Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1004/04. The contractual start date was in January 2012. The final report began editorial review in June 2015 and was accepted for publication in October 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
During the study Jenny Godson was employed within the primary care trust commissioning the dental services and involved in the procurement of the services.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Hulme et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Use of incentives in dental care
There is an increasing trend towards the use of incentives in NHS primary care including dentistry. 1 Although dentistry has long been incentivised, over the past decade commissioning of primary care dentistry has seen the introduction of refinements, with contract currency evolving from payment for units of dental activity (UDAs) towards incentive-driven or blended contracts that include incentives linked with key performance indicators such as access, quality and improved health outcome. 2 This includes (as part of the Department of Health dental contract reform programme) a series of NHS dental contract pilots which opened in 2011 with the aim of exploring how the focus could shift from treatment and repair to prevention and oral health through the introduction of a new clinical pathway and new remuneration models. 2 Although there is a burgeoning field looking at the impact of these blended contracts on the process of care, there remains limited evidence on the impact of changes in dental oral health outcomes and patient, commissioner and workforce acceptability.
The policy context
In 2003, the Department of Health set out changes in governance as part of the Modernisation Agenda in order to create the right context, incentives and operational environment for their staff and frontline teams to transform patient services. 3 The changes transformed the NHS from a centrally directed service to a more complex system with devolved local commissioners [notably, primary care trusts (PCTs)] and a delivery structure composed of diverse providers. 4 In 2002, Shifting the Balance of Power: The Next Steps5 and its subsequent delivery document gave greater authority and decision-making power to patients and front-line staff, and changed organisational roles and relationships, giving PCTs new commissioning powers. This was then followed in 2005 by Commissioning a Patient Led NHS,6 which further strengthened the lead role of PCTs as commissioners of services to meet the needs of their local communities.
NHS Dentistry: Options for Change7 set out a vision for dentistry with prevention at its heart, which was widely supported by the dental community. Personal Dental Services (PDS) pilots tested these new ways of working between 1998 and 2006. In 2006, a new dental contract emerged, essentially devolving the commissioning of dental services locally to PCTs to meet the needs of their local population. The currency of the new General Dental Services (nGDS) contracts was UDAs divided into three levels of treatment bands, with the total number of UDAs in each contract based on historical activity and agreed between PCTs and dental practices. The nGDS contracts meant that the payment mechanism changed from a one-off fee per item of service to a system whereby providers were paid an annual sum in return for delivering an agreed number of ‘courses of treatment’, weighted for complexity (UDAs). PCTs became the local commissioners of dental services and were charged with demonstrating their competencies as ‘world-class commissioners’.
The PDS pilots (1998–2006) encompassed a wide variety of configurations and were widely evaluated. 8–12 Although the evaluations were largely positive there were concerns about whether or not the PDS agreements met local needs, the absence of measures of success or appropriate goals for commissioning and missed opportunities to harness skill mix. 9,12 More recently, the health committee implicitly rejected the PDS agreements as a precursor of the nGDS contracts when it criticised the lack of piloting of the latter contracts. 13 There has been little research to date on the implementation of nGDS contracts. There were some concerns among dental practitioners,14,15 particularly on whether the nGDS contracts would allow more time for prevention16 or restrict access to new patients and those requiring complex treatment. 17
The Steele report2 examined how dental services in England could be developed over the next 5 years. The review advocated a commissioning approach to align dentistry with the rest of the NHS services, to commission for health outcomes and to develop blended contracts rewarding not only activity but quality and oral health improvement (OHImp). It recommended that payments explicitly recognise prevention and reward the contribution of the dental team to improvements to oral health, reflected in patient progression along the pathway, adherence to nationally agreed clinical guidelines and the achievement of expected outcomes. 2 Commissioners were asked to support dentists to make the best and most cost-effective use of the available dental workforce. 2
Following the Steele report2 proposals were set out to pilot different types of dental contract. 18 Alongside these proposals was the Dental Quality and Outcomes Framework (DQOF), which advocated quality as a necessary part of future dental contracts. 19 Within the framework, quality consisted of three domains: clinical effectiveness, patient experience and safety. 19
A series of NHS dental contract pilots began in 2011. The aim was to shift focus from treatment and repair to prevention and oral health through the introduction of a new clinical pathway, supported by new remuneration models. 20 The new pathway begins with an oral health assessment (OHA), following which the patient is advised of their oral risk status using a red–amber–green (RAG) traffic light rating system and given advice on maintaining or improving their oral health. A follow-up appointment or review is then set based on their risk status.
The needs assessment tool (RAG) was underpinned by the Salford and Oldham primary dental care service redesign project2 which found that the RAG scores:
-
‘Enabled the capture of oral health improvements as patients move RAG status. The project has learnt that, as some risk/modifying factors do not change, only the clinical components should be used as outcome measure
-
Motivated dentists to deliver clinical care appropriate to need through robust, consistent clinical and risk assessment
-
Incentivised dentists to perform detailed assessments and to value all patients the same through completing the same consistent, comprehensive assessment
-
Aided communication with patients through the use of the RAG status.’18
Three remuneration models were proposed in the pilot sites to identify the optimal single remuneration model. Dentists were not required to carry out a given number of UDAs but were required to adhere to the DQOF. 18 The three pilot contract types were based on (1) time spent on providing care for NHS patients as measured by the appointment time; (2) capitation payments weighted for individual patients (age, sex, deprivation) based on all care (preventative, routine and complex); and (3) capitation payments weighted for individual patients based on preventative and routine care only. 18 However, while a small element of remuneration within the models was weighted based on the DQOF, remuneration adjustments were not applied as the indicators required testing and refinements before they could be used. 18
Evidence of the effectiveness of incentive-driven contracting
Overall, the evidence of the effectiveness of use of contracting and incentives by health providers is still emerging. The Christianson and colleagues21 review found mixed results of the effect of payer initiatives that reward health-care providers for quality improvements. O’Donnell and colleagues22 found that the Quality and Outcomes Framework (QOF) within the new General Medical Services contracts in primary care incentivised performance, motivating staff towards QOF targets. Similarly, McDonald and colleagues1 found incentives to be powerful motivators in the primary care workforce. A more granular view suggests that the process-based nature of incentives may limit their long-term effects on health outcomes. 23 There is also a risk that important activities lacking a target may be underemphasised. 23,24
Within dentistry, the Tickle and colleagues’25 analysis of longitudinal data of English adults explored the impact of the nGDS contracts and found that changes to incentive structures had a substantial impact on dentists’ behaviour with respect to their treatment prescribing patterns. Significant numbers of dentists were attempting to hit their UDA contract targets in the most efficient way possible (from their perspective), by shifting towards treatments with high rewards relative to costs, as opposed to selecting on the basis of clinical factors alone. This echoed the results of Chalkley,26 who found that the introduction of the nGDS contracts in England generated a large and significant increase in activity. However, these results are tempered by a recent Cochrane review27 that found generally low-level evidence from the two randomised controlled studies included28,29 (both were UK-based studies). Brocklehurst and colleagues27 concluded that changes to remuneration may change clinical activity in primary care dentistry, but further experimental research is needed – specifically into the impact on patient outcomes.
Early findings from the most recent dental contract pilots introduced following the Steele report2 have focused on patient and practitioner views of the new clinical pathway, reporting them to be strongly supportive. 30 More recent findings20 focus on adaptation to the new system but also report positive indications about clinical benefits in terms of a reduction of risk and health improvement (measured through the RAG status and a basic periodontal examination). However, the authors have quite rightly added the caveat that there are few comparable data from outside the pilot sites. 20
Structure of the report
The project aims to evaluate a blended/incentive-driven contract model compared with traditional contracts on dental service delivery in practices in West Yorkshire, England, UK. Although the blended/incentive-driven dentist contract model pre-dates the most recent national dental contract pilots and the Steele report,2 its specification was innovative and contributed to the ethos and recommendations of the report. The model was cited within the report as an example of good practice with regard to an emphasis on quality of care, achieving health outcomes and patient-reported outcome measures (PROMs)31 while improving access to NHS dentistry. Its introduction thus widens the evidence base underpinning the proposed introduction of blended contracts in NHS primary care dentistry.
In the INnovation in Commissioning primary dENTal care delIVEry (INCENTIVE) study we used a mixed-methods approach with three interlinked projects to evaluate a blended/incentive-driven model of NHS dental service delivery compared with contemporaneous traditional contracting. These three projects addressed questions of acceptability, dental efficacy and cost-effectiveness. Included in the study were three new dental practices with a blended/incentive-driven contract and three practices under the traditional contracts (see Chapter 2).
Our qualitative work (see Chapter 3) addresses questions of acceptability using focus groups, semistructured interviews and observations with stakeholders. Qualitative exploration is useful when there is little pre-existing knowledge, in this case when it was important to find out what changes to services meant to participants. The number of stakeholder groups and budget constraints necessitated a broad, policy-focused ‘framework’ approach, useful for a structured exploration of participants’ perspectives, and provided an advantage because findings were induced from their original accounts. 32,33 This approach enabled us to cover the broad tapestry of experiences emerging from this intervention.
Our quantitative work (see Chapter 4) includes an assessment of the clinical effectiveness of the blended/incentive-driven contract comparing three newly commissioned dental practices with three existing traditional practices. In addition, we used an exploratory study to assess whether or not the traffic light (RAG) risk assessment within the model was fit for purpose.
A key question within the study is whether or not the blended/incentive-driven model of service delivery provides value for money, and our third project (see Chapter 5) assesses the cost-effectiveness of the new model compared with the traditional contract. The report concludes with a synthesis of our main findings (see Chapter 6) and a timely discussion of the implications for designing and commissioning future NHS dental services in light of the planned dental contract reform and further national testing of prototype models.
Chapter 2 Research objectives and intervention
Aim and research objectives
The overall aim of the INCENTIVE research study is to evaluate a blended/incentive-driven model of dental service provision implemented in West Yorkshire in the north of England. An ideal commissioning model will complement population-based health improvement measures with sufficient capacity to meet population needs using effective and efficient prevention and treatment to enhance the clinical status and patient-reported outcomes in the patient base. The model evaluated here uses a blended/incentive-driven approach to commission improved health outcomes through the incentivised delivery of evidence-based prevention, care pathways, skill mix and increasing access to dentistry in response to identified needs. The implementation of this novel contract provided an opportunity to evaluate an innovation in health-care delivery that was already being piloted and applied ideas from other settings offering substantial potential benefit for patients and the future commissioning and delivery of dental services throughout England.
Our primary objectives in the INCENTIVE study were to:
-
explore stakeholder perspectives of the new service delivery model
-
assess the clinical effectiveness of the new service delivery model in reducing the risk of and amount of dental disease and enhancing oral health-related quality of life (OHQoL) in patients
-
assess the cost-effectiveness of the new service delivery model in relation to OHQoL.
Over the course of this study, although our objectives have remained true to our original aim, there was a substantial move towards the introduction of blended/incentive-driven contracts in NHS primary care dentistry subsequent to the Steele report,2 specifically the introduction of the national dental contract pilots and more recent prototypes. It is important to note that the blended/incentive-driven contracts evaluated here pre-date the national dental contract pilots and the Steele report. 2 However, the specification was innovative and reflected the ethos and recommendations of the Steele report2 with regard to an emphasis on quality of care, achieving health outcomes and PROMs. 31 This evaluation therefore complements the national pilots and recent prototypes by not only providing insight into the acceptability of blended/incentive-driven contracts for all stakeholders, but also adding the important perspective of clinical effectiveness and cost-effectiveness.
The intervention
In 2007, NHS Bradford and Airedale commenced a dental service delivery procurement for three new dental practices. Providers were sought through a national procurement exercise. There was considerable interest from a wide range of providers. Nineteen pre-qualification questionnaires were submitted and, of these, 12 were invited to tender, with seven subsequently interviewed. The PCT was actively seeking bidders who both understood the principles of the Bradford and Airedale service delivery model with its focus on the delivery of OHImp, quality and activity, and had a robust business case and operational plan for delivery. The successful bidders came from a variety of provider models, an independent contractor, a dental body corporate and a not-for-profit corporate.
In 2011, 522,500 people lived in Bradford and Airedale, and population projections expect this to increase at a much higher than average rate to approximately 600,000 by 2030. The three new dental practices were carefully sited to address both oral health needs and demands for NHS dental care. The largest practice was located in an area with a predominantly white population with high levels of material deprivation; the second was also located in an area of material deprivation but with an ethnically diverse population; and the last practice was located in an affluent area (the ward is among the 10% least deprived in the country) with a predominantly white population but lacking access to NHS dental care. These communities represented a rich diversity in terms of ethnicity, material deprivation and age profile, allowing the service delivery model to be tested with a variety of practice populations and a range of providers which in turn allowed the findings to have a wider generalisability and applicability.
The Bradford and Airedale service delivery model instigated in 2007 was based on blended/incentive-driven contracts to address local NHS dental access needs and deliver quality and OHImp in addition to UDAs. The procurement remained timely and in line with subsequent recommendations of the review of NHS dentistry in Equity and Excellence: Liberating the NHS,34 that commissioning should be focused on health outcomes. This delivery system enables quality to be rewarded with payment linked to evidence-based management and monitoring of oral health outcomes. It also allows for continuous improvement through thresholds for payments and emphasis on outcomes by weighting payments. The service was, additionally, implementing quality and outcome measures that allowed us to evaluate their implementation and use.
The three practices operating under blended/incentive-driven contracts were matched with three practices operating under the traditional UDA-based contracts, by demographics, list size and number of dentists. Table 1 details differences between contracts and reimbursement as a result of the new commissioning together with the incentives and levers and how these were expected to impact on process and service delivery.
| Characteristics | Traditional practices | Incentive practices |
|---|---|---|
| Contract type | nGDS contract | A blended/incentive-driven contract |
| Mode of reimbursement | Activity-based, weighted bands of dental activity | Activity: 60% of contract value – UDAs |
| Contract currency UDAs | Incentives: 40% of contract value. (1) 20%, quality (systems, processes and infrastructure); (2) 20%, OHImp | |
| Incentives and levers | Driven by delivery of UDAs, with no incentives for preventative approach | Allocation of payment allows commissioners to incentivise key structures, processes and outcomes for quality and OHImp |
| Health professional responsible for delivery of care | Dentist (with no incentives for therapist and hygienist support) | Blended contract incentivises use of skill mix to deliver preventative focused care |
| Care pathway and recall | Prescribed by individual performers | Risk-assessed (using the RAG system) evidence-based preventative care pathway |
| Risk-assessed recall interval variations recorded | ||
| Stakeholder feedback on delivery and impact of care | Standard complaints/comments | Patient forum |
In detail, within the new practices, 60% of the contract value is apportioned to delivery of a set number of UDAs. The remaining 40% is dependent on the delivery of quality: 20% systems, processes and infrastructure [e.g. cross-infection, policies, Standards for Better Health (latterly becoming Care Quality Commission domains)] and 20% OHImp. The blended/incentive-driven contracts were aimed at ensuring evidence-based preventative interventions (based on Delivering Better Oral Health: An Evidence Based Toolkit for Prevention35) were delivered in line with identified needs for a defined population, increased access to NHS dentistry, and that care was provided by the most appropriate team member to encourage skill mix. It was intended that all the incentive-driven practices would fully utilise skill mix including, for example, dental therapists and hygienists and extended duty dental nurses.
Skill mix
One area of potential advantage in the blended incentive-driven model of delivery is more effective use of the dental team. For example, dental hygienists/therapists can carry out courses of treatments recommended by the dentist who has examined the patient. Dental hygienists can carry out treatments such as scaling and polishing, oral health promotion and fissure sealants. A dental therapist can perform additional treatments such as fillings, pulp treatment/stainless steel crowns and extractions on children. Additional skills dental nurses may be trained and competent to give preventative advice and apply preventative fluoride varnishes to teeth. Intuitively, the delegation of treatment to staff who specialise in only a specific range of treatments could reduce costs and increase access to care but this hypothesis needs testing. 36
Skill mix is advocated in several current proposals that continue a trend seen in UK dentistry over the last 20 years. 2,7,37,38 For example, dental therapists may now work in general dental practice7 and their clinical remit has expanded. 39,40 The number of training places has increased and several educational establishments have instituted programmes. The potential contribution of dental therapy is considerable. Evans and colleagues41 found that, within their current remit, therapists could undertake the treatment provided in 35% of dental visits and in 43% of clinical time. Yet dentistry has not harnessed this potential. Dentists may need models to help them employ dental hygienists/therapists profitably and fully use their skills and there have been calls to develop a system that encourages dentists to use dental hygienists/therapists differently. 42,43 The PDS pilots failed to fully involve the wider skill mix available (i.e. dental care professionals or improve their conditions to recruit and retain them). 9
Although there are few hard data to support skill mix in dentistry36 some data are beginning to emerge. A recent practice-based study found the success of fissure sealants to be comparable whether placed by dentists, hygienists or therapists. 44
There is a trend towards greater professional acceptance of therapists,43,45–49 with approximately 60–70% of dentists prepared to consider employing a therapist in the more recent studies. 50,51 Despite this, some dentists remain uncertain of the role of dental therapists. 51,52
There is also some uncertainty about public acceptance of dental therapists. Two recent surveys and a qualitative study suggest that few lay people are aware of dental therapists as a professional group. 53,54 Furthermore, even after the training of dental therapists was explained to them, only 61% of adults were willing to receive simple restorative treatment from a therapist. 53,54 The provision of dental care is influenced by the NHS contract for dentists. The existing UDA contract does not make any allowance for treatment provided by dental therapists, although since 2013 dental hygienists and therapists can carry out their full scope of practice without a prescription or the need for the patient to first see a dentist; this is known as direct access and the impact of this on dental team delivery is yet to be realised. Research is therefore needed to assess if new models of delivery and service design will encourage their use and whether or not they are acceptable to dentists and patients.
Care pathways
The Bradford and Airedale new service delivery model (incentive) was designed to encourage a care pathway approach in which all patients have an OHA on joining the practice and at each subsequent recall. Four sets of information [age group, medical history, social history (self-care, habits/diet) and clinical assessment] are used to inform a traffic light (RAG) risk assessment for patients with high (red), medium (amber) or low (green) risk of oral disease (Table 2).
| Risk | Descriptor | Example indicators |
|---|---|---|
| Red: high | High risk of disease identified through clinical assessment and social history | Clinical: active decay in more than one tooth, BPE Social history: never brushes teeth |
| Amber: medium | Medium risk of disease identified through clinical assessment and social history | Clinical: active decay in one tooth, BPE score of > 2 in two sextants Social history: brushes once per day |
| Green: low | Low risk of disease identified through clinical assessment and social history | Clinical: no active decay, BPE score of 2 confined to one sextant Social history: brushes twice a day |
Within the model, each patient follows a care pathway according to the protocol. The care pathway includes evidence-based preventative treatment and advice, suitable recall interval and restorative care as appropriate (e.g. the red risk category limits patients to stabilisation and lowering their risk status). The care pathway’s evidence base was based on the Department of Health’s Delivering Better Oral Health: An Evidence Based Toolkit for Prevention. 35 Each patient’s status is reviewed on their next OHA. Patients may therefore move between risk categories. Monitoring in practices ensures that evidence-based preventative interventions are delivered in line with identified needs and monitored access to dentistry. OHImp is assessed through the delivery of a performance framework. This framework is based on the transfer of ideas from the general practitioner contract QOF. (It is of note that this contract pre-dated the DQOF. 19)
There is little literature regarding care pathways in primary dental care, though the concept has been around for a number of years. The concepts and benefits of the care pathway approach in dental primary care were described by Hally and Pitts. 55 As a result of recommendations within NHS Dentistry: Options for Change,7 the first widely disseminated care pathway in UK dental primary care was the OHA within the National Institute for Health and Care Excellence (NICE) guidance on dental recall intervals. 56 The OHA care pathway was designed to enable more prevention within personalised care plans taking into account patients’ social and dental histories as well as clinical findings.
The type of risk assessment (the RAG traffic light system) included in the blended/incentive-driven contract in our study has hitherto not been fully evaluated. Examination of different RAG models in other dental settings is ongoing in the north-west of England. 57 Early findings from the NHS dental contract pilots suggest small improvements in risk reduction over the short term. 20
In summary, the incentive dental contracts are aimed at ensuring that evidence-based preventative interventions are delivered in line with identified needs for a defined population; ensuring increased access to dentistry; and ensuring that care is provided by the most appropriate team member to encourage skill mix. Quality indicators linked to contracts and payments have been used widely in other branches of health care, and the results are complex. The indicators can drive organisational change towards best practice, but may also be a disincentive to important but non-rewarded activities. 24 Used alongside demographic data, the indicators can measure practice performance, identify areas for development and assist sharing of best practice. 58 The indicators often increase the quantity of service provision, but not always the quality. 59 Furthermore, the indicators can affect the dynamic of professional relations and the doctor–patient interaction. 60 Although offering great potential, the DQOF with embedded quality indicators has not been comprehensively evaluated in dentistry. A recent systematic review was only able to provide a framework for how such indicators might work. 61 The blended/incentive-driven contract in West Yorkshire provides an opportunity for a comprehensive evaluation to inform the next dental contract reform.
Chapter 3 Stakeholder perspectives of the blended/incentive-driven service delivery model
Introduction
As outlined in Chapter 2, in 2007 the PCT in Bradford and Airedale commenced procurement for three new dental practices to address access to NHS dentistry and to pilot a new service delivery model. The model was based on a blended/incentive-driven contract and, although it pre-dated the Steele report2 and the NHS dental contract pilots, its specification although innovative actually reflected the ethos and recommendations of the report placing an emphasis on quality of care and achieving OHImp in accordance with the Steele report2 and Equity and Excellence: Liberating the NHS34 that followed. The successful bidders represented three provider models: an independent contractor, a dental body corporate and a social enterprise organisation.
The contract blends novel incentives to demonstrate quality and OHImp as well as volume of service (measured in UDAs) and, therefore, shares features with the reformed dental contract piloted by the Department of Health. 18 Most of the contract’s value (60%) arises from the delivery of UDAs. The remainder is divided equally between delivery of quality including systems, processes and infrastructure (e.g. infection control) and on OHImp (implementation of Delivering Better Oral Health: An Evidence Based Toolkit for Prevention35). Thus, the contract is intended to promote evidence-based preventative interventions, widen access to dentistry and encourage the use of skill mix.
A central feature of the contract is a ‘care pathway’, whereby an initial OHA for each patient joining a practice determines the risk of poor oral health and guides treatment and the frequency of recall appointments. These decisions are informed by the patient’s age, medical history, social history (e.g. self-care, habits or diet) and the clinical assessment. Patients are categorised according to RAG status with high, medium or low risk of oral disease. The treatment protocols consist of evidence-based preventative care and advice, restorative care and designated recall intervals. Patients who are considered ‘red’ are limited to stabilisation and lowering risk status. Statuses are reviewed at future appointments with the potential for patients to move between groups, for example moving from ‘red’ to ‘amber’ (see Table 2).
The three newly commissioned dental practices were in areas of high oral health need and with high demand for NHS dental care. The largest practice (practice 2) was located in an area of Bradford with a predominantly white population with high levels of deprivation. Practice 1 was in a neighbouring town in an area of material deprivation but with an ethnically diverse population (over 50% of Pakistani/Bangladeshi origin). Practice 3 was the smallest practice with only two surgeries. It was located in a predominantly white affluent area (among the 10% least deprived wards in the country), yet lacked access to NHS dental care.
In this chapter we report on the qualitative research to explore stakeholder perspectives of the new service delivery model. We describe meanings of key aspects of the model across three stakeholder groups {lay people [i.e. patients and non-patients (non-patients are defined as individuals not having a dentist)], commissioners and the primary care dental teams}, with framework analysis of focus group and semistructured interview data.
Methods
Our focus lies on the three newly commissioned dental practices working under the blended/incentive-driven contracts (incentive practices) and three dental practices working under traditional nGDS contracts (traditional practices). The traditional practices were included in the study as comparators and were matched with the incentive practices by deprivation index, age profile, size of practice and ethnicity. Details of all six practices are given in Table 3.
| Demographics | Incentive practices | Traditional practices | ||||
|---|---|---|---|---|---|---|
| Type of contract | Blended contract: UDA and incentives for health promotion/prevention activity | Working under 2006 NHS dental contract (nGDS contract) | ||||
| Practice | Practice 1 | Practice 2 | Practice 3 | Practice 4 | Practice 5 | Practice 6 |
| Established | 2008 | 2009 | 2009 | > 10 years | > 10 years | > 10 years |
| Operated as | Part of a large corporate provider | Independent provider | Part of a social enterprise organisation | Part of a large corporate provider | Independent provider | Independent provider |
| Location | Centre of large town | South-east Bradford | In an affluent market town | Centre of large town | North-west Bradford | South-west Bradford |
| Percentage of households with at least one dimension of deprivation (employment, education, health and disability, housing)a | 74.6 | 71 | 42. | 74.6 | 51 | 53.9 |
| Number of GDPs | 4 | 5 | 2 | 6 | 7 | 2 |
| Multidisciplinary team (e.g. hygienists or therapistsb) | 1 therapist | 2 therapists | 1 therapist | 2 hygienists | 1 hygienist | None |
| Number of surgeries | 5 | 5 | 2 | 7 | 6 | 2 |
| Population ethnicitya | 51.3% Pakistani/Bangladeshi | 79.4% white British | 94% white British | 51.3% Pakistani/Bangladeshi | 92.8% white British | 89.2% white British |
The qualitative study uses focus groups and semistructured interviews, supplemented with observations made during dental appointments of the delivery of dental care in the incentive practices and the traditional practices.
Purposive sampling via a sampling matrix supported recruitment of participants with different experiences of the model. The three stakeholder groups were lay people (i.e. patients and non-patients), dental teams (i.e. dental practitioners, dental care professionals and practice managers) and service commissioners.
Encounters were observed in two incentive and two traditional practices. Staff were purposively sampled across the range of skill mix so that similar numbers (15 each) of dentists and dental hygienists/therapists were observed. All eligible adult patients (aged ≥ 18 years) with appointments with the participating staff on the scheduled day of observation were invited to participate. At 2 weeks before their appointments, patients were sent a letter informing them of the study, a study information leaflet and a consent form. Patients who expressed interest in the observations were given the opportunity to ask any questions and give consent on the day of their appointment. The ‘non-participant’ observer attended appointments passively at a distance close enough to hear the conversation to take comprehensive field notes. A brief analysis of observations was conducted as soon as possible after the observation (the same day or the following day).
Observations were followed by interviews with clinicians, resulting in the participation of four dentists and four dental hygienists/therapists that took place on the same day. Staff were asked to comment on the observed encounters and share their views on what had taken place. Questions asked at the post-observation interview were influenced by the nature of the activity in the encounters and the team member’s attitude, expectations and impressions and reflections on the experience. Interviews were recorded and transcribed verbatim.
Interviews were also conducted with patients, lay people recruited through community settings, commissioners and dental team members (see Tables 4 and 5).
Lay people were recruited for the interviews in two ways. The research team gave practices information packs to mail to patients. Potential participants indicated interest in the research by returning their contact details in a Freepost envelope and were then contacted to arrange an interview. Lay people who were not patients included representatives of community groups in the locality. The researcher contacted the gatekeeper of community organisations to explain the study and provide research information and enlisted their help in recruitment. Focus groups were held with groups attending a community centre, including one aimed at parents with young children and another attended by older residents. In addition, snowball sampling entailed existing participants passing the study information and the researcher’s contact details on to acquaintances to invite them to take part. 62 The inclusion criteria for lay people were that they should be aged ≥ 16 years and willing to be interviewed. People with no natural teeth were excluded.
Ethics approval
Ethics approval was obtained from the National Research Ethics Service (NRES) Committee [London – Bromley, Research Ethics Committee (REC) reference 12/LO/0205] on 5 April 2012. Informed consent was obtained from all participants prior to any qualitative enquiry. The study was sponsored by the University of Leeds, Leeds, UK.
Data were collected between August 2012 and February 2014 by two research associates, who were social scientists rather than dentists. Interviews and focus groups followed a topic guide, partly informed by the theoretical framework (see Appendices 1 and 2) but supplemented with themes that emerged from the observations and previous interviews. Interviews with dental team members took place at the dental surgery, while interviews with patients took place in patients’ homes. All were recorded and transcribed verbatim. Interviews lasted between 15 and 70 minutes.
Theoretical framework
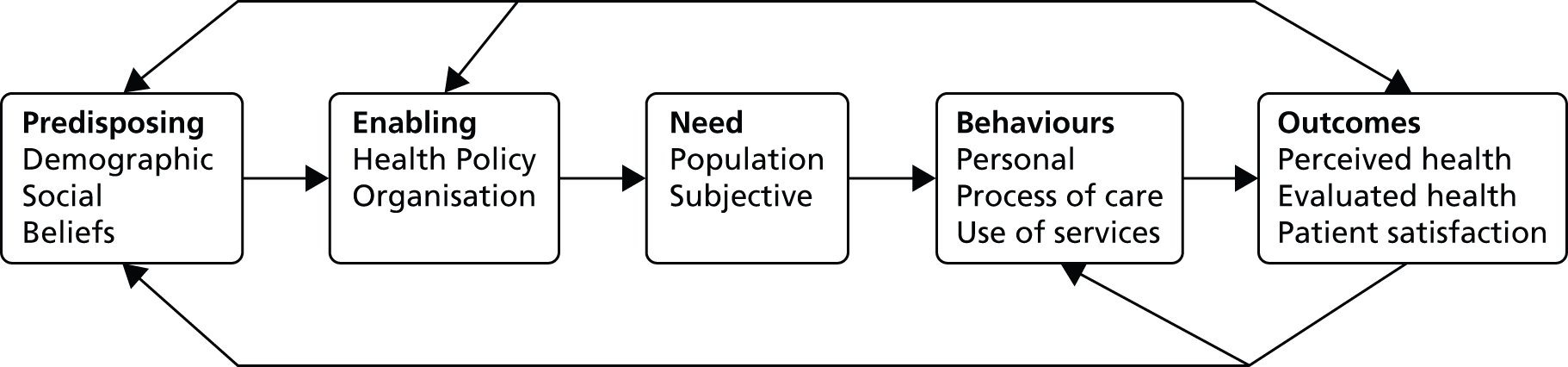
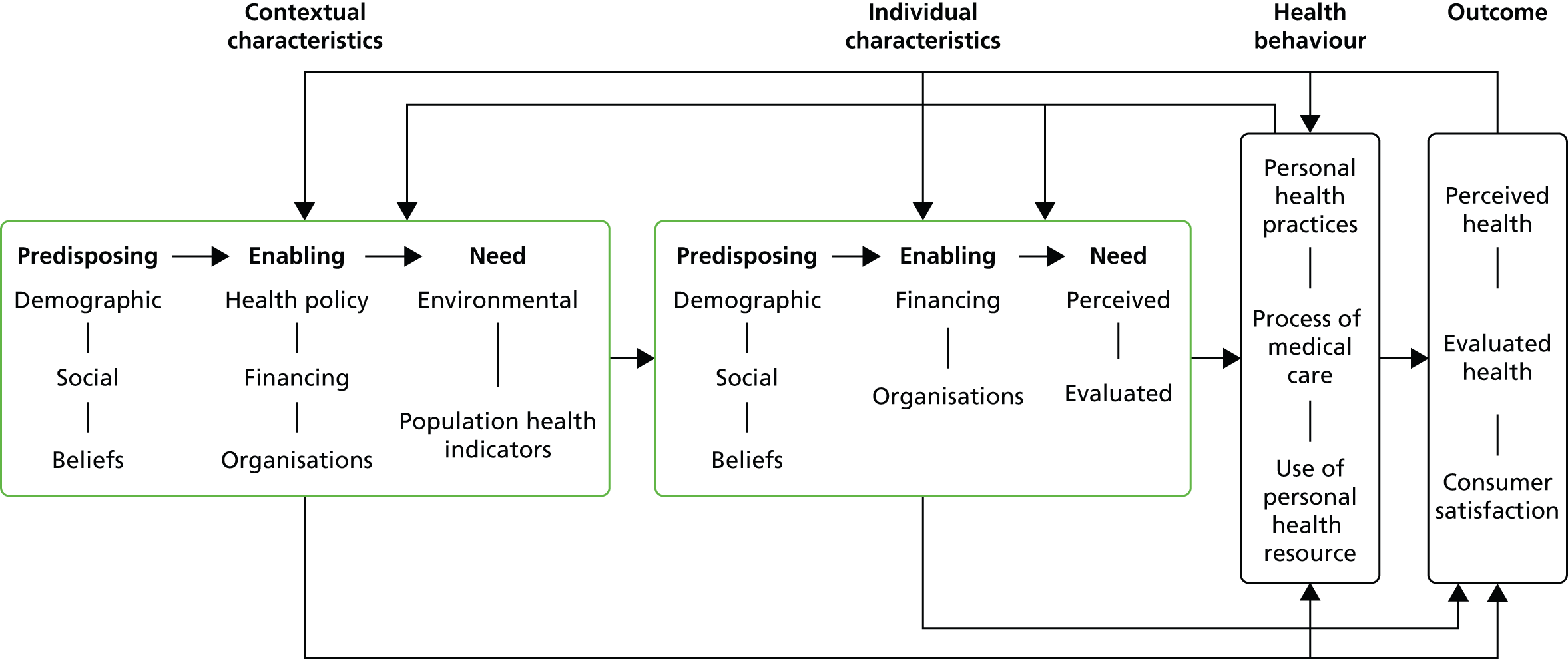
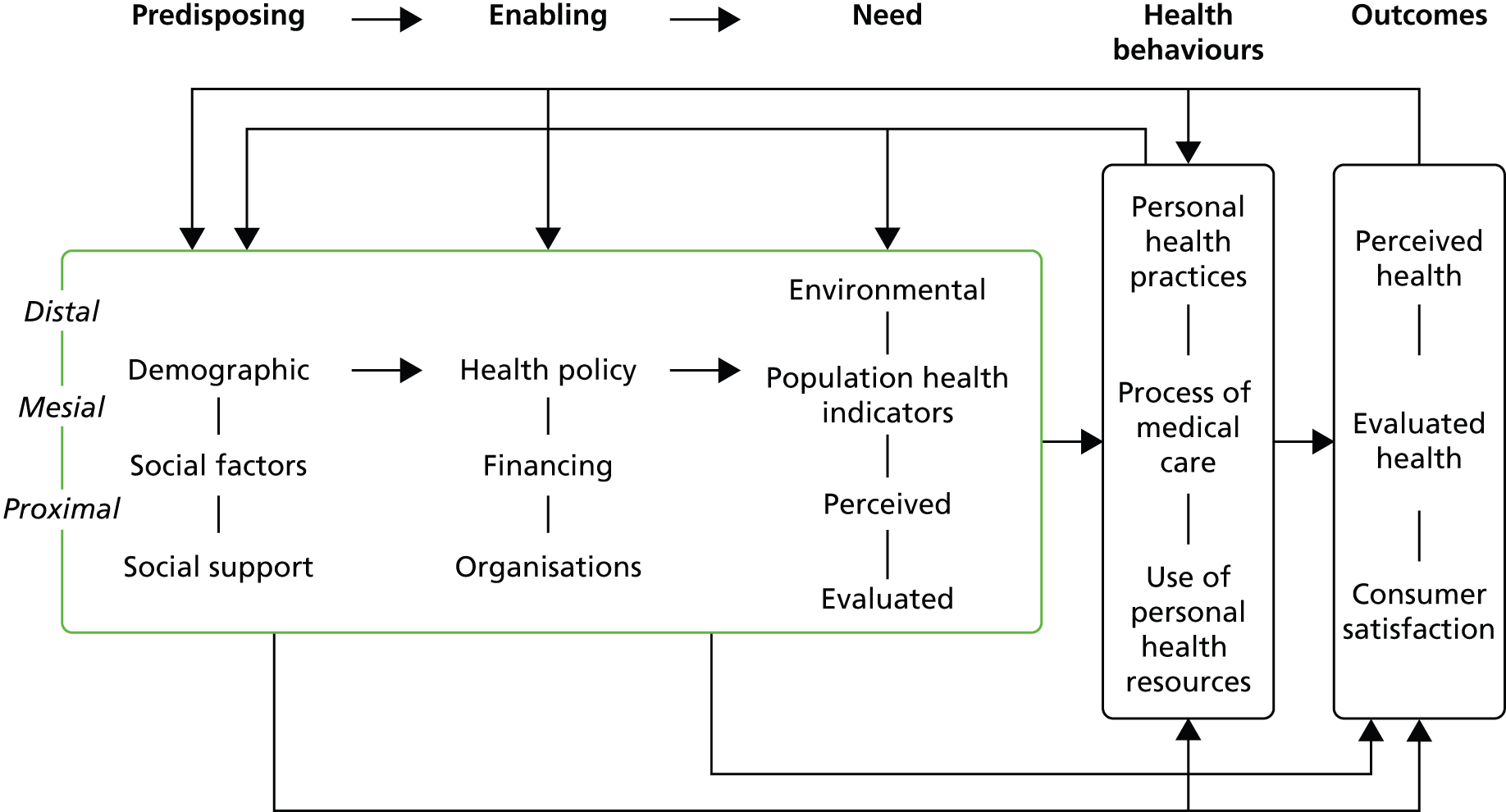
The Andersen behavioural model of access was employed as the theoretical framework for the qualitative analysis (Figure 1 shows a simplified depiction). The model sees access as ‘the use of personal health services and everything that facilitates or impedes their use’63 and distinguishes between ‘potential’ and ‘realised’ access. Potential access is measured according to enabling variables such as the availability of care or supply of health-care workers. ‘Realised access’ refers to services actually used or ‘utilisation’. 63
Originally developed 40 years ago as a model of health-care utilisation, the model has evolved in line with advances in understanding that have moved from an individual focus to incorporate the interaction between the individual, the health-care system and the external environment. 63–65 The revisions have not altered its basic foundations, but have added components to it. Later versions introduced health and patient satisfaction as desirable outcomes of health care, which were said to be determined by predisposing and enabling factors, behaviours and need. Findings from studies in many areas of health care, and dentistry in particular, support its use. 66,67
Enabling factors relate to the policies, facilities, staff and the organisation of services that might influence utilisation. 65 It is helpful to consider enabling factors as a spectrum, with different qualities of the same factors either facilitating or challenging service use. Policies, guidelines, rules, practices, contracts, resources and reform define the nature and delivery of care. Financial factors can include the funding and affordability of health care. Organisational factors refer to the structures and processes that influence the availability and distribution of health services, and the personnel and how accommodating they may be to patients’ needs.
From this perspective the blended/incentive-driven contract being evaluated in this study is an enabling factor with health policy, financial and organisational facets. The government has made policy commitments to oral health and dentistry with focus on improving the oral health of the population, particularly children, introducing a new NHS primary dental care contract and increasing access to NHS dentistry. 18,68 Other relevant drivers included the recommendations of the Steele report2 and the evidence-based prevention of Delivering Better Oral Health: An Evidence Based Toolkit for Prevention. 35
The contract replaces some of the financial emphasis on the volume of treatment with incentives for quality and changed outcomes. These incentives were based on the concept of providing care for a population rather than patients via organisational changes such as the use of care pathways, the provision of evidence-based care and the use of skill mix.
Health-care need may be seen as the potential to benefit from care and requires both a health problem and an effective intervention. 69 Health needs may include health education, disease prevention, diagnosis, treatment, rehabilitation and palliative care.
The Andersen behavioural model distinguishes between evaluated (professionally defined or normative) and perceived (personally defined or felt) need70 but recognises that there are social aspects of evaluated need, which can be influenced by technological developments and clinical guidelines.
In some versions of the model predisposing, enabling factors and need are distinguished at the contextual or individual levels. Contextual characteristics operate at a population or combined level, drawing attention to the environment or the circumstances in which health care is delivered. The most recent versions of the model have seen the context and individual levels arranged sequentially with contextual predisposing and enabling factors and need influencing similar factors for individuals.
In turn, these components could influence personal and professional health behaviours. Personal behaviours are activities that shape health status, such as oral hygiene, diet and tobacco use. Health service use is treated as behaviour in itself. Professional behaviours relate to the processes of medical care, such as health education, clinician–patient communication and prescribing behaviour. Both personal and professional behaviours may be amenable to changes via enabling factors and will influence the nature and volume of treatment provided.
The outcomes are (1) perceived and evaluated health status and (2) patient satisfaction. The maintenance and improvement of health should be the primary outcome of access and is a central target of the dental contract reform programme. 68 Perceived health status indicates how much an individual can live a ‘functional, comfortable and pain free existence’. 65 This definition is akin to OHQoL, which may be defined as ‘the impacts of oral disorders on everyday life that are important to people and of sufficient magnitude to affect perception of their life overall’. 71 However, other patient-reported outcomes could be used, such as general health perceptions. Evaluated health status requires a professional assessment of clinical status. Patient satisfaction has a bearing on patient health outcomes, with greater satisfaction being related to health improvement via adherence, involvement with treatment and continued use of services.
An important feature of the model is its recursive nature, with feedback loops so that the outcomes of access have the potential to influence future predisposing and enabling factors, population needs and use of services.
Analysis
Data were analysed in two phases. First, pen portraits of the practices are used to give the data context.
Within the second phase the principal approach used framework analysis to induce the results from the variety of original accounts across stakeholder groups within the structured policy focus of the research. 32,33 The focus of the analysis was to explore the effect of the contract as it interacted as an enabling factor with other stages of the model. Analysis adhered to the following process:
-
familiarisation with the data
-
identifying the thematic framework
-
indexing
-
charting
-
mapping and interpreting. 32
A member of the research team (MH) studied the field notes and transcripts of the post-observation interviews. This process of familiarisation (familiarisation with the data) enabled identification of emerging themes in the data set. 72 Although Andersen’s behavioural model guided the thematic framework in principle, data were not forced into an a priori model. Instead, the framework was refined as required (identifying the thematic framework). Data generated from the post-observation interviews were indexed according to the particular theme to which they corresponded (indexing) and lifted from their original text and placed under subheadings derived from the framework (charting). The themes were flexible and modified as necessary. Data were organised by theme to enable a process of constant comparison across themes and cases. The framework analysis served to either confirm or challenge the model. A form of deviant case analysis was intended to be used to add new categories or revise the model.
The validity of the findings was supported by discussion of interim and final results for triangulation and corrections with participants in focus groups. The results were also compared against existing knowledge, such as the evaluations of the NHS dental contract pilots. 30
Results
Pen portraits of the practices are presented in Table 3 to set the context of the study. The qualitative results of the principal analysis are presented in two stages. First, the major themes in the data are outlined. Second, the interactions between the themes, focusing particularly on the interactions between enabling (i.e. service organisation) and other factors, are described.
Three study practices (1, 2 and 3) were using the blended/incentive-driven contract approach, referred to as incentive. These were matched to three control practices (4, 5 and 6) operating nGDS contracts, referred to as traditional, according to the number of general dental practitioner (GDP) surgeries in the area, list size and the deprivation index and ethnicity of the local populace.
Practice 1
Practice 1 is situated in the centre of a large town several miles from Bradford. The practice is based within the one of the 10% most deprived wards in the country, with associated adverse income, living environment, education, health and employment indicators. The practice estimates that approximately 80% of its patients are eligible for benefits and a similar proportion are white British, despite the ethnicity of around 50% of the local population being of Pakistani/Bangladeshi origin. The practice was established in 2008 and is operated by a very large national corporate provider. Its team consists of four GDPs and one dental therapist.
Practice 2
Practice 2 is located at the south-east edge of Bradford, adjacent to a large council estate. Bradford ranks 16th in the most deprived local authority areas in England. The area served by the practice originally had a white British population, although it has become more ethnically diverse in recent years and has a traveller community. The people of this area had experienced difficulties with access to dental care for many years, with limited care available in the area and a local unwillingness to travel for care.
Established in 2009, the practice is owned by an independent contractor with two other practices (not part of the blended/incentive-driven contract). The practice has five surgeries, a separate decontamination room and staff training room. It employs five dentists and two dental therapists. Almost all of its treatment is provided under the NHS (99.5%).
This practice experienced a higher staff turnover than the other study practices, which was attributed anecdotally to the associates being early-career dentists eager to take up a post but not necessarily a commitment to practising in the locality in the long term. Lack of opportunities to carry out complex treatments was also thought to be a factor.
Practice 3
Practice 3 is located in an affluent market town several miles from Bradford, which has lacked NHS dental provision. It was established in 2009 and the provider is part of a social enterprise organisation. It has two surgeries, two dentists and one dental therapist. During the research, one GDP left this practice. The original practice manager was replaced, but later returned.
Three comparison practices (4, 5 and 6) continued to work under the terms of the 2006 NHS dental contract and were matched to the blended/incentive-driven practices according to the number of GDP surgeries, list size, and the deprivation index and ethnicity of the local populace.
