Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR129663. The contractual start date was in January 2019. The final report began editorial review in February 2020 and was accepted for publication in April 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Fulop et al. This work was produced by Fulop et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Fulop et al.
Chapter 1 Context
Background
There is an internationally recognised need for transparent, integrated and timely processes for identifying quality and patient safety issues across health-care systems. 1 There may be indications of persistent performance issues in a health-care organisation long before a crisis comes to the attention of the public and regulators. Attention has been placed on failing health-care organisations, the characteristics of these organisations and the factors (internal and external) that might lead to low performance. These include low leadership capability, lack of open culture, antagonistic external relationships,2–4 inadequate infrastructure, lack of a cohesive mission and system shocks. 5 A hierarchical culture and leadership focused on avoiding penalties and achieving financial targets – rather than a patient-centred mission – are characteristics identified in many failing organisations. High-quality interventions that are capable of helping struggling health-care organisations to improve are essential. 5
The Special Measures for Quality (SMQ) regime is a targeted and time-limited regime in the NHS in England that has been agreed between the national regulators, the Care Quality Commission (CQC) and NHS Improvement. The regime emerged following the Keogh Review6 into avoidable mortality in 2013. Trusts are entered into SMQ only where serious care quality failings are identified and the leadership appears unable to resolve the problems without intensive support and external input. 7–9 The SMQ regime provides trusts with oversight and interventions from NHS Improvement to help them to address specific quality failings identified in CQC inspections. The CQC then re-inspects the SMQ trust within 12 months of starting SMQ. NHS Improvement perceives SMQ as a support regime to bring about improvement (email from interviewee, NHS Improvement, October 2018). In addition, challenged providers (CPs) that are at risk of entering SMQ are placed on a ‘watch list’ and also receive support. The list of CPs, unlike the list of trusts in SMQ, is not available in the public domain.
Interventions for trusts in SMQ/CPs typically vary between trusts and may include appointment of an improvement director (ID); review of leadership capability; access to financial resources for quality improvement (QI); an improvement plan, including options for diagnostic work on assessing medical engagement; buddying with other trusts; and commissioning external expertise. These interventions may be delivered in conjunction with other interventions and within a context of significant senior leadership changes.
Commentaries on the SMQ regime have highlighted potential unintended consequences for organisations, such as difficulties with recruitment and retention, lowering of staff and patient morale, increases in financial costs, and external pressures placed on already burdened management systems. 10 A recent evaluation of the CQC inspection regime categorises eight types of regulatory impact arising from the inspection regime (Table 1). 11 The impact of CQC inspections was found to vary considerably according to the type and size of provider; however, ‘directive’, ‘stakeholder’ and ‘organisational’ influences appear most applicable to providers that are asked by the regulator to take immediate action to improve quality and enter SMQ.
| Impact mechanism | Description |
|---|---|
| Anticipatory | Providers seek to comply in advance of regulatory interactions (e.g. inspection) |
| Directive | Providers take direct actions as requested by the regulator. Legal consequences possible in cases of non-compliance |
| Organisational | Providers instigate internal processes not explicitly related to directives on account of interaction with the regulator, such as addressing leadership or culture |
| Relational | Influence of (human, interpersonal) interactions between regulatory staff and regulated providers |
| Informational | Regulatory information on performance enters the public domain and informs decision-making |
| Stakeholder | Other stakeholders take action and interact with the regulated provider |
| Lateral | Regulatory interaction results in new interorganisational actions (across boundaries), such as peer learning |
| Systemic | Regulatory information on providers is used to identify wider issues in systems of care, beyond a single provider |
Our understanding of the impact of the SMQ/CP regimes and the interventions provided by NHS Improvement to support trusts is limited. To date, to the best of our knowledge, no academic studies have independently evaluated the interventions delivered when a trust enters SMQ/CP. Here we seek to understand how trusts respond to being placed in SMQ/CPs and whether or not and how the interventions provided impact the trusts’ capacity to achieve and sustain QIs over time.
The SMQ and CP regimes were ‘in transition’ during the evaluation and writing of the report, and there were several changes:
-
Matt Hancock was appointed Secretary of State for Health and Social Care on 9 July 2018, replacing Jeremy Hunt, who had been in the role since 2012.
-
Weekly ‘Care Meetings’ with the Secretary of State to review trusts in SMQ/CP regimes were replaced by monthly meetings with no ministers present.
-
We were informed that the CP regime ended in October 2019.
Study objectives
The objective of the study was to analyse the responses of trusts to the implementation of (1) interventions for trusts in SMQ and (2) interventions for trusts in the CP regime to determine their impact on these organisations’ capacity to sustain and achieve QIs.
The study focused on the main interventions that NHS Improvement has identified as forming part of the SMQ/CP regimes:
-
appointment and use of an ID
-
buddying with other trusts
-
the opportunity to bid for central funding to spend on QI.
We also remained open to any other interventions that participating trusts identified as being part of the SMQ/CP regimes and considered these interventions within a wider context of any leadership changes.
Research questions
-
What are the programme theories (central and local) guiding the interventions delivered to trusts in SMQ/CP regimes?
-
How and why do trusts respond to SMQ/CP regimes and the interventions within these regimes?
-
Which features of trusts in SMQ/CP regimes, and their wider context, contribute to their differing performance trajectories?
-
What are the relative costs of the interventions and how do these compare with their benefits?
-
How are data used by trusts in SMQ/CP regimes, and how do data contribute to their understanding of improvements in quality and service delivery, especially in areas where performance concerns have been raised by the CQC?
-
Do trusts in SMQ/CP regimes find it more difficult to recruit and retain staff?
Research overview
This study was conducted by the Rapid Service Evaluation Team (RSET). RSET, funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research (HSDR) programme, is a 5-year research programme that aims to rapidly evaluate health and care service innovations to produce timely findings of national relevance and immediate use to decision-makers. The topic of this report was identified through discussions between the NIHR HSDR programme and the Department of Health and Social Care (DHSC). The provider policy and acute care team in the DHSC wanted to understand in greater depth how the SMQ and CP regimes were working and what lessons could be learned for the future.
There is limited knowledge about whether or not the interventions used to deliver support for trusts in SMQ/CP regimes drive improvements in quality, the costs of these interventions and whether or not the interventions strike the right balance between support and scrutiny. This study seeks to determine how provider organisations respond to these interventions, and whether or not and how these interventions impact organisations’ capacity to achieve and sustain QIs over time. Our study also provides a greater understanding of the programme theory, impact and staff views and experiences of the SMQ/CP regime.
We conducted a multisite, mixed-methods evaluation, involving eight case studies of purposively selected NHS trusts, that draws on multiple sources of national- and local-level data. The protocol was developed with input from relevant DHSC and NHS Improvement teams, by scoping relevant documents and with feedback from academic peers and patient representatives. The evaluation has been formative, with findings shared and discussed with key stakeholders during the study.
The study comprised five interrelated work streams:
-
literature review using systematic methods
-
interviews at a national level
-
multisite, mixed-method case studies
-
analysis of national indicators and workforce
-
economic analysis.
Structure of the report
Chapter 1 (background) presents the background and rationale for the evaluation. Chapter 2 (methods) presents the overarching design of the evaluation and provides an overview of the research methods employed (detailed information on methods is presented within each results chapter). Chapters 3–10 (results) present the findings of the study. With the exception of the literature review (see Chapter 3), the individual results chapters do not include discussion sections. The results are integrated and discussed in a final discussion chapter (see Chapter 11). Chapter 11 (discussion and conclusion) presents the implications and lessons learned from our findings for regulators and policy-makers, health-care providers, staff and health system leaders and for researchers conducting rapid evaluations. It discusses the strengths and limitations of the study. This chapter also proposes future areas for research and future evaluation methods.
Chapter 2 Methods
Overview
This chapter gives an overview of the methods used in the evaluation.
This chapter draws on the published study protocol by Fulop et al. 12 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Study design
We conducted a multisite, mixed-methods study that combined qualitative and quantitative approaches to analyse the implementation of interventions delivered to SMQ/CP trusts and the impact of these interventions on trust performance, quality of care, patient experience and costs. To allow the study to be undertaken within a 1-year time frame, data collection and analysis have followed a rapid research design13 involving teams of field researchers, participatory approaches and iterative data collection and analysis, with the research team meeting fortnightly to discuss progress and emergent findings.
Ethics and research governance approvals
The University College London Research and Development Office and Ethics Committee reviewed the study protocol and materials. The study was classified as a service evaluation, as defined by the NHS Health Research Authority, and did not require Research Ethics Committee approval. Guidelines for data security, confidentiality and information governance have been followed. An informed consent process, using participant information sheets and written consent, was used for recruitment to ensure informed and voluntary participation. We are aware of the sensitive nature of this research for organisations and individuals. The research team has experience in conducting research on similar sensitive topics. The independence of the research and the anonymity of participants and organisations has been upheld.
Approach to the evaluation
The study protocol12 was developed over a 6-month period (August to December 2018) through discussions with relevant teams at the DHSC and NHS Improvement, by scoping relevant documents and with feedback from academic peers and patient representatives.
This was a formative evaluation, and we took an active approach to sharing our interim findings with key stakeholders, including the DHSC, NHS Improvement central and regional teams, and CQC. For a full list of activities to date, see Report Supplementary Material 1. Key examples of ongoing engagement activity with stakeholders include:
-
presenting findings to the DHSC, NHS Improvement and CQC at their meetings and conferences
-
sharing findings with the case study trusts
-
publishing articles in peer-reviewed journals and presenting papers at academic and professional conferences
-
producing accessible summaries of our findings for wider distribution to a range of audiences, including trusts, regulators, policy-makers and patient groups.
Research methods
Our study consisted of five interrelated elements.
Literature review using systematic methods
A rapid literature review of organisational failure in the public sector was conducted to guide our empirical research, particularly with respect to data analysis (see Chapter 3). Rapid-review methodology that uses a phased search approach was followed. 14 Rapid reviews follow a systematic review approach, but some steps are adapted to reduce the time required to complete the review (i.e. using large teams to review abstracts and full texts, and extract data; in lieu of dual screening and selection, a percentage of excluded articles are reviewed by a second reviewer and software can be used for data extraction and synthesis14).
Phase 1 of the review was based on a broad search of health services, business and management journals, and a review of the grey literature (e.g. think tank reports), to develop a theoretical understanding of the main characteristics of organisational failure and turnaround, and the types of interventions implemented to improve quality. This literature was used to develop a conceptual and theoretically informed framework that could be used to inform the phase 2 research questions (RQs), search strategy, inclusion criteria and interpretation of findings. We used the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement15 to guide the reporting of the methods and findings. The review protocol was registered with PROSPERO (CRD42019131024). The full details of the review methodology are described in Chapter 3.
The review sought to answer the following RQs:
-
Phase 1
-
How are ‘failing health-care organisations’ defined?
-
What are the theoretical approaches that have been used to explain organisational failure in and outside health care?
-
How is ‘organisational turnaround’ defined?
-
Which theoretical approaches have been used to study turnaround strategies (if any)?
-
-
Phase 2 (covering health care, education and local government)
-
What are the main interventions used to improve quality?
-
Do the studies highlight any specific issues with implementation?
-
What are the interventions classified as ‘successful’?
-
Have any of these interventions been evaluated? If so, what is the impact and sustainability of improvements produced by these interventions?
-
What are the costs of these interventions?
-
Analysis of policy documents and interviews at a national level
To understand the nature of the SMQ/CP regimes and the programme theories that underpin them (i.e. the underlying assumptions and expectations about the purpose of the intervention and the anticipated impact), we conducted qualitative interviews with staff at a national level at the beginning of the evaluation. We also collected and reviewed reports and documents (n = 20) that would help us to understand the origins of the approach of the SMQ and CP regimes, the regulatory and policy context, and how these dual approaches had evolved over time (see Chapter 4). A small number of internal documents were shared with the team by NHS Improvement and interviewees early into the evaluation, which were incorporated for review.
Semistructured qualitative interviews were conducted with six staff at the national level. To identify relevant staff to invite for interview, the research team contacted representatives of key stakeholder groups – NHS Improvement, CQC and DHSC – to ask for recommendations for individuals involved in the SMQ/CP regimes. These individuals were then independently invited by e-mail to take part in a research interview. The purpose of these interviews was to better understand the nature of interventions deployed to support trusts and how the interventions were perceived by different stakeholders in relation to their programme theory/theories, and which interventions are viewed as being particularly effective, and under what conditions. The interview guide (see Appendix 1) covered three broad topic areas: (1) aims of the SMQ/CP regimes; (2) policy and interventions and (3) impact. The national interviews were professionally transcribed and analysed by a researcher (JL), who produced a thematic summary document for review by the wider project team early in the evaluation.
Multisite, mixed-method trust case studies
We conducted eight case studies (four ‘high level’ and four ‘in-depth’) using qualitative and quantitative approaches. We used a case study approach to explore the implementation of interventions in SMQ/CP trusts and reflect on any observed changes in processes and outcomes reported across specified time points (e.g. point of entry into or exit from SMQ). Case study research is common in management, business and organisational research and policy evaluations. Yin16 defined the case study as an ‘in-depth inquiry into a specific and complex phenomenon’. 16 Case studies typically employ a range of data collection methods, quantitative, qualitative or a mixture of both, to ‘construct narratives of past events, or accounts of specific cases’. 17
Sampling of case study trusts
Inclusion criteria:
-
NHS trusts (ambulance, acute, mental health and/or community providers) placed in SMQ and/or CP regimes on or before 30 September 2018.
Exclusion criteria:
-
trusts placed in SMQ and/or CP regimes (for the first time) after 30 September 2018
-
trusts placed in Special Measures for Finance (SMF) only and never in SMQ/CP regimes.
To identify potential case study trusts, we conducted a preliminary analysis of data supplied by NHS Improvement on trusts that had entered SMQ since the regime began in July 2013, up to 30 September 2018. A total of 35 trusts entered SMQ; four trusts returned to SMQ (giving 39 episodes), 25 had exited SMQ and, as of 30 September 2018, there were 14 trusts in SMQ. The ‘watch list’ of CPs was initiated in July 2015. These trusts received interventions to prevent them entering SMQ. On 30 September 2018, there were 17 trusts on this list. Since July 2015, 44 trusts have been placed on this list, with 17 trusts leaving the CP regime because they entered SMQ and one trust leaving the list and subsequently returning. A total of 59 trusts entered SMQ or became a CP between July 2013 and September 2018. As of January 2019, there were 234 trusts in England, meaning that roughly one-quarter of trusts had experience with the SMQ or CP regime (Table 2).
| Trust type | Trusts ever in the SMQ or CP regimes (n) | Trusts in SMQ (at September 2018) (n) | Trusts in the CP regime (at September 2018) (n) |
|---|---|---|---|
| Acute services only | 33 | 7 | 9 |
| Acute and community | 18 | 4 | 7 |
| Acute and mental health | 1 | 1 | 0 |
| Ambulance | 2 | 1 | 0 |
| Community and mental health | 1 | 0 | 1 |
| Mental health | 4 | 1 | 0 |
| Total | 59 | 14 | 17 |
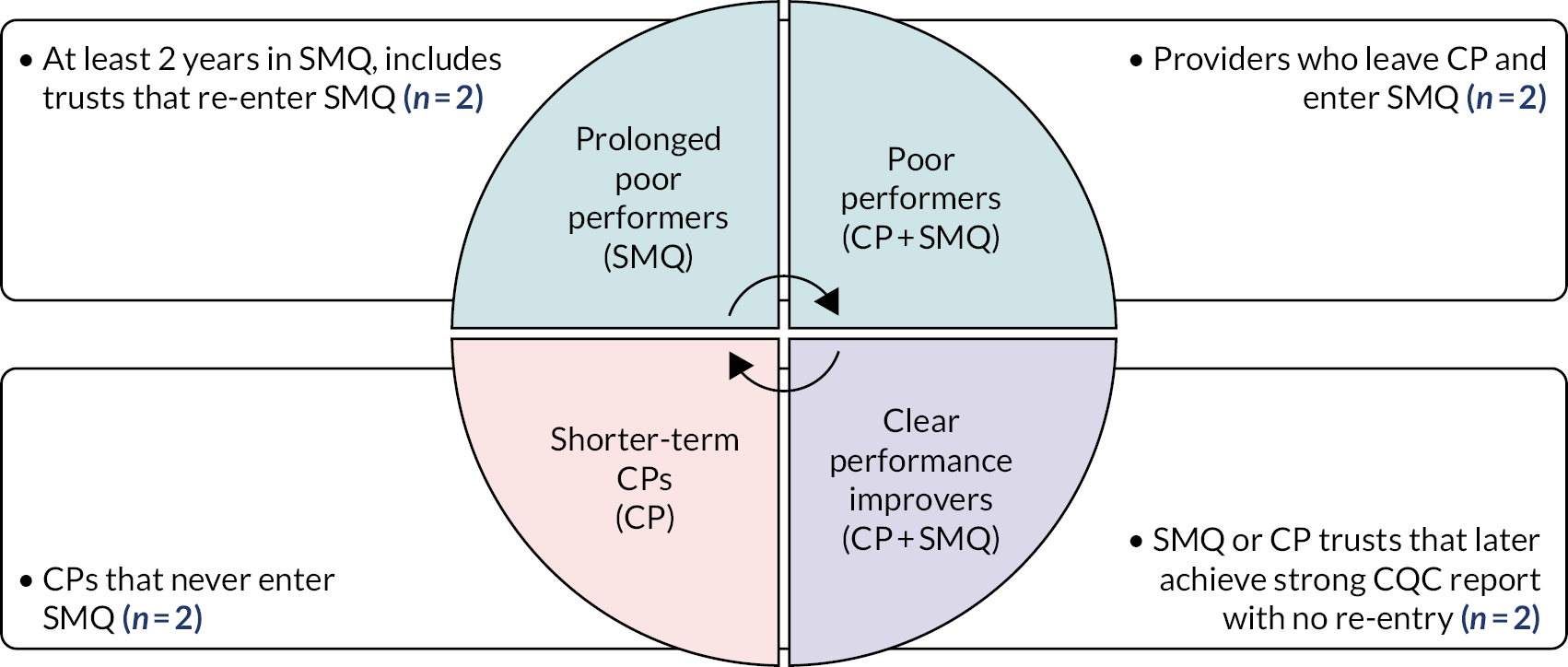
A total of 59 trusts met our inclusion criteria (see Table 2). We looked at the performance trajectories for these trusts and categorised them into four groups: prolonged poor performers, poor performers, shorter-term CPs and clear performance improvers (Table 3). Trusts were categorised based on the length of time spent in the SMQ/CP regimes and their progress over time, noting that some organisations were in the CP regime for only a short length of time and moved between categories. Therefore, although the categories are not fixed or absolute, our selected sites were in one of the categories at the time of sampling and met the criteria (e.g. re-entry into SMQ for a prolonged poor performer).
| Performance categorya | Performance category description | Trusts matching descriptionb |
|---|---|---|
| Prolonged poor performers | Trusts that have been in SMQ for ≥ 2 years since the introduction of the regime, including those trusts that re-enter SMQ after a period of exit | 19 |
| Poor performers | CP trusts that end up in SMQ | 12 |
| Shorter-term CPs | CPs that avoid entry into SMQ and have not previously been placed in SMQ. This may include trusts that merged with higher-performing providers. They are or were ‘challenged’ for < 2 years | 20 |
| Clear performance improvers | Trusts that have previously entered SMQ or CP but later achieved a good or outstanding overall CQC rating, without re-entry into either regime | 9 |
| Other trusts | Trusts that do not meet any of the other criteria (four trusts that were ‘challenged’ for a longer time, and one trust that left SMQ after a short period but has never been rated good or outstanding by CQC). These trusts were not sampled | 5 |
Given that the overall objective of the case studies was to understand dynamics within trusts and their local contexts at different ends of the performance spectrum, we purposively sampled eight case study sites, with two sites from each performance category (Figure 1). We also aimed to recruit case study sites from a range of geographical locations and types of trusts. Of the two case studies within each performance trajectory, one was conducted ‘in depth’ and one at a ‘high level’.
FIGURE 1.
Purposive sampling model for case studies. Reproduced with permission from Fulop et al. 12 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0), which permits others to share and adapt this work for any purpose, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
Case study recruitment
Trusts were invited to participate via an e-mail to the chief executive officer (CEO); the e-mail explained whether the trust would be an ‘in-depth’ or a ‘high-level’ case study and what this would entail (see Report Supplementary Material 2). To recruit eight case study trusts, a total of 12 trusts were invited to participate (Table 4). Perhaps unsurprisingly, it was more difficult to recruit to the ‘prolonged poor performer’ and ‘poor performers’ groups.
| Group | Type of sampling | Invitations to trusts |
|---|---|---|
| Prolonged poor performers | In depth | 3 (2 declined) |
| High level | 1 | |
| Poor performers | In depth | 3 (2 declined) |
| High level | 1 | |
| Short-term challenged | In depth | 1 |
| High level | 1 | |
| Clear improvers | In depth | 1 |
| High level | 1 |
Qualitative fieldwork: data collection
Qualitative fieldwork combined semistructured interviews, meeting observations and documentary analysis (Table 5). Interviews and observations were used to understand the processes used to implement the interventions based on available data to plot a chronology of the changes in quality at each site. Internal (inner) and external (outer) contextual factors potentially influencing participation in the interventions, including senior-level leadership changes and perceptions from the wider community and stakeholders in the local heath economy, were considered. In addition, we remained open to understanding the interventions that trusts perceived to be part of SMQ/CP regimes, as well as those identified by NHS Improvement as being effective for driving change. To aid the quantitative analysis, qualitative data were collected on how people within trusts use data, with an emphasis on whether or not and how data are used to track improvements in quality of care. Similarly, to facilitate the economic analysis, qualitative data were collected about resource use and costs incurred by the different interventions, and the perceived impacts on quality and additional unintended consequences of the interventions (positive or negative).
| In-depth case studies | High-level case studies | |
|---|---|---|
| Qualitative components | ||
| Non-participant observation (e.g. board meetings and operational meetings) |
|
|
| Interviews |
|
|
| Documentary analysis |
|
|
| Quantitative components | ||
| Trust use of quantitative information relating to quality of care |
|
|
| Tracking of outcome measures against improvement actions |
|
|
| Trust use of metrics to monitor impact of SMQ/CP interventions |
|
|
Sampling and recruitment within case studies
Participants
‘Vertical slicing’ was used to guide sampling in the four ‘in-depth’ case studies, with the goal of conducting interviews across different organisational tiers and with external stakeholders, including local branches of Healthwatch (London, UK). The types of interviewees who were purposively sampled were dependent on the context of each case study trust; for example, in addition to divisional/clinical directors, it was relevant to include staff from a clinical unit that the CQC had flagged as ‘inadequate’ (e.g. maternity). In the four ‘high-level’ cases, we aimed to conduct interviews at the ‘top’ of the organisation and with key external stakeholders. Senior leaders and those involved in QI at each case study trust were asked to make recommendations for interview participants. At the in-depth case study sites, it was requested that an invitation e-mail was circulated to staff to invite them to take part in the study; staff were asked to respond directly to the lead researcher to discuss further if they would like to be interviewed confidentially. Other potential participants were identified by contacting local peer organisations and through snowballing from respondents.
Non-participant observations
We observed public trust board meetings and quality-focused or performance-focused meetings at the divisional level at the four ‘in-depth’ cases after securing prior permission and gaining verbal consent from participants at the time of the meeting. We used the board QI maturity framework18 in our observations of boards and other relevant meetings to support the analysis of observational data. Our aim was to focus on critical quality incidents or service issues where progress in QI appeared to be ‘transparently observable’ or where improvements were proving especially challenging for the organisations. 19 Thus, we were open to studying a particular clinical unit that had been flagged as in need of improvement in earlier CQC inspections or a new intervention that the trust had introduced to support staff engagement in QI, such as ‘quality huddles’.
Documents
We collected and analysed documents developed by trusts to operationalise improvement efforts and recommendations from the regulator to help triangulate findings from interviews and observations. Documents included relevant meeting minutes (e.g. board meetings and operational units), quality committee meeting minutes, strategic performance documents (e.g. QI plans, where available or shared with the researchers) and business plans.
A summary of the interviews, observations and documents obtained for each case study is presented in Table 6.
| Case study site | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Data source | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Total |
| Senior team interviews | 6 | 4 | 6 | 6 | 6 | 4 | 6 | 6 | 44 |
| Divisional-level interviews | 5 | 2 | 3 | 2 | – | 1 | – | – | 13 |
| External interviews | 2 | 2 | 4 | 4 | 2 | – | 3 | 4 | 21 |
| Total interviews | 13 | 8 | 13 | 12 | 8 | 5 | 9 | 10 | 78 |
| Total meeting observations | 2 | – | 5 | 2 | – | 2 | – | – | 11 |
| Documents | 27 | 29 | 71 | 33 | 52 | 55 | 14 | 10 | 291a |
The use of data by trusts
To complement the qualitative analysis, we looked deeper into the way that data were being used by case study trusts, focusing specifically on how trusts monitor the impact of quality interventions and track improvements, and whether or not they perceive that they have the capabilities and resources to do so effectively. We assessed any changes in the way that trusts use data once being placed into SMQ or CP, including investing resources to support more accurate data collection and monitoring. We also analysed whether or not and how trusts track progress against required improvements, as these examples could offer helpful insights into whether or not trusts will be resilient to future challenges.
This work links with the qualitative analysis described above, wherein trust interviews provide on-the-ground insight into how being in SMQ/CP regimes influence their approach to the collection of data and how they monitor quality. The qualitative interview topic guides included questions focused on the trust’s use of information.
Other sources of information included CQC inspection reports; documents produced by, or on behalf of, trusts (e.g. board reports, quality accounts); NHS Improvement monthly monitoring of trusts and changes in their performance [e.g. NHS Improvement Single Oversight Framework (SOF) segmentation]; and, for wider context, the findings of the rapid literature review.
The analysis included monitoring relevant improvement actions highlighted by these documents where they can be appropriately linked to outcomes observed in data. For example, if CQC raised concerns about a stroke service, we would be interested in how the trust used data to track outcomes and to provide assurance that the quality of the stroke service was improving. There may also be evidence to suggest that pressures on some outcomes are related to performance of other providers in the local health system, which will be investigated, where feasible. For some measures, data would be available to put the trust’s changes in outcomes within a national context; possible sources include material published by the trusts (e.g. board papers), published statistics and patient-level records from Hospital Episode Statistics (HES), and national monitoring reports produced by NHS Improvement (e.g. monthly SOF segmentation spreadsheets). (Note that we have approval from NHS Digital covering all projects conducted by the RSET.)
Case study data analysis
Interviews were professionally transcribed and made centrally available, along with documents and observational data (field notes), for analysis by multiple members of the research team.
Triangulation of interview, observational, cost information, documentary and quantitative data was performed to produce eight local case studies that were analysed thematically and comparatively, consistent with suggestions in academic literature on analysing processes of change in organisations19–21 and on receptive contexts for sustaining QI in health care. 22,23
Documentary analysis was used to identify organisational strategies and variables that appear to indicate change over time (i.e. since point of entry into SMQ), such as shifts in organisational composition (e.g. workforce numbers and vacancy levels) and changes in organisational structure (e.g. new governance systems or mergers). Documentary analysis was also used to allow comparisons between central and local theories guiding QI efforts.
Throughout the data collection process, the data were summarised in the form of rapid assessment procedure (RAP) sheets (see Report Supplementary Material 3). 13 The RAP sheets were used to facilitate consistency in data collection across researchers and allowed the team to identify gaps in data collection that needed to be addressed before the end of fieldwork. The RAP sheets also facilitated analysis, allowing the researchers to readily compare specific data categories between trusts and to conduct within-case and cross-case analyses. 24
A number of conceptual frameworks guided the case study analysis. We used a board maturity framework developed in previous research, which found that boards with higher levels of maturity in relation to governing for QI were able to effectively balance short-term (external) priorities against long-term (internal) investment in QI, and engage staff and patients in the process of change. 18 We created a template for mapping meetings and papers to the ‘Organisational Maturity Framework’ developed by Jones et al. 18 (see Appendix 2), which was applied to the four in-depth case study trusts as a means of gauging their board maturity (see Chapter 7). To understand processes of QI beyond board level, especially among ‘clear improvers’ that exit SMQ and sustain change, we used the concepts of ‘absorptive capacity’ and ‘dynamic capabilities’ from the strategic management literature to identify any routines or processes that have helped staff, from senior leaders to front-line clinicians, to learn from external information about performance and quality to sustain performance objectives (see Chapter 7). 25 Absorptive capacity refers to the ability of organisations to acquire and exploit new information and knowledge, and successfully transfer it internally, across organisational subunits, to support learning and performance. 26 Dynamic capabilities refers to patterned activities and routines that require dedicated resources and long-term commitment to effect impactful change. 27 Applying such concepts has helped us to distinguish between evidence of incremental or evidence of ad hoc changes in trusts arising from externally driven SMQ interventions, and more radical or novel service innovations that improve quality and trust performance and have become embedded in new ways of working over time at trusts (see Chapter 7).
Analysis of national indicators and workforce
This quantitative component of the evaluation explored relationships between being in a SMQ/CP regime and a set of performance and workforce indicators. For workforce, we were particularly interested in whether or not trusts found it more difficult to recruit and retain staff at different levels and evidence of the impact of interventions on the staff themselves. For the case study sites, these data were combined with trust inspection information from CQC. The workforce analysis was exploratory and was subject to the construction of a consistent and comparable workforce data set and sufficient sample sizes to establish any statistical links. One of our aims was to raise hypotheses that could be tested more robustly in future studies and reflected back to the case study sites for their qualitative insights.
Economic analysis
The economic analysis aimed to quantify the costs and benefits of different combinations of interventions used in SMQ/CP regimes from an NHS perspective using a cost–consequences analysis (CCA) approach (see Chapter 9). A CCA compares interventions in which the components of incremental costs (direct or indirect) and consequences (e.g. knowledge, behaviours and processes) are computed and listed, without aggregating these results into a cost-effectiveness ratio. 28 This approach enables one to look into process measures and qualitative findings in a quantitative manner, allowing for some insight as to how potential benefits compare with the cost of interventions.
A feasibility study for the economic analysis found that:
-
A CCA was feasible, but it would be possible to evaluate different combinations of interventions only (i.e. it would not be possible to evaluate the benefits of each intervention individually). It would need to account for likely variation in the type and intensity of these interventions, for example the percentage of full-time equivalent time that the ID spends at the trust, different buddying models and varying receipt of funds spent in different ways. We will explore the impact of this variation on both costs and consequences.
-
Costs could be measured using resource use and unit cost data collected during the multisite mixed-methods study.
-
Consequences could be measured using qualitative data collected during the multisite mixed-methods study and/or combining it with quantitative data.
Cost analysis
We looked at the direct costs of the interventions at both the national level and the level of our eight case study sites. For the case studies, we examined data on funds received to support improvement (CP trusts may access up to £200,000, while SMQ trusts may access up to £500,000) and how these funds, when received, were spent. We have also considered opportunity costs that were incurred as a result of the trust being under the SMQ or CP regime.
Cost–consequences analysis
Two types of consequences were considered: primary consequences (relating to the entry and exit of the trusts in SMQ/CP regimes) and secondary consequences (relating to staff experiences and cultural changes within the trusts that were derived from the findings of the NHS staff survey 2014–18, and the financial stability of the trusts).
Presentation of findings from the case studies
To ensure the anonymity of the participating organisations and individuals in this potentially sensitive study, we present the findings in the following ways: indicating the numbers of cases in relation to particular points, rather than which cases, and for quotes we have used generalised job titles (e.g. ‘senior director’ for all executive directors) without reference to the specific case study.
Patient and public involvement
We undertook two main steps to ensure patient and public involvement (PPI) in the evaluation design. First, we presented the topic to a local research advisory panel on 16 January 2019, a group comprising 10 patient representatives and members of the public. This group was sent a three-page summary document in advance of this meeting outlining the remit of the RSET, the pipeline of current studies and an outline of the ‘Special Measures for Quality’ study. The panel were asked to reflect on the following three questions that would be explored in the meeting, as well as general points about ‘rapid evaluation’:
-
What questions would you have for staff at a hospital that was placed in SMQ by the health regulator (the CQC)?
-
What questions would you have for the senior leadership team and hospital board?
-
What questions or concerns might you have about SMQ if this was your local NHS hospital?
Two researchers (JL and JS) presented further information about the evaluation and explored these questions with the panel, which resulted in a lively discussion that was supported by a PPI and communications officer. Minutes were taken from the meeting. Questions that the panel asked of the researchers included wanting to understand why regulators were brought into health-care organisations and whether or not this occurred on an annual basis across all organisations (at trust and hospital levels), and if patients could find out about CQC reports. The panel wanted reassurance that the researchers would have access to an organisation’s leadership team, as well as historic information to find out what had arisen within the organisation over time, especially where other senior staff had left. It was noted that the model was similar to regulation in schools undertaken by Ofsted. Several key points and recommendations were summarised and reported back to the wider team to inform the study protocol:
-
Clarity about where SMQ sits (i.e. directorate, trust or hospital level).
-
Visibility and publicity about SMQ (e.g. how is it communicated to the staff and public?).
-
Access to leadership (ensure during the study).
-
Can anything be found out about preventing entry to SMQ?
-
Engage with local patient groups, such as Patient Advice and Liaison Service (PALS) (although check they are independent and separate from the complaints department) and the local Healthwatch.
The second stage involved two patient representatives (also PPI panel members) providing more detailed feedback on the revised study protocol through a process of ‘light touch’ peer review. A summary of the feedback obtained through this process and how it informed the updating of the final protocol submitted to the NIHR is presented in Appendix 3. The two patient representatives also gave feedback on the Plain English summary included in this report. Our protocol included a local involvement and engagement strategy linked to case studies. However, our rapid approach meant that we did not have time to do this.
Chapter 3 The implementation of improvement interventions for ‘low-performing’ and ‘high-performing’ organisations in health, education and local government: a phased literature review
Overview
This chapter draws on Vindrola-Padros et al. 29 ‘The implementation of improvement interventions for ‘low performing’ and ‘high performing’ organisations in health, education and local government: a phased literature review’ (submitted to the International Journal of Health Policy and Management, April 2020). The review examines underlying concepts guiding the design of interventions, processes of implementing these interventions, their unintended consequences and the impact on costs and quality of care. The purpose of the review was to inform our empirical study.
What was known?
-
There is a limited understanding of whether or not and how improvement interventions aimed at improving the performance of health-care organisations are effective.
What this chapter adds
-
Successful interventions included restructuring senior leadership teams, inspections (in schools) and internal reorganisation by external organisations.
-
Most interventions were designed and implemented at an organisational level, without considering system context.
-
Limited attention was paid to the potential negative consequences of the interventions and their costs.
Background
There may be indications of persistent performance or quality issues in a health-care organisation long before a crisis comes to the attention of the wider public and regulators. This highlights the need for transparent, integrated and timely processes for identifying quality and safety issues within organisations and across health-care systems. 1 Attention has been placed on failing health-care organisations, the characteristics of these organisations and the factors (both internal and external) that might lead to low performance. These include, for example, low leadership capability (as indicated by, for example, lack of ability to engage with staff or to be transparent), ‘closed’ culture and antagonistic external relationships. 2 There are also a number of analyses of organisational failure, and sometimes turnaround, in various sectors, for example in the corporate sector, such as Enron (Houston, TX, USA)30 and Marks & Spencer (London, UK),31 the financial crash of 2008,32 and the health sector (including failures in hospital organisation and management),33 which identify reasons for failure and how they might be addressed.
A recent systematic review5 of research on the characteristics of failing health-care organisations in multiple countries and settings identified five characteristics shared across failing organisations: (1) poor organisational culture; (2) inadequate infrastructure; (3) lack of a cohesive mission; (4) system shocks; and (5) dysfunctional external relations with other hospitals, stakeholders or governing bodies. 5 More specifically, a hierarchical culture and leadership focused on avoiding penalties and achieving financial targets, rather than a patient-centred mission, are characteristics identified in many failing health-care organisations. 34–36
Available reviews, such as that by Vaughn et al. ,5 suggest that an important next step after diagnosis of problems is the development of high-quality interventions capable of helping struggling health-care organisations to improve. However, there is limited understanding about whether or not and how improvement interventions are effective in supporting failing organisations and improving the quality of care in high-performing organisations in the public sector. The aim of this review is to examine the underlying concepts guiding the design of these interventions, processes of implementation and unintended consequences of implementing the interventions, and their impact on costs and quality of care. The review includes articles in the health-care sector, as well as other public sectors such as education and local government, to learn from the extensive research carried out in these non-health-care sectors.
Methods
Design
The review was based on the phased rapid review method proposed by Tricco et al. 14 and expanded the review of organisational failure published by Vaughn et al. 5 The rapid review method followed a systematic review approach, proposing adaptations to some of the steps to reduce the amount of time required to carry out the review (i.e. the use of large teams to review abstracts and full texts, and extract data; in lieu of dual screening and selection, a percentage of excluded articles is reviewed by a second reviewer, and software is used for data extraction and synthesis, as appropriate14).
