Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1801/1069. The contractual start date was in April 2011. The final report began editorial review in November 2013 and was accepted for publication in May 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Pinfold et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Study overview
This research study was carried out to understand how personal connections of social ties, activities and places of people with severe mental illness (SMI) were structured and had evolved in their local community. The purpose was to explore the impact of these connections on well-being, through people’s ability to utilise and exchange resources, and their influence on personal roles and identity. The study both mapped and documented what individuals described as important for well-being and explored the meaning of these connections; our epistemological approach worked between a realist stand point1 building on positivist traditions and a socially constructivist approach which emphasised changes over time and situated meanings. 2 Individual members of the research team understood the principles underpinning both of these approaches, and what they contributed to the research as a whole.
The study examined what happens in a personal network of people, place and activity connections using people’s own accounts; how community assets were used to support recovery from SMI; and the role of primary care and secondary mental health practitioners.
The research was interested in:
-
Inner resources: we approached this by describing the capacity within individuals to direct their own lives, make decisions and choices as well as reciprocally supporting others.
-
Personal relationships and social resources: we approached this by describing the personal relationships people had with others and the links and roles they had within social groups. These were positioned within specific sociocultural contexts and constitute a social framework that generates subjective meaning and value to life.
-
Meaningful activities and places as resources: we approached this by describing the everyday routines that people adopt and assessing those that were social or lone activities, those that were structured or unstructured, in meaningful place settings and their impact on well-being.
-
Organisational composition and collaboration: we approached this by describing formal organisations and groups existing within a local geographical area and the way in which these, through their practices, link together in terms of formally agreed or informally constituted working relationships.
The role of social networks for managing mental health and chronic illness has long been established. The Team for the Assessment of Psychiatric Services (TAPS) study in the 1990s3–5 documented the impact of deinstitutionalisation on the social networks of people with SMI. Studies of chronic illness have examined aspects of social support within social networks and particularly the role of the family with positive and negative impact on outcomes. 6,7 A recent conceptual framework for personal recovery in mental health8 identifies five processes including the importance of social networks as a dimension of connectedness, and having a purpose or meaning in life including roles and goals. It builds on previous conceptual work defining stages of recovery. 9,10 Having friends was important for recovery, and connecting with others through shared interests and activities can be therapeutic, although not all relationships and social interactions are experienced as positive or supportive. 11 Activities can provide structure and meaning, and the benefits of volunteering and work are well documented for people with SM1. 12 Conceptual definitions of recovery also emphasise the importance of personal responsibility in recovery – people as active agents in driving change in their lives. 9 The five ways to well-being approach13 highlights areas that are of interest for building social connections: connect, be active, take notice, keep learning and give.
People’s lives are affected by service structures, policy changes, the economy and other structural determinants. For people with SMI, primary care services and general practitioners (GPs)14 are increasingly important both as a monitor on physical health problems, incentivised through the Quality Outcomes Framework (QOF), and as a lead provider of care for people with mental health problems. Research has found a high proportion of cases of SMI are supported solely by a GP (31%) or with minimal secondary care input. 15 This was not a new finding. A review of the role of family practitioners reported about one-quarter of people with schizophrenia saw only their GP16 and only 64% of sampled service users were in contact with a psychiatrist. 17 However, there was a specific current discourse that many GPs were less keen on supporting people with SMI than other medical conditions,18 GPs lacked specialist knowledge and skills19 and they had clear ideas that the role should be limited to physical health checks and medication. 20,21 In the context of recovery-focused services, the dominance in primary care of a chronic illness management model was important to acknowledge. 22
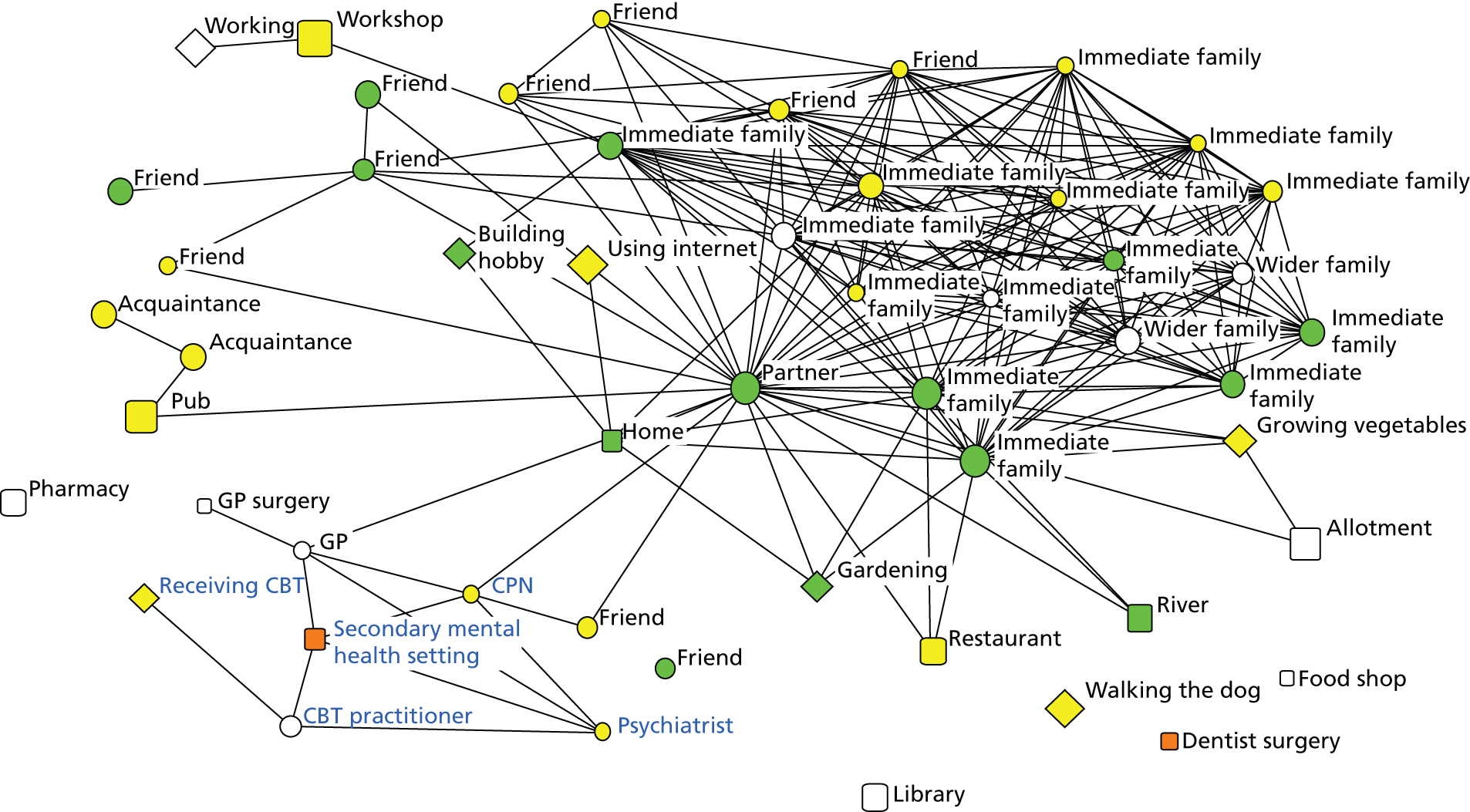
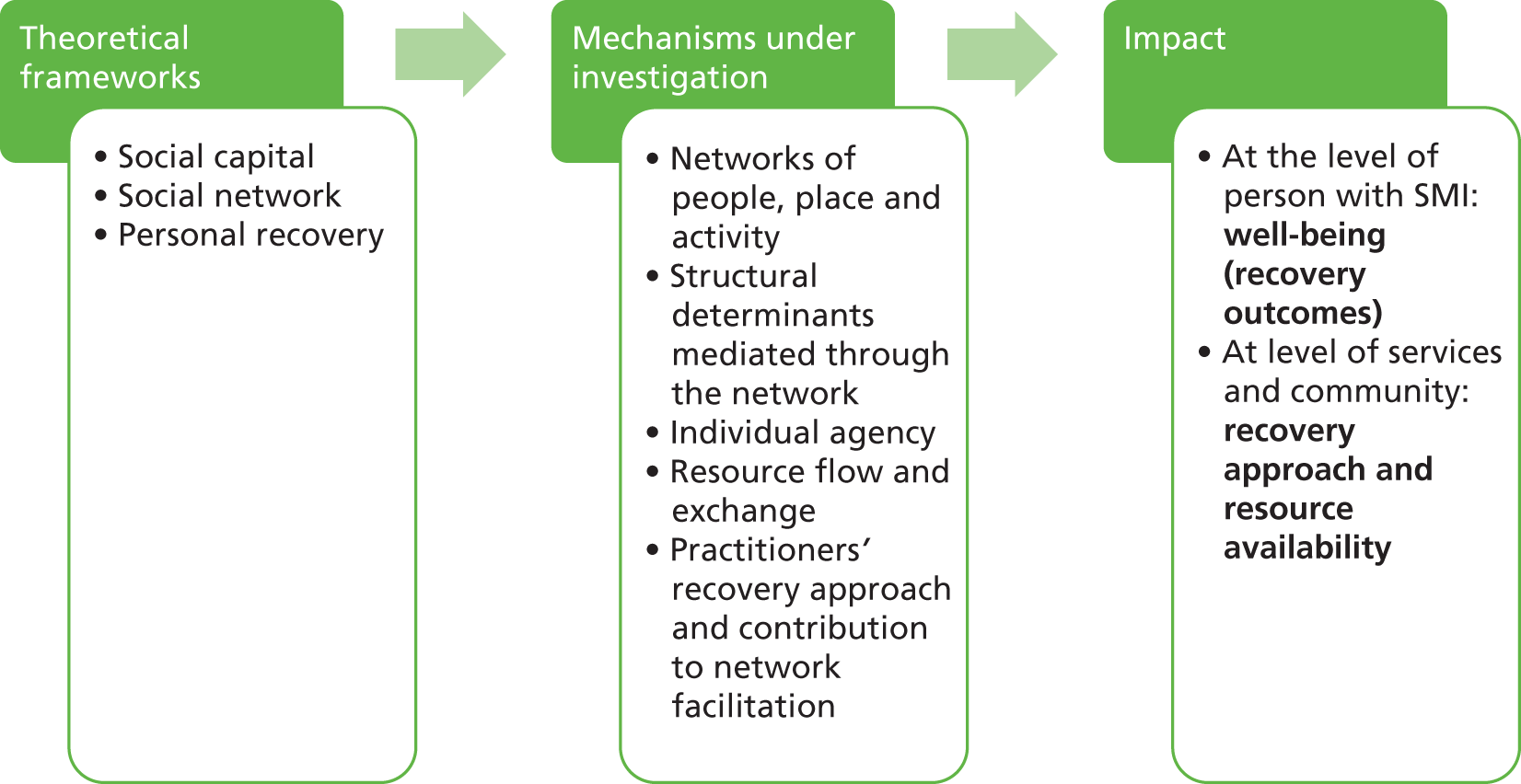
This research study considered both the individual with SMI and the systems in which they lived; it collected research data from people with SMI, community and health-care organisation leaders, and practitioners working with people with SMI to gather their own perspectives. Community health network (CHN) was conceived by the research team for the initial research proposal to help articulate the focus of the study. It was not a concept that was found in published literature. We instead started this study by exploring research that might explain connections to support health, well-being and recovery underpinned by several connected theoretical frameworks: social capital; social network analysis (SNA); and personal recovery (Figure 1). The focus of the investigation was the individual and their personal lives linking social contacts (relationships), activities (things people did) and place settings (where people went). Resource exchanges shape connections to people, places and activities and we emphasise agency and active strategy in our network approach. 23 We examined the lives of people with SMI using a network methodology and follow-up qualitative inquiry in order to understand possible health and well-being protective or facilitating factors and conditions. The study was exploratory and as such did not provide evidence to explain the variations we observe or infer causality; we can only describe the observed trends and provide possible explanations, leaving further research to test these suggestions. Our approach allowed an analytical perspective directing focus on individuals with SMI and how services and community resources may best support them, rather than taking services and systems as a departure point.
FIGURE 1.
Study approach to exploring networks of people with SMI.
Study aim
The main aim of the study has been to understand the personal network of people living with SMI from their own perspective and how their well-being, as well as mental and physical health, was supported by resource exchanges alongside roles of external structures and individual capacities using a CHN approach. Through this, we come to better understand how they could be supported by practitioners using network facilitation strategies, if these were prioritised by providers of mental health care, which could involve shrinkage or expansion of current people, place or activity connections.
Research questions
-
How do people with SMI use resources in their personal networks to support their health and well-being?
-
How do community-based practitioners and organisations support people with SMI to use their personal networks to support health and well-being?
-
How do primary care, community-based mental health providers and other organisations work together to develop effective personal networks for people with SMI to improve their overall health and well-being? What were the barriers and enablers to achieving this?
Research objectives
In order to answer the research questions, the following objectives were specified:
-
to map the personal networks utilised by people living with SMI to support their health and well-being using the CHN approach
-
to identify practitioners and organisations in primary care and community health services that contribute to developing effective personal networks for people living with SMI
-
to identify the enablers and barriers to organisations collaborating to provide effective support to people to develop their personal networks
-
to provide recommendations for practitioners, managers, service users, and health and well-being boards for organisational changes to establish and support, if appropriate, the CHN approach.
In our study the use of the term ‘network’ needs careful clarification. It has two meanings. Firstly it was used as a technical term used in SNA24,25 to describe the structure of ties between various nodes such as people and organisations. 26,27 Secondly it was used in a more general or lay sense to describe the connections to people, places and activities. Throughout the report care was taken to minimise the use of network as a general term, to avoid confusion with SNA, but at times it was included because this was an appropriate description of resource flows and connections within an individual’s life.
Policy context
The study’s policy departure point was longstanding preoccupations about the need for person-centred care provision in mental health and also three important mental health policy developments:28
-
Addressing the poor physical health outcomes of people with SMI. Research shows that this group are dying up to 25 years younger than the general population. 29–31
-
Addressing the stigma of SMI: combating stigma and discrimination through co-ordinated awareness-raising and behaviour change programmes targeting multiple audiences, including people with SMI, to address self-stigma. 32–34
-
Building recovery-focused mental health services acknowledging the importance of person-centred health and social care driven by the needs, goals and aspirations of an individual. The approach emphasises that personal recovery is different from the absence of clinical symptoms of mental illness. The individual with SMI leads the process of recovery towards ‘a life worth living’ with services supporting the development and achievement of personal goals, hopes and dreams. 35–37
These led us to the conclusion that, in order to develop appropriate person-centred services, a much greater understanding of what individuals’ personal networks of connections currently consist of and how individuals and practitioners contribute to these was needed. This would complement the primary focus of most service delivery: assessment, diagnosis and treatment with National Institute for Health and Care Excellence (NICE)-recommended interventions that emphasise medication management and psychological therapies for SMI. 38,39
Since the research project was commissioned, a new mental health strategy and implementation framework has been published30,40 and other significant mental health policy developments have been the introduction of the NHS outcomes framework31 alongside changes to commissioning arrangements within the NHS. The ambition of the strategy was that:
More people with mental health problems will recover: More people who develop mental health problems will have a good quality of life – greater ability to manage their own lives, stronger social relationships, a greater sense of purpose, the skills they need for living and working, improved chances in education, better employment rates and a suitable and stable place to live.
p. 631
Introduction of local Clinical Commissioning Groups (CCGs), health and well-being boards and directors of public health within local authorities from April 2013, informed by joint strategic needs assessments (JSNAs) of health and social care needs in the local population, provide another opportunity to reshape mental health service provision. In this structural change context there have been budget pressures, with public finance reviews driving cost reductions across all government departments in England.
Approach to literature reviewing
The academic literature context for this study was extensive. We undertook a focused and thematic background literature review of key themes that influenced how we studied the networks of people with SMI. We searched published literature and reports for factors that influence network composition, structure and outcomes, identifying in particular studies that had worked with people with mental health problems. The aim was to produce a list of potential factors for data collection to cover, or make explicit decisions to exclude. The key search terms included diagnoses and recovery as well as people-, place- and activity-related words.
An important context for the study was emerging work around recovery and mental illness that challenges services to undertake a values shift. 41 A central process within recovery theory is empowerment. 8 Personal recovery is a person-centred concept, led by the individual focusing on their strengths, not deficits;42 an active sense of self, including a determination to get better with a role for the person themselves in this process, was a feature. 43 Recovery pathways are often coproduced; people may require help to ‘own’ and lead their recovery journey but with the right kind of support can get to a place of greater self-determination. The study team were, however, aware that theory underpinning the recovery ‘movement’ was still developing, and wanted to contribute to this through empirical work rather than basing methods on it. We were also mindful of the wider pitfalls of normative assumption modelling and had been aware of assumptions such as ‘big was better’ in respect to social ties, meaningful activities and place-based connections, over-riding individual preferences linked to coping strategies, life context and health decisions. Much of the social network literature in mental health focused on social network size or number of relationships, reporting how people with psychosis tended to have smaller social networks than the general population. 44,45 Other research acknowledged that the nature of networks and their quality were as crucial as size. 46 While there may be potential benefits from larger social networks, we note the potential for negative effects of social relationships. We need to treat with caution the idea that larger social networks are a desirable and manageable outcome for all individuals. The team had therefore explicitly adopted a person-centred critical approach to the research, seeking to understand how people’s life-worlds can be examined through the lens of social, place and activity connections, and had not reviewed normalisation literature or any associated studies.
For some people and in some stages of illness, smaller networks of key contacts may be perceived as more comprehensible, manageable and meaningful, drawing on a sense of coherence theory, rather than a large network of ties that may lack emotional closeness and involve a complex set of roles or stressful relationships. Antonovsky’s sense of coherence theory regards coping and adapting in life as an active, dynamic and continuous process. A high level of sense of coherence was health promoting, predictive of how well people manage stressors and stay well. 47,48 Problems with social cognition associated with schizophrenia may also make relationships difficult to manage. 49 Moreover, the quality of relationships may be more important to well-being and recovery than the number of ties. 50 The approach was informed by critical realism and took a mixed-methods approach to enable the socially constructed and situated elements of meaning-making to be balanced against the quantitative network data. Social network studies had called for more qualitative work to understand the relative value of network characteristics and explanations for differences in network size, satisfaction, social support and well-being. 51 The mixed-methods approach adopted in this study assisted us with balancing network characteristics with meaning mapping.
Health and well-being
‘Health’ was defined in 1948 by the World Health Organization as ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. 52 This has been contested but no new international definition agreed, though the British Medical Journal reported that global conversation has suggested health be defined as ‘the ability to adapt and self-manage in the face of social, physical, and emotional challenges’ (p. 343),53 recognising health was personally defined. Well-being has been less clearly defined. 54 A recent review of well-being55 proposed ‘a new definition of wellbeing as the balance point between an individual’s resource pool and the challenges faced’ (p. 230). Resources and challenges referred to the psychological, social and physical. These definitions bring concepts of health and well-being closely together but, as in the recovery literature, allowed for individuals with significant psychiatric ‘disorders’ to achieve a sense of well-being. 56,57
It is well established that attention is needed to improve the physical health of people with SMI58 because of consistent findings that their health was poorer than the general population. 31 Health issues include a higher prevalence of cardiovascular disease,59 diabetes,60 obesity61 and a shorter lifespan, estimated at 13–30 years less than the general population. 62 Our study deliberately sought to understand the connections people with SMI have, to address the neglected focus of physical health. The reasons behind these physical health issues appear to include both lifestyle factors as well as consequences of treatment. Antipsychotic medications are linked to weight gain and metabolic dysfunction, which in turn has a negative impact on quality of life. 63 A recent systematic review of evaluations of health behaviour interventions designed to improve physical health in people with SMI found that the majority produced positive effects. 64 One of the successful mechanisms in such interventions was increased regular physical activity within the local community, but sustaining engagement was challenging. 65,66 Within this study we were interested in the potential of network interventions for addressing health inequalities. Data were collected about strategies for maintaining physical and mental well-being.
The recovery approach
The recovery approach has been adopted by secondary mental health services. Its underlying theory is still in the early stages of development and includes several threads: (1) that the outcomes of interest include non-disease-specific constructs such as having a purpose or meaning in life; (2) that individuals should be central to setting goals and decision-making; (3) that engaging in a wide and inclusive range of activities and relationships will improve outcomes;32 and (4) that practitioners and services should work alongside and support individuals with mental illness rather than impose treatments based on disease labels. 14 There was strong policy leadership for recovery-orientated practices in the UK, and staff development and training programmes were beginning to show how to work in recovery-orientated ways. 67,68 In this study we were able to explore aspects of recovery, such as community engagement,69 housing,70 employment,18 stigma71 and social skills development,72 using a network perspective. The goal is for greater social inclusion and active citizenship for marginalised groups including people with SMI. Our network-mapping approach may help shed light on the extent to which individuals are integrated into the community or living in isolation.
A key resource within recovery-orientated mental health services was practitioners, who will need new education and training and new skills such as coaching techniques. 73 Services needed to adopt a different values base, requiring significant changes to practice, services and culture. 43 A review of recovery-orientated practice guidance found lack of clarity and suggested that four practice domains provided focus: promoting citizenship; organisational commitment; supporting personally defined recovery; and working relationships. 74 Our study explores the practitioner perspective of their role in network development, assessing the place of social interventions as a treatment priority in primary and secondary care.
Social networks, social support and friendship
Within the field of mental health, literature on social networks, social support and friendship overlapped. We provide only a brief summary of key points in this section. One qualitative study which influenced this project investigated friendship in the UK. 75 It explored individual micro-social worlds to understand the ‘role of friendship as a form of social glue’ (p. 156)75 shaping social life. Acknowledging the trap of deterministic labelling, the authors did look at how factors such as gender, education, ethnicity and age impact on friendship. In using a CHN approach to understand the range of friendship resources (confidant, emotional support, practical assistance and playmate), demographic information on social ties may be important alongside establishing how, when and why different relationships matter at points in time.
Social network analysis has been used to understand connections to people, places and meaningful activities. 76,77 A fundamental assumption of SNA was the importance of dynamic structures to understand observed behaviours and outcomes: the connections that individuals had; the impact of their actions and beliefs; access to resources; and outcomes through various socially constructed mechanisms. 24,25 Social network approaches allow examination of the social structure of connections that individuals have, and have therefore been used to understand how social capital78 and social support79 are accessed. However, the approach has been critiqued as paying insufficient theoretical attention to the role of human agency and culture alongside social structures in explaining network transformations. 80 In this study we seek to understand the dynamic interplay of socially structured and creative human actions on personal networks of people with SMI.
Social network studies of people with SMI have often used counts of relationships rather than formal social network structural measures as shown by Macdonald et al. 45 and studies comparing people with SMI with the general population. 46,81 Early work in the 1990s, such as the TAPS study, found people with SMI had small networks which did not increase in size after leaving hospital but the quality of relationships improved; while living in the community was much preferred, little social integration was achieved. 11 A study in Sweden reported similar results51 and emphasised the link between negative symptoms and social interaction. This finding has been replicated in studies which had also reported a lack of social support, and unmet needs around social interaction and community belonging. 82,83 Studies which examined composition of social networks of individuals with psychosis had found them to contain fewer friends46 and more service practitioners84 than the general population, and the onset of psychosis can involve changes in social networks and the loss of friends. 85 It is the multifaceted and dynamic nature of social networks that this study explores, looking beneath a map of connections to understand the negotiated meaning, sets of choices, capacity for growth and qualities such as reciprocity.
Social networks, and change in networks, may directly influence health and well-being. 86 Increased social interaction has been associated with improved quality of life and self-esteem for people with mental illness87 and, while some social ties can be negative, on the whole studies find a correlation between larger numbers of social ties and improved outcomes in this population. 88 One of the key mechanisms of this seemed to be social support, wherein social ties provided emotional, informational, instrumental and appraisal social support, which may help improve well-being79,89,90 and provide a stress-buffering role91 related to the perception that support was available to help an individual navigate and cope with stressful situations. 92
There was well-established evidence that the characteristics of an individual’s personal social network can impact on health behaviours and outcomes, through various mechanisms that may include social influence, sense of control and perceived support. 93 The influence of social network contacts such as family and friends can directly impact health-related behaviours such as use of health services,94 while network typologies had been developed to show that resourceful networks are linked to lower alcohol abuse and higher physical activity. 95 We also noted that the quality of social relationships rather than the number of ties may provide a better indicator of well-being; not all social ties are positive and supportive. 96 Having social support available, especially in the early years of mental illness, can reduce an individual’s perception of stigmatisation or rejection due to their mental illness97 and can improve access to services. 98 However, individuals with severe and enduring mental illness tended to have limited availability of this resource. 99 Within the field of chronic illness management, researchers had used social network methodologies to understand the types of social support or ‘illness work’ within personal networks of people with long term health-limiting conditions including mental illness. 100 A study comparing family support available to people with schizophrenia with those with physical conditions found the former had much lower levels of social support available in emergencies. 101 A literature review outlined how social networks influence a number of practices of self-care in long-term illness, including how the individual perceives their illness, norms and influences around physical activity and health service access. 102 This review team highlighted the importance of home life including social connections within the home in the day-to-day management of long-term conditions. This work emphasised the importance of incorporating resources and social context within individuals’ lives into self-care plans. 103
Networks are not simply sources of support but are integral to personal identity; individuals can have different identities in different settings, and access to a wider range of settings can facilitate the development of new identities central to the recovery process. 104,105 In contrast, having fewer identities, specifically the role of a sick person or being defined by one’s mental health only, can be damaging. 106 All relationships involve a role such as husband, sister, friend, teacher; it has been argued that these role identities and expectations provide behavioural guidance which in turn can foster healthy habits and well-being. 91 Engagement in wider social networks, meanwhile, can provide identity through shared roles and belonging.
Finally, there has been some evidence in the past that outreach programmes can improve the quality and quantity of the social networks of people with mental illnesses. 107 Interventions to help support people to build new social contacts may be particularly important, and effective, for those with especially limited social networks. 86 Interventions based on strengthening social networks and community engagement for people living with SMI may improve their subjective quality of life. 108–111
Social capital
‘Social capital’ refers to the set of resources embedded and accessed through social networks which can then be used for purposive action. 112 Social resources can include material resources provided by social ties such as goods or money, reputation and social credential benefits of having a particular social contact, access to other useful contacts through a social tie or symbolic and expressive resources such as advice and reassurance. 113 The concept can be divided into two main forms; structural social capital, referring to the composition of connections and roles, and cognitive social capital, referring to beliefs, values, norms and the qualities of relationships. 114 Social capital has received attention because there was evidence that measures of social capital are related to health outcomes. 115 It has also been critiqued in its application to mental health, with differences of opinion over the merits of applying it as a population- or individual-level concept. 116
In this study we apply social capital at the level of the individual. An important distinction has been drawn in the literature between three forms of social capital that can be accessed from different contacts: bonding, bridging and linking capital. ‘Bonding social capital’ refers to close intimate ties that offer support and which are characterised by common identities, and can be seen as capital that helps people ‘get by’. 117 ‘Bridging social capital’ refers to weaker ties through which one can access different groups of individuals demographically distinct from one another,118 through which resources and information flow, and through which one can ‘get ahead’. 119 ‘Linking social capital’ meanwhile, refers to vertical connections within power hierarchies, co-operative ties between individuals on unequal levels of power. 120 When personal networks for people with SMI were considered, linking capital was less prominent in practice and studies had not addressed it. 121
Importantly, the precise mechanisms through which social capital may affect health are still not fully understood. 122 However, social capital was relevant for understanding social inclusion, recovery and the social determinants of mental health. 114,119 At the individual level, cognitive social capital, such as trust, has been shown to be inversely associated with incidence of common mental disorders. Individuals who rated their own level of resources through networks and community participation as low had a higher incidence of mental illness. Current understanding of the link between mental health and social capital uses primarily cross-sectional data, for example Webber and Huxley,123 and therefore the nature of causation is not clear and may be bidirectional: lower social capital may increase vulnerability to mental disorder and as mental illness progresses it is possible that access to social resources decreases. 124 The evidence of collective social capital’s influence on health is still inconclusive and the strongest associations have been found at the individual level. 115 It has also been shown that, at the group level, social capital links to inequality and exclusivity. When accessed through groups, the resources that some individuals obtain will come at the expense of other people. 116
There are, however, a number of conceptual issues in the definition of social capital, particularly as the construct overlaps with other social concepts, such as social support and social participation. 117 It has been suggested that social capital should be seen only as a societal or whole network concept, in order to distinguish it from social support and personal social networks. 116,118 However, at the individual level, the concept of social capital can be useful in understanding the effects on health of resources an individual can access because of their position in different networks, and bonding and bridging forms of social capital offer a distinct conceptual approach to understand what types of network are beneficial or damaging to health, and for whom. 115 This potential also extended to social capital interventions which had challenged practitioners to actively nurture and develop approaches aimed at increasing the resources available to individuals through their social networks. 125
Meaningful activities
Having a purpose or meaning in life was one dimension of recovery,8 making meaningful activities important to understand. Meaningfulness for people with SMI (and most of us) refers to the sense of achievement, connection, routine, enjoyment, autonomy and purpose that people can attain from activities. 126 This engagement in meaningful activities was associated with life satisfaction for people with mental illness,127 and feeling competent and having pleasure in daily tasks and activities was linked to subjective quality of life. 128 We suggest that participation in activities results in different emotional and cognitive responses in different individuals at different times, and that this sense of connectedness, achievement and positive identity resulting from participation can be seen as dimensions of recovery outcomes such as well-being and quality of life. For example, a 3-year prospective study in the USA found that, while recovery outcomes were sustained in fewer than one in ten people with schizophrenia, the likelihood of such favourable outcomes was associated with factors such as being employed, undertaking independent leisure activities and more daily activities. 129
There was also some evidence that engaging in meaningful activities may have a beneficial role in supporting recovery from mental illness, independent of the social support that engaging in such activities often provides. 130 Hendryx et al. 130 suggest that specific activity type may not be vital but that having a choice over what activity people engaged in could contribute to building a sense of control and that having meaningful activity may be even more important where social support is lacking.
Employment was a particularly important ‘meaningful activity’131 because it facilitates access to social interaction, a sense of identity, self-esteem and improved finances. 132 At a population level, unemployment was linked to poor mental health, while gaining employment can improve mental well-being and social inclusion. 133 While some aspects of employment can be stressful for some individuals, a 10-year study found that being in steady employment was significantly associated with a reduction in mental health service use over this time period. 134 However, individuals with SMI are much less likely to be employed than the general population,135 and face a variety of barriers to gaining employment such as poor functioning due to illness136 as well as stigma in the form of negative employer attitudes. 137 Furthermore, while we undoubtedly need to increase the level of employment for those with SMI, for some individuals certain forms of employment may be unobtainable.
Place
The final dimension explored in the literature to inform data collection was the importance of place as a therapeutic support for recovery. 138 The evidence base exploring place and mental health was weak; however, some research has linked factors such as poor housing and environmental noise to psychological distress. 139 Supportive and empowering environments in the community had been identified as enabling factors in recovery, while stigma and disempowering environments had been identified as inhibiting improvements in mental health. 140 An individual’s perception of their neighbourhood, in particular sense of cohesion, can affect mental well-being. 141
The existence of nearby green spaces such as parks and nature has been positively correlated with perceived health142 and mental health,143 particularly in urban environments linked to stress reduction and social cohesion. 144 People rate fresh air as particularly effective for improving mental health. 145 Green space can provide a buffer which reduces the impact of stress on an individual’s health and well-being146 through a number of mechanisms such as social interaction generated by recreational walking with friends. 143 In the field of sustainable development, natural capital in the form of access to resources such as green spaces was seen as one of the five forms of capital (alongside human, social, built and economic capital) that are needed for a community to flourish. 147
An important aspect of this study was rural and urban geography. Would living in the city shape networks of people with SMI in different ways from those living in rural communities? It was important not to import stereotypical views of rural148,149 or urban mental health landscapes. However, research does show higher levels of psychosis within inner cities and deprived communities,150 which could impact on our data. Neuroscientists are also interested in the impact of place. Research has shown greater rates of SMI in cities, leading to work looking at environment–gene theories and city neighbourhood studies to explore the impact of urban dwelling on mental health. 151 A promising area called social neuroscience was emerging from work linking urban upbringing and city living with stress processing. 152 By working in two distinct geographical areas, we were able to use the CHN approach to explore the impact of locality on network characteristics and report these as case studies in Chapter 7.
Stigma and discrimination
Most people living with SMI experience public stigma and discrimination153,154 and many people are also affected by self-stigma. 155 There was a large research literature documenting the conceptualisation of stigma and discrimination,34,156 as well as actions that can be taken to address public attitudes,157 self-stigma158 and discriminatory behaviours. 36 The present research did not measure stigma but the impact of stigma would probably be a feature of the world in which participants lived.
Summary
This brief review of literature relevant to personal networks of people, place and activity for people with SMI, and contextualised by the recent interest in the ‘recovery approach’, has emphasised the potential for connections in the network to generate well-being, or a range of recovery outcomes, as well as negative outcomes. We have emphasised that individuals’ networks can be seen as a means of resource exchange but we also recognise the roles of outside structures and individual capacities. The former might include the effects of structural social and financial inequalities, of policies and of geography, which may be manifested in the places and people individuals are connected to. The capacity individuals have to make decisions and engage in activities in different places includes their state of health, their cognitive abilities and their agency. Agency, a construct used to represent the ability of subjects to influence their own future and the world around them, can be seen as having three inter-related types:29
-
‘iterational’ agency or ‘habitual’ agency: ‘the selective reactivation of actors of past patterns of thought and action’ (p. 971)
-
‘projective’ agency: ‘the imaginative generation by actors of possible trajectories of action’ (p. 971)
-
‘practical-evaluative’ agency: ‘the capacity of actors to make normative judgments among alternative possible trajectories of action [in the present]’ (p. 971).
Similarly theory related to individuals’ roles and identity were potentially important when examining the network of connections of individuals with SMI. These diverse influences have not been covered in this focused review, but are considered during the analyses and interpretation of the results as we draw further on wider published literature. Finally it is worth emphasising that we have chosen to examine the worlds of those with diagnoses of SMI not because we consider the disorders to be precise entities but because as a group of individuals they face some similar challenges, including cognitive and social functioning,159 and because services are currently aligned with them as a group.
Chapter 2 Method
Ethical review and protocol changes
The study was reviewed by Central London Research Ethics Committee 4, on 2 December 2010. Favourable ethical opinion was received on 31 January 2011. We submitted four minor and three major amendments to the protocol and study materials. The study, with approval of the funder, changed in the following substantive ways:
-
The short-form health survey with 36 questions (SF-36) was replaced with the Short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS)160 and Dartmouth CO-OP charts161 (from the Dartmouth–Northern New England Primary Care Cooperative Information Project), as these were preferred by participants in piloting.
-
A survey of organisations was replaced by a practitioner interview study in response to study team concerns over survey response rates.
-
The application of study findings to a third site was replaced by dissemination events which will take place after the report is submitted, in response to feasibility concerns within the study timetable.
-
The recruitment of participants in primary care was extended to recruit through secondary mental health teams in both study sites because of slow recruitment rates.
Methodological overview
Mixed methods
In order to answer the research questions, the study used mixed methods162,163 and a three-stage synthesis process, including two context-specific case studies,164 to explore the lives of people with SMI. The study data collected from individuals with SMI aimed to be both descriptive of what was happening within personal networks using applied SNA,24,25 and be used to derive critical insights into network meaning for individuals with SMI. There were tensions in the approach adopted: we had a framework measuring incidences of connections – people, places and activities – sitting alongside reflexive analysis by lived experience researchers and the core study team. We have taken a priori research questions into the study, informed by published literature, and have carried out further consultations to understand concepts such as health and well-being or explored other published literature to make sense of emerging findings. Alongside these data sources we have integrated insights from other informants providing a practitioner perspective and organisation viewpoints. Thus the mixed-methods study has produced findings both grounded within the data and informed by deductive processing of research questions. The mixed methods were balanced, with no one approach overshadowing others either in the planning, collection of data or analysis stages. 165 Dual competency in methodological techniques166 was achieved by a team approach with all members trained in one method and some conversant in both.
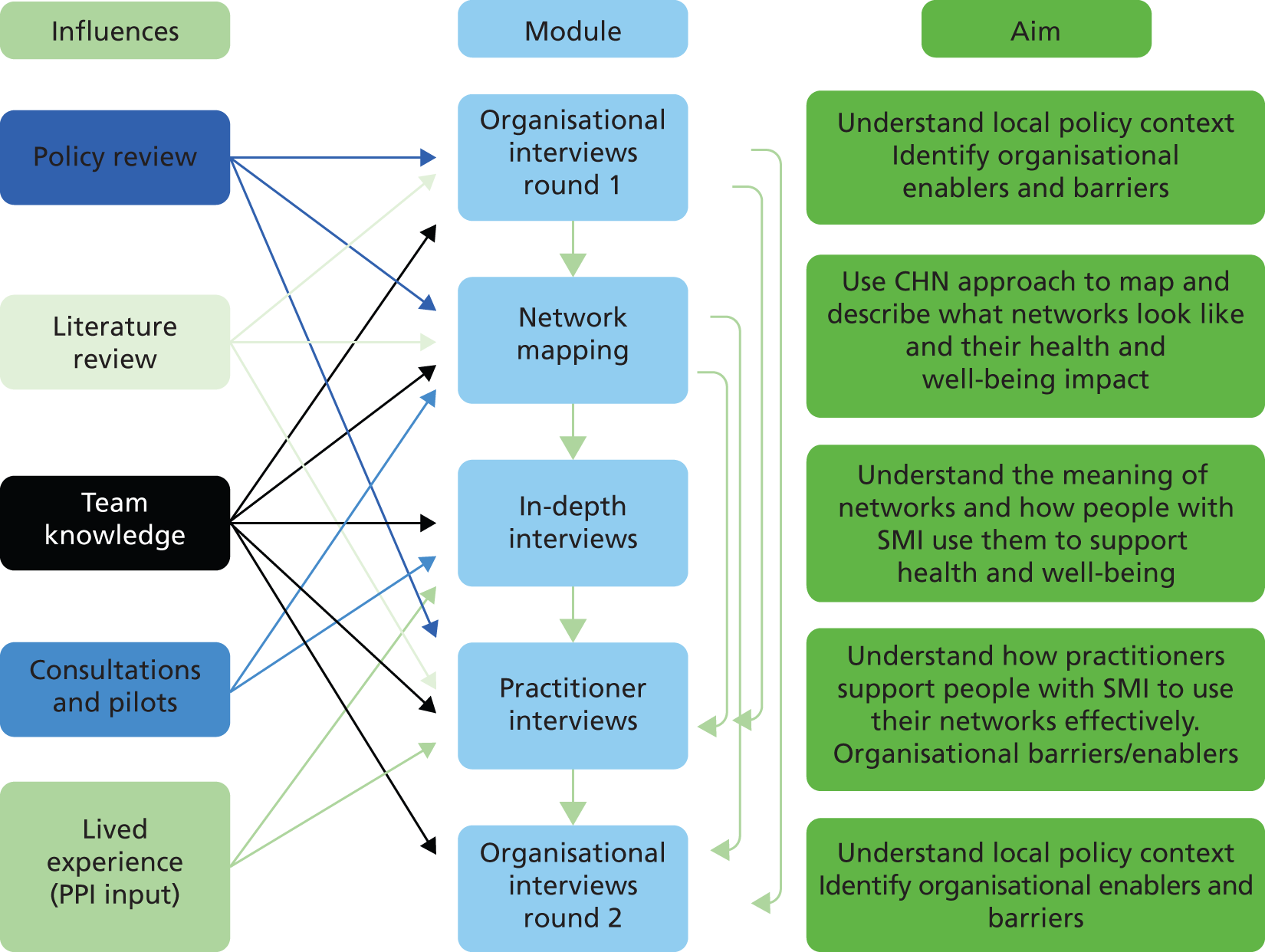
Figure 2 provides an overview of the individual data collection modules and how they inter-relate.
FIGURE 2.
Interaction between study modules: planning and data collection. PPI, patient and public involvement.
A specific focus of the study was using the CHN approach to map connections of people with SMI and follow up with interviews to explore meaning within these personal networks. In network studies, the population under investigation was often highly defined, for example examining the impact of drug use in the social networks of people with bipolar disorder. 167 However, we adopted an inclusionary and broad approach, as the study was exploratory. This broad approach does present methodological and analytical challenges because we were exploring many varying factors in people’s lives, situated in people’s own explanations, which describe heterogeneity, not network categories or types. We were mindful of these challenges and throughout the report emphasise that the work was largely descriptive and exploratory. Thus, we were cautious in our conclusions but forthcoming with potential explanations and definite recommendations based on data synthesis.
Approach to data collection and synthesis
It was important to emphasise that throughout the study, we have been grounded in emerging data and reflexive in making sense of these data. 168 We have worked iteratively and sought to explore the data by returning to literature or to further data collection and engaging our patient and public involvement (PPI) group to draw tentative conclusions. Thus, data sets were collected in sequence. First, network mapping (see Chapter 3) and in-depth interviews (see Chapter 4) were collected, as details from the former were used to recruit purposively for the latter and because the interviews involved reflecting on the mapping content and process. Second, the initial organisational interviews (see Chapter 5) and the last organisational interviews (see Chapter 7) were collected in sequence because the findings of the former, and other data sets within the study, were used both to select interviewees purposively and to refine the topics for discussion. Overall within the study the data were collected and analysed largely in parallel, as recommended, to allow for learning from one data module to inform the others throughout the data collection process. 164 The combining and synthesising of data allows the exact same phenomena to be examined from different perspectives, which should result in a more comprehensive multiperspectival understanding. Mixed methods are best suited to explore complex issues that can benefit from the integration of different types of data; it was at the synthesis stage that this approach yielded benefits. 169
Informal synthesis between the data sets took place throughout the study, as data were shared by the research team and used to both inform other modules as well as identify potential areas justifying deeper exploration; this was achieved by regular team data-sharing and discussion sessions including the PPI group members.
The formal synthesis took place in three stages. The first stage of synthesis (see Chapter 7) was the two case studies which combined data from the network mapping, in-depth interviews and organisational interviews. The goal was to understand ‘meaningfulness’ in our data: we understand this in the sense articulated by others who champion interpretive case studies as seeking not generalisable causal explanations but contextual understanding of the meaningfulness in human experience. 170 The two case studies were not designed to compare and contrast; rather they sought to explore the phenomena under study in a context-specific way. This included examining both how personal networks were influenced and moderated by the local context and also identifying and examining any salient features, within the context of each case study site, and the locally defined opportunities and resources that they might provide. The second stage involved working with our PPI group (see next section) to review the findings from Chapters 3–6 and interpret them using a reflexive methodology based on personal experiences of living with SMI. The final synthesis stage involved modelling the CHN approach to understand if it can usefully contribute to recovery theory and practice. 171 A matrix was used to test our model against data summaries from Chapters 3–7. Our model contained three dimensions: external structures and systems (shaping choice and change); individual agency (how individuals were impacted by their own agency or lack thereof); and available resources (access to people, places or activities).
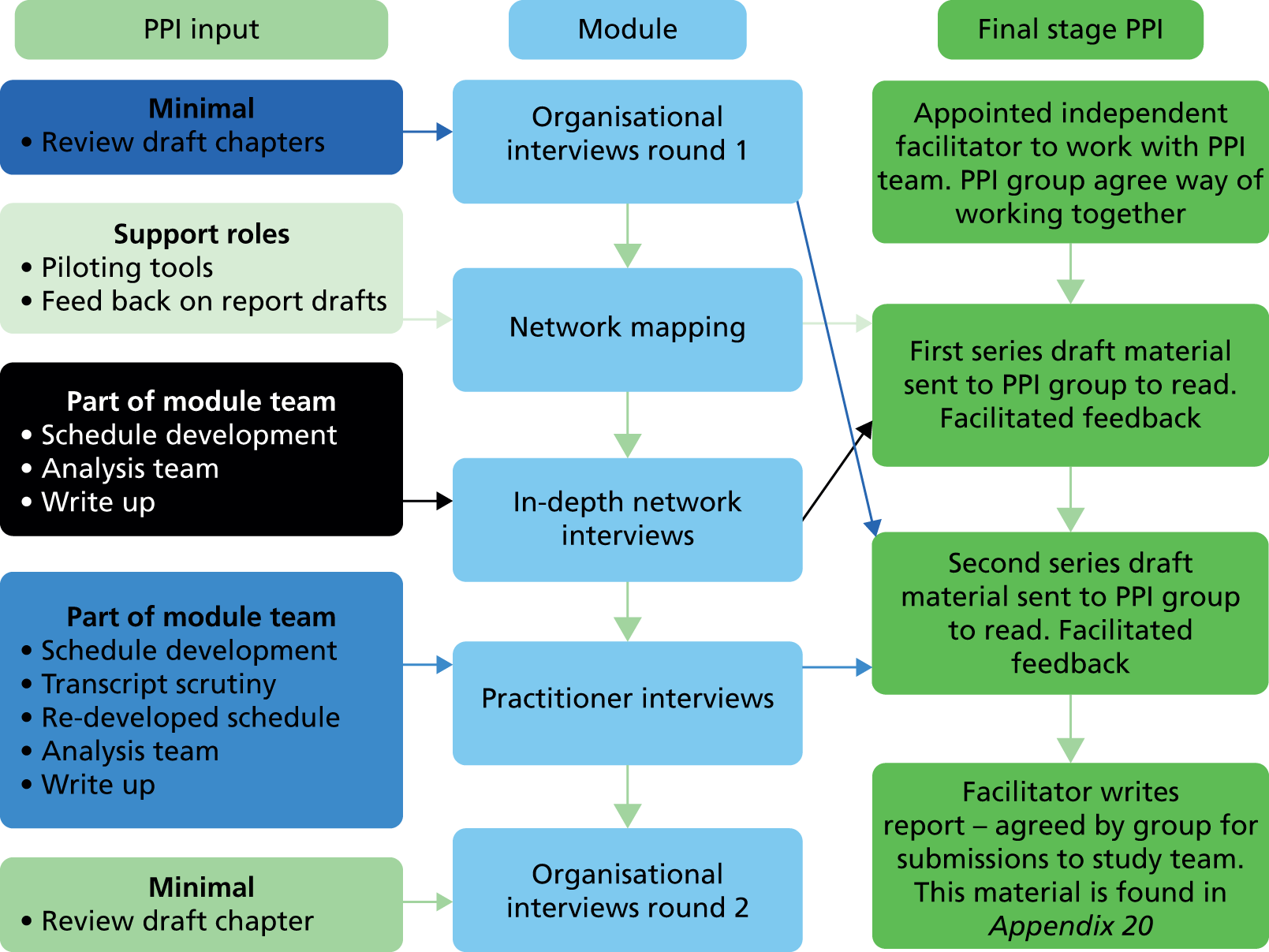
Patient and public involvement
A key part of the study methodology was the integration of lived experience expertise to understand local community resources in the two sites, the design and redesign of study materials and the interpretation of study findings. A team of six lived experience researchers worked on the study as a PPI group, with five completing the reflections analysis process at the end facilitated by an independent lived experience research consultant (full report in Appendix 1). A summary of PPI input for each module is provided in Figure 3. The two modules with the highest level of involvement in both planning and analysis were SMI in-depth (see Chapter 4) and practitioner interviews (see Chapter 6). The team were recruited to provide a diversity of perspective in terms of lived experience of schizophrenia, bipolar disorder or other psychosis as well as age and gender. We attempted but did not successfully recruit a black and minority ethnic (BME) perspective into the PPI group, which was a limitation of the study.
FIGURE 3.
Patient and public involvement in the CHN study.
Data collection and initial analysis
Organisation interviews: series 1
Over the initial months of the project, face-to-face semistructured interviews were conducted with the aim of gathering contextual information on the organisation of services, and provision of support for people with SMI in both study sites.
Data collection
Data sample
Thirty face-to-face semistructured interviews were conducted (Table 1).
| Participant type | South West | London | Total |
|---|---|---|---|
| Trust/social care leadership | 5 | 5 | 10 |
| Mental health third sector | 3 | 2 | 5 |
| Primary care | 0 | 1 | 1 |
| Community organisations | 5 | 7 | 12 |
| Commissioner | 0 | 2 | 2 |
| Total | 13 | 17 | 30 |
Recruitment
Key organisations were identified by the study team, chosen to reflect the composition of local services at both sites: health, education, sports, employment and job creation, arts and culture. Invitation to participate was via e-mail and follow-up phone calls. We used snowball sampling; where people were unavailable we asked for suggestions of alternative contacts to approach.
Development of interview guide
The study team developed a semistructured interview schedule (see Appendix 2) to explore how local organisations worked with individuals, and with each other, and make active use of individual’s networks to support well-being of people with SMI. The research themes were addressed in a focused way, and flexible space was also allowed for fresh ‘off script’ concepts to emerge. Interviews were digitally audio-recorded and transcribed verbatim.
Data analysis
A framework approach was applied with the support of the NVivo 9 (QSR International, Warrington, UK) data management tool. The framework analysis method entails organising and summarising research data resulting in a robust matrix which allows researchers to conduct analysis by case and by theme. It was a focused, well-defined approach that allows for the inclusion of a priori as well as emergent concepts, and was suited to addressing specific research questions. 172 We followed the five-step analysis process for framework analysis, with a modification to the mapping and interpretation stage, detailed below. 173
-
Familiarisation: this was carried out by two of the research team (one from each site), who had contributed to developing the interview schedule and carried out the interviews. The checking and anonymising of the transcripts contributed to the familiarisation process.
-
Identifying a thematic framework: the thematic framework combined both a priori concepts previously identified as being important for these data and inductively generated themes. The inductive generation included the two researchers who had undertaken the ‘deep familiarisation’ and two other members of the research team who had either conducted some of the interviews or listened to some of the audio recordings. Seven main ‘themes’ were generated from both the study research questions and deductive insights matching research literature and study data (care provided, change, encouraging reciprocity, organisational partnerships, organisation’s relationships with service users, personal networks, other challenges).
-
Indexing: one of the researchers who had undertaken the familiarisation process then applied the themes to the transcripts within the framework format using the NVivo 9 data management tool. The application of the coding was validated by the other researcher who had participated in the familiarisation process; they paid particular attention to contextual details that could have influenced the interpretation of the data coming from the site at which they were based. Another qualitative researcher from within the research team checked that the data were being allocated within the framework consistently.
-
Charting: this was initially conducted by the researcher undertaking the indexing, discussed with them and the researcher responsible for consistency and then validated with the wider research team.
-
Mapping and interpretation: the findings for each theme were summarised by the researcher who had applied the indexing and charting. Any divergent findings and any differences in data between the two sites were noted. Extensive discussions within the wider research team agreed that surfacing cross-cutting themes would not add any value to the products of the analytical process. The team agreed that what was most relevant in the products of the analysis was what was not there. This stage was modified to allow the researcher to re-examine the data to see whether this was an unintended consequence of the analysis process followed or these were true ‘gaps’ which may need to be addressed in other areas of data collection.
The summaries of the themes and the ‘gaps’ identified in the data were then used to answer research questions 2 and 3, the results of which are reported in Chapter 5.
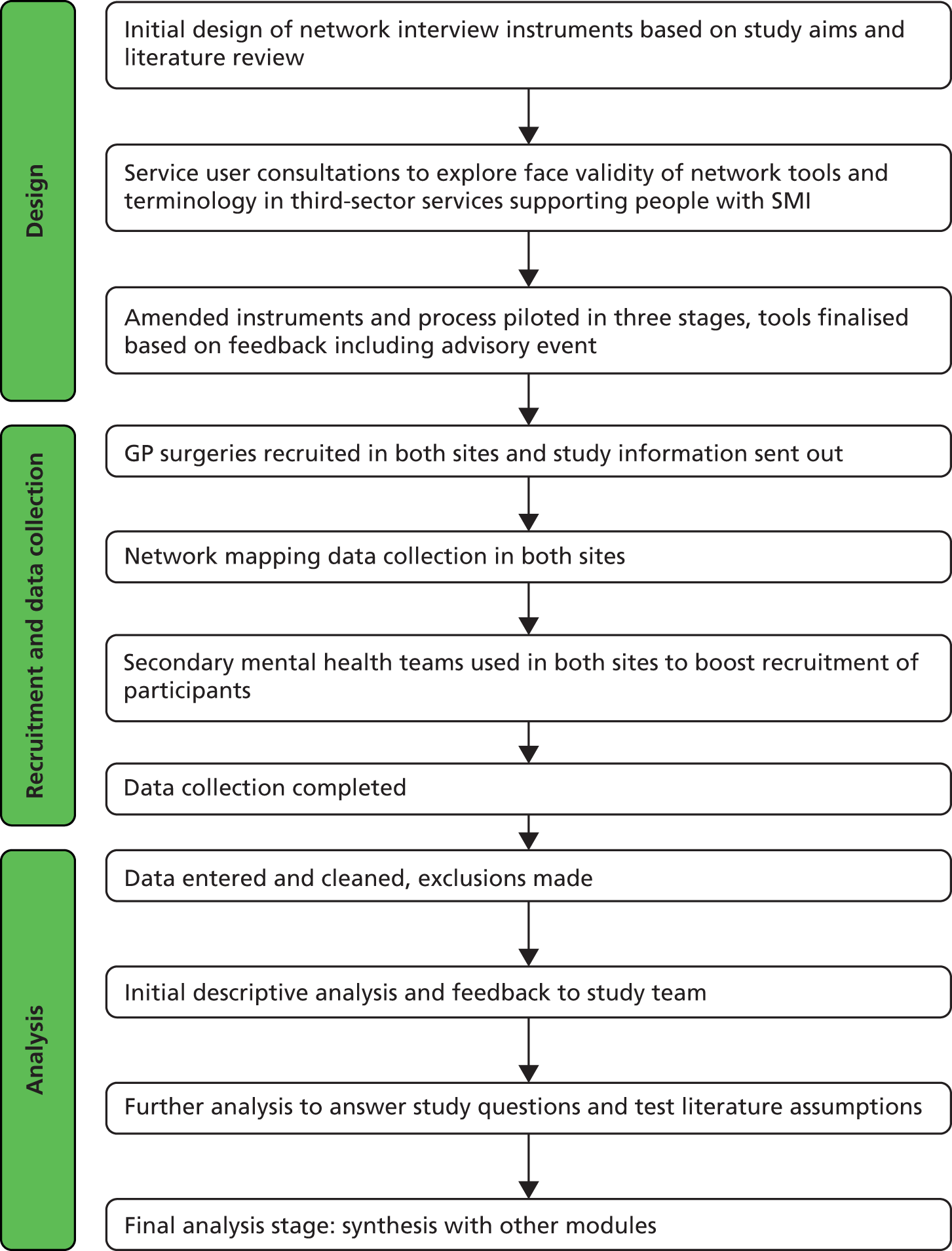
Network mapping
The primary aim of mapping interviews was to collect data from individuals with SMI on their current personal networks. This module involved a number of stages (see Figure 4), which are outlined in more detail below.
FIGURE 4.
Flow chart of network-mapping methodology.
Data collection instruments
The mapping interviews used the following instruments (a copy of these and more detailed methodological information can be found at www.mcpin.org):
-
Demographics: a questionnaire collected key sociodemographic data including age, gender, employment, relationship, education and housing status alongside background data on mental health, such as current diagnosis, medication, length of contact with services and inpatient history (see Appendix 3).
-
SWEMWBS: the short seven-item version chosen to measure current well-being asking participants about their experience of seven different thoughts and feelings over the previous 2 weeks; shows strong validity and high correlation with the longer version. 174
-
Dartmouth CO-OP charts: chosen to measure physical, social and emotional functioning for ease of completion and comprehensive dimensions. They consist of nine measures which ask about physical fitness, social activity, daily activity, pain, social support, emotional distress, quality of life, change in health and overall health. 175
-
Resource Generator UK (RGUK): this measures access to social capital within personal social networks and has four internal scales: access to domestic resources, expert advice, personal skills and problem-solving resources. It has been validated122 (see Appendix 4).
-
Health Resource Generator (HRG): consultations and pilots indicated the RGUK did not fully measure the types of resources that were relevant to the study with its particular interest in health capital. The study team therefore devised a pilot scale in the format of the RGUK and based on resources that were identified in focus group consultations to capture access to health- and well-being-related resources (see Appendix 5).
-
Community health network-generating schedule: the team developed a version of the name-generating and name-interpreting procedure used in SNA76 to map social ties, meaningful activities and meaningful places (see Appendices 6 and 7). This tool emphasised the connections within personal networks that support health and well-being.
The aim of the network-generating schedule was firstly to accurately map networks of people, place and activity, to understand how they were composed and then to understand their impact in terms of well-being. From the beginning, the team were aware of the challenges posed by this methodology when applied to participants with mental illness. Network generation was time-consuming and cognitively demanding, with concerns over accuracy of network recall having been raised by various previous studies,76 including recalling colleagues and members of groups and friends. 176 Extending the method to collect data on connection to people, places and activities and collecting the data on this population could potentially heighten these issues. The team were also aware that talking about potentially difficult relationships could cause participant distress. To tackle this, the network interview process was streamlined to have strong face validity and was designed to be as engaging as possible, with clear protocols for minimising and responding to participant distress. Studies have shown that the choice of name generator questions have a strong impact on the network mapped, impacting heavily on size, density and diversity. 177 Consultations and piloting assessed which network questions were most appropriate for mapping networks. We picked standard name generators and added extra items on the basis of consultations. These were refined based on whether or not they generated new names in piloting (if they did not, they were removed). Activity and place were ‘domain-specific’ or contextual name generators, providing extra prompts that improve recall and accuracy.
The final process is shown in Figure 5. For all three levels of network, boundaries were drawn by limiting connections to those which were current and regular interactions, or which were meaningful to the individual. The mapped networks were at a single point in time – the time of the interview. Questions used to elicit these networks can be found in Appendices 6 and 7.
The sample of 150 was based on a sample size calculation to detect differences in mental and physical health between a higher-need group, such as those in secondary mental health services, and a lower-need group, such as those supported in primary care alone, using a social networks study of day hospital and day centre service users. 46
FIGURE 5.
Final interview process chart.

Recruitment
Recruitment process
The first wave of recruitment was exclusively through primary care. Invitations to take part in the study were sent to all GP surgeries in study sites and the Primary Care Research Network (PCRN) assisted with this process. Study researchers also presented to individual practice managers directly. When surgeries responded with interest, members of the study team met relevant contacts to explain the recruitment process, including the inclusion and exclusion criteria and a recruitment log was used in primary care to document each step of the recruitment process.
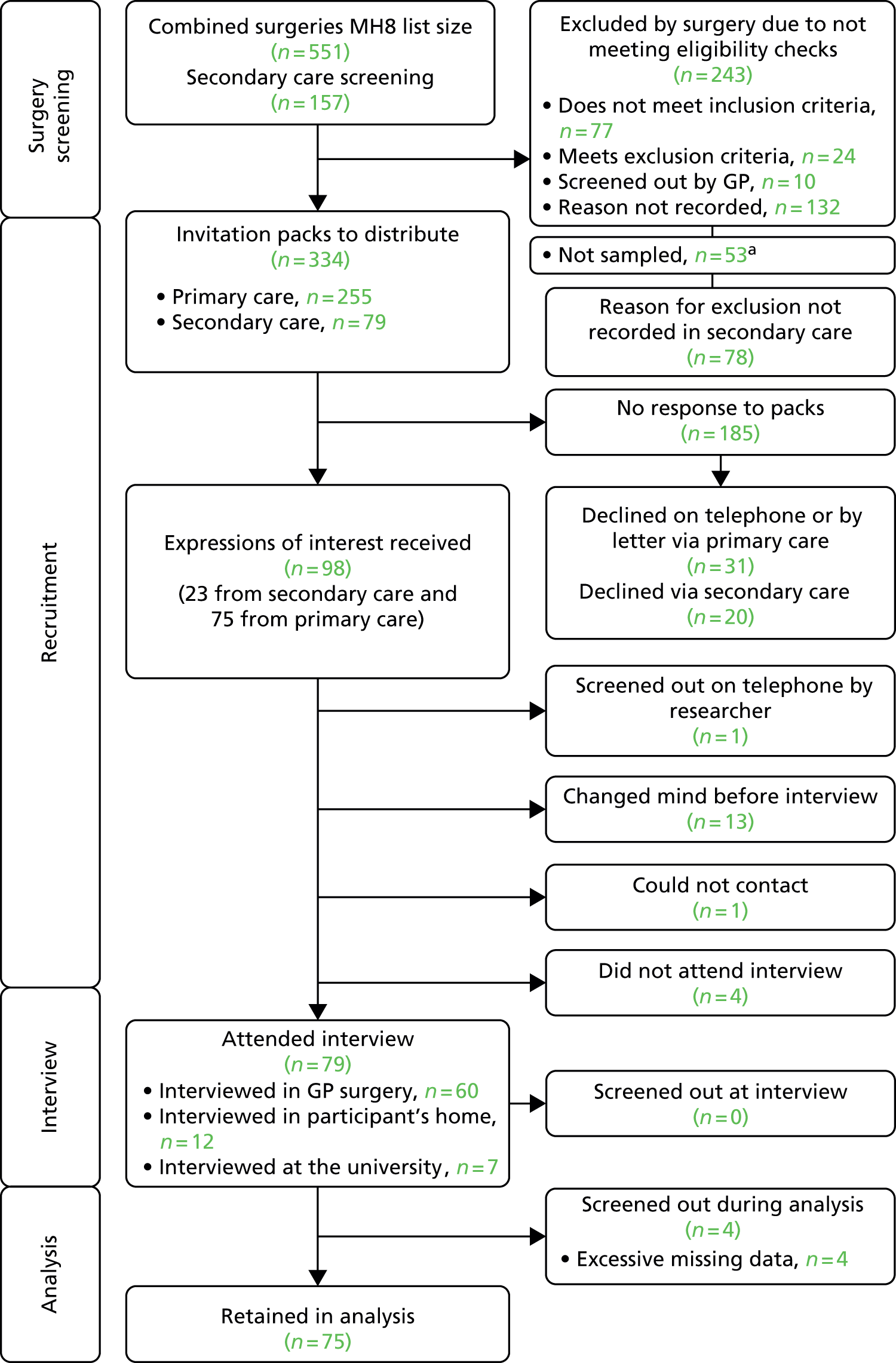
A second wave of recruitment was extended to secondary care, through early intervention services and community mental health and recovery teams, as a result of slow response rates in primary care. We targeted teams that covered the same geographical region of the South West (SW) as our GP surgeries, and those serving our London borough. The recruitment process through secondary care was that Mental Health Research Network (MHRN) staff presented the study to the team, who identified people who met our exclusion/inclusion criteria and approached them with an invitation pack. We were not able to track how many people were excluded by secondary care; we know only how many packs the teams were sent but not how many they handed out. This has impacted on our response rates, as we were unable to accurately assess how many service users were invited to take part. Our data, as presented in Figures 6 and 7, show 154 packs were given to secondary care practitioners to distribute. See Table 2 for summary of final study population by recruitment route.
| Recruitment route | SW (n = 75) | London (n = 75) | Combined (n = 150) |
|---|---|---|---|
| Primary care | 80 | 82.7 | 81.3 |
| Secondary care | 20 | 17.3 | 18.7 |
Data collection
The majority of interviews were conducted by the two study researchers; however, in London MHRN staff were trained and supervised to carry out 14 interviews and a second SW researcher did 24 interviews. All participants received a £20 high street shopping voucher as a gratuity for their time and contribution.
FIGURE 6.
Consort diagram for London recruitment. MH8, a register of patients with schizophrenia, bipolar affective disorder and other psychoses. a, In larger GP practices not all patients were sampled, we randomly selected 60 people to approach.

FIGURE 7.
Consort diagram for SW recruitment. MH8, a register of patients with schizophrenia, bipolar affective disorder and other psychoses. a, In larger GP practices not all patients were sampled, we randomly selected 60 people to approach.
Data analysis
Analysis involved detailed stages:
-
Data entry, checking and cleaning: Microsoft Excel and Access (Microsoft Corporation, Redmond, WA, USA) databases were used to store data, which were converted to SPSS (IBM SPSS Statistics for Windows, Version 21.0, IBM Corp, Armonk, NY) and UCINET (UCINET for Windows, Version 6, Analytic Technologies, Harvard, MA) for further analysis. Random accuracy checks were conducted in each site based on paper copies of data. Data were cleaned to deal with missing cases and to categorise place, activities and people (see Appendices 8 and 9).
-
Initial SPSS and UCINET analysis: this created network variables for each participant that were imported into a master SPSS file. This included use of Burt’s network efficiency to describe network density because this measure was least sensitive to network size in our data set. 26,27
-
Detailed data exploration examining descriptive and univariate statistics to draw out significant variables: this process was exploratory and reflexive, with initial results presented to team members to guide further analysis.
-
Clustering and regression models: these characterised network types and examined outcomes. Regression models were also used to study the relationship between independent variables and key outcome measures. Multicollinearity was tested using a variance inflation factor (VIF).
-
RGUK data: 149 out of 150 participants completed the resource generator. Missing data were few: out of a total of 4023 responses the total number missing from those who completed was 49, or 1.22% of total possible responses. Missing data were treated as not having access to a specific resource in line with other studies that have used the RGUK (e.g. Webber and Huxley123).
-
HRG validation process, which removed one item from the pilot scale: the distribution of scores on the scale was not normal. The majority of participants had higher scores and, therefore, the scale was split into two groups, low HRG scores from 0 to 12 (51% of respondents) and high HRG scores from 13 to 15 (49%). We had no comparative data, as the study team created and validated this scale. Missing data were treated as not having access to the resource, as with the RGUK.
The decision to use k-means clustering was based on the complexity of data and the number of available network variables that made interpretation and write-up difficult. Clusters were based on network variables only, rather than social capital or well-being data, as we were interested in describing types of network based on characteristics of people, place and activity, and relating these to health factors. Sorting individuals into small numbers of relatively homogeneous clusters provides a convenient summary of the network data, aids in interpretation and may have important theoretical and practical implications. 178
Network types were identified based on 48 selected variables covering social network, place and activity data. This number was reduced from 61 by removing highly correlated variables. The clustering procedure involves both variables and cases; with reference to previous work on creating network types. 179 We used an agglomerative clustering approach to approximate the number of clusters for the 48 variables, producing a dendrogram (see Appendix 10). The number of clusters was identified from the dendrogram based on a ‘large’ change in level, aided by the fact that three clusters made more conceptual sense to the research team when detailed analysis was carried out on each cluster. Four clusters were also tested but analysis on the three-cluster model produced stronger differences and made more conceptual sense. A k-means clustering approach was used to assign each participant to an identified cluster. Following this process, we used a frequency table (see Appendix 11) to explore the direction of variables assigned to each cluster in order to interpret and name them. In the report we refer to the clusters as network ‘types’.
Regression models180 were used to model predictors of key outcome measures (social network size, network type, RGUK score, HRG group, mental health contact type, SWEMWBS score), and the process is explained in Appendix 12. This modelling was exploratory because of the large number of sociodemographic, health status and network variables available.
Response rate
The response rate for the network interview data collection phase was disappointing. The overall response rate in London was 15.01% (80 out of 533 potential eligible participants) and in the SW 22.45% (79 out of 334). These are inaccurate, as, although we provided detailed log records to track recruitment in each GP surgery, completion of the logs by some surgeries was poor. We suggest that actual response rates based on participants successfully contacted were likely much higher but cannot accurately be estimated because of the following challenges:
-
In secondary care recruitments, teams were handed printed packs. This number was an estimate of those they told us would be eligible for the study: 75 in London and 79 in the SW. However, no records were kept on how many people were actually approached to take part. These data were requested but not recorded by the participating teams.
-
In London there were 340 packs sent by GP surgeries for which no response was received. No contact was achieved by follow-up telephone call. It was highly likely that a portion of these did not reach the participant because the surgery had the wrong address details, people on GP databases had moved away from the area, people were living in accommodation where post was less likely to reach its intended recipient and there were errors by postal services. These factors were likely to be more prevalent in London than in the SW according to feedback gathered by the study researchers. This figure was lower in the SW, with 185 packs distributed with no response received. For 61% of the potential recruitment population we have no way of knowing if they ever received our invitation to participate in the study.
We did not have data on those who did not respond or declined to participate, except that they were on the QOF GP database under the mental health indicator ‘MH8’ (MH8 is a register of patients with schizophrenia, bipolar affective disorder and other psychoses) or on team case loads in secondary care, so we cannot compare non-responders with the 150 participants on key variables to assess the likely impact of sample bias with such low response rates. We did try to obtain locality population-level data on people with psychosis but this information was not kept at borough or locality level.
In-depth interviews
Data collection
At mapping interviews, participants were asked if they would take part in the follow-up; most (127 people) consented. We selected 41 respondents to participate. People were purposively sampled to represent variation in gender, ethnicity, site, age, network size, diagnosis, length of contact with services and inpatient history (Table 3).
| Characteristic | SW (n = 20) | London (n = 21) | Total in-depth interview population (n = 41) | Network-mapping component (total study population) (n = 150) |
|---|---|---|---|---|
| Gender | ||||
| Male | 12 | 11 | 23 | 85 |
| Female | 8 | 10 | 18 | 65 |
| Age range (years) | 26–64 | 21–59 | 21–64 | 19–65 |
| Diagnosis | ||||
| Schizophrenia | 7 | 10 | 17 | 59 |
| Bipolar disorder | 8 | 7 | 15 | 65 |
| Other psychosis | 6 | 4 | 10 | 26 |
| Ethnicity | ||||
| White British | 20 | 7 | 27 | 103 |
| White other (Greek, French, Irish) | 0 | 4 | 4 | 12 |
| Asian | 0 | 3 | 3 | 7 |
| Black African/black Caribbean | 0 | 4 | 4 | 15 |
| Mixed | 0 | 3 | 3 | 13 |
| Network size range | 6–43 | 8–38 | 6–40 | 5–64 |
| Years since first mental health contact (range) | 1–45 | 3–37 | 1–45 | 1–45 |
| Has ever been an inpatient? | 15 | 15 | 30 | 122 |
Some participants were excluded because they had difficulties fully participating in the original interview process. In the later stages of sampling, a decision was made to oversample purposively from those with high levels of need, those living in supported housing, people from ethnic minorities and younger people with a diagnosis of schizophrenia in the SW, to ensure that these needs and vulnerabilities were represented, which might not have been the case if representative sampling had been used. 181
The interviews were carried out by the study’s two researchers, who undertook two pilot interviews to redefine the data collection schedule. Written informed consent was taken and participants received a £20 high street shopping voucher.
