Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/2000/11. The contractual start date was in July 2012. The final report began editorial review in April 2015 and was accepted for publication in October 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Gridley et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Dementia is a major and growing health concern across the world. With an imminent cure unlikely, providing good-quality and cost-effective care, over what is often a long period of need, is, and will remain, a major challenge for health and other care providers. The Department of Health (DH) has outlined improved quality of care in general hospitals, living well with dementia in care homes, and reduced use of antipsychotic medication as priority objectives for dementia. 1 Quality outcomes for people with dementia in the National Institute for Health and Care Excellence Quality Standards2 similarly focus on improving health outcomes through improving care processes, and two quality statements emphasise the importance of understanding people with dementia via their life stories and biographies.
Listening to people with dementia and understanding that they have rich and varied histories is essential to good care. 3 ‘Life story work’ (LSW) is used increasingly for this and involves gathering information and artefacts about the person, their history and interests, and producing a picture book or other tangible output – the ‘life story’ – including storyboards and multimedia resources. 4 LSW has been used in health and social care settings for nearly three decades, with children,5 people with learning disabilities6 and older people. 7 Since the 1990s, there has been growing interest in its potential to deliver person-centred care for people with dementia. 8,9
The approach is distinct from reminiscence and ‘biographical work’ in dementia care, because it emphasises using the life story in day-to-day care to improve communication, relationships and understanding of the individual’s past life, and in its orientation to the future. Life stories, as tangible products, are owned and held by people with dementia and can travel with them to smooth the transition to other settings, for example into acute medical care or from home to long-term care. This makes life stories distinct from biographical ‘work’ in care settings10 or the simple logging of life history details in care records.
Two systematic reviews have explored LSW in dementia care and both suggest that the approach has considerable potential. The first11 reviewed LSW with a range of user groups and reviewed four qualitative studies focused specifically on dementia. These studies suggested that life stories can help staff to understand the person they are caring for in the context of their past, which in turn can help to explain their present behaviours. Staff valued life story books as care planning and assessment resources, but there was little reporting of patients’ and carers’ views. The review’s authors noted an absence of attempts to present conflicting evidence about the value of life stories in practice. The second review identified 28 studies of LSW with people with dementia in institutional settings. 12 All interventions contained some features important for achieving an enhanced sense of identity among residents. However, the focus of the studies tended to be the impact of the life story reminiscence process, generally conducted by researchers or therapists for limited periods, rather than the routine daily use of life stories. The authors concluded that there is still much to learn about how best to deliver LSW to people with dementia and that more attention should be paid to developing a sound theoretical framework.
Subsequent studies have suggested that life stories help staff to see clients with dementia as individuals, help family carers to uphold relatives’ personhood and enable those with dementia to be heard and recognised as people with unique stories. However, these studies have been very small in scale13,14 or remain unpublished (Cohen K, Johnson D, Kaiser P, Dolan A, Lancaster University, 2008, unpublished report).
The use of life histories (sic) has been advocated in the DH Dementia Commissioning Pack15 and this, in turn, refers to a Commission for Social Care Inspection report that commended the use of life histories in care planning. 16 However, LSW for people with dementia is under-researched, with little evidence about the most cost-effective ways to implement it in different settings or with different user groups. To date, there have been no large-scale, methodologically rigorous studies of the impact of LSW on outcomes for people with dementia, carers and staff, or any attempt to establish its costs. More basically, unlike reminiscence therapy,17 the mechanisms that might make LSW effective, or the contexts in which these might apply, have not been articulated; there is, thus, no developed theory of change that underpins its use. Finally, although descriptive accounts and practice-based knowledge show LSW being used in different ways in different dementia care settings, we have no systematic knowledge about who is using it, where, how, with what effect and at what financial cost.
Despite LSW’s use in dementia care settings in the NHS and elsewhere, its outcomes for people with dementia, their carers and staff, its costs and its impact on care quality remain unevaluated. With current moves towards embedding LSW in dementia care, robust evaluation of the technique, its outcomes and costs, and how it can best be applied is urgently needed. We need to understand how LSW might improve interactions and relationships between staff, carers and people with dementia in a range of health and long-term care settings; affect service users’ and carers’ quality of life (QoL) and other individual outcomes; and reduce the use of antipsychotic drugs for behavioural ‘problems’. There is also a need to establish the likely costs and benefits of implementing LSW more widely in health and long-term care settings.
As LSW is a complex intervention, formal evaluation must be preceded by development and feasibility/pilot stage research, as recommended in the most recent Medical Research Council (MRC) guidance. 18 Our project was, therefore, planned to provide theoretical underpinnings for LSW, explore good practice in its use, establish where and how it is used in health and social care settings in England, outline its possible costs and benefits in such settings and establish the feasibility of formal evaluation.
The work was designed to generate a robust theory of change and a good practice framework to underpin growing use of LSW in dementia care for the NHS management community to use. We hoped that elucidating LSW’s potential outcomes, impact on care quality and costs might inform commissioning decisions about where and how best to use it. Future formal evaluation of LSW, building on our work, would, further, provide robust, generalisable evidence of effectiveness and costs.
The formally stated aim of the project was to carry out the development and initial feasibility stages of evaluation of a complex intervention – LSW – for people with dementia.
The objectives were to:
-
develop a theoretical model of LSW (including its potential outcomes) and establish core elements of good practice in using and applying the approach
-
benchmark the current use of LSW in dementia services in England against good practice
-
scope the potential effects and costs of using LSW in specialist inpatient and long-term care settings
-
explore the feasibility of formal evaluation of LSW in health and long-term care settings
-
disseminate findings to providers, planners, commissioners and users of dementia services.
The research questions were:
-
How might LSW improve outcomes for people with dementia, carers, staff and wider health and social care systems?
-
How cost-effective could this be?
-
Is formal evaluation of LSW feasible?
Overview of design and methods
Each main chapter describes in detail the design and methods used to address the research questions. Here, we provide a brief overview of the rationale for our choices.
Medical Research Council guidance points to the special challenges that evaluation of complex interventions poses for evaluators. 18 The guidance suggests that before formal evaluation of effectiveness and costs, understanding of the existing evidence base, a developed theory of change, process and outcome modelling, and a clear understanding of the feasibility of formal evaluation must be in place. These elements were not in place for LSW when we wrote our proposal. We thus focused on the development and initial feasibility work required before full evaluation in two main stages: (1) reviewing the evidence base and identifying and developing theory and components of good practice; and (2) data collection to support modelling of processes and outcomes and judgement about the feasibility of full evaluation. A mixed-methods approach was used throughout. Table 1 sets out how each objective was addressed by the project methods.
| Objective | Methods |
|---|---|
| 1: Develop a theoretical model of LSW, including its potential outcomes, and establish core elements of good practice in using and applying the approach | A systematic review of literature (stage 1a) published in or after 1984 on LSW with people with dementia to identify reported outcomes and their sizes, underlying theories of change and any reported elements of good practice in creating and using life stories |
| A qualitative study (stage 1b) using focus groups with people with early-stage dementia, carers and professionals, who have experience of LSW to ascertain what outcomes are experienced or expected, for whom, under what circumstances and by which causal routes; as well as participants’ views about core elements of good practice in LSW | |
| 2: Benchmark the current use of LSW in dementia services in England against good practice | A survey of health and social care providers of dementia services (stage 2a) and of informal carers (stage 2b) to establish how LSW is used in different care settings. Good practice elements identified in stage 1 will influence the survey content, enabling us to benchmark use against good practice |
| 3: Scope the potential effects and costs of using LSW in specialist inpatient and long-term care settings | Two small-scale feasibility studies (stage 2c) – one with a stepped-wedge design in care homes, the other with a pre-test post-test design in a NHS assessment unit – to examine the potential size of outcomes from and costs of using LSW in these settings. Relevant resource inputs will be identified, measured and then valued using local or national unit costs to establish the costs of LSW relative to other approaches Using these preliminary data, and assuming that we have observed any effects, we will create a probability tree for effectiveness of LSW in relation to outcomes and then a Markov model of effectiveness and cost-effectiveness of LSW (stage 2d). This will help to assess whether or not future, formal evaluation of LSW would be worthwhile |
| 4: Explore the feasibility of formal evaluation of LSW in health and long-term care settings | In addition to producing data on potential costs and outcomes of LSW, these small-scale studies (stage 2c) will provide valuable learning on the practical feasibility of formal evaluation of LSW in different settings and for two different designs |
We also planned a dissemination phase, including with a short film, produced with the advice of people with dementia, and a four-page plain English summary.
Outline of the report
Chapter 2 reports the literature review that we used to explore good practice in LSW and to develop a theory of change, while Chapter 3 reports the qualitative work with people with dementia, family carers and professionals that addressed the same issues through empirical exploration. In Chapter 4 we explain how we used the findings in Chapters 2 and 3 to identify outcomes for the feasibility study and how we chose instruments to measure them. The two national surveys of the use of LSW in health and social care settings and the experiences of carers of LSW are reported in Chapter 5. Chapter 6 reports our in-depth exploration of the feasibility of formal evaluation, while Chapters 7 and 8 report the outcomes and costs measured in the feasibility study. Chapter 9 reports the qualitative work carried out at the end of the study to explore the experiences of those who had been involved in it. The final chapter contains discussion of our results and conclusions.
Chapter 2 Review of the literature
An important element of the initial development stage of our research was a review of the existing literature to inform the development of a theoretical model of LSW, including its potential outcomes, and to establish core elements of good practice in using and applying the approach (project stage 1a, objective 1). The main research questions here were:
-
What outcomes and of what size have been reported for LSW?
-
What underlying theories of change for LSW are articulated in the literature?
-
What elements of good practice in creating and using life stories are reported in the literature?
We proposed to undertake the review following Centre for Reviews and Dissemination guidance,19 using a narrative synthesis20 of the extracted material, and a ‘realist’ approach21 – establishing what types and size of outcomes were reported, for whom, under what circumstances (including good practice components), and by which (implicit or explicit) causal routes. We further proposed synthesising evidence by the type of LSW used and the characteristics of participants and care settings.
Search strategy
The literature searches involved electronic searching of a range of databases covering the fields of health, mental health, nursing and social care (see Appendix 1, Table 8; all tables for this chapter can be found in Appendix 1). The search strategies were devised using a combination of subject indexing terms (when available), such as medical subject headings (MeSHs) in MEDLINE, and free-text search terms in the title and abstract. The search terms were identified through discussion within the research team and by scanning background literature.
The search strategies focused on the retrieval of published studies and ‘grey literature’ (dissertations, reports, etc.) in which interventions were described explicitly as life story/life history/life review or life narrative within the title/abstract. Related terms such as oral history/biography/reminiscence were not searched, in order to reduce the retrieval of irrelevant studies. The decisions to restrict the searches in this way were made after the inclusion of these wider terms was piloted. The results of the broader search were compared with those from the more focused search and a decision was taken to use the more specific terms only.
The search strategies used to identify studies are included in Appendix 2. The searches were not limited by date, but were limited to English-language results only.
The results were loaded into EndNote bibliographic software (Thomson Reuters, CA, USA) and deduplicated using several algorithms.
The reference lists of all included review articles were searched for apparently relevant additional studies.
Inclusion and exclusion criteria
As with most reviews of complex interventions, it is good practice to finesse the inclusion and exclusion criteria for selection for relevance after the first phase of searching. 22 However, we had developed some initial inclusion and exclusion criteria based on our existing knowledge of this literature, which we outlined in our proposal. These were:
-
inclusion: any published account of LSW or life stories that is also about one of the dementias and refers to outcomes; any care setting, including own home; any country (UK and non-UK); any empirical study type; any theoretical account, including guidance and training documents.
-
exclusion: opinion pieces, letters; published before 1984; not English language.
Once the project started, we further developed the inclusion and exclusion criteria in consultation with the project steering group and our project advisers. They were finalised through an iterative process during the early stages of searching and were as follows.
Inclusion criteria
Types of participants
Studies that included, and papers that were about, people with dementia or Alzheimer’s disease (including ‘confusion’ or ‘memory problems’).
Phenomena of interest
Studies that evaluated or that elucidated the theoretical underpinnings of LSW with people with dementia.
Types of outcomes
Any outcomes reported.
Study designs
Any study design, qualitative or quantitative.
Date
Studies published in or after 1984.
Exclusion criteria
-
Literature on LSW outside the dementia/Alzheimer’s context.
-
Opinion pieces and letters.
-
Studies not in English.
Selection of studies for relevance
We first went through the identified studies to assess their relevance to the aims and objectives of the review, using titles and, when available, abstracts. We developed a simple algorithm to help us in this (see Appendix 3). Two researchers (KG and GMP) worked individually and then as a pair to agreement about relevant studies.
We obtained full copies of the studies selected for relevance and read them before making a final decision about inclusion for review. Again, we developed guidelines for this process to ensure consistency across the team (see Appendix 4). Three members of the team (KG, GMP and YB) worked individually and then in pairs to agreement about relevant studies. When we could not reach agreement in pairs, the third member of the review team arbitrated.
Assessment of methodological quality
Given the limited literature on LSW and the largely scoping and qualitative nature of our research questions, we did not include or exclude papers based on their methodological quality.
Data extraction
The focus of data extraction was on outcomes that authors reported as arising, actually or potentially, from LSW, for whom these outcomes arose, explicit or implicit theoretical assumptions about causation, and any information on changes in outcomes.
We also extracted details of the type of LSW described, participants, the care setting, study design and any data or discussion related to good practice in creating and using life stories.
Data extraction headings
Data extraction headings were developed after the first reading of the included studies and were discussed both in the research team and with the project steering group. The headings were then used to create data extraction forms in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA).
For the best practice part of the review, the final data extraction headings in relation to ‘doing’ LSW were format of the LSW, contents to include, contents to exclude or avoid, style of the LSW product, which people with dementia should do LSW, who should be involved in doing LSW, when LSW should be done, and ethical issues. Headings for organisational ‘best practice’ issues were the culture of care, leadership and management support for LSW, resources and time, support for staff doing LSW, training and preparation for staff/volunteers doing LSW, and incentives.
For the theory of change review, we were interested in any causal links that authors argued – either explicitly or implicitly – existed between doing LSW and outcomes (whether for people with dementia, family members or care staff).
For this part of the review, then, the data extraction headings were type of LSW (as defined by analysis of the first stage of the review – see Results, Good practice in life story work), argued causal links between LSW and outcomes, types of primary outcomes, types of intermediate or process outcomes, and contextual influences and factors that might affect outcomes.
All data extraction for both parts of the review was carried out by one researcher (GMP). The progress and initial findings of the extraction process were shared with other members of the team and with the project steering group.
Data synthesis
All findings were analysed qualitatively and, when possible, metasynthesised. This involved aggregating or synthesising conclusions from the reviewed publications to generate a set of statements that represented that aggregation. The aim of meta-synthesis was to produce a single comprehensive set of synthesised findings. For the theory of change analysis we also used mind-mapping software in the first stages of analysis.
Results
Numbers of papers identified
The electronic searches identified 1199 records (see Appendix 1, Table 9). Following deduplication, 638 records were available to be assessed for relevance. A further 19 studies were identified at a later stage from the reference lists of papers included for review.
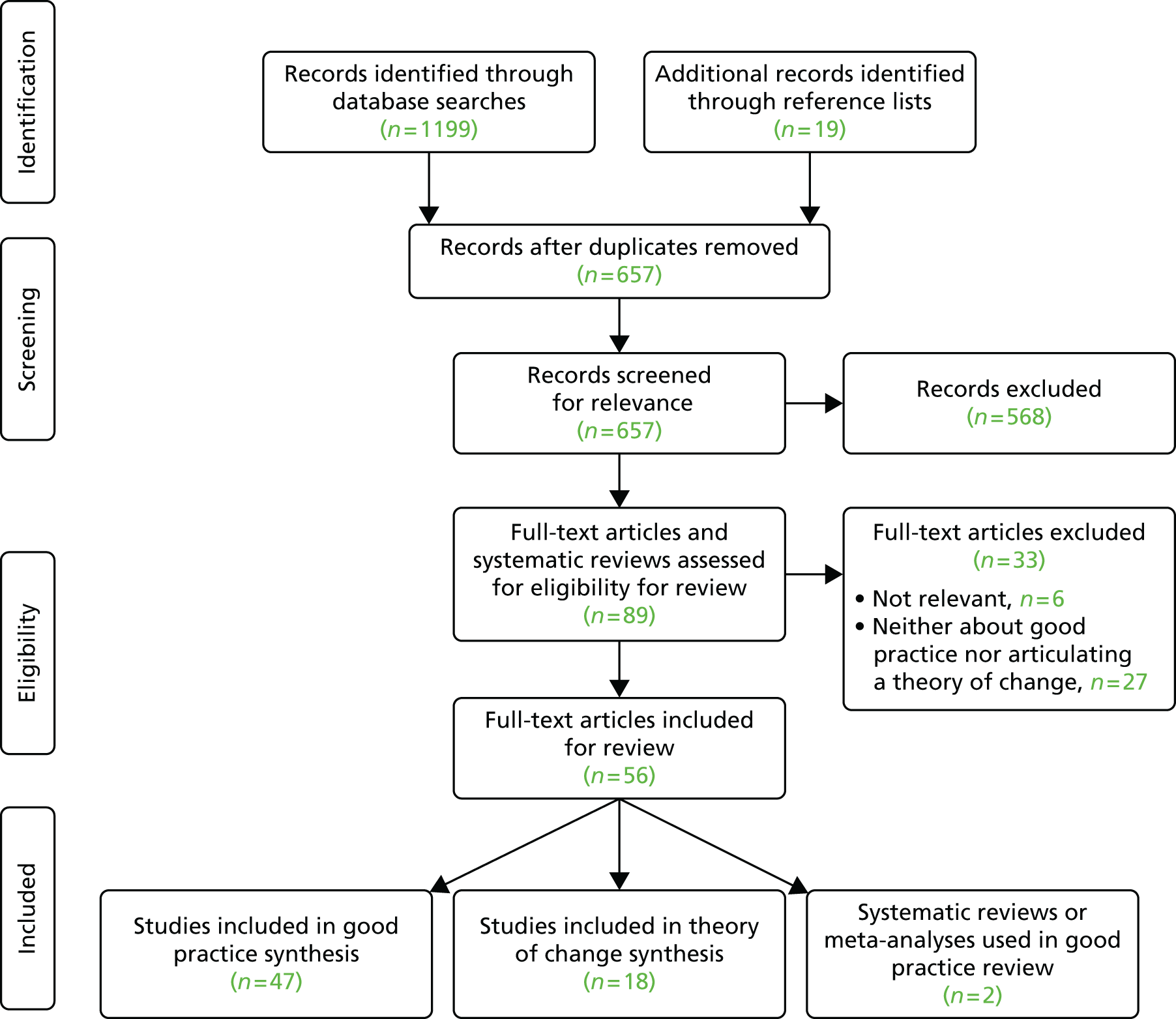
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram (Figure 1) shows the process through which the identified studies7,9–11,14,17,24–104 were reduced to a final selection of 56 papers; of these, 47 were used in the good practice review and 18 were used in the theory of change review (see Appendix 1, Table 10).
Two of the six existing systematic reviews or meta-analyses11,105 also provided material for the good practice review (see Appendix 1, Table 11).
Details of the types of primary studies included in the two reviews are in Table 12 (see Appendix 1).
As Figure 1 and the tables show, the majority of selected papers contributed to the good practice review, but few articulated any explicit or implicit explanation of why LSW might lead to better outcomes for people with dementia, their family members or care staff.
Good practice in life story work
In this part of the review we first identified which selected publications contained any ‘how to do it’ material about LSW, so that we could focus on what authors believed was good practice in relation to LSW. We looked for publications that said anything about one or more of the following issues: format of a life story, contents to include in a life story, contents to be excluded or avoided, style to be used, who should be involved in LSW, when LSW should be done, and ethical issues. We also looked for publications that said anything about the organisational context to support LSW. The issues here were culture of the care setting, leadership and management support, resources and time commitment, support for staff in settings where LSW was being done, training or preparation for staff or volunteers doing LSW, and ‘incentives’ that might encourage LSW to be undertaken.
The literature we included in this part of the review revealed a number of distinct models of LSW and ideas about best practice within them. We have tentatively labelled these as follows: narrative approaches; biographical or chronological approaches; care-focused approaches; and care-focused approaches with a narrative orientation. We deal with these approaches in separate sections below, exploring first what characterises each approach and then what the publications say about what should be done (the LSW product), when, by whom, how and with what type of involvement of which people. We then move on to discuss how each approach deals with issues around what should not be included in a life story, dealing with distress and consent to use.
We deal with the organisational context for LSW in a final subsection of this part of the chapter.
Narrative approaches to life story work
What is a narrative approach to life story work?
Publications in this category were those that most frequently talked about LSW as a process tantamount to writing a novel. Thus, LSW was not about documenting ‘objective facts’ but rather about the personal interpretation of facts24 and identifying the strength of the person living with dementia and the wisdom that they had accumulated during life. 25 As a result, the main issue in doing a life story was not accuracy, but capturing the emotions that accompanied that story, engaging with the person and hearing what they had to say about their identity and feelings. 25,26 Similarly, it was felt that there was no one way to ‘do’ LSW or to decide what content it should have; rather, it should be regarded as a process whereby doing one element of LSW might lead to another. 27,28
Given this narrative approach, it was not surprising that the person living with dementia was seen as being firmly at the centre of the work29 or as the virtual director (of a filmed life story). 30 LSW was a process, not just a form to be filled in,29 and the story produced, via a dignified and respectful process, enhanced a person-centred approach. 28 Some also felt that a narrative approach produced a life story that was easier to read and engage with, both for the person living with dementia and for those who lived and worked with them. 28,31 Further, a narrative could be a living thing that recorded not just the past but also the present. 29,30
Even in the description of an entirely carer-led life story process, a distinction was made between ‘social histories’, typically gathered in nursing homes, and the attempt in LSW to illuminate as well as report on a life. 32–34 These papers did talk about capturing facts, but also about communicating the essence of the person living with dementia and what made them unique.
Good practice in narrative approaches to life story work
Fourteen of the papers that represented a narrative approach also included details about how best to do LSW, although three of these were about the same intervention. There was a high degree of consistency about what this approach should contain and the process it should follow.
The strongest common message was that the LSW process should focus on feelings, opinions, meaning and emotions25,28,31 and reflect the themes, topics or objects that are most important to the person living with dementia. 31,35,36 This means that the person living with dementia should choose the topics and material to be included and the way in which these are presented. 35,36 This orientation was reflected in some commentators’ views that carers could be involved with creating a life story, but only with the permission of the person living with dementia. 29,36
As outlined above, we did find accounts of a strongly narrative approach to LSW that was entirely carer led, but, even here, it was argued that the emphasis should be on key themes that illustrated the person’s life rather than a list of facts about them. 32–34
Several writers also talked about the importance of the life story not just being about the past but also being a ‘living’ or continually evolving account. It should thus be able to include current hopes and future wishes,26,29 record aspects of current life,30 add new stories and ideas and allow ‘editing of the past’ to match the current viewpoint of the person living with dementia. 24,31
The emphasis on meanings and emotions underlines a need for a high degree of emotional intelligence in the person facilitating the life story production. One paper emphasised that the person who helps the person with dementia to create the life story needs to be ‘emotionally present’, prepared to be the ‘validating witness’ for the story, and receptive, open and non-judgemental about the story being told. 27 This recognised that whatever story is being told, it is of consequence to the teller and has been shared at an emotional cost. Others talked more generally about the importance of building strong rapport and a trusting relationship, without which nothing can happen. 30,35
However, this emphasis on feelings and meaning may bring up issues that the life story process cannot resolve, in and of itself. One writer clearly states that LSW should not try to resolve either past or present problems; it is not therapy, even if it might be therapeutic. The issues of material that should not be included in a life story, and with whom the life story might be shared, are thus important too. Some researchers acknowledge that, although people with dementia are likely to express a wide range of preferences in relation to sharing and privacy,25 the process might reveal issues that should never be revealed to anyone else without ‘express permission’. 27 This means that the person to whom the life story belongs must be able to choose how much of it they want to share with others. 24
When the process is carer led, carers themselves should choose to tell only the stories that they believe the person with dementia would tell, and keep private those they would keep private,32–34 thereby viewing the process in the same way that they would view surrogate decision-making. 34 By contrast, two descriptions of a narrative approach argued that, although carers could be involved in LSW, this should be only with the permission of the person living with dementia. 29,36 Although some papers included clear statements about ownership of the LSW, one gave a somewhat confused account, reflecting the experience that if ownership is not properly negotiated at the start of the process, then problems and conflict may emerge later. 30
The issue of what material should and should not be included and/or shared in a life story was also related in some writers’ accounts of which people living with dementia should or should not be offered the opportunity to do LSW. Some publications advocating a narrative approach stated that LSW could be done regardless of the stage or type of dementia26,37 – which may be true – or that it should be started as early as possible. 31 However, it is necessary to select carefully those to whom LSW is offered,38 taking into account both personal preference and the likelihood of causing distress. 26,36
Biographical or chronological approaches to life story work
What is a biographical or chronological approach to life story work?
The approach evident here is distinct from a narrative approach in its emphasis on a relatively ordered, chronological recording of the life of the person living with dementia. Writers thus talked about a final product that follows the life course, from birth to the current day, with material that is displayed or recorded chronologically, even if it is not necessarily gathered systematically. 39–42 There is thus an emphasis on remembering and memories,43 on lists of topics to be addressed39 and on timelines,41 rather than on feelings and meaning. Perhaps as a corollary to this more structured approach, there is less reference here to validation of the life portrayed (Gibson and Carson39 being a notable exception).
Good practice in biographical or chronological approaches to life story work
The more structured underlying approach here gives rise to a more directive feel to recommendations about how life stories should be recorded. Books, albums, workbooks and topic-based templates are recommended or described,39–41,43 while timelines and visual and auditory ‘prompts’ and triggers to memory are suggested as useful adjuncts. 41,42,44 There are also recommendations about ensuring that books and albums are attractive40,41 and immediately recognisable as belonging to the person living with dementia. 40
The involvement of the person living with dementia does not seem as central in these approaches as in the narrative ones. In two of the models described, the person’s memories are recorded and transcribed by others, based on audio-taped ‘life review’ sessions43 or weekly, one-to-one reminiscence sessions in which a member of care staff acts as an ‘amanuensis’. 39 One account suggests that a life story can be constructed based on what the ‘helper’ already knows about the person living with dementia, but points out that both the process and the end product are more meaningful if the person is included in the process. 41 This seems a much weaker commitment to the centrality of the person living with dementia than was evident in the descriptions of narrative approaches.
The role of family members or carers in LSW is also more evident here, with suggestions that they can encourage or facilitate the involvement of the person living with dementia40,43 or indeed that they are ‘integral’ to the process. 44 One account reported that, although family members had been initially reluctant to discuss the past with their relative, fearing that they would cause distress, they had actually managed to have meaningful and pleasant discussions while doing LSW. 40
One publication in this group (in which the production of a life story was tied in to ‘life review’) was clear that LSW was best done with people who were in the early stages of dementia and with those who were interested and had the cognitive, emotional and physical capacity to participate in life review activities. 43 By contrast, the authors who described an evaluation of a video photo show approach to LSW felt that it worked best for people with moderate to severe dementia, because they were less likely than people with lower levels of impairment to lose interest while watching the video on multiple occasions. 42
The only other practical recommendation that emerged from this set of publications was the importance of using statements rather than questions in the final LSW product; this was in relation to a video-based life story, but might well also apply to text- or audio-based products.