The review included two phases. Phase 1 was based on a broad search of health services, business and management journals, and a review of the grey literature (e.g. think tank reports) to develop a theoretical understanding of the main characteristics of organisational failure and turnaround, and the types of interventions implemented to improve quality (for an example of this approach, see Ferlie et al. 37). This literature was used to develop a conceptual and theoretically informed framework (see Table 7). The framework was used to inform the phase 2 RQs, search strategy, inclusion criteria and interpretation of findings. We used the PRISMA statement15 to guide the reporting of the methods and findings. The review protocol was registered with PROSPERO (CRD42019131024).
| Domain | Description | Disciplines (classified based on journal) | Examples in the literature |
|---|---|---|---|
| Organisational failure/success | |||
| A. Concepts used separately or in combination | |||
| 1. Failure as decline | ‘Existence-threatening decline’ in the performance of the organisation. Focus is on the organisation | Management, business | Pandit41 (2000), Mellahi and Wilkinson42 (2004) |
| 2. Failure as crisis | Focuses on the peak of failure, considering it as an acute process or sudden onset (considers the possibility of crisis denial and hidden crisis to account for more gradual representations of failure). Focus is on the organisation | Management, business | Slater43 (1984), Weitzel and Jonsson44 (1989) |
| 3. Failure as below acceptable performance levels | Organisational performance is persistently below some minimally acceptable level. Distinguishes between the minimum acceptable level of performance and performance that is ‘persistently’ below this acceptable level. Focus is on the organisation | Management, business | Hambrick and Schecter45 (1983) |
| 4. Success as a system property/structural processes involved in failure | High-performance results from properties of the system and not characteristics of the individuals. Focus is beyond the organisation and attention is paid to the structures of inspection and performance | Health services research, education | Baker et al.46 (2008), Bate et al.47 (2007), Taylor et al.48 (2015), Willmott49 (1999), Perryman50 (2005) |
| B. Theoretical frameworks | |||
| 1. Industrial organisation | Organisational failure is caused primarily by changes in the external environment, which are the result of a range of technological, economic, regulatory and demographic factors | Management, business | Mellahi and Wilkinson42 (2004) |
| 2. Organisational ecology theory | Applies a natural selection model to organisational dynamics. It is based on a biological analogy, in which organisations scan the environment and compete and recognise situations, mechanisms and processes underlying emergence, growth, regulation and demise | Management, business | Hannan and Freeman51 (1989) |
| 3. Industry life cycle theory | Organisational failure is considered a natural and objective event (i.e. likely to occur), the outcome of factors such as saturation of demand, running out of supplies, and introduction of new technology | Management, business | Klepper52 (1997) |
| 4. Organisational psychology | Views failure and success as a result of internal rather than external and environmental factors (i.e. leadership capacity, composition of top management teams, governance models, organisational arrogance and myopia) | Management, business, health services research | Mellahi et al.31 (2002), Curry et al.35 (2011) |
| 5. Failure and organisational learning/organisational culture, role of emotions | Failure is caused by lack of, limited or dysfunctional organisational learning. Preventing failure is dependent on changes in organisational culture | Health services research, education | McKiernan53 (2002), Fulop et al.54 (2005), Walshe and Shortell55 (2004), Harvey et al.25 (2015), Jones et al.18 (2017), Dixon-Woods et al.56 (2014), Willis57 (2010), Nicolaidou and Ainscow58 (2007), Leithwood et al.59 (2008) |
| 6. Failure and success within regimes of surveillance | Foucauldian outlook on surveillance, monitoring and performance, seeing external actors such as Ofsted as reproducing disciplinary power. Critique of dualisms. Focus on discourse and view of inspections (or the threat of inspections) as the mechanism through which discipline is reproduced | Education | Willmott49 (1999), Perryman60 (2005), Perryman50 (2006), Ferlie et al.37 (2012) |
| 7. Contextual factors leading to failure (internal and external) | Failure is usually caused by a combination of different factors (both internal and external). Management is unlikely to be the sole cause of decline and managers may be symptoms of failure as much as causes. Recognises the need to consider system-wide factors when addressing failure | Management, business, health services research, education | Fulop et al.54 (2005), Walshe and Shortell55 (2004), Ravaghi et al.4 (2015), Smithson et al.11 (2018), Taylor et al.48 (2015), Vaughn et al.5 (2019), Dixon-Woods et al.56 (2014), Chapman61 (2002), Chapman and Harris62 (2004) |
| Turnaround | |||
| C. Concepts | |||
| 1. Turnaround as recovery | The actions taken to bring about recovery in performance in a failing organisation | Management, business | Pandit41 (2000) |
| 2. Turnaround as a potential stage in wider analysis of organisational failure (i.e. McKieran’s six-stage model, Argyowasmy’s two-stage model) | Explains the process of decline and/or turnaround as occurring in sequential stages that may result in the survival and performance improvement or failure of an organisation | Management, business | Chowdhurry63 (2002), Fulop et al.54 (2005), Paton and Mordaunt64 (2004) |
| 3. Turnaround as a complex (non-linear) process | Considers turnaround as a complex process involving intraorganisational areas (including human relations, organisational behaviour and group-level behaviour). Considers turnaround in the context of any radical organisational change and not just recovery from a crisis | Management | Beeri65 (2009), Beeri66 (2012) |
| D. Theoretical exploration of turnaround strategies | |||
| 1. Turnaround based on replacement | Strategies put in place to reshape organisational structures | Management, business, health services research | Harvey et al.67 (2005), Fulop and Scheibl68 (2004), Paton and Mordaunt64 (2004), Walshe et al.1 (2004), Jas and Skelcher69 (2005), Ravaghi70 (2007) |
| 2. Turnaround based on retrenchment | Strategies are put in place to limit the use of resources and ‘save’ the organisation (i.e. cost cutting and asset reduction) | Management, business, health services research | McKiernan53 (2002), Greenhalgh71 (1983), Hardy72 (1987), Sutton et al.73 (1986), Ravaghi70 (2007) |
| 3. Turnaround based on renewal | Activities utilised to reorient the direction of an organisation and its vision, with the aim of ensuring long-term successful survival | Management, business, health services research | Protopsaltis et al.74 (2002), Fulop and Scheibl.68 (2004), Walshe et al.1 (2004), Boyne75 (2008), Ravaghi70 (2007) |
| 4. Turnaround based on external episodic intervention | Hands off and focused on performance outcomes and not process. Use of regular inspections | Management, business, health services research | Jas and Skelcher69 (2004), Harvey et al.76 (2006) |
| 5. Turnaround based on relational/mutual arrangements | There is agreement between all parties and it is based on monitoring | Management, business, health services research | Jas and Skelcher69 (2004), Harvey et al.76 (2006) |
| 6. Turnaround based on mandated approaches | External actors take over the organisation, allowing little room for negotiation | Management, business, health services research | Jas and Skelcher69 (2004), Harvey et al.76 (2006) |
Research questions
The review sought to answer the following RQs:
-
Phase 1 (covering health services research, management and business studies)
-
How are ‘failing organisations’ defined?
-
What are the theoretical approaches that have been used to explain organisational failure?
-
How is ‘organisational turnaround’ defined?
-
Which theoretical approaches have been used to study turnaround strategies (if any)?
-
-
Phase 2 (covering health care, education and local government)
-
What are the main interventions used to improve quality?
-
Do the studies highlight any specific issues with implementation?
-
What are the interventions classified as ‘successful’?
-
Have any of these interventions been evaluated? If so, what is the impact and sustainability of improvements produced by these interventions?
-
What are the costs of these interventions?
-
Phase 1
We used a phased search approach. 14 The first phase was broad, covering literature from the fields of health services research, management and business studies to identify overarching themes and definitions on regulation, performance and QI in health-care organisations and the public sector. Broad terms such as ‘organisational failure’, ‘organisational turnaround’, ‘special measures’ and ‘performance in organisations’ were used to identify initial relevant literature across the public sector. A second search targeted literature in the education sector. All other searches (3–5) focused on the health sector. Using a snowball technique, additional terms were found and inserted into a search strategy for five databases [MEDLINE, EMBASE™ (Elsevier, Amsterdam, the Netherlands), Cumulative Index to Nursing and Allied Health Literature (CINAHL) Plus, Web of Science™ (Clarivate Analytics, Philadelphia, PA, USA) and OpenGrey], creating longer and more complex search strategies (see Appendix 4). These databases were selected in consultation with a librarian who sought to identify the most relevant databases for the review topic.
Phase 1 focused on identifying the theoretical content from the literature on organisational failure and turnaround to develop a thematic framework to guide the review. We followed the approach for building thematic frameworks for reviews used by Ferlie et al. 37 Definitions for key concepts, such as ‘organisational failure/success’ and ‘turnaround’, were identified. Furthermore, we searched for the main theoretical frameworks used to explain these processes and synthesised their main characteristics. We sought to create a high-level overview of the different perspectives that have been used to explore failure, success and turnaround in organisations. The findings from phase 1 informed the RQs developed to guide phase 2 of the review.
Phase 2
Search strategy
The second phase was more targeted and focused only on organisational failure and turnaround in health-care, education and local government settings. The search strategy was designed in relation to the PICOS (Population, Intervention, Comparator, Outcome, Setting) framework, the findings from phase 1 and strategies used in other reviews on improvement and low- and high-performing organisations. 5,38,39 We conducted a review of published literature using multiple databases: MEDLINE, CINAHL Plus, EMBASE™ and Web of Science™. Results were combined into Mendeley (Elsevier) and duplicates were removed. The reference lists of included articles were screened to identify additional relevant publications. We also hand-searched other relevant databases, such as The King’s Fund library. We searched for relevant grey literature using OpenGrey and TRIP (a medical sciences database).
Study selection
Following rapid review methodology,37 one researcher screened the articles in the title phase and three researchers cross-checked 20% of exclusions in the abstract and full-text phases. Disagreements were discussed until consensus was reached. The inclusion criteria used for study selection were (1) focus on the delivery of interventions in failing organisations, defined as not meeting the required quality standards (self-defined); (2) focus on the delivery of interventions in high-performing organisations (self-defined); (3) describes empirical research; (4) describes a study in a health-care, education or local government setting; (5) published in last 20 years; and (6) published in English.
Data extraction and management
The included articles were analysed using a data extraction form developed in REDCap (Research Electronic Data Capture). The form was developed after the initial screening of full-text articles and piloted independently by two researchers using a random sample of five articles. Disagreements were discussed until consensus was reached. The data extraction form was finalised based on the findings from the pilot.
Data synthesis
Data were exported from REDCap and the main article characteristics were synthesised. The information that was entered in free-text boxes was exported from REDCap and analysed using framework analysis. 40 We used the thematic framework developed in the first stage of the review to guide our exploration of themes.
Results
Phase 1 thematic framework
The main components of the thematic framework are summarised in Table 7. The five waves of searches for phase 1 provided a working list of 56 relevant publications. Key examples of this literature are included in Table 7.
We found that three definitions of failure are common in the literature (as decline, crisis and below previously established performance level), but only one of these considers failures at a system level (i.e. beyond individual organisations and including multiple organisations) (see Table 7). Some authors argued that failure and success should not be considered discrete, opposite concepts, but should be understood as in a dialectical relationship (highlighting the contradictions and inherent tensions between components). The seven theoretical frameworks used to explain organisational success or failure (see Table 7) reproduce this focus on the organisation as the unit of analysis and neglect of system-level pressures, with the exception of two of the more recent ones (see Table 7, Section B – 6 and 7). Concepts of turnaround tend to privilege a linear conceptualisation of organisational recovery processes, with only one approach considering turnaround as a non-linear complex process (see Table 7, Section C– 3). Turnaround has also been explored as either an internal or an external approach, with limited discussion of the interaction between internal and external strategies.
The findings from phase 1 informed the RQs developed to guide phase 2 of the review. We sought to explore the interventions delivered in low-performing and high-performing organisations, identifying the underlying ideas that guided them, such as their conceptualisation of failure/success as an organisational or system-wide feature, the perception of turnaround as a linear or non-linear process, and the extent to which they considered the interactions between internal and external strategies to guide turnaround processes. As a result of the findings from this phase, and the consideration of success and failure in a dialectical relationship, we decided to develop a phase 2 that explored the experiences of both low-performing and high-performing organisations.
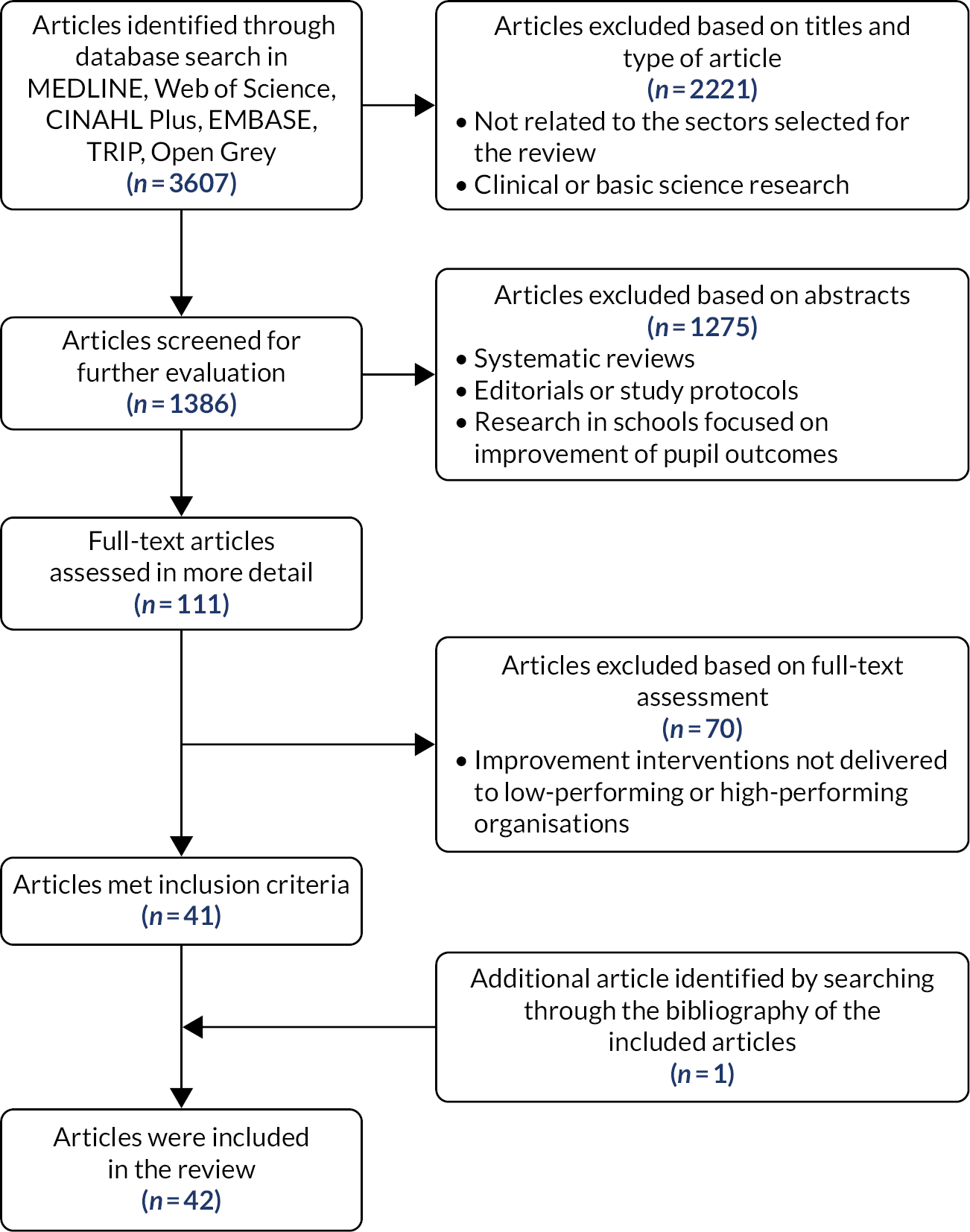
Phase 2 results
The initial search yielded 3607 published articles (Figure 2). These were screened based on their title and the type of the article, resulting in 1386 articles. These articles were further screened on the basis of their abstracts, which left 111 articles for full-text review. Full-text review of these articles led to 41 articles that met the inclusion criteria. One additional article was identified by reviewing the bibliography of the included articles, leading to 42 articles being included in the review. We excluded articles that focused on improvement in individual pupil outcomes (i.e. reading levels) and not general school performance, or articles that did not discuss specific interventions used for improvement.
FIGURE 2.
Study selection procedure.
Characteristics of the included studies
Seventeen of the studies took place in the USA, 20 were from the UK, one took place in the UK and the USA, one took place in Canada, two took place in Israel and one was a comparison across six European countries (Table 8). The publications were relatively recent, with most articles published post-2010. Study designs varied, but most studies were qualitative, followed by quantitative and mixed-methods designs.
| Characteristic | Education (n = 18) | Local government (n = 10) | Health care (n = 14) | Total (n = 42) |
|---|---|---|---|---|
| Study location |
|
|
|
|
| Publication date range | 1999–2019 | 2004–14 | 2005–18 (most 2010 onward) | 1999–2019 (most post-2010) |
| Study design |
|
|
|
|
Definitions of failure and turnaround
We examined definitions of failure and success in the articles in relation to the thematic framework that we developed in phase 1 (see Table 7). Failure/success appeared to be defined in most studies as ‘organisational performance that is persistently below or above some minimally acceptable level’45 (see Table 7, Section A – 3). Low-performing and high-performing organisations were defined as such in relation to nationally established ratings or indices (i.e. Audit Commission Comprehensive Performance Assessment ratings or Academic Performance Index). This definition distinguished between the minimum acceptable level of performance and performance that is ‘persistently’ below and above this acceptable level. The focus of this definition of failure/success tended to be on the organisation and was not applied to the wider system.
Some studies have tried to incorporate a ‘success/failure as a system property’ approach by considering the relationships between the provider organisation and other external organisations; however, even in these studies, consideration of system-level properties was limited. In most studies, failure was considered to be produced by limited or dysfunctional organisational learning (see Table 7, Section B – 5).
Preventing failure and producing improvements were dependent on changes in organisational culture. Some studies indicated that individual interventions aimed at QI were not effective if they did not address problems in organisational culture. 82
In relation to turnaround strategies, none of the 11 studies in the health-care sector described turnaround strategies imposed by external parties, yet these strategies were frequent in studies from education and local authorities. For instance, Jas69,78 argued that for turnaround to be effective in local authorities, it needed to be externally driven. In health care, most of the turnaround strategies were based on relational/mutual arrangements. Some studies framed turnaround under RRR (replacement, retrenchment and renewal), which we previously identified in phase 1 (including these three aspects of the intervention or only some of them). Replacement can refer to the replacement of executive members of a board, retrenchment is based on using stricter financial controls and focusing on performance targets, and renewal strategies could involve changing organisational culture and improving stakeholder engagement. 4 Most of the interventions that we analysed followed a renewal approach, with few examples of replacement. In local authorities, retrenchment (i.e. reduction of spending in particular areas) was seen as producing negative consequences.
Type of intervention
One of the aims of the review was to explore the types of interventions used to improve quality in low-performing and high-performing organisations. The types of interventions varied by sector, but we found overlap in a few of these. We were able to group the interventions into 10 main categories (Table 9):
-
financial incentives (including pay for performance schemes and grants)
-
external partnerships and sharing of practice
-
QI training
-
reorganisation at multiple levels, including senior leadership level, and the use of external interim managers
-
development of existing leadership and/or middle management
-
identification of organisational goals or priorities
-
use of routine data and establishment of performance standards (including dashboards)
-
standardising care practices
-
RRR (replacement, retrenchment and renewal)
-
interventions involving external inspections.
| Sectora | |||
|---|---|---|---|
| Intervention type | Education | Local government | Health care |
| Financial incentives (including pay for performance schemes and grants) | Rice et al.79 (2012); Rosenberg et al.77 (2015) | Werner et al.80 (2008) | |
| External partnerships and sharing of practice | Marsh et al.81 (2017) | Mannion et al.82 (2005) | |
| QI training | Hochman et al.77 (2016) | ||
| Reorganisation at multiple levels, including senior leadership level, and the use of external interim managers | Heck and Chang83 (2017) | Beeri66 (2012), Beeri84 (2013), Beebe13 (2014), Yapp and Skelcher85 (2007) | Mannion et al.82 (2005), Hochman et al.86 (2016) |
| Development of existing leadership and/or middle management | Meyers and Hitt87 (2018), Nicolaidou and Ainscow58 (2007), Orr et al.88 (2008), Van Gronigen and Meyers89 (2019) | Beeri84 (2013), Jas and Skelcher69 (2005), Jas78 (2013) | Gagliardi and Nathens90 (2015) |
| Identification of organisational goals or priorities | Finnigan et al.91 (2012), Chapman and Harris62 (2004) | Tsai et al.92 (2015), Hochman et al.77 (2016) | |
| Use of routine data and establishment of performance standards (including dashboards) | Mintrop and Trujillo93 (2007) | Turner et al.94 (2004) | Chang et al. 201895; Tsai et al.92 (2015), Gagliardi and Nathens90 (2015), Aboumatar et al.96 (2015) |
| Standardising care practices | Curry et al.35 (2011) | ||
| RRR (replacement, retrenchment and renewal) | Beeri65 (2009), Beeri66 (2012) | ||
| Interventions involving external inspections | Willis57 (2010), Wilmott49 (1999), Parsons97 (2013), Perryman60 (2005), Perryman50 (2006), Gorton et al.98 (2014), Ehren et al.99 (2013) | Jas and Skelcher69 (2005) | Allen et al.100 (2019), Boyd et al.101 (2016), Castro-Avila et al.102 (2019) |
Features of ‘successful interventions’
Some of the articles described interventions that produced and maintained improvements in quality. The authors reflected on the features that made these interventions successful. These included the need to (1) consider the hospital-wide co-ordination of interventions, not limited to specific departments or services; (2) establish protected time for staff to implement the changes; (3) ensure staff engagement in the identification of problems and development of the interventions (to guarantee ownership); (4) develop strong relationships with other organisations (to share good practice); and (5) identify clear goals and targets to meet as a result of the intervention and use data to monitor progress.
Issues to consider in implementation
We identified a few trends across sectors in relation to lessons learned in the design and implementation of improvement interventions for low-performing and high-performing organisations. Our review confirmed the findings of previous reviews that have stated that improvement interventions are shaped by the organisational culture, with negative cultures framed by limited ownership, lack of collaboration, hierarchies and disconnected leadership. 5 Features of organisational cultures associated successful implementation of improvement interventions include a ‘can-do attitude’ and the desire to improve on the part of staff, as well as engaged leadership. Our review also revealed interesting reflections on the need to consider processes of implementation. For instance, in the case of school inspections, Ehren et al. 99 argued that, although these might be beneficial for schools, this was contingent on the content of the feedback and how the feedback was communicated to schools after inspections. The authors found that feedback was more effective if it included detailed information on performance expectations and a clear understanding of current teaching conditions. 99 Studies on the process of carrying out inspections in health care have indicated that inspections were more reliable if carried out by larger teams and if inspectors were allowed to have discussions and received appropriate training. 101
No effects, potential negative outcomes and unintended consequences
Some of the studies in schools highlighted the negative consequences of being labelled as a failing organisation; for instance, there were important implications for recruitment and retention of both staff and pupils, relationships with parents and the community, and links with the local authority. Chapman and Harris62 found that top-down reform that treats all schools as the same is unlikely to secure long-term improvement and change, as schools should be free to select the approaches to change that suit their particular needs. External pressures were also seen as negative, as in some cases they resulted in the ‘repackaging’ or ‘recycling’ of ideas and approaches (in the case of this study, restructuring plans) that did not support the meeting of organisational goals or contribute to learning. 91
The external versus internal debate was also present in studies focusing on school inspections and special measures, and some authors argue in favour of the use of school self-evaluations rather than external inspections. 98 Recent research on the use of inspections in health care has also shown that external inspections have no effects on performance. 100,102
Costs associated with the interventions
We found that limited attention was paid to the costs of the interventions or cost savings produced by the interventions. Furthermore, the studies did not explore opportunity costs involved in implementing the interventions, the use of the time and resources to make different changes, and the extent to which the changes could have been carried out without the intervention.
Implications for future research
The articles included in the review identified gaps in research. One proposal was to explore how turnaround strategies change through time, taking into consideration the historical context of organisations. Many studies captured only a snapshot of the intervention and organisational culture, missing the nuances of how change was negotiated. Another gap identified was the need to take into account whether improvement approaches were internally or externally driven interventions by regulatory bodies, for example. The role of external partnerships in creating and sustaining improvements is currently being explored in an ongoing review,103 yet additional work is required to identify the components of interventions that might respond better to internal drive compared with those that might benefit from external support (or a combination of both). In relation to this, some articles highlighted the need to make sure that studies of these types of intervention capture the experiences of staff members across all layers of the organisation, particularly front-line staff and lower management (as many studies have focused on changes taking place at senior leadership levels).
Discussion
In this review, we sought to explore the delivery of improvement interventions for low-performing and high-performing organisations while considering the underlying concepts used to define success/failure and turnaround. We found that most improvement strategies in health, education and local government settings continue to define failure in relation to the inability of organisations to meet pre-established performance standards. Turnaround is often considered as a linear process designed to fix problems and bring organisations up to the ‘appropriate’ level. In most cases, the causes of failure and success are considered in relation to organisational features or characteristics (i.e. organisational culture and leadership arrangements) without a wider consideration of the system in which these organisations operate or their history. Improvement interventions are designed accordingly, that is are focused on specific areas of the organisation or the organisation as a whole, with limited system-level thinking.
The literature that we reviewed has hinted at the problems associated with the definitions outlined above. Some authors have highlighted the limited scope of some interventions, which did not take into consideration issues at a system level, such as regional financial pressures, fragmented care and workforce challenges (e.g. recruitment and retention in particular geographical areas). Others have questioned the roll-out of ‘one size fits all’ interventions across multiple organisations, without recognising the need to adapt improvement interventions to the local context. 62,98 The recycling of ideas from other organisations that did not suit the local context was also found in some studies.
Related to the last point, a domain of literature that did not come up explicitly in this review (because of the key words and targeted focus), yet has relevance, is the process of recycling popular ideas to support QI and performance that originate from external organisations, sectors and global institutions. This is a theme long explored by institutional theorists,who trace the flow and adoption of different types of knowledge found internationally. 104,105 The movement of management and QI ideas and innovations to support health-care delivery has received particular attention from social practice theorists, who discuss the ‘Sociology of Translation’ in health care and ‘knowledge mobilisation’; these are concepts that help us to understand why certain ideas, such as Root Cause Analysis, gain traction in health-care settings and the effort required to embed them into local practices and behaviours (e.g. Nicolini et al. 106). This review did identify some studies that observed that the re-use of ideas did not necessarily suit the local context of their application,91 a finding also supported by the knowledge mobilisation literature, which suggests that, although ideas for improvement may easily spread across boundaries, they might not achieve local buy-in and a good ‘epistemic fit’ within local contexts, especially if there is a lack of knowledge brokering and senior support to encourage organisations to be receptive to the new ideas. 107
The findings in relation to the implementation of successful interventions mirror other analyses of improvement interventions, in which success is often associated with staff engagement, protected staff time for implementation, clear priority-setting and the use of routine data to monitor progress at the board level. 18,92,108–111 There were a number of potentially negative and unintended consequences of implementing interventions, particularly for low-performing organisations. This negative effect can in part be attributed to the labelling of organisations as low performing and in need of interventions. This labelling, for instance by placing organisations in ‘recovery’ or ‘special measures’ programmes, negatively affected staff morale, retention and recruitment. It also meant that organisations came under additional scrutiny.
We were surprised by the limited consideration of the costs of designing and delivering improvement interventions, especially because many low-performing organisations appeared to be suffering from financial difficulties. In addition to a more in-depth consideration of the impact of these interventions on costs and potential cost savings, the literature that we reviewed pointed to the need to develop additional research on the changes in turnaround strategies through time and the interaction between internally driven improvements and external processes.
Conclusions
There is a recognised, limited understanding about whether or not and how improvement interventions are effective in supporting failing organisations and improving the quality of care in high-performing organisations. The aim of this review was to examine the underlying concepts guiding the design of these interventions, processes of implementation, the unintended consequences of implementing the interventions, and their impact on costs and quality of care. We learned from work carried out outside the health-care sector.
We found dominant definitions of success/failure and turnaround, which have affected the design and implementation of improvement interventions. The limitations of these definitions have been the reduced scope of the interventions, the linear perception of turnaround and failure to consider the fact that organisations operate within a wider system. Future areas of research include an analysis of the costs of delivering these interventions in relation to their impact on quality of care. These findings were used in our empirical study to identify the dominant concepts of failure/turnaround shaping interventions implemented in low-performing organisations; determine if interventions were aimed at organisational or system level or were internally driven or externally driven interventions; and explore any negative and/or unintended consequences.
Chapter 4 National policy context
Overview
This chapter discusses the SMQ/CP regimes from a national perspective and provides insights into NHS Improvement interventions and how they are operationalised in practice. We conclude this chapter by identifying themes that informed the wider evaluation, in particular the case studies.
What was known?
-
A review of research considering the impact of interventions on organisational turnaround in the health, education and local government sectors found that most improvement strategies define failure in relation to the inability of organisations to meet pre-established performance standards and that turnaround is commonly thought of as a linear process designed to fix problems and bring organisations up to the ‘appropriate’ level (see Chapter 3).
-
Understanding of the nature of the SMQ/CP regimes and the programme theories that underpin them was limited.
What this chapter adds
-
National stakeholders perceive the SMQ regime as a ‘support’ programme that aims to enable organisations to bring about improvements.
-
The CP regime was viewed as a way to provide access to additional resources for struggling organisations. CP was not intended to be a long-term intervention.
-
QI plans are a central element of SMQ/CP regimes and are intended to focus organisational leaders on quality indicators and patient outcomes (as opposed to financial stability only).
-
National teams recognise that providers might be part of ‘challenged systems’ and that this needs consideration.
Background
The aim of the work described in this chapter was to consider the SMQ/CP regimes from a national perspective to generate insights about how the current system of health-care regulation, scrutiny and intervention emerged and how it is perceived by stakeholders at the CQC and NHS Improvement, and working with NHS providers with performance challenges. The RQ we address is ‘What are the programme theories (central and local) guiding the interventions delivered to trusts in the SMQ/CP regimes?’.
Methods
To consider the SMQ/CP regimes at the national level, we undertook six semistructured interviews with senior employees at NHS Improvement, the CQC and the DHSC, including with two IDs. We reviewed documents that provided background to the SMQ regime, such as independent inquiries, policy documents and trust guidance (Table 10), to help us to obtain a broad overview of developments in regulation in England and understand the programme theory. The vast majority of these secondary documents (n = 20) were drafted in the period 2013–19 following the public inquiry into Mid Staffordshire NHS Foundation Trust. The documents, therefore, provided the team with an historical overview of the developments related to scrutinising provider performance in the NHS by arm’s-length bodies.
Interviews were conducted at the outset of the evaluation, January to February 2019, to assist the team in preparing for the case studies, health economics and quantitative evaluation components of this study. The purpose of the interviews was to understand the programme theory (or theories) underlying NHS Improvement interventions and the forms of support provided to NHS providers struggling with quality. By programme theory, we refer to an ‘overarching theory or model of how an intervention is expected to work’,120 which may include tacit assumptions about change and how it is linked to specific actions or outcomes. We wished to explore which interventions were viewed as being effective and under what conditions, and how the SMQ regime had emerged in health policy and evolved into the current regulatory approach. The interview protocols were tailored to the different health agencies that we approached and can be found in Appendix 1.
| Time point | Key events and publications |
|---|---|
| July 2008 | Health and Social Care Act 2008. Includes legislation to form a new health-care inspection body, the CQC |
| April 2010 | NHS trusts and hospitals begin to register with the new health regulator, the CQC |
| February 2013 | Independent Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry published112 |
| July 2013 | Keogh Report of 14 NHS trusts with high mortality rates published6 |
| July 2013 | 11 NHS trusts placed into ‘special measures’ |
| August 2013 | Independent Berwick review into patient safety published: A Promise to Learn – A Commitment to Act113 |
| September 2013 | The CQC begins its inspections of acute NHS trusts |
| November 2013 | The Mid Staffordshire NHS Foundation Trust public inquiry Hard Truths: The Journey to Putting Patients First114 was published – the government’s response |
| October 2014 | Publication of the NHS Five Year Forward View115 |
| August 2014 | The CQC publishes its report Special Measures: One Year On116 |
| Spring 2015 | ‘Well-led framework’ used to assess the governance of foundation trusts by Monitor |
| June 2015 | Lord Rose Review: Better Leadership for Tomorrow117 – NHS leadership review |
| Late 2015 | Emergence of the ‘challenged provider’ list to monitor NHS trusts |
| 2016 | First year of NHS Improvement. The organisation brings together Monitor, the NHS TDA, patient safety, the national reporting and learning system, and intensive support and advancing change teams. Monitor and the NHS TDA remain independent legal entities |
| November 2017 | Learning from improvement: Special Measures for Quality, published by NHS Improvement9 |
| January 2019 | Publication of the NHS Long Term Plan118 |
| August 2019 | Publication of the NHS Oversight Framework 2019/20119 |
Results
Background to Special Measures for Quality and challenged provider regimes
There is a history in public sector management of independent inspections, which are found in education from the 1990s and extending over time into local government and health and social care (see Chapter 3). The current incarnation of the health regulator, the CQC, reports to parliament via the DHSC and was founded following the Health and Social Care Act 2008. 121 From 2010 onwards, health and social care providers began to register with the CQC. Today, the regulator inspects adult social care (residential and community), NHS general practices, NHS trusts, dentists and independent providers. Registered providers pay a fee to the CQC, which accounts for the majority of the agency’s annual income.
In 2013, a number of high-profile reports highlighted major issues in standards of care within NHS hospitals. The first, the Francis Report,112 investigated in great depth the cultural and performance failings at Mid Staffordshire NHS Foundation Trust. This was followed by Sir Bruce Keogh’s review6 of 14 NHS hospitals with high mortality rates. The latter report drew attention to an absence of knowledge at the board and management level about the causes of high mortality, and raised concerns with regards to QI:
We did not see sufficient evidence to demonstrate that many Board and clinical leaders were effectively driving quality improvement. In a number of trusts, the capability of medical directors and/or directors of nursing was questioned by the review teams. Common concerns were:
poor articulation of the strategy for improving quality;
many trusts had findings from quality and safety reviews undertaken recently by internal and external parties but could not show a comprehensive and consistent approach to learning from these; and
a significant disconnect between what the clinical leadership said were the key risks and issues and what was actually happening in wards and departments around the hospitals.
NHS England, 20136 Contains public sector information licensed under the Open Government Licence v3.0
Shortly thereafter, Don Berwick and an independent group of experts in QI, patient safety and health organisations and systems were asked to review patient safety in the NHS. 113 The resulting publication, A Promise to Learn – A Commitment to Act,113 underscored the importance of regulation, yet pointed out that:
The current NHS regulatory system is bewildering in its complexity and prone to both overlaps of remit and gaps between different agencies. It should be simplified.
Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry, 2013113
The experts made 10 recommendations for the NHS to address patient safety, placing emphasis on culture change, quality assurance (QA) and continuous learning within health organisations to bring about long-term improvements in patient care. The report further suggested that the NHS regulatory system was ‘bewildering in its complexity and prone to both overlaps of remit and gaps between different agencies’ and that it should be ‘simplified’. 113 The report influenced the formation of the national Patient Safety Collaborative, a programme run by NHS England and delivered at the regional level by the Academic Health Sciences Networks.
A new CQC regulatory regime emerged following these high-profile reviews published in short succession, one intended to challenge the poor quality and complacency found within some parts of the NHS and drive a QI agenda nationally. The CQC inspections that are now a familiar feature of the health and social care system in England began in late 2013, in the wake of the Keogh and Francis investigations. 6,114 Closer working between arm’s-length health-care agencies (these organisations have a role in the processes or administrative functions of government, but operate outside of central government departments with varying levels of independence and distance from ministers122) and regulators was another important development during this period, especially between Monitor, the CQC and the NHS Trust Development Agency (TDA). A joint statement by these agencies and NHS England in May 2013123 outlined how the regulatory and assessment approach was to be delivered in future:
The Francis report makes a compelling case that the regulation of NHS trusts and foundation trusts should change in two key ways. Firstly, equal emphasis should be placed on addressing failures of quality as for failures of finance. And second, overlap and duplication in the roles of regulatory agencies must be removed.
In future, this division of roles will be simpler and clearer: the Care Quality Commission (CQC) will focus on assessing and reporting on quality; and Monitor and the NHS Trust Development Agency (TDA) will be responsible for using their enforcement powers to address quality problems. To free up time to care, the overall regulatory burden on providers will be radically reduced but, where there are failings in quality of care, there will be a stronger response.
Department of Health and Social Care124 Contains public sector information licensed under the Open Government Licence v3.0
The role of the Care Quality Commission and NHS Improvement in regulation
By June 2016, the CQC had inspected 136 NHS acute non-specialist trusts and 17 specialist trusts. 7 In this period, NHS trusts that had not obtained foundation trust status were supported by the NHS TDA, while Monitor had oversight for NHS foundation trusts. However, in 2016, NHS Improvement brought together these health agencies along with patient safety (including the national reporting and learning system) and intensive support and advancing change teams. The focus of NHS Improvement was to ensure that NHS trusts provided quality care, met the conditions of their license agreements and were financially sustainable. Although NHS Improvement and NHS England are in the process of co-joining, NHS Improvement still retains overarching responsibility for holding NHS providers to account and intervening if persistent quality challenges are identified by the CQC or through local intelligence gathered within health regions. NHS Improvement describes the organisation’s remit as ‘helping trusts to improve quality of care, finances and use of resources, operational performance, leadership and contribution to strategic change across local health systems’ (contains public sector information licensed under the Open Government Licence v3.0). 125
In practical terms, the regulatory system for health and social care in England has evolved a process of combining CQC ratings that interrogate patient safety and quality with the investigation of organisational leadership (the ‘well-led’ domain) and use of resources. The SMF regime has materialised in parallel and, although not the specific focus of this evaluation, the financial context of the NHS trusts studied for the case studies was taken into consideration. There are around 400 inspectors responsible for the regulation of hospitals, both NHS and independent providers. In an interview during the evaluation, the CQC was described as having an ‘influencing’ role within the health and social care sectors:
… the regulatory powers are there and we do use them, but we don’t see them as our main tool, we see our main tool is influencing interaction, and influencing is through meeting organisations, talking to providers, it is by inspectors producing a report, that describes all the things going on with providers and it is about producing reports on the wider sector.
CQC interviewee
The same respondent described the CQC as having a role of holding providers to account:
If we find a serious safety problem in a clinical service, you always, the next question is why has this been allowed to get to this stage? Why is it the CQC found this, rather than the trust knows it and is dealing with it itself?
CQC interviewee
The Special Measures for Quality regime
Background
The Department of Health and Social Care undertakes a variety of work to address serious failures that arise within the NHS. The department oversees national issues, such as medical or surgical devices that result in patient harm and major hospital incidents (e.g. Gosport War Memorial Hospital and Mid Staffordshire NHS Foundation Trust), as well as the SMQ programme. SMQ originated as a programme of support and oversight that was targeted at NHS providers and was imported from the Ofsted model of periodic inspections and increased intervention for failing schools in education. 60 The first NHS trusts to enter this system were 11 ‘Keogh’ trusts in July 2013. Interviewees confirmed that the SMQ regime had developed as a collective response to the publication of the Francis public inquiry into failures at Mid Staffordshire NHS Foundation Trust112 and the Keogh review of hospitals. 6 In this context, clinical system leaders had become increasingly involved in interrogating NHS provider quality, and ministers were questioning the performance of trusts in which quality and performance were not showing improvement. Monitor and the NHS TDA were tasked in this period with addressing problems flagged by the CQC; however, it was mentioned that there had been some concerns that the CQC was too ‘complicit’ and not independent enough from NHS providers to bring about ‘moral confrontation’ about poor services.
The former Secretary of State, Jeremy Hunt, was viewed by a respondent from the Department of Health and Social Care as determinedly steering a national agenda towards patient safety as a priority:
… his intellectual leap was that safety was the key to everything … And the other thing that I think Jeremy used was he met a lot of the families around Mid Staffs, and so he drew a lot from that.
DHSC interviewee
Against this backdrop, ‘Monday Care Meetings’ with the former Secretary of State were initiated and used to discuss trusts placed in SMQ with the CQC and NHS Improvement, and any other providers about which there were concerns. This created a norm of regularly reviewing and discussing trusts in which there was evidence of poor performance and quality:
The thing that we still use today that gave us some structure was the one-page piece of paper, which had all of the trusts in special measures. We traffic lit them according to how likely they were to exit… So it was very, in some ways it was very ministerially driven in the sense that the Secretary of State was chairing it, and saying tell me about [trust name], what is the plan? … So he would push and probe.
DHSC interviewee
He [the health minister] said he was making sure that action was being taken, that we were all doing our work, our jobs.
CQC interviewee
With the departure of the former Secretary of State, the Monday meetings with direct ministerial input came to an end, but appraising trusts with input from multiple health agencies continues through the adoption of official Monday meetings. At the time of writing this report, monthly meetings take place involving the DHSC, NHS Improvement and the CQC with the purpose of discussing all trusts in SMQ, but no ministers attend.