The topic guides (see Appendix 13) began by reflecting on and deepening understanding of an individual’s personal network. Each participant was presented with their visual network emotional closeness map, from the first interview, and their three network descriptor words to anchor the interview initially in the data previously provided. The topic guides then progressed to questions about changes over time and what participants did to help themselves stay well. Review of some of the early interviews by two members of the PPI group resulted in changes to the topic guide which reduced the overall number of questions and encouraged the researchers carrying out the interviews to have the confidence to allow people to talk, without worrying too much about ‘going off topic’. Interviews were digitally audio-recorded, transcribed verbatim and anonymised before analysis. The schedule was not used to elicit the social network or discuss network concepts as with some other studies167 but instead used the quantitatively mapped network as a springboard to explore how and why connections developed, the impact of illness over time, the role of practitioners and of self in shaping choices and access to resources.
Data analysis
The data analysis process took place in three stages; preliminary thematic analysis; within case, interactions between themes; and full thematic analysis and reflection. Data presented in Chapter 4 were based on the full thematic analysis but answer specific questions from emergent network dimensions prioritised as important from Chapter 3, making use of the within-case maps to support the process.
Stage 1: data immersion and theme production
Broad themes were inductively developed following the principles of working with ‘reflecting teams’, who discuss transcripts line by line, in a group, to consider all the possible layers of meaning. 182 Using this technique for data immersion allowed the academic researchers to work in partnership with the lived experience researchers. Jones states that it was more important that the members of the team work creatively and imaginatively in partnership than that they have any specific knowledge of research methods. 183
The academic researchers (two) and lived experience researchers (two) read through individually, and then as a group, three transcripts and discussed what they thought were the most important things within these transcripts. All members of the reflecting team made detailed notes on the transcripts, creating memos of their thoughts both while reading and as a result of the group discussions. The group discussion included considering whether or not differences in opinion were influenced by differences in experience and/or training. The aim of this part of the discussion was not to resolve who was ‘correct’ in a positivist sense, but to gain an understanding of the others’ perspectives. At the end of this session a list was produced of the emergent areas of what seemed to be of interest in the transcripts from the perspectives of research question 1 and what the research participants chose to talk about to the researchers.
The ‘reflecting team process’, as detailed above, was carried out twice more with one of the academics and one of the lived experience researchers on a further four transcripts. At the end of this process eight broad themes had been agreed on. Three of these were agreed to have emerged as important because interview participants had been prompted to discuss them in the initial network interviews (activities you participate in; strategies for keeping well; people). These broad themes could be considered to be deductively generated. Three broad themes were agreed to have emerged as important because of the temporal dimension that this more reflective interviewing style facilitated (past, future, changes in networks over time). One broad theme was agreed to have been inductively generated by the involvement of the lived experience researchers who identified hope and possibilities in what people had and could achieve, when the academic researchers were hearing predominantly negative narratives (building blocks to doing things for you). An eighth broad theme was introduced to cover information that was felt to be important, but which otherwise might be lost (other). Information about physical health and reflections on taking part in the network-mapping exercise were both covered by this theme.
These themes were applied, using the NVivo 10 data management tool, to all of the transcripts by two researchers who checked each other’s coding and discussed refinements to the theme definitions. The convergences, divergences and newly emergent stories within each theme were examined and discussed first within the analysis team and later with the wider research team.
For each participant a summary paragraph was also constructed blending key features of the network data from Chapter 3 with the in-depth interview material; this included three network words or phrases chosen by participants, demographical information, and diagnosis and key life events information.
Stage 2: within case, interactions between themes, analysis
We were interested in what was important to individuals and their experiences, rather than producing generalisable themes across interviews. Instead of undertaking a cross-case thematic analysis we were interested in what was important about these themes for the participants. Each broad theme, from stage 1, was allocated a colour, and visual within-case analysis was carried out for each of the participants to examine the interactions between themes within their accounts. 184 A landscape-oriented piece of white A4 paper was used for each participant185 (see Figure 8 for an example). On the left-hand side of the page factors that had been coded as being significant in participants’ ‘past’ were drawn, or written. On the right-hand side of the page the ‘future’ was represented. In the middle of the page a figure of a person was drawn and under this was listed information from ‘other’. ‘Activities’, ‘Strategies’, ‘People’, ‘Changing Networks’ and ‘Resilience’ were then all drawn or written around the remaining white space, with interactions between any of the parts of the themes being indicated with arrows.
FIGURE 8.
Example of a within-case analysis picture. Key: green, past; pink, strategies; yellow, future; orange, activities; purple, building blocks; light blue, change in networks; blue circles, people; red circles, other information, usually statements about health or beliefs; red jagged edges, particularly stressful things in life, including voices.

We asked the lived experience researcher who worked closely with the study team on this module to provide feedback on their role. The researcher summed up the involvement experience in three words:
-
energising
-
confirming (that I do have a valuable contribution to make)
-
committing (I was committed to the team and the project in the same way they were committed to supporting me in my work).
I like to think that I contributed my experiences rather than my story of living with a diagnosis of SMI. My experiences, I think, enabled me to analyse the interview transcripts in a way that was reflective of the subjective experience. I think I contributed a dry sense of humour – always helpful when the going gets tough. Being on my own recovery journey looking at the past, present and future in the analysis really fitted well with my view of peoples journeys, of which social networking and relationships are key parts.
Stage 3: axial coding and thematic analysis
The first two stages of analysis facilitated the process of data immersion and allowed the research team to consider what was important across the data set and within individual accounts, with the additional benefit of the perspective of the lived experience researchers. Qualitative components of network studies can be, and are, used to provide a greater depth of understanding of how quantitatively generated categories are experienced by individuals and to explore the heterogeneity within them. 186 A consideration of the individual in-depth interviews alongside the quantitatively derived network types and the factors that had been identified as salient by the literature review allowed individual accounts to be explored for wider meaning. Uncoded and anonymised copies of the transcripts were entered into the NVivo 10 (QSR International, Warrington, UK) data management tool. Abductive reasoning was used to produce 50 deductively (from the literature review and quantitative analysis) and inductively (from the two stages of data immersion described above) derived codes. These axial codes, which included both categories and concepts, were then applied to the transcripts by one researcher and checked, for consistency of coding, by a second. 2 The axial codes were then combined into eight thematic categories by a process of discussion and reflection between the two researchers and validation with other members of the research team; there were different categories for each of the three of the quantitatively derived network types. 187 These nine codes were specifically chosen to explore defining features of these networks in order to answer research question 1. The findings of this third stage of the analysis are reported in Chapter 4 and the implications for deepening our understanding each of the network types are discussed.
Practitioner interviews
An important aspect of the study was engaging with practitioners to explore how personal networks emphasising connections to people, place and activity were viewed both strategically and practically. The original research design was for a survey to be carried out among practitioners but concerns over poor survey response rates and the case study design led us to propose a change in methodology. The telephone interviews specifically asked about personal networks and the CHN approach as well as current concepts such as recovery.
Data collection
Semistructured interviews were conducted over the telephone with practitioners to understand their role in building and supporting personal networks. All participants at the time of interview had to be employed in a role where they had a case load including people with SMI (Table 4).
| Participant type | SW | London | Total |
|---|---|---|---|
| GP | 4 | 7 | 11 |
| Psychiatrists | 4 | 5 | 9 |
| Care co-ordinators | 9 | 6 | 15 |
| Social worker | 2 | 2 | 4 |
| Senior mental health practitioner | 2 | 2 | 4 |
| Occupational therapist | 2 | 1 | 3 |
| Psychologist team leader | 0 | 1 | 1 |
| Community psychiatric nurse | 3 | 0 | 3 |
| Third-sector staff | 5 | 4 | 9 |
| Total | 22 | 22 | 44 |
Recruitment
The sample was recruited using convenience sampling. We started with GPs, identifying participants in our recruitment surgeries. Third-sector organisations mentioned by service users in mapping interviews were contacted. The project team made presentations at secondary mental health team meetings, requesting participation from team members. The MHRN also assisted by distributing study information sheets to known contacts, particularly psychiatrists.
Development of semistructured interview guide
The semistructured interviews were designed by the research team with input from the PPI group. We undertook the following process:
-
draft schedule developed and workshop held with PPI group to review
-
pilot schedule used with two participants and transcripts reviewed
-
schedule amended by study team and data collected from 18 participants
-
workshop held with PPI group to assess schedule and data collected; six transcripts assessed
-
revised schedule used with remaining participants (n = 26) (see Appendix 14).
We found that the original schedule was not providing us with as many data as we hoped around the practitioner role and their view on network development. This had not been an issue in the pilot, where we had two engaging interviews: one with a psychiatrist, the other with a social worker. In consultation with the PPI group we revised the schedule, opening up the dialogue with questions on which all practitioners would have an opinion: factors influencing recovery and SMI. The interviews directly assessed practitioners’ views on their role within networks and network enhancement.
Interview process
To help keep track of the conversation within the interview, mind maps were created to help follow responses, identify links between points and assist with decisions over follow-up probing. An example of a mind map is provided in Figure 9.
FIGURE 9.
Example of researcher’s mind map to help navigate through interview.

Data analysis
We used a thematic analysis process before coding data in NVivo 9. The aim was to immerse ourselves in the data and look across practitioner roles for emergent themes before coding commenced; this was both a deductive process following research questions and an inductive-driven enquiry being led by the research data. 167 In total four people worked on these data before one researcher applied the final coding frame and a second researcher checked the data coding. The main coding themes were allocated to explore:
-
approaches to recovery
-
stigma
-
roles within network (practitioner, individual, others)
-
resources within networks
-
network development goals
-
challenges for network development
-
practitioner feedback on the CHN approach
-
case studies.
Query reports were discussed and agreement reached for a final coding decision.
The practitioner data were written up in Chapter 6, structured to follow the research questions, providing a similar format to the data reported in Chapter 5.
Organisation interviews: series 2
Data collection
After we had completed data collection in all the other modules, our final data gathering phase involved returning to organisations in both study sites to re-interview informants. We decided to interview strategic leaders covering commissioning, primary care, the NHS, local authority and mental health third sector (Table 5). We did not interview mainstream community resource leads (education, sports and recreation) as our interview schedule (see Appendix 15) required mental health expertise.
| Participant type | SW | London | Total |
|---|---|---|---|
| Trust/social care leadership | 2 | 2 | 4 |
| Mental health third sector | 1 | 1 | 2 |
| Primary care | 1 | 2 | 3 |
| Community organisations | 0 | 0 | 0 |
| Commissioner | 1 | 1 | 2 |
| Total | 5 | 6 | 11 |
Recruitment
We reviewed positions of responsibility among organisations and assessed appropriateness for second interviews based on job title, data collected and alternative participants. In total, out of 11 interviews, five were second interviews following up from module 1.
Development of interview guide
The second organisation interview schedule was developed by the study team following a project meeting with our advisory group and PPI group, where all study data were considered. The goal was to keep interviews to 30 minutes and to cover:
-
reaction to study data (we struggled to articulate clearly the study focus to practitioners; thus we decided to root these interviews in the data by presenting case material and seeking a reaction to this information)
-
local changes to policy and practice (in the past 18 months)
-
views on recommendations and dissemination routes.
Data analysis
The data analysis process repeated the approach outlined in Chapter 2 (section Data collection) following a modified framework approach. These data were used within the case study synthesis (see Chapter 7) to provide context for understanding the health and social care structures within which personal networks for people with SMI operate.
Synthesis
We undertook a three-stage final synthesis process. First we undertook within-case synthesis for the SW and for London, producing two site analyses. Second we commissioned the PPI group to review our findings using their lived experience to assess the relevance of our data and interpret them with reference to their own recovery journeys. Finally we brought together all data components to answer the three main research questions using a bespoke model that emerged through research team reflection. The research team, including the PPI group, found that network-mapping data, in-depth interview data, practitioner interviews and organisational leads interviews all revealed the potential of the CHN approach for understanding connectedness through people, places and activities in recovery (see Appendix 1). To test this potential, each data module write-up was reviewed by two members of the research team for evidence of individual agency, structures and systems, and access to resources for shaping people’s lives. The results of this process are found in Chapter 8.
Synthesis case studies
Social network analysis studies are increasingly incorporating and combining quantitative and qualitative data in complementary ways. 188 We did not do this formally, but instead created a hybrid approach that used network-mapping visuals as the springboard for detailed exploration of what life looks like now and in the past for someone with SMI managing their health and well-being. Within mixed-methods studies there was a danger that combining data sources could lead to clashes between the underlying assumptions of both methodological approaches. 189 We sought to overcome this using within-case synthesis by carefully integrating qualitative and quantitative data, from a variety of perspectives in a geographically bound context, working together as a study team to check each other and draw out shared meaning. The two case studies were intended to present two contrasting cases. The case studies were quantitatively driven, in that the salient features, such as the predominant characteristics of networks, were quantitatively derived. The qualitative data were used to complement this by demonstrating what these generalisable quantitative trends actually looked like in the context of individuals’ lives. The wider context was then considered and the qualitative data from organisational lead interviews (series 2), for each site, was used to examine the local barriers and facilitators for individuals when trying to develop their personal networks through the context of wider community resources. Finally the case studies consider the implications for how practitioners and organisations can help people living with SMI by using a CHN approach.
Patient and public involvement group lived experience reflexive expert review
The case for PPI in research rests on the claim that research that has involved the public at design stage and through the research cycle is likely to be of higher ethical quality and relevance to the populations that it serves. 190 PPI has further been defined as an ongoing dialogue between informed scientific and lay deliberators, each of whom adds different kinds of value to the public practice of science. 191 More recently, these ethical claims have been challenged with the suggestion that they are premised on a paradox: that once the lay voice becomes scientifically informed the ethical claim is unfounded. 192
The study team decided to approach this dilemma with an open mind. At present, the most compelling evidence for PPI in mental health research has focused on the impact of involvement in design and recruitment to studies, suggesting a correlation between the two. 193 Much less attention has been focused on the impact of PPI on the interpretation and synthesis of data as an interactive learning journey and even less on reflexive analysis around the role of lived experience in shaping findings and conclusions. Consequently, the study team decided that the recovery focus around agency within the study necessitated, on the one hand, a commitment to active involvement in the interpretation and synthesis to remain congruent with an ethics of coproduction, and on the other, reflexive critical analysis to consider the strengths and weaknesses of so doing.
We commissioned an independent lived experience PPI consultant who had not been involved with the study to facilitate and lead an interpretative review of the analysis drawing on the expertise of the existing study PPI group who had been employed on the project in a range of research roles. The reason for choosing an independent consultant was to ensure critical independence of view, blinded from the interests and research investments of the wider research team. Members of the existing PPI group were involved with a wide range of research methods awareness and project knowledge, from very little to having a role as research assistant in the data collection. All five of the PPI group had personal experience of living with schizophrenia or bipolar disorder and wider interests in mental health service development and well-being programmes. The PPI group both collaborated and consulted with the lived experience lead throughout the interpretation process according to capacity and time availability.
Three stages followed:
-
The independent PPI consultant used a clearly defined and iterative process adapted from previous life story work around personal and social recovery with people with SMI to facilitate the interpretative agency of all members of the PPI group across the range of recovery perspectives and research awareness. 194,195 This was combined with a ‘critical friendship’ approach to working with the study team in which ‘warts and all’ review was combined with working towards the greater good of research quality. This critical friendship approach to PPI has been shown in another study to improve research quality. 196
-
There was no governance requirement to go to an ethics committee for PPI. However, we felt it was important to be mindful of potential current vulnerabilities within the PPI study group. An initial telephone interview covered agreement to use lived experience to interpret the analysis and checked emotional safety around so doing. Appropriate disclosure issues were explored, as anonymous perspectives were still likely to be recognisable to the study team.
-
The PPI study group were initially given four questions by the PPI consultant, reflecting on their own recovery journey within their work on the project. Responses from each lived experience expert (LEE) were written up as an individual starting position to frame subsequent interpretation and develop the interview schedule. Reflexivity was built into the interview schedule by asking each LEE to consider how their answers were informed by their lived experience perspectives at each step. The group were asked: What was interesting in the data? What was surprising? What was missing that they might have expected to see? What was salient in relation to their experience? What did they think the conclusions and recommendations and next steps should be?
This proceeded as follows:
-
Draft report chapters from August 2013 – network and in-depth interviews – were read. This was followed by a telephone interview with the independent PPI consultant to reflect back views from reading the material. The consultant used the interview schedule to elicit feedback from all five PPI group members.
-
Second set of August 2013 draft report chapters were circulated – organisation and practitioner interviews.
-
Third telephone interview with research consultant was undertaken to reflect back views.
-
Research consultant drafted report based on all the feedback, supported by one member of the group who had also collected primary data to check accuracy of report.
-
The draft report was circulated for comment and face-to-face meeting attended by PPI group and principal investigator to discuss emerging findings.
-
Final changes were made to the draft report, which features as Appendix 1.
The original aim was to include the reflexive review as a separate chapter but on further reflection and review we considered the greatest strength of its impact on the final synthesis was at a formative rather than summative stage. The reflexive review took place at a point in time when the wider study team were still making sense of the data and was never intended be more than a positioned and situated interpretation to make the PPI collaboration within the broader work of interpretative synthesis visible; there is as yet very little formal process around recording these activities in research studies. We consider recognition of these situated limits to be a strength making the research more reflexive.
Overall synthesis
Four members of the research team, including those with quantitative and qualitative research skills, read across all the results of all of the data sets. After immersing ourselves in the data in this way we discussed what seemed to be important within it for understanding the networks of people with SMI. We inductively brought to the surface several theories about how these different elements might be functioning. These have been named ‘meta inferences’. 197 Potential interpretive inconsistencies were not avoided or ignored; following this direction ‘complementary inferences’ were used to provide insights into different aspects of the same phenomena. Therefore, when combined they provide a more complete meaning. 198 We returned to the wider literature to examine how our thoughts related to the work of others, including overarching sociological explanations, and then re-examined the data with these in mind. We first used a matrix to pull together sources of data from Chapters 3–7 in order to ‘test’ three dimensions of influence in networks: availability of resources; use of agency; and external structures and systems. These three dimensions drew on conceptions of agency23 and considerations of structure, as applied to health. 199 We explored the data for:
-
signs of enactment of different types of agency within individuals with SMI and also in practitioners and organisational leaders (the agency of others)
-
the availability of resources and their role in effecting change
-
the impact of external structures and systems enabling, and also acting as barriers to, network development.
Second, we used the products of this analysis to answer the three study research questions. We looked at how personal connections to people, places and activities were used by people with SMI, and explored practitioner roles within them as a distinct influence. We sought to understand how organisations used network approaches that extended beyond social networks to support people with SMI. Finally we addressed how wider community collaborations were built between organisations, and the partnerships forged to provide interorganisation integrated networks of support for people with SMI. The LEE report (see Appendix 1) was an additional data source at this second stage, providing insight into what the PPI group thought was most important in the data set for answering these research questions.
Our study had been primarily empirically driven, with theoretical contextualisation, and this synthesis process aimed to produce an empirically led provisional framework for understanding people’s lives and contributing the wider recovery approach. We drew on concepts in published literature as and when they deepened our understanding of these findings.
Chapter 3 Network mapping
Introduction
This chapter presents the results of network-mapping interviews and SNA analysis. It aims to answer the following protocol research question: How do people with SMI use resources in their personal networks to support their health and well-being? In doing so we created several sub-questions to investigate:
-
What characteristics made up the personal networks of people with SMI?
-
What is the mix of formal and informal health-care provision within people’s networks?
-
Do these networks differ in composition, range, size and density across subgroups?
-
How does network strength and breadth relate to well-being?
In this chapter we present results of interviews which mapped connections to people, place and activity. We explore the entire network-mapping data covering both study sites while site comparison is presented in Chapter 7. Site differences are mentioned in this chapter only where significant in regression models. We collected more information and undertook more detailed exploratory analysis than can be presented within the report. Therefore this chapter was structured by key findings:
-
three personal network types (section Network types) and exploring the study population (section Participant characteristics) to describe who has which network type
-
key characteristics of social [section Social networks (people)], place (section Connection to place) and activity (section Meaningful activity) connections among our study population and satisfaction with networks (section Satisfaction with current networks)
-
access to resources (section Networks, access to resources, well-being and mental health contact) through personal networks and their association with other outcomes (section Networks, access to resources, well-being and mental health contact).
Network types
The network-mapping cluster analysis, described in Chapter 2 (section Data analysis), generated three distinct types of network. We named these ‘diverse and active’, ‘family and stable’ and ‘formal and sparse’, based on key differences in the variables within each network type.
Diverse and active networks
Diverse and active were the largest networks, containing the most people, places and activity connections overall. They describe 36.7% of the study population (55 people). Social ties were characterised by larger numbers of friends and wider connections (acquaintances and colleagues) and a high frequency of social contact. With low social network density (ties were more loosely knit) and a high mean number of different relationships, they were also the type which most closely resembled ‘bridging capital’ in structure: weaker and wider ties to different contacts and groups.
Place connections in this network type were dominated by community-based settings such as education and work, and a higher proportion of places where social interaction was mentioned, as well as place connections which had been built through informal referral, such as recommendations from family and friends. Participants with diverse and active networks spent the majority of their waking time outside the home.
Diverse and active networks also had high levels of meaningful activity including relational activities such as socialising and physical activities such as going for walks or running. On average a fifth of these activities were externally structured (either by organisations or through involvement in formal activity groups such as book or cycling clubs). There was an even split between activities done alone and those done with other people. These networks were also characterised by higher proportions of connections made within the last 5 years. The majority of place and activity connections in this type were less than 5 years old. Participants with diverse and active networks also reported higher satisfaction with their connections.
Figure 10 illustrates a diverse and active network type. Mental and physical health settings were present, but the bulk of the network was taken up by connections to community settings and there were also a wide variety of social ties. The family network was large but did not dominate, smaller nodes indicate that many family members were seen less frequently and the existence of separate components such as the leisure centre, martial arts centre and work indicate a diverse network. In Chapter 4 we draw on a qualitative interview with SUL29, where he is known by a pseudonym, ‘Kevin’.
FIGURE 10.
An example diverse and active network (SUL29). Shape of node: type of node. Circle = person, square = place, diamond = activity. Colour of node = well-being impact. Red = very negative, orange = negative, white = neutral, yellow = positive, green = very positive. Size of node: frequency. Larger nodes = more frequently interacted with social ties/activities engaged in/places connected to. Colour of text: mental health network. Blue text = mental health nodes, black = other. Note: These diagrams have been anonymised, including changing of place names where they were too specific. Where social ties and activities were not attached to places this was because they were not interacted with or done in any specific location. Similarly activities without connections to people were those that were done alone. The participant was not located in these diagrams in order to reduce complexity of diagrams but they were connected to everything within them.
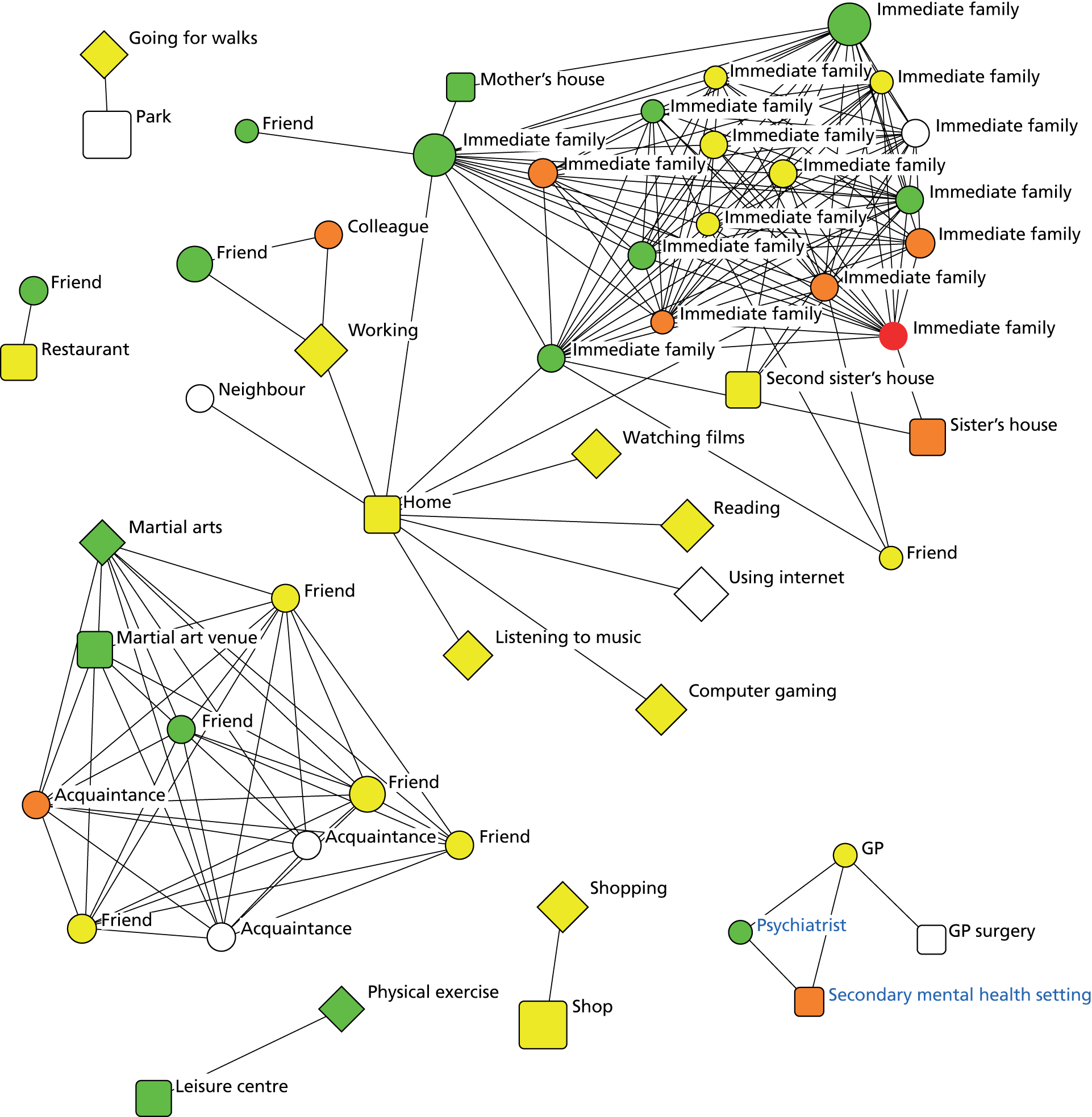
Family and stable networks
Family and stable networks were the most bonded and durable network type and describe 32% (48) of our study population. ‘Bonding capital’ refers to the presence of close ties with similar people and these networks were characterised by larger numbers of family contacts including children, partners and wider family. There were relatively few non-family ties. Stability and durability was reflected in the majority of social contacts having been known for longer than 5 years. These networks also had higher numbers of informal carers and neighbours inside the social network. Network density or the proportion of network contacts who also know each other was highest in family and stable networks.
Place connections in this type were stable, the majority on average being older than 5 years. Mental health settings make up a very low proportion of overall place connections. Participants with this network type spent most of their time at home but tended to live with others; home was rated by most as a positive place. They had similar levels of full-time and part-time employment to diverse and active networks and higher than formal and sparse networks. There were high numbers of individually structured activities (those activities where activity was structured by the individual, such as reading or walking, not part of a formal group but alone or with friends and family) and a low proportion of activities which were unstructured (such as watching TV or listening to radio).
Figure 11 is an example of a family and stable network showing a strong family-focused network where home was the key hub but it was also a social place where social interaction and social activity took place. The participant was managed by primary care for their mental health and rated this setting and their GP as negatively impacting their well-being. They also had negative wider family contacts but on the whole the network was positive and was structured around activities with family.
FIGURE 11.
An example family and stable network (SUSW56). Shape of node: type of node. Circle = person, square = place, diamond = activity. Colour of node = well-being impact. Red = very negative, orange = negative, white = neutral, yellow = positive, green = very positive. Size of node: frequency. Larger nodes = more frequently interacted with social ties/activities engaged in/places connected to. Colour of text: mental health network. Blue text = mental health nodes, black = other. Note: These diagrams have been anonymised, including changing of place names where they were too specific. Where social ties and activities were not attached to places this was because they were not interacted with or done in any specific location. Similarly activities without connections to people were those that were done alone. The participant was not located in these diagrams in order to reduce complexity of diagrams but they were connected to everything within them.
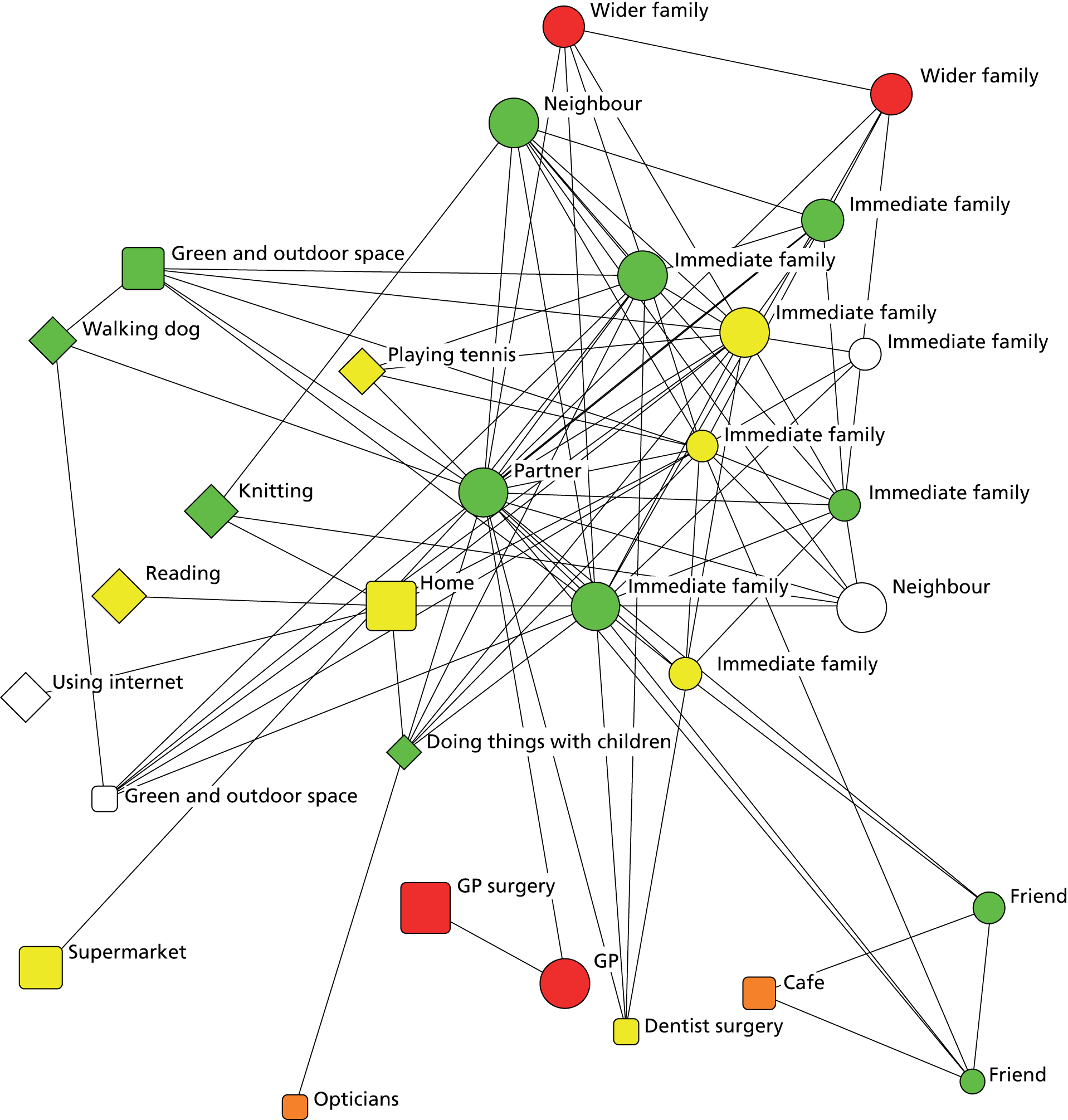
Formal and sparse networks
Formal and sparse networks were the smallest, least diverse or active of all the network types and describe 31.3% (47) of our study population. They were characterised by social networks with fewer family, friend or wider contacts and a larger proportion of the network dominated by formal contacts such as mental health or other health practitioners.
Participants with these networks spent most of their waking time at home and also tended to live alone. Place connections were dominated by high proportions of mental health and physical health settings and lower proportions of community settings. A higher number of place connections had been built through formal referral (from practitioners and organisations) and a lower proportion of places involve social interaction. Participants in this cluster had the highest number of unstructured activities such as watching TV or listening to the radio.
Figure 12 shows a formal and sparse network with fewer overall connections and in which physical or mental health settings were more dominant and most of the individual’s time was spent at home where they live alone. Although two friends visited, most activities were done alone and various local shops represented the only regular and current community setting connection. What connections the participant did have were rated positive for well-being impact.
FIGURE 12.
An example formal and sparse network (SUL13). MH, mental health. Shape of node: type of node. Circle = person, square = place, diamond = activity. Colour of node = well-being impact. Red = very negative, orange = negative, white = neutral, yellow = positive, green = very positive. Size of node: frequency. Larger nodes = more frequently interacted with social ties/activities engaged in/places connected to. Colour of text: mental health network. Blue text = mental health nodes, black = other. Note: These diagrams have been anonymised, including changing of place names where they were too specific. Where social ties and activities were not attached to places this was because they were not interacted with or done in any specific location. Similarly activities without connections to people were those that were done alone. The participant was not located in these diagrams in order to reduce complexity of diagrams but they were connected to everything within them.
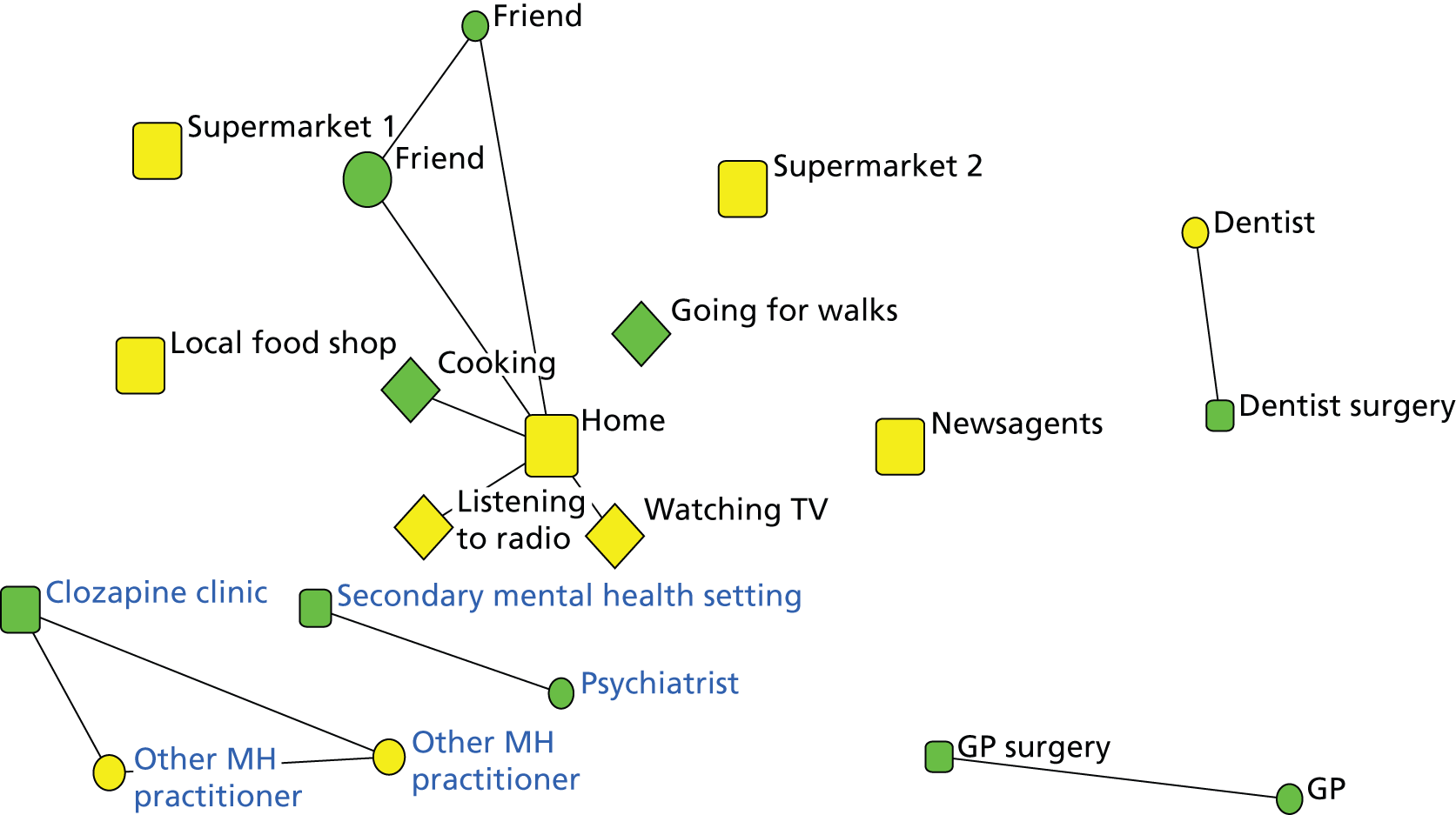
Participant characteristics
In this section we describe the 150 study participants. Asterisks in tables throughout this section indicate where differences were statistically significant across network types; only significant differences are shown.
Sociodemographics
Over half the total study population were male and over two-thirds were white British (see Table 6). Gender did not differ significantly across network type but ethnicity did differ; fewer participants who were not white British had family and stable networks. Mean age was significantly higher in formal and sparse networks and lowest in diverse and active networks.
| Variable | Level | Total study population | Diverse and active networks | Family and stable networks | Formal and sparse networks |
|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | ||
| Gender | Male | 56.7 (85) | 35.3 (30) | 30.6 (26) | 34.1 (29) |
| Female | 43.3 (65) | 38.5 (25) | 33.8 (22) | 27.7 (18) | |
| Ethnicity (χ2 = 8.59**) | White British | 69.3 (104) | 32.7 (34) | 39.4 (41) | 27.9 (29) |
| Other | 30.7 (46) | 45.7 (21) | 15.2 (7) | 39.1 (18) | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age (F = 4.01*) | Years | 46.3 (11.5) | 42.9 (12.7) | 47.8 (11.1) | 48.7 (9.5) |
Mental and physical health
Table 7 summarises mental and physical health characteristics of respondents and network type. The process of grouping diagnosis is explained in Appendix 8. We also found 88% of respondents (133 people) took medication for their mental health problem, of whom 89.5% took medication orally, 6.8% both orally and via depot injection and 3.8% via depot injection only.
Sixteen respondents (10.7%) had been admitted to hospital for physical health reasons in the last 12 months. Reasons for admission included hernia operations, kidney problems, overdose, gallstone removal, cancer treatment and a shoulder operation; 86.7% recalled receiving a physical health check from their GP or practice nurse and 50.7% were taking prescribed medication for physical health reasons.
Diagnosis was grouped as explained in Chapter 2. Groups differed significantly across network type; significantly fewer participants with psychotic disorder/schizophrenia had family and stable networks while almost half of those with manic episodes/bipolar had these networks. Mental health contact type also differed significantly; more of those participants managed only in primary care had family and stable networks and fewer had formal and sparse networks. Inpatient (but not sectioning) history differed significantly and there were fewer participants who had been a psychiatric inpatient who had family and stable networks.
We note several sociodemographic differences in these mental and physical health variables; we did not know why there were these differences in the study sample and the reasons were likely to be multiple, relating to our study design and features of the delivery of psychiatric services. Gender spread was significantly different by diagnosis; 74.6% of the psychotic disorder/schizophrenia group was male compared with 47.7% of the manic episodes/bipolar and 38.5% of the other psychoses group {χ2[degrees of freedom (df) = 2, n = 150] = 13.35, p < 0.01}. The mean age of those managed in primary care was significantly higher than those managed in secondary mental health services, at 48.8 years compared with 44.8 (t = 2.13, df = 125.51, p = 0.04). Significantly fewer participants who were not white British (23.9%) than white British participants (45.2%) were managed only in primary care [χ2(df = 1, n = 150) = 6.09, p =0.01]. Significantly more participants with schizophrenia/psychotic disorder had been an inpatient: 93.2% compared with 84.6% of those with other psychoses and 69.2% of those with manic episodes/bipolar, [χ2(df = 2, n = 150) = 11.95, p < 0.01].
Time since last psychiatric inpatient admission was used as a proxy for illness stability. The median number of years since last admission was 6 and the mode was 1. About a quarter (27%) of those who had been an inpatient had been admitted in the last 2 years, 47.8% in the last 5 years and 74.8% in the last 13 years. We found no significant difference across network type but participants in touch with secondary services had been an inpatient significantly more recently than those managed in primary care, at 7.2 years compared with 11.7 years (t = 2.81, df = 76.60, p = 0.06).
| Variable | Level | Total study population | Diverse and active networks | Family and stable networks | Formal and sparse networks |
|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | ||
| Diagnosis groups(χ2 = 14.18**) | Psychotic disorder/schizophrenia | 39.3 (59) | 42.4 (25) | 16.9 (10) | 40.7 (24) |
| Manic episodes/bipolar | 43.3 (65) | 29.2 (19) | 47.7 (31) | 23.1 (15) | |
| Other psychoses | 17.3 (26) | 42.3 (11) | 26.9 (7) | 30.8 (8) | |
| MH contact type (χ2 = 7.66*) | Primary | 38.7 (58) | 32.8 (19) | 44.8 (26) | 22.4 (13) |
| Secondary | 61.3 (92) | 39.1 (36) | 23.9 (22) | 37.0 (34) | |
| Inpatient history | Has been inpatient for MH (χ2 = 7.63*) | 81.3 (122) | 40.2 (49) | 27.0 (33) | 32.8 (40) |
| Have been under section | 63.9 (78) | 38.5 (30) | 26.9 (21) | 34.6 (27) | |
| Never been inpatient | 18.7 (28) | 21.4 (6) | 53.6 (15) | 25.0 (7) | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Time since last inpatient MH admission | Mean years since last psychiatric admission | 8.9 (8.2) | 9.5 (9.8) | 8.9 (7.2) | 8.1 (6.8) |
| Length of contact with services | Mean years since first sought help for MH problem | 20.1 (11.7) | 17.9 (12.1) | 20.9 (11.4) | 22.0 (11.4) |
Accommodation and relationship status
Table 8 summarises participant living arrangements and relationship status. We grouped housing type into three groups in which we inferred decreasing stability from ownership (most stable) to other (least stable). ‘Other’ housing types include residential homes or sheltered housing (8% of respondents), staying in a hostel (0.7%), staying with a friend or family in own room (4.7%), sofa-surfing (1.3%) or other (1.3%). We split living situation by alone or with others. ‘With others’ included living with partner/spouse (28%), parent(s) (8.7%), other family (2.7%), friends (2%), or other (8.7%). Marital status was grouped into married/in a civil partnership or cohabiting (with an intimate partner), or ‘other’. ‘Other’ statuses include separated/divorced (14.7%), single (55.3%) and widowed (0.7%).
| Variable | Level | Total population % (n) | Diverse and active networks % (n) | Family and stable networks % (n) | Formal and sparse networks % (n) |
|---|---|---|---|---|---|
| Housing type (χ2 = 17.55**) | Home ownership | 26 (39) | 33.3 (13) | 53.8 (21) | 12.8 (5) |
| Home rental | 58 (87) | 33.3 (29) | 27.6 (24) | 39.1 (34) | |
| Other | 16 (24) | 54.2 (13) | 12.5 (3) | 33.3 (8) | |
| Living situation (χ2 = 35.52***) | Alone | 50 (75) | 41.3 (31) | 10.7 (8) | 48.0 (36) |
| With others | 50 (75) | 32.0 (24) | 53.3 (40) | 14.7 (11) | |
| Children | Have children (χ2 = 27.00***) | 43.3 (65) | 16.9 (11) | 52.3 (34) | 30.8 (20) |
| Living with children (χ2 = 24.82***) | 14.7 (22) | 18.2 (4) | 77.3 (17) | 4.5 (1) | |
| Pets | Living with pets | 30 (45) | 28.9 (13) | 44.4 (20) | 26.7 (12) |
| Marital status (χ2 = 49.93***) | Married/civil partnership or cohabiting | 29.3 (44) | 22.7 (10) | 72.7 (32) | 4.5 (2) |
| Other | 70.7 (106) | 42.5 (45) | 15.1 (16) | 42.5 (45) | |
| Informal carer | Have informal carer (χ2 = 6.21*) | 28.7 (43) | 25.6 (11) | 46.5 (20) | 27.9 (12) |
We found that age decreased significantly with less stable housing type [F(df = 2, n = 147) = 8.81, p < 0.001] and participants who owned homes were significantly older (mean 51.1 years) while participants in the other housing type were youngest (mean 39.3 years). Diagnosis also significantly differed, with only 6.8% of the psychotic disorder/schizophrenia group owning a home compared with 38.5% of manic episodes/bipolar group and 38.5% of the other psychoses group χ2(df = 4, n = 150) = 18.96, p < 0.001. Participants who lived alone were significantly older (t = 3.63, df = 148, p < 0.01) and had been in touch with services for significantly longer (t = 2.55, df = 148, p = 0.01) than those who did not live alone, while significantly more of the psychotic disorder/schizophrenia group (64.4%) lived alone than the other psychoses (46.2%) or manic episodes/bipolar (38.5%) groups [χ2(df = 4, n = 150) = 8.51, p = 0.01]. Diagnosis also differed significantly by marital status, with more participants with manic episodes/bipolar and fewer of those with psychotic disorder/schizophrenia married/in a civil partnership or cohabiting [χ2(df = 2, n = 150) = 12.10, p <0.01]. The reported presence of an informal carer who provides support and assistance was significantly higher for participants who lived with others [χ2(df = 1, n = 150) = 9.42, p < 0.01], but we found no difference according to marital status; 65.9% of those married/in a civil partnership or cohabiting did not report having an informal carer. Many of our participants viewed partners and other relatives not as ‘carers’ but as ordinary family.
Table 8 shows that significantly more participants who owned their homes had family and stable networks while most participants in ‘other’ housing types had diverse and active networks. Similarly, significantly more participants who lived with others had family and stable networks and those who lived alone tended to have either diverse and active or formal and sparse networks. Significantly more participants who were married/in a civil partnership or cohabiting, and who had an informal carer, had family and stable networks. Very few participants who were married/in a civil partnership or cohabiting had formal and sparse network types.
Education and employment
Table 9 summarises education and employment status of the study participants. Only a small minority of participants did not have a formal education but fewer than 30% had full- or part-time employment. Employment percentages add to more than 100%, as some participants had more than one employment type. Qualifications included National Vocational Qualification (NVQ) level 1 or below (6.7%), General Certificate of Education (GCE)/General Certificate of Secondary Education (GCSE) O-levels or equivalent (24.7%), GCE/GCSE A-levels or equivalent (12%), higher education qualifications below degree level (12.7%) or degree level equivalent or higher (33.3%).
| Variable | Level | Total study population % (n) | Diverse and active networks % (n) | Family and stable networks % (n) | Formal and sparse networks % (n) |
|---|---|---|---|---|---|
| Education level (χ2 = 8.35*) | No formal education | 10.7 (16) | 25 (4) | 12.5 (2) | 62.5 (10) |
| Qualifications | 89.3 (134) | 38.1 (51) | 34.3 (46) | 27.6 (37) | |
| Employment status | Working full time (χ2 = 6.48*) | 15.3 (23) | 47.8 (11) | 43.5 (10) | 8.7 (2) |
| Working part time | 14 (21) | 42.9 (9) | 42.9 (9) | 14.3 (3) | |
| Volunteering | 10.7 (16) | 62.5 (10) | 18.8 (3) | 18.8 (3) | |
| In education/training | 6.7 (10) | 80 (8) | – | 20 (2) | |
| Unemployed | 15.3 (23) | 34.8 (8) | 26.1 (6) | 39.1 (9) | |
| Long-term sickness/disability (χ2 = 15.26***) | 35.3 (53) | 22.6 (12) | 26.4 (14) | 50.9 (27) | |
| Looking after family/home | 3.3 (5) | 20 (1) | 60 (3) | 20 (1) | |
| Retired | 10 (15) | 33.3 (5) | 40 (6) | 26.7 (4) |
We see from Table 9 that network types differ significantly by both education and employment (full-time employment or long-term sickness) dimensions; both more of those with no educational qualifications and those who were on long-term sickness/disability benefit, had formal and sparse networks while fewer of those who worked full time did not.
What type of individuals were in each network type?
We used multinomial logistic regression to assess which social, health and demographic variables remained significant when controlled for other variables. For categorical response variables, the computed R2 is pseudo-R2, and thus the total variation was not reported but instead approximations were reported. See Appendix 12 for the full list of variables used in this analysis.
| Network types compared | Significant independent variables | Coefficient (standard error) | Wald | p-value | Odds ratio (95% CI) |
|---|---|---|---|---|---|
| Diverse and active versus formal and sparse | Long-term sickness or disability | –1.92 (0.943) | 4.15 | 0.042 | 0.15 (0.02 to 0.93) |
| Formal and sparse versus family and stable | No formal qualifications | 4.38 (1.94) | 5.11 | 0.024 | 79.92 (1.79 to 3573) |
| Living with others | 3.74 (1.68) | 4.94 | 0.026 | 41.95 (1.55 to 1133) | |
| Diverse and active versus family and stable | Long-term sickness or disability | –3.24 (1.53) | 4.49 | 0.034 | 0.039 (0.002 to 0.785) |
| Living with others | 3.77 (1.64) | 5.28 | 0.022 | 43.2 (1.74 to 1075) | |
| Renting compared with ‘other’ housing status | 4.16 (1.77) | 5.53 | 0.019 | 64.2 (2 to 2062) |
Table 10 shows that, when controlled for other variables, only four items remain significant in the model. Participants on long-term sickness or disability benefit were significantly less likely to have diverse and active network types than the other two network types, but this was variable did not significantly affect differences between formal and sparse and family and stable network types. Participants with no formal education qualifications were significantly more likely to have formal and sparse networks compared with family and stable networks than those with formal qualifications. Participants who were living with others were more likely to have family and stable networks than both diverse and active and formal and sparse network types than those living alone. Although we found diagnostic differences in Table 7, when controlled for other variables they are no longer significant.
Well-being and functioning
The Dartmouth CO-OP charts self-assessed current functioning, health status and quality of life (Table 11). All questions were framed within the last 4 weeks from point of data collection and we used a published coding frame for comparison where lower scores refer to better functioning. 200 The CO-OP scores in our study indicated poorer health and functioning on all of eight measures than for the large community (general population) sample. 200
| CO-OP measure | Total study population mean score (SD) | Diverse and active networks mean score (SD) | Family and stable networks mean score (SD) | Formal and sparse networks mean score (SD) | Population norms,201 n = 3549, mean score (SD) |
|---|---|---|---|---|---|
| Physical fitness | 1.61 (1.35) | 1.41 (1.41) | 1.48 (1.13) | 1.91 (1.46) | 1.35 (1.25) |
| Emotional problems (feelings) | 2.07 (1.24) | 1.87 (1.23) | 1.96 (1.18) | 2.43 (1.26) | 1.37 (1.18) |
| Difficulty with daily activities | 1.57 (1.14) | 1.36 (1.06) | 1.50 (1.13) | 1.89 (1.18) | 0.68 (0.94) |
| Limited social activities (t = 3.09*) | 1.57 (1.33) | 1.33 (1.23) | 1.48 (1.13) | 1.96 (1.56) | 0.57 (0.96) |
| Experience of pain | 1.51 (1.49) | 1.27 (1.47) | 1.50 (1.44) | 1.79 (1.53) | 1.19 (1.19) |
| Overall health (t = 3.34*) | 2.14 (1.16) | 1.93 (1.23) | 2.04 (1.11) | 2.49 (1.06) | 1.63 (1.00) |
| Social support (t = 9.09***) | 1.73 (1.42) | 1.47 (1.23) | 1.35 (1.39) | 2.43 (1.44) | 1.13 (1.33) |
| Quality of life | 1.78 (0.93) | 1.69 (.96) | 1.71 (.90) | 1.96 (.93) | 1.23 (0.80) |
| SWEMWBS measure | Total population mean score (SD) | Diverse and active networks score (SD) | Family and stable networks score (SD) | Formal and sparse networks score (SD) | General population score202 |
| SWEMWBS score (F = 3.92*) | 22.3 (5.7) | 23.5 (5.6) | 23.0 (5.3) | 20.4 (6.0) | 25.3 |
We saw significant differences across network types in the three asterisked measures in Table 11, where in all cases, those with formal and sparse networks had the worst scores while those with diverse and active networks had highest overall health and least limited social activities; those with family and stable networks had the most social support.
Our SWEMWBS was lower than the general population. We present a multiple regression model on this scale in the last section.
Figure 13 indicates that, while SWEMWBS scores differed significantly across network type, all network types included participants with higher and lower well-being.
FIGURE 13.
Distribution of well-being scores within each network type.
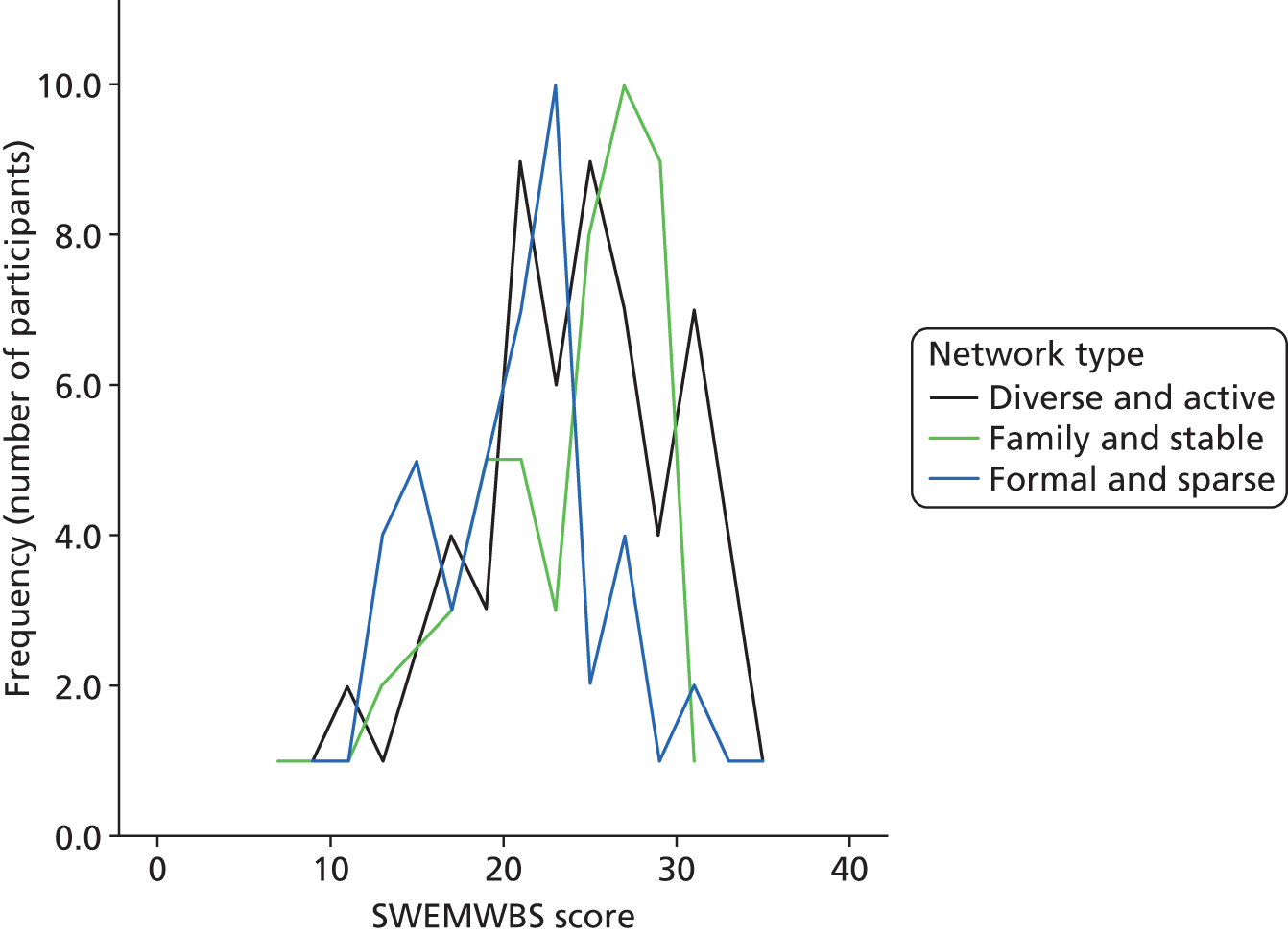
Exploring diagnosis groups in the study population
Table 12 below summarises significant differences by diagnosis, rather than network type. It shows that people with psychotic disorder/schizophrenia tended to be male, with the lowest levels of full time employment, formal education, marriage/cohabiting and home ownership and the highest levels of long-term sickness/disability and living alone.
| Variable | Psychotic disorder/schizophrenia | Manic episodes/bipolar | Other psychoses |
|---|---|---|---|
| Gender (χ2 = 13.35***) | |||
| Male n (%) | 44 (74.6) | 31 (47.7) | 10 (38.5) |
| Female n (%) | 15 (25.4) | 34 (52.3) | 16 (61.5) |
| Mean age*** (SD) | 44.5 (11.3) | 46.8 (10.8) | 49.2 (13.1) |
| Employment | |||
| Working full time n (χ2 =7.93*) | 4 | 16 | 3 |
| Long term sickness/disability** n (%) (χ2= 7.34*) | 28 (47.5) | 20 (30.8) | 5 (19.2) |
| Married or cohabiting* n (%) (χ2 = 12.10**) | 8 (13.6) | 27 (41.5) | 9 (34.6) |
| Living alone** n (%) (χ2 = 8.51**) | 38 (64.4) | 25 (38.5) | 12 (46.2) |
| Housing (χ2 = 18.96***) | |||
| Own home n (%) | 4 (6.8) | 25 (38.5) | 10 (38.5) |
| Rent n (%) | 42 (71.2) | 32 (49.2) | 13 (50) |
| Other n (%) | 13 (22) | 8 (12.3) | 3 (11.5) |
| Stayed in psychiatric ward* n (%) (χ2 = 11.95**) | 55 (93.2) | 45 (69.2) | 22 (84.6) |
Our regression model on network type did not find diagnosis to be significant, but we can see from this table a tendency for the bipolar group to have the characteristics that were associated with family and stable or diverse and active networks and for the schizophrenia group to have the variables associated with formal and sparse networks.
Network characteristics across network types
This next section moves from looking at participant characteristics to factors which were used to cluster network types. We examined a variety of network variables across people, place and activity dimensions to generate the typology, and Table 13 summarises how these differ by network type. The people, place and activity sections below describe these variables in more detail.
| Network dimension | Variable | Diverse and active networks | Family and stable networks | Formal and sparse networks |
|---|---|---|---|---|
| Summary | % participants in each type (n) | 36.7 (55) | 32.0 (48) | 31.3 (47) |
| Social networks (people) | Mean overall social network size*** (SD) | 23.9 (10.6) | 22.8 (9.1) | 12.4 (5.6) |
| Range of social network size | 9–64 | 10–44 | 5–30 | |
| Mean family group size*** (SD) | 5.3 (4.0) | 8.6 (3.7) | 3.7 (2.6) | |
| Mean friend group size*** (SD) | 8.1 (6.4) | 7.8 (5.1) | 3.3 (3.3) | |
| Mean wider group size*** (SD) | 6.1 (5.1) | 3.7 (3.9) | 1.5 (1.8) | |
| Mean formal (practitioner) group size** (SD) | 4.4 (2.9) | 2.6 (1.6) | 3.9 (2.4) | |
| Mean % of social ties who know about participant’s mental health condition** (SD) | 71.3 (23.2) | 73.4 (19.7) | 85.7 (16.1) | |
| Mean % of social ties who also use MH services (SD) | 15.8 (16.8) | 14.4 (13.2) | 16.1 (11.4) | |
| Mean number of ties in inner circle** (SD) | 5.0 (3.5) | 5.4 (3.9) | 3.0 (2.5) | |
| Mean % of social network ties rated negative (SD) | 10.9 (12.6) | 10.4 (12.1) | 10.3 (13.7) | |
| Mean frequency of contact with social ties (SD)a | 2.5 (0.5) | 2.3 (0.5) | 2.3 (0.4) | |
| Mean % of ties known for less than 5 years*** (SD) | 55.8 (18.7) | 24.7 (15.5) | 39.2 (20.8) | |
| Mean social network efficiency score*** (SD) | 0.8 (0.1) | 0.6 (0.2) | 0.8 (0.1) | |
| Mean number of relationship types*** (SD) | 6.1 (1.5) | 5.8 (1.5) | 4.5 (1.1) | |
| Places | Mean total place connections outside home*** (SD) | 10.8 (3.6) | 10.5 (4.0) | 7.5 (2.0) |
| Mean % of place connections which were community settings*** (SD) | 63.2 (11.4) | 64.4 (14.0) | 47.0 (13.8) | |
| Mean % of place connections which were physical health care settings*** (SD) | 29.7 (11.2) | 30.1 (13.6) | 41.7 (14.1) | |
| Mean % of place connections which were mental health care settings*** (SD) | 7.1 (6.2) | 5.3 (6.9) | 11.3 (8.9) | |
| Mean % of places where social interaction was mentioned*** (SD) | 76.2 (14.0) | 69.0 (17.0) | 60.5 (25.3) | |
| Mean place connection frequency*** (SD)a | 3.0 (.5) | 2.5 (0.6) | 2.9 (.6) | |
| Mean % of place connections over 5 years old*** (SD) | 37.4 (28.8) | 61.7 (21.3) | 61.0 (27.7) | |
| % of waking time spent at home** | ||||
| 0–25% | 14.5% | 8.3% | 2.1% | |
| 26–50% | 41.8% | 18.8% | 12.8% | |
| 51–75% | 30.9% | 39.6% | 31.9% | |
| 76–100% | 12.7% | 33.3% | 53.2% | |
| Activities | Mean number of meaningful activities*** (SD) | 7.5 (2.8) | 6.8 (2.9) | 4.5 (2.3) |
| Mean % of activities individually structured*** (SD) | 66.2 (19.3) | 78.9 (20.5) | 62.2 (30.0) | |
| Mean % of activities externally structured (SD) | 20.9 (19.2) | 13.2 (16.9) | 9.4 (15.0) | |
| Mean % of activities unstructured*** (SD) | 13.0 (12.5) | 7.9 (11.8) | 28.3 (27.3) | |
| Mean % of activities social*** (SD) | 50.3 (26.0) | 45.2 (25.2) | 26.2 (29.3) | |
| Mean activity frequency*** (SD)a | 2.8 (0.6) | 2.4 (0.6) | 3.0 (0.7) | |
| Mean % of activities over 5 years old*** (SD) | 56.1 (21.2) | 71.6 (23.3) | 82.2 (23.5) | |
Table 13 indicates that the three network types differ significantly not just in social network characteristics, but also in connection to places and in meaningful activities engaged with as well. We suggest that conceptually these findings highlight the importance of place and activity when examining the social in people’s lives.
Social networks (people)
Composition of social networks
We mapped all current social ties where there was regular interaction. The mean social network size was 19.9 contacts and they ranged from 5 to 64 contacts. The data were not normally distributed; we found a median size of 18 contacts and multiple modes of 13, 18 and 19 contacts.
| Group | Relationship | Mean number of contacts (SD) % total network | Mean number of contacts (SD) % total network |
|---|---|---|---|
| Family | Immediate family | 4.4 (3.1) 22.1 | 5.8 (4.1) 29.1 |
| Wider family | 1.1 (1.9) 5.6 | ||
| Partner | 0.3 (0.5) 1.6 | ||
| Friends | Friends | 6.5 (5.6) 32.5 | 6.5 (5.6) 32.7 |
| Wider contacts | Colleagues | 1.1 (2.0) 5.7 | 3.9 (4.3) 19.6 |
| Neighbours | 0.8 (1.6) 4.2 | ||
| Acquaintances | 1.9 (2.6) 9.6 | ||
| Formal contacts | Practitioners (non-mental health) | 2.1 (1.6) 10.5 | 3.7 (2.4) 18.6 |
| Clinical MH practitioners | 1.3 (1.7) 6.7 | ||
| Other MH practitioners | 0.3 (0.7) 1.4 |
We collected data on relationship type and summarised these into four relationship groups as shown in Table 14: family, friends, wider contacts and formal contacts. The largest groups of contacts were family and friends. Six per cent of participants had no family ties, 8% had no friends, 22% had no wider contacts and only 2.7% had no formal contacts.
| Significant independent variables | Coefficient (standard error) | t-value | p-value |
|---|---|---|---|
| Total number of community settings mentioned outside home | 0.021 (0.010) | 2.153 | 0.033 |
| Formally structured activities | 0.113 (0.021) | 5.389 | 0.000 |
| Time spent at home | –0.131 (0.031) | –4.163 | 0.000 |
| Family and stable networks | 0.398 (0.076) | 5.235 | 0.000 |
| Diverse and active networks | 0.342 (0.076) | 4.498 | 0.000 |
| Diagnosis dummy schizophrenia | –0.211 (0.055) | –3.799 | 0.000 |
| Mental health contact – secondary care | 0.215 (0.056) | 3.831 | 0.000 |
| White British | 0.151 (0.059) | 2.574 | 0.011 |
| Age | 0.006 (0.002) | 2.409 | 0.017 |
| SWEMWBS score | 0.009 (0.005) | 2.014 | 0.046 |
Participant characteristics, place and activity variables were included in a multiple regression model to examine variance in the natural logarithm (used instead of the original scale because of non-normal distribution) for social network size. Table 15 shows that, when controlled for other variables, social network size increased for every connection to places which were community settings, for externally/formally structured activities and also slightly with increased age and higher SWEMWBS score. It was significantly higher for participants in touch with secondary mental health services than for those managed in primary care, and significantly higher for white British participants than for those of other ethnicities. Finally, social network size decreased significantly for increased waking time spent at home and was significantly smaller for participants with psychotic disorder/schizophrenia than for those with manic episodes/bipolar. Social network size was also significantly higher for participants with family and stable networks, and those with diverse and active networks, than for those with formal and sparse network types. This model explained 62.6% of the variance in the natural logarithm of social network size.
In considering explanations for the observed variations, we were aware that the larger social networks of those in secondary mental health contact may be partly explained by the participants having significantly more practitioner contacts than those in primary care, a mean of 4.4 compared with 2.6 (t = 4.67, df = 148, p < 0.01). The larger networks of white British participants consist of significantly more friends (t = 2.48, df = 124.07, p = 0.02) and family (t = 2.50, df = 148, p = 0.01) than those of other ethnicities. The smaller networks of those with psychotic disorder/schizophrenia consist of significantly fewer friends [F(df = 2, n = 147) = 5.02, p < 0.01] and family [F(df = 2, n = 147) = 11.56, p < 0.01] but more practitioners [F(df = 2, n = 147) = 5.78, p < 0.01] than the other diagnostic groups.
We also considered mental health-related contacts within networks and these are summarised in Table 16. Participants who had a significantly higher percentage of networks comprising other mental health service users were those who had been in contact with mental health services for longer (Spearman’s r = 0.25, p = 0.02) and those who were on long-term sickness or disability benefit (t = 2.15, df = 148, p =0.03).
Participants who had significantly higher proportions of ties who knew about their mental health condition were those who were supported in secondary mental health services (t = 2.13, df = 148, p = 0.04), those who had been a psychiatric inpatient (t = 2.57, df = 148, p = 0.01) and those who were on long-term sickness or disability benefit (t = 2.92, df = 148, p < 0.01).
| Social network | Mean % of ties that the participant knows also use MH services | Mean % of ties that know about participant’s MH condition |
|---|---|---|
| Overall | 13.6 | 74.2 |
| Family group | 13.6 | 88.7 |
| Friend group | 20.6 | 75.7 |
| Wider group | 12.9 | 41.8 |
| Practitioner group | N/A | 92.2 |
Table 16 indicates how disclosure of mental health condition differs by social network group. Mental health condition was often kept from wider components of networks such as colleagues and acquaintances, as illustrated in Figure 14, which splits mental health disclosure by those who (in the participant’s perception) know (blue) about their mental health condition and those who do not (red).
FIGURE 14.
Perceived knowledge of mental health condition among network ties. Key: blue = knows about condition; red = does not know.
