populating the remaining intervention categories.
| First author, country | Intervention name in study (category) | Stated aims of intervention | Comparator name in study (category) | Stages of the care pathway at which intervention elements were delivered | Site | Who was involved in delivery? | Relevant outcomes reported (other than LOS) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-admission | Pre-operative | Perioperative | Post-operative | Post discharge | |||||||
| Abdominal surgery ( n = 2) | |||||||||||
| Kapritsou 2020,81 Greece | ERAS (ERP) | Improve recovery in terms of pain intensity, emotional response and stress biomarkers | Control (TAU) | EON EMOB |
Oncological hospital | NR | Complications, pain, emotional response | ||||
| Takagi 2019,87 Japan | ERAS (ERP) | Accelerate postoperative recovery and reduce LOS without increasing morbidity | Standard Care (TAU) | AEI | nMBP; NUT |
FM | nNGT; EON; CATH; NUT; DRA; TP; ANA; EMOB |
TEL | University hospital | NR | Complications, readmissions, QoL |
| Cardiac surgery (n = 6) | |||||||||||
| Arthur 2000,52 Canada | Preoperative intervention (Prehab) | Improve patients’ physical and psychological readiness for surgery, reducing LOS | Usual Care (TAU) | AEI; EX; REF; TEL |
Hospital, phone, patient home | Kinesiologists/exercise specialists nurses, psychologist, family | Complications, mental health, QoL | ||||
| Bennett 2020,37 UK | Cerebral oximetry (ERP) | Improve neurological and LOS outcomes | TAU (TAU) | COX | Tertiary referral cardiac centre | Anaesthetist and intra-operative team | Mental health, satisfaction | ||||
| King 2008,76 USA | Nurse-driven discharge-planning protocol (discharge planning) | Improve organisational efficiency, patient safety and patient satisfaction | TAU (TAU) | DP | DP | Post-procedure unit, hospital | Intervention registered nurses, electrophysiology physicians, mid-level providers, office staff, bedside caregivers and ancillary staff | Readmissions, patient satisfaction | |||
| Rief 2017 / Auer 2017,71,72 Germany | EXPECT (Prehab) | Optimise pre-operative expectations and improve coping with CABG | Standard medical care (TAU) | AEI; PSY |
Home or university department | Psychologists | Readmissions, complications, disability, mental health, physical function, QoL | ||||
| Sadlonova 2022,73 Germany | Multimodal perioperative intervention (ERP) | Improvements in HRQOL, self-efficacy, reductions in IL-6 and IL-8 levels and shorter lengths of ICU and hospital stay | Standard medical care (TAU) | TEL; AEI |
PSY | PSY; MM | PSY; MM | TEL | Hospital, home | Medical doctor, psychologist, other NR | QoL |
| Van der Peijl 2004,64 Netherlands | Exercise therapy (Rehab) | Facilitate recovery after surgery | Low-frequency exercise programme once a day, excluding weekends (TAU) | PT; EX |
Hospital | PT | Physical function | ||||
| Colorectal surgery ( n = 12) | |||||||||||
| Carli 2010,56 Canada | Bike/strengthening prehabilitation (Prehab) | Optimise recovery of functional walking capacity post surgery | Walking/breathing group (TAU) | EX | Patient home | NR | Mental health, physical activity, physical function, complications | ||||
| Carli 2020,55 Canada | Prehabilitation programme (Prehab) | Reduce 30-day postoperative complications in frail patients | Rehabilitation programme (Rehab) | EX | Hospital prehabilitation unit, home | Kinesiologist, nutritionist, psychology-trained nurse | Complications, mental health, physical activity, readmissions | ||||
| Bousquet-Dion 2018,54 Canada | Prehab+ (Prehab) | Improve walking capacity prior to surgery and reduce decline of physical function post-operatively | Rehabilitation (Rehab) | EX | Home and hospital | Kinesiologist, nutritionist psychologist, nursing staff | Complications, readmissions, physical activity | ||||
| Dronkers 2010,67 Netherlands | Preoperative therapeutic programme (Prehab) | Improve physical condition before surgery and improve recovery | Home-based exercise advice (TAU) | AEI; EX | Outpatient department, patient home | NR | Complications, QoL, physical activity, patient satisfaction | ||||
| Forsmo 2016,88 Norway | ERAS (ERP) | Reduce LOS | Standard Care (TAU) | AEI | CHL; PreM | ANE; FM | LAX; ANA; CATH; EON |
Hospital | MDT | Complications, mortality, readmissions, QoL | |
| Frontera 2014,82 Italy | Fast track (ERP) | Reduce LOS | Control (TAU) | nMBP | NGT; SURG; |
PONV; EON; FM; CATH |
Hospital | Clinical team | Pain, satisfaction, complications | ||
| Gillis 2014,59 Canada | Prehab (Prehab) | Reduce LOS | Rehab (Rehab) | AEI; EX; NUT; PT |
Patient home | MDT | QoL, mental health, physical function, pain, physical activity, complications, readmissions | ||||
| Khoo 2007,45 UK | Multimodal perioperative management protocol (ERP) | Reduce LOS, improve independence | Control (TAU) | NUT | ANE; FM; nNGT |
EON; EMOB; ANA; CATH |
Hospital | MDT | Complications, readmissions, satisfaction, service utilisation | ||
| Lee 2011,85 South Korea | Rehab programme (ERP) | Reduce LOS | Conventional care (TAU) | FM | EON; EMOB; LAX; CATH |
Hospital | MDT, family | Complications, pain | |||
| Lee 2013,84 South Korea | Rehab programme (ERP) | Improve recovery in hospital | Conventional care (TAU) | EMOB; EON; LAX; CATH |
Hospital | Ward nurse | Complications, readmissions, QoL, pain, mental health | ||||
| Pappalardo 2016,83 Italy | Fast-track protocol (ERP) | Reduce LOS, morbidity, mortality and improve QoL | Traditional care (TAU) | ANE; AP; TP |
nNGT; ANA | EON; EMOB; | Hospital | MDT | Complications, mortality, QoL | ||
| Vlug 2011,65 Netherlands | Fast-track programme (ERP) | Reduce LOS | SC with laparoscopy or open surgery (TAU) | AIE; EX | CHL; nFAST;PreM | ANA; FM; PONV |
EON; EMOB; FM; NUT; LAX; CATH |
Hospital: multi-site | MDT | Complications, mortality, satisfaction, QoL, readmissions | |
| Lower-limb arthroplasty ( n = 22) | |||||||||||
| Beaupre 2004,53 Canada | Preoperative exercise and education programme (Prehab) | Improve functional recovery, health related quality of life and health service utilisation | Control group (TAU) | AIE; EX; LOG |
EX; LOG |
Hospital, home | PT | Pain, physical function, QoL, mental health, social function | |||
| Borgwardt 2009,66 Denmark | Accelerated recovery programme (ERP) | Reduce LOS with good clinical outcomes | Conventional Care (TAU) | AIE; OT |
ANE | ANA | TEL | Hospital | MDT | Physical function, pain, readmissions, service utilisation, satisfaction, QoL | |
| Cavill 2016,79 Australia | Prehab programme (Prehab) | Investigate the effect of prehabilitation on functional outcomes across the continuum of care | Standard care (TAU) | AIE; EX |
EX | Local community rehab centre, home | PT | Physical function, QoL | |||
| Fransen 2018,60 Netherlands | 2-day knee (2DK) protocol (ERP) | Achieve better daily clinical and functional outcomes in the first week after surgery, and compare outcomes up to 5 years after surgery | Routine protocol (TAU) | ANE; SURG;DRA; CATH; |
EMOB; ANA |
Hospital | NR (ward staff) | Physical function, pain, mental health, physical activity, QoL | |||
| Garriga 2019,39 UK | ERAS (ERP) | Improved patient outcomes: less knee pain and better knee function, fewer surgical complications, fewer revision operations and reduced LOS | Pre-ERAS period (TAU) | x | x | x | Hospitals | NR | Complications, readmissions, physical function | ||
| Garriga 2019,40 UK | ERAS (ERP) | Improved patient outcomes: less knee pain and better knee function, fewer surgical complications, fewer revision operations and reduced LOS | Pre-ERAS period (TAU) | x | x | x | Hospitals | NR | Complications, readmissions, physical function | ||
| den Hertog 2012,75 Germany | Pathway-controlled fast track Rehab (Rehab) | Improve recovery | Standard PO rehabilitation (TAU) | EMOB; MT; PT; SW |
Hospital, rehabilitation centre | NR | QoL, complications | ||||
| Higgins 2020,41 UK | Pathway management system (ERP) | Assess impact on LOS and compare effects on PROMS | Pre-ERP (TAU) | AIE; MM |
AIE; MM |
AIE; MM; TEL |
Hospital | Clinical staff, physiotherapist | Readmissions, complications, physical function, QoL | ||
| Hoogeboom 2010,63 Netherlands | Preoperative therapeutic exercise (Prehab) | Prevent decline of functional health status when waiting for surgery | Usual PrO/PO care (TAU) | EX | Patient home | NR | QoL, pain, physical activity, complications | ||||
| Hunt 2009,42 Salmon 2013,43 UK | Rapid discharge policy (ERP) | Reduce LOS, maintain functional recovery and QoL | Comparator 1: usual care in large regional centre surgical unit. Comparator 2: usual care in treatment centre (TAU) | OT; PT |
ANA; ANE; SURG |
ANA; EMOB; PT; SW |
TEL | Hospital, outpatient clinic | MDT | QoL, physical function, mental health, pain, service utilisation, satisfaction | |
| Larsen 2008,68,69 Denmark | Accelerated perioperative care and Rehab (ERP) | Reduce LOS | Usual care | AEI; EX; GOAL; NUT; OT; SW |
AEI | PONV | EMOB; GOAL; LAX; OT; ANA; EON |
PT | Hospital | MDT, family | QoL, readmissions |
| Maempel 2015,47 UK | ERP (ERP) | Reduce LOS without adversely affecting functional recovery and ROM at 1 year post-op | Pre-ERP (TAU) | AEI; OT | AP | ANA | Hospital | MDT | Complications, readmissions, physical function | ||
| Maempel 2016,46 UK | ERP (ERP) | Improve joint function | Pre-ERP (TAU) | AEI; DP; OT |
AP | ANA; EMOB | Outpatient clinic, hospital | MDT | Readmissions, physical function, mortality | ||
| McDonald 2012,48 UK | ERP (ERP) | Reduce LOS, allow early mobilisation with satisfactory analgesia without increasing post-operative complications or affecting continuing rehabilitation | Pre-ERP period (TAU) | AEI; DP |
PreM | ANE; FM |
ANA; EMOB |
Hospital ward, clinic | Surgeon, PT, ward staff | Complications, mortality, pain, physical function | |
| McDonall, 2019,89 Australia | MyStay (ERP) | Support patient participation in their recovery after total knee-replacement surgery | Usual care (TAU) | MM | MM | Hospital | Nurses, PT | Complications, readmissions, pain, physical function, satisfaction | |||
| McGregor 2004,49 UK | Preoperative hip rehab advice (Prehab) | Aid patient recovery | Standard care (TAU) | AEI | NR | NR | QoL, pain, physical function | ||||
| Pour 2007,78 USA | Enhanced protocol (ERP) | Aid recovery | Group 3: standard incision, standard protocol. Group 4: small incision, standard protocol (TAU) | AEI; PT; OT |
ANA | ANE | ANA; DRA; EMOB; PT | Outpatient clinic, hospital | MDT, family | Complications, mental health, physical function, QoL | |
| Reilly 2005,50 UK | Accelerated recovery protocol (ERP) | Reduce pain to allow for early mobilisation | Standard care (TAU) | ANA; EMOB; EON |
AIE; TEL |
Hospital, patient home | MDT | Complications, pain, physical function | |||
| Siggeirsdottir 2005,86 Iceland | Preoperative education and training programme / rehab and nursing (ERP) | Reduce LOS | Conventional care (TAU) | AEI; EX | TP | EX; PT; OT |
Outpatient clinic, patient home | PT, OT | Complications, physical function, QoL, readmissions | ||
| Soeters 2018,77 USA | Preoperative physical therapy education (Prehab) | Achieve earlier readiness for discharge, shorter LOS, improve physical recovery | Usual care (TAU) | AEI; EX; DP; GOAL |
NR | PT | Pain, physical function | ||||
| Vesterby 2017,70 Denmark | Telemedicine support (Rehab) | Reduce LOS | Fast track (TAU) | PT; TEL | TEL; PT | Outpatient clinic, patient home | PT, support persona | Readmissions, complications, QoL, mental health, physical function | |||
| Williamson 2007,51 UK | Physiotherapy (Prehab) | Improve condition before surgery, improve recovery | Home exercise (TAU) | EX; PT |
NR | PT | Physical function, mental health, pain | ||||
| Pelvic surgery ( n = 1) | |||||||||||
| Frees 2018,58 Canada | ERAS protocol (ERP) | Reduce LOS | Standard care (TAU) | AEI | CHL; | FM; GUM; PONV |
EON | Hospital | Ward staff | Complications, readmissions, pain, QoL, satisfaction, | |
| Thoracic surgery ( n = 1) | |||||||||||
| Ferreira 2021,57 Canada | Prehabilitation programme (Prehab) | Improve post-op recovery | Rehabilitation (Rehab) | AEI; EX; NUT PSY |
Home | Kinesthesiologist, dietician, psychology-trained personnel | Readmissions, physical activity, QoL, mental health | ||||
| Surgery to remove tumours (various locations) ( n = 2) | |||||||||||
| Hempenius 2013,61 2016,62 Netherlands | Liaison Intervention in Frail Elderly (LIFE) study (PACP) | Prevent post-op delirium | Standard care (TAU) | AEI | University medical centre, teaching hospital, community hospital | Geriatric team | Complications, QoL, mortality, readmissions, mental health | ||||
| Schmidt 2015,74 Germany | Information booklet and diary (Prehab) | Develop patient empowerment to improve short- and long-term outcomes after surgery | Control group (TAU) | AEI; LOG |
Hospital | NR | Complications, pain, mental health, QoL, readmissions | ||||
| Upper abdominal surgery ( n = 3) | |||||||||||
| Dunne 2016,38 UK | Prehabilitation exercise programme (Prehab) | Improve fitness to improve recovery | Standard Care (TAU) | AEI | NR | NR | Readmissions, QoL mental health, physical function | ||||
| Jones 2013,44 UK | ERP (ERP) | Reduce morbidity and LOS | Standard care (TAU) | AEI; NUT |
DRA; FM | DRA; CATH; EON; FM; NUT; ANA |
Hospital | MDT | QoL, pain satisfaction, complications, readmissions | ||
| Kapritsou 2017,80 Greece | Fast-track recovery programme (ERP) | Improve care, improved management of stress and pain | Conventional care (TAU) | nNGT | EMOB | Oncology hospital | MDT | Mental health, pain, complications | |||
All 16 Prehab interventions included components delivered prior to admission, as did 15 of 28 ERP interventions. 41,42,44,46–48,58,65,66,68,69,73,78,86–88 The pre-admission period was used as an opportunity to help prepare patients for surgery, and this usually involved assessment, information or education, and an exercise programme. The most comprehensive pre-admission intervention content was delivered by Larsen and colleagues, and involved information, exercise, goal-setting, nutritional intervention and time with an OT and a social worker. 68,69
The pre-operative period following admission to hospital often contained intervention components in ERP approaches. The period used to directly prepare for surgery, elements such as thromboprophylaxis, absence of mechanical bowel preparation, carbohydrate loading and reduced fasting were implemented. The perioperative period was targeted exclusively by ERP interventions, with adaptations to surgical approach, anaesthesia, prevention of nausea and vomiting, catheter and drain protocols and absence of a nasogastric tube being typical intervention components.
The post-operative period, prior to discharge, featured early mobilisation in 17 studies42,43,45–48,50,60,65,68,69,75,78,80,81,83–85,87 and early oral nutrition in 13. 44,45,50,58,65,68,69,81–85,87,88
Post-discharge components were only present in 11 studies. 42,50,66,68–73,76,79,86,87 Telephone contact was employed by six of these,42,43,50,66,70,73,87 and exercise by two. 79,86
Comparators were usually described as ‘usual care’ or a similar term; however, in 12 studies an active comparator was specified: rehabilitation (n = 4 studies),54,55,57,59 home exercise (n = 2),51,67 low-frequency exercise (n = 1)64 and a walking and breathing protocol (n = 1). 56 In the case of six UBA studies, the pre-intervention period was the comparator. 39–41,46–48
Outcomes of interest included those in the domains of quality of life, mental health, physical activity, physical function, physical activity, pain, patient satisfaction, complications, readmissions, mortality and service utilisation.
Quality appraisal
Quality ratings are displayed in Table 3, with the full breakdown of scores for each item provided in Report Supplementary Material 3. There were only six studies,39,52–54,57,77,81 five of which were RCTs, that received an overall global study quality rating of ‘strong’ using the EPHPP tool. 32 Nineteen studies,37,38,40,50,51,58,60–62,66,68–75,80,82,84,85 of which 18 were RCTs, received a ‘moderate’ quality rating, and the remaining 2241–49,56,59,63–65,67,76,78,79,83,87–89 (17 RCTs) were given a weak rating.
| Study (first author, date) | Component rating (1 = strong, 2 = moderate, 3 = weak) | Global rating of paper | ||||||
|---|---|---|---|---|---|---|---|---|
| Selection bias | Study design | Confounders | Blinding of assessors and participants | Data collection methods | Withdrawals and dropouts | Is it clear how LOS and PROMs are defined? (Y/N)a | Strong = no weak ratings, Moderate = 1 weak rating, Weak = 2 + weak ratings | |
| Abdominal surgery | ||||||||
| Kapritsou 202081 | 2 | 1 | 1 | 2 | 2 | 1 | Y | Strong |
| Takagi 201987 | 2 | 1 | 1 | 3 | 3 | 1 | Y | Weak |
| Cardiac surgery | ||||||||
| Arthur 200052,a | 2 | 1 | 1 | 2 | 1 | 1 | Y | Strong |
| Bennett 202037 | 2 | 1 | 3 | 1 | 1 | 2 | Y | Moderate |
| King 200876 | 3 | 1 | 1 | 3 | 2 | 1 | Y | Weak |
| Rief; Auer 201771,72 | 3 | 1 | 1 | 2 | 1 | 1 | Y | Moderate |
| Sadlonova 202273 | 2 | 1 | 3 | 3 | 1 | 2 | Y | Moderate |
| van der Peijl 200464 | 2 | 1 | 3 | 2 | 3 | 3 | N | Weak |
| Colorectal surgery | ||||||||
| Bousquet-Dion 201854 | 2 | 1 | 1 | 2 | 1 | 2 | Y | Strong |
| Carli 201056 | 2 | 3 | 3 | 2 | 3 | 1 | N | Weak |
| Carli 202055 | 2 | 1 | 3 | 2 | 2 | 2 | Y | Moderate |
| Dronkers 201067 | 2 | 1 | 3 | 2 | 3 | 1 | N | Weak |
| Forsmo 201688 | 2 | 3 | 1 | 3 | 1 | 3 | Y | Weak |
| Frontera 201482 | 2 | 1 | 1 | 3 | 1 | 1 | N | Moderate |
| Gillis 201459 | 2 | 1 | 3 | 2 | 3 | 1 | N | Weak |
| Khoo 200745 | 3 | 1 | 3 | 2 | 3 | 1 | N | Weak |
| Lee 201185 | 2 | 1 | 1 | 1 | 3 | 1 | N | Moderate |
| Lee 201384 | 2 | 1 | 1 | 3 | 2 | 1 | Y | Moderate |
| Pappalardo 201683 | 2 | 3 | 1 | 2 | 3 | 3 | Y | Weak |
| Vlug 201165 | 3 | 1 | 1 | 2 | 3 | 1 | Y | Weak |
| Lower-limb arthroplasty | ||||||||
| Beaupre 200453 | 2 | 1 | 1 | 1 | 1 | 2 | Y | Strong |
| Borgwardt 200966 | 2 | 1 | 1 | 2 | 3 | 1 | N | Moderate |
| Cavill 201679 | 3 | 1 | 1 | 3 | 3 | 1 | Y | Weak |
| den Hertog 201275 | 2 | 1 | 1 | 2 | 3 | 1 | Y | Moderate |
| Fransen 201860 | 2 | 1 | 1 | 3 | 2 | 2 | Y | Moderate |
| Garriga 2019 (Hip)39 | 2 | 2 | 1 | 2 | 1 | 2 | Y | Strong |
| Garriga 2019 (Knee)40 | 2 | 2 | 3 | 2 | 2 | 2 | Y | Moderate |
| Higgins 202041 | 2 | 3 | 3 | 3 | 1 | 2 | N | Weak |
| Hoogeboom 201063 | 3 | 1 | 1 | 2 | 3 | 1 | N | Weak |
| Hunt 2009;42 Salmon 2013,43 | 2 | 3 | 1 | 2 | 3 | 1 | Y | Weak |
| Larsen 200868,69 | 2 | 1 | 1 | 2 | 3 | 1 | Y | Moderate |
| Maempel 201547 | 2 | 3 | 1 | 2 | 3 | 1 | N | Weak |
| Maempel 201646 | 2 | 3 | 3 | 2 | 3 | 1 | Y | Weak |
| McDonald 201248 | 3 | 3 | 1 | 3 | 1 | 3 | Y | Weak |
| McDonall 201989 | 2 | 1 | 1 | 3 | 3 | 1 | N | Weak |
| McGregor 200449 | 2 | 3 | 3 | 2 | 3 | 1 | N | Weak |
| Pour 200778 | 2 | 1 | 3 | 2 | 3 | 1 | N | Weak |
| Reilly 200550 | 2 | 1 | 1 | 2 | 3 | 1 | N | Moderate |
| Siggeirsdottir 200586 | 2 | 1 | 3 | 2 | 3 | 1 | N | Weak |
| Soeters 201877 | 2 | 1 | 1 | 2 | 1 | 1 | Y | Strong |
| Vesterby 201770 | 2 | 1 | 3 | 2 | 1 | 1 | N | Moderate |
| Williamson 200751 | 2 | 1 | 1 | 2 | 1 | 3 | N | Moderate |
| Pelvic surgery | ||||||||
| Frees 201858 | 2 | 1 | 1 | 3 | 1 | 2 | Y | Moderate |
| Thoracic surgery | ||||||||
| Ferriera 202157 | 2 | 1 | 1 | 2 | 1 | 2 | Y | Strong |
| Surgery to remove tumours | ||||||||
| Hempenius 2013; Hempenius 201661,62 | 2 | 1 | 1 | 2 | 3 | 1 | N | Moderate |
| Schmidt 201574 | 2 | 1 | 1 | 3 | 1 | 2 | Y | Moderate |
| Upper abdominal surgery | ||||||||
| Dunne 201638 | 2 | 1 | 1 | 2 | 3 | 1 | N | Moderate |
| Jones 201344 | 2 | 1 | 3 | 2 | 3 | 1 | Y | Weak |
| Kapritsou 201780 | 2 | 1 | 1 | 2 | 3 | 1 | Y | Moderate |
The component that had the highest number of ‘weak’ ratings was ‘data collection methods’ (26 studies),38,43–47,49,50,56,59,61–69,75,78–80,83,85–87,89,90 suggesting that in these studies either data collection methods were not shown to be valid, or reliability and validity were not well described. However, 17 studies were graded as ‘strong’37,39,41,48,51–54,57,58,70–74,77,82,88 for this item. While there were only seven studies45,48,63,65,71,72,76,79 with a ‘weak’ rating in the ‘selection bias’ component, no studies were rated as being ‘strong’ for this item, indicating that the selected individuals in most of the studies were ‘somewhat likely’ to be representative of the target population. 37–41,43,44,49–62,64,66–70,73–75,77,78,80–90
Thirty-eight studies were rated as ‘strong’ for study design,37–39,44,45,50–55,57–82,84–87,89 all of which were RCTs. Four RCTs49,56,83,88 received a ‘weak’ rating because they did not describe their randomisation process. All the UBA and CBA studies41,43,46–48,90 prioritised for inclusion were rated as weak for study design. The two ITS studies were rated as moderate. 39,40
The majority of studies were rated as ‘strong’ for the component considering the likelihood of possible confounding of results;38,39,43,47,48,50–54,57,58,60–63,65,66,68,69,71,72,74–77,79–85,87–90 the remaining 16 were rated as ‘weak’. 37,40,41,44–46,49,55,56,59,64,67,70,73,78,86 Most studies were rated as ‘moderate’38–40,43–47,49,50,52,54–57,59,61–72,75,77,78,80,81,83,86,90,91 regarding blinding of assessors and participants, with 13 rated as ‘weak’41,48,58,60,73,74,76,79,82,84,87–89 and only three rated as ‘strong’. 37,53,85 Thirty-two studies, including all the non-RCTs, were given a ‘strong’ rating for their reporting of numbers and reasons for withdrawals and dropouts. 38,42–47,49,50,52,56,59,61–63,65–72,75–82,84–87,89 Twelve studies were rated as ‘moderate’37,39–41,53–55,57,58,60,73,74 and only five rated as ‘weak’. 48,51,64,83,88 Though not contributing to the overall global rating of each paper, more than half of the studies (59.1%) clearly defined their LOS and PROM outcomes.
Synthesis of evidence by procedural group
The 49 studies were categorised by procedural group, with LLA (n = 22 studies39–43,46,48–50,53,60,63,66,68–70,75,77–79,86,89,91) and colorectal surgery (n = 12)45,54–56,59,65,67,82–85,88 the largest. The remaining 15 studies fell into the following categories: abdominal (n = 2),81,87 cardiac (n = 6),37,52,64,71–73,76 pelvic (n = 1),58 thoracic (n = 1),57 tumours at various sites (n = 2),61,62,74 upper abdominal (n = 3). 38,44,80 The sections below summarise the main findings for each group of studies, divided into sections dedicated to LLA studies, colorectal studies, cardiac studies, and all other studies.
Evidence from trials seeking to improve recovery from lower-limb arthroplasty
Effectiveness of ERP interventions at improving clinical outcomes (RCTs only)
Report Supplementary Material 4, Table 6 displays clinical outcome data from the seven RCTs evaluating ERP interventions in older adults undergoing elective LLA. 50,60,66,68,69,78,86,89 After imputation, standardised mean differences between ERP and TAU groups for LOS were available in three studies. 60,68,69,89 A forest plot displaying the results of meta-analysis of these three groups is displayed in Figure 2, showing that ERP interventions were associated with a reduction in LOS when compared with usual care (d = −0.79, 95% CI −1.44 to −0.15; p < 0.001). Although a large effect was estimated, wide CI and statistically significant heterogeneity for this effect (I2 = 87.7%, p < 0.001) reflect inconsistency in the evidence and suggest the true effect could be large or small. Effect sizes could not be calculated in two studies which provided variance data in the form of ranges. 50,66 In both cases, LOS was considerably lower in the ERP group – median 1 versus 6 days in the study by Borgwardt and colleagues,66 and mean 1.5 days versus 4.3 days in the study by Reilly and colleagues. 50
FIGURE 2.
Forest plot showing the results of meta-analysis of the effect of ERP vs. usual treatment on LOS following LLA.
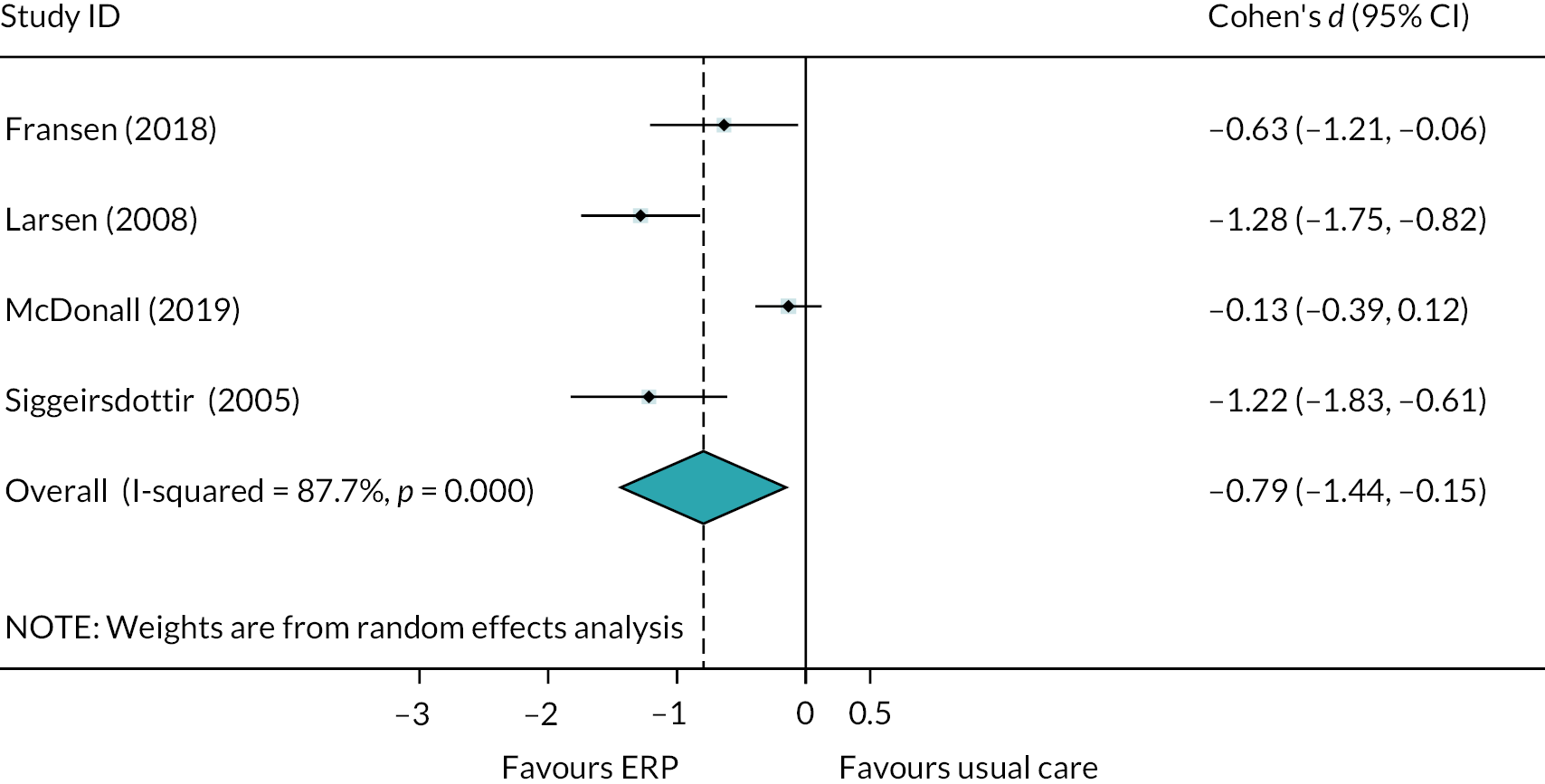
Five studies reported readmission rates for those receiving ERP interventions after LLA. 50,66,68,69,86,89 There were no readmissions in the study by Borgwardt and colleagues66 and only one, in the group receiving usual care, in the study by Siggeirsdottir and colleagues. 86 In the remaining three studies, meta-analysis indicates that the odds of being readmitted to hospital following surgery were similar whether ERP or usual care was received (OR = 1.35, 95% CI 0.40 to 4.56; p > 0.05; Figure 3).
FIGURE 3.
Forest plot showing the results of meta-analysis of the effect of ERP vs. usual treatment on the odds of readmission following LLA.
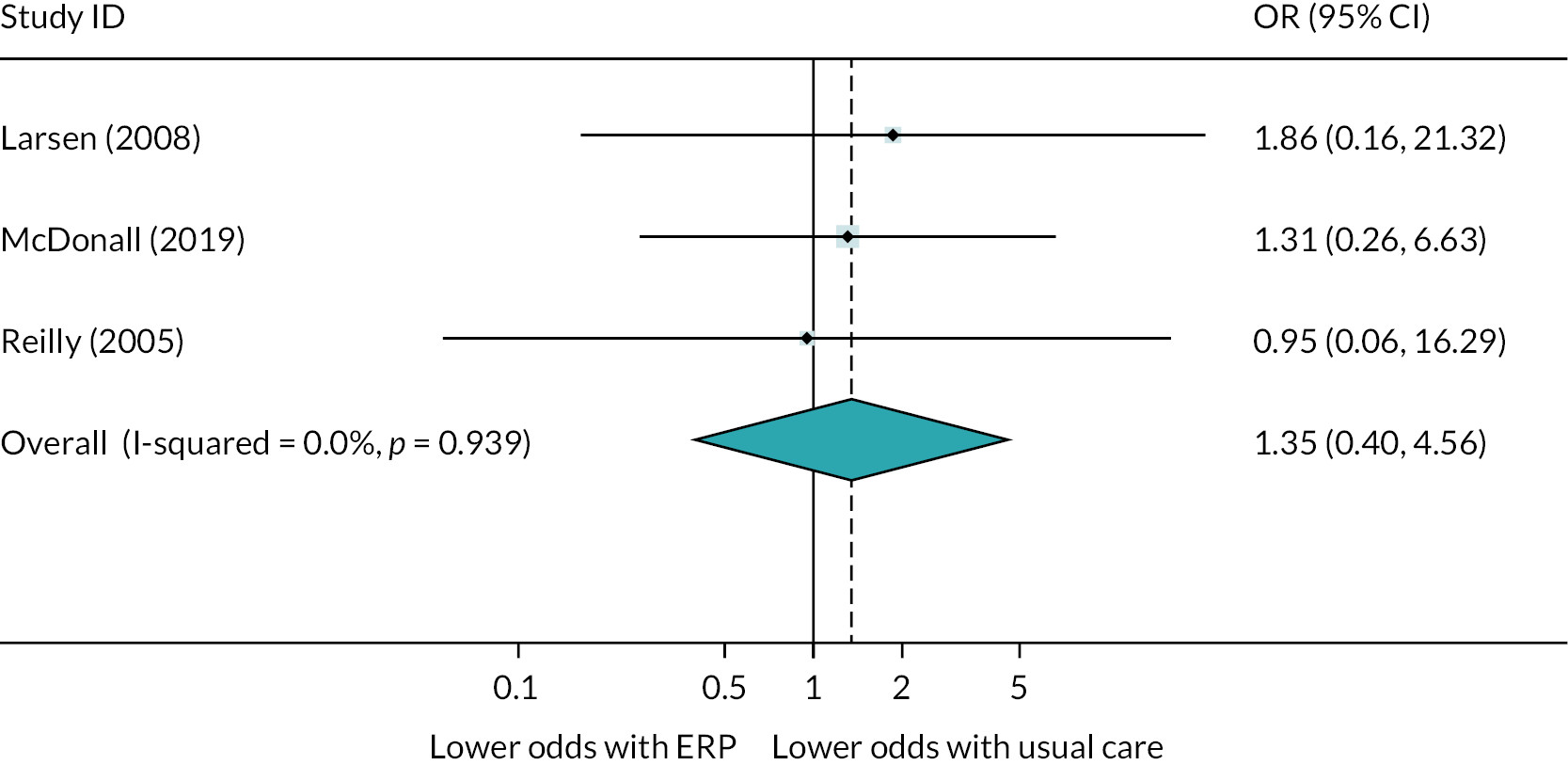
Complications were reported in four studies. 50,78,86,89 Pour and colleagues reported no short-term complications in either group, and when the remaining three studies were pooled, there was no overall difference in the odds of complications between ERP and usual care (OR = 0.90, 95% CI 0.36 to 2.26, p > 0.05; see Figure 4). CIs were notably wide in two studies,50,89 reflecting the low numbers of cases entered into the analysis.
FIGURE 4.
Forest plot showing the results of meta-analysis of the effect of ERP vs. usual treatment on odds of complications following LLA.
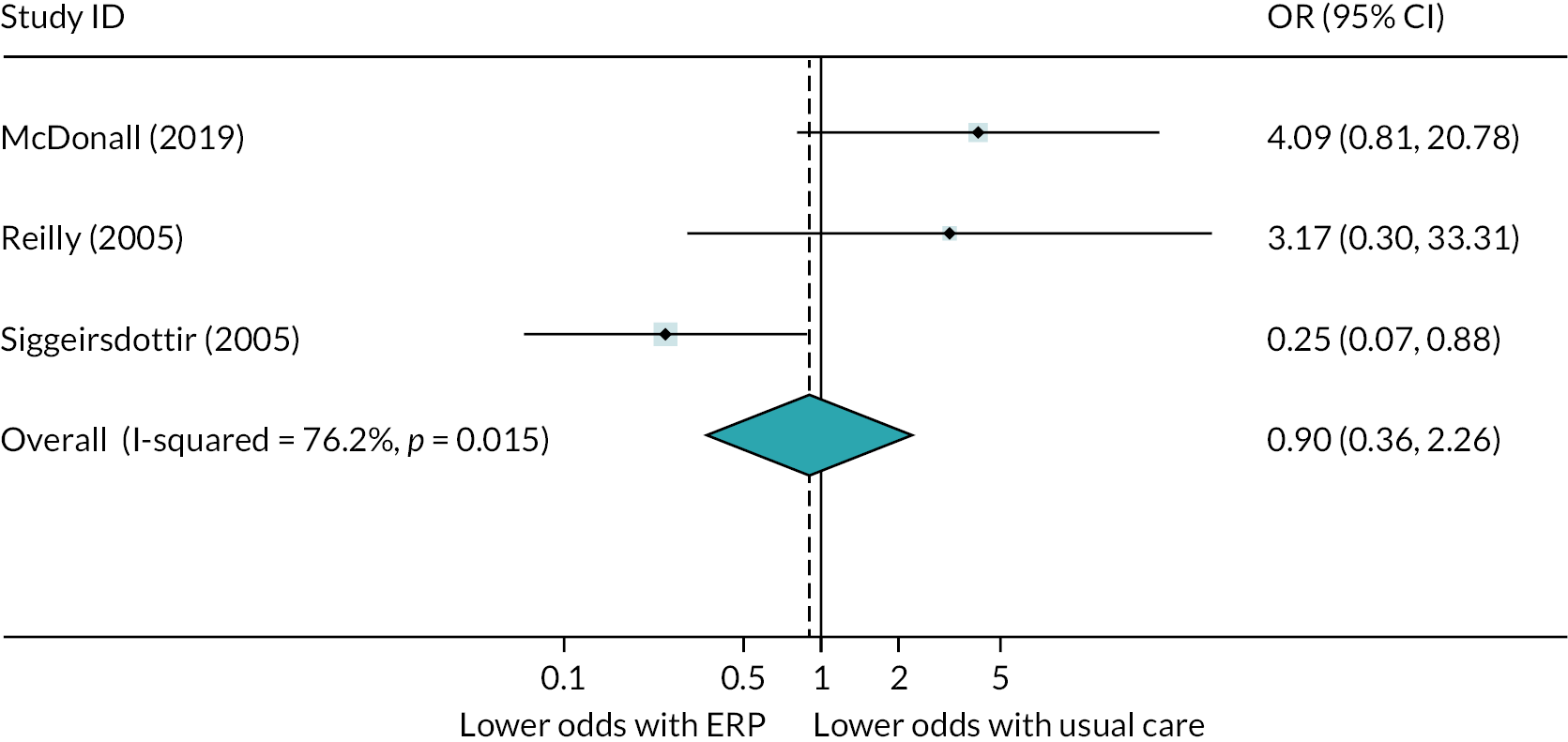
Effectiveness of ERP interventions at improving patient-reported outcomes
Report Supplementary Material 4, Table 7 displays data for patient-reported outcomes for RCTs trialling ERP interventions to improve recovery from LLA in older adults. While PROMS were reported in all studies, it was not possible to calculate effect sizes using the data provided by Pour and colleagues. 78 Pour and colleagues reported favourable outcomes in the experimental group for quality of life, functional improvement, energy and mental health. 78
Pain
It was possible to meta-analyse pain scores in three of four studies reporting this outcome,50,60,89 because data from Borgwardt and colleagues’ study were presented as a median and range and thus variance data were not imputable. 66 Pain scores tended to be reported across a range of time points, Fransen and colleagues reporting scores in the hourly intervals following surgery, and then 4 and 6 days after surgery, as well as pain change scores at 2, 6 and 12 weeks after surgery. 60 McDonall and colleagues89 reported the worst pain 3 days after surgery, and Reilly and colleagues50 reported scores from a pain diary at 6 months post-surgery, although it is unclear which specific metric was reported. The forest plot in Figure 5 displays meta-analysis of pain scores, using the 6-day post-operative data from Fransen and colleagues. 60 Overall there was evidence of a small association of ERP with lower pain scores, compared with usual care (d = −0.38, 95% CI −0.71 to −0.06; p = 0.021). The point estimate indicates a small effect, and although statistical heterogeneity was negligible and not statistically significant (I2 = 35.6%, p > 0.05) wide CIs reflect uncertainty in the true effect. Furthermore, differences in the approach to data collection, measurement time in particular, reflect the uncertainty underlying any estimate of the potential benefit of ERP for this outcome. Effect sizes for all pain metrics are available in Report Supplementary Material 4, Table 7.
FIGURE 5.
Forest plot showing the results of meta-analysis of the effect of ERP vs. usual treatment on pain following LLA.
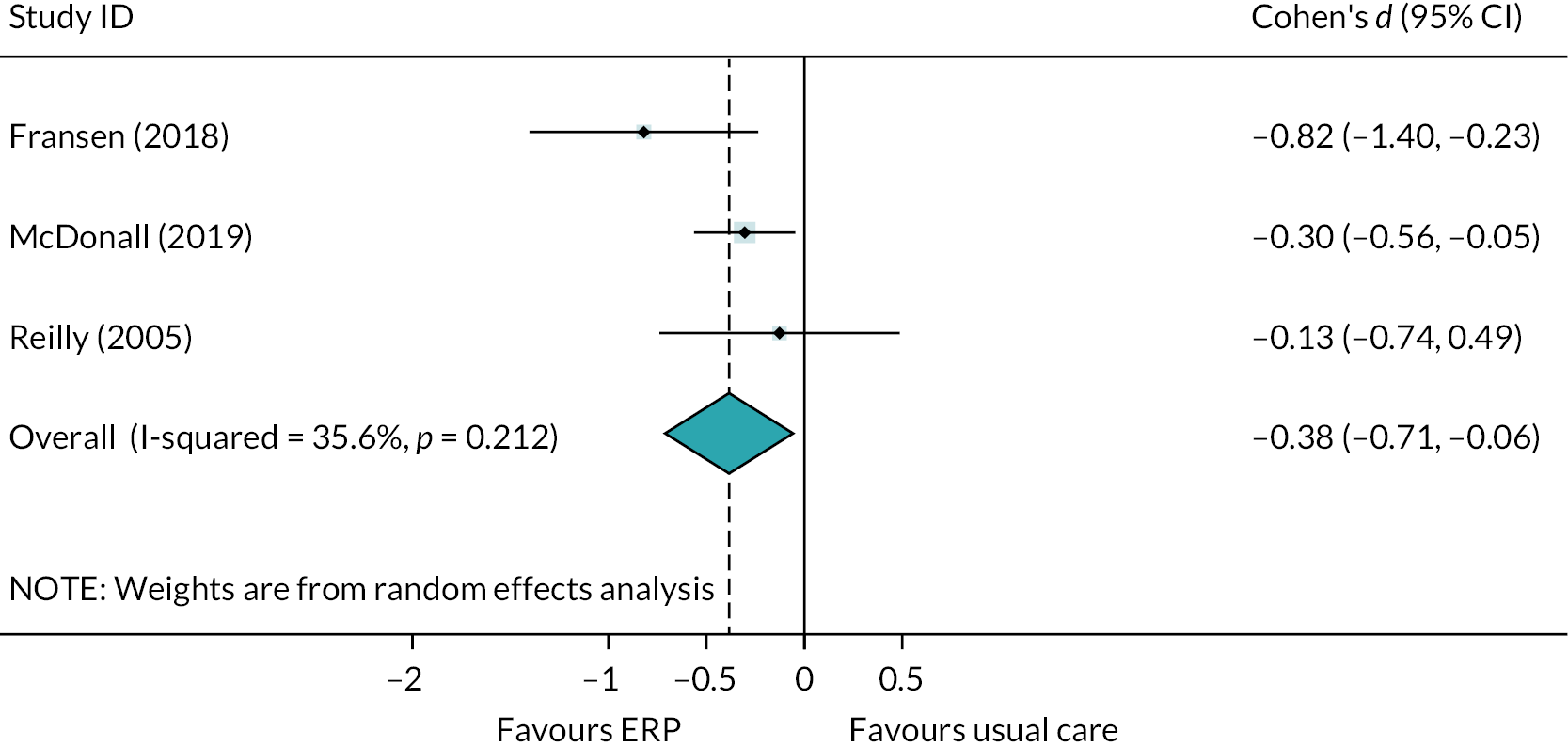
Physical function
Figure 6 is a forest plot showing the result of meta-analysis of PROMS relating to physical function following LLA. In the study by Reilly and colleagues,50 we combined 6-month data from the Oxford Knee Score and Functional outcome from the American Knee Society Scale. We used data from the 3-month time point in Fransen et al. 60 and from the 2-month time point in Siggeirsdottir et al. 86 This led to an overall pooled effect showing no benefit of ERP over usual care, despite a trend for better scores in the ERP group (d = −0.19, 95% CI −0.40 to 0.02; p > 0.05). When the 6-month follow-up data from the study by Siggeirsdottir and colleagues were entered into the analysis, the overall effect becomes statistically significant, albeit with a small effect size and uncertainty indicated by the upper CI approaching zero (d = −0.24, 95% CI −0.46 to −0.03, p = 0.024; see Figure 6B).
FIGURE 6.
Forest plots showing the results of meta-analysis of the effect of ERP vs. usual treatment on physical function following LLA. (A) Data from Siggeirsdottir et al. (2005) are from the 2-month follow-up time point; (B) data from Siggeirsdottir et al. (2005) are from the 6-month follow-up time point.

Outcomes that were not eligible for meta-analysis were as follows. Fransen and colleagues reported the mental health domain of the Short Form questionnaire-36 items (SF-36), and the sport and recreation score from the KOOS, with no differences between groups at 2, 6 or 12 weeks after discharge. 60 Quality of life was assessed in terms of the Quality of Life and Activities of Daily Living scores on the KOOS by Fransen and colleagues60 and the ability to walk and climb stairs item on the Knee Society Score questionnaire by Borgwardt and colleagues. 66 It was not possible to combine data because Borgwardt and colleagues provided median and range scores. 66 No statistically significant differences were reported between ERP and usual-care groups for any of these outcomes. Satisfaction was similar between groups in the paper by Borgwardt and colleagues;66 however, McDonall and colleagues reported that patients receiving the intervention had a higher overall satisfaction score and were more likely to recommend the health service. 89
Service utilisation was not reported by any of the studies comparing ERP with usual care.
