Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 17/05/62. The contractual start date was in February 2019. The draft manuscript began editorial review in March 2022 and was accepted for publication in May 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Noble et al. This work was produced by Noble et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Noble et al.
Chapter 1 Introduction
Overview
Emergency department (ED) visits for epilepsy are common, costly, often clinically unnecessary and typically lead to little benefit for epilepsy management. A care pathway (CP) for epilepsy, which diverts people with epilepsy (PWE) away from ED when ‘999’ is called and leads to care elsewhere, could potentially generate savings and instigate improvements in the person’s ambulatory care. A range of alternative CP configurations are possible and being considered.
This project sought to identify the optimal configuration for epilepsy, ensuring the CP is both acceptable to persons (from a particularly vulnerable target population) and feasible for delivering by the NHS. While beyond the scope of the current project, our ultimate aim is to work with the ambulance service to implement the most promising CP, rapidly evaluate it and use the evidence to transform service organisation nationally.
The current project had three-linked Work Packages (WPs) and used mixed methods. In WP1, NHS bodies were surveyed about what CPs they are considering for adults with epilepsy. We also conducted semistructured interviews with PWE and their family and friends [significant others (SOs)]. These explored the elements of postseizure care that are important to them and what concerns and expectations they have regarding an alternative CP.
In WP2, a national survey of PWE and their SOs was completed that used discrete choice experiments (DCEs). It recruited people who had had recent contact with the ambulance service for epilepsy. It aimed to identify the relative importance they placed on different care characteristics (attributes) under common seizure scenarios and the ‘trade-offs’ they were willing to make. The DCE method also allowed us to estimate the likely uptake of different CP configurations by PWE if they were implemented.
In WP3, we ran knowledge exchange (KE) with key stakeholders (ambulance clinicians and managers, neurologists, nurse specialists, commissioners and user representatives) and shared the DCE findings with them. They were asked to discuss which configuration struck the best balance between meeting users’ needs and NHS feasibility.
To maximise the impact of the project and its ability to influence practice, those considering alternative CPs for epilepsy were informed of the project, updated on its progress and had an opportunity to contribute.
The project’s aims were as follows.
Aims
Work Package 1
-
To systematically identify alternative CPs being considered by the NHS for epilepsy and describe the extent to which service users have been involved in their design.
-
To understand the decision-making processes of PWE and their SOs for seeking or not seeking ED care, and their concerns and expectations regarding alternative CPs.
-
To identify the attributes of postseizure emergency care that PWE and their SOs consider important and identify if this differs by the context in which the seizure occurs.
Work Package 2
-
To determine patient and SOs’ preferences for postseizure emergency care using DCEs and identify subgroup differences.
-
To estimate utility of different CP configurations to service users and subgroup differences.
Work Package 3
-
To hold expert workshops at which stakeholders, informed of the DCE evidence, would identify the optimal alternative CP(s) for seizures that could be recommended for implementation and evaluation.
Review of the evidence
The following sections provide a qualitative (unsystematic) review of the evidence. It helps explain the background and rationale for the project. Please note that sections of this chapter have been reproduced from McKinlay et al. 1 under licence CC-BY-4.0.
NHS context and the need to manage demand on services
Like other health systems around the world, the NHS has been operating within a context of rising demand, slow funding growth and increasing operating costs. In 2015–6, this culminated in an aggregate funding deficit of £1.85 billion for NHS providers and commissioners. 2,3 The NHS Long-Term Plan4 and the Five Year Forward View5 challenged the NHS to make substantial savings, while, at the same time, working with service users to improve care experience and outcomes and reduce health inequalities.
Avoidable attendances and epilepsy identified as an area where opportunities exist to reduce demand
One way proposed to generate savings and manage demand is by finding innovative ways to reduce clinically unnecessary use of expensive emergency health services. 6 Visits to type 1 EDs that are clinically unnecessary are termed ‘avoidable attendances’. 7 These refer to those where the patient does not require the full facilities of a type 1 ED to manage their health problem. A type 1 ED (hereafter referred to as ED) is one that offers a consultant-led 24-hour service, with full resuscitation facilities and designated accommodation for the reception of accident and emergency patients. 8 In the UK, the terms ED and accident and emergency (A&E) department are often used interchangeably, the latter being particularly common in lay parlance.
Different estimates regarding the proportion of attendances at EDs that are ‘avoidable’ are available. Using their definition (now adopted by NHS Digital9) which is based on actual care received, O’Keeffe et al. 7 conservatively estimated ~15% of adult attendances are ‘avoidable’. Based on 2018–9 attendance data, this equates to ~2.2M first ED attendances. 10
Epilepsy has been identified as one condition that accounts for some of these ‘avoidable’ visits11 and where health inequalities are implicated. 12
Epilepsy and its epidemiology
Epilepsy is the recurring tendency to have unprovoked seizures. With a prevalence of ~1%,13 this chronic relapsing condition is the UK second most common serious neurological disorder. It affects people across the age spectrum. Antiseizure medication is the mainstay of treatment. People with epilepsy, particularly the ≤ 48% who continue to experience seizures,14 are at increased risk of injury, psychological and social disadvantage and premature death. 15,16
Use of emergency hospital services for epilepsy and societal impact
In the UK, up to 20% of PWE visit an ED each year. 17–19 In England, there are around 100,000 such visits to ED each year. 20 In 2015–6, these cost the NHS ~£70 million. 21,22
One reason costs are high is because half of the PWE visiting EDs are admitted to the hospital;19,20,23–25 85% of admissions for epilepsy occur on such an unplanned basis. 26 Epilepsy and convulsions are the second leading cause of unplanned hospital admissions amongst chronic ambulatory care-sensitive conditions. 25
Re-admissions further drive costs up;27,28 ≤ 60% of PWE reattend ED within 12 months. 29 This rate of return is higher than seen for other chronic relapsing conditions, such as asthma and diabetes. 30,31 Amongst chronic ambulatory care-sensitive conditions, epilepsy is the second most common cause of unplanned hospital admissions (17%). 25
Use of emergency hospital services for epilepsy is often clinically unnecessary
Seeking emergency care for a suspected seizure, including those caused by epilepsy can be clinically appropriate, even life-saving. Reasons include a first seizure and status epilepticus. 32–34 Most PWE attending ED for a seizure do not attend for such reasons.
Our group leads the UK-wide National Audit of Seizure Management in Hospitals (NASH) initiative. 35,36 Data from > 8000 seizure-related ED attendances from 85% of UK acute hospitals were examined for the first and second rounds of NASH. Most PWE attending ED were found to have already diagnosed, rather than new epilepsy, and to be presenting with a nonemergency state not requiring the full facilities of ED.
Data23,37 indicate the leading presentations for epilepsy are a person with established epilepsy who has (1) experienced an uncomplicated seizure that is in line with their usual presentation, (2) experienced a seizure in public who cannot be ‘left at scene’ (e.g. because they are alone, in a post-ictal state, been incontinent or had a minor injury) or (3) experienced a seizure that has self-terminated, but which is different to the person’s ‘normal’ seizure(s).
While potentially dramatic and frightening, seizure presentations such as those above do not require the person to be cared for within an ED. 38–40 They will typically only require rest and reassurance and will return to baseline health without medical intervention. Respiration following a seizure usually rapidly returns to normal after convulsion cessation. Oxygen support postseizure will rarely be required,41 with supplemental oxygen only recommended if a person’s oxygen saturation level is < 94%. 40 Patients will often be left confused and aching (this is the post-ictal state), but this is not a cause for concern and usually resolves relatively rapidly leaving the patient alert.
In addition to being typically unnecessary from a clinical perspective, an ED visit after the aforementioned seizures risks iatrogenic harms arising from unnecessary investigations and interventions. 42,43 They can also be disruptive to the lives of patients, their families and hospital service functioning. The third and latest round of NASH shows that while most (~93%) ED visits for seizures last < 4 hours, a high proportion (~50%) do result in some sort of hospital admission (albeit for < 24 hours). 44
Unmet need in those with epilepsy visiting the emergency department
While the acute episodes leading PWE to visit ED do not typically require ED facilities, many of the presentations are expressions of a need for an improvement in the person’s ambulatory care.
The National Audit of Seizure Management in Hospitals20 found most (~65%) people visiting ED were not under the care of a healthcare professional specialising in epilepsy but were often requiring their support. Many patients were, for instance, on suboptimal drug treatment and thus at increased risk of experiencing avoidable seizures, side effects, psychosocial dysfunction and avoidable death. 45
Some PWE visiting ED also appear in need of enhanced self-management support, such as that provided by epilepsy nurse specialists (ENSs). This could mean the PWE and their families can learn more about their condition and how to manage seizures by themselves. 29,46–48 Unlike for other chronic conditions, there is no routine course PWE can go on to learn about epilepsy once diagnosed. Consequently, knowledge and self-management confidence can be low, particularly in those PWE who are older and those with low levels of formal education. 49,50
Momentum to reduce emergency department visits for epilepsy by introducing alternative care pathway
The policy agenda4,51,52 and the publicity given to the NASH findings21,53 created a vigour to reduce visits for seizures and enhance patient outcomes. Systematic examinations of the literature54 show there is no evidence on how to do this. An idea which has been gaining traction is for the ambulance service to assume a greater role. 55
The reason for this is that most (~90%) people who visit EDs for seizures have been transported there by an emergency ambulance. 24,35,36 Suspected seizures are the seventh most common call-out. 56 At present, ambulances convey nearly every person they attend to who has experienced a suspected seizure to ED. 56–58 This is despite most not demonstrating a clinical need for it and ambulance care guidelines not recommending it.
Dickson et al. 56 reviewed the ambulance records for suspected seizure incidents presenting to one regional English ambulance service and found medical emergencies were uncommon. The seizure had self-terminated before the emergency vehicle arrived in > 90% of cases and airways were clear. Breathing was found to be normal in > 96% of cases, and in only 8% of cases, emergency drugs were administered (by the crew or a SO beforehand). Despite this, ambulance crews still advised transport to ED in 89% of cases.
The Joint Royal Colleges Ambulance Liaison Committee (JRCALC) guidelines40 describe ambulance clinicians’ permitted scope of practice. They acknowledge the complexity of the management of seizures. Nonetheless, they state that the ‘overall risk of adverse events is low and most patients do not require the facilities of a hospital emergency department’ (p. 197). For those patients who are no longer seizing, JRCALC stipulate only that those who are pregnant, those who have experienced a first seizure and those treated with benzodiazepines should always be conveyed to ED (unless they have a care plan that states otherwise).
Conveyance decisions and factors behind high conveyance rate for epilepsy
A sizeable research literature exists on how ambulance clinicians decide whether to convey a person to ED. Two recent systematic reviews59,60 – which, between them, considered evidence up until April 2018 – have drawn this literature together. They show the complex nature of conveyance decisions, with multiple factors, beyond patient need, potentially affecting them. Oosterwold et al.’s60 conceptual framework (reproduced in Report Supplementary Material 1) summarises the macro, meso and micro factors.
Oosterwold et al.’s framework does not assert the importance or interplay between the different factors. It does, though, highlight the quality of evidence on each and opportunities for intervention. One factor associated with high-quality evidence, and which helps explain the attention being given to alternative CPs, is paramedics often lack access to alternatives to ED. This is highlighted by the following quotes from paramedics:61
We struggle for alternatives to ED. While we might be directed towards primary care, in practice they are lacking.
There was a big investment in a new urgent care centre locally but they won’t take people who’ve had a seizure. I’ve had patients … in a postictal state who need maybe half an hour until they come round … but [the centres] have this crazy idea that if somebody’s had a seizure then they need to have a CT scan … Sometimes there is no alternative but to take them to ED.
Other key factors that have been stated as contributing to high rates of conveyance and compound problems are (1) the limited external support ambulance crews receive with their conveyance decisions, (2) time pressures and (3) the limited access crews have to inform about the medical history of the person they are managing.
In terms of medical history, crews will typically not have access to the person’s full medical record. Instead, they will rely on information provided by informants on-scene and those who called for the ambulance.
Crews do increasingly have some access to NHS Summary Care Records. 62 However, in their standard form, these provide limited information pertinent to seizure care (i.e. only medications and allergies). A minority of PWE will implement procedures to overcome this limitation to information sharing, often at their own expense (e.g. by carrying a document, wearing medical alert jewellery and phone apps). However, crews still report finding information on the person’s history to be a challenge. 61 There is a National Institute for Health and Care Excellence (NICE) quality standard which states persons with epilepsy should have an agreed, written emergency care plan. 63 It only applies to adults with a history of prolonged or repeated seizures.
Regarding time pressures, some paramedics describe how under current funding arrangements they can feel able to only spend a limited amount of time ‘on scene’ to assess patients and permit them to recover. As such, transporting a person to ED can represent the most time-efficient management option. Dickson et al. 56 found that within one regional ambulance service, the mean time clinicians spent on scene for people presenting with seizures was 27 minutes. The following quotes61 show how time can sometimes impact upon paramedics’ conveyance decisions:
As a practitioner, if I don’t hit my times I’ll be pulled in by my manager, so it does pile the pressure on, forcing crews to think, ‘just put them on the truck and take them to hospital’.
If someone has a seizure outside of the home, we wouldn’t take them home … It’s not necessarily the right option for that patient … But by taking them home, which is further away, we will be tied up for longer.
There is a vision therefore of what could help: ambulance service access to some form of alternative CP whereby those seeking help for seizures judged not to require ED could be cared for within less costly, alternative environments. 64 The exact nature of the CP is not entirely clear, and most efforts are in the early stages. However, what is apparent is different English regions and services are considering different formats, and development is occurring in an unco-ordinated way.
Via positions that members of our team hold (e.g. professional bodies, scientific advisory committees and patient support organisations), we were aware of a range of packages envisioned. They included the introduction of policies for ambulance crews to leave patients at scene with the offer of a telephone call from a general practitioner (GP), a pharmacist practitioner or a nurse within 24, 48, 72 or indeed 120 hours. Other regions were considering allowing ambulance crews to transport patients home after seizures rather than taking them to ED. Others were looking to work with urgent treatment centres (UTCs), so those with seizures can be cared for within them.
‘Urgent Treatment Centre’ is the label that, following the Urgent and Emergency Care Review, has been given to most English walk-in centres, minor injury units and urgent care centres in an effort to reduce confusion. 65 Further details on them is provided in Report Supplementary Material 2.
Alternative care pathways and the ambulance service in general
The Keough Urgent and Emergency Care Review66–68 envisioned that demand on acute services could be reduced by expediting the transformation of the ambulance service. Rather than ambulances transporting most people to hospital, it envisions ambulances becoming mobile treatment centres, treating more patients at scene and making greater use of alternative CPs.
Alternative CPs are not new. Ambulance clinicians have not been obliged to transport everyone they see to ED since ~1997. Snooks et al. 69 developed some of the first CPs in 1999 and piloted them with the London Ambulance Service. These were so-called ‘see and treat’ protocols. In brief, crews were provided with protocols for different presentations. They would select the applicable protocol and work through a series of questions to establish if the presentation satisfied certain criteria. If they did, they were guided towards alternatives to ED. This ranged from them contacting the patient’s primary care team, advising the patient to contact NHS Direct, asking the patient to arrange an appointment with their GP to offering advice.
‘See and treat’ CPs are now common,70–77 and other alternative response options have also become available, such as ‘hear and treat’ (i.e. where advice is given to patients over the telephone and they are signposted to other care providers). 78,79
Recently, there have also been attempts to widen the aims of ‘see and treat’ CPs so they not only avoid unnecessary ED conveyances but also more explicitly seek to improve patient outcomes. 80–83 An illustration is the CP for hypoglycaemia developed by diabetes specialist nurses. 80 Patients with acute hypoglycaemia for whom an ambulance has been called are assessed and treated on scene by paramedics, rather than being transported to ED. Patients are then referred directly by ambulance staff to the specialist nurses, who subsequently contact the patient by telephone.
What is known about the use and risks and benefits of alternative care pathways
As is often the case with behaviour change interventions,84,85 the design and implementation of CPs have been ‘theory-lite’. The evidence on the utility of alternative CPs is nevertheless generally positive, albeit not definitive. 86–88
In their review of potential revisions to the urgent and emergency care system, the Nuffield Trust, for instance, identified greater ambulance/paramedic triage in the community as having the most positive evidence. 55 Some CP proponents highlight headline data suggesting their introduction helped ambulance services manage their own increasing demand. It is estimated that ambulance trusts saved themselves ~£74M and EDs ~£63M in 2015–6 by decreasing ED conveyance compared to 2011–2. 89 In 2018–9, England’s ambulance services managed > 8M ‘999’ calls; 6% of these received telephone advice (‘hear and treat’), 31% were treated at scene (‘see and treat’), 63% were conveyed to ED and the remaining 6% were transported to a lower-level facility (‘see and convey elsewhere’). 90
Further supporting the use of alternative CPs is the significant expert support that exists for paramedics’ ability to manage patients without conveyance. 91 There is also evidence that paramedics are willing to use CPs92 and that they can do this safely. 93 The Prehospital Outcomes for Evidence-Based Evaluation programme project looked at all types of presentations to the ambulance service94 and found that within 3 days of non-conveyance, 83% of non-conveyed cases experienced no subsequent health event (9% of patients recontacted the ambulance service, 12.6% attended ED, 6.3% were admitted and 0.3% died; patients could experience more than one event).
Finally, some studies have also indicated that CPs can be associated with increased patient satisfaction,86,87 with reports that it can be frustrating to be conveyed to ED when not needed. 95–102 For example, an initial evaluation of the aforementioned hypoglycaemia CP found patients benefitted: 88% of patients reported greater understanding of their condition and 73% felt better able to self-manage future episodes. 71 In some cases, the uptake of CPs has though been lower than anticipated69 and, to date, epilepsy is a presentation that has received little attention. 103
Potential of an alternative care pathway for epilepsy
There are several reasons for the momentum to introduce an alternative CP for epilepsy.
Firstly, the rate of transportation for seizures and subsequent hospital admissions is high and has remained so, despite wider NHS initiatives. 25 It is probable therefore that this presentation will continue to be a challenge for the NHS.
Secondly, paramedics have indicated that they are keen (if they receive additional training and the necessary support) to take on more responsibility for managing seizures. 104 This is important as acceptability of an intervention to those expected to deliver it is key to intervention feasibility. 105
Thirdly, changes to how ambulance services are funded may mean the use of CPs becomes financially incentivised and paramedics might feel able to spend more time ‘on scene’. 106
Finally, and most importantly, an alternative CP has the potential to work and improve patient outcomes. Qualitative research61,107,108 provides the beginnings of a theoretical basis for the use of an alternative CP in epilepsy. On the basis of this work, possible mechanisms by which the intervention could reasonably make a difference are that it may (1) increase awareness and likelihood that paramedics will consider non-conveyance and referral pathways as an option in appropriate cases, (2) increase paramedics’ clinical knowledge of how to make appropriate non-conveyance decisions, (3) increase paramedics’ knowledge of alternative care providers that are acceptable to service users and (4) increase paramedics’ confidence about making a non-conveyance decision and reducing anxiety about risk.
By paramedics operating as part of an integrated healthcare team, some of the CPs importantly have the potential to reduce health inequalities and improve the support PWE receive. This is likely to come by the CP introducing a mechanism by which PWE ‘in need’ are brought to the attention of specialist epilepsy services.
Despite indications that specialist input could help those attending ED,109–111 and NICE recommending it,112 most PWE (~80%) attending ED do not currently receive it. Most (~60%) are also not referred on either. 20 PWE who are older, those not known to the service and those live in the most deprived areas are the least likely to be referred. 113 The only communication regarding the event that typically occurs is a letter sent by the ED to the persons GP stating that the episode occurred. 44
Ensuring that PWE in need of specialist care receive it is a long-standing challenge in the UK. Potential reasons why persons are not always identified and supported are (1) primary care is not remunerated (as it is for other conditions) to identify PWE with uncontrolled seizures, where there is diagnostic uncertainty or treatment failure, (2) there are fewer neurologists per head than in other developed nations114 and (3) there are fewer nurse specialists than recommended. 115 An indication of the challenge is only ~50% of PWE in the UK are currently seizure-free. 14 Trial evidence indicates this should be ~70%. 116 Importantly, it is those in the most socially deprived areas who fare worst. Ashworth et al. 117 found the difference in the proportion of PWE living in the least and most deprived quintiles who were seizure-free was 12%.
Current configuration of care for those presenting with established epilepsy
While there is some variation between English regions, the information so far presented allows one to provide a broad indication as to the configuration of care an adult who presents to the ambulance service for established epilepsy is likely to receive. The ambulance crew managing them will typically not have access to relevant information about the person’s medical history and most (~70%) would ultimately be conveyed to ED. The time being cared for in ED would be ~3–4 hours. The person’s GP would typically be notified of the event by letter, but the person will not be seen by or referred on to an epilepsy specialist (such as an epilepsy nurse or neurologist).
Acceptability of alternative care pathways to target population is unknown
While a CP for epilepsy has much potential, it is unclear whether any of the CPs being considered could deliver on it. This is because their acceptability to patients and their SOs is unknown since they are not being involved in CP design. Acceptability of an intervention to its intended recipients and providers is a fundamental criterion an intervention needs to satisfy if it is to be positioned to achieve its intended outcome. 105
Care packages for epilepsy are seemingly being developed in a largely ‘top-down’ fashion. This is despite evidence that decisions about whether or not to access healthcare services can be informed by how a patient or SO perceives their situation118–120 and that patients/SOs and health professionals’ can sometimes have different views about what constitutes an ‘emergency’ situation. 121–124 It is possible therefore that the nature and content of the envisioned CPs will not align with what patients and their SOs would consider to meet their needs.
To our knowledge, only one epilepsy CP has been reported on to date. Piloted for 11 months by the Yorkshire Ambulance Service, it allowed paramedics, when they felt it appropriate, to not convey adults with known epilepsy to ED but instead directly refer them to an ENS (who would telephone the patient within 5 days). 125
An evaluation of this CP underscored the opportunities that existed to improve the management of those from the target population. Telephone consultations, for example, between the nurse specialist and patients lasted for only a median of 10 minutes. Despite this, an independent review of the nurses’ notes revealed positive action/outcomes occurred in most cases. Examples included (1) contacting the patient’s pharmacist or GP to optimise medication, (2) arranging an appointment in the neurology clinic, (3) referring the patient to a psychotherapy service and (4) booking the patient an appointment in the ENS clinic.
The problem was that over the 11-month evaluation period, < 10% of eligible PWE attended to by paramedics were put onto the CP. The reasons for this low uptake rate were not explored. An explanation is the CP’s configuration was not acceptable to PWE. To date, it has been assumed all the target population do not want to be conveyed to ED and will readily accept any alternative to ED that is offered. The actual evidence on the preferences of PWE is unclear.
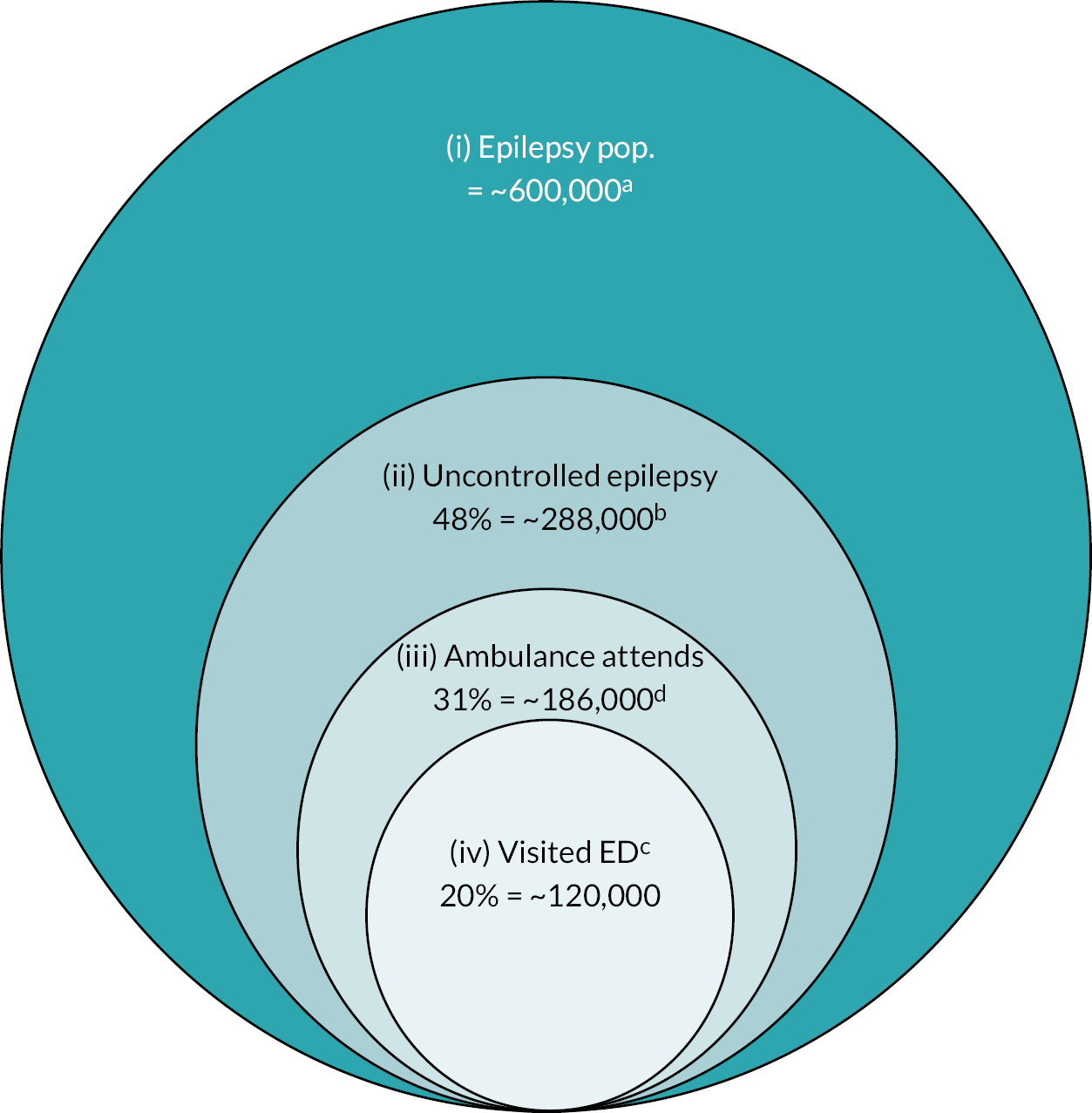
We certainly know not all people who experience a seizure will attend ED. Around 48% of PWE in the UK experienced a seizure in the past year, but less than half attended ED. 17–19 This includes people who do not seek emergency care in the first instance and others declining a visit ED even after an ambulance has attended. 95,126 Figure 1 provides a representation of this.
FIGURE 1.
Indication of experience of seizures and use of ambulance service and attendance at hospital EDs by PWE in England. Notes: Reproduced from McKinlay et al. 1 with permission. Segments of figure are not to scale. a, Based on ~1% of UK population having epilepsy13; b, Moran et al. 14 indicate 48% of PWE will have had a seizure in prior 12 months; c, When a call is received by ambulance service described as relating to a ‘convulsion’, ‘fit’, ‘seizure’, the call handler endeavours to ask standardised questions to gauge, such things as severity and potential aetiology. For those using Advanced Medical Priority Dispatch System, according to Protocol 12, one question is ‘Is s/he an epileptic?’. Most callers should be able to answer question as most (~70%) seizure calls made by relative, friend or carer. 56 Audit data from two regional ambulance services (North West Ambulance Service; Yorkshire Ambulance Service) indicate that in 2018 of those attended to ~70% of those who indicate a history of epilepsy are conveyed to ED, and 30% are not; d, Hart and Shorvon17 found that ~20% of PWE had attended an ED in the prior 12 months.
However, this does not mean that it can be assumed all PWE do not want to be conveyed to ED when it is clinically safe. The following points suggest a need to be cautious.
Firstly, the characteristics of PWE who visit ED might mean they are less ready to accept not being transported to ED during the intense and worrying moments of a seizure and aftermath. Compared to the wider epilepsy population, they have lower epilepsy knowledge, report more clinical anxiety, report greater perceived epilepsy stigma and are more likely to live in a socially deprived area. 29,127–131 Up to 20% also have an intellectual disability. 35,36
In the few studies that have interviewed PWE about their visits to ED it has been found some PWE express a need for immediate access to urgent care when they have a seizure. This includes them explaining how they and their SOs (to whom care decisions are often delegated when the patient is unconscious or lacks capacity) are often fearful of seizures, including the possibility of death and brain damage. They also say they are unsure about how to manage them. 47,48 This, they say, leads them to call for an ambulance when they are about to have, or have had, a seizure. For many, this is an established pattern of behaviour. One study found the median years diagnosed for PWE visiting ED was 11. Some telling quotes from interviews48 with PWE and SOs include:
Cancer, you’re awake. I know you can die, but you’re awake. I’d prefer something like that … Having epilepsy, you’re going into a fit. You don’t know if you’re going to wake up or die. That’s why I call [999]!
Person with epilepsy
[I was] just worried because I don’t know anything about epilepsy … I only know the bad things … I know you can die … I am so worried I decided just to ring an ambulance … better safe than sorry.
Significant other to person with epilepsy
Another important piece of evidence comes from work with paramedics. 61 It highlights that although some PWE do not want to be conveyed to ED, others may.
when they talk to us about what their preference is it’s mixed … many been taken to hospital before. They know that that’s the pattern and they expect it … they feel nervous if you start talking about them staying at home … Some feel very vulnerable and want to go through the motions of seeing the paramedic, the doctor, the nurse …
Each of the CPs being considered around the country requires financial expenditure. This is difficult to justify. This is because it is unclear whether the outlay would translate into a service that PWE and SOs would use and benefit from.
How to make the development of alternative pathway’s more rational and cost-efficient
While it is beyond the scope of the current project, our ultimate aim is to work with the ambulance service to implement the most promising CP for PWE, rapidly evaluate it and use the evidence to transform service organisation nationally. However, as patients and SOs from the target population have yet to be consulted, it is not known what sort of alternative CPs have the potential to be most effective and should be prioritised for evaluation/implementation.
What is needed is information about the target population’s preferences for seizure care, including what elements are most important to them, what things do they not want and to what extent would they be willing to give up one or more elements for the presence of others. A clearer understanding of their decision-making processes for seeking or not seeking ED care is also needed, as is information on any concerns and expectations they may have regarding alternative CPs. It would also be important to understand whether this differs according to seizure presentation. Together this information would help establish to what extent the target population is open to the possibility of alternative management and could be used to codesign a CP. It could be designed to encapsulate the features of most importance to patients and their SOs.
Patient preference information is defined by the US Food and Drug Administration as ‘qualitative or quantitative assessments of the relative desirability or acceptability to patients of specified alternatives or choices among outcomes or other attributes that differ among alternative health interventions’ (p. 6). 132 It reflects what treatment characteristics matter to patients, how much these matter and how patients make ‘trade-offs’ between them.
From an economist’s perspective, there are two approaches to the measurement of preferences: revealed and stated. The former is derived from observed market activities. Stated preferences in contrast are derived by asking persons for their views, such as via surveys. 133 An obvious advantage of the latter approach is that it can permit one to explore people’s preferences for products which remain hypothetical. In the current project, the focus has been on such stated preferences obtained by using DCEs.
Discrete choice experiments
Discrete choice experiments are one of the most popular and robust quantitative ways to obtain stated preferences. 134,135
The DCE method is an attribute-based survey methodology. It is underpinned by random utility theory and relies on the assumptions of economic rationality and utility maximisation. 136 These state that any ‘good’, including healthcare packages, can be described by their constituent characteristics – known as ‘attributes’ – and that the extent to which an individual prefers a good will depends on the levels these attributes take. 137 In the case of a healthcare package, attributes could include both process attributes (e.g. where the ambulance takes you; the healthcare professional responsible for your care) and outcome attributes (e.g. likelihood of follow-up).
Following the above-stated theories, if a person is presented with alternative ‘goods’ described by a set of attributes, it is assumed the person will make ‘trade-offs’ between attributes to select the good that yields his/her highest individual benefit, known as utility. Within a DCE, a person’s stated preferences are therefore elicited by presenting them with a scenario (e.g. having X health condition) and asking them to choose which of two (or more) care packages they prefer. Each care package is described according to the same attributes (e.g. where the ambulance takes you) and in terms of levels that vary (e.g. ED, UTC). Changing the levels (using an experimental design) produces a set of alternative care package options (choice sets), that respondents are asked to choose between.
By observing how participants change their responses across choice tasks, DCEs allow one to infer the extent to which different care attributes and levels are driving preference, the direction of their effect and the extent to which persons will accept certain ‘trade-offs’ between attributes.
To help show what a DCE looks like, we present an example in Appendix 1. It has been annotated to highlight key DCE terms.
Discrete choice experiments have increasingly been used to determine healthcare preferences, including for epilepsy. 138–140 They have been recognised as a suitable method for eliciting evidence of patient preferences to inform regulatory benefit–risk assessments of medicines. 141,142 Chief amongst the reasons for this is that they offer a robust methodology to estimate which attributes are important in decision-making.
There is also good evidence that when a DCE is designed well, the preferences expressed within them can show good congruence with real-world behaviour. 143–145 Quaife et al. 146 recently completed a meta-analysis on this topic. With a pooled sensitivity estimate of 88%, they found DCEs to be particularly good at predicting who would ‘opt-in’ to use a product or service that a respondent does not currently use. Specificity was less impressive, indicating DCEs were less good at predicting who will ‘opt out’ and not choose not to use a product or service. This did though appear to be influenced by how many choices the person had to make in the DCE.
Some key design considerations for discrete choice experiments
Good practice guidelines for designing, conducting and reporting DCEs are available. 133,147,148 One of the first and critical stages is identifying the attributes that will be used to describe the options within the DCE that people are asked to choose between and for which the DCE will provide quantitative preference weights for. The levels that the attributes take will also need determining and should be theoretically feasible.
Coast et al. 149 provide guidance for the selection of the attributes to ensure random utility theory, the psychological basis for DCEs, is not violated. Firstly, it is important that the attributes include all those that might be important for an individual in coming to a decision. Ignoring an important attribute risks an underspecified model. Selecting and defining the attributes necessitate an adequate understanding of the target population’s perspective. 150 If evidence is not already available, qualitative research can be completed with the target population to model their likely decision calculus.
Secondly, the attributes should not be too close to the latent construct that the DCE is investigating. For example, where utility is the underlying latent construct, an attribute within the DCE that is labelled as utility or expresses overall satisfaction with the good should not be included.
Thirdly, attributes should not be intrinsic to a person’s personality and should be capable of being manipulated experimentally. For example, attitude towards taking medicines is a characteristic of the person, rather than the good.
Using discrete choice experiment evidence to inform service design
As highlighted by Ryan and Farrar,151 DCEs can provide crucial information for service and policy designers and those allocating resources. Evidence on service user preference by itself is, however, potentially insufficient to help choose with confidence which CP configuration amongst the various options is best positioned to achieve its goals and should be prioritised for implementation/evaluation. This is because other feasibility factors are important.
Table 1 outlines Michie et al.’s105 so-called affordability, practicability, effectiveness, acceptability, side-effects and equity (APEASE) criteria for determining the potential of different interventions. It highlights key factors that can, to differing extents, be important in determining promise and has been used by a range of bodies to help select interventions. 152
| Item | Detail | |
|---|---|---|
| A | Affordability | Interventions often have an implicit or explicit budget. It does not matter how effective or even cost-effective it may be if it cannot be afforded. An intervention is affordable if within an acceptable budget it can be delivered to, or accessed by, all those for whom it would be relevant or of benefit. |
| P | Practicability | An intervention is practicable to the extent that it can be delivered as designed through the means intended to the target population. For example, an intervention may be effective when delivered by highly selected and trained staff and extensive resources, but in routine clinical practice, this may not be achievable. |
| E | Effectiveness (and cost-effectiveness) |
Effectiveness refers to the effect size of the intervention in relation to the designed objectives in a real-world context. It is distinct from efficacy which refers the effect size of the intervention when delivered under optimal conditions in comparative evaluations. Cost-effectiveness refers to the ratio of effect (in a way that has to be defined, and taking account of differences in timescale between intervention delivery and intervention effect) to cost. If two interventions are equally effective, then clearly the most cost-effective should be chosen. If one is more effective but less cost-effective than another, other issues such as affordability come to the forefront of the decision-making process. |
| A | Acceptability | Acceptability refers to the extent to which an intervention is judged to be appropriate by relevant stakeholders (public, professional and political). Acceptability may differ for different stakeholders. For example, the general public may favour an intervention that restricts marketing of alcohol or tobacco but politicians considering legislation on this may take a different view. Interventions that appear to limit agency on the part of the target group are often only considered acceptable for more serious problems. |
| S | Side effects/safety | An intervention may be effective and practicable but have unwanted side effects or unintended consequences. These need to be considered when deciding whether or not to proceed. |
| E | Equity | An important consideration is the extent to which an intervention may reduce or increase the disparities in standard of living, well-being or health between different sectors of society. |
The factors include affordability, practicability, effectiveness, acceptability, side effects and equity. To expand further, is the intended intervention likely to be acceptable to all those involved – including those expected to deliver it and their employing organisations? The latter will, for instance, need to be willing to assume any potential risks and consequences that may occur from the intervention if something goes wrong.
Is the envisioned intervention practicable? Can the service wanted by the intended users be implemented in the NHS? Is there the required capacity and information sharing resources? Thirdly, how effective and cost-effective will the service be in achieving the desired objectives? Fourthly, can it be afforded within budget? It arguably does not matter how acceptable or preferred an intervention is if it cannot be afforded. On a related point, if responsibility for commissioning an intervention is shared by different groups, will it be possible to get them all to agree to fund it? Fifthly, how far does one anticipate that the intervention might lead to unintended adverse outcomes? And finally, equity. How far is the intervention likely to increase or decrease known differences between the more advantaged and disadvantaged in our society?
Given the other potentially important factors raised by the APEASE model, a DCE could be seen as providing robust evidence on service user acceptability. This could then be used as the basis for discussions by informed stakeholders who would be asked to evaluate potential CP options against all the APEASE criterion. They could then advise which configuration is judged to strike the optimal balance between patient acceptability and NHS feasibility.
Current study
To achieve the project objective, we conducted a project comprised of three WPs (Figure 2). In WP1a, the CPs being considered by NHS bodies around England for epilepsy were systematically identified. In WP1b, patients and SOs were asked to describe the reasons they attend ED, their priorities for care post seizure and how this might differ by the context in which the seizure occurs and gave qualitative feedback on some CPs known to be being considered. During WP2a, the DCE was methodically designed and in WP2b completed by a sample of PWE who had had recent ambulance contact and their SOs. They were recruited by one regional ambulance service and nationally by public adverts. The DCEs determined their care preferences for three common seizure presentations to ED. In WP3, KE workshops were conducted at which the findings from WP2b were shared with stakeholder representatives. They were then asked which CP preferred by PWE and their SOs was considered NHS-feasible and should be prioritised for implementation/evaluation.
FIGURE 2.
Research project process diagram (partly revised from original due to COVID-19 pandemic). COVID-19, coronavirus disease 2019.
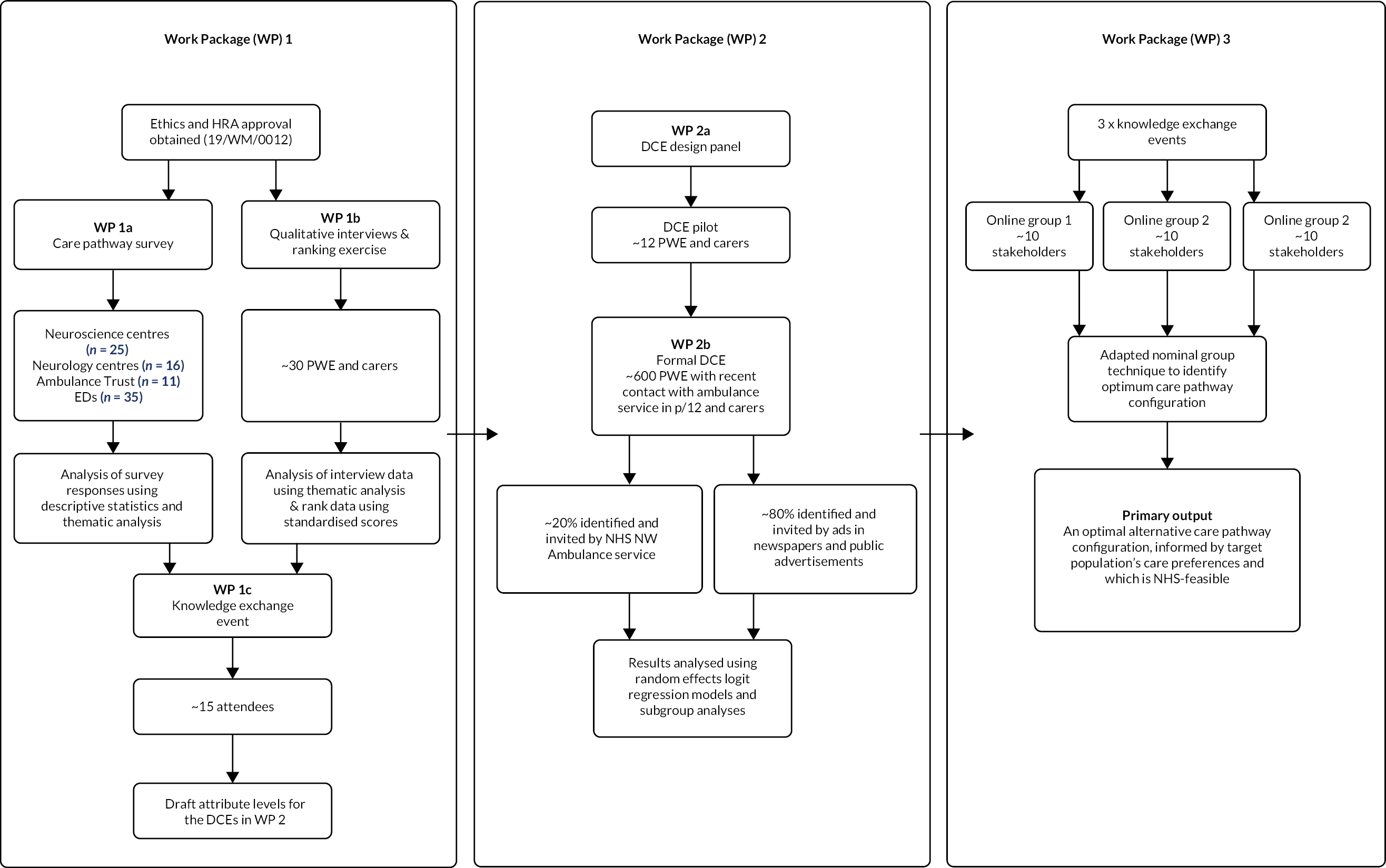
According to conceptual frameworks, such as that of Greene et al.,153 the purpose of the mixed-methods approach was both ‘development’ (seeking to use the results from one method to help develop or inform the other method) and ‘expansion’ (seeking to extend the breadth and range of inquiry by using different methods for different inquiry components). Data collection and analysis for WPs 1a and 1b were completed concurrently and independent from one another. From WP1c onwards, the design was sequential and dependent. During WP2a, the findings from the earlier stages were integrated to develop the DCE.
Chapter 2 Survey of service providers
Introduction
In the formative work, to design the DCE, it was important to consider the features of the alternative CPs already being considered by service providers. As noted in Chapter 1, a range of CPs for epilepsy are being considered across England. It was not, however, possible to readily identify all of them. No single body was co-ordinating their development or consideration and almost all activities were occurring outside of the formal research literature. It was also not clear which type of organisations or professions were leading CP initiatives.
To systematically determine what CPs were being considered, WP1a comprised a cross-sectional survey of NHS regional neuroscience centres, ambulance services and EDs in England. We asked them to what extent service users had/were involved in any service design changes. Additional questions were included to understand the extent to which their attempts to reduce unplanned hospitalisations for different ambulatory care sensitive chronic conditions aligned with the evidence on their burden.
Sections of this chapter have been reproduced from Mathieson et al. 154 under licence CC-BY-NC-ND.
Materials and methods
Design
A short piloted online survey ran from 1st April to 30th June 2019. It used a set of responsive open and closed questions. As the language for alternative CPs is still evolving and not fixed, the survey asked respondents whether the NHS organisation they were representing (or the local services they worked with) had made or were planning any changes to any policies, schemes or pathways that relate to the management of those with epilepsy (or indeed seizures generally), with a view to minimising ED visits (see Appendix 2).