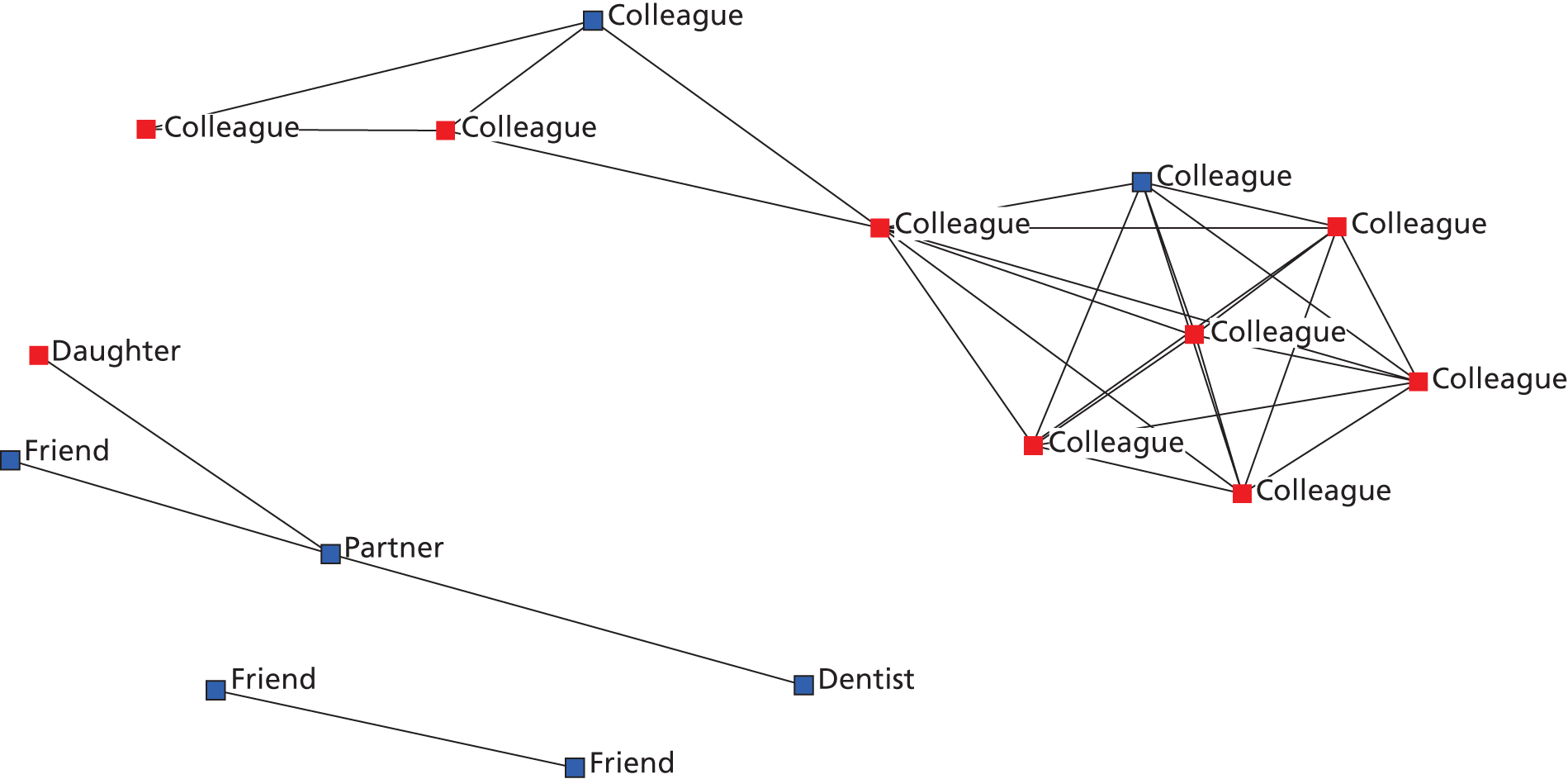
Social network ‘emotional closeness’ and well-being impact
Participants rated each social network tie by how emotionally close they felt to them through six levels using concentric circles, from inner circle (closest) to outer circle (not close at all) (see Appendix 7). Most participants (86%) had someone in their inner circle and on average 4.5 ties in the inner circle. These were primarily family (59.1%) or friends (27.6%) but practitioners (8.4%) and wider contacts (4.9%) also featured. The number of social ties within the inner circle decreased significantly with years since first mental health contact (r = –0.23 p = 0.02) and the mean number was highest for those with family and stable networks and lowest for those with formal and sparse networks [F(df = 2, n = 147)= 6.63, p < 0.01].
Participants without anyone this emotionally close had significantly fewer family contacts, with a mean of 3.1 family ties compared with 6.7 family ties (t = 3.45, df = 35.82, p < 0.01). Participants also rated each social network tie in terms of perceived impact on their own well-being, on a five-point scale from very negative (–2) to very positive (2). The majority of contacts were rated quite (37.6%) or very (26.8%) positive while only one in ten was rated as either quite (7%) or very (3.1%) negative. The proportion of negative ties did not vary significantly across network types.
Negative contacts were significantly correlated with network size (r = 0.31, p < 0.01); larger networks were more likely to contain negative contacts. The most commonly rated negative ties were colleagues, 19.2% of which were rated negative; neighbours, 18.7%; wider family, 14.3%; immediate family, 11.9%; acquaintances, 11.5%; mental health practitioners, 10.1%; non-mental health practitioners, 8.7%; partners, 6.5%; and friends 6%. Negative ties tended to be found in relationships that people had limited control over, such as colleagues, and least in those where individuals can exert more choice, such as friends and partners.
Frequency of contact with social ties (social network activity)
We measured frequency of interaction with each social tie because it was possible that participants had larger social networks of contacts but full of ties they did not regularly interact with because of illness, distance, time or other factors. ‘Interaction’ included face-to-face, phone and e-mail contact. Overall, 15.9% of contacts were interacted with on a daily basis, 32.8% at least once a week, 25.6% at least once a month and 25.3% only occasionally.
Some 23.3% of participants reported no daily contact with any individual social network tie but all participants had at least one social network tie they contacted at least once a week. We found that those participants who had no daily social network contact had significantly fewer family contacts (t = 4.79, df = 90.51, p < 0.01) and were significantly more likely to live alone [χ2(df = 1, n = 150) = 31.34, p < 0.01] and significantly less likely to be married or cohabiting [χ2(df = 1, n = 150) = 15.44, p < 0.01], and significantly more participants with schizophrenia or psychotic disorder had no daily contact with any social network tie [χ2(df = 2, n = 150) = 6.95, p = 0.03].
A ‘social network activity’ variable was created by computing mean frequency of contact with social ties and we found it decreased significantly with age (r = –0.30, p < 0.01) and was significantly lower for participants in touch with secondary mental health services (t = 2.45, df = 148, p = 0.02). It did not differ significantly across network type clusters.
Practitioner role in networks
Formal practitioner contacts comprised a mean 18.6% of total social network size. This differed significantly across network type [F(df = 2, n = 147) = 32.33, p < 0.01]; in formal and sparse networks, practitioner contacts comprised 33.0% of social networks on average compared with 19.6% of those with diverse and active networks and 12.1% of those with family and stable networks. Participants with smaller overall social networks had significantly higher proportions of practitioner ties in them (r = –0.40, p ≤ 0.01). There was also a significant difference across diagnostic groups [F(df = 2, n = 147) = 16.31, p < 0.01]. In the psychotic disorder/schizophrenia group, a mean of 28.8% of networks were composed of formal contacts, compared with 14.4% of the networks of those in the manic episodes/bipolar group and 21.82% of the social networks of those with other psychoses.
We examined three groups of practitioners: clinical mental health practitioners [psychiatrists, community psychiatric nurses (CPNs)], other mental health practitioners (third sector), and other health and social care practitioners (GPs, dentists, job advisors). While all participants in the study had a GP surgery, 70.7% had a named GP and this did not differ significantly by primary/secondary care contact or diagnosis. A total of 27.3% of participants named a dentist. A total of 22.7% of participants had at least one practitioner in their inner circle of emotional closeness: 8% had a GP, 14% had a clinical mental health professional, 3.3% had other mental health practitioners and 2.7% had other health and social care practitioners. Some individuals had more than one; for example, one participant had four clinical mental health practitioners in their inner circle. We did not find significantly more people in primary care with a GP in their inner circle.
There were no significant differences in overall network size between those who had a practitioner in their inner circle or not, but those who had a GP in their inner circle were significantly less likely to be married/in a civil partnership or cohabiting [χ2(df = 1, n = 150) = 5.41, p = 0.02]. It was possible that practitioners replaced close relationships in some networks but on the whole they seemed to complement rather than replace informal networks.
In which closeness circle, out of six, a practitioner first appeared was examined. We found that on average the first mentioned practitioner was closest in diverse and active networks and least close in family and stable networks [F(df = 2, n = 147) = 4.10, p = 0.02]. Participants who felt closer to their clinical mental health practitioners rated them as significantly better for their well-being (r = 0.34, p < 0.01).
We examined continuity of practitioner relationship. Of those participants who named GPs, 5.6% had known their current GP for less than 6 months, 48.1% for 6 months to 5 years, 20.8% for 5–10 years and 20.8% for over 10 years. Of those who named clinical mental health practitioners, 14.8% had known them for less than 6 months, 56.8% for 6 months to 5 years, 17% for 5–10 years and 11.4% for over 10 years. Participants who had known their GP for longer felt significantly closer to them (r = 0.23, p < 0.02), and rated them as having a significantly better impact on their well-being (r = 0.26, p < 0.01). Participants who had known their clinical mental health practitioners for longer felt significantly closer to them (r = 0.32, p < 0.01) and had significantly higher satisfaction with their network as a whole (r = 0.27, p = 0.01).
Social network structure: density and diversity
The structure of social networks was also examined. Participants were asked which members of their social network knew one another, to measure density; higher density refers to a larger proportion of social network members knowing each other. We considered four measures of density, all of which can be skewed by social network size, because the probability of a fully connected network decreases as network size increases. 180 Efficiency had the lowest correlation with social network size (r = 0.17, p = 0.04) and so this was selected. Higher efficiency scores equate to lower density or less connected networks. Larger numbers of wider contacts (r = 0.27, p < 0.01) and friend (r = 0.26, p < 0.01) and practitioner contacts (r = 0.24, p < 0.01) were correlated with higher efficiency but larger family networks were negatively correlated and thus more dense (r = –0.35, p < 0.01).
Density differed significantly across network types [F(df = 2, n = 147) = 17.60, p < 0.01]; family and stable networks had the lowest efficiency scores and diverse and active networks had the highest, reflecting the interconnected bonded structure of the former and the diverse settings found in the latter.
Diversity of network was considered using mean number of relationship types. On average participants had 5.5 out of a possible 9 relationship types mapped in their social networks, ranging from 3 to 9 (SD 1.5). Those with diverse and active networks had significantly more relationship types than the other networks and those with formal and sparse networks had the fewest [F(df = 2, n = 147) = 18.67, p < 0.01].
Connection to place
Personal networks were rooted in time and place, providing anchors and contexts to shape everyday living. We thus asked participants which places they connected to both currently and regularly.
Home
Home was mapped for all participants. We considered waking time spent at home, well-being impact of home and social network ties linked to home.
FIGURE 15.
The dominance of home place in networks (n = 150).

Over half of participants spent more than 50% of their waking time at home (Figure 15). This differed significantly across our three network types [χ2(df = 4, n = 150) = 17.55, p < 0.01]. Those with family and stable networks and those with formal and sparse networks both spent most of their waking time at home, but we saw from Table 8 that the latter group tended to live alone and the former with others.
Those who spent more of their time at home had significantly smaller social networks (r = –0.46, p < 0.01) including smaller friend groups (r = –0.40, p < 0.01) and wider contact groups (r = –0.34, p < 0.01). Those who spent more time at home were also significantly older (r = 0.23, p < 0.01) and had been in touch with mental health services significantly longer (r = 0.15, p < 0.05).
A total of 86.1% of participants mentioned some form of regular social interaction at home, such as regular visits from family, friends or practitioners. Participants rated home as positive for well-being on the whole. Some 74.2% rated home as positive (32%) or very positive (42.2%), 15% rated it as neutral and 10.9% rated it as negative (7.5%) or very negative (3.4%). We found significantly more participants with formal and sparse networks rated their home as positive than those with other network types [χ2(df = 2, n = 147) = 8.68, p = 0.01], and significantly more of those renting rated their home as neutral or negative than those with other housing status [χ2(df = 2, n = 147) = 7.59, p = 0.02], while significantly more participants who were not white British than white British participants also rated their home as neutral or negatively impacting well-being [χ2(df = 1, n = 147) = 6.04, p = 0.01]. A total of 41.6% of participants had lived in their current home for more than 10 years, 41.6% for 5–10 years, 17.4% for 6 months to 5 years and 6% for less than 6 months. We did not find any network or well-being differences according to time lived in current home.
Places outside the home
A total of 1449 places outside the home that people currently and regularly attended were mapped in the study. At the analysis stage, places were categorised (Table 17, or see Appendix 10 for more details). All participants were connected to a GP surgery, as this was a recruitment criterion.
| Place type | Place sub-type | % connected to at least one (n) | Mean number in each network (range) | Mean and modal well-being impact (range)a |
|---|---|---|---|---|
| Total places outside home (n = 150) | 100 | 9.66 (3–21) | 0.77, 1 (–2 to 2) | |
| Total MH settings | 61.3 | 0.73 (0–2) | 0.58, 1 (–2 to 2) | |
| Third MH settings | 9.3 | 0.09 (0–1) | 0.71, 1 (–1 to 2) | |
| Secondary MH settings | 52.6 | 0.58 (0–2) | 0.56, 1 (–2 to 2) | |
| Private MH settings | 6 | 0.06 (0–1) | 0.78, 1 (–1 to 2) | |
| Total PH settings | 100 | 3.02 (1–6) | 0.62, 1 (–1 to 2) | |
| Clinical settings | 12.7 | 0.16 (0–3) | 0.17, 0 (–2 to 2) | |
| Community settings | 90 | 1.87 (0–5) | 0.40, 0 (–2 to 2) | |
| GP surgery | 100 | 1 (1–1) | 0.63, 1 (–2 to 2) | |
| Total community settings | 100 | 5.91 (1–16) | 0.92, 1 (–2 to 2) | |
| Family and friends house | 38 | 0.57 (0–5) | 1.06, 1&2 (–2 to 2) | |
| Library | 36 | 0.36 (0–2) | 0.68, 0&1 (–2 to 2) | |
| Education setting | 8.7 | 0.09 (0–2) | 1.5, 2 (0 to 2) | |
| Physical recreation setting | 35.3 | 0.48 (0–6) | 1.3, 2 (0 to 2) | |
| Social recreation setting | 37.3 | 0.55 (0–7) | 0.98, 1 (–1 to 2) | |
| Cultural recreation setting | 15.3 | 0.24 (0–4) | 1.39, 2 (0 to 2) | |
| Spiritual setting | 20.7 | 0.23 (0–3) | 1.32, 2 (–1 to 2) | |
| Shops and markets | 89.7 | 1.75 (0–6) | 0.51, 0 (–2 to 2) | |
| Green and outdoor spaces | 64.7 | 0.96 (0–5) | 1.15, 1 (–1 to 2) | |
| Workplace (paid and voluntary) | 32 | 0.37 (0–3) | 0.89, 1 (–2 to 2) | |
| Settings connected to children | 3.7 | 0.09 (0–6) | 0.38, 1 (–2 to 1) | |
| Employment and housing services (neither PH nor MH) | 3.3 | 0.03 (0–1) | 0, –1, 0&1 (–1 to 1) | |
| Health support groups | 7.3 | 0.07 (0–1) | 1, 1 (–2 to 2) | |
| Social activity and interest groups | 10 | 0.11 (0–2) | 1, 1 (–1 to 2) | |
We found that, on the whole, places were rated as overwhelmingly positive for well-being and most network maps had only place connections they viewed positively, or which were viewed neutrally but served a function, for example shops or a GP surgery. Our analysis of place focused on connections across settings, associations with social networks and sociodemographics. Later we look at the relationship to resource access and well-being.
Across our network types we found significant differences in connection to total places outside the home [F(df = 2, n = 147) = 17.42, p < 0.01]; those with diverse and active networks connected to the most and those with formal and sparse networks the fewest. Mental health settings were most numerous in formal and sparse networks and least common in family and stable networks [F(df = 2, n = 147) = 2.12, p < 0.05]. Community settings were significantly less common in formal and sparse networks while similar numbers were found in diverse and active networks (mean 6.9) and family and stable networks (mean 7.0) [F(df = 2,n = 147) = 23.28, p < 0.01]. Those with formal and sparse networks connected to significantly fewer physical recreation settings and those with diverse and active networks connected to the most [F(df = 2, n = 147) = 5.35, p = 0.01].
Finally, some connection-building was evidenced by those who linked to more workplaces (r = 0.20, p = 0.01) and physical recreation settings (r = 0.20, p = 0.02) having significantly more social networks of contacts built within the last 5 years.
Duration of place contact
As with social networks, we also examined duration of contact to place connections and the balance between network-building and network stability. Overall, the majority of connections in participants place networks were over 5 years old (52.6%) while 47.4% had been built in the last 5 years. We found older participants had significantly more connections over 5 years old (r = 0.36, p < 0.01) and found evidence of network rupture caused by inpatient admission; those who had been inpatients in the last 5 years had significantly fewer place connections older than 5 years than those who had not been inpatients in the last 5 years (t = 3.00, df = 99.93, p < 0.01). Participants who reported decreasing health had significantly fewer place connections built within the last 5 years (r = 0.20, p = 0.01).
We also found participants who lived alone had significantly fewer new place connections built in the last 5 years (t = 2.09, df = 148, p = 0.04) and those who worked full time had significantly more new place connections (t = 4.06, df = 148, p < 0.01).
Referral to place: how were place connections built?
We examined how certain places were referred to (Table 18). Referral by others was unusual and participants tended to make their own connections; however, participants with larger friend networks (r = 0.21, p = 0.01) and larger diverse networks (r = 0.22, p < 0.01) were informally referred to a higher percentage of places; similarly those with larger practitioner networks had more formal recommendations (r = 0.30, p < 0.01). Participants in secondary mental health care were signposted to significantly more places than those in primary care (t = 8.26, df = 147.78, p < 0.01). We found informal referral to differ significantly by network type [F(df = 2, n = 147) = 4.56, p = 0.01], with the highest proportion of place connections built through informal referral in diverse and active networks and the lowest in formal and sparse networks.
| Place type | Mean % of connections built through informal referral | Mean % of connections built through formal referral | Mean % of connections built through self-referral |
|---|---|---|---|
| Community settings | 9.2 | 7.0 | 83.7 |
| Library | 0 | 3.7 | 96.3 |
| Education setting | 21.4 | 14.3 | 64.3 |
| Physical recreation setting | 13.9 | 8.3 | 77.8 |
| Social recreation setting | 9.8 | 2.4 | 87.8 |
| Cultural recreation setting | 11.1 | 5.6 | 83.3 |
| Spiritual setting | 14.3 | 0 | 85.7 |
| Green and outdoor spaces | 7.6 | 4.9 | 87.5 |
| Workplaces | 3.5 | 7.0 | 89.5 |
| Settings connected to children | 15.4 | 15.4 | 69.2 |
| Statutory services (neither MH nor PH) | 0 | 60 | 40.0 |
| Health support groups | 7.1 | 28.6 | 64.3 |
| Social activity and interest groups | 21.1 | 21.1 | 57.9 |
| Third-sector mental health settings | 7.1 | 28.6 | 64.3 |
| Community physical health settings | 6.6 | 3.8 | 89.6 |
Social interaction in place
We measured the extent of social interaction in places connected to in three categories: places where social interaction was mentioned by the participant, places were no social interaction was mentioned but was inferred as necessary (e.g. in dentist surgeries or mental health appointments social interaction was integral to the visit) and places where social interaction was not mentioned or inferred as necessary (e.g. supermarkets, libraries, parks). Overall, social interaction was mentioned in 68.9% of places, not mentioned but inferred in 12.9% and neither mentioned nor inferred in 18% of places.
The majority of places involved social interaction mentioned by the participant. We found that the number of place connections where social interaction was mentioned was correlated with more friend contacts (r = 0.49, p < 0.01), family contacts (r = 0.42, p < 0.01), practitioner contacts (r = 0.21, p < 0.01) and wider contacts (r = 0.40, p < 0.01). The number of places where social interaction was not mentioned or inferred was correlated with smaller family networks (r = –0.27, p ≤ 0.01).
Where social interaction was not mentioned but inferred, the participant did not mention it because there was no specific social tie whom they saw regularly there; for instance, at the dentist they might have seen whoever was available rather than a specific practitioner.
Social interaction was therefore a key dimension of place. However, the dominance of shops and markets in the category of no social places mentioned or inferred may skew this finding. We found that both green and outdoor spaces and spiritual settings where no social interaction was mentioned or inferred were still rated positively for well-being, with a mean positive score and a modal very positive score for both; places themselves also had a beneficial impact.
What have we learnt about place connections?
The place connection data shows us how diverse people’s lives were; people with SMI were not living in a psychiatric ghetto. These networks of place seem to be built by the individual rather than those around them. The 150 participants used 1449 places away from home that were important enough to mention at interviews for impacting on their health and well-being, mostly positively. We did not find place, as such, an important feature of network in terms of variations across the study population and impact on well-being. However, it was clear that the type of setting connected to did matter as well as social interaction in a place.
Meaningful activity
The final network level investigated was activity. Participants were asked what meaningful activities they currently and regularly undertook and whom if anyone they participated with.
What activities were the study population doing?
A total of 958 activities were mapped and 14 categories applied at the analysis stage (Table 19). We found a wide range of meaningful activities engaged in, from participants who spent all day watching TV to those who engaged in 16 diverse activities. Activities were extremely personalised and challenging to categorise. We found most participants (76%) engaged in some physical activity even if it was only going for walks. General recreation such as watching TV, reading, creative and cultural hobbies as well as multimedia use were also common. Everyday tasks such as domestic activities also featured in many networks.
| Activity type | % connected to at least one (n) | Mean and mode in each network (range) | Mean and modala well-being impact (range)b |
|---|---|---|---|
| Total activities mentioned | 100 (150) | 6.4, 5 (1–16) | 1.20, 2 (–2 to 2) |
| Volunteering and work activity | 36.7 (95) | 0.45, 0 (0–3) | 1.02, 1 (2 to 2) |
| Education, training and study | 13.3 (20) | 0.15, 0 (0–2) | 1.30, 2 (–1 to 2) |
| Physical activities | 76 (114) | 1.27, 1 (0–5) | 1.35, 2 (–2 to 2) |
| Creative and cultural hobbies | 60 (90) | 1.10, 0 (0–6) | 1.42, 2 (–1 to 2) |
| Spiritual activities | 6 (9) | 0.09, 0 (0–3) | 1.69, 2 (1 to 2) |
| Relational activity | 31.3 (47) | 0.37, 0 (0–4) | 1.38, 2 (–2 to 2) |
| Domestic activity | 43.7 (64) | 0.55, 0 (0–3) | 1, 1, (–2 to 2) |
| Multimedia use | 44.7 (67) | 0.49, 0 (0–2) | 0.77, 1 (–2 to 2) |
| Reading | 48 (72) | 0.49, 0 (0–2) | 1.33, 2 (–2 to 2) |
| General recreation | 61.3 (92) | 0.84, 1 (0–3) | 0.94, 1 (–2 to 2) |
| Shopping and spending | 15.3 (23) | 0.17, 0 (0–2) | 1.04, 2 (–2 to 2) |
| Travel and commuting | 8 (12) | 0.09, 0 (0–2) | 1.21, 2 (–1 to 2) |
| Receiving mental health and other support (e.g. CBT) | 6.6 (10) | 0.08, 0 (0–2) | 0.83, 1 (–2 to 2) |
| Miscellaneous health and well-being activities | 8.7 (13) | 0.11, 0 (0–3) | 1.41, 2 (0 to 2) |
Participants tended to rate their activities as having a positive impact on well-being, as they also did with places. We found that overall the number of meaningful activities engaged in decreased with age (r = –0.17, p = 0.03) and that those who engaged in more activities also had more friends (r = 0.41, p < 0.01), family (r = 0.18, p = 0.04) and wider contacts (r = 0.19, p = 0.02).
Across network types, participants with formal and sparse networks engaged in significantly fewer physical activities and those with diverse and active networks engaged in the most (F = 3.59, df = 147, p = 0.03).
Level of structure in activities
In order to understand activities further, we labelled them according to structure level. Unstructured activities were those that passed time without an obvious purpose, such as watching TV or listening to the radio. Individually structured activities were those where the structure was set by the participant and had an obvious purpose such as exercise, study or socialising and externally or formally structured activities were those where the structure was set by others, such as formal education, work, volunteering, exercise with a personal trainer and so on. We found 13% of activities had no structure, 71.2% were individually structured and 15.8% were externally or formally structured.
We found that larger social network size was significantly correlated with individually (r = 0.27, p < 0.01) and externally or formally (r = 0.57, p < 0.01) structured activities.
Social and non-social activity
The majority of activities were those that the participant tended to do alone (59.1%) while 40.9% were activities that the participant usually did with others.
A total of 46.7% of activities were done alone and yet were structured. We found that those who engaged in more of these ‘alone but structured’ activities had larger friend groups and connected to more places (r = 0.25, p = 0.02) including libraries, cultural recreation, spiritual settings and physical recreation settings but did not have significantly different well-being or functioning. Unstructured activities done alone were associated with smaller family networks (r = –0.18, p = 0.02) and lower perceived social support (r = 0.22, p < 0.01) and physical fitness (r = –0.18, p = 0.02). Those who engaged in more unstructured activities alone were significantly older (r = 0.16, p = 0.05) and had been in touch with mental health services for longer (r = 0.19, p = 0.02).
Activity duration
The majority (69.1%) of activities mentioned were those that participants had done for longer than 5 years, with fewer than a third (30.8%) of activities having been started within the last 5 years. We found that older participants had a significantly lower proportion of activities started in the last 5 years (r = –0.32, p < 0.01) and the percentage of newer activities to be significantly correlated to newer social networks (r = 0.26, p < 0.01) and newer place connections (r = 0.43, p < 0.01) in terms of the proportion of each that were less than 5 years old. Inpatient admission also seemed to impact on activity duration, with participants who had been an inpatient in the last 5 years having a significantly lower percentage of activities and hobbies that were older than 5 years (t = 2.36, df = 113, p = 0.02).
Summary: what we have learnt about meaningful activities
Activities mentioned as important tended to be those which were structured and which were done with other people. Those done alone or unstructured seem to be least beneficial for networks overall and we saw significant differences across network types.
Satisfaction with current networks
We asked participants how satisfied they were with their current network (Table 20).
| Satisfaction with current networks | Total study population, n (%) | Diverse and active networks, n (%) | Family and stable networks, n (%) | Formal and sparse networks, n (%) |
|---|---|---|---|---|
| Very unsatisfied | 5 (3.3) | 1 (20) | 1 (20) | 3 (60) |
| Quite unsatisfied | 18 (12) | 6 (33.3) | 7 (38.9) | 5 (27.8) |
| Neither satisfied nor unsatisfied | 20 (13.3) | 6 (30) | 4 (20) | 10 (50) |
| Quite satisfied | 75 (50) | 28 (37.3) | 24 (32) | 23 (30.6) |
| Very satisfied | 32 (21.3) | 14 (43.8) | 12 (37.5) | 6 (18.8) |
We found overall that most participants were satisfied with their current networks and there was no significant difference across network types. Participants who were more satisfied with their social network had more friends (r = 0.37, p < 0.01), family (r = 0.19, p < 0.02) and practitioners (r = 0.21, p < 0.01) but not wider contacts. Social network satisfaction was significantly positively correlated with perceived overall health (r = 0.33, p < 0.01), quality of life (r = 0.41, p < 0.01) and social support (r = 0.37, p < 0.01). Participants with more people in their inner circle of closeness (r = 0.31, p = < 0.01) were significantly more satisfied with their networks. This is consistent with our analysis of the words people used to describe their personal networks. Each participant was asked for three words to describe their network at the end of the mapping interview. We found very similar words used across the network types. This emphasises the commonalities within networks and the values that people with SMI ascribe to connections, which they overwhelmingly described as follows:
-
Formal and sparse networks were described as ‘friendly’, ‘close’, ‘supportive’, ‘reliable’, ‘positive’ and ‘caring’. A third of the 81 reflection summaries were, however, negative evaluations including ‘lonesome’, ‘sad’, ‘lacking support’ and ‘inadequate’.
-
Family and stable networks were described as ‘friendly’, ‘close’, ‘supportive’, ‘reliable’ and ‘positive’. Again a third of the 83 words selected were negative evaluations including ‘unstable’, ‘solitary’, ‘patchy’, ‘isolated’ and ‘confusing’.
-
A larger number of diverse and active networks (93) were described as ‘friendly’, ‘close’, ‘supportive’, ‘caring’, ‘trustworthy’ and ‘shared interests’, and a quarter of the evaluations were negative including ‘conflict’, ‘disjointed’, ‘frightening’, ‘limited’ and ‘sad’.
Well-being connections that were valued produced networks that contained friendship, support and emotional closeness.
For place settings, network satisfaction was significantly higher only for increased connection to community places (r = 0.23, p < 0.01) and places where social interaction was mentioned (r = 0.24, p < 0.01). For activities, satisfaction was higher only with those which were social (r = 0.21, p = 0.01) or individually structured (r = 0.18, p = 0.04).
Networks, access to resources, well-being and mental health contact
We explored the relationship between networks and access to resources. Table 21 summarises these measures across network type.
| Variable | Total study population | Diverse and active networks | Family and stable networks | Formal and sparse networks |
|---|---|---|---|---|
| RGUK score (F = 24.96***) mean (SD) | 14.2 (6.6) | 15.5 (6.0) | 17.4 (5.2) | 9.5 (5.9) |
| HRG score (χ2 = 19.90***) | % (n) | % (n) | % (n) | % (n) |
| High group (0–12) | 51 (76) | 47.3 (26) | 23.4 (11) | 83 (39) |
| Low group (13–15) | 49 (73) | 52.7 (29) | 76.6 (36) | 17 (8) |
Both RGUK score and HRG score differed significantly across network types.
Access to social capital
A key interest of the study was in how connections to people, place and activities provide access to resources. The RGUK measures access to social capital resources through personal contacts. Table 22 compares our study findings with other projects that had used the RGUK. The total possible score for the RGUK was 27, with four sub-domains: seven for domestic resources, nine for expert advice, six for personal skills and five for problem solving. It seems to suggest that access to social capital was lower for our respondents than for the general population, but it was higher than other studies involving people with SMI or depression. This could potentially be explained by our sampling locations, as all the other studies except one203 collected data in London, where people with SMI appear to have less access to social capital (as in our study), or other differences in the study populations. However, Table 21 shows the score was lower for those with formal and sparse networks than in any of the studies cited, at a mean of 9.5. Moreover, RGUK score differed significantly across diagnostic group in our study (F = 9.90, df = 158, p < 0.001); the psychotic disorder/schizophrenia group had a mean score of only 11.6, compared with 16.6 for those in the bipolar disorder group and 14.0 for those with other psychoses.
| Study authors | Total study population | Mean access to domestic resources (SD) | Mean access to expert advice (SD) | Mean access to personal skills (SD) | Mean access to problem-solving advice (SD) | Mean RGUK score (SD) |
|---|---|---|---|---|---|---|
| CHN study | SMI (n = 150) | 3.76 (2.03) | 4.82 (2.61) | 2.72 (1.70) | 2.87 (1.44) | 14.19 (6.57) |
| Dutt and Webber (2010)122 | South East Asian women with SMI (n = 54) | |||||
| First generation (n = 40) | 3.4 (2.3) | 2.8 (2.3) | 1.9 (1.6) | 2.8 (1.5) | 10.9 (6.5) | |
| Second generation (n = 14) | 4.0 (2.1) | 3.4 (2.3) | 2.0 (1.6) | 2.9 (1.7) | 12.3 (7.1) | |
| Webber and Huxley (2007)123 | General population (n = 335) | 4.88 (1.86) | 5.25 (2.47) | 3.66 (1.66) | 3.33 (1.07) | 17.24 (5.88) |
| Webber et al. (2011)198 | Individuals with depression in primary care (n = 158) (Follow-up only reported) | 4.1 (2.0) | 4.2 (2.4) | 2.7 (1.7) | 3.0 (1.2) | 13.9 (6.2) |
| Webber et al. (2014)203 | People on Care Programme Approach in England (n = 1016) | 4.03 (1.99) | 4.20 (2.36) | 2.76 (1.64) | 2.92 (1.27) | 13.9 (5.8) |
| Murray et al. (2007)204 | People with SMI in London volunteering (n = 126) (Follow-up only reported) | 3.06 (1.92) | 4.07 (2.29) | 2.48 (1.57) | 2.73 (1.25) | 12.17 (5.67) |
We examined variance in RGUK using a multiple regression model including all network and participant characteristic variables as well as network type. The variables used are presented in Appendix 12. Table 23 summarises the significant variables and shows that, when controlled for other items, RGUK scores were higher for participants who had someone in their inner circle compared with those who did not, for participants who were working full time compared with those not, for participants who had higher percentages of social ties rated as negatively impacting their well-being, for increased connection to places where social interaction was mentioned and for increases in social ties who knew about the participant’s mental health condition. It was lower for participants with higher efficiency scores (less dense networks had lower social capital), for participants who did not have any formal education qualifications, for participants in London compared with the SW site, for participants who spent more time at home and for lower physical fitness scores. Of the total variation in RGUK score, 60.7% was explained by these variables. Aspects of social ties, place connections and activities all remained significant in the final model. When examining RGUK scores across network types (see Figure 16) we found variations: people with formal and sparse networks tended to have lower scores.
| Significant independent variables | Coefficient (standard error) | t-value | p-value |
|---|---|---|---|
| Number of place connections where social interaction was mentioned | 0.423 (0.137) | 6.220 | 0.000 |
| Working full time | 3.549 (1.035) | 3.085 | 0.002 |
| Number of social ties who know about mental health condition | 0.249 (0.056) | 3.427 | 0.001 |
| Efficiency score | –9.802 (2.260) | 4.457 | 0.000 |
| Has a social contact in inner circle of emotional closeness | 4.777 (1.059) | –4.337 | 0.000 |
| No formal education qualifications | –4.241 (1.124) | 4.513 | 0.000 |
| Time spent at home | –1.252 (0.416) | –3.773 | 0.000 |
| Physical fitness score (higher score = poorer physical fitness) | –0.707 (0.267) | –3.009 | 0.003 |
| Percentage of social ties rated negative for well-being | 0.067 (0.027) | –2.645 | 0.009 |
| Site: London or SW | –1.796 (0.761) | 2.442 | 0.016 |
Figure 16 indicates how RGUK score varies within each network type and highlights the segregation of scores between network types. Few participants with diverse and active or family and stable networks had the lowest RGUK scores, while participants with formal and sparse networks tended on the whole to have low scores on this scale and very few were around or higher than the mean score of 14.19.
FIGURE 16.
Distribution of RGUK score by network type.
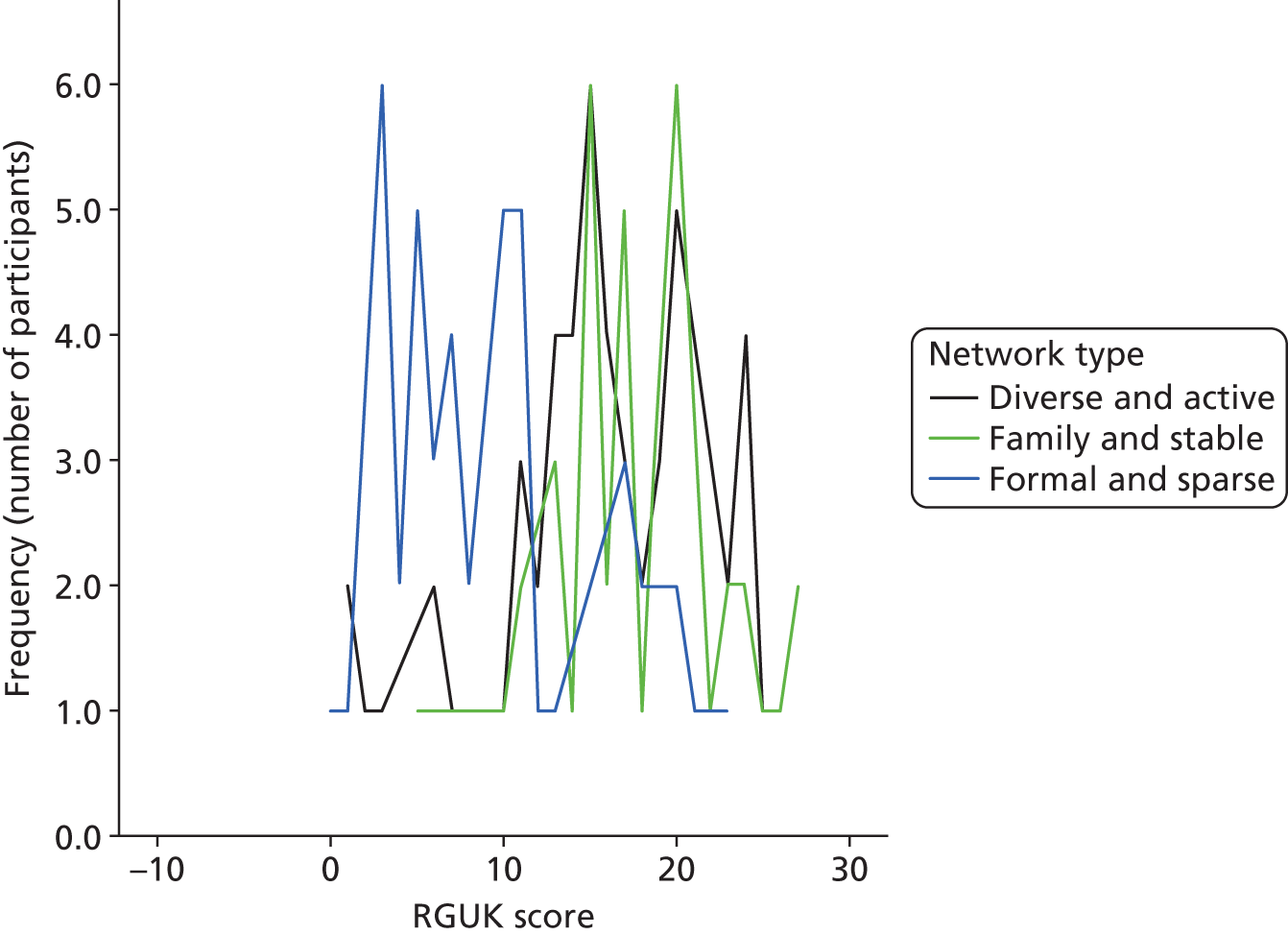
Sources of social capital
Figure 17 shows that social capital was accessed primarily through immediate family and friends, with limited resource access from practitioners. Table 24 indicates the groups for which practitioner sources of social capital were significantly higher. The percentage of resources provided by practitioners decreased significantly with time since last inpatient admission (r = –0.19, p = 0.04) and was higher for those with smaller friend (r = –0.22, p < 0.01) and family (r = –0.21, p = 0.01) networks and larger practitioner networks (r = 0.42, p < 0.01).
FIGURE 17.
Sources of social capital: % of total social capital resources accessed by relationship type.
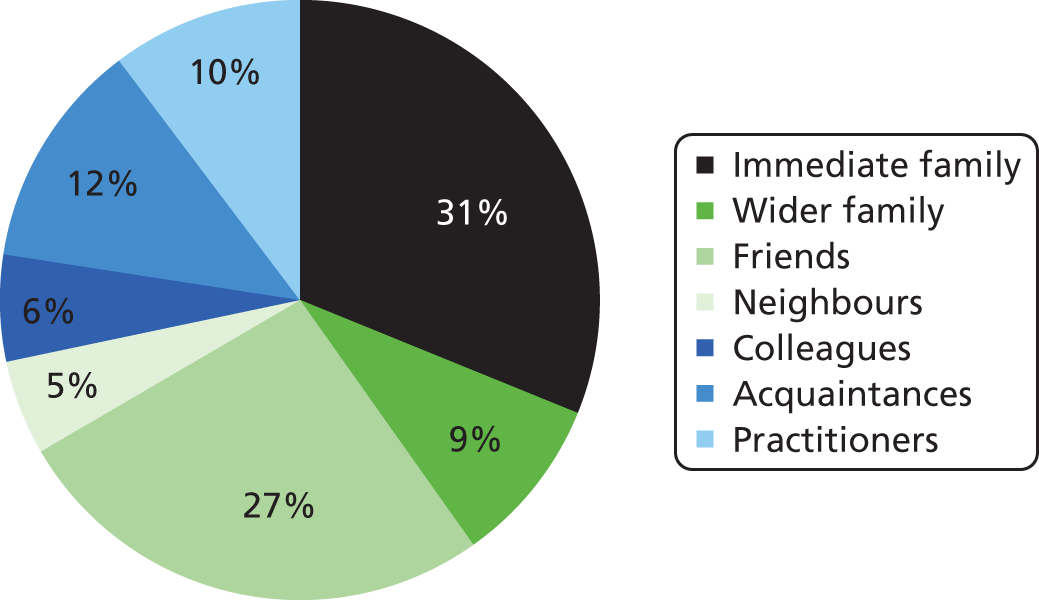
| Participant characteristics | Mean % of total social capital provided by practitioners |
|---|---|
| Ethnicity (t = 2.05*) | |
| White British | 8.3 |
| Other | 18.8 |
| Mental health contact (t = 3.94***) | |
| Primary care only | 4.0 |
| Secondary care | 14.2 |
| Working full time (t = 5.78***) | |
| Yes | 1.3 |
| No | 11.9 |
| Long-term sickness or disability (t = 3.66***) | |
| Yes | 18.8 |
| No | 5.8 |
| Married/civil partnership or cohabiting (t = 5.81***) | |
| Yes | 2.2 |
| No | 13.7 |
| Diagnosis (F = 7.53***) | |
| Psychotic disorder/schizophrenia | 17.2 |
| Manic episodes/bipolar | 5.2 |
| Other psychoses | 7.6 |
| Network type (F = 7.92***) | |
| Diverse and active networks | 10 |
| Family and stable networks | 2.8 |
| Formal and sparse networks | 18.3 |
Access to health resources
To supplement information from the RGUK looking at social capital, we created a bespoke schedule to assess access to health resources among the study population. Table 25 summarises significant independent variables explaining variance in HRG group and shows that, with increasing age and increased percentage of place connections made in the last 5 years, participants were less likely to be in the high HRG score group. Participants who were volunteering, those on long-term sickness or disability benefit and those living alone were also less likely to be in the high HRG score group, while participants with more family contacts and who engaged in more social activities were more likely to be in the high HRG score group. Sixty-one per cent of the total variance in HRG score group was explained by these variables.
| Significant independent variables | Coefficient (standard error) | z-value | p-value |
|---|---|---|---|
| Age | –0.074 (0.026) | 8.486 | 0.004 |
| Volunteering | –2.393 (0.842) | 8.074 | 0.004 |
| Long-term sickness or disability | –1.401 (0.525) | 7.138 | 0.008 |
| Living alone | –1.254 (0.519) | 5.845 | 0.016 |
| Number of family ties in social network | 0.211 (0.076) | 7.659 | 0.006 |
| Percentage of place connections less than 5 years old | –0.032 (0.011) | 8.760 | 0.003 |
| Number of activities which were social | 0.574 (0.141) | 16.560 | 0.000 |
Sources of health resources
As Figure 18 shows, health resources for those who had them were overwhelmingly provided by family and friends, although practitioner provision was higher than for RGUK. Acquaintances provided very few of these resources. Table 26 summarises for whom practitioner provision of HRG was significantly higher and it is notable that many of those in the HRG high group had formal and sparse networks.
FIGURE 18.
Sources of health resources: percentage of total health resources accessed by relationship type.

| Participant characteristics | Mean % of HRG provided by practitioners |
|---|---|
| Ethnicity (t = 2.27*) | |
| White British | 12.1 |
| Other | 21.4 |
| Working full time (t = 1.99*) | |
| Yes | 6.3 |
| No | 16.7 |
| Married/civil partnership or cohabiting (t = 4.34***) | |
| Yes | 5.9 |
| No | 19.0 |
| Diagnosis (F = 4.50**) | |
| Psychotic disorder/schizophrenia | 21.7 |
| Manic episodes/bipolar | 9.3 |
| Other psychoses | 14.8 |
| Network type (F = 7.31***) | |
| Diverse and active networks | 16.1 |
| Family and stable networks | 5.6 |
| Formal and sparse networks | 23.8 |
Networks and well-being
Only 34.1% of variance in SWEMWBS score was explained by the variables in Table 27, which indicated that SWEMWBS scores were higher for participants who had higher access to social support, were married/in a civil partnership or cohabiting and engaged in volunteer work and for males than females. It was lower for participants who had children, for increased percentage of social ties rated negative for well-being, for participants who had never been in a psychiatric inpatient ward, for those with an informal carer and for increased number of place connections in mental health settings.
| Significant independent variables | Coefficient (standard error) | t-value | p-value |
|---|---|---|---|
| CO-OP Social Support score (higher score = lower social support) | –1.342 (0.293) | –4.582 | 0.000 |
| Have children | –3.431 (0.878) | –3.909 | 0.000 |
| Married/in a civil partnership/cohabiting | 3.118 (0.938) | 3.325 | 0.001 |
| Percentage of social ties rated negative for well-being | –0.081 (0.031) | –2.622 | 0.010 |
| Never stayed in inpatient psychiatric ward | –2.408 (1.011) | –2.381 | 0.019 |
| Has informal carer | –1.885 (0.872) | –2.162 | 0.032 |
| Total number of mental health settings mentioned | –1.545 (0.589) | –2.622 | 0.010 |
| Volunteering | 3.504 (1.283) | 2.732 | 0.007 |
| Gender was male | 1.932 (0.805) | 2.399 | 0.018 |
What were the differences between primary and secondary care contact?
Because our study included both participants managed only in primary care (38.7%) and those managed in secondary care (61.3%), we considered significant differences between these populations.
Table 28 shows that, when other variables (sociodemographic, health and well-being, employment, housing and network) were held constant, participants who had a higher percentage of social ties known for less than 5 years, who had higher mean numbers of relationship types in the social network, who had a practitioner in their inner circle of emotional closeness, who spent more of their waking time at home, who engaged in more unstructured activities and who had a higher percentage of place connections which were mental health settings were more likely to be in secondary mental health service contact rather than managed in primary care. Meanwhile, participants with no formal education qualifications, who reported more limited social activities because of physical or emotional health, who had a higher mean frequency of contact with their social ties and who engaged in more activities alone were more likely to be managed in primary care.
| Significant independent variables | Coefficient (standard error) | z-value | p-value |
|---|---|---|---|
| No formal education qualifications | –4.061 (1.467) | 7.666 | 0.006 |
| CO-OP Social Activities score (higher score = more limited social activity) | –0.892 (0.349) | 6.540 | 0.011 |
| Percentage of social ties known for less than 5 years | 0.073 (0.023) | 9.688 | 0.002 |
| Mean frequency of contact with social ties | –1.581 (0.803) | 3.876 | 0.049 |
| Mean number of relationship types in social network | 1.249 (0.368) | 11.546 | 0.001 |
| Has a practitioner in inner circle of emotional closeness | 1.477 (0.835) | 3.129 | 0.077 |
| Waking time spent at home | 2.091 (0.639) | 10.721 | 0.001 |
| Number of unstructured activities engaged in | 1.443 (0.581) | 6.162 | 0.013 |
| Number of activities done alone | –0.981 (0.282) | 12.099 | 0.001 |
| Percentage of place connections which were MH settings | 0.570 (0.124) | 21.074 | 0.000 |
Discussion
Data limitations
We acknowledge that our network-mapping data were limited by potential sampling bias due to low response rates, 15.01% in London and 23.65% in the SW, and when reflecting on findings this must be taken into account.
What characterises the personal networks of people with severe mental illness?
We found great heterogeneity in the connections to people, place and activities. We see diversity in some of our participants’ lives that rebukes assumptions that the majority of this population are inactive and living in a mental health ghetto of day centres and other institutional spaces. 205 Our clustering analysis has grouped the individuals into three broad network types with distinct sets of structures and network characteristics. While the clustering is an artificial construction it is useful for showing the diversity of individuals’ people–place–activity networks. Other studies have used similar methods to identify network types, albeit on social ties only. 206–208 For example, a study on the mental health of older adults also identified that less resourceful network types, lacking friends or family, were related to poorer mental health. 179 Another study developed network types and found a more diverse and loose-knit network was more active and with better access to resources than smaller, more excluded or homogeneous networks. 46
Our network types should be interpreted in the context of two study locations; in another SMI population, network types might cluster in a different way. Moreover, while we had a ‘diverse and active’ group, the mean social network size (19.9 social contacts) was less than in studies of the ‘general population’. It was difficult to compare with other studies as methods of network size estimation varied, and often studies were interested in only one type of social tie. However, population estimates suggest, for example, 73 active ties based on listing known contacts using open questions209 and 123 active contacts based on the exchange of Christmas cards. 210 Studies that directly compare mental illness and general population networks also show smaller networks for people with mental illness. 45,109 Therefore, compared with the general population, the connections within this group were likely to be less ‘diverse and active’.
The inclusion of place and activity variables adds more detailed understanding to these network types. We can see the differing balance of formal and informal settings, and of community and health settings, in individuals’ lives. Home has emerged as an important place in networks. The extent to which people spent their time at home was significantly negatively associated with social network size and access to social capital, suggesting value in community engagement. Both participants with formal and sparse networks and those with family and stable networks spent most of their time at home, but those with the latter networks tended to live with others and also had higher access to social capital. Having more place connections outside the home, particularly those in the community, was also associated with larger social networks, and those places which were social were associated with higher social capital. Working full time was positively associated with social capital scores. This was consistent with other work, showing the importance of employment for resource generation – financial resources but also social relationships. Increased engagement in social activities was associated with having higher access to health and well-being resources.
Our participants accessed a wide variety of settings in the community. Over a third of the study population used libraries, which was more than the general population, estimated in 2009 as 12.8% of the adult population visiting once a month or more. 211 Place connections which were safe and free to access, such as parks, provided important community spaces to get out of the home, meet other people and build identities that were not defined by mental health. 212,213 Our data suggested that the community was an important resource, and fuller networks were those that connected to and made active use of community resources to enhance well-being, while people who were the most isolated were those that spent a lot of time at home doing unstructured activities, living alone and with few visitors. This may seem unsurprising, but connectedness as a dimension of recovery8 is not given the same priority in mental health services as risk assessment or medication management for SMI; social aspects of living with SMI are given minimal attention in NICE treatment guidelines. 38,39,214 Deinstitutionalisation and community connection also depends on the existence and availability of community resources and spaces outside the home to connect to, and these places being truly in the community rather than institutionalised settings,205 as well as reducing barriers to access such as stigma. 215
The importance of meaningful activity for our respondents supported findings in other studies. 127 Types of activities which were meaningful might vary from person to person216 but feeling productive, having routine and being socially engaged were key aspects of the beneficial impact of meaningful activities. 131
Our three network types might provide a useful lens through which to distil myriad network variables into types that mental health practitioners can work with more easily. It provides detail on the extent and type of connectedness that a client has, which provides a context for thinking about interventions, as well as defining some of the resources available. Our resource and well-being data indicated that both diverse and active networks and family and stable networks had healthy components to them. Although we see a tendency for people with schizophrenia/psychosis to live alone and have fewer family ties or resources, our modelling of who had each network type showed that diagnosis was not a significant explanatory variable: many participants with psychotic disorder/schizophrenia develop diverse and active networks (42% in this study). Long-term sickness and disability as an occupational status seemed to be the key variable distinguishing diverse and active from formal and sparse networks; participants who reported being long-term sick tended to have formal and sparse network types. Long-term sickness as a risk factor for poorer social connection, negative social identity and lower levels of physical and other activity was well supported in other work. 100 In these data, living alone was a key distinguishing factor determining membership of formal and sparse networks compared with family and stable networks. Living alone was likely to be a risk factor for isolation and loneliness – which themselves have well-established negative health implications200 – especially where connection to community settings outside the home was lacking. These findings are cross-sectional and exploratory; moreover, causation may be two-way: diagnosis may affect if someone is living alone or long-term sick. However, our findings indicated that it may be useful to view a person through qualities of their network in addition to the label of a diagnosis, in order to understand a person and the social support that they require. This was the approach also being advocated in the treatment of long-term conditions, recognising the central role of social support in recovery. 102,103
Employment was an indicator of access to resources, as shown in the RGUK regression model. Employment can be beneficial because it facilitates access to social interaction and provides structure, a sense of identity, self-esteem and improved finances,132 while gaining employment can improve mental well-being and social inclusion,133 but people with mental illness face discriminatory barriers in access to employment. 217 In addition, not all employment is equal, and low-paid work which lacks meaning for the individual may be no better for health and well-being than long-term sickness. 218
The networks we mapped contained contacts, places and activities that were mostly viewed as positive or neutral for well-being. The study team reflected on this and it was likely that, as our focus was health and networks to support health and well-being, adverse or difficult relationships were less readily brought to the fore through the interview questions. Despite efforts to encourage people to relate to positive and negative contacts, places and activities, we acknowledge that we might not have been fully successful in getting people to relay negative aspects of networks. Our finding may reflect the stability of our study population at time of interview, and represent individual control and agency over personal networks where individuals had pruned their networks to remove negative ties. Those with smaller networks may value any tie even where conflict or negativity exists. 96 Moreover, the existence of some negative ties is not in itself a problem if people can manage them.
Another observation was over disclosure of mental health within network settings; a recent review highlighted complexity in disclosure decisions. 219 Fewer wider contacts, including colleagues, had been disclosed to and those with formal and sparse networks had the highest level of disclosure. It may be that the ability to control this information was an important aspect of network management. Participants with formal and sparse networks had a larger proportion of practitioner contacts who knew about their mental health condition, while those who had diverse and active networks, and had greater choice over whether or not to disclose, seemed to tend not to do so.
While it was difficult to compare methods, the mean size of the social networks we mapped was larger than in many studies, including the mean size of 15.2 contacts found in the recent systematic review of individuals with psychosis. 220 This could be for a number of reasons. Our method was different: it was expansive in terms of network boundaries and included places and activities as extra prompts for social contact so we may have mapped a larger network through methods used. However, a study on people who had been in a mental institution found a larger social network size of 23. 82 Our data also suggest it was the type of relationship (close relationships) rather than the number which was most important for resource exchange and this was supported by other work. 221
Finally, the wide range of places and activities important to people in our study population underlines the personal nature of recovery from mental illness and progression towards greater citizenship;69,222 what was important varied by person and one size does not fit all. While the specific activity may differ, the literature suggests having meaningful activities in one’s life can increase life satisfaction and improve subjective quality of life in this population. 127
What was the mix of formal and informal health-care provision within people’s networks?
We considered access to social capital and to health resources to answer this question. We found these resources to be provided primarily by close informal ties such as family and friends and less so from wider and practitioner contacts. Importantly, those who lacked family and friends to provide these resources had lower resources; they did not seem to replace these resources with practitioner contacts. More health resources (HRG) were provided by practitioners than social capital resources, but their support was still a minority of overall HRG.
Elements of place, social relationships and activity all seemed to impact access to social capital. Close social ties within the inner circle seem to be particularly important. Social network contacts who know about the participant’s mental health impact positively; this was controlled for type of relationship and suggests that, regardless of relationship type, disclosure may foster the trust and reciprocity required for social capital to grow. Employment also improved access to social capital, as was found in a study of South East Asian women with SMI. 122 The finding that increased percentage of network viewed as negative contributes positively to social capital was of interest. Contacts can be disliked but still useful; we found colleagues were viewed primarily as negative, so this fits with the impact of employment. Social capital was a resource accessed through social networks so it was unsurprising that place connections which were social had an impact. Participants in the SW had higher social capital and this will be explored in the case studies (see Chapter 7).
Did these networks differ in composition, range, size and density across subgroups?
Controlled for participant characteristics, only four factors were significantly associated with network type: housing status, long-term sickness and disability, living alone or not, and formal qualifications. This was important because it suggests that, on the whole, anyone can develop a more resourceful network type regardless of their diagnosis, age, ethnicity or gender, even if influential factors might be hard to change. We find support for this idea in that formally structured activities, time spent at home and community setting connections explain variance in social network size. Longitudinal work would be required to unpick how networks develop over time. However, our work highlights the heterogeneity and complexity of networks and suggests one size does not fit all; is it also likely that mean scores will apply to a particular individual. Therefore, it may be helpful not to attempt to isolate such factors but instead to use the network approach to map networks on an individual basis, supporting a person-centred approach to interventions.
How did network strength and breadth relate to well-being?
Well-being was our only outcome measure which was not inherently social. We found activities such as engaging in voluntary work, higher social support, being married/in a civil partnership or cohabiting and being male compared with female to be significantly associated with higher well-being scores, and increased connection to mental health settings, having children, a higher proportion of negative ties, lack of psychiatric inpatient history and presence of an informal carer to be significantly associated with lower well-being. It was difficult to explain these results using our network-mapping data set without longitudinal data. We could only make suggestions such as research showing hope was a strong predictor of subjective well-being,223 which possibly explains the importance of volunteering and cohabiting relationships. We found well-being and all functioning measures including perceived physical fitness, quality of life and overall health to be lower than the general population across all three network types. Those with formal and sparse networks did the fewest physical activities and connected to the fewest physical recreation settings. This suggests that more attention was required on physical fitness and well-being for people with SMI and in particular those who were least connected through people, place or activity resources. While many networks had important connections missing from them, participants valued what connections they did have; most connections to people, places and activities were rated as positive for well-being.
Our well-being model was weak. SWEMWBS measures well-being over the previous 2 weeks,160 though subjective well-being is influenced by both short-term and long-term factors. Many of our network factors and participant characteristics were more longstanding, thus day-to-day life events could affect the score more strongly than network features. Finally we note that there was consistent perceived value in network dimensions across our data, with the words used to describe networks mostly positive descriptions. Personal networks to support well-being contain support, friendship and emotional closeness. This suggests that personal network assessment is a good way of examining strengths and assets on which to build individual plans. For the minority who saw their networks as negative and for those with negative connections, there are additional pointers for change.
What was the role of practitioners in networks?
A key answer to this question lay in evidence that improving networks can improve mental and physical health, and well-being, and that network interventions are possible. More evidence is needed, building on existing work describing effective interventions in various health settings and in mental health224,225 and the barriers practitioners face in addressing social factors in the lives of their clients. 226 The network mapping offers limited insights but the approach has potential. The process can offer a route into understanding the reasons why some networks are sparse, and into working together with individuals to identify potential routes into building connections and resources. The practitioner may have a role in strengthening both bridging and bonding capital. 117
The study looked in particular at the mix of formal and informal ties in networks. The majority of networks were not dominated by mental health: places, people or activities. Only one in four contacts was a practitioner or other mental health service user. Only two out of three participants identified a mental health place setting on their network map. In terms of social capital and health capital, most was gained from non-formal contacts such as immediate family or friends.
Mental health crises will disrupt or rupture networks, affecting activity patterns and connection to place, whether through social withdrawal, stigma227 or loss of employment and relationships. Participants who had been an inpatient in the previous 5 years had significantly lower percentages of long-term activities and place connections. In our study population, those with family and stable networks were less likely to have ever been an inpatient. We note that having family was important in personal networks and thus, where these relationships were absent, network enhancement strategies may be required to fill the gap. We observe that practitioner relationships can sometimes fill a friendship void but they did not provide access to resources in the same way as family or friend contacts. They were therefore not the solution except as a change agent, to empower, build skills and share ideas, but not to become the key network resource. A key strategy might be turning wider contacts into friendships where family were missing; practitioners might assist this process.
We also found that practitioners feature in all three network types in the inner circle of emotional closeness. To some degree, practitioners had an important role regardless of what else was in the individual’s network; they appeared in the inner circles of social networks regardless of overall social network size. We did not find significantly more people in primary care with a GP in their inner circle. GPs were in inner circles regardless of mental health contact.
While the amount of direct referral from practitioners to new place connections was low, this did not discount practitioners or informal network members encouraging participants to get involved in new things. We saw that more community place connections was associated with higher social support; it may be a two-way link where supportive network members encourage the individual to take steps themselves to make new connections. Informal contacts were more important than formal ones for referral but by far the most important factor was the individual themselves. The practitioner may be vital in helping build the confidence and resources of the individual to go and make these connections themselves. 125
How did people with severe mental illness use resources in their personal networks to support their health and well-being?
In conclusion, this chapter describes the heterogeneous social ties, places and activities that individuals with SMI draw on to access resources for health and well-being. There was evidence in the literature that connections to the community, to social ties and engaging in meaningful activities can improve access to resources, subjective well-being and quality of life. 11,111 Our study supports this evidence and gives some insight into how people, place and activity interlink. In our study the most important aspects seem to be community places which were social (and which supported engagement in activity); meaningful activities which were social and structured; and the informal network – not just the family, but friends and wider contacts too. Our data suggested most of these connections were built by the individual with limited referral by practitioners, but practitioners can have a role in encouraging or building the confidence of clients to make new connections. 228,229 Getting out of the house regularly was associated with increased access to social capital and larger social networks, yet the majority of our population spent more than half their waking time at home and had lower well-being and social capital than the general population. Therefore it seems that more needs to be done to support this group to develop and make use of personal network resources more fully. Network perspectives offer an insight into the types of connections people had and the extent of isolation, and crucially they provide detail on specific opportunities and gaps in the networks of connections that individuals have which can inform service interventions towards improving social inclusion and social capital and increasing activity levels for this group.
The next chapter will explore the meaning of these connections to answer the question of how people with SMI use personal network resources to support health and well-being more deeply.
Chapter 4 In-depth network interviews
Introduction
This chapter draws on analysis of 41 follow-up interviews conducted with people with SMI to answer the following research questions:
-
How do people with SMI use resources in their personal networks to support their health and well-being?
-
How do community-based practitioners and organisations support people with SMI to use their personal networks to support health and well-being?
To address these questions we interrogated the three network types identified and analysed in Chapter 3: formal and sparse; family and stable; diverse and active. We explored each network type to understand key features and how these evolved over time, seeking to explore five key themes identified within our literature review (see Chapter 2): agency within networks; social support; the trajectory of recovery; perceptions of stigma; and the role of social capital. We have used this qualitative analysis as the critical lens to examine complexity in networks and challenge key features identified in the quantitative analysis. In doing so, we considered the ways in which individual agency was evident in formal and sparse networks, the extent to which family support was constructive in family and stable networks, and whether or not diverse and active networks proved beneficial for well-being.
We acknowledge this is a very particular use of our qualitative data. Other analysis is also being carried out by the research team using these interviews. However, in order to answer the research questions for the report, and unpick the network categories that we generated, a focused analysis was undertaken in three distinct units. It is important to stress we do not consider particular or central features as being unique to a particular network type; each might be found in the other. For example, family is a feature in each network but was explored only in the family and stable network analysis in this chapter. What we learn about specific features for each network type may well hold true in other network types. Indeed the three network types are only a model to help us understand the diversity of individual’s lives, and people will move between categories. The purpose of this chapter is to explore in detail the heterogeneity we identified in Chapter 3, within our network framework, and assess the role individuals and others, including practitioners, play in shaping networks of connections to people, places and activities. We also examined the meaning and impact of the network interviews. Thus the focus of the analysis is on:
-
each network type, to understand how these developed exploring agency within networks and role of others, changes over time and impact of features such as stigma and severity of illness
-
understanding the impact of the network interview on participants and potential for development as a therapeutic intervention.
The characteristics of participants are provided in Table 29 to provide demographic context; in the text we refer to each person through the use of a pseudonym.
| ID | Pseudonym | Gender | Age (years) | Site | Ethnicity | Network type | Social network size | Diagnosis | Employment status | Mental health service contact | Living situation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| SUSW36 | Nigel | Male | 48 | SW | White British | Diverse and active | 40 | Bipolar | Long-term sickness/disability | Primary | Alone |
| SUSW46 | Andrew | Male | 32 | SW | White British | Diverse and active | 29 | Bipolar | Full-time work | Secondary | Alone |
| SUSW48 | Suzi | Female | 38 | SW | White British | Diverse and active | 21 | Other psychoses | Part-time work | Primary | Alone |
| SUSW53 | Michelle | Female | 42 | SW | White British | Diverse and active | 18 | Schizophrenia | Full-time work | Primary | Alone |
| SUL05 | Maggie | Female | 59 | London | White British | Diverse and active | 38 | Schizophrenia | Volunteering | Secondary | Alone |
| SUL10 | Roger | Male | 23 | London | White British | Diverse and active | 25 | Bipolar | Full-time work | Primary | Parent/parents |
| SUL23 | Donna | Female | 51 | London | Black: other | Diverse and active | 20 | Schizophrenia | Unemployed | Secondary | Alone |
| SUL28 | Ellen | Female | 32 | London | Black Caribbean | Diverse and active | 20 | Other psychoses | Education/training | Secondary | Parent/parents |
| SUL29 | Kevin | Male | 41 | London | White British | Diverse and active | 34 | Bipolar | Unemployed | Secondary | Alone |
| SUL32 | Liam | Male | 63 | London | White: any other white background | Diverse and active | 19 | Other psychoses | Retired | Primary | Alone |
| SUL39 | John | Male | 27 | London | Black African | Diverse and active | 13 | Schizophrenia | Unemployed | Primary | Alone |
| SUL48 | Zara | Female | 28 | London | White: any other white background | Diverse and active | 22 | Bipolar | Education/training | Secondary | Partner/spouse |
| SUL65 | Bryony | Female | 28 | London | White British | Diverse and active | 17 | Schizophrenia | Full-time work | Primary | Partner/spouse |
| SUL76 | Áine | Female | 56 | London | White Irish | Diverse and active | 30 | Schizophrenia | Volunteering and long-term sickness/disability | Secondary | Alone |
| SUL77 | Duncan | Male | 41 | London | Mixed white and black Caribbean | Diverse and active | 27 | Schizophrenia | Part-time work and education/training | Secondary | Other (supported housing) |
| SUSW01 | Matt | Male | 41 | SW | White British | Family and stable | 34 | Bipolar | Full-time work | Secondary | Partner/spouse |
| SUSW09 | Jackie | Female | 42 | SW | White British | Family and stable | 15 | Bipolar | Part-time work | Primary | Partner/spouse |
| SUSW16 | Ed | Male | 64 | SW | White British | Family and stable | 24 | Other psychoses | Part-time work | Primary | Partner/spouse |
| SUSW38 | Eleanor | Female | 42 | SW | White British | Family and stable | 14 | Bipolar | Long-term sickness/disability | Primary | Parent/parents |
| SUSW40 | Agnes | Female | 62 | SW | White British | Family and stable | 21 | Other psychoses | Retired | Primary | Partner/spouse |
| SUSW41 | Carl | Male | 26 | SW | White British | Family and stable | 33 | Bipolar | Unemployed | Secondary | Partner/spouse |
| SUSW51 | Nick | Male | 50 | SW | White British | Family and stable | 13 | Schizophrenia | Long-term sickness/disability | Primary | Alone |
| SUSW60 | Sam | Female | 45 | SW | White British | Family and stable | 18 | Bipolar | Part-time work | Primary | Partner/spouse |
| SUSW61 | Dora | Female | 46 | SW | White British | Family and stable | 30 | Bipolar | Long-term sickness/disability | Secondary | Other family |
| SUSW68 | Bradley | Male | 41 | SW | White British | Family and stable | 17 | Schizophrenia | Volunteering | Secondary | Partner/spouse |
| SUSW77 | Joe | Male | 34 | SW | White British | Family and stable | 18 | Schizophrenia | Long-term sickness/disability | Secondary | Parent/parents |
| SUL41 | Daniela | Female | 58 | London | White British | Family and stable | 26 | Bipolar | Part-time work, volunteering | Primary | Partner/spouse |
| SUL34 | Gavin | Male | 44 | London | Mixed white and black Caribbean | Family and stable | 12 | Schizophrenia | Long-term sickness/disability | Primary | Alone |
| SUSW10 | Gregory | Male | 53 | SW | White British | Formal and sparse | 6 | Schizophrenia | Unemployed | Primary | Alone |
| SUSW15 | Valerie | Female | 62 | SW | White British | Formal and sparse | 13 | Bipolar | Retired | Primary | Alone |
| SUSW26 | Neil | Male | 50 | SW | White British | Formal and sparse | 10 | Schizophrenia | Long-term sickness/disability | Primary | Alone |
| SUSW34 | Geoff | Male | 60 | SW | White British | Formal and sparse | 22 | Schizophrenia | Part-time work | Primary | Alone |
| SUSW42 | Bill | Male | 53 | SW | White British | Formal and sparse | 8 | Schizophrenia | Long-term sickness/disability | Secondary | Alone |
| SUL07 | Raj | Male | 48 | London | Asian: Indian | Formal and sparse | 8 | Schizophrenia | Long-term sickness/disability | Secondary | Alone |
| SUL08 | Adam | Male | 59 | London | Black African | Formal and sparse | 12 | Other psychoses | Long-term sickness/disability | Primary | Alone |
| SUL61 | Pauline | Female | 56 | London | White British | Formal and sparse | 15 | Schizophrenia | Education/training and long-term sickness/disability | Secondary | Alone |
| SUL63 | Jessica | Female | 21 | London | White: other | Formal and sparse | 17 | Bipolar | Education/training | Secondary | Parents |
| SUL64 | David | Male | 57 | London | White British | Formal and sparse | 20 | Bipolar | Part-time work | Primary | Alone |
| SUL72 | Victor | Male | 42 | London | Black African | Formal and sparse | 11 | Schizophrenia | Long-term sickness/disability | Secondary | Alone |
| SUL75 | Ali | Male | 53 | London | Asian: other | Formal and sparse | 15 | Schizophrenia | Long-term sickness/disability | Secondary | Alone |
| SUL78 | Barry | Male | 42 | London | Black African | Formal and sparse | 16 | Bipolar | Long-term sickness/disability | Secondary | Alone |
People’s experience of formal and sparse networks
The first interviews we explored were those of people categorised with formal and sparse network types. This included people who, in relation to the overall data set, had the smallest number of social ties, had proportionately more health and social care practitioners in their networks, tended to live alone and spent a high proportion of their time at home engaged in less structured activities. The size of the social networks in this group ranged from 5 contacts to 30. Those with more contacts tended to mention high numbers of formal or less active ties. We were particularly interested in examining qualitative data on these issues to understand:
-
network meaning and development of social capital
-
network dynamics, adaptations and change
-
value placed on formal support.
Network meaning and social capital
Formal and sparse networks were characterised in the quantitative analysis by a higher proportion of contacts with health and social care practitioners, potentially providing fewer opportunities to develop an identity beyond mental illness or generate social capital. However, despite more limited resource opportunities, many people in this group described ways in which they derived sense of meaning and had created identities beyond their diagnosis. The non-formal aspect of their lives was valued; although people had fewer connections, those they had were important and useful. We found that several participants had purposeful strategies to ground their lives in daily routines. We focus in this section on examples where strategies are based on non-SMI connections to explore and understand non-formal aspects of a personal network labelled ‘formal and sparse’.
Geoff (SUSW34) described his approach as doing ordinary things as much as possible. He talked about how everyday interactions with ‘ordinary working people’ helped him to learn about relationships and how to communicate. He cited ‘banter’ with (non-SMI) friends as important in terms of helping to manage his voices and dispel paranoia. This helped him in terms of emotional well-being: interacting with ordinary working people encouraged Geoff to develop a sense of routine which was manageable and had meaning for him. He discussed how his flexible job with a local greengrocer ‘creates structure for me, um, well again it’s the responsibility thing’.