The publications in this group were, overall, less reflective than those in the narrative group about how to deal with ‘difficult’ material. Some accounts simply suggested that the person might not want to discuss some things and that LSW should ‘avoid’ some types of memories or topics and concentrate on enjoyable memories;41,42 most did not refer to the possibility of difficult issues arising at all. There was, similarly, little routine acknowledgement of issues of privacy or confidentiality. The single publication in the whole review that was specifically about people living with dementia who were lesbian or gay45 talked about the person needing to feel comfortable with the level of detail included in their ‘autobiography’ and that LSW could raise issues of privacy and confidentiality. However, only one description of LSW in this subgroup talked specifically about issues of consent and future use, which, it was suggested, should be logged and recorded in the life story, and, in the case of consent (or assent), should be assured on a continuing basis. 39 Perhaps in implicit recognition of the possibility of having to deal with ‘difficult’ issues, two papers did suggest that untrained staff, or volunteers (even if trained), should not do LSW. 39,43
Care-focused approaches to life story work
What is a care-focused approach to life story work?
We defined a third group of publications about LSW based on their strong focus on practical advice about LSW done in care settings or by care staff. They are distinct from the other two groups described above by their emphasis on ‘how to do it’ and a generally lower level of reflection on ‘why’ and ‘what for’ questions about doing LSW. Indeed, only four of the publications in this section reflected on what LSW might be. One discussed the role of LSW as a device for ‘cognitive stimulation’, with the aim of maximising independence, engagement and well-being. 46 Another spoke of LSW as an opportunity to focus on ‘memory windows’ for people living with severe dementia and to identify specific and personally relevant triggers to memory. 47 A third publication spoke of the importance of seeing a life story as an ‘interactive tool-box’ for the person living with dementia, family and care staff, and not just as a source of information. 48 A single publication referred to the need for an holistic approach to underpin LSW. 49
Good practice in care-focused approaches to life story work
Many different life story formats were referred to in these publications: books, collages, photo albums, videos, digital versatile discs (DVDs), boxes of items, and albums with both text and relevant artefacts. As this might suggest, many writers argued that there should be no rigid approach to the LSW ‘product’: that the chosen format should be discussed and agreed with the person living with dementia;49 that life story ‘albums’ should be as individual as the person they were about;48 that it was important to avoid a ‘story book’ format and to include belongings and photographs;50 that any artefacts included should be personally meaningful and significant for the person living with dementia;46 and that the topics in life stories should also follow no rigid format. 51
Although these papers that were advocating a wide range of formats underlined the person-centred decision-making that should determine choice, others suggested that choice was more likely to be or should be determined by the stage of dementia51 or the care setting. 52 Thus, collages were suggested as more appropriate vehicles for life stories in continuing care settings. 52 Further, in contrast to the laissez-faire approach to format, two publications suggested the use of topic lists or templates for creating a life story. 53,54
There seems to be more emphasis in the publications in this group on other people being involved in collecting and recording information than just the person living with dementia and a life story worker. Thus, one publication states clearly that family members compiled the life story books;51 others state that staff recorded memories prompted in reminiscence sessions,54 typed up notes about memories and added photos to them54 or found or added photos and sensory objects related to the ‘main themes’ addressed during LSW. Two writers, however, do underline the importance of ensuring that information recorded by staff, and its use, should then be agreed with the person living with dementia. 49,55 One of these further states that it is the role of the care worker not to ‘steer’ the person living with dementia but to value their reflections and negotiate where in the life story content should be placed. 55
The role of family members is more prominent in this group of publications, although not all writers agree about their role. Views included that mentioned above – that family members should actually compile the life story – and an assertion that the life story should belong to the carer when the family member is living with dementia. 7 Some writers suggest that staff should gather family members’ and friends’ recollections7,47,54 and that they could provide photos or other supplementary material. 46,47,54 Only one paper suggested that the person living with dementia should be asked to give their permission before staff talked to family members and carers. 55 Overall, then, publications in this section see family member or carer involvement in LSW as unproblematic. Indeed, one suggests that staff should ensure that family members are happy with the life story’s contents, but does not make the same suggestion about the person living with dementia. 56
Perhaps because of the care-focused nature of these publications and, therefore, the possibility that they were targeted at care staff working with people living with later stages of dementia, some of them position LSW clearly within the routines and processes of the care setting. Thus, LSW is argued to start with assessment46,49 and to draw on information about the person living with dementia drawn from files, from other staff members and from interactions and observations in the care setting. 46,47,49
Only one publication in this group talked specifically about consent in relation to LSW and this emphasised that consent should be an ongoing and renegotiated process. 54 Another talked about the need to establish trust before any LSW was started. 7 Privacy and confidentiality were raised more often and particularly in relation to ‘personal’ information;7,55 one paper reported LSW where ‘sensitive’ information about the person with dementia was collected from family members but not ‘posted’ in the life story itself. 56
Responding to sensitive or difficult issues was also mentioned, with recommendations that staff helping people with dementia to do LSW should be aware of what type of material might provoke strong or upsetting emotions47,49,54 and perhaps avoid or move away from such material. 54,55 By contrast, it was also important to acknowledge or empathise with strong feelings during LSW,49,55 not least because not acknowledging ‘difficult’ things could be a barrier to understanding. 56 One publication went so far as to say that LSW could be a good vehicle for exploring feelings if staff had counselling skills. 51 Alone among all the publications included in the good practice part of our review, a publication in this subsection raised the ethical issue of the loss of close personal communication that might be experienced by the person with dementia when LSW was completed. 55
Hybrid approaches to life story work
What is a hybrid approach to life story work?
A small number of publications (five, reporting four different types of LSW9,57–60) were hybrids, in that they were mainly about LSW in care settings but included some narrative elements in the description of how LSW should be carried out. These publications were least likely of all those reviewed here so far to articulate a view about what LSW actually is. What characterised them as having elements of a narrative approach, however, was their emphasis on the centrality of the person living with dementia. They argued that a life story should reflect the issues and events of most importance to the person living with dementia,9,57 that it should use the words of the person living with dementia58 and that it should be written in the first person. 59
Good practice in hybrid approaches to life story work
Although publications in this group emphasised that there was no single format that LSW might use, in effect all were predominantly about life story books. 9,57–59 One publication emphasised the importance of making the life story product attractive to hold and look at, involving the person living with dementia in the choice of colours and design, and using high-quality materials to avoid any association with ‘childish’ activity. 58
The two publications related to life review suggested recording life review sessions to guide the process of creating the life story,57 using the Haight Life Review and Experiencing Form as a framework for the LSW process. 60 For others, objects and photographs could be ‘starting points’ for the reminiscing that informed LSW and served as illustrations for the book. 9,58 When such ‘starting points’ were absent, however, one publication suggested that finding alternatives or taking new photographs might stand in their stead. 60 Illustration might also be more useful than text in the later stages of dementia.
The authors in this section also pointed out that a life story did not have to be chronological, could include current information and details, should be kept up to date and could be edited to add new material. 9,58,59 However, one publication warned against the ‘diary/log of outings’ approach to keeping a life story up to date. 59 The life review-based publications did not talk about these sorts of issues, presumably because once a life review is finished it is considered complete.
Several authors acknowledged that LSW was not for everyone, whether because of personality or stage of dementia. Some people simply might not want to reminisce. 9 At later stages of dementia it might be difficult to do LSW,9,58,59 particularly if the work relied on life review;58 and in later stages people needed a product that they could look at rather than being involved in producing it themselves. 58 Overall, then, it was better to do LSW earlier rather than later. 9
Despite what appeared to be a commitment to the centrality of the person living with dementia, the publications in this group took different views about who should be involved in LSW and when. Those that saw the life story as a product of life review work were consistent in their view about family carer involvement. While acknowledging that family carers could contribute material to LSW, they argued that carers could not and should not direct the contents of a life story book, and that any involvement in the book should be after life review work was complete, and then only with the permission of the person living with dementia. 57 As a result, staff and participants carried out LSW. 60 There was also a suggestion that family carers should do their own life story at the same time as the person living with dementia. 57 By contrast, other publications suggested that carers could provide material for LSW, after it had been fully explained to them, and that when people living with dementia were too severely affected to do LSW themselves, then carers could contribute. 9 One also felt that templates were useful for LSW because they provided questions and prompts for staff and family members not experienced in LSW,58 suggesting that family members might themselves be doing the LSW with the person living with dementia.
Despite this divergence of views about who could be involved in doing LSW, most publications in this section were clear that the life story product was the property of the person living with dementia,9,57,58 although they were less likely to deal with access issues. One suggested that during the process of gaining consent for doing LSW, the person living with dementia should be shown an example of a life story book and be given clear examples of who might see and use the book once produced. 9 Another said that the person living with dementia should guide the current use, access to and future use of the book. 57
Only one publication in this hybrid group specifically mentioned issues of what and what not to include in the life story product, stating that the boundaries of what should be included or not should be provided by the person living with dementia and their carer and then respected during LSW. 9 Further, this publication warned that perceptions of an invasion of privacy might be more evident when a ‘task model’ of LSW was predominant.
Only two publications9,59 dealt with what to do if difficult issues came up during LSW. They counselled against ignoring expressions of emotion and underlined the importance of skilled listening, but also acknowledged that staff involved in LSW were not there to resolve problems and ‘make things better’. 9 One also talked about the importance of not letting the person with dementia get ‘trapped’ in negative memories. 59
Organisational issues around life story work
In this final section of the good practice review, we turn to what the documents said about how LSW should be organised or presented within the settings in which it was being carried out. We identified several themes here: the culture of care in the organisation; leadership and management support for LSW; the resources or time required for doing LSW; the support provided to staff involved in the setting where LSW was being carried out; and training or preparation for staff and/or volunteers doing LSW in partnership with people living with dementia. Thirty-five of the 47 publications reviewed here said something about one or more of these themes. 7,9–11,14,25,26,31–34,36–40,43–45,49,50,52,54–56,58–66,70
The culture of care
The publications that talked about the culture of care in the LSW setting were all agreed that, in order to be successfully adopted and carried out, LSW had to be embedded in and ‘match’ the culture or service philosophy of the care setting. 10,14,32,34,40,60 If LSW was being proposed from ‘outside’, then it was important to examine the culture of care implementation to ensure that this matched.
To assist the proper embedding of LSW, the care setting itself had to have an overall culture of person-centred care14,33,40 and also to believe in the importance of partnership between care staff and families. 14,33,34 One publication said that without these cultural underpinnings it was more difficult to secure staff commitment to doing LSW. 34
Furthermore, LSW had to be an integral part of everyday care and not an additional ‘task’,10,40 or one that was ‘assigned’ to some staff and not seen as a team responsibility. 32,40
Leadership and management support
Active support from the leaders, senior managers or owners of care settings was clearly seen as crucial to the successful implementation of LSW,7,11,32,34,36,39,40,44,50,52,61,62 and without this support it would probably be difficult to secure staff and/or team participation. 34,52,59,60
The appropriate commitment of leaders and managers was needed to ensure that LSW was implemented as part of a well-thought-out strategy,11 accompanied by facilitation and supervision for staff doing LSW14 as well as policies and guidelines about how LSW was to be carried out and how its products were to be used. 40,63
One particularly important study in this group specifically explored the factors that influenced implementation and argued that ‘Consistent, convinced leadership, careful prioritisation of resources and competent management (particularly over small details such as staff rosters) are all essential if lasting improvements are to be made’. 39
Resources and time needed for life story work
The major issue identified here was the time needed for doing LSW well.
Some publications talked about the actual amount of time or number of ‘sessions’ that needed to be dedicated to doing LSW: a minimum of 2 hours per week per person,39 50 hours over 6 months for each person,54 a minimum of six one-to-one sessions with the person living with dementia. 26 Others just acknowledged that LSW is time-consuming40,58 and that time has to be spent getting to know, or building trust with, the person living with dementia before starting LSW,7,11 a particular issue for those who might be working with lesbian or gay people living with dementia. 45
However, the length of each LSW session will be influenced by the attention span, motivation and emotional state of the person living with dementia at any given session. 55 It is thus presumably difficult to predict with any accuracy how long it will take to complete LSW for any given individual.
Much discussion revolved around a lack of dedicated resources or time as the biggest obstacle both to doing LSW and then to using its products in care. 7,10,11,34,39,44,49,52,56,59,60 As a corollary, adequate and dedicated resources and staff time were seen as the sine qua non for successful LSW to take place. 7,26,36,39,54,58,59
All of the comments above suggest that LSW is seen as something separate from the normal routines of care. However, one writer argued strongly that LSW should be a part of ongoing, interactive ‘joint production’, and not a ‘task’ to be completed in a given place at a given time. 9 The use of life story products should also be built into everyday routines. 59
Practical resources are also necessary to support LSW; laptops or PCs, scanners and digital cameras are essential,26 as are the skills in using them. 52 Somewhere quiet or private to do the work is also necessary, but often surprisingly hard to find in care settings. 26,39
Some publications talked about the need for trained facilitators, project workers or co-ordinators to support LSW,7,52,54,63,64 again suggesting that LSW is seen as something rather separate from everyday care.
Support for staff carrying out life story work
Related to the issue of resources and time was the theme of the nature of support offered to staff involved in doing LSW. Here, training for LSW was the main concern,7,40,58–60,65 to enable staff to both do LSW and use its products. Only two publications, however,54,65 suggested that staff might be encouraged to create their own life story.
Life story work training might not be enough in itself, however; staff might need help to develop their communication skills,40 or support and encouragement to enable them to explore the stories of people living with dementia without feeling ‘nosey’ or ‘intrusive’. 60 Appropriate supervision or mentorship should also be in place to support staff in setting appropriate professional boundaries and in case ‘difficult’ material is revealed while helping a person living with dementia to create their life story. 11,14,37,63
Finally, there was a subtheme about the importance of a team approach to LSW. LSW should be developed as a mutually supportive team effort, even if not everyone is involved in actually doing it; it should not be left to a limited number of staff whose work might be ‘sabotaged’ by others who do not understand or respect the approach. 39. 52,56,60 The role of a facilitator in developing LSW and supporting staff in this way was seen as crucial in one study that followed the implementation of LSW in a long-term care setting. 52
Training for life story work
Twenty-three of the included studies mentioned training as an issue in LSW. Most were clear that anyone doing LSW should be trained7,11,38–40,52,64,70 or that trained facilitators or ‘champions’ were essential to good practice. 32,33,39,52 Training for ‘other’ staff, or at least ensuring that all staff understood LSW and could support its use in the care setting, was also recommended. 7,31,39,52,59
Other publications placed less emphasis on the need for training, suggesting that LSW could be done with minimal training if it was accompanied by supportive supervision,66 or that volunteers could ‘graduate’ from family LSW workshop groups to run groups themselves. 33 However, one publication cautioned against the use of volunteers in LSW because of their potential vulnerability and the possibility that ‘difficult’ issues might emerge during LSW,43 while another – that had used an informal ‘monitor’ approach to rolling out LSW training to staff – had had to put in additional training to make this model work. 7
In terms of suggestions about the content of training, publications fell into two main groups.
First, there were those that were mostly practical in orientation. These recommended that training should include information about dementia itself25 and how to ‘select’ people with dementia to do LSW;38 about the different ways in which LSW might be presented;25,38,54 about technical support for LSW such as scanners and computers, library and internet resources;54,65 and about the principles of capacity and consent. 36
The second group of publications concentrated more on aspects of emotional intelligence in relation to LSW, where learning to deal with ‘difficult’ issues was predominant. This grouping included methods for recognising and dealing with difficult issues11,38,60 and emotions;9 developing communication skills and empathy;40 learning how to maintain boundaries37 or, by contrast, becoming willing to scrutinise interpersonal relationships with care home residents;60 and learning to be sensitive to family members. 56 Producing one’s own life story product54,65 or reflecting on one’s own life story more generally49 and reflective practice learning39 were possible routes to enhanced emotional intelligence in LSW practice with others, but could also be empowering for staff in their own right. 65
Underlying theories of change
One of the acknowledged weaknesses of much research that has tried to evaluate complex interventions in health and social care settings is that it has searched for improved outcomes without any pre-existing theory about why we might expect the particular intervention to affect the given outcome. 18 This is the case with LSW: there is enthusiasm for it as an approach and practitioners feel that they observe change when they use it, but it is difficult to pin down any underlying theory of change about why these changes might have occurred. There is, thus, the danger that evaluative research might choose the wrong outcomes to assess – both intermediate and final – and thus fail to demonstrate change.
This next part of our review work was, therefore, designed to develop a theory of change, based on the literature selected for review.
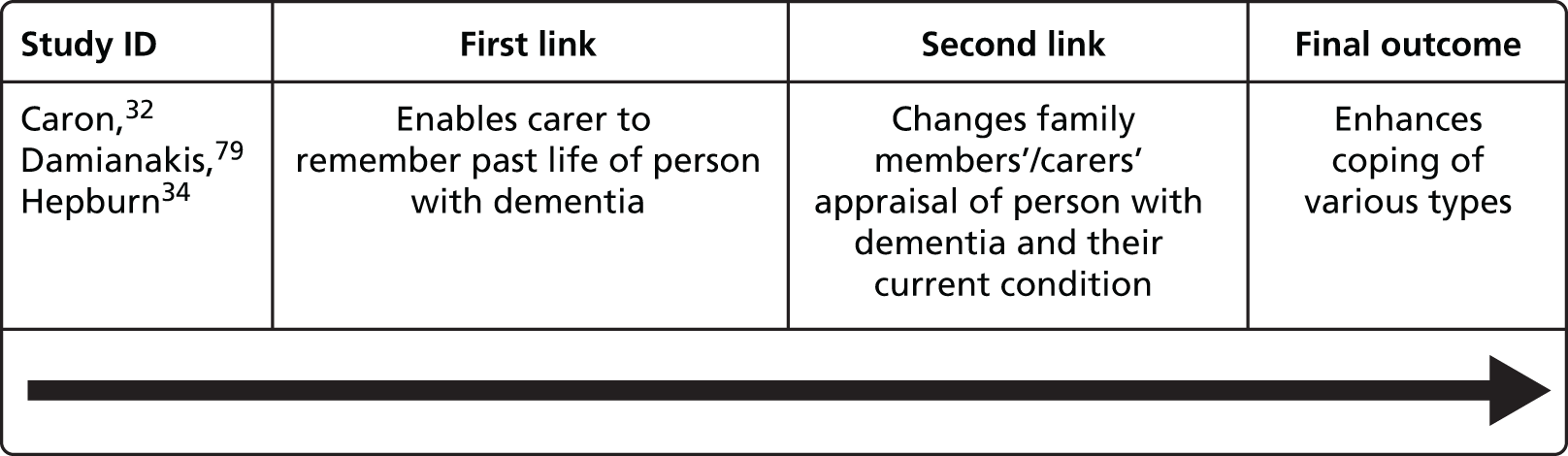
We gave an example of how we envisaged this work in our proposal:
The results of one life story project57 have been described thus: ‘The group that participated in a dyadic life review (caregiver and care receiver) seemed to gain most from the intervention, particularly in their assessment of the care receiver’s problem behaviours. Possibly . . . because they were enjoying the process simultaneously and were sharing an event again.’
p. 171106
Here, the underlying theory seemed to be that the carers’ assessment of the care receiver’s problem behaviours improved (final outcome for family carer) because the dyadic life story process (LSW) was shared (implicit causal link) and was enjoyed (implicit causal link).
This generates a theory of change that can be expressed in a linear fashion:
Type of LSW → that was a shared process → that was enjoyed → changed carer’s assessment of ‘problem behaviours’.
As this example suggests, such theoretical models are often embedded in descriptive or discursive text, rather than articulated explicitly as a hypothesis to be tested.
Analysis
In our analysis of the 16 papers that expressed an underlying theory,7,10,14,31,32,34,38,42,56,57,59,60,67–70 we identified the causal links between LSW and the outcome or outcomes that the authors were arguing for LSW, as given in the example above. In some papers there was a single such theory; in others there were several. We first summarised these theories into our Excel spreadsheet using the data headings outlined above, and then mapped them all in a mind map. This was done twice: once for the theories articulated in the introductory sections of each paper (initial theories of change) and again for the theories articulated in the discussion and concluding sections of each paper (concluding theories of change). In both cases, we concentrated on theories that the authors themselves were arguing, not on theories that they were repeating or reviewing from others’ publications.
After completing the initial mind-mapping, we synthesised the material using a set of overarching outcomes. Given that most of the papers had included some empirical work, we took the concluding theories of change as the basis for this final stage of analysis, assuming that these would be a more accurate reflection of the authors’ views about LSW, its outcomes and the routes by which it achieved these outcomes.
Theories of change
The initial mind-mapping generated complex and complicated pictures of both initial and concluding theories of change (see Appendix 1 and Boxes 1 and 2). The 18 papers outlined 26 theories of change initially, but 47 in their conclusions.
As Tables 7 and 8 show, some theories of change were relatively simple, with only one intermediate outcome between LSW and a final outcome. So, for example, concluding theory of change 3 was that LSW leads to interactions between care staff and family members, thus strengthening understanding of, and the relationship with, family members.
Others theories of change were much more complex, and sometimes argued two separate final outcomes from the same causal chain. For example, concluding theory of change 24 (final outcomes in bold) was:
24: [LSW] enables staff to gain fuller and more dynamic picture of person with dementia
24.1: which increases their knowledge of the person
24.1.1: which enables them to find out more about person’s needs and behaviour AND
24.1.2: which helps staff see person in context of whole life rather than in terms of their medical condition/physical needs AND
24.1.3: which provides a talking point between staff and person with dementia
24.1.3.1: which helps develop common bond between person with dementia and staff.
Here we see two intermediate outcomes (24, leading to 24.1) that led to two final outcomes (24.1.1 and 24.1.2) and one further intermediate outcome (24.1.3), which itself led to an additional final outcome (24.1.3.1).
As is also clear from the tables, there were overarching final outcomes in the theories of change. Our next stage of analysis was to identify these outcomes and synthesise the causal links that the literature suggested led to them. In doing this, we confined the analysis to outcomes that at least four papers identified as resulting from LSW. Then, within each outcome, we confined analysis to theories of change in which at least two studies had argued that the same or similar causal links led to these outcomes. In total, we identified seven outcomes and 12 theories of change.
The overarching final outcomes for the person with dementia were:
-
LSW supports the self-worth and empowerment of people with dementia, for example increased sense of control, pride in their lives and opportunity for reciprocity. 14,31,38,67
-
LSW affects a range of individual outcomes positively, for example anxiety, depression, agitation, mood and behaviour. 10,31,38,42,56,57,59,60,67,68
Final outcomes in relation to the care setting were:
-
LSW improves relationships between care staff and the individual person with dementia. 7,31,59,69
-
LSW leads to better care, for example more person-centred, individualised, less ‘pathological’ care on a one-to-one basis. 10,14,31,32,38,59,60,69,70
For family members and carers, the final outcomes were:
-
LSW allows more effective engagement of family members/carers within the care setting, for example enhanced communication with staff and more meaningful involvement in care planning and delivery. 7,10,32,67,69
The theories of change are summarised in Figures 2–7.
FIGURE 2.
Theories of change for increased self-worth of the person with dementia.
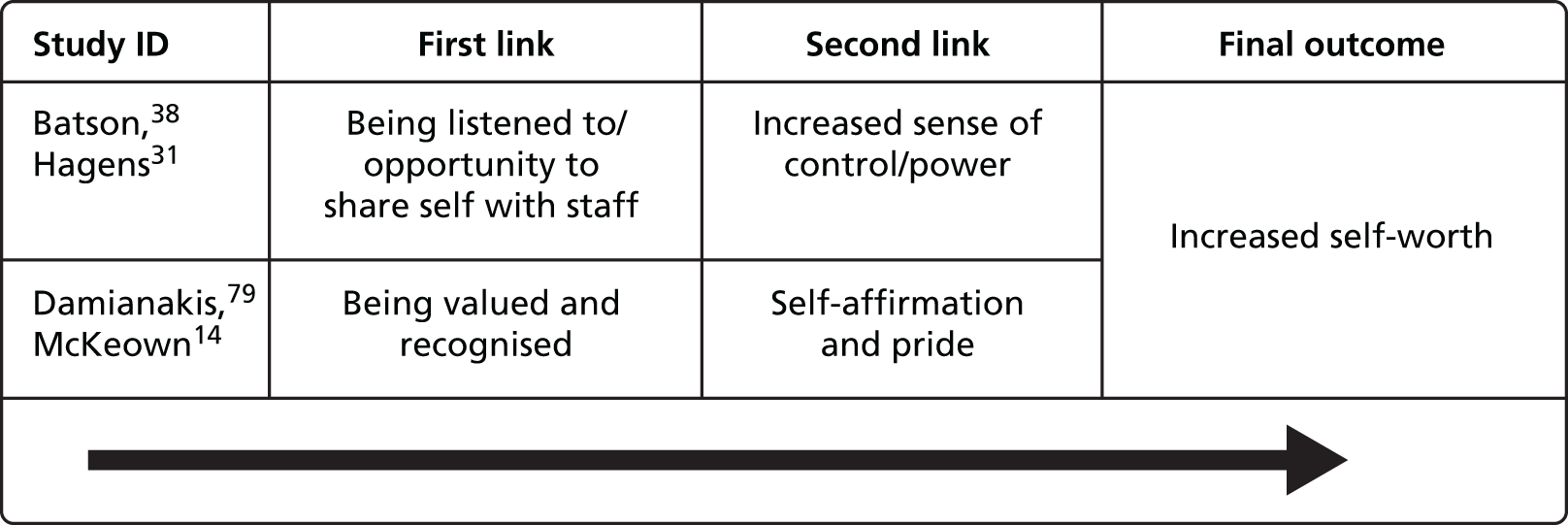
FIGURE 3.
Theories of change for improved individual outcomes for the person with dementia.
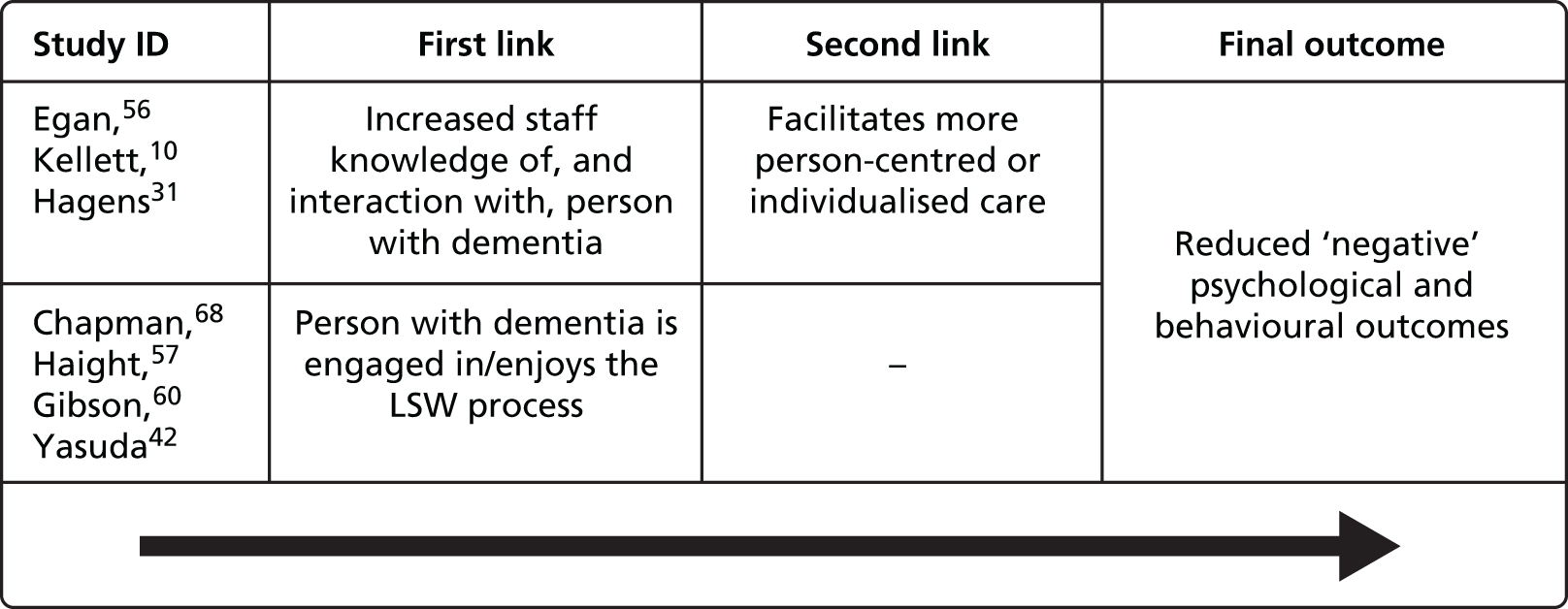
FIGURE 4.