If a change was reported to have occurred by the respondent or was planned, they were asked about its nature, to what extent service users had been involved, and how, if at all, they anticipated the change would address health inequalities. Respondents could upload a copy of any associated paperwork and inform us of what their experience with the change had been.
The time frame specified within the questionnaire for changes that had been made was the past 5 years. The time frame for future changes was the next 12 months. Five years was chosen as this corresponded with the timing of dissemination to local sites of findings from the first NASH.
Services not reporting or planning changes were asked why and shown three known care innovations and asked if they comprised usual practice within their organisation. Respondents were asked, where necessary, to consult with managers of their service to ensure responses incorporated both current and planned redesign.
All respondents were asked about the extent to which reducing unplanned hospitalisations for chronic ambulatory care sensitive conditions (generally and then by condition) was a priority for their organisation.
Survey respondents were able to indicate if they wanted to be informed of opportunities to take part in subsequent WPs.
Ethical approval was not required as the survey was deemed a service evaluation. 155
Recruitment
Personalised invitations to participate, followed by two reminders, were sent to the clinical leads/directors of England’s regional ambulance trusts (n = 10) (and to the Isle of Wight NHS Trust who provide its ambulance service),156 regional neuroscience centres (n = 25)157 and neurology centres (n = 16). 158,159 Invites were also sent to a random sample of 25% (n = 35) of England’s ‘type 1’ EDs160 (stratified by geographical area and attendance size). 161
Respondents could delegate completion of the survey to someone else within their service.
Analysis
Characteristics of the responding organisations were examined using descriptive statistics and representativeness judged against publicly available information.
To determine the different types of CPs being considered and the proportion of responding institutions considering each, the first 50% of submitted surveys was selected and imported into NVivo 10 (Lumivero, Burlington, USA). The responses given within these were read by a qualitative researcher (AM) to identify recurrent types of CP. This was used to develop an initial thematic coding framework capturing the main types. The framework was then applied to the full data corpus to identify and code all responses. Responses that reflected CPs insufficiently identified by the original coding framework were used to modify the framework. Frequent discussions between the researcher and a multidisciplinary research team helped ensure interpretations and conceptualisations of the data were credible, valid and shared.
Results
Sample
Seventy-two (82.8%) services responded: 36 (85.7%) neurology and neuroscience centres, 26 (74.3%) EDs and 10 (90.9%) ambulance services. The survey took respondents a median of 8 minutes to complete [interquartile range (IQR): 5–16.75].
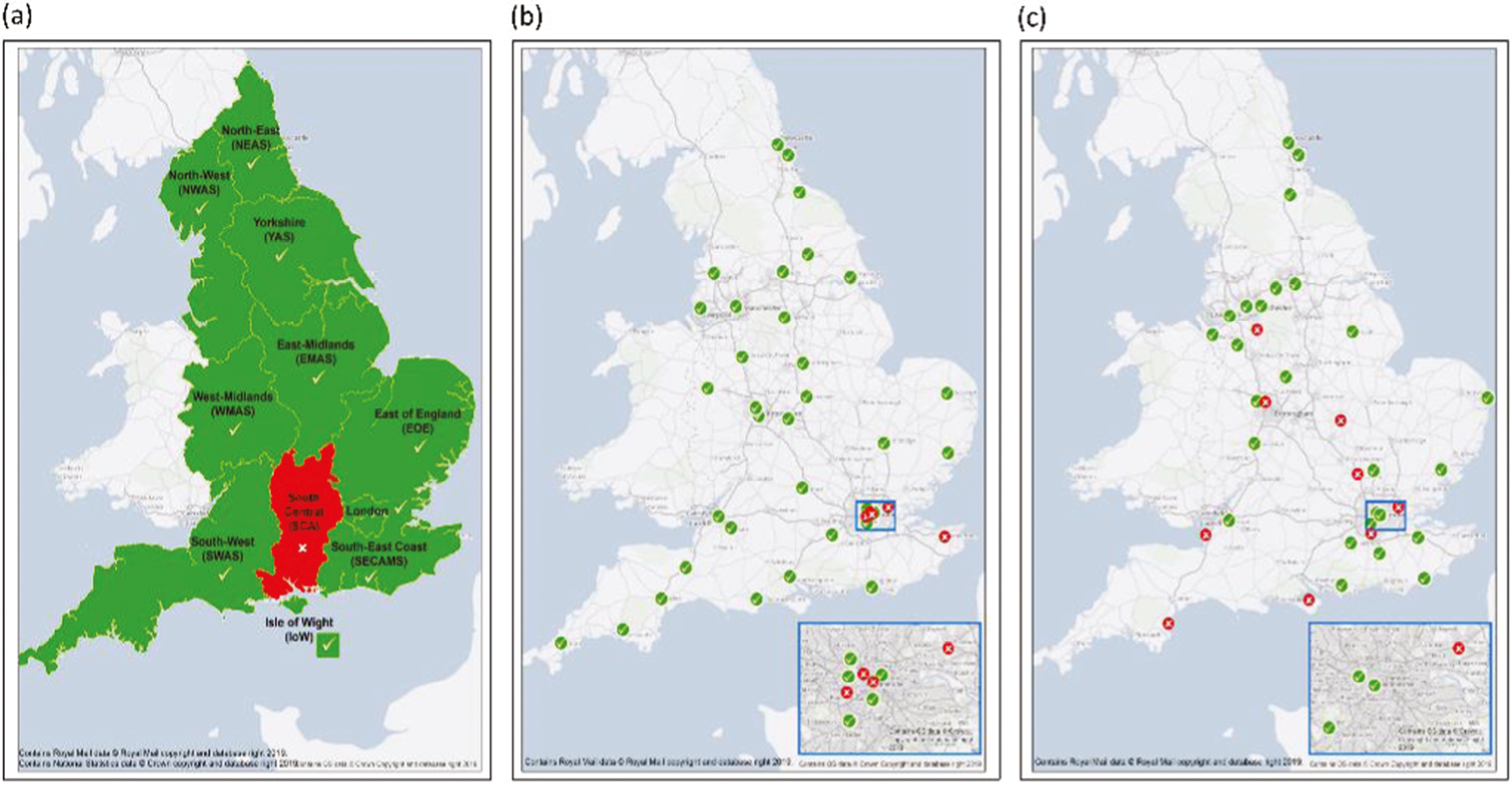
Responding services were spread across England (Figure 3), and their characteristics were similar to non-participating sites (see Report Supplementary Material 3). Responding individuals were doctors (72.2%), paramedics (13.9%) and nurses (13.9%). Analyses relating to service changes are based on responses from the 68 (94.4%) services whose responses included no missing data.
FIGURE 3.
Geographical location of (a) regional ambulance services, (b) neuroscience centres and neurology services and (c) EDs by their survey participation status.
Priority
The pooled response indicated reducing unplanned hospitalisations associated with chronic ACSs was a ‘high priority’ (median 4; IQR = 3–5). In ranking eight different ambulatory care sensitive conditions, ‘epilepsy and convulsions’ was given a pooled median rank of 3 (IQR = 2–4). Neurology/neuroscience centres gave it a median rank of 2 (IQR = 1–3), ambulances services 3.5 (IQR = 2.75–5) and EDs 4 (IQR = 3–5).
Service changes
Forty-one (60.3%) services said they or service(s) they worked with had made and/or were planning a service change(s) (see Appendix 3). Thirty-four (50.0%) reported a change(s) had occurred. Neurology/neuroscience sites (n = 30, 93.8%) were most likely to report changes, and EDs (n = 4, 15.4%) were least likely.
Types of change
Eleven change types were identified. Table 2 describes them. Most addressed the care of those with established, rather than new epilepsy. They fell into three categories according to which part of the patient’s care journey they focused on:
| Change focus | Type of service change | Description of change | Services reporting the change (n, %) | |||
|---|---|---|---|---|---|---|
| Ambulance N = 10 | ED N = 26 |
Neuro N = 32 |
Total N = 68 |
|||
| Before emergency help is sought | (1) Rapid access clinics | To help manage changes in severity or presentation, including an ability to address concerns between any scheduled appointments with specialist (wait time aim: ~1–2 weeks). Mode of delivery included telephone hotline, e-mail and face-to-face appointments or combinations thereof. Personnel delivering them was typically ENS. | 0 | 0 | 10 (31.3) | 10 (14.7) |
| (2) Educating patients and carers | Introduction of programmes to educate patients and carers on seizure first aid to increase confidence and skills and ameliorate unnecessary emergency calls for uncomplicated seizures. In some instances, this included ensuring patients (or care home if patient within one) carried a seizure care plan to aid those helping them, including ambulance crews. | 0 | 0 | 6 (18.8) | 6 (8.8) | |
| (3) Educating front-line staff | For paramedics, it was on seizure types, alternatives to ED and red flags to support decision-making and improve staff confidence. For ED staff, focus was on differentiating NEAD and on criteria for referral to onward services. | 0 | 1 (3.8) | 4 (12.5) | 5 (7.4) | |
| (4) Collaborative working | Increased working between epilepsy specialists and other services caring for persons at an increased risk of seizures/epilepsy (e.g. neuro-oncology, stroke, learning disabilities) to proactively identify patients that may need support from or referral to the epilepsy service. Changes included more straightforward referrals pathways, promoting awareness of the specialist service and participation in multidisciplinary team meetings by epilepsy specialists. | 0 | 0 | 4 (12.5) | 4 (5.9) | |
| (5) Sharing of seizure and medication data | Epilepsy services described efforts to access data on their patient’s condition between scheduled appointments to identify need for review. Changes included provision of a portal where patients could upload seizure data themselves, the use of wearable seizure detection devices and accessing data held within primary care medical records on patients’ antiepileptic prescription and collection to identify issues with non-adherence and errors. | 0 | 0 | 2 (6.3) | 2 (2.9) | |
| Individual services reporting at least one of these = 17 (25.0%) | ||||||
| When being cared for by emergency services | (6) Acute epilepsy service | ENS and/or consultant available to review attendees face to face or virtually during the emergency episode admissions. Eligibility criteria varied. For some services, focus was on those with intractable epilepsy and/or those with intellectual disabilities. | 0 | 0 | 9 (28.1) | 9 (13.2) |
| (7) Protocols to redirect away from ED | Use of protocols, with flow charts to support decision-making when managing seizures, with recommendation of non-conveyance to ED of persons with certain presentations. For those not conveyed to ED, protocols recommended leaving patients at home, ‘on scene’ or, in some instances, UTCs. A few protocols included mechanisms by which patients could be referred on to other services. In some instances, this was in the form of ambulance crews having access to a directory of local services and their contact details. In one instance, an e-referral system allowed crews to electronically notify GPs of the attendance and its details. In two areas, patients could be referred to the epilepsy service, with an ENS contacting the patient within 1–5 days by telephone. Eligibility criteria differed. In one area, it was open to anyone with established epilepsy. In another, it was only for patients already under the epilepsy service and in certain geographical locations. | 5 (50.0) | 0 | 2 (6.3) | 7 (10.3) | |
| (8) Medical record accessible to front-line staff | Paramedic access to information on patients’ medical history from their medical record. The extent of coverage, comprehensives and ease of access varied. In some instances, it was in the form of access to a generic ‘Summary Care Record’ which as a standard includes demographics, current medication and allergies. In other instances, access was to a seizure care plan that described the patient’s usual seizure presentation/s and next of kin to help the ambulance crew interpret the normality of the presentation and facilitate non-conveyance where appropriate. In some cases, paramedics had direct access to the information while on scene via internet-enabled mobile devices. In other instances, they needed to communicate with colleagues at a ‘clinic hub’ who communicated the information to them over the phone. ED staff access to information on patients’ medical history from their medical record. This came in the form of access to a seizure care plan, with the aim being that care decision could be expedited, and unnecessary investigations and admissions avoided. |
3 (30.0) | 0 | 2 (6.3) | 5 (7.4) | |
| Individual services reporting at least one of these = 19 (27.9%) | ||||||
| Follow-up care | (9) Expansion of established epilepsy service | Increased capacity to allow for shorter waiting times (aim ranged 1–8 weeks) for those with established epilepsy who were referred following an ED attendance and/or to allow more regular patient reviews. Services noted offering additional telephone appointments, several had introduced face-to-face clinics within primary care settings to increase ease of patient access. One service also allowed EDs to directly book patients into follow-up slots to reduce time associated with booking process. Several other services had implemented a process whereby the epilepsy service was automatically notified of ED attendances for seizures. In some instances, they were notified of visits only by patients under their care. In others, it was all patients. These patients’ ED attendance record would be reviewed, and the person was contacted by the epilepsy service if needed. | 0 | 1 (3.8) | 13 (40.6) | 14 (20.6) |
| (10) ‘First seizure’ clinics | Established or expanded (be it locations and/or clinic slot spaces) first seizure clinic to which acute and community services could refer. This typically included introduction of (or clarification) of referral criteria, mechanisms and proposed management of patients to promote consistency of care and avoid unnecessary tests and earlier discharge from ED if appropriate. Expansion was seen as allowing shorter wait times and thus facilitated discharge. Aimed wait time: 2–4 weeks. | 0 | 3 (11.5) | 7 (21.9) | 10 (14.7) | |
| (11) ‘NEAD’ clinic | Introduction of specialist NEAD clinic which accepted referrals from ED. | 0 | 0 | 1 (3.1) | 1 (1.5) | |
| Individual services reporting at least one of these = 23 (33.8%) | ||||||
Before emergency help is sought
Seventeen (25%) services reported such changes. These related to care planning, attempting to prevent a person’s condition from requiring emergency help. The most widely made change was the introduction of Rapid Access clinics, providing specialist epilepsy support to patients between routine appointments as needs arose. Less common changes included implementing education for PWE on seizure first aid and – to enable more proactive and risk-stratified care – access by specialist services between appointments to data on a person’s seizure control and medication.
When person is being cared for by the emergency services
Nineteen (27.9%) services reported these changes. A key change reported was, as anticipated, the introduction by ambulance services of alternative CPs to support non-conveyance to ED and alternative care arrangements for PWE with uncomplicated seizure presentations. Protocols, with flow charts, were available for the CPs with a view to supporting crews’ decision-making. For those not conveyed to ED, protocols recommended a range of differing actions from leaving patients at home, ‘on scene’ or in some instances conveying to an UTC.
A few of the protocols also included mechanisms by which patients could be referred on to other services. In some instances, this was in the form of ambulance crews having access to a directory of local services and their contact details. In one instance, an e-referral system allowed crews to electronically notify GPs of the attendance and its details. In two areas, patients could be referred to the epilepsy service, with an ENS contacting the patient within 1–5 days by telephone. Eligibility criteria differed. In one area, it was open to anyone with established epilepsy. In another, it was only for patients already under the epilepsy service and in certain geographical locations.
The other common service change under this category was the introduction or expansion of an acute neurology service. Here, an ENS or neurologist was available to review PWE once they were within the ED, either face-to-face or virtually. The aim being to facilitate discharge and identify support needs.
Follow-up care
Twenty-three (33.8%) services reported these changes, with most expanding neurology services for those with established epilepsy. These sought to reduce waiting times for ED referrals (aim 1–4 weeks). Some services offered telephonic clinics, others face-to-face appointments but within primary care locations to increase accessibility. To further minimise referral times, one neurology service allowed EDs to directly book patients into their service’s appointment slots. Two other services had implemented processes to automatically notify them of seizure-related ED attendances.
Usual practice
Nine (33.3%) of the 27 services that had not made, and did not plan, any changes, reported usual practice comprised at least one of the three presented service innovations (see Appendix 3). Five (18.5%) said epilepsy services were automatically informed of patients attending ED. Three (11.1%) used protocols to divert people presenting with an uncomplicated seizure away from ED. Two (7.4%) reported medical records for PWE were accessible to ambulance staff.
Service user involvement
Of the 34 services that had implemented a change, only 7 (21.2%) had consulted service users.
Discussion
The survey received an excellent response rate. It demonstrated the extent to which ‘calls’ for change to the care of people presenting with seizures have been heard and are starting to be responded to. Neurological and ambulance services in particular appear to be making significant efforts to bring about change.
With respect to the changes made by services, 11 types were reported. These varied in complexity and the part of the patient’s care journey they targeted. Most focused on established epilepsy, corresponding with its burden on ED. The changes typically targeted known limitations to current service provision from which ED use might arise. This included (1) inequality in referrals from acute to specialist epilepsy services,113 (2) variable seizure first aid training provision,46 (3) limited information sharing between specialist, acute and primary care services61 and (4) the challenge of a comparatively small specialist workforce114 being able to promptly learn of and respond to exacerbations in a patient’s condition.
As anticipated, one of the key planned or implemented changes was the use of alternative CPs by ambulance services. The survey showed nearly all the responding ambulance services either were considering or had implemented an alternative CP. In addition, two neuroscience services noted this as well. The survey also confirmed the lack of consistency and equity in the nature of the CPs being considered or used.
Specifically, the described CPs differed in terms of where the non-conveyed person would be taken. In some instances, they would remain at home, ‘on scene’ or in some instances taken to an UTC. The CPs differed in the extent to which they would help potentially stimulate improvements in the person’s subsequent ambulatory care. Only a few included mechanisms by which a patient would be referred for follow-up. Moreover, who it was that they were referred to, the timing of this and who was eligible to be referred also differed. The CPs noted and attributes and the levels that defined them will be used in WP2b to contribute to the design of the DCE.
Another important finding from the survey was that despite being a statutory obligation, few services had consulted service users on the proposed or intended changes. Moreover, in describing the changes and their benefits, most respondents did not report that the service change had been evaluated. Thus, even having surveyed providers, it remains unclear which CP configuration is best positioned to deliver benefits and to what extent it is acceptable to service users. This underscores the importance of the current project’s ultimate intention.
In the next chapter, service users are interviewed about their decision-making for seeking postseizure care. Their initial views of on some of the alternative CPs captured by the service provide survey are also explored.
Chapter 3 Qualitative interviews with service users
Introduction
Little is known about the views of PWE regarding postseizure care. It is not known what drives their decision-making and how this might vary depending on contextual factors, such as location and seizure type. To date, only a handful of studies have been conducted with the target population. 22,47,48,162,163 Even less is known about the views of their family and friends (to whom care decisions are often delegated when the patient is unconscious or lacks capacity). 48
The aforementioned information is needed to help design the planned DCEs. It indicates the attributes of postseizure care that PWE and their SOs regard as important and should be considered when designing the DCE. Therefore, WP1b comprised a qualitative study with patients from the target population and their SOs.
Led by LR and MM at King’s College London, it explored service users’ decision-making processes for seeking or not seeking ED care when a seizure occurs. Service users’ expectations and concerns regarding potential alternative CP configurations being considered, or indeed any experiences they might already have had of any of them, were also explored.
Please note that sections of this chapter have been reproduced from McKinlay et al. 1 under licence CC-BY-4.0.
Methods
Study design
Qualitative interviews were completed with PWE, with or without the presence of one of their SOs. Methods were guided by the COREQ checklist164 and Coast et al. 149 checklist for DCE formative work.
Feelings of stigma, the sensitive nature of the topic, lack of driving licences and anxiety about travelling due to seizures meant interviews, rather than focus groups were considered the preferable data collection mode.
The study received ethics approval by the King’s College London Psychiatry, Nursing and Midwifery Ethics Committee (LRS-18/19-10353).
Participants were reimbursed with a £20 shopping voucher for their time.
Recruitment
To be eligible, people needed to (1) be aged ≥ 18 years, (2) have a diagnosis of epilepsy for ≥ 1 year, (3) be prescribed an antiseizure medication, (4) have had emergency service contact in the previous 12 months for epilepsy (be it a visit to ED and/or ambulance contact) (living in the South-East area of England), (5) be able to provide informed consent and (6) participate in a qualitative interview in English. They could have any epilepsy syndromes or seizure type. No medical records were accessed to confirm eligibility. All were based on self-report.
Persons with severe current psychiatric disorders (e.g. acute psychosis) or life-threatening medical illness were excluded, as were those who resided within a care or nursing home or had no fixed abode. We excluded persons living in care or nursing homes since, in these circumstances, it is typically not the patient or their SOs who are responsible for care decisions when a seizure occurs.
Purposive recruitment methods were used with the intention of capturing a comprehensive range of perspectives, and recruitment was to continue until there was no new variation in observations (data saturation). Purposive sampling is a type of nonprobability sampling. Here, a researcher selects participants from their sampling frame because they have characteristics that the researcher wants present with a view to enabling a research question to be answered. It is not about creating a representative sample with the intention of making generalisations. We sought to ensure variation in age and sex of participants, as well as for those who had had recent seizures at home and in a public place to be adequately represented. Based on the previous DCE design work,139,149 we anticipated obtaining interview data from ~20 to 30 PWE.
To identify SO participants, participating PWE were asked if they wanted to choose a SO/informal carer to take part with and be interviewed with. Despite greater social isolation, up to 90% of PWE still identify a spouse, parent or friend who can act as an informal carer for them. 165 Joint interviews and eliciting the concerns of both parties to the same event are regarded as particularly appropriate for studying complex health decisions. 95,126
The first recruitment process involved AMc contacting by mail PWE who took part in the SMILE (self-management education for adults with epilepsy) trial in the South-East of England and asking them if they were interested in future projects. 166 SMILE was a phase III trial comparing a two-day education course to treatment as usual alone. Inclusion criteria were ≥ 2 seizures in the prior 12 months, having established epilepsy, being prescribed antiepileptic medication and an ability to independently complete questionnaires in English. At 12-month follow-up, no differences between trial arms on the primary (quality of life) or secondary outcome measures were found. 167 The number of people expressing an interest in future projects was ultimately lower than anticipated, with AMc receiving permission to send invites to 47 PWE. Of these, only 15 responded and were screened; eight were found to be eligible for the current study and were ultimately interviewed.
The second recruitment process was completed with the assistance of Epilepsy Action, a user-led charity in the UK. They assisted with recruitment by advertising the study on social media platforms, at in-person community events in South-East England and in their newsletters. Interested PWE were asked to contact AMc to register their interest. Of the 37 people who made contact, 21 were eligible, of whom 4 subsequently dropped out. This process provided a further 17 participants for the current study.
Recruitment concluded at 25 interviews, as no new themes were identified.
Procedure
One-off interviews were held with the participants in locations (home, public place or a university office) and at times of their choosing. Interviews were conducted by AMc – a female postdoctoral researcher with a PhD in mixed-methods psychology. She has experience of conducting interviews with PWE. No non-participants were present during the interviews.
An interview guide was used which was developed by AMc, AN, LR and MM (two research psychologists, one neurologist, and one medical sociologist, respectively). Interview guides were reviewed by two PWE and one ambulance staff member, who provided insight based on their experience and then further refined by pilot interviews with two further PWE. The topic guide is shown in Appendix 4.
All participants provided written informed consent, and interviews were audio-recorded. No field notes were taken. No prior relationships existed between the research team and participants. Participants were aware that the researcher was not affiliated with their usual care provider.
Interviews began by asking participants for contextual information about their epilepsy and recent seizures and episodes of ED care. The interviewer then sought evaluative information, asking respondents to describe positive and negative perceptions concerning emergency care and any alternative methods of care they have experienced. The researcher explored the decision-making processes that surrounded patients and SOs’ seeking or not seeking ED care following recent seizures and the reasons for their choices.
Strategic data were then obtained from respondents by describing some aspects of possible alternative CPs and asking them for their views. They were asked what they thought may be positive aspects and their concerns if they had been offered them following a stated seizure of theirs. As WP1b occurred at the same time as WP1a, the CPs discussed with the interviewees included ones already known about by the team (see Appendix 4).
Finally, at the end of the interview, AMc worked with each participant with epilepsy to complete a ranking exercise to prioritise the importance of care attributes. The findings from it are reported in Chapter 4.
Data analysis
Data collection and analyses proceeded in an iterative manner. Audio recordings were transcribed verbatim. Transcripts formed the data set. These were anonymised to protect participant confidentiality. They were not returned to participants for comment or correction.
To analyse the data, a framework approach168 was employed as it is suited to policy-oriented research examining patient experiences. 169 Transcripts were read with themes and codes identified. Data were then managed using NVivo 12 (Lumivero, Burlington, USA).
Following preliminary analysis, two matrices were developed by AMc and MM to summarise individual cases, with seven coded categories relating to decision-making (self-care, decisions by self/ambulance/public, informing others); care preferences (experiences of using emergency services, satisfaction, suggestions); and three categories regarding views and experiences relating to potential CPs. Initially, both AMc and MM summarised cases to examine consensus, with AMc completing coding. A constant comparative approach was used to interrogate the data and identify factors influencing individual participant decisions and preferences.
Where necessary, quotes with potentially identifiable information were edited to preserve anonymity and ensure clarity of meaning.
Results
Participants
Twenty-five people (15 female, 10 male), along with 5 of their SOs, completed one-off interviews between April and September 2019. Interview duration ranged from 28 to 168 minutes (mean: 69).
Report Supplementary Material 4 describes the sample’s characteristics in detail. In brief, the mean age of participants with epilepsy was 37 years (range: 19–73). Participants described their ethnicity in the following ways: White British (n = 22); white others (n = 2); Black Caribbean (n = 1). The sample was well educated, with n = 18 (72%) having postsecondary-level qualifications (beyond General Certificate of Secondary Education level) (this compares to ~44% in the UK170), and all had seen an epilepsy specialist in the prior 12 months (compared to an expected 48% based on findings from the National Audit of Seizure Management in Hospitals44). Their mean years diagnosed with epilepsy was 21 (range: 4–50); 17 (68%) were at the time being prescribed two or more antiseizure medications. Fifteen participants said they had a comorbid health condition (physical health condition: 11; mental health condition: 7), with 3 reporting dissociative seizures.
Twenty of the participants said they had a friend or family member who helped them with their epilepsy (parent: 11, child: 2, partner: 9).
Qualitative findings from interviews relating to decision-making and preference
Decision-making and care preferences after a seizure
Deciding to use emergency services after a seizure was often described by participants as being due to what they themselves perceived to be an unusual seizure presentation or because they had experienced an injury of some type.
If I have an injury off the back of the seizure, then she will call the ambulance … If it does get out of control, like for example, if it’s longer than is usual or if I go back-to-back seizures then she will call the ambulance, because one seizure is fine for me, I can just rest and relax.
p. 19, Male, age 30s
Because it was something completely different from my normal scenarios, it was best to call emergency services.
p. 18, Male, age 20s
A number of participants did though also express a desire to receive seizure aftercare from the emergency services for reasons which would likely be judged as not medically necessary. For example, one participant explained that her family contacted the ambulance because they believed she always needed oxygen after a seizure. Although it is not possible to assess the medical necessity for this without access to the patient’s medical notes, it does remain the case that oxygen support is rarely required following a seizure:40,41
I need kind of prolonged oxygen, and not every ambulance carries that, or has a policy of providing it after a seizure … that helps me recover and not go into kind of seizure after seizure.
p. 25, Female, age 40s
Seizure characteristics
Losing consciousness was reported as resulting in their informal carer calling emergency services for some participants. For example,
If I’m having a fit, a major fit, [my husband] always calls … Because he wants to be on the safe side. And I don’t have these sort of fit[s] very often. I have maybe one or two a year of those big ones.
p. 3, Female, age 50s
Assessments by ambulance staff sometimes gave reassurance of safety, and participants were therefore reassured that further care was not needed. Where participants remained conscious, many did not wish to receive further care.
One participant described an event where an ambulance was called by an emergency service call operator when he became less responsive during the phone call, ‘They just buzzed the ambulance. I cannot really remember’ (p. 27, Male, age 30s). He said on that occasion, ambulance staff arrived to do basic checks and offered to take him to a hospital, which he declined as he felt it unnecessary after a focal seizure.
Seizure location
Seven participants said one of their SOs could intervene and provide support after a seizure at home: ‘Most of my seizures are nocturnal, so when [my husband] is near … he knows to put me on my side … he just waits for the seizure to pass’ (p. 2, Female, age 40s). Most described their informal carers as being ‘experts on their epilepsy’, sometimes with years of experience, first aid knowledge or having had prior guidance from ambulance staff.
An informal carers presence often meant they completed a safety assessment and sometimes administered emergency medication. As a result, calling the emergency services was not thought necessary:
Mum deals with it as much as she can before having to call paramedics.
p. 18, Female, age 20
However, not all SOs were confident in seizure care. One participant wanted more training options for her husband to provide emergency care:
[My husband] should be trained more on what to do … they did give me midazolam before that he could put inside of my mouth. But … he’s not going to want to give it to me.
p. 29, Female, age 60s
Some participants described technology that enabled them to receive assistance at home or in public. This included a wearable device for detecting seizures that one participant used to alert a family member of seizure occurrence. Participants aged over 40 (particularly ‘young-old’, aged 60–74) were less likely to report use or awareness of any such technologies.
If I have a seizure and I am at home alone … I’ve fortunately, got my device on me that monitors me when I have a seizure, my dad will actually get texts.
p. 1, Male, age 20s
Having seizures in public was described as challenging, particularly if the person was alone. They described how the call for help in these instances would typically arise because of the good intentions of members of the public. Some had implemented strategies to try to ensure the care they received in these instances aligned with their need:
It’s frightening for people, especially if you are not just having tonic clonic seizures … they don’t know very much about complex partial seizures … I carry [epilepsy ID/seizure first seizure aid] cards around with me of my own that I’ve made up to help people, and for my own safety …
p. 8, Female, age 50s
In public areas, formal protocols of good practice (often held by public transport providers or supermarkets) occasionally influenced decisions about calling emergency services. At times, this conflicted with the preferences of PWE and their supporters: ‘It’s just because he’d had it on the bus so automatically, they had to (call an ambulance)’. This SO felt medical attention was not required: ‘[Ambulance staff] just come, check him all over and asked, ‘Did we want to take him to the hospital?’ We said ‘No.’ He’s got no cuts or nothing’ (p. 7, SO).
Another participant described being taken to ED despite having uncomplicated seizures at school. She then had a formal care plan put in place, supported by her usual care providers, which included explicit guidance on what constitutes appropriate care after a tonic–clonic seizure. She described how the plan’s implementation reduced future subsequent ED use during school hours. Five PWE also said they had a formal care plan with guidance on postseizure care that was sometimes helpful in managing decisions regarding the need for ED when in public.
One participant advocated that care plans are helpful for ambulance staff to be better equipped to provide individualised care:
If [ambulance staff] were made aware of the relevant details for each person and they were aware of the recovery time and so therefore what to expect of that person, it might be easier for them to communicate, as they’d have more understanding.
p. 20, Female, age 20s
Alternative care pathways
When discussing alternative CPs, participants highlighted how they felt the appropriateness of the different configuration options would vary on an event-by-event basis:
There shouldn’t be a set rule of that, yeah, you must go to A&E or yes, you must go to the Urgent Care Centre, it all depends on after doing the observations they do in the ambulance, where they think you should go and also how, depending on how the individual is feeling.
p. 19, Male, age 30s
Experiences of alternative care pathways
When asked if an alternative CP had ever been offered to them by ambulance staff, six PWE with informal carer support reported having previously being offered to remain where they were or to be taken home. This option was described as being ‘safe’ and reassuring.
A few participants reported occasions where they continued their journey after ambulance staff assessment. One recalled: ‘I remember in the past being, you know, [them] saying that “You must go”’ and I’m saying, ‘No, I can’t, I don’t need to.’ She was therefore thankful to carry on with her day after she had recovered from her seizure and described having ‘… a very good experience because somehow they realised what I wanted, and took me to (location redacted) which is where I was going, which was incredible, because that meant me not having to be hours in A&E department, and the worry of somebody coming to meet me and things like that’ (p. 5, Female, age 50s).
One participant who frequently had experienced seizures in public reported having regular contact with the local ambulance service who were aware of his preference to avoid ED:
As soon as you put my name into the system, it flags. They know it’s related to me or even certain description. They know ‘Okay, this is what we do … if we can try and keep you in the community, that’s what we’ll do. We’ll try and keep you away from hospital as much as possible.’
p. 1, Male, age 20s
Some participants said other attributes of care, such as medication advice and follow-up, were more important to them than avoiding ED per se. One participant, who had been diagnosed with epilepsy 6 years prior and had five tonic–clonic seizures in a short space of time, noted ‘I’d like (from the episode) to get scheduled back in with a neurologist because the last time I saw a neurologist was … the initial diagnosis’ (p. 12, Male, age 20s).
Participants were mixed in their views as to who the follow-up should be done by. Some wanted it to be with someone with epilepsy-specific knowledge, some for it to be done by their GP. Either way, it was important for participants that a system of follow-up was in place and that the system was responsive:
An appointment should be booked with the GP afterwards as like a follow-up service … What it should be is it should be classed as an emergency appointment in a few days or … they should call it like an A&E follow-up.
p. 20, Female, age 20s
The epilepsy nurse specialist, have been a great help to me in the past … to have their reassurance and their knowledge, expertise … that would be most, you know, comforting, really.
p. 10, Female, age 50s
When it came to ENSs, participants expressed concerns about their availability:
There’s not enough of these epilepsy nurses, they’re very, very busy, because more people have got the epilepsy now.
p. 29, Female, age 60s
Views about an urgent treatment centre as an alternative to emergency departments
Four participants preferred to avoid ED unless they felt there was no other option and were therefore supportive of attending an UTC instead. Some were favourable of UTCs due to perceived ease of access. In reference to the idea of a UTC, one participant explained:
That would be nice to know if there was plenty of the walk-in centres around, that if I did have a seizure outside in public or something, even with my family, if I do cut myself or put myself in danger in some way or another, that if it’s really close by, I could go to that.
p. 7, Male, age 20s
Participants did express some concerns, however, regarding the extent to which UTCs could provide an alternative to ED, mainly because of their more limited opening hours (i.e. typically 8 a.m. until 8 p.m., rather than 24 hours). Several participants for instance described how their seizures were predominantly nocturnal:
They’re only open 12 hours a day. So, if I had the seizure at night, it wouldn’t be helpful.
p. 25, Female, age 40s
Others had concerns about what would happen if their visit overran the closing time of the UTC:
If I had a seizure at … [Laughter] well, like, 4:30pm and they closed at 6:00pm, would that be the best idea?
p. 17, Male, age 20s
Three participants expressed worry about transportation after a seizure:
My … query would be would an ambulance take me there? Would I have to get there?
p. 26, Female, age 30s
Discussion
This qualitative study explored both service users’ postseizure care decision-making and their views of alternative CPs. The recruitment approach enabled the study to be rapidly completed and at low cost. It maximised on the return from previous investment by the National Institute for Health and Care Research (NIHR) in the SMILE trial. 167 It did, though, ultimately result in the recruitment of a sample that was not wide ranging in some potentially relevant characteristics. Not only were participants only from South-East England, but those who were well-educated formed the majority of the sample and all had had recent contact with an epilepsy specialist. It is possible that nature of the sample ultimately recruited did not enable us to obtain the full range of views about the topic. The noted characteristics of our participants may help explain why our findings show participants’ decision-making was mostly concordant with medical guidelines, with injury and (perceived) unusual seizure presentations being reported to be the main indicators for their ED attendances.
Despite the nature of the sample recruited, we still found potential evidence of unwanted and/or unnecessary use of emergency services following a seizure. This included potentially erroneous beliefs on the need for ED and treatments by several participants, such as routine access to oxygen following a seizure.
More than half of participants had experienced seizures in public, which may partially explain some instances of unwanted emergency service use. We found how some participants tried to triage themselves away from ED, seeking to retain autonomy by using ID cards, medical alert bracelets and digital technology. Care plans were also seen by those who had them to enhance patient autonomy by issuing guidance to others on seizure aftercare. 171,172
In line with literature on other presentations, the prehospital assessment that occurs on scene was described by participants as being critical for giving patients reassurance. 101
We presented participants with two hypothetical CP options during interviews: conveyance to a UTC instead of ED or to remain where they were, with subsequent telephone follow-up from a specialist nurse. Our findings highlight the value many patients receive from ENS support,47,50 but concerns were raised about their availability.
Concerns identified about UTCs included their ability to manage a deterioration in a person’s status. Participants also had concern regarding opening hours. They were informed that UTCs are to be open for a minimum of 12 hours a day. Most (65%) seizure presentations by those with established epilepsy occur between 8 a.m. and 8 p.m., peaking between 12 and 2 p.m. (T Baldwin, Yorkshire Ambulance Service, 30 May 2019). Nevertheless, patients still raised concerns.
Strengths of the qualitative study include the breadth and depth of issues covered with participants. It is the first study to explore service users’ views on alternative CPs.
While the sample ultimately recruited may not have included the full range of views about the topic, the evidence it provided on attributes of care that are important to PWE do nonetheless still represent the best evidence to date on this topic and the interviews generated rich qualitative evidence to support the design of the DCE, as is recommended. 173
In the next chapter, we describe how the findings from this qualitative chapter and the previous service provider survey were brought together to help develop the DCE.
Chapter 4 Formative research to develop discrete choice experiments
Introduction
This chapter reports on the formative mixed-method research that contributed to the development of the DCEs to be used in WP2b.
As with any preference elicitation technique, the validity of a DCE depends heavily on the formative work preceding it. 173 The DCE was to obtain evidence on the preferences of service users for seizure scenarios where opportunities for more non-conveyance exists. 23,37 Namely, after a person with established epilepsy has experienced: (1) a seizure at home that is in line with their usual presentation (‘Home typical seizure’); (2) a seizure in public that is in line with their usual presentation (‘Public typical seizure’) and (3) a seizure that has self-terminated, but which is different in some way to the person’s ‘normal’ seizure(s) (‘Atypical seizure’).
In Chapter 1, we outlined a range of issues that require attention when developing a DCE. Importantly, there is a natural limit to the number of attributes and levels that can be used within a DCE. The more there are, the more complex the choice task becomes, and the potential for participant burden and missing data increases. As evidence on which attributes were key was not available, in the current chapter, we report how we engaged with service users to help us better understand their decision calculus. We also report how we engaged with service providers themselves to ensure the levels used for the attributes were likely plausible (i.e. NHS-feasible and anticipated to be safe). Finally, to help ensure participants were interpreting the attributes and levels as intended and that DCE’s presentation was optimised, we describe how it was piloted.
Methods
The formative work was extensive, sequential (see Figure 2, WP1b, 1c and 2b) and informed by best practice recommendations. 149,173
Attributes of importance to service users were first identified via the ranking exercise appended to the qualitative interviews. These were then refined, and levels for them developed via a KE event with service providers (WP1c) during which the findings from WP1a and 1b were shared. A draft DCE survey was then developed and piloted with service user representatives (WP2a) and further refinements made. The process was overseen by a multidisciplinary DCE design panel that considered the evidence from the different stages and refined the DCE accordingly. The panel included expertise in DCEs (EH and DH), emergency medicine (SG), neurology (AGM), paramedical science (MJ), general practice (JMD) and psychology (AN), as well as having service user representation.
Ranking exercise methods
Design
Towards the end of the interviews reported in Chapter 3, PWE were invited to complete a ranking exercise (see Appendix 4). Using an approach previously deployed by the investigative team,174 it here involved participants being presented with five care attributes potentially relevant to the choice of CP, identified by the research team based on findings from previous studies, policy and clinical experience. These were printed on ‘show cards’, along with brief descriptors. Participants were asked to consider these and state whether they felt anything important was missing. The qualitative interviewer (AMc) helped participants recall characteristics they mentioned during their interview and wrote them onto ‘show cards’. The five attributes were:
-
‘Where the ambulance takes you’.
-
‘The healthcare professional responsible for care when you get there’.
-
‘How long you have to wait before you see that healthcare professional’.
-
‘Tests that can be carried out immediately’.
-
‘Number of people who are referred on to a health professional with specialist training in epilepsy’.
Participants were asked which of those on display were the most important in their view and would likely most affect their choice of care post seizure. To then help reduce the number of care attributes to a number manageable for a DCE and improve face validity, participants were asked to rank those selected in order of importance. Participants were encouraged to ‘think aloud’ when making their choices. Interim analysis of the ranking scores was completed to identify any areas that required further exploration within the subsequent interviews to assist with the assessment of attributes for use within the DCE.
Analysis
All ranked attributes were analysed quantitatively in Excel by EH using standardised rank scores for each attribute.
-
Rank score = (#attributes − rank + 1)/n
where:
-
rank = rank position (1 = most important)
-
n = number of attributes selected by the participant
Additional attributes nominated by individuals were categorised according to a thematic framework by EH and assessed against a set of predefined suitability criteria (Table 3). The framework was developed by EH, with assistance from AMc and the wider research team.
| Inclusion | Exclusion |
|---|---|
Attribute is:
|
Attribute is:
|
Results
Twenty-three of the PWE who were interviewed completed the ranking exercise. Five had a SO present when completing it.
In addition to the prespecified attributes, the participants together nominated 13 additional attributes for consideration (Table 4). Four were nominated by more than one participant.
| Mean score | ||
|---|---|---|
| Predefined attributes | Count selected | |
| Care provider | 19 | 0.67 |
| Where the ambulance takes you/location of care | 19 | 0.63 |
| Waiting time | 20 | 0.63 |
| Tests | 18 | 0.47 |
| Follow-up | 19 | 0.39 |
| Self-nominated attributes | Count nominated | |
| Reassurance | 3 | – |
| Contacting next of kin | 2 | – |
| Safety | 2 | – |
| Linked communicationa | 1 | – |
| Care plan awarenessa | 1 | – |
| Education | 1 | – |
| Check over | 1 | – |
| Right equipment | 1 | – |
| Going home | 1 | – |
| Training | 1 | – |
| Immediate help | 1 | – |
| Trust | 1 | – |
| Patient group/support | 1 | – |
When asked to select which were most important to their choice regarding postseizure care, the average number of attributes selected was 4.84 (range: 3–5). Waiting time was the most selected (n = 20). Care provider had the highest rank score of the predefined attributes (3.68), while safety was the highest ranked self-nominated attribute (see Table 4).
Decisions and reflections of discrete choice experiment design following ranking exercise
Discrete choice experiment panel decisions and reflections following interim analysis
The interim analysis of the ranking scores led the DCE design panel to request further qualitative exploration with subsequent participants of (1) the types of tests they were considering as important, (2) how they understood reassurance as a construct of care being provided, (3) what their understanding was of the term ‘linked communication' and (4) what overlap there was between the nominated attribute ‘care provider’ and location of care (where the ambulance takes you).
Types of tests people were considering
For some people, being in a place that has access to tests ‘just in case needed’ was reported as important. For other participants, they wanted the tests for monitoring of their condition and for the information from them to assist with their own self-management or for discussion with their routine care providers. The tests mentioned as being valued most frequently included (1) magnetic resonance imaging, ‘brain scans’ more broadly, (2) laboratory tests/blood tests and (3) electrocardiogram and blood pressure checks.
While it was acknowledged that the type of tests health professionals could carry out immediately if needed was important to patients, the design panel considered it implausible as an independent characteristic of a CP. Essential tests would be provided based on clinical necessity and were intrinsic to the emergency care episode.
‘Reassurance’ as a construct of care being provided
Participants described how reassurance was derived from various actions, including the ability for ‘someone’ (be it the paramedic or another healthcare professional) to instruct the SO what to do, intervene to stop recurrent seizures, monitor vital signs or provide immediate care in the case of injury.
The design panel considered that this evidence indicated reassurance represented the utility derived from receiving emergency care and so excluded this additional attribute from the selection process.
Understanding of the term ‘linked communication’
Upon questioning, people reported reassurance (also self-nominated) when they were cared for by one health service and found the records from their usual service were also available to the healthcare team there. One participant expressed this as meaning he ‘felt less alone and there was a team of people supporting’ him. The term ‘linked communication’ was also interpreted by some participants as a characteristic of decision-making, with some saying they wanted their healthcare professionals to involve them more in the process of their health care.
Based on the above evidence, the design panel determined that ‘linked communication’ would need to be specifically described in the DCE to ensure the survey measured preferences for a tradable characteristic of a CP, rather than ‘experience’ of accessing specialist services/decision-making. It was noted, however, that the findings of the WP1a survey (see Chapter 2) found regional variation regarding linked communication/access to medical records. The DCE design panel, therefore, proposed defining the attribute as: Access to care plan/medical notes, and proposed further discussion at the WP1c KE event to gain a clearer understanding of the importance and plausibility of this characteristic.
Overlap between attributes
Overlap was noted as existing between the predefined attributes ‘care provider’ and ‘follow-up’. Participants reported that an important aspect of ‘care provider’ was them being someone ‘with specialist training in epilepsy’. When considering follow-up, people wanted to ensure that this was by ‘someone who is connected to a neurologist’. Predefined attributes were also combined with self-nominated care characteristics by one participant: ‘Care provider’ (safe), Waiting time (monitoring) and Tests (reassurance).
