Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1009/24. The contractual start date was in October 2011. The final report began editorial review in August 2013 and was accepted for publication in June 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Spiby et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background, aims and objectives
Introduction
The concept of disadvantage is multifaceted. Within this report we will be taking a very broad definition which includes social deprivation, low income, social isolation, lone parenting, teenage parenting, drug or alcohol use, asylum seekers and refugees, mental illness, domestic abuse and safeguarding concerns. The different forms of disadvantage frequently coexist, frustrating attempts at narrower definitions. The maternal mortality rate for disadvantaged women is higher than for the general population. 1 Similarly, for babies born to disadvantaged women, the chances of dying around birth or within the first month of life are higher than for babies of women who are not in adverse circumstances. 2 Disadvantaged women have higher rates of smoking3 and formula feeding4 than other population subgroups and are less likely to access routine services such as antenatal classes. 5 Barriers include a lack of access to appropriate services (e.g. for asylum-seeking women6 and very young women7 and their partners), lack of staff training in culturally appropriate care and a lack of knowledge among health professionals about relevant interventions and services that they could refer to. 8 Recently published guidance for service provision for pregnant women with complex social factors recommends that such barriers be addressed; multiagency working should be supported and the care provided by different agencies integrated. 9
Support and care in pregnancy, labour and postpartum have positive impacts on women’s well-being and outcomes including reduced operative birth10 and increased breastfeeding rates. 10,11 In the UK, the provision of intrapartum support has traditionally been the role of the midwife. However, current midwifery staffing levels are low and it is challenging to provide women with the ongoing support they need in these vulnerable and formative months. There is evidence that a significant proportion of women are worried by feeling unsupported by health-care professionals during at least part of their labour. 12 This lack of support is often due to high workloads on busy labour wards and is unlikely to improve in the medium term, given the demographic profile of the midwifery workforce with a high number of retirements expected in the next 10 years. It is also recognised that services can offer care that is somewhat fragmented, with little co-ordination between midwives, health visitors, general practitioners (GPs) and social services, all of whom are likely to be involved in the care of families during pregnancy, birth and the early postpartum weeks. Such support and co-ordinated care is likely to be especially important in low-income communities and for young women, as women in these circumstances have lower rates of breastfeeding and increased rates of infant mortality, and are more vulnerable to problems with emotional and psychological well-being. 2
This research examines an award-winning innovative social enterprise service that has been established in one city and that is now rolling out to other sites. Based on principles derived from controlled studies conducted in other countries, the volunteer doula project offers lay support to women in vulnerable circumstances with the aim of enhancing support and improving the uptake of existing health and social services.
The lay support is offered by volunteer ‘doulas’, a term to denote women who support other women during pregnancy, birth and breastfeeding. The role is not one of a clinical professional but of a trained lay supporter and does not include the support provided by female members of the woman’s own family. Doulas offer emotional and physical support and companionship, and facilitate communications between the woman, her partner and health-care professionals and services. 13 In some situations, doula support may also include guidance with parenting. There is a substantial evidence base, derived from randomised controlled trials and other studies conducted in a diverse range of settings and systems, in countries including South America, the USA, Sweden, Finland and Belgium, that has demonstrated the benefits of doula support for childbearing women and their families. However, there is no contemporary evidence derived from UK settings.
Existing evidence
A rapid review of studies carried out prior to commencement of this research explored ‘doula support’ including systematic searches of the following databases: MEDLINE, EMBASE, Cochrane and the Cumulative Index to Nursing and Allied Health Literature. The search was not limited by country, date, methodology or language. Support during labour from trained doulas is associated with reduced length of labour,14 less pharmacological pain relief and oxytocin augmentation, and fewer instrumental or operative births. 15 In particular, instrumental and operative births are associated with increases in the risk of morbidity for women and their babies. This morbidity includes postpartum haemorrhage,16 genital tract trauma for the mother17 and increased risk of intracranial haemorrhage for babies. 18
In addition to positive impacts on labour outcomes, there is also evidence of positive impacts on breastfeeding,10 including increases in the proportion of women initiating breastfeeding and continuing with exclusive breastfeeding. 11 It is particularly noteworthy that these positive impacts have been achieved in groups where rates are frequently lower than national figures, including low-income, first-time mothers. These findings reflect the wider evidence base of breastfeeding support by peers19 and resonate with contemporary policies that encourage the implementation of peer support for breastfeeding. 20
Positive benefits for women’s psychosocial well-being include more positive feelings about labour and less anxiety,11 increased feelings of control and confidence as a mother,21 and fewer women experiencing postpartum depression and anxiety. 22 Evidence suggests that doula support during labour may also have potential positive effects on parenting behaviours and the relationship between a woman and her child,23 including increased acceptance of a baby immediately after birth and an increase in behaviours such as stroking, smiling and talking to their babies,24 and more positive parenting when babies are 2 months old. 25
All of these findings resonate with important aspects of the policy context and many also offer potential benefits to the NHS from reduced resource use, including shorter inpatient stay following normal birth than assisted birth and fewer referrals to specialist services, including mental health care. Evidence of benefit from doula care is particularly striking for women in situations of social or economic disadvantage, those with lower educational attainment and where supportive contact starts during pregnancy. There are also suggestions that the provision of doula support is associated with increased use of required health-care services. 26
The UK NHS spent £1.6B on maternity services during 2008. Part of this cost is attributable to the high rate of caesarean sections (C-sections), which increased from 12% in 1990 to 24% of all births in 2008, each costing between £1197 and £3194. 27 It was further estimated that the cost to the NHS for maternal care due to smoking in pregnancy is between £8M and £64M per year (depending on the costing approach);28 a further £12M to £23.5M per year is spent treating infant conditions attributable to smoking during pregnancy. Another study estimated that the cost of neonatal care for low birthweight babies was between £12,344 and £18,495 per child in English hospitals. 29 These items reflect those in the Quality Innovation, Productivity and Prevention (QIPP) Metrics included in the NHS Outcome Indicators for Maternity.
The impacts of doula care described above are derived from quantitative data generated by randomised controlled trials and included in systematic reviews. There is a relative dearth of qualitative evidence to enable understanding of the experience of receiving doula support. The evidence that is available from women who received doula support indicates a greater sense of participation during labour. 30 A study of the experience of receiving doula support in Sweden identified continuity, the ‘natural’ nature of the support provided and a human dimension to the birth experience as the key characteristics of doula support. Private doulas are available in the UK;31 these are usually accessed by women from higher-income groups who can afford to pay for their services, with the resulting potential to perpetuate inequalities in health and social support.
Although existing evidence from a range of countries identifies important benefits to the provision of lay support in labour, key questions remain. There is a paucity of UK evidence and doula support is rare in the UK, especially for disadvantaged women. Existing studies have as their major focus lay support in labour, yet there may be advantage in providing such support throughout the childbearing episode.
The original volunteer doula project
The first volunteer doula project was established as a social enterprise initiative and has provided support to women in situations of social disadvantage since 2005. The project developed in an area with high levels of social and economic deprivation, poor education, housing difficulties and health states lower than the general population. Women are referred to the service by health professionals, interpreters, social services workers and the Teenage Pregnancy Support Services. Support can be offered at any stage but commonly starts around the sixth month of pregnancy and continues until 6 weeks after birth. Following an initial facilitated meeting, subsequent contact occurs approximately fortnightly during pregnancy until the last month, when contact occurs weekly. This project therefore differs from many of the studies of doula support identified, several of which were limited to care in labour and the immediate postpartum period.
The original project also differs from others that have been reported elsewhere in what the doulas are trained to do. Women who volunteer to provide the doula service, who are themselves usually women from the local area with children, receive training for the role, accredited by the Open College Network (OCN). Topics included in the training are preparation for birth and the birthing process, breastfeeding, child protection, domestic abuse awareness training, cultural diversity and communication skills. The doulas are expected to work closely with existing services and to optimise women’s use of both health and social services, for example attending smoking cessation clinics, accessing Healthy Start and attending clinic appointments. Signposting women to other services is a key part of the doula’s role. Women referred to the service are matched with doulas according to personality, background, locations and availability. Volunteer doulas receive reimbursement of expenses, for example travel and childcare during training sessions. There are systems in place to provide ongoing support for the doulas through, for example, local project workers.
Descriptive data from the early years of the service indicated a range of benefit when compared with the whole population of the city; under normal circumstances, women with the deprivation profile of those cared for would expect substantially worse outcomes. There were also suggestions that experience as a volunteer doula had enabled subsequent access to employment and higher education, indicating a community development aspect to this work. 32 Descriptive data such as these informed the Department of Health’s (DH’s) decision, in March 2009, to provide 3 years’ funding (£267,000) to support roll-out and replication in up to eight additional sites. This funding supported the provision of a portfolio that informs establishing and running a volunteer doula service, including consultancy expertise for 1 year; support with issues related to human resources, volunteer recruitment and induction; ‘training the trainer’; promotional material and support; training for the first cohort in each roll-out site; and access to accredited training materials. Sites have to provide and fund their own staff. Identification of replication sites was slower than expected. By February 2011, four sites, which have substantially different service and demographic contexts from the original site, had confirmed service funding for replication.
Summary
The original doula service appeared a promising innovation, developed from an international and high-quality evidence base with demonstrable health benefits that aimed to maximise the use and efficiency of existing health and social care services. The technology, that of doula support, had been transferred from other countries, systems and settings and had been established in England for 4 years, where it had apparently been well received by women and well integrated with existing health and statutory services. It therefore met the criteria specified in the National Institute for Health Research Service Delivery and Organisation programme call for promising innovations in health care. DH funding had previously been awarded and four replication sites indicated a willingness to participate in this research. This research therefore offered the potential for an increased return on original DH investment while relating to several important policy areas.
An outline proposal was submitted to the National Institute for Health Research Service Delivery and Organisation programme on 30 March 2010 and a full proposal in October 2010. Funding was confirmed in January 2011. The research commenced in October 2011 and was carried out over a 21-month period in five settings in England.
Aims and objectives
The project aimed to answer four broad questions:
What are:
-
Objective 1: the implications for the NHS of a volunteer doula service for disadvantaged childbearing women?
-
Objective 2: the health and psychosocial impacts for women?
-
Objective 3: the impacts on doulas?
-
Objective 4: the processes of implementing and sustaining a volunteer doula service for disadvantaged childbearing women?
Specific objectives within these were:
Objective 1: implications for the NHS
-
To determine clinical and public health impacts for women and their babies, including type of delivery, low birthweight and admission to neonatal unit; to determine method of infant feeding planned during pregnancy, infant feeding initiated at birth and baby’s feeding method at 6 weeks of age; to determine impact on mothers’ smoking behaviour; and to compare these for women who have received the volunteer doula service with data for the general Hull Primary Care Trust (PCT) population, designated statistical neighbours and England averages.
-
To identify the impacts on and experiences of NHS maternity care services and providers (midwives and heads of midwifery).
-
To identify impacts on other NHS services including referral to and uptake of smoking cessation services.
-
To determine the actual and potential impacts on NHS maternity resource use of roll-out of doula support at scale.
-
To determine potential savings to the NHS through clinical events averted by the service.
Objective 2: health and psychosocial impacts on women
-
To identify underlying beliefs and theories about how the service works and the contexts in which it has more or less impact.
-
Based on this, to identify key outcomes which will allow the theories to be tested.
-
To identify the views, experiences and psychosocial impacts on women who have been recipients of the service.
-
To examine the characteristics and reasons of women who disengage from the service.
Objective 3: impact on volunteer doulas
-
To identify the views and experiences of the volunteer doulas and the impacts on their life course.
Objective 4: implementing and sustaining the service
-
To provide an independent assessment of the costs of providing a volunteer doula service, including training.
-
To identify the challenges, facilitators and barriers experienced by the manager and staff of the original initiative in establishing and maintaining the service.
-
To identify the process of agreeing funding for service costs and the main factors responsible for the positive decision.
-
To examine facilitators and barriers to implementation in the roll-out sites and the extent to which these differ between sites and from the original service.
-
To investigate the experiences of the replication package at the roll-out sites.
Chapter 2 Methods
Settings
Settings comprised five volunteer doula services, run by either the NHS or third-sector organisations: the original volunteer doula project and four roll-out sites. All are focused on providing a service for disadvantaged childbearing women. Two doula services are restricted to women from minority ethnic groups and a third serves an area with a very large minority ethnic population. All of the services work to support women in low-income communities. To protect the anonymity of individuals, the sites will be referred to throughout this report as site A (the original site) and sites W, X, Y and Z (the roll-out sites).
Sponsorship, ethics and governance
Sponsorship was provided by the University of Nottingham. Ethics approval was obtained from the University of York’s Department of Health Sciences Research Ethics Committee for preliminary data collection among key informants and from the National Research Ethics Service Committee West Midlands (see Appendix 1) for remaining components of the research. Permissions were obtained from the research and development (R&D) departments in five NHS trusts. We have endeavoured to achieve anonymity of individuals who contributed information to this evaluation and also of sites, wherever possible.
Advisory group and public involvement mechanisms
An advisory group was established and included a range of stakeholders for the doula service, public health and academic communities. Members were drawn from participating sites, across disciplines and the service user/advocacy community. We held two advisory group meetings during the course of the research and consulted individual members for advice on particular topics throughout, as needed. Advisory group members also contributed to commenting on draft data collection tools and piloting for relevance and clarity.
Two user panels were established: one of women who had received doula support and the second of doulas, both from the original site. Members of the research team met with both user panels twice, followed by e-mail consultations on draft questionnaires. Panel members contributed to identifying important issues in the experiences of women and doulas that required exploration and in pilot testing of questionnaires.
Design
Conceptual framework
This study takes a realistic evaluation perspective,33 in recognition of the complex intervention being investigated in a real-life setting. 34 The focus is therefore not so much on addressing the question ‘does it work?’ but rather on the subtler question of ‘what works for whom in what circumstances?’. The identification of Contexts, Mechanisms and Outcomes (CMOs) at an early stage of the project is key, as they were required to generate hypotheses about the circumstances under which the intervention works. These CMOs are generated both from the literature and from the beliefs of key informants, in this case doula managers and project workers in all sites and doulas and service user representatives in the original site. This approach meant that later data collection could not be fully specified until after the identification of CMOs.
Accordingly, following a description of the literature review, our methods for data collection will be described in two stages. We will first describe the methods used in the initial stage of the research and the outcomes of this stage, including the generation of CMO configurations (CMOcs). We will then present the methods for the second stage of the study, which arose from this first stage and involved some modification to our original plans.
Literature search
The original literature search was extended (see Appendix 2 for details of search strategy) to identify evidence that may suggest possible Mechanisms for how doula support might impact on women’s health and well-being. A total of 1561 abstracts were screened for relevance and full papers were obtained where appropriate, following discussion within the research team. Information extracted by team members was entered onto a Microsoft Word (Microsoft Corporation, Redmond, WA, USA) proforma and included the following:
-
which research question it informed
-
setting, content of any intervention and problem addressed
-
how outcomes were measured
-
utility for any data collection tools for women, doulas and other groups of participants
-
possible CMO pathways defined
-
additional information that would inform a general background, discussion or the health economics component.
In excess of 100 papers were reviewed and data extracted, at which point no new themes emerged and it was considered that saturation was achieved. From this data extraction, potential CMOs were identified for subsequent refinement and testing, together with those emerging from the first stage of data collection described below.
Data collection from key informants
The purpose of the first stage of data collection was to understand key features of establishing a volunteer doula service and to explore with key informants their beliefs about how the intervention works, and for whom and in which circumstances. 33
Doula service staff
Information about the research was provided directly to current and previous managers and subsequently to other doula service staff at all sites. Following provision of informed consent, digitally recorded individual interviews were carried out with the current and former managers of the original doula project and a group interview with project workers at the original site whose role includes matching women and doulas. Interviews mapped how the service works in practice and explored underlying beliefs about how it works, the contexts in which it has more or less impact and the enablers and barriers to establishing a doula service.
Individual or group interviews were then carried out with the managers and project workers in each of the roll-out services, exploring the development of the service to date and aspirations for the coming year.
Across the five sites, 25 individuals were identified who contributed to the running of the service, either in the office or in a managerial role, hereafter referred to as ‘service staff’.
Volunteer doulas
A focus group was considered to be the best way of eliciting the views and experiences of volunteer doulas so that their different perceptions could be discussed between group members. Participants were identified with the assistance of project staff in the original doula service with the aim of representing a range of views and experiences including volunteers from different training cohorts and with different sociodemographic backgrounds. Participant information leaflets were forwarded to potential participants by staff of the doula service to maintain confidentiality, with the opportunity to raise questions either via the service staff or directly with the research team. Following permission to contact/expression of interest, the focus group was arranged by the research team and held independently of project staff. Written consent was obtained from participants and the digitally recorded discussion addressed a number of areas including what might constitute a ‘good match’, which women might particularly benefit from doula support and impacts on doulas themselves from volunteering. Eight volunteer doulas (current and past) from the original doula service attended and participated in the focus group. These doulas subsequently agreed to be a doula user panel that acted as a source of advice in subsequent stages of the research, joined in a second focus group by a further three.
Service users
As with volunteer doulas, a focus group was considered to be the best way of eliciting views and experiences. Identical processes were used as for the volunteer doulas, described above. Seven women attended and participated in a focus group. These women agreed to be a women’s user panel that acted as a source of advice in subsequent stages of the research. Three women who had taken part in the first women’s focus group participated in a second group discussion.
All recordings were fully transcribed and thematically analysed to support the development of CMOcs.
Development of Context, Mechanism and Outcome configurations
Realistic evaluation seeks to address the question ‘what works for whom, in what circumstances’ by theorising the Mechanisms that might result in particular Outcomes in particular Contexts. Understanding the ‘why’ is key. 35
Initial analysis produced a lengthy list of statements from our various data sources which linked some occurrence with some outcome. These were all far too specific (e.g. ‘because Sally knew Mary she was able to access some particular resource’) and needed to be refined to a higher level of generality (e.g. being well networked increases access to resources). In many cases only two of the three CMO elements were articulated and in these there was scope for considerable debate about whether some occurrence was a Context or a Mechanism, or alternatively a Mechanism or an Outcome. Given these ambiguities, and the need to reduce the CMOs to a workable number, we decided that we would initially focus on establishing possible Mechanisms, to be developed into more general CMO configurations at the next stage.
All interview transcripts were reviewed for any evidence of a theme that we felt pointed to a Mechanism. We identified three levels of Mechanism – service level, doula level and woman level – with some Mechanisms working on more than one level.
All theorised Mechanisms identified by level are listed below:
-
service-level Mechanisms:
-
networking
-
transferable skills of staff/experienced staff
-
flexible staff
-
goodwill work and costs absorbed by host agency/organisation/other
-
service shaped to fit with local service drivers
-
responding to funding availability
-
fitting supply and demand
-
support for volunteers
-
joint/partnership/multiagency working
-
service differentiate from statutory and professional services
-
marketing
-
-
doula-level Mechanisms:
-
supported training
-
work experience
-
experience with/exposure to different backgrounds
-
choice of cases and workloads
-
supervision and support from services
-
being respected and valued and treated as an individual
-
reflection on personal experiences
-
-
woman-level Mechanisms:
-
being prepared for birth
-
doula support in labour
-
doula non-professional, non-medical support
-
doula not friend or family
-
doula someone can relate to/someone who can model behaviour
-
doula working with others as a team
-
doula exhibiting confidence in the birth process
-
doula imparting knowledge
-
doula explaining medical/technical language
-
doula as advocate
-
doula providing holistic/woman-centred support
-
doula non-judgemental, culturally aware, diplomatic and sensitive.
-
In addition to analysing the initial key informant data to identify Mechanisms, we retained a focus on the four key research questions. We organised the ensuing information into a table which captured theme (possible Mechanism), relevant research question(s), evidence (data), Mechanism level, site and data source.
One example of a dominant theme across all five sites was networking. This suggested a service-level Mechanism, possibly influenced by the Context of the service managers’ existing contacts, with a possible Outcome being referrals, volunteers or funding, thus establishing and/or sustaining a service. This potential CMOc pertains to key research objective 4:12 – to identify the challenges, facilitators and barriers experienced by the manager and staff (locality development workers) of the Goodwin volunteer doula initiative in establishing and maintaining the service – and objective 4:14 – to examine facilitators and barriers to implementation in the roll-out sites and the extent to which these differ between sites and from the original service. Table 1 is an example, an extract from the table of possible Mechanisms theorised from the key informant data, linked to research questions. Three Mechanisms are identified at the levels of service, doula and woman.
| Theme (possible Mechanism) | Research question(s) | Level(s) | Evidence (data) | Data sourcea | Site |
|---|---|---|---|---|---|
| Networking | Objective 4:12 establishing and maintaining initial service Objective 4:14 establishing and maintaining roll-outs |
Service | Networking with other organisations to recruit volunteers | 8 | W |
| Liaising with local maternity services | 11 | Z | |||
| Liaising with midwives and linking with partners/organisations | 13 | X | |||
| Service known because of pilot; also a lot of networking done | 4 | A | |||
| Partnership working; links with other organisations; attending health and social care services meetings | 15 | Y | |||
| Support for volunteers | Objective 4:12 Objective 4:14 Objective 3: impact on volunteers |
Service Doula |
Identification of need for bereavement support for volunteers | 8 | W |
| Access to six sessions of counselling via occupational health | 2 | A | |||
| Monthly volunteer meetings | 11 | Z | |||
| Flexible staff | Objective 4:12 Objective 4:14 Objective 2: health and psychosocial impacts on women |
Service Women |
Volunteers assist women with benefits queries | 13 | X |
| Postnatal support period extended beyond 6 weeks when a baby is removed from its mother | 2 | A | |||
| Text rather than phone support offered when preferred by non-English-speaking women | 4 | A |
We next focused on the Outcomes that had been identified in the literature and by key informants, with a view to selecting a subset that doulas and users considered meaningful and which could be assessed in the main data collection and used to test CMO hypotheses. This element was informed by additional insights gained during further group discussions with our two reference panels (doulas and women who had used the service). Examples of Outcomes discussed with doulas included employability and personal growth and development, and with women being linked in to services, labour and birth, and infant feeding.
The outcomes identified from stage 1 for further investigation in stage 2 are listed by level below:
-
service-level Outcomes:
-
funding
-
volunteers recruited
-
volunteers retained
-
referrals/uptake
-
balance of supply and demand (volunteers and referrals/uptake)
-
-
doula-level Outcomes:
-
role satisfaction
-
knowledge of other cultures/confidence to talk to women of other cultures
-
economic impact (e.g. impact on paid work, childcare costs)
-
increased life choices
-
knowledge of field of work
-
personal growth including self-esteem, identity, self-efficacy and confidence
-
social capital
-
-
woman-level Outcomes:
-
birth experience
-
health of mother, baby and family
-
experience of health services
-
use of appropriate services
-
self-confidence, self-esteem, self-efficacy, empowerment, confidence as a parent
-
social isolation versus social integration
-
relationship with partner.
-
Outcomes were now reunited with Mechanisms and Contexts to reformulate CMO configurations by cross-referencing the Mechanisms identified with possible relevant Contexts based on the first stage of data collection. A table was constructed for each Outcome to identify possible intersections and CMOs.
Table 2 shows an example of cross-tabulation of Mechanisms and Contexts for a specific Outcome, in this case ‘Health of mother, baby and family’. Each number in the grid represents a different CMOc. For example, CMOc2 would be ‘If a doula is experienced then not being a friend or family member will have a greater impact on women’s health outcomes (than if she is inexperienced)’. In general we found that the CMOcs were not specifying that a given Context was necessarily a prerequisite for a particular Mechanism or Outcome but rather, as in the example given for CMOc2, they were hypothesising that the impact would be greater than it would be without this Context.
| Contexts | Mechanisms | |||
|---|---|---|---|---|
| Doula non-professional/non-medical | Doula not friend/not family | Can relate to doula/doula can model behaviour | Doula imparts knowledge | |
| Woman level | ||||
| Age | 3 | |||
| Ethnicity related to language needs; communication needs | 8 | |||
| Parity and previous birth experience | ||||
| Education | 9 | |||
| Referred/self-referred (proxy for motivation) | 4 | |||
| Type of need (e.g. single, complex) | 1a | 5 | ||
| Relationship status (links to alternative of birthing alone) | ||||
| High-risk/low-risk pregnancy | ||||
| Doula level | ||||
| Ethnicity and language | 6 | |||
| Level of experience | 2 | 10 | ||
| Motivation for volunteering including past work experience | ||||
| Quality of match | 7 | |||
| Site level | ||||
| NHS vs. third sector based | ||||
| Length of time service established | ||||
| Experience/focus of staff | ||||
| Birth/maternity unit medicalised vs. natural birth | ||||
| Level of staffing | ||||
The final step involved incorporating the CMOs in the outcomes tables into CMOcs. The process of creating CMOcs was assisted by adopting the technique proposed by Jackson and Kolla36 whereby quotations are coded for each element of the CMOc. The CMOc hypothesises that there is a relationship between M and O and that this is different in different Cs. Thus questions follow the format of ‘if the right processes operate in the right conditions, then the programme will prevail’ (p. 184). 35 Contexts were defined as being at the levels of the woman, the doula and the doula service. This generated 18 service-level, 82 doula-level and 107 woman-level CMOcs. We were able to reduce this rather overwhelmingly large number by omitting all those which were not in fact testable within the research design that we were using. For example, some referred to the birth environment, about which we would have little information, and some referred to specific aspects of the doula–woman match, about which we would similarly be lacking information. A number referred to relatively rare occurrences for which we knew that our numbers would be inadequate. Those remaining were used to guide, but not to constrain, the second stage of data collection, as we were aware that considerable descriptive information would also be needed which had not necessarily yet appeared as part of a CMOc.
The initial approach was to seek to identify CMOcs that were potentially testable within our study design and within the data collection constraints. This approach was modified in the context of a limited sample size and instead we sought to explore statistically two of the three components of the CMOc and complemented this by using a qualitative and discursive approach. Testing a Mechanism–Outcome relationship may not find the expected relationship because the Mechanism ‘works’ only in certain Contexts; however, some Mechanisms (e.g. continuous labour support) may be viewed as ‘universally good/beneficial’ and therefore less dependent on Context. Linked to this is the idea that the research question is perhaps ‘what works best’. In other words, rather than the assumption that, all else being equal (i.e. programme fidelity), the doula programme does not work for some women, the assumption is that the programme has some universal benefit but works particularly well for some women.
The order below follows that of the research questions included in the original proposal.
To determine the impacts of volunteer doula support on key clinical and public health outcomes for women and their babies
Data sources
Women offered doula support
The original doula service has been collecting information and entering it into a bespoke database since 2007. Available data items include women’s age, smoking status, source of referral to the doula service, method of birth and whether or not their baby was of low birthweight. These data provided a basis for comparing women who were offered doula support with women in the same geographical area, and with other reference groups, for certain clinical and public health outcomes including health behaviours such as smoking and breastfeeding. In each case the most appropriate available comparison data sets were used.
Reference groups
Hospital Episode Statistics
Detailed analysis of Hospital Episode Statistics (HES)37 was undertaken by analysts at the Child and Maternal Health Intelligence Network (ChiMat, www.chimat.org.uk). Data items included for comparison with those from the doula service database were mode of birth, birthweight and the mother’s age, ethnicity and postcode district. Analysis was restricted to mothers whose PCT of residence was Hull (PCT code 5NX). While HES is known to have data quality issues, areas of known concern were avoided. Data were produced in line with the approach used by the Health and Social Care Information Centre when publishing data.
Maternity system at Hull and East Yorkshire Hospitals NHS Trust
Hospital Episode Statistics data indicate that 99% of women resident in Hull PCT give birth under the auspices of the Hull and East Yorkshire Hospitals NHS Trust (HEY). Data obtained from the maternity system at HEY were analysed and showed a large number of births to mothers living outside Hull. Only those mothers living in Kingston upon Hull (postcode districts HU1, HU2, HU3, HU4, HU5, HU6, HU7, HU8 and HU9) were included in our analysis. The fields available were postal area (postcode district), mode of delivery, financial year, feeding intention at delivery, smoking at delivery, ethnic category, mother’s age at delivery and admitted directly to neonatal unit. Unfortunately, because of system limitations, mother’s parity could not be reported with any accuracy. Consequently the intended analysis of parity could not, unfortunately, be carried out.
Published data
Published data were used as a comparison where local data sources were not readily available. The data sets do have some limitations, offering limited, if any, controllable variables. Published data were available at local authority or PCT, depending on subject and source.
Hull PCT and Kingston upon Hull local authority had coterminous geographical boundaries and are commonly used alongside each other in publications and analysis.
Primary Care Trust data
Published data sources38 were used including breastfeeding initiation, breastfeeding status at 6–8 weeks and smoking at delivery. 39 Comparisons were made with outcomes for demographically comparable subsamples within (1) the general Hull PCT population, (2) the designated statistical neighbours for Hull and (3) England averages. ‘Designated statistical neighbours’ are areas that have been identified as having similar key characteristics based on census data and a list of them is available from the Department for Education. Statistical neighbours were used only for published data. While there are known data quality issues with some areas, these were not considered an issue for the geographies selected.
Local authority data
Published data sources were used to compare demographic data about the mothers. The 2011 census40 provided data about age, ethnicity and population sizes. Kingston upon Hull was the reference group used.
Process
As no data dictionary was available, we met the administrative team in the Goodwin Volunteer Doula project in Hull to understand the database. This allowed confirmation of fields to be used and the interpretation of them. After a preliminary analysis and presentation of results, data quality issues were identified that required resolution prior to further analysis. Data quality checks were carried out to highlight missing data, obvious errors and conflicting observations such as the method of birth or feeding. Because of the amount of work required and resources available, data items were prioritised for checking and correction. A number of additional fields were added to the doula service’s standard report, including a flag when the mother had disengaged from the doula service, a common reason for missing data; person identification (ID); and previous number of children.
The data set on which the final analysis was based was extracted on 27 December 2012.
The data are reported from the doula database as three data sheets: ‘referral’, ‘mother’ and ‘outcome’. Data linkage across tables was possible through the creation of a unique identifier consisting of the person ID and another number based on the number of times the mother had used the service. On extraction, the fields in the doula database are represented as a ‘0’ (no), ‘1’ (yes), ‘–1‘ (not known) or blank (not known). Items were collated on the outcomes sheet, including the mother’s age, postcode district, ethnicity and previous number of children.
Additional data items were created. These included:
-
summary fields indicating feeding method at birth, feeding method at 6 weeks and mode of birth.
-
a field indicating financial year based on the baby’s date of birth; where the date of birth was missing, an assumed date of birth was created based on the date of matching. Previous analysis had indicated that, on average, the mother was matched with a doula approximately 3 months before giving birth
-
a grouping based on ethnicity where those defined as ‘white British’ were called ‘white British’ and all others were grouped into ‘non-white British’
-
mother’s age category, summarised as ‘under 20 years’, ‘20 to 24 years’, ‘25 to 29 years’, 30 to 34 years’, ‘35 to 39 years’ and ‘40 years and over’.
As the database included records for mothers who had not yet given birth, a cut-off point was established of 31 August 2012. This was the last month with almost complete data and was included in the data cleanse. Births after that date were ignored to ensure the data quality was as high as possible. Analysis of the number of live births showed they were consistent over the period reported and it was felt unnecessary to make any adjustments for this.
To determine the impacts on NHS midwives
Process
Heads of midwifery
After the research team had provided information and obtained informed consent, individual, digitally recorded telephone interviews were carried out with all heads of midwifery in the five NHS trusts providing maternity care closest to the doula service. These explored perceptions of the volunteer doula role, their voluntary status, communications and working between the doula and maternity services, and the future of doula support. Interviews were transcribed in full.
Midwives
The head of midwifery in each trust was asked to forward an e-mail from the research team to midwives asking those with experience of caring for a woman who had received doula support to attend a focus group, during working hours, at their place of work, to discuss their views and experiences. The sampling strategy was therefore purposive and midwives attended on a self-selection basis. The focus group discussion was digitally recorded and explored midwives’ views of the profile of the doula service; their experiences of providing clinical care to women supported by volunteer doulas; whether support during pregnancy, labour or following birth was most important; views of the boundaries of the doula role; and impacts on women’s use of maternity and other services. Focus group discussions were transcribed in full.
Analytical methods utilised are described later in this chapter, Qualitative data, and findings are presented in Chapter 3, The impacts on and experiences of NHS maternity care services and providers.
What are the health and psychosocial impacts for disadvantaged childbearing women?
A range of approaches was used to address this objective, with some changes to the methodology set out in the proposal, which had relied primarily on postal questionnaires. After discussion with the advisory group and our user panels, and in recognition of the high proportion of women who did not have English as a first language, or who might not be literate, we chose instead to offer a wider range of ways in which women could tell us their views. We were advised that women who were unable to speak and complete questionnaires in English might also not be able to read materials in their mother tongue. Rather than obtaining translations of consent forms and questionnaires, we decided instead to involve professional interpreting services, independent of the doula services, for the collection of data. We also hoped that this more personal approach might facilitate women’s involvement. We also decided not to offer online questionnaire completion as an option, as it was not considered likely to have a high uptake.
Our aim was to invite all women (n = 627) who had been offered doula support across all sites to contribute their views through at least one of the data collection methods: postal questionnaire, focus group discussion and assisted questionnaire completion by telephone with an interpreter if required. All information collected from women was retrospective because of resource constraints that precluded the follow-up of a prospective sample.
Data collected directly from women
Identifying and contacting women
To maintain confidentiality of information held by the doula service, women were identified from service records by local service staff, who were asked to forward invitations to participate on behalf of the research team. No service staff were directly involved in data collection.
Members of the research team consulted doula service staff in the development of guidance notes and monitoring logs for sites to complete, detailing the number of women approached, number of times approached, dates of contact, reasons for non-approach and reasons for not sending out research packs (e.g. where the woman declines).
Service staff were asked to attempt to contact all women who had ever been referred to the service (including women who subsequently failed to engage with the service but not those still in receipt of the service) in each of the five sites. Other exclusions related to women’s personal experiences where contact had the potential to increase a woman’s stress or vulnerability. The records of the doula service indicated a particular woman’s needs and circumstances. The services were asked to make the first approach using their standard practice (e.g. for a woman needing to be approached in a non-English language, approach by bilingual staff, or use of an interpreter).
The research team requested that, at the first approach, women be told about the independent evaluation and asked if they would be happy to be sent a pack containing further information about the research, including contact details for the research team, together with the questionnaire and information about the focus groups. Where a current telephone number was not available or contact could not be made after three attempts, the service was asked to send the information and questionnaire using the last known address. The research team provided doula service staff with prepared packs for forwarding to women following addition of an address label by doula service staff. The research team requested that anonymised information from the completed proforma be forwarded to the research team twice weekly. The information recorded in the proforma also provided a denominator for questionnaires sent and for calculation of response rates.
Questionnaires
It had originally been intended that questionnaires would be sent out in two waves. However, the advantages of this were subsequently judged not to outweigh the considerable extra work for the sites and so all contacts with women were made at what would have been the time for the second wave.
The packs included a covering letter from the research team, questionnaire and reply-paid envelope for direct return of the questionnaire to the research team, thus maintaining confidentiality of response. Terminology, for example the name used for the volunteer doula, varied across sites, and questionnaires and covering letters were individualised to sites accordingly. Centre codes (denoting the five sites) were printed on questionnaires. The covering letter contained all aspects pertaining to participation in the study, including the voluntary nature of participation, and contact details for the research team to enable the potential participant to ask any questions. It also informed women that they would be sent a £5 high street voucher on receipt of the completed questionnaire if they chose to provide their contact details. Contact details were not otherwise requested and were used only for the stated purpose.
Two versions of the questionnaire were developed, according to whether or not the woman accessed the support service (see Appendices 3 and 4). Completion and subsequent return of questionnaires was deemed to imply consent. Questionnaires were returned directly to the research team and the researchers’ independence from the service was stressed, as was the fact that any information provided by women would not be shared with anyone outside the research team in a way that allowed them to be identified.
Reminder postcards were sent to women by doula service staff after 3 weeks, thanking those who had already returned questionnaires and indicating that there was still time to return questionnaires, for those who had not yet done so. A phone number was given to allow women to request another copy of the questionnaire if needed; 578 women were identified for approach for completion of questionnaires.
Telephone-assisted questionnaire completion
In recognition of potential literacy issues, irrespective of preferred language, women were also offered the option of having a researcher (or interpreter appointed by the research team) telephone them to talk them through the questionnaire. If women indicated a wish for telephone-assisted completion, this information was passed from the doula service to the research team and a member of the research team or interpreter appointed by the team conducted a digitally recorded telephone completion after obtaining informed consent. The questionnaire was translated by the interpreter at the time of use. The data collection was fully structured and followed the questionnaire, which was adapted for telephone use. To make the questionnaire an acceptable length, a subset of the original questions was included. Women were interviewed in a language of their choice and translators, independent of the service, were identified for all required languages.
Questionnaire content
The questionnaire was piloted to ensure relevance and clarity with the support of members of our advisory group and women’s user panel. In addition to demographic information, for example education, employment status and whether or not the woman had a partner, questionnaires collected data in the following areas: relationship with doula and experiences of receiving doula support; health behaviours including smoking; emotional well-being, including the extent to which the woman feels in control of her life; and an assessment of the benefits and disbenefits of the service. These topic areas included those identified in work that developed CMOs in the first stage of the research.
It had always been intended that the questionnaires would include some items that would allow comparison of women’s experiences with a reference group. The Millennium Cohort Study and Family Nurse Partnership evaluation had provisionally been identified as comparators in the original proposal, but, after discussion at the first advisory group, it was apparent that these were not ideal. An alternative was identified in the surveys of women’s experiences of maternity care in England carried out by the Picker Institute, with findings available for individual NHS trusts. 41 Prior to our data collection period, the Picker Institute last conducted a survey of women’s experiences of their maternity care in 2010, and inclusion, with permission, of some of those questions thus provided a reference set of findings for those in our research.
Focus group discussions
We consulted doula service staff to identify the languages spoken by women in their sites to determine the predominant language, besides English in each site. In the roll-out sites, we planned to conduct at least one focus group in English in each site and one group in another language where the number of potential participants speaking a common language would support a focus group. In the original site, as the pool of women was potentially greater, we planned a maximum of three focus groups in English and one in another language. Participation in a focus group was offered as an alternative to questionnaire completion at site A. At the roll-out sites, because the number of women was so much smaller, it was offered as an option to all women, irrespective of questionnaire completion.
Following written consent, focus groups enabled the exploration in more depth of key topics identified through the initial data collection with the key informants and discussions with the user panels. Importantly, the group discussions allowed the exploration of those CMOs that could not be tested in questionnaires. A topic guide included the following: how doula support differed from other support; relationship with doula; doula support with feeding and use of other services; and why doula support is important. The discussion was digitally recorded.
Participant acknowledgements and reimbursement of expenses
Participants’ contributions were acknowledged with the provision of a £5 high street voucher for return of a questionnaire, a £10 voucher for participation in a focus group discussion and a £5 voucher for telephone completions. Women attending groups were informed that full reimbursement of transport costs was available. Refreshments (including lunch) were provided at the group discussions, together with a crèche facility.
Use of data collected by services
The information collected by doula services on their databases and paper-based service documents (including initial referral forms and service evaluation documents) provided an additional source of data that we had not been aware of at the time of writing our proposal.
In practice we did not find that these sources added materially to our data and they will not be reported in the body of this report, but further information about our use of these data and an overview of the findings are available in Appendix 5.
What are the impacts on volunteer doulas?
A postal questionnaire was sent to all volunteers (n = 258) trained by the five volunteer doula services, with a small number of follow-up telephone interviews to explore particular aspects of experience in questionnaire responses. In the questionnaire (see Appendix 6) we obtained some demographic information and explored the following areas: training to be a doula; becoming involved with the doula service; the doula role; workload; matching women and doulas; barriers to and challenges in supporting women; support for doulas; how the doula service fits and works with other services; impact of the doula role on women and doulas; ending the relationship with the woman; stopping volunteering; and a summary of the experience of being a doula. A second, shorter, version of the questionnaire was developed for those volunteers who had completed training but had not (yet) supported any women. This omitted sections that were not applicable and included questions about why no women had been supported and, if volunteering had ceased, the reasons for this (see Appendix 7).
The acceptability and ease of completion of the questionnaires were determined with the aid of members of the volunteer doula user panel and advisory group.
Process
To maintain confidentiality within doula services, we could not approach volunteer doulas directly. The process reported for contacting women (see To determine the impacts of volunteer doula support on key clinical and public health outcomes for women and their babies, Process) was also used to develop the sampling frame and for sending questionnaires to doulas.
The research team provided doula service staff with prepared packs for forwarding to doulas following the addition of an address label by service staff. The packs included a covering letter from the research team, questionnaire and reply-paid envelope for direct return of the questionnaire to the research team, thus maintaining confidentiality of response. The covering letter contained all aspects pertaining to participation in the study, including the voluntary nature of participation, and contact details for the research team to enable the potential participant to ask any questions. Centre codes (denoting the five sites) were printed on questionnaires.
We had originally planned for an initial and second wave of data collection to include doulas who completed training during the life of the research but for a number of reasons, including minimising demands on doula services and the protracted nature of governance processes, it became clear that a one-stage approach to this element of data collection, later than originally scheduled, was optimal.
The questionnaire asked volunteer doulas if they would be willing to take part in a telephone interview to explore any topics in more detail. Those who were willing completed a reply slip when returning the questionnaire providing their contact details and indicating their informed consent to contributing further. Respondents were not asked to provide contact details unless they wished to be contacted for participation in an interview. The sampling strategy for interviews was, therefore, a purposive one that enabled more detailed exploration of new issues identified in a questionnaire response.
Reminder postcards were sent to all volunteer doulas by doula service staff, 3 weeks after the mailing out of the questionnaires. This thanked those who had already completed questionnaires and invited completion from those who had not yet done so. If selected for participation in a telephone interview, doulas were contacted directly by a member of the research team using the details they had provided. The telephone interviews were digitally recorded (with one exception) and fully transcribed.
What are the processes of implementing and sustaining a volunteer doula service for disadvantaged childbearing women?
This component involved managers, doula service staff, local champions and commissioners at the five doula sites. Its purpose was to identify how each service works in practice and what the enablers, barriers and impacts had been. As the roll-out sites were at a relatively early stage of their development, our study had the opportunity to explore this development over time, by carrying out data collection at two time points, early in the study and later, to determine both experiences of the early stages and aspirations for the coming year and, subsequently, the extent to which these were achieved.
Doula service managers and staff
All staff employed by the doula services were identified by virtue of their professional role and invited to participate by a member of the research team. Doula service managers and staff were interviewed early in the evaluation, as already described, and a subset were reinterviewed a year later to identify changes and factors related to sustaining those services. In the proposal we had intended to limit second interviews to the roll-out sites, but it was recognised that issues of sustainability were equally important in the original site, so they were included in this aspect of data collection. A total of 11 staff contributed data.
Local champions and commissioners
Each roll-out site had at least one ‘local champion’: an individual who championed the adoption of the project and saw it through to successful commissioning. Their perspectives were considered essential to developing an understanding of this vital part of the process. At the stage of developing this research proposal, only four sites had secured local funding to become a replica service. Other sites had expressed interest but, at that stage, were unable to achieve funding. The question of what led four sites to achieve implementation of the roll-out required exploration.
Local champions and commissioners (with the exception of one site, which was not commissioned) were identified by service staff and approached by a member of the research team to take part in individual interviews. All potential participants received an information leaflet and written informed consent was obtained. Local champions were asked about the nature of their relationship with the doula service and ongoing role in it, their perceptions of the impact of the service and its future, and barriers to establishing and continuing it. Commissioners were asked to describe local commissioning arrangements and service level agreements, their relationship with the doula service, any challenges encountered in commissioning the doula services and their perceptions of the service’s future. Four champions and four commissioners contributed data.
Overview of maximum possible primary data collection
Table 3 presents the maximum primary data collection possible by method and participant group. Numbers in cells for women and doulas reflect the maximum numbers of participants and were included to inform resource requirements; numbers were informed by doula services where appropriate.
| Data source | Face-to-face/telephone interviews (n) | Questionnaires (n) | Focus groups (n) |
|---|---|---|---|
| Heads of midwifery | 5 (1 per NHS trust) | ||
| Midwives | 5 (1 per NHS trust) | ||
| Women | 600 maximum available | 12 maximuma | |
| Volunteer doulas | Maximum 10 to follow up questionnaire responses | 160 maximum available | 2b |
| Doula service managers | 11 initial and follow-up interviewsc | ||
| Project workersd | 11 | ||
| Local champions | 5 | ||
| Commissionerse | 4 |
Data analysis
Clinical and public health outcomes for women and their babies
Microsoft Excel (version 2010, Microsoft Corporation, Redmond, WA, USA) was used to summarise the data in pivot tables. Generally filters were used to remove mothers who were not supported, those who had disengaged from the service and those who gave birth (or had been expected to give birth) after 31 August 2012. Analysis of some data also required the use of ‘postnatal support only’ as a filter.
Confidence intervals were calculated using approved methodologies for public health observatories. 42 The doula service data were plotted onto bar charts alongside available comparisons, including those of designated statistical neighbours. Ninety-five per cent confidence intervals were included to indicate whether or not there were any significant differences between the doula data and comparators. Chi-squared tests were used to compare percentages of births by caesarean sections, breastfeeding at delivery and smoking in the doula population with data available from the maternity system at Hull and East Yorkshire Hospitals NHS Trust. Comparisons were made between outcomes derived from the doula database and those obtained from the maternity system at Hull and East Yorkshire Hospitals NHS Trust. Unfortunately it proved impossible to obtain all of the requisite data from the Trust data set, so we were unable to control for certain variables, such as parity.
The findings of these analyses are presented in Chapter 3, Clinical and public health impacts for women and their babies and Outcomes for women and babies, and further utilised in Chapter 7, where they have informed the economic analyses. Full details of all data sources and analytic methods for calculation of doula service and NHS costs are included in Chapter 7.
Quantitative analyses: questionnaires completed by women and doulas
On receipt of a questionnaire, each participant was assigned a unique study identity code number, for use on study documents and the Statistical Product and Service Solutions (SPSS, version 20, IBM Corporation, Armonk, NY, USA) database. Separate databases were created for women and for doulas. The women’s database included both supported and unsupported women, whether they had completed the questionnaire themselves or with assistance, with or without an interpreter. The doula database similarly included all doulas whether or not they had yet supported a woman one-to-one.
Data were analysed using SPSS. Descriptive statistics (means, frequencies, etc.) are presented where appropriate. Within-sample comparisons (e.g. of sites) were carried out as sample size allowed, using chi-squared tests for proportions and t-tests or analysis of variance to tests differences in means. When expected cell sizes were small, exact tests were used instead of chi-squared.
Comparisons with the Picker Institute maternity survey
Selected items from the Picker Institute maternity survey were included in the women’s questionnaire. A chi-squared test was used to compare the proportion of cases from the doula sample with the proportion obtained in the local maternity survey. Analyses were restricted to the original doula site because of the small numbers available at the roll-out sites. Consistent with the HES analyses, comparison data were used for the Hull PCT, a subsample of the HEY data.
Hull and East Yorkshire Hospitals NHS Trust data are based on a survey of 201 women, representing a 50% response rate for the survey. Trusts drew their sample from mothers who had had a live birth in February 2010 and were aged 16 or older. Women who gave birth in a hospital, birth centre or maternity unit, or who had a home birth, were eligible. The survey was mailed between May and June 2010, with non-responders sent up to two reminder mailings.
Qualitative data
Data collected using interviews, focus groups and free text data in questionnaires were analysed using content analysis43 to identify themes within the data, underpinned by the framework of realistic evaluation.
Each data source was treated independently. The transcripts from the interviews and focus groups were read and reread to gain a detailed familiarity with the overall accounts, and then systematically coded line by line to identify emerging themes. These themes were grouped and collapsed into higher-order conceptual themes with subthemes. For data related to women and doulas, emerging themes were considered in the light of CMO configurations. The open text questionnaire responses were tabulated using an Excel spreadsheet to show horizontally all of an individual’s responses to the questions and vertically all of the responses received to any question. This facilitated coding of themes identified in the responses on a question-by-question basis, identification of disconfirming responses and the exploration of linked patterns between questions.
For data collected from women and doulas, the final stage of the analysis was to integrate the findings of the qualitative and quantitative analyses to provide a comprehensive and integrated narrative of their experiences.
The findings related to the experiences of women and doulas are presented in Chapters 4 and 5 respectively, and those relating to implementing and sustaining the doula services in Chapter 6.
Quantitative data: costs of doula services and NHS costs
Full details of data collected and analytic method for doula service and NHS costs are included in Chapter 7.
Chapter 3 Findings: implications for the NHS
Clinical and public health impacts for women and their babies
Women supported by the original doula service
The aim of the following analysis was to identify the characteristics of the mothers who had been referred to the original volunteer doula service. Data have been pooled to produce an overall profile. At the point of extracting the data, a total of 603 mothers had been referred to the original service, of whom 599 were matched to a volunteer doula and 507 subsequently supported.
Method of referral
There were several routes of referral into the doula service. Referral sources were grouped together, as shown in Figure 1. Just over 43% of the 603 referrals were from a NHS professional and 23% by community midwives. The next largest category was ‘self-referral’.
FIGURE 1.
Method of referral summary, Hull doula mothers, all years, percentage. Source: developed from Goodwin volunteer doula database.
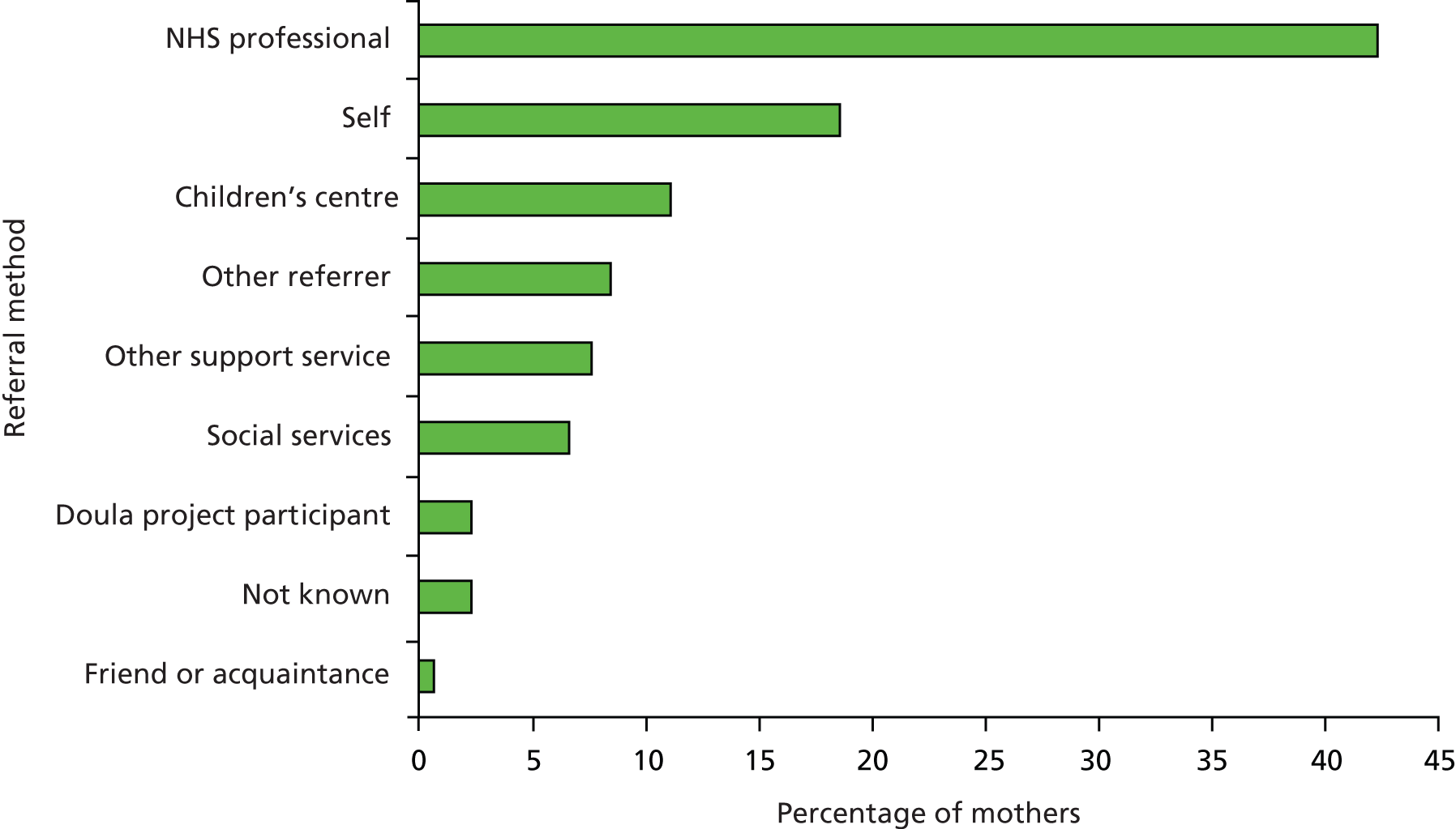
Most of the referrals by ‘other support services’ were from ‘asylum seekers/refugees support’ (3.3%) and ‘teenage pregnancy support’ (1.8%).
Mother’s postcode
Figure 2 shows the postcode districts of the 507 mothers supported by the original volunteer doula service in Hull. Most mothers lived within postcode districts HU1 to HU9, which match the boundaries of Kingston upon Hull local authority. Comparison data from HEY and the Office for National Statistics have been restricted to these postcodes.
FIGURE 2.
Mother’s postcode district, Hull doula users compared with female population, deliveries in Hull PCT and births in Hull and East Yorkshire Hospitals NHS Trust, all years, percentage. Sources: Goodwin volunteer doula database (all years); Hull and East Yorkshire Hospitals NHS Trust; Hospital Episode Statistics (HES) Copyright © 2013, reused with the permission of The Health and Social Care Information Centre. All rights reserved; Office for National Statistics (Census 2011). ONS, Office for National Statistics.

The Index of Multiple Deprivation (IMD) 2010 is a commonly accepted measure of deprivation. Kingston upon Hull is one of the 20% most deprived local authorities in England. Within Kingston upon Hull, as with most local authorities, there are differences in levels of deprivation across the area. Table 4 shows the percentage of women aged 16–44 years by postcode district in each national deprivation quintile.
| Postcode district | Deprivation quintile | ||||
|---|---|---|---|---|---|
| 1 (most deprived) | 2 | 3 | 4 | 5 (least deprived) | |
| HU1 | 99.8 | 0.0 | 0.2 | 0.0 | 0.0 |
| HU2 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| HU3 | 85.5 | 14.0 | 0.5 | 0.0 | 0.0 |
| HU4 | 43.6 | 14.5 | 24.1 | 6.7 | 11.2 |
| HU5 | 16.6 | 44.9 | 26.5 | 8.9 | 3.1 |
| HU6 | 53.4 | 5.9 | 24.8 | 15.9 | 0.0 |
| HU7 | 49.7 | 13.3 | 18.7 | 18.2 | 0.1 |
| HU8 | 37.7 | 22.3 | 19.1 | 13.3 | 7.6 |
| HU9 | 71.6 | 13.5 | 14.8 | 0.0 | 0.0 |
The majority of the population of HU1, HU2 and HU3 are in the 20% most deprived areas. It would suggest that the Goodwin volunteer doula service is used by mothers from areas of deprivation. The exception to this is the HU9 postcode district. Only 14.4% of Hull doula mothers come from this area compared with approximately 18.1% of both the deliveries in Hull PCT and babies being born in HEY to mothers from Kingston upon Hull. The children’s centre from which the Goodwin volunteer doula service operates is based in HU3 and close to HU1 and HU2.
Mother’s age
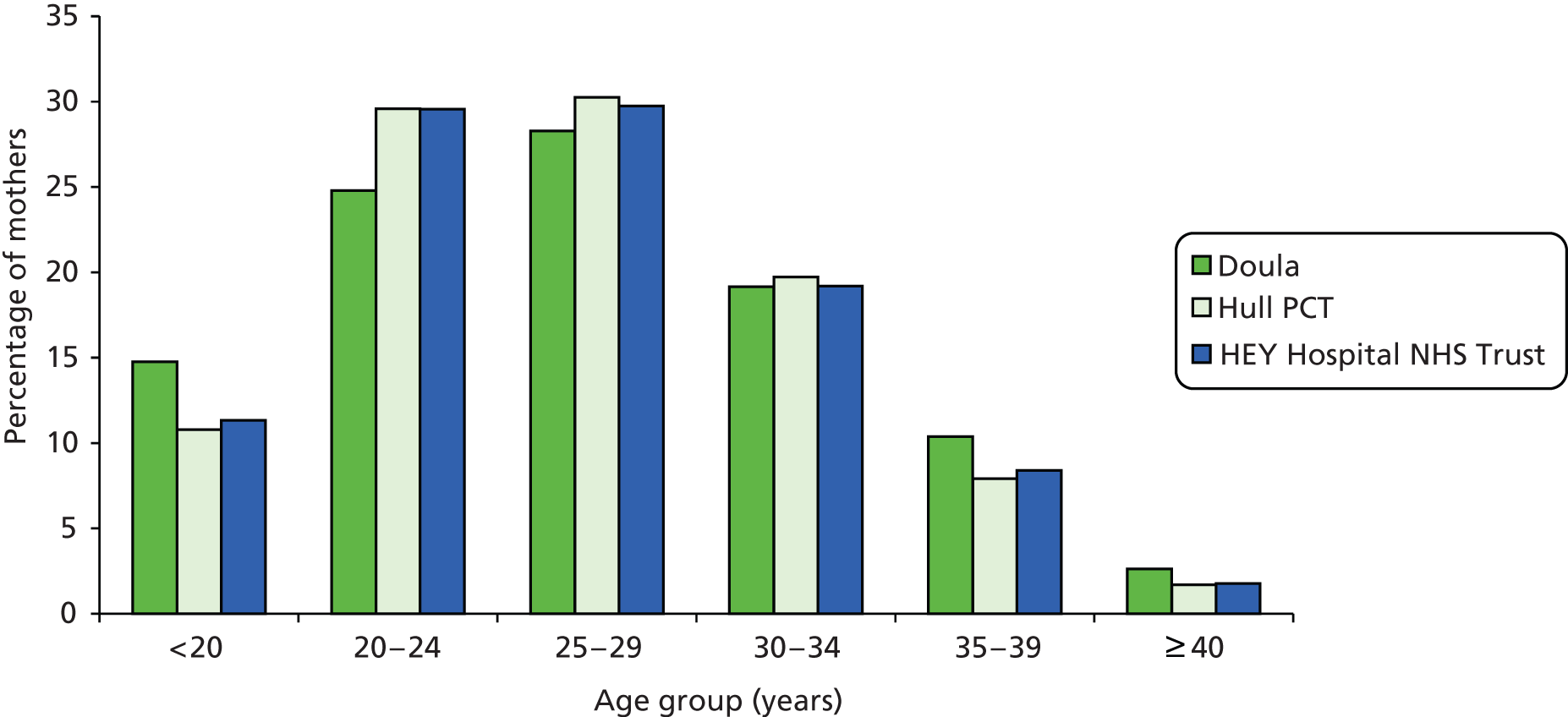
The ages of women referred to the doula service ranged from 15 to 43 years (n = 599, mean 26.7 years, mode 26 years). Figure 3 compares the age of mothers using the Hull doula service with mothers who had a child in Hull PCT and with those who lived in Kingston upon Hull and had a baby in HEY. The age profile of women offered doula support reflects the overall profile of that for Hull PCT and HEY. Mothers under 20 years of age accounted for 14.8% of all doula service users compared with 10.8% of deliveries in Hull PCT and 11.3% of deliveries to Hull mothers in HEY. Mothers aged 35 years and over were slightly over-represented among doula referrals, while those aged 20–35 years were somewhat under-represented.
FIGURE 3.
Mother’s age, Hull doula mothers compared with Hull PCT and HEY, percentage. Sources: Goodwin volunteer doula database (all years); Hull and East Yorkshire Hospitals NHS Trust, Hospital Episode Statistics (HES) Copyright © 2013, reused with the permission of The Health and Social Care Information Centre. All rights reserved.
Ethnicity
Figure 4 shows the ethnicity of mothers referred to the service. Although greater detail is available, for comparison the mothers were grouped into ‘white British’ and ‘non-white British’. ‘Non-white British’ mothers are all those mothers who are not ‘white British’. Thirty-seven per cent of women referred to the doula service were from a non-white British background. This is over twice as many as the local population rates.
FIGURE 4.
Ethnicity, Hull doula mothers compared with Hull PCT, HEY and 2011 Census, all years. Sources: Goodwin volunteer doula database (all years); Hull and East Yorkshire Hospitals NHS Trust, Hospital Episode Statistics (HES) Copyright © 2013, reused with the permission of The Health and Social Care Information Centre. All rights reserved; Office for National Statistics (Census 2011).
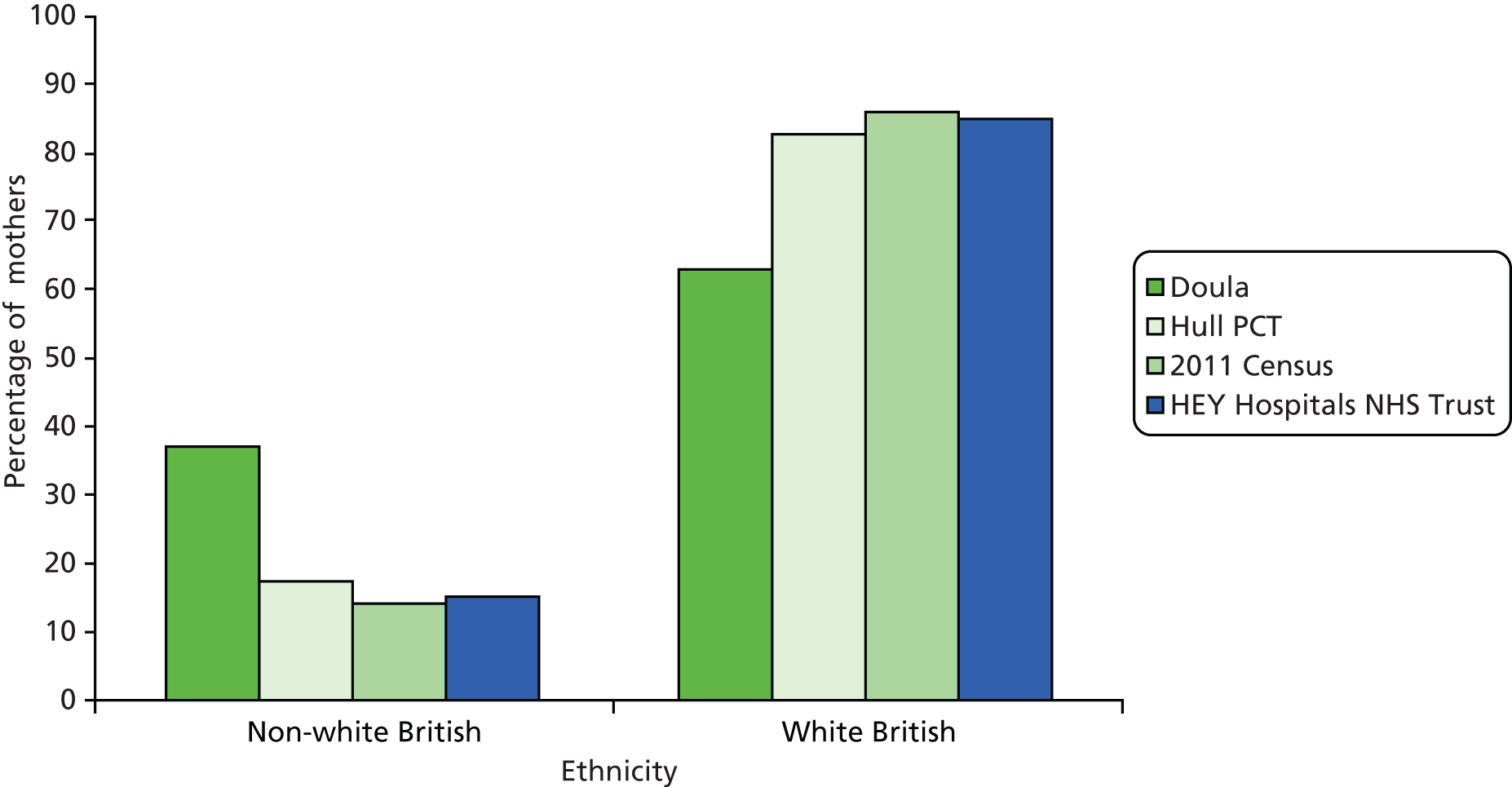
Further analysis of the doula service database showed the most frequent non-white British groups were ‘white – other’ and ‘black – African’, which each accounted for approximately 10% of the doula mothers. While definitions may vary slightly, as a comparison the 2011 Census indicated 4.0% of females (all ages) in Kingston upon Hull considered themselves as ‘white other’ and only 1.2% of females (all ages) considered themselves as either ‘black/African/Caribbean/black British: African’ or ‘mixed/multiple ethnic group: white and black African’. 46
Parity
Figure 5 shows the number of previous children born to the 387 mothers who were supported and were engaging with the doula service in Hull. The number of previous babies ranged from none to eight. Almost 45% (173) of supported and engaging users were first-time mothers. A further 28.1% of mothers had one other child.
FIGURE 5.
Previous number of children, Hull doula mothers, all years. Source: developed from Goodwin volunteer doula database.
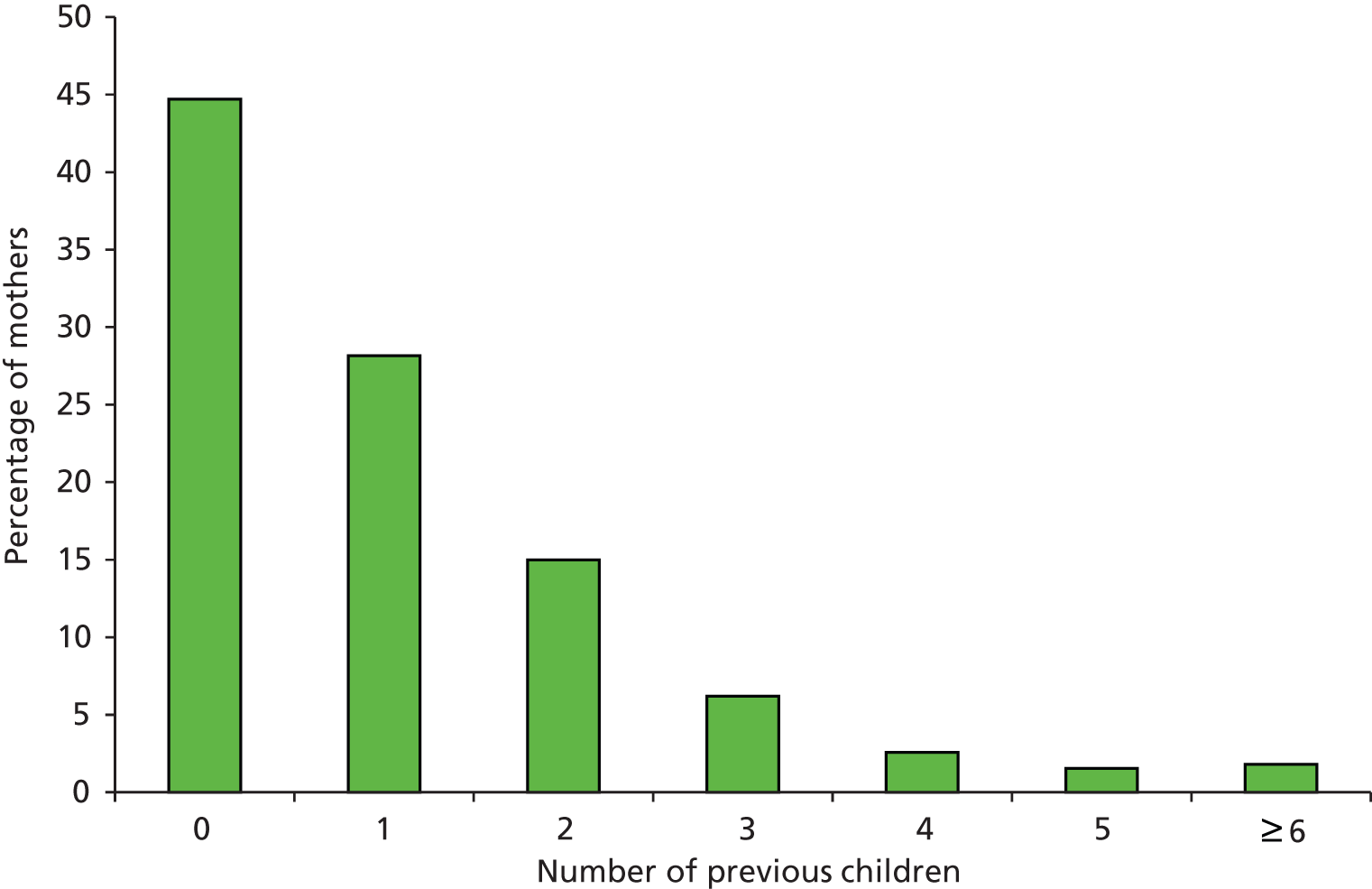
Among non-white British mothers, 46% were expecting their first baby, compared with 44% of white British mothers.