A particularly constructive relationship was reported between the DHSC and NHS Improvement, in addition to co-operation with the General Medical Council (GMC), British Medical Association and Health Education England (HEE). A Joint Strategic Oversight Group (JSOG) met on a bimonthly basis and was co-chaired by the chief inspector of the CQC and the NHS Improvement executive medical director. It brought together the different arm’s-length bodies to highlight concerns that NHS providers raised at the regional level:
What we’re asking them [regional teams] to do is work with Health Education England, the GMC and other parties, CQC and NHSE/I [NHS England/NHS Improvement] etc. to look at each organisation and raise up any that they think are slipping and might have some of the problems that would head towards special measures. They do a paper they bring it to the Joint Strategic Oversight Group …
NHS Improvement interviewee
[At the Joint Strategic Oversight Group] we discuss all the trusts in special measures and the trust or the challenge provider[s] … we discuss the regulation, jointly, how we’re going to approach regulation, because all those bodies have regulatory functions, these providers, it’s not just the CQC.
CQC interviewee
Process of entry into Special Measures for Quality
It was deemed necessary to place a health provider into SMQ where serious care quality failings were identified alongside concerns about leadership. 9 At the time of writing this report, entry to SMQ remained an option if there were concerns flagged by a CQC inspection, coupled with a lack of confidence that the regional health system and organisational leadership was able to support the trust to make improvements. Typically, the leadership of the organisations was rated as ‘inadequate’ according to the ‘well-led’ CQC rating process and at least one other domain (i.e. ‘safe’, ‘effective’, ‘caring’ or ‘responsive to people’s needs’). In this instance, national-level support is concluded to be necessary given that the organisation ‘is not safe or not in a position where it should be’ (NHS Improvement interviewee). The CQC recommends to NHS Improvement, by way of a letter, that a trust should be placed in SMQ because the CQC cannot formally place a trust in SMQ. Discussions will then begin at NHS Improvement about the interventions to be provided to the trust, such as the appointment of an ID. We were informed that the aim was that at around 12 months a re-inspection is undertaken by the CQC to ascertain whether or not improvements have been made and if their recommendations have been taken on board, although timelines often varied. Similarly, NHS Improvement decides when a trust is ready to exit SMQ, a decision made by the Provider Regulation Committee.
The challenged provider regime
Background
The CP regime originated around the time that NHS ambulance trusts first entered SMQ, in late 2015, and again ministerial input was viewed as being central. Some trusts had been ‘missed’ by the regulatory system at a time when the CQC was undertaking a large number of inspections. It was decided to have an informal ‘watch list’ of trusts that were at risk of entry into SMQ: a type of early warning system. It was commented that there was awareness within regulatory agencies that some trusts had structural issues that needed to be addressed by the wider health system. Tacit knowledge had emerged over the years, in NHS Improvement and the CQC in particular, about the warning signs that signalled that a trust might be at risk. These were described as the ‘softer things’ that the regulatory system could identify, in addition to metrics from the national staff survey, inpatient survey and reports from the GMC and HEE about poor trainee environments, leadership, culture and organisational instability. In particular, it was observed that doctors were often disengaged in challenged and poorly performing trusts, and that there may be feedback that a trust was not listening and responding to staff feedback:
… that’s more or less the genesis of the challenged providers list as an informal thing used at the top of the system to just anticipate special measures … it was one of those occasions when a minister had an idea that actually the system got taken up.
DHSC interviewee
Trusts that could potentially go into special measures in the next 12 months and that’s a judgement, it’s not based on anything hard criteria, it’s a judgement that we make, if we think a trust may be on the downward trajectory.
CQC interviewee
Therefore, the CP regime centred on collective regional and central intelligence about providers and was not dependent on the CQC as such. The JSOG was the vehicle in which decisions were made (with representation from the relevant health agencies, such as the HEE, CQC, GMC, NHS Improvement and NHS England), such as to offer interventions to a provider that might be at risk of entry to SMQ without additional support from NHS Improvement.
Process of placement on to the ‘challenged provider list’
Trusts were placed in the CP regime if quality and performance concerns were raised and a CQC inspection was scheduled to occur within the next 6–12 months. The ambition was for NHS Improvement to help the provider avoid entry into SMQ and provide additional assistance to bring about improvements, alongside increased regional monitoring. A business case was produced by the relevant regional team, which outlined why a trust should enter the CP regime, and this was escalated upwards to national decision-makers to be discussed at the JSOG:
Two fundamental questions. The first is do we think that this trust is a real risk of going into special measures, in the next 6 months? And then the second bit is, and is the region in a position to stop that happening, just giving enough support? Or does it need some more intensive sort of national support through things like improvement directors, you know, budgets to help?
NHS Improvement interviewee
I mean the regional teams don’t have vast amounts of resource and so they believe that getting them on to the challenge list means that they have access potentially to improvement director, they have access to money, from the challenge provider and special measures fund.
ID, NHS Improvement interviewee
Programme theory
In this section, we address the programme theories that guide the central (e.g. IDs, buddying and funding) and additional interventions (e.g. leadership changes) delivered to trusts in the SMQ/CP regimes. Stakeholders at NHS Improvement perceived the SMQ regime as a ‘support’ programme that enabled organisations to bring about improvements (correspondence and interviews). The intent was that SMQ would be ‘helpful’ and enable NHS providers to address the issues that had caused the poor CQC ratings, and that the QI funding would be targeted at problem areas. ‘Fundamental’ changes were expected to drive forward improvements, such as improving clinical leadership and engagement and working on the organisational culture and governance. IDs in particular were expected to proactively engage organisational leaders and develop an improvement strategy:
Special measures is meant to be about support from NHS Improvement, but also support from the wider system in helping them. So it’s meant to be a helpful regime, and it’s often portrayed as a kind of punishment that that isn’t the intention, but of course, it’s public, it’s reputational, I think it’s is often perceived as a punishment, but it’s not a punishment, it’s meant to be saying, ‘actually we just don’t think, we think you need extra help in order to move yourself out of this position’.
CQC interviewee
There was awareness that deep-seated issues typically underpinned problems in trusts’ performance and would take significant time and effort to address, especially in large and geographically dispersed providers:
… it’s leadership, governance, engagement and culture and so on. So I think the ones that really struggle have sometimes got, they’re sometimes big organisations usually more than one site and they may or may not be far apart but quite often they are, they will quite often be organisations that have kind of merged from other ones but frankly have never really merged they’ve never developed a unified culture, a sense of belonging to the overall organisation.
NHS Improvement interviewee
Interviews further suggested that if there were concerns among the regulators and arm’s-length bodies that organisational leaders were unable to address performance and quality concerns, and were not engaging staff well, such a situation could not be allowed to continue because system confidence in the provider was lacking.
The CP regime was viewed as a method for providing access to additional resources for struggling organisations and was not intended to be a long-term intervention:
It’s not an oh you’re on the naughty step this is genuinely an access to resource, help, budgeting, etc., in an aim to try and prevent them going into special measures and there’s quite a lot of examples of where we have spared them deteriorating and they’ve got better. Some we haven’t been able to stop them so that’s quite interesting in itself.
NHS Improvement interviewee
A problem with the CP intervention, however, was that it might be a ‘marginal decision’ as to whether or not to place an organisation in SMQ or CP. If an organisation was placed in the CP regime, the trust would not get the intense level of longer-term support that it might actually need:
I just wonder at times if it isn’t better to just go the whole hog and then you can probably bring about improvement faster.
NHS Improvement interviewee
For this reason, the SMQ programme was perceived by national respondents to be a deeper approach that ‘unearths a lot’ of problems and could expose local services in ‘turmoil’ and that had been problematic for years. However, there was recognition that providers might be part of ‘challenged systems’ and that this needed taking into consideration.
There were, therefore, indications that intensive support from SMQ was believed to expedite organisation-wide QIs, especially if problematic leadership and governance difficulties were promptly tackled. It was understood that instability and overreliance on interim senior leadership roles was unhelpful, although it often occurred in practice. SMQ and CP trusts were expected to produce a QI plan outlining their approach to improvement, suggesting that focusing the minds of organisational leaders on quality indicators and patient outcomes (as opposed to financial stability only) was central to the approach.
Interventions used by NHS Improvement to address performance and their perceived influence and impact
A team within NHS Improvement has responsibility for overseeing the SMQ and CP regimes and reports to the NHS Improvement medical director and the DHSC. This team works closely with a group of national IDs and has oversight of the programme budget that funds the support provided to trusts (see Chapter 6 for further information). The buddying intervention was supported by NHS Improvement’s ‘My Peer Improvement Budget’, whereas the other interventions, QI funding and IDs, were covered by the NHS Improvement SMQ and CP fund.
The interventions delivered to trusts in the SMQ/CP regimes varied from one trust to another and depended on their particular circumstances and needs. The interventions covered the appointment of an ID; a review of the trust’s leadership capability; access to funds for QI; a plan for improvement, including options for diagnostic work on assessing medical engagement; buddying with other trusts; and commissioning external expertise. As detailed throughout this report, these interventions were often delivered within a context of leadership changes at both board and senior management level.
There was said to be co-ordination, ‘open’ communication and ‘very regular contact’ between the senior leaders at the CQC and the senior leaders at NHS Improvement, and interaction at the regional level occurring between regional CQC and NHS IDs, in delivering support to NHS providers.
Improvement directors
There is an ‘NHS Improvement Director cycle’ that outlines a process for providing trusts in difficulty with 1–3 months of intensive support, followed by a further 3 months of maintenance support (NHS Improvement interviewee, January 2019). However, it was noted that some IDs have stayed in trusts for longer periods of time. The IDs we interviewed at a national level felt that they could not become too closely involved with the trusts that they were supporting, otherwise there was a risk of losing critical objectivity. There was a sense of there being an optimal period of time that an ID should work closely with a trust:
At the point that they are starting to demonstrate improvement, you have to choose the point where you start to withdraw, or there becomes a dependence. And for those trusts that are on the challenge list, it’s actually quite hard to get them off because they like the additional level of input.
ID, NHS Improvement interviewee
NHS Improvement was in a position to change IDs, and this did happen. At the same time, appointment of IDs could be resisted locally by trust chairpersons and executives, although it was said that, further down the line, it was not uncommon that a trust could shift its opinion about an appointed ID after a period of resistance, becoming more favourable towards them. At NHS Improvement, it was perceived that IDs played an ‘important role’ and played a key role in developing and tracking progress of trusts’ QI plans. Other points raised were as follows:
-
IDs are not always allocated to trusts in CP, or are allocated for shorter periods of time (e.g. 1 day per week).
-
IDs tend to cover more than one trust at a time.
Buddying (also referred to as ‘peer improvement’ within NHS Improvement)
Buddying operated on a continuum and there was not a uniform model applied centrally across trusts. Buddying could be applied at a departmental level (e.g. between maternity units) or trust wide. Some buddying arrangements were said to have worked ‘brilliantly’ with trusts in SMQ, other less so. Some NHS trusts were singled out for providing interesting models: one organisation had set itself up to provide buddying/support services to other trusts nationally. However, other trusts were deemed to be too large for buddying, and one senior respondent at NHS Improvement thought that buddying had sometimes been a ‘mistake’ and this had provided learning for NHS Improvement and for them personally.
Quality improvement funding for trusts
The following funding pots were made available to SMQ/CP trusts, which were accessible through an application made by the trust to NHS Improvement:
-
up to £500k for SMQ trusts on entry
-
up to £200k for CP trusts
-
£100k available to trusts upon exit of SMQ.
At the time of data collection, funding applications were carefully reviewed and signed-off by the executive medical director at NHS Improvement. There was an expectation that funding should be spent by trusts on activities that would ‘make a difference’ and have local impact.
Perceived influence and impact of the Special Measures for Quality and challenged provider regimes
Special Measures for Quality was viewed in central government as a ‘useful model’, although admittedly one that could first ‘destabilise’ trusts and be very disruptive. It was acknowledged that there was often a great deal of media and political interest, which could put further strain on a provider, staff and those supporting the organisation:
Quite often there’ll be resignations above board level or the exec[utive] level, there’ll be interims quite possibly in place, there’ll be people who are very worried about the position and their own personal position in this. And you know, there have to be sometimes some quite challenging conversations about how the future might look.
NHS Improvement interviewee
There were unanswered questions about trusts that re-enter SMQ or are placed in the CP regime not long after exiting SMQ, and how this might be prevented. We were informed that work was under way at NHS Improvement and the DHSC to explore wider system dynamics, especially how troubled regional health economies might contribute to a trust’s position and prolonged poor performance, financial sustainability or quality issues.
Overall, there was a lack of systematic knowledge about why some trusts re-enter SMQ and why others successfully exit and sustain QIs to achieve an overall ‘good’ or ‘outstanding’ CQC rating.
A report published by the CQC in 2014,116 which reflected on the regime after its first year, noted the following:
No single factor accounts for the improvements that have been made or for the different pace of change at individual trusts. It is important to note that the trusts did not all start from the same baseline. The size of the task was larger for some trusts than for others, especially for those covering two or more locations that are widely separated geographically. In addition, some of these trusts were known to have been struggling to provide high quality care for several years.
© Care Quality Commission 2014. Special Measures: One Year On116
It was felt that the CP regime had prevented a number of trusts from avoiding entry into SMQ:
… that’s probably one of the more powerful things that was developed and of course that all goes on behind the scenes, it’s not visible, because they never get special measures, therefore, the issue is never brought into the public domain.
CQC interviewee
However, the boundary between CP and SMQ trusts could, in practice, be blurred:
There are organisations that end up on the challenge list, that arguably should be in special measures … NHSI [NHS Improvement] make that decision, not CQC … quite often you’ve got a new chief exec[utive] going in and you need to give them a bit of airtime to get on and deliver and putting them into special measures does create a much bigger wave of people coming to review and scrutinise and want action plans, challenge doesn’t have quite such an impact, it gives them a little bit of airtime, to get on and do things.
ID, NHS Improvement interviewee
Conclusions
The insights from the national interviews and review of documents informed our understanding of the NHS Improvement interventions, their programme theory and how they were operationalised in practice. It was clear that there was not a standardised package of support for trusts and that interventions were tailored, depending on trusts’ specific needs and performance challenges. We, therefore, expected that exposure to the different interventions (e.g. buddying, IDs and funding) would be variable in practice and at the case study level of analysis.
Key themes that we identified from our analysis were as follows:
-
Following a number of public inquiries into serious health organisation failures, ministerial and health system leaders working centrally were an important influence in driving a process of greater provider accountability for patient safety, with increased scrutiny by regulators.
-
Regulatory presence at the regional level was an important influence for communicating intelligence upwards about which providers might need support.
-
Ongoing issues in trusts with leadership, governance, culture and poor staff engagement were perceived as indicators of quality and performance issues and ‘early warning’ signs.
-
There was limited knowledge about how the NHS Improvement interventions were received at a trust level, especially differences between CPs and organisations placed into SMQ.
-
The CP regime was intended to be a shorter-term support offer than the SMQ regime, yet there was uncertainty as to why it might help some trusts avoid entry into SMQ but not others.
-
There was limited knowledge about the time scales required to bring about lasting QIs, and why some organisations might fail to embed changes and later re-enter SMQ while others went on to have stronger performance trajectories.
Chapter 5 Characteristics of all Special Measures for Quality/challenged provider trusts and the eight case study trusts
Overview
This chapter describes the characteristics of all of the SMQ/CP trusts alongside the eight case study trusts during our study period.
What was known?
-
Organisational failure and turnaround have been a focus of research in the health, education and local government sectors (see Chapter 3).
-
Previous research has not addressed the characteristics of SMQ/CP trusts compared with those of other trusts.
What this chapter adds
-
The SMQ/CP trusts have slightly older populations, with more attendees living in rural areas but fewer in deprived districts. A smaller proportion are foundation trusts. Characteristics, such as size and number of separate sites providing acute care, did not differ significantly from other trusts.
-
National-level analysis found that sickness absence, staff vacancy rates, proportions of consultants and nurse–doctor ratio were not significantly different from national means at SMQ/CP trusts when they enter the regime.
-
However, they had significantly worse staff survey results for six of the nine survey domains.
-
Our case study trusts do not differ greatly from SMQ/CP trusts overall with these measures, but had significantly higher staff vacancy rates.
-
Common underlying reasons for entry into SMQ/CP among our eight case studies included issues with leadership, organisational culture, governance, workforce, finance and estates.
Background
The overarching aim of this chapter was to explore the characteristics and relative performance of trusts that enter SMQ/CP and compare them with other trusts to judge if there were any important differences. This chapter draws on both qualitative data from the case studies and quantitative data from both a national (n = 62 trusts) and a case study (n = 8 trusts) perspective.
Methods
Mixed-method case studies
Eight case study (four ‘high level’, four ‘in-depth’) trusts were purposively sampled from 59 trusts that entered SMQ or CP between July 2013, when the SMQ regime began, and September 2018. The performance trajectories of the 59 trusts were categorised into four groups: prolonged poor performers, poor performers, shorter-term CPs and clear performance improvers (see Table 3).
We sampled two sites from each performance category, with consideration given to geographical location and types of trust. The mixed-methods case studies used both qualitative and quantitative approaches (see Chapter 2). Interview, observational, documentary and quantitative data from the case studies were triangulated and analysed thematically and comparatively.
Analysis of national indicators
To investigate the characteristics of trusts that entered the SMQ/CP regime compared with those of other trusts, we considered organisational characteristics, such as the category of trust, size and numbers of sites, alongside indicators of the type of population they serve (e.g. age, rurality and deprivation). We also analysed relative performance when trusts enter SMQ or become challenged, such as against the 4-hour waiting time target for emergency departments (EDs), the 62-day cancer target and the staff survey. Among the cancer statistics, we also analysed skin cancers specifically in response to feedback from NHS England and NHS Improvement following sharing interim findings. A further group of indicators related to workforce, in particular the mix of staff employed at each trust, sickness absence and staff vacancy rates. A description of the chosen performance indicators is provided in Table 11.
| Indicator | Description | Data source and dates |
|---|---|---|
| Age | Mean age of unique attendees (admissions, ED or outpatients) | HES 2018/19126 |
| Rurality | Per cent of admissions from rural areas | HES 2018/19126 |
| Deprivation | Per cent of admissions resident in the most deprived quintile | HES 2018/19126 |
| Size of trust | Beds available | NHS England: 2018/19127 |
| Number of acute sites | HES and trust websites128 | |
| Foundation trust status | List of trusts in 2019 reported by NHS England128 | |
| ED waiting times | Proportion of attendances to type 1 ED units waiting more than 4 hours from arrival to admission, transfer or discharge | NHS England: April 2012 to September 2019129 |
| RTT times | Proportion of patients still waiting for treatment at the end of the month who have been waiting for more than 18 weeks | NHS England: April 2012 to September 2019130 |
| Cancer waiting times: all cancers | Proportion of patients waiting more than 62 days between GP referral and start of treatment | NHS England: April 2012 to September 2019131 |
| Cancer waiting times: skin cancer | Proportion of patients waiting more than 62 days between GP referral and start of treatment | NHS England: April 2012 to September 2019131 |
| Summary hospital-level mortality indicator | Standardised mortality ratio (ratio of observed to expected values by provider) | NHS England: April 2012 to July 2019132 |
| Delayed transfers of care | Delayed transfers of care as a proportion of occupied beds | NHS England: April 2012 to September 2019133 |
| Emergency caesarean section rates | Emergency caesarean sections as a proportion of all deliveries | HES: April 2012 to September 2019126 |
| Staff survey results | Responses to the staff survey combined over 10 domains | NHS England: 2015 to 2018134 |
| Consultants | Proportion of doctors at consultant grade | NHS England: October 2013 to September 2019135 |
| Nurses | Proportion of nurses among all clinical staff | NHS England: October 2013 to September 2019135 |
| Sickness absence rates | Full-time equivalent days sick divided by the number of full-time equivalent days available | NHS England: April 2013 to September 2019136 |
| Staff vacancy rates | Vacancies as a proportion of total staff in post plus vacancies | NHS England: April 2017 to September 2019137 |
Most of these measures were derived only for acute trusts owing to the nature of the service and the types of data they collect. In addition, the number of mental and community health providers and ambulance providers that have entered the SMQ/CP regimes is too small to enable meaningful comparisons with their peers. The indication of foundation trust status and staff survey results were the only indicators that used data from all types of trust. The rates of emergency caesarean sections were derived directly from patient-level HES data. The codes used to identify these are explained in the Appendix 8.
For organisational and demographic data, we compared outcomes for all trusts during the 2018/19 financial year. Demographic information came from HES and was derived from a count of all unique individuals recorded as attending ED or outpatients or admitted as an inpatient over the year. However, deprivation and rurality information were available for the inpatient data only. Differences between SMQ/CP trusts and all other acute trusts were analysed using standard two-sample t-tests for means or chi-squared tests for proportions.
We chose as our time point for performance measures the date that the trust first entered SMQ or CP, whichever was the earliest, effectively the time when concerns about quality were first officially noted since the SMQ regime started. The exceptions were staff vacancy rates and staff-mix variables (nurses and consultants) for which, because we had data from after the first trusts entered SMQ only, we chose the first time that a trust entered SMQ or CP on or after the earliest date in our data, which may have been the second time of entry.
Comparison with other trusts was not straightforward because trusts entered SMQ/CP at different times when the overall national rates may have changed. For example, two trusts may enter at different times with similar performance against the 4-hour ED target and because of changing national rates, one may be better than the national average on entry and the other significantly worse. Therefore, we calculated standardised differences between each trust’s value on entry and the national comparator using a z-scoring approach. 124 We adjusted for overdispersion with an additive hierarchical model. Where crude z-scores were skewed, we first applied a square root transformation to normalise the data before adjusting for overdispersion. Mean z-scores for the SMQ/CP sample were then compared with the baseline of zero, assuming standard normal distributions. Given that overdispersion is already accounted for in the summary hospital-level mortality indicator (SHMI) after using a log-transformation, we were able to generate z-scores from a combination of the SHMI values and the values of the two standard deviation control limits. Alongside analysing the characteristics of all SMQ/CP trusts, we also investigated the characteristics of the eight case study sites to observe how representative our selected group was of the larger population of trusts. Dates when trusts entered SMQ/CP were derived from a combination of data provided by NHS Improvement and information from the CQC website. Further details on these methods are described in the Appendix 5.
Analysis of the national staff survey
The NHS staff survey asks staff across the NHS in England about their experiences of working for their respective NHS organisations across a number of domains (Table 12). Annual survey data are available for the years 2014 or 2015 (depending on the theme) to 2018. Results cover the 230 NHS trusts that took part in the survey. Survey themes are summary scores derived from the responses to specific individual survey questions. Scores range from 0 (worst) to 10 (best). Theme results are weighted by occupational group. Details on the technical details of the survey and how theme scores are calculated can be found in the technical document published by NHS England. 138
The SMQ/CP trusts were compared with all other trusts based on the year that they entered the SMQ or CP regimes for the first time (irrespective of whether they entered as a CP or went straight into SMQ). Of 230 trusts included in the staff survey, historical data were available for 40 trusts joining SMQ/CP between 2014 and 2018 and 37 trusts joining between 2015 and 2018. The survey uses seven benchmarking groups based on trust type to allow for fair comparison between trusts.
To ascertain the relative position of a trust compared with all other trusts within a given benchmarking group, quartile ranks were derived for each theme and year based on a trust’s score and their benchmarking group. We then calculated the number of SMQ/CP trusts that were placed in the bottom quartile in the year that they joined and the year that they left SMQ/CP. The expected value was calculated as the total number of trusts that joined or left SMQ/CP over the survey period (and where historical data were available) multiplied by 0.25. Binomial confidence intervals were derived at the 95% confidence level.
| NHS staff survey theme | Years for which data are available |
|---|---|
| Equality, diversity and inclusion | 2014–18 |
| Immediate managers | 2015–18 |
| Quality of appraisals | 2015–18 |
| Health and well-being | 2015–18 |
| Quality of care | 2015–18 |
| Safe environment: bullying and harassment | 2015–18 |
| Safe environment: violence | 2015–18 |
| Safety culture | 2015–18 |
| Staff engagement | 2014–18 |
Results
Organisational characteristics and trends of all Special Measures for Quality/challenged provider trusts and the eight case study trusts
Since July 2013, when 11 trusts entered SMQ after the Keogh Review,6 a total of 62 trusts have been in either SMQ or CP, with several in both categories. The numbers in each category are shown in Table 13.
| Trust category | Number of trusts (%) |
|---|---|
| CP only, for one period | 24 (39) |
| CP for two separate periods | 2 (3) |
| CP and escalated to SMQ | 15 (24) |
| SMQ only, for one period | 14a (23) |
| SMQ for two separate periods, but never CP | 1 (2) |
| SMQ and subsequently challenged since leaving SMQ | 3b (3) |
| SMQ then subsequently CP and escalated to a second period of SMQ | 3c (3) |
Of all 47 CP trusts, 18 (38%) were escalated to SMQ. Four trusts in SMQ subsequently re-entered SMQ at a later date.
In total, 54 out of the 62 trusts (87%) in SMQ or CP have been acute trusts, with the remainder comprising three ambulance trusts and five mental health or community providers. Ten (28%) trusts in SMQ have also been in SMF. A further six trusts have been in SMF only.
Taking a snapshot of all trusts in 2018/19, the characteristics of trusts that had once been in SMQ or CP compared with the rest are shown in Table 14.
| Characteristic | Trusts not in SMQ or CP | SMQ and CP trusts | p-value for difference | Case study sites |
|---|---|---|---|---|
| Individuals attending acute trusts | ||||
| Mean age (years) of individuals attending the trustsa | 43.9 (n = 17,182,556) | 44.1 (n = 10,024,349) | p < 0.001 | 44.1 (n = 1,617,514) |
| Per cent of admissions from rural areasb | 17.2 (n = 5,606,145) | 22.7 (n = 3,244,075) | p < 0.001 | 19.6 (n = 549,039) |
| Per cent of admissions resident in the most deprived quintileb | 23.7 (n = 5,573,569) | 20.6 (n = 3,228,076) | p < 0.001 | 22.7 (n = 548,717) |
| Acute trusts | ||||
| Average number of total beds available | 696 (n = 98) | 753 (n = 53)c | p = 0.64 | 819 (n = 8) |
| Average number of acute sites | 1.98 | 1.95 | p = 0.89 | 2.13 |
| All trusts | ||||
| Per cent of foundation trusts | 70% (n = 179) | 50% (n = 62) | p = 0.005 | 50% (n = 8) |
When pooled together as a group, trusts in SMQ and CP have slightly older populations (mean age 44.1 vs. 43.9) with more attendees living in rural areas (22.7% vs. 17.2%) but fewer in deprived districts (20.6% vs. 23.7%). A smaller proportion are foundation trusts (50% vs. 70%). However, there is little difference in the size and number of separate sites providing acute care.
A breakdown by region is shown in Figure 3. SMQ/CP providers are more prevalent in the Midlands and East (33% of all trusts in the region) and South East (39%) than in other regions.
FIGURE 3.
NHS trusts by region (percentages are proportions ever in SMQ or CP): n = 242.
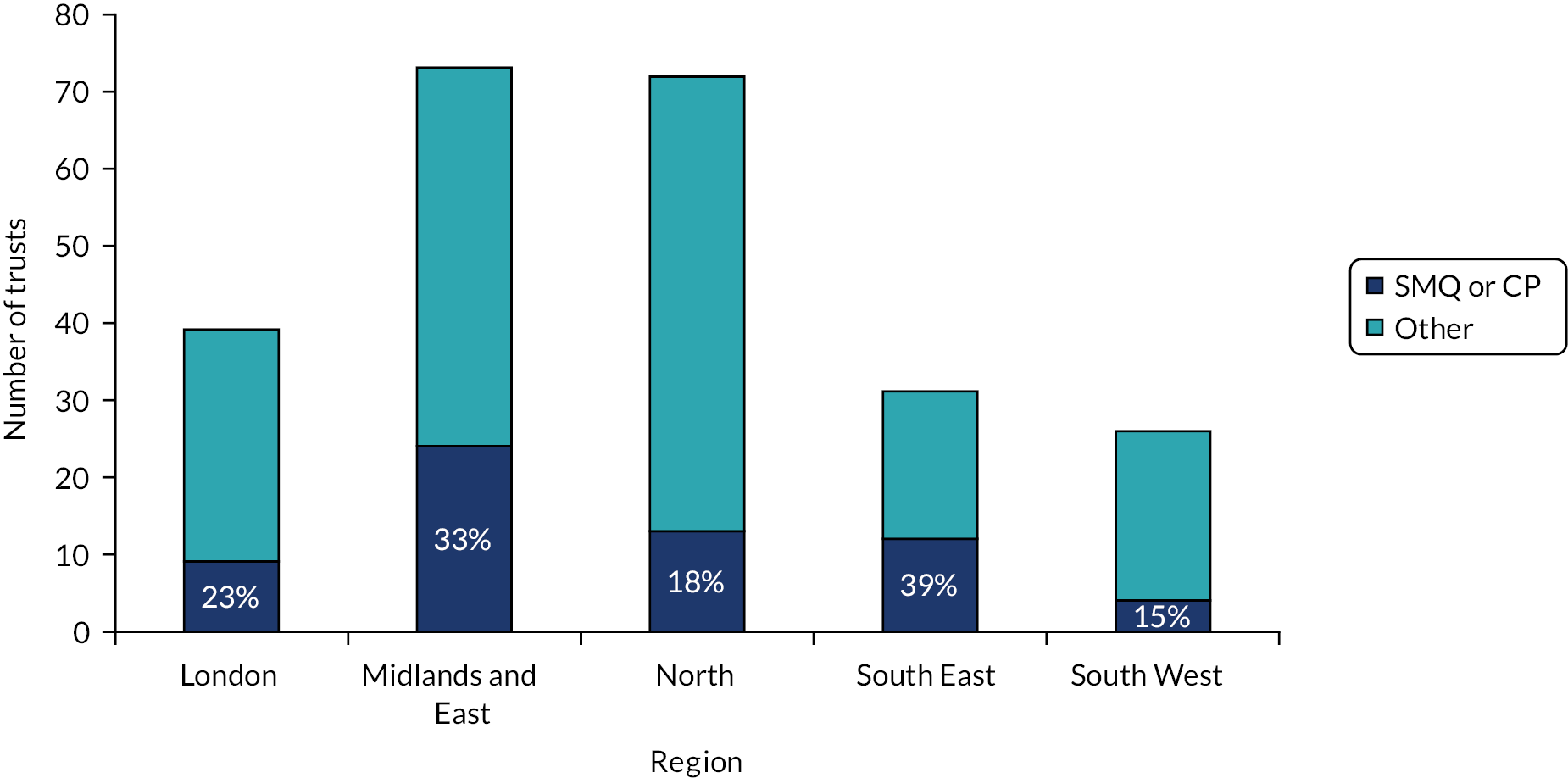
Performance characteristics
Figure 4 shows the outcomes for trusts against different national performance metrics when they first enter SMQ or enter CP (whichever is earlier).
FIGURE 4.
Outcomes for trusts when the first enter SMQ/CP. Mean z-scores compared with national value with 95% CIs (positive values reflect worse outcomes). Emergency caesarean sections data126 Copyright © [2019], NHS Digital. Re-used with permission of NHS Digital. All rights reserved.
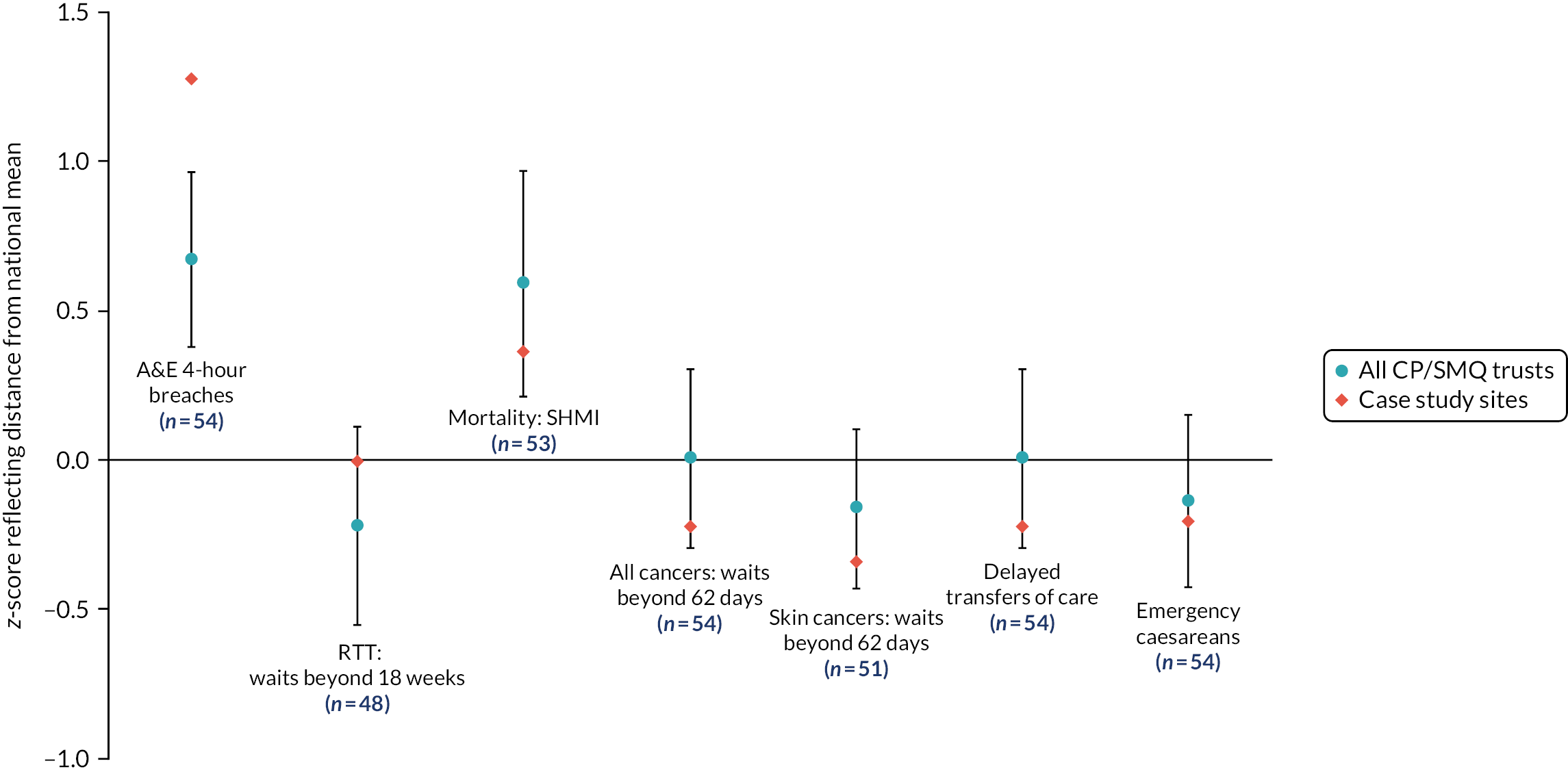
When trusts enter SMQ/CP, mean performance against the 4-hour target has been significantly worse than the national rates, as are standardised mortality rates measured with the SHMI. However, given that mortality was one of the measures used to identify the Keogh trusts in 2013,6 this would have an influence on this result. Removing the Keogh trusts, the mortality rates were no longer significantly worse.
Workforce statistics
Figure 5 illustrates outcomes for our chosen workforce metrics when trusts enter SMQ/CP. For the sickness absence rates, these reflect the first times the trusts’ enter SMQ/CP. Given that vacancy statistics were not available before April 2017, and staff-mix indicators were not available before October 2013, these are for trusts that enter SMQ/CP on or after those dates only. If this is for a second time and the first entry is before the data are available, then the values at the time of second entry are chosen. For the SMQ/CP trusts, none of these values is statistically significant compared with national values.
FIGURE 5.
Workforce statistics for trusts when they first enter SMQ or CP. Mean z-scores compared with national value with 95% CIs (positive values reflect larger numbers).

Staff survey results
For each of the domains of the staff survey, Figure 6 illustrates the number of SMQ/CP trusts in the bottom quartile of results when they enter and compared with the expected number. For six out of the nine domains, results are worse than would be expected. The only domains without significant findings are those associated with quality of appraisals, quality of care and safe-environment violence.
FIGURE 6.
Numbers of SMQ/CP trusts in the bottom quartile within each staff survey domain when they first enter SMQ or CP (whichever is earlier) compared with expected values. Error bars are 95% CIs.
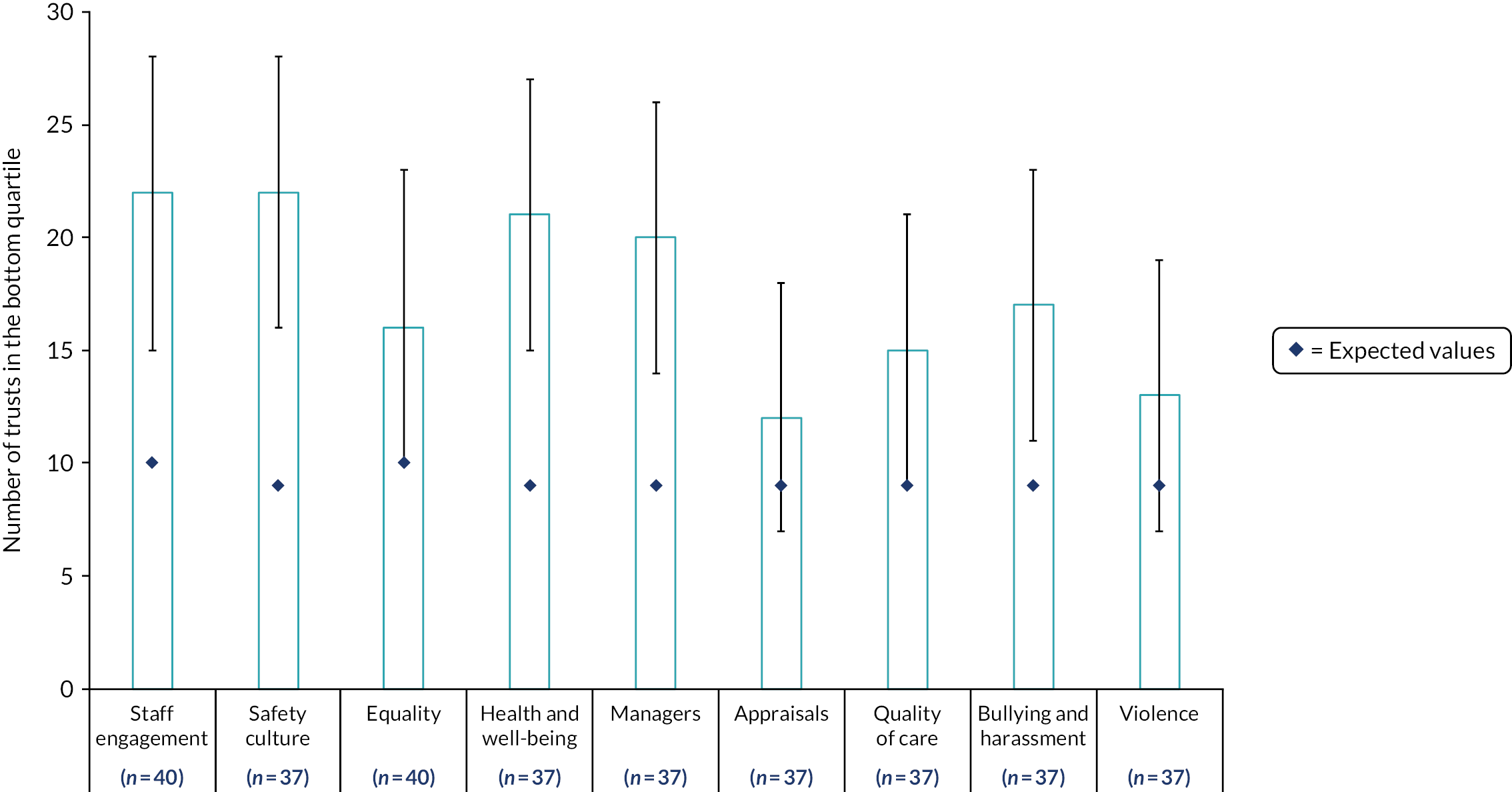
Features of trusts that re-enter (prolonged poor performers)
Four trusts in SMQ subsequently re-enter SMQ: three acute providers and one mental health/community provider. There are no consistent characteristics among the performance or workforce indicators that we have analysed for these trusts, although all are situated on the east coast and serve more rural populations than is typical. Specifically, for the three acute trusts, 46% of admitted patients were from rural areas (range 33–64%) compared with 23% from the SMQ/CP trusts as a whole.
