Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/2001/25. The contractual start date was in May 2010. The final report began editorial review in August 2012 and was accepted for publication in January 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
L Nasir received an honorarium and travel expenses for a presentation relating to this research at Case Western Reserve University, Cleveland, OH, USA. Outside this submitted work L Nasir received payment for related lectures from the School of Nursing, University of North Carolina at Chapel Hill, NC, USA and from ZHAW, Department Gesundheit, Institut für Pflege, Winterthur, Switzerland. M Fischer declared a consultancy fee from the primary care trust in which the research took place for preparation, including stakeholder consultation, in 2009 of an (unsuccessful) National Institute for Health Research (NIHR) research proposal, which predated and informed the boundary-spanning intervention researched in the present work.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Nasir et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Aims
The primary objective of this study was to explore the impact of a ‘boundary-spanning’ intervention, the Westpark Initiative (WI), on knowledge exchange processes between different sectors, organisations and professions in support of horizontal and vertical health-care integration. We undertook an in-depth, longitudinal case study of the WI that took place in four specific topic areas in a deprived area of a primary care trust (PCT) during the period 2010–12 and assessed whether or not such processes lead to improvements in the quality of health care.
Our research hypothesis was that boundary-spanning processes will stimulate the exchange and creation of knowledge between sectors, organisations and professions and that this will lead, through better integration of services, to improvements as measured by both a range of quality indicators and patient and carer experience. We describe and assess the perceived value of boundary-spanning processes in each of the four topic areas by posing the following overall question: to what extent, and by what vertical and horizontal processes, has boundary spanning facilitated knowledge exchange and creation across sectoral, organisational and professional boundaries, and what impact has this had on the quality of patient care?
Chapter 2 Background
The background to our evaluation report begins with an overview of the contemporary NHS policy context and highlights how various policy streams and wider contextual factors are combining to make the horizontal and vertical integration of services a central goal (see The contemporary NHS policy context). The origins of the ‘boundary-spanning’ concept are then explored (see ‘Boundary spanning’: origins and applications) and we describe how it has been applied both outside and within the health-care sector to date and the types of boundaries that need to be crossed to ensure high-quality health care (see ‘Boundary spanning’ in the health-care sector). We then present the findings of a review of empirical studies carried out in the health-care sector (see A review of the empirical literature), which establishes that the existing evidence base mainly relates to the characteristics of individual boundary spanners and that there is a lack of studies of how boundary-spanning processes enable knowledge exchange and creation. We then identify and describe a framework for conceptualising knowledge creation and exchange processes across boundaries, which we will later use to analyse our primary research findings (see Conceptualising knowledge creation and exchange processes across boundaries: the socialisation, externalisation, combination, internalisation model). The chapter ends with an introduction to the particular boundary-spanning intervention under study and the setting for our evaluation (see The boundary-spanning intervention under study: the Westpark Initiative).
The contemporary NHS policy context
In the health-care sector it has been recognised since the 1970s that high-quality services, particularly for patients with complex needs, cannot be provided by one health-care discipline alone or by a single sector. Today, patients in most health-care settings typically interact with a variety of health-care professionals representing many different disciplines but do not necessarily experience patient-centred care or co-ordinated teamwork. Not all multidisciplinary teams function effectively as a unit; interprofessional work groups face additional barriers to reach the level of high-functioning teams, particularly those working in a complex health-care environment. Consequently, patients commonly receive services in several settings from professionals representing a variety of disciplines and amidst a fragmented set of professional silos, all of which create barriers to truly effective multidisciplinary care. At the same time, all health-care systems face the twin challenges of improving quality while increasing efficiency. In the contemporary challenging economic climate there is an even greater imperative for health-care systems to find ways to improve both the efficiency and the quality of service provision. A recent review has highlighted that quality improvement can in some cases lead to lower costs1 and, as Crump and Adli2 have pointed out, the work of key pioneers of quality, such as Deming, Juran and Kano, has shown the scope for improving quality and reducing cost in many sectors.
Consequently, there have been a variety of initiatives to promote intersectoral and interprofessional working; collaborative multiprofessional teamworking has become a major policy objective of successive governments and an international trend. These initiatives have included:
-
the organisation of professionals into multidisciplinary teams (e.g. community mental health teams)
-
geographical colocation of services
-
shared geographical boundaries and/or merger of health- and social-care agencies
-
initiatives to promote a better understanding of each other's roles (e.g. interprofessional education)
-
the blurring of professional role boundaries in the interests of generic flexible working.
In the health-care context, as well as boundaries between different professional groups (e.g. doctors and nurses, generalists and specialists), there are also typically boundaries between organisations (e.g. acute trusts and community health service providers) and between sectors (e.g. voluntary and social service sectors). More recently, many policy recommendations and deliberations in health-care policy-making have also been reliant, to a significant extent, on successful working across such boundaries. 3 As part of the ongoing debate about how best to enable cross-boundary working, there has been increasing interest in designing patient pathways coupled with routine monitoring of patient flow, satisfaction and clinical outcomes as a recipe for a high-quality and cost-effective health service.
One major policy response has been to advocate both the horizontal and the vertical integration of health-care services. The term ‘horizontal integration’ has been utilised in many industries, particularly in business and economics; in health care it refers to building connections between similar levels of care, such as using multiprofessional teams within the same sector, for example care provided by different services all within a primary or community-based care remit. Peer-based groups working across organisational boundaries or taking part in cross-sectoral work would also be examples of horizontal integration. 4 The term ‘vertical integration’ refers to links across different levels of care, such as between acute hospital care and secondary care services. 5 We are using vertical integration to describe care pathways between generalists and specialists for named conditions. 6 As Thomas and colleagues7–9 have argued, whole-system, or comprehensive, integration aimed at reducing health-care costs and bringing care closer to home requires that vertical and horizontal integration develop in tune with each other.
Unfortunately, there is a lack of clear empirical evidence demonstrating how integration can improve service delivery and, until recently, there has been no universal definition of integration as a concept, or as a model. Furthermore, a systematic review found that there is also a lack of standardised and validated tools for evaluating outcomes of integration. 10 A recent report provides the best overview to date,11 suggesting that ‘the working definition of integrated care may be around the smoothness with which a patient or their representatives or carers can navigate the NHS and social care systems in order to meets their needs’ (p. 15) and that it has three dimensions:
-
seeks to improve the quality and cost-effectiveness of care for people and populations by ensuring that services are well co-ordinated around their needs
-
necessary for anyone for whom a lack of care co-ordination leads to an adverse impact on their own care experiences and outcomes
-
the patient's or user's perspective is the organising principle of service delivery.
Commonly cited examples of successful integrated care services include the Torbay and Southern Devon Health and Care NHS Trust (which integrates health and social care) and the Kaiser Permanente model in the USA. The National Integrated Care Pilots evaluation12 looked at 16 specific projects in the NHS and drew the following conclusions:
-
most of the pilots focused on horizontal integration rather than vertical integration and the various models depended on local circumstances
-
staff generally believed that improvement in processes was leading to improvements in the quality of care
-
patients did not appear to share the sense of improvement (possibly because the changes were driven by professionals rather than users)
-
reductions in some forms of admissions were achieved, but not in emergency admissions.
Other large-scale pilots of integrated care services are currently under way in the NHS13 and the new regulatory framework under the Health and Social Care Act includes a duty on Monitor (the NHS regulator) to ‘exercise its functions with a view to enabling the provision of healthcare services provided for the purposes of the NHS to be provided in an integrated way’. 14 More broadly, the ‘architecture and landscape of the NHS has gone through fundamental change’ (p. 2)11 as a result of what is commonly acknowledged as the most significant reform since its foundation in 1948. Newly formed clinical commissioning groups (CCGs) are expected to play a crucial role in determining how health care will be delivered by overseeing the design of local health-care services.
For the ambitions of policy-makers to be realised, processes of knowledge exchange have to improve across sectoral, organisational and professional boundaries, which can present significant barriers15 and thereby undermine attempts to integrate health-care systems, and ultimately efforts to improve quality and efficiency. ‘Boundary-spanning’ roles have been proposed as one potential solution. However, a systematic review of the diffusion of innovations in health-care literature covering the period up to early 2005 found that empirical studies exploring the role of boundary spanners were sparse. 16 Most of these had explored knowledge exchange across single (e.g. profession to profession) rather than multiple (e.g. between professions in different organisation and sectors) boundaries. In the following two sections we explore the origins of the concept of ‘boundary spanning’ and how it has been applied in the health-care sector.
‘Boundary spanning’: origins and applications
In general terms, ‘boundary spanning’ describes the role of individuals who work in groups but who have ties across boundaries that divide their colleagues. 17 Such individuals have been described as organisational liaisons and ‘key nodes in information networks’ in theories introduced by Adams18,19 and Tushman. 20 The boundary-spanning role was traditionally described as dually serving to process information and provide external representation and, as such, is delineated from the role of the formal authority in an organisation. 21
Boundary-spanning components and boundary-spanning activities are concepts described in a seminal text from organisation theory, Organisations in Action. 22 Thompson explained that boundary-spanning units are established to adjust or adapt to increasingly complex structures as a response to necessary subdivisions that result from the sheer volume of interactions in a task environment. In this theory-building treatise, the author argued that, the more an organisation's environment grows, the more it becomes complex, diverse and/or unpredictable. Thompson noted that co-ordination among organisational units is a core issue and that units developed to span across unit boundaries would be troubled by ‘adjustment to constraints and contingencies not controlled by the organisation’ (p. 67). He further wrote that boundary-spanning units, although interdependent, would be judged by the ‘disappointments they cause for elements of the task environments’ (p. 96). Boundary spanning as an act was not conceived to be serving in an easy position, and the implication is that managers may not be able to fully direct workers in such bridging positions.
In an early literature review from the 1970s,23 boundary-spanning personnel were identified by terms such as ‘input transducers’, ‘linking pins’, ‘gatekeepers’, ‘unifiers’, ‘change agents’, ‘members of extra-organisational transaction structure’, ‘regulators’, ‘liaisons’, ‘planners’, ‘innovators’ or ‘marginal men’. Although they used the term ‘boundary-spanning activity’ in the title of their journal article, the authors Leifer and Delbecq23 noted that the specific term ‘boundary spanner’ was used only once, in an unpublished manuscript, among the 28 references cited at that time (1978) describing types of boundary-spanning personnel.
Difficulty working in the potentially undefined area between units was explored further in research by Michael Tushman in 1974,24 who first examined the notion of complexity and integration efforts in the industrial setting. Tushman and colleagues are widely credited with further describing how ‘boundary roles’ evolve to function as a link to the process of innovation in a system. In a growing and differentiating organisation, such as a research and development (R&D) laboratory, certain individual communicators serve as special types of liaison agents, connecting well in a two-step process by first communicating internally within an organisation and then communicating across multiple interfaces to areas of external information and back again. This study20 explored how high-performing projects might intentionally develop boundary roles to mediate external information, especially in response to high levels of work-related uncertainty. In describing ‘boundary-spanning activities’, Tushman and Scanlan25 referred to boundary spanners as ‘internal communication stars’ (p. 290). Attempts to understand information (or knowledge) transfer, particularly with an external orientation, was enhanced by application of the concept of boundary spanning, especially in describing organisations with laboratories and R&D departments working to create and disseminate new products. 25,26
Following these early discursive papers, the conceptual background of boundary spanning, and the empirical basis of its impact, has been further explored in the organisational studies and management literatures. Boundary spanners in teams have been said to serve in ‘ambassador activities’ (p. 640) and ‘task coordinator activity’ (p. 641) at the team level,27 or have been defined as ‘employees who operate on the periphery of an organisation’ (p. 296). 28 Leaders have been in part characterised by their role in boundary-spanning activities and their emotional intelligence. 29 The role of power and trust in relationships, and the brokering of system exchanges, have also been differentiated from boundary spanning. 30,31
Boundary work in teams has been described by examining the interactions among information technology (IT) knowledge teams and other technological industries, especially in studies seeking to understand how projects are accomplished both by teams32–34 and between organisations and partnerships. 35 Success on R&D teams has been tied to vertical leaders who are skilled at boundary management and managing external relations. 36 Authors have discussed the consensus that integration drives superior performance, and that boundary spanners serve as a source of innovation across functional areas. 37 The non-routine tasks of boundary spanners and the relationship to role stress and role overload have also been described in multiple studies,28,38–40 including across samples of engineers and nurses. 41
‘Boundary spanning’ in the health-care sector
In the health-care context, ‘boundary-spanning’ interventions have been proposed as having the potential to promote the closer integration of services in the interests of improving the quality of care and/or reducing costs. However, the processes through which they can produce improved co-ordination and knowledge sharing between different professions, organisations and sectors have not been determined. This section reviews the application of the boundary-spanning concept in the field of health-care organisations, exploring how it has been operationalised as part of increasing efforts to improve the vertical and horizontal integration of health-care services.
Despite the emergence of the concept of ‘boundary spanners’ in the fields of behavioural psychology18 and organisation theory24,42 as long ago as the mid-1970s, there is a relative paucity of empirical studies exploring the role of such individuals in health-care systems and only very limited evidence exists about how such explicit attempts to improve cross-boundary knowledge exchange have an effect on the quality of health care. Although a small number of studies of boundary spanning in the health-care setting have been carried out, few have utilised rigorous empirical methods or have focused on the detailed processes by which such interventions have helped improve the vertical and horizontal integration of health-care services, and the quality of patient care. Only a study by Byng and colleagues43 utilised an evaluation framework to identify the role of link workers in efforts to improve care. Furthermore, most studies have rarely taken the time to construct theories or explanations for what they observe or find in their analyses (see Grol and colleagues44 for a critique of the atheoretical nature of the vast majority of quality research in health care and a call to researchers to make more systematic use of theories in evaluating interventions). Clearly more studies are needed that can connect boundary-spanning activity to quality improvement efforts that have a real impact on patient care outcomes.
Although contemporary policy initiatives aim for combined vertical and horizontal integration, dominant ways of thinking about how to achieve this, coupled with inadequate training of clinicians and health-care managers and the existence of sectoral, organisational and professional boundaries, are nonetheless likely to emphasise the vertical dimension. More generally, the ability of collaboration and other network forms to achieve higher quality at lower cost is seriously questioned by the substantive literature (not least because there has not been an easy transition to collaborating across traditional sectoral, organisational and professional boundaries). Collaboration places considerable demands on professionals as they learn to work for purposes other than their personal or their organisation's interests. 45,46 Disparities of objectives and positions of power, as well as diverse organisational cultures and ontological frameworks, distort collaboration47,48 and inhibit learning and change. 49 Strategically orientated networks may increase organisational advantage among partner organisations, but often do so at the cost of excluding other communities of interest. 50,51 So it is that studies of public service networks find that, even after successfully achieving new modes of working, governing organisations may simply ‘revert to type’, re-establishing traditional hierarchical control. 52 Indeed, after many years of long-term research in the field, some scholars conclude that the challenges of interorganisational collaboration are so formidable, and tendency towards collective inertia so strong, that it should be avoided as far as possible. 53
Given this overall picture, the prospects for purposeful collaboration (or integration) appear discouraging to say the least. However, there is recent evidence that more effective, nuanced forms of collaboration may be emerging, not through explicit partnerships, but from interacting networks of committed and deeply engaged participants,54 and health-care reforms in Europe now commonly emphasise community participation, interprofessional learning and collaboration across the public and independent sectors.
A review of the empirical literature
Before undertaking our fieldwork and designing our research tools we undertook a focused literature review to develop a clearer understanding of the findings from relevant empirical research studies. Our objectives were to identify empirical research that has examined boundary-spanning in health care, synthesise that literature by conducting a meta-ethnography, suggest key themes relating to boundary-spanning processes in health-care systems and establish whether current evidence suggests that these processes can contribute to improved quality and/or reduced costs. The methods we used to undertake the review are detailed in Appendix 1.
In total, 38 empirical articles15,55–91 published in a wide variety of journals were included in the review (see Appendix 1, Table 28, for summary details of each of these studies). Of the included studies, 17 were from the UK,15,56,61–64,68,70,75–77,79,80,82,83,90,91 13 were from the USA,55,58–60,65,66,71,73,84–86,88,89 four were from Canada,69,72,78,81 one was from Australia,74 one was from Ireland67 and one was from Israel. 57 Also included were two comparative case studies (one from the UK and the USA and one from the UK and South Africa). 82 Twenty-four studies (63.2%) used qualitative methods,15,55,56,58,59,61–64,66–70,75–82,87,91 of which 13 had a case study design56,58,61,62,66,69,70,75–78,79,82 and five were specifically ethnographic in their approach. 78–82 Nine studies used only quantitative research methods60,65,71–73,83–85,89 and eight utilised surveys or questionnaires;57,60,65,71,73,83,88,90 the majority (seven60,65,71,73,84,85,89) of the quantitative studies were from the USA. Five studies used a combination of qualitative and quantitative research methods. 57,74,86,88,90 Half of the studies were published since 2007,55–59,61–63,67,68,70–72,74–76,81,87,88 and the majority (n = 33, 86.8%) of research was published since 2000,15,55–59,61–72,74–78,79–83,86–88,90,91 reflecting increasing and continued interest in the subject of boundary spanning in the health services literature. Details of the direction of integration and the boundaries spanned in the included studies are shown in Table 1.
| Boundaries studied | Horizontal integration (n = 24) | Vertical integration (n = 14) |
|---|---|---|
| Sectoral | 14 | 3 |
| Organisational | 8 | 7 |
| Professional | 13 | 14 |
Overall, we found that the 14 studies of vertical boundary-spanning provide clear descriptions of how people at different levels of a health-care system relate to each other but are weak on process and evidence-based patient outcomes. 15,55,56,61–65,75–77,86,89,91 All of these studies addressed spanning professional boundaries to some degree, which may reflect contemporary research interest in examining power relations between disciplines. Top-down policy initiatives for collaboration were not found to have led to better co-ordinated services. Predefined roles for clinical boundary spanners appeared to be challenging to accomplish in reality and social (personal and political) factors played a greater than anticipated role in this. Political awareness and facilitation skills seemed important for inter- and intraprofessional working, particularly in this vertical dimension. For individuals in high-status positions, successful boundary spanning requires a willingness to work outside professional identity groups; for those in lower-status positions, gaining and communicating professional competency may be more important. In summary, although interdisciplinary and interorganisational boundary spanning is a well-described challenge, there is little research to demonstrate how effective vertical integration is accomplished by implementing boundary-spanning interventions.
Studies of horizontal integration appear to provide rather more positive support for boundary-spanning interventions than studies of vertical integration. More of the studies of horizontal integration examined the crossing of sectoral boundaries – 1357,59,60,66,67,69,71,73,82,85,87,88,90 compared with only three62,65,76 in the vertical integration articles – reflecting how non-health-care sectors experience horizontal relationships with clinical services. Efforts in the horizontal integration of primary care services are commonly implemented to improve access for patients seeking particular medical services. Boundary-spanning interventions in the form of online discussion forums, published resource guidelines and complex pathway guidelines have the potential to improve joined-up working, particularly in community settings. However, sustaining integrated solutions relies on the flexibility, adaptability and continued reflection and insight of those who are facilitating the intended change, and the receptiveness to this change in the wider environment. For individual staff, achieving boundary status is associated with accomplishment, but also ambiguity. Professionals with enhanced expertise but in new boundary-spanning posts, such as clinical nurse specialists, general practitioners (GPs) with special interests or dual specialists, may not be readily accepted either socially or politically, making system-wide integration sluggish.
The 38 empirical studies that met our inclusion criteria were then analysed using the seven iterative steps of meta-ethnography for evidence synthesis (see Appendix 1). The resulting important themes were:
-
the need for individual boundary-spanners to possess a wide range of communication skills
-
negotiating formal and informal boundary-spanning roles
-
recognising and responding to social and political influences on knowledge exchange processes
-
demonstrating evidence of the impact of boundary-spanning on the quality of patient care.
A wide range of communication skills
Martin and Tipton55 compiled a typology of communication roles from a purposive sample of non-clinical, salaried patient advocates who, as boundary spanners, might review medical charts, facilitate selection of doctors for second opinions or socialise with waiting family members. The roles were liaison, feedback/remediation, counselling and support, system monitor, troubleshooter, investigator and group facilitator. Although this research suggested, theoretically, that as boundary spanners these advocates may serve as system change agents – particularly when responding to patient complaints – the descriptive nature of the research did not build empirical evidence for vertical integration. Similarly, Abbott56 found that to be effective, nurse consultants needed to be credible leaders, be familiar with relevant policies and organisational structures, build and maintain effective relationships and apply communication skills (including facilitation of conflict).
In another mixed-methods study,57 three structural variables (team informational diversity, team boundedness and extra team links) were used to understand how to increase interorganisational boundary spanning in health promotion teams. Three types of boundary spanning were reported as being associated with team effectiveness: scouting, ambassadorial and co-ordinating. The author suggests that the most effective teams should maintain an open team configuration, invite experts and change team composition over time (including part- and full-time members). In this way, increased scouting implied greater informational diversity, and greater interorganisational team effectiveness, even in less bounded teams with more part-time members.
Tools, and processes, can serve as boundary-spanning entities as well. Three studies58–60 examined how knowledge sharing was accomplished through boundary-spanning methods. Hara and Hew58 observed an online community of practice for advanced practice nurses, finding that the non-competitive and asynchronous nature of online communication facilitated the improvement of current knowledge and validated best practice. A study of health behaviour change explored the use of referral guides along with support people external to the organisation to implement linkages in the community. 59 Connecting strategies, such as paper or electronic databases were developed to bridge primary care and community resources, especially for patient referrals. However, hurdles were discovered in both resource availability and accessibility to patients, and affordable infrastructure to support boundary-spanning activities was needed. Often boundary-spanning individuals were needed to fill in the gaps, and marshal the use of technology, when paradigm shifts in practices had not yet occurred.
As translators and diplomats, boundary spanners may serve to communicate new ideas across a divide. How that knowledge is shared, and whether or not it is adopted, is a sign of its impact. In a study of health planning staff and board members it was found that effective performance as boundary spanners improved collaboration. 60 As a study of communication strategies, staff members and board members influenced each other by the extent to which they answered each other's questions; seeking information became a mark of a good board member. Open communication appeared to enable the ability to act on shared objectives. Knowing the staff views and agency routines increased the perception of board effectiveness.
Formal and informal role negotiation
The development of new professional roles to bridge treatment areas is a relatively recent innovation in the UK. With the development of these roles comes ambiguity in task definition and efforts to build professional credibility. Examining pilots that sought to train GPs in specialist genetics and cancer roles, it was found that recruiting for such hybrid roles was difficult because of the day-to-day work of GPs; sustainability of the project was a major concern. 61 GPs with special interests were described as defining their legitimacy through relations with experts and through the motivation to extend clinical competency. However, between geneticists and GPs, the power of knowledge and jurisdiction (‘turf’) remained disputed in the professional hierarchy. Consensual divisions of labour may be backed by institutional goals, but, at the micro level, how roles were negotiated was not entirely clear. For example, a mutually agreeable role for the boundary-spanner clinician was delimited (by the specialist) to be less clinical and oriented towards a more educational role (similarly, nurse consultants are described as struggling to negotiate their role as either autonomous expert or process supporter, with a common experience of having difficulty identifying priorities56). An awareness of stakeholders' different priorities, social capital and established relationships was key for developing collaborations across organisational and sectoral boundaries. Short-term economic incentives were difficult to address with long-term preventative cost-saving calculations. In this way, politics was identified as an important aspect of role definition for boundary spanners. In these examples, beneficial evidence from putting a clinician in a boundary-spanner role was difficult to collect, and the role was constantly renegotiated within the context. When considering intentional efforts to vertically integrate services, the authors noted that colocated specialists and practitioners in hospitals had not only a supervisory relationship but also a more dialogical and informal relationship. Practitioners not located in the tertiary setting but working in primary care appeared to have more clinical–governance relationships with the hospital-based specialists. This latter relationship was considered time-consuming for the geneticist who had to check the risk assessments carried out by practitioners who might have had ‘inadequate’ training. 62 Defining a boundary-spanning role by task orientation and job description does not fully reveal the negotiations that happen on a daily basis.
Negotiating disciplinary boundaries between specialists and generalists may be mediated by disciplinary values (which may be semantic, historical, practical and unrelated to patient need or disease trajectory). In a role study in palliative care – and despite policy guidelines to share care – covert and overt tensions between services were noted, particularly in the practice of referrals. 63 Personal commitment and local organisational goals appeared to highlight dilemmas posed by uncertainty of prognosis, particularly in patients with heart failure. In these ways, boundary-spanning managers and newly appointed link workers who were perceived to have less clinical knowledge had less ability to influence others in the vertical dimension, even if supported by policy initiatives, newly funded posts or intentional clinical or managerial placement. Vertical integration may be suggested by policy, but professionals make individual decisions to collaborate, or move patients across boundaries, based on many other factors.
French64 describes four contextual factors (physical, social, political and economic) that influence how work group participants use evidence to make policy decisions. Doctors, managers and nurses working in different settings may have varying perspectives of what is needed for patient care. For example, in the social context of care, respondents reported using independent action, involvement in teaching and direct challenge to influence the care decisions by medical staff. Subterfuge and adaptation were also described as covert strategies used to influence care patterns. In the wider context of care, researchers observed that influencing commissioners, adapting decisions and informally ‘trading’ equipment were other strategies used to manage economic constraints. 64 In these ways nurses used different strategies to close gaps in services.
Finding time to engage in vertical integration activities was also a challenge for clinicians. Nurse consultants working in boundary-spanning positions were described as needing additional time to negotiate priorities and relationships, which limited the time that they were available for patient care,56 whereas cardiac surgeons reported that time constraints may contribute to inaccurate medical stories that are reported to newspapers. 65
Boundary spanners have been placed as intentional links between programmes in an effort to create a more seamless service for clients. For example, expanding the roles of mental health workers to bridge the hand-offs between the courts and components of the mental health system was a solution explored in one case. 66 Attempts to build this innovative programme as a model were complicated by the varying engagement of different stakeholders and by a lack of client health insurance (in the USA). An assessment to gauge interagency co-ordination was mentioned but not reported in detail.
For mental health link workers it was found that, although there was potential for these liaisons to improve communications between secondary education services and child and adolescent mental health services, staff were concerned that some increase in workload might result in the short term. 67
Another study examined the changing roles of practice nurses in the primary health-care setting in terms of them taking greater responsibility for the management of chronic disease. 68 The realignment of boundaries demarcating work previously carried out by GPs motivated nurses to increase their technical knowledge base to a less routine level of practice and to an increased level of professionalism, but raised some tensions in role definition.
Trust and communication, and power and conflict, were explored in a case study of multisectoral collaboration in the domain of the human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) community. 69 Boundary spanners were recognised as being in ‘dual roles’ – both collaborative partner and organisational representative – causing tensions to arise. Juggling the conversations between constituencies required a chain of conversations, which was framed as a creative process central to organising; the tension was positive and necessary for seeking change. In this case study the tenuous space between collaborators is described as a source of potential energy.
Attempts to map out a mental health safety care pathway also met challenges, because of complex assumptions about work arrangements, and attempts to connect the expectations of clinicians, managers and service users. 70 Negotiating the use of a guideline as a tool was unworkable when it was conceived of as an ideal document of standardisation. To co-ordinate services, and accommodate to variation, the pathway needed to become more abstract in its scope. As a boundary object the author describes the imprecision and looseness of the resulting pathway as an effective alignment and compromise between stakeholders. Creative solutions can resolve such tensions, while balancing the needs of standardisation with diversity of purpose. 70
Two quantitative studies71,72 in the vertical dimension measured time spent (number of hours engaging) in boundary-spanning functions as a positive characteristic of a supervisory position. Substance abuse programme directors, who were also treatment counsellors, were found to spend more time making community presentations and liaising with monitoring organisations, which the authors assume (but did not measure) may have improved treatment practices and political leverage. 71 Front-line nurse managers with a larger number of direct report staff reported lower supervision satisfaction with highly transformational leadership, except when operational hours were extended. 72 These boundary-spanning managers found more satisfaction in the transformative behaviour of performing ‘citizenship’ activities within the organisation, than simply having more time with staff, although having more time was a factor. The leadership activities that characterise boundary spanning appear to mediate contextual pressures, but further studies would need to explore this issue more fully.
Two studies73,74 used quantitative methods to evaluate the impact of perceived uncertainty on boundary-spanning behaviours. In an early field study of work units in health and welfare organisations,73 positive relationships were found between three variables: an organic management structure, frequency of boundary-spanning activity (verbal and written interactions) and perceived environmental uncertainty. The study used a composite variable of ‘organicness’ in management structure by using six scored measures, including extent of participation in strategic decisions, participation in work decisions, division of labour (specialisation), impersonality, formalisation and hierarchy of authority. Perceived environmental uncertainty was measured by questionnaire items rating whether or not subjects knew what to expect of people in the organisation. Frequency of boundary-spanning activity appeared to mediate environmental uncertainty and organisational structure. Organicness was strongly associated with frequent boundary-spanning behaviour; environmental uncertainty was not. By examining the individual as the unit of analysis, this attempt to understand the different effects of organisational structure and uncertainty made strides in adding contextual factors to the analysis of boundary-spanning activities, but limitations remain in measuring such linkages in context. Similarly, in their study of service providers working as boundary spanners in primary care partnerships in Australia, Walker and colleagues74 suggest that such individuals function to interpret environmental context for decision-makers, mediating risk and uncertainty. Service providers perceived less risk and uncertainty in the collaborative work and, so, experienced unproblematic relationships based on trust. In contrast, organisational managers perceived more risks from breaches of trust, particularly as a result of political partnerships, which also might result in more consequences and harmful uncertainties. Competitive allocation of funds and established system practices impacted these experiences, placing an importance on an institutional environment that supports trust across professions.
Social and political contextual influences on sharing knowledge
Twelve15,55,61–64,75–77,86,89,91 of the 14 studies of vertical exchanges specifically addressed the social and political contexts in which different disciplines function, particularly the two studies by Currie and colleagues. 75,76 These studies found that role and status seem to determine research uptake in professional groups, as opposed to managerial behaviour. Social and political relations between team members were identified as the medium for sharing knowledge in organisational change efforts. 76 A case study of how knowledge was shared between two NHS teaching hospitals, district general hospitals, PCTs, a strategic health authority and a university medical school took a neo-institutional perspective. 15 This study suggested that knowledge sharing could be enabled within similar organisations but that this was much more problematic across different organisations and professional groups. In this study hospital doctors were found to focus their knowledge-sharing activity on relationships with their peers within the hospital boundary and they downplayed any contribution that GPs or commissioning managers might make to service development.
The hierarchy of professional exchanges across disciplinary boundaries, and the tendency of higher-status clinicians to withhold rather than share knowledge, was described in a study of the barriers to the spread of innovation in multiprofessional health-care organisations in the UK. 77 Specialists hold overt power in the hierarchy of organisations and strong professional identity is associated with more reluctance to share knowledge. These researchers found that strong uniprofessional communities of practice can block external input from other groups and retard innovation. A key theme in both the horizontal and the vertical integration of services is therefore how credibility is inextricably linked to professional competency and expert knowledge. 77,78,92
Five ethnographic case studies78–82 examined the role of boundary spanners in horizontal integration. The advantages of observing the sociocultural and knowledge context of group work allowed these researchers to explore the factors that impede or enhance collaboration, whether in the tertiary care hospital or in the community clinic. Recognising the need for someone who sits outside of the usual routines – albeit temporarily – was noted in these studies. MacIntosh-Murray and Choo78 suggest that nursing staff – busy with prosaic tasks – may find that meetings and other forms of communication appear to be time-consuming with little time for critical thinking to solve knowledge gaps. The rhetoric of accountability (and risk of consequences) can focus busy staff on tasks rather than quality improvement and, with managerialist discourses, doers may feel burdened or disempowered by a perceived need to put in extra effort to fix problems. A boundary-spanning ‘surrogate’ was able to identify the information needs of others and act as a knowledge translator, but could not fix routines or inherent competence problems in individuals. 78 In another study,79 high workload demands in a complex environment were addressed by staffing flexible and transient teams in operating theatres; however, shared knowledge was at risk as was having a predictable knowledge composition of the teams. In this way, flexibility in coping with care delivery demands was found to undermine the acquisition of knowledge; risks to safety were implied, but evidence was not gathered to support this. Ambiguity can affect people working in boundary areas (such as volunteers working in formal organisations), which may cause confusion for the paid staff working with them. ‘Lay’ workers may be asked to share knowledge and experience but not to give advice, which poses particular tensions and the potential for conflict. 80 Salhani and Coulter81 describe how nurses in a psychiatric hospital ‘went underground’ with ‘guerrilla action’ to use a primary therapeutic nursing model to address biopsychosocial factors with patients, despite rejection from ward psychiatrists. Micropolitics and strategies to organise among the nurses were key factors in the description of interprofessional relationships in this study, as the ‘elite nurses’ intentionally expanded their jurisdictional boundaries through loyalties, logos and celebrations to oppose the dominant medical culture. In another study,82 working as ‘boundary people’ at the interface between community and statutory organisations in itself was a prized end, suggesting that empowerment may have its place in system change. In this case study, building change through ‘small steps’ and ‘good enough’ solutions were strategies used to build partnerships.
An NHS primary care-based study used a survey to examine how boundary spanners' characteristics and behaviours related to the effectiveness with which different groups jointly work together. 83 The study found that the productivity of group collaboration was predicted by boundary spanners who had frequent intergroup contact and high organisational identification. The authors suggest managerial implications (e.g. promoting individual boundary spanners to boundary positions when strong ties to their organisation can be used to overcome ineffective intergroup relations) but no interventions were tested.
Boundary-spanning strategies are used by organisations as well as individuals and groups. For hospitals in the USA, membership in a larger organisational (multihospital) system increased the likelihood that bridging strategies would be used for outreach, likely because of corporate policies to reduce costs. 84 Freestanding hospitals were less likely to seek external service linkages through planning groups or consortia. Confirming the idea that the hospital system is fragmented, this research suggested that hospitals do not have a uniform response to environmental pressures and noted that regulatory pressure did not increase boundary-spanning activity as expected. Retrenchment at the administrative level might be more likely as a response to vertical integration pressures, by increasing the size of boundary-spanning governing boards rather than increasing technical capacity. In another study of hospitals in the US health-care system85 it was found that inpatient psychiatric departments increased the number of boundary-spanning and buffering structures as they increased in size. Organisational performance was inversely related to department size as assessed by discharge rate, cost of discharge and cost per patient-day. Public hospitals had more secure government funding and were more likely to increase the number of professional staff, whereas private hospitals were more likely to use non- or paraprofessional staff to reduce costs.
Callister and Wall,86 in a mixed-methods study from the USA, specifically used conflict incidents to explore the interactions between managed-care representatives and service providers. Organisational power and status differences were the independent variables, and behavioural responses of the managed-care representatives and expressed negative emotions of providers were the dependent variables. The researchers noted that the individual boundary spanners with the most power (e.g. representatives of the larger managed-care organisation) were less compromising and collaborative when negotiating with smaller organisations, and anger resulted when decisions were blocked by a lower-status representative. Describing a ‘double power asymmetry’ the researchers also noted that the organisation that is larger and controls revenue streams can exert power over the medical doctor as provider; however, this is reversed if the boundary spanner from the managed-care organisation has a lower status (a clerk or a nurse) than the medical expertise of the provider. It is interesting to note that the boundary-spanning post can be both problematic and a proposed solution; the boundary-spanning representative in the middle of a conflict can experience stress and potential job turnover, which might be addressed by putting more doctors in boundary-spanning positions.
In a case study of successful local health partnerships,87 boundary spanning was accomplished both ‘downwards’ and ‘across and upwards’, meaning that community advisors had the responsibility for engaging multiple stakeholders, including programme recipients. Momentum was maintained for ongoing dialogue because of the trust engendered through the enthusiasm and optimistic personality of the boundary spanner. Positive results were reported as ‘100% uptake of energy efficiency measures’ and ‘high levels of satisfaction’, which were attributed to the increase in detailed local knowledge. Being a ‘community-led’ project was also held to be a positive aspect of the success of the strategic planning partnerships. The movement of knowledge across boundaries appears to be inextricable from the communicators of the process.
In another example of community partnerships, public health and faith collaborations were designed in an effort to address health disparities. 88 Boundary leaders were trained in methods of community system change at an educational institute and pre/post assessments of knowledge and skills were gathered from each participant. Despite reporting success on leadership measures of renewed sense of faith and team accomplishments in planning programmes, no impact on health disparities could be reported. Inducing plans for change can be an indicator of the effect of boundary-spanning interventions but does not provide clear and direct evidence of an impact on health outcomes, as is often demanded by stakeholders and funders.
Evidence of impact on the quality of patient care
Of the 14 studies15,55,56,61–65,75–77,86,89,91 that examined the impact on health-care quality of some form of vertical boundary-spanning intervention, only one examined patient outcomes as a result of a boundary-spanning initiative. Thompson and colleagues89 used key indicators (through retrospective chart audit) to determine the quality of peritoneal dialysis before and after a collaborative mapping project. Inpatient and ambulatory nursing representatives met to identify and change process flow charting for equipment utilisation (by patients and clinicians) across a service boundary. As an intentional quality improvement effort, patients who received care after the new jointly developed guidelines were implemented showed a decrease in transfer time between units, faster diagnosis and faster treatment of complications; plans for interdisciplinary collaboration for changing practice responses for hypovolaemia were also being monitored. In this study, how different professionals were brought together for discussions was not qualitatively examined, but the impact of the effort was well illustrated.
A postal survey and interviews90 identified five perspectives relating to the role of boundary spanners – networker, innovator, ‘cultural broker’, collaborator and leader – and explored how the factors of otherness and trust contributed to whether or not such individuals are ‘born and not bred’. The author concluded that research evidence was ‘weak on processes and effectiveness’ and failed to explain the link between individual and team behaviour and outcomes. The study confirmed the image of individual boundary spanners as being able to work in non-hierarchical decision environments by brokering resources and connecting problems to solutions; however, the link between competency and performance effectiveness was not explored.
Summary
Boundary spanning as a concept is well described in the organisational studies literature and many insights from our literature review confirm previous findings in other industries (i.e. broader insights do seem relevant to contemporary challenges relating to the vertical and horizontal integration of health-care services). However, although it is accepted that boundary spanning contributes to knowledge transfer in the technology industry, sectoral, organisational and professional boundaries in health-care systems can present significant barriers to the exchange of knowledge. 15 These can undermine attempts to integrate health-care systems and ultimately efforts to improve quality and efficiency.
Our review of the literature shows that boundary spanning is often regarded as a potential solution to the challenge of service integration. Although the 38 studies that we reviewed differed in terms of whether they took a quantitative or a qualitative stance, whether they studied boundary spanning as an informal or a formal activity and whether they focused on the co-ordination of teams within or between organisations, overall we found a quite strong normative emphasis in the literature. ‘Boundary spanning’ appeals as an ‘obvious’ solution and also tends to be quite reified through individuals being identified as ‘boundary spanners’ who extend collaboration and integration in health-care services. What is less clear, however, is how boundary spanners perform their role – or should perform their role – to improve the quality of care. But we would also note that some commentators45,46,50,51 perceive boundary-spanning processes as problematic, not just failing in implementation but also hindering and even jeopardising intended facilitation and change.
A recent review of current policy frameworks for supporting evidence-based health care93 specifically argues for greater attention to be paid to fostering ‘new boundary-spanning mechanisms to encourage knowledge flow across professional boundaries’ (p. 847) and to the means by which different professions can share and debate their ‘knowledge’ and then embed it into local practice. Our review found that, although the characteristics and experiences of individuals in formal or informal boundary-spanning roles have been studied in the health-care context, relatively little attention has been paid to date to the core focus of our study: the processes by which ‘boundary spanning’ can support horizontal and vertical health-care integration. Importantly, our review also demonstrated a lack of evidence of change in practice.
Conceptualising knowledge creation and exchange processes across boundaries: the socialisation, externalisation, combination and internalisation model
As the findings of our literature review illustrate, although the characteristics and experiences of individuals in formal or informal boundary-spanning roles have been studied in the health-care context, relatively little attention has been paid to the core focus of our study: the processes by which ‘boundary spanning’ can support horizontal and vertical health-care integration through enabling knowledge exchange (as well as knowledge creation). In the light of the limitations of the existing literature, in this section we briefly describe a conceptual framework that we shall use as a working heuristic to help analyse our findings in terms of the impact of a boundary-spanning intervention on knowledge exchange processes between different sectors, organisations and professions. Our initial data were analysed to generate candidate theories and we selected the socialisation → externalisation → combination → internalisation (SECI) model (see below) because of its distinctive combination of structure and process, and particularly the emphasis in the model on the importance of micro interactions and the impact of these at the meso and macro levels, an important theme in our emerging findings.
Outside of the health-care literature, Ikujiro Nonaka94 has proposed that organisational knowledge creation progresses in a spiral model of continual dialogue between tacit and explicit knowledge. Nonaka draws on the distinction between different types of knowledge: explicit knowledge consists of facts, rules, relationships and policies that can be faithfully codified in paper or electronic form and shared without the need for discussion, whereas tacit knowledge is engrained in the analytical and conceptual understandings of individuals (‘know what’) and also embodied in their practical skills and expertise (‘know how’). Tacit knowledge is seen as being uniquely personal and embodied, whereas shared experience and deep mutual trust facilitate the conversion and change towards the experience of a simultaneous rhythm and synchrony of action.
Although much has been written about the sharing of knowledge through artificial intelligence and computer systems, Nonaka's model emphasises the social aspects of how individuals and groups function in an organisation, and how these different types of knowledge (tacit and explicit) move across, or span, boundaries. Nonaka describes four modes of knowledge conversation – socialisation, externalisation, combination and internalisation (SECI). As demonstrated in Figure 1, the two different types of knowledge are converted from one mode to another through these four different processes. Knowledge is created and expands between individuals (i), groups (g) (or, in our terms, teams) and organisations (o) in a continuous manner of knowledge conversion through the four-stage process represented by SECI, which has been tested empirically.
FIGURE 1.
The SECI model. g, Group; i, individual; o, organisation. Source: Figure 1 entitled ‘Spiral evolution of knowledge conversion and self-transcending process’. Reproduced with permission from Nonaka I and Konno N, ‘The concept of “ba”: building a foundation for knowledge creation’ in California Management Review, vol. 40, no. 3, Spring 1998. © 1998 by the Regents of the University of California. Published by the University of California Press.
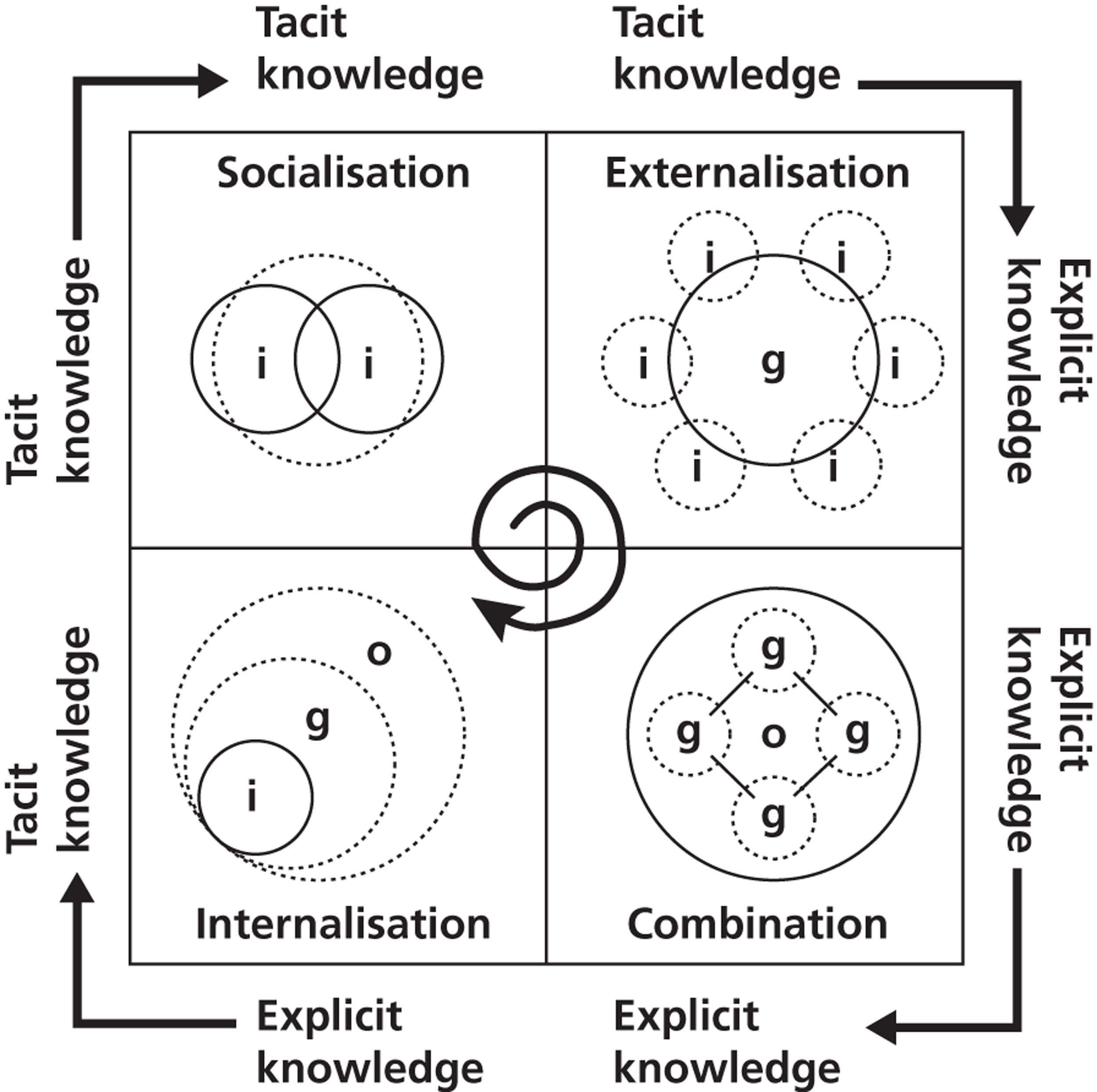
At the initial socialisation stage of the SECI model, creativity for system-wide problem-solving is potentially spurred by the sharing of tacit knowledge between individuals and builds on their own personal skills and enthusiasm. In the second stage of the process, exchanges move beyond the sharing of tacit knowledge among individuals and towards the design of explicit knowledge assets – externalisation – that can then be shared among ‘groups’ (whether teams or professions). In the third stage, explicit knowledge is clarified and put into place with more systemised approaches, including publishing documents, building databases and authoring policies: combination. Finally, systems and individuals at the internalisation stage are recognisable by their embedded routines within organisational culture and explicit skills in daily operations. Internalisation is not the final stage as the process is a continuous dynamic.
Exploring and experimenting with how to define problems, and discovering new solutions, removes individual limitations and intensifies interactions to expand the boundaries of knowledge. A knowledge outcome can include a justified belief in what is true as the team comes to a collective understanding of the new problems, different solutions and diverse tasks with which they are faced. This provides the team with an enhanced capacity to take action to improve problem-solving performance. Social practices then offer stability and routine to processes within the organisation. However, how knowledge conversation impacts on emerging social practices is not well understood. 96
Nonaka has applied this model to cross-functional teams and their business activities, particularly explaining how boundaries are spanned both inside and outside the organisation. The shared context for dynamic knowledge creation is ‘ba’ (building or place), which is an experience of interaction, not merely a physical space. Significantly for our study, Nonaka and colleagues97–99 argue that leaders can aid or impede the knowledge conversion process across organisational layers and boundaries. The ‘knowledge management system’ within an organisation is part of the context of this process.
Von Krogh and colleagues99 argue that the role of empowerment and combinations of distributed or shared leadership is not well explored in the current literature, but needs to be. Distributive leadership can initiate and shape activities and conditions by allocating resources, defining vision and describing organisational forms to link contexts, assets and processes within and across the organisation. An individual's knowledge must enlarge, and a leadership that promotes all four modes of knowledge conversion implies room for effective communicators to develop new concepts and new kinds of verbal and non-verbal language. An enabling characteristic of the organisational knowledge creation process includes chaos or fluctuation, in which crises are presented as problems needing new solutions. The challenge requires reflection and deep mutual trust, or else there will be destructive not creative chaos. 94 Von Krogh and colleagues99 therefore propose a leadership framework that combines centralised (planned, autocratic, directed) and distributed (participative, spontaneous and fluid) leadership for spanning organisational boundaries, as negotiating boundary crossings is often problematic. But little research has described how leaders can integrate SECI, knowledge assets and ba. The authors call for more attention to be paid to discovering the form and function of boundary negotiations. They also highlight the lack of research that combines the micro and macro levels in organisational processes, arguing that knowledge is not strictly individual or collective, and knowledge creation interactions should be examined at all levels. 99
To explore the complexities of how such boundaries are spanned in health care, we have chosen an ethnographic study with mixed methods. In Chapter 4 (see Multilevel, cross-case comparison: socialisation, externalisation, combination and internalisation and the four teams) we use the SECI model of knowledge creation as a holistic framework to evaluate the quality improvement activities of the four teams participating in the boundary-spanning intervention under study. We believe that the SECI model is particularly useful for analysing the barriers that boundary spanners reach across, allowing us to identify, and potentially anticipate, barriers and enablers. In the WI the four teams and team leaders and their impact will be examined by applying this SECI model and Nonaka's further theoretical developments. Primarily applied to information and technology organisations, most research and theorising related to SECI is in the management literature. We are not aware that the model has been previously applied to any health-care organisations.
The boundary-spanning intervention under study: the Westpark Initiative
As described in the WI materials, the boundary-spanning intervention was a project designed to improve services through collaboration between GPs, community services, voluntary groups and acute specialists in ‘Coxford’ during the period 2009–11. The project included the development of a network of leaders across organisational and community boundaries to facilitate knowledge exchange and was directly linked with a programme of ‘whole-system’ stakeholder conferences (in November 2009, April, July and November 2010 and April 2011, as indicated in Figure 2) to create organisational learning and change, together with community development. The project took place in Coxford PCT where there was – it is claimed – ‘sustained political support and understanding for this way of working from local statutory organisations, in partnership with voluntary sector agencies’, as explained in a letter provided by the initiative leader Chris. The WI used an annual cycle of service improvement for whole-system change, as initiated by a community leader and GP (Chris) (see Figure 2 for an overview of the annual learning cycle as we observed it).
FIGURE 2.
Westpark Initiative: cycle of service improvement, 2009–11. ICO, integrated care organisation.