Effectiveness of ERP interventions at improving clinical and patient-reported outcomes (non-RCTs only)
There were eight papers from seven non-RCTs that compared ERP interventions with usual care. 39–43,46–48 The studies by Garriga and colleagues used an ITS design to report on patients receiving hip or knee replacements as two groups, with data accessed via The National Joint Registry of England, Wales, Northern Ireland and the Isle of Man. 39,40 Despite having a very large sample size for each group of patients (nearly 500,000 patients for each type of surgery) it was unclear how many participants were analysed before and after implementation of ERAS, and no variance data were provided alongside group means, so we could not calculate effect sizes. 39,40 However, the authors reported a positive picture for both groups, with a reduction in LOS, improvement in Oxford Knee Score or Oxford Hip Score, lower rates of complications and revisions reported for each cohort with implementation of ERAS. 39,40
The study by Hunt and colleagues was presented across two papers,42,43 the authors comparing outcomes between centres with differing LOS in Belfast, Liverpool and London. The paper by Hunt and colleagues42 reports most outcomes from the study, with the paper by Salmon and colleagues focusing on patient satisfaction. 43 Where standardised mean differences were calculated, there were no statistically significant differences between outcomes except for improvement on the Oxford Hip Score in the study by Hunt and colleagues for patients in the Belfast centre compared to both control sites. 42 There was also a slight improvement on the Western Ontario and McMaster Universities’ Osteoarthritis Index (WOMAC) function scale in patients in Belfast compared to those in south west London (d = 0.23, 95% CI 0.02 to 0.44; p < 0.05). In the Belfast centre, more patients reported no problems with care than in Liverpool (18.8% more) and south west London (26.5% more), while the number reporting no problems with recovery was similar in all three centres. 43
Maempel and colleagues conducted two studies, with hip46 and knee47 replacement patients receiving different ERP packages. The study conducted with hip-replacement patients46 was considerably larger (n = 1161) than the one conducted with knee-replacement patients47 (n = 165). Median LOS was 1 day shorter in the ERP group with knee-replacement patients, with no difference in scores on the American Knee Society Global Functioning outcome. 47 In the study with hip-replacement patients, LOS was 2 days shorter in ERP patients, associated with a large effect size (d = −1.35, 95% CI −1.47 to −1.22; p < 0.001), with no differences between groups for other outcomes, including the Harris Hip Score. 46
In the study by Higgins and colleagues, it was unclear how many participants were included in each group when evaluating outcomes, therefore it was not possible to calculate effect sizes. 41 The authors reported that an ERP intervention was associated with a significantly shorter mean LOS of two days, reduction in rates of reoperation within 60 days and improvements on all PROMs, which included the Oxford Knee Score, EuroQol-5 Dimensions (EQ-5D) and quality of life VAS. 41 There were no differences in the 60-day complication rate and 30-day readmission rate.
McDonald and colleagues reported that ERP was associated with a reduction in LOS of 2 days, with a large effect size and narrow CIs (d = −1.10, 95% CI −1.20 to −1.0; p < 0.001). 48 This reduction in LOS did not come at a cost to scores on the Oxford Knee Score outcome, which was almost identical between patients receiving ERP and those receiving usual care. 48
Effectiveness of Prehab interventions at improving clinical outcomes (RCTs only)
Six RCTs evaluated the effectiveness of Prehab interventions on outcomes following LLA, compared to usual care. 49,51,53,63,77,79 It was not possible to calculate effect sizes for LOS in two studies;49,63 however, the remaining four studies could be pooled in meta-analysis. Figure 7 is a forest plot showing that pooled data indicate that there was no overall association between Prehab and LOS, despite tendency towards a small effect (d = −0.13, 95% CI −0.32 to 0.07; p > 0.05).
FIGURE 7.
Forest plot showing the results of meta-analysis of the effect of Prehab vs. usual treatment on LOS following LLA.
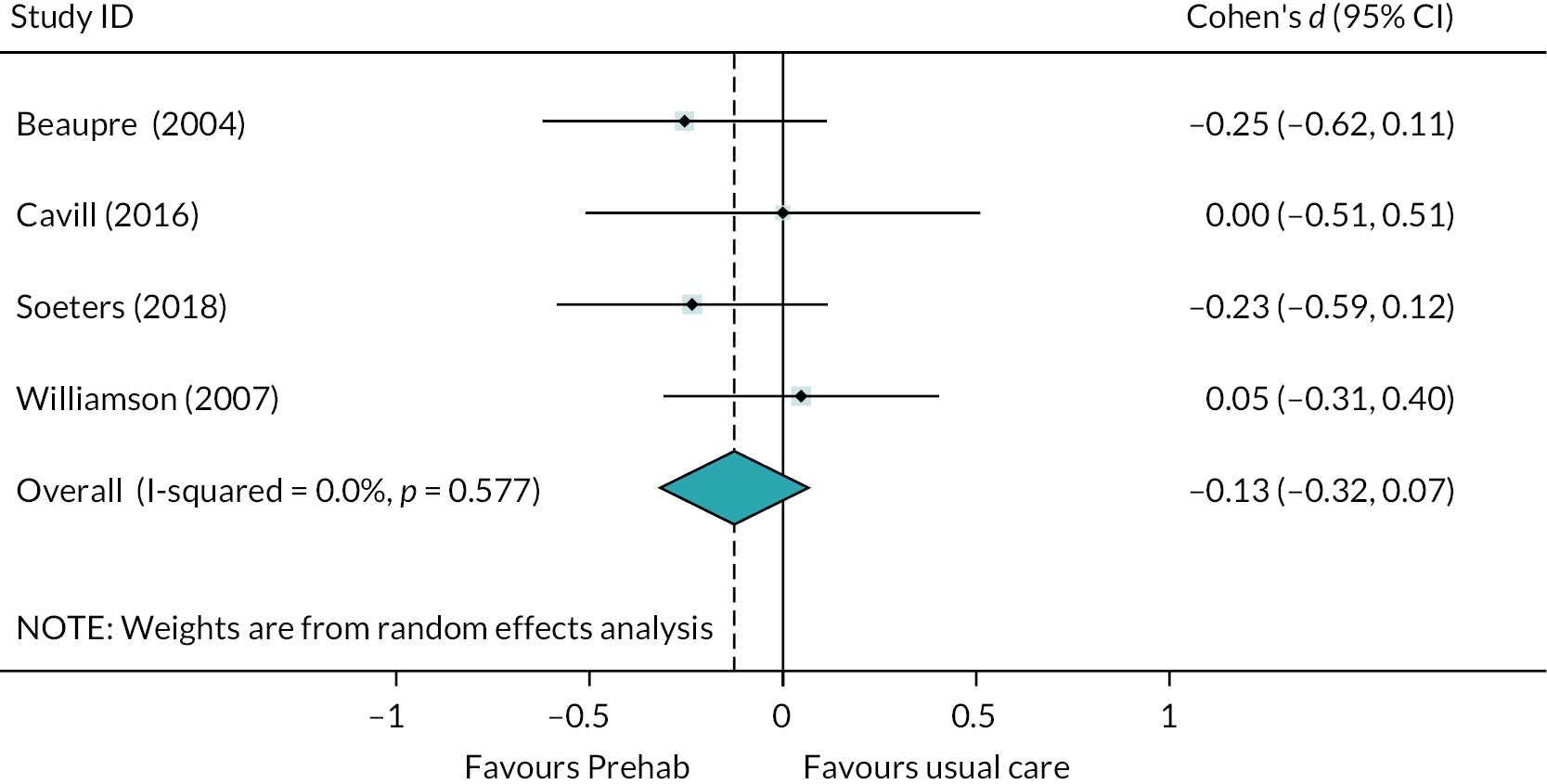
Hoogeboom et al. reported complications, with two in the intervention group and none in the control group,63 but none of the other RCTs evaluating Prehab interventions captured data on readmissions, complications or mortality.
Effectiveness of Prehab interventions at improving PROMs
Report Supplementary Material 4, Table 9 displays patient-reported outcome data from the six RCTs comparing Prehab with usual care. 49,51,53,63,77,79 Assessments of physical functioning were made in five studies. 49,51,53,77,79 using multiple measures in all but one study. 79 Measurements were taken at multiple post-operative time points (3, 6 and 12 months) in the study by Beaupre and colleagues,53 otherwise they were taken between 4 and 12 weeks after surgery.
It was possible to perform a meta-analysis of the physical functioning outcomes used in the six studies. We selected the 3-month time point and combined the Physical Component Summary score of the SF-36 with the Function score of the WOMAC to provide an input for Beaupre et al. 53 For the data provided by McGregor and colleagues49 we combined the Harris Hip Score with the Function score of the WOMAC, and for the data provided by Williamson et al. we combined the Oxford Knee Score with the WOMAC total score. 51 Meta-analysis indicates that there was an overall association between Prehab interventions and improved physical functioning scores, with a small effect demonstrated (d = −0.36, 95% CI −0.56 to −0.17, p < 0.001). However, observation of the forest plot from this analysis (see Figure 8a) indicates that the result from the paper by Soeters and colleagues77 appears to be an outlier, and thus sensitivity analysis was performed. When the large effect observed by Soeters and colleagues77 is removed, the remaining studies consistently demonstrate no difference between scores when comparing those receiving Prehab and those receiving usual care (d = 0.05, 95% CI −0.16 to 0.26, p > 0.05; see Figure 8).
FIGURE 8.
Forest plot showing the results of meta-analysis of the effect of Prehab vs. usual treatment on physical functioning PROMs following LLA. (A) Forest plot includes data from all eligible studies; (B) outlier data from Soeters et al. (2018) removed.
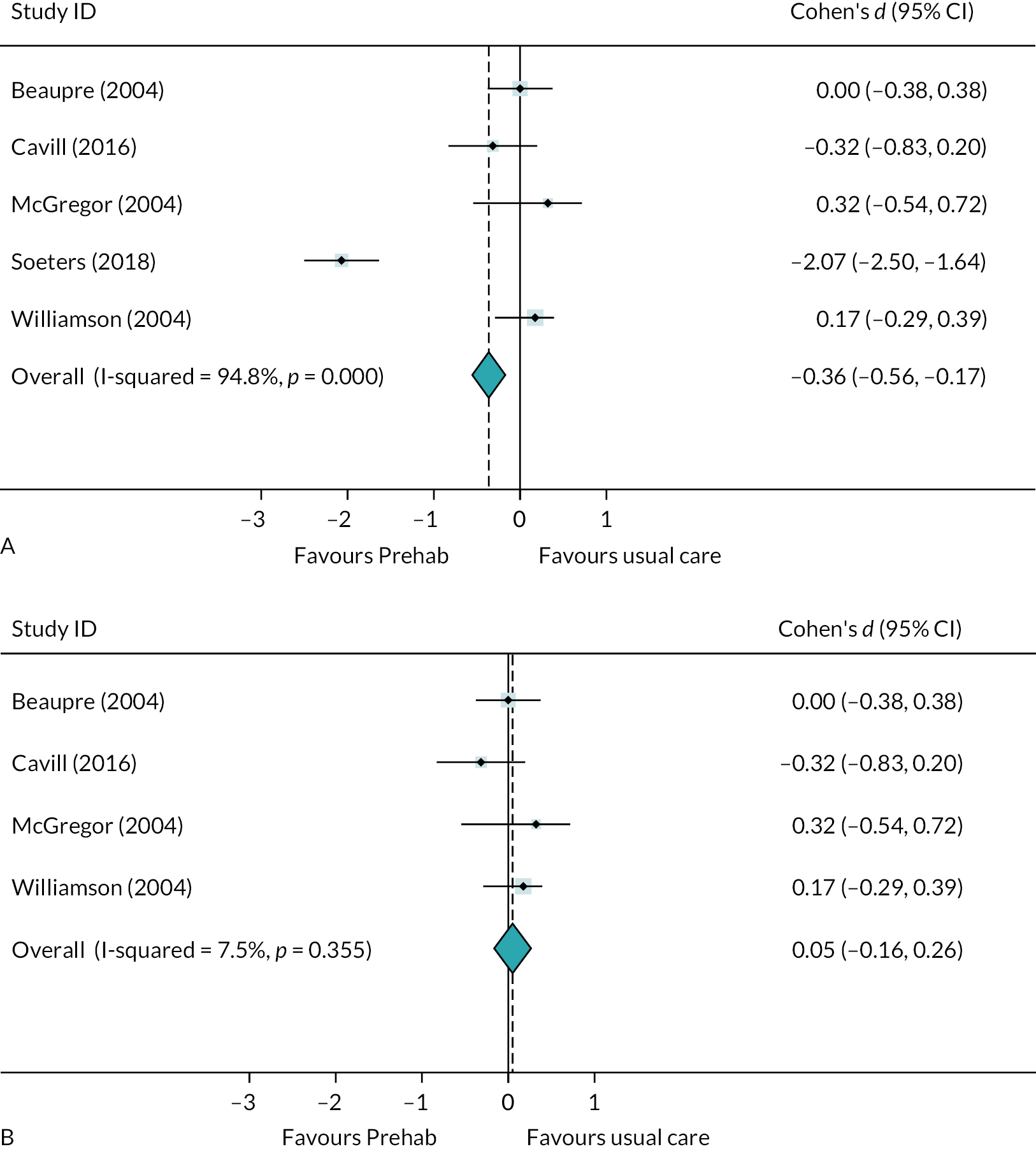
Four studies captured pain reports after discharge from hospital. 49,51,53,77 Meta-analysis reveals a lack of consistency between the four studies reporting outcomes (see Figure 9). Two studies showed no effect of Prehab on pain scores at 3 months post-operatively,51,53 one showed a large improvement in pain scores 4–6 weeks after surgery77 and one showed that pain was worse in the Prehab group after 3 months. 49 The pooled effect suggested no overall influence of Prehab on pain, with very wide CIs and an I2 value close to 100%, reflecting the inconsistency of data in the meta-analysis (d = −0.23, 95% CI −1.18 to 0.72; p > 0.05).
FIGURE 9.
Forest plot showing the results of meta-analysis of the effect of Prehab vs. usual treatment on pain scores 2–3 months after LLA.
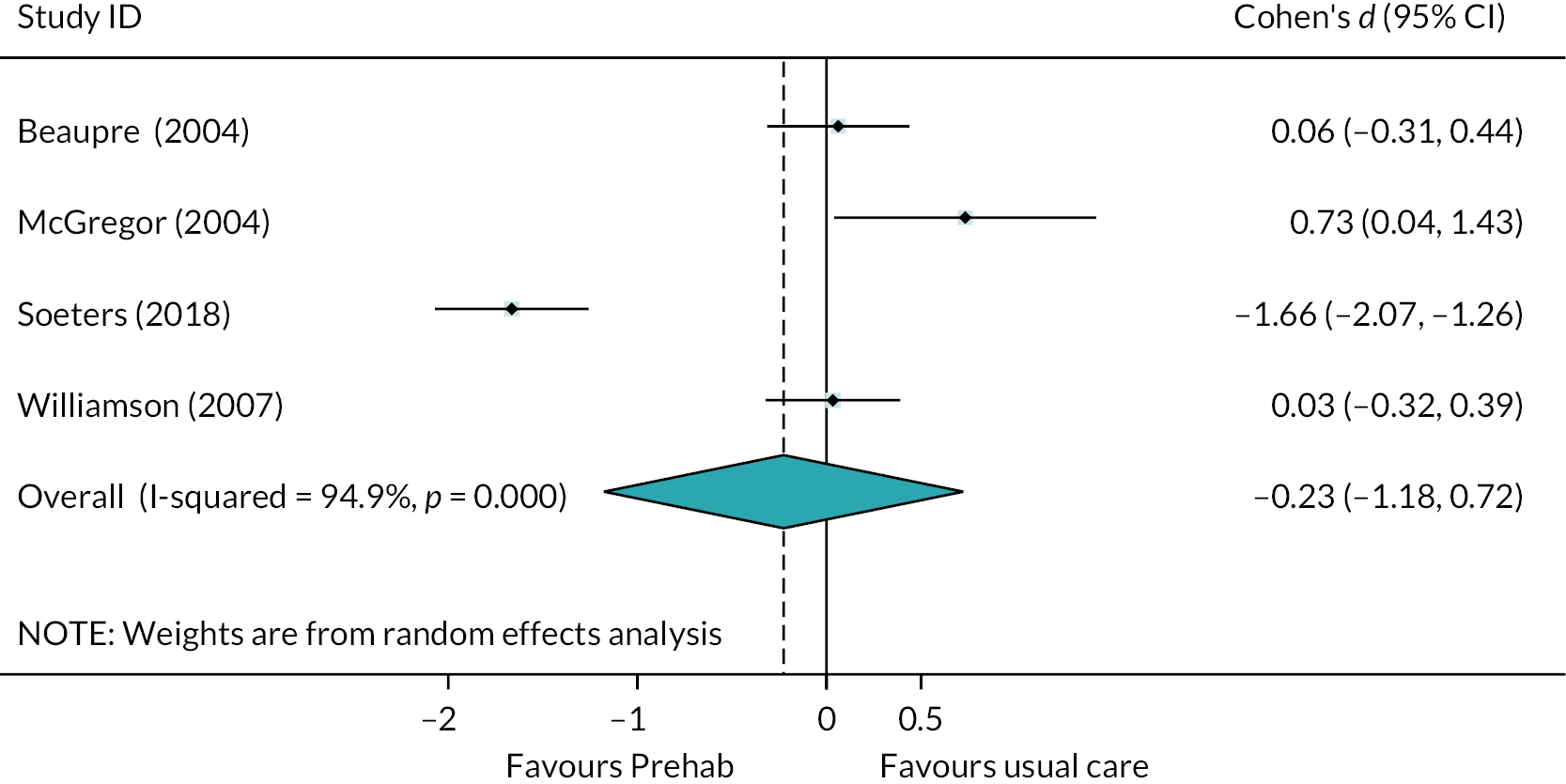
Quality of life was assessed in three studies evaluating the effects of Prehab on outcomes after lower-limb arthroplasty. 49,53,79 The general health scale of the SF-36 from Beaupre et al. ,53 the EQ-5D VAS from Cavill et al. 79 and the General Disabilities score based on the Barthel Activities of Daily Living Index from McGregor et al. 49 were pooled. Meta-analysis indicates no overall effect of Prehab on quality of life (d = 0.08, 95% CI −0.19 to 0.36, p > 0.05; see Figure 10).
FIGURE 10.
Forest plot showing the results of meta-analysis of the effect of Prehab vs. usual treatment on quality of life scores after LLA.
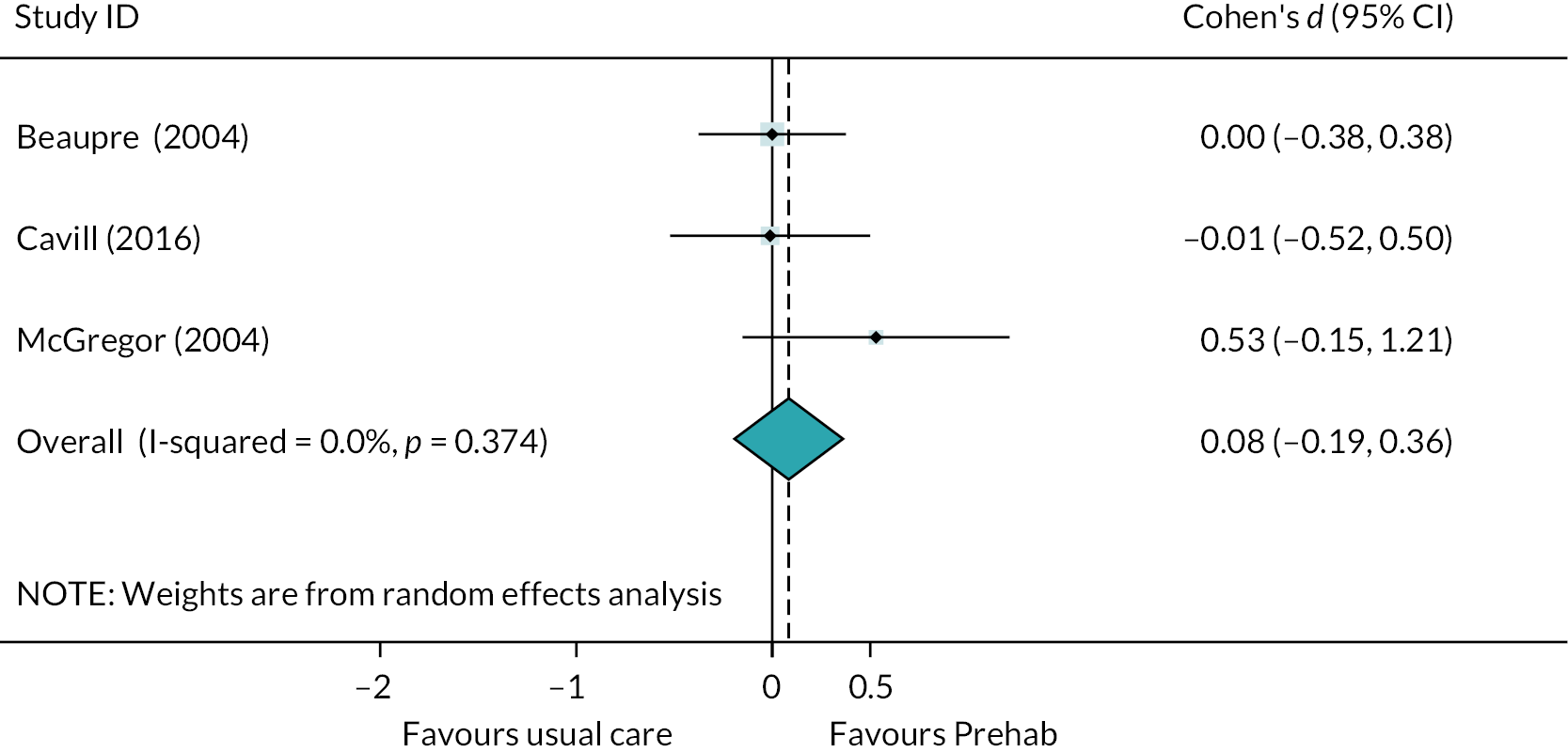
Mental health was evaluated in two studies, with Beaupre and colleagues53 reporting relevant subscales of the SF-36, and Williamson and colleagues51 reporting anxiety and depression scores on the HADS. Of the five mental health measures reported, only anxiety in the intervention group in the study by Williamson et al. improved with Prehab, as shown in Figure 11. 51 This was associated with a medium effect size, although CIs reflect uncertainty in the true magnitude of effect (d = −0.56, 95% CI −0.92 to −0.19; p = 0.03).
FIGURE 11.
Forest plot showing the effect of Prehab vs. usual treatment on mental health scores after LLA for individual measures in two studies. No meta-analysis was performed.
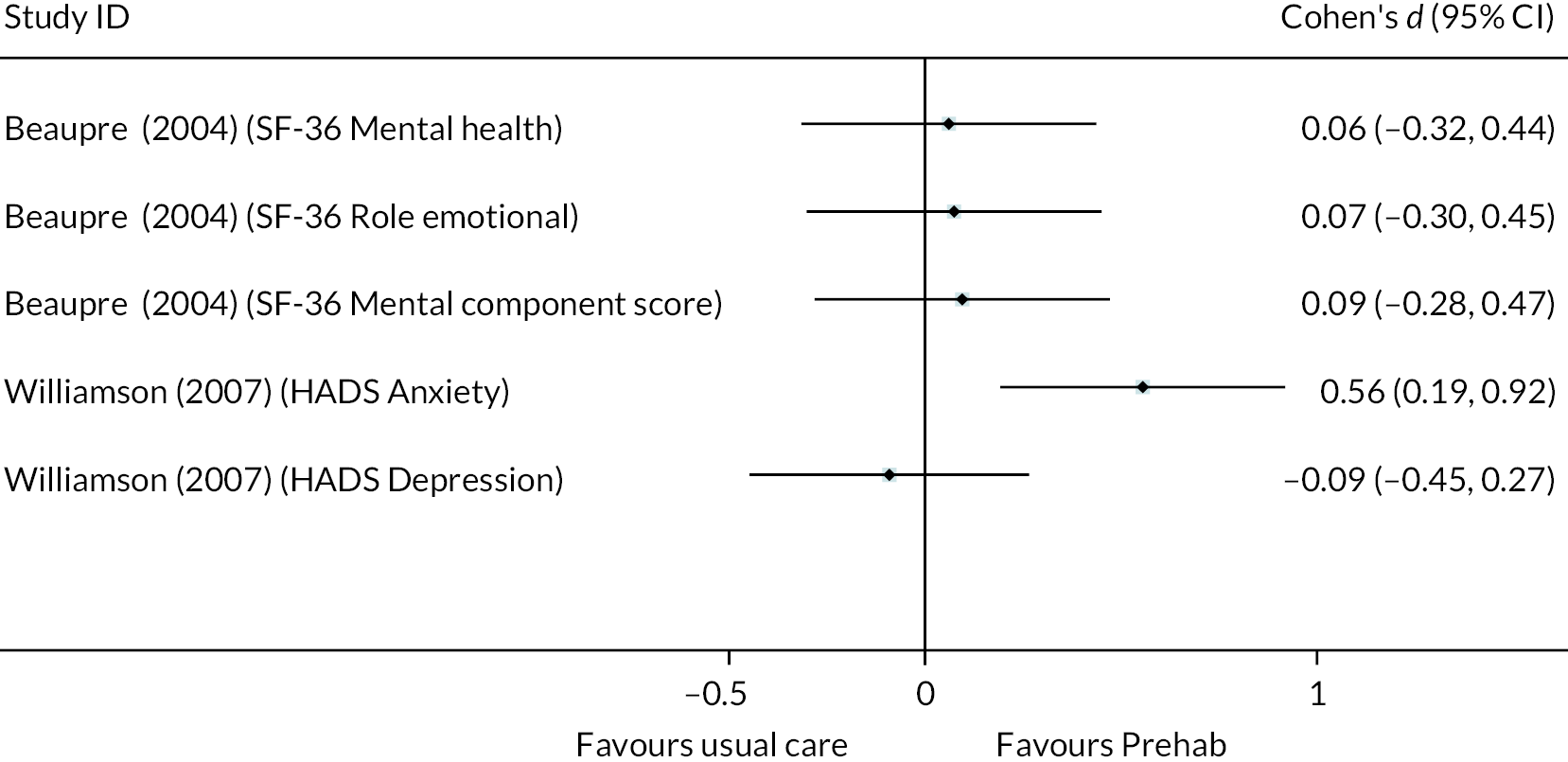
Physical activity was evaluated by Hoogeboom and colleagues, with no difference in activity levels between groups within a week of surgery. 63 Social status was assessed using the social function subscale of the SF-36 in the study by Beaupre and colleagues, and there were no differences between groups. 53
Effectiveness of Prehab versus Rehab
A single RCT compared Prehab with Rehab. 70 Vesterby and colleagues reported LOS in terms of median and range, therefore an effect size was not calculated for the difference between groups. 70 The median LOS was 1 day in the Prehab group and 2 days in the Rehab group. 70 Readmissions and unplanned visits and calls to hospital were similar between groups. In terms of PROMs, there were no differences between groups in quality of life, physical function or mental health. 70
Effectiveness of Rehab versus TAU
One RCT evaluated a Rehab intervention, compared with usual care. 75 Mean LOS was 6.5 days shorter in patients receiving Rehab intervention with similar numbers of complications in both groups. 75 In addition, those in the Rehab group achieved lower scores on the WOMAC measure, this difference associated with a large effect size (d = −1.52 95% CI −1.89 to −1.14; p < 0.001 – per-protocol analysis). 75
Summary of evidence from trials seeking to improve recovery from lower-limb arthroplasty
There were 15 RCTs evaluating interventions to improve recovery following LLA in older adults. These were split into seven studies evaluating ERP interventions, compared to usual care,50,60,66,68,69,78,86,89 six comparing Prehab with usual care,49,51,53,63,77,79 one comparing Prehab with Rehab70 and one comparing Rehab with usual care. 75 There were also seven non-RCTs evaluating the effects of ERP interventions. 39–43,46–48
There was evidence from meta-analysis to suggest that ERP interventions were associated with reduced LOS (n = 5 studies), without negative impact on readmissions (n = 3 studies) or complications (n = 3 studies). The influence on patient-reported outcomes was evaluated using a range of measures, including pain, physical function, quality of life and satisfaction. Scores tended to be better in the ERP group, or there was no difference between scores for patients receiving ERP usual care. Meta-analysis of PROMs was only possible for pain (n = 3 studies) and physical function (n = 4 studies), with evidence of a small beneficial impact on pain.
The data from non-RCTs were not combined but reflected a broadly similar story to that from the RCTs evaluating ERP interventions, in that LOS was usually improved with ERP, without detriment to, and occasionally linked with improvements in, other outcomes. However, there were issues with reporting that meant effect sizes were not readily calculable in many instances.
Four of the six RCTs evaluating Prehab interventions provided LOS data that could be pooled, indicating that this type of intervention was associated with no change in LOS compared with usual care. Other clinical outcomes, including readmissions, complications and mortality, were not reported, except in one study, so we were unable to evaluate whether Prehab interventions influenced these outcomes. However, it was possible to perform meta-analysis of various PROMs, which were better reported in this group of studies. Physical functioning was shown to be slightly improved with Prehab, but this was skewed by an outlier showing a very large effect of the intervention. When this was removed from the analysis, the remaining four studies clearly indicated no difference between Prehab and usual care.
Meta-analysis also showed there was no difference in pain scores 2–3 months after surgery (n = 4 studies), although there was very high heterogeneity between studies, and quality of life was similar between groups (n = 3 studies). For other patient-reported outcomes, where meta-analysis was not possible, there tended to be evidence of no difference between Prehab and usual care.
The single study comparing Prehab with Rehab showed no differences between groups, and the single study comparing Rehab with usual care showed large improvements in LOS and physical function.
Overall, there was a handful of studies available for the evaluation of ERP and Prehab interventions. The evidence suggests that ERP interventions can provide improvement in clinical outcomes and can offer this without detriment to, and even with improvements in, some PROMs, although further evidence is required. The data for Prehab interventions indicate that there is likely to be little impact, either positive or negative, on clinical or patient-reported outcomes.
Evidence from trials seeking to improve recovery from colorectal surgery
Effectiveness of ERP interventions at improving clinical outcomes
Report Supplementary Material 4, Table 2 displays clinical outcome data from the seven studies evaluating ERP interventions in older adults undergoing elective colorectal surgery. 45,65,82–85,88 After imputation, standardised mean differences between ERP and TAU groups for LOS were available in three comparisons from two studies. 65,84 A forest plot displaying the results of meta-analysis of these three groups is displayed in Figure 12, showing that ERP interventions were associated with a small reduction in LOS when compared with usual care (d = −0.32, 95% CI −0.56 to −0.08; p = 0.01). Heterogeneity was not statistically significant for this effect (I2 = 44.1%; p > 0.05), reflecting consistency in the evidence.
FIGURE 12.
Forest plot showing the results of meta-analysis of the effect of ERP vs. usual treatment on LOS following colorectal surgery. LOS, length of stay; LAP, laparoscopic surgery group; Open, open surgery group.
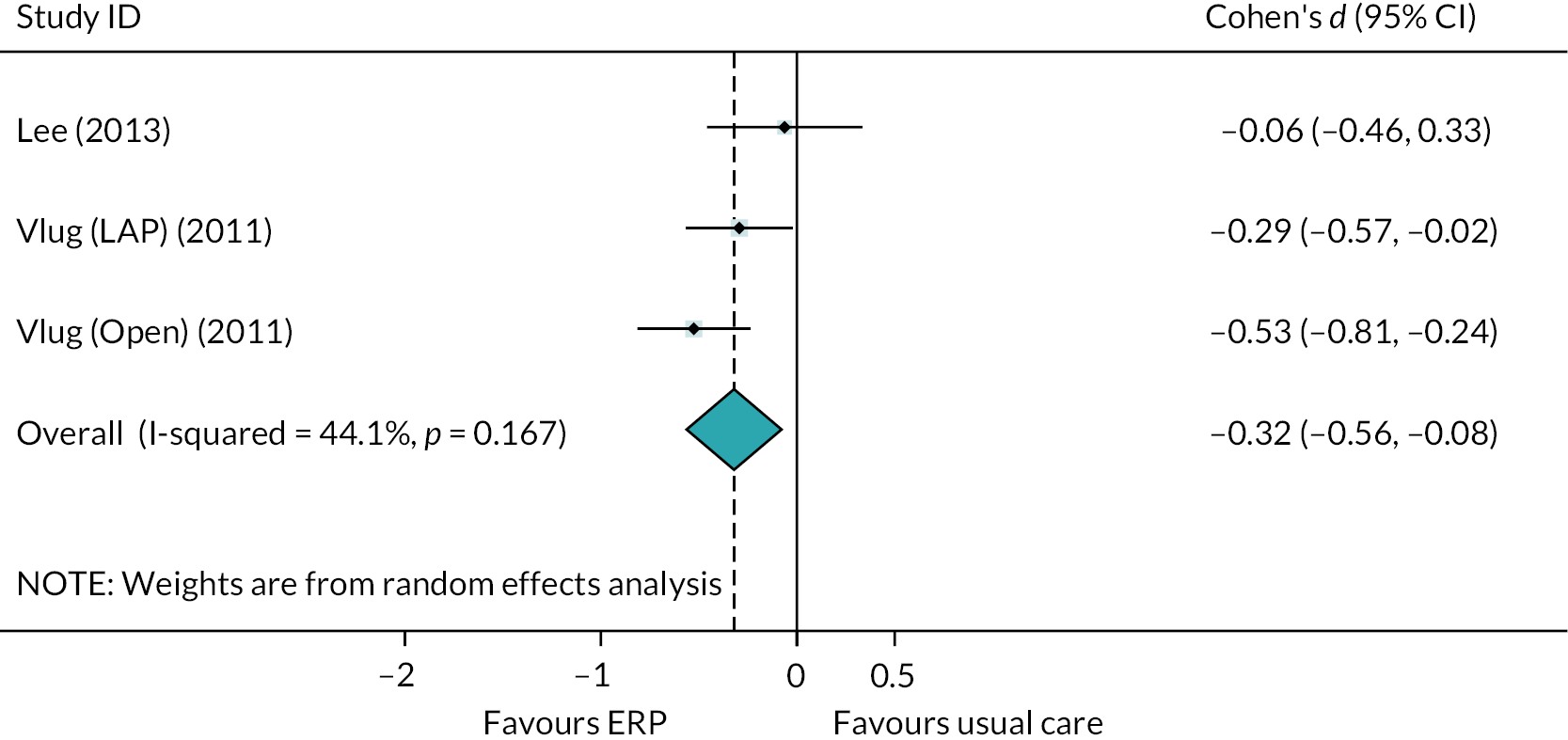
In the studies presenting data which could not be used to calculate standardised mean differences, median LOS for patients receiving ERP interventions was lower in all cases. 45,82,84,85,88 Additionally, Pappalardo and colleagues reported that patients receiving ERP had been discharged by postoperative day six, but around half of those receiving usual care had not. 83
Three studies, evaluating four comparisons, reported readmission rates following ERP interventions. 45,65,88 Figure 13 is a forest plot displaying the results of meta-analysis of readmission data, indicating the odds of readmission were similar between patients receiving ERP and usual care (OR = 1.07, 95% CI 0.62 to 1.87). In addition, there were no readmissions reported in either trial arm in the study by Lee et al. 84 Seven studies, evaluating eight comparisons, reported incidence of complications following ERP interventions. 45,65,82–85,88 Meta-analysis indicates that there was no difference in the odds of experiencing a complication between patients receiving ERP or those receiving usual care (see Figure 14) (OR = 0.83, 95% CI 0.60 to 1.15).
FIGURE 13.
Forest plot showing the results of meta-analysis of the effect of ERP vs. usual treatment on the odds of readmission following colorectal surgery. Lap, laparoscopic surgery group; Open, open surgery group.
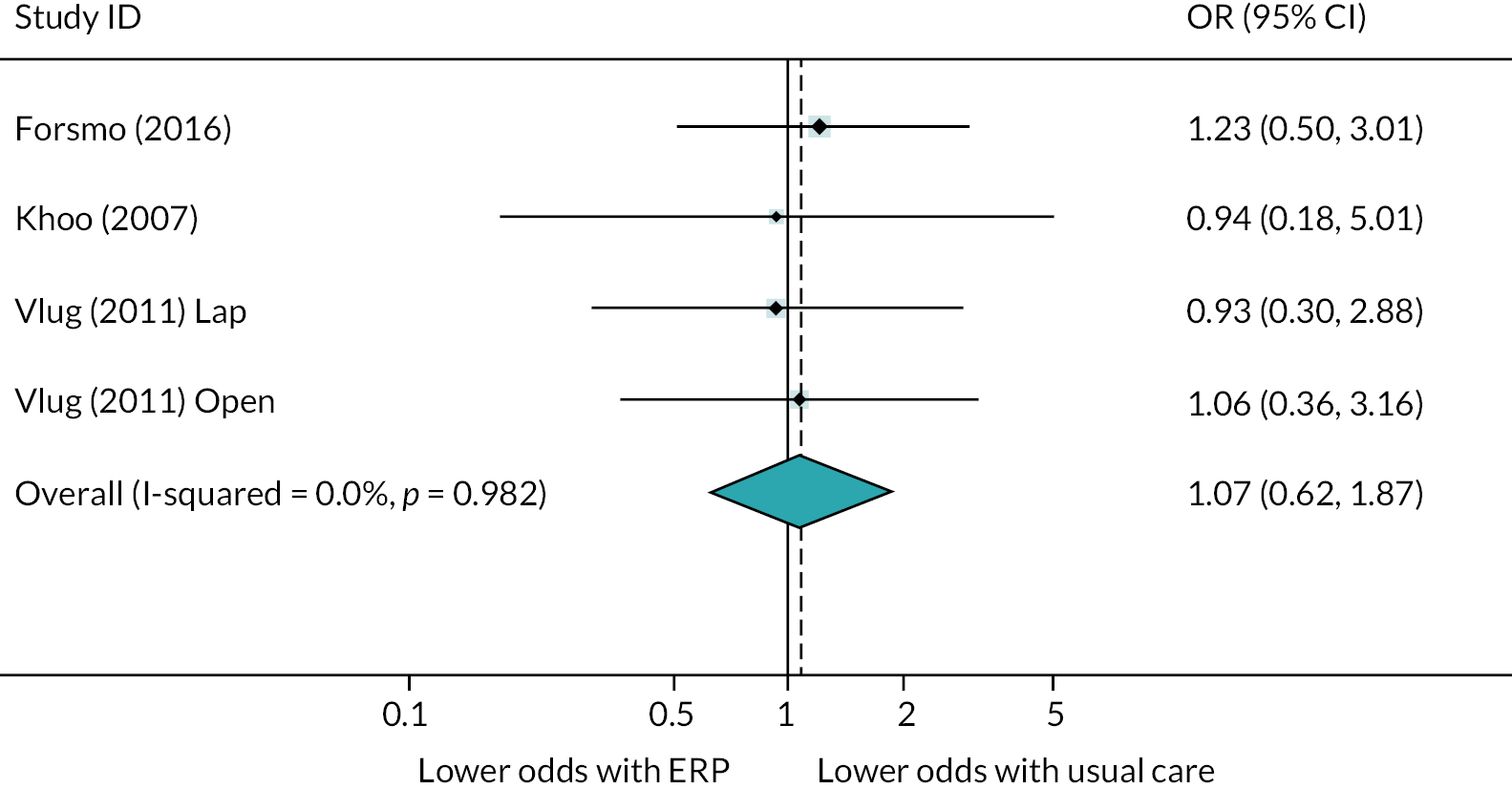
FIGURE 14.
Forest plot showing the results of meta-analysis of the effect of ERP vs. usual treatment on odds of complications following colorectal surgery. Lap, laparoscopic surgery group; Open, open surgery group.

Effectiveness of ERP interventions at improving patient-reported outcomes
Report Supplementary Material 4, Table 3 displays data for patient-reported outcomes for RCTs trialling ERP interventions to improve recovery from elective colorectal surgery in older adults. Although there were five studies collecting PROMs,65,82,84,85,88 actual outcome values were frequently unreported. It was possible to compare pain scores in two studies conducted by the same authors,84,85 with pooled data showing that pain 1 week after surgery was similar in the ERP and usual care groups (d = −0.03, 95% CI −0.31 to 0.2; p > 0.05). There were no other opportunities to combine PROMs of the same category between studies due to the absence of data provided by authors.
Outcomes that were not eligible for meta-analysis were as follows. Mean patient satisfaction scores were slightly higher in the ERP group in the study by Frontera and colleagues. 82 Khoo and colleagues45 reported that only 9% of patients randomised to the ERP group felt they would benefit from a longer inpatient stay, compared with 69% in the usual care group. Similar quality of life scores were reported between groups in the study by Pappalardo and colleagues. 83 Quality of life was similar at 10 and 30 days post-surgery in the groups in the study by Forsmo and colleagues,88 and in the study by Lee et al. 84 there was no difference in quality of life scores at 1 and 4 weeks post surgery when comparing ERP and usual-care pathways. Vlug and colleagues reported that patients fulfilled the discharge criterion of ‘accepting discharge’ sooner when they received ERP instead of usual care; this was the case in patients undergoing both laparoscopic (d = 0.56, 95% CI 0.28 to 0.84; p < 0.001) and open (d = 0.40, 95% CI 0.11 to 0.68; p = 0.003) surgery. 65
Effectiveness of ERP interventions at improving service utilisation after discharge
Khoo and colleagues reported the numbers of patients in each group who called the ward for advice or spoke to their GP and either received a prescription or advice, after discharge. 45 There were no statistically significant differences in the odds of these events taking place, despite a greater number of GP contacts in the usual care group (10 vs. 8 contacts).
Effectiveness of Prehab interventions at improving clinical outcomes
Five studies evaluated Prehab interventions, three compared to usual care54,56,67 and two compared to Rehab interventions. 55,59 Report Supplementary Material 4, Table 3 displays clinical outcome data reported in all studies. Meta-analysis was performed for two comparisons: Prehab versus TAU54,56,67 (see Figure 15 upper) and Prehab versus Rehab55,59 (see Figure 15 lower). The comparison of Prehab with TAU showed that LOS was similar between conditions (d = 0.20, 95% CI −0.06 to 0.47; p > 0.05). The pooled estimate showed no difference in LOS between patients receiving Prehab and Rehab interventions in the two studies exploring this comparison (d = −0.11, 95% CI −0.40 to 0.18; p > 0.05). 55,59
FIGURE 15.
Forest plot showing the results of meta-analysis of the effect of Prehab vs. usual treatment (top analysis) and Prehab vs. Rehab (bottom analysis) on LOS following colorectal surgery. TAU, treatment as usual.
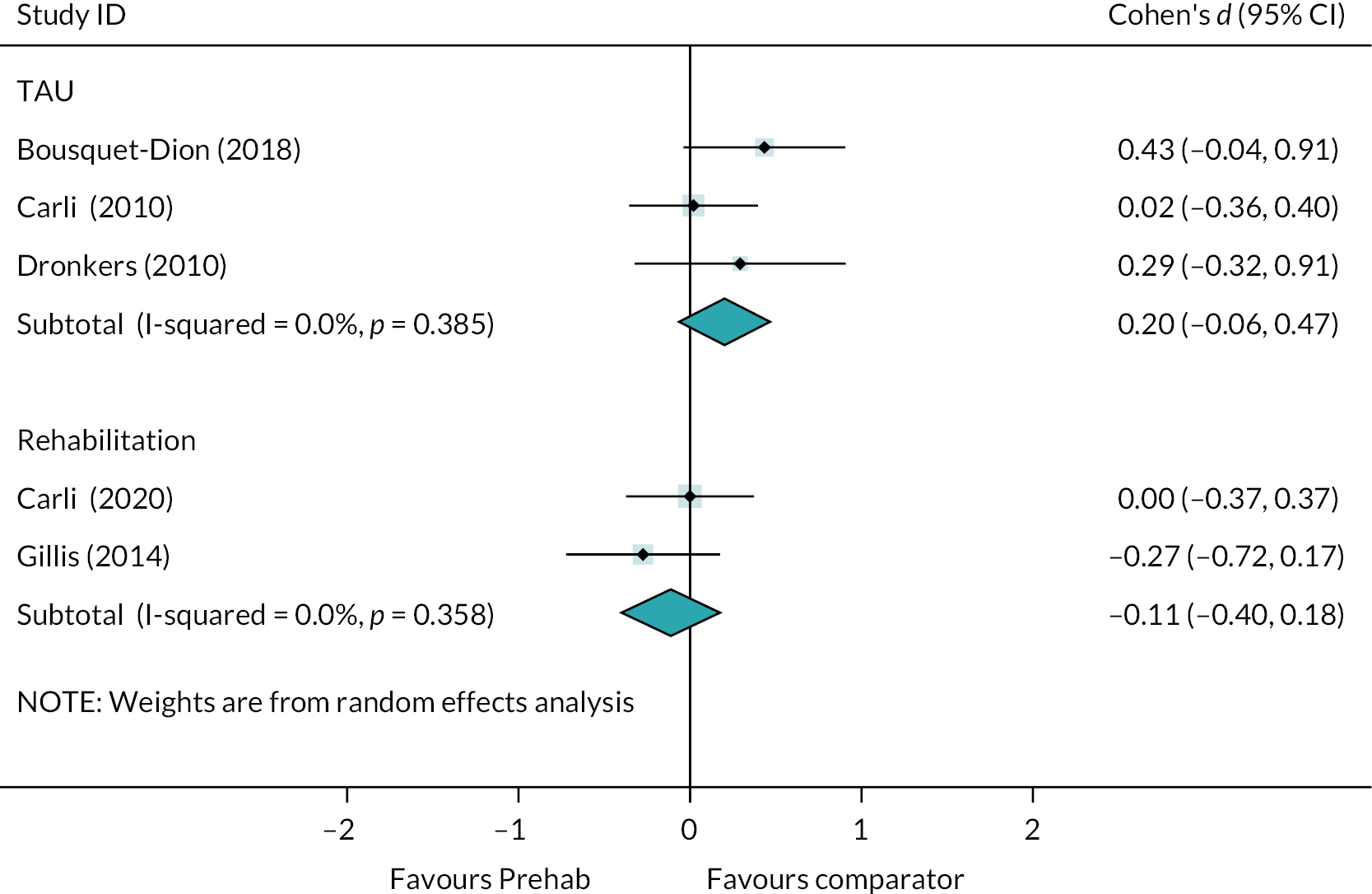
The odds of experiencing a complication was similar in Prehab and usual-care groups in the three studies exploring this association (OR = 1.33, 95% CI 0.70 to 2.53; see Figure 16). 54,55,67 Carli and colleagues55 reported that the comprehensive complication index which accounts for the number and severity of complications was similar between Prehab and Rehab groups (p > 0.05). Finally, while Gillis and colleagues saw more complications in the control group (Rehab) than the intervention group (Prehab) this difference was not statistically significant.
FIGURE 16.
Forest plot showing the results of meta-analysis of the effect of Prehab vs. usual treatment on odds of complications following colorectal surgery.