Practice 4
Practice 4 is close to practice 1 and part of a group that operates more than 200 practices in the UK. With more than 10,000 NHS patients the practice is not currently taking on any new patients. Almost all (96%) of the work is provided under the NHS. There are seven surgeries, staffed by six GDPs. Two dental hygienists are employed.
Practice 5
Practice 5 is an independent practice on the outskirts of Bradford and is the longest serving practice in the study (over 30 years). It has six dental surgeries with seven GDPs and one dental hygienist, who is available on a private basis. One dentist’s services include non-surgical procedures such as fillers.
Practice 6
Practice 6 is an independent practice run by two dentists. There are no dental hygienists or therapists, but the practice provides a full range of NHS treatments (except orthodontics) to all members of the public. It also provides private treatment including sedation for anxious patients.
Qualitative results
Observations were made during 30 dental appointments. Eighteen lay people, 15 dental team staff and a member of the commissioning team took part in the interviews and focus groups (Tables 4 and 5).
| Pseudonym | Practice | Details |
|---|---|---|
| Michael | 2 | In his early forties, recently made redundant, former army, cohabiting with partner |
| Shazia | 2 | Community worker, in her thirties, married with children |
| Katie | 2 | Mother of two, in her twenties, lives with partner, receiving benefits |
| Tony | 2 | Tony and Jeanette are a married couple. Tony is aged 66 years and is visually impaired. Jeanette (aged 65 years) is in a wheelchair following a stroke. Moved to practice 2 because their previous dentist lacked wheelchair access |
| Jeanette | 2 | |
| Ian | 3 | Married couple in their mid-forties |
| Grace | 3 | |
| Martin | 3 | Married police officer, in his forties, with two children |
| Lara | 1 | Housewife, in her thirties, married with children |
| Nanush | 1 | Married housewife with three children, in her thirties |
| Alison | Patient at a traditional practice | Working mother of one, in her thirties |
| Carol | Patient at a traditional practice | Stay-at-home mother of two, in her forties |
| Kat | Patient at a traditional practice | Stay-at-home mother of two, in her twenties. Her children attend an incentive practice |
| Natalie | No dentist | Mother of two, in her twenties, lone parent, receiving benefits |
| Johanna | No dentist | Focus group with three women in their seventies and eighties. Each had dentures to varying degrees |
| May | No dentist | |
| Mary | No dentist | |
| Ann | Discontinued incentive patient | Housewife in her fifties |
| Participants | n |
|---|---|
| Traditional practice dentists | 4 |
| Incentive practice dentists | 8 |
| Dental practice managers | 2 |
| Dental therapists | 1 |
| Commissioners | 1 |
The Andersen behavioural model framework was sustained in the data, with the only revision being the addition of trust as an outcome of access. During the analysis, the implications of the epistemological position of the model became apparent. A wider debate may be required about enabling the use of social resources for health and the position of health services within that. This debate is introduced in the discussion. The results described are supported by anonymised quotes from the data.
The qualitative results are presented in two sections. The first demonstrates the fit between the data and the Andersen model and the second examines the effect of the new contract as interactions between enabling and other factors in the model.
Predisposing factors
Predisposing factors could be characterised as demographic and social characteristics and beliefs. For example, family commitment could facilitate or hamper service utilisation and one participant (Grace) noted the effect of changing attitudes over time.
I can’t remember where I go, I wish I could. My daughter takes me to all my appointments.
Mary, no dentist
I think the danger is when you’re a professional this is what you do for a living, it’s a danger as its making an assumption that everybody else thinks it’s as important as you, and it is down to education and you know we see ourselves very much as a practice set up to educate and to inform. When you’re dealing with the demographic and you know the type of community we are working with, you’ve got to be very careful not to be patronising, you have to be very careful because you know everybody’s need is different and everybody’s circumstances, you know we shouldn’t just assume that because we think it’s important that they will.
Sarah, incentive dentist
I think and it’s something that kind of you’re very aware for your children as well aren’t you? I think when I was younger there was a different kind of attitude towards it and I only went to the dentist if there was a problem and I think attitudes have changed now and I think that its, you know you’re much more proactive in making sure that your children go and they get seen and that type of thing.
Grace, incentive patient
These data suggest that from the patients’ perspectives predisposing factors are things that either hamper or enhance their ability to access care. For the providers it involves fitting the service to what the dentist thinks the patient needs. The last quotation indicates a generational change and changing attitudes to the dentist.
Enabling factors
Compatible with the underlying framework, enabling factors fell into three subthemes of health policy, finance and organisations. The influence of health policy appeared in the data between the extremes of the changes associated with implementation of the blended/incentive-driven contract right through to an apparent lack of policy in some practices.
There’s going to be challenges in terms of its new, so you’ve constantly got perhaps a more demanding type of commissioning process. From a commissioner’s perspective as I mentioned earlier it takes more time.
Service commissioner
We don’t have any guidelines or anything.
Dentist at feedback event, traditional practice
A key part of the contract was the remuneration of dentists and thus finance was a rich theme. On the one hand traditional models of service use were problematic for the treatment of complex cases, whereas the problem for incentive practices became much more focused on the costs of OHAs and building relationships with patients that would enable more prevention.
The current [2006] contract works to an extent but means treating complex cases is difficult. I’m here to make a profit and a living. There’s no point me being here if that’s not going to happen. I’ve trained for a long time, I have laboratory costs to cover, I need to make money. Complex cases are difficult in this contract.
Adam, traditional practice dentist
The cost of doing that [OHAs] is far higher than was first anticipated, so if we were to put that as a separate issue we would say that it’s the costs prediction. The estimation of what it would cost to run this has been very underestimated, because it does take more time. It takes us away from doing, because we’re trying to get patients, encourage them, chase them so much it actually takes an hour for a clinician to build that relationship in the first place and then it’s about compliance and so that was collaboration, its maintaining that, it’s very hard to do.
Business manager, incentive practice
Computing problems featured as organisational factors.
Some of the challenges around things like the software I think have been hard and that’s been symptomatic because we’re using a software system that has to generate, its geared up for payment system as well as a clinical and reception management, patient management system and we’re trying to alter it to continue to provide some of the data that the contract demands around UDA generation but also around capturing some of the data that we want and because we’re such a small customer, it’s hard to influence that.
Service commissioner
The only disadvantage is I think in my opinion is the software, there are so many different varieties of software around and they have not prepared themselves to be really in tune or to deliver the type of things which are needed for this pilot, for this kind of service so that is very generic dental software, dental services software. Well in my opinion, the software should have been tweaked much before implementing this contract.
Amiya, incentive dentist
Need
Evaluated and environmental need and population health indicators were manifest in the data. Two localities in the study are characterised by material deprivation, poor oral health and long-standing undersupply of care. Unsurprisingly, this influenced dental treatment needs in these areas.
It would add up to perhaps eight dental visits just for one course of treatment and that will be just to stabilise the patients. There were an awful lot of extractions that were needed. Some patients do struggle obviously with substance misuse, and smoking is quite a major factor as well . . . We still do get those new patients who come in more or less the same state who require an awful lot of dental treatment.
Jennifer, incentive dentist
Treatment needs are so high and there’s a lot of neglected mouths. Some haven’t seen a dentist in years. Some have lost the motivation to maintain their oral health because of this. So there’s a lot of preparatory work.
Donna, incentive therapist
Health behaviours
Health behaviours involve personal health practices (such as teeth brushing or sugar consumption), the process of care (e.g. the delegation of care or other dental team behaviours) or the use of health resources (such as attending or not attending appointments). Personal practices can influence oral health positively or negatively:
There’s relationship between what you eat and your teeth and your health . . . They told us about what toothpaste to use and gave us some. They told us about drinking fizzy, time of day to brush teeth. I’ve changed it a bit and drink water now.
Jennifer, incentive patient
A novel aspect of the process of care involved the assessing patient’s risk of disease. Dental team members commented on the relative imprecision of the traffic light system and its three categories. However, concerns about imprecise systems were not restricted to the risk assessments.
Patients who are amber may be very red because of their diet and because of other things so a couple of amber should make it red, not amber. The software doesn’t pick out some of the differences.
Suneeta, incentive dentist
Focusing on UDAs, the three bands I think can be an issue, some of the dentists have said they think there should be more bands obviously just lumping all restorative work, apart from that needing lab work, into band 2, it could be anything from a simple filing to a very complex molar re-root canal treatment, it does seem a bit wacky.
Business manager, incentive practice
Attitudes and practices towards prevention varied appreciably among the dental teams:
All the dentists do give advice, you know the preventative advice, to all the patients whether under the contract or not.
Suneeta, incentive dentist
I have been here 12 years and have well-established relationships with my patients. I do find it hard to talk about their health – I’m trained to drill and fill.
Ian, traditional practice dentist
The use of health resources might involve attending or not attending appointments and accessing the wider dental team such as a dental hygienist.
I went through like a stage where I didn’t go for about 3 years but that was, I went back about 5 years ago, I don’t know why I didn’t go, I just stopped going and I think then you get thrown off the register.
Alison, traditional patient
They gave me an appointment because I need a filling and when it came day before I were panicking and worrying, I just cancelled it because at end of day I’m not going through that you know tight chest and I’m not going through all that because at end of day it’s not my fault is it? Sweets I’ve had.
Ann, incentive patient
I’ve started going to this one I’ve actually seen an oral hygienist, whilst I was private dental care I was never even offered to see somebody so this is the first time I’ve actually seen one.
Holly, incentive patient
Outcomes
Evaluated or perceived health and satisfaction with care were present in the data, as was the concept of trust. A dentist noticed his patients’ improved health and patients trusted and were satisfied with their dentist, although one disliked an interval of 2 years before they could have another assessment:
I think according to recalls they have improved their brushing, they are using fluoride toothpaste more, they have started smoking less so there is general improvement in their oral health as well and their attitudes towards oral health.
Manish, incentive dentist
They’re really good. I think they’ve got more of a modern approach there whereas the other ones still a bit, I don’t know seems a bit dated.
Kat, parent of an incentive patient, patient at a traditional practice
I do trust them here – they treated me, gave me root canal treatment and saved my tooth, without them, I’d have been minus a few teeth and my appearance would not have been good.
Nanush, incentive patient
The effects of the blended/incentive-driven contract: interactions in the data
The blended/incentive-driven contract changes the finance and organisation of dental practices to implement health policy. Its effects can therefore be seen as interactions between these enabling factors and other stages in the model.
Enabling and predisposing factors and need
The incentive practices were located in areas of high need, either associated with deprivation and disease or with the poor availability of NHS care.
We’d carried out quite a robust oral health needs assessment prior to commissioning these practices and we’d looked very closely at equity in terms of access to dental care, so we’d looked for places where there was very poor oral health and also looked at areas where there was limited access to services and we wanted a combination of those. The sites of the practices therefore were chosen on oral health needs, current access to NHS care, transport systems and so on.
Service commissioner
For some participants, the incentive practices marked a shift from no dental care, whereas others moved from private to NHS provision. Participants reported the impact of the new services that suited their needs in terms of location, personnel and ease of getting an appointment. Participants referred to the difficulties they had encountered accessing a NHS dentist:
Finding an NHS dentist has been really, really difficult and that’s why I have quite strong views on that to be honest with you. We lived somewhere else and we had an NHS dentist and then when we moved, you know what it’s like and then you lose your place and then you end up on a waiting list waiting for absolutely ages. Then we heard about this one.
Jane, incentive patient
Enabling and behaviour
The effects of the new contract could be detected on the processes of care, on personal health practices and the use of personal health resources. In turn, the process of care appeared to be affected in three ways: by the use of the care pathway, by increasing the amount of prevention and the use of skill mix.
The care pathways form an important feature of the Steele report,2 the reformed NHS contract pilots18 and the blended/incentive-driven model reported here. Initial OHAs for each patient guide treatment and the frequency of recall appointments. Participants reflected on their experiences with the pathways. Benefits included the clear link between the risk assessment and care pathways.
I think some of the people were saying you know if you have a red patient there’s only limited treatment options available for that patient until they start moving from red to amber or green, whichever. And I think that was quite a contentious issue, just to leave them in the state and then wait until they got more progressed through from each stage before you can start doing treatments. But I mean the actual process makes sense in the sense that you know there’s no point carrying out such complex treatment on someone who can’t, who is failing to kind of maintain that level of oral hygiene because it can just make it worse.
Amiya, incentive dentist
The blended/incentive-driven contract formalised Department of Health guidance35 from the perspective of clinicians. As treatment plans incorporated preventative treatment, these approaches became standard procedure.
Red, amber or green and then they do get the fluoride varnish, the smoking cessation and alcohol use is being taken automatically. And then obviously depending on the age groups with the fluoride varnish, depending on the categories, while the schedule of the appointments are set then and the recalls so it’s kind of, it’s part of our contract. We don’t do anything else.
David, incentive dentist
The blended/incentive-driven contract can be contrasted directly with the traditional practices (i.e. those operating under the 2006 contract). In this case the focus of care in the incentive contract had penetrated a traditional practice, causing them to reflect on their processes of care:
We are pushed towards UDAs rather than improving oral health . . . The prevention emphasis is an issue – we are expected to talk about perio disease and smoking and diet and have to squeeze that in. We did that before under the old system and it worked to an extent, but we have to do more and more without getting paid anymore. We have to do more in less time.
Sidney, traditional practice dentist
The feeling about the incentive/blended-driven contract as an enabler of preventative approaches was echoed by clinicians in all three incentive practices. Although such systems are not specific to the incentive model and reflect long-standing guidance,35 the formalisation of such procedures under this model was valued by service providers. Practitioners felt that it gave them time and space to care for patients.
By contrast, communication of the ratings was not always apparent in the observations. Moreover, patients might not be aware of it:
Thinking back to your initial assessment as well, I don’t know if your dentist, do they use the traffic light system?
No, what’s that?
There’s nothing where they kind of rate your oral health or anything like that?
No.
Katie, incentive patient
The incentive practices were not required to use multidisciplinary teams, but the successful bidders employed business models that utilised dental hygienists and dental therapists to deliver prevention-focused care. This wider use of skill mix has been advocated by repeated policy documents but not widely implemented. 7,37,73,74 One novel approach was for dentists to examine the patients and formulate treatment plans, but the practices did not deduct the value of the delegated treatment from dentists’ incomes.
The biggest advantage as well is, is that, it’s about mind set as well, if you are working in a normal practice your dentists, your associate will be charged with using the therapist, the hygienist and so therefore your dentist is, your associate is less likely to use your therapist and hygienist because they don’t want to pay for them. Here they get it for absolutely free.
Anna, incentive practice manager
They readily work with each other. I mean our therapist and the hygienist are generally busy the whole day, which they say they don’t normally get in other practices so, and we pay them on a fixed rate and the therapists are very happy with that because they’ve got full time work, they’re busy, the associates are happy because they’re not having to pay for them . . ., the patients get benefit because they get access to a therapist, . . . it may cost more for us to do it but it’s a more sensible way of running a business because everybody is working together for the same aim.
Claire, incentive practice manager
That’s definitely an advantage obviously because there’s more appointments available now so you can see more patients.
Fiona, Dentist, incentive practice
The new contractual arrangements were seen to influence personal health practices and the use of personal health resources. Lara changed her personal routines and attended the dental hygienist.
I’ve been prescribed Duraphat® [(Thepenier Pharma Industrie, SAS, Mortange, France)] fluoride toothpaste, I use interdental brushes and see the hygienist. I take advice on board and I don’t want to get told off. So I’ve changed my routine. I didn’t know you could go to a hygienist until I came here.
Lara, incentive patient
Enabling and outcomes
The blended/incentive-driven contract also influenced outcomes of perceived and evaluated health and patient satisfaction.
They managed to sort my mouth so that I can actually smile now and feel confident about my smile, I don’t feel like it’s, or people are looking at my teeth anymore which, I mean it’s a massive improvement, it makes you confidence so much more, it makes you feel better about yourself when you know that someone is helping you sort something that you know is a big problem. You feel self-confident about it.
Shazia, incentive patient
I have been working here for 2 years plus so I can see that the patients from the deprived area, yes, I think according to recalls they have improved their brushing, they are using fluoride toothpaste more, they have started smoking less so there is general improvement in their oral health as well and their attitudes towards oral health.
Jane, incentive dentist
Generally making you feel better at going, I feel much happier going to the dentist now than I did a year ago.
Carol, incentive patient
That’s really good because I don’t know maybe the hygienists have got a bit more time and if it’s something they’re trained to do that’s fine rather than taking up the dentist time which is more specialist work. I mean I know my daughters been to see the hygienist, you know about brushing her teeth and they gave her some Duraphat cream.
Grace, incentive patient
Far-reaching effects
The interactions could ripple throughout the model to have far-reaching effects. For example, the RAG ratings could influence patients’ perceptions of their own needs, leading to personal behaviour changes and satisfaction (an outcome).
I think it’s good because if you know, if someone says to you, you know on this rating you are more at risk, you’re more likely to do something about it aren’t you, as opposed to someone not saying anything to you, you know, I think you are likely to be more active. I would be more active but I think it gives people that, again it’s about having that bit more choice and a bit more involvement in your own kind of care which I think is a good thing.
Grace, incentive patient
Using the ratings to determine recall intervals liberated more time for the process of care and allowed observation of increased health but influenced patient satisfaction both positively and negatively:
The recall intervals will be according to the risk assessments that we are doing and the risk assessment is based on their medical, their social and their clinical domains and patient to understand it and they are really happy, the majority of them 99% are very happy to have the recall intervals as dictated by their risk assessment . . . The recall intervals of 2 years and a year for the green and the amber patients so we are definitely seeing more patients and as the amber ones move towards green or the reds move towards green so we would be having more appointments for the patients to be seen.
Manish, incentive dentist
2 years seemed a long time to wait . . . I sort of think umm would I be prepared to pay a premium price and go back to private care as a result of that and that’s something that I’ll have to consider really.
Martin, incentive patient
These data suggest a need to reconcile contrasting views. From the dentist’s perspective there is the ability to see more patients and hence increase access. At its best, the incentive model seems to enable greater access because it prioritises those who need treatment and rebalances appointments around need. However, the patient was not happy with waiting 2 years for another assessment and may consider seeking alternative or additional care.
In a wholly positive example, a patient satisfied with her own care encouraged her partner to attend so that professional behaviour enhanced satisfaction to change predisposing factors to increase access to care.
. . . fantastic and the dentist themselves are really friendly. They’re really understanding, I mean for me I’m not somewhat scared of the dentist as my partner and it’s made a real improvement for my partner because he’s terrified of them so, and we’ve actually managed to get him there and he’s having work done there which is an improvement, usually trying to get him through the door of the dentist was a real effort, it took a day to get him there, get him sorted and get him home again. So I mean from that point of view they’ve just been absolutely fantastic with both him and me.
Holly, incentive patient
In summary, participants’ observations are compatible with existing knowledge of access to care, but highlight possible effects of the incentive contract (Figure 2). In particular, patients’ needs were seen to influence the siting of practices. The contract had a number of direct effects on practice orientation and costs. However, participants related these effects to better health-related behaviours on the part of patients and changes in dental practice behaviours regarding assessments, prevention, patient communication, the use of skill mix, the number of patients seen and recall intervals. In turn, these changes were related to improvements in perceived and evaluated health, patient satisfaction and trust.
FIGURE 2.
Summary of stakeholders’ perspectives on the incentive contract.

Discussion
This chapter has reported the exploration of stakeholders’ views of the new contracting arrangements. There were perceptions that the blended/incentive-driven contract increased access to dental care, with the contract determining dentists’ and patients’ perceptions of need, their behaviours, evaluated and subjective health outcomes and patient satisfaction. These outcomes were then seen to feed back to shape people’s predispositions to visit the dentist. The data hint at appreciable challenges related to a general refocusing of care and especially to perceptions about preventative dentistry and use of the risk assessments and care pathways. There are also obstacles to overcome to realise any benefits of the greater deployment of skill mix. Dentists may need support in these areas and to recognise the differences between caring for individual patients and caring for segments of the population, such as that formed by the patient base of a practice.
The impact of the contract is evident as interactions with other stages in the model. There was ample evidence of such interactions.
The ratings from OHAs were seen to influence patients’ perceptions of need, which led to changes in preventative behaviour. There was also ample evidence that dentists’ behaviours were adapting in response to the contract in the desired way with greater emphasis on prevention, use of the ratings in treatment planning, adherence to the pathways and the utilisation of skill mix. Participants identified increases in the capacity of practices to deliver more care as a result. These changes were seen to improve evaluated and perceived health and patient satisfaction. These findings are compatible with the patient and staff feedback on the first year of the NHS dental contract pilots, with almost three-quarters of patients saying they had a better understanding of their oral health and had changed their behaviour. 30 Furthermore, the Department of Health has analysed matched pairs of OHAs and oral health reviews between 2011 and 2013 that suggest improved RAG ratings for small numbers of patients, even within this relatively short time span. 20
Moreover, better health and satisfaction fed back with explicit examples in which people were more predisposed to visit the dentist. These findings demonstrate the potential for the new contract to increase access to high-quality services and to improve health and provide support for the continued use of contract reform in the forthcoming prototypes. 75 However, dentists may need support and training to maximise this potential.
Several areas of the contract were also identified as requiring more careful consideration, for which NHS England, dental teams and the public may need more support if this potential is to be realised.
The practices were placed in areas of high need, in some cases related to social deprivation, although in the case of one practice unmet need had been associated with low levels of NHS dental provision in an affluent area. As well as meeting immediate needs, the perception of low availability of care may also be a barrier to access in areas that have been underserved in the past. Evidence of new services is therefore needed to break this cycle.
The geographical location of the practices was based on addressing both unmet need and local NHS demand for dental care. The commissioning process described the blended/incentive-driven contract and asked bidders to describe their business model to deliver the contract requirements. The results demonstrate direct benefits of the needs-led service commissioning that has been in place since the inception of the 2006 dental contract and which allows for local commissioning arrangements. 7,76 The forthcoming prototypes, which represent the next stage in the evolution of the NHS dental contract reform programme,75 will lack these local flexibilities. Although these local flexibilities remain with regard to dental commissioning by the NHS Executive, they are utilised less in the current commissioning arrangements. This may be a result of commissioning using a single operating model with less local knowledge applied to practice commissioning. In addition, the new system is expected to use standardised national values for capitation and activity, with weightings based on patient characteristics of age and deprivation status. The level of these weightings will be important in influencing the commissioning of new practices in areas of high need.
Successes in prevention were prominent in the data, with participants adopting a variety of preventative professional and lay preventative behaviours leading to better evaluated and perceived health. This refocus of care had also penetrated into traditional practices, with one dentist acknowledging that they were pushed towards volume of treatment rather than improving health. However, there were concerns over offering preventative advice, the complexities of accounting for the patient’s context, the time this took and the difficulties of effective prevention, especially in areas with high levels of disease.
It is interesting that these aspects of dentistry are so often presented as problems, sometimes beyond the scope of practitioners, rather than part of their job. Unlike the challenges of, for example, a difficult restoration, some dentists regard particular aspects of preventative dentistry as beyond their remit. One dentist declared ‘I do find it hard to talk about their health – I’m trained to drill and fill’. Earlier research has indicated that some dentists regard prevention as ‘not their job’ and so there is still a case for refocusing care towards prevention. 50 This is a key issue if dentistry is to achieve the necessary change indicated in the Five Year Forward View. 77 These and other data indicate that change is possible if it is encouraged by the right contractual model. Educational interventions may also be required to support contractual drivers. Neither one alone is likely to be sufficient. A Cochrane review78 concluded that educational meetings had a small effect on professional practice and health outcomes but the effects were likely to be smaller still for complex behaviours. Both a systematic review of incentives to follow best practice in health care79 and a Cochrane review of the effect of remuneration on primary care dentists’ behaviour cited within it27 concluded that financial incentives can have a ‘modest’ effect on improving the quality of health care.
The emphasis on OHAs and pathways was a key feature of the blended/incentive-driven contract and the NHS contract pilots. 30 Some patients were not aware of the RAG ratings, whereas others perceived the ratings as alerting them to their preventative needs and as a motivator. Others perceived them to be potentially disempowering. Interested to find out how the dental teams were using the RAG ratings, we specifically enquired about them when triangulating the data in focus groups with dental staff. There was near universal use of the ratings as a decision aid (as evident in the data), but their use in patient communication was said to have decreased over time. The use of RAG ratings in communication therefore remains an opportunity that might be exploited. Dental teams will clearly benefit from clarification of if and how the ratings are supposed to be communicated to patients.
The small number of categories within the rating system was a concern among dentists, especially for patients who had risk factors such as general health problems, which would not change. Some participants erroneously attributed this to the software rather than to the purpose of the OHA. Dentists’ concerns might be alleviated by the addition of new categories. Alternatively, they may become used to this system and gain confidence in over-riding the rules of the pathway. Their reluctance to do this may stem from the requirement to justify doing so. Dentists who engaged in the NHS contract reform requested reassurance about exercising clinical judgement so that ‘there would be no medicolegal repercussions arising from deviating from software recommendations provided there was evidence of clinical justification’. 80 Respondents wanted to be reassured that ‘over-riding’ software recommendations would not subsequently be used to penalise dentists. An additional category of ‘light green’ was added to the national contract pilots for instance, but dentists may need more training in working with the pathways.
A prominent feature in the data was adherence to guidance on recall intervals. There was evidence that both dentists and patients could be unhappy with longer recall intervals, although both groups were able to adapt to it, which created more space, increasing access to other patients. One view was that the extended recall intervals were too long. A dentist in a focus group acknowledged that he tended to adopt a maximum interval of annual recall, and this view was echoed by a Local Dental Committee in the recent Dental Contract Reform Engagement Exercise: Detailed Findings. 80 The dentist in the focus group could distinguish between the stakes and the probability of missing new disease with a longer recall period but did not recognise that missed diagnosis was less likely at a time of lower disease incidence. Neither the review leading to the NICE guidance56 nor a Cochrane review on recall intervals81 could find any evidence in favour of a particular time, thus the guidance was based on assessment of the risks associated with different intervals. Although there is weight of history behind the 6-month dental check-up, its risks in terms of the chances of overdiagnosis and reducing capacity may not be visible to practitioners. Dentists may require a better understanding of these population effects to help them adapt to the new system. The World Dental Federation has proposed dental education to emphasise these types of public health perspectives. 82
To some extent these problems may reflect the difficulties of any organisational change. Furthermore, dentists may be mourning their loss of individuality and clinical freedom. Again, they may need support on the nature of working with a system based on clinical guidelines and care pathways and on how to deviate from the pathways including overcoming the medicolegal implications of doing so.
One aspect of working within a framework of care pathways involves incorporating the wishes of patients with relatively strict guidelines. Participants were able to do this and indeed one patient referred to it as ‘modern’. The task of incorporation is illuminated by the work of Timmermans,83 who described how the interventions used to resuscitate people created new identities for them. For example, the passive victim receiving cardiopulmonary resuscitation with his shirt ripped open for defibrillator pads has essentially no identity, but with luck becomes a recovering middle-aged man with modesty and personal worries about family, work and recovery. These identities are primarily defined by the ‘scripts’ or protocols of resuscitation that specify the relationships of the participants (passive victim, passer-by, rescuer, paramedic, etc.). Paramedics and patients become tightly coupled to the technology, rendering the man’s more social identities less relevant, to the point where they ‘disappear into the margin of the script’. 83
Timmermans83 describes two key categories of marginality to the script. Some people may deliberately try to set themselves aside from the script, by not wishing to be resuscitated. On the other hand, there are those people (typically already in hospital) who do not get fully enrolled into the script because the medical staff determine that they are not eligible.
Of course, dental treatment is rarely so dramatic as resuscitation, yet the script can be likened to the pathways, and from this perspective an understanding of the effects of the script are helpful. First, people may exercise a legitimate right not to engage with the pathway and may choose simply to have treatment for the relief of pain, as was recognised in the Steele report. 2 Second, as patients must be active participants in their own care, dentists must reconcile the competing needs of adhering to the script and not marginalising the wishes of their patients.
Dental team members in this research talked of the need to listen to and understand their patients, and there were clear signs that patients appreciated that. Patient satisfaction and feeling sufficiently involved in decisions about their care will be indicators of patient experience in the dental prototypes. 75 This suggests a need for dental professionals to reconcile the tensions of integrating patients’ wishes into evidence-based pathways. This would involve them acquiring a stronger understanding of evidence-based care and the communication skills to listen to and negotiate with patients.
Dental therapists increased the availability of care and patient satisfaction. However, the use of skill mix is exquisitely sensitive to contracting and practice finance. 84 Practices increased the utilisation of dental therapists by not reducing the payments to individual dentists who referred their patients to them. Although seemingly paying two staff members for the same treatments, this approach incentivised referral, thus liberating dentists’ time for patient OHAs and more remunerative complex treatments. This might be further explored and evaluated in the evaluations of the forthcoming contract prototypes. 75
The impact of funding arrangements on dental practice is well known, and dentists must reconcile the business and other elements of their practices. 85,86 Revenue was a key factor in these data. Dentists could see how the new contract carried the potential for greater value for money and the reduction of unnecessary treatment. By contrast, there were concerns that the time spent with patients and therefore the costs had been underestimated. In part these additional costs were associated with longer patient OHAs, high levels of treatment needs and the need to work more quickly to maintain activity. The time taken for the OHAs was also perceived as a problem in the NHS dental contract pilot sites and was evident in reduced patient access. 75,80 Other factors were also thought to be associated with decreases in patient access in the pilots, including initial learning curves, culture change, the new pathway approaches, information technology issues and the inability of providers to monitor access. Some of this reduction in access was also attributed to the lack of financial risk carried by the practices, which will be overcome in the forthcoming prototypes by placing up to 10% of contract value at risk if there is underdelivery.
This financial risk may be particularly relevant to new practices. The NHS dental contract pilots were conducted in existing practices and experienced falls in access. However, the challenges may be even more severe in new practices (such as the blended/incentive-driven practices included in this study), where all the patients required comprehensive initial assessments and were more likely to have high treatment needs necessitating more visits. This consideration goes further than dentists’ incomes as concerns about costs were seen to influence practitioner behaviour.
These concerns support the notion of assigning contract values according to patient needs, which in the contract prototypes will be achieved by weighting the capitation element by patient characteristics of age and deprivation status. 75
Software problems loomed large in the data as they have in the national pilots. To some extent, these observations are not specific to this blended/incentive-driven contract, but reflect the difficulties of piloting any new way of working. In this case, the software was developed for a relatively small number of practices and may have needed further development. These comments echo those in the Dental Contract Reform Engagement Exercise: Detailed Findings80 in which many participants commented on software that needed to be simpler and less ‘click-heavy’. Our participants also wanted systems and software that were easier to use, more flexible and responsive than the current ones. The software used in the national pilots was refined in response to feedback like this.
The Andersen model provided a useful taxonomy for the data and allowed identification of the effects of the new contract. This fit is unsurprising as the model was developed over a 40-year period and remains among the most widely cited models of access to health care. 64,65,67,87
Theoretical models may be tested empirically or by looking for logical coherence. 88 The Andersen model is somewhat general with overlapping dimensions (need and perceived health) and others (social capital, culture, trust and social resources) not explicitly incorporated. 67 Very little is said about the demographic variables sex, age and marital status other than the fact that a particular community might have greater proportions of older people that will affect their access to health services,87 with little detail on how this might work and why. A new factor present in these data (‘trust’) is not explicit in the model but could be regarded as both a belief and an outcome of care. 89 Dimensions also overlap in the model where dissimilar concepts are grouped together (personal health practices and health service use, perceived and evaluated health and satisfaction). This is important because empirical testing demands careful specification of inclusive relationships and to a certain extent this confounded testing of this model. 67 One consequence of this might be that the model yields very different results when cross-national comparisons are made. 90
The basic taxonomic relationships in the later versions of the model place contextual before individual characteristics (Figure 3). 87 However, the variables within the demographic characteristics (socioeconomic status, ethnicity, migrant status and educational attainment) could also be properties of individuals, so the distinction between them is not always clear. An alternative approach might be to collapse this distinction and emphasise the predisposing factors and enabling resources. Figure 4 adopts this approach and allows conceptualisation of both predisposing factors and resources as proximal, mesial and distal to individuals. 67 Adding this dimension allows qualitative distinctions between broad demographic variables that are characteristics of populations and those at individual level. It also enables us to place wider social and environmental predisposing factors such as the levels of inequality in particular societies including broader social policy into the model. 91 Predisposing characteristics can also take the form of social factors that are mesial to individuals, including social capital and individual deprivation and social support networks. 92–95
In a similar vein, collapsing the distinction between contextual and individual characteristics allows us to focus on what aspects make up enabling resources and how they impact on access to services. Health policy includes the distribution and availability of resources. Thus, one strength of the Andersen model is that it forces us to think about how social resources are configured and places their configuration and use as central to population health outcomes. In this regard it can be characterised as a model of access that focuses on the success and failure of social resources for health. 96 With respect to oral health, however, it also includes the methods and techniques for delivering optimum levels of fluoride to the whole population. This might be achieved through public programmes of water fluoridation or through consumerism.
The positioning of some variables within the causal chain might also be revised. Need is seen as a function of predisposing characteristics and enabling resources. Need here can refer to the relief of symptoms or a comprehensive service including preventative care. 90 This creates difficulties in accounting for need as its effect was masked because of its relationship to predisposing characteristics and enabling resources. 67 Likewise, outcomes may overlap with need. 67 Some measures of oral health are applied both as outcomes and as indicators of need. 97 Thus the content and meaning of need at different points in the model should be considered. Harris90 argued that consumption of health services does not always reflect need as those who might benefit most might not have access to services. 98,99
Conclusions
In conclusion, the blended/incentive-driven contract influenced access to dental care. Participants associated it with increased access, greater use of skill mix and improved health outcomes. These outcomes fed back to shape predispositions to visit the dentist.
Contractual drivers to change might be supplemented with educational efforts to support the refocusing of care, perceptions about preventative dentistry, internal practice business models on the use of skill mix, the role of evidence-based dentistry, working with care pathways, communication skills and the need for a greater understanding of the difference between caring for individual patients and a population.
The Andersen model of access was broadly sustained in the data but might be enhanced by greater conceptual clarity, by not regarding contextual and individual factors in sequence and by the incorporation of additional factors.
Chapter 4 Effectiveness of the blended/incentive-driven service delivery model
Introduction
The focus of the blended/incentive-driven contracts introduced in West Yorkshire, and evaluated in this study, lies on delivery of OHImp. Although there is a burgeoning field looking at the impact of these blended contracts on the process of care,1,100,101 there remains limited evidence on the impact of changes in dental oral health outcomes.
The work of Harris and colleagues100,101 and McDonald and colleagues1 provides valuable insights into the processes by which dental teams provide treatment, but evidence is needed on the health outcomes of different ways of incentivising appropriate oral health care. Sequential systematic reviews (e.g. for the Department of Health Clinical Effectiveness and Outcomes group) have found no studies that relate methods to implement best practice on oral health outcomes. Yet such evidence is much needed to support the requirements of all recent NHS strategy documents. 34,102 Indeed, Equity and Excellence: Liberating the NHS34 focuses on improving health-care outcomes so that ‘The NHS will be held to account against clinically credible and evidence-based outcome measures, not process targets’.
One reason that other researchers may have focused on processes is because the selection of outcomes for oral health care is difficult for both theoretical and practical reasons. This study attempts to overcome these difficulties by using a series of complementary clinical measures and PROMs, which are linked by a robust and validated theoretical model.
Aim
The aim of this part of the study was to assess the effectiveness of the incentive model in reducing the risk and amount of dental disease and OHQoL in patients.
In order to assess the clinical effectiveness of the incentive model, a non-randomised study within the project compares the effectiveness of treatment in the three blended/incentive-driven dental practices with that of three existing (traditional) practices working under the nGDS contract. The traditional practices have been matched by deprivation index, age profile, size of practice, ethnicity and taking on new patients. In addition, the evaluation assesses the new risk assessment model for fitness for purpose.
The effectiveness of the new model is assessed using indicators of gingivitis and an OHQoL measure, the OHIP-14. Data are collected from patients on each of these indicators at their first visits (baseline) and then 24 months later (follow-up). A nested exploratory study assessed the dental caries experience in which enamel and dentinal caries and their treatment was recorded using the International Caries Detection and Assessment System (ICDAS) coding.
Rationale for choice of outcome measures
Wilson and Cleary103 link clinical variables to symptoms and functional limitation (analogous to health-related quality of life). Their model is directly applicable to oral health. 104,105 Changes to clinical factors (tooth decay and periodontal diseases) cause symptoms which lead to variations in OHQoL. However, individual and environmental factors intervene in these relationships by exerting independent effects. For example, the ability to understand one’s situation strongly predicted OHQoL. 105 Studying both clinical and OHQoL outcomes provides the potential not only to identify health benefits, but also to elucidate how the blended/incentive-driven contract might deliver those benefits.
Any clinical measures to assess differences in clinical status between groups must be valid, reproducible and responsive over a relatively short period of time to changes brought about by preventative treatments or improved oral health behaviours. The care pathways in this study are for up to 2 years. We therefore matched our outcome measures onto this time frame, using measures which are capable of demonstrating changes in dental and gingival health within a number of months rather than years. The health outcomes selected for this study were gingivitis (bleeding on probing, BoP), dental caries experience, oral symptoms and OHQoL.
Gingivitis was selected as the primary outcome because it affects over 90% of the population and is readily measured in a clinical examination, summarises the participant’s personal oral hygiene behaviour over the preceding days, is responsive to interventions (such as oral hygiene advice or using a new toothbrush) within 2 weeks, is a proxy for other self-care behaviours (such as the use of fluoride toothpaste), is an interim outcome for periodontitis (which is a significant public health problem)106–109 and changes are readily demonstrated over a period of 2 years. Gingivitis was recorded as the proportion of sites with BoP at baseline and at the 24 months’ follow-up.
Other periodontal outcomes were not suitable for use in this study. For example, periodontal attachment loss occurs so slowly that changes cannot be reliably detected within 2 years. 108,110 The basic periodontal examination records the worst periodontal condition in each of the six sextants of the mouth. However, this measure (and the Community Periodontal Index of Treatment Needs, its precursor) is not sufficiently precise for use in evaluative research, is not responsive to treatment of severe disease and there is the added complexity that changes in one part of a sextant can be masked by changes in other parts of the same sextant. 111
Assessment of gingivitis by way of BoP was supported by process outcome data from the incentive practices taken from the RAG system. As described in Chapter 2, the blended/incentive-driven contract was designed to encourage a care pathway approach in which all patients have an OHA on joining the practice and at each subsequent recall. Four sets of information [age group, medical history, social history (self-care, habits/diet) and clinical assessment] are used to inform a traffic light (RAG) system for patients with high (red), medium (amber) or low (green) risk of oral disease.
Secondary outcomes included assessment of dental caries experience in which enamel and dentinal caries and their treatment were recorded. In order to do this in a standardised way, the ICDAS was used to chart the number and condition of all teeth present with regard to their caries status and treatment history at baseline and follow-up. The inclusion of enamel caries allows recording of early carious lesions that may develop and heal as a result of changes in behaviour and the application of fluoride. 112–114 Although the work of Chesters and colleagues112 suggests that changes in dental caries status can readily be measured within an abbreviated (24-month) clinical trial design by including enamel caries, the measure was included as an exploratory element of the research as little is known about the prevalence and behaviour of enamel lesions in the UK population of adults attending general dental practices. However, this is an important measure in terms of OHImp and the findings of this study will help to inform future research and the suitability of enamel caries as an outcome measure in clinical dental practice. Training was provided to all practices on the use of the ICDAS following the 2009 Adult Dental Survey criteria. 114 This was supplemented with training via e-learning.
Oral health-related quality of life was recorded using the OHIP-14. 115,116 The OHIP-14 has good reliability, content and discriminative validity for use in UK dental patients117 and is responsive to the changes brought about by general dental treatments, periodontal treatment and the provision of dentures. 118–120
Methods
Design and setting
The study uses a non-randomised comparative study design. The three incentive practices were matched with three existing (traditional) practices working under the nGDS contract in West Yorkshire. The matching at practice level considered the practice in terms of deprivation index, age profile, size of practice, ethnicity profile and taking on new patients. Details of the practices are reported in Chapter 3. Patient demographics across the six practices are summarised in Table 6.
| Characteristics | Incentive practices | Traditional practices | ||||
|---|---|---|---|---|---|---|
| Blended contract: UDA and incentives for health promotion/prevention activity | Working to 2006 NHS dental contract (nGDS contract) | |||||
| Practice | Practice 3 | Practice 2 | Practice 1 | Practice 6 | Practice 5 | Practice 4 |
| Age (years) | 47.60 (17.55) | 40.30 (13.16) | 34.64 (12.08) | 40.78 (16.05) | 38.48 (13.99) | 40.99 (15.29) |
| Sex: male/female | 19/21 (47.50/52.50) | 77/75a (47.83/46.58) | 36/40 (47.37/52.63) | 15/22 (40.54/59.46) | 49/42 (53.85/46.15) | 61/55a (49.19/44.35) |
| Ethnicity: white/other | 37/3 (92.50/7.50) | 105/51a (65.22/31.68) | 49/27 (64.47/35.53) | 35/2 (94.59/5.41) | 59/32 (64.83/35.16) | 59/17a (47.58/13.71) |
| Recruitment, n | 40 | 161 | 76 | 37 | 91 | 124 |
| Loss to follow-up, n (%) | 14 (35.00) | 79 (49.07) | 56 (73.68) | 21 (56.76) | 35 (38.46) | 54 (43.55) |
From Table 6 we can see that the ethnicity balance in the 3 and 6 pairing differs from the other pairings in as much as the proportion of those who classify themselves ‘white’ is much higher than the other pairings (≈ 90/10 in 3 and 6 compared with ≈ 65/35 in 1 and 4 and in 2 and 5). The loss to follow-up differs across practices; the lowest is 35% in practice 3 and the highest 74% in practice 1. Differences in recruitment between practices are expected and reflect the number of GDPs/size of the practices.
Sample
Sample size was estimated based on powering the primary outcome measure. Based on data from the Clarkson and colleagues’ study,121 we estimated the standard deviation (SD) in percentage sites BoP across a UK cohort to be 27.5%. We assumed a within-patient correlation in baseline to follow percentage sites BoP of 0.5 and a common variance in incentive and traditional practices. We assumed a clinically meaningful mean difference in percentage sites BoP baseline to follow-up in incentive practices of 10%, versus a mean difference in percentage sites BoP baseline to follow-up in traditional practices of 0%. We fixed a type I error rate of 0.05 and a power of 0.8. A design effect was included to account for clustering of patients within the three incentive and three traditional practices, assuming an intracluster correlation of 0.2. A two-sided two independent samples t-test identified a total of 550 patients to be recruited (allowing for a 10% loss to follow-up).
Recruitment and inclusion and exclusion criteria
To achieve a recruitment of 550 new patients in the study project, recruitment was initially planned to take place over a 6-month period, although this was subsequently increased to 8 months. This figure was based on (1) six dental practices included in the study; (2) an average list size of 1000 adult patients per dentist; (3) 10% of patients per year will be new patients to the practice (estimated from the dental public health audit figures of practices in Bradford and Airedale); and (4) of these patients we estimated a minimum of 50% would agree to participate in the study over the recruitment period. Thus, at a practice level, the three incentive practices were matched with three existing traditional practices of similar size, deprivation index, age profile, ethnicity profile and taking on new patients.
At the patient level, the inclusion criteria were that patients must be:
-
aged ≥ 16 years (all the patient information leaflets were reviewed by a teenager as suitable to be easily understood for use with a broad age group in the study)
-
willing to be followed up for 24 months and give informed consent
-
a new patient to the dental practice
-
able to complete the patient-completed questionnaires.
If a translator was needed, the availability of provision of a translation service in the spoken language of the participant was via the normal dental practice access routes to such services. Study materials were not translated as the dental practices reported that those accessing the translator services are typically not literate in their mother language. Given that questionnaires were to be completed only at baseline and at 24 months, after taking advice, we concluded that the provision of a translator was sufficient, and indeed the best option to maximise inclusion. All other data collected on the participants were from routinely collected data and were not affected by the language of the participant.
With regard to exclusion criteria, and the specific handling of those who are edentulous, edentulous patients were not excluded from the sample. However, they would be considered supplementary to the core sample of 550 patients and would provide additional specific data. Postcode, age and ethnicity of all patients included within the sample were recorded and profiled during the analysis.
The practices purposefully opened their lists to recruit new patients for our study. All new patients attending the practice for the first time were invited to participate. Prior to their scheduled appointment they were sent a letter of invitation and an information sheet and provided informed consent to be part of the study. Informed consent was taken by members of the dental surgery staff who received training in taking informed consent. Patients were asked to complete the following questionnaires at their first visits and at the follow-up visit 24 months later: the European Quality of Life-5 Dimensions questionnaire, 3-level version (EQ-5D-3L; details of the EQ-5D-3L are presented in Chapter 5, Methods and Results) and the OHIP-14. The dentist undertook the clinical assessment of teeth and gingivae using the ICDAS and BoP at both visits. Family/social history was taken at the first visit only. The OHA, using the RAG system, was completed at baseline and 24 months by the incentive practices.