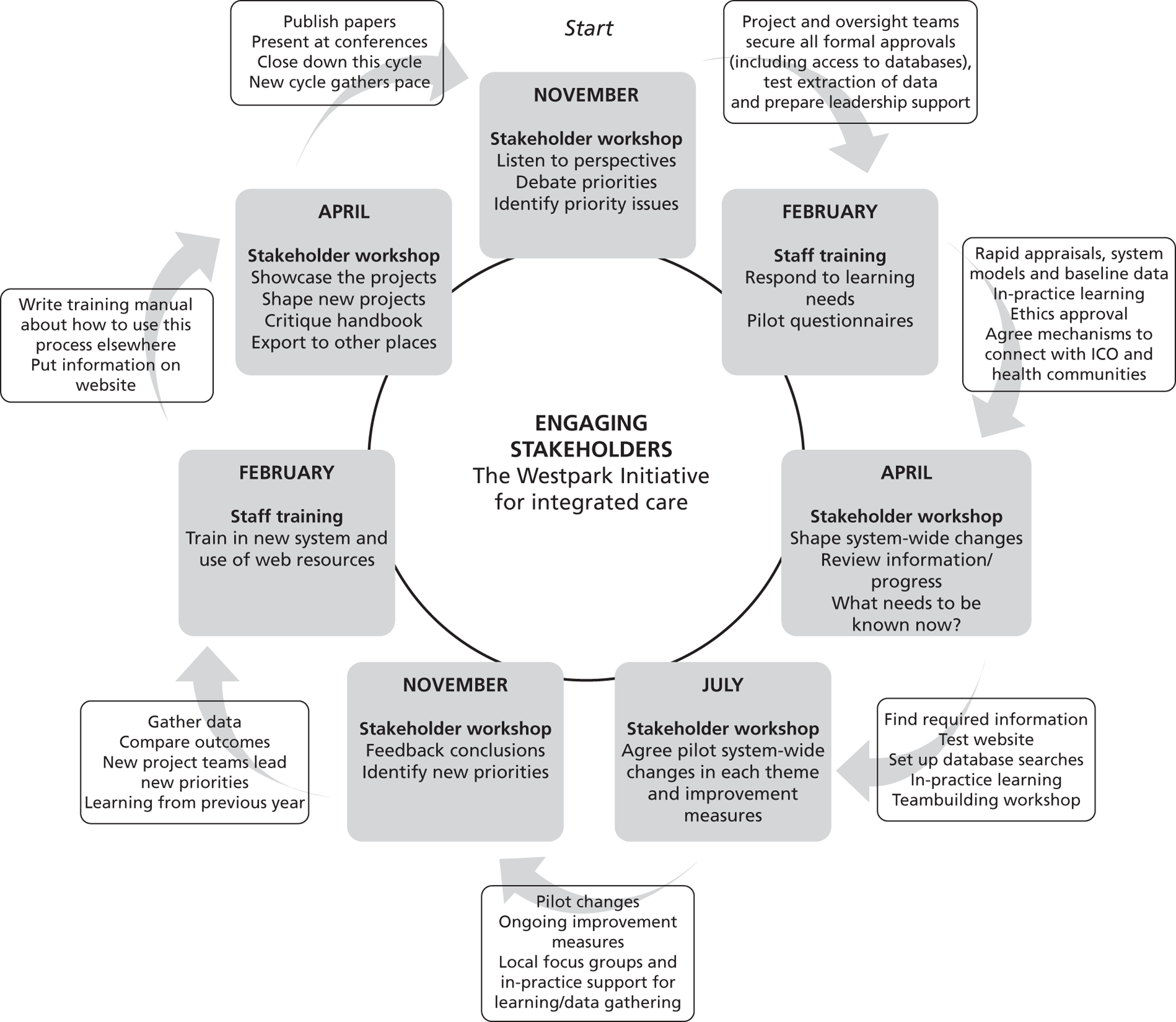
Stakeholder workshops were expected to be held quarterly, during the evening, with attendance from a wide variety of representatives from social care and the third sector as well as clinical staff from primary care and mental health.
Staff training events were held at different times for staff across the borough, with a variety of topics and sponsors. The intent was that two training events for GP surgery staff would be hosted by each of the WI teams based on their annual work.
In Coxford a set of masterclasses (local off-site educational sessions) were funded through a grant to the Development & Research (D&R) network, led by Chris, and overlapped with the WI structure, although not as a formal part of the initiative. These were designed to be monthly, during the afternoon, on a variety of topics, and all local clinical and non-clinical staff from the PCT and GP surgeries were invited. An applied research unit had been founded by the PCT in 2008 as part of a D&R network to improve practitioners' and managers' critical skills, in a cluster of GP surgeries, and to improve relationships with academics. D&R networks were introduced in the UK in 2003 by the National Educational Research Forum to serve as iterative programmes to enhance communications and increase opportunities for exchange between researchers and developers and particularly to increase capacity in local research efforts. 100 With a background as a teacher for local colleges as well as a GP trainer, Chris intended that staff could, and would, attend these training sessions to build competence in their skill set for participating in local quality improvement and research efforts. To this end, continuing professional development (CPD) credits towards a university certificate were offered as an incentive. Dates and rooms were scheduled on a monthly basis, through 2010 and 2011, with topics to be announced, although some were to be run by the local Collaboration for Leadership in Applied Health Research and Care (CLAHRC) and overlapped with WI stakeholder events.
Annual ‘residential’ retreats had been scheduled for use by the Coxford D&R network since 2008 and were usually held by invitation for GPs and PCT and primary care staff. Although not a formal part of the WI annual cycle, the booked off-site setting served as a supportive learning environment in 2009 and 2010 where Chris facilitated workshops for invited WI participants to share interdisciplinary experiences and plan for service improvement efforts. Funding for the overnight stays at the site was a factor in who was invited and how the agenda was determined from one year to the next.
From October 2009 to early 2012, three (later four) boundary-spanning multidisciplinary teams were to work to develop their own solutions to local problems through the annual cycles of shared learning represented in Figure 2. Team membership was voluntary, multidisciplinary and shifted frequently and was not assigned by work duties. Team members were invited to ‘dip in’ to masterclasses, training events, stakeholder events and residential retreats as they were able. Some time after the topics areas were agreed and the teams began work, the leader of the WI began to frame each of the teams as working to span different types of boundaries, namely between primary care and:
-
mental health care [anxiety and depression in black and minority ethnic (BME) populations]
-
social care (dementia)
-
community care (child and family health services)
-
acute care (diabetes).
The study setting
Our study took place in an area within an inner-city borough that is dominated by the Asian, particularly Punjabi, community. Although there are many Muslim and Hindu residents, the largest portion of the borough's population is Sikh (23.2%). The borough has a population of approximately 300,000 residents, > 40% of residents were born outside the UK and about 25% of adults have no academic qualifications. In the borough as a whole, many children do not speak English as a first language.
Overall, the area in which our study was conducted ranks high on all deprivation scores and is impacted by many chronic diseases, reflected in higher than expected mortality rates. The Index of Multiple Deprivation (IMD) for the study area – a summary score measuring deprivation in relation to employment, income, education, skills and training, health and disability, barriers to housing and services, and living environment and crime – was the highest in the borough. A high proportion of housing in the area is overcrowded and the area has the highest scores in the borough for child poverty and deprivation affecting older people. One particular ward within our study area had the highest percentage of low-birthweight babies (10%) born between 2002 and 2004. The area also has four wards with the highest admission rates for depression in the borough and there are also high rates of admission for psychosis. The area as a whole has the highest prevalence rate for diabetes in the borough (12.6% in males), which is also more common in people of South Asian origin.
The boundary-spanning intervention that we studied was one local project designed to build connections between community services to improve local health and well-being. Clearly the wider local context was, on one hand, a challenging one in which to implement this intervention. On the other hand there was an extensive and vibrant network of community groups active in the locality and keen to engage in projects such as the WI.
Chapter 3 Study design and methods
Our evaluation of a boundary-spanning intervention – the WI as enacted by four multidisciplinary teams – is based on a longitudinal nested case study design using mixed methods. The study protocol is provided in Appendix 2. Ethical approval for our fieldwork was granted in July 2010.
Case study research is an iterative process that includes both direct observation of processes and capturing the reflections of individuals involved in those processes (through a combination of interviews, diaries and surveys in this particular study). The method is appropriate for answering research questions inquiring why and how something happens. The nested case study design and the ethnographic stance of an embedded clinician-researcher allowed us to investigate the complexity of real phenomena – boundary-spanning processes – in the context in which they took place. Given the focus of the study an emphasis on qualitative methods was warranted as they best enable the capture of lived experiences and enabled the research team to explore meaning within interactions in a given social context. 101
Overall framework for the evaluation
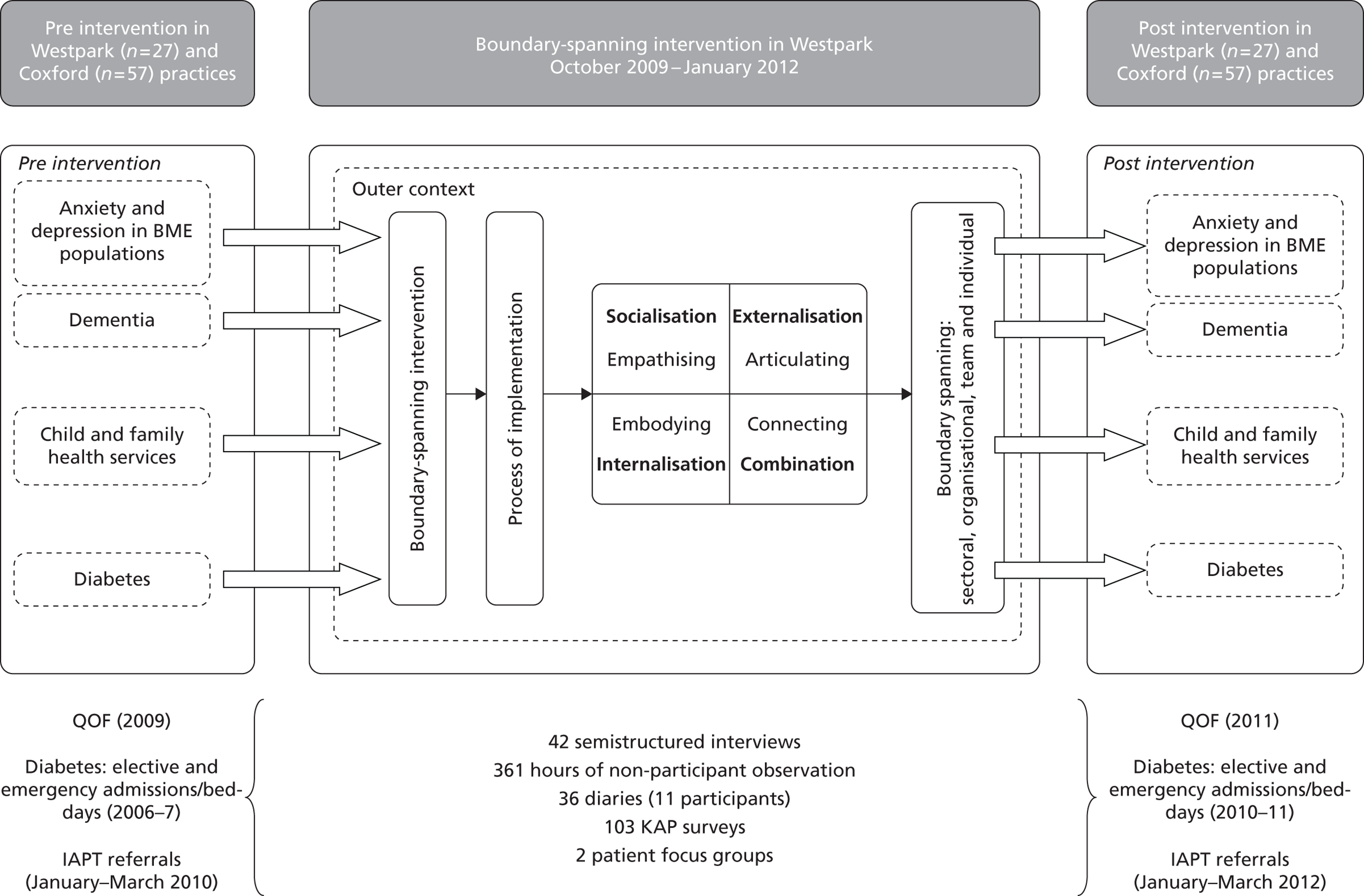
During our fieldwork we collected a range of qualitative and quantitative data (Figure 3) to study the process of implementing the boundary-spanning intervention in its local context and explore whether or not it enabled knowledge exchange across sectoral, organisational and professional boundaries in the four topic areas.
As outlined in our research protocol, our ethnographic research methods included ongoing review of project documentation, non-participant observation, semistructured interviews with the leaders of the WI and individuals in the four boundary-spanning teams, online serial diaries completed by team members, and patient focus groups. This qualitative fieldwork was supplemented with a pre- and post-survey questionnaire and secondary analyses of routine data sets. We describe each of these methods in the following sections.
FIGURE 3.
Evaluation framework. The items listed below the figure are all data sets. IAPT, Improving Access to Psychological Therapies; KAP, knowledge, attitudes and practices; QOF, Quality and Outcomes Framework.
Project documentation
Progress towards team goals in the four nested case studies was tracked through project documentation throughout the fieldwork period (July 2010 to early 2012). Researchers were included in several e-mail LISTSERVS, which included invitations to staff in Coxford to a variety of events led by the PCT. Relevant historical documents from 2009 onwards, such as presentations, reports and planning paperwork, were made available to the research team and included in our analysis.
Non-participant observation
Given the exploratory purpose of our study we observed teams in the WI in their ‘natural’ (as opposed to ‘created’) settings. As a group method of research, being able to observe individuals from the four teams interacting with each other also allowed the research team to evaluate the overall impact of the WI on boundary-spanning behaviours. Trained as a primary care clinician (nurse and family nurse practitioner), Nasir was the key observer at most events. The purpose of the observation was to identify examples of knowledge exchange and collaborative working between individuals from different parts of the health service or to note opportunities for these activities that were missed. Thus, the focus of observation was on interactions and activities. As a consistent observer, researcher interaction and feedback were invited by participants, lending an ‘embedded’ style to the field study.
Non-participant observation took place at planned stakeholder events (one every 3–4 months) once ethical approval had been granted for our study in July 2010. In total, seven stakeholder events were observed. Additional observations were carried out at four masterclasses and 10 PCT-wide meetings that overlapped the WI; 37 planning, administrative and other sessions related to the WI (attended by the WI facilitator, leaders and/or team members); and other events hosted by the WI including eight staff training events related to disease management topics and 6 days at two annual residential retreats in 2010 and 2011. A total of 361 hours were observed with written field notes (observations lasted for 128.5 hours, 203 hours and 29.5 hours in 2010, 2011 and 2012 respectively; see Appendix 3 for details).
Field notes were written in a reflective style as informed by ethnographic principles and captured four categories of material on each page:
-
Explicit activities were noted with stated agenda items matched with times, physical room layout, number of people, roles of attendees and topic being discussed.
-
Observations of mood, tone and points of perceived tension were noted in a column parallel to the agenda.
-
Boundary-spanning themes, emerging concepts and fieldworker insights were noted in coloured ink, making connections across the two main columns.
-
A ‘to do’ list was included at the bottom of each page to capture ideas of further people to interview or concepts to pursue at a later date.
This field note style allowed for multiple insights to develop and be gathered during lengthy and often complex meetings and interactions. As Tushman24 noted of the study of organisations, exploratory fieldwork requires the accumulation of a necessary background, and flexibility to make frequent adjustment to provisional hypotheses and consequent data collection. Notes were gathered during meetings and impressions noted afterward. Telephone calls and informal interactions were also written up contemporaneously in field notebooks. Analysis began during the fieldwork as qualitative data were regularly discussed to shape ongoing data collection and to allow for refined directions of inquiry. Field notes and impressions from the embedded researcher were reviewed in monthly oversight meetings with the project team and were iteratively reviewed during the analysis phase of the project.
Semistructured interviews
Semistructured interviews were conducted with individual staff identified as leading, participating in or impacted on by the WI. Participants were identified through snowball sampling beginning with the formal leaders of the WI and each of the four multidisciplinary teams and then all willing participants of each team; further interviewees were identified as the initiative proceeded. A semistructured interview guide was used to explore issues relating to the experience of participating in the initiative with a focus on boundary-spanning processes (see Appendix 4). Participants received an ethics committee-approved information sheet and signed a consent form. All scheduled interviews were audio recorded and professionally transcribed for analysis. In total, 42 formal interviews were completed with 39 participants; four participants who were highly involved in the initiative were interviewed twice, at an early stage in the fieldwork period and again at a late stage to examine their views on how boundary-spanning behaviours had developed over time (see Appendix 5 for list of interviewees).
Patient and carer focus groups
As part of our study protocol focus groups were planned with patients with conditions that may have been impacted by the work of the WI as well as their carers (see Appendix 6 for further details). The focus groups were to be held at the beginning of the data collection period, as a baseline, and repeated a year later. Despite ethics committee-approved fliers for recruitment, access to patients directly through GP surgeries was more difficult than anticipated. GPs and their practice managers were repeatedly approached and many agreed to support the identification and recruitment of appropriate patients and patient representatives. However, few primary care staff attempted to recruit patients. The reasons for this are not clear. When asked some staff stated that they were concerned to protect their patients from unnecessary intrusion. Our impression is that staff did not see the research project as a priority for them and, in some cases, we suspect that failure to recruit was an expression of resistance to what was perceived as a management initiative, in a time of great change and uncertainty of future employment in the service.
In mid-2011, following repeated unsuccessful attempts to recruit patients through GPs and practice managers, we decided to recruit individual patients directly to the focus groups but, again, although promises of access were made, similar problems were met. In January 2012 we again pursued the need for patient focus groups and were finally able to undertake these for the two most cohesive teams (diabetes and anxiety and depression for BME populations). With the benefit of hindsight, given the very marginal (if any) success of the remaining two teams (dementia and child and family health services) in achieving their objectives, it is unlikely that patient focus groups, had we been able to convene them, would have identified local changes as a result of the WI.
Participants in the diabetes and anxiety and depression in BME populations focus groups were sent an ethics committee-approved information sheet before attending. On arrival the content of the sheet was reviewed and each respondent had the opportunity to clarify any queries with a member of the research team before giving written consent to participate. Focus group discussion was structured around the semistructured topic guide included in Appendix 7. The focus group discussions were audio recorded and professionally transcribed. One focus group with seven patients with diabetes was completed in February 2012 and another focus group of two BME patients with anxiety and depression who had received counselling from the well-being service was completed in March 2012. Content and narrative analysis of the transcribed conversations elicited themes related to boundary spanning.
Online serial diaries
All members of the four boundary-spanning teams were invited to participate in online serial research diaries. A diary template was drafted by the research team and piloted with primary care staff outside Westpark before data collection began. An encrypted web link to a unique diary template was then e-mailed to invited participants every 2 weeks over a period of 2 months (a total of four diaries per participant). The diaries included both Likert-type scale questions as well as a series of prompts for narrative commentary (see Appendix 8). Completed diaries were examined for themes relating to:
-
individuals and their involvement in boundary-spanning activities over the period of their diary entries
-
participants' activities in relation to their boundary-spanning team
-
any organisational or system-wide patterns of boundary spanning.
Further analysis included examination for boundaries crossed by number and type, across time, between teams and by topic area.
Five follow-up interviews (four face-to-face and one by telephone) were conducted with those participants who completed three or four diaries; in these interviews diaries were reviewed by the researcher in dialogue with the participant on the basis of a two-page summary – prepared by the researcher – of all of the participants' diaries, which was sent to the participant before the interview. The diary follow-up interviews were audio recorded, transcribed and coded in the same manner as the semistructured interviews. The diary/interview method is useful for gaining access to informants' experiences that a researcher is generally unable to observe. Such relatively unstructured diaries followed by interviews allowed the researcher to gain insights into participants' thoughts and intentions, and also helped check the internal consistency of accounts collected through other methods. This method also elicits what Elliott102 called ‘mutedness’ or the hidden accounts that may not fit into structured categories from the researcher's point of view. Attrition rates were decreased by increased contact and debriefing efforts by the researcher. 103
In our original research protocol it was anticipated that at least three boundary-spanning team members from each of the original three teams (nine expected) would complete bimonthly research diaries. In the event, a total of 11 participants completed 36 diaries (two of the participants completed handwritten diaries on provided copies and nine completed the online version) (Table 2). Individualised e-mail and telephone reminders were provided for every diary, generally every 2 weeks until refusal or completion.
| Team | No. invited | No. participating | No. of diaries completed |
|---|---|---|---|
| Anxiety and depression in BME populations | 20 | 6 | 18 |
| Dementia | 4 | 1 | 2 |
| Child and family health services | 5 | 2 | 8 |
| Diabetes | 5 | 2 | 8 |
Questionnaire survey
A questionnaire survey provided information about the knowledge, attitudes and practices (KAP) of staff regarding the integration of services across the four topic areas of the WI at two time periods in our fieldwork (early 2011 and late 2011/early 2012). Studies on KAP are highly focused and seek to measure changes in what is known, believed and done in relation to a particular topic. In this vein our survey was designed to assess:
-
what respondents know about available local services relating to the four topic areas
-
what they think about these services
-
the ways in which they demonstrate their knowledge and attitudes through their actions (in terms of, for example, making referrals, advice-seeking, collaboration and giving information to patients).
The 52-item questionnaire (see Appendix 9) also incorporated seven items relevant to our research question from a validated instrument for assessing the quality of teamwork (the Team Climate Inventory104). The validated short Team Climate Inventory 14-item scale105 includes four factors: vision (four items), participatory safety (four items), task orientation (three items) and support for innovation (three items). Participatory safety and support for innovation were selected from the short form and the seven questions included in the survey. The single question, ‘Overall, how satisfied are you with your job’, was used with a 5-point Likert scale ranging from ‘very dissatisfied’ to ‘very satisfied’. The questionnaire was designed by the research team with advice from the leaders of the WI and pilot tested with staff from three general practices within and outside Coxford.
The questionnaire was administered as an online survey (encrypted using SurveyMonkey®; SurveyMonkey Inc., Palo Alto, CA, USA ) to all staff (clinical and non-clinical) in general practices in Westpark (26 practices) and elsewhere in Coxford (57 practices). GP surgery staff were accessed through internal e-mail LISTSERVS and practice managers and by collaborating with the trust leadership team to prepare and disseminate an invitation letter. Following a successful pilot study, the survey web link went live and weekly recruitment letters were sent to practice managers in all participating GP practices by e-mail, through handouts at local meetings and by fax. Practice managers were asked to cascade the survey invitation to all staff. Staff who completed the survey were invited to identify their practice using an optional drop-down menu in the survey. As the invitations to individual members of staff were sent via practice managers, we were not able to quantify the potential reach of the survey. Although some of the practice managers told us that they had forwarded the survey invitation, others told us that they would not ask their staff to become involved in a time-consuming activity, including questionnaire surveys. To increase recruitment, multiple invitations were sent and the online survey remained open for approximately 10 weeks at time 1 (from February 2011) and 8 weeks at time 2 (from November 2011). Recruitment rates are reported in Table 3.
| Survey open dates | No. of participants | Participant-identified locality |
|---|---|---|
| 2 February 2011–17 April 2011 | 40 | 30% Westpark, 70% Coxford |
| 28 November 2011–26 January 2012 | 63 | 25% Westpark, 75% Coxford |
Secondary data analyses: Quality and Outcomes Framework and local data sets
We conducted analyses of Quality and Outcomes Framework (QOF) indicator data for all four teams. In addition, secondary data analyses of local practice data from clinical systems were used to provide patient care outcome information relating to the anxiety and depression in BME populations and diabetes boundary-spanning teams. Comparisons were made over time and with control practices from outside Westpark (but within Coxford) to assess the impact of the WI on patient care relative to the stated objectives of the four boundary-spanning teams.
As an integral part of the project Coxford PCT was monitoring the following routine data sets with regard to patient contacts in each of the four topic areas: (1) EMIS/Vision (software systems used for practice management and patient records in primary health care developed by Egton Medical Information Systems Limited, Leeds, UK), (2) RiO (a clinical information system for community staff developed by CSE Healthcare Systems, Sheffield, UK, which is being deployed as part of the NHS National Programme for IT), (3) Adastra (a patient management system for unscheduled care across England that includes episodes of patient care in, for example, GP out-of-hours settings, walk-in centres, minor injuries units and community nurse teams; Advanced Health & Care, Ashford, Kent, UK) and (4) Secondary Uses Service (SUS) including Hospital Episode Statistics (HES), which allows practices to see how they commission services and refer patients compared with other practices locally and nationally, and also enables them to see how they care for and treat patients with particular conditions compared with other practices. We conducted secondary analyses of these data sets focusing specifically on indicators that we hypothesised could show improvements in Westpark as a result of the boundary-spanning processes observed during the fieldwork. The data sets that contributed to our analyses were as follows:
-
QOF indicators relating to the four boundary-spanning topic areas for three QOF periods (2008/9, 2009/10, 2010/11) and for each Coxford GP practice. The indicators were obtained from a pre-existing longitudinal QOF data set created by Public Health Sciences, King's College London, that has merged QOF indicator data (NHS Information Centre) with Office for National Statistics (geographical) and National Primary Care Research Centre (practice characteristics) data. 106 Four practices that did not have data for all three QOF reporting characteristics were excluded from the analysis.
-
Improving Access to Psychological Therapies (IAPT) data for referrals to psychological therapies [e.g. cognitive–behavioural therapy (CBT) for anxiety and depression, therapy for phobias] by study quarter for all Westpark practices for the period January 2010 to March 2012.
-
Diabetes admissions data (episodes and bed-days) for all Coxford (including Westpark) GP practices across 19 successive NHS quarters (April 2006 to December 2011). Practice list size from QOF [see (1) above] was merged into this data set and used to calculate number of admissions and bed-days per 10,000 registered patients.
For the analyses of QOF data relating to anxiety and depression in BME populations, dementia and child and family health services, practices where data were available over the three QOF time periods were geographically grouped into those in Westpark (n = 24) and those in the remainder of Coxford (n = 55). For the analyses of QOF diabetes indicators and diabetes admissions, practices were grouped into those that were part of the diabetes cluster in Westpark (n = 18), practices in Westpark that were not in the diabetes cluster (n = 6) and practices located in Coxford (n = 55). For the IAPT data those Westpark practices with a GP link worker were individually identified and compared with all other practices. It should be noted that GP link workers started at different times.
Quality and Outcomes Framework indicator data (true achievement) were analysed using a generalised estimating equation (GEE) model for a binomial dependent variable with unstructured covariance matrix. Parameters were fitted for area, time (the three QOF periods), their interaction (area × time) and IMD score.
The IAPT referral data are presented graphically (see Figures 5 and 6) with trend lines for each individual practice with a GP link worker and for all other Westpark practices without a link worker combined into one group and the quarterly average used. It was not possible to calculate referral rates because a register of BME patients with conditions that could be referred, or self-referred, did not exist. We have therefore made the assumption that the unknown register size has remained reasonably stable within practices across the 27-month study period. Each practice has therefore been used as its own control (before and after the introduction of the GP link worker).
The diabetes admissions data are presented graphically (see Figure 7a–d) to show trends for each practice group. A GEE first-order autoregressive model was fitted (using IBM SPSS version 20; SPSS Inc., Chicago, IL, USA) to the data (admissions, bed-days) for a Poisson-distributed dependent variable with the logarithm of the practice list size used as an offset. The correlation (ρ) between any two elements is equal to ρ for adjacent elements, ρ2 for elements that are separated by a third, and so on. ρ is constrained so that –1 < ρ < 1. Parameters for area, time (19 quarters) and their interaction (area × time) were used to statistically compare the three profiles and to calculate predicted rates. The IMD score was added to see what effect deprivation had on the model estimates.
Analytical approach
Our approach to qualitative data collection and analysis was to use a preliminary theoretical framework107 drawn from the literature review; data analysis was a combination of induction (data-driven generalisation) and deduction (theory-driven exploration of hypotheses). 108 This approach has been used previously by organisational researchers in the NHS (e.g. Fulop and colleagues109). Our fieldwork sought to provide a ‘close-to’ record of what happened once the four boundary-spanning teams began working in their topic areas.
We studied the four boundary-spanning teams throughout the WI using a combination of all of the various qualitative data collection methods described earlier (non-participant observation, interviews, focus groups, diaries and open comments in the KAP survey responses). We paid specific attention to both (1) capturing instances of knowledge creation and exchange between different sectors, organisations and professionals and then prospectively tracking how these lead (or did not lead) to the implementation of improvements aimed at increasing the quality of services and (2) the barriers to such boundary-spanning processes.
All interviews and focus groups were digitally recorded and transcribed by a professional transcriptionist, then reread by the interviewer for allegiance to the spoken word. Complete transcripts were uploaded into the qualitative data analysis and data management software NVivo 9 (QSR International, Southport, UK). Observational data were collected in the form of ethnographic field notes, which were reread for common themes that were then written as ‘memos’ and entered into NVivo. Each transcript was read and coded using the software to link common themes across interviews.
Following the end of data collection, the data sets from all of the collection methods were overlaid and themes were iteratively collated and interrogated through discussion within the interdisciplinary research team to generate a deeper understanding of boundary-spanning processes. Monthly team meetings provided a productive environment for generating themes, sense-making and enriched understanding through all stages of the study.
A series of 48 codes in three broad areas were identified before the analysis of the collated data sets:
-
historical and contextual aspects relating to the four boundary-spanning teams of the WI and common questions in the interview guide
-
boundary-spanning themes identified in the literature review (see Chapter 2, A review of the empirical literature), including sectoral, organisational and professional boundaries
-
codes relating to the four aspects of the SECI framework (see Chapter 2, Conceptualising knowledge creation and exchange processes across boundaries: the socialisation, externalisation, combination and internalisation model).
Additional ‘in vivo’ codes surfaced during transcript readings and were added to the list for a final total of 260 codes (see Appendix 10). Before and during coding members of the research team discussed code selection, reviewed coded data sets and iteratively reviewed the codebook.
A systematic method for analysing data was used, which included iteratively analysing the data within the research team as a means of sharing our evolving interpretations as the research unfolded,110 jointly exploring the significance of the findings and building theory from our qualitative, quantitative and secondary data along the lines described by Eisenhardt. 111 In terms of final findings, the intention has been to generalise in a theoretical/analytical manner rather than a statistical manner. 111–113 Our interpretation of the data was validated to some extent through feeding back our emerging findings to the leaders and participants in the WI on an ongoing and informal basis.
Chapter 4 Results
This chapter presents our results beginning with an overview of the theories of change underpinning the WI from the perspective of those leading it, together with contrasting views from key local stakeholders as these formed an important contextual variable for the story of the initiative as a whole (see The Westpark Initiative change model and local context). The early story of implementing the Westpark Initiative then describes the early stages of implementing the WI before our fieldwork commenced in July 2010. We then summarise the key findings from our KAP surveys relating to collaborative and partnership working in Coxford and the wider PCT (see Knowledge, attitudes and practices survey) and the themes that emerged from the two patient focus groups (see Patient focus groups); the results provide a broader context in which to situate our description and analysis of the specific stories of each of the four boundary-spanning teams (see The stories of the four teams). Each story focuses on the local context in which each team was working, the team's overall aims and objectives, what the team did in terms of facilitating the horizontal and vertical integration of services, the extent of patient and public involvement (PPI) in its work and the outcomes it achieved. In Participant diaries we then provide a summary of the quantitative results from the online diaries completed by participants, followed by an in-depth qualitative analysis of the reported experiences of two participants who completed four sequential diaries and a follow-up interview. Impact of the Westpark Initiative and ‘key success factors’: stakeholder perceptions presents the views of key local stakeholders on the impact of the WI and the ‘key success factors’ that they identified. Finally, we present our cross-case analysis of the four teams using the SECI framework as we seek to explain their varying success in exchanging knowledge across sectoral, organisational and professional boundaries (see Multilevel, cross-case comparison: socialisation, externalisation, combination and internalisation and the four teams).
The Westpark Initiative change model and local context
Coxford PCT has been involved in many forward-thinking quality improvement pilots in recent years, including the NHS Institute for Innovation and Improvement's Productive Series and other variations of ‘lean’ approaches. Openness to partnership working was in place long before the WI and support for evaluation of such pilots had been provided through alignment with National Institute for Health Research (NIHR) research calls and external peer review. When Chris – as a GP interested in clinical education and integrative working – was looking for a new job in 2007 he anticipated Coxford as an environment receptive to organisational change, and as the ‘the most hopeful place on the patch’ for trying to embed research in practice and improve public health. At that time the PCT was not in financial deficit.
The WI was conceived by Chris to be an integrated approach with iterative cycles of change. At the beginning of meetings he would frequently describe key attributes as including:
-
annual cycles of activity that allow people to engage and disengage
-
regular feedback
-
sharing information and perspectives about small and large projects
-
multidisciplinary leadership teams or project managers to move things forward
-
demonstrating evidence of impact
-
having a map of all of the connections.
In October 2010, when asked to explain the form of the WI, Chris responded:
Boundary-spanning multidisciplinary teams in four different directions are matched by being able to access multiple constituents which requires boundary spanning on both sides. They facilitate complex co-adaptations across boundaries which are normally impenetrable, with (1) a deeper understanding of complex problems, (2) a broader range of solutions, (3) facilitating mechanisms by which coordinated set of changes that facilitate whole-system transformation and innovation, (4) translation into policy, and then (5) ask does it translate into cost containment?
WIL2B, WI founder
In this way he felt that by enabling bottom-up solutions the WI approach could offer flexible solutions to address local issues. Chris speaks passionately about how the creative process of generating new knowledge can be experienced like a crisis, fragmenting current understanding and rebuilding a new identity, both for the individual and for ways of working.
Multidisciplinary leadership groups in each of the four topic areas were to be formed to include people from different backgrounds who had knowledge of what was happening in different parts of the wider health-care system. As Chris described the approach, members of the leadership groups would then form an action learning set that would, first, focus on accessing the research knowledge and organisational techniques needed to support and develop networking across boundaries and then, second, establish a programme of whole-system collaboration for public health and well-being, which the cohort would facilitate. Work and personal development within the action learning sets was to be supported by members maintaining diaries and participating in member weblogs, to facilitate communication and support between meetings. This network of leaders would work closely with the series of stakeholder conferences, identifying work streams and feeding back learning. In Chris's view the stakeholder conferences would bring together diverse groups of organisational and community representatives and service users in a series of four day-long workshops. These events would inform the development of the work programmes in each of the four projects, enhance learning about systemic obstacles to integrating services and initiatives and facilitate communication and exchange between diverse groups. Chris explained that the first of these whole-system events would focus on developing a number of linked priority areas in each of the topic areas. Participants would identify existing strengths and opportunities for collaboration, and identify obstacles to integrating services and approaches. The second event would then focus on reporting progress, feeding back learning from the network action learning sets and identifying means of further developing and integrating services across the locality. The third event would feed back progress from the network action learning sets and identify key learning points for further collaboration and integration of services. A further focus of this event would be to identify next steps in further developing community integration and service delivery. The whole-system events were to be organised in conjunction with a public outreach campaign, with links to local media, and supported by a public health and well-being programme website. Both the multidisciplinary leadership teams and the stakeholder conferences were being developed and funded from local organisational resources. The four multidisciplinary leadership groups – and the individuals that constitute them – were to be the focus of our research as they worked as boundary spanners in the vertical dimension to improve care pathways and in the horizontal dimension to facilitate interdisciplinary collaboration and learning.
A boundary spanner himself, for Chris, building relationships and cultivating and connecting ‘allies’ was an important part of his daily work. He recognised that the WI could lead to more efficient and cost-effective services and that framing the initiative in this way might enable it to survive the impending reorganisations (and accompanying austerities) facing commissioners and primary care services. The adaptability of the WI approach to the shifting priorities of the time was a key feature during our fieldwork. For example, in 2011, rebadging the masterclasses into topical training sessions, facilitating evening GP meetings at the site where WI meetings had been planned and negotiating a shared agenda with the newly formed GP commissioning group for the off-site retreat were important ways to keep the nature of the ‘whole-systems’ work moving forward. As Chris had said in 2010, ‘The Westpark Initiative is a framework, not a template’, and he was willing to update the approach as needed.
Chris is aware that this model can be viewed as ‘unusual’ and may be ‘misunderstood’ compared with more traditional models. As Chris describes, ‘the difficulty is it cuts across the traditional way of thinking which tends to be a silo operating bureaucracy’. As John – a trust administrator, commissioner and service improvement lead – described:
This is different in that it brings people together, and it allows systems – very often informal systems – to grow naturally out of it. It’s a much slower way, but it is in many respects a more solid way of developing, because it's based on human relations . . . it is literally a forum of bringing together people who have got some interest, involvement, or are deriving some benefit out of a particular pathway or service, to get together and jointly learn and support each other to develop or improve their particular service pathway or system.
WIA22V, commissioning manager
The iterative cycles of cross-boundary exchanges are an important aspect of the model, which John noted had the potential to increase the sustainability of any changes:
So almost every step of the way is reiterated in so many different ways, to the point that you’re almost certain that once it does get to the stage of slowly, slowly unfreezing, when it does refreeze in a different way, it’s solid. And it’s solid, and it’s balanced, because it has reached so much consensus over and over again over the same things that they fall as natural to the people involved in that system.
WIA22V, commissioning manager
Phillipa has held various leadership roles in Coxford and interviewed Chris when he came to the area as a GP and applied for the clinical director post at the PCT. She describes her receptiveness to his early interest in embedding research and evaluation in a system of relationships. They worked together as clinical directors and she believes that they share an interest in quality improvement. She describes his ‘whole-systems methodology’ as something that was discussed before 2009 and which was intentionally applied to the Westpark area as it:
Would probably benefit most from this sort of work, both in terms of the needs and demographics of the patient population, the functionality or otherwise of the relationships between general practice to start off with, but the other participants in care . . . Westpark often feels the least invested in and the least given opportunities to, and therefore there was something both political and tactical about taking that to Westpark.
WIA23W, Director of Quality and Clinical Leadership
Some other WI participants also highlighted the value of starting in what was seen a challenging locality:
That’s what I think about the project, I think that it’s getting people together from what was perceived as a difficult place to get people together and there was definitely a need and that people have been inspired by it. And I think that that is really great and I think that if they can do it there they can do it most places. I also think that it may instil the area with a sense of pride and achievement.
WIG6F, Coxford GP
However, Phillipa was less certain that the intervention would work with GPs in other localities:
They are nowhere near as suggestible and they are nowhere near as lead-able and therefore they will take a lot of convincing because they just don’t do this groupie stuff. GPs are to be in charge and if everybody else would just dance to the tail of GPs then it would all be perfectly straightforward.
WIA23W, Director of Quality and Clinical Leadership
Phillipa and John, having attended some of the events, describe their support for the WI through the period 2009–11 in terms of facilitating some of the meetings and informally ‘helping Chris and others with the thinking through about what the projects and priorities might be’ (Phillipa). As an experienced administrator, John described the traditional ‘systems’ way of introducing change as being from a top-down perspective, and contrasted this with the WI:
It’s a lot easier to sit five people down in a room and to say, ‘This is how we’re going to do things now.’ And then you force the rollout, which is how we have traditionally worked.
WIA22V, commissioning manager
Tension existed in the PCT among managers: some described relationship building (of the sort advocated by Chris) as being a time-consuming ‘luxury’ that might not have a place when budgets were having to be cut significantly. Despite visible sources of external interest and support through the NIHR (this project) and local CLAHRC, the WI was viewed by some influential local actors as a costly extra:
The whole-system stuff, in a sense, says there are no problems – we’re just going to solve everything both good and ill because it’s only about building relationships. I think when you’re trying to do that in the context of the sort of turnover and challenge and pressure that we’re on, I think that’s why people will find that increasingly difficult to sustain. Because actually, not everybody is patient enough, or feels they've got the time to embark on this long a journey
WIA23W, Director of Quality and Clinical Leadership
The early story of implementing the Westpark Initiative
In 2009 there was a concern at the level of the Coxford PCT about the lack of integration between social services and child/family well-being health-care services. It is likely that the public outcry surrounding the shocking case of ‘Baby P’ during the years 2008–9 was an influencing factor. Efforts to examine whether or not local services in Coxford were well integrated resulted in a number of ongoing conversations amongst senior managers; a desire to involve GPs in problem-solving conversations led to several grant-writing efforts, none of which was funded.
A stakeholder workshop was held in March 2009 at which ideas were sought for ways to improve care. An external consultant was employed to gather information through brief interviews across the local area and he presented his findings to staff at a 2-day residential retreat. This was held on 6 May 2009, ostensibly for the D&R network, which had been created in 2008 by the GP founder of the later WI to improve connections through a cluster of GP surgeries. Team building, projects connecting GP practices and whole-system learning were the goals of this network, and the workshop. Diabetes, child and family health, patient satisfaction with mental health services, patient access to general practice and communication for elderly care and good clinical care were identified and mapped as important areas for quality improvement.
In June 2009 a NIHR grant proposal was submitted, using ideas that arose from the workshop and including about 20 representatives from community organisations (including the Westpark Community Alliance, a local child and family health services organisation, local community centres, community nursing and mental health services). Community representatives, including actual or potential service users, were to be employed as action researchers alongside practitioners and members of the public, and community groups would be invited to ‘whole-system’ workshops as part of a whole-system approach to innovation and evaluation. This bid was unsuccessful, but the PCT went ahead anyway in the autumn with the proposed intervention.
According to the historical documents, the WI was launched on 15 October 2009, some 8 months before our formal fieldwork began, when a stakeholder event was held in a local community location, a professional facilitator was hired and representatives were invited from NHS organisations, non-NHS facilities and community-based groups from across the borough to take part in the WI. As introduced by Chris, the WI was a project designed to improve services through collaboration between GPs, community services, voluntary groups and acute specialists in the local area. The project would include the development of a network of leaders across organisational and community boundaries to facilitate knowledge exchange and to be directly linked with a programme of ‘whole-system’ stakeholder conferences to create organisational learning and change, together with community development. The project would take place in the Westpark area of the Coxford PCT where there was said to be sustained political support and understanding for this way of working from local statutory organisations, in partnership with voluntary sector agencies. From this event, three key priorities emerged as holding the most interest for stakeholders – anxiety and depression in BME populations, dementia, and child and family health services – and multidisciplinary teams began to form around each priority with their leaders appointed by the GP founder of the initiative.
Each of the three team leaders then organised focus groups with GPs and other staff in 11 of the 26 Westpark general practices in October and November 2009 to inform their perspectives on what were the key problems in the local area. None of the identified leaders had ever run focus groups before and there was no training provided, but each leader made an effort to engage GPs and secured some time to discuss the topic area. These focus group findings were documented and disseminated at a first stakeholder workshop on 25 November 2009, where the three topic areas were reviewed and next steps for the initiative were discussed. The three leaders presented at this meeting to 29 participants and a community alliance representative was invited to speak about community engagement. Evaluation of this workshop was positive, with five people commenting that ‘it would be better to have more GPs attending’ and six commenting that the anticipated work was ‘exciting’.
In December 2009 nine key people, including the three team leaders, met to determine what the three ‘project teams’ would try to accomplish and how they would further engage with GPs in their efforts to improve ‘links’ between services. Early discussion of goals included the potential for connecting dementia patients with speech therapists, using IT to connect patient information about diabetes treatments and translating cognitive screening tools into different languages. Problems were identified and solutions brainstormed; groups were vibrant, creative, and enthusiastic to improve care, but it should be noted that teams, themes and objectives were therefore not quite in place before the end of 2009.
Through awareness of local needs and funding priorities the GP founder recognised the importance of diabetes as a local health concern, one that might also be usefully addressed by the initiative. So in early 2010 a fourth team began to form, focusing on diabetes, with a request from the GP founder that a PCT-based commissioner lead the team. All four teams participated to some extent in subsequent WI meetings in 2010.
Reports from focus groups held at the start of the initiative (see above) had reported that GPs needed more training about local services and how to access them, as well as better referral systems, and that there was interest in having more link workers. As a result, in February 2010 an evening session entitled ‘How and When to Refer’ was held at a local community site; 26 people attended, including the (now four) team leaders. Small information packs about existing local services were provided to participants and the agenda included table-top brainstorming sessions to explore ways to focus the work in the four topic areas. The leader of the WI introduced researchers from two different research teams, including ours, and described the notion of ‘boundary-spanning teams’ as multidisciplinary efforts for improving service integration in Westpark. He described his hope of using the WI to test small changes for local improvement through annual cycles of applied change efforts by the three teams. All in attendance then introduced themselves by name and role. Strategies to engage GPs through, for example, teaching sessions were discussed although no GPs, practice staff or patient representatives were present at this meeting. Most present spoke about local challenges from their own perspective, including one description of frustrated efforts to effectively exchange information for child protection, which was said to be like ‘knitting smoke’. The future leader of the diabetes team was in attendance as a commissioner but was not yet recognised as part of a team. At the close of the meeting participants talked informally about the ‘enthusiasm’, ‘passion’ and ‘buzz’ that they felt from this information-sharing session, and again the feedback was positive. After the close of the meeting the team leaders met as an ‘oversight team’ to discuss plans to capture evidence of the effectiveness of their efforts.
A second stakeholder workshop was held on 22 April 2010 with 39 participants. The internal report of this event lists the fourth team – diabetes – as having developed from that time; although it is clear from our interviews that this fourth team was added to the initiative sometime before April 2010, there is no mention of the topic in the historical agenda items before this date. At this second stakeholder workshop, ‘rapid appraisal’ results were presented by the four teams. Rapid appraisals had been carried out by each team between autumn 2009 and spring 2010 during which data from local practices were gathered, including disease incidence, hospital admissions and QOF data. As part of the appraisal process, team leaders were encouraged to carry out brief literature reviews, as deemed necessary to understand local issues. Individuals varied in skill level for conducting such research and performing critical analysis; all were rather nervous public speakers. A discussion of how to achieve whole-system change with multidisciplinary teams and cross-boundary working was presented by Chris, as the meeting facilitator. Through small-group work, a matrix was constructed that mapped the ‘experiences, knowledge, skills, attitudes and service improvements’ that would be ‘desirable changes’ for change at the ‘individual, organisational, interorganisational (system-wide) and wider impact’ levels. Feedback on the event was positive, with written comments including ‘excellent opportunity to link up resources’ and hopes for ‘sustainable change’.
In keeping with PCT and D&R network tradition, a third annual 2.5-day residential workshop had been scheduled off site. Taking place on 28–30 April 2010, the retreat was organised by Chris around the theme of ‘Towards Local Health Communities’ and focused on the work of the WI. A detailed agenda shaped the small- and large-group sessions and the four team leaders had a prominent role and facilitated the small-group work during this workshop. Chris opened the first evening meeting with a description of what he termed the principles of ‘whole-system participatory action research’, namely, that all perspectives would be involved at all stages of the project and that all were welcome to engage in system change. In preparation for this workshop, each of the four teams prepared a document with their aims and objectives (see The stories of the four teams).
The first row of Figure 4 picks up the story of the WI by showing the key events and milestones for the period between the granting of ethical approval for our research study in July 2010 and the end of our fieldwork in early 2012.
FIGURE 4.
Westpark Initiative activities, local context and research activities during the fieldwork period. CFHS, child and family health services; MH, mental health.
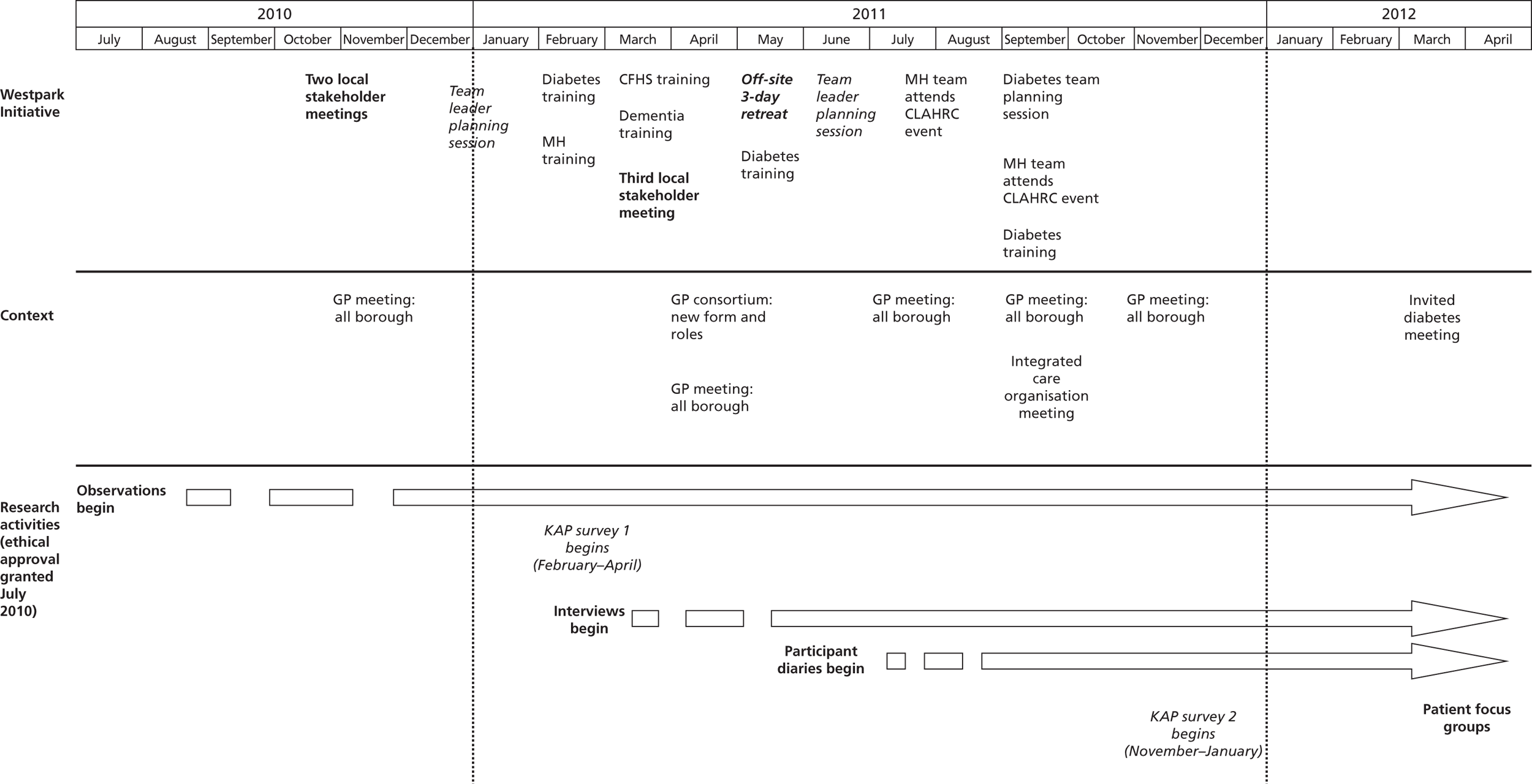
The first masterclass for the local D&R network was held in February 2010 and was called ‘Mapping Whole Systems of Care’. CPD credit towards a university certificate was offered. In March 2010 data systems training was held. The January 2011 class was cancelled and in February 2011 data collection was discussed by 15 attendees. The March and April events were ‘rearranged’. In June and July 2010 attendance ranged from 6 to 30 people, including nurses and non-clinical staff, but rarely GPs. Funding for these training events was discontinued in mid-2011. These events are not included in Figure 4 because they were not a formal part of the WI, although they were attended by many of the WI team members and were observed as part of the study. In 2011 afternoon educational sessions for all staff training were scheduled as an overlap with/possible replacement for the D&R masterclasses. In February 2011, two were hosted by members of the WI teams (diabetes and anxiety and depression in BME populations). In March 2011, two more were hosted by WI team members (child and family health services and dementia). An additional mental health redesign meeting was held in March to address changes between the acute care trust and the PCT, and both dementia and anxiety and depression team members attended. Meetings were 3–4 hours long with a full agenda that included presentations to the large group and small-group sessions about local resources, depending on the topic. Certificates of attendance were provided. Attendance ranged from 20 to 50 people with more GPs than at the masterclasses. Additional meetings appeared on the 2011 calendar (in February 2011) in response to the PCT reorganisation. GP consortia stakeholder workshops were held in April and June 2011; these were facilitated by Chris and observed by our researcher. Cancer (April 2011) and cardiovascular (May and July 2011) training was developed but was not observed for this study.