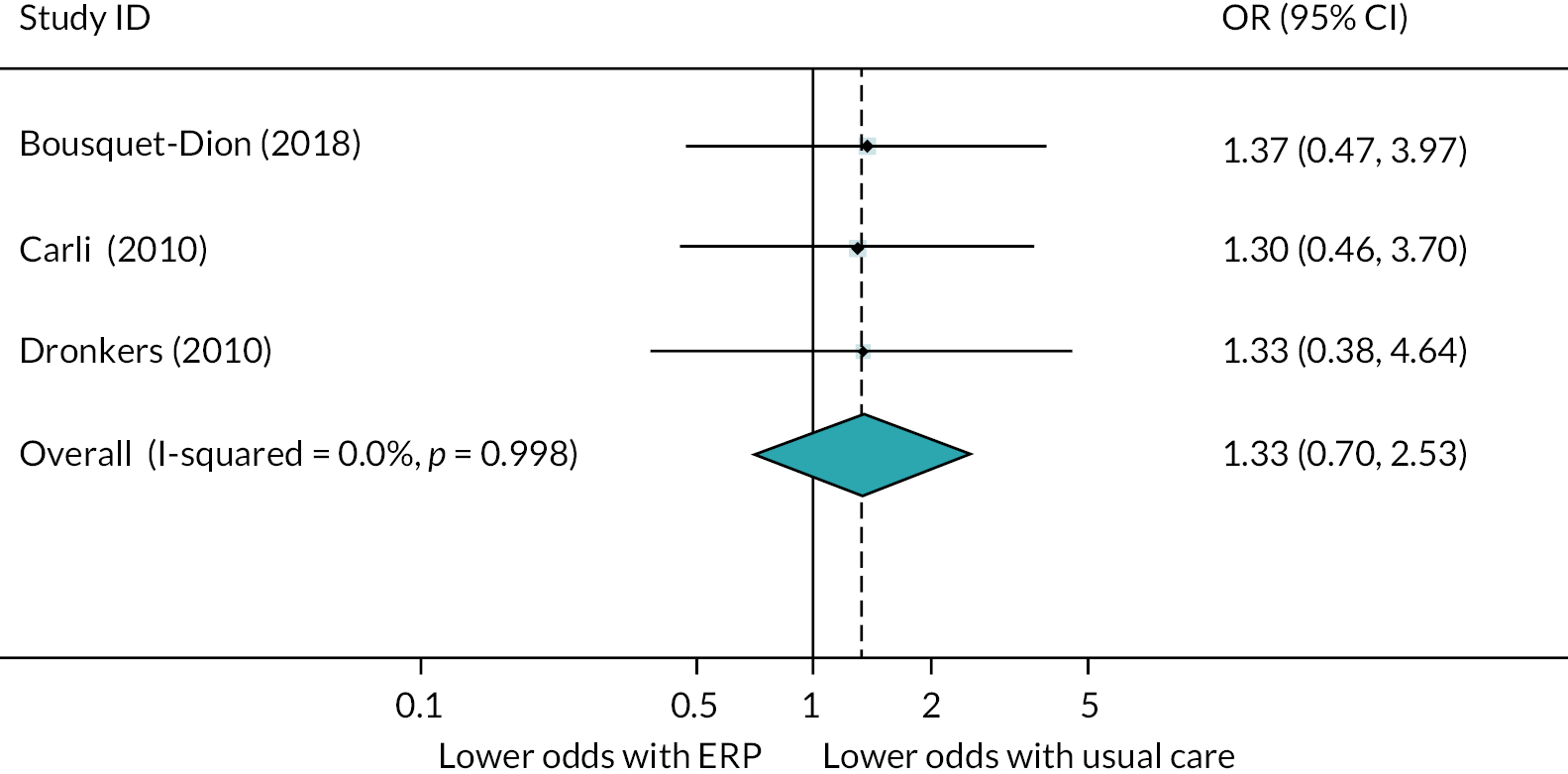
Despite a trend towards lower rates of readmissions in the Prehab groups, meta-analysis of the two studies comparing Prehab to Rehab showed there was no overall difference in the odds of experiencing a readmission to hospital following colorectal surgery (OR = 0.57, 95% CI 0.25 to 1.27; see Figure 17).
FIGURE 17.
Forest plot showing the results of meta-analysis of the effect of Prehab vs. Rehab on the odds of readmissions following colorectal surgery.
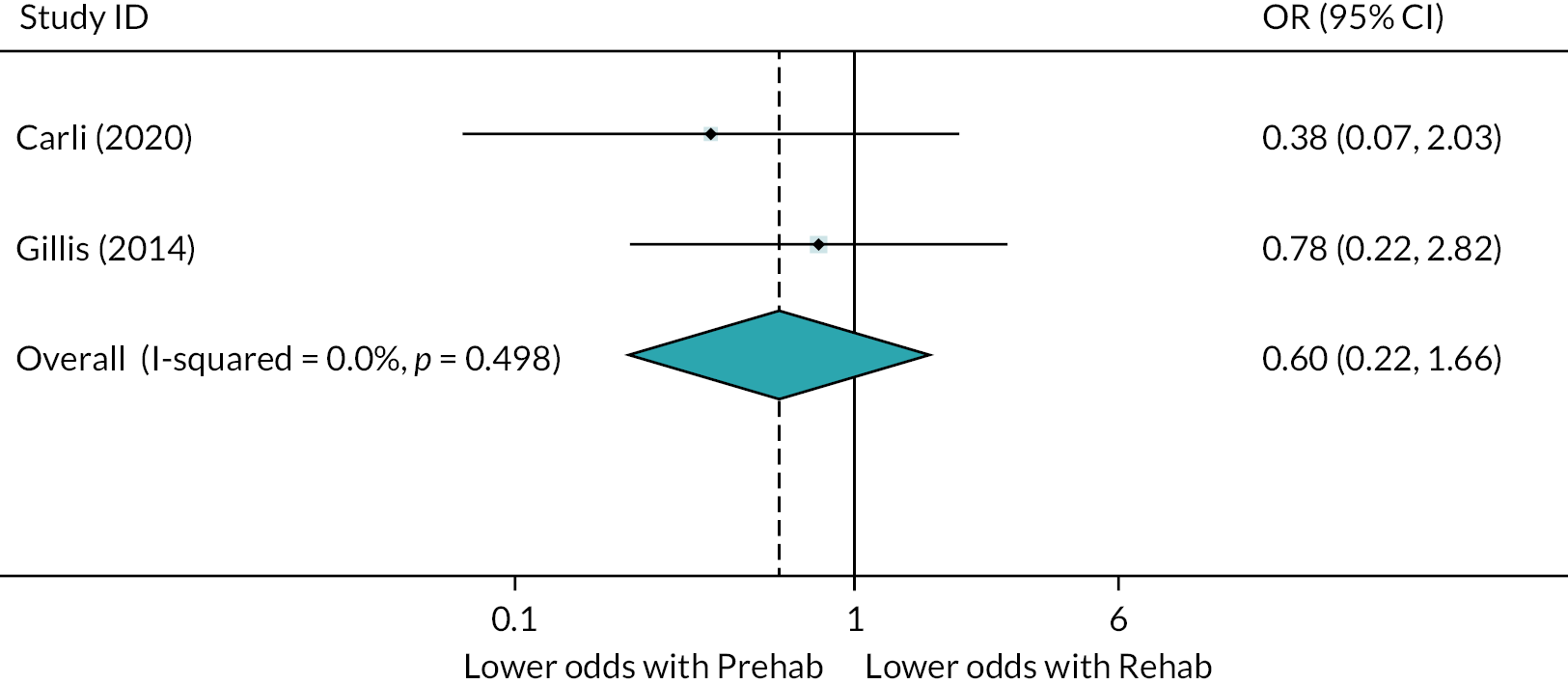
Effectiveness of Prehab interventions at improving patient-reported outcomes
Effectiveness of Prehab versus TAU
Report Supplementary Material 4, Table 5 displays data for patient-reported outcomes from the studies trialling Prehab interventions to improve recovery following colorectal surgery. In the three studies comparing Prehab interventions with usual care,54,56,67 it was possible to pool markers of physical activity after discharge. Meta-analysis of these three studies showed there was no overall effect on markers of physical activity with Prehab versus usual care (d = 0.12, 95% CI −0.15 to 0.39, p > 0.05; see Figure 18). There were no other opportunities to pool patient-reported outcomes.
FIGURE 18.
Forest plot showing the results of meta-analysis of the effect of Prehab vs. usual treatment on markers of physical activity following colorectal surgery.
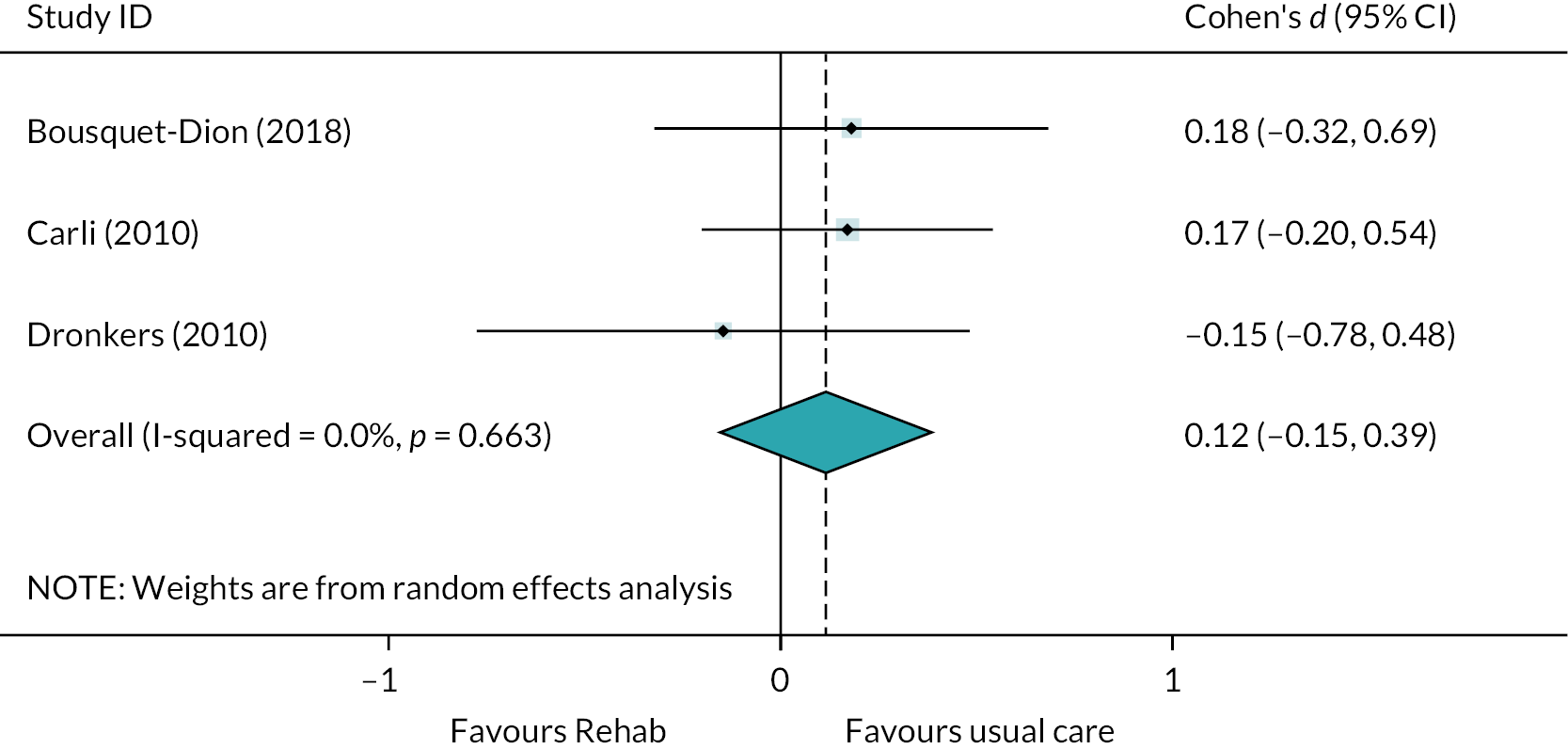
There were additional outcomes related to mental health, fatigue, quality of life, physical function and patient satisfaction. Carli et al. 56 reported anxiety and depression using the HADS, observing that Prehab was associated with lower levels of anxiety 4–9 weeks after surgery (d = −0.60, 95% CI −0.98 to −0.22; p = 0.001) but that depression was similar between groups. Dronkers and colleagues found that global health status and quality of life were similar between groups but that fatigue, assessed with the Abbreviated Fatigue Questionnaire, was greater in the Prehab group than the usual-care group, this difference associated with a large effect size (d = 0.70, 95% CI 0.06 to 1.35; p = 0.02). 67
Effectiveness of Prehab versus Rehab
It was possible to pool some outcomes reported in the two studies comparing patients randomised to a Prehab intervention with those randomised to Rehab. 55,59 Both studies used the SF-36, HADS and CHAMPS outcome measures to assess aspects of mental health, quality of life, social function, physical function and physical activity and included data at 8 weeks post surgery. 55,59 All results for individual outcomes are available in Report Supplementary Material 4, Table 5. Meta-analysis of outcomes at 8 weeks post-surgery indicates that both anxiety (d = −0.07, 95% CI −0.40 to 0.26; p > 0.05) and depression (d = −0.11, 95% CI −0.44 to 0.21; p > 0.05) on the HADS questionnaire were no different between Prehab and Rehab groups.
Meta-analysis of outcomes from the SF-36 at 8 weeks post surgery showed that Prehab was associated with an improvement in the Mental Component summary score when compared with Rehab (d = 0.38, 95% CI 0.05 to 0.71; p = 0.022). Results from the two studies were very similar, with no statistic heterogeneity (I2 = 0.0%). There was no difference in the Physical Component summary score between Prehab and Rehab groups (d = 0.08, 95% CI −0.25 to 0.41; p > 0.05).
The CHAMPS questionnaire was used in both studies to provide an indication of physical activity levels following surgery. Data were reported at 4 weeks post op by Carli et al. 55 and 8 weeks post surgery by Gillis and colleagues. 59 When pooling data from these studies, there was no overall difference in physical activity levels between those receiving Prehab versus those receiving Rehab (d = 0.07, 95% CI −0.25 to 0.40; p > 0.05).
There were no further opportunities to meta-analyse outcomes in the three studies comparing Prehab with Rehab after colorectal surgery. Additional outcomes were explored relating to additional domains of the SF-36 by Gillis and colleagues, with no differences between groups (see Report Supplementary Material 4, Table 5.)
Summary of evidence from trials seeking to improve recovery from colorectal surgery
There were 14 comparisons from 12 studies evaluating interventions to improve the recovery of older adults undergoing elective colorectal surgery. Interventions were either ERP (n = 7 studies) or Prehab interventions (n = 5) compared to either usual care or, in the case of two Prehab studies, Rehab. There were a number of examples of studies providing incomplete data or offering medians and ranges, which are not recommended to be used to impute means and standard deviations, and thus there were limited opportunities to pool data from these studies. 27
Where meta-analysis was possible, ERP studies were associated with a small reduction in LOS, without any influence on readmissions, and no effect on complications – despite a trend towards reduced complications. In terms of patient-reported outcomes, there was very poor reporting of outcomes that were purported to have been captured. There was also a heterogeneous array of outcomes across the available studies comparing ERP with TAU, such that only two studies measuring pain could be pooled. These showed no difference in pain between ERP and TAU groups. Despite this, a handful of analyses of PROMs in individual studies suggested that ERP was either associated with improved outcomes or was no worse than TAU. Only one study examined service utilisation by patients after discharge, finding no difference between groups.
When exploring the effect of Prehab on clinical outcomes, meta-analysis showed no effect on LOS, readmissions or complications compared to TAU or Rehab. The studies comparing Prehab with TAU offered few opportunities for meta-analysis. It was possible to pool data for markers of physical activity but no difference was observed between groups. One study reported an improvement in anxiety with Prehab, with another reporting increased fatigue following Prehab.
Three similar studies evaluated Prehab against Rehab, using similar outcomes and thus facilitating meta-analysis. While the anxiety and depression subscales of the HADS did not differ between groups in meta-analysis, there was evidence of an improvement in the Mental Component Summary of the SF-36 with Prehab. The Physical Component Summary score did not differ between groups, however, nor did physical activity levels.
Overall, there were limited opportunities to perform meta-analysis, and usually this was with a low number of combined studies. The available evidence suggests that ERP may be associated with shorter LOS without detriment to other clinical outcomes, and may lead to some improvement in the patient experience. Prehab interventions did not have an influence on clinical outcomes but may have some positive impact on patient mental health. However, evidence is very limited and should be interpreted with caution.
Evidence from trials seeking to improve recovery from cardiac surgery
Six RCTs evaluated interventions to improve recovery from cardiac surgery. 37,52,64,71–73,76 There were two Prehab interventions,52,71,72 two ERP interventions,37,73 one Rehab intervention64 and one discharge-planning intervention. 76
In the study by Arthur and colleagues, conducted in Canada, Prehab was compared to usual care. 52 Prehab was associated with reduced LOS (d = −0.67, 95% CI −0.92 to −0.41; p < 0.001) and improvements in the physical component of the SF-36 (d = 0.39, 95% CI 0.13 to 0.66; p = 0.04). There were no differences in the mental, social, general health, pain, vitality or emotional subscales of the SF-36.
Two papers report on the study by Rief and colleagues, one including data for LOS71 and one reporting on PROMs. 72 The trialled intervention was focused on managing patient expectations and developing psychological readiness for surgery. LOS was significantly shorter in the intervention group, associated with a large effect size (d = −2.52, 95% CI −3.12 to −1.92; p < 0.001). Readmissions and complications were similar between groups, although there was a near-statistically significant reduction in the odds of being readmitted in the intervention group (OR = 0.31, 95% CI 0.08 to 1.26; p = 0.09).
Rief and colleagues captured data for 10 PROMs, with results pointing to improvements in seven of these following the Prehab intervention. Scores for pain, disability, the SF-12 mental component, fitness for work, IPAQ-Physical Activity measure, cardiac anxiety, depression and personal control expectations on the Illness Perception Questionnaire were all improved and associated with large effect sizes in all instances (see Report Supplementary Material 4, Table 12 for details). 72
The Dutch study by van der Peijl and colleagues evaluated a Rehab intervention, compared with usual care. There were no differences in LOS, activity or functional independence between groups. 64
The two ERP trials evaluated very different approaches to improving recovery from cardiac surgery. Bennett et al. used a multimodal cerebral oximetry protocol, observing an improvement in LOS, with patients twice as likely to be discharged within 24 hours in the intervention group (OR = 2.14, 95% CI 1.15 to 3.99; p = 0.02). 37 There were also lower odds of patients experiencing worse functionality with the intervention (OR = 0.3, 95% CI 0.12 to 0.74; p = 0.01). Sadlonova and colleagues compared two active interventions with usual care, one of which was of interest to us – a combined psychological and multimedia intervention featuring bright-light therapy, noise reduction, music and virtual-reality headsets. 73 The intervention led to a moderate reduction in LOS (d = −0.62, 95% CI −1.14 to −0.09; p = 0.02) but had no effect on HRQoL or self efficacy expectations.
The discharge-planning intervention evaluated by King and colleagues involved assessment of patients’ readiness for discharge and reacting as appropriate, with the potential to initiate the discharge process sooner. 76 The intervention did not lead to a shorter length of stay, and there was no difference in the odds of being readmitted. While a survey revealed no difference in overall satisfaction, there was a statistically significantly lower overall health satisfaction score in the discharge-planning group (d = −0.72, 95% CI −1.36 to −0.08; p = 0.04).
Evidence from trials seeking to improve recovery from abdominal, pelvic, thoracic or upper abdominal surgery, or surgery to remove tumours at various sites
Evidence regarding abdominal surgery
Report Supplementary Material 4, Table 1 displays clinical outcome data from the two studies evaluating ERP interventions in older adults undergoing elective abdominal surgery, both comparing effectiveness versus usual care. 81,87 After imputation, the standardised mean differences for LOS for these two studies were available for comparison. Meta-analysis of these two studies showed a large reduction in LOS with ERP interventions, when compared with usual care (d = −0.87, 95% CI −1.29 to −0.46; p < 0.05). Heterogeneity was not statistically significant for this effect (I2 = 36.6%, p > 0.05), indicating consistency between the two studies.
Other clinical outcomes that were not eligible for meta-analysis for these two studies were as follows. Kapritsou and colleagues reported a 61% reduction in risk of experiencing a complication in the ERP group compared to TAU, but this difference was not statistically significant (OR = 0.39, 95% CI 0.14 to 1.04; p > 0.05). 81 Tagaki and colleagues saw a greater number of readmissions in the usual-care group although this difference was not statistically significant, and no deaths were reported in either group. 87
Although both studies described collecting PROMs, only Tagaki and colleagues provided data in a format allowing the calculation of an effect size. The authors reported a moderate improvement in quality of life for patients in the ERP group compared to those receiving usual care (d = 0.52, 95% CI 0.06 to 0.98; p = 0.03); however, wide CIs suggest there is uncertainty in the true effect. Kapritsou and colleagues reported decreased postoperative pain in the ERP groups, and no differences in stress or emotional response between groups. 81
Evidence regarding pelvic surgery
A single RCT was available which evaluated an intervention to improve recovery from pelvic surgery, and which collected data from PROMs. 58 This pilot study compared ERP with usual care, but reported results as medians with ranges, therefore it was not possible to calculate effect sizes for between-group differences. The authors reported that LOS was shorter and post-operative pain was lower with ERP. 58 Readmissions, complications, quality of life and satisfaction were reported to be similar between groups. 58
Evidence regarding thoracic surgery
One RCT compared Prehab with Rehab in patients undergoing thoracic surgery. 57 The authors found that LOS was similar between groups; however, there were improvements in the physical component (d = 0.61, 95% CI 0.19 to 1.02; p < 0.01), mental component (d = 0.43, 95% CI 0.02 to 0.84; p = 0.04) and total score (d = 0.51, 95% CI 0.1 to 0.92; p = 0.02) of the SF-36 when patients received Prehab. 57 There were no differences between groups when mental health, disease-specific quality of life and energy expenditure were assessed. 57
Evidence regarding upper abdominal surgery
Three RCTs evaluated interventions to improve recovery following upper abdominal surgery. 38,44,80 Two studies compared ERP with treatment as usual,44,80 and one evaluated Prehab compared to usual care. 38 Meta-analysis of the two studies evaluating ERP interventions showed that ERP was associated with a large reduction in LOS (d = −1.69, 95% CI −2.32 to −1.06, p < 0.001; see Figure 19A), while the odds of patients being readmitted following surgery was similar in both groups (OR = 0.61, 95% CI 0.27 to 1.38, p > 0.05; see Figure 19B). In the study by Jones and colleagues, there were two readmissions in the intervention group, none in the usual care group, and with one death in each group. 44 Quality of life was similar between groups in the study by Jones and colleagues, although no variance data were provided so we could not calculate an effect size. 44 Pain, sadness, stress and optimism were similar between groups in the study by Kapritsou and colleagues. 80
FIGURE 19.
Forest plot showing the results of meta-analysis of the effect of ERP vs. TAU on LOS (A) and odds of readmission (B) after upper abdominal surgery.
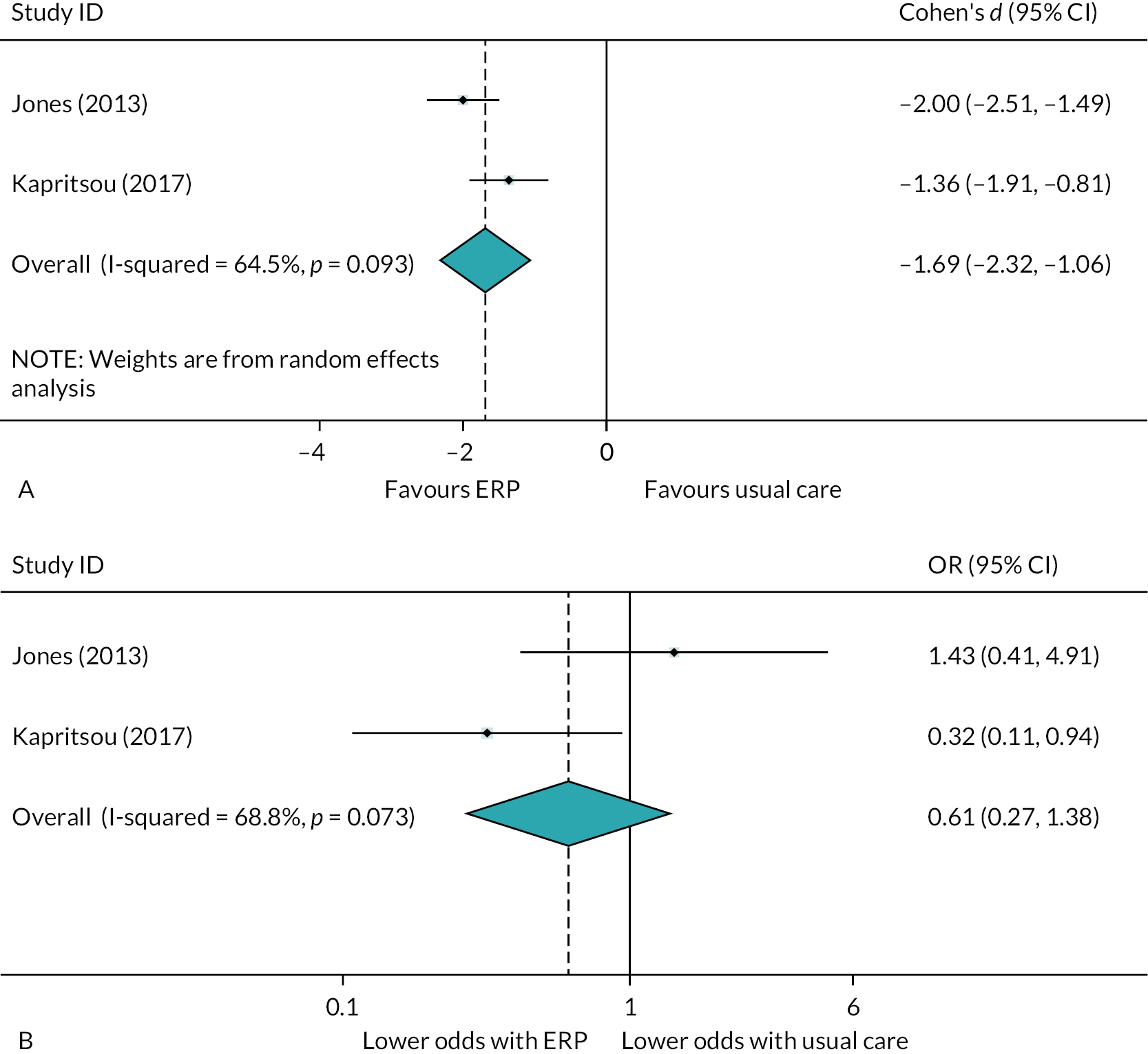
Complications
In the study comparing Prehab with usual care, both groups achieved similar scores for LOS, complications, readmissions, physical health, mental health and quality of life. 38
Evidence regarding surgery to remove tumours at various sites
Two RCTs investigated interventions to improve recovery in patients undergoing surgery for tumour removal. 61,62,74 One study evaluated an information booklet and diary,74 and the other a Prehab intervention. 61,62 In the Prehab study, Hempenius and colleagues collected information on LOS, readmissions, complications, mortality, care dependency, the MMSE and SF-36, return to pre-operative living situation, and the level of care assistance required following discharge. 61,62 Fewer patients in the experimental group were able to return to their preoperative living situation (11.8% fewer). There were no significant differences between groups for any other outcome.
In the study evaluating the information booklet and diary, LOS was shorter in the experimental group (d = −0.22, 95% CI −0.38 to −0.07; p = 0.005), while complications, readmissions and health-related quality of life were similar between groups. 74
Summary
Through extensive database and supplementary searches, we identified 125 studies pertinent to the research question: what is the impact of multicomponent interventions to enhance recovery and/or reduce LOS for older adults admitted for planned procedures on PROMs and service utilisation? We took the pragmatic decision to prioritise RCTs from any high-income country, and studies of any includable design conducted in the UK. This allowed us to synthesise the top-level evidence, and that with most relevance to the UK setting. This led to full critical appraisal and synthesis of 49 studies, including seven non-RCTs from the UK.
The largest procedural categories were studies relating to LLA (n = 22 studies) and colorectal surgery (n = 12), and the most common intervention categories were enhanced recovery protocols (ERPs) (n = 28) and prehabilitation (Prehab) (n = 16). The evidence for LLA suggested that ERP interventions were associated with reduced LOS without detriment to other outcomes, and some minimal evidence that PROMs may also be improved. However, Prehab interventions had minimal effect on LOS, other clinical outcomes or PROMs.
The evidence for colorectal surgery came from 12 RCTs, seven evaluating ERP interventions and five evaluating Prehab. Data were poorly reported, offering few opportunities to pool data, but there was potted evidence that ERP interventions were associated with small reductions in LOS and some improvement in PROMs. As with the evidence for LLA, Prehab interventions had minimal effect on outcomes compared to usual care.
The remaining evidence was characterised by small groups of two or three similar studies, which were narratively summarised. A handful of individual trials showed improvements across outcomes; however, there was not a substantial body of evidence to be able to recommend particular interventions related to particular categories of surgical procedures.
See Chapter 6 for further discussion of findings.
Chapter 3 Experiences of patients, family/carers and staff of multicomponent interventions to enhance recovery and/or reduce hospital stay
This chapter details the methods and findings from the systematic review of qualitative research, intended to answer research question 2: What are the experiences of patients receiving multi-component interventions to enhance recovery and/or reduce LOS, their family and carers and staff involved with delivering care within these interventions?
For definitions of key terms in this chapter, please see List of abbreviations.
Methods
Identification of evidence
Search strategy
For the systematic review of qualitative studies, the same search terms for the quantitative search were used but we replaced the effectiveness study type filter with a qualitative study type filter. The qualitative study filter was adapted from the ‘Best Optimisation of Sensitivity and Specificity’ qualitative filter developed by Wong and colleagues, with adaptations to include additional qualitative terminology, specifically, indexing terms (e.g. Medical Subject Heading in MEDLINE) which were unavailable when Wong and colleagues developed the filter, and the free-text terms ‘focus group’, ‘perspective’, ‘perception’, ‘themes’ and ‘thematic’. 22
The search was developed by SB in conjunction with the review team and stakeholders using MEDLINE (via Ovid) and adapted for use in other databases. The selection of bibliographic databases was tailored for the identification of qualitative studies, noting that surveys and guidance recommend using MEDLINE and CINAHL,92,93 and that Embase is considered less useful. 92 The full set of bibliographic databases searched included: MEDLINE ALL and HMIC (both via Ovid), AMED and CINAHL (both via EBSCO) and ProQuest Dissertations and Theses (via ProQuest). Searches were run in June 2021. As this review was not attempting to derive a precise measure of effectiveness based on all the relevant evidence (i.e. an aggregative synthesis), updated searches were not run. Due to the high quantity of data identified through initial searches, the identification of further studies was unlikely to significantly alter the main messages derived from the synthesis. The synthesis was based on a configurative approach, which is more interpretive and based on an appropriate sample. Bibliographic database search results were exported to EndNote 20 (Clarivate Analytics, Philadelphia, PA, USA) and de-duplicated using manual checking and the EndNote de-duplication tool.
Reference lists of all included studies were checked and forward citation searching was completed for all included studies (DC, DK) using the Science Citation Index (Web of Science, Clarivate Analytics) and Scopus (Elsevier). The results of forward citation searches were exported to EndNote 20, and reference-list checking was conducted using Microsoft Excel spreadsheets to document potentially useful studies thus identified. We further extended the supplementary searches to include checking the reference lists of topically similar systematic reviews identified by the searches. Evidence suggests this to be a potentially fruitful approach due to the imprecise use of terminology and poor-quality indexing of qualitative studies in bibliographic databases. Due to the high number of studies identified through bibliographic database searches and supplementary searches, we did not search Google Scholar or relevant websites, which represented a deviation from the protocol.
Inclusion criteria
We included papers reporting primary qualitative research exploring experiences of, or attitudes towards, multicomponent interventions which aim to enhance recovery and/or reduce length of hospital stay of older adults following admission for a planned procedure. This included the views of patients, family, carers or health/social care staff. Further details of the definitions used to describe eligible populations and interventions can be found in Chapter 2.
Study selection
After completing a calibration exercise on a sample of articles (n = 100), the inclusion criteria were applied to the title and abstract of each article independently by two reviewers (DK, DC), with disagreements resolved through discussion or referral to a third reviewer as needed. Full texts were screened in the same way (DK, DC). The screening was supported by EndNote 20 (Clarivate Analytics, Philadelphia, PA, USA).
Data extraction
Summary data were extracted for all included studies by one reviewer (DK, DC) and checked by a second (DK, DC) using Microsoft Excel 365 (Microsoft Corporation, Redmond, WA, USA). These data included information on study author, date and aim, country, study focus, type of publication, study design, participants receiving the intervention and providing their views and the name and aim of the intervention received. Extracted data also included details on the type of data collected and qualitative analysis conducted, the quantity of data available for qualitative synthesis, and a summary of the themes reported within each article.
In a deviation from our protocol, we used these data to systematically prioritise a selection of studies for full data extraction, quality appraisal and synthesis. This decision was based on the number of included studies being higher than anticipated, and the need to maintain the quality of the synthesis to ensure the review was delivered within the time-period available. The number of studies representing the voices of families, carers and staff was much smaller than the number of studies representing the views of patients, hence all were included in the synthesis. Prioritisation of the studies exploring patient views was based initially on the quantity and richness of first- and second-order data available for synthesis. Further studies were then purposively sampled to include clinical procedures, interventions to reduce hospital LOS, and participant experiences under-represented in the prioritised studies.
First- and second-order construct data relevant to research question 2 were extracted from the results and discussion sections of each prioritised article by one reviewer (DK) using Microsoft Word 365 (Microsoft Corporation, Redmond, WA, USA).
Quality appraisal
Quality appraisal was conducted alongside full data extraction, which included further detail regarding participant and intervention characteristics and study methods, and was undertaken by one reviewer and checked by a second (DK, DC) using Microsoft Excel. Quality appraisal was undertaken on the prioritised studies using an adapted version of the Wallace Checklist using the same method. 94,95 See Appendix 3 for details of summary and full data extraction.
Synthesis
Descriptive data summarising characteristics of participants, interventions and study methodology were tabulated and described narratively.
Synthesis of the first- and second-order data representing experiences of patients, families, carers and/or staff followed the principles of meta-ethnography as outlined by Noblit and Hare (1998). 96–98 This method focuses on developing new interpretations, or third-order constructs, applicable across all included studies through reciprocal translation and refutation. This process requires the identification of patterns or common themes, with refutation requiring the explanation of any findings which contradict these.
The process of meta-ethnography applied to the studies included in this review is outlined below.
Familiarisation
All included studies were read and re-read so that reviewers could familiarise themselves with their content (DK, DC, LS). This process began during full-text screening and continued throughout data extraction and synthesis.
Determining how studies relate to one another
Summary descriptive data from all studies were tabulated, enabling comparisons to be made across included studies in terms of patient characteristics, who is being interviewed, intervention received, type of qualitative analysis, and quantity and quality of qualitative data available for synthesis. The summary of themes also allowed for early exploration of similarities across studies.
Reciprocal translation
First- and second-order construct data were extracted from the studies with a high quantity of interpretative data into a Microsoft Word document by one reviewer (DK), who developed a list of descriptive ideas and concepts seen within each study. These ideas were discussed and checked by other members of the review team (LS, DC). The lead reviewer (DK) then used this list to form a descriptive coding framework within NVIVO, which was used to conduct line-by-line coding of papers with high quantity of relevant data. The process of coding this subset of studies was divided between three reviewers (DK, LS, DC). The coding conducted in a sample of 12 studies was checked for consistency by a second reviewer (DK).
A process of purposive sampling was then conducted for the articles not yet entered into the synthesis. 99 This process was achieved through discussion amongst members of the review team (DK, DC, LS) and sought articles which provided experiences of:
-
interventions or patient groups already represented in the quantitative systematic review but not yet included in the qualitative synthesis
-
types of interventions or reasons for admission not yet seen
-
participants groups whose views not yet seen
-
themes, experiences, or ideas not yet seen.
The papers identified through purposive sampling were then coded using the existing coding framework by one reviewer (DK). The stages at which different papers were entered into the coding framework is summarised below in Table 4.
| Stage of synthesis | Articles included |
|---|---|
| 1. Synthesis of articles with a large volume of interpretative findings | N = 32100–129 |
| 2. Purposive sampling: articles representing views of patient populations, interventions, or experiences not yet represented in synthesis | N = 590,130–133 |
| 3. Articles with lower quantity of descriptive data: not included in the synthesis | N = 8134–141 |
Similar concepts and ideas were merged in an iterative process to form themes, with existing coding being checked where this process yielded new interpretations or ideas (DK). Conceptually similar themes were then grouped together to form overarching constructs (DK). Throughout this process, data which refuted or challenged developing themes were explored and considered within the evolving synthesis. The synthesis was discussed with members of the review team (MN, LS, DC, SF) throughout its development.
Creating a line of argument
A line-of-argument is a model or theory which aims to summarise the relationship between the overarching constructs and contributing themes generated through the synthesis and the concepts contained within these. Here it is intended to capture the experiences of patients, their families or carers and staff of interventions intended to reduce LOS. The line-of-argument was developed by one reviewer (DK) and refined through discussion with the review team, clinical stakeholders and the patient and public involvement (PPI) group.
The stages of meta-ethnography outlined above, whilst conducted in a linear fashion, overlapped with one another in an iterative process. For further information regarding how stakeholder and patient/public involvement influenced this process, see Chapter 5.
Results
Study selection
A summary of the searching and screening process used to identify eligible articles is shown in the PRISMA diagram provided in Figure 20. Bibliographic database searches identified 6172 records. Following de-duplication, the title and abstracts of 4820 bibliographic database records were screened. Full texts were sought for 298 records; 263 of those were for records identified through bibliographic database searches and 32 identified via other sources. Eight records could not be retrieved, resulting in the full text of 287 records being screened. Two hundred and forty-four records were excluded for the reasons provided in Figure 20. Reasons for exclusion for each article are provided in Report Supplementary Material 1, Table 2. Forty-two studies (43 articles) were eligible for inclusion in this review. 90,100–141
FIGURE 20.
PRISMA diagram – review of qualitative evidence.
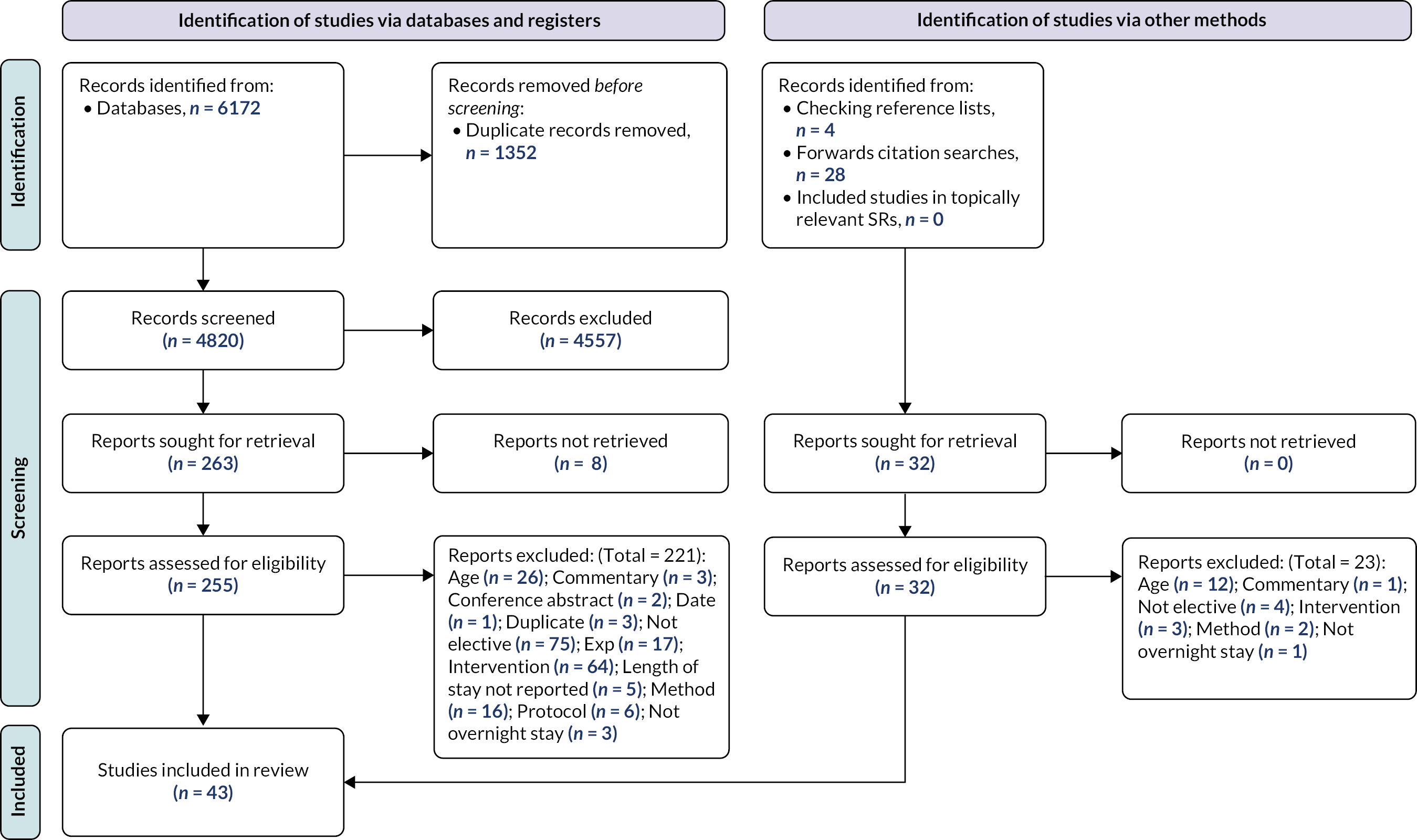
Study characteristics
Study overview: all included studies
Sixteen of the included studies were conducted within the UK,90,100,101,107,109,116,117,119,120,125,128,130,133–135,137 eight studies (nine papers) were conducted in Denmark,103–105,123,124,126,132,136,141 five studies were conducted in Australia,112,113,118,121,139 three studies in Norway,114,138,140 two studies were conducted in Canada,107,129 two in Sweden,102,122 two in the Netherlands,127,131 two in the USA,108,111 with one study being conducted in Italy,110 and one in Finland. 115
Enhanced recovery protocols (ERPs) were the most common intervention that participants were asked for their views or experiences on (n = 29 studies). 90,100,102,103,105–110,113–116,118,120,122–128,130,132,133,136,139–141 Other interventions for which views were sought included Rehab programmes (n = 4),101,129,135,137 supported discharge (n = 2)131,138 and early discharge (n = 2). 111,121 The following interventions were also each evaluated by one study: CGA,117 case management within a fast-track pathway,104 Prehab119 and staff mix,112 with one study not clearly defining their intervention. 134
Participants providing their views included patients (n = 31 studies),90,100,102,108–110,113–116,119–128,130–141 staff (n = 5),103,112,117,118,129 patients and staff (n = 2),101,107 carers (n = 3)104,105,111 and patients and carers (n = 1). 106 Interviews were the most common method of data collection (n = 37 studies);90,100–111,113,115–126,128,130–133,135–141 interviews were accompanied by observation in two studies. 105,117 Four studies collected data using focus groups112,114,127,134 and one study used interviews and focus groups. 129 Further summary details including methods of analysis, quantity of relevant data and summary of main themes for each of the included studies are provided in Appendix 3.
Below is a summary of the key characteristics of the studies prioritised for synthesis using meta-ethnography.
Participant characteristics
Thirty-four studies (35 papers) were prioritised for synthesis, including studies from the UK (n = 13),90,100,101,107,109,116,117,119,120,125,128,130,133 Denmark (n = 6),103–105,123,124,126,132 Australia (n = 3),112,113,121 the Netherlands (n = 2),127,131 Canada (n = 2),106,129 the USA (n = 2),108,111 Sweden (n = 2),102,122 Finland (n = 1),115 Italy (n = 1)110 and Norway (n = 1). 114 We prioritised all of the studies representing the views and experiences of staff (n = 7) and carers (n = 4) for synthesis using meta-ethnography. 96–98 We also prioritised 25 studies which represented patient experiences. 90,100–102,106–110,113–116,119–128,130,132,133 The total number of individuals who participated ranged from 5113 to 41. 117 The most common reason for patient admission was total hip arthroplasty (THA) and/or total knee arthroplasty (TKA); nine studies included patients admitted for hip and/or knee replacement,102,103,105,112,115,116,123–125,127,129 six studies included patients admitted for THA,90,104,106,113,119,121 and two studies included patients admitted for unilateral knee arthroplasty (UKA). 101,114 Seven studies focused on patients admitted for colorectal surgery,118,122,126,130–133 with one study representing patients admitted for the following reasons: gynaecological cancer surgery,100 hysterectomy,120 lung cancer surgery,107 saracolpopexy,108 bowel surgery,109 pancreatic surgery,110 coronary artery bypass graft (CABG) surgery,111 cancer surgery117 and liver resection. 128
Further details regarding the sample included in the prioritised studies, including mean age, percentage of female participants, ethnicity and socio-economic status and inclusion criteria, can be found in Appendix 3.
Intervention characteristics
Of the 34 studies (35 papers) prioritised for synthesis, the most common interventions participants received were fast-track, ERP or ERAS pathway (n = 26 studies),90,100,102,103,105–110,113–116,118,120–128,130,132,133 or rehabilitation (n = 2). 101,129 Single studies sought views on the following interventions: case management,104 CGA,117 early discharge,111 a perioperative care and ehealth programme,131 prehabilitation119 (Orpen) and staff mix. 112
Eight of these interventions were delivered alongside a comparator comprising usual care,90,101,104,106,108,128,131,132 key features of which included standard post-operative physiotherapy (n = 1),101 treatment as usual, case management and information (n = 1),104 usual care with placebo website (n = 1)131 and next day discharge (n = 2). 106,108 Two studies sought the views of participants within the treatment as usual condition. 106,133
Overall, interventions were poorly described, with 11 studies providing no, or minimal, description of the intervention received by participants. 100,102,106,109,111,113,122,125–127,129 Two studies provided details regarding flexibility of delivery of the intervention,101,121 four studies made reference to staff receiving training to deliver the interventions,101,104,130,133 and four studies made clear reference to the use of an intervention manual. 101,104,130,131 Information on adjuvant treatment was provided by four studies. 107,108,131,132
Intervention recipients included patients alone (n = 20),90,100,101,103,108,110,112,115–121,128–133 patients and carers (n = 5),105–107,114,123,124 or family/carers alone (n = 1). 104 Eight studies did not report this information. 102,109,111,113,122,125–127
Interventions were predominantly received in hospital (n = 20),90,103–108,110–112,114,117,118,121,128–133 including one intervention delivered via a website/mobile phone application,131 and one delivered in a pre-op hospital ward. 121 Seven studies reported the interventions had a pre-specified LOS,90,103,106,108,113,115,123,124 three studies reported that the intervention had no pre-specified LOS,112,117,132 with the remaining studies not reporting this information (n = 24). 100–102,104,105,107,109–111,114,116,118–122,125–131,133
One intervention was delivered jointly in the hospital or community,116 and one delivered both at hospital and in the patient’s home. 123,124 Ten studies did not report the location of intervention delivery,100,102,109,113,115,120,122,125,126 but it is reasonable to assume this was the hospital for eight of these. 100,102,109,113,115,120,125,127 Two interventions were delivered in the patient’s home. 101,119 Intervention characteristics for each study are reported in Appendix 3.