Discrete choice experiment panel decisions and reflections following completion of the entire ranking exercise
Attributes selected
The DCE design panel requested that the six attributes described as version 1.1 in Table 5 be taken forward for discussion at the KE event for potential use within the DCE. The panel’s decision was based on the following.
| V1.0 | V1.1 | V1.2 | V1.3 | V1.4 |
|---|---|---|---|---|
| Attributes presented in or emerging from ranking exercise | Attributes presented at KE event | Revised post 1c for use at the DCE development panel | Presented at cognitive interviews | Finally used in WP2b |
| Where the ambulance takes you Where the ambulance takes you (e.g. A&E, UTC) |
Location of care Where you are assessed and treated? |
What happens next Where you go once the paramedic has assessed you |
What happens next Where you go once the paramedic has assessed you |
What happens next Where you go once the paramedic has assessed you |
| Care provider The healthcare professional responsible for your care when you get there |
Levels (3):
|
Levels (3):
|
Levels (3):
|
Levels (3):
|
| Tests The type of tests the health professional could carry out immediately if needed |
||||
| Waiting time How long you have to wait before you see the healthcare professional |
Time The time you spend being assessed, monitored and treated |
Time How long it takes to be assessed, monitored and treated by emergency healthcare professionals today |
Time How long it takes to be assessed, monitored and treated by emergency healthcare professionals today |
|
Levels (3):
|
Levels (4):
|
Levels (4):
|
||
| Follow-up Referral to see a health professional with specialist training in epilepsy |
Involvement of specialist services Involvement of a health professional with specialist training in epilepsy |
Involvement of specialist services Involvement of a health professional with specialist training in epilepsy |
Involvement of specialist services Involvement of a health professional with specialist training in epilepsy |
Epilepsy specialists today A health professional with specialist training in neurology is available to advise the emergency healthcare professionals treating you today |
Levels (3):
|
Levels (3):
|
Levels (3):
|
Levels (2):
|
|
| Follow-up How long you have to wait for follow-up by epilepsy specialist services after this episode |
Future contact with an epilepsy specialist Length of time between the paramedic attending and contact with an epilepsy doctor or nurse |
Future contact with an epilepsy specialist Length of time between the paramedic attending and contact with an epilepsy doctor or nurse |
Additional contact with an epilepsy specialist The emergency healthcare professionals treating you today arrange for you to have an appointment with an epilepsy specialist |
|
Levels (4):
|
Levels (3):
|
Levels (3):
|
Levels (3):
|
|
| Contact with your GP The paramedic attending will contact your GP to inform them of the care you have received |
Contact with your GP Your GP will be notified that an ambulance was called out to you |
Contact with your GP Your GP will be notified that an ambulance was called out to you |
GP told Your GP will receive a written report from the ambulance service |
|
Levels (2):
|
Levels (2):
|
Levels (2):
|
Levels (2):
|
|
|
Self-nominated during ranking part 1:
‘Awareness of care plan’ ‘Linked communication’ |
Access to care plan The paramedic attending is able to access your care plan (and record the care you receive) in your epilepsy case notes |
The paramedic has access to your [a] care plan The paramedic attending is able to access a plan that explains what you require when you have a seizure |
The paramedic has access to a care plan or medical records They can read about what you require when you have a seizure |
The paramedic has access to medical records or a care plan They can read about what you require when you have a seizure |
Levels (2):
|
Levels (2):
|
Levels (2):
|
Levels (2):
|
All five predefined attributes were selected within the ranking exercise at least once by participants. However, after considering the findings from further qualitative exploration, the panel excluded the predefined attributes ‘Care provider’ and ‘Tests’ from use within the DCE. This was because they overlapped with the predefined attribute ‘Location of care’ and as such were not independent characteristics of a CP.
The panel noted that the attribute ‘Location of care’ would require detailed introduction at the beginning of the DCE experiment to ensure respondents understood the names and features of the potential level for this attribute (e.g. what an ‘Urgent Treatment Centre’ was).
The panel also recommended that the attribute ‘Waiting time’ be modified to the more neutral term ‘Time’. Moreover, they said the prose accompanying should be expanded to include time spent being assessed, monitored and treated. This was because some PWE expressed value in being in a safe location, monitored by a healthcare professional.
The attribute ‘Follow-up’ was identified as being a broader construct than initially described and so was separated to create three attributes: one relating to immediate specialist care at the time of the incident, one to future specialist care and one to non-specialist/primary care involvement.
Regarding the 12 self-nominated attributes, the panel considered that only one of them – namely ‘Access to care records’ – satisfied the eligibility criteria for use within the DCE.
Attribute levels
Based on findings from the WP 1a survey (see Chapter 2), as well as their own expertise and clinical experience, the design panel generated draft levels for the V1.1 attributes (see Table 5). They asked for these to also be considered at the WP1c KE event. In generating the levels, the panel sought to ensure the levels accounted for relevant major anticipated changes in the future – such as longer ED waiting times and more integration of services and sharing of patient records. Potential interactions, properties of the experimental design (e.g. number of choice sets) and implications for analysis (e.g. continuous/categorical levels) were also discussed when deliberating the levels.
Three attributes (i.e. Location of care, Time and Involvement of specialist services) were assigned three levels: two attributes (i.e. ‘Contact with your GP’ and ‘Access to care plan’) were binary and one (i.e. ‘Follow-up’) had four levels.
Instructions for discrete choice experiment survey
Led by AM, AN and EH, the panel generated draft instructions for the DCE and draft vignettes for the three seizure presentations that the DCEs were to be completed for (Table 6). The panel was of the view that the vignettes modelled the clinical situations faced by ambulance clinicians and did not include any details that indicated an obvious clinical driver for conveyance to ED.
| V1.1 Attributes presented at KE event |
|---|
| Home typical seizure: ‘You do not have a fever, you were not feeling unwell before the seizure. You have not been drinking alcohol or taken drugs. Not significantly injured (see previous version) Imagine you have a seizure at home. You have fully recovered and someone you know is with you. The seizure lasted no more than usual and stopped by itself. Someone called an ambulance and the paramedic is with you. Which of the following options would you prefer?’ |
| Public typical seizure: ‘You do not have a fever, you were not feeling unwell before the seizure. You have not been drinking alcohol or taken drugs. Imagine you have a seizure in a public place. You have fully recovered. The seizure lasted no more than usual and stopped by itself. Someone called an ambulance and the paramedic is with you. Which of the following options would you prefer?’ |
| Atypical seizure: ‘You are feeling unwell. For example, you may have a fever, abnormal pulse, high blood sugar, or a swollen face or tongue. The paramedic may also be concerned about past medical issues you have had in the past. You may also have wounds that need assessing or treating. You have not been drinking alcohol or taken drugs. Imagine you have a seizure. You have fully recovered and someone you know is with you. The seizure was different to usual, it may have lasted longer, and you may also have been feeling unwell before or after. Someone called an ambulance and the paramedic is with you. Which of the following options would you prefer?’ |
With regard to the instructions, it was agreed that different versions of the DCEs would need to be generated – one for completion PWE and one for completion by SOs. The language used in the two versions would need to slightly differ (e.g. for the attribute location of care ‘Where you are assessed …’ would need to be ‘Where they are assessed …’).
Knowledge exchange event methods
Design
A KE event with service provider representatives was completed. It involved representatives attending a one-day, in-person, workshop. They were asked to use their clinical experience and expertise to help refine the draft attributes, ensure the levels were plausible and provide feedback on the vignettes. The team had successfully used this approach for a previous DCE project. 139
Knowledge exchange has been defined by Wilkins and Cooper175 as comprising a two-way exchange between researchers and research users, to share ideas, research evidence, experiences and skills. It goes beyond just telling people things and should be seen as a process of listening and interaction, with a goal to generate mutual benefit.
Approval for this formative work was provided by the Health Research Authority and the National Research Ethics Service Committee West Midlands, Solihull (19/WM/0012).
Recruitment
To take part, representatives needed to be able to provide informed consent, be aged ≥ 18 years, live in the UK, work within the ambulance service (front-line or managerial role) or as a neurologist or ENS and be able to be attend and participate in the scheduled event.
Representatives were identified from those services that took part in the WP1a survey and said they and/or their service wanted to be informed about future parts of the project. A total of n = 69 respondents expressed an interest. A sampling framework was created to support the recruitment of representatives from different regions of England.
Using the framework, invitations were posted and/or e-mailed to designated contacts at n = 10 ambulance services and n = 10 neurology services. Packs included a covering letter and participant information sheet. Persons were told participation would be anonymous, and their responses would not be linked back to their organisation or service. It was possible for recipients to pass the invite onto someone they considered more suitable for participation or to ask us to. Recipients could respond to the invitation by using an enclosed response slip or by contacting the team by phone or e-mail. Repeat invites were sent to services if no response is received from them within 2 weeks. Ultimately, we sent n = 26 separate invitations after some services responded and asked us to invite someone else they nominated from their organisation.
To help ensure the voice of service users was present in all formative discussions, a representative from Epilepsy Action was also present during the meeting.
All those participating provided written informed consent and reimbursed for travel.
Process
The event was held in London in October 2019. Discussions were, at different time points, facilitated by AN and EH. In advance of the event, participants had been sent a copy of the participant information sheet, a consent form and an agenda for the day.
On the day, participants first heard short presentations from the research team (AN, AM, AMc and EH). These covered the project’s background, an introduction to the DCE method and a summary of the findings from the formative research conducted to date. Participants were then presented with the V1.1 attributes.
For each attribute, participants were asked to verify the attribute represented a characteristic of a CP, whether the levels were plausible and described appropriately (i.e. how they might describe the attribute to patients). During discussion, EH specifically enquired about the experimental potential of the attributes to ensure the utility function was adequately described and that attributes were capable of being traded. Finally, participants were asked for their views on the scenario vignettes.
Field notes were taken and the session was audio-recorded for subsequent full transcription and analysis.
Knowledge exchange event results
Participants
We formally invited 26 representatives. Fifteen confirmed a willingness to take part and were booked to attend; 13 ultimately attended and participated. Attendees included n = 6 paramedics, n = 4 consultant neurologists, n = 2 ENSs and n = 1 user group representative. All came from different organisations, and there was wide geographical spread as planned. The event lasted 6 hours, with breaks included.
Feedback from participants on draft attributes and levels
Participants agreed the six candidate attributes were all characteristics of an alternative CP. Overall, the attributes were considered likely pertinent to patients (and health professionals and policy-makers), plausible, capable of being traded and suitable for inclusion in the DCE.
Participants had the following specific feedback for the different attributes.
-
Access to care plan
Knowledge exchange participants advised that based on their experience service users might be unfamiliar with the term ‘care plan’. It was highlighted that many people do not have one. Moreover, the content of any such plan may vary between regions.
-
Location of care
Concern was raised that the attribute, as presented, might incorrectly raise an expectation amongst DCE participants that all treatment forms could be delivered at all three attribute levels. It was also considered that what treatment could be provided would depend on the role and experience of the attending ambulance clinician and where the patient was located geographically since infrastructure varies.
For these reasons, participants suggested the attribute be refined to ‘What happens next’ and that any reference to ‘treatment’ be removed. They also said that within the attribute description it be stated that ‘What happens next’ refers to the period after the patient has been initially assessed by the attending ambulance clinician. This was because an alternative CP would only be appropriate if the attending clinician had deemed this to be clinically safe.
The participants also had feedback relating to the proposed levels. Ambulance representatives stated that while it was identified as possible via the WP1a survey, transporting a patient home who had had a seizure in public, rather than conveying them to ED, was not widely offered or feasible. Thus, they recommended changing the level ‘At home/on the scene’ to ‘Stay where you are’.
In the context of an atypical seizure presentation, there was some discussion as to whether all three levels for the attribute were plausible. One epilepsy specialist representative was of the view that after an atypical seizure conveyance to ED was always necessary. This was, in part, because they believed it should mean they receive input into their care from an epilepsy specialist. For them, using the levels of ‘Stay where you are’ and ‘Urgent Treatment Centre’ were therefore inappropriate for the atypical seizure scenario.
-
Time
Knowledge exchange participants advised restricting the level used for this attribute to 2 hours when the attribute ‘Where next’ took on the level of ‘Stay where you are’ and to 3 hours when it took on the level of ‘Urgent Treatment Centre’. When ‘Where next’ took on the level of ‘ED’, the representatives said ‘4 hours +’ should be used. These changes they said would make the attribute levels more feasible and realistic. They did acknowledge though that there might be instances during periods of ‘winter pressures’ when these times might not be achievable for various reasons.
-
Involvement of specialist services
Views as to the feasibility of the different levels for this attribute varied, partly reflecting the different extents to which it was part of current practice in different regions. Participants from the ambulance service highlighted how the challenge of them contacting specialist services varied depending on the locality that they were operating within. Participants from epilepsy specialist services wanted to emphasise that working hours and capacity needed to be accounted for within the levels for this attribute. The level ‘Within 24 hours by phone’ was not considered plausible by all epilepsy specialists.
-
Follow-up
It was highlighted that the patient may be accessing the CP in a different geographical area to the one that their specialist epilepsy service was located in. Clarity on this being future contact with the patient’s specialist service (rather than that of the emergency care region) was important, as some people may not be aware that there is a local service. It was advised that the description should focus on the length of time between the emergency episode and contact with an epilepsy doctor or nurse.
-
6. Contact with your GP
Participants from the ambulance service described how what happens at present regarding this comprises more of a notification to the patients GP of the incident, rather than a full ‘report’. It was recommended that the attribute be reworded to reflect this.
Feedback from participants on seizure scenario vignettes
Knowledge exchange participants identified the vignettes as being realistic. There was some debate over the use of the term paramedic within them. Not all attending ambulance personnel are paramedics. However, the consensus was that ‘paramedic’ was from the patient perspective likely the best term and so should remain unchanged.
Decisions and reflections of discrete choice experiment design panel following knowledge exchange exercise
The panel welcomed the KE participants’ feedback. They accepted most of their suggestions. The changes served to create V1.2 of the attributes in Table 5. The details are as follows:
-
Access to care plan
The panel agreed the DCE would require an introduction that provided a detailed explanation of the term ‘care plan’ to participants and what they can contain. They also stated that the care plan attribute would need to explicitly refer to access to medical records since this is an aspiration for current practice and for many this is what ‘care plan’ in an emergency comprises.
-
Location of care
The panel, with input from clinicians within the research team, endorsed all the changes recommended by the KE participants. The exception to this was the comment from one epilepsy specialist that suggested the level ‘Stay where you are’ should not be used for the atypical seizure presentation. The reasons for the panel declining that last suggestion were as follows.
Firstly, the parameters of the atypical seizure presentation to be used within the DCE were restrictive. The presentation as described does not meet the requirements for ED care on clinical grounds (i.e. it was an epileptic seizure in a person with established epilepsy from which they had recovered from, but which was different in some way to their usual experience, and no injuries were incurred).
Secondly, the DCE was only asking for a person’s care preferences in a hypothetical situation. It was not making recommendations as to the suitability of the approach.
Finally, one reason the representative expressed a need for all atypical seizure presentations to visit ED was based on the view that not going to ED would deprive the person from input from an epilepsy specialist. This does not though reflect clinical reality. While NICE guidelines112 suggest this should happen in some form, most people with established epilepsy who visit ED are not seen or referred to a specialist. 44 Moreover, within the DCE, it was still possible for a person to stay where they were or be conveyed to an UTC and still receive specialist follow-up.
-
Time
The panel accepted the recommendations of the representatives. They noted that the experimental design would need to allow for conditions between ‘Time’ and ‘Location of care’ to ensure the choices remained plausible.
-
Involvement of specialist services
On reflection, the panel said this attribute should be refined to focus on specialist advice during the care episode, thus minimising overlap with the other attribute ‘Follow-up’.
-
Follow-up
The panel agreed that the attribute should not indicate that health professional with specialist training in epilepsy would be known to the patient.
When presented to the KE participants, the attribute ‘Follow-up’ had four draft levels (i.e. not referred; within 5 days by telephone; 2–4 weeks; and 4 weeks +). The panel on reflection stated that the level for this attribute of ‘Not referred’ be removed given the earlier noted NICE recommendation of follow-up in all cases. The panel also suggested collapsing the remaining levels to help reduce the size of the experiment to a more manageable number of choice-sets.
-
Contact with your GP
The language used for this attribute was amended in line with the participants' suggestion.
Creating survey on basis of panel decisions
EH, AM and AN developed a draft version of the DCE survey and a standardised set of instructions for piloting (experimental design reported in Chapter 5). This was hosted by the Qualtrics XM online survey platform. It included a welcome page, a participant information sheet and consent page. A filter was embedded to determine whether the participant had epilepsy themselves or was a SO. It then presented 24 DCE choice sets and a limited set of non-DCE questions. The latter, described in detail in Chapter 5, sought information on participants’ characteristics.
The instructions explained the context of the survey to participants and introduced them to the attributes and levels. Participants were asked to use their imagination as best they could if they (or the person with epilepsy they know) had not found themselves in one of the seizure scenarios used in the DCE. To promote consistency in the way SO participants completed the DCE, instruction was also made as regards ‘positionality’. They were asked to answer the DCE regarding how they would prefer for the person with epilepsy they know to be cared for.
To maximise engagement, accessibility and reduce reading burden,176 a 7-minute professionally produced animated video was developed that relayed most of the instructions. Participants were to be requested to watch it before completing the survey. The animation was narrated and included subtitles and developed with the input of service users, researchers and clinicians.
Pilot interviews
Design
The pilot involved working closely with persons from the epilepsy population to iteratively refine the draft of the DCE survey. It sought to identify any changes required to ensure survey length was acceptable and that participants completed the task as intended.
Pilotees were asked to complete the draft of the online DCE survey in the presence of a research associate (AM). Using the cognitive interview technique, pilotees were encouraged to ‘think aloud’141 when making their choices. They were also asked to consider their preferred presentation of the attributes (e.g. use of text, pictograms). Interviews were audio-recorded and field notes taken.
Recruitment
The pilotees were identified from the patient and public involvement (PPI) group that was established for the project with the support of Epilepsy Action. Persons on it were all aged ≥ 18 years and either had epilepsy or were a SO to someone with epilepsy. Beyond being willing and able to independently serve on such a group in English, no other eligibility criteria were applied. Recruitment continued until data saturation was achieved.
Results
Pilotees
Twelve PPI members were enrolled and provided feedback on the DCE survey. Saturation in terms of feedback was occurring after around six pilot interviews. However, to verify the refinements made to the DCE based on their feedback were sufficient, an additional six PPI members completed the DCE.
Feedback received and changes made to the discrete choice experiment survey
The survey was well received by the PPI members and their understanding of the majority of the DCE and wider non-DCE was as intended. Respondents did nonetheless request some changes which the panel made. The changes served to create the finalised attribute set which is labelled V1.4 in Table 5. The set is also presented in Figure 4; this time along with the images used to represent the attributes levels.
FIGURE 4.
Finalised attributes and levels used in all DCEs (V1.4) along with images.
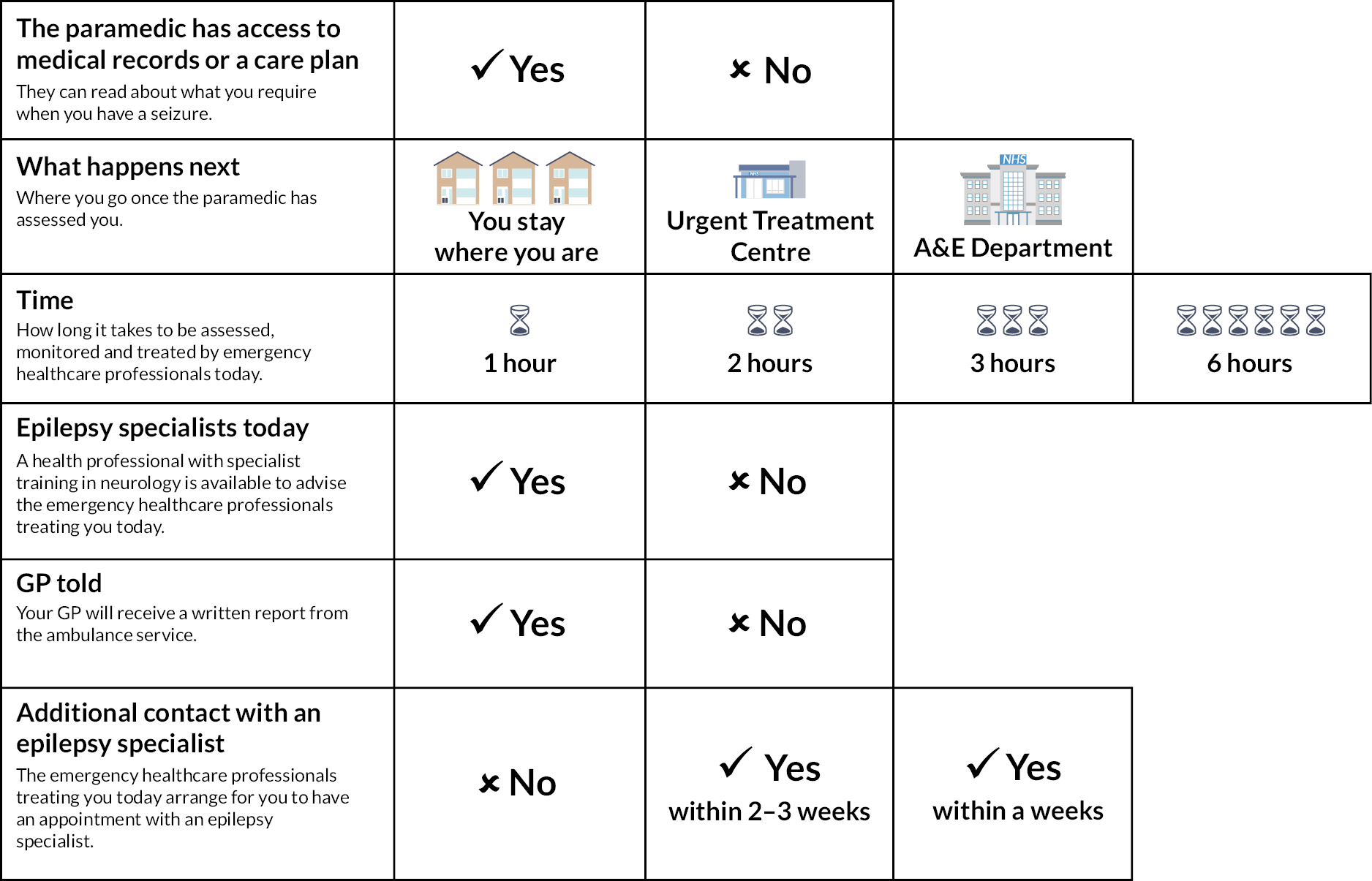
The changes made based on PPI feedback were as follows. Firstly, greater clarity of meaning for the two attributes describing current and future involvement of a health professional with specialist training in epilepsy was requested. PPI members instructed that ‘Involvement of specialist services’ be changed to ‘Epilepsy specialist today’, while ‘Future contact with an epilepsy specialist’ should be changed to ‘Additional contact with epilepsy specialist’.
There was variation in how the PPI members interpreted the two ‘yes’ levels for the attribute ‘Involvement of specialist services today’. Consequently, the panel decided to simplify this to a single ‘Yes’ level.
Patient and public involvement members also challenged the levels used for the attribute ‘Additional contact with epilepsy specialist’. They had commonly experienced ‘No’ follow-up following instances of urgent care and so requested that this level be included to help ensure face validity. The panel made this change. Finally, following the recommendation of PPI members, Contact with GP was simplified to GP told.
In addition to the above changes requested by PPI members, the DCE panel also decided it was necessary to amend the survey in view of the coronavirus disease 2019 (COVID-19) which had started to impact the UK while piloting was occurring. Government requests to ‘socially distance’ were starting, and changes in the way people were using emergency services were becoming evident. 177 Therefore, respondents were asked to make their choices based on their preferences for care outside of the pandemic, termed ‘normal times’ in the survey. Feedback was specifically received on this amendment to wording from pilots. The animation was also updated, and the close of the survey was updated to include a signpost to information on COVID-19 and epilepsy.
Discussion
This chapter has transparently and thoroughly described a substantial body of formative work to develop the DCE survey.
The breadth and depth of the formative work completed are in line with good practice. 133,147,148 Strengths include (1) its systematic approach to attribute development and refinement that ensured those selected were not only important to service users but also NHS-feasible and capable of experimental manipulation and (2) the mixed-methods approach to attribute selection and scenario development that enabled greater interpretation of the relationship between attributes and the decision-making process and maximised face validity.
Potential limitations were that the sampling frames used to recruit PWE and SOs for the qualitative investigation were subject to bias. It is also not clear what the implications are that not all of the service provider representatives invited were able to attend the KE workshop. The findings from the workshops provided part of the evidence base that was to be considered when the DCE was designed. For instance, we only wanted to use attribute levels that were considered plausible for delivery. It is possible that those who did not attend might have shared unique views on this and that this could have changed the evidence base informing the attribute levels to be used in the DCE. We would say, though, that the sample did still include representatives from across the country and from different organisations. It is not possible to present this on a map due to a concern about permitting some individuals to be identified.
In the next chapter, we describe the methods and recruitment of participants for the formal DCE survey and the experimental design used to generate the DCE choice sets.
Chapter 5 Discrete choice experiment: experimental design and survey methods
Introduction
In Chapter 4, the development and finalised selection of attributes and levels for the DCEs were reported. In the current chapter, we report on the methods used to design and administer the survey, including the design of the DCE and details of how PWE and SOs were recruited.
A key ambition was to maximise the representativeness of the sample recruited, while also aiming to permit adequately powered subgroup comparisons to be completed. Only a few studies have been conducted with the target population. This may in part be because identifying PWE who have had contact with the emergency services can be challenging, particularly those who have been seen by the ambulance service, but not conveyed.
Specifically, well-documented challenges to information sharing mean specialist services20 and GPs are not necessarily informed of ambulance attendances to, and ED visits by, the PWE for whom they care. Not all ambulance services directly inform GPs of attendances they make to patients (in part because some services do not have electronic recording systems). 178 There is also no central, ‘live’ system that can be accessed and searched to identify PWE who have had ambulance attendances or visits to EDs in England. Hospitals do maintain local electronic records of attendances at their EDs, but (historically at least) the coding within them has been insufficient to allow efficient identification of PWE from them (see Noble et al. 179).
Method
Design
The DCE survey was cross-sectional. A person with epilepsy could take part with or without one of their SOs and vice versa. People with epilepsy and SOs completed the survey independently, and the responses of any patients and SOs known to each other were not linked.
Eligibility criteria
To participate, patients needed to be aged ≥ 18 years, have had contact with the ambulance in the prior 12 months for epilepsy and have already been diagnosed with epilepsy at the time of this contact. We recruited SOs of such people who were aged ≥ 16 years. We excluded persons with a terminal condition, a severe psychiatric disorder and those who lived in a care facility.
The full inclusion and exclusion criteria are described in Table 7. These are provided according to the route by which a person was recruited. The key difference between the eligibility for the two recruitment routes is where in England the person needed to live.
| Route 1: via ambulance service | Route 2: via public adverts | ||
|---|---|---|---|
| PWE | Significant others | PWE | Significant others |
| Aged ≥ 18 years (no upper limit) | Aged ≥ 16 years (no upper limit) | Aged ≥ 18 years (no upper limit) | Aged ≥ 16 years (no upper limit) |
| Lives in North-West England | Lives in North-West England | Lives in England | Lives in England |
| Able to provide informed consent and independently complete a questionnaire in English | Able to provide informed consent and independently complete a questionnaire in English | Able to provide informed consent and independently complete a questionnaire in English | Able to provide informed consent and independently complete a questionnaire in English |
| Dx. epilepsy, Rx. ASM | Close family member or friend to person with Dx. epilepsy, Rx. ASM, aged ≥ 18 years | Dx. epilepsy, Rx. ASM | Close family member or friend to person with Dx. epilepsy, Rx. ASM, aged ≥ 18 years |
| Any syndrome or seizure type | Any syndrome or seizure type | Any syndrome or seizure type | Any syndrome or seizure type |
| Been seen by ambulance for epilepsy in prior 12 months (conveyed or not) (checked against medical record) | Person with epilepsy been seen by ambulance for epilepsy in prior 12 months (conveyed or not) (checked against medical record) | Been seen by ambulance for epilepsy in prior 12 months (conveyed or not) (self-reported) | Person with epilepsy been seen by ambulance for epilepsy in prior 12 months (conveyed or not) (self-reported) |
Ineligible:
|
Ineligible:
|
Ineligible:
|
Ineligible:
|
Sample size
Definitive sample size calculations for DCEs require the finalised design of the DCE to be known. 180 Therefore, to permit decisions regarding recruitment to be made in advance of the formative work being completed, we estimated the likely design of the DCE and used Orme’s181 commonly used182 formula. Orme’s formula is (n*t*a)/c must be ≥ 500, where n is the number of respondents, t is the number of choice tasks, a is the number of options per task and c is the number of analysis cells (for main effects, the largest number of levels for any one attribute).
We estimated that for each seizure scenario, the DCE would involve the person being asked to choose between two CP options (a = 2), that they would complete around nine choice tasks (t = 9), and that three would be the maximum number of levels for any one attribute (c = 3). Using these parameters, the required number of participants providing complete data for each of the seizure scenarios was calculated as n = 84. As the intention was for data to be obtained for three seizure scenarios, but participants would be randomised to complete a combination of just two, a minimum sample of 126 participants would be required. To allow for variation in the actual number of choice tasks and levels ultimately used, we increased this to 150. It was then further inflated to 174 to accommodate for the ~15% of participants that (based on prior epilepsy DCEs) were anticipated to have insufficient data for inclusion in the analyses. 139,140,183
As one of the study’s planned subgroup analyses was a comparison of the care preferences of PWE (and SOs) who had and had not been conveyed to ED in the prior 12 months (see Analysis), it was necessary to recruit 174 PWE (and SOs) who had visited ED in the prior 12 months and 174 PWE (and SOs) who had not. This meant the target sample size for the DCE was n = 348.
Deviations from original recruitment protocol
Original recruitment plans
When the study was designed and commissioned in 2018, the intention had been that DCE participants would be recruited only from the Merseyside region of England with persons being identified and invited to participate by the North West Ambulance Service NHS Trust (NWAS). For the reasons stated in the introduction to this chapter, the ambulance service was considered the part of the English health system best positioned to identify persons from the target population.
The plan was participants would complete the DCE via an online survey platform. This would permit use of features such as responsive questioning, animations and embedded randomisation and so help minimise participant burden and support DCE completion. Participants would be able to access the platform by themselves at a time of their choosing or by having a face-to-face appointment with a researcher. The latter would have an internet-enabled tablet computer for the participant to use.
Need to deviate from original recruitment plans
It was ultimately not possible for recruitment to proceed entirely as described in the previous section because of the COVID-19 pandemic. On 11 February 2020, the project’s Sponsor stated that non-COVID-19 research could only continue if ‘social distancing’ could be maintained. This precluded offering any face-to-face research appointments to participants. Further complications arose on 20th March 2020 when NWAS paused their support for the project. They needed to redirect resources to efforts related to COVID-19. The pause occurred at a time when NWAS had just completed an intensive participant screening process for the current project and had identified persons to be invited into the study. However, they had not physically dispatched invitation letters to them.
The above events and the uncertainty regarding how the pandemic would evolve meant it was unclear when NWAS would be able to dispatch the invitation letters. This was concerning because the time between the seizure incidents that had led to people being identified by NWAS and them being formally invited to participate in the survey was continuing to increase. This could have with potential, negative implications for uptake. Access to further NIHR ‘Service Support Costs’ for non-COVID research was also prevented.
Thus, with agreement from the Health Services and Delivery Research (HS&DR) and the project’s Steering Committee, it was decided the survey would proceed but (1) participants would be able to only complete the DCE survey online by themselves and (2) an additional recruitment route outside of the NHS’ infrastructure would be established to supplement recruitment. The NWAS recruitment route would remain in place and become active once/if permitted.
The two recruitment routes used
Route 1 – via ambulance service
North West Ambulance Service NHS Trust is the second largest of England’s 10 regional NHS Ambulance Trusts. It acted as a Participant Identification Centre for the survey. Figure 5 shows the process by which they identified and invited participants. The specifics are as follows.
FIGURE 5.
Illustration of identification and recruitment process for participants via ambulance service (with indicative figures based on prior years). AMPDS, Advanced Medical Priority Dispatch System; dx, diagnosis; ep, epilepsy; psych., psychiatric diagnosis; 12B01E, fitting with effective breathing (not verified), epileptic or previous diagnosis of fitting, < 35 years; 12C02E, fitting during pregnancy – epileptic or previous diagnosis of fitting; 12C03E, diabetic patient fitting – epileptic or previous diagnosis of fitting; 12C05E, history of stroke or brain tumour – epileptic or previous diagnosis of fitting; 12C06E, overdose/poisoning (ingestion) – epileptic or previous diagnosis of fitting; 12D01E, not breathing (after key questioning) – epileptic or previous diagnosis of fitting; 12D02E, fitting agonal/ineffective breathing – fitting history; 12D04E, fitting effective breathing (not-verified) – epileptic or previous diagnosis of fitting > 35.
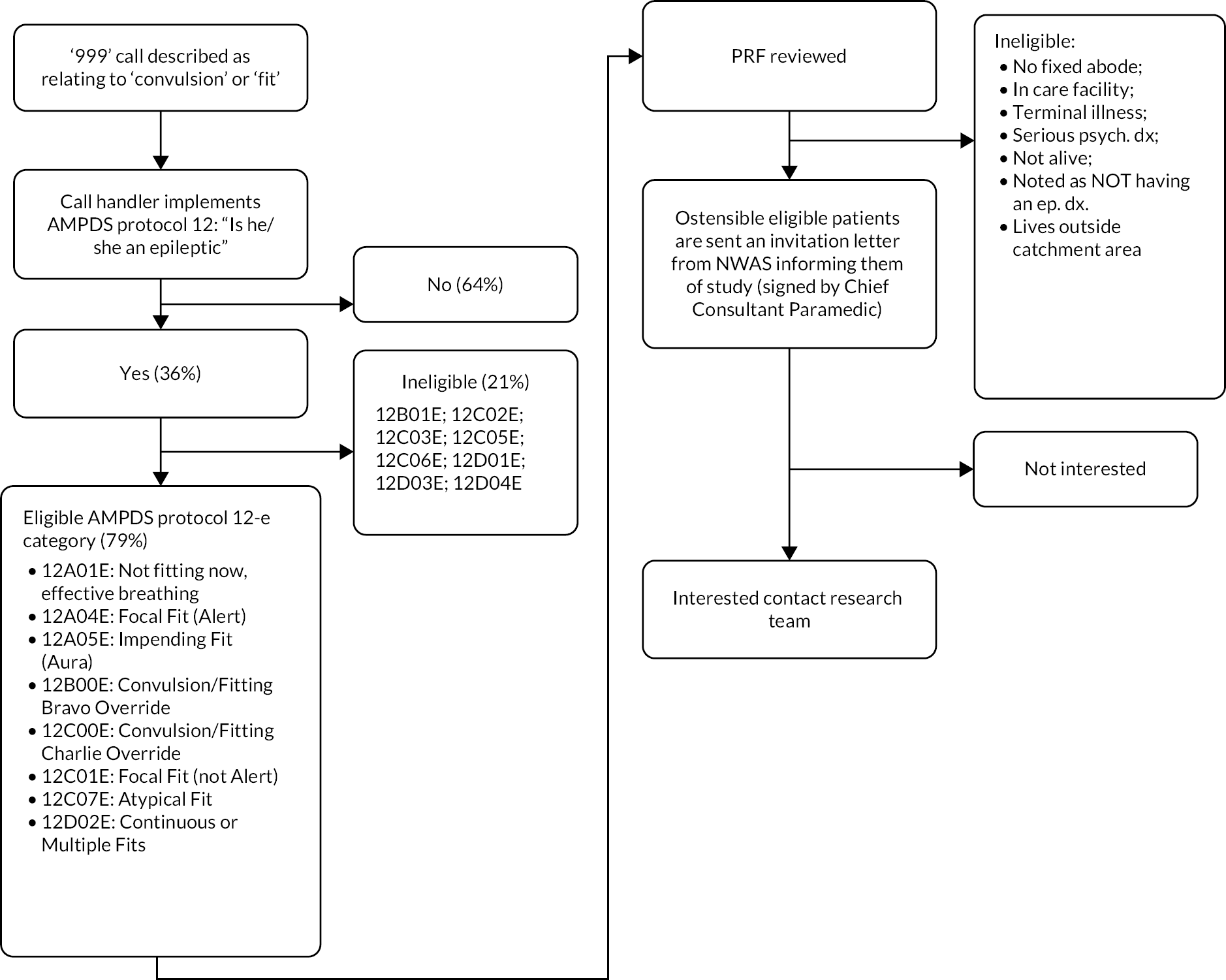
North West Ambulance Service NHS Trust first completed an electronic search of the emergency calls it had received in the prior 12 months to identify incidents coded under Advanced Medical Priority Dispatch System (AMPDS) Protocol 12 and assigned an ‘e’ suffix. Protocol 12 is used to record and manage calls which are described as relating to a convulsion. The ‘e’ suffix indicates the incident was related to a person who was reported by the caller to have epilepsy or a previous diagnosis of fitting. Further details on NWAS’ characteristics, the AMPDS and which of the Protocol 12 subcoded incidents were eligible are provided in Report Supplementary Material 5.
North West Ambulance Service NHS Trust restricted its search to mean they only identified persons with a Protocol 12 incident who were aged ≥ 18 years and living within ~30 miles of Liverpool city centre. The latter was necessary for two reasons. Firstly, to make the original plan of a researcher travelling to some participants practicable. Secondly, the Service Support Costs provided by the North-West Coast Comprehensive Research Network (NW CRN) to reimburse NWAS for the time spent identifying participants was only for persons resident within the footprint of the NW CRN. Report Supplementary Material 6 provides a map of the catchment area. Approximately 4.1M people reside within 30 miles of Liverpool city centre.
Based on prior health DCEs184 and work with the target population,22,46 we anticipated 30–60% of the PWE invited by NWAS might participate. We used the lower estimate for uptake of 30% and the target sample sizes for PWE who had (i.e. n = 174) and had not experienced conveyance to ED following ambulance attendance (i.e. n = 174) to determine how many individuals NWAS needed to identify and invite. Namely, n = 580 people who had not been conveyed to ED following attendance and n = 580 people who been conveyed to ED following attendance. As conveyance and non-conveyance to ED do not occur at the same rate, the time periods that NWAS would need to search within to identify sufficient persons from these two groups was permitted to differ.
Having completed the electronic search, two NWAS research paramedics (DW and KH, see Acknowledgements) then reviewed the ambulance report [called the Patient Report Form (PRF)] for each of the identified incidents by hand. This was to exclude persons ineligible. Those who remained had their status checked against the NHS ‘Spine’ service to further exclude any persons who had died and/or who had ‘opted out’ from contact for research.
People who continued to be eligible were posted an invitation pack by NWAS. This included a covering letter – signed by NWAS’ chief consultant paramedic – informing them about the study. A repeat invite was sent ~3 weeks later.
To identify SO participants, invited PWE were asked to identify a SO to take part with should they wish this to happen. They were asked to pass on recruitment documents to them contained within their invitation pack.
People with epilepsy and SOs interested in participating were asked to visit the survey page. A short, simple web address was provided. They could also contact the research team by phone, e-mail or by using a FREEPOST return slip included in their invitation pack. Those wanting to access the survey and take part were asked to provide – via the survey page – eConsent. 185
Each person completing the survey had the option of providing their personal details to the research team to receive a £20 shopping voucher.
Approval for this recruitment route was provided by the Health Research Authority and the National Research Ethics Service Committee, West Midlands, Solihull (19/WM/0012).
Route 2 – via public adverts
A range of participant advertisements were created for distribution via different platforms (see Report Supplementary Material 7). The specifics are as follows.
In October 2020, colour advertisements (17 cm × 3 columns wide) were placed in the print, and online versions of 15 of England’s largest regional newspapers operated by Reach PLC. The papers had a median circulation of 13,000 (IQR = 12,000–18,000). An advert appeared in at least one newspaper for each of England’s local government region, except for London (due to cost). In addition, major service user organisations affiliated in some way with epilepsy circulated the adverts within local meetings and via newsletters and on social media. Organisations included Epilepsy Action, Epilepsy Society, Brain and Spine Foundation, and the Stroke Association.
Persons interested in participating were directed via the adverts to a duplicate version of the survey page that had been created for those recruited via route 1. This permitted us to be able to differentiate how participants were recruited. Within electronic adverts, a hyperlink to the survey page was provided, while within paper versions of adverts, the link was a ‘tinyURL’.
To maximise recruitment, participants completing the survey had the option of providing their personal details so they could be entered into a prize draw to win one of four £50 shopping vouchers.
Ethical approval for this route was provided by the University of Liverpool’s Health and Life Sciences Research Ethics Committee (Ref: 7766).
Procedure
Administration
Participants completed the survey via the XM Qualtrics platform. The survey included both the DCE and a limited set of non-DCE questions.
For both recruitment routes, versions of the survey were created for people taking part as a person with epilepsy and for those participating as a SO. The main difference between the versions was the wording used for the questions and the inclusion in the SO version of some non-DCE questions about their own background.
The survey was designed to be completed within ~30 minutes. To minimise burden, participants were able to start, stop and then return to the survey. Having started the survey, they had up to 7 days to complete it before the submission was ‘locked’.
Technical telephone support was available to participants of both routes Monday to Friday, between 9 a.m. and 5 p.m.
Seizure scenarios discrete choice experiments were completed on
In Chapter 4, we presented the finalised design of the DCE survey. As described there, DCEs were created for three hypothetical seizure scenarios. Namely, a person with established epilepsy who has experienced a:
-
seizure at home that is in line with their usual presentation (‘Home typical seizure’)
-
seizure in public that is in line with their usual presentation (‘Public typical seizure’)
-
seizure that has self-terminated, but which is different in some way to the person’s ‘normal’ seizure/s (‘Atypical seizure’).
For each scenario, the participant was presented with a vignette describing the situation and asked to make 12 forced, pairwise choices. Each choice involved them identifying which of two CP options they would prefer. The two CP options were always unlabelled (i.e. option A and option B). The latter approach is common in health DCEs. It is considered most suitable when investigating trade-offs between attributes. 186 The finalised vignettes used for PWE and SOs are repeated in Table 8.
| Scenario | Participant type | |
|---|---|---|
| PWE | Significant others | |
| Public typical seizure | Story about a seizure in public Imagine you have an epileptic seizure in public. Its last no longer than usual, and you start to recover as usual. You do NOT experience an injury that requires urgent or emergency treatment. Somebody called an ambulance. The paramedic arrives and assesses you. During normal times (i.e. pre-COVID-19), which of the two care packages below would you prefer? |
Story about a seizure in public Imagine the person you know has an epileptic seizure in public. Its last no longer than usual, and they start to recover as usual. They do NOT experience an injury that requires urgent or emergency treatment. Somebody called an ambulance. The paramedic arrives and assesses them. During normal times (i.e. pre-COVID-19), which of the two care packages below would you prefer them to get? |
| Home typical seizure | Story about a seizure at home Imagine you have an epileptic seizure at home. Its last no longer than usual, and you start to recover as usual. You do NOT experience an injury that requires urgent or emergency treatment. Somebody called an ambulance. The paramedic arrives and assesses you. During normal times (i.e. pre-COVID-19), which of the two care packages below would you prefer? |
Story about a seizure at home Imagine the person you know has an epileptic seizure at home. Its last no longer than usual, and they start to recover as usual. They do NOT experience an injury that requires urgent or emergency treatment. Somebody called an ambulance. The paramedic arrives and assesses them. During normal times (i.e. pre-COVID-19), which of the two care packages below would you prefer them to get? |
| Atypical seizure | Story about a seizure different to usual Imagine you have an epileptic seizure (or seizures) that is different in some way to what you usually experience. For example, it might start differently, last longer, or be a different type. The seizure (or seizures) stops. You do NOT experience an injury that requires urgent or emergency treatment. Somebody called an ambulance. The paramedic arrives and assesses you. During normal times (i.e. pre-COVID-19), which of the two care packages below would you prefer? |
Story about a seizure different to usual Imagine the person you know has an epileptic seizure (or seizures) that is different in some way to what they usually experience. For example, it might start differently, last longer, or be a different type. The seizure (or seizures) stops. They do NOT experience an injury that requires urgent or emergency treatment. Somebody called an ambulance. The paramedic arrives and assesses them. During normal times (i.e. pre-COVID-19), which of the two care packages below would you prefer them to get? |
To minimise cognitive burden, each participant was asked to complete DCE questions for just two of the three seizure scenarios and thus make 24 forced, pairwise choices. The scenarios a participant was asked to complete DCEs on were randomly determined. The combinations they could be asked to complete DCEs on were:
-
‘Atypical seizure’ and ‘Public typical seizure’
-
‘Home typical seizure’ and ‘Atypical seizure’
-
‘Public typical seizure’ and ‘Home typical seizure’.