The second row in Figure 4 includes the key local events that took place relating to the wider context in which the WI was being implemented. On 12 July 2010 the NHS White Paper was published;114 within 2 weeks executive leaders at Coxford PCT met to discuss their response and the GP leader of the WI was asked to facilitate local discussions. An afternoon/evening pair of workshops on 22 September 2010 sought to bring a wide group of stakeholders together to plan the local response to national policy reforms of NHS commissioning and resulted in a report entitled ‘Responding to the White Paper: Towards GP Consortia and Local Health Communities’. Local priorities identified at the workshops were joined-up integrated working, patient engagement, and robust data collection and evaluation to monitor success/outcomes. The Coxford Commissioning Consortium was launched in April 2011 to implement GP commissioning.
In terms of the wider context, and despite wide and frequent discussions about the impact of proposed reforms, intense changes were experienced across the borough, and particularly within the PCT. By the time of the 2011 residential workshop two of the four WI team leaders were no longer in post and the others had reapplied to maintain similar positions.
Knowledge, attitudes and practices survey
We fielded our KAP survey to staff in all general practices in Coxford (including Westpark) in February 2011 and repeated the survey in November–December 2011. In this section we present the key results relating to respondents' knowledge about local services relating to the four topic areas (see Knowledge about available local services relating to the four topic areas); their attitudes towards these services (see Attitudes towards local services relating to the four topic areas); and their practices relating to these services (see Practices relating to local services relating to the four topic areas). The results illustrate general practice staff views on collaboration and partnership working in Westpark and Coxford and help situate the specific stories of each of the four boundary-spanning teams and their analysis in a broader local context (see The stories of the four teams).
Tables 4 and 5 summarise overall levels of job satisfaction and how confident respondents felt about making a contribution to GP commissioning. Although the small numbers of respondents make any comparisons purely speculative, those who participated in the survey in Westpark were generally more satisfied with their job and more confident about making a valuable contribution to GP commissioning than their counterparts in Coxford.
| % respondents ‘satisfied’ or ‘very satisfied’ (all staff) | |||
|---|---|---|---|
| Coxford | Westpark | ||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) |
| 92.9 | 76.6 | 100 | 100 |
| Rating average (1 = ‘strongly disagree’ to 5 = ‘strongly agree’) | |||
|---|---|---|---|
| Coxford | Westpark | ||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) |
| 3.57 | 3.49 | 4.00 | 4.13 |
Table 6 reports on responses to the seven items that we included in our KAP survey from the Team Climate Inventory. Across the seven items there was very little difference between the responses from general practice staff in Coxford and the responses from general practice staff in Westpark. The lowest ratings in both localities related to ‘searching for fresh, new ways of looking at problems’ and ‘taking time to develop new ideas’. ‘Information sharing within practices’ (our emphasis) was rated relatively highly by respondents in both localities.
| Statement | Rating average (0 = ‘strongly disagree’ to 5 = ‘strongly agree’) | |||
|---|---|---|---|---|
| Coxford | Westpark | |||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) | |
| We have a ‘we are in it together’ attitude | 4.18 | 4.11 | 4.17 | 4.19 |
| People keep each other informed about work-related issues in this practice | 4.18 | 4.26 | 4.33 | 4.13 |
| People feel understood and accepted by each other | 4.11 | 4.15 | 4.17 | 4.13 |
| There are real attempts to share information throughout the practice | 4.14 | 4.23 | 4.33 | 4.25 |
| People in this practice are always searching for fresh, new ways of looking at problems | 3.75 | 4.00 | 4.17 | 3.81 |
| In this practice we take the time needed to develop new ideas | 3.61 | 3.87 | 4.00 | 3.88 |
| People in the practice co-operate to help develop and apply new ideas | 3.86 | 3.98 | 4.08 | 4.00 |
Knowledge about available local services relating to the four topic areas
In Coxford respondents felt much more confident that they could find information that they needed to help diabetic patients than they could find information that they needed to help dementia patients. In Westpark respondents were similarly confident about diabetic patients but, on average, slightly less confident about BME patients with anxiety and depression (Table 7).
| Team | Rating average (0 = ‘strongly disagree’ to 5 = ‘strongly agree’) | |||
|---|---|---|---|---|
| Coxford | Westpark | |||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) | |
| Anxiety and depression in BME populations | 3.71 | 3.56 | 3.33 | 3.67 |
| Dementia | 2.96 | 3.25 | 3.33 | 3.93 |
| Child and family health services | 3.37 | 3.57 | 3.33 | 3.80 |
| Diabetes | 4.00 | 4.20 | 4.17 | 4.31 |
Attitudes towards local services relating to the four topic areas
Tables 8 and 9 report respondents' attitudes towards local services relating to each of the four topic areas in terms of, first, the degree of practical help when there is a crisis relating to a patient and, second, the degree of co-ordination between different services. In relation to both questions dementia services were rated as relatively less helpful and co-ordinated by respondents in both Coxford and Westpark, whereas diabetes services were consistently the highest rated on both aspects in both localities. With regard to the former question (degree of practical help) ratings increased over time for all four topic areas among Westpark respondents but decreased in Coxford in three of the four topic areas. However, small numbers of respondents make drawing firm comparative conclusions between the two areas problematic.
| Team | Rating average (0 = ‘strongly disagree’ to 5 = ‘strongly agree’) | |||
|---|---|---|---|---|
| Coxford | Westpark | |||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) | |
| Anxiety and depression in BME populations | 3.30 | 2.93 | 3.40 | 3.50 |
| Dementia | 2.64 | 2.47 | 2.67 | 3.33 |
| Child and family health services | 3.08 | 3.26 | 3.10 | 3.43 |
| Diabetes | 3.78 | 3.47 | 3.92 | 4.06 |
| Team | Rating average (0 = ‘strongly disagree’ to 5 = ‘strongly agree’) | |||
|---|---|---|---|---|
| Coxford | Westpark | |||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) | |
| Anxiety and depression in BME populations | 3.25 | 2.79 | 3.20 | 3.07 |
| Dementia | 2.38 | 2.50 | 2.75 | 2.91 |
| Child and family health services | 3.08 | 3.11 | 3.00 | 3.17 |
| Diabetes | 3.78 | 3.19 | 3.67 | 3.58 |
Table 10 reports how highly respondents rated their working relationships with a range of other health-care and non-health-care professionals. Relationships with school nurses were rated the lowest by respondents in both localities (range 2.48–3.00); dementia care teams also rated poorly (range 2.88–3.43). Relationships with community matrons were commonly rated highly (range 3.91–4.14) as were those with palliative care nurses (range 3.94–4.18) and pharmacists (range 4.23–4.56). Pharmacists were included in the time 2 survey only as was the ‘volunteer sector’, with whom working relationships were rated much lower (range 2.92–2.93).
| Staff group | Rating average (0 = ‘strongly disagree’ to 5 = ‘strongly agree’) | |||
|---|---|---|---|---|
| Coxford | Westpark | |||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) | |
| District nurses | 3.65 | 3.23 | 4.08 | 3.56 |
| Community matrons | 4.04 | 4.14 | 3.91 | 4.00 |
| School nurses | 2.95 | 2.48 | 3.00 | 2.80 |
| Palliative care nurses | 4.04 | 4.18 | 4.00 | 3.94 |
| Dementia care teams | 3.13 | 2.88 | 3.36 | 3.43 |
| Mental health-care teams | 3.68 | 3.14 | 3.67 | 3.69 |
| Diabetes specialists | 3.29 | 3.43 | 4.17 | 3.63 |
| Health visitors | 3.64 | 3.41 | 4.18 | 3.31 |
| Pharmacists | – | 4.23 | – | 4.56 |
| Physical therapists | – | 3.24 | – | 3.53 |
| Volunteer sector | – | 2.93 | – | 2.92 |
Practices pertaining to local services relating to the four topic areas
Tables 11 and 12 present findings on, first, how respondents rated their working relationships with local services specifically relating to the four topic areas and, second, the extent to which they felt that their practice made a difference to the quality of life of patients in the four topic groups. In both cases respondents typically rated dementia lowest and diabetes highest.
| Team | Rating average (0 = ‘strongly disagree’ to 5 = ‘strongly agree’) | |||
|---|---|---|---|---|
| Coxford | Westpark | |||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) | |
| Anxiety and depression in BME populations | 3.59 | 3.22 | 3.55 | 3.47 |
| Dementia | 3.10 | 3.05 | 3.25 | 3.54 |
| Child and family health services | 3.23 | 3.44 | 3.64 | 3.33 |
| Diabetes | 3.68 | 3.50 | 4.00 | 3.87 |
| Team | Rating average (0 = ‘strongly disagree’ to 5 = ‘strongly agree’) | |||
|---|---|---|---|---|
| Coxford | Westpark | |||
| Time 1 (n = 28) | Time 2 (n = 47) | Time 1 (n = 12) | Time 2 (n = 16) | |
| Anxiety and depression in BME populations | 3.91 | 3.75 | 3.58 | 4.00 |
| Dementia | 3.61 | 3.73 | 3.50 | 4.23 |
| Child and family health services | 4.07 | 4.00 | 3.75 | 3.93 |
| Diabetes | 4.56 | 4.37 | 4.50 | 4.38 |
Overall, dementia rated lowest of the four topic areas for all five questions relating to the KAP of survey respondents, whereas diabetes was consistently rated the highest of the four topic areas. In addition, working relationships with dementia care teams were rated poorly (only school nurses rated lower), whereas working relationships with diabetes specialists were rated reasonably highly. Across the five questions the responses in relation to the two other topic areas – anxiety and depression in BME populations and child and family health services – fell somewhere between these two extremes (dementia and diabetes) with no clear pattern emerging.
Patient focus groups
The two focus groups explored the perceptions of patients of the likely impact of the WI on their own experiences of care and treatment. We were particularly interested in exploring any impact on patients of specific attempts to improve the vertical and horizontal integration of services and how they had experienced connections between multiple services over the previous year.
Black and minority ethnic patients with anxiety and depression
A focus group was held in March 2012 with two patients. One participant (FG1MH01) had been seen at the women's centre in Westpark 10 years previously and she had begun to work with the Coxford women's centre as a volunteer 4 years previously. The other participant (FG1MH02) had received CBT for depression when referred by her GP a year before.
Both talked about the importance of being quickly referred and the uncertainty of the time when they were suffering with anxiety and depression but had not yet begun to receive care. Having a ‘real’ person to talk to was a particular priority too. It took the second participant 3 weeks to be seen by the well-being service after her GP told her that she might have depression. Like many patients, she was seen by her GP for another complaint (shoulder pain) and happened to mention having trouble sleeping and feeling worried and distressed. At the time she was told that it would be 10 days before she would be contacted for some type of ‘psychological help’, which ‘felt like a long time’, but when she was called in 5 days she was quite relieved:
Yes, I was given a number to call, and I was very reluctant to call that number because they have so much box ticking going on in many of these organisations, and I really was not up for anything like that, because it was at a very serious point in my life, and I really did not want to have to sit in front of anyone just checking off things and stuff. So it took me a good week before I called. Then when I called, they told me it was going to be another 10 days for someone to call me. I said, ‘Here we go.’ That’s the way I felt, ‘Here we go.’ But I think they called me within 5 days. Within 5 days really I got a phone call. I thought they were very professional on the phone, which was surprising. She told me she would be calling back, and we’ll be going through a kind of interview on the phone. All of that went exactly as she said. Then I was referred to here, immediately I was referred to here.
FG1MH02
The first participant had called a hotline, but really wanted to meet with someone immediately:
I personally was very lucky that I’d got people around me that were able to step outside of the box – because I was not a very easy patient – step outside of the box and deal with me on a really serious one-to-one level, and not what was written here, because it was not going to work in my case. I was very fortunate where that was concerned. At the beginning, in addition to the counsellor I had an advocate.
FG1MH01
Patients often have a need for advocates outside of the mental health system, perhaps through the informal support provided by family members, as well as needing more formal legal advice and links to local agencies. Both participants needed support to address issues with the local council, for instance. The first patient needed help to work out issues with her pension, with having to go to court, with harassment where she lived and with housing difficulties. As well as psychological distress, she experienced language barriers and pressing concerns in her daily life. Connections to different services were crucial for both participants:
Yeah, I myself did a lot of research on this thing. But my case probably was a very unique case, I’ve got to say. It probably was a very unique case, and that’s what my counsellor told me too. But the big thing there is that they were able to split the . . . she was able to say, ‘You know what? I’m going to deal with her mental situation . . . .’ Yeah, I think the big thing there is . . . and I remember even feeling some relief, just on the very first meeting with her, that, ‘Okay, we’re going to remove that part, don’t worry about that right now, we’re just going to look after you.’
FG1MH02
In August 2011 the WI anxiety and depression in BME populations team began recruiting former patients for a patient forum to inform its work. Given their past experiences both patients were eager to help improve mental health services for people who may struggle as they had:
My counsellor told me that they want to start this group, and she thinks I would be a good candidate if I was interested in helping them set the group up. With my experience and everything I said, ‘Yeah, why not?’ Because I think it’s important.
FG1MH01
One of the reasons I joined the [forum] and being part of helping set it up is listening to other people and their situation. I think expediency is very important, that they react right away to a call. I think I was very lucky. I’ve heard of some people who have not been that lucky. I think if I did not get that immediate intervention, it wouldn’t have been so nice . . . . Shorten time from the time you call to getting you in to see someone. When I called the very first time, I got a recording. When I called the first time, I got a recording, and the recording asked me to leave my name and number and that someone is going to call me back in 5 to 10 days, okay. Now, dependent on the urgency of that person, that 5 to 10 days is a very critical time.
FG1MH02
Having a hotline to call was an important aspect of swift services according to these two patients, and having to leave a recorded message was less of a concern if a quick response was forthcoming. They discussed together the importance of a free central number for help, but also recognised the cost barriers to implementation. As the second participant explained:
. . . to get an 0800 number available, and we were told today an 0800 number is free to the caller, but the organisation said the 0800 number has to pay for that, and they don’t know if they have those kinds of funds. This is very important, I know from working with the [refugee agency], sometimes people don’t have a phone, they don’t have money, or they have a phone and money, they need to get out of the house.
FG1MH02
Both acknowledged that their involvement in the patient forum was helping others as well as being therapeutic for them in terms of building their own confidence, something that the CBT therapist encouraged and acknowledged.
Diabetes
A focus group of diabetic patients from Westpark was held in February 2012. Seven people participated. The study information sheet was reviewed, questions regarding ethics were discussed and participants were given the opportunity to ask questions before signing the consent form. The session was recorded, transcribed and analysed for themes. The participants sat in a circle and introduced themselves, saying how long they had had diabetes, and most explained that they also cared for family members with diabetes. Six had type 2 diabetes and one had type 1 diabetes, five were women and all were of Asian descent.
Getting care all in one place and increasing their own understanding of the disease were important themes early in the group discussion:
Say 6, 7 years back, everybody was called for an annual check-up at Coxford Hospital. And then they discharged everybody and said, ‘You’ll have to go back to your local GP. They will be taking up your case, and then call you in for your check-up.’ Then any blood tests that need to be done, it was done there. In one way it’s convenient, rather than going to the hospital and waiting long. Here they give you an appointment, and then you do your tests, and you get your results. I think it’s the way forward. But what they’ve added is diabetic retinopathy, so that helps.
FG1DM05
They’ve given us little leaflets to look after ourselves now with all the results of all our bloods, which is really good because you can see where you are, which before I didn’t know what anything was.
FG1DM01
This same individual had had diabetes for 12 years and she talked about taking a short course at the Coxford Hospital 2 years previously (before the WI). Learning about food and diabetes had been helpful for her. She went on to describe the importance of quick access to the specialist nurses and how that helped with coping with the stigma of the disease:
But it was really, really good. I learnt so much information, we were able to share experiences, like this doesn’t happen. And I think initially when I was diagnosed, Indian society, being diabetic, being type 1 diabetic, oh, God forbid. God forbid you ever tell anyone. So it was absolutely disgusting . . . . Yeah. So it’s completely taboo, and it’s a shame, because now in current society people still don’t talk about it, especially because in Indian culture it’s a happening thing, it’s happening more and more. So it’s a shame. So I wasn’t able to speak to really my family other than my immediate family when I was first diagnosed. But the diabetic nurses at Coxford Hospital were absolutely amazing. I could ring them whenever I wanted, I could go and visit them any day of the week. Their offices were always open. I couldn’t see the doctor necessarily . . . . It’s stayed consistent. If I want to go and see them, if I want to make an appointment, they're always at the end of the phone. I think that's really, really nice.
FG1DM01
However, as the group continued to talk, it became clear that the care was felt to be more responsive through the hospital for the patient with type 1 diabetes than for the type 2 diabetics in the group, who found the care to be less timely:
Type 2, it’s probably a bit different, because it was the hospital, they saw you annually, and that’s it . . . . And if there’s any changes, for example, you know when they did the blood test for you, ‘Oh, your cholesterol has gone up. Oh, well, we’ll recommend you tablets, and then refer you back to your GP.’ And they would say . . . They would get the message, but not immediately. They would call you after about a month or two and say . . .
FG1DM05
Others in the group agreed that the connections between the hospital and the GPs seem to work at different speeds. When medication was being changed then time to contact was appropriately swift, but unfortunately not always informative:
Almost immediately. They always call me up, and it is almost immediate. They’ll call you in, get you a prescription. But the thing is, they don’t explain it. When I go to my NHS consultant, when he’s looking up my blood test, I like to be informed of what the changes are, even if it is every 3 months. I like to know. Just like you say, there is no support. When I got diagnosed, I had a really bad experience as well 6 years ago. And I had all the symptoms, all the symptoms that a diabetic could have had, and it was crystal clear. But I wasn’t able to get diagnosed by my GP however many times I came in. It was over a 3-month period that I was having these symptoms. So it was at a time when they didn’t really have all these monitors. I think it was about a year back when they started to introduce them, there was a big hype about all these local afternoon clinics, and they were saying, well, okay, a lot of them had free testing monitors being given out to them before these budget cuts.
FG1DM02
The participants had heard that diabetes rates were increasing in the local area and remembered that free testing monitors were frequently offered in the time period before the budget cuts, but their view was that education and support were now harder to find:
But nobody has got any information or support anywhere. Like she said, when she was first diagnosed, there’s not anywhere that . . . I had to literally do all of my reading on the internet. Diabetes . . . I got more information off the internet than I did from any of the medical professionals . . . I go to diabetes.co.uk.
FG1DM02
As the type 2 diabetics noted the shift in their services back to the GP surgery, they also began to describe their lack of confidence in the GP surgery nurse (as opposed to the diabetic specialist nurses based at the hospital). Five of the participants discussed recognising the lack of competence and continuity in their care provided at the surgery:
She hasn’t got a clue.
FG1DM02
Oh, I don’t come to see the nurse at the GP. I refuse to. I would much rather go to the hospital . . . I wouldn’t come here. But they don’t give you your prescription unless you have been to see them. So you are actually forced to come.
FG1DM06
Go to the hospital. She will do the basics, get your weight, see your feet, check your blood pressure, check your weight, and that’s about it, and everything on the system.
FG1DM05
She actually turned round to me once and said, ‘I don’t know why you’re coming here if you’re under hospital care.’ She’s not very informative. She doesn’t know, she hasn’t got much knowledge in the field of diabetes. You need specialist care.
FG1DM02
It’s very hard to get hold of her, she doesn’t do evenings. So my husband’s work, he has to take a lot of time off.
FG1DM01
In this manner, patients appear to be able to discern the difference between attentive service at a convenient location and self-selecting their care, if able, at the place where they perceive care to be the best. They also verbalised being able to recognise, and preferring, specialty-trained practitioners:
Yeah. See, they were really, really good, and you could ask questions and they actually knew, and there was a bit of banter going. It was all right. But I think with the nurse that they currently have, with me, I’ve got a running joke with the receptionist because I refuse to see her. She doesn’t even ask for me any more because I won’t. But there are some really good nurses out there who actually do know about these conditions.
FG1DM06
Can I just tell you, when [the previous doctor] was there, he had some very good nurses and staff. They were dedicated diabetic nurses.
FG1DM05
That had trained knowledge on it.
FG1DM02
As a group of diabetics with many years of experience, they were able to list the kinds of care that they knew that they should have, including blood pressure and weight monitoring and eye and kidney screening. They discussed how regular screening may have decreased recently, especially with the move of services back to primary care.
They used to do your weight . . . . Urine test they used to use, the little stick test thing for proteins. They used to do quite a bit, actually. It’s been a while now.
FG1DM02
The patients spoke about understanding the risk of hypoglycaemia and the way to treat it quickly with sugar, as well as the importance of having their eyes checked regularly. Two participants confirmed that their optician also checked their blood sugar and referred them back to their GP. The rest in the group were impressed and they began to share names of local opticians.
Making connections between services was recognised by the patients as important but not as efficient as it should be:
There was going to be a centralised database system, wasn’t there? I think that would be one step in the right direction. I know that there’s all these data protection laws and loads of negativity about it. But I think in respect of us getting the care that we deserve, everyone needs to have the same information. The last two times I’ve been to the hospital, they have written to me and cc’d in the GP. They’ve written a letter to tell them the results and what was discussed and stuff like that.
FG1DM06
The WI – and many other quality improvement efforts – have attempted to use IT solutions to co-ordinate care, but the patients in this focus group had not noticed more seamless services:
No, just about what was discussed and what my results were, because usually what used to happen was when I was going to come and see the nurse here, reluctantly, she would also send me for another blood test. And obviously I don’t have time to go out, I’m a teacher, I can’t go during term time. So there was no time. But if I’ve already had a blood test there the week before, then surely they should be able to have a look at the results here . . . . There’s not enough communication, and it’s an inconvenience against me. If something is wrong with you . . . I mean, because you could use any hospital A&E [accident and emergency]. Somebody needs to know. They could get into all of your medical records that way, knowing exactly what your past history is as well.
FG1DM06
When asked how to solve the problem of better integration of services, three of the patients suggested that they would prefer specialist care and that they believed that the hospital was where that had happened best in the past. They acknowledged recent national policy changes (e.g. GP commissioning) and the pressures of budget cuts, but they also knew how they would like care to be provided:
The step should be, like they say, like look, all the type 2s, they’re all coming to the GPs, but they’re all complaining. They’re not getting the care that they should do. So okay, you’re going to give it to the hospitals, get more consultants in there, people that know their job, know what they need, rather than have it shared here and them not know and still having to go back up to hospital to get it from the consultant. So take it off of the GPs and leave it with the hospitals where they can get their feet and their sugars and whatever they need done. I would never come to my GP. I would not be in care like they would be in care. No, they gave me the alternative, but I stayed at hospital.
FG1DM02
How you look at the doctors is generic. He is the first port of call, he has limited knowledge – I don’t know, I might be wrong. If he thinks, yes, you’ve said that, or you have some stomach problem, he’ll try to advise you and give you medication. But when it gets a bit complicated, he has to refer you to somebody specialist. That’s how they are taught. If your white blood cells are higher than normal, he can’t do anything.
FG1DM05
The participants were able to understand the difficulty in determining transitions in care between generalist and specialist services. They also discussed which health-care staff were the most informative and how to get more information about their own laboratory results. It was clear that there was no preferred discipline – whether consultant or pharmacist, doctor or nurse – but there was a consensus that they looked for practitioners who listened, explained and were readily available.
The participants also discussed the importance of receiving comprehensive care – and six of the group spoke excitedly about getting a full annual examination in India, with a body scan, a stool test and a full written report for £40–50. All agreed that this is desirable but that it is unfortunate that their UK physicians will not review the reports with them on return.
Good information is key for the patients. When discussing the use of the internet for finding information about their disease, the patients were glad to be able to find useful information, but they were not directed towards certain websites:
Pamphlets, leaflets, information sheets, somewhere to go, someone we can ring, someone who you can . . . . Not from people without having to do it myself . . . . You figure it out on your own. Yeah, who’s going to look and find for the older generation, toddling about on the internet?
FG1DM02
As the focus group wrapped up, the participants began to comment about the hour as if it was a support group and about how helpful such an experience can be.
It’s the first time I’ve been able to talk about it.
FG1DM02
This should happen more I think in the community, it should, because there are so many diabetics.
FG1DM06
The participants also asked about the study and some appeared to hope that that such discussions would continue, as they acknowledged the benefits of bringing patients together to share experiences.
Summary of focus groups
Participants in the two focus groups did not specifically identify ways in which the WI had impacted on their experiences or quality of care. However, participants were able to describe aspects of co-ordinated and timely service that they experienced as seamless care. In both focus groups quick response times through centralised telephone helplines were described as important, as was having access to a variety of services as and when necessary. Participants did not ascribe greater value to certain disciplines or professional roles but they did want more frequent access to knowledgeable practitioners who could co-ordinate their overall treatment over time, had access to their test results and could make changes to their care as needed. Where services were located was less important than oversight of patient care over time.
The stories of the four teams
In the following sections we now turn to the specific experiences of each of the four boundary-spanning teams in terms of:
-
the local context before the development of the initiative in 2009
-
their agreed aims
-
their activities from late 2009 to early 2012
-
the extent and nature of PPI in their work
-
an evaluation of their impact on the quality of health care as of early 2012.
Throughout these sections we also include some illustrative vignettes (in boxes) from the work of each of the four teams to give examples of the types of activities undertaken, challenges faced and impacts (direct and indirect) of the WI.
Anxiety and depression in black and minority ethnic populations
The local context before the development of the Westpark Initiative
The aims and objectives of this team were closely aligned with national policy in this topic area and, consequently, it was able to secure external funding for its work (from a CLAHRC, see below). Importantly, IAPT had been initiated as a programme across England in 2007. 115 Such extensive and well-funded UK government policy initiatives supported mental health services by increasing the availability of CBT and led to an increase in the number of trained psychological well-being practitioners, including members of this particular boundary-spanning team. The IAPT programme, reinforced by National Institute for Health and Care Excellence (NICE) guidelines and evidence gathered through early pilots, supported offering CBT through stepped care and encouraged self-referral, along with GP referrals, to increase access for patients. In November 2008, the IAPT programme produced guidance on commissioning for the whole community, which included efforts to reach BME communities. 116 Statistically, Westpark had a very high proportion of members of these communities, making addressing this national priority particularly important in the local area.
Team membership was very stable throughout the WI and the team had formal support for its role from senior managers. In the local well-being service, before the start of the WI, the person leading the team was already a mental health clinician and manager of a health-care team. This team leader was directly encouraged by her direct report supervisor to take part in the initiative when it began in October 2009. The same team leader was in place throughout our fieldwork period from late 2009 to early 2012, as were three key team members (all newly trained CBT therapists). Support for the team, resources for data collection, funded study days and supervisor encouragement all existed before and during the WI. Despite a disruptive local reorganisation of services, redundancies and staff changes starting in mid-2010, this team also included at most times a community development worker, a consultant psychiatrist and at least one patient representative, along with the consistent CBT therapists and team leader.
In addition, the techniques of CBT itself, including practical problem-solving techniques and facilitated reflection, appear to have positively influenced the team-building efforts of this group (which was composed of a majority of CBT therapists). Supportive co-worker relationships from their – originally colocated – clinical setting of the well-being service were sustained even after the CBT therapists moved into positions as mental health link workers in local GP surgeries (see below). Importantly, the goal of increasing access to psychological therapies for local BME patients was explicit from the beginning of the team effort, as the goals for the WI then paralleled those for the IAPT programme.
Overall aim and specific objectives
At the April 2010 stakeholder event the team set itself one overall aim with three specific objectives (Table 13). The key boundary-spanning intervention was to attach mental health workers (link workers) to general practices in Westpark to increase appropriate referrals to the IAPT service.
| Overall aim | Specific objectives as stated in the team document | Measure of impact |
|---|---|---|
| Good access to primary, secondary and other health services; monitor outcomes for equity; information |
|
Referral rate of these people to IAPT at MHWBS from Westpark GPs compared with referral rates in other Coxford localities |
What happened: team activities
In early 2009 the head of the well-being service, Satveer, encouraged the senior therapist in the mental health team, Vinoda, to meet with the leader of the WI and join a core team with the aim of building primary care connections with secondary care and planning local stakeholder workshops to increase local mental health referrals. Although not formally assigned to take part, Vinoda was already personally and professionally motivated to improve care for the local BME community in Westpark, having worked for a long time as a psychiatric nurse in the local area, which is also her childhood home. She and three members of the mental health team had already worked with the IAPT service for the previous 4 years and then together they became involved in the WI from the 2009 stakeholder meetings forward. Vinoda stepped up to join the core founding team of the WI, with a keen interest in developing her own leadership skills, with the explicit support of her supervisor.
The main boundary-spanning activity of this team was to assign CBT therapists as link workers at specific GP surgeries with the aim of impacting on the quality and quantity of referrals. Six CBT therapists were placed as link workers in Westpark, five in GP surgeries and one at the mental health and well-being location. The first took up post in 2009 (in response to the IAPT outreach goals and before the formal start of the WI) when a new GP surgery opened. Pam was placed at the new site by the well-being service to meet the IAPT goals for outreach and she also became very involved in the early stages of the WI, which she viewed as synonymous with her therapist role.
In April 2010 a first application by Vinoda to an outside funder, CLAHRC, was successful, serving as a great source of excitement and motivation for the team. In May 2010 members of the well-being service held a meeting at the new surgery in Westpark with local GPs and the team members took part in the annual residential retreat. Their digital story was used as an exemplar for the other teams during the 3-day retreat, which brought them great pride. In June 2010 outreach efforts included a newspaper article, an e-mail referral push to GPs and a practice-based commissioning (PBC) meeting. In July 2010 members presented to the newly formed GP consortium and in August 2010 the team conducted a focus group with practice managers to exchange information about well-being services. A second link worker was in place at a second surgery from April to September 2010, when she was replaced by another link worker. In November 2010 the team members attended an all-topic WI stakeholder event, presenting their work, again feeling proud that they could already demonstrate outcomes.
Bridget (WIP31E, specialist well-being advisor) joined the well-being team as an experienced advisor from outside the area in mid-2011. She is quickly aware that some GP surgeries are more reluctant than others to refer patients to the service, and attending a CLAHRC event in September 2010 only inspires her interest in fixing problems and ‘setting down a more definitive plan’. After spending 6 months with the home crisis team, 1 day a week, she describes the benefits of increased understanding from different disciplinary perspectives:
They definitely have a much greater understanding now
of what we do and don’t do as such. And I think
they’re more willing as well to pick up the
phone and discuss it with the link worker or wait until
Thursday and discuss it with them in a little more
detail before they put that referral through, which
probably really helps and it’s helped our
waiting list [decrease] as well.
A borough-wide training event was hosted by the WI and held on 3 February 2011 and was very well attended by GPs, although the focus was on system-wide infrastructure and not on improving knowledge. Another borough-wide training meeting was sponsored by the WI on 10 February 2011 and was well attended by GPs. Discussions about referrals to the IAPT service were openly facilitated and were aligned with ongoing concerns about national reforms. However, this meeting focused more on infrastructure and redesign plans in the mental health trust than on offering screening tools online or in different languages. Non-GP clinicians who had hoped to learn specifically about how to screen and refer expressed disappointment in the meeting agenda. GPs were given the consultant psychiatrist's mobile telephone number, which appeared to appease some referral concerns; however, no decisions were made by the end of the meeting.
In 2011 a follow-up application to CLAHRC was again successful, which supported the team, with some new members, with consistent and structured learning opportunities. Members of this team describe their involvement in the WI as being a ‘crucial’ part of providing micro-level support and enthusiasm for their boundary-spanning work, whereas they were more likely to credit CLAHRC with providing a macro-level structure that helped organise their efforts.
Pam (WIP10J), a CBT therapist and WI team member, agreed to be interviewed twice and completed four diaries, enthusiastically taking part in the research activities. In her diary follow-up interview she describes noticing that a patient appeared to be having memory problems, which were different from the symptoms of anxiety and depression that had prompted a referral for counselling. Having attended one of the WI educational events about dementia, the therapist recognised different clinical signs, applied a memory loss tool and then made an effort to refer the patient to the memory loss clinic:
It is a client that was referred to me by the GP for
depression. Did an assessment and became quite
concerned, and I’m really shocked that the GP
hadn’t picked this up, because quite early on in
assessment she was coming up with things that
didn’t seem right, she was forgetting things.
About session four or five, it took a long time to do
the assessment simply because she wasn’t able to
remember some of the things that we’d talked
about in previous session, or things around the house,
so the focus of the treatment went away from depression
but more to memory. It picked up in my own mind, having
had a presentation through Ganesa who works for dementia
services in Coxford. In fact one of the meetings were
actually initiated with the [Westpark surgery] GPs so
they could get dementia services to come in and do a
presentation in front of the GPs about their service.
So, in hindsight, having spoken with Ganesa and knowing
what I learnt from the presentation, bells were ringing
pretty quickly that this lady doesn’t seem as if
she’s remembering things the way we would do
ordinarily, so I did a Mini Mental State Exam in
session, and out of that quite clearly it showed that
she had . . . it was a very Mini Mental
State Examination, so it was showing mild to moderate
signs of early onset of dementia, working age dementia.
Then called Dementia Services in Westpark, they
redirected me to [service in her postcode].
When the patient returned for counselling therapy without having had an appointment for memory assessment, the therapist followed up with the clinic, located the lost chart and sent the referral through again. An increased awareness of other types of care available improved the ability to connect this patient to more appropriate services; however, it took many extra steps and time-consuming effort to get the patient seen, which contributed to the therapist not making her target of time spent with new patients. Awareness was increased, but cross-boundary working was still problematic.
Through 2011 this team struggled with multiple redesigns in services between the mental health trust and the mental health and well-being board, with many redundancies. Excitement about achieving social enterprise status evolved in the well-being service through 2011. By early 2012 social enterprise status had been approved and appeared to be imminent but because of funding constraints and interorganisational pressures it was again in question by mid-2012. Staff motivation and morale were spurred by the achievement but waned on hearing that it might not happen.
Patient and public involvement
In 2010, team members identified a previous BME patient with a willingness to engage with the wider community about her successful use of therapy for anxiety and depression. Radio programmes (in a local dialect) and a short (2-minute) film were produced that centred on this patient's story of her experiences. In addition, posters and brochures in different languages were used to reach a wide group of potential patients. By 2011, when this individual patient representative grew somewhat overwhelmed by the need to make presentations, efforts to create a patient representative forum were already under way. Team members supported the development of a patient forum by late 2011 and in 2012 team members were actively mentoring the two members of this forum with the aim of sustained PPI in their ongoing improvement work.
Team outcomes
The team had set three objectives in April 2010 at the start of the WI: to attach mental health link workers to Westpark GPs, to monitor changing patterns of referrals and to form a group to explore whole-system integration.
Pressure to provide evidence of the impact of the team's efforts came from the local trusts as well as from its involvement with research funded by this NIHR grant as well as CLAHRC (e.g. the latter expected weekly reports from team members, which ensured consistent activity and self-evaluation). Members of the team spoke of a sense of excitement over the impact that the link workers were felt to be having, as well as being overwhelmed by the need for data collection while also striving to provide clinical services. A coherent and specific goal of increasing referrals enabled this team to focus on appropriate methods for collecting useful data from the start of their work in 2010, and then to apply for more CLAHRC funding in 2011 to support this data collection process. Through 2011 and 2012 the team continued to be motivated, and partially funded by CLAHRC, to try to collect appropriate evidence, particularly around referral rates in the BME population.
Throughout the study period team members were clear about their goals but uncertain how to interpret and present data on the outcomes. They knew that referrals to the well-being service had increased but were hesitant to publish numbers for the first couple of years, partially because they were uncertain how to appropriately calculate the change over time, whether or not the ethnic distribution data were ‘clean’ and how to present the information with accuracy. They also felt that referrals from GPs were improving in quality, such that the right types of patients were being referred appropriately, although such information was not formally measured. When a previously reluctant GP began to ask for a mental health link worker in his practice, the team saw this as a success.
In February 2011, Vinoda described the outcomes at the time:
It’s not just the link workers, I think it’s everything to do with the stakeholder workshops where we’ve had practice nurses come, we’ve got health visitors that have come, we’ve got people from the voluntary sector that are making referrals. We’ve got a self-referral line which people can phone, and we’ve advertised it in different languages . . . . We’ve established links in the temples, the gurdwaras. We’re running a walk-in service in [a community centre] which is our older people service, where if someone wants to speak to one of my colleagues and wants a quick referral, we’re happy to do that. So it is a combination of stuff. But I think the GP referrals have gone up in those surgeries where there’s a link worker, and we’ve got stats to prove that.
WIL7G, BME therapy team leader
Vinoda further described signposting to the volunteer sector for domestic violence support and how waiting times for CBT had decreased from 18 months to 2–4 weeks. Persistently throughout the study period, Vinoda continued to relate how important the WI was to her own professional development, and the service:
Without the project, I don’t think we would have made such an impact, because we wouldn’t have had the time. Not just the time – especially the time, but the shared knowledge and experience and working with the other teams to do that.
WIL7G, BME therapy team leader
Informally, patient satisfaction was being catalogued as a list of small gestures (such as gifts of fruit) from thankful patients who were culturally comfortable with such exchanges. PHQ-9 data (Patient Health Questionnaire) were being collected at every patient visit for CBT counselling, but the data were sent to a distant university and were not always accessible to the staff and so changes in individual patient scores over time were not available at the time of care. In early 2012 the team drafted a report for CLAHRC, charting a 810% increase in referrals from the Westpark locality from 2008 to 2010 and a 939% increase in referrals from the Asian community in the same period. In 2007 there were < 50 referrals and in 2010 there were closer to 750 referrals. A creative variety of promotional activity was credited with impacting on professional and patient utilisation of services, as seen in increased referral rates, more appropriate referrals and perceived increases in awareness of the service among the BME population.
Our own analysis of trends in IAPT referrals is shown in Figure 5. The downward arrows indicate when the link worker started in each practice (note that for LW5 there was a link worker from April to August 2011 and then again from December 2012, and for LW1 the link worker started in January 2009). The mean profile for all other practices that did not have a link worker is shown by the dashed line (NLW). A link worker effect was not readily discernible from the figure; however, since October to December 2010 referrals have been generally higher (see Table 14 and Figure 6).
FIGURE 5.
Improving Access to Psychological Therapies referrals for individual practices with a link worker compared with all other Westpark practices. Downward arrows indicate when the link worker started.
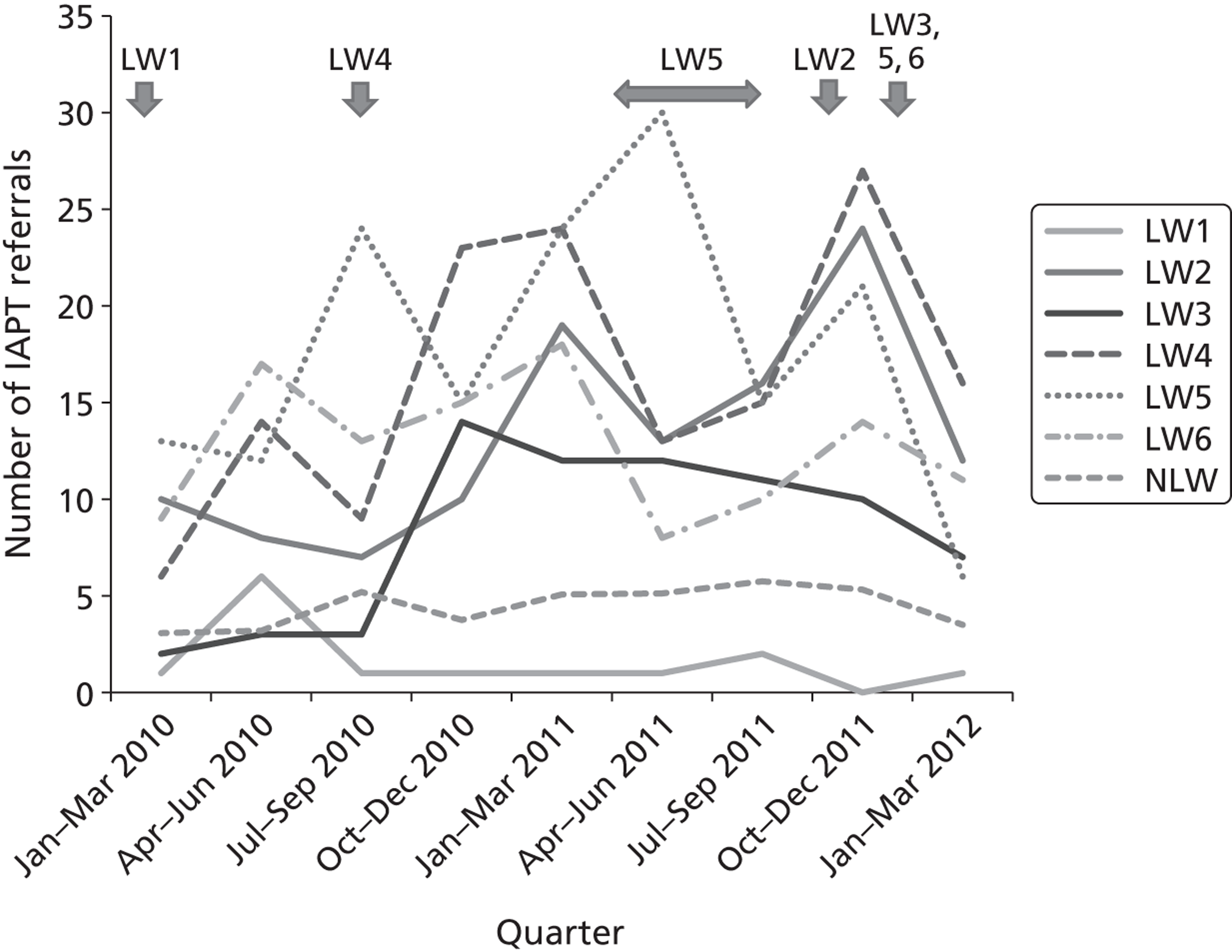
Table 14 compares the mean number of referrals of BME patients with the IAPT service in each quarter by those practices with a link worker in post at the time and those practices without a link worker. In seven of the nine quarters practices with a link worker have, on average, referred more BME patients to the IAPT service than practices without a link worker. The results show that in four of the quarters there were > 200% more referrals from practices with a link worker than from practices without a link worker.
| Practice | January–March 2010 | April–June 2010 | July–September 2010 | October–December 2010 | January–March 2011 | April–June 2011 | July–September 2011 | October–December 2011 | January–March 2012 |
|---|---|---|---|---|---|---|---|---|---|
| Link worker | 1.00 | 6.00 | 3.00 | 12.00 | 12.50 | 18.00 | 10.13 | 16.50 | 8.83 |
| No link worker | 4.24 | 5.00 | 6.58 | 5.70 | 7.70 | 5.53 | 6.93 | 6.39 | 3.50 |
Figure 6 illustrates this table in graphical form.
FIGURE 6.
Graphical representation of mean number of referrals to the IAPT service by link worker and no link worker practices, January 2010 to March 2012.
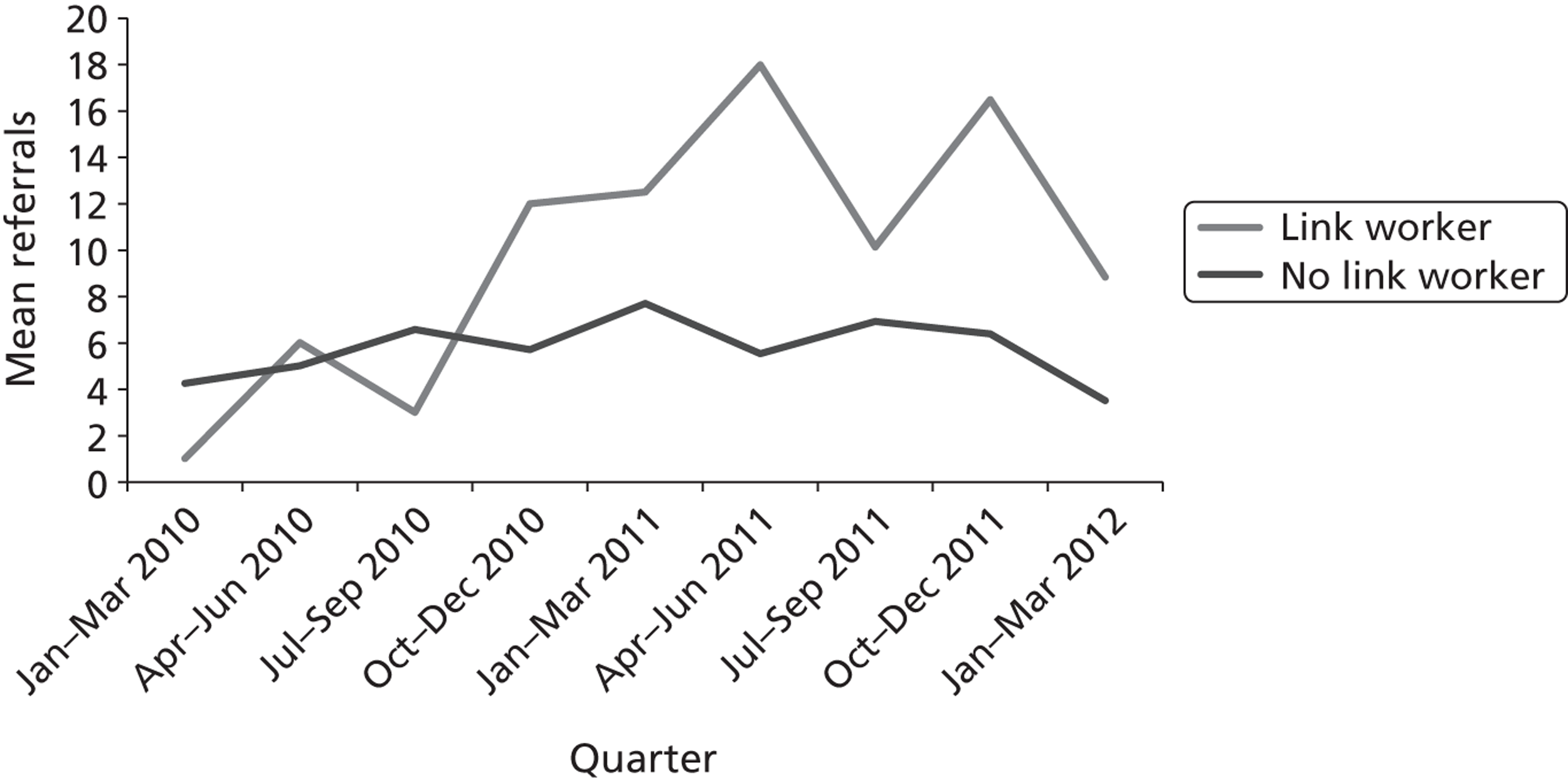
In addition, we also explored whether or not there had been any significant changes in three relevant QOF scores by comparing performance over time in the 24 Westpark practices and the 55 Coxford practices for which data were available. Performance on the three QOF depression indicators by geographical area and across three successive QOF reporting periods is shown in Table 15.
| QOF depression indicator | Coxford | Westpark | |||||
|---|---|---|---|---|---|---|---|
| 2008/9 | 2009/10 | 2010/11 | 2008/9 | 2009/10 | 2010/11 | ||
| DEP 1: % of patients on the diabetes/CHD registers for whom case finding for depression has been undertaken once in the previous 15 months | % | 84.89 | 86.42 | 87.27 | 87.13 | 83.88 | 86.37 |
| n | 12,923 | 13,271 | 14,216 | 7454 | 7773 | 8145 | |
| DEP 2: in patients with a new diagnosis of depression, recorded in the QOF year, % with assessment of severity at outset of treatment | % | 9.57 | 79.50 | 81.71 | 11.70 | 79.93 | 74.79 |
| n | 1397 | 1373 | 1126 | 295 | 243 | 181 | |
| DEP 3: in patients with a new diagnosis of depression and assessment of severity recorded in the QOF year, % who have had a further assessment of severity 5–12 weeks after the initial recording of the assessment of severity | % | 46.58 | 53.82 | 61.57 | 72.99 | ||
| n | 653 | 740 | 141 | 154 | |||
Area profiles did not differ significantly for any depression indicator. Most of the improvement in DEP 2 performance occurred between 2008/9 and 2009/10. Performance on DEP 2 dipped between 2009/10 and 2010/11 in Westpark but not in Coxford. For DEP 3 Coxford shows an increase of 7.2% and Westpark an increase of 11.4%, which is not statistically significant, and the number of patients contributing to DEP 3 is smaller than the numbers contributing to DEP 1 and DEP 2.
Dementia
The local context before the Westpark Initiative
The aims and objectives of this team were aligned with national policies relating to dementia services although it was not clear how changes to local services would be implemented and their impact measured. NICE guidelines issued in November 2006, and amended in March 2011,117 sets out best practice for person-centred dementia care. Non-discrimination, consent, involvement of carers and co-ordination and integration of health and social care were considered key priorities, as were memory assessment services. Appropriate dementia care training for all staff working in the health (including acute hospital settings), social care and voluntary sectors was also considered a priority.