Disengagement
Almost 20% of mothers who were referred to the doula service were recorded as having disengaged from the service. As a result, there were fewer records available for analysis of outcomes than expected. The majority of these analyses are based on a sample size of around 330 mothers.
Chi-squared tests were used to examine whether or not disengagement varied by ethnic group or parity (Tables 5 and 6). Mothers who disengaged were more likely to be ‘white British’ than ‘non-white British’ [χ2 = 20.3, 1 degree of freedom (df); p < 0.05] and to be first-time mothers than women with other children (χ2 = 10.6, 1 df; p < 0.05).
| Ethnicity | Disengaged n (%) | Engaged n (%) | Total n (%) |
|---|---|---|---|
| Non-white British | 28 (23.3) | 180 (46.5) | 208 (41.0) |
| White British | 92 (76.7) | 207 (53.5) | 299 (59.0) |
| Total | 120 (100) | 387 (100) | 507 (100) |
| Parity | Disengaged n (%) | Engaged n (%) | Total n (%) |
|---|---|---|---|
| No previous children | 74 (61.7) | 173 (44.7) | 247 (48.7) |
| Previous children | 46 (38.3) | 214 (55.3) | 260 (51.3) |
| Total | 120 (100) | 387 (100) | 507 (100) |
Similar comparisons found no relationship between disengagement and postcode district.
A chi-squared test was used to compare the proportion of mothers who disengaged with those who continued with the service by age group. Because the numbers were small the categories ‘35 to 39 years’ and ‘40 years and over’ were combined into ‘35 years and over’. A summary of the data can be found in Table 7. Percentages are in brackets and may not add up to 100% because of rounding. Unknown ages were removed.
| Age group (years) | Disengaged n (%) | Engaged n (%) | Total n (%) |
|---|---|---|---|
| < 20 | 32 (27.4) | 40 (10.6) | 72 (14.6) |
| 20–24 | 25 (21.4) | 90 (23.9) | 115 (23.3) |
| 25–29 | 27 (23.1) | 118 (31.3) | 145 (29.4) |
| 30–34 | 21 (17.9) | 77 (20.4) | 98 (19.8) |
| ≥ 35 | 12 (10.3) | 52 (13.8) | 64 (13.0) |
| Total | 117 (100) | 377 (100) | 494 (100) |
The age distributions of the disengaged and engaged mothers were significantly different. Disengaged mothers tended to be younger, particularly under the age of 20 years (χ2 = 15.7, 4 df; p < 0.005). Mothers under 20 years old accounted for 27.4% of disengaged mothers compared with 10.6% of those who engaged with the service.
Outcomes for women and babies
The aim of the following analysis is to compare the outcomes of the mothers and babies who were supported by the Goodwin volunteer doula service with local and statistically similar areas. While the doula database was a rich source of information, uncertainty over data quality meant consideration was restricted to key areas, following data cleansing.
For clinical outcomes related to labour reported in the next four subsections, we excluded data from women who had disengaged from the service and from those who had received support during the postnatal period only. Our analysis is therefore restricted to women who received doula support during the antenatal and/or intrapartum periods. Numbers that meet those criteria by financial year are as follows: 52 (2008/9), 53 (2009/10), 87 (2010/11), 63 (2011/12) and 66 (2012/13). Analysis of low birthweight is based on babies of 303 women because of the higher proportion of missing data. For public health outcomes (breastfeeding at birth and 6 weeks, smoking) analysis was based on 330 women supported by the doula service.
Epidural
Figure 6 shows the use of epidurals in all births (including C-section) for mothers using the Hull doula service. The use of epidurals ranged from 22.6% in 2008/9 to 35.5% in 2011/12.
FIGURE 6.
Epidurals given for all deliveries with 95% confidence intervals, Hull doula mothers, all years. Source: developed from Goodwin volunteer doula database.
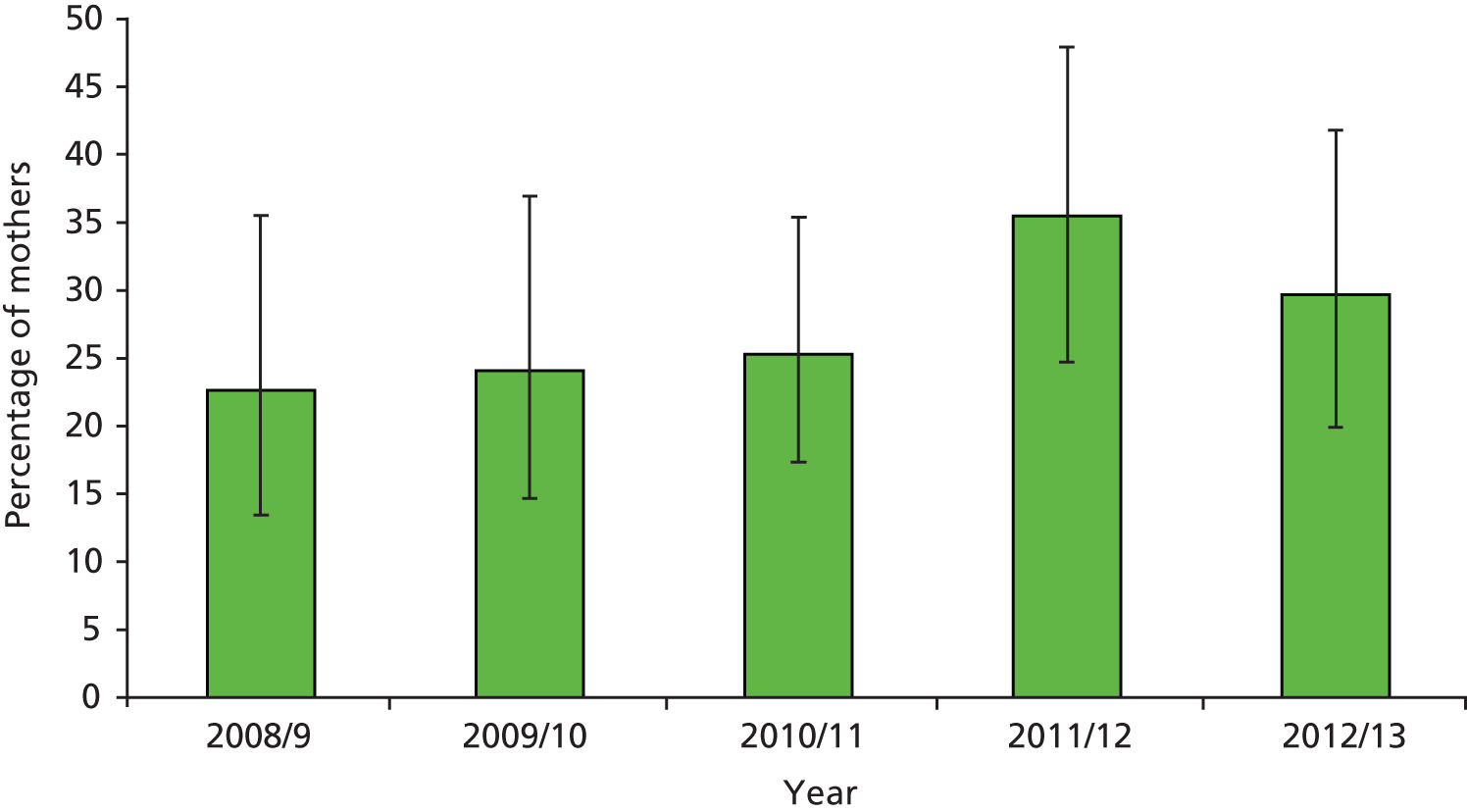
Figure 7 compares the epidural use of mothers using the Hull doula service and mothers resident in Hull PCT. The data include normal and instrumental births only and suggest that epidural use by doula mothers is lower than that by mothers from Hull PCT. However, these differences reach significance only in 2010/11.
FIGURE 7.
Epidurals for normal and instrumental deliveries with 95% confidence intervals, Hull doula mothers compared with Hull PCT, all years. Source: Goodwin volunteer doula database; Hospital Episode Statistics (HES) Copyright © 2013, reused with the permission of The Health and Social Care Information Centre. All rights reserved.

Method of delivery
Figure 8 shows method of delivery by Hull doula mothers, pooled for all years (n = 327). It shows that normal birth (operationalised as all vaginal births excluding those assisted by forceps or ventouse and also excluding all caesarean sections) accounts for 71.3% of births. A further 21.1% of births took place by C-section and 4.6% were instrumental deliveries.
FIGURE 8.
Delivery method with 95% confidence intervals, Hull doula mothers, all years. Source: Goodwin volunteer doula database.
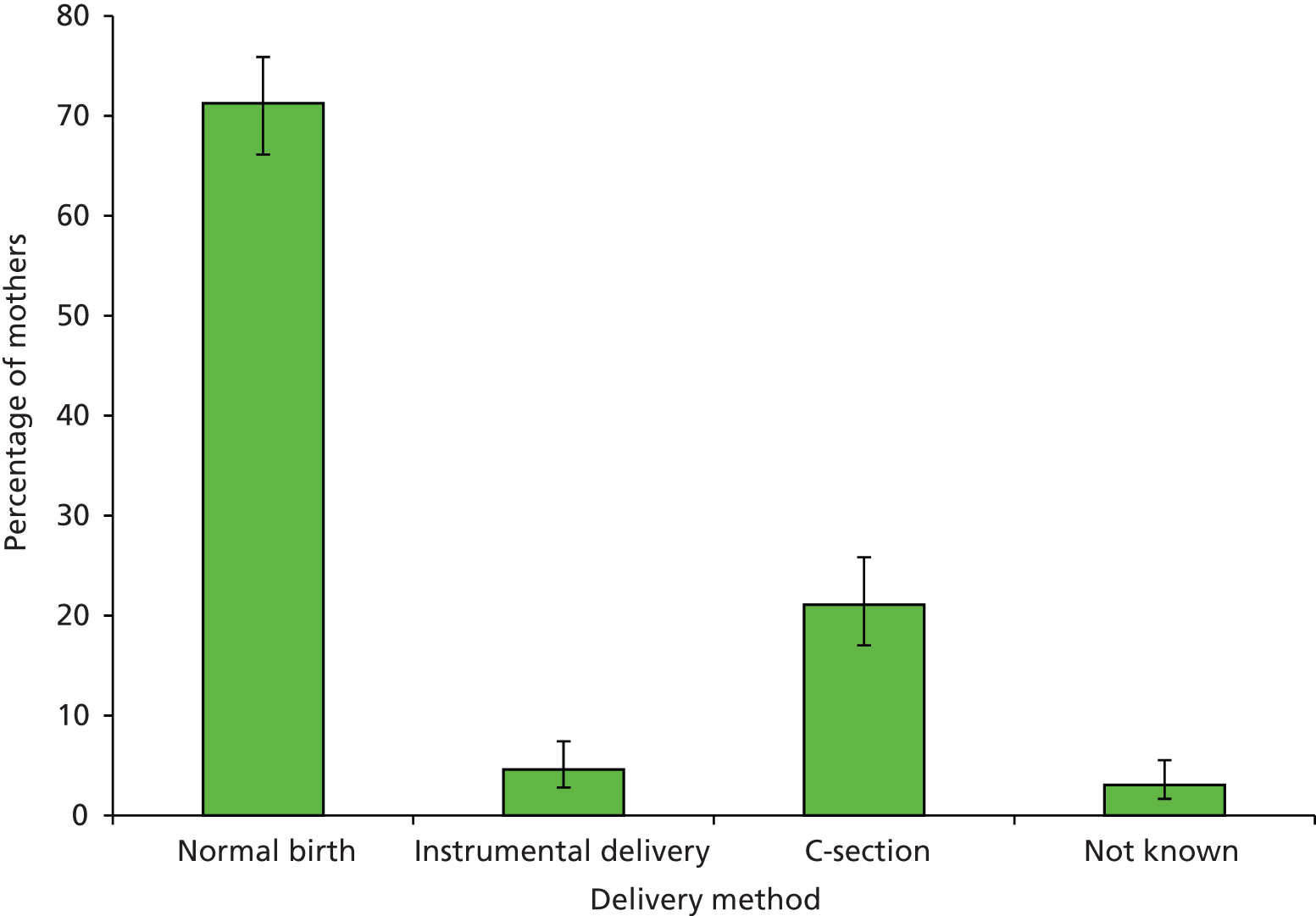
Caesarean section
Figure 9 illustrates a comparison of C-section rates for mothers using the doula service with those for mothers resident in Hull PCT and England. The percentage giving birth by C-section was lower for doula service mothers than for the other two groups, except in 2009/10. However, differences are not statistically significantly in any year, as indicated by the wide confidence intervals around the rates for the doula service mothers.
FIGURE 9.
Comparison of C-sections with 95% confidence intervals, 2008/9 to 2011/12, percentage of all deliveries. Sources: Goodwin volunteer doula database; Hospital Episode Statistics (HES) Copyright © 2013, reused with the permission of The Health and Social Care Information Centre. All rights reserved.
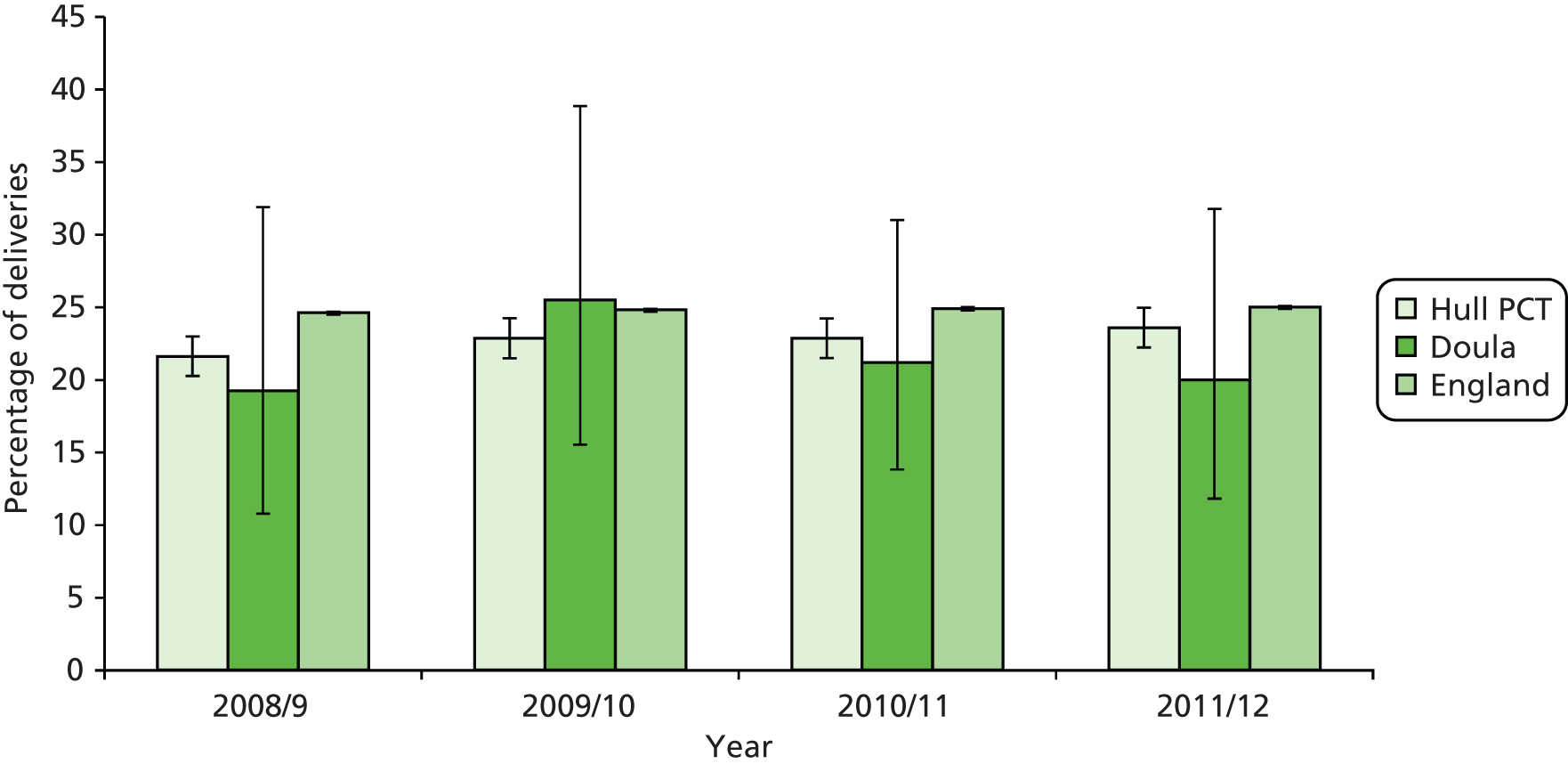
Full interpretation of C-section outcomes requires information about parity to be available. We had planned to conduct further comparisons of C-section rates by parity. We applied to the trust for these data but unfortunately a data set containing this variable could not be provided.
Babies admitted to the neonatal unit
Figure 10 compares the percentage of women using the doula service whose baby was admitted to a neonatal unit (including special care baby unit or intensive care unit) and the percentage of mothers from Kingston upon Hull whose baby was born in Hull and East Yorkshire Hospitals NHS Trust and admitted to the neonatal unit.
FIGURE 10.
Babies referred to neonatal unit with 95% confidence intervals, Hull doula mothers compared with HEY, 2009/10 to 2012/13 (quarters 1 + 2; pooled). Sources: developed from Goodwin volunteer doula database; Hull and East Yorkshire Hospitals NHS Trust.
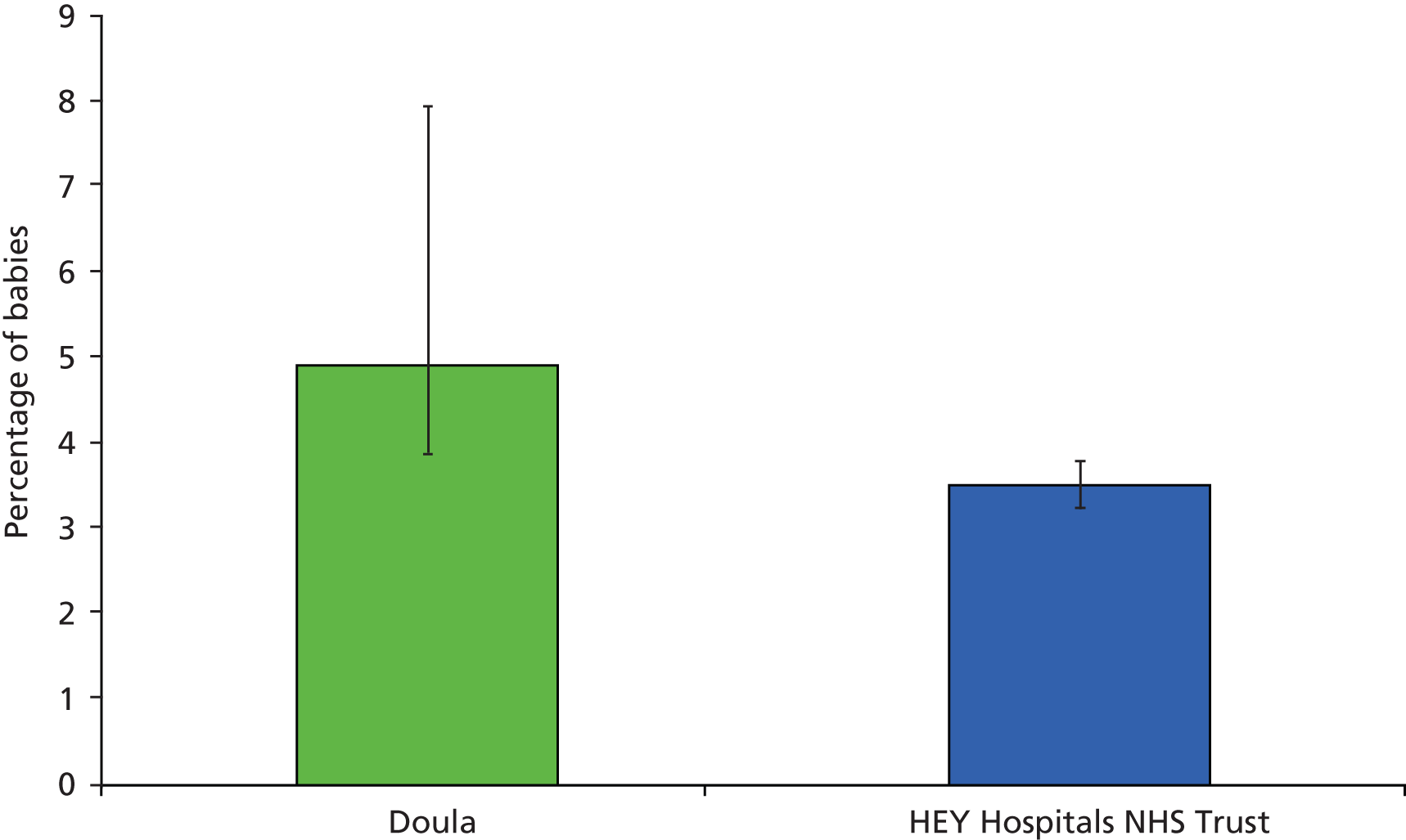
The percentage of babies of doula-supported mothers admitted to neonatal units was higher than those of mothers resident in Hull who gave birth in Hull and East Yorkshire Hospitals NHS Trust. The small numbers result in wide confidence intervals and the difference is not statistically significant.
Smoking at delivery
Figure 11 shows the percentage of doula mothers smoking between 2008/9 and 2012/13 (partial year); generally around 15% to 20% of mothers smoked at time of delivery, with 2011/12 as an exception.
FIGURE 11.
Smoking at time of delivery with 95% confidence intervals, Hull doula mothers, all years. Source: developed from Goodwin volunteer doula database.

Rates of smoking at delivery for doula service mothers were compared with those for Hull PCT and the statistical neighbours, as represented in Figure 12.
FIGURE 12.
Smoking at delivery with 95% confidence intervals, Hull doula mothers compared with Hull PCT and statistical neighbours, percentage of mothers. Sources: Goodwin volunteer doula database; Health and Social Care Information Centre Return on smoking status at time of delivery.

The percentage of mothers using the Hull doula service and smoking at time of delivery is lower than in the statistical neighbours of Hull PCT, except for Salford PCT and Stoke-on-Trent PCT in 2009/10. The confidence intervals show that the differences are not statistically significant except for the comparison with Middlesborough PCT in 2010/11 and for all services combined in 2011/12. Smoking at time of delivery has traditionally been very high in Hull PCT compared with the rest of the country. Since 2005/6, Hull has always been in the top 10% of PCTs for percentage of mothers smoking at time of delivery. During the years for which doula service data were available, it was often in the top 5%. 39
Figure 13 presents the comparison of smoking among mothers using the Hull doula service with Hull PCT and mothers from Kingston upon Hull having babies in HEY between 2008/9 and 2012/13. The overlapping confidence intervals indicate that the differences are not statistically significant except for 2011/12.
FIGURE 13.
Smoking at delivery with 95% confidence intervals, Hull doula mothers compared with Hull PCT and HEY, 2009/10 to 2012/13 (quarters 1 + 2). Sources: developed from Goodwin volunteer doula database; HEY; Health and Social Care Information Centre Return on smoking status at time of delivery.
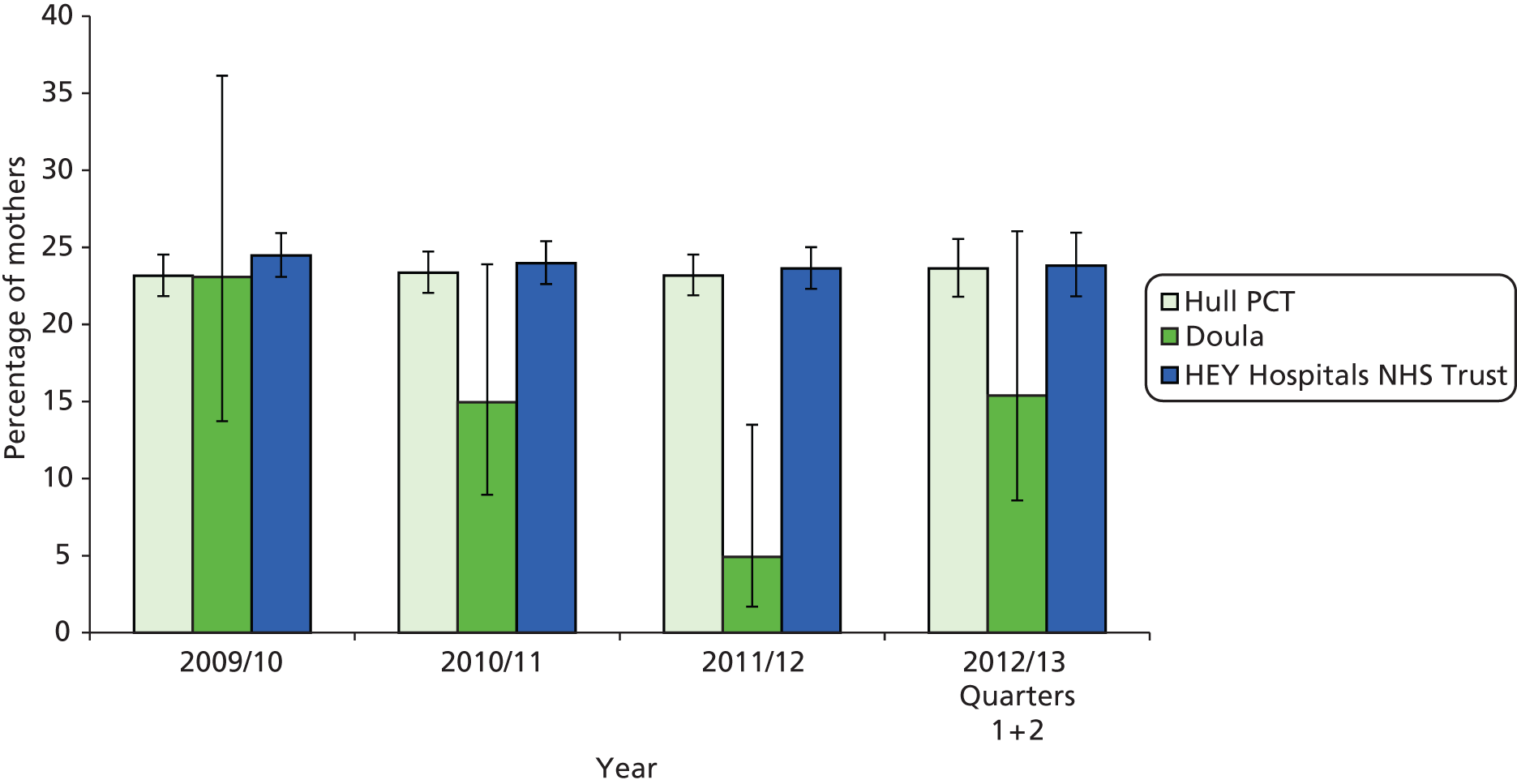
As identified earlier in Table 4, deprivation varies by postcode district.
Figure 14 shows smoking at delivery by postcode district. Hull doula mothers are compared with mothers resident in Kingston upon Hull giving birth within HEY.
FIGURE 14.
Smoking at delivery by postcode district with 95% confidence intervals, Hull doula compared with HEY, all years. Sources: developed from Goodwin volunteer doula database; HEY.

The percentage of mothers smoking at delivery is lower for doula-supported mothers across all postcode districts in Kingston upon Hull, except for HU5 and HU7. The confidence intervals indicate that these differences are statistically significant in postcode districts HU2, HU3, HU8 and HU9. As stated previously, postcode districts HU2, HU3 and HU9 have very high proportions of the populations living in the 20% most deprived areas.
Low birthweight
Figure 15 compares babies born with a low birthweight (less than 2500 g) to mothers who received the Hull doula service and to mothers resident in Hull PCT. Although only half as many babies with a low birthweight were born to doula mothers, the small numbers lead to wide confidence intervals and the difference is not statistically significant.
FIGURE 15.
Low birthweight, Hull doula mothers compared with Hull PCT, percentage of babies with 95% confidence intervals, 2009/10 to 2011/12 (pooled). Sources: Goodwin volunteer doula database; Hospital Episode Statistics (HES) Copyright © 2013, reused with the permission of The Health and Social Care Information Centre. All rights reserved.
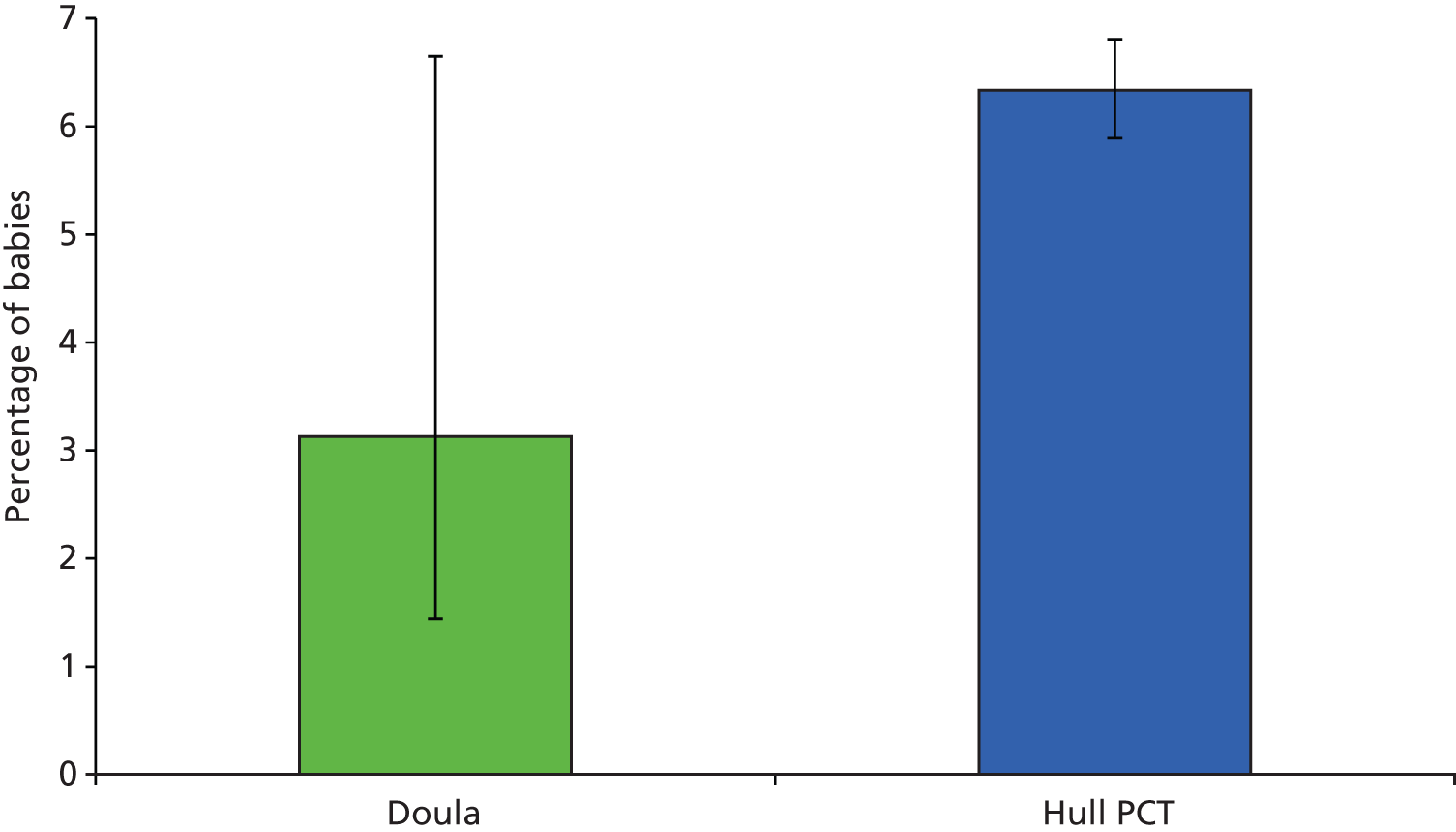
Feeding method at birth
Data reflecting feeding method recorded at birth for Hull doula mothers were pooled. The most common method of feeding was breastfeeding (71.8% of mothers), with 17.9% of mothers bottle feeding and 7.0% mixed feeding. Feeding data were not recorded for 3.3% of babies. Figure 16 shows the rates of breastfeeding initiation between 2007/8 and 2012/13 (partial year); rates exceed 70% in four of the six periods for which data are available. The wide confidence intervals reflect the small sample size.
FIGURE 16.
Breastfeeding initiation with 95% confidence intervals, Hull doula mothers, 2007/8 to 2012/13 (quarters 1 + 2). Source: developed from Goodwin volunteer doula database.
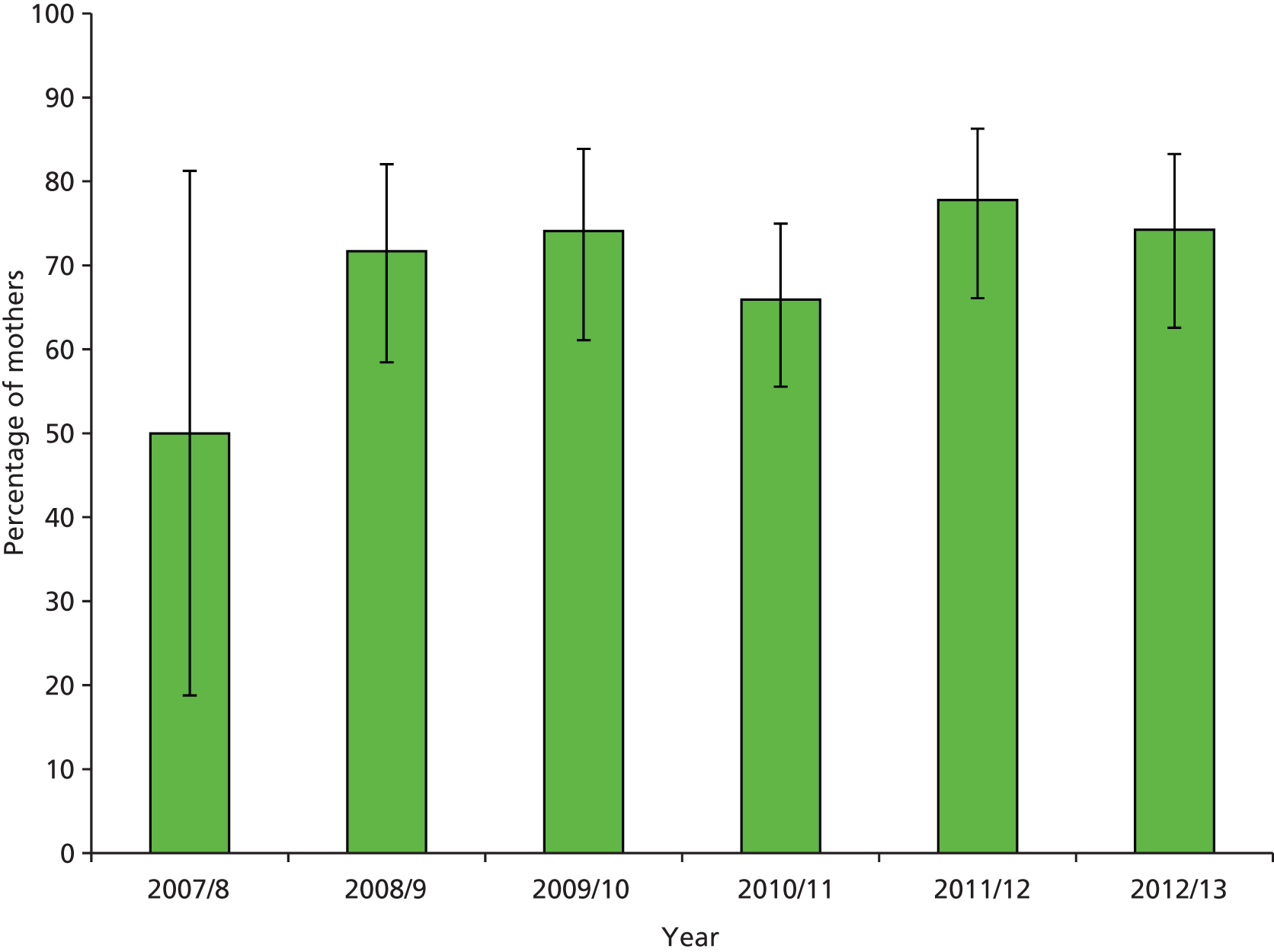
Figure 17 illustrates the comparison for breastfeeding initiation between Hull doula mothers and Hull PCT and its statistical neighbours. It shows breastfeeding initiation is higher among Hull doula mothers than in the comparison groups for each year considered, but the confidence intervals indicate that it is statistically significantly different for all groups only in 2011/12. For 2008/9, doula-supported women were significantly more likely to initiate breastfeeding than all neighbours, with the exceptions of Salford and Stoke-on-Trent; for 2009/10, a similar pattern occurred, with Salford as the exception; for 2010/11, doula-supported women were significantly more likely to initiate breastfeeding than mothers in Hartlepool and Middlesbrough PCTs; and, for the first two quarters of 2012/13, doula-supported women were significantly more likely to initiate breastfeeding than mothers in Hartlepool, Middlesbrough and Salford PCTs.
FIGURE 17.
Breastfeeding initiation with 95% confidence intervals, Hull doula mothers compared with Hull PCT and statistical neighbours, 2008/9 to 2012/13 (quarters 1 + 2). Sources: developed from Goodwin volunteer doula database; Department of Health, Integrated Performance Measure Return.
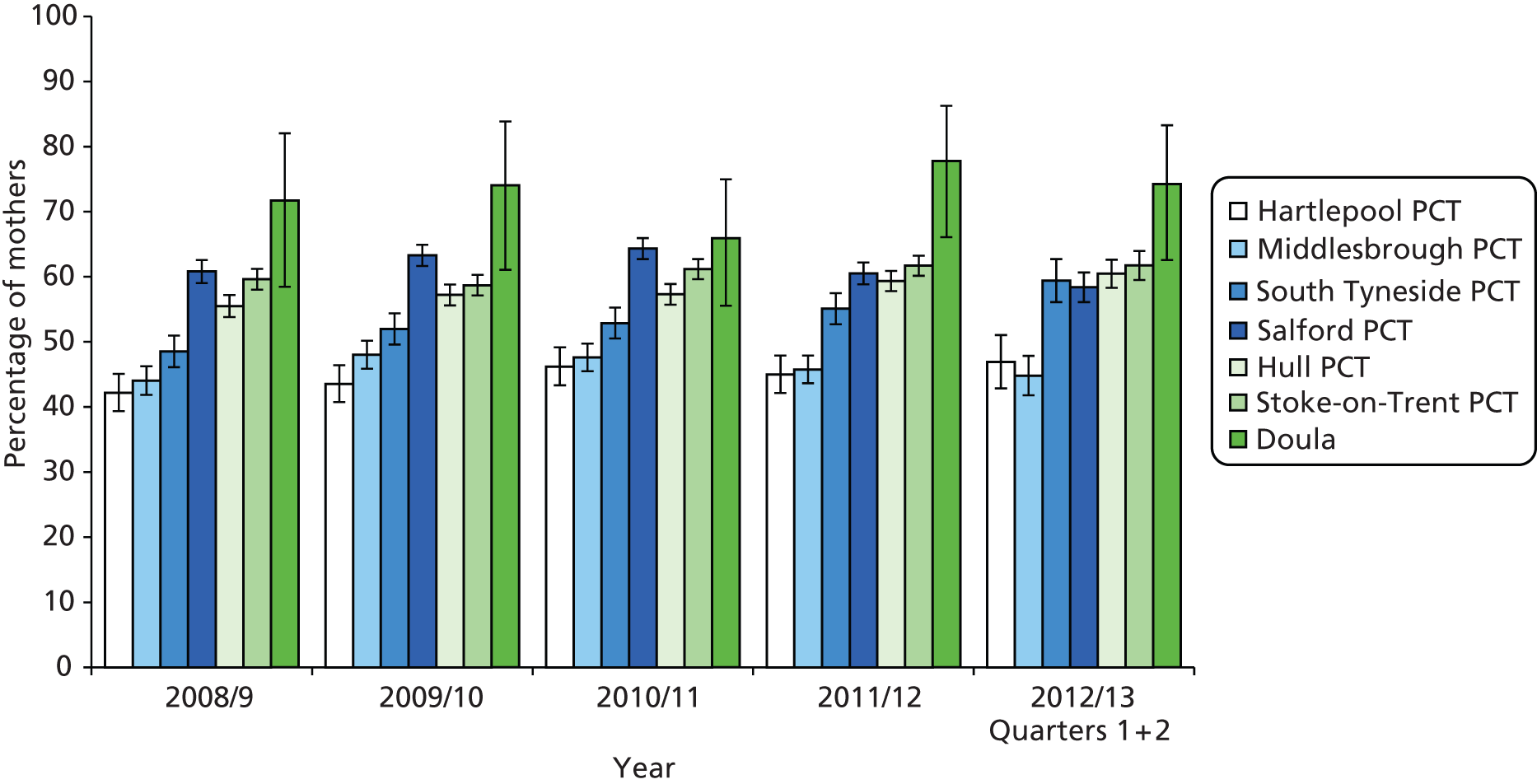
When compared with data from Hull PCT and the HEY (Figure 18), it appears breastfeeding initiation is significantly higher among women supported by the doula service, with the exception of 2010/11.
FIGURE 18.
Breastfeeding initiation with 95% confidence intervals, doula mothers compared with Hull PCT and HEY, 2008/9 to 2012/13 (quarters 1 + 2). Sources: developed from Goodwin volunteer doula database; HEY; Department of Health, Integrated Performance Measure Return.

Mothers from the Hull doula population were more likely to breastfeed at delivery (74.3%) than mothers from HEY (55.2%) (χ2 = 46.40, 1 df; p < 0.0005).
Further information about breastfeeding and postcode district is available in Appendix 8.
Infant feeding at 6 weeks
The mothers’ feeding method at 6 weeks is recorded in the doula database. The most common method was breastfeeding (42.4% of mothers) with a further 36.1% bottle feeding and 10.3% of mothers offering mixed feeding. Feeding information was missing in 11.2% of cases.
Breastfeeding at 6 weeks
Breastfeeding at 6 weeks was compared with published data related to total and partial breastfeeding at 6–8 weeks. Figure 19 provides information for total and partial breastfeeding for doula mothers compared with Hull PCT and its statistical neighbours. Figures are percentages of maternities where the feeding method is known. At the point of extracting the data from the site A doula database there were 20 mothers whose feeding method was not known for 2012/13. The percentage of doula service mothers breastfeeding at 6 weeks is significantly higher than all the statistical neighbours in each year.
FIGURE 19.
Total and partial breastfeeding at 6 weeks, doula mothers compared with Hull and statistical neighbours, 2008/9 to 2012/13 (quarters 1 + 2). Sources: developed from Goodwin volunteer doula database; Department of Health, Integrated Performance Measure Return.

Summary of findings: clinical and public health outcomes
Table 8 provides a summary of findings of comparisons for clinical and public health outcomes between mothers who received the doula service and comparison data sets.
| Outcome | Comparison group | Findings |
|---|---|---|
| Differences that are significant for all comparisons | ||
| Breastfeeding at 6 weeks | Hull PCT and statistical neighbours higher all years, all groups | Significant difference |
| Differences where there are consistent findings suggesting improved outcomes but differences are not always statistically significant | ||
| Epidural | Hull PCT lower all years | Significant difference 2010/11 |
| C-section | Hull PCT and England lower all years except 2009/10 | NS |
| Smoking at birth | Hull PCT and statistical neighbour PCTs lower than some neighbours | Significant difference 2011/12 |
| Breastfeeding initiation | Hull PCT and statistical neighbours higher than all neighbours for all years | Significant difference for all 2011/12 and compared with some neighbours in 2008/9, 2009/10, 2010/11 and 2012/13 |
| Breastfeeding at delivery | HEY higher all years | Significant difference except 2010/11 |
| Outcomes available as pooled data for all years | ||
| Babies referred to NICU | HEY higher for doula group | NS |
| Smoking at birth | HEY, by postcode lower in seven of nine postcodes | Significant difference in four of seven postcodes |
| Low birthweight | Hull PCT lower for doula group | NS |
The impacts on and experiences of NHS maternity care services and providers
Midwives
Focus groups were held with midwives in four of the five trusts providing maternity care for women offered volunteer doula support. A total of 31 midwives participated. In the fifth trust it did not prove possible to convene a group within the required time scale. Midwives who participated held a range of roles and were of varying seniority, from newly qualified midwives to managers and consultant midwives. Awareness of, and personal contact with, doula services varied within groups. Our aim had been to achieve a sample with experience of providing care to women who had received doula support. However, while interested in the topic, at several sites some participants were without such experience. Negative perceptions of paid-for doulas were voiced spontaneously at all sites. Midwives’ quotes are coded for site and participant (MW, midwife).
Midwives’ perceptions of the volunteer doula role
Midwives were asked for their perceptions of the volunteer doula role and experiences of working with volunteer doulas. There was a consensus that volunteer doulas were there to support women who might be isolated and who lacked the support of family members, acting as advocates and providing continuity:
That don’t have that family network.
Site W, MW2
There’s someone who’s going to be a constant throughout their pregnancy.
Site Y, MW1
In situations where women may be engaging with several agencies, a doula was considered to have the potential for a co-ordinating role:
It was felt that a doula was a kingpin for the pregnancy, because there was a lot going on with other people.
Site A, MW1
In terms of women’s labours, doulas were perceived to foster normality. They were expected to provide emotional and practical support; this was expected to be especially useful for women whose previous experiences of childbearing had been negative. The fact that women could form a relationship with their doulas prior to labour was a positive feature, especially as they would usually not know the midwife providing clinical care.
I think labour is something that women do worry about. But to have a relationship with somebody, it’s best that it can grow from the weeks before isn’t it?
Site W, MW2
In addition, some participants envisaged a future role of providing support in early labour.
In terms of establishing a relationship prior to the birth, around 4 weeks prior to labour was considered optimal but there was acknowledgement that that may not always be possible in situations of late referrals or pre-term labour. The doula service protocols specify that the duration of postnatal support available from volunteer doulas is 6 weeks. One midwife said that this was treated flexibly by some doula services if required by a woman’s specific situation.
Where midwives had provided care for women supported by their partner and a doula during labour, no problems were identified. It was acknowledged that some women preferred female companionship during labour and that this may be culturally more appropriate for some women and their partners. Midwives recounted circumstances where the doula had supported a woman until her partner arrived and also where the doula had supported the couple during the labour:
I think that some women want women with them.
Site Y, MW3
I’ve seen having a doula and having the partner there and work well together, so because the doula’s developed a relationship she knows where her boundaries are and what the women wants her partner to do . . . I’ve seen it working well, and the doula knows when to step back.
Site Z, MW1
Midwives’ views on boundaries and clarity about the doula role
In their consideration of the volunteer doula role, early misunderstandings had resolved but boundaries remained an important issue and midwives from more than one site observed that doulas understood where the boundaries lay:
Early on some misunderstandings but . . . now not overstepping the mark and clear where their responsibility ended . . . midwives more accepting of them . . . find them a quite a positive role.
Site A, MW3
There’s potential for conflict unless you’ve got clearly defined roles . . . I hate using the word boundaries, but everyone kind of knows.
Site Z, MW5
It was felt important that midwives understood the doula’s role and that the volunteer doula role should not include activities that may be considered ‘medical’:
I don’t think they should interfere with the medical.
Site A, MW1
I don’t think there’s any place for a doula to be giving a woman specific medical advice.
Site Y, MW3
Clarity about the role was achieved through doula training and some midwives were involved in that. Such linkages offer very different opportunities to understand the doula role from encountering doulas supporting labouring women. One roll-out site had changed the training from that introduced by the original site:
We did change the emphasis of the study sessions, because that’s what the meetings were about, the role of the doula not being to make decisions for the woman or give medical advice . . . I put emphasis on the fact that she should also be trying to encourage normality.
Site W, MW1
Potential overlaps and synergies were identified between the volunteer doula role and those of other maternity service workers, namely advocates, maternity support workers and maternity care assistants:
We have advocates here as well who quite often are sitting with women in our antenatal clinics . . . and really what is the difference for us between the advocate and the [doula], so I think it’s about getting their roles really quite clear and them more visible for all of the staff.
Site Z, MW6
Doulas are much more about being . . . a person a woman can talk to and an advocate being alongside and helping her access services which maternity support workers haven’t got the time to be taking them to children’s centres.
Site W, MW3
Matching
The extent to which midwives were aware of elements of the doula service approach, for example matching women and doulas, varied between sites and individuals. Midwives reflected on the matching process and the potential effectiveness of doulas in situations where there was not a shared language:
When you put a referral in, it’s not a case of they just put any doula, they do look at it all quite intensely . . . match the best doula for that person.
Site A, MW1
I think it’s bemused us . . . that women were placed together and both didn’t have English as the first language, but didn’t speak each other’s language, so that seemed to be a strange way of organising it.
Site W, MW1
Impacts on women of having volunteer doula support
Midwives felt that the provision of doula support helped women to take up a range of facilities and services, including non-statutory ones. One midwife recounted an example where a doula had accompanied a woman with four very young children to a local park, thus identifying benefit for the woman and her older children. It was suggested that where services were difficult for some women as outside their cultural norms, for example postnatal drop-in clinics, the doula could accompany a woman and enable access. Reducing non-attendance at appointments and generally reinforcing midwifery advice were also considered positive impacts:
But without this, having the doula to have that conversation with us, people just DNA’d [did not attend] appointments all over the place, and it was a real big issue.
Site A, MW4
In one focus group, participants discussed the potential for stigma for women having doula support if the role is not clearly understood by others. This discussion took place in the context that some participants questioned if volunteer doulas might be accompanying women to birth preparation sessions but not identifying themselves as doulas.
Endings
Although it was acknowledged that doulas should not form enduring friendships with the women they support, it was felt that this did occur. One midwife reported that she and the doula had subsequently been invited to family events such as weddings and it was thought that continuing friendships could be managed in certain circumstances, specifically if there had been a break at the end of the doula support:
Is it not the case that the voluntary doulas aren’t allowed to also become friends outside of the service?
Site W, MW1
They certainly don’t do it whilst they are actually there as a doula.
Site W, MW3
But it’s actually taking that break and I think that’s the break that is so important.
Site W, MW3
Voluntary status
Midwives made several positive comments demonstrating their respect for volunteer doulas:
I’m just amazed at the amount of time these women are prepared to give.
Site W, MW3
They do an incredible job for nothing.
Site W, MW3
They saw the benefits of voluntary status and debated the potential implications if doulas were paid:
Because otherwise you are being paid to be with somebody, it’s a lot different to volunteering to do it.
Site W, MW2
[A]nd obviously when you start paying then that gives them a right to make demands . . . so you can’t ask them for the service that the service needs, it’s much easier for them to say, well, this is what I’m prepared to offer for what I’m being paid, so it makes it a bit more mercenary.
Site Y, MW1
It was thought that payment may alter the nature of the relationship with the woman and the maternity services:
They would come under the jurisdiction of everything else, the rules and regulations and governance and we need you to do this instead if it’s busy and it wouldn’t be that supporting role any more.
Site W, MW2
I think being independent and impartial is a good thing.
Site Z, MW1
How does the volunteer doula role impact on midwives?
Knowing that volunteer doulas are supporting women had generally positive impacts for midwives and the midwifery team. Volunteer doulas were seen as an additional source of help that alleviated pressure on midwives, who could focus on particular responsibilities of their role:
So that midwives could do the things that they need to do but then they’ve got this extra pair of hands, . . . actually the relationship can work very well . . . doesn’t need to be prickly, if you know that they’re there and they are very much part of your team.
Site Z, MW4
Just for support for the woman in labour . . . [the partner] he couldn’t handle the stress of seeing her in pain but the doula was rubbing her back. But it gave me the chance to write my notes.
Site Y, MW3
It’s doing that link with the midwife, so that the midwife might go in weekly, but the doula is going in, I mean it’s taking, it’s not calling the support workers, left right and centre so it frees up the general community.
Site W, MW3
While midwives acknowledged the potential for doulas being a source of help, this was a source of some sadness for midwives, who were still keen to provide the traditional supportive elements of their role, rather than seeing them provided by another worker. The voluntary nature of doula support was considered to mitigate those concerns, to a limited extent:
The doula is actually doing the job that we would love to be doing.
Site Y, MW1
Some part of the midwifery establishment could feel threatened . . . we are already having to let go a lot of what we think should be in our remit and if we’re seeing people actually being employed to do those things that we consider we should be doing then that may intensify the feeling. Because if it’s a voluntary service it may help us not to be as upset about it as we would if they were employed, and it would make sense.
Site Z, MW7
Participants identified similarities with the introduction of maternity care assistants and identified the potential for midwifery to become a more medicalised and less holistic role:
When the MCAs, maternity care assistant came in, there was a large opposition to them, but now they’re here we can’t do without them . . . and then it’s the same for [doulas]. They’re going to be there doing the supporting, doing the one to one, and you’re going the medicalised way, so you’re just doing the fetal heart, the monitoring.
Site Z, MW1
In the context of looking after several labouring women and one woman supported by doula . . . I would probably end up being more of a functional midwife than an entire holistic midwife.
Site Y, MW3
Doula as route into midwifery
Focus group participants were aware that some midwives entered training after experience as a volunteer doula. This was generally considered a benefit to the individual and for recruitment to pre-registration education but tempered by caution for one participant:
It gives them some highlights and possibly lowlights of what the profession is about.
Site W, MW2
A true, true absolute reflection of what midwifery involves.
Site A, MW2
If a doula went into it and loved what she did and then went up to be a midwife she might be a bit disappointed because I think she’d find out that often she’d lose the thing that brought her into it all.
Site Y, MW1
Doulas as a service fix
In addition to fulfilling the requirements of their role, it emerged from examples that volunteer doulas seemed to be filling a gap in NHS services. In describing postnatal support to a woman with severe postnatal depression, the doula’s contribution was viewed very positively as helping the midwife:
So I would go in part way through the week and she would do the other half of the week, so that we were actually able to double up with it. So it actually helps the midwives in that sense, particularly if you are able to liaise with them.
Site W, MW3
Midwives suggested that volunteer doulas could be drawn in to trying to meet urgent service needs:
[Referral] sometimes, if it’s a crisis thing . . . it’s just crisis management, that’s what a lot of us do a lot of the time, and I don’t think that should be the doula.
Site A, MW4
Similarly, where an ideal system of care was not feasible, the provision of a doula service was a positive alternative:
It’s really, it’s a sort of step down from caseloading . . . in an ideal world we would have caseloading midwifery for everybody . . . so adding a doula as a constant throughout is somebody to trust.
Site Y, MW1
Profile of doula service
Several participants had never worked with and did not know much about volunteer doulas services in their local trust. This is undoubtedly caused by a range of factors including the size of the trusts, the large geographical areas served and the development of specialist teams of midwives in some trusts, who may provide care to particular groups of women. In some trusts, not all midwives were aware of which women could be referred for doula support. Participation in the focus group prompted participants in more than one site to consider women on their caseload who might benefit from doula support:
I didn’t know that they were available in the antenatal period.
Site Z, MW9
Now I’ve come, I’ve already identified two women at least that would benefit from it.
Site Y, MW3
In all sites, some participants could not easily recall when they last received updates from the doula service. This was the case across all sites, regardless of proximity to the NHS:
I do remember one about 2 years ago, where . . . somebody from the doula service came out and gave like a brief description of what they were doing . . . but generally they don’t attend on a regular basis.
Site W, MW4
We’ve all got contact numbers and we all know how to do a referral, but there’s nothing much coming back, we don’t get much feedback.
Site A, MW4
There’s about [n] women that have been attached to doulas since it started, to the [doula] project but I didn’t think we are necessarily seeing that in the labouring [women] . . . I would very much like to see it more visible, . . . it needs to be expanded and for them to maybe follow more women all the way through.
Site Z, MW4
One impact of a low or fluctuating doula service profile among midwives is that it will inevitably limit understanding of how the service operates. One issue that concerned midwives related to the perceived restricted availability of the volunteer doula service. This concern was voiced in terms that are often considered negative and that reflect inequities in service provision:
Well it’s a bit of a postcode lottery as well, it is only available to women who live in [x] geographical areas.
Site A, MW6
Because initially they only covered certain postcodes when they tried to get the service out . . . and they covered certain pockets and very few.
Site Y, MW4
Heads of midwifery
Telephone interviews were carried out with heads of midwifery (HoMs) in the five trusts providing maternity care for women offered volunteer doula support. Interviews were digitally recorded, transcribed verbatim and subjected to content analysis to identify themes. Interview duration varied between 35 and 50 minutes. To maintain anonymity of participants in unique roles, all quotes are attributed only to a head of midwifery and the site identifier omitted. All five heads of midwifery who participated in the interviews contributed quotes in the following section.
Overall experience
All HoMs reported positive experiences of volunteer doulas. This was particularly noticeable in the context that all commented on the negative perceptions of paid-for doulas that women had employed independently. These negative experiences were voiced spontaneously and often reiterated during the interview. Positive experiences of volunteer doulas were summarised as:
It’s quite simplistic really for me, kind of, what’s not to like?
HoM
No significant differences emerged between HoMs according to either the length of time for which the doula service had been running or the doula service’s source of funding.
Views of the volunteer doula role
Heads of midwifery were generally of the view that the volunteer doula service was there to support vulnerable and isolated women including those with language barriers that impeded their access to services. Their role included support, signposting and linking to other services, including advocacy and improving the quality of women’s experience.
The objectives for the role were achieved by developing a relationship with the woman where the doula was a familiar figure providing continuity through the maternity episode. Doulas were perceived as an additional route for support, providing the continuity that midwifery could no longer provide and were seen as occupying a middle ground between the woman’s family and health-care professionals:
To have that familiar face – someone that you’ve become close with, that’s been through this pregnancy with you, when you’re coming into a strange environment, you can trust . . . in today’s NHS climate, we unfortunately can’t offer that as midwives now. Not as much as we could.
HoM
They feel they have an independent person that is on their side . . . you’ve got your midwifery . . . And you’ve got whatever birthing partners from a family perspective . . . but the doula will fit between the two . . . So, it’s that sort of middle knowledge.
HoM
Opinions varied about whether or not there was one particular component of the maternity episode when doula support was especially important for women. Three HoMs felt it was important throughout, one suggested that intrapartum support was most important and one suggested support during pregnancy. The rationale for the focus on labour related to facilitating normal approaches to labour and birth but also the need to fill a gap in the language support available to women throughout labour and at all times of the day and night:
The original plan was around the intrapartum part . . . where we have a large group of women with language as a problem and we were unable to support that as well within the service over 24 hours, certainly on an individual basis for a whole period of labour.
HoM
It is probably quite important in all parts of the care . . . anecdotally the input has concentrated on the antenatal and postnatal periods . . . It’s the icing on the cake if they are there for the birth.
HoM
I think it’s more important antenatally. The more you can prepare a woman emotionally and healthwise, then the better, probably, her birth experience is going to be.
HoM
Heads of midwifery were generally of the view that appropriate women were being targeted to receive volunteer doula support. It was acknowledged that some women had particularly complex needs and that the training and the clearly defined boundaries of the role enabled doulas to support such women:
Some of the women that our volunteer doulas are targeting are pretty complex . . . if you’ve got a really complex woman you are going to have to do a little bit of work with the doula beforehand to kind of outline some of the issues.
HoM
There was considerable admiration for doulas’ significant commitment and the fact that this was provided on a voluntary basis. The voluntary status was seen as maintaining their independence in a way that would be compromised if doulas were a part of the maternity services. The importance of reimbursement of ‘out of pocket’ expenditure was agreed and the possibility of notional payments was not excluded:
I think they’re amazing women to do this . . . to give up their time for no payment whatsoever.
HoM
Integration
Heads of midwifery reflected on the future integration of doulas within or alongside their services. The vision for this varied. Some perceived a potential strategic fit for some degree of integration, while others felt strongly that independence should not be compromised:
It’s like looking at the team . . . in the team you’ve got a midwife, a maternity support worker and you have a doula, a volunteer worker, to link within that community to help us to underpin some of the barriers to early access and getting out key messages.
HoM
I wouldn’t want them to be an arm of the maternity services . . . the uniqueness of that independence is a big part of being able to support the women.
HoM
Improvements to doula service
Heads of midwifery were asked for their suggestions for improvements to the doula service. They identified the importance of a professional approach to managing the service, ensuring that women knew about the service and of achieving the appropriate flow of women referred. The importance of training was a recurrent theme in ensuring the service worked well, together with clarity about role boundaries. Midwives’ contributions to the training of doulas varied between trusts, with input into initial training identified fairly consistently and considered important. In some sites this included providing new doulas with a tour of the maternity unit. Where maternity services had been particularly involved in training, the time-consuming nature of that was identified:
It’s so important that ‘doularism’ is run properly and is regulated in some way . . . we’ve had some terrible, terrible experiences from the private doula system . . . this project has kind of restored people’s faith in the whole principle of having doulas for supporting women in their experiences.
HoM
It’s a limited service that you are implementing so it’s important to make sure that you think that through very carefully otherwise you might be inundated with the problem of having too many people referred and then women end up being disappointed at the time of their labour.
HoM
Tensions between midwifery and doulas at the service and individual levels
Few tensions were reported between volunteer doulas and midwifery services. This was considered to be thanks to clarity around roles and boundaries from the outset and an appropriate training programme.
We were very careful prior to the implementation of the project that there were clear boundaries . . . and that people really understood each other’s role . . . I think our preparation was good.
HoM
So as midwives, it’s for us to be able to, in a collaborative way, set down guidelines and standards of what the role of the doula is and what the role of the midwife is. So they’re in a supportive role.
HoM
A range of Mechanisms supported ongoing collaborative working between maternity and doula services that varied between sites. Examples included offering doula services a number of free places on study days and providing information about the doula service in maternity settings.
Linkages between services were usually characterised as informal rather than as pre-scheduled meetings. These meetings sometimes occurred through pre-existing Mechanisms such as maternity services liaison committees or midwives in specialist senior roles.
Impacts on midwives and midwifery working
Heads of midwifery were asked for their perceptions of the impacts of volunteer doula support on midwives’ work and working conditions. A further question explored impacts on the allocation of midwives to labouring women. HoMs considered that the availability of volunteer doulas was generally positive for midwives. This occurred through, for example, women being less anxious and having more positive experiences. In the context of the increasing pressures on midwifery services, doulas were perceived to provide the emotional support, previously the province of midwives, and also enabled the midwife to focus on the clinical element of their role:
If you spend your 20-minute appointment trying to sort out someone’s housing benefits, you know, you’re not addressing her needs pregnancy-wise.
HoM
If a woman feels more supported and therefore their anxieties are reduced, then obviously that makes life easier, and the care pathways more pleasant.
HoM
Overall, HoMs felt that the presence of a volunteer doula would have very little influence on the allocation of midwives to labouring women, although the potential for subtle impacts on the dynamic was acknowledged:
I think the midwives see it as an enhancement and a benefit, but not a substitute.
HoM
It probably does in a fairly subtle kind of way; I think certainly it will put the midwife on alert a little bit . . . There’s somebody there who is kind of observing your care . . . and I think it can make them behave slightly differently.
HoM
In several sites, early episodes of tension had been resolved when clarity about the respective roles was achieved.
Commissioning/funding
Doula services were supported by funding from different sources and were located in a number of host agencies. This, together with the recent changes to commissioning of maternity services, precluded firm opinions about whether or not there may be future impacts on the commissioning of maternity services in the context of doula services operating in their area. Views differed between the potential for commissioning as part of the maternity services and concerns about the impact of such an approach:
I think that if it was available to be commissioned, then we would certainly be interested in that as a service.
HoM
We certainly haven’t had any discussions with the commissioners about long-term plans or possibility of commissioning a doula service . . . They are certainly quite sympathetic to the ideas and the doula project has been discussed at the maternity network.
HoM
I would be quite anxious if the commissioners started talking too much in terms of the extent of volunteers in the services . . . You know the two should be separate in my view.
HoM
Recommendations to other heads of midwifery
Heads of midwifery were asked what recommendations they would offer their counterparts in areas considering establishing volunteer doula services. Early engagement to ensure that training was appropriate and boundaries were understood and to establish lines of communication between the two services was always mentioned. Additional suggestions included the potential support that could be achieved by linking volunteer doula services into a Trust’s wider volunteer programme.
Get in there early with them – have some part in the training as we did . . . have a very clear sort of line of communication back to the service.
HoM
Get the education and training right to link in with the trust volunteer programme. To ensure that there was professional involvement. That the midwives were given clear direction in terms of the doula role and reassurance.
HoM
Chapter 4 Findings: health and psychosocial impacts for women
Women’s data sources
The findings reported in this section are informed by several data sources: questionnaires, focus groups and individual interviews.
Sample characteristics
Sample characteristics were available only for those women who had completed questionnaires. Of the 13 women who took part in focus groups and interviews, 11 had also completed questionnaires. Quotations are accompanied by a participant identifier where the prefix denotes the data source (F = focus group or individual interview; Q = questionnaire) and the suffix denotes the site code (A = original site; W–Z = roll-out sites).
Eighty-four per cent of women who had been introduced to the service were sent the questionnaire or had their details passed on to an interpreter or member of the research team. The main reason for not contacting women was that the service had never had direct contact with the individual. The main reason for not sending the questionnaire to women who were eligible for the research was failing to make contact by telephone with women who required an interpreter. A summary of the distribution is shown in Tables 9–11, separately for women who received support from the service and those who did not. All details are available in Appendix 9 to illustrate the logistical complexities involved.
| Site | Women supported by the service | Number sent questionnaires or approached by interpreter/researcher | Questionnaires completed (any method) | % of those approached who responded |
|---|---|---|---|---|
| A | 446 | 417 | 91 | 21.8 |
| W | 51 | 50 | 14 | 28.0 |
| X | 29 | 26 | 9 | 34.6 |
| Y | 75 | 68 | 14 | 20.6 |
| Z | 26 | 17 | 9 | 52.9 |
| Total | 627 | 578 | 137a | 23.7 |
| Site | Women not supported by the service | Number sent questionnaires or approached by interpreter/researcher | Questionnaires completed (any method) | % of those approached who responded |
|---|---|---|---|---|
| A | 107 | 45 | 10 | 22.2 |
| W | 29 | 27 | 7 | 25.9 |
| X | 17 | 7 | 3 | 42.9 |
| Y | 48 | 43 | 5 | 11.6 |
| Z | 17 | 9 | 5 | 55.6 |
| Total | 218 | 131 | 30 | 22.9 |
| Site | Women introduced to the service | Number sent questionnaires or approached by interpreter/researcher (as % of women introduced to service) | Questionnaires completed (any method) | % of those approached who responded |
|---|---|---|---|---|
| A | 553 | 462 (83.5) | 101 | 21.9 |
| W | 80 | 77 (96.3) | 21 | 27.3 |
| X | 46 | 33 (71.7) | 12 | 36.4 |
| Y | 123 | 111 (90.2) | 19 | 17.1 |
| Z | 43 | 26 (60.5) | 14 | 53.8 |
| Total | 845 | 709 (83.9) | 167a | 23.6 |
The overall response rate for women’s questionnaires was 23.6% of those who were sent a questionnaire or had their details shared with interpreters or the research team. The response rate for women who had received support (23.7%) was not significantly different from the rate for those who had not (22.9%). Response rates varied significantly between sites (A, 21.9%; W, 27.3%; X, 36.4%; Y, 17.1%; Z, 53.8%). However, as will be seen from Table 9, relatively good response rates were sometimes achieved when only a reduced subset of those potentially available was contacted, notably at site Z.