Patients were contacted by the dental practice around 6–8 weeks prior to their 24-month follow-up date to arrange an appointment. Contact assumed a variety of media, including telephone, short message service (SMS) and letter, in order to optimise follow-up. Patients were contacted a minimum of three times to arrange the appointment.
Ethics approval and archiving
Ethics approval was obtained from the NRES Committee (London – Bromley, REC reference 12/LO/0205) on 5 April 2012. The study was sponsored by the University of Leeds, Leeds, UK. At the end of the study, data will be securely archived in line with the University of Leeds’ procedures for a minimum of 6 years. Data held by the research teams will be locally archived or as instructed by the University of Leeds where it is typically stored in the university’s archive facility and site data and documents. Following authorisation from the sponsor, arrangements for confidential destruction will then be made.
Intervention
Details of the blended/incentive-driven contracts for the incentive practices are described in detail in Chapter 2. In brief, within the incentive practices, the blended/incentive-driven contracts were aimed at ensuring evidence-based preventative interventions are delivered in line with identified needs for a defined population; increased access to dentistry; and that care is provided by the most appropriate team member to encourage skill mix. Within the contracts, 60% of the contract value is apportioned to delivery of a set number of UDAs. The remaining 40% is dependent on the delivery of quality: 20% systems, processes and infrastructure [e.g. cross-infection, policies, Standards for Better Health (latterly becoming Care Quality Commission domains)] and 20% OHImp.
The traditional practices operated under the nGDS contracts which are based on payment for UDAs with the number of UDAs based on historic activity and agreed between PCTs and dental practices. The nGDS contracts meant that the payment mechanism changed from a one-off fee per item of service to a system whereby providers are paid an annual sum in return for delivering an agreed number of ‘courses of treatment’ weighted for complexity.
Main outcome measures
The primary outcome of the clinical effectiveness study was the percentage of points from BoP, assuming 32 teeth per patient and 6 points per tooth, reduced by the number of missing teeth (ICDAS codes ‘97’, ‘98’, ‘99’ or ‘P’) that a patient has.
The secondary outcomes were:
-
Percentage of sound surfaces (defined as free of obvious caries, if any of the following ICDAS codes ‘00’, ‘01’, ‘02’, ‘10’, ‘11’, ‘12’, ‘20’, ‘21’ or ‘22’ are recorded), assuming 32 teeth per patient and five surfaces per tooth (reduced by the number of missing teeth a patient has).
-
Percentage of extracted and filled teeth, assuming 32 teeth per patient (reduced by the number of missing teeth a patient already has). A tooth was defined as filled if the first digit of the ICDAS code was ‘3’, ‘4’, ‘5’, ‘6’, ‘7’ or ‘8’ and the second digit of the ICDAS code was not ‘4’, ‘5’ or ‘6’. A tooth was defined as extracted if the ICDAS code was ‘97’.
-
OHIP-14 total score (integer count between 0 and 56). Each of the 14 individual questions is scored on a 0–4 scale. Any scores outside of this range are regarded as missing. If one or two of the individual questions are missing, then median imputation is used to impute the individual question scores. 122 If three or more individual questions are missing, then the total score is regarded as missing and the patient excluded from analysis.
Exploratory analyses of the RAG system were conducted to study the:
-
distributions across categories (RAG) at baseline and follow-up
-
transitions between categories from baseline to follow-up
-
proportion of risk assessments that were manually over-ridden at baseline and follow-up.
Analysis
Multiple linear regression123 is used to model the primary and secondary outcome measures. In our analysis plan we identified the difference in the measurement from baseline to follow-up as the outcome. However, given the reduced sample size because of loss to follow-up, to improve power, we used an analysis of covariance (ANCOVA) approach with follow-up measurement as the outcome and baseline measurement as a covariate. An important requirement for ANCOVA is that there must be no interaction between the groups and baseline measure. 124 Although it is plausible to assume no interaction within each incentive–traditional practice-matched pair, it is not clear if an interaction will be present across the three matched pairs. For this reason we first analyse the matched pairs separately before combining in a single analysis. Because of the reduced sample size and staff turnover, we have not been able to include practitioner-level variables in our analyses. Imputation was conducted when constructing the OHIP-14 total score as described above.
Results
Sample
Recruitment started on 1 June 2012 and the first patient entered the study on 14 June 2012. Recruitment finished on 31 January 2013. In total 550 participants were recruited to the study at baseline. However, only 291 participants attended both baseline and a follow-up appointment at 24 months. The reasons for non-attendance at the 24-month follow-up were recorded by the dental practices and are grouped as follows.
-
Patient non-response: patient did not respond to any letters, text messages (SMS) or voicemails.
-
Patient failed to attend: patient failed to attend or cancelled the appointment(s) at the last minute (i.e. ≤ 24 hours’ notice).
-
Change in patient status: patient moved away or was unable to attend because of financial difficulties or cancelled the appointment as a result of health reasons (e.g. a recent operation) or changed practice.
-
Practice decision: de-registered patients or cases in which the practice cancelled the appointment because of severe weather conditions.
-
Practice error: dentist failed to do the follow-up study/assessment.
We should note that for some de-registered patients in the ‘practice decision’ category, no further reason was provided. For others in the same group, the practice de-registered the patient for a variety of reasons that included failure to attend multiple appointments and the patient consecutively cancelling appointments. In addition, this category included de-registration because the patient had moved away. This last reason overlaps with the change in patient status category and, as such, the interpretation of these categories should be treated with caution.
Reasons for no follow-up at 24 months were available for 120 of the patients who did not attend the follow-up. From the answers provided, 27 patients were from the traditional practices and 93 patients were from the incentive practices. As shown in Figure 5, ‘patient non-response’ in both incentive and traditional practices is the most frequent reason for not completing the study (45% and 59%, respectively). In the traditional practices, one patient (4%) did not complete the follow-up because ‘patient failed to attend’, but this number was much higher in the incentive practices – 29% (27 patients). ‘Practice decision’ or ‘centre error’ are not reported in the traditional practices and even for the incentive practices the percentages are very low (4% and 9%, respectively).
FIGURE 5.
Reasons for no follow-up. (a) Incentive practice; and (b) traditional practice.
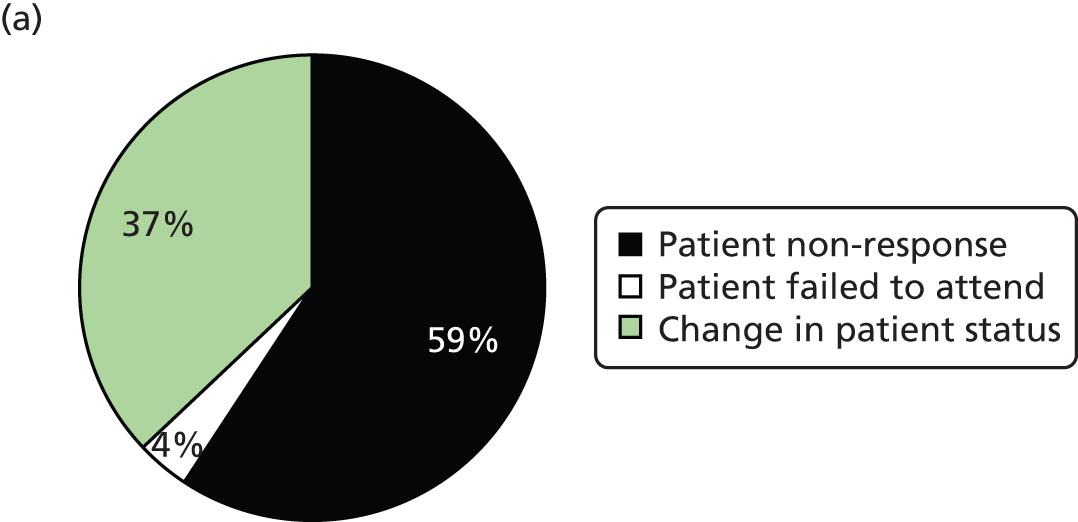
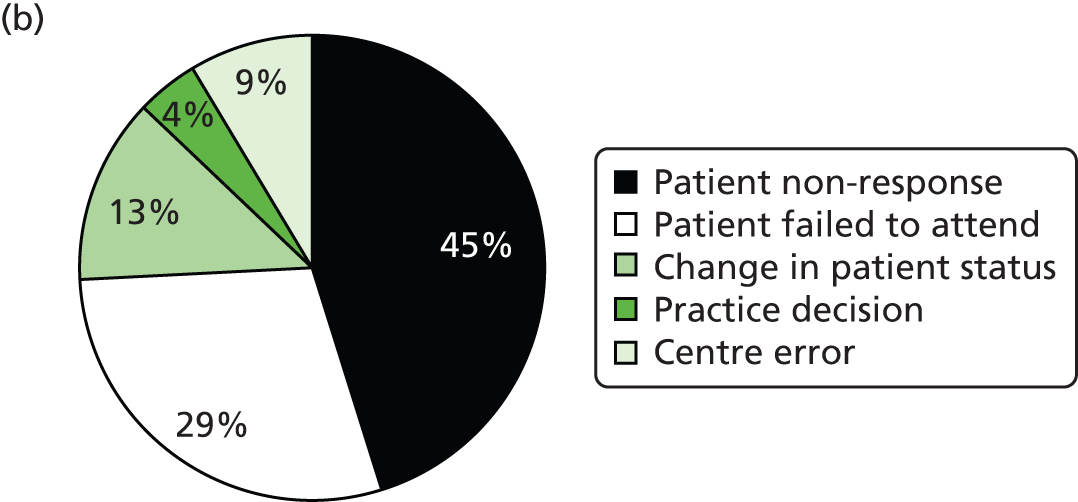
Of the 550 recruited, a BoP was measure at baseline in 529. A total of 291 participants attended both baseline and follow-up, BoP was measured at both time periods in only 270 (51.04% of those with a BoP measurement at baseline). Following quality assurance, 188 were included in the BoP analysis (incentive, n = 90; traditional practice, n = 98). Full details of the sample number available for analyses for each measure are included in Table 7.
| Measure | Incentive practices | Traditional practices | ||||||
|---|---|---|---|---|---|---|---|---|
| Blended contract: UDA and incentives for health promotion/prevention activity | Working to 2006 NHS dental contract (nGDS contract) | |||||||
| Practice | Practice 3 | Practice 2 | Practice 1 | Total | Practice 6 | Practice 5 | Practice 4 | Total |
| Recruitment, n | 40 | 161 | 76 | 277 | 37 | 91 | 124 | 252 |
| Loss to follow-up, n (%) | 14 (35.00) | 79 (49.07) | 56 (73.68) | 149 (53.79) | 21 (56.76) | 35 (38.46) | 54 (43.55) | 110 (43.65) |
| Available for scrutiny, n (%) | 26 (65.00) | 82 (50.93) | 20 (26.32) | 128 (46.21) | 16 (43.24) | 56 (61.54) | 70 (56.45) | 142 (56.35) |
| Loss to quality control: BoP, n (%) | 3 (7.50) | 29 (18.01) | 6 (7.89) | 38 (13.72) | 6 (16.21) | 16 (17.58) | 22 (17.74) | 44 (17.46) |
| Available for analysis: BoP, n (%) | 23 (57.50) | 53 (32.92) | 14 (18.43) | 90 (32.49) | 10 (27.03) | 40 (43.96) | 48 (38.71) | 98 (38.89) |
| Loss to quality control: SS, n (%) | 3 (7.50) | 28 (17.39) | 5 (6.58) | 36 (13.00) | 8 (21.62) | 16 (17.58) | 23 (18.55) | 47 (18.65) |
| Available for analysis: SS, n (%) | 23 (57.50) | 54 (33.54) | 15 (19.74) | 92 (33.21) | 8 (21.62) | 40 (43.96) | 47 (37.90) | 95 (37.70) |
| Loss to quality control: E&F, n (%) | 3 (7.50) | 28 (17.39) | 5 (6.58) | 36 (13.00) | 6 (16.21) | 15 (16.48) | 22 (17.74) | 43 (17.06) |
| Available for analysis: E&F, n (%) | 23 (57.50) | 54 (33.54) | 15 (19.74) | 92 (33.21) | 10 (27.03) | 41 (45.06) | 48 (38.71) | 99 (39.29) |
| Loss to quality control: OHIP-14, n (%) | 4 (10.00) | 32 (19.88) | 8 (10.53) | 15 (5.42) | 6 (16.21) | 20 (21.98) | 24 (19.35) | 50 (19.84) |
| Available for analysis: OHIP-14, n (%) | 22 (55.00) | 50 (31.05) | 12 (15.79) | 84 (30.32) | 10 (27.03) | 36 (39.56) | 46 (37.10) | 92 (36.51) |
Demographic and baseline outcome measures split by status (completed follow-up/loss to follow-up) are shown in Table 8. Outcomes data were manually reviewed and quality controlled by a clinician prior to the modelling reported in Table 9 and onwards. Patients with implausible data were excluded from modelling. This manual review was conducted only for those with completed follow-up, to enable comparison with those lost to follow-up. Table 8 uses outcomes data prior to this manual review and quality control process.
| Characteristics | Incentive practices | Traditional practices | ||||
|---|---|---|---|---|---|---|
| Practice 3 | Practice 2 | Practice 1 | Practice 6 | Practice 5 | Practice 4 | |
| n | 26 vs. 14 | 82 vs. 79 | 20 vs. 56 | 16 vs. 21 | 56 vs. 35 | 70 vs. 54 |
| Age (years) | 47.11 vs. 48.50 (17.58 vs. 18.12) | 41.18 vs. 39.38 (13.51 vs. 12.81) | 35.25 vs. 34.43 (14.27 vs. 11.33) | 42.50 vs. 39.48 (16.85 vs. 15.70) | 39.05 vs. 37.57 (14.47 vs. 13.33) | 44.13 vs. 36.93 (16.34 vs. 12.85) |
| Sex: male/female | 12/14 vs. 7/7 (46.15/53.84 vs. 50.00/50.00) | 37/38a vs. 40/37a (45.12/46.34 vs. 50.63/46.83) | 7/13 vs. 29/27 (35.00/65.00 vs. 51.78/48.21) | 7/9 vs. 8/13 (43.75/56.25 vs. 38.10/61.90) | 30/26 vs. 19/16 (53.57/46.43 vs. 54.29/45.71) | 30/37a vs. 31/18a (42.86/52.86 vs. 57.41/33.33) |
| Ethnicity: white/other | 24/2 vs. 13/1 (92.31/7.69 vs. 92.86/7.14) | 49/28a vs. 56/23 (59.76/34.15 vs. 70.89/29.11) | 15/5 vs. 34/22 (75.00/25.00 vs. 60.71/39.29) | 15/1 vs. 20/1 (93.75/6.25 vs. 95.24/4.76) | 40/16 vs. 19/16 (71.43/28.57 vs. 54.29/45.71) | 37/9a vs. 22/8a (52.86/12.86 vs. 40.74/14.81 |
| BoP (%) | 26.04 vs. 32.40 (20.17 vs. 18.98) | 25.09 vs. 34.39 (27.42 vs. 48.52) | 6.19 vs. 7.67 (5.79 vs. 8.18) | 22.39 vs. 32.07 (12.21 vs. 21.10) | 27.23 vs. 38.28 (23.48 vs. 36.49) | 30.66 vs. 40.56 (38.56 vs. 42.38) |
| Sound surfaces (%) | 84.44 vs. 77.60 (9.18 vs. 15.66) | 81.29 vs. 75.04 (17.13 vs. 22.78) | 77.92 vs. 85.75 (16.85 vs. 9.10) | 80.76 vs. 73.94 (17.45 vs. 13.36) | 83.06 vs. 80.21 (20.54 vs. 15.52) | 77.84 vs. 78.38 (16.86 vs. 18.71) |
| E&F (%) | 32.63 vs. 33.19 (25.56 vs. 16.80) | 39.39 vs. 44.13 (31.96 vs. 31.34) | 32.36 vs. 34.87 (23.74 vs. 29.48) | 47.41 vs. 56.01 (31.08 vs. 30.64) | 33.97 vs. 51.26 (33.11 vs. 37.11) | 44.96 vs. 39.67 (34.16 vs. 31.80) |
| OHIP-14 total score (points) | 2.50 vs. 5.79 (3.86 vs. 5.77) | 12.08 vs. 15.30 (11.11 vs. 13.67) | 12.89 vs. 11.47 (14.64 vs. 9.33) | 13.19 vs. 10.38 (14.01 vs. 13.49) | 10.43 vs. 18.69 (11.75 vs. 13.32) | 7.20 vs. 10.30 (8.74 vs. 10.23) |
| Risk assessment (RAG): red/amber/green | 8/14/4 vs. 7/5/2 (30.77/53.85/15.38 vs. 50.00/35.71/14.29) | 64/13/5 vs. 66/11/2 (78.05/15.85/6.10 vs. 83.54/13.92/2.53) | 15/5/0 vs. 44/11/0a (75.00/25.00/0.00 vs. 80.00/20.00/0.00) | |||
Those who are lost to follow-up are generally younger and more likely to be male. In terms of outcomes, those lost to follow-up have worse oral health, although this is more variable (a higher mean and SD). This was reflected in the OHIP-14 score, with those lost to follow-up having higher mean scores (indicating poorer OHQoL). In the practices that undertook a RAG rating, those lost to follow-up were more likely to have a red rating.
Bleeding on probing
Figure 6 shows a scatterplot of BoP at baseline and follow-up. The mean (SD) BoP at baseline and follow-up was 41.88 (SD 47.24) and 32.97 (SD 47.66), respectively. Eighty-two patients excluded were following manual review for quality control in addition to those lost to follow-up (see Table 7). This comprised 3, 29, 6, 6, 16 and 22 patients for practices 3, 2, 1, 6, 5 and 4, respectively. In addition, four patients with BoP in excess of 100% had BoP imputed to 100%. This gave a sample for analyses of n = 188 (n = 90, incentive practices; n = 98, traditional practices).
FIGURE 6.
Scatterplot of BoP by practice.
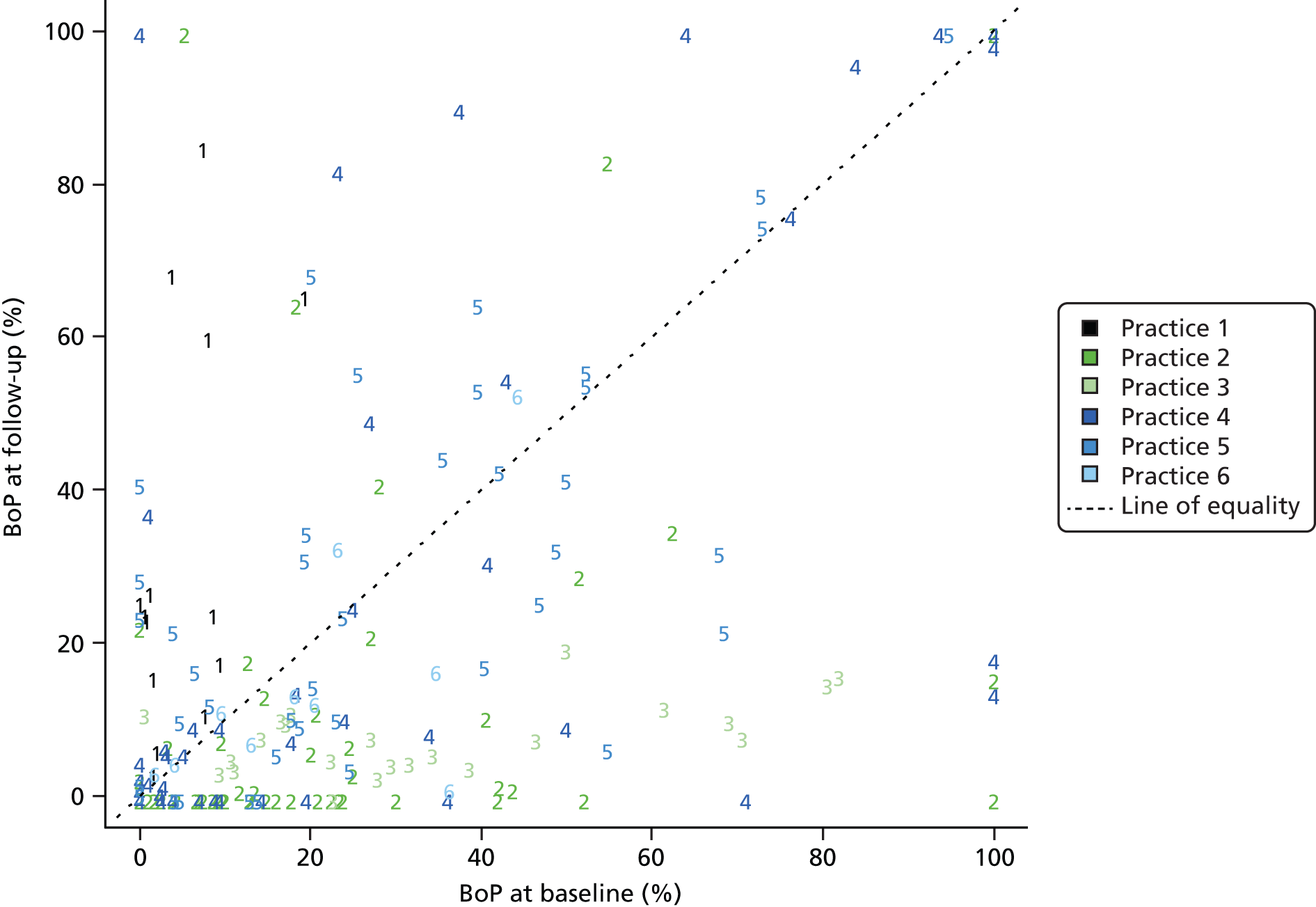
First we analysed the matched pairs separately using a baseline-adjusted ANCOVA. Table 9 relates to matched pair 1 and 4, Table 10 to matched pair 2 and 5 and Table 11 to matched pair 3 and 6.
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 29.04 | 7.50 | 14.04 to 44.04 | < 0.01 |
| Baseline | 0.71 | 0.18 | 0.47 to 0.94 | < 0.01 |
| Practice: traditional | –22.55 | 8.93 | –40.41 to –4.69 | 0.01 |
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 0.38 | 3.59 | –6.76 to 7.53 | 0.92 |
| Baseline | 0.49 | 0.09 | 0.31 to 0.67 | < 0.01 |
| Practice: traditional | 14.57 | 4.54 | 5.55 to 23.59 | < 0.01 |
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 2.10 | 3.10 | –4.24 to 8.43 | 0.50 |
| Baseline | 0.17 | 0.07 | 0.03 to 0.32 | 0.02 |
| Practice: traditional | 9.98 | 3.47 | 2.90 to 17.06 | < 0.01 |
The model in Table 9 implies that BoP was lower at follow-up for patients in traditional practice 4 (than in incentive practice 1) by an average of 22.55% [95% confidence interval (CI) 4.69% to 40.41%; p = 0.01].
The model in Table 10 implies that BoP was higher at follow-up for patients in traditional practice 5 (than in incentive practice 2) by an average of 14.57% (95% CI 5.55% to 23.59%; p < 0.01).
The model in Table 11 implies that BoP was higher at follow-up for patients in traditional practice 6 (than in incentive practice 3) by an average of 9.98% (95% CI 2.90% to 17.06%; p < 0.01).
Scatterplots of BoP at baseline and follow-up are shown for the matched pairs in Figure 7. Lines of best fit from the models described in Tables 9–11 are superimposed.
FIGURE 7.
Scatterplots of BoP by incentive vs. traditional practice. (a) Matched pair 1 and 4; (b) matched pair 2 and 5; and (c) matched pair 3 and 6.
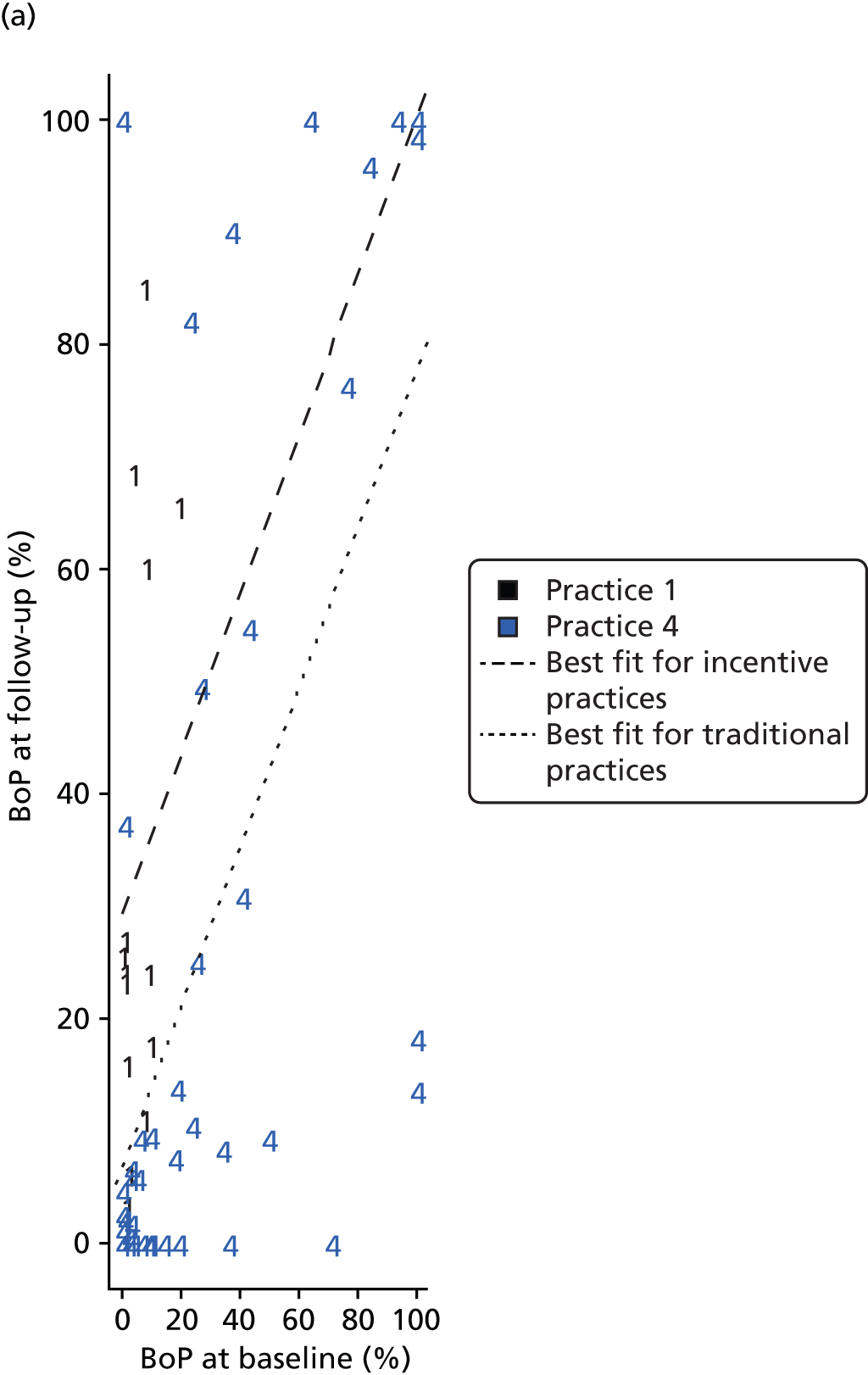
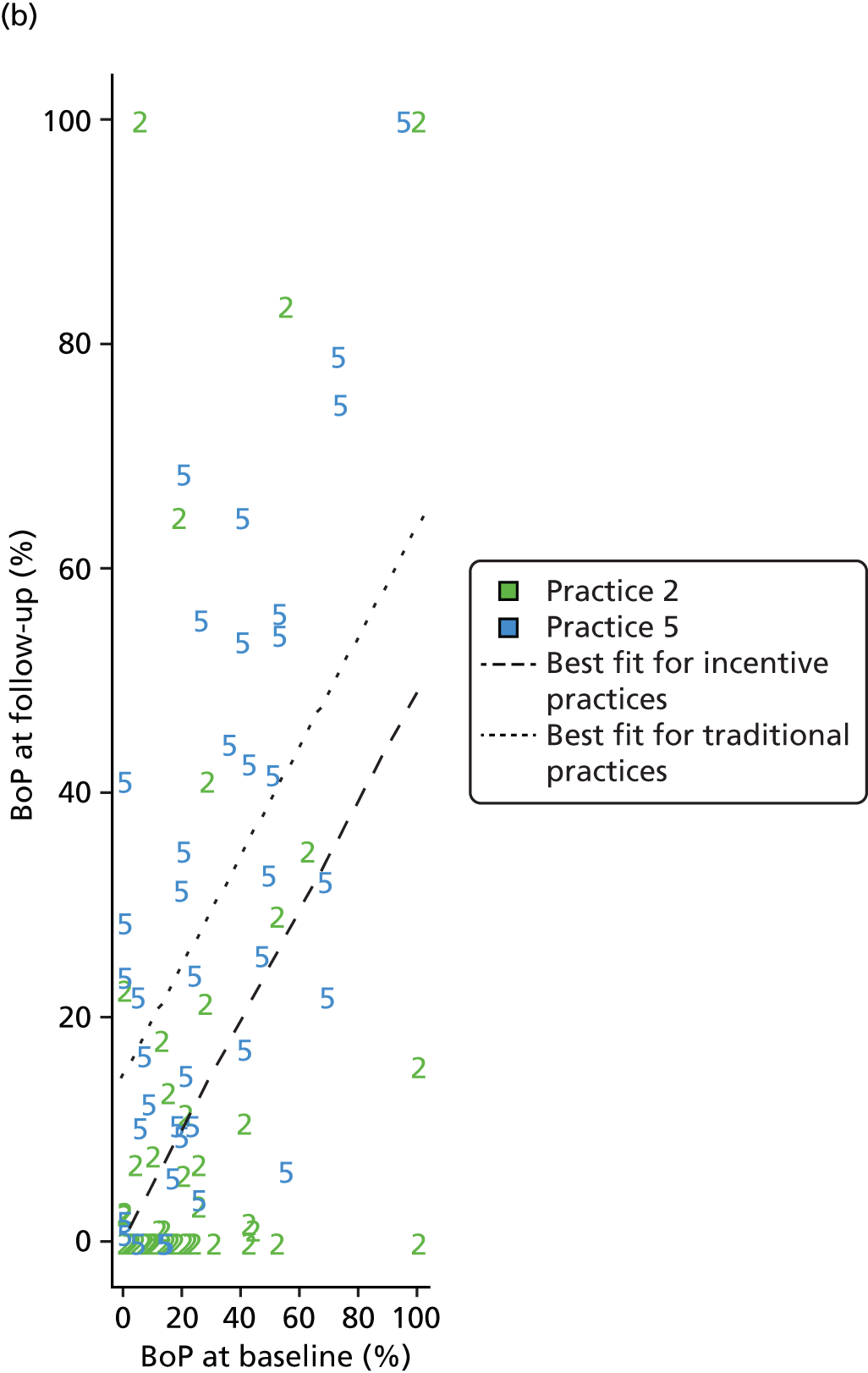
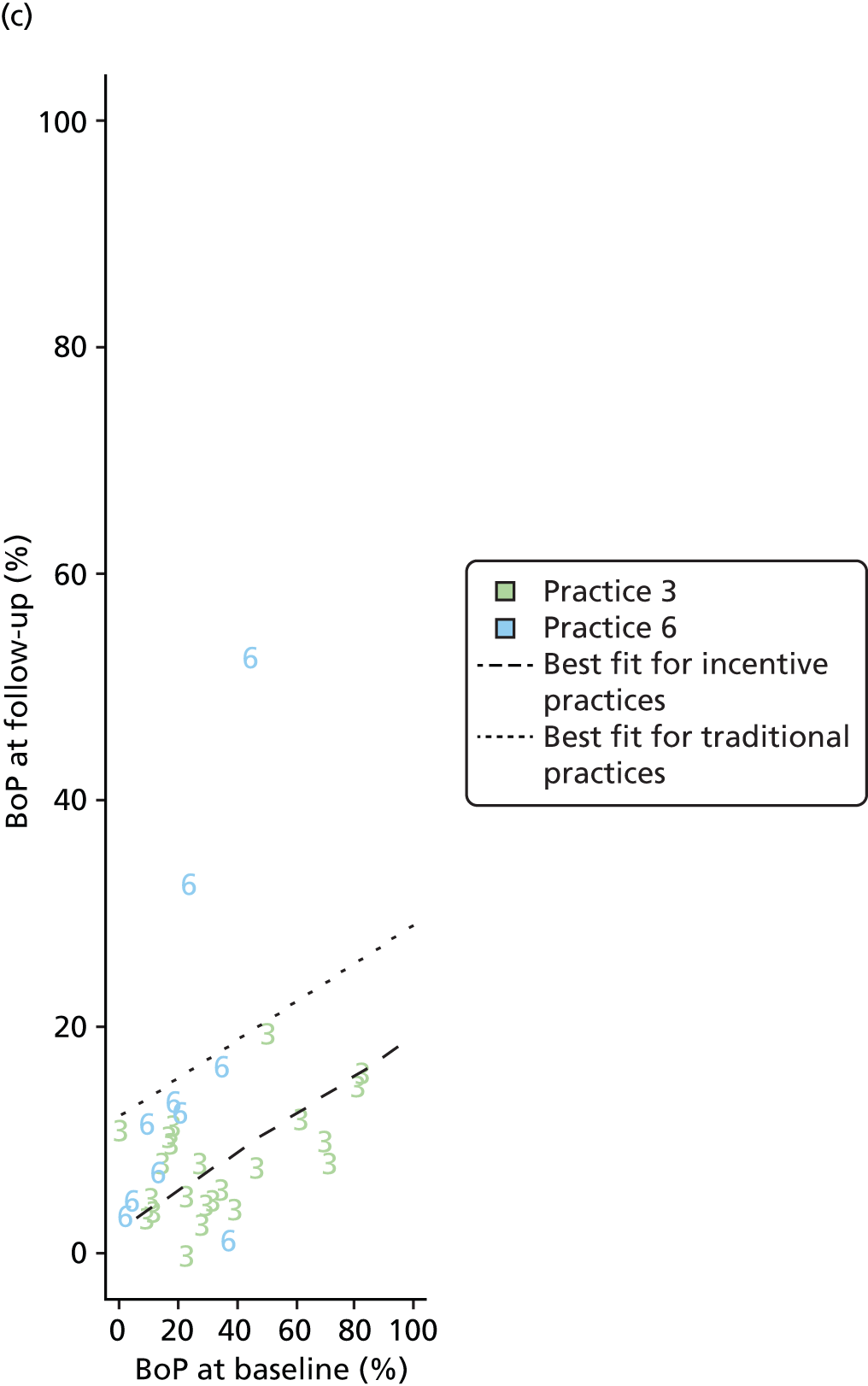
Combining the matched pairs into a single ANCOVA model produces the output shown in Table 12. This should be interpreted with caution because of the difference between the matched pairs observed in the analyses.
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 2.95 | 2.97 | –2.90 to 8.80 | 0.32 |
| Baseline | 0.48 | 0.07 | 0.35 to 0.60 | < 0.01 |
| Practice: traditional | 10.24 | 3.55 | 3.23 to 17.25 | < 0.01 |
The model in Table 12 implies that BoP was higher at follow-up for patients in traditional practices (than in incentive practices) by an average of 10.24% (95% CI 3.23% to 17.25%; p < 0.01).
A scatterplot of BoP at baseline and follow-up is shown across all the matched pairs in Figure 8. Lines of best fit from the model described in Table 12 are superimposed.
FIGURE 8.
Scatterplot of BoP by incentive vs. traditional practice across all matched pairs.
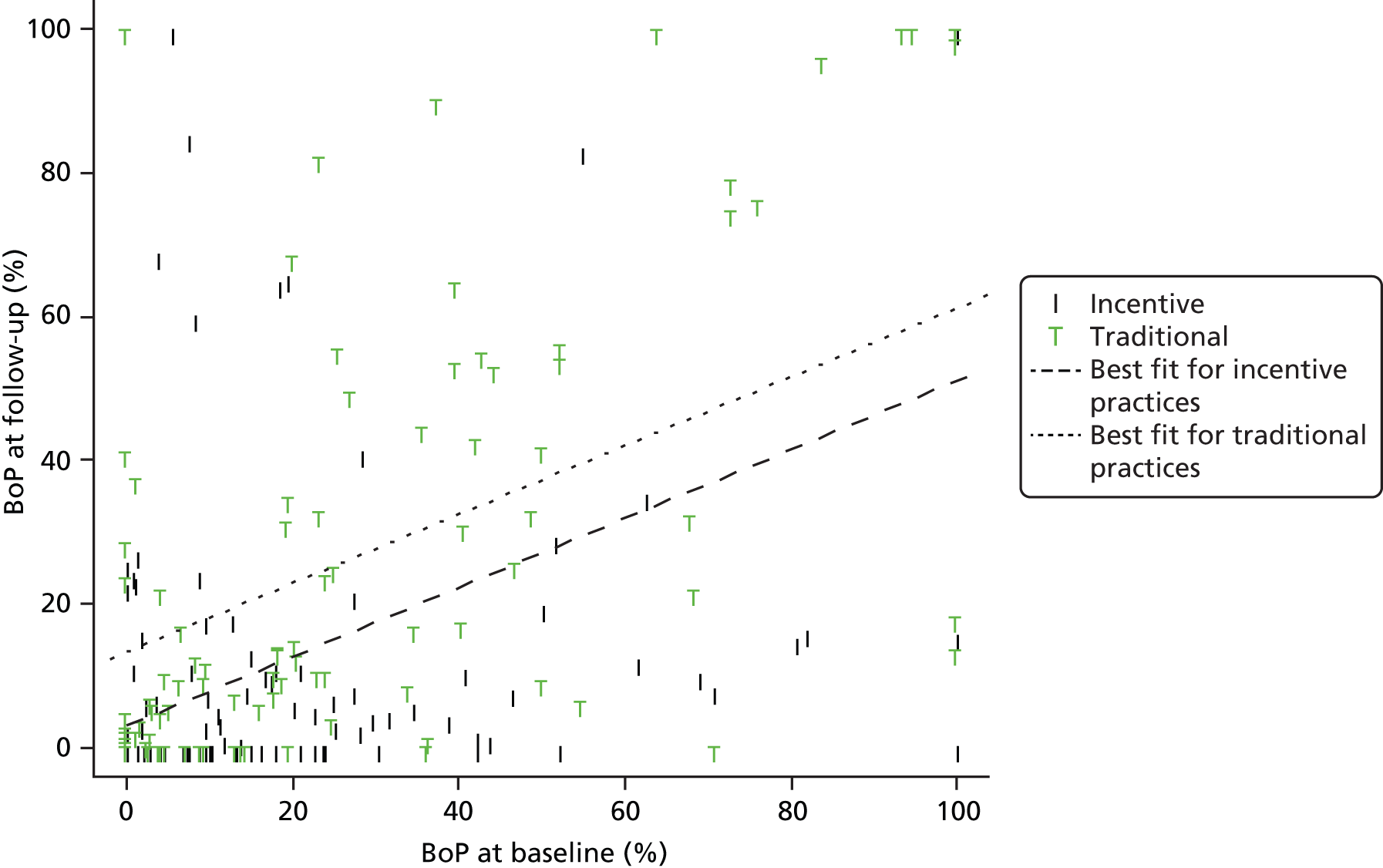
In summary, for BoP pooled across practices, the 95% CI for the effect size was 3.23 to 17.25, indicating a positive effect for incentive practices but with considerable uncertainty in magnitude. Together with reservations about the validity of pooling (because of the heterogeneity of effects across practice pairs) and differential dropout, the results should be treated with caution.
International Caries Detection and Assessment System change in sound surfaces
Figure 9 shows a scatterplot of sound surfaces at baseline and follow-up. The mean (SD) proportion of sound surfaces at baseline and follow-up was 84.52% (SD 16.45%) and 82.67% (SD 18.09%), respectively. Eighty-three patients excluded were following manual review for quality control in addition to those lost to follow-up (see Table 7). This comprised 3, 28, 5, 8, 16 and 23 patients for practices 3, 2, 1, 6, 5 and 4, respectively.
FIGURE 9.
Scatterplot of sound surfaces by practice.
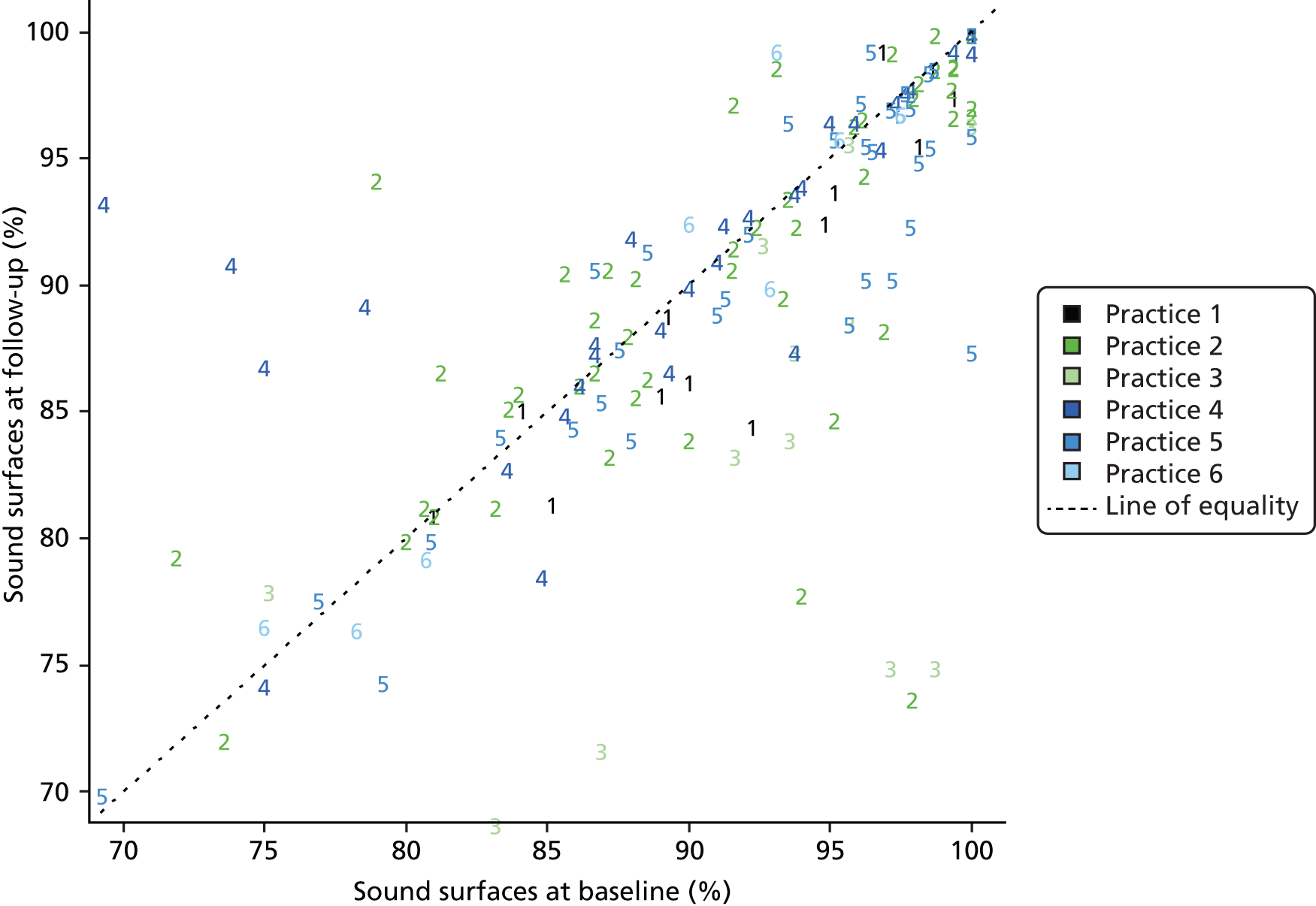
First we analysed the matched pairs separately using a baseline-adjusted ANCOVA. Table 13 relates to matched pair 1 and 4, Table 14 to matched pair 2 and 5 and Table 15 to matched pair 3 and 6.