Theories of change for improving relationships between staff and the person with dementia.

FIGURE 5.
Theories of change for improving care.
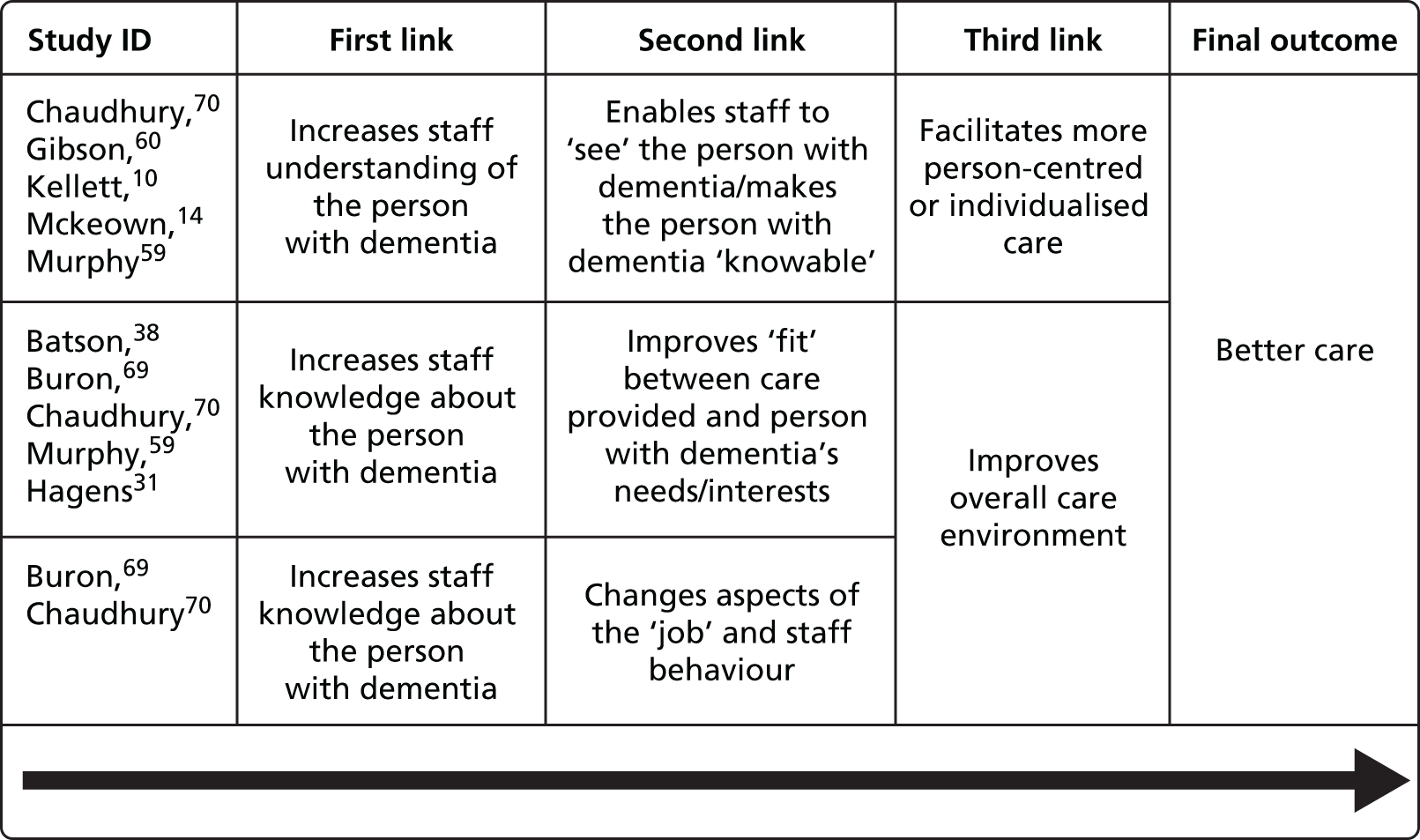
FIGURE 6.
Theories of change for more effective engagement of family/members in care setting.

FIGURE 7.
Theory of change for helping family members/carers to cope better.
The identified final outcomes from this part of the review were subsequently used to inform discussion and the final choice of outcome measures for the feasibility study (see Chapter 4).
Chapter 3 Life story work outcomes, challenges and good practice: findings from the focus groups
Introduction
The objective of this part of the study was to carry out a qualitative study of experiences of LSW, including people with dementia, family carers and professionals (objective 1). The overall aim was to develop a theoretical model of LSW, including its potential outcomes, and establish core elements of good practice in using and applying the approach.
Successful evaluation requires an understanding of what an intervention is intended to achieve and how different approaches to this intervention may determine different outcomes for different groups. 107 MRC guidance recommends drawing on existing evidence to develop a theoretical understanding of the likely process of change, but also suggests supplementing this with new primary research if there are gaps in the literature. 18 Earlier reviews of the literature on LSW concluded that more work was needed to develop a sound theoretical framework12 and, in particular, emphasised that there had so far been only limited reporting of patients’ and carers’ views. 11 We know that people living with a condition can have very different views about outcomes from policy-makers and clinicians. 108–110 This stage of the study, therefore, aimed to collect primary qualitative data about outcomes and good practice from three different perspectives: people with dementia; family carers; and staff and professionals with experience of LSW.
Aims
-
To identify potential outcomes of LSW (to be measured in the feasibility study).
-
To identify potential challenges or problems with LSW and possible solutions.
-
To establish core elements of good practice.
-
To use these findings, together with those from the review, to develop a theoretical model of LSW.
Methods
Ten focus groups were held: four with people with dementia [organised and co-facilitated by Innovations in Dementia community interest company (CIC) and KG]; three with family carers (organised and co-facilitated by Uniting Carers and KG); and three with staff, professionals and volunteers with experience of LSW, recruited through the Life Story Network CIC and co-facilitated by KG and GMP. Research ethics approval for this stage of the project was obtained from the National Institute for Health Research (NIHR) Social Care Research Ethics Committee (SCREC) for England in October 2012 (Research Ethics Committee reference number 12/IEC08/0046).
Focus groups with people with dementia
We originally planned to conduct three focus groups for each group, each with 5–10 participants. We added a fourth session with people with dementia to bring in a wider range of views and anticipating that groups of people with dementia may need to be smaller to accommodate communication and cognitive impairment. Focus groups with people with dementia were held in settings already known to and attended by participants, in order to maximise comfort and familiarity. This also meant that known and trusted group facilitators were on hand to help with the consent process and to support anyone who chose, on the day, not to take part.
Recruitment
Recruitment was purposive and designed to include people with dementia from a range of community settings and experience of LSW. Stages of recruitment were:
-
Innovations in Dementia CIC approached some groups they already worked with, as well as new contacts, via group facilitators.
-
Innovations in Dementia then visited interested groups (usually with KG) to inform potential participants about the project, answer their questions and invite them to take part (see the information sheet in Appendix 5).
-
If the group, or a number of the group’s members, were interested in taking part, a date was set for KG and Innovations in Dementia to return to conduct a focus group. Consent was taken at this stage (see below).
-
After the focus group, a further visit was planned to feedback to participants (and group facilitators).
Details of the people with dementia that took part are included in Table 13 (see Appendix 1, where other tables for this chapter can be found). In total, 25 participants with dementia (15 female and 10 male) took part across four groups.
Consent
Only people with the capacity to give informed consent were included in this stage of the project, as participation in a focus group requires an understanding of the concepts under discussion and the ability to express views. Group facilitators discussed capacity before the first visit from Innovations in Dementia to gauge whether or not at least some of the group members would have the capacity to consent. At the first visit, Innovations in Dementia and/or KG talked through the project information sheet with the group and answered any questions, and then revisited the information sheets with each individual on the day of the focus group before consent was given.
The use of written consent forms (see Appendix 5) was not straightforward, and in some cases presented an active barrier to participation. People with dementia who understood the premise of the research and expressed (verbally) that they were happy to take part sometimes struggled when presented with a lengthy consent form with a number of separate statements for them to agree to before signing. These statements are a SCREC requirement and must be included on all participant consent forms. However, asking people to agree or disagree to each of these and then sign, after they had already discussed each point (while talking through the information sheet) and indicated verbally an intention to proceed, was burdensome and fatigued some before the focus groups had even begun. Moreover, some people with dementia found it physically difficult to hold a pen and sign their names. Signing a document may also feel like a significant act for a person who is losing control over aspects of their life and we became concerned that this might be causing unnecessary worry for some of our participants. We decided therefore to build the facility for verbal consent with a witness into future consent processes with people with dementia, and received approval from SCREC to use these in the final stage of the project (see Chapter 6).
Format of the sessions and topics covered
We had planned only to include people with dementia with experience of LSW in the focus groups. However, after further consideration we agreed to include people with a range of experience of LSW. This recognised that some people with dementia may have actively chosen not to undertake LSW, while others might not have come across the idea but still have views on recording and sharing aspects of their life. To understand good practice we needed to hear from the full range of potential LSW participants, not just from those who had successfully engaged in it.
To ensure that all participants understood what we meant by LSW, we produced four specimen life stories and took these to each session to share with the group. These were:
-
a structured life story book, based on a template
-
an unstructured life story folder, with photographs and text
-
a life story box with objects, photographs and documents
-
a digital life story accessible via a touchscreen tablet.
On the advice of our advisory group, we also encouraged participants to bring in their own life story products or an object or photograph that they would be happy to share with the group. The focus groups then began with a discussion of these specific products and artefacts before moving on to more general topics such as the outcomes of recording and sharing life stories and the best ways to do this (see Appendix 6 for the topic guide). Sessions were co-facilitated by Innovations in Dementia and KG, with the existing group facilitators on hand in case participants required support from a familiar worker.
Focus groups with family carers
We held three focus groups with family carers of people with dementia with experience of LSW, all recruited through the Dementia UK network Uniting Carers. Dementia UK hosted two focus groups in London and we held a third in York. Uniting Carers and KG co-facilitated all three groups.
Recruitment
Carers were recruited through the Uniting Carers e-network as follows:
-
Invitations were circulated to the e-network of carers of people with dementia.
-
Interested carers contacted Uniting Carers who gave full information (see participant information sheet in Appendix 5) and answered carers’ questions.
-
Dates for focus groups were confirmed by telephone or e-mail and participants confirmed attendance.
-
KG and Uniting Carers co-facilitated three focus groups. Consent was taken at this stage.
-
Feedback on the overall findings from this phase of the research was circulated to participants by e-mail and comments were requested.
Table 14 (see Appendix 1) gives details of the focus groups held and the types of carers who took part. In total, 21 carers (16 female and 5 male) took part across three groups.
Consent
Written consent was given on the day of the focus groups (see Appendix 5). All participants received the information sheet in advance and again on the day of the focus group and had the opportunity to ask questions.
Format of the sessions and topics covered
Uniting Carers and KG jointly facilitated the focus groups with carers. Each began with an ‘icebreaker’ exercise and moved on to topics such as personal experiences of doing LSW, outcomes and challenges, and general views about good practice (see Appendix 6 for the topic guide).
Focus groups with professionals
Three focus groups were held with professionals from health and social care settings who had experience of doing LSW with people with dementia. The Life Story Network CIC helped to identify potential participants, as did other networks including DeNDRoN (Dementias and Neurodegeneration Network). Two focus groups were held in York and one was held in London. KG and GMP facilitated two groups together, and KG facilitated one alone.
Recruitment
Professionals were recruited as follows:
-
Invitations were circulated to a number of e-networks including the Life Story Network, local DeNDRoNs and a dementia-training network.
-
Interested professionals contacted KG, who gave full information (see participant information sheet in Appendix 5) and answered questions.
-
Dates for focus groups were confirmed and participants confirmed attendance.
-
Three focus groups were facilitated by the research team. Consent was taken at this stage.
-
Feedback on the overall findings from this phase of the research was circulated to participants by e-mail and comments were requested.
Table 15 (see Appendix 1) gives details of the focus groups held and the types of professionals who took part. In total, 27 participants (26 female and 1 male) took part across three groups.
Consent
Written consent was given on the day of the focus groups (see Appendix 5). All participants had been given the information sheet in advance but received it again on the day of the focus group and had the opportunity to ask questions.
Format of the sessions and topics covered
As well as the topics addressed with all groups, professionals were also asked about drivers of resource use in dementia care settings and what changes, if any, they would expect to see in these if LSW was carried out (see Appendix 6 for the topic guide). This material was used specifically to inform data collection in the feasibility study (see Chapter 6).
Analysis
All the focus groups were audio-recorded, with participants’ permission. They were transcribed and analysed thematically using the Framework approach. 111 The aim was to produce a realist account21 of what works, for whom and in what circumstances, from the perspectives of people with dementia, family carers and professionals.
Findings
By adopting a ‘realist’ approach, we were interested in the types of outcomes experienced or expected by different groups, as well as any situations in which such outcomes might not be achieved. By exploring the circumstance in which positive outcomes are experienced, and considering what went wrong when experiences were less positive, we also gained a better understanding of good practice. First, the findings of this stage of the research are presented in terms of outcomes – for individuals with dementia, for interpersonal relationships and for better care. Second, we examine the challenges involved in doing LSW, and what these might tell us about good practice.
The outcomes of life story work
Outcomes for people with dementia
It was clear that some people with dementia gained immense pleasure from talking about their memories. Reminiscence activities have been used in dementia care for some time8 and LSW can involve a specific form of reminiscence: that which focuses on the individual’s life history. In each focus group with people with dementia some participants told us they found it enjoyable to talk about memories. More specific to LSW, some felt that it was important to record memories, so that they had them to look back on and could share them with others:
What are you going to use them [the life story books] for?
[Pause] For memories.
For yourself?
For myself, and the family, they’ve all seen them. It’s – I think it’s nice just to have a look and think – I used to look like that once!
However, the benefits of this tool for looking back, highlighting and sharing important memories seemed to go further than simply the ‘comfort in recall’ (as one participant put it).
We asked participants in the dementia groups to bring in objects or photographs of something from their lives to act as a starting point for the discussions. Most brought things that reminded them of people or achievements that they were proud of, such as their children’s certificates or photographs from their wedding day. Highlighting and celebrating past achievements was clearly a priority and one that appeared to bring much pleasure. Moreover, each object or photograph came with a story.
The literature suggests that storytelling may be an important tool for all of us, allowing us to communicate and, in the process, reaffirm our identity. 9,112 Through storytelling we have the opportunity to review, construct and reconstruct our own identities, both in the eyes of other people and for ourselves. Yet people with dementia may find themselves increasingly left out of such conversations and storytelling,113 as illustrated here:
So, do you talk about your life much?
No, not really. Not now. Used to at one time . . . I didn’t mind. I haven’t done for a long time now.
And why’s that?
‘Cause nobody asked.
Life story work might, therefore, offer a valuable opportunity for people with dementia to continue to make and remake their identity, helping them to communicate aspects of themselves. This benefit may be of particular significance to people with impaired speech, as life story products can give visual hooks from which to hang verbal and non-verbal communication. Another participant had limited speech but was able to indicate to the group that she had a book of photographs that she valued, as it helped her to communicate with her friends and family. However, she did not see this as something to share with a wider range of people (such as care home or hospital staff): it was a private book which she used to help communicate with those close to her.
Some participants were clear that the primary purpose of LSW for them was to review their past in order to help them have a better idea of who they are today and who they might be in the future:
. . . in writing this, I can’t say that I’m writing it for posterity or for my children . . . But it is important to me . . . because I’ve never really looked back at the whole of my life at any stage, and taken stock of what I’ve done and what I aim to do, . . . it does make you think about your life . . .
DF3R3
In this way, LSW can cross over into life review;114 indeed, life review and LSW are sometimes combined, with the suggestion that making a book might help sustain the benefits of life review. 66,115 Moreover, some of the professionals we spoke to suggested that simply listening to people and validating their feelings could potentially resolve issues that were bothering a person.
Finally, in addition to celebrating past achievements and helping people to understand or reassess who they are today in the context of their histories, LSW was seen as providing an opportunity for people with dementia to achieve something today. Some of the people with dementia we spoke to were clearly very proud of the life story books they had made, seeing the process not only as an enjoyable activity but as a personal challenge they were pleased to be able to meet.
Table 2 summarises the outcomes identified for individuals with dementia. All of these potential immediate outcomes may have the potential to feed into a larger outcome, that of improved QoL, which we have added here as an hypothesised outcome.
| Immediate outcomes | Overall (hypothesised) outcome |
|---|---|
| Enjoyment/pleasure | Overall QoL |
| For identity | |
| Person is listened to/has feelings validated | |
| Issues resolved | |
| Skills maintained/independence reaffirmed |
Interpersonal relationships
Life story work tends to be a shared activity, and a number of potential outcomes were identified that went beyond the individual. Both family carers and staff suggested that LSW could bring people with dementia and others (extended family, other residents in care homes or those attending social clubs, as well as staff in these settings) together through the identification of common ground and interests. Some of the participants with dementia (although by no means all) said that they would be interested to see other people’s life stories, and both carers and staff recounted examples of life stories acting as a catalyst for relationship building.
Improved understanding and the establishment of common ground may also be important to family carers themselves seeking to connect, or reconnect, with their loved ones, as one carer explained: ‘I find it comforting, in a way, that we can still have some things in common . . .’ (CF2R7). In some cases, engaging in LSW could lead to family members learning things about their loved ones that they never knew before and found interesting or were proud of:
By . . . producing this album, I was getting to know her even more, and admiring her more as a person. So, for me, I think it probably had more beneficial – [laughs] and more impact for me than my mum.
CF1R3, son of person with dementia
In other cases, however, families learnt of things that appeared to have been concealed for good reason and there was concern about how to deal with this information.
For some, LSW provided an opportunity for an enjoyable shared activity, and a wider range of topics for conversation. Indeed, there was a suggestion from the professional focus groups that LSW might attract a wider range of visitors to care homes and hospital wards by providing new triggers for conversation. For some, however, the opportunities for conversation sparked by a life story were limited by the severity of the dementia and associated communication impairments. Nevertheless, there was a suggestion that LSW might still provide a ‘way in’ for the families and carers of people with limited speech:
And that’s when a life story book’s quite good, because they can go in. There’s no speech, but they can look at the photographs . . . I think that life story books can bring everybody in, and the children, and when she saw their faces, even though she didn’t know their names, she’d go like that and smile.
CF3R3
This could have benefits both for the person with dementia and for those around them. Even in situations when the value for the person with dementia was questioned, several family carers said that they themselves valued the life story products and the memories that the objects and images brought back.
We saw earlier that LSW might help people with dementia to express aspects of their identity to others. There was a suggestion in the focus groups that the benefits of this could go beyond the individual, challenging assumptions by helping others to understand better the person with dementia. As one woman with dementia put it:
. . . the younger ones today ought to realise it, even though I’m 82, I still feel just like I did feel when, you know? . . . even though you’re 83, you can still be falling in love . . . you don’t have to be all glamorous and young.
DF1R3
Improved understanding could have a number of benefits. Feeling understood, in itself, may be important to an individual’s well-being. In addition to this, improved understanding may alter other people’s attitudes and responses towards people with dementia. Tom Kitwood116,117 highlighted the ways in which the actions and responses of caregivers could affect the well-being of people with dementia. It was suggested in the focus groups that staff may form negative perceptions of patients or residents from reading their medical histories before meeting them, which could in turn affect how they acted towards them. Learning about people’s life stories might help to redress the balance, as this hospital occupational therapist (OT) explained:
. . . staff receive a report about who’s coming in. ‘Oh, we’ve got somebody coming in that’s done this, this, this, and this,’ and it immediately triggers those . . . negative attitudes. But . . . when people have arrived with a life story . . . once people have had a chance to look at it . . . the attitudes change completely.
PF1R1
A summary of the potential interpersonal outcomes identified in this section is given in Table 3. As with the individual outcomes, the result of any of these outcomes might be an improvement in QoL. However, these outcomes might lead to improved QoL not only for the person with dementia, but also for family carers and others involved such as wider family and friends.
| Immediate outcomes | Overall outcomes |
|---|---|
| Highlights common ground Fosters understanding Shared enjoyment Assumptions challenged |
Improved relationships Personhood recognised Overall QoL |
Outcomes for care
We saw above that LSW can provide a hook for conversations and non-verbal interaction, helping to identify common ground and build relationships. Participants in the professional and family carer focus groups, in particular, suggested that this outcome could have the additional effect of influencing the way care staff viewed the people they worked with, which in turn could improve the care they provide. As an OT explained:
I think that process of helping people recognise the common ground . . . helps humanise people again.
PF3R10
It could be argued that people receiving care should not have to be ‘humanised’; however, we know that receiving care can have a dehumanising effect and that people with dementia in particular can too often be viewed in terms of their disease first and their personhood second. 3 LSW was therefore seen by professionals and carers as a tool with the potential to remind care staff that the people they care for are people first (with equally important hopes, fears, achievements and relationships as those of the care staff themselves) and the recipients of care a distant second.
‘Seeing the person’ is an outcome in itself, implying respect and the recognition of shared humanity. In addition, it could help to personalise care, as this day centre manager suggested:
LSW in itself is maybe the way to get to that person-centred care, because by . . . helping people see the person as an individual, you can move forward to then working with them as an individual . . .
PF1R3
Life story work should tell us not only what a person has done and achieved, but what they would like to do, what they value, and how they would like to spend their time and who with. Such information is crucial to person-centred care planning. It may also shed light on the reasons why a person with dementia reacts negatively to a certain situation or approach to care. There were numerous examples given in the focus groups of people acting in ways that confused or challenged care staff until they discovered, often through LSW, that there was a perfectly rational explanation for that behaviour:
. . . one of the key factors is what somebody did for a living, what their daily routine was, you know. ‘Go on, Fred, get back to bed, it’s only 4 o’clock in the morning.’ But if you were a bus driver . . . or a postman, you were up at that time and those are the memories that stay . . . it’s about understanding the person, and then you can understand some of the behaviour, and it doesn’t challenge then.
PF1R8
Once something is understandable, it may seem less problematic. However, information pertinent to problem solving will not always be included in a life story product, particularly if the LSW is led by the person with dementia him- or herself rather than by a member of staff or carer (see Challenges and good practice, What is it for and how much control will I have?).
Even where it is difficult to understand or manage a person’s actions, LSW may still be a useful tool in helping to put people at ease without recourse to medication:
He’s rattling the doors, trying to get out, and you start talking about all his achievements, ‘cause he’s so proud of all his achievements through his life. And immediately, he comes down and PRN [pro re nata] medication [antipsychotic medication issued as and when required] isn’t needed . . .
PF1R1
Similarly, some family members found that LSW helped to calm or orientate the person they cared for:
I think it is useful for my husband, although we don’t know how much he recognises . . . but it’s about the familiarity of it . . . So it is all part of that comforting, assuring familiarity of having these things . . .
CF3R4
This carer went on to explain, further, that, although she could not know for certain whether or not the photographs of their life together were meaningful to her husband, they certainly were meaningful to her.
One effect of staff getting to know and understanding the people they work with better could be that they themselves gain more satisfaction from their work. If LSW sheds light on the ways in which a staff member can meet the needs or desires of a person better, then it may be easier for them to deliver care in a way that elicits positive feedback for them. This in turn may motivate care staff to find new ways to further the person’s well-being, as this extract indicates:
. . . the staff do get very excited when they learn new things about people and very encouraged, and, you know, it’s good for them, too.
And they start connecting, as well, and go . . .
‘Oh, I’ll have to bring that in because I was a horse rider and she was a horse rider.’
Yeah.
‘So I’ll bring in my helmet’ and finding things in common, that’s really important . . .
This suggests that measuring job satisfaction or staff motivation could be one way to assess the effectiveness of LSW.
A final area of potential outcome related to people moving from one care setting to another. We heard above how LSW could challenge the negative assumptions of staff by revealing the person behind the dementia. This effect was felt to come from seeing not only who the person was, but also who they still were and what they could still achieve. In one hospital ward, for example, they took photographs of patients taking part in activities and sent these with the person when they were discharged:
. . . those photographs went in the life story book [made on the ward and passed on] to the residential home or the nursing home. So the care staff didn’t just see Joe Bloggs who needs X, Y, and Z, but Joe Bloggs that actually can still do a bit of this and can still do a little bit of that . . .
PF2R2
Table 4 summarises the outcomes for care identified in this section, including outcomes for care staff.
| Immediate outcomes | Overall outcomes |
|---|---|
| Fosters understanding Assumptions challenged Care tailored to the needs/preferences of the individual Calming/de-escalation Smoother transition |
Personhood recognised Better care Behaviour no longer experienced as challenging (problems ‘solved’) Improved staff satisfaction/motivation |
Theory of change
As we have seen, LSW may have a variety of outcomes, arrived at via numerous different routes or mechanisms. Figure 8 shows the various mechanisms, immediate outcomes and broader consequences (overall outcomes) identified through our focus groups.
FIGURE 8.
Mechanisms and outcomes of LSW.