One hundred and sixty-six valid questionnaires were received from women who had been introduced to the doula service; the majority of them (88.0%) were self-completed. Uptake of assisted completion was lower than expected. There was an anecdotal suggestion that some of the ‘self-completed’ questionnaires were completed with the assistance of a relative, friend or support worker because of language difficulties. As shown in Table 12, 60.2% of questionnaires came from site A. Between-site analyses were limited by sample sizes, with two sites having only nine questionnaires completed by women who had been supported and two sites having 14. Women who had not used the service represented a greater proportion of respondents at the roll-out sites (between 25% and 36%) than at the original site (10%).
| Site | Completion modality | Questionnaire type (used/did not use the service) | Total n (%) | |
|---|---|---|---|---|
| Used n (%) | Did not use n (%) | |||
| A | Self-completion | 83 | 9 | 92 |
| Assisted by interpreter | 7 | 1 | 8 | |
| Total | 90 (90.0) | 10 (10.0) | 100 (100.0) | |
| W | Self-completion | 13 | 7 | 20 |
| Assisted by interpreter | 1 | 0 | 1 | |
| Total | 14 (66.7) | 7 (33.3) | 21 (100.0) | |
| X | Self-completion | 8 | 2 | 10 |
| Assisted by interpreter | 1 | 1 | 2 | |
| Total | 9 (75.0) | 3 (25.0) | 12 (100.0) | |
| Y | Self-completion | 14 | 5 | 19 |
| Assisted by interpreter | 0 | 0 | 0 | |
| Total | 14 (73.7) | 5 (26.3) | 19 (100.0) | |
| Z | Self-completion | 1 | 4 | 5 |
| Assisted by researcher | 2 | 0 | 2 | |
| Assisted by interpreter | 6 | 1 | 7 | |
| Total | 9 (64.3) | 5 (35.7) | 14 (100.0) | |
| Total | Self-completion | 119 | 27 | 146 |
| Assisted by researcher | 2 | 0 | 2 | |
| Assisted by interpreter | 15 | 3 | 18 | |
| Total | 136 (81.9) | 30 (18.1) | 166 (100.0) | |
The sample characteristics are presented in Appendix 10.
Age at time of questionnaire completion ranged from 16 to 45 years [mean 30.6 years, standard deviation (SD) 6.4 years]. Age at the time of being introduced to the doula service ranged from 15 to 44 years (mean 28.3 years, SD 6.3 years). Only 40.4% of women were giving birth for the first time (A, 33.7%, W, 52.6%, X, 45.5%; Y, 57.9%; Z, 33.3%; differences between sites not significant).
Half of the women identified their ethnicity as ‘white’ (n = 85, 51.8%); 33 were ‘Asian’ or ‘British Asian’, 30 were ‘black’ or ‘black British’, one was ‘mixed’, 15 were ‘other’ and two were not reported. Approximately half of the women were born in the UK, with a further 33 countries of birth represented across the remainder. Almost one-third of women (31.3%) had been in the UK less than 5 years at the time of introduction to the doula service. English (n = 91) was the most common of the 29 listed main languages, followed by Arabic (11), Urdu (11), Bengali (6), French (6), Igbo (4), Kurdish (4), Mandarin (3), Russian (3), Tamil (3) and Tigrinya (3).
In terms of living arrangements, 53.7% of the women reported living with a partner or husband at the time of the pregnancy and fewer (50.0%) reported having a supportive partner or husband. Almost one in five women (18.8%) reported living alone and 15.5% reported having no supportive friends or family at the time of the pregnancy, including 10 of the 28 who lived alone. Two women lived in foster care, two women lived in supported housing and three lived in temporary accommodation (hostels or ‘bed and breakfast’). Based on the services with which participants were involved at the time of being introduced, almost one-third of women (31.9%) were classified as having ‘socially complex lives’ (e.g. social services involvement, domestic abuse, housing difficulties, asylum seeker or refugee status, teenage pregnancy, mental health difficulties). 9
Age of leaving full-time education was categorised as less than 16 years (n = 17), 16 years (n = 45), 17–19 years (n = 44) or 20 years or more (n = 39). The majority of those leaving full-time education aged 20 years or more were born outside the UK (29 of 39).
The extent to which the questionnaire sample is representative of women introduced to the doula service
Site A questionnaire data were broadly comparable to the Goodwin database data for ethnicity but the questionnaires under-represented primiparous women (33.7% vs. 49.1%). Consistent with this, the mean age at introduction to the doula service was higher in the site A questionnaire sample (mean 28.1 years, SD 6.0 years; n = 95) than in the database (mean 26.7 years, SD 6.4 years; n = 595), even allowing for the time elapsed.
Experiences of the doula service
Year of introduction
Year of introduction to the doula service ranged from 2006 to 2013 (Figure 20) with the majority between 2010 and 2012 (used, 107 of 131; did not use, 26 of 29). Introductions prior to 2010 were only at the original site (used, 23; did not use, 2), reflecting the histories of the services.
FIGURE 20.
What year were you introduced to the service?

Finding out about the service and getting in touch with the service
Women had found out about the service through a diverse range of sources and commonly through more than one route; thus, where someone had contacted the service on the woman’s behalf it was not always possible to determine the source of referral.
The most common way of finding out about the doula service was being told about it by a midwife (total sample: 76 of 159; 47.8%). This was particularly pronounced at site W (15 of 21; 71.4%), where the doula service is based within the NHS maternity service. At the only site where midwifery was not the most common route (site Y), finding out about the service predominantly occurred through doula service outreach or contact with the host organisation’s affiliated services (e.g. antenatal classes: 7 of 18; 38.9%). Being told by a family member or friend was the second most common across sites (26 of 159) and comprised approximately half of women who used the service at sites X and Z (in both of these sites the Mechanism ‘word of mouth’ was identified as important in the early data collection with key informants). Only one woman reported having heard about the service via local media (newspaper/radio) and she had also seen a leaflet. Key informant data identified this route for promotion but particularly in the early stages and for recruiting doulas, yet this does not appear to have been an effective Mechanism for obtaining referrals.
Characteristics of doula support and doula qualities that women valued and experienced
Women were asked to rate several characteristics of doula support and several doula qualities according to what they had wanted and what they had experienced. It was clear from the qualitative data that what women wanted and valued most from the doula support varied considerably: it might be about pregnancy information and advice; about having a (knowledgeable) birth companion; about emotional support for someone who was lonely, frightened or lacking confidence; about breastfeeding support; or about navigating an unfamiliar health-care system. Some women wanted just one or two aspects whereas others valued the combination: ‘everything!’ (Q446A). Nonetheless, the majority of qualities were endorsed as both being important and having been provided, as shown in Figures 21–24.
FIGURE 21.
When you were wanting a doula, how important were each of the following?
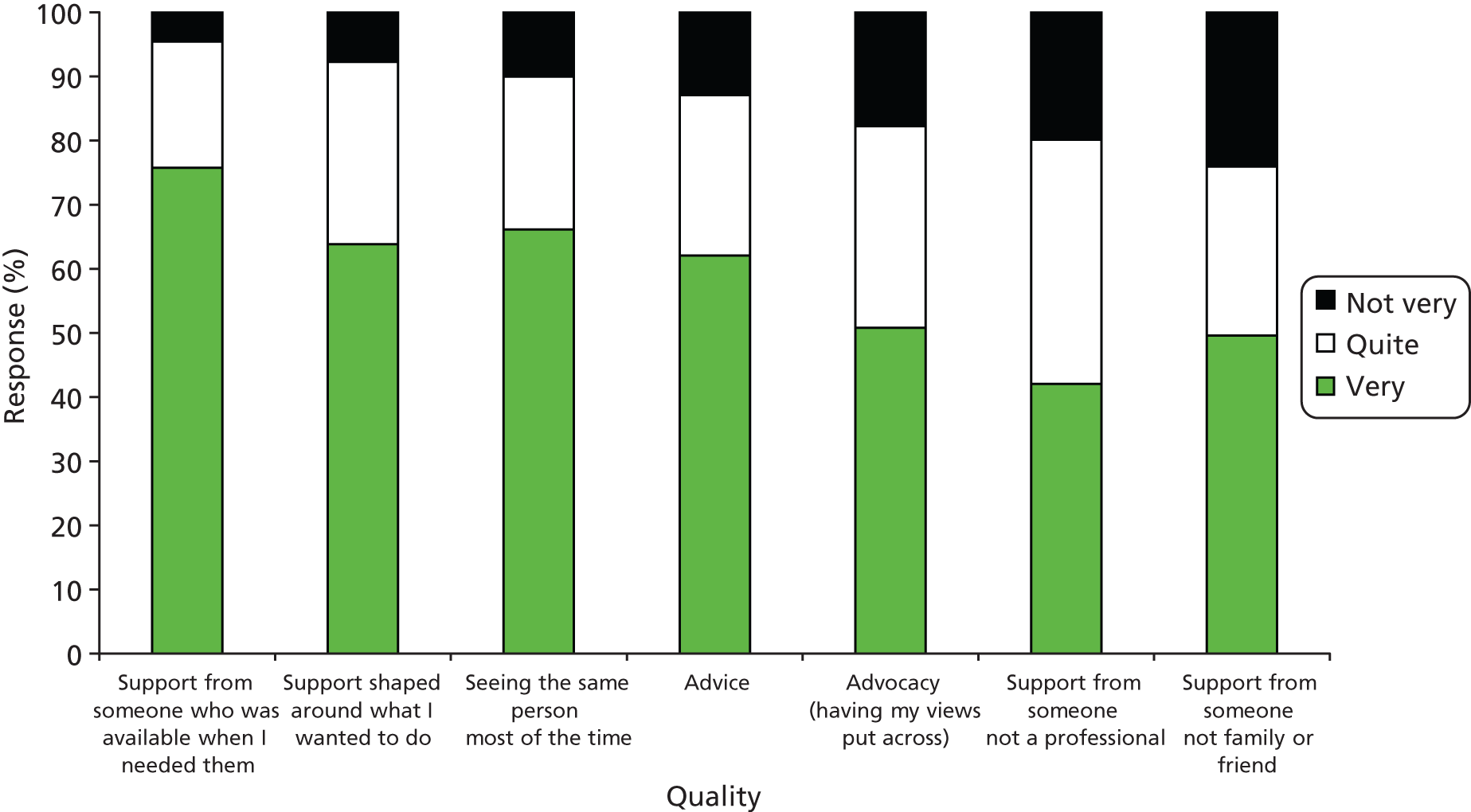
FIGURE 22.
To what extent do you feel that you got each of the following?
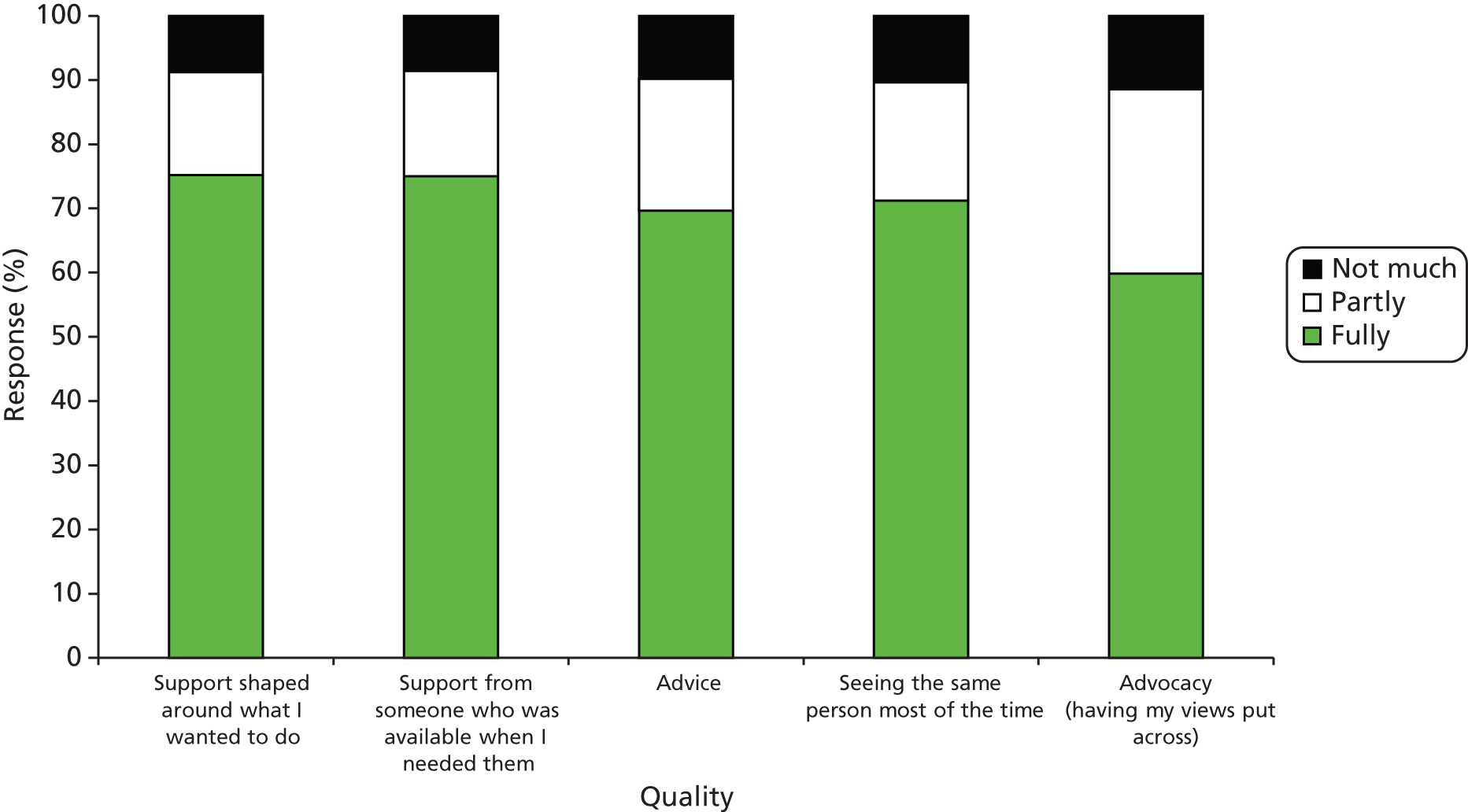
FIGURE 23.
How important was it that your doula should have each of these qualities?
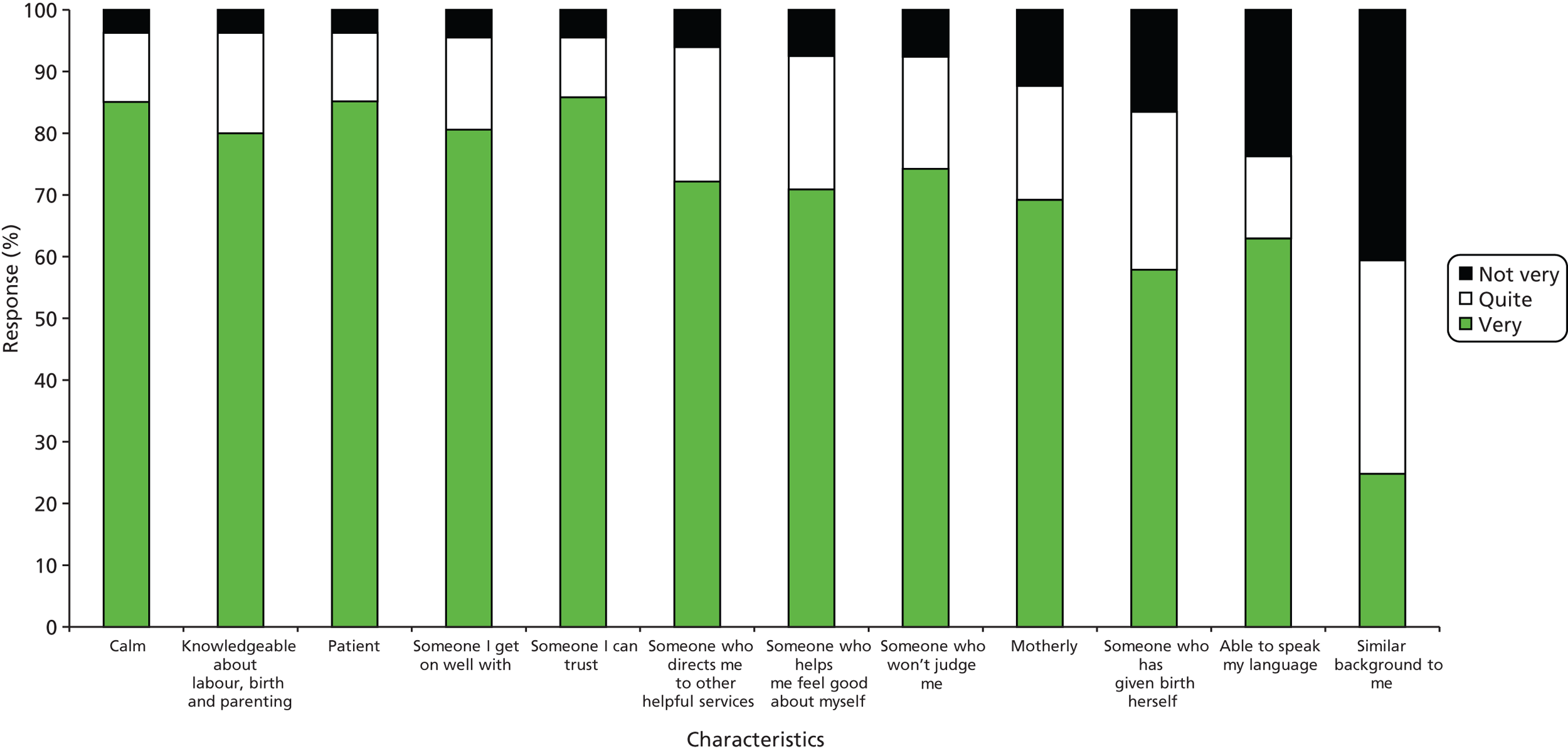
FIGURE 24.
To what extent did your doula have each of these qualities?

A few women reported that they did not receive continuity (n = 13), support shaped around what they wanted to do (n = 10) or support when they needed it (n = 6), and these women usually responded similarly across items. The listed doula qualities of ‘calm’, ‘patient’, ‘someone I can trust’, ‘someone I get on well with’ and ‘knowledgeable’ were considered important by the vast majority of women. Least important were ‘similar background to me’, ‘able to speak my language’ and ‘someone who has given birth herself’; the focus groups revealed how such factors could be fundamental to women’s experience.
Description of the doula intervention
Defining support
Early in the questionnaire, women were asked to identify whether or not they had received support for the following: during pregnancy (antenatal), labour/birth (intrapartum) and after the birth (postnatal). There were some discrepancies between these responses and subsequent endorsement of various support behaviours that were listed for each stage. Of 22 reporting no antenatal support, nine selected antenatal support behaviours, including four women who showed a similar discrepancy concerning postnatal support. Of 53 reporting no postnatal support, 32 selected postnatal support behaviours. There was some suggestion of having misunderstood the initial questions; English was a first language for one of nine supported during pregnancy and 14 of 32 supported after the birth. There was also a suggestion that discrepancies may reflect the woman not having felt supported during that period, with one woman writing ‘only had 2 visits’; this will be discussed further in (Dis)satisfaction with the service, Did the service help you in the way you hoped? of this chapter.
Stages supported/combinations of support
The distribution of combinations of support is shown in Appendix 11. Receiving doula support in all three stages (antenatal, intrapartum and postnatal support) was the most common combination, reported by 47.8% of respondents. All of the women who received postnatal support only (n = 9) were introduced to the service after the birth; the majority of these (eight of nine) were supported at site A. Of the 127 women who were introduced to the service prior to the birth, 75 (59.0%) had their birth attended by a doula; however, this varied significantly by site (A, 58.5%; W, 78.6%; X, 88.9%; Y, 42.9%; Z, 25.0%).
Late matches, operationalised as having intrapartum support without antenatal support, identified 11 women based on the initial support questions and six women based on support behaviours, three of whom were common to both. The 11 women came from site A (n = 5), site W (n = 5) and site X (n = 1), whereas the six came from site A (n = 4) and site X (n = 2). Women matched later were predominantly born outside the UK and, had they not had doula support, would have been birthing alone. Information on the combination of stages supported by site is presented in Appendix 12.
The most important stage
Both women and doulas were asked their views on the most important stage to have doula support (before the birth, during labour/birth, after the birth). Women were asked ‘If you could only have had support at one stage, which would it be?’ Responses are presented in Table 13.
| Most important stage for support | Frequency | % |
|---|---|---|
| Before the birth | 36 | 30.5 |
| During labour/birth | 60 | 50.8 |
| After the birth | 22 | 18.6 |
| Total | 118 | 100.0 |
Of the 128 women who completed the question, 118 selected one stage, as requested, the most common of which was labour/birth (50.8%), followed by antenatal (30.5%) and postnatal (18.6%). The remaining women selected antenatal and labour/birth (n = 4), antenatal and postnatal (n = 1), labour/birth and postnatal (n = 2) and all three stages (n = 3). Women were not asked to provide reasons; however, one woman selecting all three stages wrote:
I can’t pick it was all essential – removing any one part would make service pointless.
Woman Q457A
Of the 36 women who selected antenatal, 35 had received antenatal support; the remainder had postnatal only. Similarly, 21 of the 22 who selected postnatal had received postnatal support; the remainder had antenatal only. In contrast, 10% of the women favouring intrapartum support (6 of 60) had not received intrapartum support; this comprised one antenatal only, two postnatal only and three antenatal and postnatal only. Intrapartum support was the most commonly endorsed stage across all sites except site Z, where antenatal was most common. Of note, at site X all women selected labour/birth, including one who additionally selected antenatal.
Intensity of support
Women who had used the service and self-completed the questionnaire (n = 119) were asked the average weekly number of hours of doula support received.
Women on average reported having 2 hours’ support each week (median = 2.0 hours, interquartile range = 1.5 hours; n = 98); however, this ranged greatly between 0 and 10 hours. This was one of the items with the most missing data. There were some issues of recall (where women wrote ‘can’t remember’), which may also offer insights into the perceptions of support.
Some comments suggested that the service was individualised and needs-led rather than a prescriptive amount of time per week. However, this item was commonly the place where any discontent with the service was expressed:
My doula kept cancelling the day before so I only saw her twice. [Amount not reported]
Woman Q307A
I only saw her every 2–3 weeks for about 3 hours. [Amount not reported]
Woman Q385X
Was too late saw doula twice. [0 hours/week]
Woman Q449A
She only spoke to me on the phone. She never visited me. [0 hours/week]
Woman Q313A
Intensity of support and recipient characteristics
Key informant data (site A) had identified three contexts which might require more intensive doula support: (1) women in particularly complex social situations, (2) women who self-referred – seen as keen but less in need – and (3) women who lacked social support. However, none of these factors was found to be statistically associated with the intensity of support.
The distribution of average weekly hours by site is shown in Appendix 11. There was no significant difference between sites.
Support behaviours
Women were asked about the types of support provided during the antenatal, intrapartum and postnatal periods. Responses are shown in Figures 25–28.
FIGURE 25.
What support did the doula give you when you were pregnant?
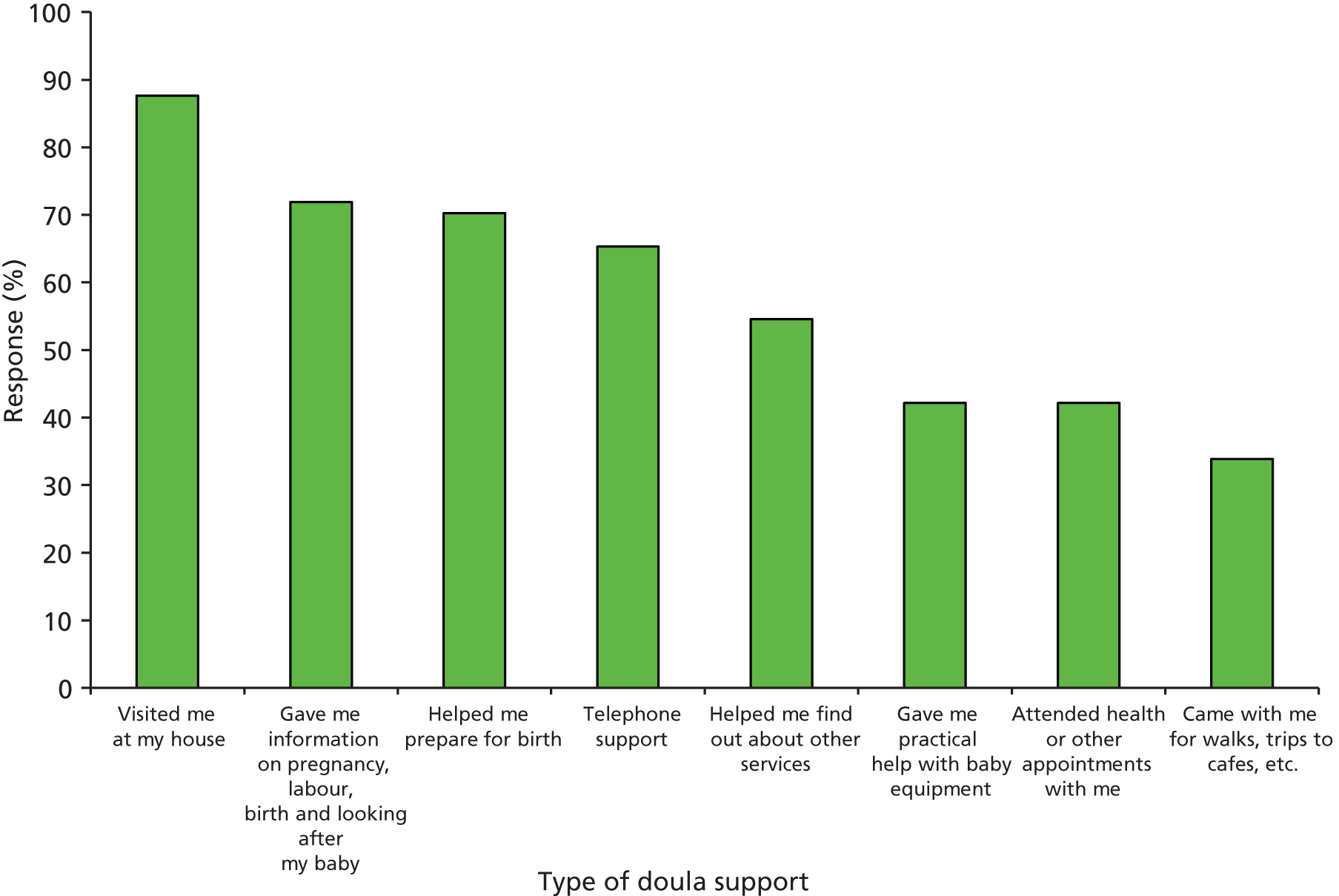
FIGURE 26.
During your labour and birth, did the doula do any of the following practical things?
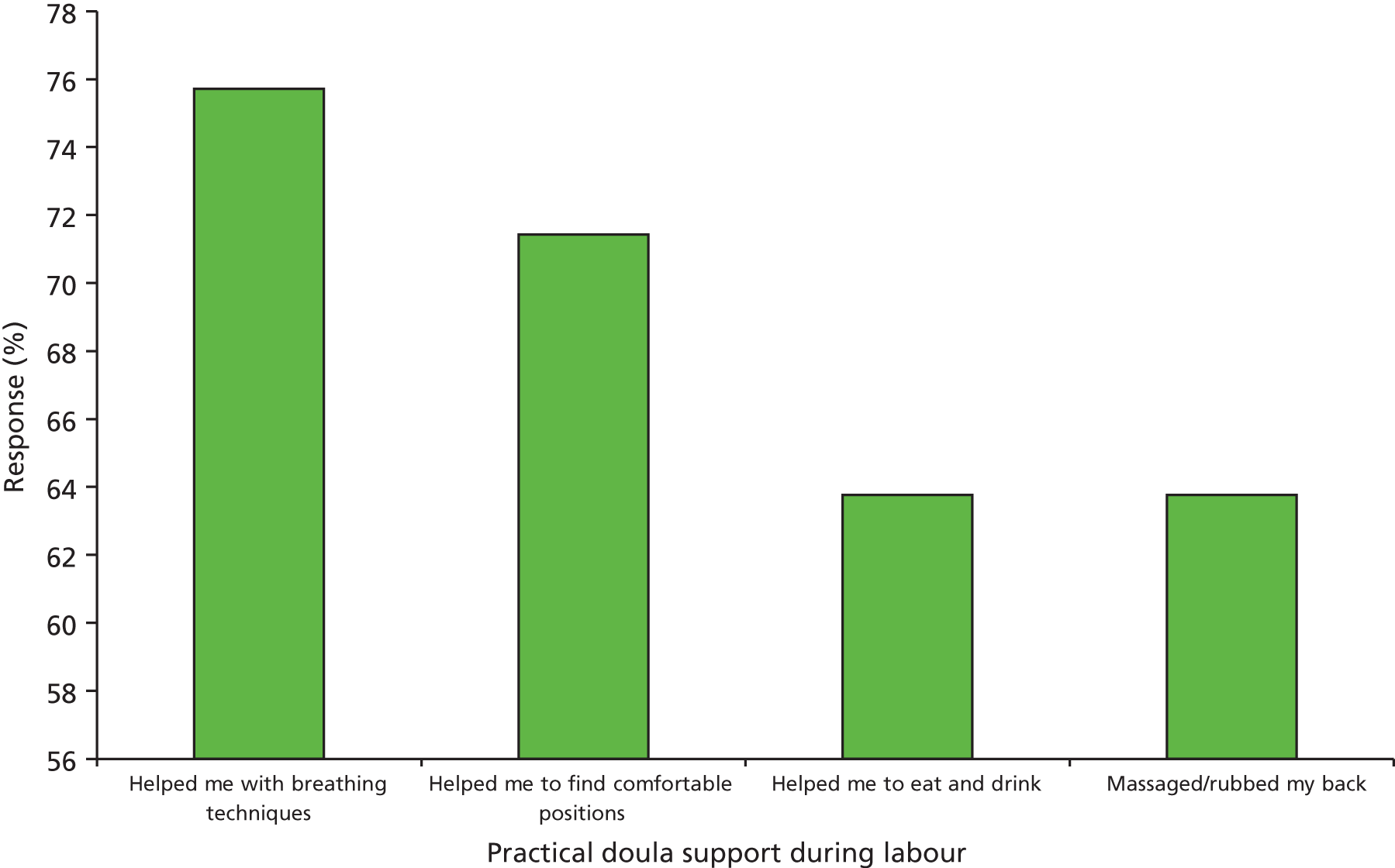
FIGURE 27.
During your labour and birth, did the doula do any of the following to support you emotionally?
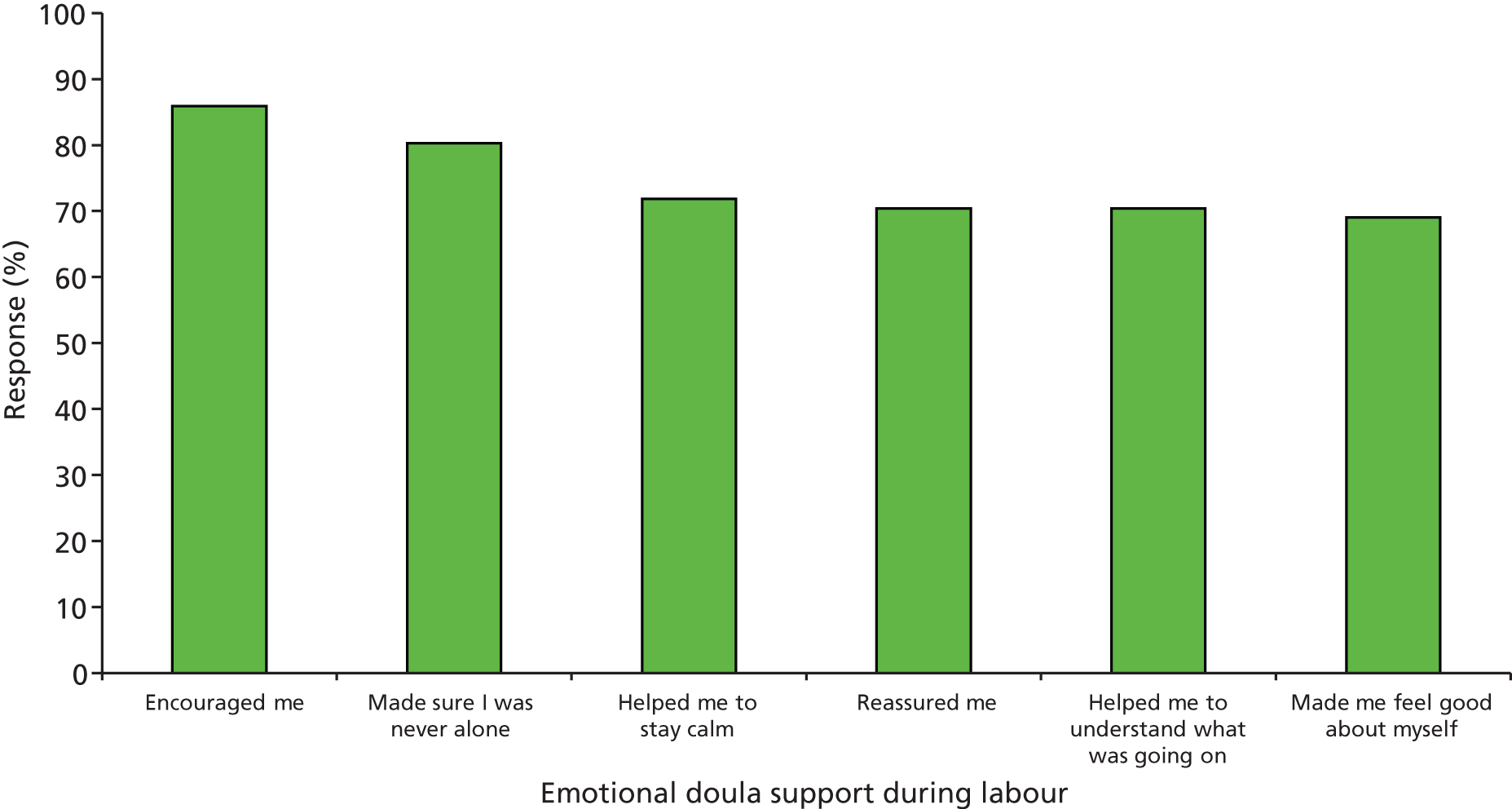
FIGURE 28.
What support did the doula give you after the birth?
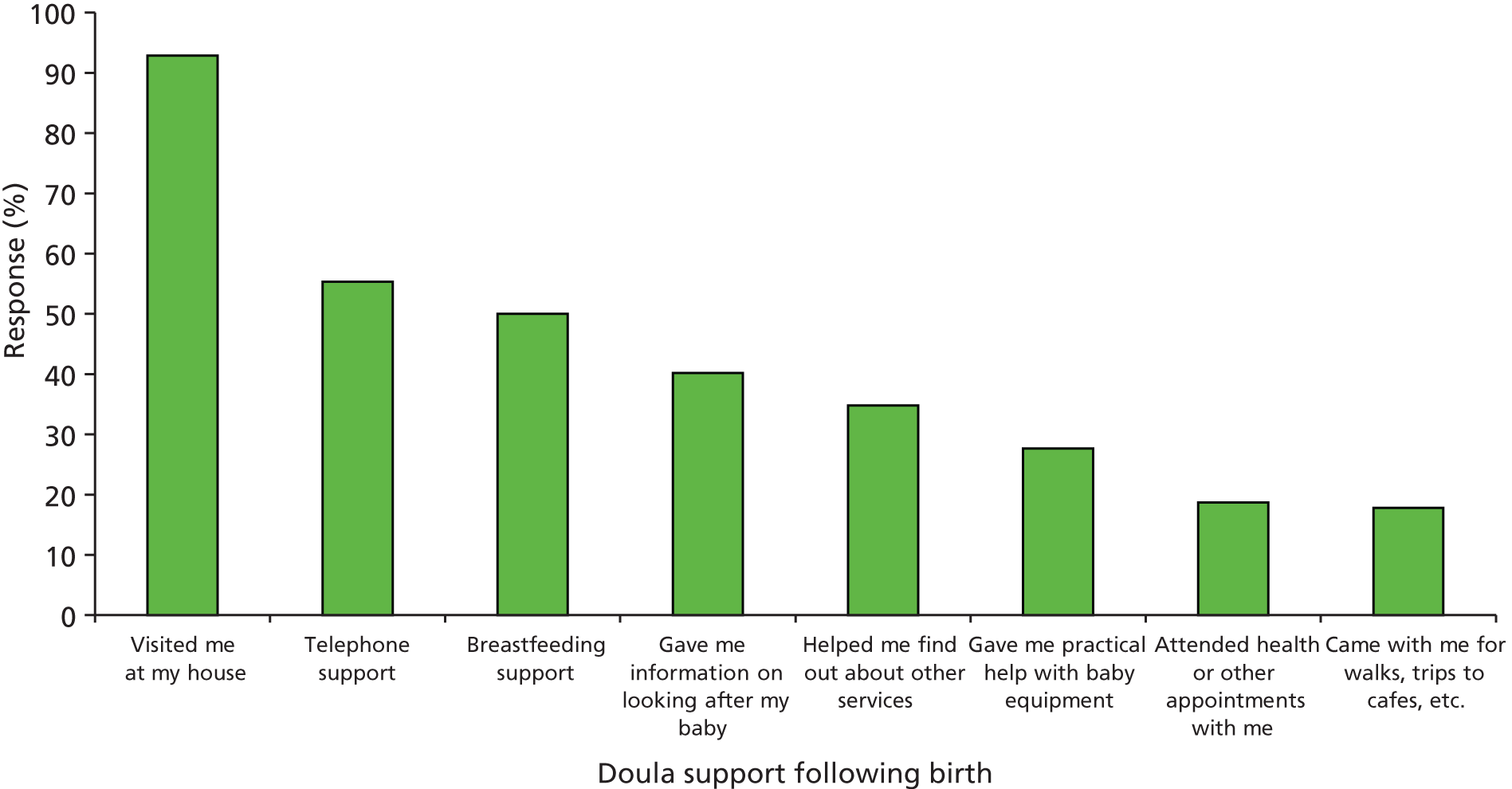
Support during pregnancy
It was striking that none of the support behaviours was endorsed by all women who were supported in that period. During pregnancy, the most common type of support was home visits (87.6%). Telephone support was reported by 65.3%. Information giving was also common (71.9%) and birth preparation was reported by 70.2% of women including 60.0% (30 of 50) of those who received antenatal support without intrapartum support. Giving information was more commonly reported by first-time mothers, but, interestingly, birth preparation did not differ by parity. This may relate to suggestions that a high proportion of the multiparous women supported had had previous bad birth experiences.
Intrapartum support
The listed practical and emotional support measures were all endorsed by the majority of women receiving intrapartum support (range: 63.8–85.9%); the most common was encouragement. In addition to the listed practical intrapartum support behaviours (see Figure 26), women listed other support measures that often spanned practical and emotional dimensions (see Figure 27):
Got a cool flannel and wiped it over my forehead because I felt too hot.
Woman Q333A
She helped to have a shower after birth and she take a photo for me and baby and daddy together.
Woman Q314A
Held my hand, kept me calm with speech.
Woman Q456A
My doula is pain killer for me.
Woman Q356Y
Talking to me, reassuring and explaining midwife speak and getting my points across.
Woman Q315A
Held my hand, was another female presence in the room.
Woman Q385X
Postnatal support
Figure 28 demonstrates that, during the postnatal period, the most common form of support was again home visits (92.9%). Attending appointments and going ‘out and about’ were only half as likely as in the antenatal period. Breastfeeding support was reported by half of the women. Other support that was described included bathing the baby (n = 4) and visiting the woman in hospital (n = 2).
The main differences in support measures across sites concerned accompanying the woman on walks and trips to cafes and introducing women to other services. Accompanying on walks and trips to cafes was most common at site A, particularly in the postnatal period, where 18 of 76 reported such support compared with none of one (W), one of six (X), 1 of 12 (Y) and neither of two (Z), although this may have reflected cultural patterns at sites W, X and Z.
Helping women to use other services
Women were asked directly about doula support in using other services. Of 83 (64.8%) who were told about a service, 22 said that their doula contacted a service on her behalf and 23 said that she accompanied them to a service, including 12 who did both. Of 45 who did not indicate that their doula had told them about a service, nine said that the doula had contacted a service on her behalf and eight said that she accompanied them to a service; none said both.
There were notable differences between sites concerning signposting. Although ‘Told me about a service’ was relatively balanced across sites (A, 55 of 86; W, 7 of 13; X, 7 of 9; Y, 11 of 14; Z, 3 of 6), ‘Contacted a service on my behalf’ was not reported by any women at site X or Z (A, 23 of 86; W, 3 of 13; Y, 5 of 14) and ‘Came with me to a service’ was more common at sites A and Y (A, 23 of 86; W, 1 of 13; X, 2 of 9; Y, 5 of 14; Z, 0 of 6).
Communication between the woman and the service and the doula
The majority of women without English as a main language communicated with the service (37 of 60) and the doula (33 of 52) without any language support. The extent to which this was a problem is unknown, as some women could speak some English or another second language. A small number of women described how, even though the doula did not speak their language, she was still able to provide valued support. One woman described how a shared cultural background helped her feel comfortable enough with her doula to disclose domestic abuse that she had not disclosed to any professional. However, another felt that the doula lacked cultural understanding:
I would like to tell you that as most women needing doulas are either asylum seekers or refugees therefore it should be really important for the doulas to be trained on different cultures and backgrounds, and interpreters should be available at all times.
Woman Q390W
How is the doula different?
Unique aspects of the doula role/what makes the doula role different?
Data collection with key informants identified several aspects of the volunteer doula role that distinguish it from other types of support. These were investigated by asking women how they think of their doula, if and how the relationship would have varied if they had met their doula sooner or later than they had, if and how the relationship was similar with the main and the back-up doula, and views on payment.
Women were asked how they thought of their doulas and were presented with a list of possibilities (Figure 29).
FIGURE 29.
How do you think of your doula?
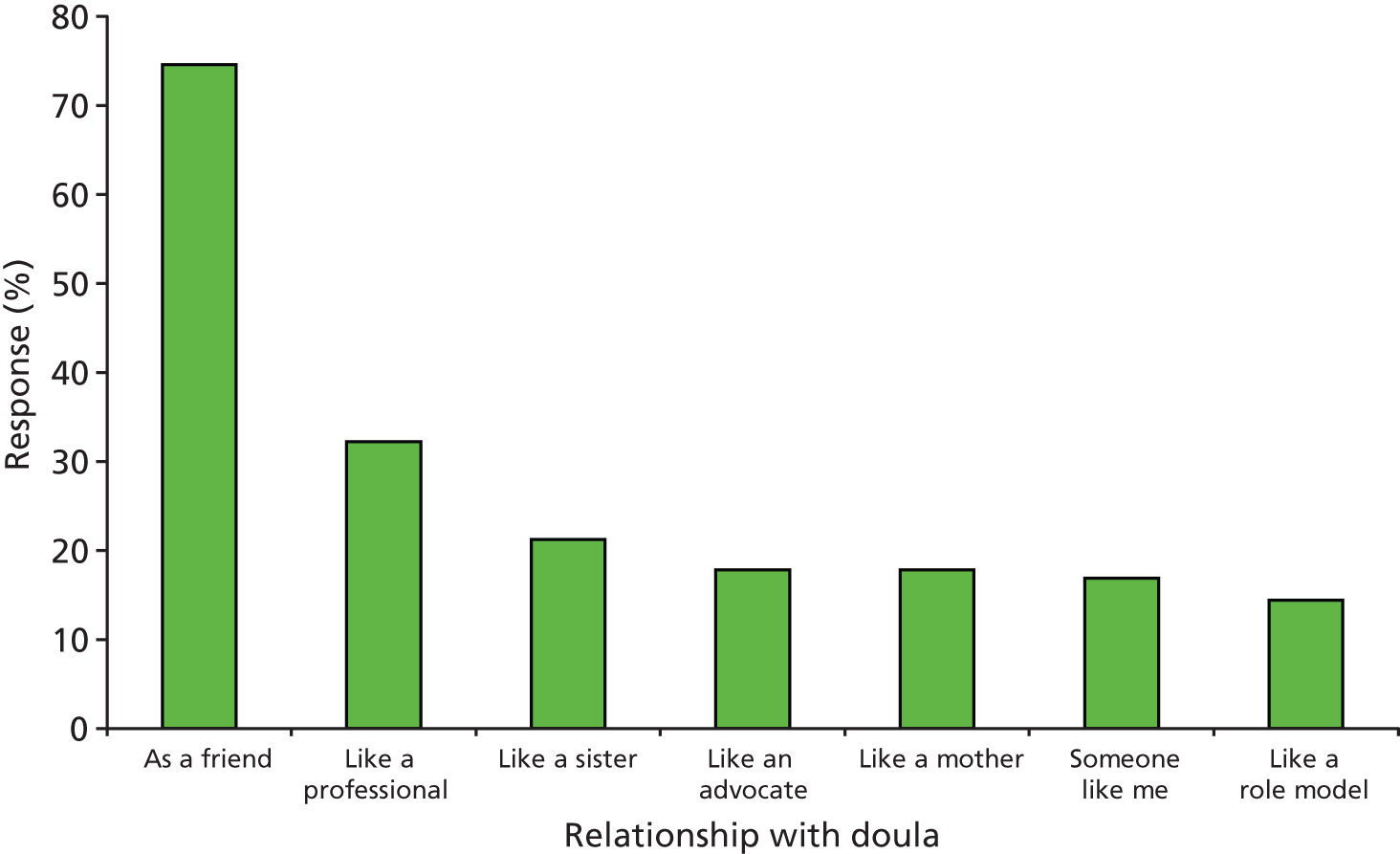
By far the most common was ‘as a friend’ (74.6%); however, discussion of the relationship’s ‘ending’ (discussed further in Impact of doulas: feelings of loss at the end of support) questioned the possibility of ‘friendship’. One woman, reflecting on the compulsory end to this relationship, characterised it sadly as ‘temporary friendship’ (F337A), a distinction echoed elsewhere.
Focus groups offered more detailed discussion of the ways in which the doula role was similar to and contrasted with support from family, partner and professionals. These discussions illustrated what women valued about the support and offered insights into the ways that it ‘worked’ for them.
Doula’s role is different from partner/family
Thirty-one per cent of women described their doula as ‘like a mother’ and/or ‘like a sister’. Of note, none of the 21 women likening the doula to a mother had a supportive mother around during their pregnancy and no-one with a supportive mother described the role in this way.
Women who had social support from a family or friend nonetheless valued the support of their doula. They pointed out how support from a doula differed from support from family or friends, who are emotionally involved in the situation and may have their own needs and agenda. In particular, family and friends would tell women what to do whereas doulas talked through options and asked what the women wanted to do. They were also better informed than family and friends about pregnancy and birth:
Your Mum, your sisters, even your husband, they are busy, everyone’s busy, and [the doulas], this is their job, and they willingly do the job, they want to help someone. And if you ask for help from your family, they are, like, forced to do that, but the [doulas] do it willingly. They were both like an angel for me.
Woman F369Z
My husband, as much as he wanted the birth that I had, he just wanted the pain to stop, but the doula, was more like, well, no, that’s not what we agreed.
Woman F337A
With your friends and family, you almost feel like you’ve got to look after them . . .
Woman F315A
[The doula is] somebody you can tell things that you can’t tell your partner about, because he’d start panicking. Whereas your doula has been there, she has done that, she has had that dodgy feeling on the boob or whatever.
Woman F337A
Doulas are different from health professionals: continuity and trust
Many women said that they had been cared for in pregnancy and postnatally by teams of midwives and health visitors and saw a different person at every appointment; the midwives at their birth were strangers. By contrast the doula provided continuity during the perinatal period. Women had time to get to know and trust their doula and to feel that they were known and understood by her; they regretted that this relationship did not exist with health professionals. Women saw doulas as a reliable and accessible source of up-to-date information. Some women were reassured to hear the same information from their doulas as from their midwives, although in many cases the doula was filling information gaps that had not been addressed by the midwives. Doulas were also contrasted with midwives in that women felt they could ask them anything, even questions that they were embarrassed to ask busy health professionals, who sometimes gave dismissive or patronising answers.
Obviously, through pregnancy, because this was my first baby, everything is completely new and, you know, you have no idea what’s going on and I had so many questions that I asked that were all silly, in my head, or embarrassing, that you wouldn’t want to ask somebody, but I think you make a relationship with [the doula] and you trust everything that they say to you and you say [it] to them . . . When you’re with your midwife . . . I think that they’ve got an agenda, things they‘ve got to do, they have to check your blood, check the baby, check this, check that and then . . . they say, is there anything else you want to ask? So that kind of [embarrassing] thing, for me, I think I won’t ask that, you know what I mean!
Woman F341Y
They also described how the doula was a person you could rely on when you needed her; this was again in contrast to midwives, who gave out their phone number but did not always answer the phone:
[The doula is] the one constant person that you get to know through it all, because I don’t know about everyone else, but I had different health visitors every time I went, different midwives every time I went, whereas the doula from when I got to know her all the way through . . . for me my doula was a stop gap between what these people should have been in the first place . . . it’s the person you tell it all once to and then sort of carries you through all the other things.
Woman F315A
I called the midwife and I wouldn’t get through and that really, really scared me and I can only imagine if other women, who are going through the same thing in a more difficult situation and the fact that I actually had a [doula] to call, to even make me feel relaxed and calm and give me that confidence, don’t worry, give me that support.
Woman F386Y
She was like a friend to me, whereas my midwife, I could only visit her when there is an appointment, or she could just examine the medical things, but an emotional support and all those things were coming from my doula.
Woman F468W
For the small proportion of women who were critical of the doula service, it was most commonly their doula’s unreliability or inability to provide continuity that was criticised: the doula had not visited or contacted them often enough, for long enough or with her full attention, or had not kept appointments. Some women were very disappointed that their doula had not turned up when expected in labour. This perceived lack of commitment was felt to undermine the very purpose of the doula’s involvement; for some women there was no meaningful emotional support, useful information or birth support:
[The doula] didn’t come regular and seemed distracted with personal matters.
Woman Q346A
The doula contacted me a few times but would have loved to have been consistent up until my labour.
Woman Q458Z
Went into labour and could not get hold of Doula and ended up with emergency C-section.
Woman Q430A
Doulas are different from health professionals: a woman-centred service
Women commented that one of the distinctive features of the doula service was that the doula focused completely on the woman and her needs with no other agenda, and had time to spend with her, unlike busy health professionals for whom you are ‘a number . . . get out, hurry up!’ (F409Y). This was true both during pregnancy and in labour, and some women described how doulas supported and comforted them in labour while the midwives focused on clinical checks. Some women explicitly perceived the doulas as filling in gaps left by overworked health professionals. Others contrasted the doulas’ non-directive information with their experience of information from health professionals. As noted above, women said they could ask the doulas anything, even things they were too shy to ask health professionals, who could make women feel like they were wasting the health professionals’ valuable time:
I think the difference is really that you have somebody who has complete time for you, it’s just that they’re there for you and they haven’t got any other pressure of things that they have to do, or go.
Woman F341Y
Having someone there to support me, who wasn’t a health professional and gave me the time I needed rather than treat me like a number.
Woman Q373Y
Midwives are so stretched [doulas] help when midwives are not present.
Woman Q427A
There are a lot of services that women are not aware of, my doula empowered me to get well informed which in turn gave me control over what I wanted, rather than someone deciding for me, which tends to happen as most health professionals take that right away.
Woman Q373Y
Doulas are different from health professionals: a flexible, personal service
The flexible and responsive nature of doula support was shown by the perception that doulas adopted multiple roles; for example, 24 of 34 women describing the doula as a professional also described her as a friend. This was summed up in a focus group:
We were like friends, she was like a sister, a friend and a mum!
Woman F366Y
Some women expressed their surprise and appreciation for the level of commitment their doulas showed, attending extremely long labours or making themselves available whenever the woman needed them. Doulas had often gone beyond the remit of their role in the support provided: they had checked a diabetic woman’s blood sugar every hour in labour when she could not manage because of drips; helped fill in benefit forms for a woman who could not read or write; taken a woman’s clothes home from the hospital to wash them; and supervised the contact visits between a woman and her older child in care:
I was stay 3 days in labour . . . she is with me all the time, like 8 hours, 7 hours a day she is staying with me and then after when I had the baby, she stay with me as well [. . .] I was 5 days in hospital. She stay with me, she’s helping me how to feed the baby, everything she’s helping me and after that 1 month she is coming at home as well, she visit me and she show me everything about the baby, she is helping me, everything.
Woman F404W
When I was in labour and needed to go to hospital it was . . . nearly 5:00 in the morning. I called [the doula] and told her about that. She only took about 15–20 minutes reaching my home. Then she took me to the hospital and stayed there with me for almost 11–12 hours . . . She helped me and took care of me just like my mother.
Woman Q455A
[The doula said] Or any time if you need me, you’re feeling depressed, give me a call, even if it is midnight, 12 o’clock in the night, you can give me a call, I can come, we can have a chat.
Woman F468W
Another aspect of the doula service that women commented on positively was the way that the doulas followed their lead and tailored the support to what they wanted, although it varied with how proactive the doula was in arranging to meet up:
They, kind of, take control of the situation without being controlling, you know? . . . She reacted to what I asked her, she’d say, what do you want to talk about next week? Is it, you know, and then she’d find the information ready for the week after.
Woman F341Y
However, there were also some women who had been disappointed at the limitations of the doula service and would have appreciated being able to ask their doula for other support, for example to help care for older children while they were in labour if necessary. One woman described how the service was presented to her entirely in terms of boundaries:
I don’t know it was quite peculiar because I didn’t know what to expect from her and when she initially turned up she went through a whole ream of things she wasn’t allowed to do but didn’t really go into the specifics of what she could do. So it was a bit strange at first. And there was a point I nearly said I don’t want to carry on with this.
Woman F385X
Understanding the relationship
Timing of match
The CMO development had identified the timing of onset of support as a potentially important Context; specifically, the intervention may not ‘work’ where the match happens late in the antenatal period and there is not time to establish a relationship (including ‘trust’) before providing intrapartum support.
Would the relationship be different if the woman and doula met sooner/later?
One-third of women self-completing questionnaires (n = 38; 33.0%) felt that the relationship would have been different if they had met the doula sooner. The proportion was highest (46.2%) at site W, where support starts considerably later in pregnancy. Overwhelmingly, women who felt the relationship would have been different felt that the relationship would have been better, either to establish the relationship sooner or to gain the benefits of doula support earlier in pregnancy.
Some women felt they would have received something different or benefited in different ways:
Although I got on very well with my doula, it wasn’t long before I gave birth and I had opted for a C-section. I think if I had met her sooner, I would have been braver to go for a normal delivery.
Woman Q373Y
Fewer women felt that the relationship would have been different if they had met the doula later (n = 25; 22.5%). These proportions were comparable across sites A, W and Y (21.4–25.0%), compared with zero at site X. Some of the women explained that this was because they met only shortly before the birth anyway. Those who felt that it would have been different felt there would not have been the chance to develop ‘trust’ or get to know each other and there was some evidence, supporting the key informant data, that this could be particularly difficult for some women:
I would have felt less able to trust and bond with her.
Woman Q332A
I wouldn’t of got to know her and wouldn’t of been as comfortable.
Woman Q448A
Less chance to bond.
Woman Q423A
Understanding the relationship: comparing the woman’s relationship with her main doula and her back-up doula
Fifty-two women (43.7%) reported having a back-up doula; this was most common at sites W and X (A, 31 of 82; W, 9 of 13; X, 5 of 7; Y, 5 of 14; Z, 0 of 1) and among women having intrapartum support (59.4% vs. 22.0%). Frequency of contact varied. Of the 32 (64.0%) who came on joint visits, 12 did so only once. One-third (3 of 9) of those who attended the birth had not previously met the woman. Two women reported having had separate visits with the back-up doula.
Women were asked if they felt as comfortable with their back-up doula as with their main doula and to provide reasons for this. Women who were not born in the UK were significantly more likely to report feeling as comfortable with the back-up doula (18 of 23, 78.3% vs. 9 of 21, 42.9%).
One woman reported feeling as comfortable because she saw both for the same amount of time. All other responses indicated a sense of similar attributes and qualities that meant that this was viewed as the ‘same service’ (Q314A) and part of the woman’s team; for example:
Because she’s got the good qualities as the main doula.
Woman Q359A
Because they’re all friendly and nice.
Woman Q361A
Very similar & supportive.
Woman Q429A
Women who did not feel as comfortable with their back-up, including two who first met the back-up at the time of labour, usually attributed this to not having met her and this meant that there had not been the opportunity to develop a relationship. In the focus groups, most women felt that they did not have a meaningful relationship with their back-up but felt that having an unknown back-up was better than having no birth partner, consistent with the views of a woman who had experienced this. Others felt that the difference was due to the back-up’s background or personality, which was consistent with key informants’ discussion on the importance of ‘matching’:
I feel [that] my [main] doula [was] like mum.
Woman Q306A
[Back-up] was more outgoing and dominating.
Woman Q334A
She was young with no children. I didn’t feel she would be as knowledgeable at the birth. Although she was very nice.
Woman Q423A
Understanding the relationship: views on payment/doulas as volunteers
Women who had received doula support were asked their views on whether or not the ‘volunteer doulas’ should be paid under two conditions: with women still receiving a free service and with women paying for the service. Whereas 75.7% of women (84 of 111) felt that doulas should be paid if the service remained free to women, this reduced to only 25.5% of women (27 of 106) if women were required to pay for the service. There were no statistically significant differences between sites in the proportion of women advocating payment of doulas provided that the service remained free to women. In contrast, when payment of doulas required payment by women, there was a statistically significant association between site and view on payment, with the roll-out sites being more positive about this scenario than site A (A, 22%; W, 40%; X, 50%; Y, 58%).
Women expressed deep appreciation that a stranger was willing to devote so much time to them as a volunteer. On the other hand some women could feel inhibited about bothering a volunteer even when they wanted her support and it was against cultural norms for a relationship to be so completely one-sided (e.g. not being allowed to give the doula even a small gift).
I felt I could not ask for more support when needed.
Woman Q380Y
Request system to contribute to doulas because I heard they do voluntary work. It used to bug me. I felt bad she is helping me for nothing.
Woman Q369Z
Some women saw an element of reciprocity in that doulas were gaining valuable job experience or clearly enjoyed their role. One woman described how she trusted the doula more because she had refused a gift (Q305A).
Women had mixed views about whether or not doulas should be paid: many felt that they deserved to be paid because they work hard supporting women in their free time and some (particularly those who were dissatisfied with the amount of support they had) thought payment would be good as it would increase the amount of time doulas could spend with a woman. Others felt that paying doulas might change their motivation, distort the relationship or make the service more vulnerable to cuts; some noted that doulas want to be volunteers to gain valuable experience and they enjoy volunteering. There was, however, a very strong view that women should not have to pay the doulas themselves, as this would be an insuperable barrier to using the service for those who need it most, or that only women who could afford it should be asked to pay.
There were reservations about the implications if women had to pay for the doula service:
Because people wouldn’t engage in it if it cost money – like paying for somebody to be your friend.
Woman Q341Y
One woman (Q394A) mistakenly believed that ‘This is part of the NHS services and should be free’.
Impacts of doula support
Women were asked about several areas of impact, informed by key informant data collection and the literature review: birth experience, pain relief in labour, skin-to-skin contact following birth, infant feeding, smoking, diet, exercise, attending antenatal classes, meeting other mothers, use and experiences of other services, postnatal mood, relationship with partner and knowledge, confidence and skills.
Comparisons with the Picker Institute maternity survey (site A)
Some of the areas of impact were measured using questions from the Picker Institute maternity survey. This allowed us to make comparisons between women who had received the doula service and data collected in the same PCT on some additional outcomes that are not routinely collected, such as methods of pain relief and feeling involved in decision making. We were able to do this only for site A, as numbers were too small in the roll-out sites. Even in site A, analysis had to be limited to the 83 women who had used the service and self-completed the questionnaire, since the relevant questions were not included in the shorter telephone version. Because of small expected values for some response options, cells were combined so that all analyses were comparing the first response option (e.g. ‘yes, always’), with all other combined responses. Tables show data for all trusts in the final column for comparison, but analyses were carried out only with respect to the Hull PCT. Columns for Hull PCT and all trusts show percentages only, not frequencies. This is because the data made available to us had been weighted so that trusts could be standardised to age and parity distributions for the country as a whole. We applied the same weighting formulae to our own data, but it made little difference to the findings, so we have presented unweighted data for site A for clarity. Nevertheless, the parity distribution of our data was significantly different from that of the local Picker survey: only 31% of site A women in our sample were primiparous, in comparison with rates of 54.7% in the local trust and 49% nationally. Our sample may also be atypical in terms of ethnicity, although ethnicity data were not available for the Picker sample.
Involvement in decision-making
A basic tenet of the doula intervention is that it gives women the confidence to make decisions for themselves and their babies, and we had therefore hypothesised that more women would report involvement in decision-making than in the PCT as a whole. We included two questions from the Picker survey that asked directly about involvement in decision-making:
Thinking about your antenatal care, were you involved enough in decisions about your care? Thinking about your care during labour and birth, were you involved enough in decisions about your care? (p. 14)41
For the question about antenatal involvement, the site A sample was limited to those women who had received antenatal support (n = 70). For the question about intrapartum decision-making, the analysis was carried out twice: once limited to women who had a doula with them for labour and birth (n = 41) and again adding in women who had not, but who had received antenatal support (n = 75). The rationale for this was that the doula’s antenatal preparation may have had an impact on this outcome even if the doula was not present.
Table 14 shows that women at site A who had had antenatal doula support were actually significantly less satisfied with their involvement in antenatal decision-making (χ2 = 6.20, 1 df; p < 0.02). The same pattern is seen in Tables 15 and 16 for involvement in intrapartum decision-making, whether limited to those who had had intrapartum doula support (χ2 = 6.15, 1 df; p < 0.05) or including those who had had antenatal support as well (χ2 = 6.19, 1 df; p < 0.02). Thus, it appears likely that doula support does have an impact, but that impact is to make women more aware of the extent to which they might potentially be involved in decisions and perhaps to raise their expectations that they will be involved, resulting in a perception of a gap between what was and what might have been.
| Response | Site A n (%) | Hull PCTa | All trustsa |
|---|---|---|---|
| Yes, always | 41 (58.6) | 76.4% | 73.7% |
| Yes, sometimes | 19 (27.1) | 19.0% | 22.0% |
| No | 10 (14.3) | 4.7% | 4.3% |
| Base size (all respondents) | 70 | 103 | 24,622 |
| Response | Site A n (%) | Hull PCTa | All trustsa |
|---|---|---|---|
| Yes, always | 24 (58.5) | 78.8% | 71.6% |
| Yes, sometimes | 13 (31.7) | 18.7% | 22.5% |
| No | 4 (9.8) | 2.5% | 5.9% |
| Base size (all respondents) | 41 | 102 | 24,518 |
| Response | Site A n (%) | Hull PCTa | All trustsa |
|---|---|---|---|
| Yes, always | 43 (61.4) | 78.8% | 71.6% |
| Yes, sometimes | 18 (25.7) | 18.7% | 22.5% |
| No | 9 (12.9) | 2.5% | 5.9% |
| Base size (all respondents) | 70 | 102 | 24,518 |
Pain relief
Women were asked to indicate all methods of pain relief used in labour from a list that included natural methods; water or a birthing pool; transcutaneous electrical nerve stimulation (TENS) machine; gas and air; pethidine or similar injection; and epidural or other.
Comparisons were made based both on women who had had intrapartum support and women who had had either intrapartum or antenatal support. No significant differences were found except that women who had a doula with them in labour were more likely to use ‘natural methods’ (59.5% vs. 39.3%). This comparison did not reach significance when women who had had antenatal, but not intrapartum, support were included. For many forms of pain relief (e.g. use of water, TENS) cell sizes were very small. Women were also asked if they had received the pain relief that they wanted. As with decision-making, it had been hypothesised that women would have greater confidence to ask for what they wanted and resist interventions that they did not want. In fact, what we found was the same effect as for decision-making: only 52.9% of site A women said that they had received the pain relief that they wanted compared with 73.4% in the local PCT. The figures were similar for women when women who had had antenatal but not intrapartum support were included and were significant (p < 0.05) in both cases.
Skin-to-skin contact
Site A women who had doula support were much more likely to have skin-to-skin contact with their baby shortly after birth. This was significant both for those whose doula had been present (92.1% vs. 75.7%) and for those supported antenatally (86.7%).
Being left alone
The Picker survey asked: ‘Were you (and/or a partner, doula or companion) left alone by midwives or doctors at a time when it worried you?’ (p. 20)41 There were no significant differences between site A women and the PCT as a whole. Within the PCT data, a total of 21.4% had been left alone at a time when it worried them, which was the same as the combined trusts average.
Impacts on women’s emotional health and well-being
Mental health and well-being were targeted through one question concerned with postnatal mood: ‘Thinking back to the weeks after your baby was born, how did you feel?’ Nearly one in five women (19.2%) reported feeling ‘depressed or low spirited most of the time’, 38.4% felt ‘sometimes cheerful and sometimes depressed or low spirited’ and 42.4% felt ‘reasonably cheerful most of the time’.
The qualitative data highlighted the significance of doula support for mental health and well-being. Some women said explicitly that the doula helped them with feelings of depression; this was not limited to those women who had been referred because of past and current mental health difficulties:
Before I got my doula I was terrified & depressed (because of the health problems) & she helped me change my view around.
Woman Q456A
She turned all my negatives into positive and encouraged me to lead a positive and happy life as this would also have impact on lives of my children . . . In a few weeks her positive attitude really influenced me and I feel I will never forget the support she gave me.
Woman Q453A
This service would have been so appreciated and needed during my 1st pregnancy and I feel if I had had a doula then I probably would not have suffered with post natal depression (as much) and highly recommend it to all 1st time mothers even if they have family support.
Woman Q353A
I could text her at 2:00 in the morning if felt down and she would reply back to me, you know, 24 hours on the phone.
Woman F319A
I think the service should be there for all mothers so won’t feel scared or lonely, or oh my god, that’s the end of life . . . I had depression . . . When I found out about [the doulas], I really needed them and they came straight to see me. That’s when I saw hope.
Woman Q369Z
Emotional support
As we have seen, many women described how the doula was someone to talk to and to listen to their concerns, in the context of a real emotional relationship. They described how important this relationship was to them in overcoming feelings of isolation and fear. This was particularly powerful for women who had little or no other support, but was also true for women who had involved partners (or sometimes even involved mothers). Doulas were described as being good and non-judgemental listeners.