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 5.49 | 3.33 | –1.19 to 12.17 | 0.11 |
| Baseline | 0.94 | 0.03 | 0.87 to 1.00 | < 0.01 |
| Practice: traditional | 1.03 | 1.61 | –2.19 to 4.25 | 0.52 |
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | –1.72 | 6.61 | –14.86 to 11.41 | 0.80 |
| Baseline | 1.00 | 0.07 | 0.85 to 1.14 | < 0.01 |
| Practice: traditional | 1.15 | 1.78 | –2.38 to 4.68 | 0.52 |
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | –5.44 | 10.05 | –26.02 to 15.15 | 0.59 |
| Baseline | 0.91 | 0.12 | 0.66 to 1.17 | < 0.01 |
| Practice: traditional | 13.49 | 4.45 | 4.38 to 22.60 | < 0.01 |
The model in Table 13 implies that the proportion of sound surfaces at follow-up was higher for patients in traditional practice 4 (than in incentive practice 1) by an average of 1.03% (95% CI –2.19% to 4.25%). This was not a significant difference between traditional and incentive practices (p = 0.52).
The model in Table 14 implies that the proportion of sound surfaces at follow-up was higher for patients in traditional practice 5 (than in incentive practice 2) by an average of 1.15% (95% CI –2.38% to 4.68%). This was not a significant difference between traditional and incentive practices (p = 0.52).
The model in Table 15 implies that the proportion of sound surfaces at follow-up was higher for patients in traditional practice 6 (than in incentive practice 3) by an average of 13.49% (95% CI 4.38% to 22.60%; p < 0.01).
Scatterplots of the proportion of sound surfaces at baseline and follow-up are shown for the matched pairs in Figure 10. Lines of best fit from the models described in Tables 13–15 are superimposed.
FIGURE 10.
Scatterplots of the proportion of sound surfaces by incentive vs. traditional practice. (a) Matched pair 1 and 4; (b) matched pair 2 and 5; and (c) matched pair 3 and 6.
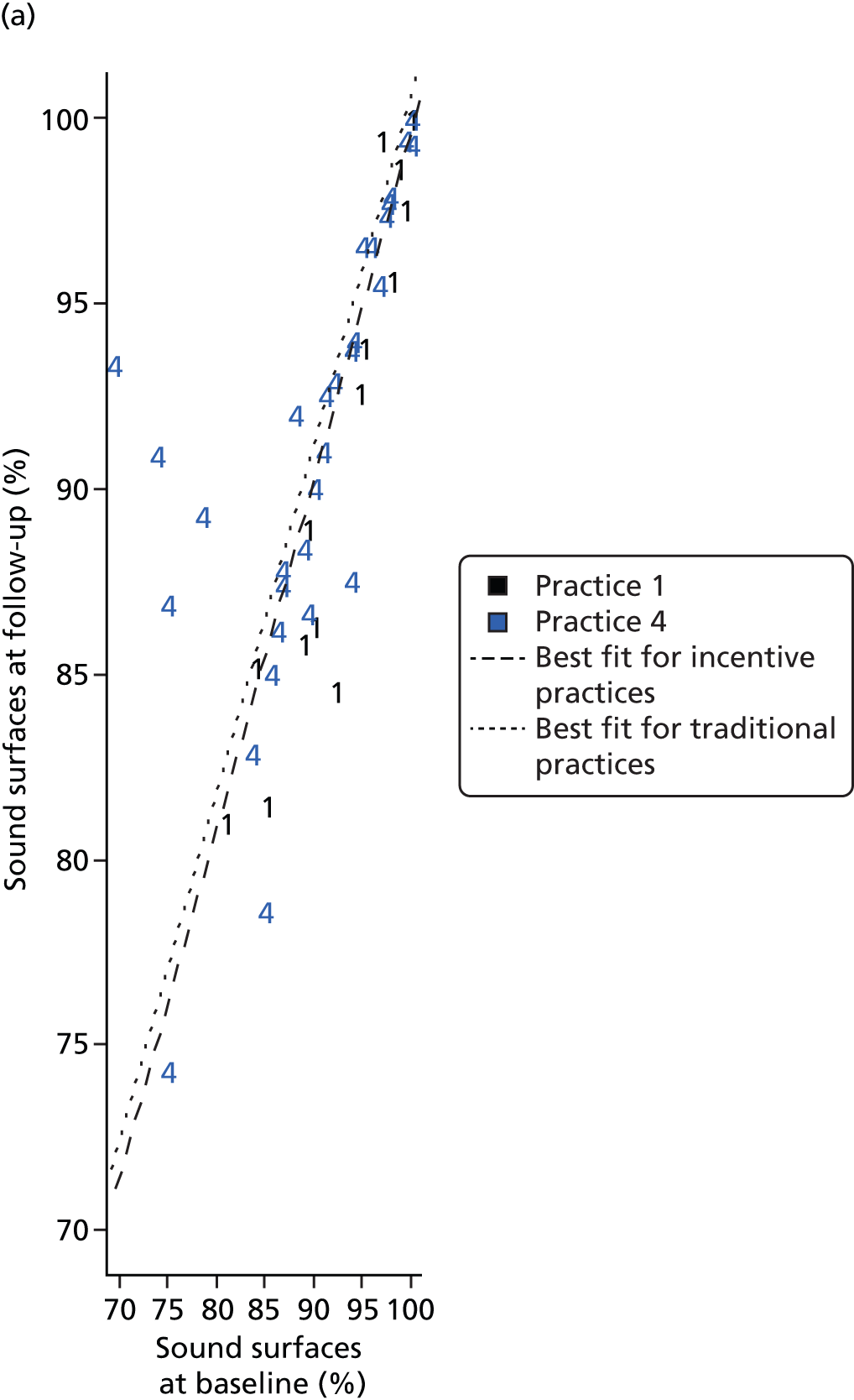

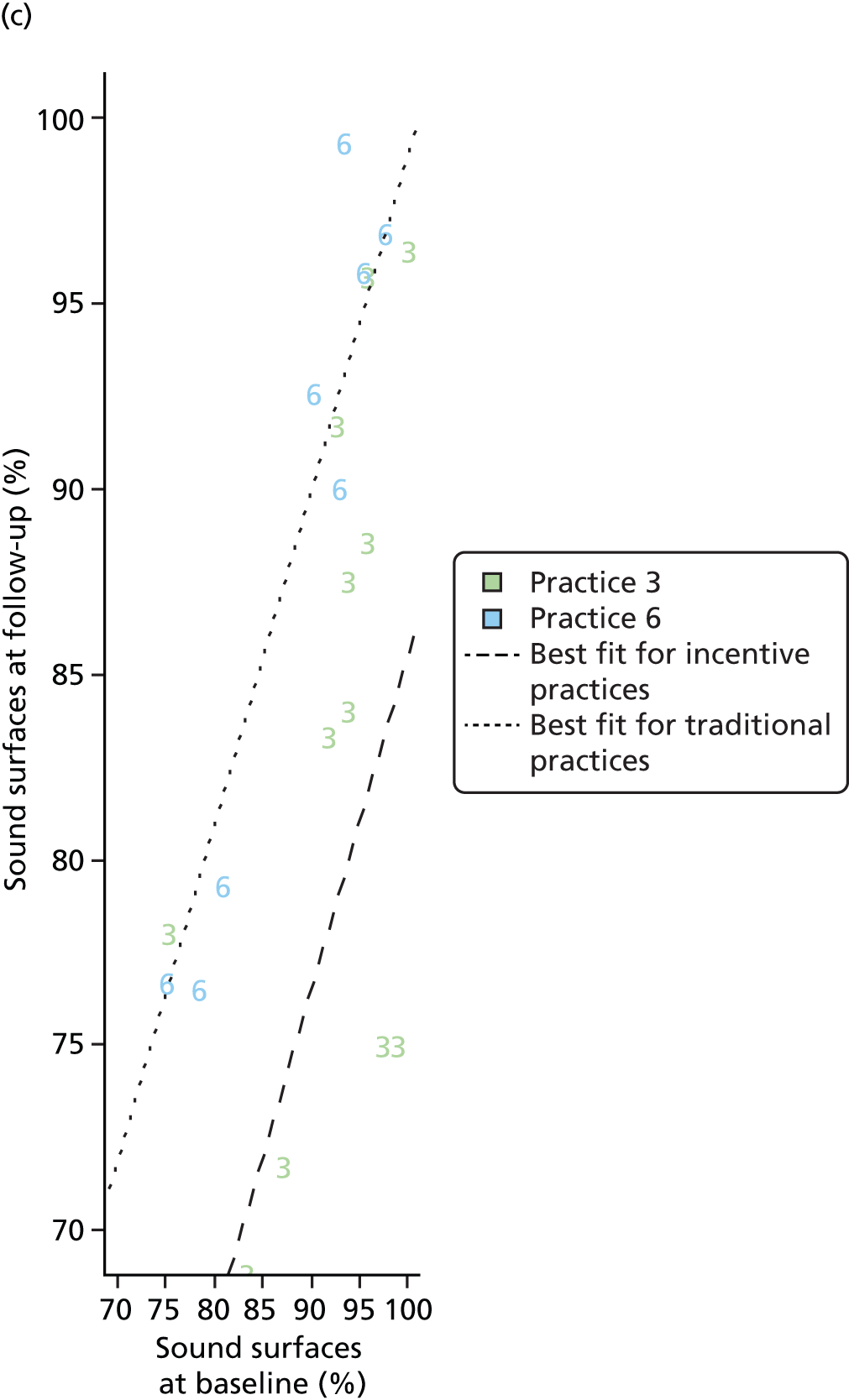
Combining the matched pairs into a single ANCOVA model produces the output shown in Table 16. This should be interpreted with caution because of the difference between the matched pairs observed in the analyses.
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | –2.62 | 3.46 | –9.44 to 4.20 | 0.45 |
| Baseline | 0.98 | 0.04 | 0.91 to 1.06 | < 0.01 |
| Practice: traditional | 4.68 | 1.27 | 2.18 to 7.18 | < 0.01 |
The model in Table 16 implies that the proportion of sound surfaces at follow-up was higher for patients in traditional practices (than in incentive practices) by an average of 4.68% (95% CI 2.18% to 7.18%; p < 0.01).
A scatterplot of the proportion of sound surfaces at baseline and follow-up is shown across all the matched pairs in Figure 11. Lines of best fit from the model described in Table 16 are superimposed.
FIGURE 11.
Scatterplot of the proportion of sound surfaces by incentive vs. traditional practice across all matched pairs.
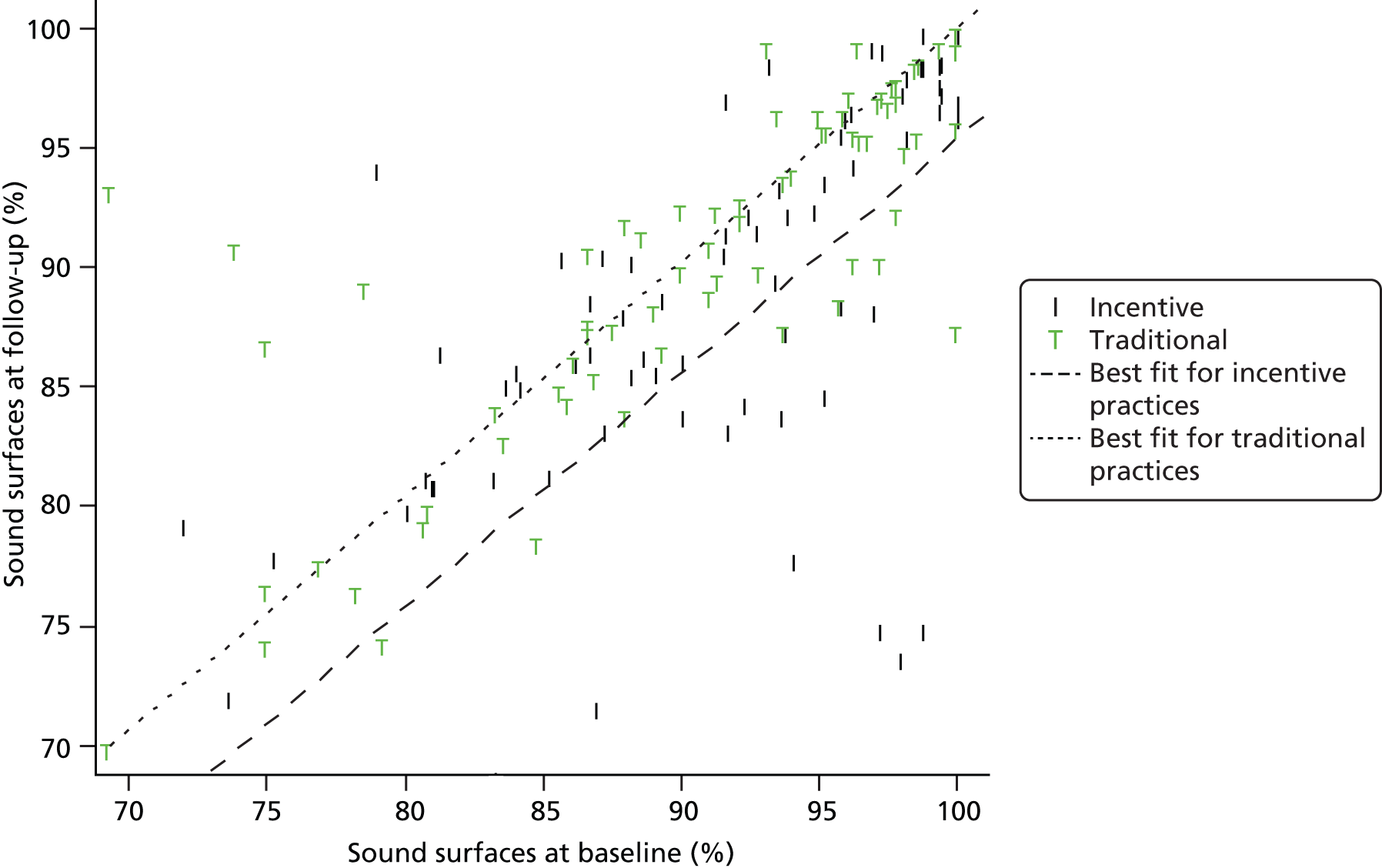
In summary, the proportion of sound surfaces (defined as caries free and having initial ICDAS codes 1 and 2) at follow-up was higher (4.68%) in traditional practices, although in two of the pairings the difference in the proportion of sound surfaces was non-significant.
International Caries Detection and Assessment System change in extractions and fillings
Figure 12 shows a scatterplot of the proportion of extractions and fillings (E&F) at baseline and follow-up. The mean (SD) of the proportion of E&F at baseline and follow-up was 29.36% (SD 27.02%) and 34.19% (SD 27.89%), respectively. Eighty-one patients were excluded following manual review for quality control in addition to those who were lost to follow-up (see Table 7). This comprised 3, 28, 5, 6, 17 and 22 patients for practices 3, 2, 1, 6, 5 and 4, respectively. In addition, 10 patients with E&F in excess of 100% had E&F imputed to 100%.
FIGURE 12.
Scatterplot of E&F by practice.
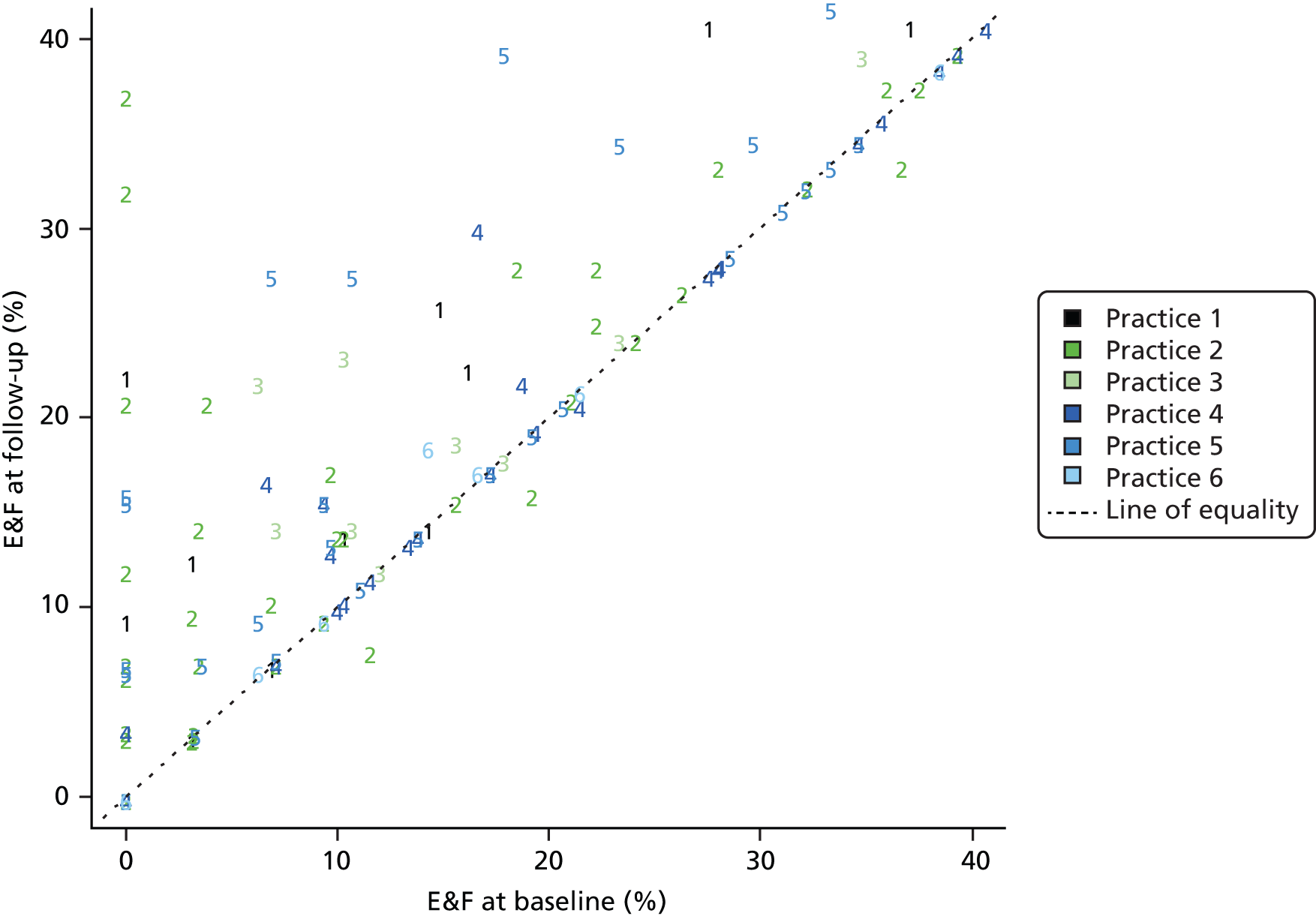
First we analysed the matched pairs separately using a baseline-adjusted ANCOVA. Table 17 relates to matched pair 1 and 4, Table 18 relates to matched pair 2 and 5 and Table 19 to matched pair 3 and 6.
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 15.34 | 2.30 | 10.72 to 19.94 | < 0.01 |
| Baseline | 1.01 | 0.04 | 0.93 to 1.09 | < 0.01 |
| Practice: traditional | –15.11 | 2.63 | –20.38 to –9.84 | < 0.01 |
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 7.32 | 2.05 | 3.24 to 11.39 | < 0.01 |
| Baseline | 0.96 | 0.04 | 0.86 to 1.05 | < 0.01 |
| Practice: traditional | –0.95 | 2.65 | –6.21 to 4.32 | 0.72 |
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 4.94 | 1.82 | 1.23 to 8.64 | 0.01 |
| Baseline | 0.97 | 0.04 | 0.89 to 1.05 | < 0.01 |
| Practice: traditional | –2.89 | 1.98 | –6.92 to 1.15 | 0.15 |
The model in Table 17 implies that the proportion of E&F at follow-up was lower for patients in traditional practice 4 (than in incentive practice 1) by an average of 15.11% (95% CI 9.84% to 20.38%; p < 0.01).
The model in Table 18 implies that the proportion of E&F at follow-up was lower for patients in traditional practice 5 (than in incentive practice 2) by an average of 0.95% (95% CI 4.32% to –6.21%). This was not a significant difference between traditional and incentive practices (p = 0.72).
The model in Table 19 implies that the proportion of E&F at follow-up was lower for patients in traditional practice 6 (than in incentive practice 3) by an average of 2.89% (95% CI –6.92% to 1.15%). This was not a significant difference between traditional and incentive practices (p = 0.15).
Scatterplots of E&F at baseline and follow-up are shown for the matched pairs in Figure 13. Lines of best fit from the models described in Tables 17–19 are superimposed.
FIGURE 13.
Scatterplot of E&F by incentive vs. traditional practice. (a) Matched pair 1 and 4; (b) matched pair 2 and 5; and (c) matched pair 3 and 6.
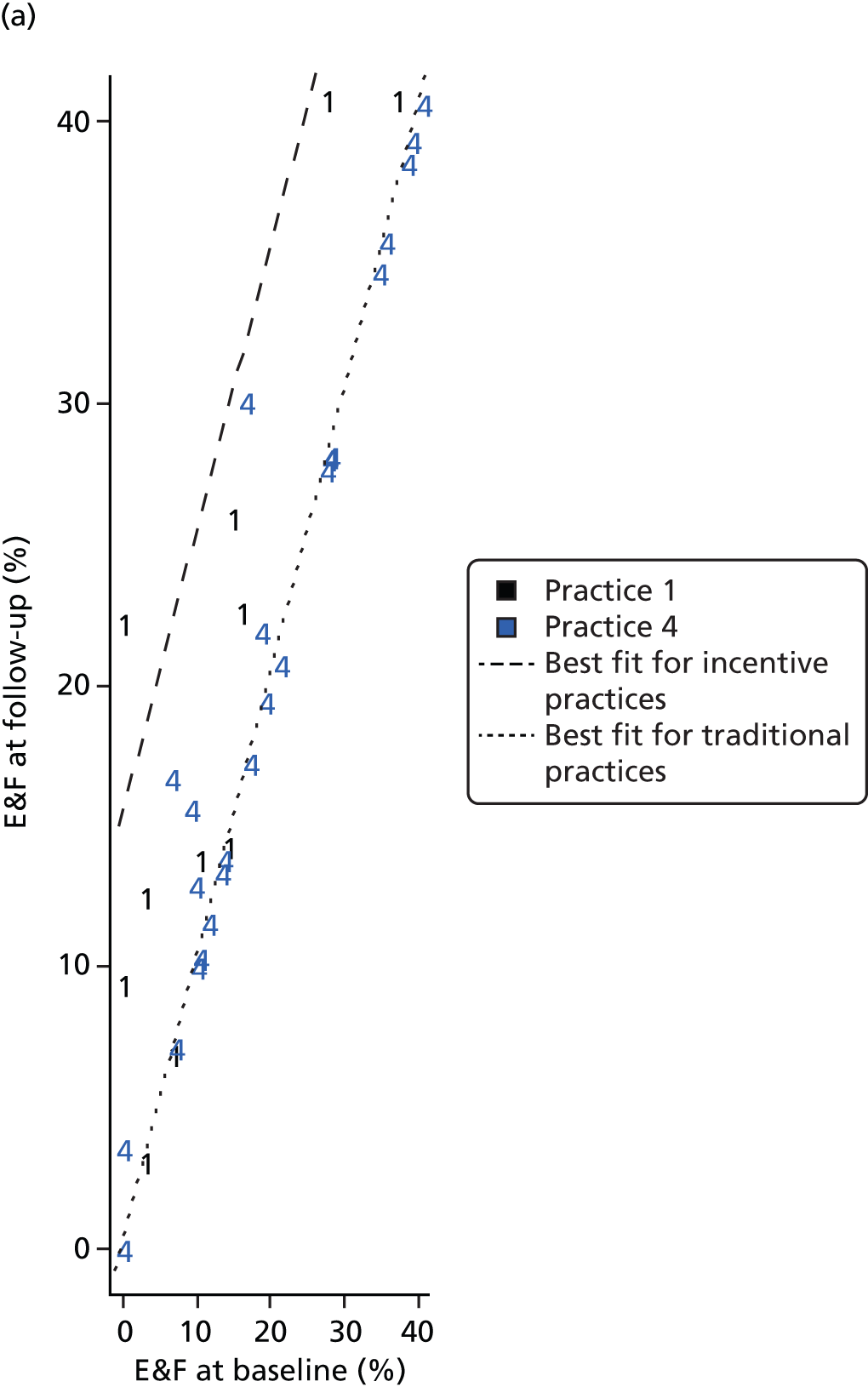
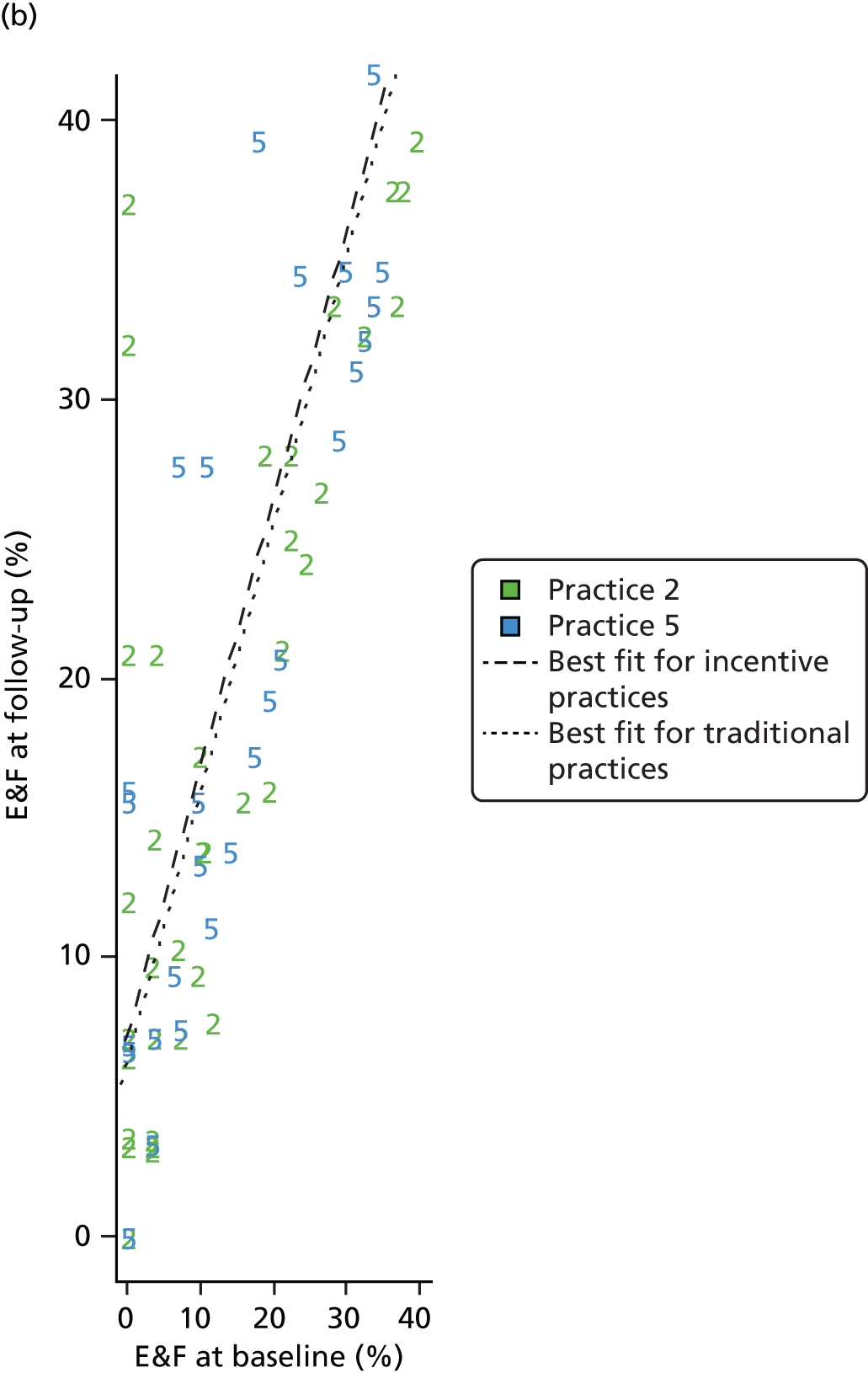
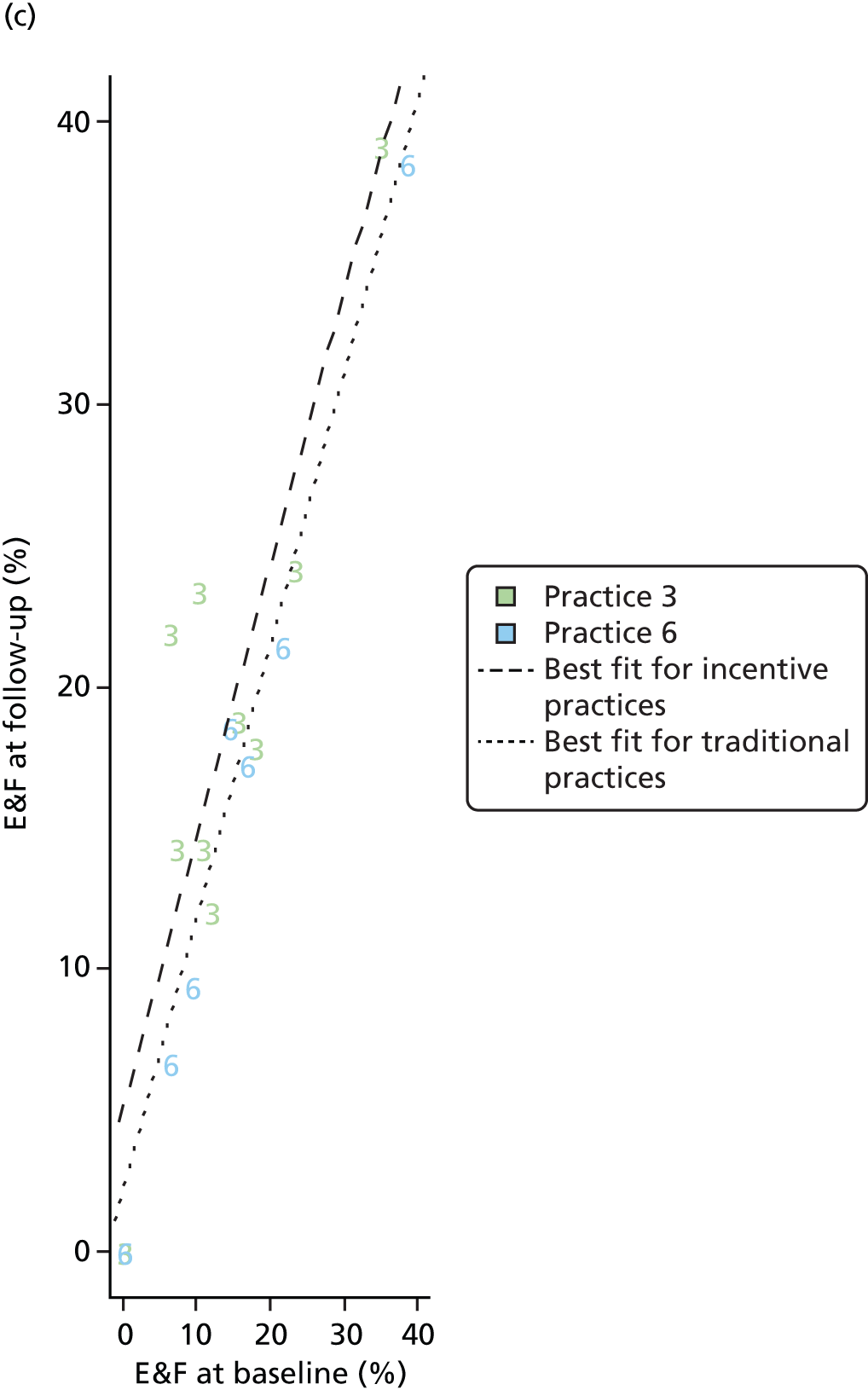
Combining the matched pairs into a single ANCOVA model produces the output shown in Table 20. This should be interpreted with caution because of the difference between the matched pairs observed in the analyses.
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 8.26 | 1.35 | 5.61 to 10.92 | < 0.01 |
| Baseline | 0.96 | 0.03 | 0.90 to 1.01 | < 0.01 |
| Practice: traditional | –4.43 | 1.57 | –7.52 to –1.34 | 0.01 |
The model in Table 20 implies that the proportion of E&F was lower at follow-up for patients in traditional practices (than in incentive practices) by an average of 4.43% (95% CI 1.34% to 7.52%; p = 0.01).
A scatterplot of the proportion of E&F at baseline and follow-up is shown across all the matched pairs in Figure 14. Lines of best fit from the model described in Table 20 are superimposed.
FIGURE 14.
Scatterplot of E&F by incentive vs. traditional practice across all matched pairs.
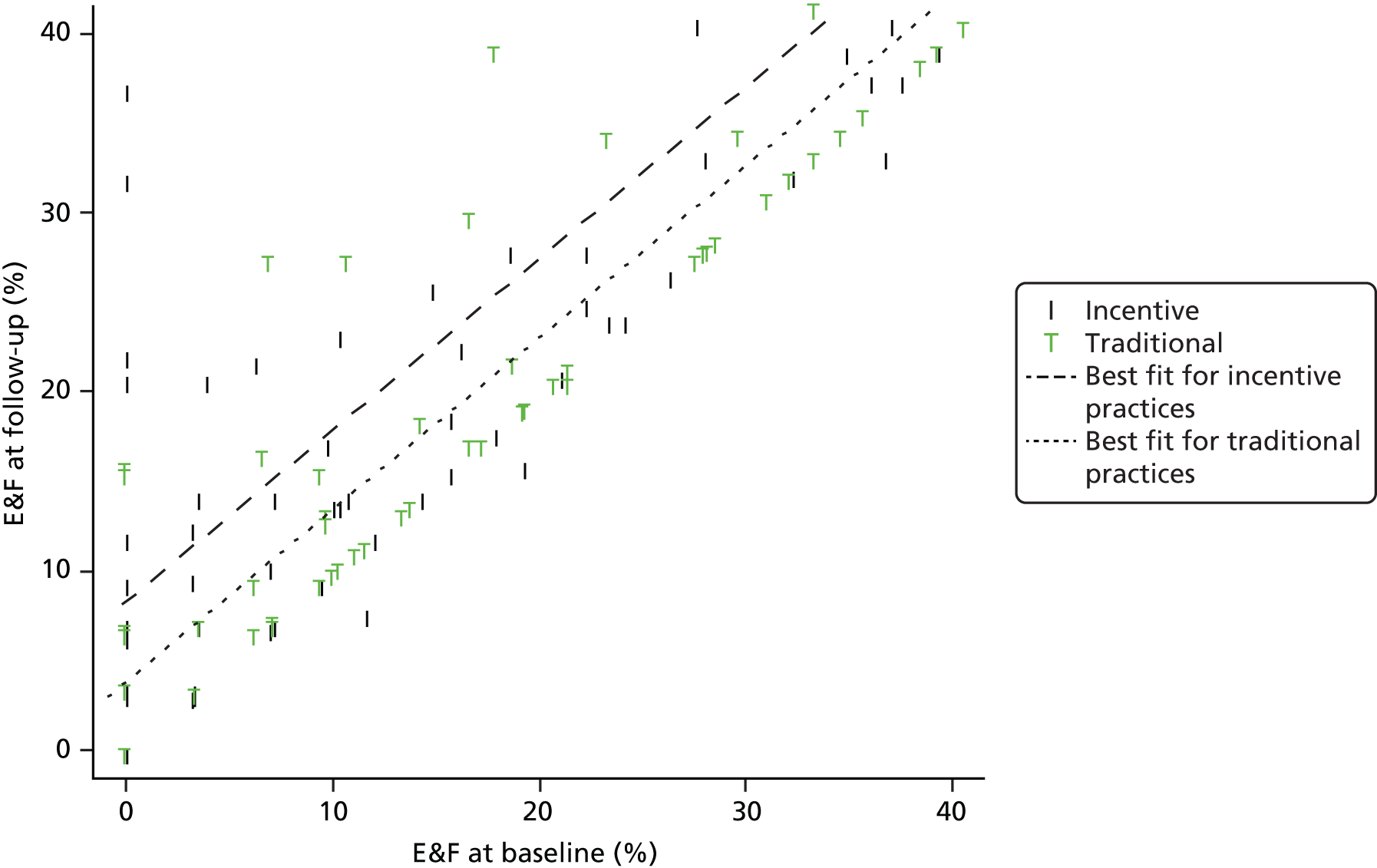
In summary, the traditional practices had a lower number of E&F at follow-up by 4.43%. However, for two of the three pairings there was no significant difference in E&F.
Oral Health Impact Profile
Figure 15 shows a scatterplot of OHIP-14 at baseline and follow-up. The mean (SD) OHIP-14 score at baseline and follow-up was 9.00 (SD 10.37) points and 6.09 (SD 8.08) points, respectively.
FIGURE 15.
Scatterplot of OHIP-14 scores by practice.
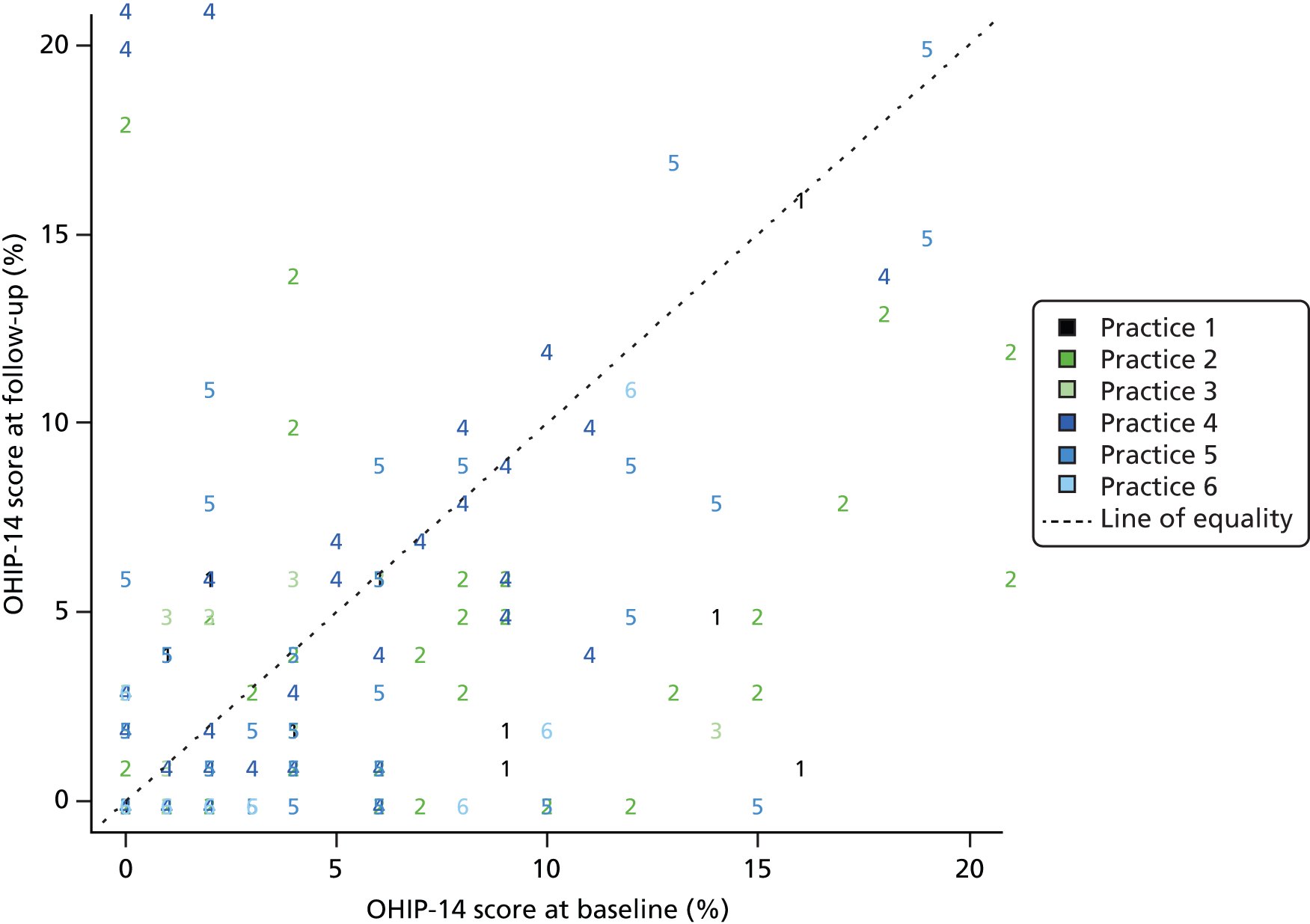
At baseline, there were three patients in whom answers to three or more questions were missing, and thus were excluded, and 12 patients in whom answers to one or two questions were missing (and were imputed as noted previously). At follow-up (excluding those lost to follow-up), there were 10 patients in whom answers to three or more questions were missing, and who were thus excluded, and 10 patients in whom answers to one or two were missing (and who were imputed as noted previously). Overall, 96 patients were excluded following manual review for quality control in addition to those who were lost to follow-up (see Table 7). This comprised 4, 32, 8, 6, 22 and 24 patients for practices 3, 2, 1, 6, 5 and 4, respectively.
First we analysed the matched pairs separately using a baseline-adjusted ANCOVA. Table 21 relates to matched pair 1 and 4, Table 22 relates to matched pair 2 and 5 and Table 23 to matched pair 3 and 6.
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | –1.81 | 1.98 | –5.78 to 2.15 | 0.36 |
| Baseline | 0.60 | 0.10 | 0.41 to 0.80 | < 0.01 |
| Practice: traditional | 5.15 | 1.99 | 1.17 to 9.14 | 0.01 |
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 0.85 | 1.22 | –1.58 to 3.28 | 0.49 |
| Baseline | 0.44 | 0.06 | 0.31 to 0.57 | < 0.01 |
| Practice: traditional | 2.74 | 1.47 | –0.18 to 5.68 | 0.07 |
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 0.51 | 1.04 | –1.61 to 2.63 | 0.63 |
| Baseline | 0.67 | 0.11 | 0.45 to 0.89 | < 0.01 |
| Practice: traditional | –1.63 | 2.04 | –5.80 to 2.53 | 0.43 |
The model in Table 21 implies that the OHIP-14 score was higher at follow-up for patients in traditional practice 4 (than in incentive practice 1) by an average of 5.15 points (95% CI 1.17 to 9.14 points; p = 0.01).
The model in Table 22 implies that the OHIP-14 score was higher at follow-up for patients in traditional practice 5 (than in incentive practice 2) by an average of 2.74 points (95% CI 5.68 to –0.18 points). This was not a significant difference between traditional and incentive practices (p = 0.07).
The model in Table 23 implies that the OHIP-14 score was lower at follow-up for patients in traditional practice 6 (than in incentive practice 3) by an average of 1.63 points (95% CI –5.80 to 2.53 points). This was not a significant difference between traditional and incentive practices (p = 0.43).
Scatterplots of the OHIP-14 scores at baseline and follow-up are shown for the matched pairs in Figure 16. Lines of best fit from the models described in Tables 21–23 are superimposed.
FIGURE 16.
Scatterplot of the OHIP-14 score by incentive vs. traditional practice. (a) Matched pair 1 and 4; (b) matched pair 2 and 5; and (c) matched pair 3 and 6.