A further five trusts re-entered as CPs after a previous period of being in CP or in SMQ. Of these, three are based in outer London and another is from the south east.
Characteristics of the eight case studies
A summary of the characteristics of the eight case study trusts is presented in Table 15. The case studies are all acute trusts, and no ambulance, mental health or solely community providers were included.
| Case | Evaluation performance segment | Foundation trust | Trust type | Urban/rural/semi urban |
|---|---|---|---|---|
| 1 | CP | Yes | Acute | Urban |
| 2 | Prolonged poor performer | No | Acute and community services | Semi urban |
| 3 | Clear improver | Yes | Acute and community services | Semi urban |
| 4 | CP to SMQ | No | Acute (teaching hospital) | Urban |
| 5 | CP | No | Acute and community services (teaching hospital) | Urban |
| 6 | Prolonged poor performer | No | Acute and community services | Rural |
| 7 | Clear improver | No | Acute and community services (teaching) | Rural |
| 8 | CP to SMQ | No | Acute (teaching hospital) | Semi urban |
As a group, the eight case study trusts have similar characteristics to the SMQ/CP trusts in general (see Table 14). However, on entry to SMQ for the first time, they had a notably higher rate of ED 4-hour breaches than other SMQ or CP sites (see Figure 4), although the differences are not significant. Vacancy rates were significantly higher for the case study sites (see Figure 5), but data existed for only three of these at their time of entry to SMQ/CP, one of which had a particularly high rate.
Underlying reasons for entry into Special Measures for Quality or challenged provider regimes (eight case studies)
From our case study analysis using RAP sheets to summarise findings from interviews and documents, we identified a number of common underlying reasons for entry into SMQ or CP among our eight case studies (Table 16). These broadly related to issues concerning leadership, organisational culture, governance, workforce, finance and estates, and chime with findings from a number of studies of characteristics of poor-performing or failing organisations (see Chapter 3).
|
|
|
|
|
|
|
|
|
|
|
|
|
Chapter 6 Implementation of targeted NHS Improvement interventions across eight case studies
Overview
This chapter provides an overview of the NHS Improvement interventions for trusts that enter the SMQ/CP regimes.
What was known?
-
There is a growing body of literature on organisational turnaround from the health, education and local government sectors, with some examples of successful interventions reported to be restructuring of senior leadership teams, inspections (in schools) and internal reorganisation by external organisations (see Chapter 3).
-
NHS Improvement supports SMQ/CP trusts through oversight and a range of interventions (see Chapter 4).
What this chapter adds
-
The type, duration and perceived value of interventions provided by NHS Improvement vary between trusts.
-
IDs were considered to be helpful when using a coaching style and offering tactical advice for interacting with the regulators. IDs were sometimes felt to bring additional demands and there were mixed views about the amount of time that IDs should spend in organisations.
-
Buddying worked best when ‘buddy’ organisations had similar contexts. Buddies were most commonly used to learn about good practice in relation to specific problems.
-
Funding was perceived as being mainly used to cover posts and external consultants and experts. Some participants felt that there was a risk that trusts might need to spend their way out of SMQ.
-
New leadership teams were a key driver for change, bringing new ideas and approaches. Previous SMQ experience was seen as helpful.
-
Other pieces of work viewed as interventions included ‘deep dives’ into data on specific topics/service areas carried out with NHS Improvement staff and responses to additional oversight and scrutiny from the regulators.
Background
The SMQ/CP regimes provide trusts with oversight and interventions from NHS Improvement to help them to address specific failings identified in CQC inspections for reasons of quality. NHS Improvement perceives SMQ/CP regimes to be support regimes that aim to bring about performance improvement (see Chapter 4). The interventions typically vary from one trust to another depending on circumstance and may include the appointment of an ID, a review of the trust’s leadership capability, access to financial resource for QI, a plan for improvement including options for diagnostic work on assessing medical engagement, buddying with other trusts and commissioning external expertise. These might be delivered in conjunction with other interventions and within a context of significant leadership changes at the board level.
Methods
This chapter primarily draws on qualitative data from the eight case study trusts, including semistructured interviews, meeting observations and documentary analysis (see Table 6). We considered the interventions perceived by NHS Improvement to be important for driving change (see Chapter 4) and remained open to understanding the interventions that trusts saw as being part of SMQ/CP regimes.
Results
The delivery of NHS Improvement interventions varied across our eight case studies. In Table 17, we have identified the interventions delivered for each case.
| Case | ||||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| ID | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Buddying | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Changes in senior management staff and/or board | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| NHS Improvement funds | ✓ | ✓ | Data not available | Data not available | ✓ | ✓ | Data not available | ✓ |
Improvement directors
Improvement directors were appointed by NHS Improvement when deemed necessary for a trust in a SMQ or CP regime. The normal cycle for an ID normally includes 1–3 months of intensive support, followed by 3 additional months of maintenance support (although this might vary by trust). Some IDs highlighted that a limit on the time that they were involved with organisations was required:
… personally I think you lose your effectiveness as an improvement director when you’ve been in an organisation for about 8 to 10 months.
Senior director, case study trust
However, this feeling was not always shared with trusts because some felt that IDs left when important work was still to be undertaken:
… our ID was withdrawn last summer, long before we had been re-inspected or let alone, come out of special measure, so I employed one of my former IDs to help us […] but the trust had to fund that itself.
Senior director, case study trust
Improvement directors can cover more than one trust at the same time and some trusts in a CP regime might not have access to an ID.
Improvement directors were used across most of the case studies included in the study, but there were mixed views in relation to their value. A few trusts viewed IDs in a negative light, indicating that they were not able to enact change, acted as a spy for the regulators or were seen as another source of demand:
Sometimes [the ID] did not feel like support, it felt like it was just another person coming in to ask, ‘have you done this?’.
Senior director, case study trust
However, in most cases, IDs were considered an asset, as capable of ‘making things happen’ (senior director, case study trust). The style used by IDs to engage with organisations (embedding themselves or maintaining distance), work with senior leadership teams and produce improvements varied. IDs deemed successful by trusts were those who used a coaching style with the senior leadership team, offered tactical advice on how to deal with the regulators, protected the senior leadership team from the regulators to ensure permanence, and gave staff confidence to make changes.
Buddying
Buddying, also referred to as peer improvement, can be arranged directly by NHS Improvement, by the ID or by the trust themselves. Buddying can be on a departmental level or trust wide. Buddying is often formalised through a memorandum of understanding. In the case of our study, we were able to identify cases of buddying in only a few of the trusts, and some of these had arranged their own buddies. The use of buddies also varied by trust, but most trusts used them to learn about good practices in relation to specific problems. The appropriateness of buddies was discussed frequently, and the first selection of buddies made by NHS Improvement was not always considered a good choice by trusts in SMQ:
They are a large metropolitan university teaching hospital and we are not and it just wasn’t compatible and wasn’t really working and the improvement work that they were doing with us was focused on things we didn’t need immediate help with.
Senior director, case study trust
The appropriateness of the matching was dependent on geographic location (with close distance seen as positive), trust type and size and experience with similar problems.
Funding
Trusts in SMQ and CP regimes had the opportunity to apply for and, if successful, access funds to help support improvement activities. Trusts labelled as CPs were able to apply for up to £200,000 and trusts in SMQ for up to £500,000. Trusts also received additional financial support when leaving SMQ (£100,000). Applications for the funds are reviewed internally at NHS Improvement and approved by the executive medical director:
… [the application] needs to be mapped to things that are going to make a difference and […] how it has impacted and made a difference.
NHS Improvement representative
Six of our eight case study trusts reported that they had access to the support funds provided by NHS Improvement. The funds were reported to be mainly used to cover the costs of external consultants and to fund posts. In some cases, trusts expressed concern that they would need to ‘spend their way out of special measures’ (senior director, case study trust). The funds were not considered to be enough to implement long-lasting QI (see Chapter 9, which includes an analysis of how funds were spent by five of the eight case study trusts).
Other relevant interventions
Changes in leadership or governance
At point of entry into SMQ/CP, leadership and governance were highlighted by the CQC as areas that required improvement in all eight case study trusts. Common issues highlighted by interview participants included instability in leadership; ‘closed’, ‘defensive’ or ‘insular’ views; a ‘disconnect’ between board and staff; and failures in governance structures and processes. Changes to leadership teams were common following entry into SMQ/CP, and only one trust had no major changes to its leadership (see Table 17). Having a new leadership team was a key driver for change in the trusts. New leadership teams were credited with being responsible for positive changes in QI, patient safety and staff morale in five case study trusts. Key benefits of a refreshed leadership team were said to be the knowledge that they bring from the other areas that they have worked in, and new ideas and approaches. Another benefit was that a new senior team was more likely to be detached from previous cultural problems in the organisation:
… it required people to come in who had a different approach and didn’t have some of the legacy of some of the history.
Senior director, case study CCG [Clinical Commissioning Group]
In four case study trusts, the new leadership teams included at least one person with previous experience of SMQ. Prior experience with SMQ was a positive factor that brought confidence that QI can be enacted, knowledge and experience of what does and does not work well and familiarity with dealing with the regulators (Box 1). Some new leadership teams included people taking on their first Medical Director (MD) or Chief Nurse (CN) roles and noted the importance of mentorship and support to help them manage both the new role and the demands of SMQ/CP. Instability in the senior leadership team and the common ‘churn’ of CEOs was thought to be a barrier to development of effective, long-term strategies for QI and patient safety. Multiple changes in the senior team over time following entry into SMQ/CP was viewed negatively because priorities and focus always change as a result. Another potential negative outcome of multiple leadership changes is that it can take time to get to know the organisation, and this may result in lost time.
Deep dives
Although we did not originally envisage deep dives as one of the NHS Improvement interventions evaluated in the study, these were frequently mentioned by interview participants. Four of the cases in the study mentioned examples of work that they had carried out with NHS Improvement staff through intensive analysis of data on specific topics/service areas. Some of these included:
-
modelling of demand and capacity for specific therapies
-
development of infection-monitoring strategies at ward level (identifying the reasons for high rates of infection and the best strategies for dealing with these taking into consideration the local context)
-
review of ED performance
-
promoting staff engagement through focus groups (linked to staff retention programme and used to identify areas for improvement)
-
analysis of organisational culture and work with staff to change perceptions of change (i.e. staff engagement workshops).
A newly appointed senior clinical director had previously been at a trust that had exited SMQ and brought with them a strategy for the trust’s improvement journey. This clinical director was able to quickly set up a purposeful working relationship with the ID that included clear boundaries and distinct goals for each of them; the clinical director would focus on overall QI and the ID would focus on working with the board:
Working with my current [ID], we sat down and I said, ‘Look, I’ve already appointed a programme director. This is what I’m going to do. This is how I’m going to do it. This is the governance structure within which I will work. Can you start with the board, because of well-led being rated inadequate?’. She started to deal with the stuff around the board conversations, which was really helpful to me because I then could get on [with QI].
The clinical director’s previous experience also guided the trust’s bid for NHS Improvement funding:
I knew what [funding] I was going after. So, I sat down with the [finance team] as soon as I got here and said, ‘Right, this is how we’re going to do it. This is what we’re going to go for’…. I’d already got the report ready for our ID to put in for my financial support for my quality improvement faculty. So, I know where I’m going. So, I think that helps, because I know the post, because it helps me negotiate it quickly… And I guess I can navigate, very easily, the regulatory conversation about the organisation, so that makes it easier for me.
System oversight and scrutiny (risk assurance)
Entry into either the SMQ or the CP regime led to an increase in regulatory assurance processes. When these processes worked well, staff viewed them as an opportunity for reflection, learning and planning for improvement (Box 2). These new processes were seen as potentially good in theory, but burdensome in practice. Some study participants highlighted the large amount of time and resources required to gather information and data for regulators and meetings designed to review progress:
… it should be helpful, but isn’t. It requires a lot of work to ‘feed’ the OAG [Oversight and Assurance Group] each month.
ID, NHS Improvement
This was further complicated if different people made simultaneous demands:
So we’ve had loads of help and I would use that in inverted commas. We’ve got the CCG crawling all over us all the time. We’ve got these improvement directors and that sometimes can be quite hard to take.
Senior director, case study trust
In addition to the increase in workload, some participants did not feel that the regulatory processes were aimed at supporting trusts, but actually contributed to blaming, ‘ritual stoning’ and fixation on the negative factors. The regulatory timelines were also considered unrealistic in many cases, with regulators demanding that lasting changes be produced in a few weeks.
One trust formed an Oversight and Assurance Group after receiving an ‘Inadequate’ rating by CQC. The group met monthly at first and bimonthly after this rating changed to ‘Requires Improvement’. The group involved a wide range of stakeholders including CQC, CCG, Healthwatch, patient groups and HEE. It initially included over 30 people, but attendance dropped off over time and engagement was limited in relation to some organisations. It was normally used by the trust as a way to formally account for progress against QI plans. A lot of work and time were required to develop papers for the Oversight and Assurance Group each month, but the meetings also acted as an opportunity for reflection.
Chapter 7 How trusts respond to being in Special Measures for Quality/challenged provider regimes
Overview
This chapter describes how trusts respond to being placed in SMQ/CP regimes and provides insights into the characteristics of trusts that improved and those that have not yet exited SMQ/CP.
What was known?
-
There is limited evidence on how the different NHS Improvement interventions are received and how effective the interventions are at delivering and sustaining performance improvement (see Chapter 3).
What this chapter adds
-
Staff have a strong emotional response when the trust is placed in SMQ/CP.
-
Entry into SMQ/CP was often thought to be necessary and ultimately can be viewed as a catalyst for change. However, some staff can view SMQ/CP as heavy-handed scrutiny or punishment.
-
There is a view that local system-wide issues also need to be addressed for a trust to make and sustain improvements in quality and performance improvement over time.
-
Trusts’ responses to being placed in SMQ/CP involved making improvements in the following eight domains: governance, accountability and leadership; service delivery; data monitoring and use of data; organisational culture and staff engagement; workforce; QI plan or strategy; QI interventions, methods or techniques; and estates and environment.
-
We have identified the key characteristics of trusts that do and do not exit SMQ/CP.
Background
The overarching aim of this chapter was to explore how trusts responded to being placed in SMQ/CP and to the interventions deployed by NHS Improvement. Using the findings from our case studies, we provide an analysis of internal and external perspectives on the SMQ/CP regimes; what trusts have undertaken to improve; and insights on the characteristics of trusts that have clearly improved and those that have yet to exit SMQ/CP, including the trusts that have struggled to change their CQC ratings.
Methods
This chapter draws on qualitative and quantitative data from the eight case studies (four in depth and four ‘light touch’). For the analysis, we drew on the findings of the literature review and considered whether the interventions were aimed at an organisational or a system level, and explored whether there were any negative and/or unintended consequences reported at the local level (e.g. in either interviews or trust documents). We also considered internal and external contextual factors and whether QI interventions themselves were internally or externally driven. Finally, we aimed to identify whether or not new ‘dynamic capabilities’ were being developed within the organisation, and whether or not trusts invested in developing their capacity to use new knowledge and innovations to drive improvements.
To consider board maturity, we created a template for mapping meetings and papers to the eight dimensions of the ‘Organisational Maturity Framework’ developed by Jones et al. 18 (see Appendix 2) and it was applied to the four in-depth case study trusts as a means of gauging their board maturity. Overall QI maturity level was assessed by the researchers against the framework as being high, medium or low.
Results
Performance journeys of the eight case studies
A summary of each case study trust’s performance improvement journey is presented in Figure 7.
FIGURE 7.
Summary of the performance improvement journeys of the eight case study trusts (to October 2019).
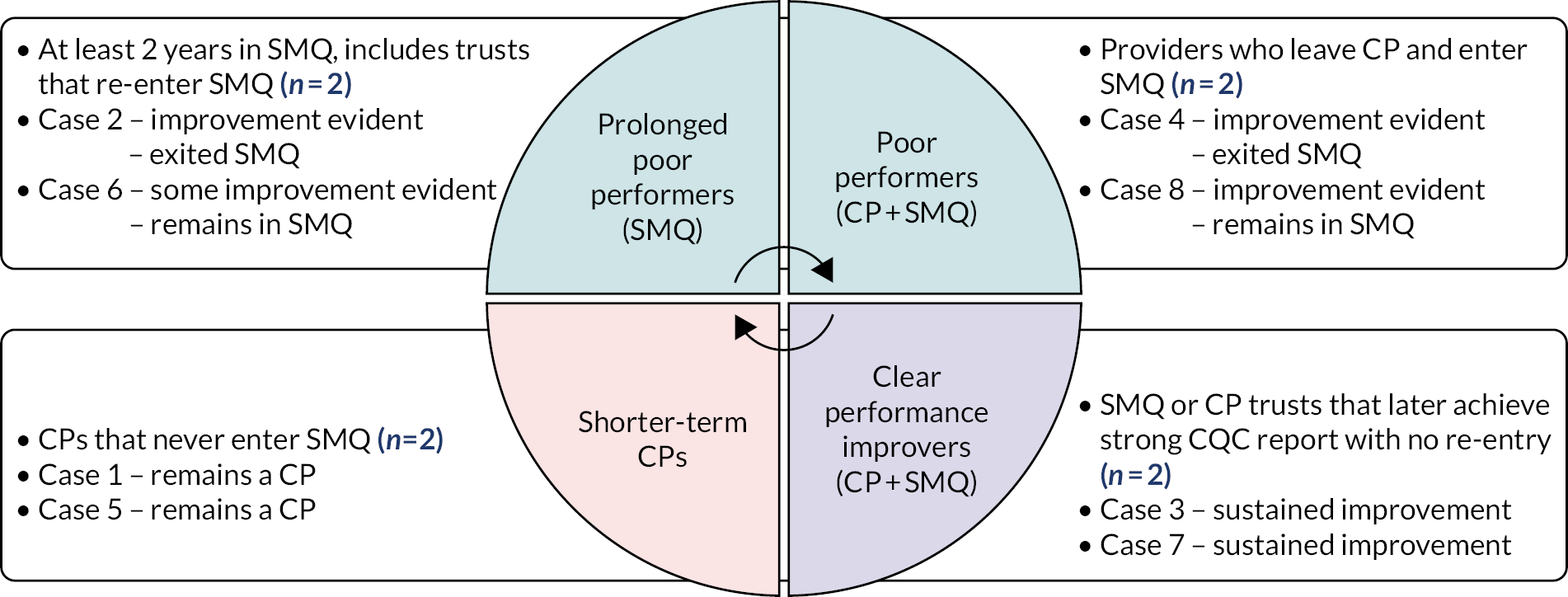
Perspectives on Special Measures for Quality/challenged provider
Internal perspectives: staff
Interview participants were asked about the impact of SMQ/CP on staff. From case study trusts that had previously been in SMQ or were currently in SMQ, the initial response of staff to the announcement that the trust would enter SMQ has been described as ‘shocked’, ‘devastated’, ‘angry’, ‘ashamed’ and ‘mortified’. These responses were attributed to staff across the organisation by interview participants from executive teams to divisional leads. Similar responses were described in the two CP case study trusts when staff learned of poor CQC reports, particularly where if it was felt that positive aspects of the organisation may have been overlooked. In two trusts, anger from staff at all levels was said to be directed at the CQC for being overly critical, for emphasising anecdotal reports and not data in their decisions or for not recognising good practice. There was also evidence of staff anger at senior management and board level for allowing the trust to reach the point at which it was necessary to enter SMQ/CP. There were, however, examples given of staff feeling ‘relief’ at the trust entering SMQ because this would force needed changes.
It was recognised that some staff were initially in denial about the need to change, ‘there’s an unrealistic assumption that life will just carry on’, and ultimately, the ability of staff to reach a point of acceptance has been cited as important for being able to move on and make positive changes (senior director, case study trust). For staff to be involved in making changes, it is important to ‘release time’ for them to focus on improvement and not just expect them to add to their existing workloads. Divisional leads noted that front-line staff were pulled out of day-to-day work to drive improvement initiatives:
… we’re taking people off the day job to run the initiatives and when services are already stretched it’s very difficult.
Front-line staff, case study trust
For the senior team specifically, it was noted that SMQ places ‘enormous pressure on senior staff’ and has an ‘impact on people’s well-being and health’. In addition, an ID noted that the senior executive team and board members are ‘very aware that their jobs are on the line’. Interviewees that were part of senior teams described stress and long hours dealing with the regulatory requirements and QA processes that come from the CQC and other groups, such as Clinical Commissioning Groups (CCGs). It was acknowledged that the pressure on the senior team is not only because of SMQ, but also the result of the problems in the trust. It was suggested that because of the pressures placed on the senior team, one of the supports that may be needed is emotional and empathic support, potentially from peers with similar experiences of SMQ.
The question of whether SMQ/CP was viewed as support or scrutiny received mixed responses: some participants felt that their trust had received the right support or were given needed ‘head space’ by NHS Improvement to make change. Others, however, saw SMQ as heavy-handed scrutiny or punishment. Ultimately, many view SMQ as ‘necessary’, ‘an opportunity and a platform to drive forward improvement’ and as a ‘catalyst for positive change’ that had a beneficial impact on the trust:
I think staff feel disappointed in that, but I think often they feel that it’s been a bit of a galvanisation for them to be heard and maybe to have some of the endemic problems solved and a bit more of a focus on improving the quality and experience and the care that patients are receiving and staff often feeling that they’re not able to give.
Senior clinical director, case study CCG
External perspectives: Healthwatch and Clinical Commissioning Groups
Local CCGs and Healthwatch are key stakeholders when considering external perspectives on SMQ/CP. These organisations are often involved in providing evidence to the CQC or escalating concerns that would have informed decisions to place the trust in SMQ/CP. These organisations also frequently interact with trusts in SMQ/CP to support and/or scrutinise improvement processes. Interviews conducted with representatives from five Healthwatch teams and four CCG teams local to case study trusts provide an insight into the perspectives of these organisations when a local trust enters SMQ/CP.
Healthwatch representatives commonly saw their role as one of ‘standing by the trust’ and to ensure that patient experience was central to the improvement process. One Healthwatch representative noted that their role in supporting the trust on their improvement journey made them feel that they were also ‘very much held to account by NHS Improvement and NHSE’ (senior director, case study Healthwatch). Healthwatch representatives described working with the SMQ/CP trusts in a range of ways, including attendance at improvement or scrutiny board meetings and Oversight and Assurance Group (OAG) meetings, participating in regular meetings with members of the senior team, and working alongside the hospital on specific aspects of patient care. They bring ‘the knowledge that we gather on the ground’ from patients and the public to these interactions (senior director, case study Healthwatch). It was also noted that Healthwatch has a role in engaging with the public ‘to support the hospital to become a successful hospital, to build that confidence of the general public’ (senior director, case study Healthwatch).
Clinical Commissioning Group representatives also see their role as ‘standing side by side’ with their local providers that enter SMQ/CP. Accordingly, there was evidence of CCGs working with trusts in SMQ/CP in a range of ways, including gathering and feeding back soft intelligence from patient discussion groups, ‘holding the mirror up’ to the trust, co-developing QA processes, providing evidence to support or challenge improvement, inputting into QI plans and directly engaging with IDs. It was noted that CCGs often share the burden of SMQ/CP with the trust:
It was incredibly time-consuming actually and obviously a big issue for us and for our governing bodies and things in terms of, you know, local people having access to good services, I mean it was a key focus of the CCG probably for a couple of years.
Senior director, case study CCG
External perspectives: patients and the public
Some interview participants noted that patients and the public can feel shocked about ‘their hospital’ being placed in SMQ and lose confidence in the services provided by the trust. Public concerns about hospitals being placed in SMQ were reported to sometimes result in general practitioners not referring to the trust and patients not wanting to attend a hospital that was in SMQ:
… nobody wanted to go there, people were holding off having their operation.
Patient group representative, case study trust
In one case, the public attitude when the trust was in SMQ was described as a ‘dangerous’ situation and the trust was very active in addressing public engagement and were supported by external groups (Healthwatch, CCGs and patient groups) to ‘start giving out positive messages and highlighting the positive things that the hospital were doing’ (patient group representative, case study trust).
Patient and public involvement in trust service development was noted by some interview participants to be very poor at the point at which the trust entered SMQ/CP. Improved engagement with patients and the public, including collaboration with Healthwatch and other patient groups who can collect and feedback patient and public views and experiences, was seen as an important part of the improvement process by four trusts. These trusts felt that it was essential that patients are included in the engagement process: ‘it’s got to involve patients, which we have been doing more and more’ (non-executive director, case study trust). Strategies introduced to improve patient and public engagement included introducing a patient voice in committee and board meetings (three trusts), asking patient panels to review plans for changes to care pathways and new units or buildings (one trust) and engagement platforms and communication initiatives that very actively seek to gather the feedback of patients and the public (one trust). Lay people have also been included in ‘walkabouts’ aimed to mirror the CQC inspections (two trusts). At two of the case studies, there was little evidence of engagement with patients and the public as part of their process of making improvements.
Role of the system in Special Measures for Quality/challenged provider regimes
Is it individual providers or whole systems that should enter Special Measures for Quality/challenged provider regimes?
Interview participants that were both internal and external to the case study trusts commented on the importance of considering wider systems when a trust was struggling and entered SMQ/CP. In several case studies, it was evident that there were systemic problems within the local region, for example workforce issues or financial pressures, and in some instances other NHS providers in the region had also been placed in SMQ. Overall, there was evidence of a mindset that is evolving from solely focusing efforts for improvement on the trust to a need to consider contextual issues and address improvement at a regional level:
One of the big failings, I think, about organisations going into special measures, is the organisation goes into special measures, not the system.
Senior director, case study trust
It was noted that ‘many of the solutions to the problem of the acute hospital lie outside the hospital’ and ‘system-wide interventions might be needed for a trust to exit SMQ’ (non-executive director, case study trust). In one case study where the trust had recently exited SMQ, several participants felt that local collaborations and ‘a whole system response to the quality issues’ at the trust had been an important factor in improvement, and yet wider system issues persisted beyond the trust’s control (e.g. quality issues within primary care and with local health transport services). Some participants from CCGs spoke of implementing system-wide approaches to QI. For example, using QI methodology across their patch and promoting a ‘mutual approach’ when measuring quality and interpreting data, and recognising the impact on the wider system of any local changes they plan to make. Accordingly, shifting focus to a regional level and strong engagement with CCGs was suggested to be a practical way to promote sustainable improvement:
I think [NHSI] have missed an opportunity by not engaging with the CCG, because had we been engaged and working alongside NHSI [NHS Improvement] and included in some of that developmental work, we could have continued the legacy that they leave behind in terms of being able to offer a sustainable improvement going forward when they are not there.
Senior clinical director, CCG
Acknowledgement of the need for system-level approaches from regulatory teams was reflected in comments from an NHS Improvement regional director who discussed a shift from providers and commissioners having individual assurance meetings with their regulators to ‘system assurance meetings’ at which all providers and commissioners meet to discuss ‘escalating items relating to finance, contract performance and quality’.
Interactions between Special Measures for Quality/challenged provider and system-wide relationships
Being placed in a SMQ/CP regime could be a catalyst for changes in system-wide relationships between organisations. Participants described different types of external collaborations across local regions that influenced processes for QI, including support from peer organisations, mergers, partnerships and alliances. It was clear that in some case study trusts historical relationships with local NHS providers and partners, such as CCGs, were dysfunctional and some participants felt that there had been a lack of transparency from the trust prior to entry into SMQ/CP. Improvement processes commonly included attempts to mend external relationships and encourage collaborative working. Changes in leadership teams can provide an opportunity to strengthen relationships with external partners. For example, in one case study the relationship with the CCG had been poor and they had not understood the ‘depth and breadth of the problem’ until the new leadership team rebuilt relationships and improved transparency, resulting in ‘a much more fluid relationship in terms of how we work together’ (senior director, case study CCG).
Improved relationships across systems that grew organically from responding to SMQ and had been sustained were described by two case study trusts that were clear improvers that exited SMQ several years ago. For one trust, SMQ forced the trust to work with its CCG and other local organisations on risk assurance in a ‘systematic and structured way’, which impacted positively on their long-term working relationships. For the other clear improver, collaborative working when the trust entered SMQ led to a formal alliance between commissioners and multiple providers. The alliance now collectively determines how services will be delivered and are responsible for improving health outcomes. Some case study trusts were already in established partnerships across local systems at the time of entering SMQ/CP, for example as members of an integrated care system. It was highlighted that it can take more time to get good working relationships with external providers when a trust enters SMQ than when trusts are members of an integrated care system in which local partners are already working together.
Entry into SMQ/CP does not always lead to improved interactions across the wider system given that examples of continued problems with regional relationships were also seen. At one trust, participants described struggling with the need to deal with multiple CCGs, and it was noted that there was less joint working after poor CQC ratings because the CCG saw itself in the role of holding the trust to account.
Being placed in Special Measures for Quality/challenged provider regimes can negatively impact a trust’s capacity to participate in local collaborations
Some participants identified a need to consider the strategic impact across the system of a trust being placed in SMQ. The trust’s capacity to participate in the development of strategy for integrated care systems, the sustainability and transformation plans (STP) and future collaborations can be negatively impacted by being placed in SMQ. One reason for this was because SMQ requires ‘a huge amount of time, internally, rather than strategically, externally’ and there is a ‘tension’ between having the capacity to deliver QI and their ability to continue to contribute to wider system change. In addition, it was reported that the SMQ label can result in the trust being viewed poorly by other local organisations and their opinions may be readily dismissed as a result. Participants were aware of ‘poor behaviour’ from partner organisations that took advantage of trusts being in SMQ. Being labelled as a SMQ trust was also said to be a barrier to obtaining tenders when local NHS providers are asked by commissioners to compete for funds and, similarly, may result in ‘bids for capital, for digital, for various things, [being] turned down because of how others in the NHS perceive you’ (senior director, case study trust).
Responses to being placed in Special Measures for Quality/challenged provider regimes
What trusts did to try and improve?
The main changes attempted by trusts to try and improve their quality and performance are grouped into eight thematic domains (Table 18). These domains are not mutually exclusive and in practice overlap, such as between governance and service improvement. Overall, trusts report making particularly strong efforts in the aftermath of CQC inspections, attending to specific recommendations from the CQC and warning and regulatory notices, such as improving compliance with staff mandatory training and appraisals, taking measures to protect patient privacy and dignity (e.g. not using mixed sex accommodation), securing medicines and hazardous substances, and reviewing staffing levels closely to ensure safety. Trusts were prioritising areas for improvement within their organisations in the light of CQC inspection reports and regulatory recommendations, often with strategic support from an ID or external expert if the resources were available. Trusts sought input from NHS agencies, such as NHS Improvement and the CQC, and often external sources of knowledge, such as from management consultancies or governance experts, particularly where financial, leadership and governance issues were particularly challenging. The following areas are not to be read in order of importance given that trusts were found to be making improvements across these dimensions in parallel.
| Domains | Empirical examples |
|---|---|
| Governance, accountability and leadership | Review of the board governance, fill senior vacant posts, create new divisional or front-line leadership or QI roles |
| Service delivery |
|
| Data monitoring and use of data | Clear use of dashboards to track local quality and performance against national metrics and expectations. More advanced and sophisticated use included visualising data to track progress and highlight any risks (clinical, safety, financial) at multiple organisational levels, from the ward to board, and attempts to measure internal ‘safety culture’ |
| Organisational culture and staff engagement | Address bullying; support growth of patient safety culture through staff training and development. Staff awards and recognition; support for completion of staff survey; use of social media to keep staff informed; listening events; senior and board presence on wards |
| Workforce | Ensure safe staff levels; appraisals improved; mandatory training up to date. Training and learning opportunities for staff |
| QI plan or strategy | Involves IDs or external expertise. Suggestions that the plan should not be transactional. Set a vision for culture change and continuous improvement centred around patient care. |
| QI interventions, methods or techniques | A variety of QI methods and tools (e.g. PDSA) and broader interventions to drive improvement, some of which are mentioned in QI plans and strategic documents |
| Estates and equipment | Strategy to improve working and patient environment to ensure safety, improve capacity and modernise services. Includes investment in equipment, addressing maintenance backlogs, removal of risks or hazards (e.g. ensuring fire safety, replacing outdated diagnostic equipment) |
Governance, accountability and leadership
Many trusts focused on improving their governance and assurance processes. Better leadership visibility came about through increasing ‘ward to board’ interactions and having members of the senior leadership team communicating more frequently with front-line staff, undertaking ward visits and ensuring that there were clearer lines of accountability with greater opportunities for senior leaders to listen to the concerns of staff:
We visited 90 areas across the trust within a 3-month period after the last report came out and drew up findings, reports, action plans and then we repeated it 3 months later and we’re now on our third iteration of walkabouts. So, by the end of the year, every area in the hospital, whether it’s clinical or non-clinical, will have been visited at least once by a team consisting of a non-executive director, a senior manager or an executive and a lay partner. Either a governor or a patient.
Non-executive director, case study trust
There was recognition across our cases for the need to ensure that there was excellent clinical leadership at divisional and ward levels, as well at the top of the organisation, to bring about improvements, and that front-line clinical staff also needed to understand why specific improvements or changes in process were necessary and be on board to deliver and lead improvements at the local level. For example, in two case studies changes in leadership were encouraged to bring about improvements to ED performance. Part of the journey of improvement was ensuring that, at all organisational levels, there was leadership accountability for managing risk, making improvements and embedded processes for assurance:
Clinical leaders taking an equal seat at our trust management board for critical decision-making.
Senior director, case study trust
Two trusts had focused on improving recognition and opportunities for ethnic minority staff; this was particularly important where there had been past issues with harassment, bullying and even reports of racism between staff. An ethnic minority leadership development programme has been instigated and trusts also mentioned deliberating creating new leadership opportunities and roles.
In terms of senior level oversight, the medical director and chief nursing roles appeared absolutely vital for re-connecting divisional and senior executive leadership tiers, ensuring that clinical engagement was trust wide. Another activity that trusts were required to enact was filling vacant senior leadership posts; several had struggled to recruit and relied on interims, which was potentially destabilising for the organisation as a whole or resulted in notable leadership gaps, such as where it was difficult to recruit a lead nurse:
… we were probably looking at 50% vacancy gaps across our senior leadership board and the layer or two below, and a lot of those had been either covered by people acting up or by more expensive interim costs.
Senior director, case study trust
Service delivery
Although CQC inspection reports resulted in what was perceived to be a large number of competing recommendations for trusts to deliver on, in reality senior leadership teams conveyed the necessity of prioritising improvements and those that focused on ensuring patient and staff safety. A trust needed first and foremost to address urgent operational issues, mitigate major risks, especially concerning the estate and workforce. Estates and equipment were frequently raised as concerns because of their immediate impact on capacity, diagnostics, the working environment and patient and staff safety (e.g. a need to increase beds, modernise facilities and improve diagnostics and, therefore, waiting times) cases:
The worst thing we can do is have 100 action plans now, to address the things that are wrong. So what we’re doing here, what I’m doing here, is pulling together one plan.
Senior director, case study trust
Examples of areas prioritised included urgent care, basic safety and fire safety, mortality, WHO surgery guidance, better safeguarding, better management of sepsis, and reducing incidents of pressure ulcers and falls. Trusts needed to meet NHS constitutional standards and compliance notices and, in our case studies, were particularly focused on the following services: ED, surgery, maternity, estates and maintenance backlogs, infection rates and control. There was a clear focus on referral to treatment (RTT) times as many trusts were in breach of these, such as on account of backlogs in diagnostics to meet cancer objectives.
A number of the case study trusts were struggling to deliver improvements within EDs in the light of rising demands and were non-compliant against the national 4-hour ED waiting target and, therefore, constitutional expectations of the regulators. Challenges were reported in ED because of rising demand, and urgent care performance was a strong performance issue for all organisations generally, as commonly experienced across the country.
How did these organisations perceive the emergency care challenge and go about making improvements within a context of deteriorating national performance and rising demands? Below are two vignettes from our case studies, which provide an overview of the performance issues (Boxes 3 and 4). The vignettes illustrate that, in some key service areas, despite concerted efforts to improve that were backed by clinical staff and organisational leaders, performance was struggling against the national 4-hour wait metric. This was a result of various inner and outer contextual factors. For example, a combination of high bed occupancy and external demand for urgent care in a busy urban setting was making progress slower than hoped for, despite investment in staff and a structured QI methodology being adopted at the service level and trust wide. In addition, some trusts had issues to resolve with ambulance turnarounds and old estates and facilities in hospital sites. Nevertheless, we found evidence in this evaluation that trusts were able to improve their ED performance trajectories following interventions (see Chapter 8).
This trust was defined as a ‘poor performer: with evidence of improvement’. While noting that poor ED performance against the 4-hour wait target was a national issue, a senior clinical director said that ED performance had remained static for the organisation for 12–18 months and described troubles at the trust’s busiest site, despite the organisation applying its QI methodologies there. The cause identified by the leadership team was growing demand and high bed occupancy (at around 99%), which resulted in negative knock-on effects and overflows within the ED department if inpatient beds were unavailable. ED attendances had increased by almost 10% over a 12-month period. The trust was struggling to make substantive improvements and comply with the national 4-hour wait target and resolve delayed transfers of care. A further 12 months later, no patients were reported to be waiting longer than 12 hours in ED and the trust had delivered a number of process and operational improvements, such as improving triage times, by providing 24/7 consultant cover and expediting ambulance handovers. The leadership team was closely monitoring 4-hour wait times and reviewing the Friends and Family Test data for ED, which was felt to be providing some encouraging findings. A target of 95% of patients being seen within 4 hours was set. There were financial implications (reduced income) to the trust of not meeting ED performance targets, yet the trust was likely to continue to struggle without additional physical capacity and beds and these were being delivered through capital investment projects.
In terms of the wider system context, the trust was in conversation with CCGs and the local authority owing to a large number of visitors to the ED not being registered with a general practitioner and a ‘transient population’; there were ongoing concerns that without improvements in social care, the local ED department would continue to be overwhelmed:
… ED performance, and that’s the one we’re struggling with at the moment. We’ve not got that right, and the reason we’re struggling is because some of the proposals that were in place for redeveloping the ED department and putting some extra beds in have proved impossible to do, because we can’t keep an ED department running at the same time.