I want to say something especially I don’t have any family here even my husband leave me alone, am really helpless. I feel sorry to say am cry every time nobody near me then doula hold my hands and give me every support which I was needed. Thank you Doula I love very much I don’t forget Doula.
Woman Q335A
One woman described how her doula followed strict rules about sharing personal experiences and that this undermined the potential for a meaningful relationship:
I found she was really quite, well, we got on but I found she was shy, or I didn’t really feel like I got to know her very well, I felt like I was saying all sorts about myself and my situation but she wasn’t giving me anything about herself. So the rapport was a bit odd . . . There was no mention of friendship. That’s why I was bit unsure about what the relationship was meant to be.
Woman F385X
Impacts of doulas: knowledge, confidence and skills
Several women reported that doula support had increased their knowledge (45.8%), confidence (54.8%) and skills (42.2%) around pregnancy, childbirth and looking after their child. There were no significant differences between sites.
We hypothesised that increasing knowledge and skills may be more relevant to primiparous women whereas a similar relationship may not be observed for confidence on the basis that multiparous women may be referred because of previous negative pregnancy and delivery experiences.
Across all three areas a greater proportion of primiparous women reported that doula support was associated with improvements in knowledge (75.0% vs. 48.4%), confidence (82.2% vs. 65.1%) or skills (62.8% vs. 48.4%); however, the difference was statistically significant only for knowledge. This fits with the earlier finding that primiparous women were more likely to report having been given information. We also hypothesised that increasing knowledge might be particularly relevant to women who were recent migrants to the UK (operationalised as having been in the UK less than 5 years prior to introduction to the doula service). Significantly more of the recent migrants reported increased knowledge (73.8% vs. 52.4%) and increased skills (73.2% vs. 46.4%) whereas there was no difference between recent migrants and other women concerning confidence (72.5% vs. 70.6%):
I chosen Doula Service, because I needed a support and an advice about English Health System. I’m from [name of country] . . . I felt very lost in English NHS system, especially in my not strong language . . . I was very happy, my doula was an English-woman, so she explained me everything about English Health System . . . I got a more informations from Doula than from NHS.
Woman Q370A
Impact of doulas: allaying fears and building confidence
Many women said they had pregnancy worries and had been afraid of birth, but the doula had helped to calm their fears. A very strong theme was how doulas supported women to believe in themselves, building up their confidence for birth and parenting through positive reinforcement:
I do not feel so scared with the help of doula.
Woman Q422W
I had someone to share my frightenedness about pain in labour birth, the most I was worried about.
Woman Q381Y
[The doula] assured me I was making good choices for my unborn/newborn baby.
Woman Q321A
She give me confidence when I was nothing and nobody with me.
Woman Q335A
I have some learning difficulties and she helped me with confidence.
Woman Q339X
Whenever they talked to me, always built up my confidence.
Woman Q369Z
We worked on my self-esteem, which made me feel less anxious and more in control.
Woman Q373Y
Women perceived that the information from their doula was balanced and non-directive:
My [doula], she never put her opinion across and she never biased anything in any way . . . if I’m saying I want to do X, or whatever, she’ll say, well, okay, you know, that’s a really good idea, you can do this, or if you think about it as well, we could do that, we could, you know, and didn’t actually ever make you feel that you were being judged, or anything in any way.
Woman F341Y
I mean she knew what I’m going to do and she told me she would support me either way, you know, if I choose bottle, she would be there for me . . . of course they were encouraging and always like presenting pluses and minuses, you know . . . The main thing she was there for you, so whatever you would do she would support you.
Woman F301A
Impact of doulas: making healthier choices
Smoking
The questions concerning smoking were answered by 91% of women who received doula support (A, 86 of 90; W, 12 of 14; X, 7 of 9; Y, 12 of 14; Z, 7 of 9). No women reported smoking at sites W, X and Z, compared with one in three at site A (28 of 84) and one in five at site Y (3 of 14). The majority (81%) reported stopping in pregnancy (19 of 31) or smoking less (6 of 31); however, only four women attributed this to doula support.
Diet and exercise
While 16.5% reported that doula support had helped to improve diet and 19.7% reported helping to take more exercise, few comments were made concerning the ways in which this was achieved. Mostly, comments were a variant of ‘advice’.
Skin-to-skin contact
Helping with skin-to-skin contact was reported by 35.4% of women. Some comments concerned giving information about skin-to-skin but the majority reflect the doula’s presence at the birth:
She hold my son skin to skin with me as soon as he was born.
Woman Q361A
Made sure I was passed my daughter straight away.
Woman Q456A
Breastfeeding
As reported in Chapter 3, breastfeeding initiation and continuation were higher among women in site A than among the local population. Interviews with key informants indicated that doula support may have particular impacts on sustaining breastfeeding rather than initiation. Within the questionnaire sample, in the first few days after giving birth, 63.2% of women exclusively breastfed, 18.0% used mixed feeding and 18.8% used formula. At 6 weeks, 42.1% exclusively breastfed, 23.3% used mixed feeding and 34.6% used only formula. As expected, white women (n = 73) were significantly less likely than non-white women (n = 60) to be giving any breastmilk either at birth (72.6% vs. 91.7%) or at 6 weeks (47.9% vs. 86.7%), although rates are still higher than might be expected for women experiencing social deprivation.
More than half of women who breastfed (54.9%) reported that doula support helped them to do so. As predicted, significantly more primiparous women than multiparous women found doula support helpful (67.6% vs. 42.0%). Contrary to our hypotheses, there were no differences with regard to this question according to country of birth (53.8% born in the UK vs. 56.0% born outside the UK), ethnicity (56.5% white vs. 54.5% non-white) or age (46.2% < 25 years vs. 55.0% 25–34 years vs. 59.3% > 34 years). No information was available on women’s previous experiences of breastfeeding or their attitudes towards breastfeeding, both of which were hypothesised to be relevant from a CMO perspective.
In the questionnaire, more comments were made concerning infant feeding than about any other outcome. The breastfeeding support given by doulas went beyond information (which doulas provided by sharing leaflets or a DVD or finding a class): they also offered encouragement when women found breastfeeding hard; gave direct help, for example with latching on; and brokered outside help, for example from the local breastfeeding service or breastfeeding peer supporters.
Impact of doulas: uptake of antenatal classes and other services
Only 44 women (36.1%) attended NHS antenatal classes; this represented 52.2% of primiparous women and 26.2% of multiparous women. Women at site A were significantly less likely to attend classes than women at other sites, even when analysis was limited to women who had been supported antenatally. Comparison of site A data with the Picker survey suggested that rates were somewhat lower than for the local trust, but the difference was not significant.
Reasons for not attending were: classes were all booked up (n = 8), attended other classes (n = 7) and not offered any NHS antenatal classes (n = 33). ‘Other’ reasons included barriers of childcare (n = 3), time (n = 1) and language (n = 1). One woman reported not wanting to attend and three reported not needing to attend, two because of medically complicated pregnancies and one in part because of doula support, suggesting a possible reason why attendance at classes was not higher overall:
I think my doula and my midwife tried to explain to me everything necessary.
Woman Q440A
We hypothesised that doula influence may be more commonly reported at sites W and Y because the host services had affiliated antenatal classes and there was some evidence to support this (A, 4.7%; W, 46.2%; X, 33.3%; Y, 57.1%; Z, 0.0%).
Some women said that their doula had accompanied them to medical appointments, antenatal classes, postnatal groups, children’s centre groups, playgroups, a domestic abuse service or a postnatal depression group. Others had given women information about a variety of local services. For some women, being accompanied the first time was essential to gain the confidence to attend:
[The doula] came with me to one of those [children’s centre group] meetings as one of our week’s things, and I wouldn’t have gone if she wasn’t going with me . . . I don’t think I would have been brave enough.
Woman F315A
Linked to this, 36.7% reported that doula support helped them to meet other mothers. Although the difference was not significant, more women at site Y reported such an effect (A, 33.8%; W, 33.3%; X, 44.4%; Y, 61.5%; Z, 16.7%).
Impact of doulas: better birth experiences
Who was present at your labour/birth, apart from health professionals?
Twenty-seven women (16.4%) had their labour/birth attended only by a doula (apart from health professionals), 21 of whom would have otherwise birthed alone. Four women did not have anyone present at their labour or birth, apart from health professionals. Of these, three reported not having who they wanted at their labour/birth. Two of these reported the reason that the doula had been unable to attend:
I did not ring my Doula worker on time.
Woman Q319A
Happened too quick. Went into labour and could not get hold of Doula and ended up with emergency C-section.
Woman Q430A
Of the remaining women (n = 134; 81.2%), who had their labour/birth attended by partner, family or friend, more than one-third (n = 48) also had their doula present.
Birth experience
Women were asked to rate their birth experience between 0 (very poor) and 5 (very good). A greater proportion of women whose birth was attended by a doula rated their experience as good (> 3; 62.2% vs. 44.8%) or very good (> 4; 31.9% vs. 20.0%); however, this difference was not significant.
How attending the labour/birth affects birth experience
Women described the birth support they received in different ways. For some the support was primarily emotional and they described how the doula encouraged, motivated, calmed or reassured them, usually in the context of a relationship developed antenatally. For some it was simply the doula’s presence making them feel safe and supported when they would otherwise have been alone or lacking a female companion. For some it was physical: massage or help with breathing. For some it was practical: having a doula meant their partner could look after other children or make arrangements for them. For others it was about advocacy when they felt unable to speak to the health professionals (advocacy is explored below in Impact of doulas: better communication with health professionals).
Many women described how the support of the doula made them feel calmer and more in control of their labour and birth and some said they needed less pain relief as a result. Others described how the doula’s support helped them come to terms with unwelcome interventions:
She made sure I was never alone, reassured me, made me feel good, and understood what was going on.
Woman Q361A
Just another female presence. I anticipated her being there, the labour was progressing fast so i was able to relax fully once she’d arrived as all my ‘team’ was there.
Woman Q385X
Encouraged me to believe in myself which made me stay longer at home during labour.
Woman Q334A
I had a home birth with no pain relief and this was only possible because of my Doula.
Woman Q312A
When I feel bad she encourage me and give a confidence: you are good, you do this very good.
Woman Q331X
I felt safe which helped me focus & concentrate.
Woman Q456A
One woman felt that the doula had saved her baby’s life by alerting the midwives to an emergency. Another woman, whose baby was taken into care at birth, described how her doula’s support had helped her to cope.
Women were asked directly in the questionnaire if there had been anything unhelpful about the doula attending the labour/birth. No women described instances that were unhelpful per se, but rather some said the doula had been unable to help much at birth or did not help in the way they would have wanted:
There is not much thing [the doula] can do. Some of the staff were not cooperating with her. [Planned caesarean]
Woman Q382A
Labour was very medicalised so she didn’t have chance to help me as much as she could. [Normal vaginal delivery]
Woman Q423A
I needed more support at birth. Doula didn’t get involved much. [Emergency caesarean]
Woman Q329Y
Comments from women who had planned caesarean sections illustrated that doula support was not only of benefit to those having natural births:
Helped calm me down.
Woman Q332A
I didn’t go through labour but my doula helped and supported me while I waited for the operation (C-section).
Woman Q386Y
Theoretically, told us about the experience.
Woman Q394A
The last of these comments came from a woman whose birth was not attended by her doula, reflecting a potential for doula support to impact birth experience without the doula being present. Similarly, one woman (Q369Z) described how her baby was unexpectedly born at home but that she had telephone support from her doula during the labour and birth, with the main and back-up doulas arriving minutes after the birth. In this situation, the woman felt that her doula had been present. These observations were consistent with comments from several women and doulas who nominated antenatal support as the most important stage of support because of birth preparation work.
Impact of doulas: empowerment
Many women commented on how the doula had changed the way they felt about their maternity care. The combination of non-directive information and building up women’s confidence through affirmation led to women developing an awareness that they had choices and feelings of being in control of their maternity care. Women experienced this as very empowering, whether they were nervous first-time mothers or mothers who had experienced a previous difficult birth. In some cases this led to them making different birth choices about pain relief or attempting a vaginal birth after caesarean.
Several mothers said that, even though the doula had not been with them during labour, the way she had given support during pregnancy meant that they could cope better in labour because they felt more in control:
The doula that I had, she was very, she was my second voice, I would tell her things and then she would do, well we could do this, well we could do that . . . She gave me the confidence to say, no, I don’t want to do that, or, yes, I want to do this, or, this is how I’m feeling right now.
Woman F337A
Made me feel in charge of my care in pregnancy and childbirth.
Woman Q444A
Gained confidence and belief in myself to deliver naturally and once my baby was born to get out the house with two babies.
Woman Q334A
Incredibly empowering that she helped me stick to my guns, give birth at home with no pain relief.
Woman Q302A
If I didn’t have a doula I would have opted for an epidural like with my other two but she suggested gas and air and if needed go from there and I’m glad I only had gas and air as I could deal with labour better.
Woman Q352A
One woman described how her doula researched the possibility of having a vaginal birth after an earlier caesarean, accompanied her to all antenatal appointments and coached her on what to say to the midwife. Although this account may raise questions about the boundaries of the doula’s role, the woman herself was extremely positive about this support:
[The doula] did her research, did everything and she was there, sitting there and it was before we went in, she told me what to say and then I had so much confidence to talk to this midwife and I was telling her, in fact, I found my voice and then when we left, she was saying, I don’t like what [the midwife] said, I’m going to find out and, you know, I found out that actually I was empowered, I didn’t have to do what the midwife told me to do, I have to do what I want to do . . . we were prepared before every antenatal, because she went for every single one with me, each time when I call her she was there, she just sits and listens and I say what she’s told me to say . . . I say it because I know it’s right.
Woman F409Y
Impact of doulas: better communication with health professionals
Some women felt a gulf between themselves and the health professionals in hospital. In these situations the doula was an effective advocate for them and they valued her role as a birth partner who could talk to health professionals on their behalf:
[The doulas] give mother second mouth, partner, to talk for her, when she need help.
Woman Q336X
Yeah, I think what my doula did was to introduce herself and say, look, she’s weak, she won’t be able to communicate with you much, so I’m here to communicate, you know, what she wants and I was very weak, I was sleepy most of the time, the only time I wake is when I actually need something and I tell her and she, you know, help pass the information around.
Woman F386Y
A friendship built on trust was formed. So during labour she encouraged me to do as the midwives suggested and I trusted her to make the right judgements.
Woman Q409Y
In some cases the doulas supported women who could not communicate with health professionals, either because of language differences (where no interpreter had been provided, especially at site Z) or because the mother felt overwhelmed and confused by medical terminology:
[The doula] also discussed waiting to clamp and cut the cord while having skin to skin with the healthcare professional – something they had been reluctant to let me do.
Woman Q457A
[Because we had a doula,] after the birth we didn’t feel useless about communicating with the midwives.
Woman Q315A
Things and terminology [the doula] was able to tell me what was happening so I understood.
Woman Q454A
One non-white woman described how being accompanied by a doula to outpatient appointments meant that she was treated more respectfully by staff than if she had been alone:
The hospital, the doctors and the nurses, if they see a [doula or community midwife] with the patient, they don’t do that [behave badly], but if the patient is alone, by themselves, even if you speak English, it’s two different things. They would listen more if you are not alone.
Woman F369Z
Impact of doulas: supporting partners and mothers’ relationships with their partners
Women were asked about potential impact of doula support for the partner through two questions: one concerning intrapartum support and one concerning the woman’s relationship with the partner.
Of the 36 women describing the impact of doula support for their partner, husband or other support person, 22 (61.1%) reported that the doula ‘made sure they were included’, 22 (61.1%) that the doula ‘showed them how to support me’ and 20 (55.6%) that the doula ‘gave them breaks from supporting me’. Occasionally, emotional impacts were also described, for example:
Helped them stay positive.
Woman Q456A
Asked if having a doula made a difference to the woman’s relationship with her partner or husband, the majority (n = 46; 59.0%) said no, 24.4% (n = 19) said yes and 16.7% (n = 13) were unsure.
Most of the comments from women with partners reflected one of five themes: having a doula to confide in meant the woman did not have to bother her partner with her worries; having a doula reduced stress because roles were shared, with the partner able to focus on looking after other children or (for a disabled mother) physical aspects of birth support; the doula supported both parents during birth, which meant the mother did not have to worry about supporting her partner herself; the doula had a direct impact on the partner by explaining things, motivating or reassuring him; or the doula had a direct impact on the relationship by helping the couple at a stressful time.
Women described how the doula service was very well received by their partners who did not want to be involved in the pregnancy or birth:
When I get pregnant first couple of months is fine, but then I feel that he is going emotionally far away from me, he’s kind of fed up, so he felt relief that there was someone else there and I was pleased that I don’t have to beg him every time. Especially when I had to go to appointments with doctors, midwives.
Woman F369Z
Well, he had to stay the first time, all through the caesarean he would stay with me and he just didn’t want to go through that again, so having someone to replace him there was a relief for him and, of course, then he could stay with my daughter.
Woman F341Y
Where the woman’s partner did want to be involved there might be a degree of suspicion or hurt feelings at first, but women described how their partners were won over by the doula and how she became a support for them both:
Yes, when I first said it to my husband he was like, does that mean I was rubbish then? I was like, no, it’s just extra support . . . he could just focus on me, rather than worrying about everything else, but, yes, it was a bit of a, yes, sore point at the beginning, but then he got to know her as well, and it was fine.
Woman F315A
[My baby] wasn’t breathing when his head popped out, so he had to go off in an incubator . . . and [my husband] knew he could call [the doula] and sob his little heart out down the phone, and 20 minutes later, she’s stood next to him, giving him that ultimate needed support.
Woman F337A
I think it’s like the pair of you though, as well, like you’re both looked after by her, not just, like you don’t have to worry about looking after him, because you’re both just sort of looked after as well.
Woman F315A
In times of stress, she helped us to keep communicating with each other and kept things calm.
Woman Q373Y
Because we all got on so well and reduced stress about what to do with our toddler. [My partner] felt much less stressed. She also reassured him about me giving birth at home.
Woman Q302A
In some cases the partner and doula would take turns supporting the mother in labour, giving each other breaks:
My partner . . . he’s coming to visit me to hospital and my doula, she stay with me 8 hours when I was in labour and is coming to visit me and he sent her to go to sleep, they help each other and after 2 hours, I will call her again, because he’s going and she’s coming again.
Woman F404W
The doula also helped couples deal with a less than optimal birth:
Helped him to understand what I had been through.
Woman Q339X
Made us closer after a difficult birth.
Woman Q427A
One woman attributed the fact that she had a partner at all to the doula’s influence:
I met my partner at 5 months pregnant. She gave me the confidence to let a man into my life.
Woman Q448A
However, one mother commented that her partner had not been fully included:
To [invite] my partner in the things and not just me.
Woman Q311A
Impact of doulas: feelings of loss at the end of support
The focus groups with volunteer doulas and the user panel carried out in the first stage of data collection identified the need to examine endings in some detail. Across women’s data sources, the feelings of loss associated with endings were identified as constituting an impact for women.
More than half of women (61.7%) reported that their doula prepared something as part of the ending. Most common was an account of the doula and woman’s time together (27.0%), followed by photographs (26.1%) and a birth story (20.0%).
One-third of women felt that support had ended too soon (33.1%), although this varied across sites (A, 30.1%; W, 14.3%; X, 33.3%; Y, 50.0%; Z, 71.4%). Similarly, when asked what they would change if they could change one thing, the most common response concerned having support for longer after the birth (n = 13), followed by staying in touch with their doula (n = 8).
Several women found that the ending was quite abrupt because they had lost track of the weeks:
I think like they say beforehand and then you get 6 weeks after, but it just flew by, like that first 6 weeks is so, I don’t know, hard and fragile, and just chaos as well, and then it was over, it is quite tough.
Woman F315A
I found it really hard actually, I kept asking if I could keep in touch with her and stuff like that, but we couldn’t . . . At least should have been able to keep their numbers or something like that, so you can have that bond, like, because once a friend they become a friend don’t they and that’s it.
Woman F319A
Yeah, it was so sad for me, because I need to more to help me at that time as well, because the service they send me letter, we stop.
Woman F404W
It happened too soon, I felt I bonded well with my doula and you get used to seeing them and receiving support and then it all stops.
Woman Q332A
I didn’t see Doula for last visit as it was cancelled. So felt it was a little abrupt and did not say goodbye and thank you face to face. Made me feel a little discarded!
Woman Q380Y
We both lost track of visits and ultimately I got a text to say that I needed an evaluation meeting with [the manager]. Wish I could have said thank you.
Woman Q315A
We hypothesised that greater preparation would facilitate endings. Comparing those women whose doula prepared something with those who did not, no statistically significant difference was found concerning feeling that the support ended too soon (31.0% vs. 37.5%) or that they lacked other sources of support when the relationship ended (14.5% vs. 16.7%). However, a greater proportion of those for whom a written account or photograph had been prepared would have liked to have stayed in touch (72.5% vs. 52.4%). This is possibly because the preparation was a reflection of the quality of the relationship, rather than a cause. Women who had received birth stories from their doulas said this was a very positive aspect of closure.
Among those who thought of their doula as a family member, the vast majority would have liked to have stayed in touch (mother, 90.5%; sister, 91.7%). This was greater than those who thought of the doula as a friend (69.0%) or professional (59.5%).
Many women said that they found the ending of doula support very hard, either because they did not yet feel confident in their postnatal role and still needed support, or because they valued the relationship as much as the support and did not want to lose it.
I had a caesarean section, so somewhat depressed at times. Wish the official time to discharge a mother who has undergone caesarean should be longer than a mother who had a natural birth.
Woman Q409Y
It seemed like ending a friendship I cherished.
Woman Q327Y
She made me feel better in myself, everything we did was great together. Felt very depressed when she was gone.
Woman Q444A
And is not fair according to your policy, that when you finish the last day that’s it, not fair at all. She was more than a doula – like family.
Woman Q336X
Women proposed two solutions: that the ending of support should be more timed to the woman’s needs (particularly in situations where she had been ill after birth and was not ready to go out to groups), or that there should be some contact permitted between doulas and women after support ended – a friendly catch-up by phone, over a coffee or at reunion meetings (although some women did have unofficial ongoing contact with their doula). They said specifically they would like to have let the doula know how they were getting on and to show her how their child was flourishing at developmental milestones. Some women framed this in terms of thanking the doula by showing her the long-term impact of her support.
It would have been nice to meet up with her when my son turned one to say she help[ed] bring him into world.
Woman Q419A
So I could show her my perfect family because of her and her help.
Woman Q427A
Just to let her know how I was coping with baby through all her advice.
Woman Q367A
Many women felt that allowing them to keep in touch would acknowledge that they had a real and meaningful relationship with the doula. Women who had formed a close relationship with their doula spoke of their sadness when it had to be broken off.
There was a day she told me that I’m not allowed to get in contact with her, that is not how they do their services, I cried, I said, God, I said, okay, what about in the future? So I just, I said, okay, maybe later I will get her again! But definitely, oh, I miss her, like, I really miss her.
Woman F366Y
What I can say is necessary to stay in touch because when someone do a good thing in life is better to have contact with him/her, like a doula you can even invite her in birthday of your baby for example.
Woman Q440A
By contrast, other women found that the support had ended at the right time, when they felt confident to cope, and some said the support had petered out naturally as they were ready to move on. This was particularly likely for women who primarily wanted information from their doula and was also particularly likely at the one site with an extended postnatal support period of 3 months.
The ending was in the right time, after I felt confident with my baby.
Woman Q408W
It was a good experience of going to coffee shop with my doula and two young girls built up my confidence to go out with my daughters with them both being so young.
Woman Q334A
Felt prepared and confident about the future.
Woman Q341Y
It was very emotional, cos we both know that something beautiful is ending. It was very nice experience.
Woman Q301A
Some women had given their doulas a small gift or card and others were unhappy that they were not allowed to do this or had not been able to; this was also seen as a potential support for feelings of closure:
It was very sad. I wasn’t even allowed to buy my Doula a gift which I didn’t understand and which upset me at the time.
Woman Q312A
Doulas’ relationship with midwives
Women who had intrapartum support were asked to rate how well the doula and midwives had worked together during labour and birth. The majority of women (80.3%) reported ‘well, most of the time’, followed by ‘well, some of the time’ (16.7%); just two women (3.0%), from two different sites, said ‘not well at all’.
It was clear that some midwives felt challenged by the presence of someone who was not a relative or friend of the woman and some did not understand the doula role:
I think the midwives were dismissive of [the doula] I think, because it’s almost, like, ‘this is my profession’.
Woman F409Y
After we had [the baby], and my doula had gone home and everything and the midwife said, you’re a bit greedy having two birth . . . you know, why did you have a doula and your husband here, like? So, yes, a bit awkward.
Woman F315A
Midwife didn’t seem to acknowledge doula.
Woman Q345X
The midwives were a little dismissive of my doula at times.
Woman Q457A
One woman suggested that midwives might use professional judgement to give less support to a woman with a doula because they would see her as already having enough support.
Others commented that midwives should see doulas as helping their work because doulas helped women stay calm and come to terms with unwelcome interventions:
In the end after all that pain, I had a caesarean, fine, but [the doula] reassured me that it was the best thing for me and the baby, and because she said that, I thought, well, that works, you know, it’s fine, I wasn’t angry . . . If a midwife told me that I probably would have been angry, because they refused to believe that I was in labour.
Woman F409Y
However, it was evident that many midwives and doulas had worked well together:
There was [co-ordination] between them, when midwife asked me to use gas inhaler or take a deep breath, Doula helped me How to use the inhaler and how to take the breath.
Woman Q304A
My midwife was lovely, she was very chatty, speaking to the doula, and speaking to my husband, and so it was really nice, it was a nice relaxed . . . I do think it’s a very selected few [midwives] that aren’t for doulas, but then a huge amount that are for doulas. It must help their job, it must help the midwives to a point, their job, because the doulas calm us.
Woman F337A
(Dis)satisfaction with the service
The majority of responses were overwhelmingly positive. However, important additional information can be learned from the women for whom the service did not work, or did not work as well. This was explored by looking in greater detail at those women who reported that the service did not help them in the way they had hoped, who would not recommend the service or who assigned a low rating to the overall doula experience.
Did the service help you in the way you hoped?
While 88.4% of all women reported that the service had helped them in the way they had hoped, the proportion was not consistent across sites; only four of seven women (57.1%) endorsed this at site Z compared with 85.7–92.3% at other sites. Of the 14 women reporting that the doula did not help in the way that she had hoped, 12 provided reasons, the majority of which concerned not having had enough support:
She was of little help because she came too late in my pregnancy and was not at the hospital for my labour and birth at all . . . I was thinking there should be a back-up doula in case of emergency.
Woman Q390W
Doula help[ed] me during labour – not before not after.
Woman Q349A
I felt that the visits were too short and not enough of them.
Woman Q380Y
I needed someone to be with me more often.
Woman Q435A
I needed more support at birth. Doula didn’t get involved much.
Woman Q329Y
Needed it earlier on in the pregnancy.
Woman Q449A
Never saw her really.
Woman Q307A
Was not contacted.
Woman Q414Z
Was only contacted a few times but would have liked more.
Woman Q458Z
For three women, their complaint was about quality rather than quantity.
Didn’t feel supported at all and had a really bad birth.
Woman Q313A
Didn’t give me information that I hoped.
Woman Q322A
I hoped the support would be more professional.
Woman Q362A
Would you recommend the service to a friend or family member?
Only five of the 133 respondents (3.8%) reported that they would not recommend the service, of whom four were from site A and one was from site W. For two of these women (Q307A and Q313A), the reasons for their response reflected not feeling supported and having limited or no face-to-face contact with the doula (discussed in Did the service help you in the way you hoped?). The remaining three women gave little explanation and gave high satisfaction ratings (4 or 5; see Overall, how would you rate your experience of being supported by a doula?). Possibly the question had been misunderstood.
Overall, how would you rate your experience of being supported by a doula?
On a 0–5 rating scale (very poor to very good), 77 women scored 5 (58.3%), 37 scored 4 (28.0%), 15 scored 3 (11.4%), two scored 2 (1.5%) and one scored 1 (0.8%). Scores below 3 were limited to site A. The percentage scoring below 4 at each site was 13.5% (A), 7.1% (W), 11.1% (X), 21.4% (Y) and 16.7% (Z).
There was some agreement between the overall doula rating and whether or not the service had helped in the way that the woman had hoped. Six out of 13 with a rating of 3 and all three women with a rating less than 3 felt it had not helped in the way they had hoped.
What factors are associated with a low rating of the doula experience?
Scores were regrouped into ‘high’ (4 and 5) versus ‘low’ (less than 4) to further investigate the association between lower ratings and various factors that were identified in the CMO configurations. No association was found for the following: self-referral, social complexity, not having whom they wanted at the birth, otherwise birthing alone and having declined any of the support offered.
Lower ratings were more common among women whose birth was not attended by a doula (22.4% vs. 6.8%); however, this appeared to partly reflect the strong association between lower ratings and having had only postnatal support (meeting before 20 weeks 7.7%, meeting at 20–30 weeks 19.0%, meeting after 30 weeks 9.1%, meeting after the birth 44.4%). Two of the five women who were matched late (operationalised as having received intrapartum support without antenatal support) assigned lower ratings.
Analysis of the key informant data and feedback from the user panels identified elements of doula support that women valued. We therefore hypothesised that women who felt that they had not experienced these would be less likely to rate doula support highly. Significant associations were found between lower ratings and not having received doula support with certain characteristics: ‘seeing the same person most of the time’; ‘support shaped around what I wanted to do’; and ‘support from someone who was available when I needed them’. There was no association between lower ratings and the doula not being ‘someone who had given birth herself’ or ‘able to speak my language’.
The association between rating and year of introduction to the service was explored at site A. Lower ratings were most common in 2010 (6 of 24; 25.0%) and 2011 (3 of 17; 17.6%). The following demographic variables were also investigated: age, education, UK born, ethnicity, parity. None of them was significant.
There was a small but significant positive correlation between intensity of support and rating of doula support. However, ratings did not always correspond with the average number of hours of weekly support. For example, the two women who reported an average of 0 hours assigned ratings of 1 and 4.
It is important to note that there appeared to be some systematic bias in ratings not being completed where women felt that they had not received the service as intended and therefore had not completed later sections of the questionnaire.
Administration of the doula services
There were both positive and negative comments about administration. Some women were impressed at how well they were matched with their doulas and how quickly they ‘clicked’. At one site (Y) they particularly commented on how the project staff really took time to get to know them before deciding on a match and on how quickly the doula support began after a referral (this was contrasted with antenatal care).
A few women found the services disorganised or overly formal. One woman with considerable needs had been referred to one of the doula services but had never heard from them and lacked the English language skills to follow this up; she was emphatic that she wished she could have had a doula to advocate for her (site Z). Another described how a member of service staff did not keep follow-up appointments (site X):
There was supposed to be an evaluation of the service shortly after I had finished seeing her and the [staff member] got in touch on a number of occasions and failed to turn up for appointments and then rang up and said ‘oh I am sorry I didn’t make it let’s make it for another time’, made another appointment and still never turned up.
Woman F385X
More awareness of the service as I was not aware until I was nearly 8 months pregnant and unfortunately the service is not readily promoted.
Woman Q373Y
To be less formal.
Woman Q382A
Less formal – tied up in data protection red tape, health + safety, etc.
Woman Q386X
Very attentive, immediate support, well organised.
Woman Q362A
More young people.
Woman Q430A
Disappointed that she didn’t have any contact with a [doula] after they first called.
Woman Q414Z
Women who commenced support and did not receive the ‘full service’
Seven women were identified where support had commenced but they had not received the service as intended, which had not been through their choice. Whereas this represented 1 of the 14 women at site W and 2 of 89 at site A, it represented almost half (4 of 9) at site Z.
Women who were not supported by the service
Comparisons between women who used the service and women who did not use the service
There were no statistically significant differences between women who used the service and women who did not use the service for any of the variables reported in the sample characteristics presented in Appendix 10.
The two groups were also compared for how they found out about the service (e.g. via the midwife or via someone who had used the service), how they were introduced to the service (i.e. self-referral or someone else got in touch on their behalf) and the point at which they first had contact with the service (i.e. before 5 months of pregnancy, 5–7 months, after 7 months or after the birth). No differences were found.
The psychological outcomes available for women who did not use the service were limited to their rating of their birth experience (as indicated using a 0–5 scale) and postnatal mood. There were no differences between groups on either of these outcomes.
The only statistically significant difference between groups was that women who did not use the service were more likely to have the birth attended by their partner or husband (76.7%) than those who used the service (52.6%) (p < 0.05). However, as indicated through women’s focus groups, it is likely that a higher proportion of women who used the service would have had their birth attended by their partner if doula support had not been available. Four women out of 135 who used the service (3%) reported birthing alone (excluding health professionals), compared with none of the women who did not use the service.
Disengaging and declining support
We have limited information from women who disengaged or declined support. Our two sources are (1) the short version of the questionnaire that was sent to women who had had contact with the service but had not been supported, some of whom had chosen not to use the service; and (2) some of the women who had used the service and, therefore, received the full length questionnaire, who reported not taking up all of the support that was offered.
Women who did not use the service
Women identified by the services as not having used the service comprised women who had chosen not to receive doula support (n = 23; 76.7%) and those whom the service had been unable to support (n = 7; 23.3%).
The 23 women who declined the service were asked to provide their reason from a list that included not needing the support, offering more or less support than the woman wanted, concerns about partner’s feelings, a language barrier, the involvement of a stranger or another person to deal with, and not wanting the particular doula offered.
Responses are shown in Table 17. No-one endorsed ‘It offered more support than I wanted’ or ‘I did not want the particular doula who was offered’; however, one woman identified the latter as the reason that the service was unable to support her.
| Reason for declining support | Site | Totala (n = 23) | ||||
|---|---|---|---|---|---|---|
| A (n = 9) | W (n = 4) | X (n = 2) | Y (n = 5) | Z (n = 3) | ||
| I did not need the support | 7 | 1 | 1 | 4 | 1 | 14 |
| I was concerned about having a stranger involved | 3 | 0 | 0 | 1 | 1 | 5 |
| I did not want another person to deal with | 1 | 2 | 0 | 1 | 1 | 5 |
| It did not offer as much support as I wanted | 1 | 1 | 0 | 0 | 0 | 2 |
| I was worried that my partner/husband would be pushed out | 1 | 0 | 1 | 0 | 0 | 2 |
| I was worried about a language barrier | 0 | 0 | 1 | 0 | 0 | 1 |
Six of the seven women reporting that the service had been unable to support them provided reasons. No details were provided by the woman from site X. Comments from site W suggested that there may have been too few active doulas to meet the number of referrals and/or that the timing or referrals or allocation of women to doulas occurred relatively late during the pregnancy:
Because I gave birth to my son earlier than the expected day and before I met the [doula].
Woman Q433W
There was no doula available at that time.
Woman Q421W
Comments from the other three women indicated that it was the nature of the support that was an issue:
Because I asked for a particular doula they said I couldn’t have a doula so the woman rights was not support[ed].
Woman Q357Z
I needed some help with picking [up] older kids from school but they said they only offer emotional support.
Woman Q326A
It did not offer as much support as I wanted.
Woman Q450Z
Some women elaborated and described additional factors that had led them to decline the support; these usually concerned the support being offered too late, feeling ‘overwhelmed’ where support would have started after the birth, changing circumstances meaning that the support was no longer necessary, and concerns that a doula might not support their birth plan:
When the time came I felt over ran with visitors and was very stressed so decided not to use a Doula, as it would be another visitor in my house I didn’t know.
Woman Q317A
I chose not to have a Doula as I felt they would tell me how to give birth and may not be happy if I needed pain relief from what the midwife explained. I was very scared about giving birth after the last 2 pregnancies before. Not saying Doulas are not good for some women just not for me.
Woman Q358A
Three women reported that finding out about the doula service sooner would have affected their decision about using it:
Because I would of know[n] her more and felt OK with her in my house.
Woman Q317A
Needed it closer to beginning.
Woman Q416Z
The women who did not use the service were asked about the level of contact that they had with the service. Of the seven women who the service was unable to support, two had been contacted by letter only and one had been contacted by telephone only. Of the 22 who chose not to use the service and reported the level of contact, two had been contacted by letter only and three had been contacted by telephone only.
Women who used the service and did not take up all of the support that was offered
Twenty-eight out of 120 women (23.3%) reported that they declined some type of support that was offered. Of these, 19 declined support at one stage only (four during pregnancy; nine during labour/birth; six after the birth), seven declined support at two stages (four during pregnancy and labour/birth; one during pregnancy and after the birth; two during labour/birth and after the birth) and two declined some form of support at all three stages.
Based on information gained during the early stages of data collection, we hypothesised that women who self-referred may be less likely to have declined support, with self-referral being seen as indicative of high levels of motivation. Although a smaller proportion of women who self-referred declined support than did those who were introduced by someone else (15.6% vs. 27.1%) the difference was not significant.
Reasons for declining support were most commonly given with respect to labour/birth support. Most commonly, those declining did not feel the need for the support, usually because they had support from their partner or a family member, or because this was not their first child:
I made up with my mum and she supported me during this stage.
Woman Q342A
I wanted it just to be me and my partner at the birth.
Woman Q330A
I wanted family to be there.
Woman Q321A
I turned down help at the birth as I had my husband for support during labour.
Woman Q347A
However, some comments concerned wariness or a lack of confidence towards having the doula support:
Wasn’t that keen on having a doula at first, more social worker thought I would benefit more, as I never knew of a doula so wasn’t [something] I could see myself having.
Woman Q434A
Some women also declined support during pregnancy, such as being accompanied to appointments, because they did not feel that they needed it. Similarly breastfeeding support was declined by one woman as unnecessary. One woman declined home visits:
Asked to stop home visits because my husband is always around. Offered to go for walks, etc, but declined.
Woman Q362A
Chapter 5 Findings: impacts on doulas
Doula questionnaire response
Response rates for doula questionnaires
All sites sent questionnaires to all doulas who had completed training, with the exception of site A, where, by negotiation, nine were omitted who either had moved abroad or had some other reason not to be contacted. Numbers received and sent by each site are shown in Table 18. Between-site differences were not statistically significant.
| Site | Sent n | Received n (%) |
|---|---|---|
| A | 127 | 35 (27.6) |
| W | 32 | 13 (40.6) |
| X | 26 | 8 (30.8) |
| Y | 48 | 24 (50.0) |
| Z | 25 | 9 (36.0) |
| Total | 258 | 89 (34.5) |
Of the 89 valid questionnaires received, 71 were from doulas who had experience of supporting women one-to-one. The remaining 18 had trained as doulas but had not (yet) supported a woman. Table 19 shows the distribution of respondents by study site and whether or not they had supported at least one woman. It will be seen that 35 (39%) were from the original site, with sites X and Z being relatively poorly represented in the overall sample. At site W, over half the respondents had not yet supported a woman.
| Site | Supported n (%) | Did not support n (%) | Total n (%) |
|---|---|---|---|
| A | 32 (91.4) | 3 (8.6) | 35 (100.0) |
| W | 6 (46.2) | 7 (53.8) | 13 (100.0) |
| X | 7 (87.5) | 1 (12.5) | 8 (100.0) |
| Y | 18 (75.0) | 6 (25.0) | 24 (100.0) |
| Z | 8 (88.9) | 1 (11.1) | 9 (100.0) |
| Total | 71 (79.8) | 18 (20.2) | 89 (100.0) |
Forty-three per cent of doulas had completed training in 2012 or in the first half of 2013 and a similar number in 2010 or 2011. The 13 who had received training earlier than 2010 were all from the original site.
Ages ranged from 18 to 65 years, with 69% being between 30 and 39 years. Mean age was 36.8 years (SD 9.4 years). Age of leaving full-time education was categorised as less than 16 years (4.5%, n = 4), 16 years (33.0%, n = 29), 17–19 years (31.8%, n = 28) or 20 or more years (30.7%, n = 27). The majority of respondents identified their ethnicity as ‘white’ (80%, n = 71); 11 were ‘Asian’ or ‘British Asian’, five were ‘black’ or ‘black British’, one was ‘mixed’ and one was ‘other’. Forty-one respondents were currently in employment, 16 full time and 25 part time. Of those not in paid employment, 13 were studying or had other major demands on their time in addition to doula activities.
A modified questionnaire was sent to volunteers who were known not to have supported any women. Of the 18 returned, five said that they had stopped volunteering as soon as they completed their training, two at site A, two at site Y and one at W. In three cases this was because a paid job had been obtained. The remaining two both found it too time-consuming, with one additionally feeling that she was not suited to the role and that the role was not what she expected. A further six were still awaiting a match: four at site W and one each at sites X and Z. Five of these six had only recently completed their training but, at site Z, training had been completed in 2010/11. Other reasons offered for not having supported a woman were all personal, for example pregnancy, moving away and the need to support a family member. At site Y two volunteers had moved into outreach work within the organisation, as an alternative to supporting women one-to-one.
Except where otherwise specified, data presented in the rest of this section necessarily refer only to respondents who had supported at least one woman. Of these 71 respondents, 40 (56%) were still active volunteers, 14 (20%) were having a break and 17 (24%) had stopped being a volunteer doula. Of those still actively volunteering, 19 were in paid employment (5 full time and 14 part time) and four were studying.
Nearly half (47%) had taken a break from volunteering at some time during their time as a doula, ranging from a few weeks to a couple of years, generally for health or family reasons. Of those currently active, 76% had never taken a break, including three who had trained before 2010 and 12 who had trained in 2010/11.
There was considerable variation in the number of women supported, ranging from 1 to 19 (including women supported in a back-up role). As would be expected, those trained more recently had supported fewer women (Table 20). In total the 69 doulas responding to this question had supported 260 women as main doula. A further 108 women had been supported in a back-up role by the 66 doulas responding to this question. Doulas at sites X and Z had supported fewer women than those at other sites, even allowing for those trained before 2010.
| When trained | Mean | n | Standard deviation |
|---|---|---|---|
| 2012–13 | 3.11 | 27 | 2.063 |
| 2010–11 | 6.07 | 28 | 4.438 |
| Before 2010 | 10.33 | 9 | 5.148 |
| Total | 5.42 | 64 | 4.414 |
As might be imagined, not having enough women to support was a source of frustration to some doulas, as one explained in a telephone interview:
Maybe there’s an issue about referrals, maybe we’re not getting enough mums through the doors to support, but whatever that reason is I think I’m a wasted resource, because I’ve been a doula for two years and I’ve only supported four mums, two properly and two as a back-up. But, I’ve had a year just gone like that I know I could have supported 16/17 as many as possible, so it’s a wasted resource I think. . . . I’m passionate about the doula scheme and my main concern is it won’t work if we don’t get consistent work, there’s no proper management of it, you get frustrated.
Doula 067X
Training
Participants were asked whether there was anything in the training that they had struggled with (Table 21). Over two-thirds of the sample said that they did not struggle with anything. The most common problem was finding the time.
| Difficulties in training | na,b | % respondents |
|---|---|---|
| Studying | 6 | 7.1 |
| Finding the time | 20 | 23.5 |
| Travel to the venue | 4 | 4.7 |
| Child care | 9 | 10.6 |
| No – did not struggle | 58 | 68.2 |
| Total respondents | 85 | |
| No response | 4 | |
| Total responses | 97 |
The majority thought that nothing was needed to help volunteers complete their training, although one-quarter felt that a choice of topics would help (Table 22).
| Help from the service during training | n a | % respondents |
|---|---|---|
| Nothing needed | 37 | 61.7 |
| Make it shorter | 6 | 10.0 |
| Provide more support | 10 | 16.7 |
| Give choice of topics | 15 | 25.0 |
| Total respondents | 60 | |
| No response | 11 | |
| Total responses | 68 |
The most important personal outcomes of training were increased knowledge, a sense of achievement and increased confidence (Figure 30). A qualification and help to get future training or employment were rated as the least important outcomes, but were still rated as ‘very important’ by approximately half the sample.
FIGURE 30.
How important were the outcomes of training for you personally?
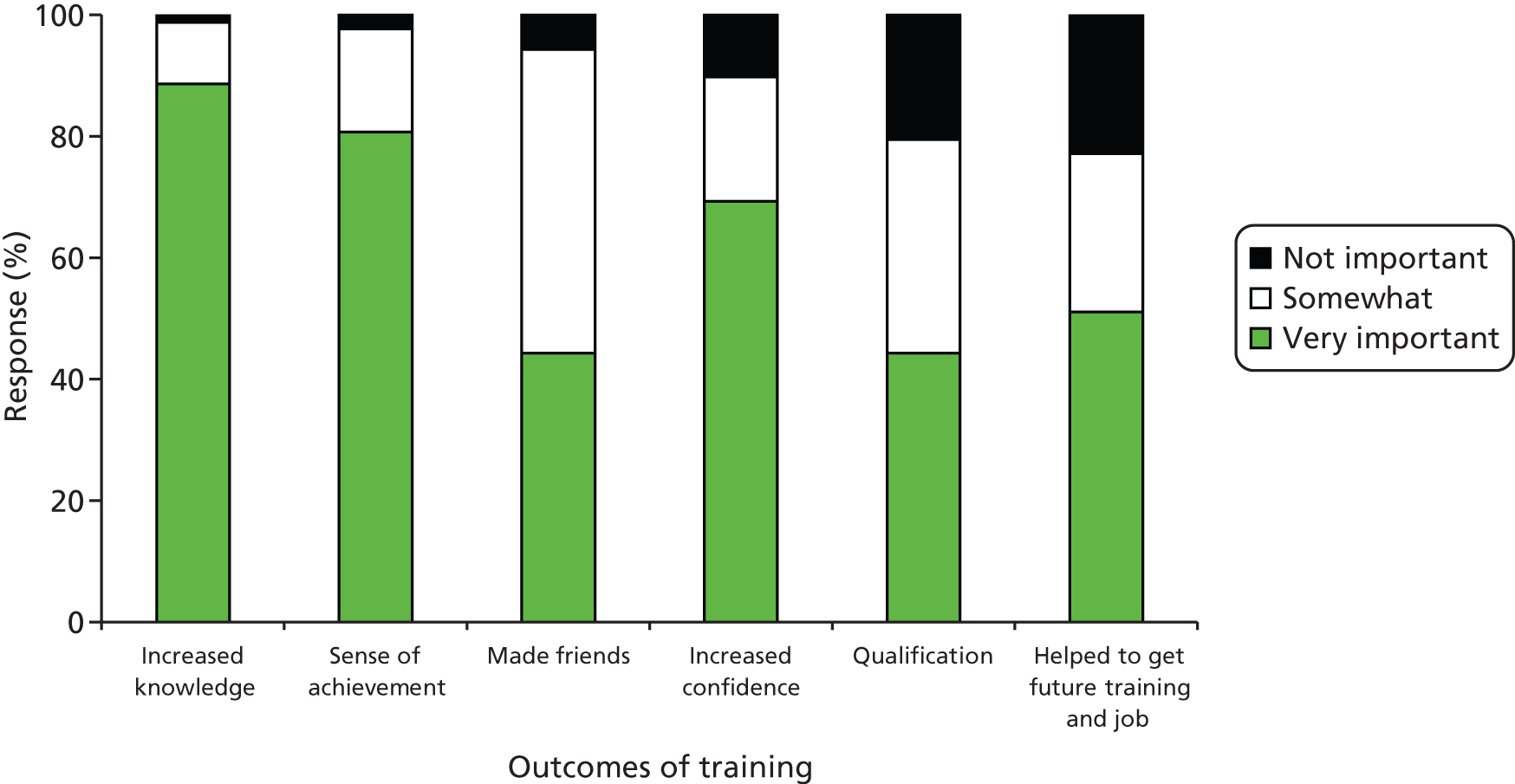
Given concerns within a number of the services about volunteers leaving soon after training, respondents were asked what was important for encouraging new volunteers to stay with the service. Figure 31 shows that views were very disparate, with none of the options offered being rated as very important by more than half the sample except for not having a long wait before being allocated to support a woman (58%).
FIGURE 31.
How important are the following for encouraging new volunteers to stay with the service?

Key informant interviews had suggested varying motivations for undertaking the training. Figure 32 shows that wanting to support women in pregnancy and during childbirth and wanting to work with socially disadvantaged women were the two main personal reasons.
FIGURE 32.
Personal reasons for becoming involved.
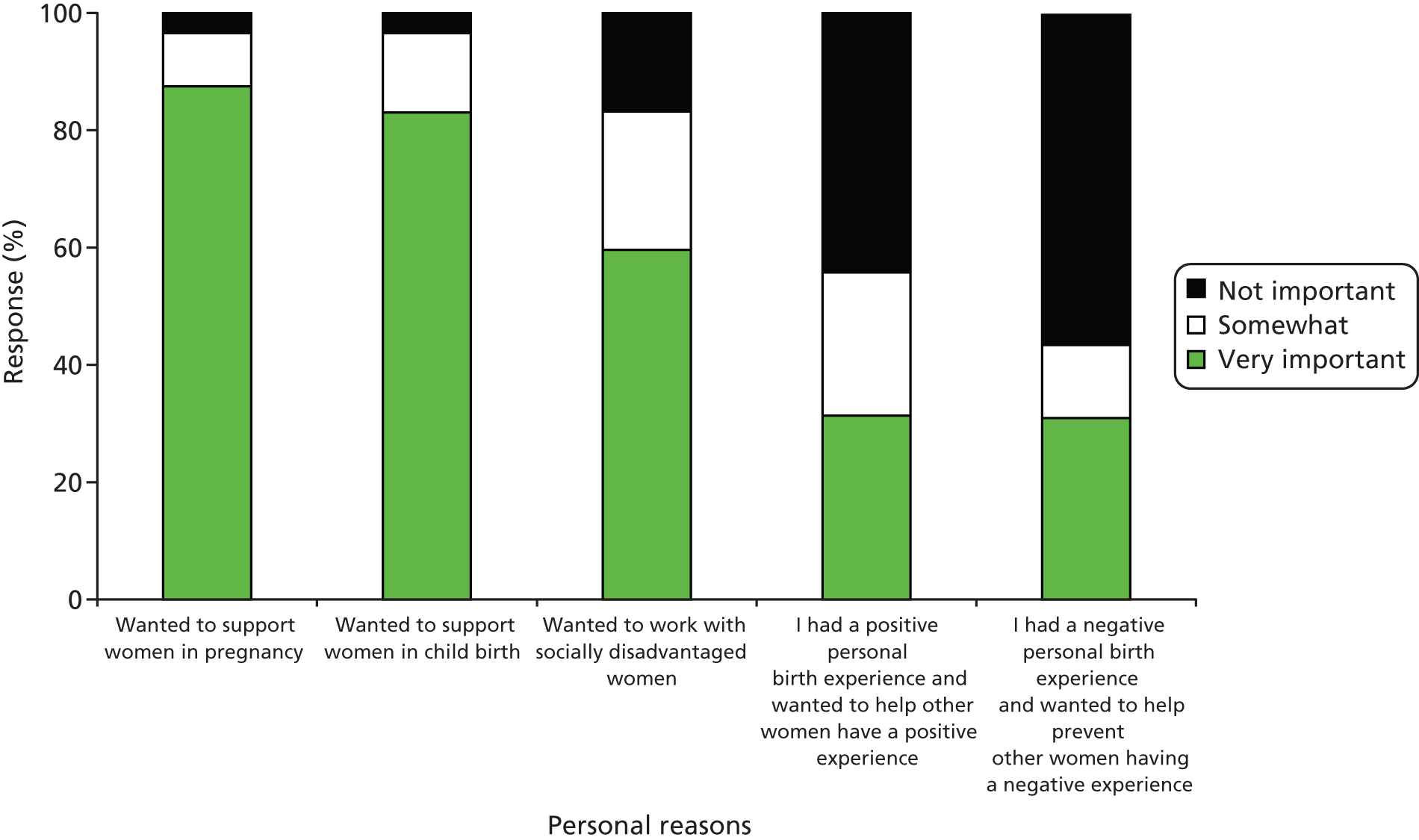
The most common work-related reason for becoming involved (Figure 33) was to use existing skills, rated as ‘not important’ by only 23.9% of respondents (n = 21). Key informant interviews had specifically drawn attention to the tendency for applicants for training to be using it as a stepping stone towards a career in midwifery. Figure 33 shows that ‘To help in applying for further training’ and ‘To help in gaining employment’ were rated as ‘very important’ by approximately one-third of the sample. Both of these reasons for undertaking doula training were more common in more recent cohorts (p < 0.01). ‘Further training’ was ‘very important’ to 15.4% of those who had trained before 2010, 37.1% of those training in 2010/11 and 47.1% of those training in 2012/13. Equivalent figures for ‘employment’ as a motivator were 7.7%, 28.6% and 37.5% (p < 0.05). However, neither of these motivators was related to whether the doula was still an active volunteer.
FIGURE 33.
Work-related reasons for becoming involved.
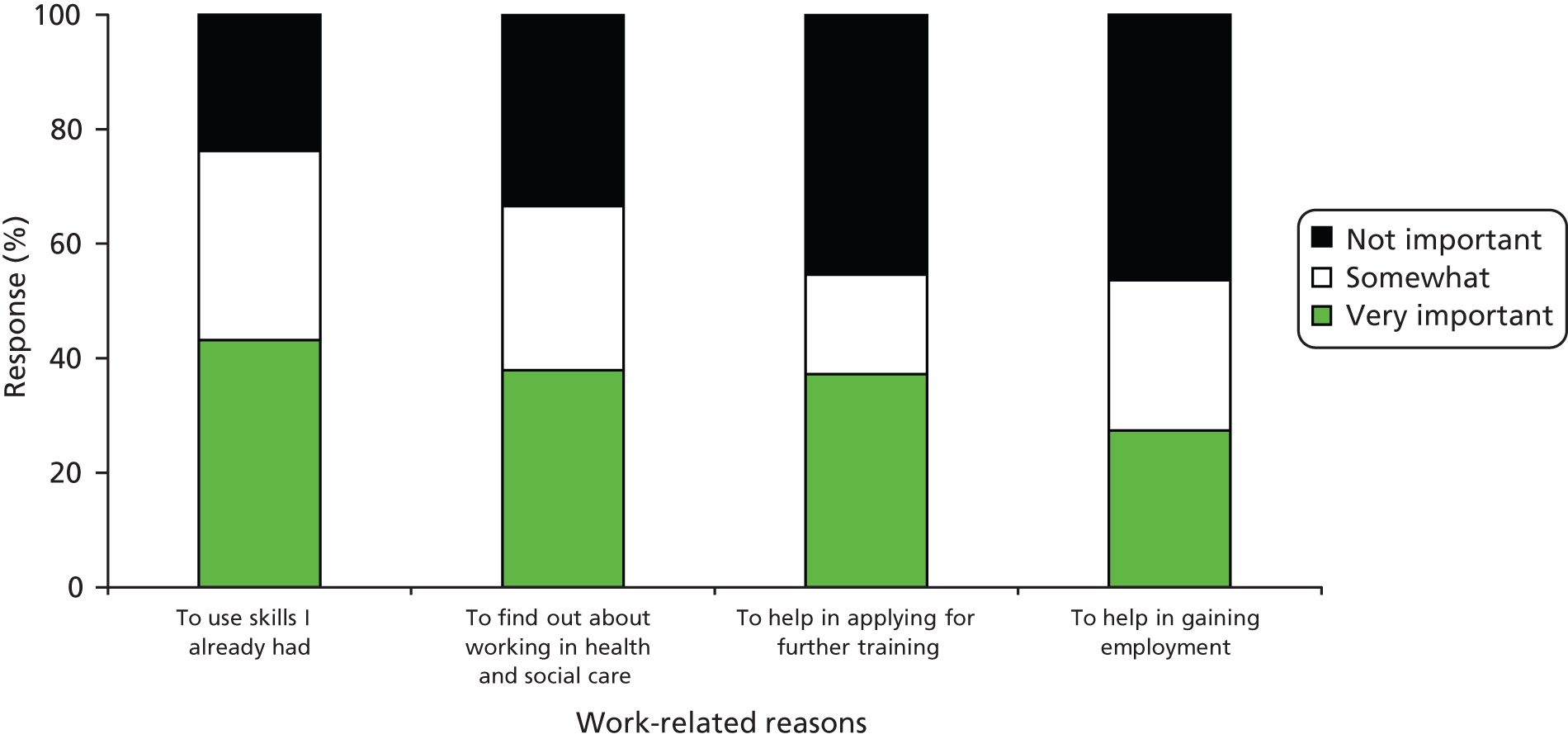
As well as being asked why they had undertaken training, doulas were also asked why they had remained involved. Enjoying their support role and the feeling that they were making a useful contribution were the most commonly endorsed personal reasons, as shown in Figure 34. Work-related reasons (Figure 35) tended not to be seen as being so important, except insofar as these were social and interpersonal aspects of the role.
FIGURE 34.
Personal reasons for remaining involved.
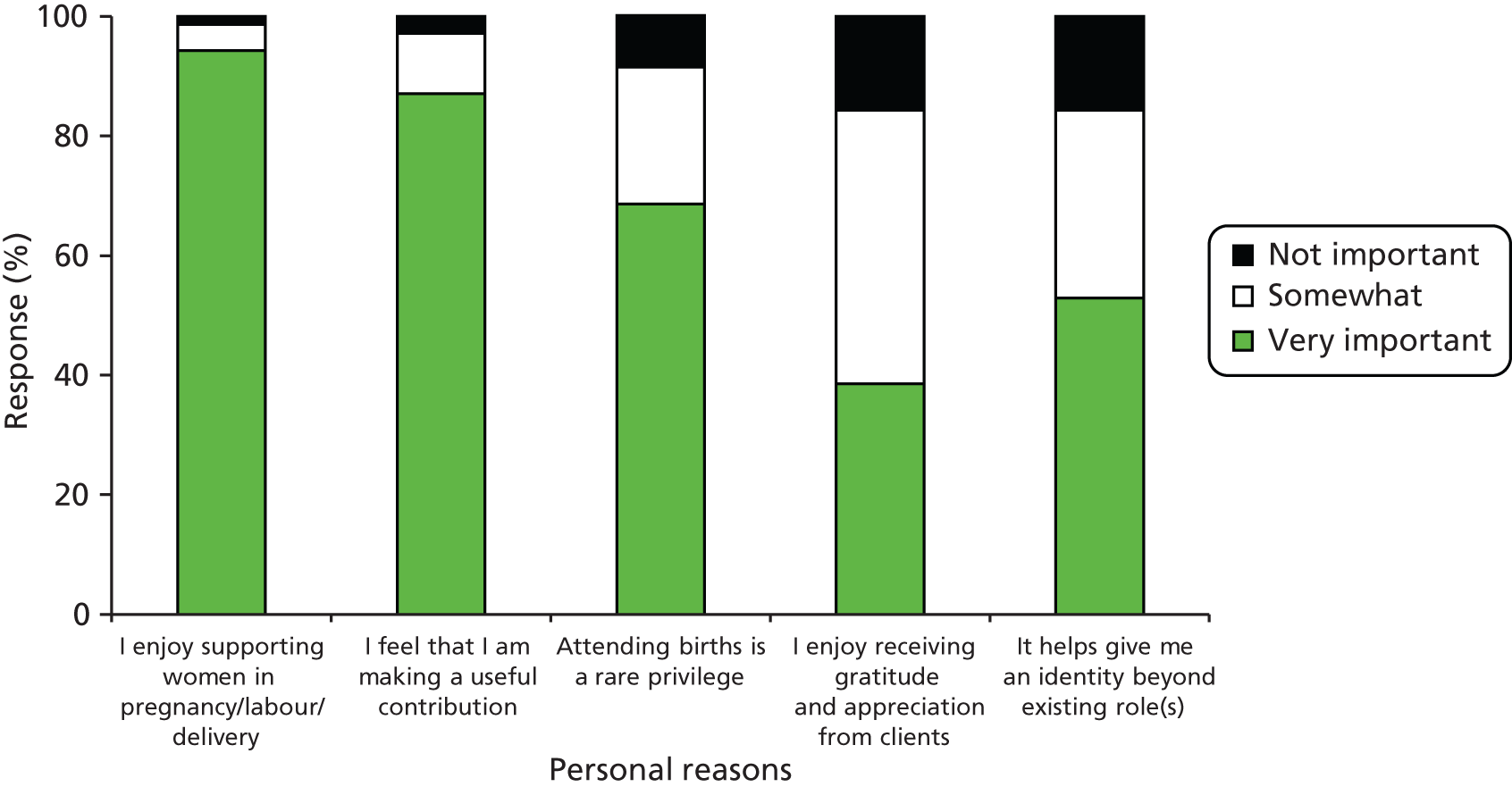
FIGURE 35.
Work-related reasons for remaining involved.
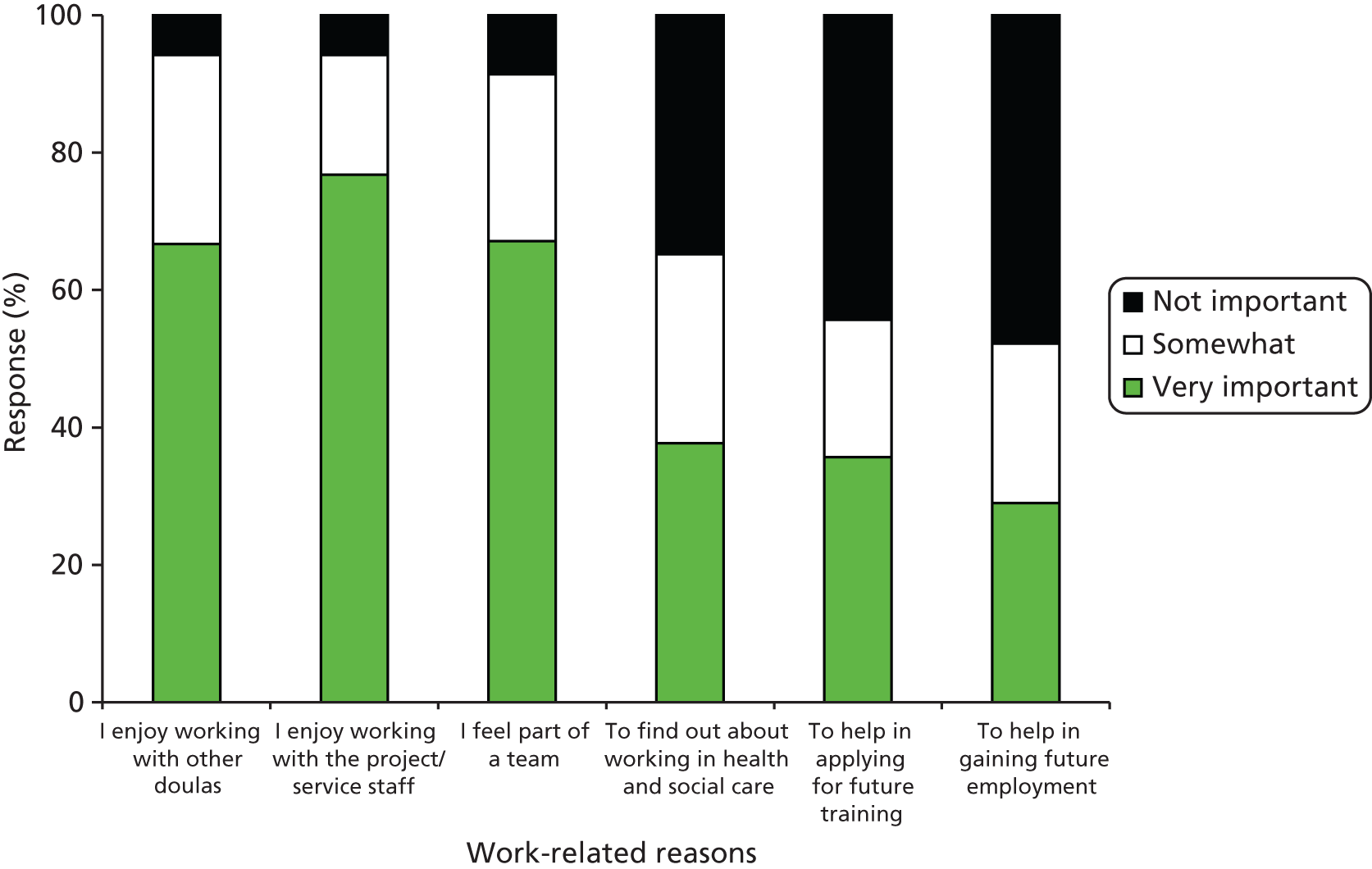
Doulas’ perceptions of the service that they provide
One of the characteristics of the volunteer doula service which marks it out from many other doula services is that support is provided from pregnancy through to 6 weeks postnatally rather than being centred on labour and birth. We were interested to see which of the three time periods (before, during or after birth) doulas thought most important. They were therefore asked ‘If the service could only provide support at one stage, which should it be?’ Responses are shown in Table 23. Only a minority (25%) selected after the birth and the remainder were almost equally divided between before and during birth.
| Response | n | % |
|---|---|---|
| Support before the birth | 35 | 39.8 |
| Support during labour/birth | 31 | 35.2 |
| Support after the birth | 22 | 25.0 |
| Total | 88 | 100.0 |
There were differences between sites, with the majorities at sites A and Y answering ‘before birth’ and the majorities at W and X answering ‘during labour/birth’. Many respondents said that it was ‘an impossible question’ and that ‘all stages are important’, but most still went on to give a single answer.
Doulas choosing ‘before birth’ (39.8%) mainly supported their choice with the argument that in the antenatal period the groundwork can be laid for all that follows:
To help prepare women for birth and beyond. To help build confidence and understanding of what is happening. Also prepare for changes ahead.
Doula 042Y
[P]rovide mums with information and support and confidence for pre-birth, labour and post-birth.
Doula 067X
Those choosing labour/birth (35.2%) generally did so because that ‘is what most women fear the most’ (060Y) and ‘so they wouldn’t have to birth alone’ (059X):
This can be a highly traumatic/emotional time when extra support can make all the difference to mothers experience and baby bonding.
Doula 035A
The smaller proportion who chose the postnatal period (25%) did so because ‘Postnatal support is vital to helping families cope with new roles and baby’ (023A) and ‘This is when a woman can be at her most vulnerable’ (003X):
That’s when I feel the reality hits on motherhood.
Doula 052Z
Doulas were also asked ‘If a service has limited resources, which of these women should be prioritised to receive doula support?’ Response options were ‘Women with complex needs’, ‘Women with no partner/husband’, ‘Women with no support locally’ and ‘Women who actively want the service’. They were asked to choose only one of these options, but many chose more than one; a total of 93 responses were given by 70 respondents, summarised in Table 24. It will be seen that there was support for all of the categories suggested, with the most popular ‘Women with no support locally’ and the least popular ‘Women with no partner/husband’.
| Response | n | % of casesa |
|---|---|---|
| Women with complex needs | 26 | 37.1 |
| Women with no partner/husband | 13 | 18.6 |
| Women with no support locally | 33 | 47.1 |
| Women who actively want the service | 21 | 30.0 |
| Total respondents | 70 | |
| Missing | 1 | |
| Total responses | 93 |
To what extent is the doula role about friendship?
The doula training emphasises that the doula’s role is time limited and that they should keep a professional distance. A number of policies underline this, such as discouraging the volunteers from revealing personal information about themselves and having no contact after the end of the period of support. However, it became apparent during initial focus groups with doulas that this created some tensions because they also saw a necessary element of befriending in their role. Responses to the question ‘To what extent is the doula role about friendship?’ produced varied answers, with the modal answer being ‘a small part’. There was significant variation by site (p < 0.005). Perhaps somewhat surprisingly, doulas at the initial site (A) were the most likely to say that friendship was a big part of the role (54.3%); this is in marked contrast to doulas at site X, where 57.1% respondents thought it was not a part of the role. However, at all sites there were some doulas who thought friendship was not part of their role and others who thought it was a small or big part. Some of the difference in doulas’ views may be explained by different conceptions of the meaning of ‘friendship’. For example, doulas at all sites talked of the key importance of trust, rapport and confidence in their work, whether or not they saw friendship as a part of their role or identified these qualities as components of friendship. Likewise, doulas who thought that friendship was a part of their role were just as likely as doulas who thought it was not part of the role to refer to the importance of professionalism and clear boundaries in their work. Words in brackets indicate the answers that doulas selected in the questionnaire:
We build trust and confidence. (not part)
Doula 064Y
Trust and care/friendship – professional. (small part)
Doula 044Z
There has to be a bond, trust but within boundaries. (small part)
Doula 071W
It is about befriending mums but knowing the boundaries and being able to cut ties at the end of the supporting stage. (big part)
Doula 009A
However, there were some real differences in doulas’ beliefs about the role of friendship. Some saw it as a separate dynamic from trust and rapport, and distinguished friendliness (which they thought was necessary) from friendship; two doulas (at sites W and X) said that they had been told not to become friends with the women they supported. Other doulas saw friendship as a key Mechanism by which trust and rapport would be achieved, so the woman would ‘open up’ and feel comfortable with her doula. A third group saw friendship as a natural and spontaneous human reaction to involvement with the woman they supported:
It is small part friendship but more a relationship of support and trust.