The majority of patients were discharged home, although this was not clearly stated in eight studies. 102,108,113,114,121,123,124,126,128 Alternative discharge destinations included temporary rehabilitation centre prior to home (n = 1),111 home or inpatient rehab (n = 1),112 and home or temporary nursing home (n = 1). 127 One study did not report this information. 129
Interviews were the most common method of data collection (n = 29). 90,100–111,113,115–126,128,130–133 Interviews were accompanied by observation in two studies. 105,117 Three studies collected data using focus groups,112,114,127 and one study used individual interviews and focus groups. 129 Quantitative data were collected alongside qualitative data collection in seven studies. 101,108,115,116,127,131,132 Further detail regarding the aims of each study, types of analysis used and recruitment method can be found in Appendix 3.
Quality appraisal
Of the 35 prioritised papers quality appraised using the Wallace checklist, the number of items on which papers scored positively ranged from eight (n = 2),106,117 to the maximum number of 14 (n = 14),110,114,115,119,124 with the mode and medium being 12 (n = 10). 90,103,105,108,109,116,126,128,130,131 The items of the checklist on which papers scored most positively were: clear reporting of the research question, appropriateness of study design, rigorous data collection, appropriate claims to generalisability, and addressing of ethical issues.
Thirty-four papers reported findings which were substantiated by the data, with only one paper rated as ‘Can’t tell’. 127 Thirty-three papers provided evidence that data analysis was rigorously conducted, with two papers awarded a ‘Can’t tell’ rating. 111,127 An adequate description of context or setting was also provided by the majority of articles (n = 31), with only three articles scoring ‘No’,103,106,117 and one article rated as ‘Can’t tell’. 125
Items of the Wallace checklist on which articles scored most poorly included the reporting of the theoretical or ideological perspective of the author. Only 14 papers were awarded a rating of ‘Yes’ for these two items. 103–105,109–111,114,115,118,119,121,123,124,126 As a consequence, it was not possible to determine if the ideological perspective had influenced the study design, methods or findings for these papers. Interventions of interest were also poorly described across prioritised studied, with only 18 papers reporting this information. 90,101,104,107,108,110,114–119,121,123,124,128,130,131 For the scores on individual items of the Wallace checklist for each paper, please see Appendix 5.
Qualitative synthesis
The translation of first- and second-order data across the 34 studies (35 articles) prioritised for the framework synthesis resulted in six overarching constructs:
-
home as the preferred place for recovery;
-
feeling safe;
-
individualisation of a standardised programme;
-
essential care at home;
-
taking responsibility; and
-
outcomes.
A number of third-order themes related to each construct. Figure 21 details the line-of-argument synthesis, illustrating the relationship between the overarching constructs and the themes contained within them.
FIGURE 21.
Line of argument.
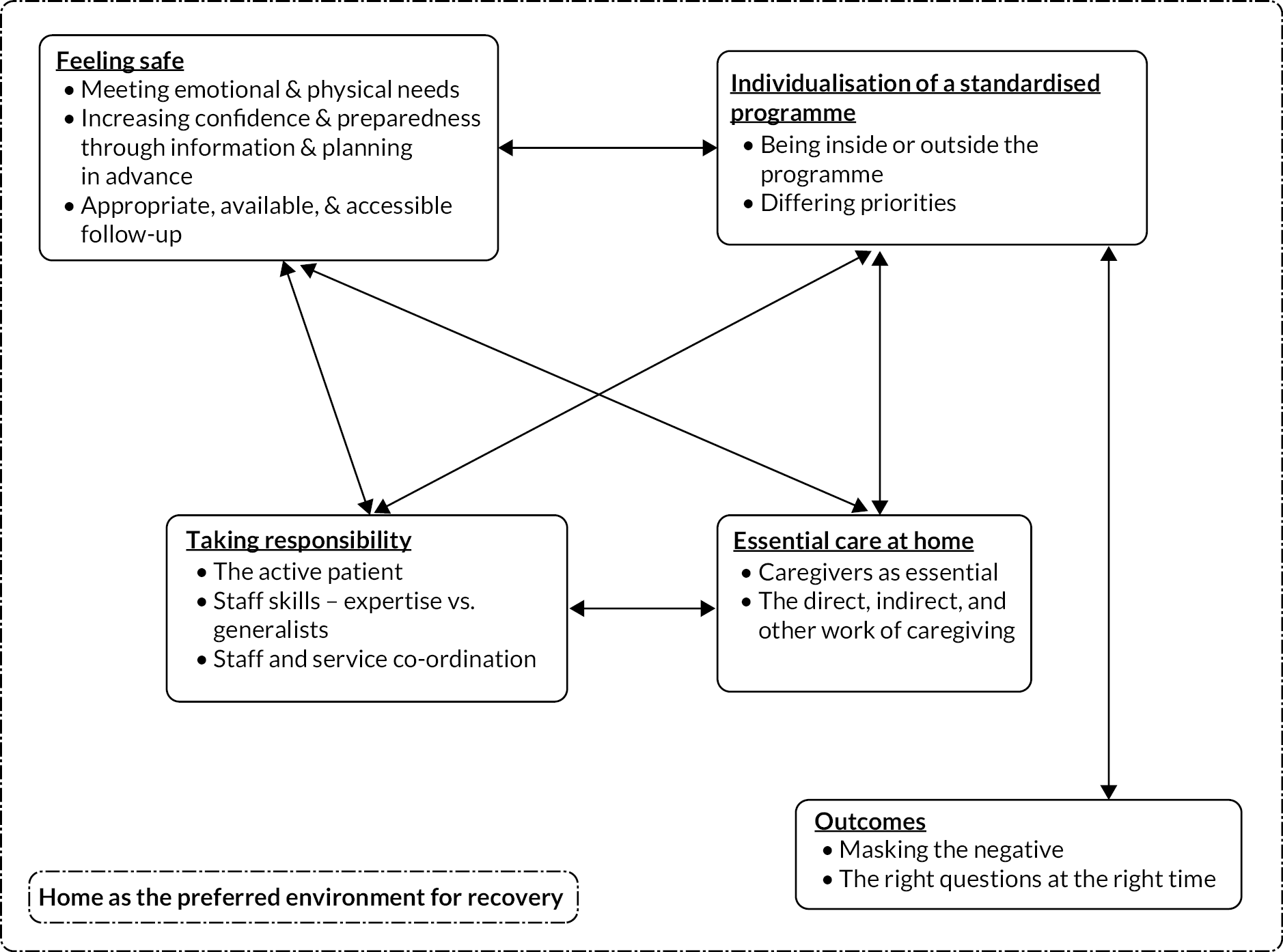
This section will first describe each of these constructs in turn, and the themes which relate to them, then describe the line of argument that suggests how they are related to one another. Appendix 4 provides an overview of the themes which relate to each construct, and the articles contributing to each theme. Full details of the first- and second-order data which contribute towards each theme can be found in Report Supplementary Material 5.
Construct: home as the preferred environment for recovery
Data from 22 studies (23 articles)90,100,101,103,104,106,108,109,111,113,114,116,121–125,127,128,130,132,133 indicated that for the majority of patients, carers and staff in included studies, home was the preferred environment for recovery. This concept links to content from the other five constructs: for example, being at home means home care becomes essential (‘Essential care at home’), follow-up must be available and accessible for people to feel safe (‘Feeling safe’) and requires patients to be active in their care (‘Taking responsibility’). Home was a familiar environment in which to recover, promoting speed of recovery and helping patients conserve resources and access support. For those for whom home is not the preferred environment, or with concerns pre-discharge, discharge home increases feelings of vulnerability, as opposed to empowerment.
Home was the preferred environment for recovery for a number of reasons. Firstly, seven studies (seven articles)100,108,114,121,123,128,130 indicated recovery was felt to be easier in a more familiar place:
The all round business of being able to get and move more easily at home, I mean there is no doubt that I began to recover the minute I got home.
[Patient, gynaecological cancer surgery]100
Seven studies (seven articles) suggested that being at home could speed or enhance recovery. 100,101,108,121,125,128,130 This could be through enhancing their feelings of control through taking charge of their own eating habits,108 or helping them feel more relaxed,100 or to sleep better. 125 This is illustrated by one 69-year-old patient discharged home following uncomplicated laparoscopically assisted left hemi-colectomy:
I’m a firm believer of being at home rather than in the hospital purely because of the ability to do what I want rather than to be part of a routine.
(Patient, colorectal cancer surgery)130
Recovering at home also allowed patients to conserve their resources, as completing activities to promote recovery could be tiring. This is illustrated by a patient talking about their recovery knee arthroplasty surgery:
I would have had to ask people to take me … and they’ve got to wait around …. It’s exhausting doing those exercises … and then having to sit in the car … sitting in that car is exhausting when you got a bad knee.
(Patient, knee arthroplasty)101
The above quote also illustrates how reliant patients can be on others for support post-discharge (see construct: ‘Essential care at home’). First- and second-order construct data from four studies (four articles) suggested that being at home could provide more social support, which was thought to enhance or aid recovery. 101,121,125,128 This is illustrated by a quote from patient who had undergone an open liver resection:
I have a very caring wife which makes a big difference I think.
(Patient, liver resection surgery)128
Second-order data from six studies suggested that, for some patients, being at home could psychologically signal recovery. 100,109,121,125,128,133 For example, Vandrevala et al. (2016)128 suggested that early discharge in particular ‘sent a powerful message to patients that they were on the path to recovery’ because they were at home, not in a hospital ward.
Home also provided a more restful recovery environment. First- and second-order data from 12 studies (12 articles) indicated that the risk of catching infections, noise leading to lack of sleep, lack of choices, and lack of privacy within the hospital environment also contributed to patients’ desire to recover at home:102,103,106,108,110,114,116,121,125,128,130,133
I was happy …. Firstly, it is nice to get back home. You always recover quicker at home. Secondly, rightly or wrongly hospital is a fairly dangerous place to be if you are going to catch anything.
(Patient, colorectal cancer surgery)130
However, data from seven studies (seven articles) showed that patient (and carer) preference for recovering at home was contingent on patients feeling well and feeling safe (see construct: ‘Feeling safe’). 106,108,109,113,128,130 Where these needs weren’t met, they preferred a longer hospital stay. For example, this patient discusses how they would prefer to stay in hospital where they felt safe because they could immediately access medical care if needed:
… like in hospital I feel safe because I know I just have to ring a buzzer and someone will be there. At home it’s not going to be like that ….
(Patient, THA)113
As discussed further within the theme ‘Appropriate, available and accessible follow-up’, first- and second-order data from seven studies (seven articles) indicated some patients worried about going home in case there was a problem, or found it difficult to be at home when there was a problem and they did not know where or how to get help. 106,108,109,113,128,130 This wasn’t just an issue for more serious or life-threatening complications. Blazeby et al. 130 suggested that even minor complications made patients feel more worried at home. Worry about potential complications is illustrated by one patient who voluntarily elected for a longer hospital stay:
That was my choice [...] I could have gone home, but at 70 years old, I just thought it might be a good thing to choose [to stay].
(Patient, sacrocolpopexy)108
However, not all patients who experienced complications wanted to return to hospital, with Hovik et al. (2018)114 describing how some patients wanted to stay at home despite dealing with adverse events such as severe nausea or high blood pressure. This indicates a need for personalised care as different patients may need different levels of support with complications at home, for example anxious patients may need more support and a named person they can contact with concerns, whereas others may need staff to contact them to ensure their health needs are being best met at home. These issues will be further discussed in the constructs ‘Individualisation of a standardised programme’ and ‘Feeling safe’.
Construct summary: home preferred place for recovery
This construct illustrates how, for some patients, home can provide a safe and familiar environment which promotes recovery through enhancing feelings of control and increasing access to required support. However, discharge home also contributed towards feelings of vulnerability in patients, with some preferring to recover in hospital if their needs for security and support at home were not addressed. This construct links with all others developed in this analysis, so the idea of ‘home as preferred’ will be interwoven in the descriptions of other constructs.
Construct: feeling safe
Thirty-three studies (34 articles) provided data illustrating how the feeling of safety was very important to both patients and carers, regardless of whether they were judged physically or medically to be safe, especially with regard to discharge. 90,100–116,118–133 Three themes contributed to this construct: ‘Meeting emotional and physical needs’, ‘Increasing confidence and preparedness through information and pre-op care’ and ‘Follow-up appropriate, available and accessible’. These themes detail different elements which may influence feelings of safety for patients and/or carers. Alongside these issues, the structure of the programme could be comforting or reassuring, and assist with feelings of safety. 104,108,110,128 However, some found the plan too rigid, which made them feel unsafe due to their individual needs not being met. This will be discussed further in the construct ‘Individualisation of a standardised programme’.
Theme: meeting emotional and physical needs
Twenty-three studies (23 articles) highlighted that meeting patients’ (and carers’) emotional and physical needs was linked to their feelings of safety and their overall experience of the programme. 90,100,101,105,107–111,113,114,116,119,120,124–126,128,130,133
First- and second-order data from five studies (five articles) explored how meeting emotional needs not only helped patients and carers feel safe, but also supported the delivery of intervention components which aimed to promote physical recovery. 100,102,112,113,120 Phillips et al. 120 described how patients did not necessarily want to mobilise, but did so with encouragement from staff, with one patient from the study discussing how this physical activity had a psychological component:
Yeah, I think a lot of it though is mental, in your own mind, that right, I’m going to do this.
(Patient, non-cancer gynaecological surgery)120
This suggests appropriate support can increase patient confidence and overcome feelings of vulnerability, and that physical and emotional health cannot be considered in isolation from one another. This idea is explored in other themes within this construct and in the ‘Taking responsibility’ construct. The below quote from an advanced nurse practitioner highlights the importance that patients place on emotional support when giving feedback about their intervention:
Patients … who’ve been through the SOLACE project, they couldn’t say nicer things … The difference it’s made …. Not just physically but the social and psychological support that becomes part of it … I think that’s clearly been a great help to a lot of people.
(Advanced nurse practitioner, lung cancer surgery)107
First- and second-order data from four studies (four articles) suggested the extent to which patients felt their emotional needs, such as a feeling of being cared for, safety, or general wellbeing, had been met by interventions varied. 107,108,116,126 Evans et al. (2021)108 described that the ERP felt rushed to some patients and ‘wasn’t perceived as an advance in care, but as an absence of care’, which is also illustrated by the quote below from a patient from Thomsen et al.:126
There was no room for questions and one is also a bit fearful. I don’t just need general information or that the doctor gives his specific message. I also need to be asked: how are you feeling.
(Patient, colorectal cancer surgery)126
The above quote suggests that, in order to support emotional needs, the intervention needs to be paced according to the needs of the patients and give them an opportunity to ask questions. Meeting emotional needs is therefore also linked to the theme of ‘Increasing confidence and preparedness through information and planning in advance’ within this construct, and the construct of ‘Individualisation of a standardised programme’.
While some patients felt their emotional needs were met, data from three studies (three articles) suggested patients could mask negative experiences, such as feeling their needs were not met, in their initial feedback (see construct: ‘Outcomes’). 90,109,125 All the patients on an accelerated discharge pathway following THA in the study conducted by Hunt et al. (2009)90 had criticisms regarding feeling overlooked by staff or uninformed, which they also tried to justify, a problem which was echoed by patients in Fecher-Jones et al.’s study:109
I suppose really the nurses have their own lives to lead and then they often, you think they’re neglecting me you know, I wish they’d come and do something.
(Patient, THA)90
I know they were ever so busy, they did plenty medically, but little things, you know, for comfort, they didn’t.
(Patient, colonic resection surgery)109
The second quote also suggests that staff may find it difficult to identify when patients are struggling (and provide appropriate support) when their workloads are high and they do not have time to check in with them in this way.
Sixteen (16 articles) indicated how a good relationship with medical staff did make a difference in whether patients or carers felt cared for emotionally as well as physically. 90,100–102,104,105,107,109,110,113,114,116,120,124,125,133 At times this was merely knowing who it was that would be medically caring for them, suggesting some basic familiarity with staff could contribute to feeling safe. This is illustrated by the below quote from a LLA patient:
When the doctors gave information I became more confident, just to put faces to some of the staff ....
(Patient, LLA)124
Alternatively, data from four studies (four articles) suggest patients and/or carers found it beneficial having a specific staff member they could build a strong relationship with, like a co-ordinator. 101,104,107,113 This concept relates to those discussed within the theme of ‘Appropriate, available and accessible follow-up’, as patients knew who to contact when they had concerns:
And she always said that if you have any problems just call me, right? And that has been very comforting. I will admit to that. We are not spring chickens any more.
(Carer, spouse of THA patient)104
However, data from six studies suggested it was not the member of staff’s seniority or particular role in the team which was of importance, but their ability to empathise, listen and connect to the patients and/or carers. 101,104,107,113,120,133
He’s [not a physiotherapist] bless him … but he’s also had injuries himself so he knows, he knows what it’s like to have a lot of pain … he’s an extraordinarily empathetic young man.
(Patient, knee arthroplasty)101
Theme: increasing confidence and preparedness through information and planning in advance
Data from 28 studies (29 articles) support this theme. 90,100,102–108,110–116,118–120,122–126,128,129,131–133 Below, the importance of pre-op care and provision of accessible and timely information is that it helps patients and carers to feel more confident and better prepared, and aligns their expectations with medical expectations. This theme also discusses the role of consistency and format of information, and discharge planning in supporting patients and carers to feel safe.
First- and second-order construct data from 13 studies (13 articles) highlighted how clear information helped patients and/or carers to feel more confident about the approaching procedure, and could reduce anxiety, linking to the idea of feeling safe. 100,102,105,108,110–112,114,116,119,122,124,129 This is illustrated by patients describing their experiences of receiving information before sacrocolpopexy surgery:
Patient 1: They made [patient instructions] clear orally as well as in the written directions …. So, I felt very comfortable going into the surgery.
Patient 2: I did not feel tense, I did not dread, I was not afraid.
(Patients, sacrocolpopexy surgery)108
Here, one patient indicates their appreciation for repeated information in different formats. Clear information was not only about managing the patient’s feelings of safety and confidence, but also to ensure they understood why they needed to do certain tasks, which meant they may be more likely to do them. This is illustrated by one female patient who was unclear as to why certain parts of her care plan were in place:
Ummm. [clicks her tongue] You see, the drinks, I don’t quite know what they do, to you. Are they full of proteins?
(Patient, non-cancer gynaecological surgery)120
The above quote indicates how lack of understanding could prevent patients from fully engaging with their recovery plan and being ‘active’ in their recovery (see theme; ‘Active patient’). In contrast, the patient in the below quote had been informed clearly about early mobilisation, and was prepared to get up and walk:
The fact that I knew what I was going to have to do when I came round. I knew I was going to have to get up … I knew that I had to get up and walk. The preparation is good.
(Patient, gynaecological cancer surgery)100
Connected to being an ‘active patient’, shared decision-making between staff and patients was difficult for patients without access to consistent and adequate information. 116,123,125 For example, this patient in Strickland et al.’s 125 study did not have enough information on what options were available, and subsequently was unable to make informed choices:
I was asking for something I couldn’t have.
(Patient, LLA)125
Being informed could also help with worries about whether a particular symptom was ‘normal’ when recovering at home, which will be discussed further in the theme: ‘Appropriate, available and accessible follow-up’.
Overall, data from four studies (four articles) suggest that the level of information provided impacted confidence or feelings of safety post-discharge. 102,114,116,122 For example, whilst Berg et al. (2019)102 described most patients as accepting of discharge due to having clear information during the pre-operative phase, Samuelsson et al. (2018)122 reported that some patients had concerns about the post-discharge phase as they felt ill-prepared.
Patients and carers from 10 studies highlighted how missing information was a particular issue for the post-discharge phase, and linked with the availability of follow-up. 90,102,104–106,111,116,126,132,133 One caregiver discussed the impact a lack of appropriate information can have on patients ability to manage their pain post discharge:
The meds, too … no one told us to make sure we take [them] …and he got really in hot water [not taking enough], so the pain came back full force, and it took longer to get it down again.
(Carer for THA patient)106
The work of carers supporting the patient at home was made more difficult when they could not get access to the information they needed to perform their home caring role, which was also echoed by our PPI group. For example, one carer in Berthelsen et al.’s (2017)104 study was described as having difficulties changing the patient’s dressing at home as she was not given enough information prior to discharge. Patients also felt this concern for those caring for them, as illustrated by the patient who had undergone hip replacement in the quote below from Hunt et al.’s (2009) study:
If you could spend a half day with us and this is what we’re going to show you what you’ll be able to … what you’ll have to do after … at least the carer would know exactly what’s going to happen.
[Patient, THR]90
Six studies suggested inconsistency of information between different staff members impacted patient confidence:105,113,116,124,126,133
… whether or not your pillow is under your knees or not at night, whether your legs should be apart or not. … because it’s your hip and your future and your recovery, I found those sort of things a bit unnerving.
[Patient, THR]113
The same patient in Heine et al.’s (2004) study said that it did not matter if the inconsistency was regarding a more minor matter, suggesting that care must be taken to ensure all aspects of information are consistent:
It’s often the small things that unravel the most. I’m inclined to agree with that.
(Patient, THR)113
First- and second-order data from four studies (five articles) discussed how having too much information, or the right information in the wrong format, could be difficult for patients or carers to handle. 105,120,123,124,133 For example, Phillips et al. 120 discuss one gynaecological surgery patient who particularly struggled with pain and linked her pain to difficulty with recalling the amount of information she was given:
… after I had some lunch I remembered that … I was told … to start off with water and liquids and I didn’t …. So I knew at that point I was in … that I’d done something wrong …. So I started to have some pain.
(Patient, non-cancer gynaecological surgery)120
However, the amount of information desired varied between patients, linking to the idea of needing to individualise care, as illustrated by two quotes from different patients in the same study below:100,102
I’m that kind of person, so that if they hadn’t given me I would have forced them to give me … I want to be prepared for what they’re going to do … I want to know about the details. (Patient 1)
In fact I want to know as little as possible about the procedure. No, I’m not really so fond of these kinds of operations. (Patient 2)
(Patients, LLA)102
The information needed to be tailored to the individual patient or carer, with adequate time or opportunity for questions. 115,119,122–124,133 Some found written information useful as a resource to refer back to,108,113–116,119,120,122,131 whereas others valued verbal instruction. 108,116,119,133
Patients from 11 studies (12 papers) indicated the timing of the information also impacted their ability to remember it, with some pre-op information classes too distant from the procedure itself, and some post-op information given to the patient when they were still affected by analgesia. 100,106,113,114,116,119,120,122–126 This is highlighted by a patient who had a longer wait between the pre-op information clinic and her procedure, and then struggled to remember instructions for the post-operative exercises she had been given:
I can’t remember [when the hip school was] because of the delay. That’s really why I’ve forgotten some of the exercises really.
(Patient, LLA)116
Data from 12 studies (13 articles) indicated that an advance plan made pre-operatively or prior to discharge could enhance feelings of safety. 100,102,104,106,113,116,118,119,121,123,124,129,133 Firstly, prehab or a pre-op visit at home helped prepare patients for their procedure and the recovery period post-discharge. 100,102,103,116,118,119,124,129,133 This pre-operative planning and thinking through could help to identify potential issues in advance and support patients to feel more confident that they know what they practically needed to do:
I was confident about coming out of hospital because I had actually walked through in my mind at the home visit … issues that hadn’t been in my mind at all … and wouldn’t have come to mind until 3 days after the op.
(Patient, THR)119
Pre-op care was important in terms of the patient gaining realistic expectations of their recovery, which could impact experience of pain (see theme: ‘The active patient’). This is illustrated by one caregiver of a patient admitted for total hip arthroplasty, who explains how they had both under-estimated the degree of post-surgical pain, which also points to the importance of realistic expectations helping patients and carers to plan:
Yeah, [the pain] was a little bit more … than I thought, because everyone said ‘Oh, the surgery is perfect, it goes great, you will be up and at ’em in no time flat’, but it’s still surgery, so it wasn’t that ….
(Carer, THR)106
Similarly, four studies discussed how advance planning could help patients and carers and feel more prepared for discharge. 113,119,121,123 This is important given that patients (and carers) needed to feel prepared for discharge. 100,113,119,121,123 For example, Specht et al. (2018)123 describe how patient confidence in going home was linked to ‘being involved and the feeling of control in the discharge planning process’.
Patients did not feel prepared when they felt rushed or their emotional needs were not met, linking with the idea that both physical and emotional needs need to be considered:
The discharge, it went fast … it was messy … I was not sure about the pills … but they also were very busy at that time.
(Patient, LLA)123
As discussed previously, consistent and adequate information was important for patient and carer confidence about post-discharge recovery, but it was also important for confidence in the discharge process itself. The below quote from a patient in Strickland et al. ’s (2018) study highlights not only the potential confusion for patients, but also the need for co-ordination between staff members and services (discussed in more detail in the construct ‘Taking responsibility’).
The surgeons tell you, you can come out the next day, the nursing staff say you are not ready to go home and you can’t go home till the physios say … so everybody you speak to tells you a different story.
(Patient, LLA)125
In addition to the importance of patients (and carers) feeling prepared for discharge, there was also a need to consider the patient’s home circumstances when planning discharge (see construct ‘Individualisation of a standardised programme’). For example, Hovik et al. 114 described how those living alone had to prepare their homes and support mechanisms for the recovery period in advance of hospitalisation.
Seven studies highlighted how carers needed to be involved in discharge and its planning to that they could effectively support the patient at home. 90,104–106,111,119,124 As will be discussed further in the ‘Essential care at home’ construct, if carers are required to support the patient in their recovery, then they need the information and support to do so:
I wasn’t there when [the physiotherapist was] there …. When we got home, he’s in his walker, there was a bit of confusion … like, put this leg first, well, what did [the physiotherapist] say?
(Carer, LLA)106
Consistency of information was important to patients, as inconsistency could make them feel more vulnerable (which is also linked to the need for service co-ordination). The format of this information could also impact understanding and memory, and it was also important to consider the needs of family carers. Planning discharge, providing information about expectations and available services, and involving carers as relevant, helps patients and carers to feel safe and less worried about discharge.
Theme: appropriate, available and accessible follow-up
Thirty studies (30 articles) contributed to this theme, which discusses how accessible and available follow-up care helped patients and carers to feel more safe and secure, even if they did not need to use it. 90,100–109,111,113–116,118–123,125–132 The difficulties in accessing follow-up, including not knowing whom to contact for particular difficulties or how, are also explored and support content within the ‘Staff and service co-ordination’ theme. Accessible and available follow-up was one of the key issues described by members of our PPI group.
Eighteen studies highlighted that patients really valued follow-up care, and that it was reassuring. 90,100,102–104,106–108,113–116,123,125,126,128,130,131
I … even just a little follow-up on it all makes you feel a lot better.
(Patient, colorectal cancer surgery)126
Four studies (four articles)109,113,119,129 particularly highlighted that this follow-up by hospital or primary carer services was even more important when patients did not have home carers, which is also supported by the idea that having a carer at home is essential for patients (as described in greater depth in the construct ‘Essential care at home’). One patient highlighted how the death of family and friends had left her isolated:
I’ve got no-one else, no-one. My friends have died, all my friends are gone. I had some lovely friends but they’re all gone. That’s the trouble isn’t it and my brother has gone who would have helped.
(Patient, THR)119
As well as follow-up care being available to patients, nine studies indicated that patients found having follow-up care booked prior to discharge helped them to feel safe:90,100,103,104,113,116,123,125,126
I didn’t want to sort of be a nuisance … [and ring them], and I was a bit worried that what would happen just in case they were any problems … it was nice to know [nurse] was going to call on Monday.
(Patient, gynaecological cancer surgery)100
The above quote also highlights how some patients or carers did not want to bother busy healthcare staff, or did not know when a particular symptom met the threshold of needing to call so did not call when needed. 100,105,106,109,126,132 Given that some are reluctant to contact of their own accord, a proactive approach by the hospital would give patients permission to voice their concerns.
… I didn’t think that it was anything worth calling about. Now I remember the nurse telling me, don’t call if you have a swollen finger. Then I thought, is a bladder infection worth calling about? I just waited until … [outpatient appointment].
(Patient discharged following colonic cancer surgery)132
Even though they said ‘you can call us’, I didn’t, because I felt that by calling on a Tuesday morning I would disturb their work.
(Patient discharged following colorectal cancer surgery)126
However, if hospitals offer a follow-up service, they must follow-through on this, as Archer et al. 100 describe in interpretation of their findings – patients may be relying on that follow-up to discuss difficulties or ask questions, and not receiving an expected service could lead to a negative experience.
Nine studies (nine articles) highlighted patient worries about difficulties in accessing follow-up care once discharged. 101,107,108,111,115,116,118,128,130 One example of this was practical concerns such as living alone or far from the hospital:
I told them I might need to stay at least one night … because we live so far out and I needed to be [at the hospital] because I did not know if I was going to react again to this medication.
(Patient, sacrocolpopexy)108
Here the patient indicates that she was involved in the process of deciding when she should go home. Thirteen studies indicated that some of the concerns experienced by patients and carers prior to discharge were well-founded, as the availability or accessibility of follow-up care could vary, even where it was part of a programme or intervention. 90,101,107,111,114–116,118,119,122,126,129,130 For example, Hovik et al. 114 described how a patient who lived alone had difficulty booking follow-up physiotherapy despite being told this was available. The accessibility of follow-up care could be a particular problem for those who were not able to travel to a service for support, as illustrated by the quote from a surgeon in Westby et al. ’s study below:
The other thing that’s non-existent for the most part is home physical therapy for … the patient who is unable to get transportation somewhere or has social issues that would preclude them from [getting there]. Those patients fall through the cracks ….
(Staff, surgeon, LLA)129
A lack of easily accessible follow-up care was also especially difficult when dealing with complications or unexpected symptoms at home (see theme ‘The active patient’), as illustrated by a patient who had been discharged following total hip arthroplasty:
The first [episode] was that night and [the second] the next morning … it scared both of us … I did not know what to do, they said to call the hospital, but you still don’t know, because I hadn’t read anything about fainting ….
(Patient, THA)106
Seven studies (seven articles) highlighted how patients and/or carers did not always know whom or what service to contact for support after discharge, though this did vary between studies, dependent on the intervention:101,111,115,116,122,126,130
It seemed to me that once you get home you felt a bit out on a limb when you tried to get back in …. This the problem. I mean you don’t really know exactly who you’ve got to contact.
(Patient, colorectal cancer surgery)130
No regrets about getting home because you could always ring physiotherapy and if there’s any issue you know drop in.
(Patient, LLA)125
Data from eight studies (eight articles) indicated that patients and carers appreciated having access to someone to whom they could ask questions or share concerns. 90,100,102–104,107,115,125 This was particularly the case when the patients or carers had a named service co-ordinator, which will be discussed further in the theme ‘Staff and service co-ordination’. This was illustrated by a study by Berthelsen et al. ,104 who specifically examined the provision of a case manager, and found carers highlighted the opportunity to telephone the manager to talk or ask questions as the most important element of the programme.
First- and second-order construct data from five studies (five articles) discussed how some patients also found it harder to measure their progress or self-motivate without some guidance through follow-up, and appreciated explicit goals or guidance which they could measure themselves against:102,113,116,123,131
Sometimes when I’m depressed, I think that there’s something wrong with me … perhaps one needs to have small goals … so that you see that things are going in the right direction, am I too slow or too fast ….
(Patient, LLA)102
But that [activity tracker] does stimulate you at the end of the day, to see where I am and oh tomorrow I have to do a bit more.
(Patient, colorectal cancer surgery)131
Construct summary: feeling safe
This construct explores the different factors which support patients and carers to feel safe throughout the hospital stay and following hospital discharge. The needs of both patients and carers need to be viewed holistically, with pre-op assessments, discharge planning and provision of information individually tailored to consider their emotional and physical needs. This can help increase patient and carer confidence by allowing them to put a post-discharge plan in place, reassuring them they have the skills and support they need to cope once they leave hospital. Follow-up care was essential for both patients and carers after hospital discharge. Both patients and carers found the opportunity to ask questions reassuring and valued being asked how they were feeling. Follow-up care also allowed medical concerns to be identified and/or addressed. Feeling safe may promote patient recovery through increasing patient and carer confidence at returning home and enabling carers to provide the support required for patients to recover at home, thus reducing the stress associated with this transition.
Construct: individualisation of a standardised programme
Thirty-one studies (32 articles) contributed to this construct,90,100,102–108,110–119,121–133 which consisted of two themes: ‘Being inside or outside the programme’ and ‘differing priorities’. Programmes generally have a structure or pathway, and some patients find comfort in the structured, predictable nature of the intervention. However, not all patients could fit within the pathway, due to experiencing complications or having needs the programme components could not adapt to. Additionally, staff could struggle to individualise care within the prescribed structure of the programme and organisational, staff and patient priorities were not always aligned, which could cause difficulties. See Report Supplementary Material 5, Table 4 for a summary of articles contributing to each theme.
Theme: being inside or outside the programme
Twenty studies (20 articles) explored how patients whose needs were met within the programme and could meet the standardised timeframes can have very different experiences and perceptions to those who are unable to, for example due to developing complications or lacking support at home. 90,102,103,107,108,110,114–118,121,122,128–131,133 This theme also explores issues related to comorbidities and complications, and weekend care.
Second-order data from two studies describe their respective patient participants as having contrasting experiences due to their individual circumstances. 108,110 Galli et al. (2015) highlighted that patients following a protocolised programme perceived they were ‘inside the right path’ whilst those who were unable to participate fully in an intervention due to more complex needs saw themselves as ‘outside’ the programme. 110
For some patients and carers, the nature of the programme being structured could be comforting or reassuring. For example, Evans et al. 108 noted that patients reported the ERP gave them a ‘sense of continuous care’ as it covered their full ‘journey’ from pre-op to post-op recovery at home, and that this made their experience more personalised, with one of their participants stating:
… you know, it just feels like, more like, there is care out there ….
(Patient, sacrocolpopexy)108
However, not all patients had this experience. Some patients were ‘outside’ the programme,110 in that they could not follow the protocol or pathway. First- and second-order data from nine studies suggested that comorbidities and/or complications were the most common reason for patients being ‘outside’ the programme. 103,108,110,117,118,121,122,128,130
Patients could feel discouraged or worried if they were not meeting the standardised milestones, or saw other patients meeting them more easily. 103,110,116,128 One patient discharged following liver resection surgery described her anxiety about not meeting expected milestones in her recovery:
The only problem with that (milestone) of course is if that doesn’t happen, because then you can get anxious because you’re thinking … if I didn’t match up to it I could feel myself thinking, oh maybe there’s something wrong.
(Patient, liver-resection surgery)128
Whether a patient experienced complications impacted whether they wanted a longer hospital LOS. Evans et al. 108 interviewed patients who had been discharged on the same day as their procedure, and those who had chosen to stay overnight, and found that those who felt more confident about their health were happier to be discharged sooner:
I was ready to come home … I knew my blood sugar had come back down to a normal level, so I was fine and felt very comfortable.
(Patient, sacrocolpopexy)108
I was really very thankful … they let me stay … I know part of the reason for that was they wanted to watch my creatinine level. But … they [also] had to treat [my blood sugar] with insulin … if I was home, I would not have … known.
(Patient, sacrocolpopexy)108
The above quote also indicates how having comorbidities could complicate the home recovery process, making it more challenging for home carers, or making patients feel more vulnerable. One patient described, in the below quote, how having comorbidities made the home recovery process more challenging. She had also discussed her partner (carer) having health issues which meant he was unable to support her as needed.
It was difficult the first few weeks … you felt you had nobody to help you, you were just on your own … in my case having [spinal-stenosis] as well … for three nights I couldn’t … get in and out of bed, just sat in the chair.
(Patient, THR)121
The above quote also suggests that the need for home support is vital (further in the theme ‘Essential care at home’), particularly given that this patient group may be more likely to have comorbidities, complications, or frailty. 6,9–16
First- and second-order data from three studies (three papers) suggested that having a procedure, or being discharged, around the weekend was another key reason for being ‘outside’ the programme, due to less availability of services both within the hospital and in the community post-discharge at the weekend. 111,112,118 Although only represented within a few studies, our PPI group highlighted it as a key difficulty.
Two of the studies112,118 highlighted that when patients had an operation on a Friday, their discharge could be delayed not because of complications, but simply because the required teams were not working over the weekend so the next step of their pathway could not be completed. Staff members from one of these studies112 discussed lower staffing levels over the weekend meaning they had to spend less time with each patient, prioritising those who would be sooner discharged:
So … they missed two full days of seeing a stoma therapy nurse and then on Monday … they should be getting out, whereas they haven’t even met the stoma therapy nurse.
(Staff, colorectal surgery)118
On weekends, we have less staffing for the same number of patients. The exact quantity is slightly different for different professions. And the way we normally prioritise is dependent on whether they (the patients) are going to go home over the weekend.
(Staff, occupational therapist, LLA)112
Patients and carers could struggle to access or arrange timely follow-up care when discharged on a Friday or at the weekend. Planned discharge on a Monday could also be challenging, as patients and carers could not contact community services on a weekend to make arrangements. The following quote from a carer illustrates the difficulty of trying to make arrangements with post-discharge services at the weekend:
… 3 o’clock on Friday that I get this bombshell of ‘find someplace’ … they wanted her out on Monday … so I made some telephone calls and went on Saturday … of course nothing could be done until Monday because the people had the weekend off.
(Carer of patient discharged following CABG)111
As suggested in the availability of follow-up theme, there could be variation in the availability of community services, regardless of when the patient was discharged (supported by 13 studies). 90,101,107,111,114–116,118,119,122,126,129,130 Where a patient did not have access to, for example, community physiotherapy which was part of the standardised plan, it could delay discharge or make the recovery process at home more challenging. This was discussed by staff in Lyon et al.,118 who cared for patients admitted for colorectal surgery within an ERP programme, and commented on how it was difficult to arrange follow-up care for patients in more rural parts of Australia and that this could delay discharge.
Data from nine studies (nine papers) suggested that when patients did not fit the standardised programme, there was variation in whether patients felt staff met their individual needs, even within the same study/programme. 108,110,114–116,121,122,130,131 For example, Judge et al. 116 described how some patients who could not mobilise quickly felt that staff listened to their worries, but others felt they were not listened to and instead were pressured to ‘conform’ to the prescribed milestones of the pathway.
Similarly, staff in four studies discussed struggling to fit all patients into the prescribed programme or meet discharge targets:103,117,118,129
It depends on their age and what other comorbidities they have.
(Staff member, colorectal surgery)118
Three studies suggested that busy staff workloads could prevent individualisation of care, as they did not have the time for longer discussion or additional care tasks. 103,122,129 For example, Berthelsen et al. 103 described how nurses reported that the only obstacles for them in providing individualised care such as additional discussion with the patients was ‘a lack of time and a busy daily schedule’. This was noticed by patients, who could then avoid requesting this kind of care, such as the below patient in Samuelsson et al. ’s study:122
You can see that the staff has a lot to do, so you feel reticent even though you need to ask a question.
(Patient, colorectal cancer surgery)122
In one study,103 staff emotionally resolved this difficulty by placing the blame on the patients themselves for being unprepared, weak, or problematic (discussed in theme ‘Differing priorities’):
Those ‘I live alone’ (voice quivering) … well you have known about this for a long time. Don’t you tell me … you haven’t put food in your freezer and you haven’t talked to your neighbour and family? Don’t you have any friends?
(Nurse, LLA)103
The above quote shows not only that some staff can struggle to empathise with the feeling of vulnerability that can come with living alone, but also that patients may benefit from support to think about the resources that they do have available to them.
One study101 suggested that a pre-op visit in the patient’s own home could help to individualise care, as staff could better understand and empathise with each patient’s context and specific needs and adjust plans accordingly:
In a … sterile clinic or environment … it doesn’t bear that much resemblance to somebody’s house … I think seeing people in their own home … being able to relate more to what the patient’s saying ’cause you can see it, it’s not just a theoretical problem ….
(Staff, physiotherapist, knee arthroplasty)101
Another study119 suggested that individualised home care could help patients to prepare for their procedure and the recovery:
it’s difficult … to translate anything that’s said [in hospital] into your home environment … I wouldn’t be able to imagine everything that I would need at home while I was sitting in hospital with somebody just talking about it.
(Patient, THR)119
However, individualising care in this way takes time and resources, which, as described above, may not be available within busy staff and service workloads.
Theme: differing priorities
Six studies (six papers) contributed to this theme, which describes how organisational, staff and patient priorities were not always aligned, and this could cause difficulties in managing individualisation of patient-care or resources. 103,112,117,119,121,129
First- and second-order data from six studies indicated the overall priorities of the organisation or healthcare systems could be mis-aligned with what staff working with patients wanted to prioritise. 103,112,117,119,121,129 Rapid discharge was cited by staff as an organisational priority which meant that their time and activities had to be directed towards this, rather than other priorities which may support other kinds of patient care:
From my perspective, allied health services are more directed at discharge planning to allow patient flow. Resources currently are more focused toward getting people home than providing a rehabilitation service.
(Staff, physiotherapist, LLA)112
As discussed in the theme ‘Being inside or outside the programme’, staff sometimes struggled to fit all patients within the programme. When LOS was the primary goal, it was not always possible to individualise care where this would increase time spent in hospital, or time spent with the patient if there were heavy workloads. This meant, for some staff, sticking as rigidly as possible to the structured plan and patients occasionally being discharged too early, and for others trying to weigh up the consequences of missing targets against the patient’s individual needs. The following two quotes from staff members highlight some of the difficulties in trying to balance these competing priorities:
He was in worse shape than we thought. He … needed to function better than he did when he was discharged … So the individual considerations can sometimes disappear.
(Staff, nurse, LLA)103
it’s weighing up those completely incongruous goals … Bugger the breach targets, but spend the time and get the patient ready, so their operation recovery are better. Or do we do it as quick as we can … hit the targets, bugger the patient?
(Site lead, CGA implementation)117
Staff from the same study as the latter quote indicated that organisational priorities could prevent innovation that did not serve these priorities, were aimed at a minority patient group who were not well-served by the existing programme, or due to time pressures. It could also mean that staff had to carefully consider how to best use resources when they were constrained by healthcare systems or insurance companies:
So you play this game with the insurance company and you get caught in the middle of the game as a patient …. One of the biggest changes we’ve seen is with rehab.
(Staff, surgeon, LLA)129
Although services in the UK do not have to contend with insurance companies, resource allocation is an increasingly pertinent one in the NHS, so staff and services must consider to whom and what resources to allocate, and how, such as through limits on number of physiotherapy sessions. This was an issue mentioned by the authors of one included UK-based study. 119
Construct summary: individualisation of a standardised programme
This construct highlights the different experiences of patients who can follow a protocolised programme versus those who are ‘outside’ the programme. It can be more difficult to accommodate patients with more complex needs, and those who experience complications or are discharged at weekends, within a standardised programme. This can cause stress for patients, who may worry that they are missing key milestones, and the people supporting them. Staff may find it hard to identify with patient feelings of vulnerability, while some patients may struggle to translate information and advice received in hospital into their home environment. Priorities may differ between patient/carer, staff and organisational groups, which may influence the extent to which personal, individualised care can be provided.
Construct: essential care at home
This construct considers the vital role of caregivers in supporting older adults during their recovery from planned surgery and is supported by 25 studies (26 articles). 90,100–106,108,110,111,113–116,119,121,123–130,132 Two themes contribute to this construct. The first theme considers how staff, carers and patients all see having care for the home recovery period as essential. The second theme highlights the direct, indirect and other work of caregiving and the emotional and physical impact this has on caregivers.
Theme: caregivers as essential
Twenty-two studies (23 articles) support this theme, which details how having a home caregiver, such as a spouse or friend, was seen by nearly all patients, carers and staff members as essential to earlier discharge and recovery at home. 90,100–106,108,110,113,114,116,119,121,123–130 The role of carers in providing reassurance and support with practical tasks is explored, alongside patient concerns around being a burden to those supporting them.
First- and second-order data from 14 studies (15 articles) indicate that the majority of patients in studies viewed having a home carer as essential for recovery at home. 90,102,103,106,108,110,114,116,119,121,123,124,126–128 This is illustrated by patients from two studies who experienced a fast-track protocol during their hospital stay:
I definitely could not have came home and been by myself.
(Patient, sacrocolpopexy)108
I think it’s important to have help in the home … one needs help with shopping and preparing food and so forth … and you are not allowed to drive a car.
(Patient, joint replacement)102
The second quote above indicates some of the practical tasks which patients require support with following hospital discharge (see theme ‘Direct, indirect and other work of caregiving’ below). However, patients also found the presence of someone to support them at home reassuring. First- and second-order data from 10 studies90,102,111,113,114,116,123,127,128,130 indicated that the uncertainty surrounding discharge provoked unease, whether this was regarding not knowing what to expect in terms of outcomes or pain following the operation,127 or finding someone who was able to provide the support required:128
My husband was very ill …. The only help available to me is my daughter and she’s got her two girls and husband at home and family to look after … I can’t really ask her to do any sort of full-time care.
(Patient, liver resection)128
[My wife]’s not a nurse by any means. And … obviously it’s a worry if there’s anything. Whereas when I’m in hospital, you’ve got teams there, if there is a problem …. So from that point of view there’s always that concern isn’t there?
(Patient, liver resection)128
These quotes also suggest that patients are aware of the additional stress providing support would place on their caregivers. Four studies (four articles) indicated that some patients felt a burden to their home carer, or worried about how they would cope with the tasks of caregiving. 113,121,128,130 One patient discussed her concerns around how both she and her partner would cope following discharge after surgery for colorectal cancer:
I felt a little bit lacking in confidence of coming home … I was just a little bit worried about how I was going to cope … how (my partner) was going to cope with this … I was afraid of putting pressure on him.
(Patient, colorectal cancer)130
This quote indicates that providing support to carers is essential, not only to ensure that they can continue with their role as caregivers, but also to reassure patients that the people they care about have adequate support. This may help alleviate any guilt experienced by patients113,128,130 associated with their reliance upon them and facilitating feelings of safety for both parties (see theme ‘The direct, indirect and other work of caregiving’).
First and second-order construct data from four studies indicated both carers105,106 and staff also viewed the role of home-care as essential:100,129
I do what I have been told to do and I keep to the routine: breakfast, do the washing up, make the beds, close the windows …. When I have finished doing that, I … shop …. It’s not difficult and I can easily manage.
(Relative of patient discharged following joint replacement)105
And the consultant explained again that if everything was OK he’d check again on the circumstances at home … he said that if [husband] was happy to have me home, then there would be no reason why I couldn’t go home.