The example of Geoff also illustrates the barriers to routine imposed by mental illness. We learnt his medication made him sleepy – ‘I just feel, I’m very very tired’ – restricting his routines but overall he recognised that listening, noticing things and ‘maybe strike up a conversation and um, that sort of thing, you know it’s quite important’. His physical health was valued and he was an active walker. Geoff acknowledged that relationships were important – ‘it’s about being needed by other people in the same way we need other people as well’ – but can feel sad that he is not in a long-term relationship. Geoff explained that, although he accepted limitations caused by SMI, his well-being was nurtured through reciprocal friendships and work. Geoff values the building of social capital that these reciprocal non-SMI relationships provide.
Adam (SUL08) was similar to Geoff with respect to age, living alone and being diagnosed with psychosis. He explained that he was purposefully spending less time with people with SMI. Although he said that he was comfortable in the company of other service users, he stressed that he was socialising with a wider range of groups: friends from the pub, a social club with his neighbours and a church community. In those social circles the issue of mental illness would rarely come up and he added that he did not want other people to think that he was ‘crazy’. At the time of the interview Adam, who had been unemployed for a long time, revealed his personal struggles with not working, because, as he phrased it, ‘work is healthy and so the more I didn’t work the more my health d . . . declined’. He mentioned routines including going to the gym and a book club, as well as applying for jobs, but believed that his age counted against him. Ordinary life goals were a motivation for Adam: he emphasised his commitment to work and his ongoing efforts to find a job, in part so he could have ‘a companion to live with because it’s not fun to live alone’. Adam described that a consequence of having more non-SMI friends was that he needed less specialist mental health support; in particular he was dismissive of psychiatrists, who he felt could do little to help him any more. However, he was reliant on his depot injection but did not like attending ‘that mental place’ as there could be ‘violent customers’; he valued instead doing ‘normal’ things: ‘I try to do things normally, in the normal way and talk to them normally.’
Geoff and Adam exemplify a recurring theme in formal and sparse networks where there was a motivation to create routines and opportunities involving people to fill gaps, such as an absence of family and employment. We found other examples in sparse and formal networks that contained less ‘social’ connectedness but where identities and meaning had been forged that were linked to skills and interests. One such example was expressed by Ali (SUL75), who described himself being ‘outside of society’. He presented himself as belonging on the margins of society, and throughout the interview he stressed that he identified with socially excluded groups and had engaged in artistic activities such as drawing sketches of the homeless. Neil (SUSW26) likewise presented himself as having an artistic identity, and reflected that, although he has not been able to work for many years, he made a useful contribution to society, for example, through writing. Neil had built cultural capital and he valued this resource. He described himself as possessing ‘a literary grounding of a thinking man’. He also said that his painting prowess had developed to the point where he felt part of an artistic community. By successfully making the activity of painting meaningful to him he was now also developing connections with people, as evidenced by going away on painting holidays, and that moving away from the chaotic SMI community was empowering.
I paint. . . . I’ve got to the stage where I think I can honestly say I am an artist. Paintings are getting good enough, now. And um I just went on holiday with a group of friends and um it was fabulous. I shed a lot of my illness there.
Formal and sparse networks also included examples of people who were embedded within the mental health system and reliant on practitioner relationships for emotional, practical and specific mental health support. These people had very limited non-formal resources to draw on. The balance of formal to informal varied in the formal and sparse network grouping, impacting on access to resources and thus social capital, and this balance changed over time.
One way this balance could change was through reduction in the proportion of formal network contacts following discharge from community mental health services. This happened to Neil, who said he was initially apprehensive when the security of such support was removed, ‘there was a time when I was not getting support. I was concerned. I thought, if only they were still here . . .’ As time developed, however, he came to feel more self-reliant and independent by moving away from the mental health system, even though this was not his personal choice at the time:
I’ve learnt to survive and I am now strong emotionally, my stress thresholds are improving daily, um, and I’m in reality and, um, whatever that reality is. I’m in this reality and, um, life is good. And, um, I, I just don’t need to be cared for any more, I just don’t need it.
But now I say what do I want them for? Namby pamby, looking after me and telling me I’m a good boy? I don’t need that. I, I believe in myself now and I’m well enough and confident enough to go out there and mix with society and not be a threat to some innocent member of the public. It doesn’t exist. It’s gone. I, I don’t need any care now, it’s not necessary. It’s all down to me.
Neil’s example demonstrates that, although people with SMI can become dependent on mental health support and the ‘going it alone’ may cause anxiety, ultimately being away from the system, at certain times, can be helpful, creating space for confidence and self-reliance to develop. It may have been that for Neil moving away from service dependency was a factor in enabling his sense of cultural capital to flourish.
The dynamics of sparse networks
All personal networks are dynamic to varying degrees; change was a feature, including fluctuations in SMI. We focus in this section on exploring the degree to which change was a feature of formal and sparse networks, drawing on examples to illustrate varying prominence of change in the accounts people shared.
Jessica (SUL63) was in her early twenties and explained that she became unwell when she left for university: ‘I don’t think that was good for me because it was a big change . . . being away from home for the first time.’ Because she was away from her immediate support network, and it was her first experience of being unwell, she reflected ‘I didn’t have a coping strategy’; as a result she had to move back to London. Jessica demonstrated resilience and determination in her interview to move forward with her goal of being a student. She had recently embarked on a new venture which was possible because of the progress she had made in her recovery. In the past, new things were ‘always related to getting unwell’ and this acted as a barrier to moving on from being ‘unwell’. However, recently she had begun an art course near home, which she experienced as positive, as she met people with ‘similar interests’ and felt ‘more of a purpose and meaning to what I do every day’. It also marked a change, providing a different type of support to the recovery group she had been attending.
Where we could share, share ideas of how to get, how to be better and . . . or how to be healthy, um, and a lot of things came from that because people were sharing experiences and giving each other advice and so you, kind of, get what works for people, what doesn’t work.
Um, no [I don’t attend any more] because I, kind of, have other activities that are meaningful and that keep me busy. And I, I can meet people through them and I don’t need to, um, I don’t need to have a social group because I, I’ve got my own social network and I’ve got friends.
Although Jessica was clear about the challenges she faced, and reflected that sometimes she would struggle ‘to keep my moods constant’, there was a clear sense of optimism for the future and strategy-building, including moving into her own home: ‘wanting to be a bit more independent’ balanced with ‘I’d still have my network close by . . .’ Jessica also reflected on the support she had and an important dilemma emerged in her account: Jessica acknowledged that support from mental health services had helped her to make changes in her life, but also had mixed feelings about the level of involvement; ‘sometimes it feels like it’s too much but I think that’s only because it reminds me that I’m not well’. We identified that Jessica had several future-forming strategies in her account affecting home, education and friendships. She explained: ‘I feel like I’m in quite a good place in terms of my mental health so, yes, things are going quite well’.
David (SUL64) provided an example of a network with a seasonal pattern of managing SMI. He described the winter months as a habitually challenging time to endure: ‘I just dread it. I mean, I absolutely dread it’. His home was transformed into a refuge away from the ‘grey, wet and dark’. His usual strategy for managing his well-being and low mood, gardening, was unavailable to him in these months so he needed an alternative routine to get out of the house. A partial solution requiring motivation and commitment was teaching gardening classes:
But this time of year . . . I mean, I have, a couple of weeks ago I was hibernating, I mean, I went and took my classes, um, but that was all. I went home to bed. . . . I was offered the classes and took them on, just as a way to get me out of bed, so . . . but, yeah, it’s not much, but I feel, well, if I’ve gone and talked, at least I have done something.
This contrasted to his routine in the summer, when, ‘given the choice, I would just potter in my garden’. David explained:
When you look at a garden, it looks like, you know, you’ve done something beautiful. Other times, when I’m very low, I can look at it and think, you know, I can’t be that bad if I’ve made a garden this beautiful. I don’t know where this fascination came from, you know. Um, but it is some to . . . and . . . I find it fascinating.
He described his strong motivation for staying physically active and this was another driving force in his commitment to address the oscillating pattern of change in his network from hibernation to long hours of exertion in his garden.
In contrast to Jessica and David, other people who had been living with SMI for many years had sparse networks that appeared to be relatively stable with limited evidence of change within them. Detailed examination of accounts however revealed potential for transformation in all networks. For example, Raj (SUL07) appeared to be settled in a routine dominated by services. However, he articulated a clear plan of self-improvement and felt that he was taking more responsibility in his life, in contrast to ‘magical thinking’, which dominated his past.
A shrinking dynamic was evident in some formal and sparse networks as home place came to dominate people’s routines at the expense of other network opportunities. Victor (SUL72), for example, felt that he was alone in life and tended to stay in his house: ‘99% of the time it’s me, myself and I.’ He reflected that his social contact was shrinking as a result of going to fewer places: ‘I don’t talk to people. I just keep to myself, I keep what’s within me I keep it to myself.’ However, he did have one notable routine taking him out into the world and providing responsibility. At the time of the interview he would periodically check on the house of his brother (who was away), which he found beneficial for his well-being: ‘yes, it is good for me. It was good because it makes me come out of the house.’ This highlights that, although formal and sparse networks may shrink, with social isolation becoming a more prominent feature, such patterns are not irreversible and routines outside the home can provide renewed meaning and purpose.
Valerie (SUSW15) had a small network and her bipolar disorder, compounded by obsessive–compulsive disorder and arthritis, left her feeling socially isolated without social backup. Yet there was an underlying determination to identify future goals. At the time of the interview, a family wedding some distance away was a major event in her life and she had set herself a new social goal:
I want to break that barrier that I don’t need to come back that night, I can stay away, for a night, and it’s not going to be the end of the world, you know?
Having access to resources for setting personal objectives was crucial, and recognising these as opportunities was also vital. Valerie acknowledged that the network-mapping exercise highlighted more positive connections in her life than she realised:
There seemed to be a lot more connections and things and she [interviewer] sparked off a connection that I didn’t realise I’d got there.
We also learnt from Valerie that an active coping strategy for managing bipolar disorder put great strain on her own well-being. She disguised her mental health condition from people living locally – a strategy we term ‘network segmentation’ – to prevent stigma.
Yeah, I would say the only people that know about my bipolar locally are medical people . . . when I’m feeling very down I make excuses like ‘oh I just don’t feel well’ or ‘I’ve got a bit of a cold’ or ‘I’ve got a chest infection’ or something. And I’m very good at putting the signs of having a cold on, do you know what I mean? . . . I haven’t, I’m just rock bottom, I just don’t want people to know you know. . . . And sometimes it can go on . . . I can be down for 6 months. It’s very difficult (tearful, and sniff). Very difficult (sniff) . . . So I just, as I say I’m very good at covering it up, but the problem is with that you can cover it up when you’re down, or if you contact them when you’re feeling like you want to go out they don’t sometimes, they don’t want to know you’ve brushed them aside so many times that when you’re feeling you want to socialise with people you tend not to be asked.
In more diverse networks that same ‘network segmentation’ strategy can work well, combating the unwanted impacts of the stigma of mental illness. However, formal and sparse networks had fewer resources within them to buffer the isolation that can result from distancing oneself from a particular social group. Within one network, signs of growth and agency can sit alongside feelings of despair plus the consequences of poor physical and mental health.
Valuing mental health supports?
The research explored the interplay in personal networks of informal support from family and friends, as well as wider ties, with formal supports from services. In this section we draw on examples to examine how people feel about mental health services being a presence in their lives. Within formal and sparse networks we found greater dominance of formal connections but these were not always well received: some individuals struggled with the loss of autonomy felt from experiencing mental illness and some people resisted any reliance on mental health services. Ali (SUL75) articulated this dilemma:
Well, the change would’ve come from when I was sectioned, 2002, and I think there’s been a complete shift towards . . . also a sense of, ah, of resentment of the Mental Health Services, but also a dependence on them. And maybe that the resentment and dependence feeding off each other, because often, when you’re dependent on someone you resent them for it, you know. You want to be your own . . . you’re not autonomous any more.
There was active engagement from services in Ali’s life. In contrast Bill (SUSW42) had limited engagement with services, which suited him, despite describing loneliness and isolation alongside paranoia. He was a man in his fifties who talked about how he was prone to feelings of guilt and isolation to such an extent that he had stopped activities he used to enjoy but again, as with other participants, was concerned to find employment and move off benefits: ‘I should be at work’ he explained. There seemed to be a disconnect between himself and health-care practitioners. Practitioners viewed him as mentally ill, whereas Bill viewed his problems in life as related to loneliness and being an outsider; he did not recognise a mental illness identity. Bill saw a GP and that was sufficient support:
I mean, I’m not going to try to get out of this job illness by claiming I’m more ill than I am, so, you know, no, I don’t think there’s much more they can do to help.
In contrast to Ali and Bill, others wanted high levels of support and welcomed having relationships with practitioners, speaking positively of the value they placed on these contacts. Pauline (SUL61) explained that her social worker and GP were highly respected relationships in her life, whose positive qualities compensated for other negative contacts, especially family:
You can’t have a family member because the family members have got no intelligence compared to the social worker, you know, and she’s trained for helping people. She’s the one that can help people. The other people can drag you down to unbelievable misery.
I’ve more trust and friendship, not friendship exactly, but respect I think the word is from these two [her GP and social worker].
So by going, dressing up smart and going to see the social worker, and coming to tell the GP about my troubles makes me feel that I’ve got the proper support in life just because they’re exceptional people as well.
It was evident that Pauline would turn to her GP and social worker for a wide range of support, whether emotional support or illness related, and these connections encouraged engagement in new activities. Both had roles as important contacts in her network as well as facilitators of network development. She explained that, although she was afflicted by voices which triggered much social anxiety – ‘they’ll start talking about fire, I’m going to be set on fire, I’m going to be run over, I’m going to get beaten up, I’m going to be scarred’ – she was still able to pursue lessons in sign language. As well as being a means of learning a new skill, it enabled her to address her extreme anxiety by being committed to supporting others and generated new social connections:
Doing the sign language is important because I’m meeting new people and that’s the thing. It’s like needing a blood transfusion, you know, for your life and, um, it’s important for me to meet new people. I’m going to be helping deaf people who are isolated, like myself, and I really understand how bad it is, you know, when you’re totally on your own and you can’t talk to people and you can’t make friends.
Pauline described the value she placed on her social worker encouraging her to engage in new activities; the latest area they were addressing together was her physical fitness. Developing new relationships was particularly valued by Pauline and she looked to her GP and social worker to help her make decisions over where, and how, to seek new connections.
Some people with formal and sparse networks turned to health-care practitioners for social contact to make up for a deficit elsewhere in their life; Gregory (SUSW10) explained that he went to see his GP sometimes, ‘just because I need to speak to someone.’ Even though he rejected his diagnosis of schizophrenia, he appreciated that his GP had broached the subject in an ‘open and tactful’ manner.
Notable elements of formal and sparse networks, alongside challenges of managing SMI, were inner strength and resilience, identified as ‘building blocks’ of recovery by one lived experience researcher. These might be very small signs of agency within the network or more substantive examples where individuals were driving actions in their networks, developing a greater sense of autonomy and independence. Practitioners were acknowledged as one influence in recognising the potential for change. Barry (SUL78) had taken the mantra of his social worker to heart: ‘don’t let life beat you’.
We summarise in Table 30 what we have learnt about formal and sparse networks in terms of five key themes highlighted in the first section of this paragraph. These were areas within our literature review (see Chapter 2) and were used to structure researcher reflection notes within the data synthesis process in order to answer the study research questions.
| Key literature area | Insights from our study data |
|---|---|
| Agency and strategies for staying well | People with formal and sparse networks demonstrated agency – taking steps to take control of their lives, making choices and finding routines that balanced demands of their illness alongside well-being needs. What form(s) this took varied from individual to individual, and changed over time: some people were in a position where they felt limited social and community engagement was actually beneficial for their well-being. Others were motivated to expand their social capital; work was identified as a goal to support well-being |
| Social support | We observed, not only in formal and sparse networks but across the data set, that the quality, not quantity, of social ties was key in terms of supporting well-being needs. The people with formal and sparse networks who appeared to be struggling the most did not generally articulate that they wanted a larger network; what they wanted was someone to fulfil emotional/social needs. Such needs cannot easily be fulfilled by practitioner contacts |
| Recovery over time | The accounts of people who had been categorised with formal and sparse networks provided rich reflections on personal recovery journeys. Times when people were very unwell provided a comparator reference point to their circumstances at the time of the interview; strategies to stay well sometimes meant limited social or community engagement. We also had feedback that the mapping process itself was a useful exercise in helping make new plans and identify potential building blocks for recovery |
| Stigma | Stigma was a feature of formal and sparse networks, partly explaining network choices to reduce engagement within the community. However, it is important to stress that different people respond to stigma in different ways, and some participants articulated a sense of resilience or a refusal to be beaten by prejudicial public attitudes or discriminatory behaviours towards the mentally ill |
| Social capital | The key agent of change, and judge of meaningful social capital, is the individual who leads (with support) new engagement with people, places or activities. It will not always be appropriate to encourage people to develop new forms of social capital when they do not feel well enough to do so or are not motivated to do so. First steps to building social capital included extending social support to develop links with wider resources that can help people ‘get on in life’; this includes work, which featured in some formal and sparse networks |
People’s experience of family and stable networks
A third of people in the study population were described as having ‘family and stable networks’ characterised by family connections, with bonded and durable links; most social and place connections were known longer than 5 years and many within the network knew each other. These were also home-focused networks and most lived with other people. Family and friends were an important resource. Mapping connections to people, places and activities, and following up these discussions by looking at how people with SMI used resources in their networks to manage well-being, revealed the multilayered influence of the family. In this section we explore family and stable networks to understand further:
-
family support and recovery
-
dependency and family support.
We have focused mainly on family relationships in this section to explore connections to people, places and activities in family and stable networks. We draw on examples to illustrate contrasting influences of family across the data set.
Family routines and support as a positive feature in personal networks
For some of the people interviewed, family life was an intrinsic part of their recovery journey, a valuable source of support for their own illness, delivered by children, partners and other relatives. It was this support that helped to give their lives a sense of structure and meaning, sharing activities and providing responsibility and purposeful roles. Families were described as providing far more than emotional support. We focus in this section on the role of families in recovery.
Jackie (SUSW09) reflected on how she had become more outgoing and that her network had grown as a result of her routine of looking after her young son. She had recently developed some close friendships and had also engaged in more activities. Routines revolving around her son stood out as positive features, providing variety and escaping spending too much time at home, which reinforced a cycle of guilt and sense of isolation. However, it was also evident that this came at a personal cost and that her determination to support her son could be challenging: ‘I’ve always said I’d never let it affect him, never show it to him, which is . . . that can be hard.’
Sometimes when you’re having a really bad day, it’s quite hard to pretend you’re not. Some days if I’m really tired I feel really like I couldn’t do something and I know that he needs to get out, that can be hard, but I do it.
Nick (SUSW51) likewise talked about how his child care routine was a positive influence. In a number of interviews there were accounts of how the pattern of family life in itself provided sense of meaning and purpose. Samantha (SUSW60) reflected that in the past she had thought that she would not be able to settle down and live an ordinary life because of her earlier experiences of bipolar disorder, but that getting married and buying a house with her husband was a significant event providing security and stability, a solid base to connect to the ‘world’ from:
We just felt this is a nice place to live, and it’s got a good feeling about it. And we’ve been there ever since and don’t want to move.
The enjoyment of her life at home was a key part of her recovery story in contrast with her experience at work, which she described as ‘extreme pressure all the time’. Samantha also explained how having a supportive and intuitive husband was helpful in terms of managing bipolar disorder on an ongoing basis:
My husband is the most important one: we’re very close. He knows all about my situation, and he’s very supportive. He seems to have got this sort of intuition as to, sort of, when if I’m sort of not quite right, if I sort of leave him to sort of cheer me up, or if I need him just to leave me alone for a bit.
There were other examples in interviews of family being central to identity and stability. Gavin (SUL34) described his uncle and father as being ‘like a rock foundation to try and help me boost myself up’. Seeing his children once a month was also identified as the highlight of his life:
I know I’m not sort of like, um, like 100%, you know, with it but at least, you know, like, you know, I can show them the love and caring and respect, do you know what I mean? And they, they, um, they understand, do you know what I mean?
Gavin identified his family as providing essential support in terms of helping him to stay well. He explained, for example that they regularly telephone him to check how he is doing:
. . . which gives me that, um, that inspiration of happiness, because like they say, it’s a serious thing. All you need is a phone call can cheer you up, you know.
The support Gavin received from his family seemed particularly important in contrast to the rest of his network. Many aspects of his life had diminished over the years, including engagement with key activities such as work. The family was a core part of Gavin’s social relationships and without them he would have been left socially isolated. Dora’s (SUSW61) interview also demonstrated the enduring value of family support, especially through times of upheaval and change. She had recently separated from her husband and had moved to a new home with her two daughters: ‘we’ve been through a lot together’, and she reflected that they had grown stronger as a result. Dora also said that it was important for her to be accepted in the local community, which was likened to ‘a goldfish bowl’ at times, for the sake of her daughters. The need to be accepted by the community felt pressuring and challenging, partly because of the stigma of mental illness, but also for a central part of her well-being. She also reflected on the impact of her illness on her eldest daughter: ‘sometimes I feel sad that they do [understand about my mental health] because it changes you as a person . . . it affected her school work. I’m sure, you know, I’m sure she would have had an easier time if this wasn’t there’. Her extended family, despite her separation from her husband, also remained important in her routine; she supported her in-laws, doing jobs for them. This evidenced again the importance of reciprocity in relationships and the different forms it can take.
The influence of family in personal networks
Our interviews revealed some challenges for recovery with respect to family support. We found that high levels of family involvement can come to dominate to the point where these relationships act as a barrier to new opportunities to build connections. A similar risk might be found with over-reliance on practitioners in formal and sparse networks, though family connections tend to last longer; the key was what roles were occupied by family and how far the individual with SMI was in control. Where family dominated to the extent that people could not imagine an alternative future and as a result lived with short-term perspectives on managing SMI, there can be a detrimental impact on personal recovery. We focus on examples that reflected on the influence of family in the network in this section.
Eleanor (SUSW38), who was in her early forties at the time of the interview, discussed having a close attachment with her mother to the extent that when she was a teenager she dreaded becoming independent and had been living at home ever since:
I’ve always had a really, really strong relation, I was always a mummy’s girl . . . And I have always had a very, very strong dependency on her. I’ve never been able to be independent in the way that other people grow up and become independent and look forward to their independence. When I was in my teens I absolutely dreaded it. I couldn’t bear to think about working or responsibility. I’ve never worked. I’ve been to interviews, but I’ve never managed to work.
Eleanor revealed that over the years she struggled to engage in activities under her own initiative but she was aiming to take more responsibility over her own recovery – ‘I think I do need to learn coping strategies’ – even though this was deemed difficult and she felt weighed down by her depression, ‘I realise now that it is down to me and I think that when I’m ready it will happen.’ We highlight that it can be challenging to break dependent relationships, and acknowledge that ‘being ready’ is an important part of recovery from SMI.
Joe (SUSW77), a man in his early thirties, discussed how he was very reliant on others to help create a sense of routine and engage in activities. He said that he felt close to his mother, who provided him with ‘organisational’, as well as emotional, support, while he revealed that ‘to do stuff’ with friends was a key strategy to help cope with his voices: ‘concentrate on that rather than concentrate on what people [voices] might be saying.’ Joe talked about potentially moving away from the small town where he lived to a nearby city because he regarded it as more ‘cosmopolitan’ and ‘job opportunities and education opportunities are better there.’ However, there were few concrete plans shared to understand how this ambition would be fulfilled. Such a move would impact on his family as well as himself and therefore barriers to change could be both internal and external to Joe.
At the time of the interview Ed (SUSW16) was recovering from a recent hospitalisation. He was experiencing an associated loss of control and found it very challenging to conceive of what his future might hold: ‘I just cannot answer that.’ His life was focused on the short term, taking one day at a time. He reflected that he could go from feeling well to unwell in a short period of time, and that he was trying to maintain a balance between being active and resting but found it difficult, as his health and well-being were delicately poised. He said that he was reliant on other people, particularly his wife, to gauge how well he was doing, but some of the support she was providing made him feel as if he was being left in the dark:
I’m fairly sure she’s doing things to support me with other people but isn’t telling me what she is doing, and I’m not necessarily aware of it so she is protecting me maybe from certain questions or dealing with certain things.
Ed’s story provided a clear sense of the impact of managing SMI for the individual and relationships within the family. Struggling to cope day to day, knowing people were supporting you, was positive but could have disempowering consequences.
It is important to state that people with SMI can restrict the opportunities of those around them at times. Bradley (SUSW68) explained that he would often devolve tasks and responsibilities in order to alleviate his own stress: creating a routine which was simplified and more manageable for him involved placing extra burden on his partner:
That’s right. I’m not going to do it if I don’t have to, sort of like thing, you know. I’ll just bung it to [name of woman: partner], some of my voices said. I’m going to laugh it off, see, but it’s quite cruel. But it’s quite funny, well, you know what I mean.
In other interviews people with family and stable networks did not always identify their family as constituting a helpful part of their life and recovery. Families were sometimes identified as a passive or unwelcome presence. Bradley (SUSW68) revealed that he had endured a difficult relationship with his mother and step-father, who had lived close by throughout his life: ‘they were cruel to me in the past, and cruel to me now.’ However, he had developed a close friendship with a man whom he described as being ‘like a father figure’, who helped him to engage in a regular exercise regime and also helped him to cope with his voices. His experience was mirrored by Jackie (SUSW09), who explained that she was estranged from parts of her family. Over recent years she has had a very negative relationship with her sister. Contrasting with this, Jackie explained that she had formed a relationship with a close friend, whom she likened to a surrogate mother and who provided her with social and emotional support lacking from her own family: ‘she accepts me for who I am and she’s just pretty laid back and always good with advice.’
Carl (SUSW41), who was in his twenties, adopted a disparaging attitude towards others and did not identify any relationships as important or significant: ‘I’ve got a very strange and maybe slightly dismissive attitude towards maybe everyone I know.’ He mentioned that he met with his mother only out of a sense of obligation, and that he did not really trust anyone, including his wife, whom he had recently married.
I’m quite happy being my own person all the time and if that means that I end up with a closer-knit circle of friends, so be it. And if it means that I get stuck at home a little bit, then so be that too.
Daniela (SUL41) described members of her family as having a less than positive influence on her well-being: ‘they’re just disruptive people to be with, I think. And when you’re feeling very bad, that’s really just more than you cope with, in my experience.’ Although she reflected that her family constituted part of her network she ‘can’t stop seeing,’ she explained how she compensated by developing her life elsewhere by deliberately adding people to her network who increased her engagement in social and cultural activities:
I wanted to find people that . . . I mean, that . . . there are certain things that I like doing in my life, like I like going to exhibitions . . . something like that. But it’s much nicer to go with somebody than go alone, and none of the people that were currently in my network were either . . . they were either not interested or not available.
The importance of family-like relationships was illustrated where challenging birth family connections can be replaced by others that can provide similar types of emotional and practical sport. We summarise in Table 31 what we have learnt about family and stable networks following five selected areas, supported by the literature review in Chapter 1.
| Key literature area | Insights from our study data |
|---|---|
| Agency and strategies for staying well | As with formal and sparse networks the motivation to control and choose social and community connections was evident but this decision-making was affected by poor motivation or reluctance to become more independent and worries over the consequences of illness or stigma. The family often provides a safety net to support well-being but for some people this can deny accessing other opportunities in the longer term |
| Social support | Family support can play a crucial role at different stages of recovery but can also be disempowering for individuals with SMI and their family members. Interviews suggested that although family ties often facilitated bonding social capital they may also restrict access to bridging social capital. Some individuals developed ‘family-like’ relationships in order to compensate for difficult family dynamics |
| Recovery over time | Family are a central support in personal recovery journeys, and where family ties are challenging (or absent) we found evidence that replacement relationships could be established. Emotional closeness was important for recovery; much of this resource is provided by family or friends |
| Stigma | Families are impacted by public attitudes to mental illness: we found evidence of courtesy stigma230 in networks. We also found families generate stigma231 and their lack of understanding can amplify the difficulties people with SMI experience. We also learnt that people often developed effective coping strategies for dealing with ‘challenging’ family relationships, sometimes aided by practitioners |
| Social capital | The social capital provided by family was often valued. We found, however, a lack of diversity in obtaining social capital from different sources where family involvement dominated, sometimes to the extent that these relationships acted as a barrier to building new connections |
Diverse and active networks
This section explores the interviews of people we found to have diverse and active networks. This includes people who, in relation to the overall data, had the largest number of social and place ties, proportionately less formal health and social care involvement in their lives, who tended to have active routines outside the home which provided a high degree of structure and many of whose connections were new. We were particularly interested in interrogating these data to understand:
-
ways in which diverse and active networks can be beneficial to well-being; in particular how people build networks over time and transferable lessons that can be learnt for those with other network types
-
potential weaknesses in diverse and active networks to explore assumptions that could be made that these are the ‘best’ network type for people with SMI.
The potential within diverse and active networks to support well-being
The interviews explored with participants the well-being impact of connections in their networks to people, places and activities. A notable aspect of diverse and active networks was efforts by individuals to manage multiple connections and maintain routines as part of managing SMI. We focus in this section on the well-being impact of networks by exploring the strategies used to support personal recovery.
John (SUL39), who was 29, explained that he had an active approach to recovery, ‘with schizophrenia, the more time you have on your hands sitting down doing nothing, the more you think about things.’ Personal resolve to create a routine to aid recovery came across strongly in the interviews. John reflected on the past and his determination to avoid relapsing back, describing it as ‘like an inner determination, isn’t it? That you don’t want to get into that situation again.’ He also underlined the importance of engaging in a range of diverse activities since becoming ill; he reflected that he had more free time, and hence opportunity, to engage in new activities such as learning to swim and speaking Arabic. He was also motivated to do so, finding out about opportunities, seeking them out. John also indicated that he had strategies for managing different parts of his network, for example he would no longer visit friends’ houses if he thought street drugs would be consumed:
I think cannabis was one of the main reasons why I ended up going into hospital and developing my medical condition, so, basically, um, I would say, um, sometimes, um, if we’re going to meet up, rather than going to his house where there’s going to be cannabis being smoked, um, we just go out for something to eat instead.
This touched on an important aspect of diverse and active networks, because they reflected a wider range of social groups and interests than other network types, and they often required more active management. One such strategy to support well-being identified in interviews involved not disclosing mental health problems to specific parts of a network, guarding against the stigma of mental illness labels. Kevin (SUL29), for instance, revealed that he purposively decided not to disclose to his martial art group his experience of bipolar disorder: ‘they might think, you know, if he’s unstable, he shouldn’t be learning a martial art, do you know what I mean?’
Um . . . (pause) what doesn’t work. My biggest thing, possibly, would be this group here [pointing at the map] . . . of me not telling them. So that-that’s . . . I wouldn’t tell them the reason why I’m not coming, or . . . um, I won’t . . . I tell them very little about my past.
Kevin’s management strategy for disclosure was to be very careful before talking about his bipolar disorder with contacts because he believed that there was a lack of widespread understanding and that he might be judged differently. He attributed multiple break-ups with past girlfriends to the fact they did not view him ‘in the same light’ when they found out about his diagnosis of bipolar disorder:
No, she-she knew I had bipolar disorder I have had a girlfriend in the past, back in-in-in my late twenties, who I told and she never looked at me again in the same light.
In his interview it was evident that Kevin found the label of being diagnosed with bipolar disorder challenging to accept and was resigned to having to manage the symptoms of mental health in the future; however, he viewed being discharged from specialist mental health services as a future goal that would represent a ‘kind of victory’. He also expressed the importance of self-determination and his own personal ‘empowerment’, and added, ‘I wouldn’t lead a passive life.’ He regarded his own recovery as a ‘slow build’ that he had developed purposively through routines to provide a sense of structure outside his home:
It is easy to isolate. See, this is why I do my martial arts. This is why I do, you know . . . go to mass on a Sunday. It’s a . . . it’s . . . go to the supermarket every night, rather than buy your shopping for a week. It’s to get you out of it [the house].
The participants’ accounts demonstrated that diverse and active networks could encompass a routine of activities in the community, activities which within themselves have meaning and enhance well-being, but also act as a safety net against social withdrawal and help to promote a sustainable recovery. This was particularly important in networks where a person was not in employment, building alternative routines and structures. Such routines were often self-initiated; Ellen (SUL28) explained that she was successful in identifying and accessing community resources to support her recovery. Her library, for example, served as a hub in terms of accessing new social groups and activities, such as a book club.
The potential durability of diverse and active networks is demonstrated by the wide variety of interests they included so that if something stopped another connection would often fill the void. Roger (SUL10) described how playing football had been a major part of his recovery, valuing the ‘camaraderie’ and that ‘being part of a team is quite, um, does make you feel more part of something and secure’. Because of a physical injury, at the time of the interview he was temporarily unable to participate in football, but found a substitute activity, of sorts, in the form of swimming with his girlfriend: ‘that’s almost as good. It’s a little less social but it’s also kind of a release.’ Roger’s narrative highlighted some of the ‘building blocks’ of diverse and active networks, and by association recovery: developing structure and routine through being active (supported by others), rather than being defined by illness, which in turn can lead to a growing sense of connectedness.
. . . after a while my mum got a bit more fed up with me being as depressed and then kind of encouraged me into going to uni and my girlfriend would be sort of more willing to push me into doing things when I was depressed rather than sort of backing off and then letting the illness be, more define me, more just pushing me into doing things and, you know, encourage me that I can do them and if I do these things then maybe I will get better quicker, you know, I think making you feel more capable rather than making you feel incapable, which you already feel.
Teaching helped him to feel part of a community:
I mean just walking to and from school, you know, the pupils wave to you, you know, yeah, you kind of feel like you’re contributing to that community, so that’s good.
The ‘good’ that Roger described translated into feelings of positive well-being for him. We note that diverse and active networks tended to contain an array of ‘building blocks’ so that if one connection closed others could be pursued. Also, people managed connections that were no longer supporting their well-being by removing them where possible.
An important aspect of accounts from people with diverse and active networks was how they had responded to problems in their past, overcoming obstacles. Memories of being treated in the mental health system were cited. Andrew (SUSW46), for example, became unemployed after a severe ‘manic’ episode, and was told by mental health professionals ‘you’ve been very ill, don’t expect to walk back into your career.’
So there’s a lot of negative suggestion I received. And so to come back from that takes a huge amount of courage and a huge amount of strength.
He defied this gloomy prognosis and at the time of the interview felt ‘strong’ and was working full time providing support for people with severe mental health problems. Practitioners acted as barriers in some networks by holding attitudes that demonstrated lack of hope and limited life expectations for their clients. Likewise Nigel (SUSW36) drew on his past experience of mental illness to help others through one-to-one mentoring:
And within that project I’m doing the one-to-one work with him, helping him because I’ve been through similar sorts of things in some ways in mental distress and now recovered bipolar even though I’m still vulnerable and need support in the system. I’m doing things to help people if I can and then to helping, and he’s helping me at the same time – it’s not just a one-way relationship, it’s a symbiotic relationship.
The well-being gains of helping others, establishing reciprocal relationships, were noted among the diverse and active group. These creative decisions demonstrated how individuals recognised the importance of connectedness as a specific strategy for managing well-being. Personal resolve to create a routine to aid recovery also came across strongly in interviews with people with diverse and active networks. We found an emphasis on generating new connections and activities, often forward looking. Part of this could entail taking personal ownership of recovery, rejecting medical explanations and treatments such as medication, as illustrated by Michelle (SUSW53): ‘I stick with my labels and don’t use the medical labels and that helps me’. The network-mapping approach supports this personalised focus. Michelle, for example, said that the initial network-mapping interview highlighted the fact that, although she had a diverse array of interests, there was a ‘big gap’ in her life and she addressed this by forming a close attachment with a dance community.
That was really useful and I’m wondering whether I’ve filled that because I’ve become aware that that was empty? So that was really useful for anyone to do I think.
There was an interesting contrast therefore between Michelle’s experience of the medicalised/diagnostic model of treatment, which she felt detracted from her sense of individuality, and the network-mapping approach, which embraced it.
Were bigger networks better for managing well-being for those with severe mental illness?
There are a lot of normative assumptions attached to studies of social networks because of the emphasis on measurement of social ties and studies that suggest larger numbers of social contacts are positive for mental health. Work assessing social capital also had this bias because resource generation was aided by social contacts and thus larger social networks provide access to more opportunities for resource generation. Our network mapping showed how connections to place and activities were also positive for generating social capital because, through connections to place, social contacts may emerge. Qualitative data also helped unpick the problematic ‘bigger was better’ narrative by exploring the complexities of optimum personal network connectedness. This is the focus of the next section, using examples that emphasise the heterogeneity of connectedness experiences.
We found not everyone felt satisfied with having a diverse and active network. Not all social ties were qualitatively equal; some were felt to be more positive, or negative, while others were considered inert. The same was true for activity and place connections. Margaret (SUL05) expressed an active desire to reduce the amount of social contact in her life; at the time of the interview she revealed she had ‘ostracised my family at the moment’. She reflected that people in her life could be emotionally draining, even ‘overwhelming’: ‘I tend to internalise other people’s problems. I’ve always done this and I find it difficult to remain emotionally detached.’ Given this, she mentioned that she would like to have fewer friends in her life in the future, stating ‘I need time to myself’. She also expressed mixed feelings about living in London: on the one hand she found it stressful and challenging to navigate, but she also acknowledged, ‘without it I’d just shrivel up . . .’ The accessible culture (museums, galleries, music) constituted an important part of her life and she considered art to have a therapeutic value, especially the ‘masters’.
Zara (SUL48) reflected on the paranoia of worrying about what the different social groups in her life, which she referred to as ‘boxes’, would discuss when she was not around. As a result she tried to keep them apart, a strategy used across the network types:
I don’t know, I’ve always been like that . . . I do, I do have paranoia about people talking about me. And especially because they, you know, if I, if I have been unwell recent, recently, or around people, and I wouldn’t want people talking about me behind my back, and if I keep people, kind of, separate then they can’t do that.
Diverse and active networks do not always hold together and when this happens people might require additional support from others, including practitioners, to buffer against negative impact on health and well-being. Suzi (SUSW48) reflected with some sadness on how her social group had become reduced by factors beyond their control:
What’s really sad and has really got me down, has got me this year, is my university friends, one by one, dropped off. There are different reasons for each of them, I suppose, but that’s how it’s happened. And I’ve tried to, sort of, keep things up a bit on Facebook [Facebook Inc., Menlo Park, CA, USA]. But no, people, some people just . . . I mean, a lot of people just, kind of, live where they are now, don’t they? And they’re not necessarily bothered about you even though you were a good mate at the time.
Diverse and active networks can also have negative elements, or aspects that need attention. We found when people with SMI were seeking out opportunities in the community this could mask issues closer to home, potentially destabilising their mental health. For example, Liam (SUL32) described how his untidy home influenced how he felt about himself, and was wary about inviting people into that private space; this was made more frustrating by health practitioners’ lack of understanding of how important this issue was for him and his inability to address the problem on his own:
I’m also escaping because my flat is in chaos. There’s a slight sense of hoarding, slight lack of elimination, slight problem about putting the place in order so it looks good. So I get up in the morning and . . . and I’m more likely to get on the phone to my girlfriend and try to arrange to meet her than I am to deal with sorting out the stuff inside my flat. So there’s . . . some of this engagement of healthy stuff is also an escape from dealing with my own stuff and getting my own stuff together. . . . If you were to walk in my flat you’d say oh, there’s something going on with this person. So, um . . . this, um . . . that’s kind of . . . remains a challenge, and it’s indicating to me that something’s not quite right with me and I need to try and work on it but I kind of avoid working on it. And if I . . . and I also feel if I put it right I’m going to . . . it’s . . . I’m going to end up making it in a mess. When I try to discuss this with health workers they kind of dismiss it. It’s like, this guy’s only going on about an untidy place, but it’s very significant for me, and I can’t get it together.
Although in this example there were frustrations about the ‘dismissive’ attitude of practitioners, it underlined how important it was for mental health workers to actively monitor connections to people, places and activities as well as their impact on well-being.
The role of practitioners in diverse and active networks
In this final section we consider the role of practitioners in diverse and active networks; although they constituted a smaller proportion of network ties, they were still present. People with diverse and active networks often emphasised the importance of practitioners for encouraging interpersonal skills and support and valuing the social aspects of people’s lives. Zara (SUL48) reflected that her social worker had played a constructive role in her recovery, describing her as ‘really helpful’; she also added that the relationship was particularly important when she had been less well and she had learnt to be more honest when she was struggling. Her experiences illustrated that, for some people with SMI, having effective ongoing social support can fulfil a vital role, and that it can be easier to talk through issues with professionals rather than family or friends:
keeping me rational and letting me talk through stuff and not [sigh] because, I guess, like, I don’t want to talk to my friends about my stuff, so, and I don’t want to talk to my partner about a lot of stuff . . .
Practitioners helped individuals develop their own coping skills. Zara highlighted that the importance of mental health workers being able to listen was more important than the actual technique or therapy used. Contrastingly, practitioners with a perceived deficit of empathy were criticised, found to be disempowering or disrespectful. Duncan (SUL77) reflected that he had negative experiences in the past of mental health workers who had been overpowering, or spent sessions obsessively making notes: ‘they don’t say a word, nothing, and that’s it, and they just write whatever they write and you don’t see it.’ Practitioners whose encouragement was viewed as unhelpful were also criticised. Kevin (SUL29) reflected on a time in the past when he was struggling and found some of the encouragement from practitioners to engage in social activities to be misplaced. He said of one mental health worker, ‘she insisted I went out and to sort of social interactions to improve my social life. It’s a bit like telling a man with a broken leg to do . . . to do a marathon’. An important emphasis in people’s own accounts was how change had to be led by them; SMI does not take away individual interests and preferences but motivation can dwindle and stigma can act as a significant barrier. Wider societal barriers, such as difficulties gaining employment or public attitudes towards mental illness, did inhibit individual agency.
In contrast to Zara, discussed above, who said she would rather talk to professionals than friends and family about her problems, for Roger (SUL10) the opposite was true: his family had become more influential and services less so.
I think in some ways it’s easier to ignore the advice of professionals actually. Although I respect their advice it kind of . . . when it’s people that are more close to you and personal then you feel more, like you’re doing something wrong by going against that advice, whereas professional advice is more like they could give that to anyone.
For John (SUL39), too, services had become less involved in his life. In the past he had a proactive CPN who supported him in recovery from hospitalisation, providing help with medication, accommodation and looking ahead to a career. Currently he said he was receiving more support and encouragement from his family, and the role of mental health services had diminished. Some people were actively shaping their support requirements for themselves. Andrew (SUSW46) reported negative experiences of mental health services but was currently in a positive psychotherapy relationship, which he arranged himself, and felt was more attuned to his needs. Michelle (SUSW53) felt well supported by a shiatsu teacher who helped her ‘see through all of my surface crap.’ This contrasted with past experiences on psychiatric wards, and patronising psychiatrists: ‘there’s no way I can reach them or they can reach me.’ The theme of individual agency being in conflict with health-care system constraints was also emphasised by Maggie (SUL05), who, reflecting on her past experience, said ‘I’ve never felt that I’ve lost control personally. It’s other people’s control that’s been imposed upon me’.
Change also featured in diverse and active networks. However, it is important to stress that recovery was not a linear one-way transition towards empowerment and agency; people with diverse and active networks could struggle with managing their networks, or aspects of them. It was thus important that services were adaptable to increasing or reducing support as required. Donna (SUL23), for example, felt stuck in the mental health system and wanted to break away, but also recognised that she was not well and needed to be supported. This sense of dependency was also paired with fear of losing independence: ‘I try to avoid the walk-in clinic, it’s fear and a fright of them trying to re-admit me back into hospital.’ Donna reflected that she would like to move on but added ‘I’m not ready yet’. It was also evident that the potential threat of discharge was one which caused her great angst, being told ‘there’s nothing more [services] could do, that would be dreadful’. Service involvement can be regarded as all or nothing by people with SMI, with discharge viewed as the loss of all support. Donna said that the ideal situation for her would be one where she could move forward and lead her own life, but with the reassurance she could call on support again if she needed it: ‘But they could say to me “yes, we’ve done so much for you, there’s nothing more you could do” that would be dreadful.’
We summarise in Table 32 what we have learnt about diverse and active networks in terms of five dimensions we have brought together in this chapter to reflect on.
| Key literature area | Insights from our study data |
|---|---|
| Agency and strategies for staying well | Diverse and active networks demonstrated higher levels of active engagement and leadership by individuals with SMI. However, driving change and decision-making was also viewed in some contexts as emotionally draining; there were times when people found it beneficial to their well-being to be less active or reduce commitments within their network |
| Social support | Interviews emphasised that everyone relies on social support. Valued social support encompassed a range of contacts for people with diverse and active networks. Having such a range of contacts buffers against social loss when valued relationships or community connections disappear, and may also mitigate against becoming dependent on one part of the network |
| Recovery over time | Diverse and active networks incorporated people at different stages of recovery. We found people who had low well-being; people who were managing recovery from recent mental health crisis; and people who had been stable for a long time. Some people were building new connections; others were seeking to reduce contacts to make their network more manageable. These networks were dynamic and varied in content, showing a high degree of active engagement in the recovery journey and awareness of their role in the recovery process |
| Stigma | Stigma was recognised as a barrier for people with diverse and active networks, who may have to deal with this challenge more than people with other network types, as they are connected to more people, places and activities. For example, decisions over disclosure at work and in social groups can impact on career development and social identity. Network segmentation was a strategy adopted to keep parts of the network separate to preserve/manage non-illness identities and reduce the impact of stigma |
| Social capital | Diverse and active networks encompassed engagement with more varied forms of social capital; and with variety often came durability. Managing this sometimes involved a greater deal of practical and emotional labour; some people preferred a simpler life that was easier to control when diversity became overwhelming |
Value of the network-mapping approach?
Towards the end of the in-depth interviews participants were asked to reflect on the process of the network-mapping exercise that they had undertaken previously. The interviewer asked them:
How did you feel about doing the mapping exercise last time?
Did doing the mapping exercise make you reflect about your life or make you want to make changes?
We briefly summarise from across the data set people’s feedback to gain a sense of the utility of the approach for individuals. We were not looking for definitive confirmation but indicators to take forward in possible further research.
Clarity and appreciation
Taking part in the exercise was described by some participants as interesting because it presented information in a different way. Kevin (SUL29) found it ‘clarifies’ a ‘complex situation’. Bradley (SUSW68) explained: ‘Yes, it was good. It was quite surprising, yes, how close I am to some of them, how not, and who knew, you know’. The value of taking part in the network-mapping exercise was explicitly referred to by some participants, including those for whom it just made them appreciate what they had. Roger (SUL10) said:
Yeah, well it’s made me realise how lucky I am in a few ways I guess, to have so many people I can draw upon. And yeah, I mean it’s made me kind of realise how important the social side of work is as well, but yeah, which I didn’t foresee happening before I got this job at all.
Bryony (SUL65) found that the exercise had made her value the people in her personal network even more. ‘I think it makes you think, like, you probably should value, value the people a bit more.’ The exercise also allowed people to express satisfaction with their personal health network overall, not just components within it. This aspect was of particular importance to Eleanor (SUSW38), who thought others might criticise the size of her personal network at 14 contacts. What was important for her was not the overall numbers, but that her personal network functioned well for her.
It reminds me of just how safe I am and that compared to millions of people I’ve got, although there aren’t like, hundreds of people all over here, like some, sort of socialite or something, I’m happy that I’ve got the family that I’ve got. I mean, you could know dozens and dozens and dozens of people but only really have one friend out of the whole lot. So I don’t think it’s a bad thing having a small group.
Sam (SUSW60) also emphasised that, although she thought others may be critical of the number of people within her personal network (the network size was 18), this was not a problem to her because this size of her personal network worked well for her. She described her network as ‘close’, ‘happy’ and ‘big enough for me’.
As I say, I’m not sort of unhappy with my map. There aren’t that many people on there. I’m sure you’ve spoken to people whose maps’ been completely filled in . . . but I don’t . . . you know that’s not something that bothers me. I don’t want to be sort of surrounded by hundreds of millions of friends all the time. I quite like my own sort of space, which is another reason I go on holiday on my own. I like to be on my own.
Value added
The utility of the network-mapping exercise went further than clarity and appreciation for some participants. The ways in which the exercise added value included raising awareness of resources; identification of gaps and vulnerabilities; and stimulus to plan proactively for the future. Several participants reported that it was worthwhile, in and of itself, just to think about what resources were available to them and how they used them to support their well-being.
Jackie (SUSW09) reflected ‘It makes you realise who’s in your life and where they come really’. Joe (SUSW77) found the clarity of people’s roles in his life beneficial: ‘Clears up what my life is and my friends and family are like. My life could be a lot worse’. Valerie (SUSW15) was relieved that, although there were lots of medical people on her personal network map, because of her physical and mental health problems, there were also ‘other connections’ as well. Undertaking the exercise had reminded her of activities that she used to enjoy, but no longer participated in, such as going to the theatre, and as a result she was now challenging herself to ‘break the barrier’ of not driving at night, so that she could do this again. Raj (SUL07) had also been motivated to make better use of the resources within his personal network including intentions to socialise with his friends more and to do a vocational course.
Mapping personal networks had made some people aware of resources within them that they could make better use of. For others, the exercise made them aware of gaps and vulnerabilities within their personal networks. Ed (SUSW15) was facing numerous uncertainties about the future and had been in contact with SMI services for only a year.
I think it clarified for me where, that actually what I thought was a network of supportive friends, really came down to two or three people.
Adam (SUL08) in undertaking the exercise had become aware that he needed more friends. He talked to his friends about the exercise and they responded by saying to let them know if he ever needed help or support. For Daniela (SUL41) the network-mapping exercise had made her more aware of distancing herself from those who had a negative impact on her well-being and an awareness that she could ‘possibly’ focus on the gaps. ‘I do everything to sort of mitigate those . . . those contacts by just emotionally removing myself from a situation’. Pauline (SUL61) also found that being aware that things were not going well with several people at the time, and seeing this mapped out, helped her to be aware that she needed more people in her life. She said that the exercise had helped make her plans to help others in the near future ‘clearer’. Agnes (SUSW40) also experienced the process as a stimulus to review her life and proactively plan for the future.
It reminded me of things, having another look at it. Um, instead of just blundering my way through life, I’m sitting down and reminding myself of how everything is.
Support
Taking part in the personal network-mapping exercise had resulted in some participants benefiting from changes they had made as a result, including socialising with their friends more and making proactive plans for the future. Donna (SUL23) had also made changes as a result of the exercise; these changes had not, however, resulted in the benefits that she desired.
It made me realise that I need to go out a bit more, maybe to talk, um, but I have done that. There’s not much improvement, um.
It was clear that a number of participants required support to both unlock the potential well-being opportunities within their personal networks and to expand them. Liam (SUL32) found the exercise ‘excellent’ but would be likely to require this type of support, as he noted in the interview: ‘But what support is going to be available to these people to help them engage with these networks that have been helpful to them?’
Bill (SUSW42) presumed that the purpose of the exercise was to show that he lacked ‘real’ friends in his life, describing his network as ‘sparse’, ‘sad’ and ‘lonesome’. He said that he could not change his life and gave a list of reasons for this, which included a lack of finance, motivation and musical skills. This individual would need support from someone else to see how he could begin to break down these obstacles and work towards what he would like to see in his personal health network.
As well as support, other suggestions were made, in the interviews, to increase the utility of the personal network-mapping exercise for those undertaking it. The first suggestion was to improve the materials used and have more time. Liam suggested that it had been very useful to have two meetings to think about and discuss the exercise. He found that he had been quite emotional in putting the details down in the first meeting. He found that the second interview, as a ‘follow up’, was more ‘powerful’, because he could be more detached and rational.
The potential value of practitioners, or other support workers, undertaking the personal network-mapping exercise with people could be clearly seen in the response from Gavin (SUL34) when he was asked if it had made him want to make changes in his life.
The impact on mapping out a network is a very serious thing. This network is not just something on paper. It’s something of life, and what it is is it shows you where you’ve been and where you can get to. Where you’ve been is everything that’s happened but where you want to get to you still have to try, and it’s on the network and it’s still there. And it’s still there with people, like I said, like, you know, social worker, people that can help you.
In summary we found broadly positive support for personal network mapping because:
-
It was person-centred, focusing on individuals and what was important to them in their lives and how this developed over time.
-
The process itself was a useful way to open up conversations about people’s interests, relationships and place connections. The visual dimension facilitated another way for people with SMI to chart and explore social recovery, emphasising the value of resources within themselves and their networks.
-
It provided a structured way to explore two abstract concepts – agency and connectedness – looking at the past, present and future.
Discussion
Our focused analysis to explore the heterogeneity of network experiences within an imposed framework of network categorisation has provided insight into the value of connectedness for people with SMI. The personal recovery literature emphasises connectedness as a key feature. 8,10,35 Our data support this and begin to look at which dimensions of connectedness are valued by individuals with SMI and the strategies adopted to develop effective networks. Effective in this context was specific for the individual, with no one-size-fits-all approach appropriate for understanding personal networks; this was the same for person-centred recovery. This poses an obvious tension in the research study that on the one hand has categorised people into ‘network types’ and at the same time has sought to explore the meaning of connectedness for each individual and their sense of well-being. The tension in analysis was managed by both looking at how useful, or not, a network-mapping exercise was as a person-centred process for managing SMI and critiquing the network types to assess how valid they appeared when explored at the level of individual explanations for how and why a network has developed.
We did find that across network types there were individuals who did not conform to the network stereotype that emerged from both the quantitative and qualitative analyses. The research team went back to the quantitative analysis on several occasions to check whether these apparent exceptions really had a formal and sparse network or a family and stable network. We found that the accounts supported the concept of network types as transient descriptors rather than bounded structures; for example, how someone might have a formal and sparse network that was moving towards a more diverse and active lifestyle as network changes were implemented, such as in the case of Jessica (SUL63).
How useful was the concept of connectedness for managing well-being for people with severe mental illness?
We learnt across networks that building connections to people, places and activities fashioned individual identities. Research has shown the importance of valuing identity formation, and understanding the complex social and political processes that exclude or include people with SMI, and the follow-on impact on their identities. 232 A recurrent theme in people’s accounts was reference to work, either as a presence with positive and negative impacts on well-being or as an absence within the network. Work connected people to important resources, such as ‘ordinary working people’ and ‘healthy activities’. It provided a benchmark identity that people were judged against, both by themselves and by others. Where work was absent, connections to interests provided an alternative role to that of being ill. Across all network types, people sought to distance themselves from the status of being mentally ill, and building connections to different groups of people, creating routines around the ‘ordinary’, helped to achieve this goal. Stigma was a barrier, and we heard how people managed non-disclosure in order to protect themselves from negative associations attached to the mental health system. However, this was not always possible and stigma was a major issue for practitioners, as it is one reason people are so reluctant to seek ongoing help for fear of being tainted with labels such as ‘mental’ or ‘crazy’. 156,227
We heard how connectedness provided people with purpose in life and routine. We also heard how people felt connected in different ways; limiting network contacts was an important well-being strategy, linked to creating manageable and coherent life-worlds,233 but so too was seeking new interests and friendships or acquaintances. Through relationships to people, places and activities, individuals with SMI develop appropriate timetables and structures that support well-being. Being able to contribute to society in a meaningful way, be that through sharing time, skills or friendship, was an important part of recovery. Friendships that involved reciprocity were highly valued by people in each network type. Quality of relationships, rather than the number of ties, emerged prominently, and people across network types explained how they are active in managing their network to rid it of troublesome contacts, where these are under their control. Where there was lack of network structure and routine, practitioners, or others, can help individuals with SMI look for ‘building blocks’ on which to plan person-centred recovery goals when they are ready to do so.
Practitioners also had a role in people’s actual routines: they were part of the connections map for people with SMI. All participants in the study had a health-care contact for managing SMI, but some was light touch through the GP and others had intensive support packages involving multiple members of a Community Mental Health Team (CMHT). We identified varying levels of engagement with practitioners. We found resistance on ideological grounds, such as believing problems were not illness based but had social origins, because of the problems caused by stigma and poor-quality staffing where practitioners lacked empathy and hope and carried a deficit view of mental illness. However, the value of connections with practitioners, and their knowledge, skills and expertise, was also identified, such as when practitioners noticed the potential for change in their client’s life, empowering new skill-building and giving confidence, or where help was provided to extend social support networks and develop new social capital, particularly through bridging contacts. We noted that an important aspect of the dynamics of personal networks was the ability of individuals themselves, and those around them, including family and friends, to identify opportunities for new connection-making and enacting internal or external resources to take advantage.
Reflecting on connectedness, one dimension identified by participants was the process of ‘moving on’ from mental illness and how developing ordinary routines supported their well-being journey(s). The fluctuating nature of mental illness meant that change was a strong feature of people’s accounts as routines were adapted around how well people felt and past illness experiences were an important reference point for future decision-making. Recovery journeys are non-linear and complex. We were particularly interested in looking for signs of active decision-making and an individual’s control over their personal network. Building blocks for change were found in all interviews, though the degree of described execution, turning ideas and plans into actions, varied. Unsurprisingly, people with formal and sparse networks and limited social support reflected on the challenges of turning their ideas and goals into plans. Those with diverse and active networks had more experiences to draw on and strategies for dealing with setbacks.
How are effective personal networks built?
In addressing the study research questions, we looked to the qualitative analysis to steer us on the role of practitioners in personal networks and how network resources are used by people with SMI to support health and well-being. Participants told us about features of effective personal networks. These included:
-
Resilience and self-determination within individuals to actively manage SMI and social recovery.
-
Management of stigma and discrimination, both anticipated and experienced, resulting from a diagnosis of SMI; having active strategies to build an identity that was not defined by mental health as well as combat stereotypes of being mentally ill.
-
Social support from friends and family, with reciprocal exchanges of support valued.
-
Identification of opportunities and having resources within networks to make use of these opportunities to build new social capital. Practitioners play a useful role, not in providing social capital, but in supporting new connections to activities and places that can lead to new social contacts.
-
Informal connections that were nothing to do with psychiatry. Ordinary relationships, activities and place settings are valued because they provide a purpose and identity that is not SMI; these may be mainstream activities or those on the ‘margins of society’, based on individual preferences and interests.
-
Strategies and plans to address an individual’s goals which are led by the person living with SMI. Others within the network will make suggestions but recovery is owned and driven by the individual. Setbacks are supported.
-
Meaning in life. Personal networks that contain routines and structures tend to provided individuals with a sense of purpose providing meaning and identity.
-
Specific pursuits and activities that generate well-being, balancing physical and mental health needs. Medication management motivated some people to do physical exercise to manage side effects; others identified cultural interests to stay healthy and ‘shed the illness’.
-
Practitioners. On the whole, formal supports were viewed positively, and across all network types health care that was provided by skilled and knowledgeable empathetic professionals was highly valued and a necessary part of managing well-being.
We have emphasised individual agency23 within the analysis: people with SMI driving changes in their lives and making decisions across each network type. This can be emotionally draining, requiring support from their social support network and clinical expertise. We found the network categorisation process was helpful in guiding individual reflection on connectedness and well-being. What emerges as important was not the relative benefits of the three network types (formal and sparse, family and stable, diverse and active) but the conversation about why the network looks that way, what were the key influences in it and where someone wanted to go next. Do people want to develop more varied connections or not? Is stability the goal, requiring reduction of some current network influences?
We also identified potential for network mapping as a therapeutic intervention tool:
-
The network-orientated approach was about unlocking the potential of a network, rather than seeking out an unrealistic ideal. Personal recovery takes many forms.
-
Network mapping was not abstract but it was applied and focused on what was important for well-being in people’s lives.
-
The tool itself was a useful way to open up conversations about meaning and identity. The visual dimension of mapping helped people chart and reflect on their connections.
-
It was also a way of exploring agency and connectedness past, present and future; how people have got where they are and where they are headed.
Chapter 5 Organisational perspectives from health and social care leaders
Introduction
This chapter provides an account of the broad context, and specific organisational working, affecting the provision and configuration of services for people with SMI across both study sites. It was based on interviews with stakeholders carried out in summer 2011. The specific focus was to gain an organisational perspective on working with people to build social capital, encourage social inclusion and maximise social support through building personal networks. The module aimed to answer the following research questions:
-
How do community-based practitioners and organisations support people with SMI to use their personal networks to support health and well-being?
-
How do primary care, community-based mental health providers and other organisations work together to develop effective networks for people with SMI to improve their overall health and well-being? What are the barriers and enablers to achieving this?
There are clear links and interactions between the perspectives of organisation leaders (presented in this chapter) and frontline practitioners (see Chapter 6) in answering the study research questions. We have not combined these data in our first-phase analysis, but do so within Chapter 8. These two stakeholder groups overlap in terms of membership and viewpoint but there is sufficient distinction in our data to present the perspectives of both organisations and individuals as distinct units of analysis.
Supporting people with severe mental illness
In addressing research question 1, we explored how leaders described their organisation’s role in supporting people with SMI. This included the experiences of mainstream community facilities as well as health and social care services, both third sector and statutory providers.
Recovery and connectedness in secondary services
The way in which an organisation approached working with people with SMI depended on its role and responsibilities in provision of specific supports for this group. We found, unsurprisingly, that secondary care providers described their role in a very different way from other organisations; there was a strong acknowledgement that the recovery approach, promoting equality and empowerment, had influenced the nature of relationships between organisations and people living with SMI in the last few years:
Over the last couple of years the recovery model also been embedded in assessments routinely carried out by mental health teams on the London site, our main agenda right now is to a recovery model of illness rather than a treatment model of mental illness.
SL114, local authority adult social care
Where recovery was emphasised, the importance of developing positive, goal-based relationships was stressed, within a person-centred biopsychosocial framework, rather than through the filters of a diagnostic, medicalised model of treatment. There was an emphasis on aiming to ‘see it through the eyes of the individual more effectively’ (SSW202, NHS). An important aspect of this had been the desire to break down traditional client and organisational relationships with ‘professionals on tap not on top’ (SD200, NHS). However, while aspects of this relationship dynamic may have evolved, there was also an acknowledgement that:
It is difficult, it is a fine balancing act in the power relationship, and service user is in a sense a little bit disadvantaged in that. But we are trying to engage with service users as much as we can; we want their opinion, we want the carer’s opinion.
SL117, NHS
Recovery-focused care was not easy to deliver. Recovery, when cited, was viewed as an overarching philosophy in secondary care services shaping organisation priorities, which caused some tensions between staff and service users. Interviews in both sites identified ongoing challenges in changing deep rooted organisational cultures and practices; there was still ‘a cohort of practitioners who promote dependent rather than independent relationships’ (SL111, NHS). There was no mention of forging interdependency within relationships between service users and the organisations there to support them.
Leadership teams in secondary care, on the whole, demonstrated awareness of the core elements of delivering recovery-focused practices, acknowledging also that more engagement was required, as people with SMI have often been left with the impression ‘they were not really listened to’ (SL100, NHS). The data were missing clear examples of how this could be achieved.
But I don’t think hand on heart that we could say that the level of engagement is where we would want it to be and that service users and people that use our services and their families and carers feel that they have as much influence around the direction of travel as they would like to see.
SW202, NHS
Organisations were aware staff needed training and support to change established practices. Also absent in our data was any discussion of how these tensions could be managed collaboratively. Such tensions were identified by leaders as individual organisational challenges, conveying a sense of silo working. There was an identified lack of interorganisational collaboration to address staff or service user resistance to change.
Another notable ‘silence’ in the data was statutory and third-sector relationships with primary care with regard to policy orientation and recovery. Our stakeholder interview with a London GP lead talked about the interface between secondary care services and primary care being patient centred in approach, but the major policy agenda of recovery was not touched on.
I guess [our role] it’s to provide services for patients that are appropriate to their needs and those that take into account both what they would like but also what is seen as being useful or right for them according to their diagnosis, so something that is seen as being evidence based, but there needs to be within that a consideration of what the patient would like as well.
SL101, NHS
In terms of social inclusion for people with SMI, primary care identified another practice void:
I know that’s been happening but I struggle to see on the ground what has actually happened. I don’t see an awful lot of change. Again it’s an area that always comes up, to do with how we do that. I haven’t seen a lot [here].
SL101, NHS
These are two illustrations of possible disconnect between mental health policy and practice on the ground from the perspective of primary care. These indications of disconnection were reinforced by the lack of use, by the interviewee, of terms associated with recovery, such as empowerment, self-determination, self-management and meaning in life.
Secondary mental health care providers, both NHS and third sector, were becoming more aware of the positive aspects of social networks for people with SMI, and there was an increasing acknowledgment that services should play a part in helping individuals to develop them, ‘to link people into networks of support and to work with them’ (SL114, local authority). A socially orientated outlook on the part of service providers was consistent with the recovery model ethos. However, there was a perception expressed in some interviews that this represented an area where people with SMI would potentially require enhanced support from organisations because of personal difficulties in sustaining personal relationships: ‘what I do see has been important for a lot of people with mental health problems is maybe they’ve lost some of that, haven’t got that wider network . . .’ (SSW200, NHS). One challenge for leaders of services, and thus the services themselves, was to see beyond generalised stereotypes to actively deliver person-centred services, working with people to overcome barriers and produce positive outcomes, hence reflecting the heterogeneity of the populations they were seeking to support. It was a challenge they were looking to meet to both aid the individual but also relieve pressure on services:
. . . the Assessment Service will look at social networks of people and what support we can tap into rather than us providing the support, so we do that all the time; the same with the Crisis Team: they will map the social network of somebody and use all the possible support that there is out there.
SL117, NHS
Secondary care organisations felt they had a role in helping people with SMI reflect on their own strengths as a means of building up their network of connections, either by embracing new forms of activity or by re-engaging with previous hobbies.
We encourage people to look at voluntary work quite a lot, because of the various benefits it can give you in terms of potentially doing something they enjoy that might give them skills towards future employment.
SSW212, third sector
So say you discover in assessment this person used to sing in a choir but hasn’t done so for 10 years – could they be encouraged to do it again or offered something? Encouraging people to go back to things they might have given up.
SL109, local authority
Social support and stigma: surviving in the context of change
Longstanding conceptual drivers frame the secondary care organisation vision for working with social networks: social support, social inclusion and reducing stigma are key themes currently. A strong linkage for organisations involves getting people ready for work: building confidence, building skills and using resources within networks to support employment-related activities. Encouraging people experiencing SMI to do something productive and take an active role in their own recovery has become an increased expectation on the part of service providers, and requires partnership working between stakeholder organisations. The personal benefits for people with SMI being engaged in productive activity, such as employment, were emphasised in interviews:
Well, I think that we as a service would feel strongly that what we do is about promoting well-being and a person’s sense of purpose and ability to contribute to be an active part of society and to be of value.
SL115, third sector
For some people it might be just a short-term goal in managing their time through something meaningful so it might be I’m linking them in for some walks for health or a local college course to develop their IT [information technology] skills or even something like a psycho educational course like a mind over mood course, to support their health and well-being and their wellness. For others it might be that they’re being made redundant and they’re looking at retraining, so there would be a piece of work done around CV [curriculum vitae], confidence-building, looking at perhaps doing a strengths analysis, have a look at their developmental needs and working on an occupational plan.
SSW209, third sector
In the London site, employment advisers had recently become embedded in some mental health teams. This had proved challenging, as there was initial resistance from clinical members of staff who ‘didn’t seem to understand why there were employment advisors within a mental health team’ (SL115, third sector). The social aspects of supporting SMI can get overlooked in the health-care system even when these dimensions are mentioned in NICE evidence-based advice on the care of adults with psychosis and schizophrenia. 39
Interviews with community leaders indicated that, outside health and social care, encouragement to engage in ‘ordinary’ activities was commonplace and the focus of their work. Engaging people with mainstream activities and providers has been established mental health policy for the past 10 years, built on principles of social inclusion. 234 The interviews captured the views of a number of mainstream community resource leaders, but they were mostly hesitant and unsure about working with people with SMI: ‘we are not at a stage where serious mental health is high on our agenda’ (SL103, other). However, an education programme highlighted elements of good practice that providers of mainstream adult education services can employ in order to ease the transition for people with SMI, to provide ongoing ‘confidence-building and reassurance’ (SL112, other).
One of the main challenges for community-based organisations was assessment, in that assessing the capabilities of people with SMI could often be difficult. One participant remarked that people with mental illness can overpresent themselves in a positive way, and ‘tell a good story’ which may be at odds with what is actually suitable or sustainable for them at the time (SSW207, other). This emphasises the distance services and systems have to close in order to build trust, and better support people with mental health problems; telling a ‘good story’ is rarely just about illness and symptoms, but is often about trust and engagement in a system of care. In addition, people with SMI may lack ‘the emotional strength or confidence’ to deal with knockbacks, ‘so that could be a negative if things don’t work out the way they should’ (SL104, third sector). A key challenge for services was to turn negatives into positives and approach ‘things that don’t work out’ as opportunities to try new strategies. There appeared to be a lack of confidence within organisations in supporting people with SMI in community resources outside health and social care. This was a challenge for statutory services, who required the community to pick up support ‘for free’ that was previously provided by mental health services. It also represents a challenge for individuals with SMI, as some interpret community organisational resistance as part of the wider stigma problems that they face in living with mental illness.
Mental health organisations spoke about a new deal with service users and families but reflected that poor service join-up could leave individuals feeling unsupported and isolated. There was an acknowledgement that recovery work should promote positive relationships between service users and organisations, but it was also underlined that this should not entail a ‘lifelong association’ (SSW208, third sector). Involvement should be limited in nature: ‘The role of services is to kind of come alongside and to try and interfere with people’s lives as little as possible whilst enabling them to get on with life and living’ (SSW210, third sector). One lead reflected: ‘we can help you help yourself and I think that has to be a message, maybe a hard one, to give’ (SL111, NHS).
Organisations acknowledged that the challenges people with SMI face include public stigma and variable access to social support. Stigma impacts through structural discrimination, for example budget cuts, as well as public attitudes or self-stigma beliefs and behaviour. There were several points raised over the role of an organisation with regard to building connections. First, concerns were shared across both sites that mental health provision has been particularly vulnerable to health spending savings. The capacity of practitioners to undertake network development activities was under threat.
Well I do know that in this borough a lot of the support services for different groups have had to close because of cuts. In terms of providing to different groups, this service offers I think 16 different languages, so we need to be mindful of what is out there.