Doula 033A
It’s about being caring and friendly but not being a friend.
Doula 077W
A friendly approach but not a friendship.
Doula 085Y
Women must trust you, an important part of this is mutual friendship.
Doula 030A
You do befriend women as you spend time getting to know them, their needs, their family, culture and it just naturally happens.
Doula 049A
A few doulas suggested that it was important or inevitable that a woman would perceive her doula as a friend, even if the doula did not share that perception, and one went on to explain that it was therefore particularly important to be clear about the boundaries of the role:
It is professional but because of the intimate nature of the role, mothers do think of us as a friend.
Doula 051Z
If the lady doesn’t see you as a friend I think they would not open up to you or want your support.
Doula 050A
I think the lady needs to feel like you are a friend to trust you. The doula needs to explain role fully though or the lady could really think you are a ‘real’ friend.
Doula 039A
Some of the doulas who felt that friendship was a small part of the role provided a clear rationale for this: doula support was time limited and voluntary and it was essential to avoid dependency.
Don’t want them to rely on you as a friend but want to empower and give confidence.
Doula 022Y
You need to build rapport and support but not get too involved as you have to leave them after 6 weeks.
Doula 018A
Doulas’ comments on friendship reflected varying interpretations of the basis of the doula role: professional, peer support, or a combination of the two.
You are providing a service and can’t possibly make friends with every mum you support.
Doula 066A
I would be relating to the women as a mum myself but also as a trained worker.
Doula 089Z
Some doulas also referred to the development of friendships with other doulas or project staff, rather than with the women they supported.
What does the back-up doula role mean to you?
In principle, every woman is allocated both a main doula and a back-up. During the initial focus group discussions with doulas, it became apparent that there were different ways of interpreting the role of the back-up and there were various ramifications of this. For some it was seen as a subordinate role and thus potentially an appropriate initiation for a newly trained doula or one with less time to offer. Some welcomed this as an opportunity to gain confidence, while others talked of feeling let down because such an allocation suggested that they were not good enough. Back-up doulas can feel undervalued. There was a lack of consistency, even within one site, in how the role was interpreted. Sometimes a doula would be assigned as a back-up only immediately before the birth and would therefore not have the opportunity to build a relationship either with the woman or with the main doula. Where there was an element of co-doula-ing, however, doulas valued the opportunity to learn from each other. This was seen not just as a more experienced doula mentoring one who was less experienced but rather as bidirectional learning because, for example, the training changes and different cohorts may have different views and information. Doulas drew attention to the lack of opportunities to discuss experiences with other doulas. (The focus group itself was greatly valued for this reason.) The main–back-up relationship was therefore seen as a potentially important way to stay in touch with other doulas’ norms. It was seen as key that the main doula keep the back-up informed so that the back-up would be fully prepared if required to step in.
The questionnaire to doulas therefore asked ‘What does the back-up doula role mean to you?’ As Table 25 shows, the majority (60%) viewed it as a reserve role. Those answering ‘other’ mainly said that both could apply depending on individual circumstances:
It depends on the family involved and how much they want/need a back-up doula. Some mums appreciate getting to know back-up well. Some mums just want one to one support.
Doula 069A
| Response | n | % |
|---|---|---|
| A reserve in case the main doula cannot attend | 42 | 60.0 |
| Someone who supports a woman jointly with the main doula | 16 | 22.9 |
| Other | 12 | 17.1 |
| Total | 70 | 100.0 |
For further insights into the way that the role was viewed, doulas were asked ‘Should the back-up always be introduced to the woman?’ As Table 26 shows, the majority thought that the back-up doula should be introduced at the second visit, but a substantial minority, mainly from site A, indicated ‘other’ with variations on this, although all agreed that it was desirable that an introduction during pregnancy should take place. This comment from site A was a minority view:
Have always only thought of my back-up doulas as an emergency only. So unless I am taken ill I will be the doula doing all visits.
Doula 039A
| Response | n | % |
|---|---|---|
| No need for woman to know the identity of back-up until/unless she’s needed | 2 | 2.8 |
| Woman should have contact details but does not need to be introduced | 5 | 7.0 |
| Introduce at the same time as the main doula | 15 | 21.1 |
| Introduce at the main doula’s second visit | 33 | 46.5 |
| Other | 16 | 22.5 |
| Total | 71 | 100.0 |
More typically doulas drew attention to the advantages primarily for the mother but also for the back-up doula:
The mum needs to be relaxed about who is around them at such a vulnerable time but needs to get to know the main doula a little first.
Doula 037A
You need to build a rapport with mum as well, or it would be like having a complete stranger at the birth should you be called.
Doula 001Y
So mum feels comfortable with both and so back-up doula feels involved.
Doula 006X
It was implicit in most comments that the back-up’s role was most likely to be during labour and birth, but a small number explicitly considered other possibilities:
I think that sometimes it is good for woman to meet back-up doula, however sometimes unnecessary. If woman wishes doula to be birth partner, I think it is good to have visit. However, if the woman just requires a few visits in pregnancy (e.g. extra support) and not birth partner, then unnecessary to introduce back-up doula (not good use of back-up doula’s time).
Doula 030A
A telephone interview with a doula at site X outlined another model:
recently they’ve changed the policy whereby they’re encouraging two doulas to support a mum, nobody is a back-up, both the doulas go in and meet the mum together.
Doula 067X
She went on to explain that she and the co-doula each have restricted availability, so:
we negotiate that we go at separate times. And that way the mum gets more out of the doula scheme than having us both there . . . she’s a lone lady this mum, she’s got no support and this way she gets two meetings as opposed to one, I think I’d really, really struggle to go three or five times in a week, I won’t, I could perhaps manage two but definitely would struggle to do three to four. It’s about managing expectations, isn’t it, I think when we set out to do doulas they said go out once a week, at least an hour, unless mum needs you again. So, the two doulas work well but they do have to be matched very carefully, if there’s no careful matching then it’s not going to work.
What is it about how the doula service works that makes it different?
This was an open-ended question answered by all of the doulas who had supported women at sites A (32 of 32) and X (seven of seven), but omitted by two of six at W, 3 of 18 at Y and four of eight at Z. Thus, at each of two sites (W and Z) there were only four responses.
At all sites, doulas described the one-to-one and woman-centred nature of their support, tailored to individual needs and delivered on the woman’s terms at a time and place of her choice:
One to one service, tailored to the woman and her family’s needs.
Doula 016Y
They noted that they were able to provide continuity when with ‘other services it may be a different face at every appointment’ (Doula 029A) and that this enabled them to build up a relationship of trust:
The service offers continuity, hand holding for 8–12 weeks within the home.
Doula 053X
The same face each time therefore building trust and confidence in the mother.
Doula 007A
Specifically, they had time for women when other services might be under pressure:
We have more time for mums and parents-to-be, quality time.
Doula 001Y
More personal service where women can talk to a ‘human being’ that has got more than 10 minutes to listen. Support in labour/birth that sometimes midwives are too busy for.
Doula 031A
Some doulas described their support as very flexible, available round the clock if needed:
Support unlimited at the mum’s convenience.
Doula 067X
It is one to one support as and when a mum needs it. My mums can contact me whenever by telephone if they have concerns.
Doula 069A
At all sites doulas highlighted the empowering nature of doula support, linked to a commitment to informed choice:
It enables women to feel supported by someone who has knowledge but not there to teach or preach at them.
Doula 023A
Demonstrate to women they are in charge of their birth experiences and have choices.
Doula 059X
It’s totally about supporting the woman with her own choices.
Doula 056Y
Doula provide true confidence and the empowerment to make decision of their own.
Doula 045Z
At three sites (A, X and Y) the doulas said that listening was an important aspect of their role and at three sites (A, Y and Z) they said that their support was non-judgemental. This was particularly marked at site Y:
We offer a non-judgemental, sympathetic [service] and we listen to anything.
Doula 017Y
We offer a support that is non-judgemental to women that maybe feel they are sometimes judged by other people.
Doula 041A
At two sites (A and X) doulas mentioned advocacy and being on a woman’s side:
Because we have relationship with mum she feels she trusts us as we always work on behalf of mum.
Doula 002X
You are on her side providing emotional and psychological support. You act as her advocate.
Doula 012A
Someone who solely concentrates on the mum . . . someone on her side.
Doula 086A
Many doulas commented on the fact that they were volunteers. For some doulas this affected the terms of their relationship with women, who they felt would be more likely to trust and relate to someone who was not a professional but a ‘peer’:
I feel we are different because we are volunteers with a non-professional interest, therefore a lot of the women we support and come into contact with feel they can maybe relate better.
Doula 033A
We are not professionals; so there is no barrier. It’s peer support.
Doula 042Y
Some expressed this in terms of the relationship being non-threatening, more friendly and relaxed, or less intrusive than other services, and without any hidden agenda:
It’s not statutory [so] mum can feel relaxed.
Doula 088Z
One to one relationship that allows a woman to relate without interference from regulatory services.
Doula 027Y
Others felt it would enhance trust because women would appreciate that the doulas were giving up their own time:
Because it is voluntary women can see how dedicated doulas are to their roles.
Doula 049A
A couple of doulas went on to equate their role with befriending or mothering:
More friendly approach as not a medical professional, we are more as a friend supporting.
Doula 036A
We are like surrogate mums to these women.
Doula 069A
It’s a non-professional mothering the mum-to-be role.
Doula 088Z
Doulas’ views on how their role affects women
Doulas were asked how they thought that doula support had an impact on women in a range of ways. Virtually all respondents (97.1%) thought that it helped women access different services and/or join different groups. Eighty-one per cent thought that it helped women to meet other mothers. Those not agreeing with these statements thought that doula support had no effect on these behaviours; none thought that it had a deleterious effect. All respondents agreed that doula support increased women’s knowledge and skills around pregnancy, childbirth and looking after a baby. This was explained in two ways. A frequent response referred to direct transmission of information from the doula to the woman. However, another prevalent response, particularly at sites Y and A, identified the woman as an active agent and the doula as an enabler, thus, for example:
Gives them choices, information and confidence.
Doula 049A
A doula encourages women to have an informed choice and they seek info together.
Doula 003X
Able to feel more confident and ask more questions.
Doula 008Y
Awareness + confidence = empowerment.
Doula 016Y
This support allows them to get better understanding of coping and knowing support sources around them.
Doula 045Z
The majority (88.4%) also thought that having doula support helps women to make lifestyle changes for the health of themselves and their babies, most frequently citing breastfeeding, smoking cessation, diet and cutting down on drugs. A similar distinction was seen in the explanations of how this was achieved. Most referred to women now having knowledge that they did not previously have, for example about how to breastfeed. Others, though, referred to women making informed choices and having confidence to make different choices.
Finally, doulas were asked to tell us about any other positive or negative effects that doula support has had for women. Most responses reinforced and summed up earlier answers.
Doula support has a positive effect by empowering woman to make choices and signposting them to other services to receive support.
Doula 014A
Women feel empowered because they’ve chosen how, when, where, instead of being told what to do.
Doula 017Y
If we have enough time to make a close relationship with the woman, our input can be amazing.
Doula 054A
Only two responses mentioned any negative effects:
Some feel a loss of friendship at the disengagement time.
Doula 028A
One lady became reliant on me, had to gradually decrease time with her.
Doula 029A
Matching issues
Interviews with doula service staff had emphasised the importance of matching the woman and the doula as a prerequisite (Context) for a good relationship to develop. However, we had some difficulty in establishing on what basis the match might be made. The questionnaire therefore asked the doulas how important they considered each of a number of attributes to be. As Figure 36 shows, ‘getting on well together’ was rated as most important, which relies on a judgement by the project staff about who will get on with whom. No other attribute was rated as ‘very important’ by more than 11 respondents. Most doulas (70.1%) rated ‘similar background’ as unimportant, reflecting perhaps the fact that most doulas are not of a similar background to the women whom they support. ‘Speaking the same language’ and ‘doula’s age’ were both rated as unimportant by nearly half the sample (41.4% and 47.1%), again perhaps showing cognitive consistency with the realities of doula and client demographics.
FIGURE 36.
How important is each of the following when allocating a doula to a woman?
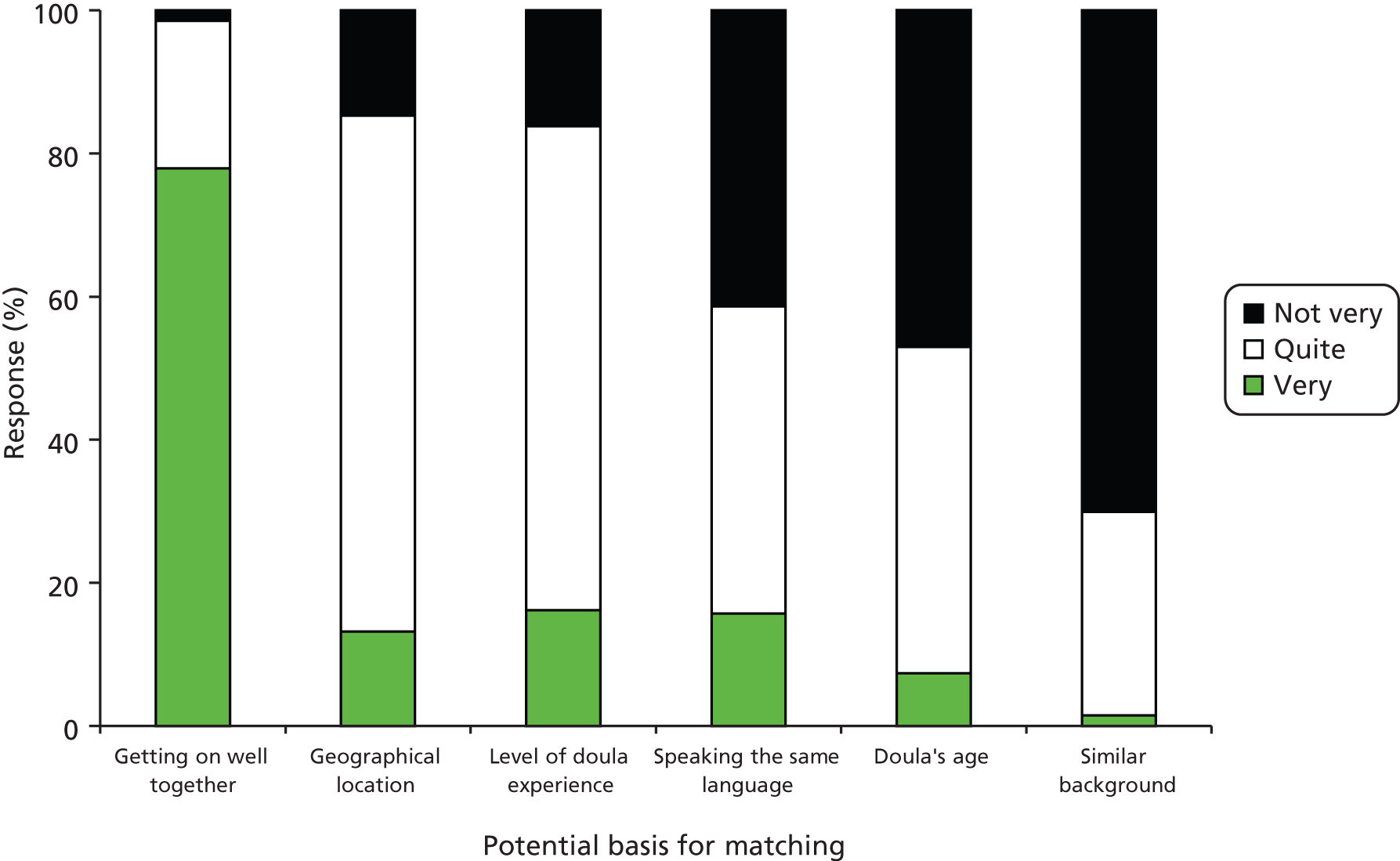
Should doulas have had a child themselves?
Doulas were also asked how important they thought it was that a doula should have had a child and/or parenting experience herself. This question was also asked of those who had not yet supported a woman. One-third of respondents (33.7%, n = 30) said it was not important, 43.8% (n = 39) ‘quite important’ and 22.5% (n = 20) ‘very important’. This varied by site, with only one doula from site A (2.9%) saying that it was ‘very important’, compared with 38.5% at W and 45.8% at Y. The reasons given for why it was not important included:
’Cause it’s not about our birth experiences.
Doula 015A
A doula can support and advocate for a woman if she has no children – that’s like saying a nurse cannot look after a patient who has had a cardiac arrest if she hasn’t had one!
Doula 049A
Be[ing] qualified and properly trained is enough to conduct and support a mother.
Doula 047Z
Those who thought that having your own experience was important mainly felt that this gave them insights and empathy that someone who had not given birth would not have:
Because if you have been through the same situation you have more understanding of what they are going through.
Doula 037A
I feel there are experiences that you cannot learn and you are able to empathise – relate to the woman better.
Doula 003X
Experience and knowledge together is a fuller package.
Doula 022Y
Two commented that they had been a doula before they had children of their own, but now felt that their experience had added to what they had to offer. Some stated their position in quite extreme terms:
Can’t preach what you haven’t practiced.
Doula 062Y
How can you give good advice, if you’ve never needed it yourself!
Doula 052Z
Some also made the point that:
The client may feel more confident in her doula if she has experienced childbirth herself.
Doula 014A
Those rating personal childbearing experience as ‘quite important’ were more likely to feel that it was ‘more of an advantage than importance’ (007A):
I don’t think it is essential for all women but some women may find it more reassuring to have someone supporting them who has personal experience of labour and pregnancy. If the doula is knowledgeable and confident this should not matter.
Doula 048A
Knowledge, empathy and professionalism matter most but the mothers I worked with were reassured that I had also given birth so knew what they were experiencing.
Doula 051Z
Matches that were ‘not the best fit’
Fifteen doulas felt that they had had matches that were ‘not the best fit’; these represented all five sites. In some cases this was put down to the doula’s own inexperience at the time or where the woman wanted something from the service (e.g. child care) which was not on offer. There were other examples where the woman was not really engaged:
The woman was hardly in contact – think she felt she had to have a doula – but didn’t want one.
Doula 039A
Only a minority of examples did specifically relate to matching, that is it was implied that a different doula–woman combination would have been more successful:
Some people you get on better with than others.
Doula 018A
Young woman who did not want support from an older doula.
Doula 027S
Could just tell the teenager wasn’t happy, but her main doula was ok for her.
Doula 017S
The woman thought I had more experience than I did and she wasn’t very keen when she found out.
Doula 080
Timing of when the mother meets the doula
In addition to the ‘who’ of matching, early key informant interviews had also talked about the ‘when’. Doulas were therefore asked ‘Do you feel that your relationship with a woman is affected by the timing of when you meet?’ Response options were ‘yes’, ‘no’ and ‘depends on the woman’s needs’. Perhaps surprisingly, just over half (5.2%, n = 37) said no, with 13.4% (n = 9) saying yes and 31.3% (n = 21) saying that it depended on the women’s needs.
All the doula services target ‘disadvantaged’ women; two are restricted to women from minority ethnic groups and a third serves an area with a very large minority ethnic population. Thus, it is to be expected that many women will not speak English, and this was borne out during data collection from women. Fifty-one per cent of the doulas (n = 36) said that they had supported a woman who did not speak English, and only seven of these (18.9%) said that they and the woman spoke the same language; one of them had also supported another non-English speaker with whom she had no common language. Thus, a substantial proportion of the volunteer doulas (30 of 71, 42.3%) had supported a woman without the benefit of a shared language. Somewhat surprisingly, the site with the highest percentage of doulas who had supported a non-English-speaking woman was site A (71%). This may reflect the greater experience of site A doulas rather than a higher proportion of non-English-speaking women.
A telephone interview with a site A doula who had worked with interpreters added to the questionnaire data:
I had had a few problems with the interpreter in that instance as well, where the interpreter sort of took over really, and didn’t interpret but actually did my role as well, in some, a little bit . . . she actually acknowledged that she had done that, and the next time I thought she was entirely different.
Doula 069A
However, she went on to make the important point that:
most of the family seem to know them [interpreters] quite well so they must come across them quite regularly, and they obviously have a really good bond with them, it’s just a little bit of an obstacle I guess, to just get the response that you would have with someone who speaks your language.
Doula 069A
A telephone interview with a bilingual doula raised the situation where one doula can communicate with the woman in her own language but the other cannot:
I’ve been interpreting, I don’t mind doing it, but I personally don’t think it’s fair on the other doula. Because I’m developing my relationship with the mum and the other doula can’t because there’s this big barrier, so I’ve had to do all the interpreting, which I don’t mind doing, but I just don’t think it’s the essence of what the doula scheme is all about.
Doula 067X
This doula also raised another issue about second language use:
with the doula scheme in X we’re allowed to use a second language in the homes but not in the hospitals.
Doula 067X
Barriers and challenges
Doulas were asked if they had ever been unable to attend a labour/birth that they had planned to attend. Twenty-eight of the 69 responding (40.6%) answered yes, although only 18 answered the following question to indicate how often this had happened. Most of those answering (89%) indicated once or twice. Reasons why this had occurred were: woman did not contact the doula (25%, n = 7); doula was not available (28.6%, n = 8); circumstances changed (25%, n = 7); labour occurred sooner than expected (28.6%, n = 8); and health professional did not allow (3.6%, n = 1). (More than one reason could be given; hence, the total is greater than 28.) Eight respondents offered additional reasons, which were in fact elaborations of those mentioned, such as the woman having a C-section or the mother having moved away ( = changed circumstances). One mentioned that the back-up doula was there in her place and another that the woman had chosen not to contact the back-up doula. In a number of cases it was apparent that the woman’s partner or other family member had been there instead. When the doula was asked how she felt about not having been able to attend, the majority said ‘disappointed’ or ‘gutted’, with some also feeling ‘guilty’ and that ‘I had let her down’. However, others, especially from sites A and Y, were able to be more philosophical:
The lady either made the decision not to let me know or had enough support. So I’m ok with that. Happy.
Doula 039A
Doulas were also asked about other, antenatal or postnatal, situations where they had been unable to support a woman in the way that they would have liked. Thirty (42.3%) said that this had occurred. Twelve (16.9%) said that this was because of the boundaries of the doula service; five (7%) because of limits placed by health professionals; ten (14.1%) because of lack of time; and 14 (19.7%) because of the complexity of the woman’s needs. (More than one reason could be given; hence, the total is greater than 30.) Additional reasons given were language and cultural barriers, barriers placed by the woman’s family, the mother disengaging and reasons personal to the doula.
Communication problems were reported by 36 doulas (50.7%). Most commonly these were with women whom they had supported (27.1%, n = 19). Four (5.7%) reported problems with a woman’s partner or husband and two (2.9%) with other family members. Communication difficulties with women or their partners or families were nearly all ascribed to lack of a shared language, but there were some additional examples given:
Mum wanted birth support and would have benefited from this however husband was not comfortable so [I] was unable to attend.
Doula 009A
Extended family dubious of service regardless of being informed – control aspect.
Doula 053X
Four doulas (5.7%) reported communication difficulties with doula service staff (two different sites); five (7.1%) with another doula; nine (12.9%) with a health professional (mainly midwives); and five (7.1%) with staff at other agencies – mostly social services.
Being ignored by one or two midwives on the labour ward once I introduced myself as a doula. Most are lovely though.
Doula 069A
Midwife failed to contact me when a mum needed me.
Doula 017Y
Interpreters not attending when booked.
Doula 018A
Have you ever felt out of your depth?
Doulas were asked if they had ever felt out of their depth. Two (2.9%), from two different sites, answered ‘often’; 18 (26.1%), from four different sites, ‘occasionally’; and 49 (71%) ‘never’. The examples given from site A reflected the increasing emphasis on women with complex problems: drug abuse; domestic violence; and babies being taken into care. However, there were also references to language problems and to inappropriate expectations.
Complex cases were also mentioned by one respondent at site Y. Comments from other sites referred to communication issues that will be explored further below, such as with a rude and non-communicating midwife (064Y) or a non-participating back-up doula (047Z). Two further comments raised training issues: one who had needed more knowledge of the benefits system (060Y) and one who felt she had not had enough practice with massage and birth positions, although ‘I revised with a fellow doula which helped’ (059X).
How the doula service fits and works with other services
Do you feel that a professional has ever misunderstood your role?
The majority of the sample (64.3%, n = 45) had never felt that a professional had misunderstood their role, which is very heartening. However, 12.9% (n = 9) said that it had happened once and 22.9% (n = 16) said that it had happened more than once. Examples given provide interesting insights into doulas’ clear perceptions of their role and its boundaries:
Midwife/social worker. They sometimes see me as a support worker rather than a volunteer.
Doula 026Y
[Thought I] was here ‘to mop her brow’. Treated like a lady’s mum. But once discussed, my role is understood.
Doula 039A
Social worker contacted me for information. Directed her to Service Manager.
Doula 054A
Others suggested that they made professionals uncomfortable:
Expecting more than we can offer, feeling threatened by our role.
Doula 003X
They don’t know the [parent organisation] and not sure why I’m there if I’m not a friend or family member or health professional.
Doula 051Z
A small number alluded to ‘teething problems’ with midwives when the service was new, with the implication that these had been overcome, and others that certain professionals were simply unaware of their role or had never heard of a doula:
Early days professionals were dubious of doula service – but through hard work and marketing we have built a good rep[utation?].
Doula 053X
In a telephone interview, one doula reinforced that these were isolated occurrences and that they could be dealt with:
It’s usually particular individuals, it’s not the midwifery team as a whole; most of them are absolutely wonderful . . . I have had three instances where the midwives have been difficult, but I have had a lot more where they have been wonderful . . . Well I actually spoke to somebody at the doula office about the recent situation . . . when I was asked if I wanted to take it further I said no, what I am going to do is try and build a relationship with that person because I will be seeing her quite regularly so I would rather change her views through building that relationship, and if I can’t I can’t.
Doula 069A
Do you feel the role of doula is clear in relation to the role of other services?
Eighty-five per cent (n = 57) felt that it was clearly a different role and, perhaps surprisingly, only 14.9% (n = 10) thought that there was overlap with other roles (four failed to answer the question). The most obvious overlap was with the midwife’s role, both the support function and that of signposting to other services:
Sign-posting – baby cares etc. HV [health visitor] and MW can also do these. I think we can free up professionals time by helping in this.
Doula 039A
More than one respondent at site Z implied that midwives took advantage of this overlap:
Midwife leaves you to it!
Doula 052Z
A small number of respondents also mentioned overlap with other voluntary organisations and one suggested that areas of overlap between different services could cause confusion to the mothers.
How well do you feel that you and midwives work together?
Six respondents answered ‘not applicable’, as their role had not yet brought them into direct contact with midwives, and one omitted the question. Of the remainder, 67.2% (n = 43) answered ‘well most of the time’, 31.3% (n = 20) ‘well some of the time’ and one person (at site A) answered ‘not well at all’. This seemed to be mainly for the reasons outlined in the earlier questions, with an additional couple of examples of particularly poor communication being given from site X and site Y:
Midwife was very rude, did not show respect for anyone, would not communicate.
Doula 064Y
Our CMOs had led to the hypothesis that role ambiguities and working relationships would be better in the sites where the service had closer NHS links, but no significant between-site differences were found for any of the three questions just reported and, as indicated, examples of friction were isolated.
How well do you feel that you and other health and social care professionals work together?
Five respondents answered ‘not applicable’, as their role had not yet brought them into direct contact with other health and social care professionals, and one omitted the question. Of the remainder, 57.1% (n = 40) said ‘well most of the time’, 32.9% (n = 23) ‘well some of the time’ and two answered ‘not well at all’. Here a significant between-site difference was found, with more problems being reported at sites W and Z. However, numbers at both of these sites were small.
Have you ever found any barriers to signposting women to other services?
Twenty-four per cent (n = 17) of respondents said that they had experienced difficulties with signposting. The reasons for them were ‘I did not know what services were available’ (four); ‘A lack of available services’ (eight); ‘Waiting times for services’ (10); and ‘Women not wanting to use the services’ (nine). Two ‘other’ reasons were given:
Frustration at services passing the buck.
Doula 001Y
Sometimes it’s too early for the mums to know what they might want.
Doula 037A
Have you ever felt there were too many other services involved in supporting a woman?
Only eight respondents answered yes to this question (11.6%). The effects of this were felt to be ‘Disrupt or interfere with other support work going on’ (four); ‘Repetition of support by different people’ (seven); ‘Contradictory support given by different people’ (six); and ‘Woman does not appreciate the support because receives so much’ (seven). One other response was:
Woman gets confused about each person’s role and what they are there for.
Doula 037A
Endings
Another theme to emerge from initial discussions with doulas concerned the ending of their period of support to women. As we have seen, doulas were conscious of the tensions caused by a ‘temporary friendship’, but were all well aware of the rules which require them to terminate their relationship with the woman once the period of support has ended. We were told about how some women may create a crisis to keep the doula involved and that women may become overdependent on their doula. This is seen as the point at which the doula needs to hand over to other networks. Doulas understood that the relationship needs to end so that they can go on to support other women. Some, nonetheless, found the ending difficult although it was felt that, with experience, it was possible to learn to distance oneself. It was also pointed out that saying goodbye may be a positive experience; they hope to leave the woman in a better position where she now has the confidence to cope without the doula. All agreed that it was important to prepare women for endings and spoke about the different strategies that they used. This was clearly a very important issue and was therefore explored further in the questionnaires.
Doulas responding to the questionnaire confirmed the importance of this topic and described three strategies to prepare a woman for the ending of support. The first was to be explicit from the outset about the end date for support, and to give reminders nearer the time, although it varied whether the doula gave these reminders frequently or just before the end. Some doulas said that they reduced their visits towards the end or involved the woman in arranging the end:
Tell them 2 weeks before, keep reminding them it’s only 6 weeks after birth, cut the hours a week down.
Doula 011X
Reminding her a few weeks beforehand – deciding a ‘last day’ together.
Doula 051Z
The second strategy was to ensure that the woman was connected, or at least signposted, to other local sources of support such as children’s centres or postnatal groups, or relevant agencies:
We look at where she can meet new people, build a support network.
Doula 072A
The third strategy was to focus on building up the woman’s own emotional strength by positive reinforcement:
Reassure her that she will be fine and is doing a great job.
Doula 009A
Doulas felt that this would leave the woman ‘prepared and empowered’ (086A), ‘self-sufficient’ (060Y) or ‘independent . . . confident’ (047Z), and some doulas described how endings were easier if the doula felt she had achieved this:
By the end the woman will hopefully no longer feel the need for you to visit.
Doula 025Y
It’s nice to see mum standing on her own two feet and that you have done your role well.
Doula 010Y
What makes for a difficult ending?
At all sites the main thing that doulas said made an ending difficult was when they had formed a bond of friendship with the woman and were not allowed to have further contact:
When you have a real friendship and both want it to continue.
Doula 028A
When you have bonded well and really helped mum through difficult times.
Doula 001Y
Never being able to see or speak to that family again.
Doula 086A
A couple of doulas said it was difficult if this relationship was one-sided:
When they want you to still be their friend.
Doula 018A
Some doulas identified a woman’s overdependence on the doula as a problem for endings. One described this as ‘giving too much support’ (034Y). Some saw this issue from the opposite point of view, in terms of unmet needs: if the woman was very isolated and not yet fully ready to cope, it was difficult for the doula to have to withdraw.
If women feel they still need you, they are lonely, low confidence.
Doula 003X
When a mum has really needed the support and doesn’t think she could cope alone . . . It’s an emotional time for both doula & woman and they sometimes feel abandoned.
Doula 066A
If you both don’t want to end the support especially if all issues not resolved.
Doula 012A
Some doulas were not confident that there was other adequate support available. In considering how endings could be done differently, many doulas responded that they did not know or that there was no way to do endings differently. Others made various suggestions, most commonly that the support should be more flexible around the mother’s needs:
Maybe offer extra time for 1st time mums – until they feel able to cope alone.
Doula 090W
6 weeks should be a guide. Sometimes a little more is needed e.g. hospital appointments for mum or baby.
Doula 039A
It was also suggested that support should be phased out rather than cut off, or that the ending of contact should not be absolute but supplemented with catch-up sessions or informal contact if the doula and woman so chose. On the other hand, a few doulas thought that ongoing contact would carry its own risks:
It’s best not to follow-up otherwise the emotional connection will be difficult to break off.
Doula 047Z
If we could stay in touch with the mother it may put the volunteer in difficult positions e.g. being called to a problem she is having or constant phone calls.
Doula 042Y
One doula suggested that articulating the reality and importance of the relationship would support feelings of closure:
You always need to remember the rules and the reasons for them, about professionalism given by the doula project, but say to the mum and family also you will never forget the time you spent together with them and that you will cherish it in your heart always.
Doula 065A
Another suggested that the doula could turn to project staff for emotional support around the ending:
Bad endings can be turned to good endings by talking to management team – getting there early for support rather than leaving it ‘til too late.
Doula 053X
Another doula said that it was easier to overcome feelings of loss if the doula went on to support another woman quickly:
Hardest part of being a doula. It is easier if meeting a new mum that week.
Doula 069A
Several of the doulas reflected that accepting endings was an inherent part of their role:
It’s a service with a natural time line. Bit like teaching a bird to fly.
Doula 088Z
Preparing something for the woman as part of the ending was the norm: 71.4% (n = 45) of those answering said that they did and 28.6% (n = 18) that they did not. (Eight did not respond.) Of these 45, 28.9% (n = 13) said that they prepared an account of the time spent together, 66.7% (n = 30) a birth story and 62.2% (n = 28) photographs. Giving a birth story was much more likely at site A (85.2%) than at other sites, and similarly giving a photograph (81.5%), but numbers responding at the other sites were all low.
Ten respondents (22.2%) indicated that they gave something else. Three, at three different sites, said that they gave a small card or gift for the mother, the baby or both. The other seven, representing all sites except W, referred to less concrete things that they gave the mother, for example:
Ensuring they are confident in accessing services.
Doula 047Z
Sum up the (positive) changes I have seen.
Doula 026Y
The majority of respondents (64.1%, n = 41) said that they had been offered a token of appreciation by women, while 23.9% (n = 23) had not (seven failed to answer this question). This was least likely at sites X and Z, although the numbers of respondents from these sites are small. Since the protocol forbids doulas to accept gifts from women, respondents were asked if an offer of a token of appreciation had ever caused any problems. Five said yes:
Mum became very upset when she was told by the doula office that I could not keep the gift.
Doula 069A
One woman wanted to prepare a meal for me and for me to bring my daughter – she was upset and possibly offended when told this was not allowed.
Doula 048A
Twenty-one of the 64 doulas answering the question (32.8%) said that they had contact or received updates beyond the official ending. This proportion was approximately the same at each site, except at site X, where it was zero. Most respondents (77.3%, n = 51) would like to have more update information on women whom they have supported. This proportion was approximately the same at each site, except at site Z, where it was zero. Fifty per cent (n = 32) said that there had been women with whom they would have liked to have stayed in touch after the official ending. Reasons given were concern about the woman (n = 11); concern about the children (n = 3); feeling that the woman needed continued contact (n = 13); and that she had no-one else (n = 7). Eighteen respondents gave additional reasons, 15 of whom alluded to friendship which either had developed or it was felt could have developed. The remaining three focused more on confirmation of progress and outcomes:
It’s nice to observe the parent parenting confidently and affirms the time spent working with her.
Doula 026Y
In a telephone interview, one doula said that her strategy was to move on immediately to a new match:
your focus has to immediately change to somebody else and that’s the only way I find to deal with that ending,
Doula 069A
Impact on doulas
Emotional impact
Has being a doula affected you emotionally in terms of revisiting your own previous experiences of childbirth?
Eleven respondents replied ‘not applicable’ to this question. Of the remaining 59, 18 (30.5%) said that they had been affected. Typical responses were:
In so many ways – I understand my own experiences now and the impact they have had on my life and am able to move on.
Doula 003X
You do revisit your experiences but it is quite a therapeutic process.
Doula 069A
Others referred to now realising that:
you don’t have to do as the staff say! It’s your birth.
Doula 039A
Where the respondent had herself had a good experience, however, there was a danger of disappointment, if events went differently for the woman she was supporting:
Feeling sad that my ‘mum’ didn’t have a birth like I had which was empowering and amazing, where my ‘mum’ had lots of drugs and a horrible time. I thought I could help her more than I did.
Doula 006X
Has being a doula exposed you to difficult experiences that have affected you emotionally?
Twenty-two out of 70 respondents (31.3%) answered yes to this question. As one might expect, some women were affected by difficult births:
Traumatic birth haunted me for a while.
Doula 051Z
There was also reference to the emotional impact when the period of support ended:
Leaving mums is very difficult. I think of all my mums regularly and wish I could get updates from the doula service about how they have got on.
Doula 069A
However, examples given in response to this question were not all negative:
Positive effect as realised how strong I can be!
Doula 023A
Made me feel lucky to have what I have.
Doula 019A
Emotionally I have felt humbled by the depth of problems that some women face and how they overcome them.
Doula 035A
Impact on health and well-being
How has being a doula affected your health and well-being?
As Table 27 shows, over half the sample considered that their health and well-being had improved as result of being a doula. The explanations given were mainly in terms of an increased sense of confidence and self-worth, and in some cases this was explicitly linked to improved health behaviours:
It made me feel good about myself that I was helping others.
Doula 049A
I am more confident. I am able to access services myself.
Doula 008Y
More confidence – I got out more, started to build a new life for myself, cycled more too!
Doula 023A
| Response | n | % |
|---|---|---|
| Positively: improved | 39 | 55.7 |
| Not affected it at all | 28 | 40.0 |
| Negatively: worsened | 2 | 2.9 |
| Both: positively and negatively | 1 | 1.4 |
| Total | 70 | 100.0 |
The small number of respondents who referred to ill effects on their health referred mainly to tiredness through juggling their doula role with other commitments or when supporting a woman during a long labour.
Social impact
How has being a doula affected you socially?
As Figure 37 shows, each of the potential social benefits of being a doula was strongly endorsed by over half of the sample.
FIGURE 37.
How has being a doula affected you socially?
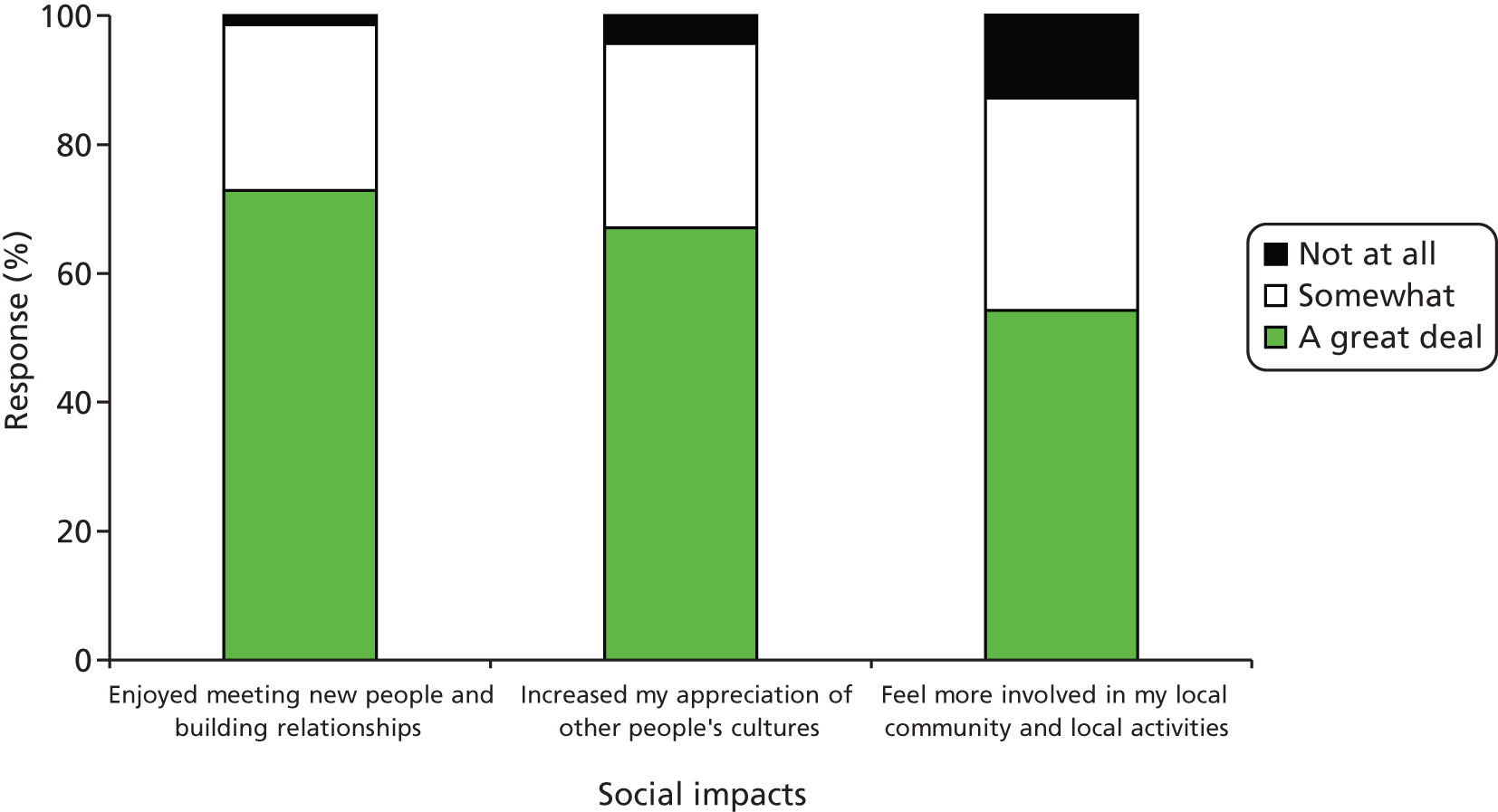
Nine respondents offered other ways in which they had been affected socially mainly becoming more confident and:
Realising that I lead a privileged life!
Doula 013A
Two alluded to negative impacts on their social lives when they were on call.
Work-related impacts
How has being a doula affected you in work-related ways?
As we have seen, many doulas were not motivated by a desire to undertake further training or employment, but most agreed ‘somewhat’ or ‘a great deal’ that being a doula had had employment-related benefits, as shown in Figure 38.
FIGURE 38.
How has being a doula affected you in work-related ways?
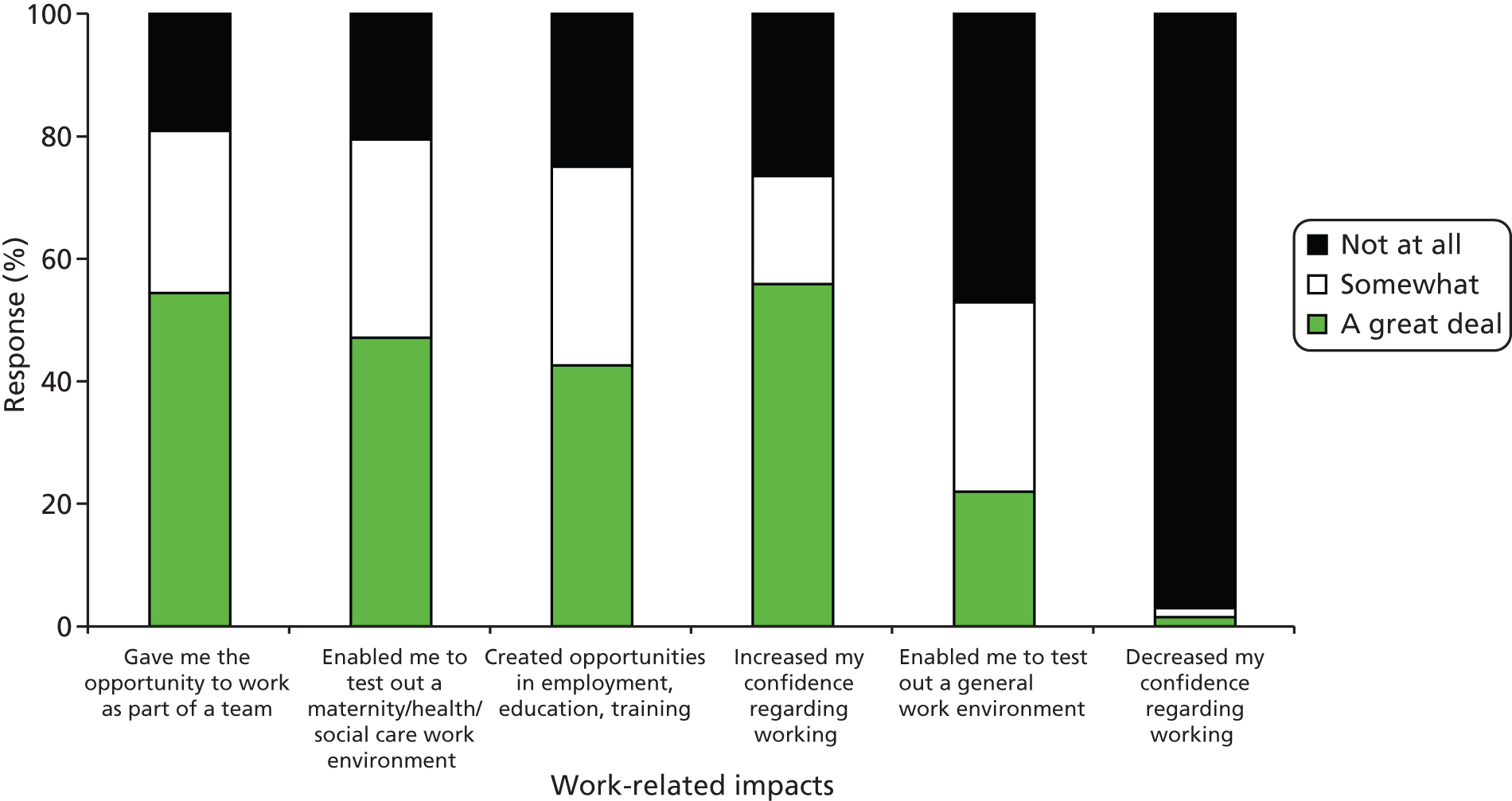
Impacts on doula’s family
How has being a doula affected your family?
Perhaps surprisingly, there was little indication of negative impact on the families (Figure 39). Being ‘less available to family’ and the ‘car being less available to family’ were each strongly agreed with by only four respondents. The most strongly endorsed impact on family (52.9%) was ‘Increased knowledge and accessing of services’.
FIGURE 39.
How has being a doula affected your family?
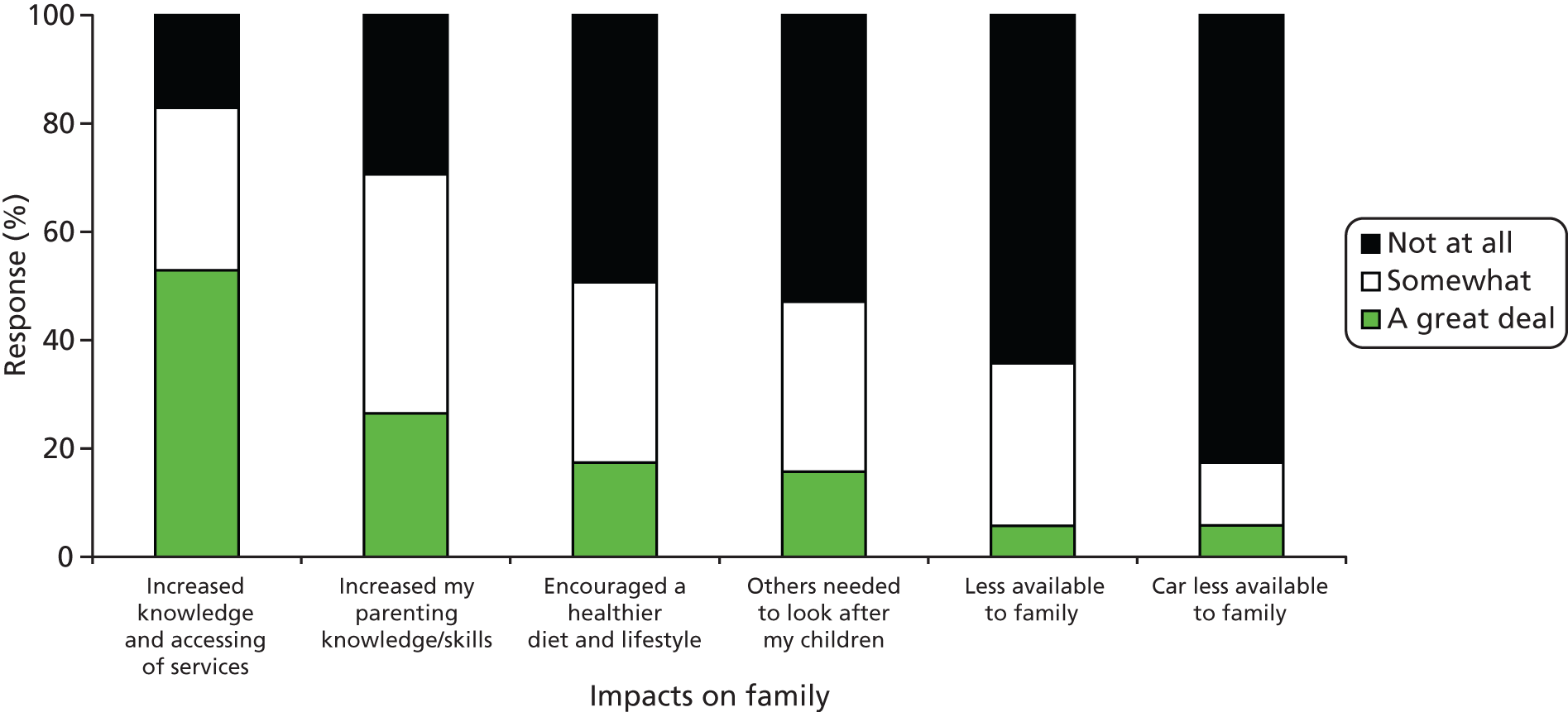
Four respondents added additional ways in which their families were affected:
Affected social life.
Doula 029A
Hope it has given them a broader understanding of people’s different experiences and encouraged them to think about what they can do to support others.
Doula 039A
My children are proud of me and have an understanding of my role and how important volunteering is.
Doula 048A
My husband has been 100% supportive. He likes me being a doula.
Doula 054A
Other impacts
An optional question invited respondents to describe any other ways in which they had been affected by being a doula and 50 of 71 (70%) responded. Most comments were positive and included a number saying that they had become less judgemental:
It has opened my eyes to how sheltered my life was. Also a lot of my opinions were misguided and ill-informed. I am a lot more open to many things and I do genuinely feel less judgemental in a positive way.
Doula 033A
A number also commented on the transferability of the skills that they had learned:
I love it. I don’t know what I would do if the service ceased to operate. It has made me a better friend and given me skills to support anyone in my life.
Doula 069A
The third category of positive comments referred to increased confidence and fulfilment:
It has made me more pro-active and has encouraged me to engage with people.
Doula 047Z
There were also references to helping with career choices: 023A was ‘now a newly qualified midwife’ while for 051Z ‘[it] helped me to decide NOT to pursue a career in midwifery.’
There were a small number of more negative comments:
It can be hard seeing how some people live and the conditions.
Doula 018A
As a grandma, there are expectations that I am available for child care from time to time. Sometimes this can be difficult.
Doula 054A
Decreased my confidence in ‘health services’, seems like a culture of ‘bullying’ in the work environment.
Doula 067X
Stopping volunteering and summing up the doula experience
Volunteers who had supported women: why did they stop?
Seventeen respondents who had supported women said that they had now stopped volunteering and all answered the subsequent question explaining why. No respondents from site X had stopped volunteering. The reasons given by those from sites A, W and Y were very similar, citing family commitments, studying, having moved away from the area, not having a car or own health problems. In contrast, at site Z the reasons given were all about the organisation and the role rather than about the individual.
The organisation was unprofessional.
Doula 051Z
Finances, lack of communication, felt uncomfortable in office and meetings, didn’t feel like I was accepted.
Doula 052Z
Am going to stop because I don’t enjoy it.
Doula 079Z
I think I have stopped, may give it one more try if they call.
Doula 089Z
It is clearly in the services’ interests to minimise attrition of trained volunteers. We therefore asked all responders (i.e. whether or not still volunteering and whether or not they had yet supported a woman) ‘What would (have) encourage(d) you to keep volunteering?’ Responses are shown in Figure 40. It will be seen that very few of these potential motivators were rated as important by the volunteers, the modal response being ‘Not at all’ for all except ‘Fewer commitments in personal life’. There were few noticeable differences between sites except that volunteers at site Z were more likely to endorse ‘More support from service/project staff’. There were also no significant differences between those still volunteering and those who had stopped, except that those who had stopped were likely to rate ‘Fewer commitments in personal life’ as very important.
FIGURE 40.
What would (have) encourage(d) you to keep volunteering? Note: Includes doulas who had not yet supported women.
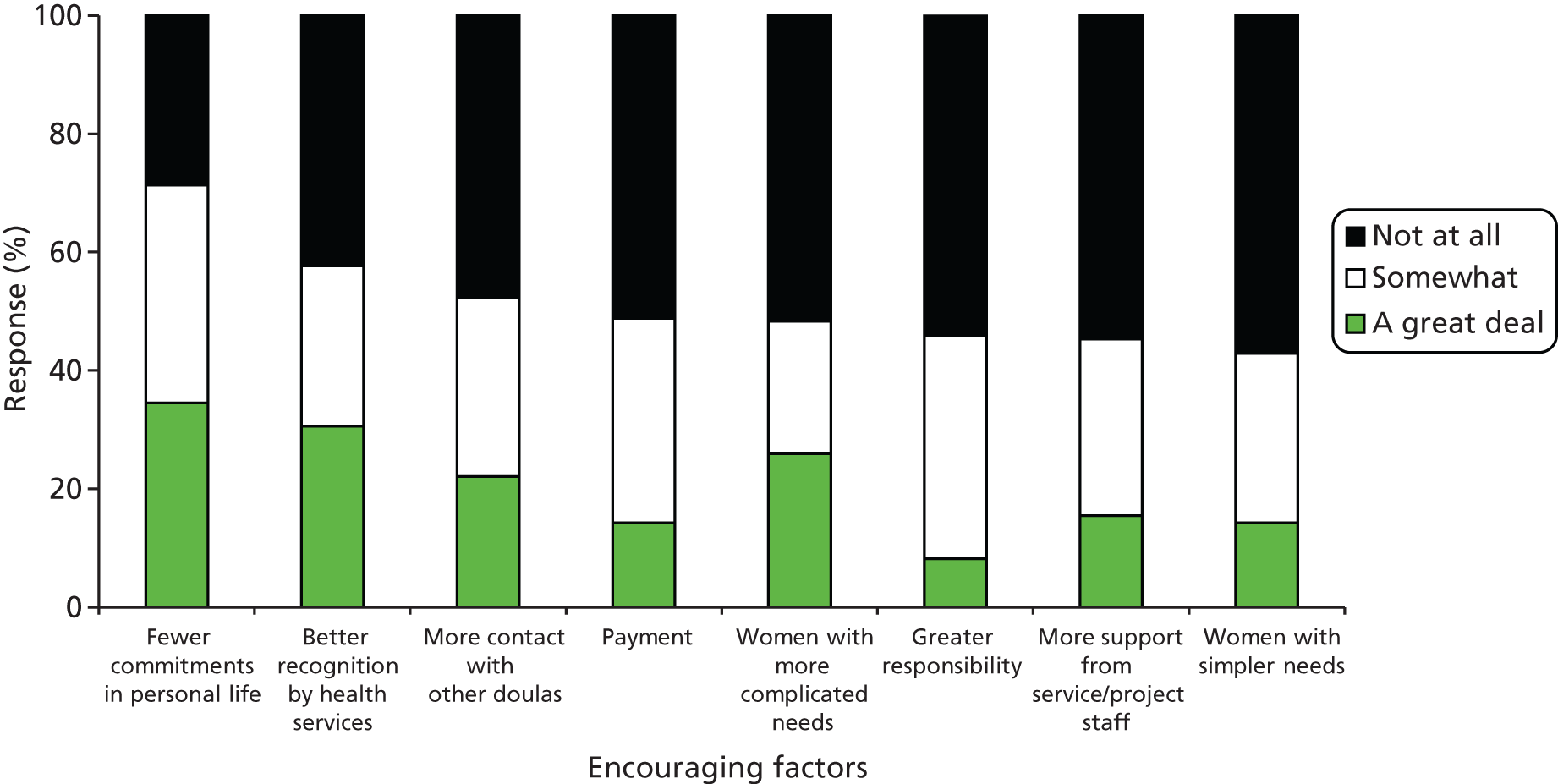
A small number of respondents offered additional motivators, with some pointing out that their reasons for stopping were intrinsic (e.g. having moved away) and not anything within the service’s control. Among those that the service could potentially act on were to have variety in the women they support; not to have to wait too long to support a woman; small group supervision; money towards childcare costs when needed; and further training. Two rather more negative comments came from site Z from doulas wanting better support from service staff and a further one from site Y from a doula who felt that the service had not been honest with her about the time commitment required.
What is the best thing about being a doula?
The overwhelming majority of doulas who answered the question ‘What is the best thing about being a doula?’ said that it was about being able to help and support women and making a difference to women and their babies:
The greatest feeling you get knowing you have made a big difference in a person’s/family’s life.
Doula 061A
Being able to share our expertise with vulnerable mums, assist and support them at a very important time in their lives.
Doula 059X
Many described it as a privilege to be allowed to share in a woman’s pregnancy and birth:
The privilege of being part of a woman’s journey from pregnancy to birth and looking after her new baby. Seeing a family blossom and a new baby thrive in that family.
Doula 027Y
Some talked in terms of ‘feeling useful to the community’ (059X) or ‘giving summat back’ (036A).
Some doulas, especially at site Y, particularly referred to the pleasure of seeing women’s confidence grow through their support:
Seeing a woman gaining confidence in her own abilities to birth her baby and care for her child.
Doula 056Y
The best thing is supporting a really vulnerable mum and within 6 weeks she becomes independent and in control especially at the birth – and to watch her grow strong with her baby and family.
Doula 053X
Some doulas framed ‘the best thing’ in terms of their own development: they had gained confidence, enjoyed meeting new people from diverse backgrounds and liked feeling they were part of a team of professionals.
I love meeting new people and I love supporting women from all ethnicities. I enjoy working with other health professionals as part of a team.
Doula 020W
A couple of doulas referred to the camaraderie of the doula service:
Contact with other doulas was essential – part of big, lovely team!
Doula 023A
Meeting the other doulas and wonderful support staff. The positivity around the service.
Doula 053X
Some doulas described the personal satisfaction of feeling needed or appreciated and pride in accomplishing what they had set out to do:
Giving help and support to someone and get the appreciation from her, especially if this woman is new in this country and doesn’t have family members or friends.
Doula 078W
When you really feel you have made a difference to someone. Some women expect to be given help, almost as a right. Others really need support and say thank you. That makes my day!
Doula 054A
What is the one thing you would change about the doula role?
There was considerable variation in answers to the question ‘What is the one thing you would change about the doula role?’ Many did not answer or said ‘nothing’. Some doulas commented on aspects of the service organisation: they would like to be offered more doula work or offered it sooner after finishing training; less paperwork; not to have to phone in every hour; or to have feedback from the women they supported. One doula said that the service should work around and not overlook family commitments of volunteers:
The fact that we are mothers with young children – we feel that sometimes late evening and night support could be a problem – so reserve two back-up doulas in order to maintain the service and not let the mother down.
Doula 047Z
At one site (A), two doulas commented on the postcode restriction of the service:
There are many women that are missing out on extra support as they live out of the area.
Doula 041A
At site W it was similarly suggested that the service should be available to young indigenous women, not only women from the black and minority ethnic (BME) community. Some doulas said they would like more support from the service: updated information, emergency back-up, more contact with other doulas. As we had been led to expect from our initial doula focus group, many doulas (55.2%) would like more contact with other doulas and this was similar across all the sites. It was also suggested that a doula co-ordinator would help to maintain motivation:
I know it isn’t possible any more but when I started in 2007 the locality workers were available on call 24/7. Very, very occasionally it would be good to have this support. The middle of the night can be lonely! If things are going wrong.
Doula 054A
Think a co-ordinator doula is needed. Someone to organise meetings, support and keep doulas motivated. Somebody just for them (to contact anytime).
Doula 071W
Overall, 34.8% of respondents had said that they thought that doulas should be paid and this was mentioned by a small number as something that they would like to see changed:
It would be nice to have some sort of payment for the time and effort that we all put in and it would be nice to be more recognised for the work we do and the differences we make.
Doula 009A
Some doulas said they would like to change some of the restrictions imposed by the services at some sites; in particular, rules about not giving women gifts and not sharing personal experiences:
That we could help them more in ways of donations, i.e. be able to give them small items or buy them a small gift when baby is born.
Doula 007A
Perhaps being able to ‘advise’ and ‘influence’ and share experiences.
Doula 067X
Several referred to the rule that doulas could not stay in touch with the women they supported:
Would like the option of some follow-up (after the 6 weeks postnatally) to be available so women don’t feel you have just moved on and forgotten them.
Doula 048A
One explained her mixed feelings about this issue:
A lot of us doulas say we don’t like the no contact with mums after the match has finished. We all know and appreciate the reasons behind it. We understand but find this the most difficult sometimes in our role as a doula. Is it something we would like to change – yes. Is it something that should change – really no.
Doula 033A
In a telephone interview, one doula pointed out:
the other thing I find really difficult particularly is trying to get mums out of the house, most of them, a lot of them don’t want to leave the house in the first month, and trying to get them to go places with you, to go to children centres and stuff is really difficult and also things like baby massage and that they don’t really want you to take your babies until they are at least 6 or 7 weeks old anyway, so that’s the bit I find most challenging about only having 6 weeks, and women in certain cultures don’t leave the house for 6 weeks anyway.
Doula 069A
A final theme was the need for the doula concept to be better known and understood:
The constant need to explain to health professionals the role we play and the importance of that role.
Doula 026Y
I would like more recognition. It would be nice when I tell someone I’m a doula for them to know that is!!
Doula 056Y
In a telephone interview, one doula said:
I’ve got this policy of telling one new person every day about what a doula is.
Doula 067X
Would you recommend being a volunteer doula to other people?
Only 2 of the 71 respondents who had supported at least one woman answered ‘no’ to this question. Both were from site Z.
Overall, how would you rate your experience of being a doula?
On a 0–5 rating scale, 49 doulas scored 5 (69%). The percentages by site were 81.3% (A), 83.3% (W), 71.4% (X), 61.1% (Y) and 25% (Z). A further 16 scored 4 (22.5%). Thus, over 90% rated their experience as either 4 or 5, including all respondents from sites A and Y. Two respondents gave a rating of 0, both from site Z.
What factors are associated with a low rating of the doula experience?
Scores were regrouped into ‘high’ (4 and 5) versus ‘low’ (< 4) to further investigate the factors associated with low scores. Based on the CMOcs developed earlier, variables investigated were degree of experience as a doula, measured in terms of both length of time since training and numbers of women supported; whether or not the doula had ever taken a break; whether or not she had ever felt out of her depth; whom the doula could talk to in an emergency; whom she could talk to for moral support; type of contact with doula service staff; satisfaction with availability of doula service staff, both during and outside office hours; satisfaction with availability of resources; whether or not more contact was wanted with other doulas; whether or not a professional had ever misunderstood her role; whether or not the doula role is distinct from other roles; and whether or not ‘volunteer’ doulas should be paid. Demographic variables were also examined: age, education and whether or not in paid employment. Ethnicity could not be considered because it was strongly correlated with site.
The very small number of low scorers (n = 6) meant that Fisher’s exact test needed to be applied, rather than a standard chi-squared analysis. Very few of the analyses were found to be statistically significant, although most showed figures in the expected directions. Those that were significant were exclusively to do with their relationships with the doula service. Low scorers were less likely to say that they were able to speak to doula service staff in an emergency or for moral support. Those who specified some other person that they could talk to for moral support were more likely to be low scorers, perhaps reflecting the fact that the service staff were not meeting this need. Respondents who said that they did not have scheduled supervision meetings were much more likely to be low scorers, as were those who did not have scheduled telephone conversations, for example before or after an initial meeting with a new woman. In the sample as a whole, five respondents said that their contacts with the doula service staff did not include telephone conversations when they needed them, and four of these were in the low-scoring group. Low scorers were also significantly less likely to say that they were able to have face-to-face conversations with staff when they needed them and more likely to say ‘I usually wait until they contact me’. All who were ‘very satisfied’ with the availability of service staff inside office hours were high scorers, whereas all who were ‘not at all satisfied’ were low scorers. The pattern was similar for availability outside office hours except that a small number of high scorers also expressed themselves as ‘not at all satisfied’. Low scorers were also less likely to feel that there were enough resources, such as interpreters and telephones, to support their work.
The difference between ‘good’ and ‘very good’
In previous work47 we have found it informative to examine differences between respondents who give maximum ratings and those who, while generally positive, still have some reservations. It was felt that comparing those scoring 5 (n = 49) with those scoring 4 (n = 16) for their doula experience may give us some insights into what it is that makes the doula experience less than optimal. We therefore re-examined the data omitting the six respondents scoring less than 4 from the analysis and comparing those scoring 5 with those scoring 4. The same list of independent variables was used as reported above for high versus low scorers. The only analysis to show a statistically significant result was that experienced doulas (those who had supported more than two women as a main doula or more than three as a back-up) were more likely to give a rating of 5 than of 4. This might be thought to be because those who are less satisfied do not stay long enough to become experienced. This was partially supported by the finding that 90.9% of those training before 2010 scored 5 compared with 78.6% of those trained in 2010/11 and 65.2% of those trained in 2012/13. However, that chi-squared analysis was not significant (p = 0.24).
Site Z: case study
Our evaluation has produced some very rich data, but, unfortunately the numbers of respondents from the roll-out sites, with smaller sampling frames, has limited what can be said about between-site differences. Despite this, however, it was apparent that among the nine respondents from site Z there was a great deal of negative feeling, mainly directed towards the organisation, which was in marked contrast to other sites. As we have seen, two took the extreme position that they would not recommend being a doula to anyone else, which did not occur at any other site, and another two qualified their answer with ‘only if the course is carried out by professional teacher’ (079Z) and ‘if it was a well organised thing’ (089Z). This last doula did in fact add that ‘the teachers brought in were very good (one in particular was EXCELLENT) but organisers so disorganised.’
Doulas who had supported a woman after training (eight of the nine at site Z), were asked to rate their experience of being a doula and at site Z only two gave the maximum rating score of 5, whereas in other sites between 61% and 83% of doulas had scored 5. Two scored 0 and two scored 3, all of whom had left or were about to. They made it clear that they enjoyed and valued supporting women: ‘I had a great connection with the mum, all that side of it actually was all I’d hoped, just the rest was not good’ (051Z). However, all four were very negative about the poorly delivered training and lack of professionalism of the staff, who were also described as ‘rude’ (079Z) and ‘disorganised’ (089Z), and that they ‘didn’t have a clue on how to support us’ (052Z). When asked about supervision meetings, one volunteer said:
I have never been invited to a supervision meeting but have been told retrospectively that it took place!