(Patient, gynaecological surgery)100
The second quote100 suggests that the presence of a partner at home can also be reassuring for staff members involved in ensuring the discharge of patients home is appropriate and safe.
Theme: the direct, indirect and other work of caregiving
This theme explores the wide range of work undertaken by home carers, which they may not have had to undertake if the patient had a longer hospital stay. This theme is supported by data from 14 studies,90,100,102,104–106,111,113,115,125,126,128,130,132 and considers the work undertaken by caregivers according to the three categories suggested by Ganske. 111 The first category details the direct work carried out, such as nursing tasks like wound care; the second category explores indirect work such as scheduling and household tasks and the final category details other responsibilities such as caring for children or maintaining employment. This theme also considers the emotional and physical impact of caring for a relative or friend on the carer.
First- and second-order construct data from five studies (five articles) highlighted that the work category of ‘direct caregiver work’ included nursing tasks like wound care, support for bathing, or managing medications. 104–106,111,113 As illustrated by the carer of a CABG surgery patient over 80 years of age, this often required carers to learn new skills, which were often physically and emotionally challenging:
I thought I had it, and I didn’t … get good blood. I think I was afraid of hurting him.
(Carer of CABG patient)111
In addition to carrying out the task itself, direct caregiver work also necessitated gaining access to, understanding and remembering medical information related to the patient’s care,100,104–106 as discussed in more detail within the ‘information’ theme. These tasks represent work which is not immediately observable but place additional stress on caregiver resources. Six studies (six articles) provided first- and second-order construct data which support the work category of ‘indirect caregiver work’,104–106,111,128,132 which included tasks which could not be described as nursing tasks, but encompassed responsibilities the carer had to perform on behalf or, or in order to care for, the patient:
I have three doctors’ appointments [to arrange] … so I called [the urologist]. And then we have to go to [cardiologist] and [cardiac surgeon].
(Carer of CABG patient)111
my schedule is full of appointments for my parents … it’s kind of a juggling act to keep everything [straight].
(Daughter of CABG patient)111
Second-order data from three studies discuss the other tasks and responsibilities beyond the patient that the carer had in their life, such as childcare or a job, which could be challenging to balance. 106,111,128 This care work had a physical cost, causing exhaustion and the exacerbation of existing health problems, particularly in elderly carers:106,111
… sometimes I’d be so tired and numb … especially at 2 or 3 or 4 o’clock in the morning and then … [only] sleep for an hour … when you’re so exhausted … your eyes hurt you’re so tired.
(Carer of CABG patient)111
In addition to this physical stress, four studies (four articles) highlighted the emotional impacts of caring, which included difficulty in witnessing a loved one in pain, stress, frustration and worry. 104–106,111 Two carers discuss their emotional responses to providing support for their family members at different stages of the recovery process following CABG surgery, and one following THA surgery:
this is twice and I don’t want to go through it again … oh I can’t even talk about [burst into tears] … seeing [him] in intensive care … oh it’s horrible. It was like going in and seeing a corpse … I wouldn’t go back again.
(Carer, CABG patient)111
I was worrying …. ‘Am I going to have to help him in and out of bed?’ because he is so much taller, and I know I could do it, but no one has ever taught me how to do it.
(Carer, THA)106
… you know you’re supposed to walk, you know you’re supposed to drink water and you know that you’re supposed to eat something to get your strength back … I’m sick of saying did you, did you, did you ….
(Carer, wife, CABG patient)111
In addition to managing their own emotional reactions arising from the trauma and challenges associated with a hospital stay and discharge, caregivers were also the recipients of anger, frustration and sadness from the people they are supporting:
There was one time when I wasn’t quick enough to provide assistance and then she was mad at me … I wasn’t close by to help her … but we had just agreed that the house needed cleaning so I was … hoover[ing] … I didn’t hear her.
(Carer, spouse, THA replacement)104
The above quote highlights how the challenge of managing multiple tasks at any one time can be frustrating for patients, when their family members are unable to provide them with timely support. Five studies highlighted that in order to fulfil their caring responsibilities and maintain their wellbeing, the carers themselves also needed support. 90,103,104,106,111 Support for home caregivers included receiving relevant information and training from the hospital,106 and support from other family members, friends and healthcare staff. One woman expressed gratitude towards her husband for the support he provided to her:
I’ve been thanking him [her husband] because he’s just been so great in going with me every day … it truly is a great help.
(Carer for CABG patient)111
First- and second-order construct data from three studies highlighted how there could also be negative emotional impacts on the carer or patient, such as conflict due to changes in their respective roles at home. 100,104,126 One patient admitted for colorectal surgery talked about the impact of role changes following her transition home:
We don’t talk much about illness in our house, and I have always been the one to take care of my husband and kids when they were ill. Now it’s me who needs looking after …. That has been a little hard.
(Patient, colorectal cancer surgery)126
However, data from two studies104,111 suggested that the emotions experienced by carers changed over time, with carers expressing more positive emotions as the patient recovered:
We have been very successful. Mom has had a much better recovery than I was worrying about.
(Carer, CABG patient)111
Construct summary: essential care at home
This construct highlights how the direct and indirect work by caregivers is vital to support patient recovery at home post-discharge. The tasks directly associated with caregiving, such as providing support with medications, changing dressings, or providing transportation to appointments, are also associated with work which is not always observable or predictable, such as making appointments and learning new skills. The transition home can be difficult for both the people providing and those receiving care, due to role changes at home and the stress associated with the additional workload of caregiving and/or being dependent on others for support. Older caregivers may have their own health needs and struggle to maintain their own wellbeing whilst supporting the patient to recover at home. Follow-up appointments may provide a way to provide practical and emotional support to caregivers, as well as patients, enabling them to manage their caregiving role.
Construct: taking responsibility
Thirty-three studies (34 papers) contributed to this construct, which represents the question of who has responsibility for care and recovery, particularly after discharge. 90,100–132 It includes the themes ‘the active patient’, ‘staff skills – expertise versus generalists’ and ‘staff and service co-ordination’. See Report Supplementary Material 5, Table 5 for a summary of articles contributing to each theme.
Theme: the active patient
This theme is supported by 30 studies and explores how patients had to be active, rather than passive, and take charge of their own care, and the ways the staff or programme components signal this to them. 90,100–104,106,107,109–111,113–116,118–132 This theme encompasses three important concepts: ‘patient attitudes and experiences’, ‘pain management’ and ‘empowerment versus vulnerability’.
The enhanced recovery programmes, by their nature, required patients to take an active rather than passive approach, as they would largely be responsible for their own recovery at home. However, two studies102,125 suggested there was variation in how much of a say patients wanted in medical decisions. For example, Berg et al. 102 described how some patients wanted to leave the decisions about surgery to medical staff, whereas others, such as the patient quoted below, wanted to actively participate:
I participated and decided when I wanted the operation. … I felt that I was participating more when it was time to do it, and it was unavoidable.
(Patient, LLA)102
But one study125 suggested this choice to be involved in decision-making may be dependent on patients receiving adequate information in empowering patients to be active patients, as discussed in the ‘Increasing confidence and preparedness through information and planning in advance’ theme.
Two studies114,123 suggested that early mobilisation emphasised the patient’s role as being active in the process of recovery. For example, the below quote highlights that not being ‘allowed’ to stay in bed was a way of communicating independence, though the language of ‘chased’ may also suggest patients can be reluctant to mobilise early and link to the idea of blame being placed on patients who do not conform to the set milestones discussed in the construct of ‘Individualisation of a standardised programme’.
Being ‘chased out of bed’ emphasised the expectation of self-care.
(Patient, TKA)114
Five studies (five papers) suggested it could be difficult for patients managing their own recovery at home to strike the balance between activity and rest. 106,114,116,123,132
You just wonder how much that you should do because I’m that sort of person you know, ‘did I overdo it? Should I have rested more with my leg up?’ and then you worry about developing problems … if you don’t mobilise.
(Patient, LLA)116
The above quote links to the ideas within the construct ‘Feeling safe’, as patients needed and wanted information (and follow-up) to manage their recovery effectively and without anxiety. If patients are ‘responsible’ for their recovery, then they need the tools to be able to do so. It also links to the importance of managing expectations, and patients having a realistic understanding of the likely trajectory of their recovery to have a better idea of, for example, the degree of pain they may be feeling in relation to rehabilitation exercises at different stages.
Seven studies indicated that both staff and patients felt that patient expectations had an impact on engagement, satisfaction, or recovery itself,106,109,114,118,125,129 which links to the earlier theme of ‘Increasing confidence and preparedness through information and planning in advance’ and the need for accurate preparations to manage expectations. Some patients’ expectations could be too high, or they could anticipate that they would feel less pain due to a planned earlier discharge than they may have experienced previously, whereas others had enough information to develop a realistic expectation, as highlighted by the contrasting quotes below.
I don’t know how many people [with TKA] I’ve had in the last little while that come in and they’re stunned that they have pain postoperatively …. They’re so not prepared for the amount of pain they have.
(Staff, physical therapist, LLA)129
My pain was as I expected it and I know how to manage it.
(Patient, LLA)125
Two studies118,129 suggested that staff felt it was important that patients had clear expectations, but that these were not always clearly communicated in a timely manner, linking to the importance of good pre-operative information (see theme ‘Increasing confidence and preparedness through information and planning in advance’). A surgeon highlighted one of the potential challenges for staff in meeting this need, linking this theme with the challenges of individualisation in the ‘Individualisation of a standardised programme’ construct:
… depending on how much time you have to spend with people and so on. You may miss the boat in terms of what they’re expecting.
(Staff, surgeon, LLA)129
The same two studies118,129 highlighted that some staff members felt that the patient’s personality or mental health was important in how well they engaged as an active patient in a programme, as illustrated by the two quotes from staff members below:
One of the most common [concurrent] diagnoses … is depression in the patients … which hugely affects motivation, adherence to the protocols, and follow-up, and it doesn’t get addressed frequently because primary care physicians don’t take the time to diagnose it appropriately.
(Staff, nurse, LLA)129
There is a group of patients who, um, basically do what they want no matter what we say.
(Staff, colorectal surgery)118
In addition, nine studies indicated both patients and staff suggested that the patient’s attitude had an impact on how well they responded to the programme. 100,101,109,113,118,125,128,129,131 This is illustrated by the patient below, who describes optimism, as opposed to pessimism, being a key part of how well you recover.
I think if you went into something with [a pessimistic] sort of mind set it must be very difficult to recover, because you’re not helping yourself. So I think the mind set is hugely important, as important as the body.
(Patient, liver-resection surgery)128
Two studies121,129 suggested that age differences could impact experiences, with Westby and Backman129 suggesting that there were differences in outcome expectations and rehabilitation needs between younger and older patients, and Reay et al. 121 suggesting that older patients were better able to cope with social restrictions caused by their recovery. One older adult discussed how she occupied her time post-discharge:
The first couple of days, uh, mainly sat down, mostly exercising; it’s in the book (the hip replacement information booklet provided). I wasn’t bored; I read quite a lot.
(Patient, THR)121
However, this does not mean to say that all older patients coped well with recovering alone, as this was also dependent on other factors such as recent loss:
I think my mental thing is more related to the loss of my wife …. Because I’m in a house on my own …. Now whether that’s had an impact on the way … I’ve recovered I don’t know … but I feel it has had an effect.
(Patient, TKA)101
The previous quote also suggests a link back to the construct of ‘Individualisation of a standardised programme’, as individual circumstances, such as recent loss, may impact experiences, and may require a different level or kind of support in home recovery.
The experience of pain and pain management was an important specific feature of being an ‘active patient’, and was a salient issue for our PPI group. This links to the need for accessible follow-up, the work of carers (when they are managing the medication), and how complications can impact perspectives.
Fourteen studies (15 papers)90,102,104,106,111,114–116,120,123–126,129,132 suggested that a number of patients and carers found it challenging to know how to manage post-operative pain when at home, including uncertainty in how to manage their pain or medication, needing more guidance or information to do so effectively. This is illustrated by the quote below from a carer who describes the impact of not understanding the need for regular pain medication to prevent pain from escalating to a more unmanageable level:
The meds, too … no one told us to make sure we take [them] … and he got really in hot water [not taking enough], so the pain came back full force, and it took longer to get it down again.
(Carer of THA patient)106
Some feared becoming addicted to the medication, or taking too much, so were reluctant to take it as described, as suggested by six studies102,106,116,120,124,129 and illustrated by the quote below.
I only took them for about a few days …. But they said you must take them because you get better quicker with pain relief. But, I just ended up taking a couple of paracetamol … because I don’t have a lot of tablets.
(Patient, non-cancerous gynaecological surgery)120
Others struggled with side effects of the medication, and tried to balance between the amount of pain they were in and the side effects they would experience (described by three studies; four articles). 106,116,123,124
It’s the painkillers you become so tired from … a total lack of energy, so it’s not easy to do anything.
(Patient, LLA)124
Being in pain could impact patients’ quality of life, including their ability to sleep and mood.
I was awake all hours of the night … not to be able to get any sleep at night is a horrible thing. (Participant 2)
Yes, it was painful it didn’t stop me sleeping but it was painful. (Participant 10)
(Patient, LLA)125
Being in pain could also impact patients’ ability to do prescribed exercises or rehab, or they struggled to find a balance between pain and movement, as indicated by five studies (six articles),106,114,120,123,124,129 and illustrated by the hip arthroplasty patient quoted below from Churchill et al.:
I pushed myself, my muscles were inflamed, and there were nights I didn’t sleep as well because I was doing too much.
(Patient, THA)106
However, there was variation between patients, even within the same studies examining the same programme or regimen, again suggesting a need to individualise information or protocols to the patient (see construct: ‘Individualisation of a standardised programme’).
I’ve hardly had any pain, I’ve really only taken the tablets that I was forced to take.
I needed more, I never had enough. I didn’t want to take an overdose either. That was the thing that felt hopeless and disconsolate … that I didn’t experience any relief so that I could relax and feel hope.
(Patient, LLA)102
These issues around pain management could impact a patient’s ability to be actively involved in their own care, due to the physical and cognitive impacts of, for example, medication side effects or pain itself. It links to the construct of ‘Feeling safe’ – patients need clear information and support to manage their pain at home, as well as a consideration of their emotional needs (such as anxieties over addiction to medication).
Another key issue for being an ‘active patient’ linked to the construct of ‘Feeling safe’ is the finding that being an ‘active patient’ could be empowering to some, but could make others feel vulnerable, suggested by 15 studies (15 papers). 90,100,106,107,109,110,114,119,122,124,126,128–130,132 For example, Thomsen et al. 126 described how some patients and carers were forced to be ‘active’ due to a lack of follow-up care, or a reluctance to contact medical staff. For some, this nurtured a feeling of being in control, but for others it could increase feelings of vulnerability and a lack of safety, particularly if they experienced complications or unexpected side effects, or promised follow-up care was not available:
I was not prepared for being continually tired. It makes me very afraid.
(Patient, colorectal cancer surgery)126
Theme: staff skills – expertise versus generalists
Four studies (four papers) contributed to this theme, which describes that there were differing views amongst staff about whether you needed a specialist for particular components of a programme, or if generalists could be trained to do them. 101,112,117,129
Three studies112,117,129 suggested that some staff members had different perceptions of the bounds of different staffing groups’ roles, and who was primarily responsible for particular tasks or even the patient themselves. For example, in Haas et al. ’s study,112 doctors and nurses generally believed it was a physiotherapist who was responsible for early mobilisation, but physiotherapists felt they were only responsible for more complex patients and nurses were otherwise well placed to mobilise patients.
Having a physiotherapist to get them out of bed in the morning, they build the confidence in the patient, they know exactly what they’re doing … and know they’re capabilities, know exactly what to do with that patient.
(Nurse, LLA patients)112
It’s the difficult ones to get up and moving that’s most challenging. That’s where physiotherapists are best placed to use their expertise.
(Physiotherapist, LLA patients)112
Similarly, in Kocman et al. ’s study,117 which aimed to introduce the CGA into the care pathway, geriatricians saw their role as supporting the general team to develop specific skills and knowledge in caring for older people, whereas those in the general team saw the geriatrician as the one to hold those skills and knowledge.
One study101 examined an intervention in which more junior rehabilitation assistants worked in patients’ homes under the (remote) supervision of a trained physiotherapist. At times, the assistants could feel out of their comfort zone, but good support and communication helped to ensure both the assistants’ and the patients’ confidence, and physiotherapists aimed to find a balance between being supported and being independent.
It’s quite nice from a physio[therapist] assistant point of view to feel like you’re making an impact independently and [the physiotherapist] trust[s] you …. But at the same time, I didn’t feel at all like I was … abandoned … it was a really nice balance.
(Assistant, TKA patients)101
Theme: staff/service co-ordination
Nine studies (nine papers) contributed to this theme about the co-ordination of staff and services. This includes within hospital teams, between hospital services, and between hospital and community-based services. 104,105,107,111,114,115,118,124,129 It also includes the importance of a co-ordinator, from the perspectives of staff and patients/carers.
Four studies105,114,118,129 suggested that, where staff teams within or between care settings did not co-ordinate, it could cause confusion for patients when they received differing instructions, linking to the construct of ‘Feeling safe’, in which inconsistent information made patients feel less safe. For example, Westby et al. 129 described how their focus group of patients spent a great deal of time discussing issues of staff and service communication, with most patient examples describing ‘how poor or a lack of communication decreased efficiency, effectiveness, and collaboration’.
Communication issues could also cause confusion for the staff themselves, as illustrated by the quote below, which could also indicate a potential lack of understanding of the ERAS protocols in place by some staff members:
Sometimes they’ll say, ‘ERAS’, and then, ‘Nil by mouth’. So sometimes it’s not always very clear in the documentation.
(Staff, colorectal surgery patients)118
Five studies (six articles) also suggested that a lack of communication between services could result in sub-optimal, less individualised, care for patients:105,111,115,123,124,129
we have this parade of people with total hips … coming through as though they’re all the same and they’re not. I think this lack of information leads to rote [physical-therapy] procedures that don’t have very much thinking going on with them.
(Staff, physical therapist, LLA)129
But three studies107,118,129 indicated that when there was a small team or a named contact person for staff, it was easier to obtain the information needed:
… because we’re small, we can call up one person … so it’s easy. I think it works well, the link from the communication we have, acute hospital stay to community back into the outpatient department.
(Staff, occupational therapist, LLA)129
Within hospital, a care co-ordinator can help ensure that the different programme components are completed in a timely way to ensure that other components are not delayed, ensure an early discharge, and be available for staff or patients should they have questions (as indicated by six studies104,107,115,118,124,129). For example, Specht et al. 124 described how patients’ discharge could be delayed if they couldn’t take part in their training because they were waiting for a dressing to be changed. Staff in Lyon et al. ’s study118 felt that an ERAS co-ordinator helped staff to follow the protocol and to answer any patient’s questions:
I suspect without an ERAS coordinator it would be futile.
(Staff, colorectal surgery patients)118
When patients have no care co-ordinator, it can fall to them or their carers to do the work of trying to chase appointments, which could be especially challenging when professionals they needed to see were not co-ordinated, linking to the theme of ‘The direct, indirect and other work of caregiving’.
I have three doctors’ appointments [to arrange] … so I called [the urologist]. And then we have to go to [cardiologist] and [cardiac surgeon].
(Carer for CABG patient)111
Somehow, I felt that medical imaging nurses had their own schedule and physiotherapists had their own and they were not at all synchronised.
(Patient, THA)115
Two studies104,107 specifically investigated patients having a care co-ordinator, and it was her availability to patients which made the biggest difference, linked to the idea of making follow-up care easily accessible. For example, Berthelsen et al. 104 described how spousal carers specifically mentioned their case manager’s constant availability, explanations of information and ability to arrange appointments with other health professionals as what they appreciated about their involvement.
There was sometimes disagreement about who had responsibility for patient care following discharge, linked to service co-ordination. This made it more difficult for patients to know whom/where to contact if they had questions or difficulties. Within the ‘Appropriate, available and accessible follow-up’ theme, it was noted that patients do not always know whom they should contact when they have a problem or an issue, suggesting that it is not clear to patients who is taking responsibility for their care post-discharge. This was also reflected in four studies103,115,122,129 related to staff, who on occasion disagreed about who had primary responsibility for the patient.
I called the … nurse who said … I should ring the primary care centre, but they say that the operation was the hospital’s responsibility. Then they said: let’s not concern ourselves about this any more; from now on you can fix this yourself.
(Patient, colorectal cancer surgery)122
Construct summary: taking responsibility
This construct focuses on responsibility for patient care and recovery, particularly after discharge from hospital. Patients had to be active, rather than passive, and take charge of their own care. The experience of pain and pain management was an important specific feature of being an ‘active patient’, with some patients reluctant to take medication, and others (and some carers) unsure of how to manage medications. For some, the experience of being an ‘active patient’ could be an empowering experience, but for others it made them feel vulnerable. Patient expectations could impact their recovery or their views on recovery. Many patients and staff felt that a positive attitude was important in recovery, but this could also become blaming towards patients who could not fit the programme or did not recover ‘well’. This construct also highlighted the importance of good staff and service co-ordination, particularly after discharge, so that patients (and carers) received consistent information and were clear on whom they needed to contact if they had difficulties or questions. However, it also highlighted that some staff/services disagreed about who had primary responsibility for the patient following discharge, and that there could be differing views on whether generalist or specialist medical staff were best placed to provide care.
Construct: outcomes
Fourteen studies (14 papers) contributed to this construct,90,100,105,106,109–111,115,123,126,128–130,132 which contains two themes, ‘masking the negative’ and ‘the right question at the right time’, which highlight the issues for both staff and patients in the way outcomes are measured, and raise questions about what best practice for measuring outcomes in this area might be. This construct is less well-supported than the other themes; however, it has been developed as a main theme due to the way it speaks to the results of the quantitative review. Details of the articles contributing to the themes supporting this construct are provided in Report Supplementary Material 5, Table 6.
Theme: masking the negative
Eight studies (eight papers)90,100,105,106,109,126,128,132 contributed to this theme, which describes how some patients give high satisfaction ratings, but this can mask concerns or things they would improve, which are then missed in quantitative evaluations.
As highlighted in the follow-up theme within the construct ‘Feeling safe’, patients and carers may not always contact their care team because they did not want to bother them. 100,105,106,109,126,132 This may lead to a skewed view of how the patient is progressing, or how the programme is working overall, as the care team then does not hear about problems or issues the patients were facing:
… even though they say that if you’ve got any problems you can ring us, well I know … I don’t like to bother people, and I probably wouldn’t have phoned unless I was really, really worried.
(Patient, gynaecological cancer surgery)100
Hip arthroplasty patients from one study90 explicitly highlighted that though patients did have criticisms of the service or care that they had received, most masked this by trying to justify the problem on the health team’s behalf:
I suppose, though really they’ve not got time and there aren’t enough physios probably, for this. But er, that’s what I feel. I think physio is very, very important, proper physio.
(Patient, THA)90
Studies contributing to this theme indicate that patients may not always raise concerns when they occur or try and excuse services which did not meet their expectations, which may make it hard for services to identify patients and/or caregivers who are struggling or dissatisfied and offer appropriate support. This highlights the importance of active follow-up by staff at key points in the patient’s recovery pathway.
Theme: the right questions at the right time
This theme explores how people’s experiences of recovery and of caring for patients can change over time, meaning that asking evaluation questions at one time point may not provide a complete understanding of patient experiences. Six studies (six papers) contributed to this theme. 110,111,115,123,129,130
One study115 noted that their LLA patients did not know how to give feedback on their experiences, particularly specific feedback for specific aspects of the service. Our PPI group also emphasised that not only did they want the opportunity to provide feedback or information, but that they wanted this communication to be acknowledged or responded to, particularly in terms of the impact it may have on changes to the service.
One study129 highlighted that it was not clear how outcomes should best be measured, with staff participants highlighting that outcomes measurements were not standardised across services, or given at all time points, which made it difficult to make comparisons. Some staff in this study suggested questionnaires were not very useful in any case, and others highlighted that the patient’s goal was often getting back to ‘normal’, and the individualised goals which mean ‘normal’ were not well captured by these tools:
… it would be nice for people to actually use the same outcome measures pre-operatively, immediately post-op … so you could actually see a difference.
(Staff, physiotherapist, LLA)129
I don’t ask patients to fill out questionnaires. That’s highly inefficient.
(Staff, surgeon, LLA)129
The point in the care pathway / duration since discharge at which patients or carers are asked for feedback can make a difference, as their experiences and views on programmes can change over time, for the negative or positive. Galli et al. 110 described the experiences of one patient who felt positively at discharge, but one month later felt angry and unhappy with her experience as she did not feel she had an effective recovery. In contrast, Ganske111 suggests that carers initially have more negative emotions and perceptions of the experience at discharge, but that they became more positive in time as they gain more confidence in their caring tasks and the patient recovers. This suggests that evaluation may need to be longitudinal to capture the full range of experiences of both patients and carers.
Construct summary: outcomes
This construct highlights how services may receive an overly optimistic picture of a patient’s recovery journey due to patient reluctance to report concerns or difficulties, or appear critical of the care they receive. Patient and carer views and experiences may also change over the course of the recovery journey, necessitating the need for repeated follow-up by services. However, this follow-up will only be useful to services and patients if the discussion reflects the potential needs of services and individual patients and/or carers at that particular stage of the intervention pathway.
Line of argument synthesis
Figure 21 presents how the different constructs are theorised to relate to each other.
‘Home as the preferred place for recovery’ is a broader, more systemic construct which has a direct impact on all aspects of the experience for patients, carers and staff, and so underlies the other concepts in the model. For example, hospital systems ‘preferring’ patients to spend less time in hospital and recover at home is one of the main reasons why these hospital interventions are in place,26 and so the responsibility for recovery then falls on patients (construct: ‘Taking responsibility’) and/or their carers (construct: ‘Essential care at home’). This idea of home being preferred will be weaved into the exploration of all constructs in this section.
‘Feeling safe’ was of great importance to patients and carers. This feeling of safety was not necessarily the same thing as being medically or physically safe, though having complications or side effects often led to feelings of a lack of safety. Patients and carers needed to have their emotional needs met, as well as the physical, in order to feel safe. What an individual needs in order to feel safe (such as the type or format of information they need) will be specific to them, which means a ‘one-size-fits-all’ approach may negatively impact some patients’ feelings of safety, though, for some, it being a very structured programme can provide feelings of safety in itself. There is also the issue of how people feel safe at home when dealing with complications or side effects, and whether the patients and carers felt there was adequate and accessible follow-up care to deal with these and any worries that they had. In these ways, the concept of ‘feeling safe’ links with ‘Individualisation of a standardised programme’, and the possible tension between the protocol of the programme and individual patient needs, felt by both patients and the staff providing their care.
Recovery at home due to shorter length of stay in hospital means there is more responsibility on the patient (and their family caregiver). Being ‘active’ in their care could help patients to feel a sense of control, but for others it could feel a vulnerable position, making them feel less safe. Having a member of staff co-ordinate care could help individualise care where needed, as well as support the emotional needs of the patient, helping them to feel safe. A co-ordinator could also support follow-up being accessible to patients. Patients (and carers) also had a need for more information to be effective ‘active’ patients, and to align their expectations with likely outcomes and timescales. This responsibility to be an active, rather than passive, patient meant the blame could be placed on patients when recovery was not on track or they had concerns, which may in part be a response to the difficulty some staff felt in individualising care within the structure of the programme.
The responsibility for recovery shifting from hospital to home, and to patients, also meant that there was a need for care at home, which often came through family caregivers. Staff, patients and carers all suggested that having home support in this way was essential. But this meant that a great deal of additional work was placed on carers. Carers needed support and information throughout the care pathway in order to be able to fulfil their roles, and patients without home support needed the support from community services instead, either through formal caregiving services or by being discharged to other healthcare settings for recovery instead of home. This also links to the construct of ‘Feeling safe’, as patients needed both physical and emotional support at home to feel safe recovering there.
Measuring patient experiences and outcomes quantitatively in these kinds of interventions and programmes could be challenging, given that patient and carer needs and perspectives could change over time, so a questionnaire at only one time point may not capture the full experience, and patients may mask their negative views, so these are not captured as fully. This may link to the themes within the construct of individualisation, as organisations, staff and patients may have differing priorities, which may cause differences between what organisations measure and what feedback patients want to give or what is important to them. Additionally, being inside or outside the programme could impact how patients viewed the programme, suggesting the importance of both considering complications when evaluating outcomes, and including patients with comorbidities in studies in order to understand the views of those who may not fit as easily within the structure of the intervention. This in turn could impact meeting patient needs, as excluding more complex patients from studies means it is not clear what this group of patients, who may be more likely to fall outside the programme, may need or what adaptations to protocols may be most appropriate.
To illustrate how the contents of the different constructs and themes presented in this line-of-argument synthesis relate to each other further, we applied the findings of this synthesis to an ERP intervention. This was used to develop the logic model used as basis for our overarching synthesis as described in Chapter 4. The patient’s attributes such as whether they have support from a family carer, live rurally, or have comorbidities, and the availability of resources such as weekend or community follow-up care, act as modifiers on the intervention. For example, having insufficient support at home from a family carer or having several complications may require more individualised support at home than for a patient with an uncomplicated recovery who has a supportive family carer. The intervention components illustrated lead to support for both emotional and physical needs, accurate expectations of recovery and outcomes, and an individualised and co-ordinated service. These then facilitate a trust in the pathway and in the staff delivering care, a feeling of safety, and the feeling of being empowered as an active participant in their own care, which then lead to positive PROMs and PREMs. However, evaluators must ensure they are measuring the right outcomes at the right time.
Summary
This systematic review of qualitative research aimed to address the research question: what are the experiences of patients receiving multicomponent interventions to enhance recovery and/or reduce LOS, their family and carers, and staff involved with delivering care within these interventions? In total 42 studies (43 articles) met the inclusion criteria for this review, with 34 studies (35 articles) prioritised for full data extraction, quality appraisal and synthesis.
Our synthesis used a meta-ethnographic approach to develop six constructs.:
-
home as the preferred environment for recovery;
-
feeling safe;
-
individualisation of a structured programme;
-
essential care at home;
-
taking responsibility; and
-
outcomes.
The first construct ‘Home as the preferred environment for recovery’ highlights the benefits, and challenges, of recovering at home for patients and carers. This construct influences the concepts discussed within the other five constructs. ‘Feeling safe’ explores the importance of ensuring the emotional and physical needs of patients and their family/carers are met, and that they are supported to develop confidence through provision of information, pre-operative care and accessible, appropriate follow-up care. ‘Individualisation of a structured programme’ discusses the importance of tailoring structured programmes, such as ERPs, to the needs of the individual patient. It also highlights the challenges that comorbidities, complications and weekend staffing levels can pose to this patient-centred process. ‘Taking responsibility’ raises key questions around roles and responsibility for the recovery process, including after discharge – exploring the role of the active patient, expert versus generalist staff and staff/service co-ordination. ‘Essential care at home’ highlights the vital role of informal caregivers in supporting patients within their own home post discharge. It also highlights the need to ensure caregivers are provided with adequate support to enable them to perform their caregiving role. The final construct ‘Outcomes’ examines how patients may not always be asked about aspects of their care or recovery that are most meaningful to them, at the right time, and that they may mask or overlook the negative aspects of their care.
We used these constructs to develop a line-of-argument, exploring the relationships between each construct and the themes contained within them, as illustrated by Figure 21.
Chapter 4 Overarching synthesis
This chapter details the methods and findings from the overarching synthesis, which aims to integrate the main findings from the quantitative systematic review (see Chapter 2) and the qualitative systematic review (see Chapter 3) to answer research question 3: Which aspects of multicomponent interventions to enhance recovery and/or reduce LOS are associated with better outcomes for older adults admitted to hospital for planned procedures? This chapter describes the methods used, results and interpretation.
Qualitative comparative analysis methods – overall approach
We drew on QCA to better understand how successful interventions ‘worked’ to inform the design of future interventions. Although QCA is named as a qualitative technique, it involves numeric data and is an approach based on set-theory. 142 Through drawing on set-theory, we can identify studies that successfully reduced length of stay as belonging to a set of studies that are distinct from studies that were unsuccessful (i.e. they belong to a different ‘outcome set’). We can also identify different sets of studies that are marked by the presence or absence of different intervention components or the implementation of (or lack of) different processes; these studies are distinguished by their ‘conditions’ (analogous to variables or features of the intervention). A goal of QCA is then to determine which sets of studies belong to both ‘condition sets’ and ‘outcome sets’ of interest and to establish the strength of relationships between these condition sets and outcome sets.
Typically, when QCA is applied to systematic reviews, the aim is to identify which condition sets can be viewed as sub-sets of outcome sets, known as a sufficient relationship. QCA allows us to recognise that there may be different pathways to successful interventions (several sufficient relationships) and the goal of QCA is to identify the simplest expression of characteristics/processes that lead to effective interventions; to find the simplest expression we draw on the laws and theorems of Boolean algebra and undertake minimisation of the solution. 143 QCA also allows us to recognise that some intervention components may only activate change in the outcome in the presence of another (conjunctural causation).
QCA is a useful approach when encountering the challenge of analysing data containing a small number of cases (i.e. studies), each with an extensive array of factors that may trigger a given outcome. 144 This ‘small N-many variables’ challenge is often faced by systematic reviewers, and over the past decade since its first application to evidence synthesis by Thomas and Harden145 QCA has been applied to an increasing number of systematic reviews to explain heterogeneity in study impacts. 146 The goals of QCA have been described as integrating the best features of the case-oriented approach, involving developing an in-depth knowledge of individual studies, with the best features of a ‘variable-oriented’ approach, where the focus is on comparing studies and identifying cross-case patterns in the data. 147 This means that QCA works best with a moderate set of studies that facilitates identifying cross-case patterns (typically ten or more studies per model) but where the number of studies allows for the researcher to develop ‘empirical intimacy’ with the set of studies and to be able to develop case-based as well as cross-case explanations for successful interventions, with QCA applications in systematic reviews typically limited to under 40 studies per model.
In undertaking this analysis, we followed guidance and stages set out elsewhere,145,148 where we:
-
identified the underlying theory and organised the cases
-
configured the datasets and developed the data tables
-
constructed the truth tables
-
checked the quality of the truth tables
-
undertook Boolean minimisation of the truth tables
-
considered logical remainders and undertook essential quality checks
-
interpreted the solution and undertook further iteration and sensitivity analysis where necessary.
To ease interpretation of the results, we provide more granular detail of these steps alongside the results.
Qualitative comparative analysis process and results
QCA stage 1 results – identification of underlying theory and organisation of cases
A fundamental principle of conducting QCA is to ensure that analytical decisions are based on theory. In our QCA, we based our theoretical framework primarily on the qualitative systematic review (see Chapter 3), the results of which were used to inform the design of a logic model. Logic models are a form of programme theory and are graphical depictions of how an intervention is expected to exert an influence on the outcome through outlining a series of assumptions about which elements of an intervention are important and how they are organised. 149 The logic model was developed based on patient perspectives represented in the qualitative evidence synthesis (see Chapter 3) as well as broader discussions within the team, with clinical stakeholders and with the PPI group, and was created to represent interventions that are implemented to support differing surgical procedures (abdominal-cavity surgery and LLA). Therefore, the logic model, and consequently the focus of the QCA, was on the implementation of common non-clinical elements of interventions to reduce LOS/enhance recovery for older adults following planned surgery (see Figure 22).
FIGURE 22.
Logic model for length of stay interventions.
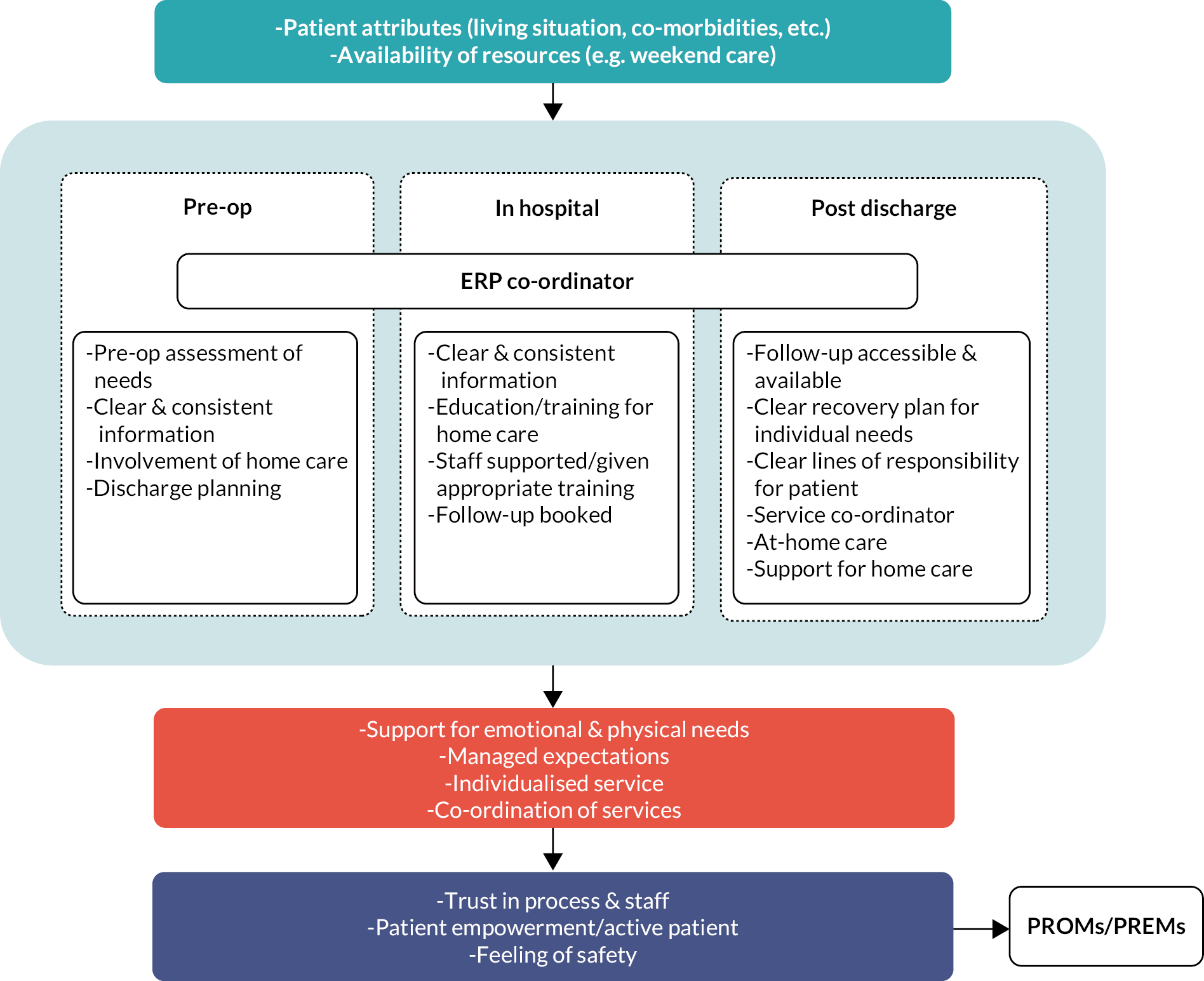
Of particular interest in this QCA is the examination of which configurations of intervention components (depicted in the orange rectangle in Figure 22) are associated with successful interventions, and how these configurations differ according to intervention focus. In addition, the presence and role of the coordinator as a focal point for coordinating care across the intervention is also of interest. We conducted an iterative process involving reading through studies to identify which conditions were reported clearly or consistently enough to be utilised in the QCA. This facilitated developing in-depth knowledge of the interventions as well as allowing us to refine the list of conditions and identify gaps in reporting. The conditions (analogous to variables) of interest were then extracted for each study.
To maximise the number of studies available for QCA synthesis, we allocated studies into successful and unsuccessful sets based on estimates of effectiveness in terms of LOS and patient-reported outcomes jointly. Studies were included if they provided data that indicated whether the intervention was effective (or not) in reducing LOS or effective in improving PROMs/PREMs, irrespective of whether the study was previously able to be incorporated into meta-analysis. For example, if a study did not provide data permitting the calculation of effect sizes for an outcome, but either stated that there was no difference between groups or provided the results of an appropriate statistical test for between-group differences, it could be included.
This resulted in a potential pool of 14 studies about recovery from lower-limb arthroplasty (LLA studies) and 24 studies about recovery following any type of surgery performed in the abdominal cavity, thus combining studies from the cardiac, abdominal, upper abdominal, pelvic and thoracic procedural groups. The studies in the abdominal surgery category were either about Prehab (n = 12 studies) or ERP (n = 12 studies) interventions. Rather than aiming to compare the effectiveness of both approaches, here we aim to understand the drivers of heterogeneity within both approaches.
The remainder of the analysis therefore focuses on three sets of studies examining the effectiveness of interventions to reduce LOS and/or accelerate recovery following elective surgery in older adults: (1) all LLA studies, (2) ERP for abdominal surgery, (3) Prehab for abdominal surgery. Individual studies are frequently referred to as ‘cases’ from hereon in, in line with QCA terminology.
QCA stage 2 results – configuration of datasets and creation of data tables
Next, we developed three data tables for the QCA models reflecting the conditions (characteristics of studies) and the outcome for studies on (1) Prehab interventions for recovery from abdominal surgery, (2) ERP interventions for recovery from abdominal surgery and (3) interventions for recovery from LLA.
We aimed to allocate studies into successful and unsuccessful sets based on their outcomes, and recognised that studies could also be partial set members (i.e. partially successful or partially unsuccessful). This involved ascribing quantitative values to effect size data based on length of stay (LOS) outcomes and PROMs, with the rules in Table 5 used to allocate studies.
| Effectiveness rating | Numeric value | Allocation criteria |
|---|---|---|
| Successful studies | 1 | Improvement (statistically significant) in at least one PROM AND LOS |
| Partially successful studies | 0.66 | Improvement in at least one PROM but NO improvement in LOS |
| Partially unsuccessful studies | 0.33 | Improvement in LOS but NOT in PROM |
| Unsuccessful studies | 0 | No improvement in either PROMs or LOS |
For each condition (components or processes that are theorised to influence intervention outcomes) a coding scheme was developed to determine whether the condition was present or absent in the cases. The scheme and the three data tables are presented in Appendix 6. As we had a limited set of cases for the number of conditions, our analytical strategy involved first creating a ‘truth table’ based on four conditions in line with guidance on the case : condition ratio outlined elsewhere;148,150 we then expected to revise this initial model based on the quality of the truth table before then seeking to produce a reduced truth table and minimised solution based on this. A ‘truth table’ sorts cases according to the configuration of conditions they exhibit.
QCA stage 3 and 4 results – construction of truth tables and undertaking quality checks
The truth tables outline the distributions of the cases across the different configurations of intervention components and processes and were created through a QCA package developed by Duşa151 in R (R Core Team, 2022). Each row in the tables represents a ‘condition set’, that is a set of cases each sharing the same configuration of characteristics. Rows with a ‘1’ in the outcome column are configurations that are viewed as triggering a successful intervention. These rows exhibit a sufficient relationship with the outcome. We set a ‘consistency threshold’ to identify these relationships at 0.79, reflecting guidance on appropriate thresholds elsewhere. 148 Those with a ‘0’ in the outcome column are viewed as triggering an unsuccessful intervention (and have consistency scores below the 0.79 threshold). On the right side of the table is a column marked consistency; this indicates the strength to which studies that belong to the condition set are also a subset of the outcome set. A value of 1 indicates perfect consistency; all cases in the configuration are full members of the condition set and the successful outcome set (a subset relationship) and there is strong evidence that interventions that share these (theory-driven) characteristics trigger a successful outcome. A value of 0 indicates perfect inconsistency and suggests there is no evidence that these intervention characteristics trigger successful outcomes. Values in between indicate some degree of ambiguity, which is expected given that we had used a fuzzy-set coding scheme, allowing studies to be partial members of sets (both outcome sets and condition sets in some of the models and iterations).
ERP interventions following abdominal surgery
We first created a model for the ERP abdominal-cavity studies, which we intended to form the basis of subsequent models. We initially looked at four conditions reflecting whether the intervention (1) provided information in different formats to participants, (2) had an emphasis on goal setting, (3) had a consistent co-ordinator role (e.g. a nurse) throughout the intervention and (4) collected a high number of PROMs.
An initial truth table was created that suggested that studies that had an emphasis on understanding patient experiences through collecting a high number of PROMs tended to be successful (see Table 6). However, on further inspection it became apparent that some configurations within the truth table included a mixture of successful and unsuccessful studies, and an alternative model was developed. This is summarised in the truth table in Table 7, which examined configurations according to whether the study (1) provided information in different formats to participants (Diff_Format), (2) had an emphasis on goal setting (Goal_set), (3) had a consistent co-ordinator role (e.g. a nurse) throughout the intervention (Nurse_Led) and (4) included efforts to support discharge (Supp_Discharge).
| Configuration | Different format | Nurse led |
Goal set | Support discharge | OUT | Number of cases | Consistency | PRI (proportional reduction in inconsistency) |
|---|---|---|---|---|---|---|---|---|
| A | 1 | 1 | 0 | 0 | 1 | 2 | 1 | 1 |
| B | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 |
| C | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 |
| D | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 |
| E | 1 | 1 | 0 | 1 | 0 | 1 | 0.33 | 0 |
| F | 1 | 1 | 1 | 1 | 0 | 1 | 0.33 | 0 |
| G | 0 | 1 | 0 | 0 | 0 | 2 | 0.165 | 0 |
| H | 0 | 0 | 0 | 0 | 0 | 3 | 0.11 | 0 |
| Configuration | Different format |
Nurse led |
Goal set |
Support discharge |
OUT | Number of cases | Consistency | PRI (proportional reduction in inconsistency) |
|---|---|---|---|---|---|---|---|---|
| A | 1 | 1 | 0 | 0 | 1 | 2 | 1 | 1 |
| B | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 |
| C | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 |
| D | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 |
| E | 1 | 1 | 0 | 1 | 0 | 1 | 0.33 | 0 |
| F | 0 | 1 | 0 | 0 | 0 | 2 | 0.165 | 0 |
| G | 0 | 0 | 0 | 0 | 0 | 3 | 0.11 | 0 |
The truth table reassuringly showed that studies that did not have any of the four conditions belonged to an unsuccessful configuration (a configuration composed of three studies). 83–85 However, the truth table also revealed that a study with all four elements conducted by73 was also unsuccessful, which challenged the assumptions outlined in the logic model (configuration F below). Further examination of the characteristics of this study showed that the study also included a distinct set of key intervention features, with the intervention’s components including light and music therapy alongside psychological intervention; all other interventions included in the dataset were evaluating changes in the type and implementation of clinical practice (e.g. changes in fluid management) as well as changes in the implementation of care practices.