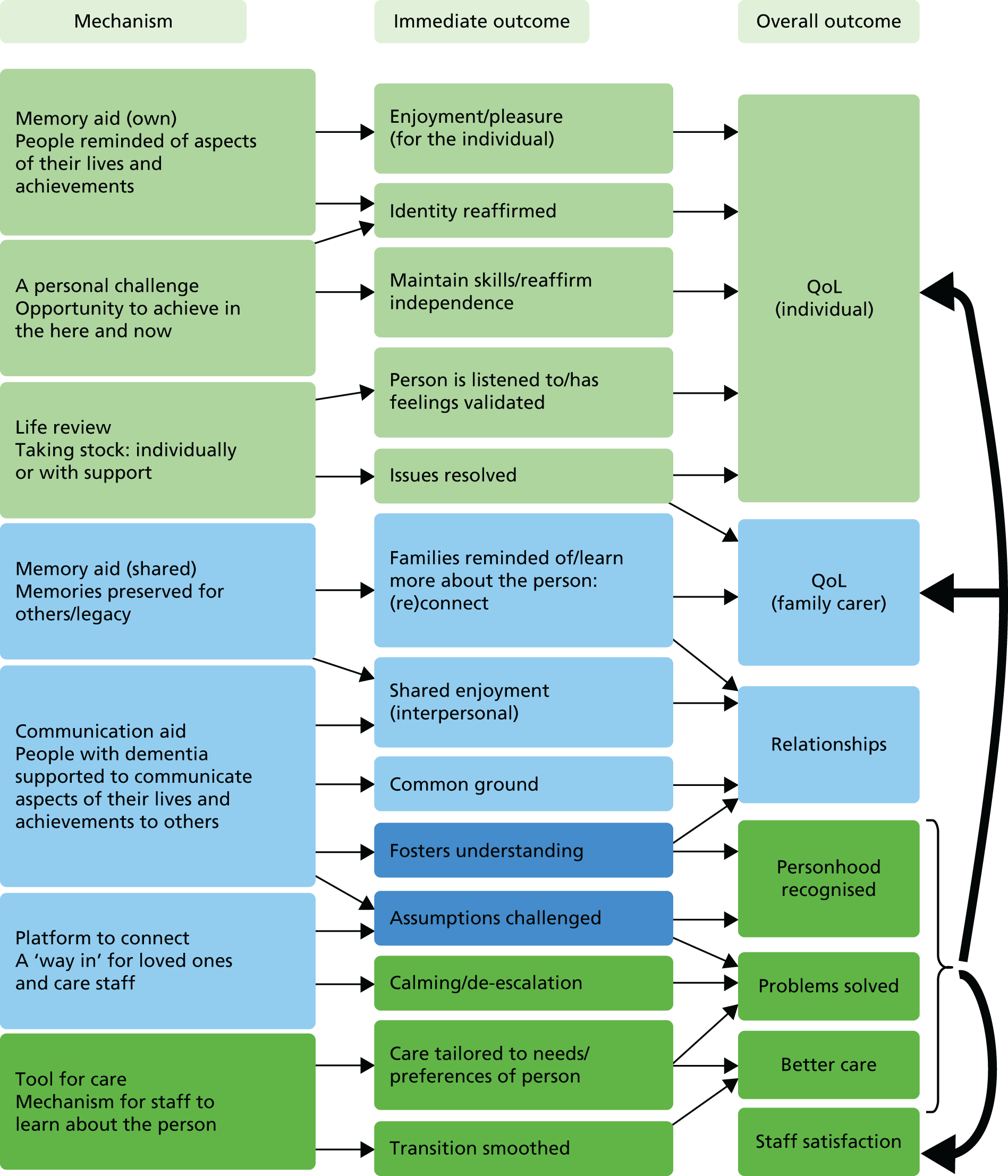
Challenges and good practice
We have outlined the ways in which our focus group participants felt LSW had been or could be beneficial. However, all of the groups agreed that LSW would not always give such benefits and that not everyone would necessarily experience benefits equally. We now look at the potential challenges associated with LSW, and what these tell us about good practice.
Not everyone wants to engage in life story work
First, not everyone thinks LSW is for them. Some people simply did not see the point:
I tend to just, sort of, say, ‘Right, this is done’ and it’s done, and then move onto the next thing, rather than talking about it a lot.
DF3R4
Others actively rejected the notion that reminiscence was a desirable thing: ‘. . . you say, “Mind your own bloody business” . . . Sometimes you want to forget’ (DF4R2). Similarly, some carers confirmed that people they cared for had not wanted to participate in LSW, with responses ranging from indifference to considerable distress:
. . . my dad’s not that interested in that sort of thing . . .
CF2R4 (daughter)
He’d rather be on his allotment.
CF2R2 (granddaughter)
. . . a couple of times, people have tried to do LSW with him . . . but it wasn’t very successful . . . he did ancestral research and he collected old postcards of Dover and so, everyone thought, oh, this is great, he – but he didn’t want to go back. And very, very early on, he really didn’t like looking at photographs, and particularly photographs of people who were dead . . . a few months on, we had another helper from the Mental Health Team who wanted to have another crack at this, but it was just as bad.
CF2R6 (wife)
Our advisers with dementia had suggested that some people might be reluctant to embark on LSW because of its focus on the past at the expense of the present and future. They were keen for people not to be ‘set in stone’ by a life story document. Some focus groups participants also flagged this up as a risk. Professionals noted that a person may actively reject an activity which they used to enjoy because they are no longer able to engage in it proficiently. There was general agreement that it would be good practice to update life story products regularly and that the life story should not be given precedence over the current expressed preferences of an individual. However, in practice there were mixed views on the practicalities of this: who would update it/would there be time? One suggestion was to combine LSW with daily reporting, as this manager of a community day service had done:
. . . [the life story includes] the important information that we need to report [such as medication use], but it also includes photographs of where we’ve taken the person. And we work with the person to compile this reporting, so they’re involved and they don’t feel like . . . ‘What’s she saying about me?’. . . we encourage them [families] to include information in the book, as well . . . we use a lot of scrapbooking techniques . . .
PF2R8
Upsetting topics and the need for staff training
Professionals and carers pointed out that families might not want to engage in LSW because it could highlight the losses that they and the people they care for had experienced. Realising that a parent no longer recognises what were once favourite holiday destinations, for example, or even members of their own family, is distressing. By contrast, this was not a strong theme among the people with dementia. However, this could be explained by a lack of insight or a perfectly understandable reluctance to imagine what it may feel like to struggle with greater memory loss as dementia progresses.
Even where differences in perception are not the issue, LSW still has the potential to cause upset, simply because delving back through people’s personal histories can be emotional and there is always the possibility of stumbling on upsetting topics. Suggestions were made for avoiding such topics, but some argued that discussing emotional subjects is not necessarily a bad thing:
But, you know, for that person to have the opportunity to have their feelings validated and acknowledged, and even if it means having to . . .
Having to cry and be upset.
. . . have those feelings again, can still be very . . .
Positive.
. . . beneficial to them.
There were mixed views in the focus groups with people with dementia about whether or not they would choose to include upsetting memories in their life stories but our advisers with dementia reiterated that those wanting to discuss difficult issues should be supported to do so. However, staff facilitating LSW are unlikely to be psychological therapists and should not be expected to handle emotional issues unsupported. Training is essential, but support should also be on hand to help handle sensitive information (including potential safeguarding disclosures) and to judge when an onward referral is required:
. . . closing the can of worms . . . for a Level 2 care staff, that could be an incredibly difficult feat to achieve . . . it’s about leadership . . . and training . . . to make sure that staff feel that they’re empowered and they’ve got the skills to be able to do it.
PF3R6
What is it for and how much control will I have?
Analysis of the outcomes that professionals, carers and people with dementia themselves hoped for indicates that people with dementia may have very different motives for embarking on LSW from, in particular, the professionals who work with them.
Professionals were concerned about recognising personhood and tailoring care to meet the needs of individuals. They also saw great potential for LSW to help ‘problem solve’, for example to help to understand and deal with behaviour that could be challenging. People with dementia, on the other hand, undertook LSW for personal reasons: to preserve memories, to share and enjoy with friends and family, to celebrate achievements or simply to prove to themselves that they could still do something like this. Even when asked directly if it might be useful for life story information to be shared more widely with care staff and professionals, there was a feeling from most that, while they had ‘nothing to hide’, this was not a priority for them personally:
I might do one for myself, just for me, my life . . .
And would you show it to people?
Yes, if they asked. Yeah, you know, I wouldn’t go out and say, ‘Look, look at this, look at this’. But if someone said, ‘Oh, what are you doing?’ I’d quite happily show it when I’d finished with it.
If you were taking a book with you about you and your life into the respite home so that they knew a bit about you, what would you put in it?
Everything about myself I suppose, and so, I left school and so forth, up to the present time. I’ve got nothing to fear. I’ve got nothing to hide.
But would you want them to know certain things about you?
Pass.
Most of the people with dementia felt that some support from professionals to help make a life story could be helpful, especially for people who did not have family carers. However, they seemed unaware of the possible motives professionals might have for encouraging a person with dementia to do this. This is important, as people may choose to put very different information in a life story for their own personal use from the information they would put in something to be used by other people. Moreover, some people felt strongly that a life story should be ‘a private thing’ (DF2R4), or at least that they should be present when other people looked at it. Good ethical practice, therefore, means that professionals should make explicit the possible uses of the life story at the start of the process and check whether or not and with whom the person is happy to share it.
Similarly, professionals need to be aware that people select what information to share based on the image of themselves they would like to project or remember. Thus, the life story product may not tell staff everything they need to know in order to solve a problem or understand behaviour. One of our focus group participants, for example, spoke at length about some difficult times in her life before revealing that she had included none of these events in her life story book:
None of that’s in my book.
What’s in your book?
. . . this book, it tells all the nice bits, but [pause] I don’t know why I did that. But that [referring to the story she had told] is the truth on it, and this [referring to the book] is also the truth . . . I suppose it’s part of me, so I should have put it in, but at the time I was doing this, I just wanted to look back at pictures, and I would still only have pictures of the nice things.
Confidentiality and data protection were common topics in our focus groups. Some felt so strongly about data protection that life story books were locked away in staff offices: ‘. . . it boils down to confidentiality. We can’t have them lying around in the lounge in case another patient picks them up or a relative sees them’ (PF2R2). However, others argued this undermined the ownership of the life story by those whose life it was about and would make the achievement of certain individual and interpersonal benefits less likely. Instead, they suggested that consent be obtained (ideally from the individual, but if they lacked capacity then from a family member or other consultee) for information to be shared and that this should specify who was allowed to see what.
One suggestion to help care staff understand how it might feel for life story information to be shared with others (or, conversely, how it might feel to make a life story and then not have easy access to it) was to encourage staff to make their own life story products. Some participants felt that this had the potential to create greater equality between staff and service users and build relationships. Rather than information flowing in only one direction, people with dementia and their families could learn about the staff working with them. This would clearly be important to some people with dementia, as was illustrated by the participant who said, when we asked her if she would like staff to know more about her, ‘I would like to know who you are [referring to the staff in the room]’ (DF2R4).
Is it ever ‘too late’?
Carers and professionals discussed a range of approaches to making and using life stories. The extent to which the people they cared for were involved in the process depended to a large degree on the severity of their symptoms, which ranged from mild to severe. The people with dementia we spoke to, on the other hand, all had capacity to consent to take part in the focus groups and, as such, tended to have only mild to moderate symptoms. This group were, therefore, all able to take an active role in making a life story (usually with some degree of support) and most identified personal motives for doing so (see Challenges and good practice, What is it for and how much control will I have?).
The experiences of family carers, many of whom had cared for a person until his or her symptoms had become very severe, confirmed that a person’s ability to take an active role in LSW could reduce over time. As a result, the motivations for doing LSW might change, along with the approaches that were most likely to give benefit. This carer, for example, initiated LSW with his mother to help her maintain her writing skills:
. . . I did it initially for my mother to have practice in writing. The story was almost secondary . . . there was a lot of confusion there. So I dictated it . . . [But] there were things that she did contribute . . .
CF2R1
As her dementia progressed, the mother’s ability to participate in making the life story deteriorated, but she did still seem to benefit from being reminded of its content:
. . . this angel from Crossroads charity . . . she took the book, took it out and read everything to my mother and my mother does respond . . . I think what she remembers is a nice feeling.
CF2R1
The outcomes of LSW in the later stages of dementia may be different from those achievable in earlier stages (more about stimulating a ‘nice feeling’ than offering people something they can actively engage in to review their life and share their memories), but such outcomes are no less important. Professionals agreed that LSW was best started early, when people are still able to express their views and take a lead in the process. However, they also felt that there could be numerous benefits (not only around problem solving, but also by raising opportunities to invoke a ‘nice feeling’) throughout the dementia journey and that it was thus never too late to get started.
It is what you do with it that counts
Family carers felt that the outcomes of LSW depended largely on whether or not care staff took on board and used life story information when planning and delivering care. Unfortunately, many life story carers were doubtful that this happened and several gave examples of lovingly crafted life story documents packed with useful information that were ignored in care settings:
. . . I put it in her bedroom, and I just, in my naivety, thought that they would share it . . . She was given dreadful antipsychotic drugs to keep her sedated, and the input from the care home was, ‘She has a condition,’ and they ignored what I’d put together . . . They didn’t use it at all.
CF3R7
Well, I don’t know if, as a carer, I, sort of, invested too much in the life story thing, thinking that the people who were helping me care for [husband] . . . would pick these things out of this, which they haven’t done, because they haven’t had time . . .
CF2R6
It is not enough simply to produce a life story and expect it to make a difference, if the route to improvement is through the actions of busy staff who may not even realise that the life story product exists.
Some participants suggested making different versions for different uses or audiences: flash cards, a collage or a one-page summary of key information that would be easily accessible to staff, for example, and a more comprehensive book or digital product that the person with dementia might enjoy looking through, sharing and adding to him- or herself. The former might also be useful for transitions, for example if a person is admitted to hospital. There are several short templates available which have been designed specifically for this purpose. However, it is important to recognise that a one-page summary or a template detailing only key facts is not the same as a comprehensive life story and is unlikely to be something owned or designed by the person with dementia him- or herself.
A good practice approach to LSW would be tailored to the individual preferences of the person with dementia. Some participants were intrigued by the digital life story we had produced and felt that this was something they would like to pursue, whereas others were put off by the technology and preferred formats they were familiar with. Few of the participants with dementia who were interested in making a life story felt that a short written summary could take the place of something more comprehensive that they themselves had created.
Organisational barriers to achieving outcomes
There was consensus among the professionals that LSW could benefit people with dementia and those who cared for them. However, they identified barriers to achieving benefits, many of which were organisational. The most common barrier discussed was lack of time, which professionals in all groups said posed a problem, if not for them then for their colleagues.
Lack of time seemed to be linked to low prioritisation, both by care staff and by their managers, so that those who viewed LSW as an optional extra struggled to find time for it once all the ‘essential’ work was complete:
. . . we work with an excellent team . . . But they’re already overwhelmed with huge amounts of paperwork and that’s where . . . we’re struggling to engage people . . . it’s another job, another thing to do . . .
PF3R3 (OT with community team)
Even when staff recognised that an investment of time in LSW could lead to benefits in the end, they felt pitted against a system that prioritised short-term targets over such longer-term gains:
We’ve got incredibly strong targets at the moment, which is having a heavy impact on our therapeutic work with the patients, because it’s more important that people are seen within a certain length of time . . .
PF1R1 (OT on acute ward)
In order to be successful, participants felt that LSW needed to be an integrated part of care rather than ‘just another task’. Training was important but, crucially, needed to be coupled with a supportive management and organisational culture:
. . . staff have been very good as well, taken it on board. I mean, the luxury I have is that when we’re in a new care home, it becomes part of what we are and what we’re doing, so they’re coming into that. . . . So, you know, they take the training very well and have done some fantastic work.
PF3R6 (care home manager)
Another factor that influenced the successful take-up of LSW by staff was their perception of its purpose: was the aim to make a useful product, or was it the process of collecting and recording information that helped build relationships and inform care? Professionals reported colleagues’ concerns that they did not have time to produce a glossy life story product. However, they themselves felt that collecting information and learning about the person behind the diagnosis was the most meaningful part of LSW, and argued that this could be undertaken concurrently with routine care (e.g. chatting to someone about their life while helping them dress). Nevertheless, focusing solely on the process could raise problems: if information is collected but never recorded or shared, how can it be used to improve care; and without a product to look through, will wider interpersonal benefits be realised?
An alternative solution to the problem of limited time was to encourage family carers to put life story documents together, which could then be used by care staff, wider family and people with dementia themselves. However, in this case staff would not be actively engaged in the collection of information from people with dementia, which was felt to be the most meaningful part of the process.
The focus groups arrived at no definitive solutions to these problems. However, we continued to grapple with them as a research team during the feasibility study, in which we observed different theory of change approaches to solving this dilemma (see Chapter 6).
Chapter 4 Choice of outcome and costs measures
Development phase
In Chapter 2 we synthesised the literature on the expected outcomes of LSW and the processes by which these outcomes were thought to be achieved. Overarching final outcomes were identified for the person with dementia, the care setting and the people (family members and care staff) providing care. However, we knew from previous reviews that there had been only limited research into LSW that includes the views of people with dementia or carers14 and that in general there was a dearth of sound quantitative and qualitative evidence.
We conducted additional primary research (in the form of qualitative focus groups) with 25 people with dementia, 21 family carers and 27 professionals, volunteers and care staff with experience of LSW. Chapter 3 sets out the findings from this research, including the outcomes expected and/or experienced by participants. Learning from both the literature review and this primary research then informed the selection of outcome measures to be used in the feasibility study in care homes and acute settings which we now outline.
Process of selection
A period of consultation preceded the selection of outcomes and outcome measurement tools. Findings from the literature review and the focus groups were discussed with both the project steering group and the advisory group; we liaised with the partner organisations that were to host the feasibility study; and we met with our specialist advisor, Professor Esme Moniz-Cook (lead author of the INTERDEM European consensus document on outcome measures for psychosocial intervention research in dementia care118). Outcomes to measure were selected in agreement with all those consulted. We then compiled and refined a list of available measures with Professor Moniz-Cook. All advisory and steering group members were asked to comment on the shortlist of outcome measures before it was finalised.
Which outcomes to measure
There was general agreement that the primary overall outcome of interest for people with dementia should be QoL, albeit that this might be influenced by intermediate outcomes such as the maintenance of skills or feeling understood. Interpersonal outcomes may also influence QoL, and impact on relationships, in particular, was felt to be worth exploring as an outcome in its own right, along with impact on identity.
For family carers, QoL was again agreed to be the primary outcome, with impact on relationships and satisfaction with care also important.
Staff approaches to care, in terms of both person-centred care and perceptions of clients with dementia, might also have an impact on QoL. It seemed important to explore these care-related outcomes in their own right, to understand whether a change in QoL was due to individual outcomes or changes to care routines. We also hypothesised that improvements to care might influence staff burnout.
Table 5 presents the outcomes that we agreed we would measure in the feasibility study.
| Group affected | Outcome to measure |
|---|---|
| People with dementia | Well-being/QoL |
| Relationships (person with dementia/carer) | |
| Identity | |
| Family carers of people with dementia | Well-being/QoL |
| Relationships (carer/person with dementia) | |
| Overall satisfaction with care | |
| Staff | Perception of clients with dementia |
| Person-centred approach to care | |
| Staff satisfaction and strain/burnout |
Selection of measurement tools
Measuring the QoL of people with dementia is notoriously challenging119 because of the difficulties a person may experience in recall, time perception, communication and insight. Generalist health-related QoL measures are not considered valid for this group and, instead, a number of dementia-specific tools have been designed. Both the DEMQOL120 and the Quality of Life – Alzheimer’s Disease (QoL-AD) measure121 have been shown to be valid and reliable QoL measures for people with mild to moderate dementia. 122 There is less evidence of their successful use with people with severe dementia. However, we were reluctant to rely on observational measures such as QUALIDEM,123 as these do not capture the voices of people with dementia. Instead, we chose to use both the self-report and proxy versions of QoL-AD and DEMQOL.
There is little precedent for quantitatively measuring the quality of relationships between carers and care recipients, particularly those with dementia. However, Professor Moniz-Cook suggested a scale [the Scale for the Quality of the Current Relationship in Caregiving (QCPR)] developed by Spruytte et al. 124 which, although not extensively tested, did have relevant subscales (measuring warmth, affection, conflict and criticism). The measurement of identity in dementia care is also a relatively underdeveloped subject. We collaborated with the School of Psychology, University of Leeds (see Appendix 7), who used the ‘I Am’ Fluency Task, developed from the Twenty Statements Task125 and adapted for use with people with Alzheimer’s disease. 126
Selection of a QoL measure for carers was more straightforward and was guided by agreement that the tool should measure care-related QoL rather than health-related QoL or carer burden. The Carer Experience Scale (CES)127 was chosen, to be supplemented by qualitative data from in-depth interviews. In the study in acute settings, the intervention site also requested that we look at carer satisfaction with the service provided, and so the Carer or Family Member Satisfaction Questionnaire was used. 128
We chose both the Approaches to Dementia Questionnaire (ADQ)129 and the Personhood in Dementia Questionnaire (PDQ)130 to measure staff approaches to care. The former had been used in a recent study of LSW131 and the latter is a newer measure intended to operationalise Tom Kitwood’s definition of personhood. The customary choice for measuring staff burnout is the Maslach Burnout Inventory,132 but we chose the Copenhagen Burnout Inventory (CBI) for its improved acceptability. 133 Data from staff measures were also supplemented by qualitative data from focus groups with staff involved in the feasibility study.
Table 6 shows the measurement tools selected for use against each outcome to be measured for each group affected (people with dementia, family carers and staff).
| Group affected | Outcome identified | Measurement tool |
|---|---|---|
| People with dementia | Well-being/QoL | DEMQOL (family carer proxy and self-report); QoL-AD (family carer proxy and self-report) and field notes |
| Relationships (person with dementia/carer) | QCPR | |
| Identity | ‘I am’ Fluency Task (care homes study only) | |
| Family carers of people with dementia | Well-being/QoL | CES and qualitative interviews |
| Relationships (carer/person with dementia) | QCPR | |
| Overall satisfaction with care | Carer or Family Member Satisfaction Questionnaire (hospitals study only) | |
| Staff | Perception of clients with dementia | ADQ |
| Person-centredness of staff | PDQ | |
| Staff satisfaction and strain/burnout | CBI; staff focus groups |
Resource use and impact on health and social care providers
We also used the learning generated from the review (see Chapter 2) and the qualitative work (see Chapter 3) to inform the data collected in the health economics element of the feasibility study (see Chapter 8). This work identified the resources that were likely to be involved in implementing LSW in hospital and care home settings as well as potential areas for resource saving, both in relation to the individuals with dementia who were recruited to the study and for the ward or care home as a whole.
We then discussed these items with our project partners and advisory group, and with staff in the feasibility study sites, to ensure their face validity in the settings in which our project was operating. So, for example, the range of prescribed medication for care home residents that we included was agreed after consultation to reflect the types of medication that might be prescribed differently if LSW was having some type of effect on the person with dementia or the care environment.
We then used standard health economics literature to identify the most appropriate data to collect in order to identify resource use, and how to ascribe costs to these resources. We also operationalised possible areas of resource savings in order to identify the type of data we needed to collect. The areas of potential resource use and savings that we explored in this part of the study were thus:
-
staff time (time spent with the person with dementia creating the life story and time spent creating the life story away from the person with dementia)
-
use of other health and social care services by study individuals
-
reported adverse events for study individuals reported
-
reported challenging behaviour episodes for study individuals
-
prescribed medication for study individuals
-
staff sickness levels for the case site as a whole
-
staff turnover for the case site as a whole
-
prescribing rates for the case site as a whole
-
number of adverse events for the case site as a whole.
Further detail about data collection methods and challenges is in Chapter 8.
Chapter 5 Surveying life story work practice
We carried out two surveys to establish how LSW is used in health and social care settings and how people with dementia and their family carers experience it (project stages 2a and 2b, objective 2). We designed the questionnaire contents to reflect the good practice elements identified in stage 1, enabling us both to benchmark use of LSW in the health and care settings and to establish how it was used in which settings.
Survey of health and social care providers
Methods
Sampling
Five parts of the health and social care pathway were the sampling frame for the survey: memory assessment services (MASs), inpatient dementia assessment services (IPAs), community dementia support services (CDSs), generalist long-term care homes and dementia-specialist long-term care homes (SCHs). Given the different numbers of each of these types of services, we planned to use proportionate sampling to generate 100 services in each category.
We explored a range of sources of national information about services to identify the best sampling frames for the five categories (see Appendix 1, Table 16). It soon became clear that we could not easily judge whether or not identified organisations had the services we were interested in, before making direct contact with them. We therefore increased the initial sample size for each to 150. For some categories, there were fewer than 150 identified services and so we took a 100% sample for these. Table 16 (see Appendix 1) shows how we generated the final sample and the stages of personal contact and filtering required.
We planned an electronic survey, and so we needed an e-mail contact for each service. We contacted all of them to identify the person best placed to complete the questionnaire. In some cases, organisations were unable or unwilling to provide an e-mail contact. We had a final sample of 567 services to which we could send the electronic survey.
Developing the questionnaire
We established benchmarks for good practice in LSW based on findings from stage 1 (see Chapters 2 and 3). This generated the domains to be covered in the questionnaire: knowledge and use of LSW; timing; type of records used; one-to-one or group work; people involved in LSW; use of LSW in the service; types of information included and excluded; temporal focus; access to the life story by different people; LSW policies and practice in the organisation; resources to support LSW; and the benefits and challenges of LSW. The questionnaire also asked for information about the service and basic sociodemographic information about the respondent.
Wherever possible, the question wording was the same as or as close as possible to that already used and tested in the questionnaire for carers (see Survey of carers of people with dementia).
The final draft was tested repeatedly within the research team and pre-piloted with members of the project advisory group. For final wording of the questionnaire, see Appendix 8.
Distributing the questionnaire
The link to the survey was e-mailed to the 567 service contacts in the first week of February 2014, with a message explaining the survey’s purpose and how to contact the research team.
Mailing to the NHS-based organisations was problematic and caused significant delay to the distribution, with the e-mails to NHS services not finally sent until mid-March 2014.
Challenges of using an electronic survey
Qualtrics (version 2013, Provo, UT, USA) is a high-quality, web-based service, with EU-based servers, making it ideal for designing, hosting and distributing research questionnaires. However, as well as the distribution problems, other challenges arose.
First, despite first contact with organisations to obtain e-mail addresses, some participants were puzzled about why they had received the survey link or how we had obtained their contact details. We sent a further e-mail explaining how we had identified them. If they responded that someone else was a more appropriate recipient, we reissued the survey to that other person.
Second, although most NHS staff have direct access to computers, this is rarely the case in social care settings, and particularly within care homes. A single e-mail address is often used for the whole care home, making it difficult to target the person who could respond to the questionnaire.
Third, e-mail addresses given were often inaccurate and bounced, requiring further personal contact with the organisation. Even after such contact, e-mail addresses were not always accurate.
Fourth, social care organisations can change significantly over short periods of time, which meant that details we were given in December 2013, when contacting the organisations personally, were no longer accurate in February 2014. Again, we used personal follow-up to deal with this. This revealed organisations that had changed e-mail provider, had closed or were no longer contracted to provide relevant dementia services, or where the nominated member of staff no longer worked there.
Response rate
Several NHS services had multiple sites, all doing LSW. In some, the service returned a questionnaire for each. In others they returned a single questionnaire but informed us that the answers applied to all the sites, in which case we replicated the responses given to all the sites. This increased the number of ‘returned’ questionnaires by eight.
Given the technical challenges of getting the survey to NHS organisations and the structural challenges of systems in flux, we adopted a rigorous approach to follow-up in order to achieve the best response rate we could. Even so, the response rates for CDSs (52%) and generalist long-term care homes (32%) were not what we would have wished. However, we achieved good response rates from the MASs (64%), IPAs (70%) and SCHs (61%) (see Appendix 1, Table 17).
Analysis
The data were downloaded from Qualtrics into IBM SPSS Statistics (version 22, IBM Corporation, Armonk, NY, USA) and cleaned. After initial frequency runs to ensure that the data were consistent, the first stage of analysis estimated the proportions of services across England carrying out LSW with people with dementia. We subsequently confined our analysis to services doing LSW currently, using bivariate approaches to explore which services were using ‘good practice’ approaches.
We used chi-squared statistics to evaluate differences between services, and examined adjusted standardised residuals to identify which cells in tables were contributing most to observed differences.
Results
How many services are doing life story work?