In 2009 the Department of Health published Living Well with Dementia: A National Dementia Strategy118 to improve three key areas: awareness, earlier diagnosis and intervention, and quality of care. Projections were that the population with dementia might double and costs for care might treble over the next three decades. Seventeen key objectives were suggested for local implementation and members of the dementia team discussed these objectives and priorities at their meetings. These discussions helped surface barriers to integrated services, especially between GPs and the local mental health trust:
GPs, they have to have such a broad spectrum. And I think the biggest fault that specialists have – and I include ourselves in that – we tend to look downwards, all we can see is our own specialism. And in terms of the referral all we can see is, ‘The GPs hasn’t filled in the right details, the right forms, the nasty man, we are not going to see the patient.’ Whereas actually from a GP’s point of view they’re seeing such a broad spectrum and we’re expecting them to do 120 things. You know for every specialty expect 120 things and I can understand why they sort of don’t want to refer on, don’t want to talk to us. So we were equally at fault.
WIP9I, assistant director mental health trust
At one of these meetings one of the team members, Amy, reported that it was anticipated that there would be an 18% increase in the population of people aged > 65 years in Coxford by 2025 and that Dementia UK had projected a 15% increase in early-/late-onset dementia from 2007 to 2020. Amy reported that in Coxford there were currently 2638 people with dementia, but only 1157 of these were recorded in the relevant QOF data set. She described that the local mental health trust provides monthly reports to the PCT including the numbers of patients referred, diagnosed, prescribed and who do not return for follow-up, and that the mental health trust had spent £4.7M per year on dementia (more than half of their £7.8M budget) and £220,000 per year on drugs for Alzheimer's disease. In March 2011, the NICE guidelines lowered the Mini Mental State Examination (MMSE) threshold score for prescribing certain medications for patients with mild cognitive impairment and supported the use of antipsychotic medications for people with mild to moderate disease. Dementia team members were well aware of these national developments and guidelines and discussed them at their training event in early 2011.
Team member Amy (WIP18R) trained as a social worker and, with many years of experience in social care, spoke of a long local history of frustrated efforts to improve integration with primary care:
I had a quick corridor conversation with Chris about
18 months ago when this was all being discussed, and
immediately it became obvious that he understood GPs and
we didn’t. [Laughs] And I think that –
and this is classic around secondary mental health-care
services or even any other silos – they
don’t understand each other. And I think that
GPs have consistently not been understood more than any
other silo . . . their world view is so
different to secondary care and so different to social
care which is my background . . .
previous to this we had made loads of attempts from the
mental health trust to invite GPs to lunch, to start
working groups, to ask them what they were doing, to ask
them what they want from us, to develop a shared care
protocol . . . we were lucky if we got
any GPs. I spent months, for example, e-mailing the
Chair of the educational committee, and months being
completely ignored.
As a social worker Amy could see many missed opportunities to connect patients to much-needed services and she eagerly aligned with the WI dementia team, but she was told that she would be made redundant in September 2011. Full of enthusiasm she continued to build connections across mental health services when she was able. Eventually she found work at the PCT to support integration between the different WI topic areas, including providing support for the diabetes team and then for the anxiety and depression in BME populations team, where she was still working in early 2012.
This team had the strong starting point of a team leader who was creative, passionate and already engaged in efforts to improve connections between primary and secondary care. Before the WI, Sandra, the team leader, had already worked for over a decade as a mental health nurse and experienced manager and was well aware of challenges unique to Westpark. In 2009, as an experienced psychiatric nurse who had just finished her degree, she returned to lead the dementia service for organic disease in older people:
We actually looked at our GP referral rate in dementia and very significantly there was a number of surgeries in Westpark that hadn’t referred in 18 months and we knew that this wasn’t right, the hypothesis was that we should have had a lot more referrals. When you looked at the population we had, the epidemiology formulas, we knew that there was an awful lot of patients that were not being referred to us, so anything to sort of try and elicit more referrals in.
WIP9I, assistant director mental health trust
Sandra had many ideas about how to improve care in the community for patients with dementia but, despite having many personal anecdotes on how she had personally connected patients swiftly to the right services, she was also aware of the barriers to integrated care for this group of patients. Early on in the WI Sandra identified the potential for a nurse in a higher band 7 position to link primary and secondary care services for older patients with dementia; a local nurse, Ganesa, working in dementia was promoted to this position with the aim of integrating services. However, Sandra did not feel that there was senior-level support for this innovative new role, portraying an outdated management structure resistant to challenges to hierarchy and authority (especially at the mental health trust and among consultant psychiatrists):
And I think they were also very, very conscious that the service was changing beyond when they were comfortable with. At the end of the day they were old-time consultants. In fact, one consultant had set up the old age service some 15/20 years ago; this was their initiative, they’d set the criteria. It’s like a lot of other places, if you’re setting up a service you generally keep your criteria for acceptance very, very rigid so you don’t flood. The only problem was we kept the criteria very, very rigid and we got a reputation for not accepting referrals.
WIP9I, assistant director mental health trust
Despite this perceived lack of support, before the WI the team leader had sought, in her own personal time, to build connections through existing committee structures with other NHS and social care staff, but with little success.
Overall aims and specific objectives
At the April 2010 WI event the dementia team set themselves four broad aims and seven more specific objectives (Table 16).
| Overall aims | Specific objectives as stated in the team document | Measures of impact |
|---|---|---|
|
|
|
What happened: team activities
The team leader, Sandra (WIL9I), aligned her personal interest in service improvement with the interests of the WI and, without initially high hopes, committed to attending events despite a lack of supervisor support. Additionally, a band 7 community nurse, Ganesa, became a coleader of the dementia team. Early in the WI, at the December 2009 multidisciplinary stakeholder event, Sandra noted some positive outcomes:
We have learned more in one short afternoon than we have in 5 years. Thank you. What was evident is that the language we use in different systems is different. We need to update our materials in this way.
WIP9I, assistant director mental health trust
Ganesa (WIL3C, specialist practitioner nurse) was hired into the band 7 nurse position seeing it as a good opportunity for career progression, although she was often observed to be reluctant to take a formal leadership role. Others are aware of her quiet manner and worry at times that leadership of the team may be difficult, especially with her reticence to speak publicly. However, through involvement in the WI Ganesa notices her personal development and the ways in which colleagues respond to her:
The other people, they can see that as well. Other
colleagues. Yeah, it affects all the team members as
well, because the other members of the team some will
come back to me asking some sort of information or
guidance . . . . Not all of them. Some
of them they have, definitely, I can say this. The
comments are like, ‘Okay, you're much
more efficient in doing the things that you have done
before’, and they are much more comfortable
coming to me asking a question, and I feel more
comfortable giving them the answer as well.
Part of her own personal development included the way in which she uses improved communication and language skills with patients:
I’m talking about the people within my ethnic
minority . . . . That has been changed
and it has been improved a lot. Because I can actually
relate my own bilinguistic skills with the clients of
the ethnic minority, and they feel much more comfortable
with me talking in my own language while I'm
assessing their needs . . . . They are
more comfortable to speak to me as well.
Improved confidence in speaking with patients and clinicians made a great difference to how Ganesa perceived the need for better integration of services:
One of my patients was being transferred from the
acute side, from the under 65 [years], the other team,
and that client only [spoke a certain Indian] language
. . . I took over the case because I
knew that he was not going to go anywhere to our team,
so he won’t be feeling that comfortable with any
member of the staff . . . with the joint
working with the adult CPN and myself, we worked
together to make him feel so comfortable in the
environment, and he was so reluctant to come to our
services because of this language barrier
. . . . He said, ‘I’m
not going to transfer my case to the older people
service because of this problem.’ I talked to
him and made sure that I reassured him, I made sure that
he understood what I said, and I listened to him very
actively with all of my communication skills, and he was
so . . . he doesn’t want to go
to the other side now. He felt so relaxed with me, he
said, ‘I want to come to your team now’,
which I thought that was an achievement.
At the April 2010 WI stakeholder event these two coleaders presented a rapid appraisal of local dementia services and the quality of care, explaining that 30% of GPs were dissatisfied with the mental health trust and 47% felt ill-informed. Although the team leaders recognised the need to increase educational offerings and access to culturally sensitive cognitive screening tools, they struggled to make this happen, possibly because they lacked a cohesive team. Additional funding or time for extensive outreach or training was not available. Sandra, Ganesa and Amy attempted to increase awareness about dementia care by Westpark GPs through outreach efforts and teaching sessions in GP surgeries in the summer of 2010:
The response from the GPs initially was not good at all, but as the WI progressed on, the GPs are much more into that. Not all of the GPs are. I can still say that there are, within the cluster of my GPs, out of six, there are four active GPs . . . which is quite a good achievement. I think it’s just the . . . lots of GPs, my personal experience is that they . . . think that the people who are over 65 [years], it is because of their illness, old age . . . . We have to go back and back, again and again, to them, just to make them aware and also doing some sort of teaching session, not with the GPs themselves, but with the other . . . the team as well. For instance, I had two sessions with two different GP surgeries, not only with the GPs, with the other professionals, the receptionist, the practice manager, the nurses, talking about the dementia itself. It’s not an age-related disease.
WIL3C, specialist practitioner nurse
Receptionists and practice managers were therefore included in outreach efforts. Forming such connections was an important aspect of the WI and later in the same year Ganesa could see a difference:
Definitely. You can actually . . . like I can ring them . . . before the thought of ringing the practice manager, it was very hard to get hold of them. But now you know them, I want to speak to them, okay, they just come to you on the phone. Definitely the relationship has been changed.
WIL3C, specialist practitioner nurse
A borough-wide staff training event for dementia was held one evening in March 2011, hosted by the members of the WI dementia team. Sandra helped facilitate the event with Chris and an occasional GP participant of the WI and a consultant psychiatrist at the mental health trust presented about early diagnosis to the (mostly) GP audience. Sandra and Amy suggested that the WI dementia team should continue working on the use of the MMSE, improving the interface (1) with dementia end-of-life care and (2) with intermediate care to avoid hospitalisation. Sandra reported that the MMSE had now been translated into two Asian languages. Chris facilitated table-top discussions and attendees discussed their developmental needs, which included requests for online decision support and integrated referral forms. Proposals for a crisis support team, specific decision support tools via e-mail, case co-ordination with adult social care services and more feedback for families were among other proposed solutions.
Daphne (WIP37K) is an occupational therapist. She and her team attend the dementia training event in March 2011 hoping to learn how to better connect with mental health services in the local area, and around the table they passionately discuss among themselves how often they see patients and family members with dementia or mental illness and how it hampers the care that they can provide. It takes too long to gain access to the home, the patient can't remember the exercises, they are verbally abused and they miss their targets for providing patient care in a set number of sessions. Knowing that the patient is inappropriate for rehabilitation yet unable to convince anyone in primary or secondary care that some type of mental health service may be needed is a frequent frustration:
What I do see is the blocks. I don’t know
that anybody understands how services work. I think we
all work differently. Our urgent responses are all
different. For example, the urgent response of my team
is within 24 hours. The urgent response of a social
services occupational therapist in another team might be
a week. So we all work completely differently, and
nobody is clear about what the route is into
services.
Daphne describes that she and her colleagues came to the meeting about dementia at the last minute after a verbal invitation to one member. They struggle with a wide variety of mental illnesses and are keen for any kind of training or help. They talk quietly among themselves but no one speaks up to the rest of the attendees, even when prompted to brainstorm local solutions. However, later Daphne recalls the meeting that she attended:
I think it’s allowed me to
. . . I mean, a few times I have tapped
in now to the well-being service . . .
because of that event. It’s been good to put
some faces to those services, because then you just
understand quite quickly how that would work, and you
can make a quick call, have a chat with somebody and see
if it’s appropriate rather than making your
blind referral. Because people know you, and people take
the time then to talk with you – or I have found
– take the time to talk with you, and perhaps
say, ‘Well, we might not be the right services
this time, but have you tried this?’ And
that’s very useful. You don’t get that
on a blank referral sheet.
The meeting ended after a long discussion about how to reorganise dementia services, with attendees reporting a better understanding of the work of local memory clinics and that self-referral was possible. Despite wide attendance by both GPs and non-GP clinicians (such as occupational therapists and pharmacists), we observed that some participants left the meeting feeling unacknowledged. Attendees appeared to increase their personal awareness of screening tools but informal networking opportunities and a facilitated discussion of streamlined referral processes were not provided. Non-medical colleagues remained quiet during the training event, although amongst themselves ideas for integration were overheard.
In late 2011 Sandra left a management post for early retirement. By early 2012 this team had no leadership and lacked a coherent goal. The infrastructure of the mental health trust had changed and it had taken over the tasks of early assessment; the attention of the Coxford PCT, now a commissioning group, moved on to other priorities.
Patient and public involvement
The dementia team did not undertake any form of PPI in its work although a local Coxford charity had been active in the locality since 1982 to support relatives. This independent organisation had merged with other services numerous times, undergoing additional changes in 2010, which made outreach to this hard-to-reach patient population even more difficult both for clinicians and for researchers.
Team outcomes
The dementia team had set itself seven objectives at the beginning of the WI (see Table 16). This team did not gather quantitative data to report in a format that could be easily communicated to identify progress toward its goals. However, Sandra reported a number of changes that she associated with the work of the WI, although the impact of many of these on the quality of care is hard to quantify. For example:
And the other thing that we’ve actually done as a result, and I think it is primarily to do with the WI, because we did a decision support tool and as the WI we actually developed some information packs, we’ve done a post-diagnostic pack that actually sits on the PCT’s website that anybody can access. Essentially all it is is just information, used by professionals but also individuals, like what is the progression of dementia, the different types of dementia. So if you’ve got a diagnosis of, say, Lewy body dementia, you can get a factsheet about Lewy body dementia.
WIP9I, assistant director mental health trust
Sanjay (WIP34H) is a local pharmacist who attended the dementia training event because it was conveniently located and offered credit for CPD. He sees himself as a competitive business owner and as a trained professional who works in the front line of primary care in recognising signs of dementia in patients, or, more often, signs of strain in an adult caregiver to an ill patient:
But also we have a lot of patients who suffer from
dementia and I thought maybe it would give me a
direction of how . . . because a lot of
families come to me and they’re at a total loss
as to what to do . . . . Family members,
they’re totally lost what to do because either
the GP doesn’t want to know because it’s
costing him too much. It’s all cost based as we
know, or there’s a long waiting list with the
units, or they want to go private. The cost of the drugs
is very, very high.
Unfortunately, despite his willingness to attend an evening event he did not feel that he received the information that he needed:
I was hoping that they would keep
. . . you know because I left my e-mail
and everything there. I was hoping I would get feedback.
I wanted it in a bullet form, ‘patient walks in
or carer walks in, they have this, this’
. . . but there was nothing. I really
thought it was a waste of money . . . .
There are no connections. Unfortunately the patient or
the carer to the pharmacy, pharmacy to the doctor, the
doctor to the social services, it’s
disjointed.
Sanjay could recognise the problems that occurred when services were not integrated and could generate ideas for community-level solutions but was unable to actually make better connections happen for patients, and he still felt disempowered after the training event.
More concrete evidence of improvement, collected through internal audit but not necessarily a direct result of the WI, was also provided by Sandra:
Our referral rate now, from the point of referral, receiving referral to initial assessment is probably 2 weeks . . . . Before it used to be 11, 13 weeks . . . . We’re seeing people very, very quickly . . . . We actually do regular audits just to make sure of that. The way the day hospitals work hasn’t changed as a direct result of the WI but they have become the Memory Assessment Service.
WIP9I, assistant director mental health trust
John (WIA2V) is a commissioner of dementia services. He is involved in the WI by having supported the very first meetings, attending annual retreats and being an administrative leader in the PCT. He was very aware of the practical and financial barriers to effective cross-boundary work and was interested in service improvement:
The interesting thing was, for the first time with
this approach, when we brought together
Alzheimer’s Concern, Westpark mental health
trust most notably, and GPs, they started to talk to
each other on some very practical ways of doing it
. . . what I found really interesting is
that the WI helped people. It made some people
compromise. Actually, it helped with their willingness
to compromise, whereas before it wouldn’t have.
And it all comes down to interpersonal relationships
. . . at least it’s shifted both
Westpark mental health trust and GPs towards a closer
position of working . . . we know
it’s directly attributable because it only
really happened to those GPs who were involved in the
discussions . . . . So I think some GPs,
a few might have changed their position towards Westpark
mental health trust, which I think is probably even more
important than having changed pathways, because pathways
haven’t really changed. They’re the same
pathways, just there’s more willingness to work
together.
Sandra did credit the WI with having helped to provide new insights into referral processes and stated that these had led to process improvements:
We have completely changed. Basically we’ve re-audited the GP referrals to us and that showed an improvement in referrals. We are also less pedantic about the information we require on a referral, there is not the necessity to do all of the blood tests. We’ve become a lot more pragmatic, we will accept a referral, go out and do an initial visit . . . . We’ve developed a decision support tool to help GPs decide whether they should be referring to us.
WIP9I, assistant director mental health trust
However, Sandra then described that the tool was on the PCT website and was not being used as often as it should be, and that a much hoped for form of electronic referral had not been accomplished:
The biggest thing that the GPs wanted was an electronic way to refer to us and that, unfortunately, is an area we have failed in. To be honest, it's certainly beyond my sphere of influence, the systems need to talk to one another, and they don’t.
WIP9I, assistant director mental health trust
When asked how patients may experience dementia services in a different way as a result of the WI, Sandra explained changes that had occurred in both routes of accessing services and referral rates although, again, she did not attribute such improvements directly to the work of the WI:
Patients can now either come through an outpatient route or through a day service route for diagnosis of dementia and we are working towards 6 weeks. From a first initial assessment to diagnosis. [Normally it was] at about 9 weeks . . . . Again, I don’t think this is all WI, but it’s everything all rolled into one.
WIP9I, assistant director mental health trust
In September 2011 Chris reported to the (now) Coxford CCG that the early diagnosis of dementia was being led by the local mental health trust (i.e. responsibility for this had passed from the WI) and that he believed this to be an ‘unexpected’ sign of a wider Coxford adoption of this as a local priority.
We explored whether or not there had been any significant changes in two relevant QOF scores by comparing performance over time in the 24 Westpark practices and the 55 Coxford practices for which data were available. Performance on the two dementia indicators by geographical area and across three successive QOF reporting periods is shown in Table 17.
| QOF dementia indicator | Coxford | Westpark | |||||
|---|---|---|---|---|---|---|---|
| 2008/9 | 2009/10 | 2010/11 | 2008/9 | 2009/10 | 2010/11 | ||
| DEM 1: practice can produce a register of patients diagnosed with dementia | % | 98 | 100 | 100 | 96 | 96 | 96 |
| n | 55 | 55 | 55 | 24 | 24 | 24 | |
| DEM 2: patients diagnosed with dementia whose care has been reviewed in the last 15 months | % | 73.46 | 79.03 | 76.37 | 72.17 | 70.33 | 79.85 |
| n | 573 | 667 | 685 | 166 | 192 | 218 | |
Nearly all practices in both areas were able to produce a register of patient diagnosed with dementia (DEM 1). DEM 2 did not vary significantly by area at the 5% level, but there was some evidence of variability (χ2 = 4.800, 2 degrees of freedom (df), p = 0.091). Most of the improvement in Coxford happened between 2008/9 and 2009/10 (from 73% to 79%), whereas in Westpark improvement occurred between 2009/10 and 2010/11 (from 70% to 80%).
However, in the web of facilitated conversations that happened over the space of 2 years, individuals could be heard saying how much they had learned and reflecting on how their ideas had changed after exposure to other professionals, which, in turn, allowed them to consider working differently.
Child and family health services
The local context before the Westpark Initiative
Representatives of a number of children's services in the local area had been seeking ways to build connections between themselves for a long time. In 2006 one particular group colocated services in Westpark to develop more integrated and holistic care, and aligned itself with the national Every Child Matters119-mandated processes and the Common Assessment Framework (CAF). 120 But as one participant described after years of attempting to provide interdisciplinary care for children in need and their families:
Integrating different professionals into a whole . . . bringing social care and mental health together becomes an issue of sharing information . . . this is like knitting smoke, I’m afraid.
SIP12L, integrated service manager
The death of ‘Baby P’ and the failure of child protection afforded by NHS and children's services professionals received great attention in the media. Concerns about such care erupted again in August 2009 when the names of the baby and his killers were publicly revealed. Complex issues related to child protection – and the need for multidisciplinary teams to share appropriate information – were a source of national concern just as this WI team's priorities were forming.
One early enabling characteristic of this team included having a leader, Francine, who was a local community matron and administrator who had come out of retirement to be involved with the WI. This individual's knowledge of the local area and ability to network across a wide range of services was an important factor in encouraging a wide range of stakeholders to attend events early in the course of the initiative. Her extensive experience naturally led to her serving as an informal mentor for the other three team leaders.
Overall aim and specific objectives
Table 18 shows the aim and specific objectives set by the child and family health services team at the April 2010 WI event.
| Overall aim | Specific objectives as stated in the team document | Measures of impact |
|---|---|---|
| To improve awareness and use of child and family health services | Need to network. Proposed actions:
|
Focus groups
|
What happened: team activities
Francine (WIL1A), a former community matron, was identified by Chris as a good leader for the child and family services team. She was well connected in the Westpark and Coxford areas and she had also held an administrative position. Francine worked effectively to build connections for the WI but when the small amount of funding that she received to lead the team ran out in early 2011 she happily returned to retirement.
An early goal of this group (objective 1a in Table 18) was to update a resource guide to local secondary, mental health and voluntary services; this was accomplished by July 2010. Unfortunately, this resource guide was not produced in any quantity, posted online or otherwise disseminated. A handful of hard copies were printed and brought to WI stakeholder events, but the guide did not reach a wide audience. A related early perceived success included talking to receptionists about disseminating the resource guide, and a receptionist in one of the Westpark practices showed facility with such signposting. In September 2011 Chris reported that training receptionists as ‘health champions’ was an ongoing redesign project. Victoria, a public health trainer from Coxford, explained the origins of the project:
A few months ago, as part of the WI, I was contacted by Chris . . . he identified three practices that were interested in having some kind of signpost-type training for their receptionists . . . . So with one of my staff, one of the health trainers, we developed a kind of training module . . . . So we did some brainstorming ourselves and with other people in the public health department about the type of things that we felt we should include in this signposting training.
WIP38L, health training co-ordinator
At the beginning of a WI stakeholder meeting one evening in November 2010 about 35 people gathered to hear about ongoing efforts to improve the integration of child and family health services. Three GPs were observed coming in late, checking their telephones for text messages and looking distracted, and only slowly engaging in small-group conversations during an introductions and brainstorming exercise. As part of the agenda, a GP was invited by the child and family health services team leader to speak about making referrals to a local service that supports families with children struggling with emotional and sometimes psychological problems. He introduced his receptionist who further described their efforts:
I personally went and visited these centres, just to
have sort of contact. When patients are just sitting
there you get to talking with them . . .
I try to incorporate this into our practice
. . . handing out leaflets
. . . pointing out posters. I was able
to find a number and give it to a family to help a
child.
Within 30 minutes all of the GPs were paying attention; one was taking notes about the topic at hand and a second was asking questions.
At a subsequent residential meeting in spring 2011, Chris, the WI founder, talked about more formal receptionist training for such signposting and a public health trainer, Victoria, was tasked with creating signpost training for receptionists. A training module including a very wide selection of health promotional topics was developed and surgeries were contacted for training; however, only three in Coxford responded and training was provided in June 2011. Time release for training was cited as a problem and practice managers were reluctant to make time to review and approve materials. Despite persistence in pursuing receptionists and practice managers for this modular training, no additional inroads were made and no practices in Westpark participated. As of early 2012, attempts to create either intranet or extranet versions of the signposting module were under way but were not resourced with funds or personnel.
Potential team members, representing community services for school-aged children, refugees, asylum seekers and women struggling with domestic violence, attended various stakeholder meetings. Although some individuals continued to attend when invited to stakeholder events, they appeared to be motivated by opportunities to represent their own services rather than by working to achieve the goals that had been set out in April 2010 (see Table 18). Ultimately no coherent team formed and, despite efforts to identify a new leader for the topic, by the time of the residential meeting in 2011 the goals of the team remained amorphous and difficult to organise around. In the event, a newly appointed team leader did not have a close professional interest in child and family health services, had no supervisory support for their involvement in the WI and was soon formally responsible for commissioning adult services; leading on this topic did not align well with her daily work and the ‘team’ did not gain cohesiveness.
Patient and public involvement
In March 2009, before the formal launch of the WI in October 2009, an organisational consultant was engaged by Chris to facilitate an interactive workshop that was widely advertised across Westpark, appealing for anyone interested in the health and well-being of children and families to attend at a local community centre. At the beginning of the workshop the Westpark Community Alliance representative offered a perspective, as did a GP, but most of the 2-hour workshop was spent in facilitated small-group discussions. Participants were asked to describe current weaknesses and strengths in the local area and then to envision a better Westpark 5 years in the future. No written minutes from this event have been traced, although user perspectives were represented in resultant events and reports. At the time, the consultant noted the number of small groups already in place locally, commenting that ‘the self-organising was just unbelievable, it was fantastic. More so than I've seen elsewhere, you know, [x] has some, but Westpark was just full of them, absolutely amazing’ (WS32012). The contribution of community-centred activity in the local area was explored by the consultant, who advised that ongoing efforts to engage with local community groups should be decentralised from the PCT. Interviewed as part of our research 2 years later, she noted that these efforts now had the PCT at the centre.
Stephanie (WIP19S) is a learning and development manager based at the PCT educational centre. Although not connected directly to clinical services, she had been approached by Chris in 2009 to help with publicising WI efforts across the borough; she continued to attend meetings through 2010 and early 2011. Stephanie describes being involved in organising training events, including trying to roll out an updated IT system (a version of RiO, an electronic care records system) to ‘transform’ and connect services across the locality. She describes herself as ‘wearing multiple hats’ and having ‘lots of strain’ because of being ‘between two worlds and pulled in different directions’. Stephanie said, ‘I see solutions others don't see because of my position, but then I'm the last one to see the implementation plan!’.
Although never part of the formal agenda, Stephanie felt the excitement of the WI but was not sure how she could contribute. Running training events meant that Stephanie met with all practice managers at a scheduled monthly forum, one of the few people in the local health-care system to do so. Stephanie had the advantage of personally building relationships with the practice managers over a 6-year period; equality and diversity updates, accreditation updates and general information flow from practices were all part of her role. In spring 2011 Stephanie noticed changes under way and knew how important it would be to maintain communication in all directions through her bridging role:
The networking is crucial for things to be developed.
And it’s not us against them, and that’s
what I think that I’ve shown, because sometimes
what would have happened is we would get the option to
go into a GP's surgery, whereas they
won’t let you in as PCT staff. So we have got
that particular network, which I felt was really good. I
could send them an e-mail and I would get x amount of
responses back very quickly, because people know who I
am.
Stephanie also recognised how receptionists and other non-clinical staff needed to be acknowledged for their important work, something that the child and family services team of the WI attempted to do:
And I’ve seen some of the things that
they’ve done, and the improvement through going
to some of the meetings that I’ve had, where the
GP’s have felt, or the staff have felt that
there has been a great improvement . . .
the receptionist to do a lot more with the patient,
which meant that because of some of that work, because
they know one another, the patients come in, the
receptionist has the most information to give a patient.
So their role becomes evolved in a sense, and it was
good to see that, and I wanted, at some point, to share
that with other practices, which I felt would have been
really good . . . I’ve felt that
the receptionists, when we met with some of them that
actually developed the WI, felt very honoured to
actually do that role, because it was their ideas that
were coming about. They were using their
initiative.
Although the WI recognised the potential of this way of increasing joined-up working, Stephanie also knew that she would in all likelihood not be the person to develop such a programme to reach out to receptionists. Stephanie was made redundant in mid-2011 and the monthly practice manager forum ceased thereafter.
Team outcomes
The child and family health services team had set itself five objectives as described at the outset of the WI in April 2010. This team did not gather quantitative data to identify progress towards their goals. They struggled to define measurable goals and lacked leadership after Francine retired. The early success in creating a community resource guide did not include the use of evaluation criteria, such as numbers of printed copies disseminated, and no updated versions were created.
Responses to the receptionist signposting training were favourable, as Victoria describes below, but developing and delivering such training programmes is very time intensive and the material needs to be constantly updated. Victoria was able to describe how, beyond the intranet, the extranet might support such efforts but she was also realistic enough to know that staffing and funding for IT development posed a major barrier looking forward:
They were particularly interested about all the different resources that are available to patients. Because we were telling them about things that they weren’t aware about, all these things. The other thing that came up was there’s so much information, how can we get up-to-date information, how can we do that. I think one way that’s sort of been addressed now is with the introduction of extranet. I mean, I’ve got no admin help . . . . Because the thing that came out to them was they wanted a general overview of the plethora of services available, because they knew about some, they didn’t know about others. And there was also information about names and contact details, but I did explain to them that if you give them a name of a certain person, sometimes they leave, and I myself struggle to keep up-to-date. I mean, they felt the content was fine, most of them. But what they said was things like notification, changes to services.
WIP38L, health training co-ordinator
We explored whether or not there had been any significant changes in one relevant QOF score by comparing performance over time in the 24 Westpark practices and the 55 Coxford practices for which data were available. Performance on the child development check indicator by geographical area and across three successive QOF reporting periods is shown in Table 19.
| QOF child and family health services indicator | Coxford | Westpark | |||||
|---|---|---|---|---|---|---|---|
| 2008/9 | 2009/10 | 2010/11 | 2008/9 | 2009/10 | 2010/11 | ||
| CHS 1: Child development checks offered at intervals that are consistent with national guidelines/policy | % | 98 | 100 | 98 | 96 | 96 | 96 |
| n | 55 | 55 | 55 | 24 | 24 | 24 | |
Nearly all practices in both areas were able to offer child development checks at intervals consistent with national guidelines/policy.
Diabetes
The local context before the Westpark Initiative
As a focus of clinical concern for many practitioners in different settings, diabetes is commonly recognised as a priority for integrated care initiatives. Multiple funding streams – at the local and national level – exist to support different aspects of the complex care that patients with diabetes may need. However, debates were taking place about which aspects of integrated care for diabetes patients needed to be prioritised in the period leading up to the White Paper114 on GP commissioning in 2010.
Locally, structured educational efforts about diabetes existed before the WI, including a local university course and certification for practitioners designed and led by local diabetic specialist nurses (and commissioned by the Coxford PCT). According to PCT documents this university course reached staff in 35 GP surgeries during the period 2004–10. A dietician-led Right Start course for Westpark patients also existed before the WI and had been offering structured sessions for patients since 2009. The PCT had also in the past commissioned a course for practitioners on initiating insulin.
The enabling characteristics of this team included consistent leadership but barriers were a lack of mentoring support for serving in such a boundary-spanning position, a lack of formal supervisory recognition for the leadership role in the WI, and work pressures to spend time on other topics (including a fear of redundancy).
Overall aims and specific objectives
The aims and specific objectives set by the diabetes team at the April 2010 WI event are shown in Table 20.
| Overall aims | Specific objectives as stated in the team document | Measures of impact |
|---|---|---|
|
|
|
What happened: team activities
This team was the last to develop within the WI and was not initially a priority topic determined from the early stakeholder meetings. As Chris, the WI founder, talked with PCT managers and local GPs, it became clear that diabetes was a major clinical concern and a cause of numerous comorbidities in the local population. Therefore, Chris and a PCT commissioner together determined that diabetes should be a focus of quality improvements and this team was named as part of the WI in early 2010.
The rapid appraisal document presented by the team leader in April 2010 proposed:
-
using cross-practice training events for GPs
-
developing out-of-hours services
-
providing hospital- and community-based care by diabetes specialist nurses.
All of these ideas were acted on in some form in the next year, despite profound system changes at the PCT resulting in leadership replacements and redundancies between 2010 and 2011.
With many disciplines involved in providing diabetic care, the membership of this group varied by professional availability and potential overlaps with existing meetings around diabetic services. Diabetic nurses and specialist nurses dropped in for some meetings, as did diabetic consultant specialists, GPs, pharmacists, dieticians and representatives from medical management. No individuals could be consistently named as part of the diabetes team for the WI, although many representatives of different services were in frequent contact as part of their formal work roles. The team leader was not able to name team ‘members’ and yet had almost daily meetings about diabetes services, alongside daily work on other topics. Tense conversations between the local hospital trust and the PCT were facilitated by the team leader in her role as a commissioner of diabetes services who brought together multidisciplinary representatives to negotiate service provision by cost, locale and provider. A specification for intermediate diabetes services was initially drafted in October 2010, but progress and take-up were slow. Resistance to change was noted among specialists, hospitalists and GPs. In early 2012 Supriya described this time period:
There have been a lot of changes in the NHS, as you know, over the last year and at that time there was a lot happening. There were meetings that we were attending where nobody knew what our future was going to be. We were in new roles, couldn’t really impact on certain things. We felt more and more distance as time went on. It started to improve, definitely it started to improve over the last 2 or 3 months, but at that time I think it was a particularly low time. Not just for me, I think a lot of people were feeling the strain.
WIL4D, PBC manager
Supriya (WIL4D), the leader of the diabetes team, worked at Coxford PCT in middle management; she was not a clinician but had a background in scientific research. A part of her remit included overseeing diabetes services across the PCT. Encouraged by the founder of the WI to take part, she was nervous about public presentations and uncertain about her leadership skills, but consistently took part in WI events.
In the summer of 2011 Supriya began to write in her diary about the sense of reaching a ‘tipping point’ and that there was now more interest in the notion of community-based diabetes services. During this time, Supriya reflected in her diary about recent personal and professional experiences that had broadened her perspective of the need that diabetic patients have for integrated services. At the same time, her line manager commented that her ‘pseudo-leadership role in the team’ was probably not associated with ‘her personal development priorities’, although that was his view of her and of the change model underpinning the WI.
In September 2011 Supriya was observed leading a meeting of different disciplinary representatives [including the district nursing service (DNS) and podiatry] who appeared to be frustrated by the lack of change, noting ongoing bureaucracy. Supriya demonstrated a calm positive manner while listening to these concerns and offered an optimistic plan towards progress; a similar experience was reflected on in her diary a month before this, demonstrating an increasingly reflective stance and ongoing personal development. A few days later Supriya noted that this conversation at the multidisciplinary meeting had prompted a number of further cross-boundary interactions that led to two new shifts in attitude from outside the usual team. Within a few days she had received calls from two previously resistant people, one a DNS at the hospital and the other a GP from the newly formed local CCG, both asking how they could move the diabetes work forward to improve care in the primary care setting. As Supriya said at the time: ‘This is now a new level of integration and working is amazingly different . . . in a good way!’.
A borough-wide training event on the topic of diabetes was held on 3 February 2011 and was very well attended by GPs. Another ripple of success was noted when the previously resistant diabetic specialist attended the third residential conference in April 2011 after never attending previous events despite multiple invitations to various multidisciplinary discussions. At this event, as part of a multidisciplinary team, the diabetologist declared for the first time a strong interest in moving diabetes care into the community; this shift in attitude was noted by many in the WI.
Additionally, 21 surgeries were involved in training through the national UK programme Year of Care (YOC) by attending at least one of three sponsored events in late 2011. In 2011, a university hospital-based pilot was initiated in 14 collaborating GP surgeries in the borough (as part of the YOC programme). The team leader spoke of her confidence and ability to provide evidence of significant involvement in the WI, to support her request as a commissioner to involve the PCT in the pilot. Another hard-won success was achieved when, despite many stops and starts, a once-weekly diabetic clinic staffed by diabetic specialist nurses was started in a community setting in the borough (although not Westpark) in early 2012.
Patient and public involvement
Through Diabetes UK there was an effort to hear patient perspectives and to encourage self-management. However, as part of the WI, patients were not directly observed participating at events.
Team outcomes
At the outset of their involvement in the WI the diabetes team had set themselves two very broad objectives and three specific measures of impact (see Table 20), which we report on in this section. Chris reported to the forming commissioning group in September 2011 that the achievement of the WI diabetes team was that 14 GP practices had collaborated to improve diabetes care and participate in the YOC, as jointly led by the hospital and the Coxford PCT.
Performance on the QOF diabetes indicators by practice group and across three successive QOF reporting periods is shown in Table 21.
| QOF diabetes indicator | Coxford | Diabetes cluster | Westpark remainder | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2008/9 | 2009/10 | 2010/11 | 2008/9 | 2009/10 | 2010/11 | 2008/9 | 2009/10 | 2010/11 | ||
| DM 2: % with diabetes whose notes record BMI in the previous 15 months | % | 91.18 | 89.70 | 90.52 | 92.42 | 96.18 | 94.16 | 90.53 | 86.73 | 88.35 |
| n | 9526 | 9835 | 10,589 | 1244 | 1359 | 1404 | 4894 | 5163 | 5386 | |
| DM 5: % with diabetes with a record of HbA1c in the previous 15 months | % | 92.91 | 92.80 | 93.54 | 91.53 | 92.29 | 91.95 | 91.25 | 86.91 | 91.24 |
| n | 9707 | 10,175 | 10,942 | 1232 | 1304 | 1371 | 4933 | 5174 | 5562 | |
| DM 7: % with diabetes in whom the last HbA1c is ≤ 10% in the previous 15 months | % | 84.41 | 77.41 | 80.02 | ||||||
| n | 8819 | 1042 | 4326 | |||||||
| DM 9: % with diabetes with record of presence/absence of peripheral pulses in the previous 15 months | % | 86.10 | 84.92 | 85.59 | 86.70 | 90.87 | 89.20 | 87.00 | 83.62 | 86.37 |
| n | 8996 | 9311 | 10,012 | 1167 | 1284 | 1330 | 4703 | 4978 | 5265 | |
| DM 10: % with diabetes with a record of neuropathy testing in the previous 15 months | % | 85.91 | 84.76 | 85.46 | 86.70 | 90.87 | 89.40 | 86.77 | 83.02 | 86.27 |
| n | 8976 | 9293 | 9997 | 1167 | 1284 | 1333 | 4691 | 4942 | 5259 | |
| DM 11: % with diabetes with a record of blood pressure in the previous 15 months | % | 96.41 | 95.75 | 96.12 | 96.36 | 97.66 | 96.58 | 95.36 | 93.05 | 94.75 |
| n | 10,073 | 10,498 | 11,244 | 1297 | 1380 | 1440 | 5155 | 5539 | 5776 | |
| DM 12: % with diabetes whose last blood pressure is ≤ 145/85 mmHg | % | 76.05 | 76.13 | 76.51 | 72.21 | 75.80 | 74.98 | 71.79 | 70.82 | 73.28 |
| n | 7946 | 8347 | 8950 | 972 | 1071 | 1118 | 3881 | 4216 | 4467 | |
| DM 13: % with diabetes with a record of microalbuminuria testing in the previous 15 months | % | 77.51 | 82.21 | 83.31 | 75.78 | 82.40 | 80.80 | 68.35 | 76.07 | 78.25 |
| n | 8098 | 8625 | 9348 | 1020 | 1114 | 1157 | 3695 | 4028 | 4250 | |
| DM 15: % with diabetes with a diagnosis of proteinuria or microalbuminuria treated with ACE inhibitors | % | 9.37 | 85.05 | 81.04 | 8.31 | 84.44 | 81.94 | 13.80 | 79.91 | 80.53 |
| n | 925 | 1217 | 1261 | 85 | 114 | 118 | 708 | 708 | 728 | |
| DM 16: % with diabetes who have a record of total cholesterol in the previous 15 months | % | 92.87 | 92.50 | 93.20 | 92.12 | 93.91 | 92.76 | 91.38 | 87.32 | 91.58 |
| n | 9703 | 10,142 | 10,903 | 1240 | 1327 | 1383 | 4940 | 5198 | 5583 | |
| DM 17: % with diabetes whose last measured total cholesterol within the previous 15 months is ≤ 5 mmol/l | % | 74.45 | 76.30 | 75.47 | 70.06 | 70.70 | 70.02 | 68.55 | 68.79 | 71.56 |
| n | 7779 | 8365 | 8829 | 943 | 999 | 1044 | 3706 | 4095 | 4362 | |
| DM 18: % with diabetes who have had influenza immunisation in the preceding 1 September to 31 March | % | 73.78 | 73.87 | 73.06 | 78.23 | 79.12 | 79.07 | 76.32 | 77.24 | 75.26 |
| n | 7709 | 8099 | 8546 | 1053 | 1118 | 1179 | 4126 | 4598 | 4588 | |
| DM 20: % with diabetes in whom the last HbA1c is ≤ 7.5% in the previous 15 months | % | 56.24 | 41.23 | 47.26 | ||||||
| n | 5876 | 555 | 2555 | |||||||
| DM 21: % with diabetes with a record of retinal screening in the previous 15 months | % | 88.75 | 85.77 | 87.03 | 90.71 | 87.54 | 89.47 | 81.89 | 76.90 | 85.50 |
| n | 9273 | 9404 | 10,181 | 1221 | 1237 | 1334 | 4427 | 4578 | 5212 | |
| DM 22: % with diabetes with a record of eGFR/serum creatinine testing in the previous 15 months | % | 93.40 | 92.69 | 93.47 | 91.90 | 93.42 | 93.29 | 91.40 | 87.33 | 91.45 |
| n | 9758 | 10,163 | 10,934 | 1237 | 1320 | 1391 | 4941 | 5199 | 5575 | |
| DM 23: % with diabetes in whom the last HbA1c is ≤ 7% in the previous 15 months | % | 42.89 | 42.43 | 30.50 | 32.41 | 33.85 | 33.25 | |||
| n | 4702 | 4964 | 431 | 482 | 2015 | 2027 | ||||
| DM 24: % with diabetes in whom the last HbA1c is ≤ 8% in the previous 15 months | % | 66.13 | 66.43 | 54.99 | 58.06 | 56.22 | 57.48 | |||
| n | 7251 | 7771 | 777 | 864 | 3347 | 3504 | ||||
| DM 25: % with diabetes in whom the last HbA1c is ≤ 9% in the previous 15 months | % | 77.86 | 78.40 | 72.26 | 72.23 | 69.31 | 71.88 | |||
| n | 8537 | 9171 | 1021 | 1074 | 4126 | 4382 | ||||
Profiles across the three QOF reporting periods varied significantly between practice groups for two indicators, DM 11 (% with diabetes with a record of blood pressure in the previous 15 months, χ2 = 22.144, 4df, p < 0.001) and DM 15 (% with diabetes with a diagnosis of proteinuria or microalbuminuria treated with angiotensin-converting enzyme inhibitors, χ2 = 11.195, 4 df, p = 0.024), and approached statistical significance for DM 21 (% patients with retinal screening in the previous 15 months, χ2 = 8.935, 4 df, p = 0.063) and DM 24 [% with diabetes in whom the last HbA1c (glycated haemoglobin) is ≤ 8% in the previous 15 months, χ2 = 5.399, 2 df, p = 0.067].
Performance dipped on DM 11 in the Coxford and Westpark practices in 2009/10, but not in the diabetes cluster, in which there was an increase in performance. There was a marked increase in performance on DM 15 for all practice groups between 2008/9 and 2009/10; performance then declined between 2009/10 and 2010/11 for Coxford (minus 4.0%) and the diabetes cluster (minus 2.5%), but not for the Westpark practices not in the diabetes cluster (plus 0.6%). Performance on DM 22 also dipped in the Coxford practices and the Westpark practices not in the diabetes cluster in 2009/10. There was greater improvement in DM 24 between 2009/10, when this indicator was first introduced, and 2010/11 in the diabetes cluster than in the other two practice groups.
Overall, therefore, those practices in Westpark that were part of the diabetes cluster performed better on three of the 17 QOF indicators (DM 11, DM 22 and DM 24) than practices in the remainder of Westpark and in the wider Coxford PCT. Practices in Westpark, but not in the diabetes cluster, performed better on DM 15, a counterintuitive finding. No statistically significant differences were found on the remaining 13 QOF indicators.
The time trends for elective admissions and bed-days and emergency admissions and bed-days based on the predicted rates (adjusting for IMD score) are shown in Figure 7.
FIGURE 7.
Admission and bed-day rates (per 10,000) by practice group over 19 NHS quarters. (a) Elective admissions; (b) elective bed-days; (c) emergency admissions; and (d) emergency bed-days.
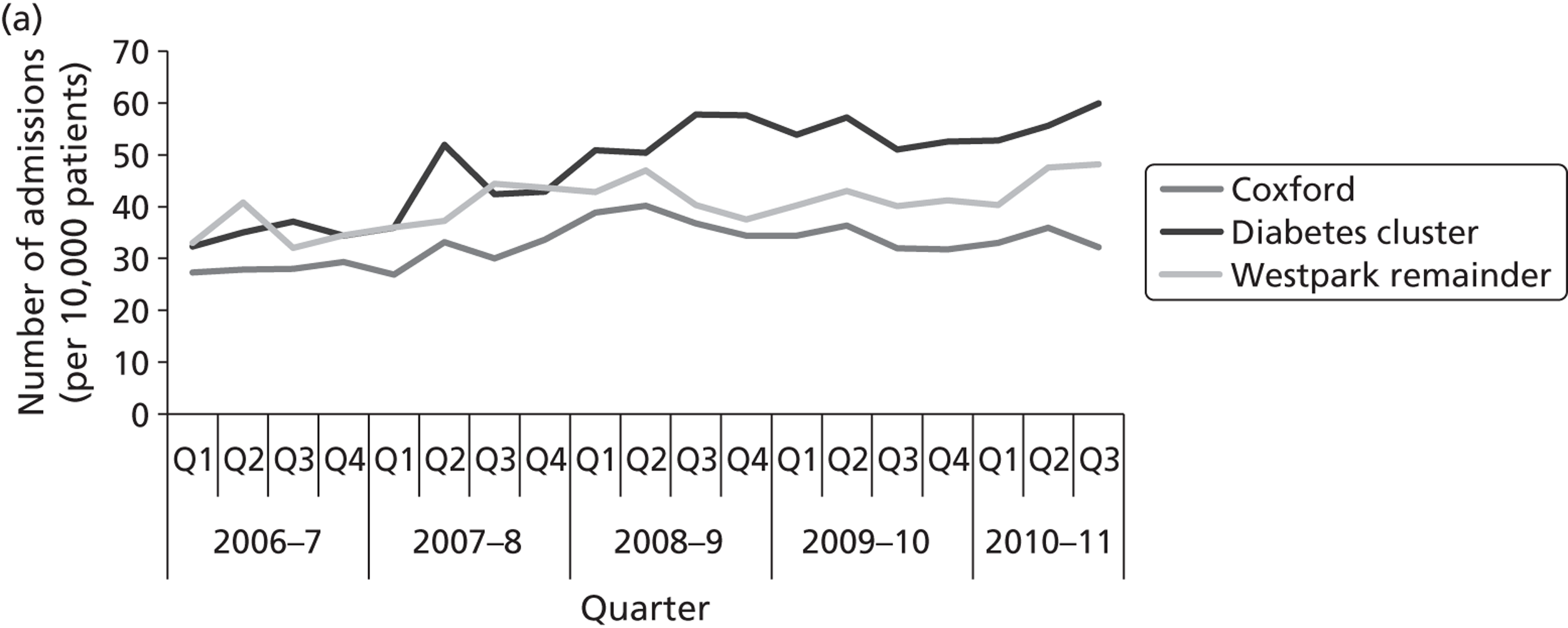
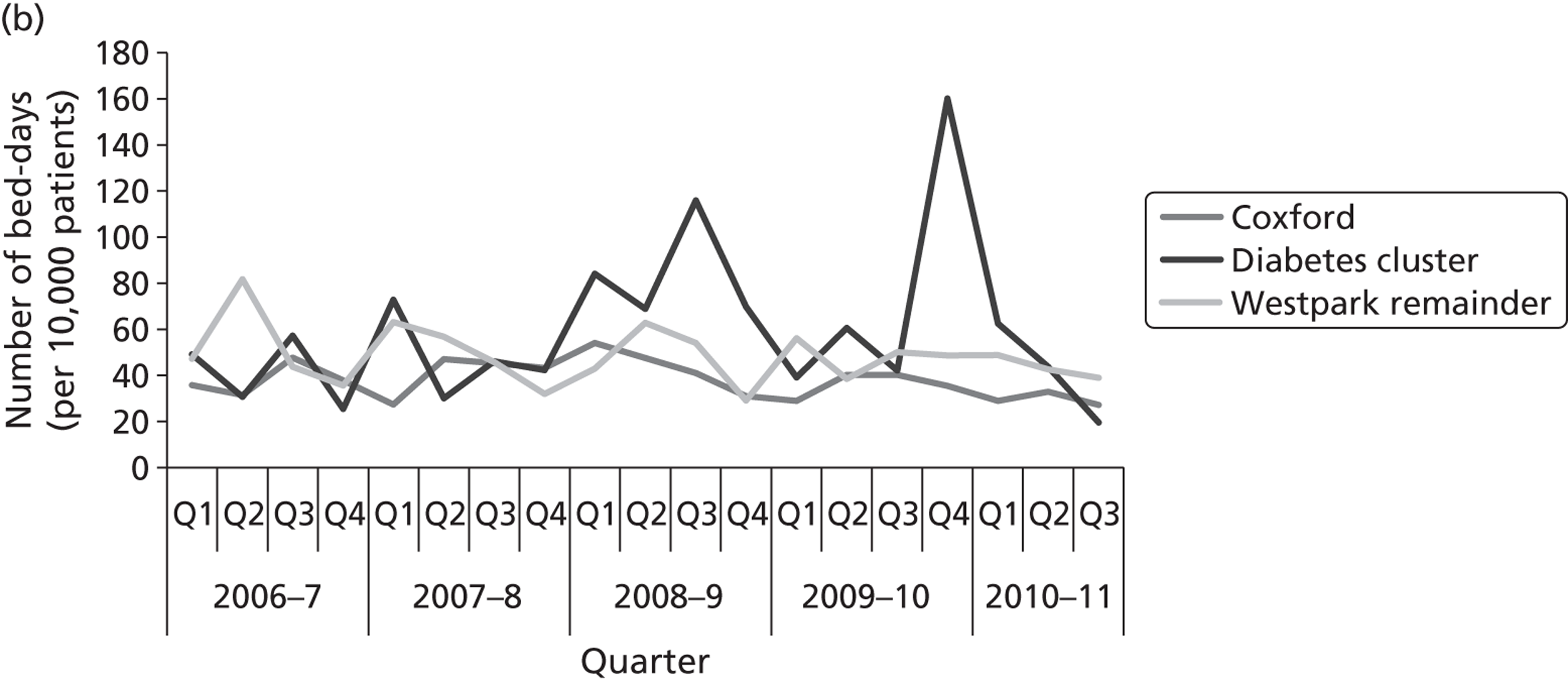
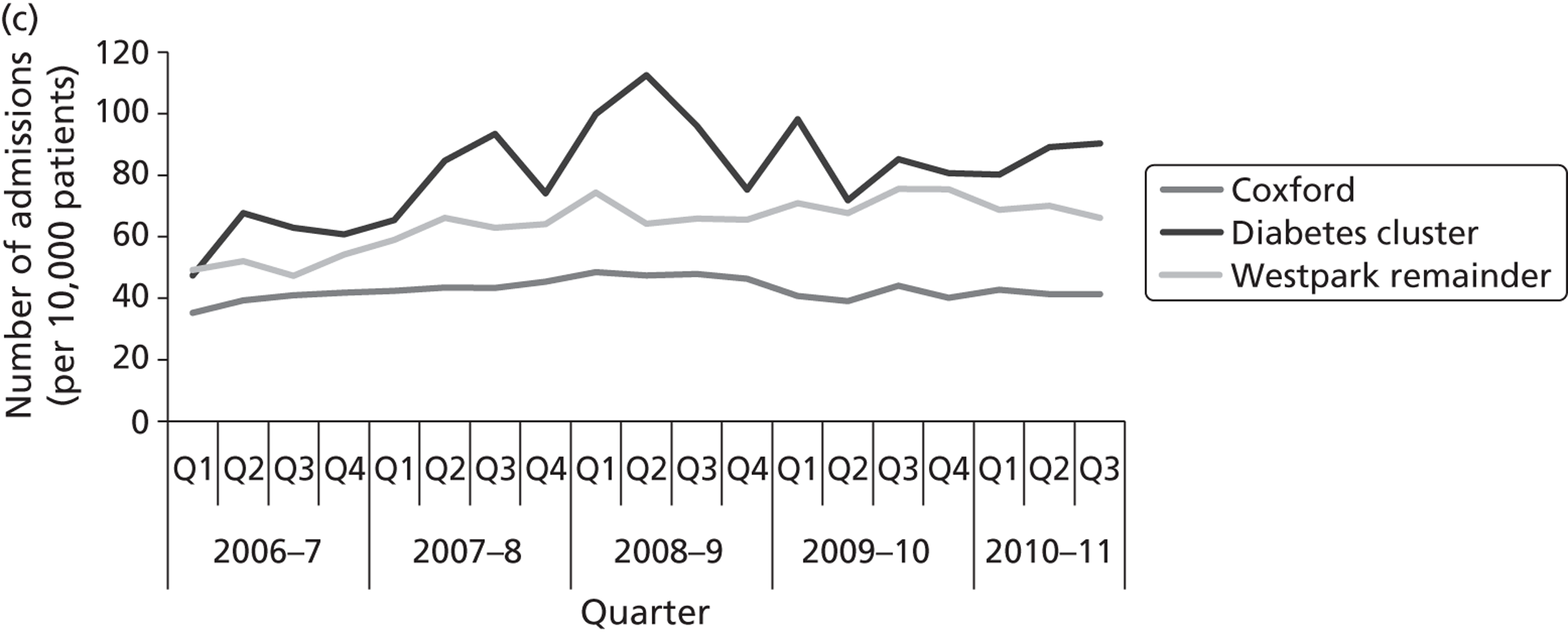
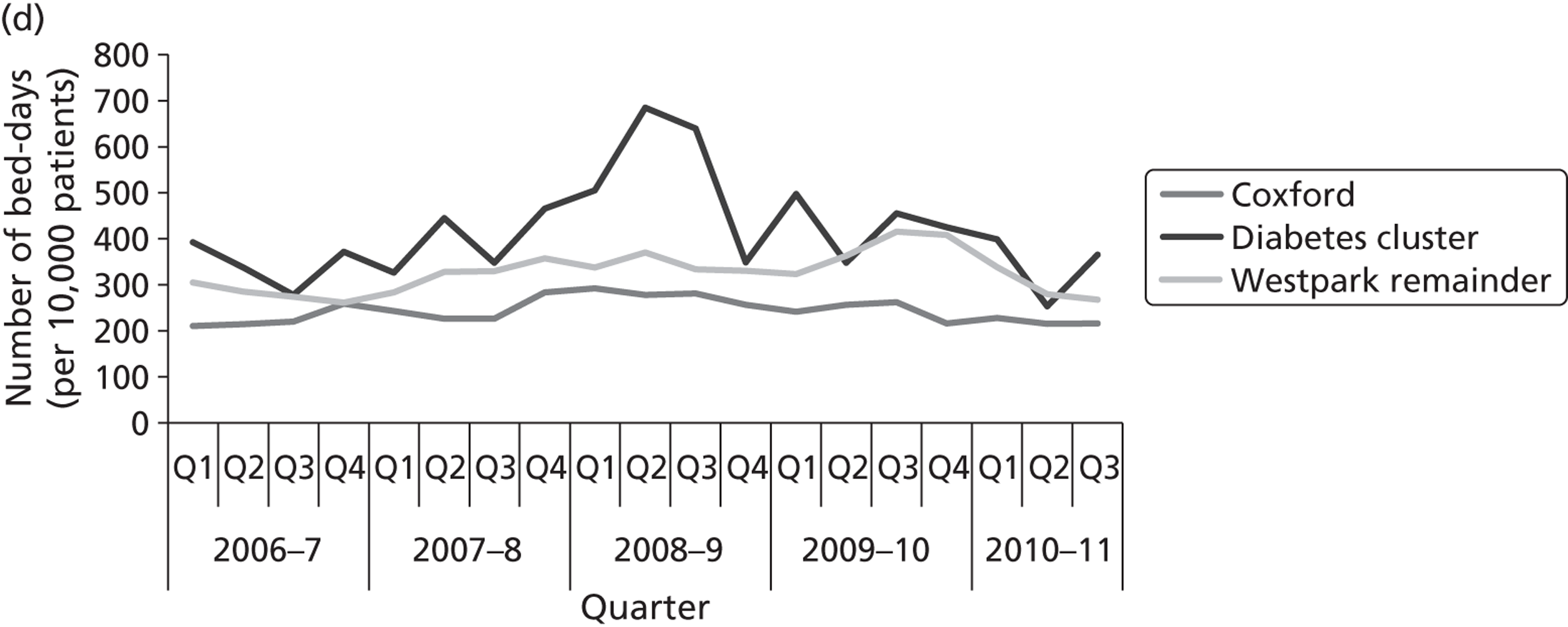
The time profiles differed significantly (p < 0.001) between practice groups for elective admissions and bed-days and emergency admissions and bed-days. The rate of elective admissions (see Figure 7a) in the diabetes cluster diverged from the rates in the other practice groups around the third quarter of 2008/9 (October to December 2008), with some convergence with the Westpark practices not in the diabetes cluster in the second quarter of 2010/11. The two spikes in elective bed-days rate for the diabetes cluster make interpretation difficult (see Figure 7b); ignoring the two spikes the profiles are closer together than in Figure 7a. The emergency admissions profile (see Figure 7c) for the diabetes cluster was more erratic than for the other two practice groups, which perhaps was not unexpected because of its small size. There was some separation between the diabetes cluster and the other two practice group profiles from the second quarter of 2007/8 until the second quarter of 2009/10 followed by a short period of convergence and then divergence in the second and third quarters of 2010/11. Emergency bed-days (see Figure 7d) largely mirrored the profile for emergency admissions with perhaps less separation.