Board member, case study trust
This trust was struggling to meet the ED national standards yet had managed to make performance improvements, which had been recognised by NHS Improvement and the CQC as ‘significant’. By 2019, the trust was no longer below the national average for ED wait 4-hour times and had maintained this position for several months. The trust had for a long time been struggling with rising demand, struggling ambulance turnaround times and poor patient flows. It had experienced ‘black breaches’ with patients being treated on trolleys in corridors and waiting more than 12 hours in ED.
The trust had undertaken a number of steps to improve patient safety and quality and turnaround patients faster. A team was put in place to assess patients arriving by ambulance improving flow into the department and staff collected observational data to monitor patients most at risk of deterioration using early warning scores. Clinical governance and leadership for urgent care had been improved by a new senior consultant appointment, which was said to have made a huge difference in terms of shaping the emergency care pathway and improving the service culture. There had been efforts to improve staff mandatory training and learning, despite heavy staff workloads. Financial investment in additional beds and staff over the winter months had increased capacity helping to supporting flow. Although issues with ED performance remained, there were signs of improvement supported by national data, regulatory assessments and observations among those interviewed at the trust for this evaluation. Finally, there was focus on improving the treatment, stabilisation and transfer of children attending ED.
Improvements in such busy emergency services was a source of pride for several senior members of staff interviewed during the evaluation, who described staff and organisational efforts as ‘herculean’ and viewed their ED units as ‘resilient’ despite rising demands:
… we’ve had to put in additional medical staff in certain areas where there was concerns over the level of activity they were working with, and we’ve had to put in some additional medical staff, so both in [ED] and actually predominantly around [ED] actually. So there’s been a number of areas where we’ve had to put in resources as a consequence of having issues highlighted.
Senior director, case study trust
Despite investment, vacancy rates and staff retention continued to remain a challenge for the very busy ED services.
Data monitoring and use of data
There have been several ways in which trusts in SMQ/CP have improved their use of data, covering how it is being collected and analysed and how findings are shared.
Many participants have referred to the inadequacy of the commonly used way of presenting outcomes as monthly Red/Amber/Green (RAG) ratings that reflect changes to a previous month. These exclude wider overall trends and may not be adequately benchmarked. Instead, they see the value of continuous monitoring techniques and the statistical process control methods promoted by NHS Improvement that are being widely implemented. Benchmarking has improved with the availability of the model hospital data, enabling trusts to view outcomes against their peers:
We obviously got the model hospital resource, which we use and which is really helpful for understanding our position in relation to benchmarks, what we need to do on that, so I think that’s been a big step forward.
Senior director, case study trust
There is also evidence of a more mature approach to understanding what data are actually describing and, rather than interpreting them as an explicit measure of quality, treating them as a prompt to investigate quality, as well as triangulating with concerns of staff and patients. Furthermore, although there is a strong incentive to focus on concerns identified by CQC, some trusts have recognised the dangers of taking their eyes off the ball elsewhere and the need to maintain or improve quality across the board.
For board-level reporting, our cases tend to focus on standard metrics (e.g. NHS Improvement provider metrics), which are limited in number and scope, and may not be the best measures for reflecting the concerns that have been raised. However, the data are often not there to support the conversations trusts want about quality: they may not exist or may require a bespoke collection that then becomes difficult to benchmark. Participants at one site identified problems with the timelines of data: some nationally benchmarked data (e.g. some audits) can be several months old before it becomes available. One trust undertakes ‘deep dives’ into hospital sites and specialties to obtain a better focus on concerns, although at others it is not clear how much capability there might be for monitoring.
Some participants recognise the problems of reporting different measures in isolation and recognise how different measures of quality interact. In particular, improving one outcome may adversely affect another, for example the potential impact of improving the speed of getting people off ambulances on ED capacity.
Organisational culture and staff engagement
Culture change was closely intertwined with senior leadership and improving staff engagement. Examples of attempts to better staff engagement included focus groups with staff and NHS Improvement support and workshops with staff. Attempts at proactive engagement with staff by new leaders was a common theme across case studies. To improve staff engagement, the board, senior executive team and managers became more ‘visible, supportive and approachable’. For example, staff observed that the senior team were often seen around the trust and used social media [e.g. Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com)] to communicate with staff and keep them informed. Many interviewees described that, previously, there had been a gap between senior leaders and front-line staff and poor communication. Some organisations measured and monitored changes in the safety culture using standardised survey tools:
… there wasn’t a great leadership strength here. The culture of the organisation became progressively closed… The governance was poor. Basically if you tried to do anything, you just got stuck somewhere in the middle of the organisation. Nobody would approve anything, so trying to get a business case through was just like running in treacle, so the clinicians were very disengaged.
Senior clinical director, case study trust
Four case study trusts had reported serious historical issues of poor culture and bullying. Within this context, some specific service areas were reported to have particular issues with a ‘bullying culture’, an issue sometimes uncovered by new incoming leaders. Overall, it was reported that bullying had to be tackled by senior leaders, and executives address reasons why staff disengaged, working to ensure that there was collective ownership of patient safety, and improving the patient experience and outcomes across the entirety of the organisation:
… evidence of serious deficits in leadership in a series of ways, both through the sort of feedback from staff about lack of staff engagement, not being listened to, bullying and harassment allegations and so on, but also clear evidence of very little clinical leadership in the organisation, so what we have focused on really is trying to get leadership culture and morale and staffing right, seeing them as the underlying themes.
Senior director, case study trust
… we committed some of the special measures money to use an external organisational development consultancy to help facilitate and mediate between [specialty team members] to develop essentially personal development plans for each of the senior staff so that they could better engage with what the organisation expected of them and work more consistently with the organisation’s values…
Senior director, case study trust
Measures taken to tackle historical issues with poor staff engagement – illustrated by poor staff survey results – included encouraging a culture of openness and transparency (measured through staff surveys, spot surveys and feedback, and Freedom to Speak Out Guardians). There was evidence of senior leaders celebrating staff successes, and especially among our clear improvers case studies. Several case study sites made efforts to improve events and facilities for doctors and trainees and improvements were demonstrated through a larger number of junior doctor applicants. Finally, there was evidence at sites that had improved of encouraging staff not only to complete mandatory training and appraisals, but also to progress their careers within the trust and develop new knowledge through QI training.
The CQC emphasises the importance of staff appraisals, and a number of case study sites discussed making particularly notable improvements here; for example, shifting the focus to staff wellness and ensuring that appraisals were not a ‘tick box’ activity, as well as taking steps to better support staff returning to work after absence because of ill health or family reasons. Culture change was recognised to take years (more than 2 years, and more likely 5–10 years), but in the short term senior teams were engendering change by celebrating staff successes, improving staff survey results (response rate and scores) and ensuring completion of mandatory training, which is closely attended to by the CQC.
Tangible evidence of improvement included improved staff survey results and completion rates and good Friends and Family Test results. Again, change appeared to take at least 12–18 months to take hold, even if the senior team were very focused on improving staff engagement and culture. Box 5 describes the staff survey as an indicator of workforce engagement. Observations at two case study sites confirmed a real drive by leaders to encourage staff to complete the national survey (e.g. ward-level initiatives to improve completion rates):
This trust was defined as a ‘clear improver’ in our sample. After a long improvement journey (which was noted as still in progress), the annual NHS staff survey found the organisation rated among the best acute trusts in the country for staff satisfaction. The trust scored highly both regionally and nationally as a place to work. There was a good response rate to the survey. These results had become a source of pride.
The internal actions or leadership behaviours that may have facilitated consistently good results over consecutive years were as follows. First, there was a widespread push for the survey to be completed and better leadership reported at the apex of the organisation by the clinical director, chief nurse and CEO, who were deemed to be visible and approachable. The staff survey was viewed as a collective drive and positive activity rather than a ‘tick box’ exercise. Fieldwork observations of several divisional level meetings provided further evidence that the trust was making strong efforts, across each division, to systematically monitor and improve workforce engagement. One example was improving the quality of staff appraisals and checking they were completed, even in busy periods: ‘1 hour with that member of staff to talk about themselves’. There was attention to, and monitoring of, stress-related absences, with the senior leaders observed asking teams what support could be provided to staff. Senior leaders also offered praise to local service leads for confronting challenging issues, ending the meeting with thanks and recognition, and noting that staff ‘can be really proud’.
… it is early days because we know with these types of programmes it is over a number of years these span with regards to changing culture and improvement and training high numbers of staff across the organisation.
Senior clinical director, case study trust
Workforce
… if you want to create the right environment to change and to improve things, you’ve got to invest in the people.
Senior director, case study trust
We found evidence that trusts in SMQ/CP performed poorer than the national average across a number of domains in the staff survey, such as engagement (see Chapter 8). Improved completion rates of the staff survey were, however, insufficient to drive QI; leaders had to actively respond to the results of staff surveys, especially if they were poor. Some organisations undertook ‘deep dives’ into results to understand specifically what was going on in areas such as staff morale and staff engagement. However, broader issues had to be tackled to reduce vacancy rates, reliance on locums and staff turnover, and improve staff retention.
Trusts were focused, therefore, on workforce planning, such as supporting e-job planning and e-roster rollout. There were diversity, equality and inclusivity interventions being put in place in recognition of historical issues. Struggling trusts have had specific issues with staff recruitment and vacancy rates, and some interviewees discussed problems with recruiting against both neighbouring trusts and other trusts around the country, with some trusts known to offer ‘golden handshakes’ and new starter incentives that they were unable to compete with. The label and ‘stigma’ attached to SMQ could further impact negatively on recruitment efforts. In the short term, trusts might address safety concerns by relying on agency staff, bank staff and locums to fill gaps and address safety concerns highlighted by CQC inspectors. But this was not viewed as a long-term solution and clearly affected overall costs, especially where new staff had to be re-trained.
Increasing the staff numbers in ED in the light of rising demands and performance pressures was one clear area of workforce investment. Changes to staff rotas to replace outmoded practices were also reported.
Quality improvement plan or strategy
Developing a structured and clear plan to take forward improvements and focus the trust’s efforts over the medium term was one area of activity in which we identified IDs playing a key role. Trusts and IDs we engaged with were, however, keen to ensure that plans were not transactional documents, but representative of positive shift in ethos and values of the trust:
… if what you do is, in your improvement plan you put, ‘Improve statutory and mandatory training’, that is the outcome measure. What you are not doing is unpicking why.
ID, NHS Improvement
… part of the problem I think in this trust is you have a list of things that people are telling you, you have to do, so the risk is it’s not a quality improvement plan, it’s actually a turnaround plan but people call it a quality improvement plan, and that list is usually a list of things the CQC want you to do, a list of things that NHSI [NHS Improvement] want you to address.
Senior clinical director, case study trust
Other trusts brought in external experts, such as management consultants or board advisors, to support the development of a detailed improvement action plan and leadership support following a CQC inspection, such as if they lacked ID input or preferred at the time to appoint their own external experts.
Quality improvement interventions, methods and techniques
Having a formal ‘method’ or strategy for QI embedded throughout the organisation is encouraged by the CQC and we found evidence of trusts looking to take a more structured approach to QI internally. We were particularly interested if trusts were investing in developing new QI capabilities and increasing their internal ‘absorptive capacity’ and receptivity to new, external knowledge to improve performance.
In several case studies, a new QI ‘team’, ‘faculty’ or ‘fellows’ were being established to support front-line staff, train staff in QI tools and progress the organisation on an improvement journey. Appendix 5 provides further details of the findings under this domain. It demonstrates the breadth of activities within trusts aimed at developing new, internal organisational capabilities and to support internal improvement. There is overlap between the other domains, such as culture, QI plans and governance, accountability and leadership.
The common factor across case studies was that these interventions relied on some form of external resource, performance management knowledge or QI expertise;139 therefore, a knowledge search and exploitation approach was evident in practice. Trusts typically wanted additional assistance to drive QI and better performance systematically following a poor CQC inspection report.
Estates and equipment
Finally, there were reports of using ‘turnaround consultants’ and external management consultancy firms to advise on financial recovery where trusts were in SMF or at risk of being so. Less available funding created problems for investing in improving hospital estates. Given that SMF was not our primary focus, we briefly draw out findings about capital investment in estates and equipment instead.
Legacy financial issues in the regional health economy were problem areas for some trusts. For one trust, a private finance initiative legacy created internal issues around financial sustainability. Funding problems were also noted at a trust that urgently needed to invest in improving a poor and decaying estate and ongoing estate improvement projects. One trust had major backlogs with maintaining and investing in equipment, which was affecting diagnostic waiting times and RTT targets. Therefore, we observe that estates and financial agreements can generate legacy issues and internal influences, such as a poor or an unsafe working environment.
Characteristics of trusts linked to clear improvement or remaining in Special Measures for Quality/challenged provider regimes
In this section, we provide a summary of characteristics of trusts that have improved and those that remain in SMQ/CP regimes. Table 19 provides an assessment of board maturity18 of four trusts that we studied in depth. This appears to indicate, as expected, that the highest board maturity was evident in the trust with the most sustained improvement. However, an analysis across all eight case studies indicates differing characteristics between the clear improvers and those that had not exited SMQ/CP. These are summarised in Tables 20 and 21.
| Case | ||||
|---|---|---|---|---|
| Board maturity category | 1 (remains challenged) | 3 (sustained improvement) | 4 (improvement evident; exited SMQ) | 6 (some improvement; remains in SMQ) |
| QI as board priority | Medium | High | High | Medium |
| Using data for improvement | High | High | High | Low |
| Familiarity with current performance | High | High | High | High |
| Degree of staff involvement | High | High | High | High |
| Degree of public/patient involvement | Medium | High | Medium | High |
| Clear systematic approach | High | High | High | Medium |
| Balance between clinical effectiveness, patient experience and safety | Medium | High | Medium | Medium |
| Dynamics | Medium | High | High | Medium |
| Example of items discussed and actions (observations and board papers) |
|
|
|
|
| Overall rating | Medium | High | Medium-high | Low-medium |
| Internal factors | External factors |
|---|---|
| More systematic use of data for QI | Established good working relationships with the regulators |
| QI method(s) and dedicated resources (develop new internal capabilities and sustain them, e.g. through ongoing staff training) | Collaborating with external partners and peers |
| Workforce: ensure safe levels and maintain staff engagement and recognition | Have been given time to embed change |
| Integrated quality, financial and risk management with clear lines of accountability | |
| Open, listening improvement culture embedded |
| Internal factors | External factors |
|---|---|
| Instability and churn at senior leadership level | Entered SMQ and CP recently |
| Absence of an organisation-wide QI strategy, methodology and culture | Improvements made but not yet embedded |
| Poor governance and risk management at all levels | Financial pressures in regional health economy |
| Poor staff engagement, retention and issues with harassment and bullying | |
| Outdated equipment and/or deteriorating estate. Lack of investment |
Chapter 8 Impact of Special Measures for Quality/challenged provider regimes on performance trajectories
Overview
This chapter describes the impact of being placed in SMQ/CP regimes from a national perspective, focusing on the analysis of changes in outcomes.
What was known?
-
There is limited previous analysis exploring the overall performance trajectories of trusts entering SMQ/CP regimes.
What this chapter adds
-
Relative to national trends, entry to SMQ/CP regimes corresponded to positive changes in 4-hour waits in EDs, mortality and delayed transfers of care. Trends in sickness and absence improved after trusts left the regimes.
-
There is some evidence that staff survey results improved over the period that trusts were in the regime.
-
The regime appeared to have no influence on RTT times or cancer waiting times.
Background
The aim of this chapter was to quantitatively explore the performance trajectories of trusts that enter either the SMQ or the CP regimes at a national level.
Methods
For the national performance indicators described in Chapter 5, we investigated the impact of SMQ/CP regimes on outcomes and, subsequently, whether or not any such impact was sustained once the trust left the SMQ/CP regime. To carry out this analysis, we divided a trust’s timeline into three:
-
the period before they first entered SMQ or were included on the CP watch list, whichever was the earlier
-
the period in which they were SMQ/CP
-
the period after they left SMQ/CP.
If a trust entered SMQ while in the CP regime, this counted as part of the same period.
We used the z-scoring approach described in Chapter 5 to standardise the deviations from the national trajectory at each point in time, and then used an interrupted time series approach to the z-scores to investigate any changes in trends. Because several trusts were still in SMQ/CP regimes, we applied two models:
-
For trusts that were still in SMQ/CP regimes by September 2019, or had only recently left, the time series had only one change point, which was at the moment when trusts entered the quality regime.
-
For trusts that had left and had more than two data points after leaving, the time series had two change points – one on entry and one on exit.
We then pooled the individual models for each trust using an approach described by Gebski et al. 140 Although the z-scoring approach reduces seasonality, we did find significant autocorrelations over time for some indicators, which we then accounted for by introducing lagged variables.
For the staff survey results, we calculated the deviations from the respective benchmarking group average for each domain on entry and exit and compared the differences in these deviations using a signed rank test. This way, we could test for any improvements that were over and above national improvements in survey results.
Results
Length of time in each regime
Of the trusts that left the SMQ regime, the average time that was spent in the regime was 27 months, with a range from 5 to 49 months (Table 22). Half of the 36 trusts were in SMQ for more than 2 years and four re-entered having previously left. Of the 26 CP trusts that did not enter SMQ, just over half (54%) did not leave CP within 1 year. Half of the trusts in SMQ were previously challenged.
| SMQ trusts (N = 36) | CP trusts that have not entered SMQ (N = 26) |
|---|---|
| 18 trusts (50.0%) had not exited within 24 months | 14 trusts (53.8%) had not exited within 12 months |
| 16 trusts (44.4%) exited within 24 months | 12 trusts (46.2%) exited within 12 months |
| Average time in SMQ = 27 months (range 5–49 months) | Average time as challenged was 14 months (range 2–41 months) |
| Two trusts (5.6%) still under the regime | |
| Four trusts re-enter SMQ, three trusts are subsequently challenged |
Impact on all SMQ/CP trusts
The results of our analysis of changes in trends of indicators before, during and after a period of SMQ/CP are shown in Table 23, which presents results for four different aspects of their trajectories:
| Indicator | Description | Trusts (n) | Value (95% CI) | Interpretation |
|---|---|---|---|---|
| ED: breaches of 4-hour target | Pre-intervention slope | 51 | 0.0054 (−0.0084 to 0.0192) | Similar to national trajectory |
| Change due to intervention | 51 | −0.1942 (−0.3045 to −0.0838) | Improvement | |
| Change in slope during intervention | 51 | −0.0198 (−0.0348 to −0.0048) | Improved trend | |
| Change in slope after intervention, relative to pre-intervention slope | 29 | −0.0648 (−0.1011 to −0.0285) | Improved trend | |
| All cancers: waits longer than 62 days | Pre-intervention slope | 54 | 0.0018 (−0.0023 to 0.0058) | Similar to national trajectory |
| Change due to intervention | 54 | −0.0246 (−0.1347 to 0.0855) | No change | |
| Change in slope during intervention | 54 | 0.0024 (−0.0025 to 0.0074) | No change | |
| Change in slope after intervention, relative to pre-intervention slope | 37 | −0.0072 (−0.0165 to 0.0021) | No change | |
| Skin cancers: waits longer than 62 days | Pre-intervention slope | 53 | 0.0003 (−0.0042 to 0.0048) | Similar to national trajectory |
| Change due to intervention | 53 | −0.0401 (−0.1612 to 0.0809) | No change | |
| Change in slope during intervention | 53 | −0.0017 (−0.0072 to 0.0038) | No change | |
| Change in slope after intervention, relative to pre-intervention slope | 37 | −0.0093 (−0.0202 to 0.0017) | No change | |
| Consultants as a proportion of doctors | Pre-intervention slope | 43 | −0.0019 (−0.0044 to 0.0005) | Similar to national trajectory |
| Change due to intervention | 43 | 0.0312 (−0.0173 to 0.0797) | No change | |
| Change in slope during intervention | 43 | −0.0036 (−0.0063 to 0.0009) | Decreasing% of consultants | |
| Change in slope after intervention, relative to pre-intervention slope | 25 | −0.0010 (−0.0081 to 0.0061) | No change | |
| Delayed transfers of care | Pre-intervention slope | 53 | 0.0085 (0.0046 to 0.0123) | Worse than national trajectory |
| Change due to intervention | 53 | −0.1114 (−0.1889 to −0.0339) | Improvement | |
| Change in slope during intervention | 53 | −0.0009 (−0.0049 to 0.0031) | No change in trajectory | |
| Change in slope after intervention, relative to pre-intervention slope | 34 | 0.0050 (−0.0025 to 0.0126) | No change | |
| Nurses as a proportion of all doctors and nurses | Pre-intervention slope | 43 | −0.0003 (−0.0018 to 0.0012) | Similar to national trajectory |
| Change due to intervention | 43 | −0.0028 (−0.0289 to 0.0232) | No change | |
| Change in slope during intervention | 43 | −0.0027 (−0.0044 to −0.0011) | Decreasing% of nurses | |
| Change in slope after intervention, relative to pre-intervention slope | 25 | 0.0076 (0.0035 to 0.0118) | Increasing% of nurses | |
| RTT | Pre-intervention slope | 53 | 0.0174 (0.0149 to 0.0200) | Worse than national trajectory |
| Change due to intervention | 53 | 0.0067 (−0.0398 to 0.0532) | No change | |
| Change in slope during intervention | 53 | 0.0022 (−0.0009 to 0.0053) | No change | |
| Change in slope after intervention, relative to pre-intervention slope | 36 | 0.0026 (−0.0096 to 0.0148) | No change | |
| Mortality: SHMI | Pre-intervention slope | 51 | −0.0032 (−0.0154 to 0.0089) | Similar to national trajectory |
| Change due to intervention | 51 | −0.0975 (−0.1835 to −0.0114) | Improvement | |
| Change in slope during intervention | 51 | −0.0207 (−0.0339 to −0.0075) | Improved trend | |
| Change in slope after intervention, relative to pre-intervention slope | 29 | −0.0259 (−0.0616 to 0.0099) | No change | |
| Sickness absence | Pre-intervention slope | 51 | 0.0043 (0.0012 to 0.0075) | Worse than national trajectory |
| Change due to intervention | 51 | −0.0263 (−0.1008 to 0.0481) | No change | |
| Change in slope during intervention | 51 | −0.0020 (−0.0053 to 0.0012) | No change | |
| Change in slope after intervention, relative to pre-intervention slope | 29 | −0.0102 (−0.0174 to −0.0031) | Improved trend | |
| Emergency caesarean section rates | Pre-intervention slope | 54 | −0.0063 (−0.0103, −0.0023) | Better than national trajectory |
| Change due to intervention | 54 | 0.1196 (0.0166 to 0.2226) | Increase | |
| Change in slope during intervention | 54 | 0.0007 (−0.0036 to 0.0050) | No change in previous trajectory | |
| Change in slope after intervention, relative to | 38 | 0.0071 (−0.0013 to 0.0155) | No change in trajectory | |
| pre-intervention slope |
-
pre-intervention slope – how trends in the indicator compare with national trends before entry to SMQ/CP
-
change due to intervention – a measure of how values of the indicator change after trusts enter SMQ/CP relative to national values
-
change in slope during the intervention – a measure of how the trajectory changes while trusts are in SMQ/CP
-
change in slope after the intervention – a measure of how the trajectory changes after a trust leaves the regime compared with what the trajectory was before it entered.
For three of these indicators (RTT time, delayed transfers of care and sickness absence), trends were significantly worse than the national trajectory before trusts entered the SMQ or CP regime for the first time. After entering the SMQ/CP regimes, trends significantly improved for ED waits and mortality, and there were significant improvements without changes in trend for delayed transfers of care. For mortality, trends also improved, even when excluding the initial 11 Keogh trusts that entered SMQ in July 2013.
There is evidence that trends in ED waits and sickness absence improved after the period in SMQ/CP. There is no evidence of trends in RTT times or cancer waits being affected by the regime. Moreover, in the case of the former, trends were worse than average before they enter. Conversely, trends in emergency caesarean section rates were improving for the SMQ/CP trusts when they entered the regime but then appeared to increase.
Proportions of consultants declined relative to national trends after trusts entered the quality regime. In addition, while in SMQ/CP, the doctor to nurse ratio increased, although this was not sustained.
The impact on the staff survey results is shown in Table 24. The number of trusts with survey results corresponding to both year of entry and year of exit is relatively small. However, allowing for general improvements in staff survey results over recent years, there are significant improvements in five of the nine domains.
| Domain | Trusts (n) | Difference in difference from the mean survey result between entry and exit | p-value |
|---|---|---|---|
| Staff engagement | 17 | 0.13 | 0.02 |
| Equality, diversity and inclusion | 17 | 0.05 | 0.19 |
| Health and well-being | 14 | 0.16 | 0.04 |
| Immediate managers | 14 | 0.16 | 0.03 |
| Quality of appraisals | 14 | 0.21 | 0.03 |
| Quality of care | 14 | 0.09 | 0.08 |
| Safe environment: bullying and harassment | 14 | 0.05 | 0.38 |
| Safe environment: violence | 14 | 0.01 | 0.79 |
| Safety culture | 14 | 0.22 | 0.01 |
Impact on case study sites
For the eight individual case study sites, outcomes against tested performance indicators are shown in Table 25. These show some evidence of individual trusts improving with respect to ED waiting, waiting times for skin cancer, delayed transfers of care, mortality and sickness absence. However, there are some trusts for which outcomes appear to have worsened once entering the regime. Notably, there is no evidence of any improvements with respect to RTT or 62-day waits for all cancers as a group.
| Indicator | Outcomes after intervention starts (all significant at the 5% level: two tailed) |
|---|---|
| ED 4-hour breaches |
|
| Cancer 62-day waits |
|
| Skin cancers 62-day waits |
|
| Delayed transfers of care |
|
| Referral for treatment waits of 18 weeks or more |
|
| Mortality: SHMI |
|
| Sickness absence |
|
| Caesarean sections |
|
Chapter 9 Cost–consequences analysis
Overview
This chapter describes a CCA to quantify the costs and benefits of different combinations of NHS Improvement interventions used in the SMQ/CP regimes.
What was known?
-
Very few studies have addressed the costs and consequences of improvement interventions in health, education and local government settings (see Chapter 3).
-
The relative costs of the NHS Improvement interventions and their consequences have not been previously evaluated.
What this chapter adds
-
At the national level, during 2018–19, the mean funds spent on trusts was £388,259 (n = 19) for trusts under the SMQ regime and £173,625 for trusts under the CP regime (n = 23). An additional £100,000 was earmarked for each trust leaving the SMQ regime (n = 4). A mean of £61,134 was spent on peer improvement for all 42 trusts under SMQ/CP regimes.
-
The largest components of NHS Improvement spending for our case studies were identified as interventions directed at ‘training on cultural change’ (33.6%), ‘workforce quality and safety’ (21.7%) and ‘governance and assurance’ (18.4%).
-
Only 15.8% of SMQ trusts exited the regime within 24 months (and did not re-enter within the next 12 months) and 65.2% of CP trusts left the CP regime after 12 months (and did not re-enter within the next 12 months).
-
The interventions delivered to trusts as part of the SMQ/CP regimes show a positive effect on staff-based measures (e.g. ‘support to staff from immediate managers’, ‘quality of staff’s appraisals’, ‘staff engagement’ and ‘staff’s experiences with safety’), while there were less improvements in the context of ‘promotion of staff’s health and well-being’, ‘staff’s satisfaction with quality of care’ or ‘organisation’s actions on quality, diversity and inclusion’.
-
The findings on the effect of SMQ/CP regimes on financial stability are not clear-cut. Most trusts that exited SMQ (68.4% of the ‘exiting’ group) experienced the same financial stability before and after exiting, although this share was lower for the group still remaining in the regime (46.2% of the ‘remaining’ group). In fact, none of the trusts in this ‘remaining’ group experienced an increase in the financial stability, whereas about 10.5% of the ‘exiting’ group did.
Background
The aim of the economic analysis was to quantify the costs and benefits of different combinations of NHS Improvement interventions used in the SMQ/CP regimes from an NHS perspective, using a CCA approach. The RQ that we addressed was, what are the relative costs of the interventions in the SMQ/CP regimes and how do these compare with their benefits/consequences? The interventions delivered to trusts in SMQ/CP regimes vary from one trust to another depending on their circumstances and needs. However, there are four common interventions: (1) the appointment of an ID, (2) a review of the trust’s leadership capability, (3) access to funds for QI and (4) a plan for improvement, including options for diagnostic work on assessing medical engagement, buddying with other trusts and commissioning external expertise. The CCA has considered these interventions depending on the availability of information, with financial information available from 2017.
Methods
A CCA is a method of health economic evaluation in which all costs, both direct and indirect, and a catalogue of different consequences of all alternatives are computed and listed separately without aggregating these results into a cost-effectiveness ratio. 141,142 This approach allows quantification of findings and process measures and compares them with the costs of particular interventions. This in turn allows researchers to get more insights on both potential costs and consequences of the intervention in a range of different dimensions. Note that, in the present study, given the small number of trusts included, the study evaluated the costs and consequences of different combinations of interventions only, not of each intervention individually. For this type of analysis, costs and outcomes have not been discounted because no modelling is involved.
Measuring costs
Direct costs
Data on intervention costs were analysed at two different levels: (1) national level and (2) across our eight individual case studies. To have a comparable time frame between the national-level analysis and the case study analysis, for the former we have kept only the trusts that were active (under the regime) during the period 2017–19. This has reduced the number of trusts in the national-level analysis from 62 to 42. Note that financial information at the national level was also available for this time period, which was another reason for choosing this approach. Of the 42 trusts in our national-level analysis, 19 trusts were in the SMQ regime and 23 trusts in the CP regime. The national-level financial data were limited to aggregate level for the following categories: (1) data for all SMQs trusts, (2) support for exited SMQs trusts, (3) CP trusts and (4) peer improvement. The peer improvement funding is for buddy trusts supporting a SMQ or CP trust. Funding is allocated based on a fully costed funding proposal submitted by trusts, setting out benefits to be achieved and approved by the MD/chief operating officer.
At the case-study level, trusts are categorised into four groups: (1) the prolonged poor performers, (2) poor performers, (3) shorter-term CPs and (4) clear performance improvers, following the performance trajectories set out earlier in this study (see Chapter 2). Given that the case studies in group 4 had received funding prior to 2017, we had to exclude them from the CCA because financial data were unavailable (NHS Improvement could provide financial data going back to 2017 only). The budgets and spending data for the selected case studies are grouped following five distinctive categories, as per the CQC framework: (1) care improvement, (2) workforce quality and safety, (3) QI training, (4) training on cultural change and (5) focus on governance and assurance (Table 26).
| Key lines of enquiry for healthcare services | What does it mean |
|---|---|
| Safe | People are protected from abuse and avoidable harm |
| Effective | People’s care, treatment and support achieves good outcomes, promotes a good quality of life and is based on the best available evidence |
| Caring | The service involves and treats people with compassion, kindness, dignity and respect |
| Responsive | Services meet people’s needs |
| Well-led | The leadership, management and governance of the organisation assures the delivery of high-quality and person-centred care, supports learning and innovation, and promotes an open and fair culture |
Ideally, the opportunity costs to be considered in our analysis would include all of the costs that were incurred because the trust was under the SMQ or CP regimes and that otherwise would not have been incurred. Such opportunity costs would include:
-
Costs that are related to additional meetings and additional training (in terms of productivity lost to participate) because of the SMQ or CP regime. The staff of the trusts under the SMQ or CP regimes have more meetings as part of drafting and implementing QI strategies and plans and, therefore, more time is lost from other activities.
-
The SMQ or CP trusts incur more inspections (resulting again in time lost from other productive activities).
-
Staff turnover in SMQ or CP trusts may also mean that more time is spent on advertising and hiring new staff.
-
Additional external audits may need to be undertaken for SMQ or CP trusts, which again contributes to costs that would otherwise not have been incurred.
-
Despite the added value that a separate analysis of opportunity costs would have brought, unfortunately, data limitations did not allow us to quantify such costs.
Measuring consequences
Two types of consequences are considered in this study: primary consequences (relating to the entry and exit of the trusts in the SMQ and CP regimes) and secondary consequences (relating to staff experiences, internal quality changes within the trusts and the trust’s financial stability). Given the aims of the regimes for trusts to exit SMQ within 24 months and CP within 12 months from the date of entry, the two primary consequences considered here are (1) exiting the SMQ regime within 24 months and not re-entering the SMQ or CP within the next 12 months, and (2) exiting the CP regime within 12 months and not re-entering CP or SMQ within the next 12 months.
The secondary consequences indicating staff experience and the internal quality changes after the intervention are derived from the NHS staff survey 2014–18138 and are organised under nine different themes (see Appendix 7). All themes are scored on a 0- to 10-point scale and reported here as mean scores. A higher score always indicates a more favourable result. Each theme includes between three and nine statements/questions.
In addition, a tenth secondary consequence on financial stability measures the financial performance of trusts on a scale from 1 to 4, where 1 reflects the strongest performance and 4 the weakest (based on the NHS Improvement – Quality Tracker). To determine if trusts under the SMQ/CP regimes became financially stable, we have chosen a threshold where those trusts that scored from 1 to 3 are considered to be financially stable and those scoring 4 are considered not to be. The choice of this threshold was based on the observed data, given that about 90% of the trusts under the SMQ/CP regimes had a score of 3 or 4.
Results
Costs
Direct costs
Table 27 presents planned budgets and expenditures associated with the SMQ/CP interventions both at the national level and for our case studies. The mean total of directly allocated funds spent per SMQ participating trust at the national level was £388,259 (this was £32,794 lower than the planned budget) and for CP trusts they were £173,625 (£69,277 more than the planned budget). The mean funds spent to support exited SMQs trusts were £80,000 and mean funds spent for the peer improvement programme were £61,134 per participating trust.
| Description | Average NHS Improvement budget, 2018/19 (£) | Average NHS Improvement funds spent, 2018/19 (£) | Difference (£) |
|---|---|---|---|
| National level (n = 42) a | |||
| SMQ trusts (n = 19) | 421,053 | 388,259 | 32,794 |
| CP trusts (n = 23) | 104,348 | 173,625 | −69,277 |
| Support to exited SMQ trusts (n = 5) | 100,000 | 80,000 | 20,000 |
| Peer improvement (n= 42) | 101,190 | 61,134 | 40,056 |
| Selected case studies (n = 5) | |||
| Prolonged poor performers (SMQ) (n = 2) | |||
| Average | 482,786 (56,871) | 443,611 (47,219) | 39,175 (9652) |
| Minimum | 442,572 | 410,222 | 32,350 |
| Maximum | 523,000 | 477,000 | 46,000 |
| Interquartile range | 40,214 | 33,389 | 6825 |
| Poor performers (CP and SMQ) (n = 1)b | |||
| Average | 499,130 (−) | 460,226 (−) | 38,904 (−) |
| Minimum | 499,130 | 460,226 | 38,904 |
| Maximum | 499,130 | 460,226 | 38,904 |
| Interquartile range | – | – | – |
| Shorter-term challenged providers (CP) (n = 2) | |||
| Average | 190,260 (1570) | 190,260 (1570) | 0.00 (0.00) |
| Minimum | 189,150 | 189,150 | 0.00 |
| Maximum | 191,370 | 191,370 | 0.00 |
| Interquartile range | 1110 | 1110 | 0.00 |
At the case study level, the average NHS Improvement funds spent on prolonged poor performers was £443,611 (£39,175 less than the planned budget), for poor performers this was £460,226 (£38,904 less than the budget) and for shorter-term CPs £190,260 (same as the budgeted amount). It should be noted that these averages are based on only five trusts in total, given the low availability of financial data. This limits the level of generalisability of the financial data by performance groups.
Table 28 details the NHS Improvement actual funds spent for our selected case studies. The majority of funds were spent on ‘training on cultural change’ (33.6%). This category included funds spent on various activities, such as (1) training and support engagement and implementation of the QI methodology; (2) training of clinical directors in understanding of their leadership and corporate responsibilities; (3) support to use Manchester Patient Safety Framework; (4) develop training materials for anti-bullying programme(s); (5) development of new advanced care practitioners; and (6) support on a ward accreditation programme.
| NHS Improvement funds that were awarded (by year) | Prolonged poor performers (SMQ) (n = 2) |
Poor performers (CP and SMQ) (n = 1) |
Shorter-term challenged providers (CP) (n = 2) | Per cent of the total NHS Improvement awarded fund |
|---|---|---|---|---|
| Care improvement | 104,000 | 59,129 | 89,400 | 14.6 |
| Workforce quality and safety | 294,621 | – | 79,750 | 21.7 |
| QI training | 95,000 | – | 106,370 | 11.7 |
| Training on cultural change | 393,601 | 122,700 | 65,000 | 33.6 |
| Focus on governance and assurance | – | 278,397 | 40,000 | 18.4 |
| Total | 887,222 | 460,226 | 380,520 | 1,727,968 |
Other categories of spending were improvements in ‘workforce quality and safety’ (21.7%) and interventions focusing on ‘governance and assurance’ (18.4%). Table 28 also shows that the current NHS Improvement funds spent on ‘care improvement’ are relatively smaller than the funds spent in other areas. The smaller investment here may also partially explain the mixed impacts that are related to patient benefit indicators, with our analysis of performance trajectories suggesting mixed impacts on patient access (see Table 25). Where there appear to be relative improvements in (1) ED 4-hour waits and (2) the delayed transfers of care (while the trust was in the SMQ or CP regime) we found worsening of 62-day cancer waiting times (despite the spending of that particular trust on care improvement). Although our sample here is small (and indicators are limited), our findings suggest that more sustainable funds need to be spent to improve patients’ outcomes. We should also note the large variability among the performance groups, which may be because of small numbers of trusts in each group.
Consequences
Primary consequences
Of the 42 trusts that were under the SMQ regime in 2017, only 15.8% exited the regime within 24 months and did not re-enter within the next 12 months (the ‘exited’ trusts), while 73.7% of the trusts were in the regime for more than 24 months (the ‘remaining’ trusts) (see Table 31). In the case of the remaining 10.5% of trusts, the primary consequences are unknown because they were still under the SMQ regime but for less than 24 months.
In terms of CP trusts, at the national level, the majority of the CP trusts, 65.2% (15 out of 23 trusts), exited this regime within 12 months and did not re-enter within the next 12 months, and only 34.8% of the trusts remained in the CP regime for more than 12 months.