Doula 051Z
The question of interest, given our realist ‘what works for whom’ approach, is why did not all volunteers at Z feel the same way? In particular, how can the following quote be squared with the extremely negative views already reported?
The supervision & training was fantastic. The supervision team are a wonderful support network. It is wonderful as I’ve grown in confidence. The team have always been very supportive and approachable.
Doula 088Z
Questionnaire data were augmented with a telephone interview with one of the doulas from this site.
Demographic variables
Age, ethnicity and education were compared. Neither age nor ethnicity distinguished satisfied (scoring 4 or 5) from dissatisfied (scoring 0–3) doulas. All the dissatisfied doulas, including the one who had never been offered a woman to support, had had more than the minimum years of education, whereas this was only true for one of those who were satisfied. There were also suggestions that at least two of the dissatisfied doulas had relevant professional experience which gave them particular insights into the shortcomings of the organisation. Possibly this may have been seen as threatening by some individuals within the organisation, thus amplifying the friction. It was hypothesised that, if the dissatisfied doulas were more likely to have a professional background, then they might be more likely to have cited ‘to use the skills I already had’ as a motivation for training than those who were satisfied. However, the hypothesis was not supported; seven of the nine respondents rated that motivator as ‘very important’ and the other two (both dissatisfied) rated it as ‘quite important’. No other demographic variables were available for comparison.
Training cohort
The doula who was interviewed had reported particular problems around the training of her cohort. All four dissatisfied doulas had trained in 2012, whereas three of the four satisfied doulas had trained in 2010. However 088Z, the positive doula quoted above, had also been part of the 2012 cohort. It was known that there had been some disruption to the normal staffing at site Z during that period, so these doulas’ experiences may not be representative of other cohorts. The doula who was interviewed had specifically reported problems in the group dynamic of her training cohort, with one individual described as constantly dominating the conversation, talking about herself, being opinionated and intimidating and with the tutors not challenging her behaviour. ‘[It’s] not useful to have one member of the group do 90% of the talking’ (doula telephone interview). A formal complaint had been made about the quality of the training and it was implied that there was some polarisation of the group thereafter into those critical of the organisation and those supportive.
There were I think 13 of us on the course and the meeting where people were airing their grievances as it were, stuff they weren’t happy about, 10 of them were saying exactly the same thing that I was saying.
Doula telephone interview
Thus, it seems likely that 088Z was not one of those 10 who were critical of the organisation, but she will almost certainly have been aware that such views were being expressed. This may account for particularly strong endorsement of the staff in her final comments: ‘fantastic’, ‘wonderful’.
Number of women supported
Of the four dissatisfied doulas, two had only supported one or two women as a back-up and had supported none as a main doula. A third had had two matches, one as main and one as back-up, but neither had developed, since one was out of area and the other wanted child care rather than a doula. Thus, neither actually met the organisation’s criteria and should never have been matched at all. She felt that this reflected poorly on the organisation. The fourth had supported two as a main doula and one as back-up. In contrast, the very positive doula, 088Z, had supported four women as a main doula since completing her training, which was more than any other doula respondent from this site. One of the nine respondents had completed training in 2011 and was still waiting to be offered a woman to support. As we saw above, volunteers at site Z had tended to support fewer women on average than those at other sites and a shortage of clients was recognised as a problem by the organisation. However, we also spoke to one woman at that site who had wanted a doula and been referred to the organisation but had never been contacted by them. Furthermore, there was a perception that such women as were available to be supported were not being shared out equally.
It did seem like there were several women [i.e. volunteers] on the [training] course who were not even getting the opportunity to work with anyone . . . it seemed to me like it was operated on the basis of who [staff member] liked the best.
Doula telephone interview
However, we were also aware from our other data sources that there were challenges at this site particularly in matching women to volunteers who could be available at the times that women wanted them, because of doulas’ family and other commitments. It may thus be that those not offered matches could not be available at the times needed, for example potentially staying with a woman during labour at night, and that this was why no matches had been offered.
Thus, it seems that the answer to ‘why did not all doulas at site Z feel the same way?’ is probably that ‘not all volunteers were treated the same way’ and that perceptions of unfair treatment have led to divided camps. A CMO can thus be hypothesised that, when staff are perceived as being unprofessional (Context), volunteers feel frustrated and marginalised (Mechanism), which leads them to be dissatisfied and to leave the organisation (Outcome). It is also interesting, that, as far as we can tell from our limited sample, negative views of the training and the organisation are restricted to one training cohort during an atypical period. This could suggest another speculative CMO, which is that a poor training experience (C) leads to a lower threshold for negative perceptions of the organisation (M) and lower role satisfaction/leaving the organisation.
Chapter 6 Findings: implementing and sustaining the service
Facilitators, challenges and barriers of establishing and sustaining the original volunteer doula service
Establishing the original service
Based on interviews with eight operational and strategic staff in the first phase of data collection, we identified 11 facilitators or ‘Mechanisms’ considered important for implementing and sustaining the site A service. In Table 28 below, these Mechanisms are listed and illustrated with quotations from the interview data.
| Mechanism number | Mechanism | Quotation |
|---|---|---|
| 1 | Skills mix and expertise of staff | I had a business, more of a business background and project development skills and we were, because we were, had a midwife on our team, a health visitor on our team, people that had worked in the community, I think it was that mixture of all the different skills that enabled us to make those links with the different agencies |
| 2 | Flexibility of staff regarding roles | I do remember at points where we didn’t have enough volunteers and I seemed to be on call a lot (laughs). So I used to do the volunteering, the doula-ing myself, and one of the other, eventually we got another paid member of staff |
| 3 | Networking (to gain referrals, volunteers and funding) | . . . we’d spent a lot of time, again, going around all the agencies to make sure that they knew we existed and that we could link into them, and I think that was done very successfully |
| 4 | Joint/partnership/multiple agency working (to gain referrals, volunteers and funding) | . . . the service that we give is unique, but it’s also not, it’s not so much stepping on their toes . . . it’s more working together and what, what, what have they lost or what have they gained and how do we fit in? . . . And so what we’ve had to do, we have team meetings and we’ve, we invited lots of the other agencies to come in and do a 15-minute slot and we’ve gone out to, like Family Nurse Partnership, and said . . . how can we work together to strengthen the support that mums and families get? |
| 5 | Differentiating the service from other professional and statutory services (to gain referrals) | We train the doulas not to advise . . . it’s all about making the mum feel a bit in control of her own situation, I think. Because they feel so bombarded by all the different organisations and you just, you know, it’s another figure in a, a system . . . but I think that that makes a lot of difference to make the mum feel as if they’re her decisions, about her baby, about her pregnancy, and the doula’s there to support the mum |
| 6 | Responding to funding availability | Initially [name of service] had sort of like five or six senior managers who just went for bids and projects and started to develop work in areas of interest and areas of expertise. We had the big Sure Start programme and, I wasn’t employed with [name of service] then, and gradually it became very clear that [name of service] was growing quickly because it had some very, very successful bids, and we did an awful lot of European funding matches against the Sure Start money that came from central government and hence built three quite large buildings |
| 7 | Goodwill work and costs absorbed by host agency/organisation/other | They provide like the free accommodation within the children’s centres and, instead, so that was kind of their in-kind funding |
| 8 | Service shaped to fit with local service drivers (to gain referrals) | . . . a lot of our service level agreements were about meeting national indicators. So we aligned our areas of service delivery with the local area agreements that were led by the council, and that was health and well-being, children and young people, employment enterprise and training, and safer stronger communities |
| 9 | Strong support for volunteers (to retain volunteers) | I think that’s one of the mainstays of this project, is that I’ve worked with other charitable organisations that have had volunteers and been in a situation where I was supporting, supporting volunteers but didn’t have the tools to do the job, and also the time to do the job. And I think my passion is to see the journey that the doulas go on and to give them an opportunity to feel supported and recognised as part of the team. We do have an open door policy where, if somebody pops in and says is there any possibility, unless we’re in meetings, one of us will free, free themselves up to actually make that doula a cup of tea and . . . sort of sit down and have a chat and say, you know ‘Is there something wrong? Can we support you if you’re having problems?’ |
| 10 | Marketing (to gain referrals) | We, we do a lot of promotional work in, in the city, letting everybody and anybody know about the service, and, and so, from that point, we, we get referrals in both from the women ourselves, so self-referrals, but we also get them from the statutory agencies, like midwives and children’s centres and Social Services and other voluntary organisations as well |
Maintaining the original service
We conducted follow-up interviews with operational and strategic staff at all five sites, approximately 1 year after the initial interviews. We revisited questions from the initial interviews, to further explore the Mechanisms identified for implementing and sustaining the services, this time specifically to explore their relevance for sustainability. Four of the Mechanisms identified in the initial interview data were identified as important for the sustaining of the site A service:
-
strong support for volunteers
-
widening criteria for referrals
-
shaping the service to fit with local service drivers
-
funding and goodwill work and costs absorbed.
Strong support for volunteers
It is essential to the services that they retain volunteers. Attrition is a problem, though, with all sites reporting concerns. While, as we reported in Chapter 5, reasons for leaving do not necessarily reflect negatively on the service, most sites recognise the need to maintain volunteers’ motivation. Sites have measures to address this that can be described as the Mechanism ‘strong support for volunteers’.
At site A, it was decided that volunteers should undertake four mandatory training sessions per year. These would include one about breastfeeding and others on topics such as substance abuse and safe sleeping. In addition to the intrinsic value of the training it was suggested that:
It re-emphasises them in their, in the, in the team and in part of being a doula. They meet the other doulas. It reinforces their value, I think, because they be, they come and they, they chat with us and they chat with each other, and I think it’s just for their ongoing, just really positive for their ongoing sense of being a part of something, which I think is probably more important than the actual training (laughs). Although of course the training is important.
Site A, doula service staff, return interview
A senior member of staff reflected on the importance of organisations supporting volunteers and made a clear connection between such support and the work done by the volunteers:
I have never in my life seen a project that manages and get such value out of volunteers but also gives so much back . . . it has crystallized the whole issue around social capital really. Which wouldn’t have meant anything to me before, I was of the view that managing volunteers was challenging and 8 out of 10 times disappointing for both the volunteer and the organisation.
Site A, doula service staff, return interview
Widening criteria for referrals
Another sustainability issue concerns referrals to the doula service. The service is keen to achieve an optimal flow of appropriate referrals. One Mechanism to achieve this is in looking to new referral sources. At site A, three new sources have recently become involved. Women from these agencies have somewhat different problems (e.g. mental health) from those that the service has traditionally supported, which is seen as positive both for women and for doulas who can expand their skills.
In addition to a flexible approach to referrals, site A are flexible with the timing and type of the support that they give to women. In the early stages, they provided women with support in the postpartum period to achieve acceptance in the maternity services and midwifery workforce. More recent developments include the availability of an early pregnancy access service in mainstream maternity services that has led to more early referrals to the local doula service. Site A has responded by adapting the support offered to accommodate this earlier referral by making initial contact and then offering telephone support in the early months.
Shaping the service to fit with local service drivers
This research has been carried out shortly after major changes to the commissioning processes for health and social care included in the Health and Social Care Act 2012,48 which has brought in new Clinical Commissioning Groups (CCGs). The commissioning uncertainties associated with these new structures have had implications for the stability of funding of the doula services. In site A there is a new commissioning emphasis on early intervention for troubled families and the doula service has responded to this with additional relationship training for all their volunteers. They have in the past similarly responded to another commissioning priority: stopping smoking.
Previously the volunteers have been supporting women very much around birthing procedures, relaxation, making sure that the women understand what is happening, making sure that they can communicate, ask questions, etc. What we have been doing in the last year is trying to enhance the training of the volunteers to start to talk to women a bit more about smoking during pregnancy, alcohol consumption during pregnancy and diet during pregnancy. Now actually I think that happened partly because the commissioner for public health changed a year and a half ago and was the lead commissioner for smoking and she saw the opportunity of these volunteers going in and supporting these women to really increase the numbers of women who were pregnant being referred to the stop smoking service for pregnant women.
Site A, doula service staff, return interview
Funding and goodwill work/costs absorbed
All sites have concerns about costs, some of which cannot be accurately foreseen, such as translation and interpretation costs. Two Mechanisms come into play to address costs: responding to funding availability, and goodwill work and costs being absorbed by another agency. There are several different funding sources and methods that sites have talked about. At site A, Investment Contract Readiness Funding is being sought for the ongoing replication work.
Challenges and barriers at the original site
Analyses of interviews with service staff at site A highlighted challenges that had been encountered in implementing the service. The first of these concerned a legacy of tensions between paid doulas and maternity service staff. A senior staff member said that:
In the context of, you know, working with, within local services and linking with other agencies is, the, the only area of tension is this business of the paid doulas going in and working with midwives and it not going so well and then volunteer doulas going in and it makes it harder for you.
Site A, doula service staff, initial interview
It was also reported that maternity services were concerned about role boundaries:
the question that I get asked most when I go is where, what is the doulas, what are the boundaries, first off. What are the doulas, what are the volunteer doulas going to be doing actually in here? Are they going to be taking the jobs of maternity assistants?
Site A, doula service staff, initial interview
Secondly, staff talked about the resource implications of the increasing number of referrals of women with Social Services involvement. These referrals require a lot more paperwork and attendance at many more meetings, including multiagency risk assessment conferences (MARACs) and case conferences. This can be quite challenging for the volunteer doulas and thus for project staff, as increased supervision and debriefings are required as well as extra training on how to record information, serious case reviews and court reports:
When you look at the referrals, before it was either self-referrals or referrals from the hospital, usually, or children’s centres. When you look now, Social Services are recommending us at MARACs. We’re getting recommended in, in childbirth, you know, written plans, case conferences, because we do make a difference for that woman engaging with other, in a multiagency approach. So it’s very different from what it [was].
Site A, doula service staff, initial interview
Smoking cessation work was also proving very challenging. Doulas felt that getting women to stop smoking was too much to aim for, and feared that being too insistent about the issue might mean women disengaging from the service. A partial solution had been found through local health champions:
We’re training up six health champions. So when the Locality Workers go in and talk to mum and say, have you, ‘who smokes in the family?’, ’cause it’s one of the questions. ‘Who comes into house and smoking?’ ‘Would you like some help asking Auntie Matilda to smoke outside?’, for example. Then they would link in with a health champion who’d go on a joint visit with the doula. So it’s them that’s actually discussing the public health outcomes. But then the doula continues to ask them at each visit, ‘and how is it going?’
Site A, doula service staff, initial interview
We revisited these problems raised in the initial interviews in the follow up interviews, to find out the extent to which they have been challenges or barriers in the sustaining of the service. The relationship with maternity services in site A was reported to be a very happy one. Former problems based on paid doulas’ interactions with midwives were no longer an issue:
I certainly think our relationship with maternity services in [name] is excellent now, we don’t have half the challenges we had when we first started, we have been accepted and recognised as a highly professional volunteers service.
Site A, doula service staff, return interview
Tensions were identified with other services and organisations. These were reported as ‘potential’ rather than ‘actual’ and included other third-sector organisations, because of competition for funding:
I think there is potential for a bit of conflict with the [another third-sector organisation] because [name] have now received funding through the Department of Health to deliver a similar type of service. So they are building that doula-ing type approach into the [name] work . . . Now in theory we should all be able to share and work together but I don’t know whether that will be a risk or challenge.
Site A, doula service staff, return interview
The resource implications in supporting an increasing number of women with Social Services involvement continued to be an issue, with paperwork being a particular challenge:
The [staff] have to be a lot more specific in how they do their report writing because they produce a day-to-day report from the doulas’ information and their information which comes to [senior staff] ready for it to go to the professionals’ meetings. So they are a lot more in-depth.
Site A, Doula service staff, return interview
Supporting women with Social Services involvement means that the service can support fewer women in total:
I think sometimes that’s where we struggle if we are looking at how many doulas we’ve got because what you are doing is saying when you’ve got eight or nine safeguarding cases, the time that you take to support them, you could quite easily have supported 12 cases that were not safeguarding.
Site A, Doula service staff, return interview
Smoking cessation work had also continued to be challenging. This seemed to be in part because it represents a culture change for the service:
It has been interesting; because it has been a culture change for the organisation, the volunteers were reluctant to take on that side of work. It wasn’t what they thought was the priority for the service. I’m sure that is what came across when you did those interviews before but I think and the managers weren’t that keen either because really, when the volunteer doula project started, it was really focusing on a natural childbirth and the impact of a natural and enjoyable birth had on parent and baby opportunity to bond. And I think and to breastfeed. And I think that then became a bit tricky because they suddenly had to start challenging women about behaviour and that is kind of changing the relationship a bit. And I think that is what the challenge was for managers in terms of how would they pass that information through to volunteers. It has taken about a year or so to for them to really realise that has to happen and that the mother’s health and behaviour during her pregnancy has a huge impact on the health of the newborn baby.
Site A, Doula service staff, return interview
Whilst progress had been made, Smoke Free Zones work was embedded into the service level agreement in 2013 and remained more successful than smoking cessation work:
definitely in terms of the smoke free stuff we are finding that women are very receptive to that and recognise it is not a good thing. But there is still a number, our stats around women smoking and being referred to the smoking service are still very low. And I don’t really know why that is to be honest, I don’t know if it is because they are lying to us or because the volunteers aren’t pushing the issues or because they genuinely aren’t smoking.
Site A, doula service staff, return interview
The return interviews with the staff also drew attention to the rising costs associated with translation and interpretation:
I think the cost that is the one that fluctuates the most is translation costs. Translation and interpretation ultimately depending on the numbers of women that are referred who don’t have English as a first language and need quite a lot of translation and interpretation support. So that fluctuates, I mean I say fluctuates it tends to go up rather than down.
Site A, doula service staff, return interview
The service had experienced some problems relating to the balancing of referrals and volunteers. It was suggested that criteria needed to be tightened in order to keep the number of referrals manageable but ‘I don’t think they like to say no to anyone actually’ (site A, doula service staff, return interview).
Alongside increasing numbers of referrals, the fluctuating availability of volunteers has to be accommodated. Service staff spoke of the stress that can arise when doulas become unavailable because of illness, family commitments or other personal reasons. No woman has ever been left unsupported, but there clearly have been ‘tense times’.
Thirdly, staff explained that it can be a problem securing the references needed for volunteers, which slows down the process of recruitment. To speed the process up, the service has begun taking verbal references and then asking for a signature on a standard reference form:
We reflect, every time we do an intake, we reflect on how that pathway has worked, have there been any difficulties and I think one of the things that we struggle with when we get the volunteers in is having references. You know, getting the written references. So what we’ve decided to do, once they have been successful, is we now take verbal references on the telephone when we’ve offered a place . . . We get a verbal reference and then we send out our standard form for them to confirm it in writing.
Site A, doula service staff, return interview
In summary, challenges and barriers to the sustainability of the original doula service include the balancing of referrals and active volunteers, which is affected in part by the increasing number of women supported who have Social Services involvement, and the changing focus or direction of the service from natural birth to public health issues, which some volunteers have found hard.
Funding for service costs
Commissioners
The original site and three of the four roll-out sites (all except site X) had been commissioned at the time of the evaluation (site W had received seed funding only). Site A was initially funded jointly by the local authority and the PCT, then by the local authority only and finally by the PCT only; site W received PCT funding; site Y was jointly funded by the local authority and the PCT; and site Z was funded by the PCT.
A total of six commissioners were interviewed whose fields covered a range of specialities within health, children, families, young people, maternity and early years.
All six of the services’ commissioners knew about the services prior to being asked to commission them. All three commissioners of the original service had prior connections with the host organisation and at site Y the commissioner had previously worked with the director.
Local champions
Four local champions were interviewed and those at sites Y and Z were involved in the commissioning process. A local champion at site Z explained that helping to secure funding had been their key role within the service:
With my commissioning hat on, with my sort of CCG board member hat on, my role was partly sort of trying to secure ongoing funding, and we had a, a sticky few months where people were saying, yes, you want to fund it but we think it might have to go out to any willing provider and go out to open tender. Well they all know this is (laughs) going to be a disaster. And we’ve managed to find a way to carry on funding it for the rest of this financial year, and we’re putting it in the commissioning, the strategic plan . . . for the next year.
Site Z, local champion
The local champion at site Y had been working as a commissioner at a point when services in the antenatal period were being commissioned, and had invited the social enterprise director to apply; that application became the basis of the local doula service. This local champion was also instrumental in protecting the service’s funding when it was under threat, by explaining to senior commissioners what the service actually comprised. This would not have been possible had this individual been less involved with the service.
Why the service was funded
The commissioners of two of the services – at sites A and Y – said that they had been able to give the services the amount of funding requested and for the time period required. Site W received only transformational seed funding, because of the rules associated with its location within a hospital trust. At site Z, 1 year’s funding had been sought, but only 8 months’ was awarded.
The commissioners of the four services were asked about how and why they had funded the services. First, what information had they needed when making a decision about funding such a service? Responses alluded to a wide range of information including:
-
epidemiological data
-
information about maternity services, including national guidance on how maternity services are working; booking targets; breastfeeding targets; pressure points identified via needs assessment; equity of access to maternity services; experiences of maternity services of disadvantaged groups
-
information about the local population: number of birth; number of births requiring interventions; breastfeeding rate; C-section rate; and area differences in these
-
information about the doula service including the number of women supported; how it supports vulnerable families; costs; and outcomes.
Second, commissioners were asked what additional considerations apply when deciding whether or not to fund a third-sector service. Responses included:
-
experience; reputation; ability to deliver/do the work
-
previous experiences with the host organisation
-
whether or not the service fits with wider remit of commissioning work
-
whether or not the service fills a gap in statutory service provision
-
whether or not the host organisation is able to take a community development approach
-
whether or not the host organisation is able to work with relevant sectors of the community
-
competitive costing.
Third, commissioners were asked specifically what had led to a positive funding decision in this case and what they had particularly liked about the services. All six commissioners said that they had chosen to fund the service because of the likely impact on two groups: the service users and the volunteers. They also alluded to wider strategic, public health and service issues. The reasons given thus fall into three categories: reaching the families most in need – the most vulnerable and deprived families and/or those least likely to access statutory maternity services; helping local women in areas of low employment into training and paid work; and fitting with wider health/public health strategies and/or filling gaps in statutory services provision. These reasons are illustrated below.
Reaching the families most in need
The women that are supported need, need a lot of support, so, in this, they build up a relationship. High numbers come from the BME population . . . and they don’t necessarily have the support networks of friends and family.
Site A, commissioner 1
Acceptability and accessibility . . . maybe didn’t have maternity services in the country they came from, so maybe felt they might have to pay if they access maternity, you know, all of these issues. So it was very important to have the local community as kind of a point of accessibility, so, really, and that kind of security and safety of having a conversation with somebody that’s not tied into the statutory service first. So that was very much part of it, as well we being, you know, ideally they’re, they’re matched up with somebody from the same, the same community, and all the advantages of that in terms of understanding language, etc. So that, those were the strengths.
Site W, commissioner
Well I think the strength of an organisation like this, sort of, they’re in the local community, they’re embedded within the community, . . . the volunteers and the people who support expectant mothers are from that community and are known in that community. So those were the strong reasons for taking that approach really, ’cos it actually got, got over some of the barriers that professionals have traditionally had in terms of those harder to reach communities.
Site Y, commissioner
It was mostly around sort of helping people to access the services, so we’re particularly targeting more vulnerable women within the community. So we did see it as a gap . . . there are very high poverty rates in [Z], as you’re probably aware . . . So it was sort of the component of helping women to access the services, to attend their appointments, and obviously then improve the outcomes for themselves and the baby.
Site Z, commissioner
Impact on volunteers
When the project first started it was for the pregnant women, and then it was found that it was having a really positive effect on the volunteers . . . these were women that lived within the communities . . . some hadn’t even finished formal education really; had left school with nothing, hadn’t worked, had babies straight away and just felt that that’s what they were, that was their lot in life. And then they would go into a doula project and suddenly find that, you know, actually they could do something, they were not stupid, and lots of them went on, I think one of the things we found was a really high number going into the sort of medical and nursing services, and quite a lot going on to be midwives, and it, it enabled them to suddenly have this opportunity to realise that, you know, educationally they could achieve way more than they actually had.
Site A, commissioner 2
There was recognition that there would be development of the volunteers and potential kind of interest and career route in, into midwifery services as well, definitely.
Site W, commissioner
At site Y the commissioner saw the doula project as a community development approach and particularly emphasised the fact that the training gave volunteers an accredited qualification which helped them to find employment. The fact that a number of volunteers had moved on was seen as positive. The experience was seen as having enhanced volunteers’ self-esteem and self-confidence. Similarly in site Z, with high levels of unemployment, especially among women, the commissioner saw volunteering with the doula project as a ‘stepping stone’ and a route into work.
Fitting with wider strategies and services
I think funding is, is, is key, the, the amount of money we have, to assist women. Midwifery services are very expensive so that would’ve been something that would’ve been taken into consideration in, in terms of deciding to go down the route of having a volunteer service.
Site A, commissioner 1
We always had a slight challenge in finding money, especially when the local authority pulled out and, you know, we knew that this project was having positive outcomes. So I think in terms of the PCT we had to work quite hard to ensure that we always got it in everything. So we always put down the doula project as a way of achieving our breastfeeding rates. So when we were doing the commissioning strategy for the PCT we needed to make sure that pregnancy was high on the agenda, which we actually did, it was one of our main target areas.
Site A, commissioner 1
I think world class commissioning was the, the kind of framework at the time where we were looking for others, I mean the whole maternity services process, specifically the commissioning of this particular element, fits that robust criteria. I mean we did, you know, it has every, in effect it has everything. It had the, the needs, it had, you know, the local needs, it had the evidence of poor outcomes for that group from a, a kind of policy, national policy perspective, it had consultation directly with women.
Site W, commissioner
It was more about my thinking, well it’s a, an area that’s a challenge for me in terms of hitting some of the key targets around maternity booking and breastfeeding, but it was all, it was about filling a gap, because maternity capacity locally, in terms of midwives, were not able to fulfil a lot of the extended role, I suppose, and the more holistic approach that is required for some of these communities. So it was really filling that deficit really in terms of having another solution to fill that gap.
Site Y, commissioner
The public health remit of the commissioner at site Z led to an awareness of wider health determinants such as poverty and unemployment. There was therefore considerable enthusiasm here for linking up with other services that might, for example, help families with budgeting and direct them towards housing and benefits advice. Thus the potential of the doula service was seen not just in terms of direct support to the mother but also in its signposting role, which it was hoped would develop and give further long-term benefit.
Processes involved in the commissioning of the services
The commissioners were also asked about challenges in the commissioning process, and what advice they would give colleagues on the commissioning of services such as the volunteer doula services. The local champions were also asked about challenges faced in their roles championing the services. When interviewed at the start of the evaluation, service staff were asked about securing initial funding. The answers to all of these questions highlight some of the processes that have been or may be important in the commissioning of such services, according to some of those involved.
Processes highlighted by commissioners
-
Joined up working with a lot of multiagency meetings.
-
Awareness of possible tensions with other services over competition for funding.
-
Looking at the wider impacts of a service and getting a service onto the agendas of all possible commissioning areas.
-
Taking a risk on services that are used by a small number of people but which have a large impact on each service user.
-
Fitting a service to a population that is not engaging with statutory services.
-
Developing the host organisation so that it can produce successful funding bids.
-
Being aware of a problem inherent in a volunteer workforce: attrition of workforce.
Processes highlighted by local champions
-
Being target focused.
Processes highlighted by service staff
-
Aligning services to local area agreements and national indicators.
-
Fitting with the local maternity service’s priorities/agenda.
-
Targeting multiple funding streams.
-
Making funding go as far as possible.
These processes identified as important in the commissioning of the services are illustrated below with extracts from some of the interviews with commissioners, local champions and service staff.
Joined-up working
You’ve got to engage all the partners from the word go, and ensure that there are regular multiagency meetings to discuss progress, and at these meetings that there is one or more of the, the volunteer doulas present, so they can, they have their voice. So for me it’s working with the statutory services, midwifery and health visiting, from the word go. Not doing it in isolation, I think, would be the key.
Site A, commissioner 1
Possible tensions due to competition for funding
The major sort of challenge was, you know, actually the initial commissioning processes and the tensions within the local community and voluntary sector environment, you know, from other organisations who thought they were potential providers but did not get the business.
Site Y, commissioner
Wider impact of services
You have to look at the wider impact of the doula service, and I think if you were working in children’s health, sometimes trying to get money for things to be commissioned, people just see it as purely something that impacts on that child or that family at this point in time. So I think what you have to do is look at those much wider social outcomes, like the effect it may have on employment rates, about linking it in absolutely to things like child poverty; and also having the awareness that it’s not just that one service really, link it in to everything you can. And I think certainly, as commissioners, we would, it didn’t matter what we were talking about or where we were within the PCT; I think you always have to keep saying, oh yes, and this, the doula project could also impact that as well, you know. If they were talking about cancer, it’s about you have to think, you know, get it in to everybody’s agenda really, just have it there and not just on what you’ve commissioned it for in the first place, like maternity; it was much, much wider than that.
Site A, commissioner 2
Commissioning small-scale/pilot services
Because of the scale of the, the project, it’s very small, so sort of internally, I suppose, it’s trying to sort of say why I think this is of value, especially getting the funding for the second year . . . I still see it as a pilot . . . until we can sort of get that evidence [of benefit].
Site Z, commissioner
It may not have significant numbers, but the impact of, of having the doulas has been significant, despite it being small. So I would ask that they wouldn’t, because it doesn’t involve huge amounts of funding and huge numbers, not to dismiss it as not being effective or of value.
Site A, commissioner 3
Fitting service to a population not accessing statutory services
The commissioner from site W spoke of the value of the doula service model for reaching population groups who did not engage with statutory services, while pointing out that the specifics of these groups would vary from place to place:
The model itself is fantastic for groups that are suspicious or reluctant to access statutory services but it’s about fitting it to your local population.
Site W, commissioner
Develop the host organisation
Before you go out to commission services like this you need to have the conversations in the local community and really have the dialogue with potential providers and put some effort into developing them as organisations that can make a successful bid, because I think very often community and voluntary sector services, you know, are small organisations or don’t always have the resources to develop a bid to the level required to be become a commissioned organisation. So the advice I would [give is to] put a lot of work into community engagement and community development.
Site Y, commissioner
Awareness of problems of volunteer workforces
At site Z the commissioner recognised the complexities of building a service based on volunteers and thus for the organisation to have strategies for ensuring that volunteers would want to stay:
having to constantly train people up ’cos they’re dropping out and going on to other things, that’s probably the biggest risk, from a commissioning point of view, is how do you actually maintain this group of women that you’ve trained, and that they’re not sort of disappearing and sort of . . . So how can we put some sort of strategies in place to try to encourage them to at least be with you for a certain period of time before moving on?
Site Z, commissioner
Facilitators and barriers to implementation in roll-out sites
Facilitators at the roll-out sites
We revisited questions from the initial interviews with staff at the four roll-out sites, to further explore the Mechanisms identified for sustaining the services. All of the Mechanisms identified in the initial site were identified as important for sustaining the roll-out sites, together with an additional Mechanism – modifying the training to aid retention of volunteers – which emerged from the return interviews data:
-
strong support for volunteers
-
modifying the training
-
flexibility in eligibility criteria
-
marketing to gain referrals
-
shaping the service to the local context
-
responding to funding availability
-
goodwill work and costs absorbed.
Strong support for volunteers
To avoid attrition of volunteers due to loss of motivation, in different ways three of the four roll-out sites employ the Mechanism of providing strong support for volunteers. At site X this involves the staff keeping volunteers up to date on service developments and making sure that they feel part of the service and feel valued:
It’s very much about keeping on top of it and making sure that they’re updated, even with the strategic developments that we have. I like them to make sure that they know what’s happening, because I like them to feel part of the project, not just the volunteers. So the catch-up sessions are really useful for that because sometimes I’ll get [the director] to come and drop in and just give the hi, this is what’s happening, this is what I’m developing and just praise them and let them know that they’re an integral part of this project; without them there is no project. So it’s just reminding them about that.
Site X, doula service staff, return interview
At site W, experienced volunteers are providing support for less experienced volunteers:
With regard to supervision I think it has always been my concern that as the project grows the amount of supervisions that is required grows as well. I have put in a business case – put it forward to the managers – for the need for having additional support for supervision. At the moment [staff member] is doing it using some of the more experienced volunteers as sort of using them to be not necessarily providing direct supervision but providing the support side of the supervision. She has set up little teams, which I think is a very creative way of doing it without having that additional person in post.
Site W, doula service staff, return interview
At site Y, volunteers are being supported in a range of ways. First, to keep their interest high, volunteers are asked to suggest topics for ongoing training. Second, at the volunteers’ request, group supervisions have been introduced, with volunteers designing their structure (despite these being requested by the volunteers, poor attendance means they have been reduced from monthly to quarterly). Third, new ideas on volunteer supervision have been introduced by a new staff member with a lot of experience in the field:
Actually we feel that the supervision is absolutely critical to the development of the project, the motivation of the volunteers, to keep them with us and to help them to reflect on their visits and to improve the quality of the support, the one-to-one support because the empowerment model is really central to what we do, the dimensions that we’ve brought in from the community parent model that we use.
Site Y, doula service staff, return interview
Fourth, plans are being developed that would both generate income and help to retain experienced doulas:
Once they’ve got their qualification and they’ve already supported women through birth, etc., so they are experienced volunteers and the possibility of them being able to offer a paid service to women who can afford to pay for it. So that’s a new income-generating arm that we are developing at the moment and several of the volunteers are very interested in that because it could generate more income for them but also helps us to retain their expertise within the programme.
Site Y, doula service staff, return interview
Modifying the training
Another Mechanism for retaining volunteers emerged at two of the roll-out sites. At site Z, they identified the problem of volunteers training but not going on to support any women. To address this they have revised the minimum number of women whom a doula must support to ‘pay back’ the training; this is considered part of the training, which is therefore now made up of a theory section followed by a practical section:
We have learned as we have gone along. We didn’t initially make the stipulation, but now we say until you have done two mums and two backups they won’t get their certificate. So this is part of the training.
Site Z, doula service staff, return interview
As we have seen, however, this plan has caused frustration for the volunteers who have not actually been offered women to support.
To address the problem of volunteers being put off at the start of the training process, site Y also made changes to the content of their training, to minimise attrition:
We’ve certainly done a fair bit of tweaking of the actual training content and what we do in the taster as opposed to what we do in the introductory. We’ve moved it around a little bit based on the evaluation from the volunteers and what we’ve then later picked up in supervision.
Site Y, doula service staff, return interview
Flexibility in eligibility criteria
Sustainability requires sufficient referrals as well as retention of volunteers. One Mechanism to address this that emerged from the return interviews at the roll-out sites is flexibility regarding eligibility criteria. Two of the roll-out sites, site X and site W, are being flexible regarding eligibility to accommodate referrals from Social Services. Site X is being flexible about when a woman is eligible to receive support. Social Services referrals are earlier than the normal 28 weeks and they are therefore making contact with the women before this date, and keeping in touch with them until this date, when doula support can begin:
We have had some from social who may refer a lot earlier than 28 weeks, they’ll send it from about 20 plus. But what we’ll do, it has been difficult because that’s quite a long time to send our doulas in. But so an example, I can give you just a recent one actually, we will touch base with the mum and I’ll usually go and see her with the midwife present or the Social Services caseworker present. And if everything’s going okay with the pregnancy at the time then we’ll reassure that we’ll come and see her 28 weeks plus, and that’s when we’ll bring the doula in. And it gives a good chance for us to select the right doula as well because we’ll know a lot more about the mum, the history, the case and what obviously we’ll be dealing with. And it just helps us to select the right doula knowing that that doula will be able to handle this case and knowing the fact her baby will be removed, just making sure that they’re well prepared as well, because the doulas will need a lot more support in those particular cases.
Site X, doula service staff, return interview
Site W is being flexible about what support a woman is eligible to receive. Additional telephone support has been provided to women with Social Services involvement:
There has been a lot of telephone support going on, yes, definitely, yes. And that has been from – well for [staff member] that has been quite time-consuming and for the women, because the women have needed a lot more than doulas other women have needed in terms of [the Locality Development Worker] support.
Site W, doula service staff, return interview
At a third roll-out site, Y, the service on offer has extended in the other direction and postnatal support is now offered until 3 months, rather than 6 weeks. This has been particularly effective for late referrals such as women who do not attend antenatal care, those who have only just moved into the area and those in homeless hostels:
Now our support continues 3 months postnatally so a late referral we no longer see as, ‘oh, well, this will be impossible to be of any use here or to make any difference’. . . . now we will embrace the late referral . . . an area of referral we thought would be very easy to just tell partner [services] we don’t accept referrals after 34 weeks and, actually, we were wrong. We’ve done some very good work with late referrals.
Site Y, doula service staff, return interview
Marketing to gain referrals
A second Mechanism to address gaining referrals, which emerged from the return interviews at the roll-out sites, is marketing. Just one site, site Z, has employed this Mechanism. Staff of the doula service and volunteers have promoted the service in GP surgeries and gained more referrals from GPs as a result. Service staff spoke of further promotional work planned with GPs:
We are looking to put a little leaflet in GP practices that says ‘Are you pregnant? Would you like a bit of help?’ Something very, very simple. So on one hand we are looking for women to self-refer but we know when it actually comes down to referrals, it is quite difficult to get women to self-refer because it is still basically a top-down system. Women listen more if the GP or midwife or social worker is saying ‘Look, you should access this service that might help you. Shall I put you in contact?’ So we have to go in both ways, to encourage more referrals from professionals but also want women to feel they can refer themselves.
Site Z, doula service staff, return interview
Shaping the service to the local context
The services at three of the four roll-out sites made reference to the changes resulting from the Health and Social Care Act 2012, specifically new CCGs and how the services fit with or can be shaped to fit with their work. At site X there were ongoing discussions with CCGs and plans to connect with them. Site Z service staff explained that the service takes a holistic approach to supporting women, rather than being clinically driven, providing ‘all sorts of social outcomes that aren’t, the CCG would acknowledge, but wouldn’t be measuring’ (site Z staff member, return interview). She also explained that the service can achieve the clinical outcomes required by the CCG and thus fit in with the CCG’s agenda. At site Y, a staff member explained the fit between the service and the CCG’s responsibility for improving voluntary work and involving communities:
I think the key with what we do is to improve the productivity of professionals because you are using early intervention to support parents within the community to stop them falling into a crisis situation which is then going to take up a lot of professional time, so it’s enabling professionals to be more effective and to focus, you know, a scarce resource more effectively rather than using volunteers to replace them with which would be a dangerous thing to do.
Site Y, doula service staff, return interview
Responding to funding availability
As well as costs that the service foresees, two of the roll-out sites identified costs which cannot be accurately foreseen: at site W administration, crèches for training and external accreditation of training; at site Z security and community interpreting training. Two Mechanisms to address the ongoing issue of funding to meet costs, including unexpected costs, were identified in the return interviews at the roll-out sites. One Mechanism is responding to funding availability. In a range of very different ways, all four of the roll-out sites demonstrated this Mechanism.
At the time of return interviews, site X was negotiating a funding route that would involve paid doulas helping to sustain the unpaid doulas service. Site Z had not trained a cohort in over a year so that all of the funding could be used to run the existing service. At site W, a trust freeze on recruiting administrative support was a strain on the service because it was lacking any such support. Site Y was working on two new sources of funding at the time of the return interviews.
Goodwill work and costs absorbed by other projects
The second Mechanism to address the ongoing issue of funding to meet costs is goodwill work and costs being absorbed by other projects. This was identified in the return interviews at two of the roll-out sites: site X and site W. At site X, the director explained that the community workers across the different services in the host organisation, including the doula service, help each other out; and similarly at site W a senior staff member spoke of staff doing more than they are paid to do:
[Project worker] is part of a community team and there are other community workers in that team, and as you would expect people support each other for different aspects of things.
Site X, doula service staff, return interview
Well I suppose you know with us it is embedded in a big organisation that is consistently having to spend less and provide more. And this is where we are all having to do more than we first were employed to do and that’s . . . it’s life.
Site W, doula service staff, return interview
When asked about the high cost of interpreters for the service, staff at site W explained the cost benefits of the service being hosted by a large organisation:
I think there are some bits, it is not the minutiae with funding here that there might be within another type of organisation. We can lose things in a big organisation in a way that is beneficial.
Site W, doula service staff, return interview
Table 29 provides a summary of Mechanisms that supported sustainability in return interviews at the original service and four roll-out sites.
| Mechanism | Site A | Site W | Site X | Site Y | Site Z |
|---|---|---|---|---|---|
| Support for volunteers | ✓ | ✓ | ✓ | ✓ | |
| Modifying training | ✓ | ✓ | |||
| Flexibility in eligibility criteria | ✓ | ✓ | ✓ | ✓ | |
| Marketing to gain referrals | ✓ | ||||
| Shaping the service to the local context | ✓ | ✓ | ✓ | ✓ | |
| Responding to funding availability | ✓ | ✓ | ✓ | ✓ | ✓ |
| Goodwill work and costs absorbed | ✓ | ✓ | ✓ |
A summary of the differences between the sustainability Mechanisms of the four roll-out sites and on the differences between the sustainability Mechanisms of the roll-out sites and the original site is:
-
All five sites employ four or five of the Mechanisms identified for sustaining a service.
-
Only one Mechanism is evident across all five sites: responding to funding availability. This perhaps reflects the fact that funding is an issue for all third-sector services.
-
All but one service – site Z – has shown flexibility regarding eligibility criteria to gain referrals.
-
Only one service – site Z – has been strategic about whom it markets the service to, to gain referrals from a specific source. (The site Z service had had a clear referral route, recently lost, which might in part explain why the service had not shown flexibility regarding referral criteria, and has begun strategically marketing to gain referrals.)
-
All but one service – site Z – has shown an emphasis on support for volunteers to aid retention. This finding reflects some of the comments from the volunteer questionnaires from site Z (see Chapter 5).
-
All but one service – site W – has shown an emphasis on shaping the service to the local context. The fact that site W has not may be due to the nature of its host organisation.
-
Two services – sites Y and Z – have modified their training to improve volunteer retention.
Challenges and barriers at roll-out sites
Three problem areas were identified in the initial interviews with staff at the roll-out sites. First, all four of the roll-out sites were experiencing funding challenges. Site X was in need of funding to train a new cohort of volunteers, which was described as a big expense, in part because of the childcare costs involved. The overall goal was to grow the service, become an established service and secure PCT funding. At site W a number of problems were mentioned that relate to funding: an ongoing lack of administrative support for the service; a plan to reduce volunteers’ supervisions from three to two over the course of the minimum post-training support work; and stopping using the site A service database because of the high costs involved in doing so. Site Y had experienced 25% funding cuts and because of this had postponed training of the next cohort. At site Z initial funding was coming to an end and it had been rather overwhelmed to discover how much work was involved in running the service:
We were really running to keep up, weren’t we, to start with, because there was so much to do, and we didn’t have the staff that [site A] have.
Site Z, doula service staff, early interview
Second, all four of the roll-out sites were experiencing some sort of tension with another service. Both site X and site W had experienced some tensions with midwifery. At site X these included midwives’ suspicion about doulas at births doing some of their work; doulas forgetting some of the boundaries addressed in the training; and doulas and midwives both writing birth plans with women and then clashing over this. At site W a history of mistrust of paid doulas by midwives on the delivery suite was cited and a site W delivery suite midwife also talked about this legacy. Sites Y and Z had both experienced tensions within the local voluntary sector over competition for funding.
Third, problems with volunteers were cited at three of the roll-out sites. At site X, these related to failing to follow procedures for contacting the service, using the designated mobile phones – a health and safety matter – and volunteers not adhering to the rules regarding expenses. At site Y, there was concern that some volunteers had unrealistic expectations of the role. At site Z, 50% of women referred wanted a doula with them for the birth, which was a much higher proportion than expected. While some volunteers were excited about this, others were not able to offer support at night. Some volunteers at site Z were also not happy with the current level of security and wanted ID badges.
In the follow-up interviews with service staff, we revisited these three problem areas raised in the initial interviews, to find out the extent to which they have been challenges or barriers in the sustaining of the services. Funding problems, experienced at all four roll-out sites, were ongoing. The site X service was still not commissioned and continued to be funded by the social enterprise host organisation. They were still unable to afford to train another cohort of volunteers, which was becoming a more pressing problem as volunteers moved on.
At the time of the follow-up interviews, site W still lacked administrative support and a business case had been written for additional support for supervision work. At site Y the effects of the changes to the commissioning system were being felt, with only short-term funding being made available:
The issue for us is that the commissioning structures that were in place with our previous contract are now not there any more so it creates instability for everybody in the NHS in that it’s changing over to now a clinical commissioning group so now it’s obviously a completely different ball game. They can’t commit to a long-term contract at the moment because of the changeover so we know . . . we’ve had it confirmed that our funding for this year but clearly it’s much more stable if you have a 3- to 5-year contract but it’s not possible because of the government changes. I mean, that’s the case for everybody at the moment.
Site Y, doula service staff, return interview
Site Z was awaiting confirmation of 1 year of funding, at the time of the return interviews, with training work on hold until then:
The funding issue has made it – the insecurity that brings and not knowing whether and when we are doing the next training. That has been difficult to manage.
Site Z, doula service staff, return interview
While funding problems were ongoing, tensions with midwives had apparently resolved at the two roll-out sites which had experienced them: site X and site W. At site X, this was ascribed to increased visibility and marketing. Doulas had attended births and supported mothers at the new birth centre so they were becoming more known and midwives were recognising the work that the service does in supporting vulnerable women:
I have to say I’ve heard a lot of good feedback from the doulas themselves, midwives are praising them, giving them really good feedback and they’ll send that back to me via email and we’ll make sure we keep a record of it. So it’s been very positive.
Site X, doula service staff, return interview
Marketing materials had been produced and circulated, which addressed the doula role and boundaries:
We’ve had good marketing material as well, I think that’s helped because on that we’ve really tried to highlight exactly what the role is, what the boundaries are, the little sections of the bottom of the leaflet saying that we don’t provide medical or clinical advice. So very much pointing out exactly what we do and what we’re here for. So I think that’s helped a lot as well.
Site X, doula service staff, return interview
At site W, relationships with midwives were similarly reported to have improved:
I think it took them a bit of a time for them to get used to it, thinking are these are private doulas, but I think once they got used to it they know that they are part of the team, part of [host organisation], and they are volunteers and as they have worked with them on delivery suite, things are changing, positive working relationships. I think we used to have this thinking ‘oh private doulas’. We have always highlighted that they have responsibilities, their role is a non-clinical role and the midwives are there clinically so knowing that they are not going to step on each other’s toes really.
Site W, doula service staff, return interview
The tensions within the voluntary sector that had been reported in initial interviews, were, however, persisting in both sites where it had been raised. In both cases the issue was concern that a large charity would take up their ideas and that they would not be able to compete for funding.
Some of the volunteer-related challenges had been successfully addressed at the time of the return interviews, while others were ongoing. Security issues in both sites had been successfully resolved by using external security companies. At site X, volunteers’ safety when going into family homes has been managed via a security company, already used by the host organisation, that volunteers phone before entering and after exiting homes.
This has relieved a lot of pressure on project staff:
in the early days it was quite a lot of a burden where doulas would ring me to say this is where I am, this is my location. I would have to call them back after an hour later and literally throughout the day and night. So it was a bit too much for me to take on. So luckily in the last year we’ve had [security company] who’ve taken over that, and they’ve been . . . really, really good.
Site X, doula service staff, return interview
At site Z an external company has similarly been contracted for nights and weekends, but the project workers are still responsible for checking doulas’ whereabouts during office hours:
because it is expensive and we don’t have funding to pay for a full system. I think [another site] are doing the same work and so I am following their advice, in daytime staff take the call, and evenings and weekends they go to the security.
Site Z, doula service staff, return interview
At site Y, staff felt that the problem of volunteers’ unrealistic expectations of the role had been successfully addressed by the time of the return interviews. They felt better able to tell volunteers the commitment expected, including support work, supervisions and training. This was ascribed to experience they had gained in running the service:
I think we recruit with a little more information as well. I think everything we do has been more informed by the fact that we are now, you know, a lot more experienced in what we are doing and so those that come on board I think are clearer as to what they will be doing.
Site Y, doula service staff, return interview
At site Z, the problem of volunteers not being able to work nights continued, with approximately 70% of the volunteers being unavailable to work at night. This clearly is a major challenge to allowing the service to meet women’s needs:
The mums who need labour support means you can be called any time 24 hours but only a few volunteers are available to support during night-time, most only in daytime 9–5, 9–6, 9–3, so it is really hard, whoever the team is that are available it is really difficult. I am going to be a bit careful who I approve next time . . . In the induction day we are making them sign an agreement that they have to be available and when I make the presentation on the open day I will make it all clearer, repeating myself. I did it all the time. But when I do the interviews I will ask the question specifically about availability and who will look after their kids and all that stuff. We can select on the recruitment.
Site Z, doula service staff, return interview
Staff at sites W and Z expressed concerns that not all volunteers were fully engaging with the role:
there are volunteers who for various personal reason just can’t offer time. And my feeling is that for whatever reason they just either have never been or are just not really engaged in the project.
Site Z, doula service staff, return interview
The return interviews with the staff at three of the roll-out sites also highlighted problems not identified at the initial interviews. A senior staff member at site X (who was not in post at the beginning of the service) talked about the service not being sufficiently linked in to the wider health/social care infrastructure. At site W there was concern that women were confused between the doula service and a new voluntary sector project with overlapping aims.
Site Z had also experienced challenges due to staffing discontinuities. A key person in the organisation had had a period of absence. At the time of the return interview another key person was just beginning a period of leave and staff were very aware of the difficulties that this created.
In summary, challenges and barriers to the sustainability of the roll-out services include funding problems; volunteer related problems; relations with other services; and staffing discontinuities. These differ somewhat from those in the original site, which, while including funding, also included balancing of referrals and active volunteers, and the changing focus or direction of the service.
Table 30 provides a summary of the barriers and challenges to sustainability of the original doula services and the four roll-out services and Mechanisms that addressed some of the initial barriers.
| Barriers and challenges | Site A | Site X | Site W | Site Y | Site Z |
|---|---|---|---|---|---|
| Funding | a | a | a | a | a |
| Balancing referrals and volunteers | a | ||||
| Changing focus/direction | Smoking cessationa Smoke Free Zones,b Mechanism unknown |
||||
| Volunteer-related problems | Not following proceduresa Security by external companyb |
Commitment to rolea | Unrealistic expectations by recruitment processb | Unavailable to support women labouring at nighta Security by external security companyb Commitment to rolea |
|
| Relations with other services (indicates type of service) | Midwivesb experience and positive feedback | Midwives by marketing materialsb | Midwives by increased understanding of roleb | Voluntary sectora | Voluntary sectora |
| Staffing discontinuities | a | ||||
| Confusion with a new voluntary sector project | c | ||||
| Insufficient linkage to wider health and social care | c |
Reflections on the differences between the challenges and barriers to sustainability of the four roll-out sites and the original site
The services do share the problem of funding, reflecting the fact that securing funding is always an ongoing concern for third-sector services. The differences between the original and four roll-out sites in barriers and challenges that are currently being encountered perhaps reflect their different durations and nature of their host organisations.
Experiences of the replication package at the roll-out sites
Service documents
Documents developed and used by the original site included those related to the recruitment and selection of doulas; service policies; information about the role for doulas and for women; equipment use and reclaiming expenditure; and documentation included in each woman’s file. All roll-out sites had also developed additional documentation of their own; some were novel and site-specific, and others were modifications of those developed by site A.
Original site database
Use and content
The database is used for providing monthly reports for funders; data on mothers, births, outcomes, etc. are exported from the database in spreadsheet form. All roll-out sites are trained in the use of the database and how to generate reports.
The database contains information about volunteer doulas, following selection and outcomes data from January 2008. Each doula’s record contains personal details; recruitment checks; training records and outline of information about women with whom they have been matched to provide support. Each woman’s record includes demographic information; doulas’ details (main and back-up) and their baby’s date of birth; contacts between the woman and doula and information about their baby’s birth; the woman and her baby’s wellbeing.
Roll-out sites’ usage of the original site database
Site X is the only roll-out site that uses the original site’s database. Site W stopped using the database before the first staff interview because it was found to be too expensive. Site Y decided to have its own database built because its work is broader than that of the original site. Site Z is developing its own database because it finds the one from the original site too restrictive.
Variations from the replication package with volunteers
The four roll-out sites deviated from the original site’s replication package in a range of different ways, including supervision, training and roles of volunteers. The quotes in the following sections illustrate these variations.
Supervisions
Three of the four roll-out sites have made changes to the replication package’s model of supervision of volunteers (which is three supervisions per woman supported). At site W, at the time of the initial interviews, the three supervisions had become two. However, by the time of the return interview, a need to increase the number of supervisions was expected as the service grows. In the meantime, experienced volunteers were providing additional non-supervision support to other volunteers:
With regard to supervision I think it has always been my concern that as the project grows the amount of supervisions that is required grows as well. I have put in a business case, put it forward to the managers, for the need for having additional support for supervision. At the moment she [the Locality Development Worker] is doing it using some of the more experienced volunteers as sort of, using them to be not necessarily providing direct supervision but providing the support side of the supervision. She has set up little teams which I think is a very creative way of doing it without having that additional person in post. But we have just another nine who have qualified and are now being matched, and there is another cohort finishing who have just had nine there, and I am very aware that the amount of supervision that is required is increasing. So I have written a business case to try to recruit some additional support, to support and provide supervision.
Site W, doula service staff, return interview
At site Z, group supervisions had been added to the individual supervisions that are part of the replication package, at the time of the return interviews:
Once a month there is group supervision, so they can come as a group and request if they particularly want an input from a particular health professional then that can come from them.
Site Z, doula service staff
A new supervision policy, one more empowering for volunteers, had been introduced at the site Y, at the time of the return interviews.
Training
Two of the four roll-out sites have made changes to the model of training of volunteers. Staff at site W in the initial interview reported both adding and removing training topics and, in particular, added more training around different cultures and faiths. They were aware that site A modified the training package as needed.
Site Y combined the original site’s OCN accredited training with its existing City & Guilds accredited training, thus creating a whole new training programme:
We’ve really sort of built a whole new training programme haven’t we?
Site Y, doula service staff, interview
Site Y also runs a taster training course as a precursor to the full training course, to help avoid volunteers dropping out after expensive training without supporting any women:
something else a bit different to the way things are done in [original site], because when I came into all of this, the background with community parents, what had shown as particularly worked well was having initial taster courses, rather than taking volunteers straight in. And you can invest a lot of time in quite expensive training, and people can drop out or you find out they’re not really suitable and all that sort of thing, that we’d, we had trialled taster courses and, where people could test the water and we could find out whether they’d be suitable during that process, and also whether they’re going to come to each of the sessions.
Site Y, doula service staff, interview
Volunteer roles
At the time of the initial interviews, site Y had also made changes to the role of the volunteers, with some carrying out outreach work:
the thing that we have put in place that has generated referrals is volunteers doing regular sessions in places where pregnant, where parent, where parent, parents-to-be will be. So we’ve got volunteers doing outreach sessions every week or every 2 weeks. So we’ve got say a, a midwife clinic who’s, the midwife who’s running her clinic at a children’s centre, the volunteer will be in the waiting room talking to those waiting to go in to see the midwife, or as they’re coming out. So have sort of a bit of a display, sharing information, trying to identify those that might need extra support. And what we found is, because they know the programme really well, they can talk about it in the best way to, to parents who might need it.
Site Y, doula service staff, initial interview
Summary of variations in use of the replication package
Table 31 presents the ways in which roll-out sites have varied from the replication package.
| Variation | Roll-out site | |||
|---|---|---|---|---|
| X | W | Y | Z | |
| Service documents differences | ✓ | ✓ | ✓ | ✓ |
| Not using original database | ✓ | ✓ | ✓ | |
| Supervision differences | ✓ | ✓ | ✓ | |
| Training differences | ✓ | ✓ | ||
| New volunteer roles | ✓ | |||
All of the roll-out sites have deviated from the replication package in one or more ways. Site Y has done so in the greatest number of ways (five). This is likely to be related to the site having meshed the replication package with an existing model, as a staff member explained:
The approach that we used was a combination of the community parent model and, and the doula model. So it’s kind of meshed the two of them together. So at the beginning of the replication process, we were already looking at a Pregnancy, Birth and Beyond community parent model. So the birth buddy aspect of it was built into that, was embedded into that, the doula aspect is one component of the, a community parent approach.
Site Y, doula service staff, return interview
We came into this with such a lot of experience of community parents, we saw things that were lacking in, in, in, in the package, although the package was fabulous, I mean there’s a huge amount of work and very beneficial, particularly around all the active birth stuff and, you know, the joint learning that went on, but there were things that stood out for me like, you know, the, the, the empowerment model, the particular personal qualities that you look for in, in volunteers and being able to support and empower another parent. The process of support and the goal setting and attachments and bonding and, there was just one session on postnatal depression which we felt, you know, there needed to be, it needed to be much wider sort of, sort of a little bit restricted in its focus from that point of view. I mean I, I have met with [name] recently, and [name] came as well, you know, from, from [original site] and, and, and, you know, the discussions that we’ve been having is that I think she’s saying that there needs to be a wider element to it rather than focusing just on the doula aspect, so it needs to be embedded in something wider. So I think those were the main things that stood out for me.
Site Y, doula service staff, return interview
While the roll-out sites have all deviated from the replication package in a number of ways, they have also stayed true to the package in other ways, and they have all sought and received support from site A, which was greatly appreciated.
Staff at site W talked about the flexibility from the original site, and site A’s ongoing helpfulness:
But now they are always there, you know, at the end of the phone to provide the support that we seek when we want to in order to clarify things or ask about things or how do you do this? What do we do about this? They have been very helpful.
Site W, doula service staff, return interview
At site Y they were very appreciative of site A’s positive attitude to the meshing of the replication package with an existing model:
what I really appreciated was they were willing to, you know, they weren’t too precious about it, it wasn’t you must do it exactly like this, you know, they were happy for us to adapt it and embed it and so, you know, and I, and their support was very helpful to the team here. Like [Service Manager] and [name] went to [the original site] and, and, you know, it was very helpful to them to go there and talk to existing people in similar roles, and that support was invaluable.
Site Y, doula service staff, return interview
Chapter 7 Health economics
Introduction
There are two main objectives of the economic analysis. The first is to describe the costs of running a volunteer doula service for pregnant women who are socioeconomically disadvantaged. The second is to evaluate the volunteer doula service across a range of observable health and clinical outcomes hypothesised to be influenced by the doula intervention. These include mode of birth, use of epidural during labour, incidence of low birthweight, rates of breastfeeding and smoking cessation.
Our analysis follows a predominantly cost–consequence approach because the volunteer doula service has a diverse range of short-term outcomes. This is defined as an analysis ‘in which costs and effects are calculated but not aggregated into quality-adjusted life-years or cost-effectiveness ratios’ (p.1176). 49 This method is used to display the key costs and consequences associated with the volunteer doula service intervention. Wherever possible we express the consequences – health and clinical outcomes – in terms of a cost differential per birth against standard NHS practice, in which the services of a doula would not be available. Comparisons of outcomes are made countrywide against practice in NHS England and, depending on data availability, outcomes in the local region in order to control better for the impact of socioeconomic circumstances. There is a paucity of economic evidence on the use of volunteer doulas in supporting pregnant women in the UK; moreover, doula support, whether it be provided by volunteer workers or otherwise, is rare in the UK, especially for disadvantaged women.
Data on running costs were gathered from service managers located at each of the five service sites. Data on clinical outcomes were gathered from the Hull Goodwin doula project database. Resource use and unit costs associated with health and clinical outcomes were estimated using various sources: NHS maternity statistics, HES, the NHS reference costs database and the PSSRU (Personal Social Services Research Unit) database.
For the second objective, the evaluation of health and clinical outcomes, the perspective of the analysis is the NHS and Personal Social Services (PSS); unless indicated otherwise, all reported currency values are expressed in 2011/12 prices. Cost inflation and price inflation, forward and backward, are assumed to match to PSSRU’s Hospital and Community Health Services (HCHS) index. 50
Methods and data
Service costs
The costs of providing the doula service were calculated from information collected from service managers of the Hull Goodwin doula project and the roll-out sites. Managers were asked to provide information relating to the costs of doula recruitment and training; doula costs (travel and telephone); and the costs of running the service including premises, equipment and consumables. This information was requested for three financial years: 2010/11, 2011/12 and 2012/13. The questionnaire issued to service managers appears in Appendix 13. The roll-out sites had some difficulties in providing information with several items missing or estimated. In some cases, costs could not be disaggregated from those of host services.
Health and clinical outcomes
Method of birth
The following data on type of birth were extracted from the Hull Goodwin doula project database. Epidural use was recorded for normal and assisted vaginal births; anaesthetic used in births by C-section was not recorded.
NHS reference costs were used to estimate the average cost by type of birth for each of the five consecutive financial years for which birth outcomes data are reported in Table 32. The estimates are activity-weighted means of average costs reported across the relevant Healthcare Resource Group (HRG) code sets. Cost data were sourced from hospital inpatient stays (elective, non-elective long stay, non-elective short stay) and hospital day cases. We also added in costing data due to excess bed-days for both inpatient types, but to avoid double-counting do not add the corresponding activity level into the denominator of the calculation. Estimates did not include costs of non-hospital births and other events such as GP consultation, antenatal and postnatal outpatient attendance.
| Financial year | Method of delivery | Total | |||||
|---|---|---|---|---|---|---|---|
| Normal | Assisted | Caesarean | Unknown | ||||
| Epidural used? | Epidural used? | ||||||
| No | Yes | No | Yes | ||||
| 2008/9 | 29 | 11 | 1 | 1 | 10 | 0 | 52 |
| 2009/10 | 27 | 7 | 1 | 3 | 13 | 2 | 53 |
| 2010/11 | 52 | 12 | 0 | 3 | 18 | 2 | 87 |
| 2011/12 | 36 | 9 | 1 | 2 | 12 | 3 | 63 |
| 2012/13 | 36 | 11 | 3 | 0 | 13 | 3 | 66 |
| Total | 180 | 50 | 6 | 9 | 66 | 10 | 321 |
Mode of birth was categorised into normal, assisted, planned caesarean and emergency caesarean. The HRG codes used to define each category are as follows: normal is NZ11A–G (i.e. NZ11A, NZ11B, . . . , NZ11G), assisted is NZ12A–G, planned caesarean combines NZ13A and NZ13B, and emergency caesarean combines NZ14A and NZ14B.
Adjustments were needed in order to obtain delivery cost estimates in 2008/9 and 2012/13. HRG codings for mode of birth recorded in 2008/9 are incompatible with those given above (a number of maternity-related HRG codes were superseded in 2009/10). Therefore, delivery costs in 2008/9 were backcast using 2009/10 estimates and PSSRU’s HCHS price index. For 2012/13, reference costings and HCHS were not yet available. We therefore forecast 2012/13 delivery costs using 2011/12 estimates and a 2012/13 prediction of 292.7 (standard error 3.77) for HCHS [obtained as the one-step-ahead prediction from the cubic regression of HCHS on annual consumer price index from 1997/8 to 2011/12 (R2 = 0.9975) using the 2012/13 consumer price index of 123.825]. 51 The full listing of estimates appears in Table 33.
| Financial year | HCHS | Method of delivery | |||
|---|---|---|---|---|---|
| Normal | Assisted | Caesarean | |||
| Planned | Emergency | ||||
| 2008/9 | 267.0 | £1546 | £2228 | £2666 | £3329 |
| 2009/10 | 268.6 | £1546 | £2228 | £2666 | £3329 |
| 2010/11 | 276.7 | £1582 | £2326 | £2709 | £3344 |
| 2011/12 | 285.7 | £1602 | £2388 | £2723 | £3467 |
| 2012/13 | 292.7 (estimate) | £1602 | £2388 | £2723 | £3467 |
Next, per birth comparisons were undertaken in which outcomes for women who had received doula support were compared with those reported countrywide for NHS England and locally for NHS Hull PCT (NHS Hull hereafter). Data for NHS England were sourced from NHS Maternity Statistics: 2011/12. 53 Data for NHS Hull were sourced from HES, but, as caesarean delivery is not separated into planned and emergency, we used instead estimates from the larger population served by HEY (available in provider-level tables that accompany NHS maternity statistics54), which includes within it the smaller population of NHS Hull. In the absence of the release of official data for 2012/13, we formed estimates equivalent to those in 2011/12. The delivery distributions are reported in Table 34.
| Method of delivery | Financial year | NHS England (%) | NHS Hull (%) |
|---|---|---|---|
| Normal | 2008/9 | 63.24 | 70.68 |
| 2009/10 | 62.80 | 69.31 | |
| 2010/11 | 62.60 | 68.98 | |
| 2011/12 | 62.12 | 67.19 | |
| 2012/13 | 62.12 | 67.19 | |
| Assisted | 2008/9 | 12.19 | 7.72 |
| 2009/10 | 12.40 | 7.85 | |
| 2010/11 | 12.50 | 8.18 | |
| 2011/12 | 12.83 | 9.24 | |
| 2012/13 | 12.83 | 9.24 | |
| Emergency caesarean | 2008/9 | 14.79 | 13.64 |
| 2009/10 | 14.80 | 14.42 | |
| 2010/11 | 14.80 | 14.27 | |
| 2011/12 | 14.83 | 13.92 | |
| 2012/13 | 14.83 | 13.92 | |
| Planned caesarean | 2008/9 | 9.79 | 7.96 |
| 2009/10 | 10.00 | 8.42 | |
| 2010/11 | 10.10 | 8.58 | |
| 2011/12 | 10.22 | 9.65 | |
| 2012/13 | 10.22 | 9.65 |
As the Hull Goodwin doula project database did not record whether caesarean deliveries were planned or emergency, we assumed that caesareans for doula-supported mothers split between emergency and planned identically with those of either comparator listed in Table 34. We examined the cost implications of varying this assumption by deriving results at either extreme, namely either all caesareans performed for doula-assisted mothers were planned or all were emergency.
Our results were formed as an aggregate across the four stated delivery types, using as unit costs the schedule given in Table 33. In the case of the doula service this is a simple sum across observed outcomes multiplied by cost. For both comparators the calculation is a weighted sum, where the weights are the empirical delivery distributions given in Table 34. The difference we report as the annual per birth cost differential.
Epidural use
Schroeder et al. 55 micro-costed epidural use in maternity at £312.14 in 2009/10 prices. Using HCHS given in Table 33, this is equivalent to £332 in 2011/12 prices. This estimate is applicable whether the method of delivery is normal or assisted.
The Hull Goodwin doula project database records administration of an epidural anaesthetic alongside the method of delivery for doula-supported mothers whenever the birth is classified as being either normal or assisted; number per financial year appear in Table 32. We combined the two delivery types and aggregated over the 5-year period 2008/9 to 2012/13 to form an estimate of the rate of epidural use by doula-assisted mothers experiencing either normal or assisted births.
We then repeated the same approach to arrive at estimates of annual per birth differentials of the cost of the doula service to NHS England and to local NHS services. These relied on using an estimate of each comparator’s rate of epidural use and multiplying by the same size cohort as the number of doula-supported mothers experiencing either normal or assisted births (i.e. a total of 245 births; see Table 32) to arrive at the expected number of epidurals.