Participant diaries
The previous section described and analysed the specific stories of each of the four boundary-spanning teams. Here we turn to the experiences of the individual boundary spanners who participated in the WI and present, first, a summary of the quantitative results from the 36 diaries completed by 11 of these individuals (see Summary results) and, second, an in-depth qualitative analysis of two examples from participants who completed four sequential diaries and a follow-up interview, one an anxiety and depression in BME populations team member (see Diary example 1) and the other from the diabetes team (see Diary example 2).
Summary results
As Table 22 shows, in terms of interactions in the past 2 weeks with other health-care professionals, representatives of the voluntary sector and patients/carers, interactions with primary health-care professionals were the most commonly reported by diary participants from each of the four topic areas (although the number of interactions was also high with patients/carers for the anxiety and depression in BME populations team and with social care for the child and family health services team). The 36 diaries recorded a total of 290 interactions and, overall, participants reported approximately eight interactions as a result of their efforts as part of the WI in each 2-week period for which they completed a diary; diabetes team members reported the highest number of interactions (10.6).
| Interaction with | Anxiety and depression in BME populations (18 diaries) | Dementia (two diaries) | Child and family health services (eight diaries) | Diabetes (eight diaries) | Total |
|---|---|---|---|---|---|
| Primary health-care professional | 43 | 7 | 13 | 27 | 90 |
| Secondary health-care professional | 17 | 5 | 7 | 12 | 41 |
| Voluntary sector | 21 | – | 8 | 15 | 44 |
| Patient/carer | 42 | – | 6 | 8 | 56 |
| Social care | 11 | 3 | 12 | 5 | 31 |
| Education | 2 | 1 | 4 | 4 | 11 |
| Housing | – | – | – | 2 | 2 |
| Other | – | – | 3 | 12 | 15 |
| Total | 136 | 16 | 53 | 85 | 290 |
| Interactions per diary | 7.6 | 8.0 | 7.6 | 10.6 | 8.3 |
Table 23 shows that face-to-face meetings, e-mails and telephone calls made up similar proportions of the reported interactions as part of the WI. In 32 diaries, respondents also indicated that on 10 occasions (diabetes: three; dementia: one; anxiety and depression in BME populations: six) at least one of the interactions in the previous 2 weeks had been with individuals or organisations that they had not contacted or been contacted by before.
| Interaction with | Face-to-face meeting | Telephone call | Document exchange | None | Total | |
|---|---|---|---|---|---|---|
| Primary health-care professional | 25 | 23 | 25 | 17 | – | 90 |
| Secondary health-care professional | 9 | 12 | 12 | 5 | 1 | 39 |
| Voluntary sector | 14 | 14 | 11 | 7 | 4 | 50 |
| Patient/carer | 19 | 13 | 17 | 9 | 1 | 59 |
| Social care | 7 | 8 | 7 | 4 | 5 | 31 |
| Education | 5 | – | 1 | 2 | 4 | 12 |
| Housing | 1 | – | – | – | 1 | 2 |
| Other | 4 | 4 | 3 | 4 | – | 15 |
| Total (%) | 84 (28) | 74 (25) | 76 (26) | 48 (16) | 16 (5) | 296 (100) |
Table 24 reports, for 33 completed diaries, the number of times that different types of boundaries – sectoral, organisational, professional and geographical – were reported to have been crossed. Professional boundaries were most likely to have been crossed at least once in each 2-week period and such boundaries were generally the most likely to have been crossed multiple times.
| No. of interactions | Sectoral | Organisational | Professional | Geographical (outside Westpark) |
|---|---|---|---|---|
| None | 8 | 10 | 4 | 5 |
| 1–3 | 22 | 17 | 16 | 23 |
| 4–6 | 2 | 2 | 7 | 4 |
| 7–10 | – | – | 3 | 1 |
| 11–15 | – | – | 1 | – |
| 16–20 | – | – | – | – |
| 21+ | – | 1 | – | – |
Table 25 shows that, for 33 completed diaries, the types of boundaries crossed were similar for each of the four topic areas.
| Team | Sectoral | Organisational | Professional | Geographical (outside Westpark) |
|---|---|---|---|---|
| Anxiety and depression in BME populations (17 diaries) | 11 | 11 | 16 | 15 |
| Dementia (two diaries) | 2 | 2 | 2 | 2 |
| Child and family health services (six diaries) | 3 | 1 | 3 | 4 |
| Diabetes (eight diaries) | 8 | 7 | 7 | 8 |
| Total | 24 | 21 | 28 | 29 |
Table 26 shows how confident diary participants from each of the four teams were feeling that the work that they were involved in to improve care in Westpark would impact on:
-
the quality of patient care
-
levels of staff motivation
-
their own personal satisfaction at work.
Respondents were generally less confident that the WI would impact on staff motivation and more confident that their work would improve the quality of patient care, with the anxiety and depression in BME populations and diabetes team members being the most confident.
| Team | Rating average (1 = ‘strongly disagree’ to 5 = ‘strongly agree’) | ||
|---|---|---|---|
| Quality of patient care | Staff motivation | Personal satisfaction | |
| Anxiety and depression in BME populations (18 diaries) | 4.33 | 3.33 | 4.00 |
| Dementia (two diaries) | 3.50 | 3.50 | 3.50 |
| Child and family health services (six diaries) | 3.66 | 3.66 | 4.00 |
| Diabetes (eight diaries) | 4.38 | 3.63 | 3.88 |
| Overall | 4.12 | 3.35 | 4.00 |
Diary example 1: anxiety and depression in black and minority ethnic populations
Pam (WIP10J) is a CBT therapist and WI team member of the anxiety and depression group. An active member throughout the study period, she agreed to be interviewed twice and completed four diaries, enthusiastically taking part in all research activities. She had been working as an office worker at a health insurance provider before becoming a therapist and was now proud to be working as a mental health link worker with patients at a Westpark general practice that was close to home. She completed four online diaries across 14 weeks in the summer of 2011 and her follow-up interview was completed in September 2011.
In June 2011, Pam wrote about how important ‘instant’ interactions between primary care colleagues were, particularly in the form of telephone calls, e-mails and regular meetings between herself and her supervisor to discuss complex patient cases. Pam described improved sharing of knowledge relating to referral pathways, especially making connections with secondary care. However, she was frustrated at having to overcome last-minute cancellations and poor co-ordination by practice managers, as well as having to travel for supervision (which meant that she lost patient care time and missed targets). As Pam wrote in her first diary, her motivation increased after effective meetings to inform GPs about local services:
Really exciting that last week I was able to arrange a meeting with GP’s and dementia services from secondary care, which took place where I work. It was exciting as dementia services have been trying for many years to get a step in the door but have been unsuccessful due to time pressures and non-responsive practice managers . . . . We were successful in increasing dementia awareness to a total of eight GP’s. They found the presentation interesting, informative and as a result many questions from both sides were clarified and resolved. The meeting has also opened up a whole new dialogue on how dementia services can cross refer care for people diagnosed with dementia to mental health services for support. As a result we are now in the process of arranging workshops for both mental health and dementia services.
As part of the work of her WI team, Pam and others had systematically visited GPs in Westpark to talk about mental health. Through these interactions they were able to recognise how services could be made more seamless:
What would happen ordinarily is a client may be just referred for depression, we do the assessment and find out that actually it’s much more severe than actually meets the criteria for primary care setting. So we have now been working very closely with the secondary care partner to ensure that if we detect there is more severity to that case then we refer accordingly to secondary care services. It’s increased much more in the last year or year and a half now . . . I find the need to be talking to secondary care services much more than I would previously.
In July, Pam again wrote about making connections with dementia services for a patient, and reported increased exchanges across professional boundaries:
Contact with dementia services in [a different borough] due to the fact that the client I was seeing resided in that borough. As she did not fit the postcode criteria which would enable her to be seen by dementia services in Coxford, making contact with another borough’s dementia services meant I was able to find out their referral process, where they were located and then were able to do a referral on to their department. The client is now doing well and is under the correct medication for working age dementia and care. This has also allowed me to share this information with other colleagues within my team should they need to do a referral.
Unfortunately, her personal motivation was negatively impacted by a lack of follow-through by her clinical supervisor:
I have been trying to apply for accreditation and my clinical supervisor has still not completed her reference which has now taken a total of 7 months, something which could have been completed in 2–3 weeks. This makes me feel extremely frustrated and angry. I feel that as a team my personal development issues are being brushed aside and this can create a feeling of being demoralised and unappreciated.
In August, further new connections were made with child and family health services and with voluntary services. At this time Pam did not report many boundaries being crossed, and she did not report feeling very motivated, but she did have a new appreciation for issues related to safeguarding:
In particular I have spoken with [local child and family support organisation] to help a client deal with domestic violence which is having an impact on the children. This has now been successfully done and [they] are in the process of offering her an appointment next week. I feel knowing what agencies are out there and what they do is really crucial so that we are able to provide the correct intervention for our clients. This was the first time I have actually worked with [this organisation] which helps families with support and difficulties they may be experiencing.
Having written about how much she learned experientially about safeguarding, in her follow-up interview she further described the challenge of bridging gaps in services and her frustration at how inefficiencies impacted her own work targets:
I didn’t have the information to hand. I then had to rely upon other health professionals, but what I found wasn’t a seamless process. I phoned one person, they didn’t know. Phoned another person, they said, ‘Oh they're not in.’ Phoned another person who said, ‘Can you call back later?’ Phoned somebody else . . . It was that kind of attitude. There should be somebody there at the end of the line. Then I phoned safeguarding, they gave me information which was not coinciding with what information the police had given me around safeguarding issues and sexual abuse. So there’s miscommunication for clarity of what should be done and what is the right protocol to follow, and that causes a lot of frustration when you have time limits placed upon you . . . . A lot of time had been spent, wasted time, calling other health professionals who weren’t able to actually give me the kind of information I needed to be able to deal with it in an efficient, effective and fast manner.
In September, Pam reported making further new links with dementia services and contacts across sectoral boundaries, and reported confidence that her boundary-spanning efforts were making a difference, especially on quality of care. Spanning boundaries, however, was not easy:
I have been trying to speak with a consultant in secondary care regarding a client I am seeing but find the process of leaving messages, returning phone calls and missing each other due to client contact rather frustrating. This often means that there is either a delay in referring on or progressing with treatment.
Pam learned new skills through cross-boundary working as part of the WI, which became crucial. Pam is able to describe the kind of flexibility needed by a boundary spanner to use her skills but also notes how supervision can serve as a barrier instead of as support:
I would think that sometimes if we can use our judgment and make that decision ourselves rather than having to duplicate. Again, there was the waste of a whole afternoon when I know that this client was quite clearly not able to function and look after themselves, because all they could think of was about killing themselves, taking tablets, going to the park and drinking, and that’s it. So if I know that this person needs to looked after by secondary care as an inpatient, why then did I have to go to the local community mental health trust, go through all that rigmarole, go through all the assessment, and then find out they still ended up as an inpatient?
The frustration felt by individual boundary spanners attempting to close gaps in patient care can come at a cost to the health-care professional and risks undermining the quality of patient care, as Pam dramatically describes:
If you look at our targets, it’s more so now that we’re working so hard to meet deadlines, and if we don’t meet our deadlines at the end of the week then there’re questions asked, ‘What were you doing? Why weren’t you able to do it?’ They’re not going to see that as justified. They’re going to say, ‘Well, you’re supposed to be achieving twenty hours, the rest of it doesn’t matter’ . . . . Today I’ve been running around after a risk client. He sent me a text this morning saying, ‘I’m going to stab myself to death.’ When you hear that, everything else becomes irrelevant, so you want to make sure that a client is looked after. In total, in between clients, I’ve had to spend an hour and a half trying to locate the client, phoning the police, getting the police and ambulance services to her home address. All of that takes time, but when I report my schedules at the end of the week they’re going to say, ‘What were you doing for two hours of that day when you could have been seeing a client?’ Are they going to understand that I was trying to look after the welfare and safety of the client because they were threatening to stab themselves?
In noting how targets now drive her work, Pam explained that, as pressure to meet targets increased in January 2011, her work in making linkages happen has decreased, and the impact will be on referral rates:
One of the key things that came up was the fact that because now we’ve all been faced with targets, our promotional GP liaison work and promoting the service has gone rock bottom . . . . Actually if we don’t continue promoting the service and increasing awareness about what we’re doing that the referrals are going to start decreasing, which is evident, that’s what’s happened, the referral rates have gone down.
Diary example 2: diabetes
Supriya (WIL4D) is a practice-based commissioner based at Coxford PCT and the leader of the diabetes team in the WI. An active member throughout the study period, she agreed to be interviewed twice and completed four diaries, enthusiastically taking part in all research activities. She has a scientific background in research but is not a clinician. Among other clinical topics she had been assigned responsibility for commissioning diabetes services, which includes negotiating contracts between primary care and secondary services and the hospital. She completed four handwritten diaries across 10 weeks in the summer of 2011 and her follow-up interview was completed in January 2012.
In early June 2011, in her first diary, Supriya writes about crossing many organisational and professional boundaries, and although none involved new contacts she reported feeling very confident about the impact of her boundary-spanning work on the quality of patient care. Involvement with Diabetes UK and the YOC pilot (with the Department of Health, the Health Foundation and the National Diabetes Support Team) was a part of her work during this time. Supriya reported that the recent training by YOC for GPs went well and that she ‘had some really good interactions with some GPs’. Supriya was also excited to have improved connections with individuals and community group representatives in the local area. Increasing disease awareness and motivating self-care for patients with diabetes are important aspects of evidence-based diabetes care and Supriya had become aware of the need to bring these concepts to both patients and practitioners:
Patients in the WI and through the LINk [Local Involvement Network] meeting I was presenting at, all said getting their [diabetes] results in advance and being involved in the decision-making is a really positive way forward and welcomed by the patients and carers. LINks were really happy to be involved in any way they can to support the diabetes work stream.
In her follow-up interview Supriya felt that her sense of confidence about impacting patient care was related to increasing her own knowledge through working with a diverse group of professionals across multiple organisations and as she provided training for local clinicians.
In her work as a commissioner of diabetes services, Supriya knew that efforts to link up services were an important way to improve care across the borough, as she outlines in one of her diaries:
I have had fantastic meetings with public health . . . 1) following from previous discussions, the new public health lead for LTCs [long-term conditions] and Active Lifestyles has arranged for a pilot on educating children at some local schools on diabetes, following the work done with asthma project. I pointed out the people that should be involved with this, including the paediatric diabetic specialist nurse and the public health lead identified school nurses, health visitors, etc. from social services; 2) the same public health lead has also agreed to put together a pack for each practice with information on different leaflets and how to get them, with recommendations on which leaflets are best for which type of patients; 3) I am also going to get the public health lead to talk to LINkS [Local Involvement Networks] to review the leaflets for YOC and simplify them and then translate them into other languages; 4) I have also met another public health lead who is working on putting a training package together for receptionists and health care assistants to do sign posting and deliver health promotion and prevention advice at GP practice.
Later in June, in the second diary, Supriya mentions an important need for collaboration with a diabetologist to bring services into the community. She also mentions frustrations with influential senior individuals who she perceived as being quite obstructive. However, she also writes about progress in making connections:
Two really exciting meetings have been with the consultant diabetologist at the Coxford Hospital and another meeting with a practice in [the north]. The diabetologist has been very indifferent to the commissioning direction for diabetes care for the last year but he has changed his approach. I hope he is being genuine and this is not just a way of getting what he wants . . . . There are frustrations in that the information governance team at the hospital are not willing to share the data. But the diabetologist is trying to get the green light himself. This data will help us determine how much money can be released from secondary care to reinvest back into primary care and community services.
At the spring residential retreat, Supriya was able to meet face-to-face with this diabetologist and her summer diaries confirm progress in sharing data between the primary care and acute trusts. Unfortunately, by the time that she was interviewed this interaction had not proved to be as productive as had been hoped.
In the third diary, Supriya also reported feeling pressurised by a pharmacist who did not think that she should be leading on a clinical topic (such sentiments had been verbalised before), frustrating her commitment to improving services.
Patient and public involvement is crucial for a commissioner working to policy guidelines, and Supriya is keenly aware of this perspective and its importance in serving local improvement efforts:
It’s given me the backing I needed. Because just very recently I was challenged on all the assumptions and the direction of travel that we’re taking with diabetes at the care committee and the clinical commissioning executive committee when I was asked, ‘What patient engagement have you done?’ And I was able to say, ‘We’ve done this huge event’, and I was able to follow that up with an e-mail with Diabetes UK and they came back immediately saying, ‘Yes, we know you've done a lot already.’
In the follow-up interview, Supriya described how she had gained an understanding of the patient perspective at a local WI event in the autumn of 2010:
We had a really multicultural group of patients attending, and carers, and they all knew exactly when was wrong with the system and what would help them manage themselves. What type of information they needed, what type . . . they even mentioned things that we hadn’t even thought of like – or we had thought of but didn’t think it was important to them – cooking for family members rather than for themselves . . . . And they knew exactly what they wanted. They knew what they wanted from GPs, they knew what they wanted from the hospital, they knew that they didn't want to go to hospital full stop, they preferred to just manage themselves.
Supriya gained that perspective through the initiative and it influenced her efforts to bridge gaps between services. This also enabled her to make a successful bid for involvement in the YOC and other funded pilots, outcomes that Supriya attributed to the WI:
And with the evidence that I had from the patient engagement and that I could ask we won the bid and we were able to launch Year of Care. So we’ve had 12 practices trained and this year we plan to get everybody else trained. So quite a significant amount of work has come from that patient engagement . . . . The patients that we invited were invited from the six groups of practices that were working specially on diabetes in the WI. And it was one of the outcomes that we wanted to achieve from the WI.
Gathering downstream evidence of the impact of PPI is rarely easy, but for Supriya it has had an important effect on enabling integration.
In her final diary, Supriya writes about overall progress on the topic of diabetes:
The practice nurses were already making good progress on YOC and knew all of their patients. I felt they were so good that they could be a leader and local trainer for YOC. One has agreed. I also had a meeting with the diabetes implementation team. The first of a series, looking to work in the same way as the WI. The focus will be to develop a practice pack with information on what services are available . . . . During one evening I was contacted by a GP in [a neighbouring borough] who was working on the integrated care pilot . . . to ask more about YOC. That felt good that I was being contacted about the project I was working on from another area.
Learning from past efforts became incorporated into the method of moving forward, and despite many hurdles and hesitations the outcome of finally realising a community-based holistic diabetic clinic was accomplished in early 2012. GP commissioners, diabetologists and specialist nurses had begun to align ways to bring diabetic care out of the hospital and into a specific community setting, and to agree how to fund such efforts. Although details of how to incorporate dieticians, podiatry and other disciplines were still being negotiated, at this point in time Supriya noted that true multidisciplinary co-ordination was weak:
And I think there’s a big fundamental issue going on at the ICO [Integrated Care Organisation] at the moment, the hospitals see themselves as an acute trust still, not as part of an ICO. And the community services again feel frustrated because they feel like the hospital services have taken over the whole agenda and community services are just sidelined and expected to just deliver and it’s not important enough. But actually, the shift that needs to happen, that the commissioners are really pushing for, is more of a shift to make the community providers a stronger partner in all of this, because that’s where we need the services. And for the acute trust to acknowledge that and work with the community providers to provide a more streamlined pathway where patients go to one place for everything almost. You know, in the ideal world. And it’s not just diabetes this is happening I’m seeing it in other areas that we’re working on as well. And I think they’re starting to realise. I don’t think the hospital have realised it yet.
When asked whether or not she felt confident that she had made an impact during her time as part of the WI, Supriya said:
My motivation comes from knowing that I can impact on patients’ lives, individually and as a population . . . . Sometimes when a practice nurse will e-mail me and say, ‘You know what, I’ve just had some patients in on Year of Care and they’ve saying how delighted and how . . . .’ I think one called it, ‘bloody marvellous, and why hadn’t we done it years ago’. Sometimes it is when I’ve arranged a really important meeting and somebody, a couple of days later, says, ‘That was a really, really good meeting. It’s about time. It’s fantastic we’re moving forward with this.’ Sometimes it’s when you finally get a breakthrough, and we’ve got a clinic starting next week. All those little things give me the motivation to just keep on going until the next one, the next high . . . . And just being that person in the middle to sort of join these people up to start to influence the whole picture. That’s what gives me the motivation.
Impact of the Westpark Initiative and ‘key success factors’: stakeholder perceptions
Impact
Given the adaptable nature of the WI, Chris formulated his own view of the successes of the initiative in ongoing and iterative ways. The expanding networks associated with the WI were seen by Chris as evidence of how professionals changed their behaviours because of the new connections being built:
So the very fact that [the diabetic specialist nurse] was there speaking with such seeming confidence and smiling a lot was a result of, I think, the work done in Westpark Initiative coupled with various prompting including my work of the last week.
WIL2B, WI founder
Although Chris pointed to improvements in gathering patient outcome data – ‘I think we're in an easier place now to produce quantitative data about that than we were a year ago or even 6 months ago’ – these have been more difficult to identify by our research team. For Chris, the focus was clearly on relationship building rather than any formal evaluation of impact on clinical or quality indicators. When a specialist agreed to share more data after the community-based diabetes clinic finally opened in the spring of 2012, Chris would point to these changes as strong evidence:
So I’m using that as another example of how there’s a legacy of people, a network of people who have been affected by it and kind of assume it is a given static long-term entity.
WIL2B, WI founder
When asked to describe the successes, Chris points to changes in the levels of engagement of GPs in Westpark:
Look at the numbers of Westpark people who are pitching up to meetings and with a smile on their face. They used to huddle in the corners looking very defensive, and they’re there talking and smiling. We’ve got all practices still engaged . . . I’m focused on what I think as the more, bigger, things which is the change in the hearts and minds and getting people on the front foot and feeling motivated and part of changing things. That has dramatically changed.
WIL2B, WI founder
Certainly, many participants noted the palpable enthusiasm at meetings, for example ‘the energy and commitment that was clearly visible’ at the 2011 retreat, as Phillipa described.
As a commissioner of dementia services in 2009, John was intrigued as to how the WI could be used to improve links between primary and secondary care. By mid-2011, John was able to describe how he felt aspects of the model could be implemented in many areas:
I mean, I wouldn’t adopt it as the main improvement approach. But what I would do, and what I have done, is I’ve taken what I thought was the most valuable stuff out of it. Certainly the idea of recurrent open-ended type workshops where you don’t necessarily go in with a preset agenda, but you do hope that certain outcomes will be achieved by the end of it, and you rely on the natural flow and the natural dynamics within that meeting to lead you to where the general group perceives to be the main issue, is certainly valuable. But there are caveats, as in any approach. And I think the value it gives to a manager or a commissioner is how you know the times and the extent to which you should use this tool.
WIA22V, commissioning manager
He further describes that, although there is no distinct – or preferred – quality improvement strategy in Coxford, and although neither dementia pathways nor clinical expectations had recently changed, he believes that the patients' journey experience theoretically may have improved ‘because things move slightly quicker’ because of better communication between providers (although no monitoring of this is carried out on a regular basis). With all the necessary tests for dementia that need to be co-ordinated, the care can improve through the personal interactions provided by the WI:
So you manage the expectation. You don’t change any of the service, but people know what to expect, and that’s different. It makes a world of difference.
WIL2B, WI founder
Despite these concerns about measuring impact, Phillipa reflected that aspects of what she terms ‘Chris's whole-systems model’ could be usefully combined with traditional aspects of management:
So we’ve constantly tried to bring those two things together . . . . And I think that’s the bit of this methodology, by being so pure in its . . . at the pure end of how you take the research around whole- system thinking, and not perhaps thinking a little bit more about how you contextualise this little bit to the systems that you’ve got, and how you also pay some regard to the other things that are going on so that you can better make it an integral part of everything, rather than this thing that's going on here, or the WI.
WIA23W, Director of Quality and Clinical Leadership
So when asked if the model is repeatable, Phillipa said:
One of the things I’m really pleased at a strategic level is that we really are trying to hang on to those sort of joint relationships at the top. So what we haven’t yet done, and we’re trying really hard not to do in a sense, is to retreat back into our specific agency corners and attempt to cross shift between each other So last week, as the executives, we all sat around from each of the agencies and had a very honest conversation about what was going on for us financially, what were we cutting, what impact might that have on somebody else, how do we try and do that. We even had a conversation about trying to create an integrated borough recovery plan and share that across each other. So we need these sorts of approaches even more. The question is: are there different ways of doing them?
WIA23W, Director of Quality and Clinical Leadership
‘Key success factors’
Key stakeholders identified four ‘key success factors’ relating to the WI; all of these were highlighted in terms of their absence from the initiative and offered as explanations for why it had not, in the views of senior interviewees, achieved as much as they had hoped.
The rhetorical tone at the end of the previous quotation is indicative of the first key success factor of the WI identified by key local stakeholders: senior leadership support. It was clear from our fieldwork that support for the WI was not forthcoming from all senior leaders. John felt that this was because its approach and appeal were problematic:
I do think it has suffered from lack of senior leadership support. And I’ve seen this on more occasions than one. And what I did notice, it’s all the pragmatic learners who didn’t see much value in it, because they can’t personally relate to that type of working, who thought it’s too fluffy, and it won’t lead to anything. And unfortunately, most of the people in this world are pragmatic learners.
WIA22V, commissioning manager
A second key success factor, measuring impact, was clearly identified by Phillipa, who was frustrated at the lack of progress in identifying ‘hard measurables’ for the WI:
The difficulties of data collection gathering and setting up data analysis systems . . . we seem to have been having some of those conversations for a very, very, very long time.
WIA23W, Director of Quality and Clinical Leadership
As she explains, the methodology of the WI means that it is difficult to define and monitor relevant metrics:
So I think the biggest challenge now is moving the overall equation towards, ‘Is it sufficiently effective, and is it sufficiently output-focused, to warrant us continuing to do it?’ We do know it delivers, but what I was saying earlier about the pace of change and this balance between consolidation and change may not necessarily work in its favour.
WIA23W, Director of Quality and Clinical Leadership
The scalability and sustainability of the WI was openly debated among senior management. Although John described the potential for increased sustainability of the changes implemented by the WI model, he also mentioned the lack of extended reach to GPs:
Aligning the work of the Trust with GPs goes beyond just the five to six GPs who are involved through the different stages of [the WI] . . . but not a lot beyond. And I would suggest that this is partly due to the leadership and the professional opinion that those GPs can leverage within their locality. Which in some cases isn't very much, or some of them may not necessarily be very highly regarded.
WIA22V, commissioning manager
A third key success factor relates to the perceived lack of structure in the WI. This was a frequent criticism by senior managers and one that became more acute as almost all jobs and titles in the PCT changed in early 2011 (anticipating restructuring changes related to national reforms and necessary cost reductions in the NHS).
A fourth key success factor was the importance of PPI:
I think in some of these whole-system methodologies can, particularly if you bring patients and carers into the centre, can bring the best way for communicating confidence in the system . . . . It’s when they aren’t confident about that because the system is fragmented, or they think they’ll have some horrific nightmare to get re-referred in, that they won’t get out in the first place.
WIA23W, Director of Quality and Clinical Leadership
The end of the Westpark Initiative or a new beginning?
Throughout the significant reorganisations in Coxford from early 2011 onwards, Chris continued as a clinical leader although his role changed to a slightly more educational position with no line authority. The trust chief executive left and had been replaced with Phillipa, now as the new borough director. John continued in an extended role in aligning service improvement with commissioning. All remained colocated at the main office of the PCT.
By February 2011, the anticipated annual cycle of the WI appeared to have come to an end, although Chris continued to envision ways that the principles of his model could be embedded in other settings. Through 2011 the diabetes team (supported by affiliation with Diabetes UK) and the anxiety and depression team (supported by affiliation with CLAHRC) continued to hold events and team meetings to address ongoing efforts in their topic areas. Triggered by financial concerns across the locality in spring 2011, discussions again took place about continuing with another iteration of the model, and internal debates on the ‘luxury’ of this sort of model ensued.
In spring 2011, roll-out of the model to other localities was widely debated but the nature of the support from the newly formed commissioning consortium was a major concern. Managers discussed whether or not the four teams should continue with the same topics and whether or not resources should be given to certain projects. Senior managers discussed how to empower staff with more direct authority, and how to determine outcomes and deliverables given the new and still emerging parameters for success in general practice.
By June 2011, John (involved since the beginning in 2009) felt that the WI was already ‘done’ and that the challenge was ‘rolling it out to the rest of the borough’. Trust and consortium leaders were discussing how to use the same infrastructure of the initiative to now engage clinical discussions among GP commissioners about the ongoing transitions in the commissioning group and to reach beyond service providers. Structuring future work around the same four teams was being debated, including the risk of continuing with only marginally involved participants attached to the WI, and ways to work differently (more effectively). As John explained, ‘So a lot of people are being carried along by virtue of inertia, or dynamics, depending whichever way you want to look at it.’ Attention to Quality, Innovation, Productivity and Prevention (QIPP) items at this point began to drive the agenda in terms of deciding where to apply attention, time and funds:
For example, BME, it will die a slow death unless it’s kept as part of a package with all the other initiatives, because it’s not on the QIPP list. Diabetes is. Mental health in general is, although not that one in particular. And dementia isn’t, but dementia has a different type of driver. Dementia has a national drive – it doesn’t sit on the QIPP agenda, but it’s very high profile for the government at the moment.
WIA22V, commissioning manager
Well aware of this complex policy environment, pragmatic aspects dominated discussions, in which Chris worked to influence this decision-making process, acting as a facilitator at commissioning meetings.
By September 2011, the WI was no longer receiving specific PCT support and had lost even part-time administrative support, and no stakeholder events were being held or planned. The conference reservation for the May 2012 retreat was cancelled. Phillipa had transitioned out of the area from her position as borough director. Chris continued to facilitate local GP and consortium meetings with a focus on integration and whole-systems thinking, and all were trying to cope with national and local policy changes. Opportunities to reinvigorate joined-up working, and new debates about geographical boundaries, were recognised by Chris as a potential opening for renewed effort. He reported:
As far as I can see, people are not ready to talk about the WI or the lessons but there seems to be an opportunity opening up in the next week or so for Westpark to readopt the processes of the WI.
WIL2B, WI founder
Although not the same as ‘political commitment’, Chris recognised some receptiveness to the idea of developing new leaders, particularly across four defined boundaries with primary care [a feature that was now being (re)attributed as the founding principle of the model]:
For example, the WI would say there are four major boundaries to cross: mental health, social care, community care and acute care from primary care, and each year you decide what you want to do in those kind of areas.
At the end of our fieldwork, Chris felt that the commissioning consortium was ready to ‘restart’ some aspects of the four streams of work, and he describes recent conversations about local changes attributed to the previous work of the WI. He thought such ‘echoes’ could be identified in recent accomplishments, and could possibly be seen as repeat patterns in the future.
Multilevel, cross-case comparison: socialisation, externalisation, combination and internalisation and the four teams
Our research took the form of longitudinal, multilevel, nested case studies and examined efforts to improve the quality of health-care services around four topic areas (see The stories of the four teams). Because of the emergent and complex nature of the WI, which involved professionals from across primary, secondary and tertiary health-care settings as well as from other sectors interacting at different times in a rapidly changing and uncertain context, finding an analytical framework for exploring our in-depth qualitative and quantitative data was a key challenge.
We endeavoured to find a framework that would allow us to analyse how the particular boundary-spanning intervention under study impacted not only on the quality of health-care services (through horizontal and vertical integration of services and our secondary analysis of routine data) but also on the multiple sectors, organisations and professionals involved in the WI. Our review of the ‘boundary-spanning’ literature did not produce a sufficiently robust framework to help analyse such a complex intervention (see Chapter 2, A review of the empirical literature). However, we have found that the SECI model of organisational knowledge creation (Figure 8 and as described in Chapter 2, Conceptualising knowledge creation and exchange processes across boundaries: the socialisation, externalisation, combination and internalisation model) may serve as a useful lens for understanding boundary-spanning activity across individual (i), group (g) (either professional or team), organisational (o) and, we would add, sectoral boundaries.
FIGURE 8.
The SECI model. g, Group; i, individual; o, organisation. Source: Figure 1 entitled ‘Spiral evolution of knowledge conversion and self-transcending process’. Reproduced with permission from Nonaka I and Konno N, ‘The concept of “ba”: building a foundation for knowledge creation’ in California Management Review, vol. 40, no. 3, Spring 1998. © 1998 by the Regents of the University of California. Published by the University of California Press.
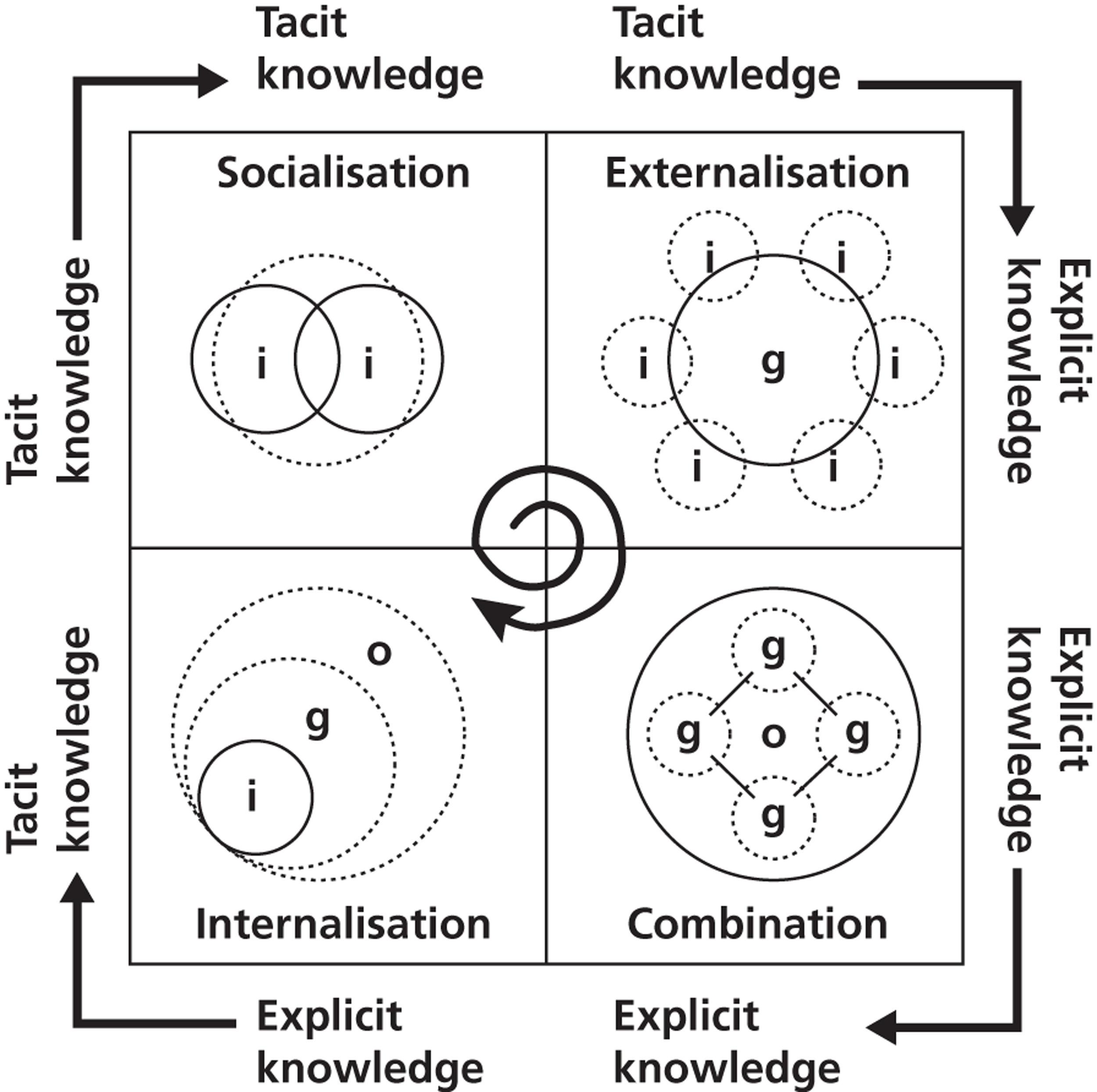
In the following sections we apply the SECI model to each of the four teams to explore the reasons for the variation in their impact across these various boundaries and provide more detailed illustrations of how the four stages of the SECI model were enacted (or not) in the WI. The chapter concludes with a summary of the findings from our cross-case analysis using the SECI model.
Anxiety and depression in black and minority ethnic populations
This team, operating in a receptive context with national policy drivers indirectly supporting its efforts, was the most successful in terms of successfully transitioning between the four stages of the SECI model. Members of this team came to the early meetings of the WI in 2009 with previous skills in counselling individuals, interacting in multidisciplinary teams and professional recognition of patterns of individual and organisational behaviour change. Perhaps unsurprisingly, socialisation between individuals was therefore easily achieved, enhanced by the WI stakeholder meetings. For example, a community health worker was not formally assigned by her organisation to be involved with the WI but was casually invited to attend an informal team session. New to the locality this individual describes the initial experience of the WI as having been ‘inspiring’ and motivating:
That was so exciting for me, because I just . . . it seemed so small when you have those meetings with just a few people. But when you look at the huge amount of time, the huge amount of space, and the amount of people that are actually all involved, when you look at every single person, it was amazing. It was so exciting . . . the WI it was definitely . . . the range of people coming in and out and contributing, even if they left and they didn’t come back, you still had that contact with them if you wanted to follow it up yourself. So I think just the spider web of . . . and range of people was the key for me to be able to get things done.
WIP11K, community worker
Including GPs and other stakeholders as part of the WI was a technique that was then used by this team to externalise and share tacit and explicit knowledge about the existing provision of care with different sectors, teams and groups. As an example, the community worker, after socialisation, identified – through conversations at WI stakeholder meetings – opportunities to develop knowledge assets in the local area relating to mental health outreach services. This individual had the resourcefulness to then develop and deliver four information sessions that reached around 30 staff members of community-level programmes and which spanned three of the teams taking part in the WI:
I ended up doing lots of other things with the other kind of groups that were involved, particularly children and families, because we had a lot of issues with mental health and people with BME backgrounds, but they often hadn’t made any connections with other people or anything like that. So basically going and making connections with the family groups that are out there in Coxford and talking to them about mental health services and things like that was actually really productive, because they hadn’t really had any information about what is mental health. So I ended up developing this mental health information kind of session for volunteers or lots of the community groups that were in Coxford, so that they would have an understanding of what mental health is and how it’s identified . . . and then that leads to dementia, because people who are under a lot of stress have mental health issues because they’re caring for people with dementia or diabetes or whatever . . . . So I just put together something, and then from there I went and initiated that with lots of the other family groups that I knew from the WI as well.
WIP11K, community worker
Delivering information sessions for GPs in this way inspired many WI participants and was acknowledged as an early success by those leading the initiative. However, this community worker was made redundant and with a new supervisor in a different programme there was no support (in time or funding) to continue such sessions.
Positioning mental health workers in GP surgeries improved knowledge exchange between primary care and mental health services. The opportunity to place such professionals at strategic junctions of knowledge flows (both horizontally and vertically) resulted in demonstrably qualitative improvements in information sharing and an increase in appropriate referrals to different services along the acute to community spectrum of care. For example (see vignette in Diary example 1: anxiety and depression in black and minority ethnic populations), an office worker in a private health insurance company was inspired to train as a CBT therapist when national policy support for IAPT services offered funds for such training. This newly trained therapist was then employed in a local GP surgery to serve the population of Westpark, which has always been her home. Working in the context of nationally determined goals and alongside like-minded mental health colleagues, the therapist's intentional aim as part of the WI was to try to improve access to psychological therapies for people of BME backgrounds. As a link worker this CBT therapist made persistent efforts to get past the practice manager to meet directly with the GPs, and initiated a meeting with all GPs in the large surgery (including three members of the local mental health team) to describe locally available mental health services. The evidence of impact of this boundary-spanning (dialoguing) meeting was described by the therapist as being able to see increased awareness by the GPs, increased multidisciplinary utilisation and improved appropriateness of referrals, a year after the meeting:
I think them knowing that there’s somebody here who they can count on for support, who will tell them the right information is really great. The other impact is then they know what we’re doing, they know all the different anxieties they can refer for. Before we weren’t getting very much referrals for things like OCD [obsessive–compulsive disorder], for instance, which is very much a lack of understanding amongst the BME communities, they don’t recognise what OCD is. So if they go and see their GPs, if they can pick that up and they can refer, we can do some good work with them and they don’t have to suffer with it. So I think increased awareness is one of the key issues with GPs. They now know little by little how to differentiate between primary care and secondary care, although I think there's a lot of work to be done in that area.
WIP10J, CBT therapist
Fine-tuning of the referral process and timing of communications continues; improved local adaptation was evident in qualitative exchanges, not just in the number of referrals. In further exchanges, the same therapist talks about the positive impact of promotional work by the mental health team to increase awareness about the counselling services: radio shows in a local dialect to reach potential patients, disseminating pamphlets and posters, meetings with GPs at their surgeries and meeting with people at the gurdwaras, the temples, the colleges, the day centres and the town hall. In an intentional reflective practice this team met regularly to ask: ‘Are we getting into every nook and cranny that we could? . . . . Trying to break down the stigma so that more people are coming forward and saying, “Yes, I have a problem and I can get help for it”.’ In this manner, outreach became more than social exchanges, and more than articulating explicit knowledge; literal efforts to document and package explicit knowledge were systematically explored. These further initiatives to systemise integration (combination) have been moderately successful, but routine internalisation remained a challenge at the end of our fieldwork.
Dementia
The WI focused on socialisation through stakeholder meetings but was largely unable to engage large numbers of GPs in either the specific topic teams or at open meetings. A PCT administrator – working on diversity and public health issues – spoke of the need for face-to-face interactions in a locality like Coxford with significant challenges. A latecomer to the WI, this individual described with enthusiasm what needed to happen – what Nonaka terms ‘socialisation’ – while also noting that no actual changes had yet resulted from the stakeholder events:
If anything is going to break through, that sort of thing is going to help, because it’s about bringing people together. So for example, what you see in dementia with the debate between GPs and the Mental Health Trust, it’s instead of letting people stay in their silos and see the world in their way, it’s making them get out and see the world another way. And that can only be helpful.
WIP15O, head of partnerships and diversity
In an example of how the WI sometimes struggled to move beyond the stage of socialisation, a community pharmacist attended a local dementia meeting hoping to hear more about how to signpost the exhausted carers of elderly parents with signs of dementia (see Vignette 6). Frustrated by identifying patients at home with poorly managed medications, and combined with concerns about how to initiate access for families into primary care, the pharmacist felt motivated to attend a nearby educational event that was part of the WI. This pharmacist was therefore already aware of the gaps in service integration and was eager to contribute to finding interdisciplinary solutions. Unfortunately, these concerns were not addressed at the locally sponsored educational session; explicit knowledge (e.g. tools for signposting) was not available. The pharmacist was able to verbalise some ways to decrease inappropriate use of acute services, and to improve signposting in primary care, including the walk-in, impromptu opportunity to advise clients at pharmacies. Our field notes document how the pharmacist's suggestions went unnoticed by others at the meeting. Interviewed after the meeting, the pharmacist spoke of his disappointment at the missed opportunity to improve services for patients with dementia. The pharmacist recalled the meeting in terms of a sense of ongoing frustration. In this manner, a multidisciplinary, face-to-face meeting did provide an opportunity for socialisation but there was no transition to explicit knowledge assets (externalisation).
As described earlier in this report, those individuals working on the topic of dementia struggled to find coherence as a team. A lack of clear membership beyond the two leaders – one of whom retired at an early stage of the WI and the other who was relatively inexperienced – meant that objectives remained unclear and there was no local champion for the work. Individual professional development was noted, as was increased awareness of services by some individuals, but putative attempts to restructure outreach services and to disseminate explicit knowledge assets (externalisation) lacked traction. Ultimately, aspirations to widely promote available services, such as educational outreach (combination), went unrealised. To illustrate (see The stories of the four teams, Dementia), producing materials in different languages was a key objective (e.g. translating clinical tools for memory assessment and disseminating dementia information in local dialects) but, although such products were created (externalisation), they were not routinely disseminated:
The leaflets we have produced and the other tools I have produced with regards to that, our assessment process, I think they are more user friendly. The information we are giving on the GP surgeries, they would not be able to get that if that had not happened. Now, all the six GP surgeries in my cluster, they have got the information on the dementia in different languages. The people, they can choose and pick whatever they want. The carers, or the patient, or anybody, they can look into those leaflets and they can go back to GP then refer to us.