In total, 73.7% of the trusts in the SMQ regime ‘remained’ in SMQ for more than 24 months, whereas for CP trusts this rate was 34.8% after 12 months (Table 29). The differences between SMQ and CP regimes may be explained by the extent of the quality failures that resulted in the trusts entering the regimes (by definition, trusts in the SMQ regime have a higher degree of quality failure and this may make it more difficult to get out of the regime). However, more analysis is needed in terms of better understanding both the determinants of the time spent in the regime and the association between particular regimes and the exit rates (especially as trusts may still fall back into the regimes again).
| Regime | Reason |
|---|---|
| 1. SMQ (n = 19) |
|
| 1. CP (n = 23) |
|
Secondary consequences
Table 30 gives the average scores for SMQ trusts across the nine themes from NHS staff survey data both at the national level and for our selected case studies. The ‘before’ observations correspond to the year before entering SMQ/CP regimes whereas the ‘after’ observations correspond to the year after exiting the SMQ/CP regimes (for the trusts still remaining in the SMQ, the last year of the data survey was 2018).
| Mean (SD) score of the ‘exiting’ trusts | Mean (SD) score of the ‘remaining’ trusts | |||||
|---|---|---|---|---|---|---|
| Description | Before | After | Difference | Before | After | Difference |
| Staff engagement (higher score = a more favourable result) | ||||||
| National level | 6.72 (0.60) | 6.81 (0.35) | 0.08 (0.41) | 6.81 (0.18) | 6.70 (0.20) | −0.08 (0.21) |
| Prolonged poor performers (SMQ) | 6.60 (−) | 6.70 (−) | 0.10 (−) | 6.70 (−) | 6.50 (−) | −0.20 (−) |
| Poor performers (CP and SMQ) | 6.80 (−) | 6.90 (−) | 0.10 (−) | 6.90 (−) | 6.80 (−) | −0.10 (−) |
| Shorter-term challenged providers (CP) | – | – | – | 7.00 (0.14) | 6.90 (0.00) | −0.10 (0.14) |
| Organisation’s actions on quality, diversity and inclusion (higher score = a more favourable result) | ||||||
| National level | 8.91 (0.44) | 8.84 (0.40) | −0.07 (0.14) | 8.96 (0.33) | 8.86 (0.30) | −0.09 (0.12) |
| Prolonged poor performers (SMQ) | 9.00 (−) | 9.00 (−) | 0.00 (−) | 9.20 (−) | 9.00 (−) | −0.20 (−) |
| Poor performers (CP and SMQ) | 9.10 (−) | 8.90 (−) | −0.20 (−) | 9.10 (−) | 9.10 (−) | 0.00 (−) |
| Shorter-term challenged providers (CP) | – | – | – | 8.50 (0.28) | 8.45 (0.21) | −0.05 (0.07) |
| Promotion of staff’s health and well-being (higher score = a more favourable result) | ||||||
| National level | 5.73 (0.53) | 5.63 (0.43) | −0.07 (0.24) | 5.85 (0.23) | 5.68 (0.20) | −0.14 (0.17) |
| Prolonged poor performers (SMQ) | 5.73 (−) | 5.63 (−) | 0.00 (−) | 5.70 (−) | 5.50 (−) | −0.20 (−) |
| Poor performers (CP and SMQ) | 5.50 (−) | 5.70 (−) | 0.20 (−) | 6.20 (−) | 6.00 (−) | −0.20 (−) |
| Shorter-term challenged providers (CP) | – | – | – | 5.85 (0.35) | 5.65 (0.21) | −0.20 (0.14) |
| Support to staff from immediate managers (higher score = a more favourable result) | ||||||
| National level | 6.56 (0.52) | 6.70 (0.43) | 0.15 (0.32) | 6.55 (0.22) | 6.52 (0.20) | −0.01 (0.17) |
| Prolonged poor performers (SMQ) | 6.50 (−) | 6.70 (−) | 0.20 (−) | 6.50 (−) | 6.40 (−) | −0.10 (−) |
| Poor performers (CP and SMQ) | 6.40 (−) | 6.80 (−) | 0.40 (−) | 6.50 (−) | 6.50 (−) | 0.00 (−) |
| Shorter-term challenged providers (CP) | – | – | – | 6.60 (0.14) | 6.55 (0.07) | −0.05 (0.07) |
| Quality of staff’s appraisals (higher score = a more favourable result) | ||||||
| National level | 5.10 (0.57) | 5.37 (0.45) | 0.24 (0.40) | 5.13 (0.42) | 5.21 (0.41) | 0.10 (0.29) |
| Prolonged poor performers (SMQ) | 5.00 (−) | 5.40 (−) | 0.40 (−) | 4.80 (−) | 4.60 (−) | −0.20 (−) |
| Poor performers (CP and SMQ) | 4.30 (−) | 5.30 (−) | 1.00 (−) | 5.30 (−) | 5.40 (−) | 0.10 (−) |
| Shorter-term challenged providers (CP) | – | – | – | 6.65 (0.07) | 5.55 (0.21) | −0.10 (0.28) |
| Staff’s satisfaction with quality of care (higher score = a more favourable result) | ||||||
| National level | 7.37 (0.23) | 7.35 (0.20) | −0.02 (0.17) | 7.38 (0.19) | 7.23 (0.22) | −0.12 (0.16) |
| Prolonged poor performers (SMQ) | 7.30 (0.00) | 7.30 (0.00) | 0.00 (0.00) | 7.40 (0.00) | 7.20 (0.00) | −0.20 (0.00) |
| Poor performers (CP and SMQ) | 7.30 (0.00) | 7.30 (0.00) | 0.00 (0.00) | 7.30 (0.00) | 7.10 (0.00) | −0.20 (0.00) |
| Shorter-term challenged providers (CP) | – | – | – | 7.55 (0.07) | 7.40 (0.00) | −0.15 (0.07) |
| Staff’s experiences with bullying & harassment (lower score = more favourable result) | ||||||
| National level | 7.78 (0.50) | 7.70 (0.40) | −0.04 (0.20) | 7.77 (0.26) | 7.66 (0.21) | −0.07 (0.21) |
| Prolonged poor performers (SMQ) | 7.70 (−) | 7.80 (−) | 0.10 (−) | 8.10 (−) | 7.60 (−) | −0.50 (−) |
| Poor performers (CP and SMQ) | 7.60 (−) | 7.80 (−) | 0.20 (−) | 7.80 (−) | 7.70 (−) | −0.10 (−) |
| Shorter-term challenged providers (CP) | – | – | – | 7.65 (0.21) | 7.55 (0.21) | −0.10 (0.00) |
| Staff’s experiences with violence (lower score = more favourable result) | ||||||
| National level | 9.32 (0.28) | 9.35 (0.23) | 0.04 (0.11) | 9.37 (0.14) | 9.39 (0.10) | 0.02 (0.11) |
| Prolonged poor performers (SMQ) | 9.20 (−) | 9.40 (−) | 0.20 (−) | 9.30 (−) | 9.40 (−) | 0.10 (−) |
| Poor performers (CP and SMQ) | 9.30 (−) | 9.40 (−) | 0.10 (−) | 9.50 (−) | 9.50 (−) | 0.00 (−) |
| Shorter-term challenged providers (CP) | – | – | – | 9.40 (0.00) | 9.40 (0.00) | 0.00 (0.00) |
| Staff’s experiences with safety (higher score = a more favourable result) | ||||||
| National level | 6.43 (0.42) | 6.52 (0.25) | 0.10 (0.31) | 6.34 (0.19) | 6.31 (0.24) | −0.02 (0.23) |
| Prolonged poor performers (SMQ) | 6.10 (−) | 6.40 (−) | 0.30 (−) | 6.40 (−) | 6.20 (−) | −0.20 (−) |
| Poor performers (CP and SMQ) | 6.40 (−) | 6.60 (−) | 0.20 (−) | 6.50 (−) | 6.40 (−) | −0.10 (−) |
| Shorter-term challenged providers (CP) | – | – | – | 6.50 (0.00) | 6.40 (0.14) | −0.10 (0.14) |
Generally, our results show that the SMQ/CP regimes had a positive effect on staff survey indicators. This is evident if we compare the differences in the mean scores before entering the regime with those after entering the regime between the trusts that have ‘exited’ the SMQ/CP regimes and the ‘remaining’ trusts. Such positive effects are generally consistent among both trusts at the national level and for each case study groups.
Table 31 shows the percentage of the trusts at the national level experiencing a change in staff survey indicators (i.e. decreasing, maintaining the same or increasing in the mean score value) before entering the SMQ/CP regimes and after exiting. The thematic fields are ranked in the descending order for a positive change (the ‘Increase’ column in Table 31) for the ‘exiting’ group.
| NHS staff survey indicators | ‘Exiting’ trusts (n = 25) (%) | ‘Remaining’ trusts (n = 17) (%) | ||||
|---|---|---|---|---|---|---|
| Decrease | Same | Increase | Decrease | Same | Increase | |
| Quality of staff’s appraisals | 24.0 | 20.0 | 56.0 | 35.3 | 17.6 | 47.1 |
| Support to staff from immediate managers | 32.0 | 16.0 | 52.0 | 47.1 | 23.5 | 29.4 |
| Staff’s experiences with safety | 28.0 | 24.0 | 48.0 | 47.1 | 17.6 | 35.3 |
| Staff engagement | 36.0 | 20.0 | 44.0 | 64.7 | 23.5 | 11.8 |
| Staff’s experiences with violence | 16.0 | 40.0 | 44.0 | 23.5 | 52.9 | 23.5 |
| Staff’s experiences with bullying and harassment | 48.0 | 24.0 | 28.0 | 52.9 | 17.6 | 29.4 |
| Promotion of staff’s health and well-being | 52.0 | 20.0 | 28.0 | 70.6 | 11.8 | 17.6 |
| Staff’s satisfaction with quality of care | 44.0 | 36.0 | 20.0 | 64.7 | 23.5 | 11.8 |
| Organisation’s actions on quality, diversity and inclusion | 60.0 | 28.0 | 12.0 | 58.8 | 35.3 | 5.9 |
Table 31 shows that the percentage of trusts experiencing a positive change in staff survey scores after being in the SMQ/CP regimes is consistently higher in the ‘exiting’ group than in the ‘remaining’ group. Hence, the highest share of trusts with a positive change in the period ‘after’ was for ‘quality of staff’s appraisals’ (56% of the ‘exiting’ group and 41% of ‘remaining’ group) and ‘support to staff from immediate managers’ (52% of the ‘exiting’ group and 29.4% of ‘remaining’ group). This indicates that the immediate interventions to improve on the management have had a considerable effect and that this effect was especially enhanced in those trusts that have exited from the SMQ/CP regimes on time.
About 44% of trusts in the ‘exiting’ group have had a positive change in ‘staff engagement’ scores (see Table 31). This indicates the likelihood of a positive effect of the SMQ/CP regime interventions on organisational culture and the orientation towards results. On the other hand, when looking at the differences in scores for the ‘remaining’ group, this is negative both at the national level and for ‘prolonged poor performers’, ‘short-term challenged’ and ‘shorter-term challenged providers’. It may be that the work pressures for staff in these trusts to perform routine jobs were greater and there was less emphasis on motivation of staff.
Although being under SMQ/CP regimes led to improvements with respect to the staff-based indicators (e.g. ‘support to staff from immediate managers’, ‘quality of staff’s appraisals’, ‘staff engagement’, ‘staff’s experiences with safety’ and ‘staff’s experiences with bullying and harassment’), this is not so for other non-staff-based indicators, such as the staff’s satisfaction with quality of care, for which only 20% of ‘exiting’ trusts and 11.8% of the ‘remaining’ trusts at the national level have had an improvement for the period 2018–19. Looking at the mean scores, we can observe that, although there is no positive change in both the ‘exiting’ and ‘remaining’ groups, the before/after difference is much lower for the ‘exiting’ group of trusts. Therefore, although these findings question the overall effect of the SMQ/CP regimes on the quality of care (at least from staff’s perspective), they also show that there is a lesser negative effect for the ‘exiting’ trusts.
Only 12% of the ‘exiting’ trusts at the national level have had a positive impact on the ‘organisation’s actions on quality, diversity and inclusion’ indicator (see Table 31), indicating that a culture of inclusion in decision-making requires time and perhaps continuous training and staff education. The results also show that there was a decrease in terms of ‘staff’s experiences with bullying and harassment’ but an increase in the number of ‘staff’s experiences with violence’. Table 31 shows that, in fact, a larger share of the ‘exiting’ trusts (48%) had an increase in the ‘staff’s experiences with bullying and harassment’. This may be because the eradication of bullying would demand a culture change that can be more difficult and can take longer to achieve than the timelines used for the analysis.
The same holds for the ‘promotion of staff’s health and well-being’ indicator, for which only 28% of ‘exiting’ trusts and 17.6% of the ‘remaining’ trusts at the national level have experienced an improvement (see Table 31). This also holds for the case study trusts for which the change in scores is very low or zero for the ‘exiting’ trusts and negative for the ‘remaining’ trusts. It can be that in improving quality of a poorly performing trust the main efforts go first in improving management and leadership and improving patient care quality, while the health and wellbeing of staff may be ranked as secondary objectives. This again calls for more attention to such indicators given that the health and well-being of staff is a crucial component that impacts directly on the performance and other quality indicators.
Financial stability
Table 32 gives the average scores for the ‘exiting’ and ‘remaining’ trusts on the financial stability before entering and after leaving the SMQ/CP regime. The figures show that for both groups there was a decrease in the mean scores over time meaning that financial stability decreases after the trust goes into the SMQ/CP regime. However, it can also be noted that the decline is smaller for the ‘exiting’ trusts.
| Description | Mean (SD) score of the ‘exiting’ trusts | Mean (SD) score of the ‘remaining’ trusts | ||||
|---|---|---|---|---|---|---|
| Before | After | Difference | Before | After | Difference | |
| National level | 2.05 (0.62) | 1.95 (0.52) | −0.11 (0.57) | 1.92 (0.49) | 1.38 (0.51) | −0.54 (0.52) |
| Prolonged poor performers (SMQ) | – | – | – | 2.0 (−) | 1.0 (−) | −1.0 (−) |
| Poor performers (CP and SMQ) | 1.00 (−) | 2.00 (−) | 1.00 (−) | 2.0 (−) | 1.0 (−) | −1.0 (−) |
| Shorter-term CPs | – | – | – | 2.00 (0.00) | 2.00 (0.00) | 0.00 (0.00) |
Table 33 details further the share of trusts as per their change in financial stability (i.e. decreased, maintained or increased) after entering the SMQ/CP regime. The table shows that for 68.4% of the ‘exiting’ trusts (13 out of 19) the financial stability remained the same, whereas for 21.1% (four trusts) it decreased and for 10.5% (two trusts) it increased. For the ‘remaining’ trusts the situation looks much worse, for which 53.8% of the trusts had a decrease in financial stability, with 46.2% staying at the same level. A similar effect is also seen for the trusts in the different performance groups, although the number of trusts here is too small for meaningful interpretations (see Table 33).
| Description | Financial stability of the ‘exiting’ trust group | Financial stability of the ‘remaining’ trust group | ||||
|---|---|---|---|---|---|---|
| Decrease | Same | Increase | Decrease | Same | Increase | |
| National level (19/13) | 21.1% | 68.4% | 10.5% | 53.8% | 46.2% | 0.0% |
| Prolonged poor performers (SMQ) (n = 1) | – | – | – | 100% (1) | – | – |
| Poor performers (CP and SMQ) (n = 1) | – | – | 100% (1) | 100% (1) | – | – |
| Shorter-term CPs (n = 2) | – | – | – | – | 100% (2) | – |
Chapter 10 Insights, lessons and advice from participants
Overview
This chapter describes the insights, lessons and advice that the interview participants in the case studies put forward for their peers and for regulators and policy-makers based on their experiences of the SMQ/CP regimes.
What was known?
-
There is limited qualitative evidence regarding direct experiences of the SMQ/CP regimes and the factors felt to be most helpful for making improvements and for sustaining change.
What this chapter adds
-
Lessons for health-care providers, staff and health system leaders suggested by participants to support sustainable change were prioritising staff, stable and mature leadership, building healthy relationships with the regulators, and consideration of improvement at a system level.
-
Lessons for regulators and policy-makers suggested by participants to support sustainable change were to address the emotional cost of SMQ/CP, deliver trust-specific support, avoid duplicate reporting, recognise that longer timelines are needed to embed change and provide system-level support.
Background
The implicit goal of the SMQ/CP regimes is to support trusts to address the quality concerns raised following CQC inspections. The quality issues, the interventions that NHS Improvement provide and the trust response vary between trusts. As a result, trusts and their external partners have differing experiences of SMQ/CP. In this chapter, we focus on participants’ reflections on their experiences of SMQ/CP and their suggestions of lessons learnt and advice for others.
Methods
The semistructured interviews conducted with internal and external participants at the eight case study trusts were drawn on for the findings described in this chapter. The full interviews were considered when drawing out lessons, with particular attention given to responses to a question in the topic guide (see Appendix 1) that specifically asked participants for their advice for other organisations seeking to improve their performance. Participants came from a range of backgrounds, including CEOs, directors of nursing, medical directors, front-line staff and external stakeholders from Healthwatch and CCGs (see Table 6).
Results
Insights for health-care providers, staff and health system leaders
Insights for health-care providers, staff and health system leaders were organised in the following themes:
-
Staff need to be considered the top priority.
-
Stable and mature leadership is required to make sustainable changes.
-
Improvement depends on the capacity to develop healthy relationships with the regulators.
-
Improvement needs to be considered at a system level through partnerships and collaboration with other organisations.
All of the trusts in the study had carried out some work on staff engagement or morale. Participants talked frequently about the importance of ‘putting staff first’ and ‘considering their needs’. A dominant assumption was that if staff were involved in identifying the changes that needed to be made, then they would experience greater ownership over them, participating in the implementation and sustainability of improvement. It was noted that both senior and front-line staff need protected time to undertake improvement work and cannot be expected to do this work on top of their usual workloads.
Interview participants also argued that trusts in SMQ or CP regimes needed to make sure that they directed their efforts at developing mature leadership teams who could remain in leadership roles throughout the implementation of the changes. Two main aspects of leadership were highlighted: (1) leadership needed to be mature and experienced enough to deal with the demands made by regulators in the light of the operational pressures prevalent in the own organisations (i.e. financial deficit, capacity issues, etc.), and (2) leaders needed to remain in the organisations or in leadership roles long enough to see the changes through. The first point entailed developing collaborative relationships with the regulators, but also knowing when to push back if demands were considered unhelpful or unrealistic. It was also related to the capacity of leadership teams to move beyond the point-by-point recommendations made by organisations, such as CQC and NHS Improvement, to the development of trust-wide improvement strategies.
The continuity of leadership teams was outlined as an issue in the light of local contexts heavily shaped by staff turnover. Some of the trusts included in our study had suffered a complete restructure of senior leadership teams and trust boards or had gone through multiple CEOs in a short amount of time. This was an issue recognised at the trust level, as well as at a more regional level by CCGs and NHS England and NHS Improvement regional representatives. There were discussions around the need to ‘protect CEOs’ to allow for this continuity and make sure planned changes were implemented. Related to this, trust leaders saw a benefit in developing collaborative and healthy relationships with the regulators by seeing them as a source of support or as ‘critical friends’.
Despite the fact that most NHS Improvement interventions had an organisational-level focus (with the exception of buddying), several trusts and CCG representatives recognised the importance of considering organisational failure and improvement at a system level. Some participants discussed the similarities in performance issues of trusts across their patch, and that improvement was not seen as sustainable until ‘systemic structural fault lines’ were resolved. Learning from other organisations was seen as beneficial, but a general belief was that organisational failure would not be resolved by buddying between two organisations. System-wide changes were needed and this required changing support structures and interventions to operate at a system level also.
Insights for regulators and policy-makers
Insights for regulators and policy fell under the following themes:
-
recognising and responding to the emotional cost of SMQ/CP
-
strategies for improvement should be trust specific
-
current requests for reporting and short timelines are barriers to sustainable improvement
-
trusts need help to support system-wide relationships.
Participants noted the emotional cost of SMQ/CP for both the senior leadership team and the front-line staff. It was suggested that owing to the pressures of SMQ/CP, emotional and empathic support may be needed alongside other support and interventions. Peer support for individuals was valued, particularly support from peers that have been through SMQ because they will be more empathic. In addition, with changes to leadership team’s common as part of SMQ/CP, some clinicians will be taking on CN or MD roles for the first time and may need additional mentorship and support. The OAG meetings were highlighted as often being an opportunity for ‘ritual stoning’, which takes an emotional toll: careful choice of a meeting chairperson who can keep participants on task and a clear focus for these meetings may diffuse this impact.
Participants felt that strategies to support improvement need to be trust specific. Participants frequently made the point that what works in one trust may not work in another. Consideration should be given to what NHS Improvement supports should be deployed at each trust, with careful matching of IDs and buddy trusts. It should be noted that some trusts valued being given space by NHS Improvement to guide the improvement themselves. For example, the organisation in case 4 did not have the common NHS Improvement supports of an ID or buddy trust and their improvement journey, which includes exiting SMQ, has been largely driven by the leadership teams’ focus on embedding a QI methodology that encourages culture change and strongly uses data to track progress and monitor trends.
Multiple concerns around current reporting processes and timelines were raised. When large numbers of CQC recommendations are made, they can be difficult to prioritise, and it may not be possible to undertake all of them (and embed changes) within current time frames. Short timelines for turnaround do not allow staff the time to accept that they need to make changes and the fact that changing staff culture and addressing issues, such as bullying, can take several years needs to be acknowledged. It was also noted that reporting to multiple bodies is time-consuming and ‘overwhelming’, and consideration is needed on how best to avoid duplication around risk assurance. As one participant from case study 5 noted, ‘we almost have had everybody and their dog through saying, “We want to check about this, we want to check about that”’.
The importance of local system-wide relationships for improvement was noted in the insights for trusts above, and it was also seen as relevant for regulators and policy-makers who can put strategies in place to support system-wide improvements. Several participants noted that it was important to include CCGs alongside trusts in improvement planning, with CCGs treated as partners of the trust in SMQ trusts and their input and feedback are incorporated into QI plans. This need has been acknowledged and a NHS Improvement regional director noted that new NHS Improvement/NHS England ‘system assurance meetings’ will start to address this issue (see Chapter 7).
Chapter 11 Discussion and conclusions
Overview
Our research used a mixed-methods approach to evaluate the responses of trusts to the implementation of interventions used within the SMQ and CP regimes and to determine their impact on these organisations’ capacity to sustain and achieve QIs.
The study focused on the main interventions that NHS Improvement deploy as part of the SMQ/CP regimes: (1) appointment and use of an ID, (2) buddying with other trusts and (3) the opportunity to bid for central funding to spend on QI. Leadership changes and other interventions identified by our case study trusts as being part of the SMQ/CP regimes were also considered.
Our RQs were as follows:
-
What are the programme theories (central and local) guiding the interventions delivered to trusts in SMQ/CP regimes?
-
How and why do trusts respond to SMQ/CP regimes and the interventions within these regimes?
-
Which features of trusts in SMQ/CP regimes, and their wider context, contribute to their differing performance trajectories?
-
What are the relative costs of the interventions and how do these compare with their benefits?
-
How are data used by trusts in SMQ/CP regimes, and how do data contribute to their understanding of improvements in quality and service delivery, especially in areas in which performance concerns have been raised by the CQC?
-
Do trusts in SMQ/CP regimes find it more difficult to recruit and retain staff?
In this chapter, we provide a summary of our principal findings, with particular attention to our RQs. We then discuss the lessons from these findings, the limitations of our study, the potential impact of our findings, and propose an evaluation framework and future research agenda.
Summary of principal findings
Our literature review (see Chapter 3) focused on the implementation of improvement interventions for ‘low-performing’ and ‘high-performing’ organisations in health, education and local government. We identified several limitations and gaps in the current literature:
-
The limitations of current commonly used definitions of success/failure and turnaround have reduced the scope of interventions researched to date.
-
Turnaround has predominantly been perceived as linear.
-
Few studies have given any consideration to factors influencing organisational performance that might be operating at a system-wide level.
-
Few studies have explored the impact of internally driven compared with externally driven interventions.
-
Few studies have included cost analyses as part of the evaluation of interventions or looked at changes in organisational performance over time.
These findings were used in our empirical study to:
-
identify the dominant concepts of failure/turnaround shaping interventions implemented in low-performing organisations
-
determine if interventions were aimed at organisational or system level
-
identify internally driven or externally driven interventions
-
explore any negative and/or unintended consequences
-
consider the issue of one size fits all and recycling interventions without adaptation.
National perspectives and the programme theories underpinning the SMQ/CP regimes (RQ1) were explored through national-level interviews and documentary analysis (see Chapter 4). This work highlighted the role of ministerial and health system leaders in driving a process of greater provider accountability, review and scrutiny following a number of public inquiries into serious health organisation failures. The key elements of the programme theory (see Chapter 4, ‘Methods’) underpinning the SMQ/CP regimes are:
-
The SMQ/CP regimes were intended to be supportive programmes that provide organisations with oversight and interventions that aim to bring about improvements in quality and patient outcomes.
-
QI plans are a central element of SMQ/CP regimes and an essential role of IDs is to proactively engage organisational leaders and support the development of the improvement strategy.
-
The CP regime was intended to be a short-term programme to provide early interventions for challenged trusts.
-
There was awareness within NHS Improvement and DHSC about types of ‘warning signs’ and indicators that could signal a trust was in real difficulty, but information was required at the regional and national levels to inform whether or not to provide external support, in addition to intelligence from the regulator, the CQC. There was evidence of cross-agency working between the CQC and NHS Improvement, in particular, with input from GMC and HEE.
The following questions raised through the national-level work were considered in the case studies:
-
Early warning signs of quality and performance issues, such as turnover of leadership, issues with governance, culture and staff engagement, were described.
-
Early intervention was deemed desirable by regulators and regional health systems to support troubled organisations.
-
The CP regime was viewed as a shorter-term intervention than the SMQ regime and was felt to help some trusts but not others, but it is not clear why this is the case.
-
Regional health systems’ influence was an important one for communicating intelligence upwards about organisations in need for support.
Our analysis of national data that examined the characteristics of SMQ/CP trusts (see Chapter 5) found that SMQ/CP trusts significantly differed from other trusts in the following ways:
-
SMQ/CP trusts have slightly older populations.
-
SMQ/CP trusts have more attendees living in rural areas.
-
SMQ/CP trusts have fewer attendees living in deprived districts.
-
A smaller proportion of SMQ/CP trusts are foundation trusts.
-
SMQ/CP trusts had significantly worse staff survey results for six of the nine survey domains.
Our case study trusts were similar to the SMQ/CP trusts overall, but had significantly higher staff vacancy rates.
From the case studies, we found that the common underlying reasons for entry into SMQ/CP included issues with leadership, organisational culture, governance, workforce, finance and estates.
Through our case study analysis, we looked closely at stakeholder perceptions of NHS Improvement interventions (RQ2):
-
Improvement directors. There were mixed views about the value of IDs. IDs were primarily thought of as an asset and viewed as helpful when using a coaching style, offering tactical advice and generating confidence to staff to deliver change. However, negative views of IDs were also evident and they could be viewed as a ‘spy’ for the regulators, an additional source of demands and unable to enact change. There were also debates about the amount of time that IDs should spend in organisations.
-
Buddying. Buddy trusts were arranged directly by NHS Improvement, the ID or the trust themselves. Buddying was primarily used to learn about good practice in relation to specific problems. This was perceived to have worked better when the buddies had similar contexts, such as trust size and being closely located.
-
Funding. Trusts in SMQ and CP could apply for funding to help support improvement activities. Qualitative data indicated that the funds were mainly used to cover posts and external consultants and experts. The funding was considered insufficient to implement long-lasting QI. Trusts needing to spend their way out of SMQ was raised as a concern by participants. For the five case studies for which we had data, approximately one-third of funds was spent on training for cultural change (see Chapter 9).
-
Changes in leadership. New leadership teams were perceived as a key driver for change. They bring new ideas and approaches, and previous SMQ experience brought experience, confidence and familiarity with regulation processes. Another key advantage of leadership change was that they were more likely to be detached from existing problems with staff and culture. Instability in the senior team was a barrier to sustainable QI.
-
Deep dives. Intensive analysis of data on specific topics/service areas carried out with NHS Improvement staff. This is used to direct change and at OAG meetings to demonstrate QI and QA.
-
System oversight and scrutiny. Regulatory assurance processes intensify when trusts enter SMQ or CP regimes. These processes had benefits for reflection and planning, but were seen as burdensome in terms of time and resources and were not always supportive. Timelines were viewed as unrealistic, especially for embedding lasting change.
Our case study analysis facilitated an exploration of how trusts responded to the SMQ/CP regimes (RQ2) and found the following:
-
SMQ/CP can have an emotional cost for staff at all levels, and it was noted that senior staff face stress and long hours dealing with regulatory requirements and QA processes.
-
Entry into SMQ/CP was often deemed necessary and can give space for an organisation to reflect and improve. In several case studies, SMQ/CP was seen as a catalyst for change. However, others perceived SMQ/CP as heavy-handed scrutiny or even punishment.
-
The impact on staff is very important (e.g. lower morale) and needs to be mitigated given that staff acceptance of problems and culture change are key elements of facilitating improvement.
-
It was acknowledged at a national level and in the case studies that local system-wide issues may need to be addressed for a trust to exit SMQ/CP.
-
SMQ can make it difficult to participate in local system development because the organisation is investing additional time and resources into SMQ and because the SMQ label can limit regional opportunities.
From the case studies, we found that trusts focus their efforts to improve across the following eight domains:
-
Governance, accountability and leadership – review of governance and accountability; increased ‘board to ward’ interactions; development of sustainable strategies for QI and patient safety; and stronger clinical leadership at senior, divisional and ward levels.
-
Service delivery – prioritising improvements that ensure patient and staff safety, focus on compliance with national standards and improved ED performance and RRT times.
-
Data monitoring and use of data – improving the use of data by addressing how it is being collected and analysed, and how findings are shared.
-
Organisational culture and staff engagement – addressing problems with organisational culture (e.g. bullying), recognising and celebrating staff, and improving lines of communication between the senior team and staff.
-
Workforce – addressing staffing levels, skill mix and retention. Ensuring safe staff levels, and introducing strategies to reduce staff turnover and improve staff retention.
-
QI plan or strategy – working with ID to develop a plan/strategy. Setting a vision for culture change and continuous improvement.
-
QI interventions, methods or techniques – a range of QI methods and tools (e.g. PDSA and WHO checklists) and broader interventions used to drive improvement. Leadership and resource commitments to embed these trust wide.
-
Estates and equipment – improvements in working and patient environments to ensure safety, improve capacity and modernise services.
Our analysis of trust performance trajectories (RQ3) utilising national level data found the following:
-
Relative to national trends, entry into the SMQ/CP regimes corresponds to positive changes in trends in ED 4-hour waits and mortality, and short-term reductions in delayed transfers of care.
-
Trends in sickness absence improve after trusts leave the SMQ/CP regime.
-
There is evidence that staff survey results improve over the period that trusts are in the regime.
-
The regime appears to have no influence on RTT or cancer waiting times.
From the case study analysis, we identified several key internal and external factors that contributed to positive performance trajectories (RQ3):
-
internal factors – systematic use of data for QI; use of QI method(s) and dedicated resources; safe workforce levels; focus on staff engagement and recognition; integrated quality, financial and risk management with clear lines of accountability; and an embedded open and listening improvement culture
-
external factors – established good working relationships with the regulators; collaborating with external partners and peers; and have had time to embed change.
We also identified several key internal and external factors that contributed to our case study trusts not yet exiting SMQ/CP (RQ3):
-
internal factors – instability and churn at senior leadership level; absence of an organisation-wide QI methodology and culture; poor governance and risk management at all levels; poor staff engagement and issues with harassment and bullying; outdated equipment and/or deteriorating estates; and problems with staff recruitment and retention
-
external factors – financial pressures in the regional health economy; recent entry into SMQ or CP recently; or improvements made but not yet embedded.
Our CCA based on case study and national data (RQ4) found the following:
-
At the national level, during 2018–19, the mean funds spent on trusts under the SMQ regime were more than two times higher than the mean funds spent during the same period for trusts under the CP regime.
-
The largest components of NHS Improvement spending for our case studies were identified as interventions directed at ‘training on cultural change’ (33.6%), ‘workforce quality and safety’ (21.7%) and ‘governance and assurance’ (18.4%).
-
Trusts under the CP regime were four times more likely to exit within the time limits (12 months) than trusts under the SMQ regime (24 months). This is probably related to the level of initial issues with which the two types of trusts enter SMQ/CP regimes.
-
The interventions delivered to trusts as part of the SMQ/CP regimes show a positive effect on staff-based measures while there were less improvements in the context of ‘promotion of staff’s health and well-being’, ‘staff’s satisfaction with quality of care’ or ‘organisation’s actions on quality, diversity and inclusion’.
-
The findings on the effect of SMQ/CP regimes on financial stability are not clear-cut. Most of the trusts that exited the SMQ experienced the same financial stability before and after exiting, while this share was lower for the group still remaining in the regime.
Our case study analyses that specifically considered data usage by trusts (RQ5) found that trusts recognise the importance of improving their use of data:
-
Trusts focus on a standard set of nationally agreed metrics for high-level reporting. The limitations, such as inadequate monitoring of the impact of QI activities, are acknowledged.
-
There is a risk that trusts will stop monitoring specific indicators when there is evidence of ‘sustained’ improvement.
-
Trusts are increasingly recognising the importance of triangulating different indicators and information sources, including ‘soft data’ from staff and patients, to get a more holistic view of quality.
Our analysis of the impact of SMQ/CP on the recruitment and retention of staff (RQ6) was based on national-level and case study-level data:
-
National-level analysis found that sickness absence, staff vacancy rates, proportions of consultants and nurse to doctor ratio at SMQ/CP trusts at the time of entering the regime were not significantly different from national means (see Chapter 5).
-
National-level analysis found that sickness absence and staff survey results improve after trusts leave SMQ/CP (see Chapter 8).
-
Workforce issues, such as staff turnover, recruitment and retention, sickness and agency spend, were identified as underlying reasons for case study trusts entering SMQ/CP (see Chapter 5).
-
Investment in their workforce was a key component of case study trusts’ response to being in SMQ/CP (see Chapter 7), with trusts striving to address gaps in staffing levels, particularly in the ED, and skill mixes, and to reduce staff turnover and improve staff retention.
-
The stigma of the SMQ label was perceived as having a negative impact on recruitment and retention of staff (see Chapter 7).
As part of our case studies, interview participants suggested several insights and lessons for stakeholders (see Chapter 10):
-
suggestions for health-care providers, staff and health system leaders to support sustainable change – prioritise staff; stable and mature leadership; establish healthy relationships with the regulators; and consider improvement at a system level
-
suggestions for regulators and policy-makers to support sustainable change – address the emotional cost of SMQ/CP; provide trust specific support; avoid duplicate reporting and short timelines; and support system-level improvements
-
early warning signs of quality and performance issues – turnover of leadership, issues with governance, culture and staff engagement.
Implications and lessons from these findings
Our study adds new empirical knowledge on the implementation and impact of the interventions delivered to SMQ/CP trusts.
Our study has identified quantitative evidence of the impact of the SMQ/CP regimes. Evidence from our analysis suggests that the SMQ/CP regimes may have a positive impact on trends in staff survey outcomes, ED 4-hour waits and mortality, as well as a short-term, but non-sustained, impact on delayed transfers of care. There may also be a delayed positive impact on trends in sickness absence occurring after trusts leave the regime. Our finding for 4-hour ED waits contrasts with a previous analysis that found no relationship between this outcome and CQC rating score. 145 Differences between these findings may be owing to combinations of using slightly different trust selections or that the previous study used data up to 2016 rather than having the advantage of the longer time period. Other patient flow indicators, such as cancer waits and RTT times, appear little affected by the regime, which could reflect the power that trusts have on their own to change these, being influenced by wider system factors that are beyond their control. There are some changes in workforce indicators, but they are not sustained.
We have gathered new information on the perceptions and value of SMQ/CP and the NHS Improvement interventions.
With regard to SMQ, there was an emotional impact on staff of the trust being labelled as failing. Although SMQ/CP could be viewed positively, with trusts feeling that they received the right support or were allowed space to make changes, others saw SMQ as heavy-handed scrutiny or punishment. Over time, and in hindsight, as a trust went on to improve and, if in receipt of support, there could be a shift to a more positive view of SMQ/CP as a needed catalyst for positive change.
The perceptions of NHS Improvement interventions of IDs, buddy trusts, funding and deep dives were mixed overall, but it was noted that each trust has it own issues and support needs and, therefore, interventions need to be tailored accordingly. Where tailoring was better (e.g. an appropriate buddy) and delivered in consultation with the trust, responses were more favourable. For example, we found that it is important to choose buddy trusts that are well matched in terms of size and location. The need for trust-specific intervention packages reflects research findings described in the literature review that one-size-fits-all interventions and recycling of interventions without adaptation are commonly viewed poorly (see Chapter 3).
Leadership teams were found to be a key driver of change and, in terms of senior-level oversight, the medical director and chief nursing roles appear vital for communication between divisional and senior executive leadership tiers, promoting trust-wide clinical engagement and overseeing QI and QA strategies. The combined effect of these roles at the apex of the organisation – CEO, MD and chief nurse – may have been overlooked in previous research that has focused on the transformational impact of hospital CEOs and single leaders as opposed to senior leadership teams. Indeed, a recent paper from Harvard Business School has suggested that NHS CEOs may have a limited impact on hospital performance overall; that ‘the organizational inertia of a large hospital is too strong for a single manager – even if this person is the CEO – to be able to impact performance within the short time period in which they are in office, and consistently across organizations’ © National Bureau of Economic Research. 146 By contrast, clinical engagement in senior management and leadership roles and ‘triumvirate’ approaches (CEO, MD and chief nurse) to leadership are valued for supporting patient-centred care and QI in health-care organisations. 18,147–149
The characteristics of trusts that improve and successfully exit SMQ/CP reflect the findings of the literature review in which successful interventions were often associated with staff engagement in the identification of problems and development of the interventions, protected staff time or ‘slack’ for implementation, clear priority-setting and the use of routine data to monitor progress at board level. 18,94,108–111,150 An important finding from both the case studies and analysis of national data on length of time taken to exit SMQ is that trusts should be given 2–3 years to implement and start to embed improvements.
Our findings highlight the importance of creating a culture of continuous learning and improvement to promote sustainable improvement. Within the internal context, the clear improvers and one trust that had exited SMQ recently indicated the importance of embedding an organisational learning and continuous improvement culture at the trust level. Organisation-wide QI plans could be helpful for setting out a vision, especially where this had been lacking previously or was unclear, as well as identifying practical steps for the organisation to make improvements; however, this had to be backed by senior leadership support and real resources aimed at introducing new organisation capabilities, such as better use of data or quality tools at the ward and board level. 151 The vision was that a cultural mindset for systematic QI and patient safety would become culturally embedded in the organisation and not be dependent on senior leaders, some of whom might move on. For a mindset to take hold long term, there needed to be constant training and investment in staff, good clinical governance and accountability structures for quality and safety and staff engagement.
Although a 1-year time frame is too short to ascertain with confidence whether or not new ‘QI’ dynamic capabilities were being fully embedded trust wide, we can suggest that some trusts were certainly making attempts to invest more resources into structured QI processes and staff training, underpinned by a QI strategy, plan or vision. The management literature has long suggested links between organisational performance and innovation and use of external knowledge. Cohen and Levinthal’s26 core argument is that ‘prior related knowledge’ is essential for an organisation to have ‘absorptive capacity’ and be able to exploit or make effective use of external knowledge. With regards to QI in health-care settings, one would anticipate, for example, that the appointment of new leaders with QI knowledge and expertise could help the trust to search for and apply new relevant knowledge to help it improve and develop new capabilities internally. We found evidence of trusts making new appointments with a QI or ‘transformational’ focus, and applying new external knowledge to drive improvement (e.g. better use of data, improvement to ED). However, more important than simply searching for new ideas was its systematic application, which required committed staff and resources. Absorptive capacity is best understood as a process dependent on what knowledge an organisation has access to. Bringing in IDs, new teams and champions that are ‘QI aware’ or well experienced in sustaining improvements could, therefore, be argued as a way to increase the absorptive capacity of trusts for performance and QI. However, if persons move on and there is a lot of churn and poor staff engagement, absorptive capacity is likely to remain limited.