SL107, other
For my other role I guess it’s a lot to do with service changes and trying to improve services to best care for people, and often it’s having to do it with money in mind. At the moment we are trying to make a lot of cuts so it’s trying to be efficient with what you’re providing and a lot of it comes down to services being reduced but how can we make it better – so it’s difficult.
SL101, NHS
Second, the sector was also worried about other government policies impacting negatively on those with SMI, such as changes to welfare benefits including housing and the work programme. The concern was about both pressure on services and impact on individual networks.
I am quite worried that [the work programme] will push people into seeking more intensive mental health support.
SSW211, third sector
However, these pressures were also regarded as potential opportunities; libraries diversifying and providing job seekers with support was one example that we were given of this. Libraries and other council services have increasingly been mainstreaming the support that was offered to all groups of disabled people, including those with SMI.
It’s not just access to books, we are the friendly face of the council and we get people who come in who are unsure about bidding for social housing for example. They used to produce a magazine to view the properties but now it’s only online so obviously if people are coming in and having difficulties using that system we will help them with that. If people are using our terminals for council business we don’t charge them and we understand we know they might need more than half an hour. Our [name] library is partnered with Work Zone, an employment agency that do training especially in retail – they’re near the [name] Centre – and help people get jobs there and that’s open to everybody.
SL108, other
Third, the networks of people with SMI were seen as vulnerable to change in line with the introduction of assertive discharge from CMHTs, resulting in individuals increasingly being moved from the care of a consultant psychiatrist to the GP.
I think the concern I always had with that is that whenever people aren’t under the CMHT they also seem to lose track of other services . . . So there’s a little bit of a gap then, so we agree that this person doesn’t need to be under the CMHT but they probably could do with some of the extra support that they were getting.
SL101, NHS
Although organisations were clear about the value of working with users of services in a network-orientated way, in a period of service reorganisation and public finance reviews, it was unclear who would, or should, take ultimate responsibility for this care strategy. One possibility was for families to become more involved, which would require organisational change in the way families were valued and supported by mental health services. The most common theme we identified across interviews was caution because of their potential negative influence on well-being and networks.
If someone [family member] is supportive and comes along to appointments or encourages them to attend appointments, that’s huge, if someone doesn’t want to let their family know that’s a big issue in itself.
SL101, NHS
The general principle is, you know, that people coexist best within families and as long as we recognise where harm is and we manage that I can’t see, I don’t think that is an issue.
SSW202, NHS
The organisation leads’ perception of family illustrated key dilemmas services and their staff face in weighing up their active role in connection-building or in encouraging that role in others.
Organisation partnerships
We investigated links between organisations to create networks of engagement and interaction to promote well-being.
An uncertain climate
The interviews, conducted in summer 2011, highlighted a number of key changes with regard to the relationship between commissioners and providers of services. The context was seen as extremely challenging across all sectors: the expectation from commissioners, and managers of contracts, was increasingly that organisations delivering mental health services will have to provide more for less, and ‘become more enterprising’ (SL102, third sector).
The biggest challenge is resources because they will be shrinking of course, and the whole big society approach and what it means, it is many tentacled, the fragmentation of what that means is just enormous. However, it seems to me it’s a real challenge to expect the third sector to be delivering services for less.
SL105, third sector
There had been a move away from long-term contracts, towards flexibility in approach. The backdrop to interviews was a time of great change, when services and organisations were in the process of being merged or decommissioned, with the function of public health shifting to the local authority, while commissioning was being restructured from primary care trusts (PCTs) to CCGs. The shift to personalised budgets was seen to have potentially huge implications for providers (especially in the third sector); ultimately when personalisation was fully realised it could mean that ‘your service will live or die by how popular it actually is’ (SL102, third sector). It would result in a demand-driven system based on choice and preferences of people with SMI rather than a supply-driven system based on what services believed was necessary, or wanted to provide. Mental health payment by results (PBR) pilots were also being established, though not in the study sites, so organisations were preparing themselves for further reforms impacting on the future finances of services.
In this demanding change context, strategic multiagency collaboration was seen as crucial to implementing improvements in mental health care. Working strategically with other organisations was considered to be essential across interviews; one participant stressed that collaborating in partnership with others helped to engender better outcomes for people with SMI: ‘we have a central role but not necessarily the most significant role for people in terms of helping them recover and live as good a life as they can’ (SSW200, NHS). The aim, from a planning and contracting perspective, was to provide individuals with a ‘seamless service’ and draw on expertise across sectors: primary, secondary and third sector (SSW200, NHS). Looking into the future, a key issue surrounding treatment and support for people with SMI was: who will take on the leadership role and co-ordinate such an interconnected care solution?
The third sector
A key stakeholder in the mental health landscape was the third-sector specialist, spanning mental health provision and generic services such as housing. There was an acknowledgement in interviews that the third sector must become more enterprising and innovative. Key factors engendering effective collaborative relationships, involving third-sector providers, were examined. One aspect that came through strongly was the need for close relationships between ‘the key individual personalities in the organisations that are involved’ (SSW08, third sector). It was also emphasised that partnerships should be established on the basis of organisations being aware of their strengths and weaknesses:
Where each organisation is aware of their strengths and weaknesses. So we work with [name of organisation] who are a large welfare to work provider, they are generic, non-mental health specialists, private sector, they rely on us because we know how to work with people with mental health problems, and have provided them with specialist support to build confidence and work on their goals, and so on.
SL102, third sector
The climate of increased competition and lack of awareness of other potential collaborative partners were identified as the main barriers preventing co-operative working being more fully realised in the third sector:
There’s an element of competition inevitably as well, business to be found.
SSW08, third sector
Well I think commissioning in the third sector has caused all this competition sometimes, so people are almost set to compete for outputs sometimes as opposed to working together, so that’s one barrier.
SL102, third sector
The evolving role of primary care
The study was particularly interested in how primary care and secondary care interfaced in both sites. The model of a hub was suggested: ‘so I guess we [primary care] sit a little bit like the hub with other services around us and depending on how unwell the patient is’ (SL101, NHS). Improving Access to Psychological Therapies services have provided primary care with a dedicated mental health service for depression and anxiety where they are mostly the lead agency, raising the profile of mental health, and the QOF provides financial incentives to regularly monitor people with SMI. However, primary care was not known as a key mental health service provider for SMI and, as one interviewee identified, joint work with GPs was ‘still a massive challenge’ (SSW208, third sector) for mental health service providers. There was a gap in our data; no one articulated a clear vision for how primary care would lead as a ‘hub’ co-ordinating care for those discharged from secondary mental health services.
There had been a policy shift encouraging discharge from secondary care to primary care for people with SMI where people were stable on medication. The evolving nature of the discharge process from secondary to primary care was discussed in interviews:
So we looked at our discharges and we worked with the GPs and sort of a lot of patients who used to be in mental health and the mental health system are now discharged back to their GP using GPs for quite a lot of the medication. The communication between primary care and secondary care has been the key in making that change.
SSW213, NHS
People who previously would have been under the CMHT forever are now being discharged back to the GPs, and the idea is that it should be easier for patients to get into the service and also out of it, so it shouldn’t be scary to be discharged into the community because it should be easy to get back into services if they become unwell again.
SL101, NHS
There was some scepticism about the motive for this change. A manager for a mental health trust at the London site identified ‘financial constraints and the difficulty in obtaining resources’ as key drivers behind people being discharged from secondary services: ‘to be able to provide services to the most needy, we had to discharge quite a significant number of people back to primary care, back to GPs’ (SL117, NHS). Services users at the ‘softer end of mental health’ have borne the brunt of this policy (SL117, NHS). The view was also expressed that, although discharging people from CMHTs into primary care was a laudable aim in itself, this tended to have a detrimental knock-on effect as other forms of support are rendered increasingly inaccessible, such as free access to public transport in London.
A key role for primary care in the management of SMI is provision of regular physical health checks. Participants representing the primary and secondary sectors acknowledged improved communication and processes for sharing blood test results of service users, along with other aspects of physical health. Limitations were also acknowledged. The physical health checks carried out in primary care were regarded as following a ‘tick box’ procedure (SL101, NHS), with not enough emphasis placed on improving access to gyms and other resources which could improve health and well-being. Interviewees expressed concerns at perceived skills deficits in primary care, illustrated by a lack of understanding of the physical health needs of people with SMI:
You know, it’s well documented isn’t it that people with severe mental health problems when they go to their GP their GP’s not really interested in physical health problems. ‘Oh, this is Joe Blogs who has schizophrenia and you know, we’ve been prescribing him this antipsychotic medication for years. We’re not really very interested in the fact that he’s come in and said, “I’ve got really bad stomach pains” ’.
SSW208, third sector
The future challenge for primary care was not only focusing on the physical and mental health needs of people with SMI, but also understanding the social factors that impact on their health and well-being. We identified poor engagement in community partnerships, for example book-prescribing programmes in London:
We found that although we had the stock we didn’t have the support from local health care at the time to send people in. It didn’t work, it was a partnership between primary care and libraries but it didn’t work. Having said that, when we did displays ourselves with all the books, we found they went out well and continue to.
SL108, other
The positive in this example was that individuals, given the opportunity, were interested in the scheme and used it. Organisations often did not know which resources were available in their local area and neither site had an online directory of local resources.
Enablers and barriers to developing organisational partnerships
A number of enablers to effective partnerships were identified, underlining the crucial importance of effective networking between organisations. An emphasis was placed on shared goals and visions across providers: ‘recovery should be at the heart of that, but that should be mirrored in the relationships that we have with our partner organisations as well’ (SSW202, NHS). Strategic partnership working was argued to be the way forward, underpinned by joint agreements if possible. Coming together collectively to achieve better outcomes for people experiencing SMI was expressed as the motivating goal, rather than individual practitioners, or organisational entities, seeking to monopolise credit:
I want us to work together more with people in groups so that we have a collective ability to heal people, rather than me saying I did it because I was a psychiatrist, so it was my psychological intervention. No it is the collective, so they might do the psychological, they might do the medication or we come in with the social, so that is why the psychosocial thing becomes really important.
SSW205, NHS
The personal aspects which engender effective organisational partnerships were also emphasised across interviews. The personal touch of organisations engaging together ‘face to face’ was viewed as a crucial element of relationship-building, fostering trust and mutual respect:
I think face-to-face relationships to be honest. Yeah, you can . . . you know there is increasingly a move in the local authority to brokerage, to call in off contracts off frameworks and having intermediaries manage that, but to be honest with you I think unless you sit down with agencies and have face-to-face conversations, networking, all of those personal ways in which, that is you know basic to any organisation and it is the nature of the working relationship that is fundamental really.
SSW201, NHS
The constantly shifting context was described as a huge impediment to partnership working. Local reorganisation, especially in London, was argued to render it more challenging for organisations to work together. Although working together and pooling resources were seen as desirable, there had, of late, been a climate of intensifying competition between third-sector providers, which made this more difficult to achieve. Lack of communication was also identified as a major barrier across interviews.
As to other barriers to joint working, I don’t know, but it’s not ideal at the moment, and people are forever doing, not mapping exercises like you’re doing, but mapping what services are available in the borough, and mapping someone’s journey through it all, and how we should all have each other’s phone numbers and talk to each other more, and we don’t, we don’t do it enough.
SL102, third sector
The difficulty of finding out what other services were actually out there, and being able to map available resources, was identified as an impediment to joined-up working. Overall, interviewees indicated that the ideal scenario for effective organisational partnerships involved co-operation, strategic working together, and shared visions and goals, along with effective communication. In stark contrast to this the reality was described as one of intensifying competition with a lack of communication or awareness between organisations, together with an unwillingness of some organisations to change and adapt. The overall picture across interviews was one where effective partnerships were needed more than ever, but in many ways were becoming more difficult to achieve.
Discussion
Through this study component we sought to explore the extent to which organisation collaborations were in place to support personal networks of people with SMI, thus forming the basis for wider health partnerships in the community. A recent report by the Mental Health Foundation235 indicated that there have been numerous cultural and institutional barriers hindering effective integrated multiagency mental health care. In summer 2011, we found very little evidence of strong interagency collaborations to tie the resources of a community together to benefit people with SMI: community facilities, mental health care, social services, primary care and physical health care. The date of data collection was important, as the sector was undergoing a rapid period of reorganisation and change. 31,236
The interviews discussed the extent to which organisations were linking together to support people with SMI. Key changes were expected, with primary care regarded as the future ‘hub’ of mental health provision, and by association the centre of organisational links, with the third sector playing a big role. There were examples of individual partnerships and collaborations but not on a large scale in either of the study sites. Overall, the impression conveyed was that a number of competing concerns – the climate of uncertainty, reorganisation of services and squeeze on resources – meant that developing organisational collaboration going forward had lost out to short-term pragmatism. Evidence from the NHS Confederation237 suggests that poor levels of access to low-intensity community services, which can enhance health and well-being, represents one of the main health inequalities faced by people who experience mental illness. Our research found that mainstream community organisations were not set up to support people with SMI; this change will not happen without focused outreach addressing stigma. The analysis suggests that network development as assessed by a CHN approach does not feature in the delivery platforms of any organisation in either study site. Third-sector organisations are in many ways best able to promote holistic practices of working, but are faced with systemic barriers, such as tightening finances and restrictive contracts, which inhibit connectedness as a philosophy and an approach.
The information provided by stakeholders has been summarised in Figure 19. There were numerous examples about the barriers and enablers to building connections, but very little about how they worked in practice or details of the key ingredients of that practice. Network development was not a recognised and embedded strategy for delivering support to people with SMI. Our analysis showed that, in respect of our specific research question, there was a gulf between vision and practice. Mental health specialist service providers want to make active use of individual networks of people when determining their support and treatment needs. However, while this was highlighted as an increasingly important ambition in terms of delivering a modern recovery-focused mental health service, it was also recognised as becoming increasingly difficult to achieve, because of system-wide constraints which impeded working with people for long terms and beyond targets agreed in national and local Commissioning for Quality and Innovation (CQUIN).
FIGURE 19.
Factors impacting network development: organisation leads overview.
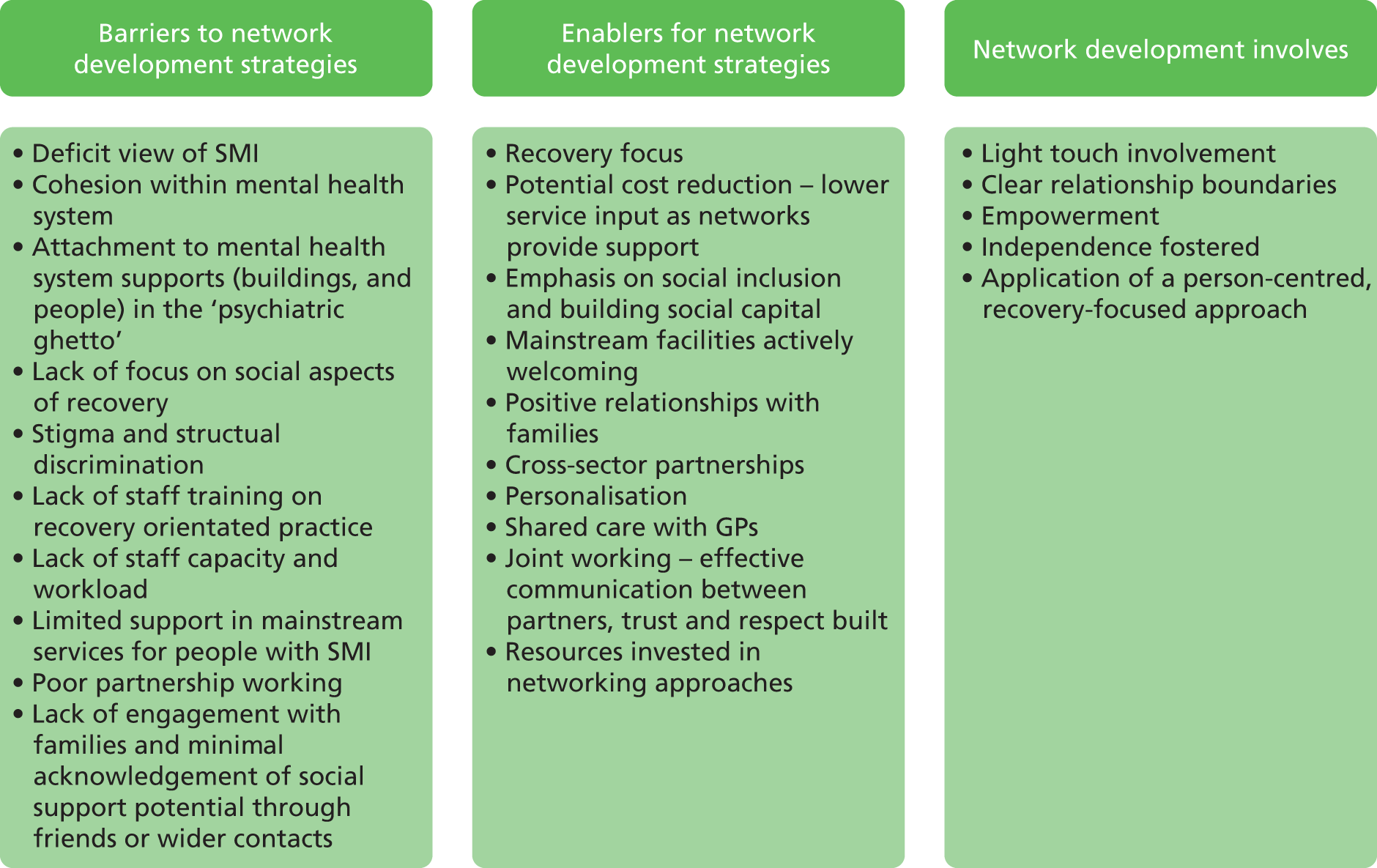
Chapter 6 The role of practitioners in personal networks of people with severe mental illness
Introduction
This chapter used interview data to explore how practitioners work with people with SMI to support their recovery. We aimed to answer the following research questions:
-
How do community-based practitioners and organisations support people with SMI to use their personal networks to support health and well-being?
-
How do primary care, community-based mental health providers and other organisations work together to develop effective personal networks for people with SMI to improve their overall health and well-being? What were the barriers and enablers to achieving this?
Social network development fits within a person-centred approach to managing SMI. This phase of the study provided a data bridge between the service user data (see Chapters 3 and 4) and stakeholder data (see Chapter 5). We sought to understand where network development sat on the practitioner agenda, if at all, for four practitioner groups: GPs, psychiatrists, care co-ordinators and third sector.
Were networks a priority in the care and treatment of people with severe mental illness?
The research engaged with practitioners from different sectors and their approach to engaging with social, place and activity connections of people with SMI was in part, unsurprisingly, shaped by the practicalities of their role. GPs had 10-minute consultation sessions to talk with the service user about concerns and possibly signpost them on. ‘I wouldn’t say the average GP would consider themselves responsible for maintaining or helping to maintain patients’ networks’ (IDL78, GP).
Psychiatrists recognised the value – ‘I think it really is important, but it’s part, it’s not the main thing I do’ (IDL46, psychiatrist) – and looked to other team members to pick up network development. Psychiatrists also spoke about being responsible for assessment and treatment to provide mental stability in order to facilitate work on psychosocial rehabilitation tasks including social networks.
I think [our role] it’s also kind of setting the tone for the way that the other members of the team work with people as well . . . our job is not just about symptom control, not just about treatment, but that’s the kind of baseline that we can help people to get to and from so that the other work takes place, you know, in terms of, say, for people who are not working, helping them to access work.
IDSW55, psychiatrist
Support workers and care co-ordinators had a case load with time allocated each week to work with people against set goals. They worked closely with an individual to strengthen connectedness, describing the role as ‘Giving them options, options that can be followed through’ (IDSW86, CPN). One care co-ordinator emphasised ‘I think people are often quite frightened by their situation, and so a lot of it’s about trying to help them, sort of, think of things in a different way, feel safe, secure and reassured, and not alone I guess is really important’ (IDSW82, recovery co-ordinator). Practitioners acknowledged that, even if they were interested in connectedness and discussions about networks, that was not the way it would be described. ‘It may not be phrased like that, people may not be talking about networks, but they would be talking about what networks are, if you know what I mean’ (IDL41, psychiatrist). Few practitioners felt they discussed an individual’s personal network development as a ‘specific therapeutic strategy’ within the team as part of case reviews or supervision, and it was the social dimension of networks that tended to be recognised as important for recovery.
I think social, one good social contact can make such a difference to somebody, a friend or a partner or someone that you’ve got a good attachment with. It’s important.
IDSW54, social worker
Referrals for aspects of network development were made but the concept of whole network enhancement was absent. There was also a lack of clarity over whether networks were viewed as outcomes in their own right or as a resource to tap into to achieve outcomes.
The practitioners whose work role was most closely allied to network development were those employed in the third sector. ‘Our contribution to this management of community health network is massive’ (IDL49, project worker). The projects they led – housing, employment, social inclusion – all used principles of network mobilisation to support person-centred goal-driven recovery. These projects guided the development of networks but still the approach was not a co-ordinated strategic endeavour considering whole-system impacts because funding was not directed in that way.
A key theme within interviews was barriers to working with people with SMI. Some of these were illness-specific factors, other organisation characteristics or system barriers, but the most uniformly mentioned challenge was time. ‘We miss out on that real nurturing sort of activity . . . we’ve got a huge pending list. We’re all very aware and conscious of that. So I’d say the main thing’s time’ (IDSW59, occupational therapist). Sufficient time to work with people in a focused way was necessary for building the essential therapeutic relationship to plan holistic treatment including engagement in wider social networks. All practitioner groups acknowledged networks as important, but the barrier of time was consistently raised, with few suggestions on how this could be overcome.
Approaches to managing severe mental illness: primary and secondary care
The interviews highlighted a clear difference between primary and secondary care approaches to mental health. It was striking that few GPs explicitly mentioned recovery in the interview and when they did it was mostly to query what we meant by the term.
What do you mean by recovery – do you mean like patients who have been sectioned under the Mental Health Act?
IDL80, GP
General practitioners spoke firstly about medication and specialist psychiatric support in the management of SMI, although most also acknowledged social factors in recovery from SMI when prompted, including risk of loneliness. ‘A lot of people with schizophrenia, for example, are often quite isolated and they don’t have friends’ (IDSW83, GP). They also spoke about the importance of family support – ‘one of the most important resources, or the most important resource, is the family and the relationship with the family’ (IDL78, GP) – housing factors – ‘Housing is a big problem, I think, it’s a big issue with them’ (IDL74, GP) – and how finance, including debt and welfare benefit problems, can impact on treatment of SMI. Overall the approach was medical management wrapped within a consultation framework that recognises service user preferences and choices within a biopsychosocial model.
A big part of it is being able to be a point of contact for the patients and maybe the person who will pick up that someone is deteriorating, or pick up that someone has a mental illness and needs to be given help, so I guess the first part is actually listening and recognising the symptoms and diagnosing, and then beyond diagnosis, I am then helpful in helping them to think through treatment options, so whether that be medication or whether that be psychological therapies.
IDL64, GP
If I saw someone with schizophrenia I may just be monitoring their schizophrenia but I wouldn’t be looking at encouraging them to go and play football, for example, at that initial stage. But maybe a year or two down the line then it may be different; you’re trying to encourage social interaction again.
IDSW45, GP
General practitioners were also very clear on their distinct role in the jigsaw of health and social care services supporting people with SMI. This role was defined by the generalist nature of family practice.
We are GPs: we are generalists; we are not specialists . . . you know, we can never replace consultants and CPNs, by the GP. But is there is a role for everyone to work together.
IDL75, GP
I think it’s quite challenging, because we’re not specifically trained to deal with the severe mental health illnesses, I think, so, we see commonly only depression, and anxiety, and these, kind of, things. And when it comes to more severe, kind of, illnesses I think they need to be assessed by the secondary care, they need to be under their care.
IDL74, GP
They recognised the importance of working closely with other systems of care for people with SMI in both health and social services. They tended to monitor physical health and review medication but seek expert advice or would defer to other specialist services for treatment decisions. One example provided was the importance of a medication helpline open 1 hour a day for GPs to call to speak with psychiatrists about any psychiatric medication queries.
The data provided a strong sense that GPs’ role in managing SMI was light monitoring and signpost or refer as required. However, some GPs have concerns about the ability of secondary mental health services to accommodate requests and acknowledge the fragility of the system when people were nearing crisis.
One of my patients who I’ve been trying to get in [hospital] for ages, he had problems with housing, he’s like . . . I mean it was just dreadful his circumstances. I used to, you know, it was at the point where I used to give him, I take sandwiches for lunch or whatever, I used to give him my, make him come in at 12 so I could give him my sandwich, you know, on a weekly basis, but it wasn’t until he jumped off the bridge that he actually got the help he needed, and that is just awful.
IDL70, GP
Some also had concerns about the skills of their colleagues.
Personally I think it’s, some GPs have absolutely no idea about mental illness, they somehow, they don’t even recognise it, which is a terrible thing to say, but that’s in my experience – I have experienced that first hand.
IDL80, GP
In secondary mental health services, most staff interviewed either work using person-centred practices, or express how they know they should be working with an ‘over-arching adoption of a recovery model, a recovery process’ (IDSW44, senior mental health practitioner). Clinical recovery and personal recovery were referred to as distinct concepts, and a strong emphasis on service user-led treatment emerged, which included staff receiving training in recovery-focused practices.
There’s been a very big emphasis in the organisation on working to a recovery model over the last 18 months to 2 years. I think that has made even experienced, sort of, staff rethink how they work with service users and what, you know, their recovery goals might be for those people they work with in a way that we didn’t before.
IDL69, psychiatrist
In practice, the recovery approach, which we defined with reference to published guidance,8 seemed to be varyingly applied by psychiatrists and care co-ordinators while most consistently practised by third sector staff. We noted variation in what factors staff thought were important for recovery. Psychiatrists cited medication and assessment first, compared with care co-ordinators, who acknowledged features of relationships: ‘I think having a therapeutic relationship with someone is [important for recovery]’ (IDL68, occupational therapist).
Psychiatrists and care co-ordinators described recovery features they had a role in providing; none talked about the personal resources or beliefs of an individual or the contacts in their network. This was in contrast to third-sector staff, who placed greater emphasis on humanity within supporting relationships and the individual’s assets themselves.
It might be for someone to be treated as a person like anyone else.
IDSW72, project facilitator
From my own observations, respect for the person’s position and belief, having a quality in a meaningful life that means something to them.
IDSW67, team leader
People need to have kind of like links within like the community, people that they can kind of rely upon.
IDL76, employment advisor
Practitioner roles in individual networks
We identified two types of role that practitioners have in personal networks of people with SMI, though not all take these up: firstly a development role assisting the person with SMI in building connections and secondly as a contact within the network who was an active agent within it.
Developing networks
Through the interviews two development mechanisms emerged to support network enhancement that all groups adopted within the boundaries of their current role:
-
referral, signposting, facilitating and linkage
-
encouragement and empowerment
We observed that some practitioners, particularly GPs, were cautious in making any network enhancement recommendations. There was a dilemma between giving information that opens up opportunities for individuals and making suggestions that turn out to be negative or harmful. This was further evidence of GP nervousness about being the prime responsible clinician for people with SMI.
I suppose, as a GP, it’s quite hard because you can signpost them to organisations that you might think would be helpful for them, but you can’t always guarantee that (a) they’re going to take up the suggestions, or (b) that it is going to be helpful.
IDSW83, GP
Making suggestions relies on having knowledge and information. The GP group in particular lack detailed knowledge of local resources for people with SMI. ‘I don’t link them into these services because I suppose I’m not really aware of them’ (IDL80, GP). The most common signposting for GPs was via a referral letter if required, or suggestions for the person to reflect on and act on themselves. GPs spoke about often not finding out if their suggestions were useful, and recommended that feedback, individual or collective, would be a positive influence and practice aid.
It would work for me better if I really have the number of patients, the majority of my patients that come in and say to me, look, doctor, I really love that; it’s really helping me.
IDL75, GP
In contrast, care co-ordinators’ and third-sector staff’s core job role is signposting. They reported being comfortable with making suggestions and ‘referring on’. Throughput of clients within services was described as a key driving force, working towards goals that will lead to onward referral out of secondary mental health services. Staff talked about using internet searches with clients to look for information and plan next steps for taking ideas forward.
I look on the internet; I search a lot of things to find classes, or activities, or gyms or . . .
IDL60, social worker
Psychiatrists tended to focus on encouraging and empowering clients to take up suggestions that they or other team members make. The approach taken also depended on a range of factors including how well a person was coping, their relationship with services, illness presentation and resource constraints.
[Some] sort of things would maybe sort of lead me to be a bit more directive, you know, and making suggestions to them, you know, for them to consider. And people that are more resourceful, further on in their recovery, it may be less important and may be more facilitating, you know?
IDSW50, psychiatrist
All groups were concerned about empowering individuals to make their own decisions, preventing the creation of dependency on them personally or the health-care system. All were mindful that individuals’ own agency was central to managing SMI.
We have to be aware that, you know, about creating dependency. So we’re always seeking to, kind of, make sure that the client is, whilst getting the best of the service, aren’t depending on us as, you know, for transport or friendships.
IDSW47, social worker
When considering whose role it was to develop CHNs, the practitioner groups all emphasised the importance of the individual service user themselves. Regardless of current health status, a large part of network development follows the interests of an individual and how engaged they seek to be with others and local resources. Interviewees gave numerous examples of how they were doing this in their own practice.
My role really is to get them, to try to build along with them, you know, the networks which is appropriate for them. But their own role really is to feel and to engage with the networks, which we agree on.
IDL62, support worker
So it’s a collaboration and co-operation of all the services involved in the care of the individual and of course with the individual taking more interest in what they would like and identify as their need. But I don’t think it’s a single person’s role, I think it’s the role of all the people involved in the care.
IDL84, psychiatrist
To my mind, you know, it’s all very well for us to go in and support people, but unless we’ve got an eye on how they’re going to live their lives without that support at the end of our time with them, then we’re failing.
IDSW42, floating support
Roles within the network
For care co-ordinators and third-sector staff, the time they spent with people on their case load included detailed work to extend community connections, tackling risks of social isolation and lack of meaningful activities. This involved direct action within networks. We understood this role as:
-
being involved directly in the network – supporting and accompanying people to make new connections
-
building skills to support network development (particularly self-confidence and self-esteem, anger management, self-care and managing anxiety), addressing both the impacts of living with mental illness and aspects of illness or symptom management.
How staff understood that role varied from walking alongside someone to being in the centre of the network and controlling it. The focus was always on empowerment, not ‘taking’ a person to an appointment but ‘accompanying’ them; however, the style of doing this varied in practice.
I think our role is, like, if you look at a spider web, we are, like, in the middle and then our responsibility is support them, linking to all the rest of the networks that are available . . . Because they will be quite, maybe, scared to go out there and, you know, join the community or even afraid of being out [of hospital], you know, stigmatised, if you like. So we have to be there constantly, you know, to reassure them. And we also have to make sure they make those small steps. Sometimes it doesn’t happen and then you try again and then eventually they make it.
IDL49, support worker
Make suggestions. Can give practical advice and health advice or dietary advice, you know, we will very much walk alongside someone, you know, I haven’t got the magical key for someone to recover – it’s what their recovery means to them.
IDSW67, team leader
A key role for care co-ordinators was skill-building and developing capacity for the individual to do more network development on their own. They were also likely to refer on to support workers to ‘do’ direct action network functions.
It’s about meaningful things. It’s about occupation things. And it’s about giving people some self-belief that they can reach out and try things that they might not have tried for a while, or they might not have even considered in the past.
IDSW81, team leader
We found that connection-building guided by practitioners mostly had an activity focus. What was notably absent in the practitioner interviews from all groups was work acknowledging the value of friendship within networks as a resource and source of support. In our data, friendship was referred to only as a gap in people’s lives, not as a resource.
Can I just say sadly, patients with mental illness, you know, tend to have less friends, they don’t have support services and things and they may have initially have had it but then people get on with their own lives, they can’t cope with it, they find it too stressful, they can’t bring people towards them – they don’t naturally have the resources to do it either.
IDL80, GP
And so with the nature of mental illness as well there’s like a lot of our clients have quite complex relationships with family and friends, and it’s not actually always in their best interest to try and nurture that network.
IDL63, social worker
However, in more general terms, network development from those most used to working in this way was seen as a positive aid reducing pressure on the practitioner in particular.
But, you know, I mean generally speaking, you know, I always try and look at what resources people have in terms of social networks, and look at how they can be improved, if needed, and you know, how they can build more networks. It is definitely really important, and actually as a worker as well, it kind of eases the responsibility on your shoulders, because, you know, you’re kind of helping people branch out and, you know, get their resources in different areas, rather than just sort of depending on you as a worker.
IDL63, social worker
Through our analysis, the team created a three-level model of practitioner network involvement. This could provide the basis for further research assessing role of practitioners within networks and the development of best-practice guidance:
-
network information point – light touch intervention communicated within a consultation session (professional expertise, information, ideas) and also providing leadership for colleagues, advocating for the approach and providing guidance
-
network resource that empowers and build skills – therapeutic interventions in groups or one-to-one sessions (so the individual can take more control)
-
network resource that co-produces outcomes with the client – embedded resource within person’s network as a network member themselves (accompany and take part in activities).
Each of these roles could place the practitioner ‘on the network map’ as a valued contact and an important resource within a personal network for someone with SMI.
Interagency networks
We try to stay in touch with the mental health team as much as possible, but most of the time it’s very difficult to link the community mental health team with a GP, with us, to work together, you know, to achieve one goal.
IDL49, support worker
It is not only individual people with SMI who can benefit from wider networks; organisations may benefit through promoting greater linkages between services sharing knowledge assets and practical resources. It was notable that physical health aspects of supporting people with SMI were mainly absent in the practitioner interviews. Very few people mentioned disease prevention or specific tasks such as monitoring weight or blood pressure. No staff mentioned links to wider health resources: dentists, physiotherapy, hygienists or chiropodists. We also observed weak linkages between different parts of professional support systems for people with SMI.
I mean, we don’t know much about them. They don’t know probably not much about us. And it would have been good if we, if I know or meet people from these agencies who are in touch with each other.
IDL46, psychiatrist
I was a bit shocked when I moved down here to find how little interagency working seems to be going on. I don’t think that we work closely enough together here.
IDSW42, floating support
We were told the following examples of interagency working, which were ‘green shoots’ to build on:
-
General practitioner surgeries have notice boards where information flyers can be displayed and third-sector agencies did visit surgeries to talk about their services and leave posters to display in waiting areas.
-
There was some communication between GPs and psychiatrists, mostly by telephone or e-mail. GPs complained about the length of written e-mails from secondary mental health staff requesting summaries of information.
-
Some services co-locate with staff from the third sector, for example employment advisors, working closely with a CMHT or recovery team.
Barriers to connection-building
The interviews uncovered many barriers and challenges related to supporting people with SMI. Each practitioner group had specific concerns related to their role. A common issue was lack of accessible resources in communities, which were felt to be both shrinking and vital for recovery. Workload pressures affected all groups but in particular care co-ordinators. Morale in this group appeared to be the lowest and some of the innovative solutions to help manage time pressures such as creating more flexible working were also viewed as a threat to working practices.
We’ve recently started having mobile working, or now we have laptops, so in theory we don’t actually have to be, sort of, in the office. . . . It’s a barrier in . . . when you’re by yourself out in the community with a laptop, you just . . . the only thing you know is what you already know. (Laugh) And there’s a lot of informal learning that happens in a multidisciplinary team. And that’s disappearing and people are just, sort of, becoming lone workers. An important challenge was access to local knowledge.
IDL60, social worker
A lot of the time there are resources available. It’s just knowing about them, and signposting patients to use them, and how to use them and access them. I think we’re pretty bad at that, on the whole, in general practice.
IDL78, GP
General practitioners had least local knowledge of community resources to aid networking but psychiatrists and care co-ordinators also recognised their limitations, particularly if they were new to an area and lived outside the communities that they worked in. One care co-ordinator talked about knowing people at the housing benefit office and the local branch of the charity Mind making referrals easier. Network enhancement is driven by personal practitioner knowledge, networking interests and skills in many services.
You, kind of, have to prioritise risk, you know, and safety management and, you know, monitoring things like mental state and medication concordance and all these things that are, you know, I guess priorities for psychiatry, if you like, but not necessarily for the person. So yes, it can, kind of, fall by the wayside slightly when you look at, kind of, the process that’s required.
IDSW85, CPN
Many practitioners acknowledged the problem: they had become constrained by addressing risk and clinical factors, leaving limited time for network development. The question for this study was: should practitioners be shifting priorities and addressing barriers to focus more specifically on health networks, facilitating access to social capital in bridging, linking and bonding relationships, or not? It was clear not all barriers were ones that were easy to address, as they were embedded within systems of care and ran throughout the psychiatric system.
Practitioner future roles in networks: the practitioner perspective
In this final section we reviewed the role that practitioners felt they should play in personal networks. When they were asked about future practitioner network roles, the overriding response was for stability of current role but new resources provided to facilitate increased time to focus better on network development among care co-ordinators. For GPs and psychiatrists, the ideal role involved combining responsibilities with others, and GPs also described clear limits around what they specifically could be expected to do.
I see my role as co-ordinating their medical care, mental health, as directed usually by the . . . if it’s mental illness, usually by the mental health team . . . I don’t see our role as actually, sort of, organising, you know, physical activity for them or joining a walking group or something like that. I mean, I’m happy to do a medical form or something if needed but I don’t see our role as actually co-ordinating their, sort of, physical exercise and things like that, no.
IDL51, GP
Third-sector staff would like to have greater capacity to work more intensively with clients, and many feel threatened by throughput pressures in services.
I think the kind of role that . . . for me personally, the role that I’ve got at the moment would be . . . is great. I think it’s a really positive one. . . . If I had fewer clients and could spend more time with each of them in a given week, that might be more beneficial.
IDSW42, floating support
All groups acknowledged the need for shared responsibility between the person themselves, their family and practitioners for network development.
I see it as my role, I see it as, it’s only part of my role, you know, I maybe only see someone 1 or 2 hours a week, what goes on in the rest of their life is, you know, it’s difficult to . . . so I think it’s their responsibility, and I have a role in it.
IDSW86, CPN
A key aspect of working with people with SMI was empowerment. Even though practitioners were keen not to create dependency on themselves or the service – ‘oh, no, I don’t need that sort of dependency! (Laughter) That’s the opposite of what I’m trying to do here!’ (IDL60, social worker) – it was a potential outcome of more focused practitioner involvement in networks. In practice many actions practitioners take can be viewed as paternalistic or creating dependency on one hand, but coaching and empowering on another. The interviews acknowledged that working with those with SMI was challenging, requiring complex solutions that address cultural, economic, social and health factors.
One solution to the service dependency trap emerged through current care co-ordination practice. The network enhancement role played by care co-ordinators was outcome focused and related to skill-building. Care co-ordinators worked within the Care Programme Approach framework, setting goals and reviewing progress against targets agreed with the client. This balanced support with realistic time restraints in a role, capacity-building principles and promoting independence. It was an approach that could be applied across all the practitioner groups. Third-sector staff also spoke about the importance of the time-limited nature of involvement, and clear outcome targets, though signs of leadership roles in networks rather than guidance roles were also present in the data. This group also had most interest in emphasising network development because that was the core aspect of their job role.
A second proposed solution to the service dependency involved a greater shift in SMI care to family practice through assertive discharge practices moving more people to primary care. In our network-mapping module 50.7% of those interviewed in the SW site, and 26.7% in London, received only primary care. Shifting care to GPs lessens mental health practitioner involvement in networks. However, there were clear weaknesses in the current system, reflected in the weight of concern expressed by practitioners over this change – not ideologically but in practical terms because of poor integration of services particularly on the primary–secondary care interface.
And I think that as a GP one of the things that I personally find, and I know my colleagues do as well, that is that you often feel you have to keep prodding the mental health services until somebody listens, does that make sense?
IDSW88, GP
General practitioners were the one group who had a clear idea on how to achieve better integrated practice in future. There was a strong sense that primary care needs an effective interface with secondary mental health services, and this does not currently exist.
The GP role is changing across the board in terms of becoming less of a gatekeeper to secondary services and more of a care navigator – helping patients understand their disease and the appropriate services available at different times during their care journey. GPs need to be aware of clear pathways of when and who to refer to at the right time also. GPs need to have a closer relationship with the mental health team.
IDL78, GP
In the context of greater responsibility for SMI within primary care, and acknowledging that networks were important – but were not the GP’s responsibility – the main suggestion was for support to be attached to primary care to deliver this function.
I personally believe there should a CPN attached to every practice, that’s the way I see it. Because they are experts in their field.
IDL70, GP
It would be nice, in a way, to have some sort of link worker in a practice that you could just, sort of, pick the phone up and say I’ve got this patient who I think might benefit from this and that and would they be able to facilitate it because I think that’s probably the most difficult thing for people, to make that first step and go along to something when they don’t know what they’re getting into and they’ve got a fear factor.
IDSW83, GP
A final important recognition from practitioners was that system-level changes would also be required if network development was to become a more prominent part of active treatment for SMI. Mental health was not currently orientated around network development and that was ‘quite damaging really’ (IDSW50, psychiatrist).
So when you say that people are concerned about risk how does that actually stop people helping service users develop their Community Health Networks?
Well, it might just make them preoccupied with assessing things like relapse indicators or signs of mental health problems and not looking at positive things, like a lot of people are doing well and resilience and coping strategies. So it changes focus. Also that is inevitably communicated to a client, you know, that these are the things that are important, you know, if you’re always asking about them, you know, and that kind of models people’s responses, you know, what to say to care co-ordinators. So there are a lot of knock-on effects from that sort of culture. It’s quite damaging, really.
Discussion
Network development was not currently part of mainstream mental health service delivery as a priority treatment strategy. Social factors impacting on recovery were viewed as important and were considered, but not systematically, and there was limited co-ordinated join-up between agencies. This illustrated that a substantial change, a cultural shift, was required to move services forward following a recovery-focused approach, as has also been highlighted elsewhere. 41 People in all the sectors we interviewed could work more effectively in relation to network enhancement, even those who felt they already were at the ‘hub’ of network development.
How did practitioners support people with severe mental illness to use their network effectively?
Reflecting on the role of practitioners there was, of course, no one-size-fits-all response as individual service users require varying levels of support, which changes over time. However, there was a role for practitioners in showing that networks were valuable, were part of recovery journeys and were a way of bringing ‘the social’ centre stage in treatment and care dialogues and monitoring processes. Social care workers can help clients build relationships and strengthen links to local communities. 238 As other components of this work show, the practitioner role was particularly influenced by the resources within people’s social networks. Practitioner interviews highlighted that staff view family as an important resource, with safeguards,239 but there was a lack of focus on friends as a recovery resource. This study has not investigated what a practitioner-led CHN network intervention would consist of, but these were under development,125 and relationship-building including friendship would be a core component. At the moment most practitioner strategies involve skill-building or connections to meaningful activities including employment; there appears to be less emphasis on addressing difficult relationships or building social connections.
Poor integrated care and support for people with SMI has recently been highlighted by the Schizophrenia Commission. 240 To facilitate effective working to enhance networks we identify a need for more holistic engagement and planning with individuals. Strategies are required for how practitioners can empower, link, facilitate, support and guide network development. Decisions were required on who was best placed to engage in network enhancement strategies; it was unlikely to be the time-poor GP unless a networking intervention within the 10-minute consultation slot could be created.
How did organisations work together to better support people with severe mental illness?
We found evidence that there were four service ‘silos’ in operation: secondary mental health services, third-sector provision, community organisations (including housing, education and leisure providers) and primary care. There was interagency communication but strategies to improve this were required; communication between primary care and the third sector was very limited and between primary and secondary care often not effective. Community resource information was vital for facilitating network development. Access to resources, through signposting, recommendations or actual referrals, currently rests mostly in practitioner’s own knowledge bank of relevant opportunities.
Several issues arise from our analysis of relevance to the support and development of networks for individuals with SMI:
-
Finding a solution for the sharing of up-to-date local network resource information is an important component of interagency support for network development.
-
When individual care is provided by different practitioners and teams (shared assessments, individual goals, records, liaison opportunities), ongoing co-ordination is needed.
-
Joint service planning and operational co-ordination between different parts of mental health provision are needed. This is particularly critical for those discharged back to primary care, given the almost total absence of interaction between primary care and the third sector.
Barriers and enablers to network development
The barriers and enablers that were recognised by organisations in Chapter 5 (see Figure 19) align with those emerging from practitioner interviews (Figure 20).
FIGURE 20.
Practitioner views on network development: barriers and enablers.
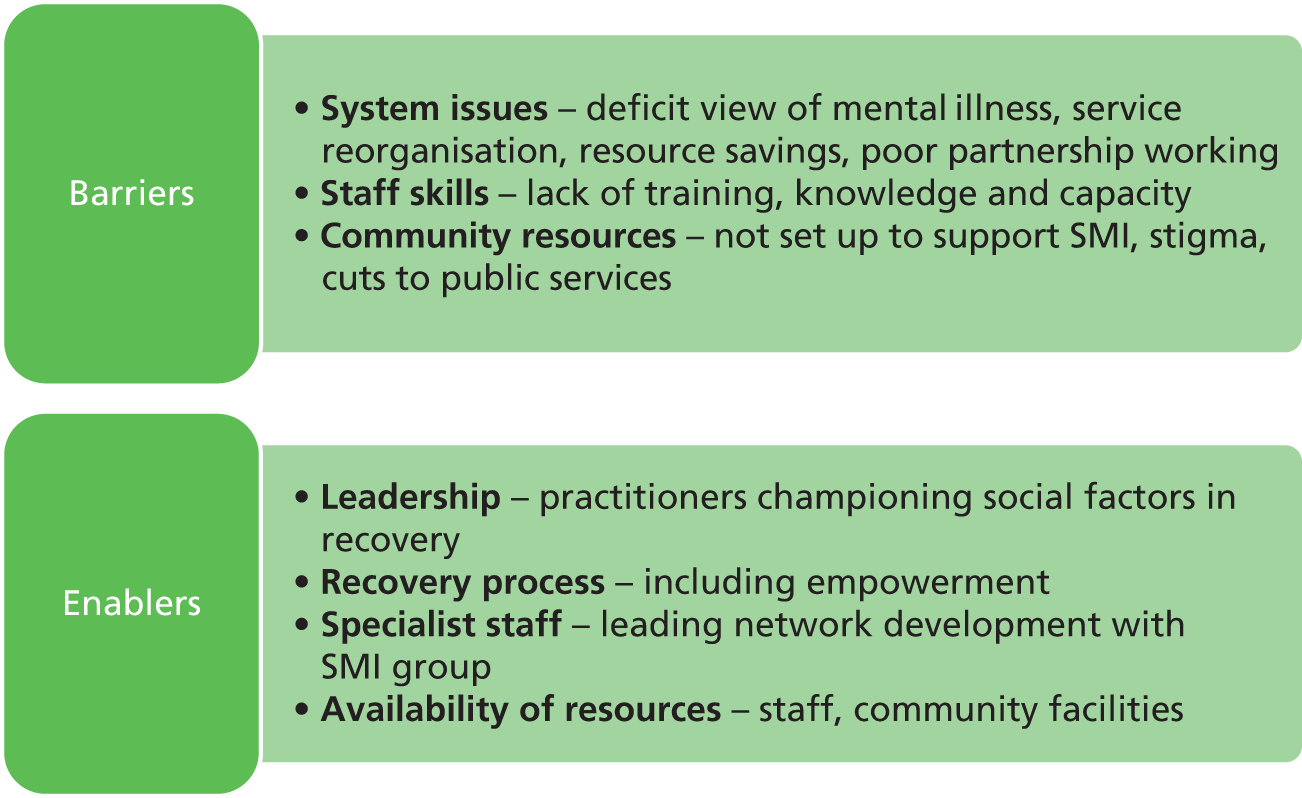
Practitioners recognised that networks were important in recovery for people with SMI but reported system-level barriers, including workloads, service reorganisation and bureaucracy of paperwork, that restrict network enhancement. We conclude that even those practitioners who were personally inspired and motivated to focus on the personal networks of people with SMI struggle to do so. There were so many system-level barriers that individual practitioner agency was squashed. We heard from practitioners how, to protect their own mental health and workloads, they could not get too involved in network development, or those were the activities they did in addition to the core role. It was acknowledged that this absence sends an unhelpful message to mental health service users: if the only attention they received from services focused on medication and relapse prevention there was a risk that individuals would not view the social aspects of their lives as important for recovery.
Chapter 7 Case studies
We worked across two locations and noticed similarities and differences in personal networks by site. We did not know what caused site differences, and could compare only the two sites, not other areas of England; however, the observations provided in this chapter emphasise a possible locality effect on networks. Influencing factors may be both structural context – services, geography and population demographics were different between sites – and the agency of individuals, and others, shaping access to network resources and well-being opportunities.
For both sites the following was presented:
-
brief description of site
-
overview of salient features of personal networks
-
two personal networks
-
structural context of personal networks, influenced by the local and organisational context and culture
-
implications for practitioners working to facilitate recovery, who may wish to develop a client’s personal network.
The South West site
Structural background to the South West site
The site was located in a predominantly rural county, with mostly small communities and limited public transport links. The area also included coastal settlements and one small city. We purposively recruited from 9 of the 109 GP surgeries and 4 secondary care teams; thus the site was one small area within a larger county. Recruitment at this site was from predominantly rural communities. The SW was chosen as a contrast to an inner London borough in order to explore how personal networks and organisational collaborations operated in two geographically and demographically different areas. The generalisability of the findings, in drawing on only two locations, is limited, but such contrasting sites helped provide an insight into if, and how, location impacted on network type and meaning.
The mental health prevalence figures for the whole county from the area’s 2012 Joint Strategic Needs Assessment (JSNA), using data from 2010, estimated 70,000 people had a common mental health problem and 1,700 had a psychotic disorder. The estimated prevalence of psychosis was 0.8 per 1000, the same as the average for the whole of England. A fifth of residents in this county lived in isolated rural communities and a further fifth lived in small or medium-sized towns. The report noted that rurality was a key challenge in providing services, particularly the availability and accessibility of public transport. The SW site had one mental health NHS trust covering the area. At the time of study data collection there were three PCTs in the county; under the new structure there are two CCGs.
How were personal networks composed in the South West?
The spread of network type significantly differed by site (χ2= 21.69, df = 2, p < 0.001) and almost half of SW networks were family and stable. Table 33 shows that network features also differed across network types in the SW site: family and stable networks had the most social ties. All network types reported high levels of time at home.
| Site (number of participants) | Diverse and active networks | Family and stable networks | Formal and spare networks |
|---|---|---|---|
| SW network types % (n) | 24 (18) | 49.3 (37) | 26.7 (20) |
| Mean social network size (SD) (F = 14.85***) | 21.4 (8.9) | 23.2 (9.7) | 10.8 (4.0) |
| Mean number of family contacts (SD) (F = 22.24***) | 4.1 (2.6) | 8.9 (3.9) | 3.8 (2.4) |
| Mean number of friends (SD) (F = 10.75***) | 9.8 (7.7) | 7.9 (5.0) | 2.3 (3.0) |
| Mean number of wider contacts (SD) | 3.2 (3.3) | 3.6 (4.2) | 3.5 (1.8) |
| Mean number of practitioners (SD) (F = 3.19*) | 4.3 (3.4) | 2.7 (1.6) | 3.5 (1.5) |
| Over 50% waking time spent at home | 66.6% | 75.9% | 90% |
| Mean number of community place connections (SD) (F = 9.92***) | 6.8 (2.9) | 7.2 (3.1) | 3.8 (1.9) |
| Mean number of meaningful activities (SD) (F = 13.68***) | 7.2 (2.7) | 6.6 (2.9) | 4.9 (2.7) |
| Mean % of activities unstructured (F = 11.30***) | 16.1 | 7.1 | 19.3 |
| Mean % of activities social (F = 8.55***) | 42.4 | 43.7 | 19.7 |
Table 34 summarises significant network differences from London. In the SW, informal networks were dense, with more longstanding place connections, carers were more common, more waking time was spent at home, connection to places outside the home were less frequent, networks had fewer wider contacts, fewer activities were done with others and there was less engagement in volunteering, training or education or study. GPs featured more prominently, as did physical activities and green and outdoor spaces; however, mental health settings were less prominent.
| Variable | SW | London |
|---|---|---|
| % (n) | % (n) | |
| Presence of an informal carer in network (χ2 = 17.25***) | 44 (33) | 13 (10) |
| % of place connections less than 5 years old (t = 2.11*) | 42.5 (27.1) | 52.2 (29.3) |
| Over half of waking time spent at home (χ2 = 9.74*) | 77 (58) | 54.7 (41) |
| Names a GP as part of network (χ2 = 18.98***) | 86.7 (65) | 54.7 (41) |
| Sees GP monthly or more frequently (χ2 = 7.68**) | 29.3 (22) | 13.3 (10) |
| Engages in education, training or study (χ2 = 6.86**) | 6.7 (6) | 20 (15) |
| Engages in volunteering (χ2 = 4.48*) | 5.4 (4) | 16 (12) |
| Mentions at least one domestic activity (χ2 = 18.93****) | 58.7 (44) | 26.7 (20) |
| Mean (SD) | Mean (SD) | |
| Number of wider social contacts (t = 2.90**) | 2.9 (3.6) | 4.1 (4.8) |
| Network efficiency ratio (t = 3.23**) | 0.7 (0.2) | 0.8 (0.1) |
| Mean number of mental health settings connected to (t = 3.74***) | 0.55 (0.6) | 0.92 (0.7) |
| Mean number of place connections where social interaction was mentioned (t = 2.76**) | 8.2 (3.4) | 6.6 (3.0) |
| Mean frequency of connection to places outside home (t = 10.31***) | 2.4 (0.5) | 3.2 (0.4) |
| Mean number of green and outdoor spaces (t = 5.82***) | 1.4 (1.2) | 0.5 (0.6) |
| Mean number of unstructured activities engaged in (t = 2.40*) | 0.7 (0.8) | 1.0 (0.9) |
| Mean number of physical activities (t = 2.08*) | 1.5 (1.2) | 1.1 (0.9) |
| Mean number of activities which are social (t = 2.10*) | 2.4 (2.0) | 3.2 (2.7) |
Site was a significant variable in our regression model, on RGUK, and participants in the SW had significantly higher access to social capital, with mean scores of 15.3 compared with 13.1 (t = 2.07, df = 145.69, p = 0.04). We found this resource to be primarily accessed through family; therefore the increased family dominance in the SW site most likely explains this finding. Yet participants in the SW obtained significantly more social capital resources from acquaintances than participants in London, 16.8% compared with 7.7% of total resources accessed (t = 3.53, df = 146, p < 0.01). It seems that acquaintance contacts involved more resource exchange in the SW than in London, possibly related to longstanding connections within the community.
Networks were also likely to be shaped by differences in participant characteristics by site. As summarised in Table 35, bipolar disorder/manic episodes were more common in the SW site (but not significantly so), ethnicity was significantly more homogeneous and significantly more participants were managed in primary care only. This site was more advanced in a policy of assertive discharge to primary care; the SMI population reflects overall lower ethnic diversity in this county (3.4% BME groups and 3% other white) than in the London borough site (22% BME groups and 20% other white), as detailed in the JSNA reports; and we acknowledge a sample bias in the SW site recruitment towards people with bipolar disorder recruited through primary care. Significantly fewer in the SW were unemployed and, although the difference was not significant, more were on long-term sickness or disability benefit; this may change with future welfare reforms. SW geography may have shaped these networks, with limited public transport links and fewer available opportunities to volunteer or engage in training. The rurality of this site was also reflected in the increased use of green and outdoor spaces, which can be beneficial for well-being.
| Variable | SW % (n) | London % (n) |
|---|---|---|
| Diagnosis | ||
| Psychotic disorder/schizophrenia | 36 (27) | 42.7 (32) |
| Bipolar disorder/manic episodes | 50.7 (38) | 36 (27) |
| Other psychoses | 13.3 (10) | 21.3 (16) |
| Ethnicity (χ2 = 55.31***) | ||
| White British | 97.3 (73) | 41.3 (31) |
| Other | 2.7 (2) | 58.7 (44) |
| Mental health contact type (χ2 = 9.11**) | ||
| Primary care only | 50.7 (38) | 26.7 (20) |
| Secondary care | 49.3 (37) | 73.3 (55) |
| On long-term sickness or disability | 41.3 (31) | 21.3 (16) |
| Unemployed (χ2 = 4.16*) | 9.3 (7) | 29.3 (22) |
We have explored the data to assess the impact of diagnosis on the SW network types. In the SW, bipolar networks were more likely to be family and stable; in London, they were more likely to be diverse and active. In the SW, bipolar networks were more likely to be supported in primary care and feature children than bipolar groups in London, but this was also the case for all diagnosis groups. There was no difference between SW and London bipolar groups in terms of HRG scores, RGUK scores or numbers of relationship types.
A detailed consideration of two networks
In this section we provide two illustrative examples, chosen to explore prominent features of SW networks, but they are neither fully representative nor meant as caricatures. In order to protect anonymity, we have changed key features. We conclude each example by considering how each of the participant’s personal network related to key dimensions of interest in the study: social support, recovery, stigma and social inclusion.
South West personal network key characteristics: Matt
The experience of the first participant, Matt (SUSW01), illustrated many of the notable features of personal networks in the SW, in that his was a family-orientated, stable network demonstrating the importance of outdoor spaces. All quotes in this section were taken from Matt’s in-depth interview, and Figure 21 provides a pictorial summary used in the analysis. Matt was a self-employed white British man in his forties, diagnosed with bipolar disorder, living with his wife and two children in a rural town. In his initial interview he described his network as ‘positive’ and ‘supportive’, providing him with ‘stability’.
FIGURE 21.
Analysis using within-case process for Matt. Key: green, past; pink, strategies; yellow, future; orange, activities; purple, building blocks; light blue, change in networks; blue circles, people; red circles, other information, usually statements about health or beliefs; red jagged edges, particularly stressful things in life including voices.

He expressed similar sentiments in his follow-up interview, saying that he was ‘fairly satisfied’ with his network, ‘my friends and family, um, and in terms of the mental health kind of provision’. Matt’s satisfaction with his network at the time of the interview was in stark contrast to past experiences. As Figure 21 shows, his experience of hospitalisation and unmanageable periods of illness caused great distress; subsequently, however, he developed active strategies that have helped him build a stable network with future goals. There was also evidence of connection-building as well as stability.
Family was a central part of his life (as shown in Figure 22) and these relationships suffered in the past when he was hospitalised: ‘the family relationship breaks down and, you know, everything goes completely awry.’ He reflected a contributing factor to his last hospitalisation was irregular contact with mental health workers and particularly his CPN: ‘I became very, very ill, it was too late, intervention happened too late’; as a consequence, he reflected, the recovery period took a long time.
The period up to and including hospitalisation for people with SMI has been shown in Chapter 3 to be a potential network rupture point. Learning from his own experience, Matt, in collaboration with practitioners, worked on creating active strategies to manage potential relapse: ‘We kind of focus mainly on the triggers and assessing . . . self-assessing my condition’. A key part of this involved looking for ‘trigger signs’ of becoming high again to facilitate early intervention. His CPN was identified as an important contact, with whom he had developed a Wellness Recovery Action Plan (WRAP). In depressive phases of his illness after being high, Matt reflected that the mindfulness approaches were helpful. An important aspect that came across was that Matt’s family were more connected to his ongoing treatment and support than in the past. He said that if he became ill again they would be likely to contact his GP or CPN at an ‘earlier stage’, and indeed that they had ‘more of an opportunity to do that now than they did before.’
With respect to Matt’s ongoing sense of well-being, it was evident that the centrality of home life and spending time with his ‘tight knit’ family were crucial. He stressed the importance of keeping up routines with his family both within the home, such a cooking and quality time, and also in activities away from the home, such as walking the family dog and growing vegetables at a local allotment. Spending time boating on a local river was also identified as an important part of family life.
Matt was self-employed and embodied an active outlook to managing his health and well-being, describing himself as a ‘practical, hands on’ person, ‘always kind of involved in some kind of project one way or another.’ His approach to staying well was underlined by ‘maintaining routine on a day-to day basis’, and, as discussed above, family and practitioners contributed to his sense of meaningful structure. Part of developing a routine which supported his health involved Matt finding the right balance and not overstretching himself. In the past he had taken on too much work at times, and such ‘stressful work situations’ were identified as ‘a major trigger’ for becoming mentally unwell.
For Matt, work provided structure, income and a sense of purpose. It also shaped his identity as a skilled craftsman producing work of a high standard. However, as we have seen, work was also a regarded as a source of stress, and awareness of this within his support network provided a useful preventative strategy.
Matt reflected on his experience of living within his wider community: both the positive and negative aspects of living in a small town. He was proud of his status as a father and family person, a self-employed craftsman and a member of the local community, which, when he was well, constituted his dominant identity. Living in a ‘tight knit’ countryside community was viewed as a safe, positive environment for ‘bringing children up’; although he had lived in more built-up places in the past, he was adamant that he did not want to raise his children in a city. In terms of his own mental health he saw some positives about the local area. One aspect he touched on was familiarity: ‘you can’t walk up the high street without probably seeing half a dozen people that you know.’ Such familiarity engendered a sense understanding: ‘they [local people] are aware of my health condition’; he added, ‘they are tolerant and accepting to a greater extent.’ However, there have been times when his identity as a skilled, self-employed family man has collided with community perceptions of the mentally ill and he has felt negatively labelled because of his mental illness:
. . . there is a stigma attached to it, but over a period of time and obviously when you’re following on from an episode when I was very low it you know, you are very anxious and paranoid about what people . . . and as a result of what you’ve done and so it does take a long period of time to get around that.
Related to his experience of stigma, Matt considered his recovery not just in the personal terms of his own health and well-being, but social recovery too, as he had gone through the process of rebuilding relationships that had become strained during past ‘high’ episodes.
It’s a huge part of the recovery certainly. Initially you know I couldn’t go out of the door for months, and you know I couldn’t deal with face-to-face contact because of what had happened . . . It just takes a period of time it’s you know rebuilding you know relationships.
Overall, Matt expressed satisfaction with his network and stressed that he wanted the future to be a continuation of the present. He considered himself ‘fairly fortunate’ in that he had a network of family and friends, who complemented his proactive outlook, who ‘steered things in the right direction’; he added, ‘I think a lot of people don’t have that advantage.’
Matt valued the stability of his network, but it is important to emphasise that it was not static and stagnating, but evolving, goal driven and future orientated. Drawing on five areas identified in our literature review (see Chapter 2) that help us understand personal networks, and answer the first study research question, we applied the learning from Matt’s case study in Table 36.
| Key area of literature | What we learn from Matt |
|---|---|
| Agency and strategies for staying well | An active, balanced routine comprising meaningful activities, is important for promoting well-being. What these are, and where the balance lies, should be self-directed by the individual |
| Social support | Practitioners have a crucial role in helping people with SMI to develop proactive, preventative strategies, linking into available family support if possible to maintain mental health |
| Recovery over time | Effective strategies for managing SMI are learnt over time, and people can draw on past experiences in shaping current decision-making and negotiating these preferences with others. Within family and stable networks the family are often a key part of the recovery journey, and they themselves have a family recovery pathway too |
| Stigma | Cohesive communities provide a measure of social support and understanding for local people with SMI; however, there can be a perceived stigma relating to public knowledge of someone’s health problems. People feel judged and labelled by their illness and the negative opinions of others at times. How people feel about community knowledge of their health problems changes over time |
| Social capital | Accessing local resources represented a crucial part of building networks, generating a sense of connectedness and strengthening belonging. Social capital and sense of inclusion can fluctuate, diminishing when unwell and growing during recovery |
South West personal network key characteristics: Nick
The experiences of Nick (SUSW51) also illustrated the importance of family networks in the SW. Nick, however, no longer had contact with specialist mental health services and had limited access to wider community resources. He was an unemployed white British man in his fifties diagnosed with schizophrenia, who described his network as ‘positive’, one where he was ‘close to kids’, but felt that he did not ‘see friends often enough’.
Nick explained that hearing voices comprised a dominant feature of his life (as shown in Figure 23) and described most of them as negative. The voices impacted on all his relationships and caused him to experience heightened stress ‘on more or less on a day-to-day basis’, which included inducing panic attacks.
FIGURE 23.
Analysis using within-case process for Nick.
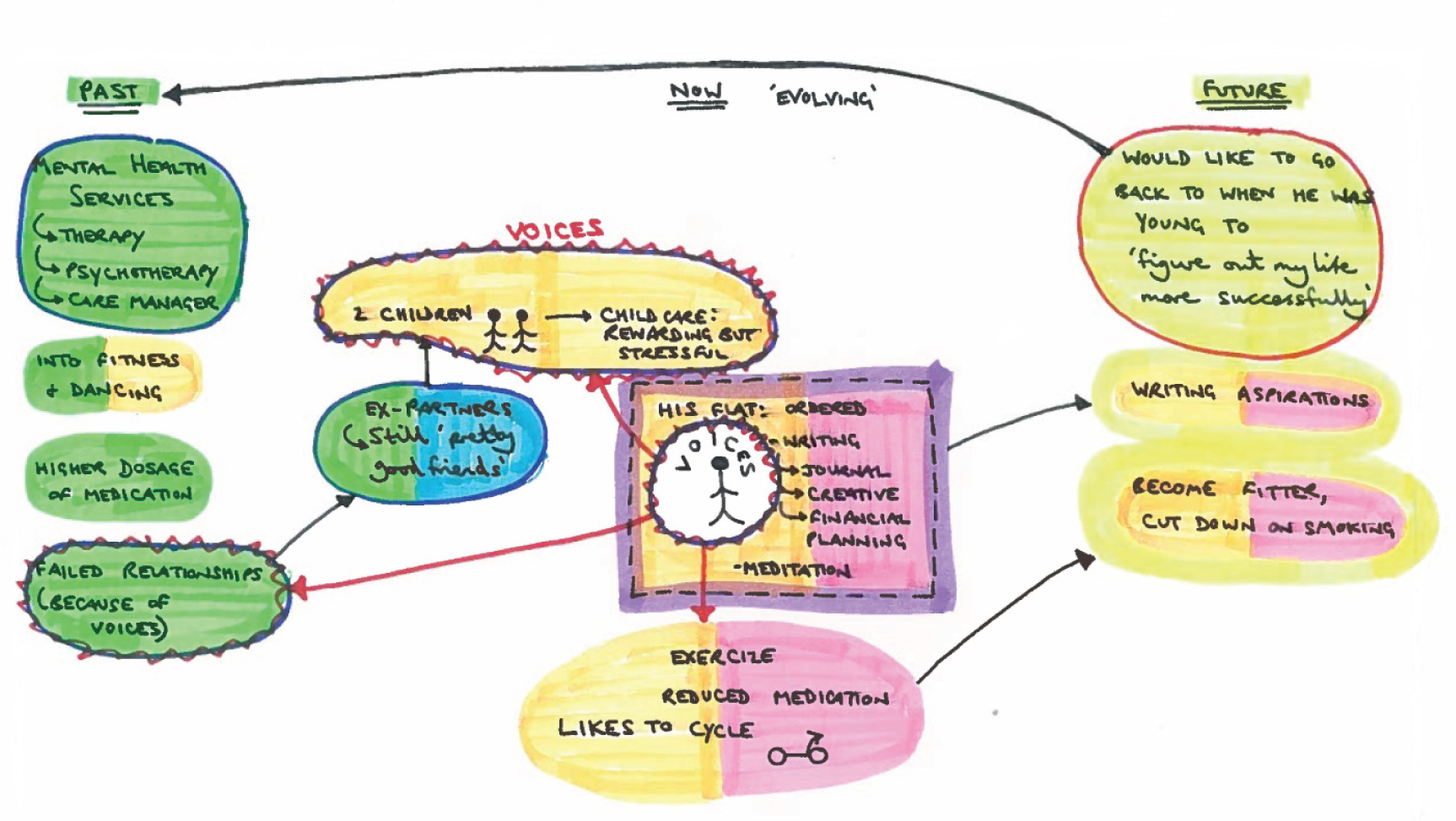
Nick lived alone and had two children, from previous relationships, with whom he was in regular and close contact (Figure 24). At the time of the interview he was proactively involved in the care of his youngest child, and talked at length about the strength of their emotional connection: ‘we play lots and lots and lots together . . . the relationship’s very close, based on quite deep feelings really.’ Nick found child care both rewarding and a source of stress. He discussed a recent experience when they went swimming together when his voices led to him having ‘something of a panic attack’ that ‘went on for several hours’ which he struggled to cope with: ‘I ended up smoking, which I don’t like doing.’
FIGURE 24.
Network map for Nick. Social network size: 13 (second-lowest quartile, mean = 19.91). RGUK score: 13 (second-lowest quartile, mean = 14.2). HRG group: lower score group. SWEMWBS score: 28 (highest quartile, mean = 22.3). See Figure 10 for key.