WIL3C, specialist practitioner nurse
In another local attempt to improve joined-up working through explicit knowledge exchange, plans to train receptionists how to signpost patients were pursued. Chris spoke with the health promotion lead and this prompted the design of a short module (externalisation) by the borough-wide training co-ordinator:
So we did three training sessions, the first one on 16 June was in the [Coxford 1] practice, and we had eight members from receptionists there, including one GP. On 29 June we went to [Westpark] practice, and it was just the practice manager and the business manager. And then on 20 July we went to [Coxford 2] practice, and there were eight members of reception and mid-team there . . . some people knew about some things, and other people didn’t. So you’ve got a mixed level of knowledge . . . . Because we were telling them about things that they weren’t aware about, all these things . . . the thing that came out to them was they wanted a general overview of the plethora of services available, because they knew about some, they didn’t know about others.
WIP38L, health training co-ordinator
This trainer spent considerable time trying to find out who to reach and how to develop an extranet as an area-wide resource, but IT support from the PCT was not forthcoming. As a result, the receptionist-training programme did not extend beyond the initial efforts described above. Practice managers blocked efforts to meet with receptionists in Westpark, stating time and space restrictions. Additional efforts floundered on mundane issues such as suitable meeting space, finding administrative support for invitations and flyers and logistical resourcing. Despite the creation and availability of local knowledge assets and support from WI leaders for disseminating health promotion information in the community, efforts continued to rely on passionate individuals and struggled to gain systemisation (combination). The training co-ordinator attempted to find funding and staff to build an intranet signposting resource, but with little success to date. When the team leader was made redundant, there was little momentum for the work and the PCT soon found other topics on which to focus.
Child and family health services
With a broad agenda, individuals working to improve services for children also struggled to form a cohesive team (socialisation), particularly as joined-up working could potentially involve a wide array of professionals from several sectors. In an effort to connect the WI to broader community involvement efforts, stakeholder meetings were held in local area centres and a wide range of patient and public representatives were invited by to attend. For example, an experienced paediatric social worker and commissioner of paediatric services describes the need to continually ‘show up’ at meetings to advocate for children's programmes, particularly for teenagers aged up to 18 years who can be missed by planning efforts that focus on younger teenagers.
If I know my job so well that I can recognise that there’s an inefficiency or a duplication, and I can get the people round the table who can actually say, ‘Yeah, you’re right’, and we can work together to put a pathway together that makes everything much more efficient, and again releases some capacity so someone can go off and do something else that’s needed, or some money that we can reinvest, that makes me happy . . . . Little things like I was in a substance misuse meeting yesterday, and we’ve worked really hard to integrate two services who 3 years ago were competitors, and both thought the other one was doing a crap job, and they could do it better, and, ‘Why don’t you just give me the money?’ And we’ve moved from they wouldn’t talk and they had no pathway between them, and kids bounced between them, and they duplicated and it was all horrible, to the fact that they now call themselves part of one service. They’ve got a joint service name. They’re colocated. They have a shared action plan.
WIP36J, commissioner of children's services
As a commissioner the need to connect resources is part of the job, but changing policies, redundancies, funding losses and local politics made the work more challenging.
A community co-ordinator (not in health care) talked of his early excitement but then quick disillusionment with what appeared to be a focus on ‘research’ rather than on local action:
Initially I went in with a very open attitude. I didn’t know what to expect. After a meeting or so I thought maybe this is going to be a practical project in the sense that there may be some attempt to resolve some of the things which patients from meetings we go to have been expressing as their concern . . . . That’s really what kept me interested at that stage. It was also the reason why I think I lost interest, quite frankly, afterwards because I think I came to feel it was a research project. I’d been maybe a bit naive, it was a bit too much a focus upon the academic side of things, and research, and research method, and so on. I was probably being a bit too impatient and I wanted the world to change in the space of 6 months or so . . . . I think I remember Chris asked for us to remain involved and lend a community presence to the whole thing but I did have the impression that this was something more for the professionals than it was for people from the community. That’s why after a while I think my interest waned.
WIP20T, co-ordinator, Westpark Community Alliance
The initial team leader left after 1 year (because of loss of funding) and the next leader, although personally committed to children through a nursing background, was professionally focused on adult services as a commissioner. Membership of the team also waned, with social care and community representatives tapping in to occasional meetings but feeling unable to align identified team priorities with their own organisation's or professional objectives. Lacking a clearly defined project that might have led to effective action, team member attrition happened fast. Solutions and potential innovations surfaced in many different areas, from a variety of stakeholders, but without the team leaders serving as ‘knowledge engineers’121 the ‘team’ was unable to move to externalisation; knowledge, ideas and plans fell through the gaps, particularly at strategic horizontal junctions. For example (see The stories of the four teams, Child and family health services), a local resource guide (a ‘dialoguing product’) was updated and made available to a small cluster of GP surgeries in the local area. The team leader met with GPs to encourage their use of the resource guide and one receptionist in particular became known for using the document to signpost patients to local services in the community:
While they haven’t fed back specific examples, what they have said is, at this particular practice, the GP, one of the lead GPs, he refers at least two clients per week back to the receptionist for using the services, one or other of the services in the booklet, and the practice, as a whole, as an entity, they have embraced the idea and they’ve got delegated responsibilities to this receptionist.
WIL1A, team leader
Unfortunately, this receptionist left her position, moving away from the area for personal reasons. Although the ‘receptionist’ example was widely cited and held up as an example of the impact of the WI, few similar examples were observed. In addition, the adoption of the resource guide was not widely replicated and no plans were ever made to disseminate it to a wider audience. In SECI terms, dialogue was demonstrated and externalised (i.e. tacit knowledge became an explicit knowledge asset in the form of the local resource guide) but was not combined or internalised beyond the initial cluster of GP practices. The efforts of this team continued to be characterised by a sense of fragmentation until the end of our fieldwork.
Diabetes
This team had the advantage of having an already clearly defined goal relating to a patient condition that is the focus of many evidence-based guidelines, including NICE guidelines, and well-established metrics (e.g. QOF indicators). However, local concerns about how to commission and fund services, in parallel with organisational reorganisations, complicated efforts to create and follow through on what might appear to have been a relatively straightforward project: opening a community-based clinic for diabetes. For example, a commissioning manager at the PCT (not a clinician or a GP) was asked to work with the WI as a member of the diabetes team. Through the series of stakeholder meetings, a broader perspective of the composition of primary care services was acquired by this individual (socialisation):
Through the WI, we were working with six practices. And what had happened, inadvertently, because I was a PBC manager as well, I happened to be working with just six GPs. And nobody else was invited to that GP commissioning meeting, it was just the GPs. And I was going round and round, and I was trying to deliver things and plan service provision with just the GPs. And every time I got close to getting anywhere near starting to implement something, I found that there was a drawback to it . . . . So eventually everybody in the group, everybody that worked in the practice, got involved at some level. So the practice nurses, health-care assistants, the practice managers, the GPs themselves, everyone. And that’s when I realised that it’s not a GP’s practice, it’s a multidisciplinary group practice.
WIL4D, PBC manager
The complexity of funding arrangements meant that few people who were working on improving diabetes services in the locality saw themselves as a member of an actual ‘team’. Personal, social and ‘political’ divisions stalled this team at the externalisation stage for a significant period of our fieldwork. In another effort to improve local joined-up working, there was an aspiration to establish and open a community-based clinic for diabetics, not least to facilitate patient access to relevant services. In the 5 years before the WI, occasional conversations had happened between primary, secondary and tertiary care professionals regarding funding, premises, personnel and a variety of other matters relating to the appropriate provision of diabetic patient care. Administrators, managers, practice nurses, specialist nurses, GPs and consultants had all, at some point, taken part in these discussions, offering their professional perspectives. A community-based nurse manager described one part of the ‘conversation’:
So we got the GPs involved, which is really important. Because the WI was being involved at the time last year it was felt that everything to do with diabetes seemed to be focused around Westpark. And we wanted to give another opportunity to another area and that’s why [neighbouring area] was chosen, because they’ve got GP’s in that area with special interest in diabetes and also the GPs were quite keen to see it happening.
WIP29C, community services
This vignette barely scrapes the surface of the deeply political stand-off between the hospital and the PCT – and the various professionals in between – as we observed at many different meetings. After more than a few years of wrangling, a clinic with a less than ideal location, and a less than ideal work plan (according to many), did finally open for half a day a week. It remains to be seen if, and how, successful this project will be, despite the very hard work of many. Despite efforts to encourage patient involvement at various stages in the planning process, the scheduled inclusion of patient representatives was particularly side-tracked because of the length of the negotiations. Therefore, after several attempts at facilitated dialogue, and continued inefficient use of resources across all services, a compromise goal was achieved. Systemising (combination) may now happen in the form of joined-up services in the community but it remains unclear whether or not routine measures of success and behaviour change (internalisation) have been embedded going forward.
Socialisation, externalisation, combination and internalisation analysis of the Westpark Initiative
The previous sections provide a sense of the process or journey of the four boundary-spanning teams through the four SECI stages and help to illustrate key differences between the teams. We conducted this cross-case analysis of our qualitative data relating to the four teams to reflect on – and try to explain – these differences. The examples cited show how knowledge exchange processes were facilitated (or not facilitated) by the work of the four WI boundary-spanning teams and the impact that they had in terms of service integration. Enablers and barriers identified by the participants are summarised in Figure 9.
FIGURE 9.
Boundary-spanning themes with regard to SECI.
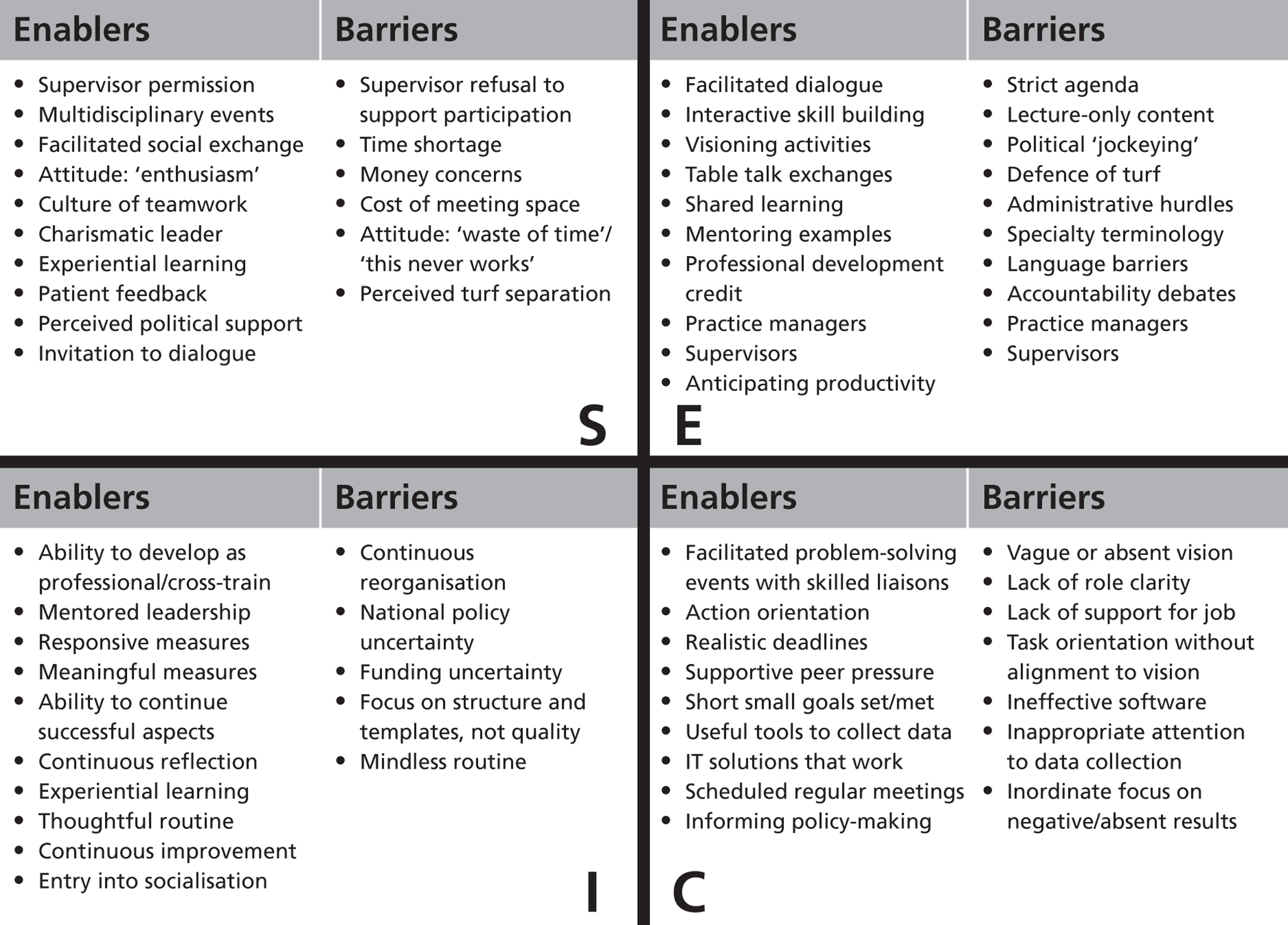
Clearly, although the four teams were invited to the same annual cycle of facilitated learning events, they varied in their ability to exchange knowledge across boundaries and then implement improvements. When considering each team, these same themes help to identify the SECI stage to which each had progressed (Figure 10).
FIGURE 10.
Four cases: boundary-spanning themes with regard to SECI.
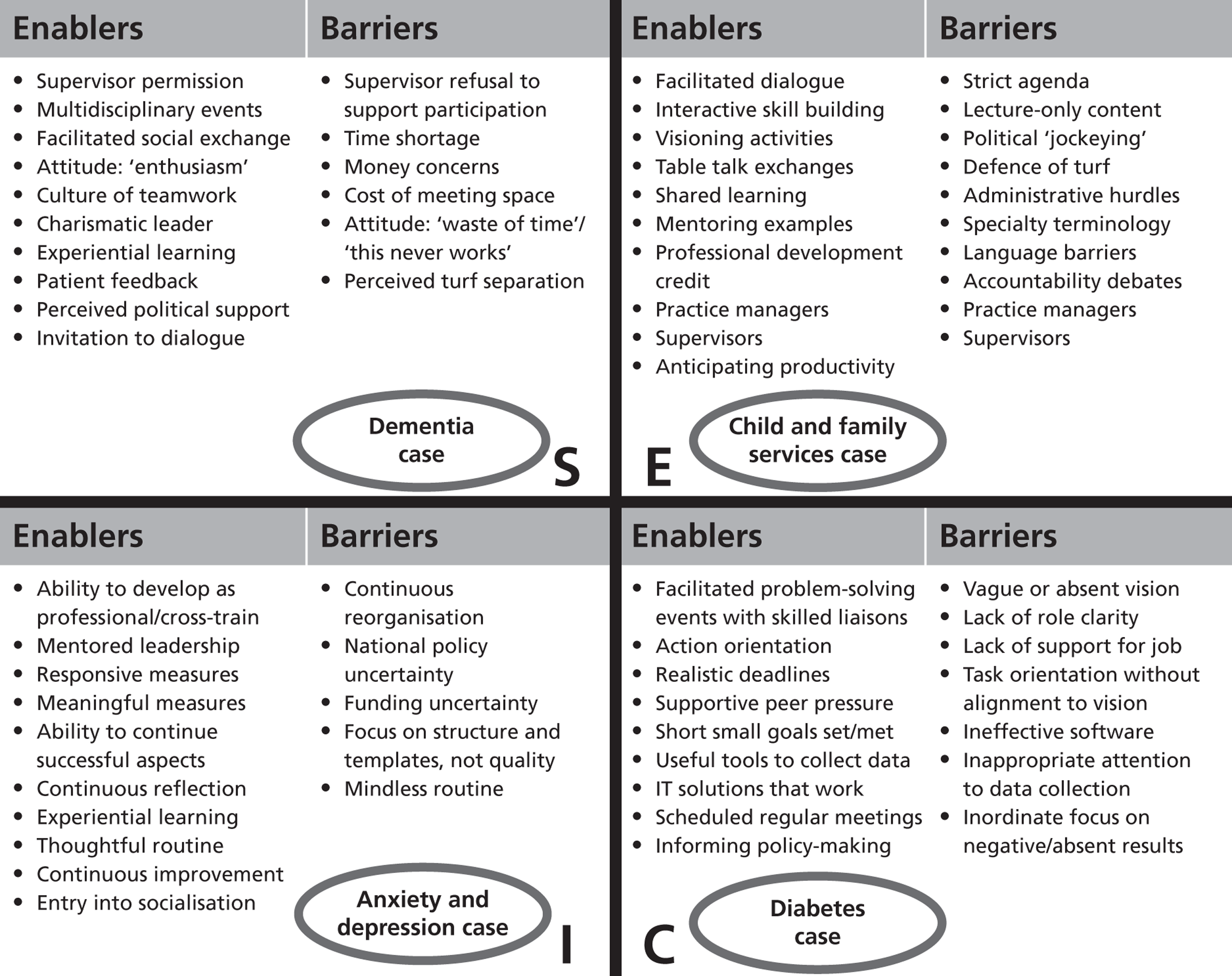
The dementia team was essentially ‘pinned’ at the socialisation stage. It was unable to establish an infrastructure for lasting knowledge exchange in explicit forms, despite translating the MMSE into a common Asian dialect and undertaking GP-led training sessions for GPs about dementia screening. The child and family services team was able to create a community resource guide to share with patients by way of receptionists but it was unable to move forward to create lasting products or receptionist training programmes; it was ‘stuck’ at the externalisation stage without formal leadership and a clear action plan. The diabetes team spent much time in the externalisation and combination stages, endeavouring to build the infrastructure for vertical integration of services through hospital specialists being based in the community. Combination goals were achieved through dialogue, and expert knowledge assets were put into place as hoped, but they had yet to be fully internalised at the time our study concluded. The anxiety and depression in BME populations team appeared to be the most successful overall, perhaps because it inherited a clearly defined goal and received structured support, despite persistent internal reorganisation. Indeed, some of the integrating efforts of this team were in place before the WI, but many innovative solutions were generated by the team as prompted and developed after interactions with the WI. This team had aspects of the internalisation stage in place but by early 2012 was struggling to keep the local infrastructure intact. None of the four teams – with this possible exception – could claim to have embedded routines within organisational culture and explicit skills in daily operations (internalisation).
Given a turbulent context (i.e. a lack of sustained leadership and inconsistent membership of three of the teams coupled with wider systemic changes), we might have predicted some of the unsuccessful boundary-spanning attempts and, based on the existing literature, it is not surprising that efforts to facilitate vertical integration in particular appear to be particularly challenging at the juncture between externalisation and combination (from dialoguing to systemising). Only one of the teams, anxiety and depression in BME populations, managed to galvanise itself in the face of a largely adverse context and ‘keep going’ through almost all of the SECI stages. As a positive outlier this one team appears to have successfully managed, in the face of the same external challenges faced by the other three teams, to blend the boundary-spanning activities enabled by the WI together with the rigour and structure demanded by CLAHRC, leading to the improved horizontal integration of primary and mental health-care services. When looking across the four teams, and at the examples from each of the four SECI stages provided earlier, four common themes emerge.
First, we would note that socialisation is only a start, and the enthusiasm of individual staff during this stage cannot be sustained without a successful transition to more explicit forms of knowledge that can be shared with groups (not least because professional satisfaction appeared to increase in situations in which explicit knowledge could be applied to directly impact outcomes). Socialisation can be successfully accomplished through the generation of enthusiasm and professional curiosity at stakeholder meetings, although even this may not be easy given time pressures and conflicting priorities, but the opportunity is brief and gaining sufficient traction to carry integration efforts forward can be challenging. Socialisation processes can also be time-consuming, particularly if boundary-spanning interventions require engagement with multiple professional groups at different times.
Second, although clinicians, staff and managers clearly recognised that socialisation is only a first step to empowering quality improvement efforts, the majority of the four teams we studied did not progress far beyond this stage. We observed instances of innovative solutions to health-care system problems emerging from the community but when they were not heard and acted on then community members quickly withdrew their commitment and interest. Administrators and managers in liaison roles can serve as boundary spanners between different professions but without successfully forming boundary-spanning teams such individuals can be left in a position of oversight of heterogeneous multidisciplinary groups that lack shared goals and clear working processes; subsequent efforts to make tacit knowledge explicit (externalisation) can then be undermined.
Third, we found that, for those teams or boundary-spanning individuals who did manage to externalise knowledge (and innovative solutions did surface in all of the four teams), horizontal and vertical integration efforts often appeared to ‘stick’ between the combination and internalisation stages of the SECI model. It was common for efforts to systemise combined forms of knowledge to hit political and logistical barriers. Despite explicit attention paid to packaging knowledge assets appropriately and tailoring delivery, systemising knowledge through, for example, training can be blocked by influential individuals at the local level (e.g. practice managers at GP surgeries in primary care). Boundary-spanning individuals may be in an ideal position to identify innovative and efficient solutions to combining sources of explicit knowledge, such as the use of an extranet to provide up-to-date information on a range of services specific to a particular patient condition, but can be undermined by their inability to secure system resources and support. Although individual boundary spanners could be well placed during each of the transitions between the four SECI stages, their success in helping to combine and internalise knowledge seemed largely dependent on their own individual capabilities and capacity, both within and external to the organisation in which they worked.
Finally, we note that none of the four teams, with the possible exception of the anxiety and depression in BME populations team, could claim to have embedded routines within organisational culture and explicit skills in daily operations (internalisation).
Chapter 5 Discussion
Our original research hypothesis was that boundary-spanning processes will stimulate the exchange and creation of knowledge between sectors, organisations and professions and that this will lead to service improvements as measured by both a range of quality indicators and patient and carer experience (see Chapter 1).
Our review of the origins of the ‘boundary-spanning’ concept and its application to date in the health-care sector (see Chapter 2) highlighted a key gap in the existing evidence base. As noted earlier in this report, although the characteristics and experiences of individuals in formal or informal boundary-spanning roles have been studied in the health-care context, relatively little attention has been paid to date to the core focus of our study: the processes by which ‘boundary-spanning’ can enable knowledge exchange to support horizontal and vertical health-care integration. This gap has made it problematic to distil recommendations or construct ‘best practice’ guidance for health-care policy-makers and leaders striving to design and implement interventions directed towards this goal.
To explore the complexities of how sectoral, organisational and professional boundaries are spanned in health care, we chose an ethnographic study with mixed methods (see Chapter 3). We selected the SECI model of knowledge creation as a holistic framework to evaluate the quality improvement activities of the four teams participating in the boundary-spanning intervention under study. We did so in the belief that the SECI model would be helpful for analysing our data, particularly in reflecting on the (until now relatively unstudied) processes of boundary-spanning (see Chapter 4), thereby allowing us to identify, and potentially anticipate, barriers to and enablers of successful knowledge exchange across different boundaries.
In the following section we reflect on the application of the SECI model in this case study by discussing the lessons learnt from how the four teams transitioned – or did not transition – through the four SECI stages, and consider wider theoretical developments that have also been introduced by Nonaka and colleagues. 95,122–124 Central to this discussion is reflecting on the varied success of the four teams and exploring the key factors and processes that shaped what each team was able to achieve, as detailed in Chapter 4. In Creating and exchanging knowledge across boundaries in the NHS we present our (1) implications for leaders of boundary-spanning interventions and (2) recommendations for further research relating to such interventions and the horizontal and vertical integration of health-care services.
Capturing and extending the learning from the socialisation, externalisation, combination and internalisation model
Overall, we have found the SECI model to be a useful lens through which to view our qualitative data, particularly in terms of thinking about processes of knowledge exchange across various boundaries. In the light of the gap in the evidence base identified by our literature review we believe that the SECI model has helped to draw out new insights and lessons for leaders of boundary-spanning interventions (see Creating and exchanging knowledge across boundaries in the NHS).
We found that the application of the SECI model of the movement of organisational knowledge allowed for nuanced analysis of multiple interactions in a complex health-care system. To our own knowledge, no researchers have previously applied this model to health care. Limitations of the SECI model have been addressed in the literature, particularly in a critique by Gourlay,125 who questioned the empirical basis for Nonaka's126 case study work beginning in 1991. Similarly, Gourlay and Nurse127 argue that the theoretical nature of the SECI mode of knowledge conversion is based on ‘semantic information’ studies that can be flawed by ‘generous interpretation’ and ‘ambiguity’. Harsh128 argues that knowledge ‘reusability’ offers a third dimension necessary to add to the two-dimensional SECI model but his critique lacks any empirical evidence and does not address any particularities of the health-care sector, as we have presented here.
The SECI model seems particularly useful, not just because it enables the study of interactions across different system levels (from individual to team to organisation) but also because it is particularly sensitive to nuanced interactions between and across these system levels: the boundary-spanning processes in which knowledge exchange takes place. SECI is therefore important not primarily for its explanatory potential (although it is helpful in this regard) but, we would argue, for how it helps in the empirical study of boundary-spanning processes. As a heuristic, we apply this to our case to study how knowledge exchange may take place across intersectoral and interorganisational boundaries. As originally developed, the SECI model applies to knowledge exchange in more stable and enduring intraorganisational settings. But what might it reveal about knowledge exchange in our case of the WI as an interorganisational and intersectoral setting, in the wider context of systemic change? In particular, as we reflected on how each of the four boundary-spanning teams had – or had not – moved through the four stages of SECI we began to ask ourselves different questions from those addressed by previous studies. Primarily these questions took the form of asking through which processes the WI as a boundary-spanning intervention had enabled each of the teams to transition between socialisation, externalisation, combination and internalisation, whether or not there was anything distinctive about applying SECI in this interorganisational context and, when teams had become ‘stuck’, what barriers they had struggled to overcome (and whether or not the WI could have done more to help them). We discuss each of these in more detail in the following sections.
Enabling teams to exchange knowledge across boundaries: why context (and ba) matters
A central factor that shaped the outcomes of the WI as a boundary-spanning intervention, and one that we explicitly included in our overall evaluation framework, was the role of ‘context’, both local and national. The early descriptions of the SECI model take no account of ‘context’. Yet as Fischer and Ferlie129 argue, in interorganisational contexts, local ‘indigenous’ knowledge, often characterised by personal and emotional involvement, interacts with, and can be significantly shaped by, external social and political contexts, including formal knowledge systems. We reflect here on how later extensions to the SECI model incorporate the role of context as a factor in explaining knowledge exchange processes and the contribution that these can make to our understanding of the varied success of the four boundary-spanning teams that we studied.
The various conceptualisations of ‘context’ originate to a large extent in the variety of different perspectives that have been brought to bear on the question of its role (e.g. organisational studies, social psychology, knowledge management and innovation studies). These different perspectives have led to different methodological approaches to studying context: broadly, on one hand, researchers have viewed contextual factors as discrete variables that can be measured; on the other hand, others view ‘context’ as a set of processes that relate both to each other and to change/improvement. By adopting Pettigrew and colleagues'130 definition we fall firmly into the latter camp:
Context refers to the ‘why’ and ‘when’ of change and concerns itself both with influence from the outer context (such as the prevailing economic, social, political environment) and influences internal to the focal organisation under study (for example, its resources, capabilities, structure, culture and politics).
p. 91
A recent review by one of the authors of this report (GR)131 argues that contemporary psychological perspectives (focusing on staff commitment to change or other social dynamics) need to be considered alongside more ‘traditional’ structural perspectives (focusing on an organisation's policies, resources or systems) of how context shapes the outcomes of quality improvement interventions such as the WI. This review found that 338 of the 476 contextual factors previously studied related to structural as opposed to psychological factors. When psychological factors had been studied this was most commonly in terms of ‘a supportive organisational culture’ at the meso (organisational) level; very few psychological factors had been studied at the micro (front-line team) level.
By contrast, we emphasise the importance of micro as well as meso contextual factors. Similarly, for Nonaka and colleagues,95,97 key to the related questions of how teams transition between the four stages of SECI and move between different levels (individual, group and organisation) is the concept of ‘ba’. ba is the energy and place where a shared context happens and where resources are concentrated so that knowledge can be created and used (Figure 11).
FIGURE 11.
‘ba’ as shared context in motion. Reprinted from Long Range Planning, 33, Nonaka et al. , SECI, ba and leadership: a unified model of dynamic knowledge creation, pp. 5–34, © 2000, with permission from Elsevier. 97
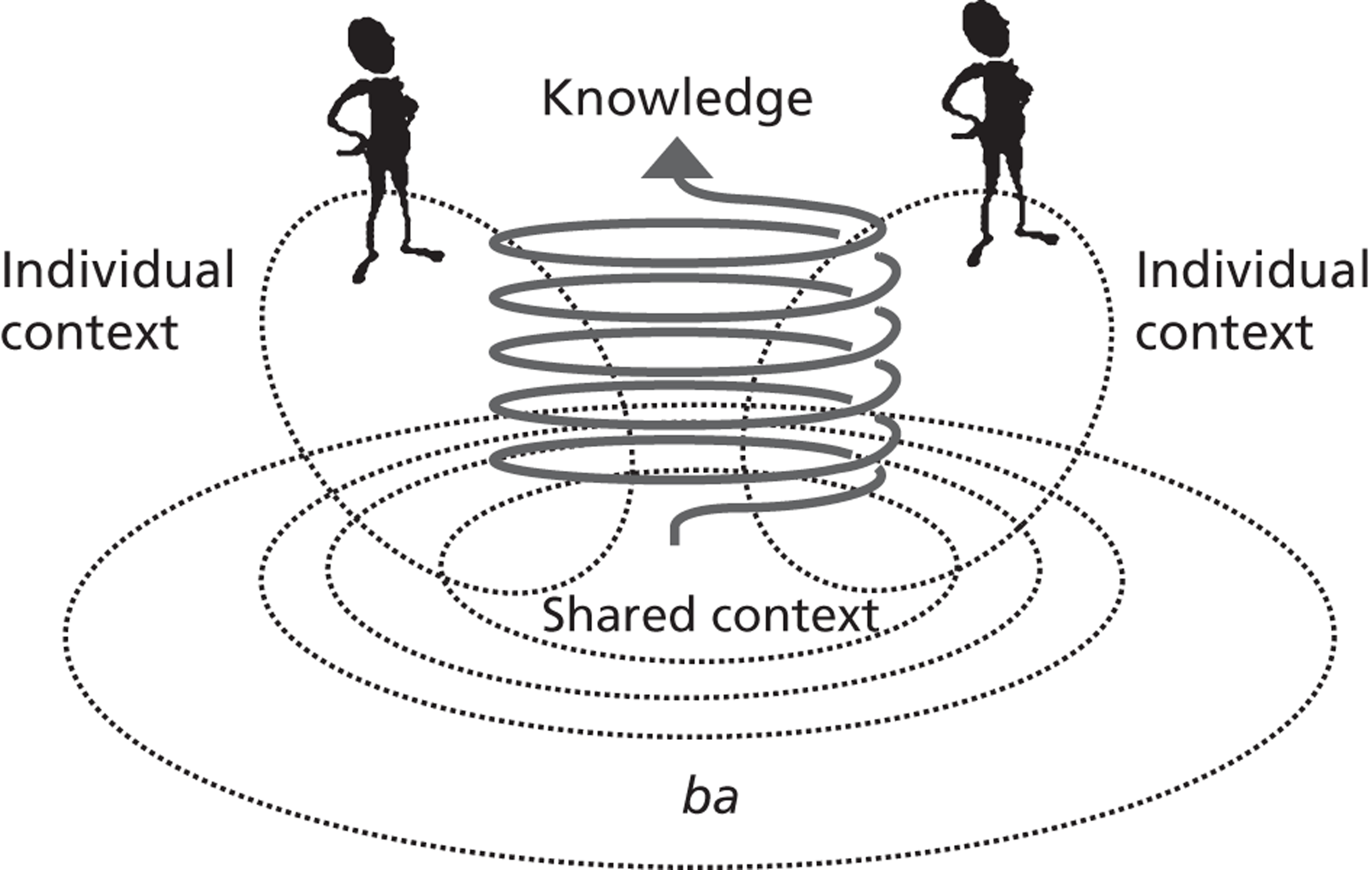
Although the four SECI stages initially provided a useful analytical lens, the concept of ‘ba’ has been helpful in explaining the differences between the stories of the four boundary-spanning teams by highlighting the role of context. For knowledge to be created, interactions must happen, and boundaries are transcended in a complex and rather fluid motion of evolving possibility. 80 Knowledge itself is boundary-less and intangible, can be both explicit and tacit and can take different forms or ‘assets’ depending on the context. Knowledge is expressed and transmitted in different ways between individuals and groups, depending on context and specific time and place, and across interfaces in a dynamic manner97,131 (Figure 12).
FIGURE 12.
Four categories of knowledge assets. Reprinted from Long Range Planning, 33, Nonaka et al. , SECI, ba and leadership: a unified model of dynamic knowledge creation, pp. 5–34, © 2000, with permission from Elsevier. 97
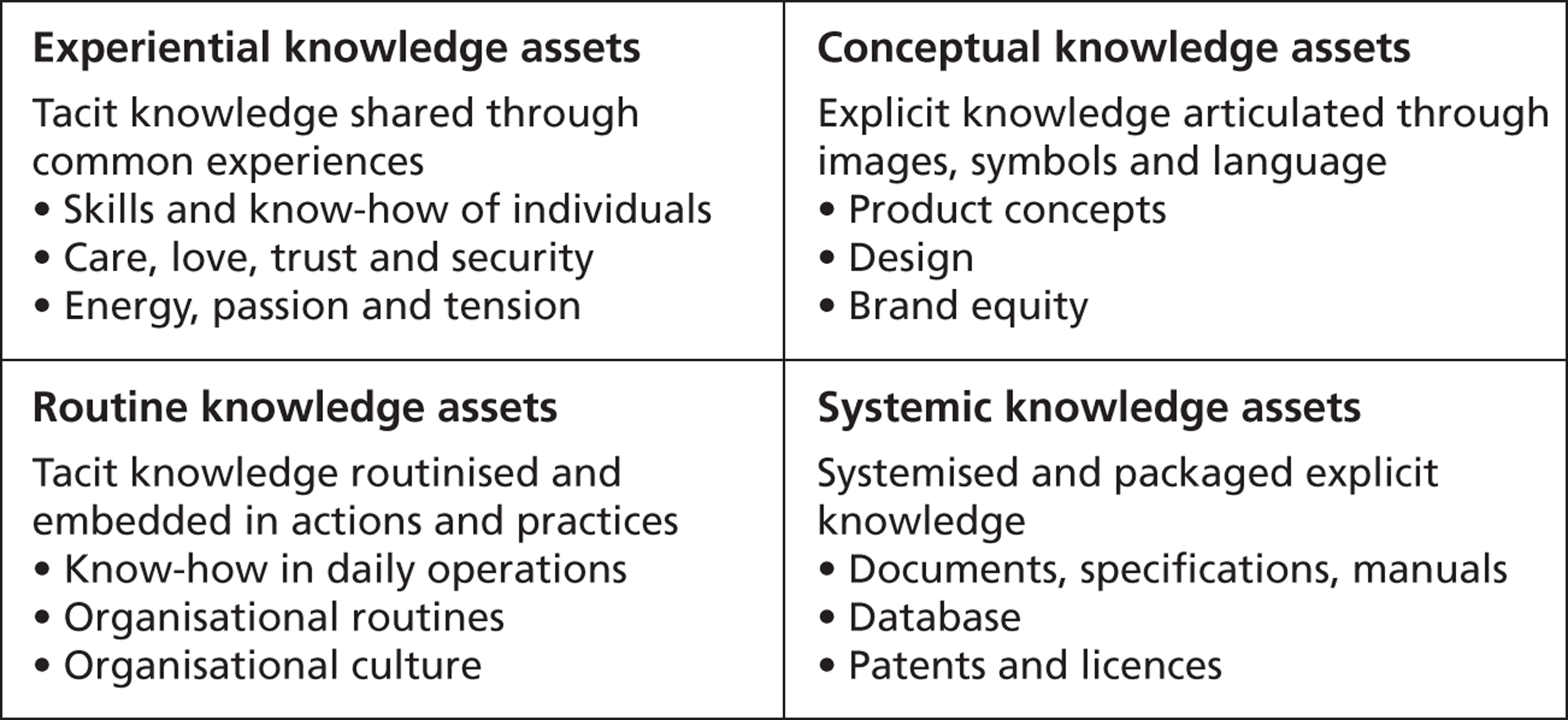
The distinction between the role of structural and psychological contextual factors at different levels (macro, meso and micro) of a health-care system is therefore also reflected, to a degree, in later elaborations of the SECI model and, importantly for our study, explicitly linked to how knowledge exchange processes are enacted and to different types of knowledge assets. We say ‘to a degree’ because the familiar macro–meso–micro distinction blurs some of the micro-psychological interactions that take place between different system and organisational levels; hence, the importance of individual boundary spanners and boundary-spanning processes. Although boundary spanning should not be seen solely as an individual role or activity, we also question the implication that ‘micro’ personal–psychological interactions take place only at the organisational margins. Our cases suggest that such interactions do indeed create important (network-like) linkages within and between systems and organisations, and not solely in the shape of individual boundary spanners. Fischer's132 article similarly argues that interactions take place in liminal areas at the ‘interstices of social relations’ where experiences, emotions and ideas are exchanged across individual, group and organisational levels. These liminal areas may function as ‘formative space(s) in which authentic, mutual relations develop, useful for organizational productivity’ (p. 1155). Their interactions are not confined to micro-level (front-line) areas but may be generated and exchanged across different organisational levels, such as in conditions of organisational turbulence.
In complex, pluralist domains such as health care, much of what constitutes useful work takes place in the micro-practices between practitioners and in their interactions with service users. Often below the radar of official organisational scrutiny, a less visible aspect of collaboration takes place in these peripheral spaces, occupied by emotionally invested participants. 133 And unlike the strategic and political advantages that may occur in formal organisational relationships, a characteristic of informal collaboration is that it is a means not only of exchanging existing knowledge, but also of creating new knowledge and innovation. Relatedly, the distributed leadership literature reveals a similarly promising perspective: groups that are deeply interconnected across formal organisational boundaries have considerable potential to achieve concerted action. When leadership develops as a distributed property of a network of interacting individuals, the knowledge, initiative and creativity that emerges between them has distinct advantages over traditional, hierarchal forms of leadership, particularly when tackling complex, interdependent problems that require innovation,36,134 such as those faced on a routine basis by the health-care practitioners that we studied.
Key activities for knowledge creation and exchange across boundaries
Nonaka and colleagues97–99,122–124,135,136 have been writing about SECI as a model of knowledge creation since 1994 and suggest that leaders play a role in facilitating how knowledge assets are developed and redefined, by moderating the conversion process, supplying energy and invoking judgments of quality. More recently, von Krogh and colleagues99 have provided suggestions for key activities or processes to support knowledge creation and exchange across boundaries. They argue that the following activities need to take place in three ‘layers’ that span formal and informal organisations:
-
core activity (the informal layer where knowledge is being created and exchanged through direct contact and collaboration between individuals):
-
look for common interests
-
emphasise and promote higher goals
-
mobilise and co-ordinate assets to convince participants of likely success
-
fix meetings and initiate discussions on priority issues
-
capture outcomes
-
-
conditional (connecting the knowledge creation and exchange processes with the overlying formal structures):
-
form teams at the right time and draw on existing links between participants
-
build non-hierarchical peer groups
-
provide experiential assets and routines
-
judge suitability of existing assets
-
connect outcomes of knowledge exchange to vision
-
connect and integrate people formally and informally*
-
provide and steer flow of assets (e.g. IT systems and data sets)*
-
set incentives to engage in knowledge creation and exchange*
-
-
structural (formal and structured processes):
-
formulate a knowledge vision that ties existing knowledge to new areas where knowledge should be sought*
-
formulate, decide on and help implement communication systems, rules and procedures*
-
balance goals for knowledge creation and exchange with economic efficiency*
-
co-ordinate access to knowledge assets across organisations and systems.*
-
The later activities marked with an asterisk are seen by von Krogh and colleagues99 as relating to ‘a formal position, process, or activity controlled by some central authority’, whereas the earlier activities in the list emerge from ‘cooperation between individuals that manifests itself in their shared direction, the alignment of their behaviour, and their mutual commitment to a particular practice’ (p. 249).
As Fischer and Ferlie129 also argue, balancing interactions between such layers (in their empirical study, particularly between core activity and structuring processes) can significantly shape the local conditions and ‘tone’ of knowledge exchange. Formal knowledge systems may provide an important background resource that can be worked with creatively and internalised; conversely, formal systems may readily proliferate, yet without their intended local effects of increasing knowledge exchange and learning.
Our empirical case suggests that ‘conditioning’ alignment between these layers may be especially important in interorganisational and intersectoral contexts. As described earlier in this report, many of the activities in the core activity layer were observed in our fieldwork and study of the four boundary-spanning teams in the WI. However, with the significant exception of the anxiety and depression in BME populations team, we would argue that the WI alone lacked many, if not all, of the key activities or processes to support knowledge creation and exchange both in the structural layer and in some of the conditional layer activities listed above. More importantly, though, ‘conditioning work’ aligning these layers appeared to be central to enabling transition beyond socialisation and externalisation to combination and internalisation.
Whereas external formal and structured processes were underdeveloped in the context of the child and family health services team, in the other three teams' contexts these structural activities developed and indeed proliferated. Notably, in the diabetes team we see a proliferation of metrics and guidelines combining external knowledge, particularly at the structural level. In the dementia team we similarly note how external knowledge was combined to produce tools and materials. As we have already noted, the anxiety and depression in BME populations team developed significant structural activities (importantly, these structural and some conditioning activities were largely provided and supported by CLAHRC). Yet combining formal knowledge in this structural layer is not sufficient, we argue, to allow teams to make the transition from the combination phase to the internalisation phase. In both the diabetes team and the dementia team, explicit and formal knowledge may have in theory been ‘combined’, but in practice it failed to move beyond a structural level to combine with local and more tacit knowledge. (In the diabetes team it was blocked by interorganisational tensions; in the dementia team it failed to move across organisational boundaries). By contrast, the anxiety and depression in BME populations team made significant progress in mobilising explicit knowledge across organisational boundaries through extensive dialogue meetings, bypassing potential barriers (such as general practice receptionists or practice administrators) to create opportunities for knowledge exchange and customisation to local contexts.
We suggest that this combination of external knowledge with more tacit knowledge is an essential aspect of the combination phase that has been overlooked in the original SECI model, yet which our interorganisational and intersectoral context reveals is highly significant. Our analysis indicates that, whereas explicit structural knowledge can readily proliferate in these contexts, considerable conditioning activities are needed to marshal resources and combine explicit knowledge with implicit knowledge – customising it for mobilisation within and between organisations. To enable the transition from the combination phase to the internalisation phase, notionally ‘combined’ explicit knowledge needs to undergo significant further elaboration and customisation.
According to our analysis, then, our teams were inhibited from progressing from socialisation to externalisation when there was insufficient shared context (ba) and lower structural processes (i.e. the child and family health services team). Conversely, when there were medium levels of shared context and higher structural processes, teams were enabled to move from implicit to explicit knowledge, combining it with formal knowledge (which tended to readily proliferate, especially in the wider context of the dementia and diabetes teams). To complete the combination phase, though, a significant activity was customising and transforming explicit knowledge – in other words, preparing it for the final stage of mobilising knowledge for internalisation. As our final example of the anxiety and depression in BME populations team indicates, the ‘combination’ phase may involve significantly more elaboration than the original SECI model suggests.
What does our case reveal about the SECI model? As a heuristic, we find that it has been helpful in allowing us to study in detail the progress of knowledge exchange in each of the teams; indeed, we advocate its further use and possible development in other interorganisational contexts. Yet our study also suggests an important limitation to the model. As originally conceptualised the combination phase suggests a quite linear (and perhaps cognitivist) progression from combined explicit knowledge to its internalisation; however, our empirical case reveals that a significant process of customisation is needed to transform explicit knowledge, developing it for potential internalisation. This activity suggests an addition to the combination phase: instead of socialisation → externalisation → combination → internalisation (SECI) we suggest socialisation → externalisation → combination and customisation → internalisation (SECCI).
In summary, although moderate to high levels of core activity in the WI initially appeared promising, knowledge creation and exchange appeared to be hampered by a general tendency for structural activities to proliferate, yet with relatively low conditional activities, and low alignment between all three levels.
Creating and exchanging knowledge across boundaries in the NHS
Implications for leaders of ‘boundary-spanning’ interventions
In the literature review in Chapter 2 we identified four main themes relating to boundary spanning in health care: the need for a wide range of communication skills, negotiating formal and informal boundary-spanning roles, recognising and responding to social and political contextual influences on knowledge exchange processes, and demonstrating evidence of impact. The review therefore established a basic framework for considering boundary-spanning processes in dynamic health-care settings. In revisiting the notion of boundary spanning through analysis of our primary data, further insights have surfaced.
Reflecting on our empirical findings in the light of the existing literature, and particularly the later developments of the SECI model described in the previous section, suggests a framework that may help to further explain what we found, as well as contributing to the design of future boundary-spanning interventions in the health-care sector. We propose that there are three interacting elements:
-
interventions such as the WI are successful at generating shared contexts for knowledge creation and exchange (ba) (i.e. they are well suited to enabling micro-boundary-spanning processes at the core activity layer) but in isolation are weaker at creating and embedding movement through the four stages of the SECI model
-
in the WI case, the Coxford PCT and wider formal organisations in the health community could have potentially provided the necessary resources and structure to facilitate the movement of the teams through the SECI stages and embed improved integration of services but, alone, are unlikely to be able to provide ba (and in our cases sometimes undermined and competed with it)
-
internal boundary-spanning team characteristics, which may enable selective drawing on external structuring ‘resources’ (e.g. CLAHRC in the case of the anxiety and depression in BME populations team) and have the potential for adapting to external constraints (similar to the activities outlined in the conditional layer).
In terms of applying this framework to our four boundary-spanning teams, then, the anxiety and depression in BME populations team was remarkably coherent with strong internal leadership; it integrated ba generation (through the WI) with sufficient ‘structuring’ (through its external CLAHRC funding) to enable it to move through the SECI stages. In contrast, in the child and family health services topic area there seemed to be a (potential) leader without a team, resulting in a much weaker shared context for knowledge exchange (ba) and very weak ‘structuring’. The dementia and diabetes teams had stronger ‘structuring’ (at least potentially) but weaker ba. The middle management roles of these two teams' leaders provided some strategic support to enable some new connections to be made; however, particularly in a time of system restructuring, the leaders were less able to create and sustain shared contexts for knowledge exchange to help their teams transition through the SECI stages.
Our overall finding, as discussed in the previous section, is therefore that, although moderate to high levels of knowledge creation and exchange through informal contact and collaboration between individuals in the WI initially appeared promising, these were generally hampered by relatively poor connections between such knowledge creation and exchange processes and the overlying formal structures present in the local Coxford and Westpark contexts. Nor is the WI atypical in NHS terms; similar initiatives and activities are being undertaken in many localities in England and so the lessons from this study are likely to have much wider applicability.
In terms of the implications for leaders of future ‘boundary-spanning’ interventions it would therefore seem crucial to recognise that, although it is relatively straightforward to enable knowledge exchange processes across professional, organisational and sectoral boundaries, it is much more challenging to align these with existing structures and systems. As highlighted by our review of the empirical literature, to do so requires a wide range of communication skills, negotiating formal and informal boundary-spanning roles, recognising and responding to social and political contextual influences on knowledge exchange processes and demonstrating evidence of impact. Beyond these, however, and as the lens of SECI helped clarify, socialisation and externalisation as forms of dialogue are just the beginning of the knowledge exchange process. Although charismatic leadership, thought leaders and empowering experiences can enable knowledge exchange in these stages, formal supervisors and managers elsewhere in the local systems act as gatekeepers and have key roles to play in enabling, or blocking, boundary-spanning initiatives during the combination and internalisation stages. Potential mechanisms to overcome the barriers encountered in the WI would, following von Krogh and colleagues,99 include:
-
connecting and integrating people formally (as well as informally)
-
providing and steering the flow of assets (e.g. IT systems and data sets)
-
setting incentives to engage in knowledge creation and exchange.
Such ‘bridging’ activities between informal knowledge creation and exchange processes and formal and structured roles and processes appear to be a crucial part of a boundary-spanning intervention. In short, although informal boundary-spanning processes (as emphasised by Chris in the WI) created the ba for knowledge exchange, a more considered approach to aligning these processes with pre-existing structures and systems was needed to move the teams through the SECI stages. Strikingly, the one team that was enabled (through CLAHRC) to align its work in this way was significantly more successful than the other three teams that we studied.
Recommendations for future research
As a key to understanding how knowledge moves and how this impacts on the quality of health care, it will be increasingly important to study exactly how problematic professional, organisational and sectoral boundaries are negotiated. 99 Boundary spanners are embedded in, and constrained by, their group identity, their organisational membership and the larger health-care system. Future empirical research of boundary spanning will need a range of tools and approaches to address these complexities and, crucially, assess the impact of such processes on health-care quality. Therefore, in order of priority, our recommendations for future research are:
-
Longitudinal studies evaluating the direct, measurable and sustained impact of boundary-spanning processes on patient care outcomes (and experiences). A variety of research designs can accomplish this task, but a move beyond purely descriptive studies of the roles and activities of individual ‘boundary spanners’ is now warranted; studying boundary spanning as a complex intervention (using the Medical Research Council framework) through a mixed-methods approach would be one potential design.
-
Based on our initial findings, a further empirically based critique and reconceptualisation of the SECI model is required, both generally and of the concept of ba particularly, so that the implications can be translated into practical ideas developed in partnership with NHS managers.
-
Following Kreindler and colleagues,137 studies of social identity dynamics during collaboration–integration efforts with a focus on identity mobilisation and context change (and how these relate to ba) may also offer valuable insights into mechanisms that explain the impact of boundary-spanning processes on the quality of health care.
-
Employing social network analysis to systematically explore the nature and composition of the interpersonal networks that emerge in boundary-spanning interventions, and the impact of these on variables such as staff well-being and team performance.