The number of respondents who had heard of LSW was highest in IPAs (100%) and MASs (97%), followed by SCHs (91%), generalist long-term care homes (82%) and CDSs (72%).
Our sampling strategy allowed us to estimate the numbers of all services that are currently carrying out LSW in England. In doing this, we made the conservative assumption that no non-respondents did LSW. We also assumed that respondents who had never heard of LSW were also not doing it. We then estimated the minimum extent of LSW across our chosen services (see Appendix 1, Table 18). This suggested that perhaps two-thirds of IPAs and just under half of SCHs offer LSW. Under one-third of MASs, just over one-fifth of generalist long-term care homes, and slightly more than one-tenth of CDSs may do LSW.
The remaining analysis is confined to the 189 services that currently did LSW, excluding those who referred people elsewhere for LSW.
How is life story work done?
Starting life story work with service users
Memory assessment services were least likely to start LSW immediately or within 1 month of people coming to the service (7%), compared with SCHs (56%) and generalist long-term care homes (52%). MASs were more likely to say that the timing of LSW depended on the individual and their readiness to start (33%) or on how long it took to confirm a diagnosis of dementia (19%).
Type of records used in life story work
Care homes and IPAs were more likely to report using a written summary type of life story record than other services (see Appendix 1, Table 19). By contrast, MASs were more likely to mention using photo albums or books that included text alongside photographs. Two-thirds (66%) of respondents gave multiple responses, suggesting a level of flexibility in the practice of LSW.
When only one type of LSW record was reported, the most common was a written summary (57%) followed by a book with a mixture of photographs and text (31%). IPAs and generalist long-term care homes were the services most likely to be using only a written summary. By contrast, MASs and SCHs were most likely to be using more than one record, with photo albums with text or books with photographs and text the most common. Numbers are small here, but do seem to reflect a more general difference in practice that is evident as we progress through the rest of the analysis.
In a group or one to one?
Almost all services (98%) said that LSW was done one to one, although 38% also referred to group-based approaches and 33% mentioned both. Generalist long-term care homes were most likely (43%) and CDSs were least likely (27%) to mention both approaches. Only three respondents reported doing LSW solely in a group and all of these were in MASs.
Some respondents referred to ‘other’ ways of doing LSW, most often that it was done by family members and carers (5%) or that it was done with family members or carers (17%). We assume by the former that staff took a minimal role in LSW, and by the latter that they worked in partnership with family members and carers.
Who is involved in life story work?
Even when people with dementia are at a late stage in their journey it is possible to involve them in LSW (see Chapters 2 and 3). Overall, 95% of respondents mentioned the involvement of the person with dementia and 95% mentioned family members or other people close to the person with dementia (‘carers’ from here on). In terms of staff involvement in LSW, the most common response was a person employed to provide care in the service (61%). Few mentioned a volunteer (3%) or someone employed specifically to do LSW (12%). Twelve per cent mentioned OTs or OT assistants and 11% mentioned activity co-ordinators. It is possible that other respondents included these types of staff in the category of people employed to provide care.
Reported involvement of the person with dementia in LSW was almost universal across the services. By contrast, although all generalist long-term care homes and 98% of IPAs said that carers were involved in LSW, only 81% of MASs reported this.
The predominant model when only two categories of people were involved was the person with dementia and a carer (53/69 cases), followed by the person with dementia plus an OT or activities co-ordinator (24/69 cases).
The role of carers was clearly important, regardless of the involvement of staff, which raises the question of what happens when people do not have carers who are available and/or willing to help.
How is the life story used?
We asked respondents both to select as many options as they wished about use of the life story in their care setting and which they felt was most important (see Appendix 1, Table 20).
Responses varied by type of service. MASs (79%) and inpatient settings (78%) were somewhat less likely than SCHs and generalist long-term care homes (both 90%) and CDSs (93%) to choose helping the person to remember important parts of their lives. By contrast, SCHs were most likely to choose helping to soothe or calm the person (85%), followed by IPAs (78%), generalist long-term care homes (77%), CDSs (73%) and MASs (61%). This difference seems likely to reflect the different stages of the dementia journey that predominate in these different settings.
Again, perhaps reflecting the nature of their work with people with dementia, IPAs (82%) and MASs (79%) were more likely than generalist long-term care homes (67%), SCHs (59%) or CDSs (47%) to say that they used the life story so that health and social care staff elsewhere could provide better care. This difference reached statistical significance (χ2 = 11.79, df = 4; p = 0.019).
Although the option of using the life story to help staff to see the person behind the dementia was a common choice, MASs were less likely than other services to choose this option (χ2 = 9.613, df = 4; p = 0.047).
When it came to choosing the most important use of the life story, similar differences between the services were also evident (see Appendix 1, Table 20). Again, these seem likely to be influenced by the type of people using the services and the nature of the service involvement.
What information is included in the life story?
Respondents were asked whether they always, sometimes or never included particular types of information in the life story.
Tables 21–24 (see Appendix 1) show the answers given across all respondents and whether or not we found significant differences between services.
Family information
Memory assessment services were less likely than other services ‘always’ to include the names and descriptions of carers, and the least likely ever to include information about reactions to or meanings of these people to the person with dementia (see Appendix 1, Table 21). IPAs included the names of carers but were less likely than other services to include their descriptions. These differences were all statistically significant.
Person’s life
The second group of questions was about including the important events, dates, places and life stages of the person with dementia (see Appendix 1, Table 22).
Differences between care settings were less evident here. MASs were much less likely than other services ‘always’ to include lists and details about life events, but more likely ‘sometimes’ to include this information. However, overall differences between services did not reach statistical significance.
Recording feelings about life events and stages was less common overall. CDSs were slightly more likely to report that they always included this information, but these differences did not reach statistical significance.
Likes and dislikes
The third group of questions was about the record made of people’s likes and dislikes (see Appendix 1, Table 23). Although this type of information was included in most life stories, preferred clothing and topics for conversation were less commonly included than information about activities and food.
Services varied substantially here. MASs were significantly less likely to say that they always included information about people’s food, clothing, activity and conversation topic preferences. CDSs were significantly more likely to record information about what people liked talking about.
Needs
Finally in this section of the questionnaire, we asked whether or not the life story recorded medical or care needs and spiritual or cultural needs (see Appendix 1, Table 24).
It was relatively unusual for life stories to include information about medical or care needs, as one might expect, given that such information would more appropriately be included in care plans. By contrast, the majority of respondents said that spiritual or cultural needs were included ‘always’ or ‘sometimes’.
There were substantial differences between services here. IPAs were most likely to report that they ‘sometimes’ included medical or care needs, while SCHs were most likely to report that they ‘always’ included this type of information. MASs and IPAs were least likely and SCHs and CDSs were most likely to report that they ‘always’ included spiritual or cultural needs.
Overall, then, there was very different patterning of the contents of life stories across different services. To some degree these may reflect both the main function of the service and the point in the dementia journey at which LSW takes place.
Leaving things out of the life story
Overall, 61% of respondents said that things were sometimes left out of the life story, with little difference between services; 62% reported that this was because some things were too private to include and 84% reported that some things were too upsetting to include. Other reasons given were related to memory problems (11 of the 32 respondents who gave an additional reason) or to the general difficulty of getting relevant information about the person with dementia (10/32). Again, there was little difference between the services.
We then asked who made the decision to leave things out of the life story. Sixty-eight per cent of those who had said that things were sometimes left out said that the person with dementia made this decision; 90% mentioned carers and 22% mentioned staff.
Services reported significantly different levels of involvement of the person with dementia in the decision [MASs (93%), CDSs (89%), IPAs (71%), generalist long-term care homes (56%) and SCHs (55%); χ2 = 10.40, df = 4; p = 0.034]. MASs were least likely to say that family members or others close to the person with dementia made the decision (73%), compared with IPAs (96%), SCHs (94%), generalist long-term care homes (89%) and CDSs (89%). However, this difference did not reach statistical significance, perhaps because numbers were small. Again, these differences may reflect the stage at which services see people with dementia and carry out LSW with them.
Is the life story static or dynamic?
Life story work literature suggests that the life story should be a dynamic product, adding material as new information about the past comes to light and as new memorable events take place.
Overall, 28% of respondents said that items relating to both past and recent events were added to the life story, suggesting that they adopted a dynamic approach to LSW (see Appendix 1, Table 25). IPAs were most likely to say that the life story was a one-off product. Along with MASs, they were also less likely to add recent events, while SCHs were most likely to refer to adding items related to recent events. This difference reached statistical significance and, again, seems likely to reflect the different work different settings would be doing with people with dementia.
Who can look at the life story and who gives permission for this?
Good practice suggests that the life story should be seen, first, as the property of the person with dementia.
Table 26 (see Appendix 1) indicates that ‘ownership’ of the life story by the person with dementia is almost, but not completely, universal. Carers in CDSs and MASs were slightly more likely than carers in other settings to be able look at the life story. The pattern of staff access to the life story was low, with only 24% of all respondents saying that all staff in the service could look at the life story. Differences between the services were very striking and statistically significant, with over two-thirds of IPAs saying that any staff could look at the life story, while no respondent in a generalist long-term care home chose this option. SCH responses were surprisingly low here.
As might be expected, IPAs were more likely to say that staff in other settings could look at the life story; indeed, some respondents in these services added further detail, pointing out that the life story was often specifically intended to accompany the person with dementia to their next, often long-term, care setting. By contrast, MASs and care homes, of whatever sort, were unlikely to suggest that staff in other care settings could look at the life story.
If the life story belongs to the person with dementia, we might expect their permission to be sought before others look at the life story. Further, seeking permission might explain some of differences in the involvement of staff in looking at the life story. We asked respondents directly about whether or not the person with dementia was asked for their permission and in what circumstances this might not happen.
There was substantial and significant variation between settings here (see Appendix 1, Table 27), mostly explained by the extent to which IPAs said that they ‘sometimes’, rather than ‘always’, asked the permission of the person with dementia. This may reflect the acute nature of confusion encountered, by definition, in IPAs. CDSs were most likely to report that they ‘always’ asked permission of the person with dementia.
Who could look at the life story did, indeed, vary according to whether or not the person with dementia was asked for their permission for this. When the person was always asked for their permission, it was less likely that any staff working in the service would be able to look at the life story (15%). By contrast, if the person with dementia was ‘sometimes’ asked to give permission, it was much more likely that any staff would be able to look at the life story (41%). These differences reached statistical significance (χ2 = 13.45, df = 2; p = 0.001).
We also asked if carers were asked to give their permission for other people to look at the life story; 54% said that carers were ‘always’ and 29% said that carers were ‘sometimes’ asked for their permission, when they were available to be asked. There were few differences between services in this aspect of LSW practice.
Although two-thirds of respondents said that the person with dementia was always asked for their permission for others to look at their life story, very few (15%) reported that this permission was formally recorded in the life story itself. CDSs (33%) were more likely than MASs (9%), SCHs (13%), IPAs (14%) and generalist care homes (19%) ‘always’ to include such a statement in the life story, but this difference did not reach statistical significance.
Access to the life story
Where is the life story usually kept?
Producing a life story is one thing; having it to hand to look at or for other people to look at so that they can understand the person with dementia in more depth is another. We asked where the life story was usually kept to give some idea of how ‘active’ the life story was (see Appendix 1, Table 28). The most common response here was that the life story was usually kept in the care record of the person with dementia (61%), followed by the person with dementia keeping the life story (44%) including those who said that it was kept in the person’s room in a residential setting. Multiple responses were possible, as we know that in some settings there is more than one copy of the life story.
There were striking differences between services, some explicable by the nature of the service and others not. As one might expect, all MASs said that the person with dementia kept the life story, and they were also much less likely to keep the life story in the person’s care record. By contrast, SCHs were significantly less likely to report that the person with dementia kept their life story and more likely to say that the life story was kept in an office or other secure place within the service. IPAs were very unlikely to keep the life story in an office or other secure place, while generalist long-term care homes were much more likely to keep it in the person’s care record. SCHs and IPAs were slightly more likely to display the life story in some form, but this difference was not statistically significant. Only one respondent (a CDS) reported that a carer kept the life story.
When respondents reported that the life story was kept in more than one place, the person with dementia was more likely to have a copy than when only one place was mentioned (73% vs. 33%). Consequently, perhaps, mentioning more than one copy was also associated with the life story being kept in an office, in the care record or being on display.
Policies and practices to support life story work
How life story work is done
We asked a range of questions about the policies and practices that underpinned how LSW was done, ordering them to avoid possible response set effects by asking questions about similar sorts of issues in different places. We then grouped responses into three thematic areas: (1) responsiveness to individual needs and wishes of the person with dementia; (2) training and supervision of those carrying out LSW; and (3) knowledge of LSW and its use across the service. Policies and practices varied considerably, depending on the type of service (see Appendix 1, Table 29).
Although many respondents (82%) said that their service offered LSW to everyone regardless of the stage of their dementia, this was significantly less likely to be the case in MASs (43%). Almost all respondents said that people with dementia who also had visual impairments were offered the opportunity to do LSW, and there was very little variation here between the services. CDSs were significantly less likely and IPAs were more likely than other services to use a template for LSW. IPAs were also much more likely to say that staff and volunteers mainly made decisions about the format and look of the life story, possibly reflecting this greater use of templates.
Most respondents reported that LSW was adapted to the strengths and needs of the person with dementia, with little variation between them. This is slightly puzzling in relation to IPAs, which were also much more likely to be using a template throughout in their LSW. We examined this further and saw that all those who said that they used a template throughout were also more likely than others (94% vs. 85%) to say that they adapted LSW to the strengths and needs of the person. This suggests that this question may have been eliciting socially desirable responses rather than responses that reflected reality.
CDSs were significantly more likely to say that they expected staff to do their own life story before doing LSW with service users. Staff in IPAs were more likely to be trained to do LSW, rather than learning how to do it ‘on the job’, but the difference between services did not reach statistical significance. There was considerable variation in the extent to which respondents said that staff or volunteers doing LSW received supervision from more senior or more experienced staff. MASs and SCHs were less likely to say that this happened, while IPAs were more likely to say that they provided this sort of oversight.
We saw earlier that some services relied on carers to carry out LSW, but only one-quarter overall said that they trained carers before they embarked on LSW. CDSs were slightly more likely to say that they did so, but this difference did not reach statistical significance.
Seventy-two per cent said that all staff and volunteers in their service knew what LSW was, with some small but non-significant differences between services.
By contrast, when it came to knowledge about how to use the life story to improve care, only two-thirds responded positively, with significant differences between the services. MAS respondents were less likely than others to feel that everyone in the service knew how to use a life story in this way, while SCHs and CDSs were slightly more likely to feel this.
Resources used to support life story work
We also asked about institutional policies that might support LSW (see Appendix 1, Table 29).
Respondents were about equally divided between those that felt that LSW was done in spare moments and those that reported dedicated and protected time for LSW. IPAs were slightly more likely to report doing LSW in spare moments and significantly less likely to report that there was protected time for it. By contrast, SCHs were slightly less likely to report doing LSW in spare moments and significantly more likely to report having protected and dedicated time.
The majority of respondents (although not all) felt that senior staff supported LSW in their service, but this did vary, with SCHs significantly more likely and MASs significantly less likely to report senior staff support. We checked whether or not this reflected the involvement of senior staff in completing the questionnaire. Indeed, three-quarters of respondents from SCHs who completed this part of the questionnaire (42/56) were managers, owners or directors of the homes. By contrast, almost three-quarters of those in MASs (16/22) were ward or team leaders or occupational therapy staff. These results thus need to be interpreted with care.
Services also varied in whether or not they reported that any staff in their service would be freed up from other work if they wanted to carry out LSW. SCHs and generalist long-term care homes were most likely and IPAs and MASs were least likely to report that this was the case. As with SCHs, respondents in care homes were mostly managers (20/26) and so perhaps were more inclined to positive responses here. However, as we saw above, generalist long-term care home respondents were not more likely to say that senior staff supported LSW.
Survey of carers of people with dementia
We also carried out a survey of carers of people with dementia to focus on the experiences of those who supported a person with dementia who had made a life story. We were interested in how the life story was used, in which settings or circumstances, and in how the life story was produced, by whom and whether or not this followed good practice identified in stage 1.
Our partnership with Dementia UK gave us access to a network of carers in contact with Uniting Carers that provided the sampling frame for the survey. Although we recognised that this was unlikely to provide a representative sample, there is no existing sampling frame from which to draw a representative sample of carers of people with dementia. For the purposes of this stage of the research, we felt that even non-representative data from the carers’ perspective would provide a valuable addition to the data collected from service providers.
The main ethical issue was the potential impact on carers of participating in the survey. Carers experience pressures on their time and energy (both emotional and physical) and it would be unethical to add to these pressures unnecessarily or excessively. We therefore worked closely with Uniting Carers to ensure that the survey and its administration had the minimum necessary impact.
Methods
Sample
The Uniting Carers database contained the details of over 700 carers of people with dementia; this included both current and past carers. Uniting Carers regularly communicated with carers in the network via e-mail, and agreed to send an e-mail to members informing them about the survey and providing a link to the questionnaire. It was then up to the carers whether or not to click the link to the survey. A copy of the e-mail is in Appendix 9. Based on previous experience, Uniting Carers expected between 10% and 20% of carers in their network to complete the survey (n = 78–156).
Survey development
Learning from stage 1 and expert advice from coapplicants and our advisory groups informed the content and design of the survey. We also pre-piloted the draft survey face to face with members of our carers’ network of advisers to ensure face validity and comprehensibility.
The questionnaire was designed to take around 15–20 minutes to complete. No explicitly emotive issues were included, and during the pre-piloting stage we asked participants to flag up any aspects of the questionnaire that could unwittingly cause distress. Some people might have been caring for more than one person with dementia or have done so in the past, so we designed the questionnaire to deal with this possibility and asked people to provide answers only about the person who they spent or had spent the most time supporting.
Once the questionnaire was finalised, we entered it into Qualtrics. A text version of the final questionnaire is given in Appendix 9.
Survey administration
The questionnaire front sheet gave more information about the project and stated clearly both that participation was optional and that by completing the questionnaire carers were consenting to the information they provided being used for the research. The research team’s contact details featured prominently so that anyone who wanted to discuss the research before deciding whether or not to take part could do so. The e-mail also made clear that we could provide paper copies of the questionnaire on request.
One reminder e-mail was circulated around the entire network 2 weeks after the first e-mail but no further correspondence was received by non-responders. Those who completed the questionnaire were asked whether or not they would like to receive a summary of the study findings in due course.
We included information about who to contact for further support at the end of the questionnaire, and repeated the research team’s contact details in case respondents had any questions or concerns.
Response rate
One hundred and three carers responded to the survey, and 96 completed enough of the survey to allow analysis of their responses. This response rate is in line with the 10–20% that Uniting Carers had predicted (see Sample). There is no way of knowing whether or not respondents were representative of all carers in the Uniting Carers network, nor would it be sensible to compare those who responded with all carers of people with dementia, even if such comparative data were available.
Of the 96 respondents, 52 were current carers and 44 had cared for someone with dementia in the past. We compared the current and ex-carers across the full range of questions and found very few differences between them. We therefore combined the results for the two groups.
Analysis
All data were imported from Qualtrics into SPSS (version 22) for analysis, which was predominantly descriptive. Bivariate analysis initially compared those who had and had not had experience of LSW. Subsequent analysis explored the experiences of the small number (n = 39) who had experience of LSW. Frequencies and chi-squared statistics are thus the main forms of analysis presented. We have also used the adjusted standardised residual to explore the main drivers of significant differences within cross-tabulations.
Results
Carer characteristics
Three-quarters of carers were female, and the majority (74%) were aged ≥ 55 years, with 40% aged ≥ 65 years. Most (98%) classified themselves as white; only two carers reported non-white ethnicity. One-third (33%) were caring for a spouse or partner and over half (57%) were caring for a parent or parent-in-law. Men were significantly more likely to be caring for a spouse or partner and women for a parent/in-law or other relation (χ2 = 4.41, df = 1; p = .036), while those aged ≥ 65 years were much more likely to be caring for a spouse or partner (χ2 = 47.89, df = 3; p< 0.000). As a result of this patterning, male carers among the respondents were significantly more likely than females to be aged ≥ 75 years (χ2 = 8.58, df = 3; p = 0.035).
These patterns are all broadly what we might expect to see in a population of carers of people with dementia.
Characteristics of the person with dementia
Sixty-three per cent of the people who were or had been supported by carers were female.
Current carers were most likely to be supporting someone aged ≥ 75 years (69%); 19% were supporting someone aged between 65 and 74 years. Forty-eight per cent reported that the person with dementia’s memory loss had become apparent between 6 and 10 years previously, with 35% reporting that this had happened between 1 and 5 years previously.
We asked those who were no longer carers how long they had cared for the person with dementia; almost two-thirds had done so for ≥ 6 years, and 21% had done so for ≥ 11 years. We also asked ex-carers how old the person with dementia had been when their memory problems had first become apparent. The majority (63%) reported that this had happened when the person was aged ≥ 75 years.
Among current carers, the largest group (44%) were those supporting someone who lived at home with them, followed by those supporting a person with dementia living in a residential or care home (23%) or nursing home (15%).
Knowledge of life story work
Three-quarters of respondents (75%) said that they had heard of LSW, but only 41% (39 carers) reported that the person they supported had ever done LSW. Carers under the age of 65 years were more likely to have heard of LSW (χ2 = 9.38, df = 3; p = 0.25) but there were no other obvious relationships between carers’ characteristics and their knowledge of LSW.
The most common source of information for carers about LSW was a voluntary organisation (46%), followed by a health or social care professional (37%). A small proportion had found out about LSW via the internet (13%) or from published material (13%). Some respondents mentioned more than one source of information.
There were no apparent relationships between whether or not LSW had been done and the characteristics of carers or those of the person with dementia.
The 36 carers who said that they had heard of LSW but that the person with dementia had not done it were asked about the reasons for this. The most important reason given (16 carers) was that LSW had never been offered to the person with dementia. Four said that it had been offered but that the person they supported was not interested in doing it and four said that they had not been sure of the benefits of doing LSW or were worried about it raising painful memories for the person they cared for. Four carers also mentioned that by the time they had heard about LSW it was ‘too late’, as the person they cared for had deteriorated too far or had died.
We explained the general principles of LSW in our questionnaire introduction. We therefore asked those who had not previously heard about LSW whether they felt that it might help or could have helped the person they supported; most (13/24) felt unsure about whether or not doing LSW might be of value.
Doing life story work
The remainder of the analysis is based on the 39 carers with experience of LSW and should be read in the light of small numbers.
Type of records used in life story work
Most carers (21/39) reported that LSW had involved only one type of record. Around one-third reported a photo album with no text and just under one-third reported the use of photos alongside written comments or stories. One-third also mentioned the use of a written summary. One-quarter mentioned that a book had been produced using a mixture of photos and stories and one-quarter mentioned the use of a memory box. Very few (n = 3) mentioned the production of a collage or similar to display. Other forms of LSW were a DVD or film (n = 1 carer) or a poem (n = 4). Some carers mentioned other forms of memory prompts such as smells or favourite plants being used to represent the person’s life.
Where only one type of record was reported, this was most likely to be a book with a mixture of photos and stories (n = 7) followed by a photo album with no text (n = 5). Four carers reported that the life story was a written summary only. A written summary combined with other type of records such as photo albums and memory boxes was the most common pattern of multiple records (n = 9).
How, where and when is life story work done and who was involved?
Most carers (34/39) said that the person with dementia had done LSW in a one-to-one situation; the remainder reported a group setting. Some carers provided additional detail here, usually reporting that they themselves had done the LSW with the person with dementia.
How the LSW was done was related to where it was done. First, most carers (n = 20) said that the LSW had been done in the home of the person with dementia or in the care home where the person lived (n = 13). One referred to LSW being done in a support group and four to a community service setting such as a memory café or day centre. When this was examined against how the LSW was done, the predominant model that emerged was of one-to-one work in the person’s own home (n = 26) or in a care home (n = 11). As these numbers suggest, some carers reported more than one setting in which the LSW had been done.
Carers themselves were the people most involved in doing the LSW (n = 34), followed by the person with dementia (n = 24). Care staff (n = 7 carers) or people paid specifically to do LSW (n = 2 carers) were also mentioned, and three mentioned volunteers. Overall, one-quarter of carers (n = 10) said that there was only one person involved, one-quarter (n = 10) said that two people were involved and the remainder reported that three or more people were involved. Nine carers reported that they were the only person involved in doing the LSW.
Carers were most likely to be involved when the LSW was done at the home of the person with dementia (n = 25) or in the care home where the person lived (n = 12). Care staff or volunteers were most likely to be mentioned (n = 8) when the LSW was done in a care home, as might be expected. In both cases in which a person paid to do LSW was involved, the work had taken place in the person with dementia’s own home.
Some carers (n = 12) said that the life story had been created before or soon after the person showed signs of memory problems. The majority (n = 18), however, reported that LSW had been done between 1 and 5 years after memory problems had become evident, and a small group (n = 8) reported that it had been done > 5 years after onset.
How is the life story used?
Most carers reported more than one use of the life story; over two-thirds reported five or more uses (see Appendix 1, Table 30).
The final column in Table 30 shows some interesting patterns. Helping the person to remember important parts of their lives was chosen most often (n = 31 carers) but when it came to the most important use, helping health and social care workers to provide better care was chosen most often.
What information is included in the life story?
Different methods of doing LSW and different uses to which the life story is put both influence and are influenced by the information that is included in the life story (see Appendix 1, Table 31). Most of the life stories carers had experienced were based more in ‘facts’ than in ‘feelings’. Thus, most reported that the names of family members and others close to the person with dementia were included, but only one-third said that the reactions of the person to these individuals were in the life story. Similarly, while many life stories included lists and details of important events, dates and so on, a record of the person’s feelings about these was much less common.
Analysis of the clustering of these different types of information showed two fairly distinct models of LSW, each accounting for around half of the responses. One concentrated on the names and descriptions of family members and the other on close people, lists and details of events, and people’s preferences for food and activities. The first model was more likely to include spiritual and care needs, people’s clothing and conversational preferences, and their feelings about family members and events. The second type tended to be more associated with a life story that was in written summary form, which was done in care homes and for which the most important use was helping health and social care workers provide better care.
Leaving things out of the life story
Just under half (n = 18) of the carers said that something had been left out of a life story, the most usual reason being that some things would have been too upsetting (nine carers) or too private (eight carers) to include. Five felt that the life story needed to be positive and, therefore, presumably, some less positive aspects of the person’s life had been excluded.
Carers were more likely to report that they had made the decision to leave something out (14 carers) than that the person with dementia made the decision (six carers). In two cases, the decision had been a joint one. Other family members (three responses) and health or social care workers (one response) were also mentioned as having influenced the exclusion of something from the life story.
Is the life story static or dynamic?
Just over one-third of carers (14) said that the life story was a ‘one-off’, with nothing added to it subsequently. Another one-third (13) said that photos, descriptions or other items about the past had been added to the life story along the way, and 10 said that items related to recent events had been added as they happened.
It was unusual for the life story to include the person’s hopes and views about the future and LSW was dominated by recollection of the past (see Appendix 1, Table 32). Overall, 16 carers reported that the life story was exclusively about the past, containing no information about the person’s current life or about their hopes and views for the future. Life stories that were classified as the second ‘type’ (see above) were more likely to include information about the person’s current life (14/19) than were those classified as the first ‘type’ (8/20) and this difference reached statistical significance (χ2 = 4.50, df = 1; p = 0.034). This perhaps reflects the use of this type of life story in care home settings.