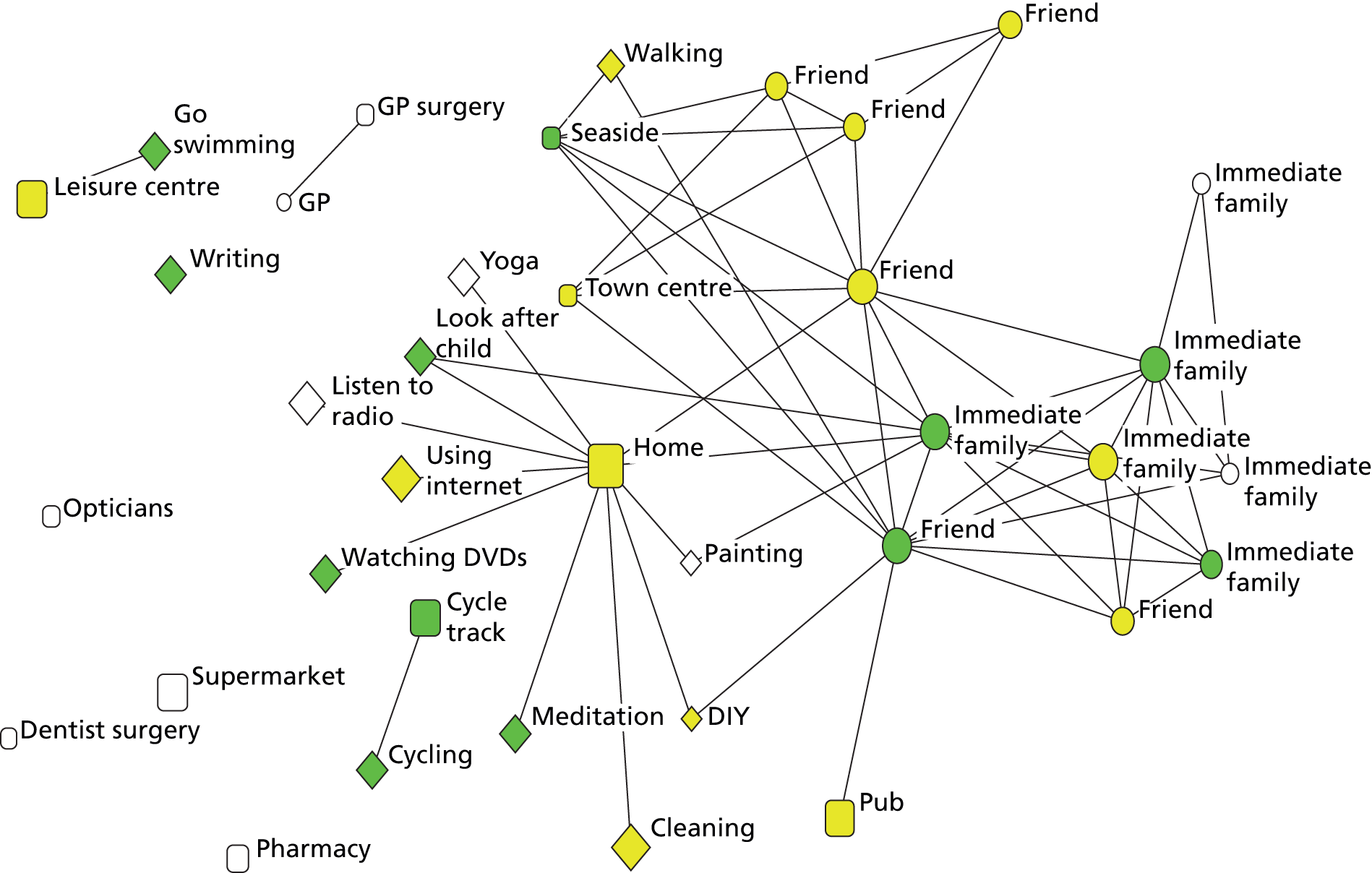
Ability to manage stressors often changes over time and a person’s stage of recovery; some people with SMI rely on social support, whereas others draw more on their own resources. Nick revealed that his network relationships could be a source of stress, and that he dealt with such life stresses largely alone; he did not have mental health practitioners or peer support groups to call on but developed his own active strategies. When he reflected on the network process it was apparent to him that there is a deficit of friendships in his life: ‘it didn’t seem like I knew enough people; I should have more, certainly more friends, really.’ Hence, his self-reliance was at least in part related to having a limited number of friends to call on, and so was out of necessity rather than choice.
As with numerous other participants who were over 50 in the SW, Nick’s contact with specialist services had ended. His mental condition was managed entirely in primary care, although he reported that he rarely discussed his mental health with his GP. He was, however, receiving medication which he believed was important in helping him to stay well. Mental health services had, in the past, featured in his life and he used to receive counselling, although he felt that it outlasted its usefulness.
Certainly over the latter stages I would keep going to talk to my counsellor about my favourite bands, and, um, there didn’t seem any point in staying there any more.
Nick presented himself as having a strong sense of self-identity and routine; his flat was likened to a well-ordered space from where he organised his life in advance: ‘I normally try to plan my day’. His routine for staying well included meticulous financial planning, as well as keeping a journal, which played an important part in developing self-awareness: ‘you get more in tune with the things that actually make sense to you’. Nick also found that having a ‘creative’ outlet had an ‘improving effect’, supporting his well-being. He explained that he wrote poetry, and had some aspirations to get his work published but was apprehensive about how his voices would react.
Having a balance of physical, creative and spiritual activities was important for Nick. Shortly before the interview he had made a conscious decision to cut down his level of smoking and to also incorporate more physical exercise in his routine, which he believed positively impacted on his SMI: ‘I think that being fitter is important to mental illness, the same as the eating well.’ This was complemented by meditation, which featured prominently in his life:
I think it makes you more calm. I think it calms as a mental activity I think it’s emotionally, it’s a nice experience. I think it takes you outside of simply, um, the external world, experiencing the external world and actually gives you an experience which you don’t get in a, most other ways.
However, Nick was also keenly aware that these strategies for staying well were solitary pursuits, and that his social life was restricted, again not always through choice. He revealed that he was keen to join a meditation group but that social anxiety was a barrier to trying this alone: ‘I’d certainly want to take somebody with me. I wouldn’t want to go on my own.’
This illustrated that, although there were a number of introspective, self-directed activities that Nick engaged in on a regular basis to manage his health and well-being, he ultimately wanted to expand this to encompass wider social resources and social interactions, but required support to achieve this. For individuals like Nick, who have limited amounts and sources of health resources within their personal network, and no specific mental health support beyond a GP, it is challenging to identify where any such resources might come from.
Drawing on five areas identified in our literature review (see Chapter 2) that help us understand personal networks, and answer the first study research question, we applied the learning from Nick’s case study in Table 37.
| Key area of literature | What we learnt from Nick |
|---|---|
| Agency and strategies for staying well | The importance of developing a self-directed routine, comprising meaningful activities, was once again underlined; this became increasingly important, but at the same time more challenging to maintain when managing stressful voices. Level of mental distress is a strong driver in shaping appropriate strategies which change over time to compensate for the impact of mental illness |
| Social support | The role of service absence is highlighted. Some people with SMI need support to engage with community resources, and there is a danger that when service contact is minimised people become increasingly isolated and less likely to engage in activities that may aid recovery |
| Recovery over time | This demonstrates how over time, especially when support from mental health services is reduced, people with SMI may have a reduced network and find it challenging to make new connections on their own, placing them at risk of isolation, particularly if they are not employed |
| Stigma | Fear of engaging in new activities, partly because of social anxiety in new situations, in which stigma can also play a part, can be a major barrier for people with SMI developing their network |
| Social capital | People who struggle with managing their SMI and experience stressors, for example hearing voices, often also have a strong sense of personal identity, in this case their own artistic capital, which can provide potential building blocks to facilitate activity- and place-based connections that in time may lever new social capital opportunities |
The commissioner and provider context
The two personal networks discussed above demonstrated contrasting levels of mental health support from services. Here we draw on data from the second round of stakeholder interviews (conducted in summer 2013) to examine how ongoing treatment, support and recovery for people with SMI in the SW site are situated within a wider provider and commissioner context. Particular attention has been paid to challenges and opportunities, and the extent to which there is a recovery-focused culture within that context.
A strong commitment to promoting a recovery-based service
Over the previous 18 months there had been a shift in the ethos and approach to provision in the SW site. The NHS Trust had taken part in a national recovery programme which had given ‘a bit more impetus to how we make our service more recovery focused’ (SSW03, NHS). Recently there had been a renewed effort to embed recovery principles within the organisation and a concerted effort to make commissioning more transparent and fit for purpose:
How we really rebase commissioning around really understanding what’s happening at the coal face, at the front line, for both the people who use our services but also our staff. [Too often in the past] services have been designed and commissioned in dark rooms rather than understanding the impact that those decisions have on people.
SSW02, NHS
The commitment to recovery-focused services at a leadership level was consistent with our practitioner interview data where staff on the ground in secondary care services were working to deliver a recovery model approach while acknowledging the challenges of doing so.
Resource challenges
In terms of promoting a recovery-orientated service in the SW, resources had been an issue. Although the aim was to keep the level of investment and spending constant, the impact of inflationary pressures combined with ‘flat cash’ meant that future available resources were effectively shrinking (SSW02, NHS). As a consequence there was an acknowledgement that ‘it does mean we have to be a bit smarter about how we do things’ (SSW03, NHS). In this climate it was envisaged that third-sector providers would have a key ‘preventative role’ to play which would remove ‘some of the burden of more specialist providers’ (SSW03, NHS). A third-sector leader emphasised that the reality from their perspective was highly challenging, with ‘commissioners expecting more for less . . . or to remodel services on less income’ (SSW04, third sector).
Interest in peer support models was high, and was viewed as both benefiting people with SMI as well as leading to potential cost savings. It was seen as a ‘win–win situation’, as people using services would ultimately get a better experience (SSW02, NHS). Within this context, services were changing their approach and working in more time-limited ways with clients: ‘moving on is much more talked about at the date of entry now’ (SSW04, third sector).
It was noted there was little scope within contracts for additional work that had been done previously. The local NHS trust was reported as having a ‘relentless’ focus on quality, effectiveness and value for money and taking the NHS forward through a combination of consolidation, integration and expansion (SSW05, NHS). Those interviewed indicated that there was potential for new services to be developed in the SW site linked to ‘step up and step down’ provision into and out of hospital. The network development agenda complements objectives to keep people well and out of hospital, making use of resources within personal networks, and the wider community, rather than relying on practitioners and services.
Improving interfacing between primary and secondary care
The need for better joined-up and closer working between primary and secondary care was emphasised and some progress had been made. Those interviewed talked about the importance of a ‘more assertive’ way of managing service users with SMI by ‘improving communication between specialist mental health services and primary care’ (SSW01, CCG and GP). One way in which this had been achieved was by attaching an experienced mental health worker, from a CMHT, to GP surgeries. This initiative had resulted in the broadening of clinical knowledge of local support resources within those surgeries. In one development an entire CMHT had also been relocated into a GP surgery in the SW site. Overall, this had been viewed as a positive development, ‘a bonus is that you can deal with things in the corridor rather than the referral management system’ (SSW02, NHS).
Discharging people into primary care had been achieved more successfully in some parts of the SW site than others. The difference in success was attributed to how confident GPs were that secondary care would be able to take people back quickly, when necessary. In order to address this situation, a single point of access electronic referral system for GPs was set up earlier in the year (2013) to provide a more co-ordinated approach; it had already reduced waiting times. However, the communication interface was still a concern; it was viewed as a priority area to address because GP confidence in the mental health system was easily undermined.
Promoting mainstream resources and recovery in the community
A key goal for services was encouraging people with SMI to engage with a wider range of resources in the community. One way this was being promoted was by looking at opportunities presented through the personalisation agenda, encompassing direct payments and personal health budgets in order ‘to support people having a much more individualised approach to their care needs’ (SSW05, NHS). A pilot had been also been agreed with the local authority to provide people with ‘independent support and advice to help them make decisions about where they want to purchase their support from’ (SSW05, NHS). This independent advocacy role was being provided by a third-sector organisation, which was seen as grounded and connected, and thus ‘more likely to be more knowledgeable about what’s out in the community than an individual member of our [NHS] staff’ (SSW03, NHS).
Their ability to identify low-cost useable resources was also emphasised. In contrast to traditional mental health daytime activities and opportunities, this approach was regarded as adding value by generating a more enterprising culture: ‘building the market a little bit and helping people deliver much more creative solutions’ (SSW05, NHS).
The theme of building independence was strong within the practitioner data set. Care co-ordinators in particular were concerned not to create dependent relationships with services. This was the starting point for all therapeutic relationships in the recovery-focused person-centred model.
The London site
Structural background to the London site
Our second site was an inner-city London borough. The borough’s JSNA for 2012 estimated just under 200,000 people registered with GPs. The population was characterised by a large proportion of young working-age residents, high levels of migration into and out of the borough, and ethnic and cultural diversity. There were also large health inequalities.
The study recruited from across the entire borough, working from 9 out of 29 surgeries and 3 secondary care teams. GP MH8 QOF data for 2012 showed that the prevalence of SMI within the borough was 1.2%, which is higher than the prevalence in London overall and higher than the mean prevalence in England. The male prevalence is higher (1.3%) than the female prevalence (1.0%) of SMI. The 2012 JSNA estimated there were 2,400 people living with SMI in the borough. The London site had one local authority and one mental health NHS trust, but both structures covered a larger region of London than one borough. At the time of study data collection there was one PCT and under the new structure there will be one CCG.
How were personal networks composed in London?
The most common network type in London was diverse and active, while fewer participants had family and stable networks in this site, as summarised in Table 38. We found less stability, but higher numbers of new place connections and wider contacts in social networks, such as colleagues and acquaintances.
| Site (number of participants) | Diverse and active networks | Family and stable networks | Formal and spare networks |
|---|---|---|---|
| London spread of network types % (n) | 49.3 (37) | 14.7 (11) | 36 (27) |
| Mean social network size (SD) (F = 12.26***) | 25.0 (11.3) | 21.3 (6.9) | 13.5 (6.3) |
| Mean number of family contacts (SD) (F = 5.36**) | 5.8 (17) | 7.6 (3.2) | 3.6 (2.8) |
| Mean number of friends (SD) (F = 3.77*) | 7.2 (5.6) | 7.4 (5.7) | 4.0 (3.4) |
| Mean number of wider contacts (SD) (F = 15.98***) | 7.5 (5.3) | 3.9 (2.6) | 1.7 (2.0) |
| Mean number of practitioners (SD) | 4.4 (2.8) | 2.4 (1.6) | 4.3 (2.7) |
| Over 50% waking time spent at home (χ2 = 19.64**) | 32.4% | 63.7% | 81.4% |
| Mean number of community place connections (SD) (F = 13.1***) | 7.0 (2.8) | 6.2 (4.0) | 3.5 (1.8) |
| Mean number of meaningful activities (SD) (F = 13.68***) | 7.7 (2.6) | 7.7 (3.3) | 4.4 (1.9) |
| Mean % of activities unstructured (F = 11.30***) | 11.4 | 13.6 | 33.9 |
| Mean % of activities social (F = 8.55***) | 54.1 | 54.5 | 28.2 |
London participants spent significantly less time at home than SW participants and connected to places more frequently (Figure 25). The community settings that London participants connected to most were workplaces, green and outdoor spaces, shops and markets, spiritual settings, social recreation settings, physical recreation settings, libraries, and family and friends’ houses.
As shown in Table 34, significantly more mental health settings, education settings and social activity or interest groups were mentioned in London. Significantly more participants also engaged in volunteering, education, training or study, and reading, and a higher number of social activities were mentioned. However, a larger number of unstructured activities were also mentioned. The mean number of physical activities was lower in London, perhaps because fewer outdoor spaces were available and costly gyms were often the only alternative. Levels of physical fitness were not significantly different by site and the number of participants who mentioned at least one physical activity did not significantly differ.
FIGURE 25.
Frequency of connection to places in community.

FIGURE 26.
Ethnicity by site.

London participants had significantly lower access to social capital and this included access to fewer domestic resources (t = 3.24, df = 145.5, p < 0.01) and personal skills (t = 3.38, df = 146.90, p < 0.01). Access to health resources did not significantly differ but in London participants accessed a significantly higher percentage of these resources from practitioners, 20.1% compared with 9.8% in the SW (t = 2.74, df = 144, p < 0.01). London networks were significantly more ethnically diverse, as shown in Figure 26. Psychotic disorder/schizophrenia and other psychoses were more common diagnoses in this site.
We found that barriers to getting the most out of networks differed by site (Figure 27). Participants in London mention mental illness, money, stigma, medication and physical health more frequently, while transport, isolation and internal factors such as lack of personal motivation and self-confidence were more frequently mentioned in the SW.
FIGURE 27.
Barriers to getting the most out of networks by site.
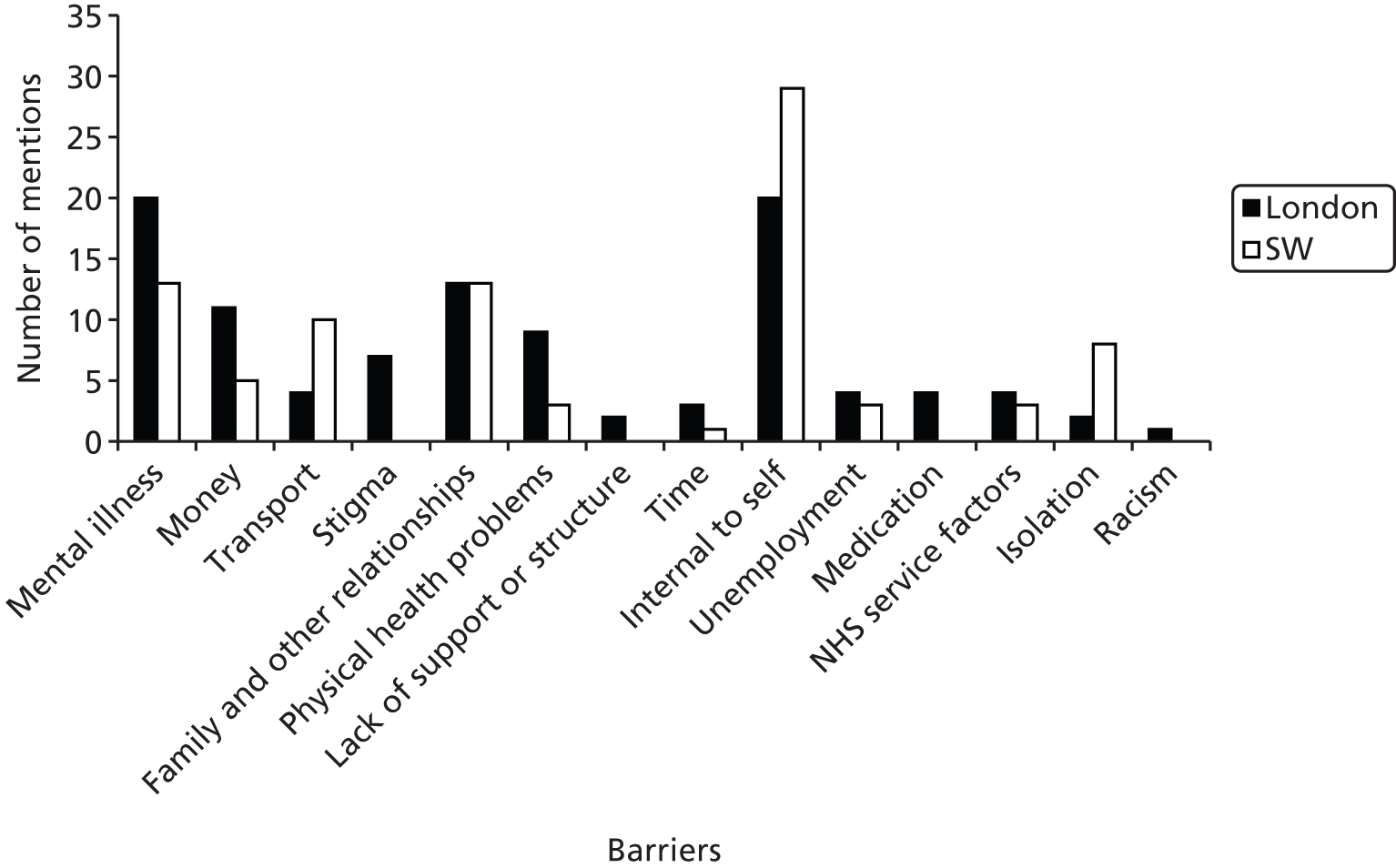
A detailed consideration of two networks
London personal network key characteristics: Raj
Raj (SUL07) illustrated a formal and sparse network, with long-term use of mental health services but limited access to social capital and wider social resources. Raj was an Asian man in his forties, diagnosed with schizophrenia, unemployed and living on his own. Although he identified only eight people in his network (Figure 28) in the initial interview, he described it in largely satisfactory and manageable terms as ‘reliable’, ‘safe’, with ‘zero chaos’.
FIGURE 28.
Network map for Raj. Social network size: 8 (lowest quartile, mean = 19.91). RGUK score: 13 (second-lowest quartile, mean = 14.2). HRG group: lower score group. SWEMWBS score: 23 (second-highest quartile, mean= 22.3)
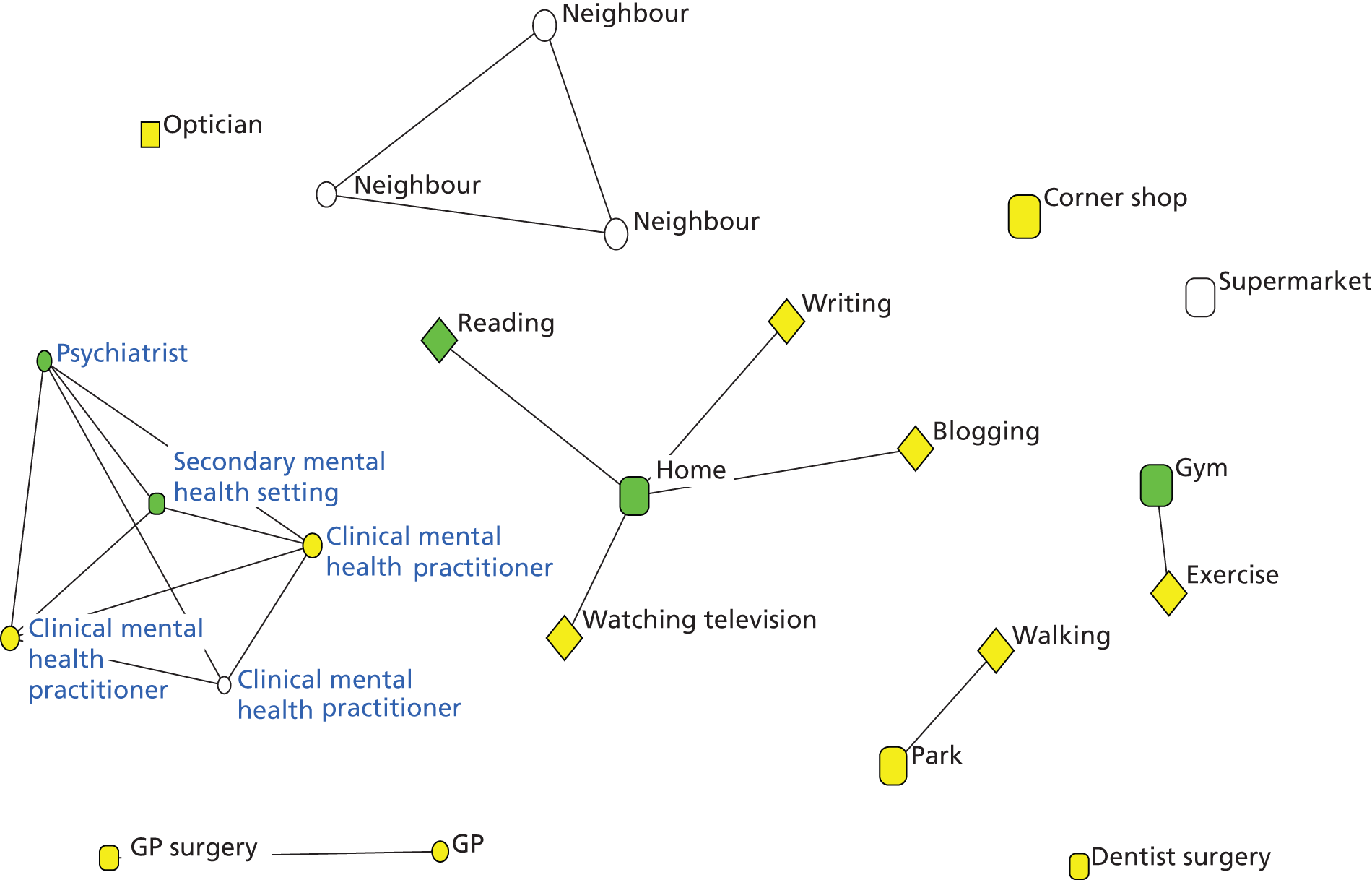
In the analysis for Raj (Figure 29) the past was shown as a strong influence on the present, with very limited reference to the future. There was a sense that Raj was surrounded by a network, partly shaped by his choices and partly by circumstances; in emotional terms, past and lost relationships constituted key features.
FIGURE 29.
Analysis using within-case process for Raj.
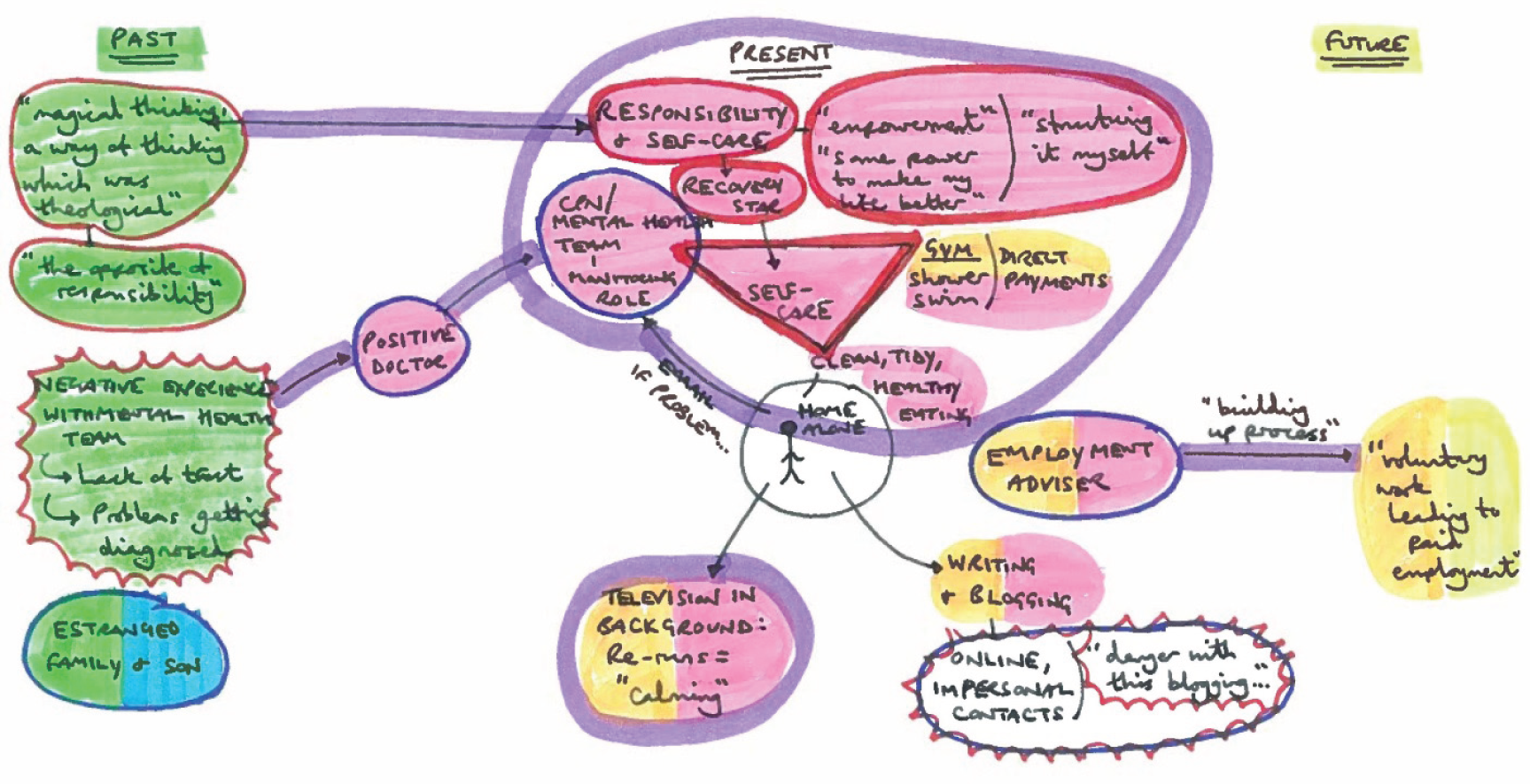
Outside the realm of health-care professionals his network was sparse. He had children but was estranged from them when they were young, but still thought of them as ‘babies’ instead of grown up, and as a consequence found it challenging to reconnect: ‘these types of emotions are not relevant now.’
Raj had been in contact with mental health services for over 20 years, and had found the ongoing level of insight and expertise he received useful: ‘professional expert cognition’ helped to identify things ‘ordinary people don’t’. He explained that he would sometimes e-mail a mental health worker during the night; writing his feelings down was a useful way of working through his ‘racing thoughts’, and collaboratively identifying ‘triggers’.
Raj explained that mental health practitioners supported him to develop active strategies to manage his mental illness on a day-to-day basis. These individuals were a dominant feature in his network, forming five out of his eight contacts (see Figure 28). Taking more responsibility and self-care had become important aspects of Raj’s life; however, he underlined that he required ‘a bit of a nudge’ from health-care professionals to enable him to maintain a sense of routine. Much of this structure came from the Recovery Star approach, which he said empowered him to be more proactive and ‘make my life better’. He explained that he had become motivated to eat more healthily, which in turn ‘impacts on my mental health so that I don’t spiral’. This was in contrast with the past, when his life was dominated by ‘magical thinking, a way of thinking which was theological’, which was ‘the opposite of responsibility’.
If I think I’m feeling depressed or something like that then I see on the star that there’s something that I can do; there are some actions I can take. For me, that self-care this includes, for example, shaving, going to the gym, maintaining a good appearance, washing my clothes.
Support from Raj’s mental health team was complemented by an employment adviser, who helped him to engage in a ‘building-up process’. In the future he aspired to see ‘voluntary work leading to paid employment or something of that sort’.
Although Raj expressed satisfaction at the support he was receiving, and the role such support played in helping him to become more self-reliant, reflecting on his past he cautioned that ongoing contact with mental health services can promote a sense of ‘client-ism’ (dependence as opposed to independence) or even resentment on the part of the service user, an ‘us against them’ attitude.
We found that home space was an important feature across networks. Raj discussed spending much of his time at home, and that his self-esteem had improved since he took charge of his home space, which helped to create more order: ‘I’ve got the confidence, because for example my house looks nice. I’ve got clean clothes, I’m having a hot shower every day, I’m shaving . . .’ This was in stark contrast with the past, when it was ‘a complete tip at home’ and he was ‘going out and keeping a façade’.
In addition to his self-care routine, writing played an important function in structuring Raj’s home life, and provided a key emotional and artistic outlet. He explained that the process of editing was ‘the absolute key’, because ‘it gives me some insight into what I was thinking at that time, what sort of things cause, like a slippage’. He also regularly blogged online, but approached this ‘virtual type of contact’ with an element of caution: ‘you can really see how there are hate mongers out there; there are people who are really not nice’.
While at home Raj also found watching, or having in the background, certain television programmes beneficial for his mental health because of the element of familiarity: ‘it’s calming’ he reflected.
Yes, because I think what’s happening is that my brain is saying that it’s matching, everything’s matching and anything, for example, I like watching reruns, programmes like Friends, I’ve seen the episode 100 times but, for me, that’s a very . . . it happens in the background.
Living alone and having time structured by lone activities in the home were key features of Raj’s network. Because of feeling anxious about the unknown, he faced barriers in accessing unfamiliar places, as well as engaging in new activities outside the home; he needed support from practitioners to achieve these. Raj had been given help to attend a gym, which was funded through direct payments and was an important part of his self-care routine, because ‘it gives me a lot of motivation for appearance, I’m very comfortable in that environment’. He added that being encouraged to go to the gym bolstered his sense of self-confidence, providing him with a sense of purpose and motivation: ‘every morning when I wake up I’ve got something to do and there’s something I can immediately do which will make me feel good about myself’.
We also observed that Raj’s network was not necessarily place-based and he could have potentially lived in another location and yet described similar connections and strategies. It is not clear how far London as a place shaped Raj’s personal network; it was more likely to have influenced his personal strategies for maintaining well-being and illness management.
Drawing on five areas identified in our literature review (see Chapter 2) that help us understand personal networks, and answer the first study research question, we applied the learning from Raj’s case study in Table 39.
| Key area of literature | What we learnt from Raj |
|---|---|
| Agency and strategies for staying well | Although people like Raj are often dependent on mental health services for formulating effective well-being strategies, there are practical ways individuals can take more responsibility. In this example, direct payments were used to access a local gym |
| Social support | The experience of living alone with SMI can be socially isolating and lacking in structure; services need to be mindful, as both features hinder recovery. Where social support networks are small, services can have a role helping people build up their informal support network |
| Recovery over time | Routines developed gradually over time such as self-care can form important building blocks for recovery. Small steps are important for skill-building and fostering self-confidence and agency |
| Stigma | A consequence of ongoing support from mental health services can leave people feeling disempowered and stigmatised, together with resentment, sometimes viewed as an ‘us against them’ mentality |
| Social capital | Home can dominate the lives of some people with SMI; when considering building social capital this can be daunting if the starting point is low. Raj had limited social contacts providing bonding capital, with no family or friend contacts mentioned |
London personal network key characteristics: Áine
The experiences of the second participant, Áine (SUL76), illustrated a contrasting experience of someone diagnosed with schizophrenia. Figure 30 provides a pictorial summary used in the analysis. Áine had also experienced long-term contact with mental health services, for over 30 years, but there was greater access to wider community resources, as well as more independently formed friendships. She was a white Irish woman in her fifties who engaged in regular voluntary work, and described her network in positive terms: ‘friendly’, ‘shared interests’ and ‘loyal’.
FIGURE 30.
Analysis using within-case process for Áine.
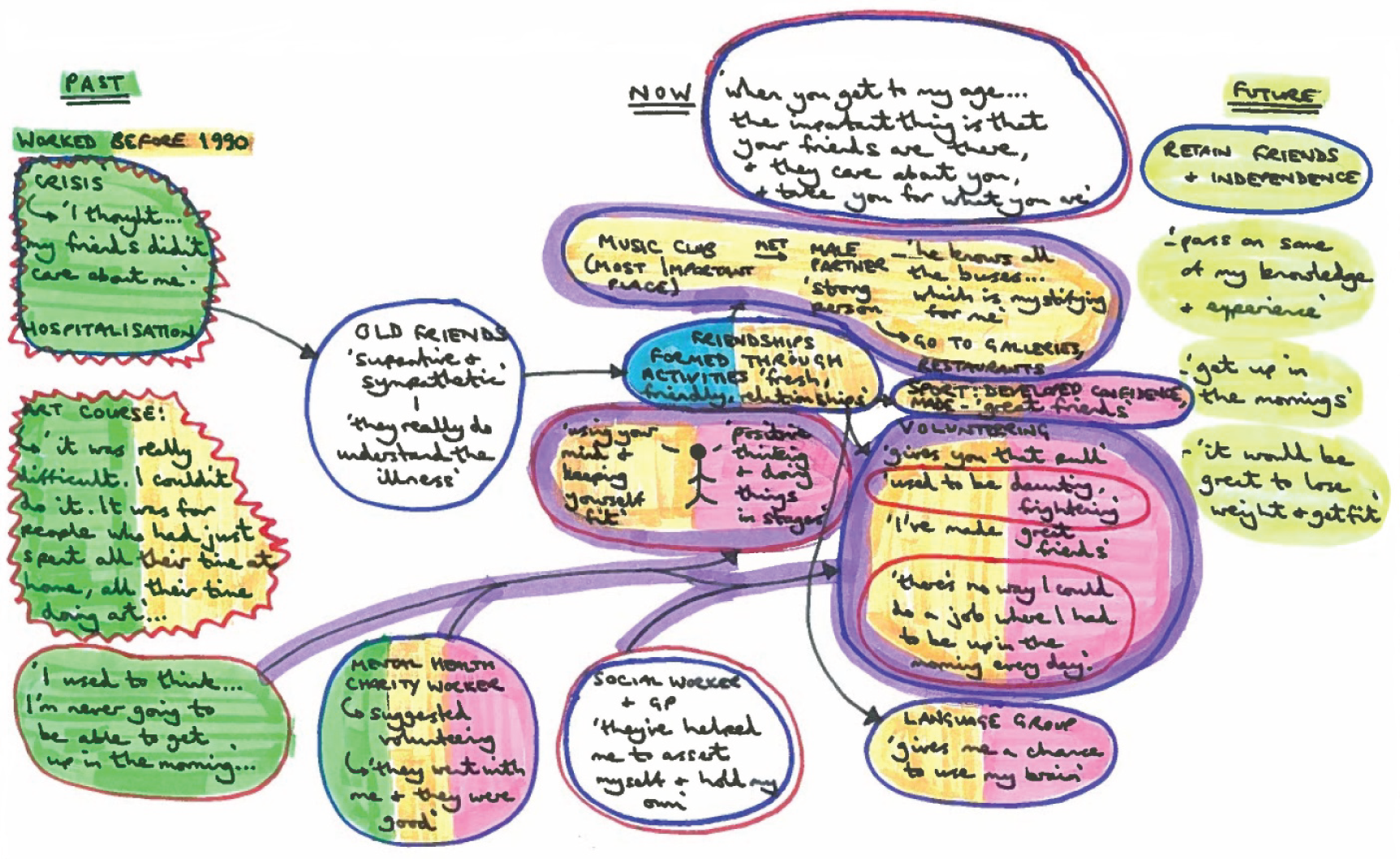
It is important to acknowledge that, although some of the data in the report show living with schizophrenia can inhibit people’s networks (such as restricting their size), this is not always the case (Figure 31).
FIGURE 31.
Network map for Áine. Words used to describe network: ‘friendly’; ‘shared interests’; ‘loyal’. Social network size: 30 (highest quartile, mean = 19.91). RGUK score: 17 (second-highest quartile, mean = 14.2). HRG group: higher score group. SWEMWBS score: 29 (highest quartile, mean = 22.3).
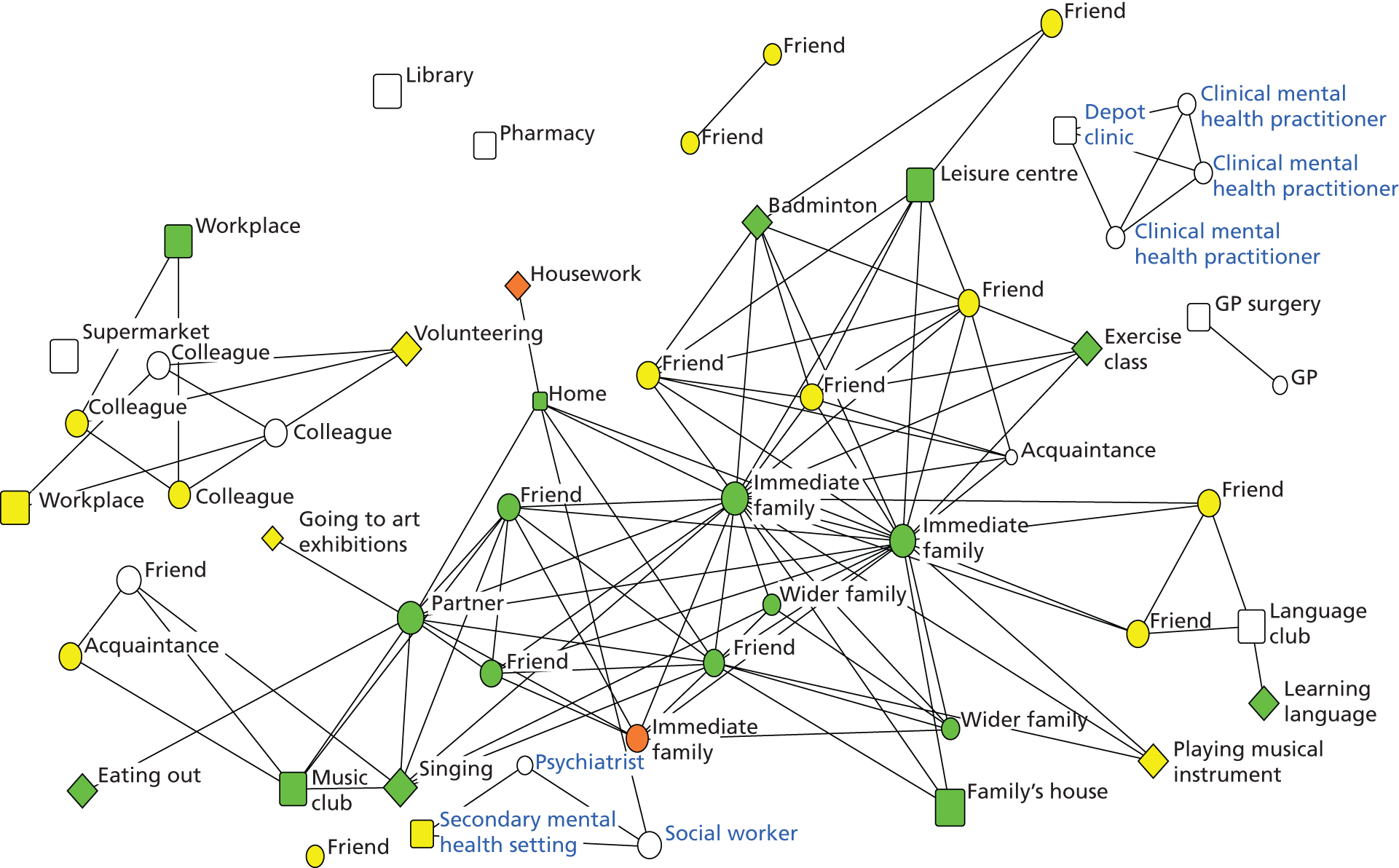
Áine attended a wide variety of places in the community; the ‘most important’ was a music club she regularly attended run by one of her friends, which was also where she met her partner. She described him as a ‘very, very supportive strong person’ and he helped to drive her network development; they regularly visited art galleries and museums together. He also assisted her in understanding bus timetables, an area she found challenging, facilitating her access to public transport, which proved essential for her in terms of accessing resources in the community.
I mean, I’m still terrible on the buses, but he knows all the buses, which is mystifying for me, and I’m only just beginning to understand that. Um, but um . . . that has been very, very good, yes. It’s been a real blessing.
Áine also had a number of longstanding friends who had been ‘supportive and sympathetic’ and ‘really understand the illness’. They had been ‘loyal’ and stuck by her when she was hospitalised because of her mental health. She also developed friendships with other people with experience of SMI; when she was in hospital she met some ‘really lovely people’. In the qualitative interview the extent to which she valued the friendships in her life was underlined throughout the session.
When you get to my age . . . the important thing is that your friends are there, and they care about you, and take you for what you are.
Áine’s story showed that the value she placed on friendship was reflected in her network maps, as not only did she maintain contacts with people from the past, but her network-building activities in the present generated new valued social contacts: volunteering, language class, music, socialising, badminton and swimming.
In terms of contact with services she had a close relationship with her social worker and GP: ‘they’ve helped me to assert myself and hold my own’; they also encouraged her to take up productive activities. Áine stressed that she aimed to improve her sense of well-being by focusing on both her physical and mental health: ‘using your mind and keeping yourself fit’. This holistic approach was complemented by ‘positive thinking and doing things in stages’.
At the time of the interview Áine had not been in paid employment for over a decade but had tried a number of activities over the years; some she developed more of an affinity with than others. Such meaningful activities, particularly volunteering, provided her with routine and structure, which, alongside close personal relationships, helped to enhance her sense of positive well-being. One exception was an art course, which she attended but did not enjoy, finding it ‘really difficult’; she reflected that ‘I couldn’t do it. It was for people who had just spent all their time at home, all their time doing art’. She tried other pursuits with more success, which highlights the importance of individuals being open to trying a variety of activities to find out what works in advancing their personal recovery journey. Playing badminton was a past time that she said she benefited greatly from: ‘the sports centre is really beautiful’; she explained that it helped to keep her fit and also helped to develop a sense of ‘real confidence’. In terms of social aspects she had made some ‘great friends’ through the sport. Another important activity in her life was attending a language group, which she said ‘gives me a chance to use my brain’. Áine illustrated how engaging in new activities, and not being afraid of setbacks, helped to generate new friendships formed around shared interests.
I suppose it’s how the friendships formed, some of them, through an activity. Um, yes, I suppose that’s true, and I think it’s more interesting if, um, you . . . you have a common interest. You do things together, that is lovely.
One of the main barriers she cited in her life was tiredness: ‘I used to think . . . I’m never going to be able to get up in the morning’. A worker for a local mental health charity suggested she should try volunteering and helped to facilitate this: ‘they went with me and they were good’. This built on her key interests and skills, and having support to make the first step was the route to success. She volunteered, at the time of the interview, at a school. Initially Áine found this to be a ‘daunting’ and frightening prospect, but had developed strength of character: ‘it gives you that pull’. She also benefited socially from her volunteer work: ‘I’ve made great friends with the teachers there . . . staff there are lovely, and the kids are friendly’. An important aspect was the flexible hours: ‘there’s no way I could do a job where I had to be up in the morning every day’ and she added if you are late ‘nobody minds, if you turn up it’s a bonus’.
Áine demonstrated wide-ranging interests, was content with her network and felt fortunate to have a group of supportive friends and practitioners in her life. There was a strong sense that the desire to engage in the key activities in her life, such as a music club and volunteering work, were self-motivated. However, it was apparent too that she needed help to maintain these structures: in terms of volunteering there was a flexible arrangement where she did not have to adhere to a rigid timetable, and she was also dependent on her partner to facilitate access to public transport. There was an over-riding sense, though, that diversity of activities and friendship groups in her network provided her with a degree of protection, helping her to avoid over-reliance on any particular elements of her network, and there was stability combined with a definite feeling of optimism for the future.
Drawing on five areas identified in our literature review (see Chapter 2) that help us understand personal networks, and answer the first study research question, we applied the learning from Áine’s case study in Table 40.
| Key area of literature | What we learnt from Áine |
|---|---|
| Agency and strategies for staying well | People with SMI often have a strong sense of internal motivation, but may need flexible and supportive structures to facilitate meaningful routines. Engaging in shared activities can be a positive way to develop a sense of self-identity |
| Social support | A balance between informal and formal networks support may be key. Everyday informal support, in Áine’s example being helped by her partner to understand bus timetables, complemented more formal service support. Practitioners should encourage people with SMI to engage in new pursuits and help reduce barriers faced in accessing mainstream community resources; provision of subsidised public transport is essential for this |
| Recovery over time | Engaging in a range of activities over time is essential in developing a sense of identity and meaning; people with SMI should not be afraid of trying new things or be disheartened by setbacks along the way. The result is a more durable network less vulnerable to collapse in the future |
| Stigma | The perceived absence of negative stigma can be important for people with SMI, as it means that the barriers to social engagement are reduced. In Áine’s example, not feeling stigmatised enabled her to engage in new activities and she did not feel demotivated, or judged, by setbacks on the way |
| Social capital | Developing a sense of connectedness and social capital through a diverse range of activities can lead to a more varied and durable network |
The commissioner and provider context
Here we draw on data from the second round of stakeholder interviews (conducted in summer 2013) to examine how ongoing treatment, support and recovery for people with SMI were situated within a wider provider and commissioner context in one London borough. In London, the assertive discharge to primary care had not begun systematically and thus more of our study population received secondary mental health care input than was found in the SW.
Transition from secondary to primary care
The London context was dominated by the agenda to transfer people with SMI away from specialist mental health team support to an enhanced primary care-based service. At the time of the interviews it was at an early stage of implementation and changes to ‘culture, attitude or practice at GP level’ (SL01, mental health commissioner).
The CCG member interviewed said that he was actively ‘looking at models to allow primary care to absorb extra capacity from community mental health teams’, which involved a detailed review of case notes to establish who might be appropriate to transfer (SL02, CCG and GP). The imagined projection was that at first there would probably be five or six extra people with SMI per practice, which was not regarded as a ‘huge demand’; however, it was emphasised that ‘the GP would be expected to look after the patient with more continuity’ (SL03, GP and mental health lead). Seeing the same GP was regarded as preferable to seeing different GPs, while the need for longer appointments was stressed to address the needs of people with SMI.
One of the main implications of this change was the necessity to ‘upskill’ health-care professionals based in primary care (SL02, CCG and GP). It was envisaged, however, that there would be extra resources available to GP practices to cope with the discharging agenda, for example an extra CPN per practice, or for a group of practices, providing ‘essentially more expertise to see and engage with patients’ (SL03, GP and mental health lead). At the time of the interviews the expectation was that this CPN would be ‘co-located’ in general practice as opposed to being based with the CMHT (SL02, CCG and GP). However, a detailed strategy for managing transition was not in place.
The transition to a more primary care-based service was seen as having a big impact on traditional services and ‘on those who are used to being managed in the service over a long period of time’ (SL06, NHS). Future care packages would be developed around PBR clusters measured against the length of stay principle, ‘rather than keeping them [service users] on ad nauseam for no particular reason’. It was also emphasised that when service users reached the end of specific interventions they would be discharged, although risk would be taken into account (SL06, NHS). Some clusters required particular ‘therapeutic input’, which was why they were still being managed by mental health teams and not primary care, and there was a dilemma concerning ‘what we do about these people’ (SL06, NHS). Barriers to discharge were also regarded as coming under increased scrutiny in the future (SL06, NHS).
The local third-sector provider identified the primary care discharge agenda as ‘something we need to respond to’, and at the heart of their evolving strategy (SL04, third sector). In anticipation, the previous year, they developed an advice and information service, a single point of access at the heart of GP surgeries, so that they could refer to non-clinical community services, allowing people to work towards recovery through non-clinical interventions. The aim of the service was ‘that GPs with one phone number can refer people to our service to deal with the psychosocial elements of their mental health’ (SL04, third sector). This service was seen as plugging a huge need, as it was stressed that links to available resources must be widely promoted to primary care practitioners to ensure effective and timely usage.
There is no way that GPs are going to be able to navigate and find their way through the literally hundreds of voluntary services in the borough, so what they need is a single point of access that will allow their patients to work towards recovery with non-clinical interventions.
SL04, third sector
Interviews highlighted potential to develop preventative services going forwards which ‘aim to stop people turning into service users’ with the focus on promoting a holistic approach (SL04, third sector). In terms of CMHTs, it was envisaged that there would be opportunities for developing new services, but the vital question was also raised of ‘how we tap into the rest of the system’ (SL06, NHS). This was consistent with the SW, where the agenda of assertive discharge and cost savings were driving innovation, and the search for new solutions to deliver support to people with SMI, from within and beyond the mental health system, was deemed crucial.
Resource implications
From a commissioning viewpoint, savings were seen as a ‘whole system concern’ and were not regarded as being confined to mental health services: resources across the community would be impacted (SL01, mental health commissioner). Although it was envisaged that the newly formed CCGs would have much influence in terms of budgets and spending, a practising GP and member of the local CCG emphasised that ‘general global cuts is the issue’, with the result that provision of all services would be affected (SL02, CCG and GP). They also added that there was a ‘particular concern that mental health gets deprioritised’ and, in effect, ‘put to one side’. This was a concern that has frequently been voiced in the mental health sector, where health-care spending has often lagged behind the global burden of disease. Across the time period for this study, community resources in the London site had closed and programmes ended.
Mental health strategy
A mental health strategy in the London site was notable by its absence. In summer 2013 there was not a borough-specific mental health strategy in place, though there were transformation programmes and discharging to primary care was a key priority. The interviews took place during a ‘transitional period’ when organisations were ‘finding their feet’ (SL02, CCG and GP). The CCG had only been operating for two months at the time of the interviews, and there was ‘not a single coherent plan or strategy’ in place (SL02, CCG and GP). The concern was that this was a rapid period of change, happening in a strategic vacuum. There was no co-ordinated approach to building the well-being of the population. The immediate priorities facing CCGs were secondary and acute care, ‘big contracts that were left over by the PCT’ (SL02, CCG and GP). In the face of huge changes, such as the transition to CCGs, ‘strategic thinking has become secondary to doing what is necessary’ (SL04, voluntary sector). Overall, the lack of a coherent mental health strategy was a cause for concern raised by the interviews, with no strategy in sight until 2014.
Chapter 8 The community health network approach
In this final analysis chapter we undertook two further steps of synthesis, to understand the potential roles of practitioners in the personal networks of people with SMI: one element of the study’s research objectives. We focused on this aspect to assess the application potential of the CHN approach. If there were indications to suggest it could be useful for recovery-focused mental health practice, it would require additional development and research. Should further work be undertaken to develop an evidence base to support connection-building strategies?
How did people with severe mental illness use their personal networks to support well-being?
Connections to social resources through people, places and activities were developed through agency within individuals themselves and those around them, but these connections were mediated by external drivers and constraints. A key finding in this study was the heterogeneity in networks reflecting differences in personal interests and capabilities as well as variance in perceived and actual local resource opportunities. For example, 1449 places were mapped in the study and most networks were not restricted to mental health connections; we had to create 14 categories to code the 958 different activities mentioned. The three network types generated by the cluster analysis provide a different lens for seeing the lives of individuals with SMI. The clustering shows that network characteristics were linked in meaningful ways. The clusters provided a way of seeing the diversity of individuals based on the lives people were living which can complement the focus on diagnosis, medication and risk management. As emphasised by the LEE analysis (see Appendix 1), importantly, many factors influencing the network types were open to change.
On the whole, our SMI population maintained connections which were manageable and coherent to them but this involved varying levels of active decision-making. Some people drove changes that shaped their lives, others sought to maintain the status quo on a daily basis, while others showed limited agency. Strategies for managing connections differ greatly: family can be the centre of a person’s recovery journey, empowering and supporting the management of well-being, or family relationships can become unhealthy and difficult to manage. The extent to which people disguise or disclose their SMI varies, as does personal acceptance or rejection of diagnostic labels of mental illness. Some prefer active, structured pursuits while others favour unstructured activities. Maintaining the status quo can mean formal and sparse networks that lack resources but are manageable and less stressful, stable family networks with large parts of the day spent at home, or networks that thrive on developing wider connections. The crucial aspect is that routines should be not only appropriate to the individual, but directed by them: practitioners can help make them manageable but what they value as meaningful must come from the individual.
In addressing the role of practitioners we developed a framework to reflect on the way people made use of agency, and how practitioners can support this (see Figure 32). This brings us to emphasise heterogeneity in the sample again. There were people with SMI making active choices and exerting control in their lives, which were not overwhelmed by wider structural factors, while others found this much more difficult. Work featured strongly in the data as a key influence shaping identity, impacting on well-being (being in employment and lack of employment) and influencing network-building. In Figure 32 we suggest a mediating role for practitioners. As we have stressed already, meaning and direction must come from the individual themselves, but practitioners have a vital connection-building role. Most importantly, they can show how connectedness (relationships with others, meaningful activities, routines that involve accessing different places) is central to recovery; if people with SMI are asked only about medication compliance and relapse plans, how will they come to value social resource within their informal social support networks and themselves as a key support? They can also help to develop flexible, balanced routines which support individuals, encouraging them to engage in previous activities, and can act as a network bridge linking individuals to new potential opportunities as well as seeking to reduce or overcome barriers. The mediating role shown in Figure 32 requires specific skills that those working in mental health should be able to tap into, or could be trained to use. Psychiatrists interviewed in the study acknowledged that if they were to work in a network development role they would need specific training. There would be cost implications for psychiatrists taking on these activities; what we felt was more important was that psychiatrists provide values-based leadership, advocating that social resources and networks are important for recovery, with other team members following up with practical interventions. GPs were keen for other people to take on responsibility for building social capital and providing social support. Care co-ordinators required capacity within their current roles to use their specialist skills for network enhancement work; none of the co-ordinators interviewed felt the way they worked needed to change, but they needed capacity to prioritise these approaches. Third-sector staff and stakeholders leading third-sector organisations emphasised that social recovery and social networks were core business in their services.
FIGURE 32.
The role of practitioners in strategies shaping personal networks.

Figure 32 emphasises two elements of agency used by people with SMI: non-transformational strategies and evaluative and future-forming strategies. The next sections consider each of these in turn.
Evaluative and future-forming active strategies
The extent to which people drive change in their networks, actively engaging in evaluating strategies and forming new plans, will vary from person to person and so too will the degree to which individuals themselves impose constraints on networks. One influence was personal beliefs about the medicalisation of mental illness. We found variation in our study population as to how far people rejected or accepted medical explanations and treatments such as medication: ‘I stick with my labels and don’t use the medical labels and that helps me’ (Michelle, SUSW53). This in turn impacted on the people, places and activities that Michelle chose to engage with, and those that she felt forced to include on her network map. Health and social services were regularly managing relationships with people who struggled to engage with the explanatory models they had on offer to explain SMI, describing their role as ‘giving them options’ (IDSW86, CPN). The balance in many people’s lives on how much choice and control they feel over their networks can relate to health and well-being. When ill-health forces people to engage with supports they did not want, such as medication or inviting health-care practitioners into their home regularly, it can lead to withdrawal if they are particularly concerned to keep their mental illness secret. We heard from people with SMI who actively segment their network to prevent friendship groups learning of their mental health status: ‘[my girlfriend] never looked at me in the same light’ (Kevin, SUL29). That individuals shape their own networks, to varying degrees, was found across this study and for all network types. Often, decisions to engage in new activities which might mean meeting new people and going to new places were based on individuals wanting to improve their life or develop their personal identity; this relates to Emirbayer’s evaluative and future-oriented forms of agency. 23 How far network behaviours were motivated by an explicit desire to increase well-being was harder to disentangle, but individuals gave us clear indications that, however unwell they were, agency in the personal networks of people with SMI is an important force to build upon.
Another example of future-forming strategies related to employment. In London in particular, we found many of those interviewed were on programmes to help them find paid work. Voluntary placements were a stepping stone towards employment; we noted from the network data that those who did voluntary work had fewer health resources. Practitioners might encourage voluntary work for those with fewer network resources to help them venture out into mainstream environments without the emphasis on friendship formation. In the SW case study, Matt (see Chapter 7) was careful to monitor his work, as work-related stress was a trigger for decline in his mental health. Employment builds social capital; it was a very important activity for people with SMI despite the external barriers people faced.
Non-transformational strategies
Individual agency changes over time, moment to moment; an individual’s sense of control over life events, over personal capabilities and over interaction with external structures such as the mental health system or welfare benefits programmes fluctuates. Understanding dimensions of agency in people with SMI was important for helping people set recovery goals.
Strategies which involved a more limited engagement were often based on choices around regular routines. Although we found evidence of 76% taking regular physical exercise including a short walk, we also heard from people who struggle to leave the house. Home as refuge was an important recurring theme in our analysis: for some people it was a base for the planning or enactment of structured activity; alternatively, home-based networks can represent withdrawal and loneliness. We found 66% of people interviewed spent over 50% of waking time at home; understanding the reason for this is crucial. Our analyses suggest that balance was essential: an over-reliance on unstructured time at home alone could lead to lower well-being and isolation; conversely, a strenuous focus on goal-setting was not appropriate for some people with SMI. Routines in leaving the house for shopping or visiting the library provided important structure for this group; they are examples of activities that provided bridging capital which in time may be cultivated further. For people who experienced social isolation, our evidence suggested that weaker ties or relationships, which often required limited active engagement to maintain, could greatly enhance well-being, serving as potential ‘building blocks’ for developing closer relationships. Practitioners, family members and friends should look for clues to how they can best empower individuals to become more engaged in strategies to manage their networks. We recognised that home can act as a network blockage, limiting people’s ability to move forward with other goals while home remained an obstacle; practitioners could begin with home space, as the network anchor, in any assessment of potential connection-building blocks to wrap new goal-setting around.
Availability of resources
Each individual varies in terms of the number of perceived and actual resources available to them in the form of people, places and activities. The great majority of social ties that individuals had were valued as beneficial to well-being. We found that even those contacts rated negatively can improve access to social capital. Some social networks were extremely small, with features of loneliness and social isolation, and others seemed fragile, with reliance on one key individual. Across all network types the quality of ties, rather than the number, was found to be the most beneficial. Having at least one close relationship was important because this provided access to social resources, as found in our RGUK regression model. Our population show agency in developing positive relationships and removing or limiting negative ones. Activities were used to provide meaning, identity and structure in lives, and those which were social also helped to build an individual’s social network and social capital resources. Places provided access to resources for well-being; they could deliver therapeutic benefit in their own right as pleasurable spaces to be in. We found on the whole that both our study sites had community resources of benefit to individuals with SMI, but individual barriers or lack of awareness of them reduced access.
The most resource-rich networks that participants had developed were those which were either diverse and active, with connections built through hobbies and social activities, as well as employment and volunteering, or family and stable networks where the presence of family offers the majority of resource provision. Neither network type will be ideal for everyone; the former may be difficult to maintain during illness and the latter was possible only where ties to family were available and desired. Formal and sparse networks were those where well-being and access to resources were lowest, and yet at certain points in an individual’s life they may be the only possible, or the least harmful, type of network to maintain. What will be important for practitioners will be working out which network type suits which of their clients at any point in time and the reasons for this. We acknowledge that a larger population sample and in different areas of the country might identify different network clusters and more network clusters. We suggest that a modified version of the CHN approach may offer a useful framework for identifying key features of networks, and we have produced a draft template to illustrate the type of questions that would be useful to ask to understand network indicators and network goals for an individual (Figure 33).
FIGURE 33.
Network development plan (draft).
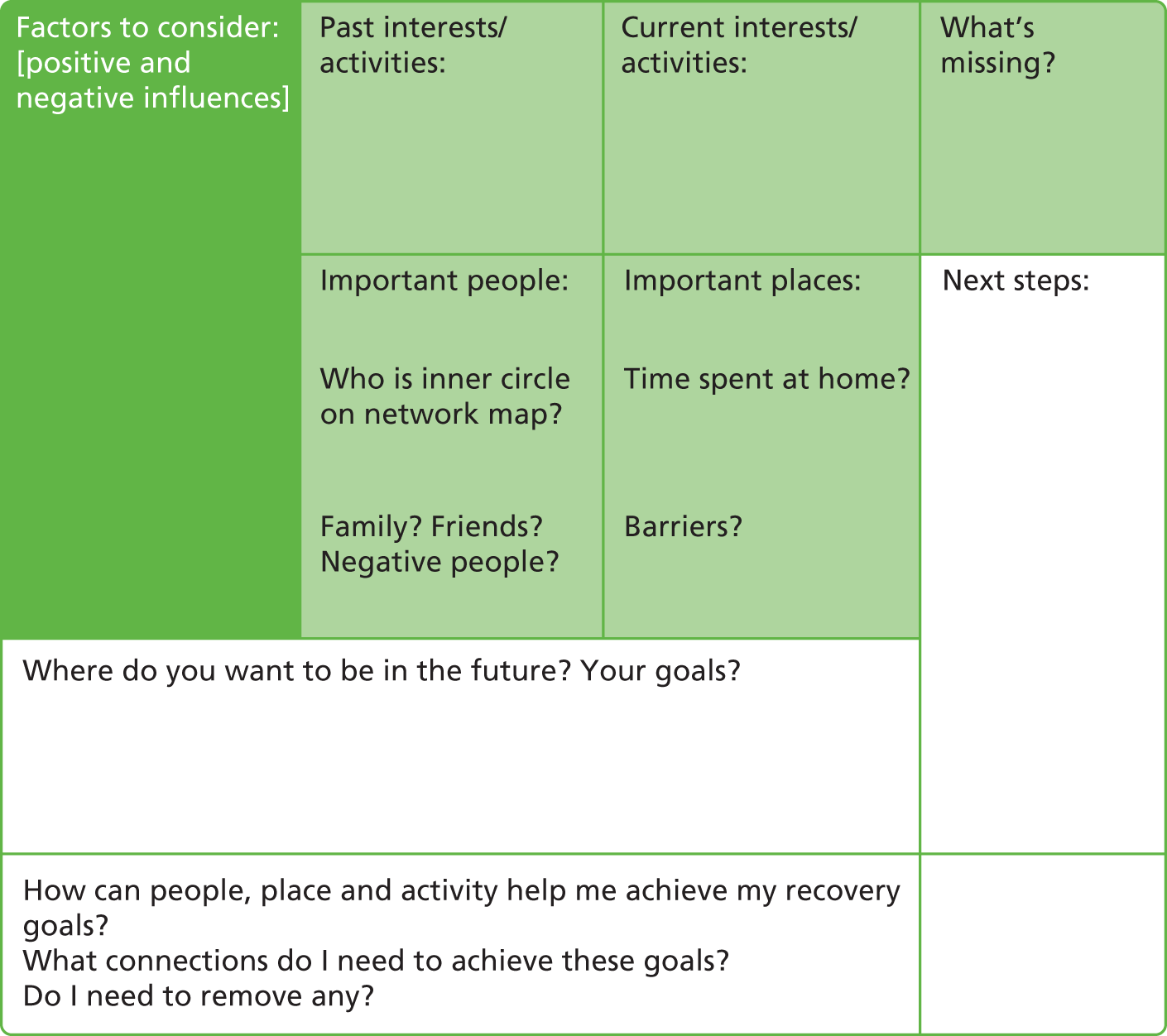
This is an example of the type of template that could be used to guide networking conversations alongside an emotional closeness map as seen in Appendix 6.
How did organisations support the personal networks of people with severe mental illness?
Practitioners play an important role in the personal networks of people with SMI and appear to complement rather than replace other connections. They were seen as important members in the networks by some individuals, but talked mainly of their role in supporting and creating networks. We found that some participants had been helped to build or to maintain their networks by practitioners, but, on the whole, networks were built by the individuals themselves and informal resources dominate. There were specific services, and staff within them, that work with people with SMI to develop social networks and community connections, particularly in the third sector. However, there were structural limitations restricting their impact. We heard frustrations too, where individuals did not believe that practitioners paid sufficient regard to the challenges they faced in changing their lives. A lack of interorganisational communication undermines the potential for best use of local resources in helping build individual networks.
Overall we found in the network maps of 150 people with SMI that referral from organisations and practitioners to place and activity resources in the community was surprisingly low. The network types provide an indication of what happened when the agency of the individual was the prime driver in network development. We found 53% of people with sparse and formal networks spent over 75% of waking time at home, and 32% spent 50–75% of waking time there. Left without practitioner intervention, individuals with formal and sparse networks seem unlikely to develop active, resourceful and satisfying networks on their own.
The interviews with practitioners showed they were concerned with people’s networks, particularly the social networks, but they did not discuss connection-building as a therapeutic strategy in itself. Network roles for practitioners emerged on two levels: first as a development role assisting people in building networks by signposting, referrals, encouraging and empowering; second as a contact within the network, an active agent within it supporting and accompanying, described as ‘walking alongside the person’ (IDL49, support worker), having a therapeutic relationship and building skills. Overall, signposting by practitioners, while an important way to open up opportunities for an individual, was a function that could be much improved, often requiring ongoing encouragement and, for some, substantial support. We summarised practitioner involvement in Figure 32.
Aside from connection-building, helping individuals manage and sustain their networks was identified as another key practitioner and organisational role. Networks can be ruptured by illness when activities are stopped or relationships damaged. Withdrawal may be an active network strategy, but organisations and practitioners have a role in challenging this where networks stagnate, encouraging the individual to adopt strategies which reverse isolation, helping them to reconnect socially and engage in meaningful activities. We found some evidence of practitioners and organisations taking on this role but many system barriers obstruct this. An increased focus on such a perspective could help individuals build more satisfying and resourceful networks, where they become active agents in reducing their social isolation, while ultimately developing a greater sense of personal independence.
A key network resource identified by organisation leads was family. What was absent from practitioner and organisation lead interviews was an acknowledgement of the importance of non-family friendship and the value of wider ties. Practitioners cited friendship as a deficit in the networks of people with SMI, but did not prioritise it as a factor for aiding recovery: ‘but a lot of people with schizophrenia, for example, are often quite isolated and they don’t have friends’ (IDSW83, GP). In contrast, the individual network interviews revealed how important friendships were in contributing to social capital, making up a third of the networks of people with SMI in this study, particularly for those with diverse and active or family and stable networks. Friendships were a way of managing SMI, in this case the voices explaining probably the best way was ‘to do stuff’ with friends, ‘concentrate on that rather than concentrate on what people (voices) might be saying.’ (Joe, SUSW77). A clearer focus on friendship, alongside the role of family where appropriate, in supporting recovery could ease pressure on services. Places and activities may also offer connection-building routes for the practitioner. It was emphasised that the key in practitioner-linked connection-building work was creating personal independence for people with SMI: growing capacity in people’s own networks to take on roles formerly provided by mental health services.
How did organisations work together to support people with severe mental illness improve well-being?
Lack of interorganisational networking was a recurrent theme from our data and acknowledged by organisations themselves. Although they recognised this was an area where they could and should do more, the climate of uncertainty, reorganisation of services and a general reduction in available resources for mental health resulted in organisational collaboration becoming less of a priority, as other factors took precedence. This lack of networking provided barriers which hindered individuals in building their networks through utilising available community resources; some functions have been duplicated while others did not exist. Where organisations did work together well the benefits of this were visible in networks, mental health services linking individuals to volunteering opportunities being one example. There was a role at every organisational level to improve personal networks: commissioning outcomes based on network improvements and better interagency networking should be commonplace; individual agencies improving their knowledge of resources they can draw on to help improve networks, and practitioners being incentivised to do the same, should likewise become a widely embedded approach.
In respect to supporting individual network development there was caution; the driving concern was a fear that, without clear boundaries, network enhancement would foster dependent relationships in the short term with health and social care staff and those were being actively discouraged. Yet developing a network offers the potential for informal ties to take over from practitioners and reduce dependency upon them, as individuals become more confident and independent. We also noted that many practitioners, however recovery focused, still had a pessimistic view of living with SMI. For example, instead of seeing the potential of network development over time to extend the social world, building wider contacts away from the mental health ghetto, network development was aligned to problems of practitioner dependency. There also appeared to be a lack of confidence within community organisations outside health and social care in supporting people with SMI, and a pessimistic and bleak view of SMI was described. This will need addressing to create non-stigmatising mainstream environments which can better support people with their recovery.
Recovery-focused practice was understood by those working in secondary mental health services but not GPs, who tended to work with a chronic disease model, even though they understood the importance of social factors. GPs have a very clear view of their role: ‘we are generalists not specialists’; the GP role in managing SMI was light monitoring of mental and physical health and signposting or referring as required. GPs did not see themselves as having a role in supporting individuals either to develop social networks or to enhance involvement in activities except possibly by signposting (termed network information resource in Figure 32) even when they could see these as beneficial for the individual.
Improved shared care241–244 has been proposed in past years. If primary and secondary mental health ‘shared care’ or ‘integrated care’ is to progress, practitioners need to be using the same language and treating people with mental health problems from the same conceptual understanding of mental illness, regardless of whether they are generalists or specialists in the field. This would mean:
-
a move towards shared understanding of the goals and outcomes aimed for by each individual person
-
having a shared understanding of which interventions are likely to help
-
being clear on one’s own and others’ roles in the shared-care process
-
systems ensuring that roles of practitioners in different teams will collectively fulfil a co-ordinated recovery programme
-
effective and appropriate knowledge and information sharing.
This was currently not the case. We found limited evidence that these five mechanisms, in either of the study sites, were embedded in practice.
Is the community health network approach useful?