Limitations of the study
There are several limitations to our study. First, we had hoped to have much greater PPI (see Appendix 6 for a fuller discussion). The involvement of service users in all aspects of quality improvement efforts, including research, is increasingly being urged by patient advocates and policy-makers alike. The WI sought patient and stakeholder views at the very beginning of the boundary-spanning intervention that we studied but it is undoubtedly a limitation of both the intervention – and therefore our evaluation – that more patients were not involved at all stages as the quality improvement strategies evolved. The two patient focus groups we did facilitate elicited some potentially interesting themes that could have helped inform our evaluation had we been able to involve patients more closely. Second, the response rate to our pre- and post-intervention KAP survey was relatively low. Although the survey responses were helpful and informed our overall analysis (see Chapter 4, Knowledge, attitudes and practices survey), we were unable to draw firm conclusions about the impact of the WI on the KAP of a large enough number and range of primary care staff in Westpark and Coxford to be significant. Finally, although our secondary analysis of routine data did allow some observations to be made of the possible impacts of the WI on the quality of patient care (see Chapter 4, The stories of the four teams), the rigour and robustness of the local data sets that we had hoped to draw on were deemed insufficient, a shortcoming that, as with the level of PPI, also impacted on the effectiveness of the WI itself. Our comparative analysis of performance between the Westpark and Coxford practices therefore relied largely on QOF indicators that were often only broadly relevant to the stated aims of the four boundary-spanning teams that we studied. Given the limitations outlined above, our evaluation largely drew on the rich, ethnographic and longitudinal data collected through a combination of semistructured interviews, non-participant observation and serial diaries completed by participants.
Chapter 6 Conclusions
Our research hypothesis was that boundary-spanning processes will stimulate the creation and exchange of knowledge between sectors, organisations and professions and that this will lead to service improvements as measured by both a range of quality indicators and patient and carer experience. We found that, although knowledge exchange was initiated and some solutions implemented by the four boundary-spanning teams that we studied, the majority of problems were merely described and not addressed. Horizontal and vertical integration (described by one participant as like ‘knitting smoke’) were not routinely accomplished outside of the efforts of a minority of individual boundary spanners. Nonetheless, there are examples from our fieldwork of two of the teams moving beyond just ‘dialogue’ and towards creating or changing systems and processes. With one exception (the anxiety and depression in BME populations team reaching its self-defined goal of increasing referrals from Westpark practices to the local well-being service) we did not find evidence of improvement on quality indicators or with regard to patient and carer experience as a result of the boundary-spanning intervention under study.
Our findings highlight the difficulties of implementing (and evaluating) programmatic change more broadly, particularly in complex and turbulent conditions, and especially in a context of low organisational support. At certain key stages there was a clear tension between, on the one hand, the WI as a boundary-spanning intervention (albeit one with some identified design limitations) with the potential to create shared spaces and facilitate knowledge exchange and, on the other hand, the Coxford PCT, an increasingly performance-managed system that tended to clash ideologically with, rather than complement, the WI.
Our analysis also suggests taking particular notice of one of the four boundary-spanning teams as a positive case. Boundary-spanning interactions in that team created important ‘spaces’ in which knowledge exchange could potentially take place. Although the WI was later destabilised (and eventually abandoned), when in its early stages it was sometimes successful at creating these spaces, team development was both impressive and resilient. In particular, this occurred where micro–meso interactions were especially responsive to wider local developments. In the case of the anxiety and depression in BME populations team, effectiveness appeared to hinge on its ability to both internalise and mobilise a ‘shared context’ for exchanging knowledge while integrating this with internal team skills and external organisational resources to enable its movement through the stages of the SECI model. In doing so the WI helped create impetus and support internal resilience and change but it was not alone sufficient to do this in the remaining three teams.
Based on our findings we conclude that successful boundary-spanning interventions are likely to require three interacting elements:
-
the generation of shared contexts for knowledge creation and exchange at the individual practitioner level
-
formal organisations in the health community providing background resources and structure to facilitate and embed improved integration of services
-
boundary-spanning teams that are able to draw on external structuring ‘resources’ and adapt to external constraints.
Acknowledgements
We are grateful to the founder of the WI for facilitating our access to the study setting during this 2-year study, his advice on the design of our study tools and his comments on our emerging analysis. We are also grateful to all of the participants in the WI who gave freely of their time to participate in one or more of our research methods.
Sari T Nasir designed Figures 2 and 13. Stephanie Waller in the National Nursing Research Unit provided invaluable administrative assistance to the project.
Finally, we are grateful for the comments and suggestions from four anonymous reviewers appointed by the NIHR Health Services and Delivery Research programme.
Contribution of authors
Laura Nasir (Research Fellow, Nursing) contributed to the conception and design of the study, the acquisition and analysis of the data, the drafting of the manuscript and gave final approval of the version to be published.
Glenn Robert (Professor, Healthcare Quality and Innovation) contributed to the conception and design of the study, the analysis of the data, the drafting of the manuscript and gave final approval of the version to be published.
Michael Fischer (Senior Research Fellow, Leadership Development) contributed to the conception and design of the study, the analysis of the data, the drafting and revising of the manuscript (critically for important intellectual content) and gave final approval of the version to be published.
Ian Norman (Professor, Nursing and Interdisciplinary care) contributed to the conception and design of the study, the analysis of the data and the drafting of the manuscript and gave final approval of the version to be published.
Trevor Murrells (Research Data Manager/Statistician) contributed to the analysis of the data, the drafting of the manuscript and gave final approval of the version to be published.
Peter Schofield (Senior Research Fellow, Primary Care and Public Health Sciences) contributed to the analysis of the data, the drafting of the manuscript and gave final approval of the version to be published.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Ovretveit J. The contribution of new social science research to patient safety. Soc Sci Med 2009;69:1780-3. http://dx.doi.org/10.1016/j.socscimed.2009.09.053.
- Crump B, Adli M. Can quality and productivity improve in a financially poorer NHS?. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b4638.
- Briefing 240. London: NHS Confederation; 2011.
- Thomas P. General medical practitioners need to be aware of the theories on which our work depend. Ann Fam Med 2006;4:450-4. http://dx.doi.org/10.1370/afm.581.
- Gröne O, Garcia-Barbero M. WHO European Office for Integrated Health Care Services . Integrated care: a position paper of the WHO European office for integrated health care services. Int J Integr Care 2001;1.
- Thomas P, Graffy J, Wallace P, Kirby M. How primary care networks can help integrate academic and service initiatives in primary care. Ann Fam Med 2006;4:235-9. http://dx.doi.org/10.1370/afm.521.
- Thomas P. Integrating primary health care: leading, managing, facilitating. Oxon: Radcliffe Publishing; 2006.
- Thomas P. The Professor Lord Darzi Interview. Lond J Prim Care 2008;1:17-22.
- Thomas P, Meads G, Moustafa A, Nazareth I, Stange KC, Donnelly Hess G. Combined vertical and horizontal integration of health care – a goal of practice based commissioning. Qual Prim Care 2008;16:425-32.
- Armitage GD, Suter E, Oelke ND, Adair CE. Health systems integration: state of the evidence. Int J Integr Care 2009;9.
- A report prepared for Monitor. London: Frontier Economics; 2012.
- National evaluation of the Department of Health's integrated care pilots. Cambridge: RAND Europe; 2012.
- Vize R. Integrated care: a story of hard won success. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e3529.
- Legislation.gov.uk . The National Health Service (Procurement, Patient Choice and Competition) (No. 2) Regulations 2013;500. www.legislation.gov.uk/uksi/2013/500/part/2/made?view=plain’ (accessed June 2013).
- Currie G, Suhomlinova O. The impact of institutional forces upon knowledge sharing in the UK NHS: the triumph of professional power and the inconsistency of policy. Publ Admin 2006;84:1-30. http://dx.doi.org/10.1111/j.0033-3298.2006.00491.x.
- Greenhalgh T, Bate P, Peacock R, Robert G, Kyriakidou O, MacFarlane F, et al. Diffusion of innovations in health service organisations: a systematic literature review. Oxford: BMJ Books; 2005.
- Ehrlich K, Horvath J. Management of Expertise 1999.
- Adams JS, Dunnette MD. Handbook of industrial and organizational psychology. Chicago, IL: Rand McNally; 1976.
- Adams JS. Interorganizational processes and organization boundary activities. Res Organ Behav 1980;2:321-55.
- Tushman ML. Special boundary roles in the innovation process. Admin Sci Q 1977;22:587-605. http://dx.doi.org/10.2307/2392402.
- Aldrich H, Herker D. Boundary spanning roles and organization structure. Acad Manag Rev 1977;2:217-30. http://dx.doi.org/10.2307/257905.
- Thompson JD. Organizations in action. New York, NY: McGraw-Hill; 1967.
- Leifer R, Delbecq A. Organizational/environmental interchange: a model of boundary spanning activity. Acad Manag Rev 1978;3:40-5. http://dx.doi.org/10.5465/AMR.1978.4296354.
- Tushman M. Organizational change: an exploratory study and case history. Ithaca, NY: New York State School of Industrial and Labor Relations, Cornell University; 1974.
- Tushman ML, Scanlan TJ. Characteristics and external orientations of boundary spanning individuals. Acad Manag J 1981;24:83-98. http://dx.doi.org/10.2307/255825.
- Tushman ML, Scanlan TJ. Boundary spanning individuals: their role in information transfer and their antecedents. Acad Manag J 1981;24:289-305. http://dx.doi.org/10.2307/255842.
- Ancona DG, Caldwell DF. Bridging the boundary: external activity and performance in organisational teams. Admin Sci Q 1992;37:634-65. http://dx.doi.org/10.2307/2393475.
- Crosno JL, Rinaldo SB, Black HG, Kelley SW. Half full or half empty: the role of optimism in boundary-spanning positions. J Serv Res 2009;11:295-309. http://dx.doi.org/10.1177/1094670508328985.
- Latendresse FJ. Individual and Organizational Characteristics That Facilitate and Restrict Boundary Spanning of Team Leaders 2006.
- Fleming L, Waguespack DM. Brokerage, boundary spanning, and leadership in open innovation communities. Organ Sci 2007;18:165-80. http://dx.doi.org/10.1287/orsc.1060.0242.
- Perrone V, Zaheer A, McEvily B. Free to be trusted? Organizational constraints on trust in boundary spanners. Organ Sci 2003;14:422-39. http://dx.doi.org/10.1287/orsc.14.4.422.17487.
- Faraj S, Yan A. Boundary work in knowledge teams. J Appl Psychol 2009;94:604-17. http://dx.doi.org/10.1037/a0014367.
- Lindgren R, Andersson M, Henfridsson O. Multi-contextuality in boundary-spanning practices. Inform Syst J 2008;18:641-61. http://dx.doi.org/10.1111/j.1365-2575.2007.00245.x.
- Ratcheva V. The knowledge advantage of virtual teams-processes supporting knowledge synergy. J Gen Manag 2008;33:53-67.
- Noble G, Jones R. The role of boundary-spanning managers in the establishment of public–private partnerships. Publ Admin 2006;84:891-917. http://dx.doi.org/10.1111/j.1467-9299.2006.00617.x.
- Pearce CL. The future of leadership: combining vertical and shared leadership to transform knowledge work. Acad Manag Exec 2004;18:47-5. http://dx.doi.org/10.5465/AME.2004.12690298.
- Hsu S-H, Wang Y-C, Tzeng S-F. The source of innovation: boundary spanner. Total Qual Manag Bus Excel 2007;18:1133-45. http://dx.doi.org/10.1080/14783360701596274.
- Stamper CL, Johlke MC. The impact of perceived organizational support on the relationship between boundary spanner role stress and work outcomes. J Manag 2003;29:569-88. http://dx.doi.org/10.1016/S0149-2063(03)00025-4.
- Mehra A, Schenkel MT. The price chameleons pay: self-monitoring, boundary spanning and role conflict in the workplace. Br J Manag 2008;19:138-44. http://dx.doi.org/10.1111/j.1467-8551.2007.00535.x.
- Marrone JA, Tesluk PE, Carson JB. A multilevel investigation of antecedents and consequences of team member boundary-spanning behavior. Acad Manag J 2007;50:1423-39. http://dx.doi.org/10.5465/AMJ.2007.28225967.
- Bacharach SB, Bamberger P, Conley S. Work-home conflict among nurses and engineers: mediating the impact of role stress on burnout and satisfaction at work. J Organ Behav 1991;12:39-53. http://dx.doi.org/10.1002/job.4030120104.
- Aldrich H, Herker D. Boundary spanning roles and organization structure. Acad Manag Rev 1977;2:217-30. http://dx.doi.org/10.2307/257905.
- Byng R, Norman I, Redfern S, Jones R. Exposing the key functions of a complex intervention for shared care in mental health: case study of a process evaluation. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-274.
- Grol RPTM, Bosch MC, Hulscher MEJL, Eccles MP, Wensing M. Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q 2007;85:93-138. http://dx.doi.org/10.1111/j.1468-0009.2007.00478.x.
- Huxham C, Vangen S. Ambiguity, complexity and dynamics in the membership of collaboration. Hum Relat 2000;53:771-806. http://dx.doi.org/10.1177/0018726700536002.
- Huxham C, Vangen S. Leadership in the shaping and implementation of collaboration agendas: how things happen in a (not quite) joined-up world. Acad Manag J 2000;11:59-75. http://dx.doi.org/10.2307/1556343.
- Eden C, Huxham C. The negotiation of purpose in multi-organizational collaborative groups. J Manag Stud 2001;38:373-91. http://dx.doi.org/10.1111/1467-6486.00241.
- Lubben M, Mayhew SH, Collins C, Green A. Reproductive health and health sector reform in developing countries: establishing a framework for dialogue. Bull World Health Organ 2002;80:667-74.
- Thomas P, Stange KCFWD. Integrating primary health care: leading, managing, facilitating. Oxford: Radcliffe Publishing; 2006.
- Hardy C, Phillips N. Strategies of engagement: lessons from the critical examination of collaboration and conflict in an interorganizational domain. Organ Sci 1998;9:217-30. http://dx.doi.org/10.1287/orsc.9.2.217.
- Hardy C. Underorganized interorganizational domains: the case of refugee systems. J Appl Behav Sci 1994;30:278-96. http://dx.doi.org/10.1177/0021886394303002.
- Addicott R, McGivern G, Ferlie E, Surrey TW. The distortion of a managerial technique? The case of clinical networks in UK health care. Br J Manag 2007;18:93-105. http://dx.doi.org/10.1111/j.1467-8551.2006.00494.x.
- Huxham C, Vangen SE. Managing to collaborate: the theory and practice of collaborative advantage. Abingdon: Routledge; 2005.
- Hardy C, Phillips N, Lawrence TB. Resources, knowledge and influence: the organizational effects of interorganizational collaboration. J Manag Stud 2003;40:321-48. http://dx.doi.org/10.1111/1467-6486.00342.
- Martin DR, Tipton BK. Patient advocacy in the USA: key communication role functions. Nurs Health Sci 2007;9:185-91. http://dx.doi.org/10.1111/j.1442-2018.2007.00320.x.
- Abbott S. Leadership across boundaries: a qualitative study of the nurse consultant role in English primary care. J Nurs Manag 2007;15:703-10.
- Drach-Zahavy A. Interorganizational teams as boundary spanners: the role of team diversity, boundedness, and extrateam links. Eur J Work Organ Psychol 2011;20:89-118. http://dx.doi.org/10.1080/13594320903115936.
- Hara N, Hew KF. Knowledge-sharing in an online community of health-care professionals. Inform Tech People 2007;20:235-61. http://dx.doi.org/10.1108/09593840710822859.
- Etz RS, Cohen DJ, Woolf SH, Holtrop JS, Ches KED, Isaacson NF, et al. Bridging primary care practices and communities to promote healthy behaviors. Am J Prev Med 2008;35:S390-7. http://dx.doi.org/10.1016/j.amepre.2008.08.008.
- Clark NM. Spanning the boundary between agency and community: a study of health planning staff and board interaction. Am J Health Plann 1978;3:40-6.
- Martin GP, Currie G, Finn R. Reconfiguring or reproducing intra-professional boundaries? Specialist expertise, generalist knowledge and the ‘modernization’ of the medical workforce. Soc Sci Med 2009;68:1191-8. http://dx.doi.org/10.1016/j.socscimed.2009.01.006.
- Martin GP, Finn R, Currie G. National evaluation of NHS genetics service investments: emerging issues from the cancer genetics pilots. Familial Cancer 2007;6:257-63. http://dx.doi.org/10.1007/s10689-007-9130-3.
- Chattoo S, Atkin KM. Extending specialist palliative care to people with heart failure: semantic, historical and practical limitations to policy guidelines. Soc Sci Med 2009;69:147-53. http://dx.doi.org/10.1016/j.socscimed.2009.02.025.
- French B. Contextual factors influencing research use in nursing. Worldviews Evid Based Nurs 2005;2:172-83. http://dx.doi.org/10.1111/j.1741-6787.2005.00034.x.
- Ankney RN, Curtin PA. Delineating (and delimiting) the boundary spanning role of the medical public information officer. Publ Relat Rev 2002;28:229-41. http://dx.doi.org/10.1016/S0363-8111(02)00129-7.
- Grudzinskas AJ, Clayfield JC, Roy-Bujnowski K, Fisher WH, Richardson MH. Integrating the criminal justice system into mental health service delivery: the worcester diversion experience. Behav Sci Law 2005;23:277-93. http://dx.doi.org/10.1002/bsl.648.
- Hunter A, Playle J, Sanchez P, Cahill J, McGowan L. Introduction of a child and adolescent mental health link worker: education and health staff focus group findings. J Psychiatr Ment Health Nurs 2008;15:670-7. http://dx.doi.org/10.1111/j.1365-2850.2008.01296.x.
- McDonald R, Campbell S, Lester H. Practice nurses and the effects of the new general practitioner contract in the English National Health Service: the extension of a professional project?. Soc Sci Med 2009;68:1206-12. http://dx.doi.org/10.1016/j.socscimed.2009.01.039.
- Hardy C, Lawrence TB, Phillips N. Swimming with sharks: creating strategic change through multi-sector collaboration. Int J Strat Change Manag 2006;1:96-112. http://dx.doi.org/10.1504/IJSCM.2006.011105.
- Allen D. From boundary concept to boundary object: the practice and politics of care pathway development. Soc Sci Med 2009;69:354-61. http://dx.doi.org/10.1016/j.socscimed.2009.05.002.
- Alexander JA, Wells R, Jiang L, Pollack H. Organizational determinants of boundary spanning activity in outpatient substance abuse treatment programmes. Health Serv Manag Res 2008;21:168-77. http://dx.doi.org/10.1258/hsmr.2007.007028.
- Meyer RM, O’Brien-Pallas L, Doran D, Streiner D, Ferguson-Pare M, Duffield C. Front-line managers as boundary spanners: effects of span and time on nurse supervision satisfaction. J Nurs Manag 2011;19:611-22. http://dx.doi.org/10.1111/j.1365-2834.2011.01260.x.
- Leifer R, Huber GP. Relations among perceived environmental uncertainty, organization structure, and boundary-spanning behavior. Admin Sci Q 1977;22:235-47. http://dx.doi.org/10.2307/2391958.
- Walker R, Smith P, Adam J. Making partnerships work: issues of risk, trust and control for managers and service providers. Health Care Anal 2009;17:47-6. http://dx.doi.org/10.1007/s10728-008-0094-8.
- Currie G, Finn R, Martin G. Accounting for the ‘dark side’ of new organizational forms: the case of healthcare professionals. Hum Relat 2008;61:539-64. http://dx.doi.org/10.1177/0018726708091018.
- Currie G, Finn R, Martin G. Spanning boundaries in pursuit of effective knowledge sharing within networks in the NHS. J Health Organ Manag 2007;21:406-17. http://dx.doi.org/10.1108/14777260710778934.
- Ferlie E, Fitzgerald L, Wood M, Hawkins C. The nonspread of innovations: the mediating role of professionals. Acad Manag J 2005;48:117-34. http://dx.doi.org/10.5465/AMJ.2005.15993150.
- MacIntosh-Murray A, Choo CW. Information behavior in the context of improving patient safety. J Am Soc Inform Sci Tech 2005;56:1332-45. http://dx.doi.org/10.1002/asi.20228.
- Finn R, Waring J. Organizational barriers to architectural knowledge and teamwork in operating theatres. Publ Money Manag 2006;26:117-24. http://dx.doi.org/10.1111/j.1467-9302.2006.00510.x.
- Merrell J. Ambiguity: exploring the complexity of roles and boundaries when working with volunteers in well woman clinics. Soc Sci Med 2000;51:93-102. http://dx.doi.org/10.1016/S0277-9536(99)00442-6.
- Salhani D, Coulter I. The politics of interprofessional working and the struggle for professional autonomy in nursing. Soc Sci Med 2009;68:1221-8. http://dx.doi.org/10.1016/j.socscimed.2009.01.041.
- Stern R, Green J. Boundary workers and the management of frustration: a case study of two Health City partnerships. Health Promot Int 2005;20:269-76.
- Richter AW, West MA, Van Dick R, Dawson JF. Boundary spanners' identification, intergroup contact, and effective intergroup relations. Acad Manag J 2006;49:1252-69. http://dx.doi.org/10.5465/AMJ.2006.23478720.
- Fennell ML, Alexander JA. Organizational boundary spanning in institutionalized environments. Acad Manag J 1987;30:456-76. http://dx.doi.org/10.2307/256009.
- Hrebiniak LG, Alutto JA. A comparative organizational study of performance and size correlates in impatient psychiatric departments. Admin Sci Q 1973;18:365-82. http://dx.doi.org/10.2307/2391669.
- Callister RR, Wall JA. Conflict across organizational boundaries: managed care organizations versus health care providers. J Appl Psychol 2001;86:754-63. http://dx.doi.org/10.1037//0021-9010.86.4.754.
- Rugkasa J, Shortt NK, Boydell L. The right tool for the task: ‘boundary spanners’ in a partnership approach to tackle fuel poverty in rural Northern Ireland. Health Soc Care Community 2007;15:221-30. http://dx.doi.org/10.1111/j.1365-2524.2006.00674.x.
- Kegler MC, Kiser M, Hall SM. Evaluation findings from the Institute for Public Health and Faith Collaborations. Public Health Rep 2007;122:793-802.
- Thompson MA, Diccion S, Hensick J, Armstrong S. Spanning organizational boundaries to improve care and service: inpatient and outpatient chronic peritoneal dialysis. J Nurs Care Qual 1996;11:9-15. http://dx.doi.org/10.1097/00001786-199612000-00004.
- Williams P. The competent boundary spanner. Publ Admin 2002;80:103-24. http://dx.doi.org/10.1111/1467-9299.00296.
- Ehrich K, Williams C, Scott R, Sandall J, Farsides B. Social welfare, genetic welfare? Boundary-work in the IVF/PGD clinic. Soc Sci Med 2006;63:1213-24. http://dx.doi.org/10.1016/j.socscimed.2006.03.005.
- Martin G, Currie G, Finn R. Bringing genetics into primary care: findings from a national evaluation of pilots in England. J Health Serv Res Policy 2009;14:204-11. http://dx.doi.org/10.1258/jhsrp.2009.008158.
- Ferlie E, Dopson S, Fitzgerald L, Locock L. Renewing policy to support evidence-based health care. Publ Admin 2009;87:837-52. http://dx.doi.org/10.1111/j.1467-9299.2009.01796.x.
- Nonaka I. A dynamic theory of organizational knowledge creation. Organ Sci 1994;5:14-37. http://dx.doi.org/10.1287/orsc.5.1.14.
- Nonaka I, Konno N. The concept of ‘ba’: building a foundation for knowledge creation. Calif Manag Rev 1998;40:40-54. http://dx.doi.org/10.2307/41165942.
- Nonaka I, von Krogh G. Tacit knowledge and knowledge conversion: controversy and advancement in organizational knowledge creation theory. Organ Sci 2009;20:635-52. http://dx.doi.org/10.1287/orsc.1080.0412.
- Nonaka I, Toyama R, Konno N. SECI, ba and leadership: a unified model of dynamic knowledge creation. Long Range Plann 2000;33:5-34. http://dx.doi.org/10.1016/S0024-6301(99)00115-6.
- von Krogh G, Nonaka I, Voelpel S. Organizational knowledge creation theory: evolutionary paths and future advances. Organ Stud 2006;27:1179-208.
- von Krogh G, Nonaka I, Rechsteiner L. Leadership in organisational knowledge creation: a review and framework. J Manag Stud 2012;49:240-77. http://dx.doi.org/10.1111/j.1467-6486.2010.00978.x.
- Education Evidence Portal . Development & Research Network (D&Amp;R) n.d. www.eep.ac.uk/dnn2/ResourceArea/DevelopmentResearchprogrammes/tabid/113/Default.aspx (accessed 12 June 2013).
- Noblit GW, Hare RD. Meta-ethnography: synthesizing qualitative studies. Newbury Park, CA: Sage Publications; 1988.
- Elliott H. The use of diaries in sociological research on health experience. Sociol Res Online 1997;2. www.socresonline.org.uk/2/2/7.html (accessed 12 June 2013).
- Symon G, Cassell C, Symon G. Essential guide to qualitative methods in organizational research. London: Sage Publications; 2004.
- Ouwens M, Hulscher M, Akkermans R, Hermens R, Grol R, Wollersheim H. The Team Climate Inventory: application in hospital teams and methodological considerations. Qual Saf Health Care 2008;17:275-80. http://dx.doi.org/10.1136/qshc.2006.021543.
- Kivimaki M, Elovainio M. A short version of the Team Climate Inventory: development and psychometric properties. J Occup Organ Psychol 1999;72:241-6. http://dx.doi.org/10.1348/096317999166644.
- Griffiths P, Murrells T, Maben J, Jones S, Ashworth M. Nurse staffing and quality of care in UK general practice: cross-sectional study using routinely collected data. Br J Gen Pract 2010;60:34-9. http://dx.doi.org/10.3399/bjgp10X482086.
- Miles MB. Qualitative data as an attractive nuisance: the problem of analysis. Admin Sci Q 1979;24:590-601. http://dx.doi.org/10.2307/2392365.
- Langley A. Strategies for theorizing from process data. Acad Manag Rev 1999;24:691-710. http://dx.doi.org/10.2307/259349.
- Fulop N, Protopsaltis G, King A, Allen P, Hutchings A, Normand C. Changing organisations: a study of the context and processes of mergers of health care providers in England. Soc Sci Med 2005;60:119-30. http://dx.doi.org/10.1016/j.socscimed.2004.04.017.
- Isabella LA. Evolving interpretations as a change unfolds: how managers construe key organizational events. Acad Manag J 1990;33:7-41. http://dx.doi.org/10.2307/256350.
- Eisenhardt KM. Building theories from case study research. Acad Manag Rev 1989;14:532-50. http://dx.doi.org/10.2307/258557.
- Eisenhardt KM. Better stories and better constructs: the case for rigor and comparative logic. Acad Manag Rev 1991;16:620-7. http://dx.doi.org/10.2307/258921.
- Yin RK. Case study research: design and methods. London: Sage; 1994.
- White Paper: equity and excellence: liberating the NHS. London: The Stationery Office; 2010.
- Clark DM. Implementing NICE guidelines for the psychological treatment of depression and anxiety disorders: the IAPT experience. Int Rev Psychiatry 2011;23:375-84. http://dx.doi.org/10.3109/09540261.2011.606803.
- Improving access to psychological therapies. Implementation plan: national guidelines for regional delivery. London: Department of Health; 2008.
- Clinical guideline 42. London: NICE; 2011.
- Living well with dementia: a national dementia strategy. Putting people first. London: Department of Health; 2009.
- Every child matters. London: The Stationery Office; 2003.
- The Common Assessment Framework for children & young people: supporting tools. Integrated working to improve outcomes for children & young people. London: The Stationery Office; 2006.
- Nonaka I, Takeuchi H. The knowledge-creating company: how Japanese companies create the dynamics of innovation. Oxford: Oxford University Press; 1995.
- Nonaka I. A dynamic theory of organisational knowledge creation. Organ Sci 1994;5:14-37. http://dx.doi.org/10.1287/orsc.5.1.14.
- Nonaka I, Byosiere P, Borucki CC, Konno N. Organisational knowledge creation theory: a first comprehensive test. Int Bus Rev 1994;3:337-51. http://dx.doi.org/10.1016/0969-5931(94)90027-2.
- Nonaka I, Toyama R. The knowledge-creating theory revisited: knowledge creation as a synthesizing process. Knowl Manag Res Pract 2003;1:2-10. http://dx.doi.org/10.1057/palgrave.kmrp.8500001.
- Gourlay S. Conceptualizing knowledge creation: a critique of Nonaka's theory. J Manag Stud 2006;43:1415-36. http://dx.doi.org/10.1111/j.1467-6486.2006.00637.x.
- Nonaka I. The knowledge-creating company. Harv Bus Rev 1991:96-104.
- Gourlay S, Nurse A, Buono AF, Poulfelt F. Challenges and issues in knowledge management. Research in Management Consulting Series, Volume 5. Greenwich, CT: Information Age Publishing; 2005.
- Harsh OK. Three dimensional knowledge management and explicit knowledge reuse. J Knowledge Manag Pract 2009;10.
- Fischer MD, Ferlie E. Resisting hybridisation between modes of clinical risk management: contradiction, contest, and the production of intractable conflict. Account Org Soc 2013;38:30-49. http://dx.doi.org/10.1016/j.aos.2012.11.002.
- Pettigrew AM, Ferlie E, McKee L. Shaping strategic change: making change in large organizations: the case of the National Health Service. London: Sage; 1992.
- Robert G, Fulop N. Draft report for the Health Foundation. London: King's College London; 2013.
- Fischer MD. Organizational turbulence, trouble and trauma: theorizing the collapse of a mental health setting. Organ Stud 2012;33:1153-73. http://dx.doi.org/10.1177/0170840612448155.
- Fischer MD. of Turbulence in the Management of Personality Disorders: An 2008.
- Bennett N, Wise C, Woods PA, Harvey JA. Distributed Leadership: a Review of Literature 2003.
- Nonaka I, Umemoto K, Senoo D. From information processing to knowledge creation: a paradigm shift in business management. Technol Soc 1996;18:203-18. http://dx.doi.org/10.1016/0160-791X(96)00001-2.
- Von Krogh G, Nonaka I, Aben M. Making the most of your company's knowledge: a strategic framework. Long Range Plann 2001;34:421-39. http://dx.doi.org/10.1016/S0024-6301(01)00059-0.
- Kreindler SA, Dowd DA, Star ND, Gottschalk T. Silos and social identity: the social identity approach as a framework for understanding and overcoming divisions in health care. Milbank Q 2012;90:347-74. http://dx.doi.org/10.1111/j.1468-0009.2012.00666.x.
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 2005;331:1064-5. http://dx.doi.org/10.1136/bmj.38636.593461.68.
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005;10:6-20. http://dx.doi.org/10.1258/1355819054308576.
- Barroso J, Gollop CJ, Sandelowski M, Meynell J, Pearce PF, Collins LJ. The challenges of searching for and retrieving qualitative studies. West J Nurs Res 2003;25:153-78. http://dx.doi.org/10.1177/0193945902250034.
- Pope C, Mays N, Popay J. Synthesizing qualitative and quantitative health evidence: a guide to methods. Maidenhead: Open University Press; 2007.
- Covey SMR, Merrill RR. New York, NY: Free Press; 2006.
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8. http://dx.doi.org/10.1186/1471-2288-8-21.
- Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy 2002;7:209-15. http://dx.doi.org/10.1258/135581902320432732.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy 2005;10:45-53. http://dx.doi.org/10.1258/1355819052801804.
Appendix 1 Literature review: methods and summary of papers
Articles were identified through multiple formal search methods including hand searching of key journals; electronic searching of main databases including the use of free-text, index terms and named author; reference scanning; and citation tracking. 138 Snowballing and identification of studies through personal contact were also used. Electronic searches of the following databases were conducted: Web of Knowledge, Web of Science, Google Scholar, PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and the digital library JSTOR®. Free-text searches included single and plural versions of boundary (boundar*) and various forms of the verb ‘to span’, such as spanner or spanning (span*). In many databases this initially yielded > 5000 articles, many related to mathematical, biological or engineering conceptualisations unrelated to the sociological meaning intended. Search terms such as ‘health’ and ‘health care’ were also used in combination to further focus and limit the selection, although this rarely yielded articles meeting the inclusion criteria. The organisational studies literature from as early as 1965 up to 2012 was explicitly included by means of hand searching of the following journals: Academy of Management Review, Administrative Science Quarterly, Organisation Studies, Organisational Science and Public Administration. The Journal of Primary Care and Community Health and Social Science & Medicine were also hand searched. Reference scanning was utilised to identify historical articles that identified the concept of boundary spanner. Citation tracking was used to forward track the key articles in the past literature. Figure 13 provides a summary of how the results of the searches of the various sources informed our overall findings.
FIGURE 13.
Summary of sources.
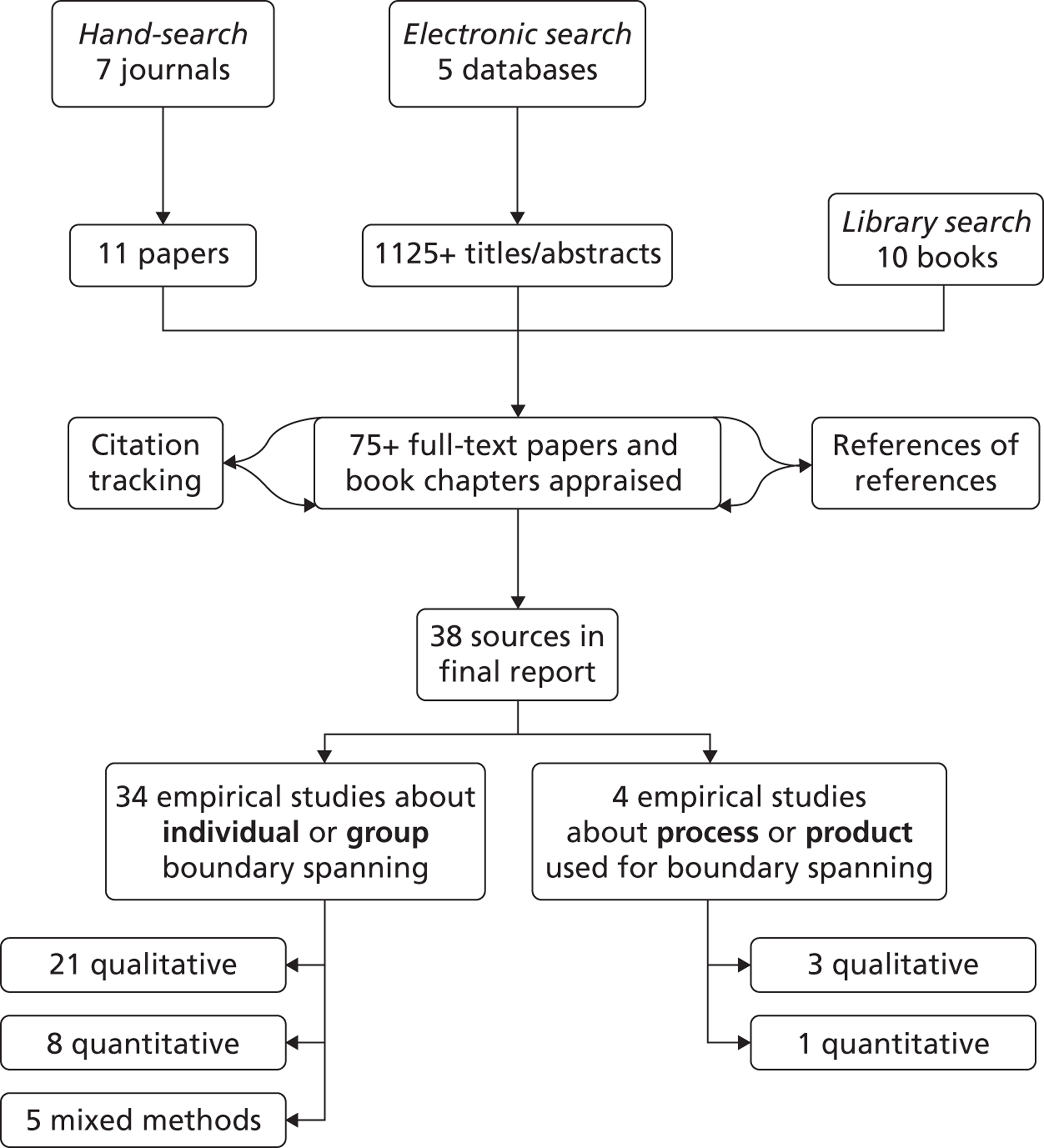
All studies that met the inclusion criteria (Box 1) were included in the initial literature review without regard for quality.
-
Relevance. Has this paper explicitly studied ‘boundary spanning’ by an individual or group in the health-care sector?
-
Specificity. Was it part of the boundary spanners' formal or informal role(s) to facilitate the vertical and/or horizontal integration of services to improve patient care?
-
Depth. Does the paper go beyond a superficial description or commentary? Is it empirical? Is it research, an enquiry, an investigation or a study that describes the role of boundary spanner(s) as applied to the vertical and/or horizontal integration of services?
-
Utility. Does the paper contribute to the understanding of how the concept of boundary spanners can be operationalised in the health-care sector to facilitate the vertical and/or horizontal integration of services?
These inclusion criteria were intentionally focused to yield empirical research specific to the intended topic of interest. Consequently, papers that explicitly described boundary-spanning related to an individual's role in an organisation were included, particularly if this was part of the main theoretical framework of the article. Boundaries in a health-care setting were included, including those between teams, networks, professionals, sectors and organisations. All selected literature had to fit the preliminary inclusion criteria and be directly related to both boundary-spanning and health care. Only papers published in peer-reviewed English-language journals were included.
Exclusion criteria included research set in the IT and software development industries or in any non-health-care setting. Research about teams with a boundary-spanning teams remit was included, although research about multidisciplinary teams was excluded, to specifically identify how boundary spanning is conceptually different from teamwork. Research about boundaries but not describing the act of bridging or spanning different areas was excluded, to identify specifically how boundary-spanning as an action or activity might be different from structural descriptions of sectors or departments within organisations. Studies particularly about collaboration or teamwork were also excluded to be distinctly clear about boundary-spanning as an intentional conceptual framework.
The search was completed in multiple iterations across 24 months until the same articles resulted. The most current search identified six new studies about boundary-spanning activity, including one in health care.
Efforts to ensure validity and reliability in qualitative research have debatable utility and rigid methods for appraising study quality may not even be beneficial. Having acknowledged these concerns, three researchers made the decision about article inclusion given the designated objectives. Careful records have been kept, using reproducible strategies, in an effort to increase overall perspective on the process. These steps and assumptions are consistent with the method of meta-ethnographic synthesis. 139
Despite all efforts to meticulously and explicitly define a search strategy, the majority of studies were identified outside of traditional database searches, which is consistent with research about search methods in qualitative reviews140 and systematic reviews. 138 Conventional ‘snowball’ tracking methods, such as references of references, as well as informal methods such as serendipitous discovery often yielded articles that were more pertinent. Once a collection of studies about boundary spanners in health care was identified in a first sift, a table of all studies was constructed; in the second sift we further identified articles that both were empirical and examined health-care integration.
Analytical framework: meta-ethnography
For the purposes of this review, the empirical studies meeting the inclusion criteria were analysed using a meta-ethnographical method for evidence synthesis. There are still relatively few examples of meta-ethnography in the health literature, but it is an ideal method to produce interpretations from a wide variety of quantitative and qualitative research findings, particularly about a complex concept. 139 The selection of articles and resultant synthesis were undertaken using the seven iterative steps of meta-ethnography as outlined by Noblit and Hare101 and described by Pope and colleagues141 (Box 2).
-
Getting started
-
Deciding what is relevant to the initial interest
-
Reading the studies
-
Determining how the studies are related
-
Translating the studies into one another
-
Synthesising translations
-
Expressing the synthesis
The first three steps included identifying the topic of interest, carrying out a purposive search and repeated reading of the studies to emphasise iterative understanding. The fourth step, determining how the studies are related, was completed by compiling a list of key ideas, key concepts and explanatory schema, in what Noblit and Hare101 term ‘reciprocal translation’. A table was produced initially (see Table 28), to organise the articles by research method, concepts of interest, key themes and conclusions. Additionally, we ascribed vertical and/or horizontal dimensions to the direction of the integration examined in each of the studies (Table 27).
| Study type | Horizontal | Vertical |
|---|---|---|
| n (%) | 24 (63) | 14 (37) |
| Qualitative | 13 | 11 |
| Quantitative | 7 | 2 |
| Mixed method | 4 | 1 |
In the table of all included studies (Table 28), each article was also ascribed as relating to spanning in any of three boundaries: professional, sectoral and organisational. A matrix was produced, tabulating recurring concepts and common themes, for comparison across all included studies and the development of a novel synthesis in the next steps. In this manner, the effort to translate studies into one another generated a comparison between different studies while still preserving the structure of relationships between concepts within any given study. As an emergent and iterative method, the fifth, sixth and seventh steps involved comparing the studies by translating comparisons and differences in the concepts, then synthesising and communicating these translations. The resultant matrix produced from the initial table further enabled comparisons and multiple conceptualisations across studies, as discussed in our analysis.
| Study | Research method | Study design | Integration | Setting | Country | Boundaries |
|---|---|---|---|---|---|---|
| Abbott 200756 | Qualitative | Four case studies; semistructured interviews with stakeholders | Vertical | Nurse consultants in a primary care setting | UK | Professional |
| Alexander et al. 200871 | Quantitative | National survey data; regression models; directors' self-reported boundary spanning | Horizontal | Outpatient substance abuse | Michigan, USA | Sectoral |
| Allen 200970 | Qualitative | Case study | Horizontal | Mental health inpatient. Mental health – acute | UK NHS | Professional, organisational |
| Ankney and Curtin 200265 | Quantitative | Survey; 25 scored questions | Vertical | Medical public information officers as boundary spanners between medical experts and journalists. Surveyed senior editors at every daily newspaper in Pennsylvania and 177 cardiac surgeons in Pennsylvania. Acute – community | Pennsylvania, USA | Professional, sectoral, organisational |
| Callister and Wall 200186 | Qualitative and quantitative | 30 semistructured interviews with managed care executive or supervisor and physician or administrative providers, plus 109 semistructured interviews related to selected conflict incidents | Vertical | Health maintenance organisation. Payer – provider | USA | Professional, organisational |
| Chattoo and Atkin 200963 | Qualitative | 27 semistructured interviews with professionals | Vertical | Nurses, cardiologists and heart failure nurses consultants. Focuses on how professionals in cardiology and specialist palliative care negotiate their disciplinary boundaries within the context of these policy moves | UK | Professional |
| Clark 197860 | Quantitative | Questionnaires by mail | Horizontal | 243 members of local health planning boards (44% provider group representatives; 51% consumer representatives); 14 local boards, three boroughs, New York City. Public health – health planning agency ‘staff’ and board member ‘outsiders’ | New York City, USA | Professional, sectoral |
| Currie and Suhomlinova 200615 | Qualitative | Interviews in two phases; observations; reviewed documents; sociological investigation (n = 29) | Vertical | Examines perceptions. Academic health centre/teaching hospital. One CEO, 15 medical consultants (digestive diseases), vascular surgery, 13 professors, interviews and observations of gastroenterology community of practice | North of England, UK | Professional, organisational |
| Health care – higher education; acute – primary care; doctors – other professionals | ||||||
| Currie et al. 200776 | Qualitative | Longitudinal comparative case study approach with semistructured interviews and observations; rather than coding the interviews through software, so that data remained contextualised, material treated holistically as narratives; telling stories | Vertical | Interviews were carried out in 11 case study sites (four cancer genetics projects, three service development projects and four GP with special interest projects) with 90 stakeholders | UK | Professional, sectoral, organisational |
| Currie et al. 200875 | Qualitative | Case study design; 11 in-depth cases of 27 mainstreaming genetics programmes; interviews | Vertical | Examines the implementation of network forms of genetics health-care delivery | UK NHS | Professional, organisational |
| Drach-Zahavy 201157 | Qualitative and quantitative | Interviews with team co-ordinators; survey data on team effectiveness; regression analysis for predicting boundary-spanning activities | Horizontal | 49 health promotion teams. Health promotion representative – community | Israel | Sectoral, organisational |
| Ehrich et al. 200691 | Qualitative | Observation clinics, one site; 16 interviews with staff from a range of disciplines | Vertical | Assisted conception unit in teaching hospital. Nursing, obstetrics, gynaecology, radiography, embryology, molecular, cytogenetics and administration, and ethics discussion groups facilitated by a specialist in medical ethics | UK | Professional |
| Etz et al. 200859 | Qualitative | Key informant field-based interviews; diary data – biweekly online; data analysis; interpretive methods | Horizontal | Health behaviour change interventions in eight practice-based research networks were examined; 2 years of data collection with comparative analysis to understand strategies used for linking primary care practice with community resources | USA | Sectoral |
| Fennell and Alexander 198784 | Quantitative | Data analysis; Hospital Administrative Environment and Structure survey data | Horizontal | 901 hospitals. Examined hospitals merging with other hospitals | USA | Organisational |
| Ferlie et al. 200577 | Qualitative | Cross-case summary tables; purposeful case study and selection – eight comparative and longitudinal cases; interpretive methods; field-based interviews | Vertical | Medicine, nursing | UK | Professional |
| Finn and Waring 200679 | Qualitative | Two ethnographic case studies | Horizontal | Teaching hospitals in English Midlands and northern England; operating theatres | UK | Professional, organisational |
| French 200564 | Qualitative | Descriptive study; groups observed – transcripts of meetings analysed; constructivist approach | Vertical | Clinical nurse specialists | UK | Professional, organisational |
| Grudzinskas et al. 200566 | Qualitative | Case study; conversation; network analysis | Horizontal | Mental health – courts | USA | Sectoral |
| Hara and Hew 200758 | Qualitative | In-depth case study with mixed methods; online observations; content analysis (narrative) method; interviews | Horizontal | Online LISTSERV involving professional nurses in critical care and advanced practice disciplines: paediatric care, trauma, general medicine, cardiology, oncology, adult critical care and surgical critical care. All had a graduate degree, with three having doctoral degrees | USA | Professional |
| Primary care – secondary care; secondary – tertiary care; primary – tertiary care | ||||||
| Hardy et al. 200669 | Qualitative | Case examination | Horizontal | Canadian Treatment Advocates Council; community | Canada | Sectoral |
| Hrebiniak and Alutto 197385 | Quantitative | Secondary data analysis | Horizontal | Medicine – 338 inpatient psychiatric departments. Acute – community | USA | Sectoral |
| Hunter et al. 200867 | Qualitative | Two focus groups; grounded theory | Horizontal | Nursing, mental health. Convenience sample of teachers, school nurses, mental health nurses, clinical psychologists, social workers and consultant psychiatrists. Community – school – mental health | Ireland | Sectoral |
| Kegler et al. 200788 | Qualitative and quantitative | Self-administered surveys by team members – pre/post assessment of knowledge and skills gained through participation; 243 semistructured telephone interviews | Horizontal | Public health – faith community. Three regional institutes with teams from Wisconsin, Pennsylvania and Los Angeles, CA, USA. Community – community | Wisconsin, Pennsylvania, Los Angeles, CA, USA | Sectoral |
| Leifer and Huber 197773 | Quantitative | Questionnaires by mail; cross-sectional field study | Horizontal | 12 work units; 182 people working in health and welfare organisation concerned with family problems, adoption, social work, etc. Each work group was semiautonomous and included clerical, managerial and caseworker personnel. Lowest two echelons of a rather tall, Midwestern state government agency. Social care | USA | Sectoral, organisational |
| MacIntosh-Murray and Choo 200578 | Qualitative | Ethnographic case study of a medical unit in a large tertiary care hospital; interviews; observation; document review; grounded theory coding | Horizontal | Acute. Staff on same unit | Ontario, Canada | Professional |
| Martin and Tipton 200755 | Qualitative | 12 semistructured interviews analysed by thematic categories; grounded theory | Vertical | Full-time patient advocacy programmes in hospitals | USA | Professional |
| Martin et al. 200762 | Qualitative | Case study in 11 pilot sites, including four of seven cancer genetics pilots | Vertical | Cancer, genetics | UK NHS | Professional, sectoral, organisational |
| Martin et al. 200961 | Qualitative | Casework; stakeholder and other interviews | Vertical | Looked at how divergent discourses were reconciled as boundaries between subprofessions were reasserted | UK | Professional |
| McDonald et al. 200968 | Qualitative | 20 interviews; themes constantly contrasted | Horizontal | Practice nurses in primary care; professional role | UK | Professional |
| Merrell 200080 | Qualitative | Ethnographic; participant observer – 18 months; interviews; thematic content analysis | Horizontal | Unpaid and paid volunteers in well woman clinics | UK | Professional |
| Meyer et al. 201172 | Quantitative | Descriptive, correlational design, cross-sectional survey, prospective work log and administrative data from a convenience sample; analysed using hierarchical linear modelling | Horizontal | 558 nurses, 31 front-line nurse managers and four acute care hospitals. Nurse – nurse manager | Ontario, Canada | Professional |
| Richter et al. 200683 | Quantitative | Survey of ‘principle groups’ of staff; questionnaire; external rating by external line manager; organisational identification | Horizontal | 53 work groups from five PCTs. GPs, nurses, and physiotherapists. Colocated teams; not managerial | UK | Organisational |
| Rugkasa et al. 200787 | Qualitative | Four focus groups; individual interviews – people from different organisations | Horizontal | Fuel poverty as a public health issue. Explores range of local partnership interventions and process of ‘spanning downwards’ | Northern Ireland | Professional (multi), sectoral, organisational |
| Salhani and Coulter 200981 | Qualitative | Ethnographic study; 48 interviews | Horizontal | Single interprofessional team over 12 months; nurse, assistant, psychiatrist, resident and social worker, etc. | Canada | Professional (multi) |
| Stern and Green 200582 | Qualitative | Case study approach – not comparative | Horizontal | Public health | UK, South Africa | Professional, sectoral |
| Thompson et al. 199689 | Quantitative | Evaluation of key indicators along health-care continuum; retrospective chart audit – patients cared for under old and new guidelines compared | Vertical | Academic tertiary care health-care system. Nursing, dialysis. Acute – secondary | USA | Professional |
| Walker et al. 200974 | Qualitative and quantitative | 63 interviews with managers and service providers participating as members of PCP committees, CEOs, managers, working party members and service providers; coded thematically; written questionnaire with follow-up interview; Trust Evaluation Scale: Smart Trust Matrix of Covey and Merrill142 | Horizontal | PCP: voluntary alliance of primary care service providers (agencies) within a Local Government Association. Social model of health. PCP is within state jurisdiction. Voluntary sector, local government area, primary care, social care | Australia | Professional, organisational |
| Williams 200290 | Qualitative and quantitative | Opportunistic postal survey (n = 10); survey of three types of boundary spanning in different policy areas: health promotion specialist, crime and community safety co-ordinators, environmental and local agenda; 21 co-ordinators | Horizontal | Health promotion specialists | South Wales, UK | Professional, sectoral, organisational |
| Local authority – voluntary sector; community – community |
The expected product of this kind of synthesis is a set of interpretations and explanations, which lead to ‘orders’ of meaning and a final ‘third-order’ interpretation. Research findings were highlighted in the matrix as a ‘second-order’ column (participants' words from the research would have been a ‘first-order’ column but were not directly utilised for our analysis as rigorous representation of primary data could not be guaranteed). Our interpretations were synthesised in the ‘third-order’ column in an effort to preserve conceptual understanding between studies. A fourth column for ‘reciprocal translation’ was used to capture key themes across different papers. 143 In this manner, the substance of each study was synthesised into a new interpretation that contributes understanding to the wider discourse beyond any individual study while also maintaining the reliability of inherent concepts. 101,139,144
Because of the relatively large number of selected articles in this review, and the inclusion of both qualitative and quantitative research, the use of meta-ethnography was combined with variant methodological aspects of critical interpretive synthesis, as developed by Dixon-Woods and colleagues145 in their large synthesis study of health care for vulnerable populations. Key processes in critical interpretive synthesis involve a dynamic and flexible search process that hedges towards purposive selection. As consistent with the steps of meta-ethnography, continual reflexivity was utilised to capture emerging themes in the literature, with a critical orientation to conceptual findings. Although transparent steps and a clear audit trail for validating process are presented here, because of the interpretative nature of the meta-ethnographic method there may be some who find limitations with such an approach. To this end, NVivo 9 software was utilised systematically to organise themes within, and across, articles with a resultant matrix for visual comparison.