The ratio used for randomisation to the different combinations was 1 : 1 : 1.
To attenuate order effects, participants were further randomised so that half received the combination of scenarios in the order described above (‘standard presentation order’) and the other half received them the other way around (‘reverse presentation order’).
All randomisation processes were completed using Qualtrics’ inbuilt automated randomisation function. The randomisation process was independent for the two recruitment routes and separate for PWE and SOs.
Instructions and guidance participants received on how to complete discrete choice experiments
Participants were instructed how to complete the DCE with the support of an animated video. It can be viewed via the following link: www.youtube.com/watch?v=T3TU4tZ46Ik. The storyboard is in Appendix 5.
Before the DCE questions were presented, all participants were shown four epileptic seizure type descriptions developed by Chapman et al. 187 (see Appendix 6, questions 4–6). They were asked to select any they (or the PWE they knew) had ever experienced. If they selected more than one type, they were asked to select their ‘typical’ seizure type. Based on pilot testing, it was stated to participants that ‘By usual, we mean what some people call their “normal”, “run of the mill” type of seizure’.
Non-discrete choice experiment questions
Appendix 6 details all the questions asked and their order.
The non-DCE questions for PWE related to their demographics (age, sex, postcode); epilepsy profile (seizure frequency in prior 12 months, seizure types, years diagnosed, prescription of emergency rescue medication); comorbidities (intellectual impairment; non-epileptic attack disorder); knowledge of, and confidence in, seizure first aid; service use (including number of ED visits and number of ambulance attendances in prior 12 months); and experience (including perceived difficulties accessing specialist care).
They were also asked who was most likely to call for an ambulance when they had a seizure; how often they were with someone who could help when they had a seizure; whether they had any way of letting healthcare professionals know what care they required in an emergency situation (e.g. via an ‘emergency care plan’); the extent of their willingness to ‘wait’ to see different healthcare providers; and their familiarity with the hypothetical seizure scenarios.
Finally, at the end of the survey, participants were asked about their experience of COVID-19 and whether they believed the pandemic and its implications had changed their willingness to access different types of NHS service.
Significant others were asked the same set of questions as PWE, but the wording was changed where necessary so that they were answering about the person with epilepsy that they knew.
Analysis
Data quality checks and curation
A member of the research team (PD) screened out any persons submitting a survey response that included any answer/s indicating they were ineligible (e.g. < 18 years old, did not live in England, insufficient contact with the ambulance service). Persons who did not submit sufficient DCE responses (defined as completion of at least one choice task from one of the DCEs) were also excluded.
For each participant, an area-based measure of social deprivation was calculated to indicate the relative social deprivation of the area in which they lived. It was calculated by using the postcode the person reported via the survey and linking this with the Index of Multiple Deprivation (IMD) 2019 score188 for their lower super output area (LSOA). Each person was classified according to the deprivation quintile they lived in (1 being the most deprived). For participants for whom an IMD was missing (because they did not supply a sufficiently complete or valid postcode), multiple imputation was performed as per Goodman and Gatward’s approach. 189
Describing sample
Reasons for exclusion, the extent of missing data and the outcomes of randomisation were calculated. These will be reported in Chapter 6, as will the characteristics of the samples recruited by the different recruitment routes and as a whole.
As data were provided by participants from two separate recruitment routes, a decision was needed about what data management approach would provide data from people most representative of the target population. Therefore, the characteristics of the participants recruited from the different routes needed to be compared to the parent population. High-quality data on the characteristics of the target population (i.e. segment 3 of Figure 1) are not available. What is available is data from the latest round of the NASH-344 on the characteristics of persons with established epilepsy prescribed antiseizure medication who are seen at ED for a seizure (i.e. segment iv of Figure 1). We compared the samples from the two different routes, and when combined, to the NASH-3 data. As will be seen when the results are presented in Chapter 6, it was judged appropriate to merge the data from the two recruitment routes to maximise representativeness.
Preference data
Experimental design
The six attributes identified in the formative work, with associated levels, resulted in 288 possible CP configurations. Twenty-four of these were paired into 12 questions, in which respondents had to choose between two possible CPs, using an efficient design generated by Ngene experimental design software (Ngene 1.2.1, Choice Metrics) using the D-error measure for an efficient design for the MNL model. This reduced the number of pairwise choices required for robust estimation while incorporating conditions on location and time, that emerged during the formative work. The Ngene syntax used is in Report Supplementary Material 8.
To ensure the CPs used in the design were plausible ‘Location of care’ and ‘Time’ were specified as individual attributes (V1.3 in Table 5), with conditional levels, rather than being combined as previously decided (V1.2 in Table 5). All three DCEs (‘Atypical seizure’, ‘Home typical seizure’ and ‘Public typical’) used the same design (12 pairwise choices that a participant would be asked to make) to describe CP options in the given seizure scenario. Figure 6 provides an example of what one of the pair-wise choice questions in the DCE looked like.
FIGURE 6.
Example of a pairwise choice question used within the DCE survey (for a participant who had epilepsy themselves). Notes: The DCE for a seizure scenario contained 12 such choice questions. For these, the attributes in the shaded left-hand column stayed constant, but the levels (i.e. the descriptions for option A and option B) varied.

Base-case analysis
The DCE data for each of the different seizure scenarios and for PWE and SOs were analysed separately. Responses to each of the DCEs were analysed in STATA, V13 (StataCorp LP, College Station, TX) using a random-effects logit model. It allowed for multiple observations (12 binary choices) from the same respondent. 190 The regression model estimated preference weights for each attribute that indicate the importance of the attributes and the direction of effect.
The following model was used to analyse the responses:
Ui = utility derived by individual
β0 = constant term
βi = estimated coefficient for each attribute (variable)
ε = error term (assumed to vary by seizure scenario)
The reference level of effects coded attributes (e.g. what happens next: stay at home) were calculated as: as −1* (sum β of other levels). Confidence intervals (95%) were determined by 1000 bootstrap replications.
Marginal rates of substitution – the rate at which respondents are willing to give up a unit change in one attribute in exchange for a unit change in another while maintaining the same level of utility – were planned for the one continuous attribute in the DCE (e.g. ‘Time’), subject to a test for linearity. We did not plan MRS on categorical attributes as the output would be arbitrary in the absence of a standardised interval scale that could be easily interpreted by stakeholders attending the KE event. The model assumed ‘Time’ was linear and continuous. This was tested by specifying a random-effects logit model with the ‘Time’ attribute included using effects coding (see Report Supplementary Material 9) and visual inspection of the output. Total utility for alterative CPs was estimated as the sum of the β coefficients for each attribute level. Care pathways were then ranked by total utility within each model.
Subgroup analysis
Preference heterogeneity was assessed using log-likelihood ratio tests of the restricted model (base case) versus unrestricted models (defined by subgroups).
A priori self-reported characteristics of interest were (1) whether the PWE had made any visits to the ED in the prior 12 months; (2) social deprivation (with participants grouped according to how socially deprived the area is within which they live); (3) contact with an epilepsy specialist within the prior 12 months; and (4) whether they (or the person they know in the case of carers) self-reported an intellectual disability. During the formative work and DCE design, we identified three further subgroups that may influence preferences: (5) problems accessing specialist services, (6) having a care plan and (7) experience of the hypothetical scenario.
Modifications to the study protocol and that participants completed the DCE in the context of a pandemic meant it also became desirable to explore the potential impact of (8) the route by which the participant was recruited and (9) participants’ views and experiences of COVID-19.
Subgroup analyses were conducted only when each group within the specified analysis had ≥ 30 participants within it. Statistical significance for the post hoc analyses was adjusted using Bonferroni correction for multiple comparisons within each seizure scenarios, with alpha set at 0.01.
Ranking of care package configurations according to preference
Using the coefficients (β) from the respective regression models, the expected utility for each of the 288 configurations was calculated for each of the three different seizure scenarios by sample (PWE or SO), as described above.
Utility can be understood as the total value a CP configuration offers a person, estimated by summing the gains or losses associated with the attribute levels the configuration has. The expected utility model was parameterised using the preference weights elicited in the DCE and attribute level selection to represent all 288 possible configurations. The β coefficients for each attribute level (derived from the DCE regression analysis) were summed to estimate the total utility for each configuration:
where β = value of the attribute coefficients represented in the individual CP.
We also investigated the contribution of individual attribute levels, by measuring the change in total utility observed by a change in a single level, while all other attributes remained equal. This is expressed as a percentage.
The 288 configurations were ranked according to expected utility. A rank of 1 indicates the configuration most favoured for that scenario, while a rank of 288 indicates the least favoured. Ranks were constructed separately for each seizure scenario and by both PWE and SOs. Thus, six different sets of ranks were generated. The rank of each CP configuration across all six models was compared visually, using a heatmap generated in Microsoft Excel.
To determine how current ambulance care was meeting participants preferences, we selected from the 288 CP configurations the one deemed to best approximate current care and its ranking for the different seizure scenarios is reported. Based on evidence presented in the earlier chapters, the configuration chosen to represent current care was, according to the six attributes and levels, comprised: (1) ‘The paramedic has access to medical records or a care plan’: no, (2) ‘What happens next’: A&E, (3) ‘Time’: 3 hours, (4) ‘Epilepsy specialists today’: no, (5) ‘GP told’: yes and (6) ‘Additional contact with an epilepsy specialist’: no. It is represented in Report Supplementary Material 10.
We anticipated service providers would be keen to understand the possibility of implementing a single CP configuration for seizures when non-conveyance was deemed clinically safe (rather than needing to offer slightly different care package configurations depending on the specifics of the seizure scenario and the person the crew was primarily liaising with ‘on scene’). To support such discussions, we determined the top-ranked care package configuration for the different seizure contexts and estimated its uptake within the other seizure contexts, by estimating: P=exp(utility CPi)/Σexp(CPj).
Discussion
In this chapter, we reported the finalised design of the DCEs and the recruitment methods. This includes the rapid revisions made to recruitment that were required when COVID-19 pandemic began impacting the UK. In providing this set of information, we conform to reporting guidelines. 191 In the next chapter, we describe the sample of participants ultimately recruited.
Chapter 6 Discrete choice experiment survey results: participants
Introduction
This chapter describes who responded to the DCE survey, from which route they were recruited, and the quality of data received.
Results
Identification and invitation
Route 1 – via North West Ambulance Service
Prior to this route being paused by the NWAS due to COVID-19, NWAS had screened n = 2634 incidents and identified n = 981 individuals for invite. Of these, n = 456 (46.5%) people were identified because of an incident that resulted in conveyance to an ED, and n = 525 (53.5%) individuals were identified due to an incident that ended with non-conveyance.
The leading reason for an incident not resulting in a person being identified for invite was that the individual had already been identified based on an earlier incident (25.7%) (Figure 7). Other key reasons included that the person resided within a care facility (19.8%); and that the person was not noted on the PRF completed by the ambulance crew at the time as having diagnosed epilepsy (18.4%). In 14.7% of cases the PRF for the incident could not be retrieved or the writing was illegible.
FIGURE 7.
Flow chart of the screening process and identification of individuals for invitation via ambulance service. n, number; NFA, no fixed abode.
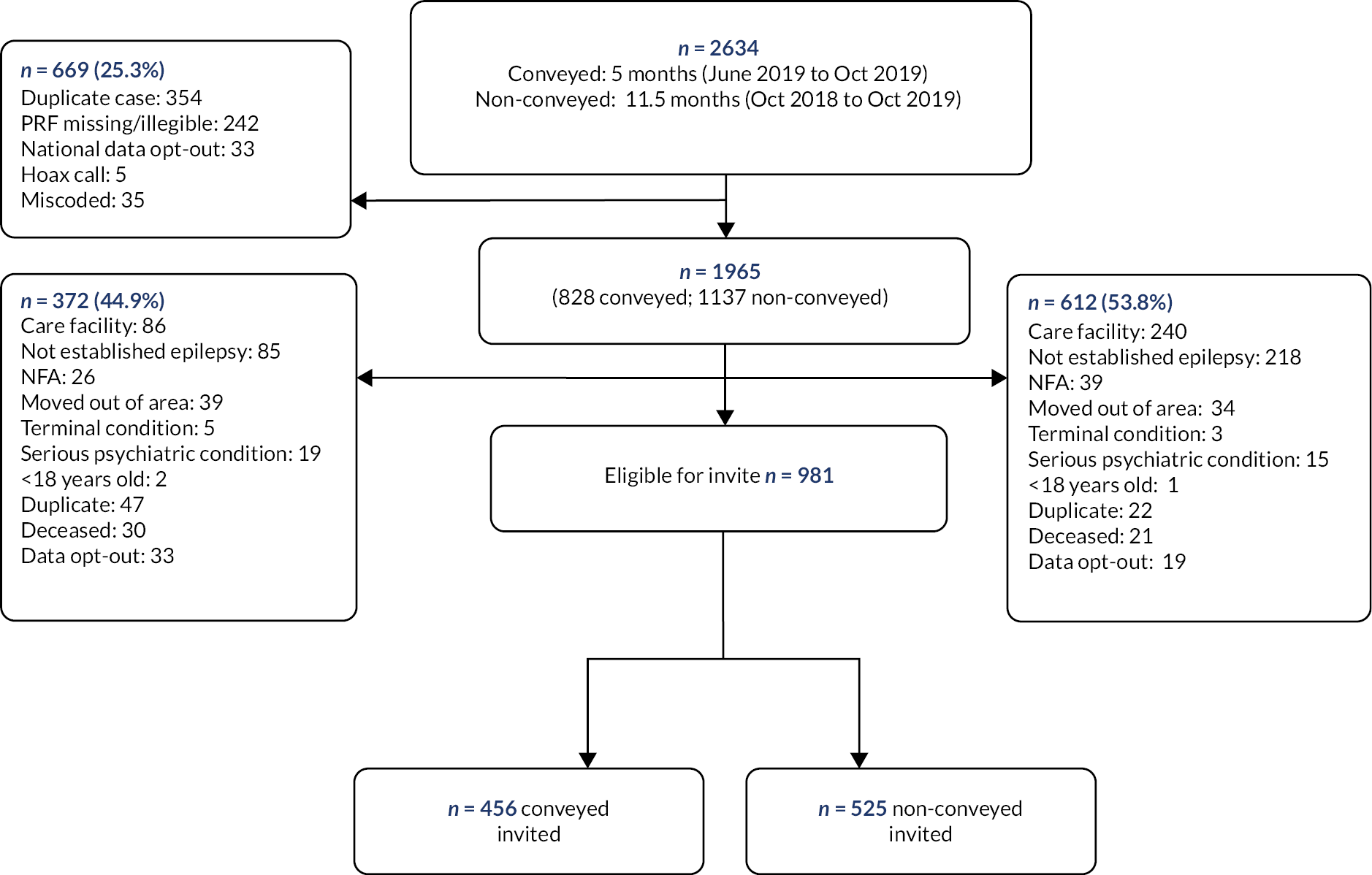
Following the NIHR’s project ‘Restart’,192 the ambulance recruitment route was reactivated and (after a further ‘status’ check) invitation packs were dispatched on 31 July 2020. A repeat was sent approximately 3 weeks later.
The time between the incidents that had led these persons to contact NWAS and them being sent an invitation ranged from 10 to 21 months. The wide range reflects the different periods of time needed to identify enough persons for invite. To identify sufficient people following a conveyed incident for invite, NWAS needed to screen 5 months of incidents (i.e. June 2019 to October 2019). In contrast, to identify a sufficient number of non-conveyed individuals, NWAS needed to screen 11.5 months of incidents (i.e. October 2018 to October 2019).
Having been sent an invitation pack, n = 18 persons informed the research team they were unable to complete the survey online. A further n = 4 persons informed the team they were ineligible.
Route 2 – via public adverts
Recruitment via public advertisement began on 13 July 2020. The major user organisations circulated adverts via their newsletters and social media between 20 July 2020 and 16 November 2020. This included utilising Facebook’s paid advertisement feature to increase the visibility of the advert. The newspaper adverts appeared between 9 and 16 October 2020. The median page number the adverts appeared on was 9 (IQR = 5–19). Alongside the print adverts, the newspapers ran electronic versions on their digital platforms. These resulted in a total of 585 ‘clicks’ through to the survey landing page.
Further details as to when and where adverts appeared in different newspapers are provided in Report Supplementary Material 11.
Participants
Recruitment
Submissions to survey
Recruitment via the ambulance service route ran for 5 months and via the public advertisement route for 5.5 months. Both closed to new recruits on 25 November 2020. During these time periods, there were a total of n = 1687 submissions via the two recruitment routes (n = 156, 9.2%, via the ambulance service route; n = 1532, 90.8%, via public advertisements). Report Supplementary Material 12 shows recruitment by time.
Usable submissions to survey
Figure 8 provides a participant flow chart. It shows that of the submissions received, n = 772 (45.7%) did not involve the person answering a single question after having consented to participate. Hence, there were n = 916 (54.3%) submissions that could be considered for analysis (n = 662 PWE; n = 254 SOs).
FIGURE 8.
Responses to survey by participant type, recruitment route and extent of completeness of response to DCE. a, NB some respondents fulfil more than one exclusion criteria.
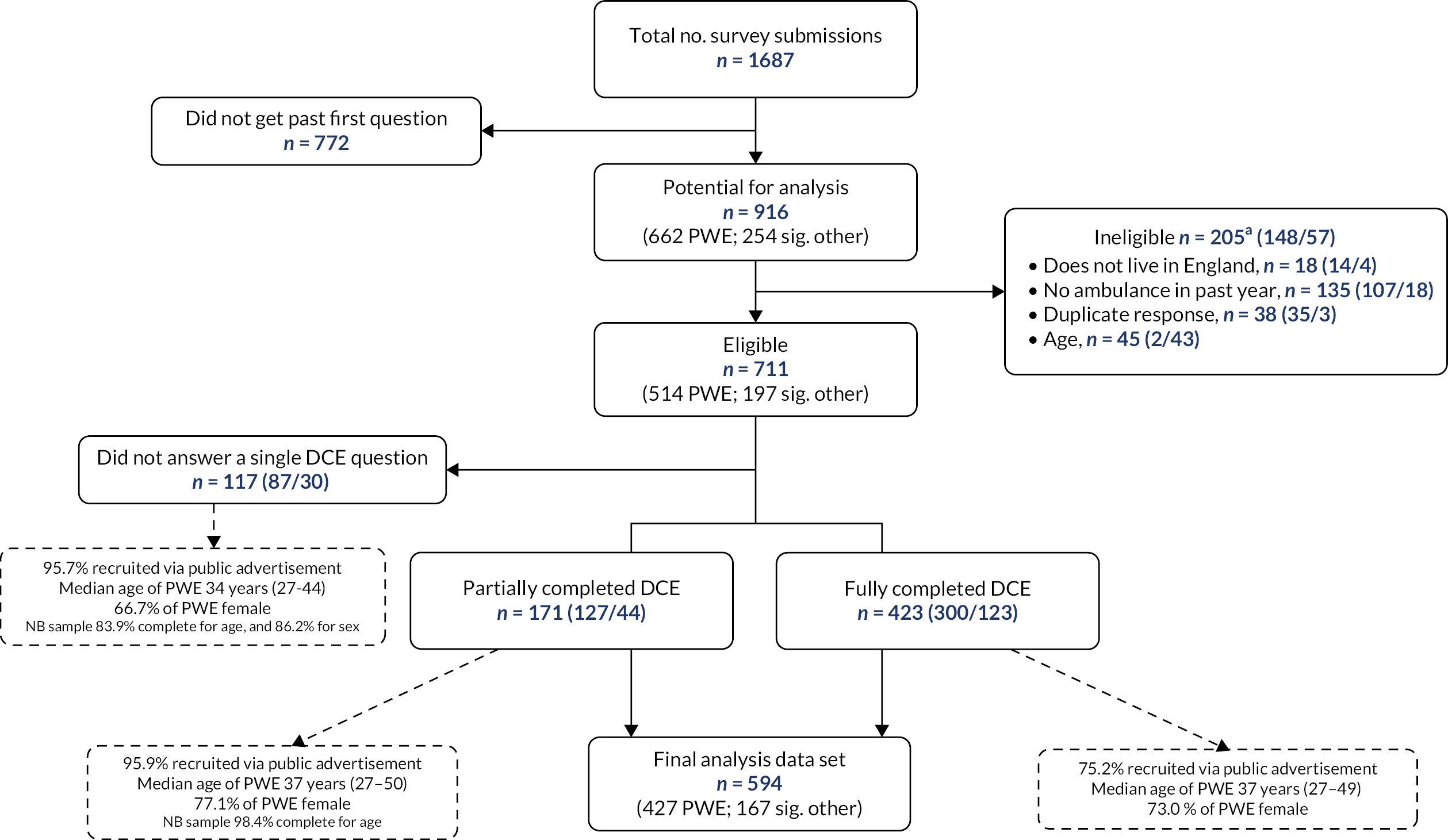
Of the n = 916 submissions, n = 205 (22.4%) (n = 148 by PWE; n = 57 by SOs) needed to be excluded as they were submitted by persons whose answers indicated they were ineligible. A further n = 117 (12.8%) submissions (n = 87 by PWE; n = 30 by SOs) were excluded as they did not involve the person answering a single DCE question.
From the two-recruitment routes, there were thus useable submissions to the DCE survey from n = 594 participants (n = 427 PWE; n = 167 SOs). Of these, most (81.1%; n = 358 PWE, n = 124 SOs) were recruited via the public advertisement route and 18.9% (n = 69 PWE, n = 43 SOs) via the ambulance service route.
Response rate
The estimated response rate for recruitment via the ambulance service route was 11.7% (112/954). The denominator here is the number of invites dispatched by the ambulance service (n = 981) minus the noted n = 4 invites sent to persons who said they were ineligible and the n = 23 submissions from persons who were ineligible. The calculation assumes the remaining invites were received by persons who were eligible, that they were sent to the correct address and treats responses by PWE and SOs as independent.
It was not possible to calculate a response rate for the public advertisement route since the denominator is unknown.
Characteristics of participants by recruitment route, sample representativeness and justification for merging
The headline characteristics of the samples recruited by the two different routes and their representativeness relative to the target population (as indicated by NASH-3) are shown in Table 9. The full characteristics of the samples are shown in Appendix 7.
| Analysis data set | Route 1, via ambulance service | Route 2, via public adverts | Combined | NASH-3 |
|---|---|---|---|---|
| N = 112 | N = 482 | N = 594 | N = 1676 | |
| Participant type, n (%) | ||||
| PWE | 69 (61.6) | 358 (74.3) | 427 (71.9) | 1676 (100) |
| SO | 43 (38.4) | 124 (25.7) | 167 (28.1) | |
| Age of PWE, median (range) | ||||
| Reported by PWE | 36 (26–51) | 37 (27–49) | 37 (27–49) | |
| Reported by SO participants | 32.5 (26–46) | 28 (23–39) | 29 (24–41) | |
| Combined | 34 (26–49) | 35 (26–48) | 35 (26–48) | 43 (29–58) |
| Missing | 1 | 45 | 46 | |
| Sex of PWE, female, n (%) | ||||
| Reported by PWE | 37 (53.6) | 280 (78.2) | 317 (74.2) | |
| Reported by SO participants | 20 (47.6) | 30 (37.0) | 50 (40.7) | |
| Combined | 57 (51.4) | 310 (70.6) | 367 (66.7) | 783 (46.8) |
| Missing | 1 | 43 | 44 | |
| Intellectual disability in PWE, yes, n (%) | ||||
| Reported by PWE | 7 (11.1) | 27 (11.4) | 34 (11.4) | |
| Reported by SO participants | 18 (42.9) | 19 (23.5) | 37 (30.1) | |
| Combined | 25 (23.8) | 46 (14.5) | 71 (16.8) | 297 (17.8) |
| Missing | 7 | 165 | 172 | |
| PWE Index of Multiple Deprivation, n (%) | ||||
| Reported by PWE | ||||
| Quintile 1 | 24 (38.1) | 60 (25.5) | 84 (28.2) | 517 (30.9) |
| Quintile 2 | 12 (19.1) | 56 (23.8) | 68 (22.8) | 395 (23.6) |
| Quintile 3 | 11 (17.5) | 40 (17.0) | 51 (17.1) | 304 (18.1) |
| Quintile 4 | 13 (20.6) | 44 (18.7) | 57 (19.1) | 292 (17.4) |
| Quintile 5 | 3 (4.8) | 35 (14.9) | 38 (12.8) | 168 (10.0) |
| Missing | 6 | 124 | 129 | |
| PWE seen epilepsy specialist in prior 12 months, yes, n (%) | ||||
| Reported by PWE | 48 (76.2) | 205 (87.2) | 253 (84.9) | |
| Reported by SO participants | 36 (85.7) | 76 (93.8) | 112 (91.1) | |
| Combined | 84 (80.0) | 281 (88.9) | 365 (86.7) | 815 (48.6) |
| Missing | 7 | 166 | 173 | |
The age of the PWE taking part in the survey, or being reported on by significant others, was similar across the two recruitment routes. Via ambulance the service, the median was 34 years (IQR = 26–49). Via the public advertisement route, it was 35 years (IQR = 26–49). However, the sex of PWE taking part in the survey, or being reported on, did differ by recruitment route.
Specifically, persons taking part via the ambulance service route were more likely to be male (48.6% of participants) than those participating via the public advertisement route (29.4% of participants). Significant other participants were also more likely to take part by the ambulance service route than by the public advertisement route. Of the participants who took part via the ambulance route, 38.4% were SOs, compared to 25.7% of the participants taking part via the public advertisement route.
Table 9 shows that combining the n = 594 participants from the two recruitment routes created a sample which was more like the target population. It had a more similar proportion of PWE in it (or that were being represented) that had an intellectual impairment (16.8%). It also had broadly the same amount of people in the different quintiles of deprivation represented within in, including from the most deprived one (28.2%). Merging the samples also meant the proportion of male PWE taking part or being represented (33.3%) better aligned with the target population data.
Figure 9 shows the geographical distribution of the participants in the merged sample. It shows a spread of participants from across England’s regions, with persons from the North West being overrepresented due to the two recruitment routes both having operated there.
FIGURE 9.
Distribution of participants in the final analysis data set by English region that they reside in. Notes: Map separates England into local government region. The figures in red relate to individuals recruited via the ambulance service route (n = 112), whereas figures in black indicate individuals recruited via the public advert route (n = 482). Postcodes for 173 individuals (n = 166 from public advert route; n = 7 from the ambulance route) were partial and did not permit confidence in determining local government region.

Even after merging the samples, the median age of the participants (35 years, IQR = 26–48) remained 8 years younger than the average for the target population. Another important difference was the much higher proportion of participants in the survey samples that had purportedly seen a health professional specialising in epilepsy in the prior 12 months. Potential reasons for this difference are proposed later in the chapter.
Further characteristics of the merged sample
The full characteristics of the n = 594 participants are shown in Appendix 7.
The median years that PWE taking part (or being represented by a SO) had been diagnosed with epilepsy was 12 (IQR = 4–26) and most (51.5%) reported having experienced 10 or more seizures (of any type) in the prior 12 months.
Most (64.8%) experienced multiple seizure types, with 79.6% selecting the tonic–clonic seizure description as best representing the type that typically led them or the person they knew to have contact with the ambulance service. A significant minority (16.8%) of PWE were noted as having an intellectual impairment.
Most (74.4%) were found to have had one to three contacts with the ambulance service in the prior 12 months for epilepsy. There was evidence of non-conveyance amongst the sample, with 36.8% of participants reporting fewer ED visits than ambulance contacts.
The main ways the SO participants knew someone with epilepsy was that they were their parent (59.4%), followed by being their spouse/partner (24.4%). The demographics, epilepsy profile and service use reported by PWE who took part in the survey and that reported by SOs on behalf of a PWE differed in some respects.
Specifically, SO participants tended to be representing PWE who were younger, more likely to be male, more likely to have an intellectual disability and more likely to be prescribed a rescue medication. The people being represented were also more likely to be said to be in the company of someone who they knew when ambulance contact occurred, tended to have had more contact with the ambulance service and when this occurred, for this to result in conveyance to ED (Table 10).
| Reported by PWE themselves (n = 427) | Reported by significant others (n = 167) | |
|---|---|---|
| Age of PWE, median (range) | 37 (27–49) | 29 (24–41) |
| Missing | 2 | 44 |
| Sex of PWE, female (%) | 74.2 | 40.7 |
| Missing | 0 | 44 |
| PWE has an intellectual disability, yes (%) | 11.4 | 30.1 |
| Missing | 128 | 44 |
| Rescue medication prescribed to PWE, yes (%) | 26.5 | 39.8 |
| Missing | 129 | 44 |
| Ambulance contacts in p/12 months, % | ||
| 1–3 | 77.2 | 67.5 |
| 4–6 | 13.8 | 17.1 |
| 7–9 | 4.4 | 6.5 |
| 10 or more | 4.7 | 8.9 |
| Missing | 129 | 44 |
| ED contacts in p/12 months, % | ||
| 0 | 15.3 | 8.9 |
| 1–3 | 64.5 | 66.7 |
| 4–6 | 13.6 | 12.2 |
| 7–9 | 3.7 | 4.1 |
| 10 or more | 3.0 | 8.1 |
| Missing | 129 | 44 |
| When ambulance comes, how often is PWE with someone who could help, % | ||
| Never | 7.4 | 1.7 |
| Rarely | 16.8 | 9.9 |
| About half the time | 20.5 | 14.9 |
| Most of the time | 35.4 | 32.2 |
| Always | 19.9 | 41.3 |
| Missing | 130 | 46 |
Randomisation and completion of allocated discrete choice experiments
Scrutiny of the randomisation outcome data showed that the randomisation function worked well. Each combination of seizure scenarios and presentation order was equally represented in the data set with useable data (see Report Supplementary Material 13).
Three hundred of the PWE (70.3%) and 123 of the SOs (73.7%) answered all of their 24 DCE questions (12 × two seizure scenarios). The remainder of the participants answered between 1 and 23 of the 24 that they were asked to do.
Of a potential 1188 DCEs (i.e. 594 participants allocated 2 each), 88% were completed. DCE completion rate ranged from 85% for the ‘Home typical seizure’ scenario when completed by PWE, to 91% for the DCE with the ‘Atypical seizure scenario’ when completed by SOs. Seventy-six per cent of participants started their second DCE. Participants were most likely to continue to a second DCE if they completed the ‘Home typical seizure’ scenario first. They were least likely to continue if the ‘Home typical seizure’ scenario came second (see Report Supplementary Material 13).
Familiarity with seizure scenarios
The majority of participants reported that they (or the person that they knew in the case of SOs) had ‘often’ or ‘sometimes’ been in each of the DCE seizure scenarios (see Appendix 8).
The extent of familiarity with the individual scenarios was similar for PWE; 69–73% said they had been in each of them. In contrast, SO participants reported more familiarity with the ‘Atypical seizure’ scenario (82%) than the ‘Public typical seizure’ (66%) or ‘Home typical seizure’ (67%) scenarios.
Experience of and feelings towards COVID-19
During the 5.5-month period of recruitment, the median daily COVID-19 infection rate was 3497 (IQR = 343–33,470) (see Report Supplementary Material 14). 193
Less than 7% of the participants believed they themselves had at some point contacted COVID-19 (see Report Supplementary Material 15). Both PWE and SOs did, however, ‘agree’ that COVID-19 had reduced their willingness to use ED after a seizure or for the person they knew to do so. For SOs, COVID-19 also meant they were less willing for the PWE that they knew to use UTCs or to attend a hospital outpatient appointment after a seizure. COVID-19 did not appear to impact on the preferences of either PWE or SOs for seeing a GP.
Discussion
The DCE survey secured usable stated preference data from approximately 600 PWE who had recent contact with the ambulance service and their SOs.
Participants were recruited from all regions of England, and the sample appeared broadly representative of the target population in most respects, except for age and extent of recent access to specialist services. It included both participants who had experience of conveyance and non-conveyance in the prior 12 months. Most participants reported they were completing DCEs on seizure scenarios that they could relate to.
As expected, SO participants were often representing a part of the target population with a different epilepsy profile than that reported by PWE taking part themselves.
The high rate of contact with an epilepsy specialist in the prior 12 months in the recruited sample requires comment; 86% reported having contact. The NASH-3 initiative reported 52% of people with established epilepsy attending ED have not had such contact. 44 The difference between our sample and NASH-3 may indicate those who taking part in the DCE represent those who are more supported from the target population. It might though more likely reflect a difference in the methods used by us and NASH in obtaining this information. This is discussed further in Chapter 9.
Finally, it was apparent that while suspected COVID-19 infection rates were low within the sample, the pandemic had changed participants willingness to use certain services. In the next chapter, we report on the stated preference data, including efforts to explore what potential impact the noted changed willingness might have had for stated postseizure care preferences.
Chapter 7 Discrete choice experiment survey results: preference data
Introduction
This chapter reports on preference data elicited by the DCEs. The aim of the DCE study was to determine patient and carer preferences for postseizure emergency care, estimate uptake of different care pathway (CP) configurations and explore potential subgroup differences.
Results
Discrete choice experiment responses
As described in Chapter 6, the survey responses from 594 participants were eligible for analysis; 72% of which were from PWE.
Each participant was asked to complete DCEs on two different seizure scenarios. The participants were therefore altogether asked to complete a total of 1188 DCEs. Of these, 1047 (88%) were completed.
Model specification: testing for non-linear effects
Table 11 shows the results of testing the linearity of the attribute ‘Time’. Model A uses a continuous specification for time, in which the results would be interpreted as linear. However, Model B suggests that when time is categorised (using effects coding to allow for estimation of all four levels), the size/direction of the coefficients moving between levels is not as expected (not linear). The most pronounced example is for SOs responding to the ‘Home typical seizure’ scenario; this indicates strongest preferences of 2 hours, rather than 1 hour as would be anticipated.
| Model statistic | PWE | Significant others | ||||
|---|---|---|---|---|---|---|
| Atypical seizure | Home typical seizure | Public typical seizure | Atypical seizure | Home typical seizure | Public typical seizure | |
| Number of observations | 2817 | 2692 | 2733 | 1139 | 1108 | 1044 |
| Number of respondents | 258 | 239 | 252 | 105 | 97 | 96 |
| Model A (time continuous) | β-coefficient | β-coefficient | β-coefficient | β-coefficient | β-coefficient | β-coefficient |
| β-coefficient of time (continuous) | −0.172a | −0.237a | −0.214a | −0.217a | −0.279a | −0.263a |
| Model B (time categorical, effects coded input) | β-coefficient | β-coefficient | β-coefficient | β-coefficient | β-coefficient | β-coefficient |
| β-coefficient of time_one (1 hourb) | 0.164 | 0.295 | 0.080 | 0.844 | −0.174 | 0.060 |
| β-coefficient of time_two (2 hours) | 0.284 | 0.192 | 0.135 | 0.295 | 0.833a | 0.509 |
| β-coefficient of time_three (3 hours) | 0.079 | 0.175 | 0.331 | −0.370 | 0.265 | 0.228 |
| β-coefficient of time_six (6 hours) | −0.526a | −0.662a | −0.545a | −0.770a | −0.924a | −0.797a |
Visual inspection of plots of the effects coded coefficients illustrates this deviation from the linear assumption by seizure contexts (see Appendix 9). The base-case model was therefore respecified as
Ui = utility derived by an individual
β0 = constant term
βi = estimated coefficient for each attribute (variable)
ε = error term (assumed to vary by seizure scenario)
While it was no longer appropriate to calculate willingness to wait (marginal rate of substitution of time), the impact on total utility of each level change was calculated as the percentage change in utility score for a categorical level change, all other attributes remaining equal, within each model.
Statistical significance of attributes and direction of their influence on preference
The results of the regression models for the preferences of PWE and SOs in the different seizure scenarios are presented in Tables 12 and 13, respectively. The β-coefficient illustrates the magnitude of preference of the attribute level. Where an attribute level does not reach statistical significance, we cannot state with certainty that that characteristic would influence a person’s preference for a CP.
| Attribute (level) | Seizure scenario | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Atypical seizure | Home typical seizure | Public typical seizure | |||||||
| β-coefficient | 95% CIa | β-coefficient | 95% CIa | β-coefficient | 95% CIa | ||||
| Access to medical records/care plan (0 = no; 1 = yes) | 0.460b | 0.346 | 0.653 | 0.539b | 0.410 | 0.783 | 0.565b | 0.435 | 0.435 |
| Convey (no – stay where you are)c | 0.067 | −0.290 | 0.400 | 0.543b | 0.230 | 0.984 | 0.407b | 0.134 | 0.748 |
| Convey (UTC) | 0.044 | −0.148 | 0.257 | −0.259b | −0.497 | −0.064 | −0.097 | −0.291 | 0.078 |
| Convey (ED) | −0.111 | −0.293 | 0.062 | −0.284b | −0.516 | −0.109 | −0.310b | −0.518 | −0.147 |
| Time (1 hourc) | 0.164 | −0.610 | 0.970 | 0.295 | −0.572 | 1.179 | 0.080 | −0.649 | 0.791 |
| Time (2 hours) | 0.284 | −0.088 | 0.716 | 0.192 | −0.240 | 0.665 | 0.135 | −0.249 | 0.559 |
| Time (3 hours) | 0.079 | −0.425 | 0.549 | 0.175 | −0.348 | 0.743 | 0.331 | −0.090 | 0.806 |
| Time (6 hours) | −0.526b | −0.738 | −0.416 | −0.662b | −0.921 | −0.558 | −0.545b | −0.754 | −0.449 |
| Epilepsy specialist advises today (0 = no; 1 = yes) | 0.591b | 0.536 | 0.751 | 0.372b | 0.298 | 0.529 | 0.353b | 0.283 | 0.487 |
| GP told (0 = no; 1 = yes) | 0.426b | 0.367 | 0.557 | 0.261b | 0.189 | 0.397 | 0.268b | 0.199 | 0.390 |
| Epilepsy specialist in future (no)c | −0.277b | −0.401 | −0.208 | −0.290b | −0.427 | −0.213 | −0.187b | −0.305 | −0.114 |
| Epilepsy specialist in future (2–3 weeks) | 0.163 | −0.126 | 0.470 | 0.153 | −0.136 | 0.499 | 0.127 | −0.121 | 0.393 |
| Epilepsy specialist in future (within 1 week) | 0.114 | −0.116 | 0.371 | 0.137 | −0.127 | 0.398 | 0.060 | −0.149 | 0.277 |
| Constant | −0.021 | −0.099b | −0.042 | ||||||
| Number of observations | 2817 | 2692 | 2733 | ||||||
| Number of respondents | 258 | 239 | 252 | ||||||
| Observations per group – minimum | 1 | 1 | 1 | ||||||
| Observations per group – average | 10.9 | 11.3 | 10.8 | ||||||
| Observations per group – maximum | 12 | 12 | 12 | ||||||
| Wald chi2(10) | 374.67 | 582.64 | 435.33 | ||||||
| Log-likelihood | −1687.92 | −1443.0 | −1604.31 | ||||||
| Attribute (level) | Seizure scenario | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Atypical seizure | Home typical seizure | Public typical seizure | |||||||
| β-coefficient | 95% CIa | β-coefficient | 95% CIa | β-coefficient | 95% CIa | ||||
| Access to medical records/care plan (0 = no; 1 = yes) | 0.456b | 0.261 | 0.779 | 0.360b | 0.035 | 0.710 | 0.584b | 0.344 | 0.937 |
| Convey (no – stay where you are)c | −0.376 | −0.977 | 0.125 | 0.729b | 0.039 | 1.684 | 0.311 | −0.323 | 1.037 |
| Convey (UTC) | 0.275 | −0.041 | 0.644 | −0.194 | −0.760 | 0.258 | −0.023 | −0.448 | 0.385 |
| Convey (ED) | 0.101 | −0.177 | 0.391 | −0.535b | −0.993 | −0.223 | −0.288 | −0.667 | 0.017 |
| Time (1 hour)c | 0.844 | −0.307 | 2.149 | −0.174 | −2.490 | 1.564 | 0.060 | −1.790 | 1.454 |
| Time (2 hours) | 0.295 | −0.305 | 0.928 | 0.833b | 0.152 | 2.183 | 0.509 | −0.178 | 1.395 |
| Time (3 hours) | −0.370 | −1.168 | 0.309 | 0.265 | −0.842 | 1.514 | 0.228 | −0.648 | 1.270 |
| Time (6 hours) | −0.770b | −1.172 | −0.575 | −0.924b | −1.380 | −0.736 | −0.797b | −1.210 | −0.573 |
| Epilepsy specialist advises today (0 = no; 1 = yes) | 0.826b | 0.727 | 1.104 | 0.356b | 0.200 | 0.606 | 0.551b | 0.408 | 0.822 |
| GP told (0 = no; 1 = yes) | 0.354b | 0.249 | 0.549 | 0.303b | 0.145 | 0.567 | 0.336b | 0.203 | 0.549 |
| Epilepsy specialist in future (no)c | −0.381b | −0.574 | −0.268 | −0.219b | −0.448 | −0.075 | −0.263b | −0.463 | −0.139 |
| Epilepsy specialist in future (2–3 weeks) | 0.395 | −0.031 | 0.873 | 0.171 | −0.636 | 0.837 | 0.163 | −0.462 | 0.686 |
| Epilepsy specialist in future (within 1 week) | −0.014 | −0.378 | 0.366 | 0.048 | −0.497 | 0.803 | 0.100 | −0.326 | 0.661 |
| Constant | −0.143b | 0.031 | −0.071 | ||||||
| Number of observations | 1139 | 1108 | 1044 | ||||||
| Number of respondents | 105 | 97 | 96 | ||||||
| Observations per group – minimum | 1 | 1 | 1 | ||||||
| Observations per group – average | 10.8 | 11.4 | 10.9 | ||||||
| Observations per group – maximum | 12 | 12 | 12 | ||||||
| Wald chi2(10) | 170.31 | 327.38 | 184.02 | ||||||
| Log-likelihood | − 662.46 | −512.11 | −575.86 | ||||||
Preferences of people with epilepsy
Across the three seizure scenarios, PWE consistently preferred a CP that involved the paramedic having ‘access to medical records or a care plan’ (see Table 12). They also consistently wanted the ‘Time’ it took to be assessed monitored and treated to be < 6 hours, for an epilepsy specialist to be available to advise their emergency healthcare professional on their care on the day of the incident, for their GP to be notified of the incident, and they wanted the CP to initiate a future appointment being booked for them with an epilepsy specialist. They did not have a significant preference as to whether this appointment occurred within 1 week of the incident or within 2–3 weeks.
There was some slight divergence across the seizure scenarios when it came to preference for ‘What happens next’. Specifically, for ‘Atypical seizure’, none of the levels reached statistical significance. However, for a ‘Home typical seizure’ and a ‘Public typical seizure’, PWE significantly preferred to ‘stay where they are’ and avoid being conveyed to ED. For a ‘Home typical seizure’, PWE also expressed a significant preference to avoid being conveyed to an UTC.
Preferences of significant others
Significant other participants, like PWE, had a consistent preference for a CP that involved the attending ambulance clinician having access to the patient’s care plan or medical record; for the duration to be < 6 hours; for an epilepsy specialist to be available to advise the emergency healthcare professionals on the day of the incident; for the patient’s GP to be notified; and for a future appointment to be arranged with an epilepsy specialist (see Table 13). Like PWE, SOs did not have a significant preference as to whether this appointment occurred within 1 week or within 2–3 weeks.
When it came to ‘Time’, SOs consistently wanted the ‘Time’ it took to be assessed monitored and treated to be < 6 hours. Uniquely, for a ‘Home typical seizure’, SOs also expressed a significant preference for the time it took to be assessed, monitored and treated at home to be 2 hours (but < 6).
With regard to ‘What happens next’, for a ‘Public typical seizure’ and an ‘Atypical seizure’, none of the attribute levels reached statistical significance. However, for a ‘Home typical seizure’, SOs did express a statistically significant preference for the patient to ‘stay at home’ and avoid conveyance to ED.
Ranking of care package configurations by preference
Highest ranking care package configurations
Figure 10 shows the top-ranked CP configuration (i.e. rank 1) for each of the six different seizure contexts. There was similarity across the seizure contexts in terms of which attribute levels featured in the top-ranked configurations. In fact, three of the contexts had the same top-ranked configuration. Thus, only four different CP configurations appear in the figure despite there being six contexts. The configurations are labelled A–D.
FIGURE 10.
Top-ranked care package configuration for the different seizure contexts. The labels for the top-ranked configurations have been given solely for the purpose of the present report. They were not labelled as such within the DCE. a p < 0.05 based on 95% CIs.