As the intervention appeared to be based on a distinct programme theory that was unlike other interventions, the remainder of the analysis is based on 11 studies, with a revised truth table shown in Table 8. Four configurations are observed as triggering a successful outcome, giving an indication that there are multiple pathways to triggering a successful outcome, although only one of these is supported by multiple studies. We can see that in this truth table, seven out of a possible 16 potential configurations of conditions are observed in the data. A study conducted by Forsmo and colleagues88 which trialled an ERAS protocol for patients who had experienced colorectal surgery was the only study in the data coded as including efforts supporting discharge; this study improved length of stay but not PROMs and was allocated to the partially unsuccessful set.
| Configuration | Different format |
Add time | Goal set |
Early mob | OUT | Number of cases | Consistency | PRI (proportional reduction in inconsistency) |
|---|---|---|---|---|---|---|---|---|
| A | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| B | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| C | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| D | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
| E | 1 | 0 | 0 | 1 | 0 | 1 | 0.33 | 0 |
| F | 0 | 1 | 1 | 0 | 0 | 6 | 0.22 | 0.12 |
| G | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
Prehab interventions for abdominal surgery
We started with a model that mirrored the conditions for the ERP studies which required further iteration due to inconsistencies within configurations. A truth table (see Table 9) consisting of four conditions was developed that reflected whether interventions (1) provided information in different formats to participants (Diff Format), (2) had an emphasis on goal setting (Goal set), (3) included additional time being spent with patients (Add time) and (4) included an emphasis on the early mobilisation of patients (Early Mob). Of 16 possible configurations, seven were observed within the data, with the largest configuration consisting of six studies that were unsuccessful which provided additional time for patients and goal-setting but did not focus efforts on early mobilisation or provide information in different formats. This suggests that configurations involving these latter two conditions may be particularly important in determining intervention success; this is explored further in the minimisation process.
| Configuration | Early mob | Goal set | Nurse led | High PROMS | OUT | Number of cases | Consistency | PRI (proportional reduction in inconsistency) |
|---|---|---|---|---|---|---|---|---|
| A | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| B | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
| C | 1 | 1 | 0 | 1 | 1 | 2 | 0.854 | 0.829 |
| D | 0 | 1 | 1 | 1 | 1 | 4 | 0.798 | 0.774 |
| E | 0 | 1 | 1 | 0 | 0 | 1 | 0.604 | 0.604 |
| F | 1 | 0 | 0 | 1 | 0 | 1 | 0.5 | 0 |
| G | 0 | 0 | 0 | 1 | 0 | 2 | 0.398 | 0 |
| H | 0 | 1 | 0 | 1 | 0 | 1 | 0.33 | 0 |
| I | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
Interventions for lower-limb arthroplasty surgery
Data from 14 studies are included in the truth table (see Table 10), which explores whether interventions (1) included an emphasis on the early mobilisation of patients (Early Mob), (2) had an emphasis on goal setting (Goal set), (3) had a consistent co-ordinator role (e.g. a nurse) throughout the intervention (Nurse_Led) and (4) collected a high number of PROMs (high PROMs). Of 16 possible configurations, nine were observed within the data. Four configurations were observed to trigger successful interventions; configuration D was close to the consistency threshold of 0.79 and included a partially successful study where there was an improvement in at least one PROM but not in LOS;51 configuration C also included a partially successful study. 78 Two of the configurations suggest that studies that had an emphasis on understanding patient experiences through collecting a high number of PROMs were also more likely to be successful, albeit with the presence of other conditions. The truth table in this case helps to separate out configurations that include fully as well as partially successful studies from those that are partially or fully unsuccessful.
| Solution consistency | PRI | Raw coverage | Unique coverage | Studies | |
|---|---|---|---|---|---|
| GOAL SETTING | 1.00 | 1.00 | 0.334 | 0.167 | Khoo44,45 |
| DIFFERENT FORMAT * ~SUPPORTING DISCHARGE | 1.00 | 1.00 | 0.668 | 0.501 | Frees;58 Jones et al.;44 Vlug Lap, Vlug Open65 |
| Solution coverage | 1.00 | 1.00 | 0.835 |
QCA stage 5 and 6 results – Boolean minimisation and incorporation of logical remainders
We applied Boolean minimisation to obtain the simplest expression of those conditions (intervention processes) that were associated with triggering a successful intervention for each truth table described above. We first developed a ‘complex solution’ based on the observed data only; however, as noted above, of the 16 possible configurations of conditions, several were left unobserved in the data. These unobserved configurations are known in QCA parlance as logical remainders and can be used to simplify the minimised solution further. We can make assumptions about the likely outcome if logical remainders were observed in the data; these assumptions can be data-driven and determined by computer algorithms to form the simplest expression (the parsimonious solution), or they can be informed by researcher input (the intermediate solution – intermediate in complexity between the complex and parsimonious solutions). For each truth table, a complex, parsimonious and intermediate solution was generated (all are available upon request), although here we focus on the results of the intermediate solution, following a growing consensus in the QCA literature around the prioritisation of the intermediate solution. 152
ERP interventions following abdominal surgery
The solution shows two pathways to triggering a successful intervention (see Table 11) – the first pathway suggests that goal-setting alone is sufficient (although not necessary) to trigger a successful intervention; the second suggests that providing information in a different format in the absence of taking efforts to support discharge leads to a successful intervention (not supporting discharge, represented by the ~ sign in the table). The interpretation of this solution is discussed later in the results. The solution has a high coverage value, and exploration of individual cases shows that the solution accounts for all cases that were full members of the effective intervention set.
| Solution consistency | PRI | Raw coverage | Unique coverage | Studies | |
|---|---|---|---|---|---|
| DIFFERENT FORMAT * ADDITIONAL TIME | 1.00 | 1.00 | 0.531 | 0.531 | Arthur,52 Tagaki,87 Reif/Auer71,72 |
| ~DIFFERENT FORMAT * ~GOAL SETTING * EARLY MOBILISATION | 1.00 | 1.00 | 0.177 | 0.177 | Kapritsou 202081 |
| Solution coverage | 1.00 | 1.00 | 0.708 |
Prehab interventions supporting abdominal surgery
This dataset included four studies that were in the successful intervention set, and the solution shows two pathways to triggering a successful intervention (see Table 12) – the first pathway suggests that providing information in a different format and spending additional time with patients is sufficient to trigger a successful intervention (the ‘and’ relationship represented by the * sign); the second pathway suggests that efforts to support early mobilisation but not providing information in different formats and not setting goals leads to a successful intervention (‘not’ represented by the ~ sign below). The interpretation of this solution is discussed later in the results. The solution has a high coverage value, and exploration of individual cases shows that the solution accounts for all cases that were full members of the effective intervention set, although it does not account for two studies that were partial members of the successful set whose characteristics were indistinguishable from less successful studies. 54,57
| Solution consistency | PRI | Raw coverage | Unique coverage | Studies | |
|---|---|---|---|---|---|
| EARLY MOBILISATION * GOAL SETTING | 0.915 | 0.907 | 0.424 | 0.424 | Larsen;68,69 Pour;78 Fransen;60 Den Hertog75 |
| GOAL SETTING * NURSE LED * PROM CONSIDERED | 0.798 | 0.774 | 0.306 | 0.306 | McDonall;89 Siggeirsdottir;86 Williamson;51 Soeters77 |
| WHOLE SOLUTION | 0.882 | 0.848 | 0.729 |
Interventions supporting lower-limb arthroplasty surgery
This dataset of 14 studies included six studies that were full members of the successful outcome set and two that were partial members, and the solution accounted for all eight of these studies (see Table 12). Two pathways were identified that triggered a successful intervention – the first accounted for four studies and suggested that a combination of early mobilisation and goal setting triggered a successful intervention; the second also accounted for four studies and suggested that goal setting, along with a consistent point of contact (e.g. a nurse) leading the intervention, along with a high number of PROMs being measured, were sufficient to trigger a successful intervention.
Additional quality checks implemented across all models
In obtaining the solutions above, some untenable assumptions may have been made about the logical remainders and we implemented an algorithm developed by Dusa151 to remove untenable and contradictory logical remainders that could be otherwise be used to generate the solution, generating an ‘enhanced intermediate solution’. Further checks on the solutions were also undertaken to ensure that the solutions did not also trigger the negation of the outcome (a possibility in QCA due to causal asymmetry). Finally, any discrepancies in coverage were also checked, with the models for both sets of abdominal studies accounting for all studies that were full members of the successful outcome set, and the model for LLA accounting for full and partial members of the successful outcome set.
QCA stage 7 – interpretation
All solutions presented explore the accompanying care processes that support interventions to reduce the length of stay within hospital and improve patient outcomes. The solutions therefore do not point to which clinical intervention components can improve these outcomes, but instead give an indication of how procedures should be implemented from the patients’ perspective.
Enhanced recovery protocols for abdominal surgery
Two pathways were identified here, with one pathway suggesting that goal-setting alone was sufficient to trigger a successful intervention, represented by two studies, one of which also appeared in the second pathway. In both studies, patients were informed of protocols and goals for different stages of their recovery, for example daily mobilisation and nutritional goals. 44,45 Such goal-setting was found to be an important way of allowing patients to measure their progress and self-motivate in the qualitative synthesis. Both the qualitative synthesis as well as the results of recent trials153 emphasise that goal-setting should be person-centred and should be viewed as shared by the patients and the clinicians. Given that both successful studies describe the clinical elements of the studies in greater detail than some of the elements around implementation (i.e. how the intervention was conducted), it is unclear the extent to which goal-setting was implemented as a joint enterprise and was person-centred in nature. 44,45
A second pathway suggested that providing information in different formats, and not implementing efforts to support discharge, triggered a successful intervention. The importance of providing information in different formats (e.g. written and orally) is congruent with the qualitative synthesis, which showed that providing information clearly helped improve the confidence of patients in self-management tasks, but also improved understanding of why tasks were important to their recovery. Efforts to support discharge were not reported in 11 ERP studies, or were similar in intervention and comparator groups, and were only present in an unsuccessful study conducted by Forsmo and colleagues. 88 The intervention involved stoma education, which was intended to allow patients to be better prepared for discharge and subsequently managing a stoma at home. This intervention was associated with reduced LOS but there was no improvement in PROMs measured.
Given that there was only one study reporting differences in efforts to support patients at or after discharge, there is insufficient evidence in the studies to fully evaluate the impact of this condition on the outcome. It may be that while there were some measures to support discharge put into place, in the case of Forsmo these did not fully prepare patients, although the description provided does not allow us to assess this further. 88 While the second pathway in this group of studies indicates that not implementing efforts to support discharge triggers a successful outcome, this suggestion is incompatible with our logic model and the reflections of PPI members and clinical stakeholders.
Prehab interventions supporting abdominal surgery
For Prehab interventions, providing information in different formats was identified as a trigger for successful intervention in one pathway, but only in combination with spending additional time with patients. This pathway once again suggests that a person-centred approach to the implementation of the intervention generates a successful outcome; here it suggests that providing information and allowing time for questions and the development of broader relationships can lead to more individualised care and improved patient outcomes. For example, in the case of one successful study supporting this pathway, in addition to education and reinforcement, monthly nurse-led telephone calls not only allowed patients time to ask questions, they also ‘provided reassurance’ to patients, emphasising that information in conjunction with creating a safe space to process information and ask questions is important in reducing length of stay and improving PROMs. 52
One study found that early mobilisation but not providing information in a different format and not incorporating goal-setting triggered a successful outcome. The intervention evaluated by Kapritsou and colleagues focused heavily on progressive mobilisation out of bed 4 hours after surgery, with four daily bouts of ambulation in the first day post-surgery, whereas conventional protocols involved far fewer bouts of ambulation from the outset. 80 Such efforts align with the qualitative evidence that early mobilisation helps crystallise the patients’ role as active patients (which may reduce the length of stay) and successful mobilisation can send a message to patients that they are on the path to recovery. While early mobilisation in this study appears to trigger success in the absence of the other two components, this may be a feature of reporting more than a form of conjunctural causality in this study given that early mobilisation may itself be viewed as a shared goal between patients and clinicians and the study reported provision of information as a core intervention feature (although this was not reported as being provided in different formats).
Interventions supporting lower-limb arthroplasty
Goal-setting was a feature of both pathways identified as triggering success for interventions supporting LLA. Among four studies, success was triggered when goal-setting was accompanied by early mobilisation, with one study noting that efforts to support early mobilisation were set around specific milestones (goals), including getting up on the day of the surgery and climbing stairs two days afterwards, and was accompanied by positive reinforcement by a case manager. 75
In a different set of studies, goal-setting was accompanied by a consistent point of care and coordination as well as a high number (4+) of PROMs measured (even if not all changed positively). We interpret this latter condition as being symbolic of a commitment by triallists to promote patient-centred care and to understand patient experiences in a holistic way; while all trials included measured a PROM as part of the inclusion criteria, there was variation in the extent to which triallists were interested in multidimensional measures. For example in one successful study included in this configuration,86 a key aim was to address a gap in evidence about the broad functioning and quality of life and levels of pain among patients who have a shorter hospital stay. In addition, the role of a consistent coordinator was also identified as crucial in this pathway alongside goal-setting and a consistent point of care, which is congruent with the qualitative research where a coordinating role was observed to be a vital one among patients and clinicians to ensure adherence to protocols and to facilitate the patient journey. Returning to the example of Siggeirsdottir and colleagues, a physiotherapist and/or OT was involved in the care of each patient, providing education from one month before the surgery, through to accompanying the patient home if needed, and conducting a number of visits after discharge (a median of four within the first 2 weeks post discharge) to ensure that the regime was being followed. 86 In the qualitative synthesis, such a regime that involves a consistent point of care helped to ensure that patients felt that their care was individualised and that follow-up care was easily accessible.
QCA summary
Summary
For ERP interventions to support recovery from abdominal surgery, goal-setting or offering information in different formats were identified as core components of studies that successfully reduced LOS and improved patient outcomes. For Prehab interventions before abdominal surgery, offering information in different formats and spending additional time with patients (e.g. to address questions) are likely to be important factors in reducing LOS and improving patient experiences (this pathway was supported by the greatest number of successful studies). Finally, for interventions focused on ERP and Prehab approaches for LLA, goal-setting along with early mobilisation or goal-setting along with a thorough approach to understanding patient outcomes holistically and a consistent point of care were identified as important for reducing LOS and improving patient outcomes. The results therefore suggest that a complex balance of intervention components trigger successful interventions: these represent both individualised approaches that allow patients to understand their treatment (e.g. through providing information in different formats), to ask questions about their treatment (through spending additional time with patients), and to build supportive relationships (through having a consistent point of care), with more exigent strategies that facilitate patients to monitor their own progress (goal-focused) and challenge themselves in recovery (through early mobilisation).
Chapter 5 End-user involvement
This chapter details how patients, members of the public and clinical stakeholders were integrated throughout each stage of the review process and identifies the impact of their involvement in review processes, decision-making and project outcomes.
Patient and public involvement and engagement
Two adults aged over 60 supported the development of the funding application and approved the final protocol for the study prior to its submission.
We met with eight adults aged 60 or over with experience of being a patient for a planned procedure with an overnight stay, and six adults with experience of caring informally (i.e. not as part of a paid role) for a patient aged 60 or over following a planned procedure with an overnight stay. Four 2-hour meetings were scheduled over the course of the project; the timings of these meetings aligned with key stages of the review (detailed below in Table 13):
-
early stages of screening – allowing for any potential changes to the inclusion criteria
-
end of screening, initial stages of data extraction – allowing for early interpretation of outcomes emerging from the quantitative systematic review
-
end of analysis for both reviews – allowing for themes to be discussed for the logic model
-
end of project – allowing for feedback on key themes and dissemination plan.
| Review stage | PPI/stakeholder involvement | Impact on project |
|---|---|---|
| Protocol development October 2018 |
1 × 2-hour in-person meeting with PPI group from previous project | The research questions for this review were derived directly from discussions with patients and clinicians during completion of our previous review and represent issues that both groups were keen to address.17 |
| May 2019 | 1 × 1-hour in-person meeting with AH | Discussed care pathway for older adults admitted for hospital procedures. Identified need to focus on support needs of patient’s post-hospital discharge. Informed focus of review. |
| July 2019 | 1 × 1.5-hour in-person meeting with patients who had supported previous review (n = 2) | Discussion on the difficulties that they, and the individuals supporting them, experienced following discharge from hospital. Also included their experiences providing support as informal carers to others who had been discharged from hospital. Discussed patient views on QoL and particular importance of this post hospital discharge. Patients approved of project plan and helped inform the selection of relevant outcomes, and thus the inclusion criteria, for the quantitative systematic review. |
| August 2019 – February 2020 | Email exchange with AH, JM, CL | Clinical stakeholders checked inclusion criteria and suggested patient and professional organisations who we could include in our dissemination strategy |
| Meeting 1, protocol revisions/checking focus of reviews 1 and 2, June 2021 | 1 × 2-hour meeting with patient group (n = 7); 1 × 2-hour individual meeting with patient; 6 × 1.5-hour individual meetings with carers | Experiences of hospital admissions and/or caring experiences shared, and factors which impacted their experience, including communication, the need to self-advocate, carers as the eyes and ears of the patient, and difficulties around discharge/post-op. These discussions helped inform our thinking for qualitative analysis and building of logic model. Perspectives on the definition of ‘length of stay’ were also discussed, with PPI members defining it as including from when they first entered hospital, while many studies define it as the period following the procedure only. |
| Feedback on analysis-in-progress | CL present at monthly team meeting | Discussion about acute post-operative pain as an outcome compared to other outcomes. Decision to de-prioritise studies in the quantitative systematic review where this was the only PROM/PREM. |
| Meeting 2, feedback on analysis-in-progress (mainly the quantitative systematic review), November 2021 | 1 × 2-hour meeting with patient group (n = 8); 1 × 2-hour meeting with carers’ group (n = 2), 2 × 2-hour individual meetings with carers | Discussed the outcomes emerging from the quantitative systematic review. Identified what was missing and what would be prioritised. QoL and anxiety felt to be very important. Discussed studies only measuring acute post-operative pain and what the group thought about the value of this as a single outcome. Discussed the difficulty of regional differences in access to post-op services, including rurality vs. urban living. Post-operative recovery phase at home raised by both carers and patients as being the most challenging where more support was often needed. This phase highlighted as being poorly represented in the studies in terms of outcomes. Carers also noted the difficulties of caregiving, such as caring for older and younger relatives at the same time, the additional challenges when the person you care for is not a relative, and the need for services to communicate with them. Discussions reinforced our thinking around deprioritising studies measuring acute pain only and highlighted where there are gaps in the evidence as well as providing materials for the discussion. |
| Feedback on analysis plans, April 2022 | Email correspondence with JM and AH | Informed how quantitative studies were grouped based on outcome, procedure and/or intervention for consideration in QCA analysis. |
| Meeting 3, feedback on initial findings of the quantitative systematic review; feedback on analysis-in-progress: qualitative evidence synthesis, May 2022 | 1 × 2-hour meeting with patient group (n = 6); 1 × individual meeting with patient; 1 × email correspondence with patient; 1 × 2-hour meeting with carers’ group (n = 2), 2 × 2-hour individual meetings with carers | Discussed patient pathway and both patients and carers highlighted that post-discharge phase at home creates the most challenges, the importance of having someone accessible to contact in this time, and good communication between the hospital and other services. Discussions reflected the findings from the qualitative evidence synthesis strengthening our arguments and providing material for discussions section. These views helped highlight outcomes and issues included in the logic model and thoughts around condition selection for QCA. |
| Feedback on analysis plans, May 2022 | Meeting with JM | Informed the merging of different types of procedures and interventions for QCA analysis. Decision made to collate all intra-abdominal studies, with LLA studies kept as a separate grouping. Discussions informed preliminary plans for dissemination of work appropriate for medical/service-related audiences. |
| Feedback on list of QCA conditions, June 2022 | Email correspondence with CL and meeting with JM | The following points were raised as important aspects of the content and/or delivery of interventions to speed up/enhance recovery which should link to better patient-reported outcomes from the clinician’s perspective: post-discharge support, carer involvement, active mobilisation, patient information, following a protocol, and person-centred PROMs. This informed the selection process of conditions included in the QCA. |
| Meeting 4 with PPI group, October 2022 | 1 × 2-hour meeting with patient group (n = 6), 1 × 2-hour meeting with carers’ group (n = 2), 1 × 2-hour individual meeting with carer | Discussed key findings from reviews 1 and 2 and overview of review 3. Discussed options for dissemination, whom we should tell and how. Discussed our potential outputs and the options for involving our PPI members in the development of these. Members to be involved in Plain English Summary editing, podcast creation and writing reflection for main report. |
| Editing of Plain English Summary and request for reflective writing for report | Sent to PPI members for comments and reflections requested. | Plain English Summary sent to PPI group and request for any comments or changes. Six members made comments which were incorporated into the final edit. Five PPI members wrote reflective comments which were added to our reflections below. |
| Reading of draft report, October 2022 | Copy of draft report circulated to all stakeholder | Comments from AH returned and changes incorporated into the report. |
As there were several months between meetings, we sent monthly or bi-monthly email updates to keep our members informed and engaged.
At the end of the project, we emailed all members individually to ask for their reflections on being involved in the project. We asked them to consider what they felt had gone well and what might have gone better.
Though we considered meeting with patients and carers together, we decided to split them into separate groups to keep numbers at each meeting at a level which would allow for good participation by all members and help ensure that people could speak more freely if they had negative experiences of, for example, caring for a family member. Splitting the group in this way allowed also for greater flexibility in identifying a mutually convenient time to meet for carers. All members could choose to meet with the researchers as part of their relevant group, or individually. Some of the PPI members were unable to attend some of the group meetings but where possible we made alternative individual meeting arrangements to give as much opportunity as possible for each member to be involved in each meeting.
All meetings were held remotely via Zoom due to uncertainty about pandemic restrictions. Remote sessions supported the inclusion of people from a wider geographical area but did mean that those without an internet connection or computer literacy could not participate. PPI members lived in the south-west, south-east, London, Midlands, and northern England, and had a range of positive and negative experiences. The carers’ group also included those members with experience of caring for their next-of-kin and those who cared for other family members or friends. Some of our carers were also able to draw on personal experiences as a patient undergoing a planned procedure.
Discussions with the PPI members helped to bring the topic to life for the research team, providing real-life examples of some of the issues described within the included studies. In particular, the patients and carers provided insights into the very real difficulties that they, and the individuals supporting them, experienced following discharge from hospital. We discussed the difficulty of regional differences in access to post-operative services, including rurality versus urban living. The post-operative recovery phase at home was felt by both carers and patients as being the most challenging where more support was often needed. These discussions helped inform our thinking for qualitative analysis and building of logic model. Further details of the impact of our discussions with patients and carers are provided in Table 13.
Stakeholders
The following clinical experts were consulted in developing the protocol and during the review:
-
A consultant geriatrician (AH) with expert knowledge in the management of adults with multiple comorbidities and complex needs, frailty syndromes and polypharmacy, and with expertise in achieving successful discharge planning and supportive home-based post-discharge interventions.
-
A consultant urological surgeon in the UK (JM), who was National Clinical Advisor to the UK Department of Health for the Enhanced Recovery Partnership Programme, and chaired the ERAS Guideline Development Group for the British Association of Urological Surgeons and authored the specialty guidelines. Recognised internationally for work in enhanced recovery following major urological surgery and has published widely within this field.
-
A clinical lead OT in neurology and neurorehabilitation in the UK. His clinical interests include Parkinson’s disease, brain injury and cognitive neuroscience.
Reflections
We had a fantastic group of both patients and carers for this project, really engaging, enthusiastic, respectful, and always with valuable comments. In a stand-alone exercise, we asked the group to provide reflections that would inform the report. They were happy for the opportunity, and some of their feedback follows below.
All in all, it had been an honour to be involved in this study and to be able here to contribute some reflections.
(Member of the carer PPI group – ID 01)
The experiences and contribution of the group have helped solidify our findings and emphasise the need for greater consideration of carers and greater focus on the transition from hospital to home. Involvement of our members throughout the project has enabled us as researchers to consider and interpret our findings at each stage from the perspective of patients and carers, reinforcing what we might already have considered and highlighting what we’d missed or what the research gaps were.
Involving other family members in what is happening is also critical as this will help everyone and help the older person feel more safe and secure and able to cope. Also having a named person to connect with by phone in case of emergency is also critical as they can then build up a relationship with this person and feel able to share their fears and worries.
(Member of the patient PPI group – ID 05)
Better communication and aftercare between those medical carers and for both patients and carers would honestly mean so much to everyone, I am sure. We have only been asked at an appointment to fill out a comment card for those visits only, nothing from hospital stays.
(Member of the carer PPI group – ID 03)
In their feedback at the end of the project several members highlighted how they felt that our findings reflected their experience.
The findings of the study matched what my experience has a been as a carer and I fully endorse the need for further research and for any examples of good practice to be shared between wards and hospitals of how early discharge and all the benefits of that which this study has proven becomes the norm when people are admitted into hospital.
(Member of the carer PPI group – ID 01)
I found the project very interesting and enjoyed participating and listening to other people’s experience of hospital care on Zoom. I agreed with the finding of the project. It is very important not to be discharged from hospital without careful planning as this may result in harm to patients’ health which may result in them having to be readmitted, costing NHS more expense.
(Member of the patient PPI group – ID 02)
I became involved in this study as I’m over 60 and have many experiences in the hospital system and some were good others were not due to not having a care plan in place after planned surgery. The strategies that are in place do not take into account your circumstances or family help. I believe the findings has highlighted this, for me I was not surprised by this as the care plans do not go far enough to the patients wellbeing.
(Member of the patient PPI group – ID 04)
It was most interesting to take part in this research project. I feel that it is a very important project and could help make a difference to the health and wellbeing of many older people together with helping staff in both hospitals and the community learn what it the best way forward.
(Member of the patient PPI group – ID 05)
The groups sessions were facilitated well, members felt able to speak openly, share experiences and question researchers in depth about the purpose of the review and how it would be used to make a difference.
It was good to meet other older people from different parts of the country, hear their views and experiences and what has helped them or has not been so good for them either.
(Member of the patient PPI group – ID 05)
The one-to-one meetings were good and gave me plenty of chance to openly express my views and were able to be at a time that I could do.
(Member of the carer PPI group – ID 01)
It was good to feel involved at all stages of the project and that our views were important and taken on board.
(Member of the patient PPI group – ID 05)
On one occasion, one member felt less able to share recent negative experiences as a group but felt comfortable to do so on a one-to-one basis with one of the researchers and this was later arranged. Group meetings also provided the opportunity for advice to be shared between members. Feedback from one carer highlighted the positive impact a group meeting can have, allowing members to bounce ideas off one another and providing the opportunity for shared experiences to provide some reassurance. Though we tried to arrange group meetings for the carers, this only happened on two occasions and not all members were able to attend and therefore had an individual meeting. One member expressed the view that they would have preferred more group meetings and that meeting one-to-one felt isolating.
I enjoyed being involved in this project but feel that as carer the fact that all the meetings bar the last one were one-to-one meetings made me feel quite isolated.
(Member of the carer PPI group – ID 01)
As a research team, we will take this feedback on board for future projects, and take steps to ensure that group meetings are prioritised where possible.
Members of the group are keen to help to share the findings from the project and have been involved in dissemination activities.
It is also really important that the results of the study are shared more widely. Having shorter stays in hospital can also save the NHS money.
(Member of the patient PPI group – ID 05)
Some members have helped to edit the Plain English Summary and provided ideas for whom to share our findings with. Some members are keen to be involved in outputs that will continue after report submission, that is by podcast.
Equality, diversity and inclusion
Future research in this area should endeavour to provide opportunities for members of the public to engage with projects of this nature in a variety of different formats, including face-to-face and online, on an individual and group basis. This will provide scope to engage with individuals according to their preferences and consider their physical capabilities, physical needs, and levels of computer literacy. Given the topic of this linked-evidence synthesis and potential related research, particular effort should continue to be made to seek and maintain relationships with people from more vulnerable and harder-to-reach sectors of the population, including individuals from black and ethnic minorities and/or those with cognitive impairment. Prior research experience and understanding should be considered when engaging with both members of the public and clinical stakeholders, and suitable training or additional support materials offered. The format and content of materials used to disseminate the findings of this research should consider the needs of these more vulnerable populations to ensure that the relevant messages are identified for each audience and that these are communicated in a way which is accessible to each group. The dissemination pathway should consider how these materials are to reach the different stakeholder groups likely to be interested in the research, again with particular emphasis on targeting harder-to-reach populations.
Chapter 6 Discussion and conclusions
This linked-evidence synthesis addressed the broad overarching question of whether multicomponent interventions designed to accelerate the recovery of older adults from elective surgery and achieve an earlier hospital discharge result in better patient outcomes. We built on previous work which established that such interventions are usually effective at reducing length of stay (LOS) without detriment to, and often improving, clinical outcomes. 17 In the current review, we focused on patient-reported outcomes (PROMs/PREMs), service utilisation and the experiences of patients, carers and staff involved in the delivery of such interventions.
We conducted two reviews and an overarching synthesis, all of which were informed by regular engagement with clinical stakeholders, older adults with experience of planned elective surgery and people who have cared for older adults undergoing surgery. The first was a review of quantitative evidence about the effect of multicomponent interventions aiming to enhance recovery/reduce LOS on PROMs, PREMs and service utilisation. The second was a review of qualitative evidence about the experiences of patients receiving multicomponent interventions to enhance recovery / reduce length of stay, their family and carers and staff involved with delivering care within these interventions. The overarching synthesis sought to identify the components of relevant interventions that are associated with better outcomes for adults admitted to hospital for planned procedures.
Summary of quantitative systematic review
For the quantitative systematic review, we identified 22,791 unique records and screened 1133 of these at full text. A total of 125 papers were eligible for inclusion, and we prioritised 53 of these, reporting on 49 studies, for full data extraction, quality appraisal and synthesis. These 49 studies were prioritised because they were either an RCT or a study conducted in the UK.
The prioritised evidence pertained to eight broad types of surgical procedure (cardiac, colorectal, LLA, pelvic, upper abdominal, abdominal, thoracic and removal of tumours at various sites), the most common being those for LLA (45% of studies) or colorectal surgery (24% of studies). These two categories were the most common in our previous review; however, there was a swing in this review to a greater proportion of studies being about LLA. 17 This may have been due to the requirement for PROMs to be measured and reported for inclusion in this review and a greater propensity, in our experience, for papers about hip and knee surgery to report such outcomes.
Studies were further grouped by intervention category, most being either ERP (59%) or Prehab (33%). There were three Rehab interventions and one each of Discharge Planning and Preoperative Assessment and Care Plan. Outcomes were categorised as LOS, complications, readmissions, mortality, morbidity, service utilisation and seven types of PROM/PREM – mental health, physical function, quality of life, physical activity, pain, patient satisfaction and social function.
The quality of evidence was generally low, with only six studies achieving a rating of ‘strong’ during quality appraisal. Furthermore, poor reporting of outcome data and intervention characteristics meant that several studies could not be included in the meta-analysis, and that a number of potential QCA conditions could not be evaluated.
Studies regarding LLA tended to show that ERP interventions were associated with reductions in LOS and occasional benefits in terms of PROMs, with no detrimental effects on any outcome. However, Prehab interventions had little influence on any outcome. This pattern was reproduced within the body of evidence regarding colorectal surgery. Studies in isolation showed promising outcomes, but there was no convincing evidence that any particular type of intervention was effective at improving clinical and patient-reported outcomes. Service utilisation was rarely reported.
Quantitative systematic review results in context
Our findings regarding clinical outcomes generally follow the wider evidence, although we previously identified more convincing associations between both ERP and Prehab interventions and improvements in clinical outcomes. 17 The requirement in the present review for quantitative studies to report PROMs/PREMs or service utilisation meant that 39 of 73 studies that were previously includable were not eligible for this review, and as such we captured a slightly different body of evidence herein. It is unclear why the evidence from the present review is less convincing in terms of clinical outcomes, particularly from Prehab interventions. We recognise that the broader literature is more conclusive on the benefits of ERP interventions, especially in terms of LOS and complications,154–156 and to a lesser extent Prehab,157 and the evidence in this review does not suggest any detrimental effects on these outcomes. However, our findings do expose the lack of high-quality evidence regarding the patient experience of care, and the longer-term impact of shorter hospital stays on patients, their carers and community services.
Regarding PROM’s, PREMs and service utilisation, to our knowledge there is a dearth of review evidence on this topic, and thus our findings are unique. Jones and colleagues systematically reviewed evidence on PROMs and experiences of enhanced recovery but specific to orthopaedic surgery. 23 They found a paucity of evidence but it indicated, similar to our review, that interventions did not compromise patient quality of life or experiences. 23 The review by Jones and colleagues was published in 2014 and called for the measurement of patient experience to be standardised with further research, sentiments which are echoed in the present review.
Strengths and limitations of quantitative systematic review
The quantitative systematic review was comprehensive and rigorous. We prioritised the best and most relevant evidence available. Despite being the best available, the evidence reviewed was,however, lacking in several aspects, expanded upon below, which limited the extent to which clear conclusions could be drawn in response to research question 1.
Prioritising a portion of the evidence available for full data extraction, critical appraisal and synthesis could be seen as a limitation; however, we believe the findings from non-RCTs conducted outside the UK would be likely to have contributed minimally to overall findings. We would not have undertaken meta-analysis of non-RCTs and although we recognise the value of before-and-after study designs in evaluating care improvement initiatives, there are inherent limitations to such study designs. An in-depth narrative synthesis of the non-prioritised studies may, however, have provided further knowledge of the types of PROMs/PREMs used, and how they are influenced by interventions of interest.
PREMs were rarely reported and usually took the form of an ad hoc survey or questionnaire. Regardless of intervention type, PROMs were rarely improved. Of the 38 studies included in the QCA, 15 saw an improvement in both LOS and at least one PROM/PREM, however in total only 36 of 152 outcomes measured across these studies were improved. Overall, the influence of enhanced recovery approaches on PROMs is inconclusive, with the approach to their measurement likely to be one limitation. We observed several potential limitations to the measurement of PROMs, including:
-
Choice of PROM. Multiple studies used similar tools such as the SF-36 to assess multiple domains including physical function, mental health, quality of life and social function. While this tool is validated and widely used, there are numerous specialist and/or bespoke tools which could have been used to provide more accurate or valid findings. 158
-
Measurement frequency. In the vast majority of studies, outcomes were measured at baseline, once post-intervention and possibly at one more follow-up point. Multiple measurement points would provide a fuller assessment of the outcome of interest. This was supported by feedback from our PPI group.
-
Not asking the right people. There were no PROMs aimed at carers, and therefore the impact of early discharge of older adults after major elective surgery, which falls heavily on carers, has not been captured. Carers in our PPI group supported this point.
-
Not asking the right questions. The qualitative evidence synthesis and our PPI group highlighted a range of important issued that were not broached by the array of PROMs and PREMs utilised in the quantitative review.
-
Incomplete reporting of outcomes. The PROMs listed in studies were sometimes not reported, and frequently were not afforded the same attention as clinical outcomes, with values absent in lieu of summary statements.
Despite identifying 42 RCTs and 7 non-RCTs from the UK, the evidence does not allow us to make firm conclusions regarding the impact of interventions to facilitate earlier hospital discharge on patient outcomes, or the subsequent effect on primary care and community services. Furthermore, there were only 14 studies conducted in the UK, of which only 6 were RCTs. While international evidence is important, it would be particularly beneficial to have more studies evaluating UK-based interventions, and especially those which evaluate the impact on service utilisation following early hospital discharge. Service utilisation was only reported in four studies.
Summary of the qualitative evidence synthesis
We identified 4820 unique records, of which 298 were sought for full-text screening. We found 43 papers that were eligible for inclusion, and prioritised 35 for quality appraisal, data extraction and synthesis, based on the quality and quantity of data provided. The evidence was dominated by ERP-type interventions (77%), with only one study about Prehab. There were two studies about Rehab, and single papers about case management, CGA, early discharge, a perioperative care and e-health programme, and a staff mix intervention. Thirteen prioritised studies were from the UK (n = 13) with Denmark (n = 6) and Australia (n = 3) next most common. Twenty-five prioritised studies captured the views of patients, and there were seven studies reporting staff views, four with the views of carers.
We used a meta-ethnographic approach for our synthesis to develop six constructs. The first construct ‘Home as the preferred environment for recovery’ highlights the benefits, and challenges, of recovering at home for patients and carers. This construct influences the concepts discussed within the other five constructs: ‘Feeling safe’, ‘Individualisation of a standardised programme’, ‘Taking responsibility’, ‘Essential care at home’ and ‘Outcomes’. ‘Feeling safe’ explores the importance of ensuring the emotional and physical needs of patients and their family/carers are met, and that they are supported to develop confidence through provision of information, pre-operative care and accessible, appropriate follow-up care. ‘Individualisation of a standardised programme’ discusses the importance of tailoring structured programmes, such as ERPs, to the needs of the individual patient. It also highlights the challenges that comorbidities, complications, and weekend staffing levels can pose to this patient-centred process. ‘Taking responsibility’ raises key questions around roles and responsibilities for the recovery process, including after discharge – exploring the role of the active patient, expert versus generalist staff, and staff/service co-ordination. ‘Essential care at home’ highlights the vital role of informal caregivers in supporting patients within their own home post-discharge. It also highlights the need to ensure caregivers are provided with adequate support to enable them to perform their caregiving role. The final construct ‘Outcomes’ examines how patients may not always be asked about aspects of their care or recovery that are most meaningful to them, at the right time, and that they may mask or overlook the negative aspects of their care.
This review represents the findings of a comprehensive search and synthesis strategy, incorporating the views and experiences of patients, families, carers and staff of interventions to reduce LOS and/or improve recovery. The resulting line of argument provides insight into aspects of the care pathway which patients and their family/carers find particularly significant and those which could be improved, which can be used to inform future clinical practice, policy-making and further research.
Qualitative evidence synthesis results in context
These findings are in line with earlier systematic reviews which did not specifically examine the experiences of older patients. In a review of qualitative evidence of experiences of ERAS programmes following surgery for a range of conditions in adults 18 years of age or over, Sibbern et al. (2017) highlighted the importance of sharing information, the dilemma presented by the need to provide individualised treatment within standardised care, the balance needed to manage burdensome symptoms during a rapid recovery and the importance of a sense of security at discharge and the role of professional support in helping patients continue their recovery plan and achieve planned discharge. 24 Another systematic review exploring staff perceptions of ERAS programmes after surgery highlighted the importance of communication and collaboration within and between services, and challenges of implementing protocol-based care and managing knowledge, and expectations of staff. 25 One difference between this review and ours is that it also highlighted the theme ‘resistance to change’, describing how some staff can be reluctant to implement new working practices. This was apparent in our review to a limited extent, with Kocman et al. (2019) finding that one reason the attempted implementation of the CGA in pre-operative assessment failed was due to the competing priorities of services and staff within an already very busy service pathway, which could be interpreted as a type of ‘resistance’ at a service, rather than specific staffing, level. It may also not have been apparent in our review due to the limited number of included studies from a staff perspective. Cohen et al. (2019) particularly highlight the need for an ERAS co-ordinator for staff, which complements the recommendation from our review of a similar co-ordinator for patients. Given that staff workloads and services are increasingly stretched with increasing numbers of patients and longer waiting lists due to the COVID-19 pandemic,3 a staff co-ordinator may ease some of the burden on other members of staff, which may also support provision of the individualised care we recommend in this review.
That both Sibbern et al. (2017) and Cohen et al. (2019) have broadly similar conclusions, despite not focusing on the experiences of older people, lends support to our conclusions as being the likely salient issues. However, as described in the background section of this report, older people are more likely to be ‘complex’ patients, for example due to being at increased risk of complications,6,9–16 which means the challenges of earlier discharge may be more pertinent for this patient group.
There is not, to our knowledge, a systematic review which specifically examines the experiences of carers of older people with these kinds of interventions, and other evidence is a little more mixed. One study159 investigating the cost-effectiveness of enhanced recovery compared to usual care found that there was no difference in the number of days that patients needed assistance from home carers, but that the carers had fewer days off work to provide this care, and concluded that caregiver burden was reduced with ERP and that earlier discharge did not result in a transfer of responsibility for recovery from the hospital to home, which is in contrast to our findings. This difference may be due to the issues we discuss with regard to outcome measurement and that ‘days off work’ may not be an appropriate metric for carers who are retired. Meulenbroeks et al. ’s systematic review160 found mixed evidence on whether caregiver-inclusive transitional care programmes for older adults with geriatric syndrome provided better value, with ‘value’ referring to not only cost-effectiveness, but also the qualitative experience of patients and staff and the quality of care. Despite finding some positive trends for improved patient and caregiver experience, they were unable to reach conclusions due to the poor quality of evidence. They also included studies for unplanned hospital admission, such as due to stroke, and there may be differing issues when there can be no pre-operative planning, for example. Given that carers in our included studies, and the carers in our PPI group, highlighted difficulties and a need for greater inclusion and consideration, further research is required which examines their perspectives to develop appropriate evidence-based support. This may be particularly important for those caring for complex older patients, who may need to deal with increased numbers of complications during the recovery period,6,9–16 the additional pressures of being a ‘sandwich’ carer supporting an elderly parent and young children,161 or their own health issues or frailty if they are also older or have their own health issues. 162
Qualitative evidence synthesis strengths and limitations
Whilst the findings of this synthesis were drawn from research representing the views of those with experience of interventions to reduce LOS for patients over the age of 60 following a planned procedure, it is probable that individuals from/representing other populations with experience of other types of hospital interventions may also be able to relate to aspects of our findings. The synthesis represents the views of patients admitted for a diverse range of procedures, who experienced a variety of different types of interventions. Five of the six constructs identified in the final synthesis were supported by at least 21 high- to moderate-quality studies. The exception to this was the construct ‘Outcomes’, which was supported by 14 studies, of which 13 were of high/moderate quality. Despite this construct being supported by fewer studies, we felt that the importance of the concepts represented within merited representation through a separate, stand-alone construct, particularly given that a lack of adequate outcome reporting limited the systematic review of quantitative evidence.
Whilst views of ERP/ERAS-style interventions dominated the synthesis, we accounted for this by incorporating views of other types of interventions early in the synthesis and by comparing and contrasting experiences across different types of interventions. Most of the articles included within the synthesis represented the views/experiences of patients. This reflects the poor reporting of the characteristics of the patients being supported, including age and reason for admission, within articles reporting the views of carers and staff. This meant these papers did not meet the inclusion criteria for this review and resulted in the views of carers/families and staff being under-represented in the synthesis.
This systematic review was conducted and reported in accordance with best-practice guidelines. Due to the high number of studies identified through searches, we did not conduct searches of Google Scholar or relevant websites. In addition, the high number of studies eligible for inclusion in the qualitative evidence synthesis meant that we prioritised the studies with the highest quantity of interpretative data across different population and intervention groups for inclusion in the synthesis. This meant that eight articles were not quality appraised or incorporated into the final line of argument; however, summary details of these studies were extracted and included in Appendix 3. The analyses of these eight studies were also primarily descriptive in nature and represented experiences of patients of interventions already included within the synthesis, thus their findings are unlikely to alter our main findings. These pragmatic decisions were necessary to ensure the linked-evidence synthesis could be undertaken within the timeframe and resources available.
Summary of overarching synthesis
The overarching synthesis aimed to bring together the evidence from the first two reviews in order to develop an understanding of the aspects of interventions or their delivery which can lead to better patient outcomes. We performed a QCA, and through this process were able to draw out additional key points relevant to the research question.
Using the findings of the qualitative evidence synthesis and informed by consultation with clinical stakeholders and our PPI group, we developed a logic model outlining the theory by which improved patient outcomes may be achieved. We then drew out the individual components of the logic model and, in discussion with clinical stakeholders and following checking of papers, shortlisted those which were both likely to be the most influential in determining success and able to be identifiable within the quantitative evidence. We then examined the studies in the quantitative review for evidence of these.
The results suggest that a complex balance of intervention components trigger successful interventions: these represent both individualised approaches that allow patients to understand their treatment (e.g. through providing information in different formats), to ask questions about their treatment (through spending additional time with patients), and to build supportive relationships (through having a consistent point of care), with more exigent strategies that facilitate patients to monitor their own progress (goal-focused) and challenge themselves in recovery (through early mobilisation).
Overarching synthesis strengths and limitations
A strength of this QCA is that the focus on patient perspectives generated from the qualitative evidence synthesis was instrumental in the design of the logic model, which in turn formed the basis of the QCA. The components identified are those that could be implemented to support a range of intervention approaches that aim to reduce the LOS following surgery, and the components identified are supported by the insights provided through the qualitative evidence synthesis and conversations with clinical stakeholders and people with relevant experience of elective procedures involving overnight stays at hospital.
Given the focus on the factors that are experienced and known to patients, a substantial limitation of the synthesis, however, is its focus on non-clinical implementation factors, and the synthesis does not give any direct indication of the efficacy of different clinical procedures that may also influence LOS and patient-reported outcomes, which would be largely unseen or unknown to most patients. A further limitation is that each model identified a slightly different set of components as being important in triggering successful interventions. Attempts at an overall model based on all 36 studies were not fruitful and may reflect the fact that different components are differentially important depending on the implementation stage [pre-operation vs. across the patient journey (ERP)] and the type of surgery (abdominal cavity vs. LLA).
An important limitation is around the QCA approach itself and its capacity to consistently and correctly reveal complex causal relationships, including around the stability of QCA solutions when new evidence is added, and the generalisability of the solutions to alternative datasets. Similarly, there exist critiques based on simulated datasets where the causal processes are known around whether QCA does identify the correct solution;163 although these critiques also do not take into account that QCA solutions cannot be generated in the absence of theoretical and case-based knowledge. In the present QCA, the synthesis primarily rests on programme theory generated from a synthesis of patient perspectives on interventions to reduce LOS/enhance recovery, which forms a strong basis for the analytical decisions made and the interpretation of the results.
This QCA is also not immune to issues around the reporting of interventions and the influence of lower-quality studies. In terms of the latter, several of the studies were of moderate or weak quality, with none of the studies included in the ERP analysis deemed to be of high quality. There was little relationship between the quality of the study and its effectiveness in models and therefore some of the components identified as important for a successful intervention were identified through evidence from weak studies. Similarly, most studies screened patients with more challenging profiles out of the intervention, therefore the extent to which the results are generalisable to patients with more complex needs is unclear. In terms of reporting, it was clear that many of the trials were not directly interested in reporting the implementation of clinical components, and the identification of intervention components in some cases was based on sparse data. Several of the trials also regarded quantitative data on patient experience as ancillary process evaluation data and not a core metric in of its own right, and the triallists generally offered little reflection.
Finally, in developing the list of conditions for the final QCA we had to discard or combine a number of desirable elements identified within the logic model. This was either due to poor or absent reporting within the quantitative studies, or because some individual elements were too specific or numerous to be operationalised in the analysis. For example, the item ‘efforts to support discharge’ was developed to capture multiple possible actions or intervention components that could have been implemented to support patients including discharge planning, assessment of the home environment, telephone support, education and information to support rehabilitation at home, nurse visits, etc. Other conditions such as ‘goal-setting’ involved a level of interpretation during coding, for example when patients performed a graded exercise programme. Therefore, it is important to note the limitations involved when coding conditions in the development of the truth tables.