Data for NHS England for normal deliveries and assisted deliveries were constructed using extracts from NHS maternity statistics. Table 35 gives the numbers of births recorded across NHS England of each delivery type – normal and assisted – and for each of those the number in which an epidural was used: normal + epidural and assisted + epidural. The percentage of epidural use combined across the two delivery types is also included.
| Method of delivery | 2008/9 | 2009/10 | 2010/11 | 2011/12 |
|---|---|---|---|---|
| Normal | 290,143 | 327,315 | 339,214 | 347,104 |
| Normal + epidural | 32,254 | 34,191 | 36,366 | 38,595 |
| Assisted | 58,987 | 64,458 | 67,747 | 72,130 |
| Assisted + epidural | 25,140 | 26,666 | 27,594 | 30,433 |
| Combined | 16.4% | 15.5% | 15.7% | 16.5% |
In addition to NHS Hull we considered other, potential, local area-level NHS comparators, being those PCTs defined to be its statistical neighbours: NHS Hartlepool, NHS Middlesbrough, NHS Salford, NHS South of Tyne – South Tyneside PCT and NHS Stoke-on-Trent. Data for these geographies were sourced from HES and appear in Table 36. The extraction was based on the presence of Y81.X, the identifiers for epidural procedures, among the R19–24 coded set of episodes of normal and assisted deliveries. Data for NHS Stoke-on-Trent were only partially complete and are therefore not reported.
| Region | Method of delivery | 2008/9 | 2009/10 | 2010/11 | 2011/12 |
|---|---|---|---|---|---|
| NHS Hull | Normal | 2495 | 2480 | 2511 | 2519 |
| Normal + epidural | 800 | 754 | 745 | 729 | |
| Assisted | 256 | 263 | 280 | 327 | |
| Assisted + epidural | 206 | 197 | 208 | 253 | |
| Combined percentage | 36.6 | 34.7 | 34.1 | 34.5 | |
| NHS Hartlepool | Normal | 801 | 803 | 746 | 766 |
| Normal + epidural | 47 | 43 | 63 | 54 | |
| Assisted | 103 | 95 | 92 | 113 | |
| Assisted + epidural | 24 | 40 | 28 | 40 | |
| Combined percentage | 7.9 | 9.2 | 10.9 | 10.7 | |
| NHS Middlesbrough | Normal | 1319 | 1369 | 1366 | 1323 |
| Normal + epidural | 152 | 147 | 135 | 140 | |
| Assisted | 178 | 204 | 212 | 221 | |
| Assisted + epidural | 99 | 108 | 111 | 102 | |
| Combined percentage | 16.8 | 16.2 | 15.6 | 15.7 | |
| NHS Salford | Normal | 2275 | 2315 | 2425 | 2283 |
| Normal + epidural | 417 | 387 | 356 | 267 | |
| Assisted | 366 | 411 | 491 | 487 | |
| Assisted + epidural | 231 | 257 | 295 | 244 | |
| Combined percentage | 24.5 | 23.6 | 22.3 | 18.4 | |
| NHS South of Tyne – South Tyneside PCT | Normal | 1071 | 1056 | 1081 | 1010 |
| Normal + epidural | 101 | 120 | 120 | 102 | |
| Assisted | 218 | 253 | 265 | 213 | |
| Assisted + epidural | 90 | 122 | 108 | 74 | |
| Combined percentage | 14.8 | 18.5 | 16.9 | 14.4 |
Breastfeeding
The following data on breastfeeding outcomes (Table 37) were extracted from the Hull Goodwin doula project database.
| Financial year | Feeding | |||||
|---|---|---|---|---|---|---|
| At birth | At 6 weeks | |||||
| EBF | Mixed | Bottle | EBF | Mixed | Bottle | |
| 2008/9 | 73.1 | 5.8 | 21.2 | 47.1 | 7.8 | 45.1 |
| 2009/10 | 76.9 | 5.8 | 17.3 | 44.2 | 15.4 | 40.4 |
| 2010/11 | 67.4 | 15.1 | 17.4 | 45.8 | 7.2 | 47.0 |
| 2011/12 | 80.3 | 3.3 | 16.4 | 47.5 | 23.7 | 28.8 |
| 2012/13 | 79.0 | 3.2 | 17.7 | 54.3 | 4.3 | 41.3 |
| Average | 74.8 | 7.3 | 17.9 | 47.4 | 11.7 | 40.9 |
Over the 5-year period 2008/9 to 2012/13, the at-birth and 6-week rates of exclusive breastfeeding by doula-supported mothers averaged, respectively, 74.8% and 47.4%. These were contrasted against the at-birth exclusive breastfeeding rates for NHS England and for NHS Hull of, respectively, 73.1% and 57.4% (averaged over the period 2008/9 to quarter 2 of 2012/13) and the 6- to 8-week rates of, respectively, 31.9% and 24.3% (England averaged over the calendar years 2010–12, Hull averaged over the calendar years 2009–12). 56 These figures showed greater persistence in exclusive breastfeeding up to 6 weeks by doula-supported mothers and so our economic comparisons were based on 6-week differentials.
We applied the economic model given by Renfrew et al. 57 to estimate whether or not there are NHS costs avoided that accrue to the doula service, based on observed exclusive breastfeeding (EBF) 6-week data against the comparators NHS England and NHS Hull. We aggregated across primary and secondary care costs, doing so for two selected health outcomes taken from the Renfrew et al. study: gastrointestinal infection and lower respiratory tract infection. For a given health outcome, the per birth cost differential is given by the formula:
where c denotes the per unit outcome cost, b1 the doula service EBF 6-week rate, r the component odds ratio in favour of EBF and s the overall disease incidence. The outcome non-EBF incidence rate, represented by x in the above formula, is defined by
and was calculated using b0, which, in our case, is the comparator’s EBF 6-week rate given previously. Table 38 lists the parameter values of r, s and c at which our estimates were formed.
| Parameter | Value | Source |
|---|---|---|
| Gastrointestinal infection | ||
| Primary care | ||
| r | 0.28 | See appendix 12 of Renfrew et al. (2012)57 |
| s (England) | 4.682% | See appendix 12 of Renfrew et al. (2012)57 |
| s (Hull) | 8.125% | See ‘North region’ estimate, Table 16.1 in appendix 16 of Renfrew et al. (2012)57 |
| c | £43 | GP consultation length averaging 11.7 minutes, Curtis (2012)50 |
| Secondary care | ||
| r | 0.39 | See appendix 12 of Renfrew et al. (2012)57 |
| s (England) | 1.69% | Table 8 of Infant Feeding Profiles 2010 to 201156 |
| s (Hull) | 1.15% | Table 8 of Infant Feeding Profiles 2010 to 201156 |
| c | £1052 | HCHS upscale of Renfrew et al.’s (2012)57 cost |
| Lower respiratory tract infection | ||
| Primary care | ||
| r | 0.69 | See appendix 12 of Renfrew et al. (2012)57 |
| s (England) | 23.433% | See appendix 12 of Renfrew et al. (2012)57 |
| s (Hull) | 19.082% | See ‘North region’ estimate, Table 16.4 in appendix 16 of Renfrew et al. (2012)57 |
| c | £43 | GP consultation length averaging 11.7 minutes, Curtis (2012)50 |
| Secondary care | ||
| r | 0.7 | See appendix 12 of Renfrew et al. (2012)57 |
| s (England) | 6.33% | Table 2 of Infant Feeding Profiles 2010 to 201156 |
| s (Hull) | 7.28% | Table 2 of Infant Feeding Profiles 2010 to 201156 |
| c | £1078 | HCHS upscale of Renfrew et al.’s (2012)57 cost |
Smoking cessation
Smoking prevalence and smoking cessation among doula-supported mothers may be estimated from questionnaires completed by women who accepted the offer of doula support; 32.6% of the women (28 of 86) were smokers and 60.7% (17 of 28) reported that they had stopped smoking during pregnancy. These contrasted with 2010 NHS England figures: prevalence 22% and cessation rate 45.5% (table 11.4)4 (note that for purposes of comparability the category of smoking behaviour in the year prior to conception is not included here). Corresponding figures for NHS Hull do not seem to be available.
To compare maternal and infant health outcomes attributable to smoking alongside financial cost we used the costing tool that accompanies the National Institute of Health and Care Excellence (NICE) guidance on smoking cessation in pregnancy. 58 Although the tool’s original purpose was to evaluate and compare savings due to NHS campaigns to stop smoking in pregnancy, it was adapted to examine cost savings in our prevalence–cessation circumstance. This was done essentially by ignoring the tool’s intervention settings, but ensuring that the percentage quit rate was set such that it generated exactly the assigned smoking cessation rate. The maternal complications attributable to smoking include ectopic pregnancy, premature rupture of membrane, placenta praevia, placental abruption, pre-term delivery and pre-eclampsia. The infant complications attributable to smoking include low birthweight, respiratory distress and sudden infant death syndrome.
For a given prevalence–cessation pair we used the costing tool to compute the savings to the NHS across the adverse health outcomes attributable to cessation of smoking. We removed any savings attributable to the avoidance of ectopic pregnancy because this outcome precedes involvement of the doula. We then examined the impact that a decline in the smoking cessation rate has.
To illustrate the settings, suppose that cohort size is 1000. At a prevalence of 32.6%, then, 326 pregnant women will be current smokers. Of these, 198 (60.7% of 326) will quit smoking prior to giving birth. Thus, out of the total of 1000 women, 128 will continue to smoke. Repeating this calculation, assuming a 10% reduction in the cessation rate to 50.7%, finds 16 fewer quitters.
Attributing to doulas the entirety of any gain to the NHS from smoking cessation may not be a tenable assumption. From the above mentioned Infant Feeding Survey 2010 data, 90% of quitters gave up on confirmation of pregnancy, whereas only 10% of all quitters gave up later in pregnancy and stayed quit. In questionnaires completed by women for this research, data reflected a similar pattern, with only 12% of quitters (2 of 17) attributing their smoking cessation to their doula. Accordingly, we attributed 10% of any gains from smoking cessation as the portion accruing on average to doula support.
Neonatal intensive care
Data on admission to Hull’s neonatal intensive care unit (NICU) were extracted from the Hull Goodwin doula project database. A total of 15 babies of doula-supported mothers were admitted to NICU over the 5-year period 2008/9 to 2012/13. With data available for a total of 321 doula-assisted births over this period, this yielded an admission rate to NICU of 4.67%.
Hull Royal Infirmary provides a level 3 NICU and neonatal care services for the population covered by HEY. For the calendar year 2011, Watkinson and Davis59 reported a total of 492 babies admitted to the infirmary’s NICU. We estimated the number of babies born in the trust in the 2011 calendar year by taking the reported birth counts by financial years 2010/11 (5661 births) and 2011/12 (5822 births) reported in Tables 32–45 in the provider-level data that accompany NHS Maternity Statistics: 2011/12 and apportioning one-quarter of those in 2010/11 and three-quarters of those in 2011/12 to 2011. This yielded an admission rate estimate of 8.51% in 2011 (492 of 5781.75). We assumed this estimate applies in each financial year of our data.
Critical care tables in NHS Reference Costs list cost per cot day, by each neonatal care type; HRG codes XA01Z–XA05Z. Aggregated across each care type, the average cost per cot day is given in Table 39.
| Financial year | Cost |
|---|---|
| 2008/9 | £658 |
| 2009/10 | £658 |
| 2010/11 | £660 |
| 2011/12 | £630 |
| 2012/13 | £630 |
Modi61 presents nationwide NICU discharge data giving median length of stay by gestational age at birth for the calendar year 2011 and for the 9 months to September 2012. The weighted average of these results across gestational age and in combination across the full 21-month period yields an averaged median length of stay of 15.41 days.
Results
Doula service costs
Service provision
Service provision comprised costs incurred in running and maintaining the doula service. Despite the heterogeneous nature of the services, the major item of cost was staff salaries, wages and on-costs, amounting variously to between 50% and 70% of overall yearly budgets, and to a grand average per financial year of approximately 60%. In the case of one roll-out service, the costs of two half-time staffing positions represented an even higher proportion of overall costs, but this was mainly because service costs were largely absorbed by its parent organisation. In contrast to the six whole-time equivalent staff supporting the doula service at site A, the numbers at roll-out sites ranged between 0.5 and 1, although it was not always possible to make these calculations separately from their host organisations. One roll-out service located beneath a larger umbrella of NHS-provided maternity services had all its costs subsumed within its host organisation. The ability to absorb costs elsewhere in the system has its advantages. For example, costs associated with language interpretation totalled £9600 in service A across the three surveyed financial years, yet for two other services this item of cost was entirely absorbed by their host organisations.
Other possible service provision items included equipment (computers, printers, mobile phones, etc.), consumables (telephone calls, postage, stationery, licences, insurances, etc.), building, premises and rent, among others. The rent in the case of service A was substantial, averaging approximately 15% of total budget per financial year.
Free support
Free or in-kind support represented an important, potentially necessary supplement received by all services to varying degrees. Sharing of office space and rental costs, either in full or in part, were indicated by two services. Indeed, one service estimated the value of its office accommodation at well over 50% of its total of freely received support, where the latter represented approximately one-third of its overall grant-funded income received over the 3 financial years of data. Training venue access was another listed item of free support. Volunteer teaching featured too, with sessions received through NHS-led services. These included sessions on local safeguarding, smoking cessation and interpreting as well as sessions given by midwives. For 2 financial years, one roll-out service reported receiving 90 hours of volunteer teaching. It estimated the worth of that provision to be approximately 20% of its combined budget over that period.
An important budgetary supplement is external grant income with, for example, service A securing approximately 20% of its 2010/11 and 2011/12 budgets through breastfeeding support funding.
Unpaid out-of-hours work
Offsetting in-kind provisions was unpaid out-of-hours work by salaried staff. Out-of-hours cover arrangements varied; one service, for example, had salaried staff available on call out of hours in case of an emergency. Service A defined its out-of-hours system: all staff are on call on weekdays from 17.00 to 20.00 and from 16.30 on Friday to 09.00 on Monday; on-call is staffed on a rota basis. Furthermore, the service manager is on call 24 hours of every day and can attend births. Actioned calls are offered back to staff as time off in lieu.
One of the roll-out services differed in that, in its initial years, any call taken by 24-hour on-call staff was offered back as time off in lieu whether actioned or not. Uptakes of on-call time were not specified by services; however, estimates of total unpaid staff overtime not counterbalanced with time off in lieu arrangements varied between 8 and 15 hours per week for the three services that provided information.
Volunteer recruitment and training
To attract a new cohort of volunteers, each service utilised advertising, promotional materials and marketing or recruitment events. However, expressed as a portion of budget these drives are small: in the region of 1–2%. Documentation fees included enhanced Disclosure and Barring Service checks for the incoming cohort when establishing a training group and outgoing volunteer training programme accreditation fees such as those for the OCN or City & Guilds. Each service reported accreditation fees averaging around £1000 per financial year. This fee typically comprised an overarching component due to the service acting as a training centre and a per cohort component that depended on volunteer numbers.
When running training sessions there were costs associated with training materials, catering and provision of child care for volunteers. Training materials at service A averaged over £2000 per financial year, as did their childcare provision. For one roll-out service, training materials averaged over £300 per financial year, with childcare costing £1500 in 2011/12. At another, the first of two cohorts commenced during 2011/12; training materials cost £1000 per financial year; childcare cost over £2000 in 2011/12 but was reduced to 30% of this figure in 2012/13; and catering cost £800 in 2011/12 and £1000 in 2012/13. At a third service, childcare was the more costly item at £1200 in 2010/11 and £900 in 2011/12.
Travel expenses associated with training can be substantial. These were incurred in two main ways: (1) costs associated with travel to initial screening interviews to assess suitability to enter the programme (either by reimbursing salaried staff for undertaking home visits or by reimbursing applicants for travel to interview) and (2) costs associated with travel to and from training sessions. One roll-out service had combined training travel costs of £600 across 3 financial years; another service specified training travel as £400 in 2011/12 and £1600 in 2012/13. Service A identified staff travel totalling £6300 in the 3 financial years, but not the portion of this due to screening interviews. Service A identified volunteer travel costs as totalling almost £18,000 across the three financial years; however, this figure was essentially the combined reimbursement of all expenses incurred by doulas (travel, mobile phone, etc.), whether that be in a cohort undertaking training or in doulas actively supporting women. Another roll-out service recorded aggregate volunteer doula support over the 3 financial years totalling almost £20,000 but did not give an itemised breakdown.
Only one service reported incurring costs associated with hiring of a training venue, whereas most report that as support in kind. Trainer fees were split between internal and external providers. Fees for the latter were reported to be £150 per financial year at service A, £720 per trainee cohort at one roll-out site and between £600 and £700 per financial year elsewhere.
Over the 3 financial years, one service reported aggregate volunteer recruitment costs of £2200 and aggregate training costs of over £16,000, but itemised breakdowns are not available in either case.
In regard to ongoing training of volunteer doulas only one roll-out service reported incurring costs in this category, totalling £800 over the 3 financial years.
Volunteer numbers
Training completion rates varied between services where data were available; at service A for 2012/13, a completion rate of 96.7% (29 of 30) was reported, with a figure of 80% (29 of 36) reported in one of the roll-out sites. At 1 year, retention rates for doulas varied: 85% (33 of 39) and 70% (25 of 36) for two services. In one roll-out service in 2010, six of seven recruits completed training, of whom four went on to provide support to women and, in 2011, 15 of 16 recruits completed training, of whom 11 went on to provide support. In 2012, 10 of 15 recruits completed training, of whom five had since provided support. In 2013, 9 of 12 recruits completed training but had not yet provided active support. For another roll-out service, 13 recruits had completed training for each of their first two intakes. Out of the first cohort (trained in 2011/12) four remained as active volunteer doulas to late 2013 and of the second cohort (trained in 2012/13) 12 continued.
At the beginning of the financial year 2012/13, service A had 53 trained volunteers, of whom 11 were inactive and 11 were taking a break. By the end of the financial year, and with numbers boosted by two training intakes during the year, numbers of trained volunteers had risen to 81; of these, 27 were inactive and seven were taking a break. For 9 months of the year a total of 30 volunteers were actively involved in supporting women, which increased to 47 in the remaining months, averaging 34.25 active doulas per month over the course of the financial year. Given total volunteering costs of £8000 for service A in 2012/13, this equals an average cost incurred of £234 per active volunteer doula. Expressed per client match, for 2012/13 the cost averages to £121 (using 66 births as divisor, see Table 32). This contrasts with one roll-out site, for which £98 per match was budgeted in 2012/13.
Health and clinical outcomes
The following section draws on outcome data available from service A database, as described in Chapters 2 and 3.
Method of birth
The delivery data given in Table 32 for the doula-supported women when averaged across the 5 financial years 2008/9 to 2012/13, and ignoring the 10 deliveries categorised as unknown, yielded rates for normal births of 74% (230 of 311), for assisted births of 4.8% (15 of 311) and for caesarean births of 21.2% (66 of 311). Focusing on caesarean births, the rate in the doula-supported group compares favourably, although not significantly so, against the simple average rates computed from the data given in Table 33 of approximately 25% for NHS England and 23% locally for NHS Hull.
Per birth, and aggregated across the four delivery types, the cost differentials between doula-assisted deliveries and NHS England, and between doula-assisted deliveries and deliveries in NHS Hull, are given in Table 40 by financial year. Negative values indicate a cost saving to the NHS arising from the doula service.
| Financial year | NHS England | NHS Hull |
|---|---|---|
| 2008/9 | –£164 | –£63 |
| 2009/10 | –£53 | +£41 |
| 2010/11 | –£148 | –£60 |
| 2011/12 | –£168 | –£89 |
| 2012/13 | –£161 | –£81 |
In the absence of the type of caesarean recorded in the Hull Goodwin doula project database, the results appearing in Table 40 were based on the assumption that caesareans split between emergency and planned identically to that of the comparator as recorded in Table 34. In contrast, cost differences are given in Table 41 corresponding to either extreme; namely, that either all caesareans performed on doula-supported mothers are planned or all are emergency.
| Financial year | NHS England | NHS Hull | ||
|---|---|---|---|---|
| All planned | All emergency | All planned | All emergency | |
| 2008/9 | –£215 | –£87 | –£384 | –£16 |
| 2009/10 | –£121 | +£47 | –£340 | +£103 |
| 2010/11 | –£203 | –£68 | –£386 | –£9 |
| 2011/12 | –£228 | –£80 | –£398 | –£28 |
| 2012/13 | –£223 | –£70 | –£398 | –£18 |
It is not surprising, given the additional costs resulting from emergency versus planned caesareans, that savings to the NHS diminish if more caesareans are undertaken on an emergency basis. However, even if all caesareans to doula-supported mothers were performed as emergency procedures, there is still a small cushion of savings accruing to the NHS resulting from the doula service when aggregated across all delivery types relative to both comparators, the results for 2009/10 set aside.
Epidural use
Combining normal and assisted deliveries in Table 32, for the 5-year period 2008/9 to 2012/13 epidural use amongst doula-supported mothers occurred in 57 of 245 deliveries, yielding an estimated rate of use of 23.3% (SD 2.7%). Comparison with, for example, NHS England, for the expected number of epidurals when scaled to the same cohort size of 245 is, using figures derived from Table 35:
Accordingly, we estimated that epidural use by doula-supported mothers incurs further costs relative to NHS England averaging approximately £24 per birth [£332(57–39.3)/245]. Similar calculations using data given in Table 36 for NHS Hull and for the combined statistical neighbours are reported in Table 42.
| Service | % (SD) | Expected number per cohort | Per birth differential cost |
|---|---|---|---|
| Doula service | 23.3 (2.7) | 57 | |
| NHS England | 16.0 (0.03) | 39.3 | +£23.99 |
| NHS Hull | 35.0 (0.5) | 85.7 | –£38.84 |
| Statistical neighbours | 17.8 (0.2) | 43.7 | +£18.04 |
Positive values for the cost differential indicate an additional cost burden to the NHS relative to the comparator, whereas a negative value indicates a cost saving to the NHS relative to the comparator. As the epidural rate of the doula service in normal and assisted births is placed between those of NHS Hull and NHS England, then, depending on which comparator is picked, either result – a cost saving or a cost burden – may occur.
Breastfeeding
The estimate of overall potential NHS cost avoided when comparing the doula service EBF outcomes with those of NHS England is £6.66 per birth. Compared with NHS Hull, the estimate is £9.59 per birth. Summaries by health outcome are given in Table 43. Negative values imply that NHS costs are avoided, or saved.
| Outcome | NHS England | NHS Hull |
|---|---|---|
| Gastrointestinal infection | ||
| Primary care | –£0.29 | –£0.71 |
| Secondary care | –£2.09 | –£2.00 |
| Lower respiratory tract infection | ||
| Primary care | –£0.54 | –£0.64 |
| Secondary care | –£3.74 | –£6.25 |
| Total | –£6.66 | –£9.59 |
Estimates of savings experienced against either comparator in gastrointestinal infection are, on aggregate, very similar. The main contributor to NHS savings relates to a reduction in the secondary care treatment of infants’ lower respiratory tract infection due to the higher EBF 6-week rate among doula-supported mothers.
Smoking cessation
Table 44 lists estimates of the number of cases of adverse health outcomes avoided as a result of a rate of cessation of smoking of 60.7% among a population of doula-supported women with a 32.6% prevalence of smoking. In all cases, with the exception of pre-eclampsia, maternal and infant outcomes worsen as the smoking cessation rate falls as the relative risk of these outcomes occurring is greater for smokers than it is for non-smokers. 28
| Number of complications | Smoking cessation rate 60.7% | Smoking cessation rate 50.7% |
|---|---|---|
| Number of maternal complications | ||
| Premature rupture of membrane | 13.06 | 11.75 |
| Placenta praevia | 1.06 | 0.96 |
| Abruption placenta | 0.61 | 0.55 |
| Pre-term delivery | 7.66 | 6.89 |
| Pre-eclampsia | –2.01 | –1.59 |
| Number of infant complications | ||
| Low birthweight | 9.43 | 8.45 |
| Respiratory distress | 4.01 | 3.59 |
| Sudden infant death syndrome | 1.39 | 1.31 |
| Total per birth saving | £69.70 | £63.33 |
In 2011/12 prices, Table 44 presents the costed savings on health that contribute positive savings to the NHS of £70 per birth, which drop back to £63 per birth should the cessation rate fall by 10 percentage points. Thus, NHS spending up to these levels per pregnant smoker would retain positive cost savings to the NHS. Finally, of the total gain we attributed a 10% portion to the doula service; namely, a saving of £7 per birth on average.
Neonatal intensive care unit
Since 2008/9, 15 of 321 babies (4.67%) born to doula-supported mothers have been admitted to Hull’s NICU. We applied national costing estimates in NHS Hull and assumed the local admission rate to be 8.51% as estimated for HEY. Table 45 gives the average cost differential between NICU use by babies born to doula-supported mothers and expected use across NHS Hull. Negative values indicate a cost saving to the NHS.
| Financial year | NHS Hull | +1 | 75% cost |
|---|---|---|---|
| 2008/9 | –£278 | –£82.81 | –£188.96 |
| 2009/10 | –£664 | –£464.90 | –£633.43 |
| 2010/11 | –£267 | –£147.48 | –£160.55 |
| 2011/12 | –£179 | –£17.10 | –£78.49 |
| 2012/13 | –£518 | –£363.62 | –£469.86 |
A small number of babies born to doula-supported mothers are admitted to neonatal intensive care each year. Reflecting on this uncertainty, the column in Table 45 labelled ‘+ 1’ gives cost differentials for the experiment that raises the admittance numbers by one more baby across each financial year. Averaging the difference in cost differences across the 5 years, one additional baby admitted from the doula-supported group reduces the savings differential to the NHS by £166.
Our construction of NICU cost implies that roughly one-half of all admissions are to lower level special care, one-quarter to high dependency and one-quarter to intensive care; this split follows the relative weightings seen on cot day counts across HRG codes. To simulate the circumstance that babies of doula-supported mothers might need higher levels of care when in NICU, we raised the per day cost applicable to this cohort to its upper quartile value (approximately equivalent to an additional £100 in 2011/12 prices in each year in Table 40). The results in the column of Table 45 labelled ‘75% cost’ show an expected reduction in savings to the NHS, but savings accruing to the doula service are nevertheless still made.
Costing summary
In the following section, service site cost aggregates are presented in Table 46 for the Goodwin volunteer doula service so that potential cost savings can be contextualised by the costs associated with running a mature volunteer doula service.
| Item | 2010/11 | 2011/12 | 2012/13 |
|---|---|---|---|
| Service provision | 148,768 | 152,176 | 155,840 |
| Volunteer recruitment | 3990 | 1492 | 2374 |
| Volunteer training | 4681 | 5916 | 5612 |
| Volunteer support | 6399 | 8875 | 11,229 |
| Total | 163,837a | 168,459 | 175,055 |
Service costs
Table 47 gives the total financial year expenditure per birth in the Hull Goodwin doula service and forms a per birth weighted average across the 3 reporting years. While the provider in this case is located in the third sector, we shall assume for purposes of illustration that its funding is entirely from the NHS, although this has not always been the case for this or other doula services.
| Financial year | Total expenditure (£) | Number of births | Expenditure per birth (£) |
|---|---|---|---|
| 2010/11 | 163,837a | 87 | 1883.18 |
| 2011/12 | 168,459 | 63 | 2673.95 |
| 2012/13 | 175,055 | 66 | 2652.35 |
| Total | 507,351 | 216 | 2348.85 |
Based on these figures, the average cost to the doula service per woman supported is approximately £2439, excluding women who received only postnatal support and women who disengaged from the service.
Health and clinical outcomes
In Table 48, summary estimates of the per birth cost differentials across the health and clinical outcomes of the doula service compared with NHS England and NHS Hull are listed. A cost differential displaying a positive value indicates an additional cost burden on the NHS, whereas a negative value indicates a cost saving to the NHS.
| Outcome | NHS England | NHS Hull |
|---|---|---|
| Method of birth | –£138.80 | –£50.40 |
| Epidural use | +£23.99 | –£38.84 |
| Breastfeeding | –£6.66 | –£9.59 |
| Smoking cessation | –£6.97 | N/A |
| NICU | N/A | –£381.20 |
The entries in the method of birth row were obtained as the simple average of the results that appear in Table 42. The entry in the NICU row was derived as the simple average taken across the first column of Table 45.
Treating each health or clinical outcome as equally important, we estimated the financial impact of volunteer doula support versus standard practice across health and clinical outcomes by adding up the columns of Table 48. In this calculation, we excluded epidural use in normal and assisted births, as this component had already been accounted for in the HRG code sets used to construct the per birth cost differential for method of birth. For example, selecting NHS Hull as the localised, socioeconomically similar comparator, the impact on the NHS across health and clinical outcomes versus standard practice was a net contribution to savings of £487 per birth (we have imputed £6.97, the NHS England estimate, as the saving difference for smoking cessation in NHS Hull).
Net cost to the NHS
Expressed per birth, and in the postulated scenario where all doula service funding is derived from NHS sources, the net cost to the NHS of a volunteer doula service is estimated by subtracting the estimated contribution to savings (£487) from the estimated average service cost (£2349), giving £1862 per doula-supported birth.
Doula payment
The doulas in this intervention provide their labour voluntarily, so from the NHS + PSS perspective the time spent by the doula in client support is a free resource and therefore imposes no cost burden.
On the other hand, if the perspective is (momentarily) widened such that the doula’s opportunity cost of time forgone on other activities could now be included in the cost schedule, then some portion of that time may involve productive activity involving paid employment and so could be costed at that level. However, when we surveyed the extent to which their role as doula affected their ability to take on paid work or devote additional hours to their existing work, 77.9% (53 of 68) responded that there had never been any effect on this. Only 4.4% (3 of 68) recorded a frequent impact; the remaining 12 doulas reported that they had sometimes been affected.
Departing from the volunteer model to one in which doulas are paid as employees by the NHS, the previous result (showing little hindrance if seeking additional time for productive labour) suggests that the reservation wage to work as a doula may be in the region of the minimum wage. This is also in line with responses to questionnaires completed by doula-supported mothers, in which exactly one-half favoured doulas being paid an hourly wage similar to that of a maternity support worker (£7–10 per hour), with the next most popular response (31%, 24 of 78) suggesting pay be at the minimum wage, £6 per hour. The remaining 13% (10 of 78) suggested wages be similar to those of a newly qualified midwife (£11–14 per hour).
The implications for service costs of an NHS-paid doula model are illustrated with one example in the context of service A. Assuming a wage rate of £8 per hour with 30% add-on costs, an active list averaging 34.25 doulas at any one time and contact with client and service totalling 4 hours per week on average [from responses to questions 5(a), 5(b) and 6(a) in the doula questionnaire] would add approximately a further £74,000 to total costs per year.
Discussion of costs to the NHS
Service costs
The per birth cost to the NHS of the volunteer doula service for disadvantaged childbearing women was estimated to be £2349. This figure was arrived at using Hull Goodwin expenditure data, where this, the original service, is based within the third sector and is a mature service, relative to the roll-out sites.
Health and clinical outcomes
The per birth contribution to NHS savings resulting from improvements in health and clinical outcomes resulting from doula assistance was estimated to be £487. This figure was arrived at by aggregation across a number of health and clinical outcomes hypothesised to be influenced by the doula intervention. It is worth noting that those outcomes may not necessarily be exhaustive, for there may be benefits from doula support that exist beyond the maternity episode that may be of wider societal benefit for women, and indeed for doulas.
The major contributor to the estimate was NICU use and this was shown to be sensitive to changing assumptions. For example, one additional NICU admission per year (see the ‘+ 1’ column in Table 45) reduces to £282 per birth the estimate of the net contribution to savings versus standard practice in NHS Hull.
Births by C-section among women who received doula support from the Hull Goodwin service were fewer than both comparators, but only marginally so: 21.2% versus 25% (NHS England) and 23% (NHS Hull). Despite the modest improvement, cost savings due to the doula service were evidenced even in the sensitivity analysis scenario in which all caesareans were assumed to be performed as emergency procedures. Contrasting the marginal difference observed here are two US studies, by Kennell et al. 15 and Kozhimannil et al. ,62 in which the differences between the two caesarean rates were of the order of 10%, in favour of doula support. If this level of improvement were translated into the UK context, then the contribution to cost savings due to the doula service would be substantial.
Epidural use among doula-supported women in Hull for normal or assisted birth averaged 23.3%. This was a higher rate of use than that observed throughout NHS England (16%) but does represent a one-third reduction on the rate of use seen in the local region NHS Hull (35%). When the doula service was compared against the local comparator, NHS Hull, less epidural use resulted in cost savings to the NHS. However, this reversed when the comparison was with countrywide practice. There was, of course, statistical uncertainty about both estimates due to small sample size. Finally, we note a similar epidural rate of 27.9% (n = 1079) reported in a recent study by Kozhimannil et al. 62 for doula-supported births to women of lower socioeconomic standing, where the cohort in that study was of Medicaid recipients in Minneapolis, MN, USA.
Costing summary
The net per birth cost to the NHS from doula support to disadvantaged childbearing women was estimated to be £1862. The caveats already noted on the relevance, weighting and uncertainty affecting each component in this calculation will be inherited by the net estimate.
Chapter 8 Discussion
Introduction and summary of primary data collection
This research provides the largest independent evaluation of trained volunteer doula services in England and involved the original site and four replication sites. Apart from one study that was carried out at the same time as our own and evaluated a single doula service in England,63 other studies of doula support have been conducted in non-UK settings, with different health-care systems and where the package of doula support has differed from that evaluated here and in some contexts where doulas may receive payment, either from funds or directly from clients. Our research used the conceptual framework of realistic evaluation,33 in recognition of the complex intervention being investigated in a real-life setting and took a pragmatic approach, utilising both quantitative and qualitative data, contributed by a wide range of individual participants and organisations. Our multiple approaches to data collection have provided a rich data source that encompasses the perceptions and experiences of women and doulas with a range of characteristics and perspectives. Focus groups and interviews yielded additional useful information and allowed exploration of CMOcs that were not possible by questionnaire. Doula service staff, local champions, commissioners, midwives and HoMs generally welcomed participation and, while there were practical challenges in arranging some data collection episodes, these constituencies engaged with the research in a supportive way that enables us to be confident that we have captured these perspectives comprehensively. Table 49 provides a summary of the primary data collection achieved. Where our findings have important limitations or potential for bias exists, we highlight these below.
| Data source | Face-to-face/telephone interviews (n) | Questionnaires (n) | Focus groups (n) |
|---|---|---|---|
| HoMs | 5 | 0 | 0 |
| Midwives | 0 | 0 | 4 groups (31 midwives) |
| Women | 0 | 166 (including telephone completion) | 2 groups preliminary data collection (7 women) 5 groups main data collection (13 women) |
| Volunteer doulas | 6 | 89 (71 of whom had supported women after training) | 2 groups preliminary data collection (11 doulas) |
| Doula service managers | 6 managers (11 interviews) | 0 | 0 |
| Doula service staff | 11 | 0 | 0 |
| Local champions | 4 (2 at X, 1 each at Y and Z)a | 0 | 0 |
| Commissioners | 4 (sites A, W, Y, Z)b | 0 | 0 |
| Total | 41 interviews | 255 participants completed questionnaires | 13 focus groups; 62 participants |
Challenges, strengths, limitations
Disadvantage
As noted in Chapter 1, the term ‘disadvantage’ covers a range of social, economic and psychological states which frequently coexist. Our evidence suggests that the doula services are indeed successfully engaging with women who are disadvantaged, as can be seen by data from a range of sources. Referrals to the original service were in areas with higher than average material deprivation as categorised by the IMD. The IMD comprises seven dimensions of deprivation: income; employment; health and disability; education, skills and training; barriers to housing and services; living environment; and crime. In several of the sites we included, other initiatives that target women in disadvantage were evident, for example Family Nurse Partnership programmes.
Referrals to the original doula service reflected higher rates for younger women and lower proportions of white British women than in the local population of childbearing women. Midwives described the positive features of doula support for isolated women without family networks or other support; they perceived that doulas supported access to and uptake of services, for women who may have otherwise found it difficult. Through women’s questionnaire responses, it was evident that a higher proportion of women who engaged with doula services were born outside the UK than national rates for women giving birth in England. A large proportion of women referred for doula support lived alone or had no supportive friends or family available to them. Women also reported their difficulties and thus disadvantage in trying to access services due to language or cultural barriers. Doulas also spoke of the difficult lives of some of the women they supported.
Ethics and governance issues
As with any research of this scale, considerable effort was invested in the ethics and research governance processes. The particular nature of the service being researched, that is one that comprises volunteer doulas working in the main from third-sector agencies, provided challenges in ensuring the appropriate governance mechanisms were pursued, as NHS governance staff are generally unfamiliar with the role of doulas and do not frequently encounter research that evaluates services provided by trained volunteers, based in non-NHS agencies. Some of the third-sector agencies were unclear of their status and governance requirements, if they received some funding contribution from NHS organisations. Finding answers to those queries required them to seek advice which added to the time required for governance approvals.
We encountered delays while trying to achieve portfolio adoption, until our research was reallocated within a team. We also encountered situations where NHS R&D departments would not initiate review, if, for example, staff were due for annual leave, because of the time targets they are required to meet.
We are aware that the NIHR is familiar with these issues but report them here because governance processes continue to result in serious delays and threats to timetables.
Patient and public involvement
We described our convening of two user panels in Chapter 2, section Advisory group and public involvement mechanisms, and their contributions to identifying important topics to be explored: in advising on approaches to data collection and in testing out data collection instruments for feasibility and acceptability. Public involvement in our research was further strengthened by a multidisciplinary advisory group that comprised a range of stakeholders including staff of doula services, women who had received doula support and doulas, in addition to maternity service commissioners, NHS staff and academic experts. These individuals provided advice both in and between meetings and also supported our research in their local constituencies, where applicable.
Measurement of clinical and public health outcomes
Measurement of public health outcomes was possible only for the original site, as numbers were too small at the roll-out sites. Even so, the sample size available in the Goodwin database was rather lower than we had expected and thus, for some clinical and public health outcomes, estimates of effect are very wide. The data held in the Hull doula database had a substantial data cleanse, routine checks were carried out for inconsistencies and data were checked against manual records. However, the limitations of the relatively small sample of doula-supported mothers must be noted in interpreting outcomes. We were constrained by what was available and inevitably use of comparisons is less robust than determining effects through prospective randomised controlled trials. In our application, we were always clear that such a trial was impossible for a range of reasons including the provision of DH funding to support roll-out and the fact that doula services were not in equipoise. Given the impossibility of a randomised controlled trial, the use of reference data sets of routinely collected data, available through the public health observatories, provided the most robust alternative. The data used were produced at different geographies, hence the use of PCT, local authority and trust data to strengthen comparisons.
Hull PCT and Kingston upon Hull local authority were considered coterminous and were used, as comparisons are often made in these situations. Other data were derived specifically from the maternity database at HEY. When this data source was used, the data were filtered to include only mothers who were resident in Kingston upon Hull. Analysis of deliveries in HES shows that 99.2% of deliveries to mothers who were resident in Hull PCT took place in HEY. No data quality issues were identified in the published data used for comparison. Data published by the Office for National Statistics, the DH and the Health and Social Care Information Centre have undergone quality assurance before publication. While some PCTs have known data quality issues relating to breastfeeding, this was not the case for the Hull PCT or its statistical neighbours. Data from HES are known to have some data quality issues, some fields more than others. Areas of known concern were avoided.
Data from doulas and women
We were surprised by the lower than expected response to questionnaires among doulas, especially in the context of the demonstrated commitment to the role. This constitutes a limitation to the interpretation of findings, although we were able to identify and offer explanations for both positive and negative experiences of the doula role. We can only hypothesise that our distance as researchers with information brokered through a third party may have contributed to the low response rate. It may also have been that doulas perceived our research as a potential threat to their organisation and thus did not engage.
We had expected a low response rate from women offered doula support and this was our experience. The implications of this low response rate must be noted. Despite multiple options for providing their views, response rates to our questionnaires were low, with 23.6% of women completing questionnaires out of the 84% of women who had been introduced to the service and sent a questionnaire. The proportion of multiparous women was higher than expected; unfortunately we do not have information about their previous childbearing experience. We suggest that reasons for the low response include the fact that women who were eligible to receive doula support were in groups traditionally hard to engage in research. They may well be suspicious of strangers asking questions and may worry about the implications of answers or even of responding, for example with regard to benefit entitlement or applications to stay in the UK. We had hoped that approaching women via an organisation previously known to them and reassuring them of confidentiality would help to maximise response rates. We also tried to ensure that potential participants understood that their responses would not be fed back to the doula services. We knew that some of the services focused their support on women from BME communities that would include some women unable to read and write in either English or their own language. That was part of the rationale for offering a variety of different ways in which women could take part. We also appreciate that some topics, for example emotional well-being, are sensitive ones about which women from some cultures may feel diffident about providing information. We realised that some of our potential participants had accessed the service several years previously and may well have moved from the address recorded while they were in receipt of doula services. That was borne out by the proportion who could not be contacted via the information held by the doula service. We do, however, feel that the number of women included who gave their first language as other than English (45.2%) is a strength of this research.
Low response generally means that those who are less articulate and those without strong feelings, in either direction, are less likely to offer a view. Since so many of the women were so positive about the service, it may be that we have failed to get responses from those who did not rate it so positively. It was evident, in at least one focus group, that women saw their attendance as a way to repay to the service the benefit that that they had received. Those who did not think that they owed the service anything will not have been motivated in this way. Thus, although we were as facilitative as we could be to enable women to attend the focus groups (e.g. providing transport, lunch, crèche and financial acknowledgement), it was evident that for many women the effort of getting themselves and their children to a specific place at a specific time was quite substantial.
In the absence of randomly derived groups, we had given considerable thought and taken advice on the identification of potential comparison groups against which, for example, women’s experiences of labour could be compared and from which we could identify questions acceptable to women that could be incorporated into our questionnaire survey. In using the Picker survey41 as our comparison, we were aware of some differences between the Picker sample and our own. These included the different years over which experience of the maternity service was compared (i.e. women responding to Picker gave birth in January and February 2010) and that Picker outcomes relate to a sample rather than all women giving birth at the trust; our sample was drawn from women who had experienced maternity care during all of the years in which the original doula service was available. Picker respondents are generally more likely to be older, white mothers, who may rate maternity services more positively than younger and non-white women (Anderson, Public Health England, 2013, personal communication). However, there were also similarities in that both were postal questionnaires (generally associated with a low response rate) and the means of maximising response rates for both questionnaires was informed by consultation with service users. In addition, the questions from the Picker survey included in our questionnaire have been utilised in several national surveys of maternity care.
Language support
Interestingly, the possession of a common language for communication is not considered essential by a significant proportion of women and doulas. Some midwives appeared to see the doula’s main purpose as language support and were thus mystified when a doula did not share a common language with the woman that she was supporting. There were also suggestions that some midwives might be more comfortable with the idea of a doula fulfilling a role as an intermediary which complemented their own role rather than challenging it.
A particular challenge in this research was involving women who were not fluent in English. Over half of the doulas had supported women who did not speak English. Of the women on the database of the original site, 37.1% were not ‘white British’ and, across all the sites, 45.2% of women completing questionnaires identified themselves as having a first language other than English. To identify these women, we were dependent on service records to tell us that the woman required an interpreter. We were surprised that smaller numbers of women than expected apparently required language support for their participation. Doula service documentation concerning language was largely limited to the need for an interpreter, rather than documenting the main language(s) spoken, which led to under-reporting of languages that could be pursued for the non-English-language focus groups. It is also possible that the need for language support was under-reported for pragmatic reasons: the financial implications of interpreter support; the greater complexity of involving an interpreter; and possibly as a strategy to encourage communication in English language and social integration. It is also the case that participation in research may require a different vocabulary than is required to engage with services.
Working with third-sector agencies
The organisations that host the doula service were generally of small to modest size with insecure funding in the longer term. Staffing levels in all of the doula services are low and administrative support limited. Priorities for these services include securing their own funding, training and running the service on a day-to-day basis.
We were aware that, in seeking the doula services’ support in steps towards data collection, we were placing additional burdens on them. Despite the provision of some funding for administrative support, it appeared difficult for services to put this to positive use within a short time scale. We identify these as issues that researchers may wish to consider in future research with such services.
Prior to commencing the research, we had been given to understand that the database at the original site would yield data for approximately 600 women and that data quality was considered good. The database and reports available from that system were, of course, designed for service provision rather than for evaluation; thus we identified the need for work to quality assure the data set before extraction could begin. Following completion of data cleaning and other aspects of quality assurance, it became apparent that outcome data were not available for as many doula service recipients as we had been given to understand. Further reflections, which may be of interest to researchers, on conducting research into volunteer roles and with third-sector agencies are included in Appendix 14.
Challenges with realistic evaluation
Realistic evaluation emphasises that interventions are intrinsically theory based: a given intervention is implicitly meant to tackle an underlying ‘social problem’ and people have, often unspoken, assumptions (theory) about how and why change happens (Mechanisms). The initial work in a realistic evaluation is to make the theory explicit. Identifying what different people see as the problem that is being addressed by the intervention was an important first step, achieved through our early interviews with doula service staff and focus groups with women’s and doulas’ user panels. Through initial data collection we identified each service’s key features and how they operationalised doula support. By defining the interventions we hypothesised the implicit CMOs at each site. These then had to be rendered accessible to key informants and we adopted the approach of working backwards from Outcomes to elicit informants’ beliefs about Mechanisms that would achieve those from a range of starting points or Contexts.
Published accounts of the use of realistic evaluation most commonly investigate interventions that occur at a system level. Furthermore, these are commonly investigated using a more discursive (qualitative) approach. The study of the Scottish policy initiative Keeping Childbirth Natural and Dynamic64 provides an example of this approach to programme evaluation. In our research, CMOcs were constructed at different levels of Context: woman level, doula level and doula service level. There is rather less literature on the application of realistic evaluation where an intervention is targeted at the individual level, as is the case with volunteer doulas.
Some may question the extent to which realistic evaluation is consistent with a quantitative paradigm unless considerably larger data sets are used. Further, how ‘testable’ are CMO configurations within the quantitative paradigm? The characteristics (Contexts) that have been identified as ‘for whom’ and ‘in what circumstances’ occur in combination, so bivariate analyses are unable to tease out the possible interactions that a realistic evaluation approach seeks to disentangle.
Context, Mechanism and Outcome configurations can be challenging to create or propose for several reasons. The CMO can ‘slide’; that is, a Context may sometimes be viewed as a Mechanism (e.g. provision of support), a Mechanism may sometimes be viewed as an Outcome (e.g. self-efficacy) and an Outcome may, itself, become a Mechanism for a longer-term Outcome.
A further challenge is discriminating between the description of the active intervention and the Mechanism; at times these appear to be the same, but the description of the intervention concerns its components, whereas the Mechanism describes the process by which the intervention (or its component parts) works. There are suggestions that the Mechanism must relate to how the intervention impacts on individual’s reasoning,33 but for some interventions this may not be achievable. An example from our research may be where accompanying a woman to appointments is the simplistic view of the Mechanism (and describes the intervention) but the Mechanism is reducing barriers to access, whether they are linked to lack of knowledge of the system, lack of transport for access or anxiety, but they do not relate to reasoning.
Another challenge is accessing the elements of the CMOc so that they are testable. This is particularly challenging when the intervention occurs at an individual level: the Context can be highly sensitive and the Mechanism can be subconscious. Participants are more likely to identify reasons for the intervention not ‘working’ that are at the doula or site level, rather than the woman level, for example engagement or motivation. However, the approach to data collection is also important: focus groups led to greater discussion of woman-level factors (Context) than obtained in the questionnaire and this reflects both the richness of data gathered in conversation and also the positive contribution of different but complementary approaches to data collection in our research.
The nature of replication
Interviews with key informants in the first stages of data collection identified that the roll-out sites were not, in fact, replicating the original doula service to the extent that we had been led to expect. This is perhaps inevitable when a concept is transplanted into a different setting and need not be seen as a problem in terms of achieving the wider goal of supporting disadvantaged childbearing women. However, it is of importance in terms of a Realist Evaluation because it means that key components of context and intervention may differ, as may the underlying social problem being addressed and different Mechanisms may be called into play. Thus, if different services are trying to address different problems, then it may well be that different Outcomes are of relevance and different Mechanisms are engaged to achieve these. Some differences were, in fact, found between sites on views of the underlying social problem, for example at the woman level, women birthing alone, high smoking rates, low breastfeeding rates and high infant mortality, or worklessness in the local community at the doula level.
Services were based in a range of host agencies, with different degrees of autonomy and funded from a range of sources; they used different names for the volunteer doulas; they served significantly different populations; they had amended training from that provided by the original service; and they did not use the bespoke database developed by the original service but developed their own or modified documentation used by the original site. Therefore, programme implementation varied considerably, together with the size of the doula services and their staffing configurations.
Differences extended beyond those that might be expected to develop to meet local needs. Rather than aspiring to intervention fidelity (or true replication), sites had developed services that were shaped by the existing skills, knowledge and expertise of the local service staff and organisation; local funding priorities; and relationships with other local services, both statutory and third-sector services. These were often positively influenced by the nature of the doula services’ host organisations, variously an NHS maternity service and third-sector organisations of varying sizes and with different core business including advocacy, community parenting and neighbourhood regeneration.
Services differed in other unforeseen ways related to the women supported, the focus of the doula’s role and referral criteria. Examples included that in some settings volunteers do outreach sessions in clinics rather than one-to-one support work; the relative weights given to different aspects of the role, for example the extent to which labour and birth is the focus of the service; the extent to which services dealt with women in particularly complex social situations; the point at which services were willing to accept referrals; and whether or not they were willing to provide support limited to the postnatal period. Interviews with commissioners and heads of midwifery services, in particular, identified that the underlying problems that the intervention is seen as addressing varied between sites, with implications for theorised Mechanisms of how and why the intervention is effective.
Discussion of findings
The following section will consider the findings, in the light of the available evidence, from the perspectives of women offered doula support, doulas and doula services; this will be followed by consideration of NHS perspectives, in particular those related to maternity services. As we have described above, the multiplicity of Contexts, Mechanisms and Outcomes identified makes it unhelpful to discuss individual CMOs and CMOcs.
Women’s perspectives
Being referred to the service
Women were referred to the service because they were isolated, alone or unsupported, had existing health problems or had particular concerns about labour and giving birth. We have some information about women who did not take up the offer of doula support or who discontinued it. The reasons for discontinuation varied but, from comparisons between women who engaged and who discontinued from the original site, it is interesting to note that younger women, those who were white British and those having their first child were more likely not to continue with doula support. This may be because the doula service is not the only source of support for women with some of those characteristics. In some locations, including site A, the Family Nurse Partnership service is well established, criteria are generally well known and referral systems are well established and mainstreamed. A further reason for disengagement may be that some women may prefer the additional input from a health-care professional, for example a teenage pregnancy specialist midwife, whose role may be better known than a volunteer doula.
Women were referred to doula services by a range of routes and, in respect to the original service, most frequently by community midwives. The proportion of women who were offered doula support but did not accept it was perhaps higher than might be expected among a group of women who may have limited alternative sources of support. This is an area that merits further exploration to inform marketing of services and information materials and to understand more about barriers to uptake.
The doula services place emphasis on trying to achieve optimum matches between women referred and doulas and also on facilitation of initial meetings. These would appear to be beneficial activities that avoid the difficulties of establishing contact between volunteers and women referred to services encountered in a randomised controlled trial of peer-mentoring for disadvantaged first-time mothers conducted in Northern Ireland. 65 In that study, despite living in the same geographical area, 25% of peer mentors reported difficulties establishing initial contacts with women, which could lead to reduced morale among the mentors, especially in the early days of the programme.
The nature of doula support
For women who accepted and continued with the doula service, their experiences of doula support were generally positive across a range of domains including practical and emotional support during labour, positive psychosocial impacts and being able to access other services. Women described themselves as gaining in confidence and ability to make decisions as a parent; this appears to be enabled through the doulas’ approach, which involves listening, is non-judgemental and non-directive, and supports the woman’s own choices. Women who received doula support appeared to benefit from the flexibility and continuity in relationships that they did not encounter among maternity professionals. 63 Through an approach based on building trust, listening and enabling (Mechanisms), women described experiences that demonstrated improvements in emotional well-being (Outcomes) and being supported to access services (Outcomes) which they might not otherwise have done, for example breastfeeding counsellors and children’s centres.
Similar sentiments were expressed by women who participated in the other independent UK evaluation of volunteer doula support. In that evaluation, doula support was reported by women as making them feel better informed, providing support for women who would otherwise have been alone for labour, and relieving isolation, based on relationships built on trust and confidence. 64
Some groups of women may require assistance to navigate and get the best out of the NHS maternity system. This may include women without previous experience of UK maternity services, women who do not speak English or women who are unsure of what they can ask for and expect to receive. Barriers to access for care include difficulties with communication, the involvement of multiple agencies and a lack of knowledge of the system of care. The NICE guideline Pregnancy and complex social factors9 (including women who may be recent migrants or who do not speak English) calls for models that overcome such barriers and facilitate access. It would appear that volunteer doula services make a contribution to this, in the main, from outside the NHS system through, for example, the co-ordinating support that a doula may provide for women engaging with a number of agencies and supporting women in making choices in maternity care; this finding was also identified in the other independent UK evaluation. 63
Women reported few frustrations with doula support or doula services. These appeared to relate to individual situations where the service or an individual had not provided support in the quantity or at the time expected. Some women found the doula service’s rules restrictive, for example that doulas were not allowed to disclose personal information or to accept small gifts. There were isolated criticisms about cultural awareness and also recommendations that doulas should be available who shared a common language with the woman, but the latter was by no means an issue for everyone.
Doulas’ perspectives
A response rate of 34.5% was achieved. It included doulas who had experience of supporting women and a smaller number who had not. Doulas came from a wide age range and different ethnic groups and included women in employment and education. Among doulas who had not supported women, some had discontinued because paid work became available; others had not yet had an opportunity to provide doula support.
Almost all doulas felt that their role helped women to access other services and increased women’s knowledge and skills related to childbearing and looking after their baby. When considered against a framework of social capital theory,66 both bonds and bridges were formed within and between groups and also among individuals. The most important factor that allowed them to achieve that was that they ‘got on well’ with women they were matched with, rather than having a shared language, being of a similar background or living in the same geographical location. Where matches had not been optimal, this was ascribed to the doula’s inexperience at that time or women hoping for support in areas that the doula service could not provide. In a small number of situations, there were suggestions that, with other partnerships, things might have been better. Doulas did not feel that their relationship with a woman was affected by when they met.
Some doulas had experienced communication problems with health and social care professionals, especially in the early days of the service, but these were rare. Doulas were mostly of the view that the role was distinct from other roles; just under 15% felt there were some overlaps, predominantly with that of midwives.
Reasons why doulas stopped volunteering varied. In three sites, volunteering had been discontinued for personal reasons; at site X there were no discontinuations of volunteering; at site Z, reasons for discontinuation related to the organisation of the service and the role.
With two exceptions, all would recommend being a doula to other people, and over 90% rated their experience very highly. Low ratings were associated with perceptions of the doula service, including the staff and their availability.
There are parallels between women and doulas for positive experiences and outcomes. Our findings support existing evidence67 that experience as a volunteer doula has positive impacts for the majority of volunteers, across a number of domains including the doula’s own health and well-being, and for their wider social context. Training appears to prepare them well for the role, as reported elsewhere,63 and to be a Mechanism that supports satisfaction with the role, together with positive experiences. Satisfaction with, and being supported by, their doula service are also Mechanisms that support positive experiences (Outcomes).
Doula services
Maintaining an appropriate flow of referrals and volunteers
A finding that emerged was the importance of doula services maintaining a high profile with potential sources of referrals. The doula services had limited resources at their disposal and their staff sometimes had multiple components to their role. It may be that these factors contributed to the fluctuations in the external profile of the doula services, with consequent impacts on recruitment of volunteers and referrals of women. The regular updates to maternity services that had been a feature of doula services’ early stages of development had diminished, leaving maternity staff unfamiliar with them and, thus, less likely to refer women. Information available within the original service’s database demonstrated that midwives were the most common source of referral to doula services, although interestingly their role as a route of referral was not commented on by participants in midwives’ focus groups. If midwives are not aware that they are a key source of referrals, low numbers of referrals are likely to continue. Without regular updates, relationships between services may suffer and referrals of appropriate women may not continue. The need to keep reminding midwives about the doula service was reported elsewhere. 63 Maintaining an external profile is also likely to contribute to sustaining a steady flow of volunteers, thus addressing the service challenge of balancing women referred to the service with the numbers of available volunteers.
To retain volunteers and to avoid demotivation,67 it would appear optimal that they achieve experience in the role within a relatively short time of completing training and that services should have processes in place to support this. This did not appear to be the case in all sites, leaving doulas questioning the service’s systems, why they had committed effort to the training and whether or not it was worthwhile to continue. Realistic evaluation asks ‘what works for whom under what circumstances?’ As with any intervention, there may be problems in that its theoretical base may be flawed or its implementation incorrect. This would seem to be an example where the problem is one of implementation rather than a fundamental problem with the programme itself, but it also reflects the importance of balancing supply and demand in order for the programme to succeed.
Doula support during labour
Much of the previous work related to doulas in other countries and health-care systems has focused on the presence of the doula to provide support during labour. 26 In some of those settings, midwives were not available and staffing complements were described as limited. The starting point and continuing emphasis of some of the doula services in this research was that labour was a priority area for doula support. Data collected from women across all sites identified that they derived benefits from doula support in labour through (female) companionship (reflecting research from a range of settings, e.g. by Pascali-Bonaro and Kroeger68), the doula’s supportive presence and being able to achieve the birth they wanted. However, when comparisons of the experiences of women who received doula support at site A are made with a sample of women from that city who completed the Picker Institute questions, we have some interesting findings that may appear contradictory. Women who had doula support reported feeling less involved in decision-making relating to both antenatal and intrapartum care, and more of the doula-supported women indicated that they did not receive the pain relief method they wanted, than the Hull Picker respondents. These findings must be interpreted with caution, beyond that associated with the limitations of use of the Picker reference data discussed previously. They may be interpreted as doulas encouraging inappropriate expectations or directing women’s choices in ways that may not be in line with their wishes, if, for example, the woman’s situation during labour is different from that expected, or of failing to advocate or enable a woman to engage in discussion of this. However, there were no reports from women that would support this interpretation and a number to the contrary. An alternative explanation is that, in line with the findings of feeling less involved with decisions about their care, doula-supported women were less satisfied with pain relief decisions because they had a greater understanding of the options that might have been available.
Doula support other than during labour
It is important to note that approximately 40% of doulas reported that there had been at least one occasion on which they had not attended a labour and birth that they had planned to attend, because of not being contacted when women went into labour or unavailability on their part. While non-attendance was often disappointing for the doula, it was noteworthy that support during pregnancy was sometimes sufficient to help a woman to achieve her goals for labour and birth; the presence of the doula in labour was not always essential for that.
Although many people consider labour support as the raison d’être of such services, we became increasingly aware that this was not necessarily how it was seen by women who contributed their views to this research. When asked if they could access support at only one stage which that would be, slightly over 30% women stipulated support before birth and slightly under one-fifth indicated support after giving birth as their preference. When volunteer doulas were asked the same question, support before birth was, in fact, the most popular answer (40%) on the grounds that antenatal preparation can set a woman up for what is to follow. Some doula services will accept referrals of women who have already given birth and women take up those offers. It could be argued that some women’s situations may be so difficult that any supportive contact may be welcomed but we have clear evidence, in regard to their labour experiences, that women still benefited from doula support (received during pregnancy) even if the doula was not present during labour. Women reported a range of support from their doula during pregnancy including help with preparing baby equipment, preparing for labour, being accompanied to appointments and going out into their community. Following birth, women reported support with breastfeeding, receiving information about and practical help with looking after their new baby. Women also benefited from improved communication with professionals as a consequence of doula support, receiving information about other services and help to access community and health service resources; all of these are independent of the intrapartum component of doula support.
It is important that the positive benefits of doula support outwith labour are not overlooked and that assumptions not be made about what might be achieved in improving a woman’s well-being if, for example, she is referred to the service later than usual or if she does not have doula support in labour. It is also important, when marketing the service with other agencies and also when discussing the service with women, that there be shared understandings of what doula services can provide and whether or not labour support is a key focus.
Signposting women to services
One aspect of the doula role is to signpost women to use of appropriate services. If this is considered using antenatal classes as an example, the relatively low rates of attendance across the sites and particularly at site A could be interpreted as a failure of the doula service in that regard. We would suggest that such an interpretation fails to take into account the complexities of the situation and offer alternative interpretations. While some women reported that their doula facilitated their access to antenatal classes, others may achieve the outcomes of being informed and confident about labour and gain the social support that antenatal classes aim to provide69 through the information provided by and support of their doula. Women may therefore feel that they do not need to attend antenatal classes.
However, it is important that services note that, while doulas generally felt well-prepared by their training, almost one-quarter had experienced problems in effecting the signposting element of their role; reasons varied from resistance on the part of the woman to the doula’s own lack of knowledge of the services. Doula services may wish to review the training related to this.
Friendship and endings
In the peer-mentoring trial described in Discussion of findings, Women’s perspectives, above,65 the role of mentors, who were trained and received a payment of £6 per hour for their activity, was to identify women’s health and social needs, to ensure that women were aware of health promotion information and to provide social support; there are therefore similarities with the doula role. Peer mentors reported that developing the relationship and external influences could be challenging. Interestingly, peer mentors shared information about their own families as a means of developing trust and rapport with their clients, and friendship was considered by midwives to be a positive feature in the relationship between mentors and clients. This approach differs from that in the doula services we explored, where we found evidence that doulas and women identified inconsistencies in how the doula role related to friendship. This friendship was externally bounded by rules that prohibited reciprocity of information and dictated discontinuation. While some women and doulas were untroubled by this, for others it was associated with distress for some women and disquiet for doulas. Doulas managed the ending of the period of support in a range of ways that included ensuring that women were linked in to other services and building up a woman’s confidence to access these. Endings were inevitable but difficult, especially where follow-on services were not easily identifiable and where women may have become over-reliant on their doula’s support. Although the preparation for endings differed between doulas, there was a clear sense that the suddenness after a period of quite intense relationship could be difficult.
It may be helpful to compare the doula role with that of other sources of volunteer support available to childbearing women. Roles such as breastfeeding counsellors or peer supporters also adopt non-directive approaches but those relationships are usually of a shorter duration and, it is argued, do not require an intense relationship to have been built and sustained over a period of several weeks. Such support is also focused on one particular element of the woman’s needs, in comparison with volunteer doula support, which encompasses a number of areas and is of a longer duration. Endings may therefore not be an issue with other volunteer roles, as these will often occur when a problem has been resolved. The negative impact of endings was compounded when there was no opportunity for women to express their gratitude to doulas with a token of thanks or other formal marking of the end of their support. Women were generally very appreciative of their doula’s support but were aware of the lack of opportunity for any reciprocity; this resonates with the findings of other research70 that women did not wish to be a burden to other women. This also reflects evidence related to support transactions and feelings of obligation. 71 Suggestions were voiced by doulas, women and midwives about how this issue could be dealt with; these included having a break between the end of the period of doula support and before further social contact between the woman and doula, informal catch-ups or the opportunity to mark birthdays and to provide or receive an update on the family’s progress. Doula services may wish to give further consideration to this aspect of their guidance.
Doula services: surviving and adapting
As we noted, the doula services are located within a range of host organisations. There is strength in that doula services may be part-supported by the host, which bears some costs, but may also be a threat if the host service itself is destabilised. The influence of the host organisations’ core businesses and their experiences have understandably shaped the direction of doula services. Doula services have had to be flexible to survive in a financially constrained climate where they may be competing for funds against both statutory and other third-sector agencies. To do this, in some services there has been a shift in emphasis to meet commissioners’ changes of policy, for example from a focus on supporting normality in labour to becoming active in changing smoking behaviours.
Capturing processes and outcomes
While a bespoke database was available as part of the replication package, it was not utilised by all services. As doula services continued to experience challenges in securing funding, it would appear important that robust systems are in place to monitor service use, the characteristics of women referred and outcomes for women and babies recorded for subsequent analysis and reporting. We would recommend that services consider whether or not their processes and systems enable the collation of such data, in addition to service support.
Payment for doulas
Volunteer doulas entered an arena where the negative perceptions of paid for doulas were frequently voiced. We found that the volunteer status is respected by all parties – women and maternity service staff – and the independent status is highly regarded, even when doula services are located within the NHS. When women and midwives considered payment, even of a token nature, this met with a cautious response, due to a sense not that doulas did not deserve payment, but that payment might result in recruitment of individuals without the same altruism as the volunteer doulas, which might, in turn, influence the doula’s relationship with the woman. Over three-quarters of women respondents supported payment, provided women were not charged, and one-quarter supported payment if women were charged. Payment of doulas was also seen to preclude access for some women for whom payment would be impossible. There appears, therefore, little evidence to require a change from the current voluntary basis.
A professional service
The majority of women would recommend the doula service to a friend or family member and nearly all doulas would recommend being a volunteer doula to others. Overall ratings of the experience of being supported by a doula were high, as were ratings of being a doula.
However, doula services are working in challenging situations and some of the women they support are in situations of considerable social complexity. For that reason, they must be perceived as being professional in approach, albeit when delivering a volunteer programme. This offers reassurance to other service leads, for example HoMs, and also to their own volunteers and women referred to the service. Women were critical of the doula service if they perceived it as unreliable, where it did not provide continuity or where they did not receive as much support as they wished. A higher proportion of women (and volunteer doulas) felt that the service had not worked for them at site Z than at other sites.
The importance of providing a professional service should not, however, be confused with the para-professional role for the volunteer doulas, as is the case for some doulas in the USA,72 or of moving towards professional care in the space between ‘natural’ (family/friend) and professional (midwife) support in the Swedish study by Lundgren et al. 73 where doulas were paid from a fund to provide support. Our research is more usefully viewed within the body of evidence of community-based and volunteer-provided programmes.
NHS maternity services
Positive working relationships
Heads of midwifery and midwives who attended focus groups voiced negative perceptions and experiences of paid-for doulas. Their experiences of the volunteer doula services were, by contrast, generally positive. Positive working relationships were usually achieved between doulas and midwives at both the individual and service levels. When present during episodes of hospital care, doulas supported communication between the woman and health-care professionals and advocated for her preferences.
Midwives considered that the relationship between doulas and themselves was facilitated by midwifery contributions to doulas’ training. The other key issue, as reported similarly by Granville and Sugarman,63 related to boundaries. Relationships were positive where doulas understood the boundaries of their role and kept within those. HoMs recommended early engagement with new doula services and midwifery involvement in the training of doulas.
Midwives and HoMs acknowledged the support that volunteer doulas provided to women as beneficial and also felt that volunteer doulas were of help to midwives and maternity teams in their own increasingly pressured work situations and that, in particular, the presence of a doula enabled midwives to focus on their core role. Granville and Sugarman also found positive perceptions of the volunteer doula role among midwives and suggest that volunteer support has the potential to reduce women’s dependency on professionals and their use of overstretched services. 63 There were suggestions that midwives were starting to see volunteers as an integral part of the care team, as described in the recent review of volunteering in health and social care, carried out by The King’s Fund. 67
The organisation of midwifery and maternity services
Service pressures and changes in the organisation of midwifery mean that women often experience discontinuities at a time when seeing a familiar face is important. In contrast to some of their experiences of midwives, women felt that they could trust the doula to be available to them, for example to reply when contacted. A further key difference between women’s experiences of doulas and of health professionals was that women felt that doulas provided a service that was focused on them, flexible and personal.
We suggest that the positive experiences of the doula role and satisfaction with the information they provide may result in lower ratings of perceptions of NHS staff. There were suggestions from a range of our data sources that, if women are accompanied by a doula, the midwife may see that as an opportunity to do other elements of her role or to direct support to other labouring women who are without doula support. Women supported by doulas may also feel more able to articulate their wishes about how health professionals conduct their labour and birth. Some midwives spoke regretfully of the aspects of their role that they could no longer fulfil in terms of supporting women, that is of providing continuous support to labouring women. It may be that the continuity and focused nature of support from the doula renders a woman more likely to be dissatisfied with what is available from the statutory services when the busyness of the clinical setting and discontinuities within it are often apparent.
There appears to be a benefit to midwives and maternity services in having this additional worker in an increasingly pressured environment that, as maternity staff and managers acknowledge, cannot provide the continuity that vulnerable women, in particular, need. The volunteer doula service is an example of volunteer agencies working in partnership with statutory provision in roles that offer emotional and practical support, build confidence and encourage engagement in groups of individuals who may find it difficult to access services. 74 However, there is a need for caution to avoid volunteer doula services being utilised inappropriately at a local level to fill gaps in statutory service provision.