The three contexts that had the same top-ranked CP configuration – namely, A – were when PWE considered an ‘Atypical seizure’ and when SOs considered a ‘Home typical seizure’ and a ‘Public typical seizure’. The probability of preferring the alternative (highest-ranked) CP over the current practice configuration ranged from 0.75 to 0.94.
For all contexts, the highest-ranked configuration included the paramedic having access to medical records or a care plan, an epilepsy specialist being available to advise the attending paramedic, the patients GP being notified of the incident and an appointment with a specialist within 2–3 weeks being booked for the patient. The only attributes that varied within the four top-ranked configurations were ‘What happens next’ and ‘Time’, which is explained by the differences in statistical significance of these attributes between across scenarios.
With respect to ‘What happens next’, none of the top-ranked configurations for the six scenarios involved the person being conveyed to ED. For five of them, the top configuration involved the patient staying ‘where they were’. For the remaining one – namely, for an ‘Atypical seizure’ being considered by a SO – the top configuration involved the patient being conveyed to a UTC. For this scenario, SOs did not have a significant preference for any location, but the location with the greatest positive coefficient was UTC.
The preferred ‘Time’ level varied between the contexts. PWE preferred 2 hours for an ‘Atypical seizure’, as did SOs for a ‘Home typical seizure’ and a ‘Public typical seizure’. For a ‘Home typical seizure’, PWE preferred 1 hour, as did SOs for an ‘Atypical seizure’. For the remaining context – namely, a ‘Public typical seizure’ – PWE preferred 3 hours.
How care package configuration approximating current care positioned within rankings
The top-ranked configurations differed in important ways from how current care is typically configured. The only attribute level within all the top-ranked configurations consistent with much of current practice was that participants wanted the patient’s GP to be notified of the incident. It is unsurprising therefore that for all six seizure contexts, the CP configuration representing current care was amongst those least favoured.
For PWE, the highest rank the current care configuration achieved across the six contexts was 230/288. For SOs, the highest rank it achieved was 220. The only CP configurations that ranked lower than the current care configuration was those which did not involve the patient’s GP being notified of the incident (see Report Supplementary Material 16).
Figure 11a and b show a heatmap of the rankings by seizure scenario and participant type and where current care appears (horizontal line Figure 11b). This data visualisation shows how preference varies across the 288 CPs and indicates even minor changes (i.e. single attribute level changes) would be estimated to result in a CP configuration that was typically more favoured by participants than current care. It also confirms how not all attribute level changes would be equal in the extent to which they result in a CP that aligns with participant preference.
FIGURE 11.
Heatmap of the ranking of 288 CP configurations across the six seizure contexts according to extent to which they align with service user preference. (a) Care pathway configurations ranked 1–144; (b) CP configurations ranked 145–288. Green = highest rank/most preferred; red = lowest rank/least preferred; vertical black line at rank 271 represents current care configuration.
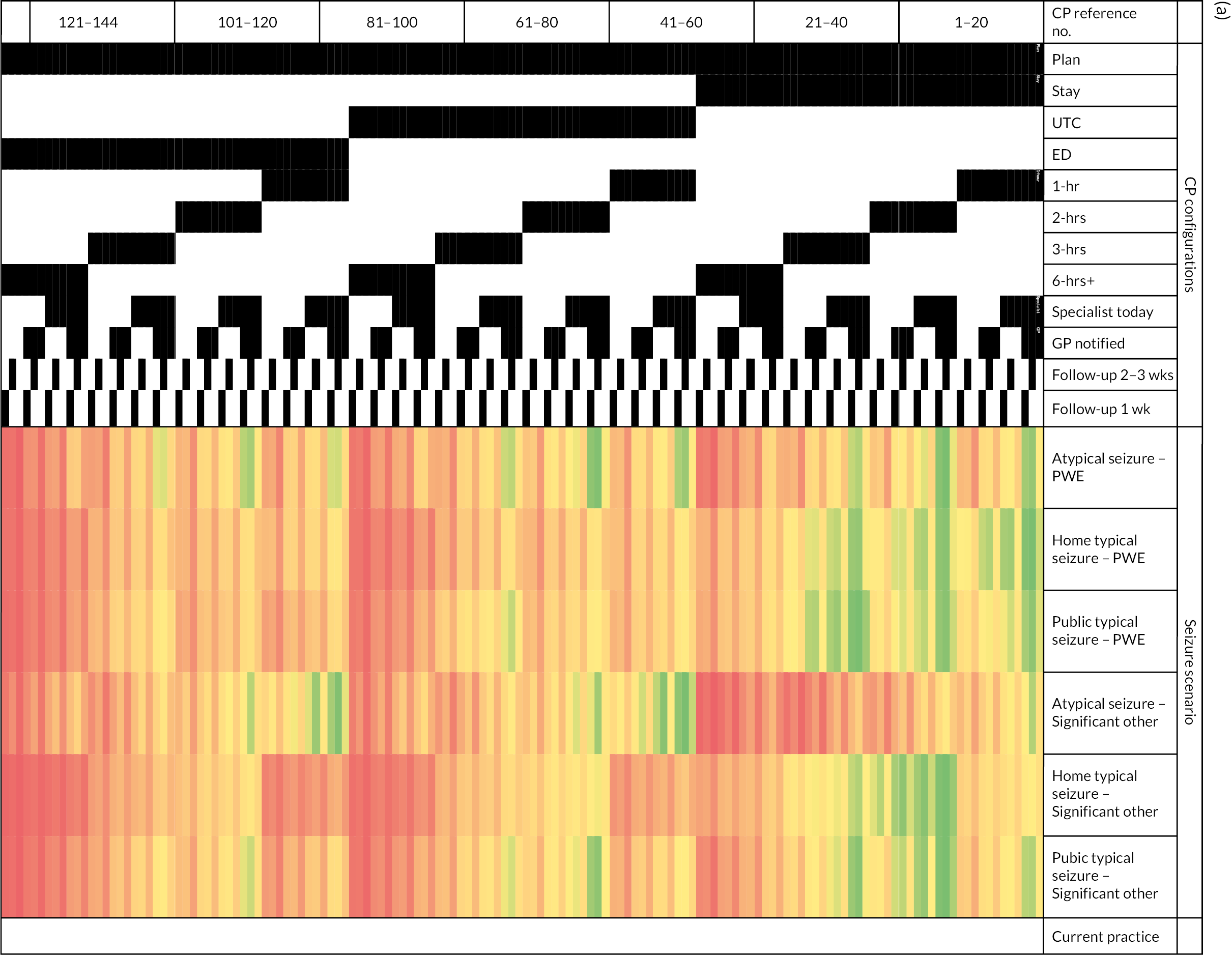

Estimated uptake of top-ranked care package configurations across seizure contexts
We estimated the uptake of each of the top-ranked configurations across all the other seizure contexts. Table 14 shows the proportion of people for the different seizure scenarios that would be estimated to favour configuration A, B, C, D or current care if these were all available. It shows configurations A–D would all be expected to have reasonable uptake across the six scenarios. Each would be expected to be selected more often by services users than current care.
| Seizure context | Proportion estimated to select different care package configurations | |||||
|---|---|---|---|---|---|---|
| Participant type | Seizure scenario | Current care | A | B | C | D |
| PWE | Atypical seizure | 4 | 27 | 24 | 22 | 23 |
| Home typical seizure | 3 | 27 | 30 | 27 | 13 | |
| Public typical seizure | 4 | 26 | 24 | 31 | 15 | |
| SO | Atypical seizure | 1 | 15 | 26 | 8 | 50 |
| Home typical seizure | 2 | 47 | 17 | 27 | 7 | |
| Public typical seizure | 3 | 34 | 22 | 25 | 16 | |
Subgroup analysis
Planned analyses
A priori subgroup analyses could be completed for 17 of the 21 (7 subgroups × 3 seizure scenarios) planned with PWE. None could be completed for SOs due to insufficient cases. The results are summarised in Appendix 10.
It was found that for the seizure scenario ‘Home typical seizure’ whether a person had visited ED in the prior 12 months was associated with preference. Those who had visited ED in the prior 12 months had a statistically significant preference to avoid ED, whereas those who had not did not show a statistically significant preference to avoid it. Whether a person had or had not visited an ED in the prior 12 months was not associated with their preference for the ‘Atypical seizure’ scenario. Its association with preferences for the ‘Public typical seizure’ scenario could not be tested due to insufficient cases.
The following factors were not found to be significantly related to preference: social deprivation; whether the PWE reported an intellectual impairment; whether someone had had contact with specialist services in the prior 12 months; whether they reported experience of the seizure scenario; and whether they had a care plan.
What was found to be important was whether they reported having had previous problems accessing specialist services. It was associated with their preferences for care in the ‘Atypical seizure’ scenario and the ‘Public typical seizure’ scenario (see Appendix 10).
Specifically, for an ‘Atypical seizure’ PWE who reported no problems accessing specialist services had a significant preference for assessment, monitoring and treatment of 2 hours, and a follow-up appointment with an epilepsy specialist within 1 week. In contrast, participants who had experienced problems preferred to be conveyed to a UTC and spend less time being assessed, monitored and treated (1 hour). However, they did prefer to wait longer for follow-up with an epilepsy specialist (i.e. 2–3 weeks rather than within 1 week). In the scenario of a ‘Public typical seizure’, those who reported no problems accessing services had a significant preference to avoid going to the ED, compared to those who reported problems, where none of the options for ‘What happens next’ made a statistically significant contribution to preference.
Post hoc analyses
Post hoc subgroup analyses were, for the most part, only possible for PWE (see Appendix 10). These showed the routes by which PWE had been recruited were not significantly associated with preference. Willingness to access health services (A&E, UTC, outpatient department, GP) during the pandemic had no impact on preferences for CPs, except for when PWE considered a ‘Home typical seizure’. For that scenario, the attribute ‘What happens next’ was no longer associated with preference for participants who said they were less willing to use an UTC due to COVID-19.
Discussion
The DCE successfully elicited the preferences of PWE and their SOs across three different seizure scenarios. In the main, the preferences they expressed did not appear to be obviously influenced by them completing the DCE in the context of the pandemic.
In all instances, participants preferred care where the paramedic had access to medical records or a care plan; where a health professional with specialist training in neurology was available to advise crews; where the GP receives a report from the ambulance service; and where the incident results in an appointment being arranged for them with an epilepsy specialist in the future. In terms of ‘What happens next’, there was a pattern for both participant groups to want to avoid conveyance to ED and preferring to remain where they were, or in one instance to go to a UTC instead. With regard to ‘Time’, everyone wanted to avoid the longest care duration of 6 hours in all seizure scenarios.
The findings provide important insights for discussions regarding implementation. Firstly, the ideal CP configuration for the seizure contexts differed markedly from current care in almost all respects.
Secondly, not all attributes had equal strength of influence on participants’ preference. The DCE findings state the expected magnitude of benefit for utility of different individual attribute changes. The attribute levels which had the most consistently strong patterns of influence were having a specialist advise the emergency clinicians on the day and providing crews with access to medical records or a care plan.
Thirdly, while there were some slight differences in the care preferences of people for the different seizure scenarios, the findings do suggest commonality across them. This, along with the finding that care preferences, does not appear markedly different between certain specified subgroups; it means a single CP configuration might theoretically be deployable for all the seizure scenarios and service users. A single configuration might be pragmatically attractive to service providers.
In the next chapter, we describe how we held expert workshops at which stakeholders, informed of the DCE evidence, were asked identify the optimal alternative CP(s) for seizures that could be recommended for implementation and evaluation.
Chapter 8 Knowledge exchange events
Introduction
In seeking to identify which CP configuration(s) should be prioritised for implementation and evaluation, it was anticipated that factors beyond patient preference would also be important. Factors such as known or expected affordability, practicability, effectiveness, side effects, equity and acceptability to providers. 105 Therefore, in this chapter, we report on KE workshops that were completed with people whose professional positions meant they could develop, fund, implement, support or run an alternative CP for seizures. The workshops sought to disseminate the DCE to them and then utilise their expertise and experience to help understand which CP(s) was judged to represent the optimal balance between service user preference and NHS feasibility.
Methods
Design
The design adopted was relatively novel. It was informed by experience within the investigator team of completing KE endeavours and findings from the literature. Wilkins and Cooper’s175 definition of KE noted in Chapter 2 informed our approach. Our study design asked stakeholders to consider and debate the findings from the DCEs on service user preference, for them to share their views on the feasibility of users preferred attribute levels and to then identify together what they considered to be the optimal CP configuration.
Because of the following assumptions, a group, rather than an individual, approach to KE was considered preferable: a group of people should be less likely to arrive at a wrong decision than a single individual is; a group is more likely to lend some authority to the decision produced and decisions are improved when opinions are openly discussed, potentially challenged and views need to be justified. 194
Eligibility criteria
For the workshops, we sought a group of informed individuals/‘experts’ deemed to have a high level of knowledge and clinical experience of epilepsy, neuroscience and urgent and emergency care policy and practice. Persons from the following groups were considered the key stakeholder groups in this regard: ambulance clinicians, epilepsy specialists (neurologists, ENS and neuropsychiatrists), emergency medicine consultants, GPs, commissioners and managers.
To take part, persons needed to be aged ≥ 18 years, live in the UK and be able to provide informed consent and participate independently in English in a workshop.
At each workshop, we sought to have persons from each of the different groups represented. Evidence suggests heterogeneity in a decision-making group can lead to a better performance than homogeneity in terms of considering all relevant aspects of the topic. 195 We also sought to have representatives from a range of different English regions present at each workshop. This was important since ambulance regions can differ in their non-conveyance rates. 92 Moreover, infrastructure relevant to CP has historically differed between regions. 196
In addition to the participant groups noted above, at each workshop, we also sought to have at least one service user representative and for them to be an active participant. Their representation was primarily with the intention of helping the other participants, where needed, interpret the reasons for the preferences that service users expressed within the survey. It was not about seeking further evidence on the preferences of service users.
Deviations from original protocol
Original plans
When the study was designed and commissioned in 2018, the intention had been that two half-day face-to-face KE workshops would be hosted. They would be run between January and March 2021. There were to be 40–50 representatives at each workshop.
The events were to start with a presentation of the project’s findings. A version of the nominal group technique (NGT) would then be used to organise proceedings and manage breakout groups. NGT – used by the James Lind Alliance for their priority setting exercises197 – is a well-established and adaptable technique that can help ensure all delegates have the opportunity to articulate their views on the topic being discussed.
Need to deviate from original plan
It was not possible to complete the workshops as planned. The COVID-19 pandemic, government regulations and the project’s Sponsor stated face-to-face meetings and non-essential travel were not permitted. The Sponsor asked that the workshops be completed remotely using video-conference technology. This change was done with the agreement of the HS&DR and the project’s Steering Committee.
Knowledge exchange events had been completed online before, as had NGTs198 (albeit to a lesser extent). Nevertheless, we needed to deviate from the original plan in terms of how the workshops were run. Firstly, the number of workshop participants needed to be smaller to ensure high-quality data. 199,200 Moreover, to minimise participant burden, the workshops needed to be shorter. Three smaller workshops of around 2 hours in duration each were therefore run.
Each workshop was limited to six to eight participants. To enable this, participation was restricted to ambulance and neuroscience clinicians, commissioners and service user representatives. The justification for excluding emergency medicine and general practice representatives was WP1a indicated they were less likely to be the clinicians delivering an alternative CP.
To maximise participation by what were often front-line clinicians, we also decided to run the workshops in the spring, rather than winter of 2021. The median for COVID-19 daily infections in England in April and May 2021 was down to 2490 (IQR = 2155–2796) (see Report Supplementary Material 14).
Recruitment
Clinical representatives were recruited from organisations participating in the WP1a survey of service providers. Commissioning and managerial representation was secured by asking the National Ambulance Commissioners Network and the Association of Ambulance Chief Executives National Ambulance Strategy and Transformation group (NASAT) to circulate an advert to appropriate members. NASAT comprises strategy and transformation directors with senior clinicians from each ambulance service being represented. Service user representation was secured by inviting members from the project’s PPI group.
Fifty people were ultimately selected and sent invitation packs that included a participant information sheet. A sampling matrix was used to facilitate broadly equal recruitment of persons from the different target groups. We intentionally sought to over-recruit by ~30% with the anticipation that some would not attend workshops they were scheduled to attend. 201
Persons receiving the invites could pass on the invitation to someone else if they themselves were not able, willing or suitable to take part. Repeat invites were sent if no response was received from them within 2 weeks. Those willing to participate were asked to inform the research team who sent them a link to an e-consent form.
To promote transparency, records of the workshops were kept, and they were audio-recorded and subsequently transcribed verbatim.
The KE workshops received Health Research Authority approval and approval opinion from the NRES Committee, West Midlands, Solihull (19/WM/0012).
Service user representatives were offered a shopping voucher of £20 as an acknowledgement of their time.
Procedure
Overview of structure and facilitation
Figure 12 illustrates the three-part structure of the workshops. Workshops were facilitated by BM, a university-based qualitative research assistant with a specialist interest in health services research but no specialist knowledge of the ambulance service. BM had not had any involvement in any other WP.
FIGURE 12.
Structure of WP3 KE workshops.
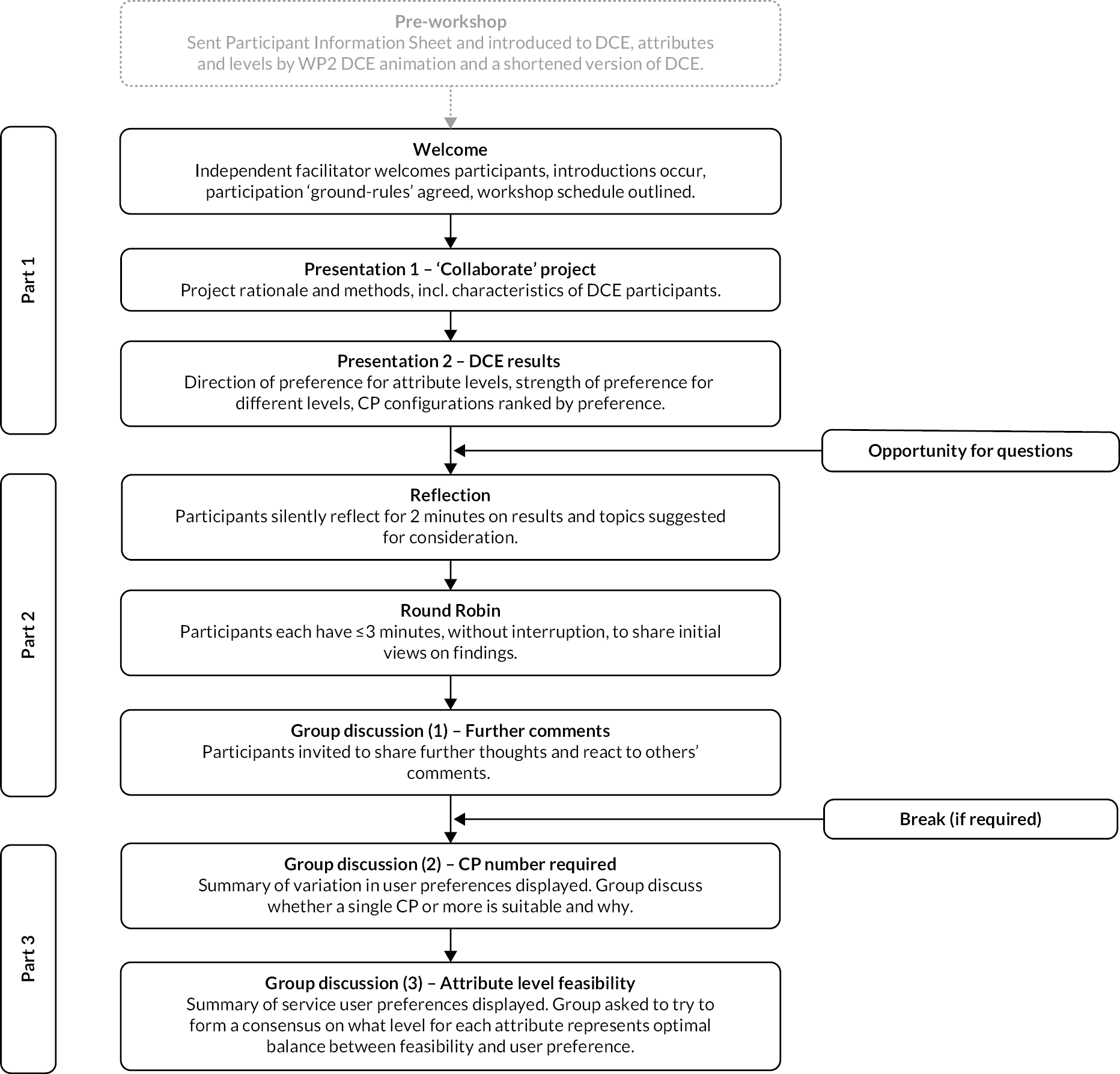
Part 1 of knowledge exchange workshops
Participants were shown two presentations. The first, by AN, briefly outlined the rationale for the project and purpose of the event. The second, by EH, shared detailed, yet distilled evidence from the DCE survey on user preference. Its content is shown in Report Supplementary Material 17.
The presentations were prerecorded to reduce opportunity for technical difficulties and to standardise the evidence the different groups received. AN and EH were present at each workshop to address questions delegates had.
Extensive consideration was given to how best to share the DCE evidence. In advance of the workshop, participants were sent instructions relating to the purposes of the workshops. They could also view the animation on the DCE seen by WP2 participants and could complete a shortened version of the WP2 DCE.
Part 2 of knowledge exchange workshops
Nominal group techniques were used here to secure participants’ views on the findings. Firstly, there was a period of ‘reflection’. It comprised of 2 minutes of silence and ensured each participant was given some dedicated time to consider the items for discussion. This was followed by a ‘round robin’ phase. It provided each participant with a protected opportunity to give their views. Participants were asked to feedback on their reactions to the DCE evidence and on potential barriers and facilitators to change for the different CP configurations. They were encouraged to consider factors such as supply constraints, acceptability to staff, possible cost, geographical considerations and the potential of the different CPs to redress healthcare inequalities. When considering the feasibility of the different attribute levels, participants were asked to have a time frame of the next 5–10 years in mind.
Once all participants had spoken via the ‘round robin’ phase, a ‘clarification’ phase occurred during which participants could discuss matters openly and respond to each other.
All discussions during part 2 were supported by a piloted topic guide (see Report Supplementary Material 18).
Part 3 of the knowledge exchange workshops
This final part sought to identify participants’ views on the optimal CP configuration. Each workshop group was asked whether they as a group would recommend the development of one or more CPs for use with the different seizure presentations. To support their decision-making, they were shown a summary slide of the DCE evidence on the extent of variation in preference by seizure context. During this stage of specifying CP configuration, the group were prompted to discuss any interdependence between attributes, and scenarios in which the CP configuration may require more flexibility.
If a group ultimately recommended a single CP be developed, they were asked to identify for each attribute what level was considered to represent the optimal balance between NHS feasibility and service user preference. In doing so, they would create a CP configuration. If participants recommended more than one CP be developed for different seizure scenarios, then they repeated the attribute level specification process for each.
Analysis
The CP configuration(s) specified as representing the optimum by the different workshop groups were recorded and are presented in a matrix, alongside the DCE evidence.
The qualitative data from parts 1, 2 and 3 were thematically analysed using an approach informed by the work of Braun and Clarke. 202 It enabled scrutiny of the data to capture delegates’ views and justifications for their preferences. It was conducted deductively (with the identification of pre-existing themes underpinned by previous research) and inductively (with the identification of themes grounded in the data to identify patterns and themes related to the study objectives).
Beth Morris led the qualitative analysis and was supported by AN. Familiarity with the data was developed by them independently listening to the audio-recordings and reading the transcripts. BM generated codes through open coding and categorised these thematically. AN reviewed the codes and their application and suggested alternative interpretations until consensus was reached about the interpretation that best fitted the data.
Quotations are presented within the body of the results section to illustrate themes. There has been minor editing to preserve anonymity and ensure clarity of meaning.
When presenting quotes from neuroscience representatives, those from ENSs are presented separately to those of neuroscience doctors (i.e. neurologists and neuropsychiatrists). This is to preserve potentially different views. The merging of comments from neurology and neuropsychiatry was required to help maintain anonymity.
When describing participants’ views on the feasibility of different attribute levels a brief reminder is given each time as to the preferences of service users (as determined by the DCE).
Findings from part 3 of the workshop were used to refine the list of possible attribute levels that a CP for this target population would be recommended to assume. This would reduce the number of CP configurations for consideration from the possible to 288 (presented in Chapter 7) to only those which stakeholders considered optimal and feasible. Descriptive statistics were used to describe the expected utility of these remaining configurations.
Results
Participants
From the 50 representatives invited, 35 confirmed a willingness to take part and were booked to attend a workshop. Twenty-seven of these ultimately attended a workshop: 14 females and 13 males. They included 10 ambulance clinicians (from 7 different regional services), 8 neuroscience representatives [from 5 different ambulance regions (3 neurologists, 1 neuropsychiatrist and 4 ENSs)], 5 commissioners (from 4 different ambulance regions) and 4 PPI representatives (from 4 different ambulance regions).
Two of the workshops lasted 2 hours, while one lasted 2.5 hours. One had 8 participants, one 10 and the other 9.
Themes
Analysis of the transcripts provided insights into the extent to which the DCE evidence aligned with the representatives’ clinical, professional or lived experience and the perceived feasibility of the preferred attribute levels. These shall be expanded upon in the following sections (with additional illustrative quotes for the themes being provided in Report Supplementary Material 19).
Reactions to discrete choice experiment survey findings
Some participants said the DCE evidence aligned with their clinical or lived experience. For others, the evidence was revealing. Either way, both sections welcomed users’ preferences being formally documented for the first time and said it represented important evidence for ambulance services to change their provision:
I thought it was … quite sobering that … patients … presenting to us with epilepsy don’t, don’t really kind of want what we’re currently doing. So, there’s, there is clearly a burning platform I think for us to erm to change and do something different.
Paramedic, Female 1
Participants were keen to highlight that, as for CPs already used for other presentations, whether and the extent to which a CP is used by a clinician will be ultimately based on clinical judgement at the time. It would not be appropriate to mandate use based on the case description alone. To illustrate this, participants highlighted hypothetical examples of how factors beyond immediate case description might need accounting for:
… crews are going to be faced with not just the clinical condition in front of them you know, but [also potentially unforeseen] patient safety and dignity issues that might also impact on what care provision is appropriate.
Commissioner, Female 2
Feasibility of attribute levels and number of care package configurations required for seizure scenarios
Participants believed the different attribute levels preferred by participants would broadly speaking be feasible to implement in the NHS in the next 5–10 years. Moreover, they believed that a single CP for all the seizure scenarios was preferable and justifiable. They were of the view that there was sufficient commonality in service user preferences across the seizure contexts for this to occur. They considered a single CP would also be preferable from an administrative and commissioning perspective:
There are some challenges for ambulance staff in terms of quality versus performance … but er, I think for a lot a lot of ambulance services it’s [preferred CP configurations] probably not that, that far of a stretch actually.
Paramedic, Male 1
As shown in Figure 13, the three workshop groups were of the same view as to which configuration represented the optimum. It comprised ambulance clinicians having access to medical records, the person typically staying where they were, the time taken being < 6 hours (be it 1, 2 or 3 hours), for crews to be able to be advised by a specialist on the day, for the GP to be notified and for the incident to result in an appointment being made for the patient to subsequently have a follow-up appointment with an epilepsy specialist (be it within 1 or 2–3 weeks).
FIGURE 13.
Attribute levels specified by KE groups as representing optimal balance between NHS feasibility and service user preference. For columns presenting ‘Summary of evidence from DCE’: a green cell indicates an attribute level the respondents significantly preferred for the CP to have in that scenario; a red cell means an attribute level that respondents significantly preferred to not have in the CP for the scenario; white cells indicate those that did not reach statistical significance.
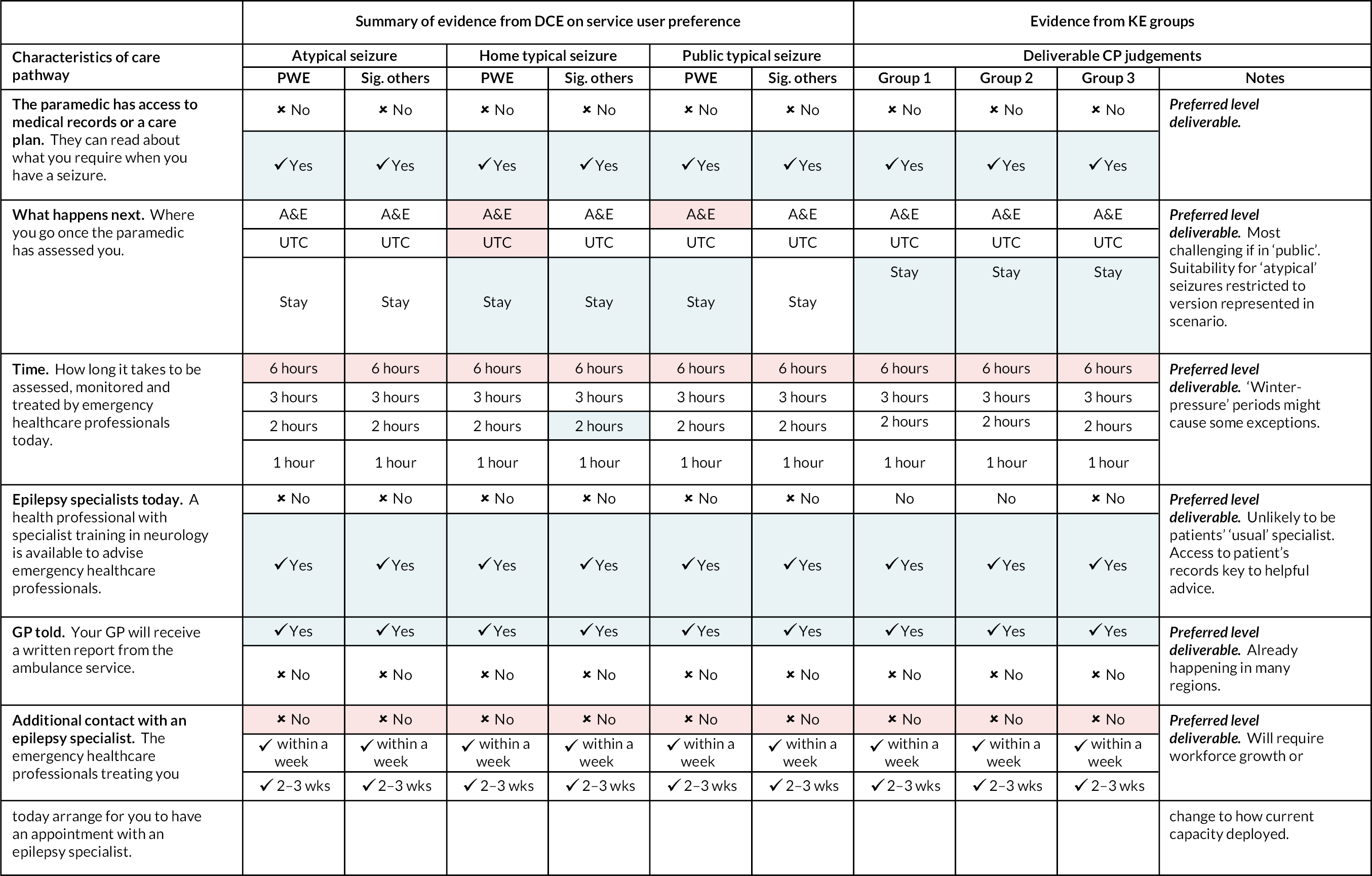
While the groups considered it to be NHS-feasible, they did note some instances when some of its preferred attribute levels might not be achievable and so some flexibility in permitted attribute levels would be required. These instances mainly centred around periods of ‘winter pressure’ and when a specialist who knew the PWE being attended to was not available to advise paramedics. Their qualifying statements are noted in Figure 13.
The specific feedback that the participants had for the feasibility of the different attribute levels is as follows. Their comments informed why they believed a CP could, in due course, be offered that was largely in line with service users’ preference.
Attribute 1: the ambulance clinician has access to medical records or a care plan
Reminder of DCE findings: Service user representatives wanted ambulance clinicians to have access to their medical records or a care plan across the seizure scenarios.
The consensus was this was achievable in the next 5–10 years. Indeed, some stated that it could happen sooner. Their justification being that in some regions, mechanisms were in place for the sharing of more rudimentary medical records (e.g. NHS Summary Care Records) with crews:
we’ve got access to Summary Care Records, and we’ve got access to a system called ‘Co-ordinate my Care’ … a purpose-built platform for er sharing care plans. [So implementing medical record or care plan access is] Very doable. You could do it tomorrow.
Paramedic, Female 1
Participants believed the key benefit of ambulance clinicians having access to such information was it could help them identify persons suitable for consideration of non-conveyance and increase their confidence:
[It could] give them that bit of reassurance … [paramedics] don’t work in an ED department where there’s somebody on hand to ask the question and get that second opinion … for me, it doesn’t have to be that physical person, it can be that well documented care plan that will give them the confidence to make that decision.
Paramedic, Male 3
In the future, the information was seen as also holding the potential to positively influence the vehicle/crew type that was dispatched:
… if this person’s preferred place of care is at home and … they have a history of epilepsy, you may well think actually we need to send a response vehicle with a senior clinician on it to this patient rather than a double crewed ambulance erm, to make sure that we’re providing exactly the right response …
Paramedic, Male 6
All participants were united in stating the information from the medical record that crews were given access to needed to be pertinent and concise:
… in the heat of the moment to kind of trawl … years of clinic letters or hand-written medical notes is you know, only half useful … the development of a very specific document … a care plan is where er, significant gains can be had.
Neuroscience doctor, Male 1
In terms of what was pertinent, participants said it should cover ‘the baseline for that patient as an absolute minimum’ and have ‘some representation of that patient’s wishes’ (Paramedic, Male 6).
Ambulance clinicians can differ widely in terms of their training and experience. 61,108 For this reason, participants emphasised the information needed to be in a format and language accessible to all. Participants also reflected on some limitations of what is already being made available to crews for other presentations. They said lessons should be learnt to ensure the information provided is consistent and easy to use:
We cover over 30 CCG [clinical commissioning group] footprints, so we’ve got er over 30 variations in documentation that we may see on scene.
Paramedic, Male 6
Attribute 2: what happens next – are patients conveyed and, if so, where to?
Reminder of DCE findings: Service user representatives expressed a tendency to prefer being cared for ‘where they were’ and avoid ED. For typical seizures at home, PWE and SOs had a statistically significant preference to remain where they were. PWE also significantly preferred avoiding ED and UTCs for seizures occurring at home and to avoid ED for typical seizures in public.
Workshop participants were mostly in agreement that it was feasible to follow service users’ preferences to stay where they were following a typical seizure and that this is becoming more common practice:
… do we think this is feasible … patients with diagnosed epilepsy with a typical seizure presentation 100%. We would engage with this … I think that’s absolutely been the best option for a while [stay at home] and paramedics are gaining confidence in that in their current practice.
Paramedic, Female 2
Participants were more circumspect in their support for the preference of PWE (1) to stay where they were following typical seizures in public and (2) to not be conveyed to ED following an atypical seizure. It was noted how caring for patients where they are after an atypical presentation, rather than conveying them to ED, would represent a major change in practice for many clinicians:
… with atypical seizure presentations, most of us have quite low thresholds to take patients to ED.
Paramedic, Female 2
Much discussion was also had about the range of possible presentations that can be captured by the term ‘atypical’. They stated the CP preferred by services users might be suitable for some, but not all of them. They acknowledged the parameters of the atypical seizure scenario used in the DCE and agreed that for this specific variation, the patient staying where they were should be feasible.
The difficulty with referring to ‘atypical’ is it’s a wide term. If a patient’s seizure lasted 30 seconds longer than normal that may be construed as atypical, but they are probably still safe to stay at home …
Paramedic, Male 4
Because of the potential elevated risk of atypical seizure presentations, participants highlighted how consideration might need to be given as to which grades of ambulance clinician would be permitted to use the CP for them. They highlighted this was already done for some CPs used for other presentations. They also noted that the issue would become most pertinent during periods of high demand when ambulance services are sometimes supported by voluntary staff and private services.
… there aren’t just paramedics throughout ambulance trusts, there are non-registrants that go out to patients on their own as well …
Paramedic, Female 3
Attribute 3: time taken to be assessed, monitored and treated
Reminder of DCE findings: Service users, across all seizure scenarios, expressed a statistically significant preference to avoid being assessed, monitored and treated by an emergency healthcare professional for more than 6 hours. SOs also had a significant preference, following a typical seizure at home, for the time to be 2 hours.
Workshop participants believed a CP that reflected patient preferences for time would be feasible:
… absolutely achievable and probably for the most part er, that is something that we achieve with … cases already.
Paramedic, Male 4
They also highlighted how this could theoretically be achieved if the seizure occurred in public:
where would you allow them to recover safely … One thought was in the back of an ambulance …
ENS, Female 3
Nonetheless, participants did highlight how feasibility might reduce during periods of high demand and that there might be operational challenges if crews stay with persons for long recovery times (rather than being available to respond to other incidents):
… there will always be tensions between you know, call volumes … some days it would be possible to, to maintain that kind of stance [2-hour timeframe] but on other days … It just may not always be possible …
Commissioner, Female 2
Attribute 4: paramedic access to specialist advice on the day of seizure presentation
Reminder of DCE findings: Across all seizure scenarios, service user participants expressed a statistically significant preference for their emergency healthcare professional to have access to a healthcare professional with specialist training in neurology for advice. The attribute did not specify that the professional would be someone they had previously received care from.
While workshop participants believed this to be feasible within the next 5–10 years, they were not in consensus as to who should be providing the advice. Some epilepsy service representatives believed that for the specialist – be it an epilepsy nurse or neurologist – to offer meaningful support they needed to be personally familiar with the patient. With existing capacity, they stated this would not be likely to happen:
… if it’s not someone who knows them or who really understands their epilepsy and their background then actually the value of that specialist advice I think is massively diminished.
Neuroscience doctor, Female 1
They were of the view that access to medical records that include high-quality emergency seizure care plans would be more helpful than specialist advice:
… if they’ve got a seizure care plan, if they know their treatment plans and it’s all written out, actually they [crews] won’t need this … they don’t need the specialist advice.
Neuroscience doctor, Male 1
However, it was acknowledged that not all PWE being attended to by the ambulance service are ‘known’ to a specialist. They might not have been seen by them for a substantial period, or indeed ever, in some instances. Moreover, as reflected by a service user representative at the workshop, even some of those that are ‘known’ to specialist services do not currently have emergency seizure care plans:
I don’t have a care plan, and I do wonder how many other people with epilepsy don’t really have a care plan.
PPI, Female 2
In contrast, ambulance clinicians were keen to emphasise any sort of advice from an epilepsy specialist would be welcomed – be it from a healthcare professional who knew the patient or not. They emphasised how they work in a largely isolated way and so would value access to any sort of additional expertise to decisions:
… when you’re working in the ambulance setting … you can’t just kind of pop out to like the, the cubicle and catch your colleague …
Paramedic, Female 1
They felt access could be particularly helpful when crews were managing atypical seizure presentations and for newly qualified paramedics. Whoever it is that provides the specialist advice, it was agreed that any scaled system of support would need to be robust for ambulance clinicians to have confidence utilising it:
… there’s got to be a reaction, there’s got to be someone picking up that phone [when you call for advice] … otherwise you get a couple of er hangings on or no pick up and very quickly that can … lead to lack of confidence … crews … saying … you know don’t bother … it’s never working and we just end up conveying anyway …
Commissioner, Male 1
In terms of how access would occur, ambulance participants explained the infrastructure is already in place in many areas as they use it to access advice from different specialities for other presentations.
Attribute 5: general practitioner informed of seizure presentation via report from ambulance clinician
Reminder of DCE findings: Service user representatives for all seizure scenarios expressed a significant preference for the patient’s GP to receive a written report from the ambulance service.
There was a consensus at the workshops that this would be feasible in the next 5–10 years. In fact, participants pointed out that in those regions where crew members complete patient report records electronically, it was already happening:
When we discharge someone on the scene, the GP is automatically emailed … as long as we can trace the patient on the [system] a … record from us of our attendance. So yeah absolutely, easily achievable …
Paramedic, Male 3
… we’re a little bit behind the curve on erm, electronic er report forms, but I, I don’t think that would hold us back in the, the timescales that we’re talking about.
Paramedic, Female 1
Attribute 6: additional contact with an epilepsy specialist arranged by ambulance service
Reminder of DCE findings: Service user representatives had a statistically significant preference for the emergency healthcare professional treating them on the day to arrange for them to have a follow-up appointment with an epilepsy specialist. They did not have a significant preference for whether the appointment occurred within one or within 2–3 weeks.
Overall, workshop participants believed this attribute level was feasible to achieve in the next 5–10 years.
Neuroscience representatives highlighted how other parts of the urgent and emergency care system – particularly ED staff – can already arrange follow-up clinic appointments for the patients they see. Extending this to ambulance crews was considered viable.
Ambulance clinicians said they already arrange follow-up appointments for other presentations with different specialities. They stated they would prefer for the referral process to be via an online service. If telephone calls were required to arrange it, they wanted this be delegated to another part of the service, such as to those within the ambulance service’s central hub, NHS 111 or primary care:
Yeah, it’s absolutely doable and we do it for other areas and er other clinical conditions.
Paramedic, Male 3
what we don’t want to do is leave our crew on scene … chasing telephone numbers and referrals and doing lots in the back of an ambulance.
Paramedic, Male 6
Neuroscience representatives wanted to note that the feasibility of the patient having an appointment with a specialist could vary between regions and potential inequities in access existed. It was highlighted how some services were already struggling to meet wait time standards for the referrals they were receiving from more traditional referral routes. This issue was not, however, deemed to be an insurmountable barrier. Participants believed that with expansion in capacity and/or a change in how existing resources were utilised, that providing the desired follow-up would be feasible:
Where there isn’t a larger group of epilepsy nurses or epilepsy specialists, then they would have to look at investing and training and setting up services. But I think that would be possible …
ENS, Female 3
… we’ve looked at the way we run our services and made quite a radical change … we’re not booking routine follow-up appointments … they can contact us. … that’s allowing more capacity … that’s now our mission – that we get back to calls within the day because they’re, they’re patients or healthcare professionals that really need to speak to us.
ENS, Female 2
Optimal and feasible configurations
In the last section, we reported on how stakeholders advised on which attribute levels were optimal. We used their feedback to restrict the levels that the attributes could take and understand how many CP could be generated and their expected utility.
With the restrictions applied, the number of CP that could be constructed reduced from 288 to 18. Table 15 – under the column titled ‘Base case’ – shows the expected utility of the 18 configurations in the different seizure contexts (i.e. seizure scenario × participant type). The descriptive statistics relating to where these configurations would be expected to rank based on their utility shows that for each scenario the 18 configurations include the configuration expected to be most preferred by service providers in each seizure context (i.e. rank 1). Moreover, all 18 configurations would be expected to hold more utility for service users than current care does.
| Base case | Situation one | Situation two | ||
|---|---|---|---|---|
| Optimal and feasible | Specialist advice not available today, assumed to be contained in care plan | ‘Winter pressures’/times of strain of NHS resources | ||
| Attributes | ||||
| The paramedic has access to medical records or a care plan | Yes | Yes | Yes | |
| What happens next | Stay, UTC, ED | Stay, UTC, ED | Stay, UTC, ED | |
| Time | 1,2,3 | 1,2,3 | 1,2,3, 6 + | |
| Epilepsy specialists today | Yes | No | Yes, No | |
| GP told | Yes | Yes | Yes | |
| Additional contact with an epilepsy specialist | 2–3 weeks, 1 week | 2–3 weeks, 1 week | 2–3 weeks, 1 week | |
| Count of CP configurations | 18 | 18 | 12 | |
| Median rank (range) | Median rank (range) | Median rank (range) | Current care configuration rank | |
| PWE | ||||
| Atypical seizure | 9.5 (1–19) | 66.5 (34–99) | 139.5 (70–210) | 248 |
| Home typical seizure | 42.5 (1–60) | 86 (10–107) | 183.5 (59–236) | 247 |
| Public typical seizure | 30.5 (1–71) | 74 (10–136) | 158.5 (49–240) | 230 |
| Significant other | ||||
| Atypical seizure | 28 (1–138) | 97 (15–231) | 167.5 (67–261) | 253 |
| Home typical seizure | 47.5 (1–162) | 79 (4–205) | 219.5 (91–264) | 220 |
| Public typical seizure | 15 (1–61) | 64.5 (12–144) | 180 (88–247) | 239 |
Stakeholders also identified two specific situations in which some attributes might need to assume less than optimal levels to ensure feasibility, namely, (1) during periods of ‘winter pressures’ (or strains on NHS resources) when the optimal level for ‘Time’ might not be feasible and preferences for conveyance might not be possible due to the person attending the scene not being a qualified paramedic and (2) when advice contained in the care plan might be considered appropriate/or sufficient to negate the need for advice for paramedics on the day from an epilepsy specialist.