Implications for policy and practice
Our findings support the use of ERP interventions and, to a lesser extent, Prehab interventions, as effective means of reducing LOS for older adults undergoing elective surgery requiring an overnight stay in hospital. Shorter stays are achieved without detriment to other clinical outcomes (e.g. complications, readmissions), but our findings reflect ongoing uncertainty over the impacts of earlier discharge on patients and carers, or service utilisation.
Despite the lack of quantitative evidence to allow the evaluation of patient outcomes and service utilisation, the rich qualitative evidence exploring the support patients, families and carers may need before, during and after hospital admission presents compelling arguments. The overarching synthesis reinforced many of these suggestions, pointing to the need for individualised approaches to care that allow patients to understand their treatment, to ask questions about their treatment, and to build supportive relationships, with strategies that facilitate patients to monitor their own progress, and challenge themselves in recovery, being warranted. These suggestions accord strongly with recommendations outlined in NICE guideline 180, about perioperative care in adults. 164
Our findings should inform policy-making with regard to:
-
informing how the support needs of patients, carers and families are assessed and managed before, during and after the hospital stay
-
the commissioning of appropriately structured services to ensure that patients and carers/families receive appropriate follow-up support following discharge
-
establishing minimum national outcome criteria to ensure that the PROMS reflect information which both is useful to inform the evaluation of services and captures recovery outcomes which are meaningful to patients and carers themselves
-
clarifying core responsibilities of hospital and community staff across the patient care pathway and how these could be adapted according to individual service models
-
considering how patients with more complex needs, including those with multiple comorbidities/conditions, who experience complications, and those who are isolated can be better supported within structured care pathways, including post-discharge support.
Regarding clinical practice, these findings may help support hospital and community-based health and social care staff to provide person-centred care which:
-
is based upon an assessment of emotional and physical wellbeing of patients and their family/carers before, during and after the patient’s hospital stay
-
considers the separate responsibilities of the patients, carers and staff to promote patient recovery and the information, training and/or support each group may require to fulfil these
-
considers the health and wellbeing needs of carers as separate individuals
-
promotes the involvement of family and/or carers throughout the patient care pathway
-
is oriented around recovery goals which are both clinically and personally meaningful to the patient and/or their carer/family
-
promotes the adaptation of protocolised hospital interventions to accommodate the individual needs of patients with more complex needs
-
includes the time and resources staff need to fulfil holistic, individualised care for patients.
Our findings may also be useful to managers across primary and secondary health and social care settings to evaluate the extent to which their existing services align with the findings and recommendations of this linked-evidence synthesis.
Suggested research priorities
We suggest the following research priorities:
-
Addressing the overdue requirement to effectively capture patient and carer outcomes and experiences of interventions to achieve earlier discharge. In particular, the views of carers who may shoulder the majority of the burden of aftercare were not represented alongside any trials included in the quantitative review.
-
As part of this, establishing a core-set of PROMs which more accurately capture aspects of recovery which are meaningful to patients and the time-points at which these should be assessed, particularly post hospital discharge.
-
Gathering evidence (particularly UK-based) about the direct consequences of earlier discharge on use of services outside hospital. This should include an evaluation of the systemic impact of the work associated with the increased emphasis on creating individualised support plans for patients and carers on the health and social care services supporting these individuals post-discharge. Specific professional groups to consider include, but may not be limited to, social workers, OT, physiotherapists, community support workers, community nurses and GP.
-
Supporting the adaptation of protocolised interventions to meet the needs of older patients admitted to hospital for a planned procedure, who have complex needs such as frailty, living alone or comorbid conditions, who may be at greater risk of experiencing complications pre- or post-discharge.
Equality, diversity and inclusion
Participant representation
Compared to younger patients, older adults admitted to hospital for elective procedures face disrupted discharge trajectories out of hospital due to transport difficulties, they may be in poor physical health or living with frailty, they may be socially isolated or have living arrangements requiring additional support following discharge.
Our research question sought to understand the impact of interventions that aim to expedite the discharge of older adults from hospital back into the community, often as early as a day or two after major surgery. Our systematic reviews focused on the influence of the interventions on the experiences of patients and their families and carers. Though we intended to explore the impact of age, gender and frailty within the quantitative evidence, the paucity of high-quality data on PROMS and PREMs prevented this. Our qualitative evidence synthesis highlights the vital role of informal caregivers in supporting patients within their own home post discharge. It also highlights the need to ensure caregivers are provided with adequate support to enable them to perform their caregiving. Although the underlying construct from the qualitative synthesis is that home is the preferred environment for recovery, patients without access to informal carers or whose informal carers have their own complex circumstances may experience health inequity.
Research team and wider participation
Our team is small, making it difficult to ensure diversity across a range of groups; we also do not feel comfortable asking team members to disclose information on diversity unless they wish to share this. However, we did recruit a PPI group of patients with experience of a hospital stay following a planned procedure and people who have cared for a family member undergoing such an experience. The PPI group brought a broad range of backgrounds and experiences to the review. Further details of the activities undertaken with the PPI group and the impact of these activities on the project can be found in Chapter 5.
There was a range of experiences and expertise within the team. The project provided opportunities for the development of skills in quantitative evidence synthesis, QCA, project management and report-writing.
Patient and public involvement
PPI was included throughout the project. Full details of this involvement can be found in Chapter 5.
Acknowledgements
We would like to thank Sue Whiffin for administrative support and proofreading. Thank you to Rebecca Abbott for proofreading. Thank you to the patients and members of the public who provided us with the benefit of their expertise, insight and experience.
Contributions of authors
Debbie Kinsey (https://orcid.org/0000-0001-9578-4001) was involved in the screening, data extraction, critical appraisal, synthesis for both the quantitative and qualitative reviews. She led the qualitative evidence synthesis and developed the logical model for the overarching synthesis. She co-led PPI, drafted key sections of the final report and read and edited all sections of the final report.
Samantha Febrey (https://orcid.org/0000-0002-4944-664X) was involved in the screening, data extraction, critical appraisal, synthesis for the quantitative systematic review and the overarching synthesis, and screening for the qualitative review. She co-led PPI, drafted key sections of the final report and read and edited all sections of the final report.
Simon Briscoe (https://orcid.org/0000-0002-6982-4521) was involved in direction/conception, designing and conducting database and supplementary searches, screening, data extraction and, critical appraisal. He also managed the reference library, drafted sections of the final report and critically read and edited all sections of the final report.
Dylan Kneale (https://orcid.org/0000-0002-7016-978X) supported the direction/conception, he led the overarching synthesis, drafted key sections of the final report and critically read and edited all sections of the final report.
Jo Thompson Coon (https://orcid.org/0000-0002-5161-0234) led the application for funding, was involved in direction/conception, advised on all stages of conducting the review, and critically read and edited all sections of the final report.
Daniele Carrieri (https://orcid.org/0000-0002-3143-8430) supported the screening, data extraction and critical appraisal for both reviews. He contributed to the qualitative evidence synthesis and critically read and edited key sections of the final report.
Christopher Lovegrove (https://orcid.org/0000-0003-2530-1988) supported the direction/conception, contributed to synthesis and interpretation, and critically read and edited all sections of the final report.
John McGrath (https://orcid.org/0000-0001-9416-9912) supported direction/conception, contributed to synthesis and interpretation, and critically read and edited all sections of the final report.
Anthony Hemsley (https://orcid.org/0000-0002-5595-4528) supported direction/conception, contributed to synthesis and interpretation, provided links to expert clinical advisors, and critically read and edited all sections of the final report.
GJ Melendez-Torres (https://orcid.org/0000-0002-9823-4790) supported the direction/conception, provided expertise and input around network meta-analysis and critically read and edited all sections of the final report.
Liz Shaw (https://orcid.org/0000-0002-6092-5019) was involved in all stages including direction/conception, planning searches, screening, data extraction, critical appraisal, synthesis, and write-up. She oversaw the qualitative evidence synthesis and the development of the logic model for the overarching synthesis, drafted key sections of the final report and read and edited all sections of the final report.
Michael Nunns (https://orcid.org/0000-0001-5500-0911) was involved in all stages including direction/conception, planning searches, and screening, data extraction, critical appraisal, synthesis and write-up for the quantitative systematic review and the overarching synthesis. He led the quantitative data analysis and synthesis, drafted key sections of the final report and read and edited all sections of the final report.
Ethics statement
This mixed-evidence synthesis consisted of two reviews of existing evidence and thus did not require ethical approval.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Information governance statement
During the conduct of this report, we were not required to handle any personal information.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS Digital 2016.
- ONS 2020. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/subnationalpopulationprojectionsforengland/2018based (accessed February 2023).
- BMA 2022. www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/nhs-backlog-data-analysis (accessed February 2023).
- Flinders S, Sarah S. Nuffield Trust; 2022.
- Age UK . Painful Journeys: Why Getting to Hospital Appointments Is a Major Issue for Older People n.d.
- Bakker FC, Robben SH, Olde Rikkert MG. Effects of hospital-wide interventions to improve care for frail older inpatients: a systematic review. BMJ Qual Saf 2011;20:680-91. https://doi.org/10.1136/bmjqs.2010.047183.
- Age UK . Loneliness and Isolation: Evidence Review n.d.
- Shepperd S, Lannin NA, Clemson LM, McCluskey A, Cameron ID, Barras SL. Discharge planning from hospital to home. Cochrane Database Syst Rev 2013. https://doi.org/10.1002/14651858.CD000313.pub4.
- Buurman BM, Hoogerduijn JG, de Haan RJ, Abu-Hanna A, Lagaay AM, Verhaar HJ, et al. Geriatric conditions in acutely hospitalized older patients: prevalence and one-year survival and functional decline. PLOS ONE 2011;6. https://doi.org/10.1371/journal.pone.0026951.
- Elia M, Zellipour L, Stratton RJ. To screen or not to screen for adult malnutrition?. Clin Nutr 2005;24:867-84. https://doi.org/10.1016/j.clnu.2005.03.004.
- Healey F, Oliver D. Preventing falls and injury in hospitals. The evidence for interventions. Health Care Risk Rep 2006;6:12-7.
- Lim SC, Doshi V, Castasus B, Lim JK, Mamun K. Factors causing delay in discharge of elderly patients in an acute care hospital. Ann Acad Med Singap 2006;35:27-32.
- An Analysis of Research on Preventing Falls and Falls Injury in Older People: Community, Residential Care and Hospital Settings. Canberra: Australian Government Department of Health and Ageing; 2004.
- Vanderwee K, Clays E, Bocquaert I, Gobert M, Folens B, Defloor T. Malnutrition and associated factors in elderly hospital patients: a Belgian cross-sectional, multi-centre study. Clin Nutr 2010;29:469-76. https://doi.org/10.1016/j.clnu.2009.12.013.
- Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc 2011;59:266-73. https://doi.org/10.1111/j.1532-5415.2010.03276.x.
- Edwards N, Lewis R. Improving Length of Stay: What Can Hospitals Do?. London: Nuffield Trust; 2015.
- Nunns M, Shaw L, Briscoe S, Thompson Coon J, Hemsley A, McGrath JS, et al. Multicomponent Hospital-Led Interventions to Reduce Hospital Stay for Older Adults Following Elective Surgery: A Systematic Review. Southampton (UK): NIHR Journals Library. Southampton UK; 2019.
- Olde Rikkert MGM, van der Wees PJ, Schoon Y, Westert GP. Using Patient Reported Outcomes Measures to Promote Integrated Care. Int J Integr Care 2018;18. https://doi.org/10.5334/ijic.3961.
- Øvretveit J, Zubkoff L, Nelson EC, Frampton S, Knudsen JL, Zimlichman E. Using patient-reported outcome measurement to improve patient care. Int J Qual Health Care 2017;29:874-9. https://doi.org/10.1093/intqhc/mzx108.
- Hestevik CH, Molin M, Debesay J, Bergland A, Bye A. Older persons’ experiences of adapting to daily life at home after hospital discharge: a qualitative metasummary. BMC Health Serv Res 2019;19. https://doi.org/10.1186/s12913-019-4035-z.
- Feldman LS, Lee L, Fiore J. What outcomes are important in the assessment of Enhanced Recovery After Surgery (ERAS) pathways?. Can J Anaesth 2015;62:120-30. https://doi.org/10.1007/s12630-014-0263-1.
- Wong SS, Wilczynski NL, Haynes RB. Hedges Team . Developing optimal search strategies for detecting clinically relevant qualitative studies in MEDLINE. Stud Health Technol Inform 2004;107:311-6.
- Jones EL, Wainwright TW, Foster JD, Smith JR, Middleton RG, Francis NK. A systematic review of patient reported outcomes and patient experience in enhanced recovery after orthopaedic surgery. Ann R Coll Surg Engl 2014;96:89-94. https://doi.org/10.1308/003588414x13824511649571.
- Sibbern T, Bull Sellevold V, Steindal SA, Dale C, Watt-Watson J, Dihle A. Patients’ experiences of enhanced recovery after surgery: a systematic review of qualitative studies. J Clin Nurs 2017;26:1172-88. https://doi.org/10.1111/jocn.13456.
- Cohen R, Gooberman-Hill R. Staff experiences of enhanced recovery after surgery: systematic review of qualitative studies. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-022259.
- NHS England . The NHS Long Term Plan 2019.
- 2022. www.training.cochrane.org/handbook (accessed February 2023).
- Bethel AC, Rogers M, Abbott R. Use of a search summary table to improve systematic review search methods, results, and efficiency. J Med Libr Assoc 2021;109:97-106. https://doi.org/10.5195/jmla.2021.809.
- World Health Organization . World Report on Ageing and Health 2015.
- ERAS Society . List of Guidelines n.d. https://erassociety.org/guidelines/ (accessed February 2023).
- World Bank List of Economies 2021. https://datacatalogfiles.worldbank.org/ddh-published/0037712/DR0090755/CLASS.xlsx (accessed February 2023).
- Effective Public Health Practice Project . Quality Assessment Tool for Quantitative Studies 1998.
- Altman DG, Bland JM. How to obtain the confidence interval from a P value. BMJ 2011;343.
- Cohen J. A power primer. Psychol Bull 2016;112:155-9. https://doi.org/10.1037//0033-2909.112.1.155.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60.
- Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to Meta-Analysis. Chichester: John Wiley; 2009.
- Bennett SR, Smith N, Bennett MR. Cerebral oximetry in adult cardiac surgery to reduce the incidence of neurological impairment and hospital length-of-stay: a prospective, randomized, controlled trial. J Intensive Care Soc 2020;23:109-16. https://doi.org/10.1177/1751143720977280.
- Dunne DF, Jack S, Jones RP, Jones L, Lythgoe DT, Malik HZ, et al. Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg 2016;103:504-12. https://doi.org/10.1002/bjs.10096.
- Garriga C, Murphy J, Leal J, Arden NK, Price AJ, Prieto-Alhambra D, et al. Assessment on patient outcomes of primary hip replacement: an interrupted time series analysis from ‘The National Joint Registry of England and Wales’. BMJ Open 2019;9.
- Garriga C, Murphy J, Leal J, Price A, Prieto-Alhambra D, Carr A, et al. Impact of a national enhanced recovery after surgery programme on patient outcomes of primary total knee replacement: an interrupted time series analysis from ‘The National Joint Registry of England, Wales, Northern Ireland and the Isle of Man’. Osteoarthritis Cartilage 2019;27:1280-93.
- Higgins M, Jayakumar P, Kortlever JTP, Rijk L, Galvain T, Drury G, et al. Improving resource utilisation and outcomes after total knee arthroplasty through technology-enabled patient engagement. Knee 2020;27:469-76.
- Hunt GR, Crealey G, Murthy BV, Hall GM, Constantine P, O’Brien S, et al. The consequences of early discharge after hip arthroplasty for patient outcomes and health care costs: comparison of three centres with differing durations of stay. Clin Rehabil 2009;23:1067-77. https://doi.org/10.1177/0269215509339000.
- Salmon P, Hunt GR, Murthy BV, O’Brien S, Beverland D, Lynch MC, et al. Patient evaluation of early discharge after hip arthroplasty: development of a measure and comparison of three centres with differing durations of stay. Clin Rehabil 2013;27:854-63.
- Jones C, Kelliher L, Dickinson M, Riga A, Worthington T, Scott MJ, et al. Randomized clinical trial on enhanced recovery versus standard care following open liver resection. Br J Surg 2013;100:1015-24. https://doi.org/10.1002/bjs.9165.
- Khoo CK, Vickery CJ, Forsyth N, Vinall NS, Eyre-Brook IA. A prospective randomized controlled trial of multimodal perioperative management protocol in patients undergoing elective colorectal resection for cancer. Ann Surg 2007;245:867-72. https://doi.org/10.1097/01.sla.0000259219.08209.36.
- Maempel JF, Clement ND, Ballantyne JA, Dunstan E. Enhanced recovery programmes after total hip arthroplasty can result in reduced length of hospital stay without compromising functional outcome. Bone Joint J 2016;98-b:475-82. https://doi.org/10.1302/0301-620x.98b4.36243.
- Maempel JF, Walmsley PJ. Enhanced recovery programmes can reduce length of stay after total knee replacement without sacrificing functional outcome at one year. Ann R Coll Surg Engl 2015;97:563-7. https://doi.org/10.1308/rcsann.2015.0016.
- McDonald DA, Siegmeth R, Deakin AH, Kinninmonth AWG, Scott NB. An enhanced recovery programme for primary total knee arthroplasty in the United Kingdom: follow up at one year. Knee 2012;19:525-9. https://doi.org/10.1016/j.knee.2011.07.012.
- McGregor AH, Rylands H, Owen A, Doré CJ, Hughes SP. Does preoperative hip rehabilitation advice improve recovery and patient satisfaction?. J Arthroplasty 2004;19:464-8. https://doi.org/10.1016/j.arth.2003.12.074.
- Reilly KA, Beard DJ, Barker KL, Dodd CA, Price AJ, Murray DW. Efficacy of an accelerated recovery protocol for Oxford unicompartmental knee arthroplasty--a randomised controlled trial. Knee 2005;12:351-7. https://doi.org/10.1016/j.knee.2005.01.002.
- Williamson L, Wyatt M, Yein K, Melton J. Severe knee osteoarthritis: a randomized controlled trial of acupuncture, physiotherapy (supervised exercise) and standard management for patients awaiting knee replacement. Rheumatology 2007;46:1445-9.
- Arthur HM, Daniels C, McKelvie R, Hirsh J, Rush B. Effect of a preoperative intervention on preoperative and postoperative outcomes in low-risk patients awaiting elective coronary artery bypass graft surgery. A randomized, controlled trial. Ann Intern Med 2000;133:253-62. https://doi.org/10.7326/0003-4819-133-4-200008150-00007.
- Beaupre LA, Lier D, Davies DM, Johnston DB. The effect of a preoperative exercise and education program on functional recovery, health related quality of life, and health service utilization following primary total knee arthroplasty. J Rheumatol 2004;31:1166-73.
- Bousquet-Dion G, Awasthi R, Loiselle S, Minnella EM, Agnihotram RV, Bergdahl A, et al. Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol 2018;57:849-59. https://doi.org/10.1080/0284186x.2017.1423180.
- Carli F, Bousquet-Dion G, Awasthi R, Elsherbini N, Liberman S, Boutros M, et al. Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: a randomized clinical trial. JAMA Surgery 2020;155:233-42. https://doi.org/10.1001/jamasurg.2019.5474.
- Carli F, Charlebois P, Stein B, Feldman L, Zavorsky G, Kim DJ, et al. Randomized clinical trial of prehabilitation in colorectal surgery. Br J Surg 2010;97:1187-97. https://doi.org/10.1002/bjs.7102.
- Ferreira V, Minnella EM, Awasthi R, Gamsa A, Ferri L, Mulder D, et al. Multimodal prehabilitation for lung cancer surgery: a randomized controlled trial. Ann Thorac Surg 2021;112:1600-8. https://doi.org/10.1016/j.athoracsur.2020.11.022.
- Frees SK, Aning J, Black P, Struss W, Bell R, Chavez-Munoz C, et al. A prospective randomized pilot study evaluating an ERAS protocol versus a standard protocol for patients treated with radical cystectomy and urinary diversion for bladder cancer. World J Urol 2018;36:215-20.
- Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 2014;121:937-47. https://doi.org/10.1097/aln.0000000000000393.
- Fransen BL, Hoozemans MJM, Argelo KDS, Keijser LCM, Burger BJ. Fast-track total knee arthroplasty improved clinical and functional outcome in the first 7 days after surgery: a randomized controlled pilot study with 5-year follow-up. Arch Orthop Trauma Surg 2018;138:1305-16. https://doi.org/10.1007/s00402-018-3001-2.
- Hempenius L, Slaets JP, van Asselt D, de Bock GH, Wiggers T, van Leeuwen BL. Outcomes of a geriatric liaison intervention to prevent the development of postoperative delirium in frail elderly cancer patients: report on a multicentre, randomized, controlled trial. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0064834.
- Hempenius L, Slaets JP, van Asselt D, de Bock TH, Wiggers T, van Leeuwen BL. Long term outcomes of a geriatric liaison intervention in frail elderly cancer patients. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0143364.
- Hoogeboom TJ, Dronkers JJ, van den Ende CH, Oosting E, van Meeteren NL. Preoperative therapeutic exercise in frail elderly scheduled for total hip replacement: a randomized pilot trial. Clin Rehabil 2010;24:901-10. https://doi.org/10.1177/0269215510371427.
- van der Peijl ID, Vliet Vlieland TP, Versteegh MI, Lok JJ, Munneke M, Dion RA. Exercise therapy after coronary artery bypass graft surgery: a randomized comparison of a high and low frequency exercise therapy program. Ann Thorac Surg 2004;77:1535-41. https://doi.org/10.1016/j.athoracsur.2003.10.091.
- Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, et al. LAFA study group . Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 2011;254:868-75. https://doi.org/10.1097/SLA.0b013e31821fd1ce.
- Borgwardt L, Zerahn B, Bliddal H, Christiansen C, Sylvest J, Borgwardt A. Similar clinical outcome after unicompartmental knee arthroplasty using a conventional or accelerated care program: a randomized, controlled study of 40 patients. Acta Orthop 2009;80:334-7. https://doi.org/10.3109/17453670903035559.
- Dronkers JJ, Lamberts H, Reutelingsperger IM, Naber RH, Dronkers-Landman CM, Veldman A, et al. Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil 2010;24:614-22. https://doi.org/10.1177/0269215509358941.
- Larsen K. Efficacy, Effectiveness, and Efficiency of Accelerated Perioperative Care and Rehabilitation Intervention After Hip and Knee Arthroplasty 2008.
- Larsen K, Sørensen OG, Hansen TB, Thomsen PB, Søballe K. Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthop 2008;79:149-59. https://doi.org/10.1080/17453670710014923.
- Vesterby MS, Pedersen PU, Laursen M, Mikkelsen S, Larsen J, Søballe K, et al. Telemedicine support shortens length of stay after fast-track hip replacement. Acta Orthop 2017;88:41-7. https://doi.org/10.1080/17453674.2016.1256939.
- Auer CJ, Laferton JAC, Shedden-Mora MC, Salzmann S, Moosdorf R, Rief W. Optimizing preoperative expectations leads to a shorter length of hospital stay in CABG patients: Further results of the randomized controlled PSY-HEART trial. J Psychosom Res 2017;97:82-9. https://doi.org/10.1016/j.jpsychores.2017.04.008.
- Rief W, Shedden-Mora MC, Laferton JA, Auer C, Petrie KJ, Salzmann S, et al. Preoperative optimization of patient expectations improves long-term outcome in heart surgery patients: results of the randomized controlled PSY-HEART trial. BMC Med 2017;15. https://doi.org/10.1186/s12916-016-0767-3.
- Sadlonova M, Nagel J, Becker S, Neumann S, Staab J, Meyer T, et al. Feasibility and preliminary efficacy of perioperative interventions in patients undergoing coronary artery bypass grafting: the randomized controlled I-COPE trial. European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Thoracic Surgery 2022;62. https://doi.org/10.1093/ejcts/ezac041.
- Schmidt M, Eckardt R, Scholtz K, Neuner B, von Dossow-Hanfstingl V, Sehouli J, et al. patient empowerment improved perioperative quality of care in cancer patients aged ≥ 65 years: a randomized controlled trial. PLOS ONE 2015;10.
- den Hertog A, Gliesche K, Timm J, Mühlbauer B, Zebrowski S. Pathway-controlled fast-track rehabilitation after total knee arthroplasty: a randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch Orthop Trauma Surg 2012;132:1153-63. https://doi.org/10.1007/s00402-012-1528-1.
- King TL. The Impact of a Nurse-Driven Evidence-Based Discharge Planning Protocol on Organizational Efficiency and Patient Satisfaction in Patients with Cardiac Implants. Orlando: University of Central Florida; 2008.
- Soeters R, White PB, Murray-Weir M, Koltsov JCB, Alexiades MM, Ranawat AS. Hip and Knee Surgeons Writing Committee . Preoperative physical therapy education reduces time to meet functional milestones after total joint arthroplasty. Clin Orthop Relat Res 2018;476:40-8. https://doi.org/10.1007/s11999.0000000000000010.
- Pour AE, Parvizi J, Sharkey PF, Hozack WJ, Rothman RH. Minimally invasive hip arthroplasty: what role does patient preconditioning play?. J Bone Joint Surg Am 2007;89:1920-7. https://doi.org/10.2106/jbjs.F.01153.
- Cavill S, McKenzie K, Munro A, McKeever J, Whelan L, Biggs L, et al. The effect of prehabilitation on the range of motion and functional outcomes in patients following the total knee or hip arthroplasty: a pilot randomized trial. Physiother Theory Pract 2016;32:262-70. https://doi.org/10.3109/09593985.2016.1138174.
- Kapritsou M, Papathanassoglou ED, Bozas E, Korkolis DP, Konstantinou EA, Kaklamanos I, et al. Comparative evaluation of pain, stress, neuropeptide Y, ACTH, and cortisol levels between a conventional postoperative care protocol and a fast-track recovery program in patients undergoing major abdominal surgery. Biol Res Nurs 2017;19:180-9. https://doi.org/10.1177/1099800416682617.
- Kapritsou M, Papathanassoglou ED, Konstantinou EA, Korkolis DP, Mpouzika M, Kaklamanos I, et al. Effects of the enhanced recovery program on the recovery and stress response in patients with cancer undergoing pancreatoduodenectomy. Gastroenterol Nurs 2020;43:146-55. https://doi.org/10.1097/SGA.0000000000000417.
- Frontera D, Arena L, Corsale I, Francioli N, Mammoliti F, Buccianelli E. Fast track in colo-rectal surgery: preliminary experience in a rural hospital. G Chir 2014;35:293-301.
- Pappalardo G, Coiro S, De Lucia F, Giannella A, Ruffolo F, Frattaroli FM. Open sphincter-preserving surgery of extraperitoneal rectal cancer without primary stoma and Fast Track Protocol. G Chir 2016;37:257-61. https://doi.org/10.11138/gchir/2016.37.6.257.
- Lee SM, Kang SB, Jang JH, Park JS, Hong S, Lee TG, et al. Early rehabilitation versus conventional care after laparoscopic rectal surgery: a prospective, randomized, controlled trial. Surg Endosc 2013;27:3902-9.
- Lee TG, Kang SB, Kim DW, Hong S, Heo SC, Park KJ. Comparison of early mobilization and diet rehabilitation program with conventional care after laparoscopic colon surgery: a prospective randomized controlled trial. Dis Colon Rectum 2011;54:21-8. https://doi.org/10.1007/DCR.0b013e3181fcdb3e.
- Siggeirsdottir K, Olafsson O, Jonsson H, Iwarsson S, Gudnason V, Jonsson BY. Short hospital stay augmented with education and home-based rehabilitation improves function and quality of life after hip replacement: randomized study of 50 patients with 6 months of follow-up. Acta Orthop 2005;76:555-62. https://doi.org/10.1080/17453670510041565.
- Takagi K, Yoshida R, Yagi T, Umeda Y, Nobuoka D, Kuise T, et al. Effect of an enhanced recovery after surgery protocol in patients undergoing pancreaticoduodenectomy: a randomized controlled trial. Clinical Nutrition (Edinburgh, Scotland) 2019;38:174-81. https://doi.org/10.1016/j.clnu.2018.01.002.
- Forsmo HM, Pfeffer F, Rasdal A, Sintonen H, Korner H, Erichsen C. Pre- and postoperative stoma education and guidance within an enhanced recovery after surgery (ERAS) programme reduces length of hospital stay in colorectal surgery. Int J Surg 2016;36:121-6.
- McDonall J, de Steiger R, Botti M, Htchinson AF, Livingston PM, Redley B, et al. Patient activation intervention to facilitate participation in recovery after total knee replacement (MIME): a cluster randomised cross-over trial. BMJ Quality and Safety 2019;28:782-92.
- Hunt GR. Early discharge following hip arthroplasty: patients’ acceptance masks doubts and concerns. Health Expect 2009;12:130-7.
- Williamsson C, Karlsson N, Sturesson C, Lindell G, Andersson R, Tingstedt B. Impact of a fast-track surgery programme for pancreaticoduodenectomy. Br J Surg 2015;102:1133-41. https://doi.org/10.1002/bjs.9856.
- Booth A. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0249-x.
- Centre for Reviews and Dissemination . Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care 2008.
- Wallace A, Croucher K, Quilgars D, Baldwin S. Meeting the challenge: developing systematic reviewing in social policy. Policy Polit 2004;32:455-70. https://doi.org/10.1332/0305573042009444.
- Moore DA, Nunns M, Shaw L, Rogers M, Walker E, Ford T, et al. Interventions to improve the mental health of children and young people with long-term physical conditions: linked evidence syntheses. Health Technol Assess 2019;23:1-164. https://doi.org/10.3310/hta23220.
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-21.
- Noblit GW, Hare RD. Meta-Ethnography: Synthesizing Qualitative Studies. Newbury Park, CA: Sage; 1998.
- Sattar R, Lawton R, Panagioti M, Johnson J. Meta-ethnography in healthcare research: a guide to using a meta-ethnographic approach for literature synthesis. BMC Health Serv Res 2021;21:1-13.
- Suri H. Purposeful sampling in qualitative research synthesis. Qual Res J 2011;11:63-75.
- Archer S, Montague J, Bali A. Exploring the experience of an enhanced recovery programme for gynaecological cancer patients: a qualitative study. Perioper Med (Lond) 2014;3. https://doi.org/10.1186/2047-0525-3-2.
- Barker KL, Room J, Knight R, Dutton SJ, Toye F, Leal J, et al. Outpatient physiotherapy versus home-based rehabilitation for patients at risk of poor outcomes after knee arthroplasty: CORKA RCT. Health Technology Assessment (Winchester, England) 2020;24:1-116.
- Berg U, Berg M, Rolfson O, Erichsen-Andersson A. Fast-track program of elective joint replacement in hip and knee—patients’ experiences of the clinical pathway and care process. J Orthop Surg Res 2019;14:N.PAG-N.PAG. https://doi.org/10.1186/s13018-019-1232-8.
- Berthelsen CB, Frederiksen K. Orchestrating care through the fast-track perspective: a qualitative content analysis of the provision of individualised nursing care in orthopaedic fast-track programmes. Int J Orthop Trauma Nurs 2017;24:40-9. https://doi.org/10.1016/j.ijotn.2016.04.006.
- Berthelsen CB, Kristensson J. A sense of security: Spouses’ experiences of participating in an orthopaedic case management intervention (the SICAM-trial). Int J Orthop Trauma Nurs 2017;24:21-30. https://doi.org/10.1016/j.ijotn.2016.06.002.
- Berthelsen CB, Lindhardt T, Frederiksen K. Maintaining unity: relatives in older patients’ fast-track treatment programmes. A grounded theory study. J Adv Nurs 2014;70:2746-56. https://doi.org/10.1111/jan.12407.
- Churchill L, Pollock M, Lebedeva Y, Pasic N, Bryant D, Howard J, et al. Optimizing outpatient total hip arthroplasty: perspectives of key stakeholders. Can J Surg 2018;61:370-6. https://doi.org/10.1503/cjs.016117.
- Collaco N, Henshall C, Belcher E, Canavan J, Merriman C, Mitchell J, et al. Patients’ and healthcare professionals’ views on a pre- and post-operative rehabilitation programme (SOLACE) for lung cancer: a qualitative study. J Clin Nurs 2021;10.
- Evans S, Snook L, Yates T, Bundy H, Abimbola O, Myers EM. Patient experience with enhanced recovery and early discharge after minimally invasive sacrocolpopexy: a qualitative study. Int Urogynecol J 2021;32:387-94. https://doi.org/10.1007/s00192-020-04431-0.
- Fecher-Jones I, Taylor C. Lived experience, enhanced recovery and laparoscopic colonic resection. Br J Nurs 2015;24:223-8.
- Galli E, Fagnani C, Laurora I, Marchese C, Capretti G, Pecorelli N, et al. Enhanced Recovery After Surgery (ERAS) multimodal programme as experienced by pancreatic surgery patients: findings from an Italian qualitative study. Int J Surg 2015;23:152-9. https://doi.org/10.1016/j.ijsu.2015.09.071.
- Ganske KM. Caring for octogenarian coronary artery bypass graft patients at home: family perspectives. J Cardiovasc Nurs 2006;21:E8-E13. https://doi.org/10.1097/00005082-200603000-00016.
- Haas R, O’Brien L, Bowles KA, Haines T. Health professionals’ perceptions of the allied health role in the acute setting following hip and knee joint replacement surgery: a qualitative study. Disabil Rehabil 2020;42:93-101.
- Heine J, Koch S, Goldie P. Patients’ experiences of readiness for discharge following a total hip replacement. Aust J Physiother 2004;50:227-33.
- Hovik LH, Aglen B, Husby VS. Patient experience with early discharge after total knee arthroplasty: a focus group study. Scand J Caring Sci 2018;32:833-42.
- Jansson MM, Harjumaa M, Puhto AP, Pikkarainen M. Patients’ satisfaction and experiences during elective primary fast-track total hip and knee arthroplasty journey: a qualitative study. J Clin Nurs 2020;29:567-82. https://doi.org/10.1111/jocn.15121.
- Judge A, Carr A, Price A, Garriga C, Cooper C, Prieto-Alhambra D, et al. NIHR Journals Library. Health Services and Delivery Research 2020;1.
- Kocman D, Regen E, Phelps K, Martin G, Parker S, Gilbert T, et al. Can comprehensive geriatric assessment be delivered without the need for geriatricians? A formative evaluation in two perioperative surgical settings. Age Ageing 2019;48:644-9. https://doi.org/10.1093/ageing/afz025.
- Lyon A, Solomon MJ, Harrison JD. A qualitative study assessing the barriers to implementation of enhanced recovery after surgery. World J Surg 2014;38:1374-80.
- Orpen N, Harris J. Patients’ perceptions of preoperative home-based occupational therapy and/or physiotherapy interventions prior to total hip replacement. Br J Occup Ther 2010;73:461-9.
- Phillips E, Archer S, Montague J, Bali A. Experiences of enhanced recovery after surgery in general gynaecology patients: an interpretative phenomenological analysis. Health Psychol Open 2019;6. https://doi.org/10.1177/2055102919860635.
- Reay PA, Horner B, Duggan R. The patient’s experience of early discharge following total hip replacement. Int J Orthopa Trauma Nurs 2015;19:131-9. https://doi.org/10.1016/j.ijotn.2015.02.003.
- Samuelsson KS, Egenvall M, Klarin I, Lokk J, Gunnarsson U, Iwarzon M. The older patient’s experience of the healthcare chain and information when undergoing colorectal cancer surgery according to the enhanced recovery after surgery concept. J Clin Nurs 2018;27:e1580-8.
- Specht K, Agerskov H, Kjaersgaard-Andersen P, Jester R, Pedersen BD. Patients’ experiences during the first 12 weeks after discharge in fast-track hip and knee arthroplasty: a qualitative study. Int J Orthopa Trauma Nurs 2018;31:13-9.
- Specht K, Kjaersgaard-Andersen P, Pedersen BD. Patient experience in fast-track hip and knee arthroplasty--a qualitative study. J Clin Nurs 2016;25:836-45.
- Strickland LH, Kelly L, Hamilton TW, Murray DW, Pandit HG, Jenkinson C. Early recovery following lower limb arthroplasty: qualitative interviews with patients undergoing elective hip and knee replacement surgery. Initial phase in the development of a patient-reported outcome measure. J Clin Nurs 2018;27:2598-608.
- Thomsen TG, Holge-Hazelton B. Patients’ vulnerability in follow-up after colorectal cancer: a qualitative action research study. Cancer Nurs 2017;40:152-9.
- van Egmond JC, Verburg H, Vehmeijer SB, Mathijssen NM. Early follow-up after primary total knee and total hip arthroplasty with rapid recovery: focus groups. Acta Orthop Belg 2015;81:447-53.
- Vandrevala T, Senior V, Spring L, Kelliher L, Jones C. ‘Am I really ready to go home?’: a qualitative study of patients’ experience of early discharge following an enhanced recovery programme for liver resection surgery. Support Care Cancer 2016;24:3447-54. https://doi.org/10.1007/s00520-016-3158-6.
- Westby MD, Backman CL. Patient and health professional views on rehabilitation practices and outcomes following total hip and knee arthroplasty for osteoarthritis: a focus group study. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-119.
- Blazeby JM, Soulsby M, Winstone K, King PM, Bulley S, Kennedy RH. A qualitative evaluation of patients’ experiences of an enhanced recovery programme for colorectal cancer. Colorectal Dis 2010;12:e236-42.
- den Bakker CM, Huirne JA, Schaafsma FG, de Geus C, Bonjer HJ, Anema JR. Electronic health program to empower patients in returning to normal activities after colorectal surgical procedures: mixed-methods process evaluation alongside a randomized controlled trial. J Med Internet Res 2019;21.
- Krogsgaard M, Dreyer P, Egerod I, Jarden M. Post-discharge symptoms following fast-track colonic cancer surgery: a phenomenological hermeneutic study. Springerplus 2014;3.
- Short V, Atkinson C, Ness AR, Thomas S, Burden S, Sutton E. Patient experiences of perioperative nutrition within an enhanced recovery after surgery programme for colorectal surgery: a qualitative study. Colorectal Dis 2016;18:O74-80.
- Bin Sheeha B, Williams A, Johnson DS, Granat M, Jones R. Patients’ experiences and satisfaction at one year following primary total knee arthroplasty: a focus-group discussion. Musculoskeletal Care 2020;18:434-49. https://doi.org/10.1002/msc.1478.
- Heaton J, McMurray R, Sloper P, Nettleton S. Rehabilitation and total hip replacement: patients’ perspectives on provision. Int J Rehabil Res 2000;23:253-9. https://doi.org/10.1097/00004356-200023040-00001.
- Jorgensen LB, Fridlund B. Restoring integrity – a grounded theory of coping with a fast track surgery programme. Int J Qual Stud Health and Well-Being 2016;11.
- Kadiri SB, Kerr AP, Oswald NK, Budacan AM, Flanagan S, Golby C, et al. Fit 4 surgery, a bespoke app with biofeedback delivers rehabilitation at home before and after elective lung resection. J Cardiothorac Surg 2019;14.
- Lie I, Bunch EH, Smeby NA, Arnesen H, Hamilton G. Patients’ experiences with symptoms and needs in the early rehabilitation phase after coronary artery bypass grafting. Eur J Cardiovasc Nurs 2012;11:14-2.
- Rattray M, Ben D, Marshall AP, von Papen M, Roberts S. Evaluation of an intervention to improve nutrition intake in patients undergoing elective colorectal surgery: a mixed-methods pilot study. Nutrition 2021;84. https://doi.org/10.1016/j.nut.2020.111015.
- Sjoveian AKH, Leegaard M. Hip and knee arthroplasty: patient’s experiences of pain and rehabilitation after discharge from hospital. Int J Orthopa Trauma Nurs 2017;27:28-35.
- Uhrenfeldt L, Hoybye MT. Care interaction adding challenges to old patients’ well-being during surgical hospital treatment. Int J Qual Stud Health Well-Being 2015;10.
- Schneider CQ, Wagemann C. Set-Theoretic Methods for the Social Sciences: A Guide to Qualitative Comparative Analysis. Cambridge: Cambridge University Press; 2012.
- Thiem A, Duşa A. Boolean minimization in social science research: a review of current software for Qualitative Comparative Analysis (QCA). Soc Sci Comput Rev 2013;31:505-21.
- Ragin CC. Redesigning Social Inquiry: Fuzzy Sets and Beyond. New York: Wiley Online Library; 2008.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-45.
- Sutcliffe K, Kneale D, Thomas J. Using Qualitative Comparative Analysis (QCA) in diverse ways to explore intervention complexity: how two QCA approaches were valuable within a single review n.d. https://doi.org/10.1002/14651858.CD201901.
- Rihoux B. Qualitative Comparative Analysis (QCA) and related techniques: recent advances and challenges. Methoden Der Vergleichenden Politik-Und Sozialwissenschaft 2009;3:65-8.
- Kneale D, Sutcliffe K, Thomas J. Critical Appraisal of Reviews Using Qualitative Comparative Analyses (CARU-QCA): a tool to critically appraise systematic reviews that use qualitative comparative analysis 2019.
- Kneale D, Thomas J, Harris K. Developing and optimising the use of logic models in systematic reviews: exploring practice and good practice in the use of programme theory in reviews. PLOS ONE 2015;10.
- Marx A, Dusa A. Crisp-set qualitative comparative analysis (csQCA), contradictions and consistency benchmarks for model specification. Methodological Innovations Online 2011;6:103-48.
- Duşa A. QCA with R: A Comprehensive Resource. Dordrecht: Springer; 2019.
- Sutcliffe K, Kneale D, Thomas J. ‘Leading from the front’implementation increases the success of influenza vaccination drives among healthcare workers: a reanalysis of systematic review evidence using Intervention Component Analysis (ICA) and Qualitative Comparative Analysis (QCA). BMC Health Serv Res 2022;22:1-13.
- Porserud A, Lundberg M, Eriksson J, Nygren Bonnier M, Hagströmer M. Like I said, I would not have likely gotten up otherwise: patient experiences of using an activity board after abdominal cancer surgery. Disabil Rehabil 2023;45:1022-9.
- Greer NL, Gunnar WP, Dahm P, Lee AE, MacDonald R, Shaukat A, et al. Enhanced recovery protocols for adults undergoing colorectal surgery: a systematic review and meta-analysis. Dis Colon Rectum 2018;61:1108-18.
- Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surgery 2017;152:292-8.
- Deng Q-F, Gu H-Y, Peng W-y, Zhang Q, Huang Z-D, Zhang C, et al. Impact of enhanced recovery after surgery on postoperative recovery after joint arthroplasty: results from a systematic review and meta-analysis. Postgrad Med J 2018;94:678-93.
- McIsaac DI, Gill M, Boland L, Hutton B, Branje K, Shaw J, et al. Prehabilitation in adult patients undergoing surgery: an umbrella review of systematic reviews. Br J Anaesth 2021;128:244-57.
- Churruca K, Pomare C, Ellis LA, Long JC, Henderson SB, Murphy LED, et al. Patient-reported outcome measures (PROMs): a review of generic and condition-specific measures and a discussion of trends and issues. Health Expect 2021;24:1015-24. https://doi.org/10.1111/hex.13254.
- Lee L, Mata J, Ghitulescu GA, Boutros M, Charlebois P, Stein B, et al. Cost-effectiveness of enhanced recovery versus conventional perioperative management for colorectal surgery. Ann Surg 2015;262:1026-33. https://doi.org/10.1097/sla.0000000000001019.
- Meulenbroeks I, Epp J, Schroeder L. The value of caregiver inclusive practices in geriatric transitions of care: a systematic review. Health Policy 2021;125:888-98.
- Riley LD, Bowen CP. The sandwich generation: challenges and coping strategies of multigenerational families. Family J 2005;13:52-8.
- Doran T, Drever F, Whitehead M. Health of young and elderly informal carers: analysis of UK census data. BMJ 2003;327.
- Lucas SR, Szatrowski A. Qualitative comparative analysis in critical perspective. Sociol Methodol 2014;44:1-79.
- NICE 2020. www.nice.org.uk/guidance/ng180 (accessed February 2023).
Appendix 1 Search strategy for MEDLINE
Database: MEDLINE ALL
Host: Ovid
Hits: 8446
Strategy:
-
((older or frail or elderly) adj2 (person* or people or patient* or population* or adult*)).tw.
-
geriatric*.tw.
-
*aged/
-
*“Aged, 80 and over”/
-
*frail elderly/
-
*Geriatrics/
-
or/1-6
-
((eye* or sclera or iris or retina or cataract or ophthalmol*) adj3 (surgery or surgical* or procedur*)).tw.
-
exp *ophthalmologic surgical procedures/
-
((heart or cardiac or coronary) adj3 (surgery or surgical* or procedur* or transplant* or angiography or angioplasty or bypass)).tw.
-
(aortic adj3 (replacement or surgery or surgical* or procedur*)).tw.
-
(carotid adj3 endarterectomy).tw.
-
((arterial or artery or arteries) adj3 (bypass or surgery or surgical* or angioplasty or embolectomy)).tw.
-
*coronary artery bypass/
-
((urinary or urologic* or genitourinary or bladder or prostate) adj3 (surgery or surgical* or procedur*)).tw.
-
(urethrotomy or prostatectomy).tw.
-
exp *Urologic Surgical Procedures/
-
(meningioma* adj3 (surgery or surgical* or procedur*)).tw.
-
craniotomy.tw.
-
*craniotomy/
-
((lung or thoracic or thorax or cardiothoracic or pulmonary or chest or diaphragm) adj3 (surgery or surgical* or resection* or procedur*)).tw.
-
(thoracotomy or pneumonectomy).tw.
-
*Thoracic Surgery/
-
(“bile duct” adj3 (resection* or surgery or surgical* or procedur*)).tw.
-
((pancreas or pancreatic) adj3 (surgery or surgical* or resection* or procedur*)).tw.
-
(pancreatectomy or pancreaticoduodenectomy).tw.
-
*Pancreatectomy/
-
“endovascular aortic aneurysm repair*”.tw.
-
“endovascular abdominal aneurysm repair*”.tw.
-
((hip or knee or “lower limb*”) adj3 (replacement* or restructur* or arthroplasty or hemiarthroplasty or surgery or surgical* or procedur*)).tw.
-
*arthroplasty, replacement, hip/
-
*arthroplasty, replacement, knee/
-
((colorectal or colon or colonic or rectal or rectum or bowel or intenstin*) adj3 (surgery or surgical* or resection* or procedur*)).tw.
-
Colorectal Surgery/
-
or/8-34
-
7 or 35
-
(“enhanced recovery after” adj3 surgery).tw.
-
ERAS.tw.
-
((enhanced or early or earlier) adj3 (recovery or mobili?ation or ambulation or rehab*)).tw.
-
ERP.tw.
-
(“proactive care” adj2 “older people”).tw.
-
POPS.tw.
-
(“fast track” adj3 (surgery or surgical* or program* or management or “patient care”)).tw.
-
(multimodal adj3 (rehab* or perioperative or postoperative or “post operative” or optimi?ation or care or convalesc*)).tw.
-
(optimal adj2 (“preoperative assessment” or “preoperative management”)).tw.