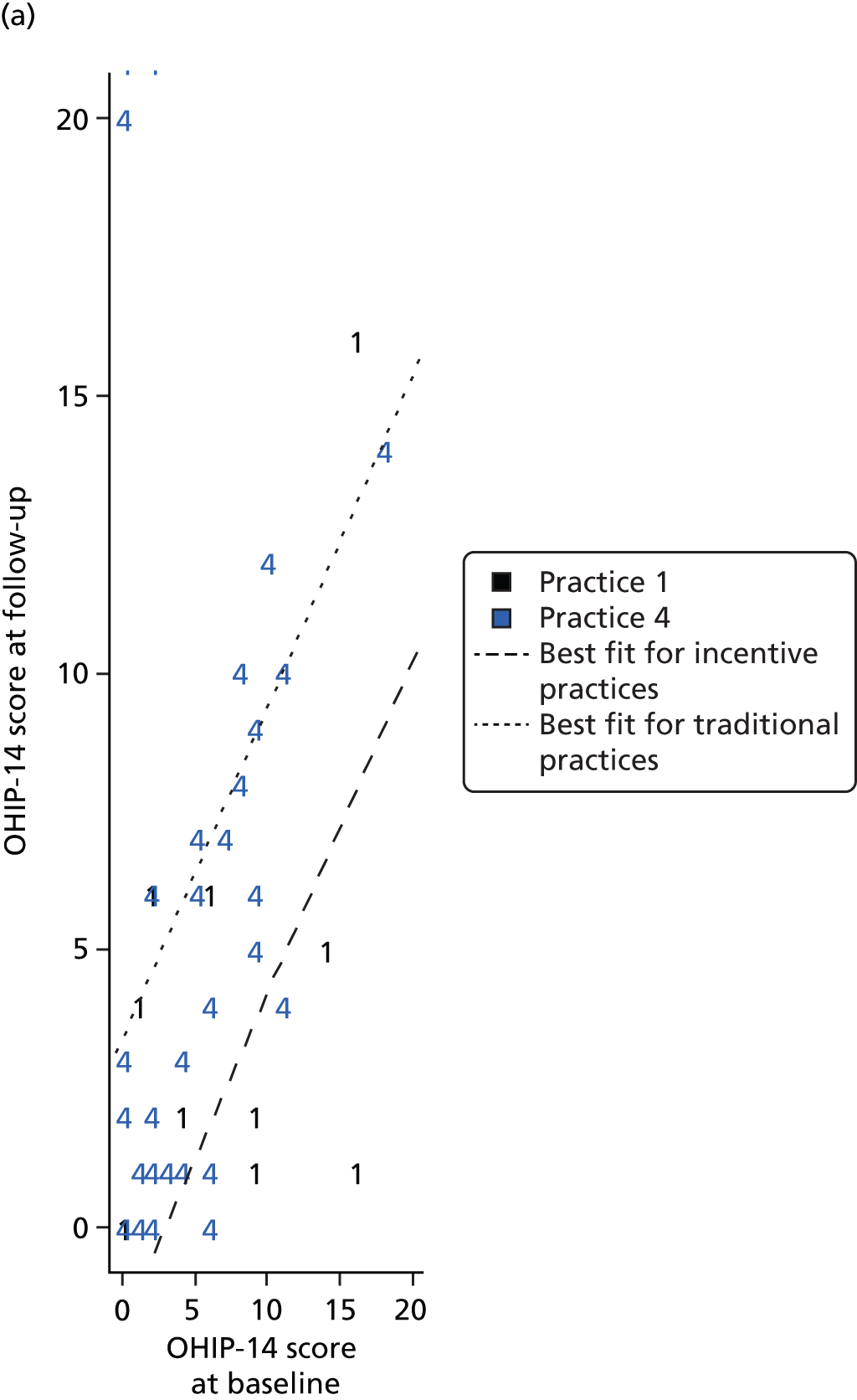

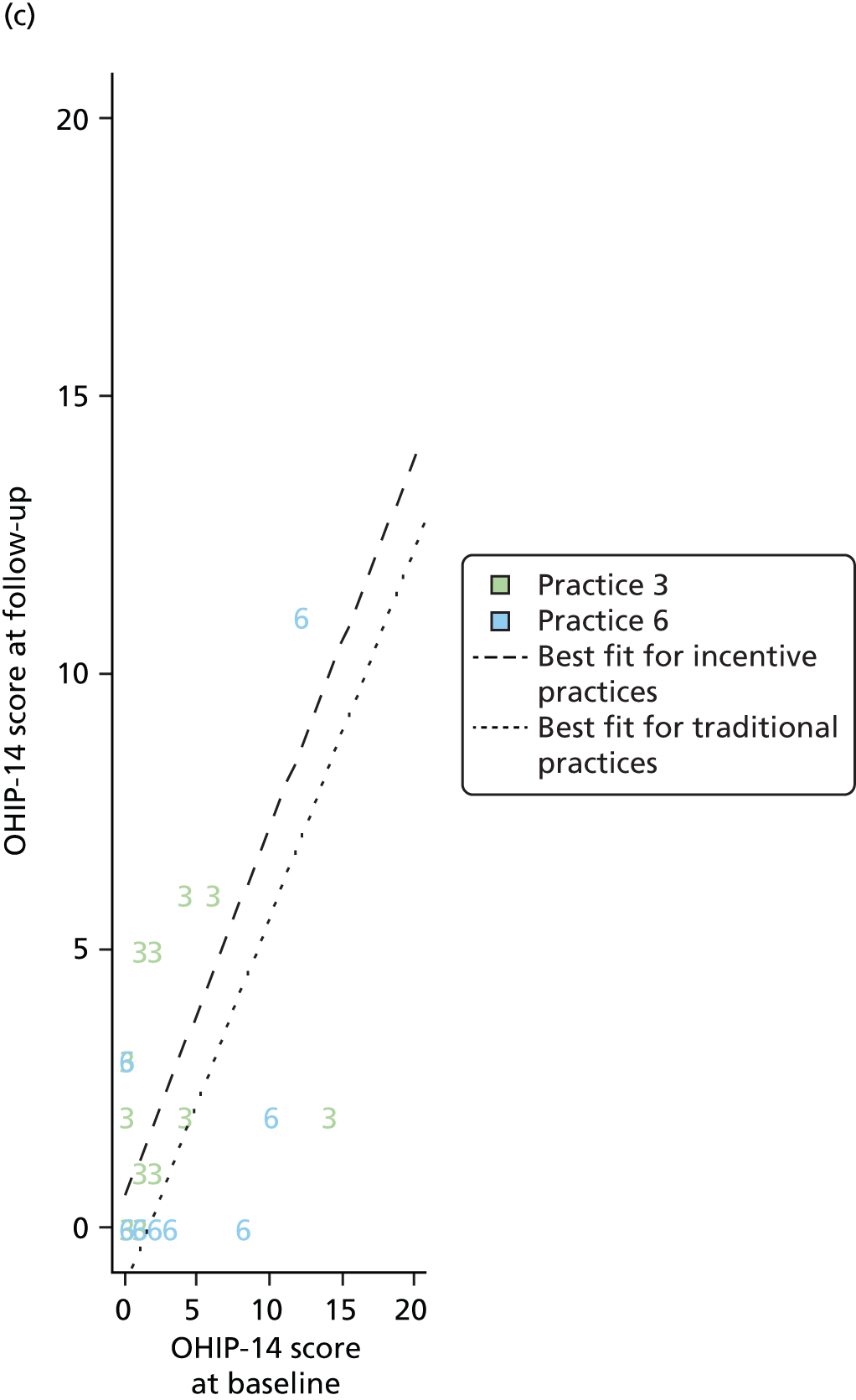
Combining the matched pairs into a single ANCOVA model produces the output shown in Table 24. This should be interpreted with caution because of the difference between the matched pairs observed in the analyses.
| Measure | Coefficient | SE | 95% CI | p-value |
|---|---|---|---|---|
| Intercept | 0.27 | 0.79 | –1.29 to 1.84 | 0.73 |
| Baseline | 0.49 | 0.05 | 0.40 to 0.58 | < 0.01 |
| Practice: traditional | 3.05 | 0.94 | 1.20 to 4.90 | < 0.01 |
The model in Table 24 implies that the OHIP-14 score was higher at follow-up for patients in traditional practices (than in incentive practices) by an average of 3.05 points (95% CI 1.20 to 4.90 points; p < 0.01).
A scatterplot of OHIP-14 score at baseline and follow-up is shown across all the matched pairs in Figure 17. Lines of best fit from the model described in Table 24 are superimposed.
FIGURE 17.
Scatterplot of OHIP-14 score by incentive vs. traditional practice across all matched pairs.
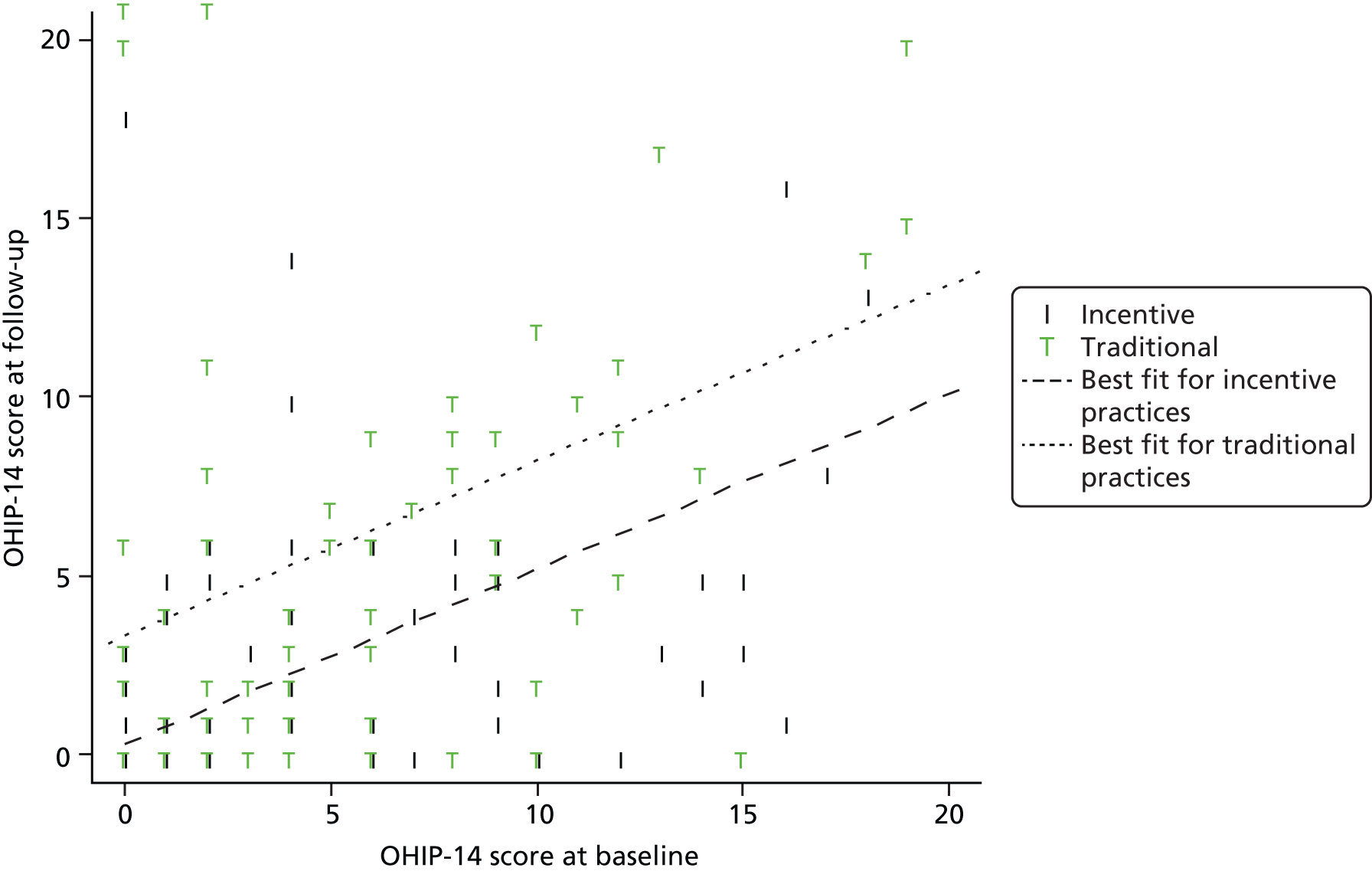
In summary, overall, OHIP-14 total scores at follow-up score were 3.5 points higher in traditional practices, indicating worse OHQoL. Again, for two of the three pairings there was no significant difference.
Risk assessment traffic light system
Table 25 shows the distribution of risk assessments in the RAG categories at baseline and follow-up. All patients who reported a risk assessment rating are included regardless of whether or not they had BoP assessment at baseline and follow-up, or whether or not they were excluded from modelling work following manual data review for quality control.
| Risk assessment | Red | Amber | Green | Total |
|---|---|---|---|---|
| Baseline | 207 (73.93) | 60 (21.43) | 13 (4.64) | 280 (100) |
| Follow-up | 49 (44.14) | 43 (38.74) | 19 (17.11) | 111 (100) |
Table 25 implies that the most common risk assessment category at both baseline and follow-up was red (73.93% and 44.14%, respectively) and the least common risk assessment category in both time periods was green (4.64% and 17.11%, respectively). The table suggests a possible improvement in risk assessment category from baseline to follow-up, with increasing proportions of patients in amber and green categories as opposed to red. However, the inclusion of patients lost to follow-up in the baseline assessments may also account for these changes.
At the practice level, there were two, one and no incomplete risk assessment traffic lights in practices 1, 2 and 3, respectively. At follow-up (excluding those lost to follow-up) the figures were 7, 14 and 1, respectively.
Table 26 shows the transitions between categories from baseline to follow-up.
| Risk assessment | Follow-up | Total | ||
|---|---|---|---|---|
| Red | Amber | Green | ||
| Red | 47 | 26 | 3 | 76 (68.47) |
| Amber | 2 | 14 | 10 | 26 (23.42) |
| Green | 0 | 3 | 6 | 9 (8.11) |
| Total | 49 (44.14) | 43 (38.74) | 19 (17.11) | 111 (100) |
Table 26 implies that, in general, patients’ risk assessments improve from baseline to follow-up. Of the 76 patients in the red category at baseline who attended follow-up, only 47 (61.84%) remained red, with 26 (34.21%) moving to amber and three (3.95%) moving to green. Of the 26 patients in the amber category at baseline attending for follow-up, 10 (38.46%) moved to green and only two (7.69%) moved to red. Of the nine patients in the green category at baseline who attended follow-up, six (66.67%) remained green, with the other three (33.33%) moving to amber. Those patients who were red at baseline were less likely to attend follow-up (76 of 207, 36.71%) than those who were amber (26 of 60, 43.33%) or green (9 of 13, 69.23%) at baseline.
Table 27 shows the distribution of risk assessments that were manually over-ridden at baseline and follow-up.
| Risk assessment | Red | Amber | Green | Total |
|---|---|---|---|---|
| Baseline | 4 (30.77) | 8 (61.54) | 1 (7.69) | 13 (100) |
| Follow-up | 3 (37.50) | 4 (50.00) | 1 (12.50) | 8 (100) |
Table 27 implies that very few risk assessments were over-ridden [13 of 280 (4.64%) at baseline and 8 of 111 (7.21%) at follow-up]. Although it would be unwise to overinterpret the data given these small numbers, over-rides to red or amber are more common than over-rides to green (92.31% vs. 7.69% at baseline compared with 87.50% vs. 12.50% at follow-up).
At the practice level, there were 10, 1 and 1 incomplete manual over-ride records at practices 1, 2 and 3, respectively. At follow-up (excluding those lost to follow-up) the figures were 9, 15 and 1, respectively.
Dental practitioners were asked to give reasons for any over-rides made in the risk assessment and thus the changed care pathway. Over-rides to a lower risk tended to be characterised by general comments about improved oral health, the patient’s commitment to improved oral health and reference to caries. The following are typical responses:
-
oral health improved
-
oral hygiene improved; patient is caries free
-
moderate risk for periodontitis and caries
-
patient currently amber, but committed to improving oral health
-
minor calculus present in two quadrants plus heavy calculus in one gives red, but as everything else is healthy and the patient is highly motivated moved to amber
-
minimum calculus present and committed to improving
-
more carious teeth last visit.
There were, however, examples of over-rides related to family health conditions or medication that put the patient in a higher risk category than the dentist thought warranted:
-
patient on hay fever tablets – computer placed on red pathway, over-ride to amber
-
diabetes in the family – placed on high risk, over-ride to medium risk.
The over-rides that placed patients on higher risk than indicated by the RAG system included changes based on the result of investigations within the dental appointment (specifically radiographs) and the patient’s lack of commitment to their OHImp evidenced through attendance at the dentist:
-
after further investigation of the bitewing radiographs taken, bone loss found, which makes the patient high risk because of compromised periodontal health
-
patient failed to attend for treatments
-
irregular attender.
In summary, using the RAG system (incentive practices only), among those who attended both baseline and follow-up there was an improvement with 68% red at baseline and 44% red at follow-up. Those who were red at baseline were less likely to attend follow-up. A total of 36.71% of those who were red at baseline attended follow-up; 69.23% of those who were green at baseline attended follow-up. There were very few decision over-rides on the RAG system.
Discussion
The matched pair design was chosen to help control for important differences between practices in the absence of a randomised design. However, there are acknowledged limitations inherent in not using a randomised controlled trial. We match practices on deprivation of location of the practice, the ethnic mix of the location, the practice profile of patient age and size of the practice. In practice, the matching process was successful in as much as it resulted in pairs being balanced in terms of ethnicity. Although not matched for sex, the pairings were well matched in this area. One area that did show differences was the average age of patients. However, it is important to note that we matched on the practice profile of existing patients; the profile of participants indicated that the age of new patients differed. Practice 1 had the lowest mean age, at 34.64 years (matched with practice 4, at 40.99 years), whereas practice 3 had the highest, at 47.60 years (matched with practice 6, at 40.78 years).
In terms of baseline oral health, the matching produced relative balance in terms of BoP and caries, with the exception of the 1 and 4 pairing, with practice 1 showing far lower BoP, which is indicative of better oral health. For those patients who were included in the baseline and follow-up analysis, a mean score of BoP at follow-up of 6.19 was recorded for practice 1, compared with a mean score of 30.66 for practice 4. In respect of OHIP-14 scores, pairings were relatively balanced with the exception of pair 3 and 6 (mean OHIP-14 score of 2.5 points in practice 3 vs. 13.19 points in practice 6 for those patients who are included in the baseline and follow-up). Despite the pairings being matched for practice size, recruitment rates in matched pairs differed, especially in pairs 2 and 5 and 1 and 4.
If we pool our results across the three pairings, the results are mixed. Our primary outcome, BoP, is assessed to be in favour of the incentive practices as are the OHIP-14 score results. Conversely, the proportions of sound surfaces and E&F taken from the ICDAS data are in favour of the traditional practices. However, the numbers of patients available for analyses for pairs 1 and 4 and 3 and 6 were unbalanced. This leads us to question whether or not it is robust to pool the three pairings in single analyses. If we are not willing to pool them, then the only pairing with balanced numbers for analyses is the 2 and 5 pairing. The results from this single pairing show a significant difference only for the primary outcome, BoP, in favour of the blended/incentive-driven contract. It is of note, whether the pooled analyses or only the analyses from the balanced pairing are used, that the primary outcome of BoP is significantly in favour of incentive practices, which gives a degree of confidence in this result.
Loss to follow-up also differed among practices, ranging from 35% to 74%. Even at the lower end of the range this was far higher than the 10% expected;119 this was despite dental practices using a variety of media to contact patients to optimise attendance at 24-month appointments (letter by post, telephone and SMS). Individual practices also opened their surgeries out of usual hours (evening and weekend) to encourage study participants to attend the 24-month recall appointment. Although we do not have a complete record of reasons for non-attendance, patients not responding to contact from the dental practices was the most frequently cited reason across incentive and traditional practices. Within the incentive practices there was also a substantial number of patients who failed to attend pre-booked appointments. One potential explanation for the difference in loss to follow-up rates between our study and other studies is that all participants in the study were new patients rather than existing patients who were regular attenders, as in most previous studies. It is also of interest that the practice with the lowest loss to follow-up was in an affluent area and had the oldest study population. Conversely, the practice with the highest loss to follow-up is based in one of the 10% most deprived wards in the country, with associated adverse income, living environment, education, health and employment indicators. The practice estimates that approximately 80% of its patients are eligible for benefits. The study population was the youngest of all the practices.
With regard to data quality, within the study training was provided for all team members in completion of the ICDAS and BoP charts. This initially took place prior to recruitment of patients. The training was provided by an experienced clinician on the study team. Training took place on the individual practice premises over a period of weeks. The training was competence based, with practices encouraged to request follow-up training until all personnel felt competent in the use of the indices. For some practices this was a single training session before recruitment began, for others this was two or three sessions. Online training materials were made available and materials from the training presentations were kept by the practices. Prior to follow-up at 24 months, all practices undertook repeat training to ensure comparability. Despite this training, the quality of the data for the ICDAS has proved to be variable. Although the majority of charts were completed to an acceptable standard, a number of issues were evident which give cause for caution in interpretation of the results. For example, in some instances teeth with obvious caries or fillings at baseline were charted as sound at follow-up, even allowing for errors in the transposition of adjacent teeth. Indeed, concerns about the implausibility and missing data meant that all the charts for those who completed baseline and follow-up were manually reviewed and quality controlled by an experienced clinician. The manual review of data resulted in the exclusion of 71 patients from the analyses. Thirty-five of those patients have impossible transitions such as dentine caries at baseline charted as sound at follow-up (n = 22); teeth charted as missing at baseline charted as sound at follow-up (n = 5); and restoration charted at baseline as sound at follow-up (n = 8). Charting errors were found in a further 17 records [partial data missing, n = 14; single-digit coding, n = 2; ‘illegal’ code, n = 1 (an illegal code is one not on the ICDAS range of response codes)]. Nineteen charting pairs were missing either the baseline or the follow-up chart.
It should be noted that all ICDAS charts were completed by the dental practitioners using a paper form. Given the comprehensive training provided, future studies should consider electronic completion, which has built-in automatic error checks. We had intended to use this electronic capture in this study, but, unfortunately, in some cases computer terminals were not within the dental surgery. As a result of this, and to ensure no bias resulting from method of completion, we used the paper form of the ICDAS in all practices.
Use of the ICDAS was exploratory in the study. It has proved to be illuminating in as much as there are lessons to take forward. The data suggest that there are issues in relation to the capability within practices of recording this clinical outcome accurately. Indeed, the lack of confidence in the quality of the ICDAS data means that we have not explored the enamel transitions in the way that we would have wanted to. Indeed, changes in the ICDAS scores may be the result of multiple factors, such as attrition of study participants, diagnostic inaccuracies, poor completion, complexity of the ICDAS, difficulty in diagnosing enamel caries in general dental practice, errors in syntax or the relatively short time frame of the study.
The traffic light (RAG) risk assessment showed improvement from baseline to follow-up, which suggests a degree of responsivity. However, more work is needed to validate this as there may be some operator bias. One of the concerns a priori was that it would be impossible for some patients with particular irreversible medical conditions to move out of the red category. In our sample there were very few over-rides, and from the small number that had been over-ridden we are unable to ascertain whether or not this a priori concern was borne out. Explanations for over-rides, especially moves away from red, suggest other reasons. Only one patient score was over-ridden because of a family medical condition (diabetes). It is of note that those who were red at baseline were less likely to attend follow-up.
Conclusions
Although the study results favour the blended/incentive model, this is with the caveats relating to sample size and data quality, given that 16% of participants were excluded from the analyses of the primary outcome for issues of data quality. However, a large proportion of people in this study who had access to a dentist did not follow up on oral care. These individuals were more likely to be younger males and have poorer oral health. Within this patient group, although access to dental services was increased this did not appear to facilitate continued use of services. Further work is required to understand how best to promote and encourage appropriate dental service attendance, especially among those with a high level of need to avoid increasing health inequalities.
Should services consider an oral health-related outcome measure of clinical effectiveness, this study would support the use of BoP as a potential measure. However, further work is required to validate this information. In terms of a dental caries, the need for further work is indicated for both accuracy and validity of recording.
Chapter 5 Economic study
Introduction
In order to assess value for money of the new blended/incentive-driven contract, this part of the study provides an economic evaluation of a new service delivery model (incentive) compared with the standard (traditional) practice model. The evaluation identifies within-study incremental cost-effectiveness ratios (ICERs) for the incentive model compared with traditional practice. Use of these ratios enables comparison of any additional financial costs imposed by the new model over standard care practice with any additional benefits it delivers.
The primary analyses take the perspective of the commissioners of the service, taking into account differences in contractual payments. Secondary analysis takes the perspective of the service provider including the cost of dental practitioners’ time and treatment materials. The price year is 2012.
The EQ-5D-3L was used in the analyses to derive quality-adjusted life-years (QALYs). 125,126 However, given the apparent insensitivity of the EQ-5D-3L in oral health,127 the OHIP-14, an OHQoL measure, was also used. 115,116 The analyses will show the cost per QALY and cost per unit change in the OHIP-14 score of the incentive model compared with that of the traditional care practice.
The OHIP-14 measure has been used extensively in cost-effectiveness analyses in oral health (see, for example, Stone and colleagues127 and Hulme and colleagues128). However, in the UK the recommended outcome measure in cost-effectiveness analysis is the QALY. 129 Calculation of QALYs requires a preference-based measure. At the present time there is no preference-based measure specific to oral health and, given that OHIP-14 is not preference based, QALYs cannot be derived directly from it. Within this study the OHIP-14 scores will also be mapped using regression techniques to the baseline EQ-5D-3L scores. Our analysis explores the potential for estimating utility scores that can be used to produce QALYs based on responses to the OHIP-14.
Methods
Outcome measures
Patient health-related quality of life was assessed using the OHIP-14115,116 and the EQ-5D-3L. 125,126 Patients completed both measures at baseline and at the end of the 24-month assessment period.
The OHIP-14 is a non-preference-based measure of the impact of oral disorders on individuals’ well-being. 115 It contains 49 questions (seven questions for each of the seven dimensions of impact of an oral condition) based on a theoretical model of oral health. 130 The OHIP-14 used here is a shorter version based on a subset of two questions for each of the seven dimensions. 116 The OHIP-14 questionnaire asks patients to rate the problems they had with their mouth, teeth or gums in the last 6 months. It consists of 14 items that capture seven dimensions of functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap. Response options to each of these items ranged between 0 and 4, with 4 = very often, 3 = fairly often, 2 = occasionally, 1 = hardly ever and 0 = never. The total OHIP-14 score was calculated using the additive method (i.e. the sum of the responses to the 14 items). This method was selected because of its operational simplicity and its effectiveness in measuring OHQoL between groups. 117 The total OHIP-14 score ranges between 0 and 56 points, with lower scores indicating better OHQoL.
The QALYs were estimated using the EQ-5D-3L. The EQ-5D-3L is a standardised generic instrument for use as a measure of health outcome. 126 It can be applied to a range of health conditions and treatments, and provides a health-state profile or a utility value index for an individual. In the EQ-5D-3L questionnaire, patients were asked to rate their health on five health-state dimensions. These dimensions were mobility (e.g. walking about); self-care (e.g. washing or dressing); usual activities (e.g. work, study, housework, family or leisure activities); pain/discomfort; and anxiety/depression. Each of the five health states has a three-level response (1 = no problems, 2 = some/moderate problems or 3 = extreme problems/unable). The item responses were converted to health-state utility values using an algorithm derived from a UK tariff. 131 The health-state values could take negative values (i.e. worse than death), but could not exceed 1 (i.e. full health). These utility values were then used to estimate QALYs using the area under the curve approach, in which 1 QALY is the equivalent of 1 year of full health. As any effects were observed over 2 years, discounting the QALY and OHIP-14 score was necessary. The recommended rate of 3.5% was used. 129
For the mapping exercise, we used baseline data from the EQ-5D-3L, OHIP-14 and information on other controls, including date of birth and sex. To simplify the analysis, the responses to each of the OHIP-14 items were recoded into three wide groups: ‘never’, ‘hardly ever’ and ‘occasionally/fairly often/very often’. These groups were also converted into indicator variables with values of zero indicating that there was no response in that group and values of 1 indicating a positive response in that group. Age was calculated in years using the reported year of birth and sex was coded 1 for male and 0 for female.
Resource use and costs
To recap, as set out in Chapter 2, within the incentive practices, 60% of the contract value is apportioned to delivery of a set number of UDAs. The remaining 40% is dependent on the delivery of quality: 20% systems, processes and infrastructure (e.g. cross-infection, policies, Standards for Better Health latterly becoming Care Quality Commission domains) and 20% OHImp. With the traditional practices, contracts are drawn up to deliver a set number of UDAs for an agreed financial value. Thus, all practices were paid the cost of the UDAs claimed, but incentive practices also received a ‘fixed’ cost equivalent to 40% of the total contract value (TCV).
Units of dental activity are based on three treatment bands (band 1: diagnosis, treatment planning and maintenance; band 2: simple treatment, e.g. fillings; and band 3: complex treatment, e.g. bridges or crowns). Each band attracts a set number of UDAs (band 1 = 1 UDA; band 2 = 3 UDAs; band 3 = 12 UDAs) and UDAs awarded for completed treatments. 2
It is important to note that the value of UDAs (i.e. the payment made for each UDA) varies between dental practices and thus UDA values vary from provider to provider. Typically, the greater the need for NHS dentists in an area the higher the UDA value.
For the analysis from the commissioner’s perspective, NHS England provided us with the financial value of UDAs for the traditional practices in the relevant years. The UDA value assigned to the incentive practices in this analysis includes the 40% of the contract value paid to the practices dependent on delivery of quality (systems, processes and infrastructure) and OHImp.
Information on the number, and value, of UDAs claimed per patient within the study was collected from recorded appointment history data from the practices.
The analysis from the service provider’s perspective included information on the number and duration of appointment; the type of treatment; and the dental professional carrying out the appointment/treatment. This information was provided by the dental practices and taken from the appointment history of each patient. Material costs such as the cost of radiographic film or the cost of filling materials are based on the Kent Express Catalogue132 and are shown in Table 28. The salaries of the different staff involved in the treatment were obtained from national sources such as the Pay Circular134 and the NHS Agenda for Change135 and overhead costs were calculated using the same method as in Hulme and colleagues128 (Table 29). Costs and salaries are adjusted for inflation using the CCEMG-EPPI (Campbell and Cochrane Economics Methods Group – Evidence for Policy and Practice Information and Co-ordinating Centre) cost converter. 136 Discounting of costs was also necessary and a discount rate of 3.5% was used. 129
| Material | Description | Cost (£) | Source |
|---|---|---|---|
| Radiograph | Optimum film | 0.33 | Kent Express Catalogue (2014)132 |
| Periapical film | 0.28 | ||
| Amalgam filling | 1 spill | 0.90 | |
| Dycal® Radiopaque calcium hydroxide cements liner [DENTSPLY International, York, PA, USA (base 13 g and catalyst 11 g)] | 21.20 | ||
| Laboratory | |||
| Denture | Full upper or lower only with standard teeth (× 2 for full over full) | 167.05 | MGill price list (2011)133 |
| Crown | – | 116.00 | |
| Bridge | – | 131.00 | |
| Staff | Per hour (£) | Source | |||
|---|---|---|---|---|---|
| Dentist | 32.89 | Pay Circular (M&D) 1/2011 reference134 | |||
| Therapist | 16.59 | NHS Agenda for Change pay scales–2011/2012135 | |||
| Hygienist | 13.56 | ||||
| Oral health educator | 11.17 | ||||
| Overheads | % of income | Dentist | Therapist | Hygienist | Oral health educator |
| Wages and National Insurance (per hour) | 17.42 | £32.89 | £16.59 | £13.56 | £11.17 |
| Overheads (per hour) | 12.77 | £24.11 | £12.16 | £9.94 | £8.19 |
Cost-effectiveness
The outcome of the cost-effectiveness analyses was the incremental cost per unit change in the OHIP-14 score and the cost per QALY. We present ICERs representing the ratios of the incremental cost and incremental benefits (OHIP-14 points/QALYs) between incentive and traditional care practices. The ICER represents the additional cost per one unit of outcome gained, in this case per OHIP-14 point lost/QALY gained for incentive versus traditional practices. As a guideline rule, NICE129 accepts as cost-effective those interventions with an ICER of < £20,000 per QALY. The NICE guidelines129 state that, in general, a treatment that costs > £30,000 per QALY would not be considered cost-effective. In addition, we present cost-effectiveness plane scatterplots showing the uncertainty surrounding the cost-effectiveness estimates. The cost-effectiveness planes were derived using bootstrapping with replacement. This stochastic uncertainty analysis involved running 10,000 bootstrapped estimates of the incremental costs and QALYs/OHIP-14 scores. The bootstrap approach is a non-parametric method that treats the original sample as though it was the population and draws multiple random samples from the original sample. Cost-effectiveness acceptability curves (CEACs) were also generated to illustrate the probability that each treatment would be cost-effective given a range of acceptable threshold values. 137
Sensitivity analyses were further carried out to account for uncertainty in the cost values. For the commissioner’s perspective, we performed one-way sensitivity analyses by assuming either no change or a 3% increase in the TCV per (financial) year or a 0%, 10% increase or 10% decrease in the number of patients treated per year. For the analysis from the service provider’s perspective, costs were altered by ± 20%. Although these values are essentially arbitrary, it was considered likely to represent any uncertainty in the cost values.
Missing data
Following Slade and colleagues,122 we used median imputation if one or two OHIP-14 item scores were missing. Participants in whom more than two components of the OHIP-14 were missing or or for whom EQ-5D-3L at baseline and follow-up was missing are excluded from the analysis. Multiple imputation was also used to attempt to deal with missing EQ-5D-3L/OHIP-14 scores at follow-up; however, the missing values were not missing at random, making this technique not appropriate to use here (see Appendix 3 for more details).
Mapping the Oral Health Impact Profile-14 to the European Quality of Life-5 Dimensions questionnaire
In mapping the OHIP-14 to the EQ-5D-3L, we used the methods set out by Brennan and Spencer. 138 Using baseline data, we split the data into estimation and validation samples. We ran different types of models in which the observed EQ-5D-3L was the dependent variable and the OHIP-14 items, age, age squared (to account for a potential non-linear relationship between age and the EQ-5D-3L) and sex were the independent variables.
First, we ran an ordinary least squares (OLS) regression. A common phenomenon observed in the health profile (EQ-5D-3L) is that its distribution is skewed to the left (i.e. a large proportion of the sample is at full health – known as a ceiling effect), which we also observed in the data (Figure 18 shows an illustration).
FIGURE 18.
Distribution of observed EQ-5D-3L.
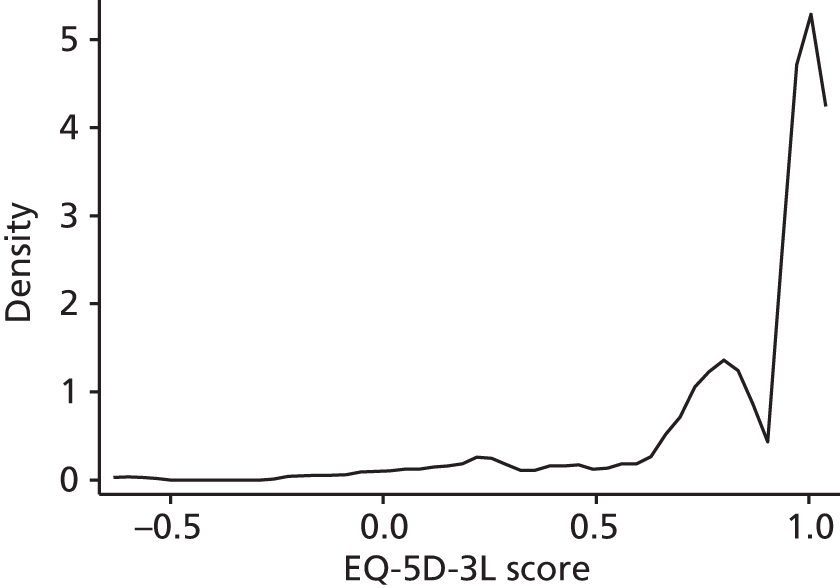
This ceiling effect makes OLS regression inappropriate as it will give biased and inconsistent results. The Tobit model is proposed as a solution, often used in ‘mapping’ studies. 138,139 Simply, in the Tobit model the unobservable EQ-5D-3L linearly depends on the independent variables. Then, the observable EQ-5D-3L is equal to the unobserved one whenever the true unobservable EQ-5D-3L is greater than or equal to the ceiling value (1 in our case). The Tobit model also assumes that the error terms are normally distributed with uniform variance (homoscedasticity), but evidence suggests that the distribution of utility scores does not follow these assumptions. 140 Therefore, results from Tobit should be interpreted cautiously. A more flexible approach to address the fact that utility scores usually have mixed distributions (i.e. the majority of observations are at the ceiling and there is a left-skewed distribution not at the ceiling) is the two-part model (TPM). In the TPM, the respondents reporting full health in all five health states of the EQ-5D-3L are modelled separately from those reporting all other EQ-5D-3L scores. The logic is that individuals reporting full health in all states are different in some fundamental way from others who report at least one problem in any of the EQ-5D-3L dimensions. For this reason, in the first stage we used the logit regression to estimate the probability of reporting full health in the whole sample, whereas in the second stage OLS regression was used to estimate an EQ-5D-3L score for those without full health.
The possibility of adding more control variables was also examined as there was available information on the risk of an oral disease. However, the high number of missing values in these variables at baseline made most of the estimations impossible.
All analyses were conducted using Stata (StataCorp LP, College Station, TX, USA) and Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA).
Results
Sample
A total of 550 patients were recruited in this study (see Chapter 4). A total of 210 of those patients were included in the cost-effectiveness analyses. In detail, four patients withdrew prior to their appointment, five patients did not have appointment history data at baseline and/or follow-up (hence costs could not be estimated) and 289 patients did not complete the follow-up assessment. From the remaining 252 patients, 42 patients had more than two components of the OHIP-14 missing or were missing EQ-5D-3L at baseline and follow-up, and were excluded from the analysis (13 patients at baseline and 10 patients at follow-up had two or fewer OHIP-14 item scores missing so we were able to impute the missing data and include these in the analysis). Therefore, for 210 patients (108 from incentive practices and 102 from traditional practices) data were complete [costs, EQ-5D-3L and OHIP-14 (after imputation for those with only one missing item)] and were included in the cost-effectiveness analyses. Baseline characteristics of the patients are presented in Table 30. There are no statistically significant differences in age, sex or ethnicity between those included in these analyses and those lost to follow-up.
Resource use and costs
Table 31 shows the average number of UDAs per person over the 2 years of the study. There are negligible differences in the average number of UDAs per person if the treatment/appointment was carried out by a dentist. It is difficult to draw conclusions for the therapist and hygienist as some of the incentive and/or traditional practices did not have these dental professionals. Table 32 shows the average number of appointments per person over the study. Patients in the incentive practices had more appointments, on average, than those in the traditional practices. The picture is similar when looking at the appointments carried out by a dentist. Patients in both groups had, on average, the same number of appointments with an oral health educator. Again, it is not possible to compare incentive with traditional practices with regards to the number of appointments performed by the rest of the dental professionals.
| Dental profession | Incentive practices, mean (SD) | Traditional practices, mean (SD) |
|---|---|---|
| All | 11.23 (8.08) | 10.74 (8.23) |
| Dentist | 10.70 (8.07) | 10.58 (8.25) |
| Therapist | 0.65 (1.66) | N/A |
| Hygienist | N/A | 4.05 (6.10) |
| Oral health educator | 0.80 (1.30) | 0.00 (–)a |
| Dental profession | Incentive practices, mean (SD) | Traditional practices, mean (SD) |
|---|---|---|
| All | 8.89 (4.50) | 6.63 (2.93) |
| Dentist | 7.13 (4.02) | 6.56 (2.95) |
| Therapist | 2.28 (1.60) | N/A |
| Hygienist | N/A | 1.50 (1.00) |
| Oral health educator | 1.00 (0.00) | 1.00 (–)a |
For the patients who were lost to follow-up (and those for whom we had appointment data), the average number of dental appointments was 7.97 (SD 5.34; n = 152) for the incentive practices and 4.99 (SD 3.53; n = 131) for the traditional practices. Treatment within these appointments included fillings, dentures and crowns. For example, 72% of patients in the incentive practices and 60% in the traditional practices had one or more fillings; 77% and 69%, respectively, had radiographs taken; 8% and 20%, respectively, had dentures made; and 6% and 5%, respectively, had a crown.
For the 210 people included in the health economics study, the mean time spent with the dental professional by group is presented in Table 33. On average, dentists in the incentive practices spent less time with patients than dentists in the traditional practices and therapists in incentive practices spent more time with patients than therapists in traditional practices.
| Dental profession | Time (minutes) | |
|---|---|---|
| Incentive practices, mean (SD) | Traditional practices, mean (SD) | |
| Dentist | 16.91 (7.35) | 24.44 (10.46) |
| Therapist | 23.89 (10.49) | N/A |
| Hygienist | N/A | 21.25 (8.54) |
| Oral health educator | 22.00 (4.47) | 20.00 (–)a |
Costs from the perspective of the commissioner
The UDA value paid for each of the practices is shown in Table 34 (the incentive UDA value includes the 40% of the contract dependent on quality and processes).
| Practice | Pounds sterling (£) |
|---|---|
| Incentive practice | |
| 1 | 33.69 |
| 2 | 33.62 |
| 3 | 33.62 |
| Traditional practice | |
| 4 | 27.31 |
| 5 | 25.47 |
| 6 | 28.80 |
The mean per-person cost over the study for the incentive practices is £459.77 and for the traditional practices is £281.57 (Table 35).
| Practice | Cost (£), mean (SD) |
|---|---|
| Incentive practice | |
| 1 | 518.37 (269.04) |
| 2 | 507.22 (287.06) |
| 3 | 286.26 (181.37) |
| Traditional practice | |
| 4 | 291.99 (206.09) |
| 5 | 256.36 (203.20) |
| 6 | 370.29 (319.10) |
Costs from the perspective of the dental provider
As highlighted earlier, the costs to the dental provider are made up of the practitioners’ time, materials and laboratory costs. In addition, the dental surgeries receive a payment for UDAs delivered (incentive and traditional practices). The sum of these payments is subtracted from the costs accruing to the dental provider (time/materials/laboratory costs). These payments are the cost to the commissioner detailed in the previous section.
The mean cost of the materials and any laboratory cost per person are presented in Table 36.
| Materials | Incentive practices: cost (£), mean (SD) | Traditional practices: cost (£), mean (SD) | ||||
|---|---|---|---|---|---|---|
| Dentist | Therapist | Oral health educator | Dentist | Hygienist | Oral health educator | |
| Radiographic film | 0.75 (0.46) | 0.32 (0.00) | N/A | 0.54 (0.34) | N/A | N/A |
| Periapical film | 0.46 (0.26) | 0.27 (0.00) | N/A | N/A | N/A | N/A |
| Filling | 8.59 (7.87) | 4.95 (3.78) | N/A | 8.98 (6.34) | N/A | N/A |
| Denture | 243.67 (123.31) | N/A | N/A | 234.71 (110.26) | N/A | N/A |
| Crown | 134.53 (44.49) | N/A | N/A | 162.98 (76.56) | N/A | N/A |
| Bridge | 132.93 (–) | N/A | N/A | N/A | N/A | N/A |
The costs are combined with the cost of the time spent by the different dental professionals, and the per-patient cost of UDAs (see Table 35) to find the per-patient cost from the perspective of the service provider. The mean per-person cost from the perspective of the service provider for the incentive practices is –£209.26, whereas for the traditional practices the mean cost is –£116.21 (Table 37).
| Resource | Incentive practices: cost (£), mean (SD) | Traditional practices: cost (£), mean (SD) |
|---|---|---|
| Time of dental professionals | 195.63 (102.92) | 107.02 (55.55) |
| Materials and laboratory costs | 54.88 (114.47) | 58.34 (111.25) |
| Total | 250.51 (186.85) | 165.37 (146.28) |
| Payment to providers | 459.77 (278.42) | 281.57 (218.71) |
| Total mean health-care costs | –209.26 (123.36) | –116.21 (99.16) |
Outcome (quality-of-life) data
Overall, improvement in the OHIP-14 scores between baseline and follow-up is observed in both the incentive and traditional practice groups (Table 38). However, no statistically significant difference in EQ-5D-3L score was found between groups or over time. There are no statistically significant differences in the OHIP-14 scores between groups, but there are statistically significant differences (at the 5% level) in these scores over time in both groups.
| Time point | Incentive practices (n = 108) | Traditional practices (n = 102) |
|---|---|---|
| Baseline, mean (SD) | 8.99 (10.30) | 9.12 (10.98) |
| Follow-up (24 months), mean (SD) | 5.60 (7.58) | 7.38 (8.89) |
| Change, mean (p-value) | 3.39 (< 0.001) | 1.74 (0.051) |
In addition, the changes in the EQ-5D-3L scores by group (or over time) are negligible (Table 39), making it difficult to draw any conclusions about the impact of the new care practice on the patients’ general health-related quality of life.
| Time point | Incentive practices (n = 108) | Traditional practices (n = 102) |
|---|---|---|
| Baseline, mean (SD) | 0.880 (0.250) | 0.896 (0.232) |
| Follow-up (24 months), mean (SD) | 0.882 (0.207) | 0.897 (0.257) |
| Change, mean (p-value) | –0.018 (0.235) | 0.014 (0.552) |
Cost-effectiveness results
Table 40 shows the costs, from the commissioner’s perspective, and changes in OHIP-14 scores for each of the two groups. The traditional practices had lower costs and higher OHIP-14 scores (i.e. patients in the traditional practices had worse OHQoL). This represents an estimated cost of £199.22 per 1-point decrease (improvement) in OHIP-14 score for the incentive practices.
| Practice | Costs (£), mean (SD) | OHIP-14 score (points), mean (SD) | |
|---|---|---|---|
| Incentive | 459.77 (278.42) | 7.110 (7.673) | |
| Traditional | 281.57 (218.71) | 8.005 (8.699) | |
| Incremental cost (£) | Incremental OHIP-14 score | ICER (£/OHIP-14 point) | |
| Incentive vs. traditional practices | 178.20 | –0.895 | 199.22 |
Similarly, Table 41 shows the costs from the service provider’s perspective. In incentive practices, costs to the dental providers were lower (a greater surplus once costs and income from payments for services delivered had been taken into account) and health outcomes were better. Thus, from the dental provider’s perspective incentive dominates traditional practice.
| Practice | Costs (£), mean (SD) | OHIP-14 (points), mean (SD) | |
|---|---|---|---|
| Incentive | –209.26 (123.36) | 7.110 (7.673) | |
| Traditional | –116.21 (99.16) | 8.005 (8.699) | |
| Incremental cost (£) | Incremental OHIP-14 score | ICER (£/OHIP-14 point) | |
| Incentive vs. traditional practices | –93.05 | –0.895 | –104.03 (incentive dominates) |
Similarly, Tables 42 and 43 show the costs and QALYs for each of the two groups. They also provide the incremental costs and benefits (expressed as QALY gains) as well as the ICER. Any interpretation in this case should be tempered given the negligible differences in QALY gains between the two groups.
| Practice | Costs (£), mean (SD) | QALYs, mean (SD) | |
|---|---|---|---|
| Incentive | 459.77 (278.42) | 1.659 (0.451) | |
| Traditional | 281.57 (218.71) | 1.660 (0.342) | |
| Incremental cost (£) | Incremental QALYs | ICER (£/QALY) | |
| Incentive vs. traditional practices | 178.20 | –0.0008 | Incentive dominated |
| Practice | Costs (£), mean (SD) | QALYs, mean (SD) | |
|---|---|---|---|
| Incentive | –209.26 (123.36) | 1.659 (0.451) | |
| Traditional | –116.21 (99.16) | 1.660 (0.342) | |
| Incremental cost (£) | Incremental QALYs | ICER (£/QALY) | |
| Incentive vs. traditional practices | –93.05 | –0.0008 | 122,089.48 |
Figure 19 shows the cost-effectiveness plane for incentive care practice compared with traditional care practice using the QALY outcome measure from the commissioner’s perspective. The sample estimates are spread mainly in the north-west and north-east quadrants, suggesting that incentive care practice is unlikely to be cost-effective from the commissioner’s perspective. Iteration results seem to be equally spread in north-east and north-west quadrants, making it difficult to draw conclusions on which of the two care practices leads to better general health-related quality of life. Similarly, Figure 20 shows the cost-effectiveness plane for incentive care practice compared with traditional care practice using the QALY outcome measure from the perspective of the service provider. Iteration results in this case are spread in the south-west and south-east quadrants, indicating that incentive practices had lower costs than traditional dental practices.