Throughout the study, we have sought to assess if the methodology we were employing might be useful for practitioners in terms of network enhancement strategies. We cannot answer this directly from the study data. However, we note that those interviewed mostly consented to follow-up and in the in-depth interview were directly asked how the mapping exercise had felt (see Chapter 4). We heard it helped people make assessments such as ‘It made me realise that I need to go out a bit more’ (Donna, SUL23) but we were also reminded how potentially sensitive and far-reaching the approach was: ‘This network is not just something on paper. It’s something of life, and what it is, is it shows you where you’ve been and where you can get to’ (Gavin, SUL34).
We have presented the networks of people with SMI as resulting from the pushes and pulls of structural determinants and individual agency. The role of the practitioner as a node in these networks in helping maintain the network and as an agent of change has been highlighted. That individuals value these aspects of their lives is a powerful reason for an increased focus on this perspective. We present the approach as having the potential to facilitate new conversations and ways of working with clients, especially those who are isolated or others who feel their networks are shrinking or are a struggle to maintain. However, even clients who feel satisfied with the status quo can, through this framework, become aware of gaps, barriers and potential future vulnerabilities within their networks. While much of networking is the responsibility of the individual, there are important roles at the practitioner and organisational levels; there also remain system-level barriers preventing the best use of resources in an individual’s life as well as those they are not yet connected to.
Chapter 9 Conclusion
The CHN study collected and analysed large amounts of data from individuals, practitioners and organisation leads. In this chapter we summarise our key findings and present implications for commissioners, services and practitioners alongside suggestions for further research.
Summary of main findings
This summary follows the order in which data appeared in the report. We start with individual personal networks, findings from interviews with organisation leaders and practitioners and insights from two case studies. We have found:
-
Three types of personal networks of people with SMI were generated by k-cluster analysis, which we carried out in order to understand heterogeneity within, and similarities between, people in our sample in terms of network characteristics: diverse and active; family and stable; formal and sparse. These incorporated dimensions of people, place and activity, an approach that was broader than measuring social ties alone.
-
Only a few factors in our data set explained variance in network type, and the significant factors found could potentially be altered: living alone or not; housing status; formal education; and long-term sickness or disability. These are hard factors to change but deserve attention. Network type differed significantly by diagnosis but, when it was controlled for other factors, diagnosis did not explain variance; though participants with a schizophrenia/psychosis diagnosis had significantly fewer social ties than other diagnostic groups, 42% of this group had diverse and active network types.
-
There were some key observations about network types:
-
Diverse and active networks had higher numbers of people, place and activity connections. Those with these networks had the highest proportion of new connections and the highest network satisfaction. Qualitative analysis found active management of connections, resources and network opportunities but that big was not always better. Diversity and variety could be associated with enhanced personal well-being and more durable networks, but for some people connectedness caused stress and distress. Manageable routines were important and stigma featured prominently; as networks diversified, the potential for mental health discrimination increased.
-
Family and stable networks had the highest access to social capital and health resources, but lower levels of activity and place connection than diverse and active networks. Participants with these networks spent most of their time at home but tended to live with others. Qualitative analysis found high levels of social support and building blocks for wellness and recovery through family connections; however, such support could restrict access to social capital and well-being resources. Reciprocal relationships were highly valued.
-
Formal and sparse networks were significantly smaller with lower access to social capital and health resources, poorer functioning and well-being. They were the least active, having fewer friends, family and wider contacts, and practitioner contacts were more dominant. Qualitative analysis found mental illness featured most strongly in these networks framing decisions and experiences. We found agency in some of these networks, despite limited resources, and potential building blocks for recovery; others needed help identifying potential opportunities. Sparse networks were sometimes considered beneficial for supporting individual well-being. Strength was also gained from identities developed away from diagnostic labels and there were signs of resilience and determination to move on from mental illness. These networks also revealed the resentment that some people feel when relying on practitioners to support mental health and well-being.
-
-
Role of practitioners within current networks of people with SMI varied. We found more than one in five participants named a practitioner within their inner circle of emotional closeness and they formed a portion of social contacts in all network types: formal and sparse networks 33%; diverse and active networks 20%; family and stable networks 12%. Practitioners tended to complement rather than replace informal network contacts, and had a role too in larger networks, but did not replace social or health capital where this was missing from informal ties. This was consistent with practitioner accounts that their role was not to provide social support but to encourage clients towards ‘taking control’ (IDSW59, occupational therapist) to build networks and recovery: ‘we will very much walk alongside someone, you know, I haven’t got the magical key for someone to recover – it’s what their recovery means to them’ (IDSW67, team leader).
-
We investigated social capital among the study population. The mean social capital score was 14.2, which was higher overall than other studies of mental health social capital, but lower than the general population, and there was variation across network type and between study sites. In the schizophrenia/psychosis group it was 11.6, in the bipolar group 16.6. We found social capital and health resources to be provided primarily by close informal ties such as family and friends and less so from wider and practitioner contacts overall, although they were more prominent in networks lacking informal social support. Importantly, those who lacked family and friends had lower resources overall. We noted that connections to activities including employment and place were important providing gateways to social ties.
-
The social networks in our study population had a mean of 19.9 contacts, ranging from 5 to 64 contacts. However, formal and sparse networks had only 12.4 contacts on average. Our data suggest it was the type of relationship (close relationships) rather than the number which was most important for resource exchange.
-
The qualitative interviews helped us to explore heterogeneity within the study population. We found individual agency across all network types and surface tensions, including relationships with practitioners or families; dealing with the impact of stigma; and employment and financial frustrations. The value of connectedness, countering the risk of isolation and loneliness, within personal networks for supporting recovery was evident, shaping identity, providing meaning to life and sense of belonging, gaining access to new resources, structuring routines and helping individuals ‘move on’ in their recovery journey.
-
Managing a personal network was a complex interplay of personal and external factors. Evidence showed how relationships, places and activities in networks could be used to build new network connections, and withdrawal was also a strategy. Identities were closely bound to activities and roles. Participants acknowledged their own responsibility to develop their networks – ‘it is down to me’ (Eleanor, SUSW38); ‘It’s all down to me’ (Neil, SUSW26) – and it was also evident that practitioners have an important role in assisting the process.
-
Networks in London showed more bridging capital properties, with higher numbers of wider contacts and access to more diverse relationships and place types. These networks had fewer family contacts and lower social capital.
-
Networks in the SW showed more features of bonding capital, with close family and friend ties and dense interconnected lives. Challenges for practitioners lay in working with individuals who had networks where family ties were negative or absent.
-
Service providers were keen to promote a recovery-focused approach but we found a distance between recovery policy and practice. In particular, the social aspects of supporting SMI get overlooked in the health-care system. In a demanding and changing context, strategic multiagency collaboration was seen as crucial; however, we found limited organisational partnerships or collaborations.
-
Health-care and third-sector practitioners, including GPs and psychiatrists, recognised social factors were important in recovery but reported system-level barriers (workload, administrative bureaucracy, limited contact time with clients) in addressing these issues. Skilled care co-ordinators acknowledged the importance of network development, and many reported they used to do more in past roles, but currently did not believe they had enough time to focus sufficiently on ‘the social’.
-
We suggest the CHN approach provides a useful ‘way in’ to working with people with SMI to develop personal networks, emphasising meaningful people, places and activities. Using a person-centred networking approach is supportive of recovery-focused practice in that it helps to identify varying levels of agency in people with SMI, from limited engagement to active evaluative and future-forming strategies, as well as addressing barriers to change.
Discussion
The CHN study argues that network development should be seen as an integral part of recovery for people with SMI, through encouraging increased connections and engagement in meaningful activities. 8 Working within an individual’s personal network could help services to emphasise a person-centred and strength-focused approach that the recovery approach advocates. 41,42 The importance of employment for people with SMI245 was supported in our data, with those in employment having increased social capital. Those working tended to have diverse and active networks, and this included people with schizophrenia/psychosis. Research has found that people with SMI, and particularly schizophrenia, tend to have low rates of employment. 12 Our data showed that any activities leading towards work (volunteering, education, part-time or full-time work), which meant people were not categorised as long-term sick or disabled, were beneficial for building diverse networks which helped build social capital.
We found evidence that social networks for this population were larger, more diverse and more socially integrated today than those found in the TAPS study following deinstitutionalisation policies of community care in the 1990s. 3–5 However, many of our participants remained isolated in formal and sparse networks with low activity levels and our population overall had lower perceived social support than in the general population. 245 There is a serious concern that selection bias, likely to have occurred as part of our low recruitment rates, might mean that the population we studied was more connected than an average population of individuals with SMI.
Mapping the structure of networks has allowed us to understand how social capital and health resources were accessed. We found networks with both bonding117 and bridging118 capital. It seemed that a mixture of each was healthiest; our diverse and active, and family and stable networks had some elements of both. Our social capital scores were slightly higher than other SMI populations198 but lower than the general population. 123 Lower access to resources may be a vulnerability factor for mental ill-health, or a result of social withdrawal due to mental illness, or the relationship may work in both directions;123 our study cannot draw any conclusions on the direction of observed relationships. However, access to resources was important for the provision of support and had wider benefits, such as helping people attain goals such as gaining employment through informal contacts. 246 Our data suggested more needed to be done to help individuals build their social capital.
The qualitative insights we present highlight the importance of understanding the meaning of network characteristics51 and show how networks were often managed through agency of individuals and others,80 which also applied to networks we have described as formal and sparse. The level of agency that people could draw on varied, underlining the heterogeneity of this population. Networks were actively managed in terms of segregation of components, removal of negative ties and mental health disclosure, the latter linking to the impact of mental health stigma. 32,227 Network configuration also seemed to reflect what was coherent and manageable for the individual. 47 Understanding why networks are the way they were, without an assumption that they need to stay that way, may not always reveal new information for the practitioner but visual network mapping may offer new ways of conversing and understanding the meaning of connections, to plan goals holistically. We suggest the systematic collation of network data would provide a useful framework for planning interventions and setting person-centred outcomes.
Our population has poorer well-being202 and functioning201 than the general population, while our limited data on hospitalisation for physical health issues reflects the poor physical health of this population, and the need for greater attention on the part of services to improve it. 58 We heard varying views from participants about antipsychotic medication: it kept mental health symptoms stable and allowed networks to be (re)built; conversely the side effects of medication could make maintaining active networks difficult. The breadth of physical activities and interests found in our activity data suggests how this might be achieved: supporting individuals to increase engagement in activities of interest to them, as well as identifying local community spaces where these activities can be engaged in, while addressing potential barriers, facilitates greater social contact and connectedness, and enhances personal well-being.
Finally, we believe our study’s approach and findings support current government mental health policy and the No Health without Mental Health strategy. 30,40 Our data were closely aligned to the objective in this strategy that people with mental illness should have a ‘greater ability to manage their own lives, stronger social relationships, a greater sense of purpose, the skills they need for living and working, improved chances in education, better employment rates and a suitable and stable place to live’ (p. 21). 30 A modified CHN approach offers potential insights into how to meet these policy aims, addressing inequalities in mental health, physical health, stigma, social inclusion and quality of life for people with SMI.
Research limitations
This study has several strengths but there have been many challenges. In terms of strengths, it has worked innovatively with lived experience researchers to synthesise research findings. It has adapted a standard SNA framework and created multiple layers of data to explore connections and interactions: people, places and activities. In doing so it has applied SNA principles to multiple aspects of people’s lives. However, the data set was limited by a number of important factors that need to be considered when interpreting the data.
First, in relation to the networking methodology, the data were limited to the source questions used to elicit information from participants. Studies which map people’s social networks lack a consistent methodology; the questions used to ties identify, and boundaries around what constitutes a network, vary greatly, making comparison of studies findings problematic. We had to create our own bespoke data collection process for network mapping, and set boundaries round the networks under investigation. We undertook extensive piloting in an attempt to reduce cognitive load and recall error but, as with all network-mapping studies, our data were limited by the memory and perception of the participant on the day of interview. The use of place and activity (who did you see there? who did you do that with?) provides additional prompts for recall that many other network-mapping studies do not have. We were interested in the network only from the perspective of the person with SMI. It was the connections that were important to them that we wanted to map, followed up in depth to understand why. No verification of data from third parties was undertaken; this was not a limitation but a point of method and approach in this study grounded in the views of people with SMI.
Second, we worked in two contrasting regions in an attempt to understand heterogeneity but cannot generalise these findings to other areas. If this study were undertaken in different regions of England it is possible other network types would emerge; we can ground our findings only in the two study site locations and within the population we recruited. The LEE group point out in Appendix 1 that they have based their reflections on available data and would like to see how far the approach based on network types can aid recovery-orientated practice in a more applied study moving towards the development of an intervention.
Third, the bias in our data was from several sources but particularly recruitment sample bias. We were not working with a randomly sampled study population. In each site we recruited only from practices agreeing to participate, and overall response rates of individuals with SMI were poor: 23.65% in the SW and 15.01% in London. These figures are likely to be lower than the actual response rate because, despite attempts to keep detailed recruitment records with surgeries and CMHTs, we do not know how many people were actually invited (received or presented with an invitation) to take part and therefore how many declined to participate. We struggled with a number of London GP surgeries in particular, whose capacity to support the research process was severely limited, resulting in inaccurate screening, poor follow-up of non-responding participants and poor record-keeping hindering an accurate response rate calculation. These difficulties have also been reported by other studies. 247 In the SW a disproportionate number of older and middle-aged men with bipolar disorder participated and to compensate we approached secondary care teams to identify a younger population, including people with schizophrenia. We attempted to find population-level data to assess how representative our data were compared with people with SMI registered with primary care services, using indicators such as age, gender, ethnicity and diagnosis, but these data were not collated at a borough or county level. We do believe we have oversampled people with bipolar disorder in the SW based on a comparison of our data with another national study. 15 It reported, from data collected in 64 GP surgeries of people with SMI, that 56% were diagnosed with schizophrenia and 38% with bipolar disorder; in our study we had 51% of people in the SW with bipolar disorder but only 36% in London. We compared our respondents with this sample identified in a primary care notes review study and found a higher proportion of non-white participants (provided by the London respondents), similar gender proportions, a higher length of contact with services (20.1 years compared with 17.3 years) and a larger proportion of people living alone (50% in this study compared with 33.3%) but similar proportions with a partner or married. We found more people within employment: 29.3% in our sample compared with 12.6%.
Interview bias was addressed by careful co-ordination between the study’s two researchers. Both network mapping and network interview transcripts were shared in the first phases of each module to assist quality control and consistency. This ‘checking in’ happened across the study, supervisors listened to transcripts to pick up on inconsistencies in qualitative interviews and the PPI group also reviewed transcripts and provided feedback.
We undertook a cross-sectional descriptive pilot study and gained insights into changes over time from the qualitative analysis, but we cannot make any causal inferences. We acknowledge that causation will be complex and bidirectional. The descriptions we have brought to the surface through network types, however, provide a platform for other research in this area to explore further.
We were also limited by lack of data on clinical features of our population such as current symptomology of mental illness. We had to use proxy indicators of severity such as time since last inpatient admission. In future studies we would recommend including a formal clinical measure of mental health functioning, as this may explain additional variance in the regression models presented. Finally, it is worth noting, the bespoke scale we created – the HRG – did not prove to be useful in explaining variation in access to health capital across the sample population. It will require further development work if it is to be used to measure health as opposed to social capital.
Reflections on patient and public involvement
The study involved a PPI group at various stages of the research process. In the final reporting stage we used reflections from people’s own experience of recovery specifically as a ‘way in’ to the project data. The value of these contributions included scientific and non-scientific perspectives. This suggests that, while the distinction between different kinds of informed deliberator is a good place to start in PPI coproduction,192 there was also a third space of interaction opened up between different kinds of knowledge which may mutually enrich each other. The collaboration with the LEE group was important for delivering a reflexive review that remained connected to the study data yet still added value through powerful insights from lived experience. Conversations with the least scientifically informed also yielded key insights that shaped the interpretation. This may suggest that the ethical contribution of PPI as knowledge coproduction was more complex than some commentators suggest,193 requiring both perspectives rather than an either/or approach to the range of ways in which lived experience expertise can inform the public practice of science.
Our conclusions
From our qualitative data analysis, we see potential for people with SMI to become even more active managers of their own networks regardless of current network type; the building blocks of hope that the lived experience researchers first identified are found across the data set. The health and social care system currently did not deliver multiagency integrated networking solutions to support SMI and recovery. We also found competing tensions in policy agendas shaping provision of mental health services; primary and secondary care were not using the same approach to the management of SMI. The network types we have produced could be a very useful way of viewing the lives of people with SMI; understanding the dynamics of an individual’s connections with people activities and places, alongside diagnosis, provides a more person-centred approach to plan treatment and care.
Commissioner, organisation and practitioner level
The health and social care system for people with SMI is undergoing rapid change. Such change offers up opportunities to develop new solutions for how services support recovery but there are risks if there is no clear planning on how changes to community resources might impact on vulnerable groups. In such periods of flux, understanding the resources that individuals have and where they come from is of value, particularly if these are fragile and reliant on services. Offering values-based leadership to people with SMI is a very important role for both organisations and the practitioners who work within them; creating joint mental health strategies to guide these practices across current service silos is vital. We found evidence for a strong vision for delivering recovery-focused services in secondary mental health care and the third sector, but not in primary care. There was a lack of strategy across the service silos.
Practitioners understand and value aspects of social recovery from SMI but many, particularly GPs, and also community mental health practitioners, did not believe they had the time in their job role to focus on ‘the social’. Service systems appeared to thwart the agency of practitioners and created obstacles to person-centred outcome-focused care, even within the third sector, whose practitioners wanted to work in this way far more but found it was not currently feasible within available commissioning arrangements. This identified lack of focus on social recovery was a barrier to working using a networking approach. This study suggests that an alignment between the recovery approach and a networking model using the CHN method could be useful in the delivery of mental health care, although more work is required to adapt a research process into a clinical intervention. This constitutes an area that newly formed bodies such as Public Health England, local health and well-being boards and CCGs may all be interested in: mapping community assets and the potential within individuals to become more active managers in their recovery journey.
Individual network level
A striking issue emerging in our work was how heterogeneous people with SMI were and the implications for working with people to manage their health problems. Yet network types were found which reflected connectedness patterns that could guide the work of practitioners. We found connections to people, places and activities to be an important aspect of individual’s lives which impacted on access to resources used to support well-being, and were not related to diagnosis. Individual agency in developing and maintaining networks was uncovered but most people required some support, even if this support was received reluctantly. Many with SMI were living out the majority of their lives away from mental health services and away from other people using services. However, a minority had significant proportions of their social network formed by mental health-related contacts.
Identifying the building blocks of individual agency that can be enhanced or nurtured with the help of others was a vital aspect of recovery, particularly where individuals lacked belief in both themselves and inner resources. The change agent might be within a person, drawing on their interests, identity and goals. Change agents might also be found in family, friend, wider contact or practitioner relationship groups.
Developing the personal networks of individual’s with SMI was not identified as an organisational priority alongside management of medication and symptoms. While this remains the case it seems unlikely that this population will be able to build personal networks that make use of the full potential of inner and external resources. We note that there was potential in all networks to develop.
Network theory
This pilot study attempted to combine applied SNA to identify form and structure in networks, with qualitative data collection based on a hybrid approach of two traditions. It has merged qualitative SNA, unpicking meaning in network structures, and narrative research, exploring meaning in people’s lives, using the emotional closeness map as a ‘way in’ to the conversations that explored connectedness, well-being and recovery. Our network mapping was guided by SNA theory,24 as it offered a framework to measure connections (or a lack of connections) using name-generating and name-interpreting procedures. 76 The benefits of the approach were that networks provide a top-down view, generated by the individual, of their current social world and meaningful activities. Once mapped, these networks were reflected on and we found this perspective helped conversations about how resources in the wider community impact on, or were used to support, both mental and physical health. This approach allows for consideration of what connections are important to individuals as well as what is missing; the latter provides a springboard to goal-planning. Including place and activity dimensions to create a multidimensional network, although time-consuming, added to the explanatory potential of network types. We found that many participants reported the mapping interview procedure useful in terms of their own thinking and understanding about their networks, and at follow-up interviews some had already begun to make changes. This framework has therapeutic potential, is a whole-person rather than illness-focused approach and could help both individuals and practitioners to consider new opportunities, or steps toward these, that improve well-being, promote recovery and increase access to resources.
The analysis we undertook also took a person-centred focus for understanding the lives of people with SMI, as recommended in the recovery literature,74 through drawing out what was important to people and understanding why in terms of impact on well-being. The qualitative follow-up interviews were particularly helpful in understanding the dynamics of networks, how things change over time and the role of self or others in shaping ‘form’ or ‘content’, and why.
Aside from the individual’s perspective, the structure and composition of networks that this approach provides gives insights for practitioners into stage of recovery for an individual. 9 This can help identify areas of potential to address through goal-setting: isolation or lack of diversity, lack of family or friends can all be identified. The dimension of activity offers an insight into the individual’s identity beyond mental health. Through identifying what is meaningful and important to each person, interventions to build new connections can be targeted. Place is an important dimension because it situates the individual’s network inside the context of their local area; networks are constrained by and enabled by environment (social, cultural, economic). Both opportunities, such as local groups related to an individual’s interests, and barriers, such as transport, antisocial neighbours and safety, can be identified through consideration of place networks. People, place and activity networks interact. A framework can help both the individual and practitioners to build new connections that improve well-being, promote recovery and increase access to resources.
Implications for commissioners, services and practitioners
In line with National Institute for Health Research (NIHR) guidance the report does not make policy and practice recommendations. The study was an exploratory pilot and as such can only offer preliminary evidence for commissioners, services and practitioners about the CHN approach to understand personal networks and implications for practice. However, the study did provide evidence about the social dimension in recovery and its importance alongside NICE guidelines for schizophrenia and bipolar disorder addressing medication use, psychological therapies and service experience. The following potential steps are noted:
-
Developing the CHN methodology as a tool to support recovery. This study suggests an alignment between recovery-focused practice and a networking model using the CHN approach could be useful in the delivery of mental health care. Important elements of personal networks were recognised within recovery frameworks, and practitioners draw on aspects of this work in current practices, particularly meaningful activities and social networks. The lack of a framework and emphasis on this work could be addressed by adopting the CHN model, although more work is required to adapt a research process into a clinical intervention. There are few practical resources guiding practitioners in how to build recovery programmes; insights from a CHN approach could help structure person-centred planning and help them reflect on the challenges of doing so.
-
The need for improved organisational collaborations. Several service silos were in operation: secondary mental health care, local authorities, voluntary services, including mainstream community resources, and primary care. We found there was a significant community resource knowledge gap; many practitioners rely on their own interests and personal connections to build a personal knowledge bank of community opportunities that they use to support clients. A system that can encourage interorganisational information sharing, and ideally practitioner and service use feedback on the value of local community resources, is recommended. It was acknowledged that keeping such a system updated was a major challenge
-
Supporting people with SMI to make active use of network resources. People with SMI should be empowered to make even more active use of the resources in their networks. These resources include relationships with friends and families; other health-care facilities; and non-health resources in the community, which may be free but have other barriers. Local authorities and health services can make resources more accessible and practitioners need to see enhancing personal networks as a means to mobilising resources to achieve recovery.
-
A mediating role for practitioners in sustaining and developing networks. Meaning and direction must come from people with SMI themselves, many of whom may become independent, but practitioners have a vital connection-building role in terms of helping to develop both flexible, balanced routines and achieving new roles. In part this role is showing that networks and the resources within them matter to recovery, alongside medication and psychological therapies. Support can include encouragement to develop previously valued and potentially beneficial network elements: activities, social interactions and places. For those with formal and sparse networks, practitioners were a key resource, sometimes the only resource, and helping them to reduce barriers to network development may be critical. Practitioner network roles have to take into account appropriate responsibilities for network development. For example, the consultant psychiatrist could be the leader and champion for network interventions but support workers and care co-ordinators deliver these supports.
-
We acknowledge the risk that we were perpetuating silo working but we have listed recommendations under service elements. We suggest some specific tasks.
-
Primary care: An important hub in the networks of people with SMI was, and will increasingly be, primary care. GPs need a greater understanding of the value of personal networks in recovery, particularly for those who have been discharged from secondary care; they also need to develop closer working relationships with third-sector providers.
-
Secondary mental health care: Skilled care co-ordinators acknowledge the importance of network development, but need to be required to make it a key part of their role. Efforts to embed recovery-focused practices can draw on network enhancement strategies, and creating shared care processes with primary care and the third sector will become fundamental in the management of SMI.
-
Mental health third-sector services: Currently they support network development working alongside people with SMI, linking, facilitating, empowering and encouraging, but often in isolation from other services. They could develop these models further and include peer elements, and are likely to be able to be more efficient if more closely linked to primary and secondary care.
-
Local authorities: Social services provide crucial support to people with SMI including housing, employment and welfare support. These services tended to operate separately from health systems, and staff related how mental health was not really on their agenda and thus specific services or supports for this group were not a priority. Their impact on networks can be significant, as employment, stable housing and welfare support were crucial resources. In addition, local authorities have new responsibilities for well-being through directors of public health. The creation of a mental health intelligence network is an ideal focus for well-being outcome data, including resources data on social capital and social networks.
-
Commissioning: A crucial gap in practice was the lack of any overarching framework for the provision of services to people with SMI following a recovery approach. Social outcomes of care were largely absent in the current NHS outcomes framework, which applies only to secondary care. Building a set of social outcome indicators for SMI and including network indicators that operate across the service silos would incentivise joint working and promote social inclusion. One new model worth exploring is for primary care and third-sector providers to be jointly commissioned to provide care for those individuals with SMI at lower risk or predominantly requiring a recovery approach. Payment or incentive systems would need to be developed; existing direct payments or emerging PBR tariffs could be utilised.
-
Recommendations for research
-
This study has begun to explore the role of agency within networks of people with SMI and how agency was impacted by network structure. We recommend further research be carried out to understand agency within personal networks. This is both to understand the role of agency in networks and how it is affected by network structures as well as to understand how it varies for different groups of people with SMI such as Afro-Caribbean men on discharge from hospital, mothers with bipolar disorder and single men aged over 45. Such an understanding would help build an evidence base for how best to support network development and the role of self, practitioners and others in this process. We learnt that practitioners are hard pressed to do one-to-one social intervention-type work with clients, because of capacity constraints; thus, identifying key skills to create further self-sufficiency and resilience within people with SMI so they can access informal resources to support recovery would be central in this further research.
-
For research in this area to be most effective, and comparable, it is recommended that a standardised tool be developed to collect network data in enough detail to provide insight to resource access, identity and recovery. Our study tool needs refinement because of the length of time required to collect data. More data on social media use should be collected.
-
We have begun to find differences in networks comparing people from BME and ‘white other’ communities with the white British population. The qualitative data collected should be reanalysed to look specifically at meaning in networks by ethnicity, and follow-up research should be carried out to understand how a networking approach might support initiatives to improve services and support networks for people from BME communities.
-
We recommend research be undertaken to develop the CHN-mapping technique as a formulation and therapeutic intervention. We believe there is potential for this to be used in primary care, secondary care and shared care models of mental health provision. Research could also look at which practitioners are best placed to deliver CHN mapping, including peer support workers within this assessment. It could also look at the qualities of friendship within networks that best support recovery.
-
In particular we suggest that network mapping be evaluated as a strategy for managing transitions in care at key discharge points in the recovery pathway (inpatient unit, secondary care discharge) against treatment as usual. This is particularly relevant in a policy context of increased assertive discharge to primary care services for people with SMI. Such a tool could provide the basis for ongoing care shared between general practice and the third sector in the absence of secondary services input.
Acknowledgements
This research would not have been possible without the many people who participated in our piloting phase and data collection modules. We are very grateful to all the mental health service users and practitioners who took part, as well as the MHRN and PCRN staff who assisted recruitment and staff in GP surgeries; also to Dr Deborah Shenton, who collected data in the SW. We thank our advisory group members for their guidance, and colleagues in our workplaces for engaging in discussions around the CHN approach. We acknowledge the support and guidance of Professor Martin Everett (Chair in Network Analysis) and Dr Elisa Bellotti (Lecturer) of the School of Sociology and Mitchell Centre for Social Network Analysis at the University of Manchester. Both have provided expert input into data collection, data analysis and write-up of the network-mapping module. We thank Dr Josip Car, Director of the Global eHealth Unit, Imperial College London, and Dr Michael Phelan, Clinical Director, West London Mental Health Trust, for their guidance and support in delivering the research in London, and piloting our data collection schedules with us. Thanks to Ms Louise Howard, Senior Lecturer in Mental Health Nursing, Kingston University and St George’s, University of London, for comments on the report and ideas for dissemination. Our PPI group have been a vital part of this study; two members are authors on the report and we gratefully acknowledge the contributions of all members: Ms Alice Meek, Ms Elaine Hewis, Mr Roger Smith and Mr Simon Love. We would also like to acknowledge the helpful reviewer comments which we received through the NIHR review process.
Contribution of authors
Dr Vanessa Pinfold, Research Director, McPin Foundation, London. Chief investigator with responsibility for designing and managing the study, leading data analysis in Chapters 4 and 6, contributing to data analysis of all sections and leading writing of the final report.
Mr Daryl Sweet, Senior Researcher, McPin Foundation, London. Lead researcher in London, leading data analysis and writing of Chapter 3 including SNA and contributing to all sections of the report, particularly Chapters 2 and 8.
Dr Ian Porter, Primary Care Researcher, Primary Care Group, Peninsula Schools of Medicine and Dentistry, Plymouth University, Plymouth. Lead researcher in Plymouth, leading data analysis and writing of Chapters 5 and 7, and contributing to all sections of the report through critical review.
Dr Cath Quinn, Senior Research Fellow, Primary Care Group, Peninsula Schools of Medicine and Dentistry, Plymouth University, Plymouth. Qualitative researcher supporting data analysis for Chapters 4 and 5.
Professor Richard Byng, Primary Care Group, Peninsula Schools of Medicine and Dentistry, Plymouth University, Plymouth. Site lead in Plymouth providing leadership for study synthesis and conceptual frameworks, contributing to detailed report editing.
Dr Chris Griffiths, Senior Research Officer, Rethink Mental Illness, London. Study co-ordinator providing feedback and edits on all report chapters.
Ms Julie Billsborough, freelance lived experience researcher. Member of LEE group authoring Appendix 1, study researcher collecting data for Chapter 6, commenting in detail on entire report and writing plain English summary.
Dr Doyo Gragn Enki, Research Fellow in Statistics, Peninsula Schools of Medicine and Dentistry, Plymouth University, Plymouth. Study statistician undertaking regression modelling and k-cluster work in Chapter 4.
Ruth Chandler, Service User and Carer Involvement Coordinator, Research and Development, Sussex Partnership NHS Foundation Trust. Lead for LEE group authoring Appendix 1 and providing critical review of entire report.
Dr Martin Webber, Director, International Centre for Mental Health Social Research, University of York. Advisor for RGUK analysis, undertaking validation analysis for HRG and providing detailed feedback on Chapter 3.
Dr John Larsen, former Head of Evaluation, Rethink Mental Illness, London. Advisor, providing detailed feedback on conceptual development of the study as presented in the report and Chapter 4.
Professor John Carpenter, Professor of Social Work and Applied Social Sciences, University of Bristol. Advisor, providing detailed feedback on entire report.
Professor Peter Huxley, Director of Centre for Social Work and Social Care Research, University of Swansea. Advisor, providing detailed feedback on Chapter 3.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. London: Sage; 2006.
- Leff JP, Thornicroft G, Coxhead N, Crawford C. The TAPS Project. 22: A five-year follow-up of long-stay psychiatric patients discharged to the community. Br J Psychiatry Suppl 1994;165:13-7.
- Leff J, O’Driscoll C, Dayson D, Wills W, Anderson J. The TAPS Project. 5: The structure of social-network data obtained from long-stay patients. Br J Psychiatry 1990;157:848-52. http://dx.doi.org/10.1192/bjp.157.6.848.
- Leff J, Trieman N. Long-stay patients discharged from psychiatric hospitals: social and clinical outcomes after five years in the community. The TAPS Project 46. Br J Psychiatry 2000;176:217-23. http://dx.doi.org/10.1192/bjp.176.3.217.
- Rosland AM, Heisler M, Piette JD. The impact of family behaviors and communication patterns on chronic illness outcomes: a systematic review. J Behav Med 2012;35:221-39. http://dx.doi.org/10.1007/s10865-011-9354-4.
- Ell K. Social networks, social support and coping with serious illness: the family connection. Soc Sci Med 1996;42:173-83. http://dx.doi.org/10.1016/0277-9536(95)00100-X.
- Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry 2011;199:445-52. http://dx.doi.org/10.1192/bjp.bp.110.083733.
- Andresen R, Caputi P, Oades L. Stages of recovery instrument: development of a measure of recovery from serious mental illness. Aust N Z J Psychiatry 2006;40:972-80. http://dx.doi.org/10.1080/j.1440-1614.2006.01921.x.
- Andresen R, Oades L, Caputi P. The experience of recovery from schizophrenia: towards an empirically validated stage model. Aust Psychiatry 2003;37:586-94. http://dx.doi.org/10.1046/j.1440-1614.2003.01234.x.
- Tew J, Ramon S, Slade M, Bird V, Melton J, Le Boutillier C. Social factors and recovery from mental health difficulties: a review of the evidence. Br J Soc Work 2012;42:443-60. http://dx.doi.org/10.1093/bjsw/bcr076.
- Marwaha S, Johnson S. Schizophrenia and employment. Soc Psychiatry Psychiatr Epidemiol 2004;39:337-49. http://dx.doi.org/10.1007/s00127-004-0762-4.
- Aked J, Marks N, Cordon C, Thompson S. Five Ways to Well-Being: A Report Presented to the Foresight Project on Communicating the Evidence Base for Improving People’s Well-Being. London: New Economics Foundation (NEF); 2009.
- Mason VL, Shaw A, Wiles NJ, Mulligan J, Peters TJ, Sharp D, et al. GPs’ experiences of primary care mental health research: a qualitative study of the barriers to recruitment. Fam Pract 2007;24:518-25. http://dx.doi.org/10.1093/fampra/cmm047.
- Reilly S, Planner C, Hann M, Reeves D, Nazareth I, Lester H. The role of primary care in service provision for people with severe mental illness in the United Kingdom. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0036468.
- Nazareth ID, King MB. Schizophrenia: community care and the family physician. Int Rev Psychiatry 1992;4:267-71. http://dx.doi.org/10.3109/09540269209066327.
- Nazareth I, King M, Davies S. Care of schizophrenia in general practice: the general practitioner and the patient. Br J Gen Pract 1995;45:343-7.
- Album D, Westin S. Do diseases have a prestige hierarchy? A survey among physicians and medical students. Soc Sci Med 2008;66:182-8. http://dx.doi.org/10.1016/j.socscimed.2007.07.003.
- Lester H, Tritter JQ, Sorohan H. Patients’ and health professionals’ views on primary care for people with serious mental illness: focus group study. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.38440.418426.8F.
- Bindman J, Johnson S, Wright S, Szmukler G, Bebbington P, Kuipers E, et al. Integration between primary and secondary services in the care of the severely mentally ill: patients’ and general practitioners’ views. Br J Psychiatry 1997;171:169-74. http://dx.doi.org/10.1192/bjp.171.2.169.
- Burns T, Greenwood N, Kendrick T, Garland C. Attitudes of general practitioners and community mental health team staff towards the locus of care for people with chronic psychotic disorders. Int J Psychiatry Clin Pract 2000;6:67-71.
- Lester H, Gask L. Delivering medical care for patients with serious mental illness or promoting a collaborative model of recovery?. Br J Psychiatry 2006;188:401-2. http://dx.doi.org/10.1192/bjp.bp.105.015933.
- Emirbayer M, Mische A. What is agency?. Am J Sociol 1998;103:962-1023. http://dx.doi.org/10.1086/231294.
- Knoke D, Yang S. Social Network Analysis. New York, NY: Sage; 2008.
- Scott J, Carrington PJ. The SAGE Handbook of Social Network Analysis. London: Sage; 2011.
- Burt RS, Nohria N, Eccles RG. Networks and Organizations: Structure, Form and Action. Boston, MA: Harvard Business School Press; 1992.
- Burt RS. Structural Holes: The Social Structure of Competition. Cambridge, MA: Harvard University Press; 2009.
- New Horizons: A Shared Vision for Mental Health. London: HMSO; 2009.
- Brown S, Kim M, Mitchell C, Inskip H. Twenty-five year mortality of a community cohort with schizophrenia. Br J Psychiatry 2010;196:116-21. http://dx.doi.org/10.1192/bjp.bp.109.067512.
- No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: HMSO; 2011.
- NHS Outcomes Framework 2012 to 2013. London: HMSO; 2012.
- Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: ignorance, prejudice or discrimination?. Br J Psychiatry 2007;190:192-3. http://dx.doi.org/10.1192/bjp.bp.106.025791.
- Thornicroft G. Physical health disparities and mental illness: the scandal of premature mortality. Br J Psychiatry 2011;199:441-2. http://dx.doi.org/10.1192/bjp.bp.111.092718.
- Pinfold V, Thornicroft G, Huxley P, Farmer P. Active ingredients in anti-stigma programmes in mental health. Int Rev Psychiatry 2005;17:123-31. http://dx.doi.org/10.1080/09540260500073638.
- Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychiatr Rehabil J 1993;16:11-23.
- Perkins R, Slade M. Recovery in England: transforming statutory services?. Int Rev Psychiatry 2012;24:29-3. http://dx.doi.org/10.3109/09540261.2011.645025.
- Whitwell D. The myth of recovery from mental illness. Psychiatr Bull 1999;23:621-2. http://dx.doi.org/10.1192/pb.23.10.621.
- National Institute for Health and Clinical Excellence . Bipolar Disorder: The Management of Bipolar Disorder in Adults, Children and Adolescents, in Primary and Secondary Care 2006.
- National Institute for Health and Clinical Excellence . Schizophrenia: Core Interventions in the Treatment and Management of Schizophrenia in Adults in Primary and Secondary Care 2009.
- No Health without Mental Health: Implementation Framework. London: HMSO; 2012.
- Shepherd G, Boardman J, Slade M. Making Recovery a Reality. London: Sainsbury Centre for Mental Health; 2008.
- Slade M. Personal Recovery and Mental Illness: A Guide for Mental Health Professionals. Cambridge: Cambridge University Press; 2009.
- Tooth B, Kalyanasundaram V, Glover H, Momenzadah S. Factors consumers identify as important to recovery from schizophrenia. Australas Psychiatry 2003;11:S70-S77. http://dx.doi.org/10.1046/j.1440-1665.11.s1.1.x.
- Albert M, Becker T, McCrone P, Thornicroft G. Social networks and mental health services utilisation: a literature review. Int J Soc Psychiatry 1998;44:248-66. http://dx.doi.org/10.1177/002076409804400402.
- Macdonald EM, Hayes RL, Baglioni AJ. The quantity and quality of the social networks of young people with early psychosis compared with closely matched controls. Schizophr Res 2000;46:25-30. http://dx.doi.org/10.1016/S0920-9964(00)00024-4.
- Catty J, Goddard K, Burns T. Social services and health services day care in mental health: the social networks and care needs of their users. Int J Soc Psychiatry 2005;51:23-34. http://dx.doi.org/10.1177/0020764005053267.
- Antonovsky A. Health, Stress, and Coping. San Francisco, CA: Jossey-Bass; 1979.
- Antonovsky A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well. San Francisco, CA: Jossey-Bass; 1987.
- Harvey PD, Penn D. Social cognition: the key factor predicting social outcome in people with schizophrenia?. Psychiatry (Edgmont) 2010;7:41-4.
- Schön UK, Denhov A, Topor A. Social relationships as a decisive factor in recovering from severe mental illness. Int J Soc Psychiatry 2009;55:336-47. http://dx.doi.org/10.1177/0020764008093686.
- Brunt D, Hansson L. The social networks of persons with severe mental illness in in-patient settings and supported community settings. J Mental Health 2002;11:611-21. http://dx.doi.org/10.1080/09638230021000058175.
- Preamble to the Constitution of the World Health Organization n.d. www.who.int/about/definition/en/print.html (accessed 8 December 2014).
- Godlee F. What is health?. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d4817.
- Schrank B, Bird V, Tylee A, Coggins T, Rashid T, Slade M. Conceptualising and measuring the well-being of people with psychosis: systematic review and narrative synthesis. Soc Sci Med 2013;93:9-21. http://dx.doi.org/10.1016/j.socscimed.2013.05.011.
- Dodge R, Daly AP, Huyton J, Sanders LD. The challenge of defining wellbeing. Int J Wellbeing 2012;2:222-35. http://dx.doi.org/10.5502/ijw.v2i3.4.
- Weich S, Brugha T, King M, McManus S, Bebbington P, Jenkins R, et al. Mental well-being and mental illness: findings from the Adult Psychiatric Morbidity Survey for England 2007. Br J Psychiatry 2011;199:23-8. http://dx.doi.org/10.1192/bjp.bp.111.091496.
- Schrank B, Riches S, Bird V, Murray J, Tylee A, Slade M. A conceptual framework for improving well-being in people with a diagnosis of psychosis. Epidemiol Psychiatr Sci 2013. http://dx.doi.org/10.1017/S2045796013000462.
- Phelan M, Stradins L, Morrison S. Physical health of people with severe mental illness: can be improved if primary care and mental health professionals pay attention to it. BMJ 2001;322. http://dx.doi.org/10.1136/bmj.322.7284.443.
- Osborn DP, Nazareth I, King MB. Risk for coronary heart disease in people with severe mental illness: cross-sectional comparative study in primary care. Br J Psychiatry 2006;188:271-7. http://dx.doi.org/10.1192/bjp.bp.104.008060.
- De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. prevalence, impact of medications and disparities in health care. World Psychiatry 2011;10:52-77.
- McElroy SL. Obesity in patients with severe mental illness: overview and management. J Clin Psychiatry 2009;70:12-21. http://dx.doi.org/10.4088/JCP.7075su1c.03.
- Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time?. Arch Gen Psychiatry 2007;64:1123-31. http://dx.doi.org/10.1001/archpsyc.64.10.1123.
- Deakin B, Ferrier N, Holt RI, Millar H, Nutt DJ, Reynolds G, et al. The physical health challenges in patients with severe mental illness: cardiovascular and metabolic risks. J Psychopharmacol 2010;24:1-8. http://dx.doi.org/10.1177/1359786810374863.
- Happell B, Davies C, Scott D. Health behaviour interventions to improve physical health in individuals diagnosed with a mental illness: a systematic review. Int J Mental Health Nurs 2012;21:236-47. http://dx.doi.org/10.1111/j.1447-0349.2012.00816.x.
- Eldridge D, Dawber N, Gray R. A well-being support program for patients with severe mental illness: a service evaluation. BMC Psychiatry 2011;11. http://dx.doi.org/10.1186/1471-244X-11-46.
- Smith S, Yeomans D, Bushe CJ, Eriksson C, Harrison T, Holmes R, et al. A well-being programme in severe mental illness. Reducing risk for physical ill-health: a post-programme service evaluation at 2 years. Eur Psychiatry 2007;22:413-18. http://dx.doi.org/10.1016/j.eurpsy.2007.07.002.
- Slade M. 100 Ways to Support Recovery: A Guide for Mental Health Professionals. London: Rethink Mental Illness; 2009.
- Roberts G, Boardman J. Becoming a recovery-oriented practitioner. Adv Psychiatric Treat 2014;20:37-4. http://dx.doi.org/10.1192/apt.bp.112.010652.
- Sayce L. From Psychiatric Patient to Citizen. London: St Martin’s Press; 2000.
- Fakhoury W, Priebe S. Deinstitutionalization and reinstitutionalization: major changes in the provision of mental healthcare. Psychiatry 2007;6:313-16. http://dx.doi.org/10.1016/j.mppsy.2007.05.008.
- Henderson C, Thornicroft G. Stigma and discrimination in mental illness: time to change. Lancet 2009;373:1928-30. http://dx.doi.org/10.1016/S0140-6736(09)61046-1.
- Noordsy D, Torrey W, Mueser K, Mead S, O’Keefe C, Fox L. Recovery from severe mental illness: an intrapersonal and functional outcome definition. Int Rev Psychiatry 2002;14:318-26. http://dx.doi.org/10.1080/0954026021000016969.
- Bora R. Empowering People: Coaching for Mental Health Recovery. London: Rethink Mental Illness; 2012.
- Le Boutillier C, Leamy M, Bird VJ, Davidson L, Williams J, Slade M. What does recovery mean in practice? A qualitative analysis of international recovery-oriented practice guidance. Psychiatr Serv 2011;62:1470-6. http://dx.doi.org/10.1176/appi.ps.001312011.
- Spencer L, Pahl RE. Rethinking Friendship: Hidden Solidarities Today. Princeton, NJ: Princeton University Press; 2006.
- Marsden PV, Lin N. Social Structure and Networks Analysis. Beverly Hills, CA: Sage; 1982.
- Marsden PV. Core discussion networks of Americans. Am Sociol Rev 1987;52:122-31. http://dx.doi.org/10.2307/2095397.
- Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Soc Sci Med 2001;52:1501-16. http://dx.doi.org/10.1016/S0277-9536(00)00259-8.
- Heaney CA, Israel BA, Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: John Wiley & Sons; 2008.
- Emirbayer M, Goodwin J. Network analysis, culture, and the problem of agency. Am J Sociol 1994;99:1411-54.
- Cohen CI, Sokolovsky J. Schizophrenia and social networks: ex-patients in the inner city. Schizophr Bull 1978;4:546-60. http://dx.doi.org/10.1093/schbul/4.4.546.
- Forrester-Jones R, Carpenter J, Coolen-Schrijner P, Cambridge P, Tate A, Hallam A, et al. Good friends are hard to find? The social networks of people with mental illness 12 years after deinstitutionalisation. J Mental Health 2012;21:4-14. http://dx.doi.org/10.3109/09638237.2011.608743.
- Middelboe T, Mackeprang T, Hansson L, Werdelin G, Karlsson H, Bjarnason O, et al. The Nordic Study on schizophrenic patients living in the community: subjective needs and perceived help. Eur Psychiatry 2001;16:207-14. http://dx.doi.org/10.1016/S0924-9338(01)00566-1.
- Meeks S, Murrell SA. Service providers in the social networks of clients with severe mental illness. Schizophr Bull 1994;20:399-406. http://dx.doi.org/10.1093/schbul/20.2.399.
- MacDonald E, Sauer K, Howie L, Albiston D. What happens to social relationships in early psychosis? A phenomenological study of young people’s experiences. J Mental Health 2005;14:129-43. http://dx.doi.org/10.1080/09638230500060052.
- Cornwell B, Laumann EO. The health benefits of network growth: new evidence from a national survey of older adults. Soc Sci Med n.d. www.sciencedirect.com/science/article/pii/S0277953613005170 (accessed 8 December 2014).
- Eklund M, Hansson L. Social network among people with persistent mental illness: associations with sociodemographic, clinical and health-related factors. Int J Soc Psychiatry 2007;53:293-305. http://dx.doi.org/10.1177/0020764006074540.
- Becker T, Thornicroft G, Leese M, McCrone P, Johnson S, Albert M, et al. Social networks and service use among representative cases of psychosis in south London. Br J Psychiatry 1997;171:15-9. http://dx.doi.org/10.1192/bjp.171.1.15.
- Agneessens F, Waege H, Lievens J. Diversity in social support by role relations: a typology. Soc Netw 2008;28:427-41. http://dx.doi.org/10.1016/j.socnet.2005.10.001.
- Alcalay R. Health and social support networks: a case for improving interpersonal communication. Soc Netw 1983;5:71-88. http://dx.doi.org/10.1016/0378-8733(83)90016-3.
- Cohen S, Wills T. Stress, social support, and the buffering hypothesis. Psychological Bull 1985;98:310-57. http://dx.doi.org/10.1037/0033-2909.98.2.310.
- Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav 2011;52:145-61. http://dx.doi.org/10.1177/0022146510395592.
- McKinlay JB. Social networks, lay consultation and help-seeking behavior. Soc Forces 1973;51:275-92. http://dx.doi.org/10.1093/sf/51.3.275.
- Shiovitz-Ezra S, Litwin H. Social network type and health-related behaviors: evidence from an American national survey. Soc Sci Med 2012;75:901-4. http://dx.doi.org/10.1016/j.socscimed.2012.04.031.
- Cohen S, Gottlieb B, Underwood L, Cohen S, Underwood L, Gottlieb B. Social Support Measurement and Intervention. New York, NY: Oxford University Press; 2000.
- Green G, Hayes C, Dickinson D, Whittaker A, Gilheany B. The role and impact of social relationships upon well-being reported by mental health service users: a qualitative study. J Ment Health 2002;11:565-79. http://dx.doi.org/10.1080/09638230020023912.
- Mueller B, Nordt C, Lauber C, Rueesch P, Meyer P, Roessler W. Social support modifies perceived stigmatization in the first years of mental illness: a longitudinal approach. Soc Sci Med 2006;62:39-4. http://dx.doi.org/10.1016/j.socscimed.2005.05.014.
- Lam JA, Rosenheck R. Social support and service use among homeless persons with serious mental illness. Int J Soc Psychiatry 1999;45:13-28. http://dx.doi.org/10.1177/002076409904500103.
- Hultman CM, Wieselgren I, Öhman A. Relationships between social support, social coping and life events in the relapse of schizophrenic patients. Scand J Psychol 1997;38:3-13. http://dx.doi.org/10.1111/1467-9450.00002.
- Vassilev I, Rogers A, Blickem C, Brooks H, Kapadia D, Kennedy A, et al. Social networks, the ‘work’ and work force of chronic illness self-management: a survey analysis of personal communities. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0059723.
- Magliano L, Fiorillo A, De Rosa C, Malangone C, Maj M. Family burden in long-term diseases: a comparative study in schizophrenia vs. physical disorders. Soc Sci Med 2005;61:313-22. http://dx.doi.org/10.1016/j.socscimed.2004.11.064.
- Vassilev I, Rogers A, Sanders C, Kennedy A, Blickem C, Protheroe J, et al. Social networks, social capital and chronic illness self-management: a realist review. Chronic Illn 2011;7:60-86. http://dx.doi.org/10.1177/1742395310383338.
- Rogers A, Vassilev I, Sanders C, Kirk S, Chew-Graham C, Kennedy A, et al. Social networks, work and network-based resources for the management of long-term conditions: a framework and study protocol for developing self-care support. Implement Sci 2011;6. www.biomedcentral.com/content/pdf/1748-5908-6-56.pdf (accessed 8 December 2014).
- Davidson L, Strauss JS. Sense of self in recovery from severe mental illness. Br J Med Psychol 1992;65:131-45. http://dx.doi.org/10.1111/j.2044-8341.1992.tb01693.x.
- Pettie D, Triolo AM. Illness as evolution: the search for identity and meaning in the recovery process. Psychiatry Rehabil J 1999;22:255-62. http://dx.doi.org/10.1037/h0095236.
- Bentall RP. Madness Explained: Psychosis and Human Nature. London: Penguin; 2004.
- Thornicroft G, Breakey WR. The COSTAR programme. 1: improving social networks of the long-term mentally ill. Br J Psychiaty 1991;159:245-9. http://dx.doi.org/10.1192/bjp.159.2.245.
- Björkman T, Hansson L. Predictors of improvement in quality of life of long-term mentally ill individuals receiving case management. Eur Psychiatry 2002;17:33-40. http://dx.doi.org/10.1016/S0924-9338(02)00621-1.
- Hansson L, Middelboe T, Sørgaard KW, Bengtsson-Tops A, Bjarnason O, Merinder L, et al. Living situation, subjective quality of life and social network among individuals with schizophrenia living in community settings. Acta Psychiatr Scand 2002;106:343-50. http://dx.doi.org/10.1034/j.1600-0447.2002.02346.x.
- Hansson L. Determinants of quality of life in people with severe mental illness. Acta Psychiatr Scand 2006;113:46-50. http://dx.doi.org/10.1111/j.1600-0447.2005.00717.x.
- Sibitz I, Amering M, Unger A, Seyringer ME, Bachmann A, Schrank B, et al. The impact of the social network, stigma and empowerment on the quality of life in patients with schizophrenia. Eur Psychiatry 2011;26:28-33. http://dx.doi.org/10.1016/j.eurpsy.2010.08.010.
- Lin N. Connections 1999;22:28-51.
- Di Nicola P, Stanzani S, Tronca L. Personal networks as social capital: a research strategy to measure contents and forms of social support. Ital Sociol Rev 2011;1:1-15.
- McKenzie K, Whitley R, Weich S. Social capital and mental health. Br J Psychiatry 2002;181:280-3. http://dx.doi.org/10.1192/bjp.181.4.280.
- Eriksson M. Social capital and health: complications for health promotion. Global Health Action 2011;4. www.ncbi.nlm.nih.gov/pmc/articles/PMC3036711/ (accessed 8 December 2014).
- Henderson S, Whiteford H. Social capital and mental health. Lancet 2003;362:505-6. http://dx.doi.org/10.1016/S0140-6736(03)14150-5.
- Almedom AM. Social capital and mental health: an interdisciplinary review of primary evidence. Soc Sci Med 2005;61:943-64. http://dx.doi.org/10.1016/j.socscimed.2004.12.025.
- Lofors J, Sundquist K. Low-linking social capital as a predictor of mental disorders: a cohort study of 4.5 million Swedes. Soc Sci Med 2007;64:21-34. http://dx.doi.org/10.1016/j.socscimed.2006.08.024.
- Elgar FJ, Davis CG, Wohl MJ, Trites SJ, Zelenski JM, Martin MS. Social capital, health and life satisfaction in 50 countries. Health Place 2011;17:1044-53. http://dx.doi.org/10.1016/j.healthplace.2011.06.010.
- De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental illness: a systematic review. J Epidemiol Community Health 2005;59:619-27. http://dx.doi.org/10.1136/jech.2004.029678.
- Moore S, Bockenholt U, Daniel M, Frohlich K, Kestens Y, Richard L. Social capital and core network ties: a validation study of individual-level social capital measures and their association with extra- and intra-neighborhood ties, and self-rated health. Health Place 2011;17:536-44. http://dx.doi.org/10.1016/j.healthplace.2010.12.010.
- Dutt K, Webber M. Access to social capital and social support among South East Asian women with severe mental health problems: a cross-sectional survey. Int J Soc Psychiatry 2010;56:593-605. http://dx.doi.org/10.1177/0020764009106415.
- Webber MP, Huxley PJ. Measuring access to social capital: the validity and reliability of the Resource Generator-UK and its association with common mental disorder. Soc Sci Med 2007;65:481-92. http://dx.doi.org/10.1016/j.socscimed.2007.03.030.
- Portes A, Landolt P. Social capital: promise and pitfalls of its role in development. J Latin Am Stud 2000;32:529-47. http://dx.doi.org/10.1017/S0022216X00005836.
- Webber M, Reidy H, Ansari D, Stevens M, Morris D. Enhancing social networks: a qualitative study of health and social care practice in UK mental health services. Health Soc Care Community 2014.
- Leufstadius C, Erlandsson L, Björkman T, Eklund M. Meaningfulness in daily occupations among individuals with persistent mental illness. J Occup Sci 2008;15:27-35. http://dx.doi.org/10.1080/14427591.2008.9686604.
- Goldberg B, Brintnell ES, Goldberg J. The relationship between engagement in meaningful activities and quality of life in persons disabled by mental illness. Occup Ther Mental Health 2002;18:17-44. http://dx.doi.org/10.1300/J004v18n02_03.
- Aubin G, Hachey R, Mercier C. Meaning of daily activities and subjective quality of life in people with severe mental illness. Scand J Occup Ther 1999;6:53-62. http://dx.doi.org/10.1080/110381299443744.
- Carter GBC, Milton DR, Ascher-Svanum H, Faries DE. Sustained favorable long-term outcome in the treatment of schizophrenia: a 3-year prospective observational study. BMC Psychiatry 2011;11. http://dx.doi.org/10.1186/1471-244X-11-143.
- Hendryx M, Green CA, Perrin NA. Social support, activities, and recovery from serious mental illness: STARS study findings. J Behav Health Serv Res 2009;36:320-9. http://dx.doi.org/10.1007/s11414-008-9151-1.
- Argentzell E, Håkansson C, Eklund M. Experience of meaning in everyday occupations among unemployed people with severe mental illness. Scand J Occup Ther 2012;19:49-58. http://dx.doi.org/10.3109/11038128.2010.540038.
- Dunn EC, Wewiorski NJ, Rogers ES. The meaning and importance of employment to people in recovery from serious mental illness: results of a qualitative study. Psychiatric Rehabil J 2008;32:59-62. http://dx.doi.org/10.2975/32.1.2008.59.62.
- Evans J, Repper J. Employment, social inclusion and mental health. J Psychiatric Mental Health Nurs 2000;7:15-24. http://dx.doi.org/10.1046/j.1365-2850.2000.00260.x.
- Bush P, Drake R, Xie H, McHugo G, Haslett W. The long-term impact of employment on mental health service use and costs for persons with severe mental illness. Psychiatric Serv 2009;60:1024-31. http://dx.doi.org/10.1176/appi.ps.60.8.1024.
- Perkins R, Rinaldi M. Unemployment rates among patients with long-term mental health problems: a decade of rising unemployment. Psychiatric Bull 2002;26:295-8. http://dx.doi.org/10.1192/pb.26.8.295.
- Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, Perkins D, et al. Barriers to employment for people with schizophrenia. Am J Psychiatry 2006;163:411-17. http://dx.doi.org/10.1176/appi.ajp.163.3.411.
- Stuart H. Mental illness and employment discrimination. Curr Opin Psychiatry 2006;19:522-6. http://dx.doi.org/10.1097/01.yco.0000238482.27270.5d.
- Pinfold V. Building up safe havens all around the world: users experiences of living in the community with mental health problems. Health Place 2000;6:201-12. http://dx.doi.org/10.1016/S1353-8292(00)00023-X.
- Evans GW. The built environment and mental health. J Urban Health 2003;80:536-55. http://dx.doi.org/10.1093/jurban/jtg063.
- Nelson G, Lord J, Ochocka J. Empowerment and mental health in community: narratives of psychiatric consumer/survivors. J Community Appl Soc Psychol 2001;11:125-42. http://dx.doi.org/10.1002/casp.619.
- Gale CR, Dennison EM, Cooper C, Sayer AA. Neighbourhood environment and positive mental health in older people: the Hertfordshire Cohort Study. Health Place 2011;17:867-74. http://dx.doi.org/10.1016/j.healthplace.2011.05.003.
- Maas J, Verheij RA, Groenewegen PP, De Vries S, Spreeuwenberg P. Green space, urbanity, and health: how strong is the relation?. J Epidemiol Comm Health 2006;60:587-92. http://dx.doi.org/10.1136/jech.2005.043125.
- Sugiyama T, Leslie E, Giles-Corti B, Owen N. Associations of neighbourhood greenness with physical and mental health: do walking, social coherence and local social interaction explain the relationships?. J Epidemiol Community Health 2008;62. http://dx.doi.org/10.1136/jech.2007.064287.
- Groenewegen PP, van den Berg AE, Maas J, Verheij RA, De Vries S. Is a green residential environment better for health? If so, why?. Ann Assoc Am Geographers 2012;102:996-1003. http://dx.doi.org/10.1080/00045608.2012.674899.
- Lauber C, Nordt C, Falcato L, Rössler W. Lay recommendations on how to treat mental disorders. Soc Psychiatry Psychiatric Epidemiol 2001;36:553-6. http://dx.doi.org/10.1007/s001270170006.
- van den Berg AE, Maas J, Verheij RA, Groenewegen PP. Green space as a buffer between stressful life events and health. Soc Sci Med 2010;70:1203-10. http://dx.doi.org/10.1016/j.socscimed.2010.01.002.
- Manzi T, Lucas K, Lloyd-Jones T, Allen J, Lucas K, Lloyd Jones T, et al. Social Sustainability in Urban Areas Communities, Connectivity and the Urban Fabric. London: Routledge; 2010.
- Parr H, Philo C, Burns N. Social geographies of rural mental health: experiencing inclusions and exclusions. Trans Inst Br Geographers 2004;29:401-19. http://dx.doi.org/10.1111/j.0020-2754.2004.00138.x.
- Philo C, Parr H, Burns N. Rural madness: a geographical reading and critique of the rural mental health literature. J Rural Stud 2003;19:259-81. http://dx.doi.org/10.1016/S0743-0167(03)00005-6.
- Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J, et al. Incidence of Schizophrenia and Other Psychoses in England, 1950–2009: A Systematic Review and Meta-Analyses 2012. www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0031660 (accessed 22 October 2014).
- Krabbendam L, Van Os J. Schizophrenia and urbanicity: a major environmental influence – conditional on genetic risk. Schizophr Bull 2005;31:795-9. http://dx.doi.org/10.1093/schbul/sbi060.
- Lederbogen F, Kirsch P, Haddad L, Streit F, Tost H, Schuch P, et al. City living and urban upbringing affect neural social stress processing in humans. Nature 2011;474:498-501. http://dx.doi.org/10.1038/nature10190.
- Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry 2000;177:4-7. http://dx.doi.org/10.1192/bjp.177.1.4.
- Dickerson FB, Sommerville J, Origoni AE, Ringel NB, Parente F. Experiences of stigma among outpatients with schizophrenia. Schizophr Bull 2002;28:143-55. http://dx.doi.org/10.1093/oxfordjournals.schbul.a006917.
- Brohan E, Elgie R, Sartorius N, Thornicroft G. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophr Res 2010;122:232-8. http://dx.doi.org/10.1016/j.schres.2010.02.1065.
- Link BG, Phelan JC. Conceptualizing stigma. Ann Rev Sociol 2001;27:363-85. http://dx.doi.org/10.1146/annurev.soc.27.1.363.
- Evans-Lacko S, Malcolm E, West K, Rose D, London J, Rüsch N, et al. Influence of Time to Change’s social marketing interventions on stigma in England 2009–2011. Br J Psychiatry 2013;202. http://dx.doi.org/10.1192/bjp.bp.113.126672.
- Corrigan PW, Larson JE, Ruesch N. Self-stigma and the ‘why try’ effect: impact on life goals and evidence-based practices. World Psychiatry 2009;8:75-81.
- Dickerson FB, Sommerville J, Origoni AE, Ringel NB, Parente F. Outpatients with schizophrenia and bipolar I disorder: do they differ in their cognitive and social functioning?. Psychiatry Res 2001;102:21-7. http://dx.doi.org/10.1016/S0165-1781(01)00247-5.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick–Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. http://dx.doi.org/10.1186/1477-7525-5-63.
- Nelson EC, Wasson J, Kirk J, Keller A, Clark D, Stewart A, et al. Assessment of function in routine clinical practice: description of the COOP Charts method and preliminary findings. J Chron Dis 1987;40:55S-6S.
- Bergman MM. Advances in Mixed Methods Research: Theories and Applications. New York, NY: Sage; 2008.
- Moran-Ellis J, Alexander VD, Cronin A, Dickinson M, Fielding J, Sleney J, et al. Triangulation and integration: processes, claims and implications. Qual Res 2006;6:45-59. http://dx.doi.org/10.1177/1468794106058870.
- Yin RK. Case Study Research: Design and Methods. London: Sage; 2009.
- Hammersley M, Bergman M. Advances in Mixed Methods Research: Theories and Applications. Thousand Oaks, CA: Sage; 2008.
- Denzin NK. Moments, mixed methods, and paradigm dialogs. Qual Inq 2010;16:419-27. http://dx.doi.org/10.1177/1077800410364608.
- McDonald LJ, Griffin ML, Kolodziej ME, Fitzmaurice GM, Weiss RD. The impact of drug use in social networks of patients with substance use and bipolar disorders. Am J Addict 2011;20:100-5. http://dx.doi.org/10.1177/10.1111/j.1521-0391.2010.00117.x.
- Finlay L, Gough B. Reflexivity: A Practical Guide for Researchers in Health and Social Sciences. London: John Wiley & Sons; 2008.
- Tariq S, Woodman J. Using mixed methods in health research. JRSM Short Rep 2013;4. http://dx.doi.org/10.1177/10.1177/2042533313479197.
- Greene JC. Toward a methodology of mixed methods social inquiry. Res Schools 2006;13:93-8.
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. London: Sage; 1994.
- Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. J Admin Governance 2009;4:72-9.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Stewart-Brown S, Tennant A, Tennant R, Platt S, Parkinson J, Weich S. Internal construct validity of the Warwick–Edinburgh mental well-being scale (WEMWBS): a Rasch analysis using data from the Scottish health education population survey. Health Qual Life Outcomes 2009;7:15-22. http://dx.doi.org/10.1186/1477-7525-7-15.
- Eaton T, Young P, Fergusson W, Garrett JE, Kolbe J. The Dartmouth COOP Charts: a simple, reliable, valid and responsive quality of life tool for chronic obstructive pulmonary disease. Qual Life Res 2005;14:575-85. http://dx.doi.org/10.1007/s11136-004-0624-2.
- Brewer DD, Webster CM. Forgetting of friends and its effects on measuring friendship networks. Soc Netw 2000;21:361-73. http://dx.doi.org/10.1016/S0378-8733(99)00018-0.
- Campbell KE, Lee BA. Name generators in surveys of personal networks. Soc Netw 1991;13:203-21. http://dx.doi.org/10.1016/0378-8733(91)90006-F.
- Everitt BS. Making Sense of Statistics in Psychology: A Second-Level Course. Oxford: Oxford University Press; 1996.
- Fiori KL, Antonucci TC, Cortina KS. Social network typologies and mental health among older adults. J Gerontol B: Psychol Sci Soc Sci 2006;61:25-32. http://dx.doi.org/10.1093/geronb/61.1.P25.
- Kutner MH, Nachtsheim CJ, Neter J, Li W. Applied Linear Statistical Models. New York, NY: McGraw-Hill; 2005.
- Green J, Thorogood N. Qualitative Methods For Health Research. London: Sage; 2013.
- Jones K, Rapport F. New Qualitative Methodologies in Health and Social Care Research. New York, NY: Routledge; 2004.
- Jones K. Mission drift in qualitative research, or moving toward a systematic review of qualitative studies, moving back to a more systematic narrative review. Qual Report 2004;9:95-112.
- Ayres L, Kavanaugh K, Knafl KA. Within-case and across-case approaches to qualitative data analysis. Qual Health Res 2003;13:871-83. http://dx.doi.org/10.1177/1049732303013006008.
- Buckley CA, Waring MJ. Using diagrams to support the research process: examples from grounded theory. Qual Res 2013;13:148-72. http://dx.doi.org/10.1177/1468794112472280.
- Rice E, Holloway IW, Barman-Adhikari A, Fuentes D, Brown CH, Palinkas LA. A mixed methods approach to network data collection. Field Methods 2014;26:252-68. http://dx.doi.org/10.1177/1525822X13518168.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Edwards G. Mixed-Methods Approaches to Social Network Analysis. London: National Centre for Research Methods; 2010.
- Fischer M. Social network analysis and qualitative comparative analysis: their mutual benefit for the explanation of policy network structures. Methodol Innov Online 2011;6:27-51. www.pbs.plym.ac.uk/mi/pdf/31-08-11/3.%20Fischer%20-%20pp27-51.pdf.
- Staley K. Exploring Impact: Public involvement in NHS, Public Health and Social Care Research. London: National Institute for Health Research; 2009.
- Szmukler G, Staley K, Kabir T. Service user involvement in research. Asia Pac Psychiatry 2011;3:180-6. http://dx.doi.org/10.1111/j.1758-5872.2011.00145.x.
- Ives J, Damery S, Redwod S. PPI, paradoxes and Plato: who’s sailing the ship?. J Med Ethics 2013;39:181-5. http://dx.doi.org/10.1136/medethics-2011-100150.
- Ennis L, Wykes T. Impact of patient involvement in mental health research: longitudinal study. Br J Psychiatry 2013;203:381-6. http://dx.doi.org/10.1192/bjp.bp.112.119818.
- Chandler R, Hayward M. Voicing Psychotic Experiences: A Reconsideration of Recovery and Diversity. Brighton: OLM-Pavilion; 2009.
- Chandler R, Bradstreet S, Hayward M. Voicing Caregiver Experiences: Narratives of Wellbeing and Recovery 2013. www.sussexpartnership.nhs.uk/gps/policies/finish/2301/8950 (accessed 8 December 2014).
- Slade M, Bird V, Chandler R, Fox J, Larsen J, Tew J, et al. The contribution of advisory committees and public involvement to large studies: case study. BMC Health Serv Res 2010;10. www.biomedcentral.com/1472-6963/10/323 (accessed 8 December 2014).
- Tashakkori A, Teddlie C, Bergman MM. Advances in Mixed methods Research. London: Sage; 2008.
- Webber M, Huxley P, Harris T. Social capital and the course of depression: six-month prospective cohort study. J Affect Disord 2011;129:149-57. http://dx.doi.org/10.1016/j.jad.2010.08.005.
- Cockerham WC. Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav 2005;46:51-67. http://dx.doi.org/10.1177/002214650504600105.
- Cacioppo JT, Hawkley LC. Social isolation and health with an emphasis on underlying mechanisms. Perspect Biol Med 2003;46:S39-S52. http://dx.doi.org/10.1353/pbm.2003.0049.
- Jenkinson C, Mayou R, Day A, Garratt A, Juszczak E. Evaluation of the Dartmouth COOP Charts in a large-scale community survey in the United Kingdom. J Public Health 2002;24:106-11. http://dx.doi.org/10.1093/pubmed/24.2.106.
- McFall SL, Garrington C. Understanding Society: Early Findings from the First Wave of the UK’s Household Longitudinal Study. Colchester: Institute for Social and Economic Research, University of Essex; 2011.
- Webber M, Corker E, Hamilton S, Weeks C, Pinfold V, Rose D, et al. Discrimination against people with severe mental health illness and their access to social capital: findings from the Viewpoint Survey. Epidemiol Psychiatric Sci 2014;23:155-65. http://dx.doi.org/10.1017/S2045796013000243.
- Murray J, Easter A, Bellringer S. Evaluation of Capital Volunteering. Fourth Interim Report: Outcomes at Twelve Months. London: Health Service & Population Research Department, Institute of Psychiatry, King’s College London; 2007.
- Wolch J, Philo C. From distributions of deviance to definitions of difference: past and future mental health geographies. Health Place 2000;63:137-57. http://dx.doi.org/10.1016/S1353-8292(00)00019-8.
- Wenger GC. A network typology: from theory to practice. J Aging Stud 1991;5:147-62. http://dx.doi.org/10.1016/0890-4065(91)90003-B.