The importance of organisational culture and staff engagement have been highlighted as critical for delivering QIs. This finding mirrors findings from our (see Chapter 3) and other5 reviews that concluded that successful improvement interventions are dependent on organisational culture and research that shows that positive organisational and workplace cultures are associated with improved patient outcomes across many studies, settings and countries. 152
Implications from the cost–consequences analysis
The CCA has shown that the trusts that remain under SMQ/CP regimes beyond the time limits do not perform as well in terms of staff indicators and financial stability compared with trusts that exit on time. Moreover, we show that a small percentage of trusts (15%) are able to exit the SMQ regime within the time limit. This is likely to be because of the extent of problems within these trusts and also highlights that it takes time to embed change and make improvements. Jones et al. 111 note that there is growing awareness that organisational improvement is a long journey, and it can be difficult to maintain momentum. Our findings indicate the need for more research to better understand the timescales of improvement and for the consideration of what interventions might be most helpful to specifically support trusts that remain in SMQ/CP for long periods of time.
Our findings have important implications for data usage by trusts in SMQ/CP. With potentially vast numbers of data available for monitoring quality, it is understandable that there is a tendency to rationalise by focusing on a standard set of nationally agreed metrics for high-level reporting. The limitations of this are recognised by trusts, including the risk that the impact of improvement actions is not adequately monitored. Bespoke data collections for specific purposes may, therefore, be valuable and, in the absence of a peer group, may need to be benchmarked against past history. There is also the issue of when to stop collecting and monitoring such data. CQC want to create a system that sustains continuous improvement. However, there is evidence of some trusts stopping monitoring indicators when there is evidence of ‘sustained’ improvement.
There is increased recognition of what should be monitored at the system level and what can be undertaken locally at the trust. However, the appropriate data can be hard to capture, although the new initiative by NHS Improvement to provide system-level indicators is a positive step in this direction. Triangulation of different indicators and sources of information, such as more anecdotal information from staff and patients, is also being recognised as a useful way of using data more holistically to understand quality. This also means looking more widely across the system to understand whether or not any improvement actions are having negative impacts elsewhere. With several indicators and statistical process control tools, there are potentially large numbers of signals of potential concerns that could be followed up. Chasing all these could be time-consuming; therefore, it would be useful to have efficient ways of prioritising, for example by detecting likely false positives. 124 However, any improvements in the use of data need to be supported by adequate IT systems and analytical capability. 153
A novel outcome of this evaluation is the greater understanding of the role of local systems in SMQ/CP. Research exploring the role of wider systems in organisation improvement was identified as a gap in the existing literature (see Chapter 3). Through the national interviews (see Chapter 4) and case studies (see Chapter 7) we repeatedly found reference to the importance of local health-care systems and peer organisations in performance improvement. Shifting the improvement focus to a regional level, with strong engagement with CCGs and better support from neighbouring NHS providers, may be a practical way to promote sustainable improvement over the long term in the outer context. Participants highlighted the need to consider system-wide issues when the trust is placed in SMQ/CP and involve peers and partners to a greater extent in improvement planning. It is also important to note that we found that Healthwatch and CCG’s share the burden of SMQ with the trust, workloads for QA are high and these organisations also feel they are being held to account. A system-wide approach to improvement fits with the NHS Long Term Plan,118 which encourages collaboration between providers in local health systems. In addition, NHS England and NHS Improvement have introduced operating models for oversight that place a greater emphasis on system working with monitoring and support now directed at both providers and CCGs. 119
Through this evaluation, we identified negative unintended consequences of the SMQ/CP regimes. The stigma of the SMQ label contributes to the lowering of staff morale, exacerbates existing problems with the recruitment and retention of staff, can negatively impact on how a trust is viewed and treated by local peers and partners and may be a barrier to obtaining competitive funding. Duplicate reporting, overwhelming workloads and stress were also seen as a result of SMQ/CP and the associated regulatory requirements from both the CQC and other organisations requesting QA. Another unintended consequence of being placed in SMQ was the negative impact on the trust’s capacity to participate in local collaborations owing to the time and focus required for regulatory requirements. Difficulties with recruitment and retention for trusts in SMQ, excessive workloads and strain on management systems and lower staff and patient morale were also noted by in a commentary by Rendel et al. 10 The literature review (see Chapter 3) identified studies in the education sector where negative impacts on recruitment and retention of both staff and pupils were seen when schools were labelled as failing.
Implications for the use of early intervention strategies
Early warning signs of poor performance recognised at a national level (see Chapter 4) overlap with the underlying reasons for entry into the SMQ/CP regimes that were identified in case studies (see Chapter 5), which included issues with leadership, organisational culture, governance, workforce, basic safety, finance and estates, and have also been highlighted in the wider literature (see Chapter 3). Trusts in CP were more likely to exit CP on time than trusts in SMQ; this may be because the goal of the CP regime is to provide early intervention before performance and quality issues escalate.
Lessons for performance improvement
The key overarching lessons that we have identified for regulators, policy-makers and trusts are detailed in the following sections.
Regulatory bodies
-
Time is needed to implement and embed sustainable changes – 2–3 years not 1 year – and staff should be given ‘slack’ to develop and implement changes.
-
Strategies to support improvement need to be more trust specific.
-
Duplication of reporting requirements to different regulatory bodies should be reduced.
-
Consideration should be given to the ‘fit’ of IDs with the context of the trust they work with and discussed with the trust involved.
-
Consideration should be given to the provision of sustainable funds required to improve patients’ outcomes.
Trust leadership
-
Stable leadership is needed once the new team is established because of the time it takes to make improvements, otherwise problems are perpetuated.
-
Inclusion of people with previous experience with SMQ in senior leadership teams can help manage regulatory requirements and bring knowledge and confidence to enacting change.
Staff and culture
-
Staff engagement and an organisational culture that supports learning are key to sustainable improvement.
Emotional costs and stigma
-
Ways to mitigate the emotional cost and stigma of SMQ are needed; for example, the way trusts are informed they are in SMQ. The name of the regime could be changed to intensive support as opposed to ‘special measures’ and provide emotional support for leaders who require it.
Quality improvement strategies and capabilities
-
Development of organisation-wide QI strategies and capabilities is important.
Local systems
-
Poor organisational performance needs to be considered at both organisational and system levels (considering the factors that might be hindering improvement at the regional level).
-
Trusts in SMQ/CP need support from other organisations in the system.
Patients and the public
-
Engagement with patients and the public should be emphasised as an important part of the process of making improvements.
-
Involvement from Healthwatch and CCGs can help to bring feedback from patients and the public and supports a focus on patient experience as part of QI.
Strategies to support sustainable improvement
We found that trusts focused their QI objectives in eight domains. Here, we highlight the strategies within each domain that were seen as particularly effective in achieving sustainable improvements.
Governance, accountability and leadership
-
Address poor existing governance structures (e.g. lack of clear lines of reporting, poor clinical engagement).
-
Financial investment (e.g. external advisors and reviews) has been effective in improving governance.
-
Provide transparency, assurance, risk management and financial management with clear lines of accountability for quality and performance: ‘board to ward’.
-
Senior teams need to encourage accountability for patient safety and quality at all levels and embed an open and listening improvement culture.
-
It is important that staff understand why specific changes to processes are necessary and become engaged in governance meetings and structures.
-
Effective leadership teams are stable, ‘visible, supportive and approachable’, work as a team and encourage learning and application of new knowledge.
-
Effective clinical leadership is needed, through the MD and CN roles and/or reorganisation of governance pathways.
-
Senior teams need to establish good working relationships with the regulators and facilitate positive collaborations with external partners and peers.
Service delivery
-
Ensure compliance with national standards and CQC and NHS Improvement recommendations.
-
Prioritise service-level improvements that will ensure patient and staff safety.
Data monitoring and use of data
-
Ensure systematic use of data across the organisation for QI and QA.
-
Focus on understanding what data are describing and triangulate standard metrics with other sources of information, including the concerns of staff and patients.
-
Treat data as a prompt to investigate quality.
-
Consider bespoke data collection for specific purposes.
Organisational culture and staff engagement
-
Improvement relies on better staff morale and culture.
-
How accepting leaders and staff are of the need to change varies – for effective change, leaders and staff need to accept and input into improvement plans.
-
Positive engagement and investment in staff are essential:
-
Develop strategies for better communication/listening to staff concerns.
-
Address ‘bullying’ or ‘insular’ cultures.
-
Promote staff appraisals, celebrate staff success and widen opportunities for education and training.
-
Support growth of patient safety culture through staff training and development.
-
Close communication gaps between the senior executive team and front-line staff, for example listening events and increased senior and board presence on wards.
-
Encourage a culture of openness and transparency.
-
Workforce
-
Address problems with staffing levels to ensure patient safety:
-
Staff appraisals.
-
Improved workforce planning.
-
Financial investment to increase staff numbers.
-
Quality improvement plan or strategy
-
Leadership teams need to establish a vision for culture change and continuous improvement.
-
Develop a deeper understanding of problem areas and causation.
-
IDs playing a key role in developing the QI plan/strategy for the trust.
-
Allow staff dedicated time to work on QI and do not expect them to undertake QI activities on top of their existing work.
Quality improvement interventions, methods or techniques
-
Use of a formal ‘method’ or strategy for QI that is embedded throughout the organisation.
-
Dedicated resources are needed for QI: trusts need to develop new internal capabilities.
-
Receptive to new, external knowledge to improve performance.
Estates and equipment
-
Strategies and financial investment are needed to improve working and patient environments to ensure safety, improve capacity and modernised services.
System-level facilitators and barriers to quality improvement
The importance of the local system in performance improvement has been an important finding in this study. Here we highlight the local system-level factors that are facilitators of and barriers to improvement for trusts in SMQ/CP.
Facilitators of improvement
-
Positive engagement with system peers and partners:
-
In some cases, providers were already working together, for example in integrated care systems.
-
-
Whole local system response to quality issues.
-
QA that is linked to strong governance and data collection processes across the system.
-
Supportive OAG meetings involving local system peers and partners.
-
Financial sustainability planning across the system.
Barriers to improvement
-
It can take time and considerable effort to build/rebuild external relationships.
-
System-wide issues that are difficult to address, for example workforce and financial pressures.
-
OAG meetings can be a ‘ritual stoning’ for the trust.
Study strengths and limitations
To the best of our knowledge, this is the first study of the response to and impact of the SMQ/CP regimes. The key strength of the study is the mixed-methods approach, which has allowed us to look at SMQ/CP at a national level through a quantitative study of impacts and a CCA across all trusts in SMQ/CP, as well as eight case studies that have utilised both qualitative and quantitative methodologies. Another strength of the study has been the development of the protocol with input from key stakeholders (DHSC and NHS Improvement) and PPI feedback. In addition, the evaluation has been formative, with findings shared and discussed with key stakeholders during the study. There are, however, several potential limitations of our evaluation. The study duration of 1 year has meant that we had only a partial view of the process and could not study longitudinally any developments within the eight case studies, their strategic responses to performance issues and how far their dynamic capabilities have been embedded. The rapid approach has also meant that patient input and engagement at a local case study level has not been possible. We also have to caution that we were not able to interview senior leaders who had left an organisation, although our analysis of trust board papers and successive CQC reports offered a longer-term view of internal trust issues and how they were tackled over time. In addition, some data were retrospective and changes in policies have occurred over the course of the study period. It is also possible that access to case study sites was constrained because of the sensitive nature of the research topic. In addition, our interviews with external stakeholders did not include local health-care providers who may have offered different views. The generalisability of the study is to some extent limited by the types of services provided by the case study sites; for example, no trusts providing mental health services or ambulance trusts were included and these may differ from acute trusts in a number of ways, including reasons for entering SMQ/CP or types of quality issues.
The small number of case study sites may make it difficult to draw general conclusions about the use of data, although our sampling is in line with many other high-quality examples of case study research that apply mixed methods and may have less than eight organisations to compare. Within the trusts themselves, we have been pragmatic about access to relevant data and have worked with what we could obtain from national and publicly available data sets. For quantitative analysis of impact, we studied a few indicators only, many relating to patient flows and waiting times, and our ability to measure effects on the workforce was limited by the information that was available to us. The staff survey, in particular, was available only from 2014 to 2018, with most domains from 2015. This meant that there were a limited number of trusts for which we could identify results both at the beginning and at the end of the improvement regimes to observe how they might have changed. In addition, the results may not accurately reflect views at the time the regimes started or ended given that annual surveys were used. In our analysis of indicators, we treated the CP and SMQ regimes identically and did not investigate any differences in how they might separately influence outcomes. Our analysis of characteristics of those who re-enter is based on a very small sample. The economic component of the study was not able to disentangle the individual effects of each intervention owing to their complex nature and implementation approaches that were unique to each case study site. In addition, limitations of available data meant that it was not possible to conduct a separate analysis of opportunity costs. It also meant that important aspects, such as patient benefits (e.g. patients’ improved safety and access), were only partially considered as consequences in the CCA (we did consider indicators such as ED waits, delayed transfers of care or 62-day cancer waiting time) because of the limited information available.
Lessons about the conduct of rapid evaluations
Our study followed a rapid research design that has allowed it to be completed within a 1-year time frame. The lessons around the conduct of rapid evaluations we have identified are:
-
There is an evident trade-off between guaranteeing the breadth and guaranteeing the depth of data.
-
For findings to be shared on a regular basis, dissemination feedback loops need to be discussed with stakeholders before the study begins, as well as during the study, and these need to be built into the design.
-
RAP sheets facilitate the collection and analysis of data across researchers and across case studies. However, transcripts and field notes should be maintained for future in-depth studies (if desired) because RAP sheets might not be able to capture all of the relevant detail/complexity.
-
Data collection and analysis need to be carried out in parallel to ensure consistency across researchers, to share interim findings with stakeholders, to address gaps in data collection before fieldwork has ended, and to reduce the amount of time required for analysis after fieldwork has ended.
-
Need to build in sufficient time for reflection and discussions in relation to interpretation of the data – this is more challenging in a rapid study.
-
Opportunities for more comprehensive PPI, such as local engagement linked to case studies and Research Advisory Panel member involvement with the analysis and interpretation of findings, was not feasible within the 1-year time frame for the rapid evaluation, although patient experts informed the design of the original protocol and fed back on the final report. More integrated PPI strategies that are feasible within rapid evaluation approaches should be explored.
-
Less ability to explore patient perspectives or clinical data.
Conclusions, suggestions for future research and lessons for future evaluations
High-quality interventions that successfully support struggling health-care organisations are essential and an issue that is an international concern. Through our evaluation, we have delivered a greater understanding of the programme theory, impact and staff views and experiences of the SMQ/CP regimes, with formative feedback shared with key stakeholders. Lessons for trusts on responding to interventions in SMQ/CP regimes, as well as lessons for the DHSC and NHS Improvement on how to support these, trusts have been proposed. These lessons are timely because the oversight model is currently being redesigned by NHS England and NHS Improvement.
Given both the rapid nature of this study and that the findings have raised further questions, we propose that future areas of research should include the following:
-
Evaluation of the impact of the new NHS Improvement/NHS England operating framework,119 particularly with its emphasis on system improvement.
-
Evaluate SMQ/CP at the local system level and expand the range of stakeholders external to the trust giving viewpoints on SMQ/CP, including local government and other health service providers.
-
Study of trusts in SMF and an exploration of the link between SMQ and SMF.
-
Further research to understand the impact of SMQ on the financial stability of trusts in SMQ/CP.
-
Research to delineate the timescales required for sustainable improvement.
-
Longitudinal empirical data collection to look at the sustainability of improvement over time and improve our understanding of why some trusts re-enter SMQ (e.g. follow-up case studies or additional observations through embedded research154).
-
Consider what interventions are most helpful to trusts that remain in SMQ/CP for long periods.
-
Further research on the early detection of trusts in difficulty as well as early intervention/prevention to determine which strategies are effective.
An exploration of how to engage with patients and the public when a trust goes into SMQ.
Reflections on the methods used in this study have led us to draw out the following lessons for future evaluations:
-
Use mixed-methods approaches, combining quantitative and qualitative data, for example structured use of board reports (including papers) and CQC inspection reports can provide insights about trust’s trajectories, which are helpful and powerful if combined with quantitative indicators derived from nationally available routine data. Mixed-method case studies are, therefore, most valuable for insights that have depth and internal validity.
-
Data collection for monitoring could be tailored to the concerns in each organisation and be used not only for internal monitoring (which happens to an extent already) but also to feed into the overall evaluation framework. It would mean using different measures for different trusts but would have the advantage of greater specificity. In the national analysis provided in this study, we have used the same metrics for all trusts, which has been important for making comparisons, although the metrics may not always be closely related to the actual improvements that a trust needs to make.
-
If possible, conduct evaluations prospectively in ‘real time’ using sequential monitoring techniques for assessing whether or not is something is working while under the regime. Such techniques would also have value in identifying longer-term impact, that is whether or not any improvements are sustained after they leave, and pick up any deterioration against these indicators.
-
When considering system-wide impacts, it will be extremely important to know the financial stability of the trusts under the SMQ/CP regime. We have looked at this by using a simple scale measure for such stability before, during and after the regime. However, it would be equally important to link this indicator to changes in direct/indirect costs and also to additional opportunity costs that are raised while a trust is in the SMQ or CP regime. It was not possible to make this link retrospectively, but this could be accounted for if all such indicators are to be part of routinely reported data.
Acknowledgements
We are grateful to all of the participants who took part in this study and to our contacts at each case study trust who helped to co-ordinate our interactions with the trusts and provided documents. We also thank the DHSC and NHS Improvement teams who discussed the development of study with us and the members of the NIHR CLAHRC North Thames Research Advisory Panel who contributed a PPI viewpoint to inform protocol development, in particular Raj Mehta and Fola Tayo who also reviewed the Plain English summary in this report. We thank Christine Taylor for her contributions to project management and administrative support. We thank Kieran Walshe who reviewed the study protocol, and are grateful to Kieran Walshe, Ewan Ferlie and Gill Harvey for reviewing the rapid review study protocol and the findings from phase 1 of the review. Their feedback was used to inform the design and development of the searches carried out for phase 2. We thank Angus Ramsay for undertaking a critical review of the draft report.
Contributions of authors
Naomi J Fulop (https://orcid.org/0000-0001-5306-6140) (Professor of Health Care Organisation and Management) was the principal investigator and led the study. She contributed to the conception and design of the study, the theoretical framework, the rapid review (see Chapter 3), overall data analysis and interpretation, and is lead author of the final report.
Estela Capelas Barbosa (https://orcid.org/0000-0001-8282-131X) (Research Associate – Health Economist) contributed to the conception and design of the study, the conduct of the rapid review (see Chapter 3) and the data collection and analysis for the CCA (see Chapter 9). She also contributed to Chapters 1 and 2.
Melissa Hill (https://orcid.org/0000-0003-3900-1425) (Senior Social Scientist) contributed to qualitative fieldwork (two case studies), data analysis and interpretation and the write-up of the final report. She contributed to Chapters 1, 2, 6, 7, 10 and 11.
Jean Ledger (https://orcid.org/0000-0003-2523-7971) (Research Fellow) contributed to the conception and design of the study, theoretical framework, qualitative fieldwork (four cases studies), the rapid review (see Chapter 3), data analysis and interpretation and the overall write-up of the final report. She led the analysis and writing for Chapters 4 and 7 and contributed to Chapters 1, 2, 3, 6, 10 and 11.
Pei Li Ng (https://orcid.org/0000-0001-8411-220X) (Research Project Manager) managed the project and provided administrative support.
Christopher Sherlaw-Johnson (https://orcid.org/0000-0002-4851-6060) (Senior Fellow) provided oversight for the quantitative analysis. He contributed to the conception and design of the study, the rapid review (see Chapter 3), data collection, data analysis and interpretation, and the overall write-up of the final report. He led the analysis and writing for Chapters 5 and 8 and contributed to Chapters 1, 2, 3, 10 and 11.
Lucina Rolewicz (https://orcid.org/0000-0003-4308-2408) (Researcher) conducted the quantitative analysis and contributed to Chapters 5 and 8.
Laura Schlepper (https://orcid.org/0000-0002-3242-8904) (Research Analyst) conducted the quantitative analysis and contributed to Chapters 5 and 8.
Jonathan Spencer (https://orcid.org/0000-0001-6660-6919) (Research Analyst) contributed to the conception and design of the study, the rapid review (see Chapter 3), quantitative data collection and analysis. He contributed to Chapters 1, 2, 3, 5 and 8.
Sonila M Tomini (https://orcid.org/0000-0002-4241-2121) (Research Fellow – Health Economics) contributed to the data collection and led the CCA and write-up (see Chapter 9). She also contributed to Chapter 11.
Cecilia Vindrola-Padros (https://orcid.org/0000-0001-7859-1646) (Senior Research Fellow) contributed to the conception and design of the study, theoretical framework, qualitative fieldwork (two case studies), data analysis and interpretation and the write-up of the final report. She led the conduct and writing of the rapid review (see Chapter 3) and the analysis and writing for Chapters 6 and 10. She also contributed to Chapters 1, 2, 7 and 11.
Steve Morris (https://orcid.org/0000-0002-5828-3563) (Professor of Health Economics) provided oversight for the economic analyses (see Chapter 9). He contributed to the conception and design of the study and overall analysis and interpretation, and the write-up of the final report.
All authors contributed to integrating the findings of the study. All authors made critical revisions to the report for important intellectual content and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Publication
Fulop N, Capelas Barbosa E, Hill M, Ledger J, Sherlaw-Johnson C, Spencer J, et al. Special measures for quality and challenged providers: study protocol for evaluating the impact of improvement interventions in NHS trusts. Int J Health Policy Manag 2020;9:143–51.
Vindrola-Padros C, Ledger J, Hill M, Tomini S, Spencer J, Fulop NJ. The special measures for quality and challenged provider regimes in the English NHS: a rapid evaluation of a national improvement initiative for failing healthcare organisations. Int J Health Policy Manag 2022;11:2917–26. https://doi.org/10.34172/IJHPM.2022.6619
Vindrola-Padros C, Ledger J, Capelas Barbosa E, Fulop NJ. The implementation of improvement interventions for ‘low performing’ and ‘high performing’ organisations in health, education and local government: a phased literature review. Int J Health Policy Manag 2022;11:874–82. https://doi.org/10.34172/IJHPM.2020.197
Data-sharing statement
This study used HES data obtained from NHS Digital under a data sharing agreement and are reused with their permission. HES data may be obtained from NHS Digital under a similar process but we are unable to share it per the terms of our agreement.
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Walshe K, Harvey G, Hyde P, Pandit N. Organizational failure and turnaround: lessons for public services from the for-profit sector. Public Money Manag 2004;24:201-8. https://doi.org/10.1111/j.1467-9302.2004.00421.x.
- Hockey PM, Bates DW. Physicians’ identification of factors associated with quality in high-and low-performing hospitals. Jt Comm J Qual Patient Saf 2010;36:217-23. https://doi.org/10.1016/S1553-7250(10)36035-1.
- Speroff T, Nwosu S, Greevy R, Weinger MB, Talbot TR, Wall RJ, et al. Organisational culture: variation across hospitals and connection to patient safety climate. Qual Saf Health Care 2010;19:592-6. https://doi.org/10.1136/qshc.2009.039511.
- Ravaghi H, Mannion R, Sajadi HS. Organizational failure in an NHS hospital trust: a qualitative study. Health Care Manag 2015;34:367-75. https://doi.org/10.1097/HCM.0000000000000087.
- Vaughn VM, Saint S, Krein SL, Forman JH, Meddings J, Ameling J, et al. Characteristics of healthcare organisations struggling to improve quality: results from a systematic review of qualitative studies. BMJ Qual Saf 2019;28:74-8. https://doi.org/10.1136/bmjqs-2017-007573.
- NHS England 2013. https://www.basw.co.uk/system/files/resources/basw_85333-2_0.pdf (accessed 23 June 2023).
- Care Quality Commission (CQC) . The State of Care in NHS Acute Hospitals 2014 to 2016: Findings from the End of CQC’s Programme of NHS Acute Comprehensive Inspections 2017. www.cqc.org.uk/publications/major-report/state-care-nhs-acute-hospitals (accessed January 2020).
- Care Quality Commission (CQC) . Quality Improvement in Hospital Trusts: Sharing Learning from Trusts on a Journey of QI 2018. https://www.basw.co.uk/system/files/resources/basw_85333-2_0.pdf (accessed 23 June 2023).
- NHS Improvement 2017. https://improvement.nhs.uk/documents/1902/Learning_from_improvement_-_SMQ_FINAL.pdf (accessed January 2020).
- Rendel S, Crawley H, Ballard T. CQC inspections: unintended consequences of being placed in special measures. Br J Gen Pract 2015;65:e640-1. https://doi.org/10.3399/bjgp15X686809.
- Smithson R, Richardson E, Roberts J, Walshe K, Wenzel L, Robertson R, et al. Impact of the Care Quality Commission on Provider Performance: Room for Improvement? 2018. www.kingsfund.org.uk/publications/impact-cqc-provider-performance (accessed January 2020).
- Fulop N, Barbosa EC, Hill M, Ledger J, Sherlaw-Johnson C, Spencer J, et al. Special measures for quality and challenged providers: study protocol for evaluating the impact of improvement interventions in NHS trusts. Int J Health Policy Manag 2020;9:143-51. https://doi.org/10.15171/ijhpm.2019.100.
- Beebe J. Rapid Qualitative Inquiry: A Field Guide to Team-based Assessment. London: Rowman and Littlefield; 2014.
- Tricco AC, Langlois EV, Straus SE. Rapid Reviews to Strengthen Health Policy and Systems: A Practical Guide. Geneva, Switzerland: World Health Organization, Alliance For Health Policy And Systems Research; 2017.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339. https://doi.org/10.1136/bmj.b2535.
- Yin RK. Validity and generalization in future case study evaluations. Evaluation 2013;19:321-32. https://doi.org/10.1177/1356389013497081.
- Giacomini M. The SAGE Handbook of Qualitative Methods in Health Research. London: SAGE Publications Ltd; 2010.
- Jones L, Pomeroy L, Robert G, Burnett S, Anderson JE, Fulop NJ. How do hospital boards govern for quality improvement? A mixed methods study of 15 organisations in England. BMJ Qual Saf 2017;26:978-86. https://doi.org/10.1136/bmjqs-2016-006433.
- Pettigrew AM. Longitudinal field research on change: theory and practice. Organ Sci 1990;1:267-92. https://doi.org/10.1287/orsc.1.3.267.
- Nelson L. Managing the human resources in organisational change: a case study, research and practice. Hum Resour Manage 2005;13:55-70.
- Buchanan D, Fitzgerald L, Ketley D, Gollop R, Jones JL, Lamont SS, et al. No going back: a review of the literature on sustaining organizational change. Int J Manag Rev 2005;7:189-205. https://doi.org/10.1111/j.1468-2370.2005.00111.x.
- Fulop NJ, Robert G. Context for Successful Quality Improvement: Evidence Review 2015. www.health.org.uk/publications/context-for-successful-quality-improvement (accessed February 2020).
- Robert G, Fulop NJ. Perspectives on Context. A Selection of Essays Considering the Role of Context in Successful Quality Improvement. London: The Health Foundation; 2014.
- Eisenhardt KM. Building theories from case study research. Acad Manag Rev 1989;14. https://doi.org/10.2307/258557.
- Harvey G, Jas P, Walshe K. Analysing organisational context: case studies on the contribution of absorptive capacity theory to understanding inter-organisational variation in performance improvement. BMJ Qual Saf 2015;24:48-55. https://doi.org/10.1136/bmjqs-2014-002928.
- Cohen WM, Levinthal DA. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q 1990;35. https://doi.org/10.2307/2393553.
- Winter SG. Understanding dynamic capabilities. Strat Manag J 2003;24:991-5. https://doi.org/10.1002/smj.318.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Vindrola-Padros C, Ledger J, Barbosa EC, Fulop NJ. The implementation of improvement interventions for ‘low performing’ and ‘high performing’ organisations in health, education and local government: a phased literature review. International Journal of Health Policy and Management 2022;11:874-82.
- McLean B, Elkind P. The Smartest Guys in the Room: The Amazing Rise and Scandalous Fall of Enron. New York, NY: Portfolio; 2003.
- Mellahi K, Jackson P, Sparks L. An exploratory study into failure in successful organizations: the case of Marks & Spencer. Br J Manag 2002;13:15-29. https://doi.org/10.1111/1467-8551.00220.
- Carmeli A, Schaubroeck J. Organisational crisis-preparedness: the importance of learning from failures. Long Range Plann 2008;41:177-96. https://doi.org/10.1016/j.lrp.2008.01.001.
- Filochowski J. Too Good to Fail. Harlow, UK: Pearson Education Ltd; 2013.
- Hafner JM, Williams SC, Morton DJ, Koss RG, Loeb JM. From bad to better: a qualitative assessment of low-performing hospitals that improved their smoking cessation counseling performance. J Clin Outcomes Manag 2008;15:329-37.
- Curry LA, Spatz E, Cherlin E, Thompson JW, Berg D, Ting HH, et al. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. Ann Intern Med 2011;154:384-90. https://doi.org/10.7326/0003-4819-154-6-201103150-00003.
- Brewster AL, Cherlin EJ, Ndumele CD, Collins D, Burgess JF, Charns MP, et al. What works in readmissions reduction: how hospitals improve performance. Med Care 2016;54:600-7. https://doi.org/10.1097/MLR.0000000000000530.
- Ferlie E, Crilly T, Jashapara A, Peckham A. Knowledge mobilisation in healthcare: a critical review of health sector and generic management literature. Soc Sci Med 2012;74:1297-304. https://doi.org/10.1016/j.socscimed.2011.11.042.
- Jones E, Lees N, Martin G, Dixon-Woods M. Describing methods and interventions: a protocol for the systematic analysis of the perioperative quality improvement literature. Syst Rev 2014;3. https://doi.org/10.1186/2046-4053-3-98.
- Portela MC, Pronovost PJ, Woodcock T, Carter P, Dixon-Woods M. How to study improvement interventions: a brief overview of possible study types. BMJ Qual Saf 2015;24:325-36. https://doi.org/10.1136/bmjqs-2014-003620.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Pandit NR. Some recommendations for improved research on corporate turnaround. Management 2000;3:31-56.
- Mellahi K, Wilkinson A. Organizational failure: a critique of recent research and a proposed integrative framework. Int J Manag Rev 2004;5:21-4. https://doi.org/10.1111/j.1460-8545.2004.00095.x.
- Slatter S. Corporate Recovery: A Guide to Turnaround Management. London: Penguin; 1984.
- Weitzel W, Jonsson E. Decline in organizations: a literature integration and extension. Adm Sci Q 1989;34:91-109. https://doi.org/10.2307/2392987.
- Hambrick DC, Schecter SM. Turnaround strategies for mature industrial-product business units. Acad Manage J 1983;26:231-48. https://doi.org/10.2307/255972.
- Baker GR, MacIntosh-Murray A, Porcellato C, Dionne L, Stelmacovich K, Born K. High Performing Healthcare Systems: Delivering Quality by Design. Toronto, ON: Longwoods Publishing; 2008.
- Bate P, Mendel P, Robert G. Organizing for Quality: The Improvement Journeys of Leading Hospitals in Europe and the United States. Abingdon: Radcliffe Publishing Ltd; 2007.
- Taylor N, Clay-Williams R, Hogden E, Braithwaite J, Groene O. High performing hospitals: a qualitative systematic review of associated factors and practical strategies for improvement. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0879-z.
- Willmott R. Structure, agency and school effectiveness: researching a ‘failing’ school. Educ Stud 1999;25:5-18. https://doi.org/10.1080/03055699997936.
- Perryman J. Panoptic performativity and school inspection regimes: disciplinary mechanisms and life under special measures. J Educ Pol 2006;21:147-61. https://doi.org/10.1080/02680930500500138.
- Hannan MT, Freeman J. Organizational Ecology. Cambridge, MA: Harvard University Press; 1989.
- Klepper S. Industry life cycles. Industrial and Corporate Change 1997;6:145-82. https://doi.org/10.1093/icc/6.1.145.
- McKiernan P. The Oxford Handbook of Strategy, Vol. Ii. New York: Oxford University Press; 2002.
- Fulop N, Protopsaltis G, King A, Allen P, Hutchings A, Normand C. Changing organisations: a study of the context and processes of mergers of health care providers in England. Soc Sci Med 2005;60:119-30. https://doi.org/10.1016/j.socscimed.2004.04.017.
- Walshe K, Shortell SM. When things go wrong: how health care organizations deal with major failures. Health Aff 2004;23:103-11. https://doi.org/10.1377/hlthaff.23.3.103.
- Dixon-Woods M, Baker R, Charles K, Dawson J, Jerzembek G, Martin G, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106-15. https://doi.org/10.1136/bmjqs-2013-001947.
- Willis L. Is the process of special measures an effective tool for bringing about authentic school improvement?. Manag Educ 2010;24:142-8. https://doi.org/10.1177/0892020610379314.
- Nicolaidou M, Ainscow M. Understanding failing schools: perspectives from the inside. Sch Effect Sch Improv 2007;16:229-48. https://doi.org/10.1080/09243450500113647.
- Leithwood K, Harris A, Hopkins D. Seven strong claims about successful school leadership. Sch Leader Manag 2008;28:27-42. https://doi.org/10.1080/13632430701800060.
- Perryman J. School leadership and management after special measures: discipline without the gaze?. Sch Leader Manag 2005;25:281-97. https://doi.org/10.1080/13634230500116355.
- Chapman C. Ofsted and school improvement: teachers’ perceptions of the inspection process in schools facing challenging circumstances. Sch Leader Manag 2002;22:257-72. https://doi.org/10.1080/1363243022000020390.
- Chapman C, Harris A. Improving schools in difficult and challenging contexts: strategies for improvement. Educ Res 2010;46:219-28. https://doi.org/10.1080/0013188042000277296.
- Chowdhury SD. Turnarounds: a stage theory perspective. Can J Adm Sci 2009;19:249-66. https://doi.org/10.1111/j.1936-4490.2002.tb00271.x.
- Paton R, Mordaunt J. What’s different about public and non-profit ‘turnaround’?. Public Money Manag 2004;24:209-16. https://doi.org/10.1111/j.1467-9302.2004.00422.x.
- Beeri I. The measurement of turnaround management strategies in local authorities. Public Money Manag 2009;29:131-6. https://doi.org/10.1080/09540960902768046.
- Beeri I. Turnaround management strategies in public systems: the impact on group-level organizational citizenship behavior. Int Rev Adm Sci 2012;78:158-79. https://doi.org/10.1177/0020852311430284.
- Harvey G, Hyde P, Walshe K. Investigating ‘Turnaround’ in NHS Organisations Supported by the Performance Development Team (PDT) of the Modernisation Agency. Manchester: Centre For Public Policy And Management, Manchester Business School, University Of Manchester; 2005.
- Fulop N, Scheibl F, Edwards N. Turnaround in Health Care Providers. London: London School of Hygiene and Tropical Medicine; 2004.
- Jas P, Skelcher C. Performance decline and turnaround in public organizations: a theoretical and empirical analysis. Br J Manag 2005;16:195-210. https://doi.org/10.1111/j.1467-8551.2005.00458.x.
- Ravaghi H. Organisational Failure and Turnaround Process in NHS Hospital Trusts. PhD Thesis 2007.
- Greenhalgh L. Managing the job insecurity crisis. Hum Resource Manag 1983;22. https://doi.org/10.1002/hrm.3930220409.
- Hardy C. Investing in retrenchment: avoiding the hidden costs. Calif Manage Rev 1987;29:111-25. https://doi.org/10.2307/41162134.
- Sutton RI, Eisenhardt KM, Jucker JV. Managing organizational decline: lessons from Atari. Organ Dyn 1986;14:17-29. https://doi.org/10.1016/0090-2616(86)90041-0.
- Protopsaltis G, Fulop N, Meara R, Edwards N. Turning Around Failing Hospitals. London: The NHS Confederation; 2002.
- Boyne G. Managing To Improve Public Services. Cambridge: Cambridge University Press; 2008.
- Harvey G, Hyde P, Fulop N, Edwards N, Filochowski J, Walshe K. Recognising, Understanding and Addressing Performance Problems in Healthcare Organisations Providing Care to NHS Patient. London: Department of Health and Social Care; 2006.
- Rosenberg L, Christianson MD, Hague Angus M. Improvement efforts in rural schools: experiences of nine schools receiving school improvement grants. Peabody Journal of Education 2015;90:194-210. https://doi.org/10.1080/0161956X.2015.1022109.
- Jas P. The role of interim managers in performance improvement: evidence from English local authorities. Public Money Manag 2013;33:15-22. https://doi.org/10.1080/09540962.2013.744890.
- Rice JK, Malen B, Baumann P, Chen E, Dougherty A, Hyde L, et al. The persistent problems and confounding challenges of educator incentives: the case of TIF in prince George’s county, Maryland. Educational Policy 2012;26:892-933. https://doi.org/10.1177/0895904812465708.
- Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. JAMA 2008;299:2180-7. https://doi.org/10.1001/jama.299.18.2180.
- Marsh JA, Bush-Mecenas S, Hough H. Learning from early adopters in the new accountability era: insights from California’s core waiver districts. Educ Adm Q 2017;53:327-64. https://doi.org/10.1177/0013161X16688064.
- Mannion R, Davies HT, Marshall MN. Cultural characteristics of ‘high’ and ‘low’ performing hospitals. J Health Organ Manag 2005;19:431-9. https://doi.org/10.1108/14777260510629689.
- Heck RH, Chang J. Examining the timing of educational changes among elementary schools after the implementation of NCLB. Educ Adm Q 2017;53:649-94. https://doi.org/10.1177/0013161X17711480.
- Beeri I. Governmental strategies towards poorly-performing municipalities: from narrow perceptions to ineffective policies. Lex Localis - Journal of Local Self-Government 2013;11:33-52. https://doi.org/10.4335/220.
- Yapp C, Skelcher C. Improvement boards: building capability for public service improvement through peer support. Public Money Manag 2007;27:285-92. https://doi.org/10.1111/j.1467-9302.2007.00596.x.
- Hochman M, Briggs-Malonson M, Wilkes E, Bergman J, Daskivich LP, Moin T, et al. Fostering a commitment to quality: best practices in safety-net hospitals. J Health Care Poor Underserved 2016;27:293-307. https://doi.org/10.1353/hpu.2016.0008.
- Meyers CV, Hitt DH. Planning for school turnaround in the united states: an analysis of the quality of principal-developed quick wins. Sch Effect Sch Improv 2018;29:362-82. https://doi.org/10.1080/09243453.2018.1428202.
- Orr MT, Berg B, Shore R, Meier E. Putting the pieces together: leadership for change in low-performing urban schools. Educ Urban Soc 2008;40:670-93. https://doi.org/10.1177/0013124508324018.
- VanGronigen BA, Meyers CV. How state education agencies are administering school turnaround efforts: 15 years after no child left behind. Educ Pol 2019;33:423-52. https://doi.org/10.1177/0895904817691846.
- Gagliardi AR, Nathens AB. Exploring the characteristics of high-performing hospitals that influence trauma triage and transfer. J Trauma Acute Care Surg 2015;78:300-5. https://doi.org/10.1097/TA.0000000000000506.
- Finnigan KS, Daly AJ, Stewart TJ. Organizational learning in schools under sanction. Educ Res Int 2012;2012. https://doi.org/10.1155/2012/270404.