When CP configurations were generated without allowing them to include specialist advice being provided to paramedics on the day (situation one), overall utility of the CPs reduced (as indicated by change in median rank) (see Table 15, column ‘Situation one’). Nevertheless, in all the seizure scenarios, each of the CP configurations remained preferable to current practice (as indicated by the range of rank scores relative to the rank for the current care configuration).
An even greater reduction in utility was seen when CP configurations were generated using the CP attribute levels that might be necessary during periods of ‘winter pressure’ (situation two). In some instances, the CP configurations that were possible remained preferable to current practice. However, for three of the seizure scenarios (as indicated by the range of rank scores), the reduction in utility was sufficient to mean some of the configurations generated using the restricted attribute levels would result in a CP worse than current care in expected utility. Specifically, seven CPs configuration were found to rank lower than current practice for at least one seizure scenario/group (see Table 15, column ‘Situation two’).
Discussion
Three constructive KE workshops were conducted with key stakeholder groups. Stakeholders were found to be broadly of the view that the attribute levels favoured by service users for the different seizure scenarios were largely feasible within 5–10 years, if not sooner. Importantly, there was also consensus amongst workshop participants that there was sufficient consistency in the preferences of service users to endeavour to implement and evaluate a single CP for epilepsy.
Across the workshops, the CP configuration they said should be prioritised for implementation comprised of ambulance clinicians having access to medical records; the person staying where they are; the time taken being < 6 hours (be it 1, 2 or 3 hours); for crews to be able to be advised by a specialist on the day; for the GP to be notified; and for the incident to result in an appointment being made for the patient to subsequently have a follow-up appointment with the specialist (either within 1 or 2–3 weeks).
Having said this, stakeholders did highlight instances when the optimal CP configuration identified for implementation might not be feasible in its entirety and result in a CP being offered that did not fully align with service users’ preferences. The stakeholders helped surfaced two possible scenarios in which this might occur and said attribute levels would need to be permitted to flex in these instances. Specifically, during periods of ‘winter pressure’ crews might not always be able to wait with patients for as long as preferred, or there might not be crew members available who would be qualified to use the CP. Moreover, in instances in which some neuroscience representatives would want the specialist advice offered to crews to only be given by a healthcare professional that knew the patient (which might not always be possible) and who consider a well-developed ‘care plan’ to be sufficient to negate the need for specialist advice on the day.
In the next, and final, chapter, we discuss and seek to integrate the findings from the different WPs. We discuss strength and weakness of the approaches used and highlight potential clinical and research implications of the project’s findings.
Chapter 9 Discussion
Principal findings
Survey of service providers
The cross-sectional survey – to which over 72 services responded – confirmed the impressions that instigated the ‘Collaborate’ project. Specifically, nearly all responding ambulance services were considering, or were working towards implementing an alternative CP for crews to use for epilepsy. Moreover, there was a lack of consistency and equity in the nature of the CPs being considered.
The CP configurations being considered differed in terms of where the non-conveyed person would be taken. In some instances, they would remain at home, in some ‘on scene’ or in others taken to an UTC. The CPs also differed in the extent to which they would help potentially stimulate improvements in the person’s subsequent ambulatory care and potentially address known health inequalities. Only a few included a mechanism by which the patients would be referred for a review of their epilepsy, and then they differed in terms of eligibility, timing and who conducted the review.
A final important finding was that, despite being a statutory obligation, almost none of the responding services had consulted service users on the proposed or intended changes. Thus, even having surveyed providers, it remained unclear which CP configuration was best positioned to deliver benefits since the extent to which they were acceptable to service users was unknown. This underscored the need for the subsequent WP elements.
In helping clarify the characteristics of the CP configuration being considered, the survey provided the evidence needed to help us to ensure that the CP options presented to PWE and SOs within the DCEs were plausible options. This ensure were therefore modelling preference for realistic CP configurations.
Qualitative interviews with service users and ranking exercise
In-depth interviews were completed with 30 service users. They provided important insights into some of the challenges PWE continue to experience, how disruptive seizures can be and how a lack of information transfer and co-ordination among services poses challenges for this population.
The interviews also highlighted some concerns that service user would have with some potential CP configurations. These would be important to address, even if it were simply addressing possible misunderstandings on their behalf (e.g. that the opening times of UTCs should be sufficient to capture most seizure incidents in people with established epilepsy).
One of the additional purposes of the interviews was to help identify attributes of care that were important to service users and which would need to be used to describe the CP options presented within the DCE. To do this, the interviewer worked with participants to complete a ranking exercise, towards the end of the interview. The approach helped us manage the tension that can exist between the complex and nuanced findings produced by qualitative research and the reductive nature of attribute development. 149 The exercise was important as service users identified attributes of potential importance that the research team and literature had not initially considered.
What emerged from the interviews and ranking exercise was an approximation of the factors contributing to the ‘decision calculus’ that service users use when considering postseizure care options. At this stage, while their relative weight of importance was not known, it was becoming apparent that service users would likely want to know where the CP would take them (or not, in the case of non-conveyance); whether the ambulance crew would have access to their medical records or care plan; how long it would take for them to be assessed, monitored and treated during the emergency episode; the extent to which the emergency care provider could request advice from an epilepsy specialist (e.g. epilepsy nurse, consultant); to what extent the CP would mean their usual care providers would be informed of the incident; and, finally, whether any follow-up from a epilepsy specialist would be instigated.
Discrete choice experiment survey
Aided by the evidence from the survey and qualitative interviews, a DCE survey was developed and completed by almost 600 service user participants. It elicited care preferences for three hypothetical seizure scenarios (‘Home typical seizure’, ‘Public typical seizure’ and ‘Atypical seizure’). The findings were illuminating.
For all seizure scenarios, both PWE and SOs (i.e. close family and friends) were found to want a CP configuration that differed markedly from what they are currently offered. Specifically, in all instances, they preferred: for the paramedic to have access to their medical records or a care plan; for a health professional with specialist training in neurology (be it an epilepsy nurse, neurologist and not someone necessarily known the patient) to be available to advise paramedics; for their GP to receive a report from the ambulance service; and for the incident to result in an appointment being arranged for them with an epilepsy specialist in the future. Whether an appointment occurred within 1 week or within 2–3 weeks was not found to be a significant determinant of preference. In terms of ‘What happens next’, there was a pattern of preferring to avoid conveyance to ED and to remain where they were, or in one instance to go to a UTC. With regard to ‘Time’ (i.e. how long the CP involved the person being assessed, monitored and treated), everyone wanted to avoid the longest duration of 6 hours in all seizure scenarios.
That service users want something clearly different to what is currently offered was most starkly illustrated when we ranked 288 different CP configurations according to their expected utility to service users. The configuration representing current care was amongst the least favoured in all scenarios.
Perhaps more positively, the DCE indicate the improvement in CP utility that would be expected to result from specific attribute changes for each seizure scenario. If only limited changes are considered possible, these could help service providers identify which changes to prioritise. The attribute levels with the most consistent and largest impact on preference across the scenarios were (1) providing the crews with access to medical records or a care plan and (2) having a specialist who is able to advise the ambulance crew during the episode. Table 16 shows the expected utility for each individual configuration.
| Context | CP configuration | PWE | SO | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Atypical seizure | Home typical seizure | Public typical seizure | Atypical seizure | Home typical seizure | Public typical seizure | |||||||||
| ID number | Brief description of configurationa | Utility | Rank | Utility | Rank | Utility | Rank | Utility | Rank | Utility | Rank | Utility | Rank | |
| CP configurations based on optimal attribute levels | 14 | Plan, stay, 2 hours, specialist, GP, 2–3 weeks | 1.992 | 1 | 2.060 | 3 | 1.855 | 3 | 1.950 | 33 | 2.751 | 1 | 2.452 | 1 |
| 62 | Plan, UTC, 2 hours, specialist, GP, 2–3 weeks | 1.968 | 2 | 1.257 | 45 | 1.352 | 30 | 2.602 | 7 | 1.828 | 22 | 2.118 | 4 | |
| 15 | Plan, stay, 2 hours, specialist, GP, 1 week | 1.942 | 3 | 2.044 | 4 | 1.788 | 5 | 1.542 | 66 | 2.628 | 2 | 2.390 | 2 | |
| 63 | Plan, UTC, 2 hours, specialist, GP, 1 week | 1.919 | 4 | 1.242 | 50 | 1.285 | 34 | 2.193 | 20 | 1.705 | 29 | 2.056 | 7 | |
| 2 | Plan, stay, 1 hour, specialist, GP, 2–3 weeks | 1.871 | 5 | 2.163 | 1 | 1.800 | 4 | 2.499 | 10 | 1.744 | 27 | 2.004 | 10 | |
| 50 | Plan, UTC, 1 hour, specialist, GP, 2–3 weeks | 1.848 | 6 | 1.361 | 36 | 1.297 | 32 | 3.150 | 1 | 0.821 | 105 | 1.670 | 27 | |
| 3 | Plan, stay, 1 hour specialist, GP, 1 week | 1.822 | 7 | 2.148 | 2 | 1.733 | 8 | 2.091 | 26 | 1.622 | 35 | 1.941 | 11 | |
| 110 | Plan, ED, 2 hours, specialist, GP, 2–3 weeks | 1.814 | 8 | 1.233 | 53 | 1.138 | 54 | 2.427 | 11 | 1.487 | 41 | 1.853 | 14 | |
| 51 | Plan, UTC, 1 hour, specialist, GP, 1 week | 1.798 | 9 | 1.345 | 40 | 1.230 | 41 | 2.742 | 4 | 0.699 | 121 | 1.608 | 30 | |
| 26 | Plan, stay, 3 hours, specialist, GP, 2–3 weeks | 1.786 | 10 | 2.043 | 5 | 2.051 | 1 | 1.285 | 91 | 2.182 | 10 | 2.172 | 3 | |
| 111 | Plan, ED, 2 hours, specialist, GP, 1 week | 1.764 | 11 | 1.218 | 57 | 1.071 | 63 | 2.019 | 30 | 1.365 | 54 | 1.791 | 19 | |
| 74 | Plan, UTC, 3 hours, specialist, GP, 2–3 weeks | 1.763 | 12 | 1.240 | 51 | 1.548 | 13 | 1.937 | 34 | 1.259 | 63 | 1.838 | 16 | |
| 27 | Plan, stay, 3 hours, specialist, GP, 1 week | 1.737 | 13 | 2.027 | 6 | 1.984 | 2 | 0.877 | 138 | 2.060 | 13 | 2.109 | 6 | |
| 75 | Plan, UTC, 3 hours, specialist, GP, 1 week | 1.713 | 14 | 1.225 | 56 | 1.481 | 20 | 1.529 | 68 | 1.137 | 68 | 1.776 | 21 | |
| 98 | Plan, ED, 1 hour, specialist, GP, 2–3 weeks | 1.694 | 15 | 1.336 | 42 | 1.083 | 62 | 2.975 | 2 | 0.481 | 147 | 1.405 | 57 | |
| 99 | Plan, ED, 1 hour, specialist, GP, 1 week | 1.644 | 16 | 1.321 | 43 | 1.016 | 71 | 2.567 | 8 | 0.358 | 162 | 1.343 | 61 | |
| 122 | Plan, ED, 3 hours, specialist, GP, 2–3 weeks | 1.608 | 17 | 1.216 | 58 | 1.334 | 31 | 1.762 | 45 | 0.919 | 96 | 1.573 | 34 | |
| 123 | Plan, ED, 3 hours, specialist, GP, 1 week | 1.559 | 19 | 1.201 | 60 | 1.267 | 37 | 1.354 | 84 | 0.797 | 107 | 1.511 | 42 | |
| CP configurations without specialist advice today being permitted | 20 | Plan, stay, 2 hours, GP, 2–3 weeks | 1.401 | 34 | 1.688 | 16 | 1.502 | 17 | 1.124 | 110 | 2.395 | 4 | 1.901 | 12 |
| 68 | Plan, UTC, 2 hours, GP, 2–3 weeks | 1.377 | 38 | 0.885 | 96 | 0.999 | 72 | 1.776 | 44 | 1.472 | 42 | 1.568 | 35 | |
| 21 | Plan, stay, 2 hours, GP, 1 week | 1.351 | 44 | 1.672 | 17 | 1.435 | 24 | 0.716 | 158 | 2.272 | 8 | 1.839 | 15 | |
| 69 | Plan, UTC, 2 hours, GP, 1 week | 1.328 | 49 | 0.870 | 99 | 0.932 | 84 | 1.368 | 82 | 1.349 | 56 | 1.505 | 43 | |
| 8 | Plan, stay, 1 hour, GP, 2–3 weeks | 1.280 | 56 | 1.791 | 10 | 1.447 | 23 | 1.673 | 54 | 1.388 | 52 | 1.453 | 50 | |
| 56 | Plan, UTC, 1 hour, GP, 2–3 weeks | 1.257 | 59 | 0.989 | 76 | 0.944 | 82 | 2.324 | 15 | 0.465 | 151 | 1.119 | 92 | |
| 9 | Plan, stay, 1 hour, GP, 1 week | 1.231 | 63 | 1.776 | 13 | 1.380 | 28 | 1.265 | 94 | 1.265 | 61 | 1.391 | 58 | |
| 116 | Plan, ED, 2 hours, GP, 2–3 weeks | 1.223 | 64 | 0.861 | 101 | 0.785 | 111 | 1.601 | 59 | 1.131 | 71 | 1.303 | 64 | |
| 57 | Plan, UTC, 1 hour, GP, 1 week | 1.208 | 66 | 0.973 | 81 | 0.877 | 95 | 1.916 | 37 | 0.343 | 164 | 1.057 | 102 | |
| 32 | Plan, stay, 3 hours, GP, 2–3 weeks | 1.195 | 67 | 1.671 | 18 | 1.698 | 10 | 0.459 | 187 | 1.826 | 23 | 1.621 | 29 | |
| 117 | Plan, ED, 2 hours, GP, 1 week | 1.174 | 71 | 0.845 | 104 | 0.718 | 122 | 1.193 | 100 | 1.009 | 87 | 1.240 | 74 | |
| 80 | Plan, UTC, 3 hours, GP, 2–3 weeks | 1.172 | 72 | 0.868 | 100 | 1.195 | 46 | 1.111 | 111 | 0.903 | 98 | 1.287 | 65 | |
| 33 | Plan, stay, 3 hours, GP, 1 week | 1.146 | 76 | 1.655 | 19 | 1.631 | 11 | 0.051 | 231 | 1.704 | 30 | 1.559 | 37 | |
| 81 | Plan, UTC, 3 hours, GP, 1 week | 1.122 | 80 | 0.853 | 103 | 1.128 | 57 | 0.703 | 161 | 0.781 | 109 | 1.225 | 77 | |
| 104 | Plan, ED, 1 hour, GP, 2–3 weeks | 1.103 | 83 | 0.964 | 84 | 0.730 | 120 | 2.149 | 22 | 0.125 | 192 | 0.854 | 134 | |
| 105 | Plan, ED, 1 hour, GP, 1 week | 1.053 | 90 | 0.949 | 88 | 0.663 | 136 | 1.741 | 48 | 0.002 | 205 | 0.792 | 144 | |
| 128 | Plan, ED, 3 hours, GP, 2–3 weeks | 1.018 | 92 | 0.844 | 105 | 0.981 | 76 | 0.936 | 127 | 0.563 | 137 | 1.022 | 107 | |
| 129 | Plan, ED, 3 hours, GP, 1 week | 0.968 | 99 | 0.829 | 107 | 0.914 | 89 | 0.528 | 179 | 0.440 | 153 | 0.960 | 117 | |
| CP configurations considered plausible during ‘winter pressures’ | 38 | Plan, stay, 6 hours, specialist, GP, 2–3 weeks | 1.181 | 70 | 1.206 | 59 | 1.175 | 49 | 0.885 | 137 | 0.993 | 91 | 1.146 | 88 |
| 86 | Plan, UTC, 6 hours, specialist, GP, 2–3 weeks | 1.158 | 74 | 0.404 | 178 | 0.672 | 130 | 1.536 | 67 | 0.070 | 201 | 0.812 | 139 | |
| 39 | Plan, stay, 6 hours, specialist, GP, 1 week | 1.132 | 78 | 1.191 | 61 | 1.108 | 60 | 0.477 | 184 | 0.871 | 100 | 1.084 | 99 | |
| 87 | Plan, UTC, 6 hours, specialist, GP, 1 week | 1.108 | 81 | 0.388 | 183 | 0.605 | 147 | 1.128 | 108 | −0.052 | 209 | 0.750 | 149 | |
| 134 | Plan, ED, 6 hours, specialist, GP, 2–3 weeksb | 1.004 | 94 | 0.380 | 184 | 0.458 | 170 | 1.361 | 83 | −0.270 | 230 c | 0.547 | 178 | |
| 135 | Plan, ED, 6 hours, specialist, GP, 1 weekb | 0.954 | 102 | 0.364 | 186 | 0.391 | 186 | 0.953 | 125 | −0.392 | 240 c | 0.485 | 189 | |
| 44 | Plan, stay, 6 hours, GP, 2–3 weeks | 0.590 | 177 | 0.834 | 106 | 0.822 | 104 | 0.059 | 229 | 0.637 | 128 | 0.596 | 171 | |
| 92 | Plan, UTC, 6 hours, GP, 2–3 weeksb | 0.567 | 180 | 0.032 | 228 | 0.319 | 196 | 0.710 | 159 | −0.286 | 232 c | 0.262 | 213 | |
| 45 | Plan, stay, 6 hours, GP, 1 weekb | 0.541 | 186 | 0.819 | 109 | 0.755 | 115 | −0.349 | 261 c | 0.515 | 142 | 0.533 | 182 | |
| 93 | Plan, UTC, 6 hours, GP, 1 weekb | 0.518 | 190 | 0.016 | 231 | 0.252 | 206 | 0.302 | 205 | −0.408 | 241 c | 0.199 | 223 | |
| 140 | Plan, ED, 6 hours, GP, 2–3 weeksb | 0.413 | 204 | 0.007 | 233 | 0.105 | 229 | 0.535 | 176 | −0.626 | 254 c | −0.003 | 241 c | |
| 141 | Plan, ED, 6 hours, GP, 1 weekb | 0.363 | 210 | −0.008 | 236 | 0.038 | 240 c | 0.127 | 219 | −0.749 | 264 c | −0.066 | 247 c | |
There were instances of variation between seizure scenarios and participant types in terms of exact preference. These are important to note and will be discussed shortly. However, what was most apparent was the sizeable similarity across and between them in terms of what care attributes were important. This raised the possibility that a single CP configuration might be possible to deploy for all target seizure scenarios. This was something explored with stakeholders in the WP3 workshops.
Interestingly, the slight differences that did exist between seizure scenarios and participant types in terms of the direction and strength of effect different attributes appeared to hold face validity. For instance, in terms of the different seizure scenarios, participants ascribed most value to paramedics having access to a patient’s medical records or a care plan when a seizure occurred in public. Our PPI group helped the research team interpret this. They said it was likely because, in public, a PWE is more likely to be unaccompanied by a SO who could share medical history information. Also, it is in these instances that the call for an ambulance would often have been made by a concerned member of the public and the presence of the medical record would provide important context for the incident. Indeed, it could help avoid misinterpretation of the episode. There is the risk that unusual behaviour associated with some seizures can be misinterpreted (e.g. as stemming from intoxication, mental illness or representing disorderly conduct). 203–205
Participants also expressed a stronger preference for an epilepsy specialist to be able to advise the paramedics on the day and for their GP to notified of the event when the seizure presentation was atypical. Our PPI group again helped the research team interpret this. They were of the view that this made intuitive sense. They stated that while still potentially distressing, typical seizures are the manifestations PWE and SOs would have most knowledge of. Consequently, they are the ones they might feel most comfortable in managing. Atypical seizures, however, were the manifestations they would be most concerned about and thus would likely most value specialists guiding paramedics on. The PPI members said the need for attention from an epilepsy specialist after an atypical seizure was a key message frequently relayed to them by their own usual care providers and by seizure first aid resources.
Responsibility for care decisions after a seizure is often delegated to SOs and so it was important to capture their preferences. We found few differences existed between PWE and SOs. The degree of similarity in their preferences lends further support to the possible deployment of a single CP configuration for the target population.
The similarity for the most part in the views of PWE and SOs is perhaps remarkable. SOs were after all instructed to express via the DCE their preferences for the care of the PWE they knew (even if it was different to what they expect the PWE they knew would say). Also, SOs were (as we had anticipated) often ‘representing’ a different part of the target population.
One of the areas of divergence that did exist between PWE and SOs in their preferences related to the attribute ‘Time’ for a ‘Home typical’ seizure. Like PWE, SOs wanted the ‘Time’ it took to be assessed monitored and treated to be < 6 hours. Uniquely though, SOs also expressed a preference for the time to be 2 hours, rather than 1.
This desire for a longer time period in the presence of a paramedic may be explained by the different epilepsy profile of the PWE known by the SOs. For example, they were more likely to have an intellectual disability. This may lead to slightly different care preferences since some epilepsy syndromes with unique presentations are more common in those with an intellectual disability (e.g. Lennox–Gastaut syndrome). 206 The presence of an intellectual disability may also be important because it can take more time to be confident if a person with one is beginning to recover to their baseline health following a seizure (e.g. due to possible communication difficulties). 207 Another characteristic of the PWE known by the SOs that may also be important is they were more likely to be prescribed a rescue medication. Administration of benzodiazepines following a seizure is associated with longer recovery times. 208,209 The aforementioned explanations do, however, remain speculative since we did not have the sample size to formally test them (see Strengths and limitations).
The other notable difference between PWE and SOs in their preferences was for the attribute ‘What happens next’ when imagining an ‘Atypical seizure’. PWE preferred to ‘Stay where they were’, with going to an UTC or an ED associated with increasing reductions in utility from their perspective. For SOs, staying at home was associated with disutility (i.e. preference to avoid). They instead preferred conveyance to a UTC, followed by ED.
This may again be explained by the different epilepsy profiles of the PWE they knew. Rescue medication was more highly prescribed amongst this group, and they reported having had more contact with the ambulance service in the prior 12 months. Ambulance guidelines40 recommend conveyance to a health facility for all those treated with benzodiazepines (unless they have care plan that states otherwise). Awareness of this amongst the SOs might explain their preference for a UTC.
Knowledge exchange event
Three KE events were run with 27 stakeholder representatives (ambulance clinicians, neurologists, epilepsy nurses and commissioners). Having shared the key DCE findings with them, we asked the stakeholders to reflect on which attribute levels represented the optimum balance between service user preference and NHS feasibility.
Stakeholders were found to be broadly of the view that the attribute levels favoured by service users for the different seizure scenarios were largely feasible. Importantly, there was also consensus amongst workshop participants that there was sufficient consistency in the preferences of service users across the seizure scenarios to focus on developing a single CP for epilepsy.
That workshop participants considered service users preferences to be largely feasible may be attributable to the detailed formative work we completed for the DCE survey. WP1c helped ensure the attribute levels and combinations of them presented within the DCE were anticipated to all be within the bounds of realism and likely to be safe.
Across the three KE events, the CP configuration which stakeholders said should be prioritised for implementation was comprised of ambulance clinicians having access to medical records; the person largely staying where they are (if judged to be clinically appropriate); the time being < 6 hours (be it 1, 2 or 3 hours); for crews to have access to specialist advice during the episode; for the GP to be notified of the incident; and for the episode to generate a follow-up appointment with an epilepsy specialist (either within 1 or 2–3 weeks).
Based on stakeholders’ judgement regarding the optimal attribute levels, 18 possible CP configurations can be constructed. The DCE evidence permitted us to estimate their utility and where they would rank out of 288 possible CP configurations (with rank 1 being the one best aligned with service users’ preferences). It was found all 18 of the CPs would be expected to carry high utility. The configurations would be estimated to have a median rank for PWE of 9.5 (range 1–19) for an ‘Atypical seizure’, 30.5 (range 1–71) for a ‘Public typical seizure’ and 42.5 (range 1–60) for ‘Home typical seizure’. The configuration representing current care was ranked by PWE as low as 230/288 for a ‘Public typical seizure’, 247/288 for a ‘Home typical seizure’ and 248/288 for an ‘Atypical seizure’. Thus, any of the 18 CPs should mean that users would be being offered a preferable CP.
Stakeholders also offered other important insights which further underlined the value of the KE exercise. One of these was that while they said the attribute levels so far noted were optimal and, on the whole, would be NHS-feasible, there were circumstances during a calendar year or location when these targets might not be achievable. Thus, flexibility for some of the attributes might be required to maintain deliverability. Namely, during periods of intense pressure on the NHS and if a specialist known to the patient being cared for is not available to provide advice to crews.
To support subsequent discussions about what to do during these periods and what impact the changes could have, we estimated the utility and rankings of the amended CP configurations. The changes to attribute levels did reduce expected utility and as the DCE findings discussed earlier would suggest, the impact of these changes was not equal.
Of most concern was the reduction in utility of the CPs seen when restrictions were placed on attributes so they assumed the levels expected to be needed during periods of ‘winter pressure’. One of these related to increased ‘Time’ for assessment, monitoring and treatment. The change in attribute levels in this circumstance were sufficient to mean seven of the CPs that could be generated could be perceived as ‘worse’ than current practice by service users. This finding highlights the disutility (utility loss) attributable to the increase in time (6 + hours) experienced during ‘winter pressures’. The reduction in utility was less pronounced if the only attribute restriction was that the CP was not permitted to involve a specialist being available to advise attending paramedics.
In addition to helping understand optimal attribute levels, stakeholders also provided granular information that could be helpful for implementation of a new CP configuration (e.g. how best to ‘brand’ it to ambulance crews, what grades of clinicians could to use it and which ambulance performance measures might need to evolve to ensure they support CP use). They also identified which attribute levels likely require the most attention in terms of work and investment to make them a reality. Namely, seizure care plans/access to information about the person’s medical history and how best to use existing specialist capacity.
Strengths and limitations
Survey of service providers
This survey received an excellent response rate of 82%. This is likely attributable to the importance of the problem and concern about the inadequacy of current practice. What also might be important was the survey’s short duration, the manner of invitation and that the survey was carefully piloted. Another strength of the survey is that we asked responding services who reported no planned or recent CP changes about what ‘usual care’ looked like for them. This helped ensure we identified already embedded changes made by the more innovative service providers prior to the 5-year period asked about.
The survey also asked respondents to report on changes their service or ones they work with had or were planning to make. We took this comprehensive approach since we were aware some of the CP changes might lead to service providers other than those primarily responsible for instigating the CP change being asked to deliver them or support it (e.g. for epilepsy specialists to receive referrals from the ambulance service). A potential limitation to this approach is that we cannot rule out ‘double-counting’ of changes (e.g. multiple neurology centres or EDs might report a change being instigated by one regional ambulance service). If this did occur, our estimate on the number of services making or considering a CP change might be exaggerated.
Qualitative interviews with service users and ranking exercise
Going into the DCE phase, the qualitative interviews presented the best available evidence on attributes of importance to service users. This was preferable to relying on expert judgement or researcher opinion.
For the interviews a purposive sample was sought to try to obtain the full range of views about the topic. It is probable that the sample we eventually recruited did not include the full range of views about the topic. Not only were participants drawn from only one English region, but they were also well educated (72% had post-secondary level qualifications compared to ~44% in the UK general population170). This may explain why our findings showed participants’ decision-making was mostly concordant with medical guidelines.
Discrete choice experiment survey
A key strength of the DCE was its rigorous development and thorough description. 173
The strengths of the formative work include (1) the systematic approach to attribute development and refinement that ensured those selected were important to service users, but also NHS-feasible and capable of experimental manipulation, (2) a mixed-methods approach to attribute selection and scenario development, that enabled greater interpretation of the relationship between attributes and the decision-making process and maximised face validity of the vignettes and (3) that its conduct aligned with good practice guidelines. 149,173
An indicator of the strength of the formative work is that having read the seizure scenarios vignettes, ~70% of the PWE said they were familiar with them. A potential limitation of the formative work was that the sampling frames used to recruit PWE and SOs for the qualitative interviews was subject to bias.
When the COVID-19 pandemic began to impact the UK, rapid revisions to the recruitment methods for the formal DCE were required to ensure it could continue. We described in detail what changes were made, their rationale and how the DCE survey was ultimately administered. In providing this information, we conform to reporting guidelines. 191
Our revised approach enabled us to secure usable stated preference data from approximately 600 PWE who had recent contact with the ambulance service and their SOs – a population that is challenging to identify and potentially vulnerable. The sample size was sufficient to examine preferences for all seizure scenarios and for all participant types. It was though insufficient to allow us to complete all the subgroup analyses of interest.
A key strength to our DCE was the representativeness of the sample we recruited. This is likely in part because SOs could still participate in the DCE even if the PWE they knew could not (e.g. due to a lack of capacity). When we compared our sample’s headline characteristics to the target population, we found limited differences. Nevertheless, given how important sample representativeness is to the generalisability of our findings, in the subsequent paragraphs, we consider ways in which our methods might have led it to differ from the parent population.
Firstly, under the revised recruitment and survey approach, all participants were asked to complete the DCE online by themselves. Online self-completion is the most common approach used for DCEs. 134 Ninety-six per cent of households in Great Britain report internet access. 210 Nevertheless, there is the possibility that the revised approach could have excluded from participation a minority of people who could not or did not want to participate in this way. Digital exclusion is linked to wider inequalities in society and is more likely to be faced by people over 65, those on low incomes, and disabled people. 211 Our sample was certainly 8 years younger than the target population, and this could be due to the manner of DCE completion. It is hard to know how the slightly younger age of our participants impacts on preferences. With regard to the other factors that can be associated with digital exclusion, it is pleasing to note our sample was at least comparable to the target population in terms of social deprivation.
Secondly, rather than recruiting most participants directly from the ambulance service, we, in the end, recruited most of our DCE participants by public advertisement. This included the adverts being circulated by epilepsy user groups to their affiliates. The approach enabled recruitment of a sufficient number of participants during the COVID-19 pandemic and permitted us to capture the views of people from across England. Nevertheless, it has been contended that people affiliated with user groups might differ in important ways from those who are not. It is important to note that our DCE subgroup analyses did not detect any significant differences in the care preferences of participants recruited by public advert and those recruited directly from the ambulance service.
Thirdly, participants completed the DCE within the pandemic. Concerns regarding acquiring an infection and requests to ‘socially distance’ could have influenced the preferences people expressed. Our results do not support this possibility. While the pandemic had changed some participants willingness to access certain NHS services at the time, this did not for the most part alter their preferences for postseizure care during ‘normal times’.
Finally, one notable difference between our sample and the target population was the large proportion (86%) of our participants that reported contact with an epilepsy specialist in the 12 months prior to recruitment. The NASH-3 initiative reported only 52% of PWE attending ED would be expected to have had such contact. 44 This may suggest those who took part in the study represented those who are more supported from the target population. However, it may also reflect a difference in methods.
Specifically, we asked participants whether ‘they had seen or spoken to a doctor or nurse that specialises in epilepsy? (such as a neurologist or epilepsy nurse specialist)’. NASH, in contrast, relied on what, if anything, was recorded within the ED records regarding the extent of contact the person had had. It is also possible that during the period of recruitment, specialist services were initiating more contact with PWE in the communities they served due to the pandemic (e.g. to inform them as to how get in contact during periods of COVID-19-related restrictions, to rearrange booked appointments or offer more general advice regarding how to manage epilepsy in the context of the pandemic). We know some services were doing this.
Knowledge exchange events
For WP3, we developed and then used a novel approach that allowed us to work, during a global pandemic, efficiently and collaboratively with representatives from key stakeholder groups.
Strengths include the standardised approach used to share the DCE evidence and the efforts given to ensuring the information was presented in an accessible way. The composition of the groups at the events was also a strength. Different stakeholder groups and persons from different regions of the country sometimes expressed different priorities and experiences. It was important that other stakeholders were aware of these prior to the group making their judgements as to which CP(s) represented the optimal configuration.
The use of well-established NGTs was also a strength. Despite the short duration of the events and that participants were not familiar with one another, each participant shared and discuss their views openly and constructively. Moreover, there were no instances of particular participants dominating the conversation. 200
It was reassuring that the stakeholders at the event largely identified the attribute levels preferred by service users as all being deliverable and realistic. This is likely to be attributable to the robust formative works that informed the DCE.
The KE workshops built on the evidence obtained by the preceding WPs. They enabled the project to identify the configuration/s that appear to strike the optimal balance between service user preference and NHS feasibility and are the strongest candidates for implementation and evaluation. This addressed an important information gap which determined the need for the current project. It is important to acknowledge, though, that their identification is ultimately based on an informed judgement made by stakeholders. It remains to be determined how well they will work in practice. Evidence from the different WPs emphasised how a range of contextual factors might influence whether a CP would operate effectively. Realist evaluation methods could ultimately help understand for whom the candidate CPs do work, to what extent, in which circumstances and how and why. A final, potential limitation of WP3 is that due to the need to restrict participant numbers, there were no representatives at the events from general practice or emergency medicine. They might have shared views and experiences that could have changed the judgement of the group with regard to optimal CP.
Conclusions
By working collaboratively with service users from the target population and with ambulance clinicians, epilepsy specialists and commissioners from around the country, this project has provided clear answers to pressing service delivery questions.
It has shown that for three common seizure scenarios, PWE appear open to paramedics not conveying them to ED. The project also showed in stark terms just how poorly current care aligns with service users’ actual preferences. This, together with existing evidence on how current care is not addressing health inequalities in the target population, helps makes a convincing case for change.
What our project has also signalled is what sort of postseizure care service users do want. It also shows there appear to be limited differences in their preferences for different seizure scenarios. This supports the deployment of a single CP configuration. Broadly speaking, service users want a CP where ambulance clinicians have access to their medical records; they largely prefer to stay where they are rather than being conveyed to ED or a UTC; the time taken for them to be monitored, evaluated and treated is < 6 hours; where crews can be advised by a specialist on the day; their GP is notified of the incident; and the episode results in an appointment being made for them to have a follow-up appointment with an epilepsy specialist (be it within 1 or 2–3 weeks).
Service providers and commissioners were found to be of the view that such a CP configuration could be NHS-feasible within 5–10 years. They identified which attribute levels require the most work for the CP to become a reality.
Not all organisations will be able to immediately deliver the whole CP preferred by service users. Our findings allowed us to infer the expected improvements in utility to service users that individual attribute changes could generate. These inferred estimates could help organisations determine which aspects of the CP to prioritise for development and/or delivery. The attribute levels which had the most consistently strong, positive patterns of influence on stated preference were providing crews with access to the medical records of the PWE being attended to or a care plan and having a specialist be able to advise the emergency clinicians on the day. What had one of the strongest negative impacts on preference and could create disutility was when the time the CP required for the patient to be assessed, monitored and treated was 6 or more hours.
Implications for NHS service commissioning, policy and practice
-
The project has identified what appears to be the optimal CP configuration, namely, acceptable to service users in principle and likely NHS-feasible. To our knowledge, no CP that aligns with this configuration is currently being offered by the NHS. The configuration represents the most promising candidate for ultimate implementation.
-
Our project was not designed to formally test the efficacy of this or any other CP configuration. Our project thus provides limited justification to formally commission a service to offer it. An evaluation of the CP’s efficacy would first be recommended.
-
Pressures on EDs212 and ambulance services213 have intensified since the final KE element of our project was completed. This may incentivise ambulance services to implement an alternative CP before an evaluation has been undertaken.
-
The pressures on acute services are likely to garner further support from service users for an alternative CP. Service users had a consistent preference for a CP in which care is completed within 6 hours. This might now only be consistently achievable if conveyance to the ED is avoided.
-
Should service providers and commissioners be minded to use our findings to inform their choice on which CP configuration to offer, we recommend they factor in an element of evaluation themselves to help understand the CP’s benefits and risks.
-
Not all ambulance services would have access to the infrastructure and relationships with partner organisations to immediately implement the CP configuration considered optimal. Our findings on the extent to which attributes have different degrees of influence on service users’ preference could help stakeholders determine which areas requiring development should be prioritised.
-
The attribute levels which had the most consistently strong pattern of influence on preference and support non-conveyance choices were having a specialist available to advise the emergency clinicians on the day, providing crews with access to the medical records or a care plan for the person they were attending and keeping the time required for the person to be assessed, monitored and treated below 6 hours. Commissioners, policy and service providers could support the development of the systems – such as shared record initiatives – to permit these attribute levels to be offered. The time and effort that would be needed to develop such systems should not be underestimated.
-
Secondary findings from the project provide evidence on how to ‘brand’ a CP to ambulance clinicians to maximise engagement and which ambulance performance measures might need to continue to evolve to facilitate use (i.e. increasing focus on care and outcomes, rather than time targets). They also highlight areas where additional investment might be needed to help ensure service delivery is resilient to ‘winter pressures’ and do not mean the attribute levels change to mean the CP offered now provides ‘disutility’ from the service users’ perspective (i.e. it is worse than the current CP being offered to service users).
-
Identifying eligible people for the DCE survey via the NHS ambulance service directly was a time-consuming process. It required clinical staff from the ambulance service to be trained and then spend substantial time reviewing ambulance records to determine persons eligible for invitation. One reason why was that much of the key data on the ambulance records (PRFs) regarding the patients’ eligibility/characteristics was contained within scanned, ‘hand-written’ free text. This was frequently challenging to decipher and precluded ‘key word’ searches to support the screening process. The ambulance trust we recruited via has since started utilising electronic PRFs. This could speed up identification. Our experience indicates commissioners and services should support the continued implementation, development and use of such systems.
-
There are additional steps service providers and policy-makers could take to support research activity to occur within the ambulance service in a timely way and reduce bureaucracy. Even with an electronic PRF system, our project would still need clinical staff from the ambulance service to review the ePRFs. What could be more efficient would be to embed processes within the records system that ‘strip’ records of confidential data (e.g. names and addresses). This would enable trained individuals not involved in a person’s care to have access to now anonymised records and complete the screening. The Pandemic Respiratory Infection Emergency System Triage (PRIEST) study214 offers important insights on how to do this.
Recommendations for research
-
Using the attribute levels specified by stakeholders as representing the optimum, one of the possible (18) CP configurations should be developed and evaluated for its efficacy.
-
A cluster-randomised controlled trial would be likely to provide the most rigorous evaluation of its efficacy. However, it might not provide evidence soon enough to affect service developments. 215 Alternative evaluation approaches may thus be needed.
-
Evidence from the different elements of the project also emphasises how a range of contextual factors might influence whether a CP would operate effectively. Realist evaluation methods could help understand for whom it does work, to what extent, in which circumstances and how and why.
-
Any evaluation should consider the effects of the CP on short-term (e.g. rates of recontact with urgent and emergency care services, death) and longer-term outcomes (e.g. PWE ‘unknown’ to specialists brought to their attention, improvements in epilepsy outcomes, cost-effectiveness).
-
Data sets that link routine emergency care records with wider care records are beginning to emerge in some English regions. 216 These might enable an efficient evaluation of a CP.
-
This project has considered one important barrier to increased safe non-conveyance. There are other factors that warrant research attention. One is how to address crews’ requests for additional support to allow them to identify persons suitable for non-conveyance. There is also potential to intervene earlier by ensuring PWE and their supporters have the knowledge and confidence to manage certain seizures by themselves, without calling an ambulance.
Additional information
Acknowledgements
We thank the people who so generously participated in this study. We also thank paramedic colleagues at the North West Ambulance Service – Deborah Webb, Kirsty Hardman and Steve Bell – for helping identify persons eligible for invite into the formal DCE survey. Similarly, we are grateful to the user groups Epilepsy Action, Epilepsy Society and the Brain and Spine Foundation for helping circulate the public adverts. We also acknowledge the support and guidance we received from our study’s steering committee [Prof. Tom Quinn (chairperson), Mr Trevor Baldwin, MrsJayne Burton, Prof. Verity Watson, Mr Nigel Rees, Mrs Juliet Bransgrove, Mr Sam Burton and Professors Dan Horner and Khalid Hamandi] and Patient and Public Involvement volunteers. Finally, we acknowledge Ms. Fiona Biermann who kindly narrated the animation.
Contributions of authors
Adam J Noble (https://orcid.org/0000-0002-8070-4352) (Senior Lecturer in Health Services Research) was chief investigator, conceived the study, led its design, supervised and co-ordinated the study, the interpretation of the data and, with Emily Holmes, the writing of the final report.
Pete Dixon (https://orcid.org/0000-0002-2150-5580) (Research Associate, Public Health, Policy and Systems) contributed to the running of, and recruitment for, the Discrete Choice Experiment survey, data curation and description of the participants and reviewed the final report.
Amy Mathieson (https://orcid.org/0000-0002-5360-3644) (Research Associate, Public Health, Policy and Systems) contributed to the running of, and recruitment for, the survey of service providers and the Work Package 1 knowledge exchange workshop. She also helped with the development of the Discrete Choice Experiment survey and the initial stages of recruitment for it and reviewed the final report.
Leone Ridsdale (https://orcid.org/0000-0002-2234-2859) (Professor of Neurology and General Practice) helped in the design of the study, oversaw the running of the Work Package 1 qualitative interviews and reviewed the final report.
Myfanwy Morgan (https://orcid.org/0000-0001-5532-8941) (Professor of Medical Sociology) helped in the design of the study, oversaw the running of the Work Package 1 qualitative interviews with Leone Ridsdale, supervised analysis and reviewed the final report.
Alison McKinlay (https://orcid.org/0000-0002-3271-3502) (Research Associate) was responsible for the day-to-day conduct of the Work Package 1 qualitative interviews, analysis and helped write the final report.
Jon Dickson (https://orcid.org/0000-0002-1361-2714) (Senior Clinical Lecturer) contributed to the design of the research, its conduct and interpretation and reviewed the final report.
Steve Goodacre (https://orcid.org/0000-0003-0803-8444) (Professor of Emergency Medicine) contributed to the design of the research, its conduct, particularly the involvement of stakeholders, interpretation and reviewed the final report.
Mike Jackson (https://orcid.org/0000-0002-0228-3089) (Chief Consultant Paramedic) contributed to the design of the research, supported the involvement of the North-West Ambulance, and reviewed the final report.
Beth Morris (https://orcid.org/0000-0001-5346-4173) (Research Assistant) contributed to the running of, and recruitment for, the Work Package 3 knowledge exchange workshop. She also led with the analysis of the qualitative data from this package and helped write the final report.
Dyfrig Hughes (https://orcid.org/0000-0001-8247-7459) (Professor in Pharmacoeconomics) contributed to the design of the study, supervised the collection of the discrete choice experiment data and its analysis and reviewed the final report.
Anthony Marson (https://orcid.org/0000-0002-6861-8806) (Professor of Neurology) contributed to the design of the research, its conduct, particularly the involvement of stakeholders, interpretation and reviewed the final report.
Emily Holmes (https://orcid.org/0000-0002-0479-5336) (Research Fellow, Pharmacoeconomics), with Adam J Noble, led the design of the study, the development of the Discrete Choice Experiments, analysed the data from them and helped write the final report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/HKQW4129.
Primary conflicts of interest: Adam J Noble was a member of Health Services and Delivery Research (HS&DR) Commissioned Panel, HS&DR Funding Committee and RfPB North West Committee. Steve Goodacre was a member of HTA PCCPI Methods Group, NIHR CTU Standing Advisory Committee, HTA Prioritisation Committee B Methods Group, HTA Prioritisation Committee A Methods Group, HTA Commissioning Committee, HTA Efficient Study Designs – 2, HTA IP Methods Group, HTA Remit and Competitiveness Group, HTA Post-Funding Committee teleconference (POC members to attend), HTA Funding Committee Policy Group (formerly CSG), HTA Clinical Evaluation and Trials Committee and HTA Programme Oversight Committee. Steve Goodacre is also a NIHR Senior Investigator. Dyfrig Hughes was a member of HS&DR Commissioned – Panel Members, HTA Funding Teleconference Members, EME – Funding Committee Members and HTA Clinical Evaluation and Trials Committee. Anthony Marson is a NIHR Senior Investigator and also part funded by NIHR ARC North West Coast. He has no SI projects of relevance to declare.
Patient and public involvement
People with epilepsy (PWE) and their family and friends were at the centre of this project as participants, but also as patient and public involvement (PPI) representatives. As shown below, PPI has been embedded in this project from start to finish.