- Wenger GC. Review of findings on support networks of older Europeans. J Cross Cultural Gerontol 1997;12:1-21. http://dx.doi.org/10.1023/A:1006597110040.
- Wenger GC, Tucker I. Network variation in practice: identification of support network type. Health Soc Care Community 2000;10:28-35. http://dx.doi.org/10.1046/j.0966-0410.2001.00339.x.
- Roberts SG, Dunbar RI, Pollet TV, Kuppens T. Exploring variation in active network size: constraints and ego characteristics. Soc Netw 2009;31:138-46. http://dx.doi.org/10.1016/j.socnet.2008.12.002.
- Hill RA, Dunbar RI. Social network size in humans. Human Nature 2003;14:53-72. http://dx.doi.org/10.1007/s12110-003-1016-y.
- Report for Department of Culture, Media and Sports quoted 26 January 2011 n.d. www.bbc.co.uk/news/uk-england-12239388 (accessed 14 March 2014).
- Tucker I. Mental health service user territories: enacting ‘safe spaces’ in the community. Health 2010;14:434-48. http://dx.doi.org/10.1177/1363459309357485.
- Parr H. Mental health, public space, and the city: questions of individual and collective access. Environ Plann D 1997;15:435-54. http://dx.doi.org/10.1068/d150435.
- Psychosis and Schizophrenia in Adults: Management and Treatment. London: NICE; 2014.
- Corrigan PW. Empowerment and serious mental illness: treatment partnerships and community opportunities. Psychiatric Q 2002;73:217-28. http://dx.doi.org/10.1023/A:1016040805432.
- Eklund M, Erlandsson LK, Persson D. Occupational value among individuals with long-term mental illness. Can J Occup Ther 2003;70:276-84.
- Corrigan PW, Markowitz FE, Watson AC. Structural levels of mental illness stigma and discrimination. Schizophr Bull n.d.;30:481-91. http://dx.doi.org/10.1093/oxfordjournals.schbul.a007096.
- Broom D, D’Souza R, Strazdins L, Butterworth P, Parslow R, Rodgers B. The lesser evil: bad jobs or unemployment? A survey of mid-aged Australians. Soc Sci Med 2006;63:575-86. http://dx.doi.org/10.1016/j.socscimed.2006.02.003.
- Brohan E, Henderson C, Wheat K, Malcolm E, Clement S, Barley EA, et al. Systematic review of beliefs, behaviours and influencing factors associated with disclosure of a mental health problem in the workplace. BMC Psychiatry 2012;12. www.biomedcentral.com/1471-244X/12/11/ (accessed 8 December 2014).
- Palumbo C, Matanov A, Valpe U, Priebe S. Characteristics of social networks of patients with psychotic disorders: a systematic literature review. Eur Psychiatry 2013;28. www.sciencedirect.com/science/article/pii/S0924933813768019 (accessed 8 December 2014).
- Cohen S. Social relationships and health. Am Psychologist 2004;59:676-84. http://dx.doi.org/10.1037/0003-066X.59.8.676.
- Barham P, Hayward R. From the Mental Patient to the Person. London: Routledge; 2002.
- Werner S. Subjective well-being, hope, and needs of individuals with serious mental illness. Psychiatry Res 2012;196:214-19. http://dx.doi.org/10.1016/j.psychres.2011.10.012.
- Valente TW. Social Networks and Health: Models, Methods, and Applications. Oxford: Oxford University Press; 2010.
- Siegel DE, Tracy EM, Corvo KN. Strengthening social networks: intervention strategies for mental health case managers. Health Soc Work 2010;19:206-16.
- Biegel DE, Tracy EM, Song LY. Barriers to social network interventions with persons with severe and persistent mental illness: a survey of mental health case managers. Community Mental Health J 1995;31:335-49. http://dx.doi.org/10.1007/BF02207520.
- Thornicroft G. Shunned: Discrimination against People with Mental Illness. New York, NY: Oxford University Press; 2006.
- Moore S, Salsberg J, Leroux J, Kawachi I, Takao S, Subramanian SV. Global Perspectives on Social Capital and Health. New York, NY: Springer; 2013.
- Whitley R, McKenzie K. Social capital and psychiatry: review of the literature. Harvard Rev Psychiatry 2005;13:71-84. http://dx.doi.org/10.1080/10673220590956474.
- Angermeyer MC, Schulze B, Dietrich S. Courtesy stigma. Soc Psychiatry Psychiatr Epidemiol 2003;38:593-602. http://dx.doi.org/10.1007/s00127-003-0680-x.
- Hamilton S, Lewis-Homes E, Pinfold V, Henderson C, Rose D, Thornicroft G. Discrimination against people with a mental health diagnosis: qualitative analysis of reported experiences. J Mental Health 2014;23:88-93. http://informahealthcare.com/doi/abs/10.3109/09638237.2014.880408 (accessed 8 December 2014).
- Parr H. Interpreting the ‘hidden social geographies’ of mental health: ethnographies of inclusion and exclusion in semi-institutional places. Health Place 2000;6:225-37. http://dx.doi.org/10.1016/S1353-8292(00)00025-3.
- Larsen JA. Finding meaning in first episode psychosis: experience, agency, and the cultural repertoire. Med Anthropol Q 2004;18:447-71. http://dx.doi.org/10.1525/maq.2004.18.4.447.
- Social Exclusion Unit . Mental Health and Social Exclusion 2004.
- Mental Health Foundation . Crossing Boundaries: Improving Integrated Care for People With Mental Health Problems 2013. www.mentalhealth.org.uk/content/assets/PDF/publications/crossing-boundaries.pdf?view=Standard (accessed 14 March 2013).
- Healthy Lives Healthy People: Our Strategy for Public Health in England. London: HMSO; 2010.
- NHS Confederation . A Primary Care Approach to Health and Wellbeing 2012. www.nhsconfed.org/Publications/Documents/Case-study-report-on-Sandwell.pdf (accessed 15 March 2014).
- Huxley P, Evans S, Beresford P, Davidson B, King S. The principles and provisions of relationships: findings from an evaluation of support, time and recovery workers in mental health services in England. J Soc Work 2009;9:99-117. http://dx.doi.org/10.1177/1468017308098434.
- Pinfold V, Rapaport J, Bellringer S. Developing partnerships with carers through good practice in information-sharing. Mental Health Rev J 2007;12:7-14. http://dx.doi.org/10.1108/13619322200700015.
- The Abandoned Illness: A Report by the Schizophrenia Commission. London: Rethink Mental Illness; 2012.
- Abrahams S, Alder DA, Bartels SJ. Better practices in collaborative mental health care: an analysis of the evidence base. Can J Psychiatry 2006;51:7S-72S.
- Byng R, Jones R, Leese M, Hamilton B, McCrone P, Craig T. Exploratory cluster randomised controlled trial of shared care development for long-term mental illness. Br J Gen Pract 2004;54:259-66.
- Byng R, Norman I, Redfern S, Jones R. Exposing the key functions of a complex intervention for shared care in mental health: case study of a process evaluation. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-274 (accessed 8 Dcember 2014).
- Reilly S, Planner C, Gask L, Hann M, Knowles S, Druss B, et al. Collaborative care approaches for people with severe mental illness. Cochrane Database Syst Rev 2012. http://dx.doi.org/10.1002/14651858.CD009531.
- Bevan S, Taskila T, Steadman K, Gulliford J, Thomas R, Moise A. Working with Schizophrenia: Pathways to Employment, Recovery and Inclusion. London: The Work Foundation; 2013.
- Flap H, Volker B. Goal specific social capital and job satisfaction: effects of different types of networks on instrumental and social aspects of work. Soc Netw 2001;23:297-320. http://dx.doi.org/10.1016/S0378-8733(01)00044-2.
- Ewing G, Rogers M, Barclay S, McCabe J, Martin A, Todd C. Recruiting patients into a primary care based study of palliative care: why is it so difficult?. Palliat Med 2004;18:452-9. http://dx.doi.org/10.1191/0269216304pm905oa.
Appendix 1 Lived experience reflections on community health network: project report
Note: This report was commissioned by the chief investigator to aid the study synthesis process; it has not been edited but is provided as received. The LEEs saw draft chapters in August 2013, not full analysis. This is particularly an issue for network mapping (see Chapter 3) and in-depth interview analysis (see Chapter 4) where substantial new analysis has been undertaken since the LEEs reviewed the drafts. We draw on the insights provided by the PPI group in Chapter 8.
The aim of this consultation was to facilitate reflection on and interpretation of the research findings from the CHN project from the perspectives of the LEEs who had worked on the study. We have not attempted to produce a comprehensive synthesis of the findings. Rather, our aim was to prioritise the results that mattered most to the LEEs and give reasons for this selection. The meaning of study findings and the recommendations below were grounded in each LEE’s lived experience and understanding of recovery. Because there is no one size fits all on recovery, the task was not to force consensus, although consensus is given weight where it occurs. This process was facilitated by a lived experience researcher independent of the project.
How we worked together
Five LEEs were contacted by e-mail and telephone in Week 1 of the interpretation phase to agree a collective method. LEEs varied on research experience, location and existing work commitments. The goal was to think through the subjective meaning of the results. It was also agreed that recovery means different things to people and that the project needed to preserve these differences. After initial contact, it was agreed that each LEE would start by thinking about baseline questions individually and send private responses to the facilitator. It was agreed that LEEs would either write responses or take part in a telephone interview using the same schedule. This process was repeated for each of the reports, generating an individual study interpretation for each LEE. The group met to collectively steer the facilitator’s organisation of the LEEs interpretations. We chose this way of working to embed a recovery ethos into our report as a work of coproduction.
Ethical considerations
PPI consultancy is not bound by the same stringent ethics protocol that exists for research participants. Nevertheless, the sensitivity of the questions around lived experience required due consideration of the LEEs current vulnerabilities. Each LEE was informed about how their responses would be used in the study, report and potential publications.
Although responses to the questions would be anonymised in the published report, LEEs were advised that in a small group their responses may be recognised by each other and by some other members of the research team. Each was advised not to disclose more than they were comfortable with sharing and was given the option to amend and take back responses throughout. The group meeting was also used to check comfort with disclosure. This resulted in significant revisions to the final document suggesting that it is important to build in this option when drawing directly on lived experience in a research task. Each LEE was asked about the availability of emotional support should reflection on lived experience become upsetting and advised that they could withdraw at any time or not answer questions they did not wish to. Each LEE was offered payment for their time.
Interview 1: initial views
Initial views on recovery from the LEEs ranged from symptom reduction; being useful and able to take an active part in society; a process of rebuilding and self-determination with continued symptoms to a journey of discovery and on-going process of evaluation.
Work was a key part of recovery for the five LEEs and where this was not going well this was listed as an obstacle to recovery. Each LEE said their lived experiences influenced their various roles throughout the project from constructing the interview schedules, data collection and analysis of transcripts which also structured their responses to the reports. All LEEs expressed mixed feelings on the interaction between lived experience and the research focus on mapping social networks as this could both unlock unidentified sources of personal and social recovery and further identify lack of support in their current or past situation.
Interview 2 and 3: the reports
Mixed perspectives on friendship, project roles and recovery were key to subsequent interpretation of the reports. Seven further questions were developed during the initial interview and circulated with the Network Mapping draft (chapters 3 and 4) in Week 2 and stakeholder (chapter 5) and practitioner (chapter 6) in Week 3. The LEEs were asked to give first impressions, prioritise five most and least important points from each report, comment on any surprises and give reasons for these choices.
First impressions: network mapping and in-depth interviews
Significance versus importance
The LEEs expressed differing views on how to prioritise the relationship between statistical significance and interpretative importance. The comprehensiveness of the report was itself regarded as an important outcome because of the potential effect it could have on practice change. However, the wealth of quantitative data also presented an interpretative challenge:
The report doesn’t answer that much in itself as there could be many reasons for the same outputs.
One LEE suggested that statistical insignificance had been over reported which made it difficult to focus on the results that mattered. Another found some of the insignificant results unexpected and included them in priorities. Alternatively, all of the LEEs welcomed the statistically significant findings about the relationship of work to well-being as confirmation of existing research but did not rank it as important because these findings are already well known. Thus the importance of work to LEEs did not appear as a theme in its own right but was nevertheless active in the interpretation. LEEs also pointed to the findings around the over representation of ethnic groups in secondary services as both significant and very important but, because all LEEs were white British they struggled to interpret further from their lived experience.
All LEEs struggled with data volume in the network mapping and suggested that key terminology like social capital would need explaining in lay summaries. Despite these challenges, everyone did form a view about what was most important but found it more difficult to say what was least important. This question was only partially answered by LEEs
First impressions: practitioner and stakeholder reports
Data blindness on friendship in social networks
In stark contrast, the LEEs found the qualitative practitioner and stakeholder data much easier to process. Whereas, the network mapping offered multiple interpretative options, what was most important on first impression of the qualitative data was not there at all, that is the almost unilateral absence of evidence to demonstrate practitioner and stakeholder awareness of the importance of friendship in social networking for personal and social recovery.
LEEs acknowledged that social capital had a wider application than friendship but, given the importance of friendship to their recovery, they were disappointed by lack of recognition of this key area of human relationships. Although the qualitative reports showed realisation amongst practitioners and stakeholders that people with SMI had fewer friends, this insight appeared compartmentalised from practice and at distinct odds with the wealth of data within the network mapping. While it was difficult to conceptualise an absence as a concrete result, the LEEs were unanimous in prioritising it as a key if not the most important study finding.
Further themes from all reports were as follows:
Diagnostic differences on lifestyle and opportunity
For two of the LEEs, diagnostic comparisons were the differences that mattered most in the network mapping.
What I first noticed are the differences between the diagnostic groups on home ownership. That’s the thing that stood out for me. I concentrated more on these differences rather than differences between the 2 locations.
One LEE reported unease on first impression about organising people’s experiences under diagnostic labels as a continuation of the medical mode of interpreting and categorising experience:
When I read the report I don’t particularly see it in relation to diagnosis, rather in relation to people. I think listening/reading transcripts of their lived experience was very important. I did find it a challenge seeing the diagnosis at the top of each transcript in the same way that seeing the breakdown of data into schizophrenia and psychotic disorder, bipolar disorder and manic episodes and other psychoses.
Another LEE stated that diagnostic differences were the least important as the focus of the report was what people do to support recovery regardless of symptoms. For two LEEs the practical and educational implications of the report were most important although all had something to say about this. Nevertheless, for three LEE there was also a clear sense in which diagnostic differences were statistically significant findings which made some important health inequalities in social capital visible.
LEEs commented in particular on the diagnostic differences in lifestyle. For example, ‘only 6.8% of participants in the schizophrenia and psychotic disorder group owned a home . . . compared to 38.5% of those in the bipolar and manic episodes group’. This could be to do with severity of illness. A far higher percentage of participants with schizophrenia had been inpatients compared with those with a bipolar diagnosis and this may have had an adverse effect on their accommodation status. The impact of cognitive deficit for people with schizophrenia on lifestyle planning could also be higher. Crucially, well-being did not differ across the three diagnostic groups implying that it is not the severity of illness that mattered most to well-being. Rather, differences in well-being were linked to social factors such as employment, children and gender. Although some of these statistics made difficult reading to the LEEs, it was also suggested that the majority of these factors were open to change and could be acted on within a recovery focus to living well with continued symptoms of SMI. The LEEs were unanimous in suggesting that more support for accessing and maintaining employment was needed for people with SMI to reduce these lifestyle inequalities. For example, services open outside working hours to reduce time taken off and education for employers on how to get the best from staff with SMI.
Diagnostic differences on network stability and closeness
There was broad consensus that the quantitative evidence showed that network stability over time (10 years) was most important to subjective well-being. However, network emotional closeness was also seen as of equally high priority as people are more likely to confide in people they trust.
Pets were singled out as a potential source of network stability and closeness in so far as they provide non-judgemental companionship. Activities associated with pet ownership such as walking, buying food and visiting vets could offer purposeful opportunities to expand social networks. It would be interesting to see further research into whether those who are not in a relationship are still on a more positive recovery journey because they have pets.
LEEs were keen not to emphasise clinical factors when it came to developing targeted supports for people with SMI to improve their social capital. Paranoia, depression and social anxiety were also prioritised as obstacles to developing network stability and closeness. Although there was no significant difference in well-being linked to diagnosis, LEEs suggested that some symptoms have a social impact on network stability across the range of diagnoses. For example, it is harder to feel motivated to invest time and effort in other people if one is very depressed and it should go without saying that paranoia and social anxiety might make relationship-building more difficult than for people without these symptoms.
Diagnostic differences on network size, closeness and duration
Network size was also seen as an important factor in so far as participants who had larger networks and more people in their inner circle of closeness were significantly more satisfied with their networks. However, it was the number of contacts in the inner circle that was significantly correlated with higher well-being, suggesting that quality rather than quantity was most important. Participants with a diagnosis of schizophrenia also had lower number of contacts in the inner circle, suggesting that they might require more help to maintain and develop relationships over time. Cognitive deficit was singled out as a particularly challenging obstacle to relationship-building for this group which could require targeted support.
One LEE found these results particularly important. They confirmed expectations that network size of people with bipolar would be larger than for people with schizophrenia. However, the differences in size between weekly and daily networks suggested that diagnostic differences might also point to different kinds of social disablers to routine contact, perhaps greater effects of diagnostic labelling and stigma on daily contacts for people with schizophrenia and possibly more duty-driven weekly contact from people around them. People with a diagnosis of bipolar, alternatively, might find it easier to strike up daily short term relationships but could more easily sabotage them.
The most puzzling finding here was the larger inner circles for people with more inpatient stay which seemed at odds with findings for people with schizophrenia. LEEs suggested that possibly network stability could also be maintained through the social effects of having a serious problem but that such stability could also be a function of a highly medicalised social world. Exceptionally, people with bipolar managed in secondary care also had larger social networks than in primary care. Nothing else showed that secondary care improved the size of social networks for other diagnoses which seemed to have been reduced in secondary care. This could be an effect of greater monitoring and compassionate support in secondary services for people with bipolar.
Age and health inequalities
Another striking finding was the negative correlation between older age on social network activity. Against the general population, age was more statistically important than mental health in the reduction of social networks over time, suggesting that older people with SMI too could be at greater risk of becoming more socially isolated than peers. It is already known that there are greater levels of bereavement for the ageing population which would inevitably impact on network stability in both the inner and outer circles of closeness. However, LEEs also suggested that living with SMI at any age made it more difficult to access appropriate physical care which could also stack up into greater comorbidity in later life, potentially reducing physical capacity to maintain social capital earlier for people with SMI.
The mean age of participants was in their 40s which prompted some curiosity from LEEs about what would have been found with a younger population. Although this study did not include social media, LEEs suggested that the increasing importance of networking sites, like Facebook, to young people’s social networking activity and sense of social capital should not be underestimated in future research. Further, virtual networking via e-mail and websites of common interest had been of real value to three LEEs as an in between recovery space, that is, connectivity they could maintain at home between outside networks or employment even when they felt unwell.
Gender differences on network composition
Two LEEs noted that men had subjectively better quality ties but women had greater network size. This challenged gender stereotypes of women’s social networks as more co-operative and nurturing. It was speculated that men might demand more from their environment and/or might be perceived as more helpless, thus eliciting a more nurturing response from others. It was suggested that it might be more striking to perceive a man as helpless in relation to gender stereotypes of masculinity thus eliciting a greater sense of need. Alternatively, the gender stereotype of women as primary caregivers could work against them as not in so much need of nurture and support within their networks and against men as non-nurturing. The reports did not support further interrogation of these ideas. Nevertheless, it was suggested that a finding that was significant for so many people with SMI should be investigated further and that gender awareness around social networking should be part of any training developed as a result of the research.
Family, home life and parenting
LEEs welcomed recognition of the importance of family in stakeholder reports. Families could be a valued part of a person’s social capital but could also actively impede it or need extra support and education from services to most ably help the person with SMI. LEEs suggested that, unless the person lived alone, time spent at home needed to be cross referenced to quality of family life and impact on social networking behaviours. One LEE suggested that if home life was very poor this could lead to increased social networking as a form of escape. However, families that ‘wrapped the person in cotton wool’ could also be unhelpful. Broader discussion about the effect of home and family life on mental health suggested that this could be negative if someone turned into a ‘couch potato’ but could also be a refuge or place of safety which could resource social networking.
Two LEEs prioritised the findings about negative correlation between well-being and parenting as particularly surprising:
Do we know what proportion of those interviewed had children and were allowed to keep them? The ability for parents to stay with their children in a parenting role when they have a diagnosis of SMI is something that interests me . . . It’s interesting that, in my experience and talking with other mums, having children is quite often the reason given for preserving one’s life.
There was further curiosity about the role children played in their parent’s networking. Children give many reasons to develop social capital, e.g. contacts with other parents through schools, hobbies, etc. However, children may also view parents positively or negatively as part of their social capital The LEEs were interested to know more about how SMI is explained to children and their friends and how children describe their parent with SMI to their friends.
Location differences on network composition
Diagnostic, gender and age differences were more statistically significant than location differences. This led one LEE to suggest that perhaps the social difficulties faced by people with SMI were common. For two LEEs, differences in location were still more important. In group discussion, it was suggested that the urban/rural divide was also not straightforward in comparing samples as there were also a small city in the rural location. Nevertheless, some statistical differences between locations were intriguing. For example, there was a correlation between network size and well-being in the SW but not in London. Potential reasons for this were discussed in relation to cost of living in London, feeling anonymous in a crowd and not belonging anywhere. There were more long-term relationships in the rural sample which could support a greater sense of belonging and network stability. It was suggested that familiarity growing up around the same people could engender more community responsibility. Curiously, network stability in the inner circle correlated with well-being in London but not in the SW and people in the SW were less satisfied with their social networks overall. It was suggested that in a tight knit rural community there is no escape from being known which, when stigma is also present, could disable social networking for people with SMI from the start. Further, everyone knowing everyone’s business can be stifling and anonymity in a crowd could be viewed as exciting if a person were seeking to develop new networks or leave poor relationships behind.
There was debate about whether greater network size afforded more choice about who was accepted into the inner circle which could also engender more selectivity about the quality of these relationships. In group discussion, it was considered whether there might be a sense in which the urban streets could be viewed as paved with gold from a rural location, as promising more choice from a larger pool. Interestingly, there were no significant differences between sites on the overall number of place connections made and no correlation between size of place connection and well-being. This finding appeared to weigh against the greater choice theory but, as more than one LEE pointed out, satisfaction and well-being are not the same. Perceived difference in choice could account for dissatisfaction whether this affected well-being or not. LEEs also pointed to location discrepancies on availability of paid work, suggesting that differences between voluntary and paid opportunities might explain some of the higher dissatisfaction with networks in the SW.
Importance of individually generated place connections and individually structured activities
One of the biggest surprises was that the majority of place connections were built by the individual, most likely through their own interests and proximity to a place and everyday routines. At face value, this finding appeared to suggest that people with SMI did not need support with developing social capital. However, this was not borne out by the diagnostic, gendered and age differences. Further, the amount of places attended outside the home had no bearing on well-being suggesting that it may be what people get out of going to specific places that is more important. Only individually structured activities were significantly positively correlated with well-being, i.e. activities need to have some structure or a goal to be beneficial. Unsurprisingly, the data showed that those who worked full time had significantly higher well-being that those who did not. Thus LEEs speculated that paucity of practitioner structured activities and/dominance of the medical model could also account for the high prevalence of individually generated activities which might not by themselves always be linked to well-being or any kind of meaningful activity.
Current levels of service support for maintaining and developing social capital in primary and secondary care
All LEEs agreed that recovery orientated practitioners would be ideally placed to encourage connection building that worked in support of people’s personal choices and interests and to help with goal setting to develop structured activities and self-management techniques. The qualitative data showed variable recognition of this. There was a strong investment from stakeholders in recovery as a management and strategic ideal but something of a bypass in translation between this and practitioner behaviour where highly medicalised language and practices often dominated.
The LEEs also identified a mismatch between recovery rhetoric and application across both Chapters 6 and 7. There was a strong feeling that practitioners who really understood recovery as living a meaningful life with continued presence of symptoms would not need the importance of friendship pointing out. However, it was also clear that sometimes recovery was misunderstood by professionals, for example as setting goals for rather than with service users. The LEEs observed that quite often reports demonstrated a superficial understanding of recovery. For example, frequent references to ‘the recovery model’ in the stakeholder’s report showed lack of understanding of the most basic point; that is there is no model that can adequately capture what recovery means to each individual. The closest thing to a model is person-centred practice. One LEE suggested that sometimes a practitioner could implicitly understand this, for example, a GP might ask questions about friends, family and other relationships as part of their routine ‘bedside manner’ but not have conceptualised this as part of a recovery approach. Practitioners also appeared to recognise the loneliness of people with SMI but did not often appear to take the extra step of acting on this information.
The LEEs agreed that the reports showed that mental health services do not do enough proactively to help people keep in touch with contacts and maintain and develop meaningful activities in the community. This may be particularly important for those who need inpatient treatment or have lost contacts because of their mental health. Differences between secondary and primary care were also key to LEEs in making sense of the lack of awareness of social networking amongst practitioners:
This is interesting – do practitioners look at people’s networks. Certainly when I was unwell, no-one made even the slightest attempt to examine my social networks. I think somewhere in the report, it mentioned that participants receiving care from just primary services were less likely to ‘get their networks looked at’. This surely has implications for those receiving primary services.
LEEs expressed concern that cuts and closures of voluntary services would result in an even poorer, crisis- driven mental health service. The reports showed that financial constraints and difficulty obtaining resources often led to earlier discharge of significant numbers of people from secondary services back to GPs to provide services to the most needy. Again, people receiving services from primary care were seen as particularly vulnerable to falling through the net of finite resources.
The data showed people with SMI did not necessarily go to GPs with an awareness of the importance of social networks. There was concern from two LEEs about the high numbers of people in the SW who did not know why or did not say why they had visited their GP. It was also a source of comment that only 10 per cent of people’s social networks in primary care were with other people using mental health services. There were mixed views about this. One recounted the detrimental effects on her mental health of being referred to a mental health support group. However, LEEs also spoke about long-term friendships with other people with SMI as key sources of network stability and closeness. LEEs talked about getting the balance right for each individual. Joining groups explicitly set up for people with SMI could be helpful in facilitating an initial sense of belonging somewhere for people who are very isolated, paranoid and/or socially anxious which could then be used as a platform to access community groups and activities with greater confidence. However, joining mental health groups could be less helpful if that is all a person does, fostering a sense of dependence and sick role.
The qualitative data showed considerable hesitance on behalf of practitioners to refer to community groups as they had no way of knowing whether they would help or not. There was a risk that a community group would have little understanding or acceptance of SMI, potentially making things worse. However, there was also limited local knowledge of community resources for people with SMI including voluntary services. LEEs suggested that people with SMI evaluated their experiences of participating in community and third-sector groups and contributed on-going feedback to an electronic resource for practitioners to keep the resource in date.
Communication between secondary and primary services was high priority, with discharge again seen as a point of increased vulnerability where GPs did not always feel knowledgeable enough to help or felt they lacked understanding of SMI. Good ideas in the report for managing this more effectively included locating a CPN or link worker in GP surgeries. Advance statements in primary and secondary care could also help with maintaining existing relationships during a period of crisis rather than leave it to the person with SMI to start again on discharge.
Face-to-face contact was also flagged up as key to relationship building. Stakeholders could be more proactive here by inviting key members of voluntary organisations to meetings, where they could talk about their services and hold an annual ‘getting-to-know-you’ event and allow mental health service staff time off to attend. LEEs also suggested producing guidelines and leaflets for all relevant agencies.
Recommendations
-
Further research would help to understand more rigorously the statistical differences on diagnosis, age, gender and lifestyle prioritised above, curiosities expressed about home, parenting, family life and the ethnic differences on secondary and primary care not examined by this report.
-
LEEs also suggested that many results were sufficient to ground training focused on implementing network mapping sensitive to common symptoms and problems faced by people with SMI and developing databases of community resources for practitioners.
-
Peer support could help people with SMI develop strategies for navigating social relationships whereas service user-led recovery training could help practitioners see the value of working with clients on their social networks to develop self-management strategies and support lifestyle goals such as employment and a decent place to live.
-
Stakeholders need to take a whole-systems approach to optimising best use of finite resource between primary and secondary care. Link workers in GP surgeries and encouragement of advance statements could be piloted as an approach to communication break down between secondary and primary services, maintaining and developing continuity of social network and as a way of sharing knowledge about SMI for people managed solely in primary care.
Reflections: social mapping as a mental health support and/or self-help tool
In reflection, differentiating between inner and outer circles of closeness was regarded by all LEEs as a helpful and meaningful way of understanding a person’s social world which could be used in primary and secondary care as a self-help tool or as something a practitioner explored with an individual.
The LEEs suggested that as a self-help tool mapping social networks would be useful to people some way along with their recovery but that not everyone was in a place of readiness to do this alone. All of the LEEs suggested that a practitioner approach to mapping social networks would need to be carefully thought through and sensitively delivered to build confidence around further social networking rather than further undermine it. Mapping social networks could be a deeply depressing activity, especially if the network were very small. As one LEE put it, nobody wants to be seen as ‘Billy no mates’, yet mapping also contained the potential to see and build on the strengths and resources people already bring to their recovery pathways.
Micro mapping
It was also noted by one LEE that many of the everyday networks and brief interactions that support well-being in a community were not included in the report but could usefully be drawn on when supporting someone with SMI. For example noting regular interactions with a local shopkeeper, persons met frequently walking a dog, taxi drivers or people using the same bus route or train and the virtual relationships described above. It was suggested that the micro effects of these kinds of interaction (or lack of) could greatly contribute to person’s sense of well-being or impede it in connection with a specific place, meaningful activity or regular geography. The style of interaction in these micro relationships could be important to the on-going expansion or limitation of a person’s social world. For people who choose to disclose, it was suggested that there are ways of talking to less close people about a mental health diagnosis which can be more or less stigma busting which could be supported by mental health and/or peer workers.
Toxicity mapping
Most LEEs pointed out that all relationships and activities contained the potential to be enabling or disabling. As well as mapping for strengths, people with SMI could be supported to map for toxicity. That is, unhelpful social influences and relationships. LEEs were divided on how far toxicity was a useful term. Two suggested that this accurately named some of the less helpful social influences in their lives and two suggested that this term could be stigmatising of the person identified as a toxic influence. It is rarely black and white and could be more helpful to identify toxic behaviours within networks and develop assertiveness strategies for dealing with them. Ultimately, it would be down to the person with SMI how they named less helpful relationships in their networks.
Finally, all of the LEEs agreed that social network mapping would have been helpful to them if they had accessed it when first unwell:
Looking at the mapping of people’s social networks exercise has been really interesting. It made me realise that something was missing from my mental health treatment. I really wish someone had done this for me when I was unwell and then taken steps to help me expand my networks.
Ultimately, it does not cost much to sit down with someone and find out what their human resources already are and how they could improve on them. In this sense, social network mapping holds out real hope in these gloomy economic times for services to improve social capital and become recovery orientated in practice as well as strategic vision.
Appendix 2 Interview guide: stakeholder interviews (series 1)
Appendix 3 Service user participant demographics
Appendix 4 Resource Generator United Kingdom (RGUK)
Appendix 5 Health Resource Generator (HRG)
Appendix 6 Community Health Network name generator
Service user interviews – series 1.
Start recording.
1) Name-generating questions
Script:
-
I’m going to ask you a series of questions to find out the names of people you know. The people you name can have a positive or negative influence in your life.
-
For each question please only name people you haven’t mentioned yet.
-
You can provide any one known to you in any capacity – family, friend, neighbour, acquaintance, health or social care practitioners.
-
Please only include people you currently and regularly interact with.
-
If you would like to use false names you are welcome to do so, as long as you can remember who you have named a false name. However you do not need to do this as we will keep the data completely confidential.
-
Each name written on a new PEOPLE card and place in front of participant.
-
Participant is probed to only name people not already named.
-
After each question research probes ‘anyone else?’ until participant says no.
-
– Who are the people you currently particularly enjoy seeing?
-
– Who do you currently have to see but would prefer not to?
-
– Most people discuss important matters with other people. Who are the people with whom you discuss matters with?
-
– If you needed to obtain advice, help or support with a health or emotional problem, who would you approach?
-
– Who approaches you for advice/help or support with health or emotional problems?
-
– Which health or social care practitioners do you see regularly?
-
– Who has recently helped you with tasks, such as housework, shopping, filling out forms, and finding out information?
-
– Who do you help with these kinds of tasks?
-
– Who else do you often interact with?
-
Probe: Any other family, friends, neighbours, acquaintances, health or social care practitioners?
-
-
– Who are the people you currently see with whom you find encounters difficult or stressful?
-
2) Place-and activity-generating questions
Script:
-
I’m now going to ask about the sort of places you currently go to in your community and the sort of activities you engage in regularly.
-
These places and activities can be both positive and negative.
-
All places should be places you currently and regularly go to, and all activities should be things you currently and regularly do.
-
Researcher lists places named on PLACE cards and activities on ACTIVITY cards.
-
Any names mentioned at this stage (such as doctor) are added to a PEOPLE card.
-
– Where do you regularly go in the course of a week that is important to your health and wellbeing? Prompt: recreation/leisure, routine tasks and activities.
-
– When you have problems with your physical health where do you go?
-
– Where do you go for support from mental health practitioners?
-
– Are you using any other community based health services, such as dentists, pharmacies, opticians, podiatrists, therapists? If so, please name all that you are currently in contact with.
-
– Are you using any private health services? If so, please name all services that you are currently in contact with.
-
– Are you using any other social or health services that you have not already mentioned? If so, please name all those that you are currently in contact with.
-
– Do you currently attend any groups, clubs, societies, third-sector organisations? If so, please name all those that you are currently attend.
-
– Do you currently attend any other facilities in your local area, such as parks, leisure centre, library, community centres? If so, please name all those that you currently attend.
-
– What shops do you regularly go to?
-
– Where do you go when things are difficult?
-
– What places do you go to that you feel are bad for your health and wellbeing?
-
– Do you use the internet regularly? Are you part of any online group, blog or society?
-
– What are the other hobbies or activities you do on your own?
-
– Any other activities important to you that we have not mentioned? [Write on activity card/place card as appropriate.]
-
3) Place-interpreting questions
-
Researcher hands a HOME AND PLACE card to participant to refer to interpreter questions.
Script:
-
I’m now going to ask you some questions about each place you have mentioned.
-
The questions I will ask are on the cards in front of you.
-
First we will start with your home.
-
Researcher starts with HOME card and completes the questions on it.
-
The questions on each place card is then completed.
-
Each new activity mentioned is written on an ACTIVITY card.
-
Any new names mentioned are written on a PEOPLE card.
4) Activity-interpreting questions
-
Researcher hands an ACTIVITY card to participant to refer to interpreter questions.
Script:
-
I’m now going to ask you some questions about the activities you have mentioned.
-
The questions I will ask are on the cards in front of you.
-
Each ACTIVITY card is then completed.
-
Any new names mentioned are written on a PEOPLE card.
[Suggest Break]– ‘Would you like to take a break or are you happy to continue?’
5) Mapping network
-
Participant is shown the map which will be A2 or A3 depended on network size.
-
Use A2 for larger networks – over 30 contacts.
Script:
-
I’m now going to ask you to place all the names we’ve generated on this map according to how close you feel they are to you.
-
Please put those you feel closest to in the inner circles and those you feel less close to in the outer circles.
-
You can also place people outside the circle completely if you do not feel close to them at all, but please write everyone down somewhere.
-
After you’ve written everyone down I will ask you to draw lines between each person who knows each other – so please group people who know each other together in the same zone of the map.
-
– All names are written on map by going through PEOPLE cards – researcher can take lead on this where necessary.
-
– Lines are drawn between each person who knows each other – each name is connected to others systematically starting with inner circle. Circles are drawn around groups in which everyone knows each other. Researcher probes to make sure everyone who knows each other is connected by going round each name and asking who they know. Coloured pens used to help keep map readable.
-
– Inner circle – participant asked if they can rank inner circle by closeness – score put beside each.
-
– Participant asked if anyone is missing – if so, complete a PEOPLE card and add to map.
-
6) Well-being scale
-
Participant is shown laminated Likert scale for card sort.
Script:
-
I’m now going to ask you to rate each person, place and activity based on how you feel it generally affects you health and wellbeing – both your mental and physical health.
-
People, places and activities are done separately.
-
Participant asked to sorted them into piles along the Likert scale.
-
Cards are then marked with score from –2 to +2.
-
– In general how do you rate each person/place/activity in terms of how they effect your health and wellbeing: Very positive – Positive – Neutral – Negative – Very negative, as shown on the scale in front of you?
-
– We want to look at the range of effect that each person/place/activity has on you over time. Using the same scores, could you rate each person over time?
-
– At their best, how do you rate do you rate this person/place/activity on your health and wellbeing?
-
– At worst how do you rate them?
-
-
For 2 and 3, participant is given pile of cards and asked to mark the range themselves for each card.
-
If they cannot do this, the researcher goes through it for them.
7) Name interpreter questions
-
Researcher hands a PEOPLE card to participant to refer to interpreter questions.
Script:
-
For each of the names you’ve mentioned, I am going to ask you a series of questions which you can see on the card in front of you.
-
Please answer with the category that fits best.
-
Researcher goes through interpreter questions (on cards) for each named contact.
8) Open-ended questions
-
This section is for recorded transcription not note taking.
-
Thinking about the map in front of you, what 3 words would you use to best describe your network? [if necessary show participant pre-prepared list of words]
-
What is your overall satisfaction with your current network we have mapped? From Very satisfied – Satisfied – Neither satisfied/unsatisfied – Unsatisfied – Very unsatisfied. [show participant this scale]
-
Why is this?
-
-
Is your network changed much from 6 months ago? From Not at all – Slightly – Moderately – Quite a bit – Extremely [show participant this scale].
-
Why is this?
-
-
Are there any barriers to getting the most out of your network?
-
Who are the key people, places and activities you would miss the most if they were not in your life anymore?
-
Closing.
-
Recording stopped.
Appendix 7 Name interpreter cards and emotional closeness map
Name interpreter cards
Emotional closeness map
Appendix 8 Data exclusions
Data exclusions
Some exclusions were made at the analysis stage because of missing data or diagnosis.
Participants were asked to self-report diagnosis. Where diagnoses fell outside the study inclusion criteria or seemed conflicting (for example, two participants ticked both schizophrenia and bipolar disorder), these diagnoses were checked by asking the GP surgery to review medical notes. A total of 18 participants were checked for diagnosis. The table below outlines the diagnoses checked and the resulting diagnosis or exclusion decision.
Diagnosis checking
| Site | Reported diagnosis | Diagnosis in medical notes | Action |
|---|---|---|---|
| London | Bipolar disorder and schizophrenia | Schizophrenia | Diagnosis changed to schizophrenia |
| London | Bipolar disorder and schizophrenia | Severe depression with psychosis | Diagnosis changed to severe depression with psychosis |
| London | Depression and anxiety | Schizophrenia | Diagnosis changed to schizophrenia |
| London | Depression | Depression | Participant excluded from analysis |
| London | Recurrent brief depression | Bipolar disorder | Diagnosis changed to bipolar disorder |
| SW | Missing diagnosis | Paranoid ideations (2004), psychosis influenced by drugs (2011) | Diagnosis changed to other |
| SW | Major depression with periods of mania | Bipolar | Diagnosis changed to bipolar disorder |
| SW | Don’t know | Schizophrenia | Diagnosis changed to schizophrenia |
| SW | Don’t know | Schizophrenic disorder | Diagnosis changed to schizophrenia |
| SW | Missing diagnosis | Schizophrenia | Diagnosis changed to schizophrenia |
| SW | Anxiety | Delusion disorder | Diagnosis changed to delusional disorder |
| SW | Depression | Bipolar | Diagnosis changed to bipolar disorder |
| SW | Don’t know | Schizophrenia | Diagnosis changed to schizophrenia |
| SW | Not sure | Severe depression with psychosis | Diagnosis changed to severe depression with psychosis |
| SW | Schizophrenia, bipolar and psychotic disorder | Schizophrenia | Diagnosis changed to schizophrenia |
| SW | Severe depression | Bipolar | Diagnosis changed to bipolar disorder |
| SW | Chronic depression | Bipolar | Diagnosis changed to bipolar disorder |
| SW | Don’t know | Bipolar | Diagnosis changed to bipolar disorder |
Other exclusions
Two further participants in the London site were removed at the analysis stage, one because of excessive incomplete data (SUL49) and the other (SUL12) because of lack of service or medication use in the last 2 years. The latter was an early participant, and telephone screening by the researcher was tightened following this interview, to correct GP surgery failure to screen out such participants.
In the SW, a total of four participants were excluded because of excessive missing data.
Appendix 9 Data cleaning
Data cleaning
Network data were input into six separate sheets in Microsoft Excel:
-
Sheet 1: edgelists of social network connections including each connection between ego and alter as well as each connection between alters. Closeness score values were also input.
-
Sheet 2: attributes for each alter (age, gender, well-being impact, etc.).
-
Sheet 3: edgelists of connections to each place mentioned as well as each alter connected to the place. Also input was the type of connection between the alter and each place (referred/suggested, go with, see there, regularly visit and live with).
-
Sheet 4: attributes of each place (frequency visited, well-being impact, etc.).
-
Sheet 5: edgelists of connections to each activity mentioned and connections between alters and activity (people with whom the participant did the activity).
-
Sheet 6: attributes of each activity (frequency done, well-being impact, etc.).
Accuracy checks were conducted against the physical copies of data once data entry was complete, on 10 randomly selected sets of network data per site.
The social network data were reviewed to remove any contacts whom the participant said they no longer saw, in order to maintain consistency across data sets of a current social network. Additional categories were added to code mental health professionals on sheet 2, to code if the participant was living with children, and to code by secondary care contact or primary care contact only. A variety of cleaning procedures were then applied to summarise and categorise social network and place and activity data using exploratory procedures within Excel and SPSS before importing these matrix data into a global SPSS file with participant demographic data. These procedures included summary statistics based on network data for network size, composition and well-being impact, as well as detail on activity and place for each participant such as referral route summaries, types, social interaction and well-being impact.
Place and activity categories
Because the responses to places and activities were open ended, a number of categories were applied to each to aid analysis. These codes were both based on the collected data and pre-determined based on the study aims. The tables below summarise these categories with examples.
Place
| Code | Mental health setting | Physical health setting | Primary care setting | Community setting | Referral | Social interaction |
|---|---|---|---|---|---|---|
| 0 | No | No | No | No | No | No |
| 1 | Voluntary (e.g. local Mind) | Clinical (e.g. hospital) | Attending for mental health | Family and friends’ houses (e.g. mother’s house) | Informal | Inferred |
| 2 | Secondary (e.g. CMHT) | Community (e.g. dentist) | Attending for physical health | Library | Formal | Mentioned |
| 3 | Other (e.g. private) | Attending for both | Education (e.g. university, adult education centre) | |||
| 4 | Not clear attending reason | Physical recreation setting (e.g. football club or gym) | ||||
| 5 | Social recreation setting (e.g. pub, café) | |||||
| 6 | Cultural recreation setting (e.g. museum, cinema) | |||||
| 7 | Spiritual setting (e.g. church, mosque) | |||||
| 8 | Shops and markets (e.g. cornershop, supermarket) | |||||
| 9 | Green or outdoor spaces (e.g. park, forest, seaside) | |||||
| 10 | Workplace (including voluntary and paid) | |||||
| 11 | Places connected to children (e.g. children’s school/nursery) | |||||
| 12 | Social activity groups (e.g. book club) | |||||
| 13 | Statutory services (non MH/PH) (e.g. housing office) |
Activity
| Code | Social | Type | Structure level |
|---|---|---|---|
| 0 | No | Work and volunteering | Unstructured |
| 1 | Yes | Education, training and studying | Individual structured |
| 2 | Physical activities (e.g. walking, running, sport) | Formally or externally structured | |
| 3 | Creative activities and hobbies (e.g. writing, painting, guitar) | ||
| 4 | Cultural activities and hobbies (e.g. going to museums and cinema) | ||
| 5 | Spiritual (e.g. prayer) | ||
| 6 | Relational (socialising, seeing friends, sexual intercourse, providing care) | ||
| 7 | Domestic (housework, baking, DIY) | ||
| 8 | Multimedia use (PC, internet, video gaming) | ||
| 9 | Reading | ||
| 10 | General recreation (e.g. watching television) | ||
| 11 | Shopping, spending | ||
| 12 | Travel (including commuting) | ||
| 13 | Receiving mental health or other support |
Categorising diagnosis
Following diagnosis checking, diagnoses were first simplified and then clustered for analysis.
Simplifying involved prioritising the primary diagnosis where more than one diagnosis was ticked by the participant, using the method below. Schizophrenia and bipolar were prioritised where extra diagnoses were ticked.
| Multiple diagnoses | Percentage of total responses | New diagnosis |
|---|---|---|
| Bipolar disorder, severe depression with psychosis | 4 | Bipolar disorder |
| Bipolar disorder, psychotic disorder | 2 | Bipolar disorder |
| Bipolar disorder, psychotic disorder, manic episodes | 0.7 | Bipolar disorder |
| Bipolar disorder, manic episodes, severe depression with psychosis | 0.7 | Bipolar disorder |
| Bipolar disorder, delusional disorder | 0.7 | Bipolar disorder |
| Bipolar disorder, manic episodes | 0.7 | Bipolar disorder |
| Psychotic disorder, manic episodes | 0.7 | Psychotic disorder |
| Schizophrenia, other | 0.7 | Schizophrenia |
| Schizophrenia, psychotic disorder | 0.7 | Schizophrenia |
| Schizophrenia, severe depression with psychosis | 0.7 | Schizophrenia |
| Schizophrenia, psychotic disorder, severe depression with psychosis | 0.7 | Schizophrenia |
| Schizophrenia, bipolar disorder, psychotic disorder, severe depression with psychosis | 0.7 | Schizophrenia and bipolar disorder |
| Severe depression with psychosis, psychotic disorder | 0.7 | Severe depression with psychosis |
| Severe depression with psychosis, psychotic disorder, manic episodes | 0.7 | Severe depression with psychosis |
| Severe depression with psychosis, delusional disorder | 0.7 | Severe depression with psychosis |
| Total multiple diagnoses simplified | 14.6 |
Finally, diagnoses were clustered in order to allow for analysis between meaningfully large groups. The following diagnoses were clustered together:
-
schizophrenia and psychotic disorder
-
bipolar and manic episodes
-
severe depression and psychosis, delusional disorder, schizoaffective disorder.
Exploratory analyses were run on basic measures such as network size, density and social capital scores to confirm that meaningful differences between these clusters existed.
Pre- and post-clustering diagnoses
| Simplified diagnosis | n (%) |
|---|---|
| Schizophrenia | 54 (36) |
| Bipolar disorder | 64 (42.7) |
| Schizoaffective disorder | 4 (2.7) |
| Psychotic disorder | 5 (3.3) |
| Delusional disorder | 2 (1.3) |
| Manic episodes | 1 (0.7) |
| Severe depression with psychosis | 20 (13.3) |
| Clustered diagnosis | |
| Schizophrenia and psychotic disorder | 59 (39.3) |
| Bipolar disorder and manic episodes | 65 (43.3) |
| Other psychoses | 26 (17.3) |
Appendix 10 Dendrogram created using agglomerative clustering approach
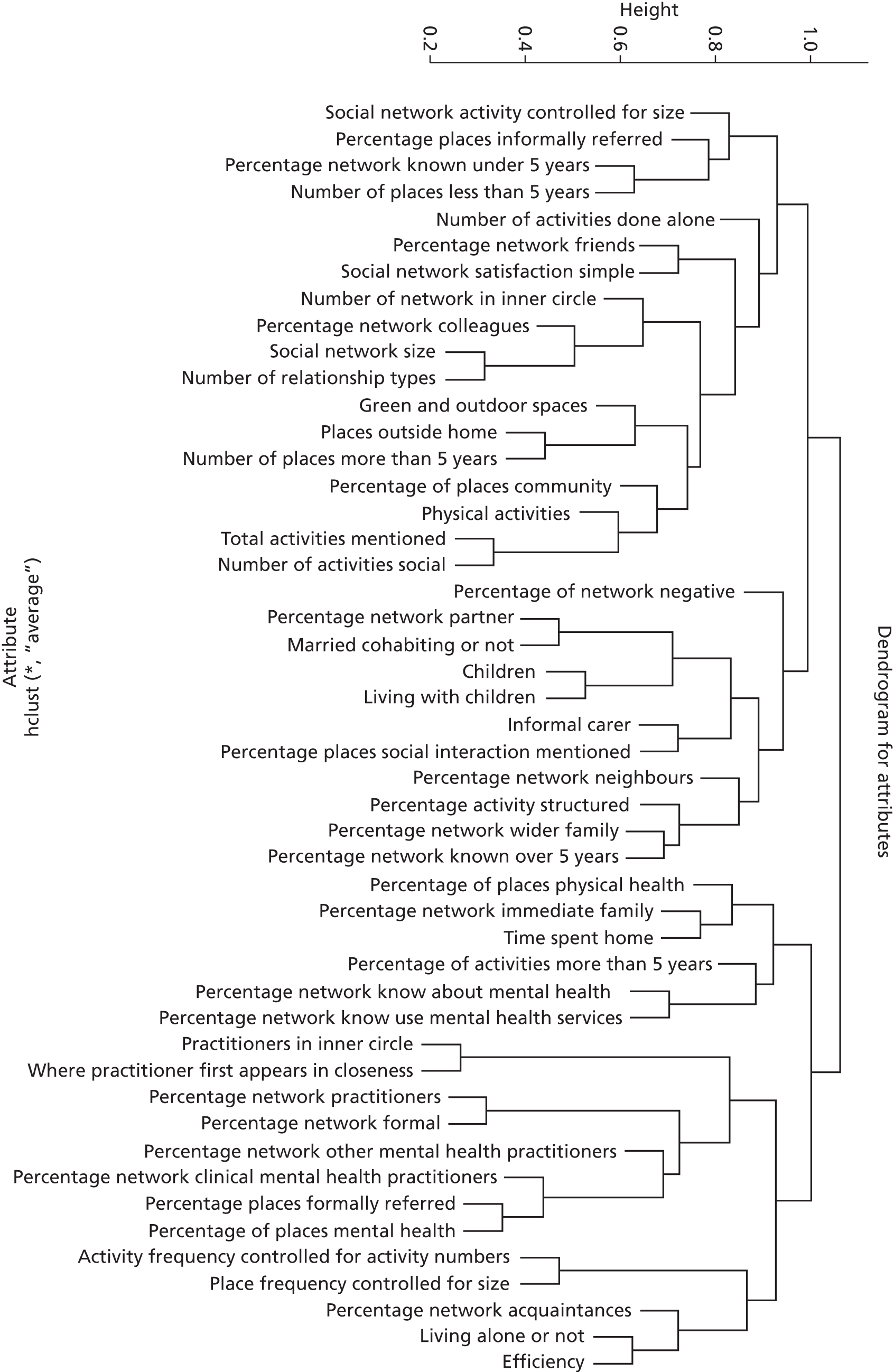
Appendix 11 Frequency table based on clustered variables used to name each cluster
| Variable | Cluster assigned to by k-means analysis | Cluster 1 (named diverse and active) | Cluster 2 (named family and stable) | Cluster 3 (named formal and sparse) |
|---|---|---|---|---|
| Percentage of social network consisting of friends | 1 | 32.2 | 33.2 | 23.6 |
| Percentage of social network consisting of colleagues | 1 | 8.9 | 2.1 | 1.9 |
| Percentage of social network consisting of acquaintances | 1 | 12.7 | 6.5 | 7.8 |
| Mean overall social network size | 1 | 23.9 | 22.8 | 12.4 |
| Social Network Satisfaction Binary | 1 | |||
| Percentage satisfied | 76.4 | 75 | 61.7 | |
| Percentage not satisfied | 26.6 | 25 | 38.3 | |
| Mean number of relationship types in social network | 1 | 6.1 | 5.8 | 4.5 |
| Mean number of social network members in inner circle | 1 | 5.0 | 5.4 | 3.0 |
| Mean frequency of contact with social network contacts (social network activity) | 1 | 2.49 | 2.34 | 2.31 |
| Mean number of places connected to outside the home | 1 | 10.7 | 10.9 | 7.4 |
| Percentage of place connections consisting of community settings | 1 | 64.3 | 63.5 | 47.2 |
| Percentage of place connections built through informal referral (recommendation from informal network) | 1 | 7.1 | 4.2 | 2.3 |
| Mean number of green and outdoor spaces connected to | 1 | 0.9 | 1.5 | 0.47 |
| Mean total number of meaningful activities mentioned | 1 | 7.5 | 6.8 | 4.6 |
| Mean number of physical activities engaged in | 1 | 1.5 | 1.4 | 0.9 |
| Mean number of meaningful activities done alone | 1 | 3.6 | 3.7 | 3.5 |
| Mean number of meaningful activities done with others | 1 | 3.9 | 3.1 | 1.2 |
| Mean number of relational activities mentioned | 1 | 0.6 | 0.3 | 0.1 |
| Mean number of family and friends houses mentioned | 1 | 0.6 | 0.8 | 0.3 |
| Percentage of place connections less than 5 years old | 1 | 62.5 | 38.3 | 28.9 |
| Percentage of places where social interaction engaged in | 1 | 68.6 | 75.9 | 61.3 |
| Mean number of domestic activities mentioned | 2 | 0.4 | 0.9 | 0.5 |
| Percentage of place connections more than 5 years old | 2 | 37.0 | 61.7 | 60.9 |
| Percentage who are married/in a civil partnership or cohabiting | 2 | 18.2 | 66.7 | 4.3 |
| Percentage who have children | 2 | 20 | 70.8 | 42.6 |
| Percentage who are living with children | 2 | 7.3 | 35.4 | 2.1 |
| Percentage who mention an informal carer | 2 | 20 | 41.7 | 25.5 |
| Percentage of social network consisting of immediate family | 2 | 17.5 | 28.0 | 27.2 |
| Percentage of social network consisting of wider family | 2 | 3.1 | 9.2 | 2.7 |
| Percentage who have an intimate partner | 2 | 21.8 | 60.4 | 10.6 |
| Percentage of social network consisting of neighbours | 2 | 3.9 | 5.7 | 3.1 |
| Percentage of social network who also use mental health services | 2 | 13.2 | 14.4 | 14.3 |
| Percentage of social network rated negative for well-being | 2 | 10.9 | 10.4 | 10.3 |
| Percentage of social network known for over 5 years | 2 | 44.2 | 75.3 | 60.7 |
| Proportion of waking time spent at home | 2 | |||
| 0–25% | 14.5% | 8.3% | 2.1% | |
| 26–50% | 41.8% | 18.8% | 12.8% | |
| 51–75% | 30.9% | 39.6% | 31.9% | |
| 76–100% | 12.7% | 33.3% | 53.2% | |
| Percentage of activities which are individually structured | 2 | 66.2 | 79.4 | 60.5 |
| Percentage of activities that have been done for more than 5 years | 2 | 56.0 | 71.6 | 81.8 |
| Percentage of place connections consisting of physical health settings | 2 | 19.0 | 17.7 | 27.6 |
| Percentage who are living alone | 3 | 56.4 | 16.7 | 76.6 |
| Percentage of social network consisting of non-mental health and social care practitioners | 3 | 9.2 | 8.8 | 18.7 |
| Percentage of social network consisting of clinical mental health practitioners | 3 | 8.1 | 2.7 | 12.2 |
| Percentage of social network consisting of other mental health practitioners | 3 | 2.2 | 0.5 | 2.1 |
| Percentage of social network who know about your mental health condition | 3 | 70.8 | 73.4 | 85.7 |
| Social network efficiency (lower = more dense) | 3 | 0.8 | 0.6 | 0.8 |
| Percentage who have a practitioner in their inner circle of closeness | 3 | 30.9 | 12.5 | 23.4 |
| Mean ring where practitioner first appears in closeness map (higher score = closer ring) | 3 | 4.38 | 3.48 | 3.72 |
| Percentage of network which is formal connections | 3 | 19.4 | 12.1 | 33 |
| Percentage of social network known for less than 5 years | 3 | 55.8 | 24.7 | 39.2 |
| Percentage of places which are mental health settings | 3 | 7.4 | 5.1 | 11.5 |
| Percentage of place connections formally referred to | 3 | 10.7 | 6.2 | 17 |
| Mean frequency of connection to places outside the home | 3 | 3.0 | 2.5 | 2.9 |
| Mean frequency of engagement in meaningful activities | 3 | 2.8 | 2.4 | 3.0 |
Appendix 12 Regression models
We modelled the following outcomes: social network size, network type, RGUK score, HRG group, mental health contact type, SWEMWBS score.
The study was exploratory and we had many potential independent variables (IVs). Therefore various iterations of each model were included.
For all appropriate models, VIF was used for checking multicollinearity and no problems were found in the final models presented below.
The variables listed below were included as IVs in all regression models except where the variable below was the dependent variable in the model, with the exceptions listed below.
Participant characteristics: (1) Participant age. (2) Gender. (3) Site (London/SW). (4) Ethnicity (white British/other). (5) Working full time or not. (6) Working part time or not. (7) Volunteering or not. (8) Unemployed or not. (9) Long-term sickness or disability (yes/no). (10) No formal education (yes/no). (11) Married/in a civil partnership or cohabiting (yes/no). (12) Have children or not. (13) Living with children or not. (14) Living with others or alone. (15) Have informal carer or not. (16) Housing status – three levels: ownership, renting, other.
Health, well-being and functioning variables: (1) Diagnosis – three levels: psychotic disorder/schizophrenia, bipolar disorder/manic episodes, other psychoses. (2) Mean number of years since first contact with mental health services. (3) Psychiatric inpatient history – three levels: never been inpatient, inpatient voluntarily, inpatient under section. (4) Mean number of years since last psychiatric admission. (5) Mental health contact type (primary only/secondary care). (6) CO-OP physical fitness score. (7) CO-OP feelings score. (8) CO-OP daily activities score. (9) CO-OP social activities score. (10) CO-OP pain score. (11) CO-OP overall health score. (12) CO-OP social support score. (13) CO-OP quality of life score. (14) SWEMWBS score.
Network type: Three levels: diverse and active, family and stable, formal and sparse.
Social network variables: (1) Number of friends. (2) Number of family contacts. (3) Number of practitioner contacts. (4) Number of wider contacts. (5) Percentage of network known for less than 5 years. (6) Mean frequency of contact with social network contacts. (7) Have someone in inner circle of closeness (yes/no). (8) Number of people in inner circle. (9) Mean well-being impact of social network. (10) Mean closeness of social network. (11) Number of relationship types in social network. (12) Number of contacts who also use mental health services. (13) Number of contacts who know about participant’s mental health condition. (14) Social network efficiency score. (15) Percentage of social network consisting of negativeties. (16) Practitioner in inner circle (yes/no). (17) Where practitioner first appears in closeness map.
Place variables: (1) Percentage of waking time spent at home. (2) Number of community setting connections. (3) Number of mental health setting connections. (4) Number of physical health setting connections. (5) Number of places where social interaction mentioned. (6) Mean frequency of connection to places mentioned. (7) Percentage of place connections less than 5 years old.
Activity variables: (1) Number of unstructured activities. (2) Number of individually structured activities. (3) Number of formally structured activities. (4) Number of physical activities. (5) Number of activities done with others. (6) Number of activities done alone. (7) Mean frequency of engagement in activities. (8) Percentage of activities less than 5 years old.
Other: (1) Network satisfaction (satisfied or not).
For social network size, the social network variables listed above were not included as IVs. Network types were included as IVs because, although the social network variables were used (with others) to create them, they did not show high collinearity and therefore were assumed independent. Including them allowed us to understand if network types were significantly different in size even when controlled for sociodemographic and health variables.
For network type, only participant characteristics and health, well-being and functioning variables were included as IVs.
For SWEMWBS score regression, the CO-OP variables were not included as IVs.
Appendix 13 Qualitative schedule: service user interview (series 2)
Appendix 14 Practitioner schedule 2
Community Health Networks
Practitioner Schedule
Version 8: 22 November 2012
Section one: background information
Your job title:
Your professional background: (e.g. nurse, psychiatrist, social worker, GP)
Length of time in current role:
Length of time qualified:
Gender: male female
Ethnicity:
Main approaches (skills) used with clients (e.g. motivational interviewing, cognitive–behavioural therapy, recovery practice)
Tools (schedules, techniques) used with clients to assess progress, set goals, measure outcomes
Our definition of severe mental illness is experience of psychosis, schizophrenia or bipolar disorder
Recovery and your role
What factors are important in recovery from severe mental illness?
Probe ideas:
-
Role of social factors (poverty, discrimination, environment, upbringing, housing, relationships, debt)
-
Ensure focus is on SMI
What do you do to help people with severe mental illness to recover?
Probe ideas:
-
social aspects of support if these are not mentioned
Ask for a case study linking to one of the strategies they mention and probe WHY this strategy is important for recovery and promoting wellbeing?
For GPs
How do you see the role of the GP changing now that mental health services are discharging more people from primary care? A recent study suggested 31% people with SMI on primary care case loads only see a GP (Prof Helen Lester PARTNERS1 study).
How do you feel about having a more central role in managing severe mental illness?
For psychiatrists
Do you see the role of the psychiatrist changing within restructured mental health services?
How do you feel about these changes for people with severe mental illness?
For others
Do you see your role changing within restructured mental health services?
How do you feel about these changes for people with severe mental illness?
Community health networks questions
The rest of the questions are about community health networks. We refer to these as networks in the questions below.
Our working definition of a community health network is the resources a person connects with through people, places and activities and the potential of these to support or hinder wellbeing.
We are considering networks in their broadest sense to generate wellbeing – capturing friendship, walking in the park, going to a work programme, volunteering, visiting a CPN in a clinic, seeing the optician, going to art classes . . .
Question 5
How do you link people with severe mental illness with local network opportunities?
How central to what you do is working to build people’s networks?
[We are seeking to understand if they think it’s part of their job or someone else’s. If not their role whose is it?] This is a very important aspect of the schedule. We need to know about role boundaries – are they a node in the network – how much guiding and facilitating do they do? What is their responsibility vs. individual’s vs. other people such as families and friends?
Question 6
Does your network role vary with different clients – how and why?
Ask for a case study where they are helping someone manage their mental health
Ask for a case study where a person with SMI will be presenting with a physical health issue (if appropriate)
Question 7
What are the boundaries around your role in terms of developing networks? What determines these?
Probe ideas:
-
To what extent do you think it is the role of the practitioner (statutory and vol sector – any paid person) or that of the person themselves to build, maintain and manage networks?
-
Or the role of the person’s friends, neighbours, family to build, maintain and manage networks?
-
How do you balance your input and that of others?
Question 8
Do you discuss network development as a therapeutic strategy with colleagues in individual cases?
Question 9 – BARRIERS AND FACILITATORS
Thinking about your work currently, what are the barriers to working on building networks?
[Make sure we probe on interagency barriers and enablers as this is important for the funder]
Probe ideas:
-
Barriers and enablers at an inter-organisational/inter-team level
-
Links with other organisations and within organisations
-
Barriers at practitioner level
-
Barriers at client level
-
Are there any skill gaps for practitioners such as yourself in working in this way?
-
If conversation is hard might like to ask for case study examples
[there are lots of things that might get mentioned here – barriers relating to clients, systems, their skill level, practical things like time]
Are there any things that help you work to build people’s networks?
Probe:
-
The enablers
-
Positive developments maybe policy level or practical
Question 10 – THE FUTURE IDEALLY
Ok so we are going to forget the real world and think ideal . . .
In an ideal world, what would your role be in helping a person develop their network to support well-being?
[This is important – we need to find out about their perceived role – where does their responsibility begin and end for building or maintaining CHN]
What, if anything, would need to change to support you working in this way?
Probe ideas:
-
Do you need new skills and tools to do this – or do you already have all the info it’s just about facilitating working in this way?
-
Could mapping a client’s community health network and developing action plans from this be useful?
-
Do you need to work with others – individual practitioners or organisations to support network development?
-
How can you work better together as part of a network?
-
What do you see as the advantage of active links with a variety of organisations?
Question 11 – We have been using the term community health network in the study.
What does this term mean to you?
Appendix 15 Interview schedule: stakeholder interviews (series 2)
Part 1: recent changes
-
What have been the key changes over the past 18 months in terms of the way your organisation supports people with SMI?
-
– What are the impacts on the ground? What has changed?
-
– What are the current opportunities for developing services to support SMI?
-
– Do you have any concerns about reorganisation of services and cuts?
-
– What about staff morale?
-
– Do you have a local mental health strategy and plan detailing how organisations work together to commission and deliver services? Probe: when will a local plan exist? If answer is overly positive or negative challenge the view with our data.
-
Part 2: network data
Diagrams introduced – One thriving network and one higher need network with summary scores and quotes. Introduce in summary the data collected and variation in networks. What is their initial reaction and impression?
-
What is the role of your organisation (the CCG, foundation trust, local council, housing association etc.) within these networks? (Both when lower and higher need)
-
What would you like the role of your organisation to be within these networks to promote people’s health and wellbeing?
-
Probe: What needs to change to achieve this?
-
Probe: What is a healthy balance between support from organisations and personal independence for service users? What should your role be in network development? What is the role for others?
-
-
Is this approach useful for mapping networks and could it make a difference to or help inform your organisation’s way of working? Could network mapping have an impact on service provision? Is it relevant? Is it a priority? Could that change?
Part 3: reaction to pre read
-
The pre read bullet points summarise some of our main findings, do these findings fit with your experience?
-
Probe – bring pre read out if necessary.
-
Probe around examples of how it fits with their work or does not fit.
-
Part 4: recommendations
-
How would you like to see organisations working together to improve access to social resources and health and wellbeing opportunities for people with SMI?
-
Probe for specific ways this can work.
-
-
What would you suggest we need to do in order to communicate our findings locally – who needs to receive them and how?
-
Probe around resources for GP, mental health trusts, service user and carer networks as well as wider community audiences.
-
Glossary
This is not a full glossary but contains key terms used in the report, where clarification might be required, on how the study team have applied a particular term. Where words appear in bold, they are also defined in this glossary.
- Alters
- These are the people in an individual’s personal network: the ties to which an individual is connected.
- Community health network
- This term was devised by the study team when submitting the original research proposal for funding; it is not a term found in published literature. It refers to the multilevel focus of networks taken in this research considering connections through people, places and activities.
- Ego
- In social network analysis, ego refers to the individual at the centre of the network: the person whose personal network is being studied.
- Joint Strategic Needs Assessment
- Joint Strategic Needs Assessments analyse the health needs of populations, physical and mental health, as well as the well-being of individuals and communities, to inform and guide commissioning of health, well-being and social care services within local authority areas.
- Network density
- Network density means how interconnected a person’s social network is: the proportion of possible ties between the alters in an ego’s network that actually exist. The more a person’s social network ties know (are connected to) each other, the denser the network. We measure this structural feature in our study using a network efficiency score.
- Network enhancement or network development or connection-building(used interchangeably)
- These refer to a person-centred goal-led approach for practitioners to work with people with severe mental illness to actively manage their network of connections to people, places and activities. It does not imply normative assumptions that healthy networks should grow, but looks at active steps to manage networks at a point in time and could include strategies to reduce connections to enhance well-being. Rather than a top-down intervention approach, we use these terms in relation to personal goals and building individual agency to achieve them.
- Patient
- We tended not to use this term in the report to describe people with mental health problems using services. However, this is a term used widely by general practitioners, and it features in many of the direct quotations. It also appears to describe hospital treatment when people were inpatients.
- Personal network
- We use the term ‘personal network’ to refer to individual-level social networks. Personal networks in this study were an individual’s connections to people, place and activity, mapped using the community health network approach. We use this term rather than the commonly used ‘egonetwork’ as ‘personal network’ has more conceptual clarity to the non-network specialist.
- Patient and public involvement
- This term is used by the funder – the National Institute for Health Research Health Services and Delivery Research programme – to describe the involvement of direct beneficiaries of any research, within a research project. In this study, patient and public involvement is the involvement of people with mental health problems who had worked in various roles alongside the research team and as part of the study team.
- Resources
- Resources were measured in three ways in our study: (1) assets within the community including both people and places – a library, a park, the clinic, dentist, general practitioner, gym instructor; (2) social capital or health assets accessed/exchanged within individual lives including personal resources – friends, family and colleagues; (3) inner resources such as self-esteem, self-confidence, inner determination that have been collectively assessed in this study to understand the impact on well-being.
- Severe mental illness
- Also known as serious mental illness or severe and enduring mental health problems, this was defined using the diagnostic criteria in the Mental Health 8 indicator under the primary care Quality Outcomes Framework, with a focus on adults of working age and excluding those with a primary diagnosis of personality disorder or dementia and those with chaotic drug or alcohol use.
- Social capital
- In this report we focus on social capital measured at an individual rather than community level. Seen in this way, social capital refers to the availability of social resources that were accessed by an individual through their social network.
- Social network
- In the formal sense used in social network analysis, social network refers to features regarding the specific structures and features of social ties between sets of actors that make up a network. The term is also often understood in a lay sense to refer to social relationships more generally.
- Well-being
- Well-being is a term with various meanings. In this report, we use well-being in reference to the Short Warwick–Edinburgh Mental Well-being Scale, which defines mental well-being as individuals realising their own abilities, coping with ordinary stresses of life and working efficiently and purposefully, as well as making a contribution to the community.
List of abbreviations
- BME
- black and minority ethnic
- CCG
- Clinical Commissioning Group
- CHN
- community health network
- CMHT
- Community Mental Health Team
- CPN
- community psychiatric nurse
- df
- degrees of freedom
- GCE
- General Certificate of Education
- GCSE
- General Certificate of Secondary Education
- GP
- general practitioner
- HRG
- Health Resource Generator
- IV
- independent variable
- JSNA
- joint strategic needs assessment
- LEE
- lived experience expert
- MHRN
- Mental Health Research Network
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PBR
- payment by results
- PCRN
- Primary Care Research Network
- PCT
- primary care trust
- PPI
- patient and public involvement
- QOF
- Quality Outcomes Framework
- RGUK
- Resource Generator United Kingdom
- SMI
- severe mental illness
- SNA
- social network analysis
- SW
- South West
- SWEMWBS
- Short Warwick–Edinburgh Mental Well-being Scale
- TAPS
- Team for the Assessment of Psychiatric Services
- VIF
- variance inflation factor