-
((accelerated or optimi?ed or rapid or “fast track”) adj3 (care or rehab* or recovery or mobili?ation or ambulation or convalesc*)).tw.
-
((improved or improving) adj2 recovery).tw.
-
“comprehensive geriatric assessment*”.tw.
-
“short acting an?esthetic*”.tw.
-
((integrated or managed) adj1 “care pathway*”).tw.
-
((multidisciplinary or “multi disciplinary”) adj1 assessment*).tw.
-
((physiotherap* or exercise*) adj3 (augment* or increas* or “higher frequency”)).tw.
-
(“pressure ulcer*” adj3 “risk assessment”).tw.
-
((nutrition* or feed* or eat*) adj3 support*).tw.
-
*Nutritional Support/
-
((support* or community) adj3 discharg*).tw.
-
(discharg* adj3 plan*).tw.
-
(rehab* adj3 (home or community)).tw.
-
or/37-58
-
((length or duration) adj4 stay adj8 (reduce* or reduction* or reducing or shorter or shortening or “positive effect*” or prolong* or increas* or decreas* or improve* or improving or “patient outcome*” or “clinical outcome*” or “clinical indicator*” or “outcome measure*”)).tw.
-
(hospital* adj3 stay adj8 (reduce* or reduction* or reducing or shorter or shortening or “positive effect” or prolong* or increas* or decreas* or improve* or improving or “patient outcome*” or “clinical outcome*” or “clinical indicator*” or “outcome measure*”)).tw.
-
(time adj3 discharg*).tw.
-
*“Length of Stay”/
-
or/60-63
-
59 or 64
-
(randomis* or randomiz* or randomly).tw.
-
rct*.tw.
-
(trial* or controlled or “control group*” or “intervention group*”).tw.
-
((single or doubl* or tripl* or treb*) and (blind* or mask*)).tw.
-
(“4 arm” or “four arm”).tw.
-
((before adj4 after) or “BA stud*” or “CBA stud*”).tw.
-
(“pre post” or “pre test*” or pretest* or posttest* or “post test*” or (pre adj3 post)).tw.
-
(interrupt* adj2 “time series”).tw.
-
(“time points” adj3 (over or multiple or three or four or five or six or seven or eight or nine or ten or eleven or twelve or month* or hour* or day* or “more than”)).tw.
-
((“quasi experiment*” or quasiexperiment* or “quasi random*” or quasirandom* or “quasi control*” or quasicontrol*) adj3 (method* or stud* or design*)).tw.
-
randomized controlled trial.pt.
-
controlled clinical trial.pt.
-
or/66-77
-
(quality adj2 (life or wellbeing or “well being”)).tw.
-
(hql or hqol or “h qol” or hrqol or “hr qol”).tw.
-
“Quality of Life”/
-
(qaly* or qald* or qale* or qtime*).tw.
-
quality-adjusted life years/
-
(“disability adjusted life” or daly*).tw.
-
(sf36 or “sf 36” or “short form 36” or “shortform 36” or “sf thirtysix” or “sf thirty six” or “shortform thirtysix” or “shortform thirty six” or “short form thirtysix” or “short form thirty six”).tw.
-
(sf6 or “sf 6” or “short form 6” or “shortform 6” or “sf six” or sfsix or “shortform six” or “short form six”).tw.
-
(sf12 or “sf 12” or “short form 12” or “shortform 12” or “sf twelve” or sftwelve or “shortform twelve” or “short form twelve”).tw.
-
(sf6D or “sf 6D” or “short form 6D” or “shortform 6D” or “sf six D” or sfsixD or “shortform six D” or “short form six D”).tw.
-
(sf20 or “sf 20” or “short form 20” or “shortform 20” or “sf twenty” or sftwenty or “shortform twenty” or “short form twenty”).tw.
-
(euroqol or “euro qol” or eq5d or “eq 5d” or “eq 5d 3l” or “eq 5d 5l”).tw.
-
AQoL.tw.
-
(“health* year* equivalent*” or hye or hyes).tw.
-
(utilit* adj3 (analys* or assess* or estimat* or scor* or valu*)).tw.
-
(“health utility index” or hui or hui1 or hui2 or hui3).tw.
-
disutili*.tw.
-
“standard gamble*”.tw.
-
(“time trade off” or “time tradeoff” or tto).tw.
-
or/79-97
-
78 or 98
-
36 and 65 and 99
Appendix 2 Matrices for network meta-analysis feasibility assessment
The tables below display attempts to identify clusters of studies with the same comparison, outcome categories and measurement time points that could have made network meta-analysis feasible. The two largest groups of studies were assessed, colorectal and lower-limb arthroplasty. There was no comparison where network meta-analysis would have been feasible.
| Comparison | IN-HOSPITAL | DISCHARGE TO 30D | 31D TO 6MO | 6MO PLUS | ||||
|---|---|---|---|---|---|---|---|---|
| Pain | QOL | MH | PF | PA | MH | PA | N/A | |
| ERP vs. TAU | Two studies | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Prehab vs. TAU | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Prehab vs. Rehab | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Rehab vs. TAU | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Comparison | IN-HOSPITAL | DISCHARGE to 30D | 31D TO 6MO | 6MO PLUS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pain | Pain | QoL | MH | PF | Sat | PA | Pain | QoL | Pain | |
| ERP vs. TAU | 3 studies | 4 studies | 3 studies | |||||||
| Prehab vs. TAU | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 4 studies | N/A | N/A |
| Rehab vs. TAU | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
Appendix 3 Qualitative review – summary of all included studies
| First author date; country [publication status] | Study aim | Reason for patient admission; intervention category | Intervention aim | Deliverers of intervention (name of profession), N, age range | Participants providing views [N], age range, profession | Data collection method | Data analysis (interpretive/descriptive): quantity of relevant data | Summary of themes |
|---|---|---|---|---|---|---|---|---|
| Archer 2014; UK [JAP]100 | Experience of ERP for women at an East Midlands regional cancer centre | Gynaecological cancer open surgery; ERP | ‘Enhanced’ or ‘fast-track’ recovery combines several perioperative interventions to reduce the length of inpatient stay in hospital and promote early recovery after surgery | NR | Patients [14], 53–80 (mean 66) | Interviews | IPA (interpretive): high | Two main themes (with subthemes): (1) Taking part in the programme; (2) Home (going home; the follow-up call) |
| Barker 2020; UK [JAP]101 | 1. Design screening tool to guide patient selection for trial. 2. Evaluate multicomponent rehabilitation programme delivered in patients’ homes compared to standard outpatient physiotherapy rehabilitation over 12 months | UKA; Rehabilitation programme | Improve function and participation in activities for participants at risk of a poor outcome | UK-registered PT/OTs, + rehabilitation assistants across 14 NHS Trusts in England | Patients and staff. Patients [10], 64–90. Staff [11] (5 physios and 6 rehab assistants) | Individual interviews | TA (descriptive/interpretive): high | Staff themes (Enjoying the above and beyond. See the person in their own world. Developing people skills. Thinking outside the cubicle. Treading a fine line between patient and friend. Feeling outside my comfort zone. Needing a support network) |
| 3. Explore patients’ and clinicians’ perceptions of the community-based rehabilitation programme. 4. Compare cost-effectiveness of the intervention to TAU | Patient themes: the benefits of having treatment at home (it was a relief not travel; I got an hour’s work done in an hour; they can work with your surroundings; I wouldn’t have done it on my own; there is nothing like company) | |||||||
| Challenges of having treatment at home (they put me through my paces; feeling at sea now that it is over). Factors that might have effected outcome (my get up and go has got up and gone; a variable social life; if you take to the person it goes a long way; a lot would shirk from putting on a pair of running shoes) | ||||||||
| Berg 2019; Sweden [JAP]102 | Explore patients’ perspective and experiences of undergoing THR and TKR surgery within the entire fast-track care process | THR or TKR; ERP | Reduce physiological and psychological stress related to surgery, enhancing early mobilisation and rapid recovery | Hospital staff (not specified) | Patients [24], 44–85 (mean 65 years) | Individual interviews | Inductive content analysis (descriptive): High | Findings split into chronological phases of fast-track pathway (preparation, hospital stay for surgery, and recovery after discharge) with categories within each phase (e.g. early mobilisation, managing daily life, etc.) |
| Berthelsen 2014; Denmark [JAP]105 | Generate substantive GT of relatives’ pattern of behaviour in older patients fast-track treatment programmes during total joint replacement | Joint replacement; ERP | Enhancing recovery by implementing evidence in key areas, such as analgesia, reduction of surgical stress, nutrition and mobilisation | Hospital staff (not specified) | Family carers [7], 40–60 | Non-participant observation and interviews | GT (interpretive): Low | Theory of Maintaining Unity with three behavioural modes: protecting mode, substituting mode, and adapting mode |
| Berthelsen 2017; Denmark [JAP]104 | Explore and describe spouses’ experiences of participating in a case management intervention during older patients’ fast track total hip replacement programmes and discover which intervention elements they found useful | THR; case management | Case management intervention directed towards spouses of older patients undergoing total hip replacements in a fast-track programme | Case manager (nurse from orthopaedics specialising in fast-track) | Spouses [10], 64–78 (mean 71.2) | Interviews | Directed content analysis (descriptive): high | Findings described according to pre-determined codes: spouses’ overall experience of participating in the intervention; involvement by case manager; most meaningful part of participating; problematic issues; changes to be made; the spouses’ role as an active participant; specific intervention elements that were found to be useful |
| Berthelsen 2017; Denmark [JAP]103 | Illuminate orthopaedic nurses’ perceptions and experiences of providing individual nursing care for older patients in standardised fast-track programmes after THA/TKA | THA/TKA; ERP | Evaluate beneficent effect on convalescence achieved by adding multimodal evidence-based care principles and combining these with optimised logistics | Nurses (plus other hospital staff) | Staff – nurses responsible for patient care on fast-track programme [10], 25–43 (mean 34) | Interviews | Manifest and latent content analysis [descriptive (manifest) and interpretive (latent)]: high | Manifest findings overall categories: Nurses’ description of the fast-track programme; possibilities for providing individual nursing care; consequences of providing individual nursing care. Latent findings main theme: orchestrating care through the fast-track perspective; overall themes: |
| identifying and legitimising relevant individual care in the fast-track programme; struggling to fit all patients into the fast-track programme; justifying care-related actions in the fast-track programme | ||||||||
| Bin Sheeha 2020; UK [JAP]134 | Understand patient experiences, outcomes and satisfaction post-TKA | TKR; unclear | NR | NR | Patients [7], 70–82 (mean 76.71) | Focus group | TA (descriptive): med | Four main themes (with several subthemes): (1) recovery experience; (2) experience before TKA; (3) ADL changes 1 year post-TKA; (4) outcome expectations following TKA |
| Blazeby 2010; UK [JAP]130 | Understand patients’ views and experiences of surgery for colorectal cancer within an ERP | Laparoscopic or open surgery for adenocarcinoma of the colon or rectum; ERP | Improve short-term clinical, economic and patient-reported outcomes | Nurses (plus other hospital staff during hospital stay) | Patients [20], mean age 73.8 (8.2 SD) | Interviews | Constant comparison techniques derived from GT (descriptive): high | Findings described in two sections: participants’ views of the enhanced recovery programme; social support at home |
| Churchill 2018; Canada [JAP]106 | Gain insight into patient and caregiver perspectives regarding the advantages and disadvantages of outpatient THA to identify areas of care that can be improved | THA; ERP | Cost savings, potential improvement in patient satisfaction and more rapid independence for patients | NR (various hospital staff implied) | Patient–carer dyads, inpatient pathway = 6 dyads [patient mean age 69 (12) and carer mean 59 (15)]. Outpatient pathway = 6 dyads [patient mean age 63 (5) and carer mean 62 (7)] | Interviews | Thematic and content analysis (descriptive): high | Three main themes: (1) supporting the transition home, (2) challenges for transitioning home and (3) unique considerations for same-day discharge. Also subcategories within them and explored for inpatient vs. outpatient participants |
| Collaco 2021; UK [JAP]107 | Explore patients’ experiences of the rehabilitation intervention service (SOLACE) and experiences/views of healthcare professionals (HCPs) linked to SOLACE | Surgery for early-stage lung cancer; ERP | Enhanced support for early-stage surgical lung cancer aiming to reduce morbidity and mortality / improve physical, psychological and social health and wellbeing. Optimise patients’ health and fitness levels prior to, and following surgery, with long-term aim of preventing hospital readmissions and improving LOS | All NR (includes specialist Macmillan nurses) | Patients and staff, patients [17] (median age = 70). Staff [8] (4 nurses, 1 advanced therapist practitioner, 1 surgeon, 1 respiratory, 1 physician) | Interviews | TA. (descriptive): high | Key themes: (1) experience of SOLACE service; (2) engagement with SOLACE; (3) barriers to patient uptake of rehabilitation classes; and (4) follow-up pathways |
| den Bakker 2019; Netherlands [JAP]131 | Evaluate whether recovery-orientated eHealth intervention was executed as planned to assist with interpreting future trial outcomes and determine important factors for program scale-up | Colorectal surgery; supported discharge | To partially substitute guiding and monitoring of long-term recovery including resumption of normal activities and work of colorectal patients | NR | Patients [14], 45–76 (mean 62) | Interviews | TA (descriptive): med | Findings reported using the four constructs of the Unified Theory of Acceptance and Use of Technology (UTAUT): performance expectancy; effort expectancy; social influence; facilitating and inhibiting conditions. Performance expectancy also includes sub-themes (guidance and support; information provision; communication; functionality) |
| Evans 2021; USA [JAP]108 | Describe patient experiences with an ERP after minimally invasive SCP | Minimally invasive SCP; ERP | Expedite recovery | NR | Patients [14], IQR (58–69.25) (mean 65.5) | Interviews | Constant comparative method, guided by GT (interpretive/descriptive): high | Five main themes: (1) feeling prepared and adequately educated; (2) convenience of at-home recovery and importance of social support; (3) trust in care and decision-making; 4) staying or going; (5) challenges of catheter care |
| Fecher-Jones 2015; UK [JAP]109 | Explore patients’ lived experience of undergoing laparoscopic colonic resection on an ERP | Laparoscopic colonic resection; ERP | Optimise patient recovery by combining both ERP and laparoscopic surgery, there is the potential to improve patients’ quality of life with regard to pain and fatigue | NR | Patients [11], 52–92 (mean 75) | Interviews | Lindseth and Norberg (2004) phenomenological method of analysis (interpretive): high | Overarching themes (and subthemes): expectation (laparoscopic surgery, what would be expected of them, how they would feel, discharge, hospital environment); control (desire to be in control of recovery, desire to regain control of physical function); needing comfort (feeling pressure to look after themselves, need for psychological support); and regaining wellness (desire to put experience behind them, worry caused by physical symptoms, not wanting to rely on others) |
| Galli 2015; Italy [JAP]110 | Capture experience of patients undergoing pancreatic surgery who received perioperative care based on the ERAS programme | Pancreatic surgery; ERP | Attenuate patient stress response before, during, and after surgical procedures, facilitating maintenance of physiological organ functions and allowing patients to achieve early recovery | Surgeon and RN at pre-admission counselling meeting, anaesthesiologist, other deliverers NR but list of key interventions implies multidisciplinary | Patients [13], 46–77 (mean 65) | Interviews | TA (interpretive): high | Four themes: feeling prepared to face surgery; being actively ‘inside’ or ‘outside’ the programme; healing at home: the best setting; ‘perceiving the ordinary as extraordinary’: reaching independence once at home |
| Ganske 2006; USA [JAP]111 | Describe the lived experience of caring for very elderly (80 years or older) CABG patients during convalescence at home | CABG; early discharge | NR | NR | Carers [12], 46–83 (5 wives and 7 daughters of patients) | Interviews | Lincoln and Guba as guide: prolonged engagement with persistent observation, peer expert debriefing+ validation, investigator transcription/review of text for errors, reflective journaling, and informal member checks (descriptive): high | Three main themes: work; personal reaction to caregiving; experiences with formal care |
| Haas 2020; Australia [JAP]112 | Describe health professionals’ perceptions of role of allied health during the acute phase following elective LLA surgery to inform the development of efficient allied health service models | Elective TKA or THA; staff mix | Improve patient outcomes and reduce length of stay and the associated costs | MDT (unclear which professions classed as “allied health”) | Staff [25], 20–60, professions = PT (3), OT (2), allied health assistant (1), social worker (1), nurse (11), medical (7) | Focus groups (three groups: allied health staff (6), medical professionals (7), nursing and allied health (14) – 2 allied health staff attended groups 1 and 3) | TA (descriptive): high | Findings split into five areas of practice: (1) aims of allied health after joint replacement; (2) facilitation of early mobilisation; (3) professional roles; (4) intervention to patients awaiting rehabilitation; (5) overlapping 7-day allied health service vs. limited weekend service |
| Heaton 2000; UK [JAP]135 | First, to describe the rehabilitation process associated with this procedure. Second, to elicit patients’ views on their needs and goals. (Third aim related to postal survey) | THR; rehabilitation programme | NR | OT, PT, nurse, consultant. Further details NR | Patients, Site 1: N = 30, age = 66.43. Site 2: N = 28, age = 66.17 | Interviews | TA assumed (descriptive): med | Findings described under two main headings (with subheadings): (1) goal attainment; (2) effectiveness of rehabilitation provision (information; equipment; therapy; other provision) |
| Heine 2004; Australia [JAP]113 | Understand experiences of people undergoing a THA, in relation to their pending discharge | Elective THA; ERP | Shorter hospital stays and clinical pathways have been promoted widely in hospitals to reduce health-care costs and promote patient care | NR | Patients [5], 43–79 (mean 66.4) | Interviews | GT (interpretive): high | Three major categories (with subcategories): feeling safe; confidence (staff influences; consistent information; preoperative information); family and friends (reluctance to return home alone; the different roles of family members) |
| Hovik 2018; Norway [JAP]114 | Explore experience of patients undergoing TKA in a fast-track pathway during the first 2 weeks after surgery | Elective TKA; ERP | Reduce convalescence time and complication rates (including reduced morbidity and mortality), increase patient satisfaction and reduce time to full physical function | Nurses, surgeon, anaesthesiologist, PT | Patients [13], 40–79 (mean 64.2) | Focus groups | Systematic text condensation (interpretive): high | Four main themes: (1) the value of coming home; (2) security and predictability; (3) feeling empowered by sharing experiences; (4) no pain, no gain |
| Hunt 2009; UK [JAP]90 | Describe patients’ experience of accelerated discharge after hip arthroplasty to test acceptability to patients of economically driven shortening of post-operative stay | THR; ERP | Shorten LOS | For Belfast ERP – surgeon, PT plus telephone helpline with NR staff type | Patients, Belfast (ERP group [15], 57–82 (mean 70); Liverpool [20] usual care): 48–88 (mean 71) | Interviews | Inductive analysis, categories developed on basis of what patients said (interpretive): high | Findings presented in two main sections: (1) complaints; (2) length of stay and post-discharge experience |
| Jansson 2020; Finland [JAP]115 | Explore patient satisfaction with process of treatment and care and identify experiences that patients perceive during elective primary fast-track THA/TKA journey | TKA or THA; ERP | NR | NR all, but includes anaesthesiologist and PT | Patients, THA [9], 52–74 (mean 66.2). TKA [11], 56–76 (mean 68.1) | Interviews | Inductive content analysis (interpretive): high | Eight main categories: (1) patient selection, (2) meeting the Health Care Guarantee, (3) patient flow, (4) post-discharge care, (5) patient counselling, (6) transparency of the journey, (7) communication and (8) feedback |
| Jorgensen 2016; Denmark [JAP]136 | Present a theory on how patients predominantly cope with a fast-track THA programme | THA; ERP | Focusing on preoperative optimisation and patient education, reducing surgical stress response, optimising pain relief, and enforcing mobilisation and nutritional support. Reducing hospitalisation time | NR (includes care co-ordinator who is a specially trained nurse or PT) | Patients [14], 52–78 (mean 62.64) | Interviews | GT (interpretive): med/high | Findings expressed as four types of coping behaviour: (1) exceeding the boundaries of capability; (2) protecting the boundaries of capability; (3) challenging the boundaries of capability; (4) accepting the boundaries of capability |
| Judge 2020; UK [JAP]116 | Determine effect of hospital organisation, surgical factors and ERAS pathway on patient outcomes and NHS costs of hip and knee replacement. Qualitative aims: (1) understand organisational processes that help or hinder the implementation of ERAS programmes for hip/knee replacement; (2) explore patients’ experiences of ERAS for hip and knee replacement | THR or TKR; ERP | Improve patient care, preoperatively, perioperatively and postoperatively | Range of staff at each site, inc. nurses, PTs (2 sites have central coordinator for patient) | Patients [37], 36–90 (mean = 66.41) | Interviews | Inductive TA (descriptive): high | Findings presented in sections related to patient journey: referral process; preoperative preparation; waiting for operation; anaesthesia; pain management; inconsistencies in information; early postoperative mobilisation; discharge; postoperative; physiotherapy exercises; pain relief; post-discharge support; family; the future |
| Kadiri 2019; UK [JAP]137 | Develop a bespoke pulmonary rehabilitation app and test its feasibility and acceptability to patients | Curative lung cancer surgery; rehabilitation programme | Therefore, there is a need for a [rehabilitation] service that can be delivered immediately at the convenience and in the control of the patient | App (plus instruction on app from medical team) | Patients, N = 13 (age NR, from wider sample of 31) | Interviews | Content analysis. (descriptive): low | Five main qual themes: (1) ease of use/instructions; (2) positive features of the app; (3) motivation for taking part in the study; (4) perceived impact upon fitness levels; (5) problems and tips for improvement |
| Kocman 2019; UK [JAP]117 | Design, pilot and formatively evaluate approach to improving care for frail older patients in areas of the hospital where CGA is not part of the clinical tradition | Cancer surgery; CGA | Identifies medical, social and functional needs, and the development of an integrated/co-ordinated care plan to meet those needs | Clinicians involved in care of older patients | Staff [41], lead clinicians and their collaborators from multiple clinical specialisms | Interviews and ethno-graphic observation | Normalisation process theory (descriptive): med | Findings described under two headings: (1) factors supporting change; (2) key challenges in delivering CGA |
| Krogsgaard 2014; Denmark [JAP]132 | Obtain knowledge of patients’ experiences of postoperative symptoms during initial 2 weeks following fast-track colonic cancer surgery | Colonic cancer surgery; ERP | NR directly (components of fast-track given) | Full team NR but includes nurse and implied other clinicians | Patients [7], 55–82 (mean 70.71) | Interviews | Analysis: naïve reading, structural analysis, and critical analysis and discussion (interpretive): med/high | Two main themes (with subthemes): (1) symptoms permeate everyday life (daily activities driven by own motivation; symptoms limit activity and cause concern; symptoms are managed by own experiences); (2) experience of grief (stunned by cancer diagnosis; chaotic thinking) |
| Lie 2012; Norway [JAP]138 | Explore CABG patients’ symptoms and needs in early rehabilitation phase | CABG; supported discharge | NR in this paper | Nurses | Patients [93], 39–77 (mean 62) | Interviews | Qualitative, manifest content analysis in accordance with Graneheim and Lundman (descriptive): low | Findings presented in following sections: physical experiences; experiences with prescribed discharge medications; psychological experiences: anxiety and/or depression; experiences with sexuality; patient-defined experiences |
| Lyon 2014; Australia [JAP]118 | Elicit barriers to implementation and functioning of ERAS program at Royal Prince Alfred Hospital | Colorectal surgery; ERP | Reducing morbidity, allowing earlier safe discharge after colorectal surgery, and reducing the amount of time to return to normal daily function | NR – range of clinicians implied (including types interviewed) | Staff [18], professions = colorectal consultants, nurses (ward and nursing managers), allied health staff (PT, dietician, stoma nurse, ERAS coordinator, care coordinator), service improve coordinator | Interviews | GT (descriptive): low | Four main themes: (1) patient-related factors; (2) staff-related factors; (3) practice-related issues; (4) resources |
| Orpen 2010; UK [JAP]119 | Focus on patients’ perceptions and experience of intervention to increase health professionals’ understanding of what is important or not important in supporting patients preparing for hip-replacement surgery | THR; prehabilitation | Provides therapists with valuable information about patients’ preoperative function in their daily environment. The intervention facilitates decision-making about patients’ equipment requirements and discharge planning. Treatment plans are drafted and equipment or adaptations supplied prior to admission in order to facilitate a streamlined inpatient stay and discharge process. Information helps to give patients a sense of control over their pending surgery and discharge planning is commenced in collaboration with the patient prior to his or her hospital admission | OTs and PTs | Patients [11], age range, 53–85 (mean 67.73) | Interviews | Colaizzi’s (1978) seven-step framework for phenomenological data analysis (descriptive): high | Five main themes: (1) preoperative equipment use increases independence, progress and confidence; (2) individual needs are better met through timely visits; (3) competent therapist home intervention offers reassurance regarding surgery; (4) knowing one’s home environment is suitable increases confidence in planning hospital discharge after surgery; (5) levels of social support require preoperative assessment |
| Phillips 2019; UK [JAP]120 | Explore experiences of women who had undergone general gynaecological surgery, focusing on experiences of ERAS pathway, identify factors to address when scaling these programmes | Elective open surgery (hysterectomy); ERP | Improve clinical outcomes and quality of care post-surgery | NR | Patients [7], 48–77 (mean 66) | Interviews | IPA (descriptive/interpretive): high | Three main themes: (1) meeting informational needs; (2) taking control of pain; (3) mobilising when feeling fragile |
| Rattray 2021; Australia [JAP]139 | Assess timing to and type of nutrition used, and patients’ energy and protein intake after surgery, pre- and postintervention, gain insight into the potential effects of the intervention | Colorectal and/or small bowel surgical procedure; ERP | Improve dietary practices and intake among patients who have undergone colorectal surgery | Range of staff, as well as education sessions for staff | Patients, Qmual interviews [18]: age range NR | Interviews | Content analysis (descriptive): low/med | No themes. Brief paragraph describing responses to the intervention, and a table of seven points with illustrative quotes (only one quote is age 60+) |
| Secondary aims: assessing feeding-related outcomes (e.g. vomiting incidence, time to first flatus and bowel motion) pre- and postintervention + exploring patient perceptions of the intervention (i.e. acceptability) | ||||||||
| Reay 2015; Australia [JAP]121 | Describe post-discharge experience of elderly patients following THR | THR; early discharge | NR (reduced length of stay, hospital resources) | NR, but includes pre-op clinic with MDT | Patients [10], aged over 65 (range/mean NR) | Interviews | (1) Reading participant’s transcripts, (2) identified naïve meaning units, (3) words and phrases irrelevant to discharge experience eliminated, (4) these grouped together according to similarities, which resulted in major meaning units, (5) these were transformed into disciplinary meaning units (descriptive/interpretive): high | Four major ‘meaning units’: (1) inadequate assessment of suitable adaptive aids and person needs; (2) frustration; (3) coping with the physical and mobility restrictions; (4) limited social interaction |
| Samuelsson 2018; Sweden [JAP]122 | Describe how older patients experience the healthcare chain and information given before, during and after colorectal cancer surgery | Colorectal cancer surgery; ERP | Reduce postoperative complications and encourage fast rehabilitation in close cooperation with the patient | NR | Patients [16], 8 men (median age 82.5, range 76–89); 8 women (median age 82.5, range 78–84) | Interviews | Inductive content analysis (interpretive): high | Findings presented under themes (and subtheme): (1) the time during primary investigation (varying quality of primary care investigations; lack of understanding of the information received; lack of control); (2) stay in hospital (lack of personalised information; obstacles to recovery; need for reflection); (3) rehabilitation and recovery at home (lack of individualised rehabilitation; lack of self-care information; varying quality of follow-up and unclear responsibility) |
| Short 2016; UK [JAP]133 | Explore perioperative nutrition experiences of colorectal surgical patients to identify barriers and facilitators to the integration of nutrition within ERAS | Elective colorectal resection; ERP | Improves clinical outcomes across surgical disciplines compared with standard care | NR | Patients [16], 32–83 (median 68) | Interviews | Inductive TA (interpretative/descriptive): high | Findings presented by stage of op: preoperative information; preoperative fasting; carbohydrate loading and nutritional drinks; postoperative diet; discharge |
| Sjoveian 2017; Norway [JAP]140 | Describe patients experience pain and manage the rehabilitation process the first 6 weeks after discharge | THA or TKA; ERP | Limit morbidity and quickly restore the body’s normal functions after surgery | NR for all elements, but includes nurses, PTs, orthopaedists | Patients [12], 45–79 (mean 68.42) | Interviews | Qualitative content analysis (descriptive): high | Categories derived from research questions with three subthemes: (1) pain while moving and resting; (2) assisted daily living; (3) lack of continuity in pain assessment |
| Specht 2016; Denmark [JAP]124 | Explore lived experience of patients in fast-track primary unilateral THA/TKA from first visit at the outpatient clinic until discharge | THA or TKA; ERP | Prevent complications and to support speedy recovery after surgery | Nurse specialists, surgeon, anaesthesiologist, PT, community physiotherapy (if needed) | Patients [8], 42–82 (mean 63). Same sample as Specht 2018 | Interviews (and observation) | Inspired by Paul Ricoeur: three analytical levels (1) naive reading, (2) structural analysis, (3) critical interpretation and discussion (interpretive): high | Three themes: (1) dealing with pain; (2) feelings of confidence or uncertainty – the meaning of information; (3) readiness for discharge |
| Specht 2018; Denmark [JAP]123 | Explore lived experience of patients in fast-track THA/TKA during first 12 weeks after discharge | THA or TKA; ERP | Fast-track aims to supply best evidence-based practice and seeks to optimise preoperative patient information, multimodal opioid-sparing analgesia, fluid management/nutrition and rehabilitation | Nurse specialists, surgeon, anaesthesiologist, PT, community physiotherapy (if needed) | Patients [8], 42–82 (mean 63). Same sample as Specht 2016 | Interviews | See Specht 2016 | Three themes (with subthemes): (1) dealing with transition between hospital and home (home is where the heart is; shared decision-making in discharge planning); (2) pain and self-management of pain (pain is like a roller coaster; learn it the hard way; need for a closer link back to the hospital); (3) challenges in rehabilitation (motivation and discipline – back in the saddle; confidence and uncertainty during rehabilitation) |
| Strickland 2018; UK [JAP]125 | Explore patients perspective of surgery and early recovery when undergoing LLA | THA or TKA; ERP | Reduce perioperative pain and opiate consumption and make cost savings to the healthcare system through reduced LOS and associated healthcare costs | NR | Patients [30], 45–92 (mean 70.97) | Interviews | Narrative TA method (descriptive/interpretive): high | Seven themes: (1) improving function and mobility; (2) pain; (3) experiences of health care; (4) support from others; (5) involvement and understanding of care decisions; (6) behaviour and coping; (7) fatigue and sleeping |
| Thomsen 2017; Denmark [JAP]126 | Identify the perspectives of fast-track colorectal cancer surgery patients on challenges experienced in the transition from being hospitalised with cancer to being a cancer survivor | Colorectal cancer surgery; ERP | NR | NR | Patients [12], 60–81 (mean 72.42) | Interviews | Following interpretive description (interpretive/descriptive): med | Overarching theme of ‘vulnerability due to the feeling of being alone in a fragile situation’. Four subthemes: restore an everyday life; participate in follow-up program; get relevant information; manage contact with relevant health professionals |
| Uhrenfeldt 2015; Denmark [JAP]141 | Explore how wellbeing of old hospitalised patients affected by interaction with staff during fast-track surgical treatment and hospital admission for colon cancer | Colorectal cancer surgery; ERP | Reduced LOS and complications, and improve postoperative recovery | NR | Patients [9], all over age 74 (further details NR) | Interviews | (1) Overview of sample/organising data, (2) transcribe field notes, (3) read individually and together to identify repeating/deviating patterns, (4) themes developed, scrutinised, and refined, (5) themes illustrated through case stories (interpretive/descriptive): med/low | Three main care challenges from patients’ perspectives: (1) wellbeing as a matter of different perspectives; (2) vulnerability in contrast to wellbeing; (3) staff mix influences on the care encounter |
| van Egmond 2015; Netherlands [JAP]127 | Examine which problems patients encountered during first 6 weeks after primary TKA or THA surgery with rapid recovery | THA or TKA; ERP | NR | NR | Patients [19], mean age = 69.9 (6.5). (TKA: n = 9, age = 68.2; THA: n = 10, age = 71.4) | Focus groups (separate groups for TKA and THA patients) | Describing and summarising reactions of patients on the various topics (descriptive): high | Findings presented under topics: pain; physical therapy; sleep; wound; home care services/nursing home; functional devices; attainability of the hospital; anticoagulation; complications |
| Vandrevala 2016; UK [JAP]128 | Ascertain patients’ expectations and experiences of fast-track surgery and recovery at home within the setting of an ERP | Open liver resection; ERP | Achieving the best possible recovery – reducing post-operative complications and length of hospital stay and improving patient satisfaction | NR (but is in other paper describing RCT) | Patients [20], 42–83 (mean 63) | Interviews | Interviews transcribed verbatim and analysed using TA (interpretive/descriptive): high | One overarching theme: ‘anticipation of surgery: renewed hope’. Three main themes (with subthemes): (1) expectations of ERP and early discharge; (2) perception of factors that facilitate recovery in ERP; (3) realities of the experience |
| Westby 2010; Canada [JAP]129 | Explore patient and health professional experiences with current rehabilitation practices and outcomes following THA and TKA to inform development of clinical practice guidelines applicable for North America | THA or TKA; rehabilitation programme | NR | NR | Staff (patient and carer views assessed in study but not included in review due to no mean age), staff [44] (AHPs = 30, surgeons = 9, physicians = 5) | Focus groups and interviews | Thematic content analysis concurrently with data collection to allow for revision of questions and development of new lines of inquiry (interpretive): low/med | Six major themes: (1) let’s talk; (2) expecting the unexpected; (3) it’s attitude that counts; (4) it takes all kinds of support; (5) barriers to recovery; (6) back to normal. Different participant groups (patients, AHPs, surgeons, physicians) each have their own specific subthemes |
Appendix 4 Articles contributing to constructs and themes
| Construct | Theme | Number of studies contributing to theme | Supporting studies |
|---|---|---|---|
| Home as the preferred environment for recovery | NA | 22 | 90,100,101,103,104,106,108–111,113,114,116,121–125,127,128,130,132,133 |
| Feeling safe | Meeting emotional and physical needs | 23 | 90,100–105,107–111,113,114,116,119,120,124–126,128,130,133 |
| Increasing confidence and preparedness through information and planning in advance | 28 | 90,100,102–108,110–116,118–120,122–126,128,129,131–133 | |
| Appropriate, available and accessible follow-up | 30 | 90,100–109,111,113–116,118–123,125–132 | |
| Individualisation of a structured programme | Being inside or outside the programme | 20 | 90,102,103,107,108,110–112,114–118,121,122,128–131,133 |
| Differing priorities | 6 | 103,112,117,119,121,129 | |
| Essential care at home | Caregivers as essential | 20 | 90,100,102,103,105,106,108,110,113,114,116,119,121,123–130 |
| The direct, indirect and other work of caregiving | 13 | 90,100,104–106,111,113,115,125,126,128,130,132 | |
| Taking responsibility | The active patient | 29 | 90,100–104,106,107,109–111,113–116,118–132 |
| Staff skills – expertise vs. generalists | 4 | 101,112,117,129 | |
| Staff and service co-ordination | 18 | 103–105,107,108,111,114–116,118,122,124–130 | |
| Outcomes | Masking the negative | 8 | 90,100,105,106,109,126,128,132 |
| The right questions at the right time | 6 | 110,111,115,123,129,130 |
Appendix 5 Quality appraisal of prioritised qualitative studies using Wallace checklist
| Author, date | Item on Wallace checklist | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Is the research question clear? | Is the theoretical or ideological perspective of the author (or funder) explicit? | Has this influenced the study design, methods or research findings? | Is the study design appropriate to answer the question? | Is the context or setting adequately described? | Is the sample adequate to explore the range of subjects and settings, and has it been drawn from an appropriate population? | Was the data collection adequately described? | Was data collection rigorously conducted to ensure confidence in the findings? | Was there evidence that the data analysis was rigorously conducted to ensure confidence in the findings? | Are the findings substantiated by the data? | Has consideration been given to any limitations of the methods or data that may have affected the results? | Do any claims to generalisability follow logically and theoretically from the data? | Have ethical issues been addressed and confidentiality respected? | Are the interventions of interest clearly described? | |
| Archer, 2014100 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Barker, 2020101 | Y | N | NA | Y | Y | CT | Y | Y | Y | Y | NA | Y | Y | Y |
| Berg, 2019102 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Berthelsen, 2014105 | Y | Y | Y | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | N |
| Berthelsen, 2017103 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Berthelsen, 2017104 | Y | Y | Y | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | Y |
| Blazeby, 2010130 | Y | N | N | Y | Y | Yb | Y | Y | Y | Y | Y | Y | Y | Y |
| Churchill, 2018106 | Y | N | NA | Y | N | CT | N | Y | Y | Y | Y | Y | Y | N |
| Collaco, 2021107 | Y | CT | NA | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | Y |
| den Bakker, 2019131 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Evans, 2021108 | Y | NR | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Fecher-Jones, 2015109 | Y | Y | Y | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | N |
| Galli, 2015110 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Ganske, 2006111 | Y | Y | Y | Y | Y | Y | Y | Y | CT | Y | N | Y | Y | N |
| Haas, 2020112 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | CT |
| Heine, 2004113 | Y | N | NA | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | N |
| Hovik, 2018114 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Hunt, 200990 | Y | CT | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Jansson, 2019115 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Judge, 2020116 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Kocman, 2019117 | Y | N | NA | Y | N | CT | N | Y | Y | Y | N | Y | Y | Y |
| Krogsgaard, 2014132 | Y | N | CT | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Lyon, 2014118 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Orpen, 2010119 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Phillips, 2019120 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N |
| Reay, 2015121 | Y | Y | Y | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | Y |
| Samuelsson, 2018122 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Short, 2016133 | Y | CT | CT | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Specht, 2016124 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Specht, 2018123 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Strickland, 2018125 | Y | N | NA | Y | CT | CT | Y | Y | Y | Y | Y | Y | Y | N |
| Thomsen, 2017126 | Y | Y | Y | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | N |
| van Egmond, 2015127 | Y | N | NA | Y | Y | Y | Y | Y | CT | CT | Y | Y | Y | N |
| Vandrevala, 2016128 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Yc |
| Westby, 2010129 | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
Appendix 6 Coding scheme and three data tables for qualitative comparative analysis
| Study | Is pre-op info provided in different formats? | Is the intervention nurse-led or co-ordinated through a defined role? | Is additional time spent with patients as part of the intervention? | Are goal-setting strategies used? | Are patients able to ask for additional pain relief? | Are more challenging/complex/risky patients screened out? | Early mobilisation of patient a feature of the intervention? | Efforts to support discharge included in intervention? | High quality | Effectiveness rating | Number of PROMs considered | Number of PROMs improved |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coding rules | 1 = Yes 0 = No |
1 = Yes 0 = No |
1 = Yes 0 = No |
1 = Yes 0 = No |
1 = Yes 0 = No |
1 = Yes 0 = No |
1 = Yes 0 = No |
1 = Yes 0 = No |
1 = high 0.66 = moderate 0 = low |
See coding scheme in text | 1 = 4+ 0.66 = 3 0.33 = 2 0 = 1 |
1 = All and study had 3+ PROMS |
| 0.66 = all for study assessing low number | ||||||||||||
| (1 or 2) or at least half for study assessing high number | ||||||||||||
| (3+) 0.33 = less than half 0 = none |
||||||||||||
| Lower-limb arthroplasty studies | ||||||||||||
| Borgwardt66 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0.66 | 0.33 | 0.66 | 0 |
| Pour78 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0.66 | 1 | 0.66 |
| Den Hertog75 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0.66 | 1 | 0 | 0.66 |
| Vesterby70 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0.66 | 0 | 0.33 | 0 |
| Fransen60 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0.66 | 1 | 1 | 0.33 |
| McDonall89 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0.33 |
| Reilly50 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0.66 | 0.33 | 0.66 | 0 |
| Siggeirsdottir86 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0.66 | 1 |
| Beaupre53 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0.33 | 1 | 0 |
| Cavill79 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0.33 | 0 |
| McGregor49 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0.33 | 1 | 0 |
| Williamson51 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0.66 | 0.66 | 1 | 0.33 |
| Soeters77 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0.66 | 1 |
| Larsen68,69 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0.66 | 1 | 0.33 | 0.66 |
| Abdominal Prehab studies | ||||||||||||
| Kap 202081 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0.33 | 0.33 |
| Tagaki87 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0.66 |
| Arthur52 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0.33 |
| Bousquet-Dion54 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0.66 | 0.66 | 0.33 |
| Carli 201056 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0.33 | 0 |
| Dronkers67 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0.66 | 0 |
| Schmidt74 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0.66 | 0.33 | 0.66 | 0 |
| Dunne38 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0.66 | 0 | 0.66 | 0 |
| Reif72 Auer71 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0.66 | 1 | 1 | 0.66 |
| Gillis59 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| Ferreira57 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0.66 | 1 | 0.33 |
| Carli 202055 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0.66 | 0 | 1 | 0 |
| Abdominal enhanced recovery protocol studies | ||||||||||||
| Lee 201384 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0.66 | 0 | 0.66 | 0 |
| Vlug Lap65 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0.66 |
| Vlug Open65 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0.66 |
| Jones44 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0.66 | 0.33 |
| Kapritsou 201780 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0.66 | 0.33 | 0.66 | 0 |
| Sadlonova73 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0.66 | 0.33 | 0.33 | 0 |
| Forsmo88 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0.33 | 0 | 0 |
| Lee 201185 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0.66 | 0 | 0 | 0 |
| Pappalardo83 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0.33 | 0 | 0 |
| Frees58 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0.66 | 1 | 1 | 0.33 |
| Khoo45 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0.33 |
| Bennett37 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0.66 | 0 | 0.66 | 0 |
Glossary
- Abdominal
- Relating to the abdomen, that is, the anatomical region between the thorax (chest) and pelvis, including the stomach, small and large intestines, pancreas, liver and gallbladder.
- Cardiac
- Relating to the physiology of the heart.
- Care pathway (or patient care pathway)
- Separated into five distinct phases in relation to a hospital admission: pre admission; after admission but before treatment; perioperative/during treatment; postoperative but before discharge; and post discharge.
- Colorectal
- Relating to the physiology of the rectum, anus and colon.
- Comprehensive geriatric assessment
- A multidisciplinary diagnostic and treatment process that identifies the medical, psychosocial and functional limitations of an older person. The aim of a comprehensive geriatric assessment is to develop a co-ordinated and integrated plan for the needs of the patient.
- Enhanced recovery after surgery
- A multidisciplinary approach to caring for surgical patients involving surgeons, anaesthetists, nurses and allied health professionals. Enhanced recovery after surgery programmes typically follows a protocol involving preoperative assessment, minimally invasive surgery wherever possible, and a structured approach to postoperative care. The aims of enhanced recovery after surgery include improving patient experience and reducing postoperative complications and hospital length of stay. It is associated with the Enhanced Recovery After Surgery Society.
- Enhanced recovery protocol (or programme or pathway)
- A multicomponent intervention that includes the delivery of healthcare components at multiple stages of the patient care pathway.
- Hospitalist
- A physician in the USA who specialises in the general medical care of hospitalised patients, both within hospital and in related outpatient care.
- Inpatient
- A person admitted to hospital for at least one night.
- Kinesiologist
- A care professional with training in kinesiology, which is the study of human body movements, performance and function, combining knowledge from biomechanics, anatomy, physiology, psychology and neuroscience. It is not a licensed or officially recognised profession in most countries.
- Length of stay
- The time a patient stays in hospital, usually measured in days.
- Lower-limb arthroplasty
- The surgical reconstruction or replacement of joints of the lower limb, most commonly the hip or knee.
- Multicomponent intervention
- An intervention that has two or more components that could otherwise be delivered as independent interventions.
- Patient-reported experience measures
- assess the quality of healthcare experiences from the patient’s perspective.
- Patient-reported outcome measures
- assess the health status or health-related quality of life of a patient at a single point in time. Usually collected through short, self-completed questionnaires.
- Pelvic
- Relating to the pelvis, that is, the lower part of the torso between the abdomen and thighs.
- Prehabilitation (or ‘Prehab’)
- The process of preparing a patient for a medical intervention such as a surgical procedure. This can involve physical strengthening, making dietary changes or engaging with learning materials. The aim of prehabilitation is to optimise the patient’s physical health and wellbeing before a medical intervention with a view to facilitating a rapid recovery after the intervention.
- Rehabilitation (or ‘Rehab’)
- The assisted process of recovery following a medical intervention. Rehabilitation can involve physical, occupational and mental health therapies that aim to improve a patient’s post-treatment recovery.
- Sacrocolpopexy
- Operation to treat a prolapse of the vaginal vault in women who have had a hysterectomy.
- Staff mix
- In a hospital setting, the organised deployment of various clinical and non-clinical staff roles with the aim of optimising patient care, including reducing length of hospital stay.
- Thoracic
- Relating to the anatomical region of the chest (or thorax), in particular the heart and lungs.
- Upper abdominal
- Relating to the upper abdomen, that is, the anatomical region containing the stomach, spleen, pancreas, kidneys, liver and gallbladder.
- Vascular
- Relating to the system of vessels that move fluids around the body, including the arteries, veins, lymph vessels and lymph nodes.
List of abbreviations
- AMED
- Allied and Complementary Medicine Database
- CABG
- coronary artery bypass graft
- CBA
- controlled before-and-after trial
- CGA
- comprehensive geriatric assessment
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- EPHPP
- Effective Public Health Practice Project
- EQ-5D
- EuroQol-5 Dimensions
- ERAS
- enhanced recovery after surgery
- ERP
- enhanced recovery protocol
- GP
- general practitioner
- HMIC
- Health Management Information Consortium
- LLA
- lower-limb arthroplasty
- LOS
- length of stay
- OR
- odds ratio
- OT
- occupational therapist
- PACP
- preoperative assessment with care plan
- PPI
- patient and public involvement
- PREM
- patient-reported experience measure
- PRISMA
- Preferred Reporting Items for Systematic reviews and Meta Analyses
- PROM
- patient-reported outcome measure
- PT
- physiotherapist
- QCA
- qualitative comparative analysis
- RCT
- randomised controlled trial
- SD
- standard deviation
- SF-36
- Short Form questionnaire-36 items
- THA/TKA
- total hip/knee arthroplasty
- THR/TKR
- total hip/knee replacement
- UBA
- uncontrolled before-and-after trial
- UK
- United Kingdom
- WOMAC
- Western Ontario and McMaster Universities’ Osteoarthritis Index
Notes
-
Quantitative review full text excludes with reasons for exclusion
-
Non-prioritised studies eligible for inclusion in the quantitative review
-
Qualitative review full text excludes with reasons for exclusion
-
Tables of results for all prioritised studies in the quantitative review
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/GHTY5117).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