There are an increasing number of roles in maternity care settings and thus the potential for women to engage with a greater number of professional and voluntary workers. This was reported as a concern for health professionals in one area. 63 The addition of volunteer doulas does not seem to have been detrimental to women in that regard in our research, although, as we found, there is the potential for confusion for other workers, and a minority of women clearly do not wish to have to deal with yet another person. Midwives who remembered the introduction of maternity care assistants and the resistance encountered at that time recognised parallels in the recent introduction of volunteer doulas. They also acknowledged how the integration of maternity care assistants into the team had occurred with time and envisaged similar for volunteer doulas.
Challenges in the maternity services
A challenge for maternity service commissioners and providers is how policy imperatives can be addressed in a service that will, at least in the medium term, experience resource constraints and a dwindling workforce. NICE guidance9 specific to pregnancy for women in situations of social complexity identified the following research questions: ‘What effect does involving 3rd sector agencies in providing support and coordination of care for vulnerable women have on outcomes?’ and ‘Is intervention and/or family support provided by statutory and 3rd sector agencies effective in improving outcomes for women and their babies?’ (p. 46).
Our research makes a contribution to answering these questions. Our work also provides evidence of beneficial impacts on women’s emotional well-being: an important policy imperative recently announced. 9
Other schemes that support disadvantaged women
We acknowledged, in Chapter 8, Women’s perspectives, the availability of the Family Nurse Partnership programme, which provides support to young women who meet specific criteria; this programme is available in some but not all areas. In that programme support is provided by salaried nurses specifically trained for that role. 75
There are a number of other peer-based approaches. We note some similarities between the volunteer doula role and other community-based support programmes for women who may find it difficult to access or engage with services. 74 A randomised controlled trial of pregnancy outreach workers, working from a base in the maternity services, found that support has a modest effect on maternal mental health for women with identified social risk factors. 76 In that trial, all women accessing maternity services are assessed for social risk in addition to medical and obstetric risk. Women who have been assessed and identified as being at social risk and who have been randomly allocated to the intervention arm of the trial are referred to a pregnancy outreach worker for a programme of support that includes home visits and that aims to support changes in behaviours such as smoking and breastfeeding and to ensure that available benefits are accessed. Workers are trained to a National Vocational Training Level 3 standard and have access to ongoing support.
A befriending scheme that supports pregnant asylum-seeking and refugee women comprises a package of support from a befriender that lasts from early pregnancy to 2 months after birth. 77 When applying to become befrienders, women who are themselves often asylum-seekers or refugee mothers receive a 4-half-day training programme. Befrienders are matched with their clients as closely as possible for cultural background and shared language and are expected to meet clients for up to 3 hours per week. Referrals to the service are received from community midwives and early years services. Early findings suggest that clients value befrienders’ support for a range of reasons and activities reported include help for clients to access a range of services and being accompanied to appointments. This scheme, which commenced in 2011, has exceeded some of its initial targets for volunteers and clients, and volunteers are also experiencing benefits from their experiences in the role.
Clinical and public health outcomes for women and their babies
Our findings suggest some improvements in clinical and public health outcomes, but these do not always reach statistical significance and must be considered in the light of the limitations described above. Information available from the original site prior to the start of this research suggested positive impacts on C-section and epidural rates. Reduced C-section rates were reported in studies of doula support in non-UK settings, for example by Kennell et al. 15 and Madi et al. 78 We have not found significant differences but, it must also be noted, we have not observed any worrying trends in any of the outcomes examined that would seriously call into question the safety of doula support. In the context of concerns about C-section rates in the UK, where significant reductions in rate are unlikely to be achieved, it is worth considering practices that may help to avoid increases. Furthermore, we are aware that some women supported by the doula service, especially at the original site, are not typical and that some multiparous women have had previous difficult birth experiences which may increase their chances of a C-section. Unfortunately, we do not have the data available to investigate this hypothesis further but it merits inclusion in further research.
For both epidural use and the prevalence of smoking during pregnancy, Hull is an area with higher rates than the comparators used. Interpretation of non-statistically significant reductions in epidural use is compromised by the necessary exclusion from the analysis of women who had a C-section. Apart from planned C-section, the decision to use an epidural usually precedes that of mode of birth and cannot be considered independent. It is known that women who have an epidural are significantly less likely to have a normal vaginal birth. 79 It is quite plausible that doula support may improve the likelihood that a woman with an epidural will go on to have a vaginal birth and this hypothesis could usefully be examined in future research.
It is difficult to attribute smoking cessation findings to doula support when so few women reported doula involvement in conjunction with changes to their smoking behaviour. In some sites, it appears that involvement in smoking cessation work has not always been a prominent or easy part of the doula role; thus the relatively low level of doulas’ involvement may be attributed in part to that.
The impacts on breastfeeding appear more convincing, although breastfeeding rates, while generally lower among disadvantaged women,4 are higher among women from some minority ethnic communities. Nevertheless, breastfeeding rates are encouraging and compare well with those for similar groups of women reported in UK national infant feeding surveys. 4 Doula activity is reported that includes direct support, signposting to other sources of support and obtaining specialist help for women in situations of difficulty. It would appear that the doulas’ non-directive approach may have been an enabling factor, as is their practical support for skin-to-skin contact between mothers and babies at birth. Doula-supported women at the original site were significantly more likely to hold their babies skin to skin at birth than the Picker survey comparison group. Peer support, generally provided on a voluntary basis, has been found to support the initiation of breastfeeding. 80 The impact of peer support is less clear for continuing breastfeeding. 81 A randomised trial of peer support (mother to mother) provided by telephone was acceptable and associated with significant increases in breastfeeding rates at 3 months postpartum, compared with standard support provided in the main by hospital-based health-care professionals. 82 In a trial where doula support in a non-UK setting was restricted to labour only, increases in breastfeeding at 6 weeks were hypothesised to be due to increased empowerment by the doula during labour that increased women’s sense of confidence and thus ability to breastfeed. 11
Costs to the NHS
We utilised a predominantly cost–consequence approach when evaluating the impact of doula support across key health and clinical outcomes. In the absence of a primary outcome, for example the quality-adjusted life-year, a fully aggregated incremental analysis was not possible. In this approach, we deliberately did not assign a priority to one health or clinical outcome compared with another, as we were aware that priorities and challenges may vary between geographical areas.
Our findings suggest some improved outcomes associated with doula support. It is noteworthy that these improvements are achieved through relatively small amounts (in numbers of hours) of volunteer support. These improvements have the potential to reduce NHS costs if doula services do not receive NHS funding. If, however, NHS funding into the original doula service is considered, then the net per birth cost to the NHS was estimated to be £1862. We do, however, have some reservations about this calculation. Historically, volunteer doula services have not always been NHS commissioned and funded, and the context of a third-sector agency is very different from being a part of mainstream NHS services. As our study has demonstrated, doula services have needed to expend considerable energy and staff time in securing their funding, often from multiple sources. Funding insecurity adds costs both directly through staff time and indirectly through inhibiting planning and the efficiencies that come with that. Furthermore, the figures presented are based on only one service, since the roll-out sites were not yet in a position to provide comparable data. A final caveat is that the costing of benefits to the NHS is necessarily based only on outcomes that can be measured in the short term. Such estimates exclude the positive impacts of psychosocial outcomes and other benefits to women that may persist beyond the maternity episode, and the wider societal benefits for women, families and doulas.
Implications for practice
These will be considered from the perspectives of doula services and NHS maternity care.
Doula services
Existing doula services
We identified several features that could be considered good practice in the existing doula services. It is important that doula services maintain a high profile in relation to statutory services and potential volunteers. This requires time and other resources in order to optimise the balance between a steady rate of referrals to the service and the right number of volunteers. An imbalance results in either disappointed women or disappointed or stressed volunteers. This is particularly challenging to achieve when short-term funding makes it difficult to plan ahead, as training a new cohort of volunteers is a substantial investment. In addition, a professional approach is requisite for dealings with statutory services, volunteers and clients. Doulas must retain an awareness of the boundaries of their role to avoid confusion for women and concern among professionals.
Aspects of the doula role that merit further consideration are principally the signposting function and, above all others, management of the end of doula support and how that is best achieved from the perspectives of both women and doulas.
Doula services described the continuing challenge of securing funding to be able to continue the service. This is a pressure on the existing service and its staff and affects decisions and activity, for example whether or not a new cohort of volunteers can and should be trained. However, it could usually be assumed that applications for funding are more likely to be successful if based on high-quality data. It is vital that doula services have robust information management and other systems that support both the process, that is service provision, and also the evaluation and outcome measurement function.
New doula services
For organisations considering setting up a doula service, from our research we would suggest that the following are important requisites. The service needs a manager and team with a flexible approach and adequate administrative support. Stability within the staff of the service is important. The doula service needs to be hosted by a larger organisation that is linked in to maternity/early years/neighbourhood services and that will be prepared to either accommodate some of the doula service’s costs or provide support in kind. Doula services need local champions who can represent their interests and expertise in other fora, including commissioning. Doula services must be able to deliver a training package professionally, with midwifery involvement, and a package that establishes the boundaries of the doula role and must be able to provide ongoing support and supervision to its volunteers. It must provide doulas with early opportunities to work in the role following training. A doula service will need to establish systems to maintain its profile in the local area and with other agencies, to support referrals and networking and to maintain these even when the service is established. Doula services require robust recruitment strategies and practices and will need to articulate clearly the expectations of the role and the philosophy of their service, for example whether the focus is on labour or all aspects of support. The doula service must be prepared to develop clear criteria for referral, review these if required and provide regular updates to key referring agencies. The service must be sure that it can establish systems that capture process and outcome data to support regular summary reports. Maternity services should engage early with doula services, contribute to training and offer a welcome into the local maternity community. Doula services should consider joining or establishing a formal network to enable shared learning, mutual support and to minimise reinvention where experience exists.
At this stage, we do not feel in a position to recommend roll-out of doula services at scale. This is not, in any way, a criticism of existing services, but our research has identified just how much needs to be in place to enable a doula service to be established and to keep working. At this point, while we have evidence that generally women and doulas accrue positive impacts from doula support, available clinical and public health outcome data are not sufficiently robust to make such recommendations. However, this research has generated considerable learning that would inform the design of a randomised controlled trial and we would recommend that future roll-out of doula services take place within a framework of controlled evaluation.
NHS maternity services
Midwives need to be aware of their role as a key route of referral to the service and to be familiar with the criteria for referral to their local doula service. Where doula services are being considered for a locality, midwifery staff should accept opportunities for involvement from an early stage, including the opportunity to contribute to training.
Ensuring that communication systems are established to support the two-way flow of information is in the best interests of both doula and maternity services. These systems need to be continued, to cope with changes in personnel of both services.
While efforts to accommodate and integrate volunteer doulas within maternity services are generally to be encouraged, it is important that doulas are not utilised inappropriately to fill gaps in pressurised services. Neither does current evidence support the assimilation of volunteer doulas as (paid) members of the NHS workforce, as their independence is highly valued. The challenging experiences that volunteer breastfeeding counsellors encountered in a transition to their incorporation into statutory services offer important warnings in this regard. 83
Conclusion
In summary, we have carried out a comprehensive evaluation of five doula services drawing on a wide range of quantitative and qualitative data. Given the impossibility of a randomised controlled trial at the point of designing this research, we have drawn on a range of reference data to contextualise our findings. A cost–consequence analysis has identified outcomes with potential areas of saving for the NHS. Where NHS funding supports a doula service, a net increase in NHS costs is estimated, based on the running costs of an independently run, established third-sector service. In practice, these costs are not all likely to be borne by the NHS.
Research recommendations
We recommend further evaluation of impacts on clinical and public health outcomes in 2–3 years’ time, when more data are available from women, babies and doulas, and to include the roll-out sites. To support this, the most important recommendation is that doula services ensure that appropriate processes and systems are in place to support data collection. It also appears important to determine the reasons for failure to accept the offer of doula support in areas where such services are available. Further research would also enable re-exploration of issues related to sustaining a volunteer doula service when new commissioning arrangements are better established and allow exploration of any doula services that have discontinued, if that occurs.
To avoid the limitations of non-randomised designs and in the context of challenges in setting up and sustaining replica services, further research should explore the design and feasibility of a randomised controlled trial of volunteer doula support that incorporates a cost-effectiveness analysis. We would recommend that consideration be given to introducing future volunteer doula services within a framework of controlled evaluation.
Acknowledgements
The research team would like to thank everyone who participated in and supported this research, namely women and doulas, staff and those associated with the doula services, midwives and HoMs.
We thank Jenny Brown, Sue Collins, Julie Corden, Laura Iannuzzi and Lindsay McLoughlin for administrative support and we also thank members of our advisory group and service user and doula reference panels.
Contributions of authors
Helen Spiby (Professor in Midwifery, midwife and health services researcher) responsible for analysis of midwives and HoMs data, contributed to writing of all chapters in the report, overall responsibility for the research.
Josephine M Green (Professor in Psychosocial Reproductive Health, psychologist and health services researcher) responsible for analysis of quantitative data for doulas, advised on analysis of quantitative data for women, contributed to writing of all chapters in the report.
Zoe Darwin (research fellow) responsible for analysis of women’s quantitative date, contributed to writing Chapter 4 in the report.
Helen Willmot (research fellow) responsible for analysis of doula service data, contributed to writing Chapter 6 in the report.
David Knox (workforce intelligence specialist, Public Health England) responsible for analysis of clinical and public health outcomes, writing of related sections in the report.
Jenny McLeish (advocate for disadvantaged childbearing women, freelance researcher) contributed to the analysis of women’s qualitative data and writing of relevant sections for the report.
Murray Smith (Associate Professor, econometrician) responsible for the health economics component and calculation of doula service costs, contributed to writing of related sections in the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Lewis G. Saving Mothers’ Lives: Reviewing Maternal Deaths to Make Motherhood Safer – 2003–2005. The Seventh Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. London; 2007.
- Perinatal Mortality 2009. London: CEMACH; 2009.
- Lumley J, Chamberlain C, Dowswell T, Oliver S, Oakley L, Watson L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev 2009;3.
- McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ. Infant Feeding Survey 2010. London: Health and Social Care Information Centre; 2012.
- Howie L, Carlisle C. ‘I felt like they were all kind of staring at me’. RCM Midwives 2005;8:304-8.
- McLeish J. Maternity experiences of asylum seekers in England. Br J Midwifery 2005;13:782-5. http://dx.doi.org/10.12968/bjom.2005.13.12.20125.
- De Jonge A. Support for teenage mothers: a qualitative study into the views of women about the support they received as teenage mothers. J Adv Nurs 2001;36:49-57. http://dx.doi.org/10.1046/j.1365-2648.2001.01942.x.
- Reynolds F, Shams M. Views on cultural barriers to caring for South Asian women. Br J Midwifery 2005;13:236-42. http://dx.doi.org/10.12968/bjom.2005.13.4.17987.
- Pregnancy and Complex Social Factors: A Model for Service Provision for Pregnant Women with Complex Social Factors. London: Royal College of Obstetricians and Gynaecologists; 2010.
- Nommsen-Rivers LA, Mastergeorge AM, Hansen RL, Cullum AS, Dewey KG. Doula care, early breastfeeding outcomes, and breastfeeding status at 6 weeks postpartum among low-income primiparae. J Obstet Gynecol Neonatal Nurs 2009;38:157-73. http://dx.doi.org/10.1111/j.1552-6909.2009.01005.x.
- Hofmeyr GJ, Nikodem VC, Wolman WL, Chalmers BE, Kramer T. Companionship to modify the clinical birth environment: effects on progress and perceptions of labour, and breastfeeding. Br J Obstet Gynaecol 1991;98:756-64. http://dx.doi.org/10.1111/j.1471-0528.1991.tb13479.x.
- Redshaw M, Rowe R, Hockley C, Brocklehurst P. Recorded Delivery: A National Survey of Women’s Experience of Maternity Care 2006. Oxford: National Perinatal Epidemiology Unit; 2007.
- Hodnett ED, Gates S, Hofmeyr GJ, Sakala C. Continuous support for women during childbirth. Cochrane Database Syst Rev 2007;3.
- Campbell DA, Lake MF, Falk M, Backstrand JR. A randomized control trial of continuous support in labor by a lay doula. J Obstet Gynecol Neonatal Nurs 2006;35:456-64. http://dx.doi.org/10.1111/j.1552-6909.2006.00067.x.
- Kennell J, Klaus M, McGrath S, Robertson S, Hinkley C. Continuous emotional support during labor in a US hospital: a randomized controlled trial. JAMA 1991;265:2197-201. http://dx.doi.org/10.1001/jama.1991.03460170051032.
- Stones RW, Paterson CM, Saunders NJ. Risk factors for major obstetric haemorrhage. Eur J Obstet Gynecol Reprod Biol 1993;48:15-8. http://dx.doi.org/10.1016/0028-2243(93)90047-G.
- Lydon-Rochelle M, Holt VL, Martin DP, Easterling TR. Association between method of delivery and maternal rehospitalization. JAMA 2000;283:2411-16. http://dx.doi.org/10.1001/jama.283.18.2411.
- Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med 1999;341:1709-14. http://dx.doi.org/10.1056/NEJM199912023412301.
- Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breastfeeding mothers. Cochrane Database Syst Rev 2007;1.
- A Peer-support Programme for Women who Breastfeed. London: NICE; 2008.
- Langer A, Campero L, Garcia C, Reynoso S. Effects of psychosocial support during labour and childbirth on breastfeeding, medical interventions, and mothers’ wellbeing in a Mexican public hospital: a randomised clinical trial. Br J Obstet Gynaecol 1998;105:1056-63. http://dx.doi.org/10.1111/j.1471-0528.1998.tb09936.x.
- Wolman WL, Chalmers B, Hofmeyr J, Nikodem VC. Postpartum depression and companionship in the clinical birth environment: a randomized, controlled study. Am J Obstet Gynecol 1993;168:1388-93. http://dx.doi.org/10.1016/S0002-9378(11)90770-4.
- Gordon NP, Walton D, McAdam E, Derman J, Gallitero G, Garrett L. Effects of providing hospital-based doulas in health maintenance organization hospitals. Obstet Gynecol 1999;93:422-6. http://dx.doi.org/10.1016/S0029-7844(98)00430-X.
- Sosa R, Kennell J, Klaus M, Robertson S, Urrutia J. The effect of a supportive companion on perinatal problems, length of labor, and mother–infant interaction. N Engl J Med 1980;303:597-600. http://dx.doi.org/10.1056/NEJM198009113031101.
- Gilbert S. Benefits of Assistant for Childhood Go Far Beyond the Birthing Room. Report of Conference Study. New York Times 1998.
- Mottl-Santiago J, Walker C, Ewan J, Vragovic O, Winder S, Stubblefield P. A hospital-based doula program and childbirth outcomes in an urban, multicultural setting. Matern Child Health J 2008;12:372-7. http://dx.doi.org/10.1007/s10995-007-0245-9.
- Department of Health . 2009–10 Reference Costs Publication 2011. www.gov.uk/government/uploads/system/uploads/attachment_data/file/216305/dh_123501.pdf (accessed December 2014).
- Godfrey C, Pickett K, Parrott S, Mdege N, Eapen D. Estimating the Costs to the NHS of Smoking in Pregnancy for Pregnant Women and Infants. University of York: Public Health Research Consortium; 2010.
- Mistry H, Dowie R, Franklin RCG, Jani BR. Costs of neonatal care for low-birthweight babies in English hospitals. Acta Pædiatrica 2009;98:1123-9. http://dx.doi.org/10.1111/j.1651-2227.2009.01316.x.
- Campero L, Garcia C, Diaz C, Ortiz O, Reynoso S, Langer A. ‘Alone, I wouldn’t have known what to do’: a qualitative study on social support during labor and delivery in Mexico. Soc Sci Med 1998;47:395-403. http://dx.doi.org/10.1016/S0277-9536(98)00077-X.
- Goedkoop V. Side by side: a survey of doula care in the UK in 2008. MIDIRS Midwifery Digest 2009;19:217-18.
- Byrom S, Gaudion A, Byrom S, Edwards G, Bick D. Essential Midwifery Practice: Postnatal Care. Chichester: Wiley Blackwell; 2010.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- McCourt C. Research and theory for nursing and midwifery: rethinking the nature of evidence. Worldviews Evid Based Nurs 2005;2:75-83. http://dx.doi.org/10.1111/j.1741-6787.2005.05003.x.
- Pawson R, Manzano-Santaella A. A realist diagnostic workshop. Evaluation 2012;18:176-91. http://dx.doi.org/10.1177/1356389012440912.
- Jackson SF, Kolla G. A new realist evaluation analysis method: linked coding of context, mechanism, and outcome relationships. Am J Eval 2012;33:339-49. http://dx.doi.org/10.1177/1098214012440030.
- Hospital Episode Statistics n.d. www.hscic.gov.uk/hes.
- Department of Health . Breastfeeding Statistics 2012. http://webarchive.nationalarchives.gov.uk/20130402145952/http://transparency.dh.gov.uk/2012/11/29/breastfeeding-data-download/ (accessed 18 December 2014).
- Health and Social Care Information Centre . Smoking at Time of Delivery 2012. www.hscic.gov.uk/searchcatalogue?q=title%3A%22Statistics+on+Women%27s+Smoking+Status+at+Time+of+Delivery%22&area=&size=10&sort=RelevanceDesc (accessed 18 December 2014).
- Office for National Statistics . 2011 Census, Detailed Characteristics for 2011 Census Merged Wards and Middle Layer Super Output Areas in England and Wales 2013 2013. www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-315005 (accessed December 2014).
- Care Quality Commission . National NHS Patient Survey Programme: Survey of Women’s Experiences of Maternity Services 2010 2010.
- Public Health England . Analytical Tools for Public Health: Commonly Used Public Health Statistics and Their Confidence Intervals n.d. www.apho.org.uk/default.aspx?RID=39403 (accessed December 2014).
- Grbich C. Qualitative Research in Health, an Introduction. London: Sage; 1999.
- Department for Communities and Local Government . English Indices of Deprivation 2010 2011. www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed December 2014).
- Office for National Statistics . Population Estimates for UK, England and Wales, Scotland and Northern Ireland, Mid-2010 2011. www.ons.gov.uk/ons/rel/pop-estimate/population-estimates-for-uk--england-and-wales--scotland-and-northern-ireland/mid-2010-population-estimates/index.html (accessed December 2014).
- Nomis . Census Data DC2101EW: Ethnic Group by Sex by Age 2011 2013. www.nomisweb.co.uk/census/2011/dc2101ew (accessed December 2014).
- Green JM, Spiby HJM, Hucknall C, Richardson Foster H. Converting policy into care: women’s satisfaction with the early labour telephone component of the All Wales Clinical Pathway for Normal Labour. J Adv Nurs 2011;68:2218-28. http://dx.doi.org/10.1111/j.1365-2648.2011.05906.x.
- Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. JAMA 1996;276:1172-7. http://dx.doi.org/10.1001/jama.1996.03540140060028.
- Health and Social Care Act 2012: Elizabeth II. London: The Stationery Office; 2012.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: Personal Social Services Research Unit; 2012.
- Office of National Statistics . Consumer Price Inflation, Briefing Note, May 2013. Table 6a CPI All Items: 1997 to 2013 2013. www.ons.gov.uk/ons/rel/cpi/consumer-price-indices/briefing-note-may-2013/index.html (accessed December 2014).
- Department of Health . 2010–11 Reference Costs Publication 2012. www.gov.uk/government/publications/2010-11-reference-costs-publication (accessed December 2014).
- Health and Social Care Information Centre . NHS Maternity Statistics, England: 2011 12 2012. www.hscic.gov.uk/catalogue/PUB09202 (accessed December 2014).
- Health and Social Care Information Centre . NHS Maternity Statistics, England: 2010 11 2011. www.hscic.gov.uk/pubs/maternity1011 (accessed December 2014).
- Schroeder L, Petrou S, Patel N, Hollowell J, Puddicombe D, Redshaw M, et al. Birthplace Cost-Effectiveness Analysis of Planned Place of Birth: Individual Level Analysis 2011.
- Department of Health . Infant Feeding Profiles 2010 to 2011 2013. www.gov.uk/government/publications/infant-feeding-profiles-2010-to-2011 (accessed December 2014).
- Renfrew M, Pokhrel S, Quigley M, McCormick F, Fox-Rushby J, Dodds R, et al. Preventing Disease and Saving Resources: The Potential Contribution of Increasing Breastfeeding Rates in the UK 2012. www.unicef.org.uk/Documents/Baby_Friendly/Research/appendices_preventing_disease_saving_resources.pdf (accessed December 2014).
- National Institute for Health and Care Excellence . Quitting Smoking in Pregnancy and Following Childbirth 2010. www.nice.org.uk/guidance/ph26 (accessed December 2014).
- Watkinson M, Davis K. National Neonatal Audit Programme, Annual Report 2011, Extended on-Line Version: July 2012 2012. www.rcpch.ac.uk/child-health/standards-care/clinical-audit-and-quality-improvement/national-neonatal-audit-programme#resources (accessed December 2014).
- Department of Health . NHS Reference Costs: Financial Year 2011 to 2012 2012. www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012 (accessed December 2014).
- Modi N. Developments over the Last Year n.d. www.imperial.ac.uk/resources/FC1C1061-843D-4DF4-A74D-D9E9DB0054BF/uknc_nm.pdf (accessed December 2014).
- Kozhimannil KB, Hardeman RR, Attanasio LB, Blauer-Peterson C, O’Brien M. Doula care, birth outcomes, and costs among Medicaid beneficiaries. Am J Public Health 2013;103:e113-21. http://dx.doi.org/10.2105/AJPH.2012.301201.
- Granville G, Sugarman W. ‘Someone in My Corner’: A Volunteer Peer Support Programme for Parenthood, Birth and Beyond 2012.
- Cheyne H, Abhyankar P, McCourt C. Keeping Childbirth Natural & Dynamic: Evaluation of a National Maternity Care Programme in Scotland. Stirling: Nursing, Midwifery and Allied Health Professionals Research Unit, University of Stirling; 2013.
- Murphy CA, Cupples ME, Percy A, Halliday HL, Stewart MC. Peer-mentoring for first-time mothers from areas of socio-economic disadvantage: a qualitative study within a randomised controlled trial. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-46.
- Narayan-Parker D. Bonds and Bridges: Social Capital and Poverty. Washington, DC: World Bank Publications; 1999.
- Naylor C, Mundle C, Weaks L, Buck D. Volunteering in Health and Care: Securing a Sustainable Future. London: The King’s Fund; 2013.
- Pascali-Bonaro D, Kroeger M. Continuous female companionship during childbirth: a crucial resource in times of stress or calm. J Nurse Midwifery 2004;49:19-27. http://dx.doi.org/10.1016/j.jmwh.2004.04.017.
- McMillan AS, Barlow J, Redshaw M. Birth and Beyond: A Review of the Evidence about Antenatal Education. London: Department of Health; 2009.
- Podkolinski J, Clement S. Psychological Perspectives on Pregnancy and Childbirth. London: Churchill Livingstone; 1998.
- Bolger N, Zuckerman A, Kessler R. Invisible support and adjustment to stress. J Pers Soc Psychol 2000;79:953-61. http://dx.doi.org/10.1037/0022-3514.79.6.953.
- Lantz PM, Low LK, Varkey S, Watson RL. Doulas as childbirth paraprofessionals: results from a national survey. Womens Health Issues 2005;15:109-16. http://dx.doi.org/10.1016/j.whi.2005.01.002.
- Lundgren I. Swedish women’s experiences of doula support during childbirth. Midwifery 2010;26:173-80. http://dx.doi.org/10.1016/j.midw.2008.05.002.
- Coe C, Barlow J. Supporting women with perinatal mental health problems: the role of the voluntary sector. Community Pract 2013;86:23-7.
- Department of Health . Evaluation of Family Nurse Partnership Programme 2012. www.gov.uk/government/publications/evaluation-of-family-nurse-partnership-programme (accessed December 2014).
- Kenyon S, Jolly K, Hemming K, Ingram L, Blissett J, Dann S, et al. Effects of additional lay support for pregnant women with social risk factors on antenatal attendance and maternal psychological health: a randomised controlled trial (ELSIPS). Arch Dis Child Fetal Neonatal Ed 2014;99. http://dx.doi.org/10.1136/archdischild-2014-306576.49.
- Mccarthy R, Haith-Cooper M. Evaluating the impact of befriending for pregnant asylum-seeking and refugee women. Br J Midwifery 2013;21:404-9. http://dx.doi.org/10.12968/bjom.2013.21.6.404.
- Madi BC, Sandall J, Bennett R, MacLeod C. Effects of female relative support in labor: a randomized controlled trial. Birth 1999;26:4-8. http://dx.doi.org/10.1046/j.1523-536x.1999.00004.x.
- Anim-Somuah M, Smyth R, Jones L. Epidural versus non-epidural or no analgesia in labour. Cochrane Database Syst Rev 2011;12.
- Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D. A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding. Health Technol Assess 2000;4.
- Spiby H, McCormick F, Wallace L, Renfrew MJ, D’Souza L, Dyson L. A systematic review of education and evidence-based practice interventions with health professionals and breast feeding counsellors on duration of breast feeding. Midwifery 2009;25:50-61. http://dx.doi.org/10.1016/j.midw.2007.01.006.
- Dennis CL. Breastfeeding peer support: maternal and volunteer perceptions from a randomized controlled trial. Birth 2002;29:169-76. http://dx.doi.org/10.1046/j.1523-536X.2002.00184.x.
- Aiken A, Thomson G. Professionalisation of a breast-feeding peer support service: issues and experiences of peer supporters. Midwifery 2013;29:e145-51. http://dx.doi.org/10.1016/j.midw.2012.12.014.
Appendix 1 Ethics approval letter
Appendix 2 Search strategy
Databases searched
AMED (Allied and Complementary Medicine) (Ovid).
CINAHL (Cumulative Index to Nursing and Allied Health Literature) (EBSCOhost).
The Cochrane Library:
-
Cochrane Database of Systematic Reviews (CDSR)
-
Database of Abstracts of Reviews of Effects (DARE)
-
NHS Economic Evaluation Database (NHS EED)
-
Health Technology Assessment (HTA) Database
-
Cochrane Central Register of Controlled Trials.
EMBASE (Ovid).
HMIC (Health Management Information Consortium) (Ovid).
Maternity and Infant Care (Ovid).
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (Ovid).
Limits
No limits were applied in terms of language, study design or date of publication.
All databases were searched from the date of inception until the most recent date available (full details provided below).
Search strategies
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (Ovid)
1948 to October week 4 2011.
Date of search: 8 November 2011.
Number of records found: 1347.
-
(doula or doulas).ti,ab. (133)
-
(labour attendant$ or labor attendant$).ti,ab. (6)
-
(labour companion$ or labor companion$).ti,ab. (10)
-
(labour assistant$ or labor assistant$).ti,ab. (2)
-
(birth companion$ or childbirth companion$).ti,ab. (10)
-
(birth assistant$ or childbirth assistant$).ti,ab. (15)
-
birth partner$.ti,ab. (11)
-
supportive companion$.ti,ab. (17)
-
monitrice$.ti,ab. (7)
-
childbirth support$.ti,ab. (5)
-
((birth or birthing) adj1 support$).ti,ab. (46)
-
(labo?r adj1 support$).ti,ab. (109)
-
((childbearing or child-bearing) adj1 support$).ti,ab. (7)
-
((intrapartum or perinatal$) adj1 support$).ti,ab. (44)
-
((prenatal$ or antenatal$) adj1 support$).ti,ab. (59)
-
(pregnan$ adj1 support$).ti,ab. (174)
-
(pregnan$ adj1 outreach).ti,ab. (5)
-
labo?r coach$.ti,ab. (12)
-
(((continuous or continual) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (55)
-
(advocacy adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (38)
-
(befriend$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (1)
-
(human support adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (1)
-
(emotional$ support$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (32)
-
((paraprofessional? or allied health personnel or allied health worker? or support worker? or home health aide?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (15)
-
(trained adj3 (volunteer? or health worker? or mother?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (21)
-
((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or attendant? or aide or aides or support$ or person or people or helper? or carer? or caregiver? or care giver? or assistant?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (105)
-
maternity assistant?.ti,ab. (2)
-
((peer or community) adj2 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (330)
-
(((peer or community) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (193)
-
community parent$.ti,ab. (46)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 (1403)
[All terms relating to doulas]
-
exp animals/ not humans/ (3707268)
[Excludes animal-only studies]
-
31 not 32 (1347)
[Final results set]
Key
/ = indexing term [medical subject heading (MeSH) heading]
$ = truncation
? = embedded truncation or single character truncation
.ti,ab. = terms in either title or abstract fields
adj = terms adjacent to each other (same order)
adj1 = terms within one word of each other (any order)
adj2 = terms within two words of each other (any order)
AMED (Allied and Complementary Medicine) (Ovid)
1985 to November 2011.
Date of search: 8 November 2011.
Number of records found: 30.
-
(doula or doulas).ti,ab. (3)
-
(labour attendant$ or labor attendant$).ti,ab. (1)
-
(labour companion$ or labor companion$).ti,ab. (0)
-
(labour assistant$ or labor assistant$).ti,ab. (0)
-
(birth companion$ or childbirth companion$).ti,ab. (0)
-
(birth assistant$ or childbirth assistant$).ti,ab. (0)
-
birth partner$.ti,ab. (2)
-
supportive companion$.ti,ab. (0)
-
monitrice$.ti,ab. (0)
-
childbirth support$.ti,ab. (0)
-
((birth or birthing) adj1 support$).ti,ab. (1)
-
(labo?r adj1 support$).ti,ab. (4)
-
((childbearing or child-bearing) adj1 support$).ti,ab. (1)
-
((intrapartum or perinatal$) adj1 support$).ti,ab. (3)
-
((prenatal$ or antenatal$) adj1 support$).ti,ab. (2)
-
(pregnan$ adj1 support$).ti,ab. (2)
-
(pregnan$ adj1 outreach).ti,ab. (0)
-
labo?r coach$.ti,ab. (0)
-
(((continuous or continual) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
(advocacy adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
(befriend$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
(human support adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
(emotional$ support$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (3)
-
((paraprofessional? or allied health personnel or allied health worker? or support worker? or home health aide?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
(trained adj3 (volunteer? or health worker? or mother?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or attendant? or aide or aides or support$ or person or people or helper? or carer? or caregiver? or care giver? or assistant?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (1)
-
maternity assistant?.ti,ab. (0)
-
((peer or community) adj2 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (5)
-
(((peer or community) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (3)
-
community parent$.ti,ab. (3)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 (30)
CINAHL (Cumulative Index to Nursing and Allied Health Literature) (EBSCOhost)
1982 to date.
Date of search: 8 November 2011.
Number of records found: 1496.
-
doula or doulas or (MH “Doulas”)
-
“labour attendant*” or “labor attendant*”
-
“labour companion*” or “labor companion*”
-
“labour assistant*” or “labor assistant*”
-
“birth companion*” or “childbirth companion*”
-
“birth assistant*” or “childbirth assistant*”
-
“birth partner*”
-
“supportive companion*”
-
monitrice*
-
“childbirth support*”
-
(birth or birthing) n1 support*
-
labo?r n1 support*
-
(childbearing or “child-bearing”) n1 support*
-
(intrapartum or perinatal*) n1 support*
-
(prenatal* or antenatal*) n1 support*
-
pregnan* n1 support*
-
pregnan* n1 outreach
-
“labo?r coach*”
-
((continuous or continual) n1 support*) and (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
advocacy n5 (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
befriend* n5 (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
“human support” n5 (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
“emotional* support*” n5 (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
(paraprofessional* or allied health personnel or allied health worker* or support worker* or home health aide*) n5 (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
(trained n3 (volunteer* or health worker* or mother*)) n5 (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
(lay or voluntary or volunteer* or untrained or unlicensed or nonprofessional* or non professional*) n5 (worker* or attendant* or aide or aides or support* or person or people or helper* or carer* or caregiver* or care giver* or assistant*) n5 (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
“maternity assistant*”
-
(peer or community) n2 (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
((peer or community) n1 support*) and (labo?r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
-
“community parent*”
-
s1 or s2 or s3 or s4 or s5 or s6 or s7 or s8 or s9 or s10 or s11 or s12 or s13 or s14 or s15 or s16 or s17 or s18 or s19 or s20 or s21 or s22 or s23 or s24 or s25 or s26 or s27 or s28 or s29 or s30
Key
MH = indexing term (MeSH heading)
* = truncation
? = embedded truncation
“ ”= phrase search
n1 = terms within one word of each other (any order)
n2 = terms within two words of each other (any order)
The Cochrane Library
Issue 11 of 12 November 2011.
Date of search: 15 November 2011.
Number of records found:
-
CDSR (11)
-
DARE (20)
-
NHS EED (23)
-
HTA Database (5)
-
Cochrane Central Register of Controlled Trials (170)
Cochrane Database of Systematic Reviews (CDSR) strategy
The search for the CDSR database was limited to title and abstract fields only so that the extensive references in each Cochrane review were not also searched by the strategy.
(doula or doulas):ti,ab
(“labour attendant*” or “labor attendant*”):ti,ab
(“labour companion*” or “labor companion*”):ti,ab
(“labour assistant*” or “labor assistant*”):ti,ab
(“birth companion*” or “childbirth companion*”):ti,ab
(“birth assistant*” or “childbirth assistant*”):ti,ab
(“birth partner*”):ti,ab
(“supportive companion*”):ti,ab
(monitrice*):ti,ab
(“childbirth support*”):ti,ab
((birth or birthing) NEAR/1 support*):ti,ab
(labo*r NEAR/1 support*):ti,ab
((childbearing or “child-bearing”) NEAR/1 support*):ti,ab
((intrapartum or perinatal*) NEAR/1 support*):ti,ab
((prenatal* or antenatal*) NEAR/1 support*):ti,ab
(pregnan* NEAR/1 support*):ti,ab
(pregnan* NEAR/1 outreach):ti,ab
(“labo*r coach*”):ti,ab
(((continuous or continual) NEAR/1 support*) and (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
(advocacy NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
(befriend* NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
(“human support” NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
(“emotional* support*” NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
((paraprofessional* or allied health personnel or allied health worker* or support worker* or home health aide*) NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
((trained NEAR (volunteer* or health worker* or mother*)) NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
((lay or voluntary or volunteer* or untrained or unlicensed or nonprofessional* or non professional*) NEAR (worker* or attendant* or aide or aides or support* or person or people or helper* or carer* or caregiver* or care giver* or assistant*) NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
(“maternity assistant*”):ti,ab
((peer or community) NEAR/2 (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
(((peer or community) NEAR/1 support*) and (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)):ti,ab
(“community parent*”):ti,ab
#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30
Database of Abstracts of Reviews of Effects (DARE), NHS Economic Evaluation Database (NHS EED), Health Technology Assessment (HTA) Database and Cochrane Central Register of Controlled Trials strategy
All fields were searched for these databases as it is not clear what fields are indexed as belonging to the abstract field in the DARE, NHS EED and HTA databases.
doula or doulas
“labour attendant*” or “labor attendant*”
“labour companion*” or “labor companion*”
“labour assistant*” r “labor assistant*”
“birth companion*” or “childbirth companion*”
“birth assistant*” or “childbirth assistant*”
“birth partner*”
“supportive companion*”
monitrice*
“childbirth support*”
(birth or birthing) NEAR/1 support*
labo*r NEAR/1 support*
(childbearing or “child-bearing”) NEAR/1 support*
(intrapartum or perinatal*) NEAR/1 support*
(prenatal* or antenatal*) NEAR/1 support*
pregnan* NEAR/1 support*
pregnan* NEAR/1 outreach
“labo*r coach*”
((continuous or continual) NEAR/1 support*) and (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
advocacy NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
befriend* NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
“human support” NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
“emotional* support*” NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
(paraprofessional* or allied health personnel or allied health worker* or support worker* or home health aide*) NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
(trained NEAR (volunteer* or health worker* or mother*)) NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
(lay or voluntary or volunteer* or untrained or unlicensed or nonprofessional* or non professional*) NEAR (worker* or attendant* or aide or aides or support* or person or people or helper* or carer* or caregiver* or care giver* or assistant*) NEAR (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
“maternity assistant*”
(peer or community) NEAR/2 (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
((peer or community) NEAR/1 support*) and (labo*r or birth or childbirth or prenatal* or antenatal* or perinatal* or intrapartum or birthing or pregnan*)
“community parent*”
#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30
Key
* = truncation
“ ”= phrase search
:ti,ab = terms in either title or abstract fields
near/1 = terms within one word of each other (any order)
near/2 = terms within two words of each other (any order)
next = terms are next to each other
EMBASE (Ovid)
1980 to 2011 week 44.
Date of search: 8 November 2011.
Number of records found: 1333.
-
(doula or doulas).ti,ab. or doula/ (123)
-
(labour attendant$ or labor attendant$).ti,ab. (7)
-
(labour companion$ or labor companion$).ti,ab. (12)
-
(labour assistant$ or labor assistant$).ti,ab. (2)
-
(birth companion$ or childbirth companion$).ti,ab. (12)
-
(birth assistant$ or childbirth assistant$).ti,ab. (13)
-
birth partner$.ti,ab. (11)
-
supportive companion$.ti,ab. (20)
-
monitrice$.ti,ab. (7)
-
childbirth support$.ti,ab. (6)
-
((birth or birthing) adj1 support$).ti,ab. (46)
-
(labo?r adj1 support$).ti,ab. (105)
-
((childbearing or child-bearing) adj1 support$).ti,ab. (6)
-
((intrapartum or perinatal$) adj1 support$).ti,ab. (50)
-
((prenatal$ or antenatal$) adj1 support$).ti,ab. (68)
-
(pregnan$ adj1 support$).ti,ab. (185)
-
(pregnan$ adj1 outreach).ti,ab. (5)
-
labo?r coach$.ti,ab. (12)
-
(((continuous or continual) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (54)
-
(advocacy adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (35)
-
(befriend$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
(human support adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (2)
-
(emotional$ support$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (39)
-
((paraprofessional? or allied health personnel or allied health worker? or support worker? or home health aide?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (15)
-
(trained adj3 (volunteer? or health worker? or mother?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (20)
-
((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or attendant? or aide or aides or support$ or person or people or helper? or carer? or caregiver? or care giver? or assistant?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (79)
-
maternity assistant?.ti,ab. (1)
-
((peer or community) adj2 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (339)
-
(((peer or community) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (179)
-
community parent$.ti,ab. (50)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 (1389)
-
(animal/ or nonhuman/) not exp human/ (4294597)
-
31 not 32 (1333)
Key
/ = indexing term (EMTREE heading)
$ = truncation
? = embedded truncation
.ti,ab. = terms in either title or abstract fields
adj = terms adjacent to each other (same order)
adj1 = terms within one word of each other (any order)
adj2 = terms within two words of each other (any order)
HMIC (Health Management Information Consortium) (Ovid)
1979 to September 2011.
Date of search: 8 November 2011.
Number of records found: 111.
-
(doula or doulas).ti,ab. (2)
-
(labour attendant$ or labor attendant$).ti,ab. (0)
-
(labour companion$ or labor companion$).ti,ab. (0)
-
(labour assistant$ or labor assistant$).ti,ab. (0)
-
(birth companion$ or childbirth companion$).ti,ab. (2)
-
(birth assistant$ or childbirth assistant$).ti,ab. (0)
-
birth partner$.ti,ab. (4)
-
supportive companion$.ti,ab. (0)
-
monitrice$.ti,ab. (0)
-
childbirth support$.ti,ab. (0)
-
((birth or birthing) adj1 support$).ti,ab. (4)
-
(labo?r adj1 support$).ti,ab. (4)
-
((childbearing or child-bearing) adj1 support$).ti,ab. (0)
-
((intrapartum or perinatal$) adj1 support$).ti,ab. (4)
-
((prenatal$ or antenatal$) adj1 support$).ti,ab. (3)
-
(pregnan$ adj1 support$).ti,ab. (5)
-
(pregnan$ adj1 outreach).ti,ab. (0)
-
labo?r coach$.ti,ab. (0)
-
(((continuous or continual) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (2)
-
(advocacy adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (1)
-
(befriend$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (1)
-
(human support adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
(emotional$ support$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (2)
-
((paraprofessional? or allied health personnel or allied health worker? or support worker? or home health aide?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (3)
-
(trained adj3 (volunteer? or health worker? or mother?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (1)
-
((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or attendant? or aide or aides or support$ or person or people or helper? or carer? or caregiver? or care giver? or assistant?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (1)
-
maternity assistant?.ti,ab. (0)
-
((peer or community) adj2 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (47)
-
(((peer or community) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (24)
-
community parent$.ti,ab. (4)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 (111)
Key
$ = truncation
? = embedded truncation
.ti,ab. = terms in either title or abstract fields
adj1 = terms within one word of each other (any order)
adj2 = terms within two words of each other (any order)
Maternity and Infant Care (Ovid)
1971 to October 2011.
Date of search: 8 November 2011.
Number of records found: 1149.
-
(doula or doulas).ti,ab. or doulas.de. (394)
-
(labour attendant$ or labor attendant$).ti,ab. (8)
-
(labour companion$ or labor companion$).ti,ab. (20)
-
(labour assistant$ or labor assistant$).ti,ab. (6)
-
(birth companion$ or childbirth companion$).ti,ab. (24)
-
(birth assistant$ or childbirth assistant$).ti,ab. (18)
-
birth partner$.ti,ab. (43)
-
supportive companion$.ti,ab. (16)
-
monitrice$.ti,ab. (7)
-
childbirth support$.ti,ab. (7)
-
((birth or birthing) adj1 support$).ti,ab. (55)
-
(labo?r adj1 support$).ti,ab. (134)
-
((childbearing or child-bearing) adj1 support$).ti,ab. (8)
-
((intrapartum or perinatal$) adj1 support$).ti,ab. (22)
-
((prenatal$ or antenatal$) adj1 support$).ti,ab. (49)
-
(pregnan$ adj1 support$).ti,ab. (67)
-
(pregnan$ adj1 outreach).ti,ab. (4)
-
labo?r coach$.ti,ab. (8)
-
(((continuous or continual) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (57)
-
(advocacy adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (28)
-
(befriend$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (0)
-
(human support adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (2)
-
(emotional$ support$ adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (36)
-
((paraprofessional? or allied health personnel or allied health worker? or support worker? or home health aide?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (12)
-
(trained adj3 (volunteer? or health worker? or mother?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (8)
-
((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or attendant? or aide or aides or support$ or person or people or helper? or carer? or caregiver? or care giver? or assistant?) adj5 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (48)
-
maternity assistant?.ti,ab. (4)
-
((peer or community) adj2 (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (156)
-
(((peer or community) adj1 support$) and (labo?r or birth or childbirth or prenatal$ or antenatal$ or perinatal$ or intrapartum or birthing or pregnan$)).ti,ab. (93)
-
community parent$.ti,ab. (2)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 (1149)
Key
$ = truncation
? = embedded truncation
.de. = descriptor
.ti,ab. = terms in either title or abstract fields
adj1 = terms within one word of each other (any order)
adj2 = terms within two words of each other (any order)
Appendix 3 Women’s questionnaire supported
Appendix 4 Women’s questionnaire unsupported
Appendix 5 Service evaluation documents: use and findings
Service documents were available from all five services. We reviewed all documents used by each doula service and obtained anonymised copies of those that related to women’s referrals and evaluations of doula services; these were not linked with any other sources of data such as women’s questionnaires. In the original site, documents were sampled on a 1 : 5 ratio because of the higher number of women who had used that service. Information from the referral and evaluation documents was reviewed to identify particular themes within free text comments.
Referral forms
Forms that documented reasons for women’s referral to the doula service were available as follows: site A, 120; site W, 23; site X, 38; site Y, 115; site Z, 10.
From the referral forms, the most frequent reasons why women were referred to the service were because they lacked social support or a birth partner. This was generally for one or more of the following reasons: no partner or no family support; they had recently arrived in the area or in the UK; they spoke limited English; their husband was away working or in prison; their husband did not want to attend the birth; or their husband needed to look after other children. The second most common theme was depression and other mental health difficulties. The involvement of social services because of child protection concerns was an important factor in sites A, W and Y and the need for support to achieve a vaginal birth after C-section was a reason in sites X and Y. In addition, site Y had a large number of referrals where the mother was young or a care leaver and, in comparison with other sites, a large number involving domestic abuse.
Evaluation forms
Information on the evaluation forms was collected and entered on to the form by doula service staff at the end of the woman’s period of doula support. Responses were coded by the research team and themes identified within women’s experiences. We explored responses within sites to identify any common themes. Individual evaluation forms were not coded. Forms were available from sites as follows: site A, 56; site W, 23; site X, 19; site Y, 31; site Z, 10.
At each site the service evaluations were overwhelmingly positive: most would recommend the service to others and said there was nothing more the doula could have done to make it better. Site X had the largest number of negative comments.
The following reflect the positive views documented in the service evaluations:
[Doula] was faultless, she was like having a best friend.
Like an angel. If it hadn’t been for [doula] I don’t know what would have happened. She was like a miracle.
She was understanding, offered support, was available on phone, she was caring and kind and she never judged me.
Turned what could have been an awful experience into a fantastic one.
A very good person and I will never forget her, as I was at such a difficult time.
Particular themes at individual sites
Site A: Looked forward to visits once a week, someone to talk to, created birth plan, breastfeeding support and taking woman to children’s centre or other group.
Site W: Advocacy at the hospital.
Site Y: Building confidence, empowerment, overcoming fears of labour/birth
Site Z: Language support at the hospital – ‘She helped me speak and translate my language, she was there for me.’
There was no theme identifiable at site X.
The nature of doula support
During pregnancy, doulas provided information, helped women with birth plans, supported confidence building and calmed women’s fears. During the labour and birth, doulas provided emotional and practical support including massage; supporting the use of different positions and mobility during labour; providing comfort; building confidence; providing information; encouragement; reassurance; and calm. Following the baby’s birth, the doula gave the family space and support in ways that suited them (both telephone calls and home visits) and listened to accounts of the birth including when birth had not progressed as planned. Doulas provided information and support for breastfeeding women, including arranging a breastfeeding supporter to visit. They provided reassurance and accompanied women to other services, for example children’s centre.
The few negative comments related to receiving less support than expected and communication difficulties, for example ‘We had a bit of communication problem. [The doula] couldn’t speak my own mother tongue . . . Please . . . Please get more non-English-speaking volunteers.’
Appendix 6 Doula questionnaire: supported women
Appendix 7 Doula questionnaire: not (yet) supported women
Appendix 8 Breastfeeding by postcode district
As identified earlier in Table 4, deprivation varies by postcode district. Figure 41 compares breastfeeding initiation by postcode district. Hull doula mothers are compared with mothers resident in Kingston upon Hull and having a baby in HEY.
FIGURE 41.
Breastfeeding initiation by postcode district with 95% confidence intervals, Hull doula mothers compared with HEY (all years).

The percentage of mothers initiating breastfeeding is higher for the doula mother group across all postcode districts in Kingston upon Hull. The confidence intervals indicate the percentage of mothers initiating breastfeeding and using the Goodwin volunteer doula service is significantly higher in postcode districts HU3, HU6 and HU7. As identified in Table 4, over 85% of the female population of HU3 aged 16 to 44 years live in the most deprived quintile. The postcode districts of HU6 and HU7 both have approximately 50% of their female population aged 16 to 44 years living in the most deprived quintile.
Appendix 9 Women’s sampling frame and distribution
| Contact made by doula service | Type of questionnaire | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Supported | Not supported | Pooled (supported and not supported) | ||||||||||||||||
| Site | ||||||||||||||||||
| A | W | X | Y | Z | Total | A | W | X | Y | Z | Total | A | W | X | Y | Z | Total | |
| Do not contact – because of duplicate | 12 | 0 | 0 | 0 | 0 | 12 | 2 | 0 | 0 | 0 | 0 | 2 | 14 | 0 | 0 | 0 | 0 | 14 |
| Do not contact – because ‘never had contact with the service’ | 0 | 0 | 0 | 0 | 0 | 0 | 52 | 0 | 7 | 0 | 0 | 59 | 52 | 0 | 7 | 0 | 0 | 59 |
| Do not contact – because of circumstances | 5 | 0 | 2 | 2 | 1 | 10 | 5 | 0 | 3 | 0 | 0 | 8 | 10 | 0 | 5 | 2 | 1 | 18 |
| No reply (sent) | 108 | 17 | 0 | 3 | 4 | 132 | 12 | 9 | 0 | 19 | 0 | 40 | 120 | 26 | 0 | 22 | 4 | 172 |
| Telephone number not in use (sent) | 174 | 0 | 0 | 40 | 2 | 216 | 17 | 0 | 0 | 21 | 1 | 39 | 191 | 0 | 0 | 61 | 3 | 255 |
| No reply/telephone number not in use (sent) [sum of 2 rows above; not all sites separated these] | 282 | 17 | 0 | 43 | 6 | 348 | 29 | 9 | 0 | 40 | 1 | 79 | 311 | 26 | 0 | 83 | 7 | 427 |
| No reply/telephone number not in use – not sent because no current address details | 4 | 0 | 1 | 0 | 0 | 5 | 1 | 0 | 0 | 4 | 1 | 6 | 5 | 0 | 1 | 4 | 1 | 11 |
| No reply/telephone number not in use – not sent because interpreter required | 0 | 1 | 0 | 4 | 6 | 11 | 0 | 1 | 0 | 0 | 6 | 7 | 0 | 2 | 0 | 4 | 12 | 18 |
| Reached – declined | 4 | 0 | 0 | 1 | 2 | 7 | 0 | 1 | 0 | 1 | 1 | 3 | 4 | 1 | 0 | 2 | 3 | 10 |
| Reached – accepted (sent) | 119 | 32 | 24 | 25 | 3 | 203 | 13 | 18 | 5 | 3 | 5 | 44 | 132 | 50 | 29 | 28 | 8 | 247 |
| Reached – accepted (completion with researcher) | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| Reached – interpreter to contact | 16 | 1 | 2 | 0 | 6 | 25 | 3 | 0 | 2 | 0 | 3 | 8 | 19 | 1 | 4 | 0 | 9 | 33 |
| Outcome unclear from log | 4 | 0 | 0 | 0 | 0 | 4 | 2 | 0 | 0 | 0 | 0 | 2 | 6 | 0 | 0 | 0 | 0 | 6 |
| Total per site with details held by services a | 446 | 51 | 29 | 75 | 26 | 627 | 107 | 29 | 17 | 48 | 17 | 218 | 553 | 80 | 46 | 123 | 43 | 845 |
| Number sent for self-completion | 401 | 49 | 24 | 68 | 9 | 551 | 42 | 27 | 5 | 43 | 6 | 123 | 443 | 76 | 29 | 111 | 15 | 674 |
| Self-completed (postal) | 83 | 13 | 8 | 14 | 1 | 119 | 9 | 7 | 2 | 5 | 4 | 27 | 92 | 20 | 10 | 19 | 5 | 146 |
| Completed with researcher | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| Completed with interpreter | 8 | 1 | 1 | 0 | 6 | 16 | 1 | 0 | 1 | 0 | 1 | 3 | 9 | 1 | 2 | 0 | 7 | 19 |
| Completed (any method) | 91 | 14 | 9 | 14 | 9 | 137 | 10 | 7 | 3 | 5 | 5 | 30 | 101 | 21 | 12 | 19 | 14 | 167 |
| Response rate – self-completion only | 20.7 | 26.5 | 33.3 | 20.6 | 11.1 | 21.6 | 21.4 | 25.9 | 40.0 | 11.6 | 66.7 | 22.0 | 20.8 | 26.3 | 34.5 | 17.1 | 33.3 | 21.7 |
| Response rate – vs. any contacted | 21.2 | 27.5 | 33.3 | 19.2 | 36.0 | 22.6 | 20.8 | 24.1 | 42.9 | 10.4 | 29.4 | 20.1 | 21.2 | 26.3 | 35.3 | 15.7 | 33.3 | 22.1 |
| Response rate – vs. any logged | 21.0 | 27.5 | 31.0 | 18.7 | 34.6 | 22.3 | 9.5 | 24.1 | 17.6 | 10.4 | 29.4 | 13.9 | 18.7 | 26.3 | 26.1 | 15.4 | 32.6 | 20.1 |
| Number sent or approached by interpreter/researcher | 417 | 50 | 26 | 68 | 17 | 578 | 45 | 27 | 7 | 43 | 9 | 131 | 462 | 77 | 33 | 111 | 26 | 709 |
| Response rate across all types | 21.8 | 28.0 | 34.6 | 20.6 | 52.9 | 23.7 | 22.2 | 25.9 | 42.9 | 11.6 | 55.6 | 22.9 | 21.9 | 27.3 | 36.4 | 17.1 | 53.8 | 23.6 |
Appendix 10 Sample characteristics of women completing questionnaires (n = 166)
| Variable | All women (n = 166) | Used (n = 136) | Not used (n = 30) | |||
|---|---|---|---|---|---|---|
| n for whom data available | n (%) | n for whom data available | n (%) | n for whom data available | n (%) | |
| Current age (years) | 162 | Mean 30.6 (6.4), range 16–45 | 132 | Mean 30.9 (6.1), range 16–45 | 30 | Mean 29.7 (7.5), range 17–44 |
| Age at introduction to doula service (years) | 157 | Mean 28.3 (6.3), range 15–44 | 128 | Mean 28.4 (6.1), range 15–44 | 29 | Mean 27.7 (7.0), range 15–40 |
| Resides with partner | 149 | 80 (53.7) | 119 | 63 (52.9) | 30 | 17 (56.7) |
| Resides alone | 149 | 28 (18.8) | 119 | 23 (19.3) | 30 | 5 (16.7) |
| Housing – hostel/B&B/supported/foster care/friend | 149 | 10 (6.7) | 119 | 7 (5.9) | 30 | 3 (10.0) |
| Supportive partner/husband | 148 | 74 (50.0) | 119 | 56 (47.1) | 29 | 18 (62.1) |
| No-one supportive | 148 | 23 (15.5) | 119 | 20 (16.8) | 29 | 3 (10.3) |
| Primiparous (first child) | 141 | 57 (40.4) | 111 | 46 (41.4) | 30 | 11 (36.7) |
| Time in UK at introduction to doula service | ||||||
| Since birth | 160 | 85 (53.1) | 130 | 66 (50.8) | 30 | 19 (63.3) |
| > 5 years | 25 (15.6) | 20 (15.4) | 5 (16.7) | |||
| 1–5 years | 34 (21.3) | 30 (23.1) | 4 (13.3) | |||
| < 1 year | 16 (10.0) | 14 (10.8) | 2 (6.7) | |||
| Ethnicity | ||||||
| White | 164 | 85 (51.8) | 134 | 73 (54.5) | 30 | 12 (40.0) |
| Mixed | 1 (0.6) | 0 (0.0) | 1 (3.3) | |||
| Asian/Asian British | 33 (20.1) | 26 (19.4) | 7 (23.3) | |||
| Black/black British | 30 (18.3) | 22 (16.4) | 8 (26.7) | |||
| Other | 15 (9.1) | 13 (9.7) | 2 (6.7) | |||
| Main language | ||||||
| English | 163 | 91 (55.8) | 134 | 73 (54.5) | 29 | 18 (62.1) |
| English and another | 9 (5.5) | 6 (4.5) | 3 (10.3) | |||
| Non-English | 63 (38.7) | 55 (41.0) | 8 (27.6) | |||
| Age left school or college (years)a | ||||||
| ≤ 15 | 145 | 17 (11.7) | 119 | 12 (10.1) | 26 | 5 (19.2) |
| 16 | 45 (31.0) | 37 (31.1) | 8 (30.8) | |||
| 17–19 | 44 (30.3) | 35 (29.4) | 9 (34.6) | |||
| ≥ 20 | 39 (26.9) | 35 (29.4) | 4 (15.4) | |||
| Social complexityb | 166 | 53 (31.9) [excluding MH 49 (29.5)] | 136 | 46 (33.8) [excluding MH 42 (30.9)] | 30 | 7 (23.3) [excluding MH 7 (23.3)] |
Appendix 11 Average weekly hours doula support by site
FIGURE 42.
How many hours of doula support did you have each week (on average)? Note: site Z excluded from analyses because of low numbers.
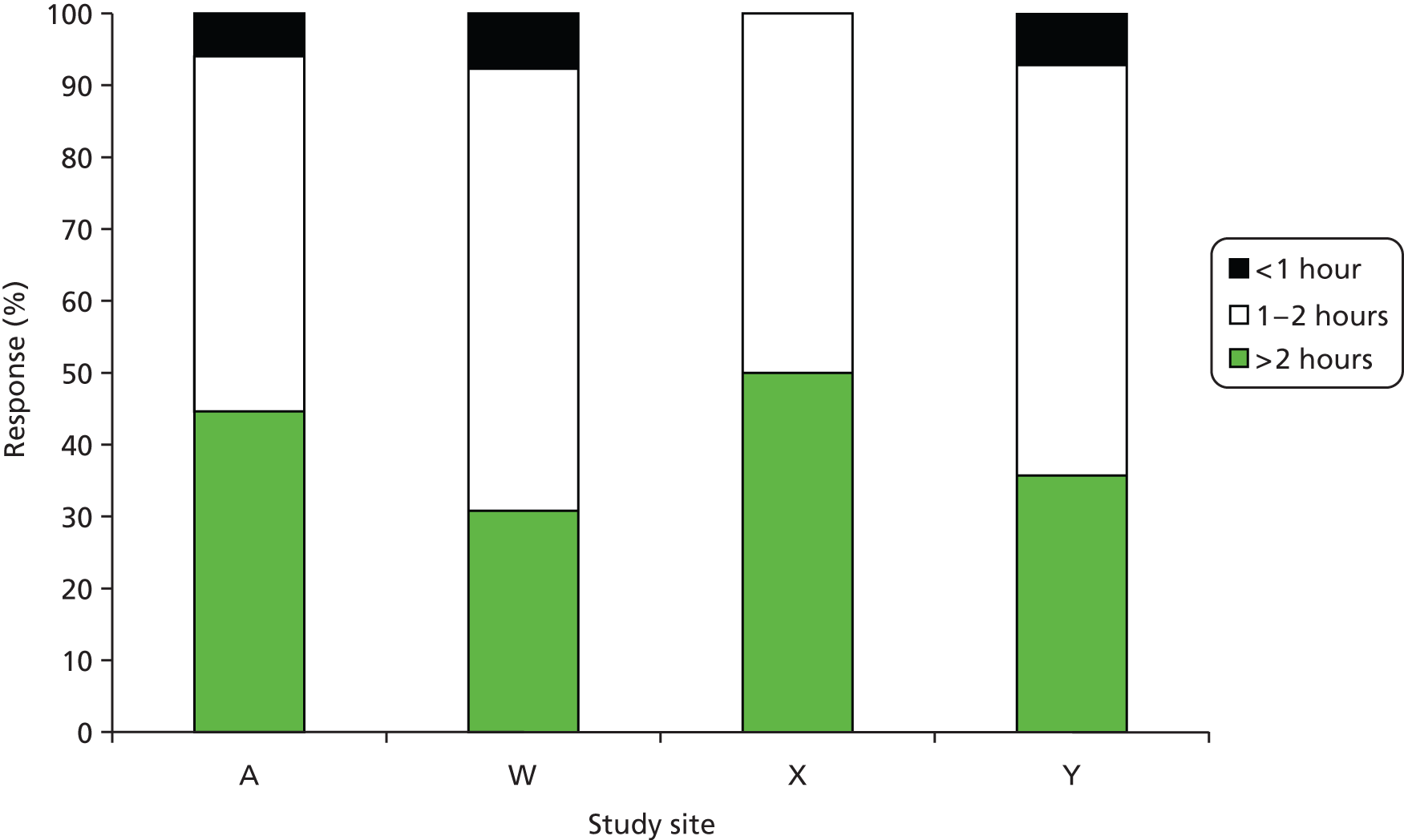
Appendix 12 Combinations of stages supported, presented by site (n = 166)
| Study site | Stages supported | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| None | Postnatal only | Intrapartum only | Intrapartum and postnatal | Antenatal only | Antenatal and postnatal | Antenatal and intrapartum | All three stages | ||
| A | 10 | 8 | 1 | 2 | 9 | 25 | 2 | 43 | 100 |
| W | 7 | 0 | 0 | 0 | 0 | 3 | 0 | 11 | 21 |
| X | 3 | 0 | 2 | 0 | 1 | 0 | 1 | 5 | 12 |
| Y | 5 | 0 | 0 | 0 | 0 | 8 | 1 | 5 | 19 |
| Z | 5 | 1 | 0 | 0 | 6 | 0 | 1 | 1 | 14 |
| Total (%) | 30 (18.1) | 9 (5.4) | 3 (1.8) | 2 (1.2) | 16 (9.6) | 36 (21.7) | 5 (3.0) | 65 (39.2) | 166 (100.0) |
Appendix 13 Service managers’ questionnaire
Appendix 14 Reflections on conducting research on volunteer roles and with third-sector agencies
Data collection from women
The preparatory work was a more resource-intensive task than expected. Not all of the roll-out sites used the database that was provided as part of the roll-out package and not all of the sites had established administrative systems. Difficulties were encountered in determining the type of questionnaire (‘supported’ or ‘not supported’) a woman required and appropriate type of completion (i.e. whether or not completion with an interpreter was required).
We had provided detailed, step-by-step guidance for sites in the hope that this would maintain a consistent process and be a source of support to service staff. We became aware that not all sites carried out the initial approach to women who had been offered doula support in the way we had requested and described in the guidance proforma. Interpreters were rarely used for initial contacts even when the woman’s language was not spoken by service staff. Feedback from one of the sites was ‘The guidance for telephoning was really too long’ (site Y).
We had requested regular return of monitoring logs, as these triggered contacts with participants who required assisted completion of questionnaires. The logs were not completed accurately in some sites and were not always returned to the required schedule. Timescales therefore suffered and considerable additional effort was expended by the research team in following up to achieve progress with the doulas’ and women’s data collection.
Ongoing service responsibilities had to take priority, with consequent impacts on the research timetable. While goodwill and positive relationships were sustained, requests for information, or for actions to be effected, frequently encountered delays. Despite the provision of some funding for administrative support, it appeared difficult for services to put this to positive use within a short time scale. We identify these as issues that researchers may wish to consider in future research with third-sector agencies.
Site A database
We also encountered challenges in accessing the data from site A’s database in a useable form. The lack of a data dictionary or guidance notes was a concern. The system was utilised by several members of staff who had a range of other responsibilities. There was the potential for different interpretation of data items. Similarly the reporting functionality of the database was limited and required considerable modification to render it useable.
Modifications were made by the service’s information technology consultant to deal with multiple records for women who had accessed the service on more than one occasion, and missing data items.
Empirical research of this nature is not a mainstream activity in third-sector organisations, which, despite prior discussion, may find project duration longer than optimal, when they are under pressure to provide evidence of measurable impacts from their service.
List of abbreviations
- BME
- black and minority ethnic
- CCG
- Clinical Commissioning Group
- CMO
- Context, Mechanism and Outcome
- CMOc
- Context, Mechanism and Outcome configuration
- C-section
- caesarean section
- df
- degree of freedom
- DH
- Department of Health
- EBF
- exclusive breastfeeding
- GP
- general practitioner
- HCHS
- Hospital and Community Health Services
- HES
- Hospital Episode Statistics
- HEY
- Hull and East Yorkshire Hospitals NHS Trust
- HoM
- head of midwifery
- HRG
- Healthcare Resource Group
- ID
- identification
- IMD
- Index of Multiple Deprivation
- MARAC
- multiagency risk assessment conference
- NICE
- National Institute for Health and Care Excellence
- NICU
- neonatal intensive care unit
- OCN
- Open College Network
- PCT
- primary care trust
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- R&D
- research and development
- SD
- standard deviation
- SPSS
- Statistical Product and Service Solutions
- TENS
- transcutaneous electrical nerve stimulation