Who can look at the life story and who gives permission for this?
The majority of carers said that they and the person with dementia were able to look at the life story (34 in both cases). Family members were next most likely to have access (32 responses). Only 17 carers reported that selected health and social care staff could look at the life story, and 14 that any health or social care staff could look at it.
Eighteen carers reported that the person with dementia had given explicit permission for the life story to be seen by others (or not); eight reported that the person with dementia had not given explicit permission and 11 did not know or could not remember. Rather more carers (27/39) reported that they had given permission. However, the majority of carers said that there was no written statement of permission included in the life story record that allowed others to look at the life story or that they could not remember such a statement.
Access to the life story
Where is the life story usually kept?
We saw earlier that some carers reported more than one life story record. This is reflected in 12 people reporting that there was a life story record in more than one place (see Appendix 1, Table 33). The most common combination was when the carer had a copy of the life story and a copy was also kept at the care home where the person with dementia lived.
Looking at and using the life story
Finally, we look at the active use of the life story, indicated by how often people actually looked at it (see Appendix 1, Table 34).
We saw earlier that the use of the life story to enable care staff to look after the person with dementia was, for many carers, the most important reason for having a life story. Despite this, carers reported that use of the life story by care staff was relatively low, and lack of knowledge about whether it was ever used was relatively high. Even for carers and people with dementia, however, use was not as high as might have been expected. Only one-third of carers said that they or the person with dementia looked or had looked at the life story at least every week, and of these very few reported daily use (two and three responses, respectively).
Chapter 6 Exploring feasibility
This element of our work related to stage 2c in our proposal: scoping the potential effects and costs of using LSW in specialist inpatient and long-term care settings (objective 3) and exploring the feasibility of formal evaluation (objective 4).
Medical Research Council guidance18 confirms that assessment of feasibility and piloting of methods is vital preparatory work in developing and evaluating complex interventions. In this stage of our work we were interested, first, to see whether or not we could observe any effects from and costs of using LSW and, second, to test the feasibility of large-scale formal evaluation of LSW. We piloted two different study designs in two different settings to address our objectives:
-
a stepped-wedge trial design in independently provided care homes
-
a pre-test post-test design, with controls, in NHS mental health assessment units that specialised in the care of people with dementia.
In this chapter, we present the findings of the assessment of feasibility in both settings. The measured outcomes and costs are reported in Chapters 7 and 8.
The aims of the feasibility elements of the work were to:
-
establish the likely rates of recruitment and retention
-
identify any problems service providers experienced in delivering the intervention
-
assess the feasibility of measuring the outcomes of LSW in these settings
-
assess the feasibility of collecting data on the costs of LSW in these settings.
Methods
Study 1: a stepped-wedge trial design in independently provided care homes
Design
We chose a stepped-wedge design to allow us to test the feasibility of not only evaluation but also rolling out the LSW approach to these new care settings. In this design, each setting receives the intervention at some point during the period of the study (ensuring equity), but roll-out is staggered, rendering implementation across multiple sites more straightforward than attempting a simultaneous start. 134
We worked with a single, not-for-profit care home provider that was keen to introduce LSW across its services. The provider selected a purposive sample of six care homes. None of the homes currently practised LSW but all had managers who were disposed to introduce it.
The project was designed so that one care home introduced LSW each month for 6 months, with baseline data collected immediately before implementation and follow-up data collected 1 month, 2 months and 6 months after LSW was due to begin. The first care home entered the study in January 2014 (with training taking place in the previous month) and the following care homes entered at monthly intervals; thus, care home 6 entered the study in June 2014.
Intervention
A training package was designed, informed by the findings on good practice from the development stage of the project (see Chapters 2 and 3). This consisted of:
-
a 2-hour training session for care home staff (delivered by the care provider’s dementia care consultant)
-
printed guidance and hand-outs on good practice in LSW
-
a template, ‘some important things’, to help staff get started (it was emphasised in the training that the template need not be followed – the form LSW takes should be led by the needs and desires of the individual – but it could be used as a starting point).
Sample
Ten residents with dementia or dementia-like symptoms (and their family carer, if they had one) in each of the six care homes were randomly selected and invited to join the study. All staff who undertook the LSW training were also invited to take part.
Study 2: a pre-test post-test design, with controls, in NHS mental health assessment units that specialised in the care of people with dementia
Design
The stepped-wedge approach was not appropriate in the acute settings, as we were working with three mental health assessment units in which LSW was reported to be a routine part of care for all patients with dementia already. We instead opted for a pre-test post-test design in the acute settings, with a comparison setting providing a control, and collecting data over a 6-month period from baseline. All three wards in the intervention site joined the study in February 2014 and the comparison site joined in April 2014.
Intervention
In the intervention site, a group that included the NHS trust’s clinical lead for psychological therapies for older people had initiated LSW some years previously. In October 2013, we attended the trust’s Service Line Planning Group meeting for older people’s services and agreed with service managers to focus on three short-stay assessment units for older people with mental health problems where LSW (usually in book form) was routinely practised.
In the comparison site, LSW was not practised but the ward manager was keen to introduce it. We agreed that, once the 6-month participant recruitment period was over, the project team would support the ward to access LSW training.
Sample
Ten people with dementia (and their family carer, if they had one) were to be recruited sequentially from each of three inpatient assessment units that practised LSW as or soon after they were admitted and 10 were to be recruited sequentially from each of three comparison sites as or soon after they were admitted. In addition, data were to be collected from a cross-section of staff on the wards at three time points over the 6-month period.
Process (both studies)
Quantitative data collection
We planned to measure selected outcomes for all participants with dementia and family carers at baseline (for those in the LSW groups, before any LSW had commenced) and then follow them up at 1 month, 2 months and 6 months after baseline, wherever they were then living. We had originally considered training staff on site to use some of the outcome measures, but it soon became clear that this would not be workable without additional funds to backfill staff time. Two researchers in the project team (KG and JB), supported by a research assistant employed on a casual basis (LC) for the care homes study, collected data at all time points.
Innovations in Dementia provided advice on consent and data collection processes with people with dementia, and observed the researchers in action at one care home to ensure that ethical practices were in operation.
We also planned to collect data from participants’ care records about dementia diagnosis and severity at baseline, and on relevant drug use and adverse events for the 3 months prior to entering the study and the final 3 months of follow-up.
Levels of staff burnout, staff assessments of personhood and staff approaches to working with people with dementia were assessed using existing measures. In care homes, consenting staff provided baseline data and were followed up after 1 month, 2 months and 6 months. In the hospitals, cross-sectional data were collected at three time points over the 6-month study period.
Qualitative data collection
We gathered in-depth, qualitative information about experiences of LSW and the processes involved in its evaluation from carers, staff and (where possible) participants with dementia. The aims here were to:
-
develop a qualitative understanding of causal links between LSW and the outcomes measured in the quantitative element of the study
-
explore the acceptability of the processes involved in evaluation
-
understand any implementation issues, including barriers and facilitators to LSW, and any unanticipated consequences (including how these could be managed in future).
We conducted a mix of face-to-face and telephone interviews with family carers (guided by their stated preferences) and guided conversations with participants with dementia who were able to communicate verbally (and were happy to do so). We also conducted focus groups with staff, covering both their views on the use of LSW and their experiences of taking part in the study.
Ethical approach
Research ethics approval for the feasibility study stage of the project (including the qualitative work discussed in Chapter 9) was obtained from the NIHR SCREC on 28 November 2013 for people with the capacity to consent to take part, and on 2 December 2013 for those without the capacity to consent.
Findings of the feasibility studies
Selection and recruitment of sites
Recruitment of care home study sites
As planned, we recruited six care homes to the study through the care home provider already partnered with the project. Selection of sites was purposive, to provide a range of research settings (some more and some less research ready) all within 2.5 hours’ travel of York. Recruitment was initially straightforward: the coapplicant on the project made the initial approach to regional managers, who in turn approached individual care home managers. In April 2013, when the Social Policy Research Unit held a meeting for the care homes for them to learn more about the project and contribute to the design of the study, all six sites were enthusiastic about taking part. However, by the time fieldwork was due to commence, managers had changed in two of the six sites and a further two sites had withdrawn, citing staffing and capacity issues. Both of the sites that withdrew were replaced before fieldwork started (CH1 and CH6), using the same purposive sampling criteria.
The researchers visited each care home in advance to familiarise themselves with the setting, to ensure that managers were still committed to the research and to build rapport with staff. Nevertheless, the change in management at two sites did appear to have an adverse effect, as both seemed less engaged in the research for the remainder of the study period. Indeed, continuity continued to be an issue at both of these sites throughout the fieldwork, with the new care manager in one home leaving part way into the study and both the care manager and the business manager leaving the other before final follow-up was carried out.
Table 35 in Appendix 1 summarises the characteristics of the six care homes that were finally included.
The ethical issues regarding the assessment of people for dementia in a research project, when no formal diagnosis exists, are considerable. This is particularly the case in relation to people who live in residential care homes where diagnosis may have considerable financial consequences for those who are self-payers. We also know that diagnosis rates are below 50% in England. 135 However, even when a formal diagnosis had been made for a care home resident, this was not always recorded in the resident’s care records. We therefore decided to rely on the professional views of the care home managers in relation to the assessment of the presence of dementia and/or cognitive impairment.
Recruitment of specialist mental health assessment units
As planned, we recruited the three intervention sites through the NHS trust already partnered with the project. The site had six eligible wards and the final decision about which three to include was taken by the older people’s service-level managers after a meeting with the research team. As ward managers themselves did not actively opt into the study, this may have influenced ongoing engagement.
The research team visited each ward before fieldwork started, meeting ward managers and available staff. However, as ward staff work shifts and a high proportion of bank staff work on the wards, it was not possible to meet the entire staff team before the research started. Again, this may have affected engagement with the project.
There was one change of manager at one of the intervention wards immediately before the study commenced but this did not appear to influence engagement.
Recruitment of a comparison site was less straightforward. We had originally planned to recruit three comparable mental health assessment units through the survey of care providers. However, it took longer than anticipated to identify the survey sample, and, once the sample was identified, responses from the NHS in particular were slow to come in (see Chapter 5). It was not possible to recruit through the NHS Portfolio at this point, as we had not yet received research ethics approval for this stage of the project. We opted instead to utilise existing contacts and relevant networks to identify comparable sites. However, comparable sites were not in abundance. There seemed to be two main reasons for this. First, there has been a recent move towards greater community provision, meaning that fewer trusts now appear to provide inpatient mental health assessment. Second, several of the sites that expressed an interest already employed LSW in some form on their wards and so were ineligible as comparators.
The site eventually recruited was identified through a national database of clinical psychologists and related practitioners. The trust had only one mental health assessment unit but this was larger than the three intervention wards in total. Further, the ward manager and local principal investigator agreed to continue recruitment until we had reached the target of 30 comparison patients (as opposed to 10 patients per ward, in the intervention sites) or the 6-month recruitment period ended, whichever came first. Table 36 (see Appendix 1) summarises the characteristics of the specialist mental health assessment units recruited for this part of the study.
Selection and recruitment of staff
Care homes
All staff taking the LSW training in the care homes were invited to join the study. Signing up to the project involved agreeing to complete three questionnaires (the ADQ,129 the PDQ130 and the CBI;133 see Chapter 4) at baseline and three follow-up points over 6 months. There was also the option of taking part in a focus group at the end of the study, but it was stressed that staff could choose to opt in or out of this nearer the time.
Recruitment was undertaken directly by the research team who visited each care home before the training. Recruitment was most successful when the researchers were allocated a dedicated room to talk through the project with each member of staff, either individually or in small groups. It was also most successful when staff were granted time from their caring responsibilities to consider their decision and, if they consented, complete the baseline measures there and then. In CH2, this time and space was not available and recruitment here was poor. At CH3, the manager led by example in a communal dining area, making time to sit with the researchers and go through the information sheet. She then encouraged her staff to meet with the researchers (allocating a dedicated room) but emphasised that whether or not they decided to join the study was optional.
Obviously, staff recruitment was also affected by numbers of staff allocated (usually by a manager) to take the LSW training and who were also available when researchers were recruiting at the home. Both varied considerably. In total, 51 staff were recruited across the six homes (see Appendix 1, Table 37).
Specialist mental health assessment units
The research team carried out recruitment of staff in these settings. As explained earlier, the aim of the study in relation to staff differed from that for staff in care homes. Rather than investigating change over time, we were interested in identifying overall differences in staff groups between the sites that did LSW and those that did not. We thus planned to collect cross-sectional data at three time points over an 8-month period (February–September 2014) and use this to calculate an overall average for the staff teams at each site. The measures were the same as those used in care homes and staff were also informed about the optional focus group to be held towards the end of the study.
All staff members working on the ward on the day of our visit, from managers to bank staff, were invited to take part. The numbers working each shift differed between sites. However, the numbers completing questionnaires depended less on the size of the staff team and more on the activities staff were engaged in; often they were allocated to work one to one with a patient or were required to accompany patients off-site, effectively excluding them from involvement. In such circumstances we left recruitment packs for individuals, including pre-paid envelopes for them to return completed questionnaires, but we did not receive any additional responses using this approach.
As with the care home sites, the most effective means of recruiting staff in the acute sites was through face-to-face discussion in a dedicated room. When there was no space allocated for these discussions, or for staff to use while completing questionnaires, recruitment was less successful. Table 38 (see Appendix 1) shows the numbers of staff who completed questionnaires at each time point; in total, 47 staff over four wards were recruited.
Not all of those completing questionnaires at time points 2 and 3 were new recruits: all staff members working on the ward at each time point were invited to complete the questionnaires, regardless of whether or not they had already participated at an earlier time point.
In summary, the recruitment of staff was relatively successful in both care homes and hospital settings but was influenced by a number of factors:
-
dedicated space for staff to read the information, ask questions and complete questionnaires
-
availability of staff to meet the researchers on the day
-
manager leading by example
-
communication to staff that research was taking place on that day.
Selection and recruitment of people with dementia and family carers
People with dementia in care homes
We planned to select 10 eligible residents from each care home, using random selection, and invite them to join the study, either directly (if they had capacity to give informed consent) or through a consultee. After we met with representatives from the included care homes in April 2013, it was agreed to keep the eligibility of care home residents as broad as possible. At this meeting, three basic criteria were set for inclusion/exclusion, as follows.
-
Include:
-
residents with dementia or suspected dementia.
-
-
Exclude:
-
residents considered by the care home manager to be reaching the end of their lives
-
residents who had been at the care home for < 3 months (in order to ensure that 3 months’ baseline data were available from the person’s care records).
-
In addition, recognising the importance of learning throughout the feasibility study, it was agreed that if managers identified further reasonable grounds for exclusion once selection began, these would be considered by the research team and, if agreed, applied throughout.
Ten eligible residents were to be randomly selected in each care home in the month prior to the intervention being introduced. However, obtaining a sampling frame of eligible residents from each care home was challenging, as pertinent information to establish eligibility (whether a person had dementia or suspected dementia) was not routinely recorded in care records. We decided therefore to ask each care home manager to make an assessment based on their knowledge of their residents and supply the research team with an anonymous list of all residents they considered to be eligible.
A researcher at the University of York who was independent of data collection and analysis then randomly selected residents, using the eligible participants’ room numbers and a random number table. These allocations were communicated back to the researchers. In the case of CH3, the independent researcher was unavailable and so resident numbers were picked out of a hat by the two researchers in the presence of two members of staff.
The situation of people with dementia can change so suddenly that it is not always possible to exclude potentially ineligible residents before selection. For example, one resident, who was well when the random selection took place, became severely ill the following week and died soon after. Further, in two care homes, staff felt unable to approach some selected residents because a change in the residents’ circumstances meant that the approach might now cause distress. We therefore added a further selection criterion, whereby residents were not entered for random selection if care staff had reason to believe that approaching the resident or (where necessary) their consultee would cause distress.
This openness to amending the criteria meant that we had to select some additional residents after the original selections, by generating a new random number table from the remaining eligible participant list. This approach does not meet the criteria for full randomisation but as this was feasibility work, and as participants were difficult to recruit, we felt it appropriate to randomly generate further participants where necessary. We also set a limit of selecting a maximum of two additional residents per care home, to preserve as much of the random approach to selection as possible.
Table 39 (see Appendix 1) shows the numbers of residents selected and reselected at each care home and the final numbers invited to take part (either directly or via a consultee).
Recruitment
The first 10 randomly selected residents were approached by a researcher and invited to take part in the study.
In consultation with care home staff, a researcher (supported where necessary by Innovations in Dementia) looked into what arrangements were necessary to support each potential participant to understand and retain information about the research, to weigh up this information and to communicate their decision (e.g. through the use of communication aids or the support of a trusted member of staff or family). If the person had capacity to consent, the researcher supported them to read through the participant information leaflet (see Appendix 10) and answered any questions they had. The information sheet was clear and easy to read, and project advisers with dementia had contributed to its design. If the person wanted to take part in the study, they were asked to complete a consent form or to give verbal consent witnessed by a family member or member of staff (see Appendix 10).
If the researcher had reason to believe that the resident did not have capacity to give informed consent, a consultee was identified and asked to advise on the potential participant’s wishes. Again, this decision was made in consultation with care home staff and Innovations in Dementia, but responsibility for the final decision lay with the researcher. In most cases, consultees were family members or close friends (i.e. personal consultees). Nominated consultees (members of staff who knew the person well) were approached only if no close family or friends could be identified or if those approached felt that staff knew the person better than they did.
Contacting personal consultees was not always straightforward as, for data protection reasons, the researchers could not be given contact details without the consultee’s agreement, and so care home staff had to make initial contact. We gave care homes consultee information sheets and asked them to make contact in whichever way they felt was most appropriate (passing information sheets on when the consultee came to visit, telephoning the consultee or sending an information sheet through the post). Success was patchy and we had to send several reminder calls and e-mails to prompt care homes to contact potential consultees and let us know the outcome.
At this stage, potential consultees were simply asked whether or not it was acceptable for a researcher to make contact to explain more about the study (i.e. consent to contact). However, this proved to be a critical gateway (or barrier) to recruitment, as the majority of the people with dementia selected for the study did not have capacity to give informed consent (43/59). Without agreement from the potential consultee that we could make contact, we could not progress (effectively excluding the person with dementia from the study). Moreover, the indirect nature of first contact means that we do not know the reasons for refusal or non-response from those who did not agree to initial contact.
Some consultees actively advised against including the person they cared for, for reasons that included the person with dementia’s mental health status, lack of interest and current physical health.
Table 40 (see Appendix 1) summarises the numbers of people with dementia selected in each care home who had capacity to consent and their decisions, as well as those without capacity and the responses of consultees. The majority (14/16) of people with capacity to make a decision consented to take part, whereas fewer than two-thirds (25/43) of the people without capacity were included. Of these, seven were not included on consultee advice and a further 11 were effectively excluded because potential consultees did not agree to the researchers contacting them in the first place. In total, we recruited two-thirds (39/59) of potential participants (66%) sampled.
Family carers of people with dementia in care homes
If a person with dementia was recruited to the study, we also invited a family carer or close friend to take part, as findings from our focus groups and literature review suggested that carers’ QoL and relationships could be affected by LSW. Often, where a person with dementia did not have capacity to give informed consent, the family carer was the same person who had been contacted as a personal consultee. However, this was not always the case; in some families one person visited regularly but someone else took responsibility for managing the person’s affairs, and we were guided by the family as to who should be involved in which capacity. For the 14 people with dementia who consented to join the study themselves, we needed to make contact with the family carers to invite them to take part in their own right, and this was again a lengthy process relying on care home staff having time to obtain consent to contact. Once this was obtained further information (see information sheets in Appendix 10) could be given via post or e-mail and consent discussed over the telephone or in person. Written consent was always obtained (see carer consent forms in Appendix 10).
Table 41 (see Appendix 1) shows the number of family carers recruited against the numbers of people with dementia included and gives the reasons for the lower number of carers. In total, we recruited 31 family carers.
In summary, the factors contributing to success of recruitment of people with dementia and of family carers were:
-
capacity of the person with dementia to consent directly
-
time and enthusiasm of care home staff for making contact with potential consultees/carer participants and obtaining consent to contact
-
consultees’ concerns about health issues (mental and physical) and how these might be affected by the research.
People with dementia in specialist mental health assessment units
Recruitment from the mental health assessment units (hereafter referred to as ‘wards’) was intended to be sequential and followed similar inclusion/exclusion criteria to those applied in care homes, as follows.
-
Include:
-
new patients with dementia (i.e. new to the model of care, so patients transferred from one of the other study wards were excluded).
-
-
Exclude:
-
patients considered by the ward manager to be reaching the end of their lives
-
if there was reason to believe that approaching the patient or (where necessary) their consultee would cause distress.
-
Wards agreed to notify the research team when a new patient with dementia was admitted and our links in the trusts’ own research teams also agreed to track eligible admissions. A researcher contacted the wards each week for details of any new admissions who might be eligible for the study. After some discussion about the slow start to recruitment, an e-mail reminder was also sent at the start of each week reminding the ward manager (or a nominated member of staff) of the eligibility criteria and asking them to notify us of any new patients who might meet these. Where possible, we cross-checked these figures with admissions figures from the on-site research team/trials unit at our sites but suspect strongly that we were not notified of all new admissions.
We were advised by service managers not to assume capacity to consent in the ward sites, as the majority of patients admitted did not have the capacity to make complex decisions. Instead, we asked ward staff to give an initial assessment (which would later be confirmed by a researcher in consultation with the individual and/or their consultee). Ward staff considered that none of the patients identified as potentially eligible had capacity to consent, so we sought a consultee in every case.
As in the care homes, data protection issues meant that consultees had to be contacted through the wards. However, this approach was even less successful in the wards than it had been in the care homes. The most frequent reason given for delays in staff obtaining consent for a researcher to contact a potential consultee was lack of time, as this extract from our field notes about one of the intervention wards illustrates:
20th May 2014 – Recruitment has stalled somewhat at this site. Despite being notified of four new patients on the ward we have heard nothing about whether they would like to [be contacted about] the study. Moreover, it appears that LSW is not happening, at least while the ward is very busy . . .
2nd June 2014 – Had a long chat with [name], a nurse on the ward. She said that the staff have been so busy recently that they haven’t had any time to approach any of the family members about the research (or do much LSW) . . . She said really they could do with someone on the ward whose job it is to do this (not clear if she is talking about LSW or recruitment for the research – possibly both). It turned out that several new people had been admitted to the ward in May that we hadn’t been told about . . .
Field notes
As a result of such delays we developed our exclusion criteria further.
-
Exclude:
-
patients whose consultee has not been approached 2 months after admission
-
patients whose consultee has not been approached 1 month after recruitment period finished (or the month recruitment ended at the comparison site, to allow sufficient time for follow-up).
-
It also transpired that some ward staff were reluctant to approach some families because of concerns that this could cause distress, given the already-stressful situation the families were in. People with dementia tend to be admitted to a mental health assessment unit only when they and/or the people who care for them reach crisis. Their family carers are thus likely to be at a different point on the dementia journey from the families of people who have been living in long-term care. Indeed, we saw from the responses of consultees we did make contact with that ward admission was not always felt to be a good time to be engaging in research, either because the person they cared for was already distressed or because they themselves were overburdened with form filling and other caring responsibilities. Reasons given by consultees who decided not to proceed with the research included:
-
Wife said she was tired and worried about her husband.
-
Daughter did not want people ringing her when she was busy.
-
Husband said that as long as his wife was getting good care he was not interested in taking part in research.
-
Partner said he did not want the patient to be involved because he was already distressed by the things people were asking him on the ward.
-
Son said it was not the sort of thing his dad would want (or would ever have wanted) to get involved with as he was quite wary of authority figures/people asking questions.
Reasons given by staff for not approaching potential consultees included:
-
Staff member rang to say that the patient’s wife was poorly at that moment so they decided not to approach her.
-
Staff were reluctant to approach niece as the person had just had a fall and it would seem as if they had got their priorities wrong.
-
Staff forgot to ask family member about the research last time she was in and now they did not want to approach her because she herself was poorly.
Table 42 (see Appendix 1) sets out the numbers of potentially eligible participants and the stages they moved through before inclusion in the study. From an initial pool of 50 patients, we received consultee advice to include just 12 patients (24%). Sixteen potential participants were lost simply because the research team did not receive consent to contact (which could be arranged only by busy ward staff) in time and a further 15 were lost because consultees actively (or passively, by not responding) declined/advised against inclusion, or because the patients’ circumstances changed after the consultee was approached.
There was a similar refusal rate among consultees for people with dementia on wards (48%) as there was among consultees for residents in care homes (42%), but, coupled with the high numbers of consultees who were never approached by staff and the fact that none of the patients had capacity to consent themselves, the recruitment rate on the wards was much lower than in the care homes.
Four potential participants were excluded because of doubt over their diagnoses. Although we had expected some uncertainty about diagnosis in the care homes, we had not anticipated this in the hospital sites. However, questions about diagnosis were largely related to newly admitted patients, so this is perhaps not surprising, given the focus on assessment in these settings.
However, even for patients for whom diagnosis was secure, there was little in their notes about severity. Discussion with the on-site research team suggested that this was because many patients on the wards were not able to undertake the Mini-Mental State Examination. 136 The information we did receive about severity of dementia was, therefore, more likely to be based on a consultant’s clinical judgement (found, for example, by the on-site research team searching through correspondence).
This uncertainty and inconsistency in recording makes it difficult to envisage receiving accurate data on dementia severity for a full trial without conducting additional assessment with participants specifically for the research.
Not all consultees who agreed to participation were happy for the person with dementia to be approached to answer questions about their QoL and relationships. In most cases, consultees agreed to a researcher meeting the person and seeing if they were able to answer any questions, but in some cases consultees said that they would prefer the person not to be approached. In such cases the person could still be included in the study, but data were collected from proxies and/or their care records only, reducing further the amount of information available.
In summary, the recruitment of and gathering of data from people with dementia in specialist mental health settings was less successful than in care homes. The main reasons for this were that:
-
None of the patients on the wards had capacity to consent and so, without consultee agreement, they could not be approached.
-
Researchers could not make contact with over one-third of patients’ potential consultees because they were never approached by staff for consent to contact.
-
Even when consultees agreed to the person with dementia being approached, some placed restrictions on the type and nature of data to be collected.
The recruitment process through the mental health assessment units was also labour intensive, with multiple telephone calls and e-mails often leading to nothing, as the following extract from our field notes illustrates.
. . . email on 3rd March said two people had been admitted to [ward] in the previous fortnight – one of them . . . is potentially eligible (the other has been transferred out).
KG tried to ring on 5th March but was asked to ring back on Friday 7th.
Rang on 7th March – manager not available – staff member said they would pass on a message for [manager] to ring me. Not heard by afternoon so rang at 4.40 pm but no-one answered.
Spoke to manager on 11th March . . . said [staff member 1] would ring me back that day but no-one did.
I rang again the next day (12th March) and spoke to [staff member 2] who said that manager is now away until Monday, [staff member 1] is also off and [staff member 3, who might be able to answer my questions] is currently busy. I asked for [staff member 3] to ring me back and left my mobile number . . . [no phone call received]
Rang on 21st March but [manager] not there.
Rang again on the 24th – left a message for [manager] to ring me back. Rang again in afternoon and spoke to [manager] who explained the patient had since had a fall and they were reluctant to approach him.