FIGURE 19.
Cost-effectiveness plane for incentive care practice compared with traditional care practice (outcome measure: QALY, commissioner’s perspective).
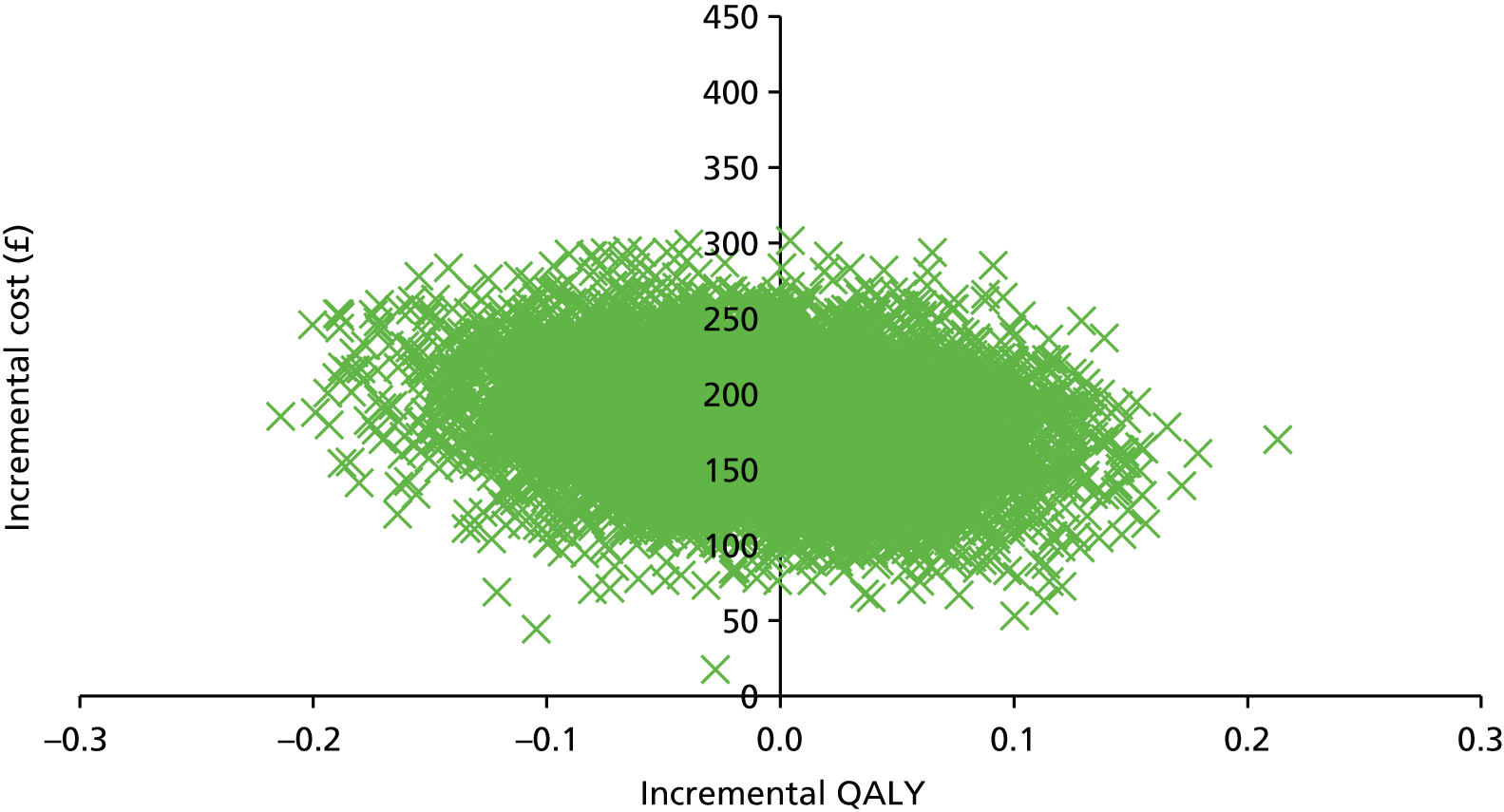
FIGURE 20.
Cost-effectiveness plane for incentive care practice compared with traditional care practice (outcome measure: QALY, service provider’s perspective).
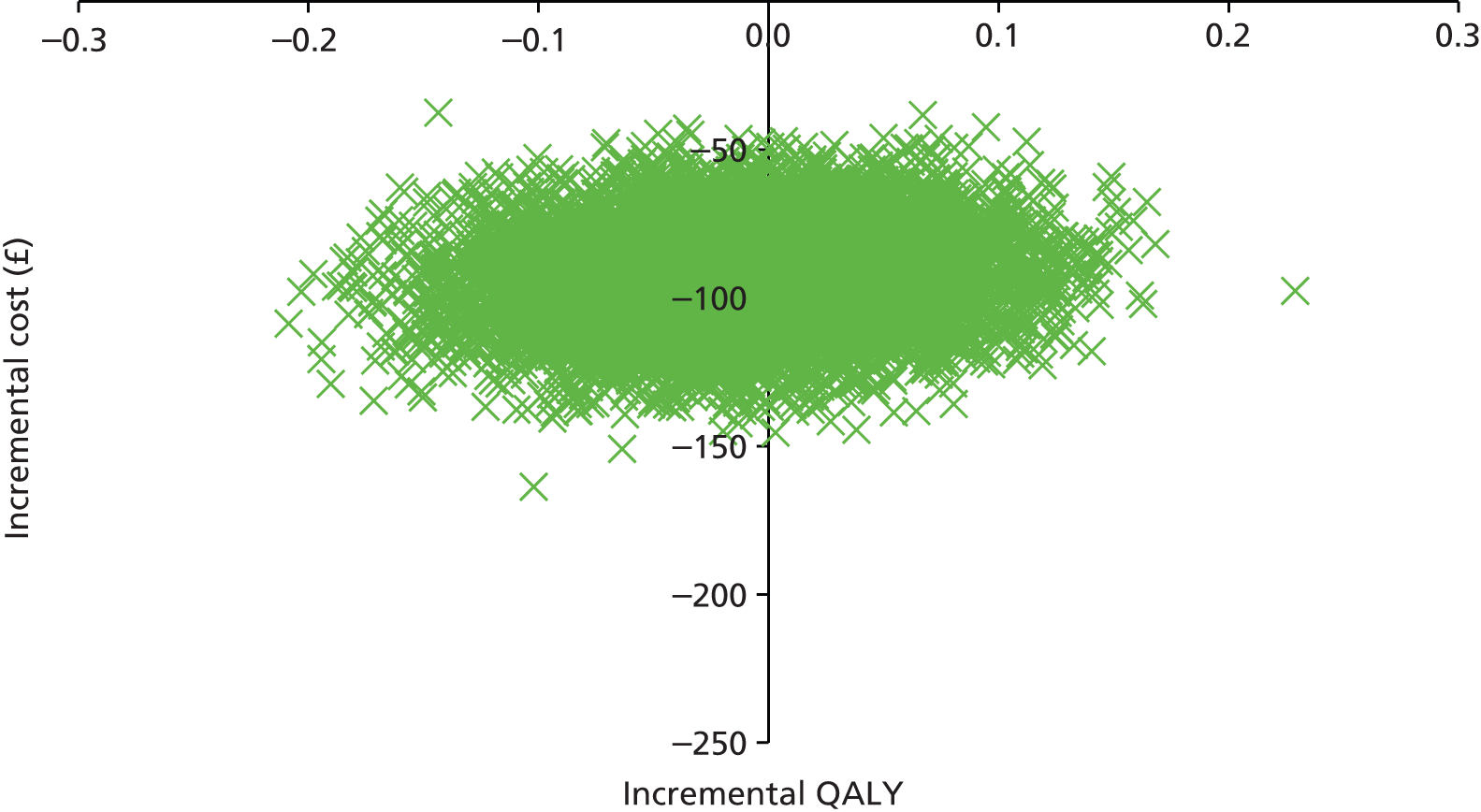
Figures 21 and 22 show the cost-effectiveness plane for incentive care practice compared with traditional care practice using the OHIP-14, from the commissioner’s and service provider’s perspectives, respectively. From the commissioner’s perspective, the estimated ICERs are mostly located in the north-east quadrant, implying that incentive is more effective with regards to improving OHQoL, but more expensive than traditional care practice. For the service provider, the ICERs are mostly spread in the south-east quadrant, suggesting, again, that incentive is more effective than traditional care practice in terms of improving OHQoL.
FIGURE 21.
Cost-effectiveness plane for incentive care practice compared with traditional care practice (outcome measure: OHIP-14 score, commissioner’s perspective).
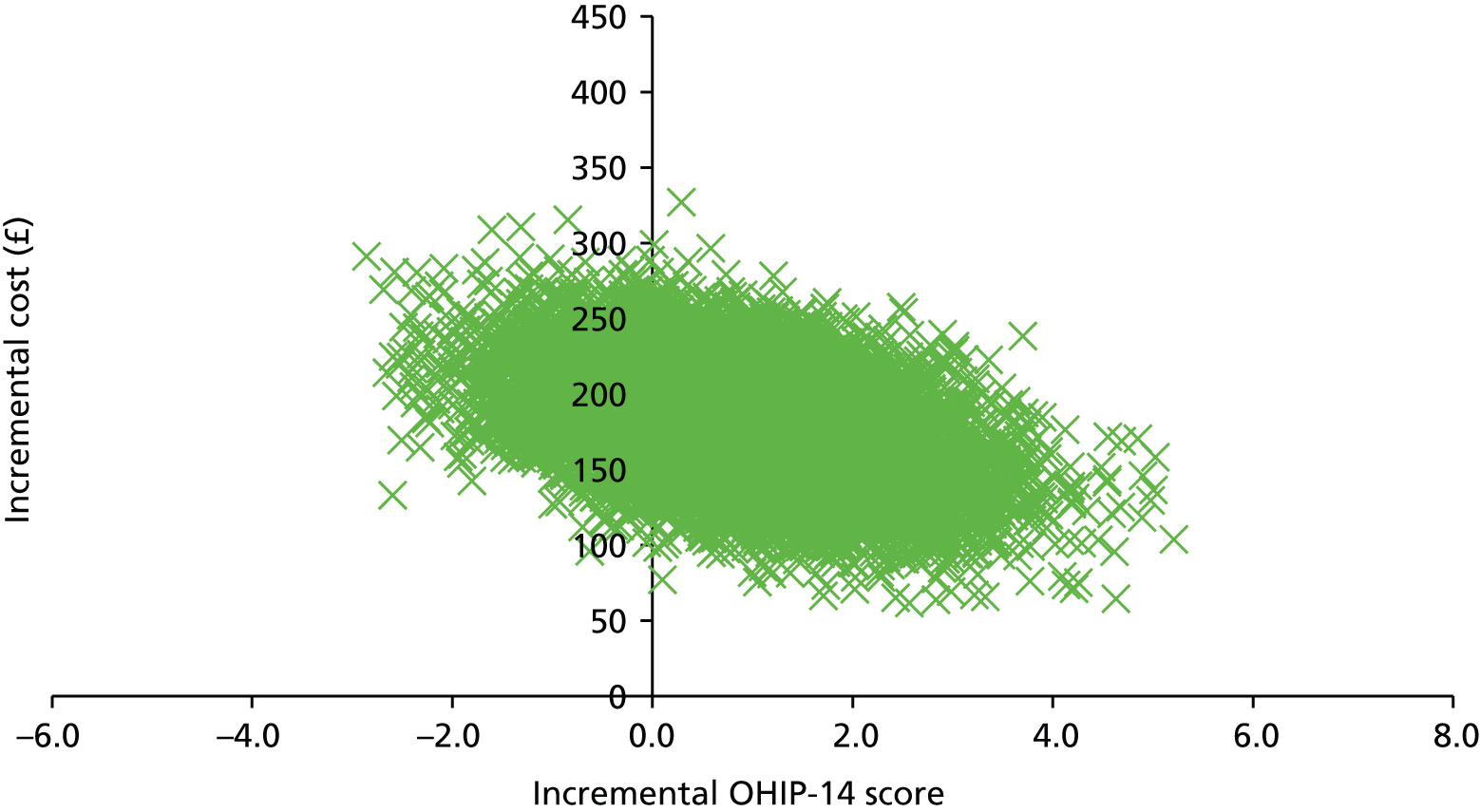
FIGURE 22.
Cost-effectiveness plane for incentive care practice compared with traditional care practice (outcome measure: OHIP-14 score, service provider’s perspective).
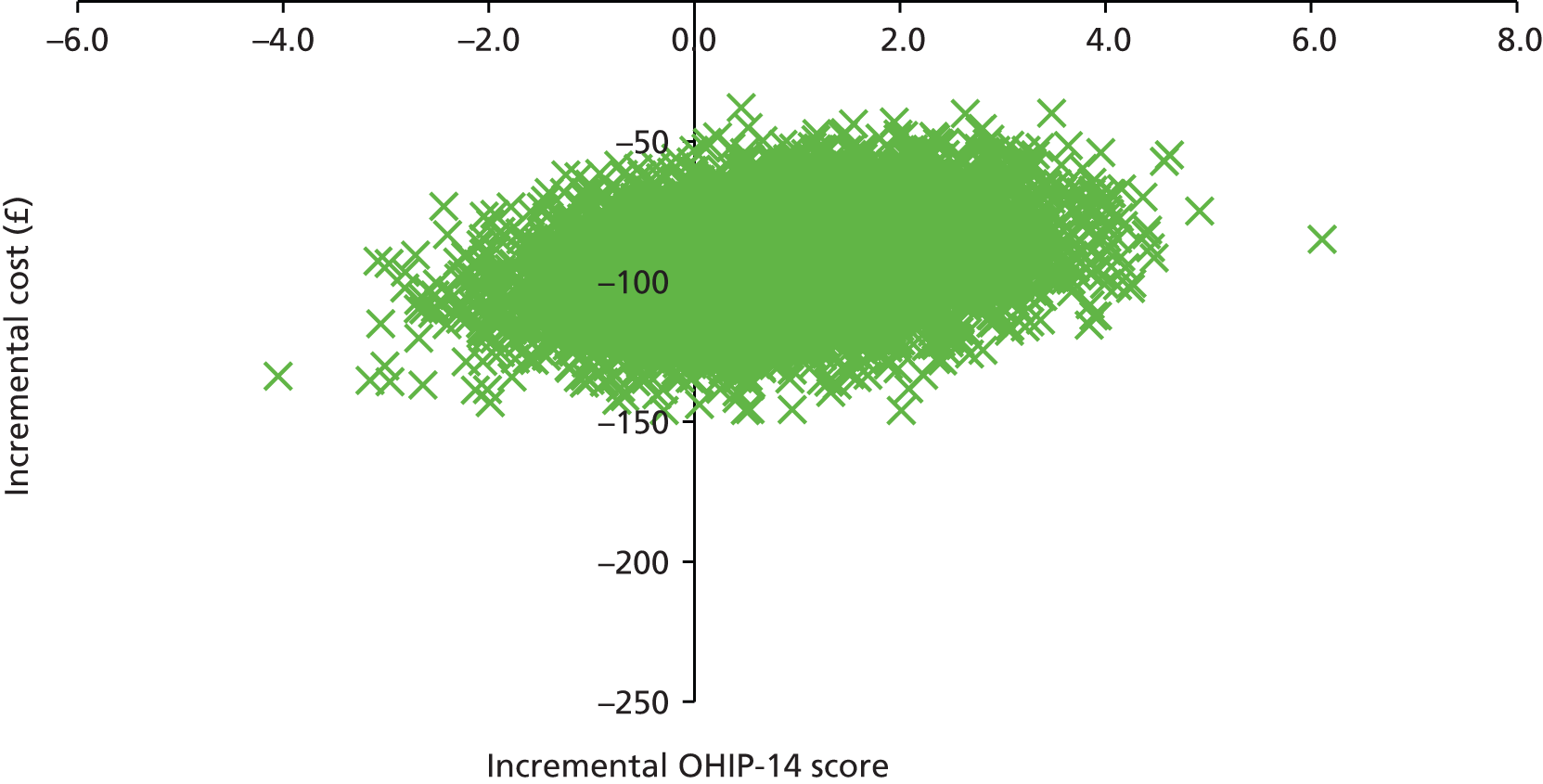
To account for uncertainty around mean incremental costs and effectiveness, we conducted sensitivity analyses and non-parametric bootstrapping (Tables 44 and 45). From the commissioner’s perspective, the univariate sensitivity analysis varied the TCV per year by 0% or 3%. We also looked at the case that the number of patients treated remained the same per year or increased/decreased by 10%. From the service provider’s perspective, we added and subtracted 20% of the total costs and assessed the subsequent impact on the ICERs. The ICER estimates from the bootstrapping were similar to those of the deterministic base-case scenario from both perspectives.
| Incentive vs. traditional practices | Incremental cost (£) | Incremental OHIP-14 | ICER (£/OHIP-14 point) |
|---|---|---|---|
| TCV 0% change per year | 177.09 | –0.895 | 197.97 |
| TCV 3% increase per year | 187.99 | –0.895 | 210.16 |
| Number of patients treated 0% change per year | 179.34 | –0.895 | 200.49 |
| Number of patients treated 10% increase per year | 179.72 | –0.895 | 200.92 |
| Number of patients treated 10% decrease per year | 199.26 | –0.895 | 222.76 |
| Bootstrapping (10,000 replications) | 179.75 | –0.862 | 208.59 |
| Incremental cost (£) | Incremental QALY | ICER (£/QALY) | |
| TCV 0% change per year | 177.09 | –0.0008 | Incentive dominated |
| TCV 3% increase per year | 187.99 | –0.0008 | Incentive dominated |
| Number of patients treated 0% change per year | 179.34 | –0.0008 | Incentive dominated |
| Number of patients treated 10% increase per year | 179.72 | –0.0008 | Incentive dominated |
| Number of patients treated 10% decrease per year | 199.26 | –0.0008 | Incentive dominated |
| Bootstrapping (10,000 replications) | 180.42 | –0.0088 | Incentive dominated |
| Incentive vs. traditional practices | Incremental cost (£) | Incremental OHIP-14 | ICER (£/OHIP-14 point) |
|---|---|---|---|
| 20% increase in costs | –111.66 | –0.895 | –124.83 (incentive dominates) |
| 20% decrease in costs | –74.44 | –0.895 | –83.22 (incentive dominates) |
| Bootstrapping (10,000 replications) | –92.76 | –0.830 | –111.82 (incentive dominates) |
| Incremental cost (£) | Incremental QALY | ICER (£/QALY) | |
| 20% increase in costs | –111.66 | –0.0008 | 146,507.37 |
| 20% decrease in costs | –74.44 | –0.0008 | 97,671.58 |
| Bootstrapping (10,000 replications) | –92.79 | –0.0098 | 9483.68a |
Figures 23 and 24, the CEACs, show the probability that the incentive care practice will be cost-effective compared with traditional care practice given a range of threshold values between £0 and £60,000 per QALY. The curve is based on 10,000 replications. Using the threshold of £20,000 that is recommended by NICE, from the commissioner’s (service provider’s) perspective the probability that incentive care practice is effective is 0.37 (0.47), compared with a probability of 0.63 (0.53) for the traditional care practice. At lower levels of willingness-to-pay thresholds (< £18,000) there is a lower (higher) probability of the incentive care practice being cost-effective from the commissioner’s (service provider’s) perspective. It is worth reiterating at this point that, although we have presented the sensitivity analysis and bootstrapping results, the results should be interpreted with caution given the negligible difference between the QALYs in incentive and traditional practices.
FIGURE 23.
Cost-effectiveness acceptability curve based on bootstrap replications for incentive compared with traditional practice care (outcome measure: QALY, commissioner’s perspective).
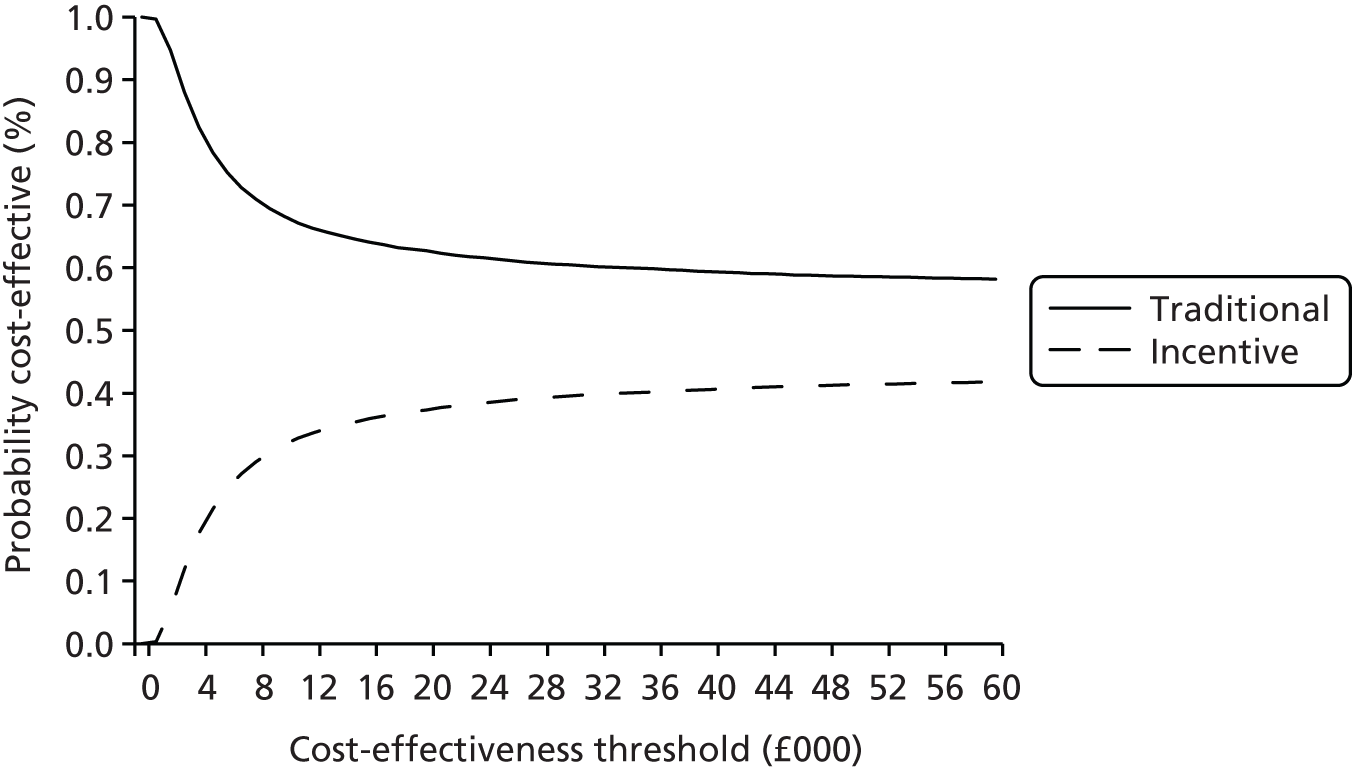
FIGURE 24.
Cost-effectiveness acceptability curve based on bootstrap replications for incentive compared with traditional practice care (outcome measure: QALY, service provider’s perspective).
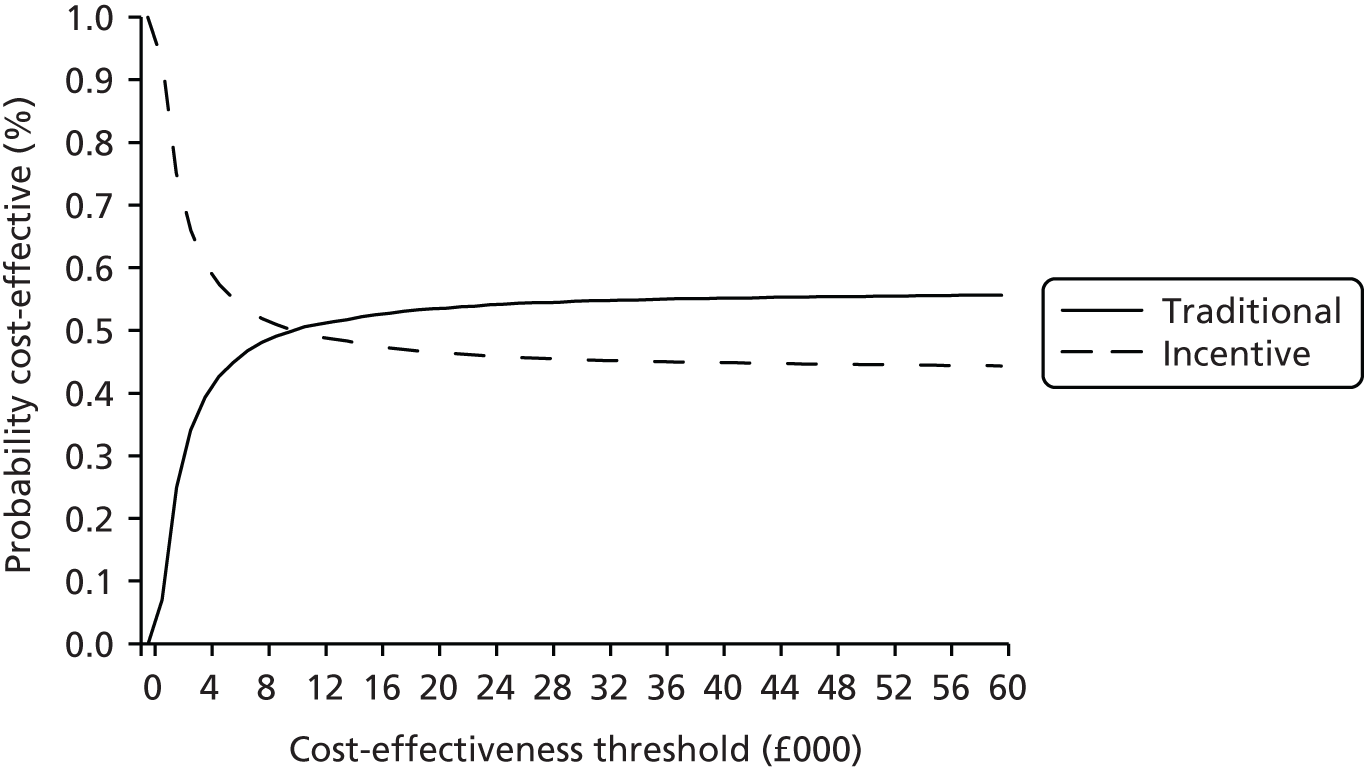
Results mapping
Characteristics of patients
As described in the earlier Methods section, for this analysis we used only baseline data. We included all participants who had fully completed the EQ-5D-3L and OHIP-14 questionnaires. Details of our sample in this part of the analysis are reported in Table 46. Females accounted for slightly more than half of the sample (50.8%) and the mean age was 40.4 years. The mean EQ-5D-3L was 0.852 with a 95% CI of 0.829 to 0.875. Many patients, more than 30%, reported no symptoms in all OHIP-14 items. Only a few reported that the symptoms occurred ‘occasionally/fairly often/very often’, with responses ranging from 0.77% for ‘trouble in pronouncing words’ to 14.09% for ‘felt self-conscious’. Symptoms were ‘hardly ever’ for a bigger percentage of the sample, ranging from 18.34% for ‘unable to function’ up to 54.74% for ‘uncomfortable eating’. The mean values for the OHIP-14 items ranged from 0.203 for ‘unable to function’ to 0.710 for ‘uncomfortable eating’.
| Variable | n | Per cent | Mean | 95% CI | |
|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||
| Trouble pronouncing words | 519 | 0.216 | 0.179 | 0.253 | |
| Never | 79.19 | ||||
| Hardly ever | 20.04 | ||||
| Occasionally/fairly often/very often | 0.77 | ||||
| Sense of taste worsened | 519 | 0.268 | 0.226 | 0.309 | |
| Never | 74.95 | ||||
| Hardly ever | 23.31 | ||||
| Occasionally/fairly often/very often | 1.73 | ||||
| Painful aching in mouth | 513 | 0.639 | 0.590 | 0.689 | |
| Never | 40.94 | ||||
| Hardly ever | 54.19 | ||||
| Occasionally/fairly often/very often | 4.87 | ||||
| Uncomfortable eating | 517 | 0.710 | 0.657 | 0.762 | |
| Never | 37.14 | ||||
| Hardly ever | 54.74 | ||||
| Occasionally/fairly often/very often | 8.12 | ||||
| Felt self-conscious | 518 | 0.708 | 0.648 | 0.769 | |
| Never | 43.24 | ||||
| Hardly ever | 42.66 | ||||
| Occasionally/fairly often/very often | 14.09 | ||||
| Felt tense | 514 | 0.533 | 0.479 | 0.587 | |
| Never | 53.89 | ||||
| Hardly ever | 38.91 | ||||
| Occasionally/fairly often/very often | 7.20 | ||||
| Diet unsatisfactory | 519 | 0.362 | 0.315 | 0.410 | |
| Never | 67.24 | ||||
| Hardly ever | 29.29 | ||||
| Occasionally/fairly often/very often | 3.47 | ||||
| Interrupt meals | 515 | 0.400 | 0.352 | 0.448 | |
| Never | 63.50 | ||||
| Hardly ever | 33.01 | ||||
| Occasionally/fairly often/very often | 3.50 | ||||
| Difficulty relaxing | 517 | 0.478 | 0.428 | 0.527 | |
| Never | 56.09 | ||||
| Hardly ever | 40.04 | ||||
| Occasionally/fairly often/very often | 3.87 | ||||
| Been embarrassed | 520 | 0.621 | 0.562 | 0.680 | |
| Never | 49.62 | ||||
| Hardly ever | 38.65 | ||||
| Occasionally/fairly often/very often | 11.73 | ||||
| Irritable with other people | 518 | 0.392 | 0.341 | 0.442 | |
| Never | 66.02 | ||||
| Hardly ever | 28.76 | ||||
| Occasionally/fairly often/very often | 5.21 | ||||
| Difficulty doing usual jobs | 520 | 0.262 | 0.220 | 0.303 | |
| Never | 75.58 | ||||
| Hardly ever | 22.69 | ||||
| Occasionally/fairly often/very often | 1.73 | ||||
| Life less satisfying | 519 | 0.432 | 0.379 | 0.484 | |
| Never | 63.01 | ||||
| Hardly ever | 30.83 | ||||
| Occasionally/fairly often/very often | 6.17 | ||||
| Unable to function | 518 | 0.203 | 0.166 | 0.239 | |
| Never | 80.69 | ||||
| Hardly ever | 18.34 | ||||
| Occasionally/fairly often/very often | 0.97 | ||||
| EQ-5D-3L | 507 | 0.852 | 0.829 | 0.875 | |
| Age (in years) | 528 | 40.4 | 39.11 | 41.76 | |
| Sex | 528 | ||||
| Female | 50.76 | ||||
Regression results
Figure 25 shows the actual versus the predicted health-state values. The graphs are presented separately for the OHIP-14 items as continuous and categorical variables. OLS, Tobit and the TPM seem to perform similarly in the categorical model. In the continuous model, the TPM seems to better predict the EQ-5D-3L values than OLS and Tobit.
FIGURE 25.
Actual vs. predicted health-state values. (a) OLS continuous model; (b) OLS categorical model; (c) Tobit continuous model; (d) Tobit categorical model; (e) two-part continuous model; and (f) two-part categorical model.
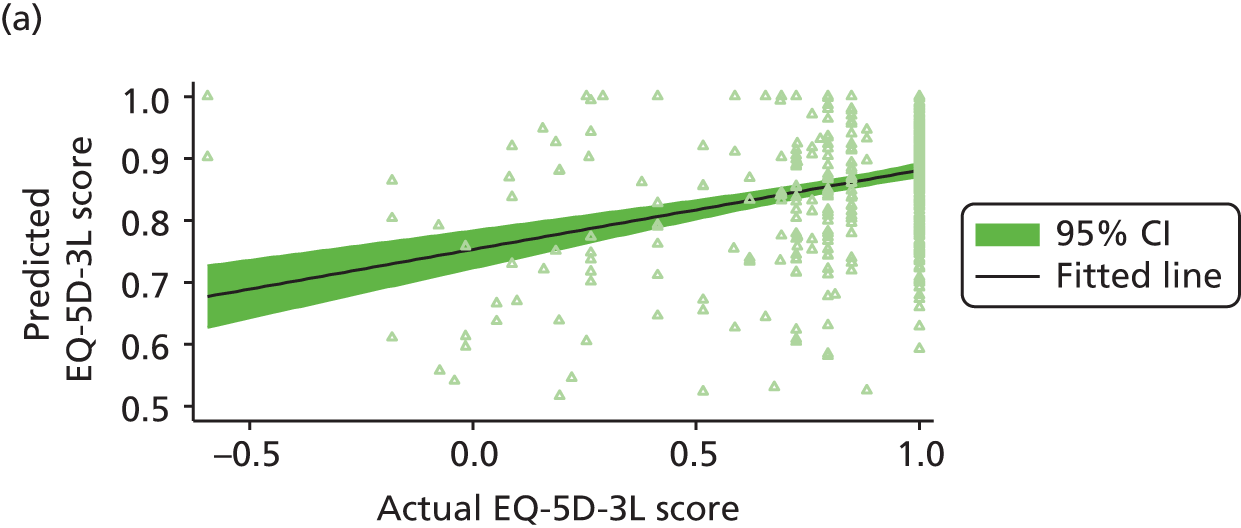
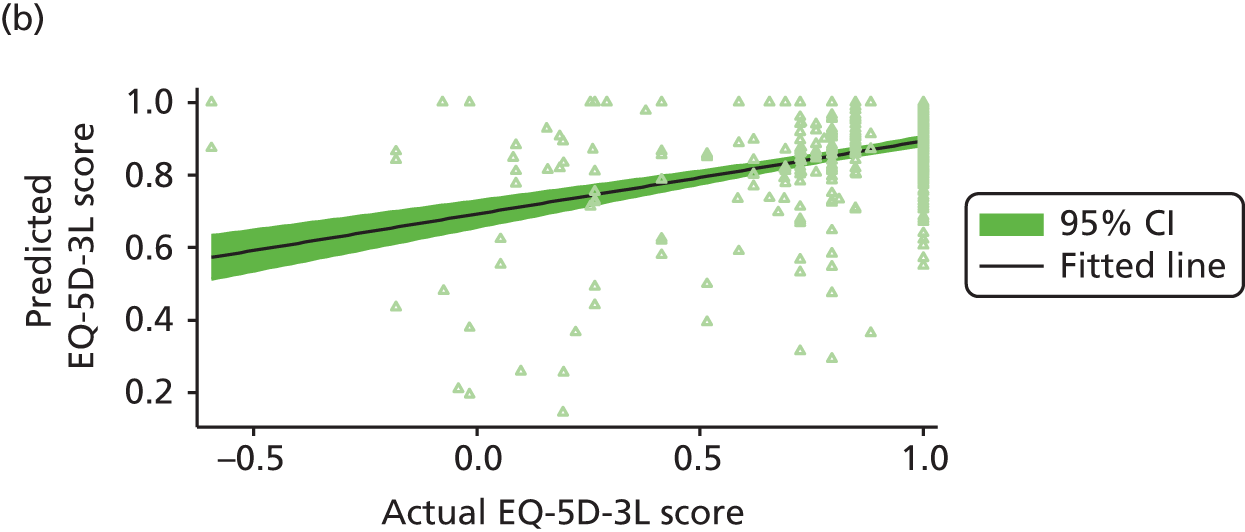
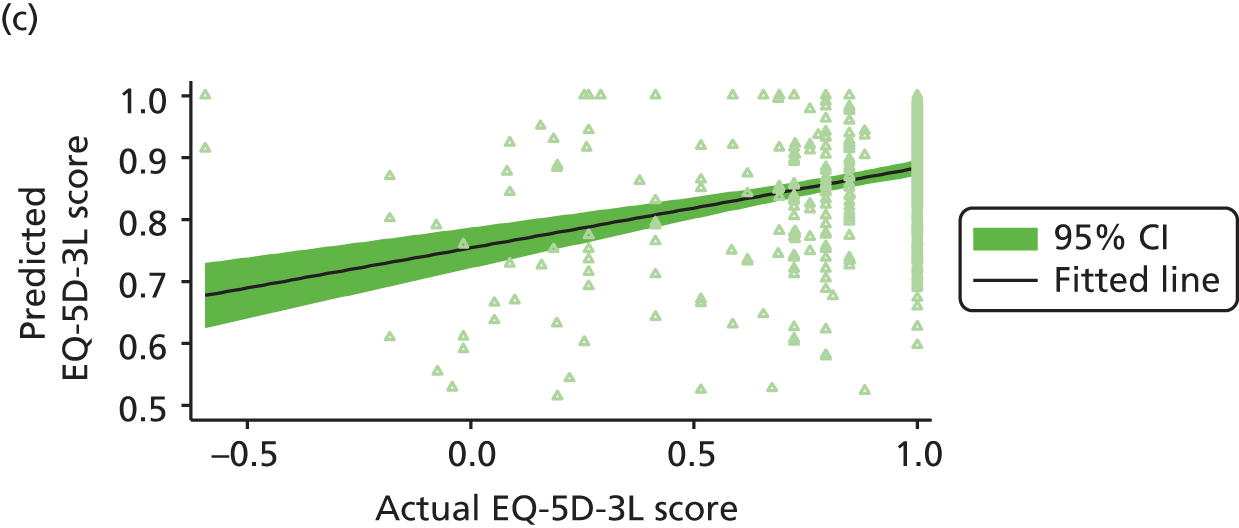
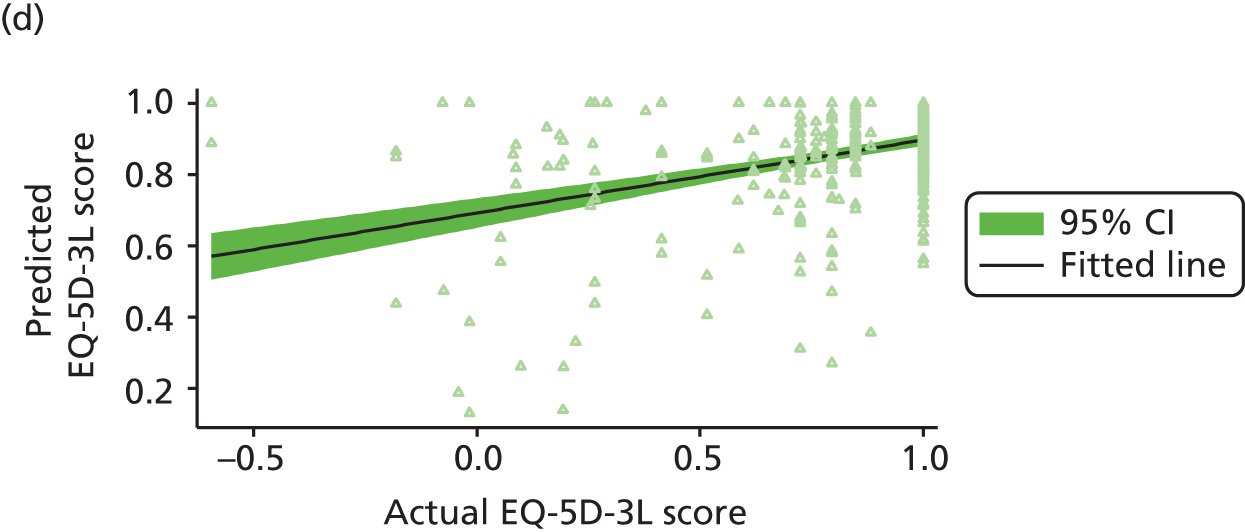
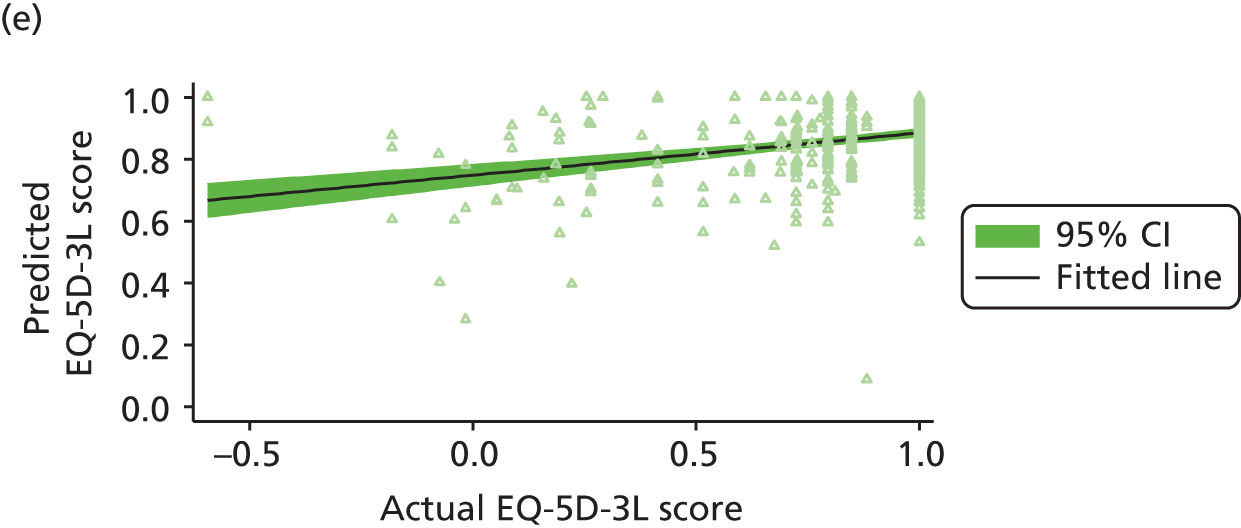
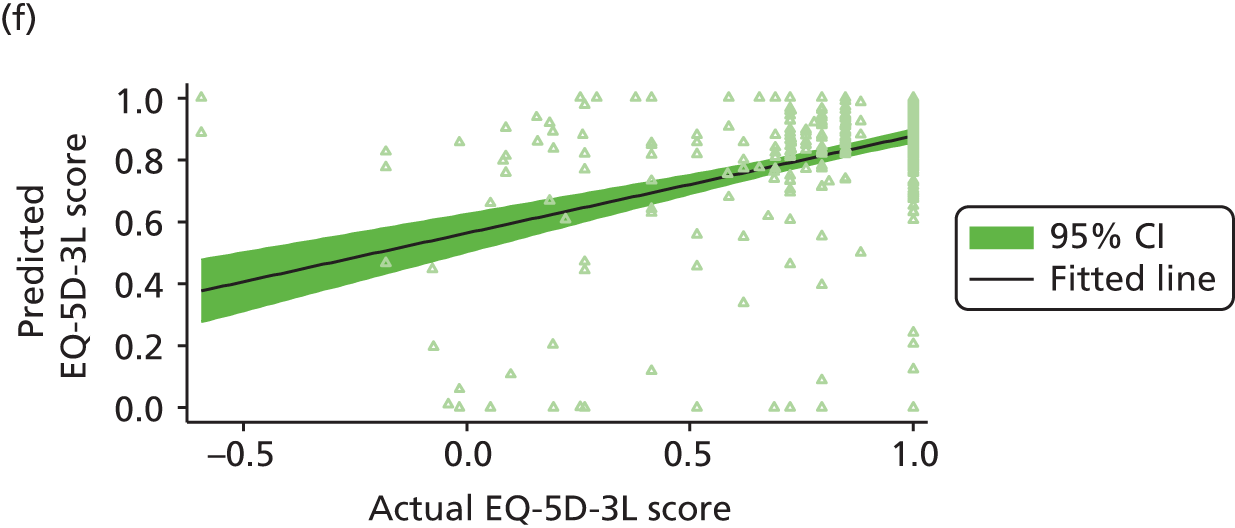
In support of Figure 25, Table 47 shows the mean values of the observed and predicted EQ-5D-3L scores, for different ranges of observed health-state values for the continuous model. At high levels of observed EQ-5D-3L (> 0.8), the mean observed value exceeds the fitted one. The mean observed value is less than the fitted value at any other level of observed EQ-5D-3L. Similar results are reported for the categorical model (see Appendix 3, Table 52 for more details) with the only exception that the predicted mean is smaller for low levels of EQ-5D-3L than the one we obtained from the continuous model in the TPM.
| Observed health-state category | n | Observed values | Fitted values | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OLS | Tobit | TPM | |||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | ||
| < 0.70 | 28 | 0.33 | 0.22 to 0.43 | 0.81 | 0.75 to 0.86 | 0.81 | 0.75 to 0.87 | 0.81 | 0.75 to 0.86 |
| 0.70–0.80 | 24 | 0.76 | 0.75 to 0.78 | 0.83 | 0.78 to 0.88 | 0.84 | 0.79 to 0.89 | 0.84 | 0.79 to 0.88 |
| > 0.80 | 151 | 0.98 | 0.97 to 0.99 | 0.88 | 0.86 to 0.89 | 0.88 | 0.87 to 0.90 | 0.88 | 0.86 to 0.90 |
| All | 203 | 0.86 | 0.83 to 0.90 | 0.86 | 0.85 to 0.88 | 0.87 | 0.85 to 0.88 | 0.87 | 0.85 to 0.88 |
Finally, in Table 48 we report the mean forecast errors for both the categorical and continuous models. Mean forecast errors relative to the mean observed health-state value were higher (in absolute values) when fitted to the categorical model but the magnitude varies depending on the type of regression used. The forecast errors were higher for the continuous model at each of the different levels of observed health-state value except for the TPM.
| Observed health-state category | n | OLS | Tobit | TPM | |||
|---|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | ||
| Continuous model | |||||||
| < 0.70 | 28 | –55.85% | –66.47% to –45.24% | –56.10% | –66.65% to –45.55% | –55.68% | –66.68% to –44.69% |
| 0.70–0.80 | 24 | –8.36% | –13.79% to –2.93% | –8.59% | –14.12% to –3.05% | –8.6% | –13.76% to –3.45% |
| > 0.80 | 151 | 11.77% | 9.88% to 13.66% | 11.59% | 9.68% to 13.49% | 11.58% | 9.5% to 13.66% |
| All | 203 | 0.06% | –3.77% to –3.89% | –0.13% | –3.97% to 3.7% | –0.08% | –3.97% to 3.8% |
| Categorical model | |||||||
| < 0.70 | 28 | –53.38% | –66.17% to –40.59% | –53.51% | –66.3% to –40.73% | –38.51% | –66.68% to –44.69% |
| 0.70–0.80 | 24 | –8.25% | –16.12% to –0.39% | –8.51% | –16.44% to –0.58% | –3.75% | –13.76% to –3.45% |
| > 0.80 | 151 | 10.60% | 8.64% to 12.56% | 10.37% | 8.4% to 12.35% | 13.38% | 9.5% to 13.66% |
| All | 203 | –0.45% | –4.33% to 3.42% | –0.67% | –4.54% to 3.2% | 4.2% | –3.97% to 3.8% |
Discussion
A total of 210 participants were included in the cost and cost-effectiveness analyses. There were no statistically significant differences in age, sex or ethnicity between those who were included in these analyses and those lost to follow-up. It is of note that those lost to follow-up had multiple appointments. Specifically, those in the incentive practices had attended, on average, around eight appointments. Of those lost to follow-up with details available of their appointment, 72% of participants in the incentive practices and 60% in the traditional practices had one or more fillings. Reasons for not attending follow-up were outlined in Chapter 4. As stated in Chapter 4, although we do not have a complete record of reasons for non-attendance, patients not responding to contact from the dental practices was the most frequently cited reason across incentive and traditional practices. Within the incentive practices there was also a substantial number of patients who failed to attend pre-booked appointments. Given the multiple appointments that this group did attend prior to the 24-month follow-up and the treatment carried out there are two likely explanations for non-response for follow-up and/or non-attendance at pre-booked appointments. The first is that participants did not feel that the recall was timely given their previous dental treatment. The second is that the problem they had visited the dental surgery for had been rectified and, in the absence of any current dental problems, they did not wish to visit the dentist for a ‘check-up’ (this aligns with previous figures that suggest that around one-third of the population in the UK go to the dentist only when they have a problem). 2 In the absence of further details outlining the reasons for no follow-up, the explanations we propose are speculative but have implications for research and practice. If the first scenario holds, the time over which treatment is delivered warrants further consideration in planning future research in dentistry that includes a follow-up visit. If the second scenario or explanation holds, then this has implications for how to encourage appropriate preventative dental visits.