Appendix 2 Protocol (extract)
Note: reference citations have been removed from this extract to avoid breaking the anonymity of the case study site.
FACILITATING KNOWLEDGE EXCHANGE BETWEEN HEALTH CARE SECTORS, ORGANISATIONS AND PROFESSIONS: STUDYING ‘BOUNDARY-SPANNING’ PROCESSES AND THEIR IMPACT ON HEALTH CARE QUALITY
Methods
a. Setting
Our case study is a project designed to improve services through collaboration between general practitioners, community services, voluntary groups and acute specialists. The project includes the development of a network of leaders across organisational and community boundaries to facilitate knowledge exchange, and is directly linked with a programme of ‘whole system’ stakeholder conferences to create organisational learning and change, together with community development. The project is being led in an area where there is sustained political support and understanding for this way of working from local statutory organisations, in partnership with voluntary sector agencies. Four topic areas will be covered by the project which will form our case study:
-
Dementia.
-
Child & Family Health.
-
Depression & anxiety in people from black and minority ethnic backgrounds.
-
Diabetes.
The WI project itself is bringing people from all parts of the health care system together at ‘stakeholder conferences’ on four occasions to share their experiences, consider data, exchange views and agree actions to be completed as they relate to each of the four topic areas. Preparation for the project began with focus groups to understand different perspectives and a stakeholder conference to set the scene; these events were attended and observed by a member of the research team (Robert). The next stakeholder conference will aim to shape the agreed priorities in each of the four topic areas (and will again be observed by the research team), with a final conference planned where the findings from the project will be disseminated.
b. Design
We will use an in-depth longitudinal, case study approach. Our extensive fieldwork will encompass the four specific topic areas in which boundary-spanning activities will be undertaken as part of the case study. Research methods will include ethnographic fieldwork through: non-participant observation, interviews centred on individuals in the boundary-spanning groups, participant (boundary-spanning individual) diaries, ongoing review of project documentation, and patient & carer focus groups. This qualitative fieldwork will be supplemented with a Knowledge, Attitude and Practice (KAP) questionnaire delivered at two time points 6–12 months apart and secondary analyses of routine datasets.
Organisational case studies are a preferred research method within complex and dynamic contexts where it is difficult to isolate variables or where there are strong interactions between variables. The case study can generate hypotheses from exploratory data which can then be tested in wider samples using different methods, and – particularly relevant to this proposal – they address questions of process as opposed to the input–output model of much quantitative research. Process research is characterised by the dynamic study of behaviour within organisations, focusing on organisational context, activity and actions which unfold over time. Making sense of processes will be especially useful for examining the role of boundary spanners in the dynamic context of cross-boundary working. Our case study research strategy is therefore particularly well suited for a detailed investigation of people in different organisations, in their local context, and over time.
The proposed study will explicitly set out to explore the theoretical framework (theories, assumptions, key concepts) for boundary-spanning that underpins the case study. For example, previous work involving the lead applicant (Robert) has presented different conceptual and theoretical bases for the spread of innovation in service organisations, ranging from unpredictable and emergent (bottom-up) processes, through negotiated and enabled facilitation, and onto the scientific and planned (top-down) interventions. Through our fieldwork we will seek to make the framework operating in the case study explicit and explore whether it is appropriate (based on our review of the research evidence and empirical data) to meet the agreed priorities in each of the topic areas. The rationale for highlighting the importance of these underlying frameworks is that – as a number of influential researchers have proposed – behaviour does not occur by chance but is guided by ‘mental models’ and intrinsic ‘theories of action’. A key part of our assessment of the boundary-spanning processes under study will therefore be to surface the mental models/theories in action that the participants are acting on. We will explore whether the models imparted during the case study have actually been translated into practice and are appropriate for facilitating knowledge exchange and leading, and spreading and sustaining high quality health care on the ground.
Strategy for reviewing literature:
Phase I: Literature review (see flow diagram in Annex 1): our literature review of key management, organisation and knowledge management journals and books will update and extend the previous review undertaken by the lead applicant and colleagues by identifying state of the art concepts, models and theories in relevant fields and establish the form and extent to which these are present in the selected case study. A search of the literature will be conducted using key electronic databases including Medline, the Applied Social Sciences Index and Abstracts (ASSIA), and the Web of Science. Searches will include a wide range of ‘boundary-spanning’ synonyms in any team context in the health care sector, and also include hand-searching of the key management, organisation and knowledge management journals and texts. The search will then be extended to additional terms to include ‘multidisciplinary’, ‘interprofessional’ ‘healthcare’, ‘teamwork’, ‘collaboration’ and ‘primary care’ synonyms alone and in combination. Through the scoping phase search terms may be changed to provide the most relevant references for the health care context. In addition to this conventional literature review we would conduct a review and content analysis of other relevant NHS programmes or projects seeking to facilitate knowledge exchange and support vertical and horizontal integration of health care services; this will enable us to identify and compare key themes, focal knowledge and skills, and delivery methods. This will help reveal where our chosen case study is unique, and identify any differences in themes, focal skills and methods. This scoping review would be undertaken primarily through the relevant formal and informal networks.
c. Data collection
(See flow diagram in Annex 1 for summary of six phases to the research.).
Our approach to data collection and analysis will be to use a preliminary theoretical framework drawn from the literature review; data analysis will be a combination of induction (data-driven generalisation) and deduction (theory-driven exploration of hypotheses). This approach has been used previously by organisational researchers in the NHS. Our fieldwork will seek to provide a ‘close-to’ record of what happens once the boundary-spanning groups are working in the four topic areas. In order to capture this we will (a) study the cohort of boundary-spanning groups throughout the project by means of a combination of all of the various qualitative data collection methods described below, and (b) assess the value of the constituent parts of the project (for example, the leadership training, opportunities for joint reflection on amalgamated data, cycles of inquiry and action, and work on identified quality improvement projects) from the perspective of the participants themselves by means of semi-structured interviews and participant diaries. We will pay equal attention to capturing instances of (a) knowledge creation and exchange between different sectors, organisations and professions and then prospectively track how these lead (or not) to the implementation of improvements in the quality of service provision, and (b) the barriers to such processes.
Phase 2: Induction, familiarisation and relationship building: firstly, we would make contact and meet with the formal leaders of the WI project and identify early ‘key informants’ associated with each of the four topic areas – including voluntary and community groups and service users – to help get an early ‘lie of the land’ and begin to develop relationships and clarify expectations and fruitful lines of inquiry. We would also conduct a contextual inquiry to gain an appreciation of the socio-organisational environment within which the boundary-spanning processes we will be studying are situated and embedded. This will include discussions with participants to recapitulate on the history, origins and rationales of the project and understand the contexts within which it has unfolded to date. It should be noted that we would anticipate that much of this familiarization and relationship building will have been completed before a research grant may be awarded through our ongoing attendance at the management team meetings for the project from November 2009 onwards. Secondly, we would undertake a content analysis of the documentation relating to the WI project to: a) identify aims and objectives, key terms, themes and methods being employed, and b) begin to surface, describe and make explicit the ‘espoused’ theories and models underlying the chosen approach to boundary spanning (assumptions, values, concepts). As argued earlier, making the (often) implicit explicit in this way will be crucial to the evaluation process. As part of this first phase we will be able to draw on secondary data provided, including routine data, business plans, previous related schemes and any evaluation reports.
Phase 3: Scoping Observation and Tool Design: to help inform our overall study of the impact of boundary-spanning processes we will begin our scoping observations as soon as ethics is approved. Individuals involved in the boundary-spanning intervention under study will be conducting focus groups with their own established patient reference groups to collect the perceptions of services provided for patients and their informal carers. As part of the intervention, focus groups will also be initiated with staff and practitioners in local GP surgeries to determine what service improvements may be worth developing and delivering. Discussions between team members at these focus groups, and at their team meetings, will be observed, and it is expected that this will be an iterative process throughout the intervention. Further, our research interviews (see Phase 4) with team members who conducted and participated in focus groups will deepen our understanding of how sectoral, organisational and professional boundaries impact upon the lived experiences of staff and practitioners, and how efforts to enable vertical and horizontal integration of services might improve those experiences; the findings from the focus groups that are undertaken as part of the boundary-spanning intervention under study will therefore help us both refine our overall research approach (including assisting with the design of several of our later research tools) and inform our final evaluation of the project. We will conduct a Knowledge, Attitudes and Practices (KAP) questionnaire survey relating to the four topic areas (and any additional topic areas) which will be sent to a stratified, random sample of named staff (including GPs, nurse practitioners and other staff groups) in (a) each of the general practices in Westpark, (b) the remaining practices elsewhere in the wider PCT, and (c) practices in neighbouring primary care trusts. KAP studies are highly focused and seek to measure changes in what is known, believed and done in relation to a particular topic. In this vein the questionnaire will be designed to assess: what respondents know about available local services relating to the four topic areas; what they think about these services; and the ways in which they demonstrate their knowledge and attitudes through their actions (in terms of, for example, making referrals, advice-seeking, collaboration and giving information to patients). The questionnaire will also directly explore respondents' views as to the nature and extent of the vertical and horizontal integration of services in relation to the four topic areas, the formal and informal networks of which they are part relating to each topic area, and any specific knowledge exchange activities in which they are already involved. The questionnaire will be designed by the core research team in conjunction with local stakeholders (ensuring a wide range of perspectives) and piloted with staff from 3 general practices in Coxford and a neighbouring PCT.
Phase 4: Programme engagement and immersion (‘deep dive’) and ‘thick/rich description’: following our initial assessment and the design of our research tools, our in-depth qualitative fieldwork will comprise: non-participant observation, participant interviews, participant diaries, and ongoing collation and analysis of project-related documentation. All of our qualitative research will be grounded in the real-life experiences and events of the boundary-spanning individuals and groups, and the participants in the wider project in each of the four topic areas; this ‘actor centred’ approach will allow us to focus on the interactive, pedagogic and political processes which shape the individual (and collective) development and impact of the boundary-spanning individuals and teams (thereby taking in the ‘facts on the ground’). Given that knowledge is mainly tacit knowledge and is shared face-to-face in real time as problems arise, it will be necessary to complement a standard interview-based approach with observation of knowledge exchange and creation within the case studies. This would involve observing the boundary-spanning individuals and groups in situ; two members of the research team would therefore attend the (a) action learning sets and (b) stakeholder conferences to observe them in action and to interact informally and get ‘live commentary’ from those who are participating in them. Contemporaneous field notes would be supplemented by the use of either an audio diary or written notes by the researchers immediately after each observation ‘event’. These field notes and audio diaries will be analysed (see section below) as part of the overall research evaluation. In parallel to the observational fieldwork we would undertake tape-recorded, semi-structured participant interviews in order to compare what was/is being provided in terms of support for cross-boundary knowledge exchange and creation (and the way it was/is provided) with what participants felt they needed and wanted. The specific questions to be asked at these interviews will be developed and refined as the data collection process unfolds and will, wherever possible, be ‘grounded’ in critical incidents and the real-life experiences and events of participants. Questions will however largely focus on the ‘how’ and ‘why’ to elicit rich information about boundary spanning and knowledge exchange processes targeted at the improvement priorities identified in each of the topic areas, and will include exploration of the interactions of stakeholders with each other, and highlight any barriers to knowledge sharing between stakeholders. Selecting participants to be interviewed will be via a ‘360-degree’ approach for systematic coverage of the whole system; the four leaders of the boundary-spanning groups in each of the topic areas would be the focus of the approach and the first to be interviewed. The ‘360-degree’ method for gathering feedback is often associated with annual performance appraisals of staff by seeking input from all members of an individual's work group, including those with both higher and lower levels of line authority and those serving in different roles. For the purposes of this research, we will apply the concept of ‘360-degree’ to identify participants to interview across the sectoral, professional and organisational boundaries represented within the project; in this way all participants being interviewed are considered key stakeholders in the boundary-spanning group work. This will mean that any individuals who come into contact with one or more of the four boundary spanner leaders as a direct consequence of the boundary-spanning group work during the case study would be invited to participate; this might include hospital consultants, GPs, nurses, managers and voluntary sector workers. Where relevant we would conduct repeat interviews with key individuals and members of the groups at various points in order to monitor any change of attitudes or experiences over time. The qualitative fieldwork will also include in-depth, embedded case studies of four individual boundary spanners (the leader and two other members) drawn from each of the four topic areas to enable an assessment of (a) the impact of the project on the individual development of the participants, as well as (b) the impact of the boundary-spanning activities on a sample of specific quality improvement priorities pertaining to their specific topic area. We will adopt an ‘autoethnography’/narrative autobiography approach that will draw largely on the self-completed diaries that members of the boundary-spanning groups will be asked to maintain as part of their training and activities throughout the project. Diaries as a research method are ideal for capturing details that exist in complex social structures, beyond so-called technical work or formal procedures. As an ethnographic method, diaries can provide scientific observations in situations where a researcher cannot be present and capture reflections upon interpersonal processes. Other than the nominated leaders of the four groups, at least two additional boundary spanners from each of the four topic areas who will be invited to complete a diary will be identified by their roles which cross across known organizational, sectoral and/or professional boundaries; each will be asked to record weekly to fortnightly diaries which address knowledge, attitudes and practices in their work and how they perceive these to be changing (or not) as a result of the project (with specific reference to improving the vertical and horizontal integration of services). Diaries will be brief and semi-structured, directing responses to a few specific questions about progress towards self-defined goals over time, reflection about knowledge exchange and creation processes within and across groups, and include an open-ended question allowing for subjective narrative. Professional time spent recording diaries will be kept brief to ensure on-going involvement of participants. Further, at the onset of the study, and in an effort to decrease attrition due to time burden, respondents will be invited to collaborate in formalizing the diary design to ensure the most convenient format and timing for diary recording. Finally, as part of the qualitative fieldwork we will collect and analyse relevant documentation such as the minutes of meetings and email discussion lists on an ongoing basis.
Phase 5: End of project evaluation: this will comprise a repeat of the earlier questionnaire survey, secondary analyses of routine datasets and our own patient & carer focus groups. We will repeat our questionnaire survey in (a) each of the general practices in Westpark, (b) the remaining practices elsewhere in Coxford, and (c) practices in neighbouring primary care trusts, and observe any differences in responses from each of – and between – these groups compared with the baseline assessment (see above). As an integral part of the WI project will be monitoring on a PCT-wide basis the following routine datasets with regard to patient contacts in each of the four topic areas: (a) EMIS/Vision (software systems used for practice management and patient records in primary health care), (b) RiO (a clinical information system for community staff which is being deployed throughout London as part of the National Programme for IT), (c) Adastra (a patient management system for unscheduled care across England that includes episodes of patient care in, for example, GP Out-of-Hours, Walk-in Centres, Minor Injuries Units, and Community Nurse Teams), and (d) Secondary Uses Service (SUS) including Hospital Episode Statistics (HES) which allows practices to see how the way they commission services and refer patients compares with other practices locally and nationally, and also enables them to see how they care and treat on patients with particular conditions compares to other practices. The data to be monitored by the PCT will be determined by the priorities for improvement identified by participants in the project once the work in the topic areas begins in spring 2010. We will conduct secondary analyses of these datasets which will focus specifically on indicators that we would hypothesise – as a result of the boundary-spanning processes that we observe during our fieldwork – should see improvements in the quality of patient care over the course of the project in the participating general practices in Westpark (compared with the PCT as a whole). However, whilst knowledge exchange can empower an individual to avoid costly referrals it can also potentially raise awareness of hidden problems and precipitate referrals; our secondary analyses of the datasets will examine both of these scenarios.
Finally, we will undertake focus groups at the end of the project with patients & carers from each of the topic areas. These focus groups will explore the perceptions of the patients & carers as to the real (or perceived to be likely) impact of the improvements made and reported as part of the project on their own experiences of care and treatment in Westpark (with particular regard to the impact on patients & carers of specific attempts to improve the vertical and horizontal integration of services).Their experiences and degree of integration of services will be explored through semi-structured questions.
d. Data analysis
As stated in the ‘aims and objectives’ above, our research hypothesis is that boundary-spanning processes will stimulate the exchange and creation of knowledge between sectors, organisations and professions and that this will lead to service improvements (as measured by a range of quality indicators including patient and carer experience). We will describe and assess the perceived value of boundary-spanning processes in each of the four topic areas by posing the following overall question: to what extent – and by what vertical and horizontal processes – has boundary spanning facilitated knowledge exchange and creation across sectoral, organisational and professional boundaries, and what impact has this had on the quality of patient care? In seeking to test our hypothesis we will undertake four specific and related activities (details of which are provided above): (i) provide a rich ethnographic account of all the boundary-spanning processes (horizontal and vertical) that occur within each of the four topic areas as we observe and follow them throughout the duration of the overall project; (ii) monitor a range of routine datasets and quality indicators pertaining to the four topic areas across the whole PCT, including making comparisons between (a) the general practices in Westpark and (b) practices from the remainder of the PCT; (iii) undertake a repeated project questionnaire survey of selected staff in (a) each of the general practices in Westpark, (b) practices elsewhere in Coxford, and (c) practices in neighbouring PCTs; and (iv) conduct focus groups with patients and carers in each of the four topic areas as to their experiences of care and treatment.
The research team will iteratively analyse the data from the four activities above and share our evolving interpretations as the research unfolds, jointly exploring the significance of the findings and building theory from our qualitative, quantitative and secondary data along the lines described by Eisenhardt. In terms of our final findings our intention is to generalize in a theoretical/analytical rather than statistical manner. The research team is experienced in the use of framework analysis as a means of managing and organizing complex qualitative datasets and we will use this approach in order to assist our development of key themes reflecting the perceptions of interviewees from the various sources described above, our observational data and issues evident in documentation. Transcripts, fieldnotes and document content analysis will be entered into ‘Framework’ software to assist data interpretation. In presenting our findings, temporal bracketing and narrative strategies will be utilized in a holistic analysis so that data remains contextualized. Our interpretation of the data will be checked through feeding back our initial findings to the leaders and participants in the project. Completion of this process is essential if the proposed combination of (largely) case study-based research is to result in more than interesting vignettes from each of the topic areas and boundary-spanning groups. Our overall aim is to make a wider contribution to the theory and practice of implementing quality improvements through the vertical and horizontal integration of services.
Plan of Investigation
Annex 1 presents an overview of the research timetable and its six constituent phases. The milestones in column one in the table below provide an overview of activities over the duration of the WI project. Column two in the table indicates when the various research activities will be undertaken but is not intended to reflect the ongoing observational work, or sharing and sense-making of emerging findings between the research team that will characterise the work throughout. The WI project began in Autumn 2009 with focus groups led by the PCT to understand different perspectives and a Stakeholder Conference to consider these different perspectives; this latter event was attended and observed by a member of the proposed research team (Robert) and the proposed full-time researcher on the proposal (Nasir) was an invited observer of the management team for the WI project and attended stakeholder meetings in the period December 2009 to spring 2010. An application for NHS research ethics approval was initially submitted March 2010 and approved in July 2010 (see section below).
| WI project milestones | Planned research activities (excluding ongoing observational fieldwork and sense-making) |
|---|---|
| 2010 Spring | |
| Rapid Appraisals for deep
understanding Systems modelling. Set up database searches Learning Events Stakeholder Conference to shape pilot changes Residential workshop |
Update and extend literature review Map contemporary projects Induction and familiarization:
|
| 2010 Summer/Autumn/Winter | |
| Focus groups with stakeholders Stakeholder Conference to agree plans Pilot changes Stakeholder Conference to feedback conclusions and start a new cycle of inquiry and action |
Baseline assessment and tool design:
|
| 2011 Spring/Summer/Autumn | |
| Learning Events & Web-based Educational
materials Stakeholder Conference to disseminate findings |
End of project evaluation
|
| 2011 Autumn/Winter to 2012 Spring | |
Analysis, writing up and dissemination:
|
|
Service users/public involvement:
Appropriate means of access for exploring patient experience will be consistently discussed in the field and within the research team, always with consideration of ethical parameters. The boundary-spanning intervention under study (through four multidisciplinary teams) will design and implement their own service user involvement thorough invitations to attend topic specific focus groups and local stakeholder events. Our field-based researcher will collect data pertaining to patient and public involvement in the intervention through non-participant observation. The WI project will be evaluated for its ability to include services users in their iterative cycles of service improvement by each of the four topic groups. Additionally, at the end of our study we will conduct focus groups with patients and carers in the local area to qualitatively explore their experience of efforts to integrate care across sectoral, organisational, and professional boundaries.
Annex 1: Flow diagram
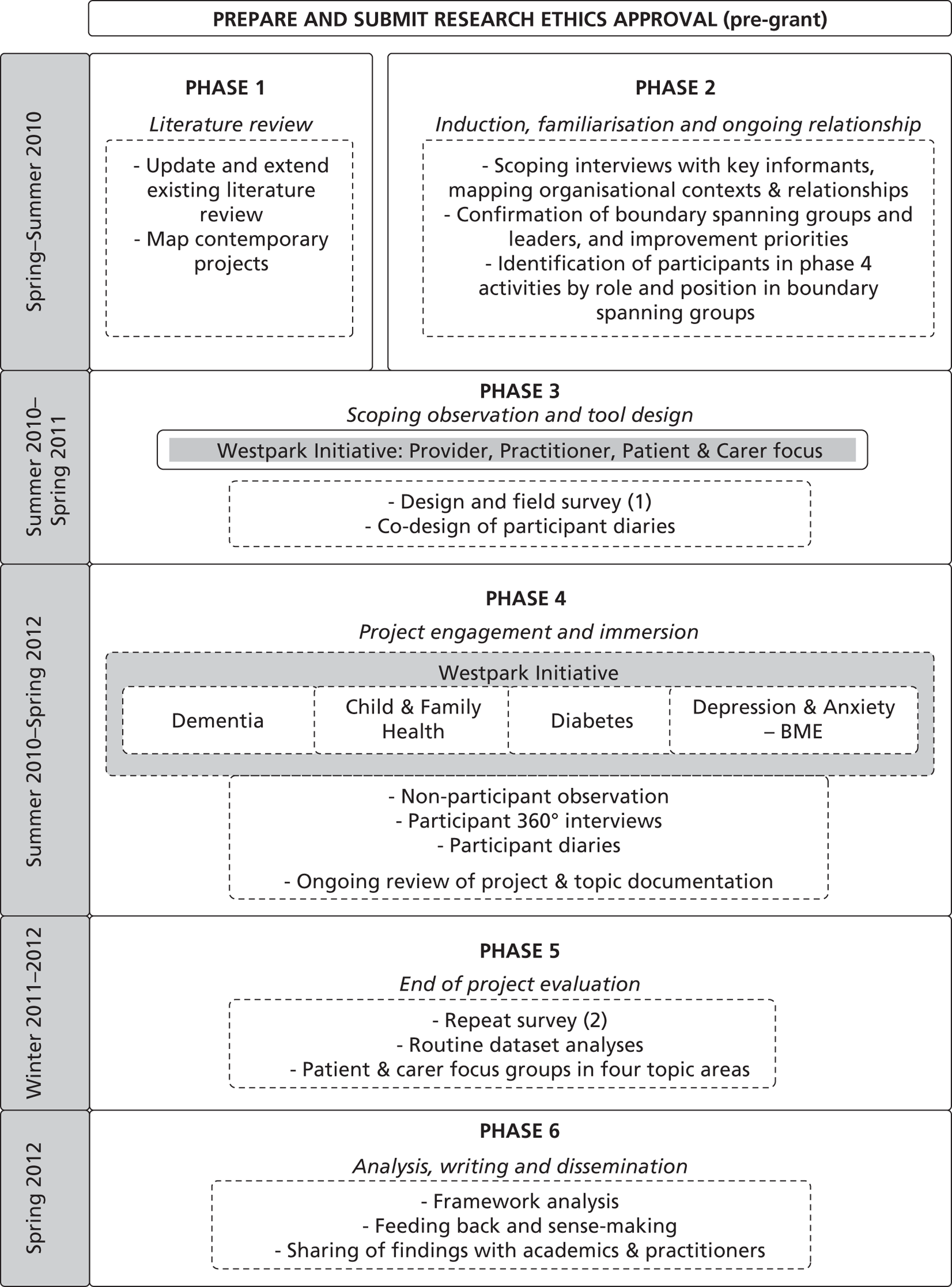
Appendix 3 Observation
| Date | Event | Purpose (researcher tasks) | Hours |
|---|---|---|---|
| 25 November 2009 | Stakeholder event | Observation; scoping | 4 |
| 10 December 2009 | WI team leader meeting | Observation; scoping | 2.5 |
| 10 February 2010 | Stakeholder event | Observation | 3 |
| 10 February 2010 | WI team leader meeting with GP founder | Observation; also, conversations with team leaders after event | 2.0 |
| 11 February 2010 | Masterclass | Observation | 4.5 |
| 10 March 2010 | Masterclass | Observation | 4 |
| 22 April 2010 | Stakeholder event | Observation | 5 |
| 28–30 April 2010 | Off-site retreat | Observation; scoping; after-meeting conversations with participants | 34 |
| 17 June 2010 | Masterclass | Observation | 4 |
| 17 June 2010 | Applied research unit meeting | Observation | 2 |
| 23 June 2010 | Meeting with WIP14N | To discuss possible outcome measures | 1 |
| 23 June 2010 | Meeting at PCT: research team with GP Founder | To discuss possible outcome measures | 2 |
| 23 June 2010 | Meeting with WIP11K | To discuss possible outcome measures | 1 |
| 23 June 2010 | Meeting with WIP13M | To discuss possible outcome measures | 1 |
| 23 June 2010 | Joint PBC meeting | Observation | 3 |
| 30 June 2010 | Telephone conversation WIA5E | To discuss how meeting evaluations are carried out internally | 1 |
| 1 July 2010 | CLAHRC event | To observe anxiety and depression team; discussion of possible outcome measures | 8 |
| 7 July 2010 | Meeting with WIA16P | To discuss possible outcome measures | 1 |
| 7 July 2010 | Masterclass | Observation | 2 |
| 7 July 2010 | Meeting with WIL2B | To discuss possible outcome measures | 1 |
| 7 July 2010 | Applied research unit meeting | Observation | 1 |
| 8 July 2010 | Stakeholder event | Observation | 4 |
| 6 October 2010 | Meeting with GP founder | To discuss outcome measures | 4 |
| 8 October 2010 | GP conference – GP founder presents to wide audience, presentation of model | Observation | 2 |
| 8–9 October 2010 | GP conference | Observations of GP founder interacting with other GPs | 8 |
| 20 October 2010 | Team leader meeting – planning session | Observation | 4 |
| 22 October 2010 | Meeting with GP founder | Discuss conceptual model (codesign tools) | 2 |
| 17 November 2010 | Local GP meeting | GP consortia topics (piloting tools) | 3 |
| 18 November 2010 | Stakeholder event | Presenting/planning (codesign tools) | 7 |
| 25 November 2010 | Stakeholder event | Presenting/planning (recruiting) | 7.5 |
| 14 January 2011 | WI team meeting | Planning session | 3.5 |
| 3 February 2011 | Diabetes staff training | Led by boundary-spanning team leader | 4 |
| 3 February 2011 | Interview WIL1A | Data collection | 1 |
| 4 February 2011 | Interview WIL2B | Data collection | 4 |
| 8 February 2011 | Interview WIL3C | Data collection | 1.5 |
| 8 February 2011 | Interview WIL4D | Data collection | 2 |
| 8 February 2011 | Interview WIA5E | Data collection | 1 |
| 10 February 2011 | Mental health staff training | Led by boundary-spanning team leader | 4 |
| 12 February 2011 | Interview WIG6F | Data collection | 2.5 |
| 14 February 2011 | Interview WIL7G | Data collection | 2 |
| 14 February 2011 | Interview WS32012 | Data collection | 3 |
| 17 February 2011 | Staff training – data management | Led by GP founder | 2 |
| 18 February 2011 | Interview WIL9I | Data collection | 2 |
| 21 February 2011 | Interview WIP10J | Data collection and tour | 3 |
| 23 February 2011 | Interview WIP11K | Data collection | 2 |
| 23 February 2011 | Interview WIP12L | Data collection and tour | 2.5 |
| 1 March 2011 | Interview WIP13M | Data collection | 1 |
| 1 March 2011 | Interview WIP14N | Data collection | 1 |
| 1 March 2011 | Interview WIP15O | Data collection | 1 |
| 3 March 2011 | Child and family health services training event | Led by boundary-spanning team leader (attended by GR) | 4 |
| 10 March 2011 | Dementia training event | Led by boundary-spanning team leader | 5 |
| 17 March 2011 | Interview WIA16P | Data collection | 1.5 |
| 31 March 2011 | Stakeholder event | (Researcher presents) | 5 |
| 5 April 2011 | Interview WIA17Q | Data collection | 1.5 |
| 7 April 2011 | Local GP meeting | Local planning session | 6.5 |
| 7 April 2011 | Conversation with patient/citizen | At local planning session | 0.5 |
| 7 April 2011 | Interview WIP18R | Data collection | 2 |
| 8 April 2011 | Interview WIP19S | Data collection | 2 |
| 8 April 2011 | Interview WIP20T | Data collection and tour | 2.5 |
| 8 April 2011 | Interview WIP21U | Data collection | 1 |
| 11 May 2011 | Retreat | Planning workshops | 6 |
| 12 May 2011 | Retreat | Groups, seminars, meals | 16 |
| 13 May 2011 | Retreat | Groups, presentations | 10 |
| 24 May 2011 | Meeting with diabetes team leader | Data discussion | 2 |
| 25 May 2011 | Diabetes staff training | Observation; boundary-spanning team leader observed | 5 |
| 13 June 2011 | Interview WIA22V | Data collection | 1 |
| 13 June 2011 | Interview WIA23W | Data collection | 1.5 |
| 20 June 2011 | Meeting with diabetes team leader | Data discussion | 1 |
| 23 June 2011 | WI leader planning session | Regroup | 3 |
| 23 June 2011 | Interview WIL24X | Data collection | 2 |
| 24 June 2011 | Interview WIP25Y | Data collection | 1 |
| 24 June 2011 | Meeting with WI founder | Data discussion | 3.5 |
| 6 July 2011 | Mental health team leaders attend CLAHRC event | Boundary-spanning team leader presents and group attends | 9 |
| 7 July 2011 | WI leader planning meeting | Planning | 3 |
| 21 July 2011 | Local GP meeting | Local planning session (attended by GR) | 3 |
| 8 September 2011 | Diabetes team meeting | Team planning session | 3 |
| 9 September 2011 | Talk with diabetes team leader | Data discussion | 2 |
| 19 September 2011 | Talk with diabetes team leader | Data discussion | 2 |
| 27 September 2011 | Local GP meeting | Planning session | 3 |
| 29 September 2011 | Mental health team leaders attend CLAHRC event | Boundary-spanning team leader presents and group attends | 3 |
| 29 September 2011 | Diabetes staff training | Boundary-spanning team leader presents | 4.5 |
| 30 September 2011 | Interview (repeat) WIL2B | Data collection | 3 |
| 30 September 2011 | Integrated care organisation meeting | Boundary-spanning team project | 2.5 |
| 4 October 2011 | Interview WIP28BPD | Data collection | 1.5 |
| 7 October 2011 | Meeting with GP founder | Discuss data collection | 4 |
| 10 October 2011 | Interview WIP29C | Data collection and tour | 3 |
| 11 October 2011 | Interview WIP30D | Data collection | 1.5 |
| 11 October 2011 | Interview WIP31E | Data collection | 1 |
| 14 October 2011 | Interview WIP32FA + WIP32FB | Data collection | 3 |
| 17 October 2011 | Interview WIP33G | Data collection | 2 |
| 19 October 2011 | Interview (follow-up) WIP10J | Data collection | 2 |
| 25 October 2011 | Interview WIP34H | Data collection | 1 |
| 31 October 2011 | Interview WIP 35I | Data collection | 1 |
| 2 November 2011 | Meeting with GP founder | Discuss data collection | 1 |
| 9 November 2011 | Interview WIP36J | Data collection | 1.5 |
| 11 November 2011 | Meeting with GP founder | Discuss data collection | 1 |
| 16 November 2011 | Meeting with team participants | Discuss data collection | 1 |
| 17 November 2011 | Meeting with GP founder | Discuss data collection | 1 |
| 18 November 2011 | Meeting with GP founder | Discuss data collection | 1 |
| 21 November 2011 | Interview WIP37K | Data collection | 1 |
| 22 November 2011 | Local GP meeting | Observe | 3 |
| 25 November 2011 | Meeting with participant | Discuss current issues | 2 |
| 2 December 2011 | Meeting with GP founder | Discuss data collection | 2 |
| 5 December 2011 | Meeting with diabetes team leader | Discuss data collection | 1 |
| 12 December 2011 | Meeting at PCT | Discuss secondary data collection | 3 |
| 19 January 2012 | Telephone conversation – public health | Discuss current issues/access | 1 |
| 20 January 2012 | Meetings at PCT/interviews: follow-up WIL4D, WIL24X | Discuss current issues, data collection | 6 |
| 14 February 2012 | Interview WIP38L | Data collection | 2 |
| 16 February 2012 | Focus group at GP surgery | Observe staff, setting, patients | 2.5 |
| 29 February 2012 | Telephone conversation – patient representative | Discuss current issues/access | 1 |
| 26 March 2012 | Meeting with GP founder | Discuss current Issues | 3 |
| 28 March 2012 | Meeting at PCT | Researcher panel discussions with staff | 3 |
| 2 April 2012 | Meetings at well-being service | Discuss secondary data collection | 1.5 |
| 2 April 2012 | Interview (repeat) WIP18R | Data collection | 2 |
| 16 May 2012 | Mental health training in Coxford | Observe | 3.5 |
| 29 May 2012 | Interview WIP39M | Data collection | 4 |
Appendix 4 Interview schedules
Thank you for taking the time to meet with me for this research study. This interview is being recorded. This conversation, and others, will be transcribed and analysed by a research team at King's College London and the National Nursing Research Unit. Your responses with identifiable information will not be shared with others outside the research team or with any NHS staff. The recorder is on.
-
Please tell me about the WI. What is it all about?
-
I'd like to ask you some questions about your involvement with the WI project.
-
(a) When did you first hear about the project?
-
(b) Why did you get involved with the WI?
-
(c) At that time, what did you hope the WI might accomplish?
-
-
Now that you have been involved with the WI for a while, what do you think about how it has affected you?
-
(a) In what ways has your thinking changed due to this project?
-
(b) In what ways has your daily work changed due to this project?
-
(c) In what ways has your workplace changed due to this project?
-
(d) In what ways has the quality of care for your patients changed due to this project?
-
-
What has gone well, been improved or been implemented because of your involvement in the WI?
-
(a) What are the achievements? Can you give specific examples?
-
-
What has helped or facilitated the projects you have been involved with as part of the WI?
-
(a) Can you give specific examples?
-
-
What barriers or challenges have you experienced as part of your involvement in the WI?
-
(a) What are the disappointments? Can you give specific examples?
-
-
If the WI had never happened what would be different now?
-
(a) For you?
-
(b) For your patients?
-
(c) For the system in which you work?
-
Could you describe an example?
-
-
-
Up to now, what do you think has been the overall impact of the WI?
-
(a) Why?
-
-
Given everything that is happening now, is the WI still relevant today?
-
(a) On a scale from 0 to 10, 0 being not relevant at all and 10 being the most relevant, how would you rate the relevance of the WI?
-
(b) Why or how so?
-
-
Is there anything else you would like to share, as related to your work with the WI?
-
Is there anyone that you would suggest we need to talk to about this subject?
Thank you very much for your time and willingness to take part in this research study. I am turning off the recorder now.
Appendix 5 Interviewees
| Participant by ID | Date | WI team | Professional role | Role in WI | Interview type (first, follow-up or post diary) | Diary (yes or no) | Westpark or Coxford based | Current clinical role |
|---|---|---|---|---|---|---|---|---|
| WIL1A | 3 February 2011 | CFS | Former community matron | Team leader | First | No | Westpark | No |
| WIL2B | 4 February 2011 | All | GP; clinical lead | Founder and leader | First | No | Coxford | Yes |
| WIL3C | 8 February 2011 | Dementia | Specialist practitioner nurse | Team coleader | First | No | Westpark | Yes |
| WIL4D | 8 February 2011 | Diabetes | PBC manager | Team leader | First | Yes | Coxford | No |
| WIA5E | 8 February 2011 | All | Commissioner/administrator | Administrator | First | No | Coxford | No |
| WIG6F | 12 February 2011 | All | GP; GP tutor | Participant | First | No | Coxford | Yes |
| WIL7G | 14 February 2011 | ADBME | BME therapy team leader; nurse | Team leader | First | No | Westpark | Yes |
| WS32012 | 14 February 2011 | None | Therapist; organisational behaviourist | External consultant | First | No | None | Yes |
| WIL9I | 18 February 2011 | Dementia | Assistant director mental health trust | Coleader | First | No | Westpark | Yes |
| WIP10J | 21 February 2011 | ADBME | CBT therapist; mental health worker | Team member | First | Yes | Westpark | Yes |
| WIP11K | 23 February 2011 | ADBME | Community worker | Team member | First | No | Westpark | Yes |
| WIP12L | 23 February 2011 | CFS | Integrated service manager; child and family services organisation | Team member | First | Yes | Westpark | Yes |
| WIP13M | 1 March 2011 | All | Interim director of ICT | Participant | First | No | Coxford | No |
| WIP14N | 1 March 2011 | IT | PBC manager | Team leader | First | No | Coxford | No |
| WIP15O | 1 March 2011 | None | Head of partnerships and diversity | Participant | First | No | Coxford | No |
| WIA16P | 17 March 2011 | All | PBC manager | Administrator | First | No | Coxford | No |
| WIA17Q | 5 April 2011 | None | Clinical director | Participant | First | No | Coxford | No |
| WIP18R | 7 April 2011 | Dementia | Social worker | Team leader | First | Yes | Westpark | Yes |
| WIP19S | 8 April 2011 | None | Learning and development manager | Participant | First | No | Westpark | No |
| WIP20T | 8 April 2011 | None | Co-ordinator, Westpark Community Alliance | Participant | First | No | Westpark | No |
| WIP21U | 8 April 2011 | CFS | Strategic manager | Participant | First | No | Coxford | No |
| WIA22V | 13 June 2011 | None | Commissioning manager – older people | None | First | No | Coxford | No |
| WIA23W | 13 June 2011 | None | Director of Quality and Clinical Leadership; former nurse | None | First | No | Coxford | No |
| WIL24X | 23 June 2011 | CFS | Commissioner; midwife | Team leader | First | Yes | Coxford | No |
| WIP25Y | 24 June 2011 | None | Head of medicine management; pharmacist | Participant | First | No | Coxford | No |
| WIP26ZPD | None | ADBME | CBT therapist; mental health worker | Participant | None | No | Westpark | Yes |
| WIP27APD | None | ADBME | CBT therapist; mental health worker | Participant | None | Yes | Westpark | Yes |
| WIP28BPD | 4 October 2011 | ADBME | Community worker | Participant | Post diary | Yes | Westpark | Yes |
| WIP29C | 10 October 2011 | Diabetes | Community services | Participant | First | No | Westpark | No |
| WIP30D | 11 October 2011 | ADBME | Mental health home treatment | None | First | No | Coxford | Yes |
| WIP31E | 11 October 2011 | ADBME | Specialist well-being advisor | Participant | First | No | Coxford | Yes |
| WIP32FA | 14 October 2011 | None | Retired chief nurse | None | First | No | Coxford | No |
| WIP32FB | 14 October 2011 | None | Retired medical officer | None | First | No | Coxford | No |
| WIP33G | 17 October 2011 | Diabetes | Diabetic specialist nurse | None | First | No | Coxford | Yes |
| WIP34H | 25 October 2011 | None | Pharmacist | None | First | No | Coxford | Yes |
| WIP35I | 31 October 2011 | Diabetes | Lead dietician | None | First | No | Westpark | Yes |
| WIP36J | 9 November 2011 | CFS | Commissioning – children | Participant | First | No | Coxford | Yes |
| WIP37K | 21 November 2011 | Mental health | OT rehabilitation staff | Participant | First | Yes | Coxford | Yes |
| WIP38L | 14 February 2012 | CFS | Public health; health training co-ordinator | Participant | First | No | Coxford | No |
| WIP39M | 29 May 2 2012 | Mental health | Head of service | Participant | First | No | Westpark | Yes |
| WIL2BFU | 30 September 2011 | All | GP; clinical lead | Leader | Follow-up | No | Coxford | Yes |
| WIL4DPD | 20 January 2012 | Diabetes | PBC manager | Leader | Post diary | Yes | Coxford | No |
| WIP10JPD | 19 October 2011 | ADBME | CBT therapist; mental health worker | Team member | Post diary | Yes | Westpark | Yes |
| WIP18RPD | 2 April 2011 | Diabetes + ADBME | Social worker | Participant | Post diary | Yes | Westpark | Yes |
| WIL24XPD | 20 January 2012 | CFS | Commissioner; midwife | Participant | Post diary | Yes | Coxford | No |
| FG1DM01 | 16 February 2012 | Diabetes | Patient | Patient focus group | None | No | Westpark | No |
| FG1DM02 | 16 February 2012 | Diabetes | Patient | Patient focus group | None | No | Westpark | No |
| FG1DM03 | 16 February 2012 | Diabetes | Patient | Patient focus group | None | No | Westpark | No |
| FG1DM04 | 16 February 2012 | Diabetes | Patient | Patient focus group | None | No | Westpark | No |
| FG1DM05 | 16 February 2012 | Diabetes | Patient | Patient focus group | None | No | Westpark | No |
| FG1DM06 | 16 February 2012 | Diabetes | Patient | Patient focus group | None | No | Westpark | No |
| FG1DM07 | 16 February 2012 | Diabetes | Patient | Patient focus group | None | No | Westpark | No |
| FG1MH01 | 19 March 2012 | ADBME | Patient | Patient focus group | None | No | Westpark | No |
| FG1MH02 | 19 March 2012 | ADBME | Patient | Patient focus group | None | No | Westpark | No |
Appendix 6 Patient focus groups and patient and public involvement in the Westpark Initiative
Patient and public involvement was originally a core component of the boundary-spanning intervention under study. Indeed, the WI was launched with a stakeholder event to coproduce the topic areas and priorities within each topic. However, as we have described, the WI fragmented halfway through and, although its methods were adopted in various ways by other local initiatives, we subsequently observed how the patient groups that had initially been part of the original three topic groups drifted away. Capturing and explaining what happened to the original aspirations relating to PPI has nonetheless been a focus of our fieldwork.
We have had extensive research interactions with various local PPI groups that were, to varying extents, involved with the boundary-spanning intervention under study. We have conducted informal and formal interviews with members of many groups that represent patients in the local area, including Coxford LINk, a Westpark domestic violence community group, a Westpark child and family services organisation and individual patient representatives from local services and GP surgeries. Certain individuals from these and other patient groups were invited to specific stakeholder meetings – a component of the intervention under study – and our informal conversations with them have been captured in our field notes. Additionally, the semistructured interviews with community-based staff included asking the respondents to describe any impact of the intervention on the quality of patient care; efforts to measure outcomes related to patient care; and any increase in staff understanding of the patient perspective. In combination, these data sources allowed us to approach the impact of the intervention on patient experience from multiple perspectives (as in the 360-degree view that we suggested in our initial proposal) and to include this important outcome in our final report.
At the initial protocol stage a pre/post design exploring patients' experiences appeared to offer one approach to collecting data to address the aims of the study. But because of the fast-changing nature of the boundary-spanning intervention under study, as described in this report, it transpired that this approach was unlikely to have generated insights to inform our overall evaluation of the intervention. Our original plans to conduct pre and post patient focus groups have therefore not been fully implemented. We also faced considerable challenges in establishing and conducting these focus groups in the specific topic areas (e.g. open invitations for patient groups to participate were found not to be a structured part of the intervention as we had initially anticipated). Our efforts to establish focus groups were pursued immediately after ethical approval was granted. At every subsequent stakeholder event team leaders, GPs and practice managers were approached by the research team to help identify appropriate ways to reach patients in their local practice areas; most agreed to help but follow-through was not forthcoming. The barriers we faced in recruiting patients to participate in focus groups at an early stage of our project are similar to those faced by the intervention itself; indeed, one of our findings is the lack of significant PPI in the intervention as a whole (including examples from our 361 hours of observational fieldwork in which clear opportunities for the teams to engage with, and involve, patient groups were not grasped).
Nonetheless, our qualitative data do include positive examples of PPI in the intervention. Also, although some patients had declined to be interviewed for our research, patient representatives have been central to the work of one of the topic groups – the anxiety and depression in BME populations group – and patient views have been incorporated in all of their outreach efforts and other initiatives. We have examined and reported their efforts in our final report.
The two patient focus groups that were completed at the end of the study further enhanced our understanding of how boundary-spanning activities more broadly were perceived and experienced by patients/carers. A focus group of diabetic patients from Westpark was held in February 2012. Seven people participated (Table 29).
| Patient | Diabetes type | Gender | Time since diagnosis |
|---|---|---|---|
| FG1DM01 | Type 2 | Female | 12 years |
| FG1DM02 | Type 1 | Female | 6 years |
| FG1DM03 | Type 2 | Male | ? |
| FG1DM04 | Type 2 | Female | 20 years |
| FG1DM05 | Type 2 | Female | 12 years |
| FG1DM06 | Type 2 | Female | 11 years |
| FG1DM07 | Type 2 | Male | ? |
Appendix 7 Patient and carer focus group discussion guide
INTRODUCTION SCRIPT: To be read by researcher/group facilitator:
You have been invited to take part in this research study because you have received care for diabetes in [Westpark]. Our study is looking at how links happen across organisations and how to make your health care better.
For this discussion group I will invite you to share as much or little as you feel comfortable sharing with the other patients and carers in this group. This conversation will be tape-recorded for only the researchers to hear. Any recording of you taken today will not be used without your express consent.
I cannot guarantee the confidentiality of the discussion groups. You may choose not to speak, or may leave the discussion at any time, for any reason, without explanation. I do ask that each you respect the experience of everyone else in the group by not sharing the stories you hear today with others outside of this room. Please raise your hand if you can agree with this ground rule. Thanks.
QUESTIONS FOR DISCUSSION:
-
Please introduce yourself and tell us how long you have had diabetes.
-
Thinking about your experiences as a diabetes patient, what have been some of the different services, staff, departments or types of care that you used recently?
-
Thinking back, what sticks in your mind about what went well about being able to receive different kinds of services from different kinds of clinicians or practitioners?
-
Thinking back, do you think you received good care? Why or why not?
-
Now think about what needed to happen so that you could get these different kinds of services.
-
(a) PEOPLE – Which staff have been MOST helpful to you?
-
Who helped you to get this service?
-
Did someone coordinate?
-
Was it this person's job assignment to help you?
-
Who helped you to know what was going to happen next?
-
Did you always know who to call if you weren't sure about something?
-
Can you give a specific example?
-
-
(b) PROCESSES – How well ORGANISED has your care been?
-
Was care co-ordinated for you – if so, can you describe how?
-
What sort of process had to happen so that you could get this service?
-
Was there some sort of structure in place to help you get this service? Can you describe it?
-
How well or poorly was information about your care shared between areas?
-
Did something happen that seemed unplanned but was helpful?
-
Were there any mix-ups? How were they solved?
-
Can you give a specific example?
-
-
(c) TIMING AND ANTICIPATION – Did everything go smoothly? How so?
-
Were there any misunderstandings? How were they sorted out?
-
How clear were your expectations of what might happen?
-
How uncertain were you about the next steps in your care?
-
Did something happen that you didn't expect?
-
Can you give a specific example?
-
-
-
If I had asked you these questions 12 months ago, with respect to a similar type of care, would the processes you described have been the same or different?
-
(a) If different – in what ways? What has changed?
-
-
Do you think the quality of care has improved over the last year? Have things gotten better?
-
Thinking back to the people and processes related to your care, what part of these services could have been better or improved upon? If you were asked to advise the NHS on what it should do about increasing linkages between people and sections of the organisation, for better patient care, what would you suggest?
-
When thinking about making good connections for better care, is there anything else you think we should know about?
-
Is there anything you would like to add?
CLOSURE SCRIPT: To be read by researcher/group facilitator:
Thank you very much for your time and willingness to share your experiences with us today. We will include your comments in our data to describe how patient care may be improved by boundary-spanning processes in health-care organisations.
Appendix 8 Diaries
Appendix 9 Staff knowledge, attitudes and practices survey
Staff knowledge, attitudes and practices survey (PDF download)
Appendix 10 Final codebook
List of abbreviations
- BME
- black and minority ethnic
- CBT
- cognitive–behavioural therapy
- CCG
- clinical commissioning group
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- CPD
- continuing professional development
- D&R
- Development & Research
- df
- degrees of freedom
- DNS
- district nursing service
- GEE
- generalised estimating equation
- GP
- general practitioner
- HbA1c
- glycated haemoglobin
- IAPT
- Improving Access to Psychological Therapies
- ICO
- integrated care organisation
- IMD
- Index of Multiple Deprivation
- IT
- information technology
- KAP
- knowledge, attitudes and practices
- MMSE
- Mini Mental State Examination
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PBC
- practice-based commissioning
- PCT
- primary care trust
- PPI
- patient and public involvement
- QIPP
- Quality, Innovation, Productivity and Prevention
- QOF
- Quality and Outcomes Framework
- R&D
- research and development
- SECI
- socialisation → externalisation → combination → internalisation
- WI
- Westpark Initiative
- YOC
- Year of Care