Design of the research
The project arose as the research team heard of moves towards alternative CPs for ambulance users and were aware that the views of PWE were not being considered. Epilepsy Action – the largest UK user group associated with epilepsy – were also aware and concerned. We thus held a PPI event with the support of Epilepsy Action and the ‘Brain and Spine Foundation’. The context and proposed study were shared with 23 PWE and their SOs (family, friends). Ten of the representatives had had seizures in the prior year and eight had visited a hospital ED. They gave feedback on a draft of the project and suggested changes and ways to ensure it would answer the questions they had, including on ways to capture some indication of the views of PWE who could not themselves due to a severe learning disability. Users were disappointed by the current trajectory and welcomed the current study. Asked how important the proposed project was on a scale from 1 to 10 (10 = extremely important), the average rating was 9. After the project was commissioned, PWE and SOs continued to be actively involved at every stage of its completion.
Developing participant information resources
In the study development stages, we worked with PPI users from Epilepsy Action to develop recruitment materials.
Management of the research
The study was supported and directed by an Independent Steering Committee and a DCE development panel. Both included two service users. A study PPI group of 15 volunteers whose lives were impacted in some way by epilepsy was also informed. They were all supported in their role by Epilepsy Action who have an active PPI scheme. Service users were reimbursed for travel and time according to the INVOLVE framework. One of the key roles of the PPI group was scrutinising the draft version of the DCE survey and sharing their views on its ease of understanding.
Analysing the research and dissemination of research findings
As the results of the study were secured, the service users on the study Steering Group and PPI group were all actively engaged with and helped with our interpretation of the results. Having now finished the study and as we are moving towards dissemination, we shall be seeking to work with users to help us share the findings, including co-presentation at conferences and meetings.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethics approval for WP1b was received from the King’s College London Psychiatry, Nursing and Midwifery Ethics Committee (LRS-18/19-10353). Approval for WP components 1c, 2a, 2b (recruitment via the North West Ambulance Service) and 3 was provided by the Health Research Authority and the National Research Ethics Service Committee, West Midlands, Solihull (19/WM/0012). Approval for WP2b’s recruitment via public advert was provided by the University of Liverpool’s Health and Life Sciences Research Ethics Committee (ref: 7766). Informed consent was obtained from all participants.
Information governance statement
The University of Liverpool is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Liverpool is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here https://www.liverpool.ac.uk/legal/data_protection/.
Publications
Noble AJ, Mathieson A, Ridsdale L, Holmes EA, Morgan M, McKinlay A, et al. Developing patient-centred, feasible alternative care for adult emergency department users with epilepsy: protocol for the mixed-methods observational ‘Collaborate’ project. BMJ Open 2019;9(11):e031696.
McKinlay A, Morgan M, Noble A, Ridsdale L. Patient views on use of emergency and alternative care services for adult epilepsy: a qualitative study. Seizure 2020;80:56–62.
Mathieson A, Marson AG, Jackson M, Ridsdale L, Goodacre S, Dickson JM, Noble AJ. Clinically unnecessary and avoidable emergency health service use for epilepsy: a survey of what English services are doing to reduce it. Seizure 2020;76:156–60. https://doi.org/10.1016/j.seizure.2020.02.012
Holmes E, Dixon P, Mathieson A, Ridsdale L, Morgan M, McKinlay A, et al. Developing an alternative care pathway for emergency ambulance responses for adults with epilepsy: a discrete choice experiment to understand which configuration service users prefer. Part of the COLLABORATE project. Seizure 2024;118:28–37. https://doi.org/10.1016/j.seizure.2024.04.008
Noble AJ, Morris B, Dixon P, Mathieson A, Ridsdale L, Morgan M, et al. Service users’ preferences and feasibility – which alternative care pathway for adult ambulance users achieves the optimal balance? Workshops for the COLLABORATE project. Seizure 2024;118:17–27. https://doi.org/10.1016/j.seizure.2024.04.010
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- McKinlay A, Morgan M, Noble A, Ridsdale L. Patient views on use of emergency and alternative care services for adult epilepsy: a qualitative study. Seizure 2020;80:56-62.
- House of Commons Committee of Public Accounts . Financial Sustainability of the NHS: Forty-Third Report of Session 2016–17, HC 887 2017. www.publications.parliament.uk/pa/cm201617/cmselect/cmpubacc/887/887.pdf (accessed 1 January 2018).
- The King’s Fund . Nine Things We Learnt About Provider Finances in 2016 17 2017. www.kingsfund.org.uk/publications/nine-things-NHS-provider-finances-2016-17 (accessed 1 January 2018).
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 1 January 2018).
- NHS . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/ (accessed 14 May 2019).
- McHale P, Wood S, Hughes K, Bellis MA, Demnitz U, Wyke S. Who uses emergency departments inappropriately and when – a national cross-sectional study using a monitoring data system. BMC Med 2013;11.
- O’Keeffe C, Mason S, Jacques R, Nicholl J. Characterising non-urgent users of the emergency department (ED): a retrospective analysis of routine ED data. PLOS ONE 2018;13.
- NHS . NHS Data Model and Dictionary: EMERGENCY CARE DEPARTMENT TYPE 2021. https://datadictionary.nhs.uk/attributes/emergency_care_department_type.html (accessed 9 August 2021).
- NHS Digital . Non-Urgent A&Amp;E Attendances 2021. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/innovative-uses-of-data/demand-on-healthcare/unnecessary-a-and-e-attendances#definitions (accessed 9 August 2021).
- NHS Digital . NHS Digital. Hospital Accident and Emergency Activity 2018–19 2019.
- Miles J, O’Keeffe C, Jacques R, Stone T, Mason S. 17 Exploring ambulance conveyances to the emergency department: a descriptive analysis of non-urgent transports. Emerg Med J 2017;34:A872-3.
- NHS England . NHS Outcomes Framework Indicators: Feb 2017 Release 2017. www.gov.uk/government/statistics/nhs-outcomes-framework-indicators-feb-2017-release (accessed 1 January 2018).
- Ridsdale L, Charlton J, Ashworth M, Richardson MP, Gulliford MC. Epilepsy mortality and risk factors for death in epilepsy: a population-based study. Br J Gen Pract 2011;61:e271-8.
- Moran NF, Poole K, Bell G, Solomon J, Kendall S, McCarthy M, et al. Epilepsy in the United Kingdom: seizure frequency and severity, anti-epileptic drug utilization and impact on life in 1652 people with epilepsy. Seizure 2004;13:425-33.
- Jacoby A, Snape D, Baker GA. Determinants of quality of life in people with epilepsy. Neurol Clin 2009;27:843-63.
- Institute of Medicine . Epilepsy Across the Spectrum: Promoting Health and Understanding 2012.
- Hart YM, Shorvon SD. The nature of epilepsy in the general population. II. Medical care. Epilepsy Res 1995;21:51-8.
- Jacoby A, Buck D, Baker G, McNamee P, Graham-Jones S, Chadwick D. Uptake and costs of care for epilepsy: findings from a U.K. regional study. Epilepsia 1998;39:776-86.
- Kitson A, Shorvon S, Group CSA. Services for Patients with Epilepsy. London; 2000.
- Dixon PA, Kirkham JJ, Marson AG, Pearson MG. National Audit of Seizure management in Hospitals (NASH): results of the national audit of adult epilepsy in the UK. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-007325.
- House of Commons Committee of Public Accounts . Services to People With Neurological Conditions (HC 502) 2015. www.publications.parliament.uk/pa/cm201516/cmselect/cmpubacc/502/502.pdf (accessed 12 October 2022).
- Ridsdale L, McCrone P, Morgan M, Goldstein L, Seed P, Noble A. Can an epilepsy nurse specialist-led self-management intervention reduce attendance at emergency departments and promote well-being for people with severe epilepsy? A non-randomised trial with a nested qualitative phase. Health Serv Deliv Res 2013;1:1-128. https://doi.org/10.3310/hsdr01090.
- Reuber M, Hattingh L, Goulding PJ. Epileptological emergencies in accident and emergency: a survey at St James’s University Hospital, Leeds. Seizure 2000;9:216-20. https://doi.org/10.1053/seiz.2000.0386.
- Ryan J, Nash S, Lyndon J. Epilepsy in the accident and emergency department: developing a code of safe practice for adult patients. South East and South West Thames Accident and Emergency Specialty Sub-committees. J Accid Emerg Med 1998;15:237-43.
- Bardsley M, Blunt I, Davies S, Dixon J. Is secondary preventive care improving? Observational study of 10-year trends in emergency admissions for conditions amenable to ambulatory care. BMJ Open 2013;3.
- Bruce M, Griffiths C, Brock A. Trends in mortality and hospital admissions associated with epilepsy in England and Wales during the 1990s. Health Stat Q 2004;21:23-9.
- Whiston S, Coyle B, Chappel D. Health Needs Assessment for Long Term Neurological Conditions in North East England. Stockton on Tees: North East Public Health Observatory; 2009.
- National Institute for Health and Care Excellence (NICE) . Services for the Diagnosis and Management of the Epilepsies in Adults, Children and Young People: Commissioning Guide 2013. www.nice.org.uk/guidance/qs26/resources/services-for-the-diagnosis-and-management-of-the-epilepsies-in-adults-children-and-young-people-commissioning-guide-317820637/chapter/3-Assessing-service-levels-for-the-diagnosis-and-management-of-the-epilepsies#ftn.footnote_19 (accessed 1 January 2018).
- Noble AJ, Goldstein LH, Seed P, Glucksman E, Ridsdale L. Characteristics of people with epilepsy who attend emergency departments: prospective study of metropolitan hospital attendees. Epilepsia 2012;53:1820-8.
- Egede LE. Patterns and correlates of emergency department use by individuals with diabetes. Diabetes Care 2004;27:1748-50. https://doi.org/27/7/1748.
- Emtner M, Hedin A, Andersson M, Janson C. Impact of patient characteristics, education and knowledge on emergency room visits in patients with asthma and COPD: a descriptive and correlative study. BMC Pulm Med 2009;9. https://doi.org/10.1186/1471-2466-9-43.
- National Society for Epilepsy . When to Dial 999 2012. www.epilepsysociety.org.uk/AboutEpilepsy/Firstaid/Whentodial999 (accessed 9 February 2020).
- British Epilepsy Association . What to Do When Someone Has a Seizure 2013. www.epilepsy.org.uk/info/firstaid (accessed 12 October 2022).
- NHS Choices . What to Do If Someone Has a Seizure (Fit) 2013. www.nhs.uk/Livewell/Epilepsy/Pages/Ifyouseeaseizure.aspx (accessed 12 October 2022).
- Pearson M, Marson T, Dixon P, Scott K. National Audit of Seizure Management in Hospitals: St Elsewhere’s Clinical Report 2014. www.nashstudy.org.uk/Newsletters/St%20Elsewhere%27s%20Clinical%20Report%20NASH%202.pdf (accessed 1 January 2018).
- Pearson M, Marson T, Dixon P, Billington K. National Audit of Seizure Management in Hospitals: St Elsewhere’s Clinical Report 2012. www.nashstudy.org.uk/Newsletters/St%20Elsewhere%27s%20NASH%20Report.pdf (accessed 1 January 2018).
- Girot M, Hubert H, Richard F, Chochoi M, Deplanque D, Derambure P, et al. Use of emergency departments by known epileptic patients: an underestimated problem?. Epilepsy Res 2015;113:1-4.
- Epilepsy Action . What to Do When Someone Has a Seizure 2016. www.epilepsy.org.uk/info/firstaid/what-to-do (accessed 4 April 2019).
- NHS Choices . What to Do If Someone Has a Seizure (Fit) 2017. www.nhs.uk/conditions/what-to-do-if-someone-has-a-seizure-fit/ (accessed 4 April 2019).
- Joint Royal Colleges Ambulance Liaison Committee/Association of Ambulance Chief Executives . JRCALC Clinical Guidelines 2019.
- Osborne A, Taylor L, Reuber M, Grünewald RA, Parkinson M, Dickson JM. Pre-hospital care after a seizure: evidence base and United Kingdom management guidelines. Seizure 2015;24:82-7.
- Limm EI, Fang X, Dendle C, Stuart RL, Egerton Warburton D. Half of all peripheral intravenous lines in an Australian tertiary emergency department are unused: pain with no gain?. Ann Emerg Med 2013;62:521-5.
- Allen L, Jones CT. Emergency department use of computed tomography in children with epilepsy and breakthrough seizure activity. J Child Neurol 2007;22:1099-101.
- Taylor C, Dixon P, Powell G, Buchanan M, Pullen A, Pearson M, et al. St Elsewhere’s Data Analysis and Methodology Report 2020 (NASH3) 2020. www.nashstudy.org.uk/Newsletters/NASH3%20St%20Elsewhere%20Report%202020.pdf (accessed 9 August 2021).
- Hanna JN, Black M, Sander JW, Smithson H, Appleton R, Brown S, et al. National Sentinel Clinical Audit of Epilepsy-related Death. London: The Stationery Office; 2002.
- Noble AJ, Marson AG, Tudur-Smith C, Morgan M, Hughes DA, Goodacre S, et al. Seizure first aid training’ for people with epilepsy who attend emergency departments, and their family and friends: study protocol for intervention development and a pilot randomised controlled trial. BMJ Open 2015;5.
- Noble AJ, Morgan M, Virdi C, Ridsdale L. A nurse-led self-management intervention for people who attend emergency departments with epilepsy: the patients’ view. J Neurol 2013;260:1022-30.
- Ridsdale L, Virdi C, Noble A, Morgan M. Explanations given by people with epilepsy for using emergency medical services: a qualitative study. Epilepsy Behav 2012;25:529-33. https://doi.org/10.1016/j.yebeh.2012.09.034.
- Ridsdale L, Kwan I, Cryer C. The effect of a special nurse on patients’ knowledge of epilepsy and their emotional state: Epilepsy Evaluation Care Group. Br J Gen Pract 1999;49:285-9.
- Ridsdale L, Kwan I, Cryer C. Newly diagnosed epilepsy: can nurse specialists help? A randomized controlled trial: Epilepsy Care Evaluation Group. Epilepsia 2000;41:1014-9.
- NHS England . Next Steps on the NHS Five Year Forward View 2017. www.england.nhs.uk/wp-content/uploads/2017/03/NEXT-STEPS-ON-THE-NHS-FIVE-YEAR-FORWARD-VIEW.pdf (accessed 1 January 2018).
- Alderwick H, Dunn P, McKenna H, Walsh N, Ham C. Sustainability and Transformation Plans in the NHS: How Are They Being Developed in Practice?. The King’s Fund; 2016.
- National Institute for Health and Care Excellence (NICE) . Epilepsy in Adults: Briefing Paper 2012. www.nice.org.uk/guidance/qs26/documents/epilepsy-in-adults-briefing-paper2 (accessed 1 January 2018).
- Centre NCG . Pharmacological Update of Clinical Guideline 20 – The Epilepsies: The Diagnosis and Management of the Epilepsies in Adults and Children in Primary and Secondary Care – Methods, Evidence and Recommendations 2012. www.ncbi.nlm.nih.gov/pubmedhealth/PMH0068980/ (accessed 1 January 2018).
- Imison C, Curry N, Holder H, Castle-Clarke S, Nimmons D, Appleby J, et al. Shifting the Balance of Care: Great Expectations 2017. www.nuffieldtrust.org.uk/files/2017-02/shifting-the-balance-of-care-summary-web-final.pdf (accessed 31 March 2019).
- Dickson JM, Taylor LH, Shewan J, Baldwin T, Grünewald R, Reuber M. Cross-sectional study of the prehospital management of adult patients with a suspected seizure (EPIC1). BMJ Open 2016;6.
- Day J. Care Given to Patients Treated for Epileptic Seizure by the London Ambulance Service. London: London Ambulance Service Clinical Audit and Research Unit; 2011.
- Marks PJ, Daniel TD, Afolabi O, Spiers G, Nguyen-Van-Tam JS. Emergency (999) calls to the ambulance service that do not result in the patient being transported to hospital: an epidemiological study. Emerg Med J 2002;19.
- Ebben R, Vloet L, Speijers RF, Tönjes NW, Loef J, Pelgrim T, et al. A patient-safety and professional perspective on non-conveyance in ambulance care: a systematic review. Scand J Trauma Resusc Emerg Med 2017;25.
- Oosterwold J, Sagel D, Berben S, Roodbol P, Broekhuis M. Factors influencing the decision to convey or not to convey elderly people to the emergency department after emergency ambulance attendance: a systematic mixed studies review. BMJ Open 2018;8.
- Noble A, Snape D, Goodacre S, Jackson M, Sherratt F, Pearson M, et al. Qualitative study of paramedics’ experiences of managing seizures: a national perspective from England. BMJ Open 2016;6.
- NHS Digital . Summary Care Records (SCR) 2020. https://digital.nhs.uk/services/summary-care-records-scr (accessed 17 August 2021).
- National Institute for Health and Care Excellence (NICE) . Epilepsy in Adults. Quality Standard [QS26] 2013. www.nice.org.uk/guidance/qs26/chapter/Quality-statement-6-Prolonged-or-repeated-seizures (accessed 9 August 2021).
- International League Against Epilepsy – UK Chapter . Emergency Health Services for Epilepsy: The Proceedings of an Expert Workshop 2016. http://ilaebritish.org.uk/epilepsy-emergency-care/ (accessed 1 January 2018).
- NHS England . Urgent Treatment Centres – Principles and Standards Superseded 2017. www.england.nhs.uk/wp-content/uploads/2017/07/urgent-treatment-centres%E2%80%93principles-standards.pdf (accessed 15 January 2022).
- Urgent and Emergency Care Review Team . Transforming Urgent and Emergency Care Services in England 2013. www.nhs.uk/nhsengland/keogh-review/documents/uecr.ph1report.appendix%201.evbase.fv.pdf (accessed 19 March 2019).
- NHS England . Transforming Urgent and Emergency Care Services in England: Clinical Models for Ambulance Services. Urgent and Emergency Care Review Programme Team 2015. www.nhs.uk/nhsengland/keogh-review/documents/uecr-ambulance-guidance-fv.pdf (accessed 1 January 2018).
- NHS England . High Quality Care for All, Now and for Future Generations: Transforming Urgent and Emergency Care Services in England-Urgent and Emergency Care Review End of Phase 1 Report 2013. www.england.nhs.uk/wp-content/uploads/2013/06/urg-emerg-care-ev-bse.pdf (accessed 1 January 2018).
- Snooks H, Kearsley N, Dale J, Halter M, Redhead J, Cheung W. Towards primary care for non-serious 999 callers: results of a controlled study of ‘Treat and Refer’ protocols for ambulance crews. Qual Saf Health Care 2004;13:435-43.
- National Audit Office . Improving Emergency Care in England. HC 1075 Session 2003–2004 2004. www.nao.org.uk/wp-content/uploads/2004/10/03041075.pdf (accessed 1 January 2018).
- East of England Ambulance Service NHS Trust . Conveyance and Discharge of Care Policy 2011. www.eastamb.nhs.uk/Policies/clinical/conveyance-and-discharge-policy.pdf (accessed 1 January 2018).
- Isle of Wight NHS Trust . Ambulance Service Conveyance Policy 2013. www.iow.nhs.uk/Downloads/Policies/Ambulance%20Service%20Conveyance%20Policy.pdf (accessed 1 January 2018).
- East Midlands Ambulance Service NHS Trust . Quality Account 2016 17 2017. www.emas.nhs.uk/EasySiteWeb/GatewayLink.aspx?alId=4519 (accessed 1 January 2017).
- North East Ambulance Service NHS Foundation Trust . Quality Account for the Year Ending 31st March 2012 2012. www.neas.nhs.uk/media/63718/102878_-_quality_report.pdf (accessed 1 January 2018).
- North West Ambulance Service NHS Trust . Paramedic Pathfinder and Community Care Pathways 2014. www.nwas.nhs.uk/DownloadFile.ashx?id=286&page=16586 (accessed 1 January 2018).
- South East Coast Ambulance Service NHS Foundation Trust . Trust Board Report, NHS Pathways Triage System, Post Implementation Report 2012. www.secamb.nhs.uk/about_us/idoc.ashx?docid=1b1f14cf-520d-479f-a022 (accessed 1 January 2018).
- South Central Ambulance Service NHS Foundation Trust . Clinical Services Policy and Procedure (CSPP No. 7), Care Pathway and Policy Procedures 2016. www.scas.nhs.uk/wp-content/uploads/Care-Pathway-Policy.pdf (accessed 1 January 2018).
- Eastwood K, Morgans A, Smith K, Stoelwinder J. Secondary triage in prehospital emergency ambulance services: a systematic review. Emerg Med J 2015;32:486-92.
- Brotherton J. Emergency Services Review Good Practice Guide for Ambulance Services and Their Commissioners. Office of the Strategic Health Authorities; 2009.
- Walker A, James C, Bannister M, Jobes E. Evaluation of a diabetes referral pathway for the management of hypoglycaemia following emergency contact with the ambulance service to a diabetes specialist nurse team. Emerg Med J 2006;23:449-51.
- Mikolaizak AS, Simpson PM, Tiedemann A, Lord SR, Caplan GA, Bendall JC, et al. Intervention to prevent further falls in older people who call an ambulance as a result of a fall: a protocol for the iPREFER randomised controlled trial. BMC Health Serv Res 2013;13.
- Snooks HA, Anthony R, Chatters R, Dale J, Fothergill RT, Gaze S, et al. Paramedic assessment of older adults after falls, including community care referral pathway: cluster randomized trial. Ann Emerg Med 2017;70:495-505.e28.
- Rees N, Bulger J, Dewar R, Edwards A, Evans B, Moore C, et al. Transient ischaemic attack 999 Emergency Referral (TIER): feasibility trial. Emerg Med J 2016;33:e13.1-13.
- Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med 2008;35:358-62.
- Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implement Sci 2010;5.
- Fisher JD, Freeman K, Clarke A, Spurgeon P, Smyth M, Perkins GD, et al. Patient safety in ambulance services: a scoping review. Health Serv Deliv Res 2015;3:1-250.
- Turner J, Coster J, Chambers D, Cantrell A, Phung V, Knowles E, et al. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv Deliv Res 2015;3.
- Snooks HA, Dale J, Hartley-Sharpe C, Halter M. On-scene alternatives for emergency ambulance crews attending patients who do not need to travel to the accident and emergency department: a review of the literature. Emerg Med J 2004;21:212-5.
- National Audit Office . NHS Ambulance Services HC 972 2017. www.nao.org.uk/wp-content/uploads/2017/01/NHS-Ambulance-Services.pdf (accessed 19 June 2017).
- NHS England . Ambulance Quality Indicators Data 2018–19 2019. www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality-indicators/ambulance-quality-indicators-data-2018-19/ (accessed 5 February 2024).
- House of Commons Health Committee . Winter Pressure in Accident and Emergency Departments, 2016 HC 277 2016. https://publications.parliament.uk/pa/cm201617/cmselect/cmhealth/277/277.pdf (accessed 15 January 2022).
- O’Cathain A, Knowles E, Bishop-Edwards L, Coster J, Cum A, Jacques R, et al. Understanding variation in ambulance service non-conveyance rates: a mixed methods study. Health Serv Deliv Res 2018;28.
- Turner J, Coster J, Chambers D, Phung V-H, Knowles E, Bradbury D, et al. What evidence is there on the effectiveness of different models of delivering urgent care? A rapid review. Health Serv Deliv Res 2015;3.
- Coster J, O’Cathain A, Jacques R, Crum A, Siriwardena AN, Turner J. Outcomes for patients who contact the emergency ambulance service and are not transported to the emergency department: a data linkage study. Prehosp Emerg Care 2019;23:566-77.
- Keene T, Davis M, Brook C. Characteristics and outcomes of patients assessed by paramedics and not transported to hospital: a pilot study. Australas J Paramed 2015;12:1-8.
- Machen I, Dickinson A, Williams J, Widiatmoko D, Kendall S. Nurses and paramedics in partnership: perceptions of a new response to low-priority ambulance calls. Accid Emerg Nurs 2007;15:185-92.
- NHS England . Friends and Family Test Data – January 2020 2020. https://www.england.nhs.uk/publication/friends-and-family-test-data-january-2020/ (accessed 5 February 2024).
- King R, Oprescu F, Lord B, Flanagan B. Patient experience of non-conveyance following emergency ambulance service response: a scoping review of the literature. Australas Emerg Care 2020;S2588-994X.
- Jones CM, Wasserman EB, Li T, Shah MN. Acceptability of alternatives to traditional emergency care: patient characteristics, alternate transport modes, and alternate destinations. Prehosp Emerg Care 2015;19:516-23.
- Ipsos Mori . North East Ambulance Service Patient Experience Survey 2017. www.neas.nhs.uk/media/136931/neas_2017_presentation_version_3_final.pdf (accessed 12 January 2021).
- Togher FJ, O’Cathain A, Phung VH, Turner J, Siriwardena AN. Reassurance as a key outcome valued by emergency ambulance service users: a qualitative interview study. Health Expect 2015;18:2951-61.
- Scuffham PA, Moretto N, Krinks R, Burton P, Whitty JA, Wilson A, et al. Engaging the public in healthcare decision-making: results from a Citizens’ Jury on emergency care services. Emerg Med J 2106;33:782-8.
- Snooks H, Foster T, Nicholl J. Results of an evaluation of the effectiveness of triage and direct transportation to minor injuries units by ambulance crews. Emerg Med J 2004;21:105-11.
- Sherratt FC, Snape D, Goodacre S, Jackson M, Pearson M, Marson AG, et al. Paramedics’ views on their seizure management learning needs: a qualitative study in England. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014024.
- Michie S, West R, Campbell R, Brown J, Gainforth H. ABC of Behaviour Change Theories. London: Silverback Publishing; 2014.
- NHS England . Commissioning for Quality and Innovation (CQUIN) Indicator Specification 2017–2019 2017. www.england.nhs.uk/publication/cquin-indicator-specification/ (accessed 1 January 2018).
- Burrell L, Noble A, Ridsdale L. Decision-making by ambulance clinicians in London when managing patients with epilepsy: a qualitative study. Emerg Med J 2013;30:236-40.
- Sherratt F, Snape D, Goodacre S, Jackson M, Pearson M, Marson A, et al. Paramedics’ views on their seizure management learning needs: a qualitative study in England. BMJ Open 2017;7.
- Luciano AL, Shorvon SD. Results of treatment changes in patients with apparently drug-resistant chronic epilepsy. Ann Neurol 2007;62:375-81.
- Leach JP, Lauder R, Nicolson A, Smith DF. Epilepsy in the UK: misdiagnosis, mistreatment, and undertreatment? The Wrexham area epilepsy project. Seizure 2005;14:514-20.
- Smith D, Dafalla B, Chadwick DW. The misdiagnosis of epilepsy and the management of refractory epilepsy in a specialist clinic. QJM: Mon J Assoc Physicians 1999;92:15-23.
- National Institute for Health and Care Excellence . The Epilepsies: The Diagnosis and Management of the Epilepsies in Adults and Children in Primary and Secondary Care. NICE Clinical Guideline 137 2012. http://guidance.nice.org.uk/CG137/NICEGuidance/pdf/English (accessed 19 March 2018).
- Grainger R, Pearson M, Dixon P, Devonport E, Timoney M, Bodger K, et al. Referral patterns after a seizure admission in an English region: an opportunity for effective intervention? An observational study of routine hospital data. BMJ Open 2016;6.
- Morrish PK. Inadequate neurology services undermine patient care in the UK. Br Med J 2015;350.
- Epilepsy Action . Epilepsy in England: Time for Change 2009. www.epilepsy.org.uk/sites/epilepsy/files/images/campaigns/Epilepsy_in_England_-_Time_for_change_report.pdf (accessed 19 June 2017).
- Sander JW. The use of antiepileptic drugs – principles and practice. Epilepsia 2004;45:28-34.
- Ashworth M, Seed P, Armstrong D, Durbaba S, Jones R. The relationship between social deprivation and the quality of primary care: a national survey using indicators from the UK Quality and Outcomes Framework. Br J Gen Pract 2007;57:441-8.
- Frostholm L, Fink P, Christensen KS, Toft T, Oernboel E, Olesen F, et al. The patients’ illness perceptions and the use of primary health care. Psychosom Med 2005;67:997-1005.
- Lowe R, Porter A, Snooks H, Button L, Evans BA. The association between illness representation profiles and use of unscheduled urgent and emergency health care services. Br J Health Psychol 2011;16:862-79.
- Martin R, Leventhal H. Handbook of Clinical Health Psychology. Washington, DC: American Psychological Association; 2004.
- Ross J, Stefan H, Schäuble B, Day R, Sander JW. European survey of the level of satisfaction of patients and physicians in the management of epilepsy in general practice. Epilepsy Behav 2010;19:36-42.
- Booker MJ, Purdy S, Shaw ARG. Seeking ambulance treatment for ‘primary care’ problems: a qualitative systematic review of patient, carer and professional perspectives. BMJ Open 2017;7.
- Whitehead K, Kandler R, Reuber M. Patients’ and neurologists’ perception of epilepsy and psychogenic nonepileptic seizures. Epilepsia 2013;54:708-17.
- Thompson R, Linehan C, Glynn M, Kerr MP. A qualitative study of carers’ and professionals’ views on the management of people with intellectual disability and epilepsy: a neglected population. Epilepsy Behav 2013;28:379-85.
- Dickson JM, Rawlings GH, Grünewald RA, Miles K, Mack C, Heywood T, et al. An alternative care pathway for suspected seizures in pre-hospital care: a service evaluation. Br Paramed J 2017;2:22-8.
- Burstein JL, Henry MC, Alicandro J, Gentile D, Thode HC, Hollander JE. Outcome of patients who refused out-of-hospital medical assistance. Am J Emerg Med 1996;14:23-6.
- Bautista RE, Glen ET, Wludyka PS, Shetty NK. Factors associated with utilization of healthcare resources among epilepsy patients. Epilepsy Res 2008;79:120-9. https://doi.org/10.1016/j.eplepsyres.2008.01.003.
- Allard J, Shankar R, Henley W, Brown A, McLean B, Jadav M, et al. Frequency and factors associated with emergency department attendance for people with epilepsy in a rural UK population. Epilepsy Behav 2017;68:192-5.
- Public Health England . The NHS Atlas of Variation in Healthcare: Reducing Unwarranted Variation to Increase Value and Improve Quality 2016. www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=2&cad=rja&uact=8&ved=0ahUKEwiO7OnKgszUAhVBKVAKHYAsBH8QFggtMAE&url=http%3A%2F%2Ffingertips.phe.org.uk%2Fdocuments%2FAtlas_2015%2520Compendium.pdf&usg=AFQjCNGHTh-dyojlDBlL8oAItOVWTmRTYw&sig2=66tZEpM1wbh87_PyaqDOoQ (accessed 19 June 2017).
- QIPP/Right Care . The NHS Atlas of Variation in Healthcare 2010. https://fingertips.phe.org.uk/documents/Atlas_2010%20Compendium.pdf (accessed 5 February 2024).
- Right Care . The NHS Atlas of Variation in Healthcare: Reducing Unwarranted Variation to Increase Value and Improve Quality 2011. www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&cad=rja&uact=8&ved=0ahUKEwjmgOTshMzUAhWgHsAKHfeAD3YQFggtMAA&url=https%3A%2F%2Ffingertips.phe.org.uk%2Fdocuments%2FAtlas_2011%2520Compendium.pdf&usg=AFQjCNGpPwHEBvLA8VsAaRQVp3svjjRJjw&sig2=v5aebVj6Gimqtp9-b-l9gw (accessed 19 June 2017).
- Food and Drug Administration . Patient Preference Information – Voluntary Submission, Review in Premarket Approval Applications, Humanitarian Device Exemption Applications, and De Novo Requests, and Inclusion in Decision Summaries and Device Labeling: Guidance for Industry, Food and Drug Administration Staff, and Other Stakeholders 2016. www.fda.gov/media/92593/download (accessed 10 August 2021).
- Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health: a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 2011;14:403-13.
- Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past, present and future. PharmacoEcon 2019;37:201-26.
- van Overbeeke E, Janssens R, Whichello C, Schölin Bywall K, Sharpe J, Nikolenko N, et al. Design, conduct, and use of patient preference studies in the medical product life cycle: a multi-method study. Front Pharmacol 2019;10.
- Hall J, Viney R, Haas M, Louviere JJ. Using stated preference discrete choice modelling to evaluate health care programs. J Bus Res 2004;57:1026-32.
- Lancaster K. New approach to consumer theory. J Polit Economy 1966;74:132-57.
- Manjunath R, Yang J-C, Ettinger AB. Patients’ preferences for treatment outcomes of add-on antiepileptic drugs: a conjoint analysis. Epilepsy Behav 2012;24:474-9.
- Powell G, Holmes EA, Plumpton CO, Ring A, Baker GA, Jacoby A, et al. Pharmacogenetic testing prior to carbamazepine treatment of epilepsy: patients’ and physicians’ preferences for testing and service delivery. Br J Clin Pharmacol 2015;80:1149-59.
- Wijnen BFM, de Kinderen RJA, Colon AJ, Dirksen CD, Essers BAB, Hiligsmann M, et al. Eliciting patients’ preferences for epilepsy diagnostics: a discrete choice experiment. Epilepsy Behav 2014;31:102-9.
- Mühlbacher AC, Juhnke C, Beyer AR, Garner S. Patient-focused benefit-risk analysis to inform regulatory decisions: the European Union Perspective. Value Health 2016;19:734-40.
- US Food and Drug Administration . Patient Preference Information – Voluntary Submission, Review in Premarket Approval Applications, Humanitarian Device Exemption Applications, and De Novo Requests, and Inclusion in Decision Summaries and Device Labeling. Guidance for Industry, Food and Drug Administration Staff, and Other Stakeholders 2016. www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm446680.pdf (accessed 1 January 2018).
- Linley WG, Hughes DA. Decision-makers’ preferences for approving new medicines in Wales: a discrete-choice experiment with assessment of external validity. PharmacoEcon 2013;31:345-55.
- Telser H, Zweifel P. Validity of discrete-choice experiments evidence for health risk reduction. Appl Econ 2007;39:69-78.
- Ryan M, Watson V. Comparing welfare estimates from payment card contingent valuation and discrete choice experiments. Health Econ 2009;18:389-401.
- Quaife M, Terris-Prestholt F, Di Tanna GL, Vickerman P. How well do discrete choice experiments predict health choices? A systematic review and meta-analysis of external validity. Eur J Health Econ 2018;19:1053-66.
- Johnson FR, Lancsar E, Marshall D, Kilambi V, Mühlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health 2013;16:3-13.
- Hauber AB, González JM, Groothuis-Oudshoorn CG, Prior T, Marshall DA, Cunningham C, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health 2016;19:300-15.
- Coast J, Al-Janabi H, Sutton EJ, Horrocks SA, Vosper AJ, Swancutt DR, et al. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ 2012;21:730-41.
- Mangham LJ, Hanson K, McPake B. How to do (or not to do) … Designing a discrete choice experiment for application in a low-income country. Health Policy Plan 2009;24.
- Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ Open 2000;320:1530-3.
- Michie S, West R, Rogers MB, Bonell C, Rubin GJ, Amlôt R. Reducing SARS-CoV-2 transmission in the UK: a behavioural science approach to identifying options for increasing adherence to social distancing and shielding vulnerable people. Br J Health Psychol 2020;25:945-56.
- Greene JC, Caracelli VJ, Graham WF. Toward a conceptual framework for mixed-method evaluation designs. Educ Eval Policy Anal 1989;11:255-74.
- Mathieson A, Marson AG, Jackson M, Ridsdale L, Goodacre S, Dickson JM, et al. Clinically unnecessary and avoidable emergency health service use for epilepsy: a survey of what English services are doing to reduce it. Seizure 2020;76:156-60.
- Medical Research Council and Health Research Authority . Is My Study Research? 2019. www.hra-decisiontools.org.uk/research/ (accessed 11 August 2021).
- Association of Ambulance Chief Executives . Structure of the UK Ambulance Services 2021. https://aace.org.uk/uk-ambulance-service/ (accessed 12 August 2021).
- NHS England . D04. Neurosciences 2017. www.england.nhs.uk/wp-content/uploads/2013/06/d04-neurosci-spec-neuro.pdf (accessed 1 January 2018).
- Association of British Neurologists . Acute Neurology Services Survey 2017 2017. www.theabn.org/media/Documents/Acute%20Neurology/ABN%20acute%20neurology%20survey%20final%2013%20March%202017.pdf (accessed 1 March 2019).
- Brain and Spine Foundation . List of Neurocentres in the UK n.d. www.brainandspine.org.uk/wp-content/uploads/2018/03/BSF_List-of-Neurocentres-in-the-UK.pdf (accessed 25 April 2019).
- Health and Social Care Information Centre . Summary Report 7, Hospital Accident and Emergency Activity, 2016–17 2017.
- NHS Digital . Hospital Accident and Emergency Activity: 2017–18 2018. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-accident-emergency-activity/2017-18 (accessed 5 February 2024).
- Peterson CL, Walker C, Coleman H. ‘I hate wasting the hospital’s time’: experiences of emergency department admissions of Australian people with epilepsy. Epilepsy Behav 2019;90:228-32.
- Male LR, Noble A, Snape DA, Dixon P, Marson T. Perceptions of emergency care using a seizure care pathway for patients presenting to emergency departments in the North West of England following a seizure: a qualitative study. BMJ Open 2018;8.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57.
- Walker ER, Bamps Y, Burdett A, Rothkopf J, Diiorio C. Social support for self-management behaviors among people with epilepsy: a content analysis of the WebEase program. Epilepsy Behav 2012;23:285-90.
- Kralj-Hans I, Goldstein LH, Noble AJ, Landau S, Magill N, McCrone P, et al. Self-Management education for adults with poorly controlled epILEpsy (SMILE (UK)): a randomised controlled trial protocol. BMC Neurol 2014;14.
- Ridsdale L, Wojewodka G, Robinson E, Noble AJ, Morgan M, Taylor S, et al. The effectiveness of a group self-management education course for adults with poorly controlled epilepsy, SMILE (UK): a randomised controlled trial. Epilepsia n.d.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage Publications; 2003.
- Smith J, Firth J. Qualitative data analysis: the framework approach. Nurse Res 2011;18:52-6.
- Office for National Statistics . A Comparison of the 2011 Census and the Labour Force Survey (LFS) Labour Market Indicators 2012. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/acomparisonofthe2011censusandthelabourforcesurveylfslabourmarketindicators/2012-12-11 (accessed 25 May 2016).
- West London Mental Health NHS Trust . Policy: S42 Seizure and Epilepsy Policy 2018. www.westlondon.nhs.uk/wp-content/uploads/2018/12/S42-Seizures-and-Epilepsy-policy.pdf (accessed 1 April 2020).
- National Institute for Health and Care Excellence . Epilepsy in Children and Young People – Quality Statement 4: Epilepsy Care Plan 2013. www.nice.org.uk/guidance/qs27/chapter/Quality-statement-4-Epilepsy-care-plan (accessed 12 August 2021).
- Hollin IL, Craig BM, Coast J, Beusterien K, Vass C, DiSantostefano R, et al. Reporting formative qualitative research to support the development of quantitative preference study protocols and corresponding survey instruments: guidelines for authors and reviewers. The Patient-Patient-Centered Outcomes Research 2020;13:121-36.
- Poolman M, Roberts J, Wright S, Hendry A, Goulden N, Holmes EAF, et al. Carer administration of as-needed subcutaneous medication for breakthrough symptoms in people dying at home: the CARiAD feasibility RCT. Health Technol Assess 2020;24.
- Wilkins T, Cooper I. Lessons from coordinating a knowledge-exchange network for connecting research, policy and practice. Research for All 2019;3:204-17.
- Department for Business Innovation and Skills . The 2011 Skills for Life Survey: A Survey of Literacy, Numeracy and ICT Levels in England 2012. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/36000/12-p168-2011-skills-for-life-survey.pdf (accessed 30 November 2021).
- HM Government . Social Distancing Review: Report 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/999413/Social-Distancing-Review-Report.pdf (accessed 17 January 2022).
- Porter A, Badshah A, Black S, Fitzpatrick D, Harris-Mayes R, Islam S, et al. Electronic health records in ambulances: the ERA multiple-methods study. Health Serv Deliv Res 2020;8.
- Noble A, Nevitt S, Holmes E, Ridsdale L, Morgan M, Tudur-Smith C, et al. Seizure first aid training for people with epilepsy attending emergency departments and their significant others: the SAFE intervention and feasibility RCT. Health Serv Deliv Res 2020;8.
- Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. PharmacoEcon 2008;26:661-77.
- Orme B. Getting Started with Conjoint Analysis: Strategies for Product Design and Pricing Research. Madison, WI: Research Publishers LLC; 2010.
- de Bekker-Grob EW, Donkers B, Jonker MF, Stolk EA. Sample size requirements for discrete-choice experiments in healthcare: a practical guide. Patient 2015;8:373-84.
- Lloyd A, McIntosh E, Price M. The importance of drug adverse effects compared with seizure control for people with epilepsy: a discrete choice experiment. PharmacoEcon 2005;23:1167-81.
- Watson V, Becker F, de Bekker-Grob E. Discrete choice experiment response rates: a meta-analysis. Health Econ 2017;26:810-7.
- Medicines and Healthcare products Regulatory Agency, Health Research Authority . Joint Statement on Seeking Consent by Electronic Methods 2018. www.hra.nhs.uk/documents/1588/hra-mhra-econsent-statement-sept-18.pdf (accessed 13 August 2021).
- de Bekker-Grob EW, Hol L, Donkers B, van Dam L, Habbema JD, van Leerdam ME, et al. Labeled versus unlabeled discrete choice experiments in health economics: an application to colorectal cancer screening. Value Health 2010;13:315-23.
- Chapman SC, Horne R, Eade R, Balestrini S, Rush J, Sisodiya SM. Applying a perceptions and practicalities approach to understanding nonadherence to antiepileptic drugs. Epilepsia 2015;56:1398-407.
- Ministry of Housing CLG . English Indices of Deprivation 2019 2019. www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed 13 August 2021).
- Goodman A, Gatward R. Who are we missing? Area deprivation and survey participation. Eur J Epidemiol 2008;23:379-87.
- Ryan M, Gerard K, Amaya-Amaya M. Using Discrete Choice Experiments to Value Health and Health Care. Dordrecht: SpringerLink; 2008.
- Sharma A, Minh Duc NT, Luu Lam Thang T, Nam NH, Ng SJ, Abbas KS, et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J Gen Intern Med 2021;36:3179-87.
- National Institute for Health Research . A Framework for Restarting NIHR Research Activities Which Have Been Paused Due to COVID-19 2020. www.nihr.ac.uk/documents/restart-framework/24886 (accessed 13 August 2021).
- Public Health England . COVID-19: Cases in United Kingdom 2021. https://coronavirus.data.gov.uk/ (accessed 5 February 2024).
- Black N, Murphy M, Lamping D, McKee M, Sanderson C, Askham J, et al. Consensus development methods: a review of best practice in creating clinical guidelines. J Health Serv Res Policy 1999;4:236-48.
- Jackson S. Group Processes and Productivity. Newbury Park, CA: Sage Publications; 1992.
- National Audit Office . NHS Ambulance Services 2017. www.nao.org.uk/wp-content/uploads/2017/01/NHS-Ambulance-Services.pdf (accessed 16 August 2021).
- James Lind Alliance . JLA Guidebook 2021. www.jla.nihr.ac.uk/jla-guidebook/ (accessed 16 August 2021).
- Lago PP, Beruvides MG, Jian J, Canto AM, Sandoval A, Taraban R. Structuring group decision making in a web-based environment by using the nominal group technique. Comput Ind Eng 2007;52:277-95.
- Cantrill J, Sibbald B, Buetow S. The Delphi and nominal group techniques in health services research. Int J Pharm Pract 1996;4:67-74.
- McMillan SS, Kelly F, Sav A, Kendall E, King MA, Whitty JA, et al. Using the Nominal Group Technique: how to analyse across multiple groups. Health Serv Outcomes Res Methodol 2014;14:92-108.
- Webb C, Doman M. Conducting focus groups: experience from nursing research. Junct: J Them Dialog 2008;10:51-60.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Epilepsy Action . Increasing Seizure Awareness for UK Police Officers 2021. www.epilepsy.org.uk/news/news/increasing-seizure-awareness-uk-police-officers (accessed 10 February 2022).
- Epilepsy Scotland . Epilepsy and the Justice System 2019. www.epilepsyscotland.org.uk/epilepsy-and-the-justice-system/ (accessed 10 February 2022).