Cost and cost-effectiveness
The cost-effectiveness analyses were undertaken from two perspectives: the commissioner and the service (dental) provider. The analyses from each perspective uses two distinct outcomes: first, use of the OHIP-14 scores and, second, QALYs derived from the EQ-5D-3L. The analyses revealed negligible between-group differences in QALY gains, and no statistically significant difference in the EQ-5D-3L score was found between groups or over time. Although the EQ-5D-3L is the NICE-recommended outcome of choice for economic evaluation,129 the apparent insensitivity of the EQ-5D-3L in oral health led to the use of the OHIP-14. 127 The EQ-5D-3L has been reported to have adequate construct and convergent validity, but may not be as sensitive as specific measures of OHQoL. 142–144
Although we found no statistically significant differences in the OHIP-14 scores between groups, there were statistically significant differences (at the 5% level) in these scores over time in both groups, suggesting an overall improvement in OHQoL for both the incentive and the traditional groups. The magnitude of change in scores did not achieve the level that corresponds to a minimal important difference (MID). The MID is defined as ‘the smallest difference in scores in the domain of interest which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in the patient’s management’. 145 Locker and colleagues118 suggest a 5-point difference in OHIP-14 score could be considered the MID. In this study, the mean improvement in OHQoL over the 24 months was 3.39 in incentive practices and 1.74 in traditional practices. However, it is important to note that the OHIP-14 score is a secondary outcome; the study was powered on changes in BoP and thus changes in OHIP-14 scores should be treated with caution.
Given the negligible between-group differences, in the EQ-5D-3L and the derived QALY at least, the cost of the two services was driving the cost-effectiveness ratios. The cost of the incentive practices from the commissioner’s perspective is based on the contractual terms, which specify a UDA value and payment for quality indicators (systems, processes, infrastructure) and OHImp. In these analyses the UDA values assigned to the incentive practices included the payment for quality indicators. Traditional practices are based purely on UDAs – no additional payment is made. The value of the UDA is based in part on the practice location, for example whether or not it is in an area of need, and, for the traditional practices, historical data relating to previous work carried out. (In the cases of the incentive practices, these were brand-new practices when the contract terms were agreed and thus there were no historical data to take account of.) The incentive practices were located in areas where there was no, or limited, provision of NHS dentistry with the aim of increasing access to NHS dentistry, and this is likely to have been influential in negotiation of the UDA payment value, which was higher in the incentive practices than in the traditional practices.
In fact, over the study period, for the 210 participants included in the economic analysis, the incentive practices showed, on average, a higher number of UDAs claimed per patient than the traditional practices (11.23 vs. 10.74); this was accompanied by an overall higher number of appointments per patient (8.89 vs. 6.63). The differences in the number of appointments might in part be explained by skill mix within the two different types of practice. The blended/incentive-driven contracts were designed to facilitate provision of dental care by the most appropriate team member to encourage skill mix. It was intended that all the incentive-driven practices would fully utilise skill mix including, for example, dental therapists, hygienists and extended-duty dental nurses. There are indications in our data that more use was made of skill mix within the incentive practices with fewer appointments with the dentists and more appointments with the dental therapist in incentive practices. The dentists within the traditional practices had a marginally higher number of appointments per patient and the mean duration of those appointments was over 40% higher (16.91 minutes in incentive vs. 24.44 minutes in traditional). Within the incentive practices, on average, patients saw the therapist 2.28 times over the 24 months; in the traditional practices, on average, patients saw the hygienist 1.5 times. The difference in use of different practitioners will inevitably be because of staff configuration and thus the availability of, for example, dental therapists and hygienists. For example, one traditional practice did not employ any dental therapists or dental hygienists. However, the incentive practices were actively encouraged to increase skill mix as part of the bidding process for the dental contracts, which might go some way to explain the more prevalent use of dental therapists and the fewer appointments with dentists in the incentive practices.
Mapping from the Oral Health Impact Profile-14 to the European Quality-of-Life-5 Dimensions questionnaire
There are two areas worthy of particular discussion with regards to the mapping exercise. The first is the choice of the model for mapping from the OHIP-14 to the EQ-5D-3L. The second is the strengths and weaknesses of this approach.
We presented results from OLS, Tobit and TPMs in order to account for the prevalence of full health-state values in the sample – the ceiling effect. Estimation results did not seem to differ, at least in terms of significance, but when looking at the plots of the fitted versus the observed health-state values, the TPM seems to be the best way to proceed; the regression line is closer to the observed outcomes especially when the OHIP-14 is continuous (i.e. each subgroup of the 14 questions is a dummy variable). When the OHIP-14 is included as a categorical variable in the estimation, the results between the different techniques are more obscure.
The availability and inclusion of more personal characteristics such as ethnicity or marital status in the estimation analysis can potentially improve the estimation results. For example, it can be argued that black minorities face worse health than their white counterparts146 or that having a partner can improve an individual’s health, especially among the older population, as one partner can act as a carer for the other. In this study, marital status was not available and the response rate to the ethnicity question was low, making it impossible to test these arguments.
The mapping exercise shows that it is possible to perform economic evaluations when a general health-state outcome is not available using mapping but the approach has severe limitations, especially for those patients reporting a low EQ-5D-3L score. This is because, consistent with other mapping studies,138,147 we fail to predict correctly low levels of EQ-5D-3L (i.e. the mean of the predicted EQ-5D-3L is by far greater than the mean of the observed EQ-5D-3L). This, however, may be related to the different time frame set for the two measures; the OHIP-14 asks about problems with oral health in the ‘last 6 months’, whereas the EQ-5D-3L asks about health ‘today’. It may also be related to how well an oral health measure can predict a more general heath outcome such as the EQ-5D-3L. It would be interesting to explore how much information from the OHIP-14 is ‘transferred’ to the EQ-5D-3L, but this remains for future research.
Conclusion
Although the cost analysis from the commissioner’s perspective has shown the incentive group to attract higher costs, overall OHQoL was higher for participants in the incentive practices than it was for those in the traditional practices. This represents an estimated cost of £199.22 per 1-point decrease (improvement) in the OHIP-14 score for incentive practices. However, this is caveated in as much as the improvement did not represent a MID. It is also important to note that the OHIP-14 score is a secondary outcome; the study was powered on changes in BoP and thus changes in OHIP-14 scores should be treated with caution. In addition, interpretation of the cost per QALY results should be treated with caution given the negligible differences in the QALYs. It should also be noted that the time frame in which participants were followed was relatively short, at 24 months. The blended/incentive-driven service model’s aim of quality and OHImp and the move towards preventative dentistry requires behaviour change by both the dental provider and the patient; the long-term impact of blended/incentive-driven contracts on OHQoL will likely provide better insight into the achievement of these aims.
There are indications that skill mix was utilised in the incentive practices to a greater extent than in the traditional practices. Although, on average, incentive patients saw practitioners more times over the study period, in the incentive practices the number and duration of appointments with dentists was lower as use was made of dental therapists. This would warrant further research to explore OHImp and potential cost savings from the use of dental therapists, hygienists and extended-duty dental nurses.
The acceptability of the blended/incentive-driven contract to dental providers is important. The analysis from the perspective of the provider, including the time spent in appointments with patients and the materials and laboratory costs, indicated that despite the increased number of appointments per patient, overall the new contract was estimated to provide greater financial returns than those observed in the traditional practices. However, for the incentive practices in this study, although the analysis included overheads (included in the practitioner time element of the analysis), the costs associated with setting up the new dental practices were not included and these are unlikely to be insubstantial.
Chapter 6 Discussion and conclusions
Introduction
Primary care dental services have been contracted by the NHS since its inception in 1948. Initially, contracts were centrally determined and relatively undemanding in terms of performance monitoring. 85 However, since the 1990s, contracts have evolved. The PDS pilots (1998–2006)148 encompassed a wide variety of configurations, but concerns were expressed about how they met local needs for service provision, the absence of measures of success or appropriate goals for commissioning and missed opportunities to harness skill mix. 2,9 In 2006, the current nGDS contracts were introduced with dental commissioning devolved to a local level. The nGDS contracts are activity based, with weighted bands of dental activity. However, there are concerns among dental practitioners about whether or not the nGDS contracts have achieved their goal and some believe that insufficient time is allocated for prevention16 and that they restrict access to new patients and those requiring complex treatment. 17 More recently, in 2011, as part of the Department of Health dental contract reform programme, a series of NHS dental contract pilots were initiated, with the aim of exploring how the focus can shift from treatment and repair to prevention and oral health by introducing a new clinical pathway and new remuneration models. 2 The forthcoming prototypes represent the next stage in the evolution of the NHS dental contract reform programme. 75 This evolution is set in the context of a substantial increase in demand for dental care and barriers to dental attendance which include access, cost and dental anxiety. 11
The aim of this project was to evaluate a new model of dental service provision implemented in West Yorkshire in the north of England. The model uses a blended/incentive-driven approach to commission improved health outcomes through the incentivised delivery of evidence-based prevention care pathways, utilising a wider skill mix and increasing access to dentistry in response to identified local NHS dental needs. Our objectives were (1) to explore stakeholder perspectives of the new service delivery model; (2) to assess the effectiveness of the new service delivery model in reducing the risk of and amount of dental disease and enhancing OHQoL in patients; and (3) to assess the cost-effectiveness of the new service delivery model in relation to OHQoL.
There has been a substantial move towards the introduction of blended, incentivised contracts in NHS primary care dentistry following the Steele report,2 specifically the introduction of the national dental contract pilots and more recently the proposed prototypes. Although the contract evaluated in this project pre-dates the NHS dental contract pilots, it reflects the ethos of the report on which the national pilots were based,2 providing an opportunity to evaluate an innovation in health-care delivery and complementing the pilots with greater granularity. It therefore offers substantial potential benefit for patients and the future commissioning and delivery of dental services throughout England.
Principal findings
Using a non-randomised study design we compared the effectiveness of treatment in the three newly commissioned blended/incentive-driven (incentive) dental practices with three matched existing (traditional) practices working under the nGDS contract. Gingivitis was selected as the primary outcome because it affects over 90% of the population, is readily measured in a clinical examination, summarises the participant’s personal oral hygiene behaviour over the preceding days, is responsive to interventions (such as oral hygiene advice or using a new toothbrush) within 2 weeks, is a proxy for other self-care behaviours (such as the use of fluoride toothpaste) and is an interim outcome for periodontitis (which is a significant public health problem)107–109 and because changes are readily demonstrated over a period of 2 years. Secondary outcomes included assessment of caries, quality of life and cost-effectiveness.
The results of the quantitative analysis were mixed. We found that the results of the assessment of BoP favoured the blended/incentive-driven model of service delivery, although the results should be treated with caution given the high attrition and issues of data quality.
The health economics analyses showed the blended/incentive-driven contract was more costly for the commissioner. In respect of our secondary measure of quality of life, overall OHQoL, assessed using the OHIP-14, was higher for participants in the blended/incentive-driven practices than it was in practices under the traditional UDA-based contract, but it did not represent a minimal important clinical difference. It is also important to note that the OHIP-14 is a secondary outcome; the study was powered on changes in BoP and thus changes in OHIP-14 scores should be treated with caution. The differences within and between groups for the EQ-5D-3L were negligible. The last result was not entirely unexpected. Although the EQ-5D-3L is the NICE-recommended outcome of choice for economic evaluation,130 the apparent insensitivity of the EQ-5D-3L in oral health led to use of the OHIP-14. 129 The EQ-5D-3L has been reported to have adequate construct and convergent validity, but may not be as sensitive as specific measures of OHQoL. 143,145
Use of the ICDAS was exploratory in the study. It has proved to be illuminating in as much as there are lessons to take forward. Although the majority of charts were completed to an acceptable standard, a number of issues were evident which give cause for caution in interpretation of the results. For example, in some instances teeth with obvious caries or fillings at baseline were charted as sound at follow-up, even allowing for errors in the transposition of adjacent teeth. Lack of confidence in the quality of the ICDAS data means that we have not explored the enamel transitions in the way that we had originally planned to.
As highlighted earlier, in addition to problems with data quality for the ICDAS, data quality for BoP was also an issue, with a substantial number of participants excluded from the analysis following quality assurance. Dentition charting has been highlighted as a problem with the national dental contract pilots. 2 Early on it was found that data on charting were incomplete or absent for many patients. 30 These findings are interesting in as much as in our study charting was completed by the dental practitioners using a paper form. For the ICDAS, in particular, we had intended to use electronic charting, which incorporates built-in automatic error checks. However, in the pilots there was a requirement for practices to keep patient records in electronic form and they reported that ‘the evidence to date, however, suggests there have been inconsistencies in the quality of electronic data recording from practice to practice and within practices, from clinician to clinician’. 20 It would seem that charting and dentist recording of data is a challenge whether paper based or electronic and despite the training given in the INCENTIVE study, many of the issues the pilot sites experienced appear to be replicated in our study, including misinterpretation and lack of understanding of what is required.
In relation to access to dental services, within our qualitative study we identified perceptions that the blended/incentive-driven contract increased access to dental care, with the contract determining dentists’ and patients’ perceptions of need, their behaviours, evaluated and subjective health outcomes and patient satisfaction. These outcomes were then seen to feed back to shape people’s predispositions to visit the dentist. However, an important, and unexpected, finding of the study was the high ‘fail to return’ rate. A large proportion of people in the study who had access to a dentist did not follow up on oral care. These individuals were more likely to be younger males and have poorer oral health. Within this patient group, although access to dental services increased, this did not appear to facilitate continued use of services. Although the reasons for non-attendance recorded by the dental practices was incomplete, of the reasons recorded the most frequently cited was no response to contact from the dental practices and, in the blended/incentive-driven practices, a substantial number also failed to attend pre-booked appointments. Interestingly, those lost to follow-up had multiple appointments and treatments, including fillings, crowns and bridges. One possible explanation for this may be that the problem they had visited the dental surgery for had been rectified and, in the absence of any current dental problems, they did not wish to visit the dentist for a ‘check-up’. Indeed, one patient talks about attitudes in the past which meant she only went to the dentist if there was a problem, although she goes on to say that she thinks attitudes have changed now. A dental therapist talks about high levels of need and there being ‘a lot of neglected mouths. Some haven’t seen a dentist in years. Some have lost their motivation because of this’. Another patient recalls not going to the dentist for about 3 years, saying ‘I don’t know why I didn’t go, I just stopped going and I think then you get thrown off the register’. This aligns with previous figures that suggest around one-third of the population in the UK go to the dentist only when they have a problem. 2
The failure of some individuals to attend pre-booked appointments may, in part, be attributed to dental anxiety, a recognised barrier to dental attendance. 11 One patient spoke about cancelling an appointment for a filling because she was ‘panicking and worrying’. Another talked about her partner being ‘scared to death of the dentist’ and how ‘trying to get him through the door of the dentist was a real effort’.
Another possible explanation for the unexpected high loss to follow-up within our study, and indeed the difference between estimated and actual loss to follow-up, is that all the patients in the study were new patients. This suggests that we had inadvertently selected a sample that were not regular dental attenders, although this may still be representative as one-third of the population falls into this classification. 2 The study sample size (including allowance for attrition) was powered on a previous study. 121 In the study by Clarkson and colleagues,121 the authors outline their inclusion criteria; eligible patients were dentate adults who had already made an appointment for a routine check-up and had in whom probing of gingiva was not contraindicated at the time of the appointment. This indicates that their sample included primarily regular dental practice attenders rather than new patients who may not have attended a dental appointment for some time. It also indicates, given that contrandication to probing of gingiva was an exclusion criterion, that their sample had better oral health than those included in our study.
Furthermore, groups of new patients might be likely to include a larger proportion of patients who are migrants. Most research on the dental attendance of migrants has been conducted in the USA or Australia. This work consistently describes the barriers to access among migrants. 149,150 Brennan and Spencer149 noted that service utilisation patterns were related to cultural factors within populations and it may be that groups who have little history of dental attendance do not adopt this behaviour immediately.
The low rate of reattendance for regular dental care (thereby implying a pattern of emergency care) provides support for the care pathway approach recommended in the Steele report,2 which legitimises irregular dental attendance for those who choose it. High proportions of patients adopting this pattern will shape the practices in these areas. Such practices will be characterised by the provision of more emergency care and more of the time-consuming initial assessments. This burden might be considered in the commissioning of services in these areas.
Skill mix was of particular interest in our study given one of the aims of the blended/incentive-driven contract is to improve health outcomes through wider skill mix utilisation. In England there has been a steady shift in the make-up of the dental practice team with an expansion of numbers of, for example, dental therapists and dental hygienists. 151 Our analyses indicate that skill mix was utilised in the blended/incentive-driven practices to a greater extent than the practices under the traditional nGDS contract. While on average incentive patients saw dental practitioners more often over the study period, in the incentive practices the number and duration of appointments with dentists was lower, as use was made of dental therapists. The difference in use of different practitioners will inevitably be influenced by current staff configuration and thus the availability of, for example, dental therapists and hygienists. However, the incentive practices were actively encouraged to increase skill mix as part of the bidding process for the dental contracts, which may go some way to explain the more prevalent use of dental therapists and the lower number of appointments with dentists in the incentive practices. Collectively, the patients in incentive practices had, on average, more appointments than patients in the traditional practices. In this regard the commissioning strategy was seen to be effective.
There are obstacles to overcome to realise any benefits of the greater deployment of skill mix. Dentists may need support in these areas and to recognise the differences between caring for individual patients and caring for segments of the population, such as that formed by the patient base of a practice. In addition, one incentive practice experienced a higher turnover of its dentists than the other practices, which was attributed in part to lack of opportunities to carry out complex treatments. This echoes evidence from elsewhere of tension between ‘acknowledging that less qualified practitioners can contribute directly to dental treatment and the unwelcome consequences of a modularised approach’. 152
Intuitively, the delegation of treatment to staff specialised in only a specific range of treatments could reduce costs and increase access to care. 132 The acceptability of the blended/incentive-driven contract to dental providers is clearly important, not least because of the financial implications. Primary care dentist practices, unlike many other medical providers in the UK, are operated as businesses,84 with NHS provision of dental services governed using quasi-market principles. 90 It has been suggested that under the current nGDS contract remuneration structure there are financial barriers that ‘prevent the profitability and effective use of skill mix’. 84 Our analyses included assessment of costs from the perspective of the dental provider. This included the time spent in appointments with patients and the materials and laboratory costs. The analysis showed that, despite the increased number of appointments per patient, overall, the new contract was estimated to provide greater financial returns than those observed in the traditional practices. However, for the incentive practices in this study, although the analysis included overheads (included in the practitioner time element of the analysis), the costs associated with setting up the new dental practices were not included and are likely to be substantial.
The unit of analysis for the costs in this study was the practice; the financial implications for the individual GDPs in the practices are unclear given that one of the most important barriers is referral by the dentist to, for example, a dental therapist, preventing further earning potential for additional band 1 treatments. 84 However, in the qualitative study dental therapists were perceived to increase the availability of care and patient satisfaction. Practices increased the utilisation of dental therapists by not reducing the payments to individual dentists who referred their patients to them. Although seemingly paying two staff members for the same treatments, this approach incentivised referral, thus liberating dentists’ time for patient OHAs and more remunerative complex treatments. This might be further explored and evaluated in the evaluations of the forthcoming contract prototypes. 75
The data hint at appreciable challenges related to a general refocusing of care and especially to perceptions about preventative dentistry and use of the risk assessments and care pathways. The quantitative data from the RAG assessment showed > 30% of the participants in our sample to be in the highest risk category (red) and < 7% in the lowest category (green) at baseline. There was an improvement from baseline to follow-up which suggests a degree of responsivity. In addition, there were very few over-rides of the RAG system (4.64% at baseline and 7.21% at follow-up). Although it would be inappropriate to make direct comparisons with findings from the dental contract pilots with regard to changes over time, the proportion of patients in each category at the initial OHA (6% in green and 26% in red for the national pilots and 7% and 30% in the INCENTIVE study) indicate a similar distribution of patients. 30 One of the concerns a priori in our study was that for individuals with particular irreversible medical conditions it was not possible to move out of the amber category. Unfortunately, because of the small number of pathways that had been over-ridden, we are unable to ascertain whether or not this a priori concern was borne out. Explanations for over-rides, especially moves away from red, suggest other reasons. Only one patient score was over-ridden because of a family medical condition (diabetes). It is of note that those who were red at baseline were less likely to attend follow-up.
The OHA RAG system is key to the current national dental contract pilots and integral to the incentive contract. Within our study, practitioners were concerned that it was not sufficiently precise and, as illustrated above, rarely overrode the assessments, even though they could. In practice applications, dentists’ assessments may be prone to allocation bias as treatments are apportioned according to the ratings, and to measurement bias changes in status which are used for contract monitoring. Further research is required to validate the RAG assessment, but in its primary guise for risk assessment, and also in this application as a tool for evaluation.
Strengths and limitations
Overall the evidence of the effectiveness of use of contracting and incentives in health providers is still emerging, with further experimental research needed – specifically the impact on patient outcomes. 27 The study design reported here has enabled a direct comparison of practices offering incentive-driven preventative dentistry with those offering traditional, solely activity-driven dentistry operating under the nGDS. This enhances early findings from the ongoing national dental contract pilots introduced following the Steele report2 which have focused on patients’ and practitioners’ views of the new clinical pathway, reporting them to be strongly supportive. 30 Within more recently reported findings focus has lain on adaptation to the new system but these findings also report positive indications about clinical benefits in terms of a reduction of risk and health improvement (measured through the RAG system and a basic periodontal examination). This study adds value to the current evidence base of blended/incentive-driven contracts. The study is the first to systematically evaluate the impact of a dental service provision on oral health outcomes by comparing those operating under the traditional nGDS and those driven in part by incentives that have been developed in partnership with the dental practices.
One of the challenges in undertaking the study was the pragmatic study design. Neither the practices nor the participants in the study were randomised. There will inevitably be a degree of bias given that all the practices were self-selected. The three incentive practices had competitively tendered to operate practices under the new contract, and as such may be thought of as early adopters and may well be atypical of dental practices in England. Similarly, while the traditional practices were matched to the incentive practices, they chose to take part in the study. One stumbling block when recruiting traditional practices was that all the study participants had to be new patients. For some practices this was not viable and as such those practices declined our invitation to take part in the study.
The study is also limited by the high loss to follow-up. As highlighted, attrition was much higher than anticipated. Although we have been able to shed some light on reasons for this, it has meant that two of the three matched practices were unbalanced in terms of participant numbers (pairs 1 and 4 and 3 and 6). This leads us to question if it is robust to pool the three pairings in single analyses. If we are not willing to pool them then the only pairing with balanced numbers for analyses is the 2 and 5 pairing. Although there is some reassurance that the effect size for the primary outcome (BoP, pooled across practices) is similar to that included in the original power calculation (10.24% observed vs. 10% in calculation) and achieves statistical significance (p < 0.01) this cannot guarantee the study achieved power of 80% for the primary outcome (as originally specified in the study design). The original power calculation required numbers available for analysis of 500 participants split equally across incentive and traditional practices, whereas 188 were available for analysis (37.60% of those required to achieve power of 80% at a significance level of 5%). There was some further indication of differential dropout among males and younger patients. Post-hoc power analysis is best avoided. 153 Instead, consideration of a sample is better based on CIs. For the primary outcome (BoP pooled across practices) a 95% CI for the effect size was 3.23% to 17.25%, indicating a positive effect for incentive practices but with considerable uncertainty in magnitude. Together with reservations about the validity of pooling (because of heterogeneity of effects across practice pairs) and differential dropout, results should be treated with caution and followed up with further study. However, this loss to follow-up also exemplifies the challenges of running a dental practice in order to improve patients’ oral health, and from this perspective the data have greater external validity than a highly controlled study with artificially high rates of reattendance.
For the cost-effectiveness analysis there remains a tension between use of a preference-based utility measure as recommended by NICE129 and use of a condition-specific measure that is posited to be more sensitive to changes in oral health. The OHIP-14 measure has been used extensively in cost-effectiveness analyses in oral health (see, for example, Stone and colleagues127 and Hulme and colleagues128), but is not preference based and therefore cannot be used to produce QALYs. At the present time there is no preference-based measure specific to oral health. In this study the OHIP-14 scores were mapped using regression techniques to the baseline EQ-5D-3L scores to explore the potential for estimating utility scores that can be used to produce QALYs based on responses to the OHIP-14. Unfortunately, consistent with other mapping studies,139,147 we fail to predict correctly low levels of the EQ-5D-3L, that is the mean of the predicted EQ-5D-3L is far greater than the mean of the observed EQ-5D-3L. This, however, may be related to the different time frame set for the two measures; the OHIP-14 asks about problems with oral health in the last 6 months whereas the EQ-5D-3L asks about health ‘today’. It may also be related to how well an oral health measure can predict a more general heath outcome such as the EQ-5D-3L.
It should also be noted that the time frame in which participants were followed was relatively short, at 24 months. Although we have confidence that changes to the primary outcome (BoP) can be readily demonstrated over a period of 2 years, the blended/incentive-driven service model’s aim of quality and OHImp and the move towards preventative dentistry requires behaviour change by both the dental provider and the patient; the long-term impact of blended/incentive-driven contracts on OHQoL will likely provide better insight into the achievement of these aims.
The selection of outcomes in evaluative research is difficult, and the rationale for our choice is presented in Chapter 4. BoP was selected because it is responsive to change and readily measured. It can be changed by dental teams’ behaviours, including preventative advice and treatment, but is also subject to changes in patients’ behaviours and measurement error. It is quite likely that the influence of patient behaviours and measurement error would be random and would attenuate the apparent relationships between the contract types and the patient outcome. The estimates of the treatment effect may therefore be underestimated in this study. It is possible that measurement bias may have favoured one or other contract type, but this seems unlikely. The contract type was associated with improvements in this clinical outcome. Few other studies have assessed clinical outcomes in relation to dental contracts. Nevertheless, the utility of BoP as a surrogate for other oral health outcomes warrants further investigation.
Caries and treatment increments (measured with the ICDAS) were selected as a secondary outcome because changes in caries levels may be modest among adults at times of low caries incidence. Furthermore, there were no data on the responsiveness of the ICDAS on which to base power calculations. The ICDAS may need more evaluation and greater utility before it can be used for this purpose.
The effects of the mouth on everyday life (as measured with the OHIP-14) correlate only weakly with clinical status. The OHIP-14 is therefore unlikely to be measurably affected by dental treatment or to reach a minimally important difference in a natural experiment for which patients were arriving with different levels of impact and receiving different interventions. It was included as a secondary outcome to incorporate patient-reported outcomes and for inclusion in the health economic analysis.
A further potential limitation in the economic evaluation is the use of national salary costs for the dental workforce rather than actual contractual agreements between the workforce and provider. Within any economic evaluation there is tension between making the evaluation specific to a particular setting and the generalisability of the results across settings. This is particularly pertinent to primary care dentistry as dental practices assume different commercial guises (e.g. social enterprises, independent providers and large corporate providers). Within these models there are a wide range of workforce contracts. For example, therapists may be salaried, on an activity-based contract linked to UDAs or paid an hourly rate. The type of contract adopted varies within and across providers. In this case we took a pragmatic view. Although we included the actual commissioning contracts for the practices (i.e. UDA values for each of the traditional practices and the actual contracts for the incentive practices), we assumed national salary rates to increase generalisability.
Within our qualitative study we used the Andersen model of access. It provided a useful taxonomy for the data and allowed identification of the effects of the new contract. This fit is unsurprising as the model was developed over a 40-year period and remains among the most widely cited models of access to health care. 63,64,67,87 However, although the model was broadly sustained in the data it might be enhanced by greater conceptual clarity, not regarding contextual and individual factors in sequence and by the incorporation of additional factors.
Patient and public involvement
We were committed to patient and public involvement (PPI) throughout the INCENTIVE research cycle and patient contributors worked as integral members of the research team from conception of the research idea to shape our research questions and aid delivery, project management and final data interpretation through to reporting. They ensured our research was of relevance to patients and the NHS and would contribute to shape and improve reform of the dental contract to maximise a service designed to address patient needs in terms of improved oral health outcome through a paradigm shift from restorative to preventative oral health care and access to NHS services. Details of how PPI input informed different parts of the study are detailed below.
Identification and/or prioritisation of the research questions and development of the research design
We worked closely with two PPI contributors, each bringing a unique perspective as current users of dental services but covering different age and societal groups – middle-aged participants and parents (Susan) and working young adults/students (Alex) – that we considered may have differing expectations and use of dental services that would be of relevance to INCENTIVE. We also sought specific advice from a third PPI advisor (Rosie, 84 years of age) on an ad hoc basis; she did not attend the advisory group meetings.
The qualitative enquiry was informed from discussions with the PPI contributors and the sampling matrix was codesigned to include criteria linked to the objectives of the programme including demographic factors (age, sex, ethnicity, socioeconomic status). Access to dental services was seen as a priority by the PPI contributors and they were central in ensuring that we also collected data from non-patients to understand barriers to access to NHS dentistry. Rosie helped shape the inclusion of elderly patient groups, lobbying for a broad entry criteria and to ensure that patients > 65 years were included in the cohort. Susan and Alex welcomed the idea that we were addressing the utilisation of the wider skill mix in our analysis of the contracts.
Our PPI contributors regularly attended the project advisory group meetings and had additional input on a needs basis; for example, they made a significant contribution to the preparation and internal development and review of the ethics application to ensure it was understandable yet not patronising, to ensure informed consent was readily achievable and the study not too onerous for participants by carefully considering the volume of paperwork participants would need to complete.
Dissemination
The PPI contributors codeveloped the participant information leaflets and are currently assisting in the preparation of materials for the dissemination event and ensuring that the study material will improve participant understanding of the importance of INCENTIVE in redesigning the dental contracts as we move forward. Our PPI contributors have ensured our dissemination strategies are inclusive and accessible to research participants, patients and the public.
Patient and public involvement identification and training
Two INCENTIVE PPI advisors sit on the study advisory group, and all PPI advisors were willing to be contacted by the researchers to contribute to individual work packages as required.
Patient and public involvement contributor training and mentorship
The INCENTIVE PPI contributors were offered training and mentorship to increase their confidence in working in partnership. Similarly, the INCENTIVE research team were also trained in how to work with PPI contributors as equal partners. We provided mentorship and personal support to PPI contributors before and after meetings, addressing queries, language and documentation. The PPI contributors were also provided with a ‘jargon buster’. The researchers received training to facilitate inclusive project meetings with PPI representatives by knowledge transfer from the ‘getting involved in shaping research and building partnerships’ workshop.
Throughout we adhered to INVOLVE guidelines and reimbursed PPI members according to INVOLVE recommendations. 154
Conclusions
The policy context in which the INCENTIVE study was funded has remained remarkably constant in its aims for NHS dentistry over the course of the research. The Steele report of 20092 examined how dental services in England could be developed, advocating a commissioning approach to align dentistry with the rest of the NHS services, to commission for health outcomes and to develop blended contracts rewarding not only activity but quality and OHImp. The report recommended that payments explicitly recognise prevention and reward the contribution of the dental team to improvements in oral health, reflected in patient progression along the pathway, adherence to nationally agreed clinical guidelines and the achievement of expected outcomes. 2 Commissioners were asked to support dentists to make the best and most cost-effective use of the available dental workforce. 2 Despite pre-dating the Steele report2 the incentive contracts introduced in West Yorkshire proved themselves to be forerunners of these new blended contracts.
Since the Steele report2 we have seen the development of the national dental contract pilots which sat alongside the incentive contract. Currently national dentistry is moving apace towards a more advanced stage which would test a prototype of a potential new system. 75 The aim of the prototype retains the same ethos as set out in the Steele report2 with focus lying on the shift of NHS dentistry towards prevention and oral health rather than treatment and repair through a new clinical pathway and new remuneration models. The prototypes have three elements: (1) the use of comprehensive assessments in a pathway approach; (2) remuneration for quality of care and remuneration to encourage continuing care; and (3) prevention as well as activity. They aim to test different balances of remuneration for the different elements and will form a stage in the evolution of the contract rather than preparing a large one-off change. With this in mind the findings of this study remain directly relevant to the further evolution of the NHS dental contract. Some of those findings relate to access to care, the use of gingivitis as an outcome measure, the use of the RAG system in risk assessment, communication and contract monitoring.
Findings from the evaluation of the national dental pilots have been relatively positive, although they highlight challenges in a number of areas including use of the OHA, data and feedback, and skill mix. Although the two evaluations (the evaluation of the national dental contract pilots and the INCENTIVE study) differ in many respects, our conclusions below highlight where findings converge and lessons for future commissioning of NHS dentistry. The final sections summarise the recommendations for future research and implications for practice.
Access and inequalities
Access can be assessed using list size as a proxy (as in the national dental contract pilot evaluation). 20 The incentive practices were new practices and, therefore, still establishing their patient base, thus we were unable to assess increased access in this way. However, the siting of the incentive practices in areas of high need associated either with deprivation and disease or with the poor availability of NHS care meant that access to dental services increased within these communities. But many people who had access to a dentist in these practices, and many of the new patients included in the study in traditional activity-based practices, did not continue with their oral care. These individuals were more likely to be young men and have poorer oral health.
The qualitative data suggested that this was in part a consequence of taking on many new patients who might not wish to receive continued care. Some patients may also have come from minority ethnic groups not used to attending the dentist regularly. Thus, although the new practices increased access, further work is required to understand how best to promote and encourage appropriate dental service attendance especially among those with high level of need to avoid increasing health inequalities.
Oral health assessment and skill mix
As described earlier in the chapter (see Principal findings), use of the RAG risk assessment in our study showed improvement from baseline to follow-up which suggests a degree of responsivity. Although the RAG ratings were used in risk assessment, participants were concerned that it was not sufficiently precise and rarely over-rode the assessments, even though they could. In practice, dentists’ assessments may be prone to allocation bias as treatments are apportioned according to the ratings, and to measurement bias where changes in status are used for contract monitoring. The risk assessments were less frequently used as an aid to patient communication. Within the national pilots sites, communication of the care pathway from practitioner to patient was also mixed. 20 Further research is required to validate the RAG assessment, in the following guises: risk assessment, communication aid, contract-monitoring tool and also as a tool for evaluation.
The evaluation of the national pilots also reports that the pathway model takes longer to operate per patient than the previous model. Within the INCENTIVE study, although patients had a greater number of appointments in incentive practices, the duration of the appointment was on average shorter than the practices operating under the UDA-based contract. The incentive practices were set up in areas of high need and poor access to dental services and therefore it is not surprising that they had more appointments and a higher level of treatment. Although it is not possible to draw any firm conclusions from the figures, the qualitative data hint at appreciable challenges related to a general refocusing of care and especially to perceptions about preventative dentistry and use of the risk assessments and care pathways. There are also obstacles to overcome to realise any benefits of the greater deployment of skill mix. One potential solution would be for contractual drivers to change to be supplemented with educational efforts to support the refocusing of care, perceptions about preventative dentistry, internal practice business models on the use of skill mix, the role of evidence-based dentistry, working with care pathways, communication skills and the need for a greater understanding of the difference between caring for individual patients and a population.
Clinical effectiveness and clinical outcomes
The findings with respect to the clinical effectiveness of the blended/incentivised contracts are mixed. Although the results of the primary outcome of gingivitis (BoP) favour the blended/incentivised model, and there is some reassurance that the effect size is similar to that included in the original power calculation, the results should be treated with caution given the reduced sample size and data quality issues (discussed in more detail in Data quality), and reservations about the validity of pooling data.
Few studies have assessed the clinical effectiveness of contracting in dentistry; for example, the national pilots’ evaluation looks at clinical response using the RAG status between assessment and review. 20 Should services consider an oral health-related outcome measure of clinical effectiveness, despite the challenges, this study would support the use of BoP. BoP is readily measured and responsive to change. It can be changed by dental teams’ behaviours including preventative advice and treatment but is also subject to changes in patients’ behaviours and to measurement error. Random changes in patient behaviours and measurement error would attenuate the apparent relationships between the contract types and BoP identified in this study. The estimates of the treatment effect may therefore be underestimated. It is possible that measurement bias may have favoured one or other contract type, but this seems unlikely. Few other studies have assessed clinical outcomes in relation to dental contracts. Nevertheless, the utility of BoP as a surrogate for other oral health outcomes warrants further investigation.
Data quality
The data quality issues with BoP were also seen within the ICDAS. In respect of caries assessment, which favoured the traditional practices, although the majority of ICDAS charts were completed to an acceptable standard, a number of issues were evident that give cause for caution in interpretation of the results.
Use of the ICDAS was exploratory and changes in the ICDAS scores may be the result of multiple factors, such as attrition of study participants, diagnostic inaccuracies, poor completion, complexity of the ICDAS, difficulty in diagnosing enamel caries in general dental practice, errors in syntax or the relatively short time frame of the study. Further work is indicated on both the utility and the validity of recording dental caries and treatment experience with an indicator such as the ICDAS as a contract outcome. The precision of this system (the number of categories and levels) mean that it is time-consuming to use and dental caries and treatment experience may not change sufficiently quickly for contract monitoring. Standardisation of the dental practice software could facilitate the use of this and other clinical outcomes.
Data quality and dentist data recording have recently been flagged as challenges within the dental contract pilots, with the recommendation that there should be a strong driver in the contract for data to be collected accurately and for appropriate training and support provided for practices. 20 Evidence from the INCENTIVE study supports this.
Cost-effectiveness
The economic analysis showed the INCENTIVE arm of the study to attract a higher cost for the dental commissioner but to be financially attractive for the dental provider at the practice level. Caveats also apply to these findings given the high attrition rate and further research that is required to assess the financial impact of the contract, in particular the impact of an increase of skill mix on the individual practitioner, in order to support the model.
Finally, within dentistry, the OHIP-14 measure has been used extensively in cost-effectiveness analyses in oral health but cannot be used to produce QALYs. Within this study the OHIP-14 scores were mapped using regression techniques to the baseline EQ-5D-3L scores to explore the potential for estimating utility scores that can be used to produce QALYs based on responses to the OHIP-14. Unfortunately, consistent with other mapping studies, we fail to predict correctly low levels of EQ-5D-3L. This suggests that there is a need for the development of a condition-specific utility measure for use in oral health for economic evaluation.
Recommendations for future research
Further research is required to:
-
understand how best to promote and encourage appropriate dental service attendance, especially among those with a high level of need to avoid increasing health inequalities
-
assess the financial impact of the contract and particularly the increase of skill mix on the individual practitioner in order to support the model
-
validate the RAG assessment as a risk assessment, communication aid and contract-monitoring tool and as a tool for evaluation
-
explore further the utility of BoP as a surrogate for other oral health outcomes
-
explore both the utility and the validity of recording dental caries and treatment experience with an indicator such as the ICDAS as a contract outcome
-
develop a condition-specific utility measure for use in oral health for economic evaluation.
Implications for practice
-
The blended/incentive-driven contracts were perceived to increase access to dental care, with the contract determining dentists’ and patients’ perceptions of need, their behaviours, evaluated and subjective health outcomes and patient satisfaction.