Field notes
-
Exclude In this instance, it took 3 full weeks (and eight telephone calls) to speak to someone on the ward about obtaining consent to contact a family member. Eventually staff decided not to approach the family as, during the 3-week period since the research team had been notified of the patient’s admission, the patient had fallen, and it was felt that approaching his family would now cause distress.
Family carers of people with dementia in mental health assessment units
As in the study in care homes, we also invited the family carers of participants with dementia to join the study. In all cases this was the same person who was contacted as a personal consultee. However, carers were given a separate information sheet regarding their own participation (see Appendix 10) and it was stressed that their inclusion was voluntary and would not affect whether or not the person they cared for could take part. Information was given via whatever means carers felt would be most convenient for them (by e-mail, by post or face to face). No carers joined the study without at least one telephone conversation in which they had the opportunity to ask questions and researchers could explain the consent process. As with the care homes study, all included carers gave written consent to take part (see carer consent forms in Appendix 10).
Table 43 (see Appendix 1) shows the number of family carers recruited against the numbers of people with dementia included and gives the reasons for the lower number of carers. In total, we recruited 10 family carers across the four wards.
Delivery of the intervention
Implementation of life story work in care homes
The stepped-wedge design relies on an intervention being implemented at each site in turn over the period of a study. Our first observation in this feasibility study was that implementation varied considerably from care home to care home, despite the commitment of the care home provider (including training and resources) being the same at each site.
The training emphasised the role of all care home staff in making LSW a routine part of care rather than an additional ‘task’ to be completed. In keeping with this, homes were encouraged to enter as many staff as possible for the training, which ran twice at each care home at times agreed to be convenient with managers. It was also limited to 2 hours so that staff could attend without being kept too long from their core duties.
The numbers attending the training at each site ranged from 6 to 15. However, in care homes that went on to implement the intervention (carrying out at least some LSW with at least half of the study participants), one individual co-ordinated and in most cases also carried out the majority of the LSW single-handedly. In three care homes this person was the activities co-ordinator; in a fourth the activities co-ordinator left near the start of the project but another member of staff then took on LSW, fitting it around her other responsibilities. At these care homes other care staff were supportive of the process but found little time to engage in it themselves.
In the two remaining care homes the activities co-ordinators set up systems to support care staff to collect life story information during their day-to-day routines. Both created a folder for each resident: in one, care staff were then issued with notepads to note down life story information gleaned during everyday interactions and were encouraged to add this to the folders. In the other home, staff were allocated 20 minutes’ protected time per day to work with named residents. However in both cases, according to the logs that assessed how long staff spent on LSW (see Chapter 8), it was still the activities co-ordinators who collected most information and they alone who spent time constructing the life story products.
Thus, although care staff did spend time talking to and learning about residents as part of their day-to-day routines, they found it difficult to find time to put this information into a format that could be used by others or enjoyed by the individual or their family. If we refer back to the potential challenges identified in the development phase of this study (see Chapter 3), this supports the argument that outcomes for care, as well as wider interpersonal benefits to people with dementia and their carers, may be lost if staff have time only to focus on the process of collecting life story information without then having time to do anything with it. Sites that appeared to have the most success in implementing LSW were those that combined a shared responsibility among staff to collect information with a designated worker who took responsibility, and had dedicated time, for pulling information together and presenting it in a way that others, including the people with dementia themselves, could use.
The approaches to LSW undertaken in each care home also varied and, crucially, tended to differ from the approaches often depicted in LSW literature and envisaged by those discussing the outcomes of LSW in our earlier focus groups. In Chapter 3 we set out a range of approaches to LSW or ‘mechanisms’ through which LSW was intended to produce an outcome. These ranged from approaches focusing on the individual, such as LSW as a personal memory aid, a personal challenge or an approach to life review, through more interpersonal approaches, such as LSW as a shared memory aid, communication aid or platform to enhance connection between people with dementia and others, to LSW as a tool for care. The training given by the care home provider emphasised the full range of possible outcomes.
A template entitled ‘some important things’ was provided, which staff could use as a starting point. However, it was emphasised that completing this did not constitute LSW: it could be a useful tool to get the process started, but the approach and resultant products should be individually tailored and informed by the needs and preferences of the person with dementia. This tailored approach was taken in four care homes (in that personalised books, boxes or other items were created) but in all cases the design and construction of the life story products were led by staff, not by people with dementia or family carers. It appeared that in almost all cases residents were not considered to have the capacity to take a lead in the LSW themselves. This reduced the chances of seeing the outcomes anticipated by the people with dementia who took part in our focus groups, many of whom had a greater degree of capacity than those in the feasibility study, and who thought that LSW could provide a satisfying personal challenge or opportunity for reflection on achievements and identity. Moreover, family carers were only sporadically involved – perhaps to provide some photographs or view the ‘finished’ product – and so improvements to their QoL and relationships with the people with dementia also seemed unlikely. As evidenced in the focus groups with staff at study sites, the primary intention was that life story information could be used to improve care, which in turn might improve residents’ QoL (see Chapter 9).
The organisational context at individual sites appears to have influenced the success or otherwise of the implementation of LSW. Although the care home provider as a whole was supportive of LSW (indeed, they provided the initial training and guidance), care home managers were essentially left to their own devices after this to bring about change in their own settings. In homes where managers proactively led this process and/or actively supported individual members of staff to dedicate time and energy to LSW, there was a degree of success.
A key factor appeared to be the consistency of management, with all four care homes that had retained the same managers from initial sign up to the 6-month follow-up seeing the most success. In the two sites where there had been a change in management there was less sense of ownership of the intervention, and while, ostensibly, managers had sanctioned staff to undertake LSW, there seemed to be confusion about whose responsibility this was, as this extract from field notes suggests:
Popped up to see business manager who didn’t recognise me (and didn’t seem to be expecting me), and who also said she didn’t know about any LSW, but the care manager [who was currently off site] would . . . She said the staff would know if they’d done any LSW.
Field notes
At some of the sites that did undertake LSW, staff were also unsure at the start about how they should proceed, but were supported by managers, or enthusiastic/more experienced individuals who the managers encouraged to take a lead, as illustrated in this field note:
Spoke to manager on [date] who said that staff are feeling a bit overwhelmed and as a result are struggling to get going with LSW (they have lots of good ideas but are struggling/or don’t have the confidence to put these into action). Has decided to back fill the activities coordinator for two full days to support the other staff to get going with LSW. The activities coordinator is experienced in this sort of work.
Field notes
In one of the sites, staff had only recently finished a previous project that had left them feeling disillusioned, and this ‘project fatigue’ was cited as a reason why there was little enthusiasm for LSW (see Chapter 10).
Table 44 (see Appendix 1) summarises the approach to and organisational context of LSW implementation in the homes.
In summary, the factors that influenced the implementation of LSW in the care homes were:
-
Care staff finding it difficult to find the time to put life story information into a format that could be used by others or enjoyed by the individual or their family.
-
Sites that combined a shared responsibility among staff to collect information with a designated worker who had dedicated time to compile and present information appeared most successful in implementing LSW.
-
The design and construction of life story products being led by staff, not people with dementia or family carers, might have reduced the chances of seeing certain types of outcomes such as improved relationships or carer QoL, thought to be associated with LSW.
-
In sites where there had been a change in management, there was less sense of ownership of the intervention and some confusion about whose responsibility LSW was.
It should be noted that the above relates only to whether or not and in what ways care homes undertook the collection of information and creation of products necessary for LSW. It does not cover how life story information or products were used, something that the participants in our development stage focus groups (see Chapter 3) felt was key to achieving positive outcomes from LSW. Qualitative data about the use of life story information and products were collected through interviews and discussions with people with dementia and carers and focus groups with staff at study sites towards the end of the study (see Chapter 9).
Life story work on mental health assessment units
In the three ‘intervention’ wards, LSW was considered a routine part of care and we were not, therefore, expecting to see any marked differences in the use of, or commitment to, LSW between the three wards. Instead, we wanted to assess how feasible it was to compare individual outcomes and costs on these three wards with those on a ward where LSW was not done. However, it soon transpired that the three intervention wards were not using LSW in similar ways or to a comparable extent: indeed, there appeared to be as great a difference between these wards as there was between them and the ‘comparison’ site. As such, rather than considering the wards as three intervention sites and one comparison site, it makes more sense to consider them as a continuum: from a ward that does LSW with most patients with fairly routine procedures for this to a ward that does no LSW at all (the comparison site); and two in between that did some LSW elements. Table 45 (see Appendix 1) summarises the approaches at each site.
The resources available to do LSW at each of the wards differed considerably. In intervention ward (IW) 2, LSW was a core part of the work of three part-time occupational therapy technical instructors (OTTIs). They had dedicated time and access to a computer and scanner to produce the life story documents and were able to collect and use life story information during activities they ran with patients on the ward. IW1 and IW3 had had similar resources in the past but these had been lost some time before the research began and, thus, during the study period, IW1 nursing staff and assistants had no additional support to undertake LSW and IW3 had access to an OT only 1 day per week. Chapter 9 provides a more thorough discussion of the reasons staff on IW1 and IW3 found it harder both to find time to undertake LSW and to participate in the research, but one factor was clearly the additional resource on IW2. By way of illustration, permission for the research team to contact the consultees of three out of the five patients recruited through IW2 was obtained not by ward staff but by the OTTIs. Without their support it is likely that recruitment on IW2 would have been no higher than it was on the other wards.
Chapter 7 Measuring outcomes
In this chapter we continue the reporting of our feasibility work, examining the challenges of collecting outcome data and reporting what, if any, effects we detected from the use of LSW in our chosen care settings.
Completion of outcome measures
People with dementia in care homes
Completion of outcome measures by people with dementia was challenging for a number of reasons, including:
-
the capacity and frailty of the participants
-
the context in which data collection took place (care homes getting on with their daily routines)
-
the geographic location of the research settings, compared with that of the research team.
Some participants withdrew (or were withdrawn) from the study as it progressed and some died before the 6-month follow-up point. Of the 39 people with dementia recruited, 34 remained at 6-month follow-up (see Appendix 1, Table 46).
The measures chosen were all designed to be completed by people with dementia but completion rates leading to usable data were low and varied between the measures (see Appendix 1, Table 47).
The main reason for participants not completing a measure was that they were not able to understand and/or respond to the questions. Although both DEMQOL120 and QoL-AD121 have been shown to be valid and reliable QoL measures for people with mild to moderate dementia,122 there is less evidence of their successful use with people with severe dementia.
In the care homes, we had most success with QoL-AD, which is a simple 13-question measure that we administered in interview form with a large-type visual aid (one question per page). Indeed, a higher proportion of participants with dementia were able to complete this at baseline (64%) than were able themselves to give informed consent (36%). DEMQOL, on the other hand, is a much longer tool (29 questions). Again, it was administered in interview form, but the only visual aid was a picking list of answer options. At baseline, only 31% of participants were able to complete this measure to produce usable data.
At baseline and the first two follow-up visits, we administered QoL-AD first, and on a small number of occasions, after completing QoL-AD, participants mentioned that they were tired, or did not want to answer any more questions. In order to test whether or not DEMQOL was indeed more difficult to complete, or whether or not participants were fatigued after completing QoL-AD first, we decided to administer DEMQOL first for some participants at the final follow-up to see if this affected completion rates. Two participants were able to complete both QoL-AD and DEMQOL at this follow-up when previously they had completed only QoL-AD, but the numbers involved were so small as to make this inconclusive.
Another reason for low completion rates of DEMQOL appeared to be the subject matter of some of the questions. This is rarely mentioned in the literature, but we found that, for example, asking people in quick succession whether they had lately felt sad (question 7), lonely (question 8) and then distressed (question 9) could trigger sadness. On one occasion (plus on two occasions in hospital wards) DEMQOL was abandoned specifically for this reason.
The closed-question format of the measures might also have affected completion rates. Often participants understood our questions but wanted to answer us fully (i.e. qualitatively), giving us examples of why they felt a certain way and caveats about how and when those feelings arose. It was difficult to bring some participants back to the picking list of answers (for QoL-AD the options are ‘poor’, ‘fair’, ‘good’ and ‘excellent’; for DEMQOL they are ‘a lot’, ‘quite a bit’, ‘a little’ and ‘not at all’). The guidance notes for DEMQOL instruct the interviewer in such circumstances to ‘repeat the question and the response options verbatim and ask them to choose . . . reiterate that they need to choose [and]. . . if they still don’t choose one of the response options . . . mark the questionnaire as missing. . .’. 137 In some cases, then, participants clearly understood the questions and were able to answer in their own words, but their responses were not recorded because they were unable to pick a response.
For QoL-AD this happened so often that we decided to record verbatim answers when these were given, and a third member of the research team (not involved in data collection) coded them for consistency. We adopted this approach in the interests of inclusivity, as the majority of participants did appear to be able to respond to QoL-AD (albeit sometimes in this semiqualitative way). Without this approach, precious data from people with dementia would have been lost.
Discrepancies between proxy and self-report are well documented, with proxies typically rating the QoL of the person with dementia lower than the person him- or herself would rate it. 138 We were, therefore, reluctant to rely solely on proxy estimates of QoL when these additional verbatim responses from people with dementia themselves were available.
Completion of the Scale for the Quality of the Current Relationship in Caregiving (QCPR): 14-item-version5 by participants with dementia was the least successful of all the measures. The items in this measure are translated for use in English from a validated Dutch measurement tool. The language in the answer scale was particularly difficult for our first set of participants to understand, spanning from ‘1 = totally not agree’ to ‘5 = totally agree’. Agree/disagree scales are cognitively complex for the general population, regardless of dementia, as they confound attitudinal position with strength of feeling. 139
After our first attempt to use the measure, we amended the answer scale to the more conventional ‘1 = strongly disagree’ to ‘5 = strongly agree’. However, participants still struggled to put their initial responses into this format. The subject matter of the measure served to compound difficulties, as the questions ask how well the person gets on with their family carer. Asking participants to clarify a response by saying to what degree they ‘agreed’ or ‘disagreed’ was inevitably confusing. We soon abandoned the answer scale altogether and opted instead simply to record verbatim answers and code post hoc, using the same approach as with QoL-AD.
Even accepting verbatim answers, the completion rate of the QCPR was lower than either DEMQOL or QoL-AD at each time point. One reason for this could be that completion of the QCPR relies on the participant being able to bring to mind their relationship with their family carer. This was facilitated for some participants at baseline when the carer was present (a number of carers combined a visit to the care home with a meeting with the researchers to go through the consent process in person). In contrast, although carers were always invited to follow-up sessions, they did not always attend these (choosing instead to complete proxy and carer-specific measures over the telephone or by post), and without the carer present, participants sometimes found it hard to bring to mind a close relationship. In addition, if people had experienced difficulty in answering QoL-AD or DEMQOL questions, or had become distressed when talking about relationships, we did not attempt the QCPR.
Participants’ ability to understand and respond to the questions in the measures was not the only reason that some data are missing. Data collection had to fit around the routines and other priorities of care homes, and residents also had their own preferences and choices of daily activities. As the researchers often had to travel for ≥ 2 hours to attend research sites, it was not always possible to return on another occasion to complete data collection after interruptions.
Davies et al. ,140 focusing on the recruitment and retention of research sites, have argued that care homes can be particularly challenging environments in which to conduct research. We would add that the routines and competing priorities in these settings pose challenges to data collection itself. Despite agreeing all visits in advance, for example, it was not unusual for researchers to arrive to find alternative activities under way that meant residents were not free to speak to them. The general frailty and ill health of many residents also meant that illness, falls or unplanned hospital admissions could foil a planned data collection session.
Participants were not able to self-complete measures in their own time, and therefore we were reliant on obtaining face-to-face access to people who often required a considerable amount of time and support to participate, and might not, in the end, be available at all on the days planned.
Quality of life measures with people with dementia are intended to measure overall or health-related QoL at a specific time point (DEMQOL asks participants to consider ‘the last week’; QoL-AD asks about ‘your current situation’). The assumption is that QoL is something relatively stable over these short time periods. However, Trigg et al. ,141 when considering the discrepancies between self-report and proxy assessments of QoL, comment that the assessments people with dementia make are probably feeling-centred.
Whilst observational or proxy ratings commonly provide QoL judgements based upon an appraisal of the patient’s functional performance, the dementia patient may be appraising the situation on the basis of the mood states and feelings these activities produce . . .
Feelings can change throughout the day, and during fieldwork we observed for ourselves several examples where people who were cheerful in the morning seemed very low in the afternoon, and vice versa. Time of day and night thus influence the answers given to QoL measures. Another example of the possible wide variability of QoL for people with dementia arose when we arrived at one care home while a singing activity was under way. The only time we could administer the measures was directly after this group: perhaps not surprisingly, participants were in a good mood, and they answered the QoL questions very positively. This may tell us something about the singing activity, but we are not sure that it tells us much about LSW.
There is a possibility that LSW (and other enjoyable or meaningful activities) may have an impact on the feelings of people with dementia ‘in the moment’. If QoL measures are administered immediately after an enjoyable activity, it may be that the measures pick up the effect of this. However, people in care homes may engage in such activities most days; might the responses therefore tell us more about what the person has been doing that day than any longer-term effect of the intervention?
During the study, both staff and family carers suggested to us that the tools we were using missed the true benefits of LSW, which occurred ‘in the moment’ and thus could be fleeting. LSW was used either to lift a person’s mood (albeit often temporarily) or to calm a person who was anxious or exhibiting behaviour that challenged. Both were seen as valuable outcomes, but were not expected necessarily to change a person’s QoL in the longer term.
Completion of outcome measures by people with dementia in hospital wards
In total, 12 people with dementia were recruited across three interventions and one control ward, 11 of whom remained at 6-month follow-up (see Appendix 1, Table 48).
Of the 12 recruited people with dementia, not all consultees gave permission to approach the person themselves. In four cases we were advised not to approach the person themselves, and given permission to collect information from care records only. This was extended to another participant after the first follow-up, as he had recently been sectioned and his wife felt it inappropriate for us to approach him again.
Table 49 (see Appendix 1) shows the low completion rates at baseline and follow-up for the three measures used in the hospitals study.
The main factor influencing completion of outcome measures in hospital wards was capacity. However, this barrier was compounded by the geographical spread of participants, as they were discharged to different settings. We then needed to obtain approval from both family carers and residential care or nursing homes before collecting data in the new settings.
Gaining access to these new sites was not always straightforward. Davies et al. 140 found that researchers wanting to conduct research involving care homes had to approach at least 40% more care homes than they needed in order to recruit the required number of sites. We needed access to the specific care homes into which participants had been discharged, but the care homes were not always receptive to this.
A researcher might have to make several telephone calls to arrange a visit, and then travel for a number of hours, in order to meet a person and support them to complete some or all of the questionnaires, if the person was able. In this way, a whole day could be spent completing one measure with one participant. We decided that this was not a good use of time and, after reviewing this as a team, reduced the follow-up time points from baseline for the hospital-recruited participants to two: one at between 1 and 2 months and one at 6 months.
We encountered similar issues to those in care homes in terms of the acceptability of the measures and their usefulness for our research.
Completion of outcome measures by family carers of people with dementia in care homes
Completion of outcome measures by family carers was more straightforward, with no capacity issues and face-to-face administration not always necessary. Nevertheless, some issues regarding acceptability did arise which may have affected completion rates and warrant further exploration.
In total, 31 family carers of people in care homes were recruited and 25 remained in the study at 6-month follow-up (see Appendix 1, Table 50). One additional carer joined the study for the purpose of a final interview only, and did not complete the questionnaires.
Carers were asked to complete a measure of their carer-related QoL (the CES),127 the QCPR from their own perspective (i.e. how they viewed their relationship with the person they cared for) and two proxy measures of QoL for the person with dementia: QoL-AD proxy and DEMQOL proxy.
Table 51 (see Appendix 1) shows the completion rates at baseline and follow-up for the two carer measures and two proxy measures by carer of people with dementia recruited through care homes.
We opted to give carers a choice of completion options for all of the measures, in recognition that flexibility is often paramount for busy carers juggling work, family and caring responsibilities. While the CES and QoL-AD proxy were designed for self-completion, DEMQOL proxy and the QCPR were designed for face-to-face administration. We suggested to carers that we should administer baseline measures face to face or over the telephone in order to familiarise them with the format and requirements. After this, we offered the opportunity for them to complete follow-up measures in their own time and post responses back (in the freepost enveloped provided).
Although a high proportion of the carer measures and proxy measures were completed, carers often fed back that they did not enjoy completing the measures or did not see their relevance. We therefore included questions about this in the qualitative interviews at the end of the feasibility study (see Chapter 9).
Completion of outcome measures by family carers of people with dementia in hospital wards
In total, 10 family carers of people with dementia were recruited and seven remained in the study at the6-month follow-up (see Appendix 1, Table 52). An additional carer was recruited at IW1 for interview only.
Carers were asked to complete the same carer measures and proxy measures used in care homes, but were given an additional questionnaire to be completed when the person they cared for was discharged from the hospital (the Carer Satisfaction Questionnaire128).
Table 53 (see Appendix 1) shows the completion rates at baseline and follow-up for these measures by carers of people with dementia recruited through hospital wards.
Carers in these settings appeared to find the outcome measures even less acceptable than those recruited through care homes, and one who consented to the study then refused to complete them at all. This extract from our field notes explains why:
Started QoL-AD but [carer] wouldn’t pick answers, and said very specifically she didn’t like the questionnaires, that there wasn’t much difference between poor and fair but there was a huge difference between poor and none (e.g. relationship with family or friends or marriage). Stopped before the end . . . Showed her Quality of Relationships scale but she started crying and said a year ago she had a relationship but not now . . . she thought questions were inappropriate and wrong and she couldn’t answer them. Tried carer experience scale but again couldn’t pick, and said question about fulfilment was offensive and abusive, and that she had no control over the care (she’d just brought in some cereal for husband but staff had said he hadn’t used the old stuff yet because he didn’t get up until lunchtime, she asked them to give it to him anyway). She just raised her hands in the air, exasperated at the final question.
Field notes
Moreover, despite reading the participant information sheet and discussing the study with a researcher, it appeared that several carers found the use of follow-up questionnaires repetitive. At least one carer did not understand the 6-month span of the study, or the need for follow-up, and withdrew from the study after the first follow-up.
Completion of outcome measures by care home staff
In total, we recruited 50 care staff over six care homes, with 45 retained until the 6-month follow-up (see Appendix 1, Table 54).
Table 55 (see Appendix 1) shows the completion rates for the three measures care home staff were asked to complete at baseline and three follow-up points.
All three measures – the ADQ, the PDQ and the CBI – were self-completion questionnaires, but when possible a researcher sat with staff members as they filled them in, in order to answer any questions they had and to receive any feedback.
As with some of the family carers, a misconception among some staff was that completion of the measures was a one-off task (despite the researchers talking through information sheets that explained otherwise). Therefore, when it came to the first follow-up a number of staff members commented that they had already completed the measures – implying that there was no need to do this again. Others were concerned (again, despite assurances to the contrary in the information sheets) that the information they provided would reach their managers or higher in the care home provider organisation, and be used in performance management.
Hospital staff did not raise these sorts of concerns. This difference perhaps reflects the limited exposure that care home staff have to research, compared with that of hospital staff. Care home staff seemed generally more suspicious of the research process, and they were less likely to accept the associated reassurances involved. There was also a more limited understanding of research processes, such as in one notable example when a staff member completed one of the measures ‘on behalf’ of her colleague (who was busy), despite this being an attitudinal questionnaire and thus unique to the individual.
The shift patterns and busy work schedules of care home staff made follow-up particularly tricky and accounts for much of the loss to follow-up in this group. If staff who signed up to the project were not available when researchers visited to collect follow-up data, there was little option other than to leave packs for individuals to self-complete and return in the pre-paid envelope provided. However, this was an unsuccessful approach: very few packs were returned, even when researchers had handed them to staff in person.
In response to the poor rates of follow-up by month 2 in most sites, the team decided to write to each care home, enclosing packs for each of the members of staff who had not completed follow-up, asking participants if they would like remain in the study and, if they did, to complete and return the enclosed questionnaires. This was also unsuccessful: only three participants responded to the letter, and another one after the final follow-up, across all six care homes.
Completion of outcome measures by hospital staff
Cross-sectional data were collected from staff working on the wards at three time points. There are no withdrawal rates for this group, as recruitment was done each time afresh; all staff on the wards on the day of the research visit were approached for consent and all staff who consented completed the measures. Some staff thus completed the measures more than once, if they happened also to be on duty on a subsequent visit of the researchers. When this happened, we calculated average values for their repeated measures.
As with the family carers in the care home study, staff did not always like the questionnaires and had much to say about their acceptability and relevance. The wording of the questions was described as ‘extreme’, ‘horrible’ and ‘shocking’. One manager noted that the questionnaires were ‘a bit simplistic for staff at this level on a specialist dementia ward’:
[He said the measures] seem to be aimed at agency staff, or staff on generic medical wards, or possibly unqualified staff. You would hope that anyone with those sorts of attitudes is rooted out before they get to a ward like this. Nurse filling in questionnaires at the same time agreed.
Field notes, IW3
Members of staff also noted that many of the answers depended on the situation, and in some cases felt that they could not answer them at all:
Decided to leave question number 16 on Personhood in Dementia questionnaire blank – said that sometimes if people can become quite vocal when they are agitated and may benefit from some one-to-one time with staff, which also gives other residents a bit of respite if the person is making a lot of noise, but this is different from isolating people.
Field notes, IW3
Other staff expressed similar reservations about this particular question (and others):
She also commented on the questionnaire about personhood that some of the questions are ‘horrible’. Commented on Q16 – didn’t like the wording so put strongly disagree, but said that she does think that sometimes it’s in people’s best interests to spend some time on their own (i.e. it was the wording that made her strongly disagree, not the content of the question).
Field notes, IW2
Several people commented that the questionnaires lumped everyone together, whereas people with dementia can be very different, with some responding well to a strict routine, for example, and others not.
Analysis
All of the data were recorded initially in Excel spreadsheets and then prepared for analysis and imported into SPSS version 22. Where instructions were provided for calculating overall scores and subscale scores, these were embedded in the Excel spreadsheet, with the exception of DEMQOL, which has separate SPSS instruction files for conversion and for imputation of missing values.
Once prepared and entered into SPSS, the data were tested for normality. When normal distributions were evident, we used paired t-tests to examine change over time in the care home participants and, when appropriate, in the hospital participants. We also used simple independent sample t-tests to examine differences in staff morale and attitudes between the comparison and intervention wards. When normality was not evident, appropriate non-parametric tests were used.
For most measures, we did not have data for baseline and all follow-up points. Where this was so, cases were omitted from the analysis on a case-wise rather than list-wise basis. This enabled us to make the most use of the valuable data that we had managed to collect.
Quality of life for the person with dementia
QoL-AD measure
The QoL – AD produced the largest amount of usable data on QoL for the person with dementia.
Because the person with dementia did not always answer all questions, and because some questions were not relevant to people living in care homes (e.g. ability to do chores around the home), we converted total QoL-AD scores into an average, using the number of completed questions as the denominator, and then scaled the score back up. Given that the QoL-AD produces a simple additive total score, we felt that this was acceptable and, again, this allowed us to use all of the data we had collected rather than discarding large numbers of questionnaires that had missing data.
Higher scores indicate better QoL (with total scores ranging from 13 to 52). Negative mean differences, therefore, indicate improvement.
QoL-AD proxy in care homes
Paired data were available from 23 carers at baseline and first follow-up, 21 at baseline and second follow-up and 19 at baseline and third follow-up. These data were not normally distributed.