- Tsai TC, Jha AK, Gawande AA, Huckman RS, Bloom N, Sadun R. Hospital board and management practices are strongly related to hospital performance on clinical quality metrics. Health Aff 2015;34:1304-11. https://doi.org/10.1377/hlthaff.2014.1282.
- Mintrop H, Trujillo T. The practical relevance of accountability systems for school improvement: a descriptive analysis of California schools. Educ Eval Pol Anal 2007;29:319-52. https://doi.org/10.3102/0162373707309219.
- Turner D, Skelcher C, Whiteman P, Hughes M, Jas P. Intervention or persuasion? Strategies for turnaround of poorly-performing councils. Public Money Manag 2004;24:217-26. https://doi.org/10.1111/j.1467-9302.2004.00423.x.
- Chang AM, Cohen DJ, Lin A, Augustine J, Handel DA, Howell E, et al. Hospital strategies for reducing emergency department crowding: a mixed-methods study. Annals of Emergency Medicine 2018;71:497-505.e4.
- Aboumatar HJ, Chang BH, Al Danaf J, Shaear M, Namuyinga R, Elumalai S, et al. Promising practices for achieving patient-centered hospital care: a national study of high-performing US hospitals. Med Care 2015;53:758-67. https://doi.org/10.1097/MLR.0000000000000396.
- Parsons C. Challenged school – challenged society: stacking the odds against the poor. Educ Rev 2013;65:267-83. https://doi.org/10.1080/00131911.2013.772127.
- Gorton J, Williams M, Wrigley T. Inspection judgements on urban schools: a case for the defence. Urban Rev 2014;46:891-903. https://doi.org/10.1007/s11256-014-0309-2.
- Ehren MCM, Altrichter H, McNamara G, O’Hara J. Impact of school inspections on improvement of schools — describing assumptions on causal mechanisms in six European countries. Educ Asse Eval Acc 2013;25:3-43. https://doi.org/10.1007/s11092-012-9156-4.
- Allen T, Walshe K, Proudlove N, Sutton M. Do performance indicators predict regulator ratings of healthcare providers? Cross-sectional study of acute hospitals in England. Int J Qual Health Care 2019;1. https://doi.org/10.1093/intqhc/mzz101.
- Boyd A, Addicott R, Robertson R, Ross S, Walshe K. Are inspectors’ assessments reliable? Ratings of NHS acute hospital trust services in England. J Health Serv Res Policy 2017;22:28-36. https://doi.org/10.1177/1355819616669736.
- Castro-Avila A, Bloor K, Thompson C. The effect of external inspections on safety in acute hospitals in the National Health Service in England: a controlled interrupted time-series analysis. J Health Serv Res Policy 2019;24:182-90. https://doi.org/10.1177/1355819619837288.
- Millar R, Greenhalgh J, Rafferty AM, McLeod H, Mannion R. 2019. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019149009 (accessed December 2019).
- Sahlin-Andersson K, Engwall L. The Expansion of Management Knowledge: Carriers, Flows, and Sources. Redwood City, CA: Stanford University Press; 2002.
- Sahlin K, Wedlin L. The SAGE Handbook of Organizational Institutionalism. London: SAGE Publications Ltd; 2008.
- Nicolini D, Mengis J, Meacheam D, Waring J, Swan J. Mobilizing Knowledge in Healthcare: Challenges for Management and Organization. Oxford: Oxford University Press; 2016.
- McGivern G, Dopson S, Ferlie E, Bennett C, Fischer M, Fitzgerald L, et al. Mobilizing Knowledge in Healthcare: Challenges for Management and Organization. Oxford: Oxford University Press; 2016.
- Jha AK, DesRoches CM, Kralovec PD, Joshi MS. A progress report on electronic health records in US hospitals. Health Aff (Millwood) 2010;29:1951-7. https://doi.org/10.1377/hlthaff.2010.0502.
- Millar R, Mannion R, Freeman T, Davies HT. Hospital board oversight of quality and patient safety: a narrative review and synthesis of recent empirical research. Milbank Q 2013;91:738-70. https://doi.org/10.1111/1468-0009.12032.
- Bismark MM, Studdert DM. Governance of quality of care: a qualitative study of health service boards in Victoria, Australia. BMJ Qual Saf 2014;23:474-82. https://doi.org/10.1136/bmjqs-2013-002193.
- Jones B, Horton T, Warburton W. The Improvement Journey: Why Organisation-Wide Improvement in Health Care Matters, and How to Get Started 2019. https://www.health.org.uk/publications/reports/the-improvement-journey (accessed January 2020).
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/279124/0947.pdf (accessed January 2020).
- National Advisory Group on the Safety of Patients in England . A Promise to Learn – A Commitment to Act. Improving the Safety of Patients in England 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/226703/Berwick_Report.pdf (accessed January 2020).
- Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file /279124/0947.pdf (accessed January 2020).
- NHS England 2014. https://www.england.NHS.uk/publication/nhs-five-year-forward-view/ (accessed January 2020).
- Care Quality Commission (CQC) 2014. https://www.cqc.org.uk/sites/default/files/20140801_special_measures_one_year_on_report_final.pdf (accessed January 2020).
- Rose L. Better Leadership for Tomorrow 2015. https://www.Gov.Uk/government/publications/better-leadership-for-tomorrow-nhs-leadership-review (accessed January 2020).
- NHS England . The NHS Long Term Plan 2019. https://www.longtermplan.nhs.uk (accessed January 2020).
- NHS England and NHS Improvement 2019. https://improvement.nhs.uk/resources/nhs-oversight-framework-201920 (accessed January 2020).
- Maden M, Cunliffe A, McMahon N, Booth A, Carey GM, Paisley S, et al. Use of programme theory to understand the differential effects of interventions across socio-economic groups in systematic reviews-a systematic methodology review. Syst Rev 2017;6. https://doi.org/10.1186/s13643-017-0638-9 (accessed January 2020).
- Great Britain . Health and Social Care Act 2008. Chapter 1 2008. https://www.legislation.gov.uk/ukpga/2008/14/contents (accessed January 2020).
- Gov.UK n.d. https://www.gov.uk/guidance/public-bodies-reform#:~:text=An%20arm%27s%20length%20bodies%20(%20ALBs,classified%20by%20the%20Cabinet%20Office (accessed 22 June 2023).
- Department of Health and Social Care (DHSC) . The Regulation and Oversight of NHS Trusts and NHS Foundation Frusts 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/200446/regulation-oversight-NHS-trusts.pdf (accessed January 2020).
- Spiegelhalter D, Sherlaw-Johnson C, Bardsley M, Blunt I, Wood C, Grigg O. Statistical methods for healthcare regulation: rating, screening and surveillance. J Roy Stat Soc Stat Soc 2012;175:1-47. https://doi.org/10.1111/j.1467-985X.2011.01010.x (accessed January 2020).
- NHS Improvement 2017. https://www.gov.uk/government/publications/nhs-improvement-annual-report-and-accounts-201617 (accessed January 2020).
- NHS Digital 2019. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics (accessed January 2020).
- NHS England n.d. https://www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/ (accessed January 2020).
- NHS England n.d. https://www.nhs.uk/servicedirectories/pages/nhstrustlisting.aspx (accessed January 2020).
- NHS England n.d. https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ (accessed January 2020).
- NHS England n.d. https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/ (accessed January 2020).
- NHS England n.d. https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/ (accessed January 2020).
- NHS England n.d. https://digital.nhs.uk/data-and-information/publications/statistical/shmi (accessed January 2020).
- NHS England n.d. https://www.england.nhs.uk/statistics/statistical-work-areas/delayed-transfers-of-care/ (accessed January 2020).
- NHS England n.d. https://www.nhsstaffsurveys.com/results/results-archive/ (accessed January 2020).
- NHS England n.d. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics (accessed January 2020).
- NHS England n.d. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates (accessed January 2020).
- NHS England n.d. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-vacancies-survey (accessed January 2020).
- NHS Staff Survey Coordination Centre 2019. https://www.nhsstaffsurveys.com/Page/1064/Latest-Results/2018-Results/ (accessed January 2020).
- Ferlie E, Dopson S, Bennett C, Fischer MD, Ledger J, McGivern G. The Politics of Management Knowledge in Times of Austerity. New York, NY: Oxford University Press; 2019.
- Gebski V, Ellingson K, Edwards J, Jernigan J, Kleinbaum D. Modelling interrupted time series to evaluate prevention and control of infection in healthcare. Epidemiol Infect 2012;140:2131-41. https://doi.org/10.1017/S0950268812000179 (accessed January 2020).
- Drummond M, Sculpher M, Torrance G, O’Brien B, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Brazier J, Ratcliffe J, Tsuchiya A, Salomon J. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford: Oxford University Press; 2007.
- Care Quality Commission (CQC) 2022. https://www.cqc.org.uk/guidance-providers/healthcare/key-lines-enquiry-healthcare-services (accessed 23 June 2023).
- NHS Improvement n.d.
- Allen T, Walshe K, Proudlove N, Sutton M. Measurement and improvement of emergency department performance through inspection and rating: an observational study of emergency departments in acute hospitals in England. Emerg Med J 2019;36:326-32. https://doi.org/10.1136/emermed-2018-207941 (accessed January 2020).
- Janke K, Propper C, Sadun R. The Impact of CEOs in the Public Sector: Evidence from the English NHS. Cambridge, MA: National Bureau of Economic Research; 2019.
- Fielden J. A medical director’s perspective on healthcare leadership. Future Hosp J 2015;2:190-3. https://doi.org/10.7861/futurehosp.2-3-190 (accessed January 2020).
- Willcocks SG, Wibberley G. Exploring a shared leadership perspective for NHS doctors. Leadersh Health Serv 2015;28:345-55. https://doi.org/10.1108/LHS-08-2014-0060 (accessed January 2020).
- Dickinson H, Snelling I, Ham C, Spurgeon PC. Are we nearly there yet? A study of the English National Health Service as professional bureaucracies. J Health Organ Manag 2017;31:430-44. https://doi.org/10.1108/JHOM-01-2017-0023 (accessed January 2020).
- Jones L, Pomeroy L, Robert G, Burnett S, Anderson JE, Morris S, et al. Explaining organisational responses to a board-level quality improvement intervention: findings from an evaluation in six providers in the English National Health Service. BMJ Qual Saf 2019;28:198-204. https://doi.org/10.1136/bmjqs-2018-008291 (accessed January 2020).
- Fulop NJ, Ramsay AIG. How organisations contribute to improving the quality of healthcare. BMJ 2019;365. https://doi.org/10.1136/bmj.l1773 (accessed January 2020).
- Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G. Association between organisational and workplace cultures, and patient outcomes: systematic review. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-017708 (accessed January 2020).
- Bardsley M. 2016. https://www.health.org.uk/publications/understanding-analytical-capability-in-health-care (accessed January 2020).
- Vindrola-Padros C, Pape T, Utley M, Fulop NJ. The role of embedded research in quality improvement: a narrative review. BMJ Qual Saf 2017;26:70-8. https://doi.org/10.1136/bmjqs-2015-004877 (accessed January 2020).
- NHS Digital n.d. https://digital.nhs.uk/data-and-information/publications/statistical/shmi (accessed 23 June 2023).
Appendix 1 Interview topic guides
Interview topic guide: national interviews – DHSC and NHS Improvement (version 4.0, 10 January 2019)
General introduction and background
-
To begin, could you tell me about your professional background? [PROMPT]
-
How long have you worked at DHSC/NHS Improvement?
-
How long have you been in this particular role?
-
-
What are your main areas of responsibility? [PROMPT]
-
Do you have specific responsibilities in relation to NHS provider performance and/or quality?
-
-
In terms of this organisation’s governance, what committees or teams do you report to and how often is this? [PROMPT]
-
Board.
-
Senior officials.
-
The Special Measures Regime: general (20 minutes)
We are looking at the special measures regime for quality and the impact of different types of interventions delivered within trusts by NHS Improvement.
-
What do you see as the main aim of the Special Measures programme for Quality?
-
Could you describe the typical process when NHS trusts enter Special Measures for Quality?
-
Do you have a view on why some NHS trusts fall into the special measures regime for quality? [PROMPT]
-
Are there warning signs that you have observed in practice?
-
-
When a trust has entered Special Measures for Quality, how does NHS Improvement work with other organisations such as the CQC to support that trust to improve? [PROMPT]
-
Do the CQC and NHS Improvement work jointly together to share information? If so, how does work in practice and what data or information is shared?
-
Do you collect specific data for trusts in Special Measures for Quality – beyond that which is already routinely collected in the NHS? If so, please explain.
-
Does NHS Improvement also engage local commissioners or other local health system leaders when a trust enters Special Measures for Quality?
-
-
Why do you think some NHS trusts struggle to leave Special Measures and require external support for a longer time, for example over 18 months?
-
Could you describe the process for identifying when a NHS trust is placed on the ‘challenged provider’ list?
-
Do you have a view on why some NHS trusts end up on the ‘challenged provider’ list but avoid entering Special Measures?
Policy and interventions (NHS Improvement)
We would like to understand more about the specific quality support mechanisms or interventions issued by NHS Improvement to trusts that enter the Special Measures regime for Quality or are placed on the challenged provider list.
-
What are your perceptions of the interventions used by NHS Improvement to improve quality in NHS trusts placed in Special Measures for Quality, such as:
-
appointment of an ID
-
buddying with another (higher performing) trust
-
access to funds to spend on quality improvement
-
senior executive and/or board leadership change.v
-
-
What are the aims of each of these different mechanisms?
-
What outcomes or impacts do you expect from each of these? [PROMPT]
-
How are these achieved locally?
-
-
What is the process for choosing the types of support mechanisms or interventions that trusts receive? [PROMPT]
-
To what extent are trusts involved in these discussions?
-
Is the process different for challenged and special measures trusts?
-
-
In your opinion, is it better to deliver some of these interventions or support mechanisms together – as a bundle of support for example? [PROMPT]
-
Do you have a sense of which intervention – or combination of interventions – work well in NHS organisations in Special Measures or challenged? Why is this?
-
-
Do you know where the specific interventions used in the Special Measures regime originate from, such as the policies or frameworks that have encouraged their use over time?
-
Do you observe any of the improvement interventions listed above to work better in certain types of trusts or contexts than others? [PROMPT]
-
ambulance or mental health trust or an acute trust
-
rural or urban areas
-
small or large trusts
-
different organisational cultures or health system contexts
-
-
In your experience, how do NHS organisations receiving the NHS Improvement support interventions tend to respond?
-
Does their response change over time?
-
-
What are the common difficulties or barriers that NHS organisations face when in Special Measures for Quality and implementing these support interventions?
-
Has the implementation of these interventions ever led to any unanticipated negative outcomes in any NHS trusts?
-
What types of actions do you think NHS leaders, CEOs and the board should undertake to exit Special Measures or leave the challenged provider list and sustain exit?
-
Do you have any other comments about the role of CEOs and the board in supporting health-care organisations to promote quality improvement over time? [PROMPT]
-
For example, what organisational skills or capabilities they should seek to develop?
-
-
Are there any other quality improvement interventions or NHS policies that we should be aware of in this study and support quality improvement in challenged NHS trusts or those in Special Measures?
-
Is there anything you would like to add that we have not covered?
Interview topic guide: national interviews – CQC (version 4.0, 10 January 2019)
General introduction and background
-
To begin, could you tell me about your professional background? [PROMPT]
-
How long have you worked at the CQC?
-
How long have you been in this particular role?
-
-
What are your main areas of responsibility?
-
In terms of this organisation’s governance, what committees or agencies do you report to and how often is this? [PROMPT]
-
Board.
-
NHS agencies or central government (e.g. NHS Improvement/NHS England/DHSC).
-
The Special Measures Regime: general
We are looking at the special measures regime for quality and the impact of different types of interventions delivered within trusts by NHS Improvement.
-
What do you see as the main aim of the Special Measures regime for Quality?
-
Could you describe the typical process that occurs when NHS trusts enter Special Measures for Quality, from a regulatory perspective? [PROMPT]
-
How is a decision reached about whether to place a trust in Special Measures for Quality? For example, if it receives an ‘inadequate’ rating.
-
What evidence or type of informs the decision?
-
-
Once a trust enters Special Measures for Quality, how does the CQC work with other organisations in the health system to make improvements at that trust, for example:
-
How do the CQC and NHS Improvement work jointly?
-
What information is shared?
-
-
How does the CQC monitor a trusts performance after they are placed in Special Measures for Quality? [PROMPT]
-
Do you collect specific types of data for trusts in Special Measures for Quality to track improvements?
-
Does a trust have to collect or send specific data to the CQC?
-
-
Does the CQC follow up at intervals with the trust?
-
Could you explain how the process of re-inspection of a trust in Special Measures works in practice?
-
Does the CQC also have a role in identifying NHS trusts on the ‘challenged provider’ list? [PROMPT]
-
[If so]: how does the CQC work with NHS to address quality issues in challenged provider?
-
-
Does the CQC have a role in decisions about whether, and when, a trust exits or stays in Special Measures for Quality?
-
Does the CQC have a role in decisions about whether and when a trust leaves the Challenged Provider ‘watch list’?
-
Specific interventions
-
What are your perceptions of the interventions used by NHS Improvement to improve quality in NHS trusts placed in Special Measures for Quality, such as the following: [PROMPT]
-
Appointment of an ID.
-
Buddying with another (higher performing) trust.
-
Access to funds to spend on QI.
-
Senior executive and/or board leadership change.
-
[PROMPT]: Any others not listed?
-
-
Do you know where the specific interventions used in the Special Measures regime originate from – such as which policies or frameworks have encouraged their use over time?
-
What outcomes or impacts do you expect from each of these?
-
Do you have a sense of which type of intervention – or combination of interventions – works well in NHS organisations with quality issues? And why?
-
Do some quality improvement interventions work better in certain types of trusts or local health systems than in others? [PROMPT]
-
ambulance or mental health trust or an acute trust
-
rural or urban areas
-
different organisational cultures or health system contexts?
-
-
In your experience, how do NHS organisations receiving the NHS Improvement support interventions respond initially?
-
Does their response change over time?
-
What are some of the barriers they face when implementing these interventions?
-
-
In your view, do the interventions lead to sustainable quality improvement in trusts over time? [PROMPT]
-
In your view, how attributable are improvements in quality to the NHS Improvement interventions discussed above?
-
-
Has the implementation of these interventions ever led to any unanticipated negative outcomes in any NHS trusts?
-
What types of actions would you recommend trust CEOs and boards undertake to improve quality and exit Special Measures permanently?
-
Do you have any other comments about the role of NHS system leaders, CEOs or trust boards in supporting health-care organisations to promote quality improvement over time? For example, the organisational skills or capabilities they should seek to develop.
-
Is there anything you would like to add that we have not covered?
Interview topic guide: trust case studies (internal interviewees) (version 2.0, 24 February 2019)
Introduction/warm-up
-
What is your role in this organisation?
-
How long have you worked here for?
-
To confirm, were you working in this organisation when it was placed on the challenged provider list?
Special Measures for Quality/Challenged Provider: background
-
Could you describe any specific quality issues that have been previously identified in this trust in CQC inspections?
-
Have any other issues been identified in this trust by NHS Improvement or the Department of Health and Social Care?
-
Was this during a visit from a regional team or central team?
-
Do you think it was necessary for this organisation to be placed in SMQ/CP?
-
What has been the short-term impact of being placed in SMQ/CP?
-
How did staff respond to the news?
-
Was there an impact on recruitment or workforce retention?
NHS Improvement interventions
-
[Unprompted]: Has this organisation received support from NHS Improvement to make changes in performance and quality?
-
[If yes, please describe]
-
When did this begin?
-
[Prompted]: Has this organisation received any of the following interventions from NHS Improvement?
-
appointment of an Improvement Director
-
appointment of a ‘buddying’ trust
-
funding dedicated to quality improvement activities.
-
-
[For each of the above that is mentioned] Do you recall when this intervention began?
-
[For each of the above that is mentioned] Do you recall for how long the intervention was received?
-
What was your experience of the intervention?
-
Do you think the intervention(s) supported this organisation to make changes? [If so] how?
-
Have changes in senior leadership or governance been recommended by NHS Improvement, an ID or the regulator?
-
Did an ID develop a quality improvement plan with this organisation? [If so]:
-
Was this plan helpful?
-
Were any recommendations unhelpful?
-
Were any recommendations particularly challenging to implement?
-
Deployment of resources to deliver QI and opportunity costs
-
Have there been direct costs to this organisation of being placed on in SMQ/CP?
-
Have there been direct costs to this organisation to implement the kinds of improvements recommended by NHS Improvement or the CQC? If so, could you provide some examples?
-
[If not discussed above]: Has this organisation applied for QI funds from NHS Improvement to drive quality improvement locally?
-
If so, how was this money allocated locally? What was it used for?
-
Has this organisation changed how you allocate staff time or resources in the organisation?
-
Do any new activities prompt a trade-off in terms of staff time or resources?
Quality improvement knowledge and organisational capabilities for QI
-
Have you applied any quality improvement methodologies in this organisation? For example, Lean, Virginia Mason, PDSA cycles, IHI.
-
Do you use any other management tools or information systems to monitor quality improvements in the organisation?
-
Have you started to collect any new types of data to monitor changes in performance since being placed in SMQ/CP?
-
Have you implemented any service innovations to support better outcomes, quality or patient experience since being placed in SMQ/CP?
-
Has this organisation brought in external management consultants or external experts to support performance or quality improvement? If so, did this bring about any changes locally?
-
Does the organisation engage with patients and the public around quality issues? If so, how does this work in practice?
Local health economy and stakeholders (outer context)
-
Does this organisation have any important strategic or collaborative partnerships with other local providers or commissioners?
-
If so, how does this arrangement work in practice?
Wrap up questions
-
On reflection, what has been most helpful to this organisation to support any changes in quality and performance over time? [PROMPT]
-
funding
-
NHS Improvement interventions
-
leadership/governance changes
-
other.
-
-
What advice would you give to other health-care organisations seeking to improve their performance and avoid entry into SMQ/CP?
-
Anything else we should be aware of or that you would like to add?
Interview topic guide: trust case studies (external interviewees) (version 2.0, 26 March 2019)
Preliminaries
-
Ensure participant has reviewed information sheet and signed consent form/sends digitally in case of telephone interview.
-
Explain plans for feedback and dissemination.
-
Seek permission to record.
Questions
Introduction/warm-up
-
What is your role in this organisation?
-
How long have you worked here for?
-
What are your main responsibilities?
Special Measures for Quality/Challenged Provider
-
Have you had any formal involvement with [trust name] since it has been in SMQ/on the CP list?
-
Have you reviewed the case of [trust name] in relation to the SMQ or CP regimes?
-
Are there any specific quality issues that you are aware of in this trust?
-
Do these quality issues have any impact on your organisation or you in your professional role?
-
Do you think it was necessary for this organisation to be placed in SMQ/on the CP list?
-
In your opinion, what is the purpose of the SMQ/CP regime? What are the outcomes it hopes to achieve and how will it achieve them?
-
What was the short-term impact of this trust being placed in SMQ/on the CP list? Has this had an impact on the local system?
-
Has this had an impact on local staff, patients or the public in your view?
-
Has your organisation worked with the trust to help it make changes in practice in response to the trust being placed in SMQ or CP? If so, please can you give an example.
-
Are there any local or regional collaborations within this health system to support quality improvement, including in [trust name]?
-
Are you aware of any financial or capital investments to drive quality improvements in [trust name] that have been made since it was placed in SMQ or on the CP list?
-
Do you have regular meetings with other organisations, such as NHS Improvement and CQC, in relation to trusts in SMQ or CP in your region to discuss NHS provider performance and quality? If so, how often is this? What is usually discussed at meetings? Who attends?
-
What specific data for trusts in SMQ in your area do you collect and discuss on a regular basis?
NHS Improvement interventions
-
Are you aware of any interventions used by NHS Improvement to improve quality in NHS trusts placed in Special Measures for Quality, such as: [PROMPT]
-
appointment of an ID
-
buddying with another (higher performing) trust
-
access to funds to spend on quality improvement
-
senior executive and/or board leadership change.
-
-
Are you aware of any other formal or informal quality improvement interventions?
-
[If aware] In your experience, how do NHS organisations receiving the NHS Improvement support interventions tend to respond?
-
What are the common difficulties or barriers that NHS organisations in your region face when in SMQ or CP and implementing these support interventions?
Wrap up questions and close
-
On reflection, what is most helpful to organisations in your region to bring about lasting changes in quality and performance over time? [PROMPT]
-
funding
-
NHS Improvement interventions
-
leadership/senior management team changes
-
other.
-
-
What advice would you give to other regions with health care organisations seeking to improve their performance and avoid entry into Special Measures for Quality or the CP list?
-
Anything else we should be aware of or that you would like to add? Is there anyone else you would recommend we speak with about these issues in the local health system?
Appendix 2 Board maturity framework observation template
Template for mapping meetings and papers to the ‘Organisational Maturity Framework’ adapted from Jones et al. 18 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
| Dimension | Notes |
|---|---|
| 1. QI as a board priority | |
|
|
| 2. Using data for improvement | |
|
|
| 3. Familiarity with current performance | |
|
|
| 4. Degree of staff involvement | |
|
|
| 5. Degree of public/patient involvement | |
|
|
| 6. Clear systematic approach | |
|
|
| 7. Balance between clinical effectiveness patient experience and safety | |
|
|
| 8. Dynamics | |
|
Appendix 3 Summary of actions from the patient and public involvement peer review process
| PPI ‘light touch’ peer review of SMQ protocol | |
|---|---|
| Recommendation | Action |
| Include analysis of which interventions work better than others | We updated one of our RQs to ask what features of trusts in SMQ/challenged provider regimes contribute to their differing performance trajectories. We reworked our quantitative analysis section to try to look at improvement actions against different outcomes. We may be able to compare these outcomes with trusts that have not received this intervention to better understand the impact of the intervention |
| Include investigation of what data trusts use to track improvements | We will also be asking the trusts what type of data they use, which may highlight differences between trusts and something that works well |
| More clarity about RSET SMQ project team organisation | We added a section on project management of peer review of SM protocol |
| How does SMQ impact (1) patient referrals, (2) patient choices of provider and (3) staff recruitment and retention | We will be conducting interviews with patient groups, which may uncover some of this (although it is not the main intention of the interview), we will also be undertaking an exploratory study to see if there is an effect on staff retention/recruitment within trusts in SMQ |
| Include a brief lay summary of all RSET outputs | We have updated our dissemination plan to include the production of more accessible outputs that would summarise results for a range of audiences, including patient groups |
Appendix 4 Snowball technique for five waves of searches (phase 1)
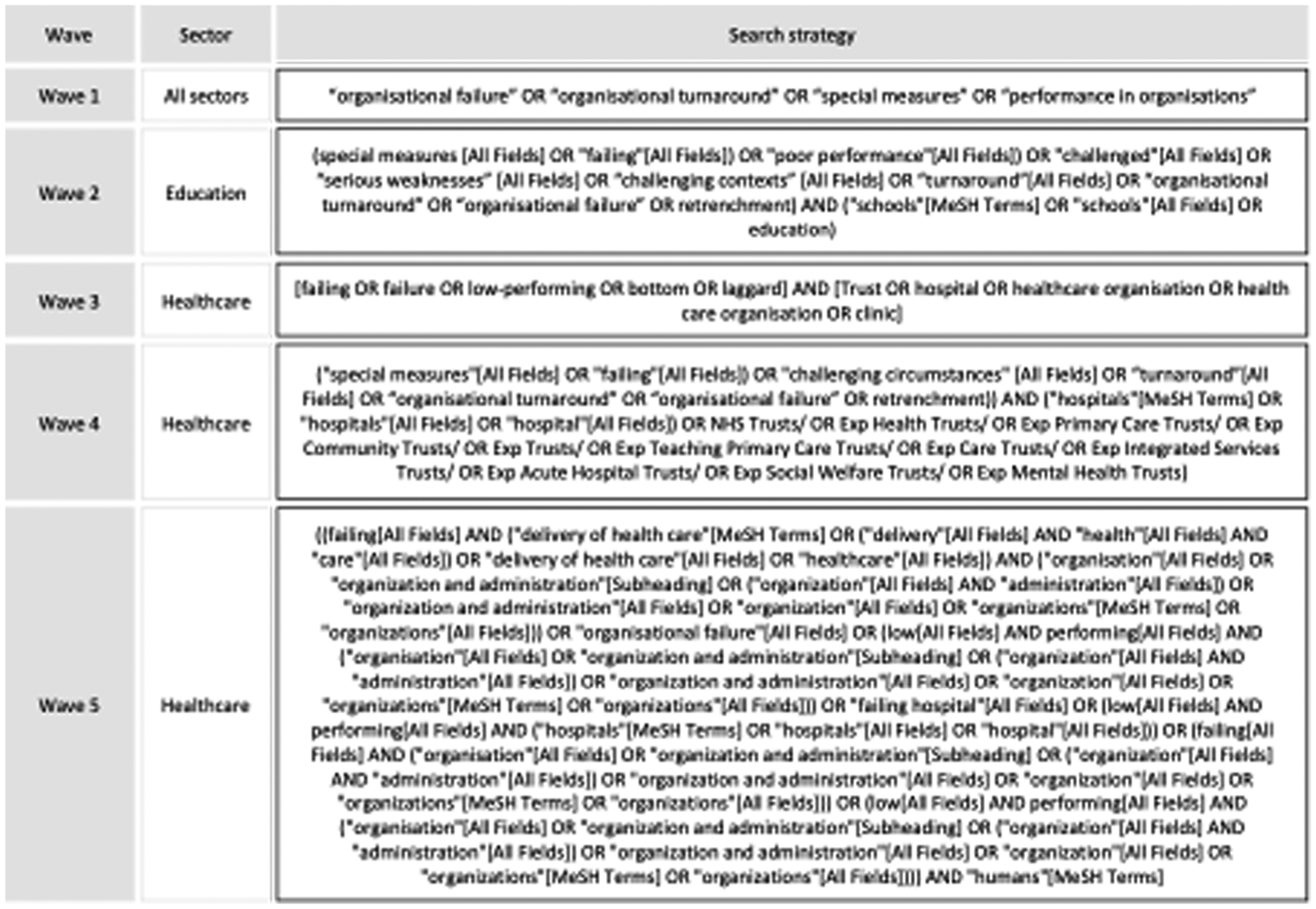
Appendix 5 Further details on the statistical aspects of the analysis
z-scoring methodology
We applied a z-scoring approach to standardise the deviations of a trust’s outcomes from the national mean. This was necessary because national means change seasonally and often follow trends that consistently increase or decrease over time.
z-scores are calculated from the following formula:
The indicators we analysed were binomial, representing rates or proportions and the scores we calculated with the above formula were skewed. Therefore, we reduced skewness using a square root transformation of the data.
The z-scoring formula for our transformed binomial observations, therefore, becomes:
where p is the observed proportion, π is the expected proportion and n is the size of the population (i.e. the number of trusts). The direction of the skewness depends on the proportion being used. With any proportion, there is a choice between using p or 1 – p, and the square root transformation works best if we choose the smaller of these for our observations (i.e. we work with breaches of the 4-hour ED target rather than percentage achievement).
In all cases, we found that z-scores calculated in this way were over dispersed. To overcome this, we assumed additive overdispersion and adjusted these z-scores accordingly. 124
z-scores from the SHMI mortality indicator
Although the SHMI is already standardised against an expected value of 1, the variances change from one period to the next, so that similar values may be an outlier one-quarter, but within acceptable limits for another quarter. To adjust for changing variances we, again, applied a z-scoring approach but used a different methodology as SHMI control limits already adjusted for additive overdispersion and a log transformation rather than a square root transformation is used to overcome skewness.
For the SHMI, additive overdispersion is assumed whereby, for a SHMI value y:
and:
where:
Therefore:
We can find the denominator from the two standard deviation upper or lower limits quoted for y in the published data. 155
If u denotes the upper limit, then the z-score at the upper limit:
so that:
Therefore:
Interrupted time series
Using our z-scoring approach for each indicator, we created time series for each challenged or special measures trust. The interrupted time series method enabled us to analyse trends in these z-scores, and whether or not there were any significant changes to these trends after trusts entered the regime and any further changes once they had left. Separate time series were analysed for each trust and then pooled to create overall trends for each indicator. 140
The data series were monthly with two exceptions, ED 4-hour waits and SHMI, for which we used quarterly data because of what was available (monthly data are now being collected but did not go back far enough for these indicators). The length of the pre-intervention period was chosen as 18 months for each indicator, and 24 months for the cancer waiting time indicators owing to their greater stability.
We tested for autocorrelations by calculating Durbin–Watson statistics for each series. There was less evidence of autocorrelations among the ED, cancer and caesarean section indicators, but clear evidence with the others. (The SHMI is clearly autocorrelated because, although it is reported quarterly, each value refers to a whole year, which means successive quarters overlap by 9 months.) For the series for which there was evidence of autocorrelation, we accounted for it by introducing appropriate lagged variables into the models.
We applied two interrupted time series models. For trusts that were still in SMQ/CP by September 2019, or had only recently left, the time series had only one change point at the moment when trusts entered the quality regime. For trusts that had left and had more than two data points after leaving, the time series had two change points: one on entry and the other on exit.
If the trust enters the regime at time t1, the first case the model had the form:
where T is the time since the start of the series; I is a binary variable that = 1 for T > t1; T* is the time since the regime starts: = 0 for T < t1; and = T – t1 for T ≥ t1.
If the trust leaves the regime at time t2, then the second model applies and has the form:
where:
T* = 0 for T < t1 and T ≥ t2;
T* = T – t1 for t1 ≤ T < t2
T** is the time since the trust leaves the regime: = 0 for T < t2 and = T – t2 for T ≥ t2
With this formulation, β4 reflects the degree to which the trend after exit differs from the trend before the trust enters the regime, and thus any longer-term impact on trend.
All analyses and calculations were performed using combinations of Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA; 2016) and SAS® software (version 9.4) (SAS Institute Inc., Cary, NC, USA).
Appendix 6 Summary of quality improvement interventions, methods and techniques utilised by trusts
| QI method/tool/intervention | Theme | Service area | Number of sites | Internal/external resource or QI knowledge | Analysis |
|---|---|---|---|---|---|
| NHS Improvement Emergency Care Improvement Programme Team/emergency care intensive support | Service quality improvement | ED | 2 | External: NHS Improvement | Well-regarded support service from NHS Improvement. External input where unit/trust struggling with rising demand and improvement |
| Lean and/or Kaizen | Service efficiency and Quality improvement | Trust-wide or specific Service improvements (e.g. RTTs) | 4 |
|
Well-known methodology in the NHS and viewed as a structured, systematic approach to improving quality and organisational processes. Applied to local services |
| Virginia Mason | Service and quality improvement | Trust wide | 2 |
|
Approach has gained popularity and traction across the NHS. NHS Improvement endorsed approach. Complementary with lean principles. Method for continuous quality improvement in local services |
| Well-led review and turnaround | Leadership and governance | Senior team and board | 1 | Usually large management consultancy firms | External, independent reviews of top teams and boards. May result in detailed reports and quality action plans. Overlap with leadership development and governance reviews (below) |
|
Leadership, culture and governance: most often at senior level | Trust and service leaders; for example, clinical directors, senior nurses and senior managers. Senior executive team and board | 4 | External: e.g. university providers, governance experts, consultants | Focused programmes may be for staff more widely or focused on the senior leadership team and board. Can take the form of coaching, mentorship, intensive support by an external supplier and away days. Typically focuses on good governance, values and culture. At board level – support better working with senior team |
| Ward ‘huddles’ and ‘safety huddles’ | Patient safety and staff engagement | Service and departmental level | 3 | Internal: local QI champions and clinical teams | Encourage regular checks and local communication practices to support patient safety at ward level |
| QI fellows and/or QI unit or embedded team within the trust. May have a transformation focus | Building QI capabilities and awareness among staff | Trust wide and service level | 4 |
|
Investment in permanent QI teams, ‘academies’, ‘faculty’ and ‘fellows’ to support staff training in QI methods. Aims to encourage a safety and improvement culture using structured approaches to continuous improvement (e.g. PDSA). May also focus on specific service improvement projects (e.g. in ED) or wider transformation. Aim to building organisational QI capabilities |
| (WHO) Five Steps to Safer Surgery/checklist | Service quality and patient safety | Surgical teams and services | 3 |
|
Organisations to use WHO surgical safety checklist and guidelines to improve safety of patients undergoing surgery |
| Staff engagement listening events | Staff morale and engagement | Trust and service level (e.g. ED), support for junior doctors | 2 | Internal | Aims to improve staff engagement and listen to concerns, including of trainees and new staff |
| Quality, service improvement and redesign | Service and quality improvement | Trust wide | 2 | External: NHS Improvement quality, service improvement and redesign college | Practitioner-focused training for clinical and non-clinical staff to develop quality and efficiency improvement capability to apply in organisations and/or health systems. Focus on capacity building |
| ‘Model for Improvement’ (developed by the Institute of Healthcare Improvement, USA) | Service and quality improvement | Trust wide | 1 | External: Institute of Healthcare Improvement | Structured model applying Plan-Do-Study-Act (PDSA) cycle approach |
Appendix 7 Themes from the NHS staff survey
|
Appendix 8 Identification of deliveries and emergency caesarean sections within Hospital Episode Statistics Inpatient Care data
Patient selection criteria:
-
Type of episode is classed as a “delivery episode” (EPITYPE = 2) or “other delivery event” (EPITYPE = 5).
-
Place of delivery is an NHS hospital (DELPLAC_1 ≠ 1, 5, 6).
-
Episode has finished (EPISTAT = 3).
-
Patient classed as: “ordinary admission” (CLASSPAT = 1), “day case admission” (CLASSPAT = 2) or “mothers and babies using only delivery facilities” (CLASSPAT = 5).
All deliveries are identified by any of the following OPCS procedure code occurring within any of the fields OPERTN_01 to OPERTN_24:
-
R17: Elective caesarean delivery;
-
R18: Other caesarean delivery;
-
R19: Breech extraction delivery;
-
R20: Other breech delivery;
-
R21: Forceps cephalic delivery;
-
R22: Vacuum delivery;
-
R23: Cephalic vaginal delivery with abnormal presentation;
-
R24: Normal delivery;
-
R25: Other methods of delivery, including:
-
R251: Caesarean hysterectomy;
-
R252: Destructive operation to facilitate delivery;
-
R258: Other specified;
-
R259: Unspecified.
-
Emergency caesarean sections are identified by one of the following:
-
R18 (Other caesarean delivery);
-
R251 (Caesarean hysterectomy).
List of abbreviations
- CCA
- cost–consequences analysis
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CP
- challenged provider
- CQC
- Care Quality Commission
- DHSC
- Department of Health and Social Care
- ED
- emergency department
- GMC
- General Medical Council
- HEE
- Health Education England
- HES
- Hospital Episode Statistics
- HSDR
- Health and Social Care Delivery Research
- ID
- improvement director
- JSOG
- Joint Strategic Oversight Group
- NIHR
- National Institute for Health and Care Research
- OAG
- Oversight and Assurance Group
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- QA
- quality assurance
- QI
- quality improvement
- RAP
- rapid assessment procedure
- RQ
- research question
- RSET
- Rapid Service Evaluation Team
- RTT
- referral to treatment
- SHMI
- summary hospital-level mortality indicator
- SMF
- Special Measures for Finance
- SMQ
- Special Measures For Quality
- SOF
- Single Oversight Framework
- TDA
- Trust Development Agency
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/GQQV3512).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