-
A large proportion of people in the study who had access to a dentist did not follow up on oral care. This supports the care pathway approach recommended in the Steele report,2 which legitimises irregular dental attendance for those who choose it.
-
For dental practitioners, there are challenges within the blended/incentive-driven contracts related to a general refocusing of care around preventative dentistry, risk assessment and a care pathway approach rather than the focus on treatment inherent in the UDA-based contract.
-
There are obstacles to overcome to realise the benefits of the greater deployment of skill mix. Intuitively, the delegation of treatment to staff specialising in only a specific range of treatments could reduce costs and increase access to care but, as previous research indicates, there may be financial barriers that prevent the profitability and effective use of skill mix.
-
Data quality and dentist data recording, particularly dentition charting, was challenging. This supports the view that there should be a strong driver in the contract for it to be collected accurately and appropriate training and support provided for practices.
Acknowledgements
The project was developed and overseen by a multidisciplinary research group at the Universities of Leeds and Sheffield. We would like to thank our advisory group members who helped steer the project and provided valuable feedback at key points: James Steele (chairperson), Sue Gregory, Lynn Windle, Ian Kirkpatrick, Kate Jones, Susan Neal, Alex Pavitt, Paul Carder and Rebecca Harper.
We would like to thank all those people who took part in this project: the dental teams, the patients, members of the public and the commissioners.
Thanks go to Jenny Porritt and to Mel Hall for their contribution to the data collection for the qualitative study. We are grateful for the support provided by Tom Fleming for setting up our databases and Judy Wright who developed and ran our literature searches. A special thanks to Denise Womersley for the administrative support she provided.
Finally, we would like to acknowledge the input to the original proposal from Richard Edlin.
Contributions of authors
Professor Claire Hulme (Director, Academic Unit of Health Economics, University of Leeds) was the principal investigator for the project and is responsible for the integrity of the report as a whole.
Professor Peter Robinson (Professor of Dental Public Health, School of Clinical Dentistry, University of Sheffield) was lead for the qualitative study (see Chapter 3).
Professor Gail Douglas (Professor of Dental Public Health, School of Dentistry, University of Leeds) oversaw use of the ICDAS including training and provided clinical advice in the effectiveness study (see Chapter 4).
Dr Paul Baxter (Senior Lecturer in Biostatistics, Division of Biostatistics, University of Leeds) lead for the clinical effectiveness analysis (statistics).
Dr Barry Gibson (Senior Lecturer, School of Clinical Dentistry, University of Sheffield) contributed to the qualitative study.
Dr Jenny Godson (Regional Consultant in Dental Public Health, Public Health England) provided advice/input in dental public health commissioning.
Dr Karen Vinall-Collier (Lecturer, School of Dentistry, University of Leeds) was the study co-ordinator.
Dr Eirini Saloniki (Research Fellow, Academic Unit of Health Economics, University of Leeds) contributed to the health economics analysis.
Mr David Meads (Associate Professor in Health Economics) contributed to health economics.
Professor Paul Brunton (Professor of Restorative Dentistry) contributed to the methodology.
Professor Sue Pavitt (Professor of Applied Health & Translational Research, School of Dentistry, University of Leeds) contributed to the methodology and PPI.
Publications
Pavitt SH, Baxter PD, Brunton PA, Douglas G, Edlin R, Gibson BJ, et al. The INCENTIVE protocol – an evaluation of the organisation and delivery of NHS dental health care to patients – innovation in the commissioning of primary dental care service delivery and organisation in the UK. BMJ Open 2014;4:e005931.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- McDonald R, Cheraghi-Sohi S, Tickle M, Roland M, Doran T. The Impact of Incentives on the Behaviour and Performance of Primary Care Professionals. London: Queen’s Printer and Controller of HMSO; 2010.
- NHS Dental Services in England: An Independent Review Led by Professor Jimmy Steele. London: Department of Health; 2009.
- Governing the NHS: A Guide for NHS Boards. London: Department of Health; 2003.
- Storey J, Bate P, Buchanan D, Green R, Salaman GJ, Winchester NJ. New Governance Arrangements in the NHS: Emergent Implications. Milton Keynes: The Open University; 2008.
- Shifting the Balance of Power: The Next Steps. London: Department of Health; 2002.
- Commissioning a Patient Led NHS. London: Department of Health; 2005.
- NHS Dentistry: Options for Change. London: Department of Health; 2002.
- Goodwin N, Morris AJ, Hill KB, McLeod HS, Burke FJ, Hall AC. National evaluation of personal dental services (PDS): the perspective of dentists and professionals complementary to dentistry. Br Dent J 2003;195:640-3. http://dx.doi.org/10.1038/sj.bdj.4810781.
- Hall AC, Hill KB, Goodwin N, Morris AJ, Burke FJ. National evaluation of personal dental services and professionals complementary to dentistry. Br Dent J 2003;195:651-3. http://dx.doi.org/10.1038/sj.bdj.4810783.
- McLeod HS, Morris AJ. Evaluation of personal dental services (PDS) first wave pilots: the alternative to general dental services (GDS) offered by the capitation-based pilots. Br Dent J 2003;195:644-50. http://dx.doi.org/10.1038/sj.bdj.4810782.
- Hill KB, White DA, Morris AJ, Hall AC, Goodwin N, Burke FJ. National evaluation of personal dental services: a qualitative investigation into patients’ perceptions of dental services. Br Dent J 2003;195:654-6. http://dx.doi.org/10.1038/sj.bdj.4810784.
- Newton JT, Alexandrou B, Bate BD, Best H. A qualitative analysis of the planning, implementation and management of a PDS Scheme: lessons for local commissioning of dental services. Br Dent J 2006;200:625-30. http://dx.doi.org/10.1038/sj.bdj.4813643.
- Dental Services. Fifth Report of Session 2007–08. London: The Stationery Office; 2008.
- Baird WO, Jackson RJ, Worthington LS, Robinson PG. Perspectives of general dental practitioners ahead of the ‘new ways of working’. Br Dent J 2007;202:614-15. http://dx.doi.org/10.1038/bdj.2007.470.
- Jacobs L. NHS dentistry in the United Kingdom: past, present and future. Alpha Omegan 2007;100:75-9. http://dx.doi.org/10.1016/j.aodf.2007.04.007.
- Chestnutt IG, Thomas DR, Patel R, Treasure ET. Perceptions and attitudes to a fundamental reform of general dental services in Wales. Prim Dent Care 2007;14:13-8. http://dx.doi.org/10.1308/135576107779398228.
- Milsom KM, Threlfall A, Pine K, Tickle M, Blinkhorn AS, Kearney-Mitchell P. The introduction of the new dental contract in England – a baseline qualitative assessment. Br Dent J 2008;204:59-62. http://dx.doi.org/10.1038/bdj.2008.1.
- NHS Dental Contract: Proposals for Pilots (December). London: Department of Health; 2010.
- Dental Quality and Outcomes Framework (May). London: Department of Health; 2011.
- NHS Dental Contract Pilots – Learning After the First Two Years of Piloting (February). London: Department of Health; 2014.
- Christianson J, Leatherman S, Sutherland K. Financial Incentives, Healthcare Providers and Quality Improvements: A Review of the Evidence. London: The Health Foundation; 2007.
- O’Donnell CA, Ring A, McLean G, Grant S, Guthrie B, Gabbay M, et al. The New GMS Contract in Primary Care: The Impact of Governance and Incentives on Care. Final Report. Southampton: NIHR Service Delivery and Organisation programme; 2011.
- Langdown C, Peckham S. The use of financial incentives to help improve health outcomes: is the quality and outcomes framework fit for purpose? A systematic review. Public Health 2014;36:251-8. http://dx.doi.org/10.1093/pubmed/fdt077.
- Maisey S, Steel N, Marsh R, Gillam S, Fleetcroft R, Howe A. Effects of payment for performance in primary care: qualitative interview study. J Health Serv Res Policy 2008;13:133-9. http://dx.doi.org/10.1258/jhsrp.2008.007118.
- Tickle M, McDonald R, Franklin J, Aggarwal V, Milsom K, Reeves D. Paying for the wrong kind of performance? Financial incentives and behaviour changes in National Health Service dentistry 1992–2009. Community Dent Oral Epidemiol 2011;39. http://dx.doi.org/10.1111/j.1600-0528.2011.00622.x.
- Chalkley M. Incentives for dentists in public service: evidence from a natural experiment. J Public Adm Res Theory 2010;20:i207-23. http://dx.doi.org/10.1093/jopart/muq025.
- Brocklehurst P, Price J, Glenny AM, Tickle M, Birch S, Mertz E, et al. The effect of different methods of remuneration on the behaviour of primary care dentists. Cochrane Database Syst Rev 2013;6. http://dx.doi.org/10.1002/14651858.cd009853.pub2.
- Clarkson JE, Turner S, Grimshaw JM, Ramsay CR, Johnston M, Scott A. Changing clinicians’ behaviour: a randomized controlled trial of fees and education. J Dent Res 2008;87:640-4. http://dx.doi.org/10.1177/154405910808700701.
- Coventry P, Holloway PJ, Lennon MA, Mellor A, Worthington HV. A trial of a capitation system of payment for the treatment of children in the General Dental Service. Final report. Community Dent Health 1989;6:1-63.
- NHS Dental Contract Pilots – Early Findings. London: Department of Health; 2012.
- Transparency in Outcomes – A Framework for the NHS. London: Department of Health; 2010.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage Publications Inc.; 2003.
- Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Delivering Better Oral Health: An Evidence Based Toolkit for Prevention. London: The Stationery Office; 2009.
- Galloway J, Gorham J, Lambert M. The Professionals Complementary to Dentistry: A Systematic Review and Synthesis. London: University College London; 2002.
- Modernising NHS Dentistry – Implementing the NHS Plan: Briefing Dentists and NHS Managers. London: Department of Health; 2000.
- British Dental Association’s Independent Local Commissioning Working Group Report. London: British Dental Association; 2009.
- Developing the Dental Team: Curricula Frameworks for Registrable Qualifications for Professionals Complementary to Dentistry (PCDs). London: General Dental Council; 2004.
- Scope of Practice. London: General Dental Council; 2009.
- Evans C, Chestnutt IG, Chadwick BL. The potential for delegation of clinical care in general dental practice. Br Dent J 2007;203:695-9. http://dx.doi.org/10.1038/bdj.2007.1111.
- Harris R, Burnside G. The role of dental therapists working in four personal dental service pilots: type of patients seen, work undertaken and cost-effectiveness within the context of the dental practice. Br Dent J 2004;197:491-6. http://dx.doi.org/10.1038/sj.bdj.4811749.
- Jones G, Evans C, Hunter L. A survey of the workload of dental therapists/hygienist-therapists employed in primary care settings. Br Dent J 2008;204. http://dx.doi.org/10.1038/bdj.2007.1205.
- Nilchian F, Rodd HD, Robinson PG. The success of fissure sealants placed by dentists and dental care professionals. Community Dent Health 2011;28:99-103.
- Woolgrove J, Harris R. Attitudes of dentists towards delegation. Br Dent J 1982;153:339-40. http://dx.doi.org/10.1038/sj.bdj.4804939.
- Woolgrove J, Boyles J. Operating dental auxiliaries in the United Kingdom – a review. Community Dent Health 1984;1:93-9.
- Hay IS, Batchelor PA. The future role of dental therapists in the UK: a survey of district dental officers and general practitioners in England and Wales. Br Dent J 1993;175:61-6. http://dx.doi.org/10.1038/sj.bdj.4808225.
- Sprod A, Boyes J. The workforce of professionals complementary to dentistry in the general dental services: a survey of general dental practices in the South West. Br Dent J 2003;194:389-97. http://dx.doi.org/10.1038/sj.bdj.4810005.
- Gallagher JL, Wright DA. General dental practitioners’ knowledge of and attitudes towards the employment of dental therapists in general practice. Br Dent J 2003;194:37-41. http://dx.doi.org/10.1038/sj.bdj.4802411.
- Dyer T, Robinson PG. General health promotion in general dental practice – the involvement of the dental team. Part 2 – a qualitative and quantitative investigation of the views of practice principals in South Yorkshire. Br Dent J 2006;201:45-51. http://dx.doi.org/10.1038/sj.bdj.4813774.
- Ross MK, Ibbetson RJ, Turner S. The acceptability of dually-qualified dental hygienist-therapists to general dental practitioners in South-East Scotland. Br Dent J 2007;202:146-7. http://dx.doi.org/10.1038/bdj.2007.45.
- Nilchian F, Rodd HD, Robinson PG. Influences on dentists’ decisions to refer paediatric patients to dental hygienists and therapists for fissure sealants: a qualitative approach. Br Dent J 2009;207. http://dx.doi.org/10.1038/sj.bdj.2009.856.
- Dyer TA, Robinson PG. Exploring the social acceptability of skill-mix in dentistry. Int Dent J 2008;58:173-80.
- Dyer TA, Robinson PG. Public awareness and social acceptability of dental therapists. Int J Dent Hyg 2009;7:108-14. http://dx.doi.org/10.1111/j.1601-5037.2008.00340.x.
- Hally JP, Pitts NB. Developing the first dental care pathway: the oral health assessment. Prim Dent Care 2005;12:117-21. http://dx.doi.org/10.1308/135576105774342947.
- Dental Recall Interval between Routine Dental Examinations: Clinical Guideline 19. London: NICE; 2004.
- Harris R, Bridgman C. Introducing care pathway commissioning to primary dental care: the concept. Br Dent J 2010;209:233-9. http://dx.doi.org/10.1038/sj.bdj.2010.770.
- Subramanian DN, Hopayian K. An audit of the first year of screening for depression in patients with diabetes and ischaemic heart disease under the Quality and Outcomes Framework. Qual Prim Care 2008;16:341-4.
- Strong M, South G, Carlisle R. The UK Quality and Outcomes Framework pay-for-performance scheme and spirometry: rewarding quality or just quantity? A cross-sectional study in Rotherham, UK. BMC Health Serv Res 2009;9. http://dx.doi.org/10.1186/1472-6963-9-108.
- Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med 2008;6:228-34. http://dx.doi.org/10.1370/afm.844.
- Gonzalez GZ, Klazinga N, Asbroek GT. Performance indicators used to assess the quality of primary dental care. Community Dent Health 2006;23:228-35.
- Faugier J, Sargeant M. Sociology of health and illness. J Adv Nurs 1997;26:790-7. http://dx.doi.org/10.1046/j.1365-2648.1997.00371.x.
- Andersen RM, Davidson PL. Ethnicity, aging, and oral health outcomes: a conceptual framework. Adv Dent Res 1997;11:203-9. http://dx.doi.org/10.1177/08959374970110020201.
- Andersen R. A Behavioral Model of Families’ Use of Health Services. Chicago, IL: University of Chicago; 1968.
- Andersen R. Revisiting the behavioral model and access to medical care: does it matter?. J Health Soc Behav 1995;36:1-10. http://dx.doi.org/10.2307/2137284.
- Goldsmith L. A critical history of Andersen’s behavioral model of health services use: a reflection of how we study access to health care. Acad Health Serv Res Health Policy 2002;19.
- Baker SR. Applying Andersen’s behavioural model to oral health: what are the contextual factors shaping perceived oral health outcomes?. Community Dent Oral Epidemiol 2009;37:485-94. http://dx.doi.org/10.1111/j.1600-0528.2009.00495.x.
- Improving Dental Care and Oral Health – A Call for Action. London: NHS England; 2014.
- Culyer AJ. Need: the idea won’t do – but we still need it. Soc Sci Med 1995;40:727-30. http://dx.doi.org/10.1016/0277-9536(94)00307-F.
- Bradshaw J, McLachlan G. Problems and Progress in Medical Care. Oxford: Oxford University Press; 1972.
- Locker D, Allen F. What do measures of ‘oral health-related quality of life’ measure?. Community Dent Oral Epidemiol 2007;35:401-11. http://dx.doi.org/10.1111/j.1600-0528.2007.00418.x.
- Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. JOAAG 2009;4.
- Looking Ahead: Changes to Dental Provision in the UK and the Implications for the General Dental Council. A Policy Horizon Scanning Report. London: General Dental Council; 2013.
- NHS Dentistry: Delivering Change. London: Department of Health; 2004.
- Dental Contract Reform: Prototypes Overview Document. London: Department of Health; 2015.
- Primary Dental Care Services: Implementation of Local Commissioning. London: Department of Health; 2005.
- Five Year Forward View. London: NHS England; 2014.
- Forsetlund L, Bjørndal A, Rashidian A, Jamtvedt G, O’Brien MA, Wolf FM, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2009;15. http://dx.doi.org/10.1002/14651858.cd003030.pub2.
- Karlsberg Schaffer SK, Sussex J, Feng Y. Incentives to Follow Best Practice in Health Care. London: Office of Health Economics; 2015.
- Dental Contract Reform Engagement Exercise: Detailed Findings. London: Department of Health; 2015.
- Beirne P. Recall intervals for oral health in primary care patients. Cochrane Database Syst Rev 2007;17. http://dx.doi.org/10.1002/14651858.cd004346.pub3.
- Glick M, da Silva OM, Seeberger GK, Xu T, Pucca G, Williams DM, et al. FDI Vision 2020: shaping the future of oral health. Int Dent J 2012;62:278-91. http://dx.doi.org/10.1111/idj.12009.
- Timmermans S. Saving lives or saving multiple identities?: the double dynamic of resuscitation scripts. Soc Stud Sci 1996;26:767-97. http://dx.doi.org/10.1177/030631296026004003.
- Brocklehurst PR, Tickle M. Is skill mix profitable in the current NHS dental contract in England?. Br Dent J 2011;210:303-8. http://dx.doi.org/10.1038/sj.bdj.2011.238.
- Harris R, Mosedale S, Garner J, Perkins E. What factors influence the use of contracts in the context of NHS dental practice? A systematic review of theory and logic model. Soc Sci Med 2014;108:54-9. http://dx.doi.org/10.1016/j.socscimed.2014.01.032.
- Harris R, Holt R. Interacting institutional logics in general dental practice. Soc Sci Med 2013;94.
- Andersen R, Davidson P, Andersen R, Rice T, Kominski G. Changing the US Health Care System: Key Issues in Health Services Policy and Management. San Francisco, CA: Jossey-Bass; 2001.
- Gerson E, Maines D. Social Organization and Social Process. New York, NY: Aldine De Gruyter; 1991.
- Dyer T, Owens J, Robinson PG. The acceptability of care delegation in skill-mix: the salience of trust. Health Policy 2014;117:170-8. http://dx.doi.org/10.1016/j.healthpol.2014.02.013.
- Harris R. Operationalisation of the construct of access to dental care: a position paper and proposed conceptual definitions. Community Dent Health 2013;30:94-101.
- Peacock M, Bissell P, Owen J. Dependency denied: health inequalities in the neo-liberal era. Soc Sci Med 2014;118:173-80. http://dx.doi.org/10.1016/j.socscimed.2014.08.006.
- Locker D. Deprivation and oral health: a review. Community Dent Oral Epidemiol 2000;28:161-9. http://dx.doi.org/10.1034/j.1600-0528.2000.280301.x.
- Page LAF, Thomson WM, Ukra A, Farella M. Factors influencing adolescents’ oral health-related quality of life (OHRQoL). Int J Paediatr Dent 2013;23:415-23.
- Spencer N, Bambang S, Logan S, Gill L. Socioeconomic status and birth weight: comparison of an area-based measure with the Registrar General’s social class. J Epidemiol Community Health 1999;53:495-8. http://dx.doi.org/10.1136/jech.53.8.495.
- Shohaimi S, Luben R, Wareham N, Day N, Bingham S, Welch A, et al. Residential area deprivation predicts smoking habit independently of individual educational level and occupational social class. A cross sectional study in the Norfolk cohort of the European Investigation into Cancer (EPIC-Norfolk). J Epidemiol Community Health 2003;57:270-6. http://dx.doi.org/10.1136/jech.57.4.270.
- Gerhardt U. Ideas About Illness: An Intellectual and Political History of Medical Sociology. London: Macmillan Education Ltd; 1989.
- Tsakos G, Pine CM, Harris R. Community Oral Health. London: Quintessence Publishing; 2007.
- Gulliford M, Morgan M, Hughes D, Beech R, Figeroa-Munoz J, Gibson B, et al. Access to Health Care: Report of a Scoping Exercise for the National Co-ordinating Centre for NHS Service Delivery and Organisation R & D (NCCSDO). London: National Co-ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO); 2001.
- Tudor Hart J. The Inverse Care Law. Lancet 1971;297:405-12. http://dx.doi.org/10.1016/S0140-6736(71)92410-X.
- Harris RV, Pender SM, Merry A, Leo A. Unravelling referral paths relating to the dental care of children: a study in Liverpool. Prim Dent Care 2008;15:45-52. http://dx.doi.org/10.1308/135576108784000294.
- Harris RV, Dancer JM, Smith D, Campbell S. The use of conversation mapping to frame key perceptual issues facing the general dental practice system in England. Community Dent Health 2009;26:84-91.
- High Quality Care for All. NHS Next Stage Review Final Report. London: Department of Health; 2008.
- Wilson IR, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. J Am Med Assoc 1995;273:59-65. http://dx.doi.org/10.1001/jama.1995.03520250075037.
- Baker SR, Pearson NK, Robinson PG. Testing the applicability of a conceptual model of oral health in housebound edentulous older people. Community Dent Oral Epidemiol 2008;36:237-48. http://dx.doi.org/10.1111/j.1600-0528.2007.00394.x.
- Baker SR, Mat A, Robinson PG. What psychosocial factors influence adolescents’ oral health?. J Dent Res 2010;89:1230-5. http://dx.doi.org/10.1177/0022034510376650.
- Coventry J, Griffiths G, Scully C, Tonetti M. Periodontal disease. BMJ 2000;321:36-9. http://dx.doi.org/10.1136/bmj.321.7252.36.
- Alexander AG, Leon AR, Ribbons JW, Morganstein SI. An assessment of the inter-and intra-examiner agreement in scoring gingivitis clinically. J Periodont Res 1971;6:146-51. http://dx.doi.org/10.1111/j.1600-0765.1971.tb00602.x.
- Cowell CR, Saxton CA, Sheiham A, Wagg BJ. Testing therapeutic measures for controlling chronic gingivitis in man: a suggested protocol. J Clin Periodontol 1975;2:231-40. http://dx.doi.org/10.1111/j.1600-051X.1975.tb01747.x.
- Robinson PG, Deacon SA, Deery C. Manual versus powered toothbrushing for oral health. Cochrane Database Syst Rev 2005;2. http://dx.doi.org/10.1002/14651858.cd002281.pub2.
- Watts TL. Periodontal inflammation and attachment loss: a critical problem for biological studies. Oral Dis 1995;1:254-8. http://dx.doi.org/10.1111/j.1601-0825.1995.tb00190.x.
- Mombelli A. Clinical parameters: biological validity and clinical utility. Periodontol 2005;39:30-9. http://dx.doi.org/10.1111/j.1600-0757.2005.00117.x.
- Chesters RK, Pitts NB, Matuliene G, Kvedariene A, Huntington E, Bendinskaite R. An abbreviated caries clinical trial design validated over 24 months. J Dent Res 2002;81:637-40. http://dx.doi.org/10.1177/154405910208100912.
- Ekstrand KR, Bakhshandeh A, Martignon S. Treatment of proximal superficial caries lesions on primary molar teeth with resin infiltration and fluoride varnish versus fluoride varnish only: efficacy after 1 year. Caries Res 2010;44:41-6. http://dx.doi.org/10.1159/000275573.
- Ismail AL, Sohn W, Tellez M, Willem JM, Betz J, Lepkowski J. Risk indicators for dental caries using the International Caries Detection and Assessment System (ICDAS). Community Dent Oral Epidemiol 2008;36:55-68.
- Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health 1994;11:3-11.
- Slade G. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 1997;25:284-90. http://dx.doi.org/10.1111/j.1600-0528.1997.tb00941.x.
- Robinson PG, Gibson B, Khan FA, Birnbaum W. Validity of two oral health related quality of life measures in a UK setting. Community Dent Oral Epidemiol 2003;31:90-9. http://dx.doi.org/10.1034/j.1600-0528.2003.00051.x.
- Locker D, Jokovic A, Clarke M. Assessing the responsiveness of measures of oral health-related quality of life. Community Dent Oral Epidemiol 2004;32:10-8. http://dx.doi.org/10.1111/j.1600-0528.2004.00114.x.
- Jowett A, Rawlinson A, Orr S, Robinson PG. The psychosocial impact of periodontal disease and its treatment with 24 hour root surface debridement. J Clin Periodontol 2009;36:413-18. http://dx.doi.org/10.1111/j.1600-051X.2009.01384.x.
- Pearson NK, Gibson BJ, Davis DM, Gelbier S, Robinson PG. The effect of a domiciliary denture service on oral health quality of life: a randomised controlled trial. Br Dent J 2007;203. http://dx.doi.org/10.1038/bdj.2007.569.
- Clarkson JE, Young L, Ramsay CR, Bonner BC, Bonetti D. How to influence patient oral hygiene behaviour effectively. J Dent Res 2009;88. http://dx.doi.org/10.1177/0022034509345627.
- Slade GD, Nuttall N, Sanders AE, Steele JG, Allen PF, Lahti S. Impacts of oral disorders in Australia and the United Kingdom. Br Dent J 2005;198:489-93. http://dx.doi.org/10.1038/sj.bdj.4812252.
- Fox J. Applied Regression Analysis and Generalized Linear Models. New York, NY: Sage; 2008.
- Blance A, Tu YK, Baelum V, Gilthorpe MS. Statistical issues on the analysis of change in follow-up studies in dental research. Community Dent Oral Epidemiol 2007;35:412-20. http://dx.doi.org/10.1111/j.1600-0528.2007.00407.x.
- Williams A. Euroqol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. http://dx.doi.org/10.1016/0168-8510(96)00822-6.
- Stone S, McCracken G, Heasman P, Staines S, Pennington M. Cost-effectiveness of personalized plaque control for managing the gingival manifestations of oral lichen planus: a randomized controlled study. J Clin Periodontol 2013;40:859-67. http://dx.doi.org/10.1111/jcpe.12126.
- Hulme C, Yu G, Browne C, O’Dwyer J, Craddock H, Brown S, et al. Cost-effectiveness of silicone and alginate impressions for complete dentures. J Dent 2014;42:902-7. http://dx.doi.org/10.1016/j.jdent.2014.03.001.
- Guide to the Methods of Health Technology Appraisal. London: NICE; 2013.
- Locker D. Measuring oral health: a conceptual framework. Community Dent Health 1988;5:5-13.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. http://dx.doi.org/10.1097/00005650-199711000-00002.
- Kent Express . Kent Express Dental Supplies 2014. www.kentexpress.co.uk/gb-en/kent/default.aspx?did=kent (accessed 2 September 2015).
- MGill . 2011 Price List 2011. http://mgill.co.uk/Price_list/index.html (accessed 2 September 2015).
- NHS . Pay Circular (M&Amp;D) 1 2011 2011. www.nhsemployers.org/~/media/employers/publications/pay%20circulars/pay%20circular%20_MD_%201-2011.pdf.
- NHS Agenda for Change Pay Scales – 2011/2012. London: Royal Collage of Nursing; 2011.
- Campbell and Cochrane Economics Methods Group (CCEMG) and the Evidence for Policy and Practice Information and Coordinating Centre (EPPI-Centre) . CCEMG–EPPI-Centre Cost Converter 2014. www.eppi.ioe.ac.uk/costconversion/ (accessed 2 September 2015).
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. http://dx.doi.org/10.1002/hec.635.
- Brennan D, Spencer AJ. Mapping oral health related quality of life to generic health state values. BMC Health Serv Res 2006;6. http://dx.doi.org/10.1186/1472-6963-6-96.
- Sullivan P, Ghushchyan V. Mapping the EQ-5D index from the SF-12: US general population preferences in a nationally representative sample. Med Decis Making 2006;26:401-9. http://dx.doi.org/10.1177/0272989X06290496.
- Austin PC. Bayesian extensions of the Tobit model for analysing measures of health status. Med Decis Making 2002;22:152-62. http://dx.doi.org/10.1177/0272989X0202200212.
- Adult Dental Health. Survey. Leeds: The Health and Social Care Information Centre; 2009.
- Heydecke G, Locker D, Awad MA, Lund JP, Feine JS. Oral and general health-related quality of life with conventional and implant dentures. Community Dent Oral Epidemiol 2003;31:161-8. http://dx.doi.org/10.1034/j.1600-0528.2003.00029.x.
- Broder HL, Slade G, Caine R, Reisine S. Perceived impact of oral health conditions among minority adolescents. J Public Health Dent 2000;60:189-92. http://dx.doi.org/10.1111/j.1752-7325.2000.tb03326.x.
- Allen PF, McMillan AS, Walshaw D, Locker D. A comparison of the validity of generic- and disease-specific measures in the assessment of oral health-related quality of life. Community Dent Oral Epidemiol 1999;27:344-52. http://dx.doi.org/10.1111/j.1600-0528.1999.tb02031.x.
- Jaeschke, Singer J, Guyatt GH. Measurement of health-status – ascertaining the minimal clinically important difference. Control Clin Trials 1989;10:407-15. http://dx.doi.org/10.1016/0197-2456(89)90005-6.
- Borrell L, Kiefe C, Williams D, Diez-Roux A, Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Soc Sci Med 2006;63:1415-27. http://dx.doi.org/10.1016/j.socscimed.2006.04.008.
- Wolfe F, Michaud K, Wallenstein G. Scale characteristics and mapping accuracy of the US EQ-5D, UK EQ-5D, and SF-6D in patients with rheumatoid arthritis. J Rheumatol 2010;37:1615-25. http://dx.doi.org/10.3899/jrheum.100043.
- Primary Care: The Future: Choice and Opportunity. London: The Stationery Office; 1997.
- Brennan D, Spencer SJ. Variation in dental service provision among adult migrant public-funded patients. Aust N Z J Public Health 1999;23:639-42. http://dx.doi.org/10.1111/j.1467-842X.1999.tb01551.x.
- Riggs E, Gussy M, Gibbs L, van Gemert C, Waters E, Kilpatrick N. Hard to reach communities or hard to access services? Migrant mothers’ experiences of dental services. Aust Dent J 2014;59:201-7. http://dx.doi.org/10.1111/adj.12171.
- A Strategic Review of the Future Dentistry Workforce. London: CFWI; 2013.
- Bullock A, Firmstone V. A professional challenge: the development of skill mix in UK primary care dentistry. Health Serv Manage Res 2011;21:190-5. http://dx.doi.org/10.1258/hsmr.2011.011011.
- Levine M, Ensom MH. Post hoc power analysis: an idea whose time has passed?. Pharmacotherapy 2001;4:405-9. http://dx.doi.org/10.1592/phco.21.5.405.34503.
- Briefing Notes for Researchers: Involving the Public in NHS, Public Health and Social Care Research. Eastleigh: INVOLVE; 2012.
Appendix 1 Theoretical framework
Appendix 2 Topic guides
Appendix 3 Lost to follow-up and missing at random
In Figure 26 we can see the distribution of missing EQ-5D-3L scores in the sample over the study. More than half of the patients at follow-up had all or some of the EQ-5D-3L components missing (279 and 12 patients, respectively, each highlighted in the figure with a dashed line box). From the patients who did the follow-up, 16 (10) had all (some) EQ-5D-3L items missing and with regards to the missing OHIP-14 items: 16 patients had all items missing and only two patients had some items missing. Adding to this, those patients who did not complete the study had worse OHQoL (i.e. a higher total OHIP-14 score) than the patients who did complete the study in either traditional or incentive practices (Table 49). Differences in either OHIP-14 or EQ-5D-3L scores between those who did and those who did not complete the study are mostly significant at the 5% level, suggesting that many patients in this study only visited the practice when they had a problem and did not come back.
FIGURE 26.
Distribution of missing EQ-5D-3L scores in the study.
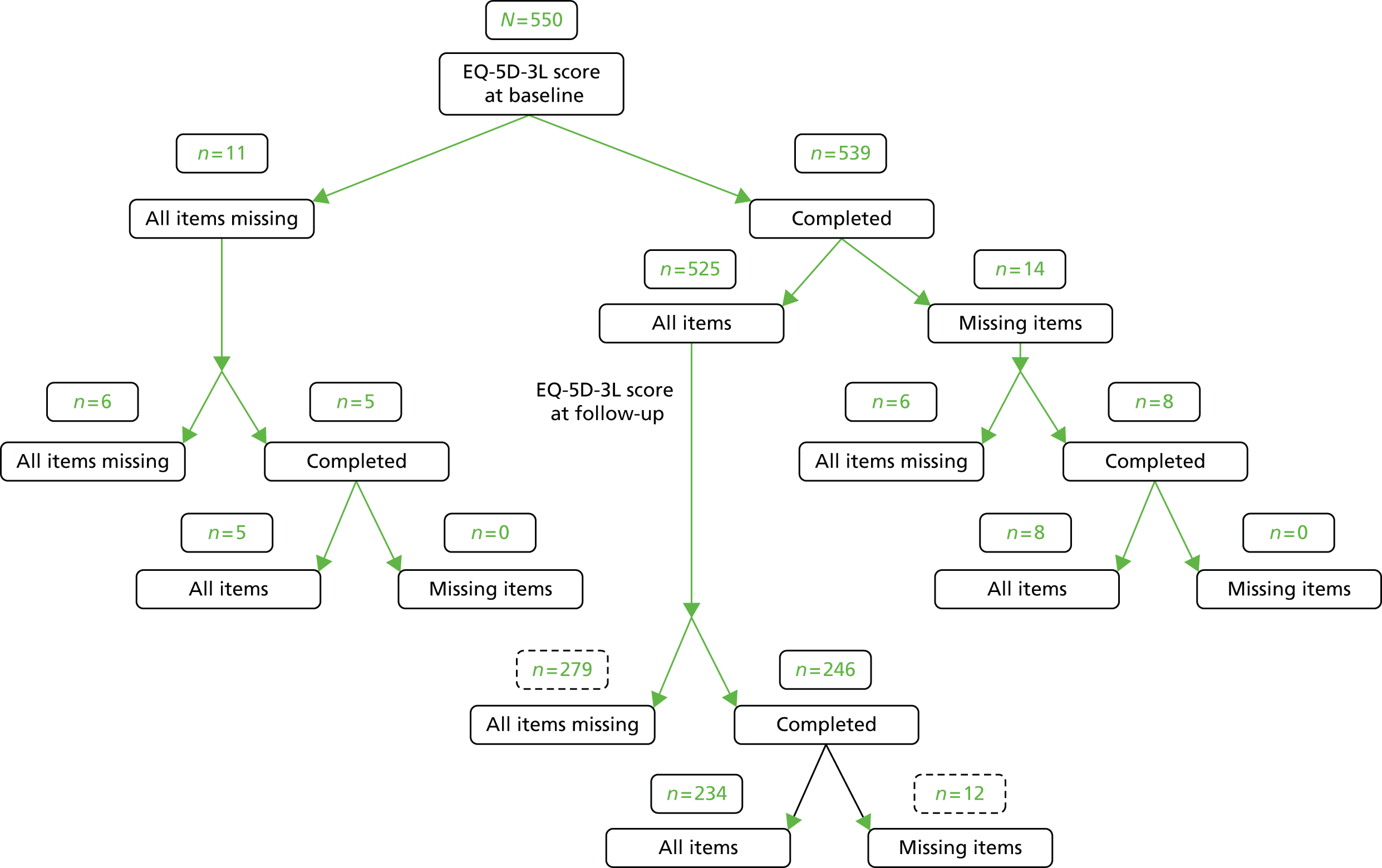
| Practice | Complete (n = 210), mean (SD) | Lost to follow-up (n = 340), mean (SD) | Change, mean (p-value) |
|---|---|---|---|
| Baseline (OHIP-14) | |||
| Traditional | 9.12 (10.98) | 12.30 (2.12) | –3.18 (0.033) |
| Incentive | 9.00 (10.30) | 13.52 (12.45) | –4.52 (0.002) |
| Baseline (EQ-5D-3L) | |||
| Traditional | 0.896 (0.232) | 0.835 (0.020) | 0.061 (0.135) |
| Incentive | 0.880 (0.250) | 0.828 (0.023) | 0.052 (0.047) |
Complementary results mapping
Tables 50 and 51 show the regression results of health-state values by OHIP-14 score for the continuous model and categorical model, respectively. Table 52 shows the mean observed and fitted health-state values within categories of observed health-state values for the categorical model.
| Variable | OLS | Tobit | TPM |
|---|---|---|---|
| Trouble pronouncing words | –0.028 (0.042) | –0.028 (0.040) | –0.014 (0.039) |
| Sense of taste worsened | –0.047 (0.039) | –0.048 (0.038) | –0.013 (0.032) |
| Painful aching in mouth | –0.077* (0.032) | –0.079** (0.031) | –0.093* (0.030) |
| Uncomfortable eating | –0.014 (0.030) | –0.015 (0.028) | –0.011 (0.026) |
| Felt self-conscious | –0.030 (0.030) | –0.033 (0.029) | –0.015 (0.028) |
| Felt tense | 0.047 (0.035) | 0.046 (0.034) | 0.014 (0.031) |
| Diet unsatisfactory | –0.0003 (0.043) | 0.001 (0.042) | –0.013 (0.041) |
| Interrupt meals | 0.059 (0.044) | 0.058 (0.043) | 0.065 (0.040) |
| Difficulty relaxing | –0.029 (0.040) | –0.029 (0.039) | –0.037 (0.040) |
| Been embarrassed | –0.031 (0.040) | –0.029 (0.038) | –0.032 (0.034) |
| Irritable with other people | –0.004 (0.045) | –0.002 (0.043) | –0.008 (0.043) |
| Difficulty doing usual jobs | 0.076 (0.058) | 0.078 (0.056) | 0.071 (0.056) |
| Life less satisfying | –0.079*** (0.043) | –0.082*** (0.042) | –0.060 (0.039) |
| Unable to function | –0.058 (0.053) | –0.058 (0.051) | –0.026 (0.049) |
| Sex (male) | 0.007 (0.031) | 0.011 (0.028) | 0.017 (0.026) |
| Age (years) | –0.008*** (0.005) | –0.008*** (0.005) | 0.006 (0.004) |
| Agesq (years) | 0.0001 (0.00001) | 0.0001 (0.0001) | 0.0004 (0.0004) |
| Constant | 1.1275* (0.106) | 1.181* (0.100) | 1.142* (0.089) |
| F-stat (p-value) | 3.07 (0.000) | 3.31 (0.000) | 3.13 (0.000) |
| Variable | OLS | Tobit | TPM |
|---|---|---|---|
| Trouble pronouncing words | |||
| Hardly ever | –0.054 (0.044) | –0.055 (0.040) | –0.027 (0.039) |
| Occasionally/fairly often/very often | 0.646* (0.223) | 0.678* (0.225) | 0.504** (0.217) |
| Sense of taste worsened | |||
| Hardly ever | –0.051 (0.036) | –0.050 (0.034) | –0.031 (0.033) |
| Occasionally/fairly often/very often | –0.211 (0.199) | –0.242 (0.207) | –0.027 (0.207) |
| Painful aching in mouth | |||
| Hardly ever | –0.027 (0.032) | –0.031 (0.290) | –0.043 (0.028) |
| Occasionally/fairly often/very often | –0.407* (0.107) | –0.405* (0.102) | –0.414* (0.105) |
| Uncomfortable eating | |||
| Hardly ever | –0.014 (0.033) | –0.015 (0.030) | –0.009 (0.026) |
| Occasionally/fairly often/very often | 0.065 (0.081) | 0.058 (0.075) | 0.034 (0.075) |
| Felt self-conscious | |||
| Hardly ever | –0.024 (0.033) | –0.025 (0.030) | –0.024 (0.030) |
| Occasionally/fairly often/very often | –0.096 (0.072) | –0.100 (0.068) | –0.065 (0.070) |
| Felt tense | |||
| Hardly ever | 0.031 (0.107) | 0.028 (0.031) | 0.012 (0.030) |
| Occasionally/fairly often/very often | 0.074 (0.045) | 0.075 (0.101) | –0.023 (0.087) |
| Diet unsatisfactory | |||
| Hardly ever | –0.011 (0.150) | –0.010 (0.042) | –0.006 (0.041) |
| Occasionally/fairly often/very often | 0.127 (0.042) | 0.152 (0.154) | –0.006 (0.156) |
| Interrupt meals | |||
| Hardly ever | 0.088** (0.157) | 0.088** (0.040) | 0.077 (0.040) |
| Occasionally/fairly often/very often | –0.064 (0.128) | –0.079 (0.151) | 0.019 (0.167) |
| Difficulty relaxing | |||
| Hardly ever | –0.044 (0.035) | –0.045 (0.033) | –0.054 (0.034) |
| Occasionally/fairly often/very often | 0.087 (0.180) | 0.085 (0.170) | 0.074 (0.193) |
| Been embarrassed | |||
| Hardly ever | –0.039 (0.044) | –0.038 (0.040) | –0.023 (0.039) |
| Occasionally/fairly often/very often | 0.024 (0.082) | 0.031 (0.078) | 0.031 (0.067) |
| Irritable with other people | |||
| Hardly ever | –0.003 (0.047) | –0.003 (0.044) | 0.007 (0.046) |
| Occasionally/fairly often/very often | 0.021 (0.122) | 0.027 (0.116) | –0.062 (0.119) |
| Difficulty doing usual jobs | |||
| Hardly ever | 0.074 (0.058) | 0.075 (0.055) | 0.091*** (0.055) |
| Occasionally/fairly often/very often | –0.011 (0.127) | –0.015 (0.120) | –0.076 (0.101) |
| Life less satisfying | |||
| Hardly ever | –0.019 (0.043) | –0.020 (0.040) | –0.043 (0.041) |
| Occasionally/fairly often/very often | –0.297* (0.101) | –0.310*** (0.098) | –0.188*** (0.098) |
| Unable to function | |||
| Hardly ever | –0.031 (0.051) | –0.030 (0.047) | 0.018 (0.042) |
| Occasionally/fairly often/very often | –0.203 (0.199) | –0.207 (0.186) | –0.142 (0.181) |
| Sex (male) | 0.008 (0.030) | 0.011 (0.027) | 0.019 (0.025) |
| Age (years) | –0.007 (0.005) | –0.007 (0.004) | –0.005 (0.004) |
| Agesq (years) | 0.00004 (0.0001) | 0.0001 (0.0001) | 0.0002 (0.0004) |
| Constant | 1.120* (0.104) | 1.128* (0.095) | 1.086* (0.089) |
| F-stat (p-value) | 5.91 (0.000) | 6.48 (0.000) | 10.91 (0.000) |
| Observed health state | Observed values | Fitted values | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OLS | Tobit | TPM | |||||||
| Category | n | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI |
| < 0.70 | 28 | 0.33 | 0.22 to 0.43 | 0.79 | 0.70 to 0.87 | 0.79 | 0.70 to 0.88 | 0.66 | 0.53 to 0.79 |
| 0.70–0.80 | 24 | 0.76 | 0.75 to 0.78 | 0.83 | 0.76 to 0.90 | 0.83 | 0.76 to 0.91 | 0.79 | 0.68 to 0.91 |
| > 0.80 | 151 | 0.98 | 0.97 to 0.99 | 0.89 | 0.87 to 0.90 | 0.89 | 0.88 to 0.91 | 0.87 | 0.84 to 0.89 |
| All | 203 | 0.86 | 0.83 to 0.90 | 0.87 | 0.85 to 0.89 | 0.87 | 0.85 to 0.89 | 0.83 | 0.80 to 0.86 |
List of abbreviations
- ANCOVA
- analysis of covariance
- BoP
- bleeding on probing
- CCEMG–EPPI
- Campbell and Cochrane Economics Methods Group – Evidence for Policy and Practice Information and Co-ordinating Centre
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- DQOF
- Dental Quality and Outcomes Framework
- E&F
- extractions and fillings
- EQ-5D-3L
- European Quality of Life-5 Dimensions questionnaire, 3-level version
- GDP
- general dental practitioner
- ICDAS
- International Caries Detection and Assessment System
- ICER
- incremental cost-effectiveness ratio
- INCENTIVE
- INnovation in Commissioning primary dENTal care delIVEry
- MID
- minimal important difference
- nGDS
- new General Dental Services
- NICE
- National Institute for Health and Care Excellence
- NRES
- National Research Ethics Service
- OHA
- oral health assessment
- OHImp
- oral health improvement
- OHIP-14
- Oral Health Impact Profile
- OHQoL
- oral health-related quality of life
- OLS
- ordinary least squares
- PCT
- primary care trust
- PDS
- Personal Dental Services
- PPI
- patient and public involvement
- PROM
- patient-reported outcome measure
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- RAG
- red–amber–green
- REC
- Research Ethics Committee
- SD
- standard deviation
- SMS
- short message service
- TCV
- total contract value
- TPM
- two-part model
- UDA
- unit of dental activity