- Epilepsy Foundation . Criminal Justice: Arrest for Seizure-Related Behaviors 2014. www.epilepsy.com/sites/core/files/atoms/files/Criminal%20Justice%20Seizure%20Arrest%2012.%202014.pdf (accessed 10 February 2022).
- Cross JH, Auvin S, Falip M, Striano P, Arzimanoglou A. Expert opinion on the management of Lennox-Gastaut syndrome: treatment algorithms and practical considerations. Front Neurol 2017;8.
- Whitten E, Griffiths A. Implementing epilepsy guidelines within a learning disability service. Seizure 2007;16:471-8.
- Allen JE, Ferrie CD, Livingston JH, Feltbower RG. Recovery of consciousness after epileptic seizures in children. Arch Dis Child 2007;92:39-42.
- Ohira J, Yoshimura H, Morimoto T, Ariyoshi K, Kohara N. Factors associated with the duration of the postictal state after a generalized convulsion. Seizure 2019;65:101-5.
- Office for National Statistics . Internet Access – Households and Individuals, Great Britain: 2020 2020. www.ons.gov.uk/peoplepopulationandcommunity/householdcharacteristics/homeinternetandsocialmediausage/bulletins/internetaccesshouseholdsandindividuals/2020 (accessed 13 August 2021).
- Local Government Association . Tackling the Digital Divide: House of Commons, 4 November 2021 2021. www.local.gov.uk/parliament/briefings-and-responses/tackling-digital-divide-house-commons-4-november-2021 (accessed 15 February 2022).
- NHS England and NHS Improvement . A&Amp;E Attendances and Emergency Admissions January 2022 Statistical Commentary 2022.
- NHS England and NHS Improvement . Statistical Note: Ambulance Quality Indicators (AQI) 2022.
- Marincowitz C, Sutton L, Stone T, Pilbery R, Campbell R, Thomas B, et al. Prognostic accuracy of triage tools for adults with suspected COVID-19 in a pre-hospital setting: an observational cohort study. Emerg Med J 2022;39:317-24. https://doi.org/10.1136/emermed-2021-211934.
- Ioannidis JP. Effect of the statistical significance of results on the time to completion and publication of randomized efficacy trials. JAMA 1998;279:281-6.
- Mason S, Stone T, Jacques R, Lewis J, Simpson R, Kuczawski M, et al. Creating a real-world linked research platform for analyzing the urgent and emergency care system. Med Decis Making 2022;42:999-1009. https://doi.org/10.1177/0272989X221098699.
Appendix 1 Annotated example of a discrete choice experiment binary choice task
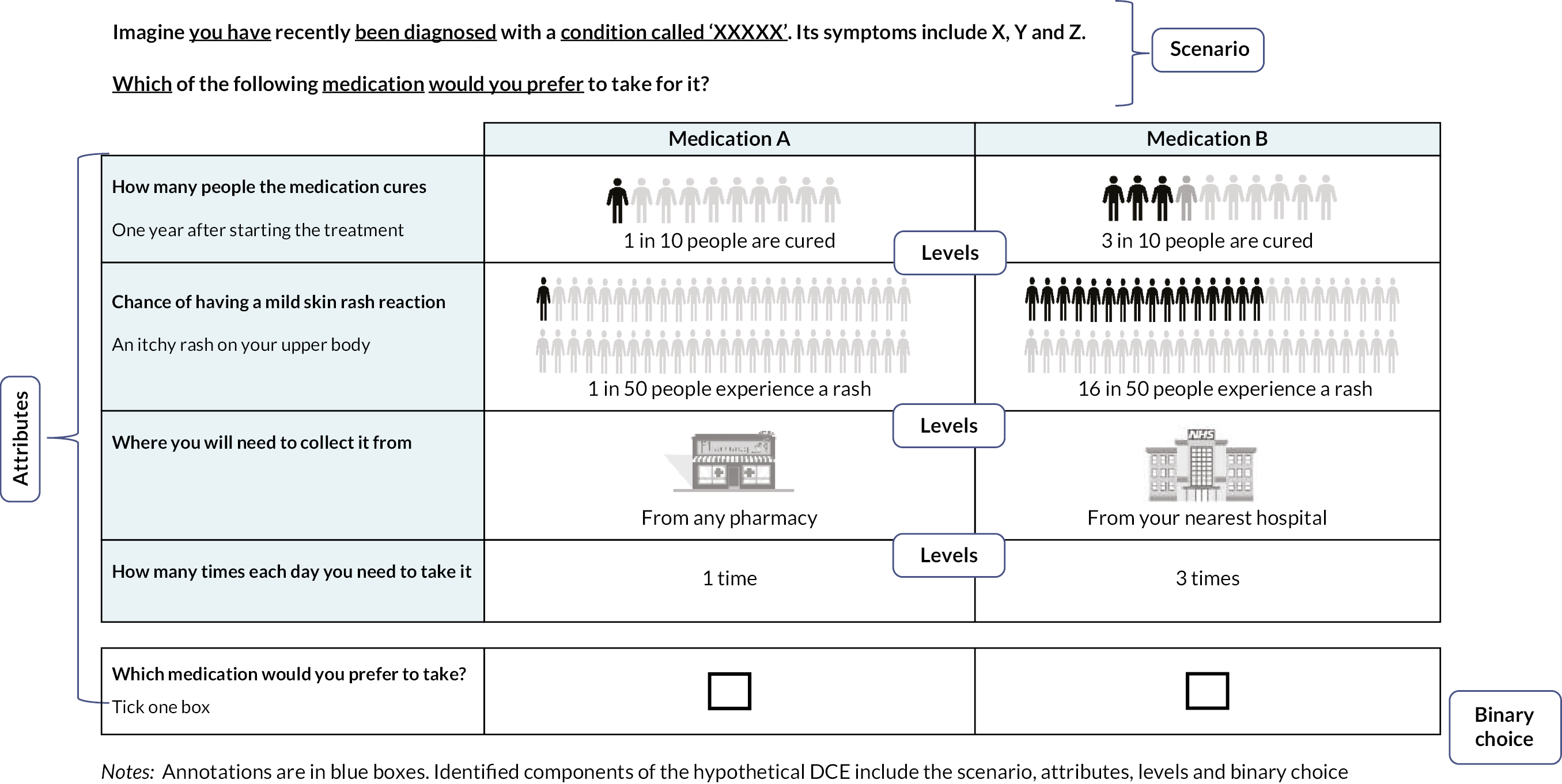
Appendix 2 Questions included in survey of services
Sections of this appendix have been reproduced from Mathieson et al. 154 under licence CC-BY-NC-ND.
| Purpose | Questions | Answer | |
|---|---|---|---|
| Priority | How much of a priority would you say reducing unplanned hospitalisation for chronic ambulatory care sensitive conditions is for your service?a | 1 = Not a priority, 2 = Low priority, 3 = Moderate priority, 4 = High priority, 5 = Very high priority | |
| Order these conditions in terms of how much priority the urgent and emergency care system should be giving each of them, so as to reduce associated emergency admissions | (Position 1 = most important; position 8 = least important)
|
||
| Changes | Past | Has your service (or any local service you may work with) made changes (within the last 5 years) to how people with suspected seizures/epilepsy are cared for that could reduce clinically unnecessary and/or avoidable unplanned health service use? | Yes/No/Don’t know |
If Yes…
|
|||
| Future | Is your service (or any local service you may work with) considering or planning to implement any changes (within the next 12 months) to how people with suspected seizures/epilepsy are cared for? | Yes/No/Don’t know | |
If Yes…
|
|||
| Service user involvement c | Were service users involved in any way in informing this service change? By ‘service users’ we mean representatives from the target population, for example patients, carers, persons from relevant user groups |
Yes/No/Don’t know | |
If Yes, how:
|
|||
| Barriers d | If your service has not recently made, nor is planning to make, any service changes to reduce clinically unnecessary and/or avoidable visits for suspected seizures/epilepsy, why might this be? | Free-text response. | |
| Usual practice questions e | What some services have recently introduced to reduce clinically unnecessary and/or avoidable visits for suspected seizures/epilepsy might already be part of usual practice in your service. Please indicate whether any of these are usual practice within your service or local area. |
|
|
Appendix 3 Organisations reporting of implemented or planned service changes to how people with suspected seizures/epilepsy are cared for that could reduce clinically unnecessary and/or avoidable unplanned health service use
| Service type | ‘Has your service (or any local service you may work with) made changes …?’ | ‘Is your service (or any local service you may work with) considering or planning to implement any changes …?’ | Did the service report an implemented and/or planned change? | Did the service report that usual practice included ≥ 1 of the noted service changes?a | Did the service report an implemented and/or planned change or usual practice as including ≥ 1 of the noted service changes? | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Yes (n, %) | No (n, %) | Don’t know (n, %) | N | Yes (n, %) | No (n, %) | Don’t know (n, %) | N | Yes (n, %) | Nob (n, %) | N | Yes (n, %) | No (n, %) | N | Yes (n, %) | Nob (n, %) | |
| Ambulance | 10 | 7 (70.0) | 3 (30.0) | – | 10 | 1 (10.0) | 5 (50.0) | 4 (40.0) | 10 | 7 (70.0) | 3 (30.0) | 3 | 2 (66.7) | 1 (33.3) | 10 | 9 (90.0) | 1 (10.0) |
| ED | 26 | 4 (15.4) | 16 (61.5) | 6 (23.1) | 26 | – | 13 (50.0) | 13 (50.0) | 26 | 4 (15.4) | 22 (84.6) | 22 | 7 (31.8) | 15 (68.2) | 26 | 11 (42.3) | 15 (57.7) |
| Neuro | 32 | 23 (71.9) | 6 (18.8) | 3 (9.4) | 32 | 20 (62.5) | 8 (25.0) | 4 (12.5) | 32 | 30 (93.8) | 2 (6.3) | 2 | – | 2 (100) | 32 | 30 (93.8) | 2 (6.3) |
| Total | 68 | 34 (50.0) | 25 (36.8) | 9 (13.2) | 68 | 21 (30.9) | 26 (38.2) | 21 (30.9) | 68 | 41 (60.3) | 27 (39.7) | 27 | 9 (33.3) | 18 (66.7) | 68 | 50 (73.5) | 18 (26.5) |
Appendix 4 Topic guide for WP1 interviews
Please note sections of this appendix have been reproduced from McKinlay et al. 1 under licence CC-BY-4.0, while the ranking exercise task used an approach previously deployed by the investigative team174 and is reproduced under licence CC-BY-4.0.
| Topics | Questions |
|---|---|
| Introduction |
|
| Carers |
|
| Seizures | Perhaps first you could tell me about your seizures …
|
| Decision-making |
|
Public place:
|
|
Home:
|
|
| Emergency Services/A&E |
|
| Views of A&E | If you had to use emergency services again, are there any changes that you would like to see in the way this service is provided? (Prompt if needed: and how about A&E?)
|
| Alternatives to A&E | When you have had a seizure and contact has been made with emergency services (i.e. 999/paramedics/111), have you ever been offered an alternative to A&E? If so, what?
|
| Are you familiar with something called an urgent treatment centre? Extra Explanation, only if needed: The term urgent treatment centres is a relatively new one, but it has been suggested as a potential alternative to A&E. To give you a feel of what they are, the idea is that: They will be open at least 12 hours a day, 7 days a week. Staffed by GPs and nurses. Be able to issue prescriptions and have access to some common, but basic equipment, such as ECGs to test heart function and in some cases X-ray machines. If yes, have you ever been to one before? If no, you might be more familiar with terms like ‘walk-in centres’ and ‘minor injury units’. These are to be relabelled urgent treatment centres. How many there are located near you, and where they are, varies. Some are located next to GP practices, some are on hospital sites What might be your expectations of such a centre be? Would you have any concerns about this? If so, what kind? Would anything change how you felt about this CP? That is, seizure type, recent changes in meds. Another option that is being considered instead of always taking PWE to A&E following a seizure, is for the person to be left at home or taken home if they were out. They would then be telephoned within say 24 hours by an epilepsy nurse specialist. The nurse would be phoning to see how the person was recovering and whether needed any additional support, such as a change in medication, advice or to be booked in to see a neurologist. Extra Explanation, only if needed/not seen an ENS before: An epilepsy nurse is a registered nurse who typically has extra experience or qualifications in neurology. Their role varies but they can provide information regarding epilepsy and its management, they can help monitor and change medication, order tests and act as a first point of contact for patients and GPs. They advise people in a variety of settings, including in outpatient clinics and over the phone. What might be your expectations be over this sort of alternative to being taken to A&E? Would you have any concerns about this? If so, what kind? Would anything change how you felt about this CP? That is, seizure type, recent changes in meds |
|
| Rank |
|
| Characteristics | Now I have some final short-answer questions to run through about you …
|
|
|
| Closing |
|
| *Ranking exercise | We are keen to understand what type of care people would prefer when they have a seizure. Here are some factors** that you have mentioned/or we think may be important … Interviewer displays show cards in a random order in front of the participant. Looking at these cards: 1. Is there anything missing? Are there any other factors what would affect your choice? Interviewer writes additional factors on blank cards and places them alongside the pre-defined cards in front of the participant. Record any self-nominated factors on the interview record sheet. 2. Which are the most important factors in your opinion? Can you pick up all the cards that would most likely affect your decision? Explain that these factors can have been experienced, or not; and include any that were self-nominated in this exercise. Clear the remaining cards from the table. 3. Now, can you rank these in order of most important to least important? Check the order the interviewer places the cards is that is. So, you think ‘X’ at the top is the most important? Encourage the participant to ‘think aloud’ and explain their ranking. If participants find it hard to rank certain factors, or align them side by side, explore why. Record the rank scores on the interview record sheet. |
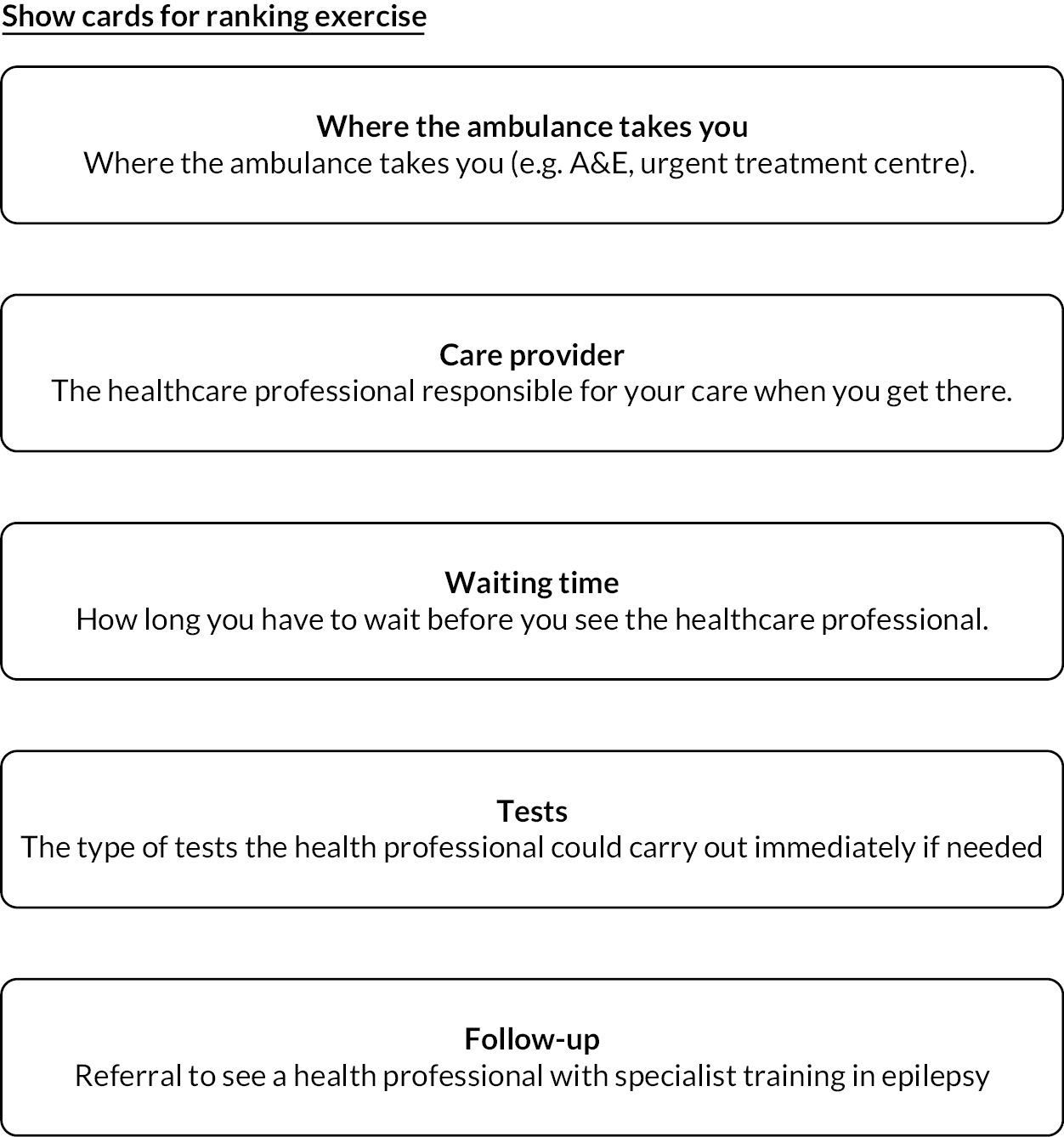
Ranking exercise interview record sheet
Participant ID: _ _/_ _/ _ _
Interviewer ID _ _
| Factor* | Rank results (insert 1–5) 1 = most important 5 = least important X = not selected |
|---|---|
| Anything else? Write here: | |
| Anything else? Write here: | |
| Anything else? Write here: | |
| Anything else? Write here: | |
| Anything else? Write here: | |
| Anything else? Write here: | |
| Where the ambulance takes you | |
| Care provider | |
| Waiting time | |
| Tests | |
| Follow-up |
Appendix 5 Screenshots from animation along with accompanying narration

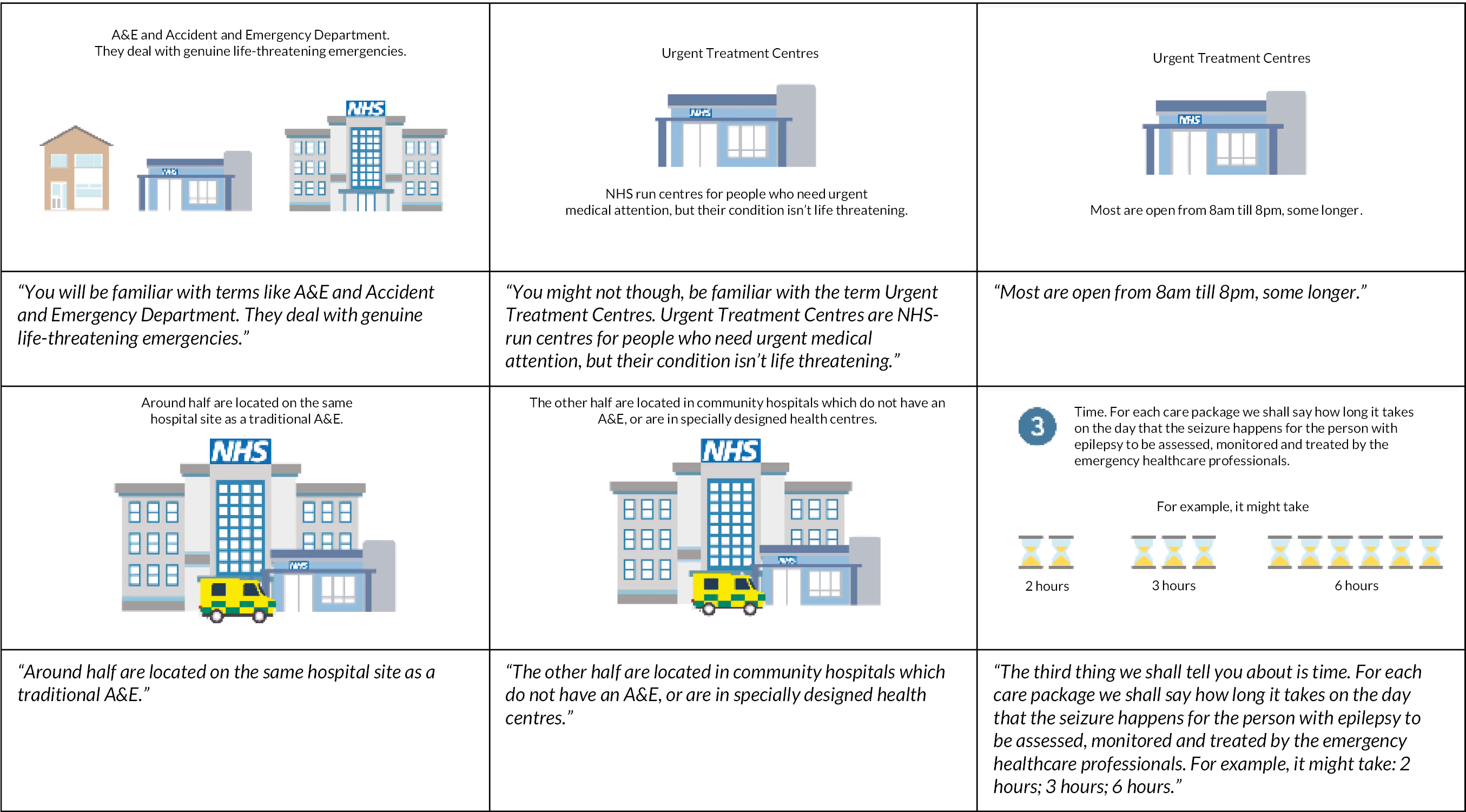

Appendix 6 Non-discrete choice experiment questions asked of participants by survey in order of appearance
| Number | Question | Answer options | |
|---|---|---|---|
| PWE | SOs | ||
| 1 | 1 | Are you doing this survey because you have epilepsy or because you know someone who has epilepsy? |
|
| 2 | 2 | Please tell us your date of birth |
|
| 3 | 3 | Are you male or female? |
|
| 4 | 4 | For PWE: Here are some types of epileptic seizure. Which have you ever experienced? (You can select more than one. Please select the one(s) that come closest to what you have experienced) For ‘significant other’: Below are some different types of epileptic seizures. Which type(s) do you think the person with epilepsy that you know has ever experienced. (You can select more than one. Please select the one(s) that come closest to what you believe they have experienced) |
|
| 5 | 5 | (Presented if > type selected for Q4) For PWE: In the past 2 years, which of these types of epileptic seizures would you say is your usual type(s)? By usual, we mean what some people call their ‘normal’, ‘run of the mill’ type of seizure (You can select more than one.) For ‘significant other’: In the past 2 years, which of these types of seizure would you say is their usual type(s)? By usual, we mean their ‘normal’, ‘run of the mill’ type of seizure of seizure. (You can select more than one) |
|
| 6 | 6 | (Presented if > 1 type also selected for Q5) For PWE: Which one of these types is mostly likely to lead you to have contact with the emergency health services? (Select just one) For ‘significant other’: Which one of these seizure types would mostly likely lead the person you know with epilepsy to have contact with the emergency health services? (Please select only one) |
|
| 7–18 | 7–18 | DCE questions for first scenario randomised to (see Table 8 for scenarios) |
|
| 19–30 | 19–30 | DCE questions for second scenario randomised to (see Table 8 for scenarios) |
|
| 31 | 31 |
What is your home postcode?
(If you do not know it, please type in your address, including the area, village or town name. You do not need to tell us your house or flat name or number.) |
|
| – | 32 |
For ‘significant other’:
How do you know the person with epilepsy that led you to take part in this study? The person I know is my … |
|
| – | 33 |
For ‘significant other’:
How old is the person with epilepsy that you know? (If you do not know exactly, please give us your best guess) |
|
| 34 |
For ‘significant other’:
Are they male or female? |
|
|
| 32 | 35 | For PWE: Do you have a learning disability? For ‘significant other’: Do they have a learning disability? |
|
| 33 | 36 | For PWE: How old were you when you were first diagnosed with epilepsy? (This might be different to when you had your first seizure) For ‘significant other’: How old were they when they were first diagnosed with epilepsy? (If you do not know exactly, please give us your best guess. The answer might be different to when they had their first seizure) |
|
| 34 | 37 | For PWE: Have you ever been diagnosed with non-epileptic attack disorder (NEAD)? (even if the diagnosis might have proved to be wrong). [Other names used are non-epileptic seizures (NES), non-epileptic events, psychogenic seizures, functional seizures, dissociative seizures, pseudoseizures or pseudoepileptic seizures] For ‘significant other’: Have they ever been diagnosed with non-epileptic attack disorder (NEAD)? (even if the diagnosis might have proved to be wrong). (Other names used are non-epileptic seizures …) |
|
| 35 | 38 | For PWE: Are you prescribed an emergency rescue medicine for your epilepsy? (This would be a medicine that you or someone close to you carries around and uses during or straight after a seizure) For ‘significant other’: Are they prescribed an emergency rescue medicine for their epilepsy? (This would be a medicine that they or someone close to them carries around and uses during or straight after a seizure) |
|
| 36 | 39 | For PWE: In an emergency situation, do you have some way of letting healthcare professionals know what care and support you need? (For example, you might have a ‘care plan’ that they can see, have a way of sharing your medical records with them or you might carry instructions personal to you) For ‘significant other’: In an emergency situation, do they have some way of letting healthcare professionals know how to care and support them? (For example, they might have a ‘care plan’ that they can see, have a way of sharing their medical records with them or carry instructions personal to them) |
|
| 27 | 40 | For PWE: How many epileptic seizures (of any type) have you had in the past 12 months? (If you are unsure, please give us your best guess) For ‘significant other’: How many epileptic seizures (of any type) would you say they have had in the past 12 months? (If you do not know exactly, please give us your best guess) |
|
| 28 | 41 | For PWE: In the past 12 months, how many times have you been to a hospital emergency department because of your epilepsy? (If you are unsure, please give your best guess) For ‘significant other’: In the past 12 months, how many times have they have been to a hospital emergency department because of epilepsy? (If you are unsure, please give your best guess) |
|
| 29 | 42 | For PWE: In the past 12 months, how many times has an emergency ambulance come to you because of epilepsy? (Please include even those times when the ambulance was not called by you or someone you know) For ‘significant other’: In the past 12 months, how many times has an emergency ambulance come to them because of epilepsy? (If you are not sure, please give us your best guess. Please do include any times as well when an ambulance might have been called for by someone else) |
|
| 30 | 43 | For PWE: In the past 12 months, have you seen or spoken to a doctor or nurse that specialises in epilepsy? (such as a neurologist or epilepsy nurse specialist) For ‘significant other’: In the past 12 months, have you or the person you know with epilepsy seen or spoken to a doctor or nurse that specialises in epilepsy? (such as a neurologist or epilepsy nurse specialist) |
|
| 31 | 44 | For PWE: Do you ever have problems accessing the epilepsy specialist services in your area? For ‘significant other’: Do you know whether they ever have problems accessing the epilepsy specialist service in their area? |
|
| 32 | 45 | For PWE: Do you believe you have had enough support so you and those close to you know what to do when a seizure happens? For ‘significant other’: Do you believe they have had enough support so that they and those close to them know what to do when a seizure happens? |
|
| 33 | 46 | For PWE: How long would you be prepared to wait to see a doctor in an NHS Urgent Treatment Centre? For ‘significant other’: How long would you yourself be prepared to wait with the person you know with epilepsy to see a doctor in an NHS Urgent Treatment Centre? |
|
| 34 | 47 | For PWE: How long would you be prepared to wait to see a doctor in a NHS hospital Emergency Department? For ‘significant other’: How long would you yourself be prepared to wait with the person you know with epilepsy to see a doctor in the NHS hospital Emergency Department? |
|
| 34 | 48 | ‘When it comes to caring for someone after a seizure, do you think the following sentence is true or false’: ‘If a person with epilepsy has a simple, uncomplicated seizure, there is no need to call a doctor or ambulance’ |
|
| 35 | 49 | For PWE: ‘How often have you found yourself in the situations below’ ‘You have an epileptic seizure in a public place and an ambulance comes. The seizure lasts no longer than usual and you recover as usual. You have NOT experienced an injury that requires urgent or emergency treatment’ For ‘significant other’: ‘How often would you say the person you know with epilepsy has found themselves in the situations below? (If you are not sure, please give us your best guess)’ ‘They have an epileptic seizure in a public place and an ambulance comes. Their seizure lasts no longer than usual and they recover as usual. They have NOT experienced an injury that requires urgent or emergency treatment’ |
|
| 36 | 50 | For PWE: ‘You have an epileptic seizure at home and an ambulance comes. The seizure lasts no longer than usual and you recover as usual. You have NOT experienced an injury that requires urgent or emergency treatment’ For ‘significant other’: ‘They have an epileptic seizure at home and an ambulance comes. Their seizure lasts no longer than usual and they recover as usual. They have NOT experienced an injury that requires urgent or emergency treatment’ |
|
| 37 | 51 | For PWE: ‘You have an epileptic seizure (or seizures) that is different to what you usually experience. An ambulance comes. The seizure (or seizures) has stopped. You have NOT experienced an injury that requires urgent or emergency treatment’ For ‘significant other’: ‘They have an epileptic seizure (or seizures) that is different to what they usually experience. An ambulance comes. The seizure (or seizures) has stopped. They have NOT experienced an injury that requires urgent or emergency treatment’ |
|
| 38 | 52 | For PWE: Thinking about all the times an emergency ambulance has come to you for epilepsy, how often have you been with someone you know who could help? For ‘significant other’: Thinking about all the times an emergency ambulance has come to them for epilepsy, how often have they been with someone they know who could help? (If you are unsure, please give your best guess) |
|
| 39 | 53 | For PWE: When an emergency ambulance has come to you for epilepsy, who has been most likely to call for it? For ‘significant other’: When an emergency ambulance has come to them for epilepsy, who has been most likely to call for it? |
|
| 40 | 54 | Do you think the coronavirus (COVID-19) has changed your willingness to access/your willingness for the person with epilepsy to access NHS services? Please read each of the statements below and indicate to what extent you agree or disagree. For PWE: I am less willing to go to A&E following a seizure, due to the coronavirus. For ‘significant other’: I am less willing for them to go to A&E following a seizure, due to the coronavirus. |
|
| 41 | 55 | For PWE: I am less willing to go to an UTC following a seizure, due to the coronavirus. For ‘significant other’: I am less willing for them to go to an UTC following a seizure, due to the coronavirus. |
|
| 42 | 56 | For PWE: I am less willing to go to an outpatient appointment, to see an epilepsy specialist, due to the coronavirus. For ‘significant other’: I am less willing for them to go to an outpatient appointment, to see an epilepsy specialist, due to the coronavirus. |
|
| 43 | 57 | For PWE: I am less willing to go to see my GP following a seizure, due to the coronavirus. For ‘significant other’: I am less willing for them to go to see my GP following a seizure, due to the coronavirus. |
|
| 44 | 58 | Do you believe you have had the coronavirus (COVID-19)? |
|
| 45 | 59 | Do you believe someone close to you has had the coronavirus (COVID-19)? |
|
Appendix 7 Detailed description of participants’ demographics and epilepsy characteristics by recruitment route and when combined
Appendix 8 Familiarity to participants of seizure scenarios used within discrete choice experiments
Appendix 9 Testing for non-linear effects of time: plot estimated coefficients for time by scenario and sample
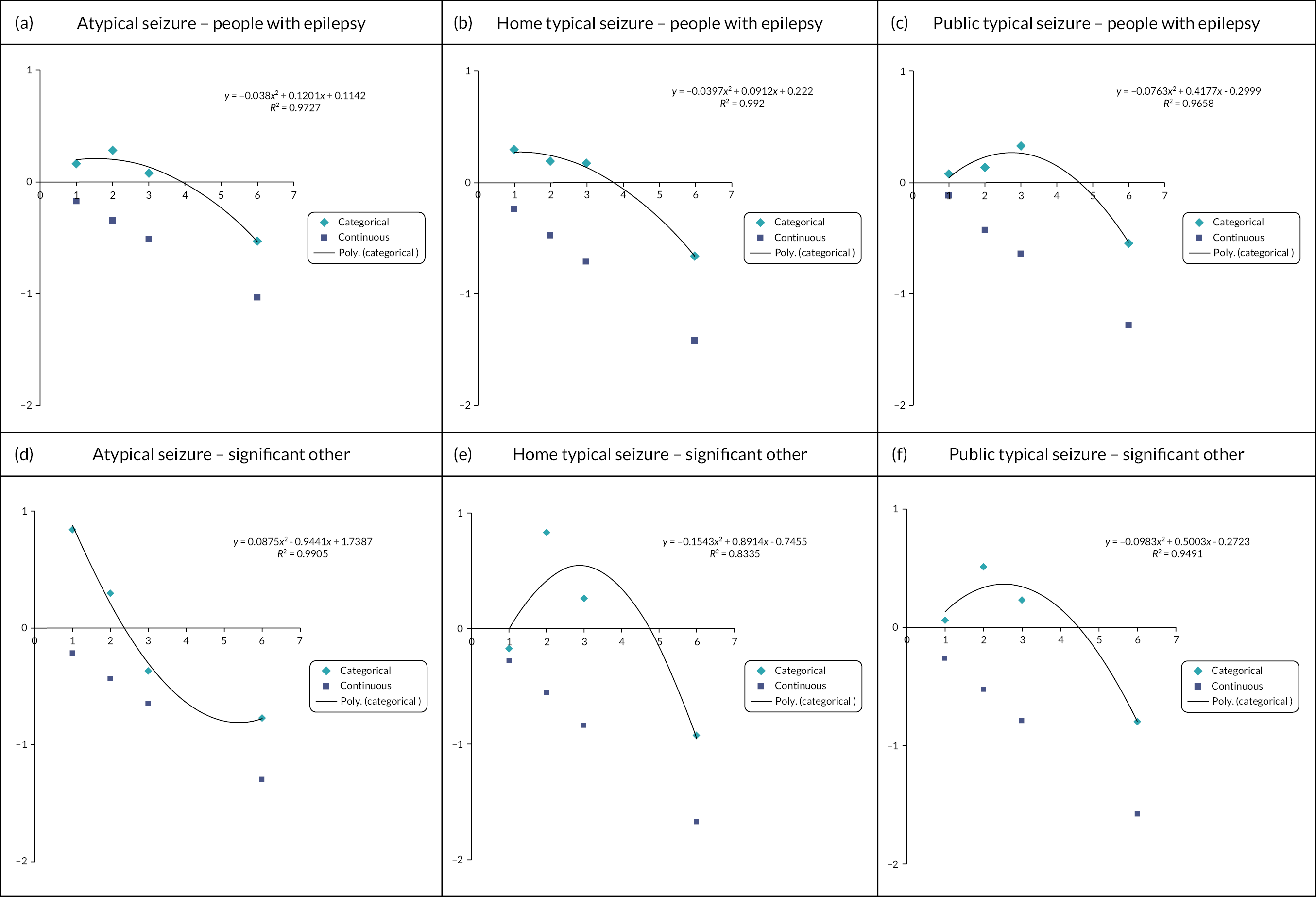
Appendix 10 Results from discrete choice experiment subgroup analyses
Summary of subgroup analysis to explore preference heterogeneity
| Atypical seizure | Home typical seizure | Public typical seizure | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| m1 n |
m2 n |
m3 n |
LLR p-value |
m1 n |
m2 n |
m3 n |
LLR p-value |
m1 n |
m2 n |
m3 n |
LLR p-value |
||
| Planned subgroup analysis (PWE) | |||||||||||||
| (1) Any visits to ED in past 12 months (no = m2; yes = m3) | 204 | 32 | 172 | 0.3102 | 198 | 31 | 167 | 0.0030 | 194 | 29 | 165 | N/A | |
| (2) Social deprivation (IMD decile 1–4 = m2; IMD decile 5–10 = m3) | 205 | 101 | 104 | 0.5308 | 198 | 97 | 101 | 0.3708 | 193 | 94 | 99 | 0.4478 | |
| (3) Contact with epilepsy specialist in past 12 months (no = m2; yes = m3) | 204 | 22 | 182 | N/A | 198 | 37 | 161 | 0.0476 | 194 | 31 | 163 | 0.0552 | |
| (4) Intellectual disability (no = m2; yes = m3) | 205 | 182 | 23 | N/A | 199 | 169 | 30 | 0.0434 | 194 | 179 | 15 | N/A | |
| (5) Problems accessing specialist services (no or don’t know = m2; yes = m3) | 204 | 106 | 98 | 0.0033 | 198 | 111 | 87 | 0.1221 | 194 | 111 | 83 | 0.0056 | |
| (6) Care plan (no or don’t know = m2; yes = m3) | 204 | 133 | 71 | 0.8565 | 198 | 131 | 67 | 0.4481 | 194 | 122 | 72 | 0.1814 | |
| (7) Experience of scenario (never = m2; often or sometimes = m3) |
2 | 56 | 147 | 0.5956 | 197 | 60 | 137 | 0.1244 | 194 | 50 | 144 | 0.0164 | |
| Post hoc analysis (PWE) | |||||||||||||
| (1) Sampling frame (NWAS = m2; public advert = m3) | 258 | 48 | 210 | 0.3575 | 239 | 40 | 199 | 0.1393 | 252 | 44 | 208 | 0.6919 | |
| (2) Willingness to access health care during coronavirus pandemic (strongly agree/somewhat agree = m2; neutral, disagree/strongly disagree = m3) | … A&E | 170 | 104 | 66 | 0.8947 | 171 | 109 | 62 | 0.4294 | 163 | 103 | 60 | 0.4605 |
| … UTC | 168 | 93 | 75 | 0.7671 | 165 | 100 | 65 | 0.007 | 161 | 95 | 66 | 0.9519 | |
| … OPD | 143 | 58 | 85 | 0.7459 | 143 | 62 | 81 | 0.5417 | 142 | 54 | 88 | 0.817 | |
| … GP | 157 | 61 | 96 | 0.7105 | 149 | 58 | 91 | 0.3456 | 153 | 55 | 97 | 0.7544 | |
| Post hoc analysis (Significant other) | |||||||||||||
| (1) Sampling frame (NWAS = m2; public advert = m3) | 105 | 30 | 75 | 0.2474 | 97 | 28 | 69 | N/A | 96 | 28 | 68 | N/A | |
| (2) Willingness to access health care during coronavirus pandemic (strongly agree/somewhat agree = m2; neutral, disagree/strongly disagree = m3) | …. A&E | 75 | 50 | 25 | N/A | 66 | 47 | 19 | N/A | 65 | 39 | 26 | N/A |
| … UTC | 75 | 43 | 32 | 0.0298 | 66 | 43 | 23 | N/A | 66 | 36 | 29 | N/A | |
| … OPD | 64 | 26 | 38 | N/A | 60 | 22 | 38 | N/A | 54 | 22 | 32 | N/A | |
| … GP | 66 | 21 | 45 | N/A | 59 | 19 | 40 | N/A | 57 | 20 | 37 | N/A | |
Summary of regression models for subgroups reaching statistical significance
| Attribute (level) | Home typical seizure – PWE | Atypical seizure – PWE | Public typical – PWE | Home typical seizure – PWE | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Any visits to ED in past 12 months | (5) Problems accessing specialist services | (5) Problems accessing specialist services | (ii) Willingness to access UTC during coronavirus pandemic | |||||||||||||
| No | Yes | No/don’t know | Yes | No/don’t know | Yes | Agree | Neural/disagree | |||||||||
| β-coefficient | p-value | β-coefficient | p-value | β-coefficient | p-value | β-coefficient | p-value | β-coefficient | p-value | β-coefficient | p-value | β-coefficient | p-value | β-coefficient | p-value | |
| Access to medical records/care plan | 0.770 | 0.060 | 0.499 | 0.000 | 0.440 | 0.000 | 0.600 | 0.000 | 0.587 | 0.000 | 0.559 | 0.000 | 0.464 | 0.003 | 0.531 | 0.002 |
| Convey (UTC) | –11.22 | 0.992 | –0.152 | 0.189 | –0.220 | 0.187 | 0.371 | 0.013 | –0.050 | 0.726 | –0.067 | 0.655 | –0.188 | 0.247 | –0.460 | 0.023 |
| Convey (ED) | –7.726 | 0.991 | –0.244 | 0.032 | –0.335 | 0.016 | 0.013 | 0.923 | –0.378 | 0.004 | –0.149 | 0.297 | –0.227 | 0.188 | –0.525 | 0.004 |
| Time (1 hour)^ | –41.02 | 0.507 | –0.847 | 1.114 | 0.256 | 0.180 | ||||||||||
| Time (2 hours) | 16.42 | 0.992 | 0.203 | 0.381 | 0.722 | 0.032 | –0.136 | 0.614 | 0.207 | 0.453 | 0.129 | 0.667 | 0.116 | 0.724 | 0.597 | 0.151 |
| Time (3 hours) | 24.78 | 0.992 | 0.011 | 0.968 | 0.689 | 0.077 | –0.411 | 0.225 | 0.196 | 0.569 | 0.280 | 0.440 | –0.333 | 0.433 | 0.889 | 0.069 |
| Time (6 hours) | –0.188 | 0.487 | –0.721 | 0.000 | –0.564 | 0.000 | –0.567 | 0.000 | –0.659 | 0.000 | –0.589 | 0.000 | –0.884 | 0.000 | –0.513 | 0.001 |
| Epilepsy specialist advises today | 2.398 | 0.990 | 0.402 | 0.000 | 0.547 | 0.000 | 0.771 | 0.000 | 0.331 | 0.000 | 0.448 | 0.000 | 0.471 | 0.000 | 0.315 | 0.001 |
| GP told | 2.226 | 0.990 | 0.306 | 0.000 | 0.530 | 0.000 | 0.395 | 0.000 | 0.277 | 0.000 | 0.341 | 0.000 | 0.241 | 0.003 | 0.344 | 0.000 |
| Epilepsy specialist in future (2–3 weeks) | –14.60 | 0.992 | 0.226 | 0.172 | –0.190 | 0.423 | 0.536 | 0.006 | 0.184 | 0.360 | 0.165 | 0.436 | 0.400 | 0.092 | –0.256 | 0.385 |
| Epilepsy specialist in future (within 1 week) | 14.95 | 0.992 | 0.084 | 0.539 | 0.433 | 0.039 | –0.221 | 0.166 | 0.041 | 0.803 | 0.076 | 0.658 | 0.029 | 0.882 | 0.425 | 0.095 |
| Constant | 1.750 | 0.992 | –0.154 | 0.006 | 0.007 | 0.917 | –0.113 | 0.101 | –0.096 | 0.152 | 0.007 | 0.919 | –0.212 | 0.011 | –0.079 | 0.392 |
| Number of observations | 372 | 2004 | 1272 | 1176 | 1332 | 996 | 1200 | 780 | ||||||||
| Number of respondents | 31 | 167 | 106 | 98 | 111 | 83 | 100 | 65 | ||||||||
List of abbreviations
- A&E
- accident and emergency
- AMPDS
- Advanced Medical Priority Dispatch System
- APEASE
- affordability, practicability, effectiveness, acceptability, side-effects and equity
- COVID-19
- coronavirus disease 2019
- CP
- care pathway
- DCE
- discrete choice experiment
- ED
- emergency department
- ENS
- epilepsy nurse specialist
- FTE
- full-time equivalent
- GP
- general practitioner
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- KE
- knowledge exchange
- NASAT
- National Ambulance Strategy and Transformation group
- NASH
- National Audit of Seizure Management in Hospitals
- NEAD
- non-epileptic attack disorder
- NGT
- nominal group technique
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NWAS
- North West Ambulance Service NHS Trust
- NW CRN
- North-West Coast Comprehensive Research Network
- PPI
- patient and public involvement
- PRF
- Patient Report Form
- PWE
- people with epilepsy
- SMILE
- self-management education for adults with epilepsy
- SO
- significant other
- UTC
- urgent treatment centre
- WP
- Work Package
Notes
-
Oosterwold et al .’s conceptual framework of factors affecting the decision of ambulance service personnel regarding conveying adult patients to an emergency department
-
Characteristics of services that did and did not respond to service evaluation survey (based on reports focusing on varied time periods; range 2004–18)
-
Further details relating to NWAS and the management of calls relating to seizures
-
Examples of materials used for public advert recruitment route
-
Care package configuration within DCE that was selected for analysis purposes to represent current practice configuration (based on evidence presented in Chapter 1)
-
Seizure scenario sets and presentation order participants were randomised to response rates
-
Confirmed COVID-19 confirmed cases in UK by date (31/01/2020 to 10/06/2021)
-
How current practice was ranked across seizure scenarios in terms of preference
-
Screenshots and narration from presentation shown to WP3 KE workshop participants on the results from the DCE survey
-
Additional quotes from WP KE workshop groups illustrating some of the themes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/HKQW4129).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