Median score at baseline was 26.5, at first follow-up 25.5, at second follow-up 24.5 and at third follow-up 25.0. The Wilcoxon signed-rank test for related samples showed no significant changes between baseline and any follow-up point.
QoL-AD completed by person with dementia in care home
Paired data were available for 23 people with dementia at baseline and first follow-up, 23 at baseline and second follow-up and 18 at baseline and third follow-up.
The first thing to note is the higher average scores reported by people with dementia than by the proxies. The mean score was 37.22 at baseline, 35.94 at first follow-up, 35.82 at second follow-up and 35.79 at third follow-up. The data were also normally distributed, which allowed us to use t-tests.
Although the mean scores showed slight deterioration over time in QoL as reported by people with dementia, t-tests showed no significant changes. Between baseline and first follow-up, the mean difference was 1.27 (t = 1.12, df = 22; p = 0.274); between baseline and second follow-up it was 1.91 (t = 1.01, df = 22; p = 0.324); and between baseline and third follow-up it was 0.89 (t = 1.15, df = 17; p = 0.266).
QoL-AD in hospital wards
There were proxy QoL-AD data for only one person in the control ward and only baseline data provided by two people with dementia themselves, so we could not make the planned direct comparison here. We therefore looked at change over time only for the respondents in the intervention wards when a family member had completed the proxy measure.
Numbers were small: seven proxy measures at baseline and first follow-up, six at baseline and final follow-up, and none with data at all time points. There were no follow-up data for the intervention wards from people with dementia themselves.
No differences were evident in the proxy data between baseline and any of the follow-up stages.
Dementia quality of life measure (DEMQOL)
DEMQOL allows the imputation of missing values when at least half the questions are answered, and provides SPSS instructions for doing so. Despite this, we could calculate overall DEMQOL scores for only a few people with dementia. Data collection was somewhat more successful when carers completed the proxy DEMQOL.
Higher values of the total DEMQOL score indicate higher QoL. Negative mean differences thus indicate improvement.
DEMQOL proxy in care homes
We had paired data for 18 people at baseline and first follow-up, for 17 at baseline and second follow-up and for 13 at baseline and third follow-up. Minimal differences were evident between baseline and first follow-up (mean difference = 0.77; t = 0.25, df = 18; p = 0.804) and between baseline and third follow-up (mean difference = –0.19; t = –0.06, df = 13; p = 0.952). There was a larger difference between baseline and second follow-up but this was not statistically significant (mean difference = 5.83; t = 1.36, df = 17; p = 0.192).
DEMQOL completed by person with dementia in care homes
We had enough data to calculate overall DEMQOL scores for 12 people at baseline and for each set of follow-up comparisons. Analysis suggested a small improvement in QoL over time, such that by the third follow-up the difference from baseline reached statistical significance. The mean difference between baseline and first follow-up was 0.99 (t = 0.330, df = 11; p = 0.747), between baseline and second follow-up was –1.57 (t = –0.527, df = 11; p = 0.609) and between baseline and third follow-up was –5.96 (t = –2.328, df = 11; p = 0.04).
We reran the analysis solely for the 10 people with dementia who had DEMQOL scores at baseline and all three follow-up points. This showed a similar pattern, with an improvement between baseline and third follow-up but this did not reach statistical significance (mean difference = –5.44; t = –1.775, df = 9; p = 0.110).
DEMQOL proxy in hospital wards
There were paired data for DEMQOL proxy in the control hospital for only one case.
In the intervention hospital, there were paired data for five people between baseline and first follow-up and for six people between baseline and final follow-up. There were only very small differences between baseline and any of the follow-up points and none was statistically significant.
DEMQOL completed by person with dementia in hospital wards
One person completed enough of DEMQOL at baseline to calculate an overall score, but did not complete any follow-up.
Quality of relationships for the person with dementia and their family carers
The QCPR measure generates two subscale scores: a positive subscale based on warmth and affection in the relationship and a negative subscale based on conflict and criticism. The latter is deducted from the former to give an overall measure of the quality of the relationship. A higher score on the positive scale indicates positive relationships and a higher score on the negative scale indicates negative relationships.
QCPR
Quality of relationships in care homes
Only small numbers of people with dementia generated data on both subscales at baseline and any follow-up point; t-tests showed no differences from baseline to any point of follow-up, on either subscale or on the total.
We had paired data for 22 carers from baseline to first follow-up, 18 from baseline to second follow-up and 18 from baseline to third follow-up. t-Tests showed no differences from baseline to any point of follow-up, on either subscale or on the total.
Quality of relationships in hospital wards
There were insufficient data collected from control wards to analyse effect on quality of relationships.
Data from family members in the intervention wards (six at baseline and first follow-up, and five at baseline and final follow-up) were analysed. t-Tests showed no differences from baseline to any point of follow-up, on either subscale or on the total.
Staff burnout
CBI measure
The CBI measure has three subscales: work-related burnout, personal burnout and client-related burnout. In all cases, higher scores indicate higher levels of burnout. Negative mean differences thus indicate a negative outcome (higher mean burnout at follow-up).
In care homes, the intention was to track change in burnout for individual members of staff before and after LSW was introduced to the care setting. In the hospital wards, with the different research design, the intention was to ask whichever members of staff were available at a given point to complete the measure in order to assess the overall morale of the workplace. The underlying hypothesis was that we might expect better overall morale in the intervention wards because they used LSW.
Staff burnout in care homes
We had paired data for 26 members of staff for baseline and first follow-up, for 17 for baseline and second follow-up and for 15 for baseline and third follow-up.
None of the paired t-tests showed any difference between baseline and any follow-up point on any of the subscales.
Staff burnout in hospital wards
Nineteen staff in the control hospital and 63 staff in the intervention hospital contributed data to this analysis. There were no obvious differences between the two settings on any of the subscale mean scores.
Attitudes to dementia
ADQ measure
The ADQ produces an overall score and two subscale scores: one that is said to reflect ‘hope’ and one that is said to reflect ‘person-centredness’. The authors of the questionnaire state that ‘it is hope that especially predicts staff behaviour e.g. engagement in social interaction with residents, involvement in purposeful activity and stimulation, and the quality of physical care interactions’. 129
In all cases, higher scores indicate positive attitudes. Negative mean or median differences, thus, indicate improvement.
ADQ in care homes
There were paired data for 27 staff members at both baseline and first follow-up, for 17 at baseline and second follow-up and for 18 at baseline and third follow-up. Only seven members of staff completed the measure at both baseline and all follow-up points.
Although the overall scores were normally distributed at baseline, first and second follow-up, they were not at third follow-up. Neither of the subscale scores was normally distributed at any point. We therefore carried out non-parametric analyses.
Analysis showed a statistically significant positive change in overall score between baseline and first follow-up (overall score median at baseline = 83, at first follow-up = 87; Wilcoxon signed-rank test z = –2.863, p = 0.004). Although overall median scores at second and third follow-up were also higher (improved) than at baseline (84 and 85, respectively), these values were not significantly different from baseline.
The difference between baseline and first follow-up appeared to be accounted for by an increase in the person-centred subscale, which also changed significantly between these points (person-centred subscale at baseline = 51, at first follow-up = 53; Wilcoxon signed-rank test z = –2.268, p = 0.023). There were no other significant changes in the person-centred subscale and none at all in the ‘hope’ subscale.
ADQ in hospital wards
We collected measures from 10 different staff members in the comparison wards and 47 staff members in the intervention wards. Analysis of median values in the two settings using the Mann–Whitney U-test showed no significant difference between them.
Personhood in dementia
PID measure
The PDQ is a 20-item test of people’s beliefs about personhood in dementia. Higher scores indicate more positive views; thus, negative mean or median differences indicate a positive outcome.
PID in care homes
Paired data were available for 21 staff members at baseline and first follow-up, and for 16 at both baseline and second follow-up and baseline and third follow-up. The data were not normally distributed, so we used non-parametric techniques to explore change between baseline and the three follow-up points.
The median score for all staff who completed a questionnaire was 130.5 at baseline, 134.0 at first follow-up, 135.5 at second follow-up and 136.5 at third follow-up, so showing a consistent improvement over time.
When paired data were analysed, these showed no significant change between baseline and first follow-up (Wilcoxon signed-rank test z = –0.435, p = 0.664) but significant change between baseline and second follow-up (Wilcoxon signed-rank test z = –2.303, p = 0.021). Although third follow-up continued in the same positive direction, the difference from baseline did not reach statistical significance (Wilcoxon signed-rank test z = –1.527, p = 0.127).
PID in hospital wards
In total, we had completed measures for 13 different staff in the comparison wards and 40 staff in the intervention wards. Again, the data were not normally distributed.
There were no differences between the two settings in their median scores.
Carers’ experiences
CES
The CES assesses a range of issues for family carers or others who provide support to the person with dementia. It covers the extent to which carers feel that they can carry out activities outside caring, the support they receive from others in their network and from statutory organisations, the fulfilment they get from caring, the amount of control that they feel they have over caring and how well they get on with the person they are supporting.
Higher scores indicate better experiences; therefore, negative mean differences indicate positive change between baseline and follow-up.
CES in care homes
There were data for 23 carers at baseline and first follow-up, for 19 carers at baseline and second follow-up and for 14 carers at baseline and third follow-up.
The data were not normally distributed at baseline, but were at all three follow-up points. Visual inspection of the baseline normality plots suggested that the variation from normality was within tolerable limits, but we carried out both parametric and non-parametric tests to ensure robustness.
Both the t-tests and the Wilcoxon signed-rank test suggested that there was a significant deterioration in carers’ experience between baseline and first follow-up [mean difference = 6.547, 95% confidence interval (CI) 1.08 to 12.015; t = 2.484, df = 22; p = 0.021; Wilcoxon signed-rank test z = –2.128, p = 0.033]. The t-tests also showed a difference between baseline and second follow-up that approached conventional levels of significance (mean difference = 7.206, 95% CI –0.175 to 14.587; t = 2.051, df = 18; p = 0.055), although this was not replicated in the non-parametric analysis (Wilcoxon signed-rank test z = –1.587, p = 0.113). Neither type of test showed any significant difference between baseline and third follow-up, although in both cases the deterioration in carers’ experience scores continued.
CES in hospital wards
There were data for 7 of the 10 carers at baseline and first follow-up, and for five at baseline and final follow-up (at both follow-ups, only one carer was in the comparison ward group). Our analysis is thus confined here to carers of people who were in the intervention wards.
The mean difference in scores showed no change in carers’ experiences between baseline and first follow-up. However, there was a large and significant improvement in their experience between baseline and final follow-up (mean difference = –14.58, 95% CI –26.24 to –2.92; t = –3.47, df = 4; p = 0.026).
This was in contrast to the results for carers of people with dementia in care homes and may well reflect the acute nature of the person with dementia’s condition when they were admitted to hospital.
Chapter 8 The costs of life story work
Introduction
The aim of this element of the project was to investigate the potential costs of using LSW in specialist inpatient and residential care settings by identifying and measuring relevant resource inputs, and valuing them by applying local or national unit costs. 142–144 We hoped to establish the size of organisations’ investments in LSW, the potential for savings from reductions in the use of other health and social care resources, and the main drivers of costs.
We also aimed to test the feasibility of different methods of collecting resource-use data, using both routine records and specially designed data collection forms for completion by staff.
Methods
Focus groups and meetings with staff from the sites identified the resources that staff felt were particularly important and specific to developing and using LSW (such as training in LSW, developing and using life stories, and physical resources for creating products), as well as potential areas for resource saving (service use, adverse incidents and prescribing).
The hospital intervention wards and care homes were issued with paper log-sheets to record the time that staff, family carers and volunteers spent working on LSW and using it with patients and residents. The log-sheets also included a section to record the materials and equipment used.
Data collection forms based on the Client Socio-Demographic and Service Receipt Inventory (CSDSRI)145 were used to collect resource-use data. Care home staff completed these from care records. In the intervention wards, an on-site research team provided additional support for data collection; in the comparison ward, the local trials unit collected data.
The same teams collected ward-level data from routine records about staff sickness and turnover, prescribing and falls or other incidents. At the care homes, the business manager provided this information. The format of this data request was left deliberately open to assess which data were available and in what formats, and therefore what data would be feasible to collect in a formal evaluation.
Challenges of data collection
This section describes the challenges of data collection and the feasibility of collecting similar data using these methods in a large evaluation.
Training in life story work
One trainer (the dementia care consultant for the care home provider) was responsible for developing and delivering the LSW training in the six care homes. She provided information on the time spent developing, organising and delivering the training. Five of the six care homes provided information on the members of staff who attended the training and their approximate salary levels.
Hospital intervention wards routinely used LSW and so training was not necessary.
Development and use of life stories, and materials used
Care homes
All staff were asked to log the time they spent on LSW with each participant. This included time spent with the resident/patient creating and using the life story, as well as time spent creating the life story while the resident/patient was not present, for example sticking photographs into a booklet. Time spent by all staff members as well as by volunteers, students and residents’ family members should have been included.
The LSW log-sheets for care homes were completed with few problems in three care homes. However, it was not usually possible to tell whether LSW required additional resources or the redirection of existing resources; sometimes, life story information was collected or discussed during a meal time or other routine activity. The information collected was useful in shedding light on how LSW was used as part of routine care, but not in identifying additional, LSW-specific resource use.
The person who co-ordinated, and in most cases carried out, the majority of the LSW completed the logs in these three care homes, even when recording another person’s time spent working on the life stories. We originally anticipated that the logs would be kept in residents’ care records and be completed by whichever staff members engaged in LSW. However, in each care home one member of staff took responsibility for the LSW, and kept the logs with the products as they were made. This staff member kept the products until they were ‘finished’ and given to the resident. Had residents been more involved in the LSW process, and the product kept in their room while it was in progress, keeping the log in their care records might have been more practical.
The majority of the activity recorded on the LSW logs related to the collection of life story information and the construction of life story products. However, life story ‘work’ also covers the use of the life story to improve care and QoL. This is much harder to capture and might arguably involve a wide range of people. Were the life story products used to trigger conversations with previously unresponsive residents, for example, or to understand why a person exhibited behaviour that challenged? There was little evidence of this type of use of the life story in the logs (or the reporting of adverse incidents and challenging behaviour) but staff did identify this use as important in the end of study focus groups (see Chapter 9). We cannot assume, therefore, that the life stories were not used in this way. To capture this routine use of LSW in everyday care, a different approach may be required, such as observation or ethnographic methods.
Life story work logs were not completed at all in the two care homes that did very little LSW and where no single individual took responsibility for it. In the final care home, the activities co-ordinator reported that extensive LSW logs were completed not just for study participants but for all care home residents, for the first 2 weeks of the study. After this, the logs were considered too time-consuming. None was provided to the research team.
Hospital wards (intervention wards only)
Completed LSW logs were received from one of the three intervention wards. In this ward, three OTTIs took responsibility for LSW, although they were not based on the ward continuously. One OTTI completed the logs but covered the activities of all three. The OTTI explained that the logs did not capture any LSW activity undertaken by nursing or other ward staff. For example, ward staff routinely used life story information to put patients at ease while they were providing personal care, or for ‘de-escalation’ (i.e. calming or distracting a person when they became agitated, without recourse to medication).
Thus, LSW logs were missing from two intervention wards and those that were returned did not capture all use of the life story for all staff.
Service use, adverse incidents and challenging behaviour
Care homes
At baseline, a researcher and member of care staff together completed the data collection forms for service use, challenging behaviour and adverse incidents, with the staff member navigating participants’ care records and the researcher entering information into the forms. However, this process was labour intensive (taking two people up to half an hour to collect data for each participant). The research team concluded that it would not be feasible to employ this approach in a full trial.
For the follow-up data collection, we issued the forms to care homes in advance and asked them to enter the information without the researcher’s support. This resulted in some inconsistent and incomplete data collection. In some cases, the dates of incidents were outside the requested period, despite the dates of the follow-up period being pre-printed on the form. One possible reason for this is that care records were on paper in ring binders, which can be difficult to navigate.
Some adverse incidents and episodes of behaviour that challenges were recorded in separate sections of the care records, while others were recorded in the ‘daily records’, which were lengthy and not always filed in date order. Care staff would thus have found providing complete and accurate data very time-consuming. Without appropriate training and ring-fenced time, it is unlikely that care home staff could provide data for a full evaluation. If researchers were to collect these data without the support of care staff, ethical approval for unsupervised access to care records would be needed and explicitly agreed to by participants or their consultees.
Hospital wards
For intervention wards, the trust’s central research team offered to provide data on service use, adverse incidents and challenging behaviour. Data collection forms were converted to Excel spreadsheets in accordance with the team’s preferences. Despite the small numbers of patients with dementia recruited to the study from each ward, it proved labour intensive to collect the required data. Indeed, the process highlighted issues with record keeping that this NHS trust is now looking to address.
As with the care homes, incidents and behaviour that challenges were usually entered only in the patients’ daily care records (which in the intervention wards were paper records) rather than being reported separately. The trust’s research team searched through large quantities of paper records. For one patient they found over 250 entries of behaviour that challenged; they entered every incident onto the spreadsheet, but this was time-consuming and clearly would not be feasible with a larger number of participants.
The trials unit covering the comparison ward found it easier to gather the information requested, as their records were electronic and could be accessed remotely. However, it was still time-consuming to collect the information, with at least three entries per participant per day.
The intervention wards used a 25-point challenging behaviour scale to identify incidents,146 which might mean that they considered a wider range of incidents than the comparison ward. In a full trial it would be important to standardise the data collected.
We planned to collect data on service use, falls/other incidents and behaviour that challenges for 6 months after admission. When patients were discharged before 6 months, we tried to collect data from the care home or other discharge destination. This proved difficult, perhaps because the research team had no prior relationship with these organisations and they were not engaged with the project (see Chapter 6). Follow-up data were provided by only one of these organisations: the one the researcher visited in person.
Prescribed medication
Care homes
We developed a list of relevant antipsychotic, anxiety, hypnotic and antidepressant medications, in consultation with the care home provider, the project advisory group and a general practitioner (GP). The list was intended to represent medications that might be prescribed differently as a result of LSW. We designed a data collection form so that data could be collected from care home medical administration record sheets and then costed.
Care home managers anticipated that collecting these data would be time-consuming, as multiple paper records (which were stored separately from the care record files) would need to be retrieved for each participant. To minimise disruption, in one home the researcher agreed to collect data on baseline and follow-up medication use on a single day, at the 6-month follow-up visit. However, many medical administration record sheets had been archived and were not easily located.
In five care homes, on-site staff located the medical administration record sheets and extracted the data themselves. However, the results were variable, with forms not returned for all participants, those that were returned having gaps in the dates covered and/or entries made for medications not on the list of relevant medications. Again, it does not appear to be feasible to expect care staff to provide this type of data without training and ring-fenced time.
Hospital wards
The hospital sites were asked to report all medication, both routine and as required (PRN), during the patient’s stay on the ward. At the comparison trust this information was recorded electronically. Although it was easier to access data here than in the care homes, extraction and reporting took considerable time.
Medication for anxiety and depression (including antipsychotics) was also reported on the incident sheets. For the intervention wards, data on prescribed medication were provided as part of the incident reporting.
Care-home- and ward-level data
All study care homes and wards were asked to provide data about staff sickness and turnover, prescribing rates and incidents at care home or ward level. The purpose was to explore the feasibility of collecting these data, as well as to understand any impacts of LSW on the care home or ward and vice versa.
Care homes
We asked the six care homes to provide data for the whole care home for the 6 months from baseline. We did not suggest how this should be done; rather, we were interested in understanding how these records were kept and their accessibility. By the end of the fieldwork period (January 2015), one care home had provided all of the information requested, another had provided details of staff sickness and a third had given information on prescribing. Data were provided on staff sickness as number of hours per month, on prescribing as number of residents receiving named antipsychotic drugs and on incidents as total recorded incidents including falls.
Hospital wards
The control ward provided details of staff sickness and turnover, and incidents, but not prescribing. Data on sickness were provided as number of days over the 6-month period, and incidents as number of falls and number of other incidents.
All three intervention wards provided data on staff sickness, prescribing and falls, and one ward provided data on staff turnover. Staff sickness was reported as percentage of staff off sick over the 6-month period, to comply with the NHS trust reporting requirements for monitoring target sickness levels, and could not easily be reported as number of days. Data were provided on falls but not on other incidents. This was because not all behaviour that challenges was recorded as an incident, for example if such behaviour was ‘usual’ for that patient.
Results
This section presents the costs associated with training in LSW; developing and using LSW products; numbers of adverse incidents and behaviour that challenges; use of the NHS and other services; and use of prescribed medication.
Development and delivery costs of life story work training (care homes only)
The development of LSW training materials by the dementia care consultant took the equivalent of 1 working day, and a further day was spent developing the training sessions for care homes. There was no refresher training during the study period, although telephone support was available if required. The one-off costs for this activity ranged from £421 to £765, depending on the assumptions made about staff salary costs (see Appendix 1, Table 56).
All care homes received the training. Each training session lasted 2 hours and was repeated on consecutive days to ensure that as many staff as possible attended. Five care homes provided details of the staff members who attended the sessions and their approximate hourly wage rates. Sessions were attended by a variety of staff, including National Vocational Qualification-qualified and -unqualified care assistants; activity co-ordinators; team leaders; and non-care staff including a laundry worker, a chef and a housekeeper (see Appendix 1, Table 57).
The cost of receiving the training in a care home ranged from £950 to £1581, based on different assumptions about hourly rates (see Appendix 1, Table 58). The mean based on actual salary costs only was £1065; that based on unit costs per hour (including all overheads) of comparable staff142 was £1449.
Costs of developing and using life story products
This section describes the costs associated with staff developing and using the life story in care homes and hospital wards.
Logs were completed, at least in part, for 17 study participants (11 care home residents from three care homes and six hospital patients from one ward) and for an average of 80 days (approximately 11 weeks, range 13 days to 27 weeks). In care homes, they were completed for longer, on average, than in the hospital ward (16 weeks and 3 weeks, respectively). This may be because participants on the hospital ward were there temporarily, whereas participants in the care homes lived there, or because researchers visited care homes for multiple follow-ups and were therefore more visible to staff. As outlined above, the logs in the hospital setting were completed by an OTTI who was not based on the ward itself but who had dedicated time to do LSW.
The average number of hours spent on LSW per participant (including creating and using the life story) over the periods logged was 6.5 hours (6.7 hours in care homes and 6.1 hours in the hospital ward). In the care homes, the main member of staff involved in LSW, according to the logs, was the activity co-ordinator (or another staff member carrying out that role), who spent, on average, 4.1 hours on LSW per participant over the logged period. In the hospital ward the OTTI spent 6 hours per patient on average.
In one care home, care workers were involved in LSW with two residents, for half an hour and 1 hour, respectively. In the hospital ward, a nursing assistant was involved for 1 hour with one patient.
Occasionally in the care homes, a volunteer or student would be involved with LSW; for the five residents they were involved with, they spent on average 1.7 hours per resident. No volunteer or student involvement in LSW was recorded in the hospital ward.
Family members were also sometimes involved, more commonly in the hospital ward (5/6 patients compared with 6/11 residents), but with a similar average time of just over 1 hour per person across the logged periods.
Adjusting the averages to reflect the length of time over which LSW activity was logged revealed that the average time per week staff spent on LSW with residents of the care homes was 24 minutes, compared with 2 hours in the hospital ward. In addition, residents’ families were involved for 6 minutes per week, on average, compared with 24 minutes per week for hospital patients.
Some logs clearly indicated how much time staff spent physically creating the life story product (such as a scrapbook or memory box), whereas others did not. From the limited information available, staff in the hospital ward spent considerably longer on creating the life story product (e.g. scanning photographs or searching for relevant pictures on the internet, and sticking photographs into a scrapbook) than care home staff. In the ward, staff spent on average a total of 3.3 hours creating the product, whereas care home staff spent 1.3 hours, possibly reflecting the dedicated time that staff doing LSW on the ward had for this activity, as a part of their usual role.
When converted into hours per week, ward staff spent just over 1 hour and care home staff, on average, spent just over 5 minutes per week creating the life story product. This difference arises in part because patients spent less time on the ward and so the time spent on creating the life story product is averaged over a shorter time period than for care home residents. Life story products created in hospital may be used after discharge (so the ‘payback’ from the initial time investment could be spread over a longer time period) but we did not collect these data in this study.
The average costs (Table 7) show that creating and using LSW was not an expensive activity in terms of overall monetary costs, but the intensive activity to create the product on the ward, presumably to complete it before the patient was discharged, might have substantial opportunity costs. However, on the ward LSW was done by staff based in another team, with dedicated time for LSW and a remit to do this as part of their usual routine.
| Type of costa | Care homes (£) | Hospital ward (£) | All (£) |
|---|---|---|---|
| Cost of creating life story products | |||
| Staff cost per participant | 10.63 | 36.95 | 22.59 |
| Staff hours per week per participant | Just over 1 hour | Just over 5 minutes | – |
| Cost of using LSW | |||
| Staff cost per participant | 37.42 | 68.21 | 48.29 |
| Staff cost per participant per week | 9.40 | 22.60 | 14.06 |
Changes in the number of adverse incidents and challenging behaviour
We received data on adverse incidents or behaviour that challenges for 32 residents from five care homes, and for three patients from the control ward and eight patients from three intervention wards.
Care homes
Incidents and examples of logged behaviour in the care homes included falls; residents being agitated, distressed or unsettled; verbal abuse of other residents or staff; shouting; slapping, pushing or biting another resident or member of staff; unco-operativeness with care or refusing to take medication; and taking items from other residents/flats.
The highest number of incidents reported in any 3-month period for one resident was 18. The data are based on only 32 residents, but appear to suggest a decrease in the number of residents with one or more reported incidents over the 3-month data collection period (see Appendix 1, Table 59).
Hospital wards
In the hospital control ward, the number of incidents per patient was recorded over approximately 6 months. In the three intervention wards, the number of incidents per patient was recorded over, on average, 12 weeks.
Data were reported for three patients from the control ward and for one, four and three patients from the three intervention wards (see Appendix 1, Table 60). The types of incidents were similar to those in the care homes except for falls; only one fall was recorded in the control ward and three were recorded in the intervention wards. The highest number of incidents reported for a single patient was 255 over 16 weeks.
Changes in use of the NHS and other services
Care homes
We received data for 38 residents from six care homes about the use of the NHS and social care services, residents’ trips out with family and safeguarding referrals. These are reported as totals across all care homes to give an indication of the size of any changes.
Table 61 (see Appendix 1) shows there were very few hospital admissions either before or after the implementation of LSW. Table 62 (see Appendix 1) shows that there were fewer reported attendances at hospital outpatient services after than before implementation of LSW. Table 63 (see Appendix 1) shows that there was little difference before and after implementation of LSW in the number of telephone calls to participants’ GPs for advice or to the NHS 111 service.
Table 64 (see Appendix 1) gives the number of appointments that primary care and community-based health and social care professionals attended at the care homes. GPs and district nurses undertook the most appointments. Except for the dietitians, the number of visits by all staff, particularly GPs, reduced during the follow-up period.
Table 65 (see Appendix 1) shows the number of visits study participants made to the GP and other professionals outside the care home, and trips out with family or friends. There were no attendances at day centres (NHS, local council, for profit or not for profit). The number of trips out with family or friends appeared to increase after the implementation of LSW.
Data were collected on the number of safeguarding referrals made. One initial report was completed in the baseline period and one in the follow-up. There were no investigations and no visits from the local council safeguarding teams and the Care Quality Commission was not informed of any incidents.
Hospital wards
Tables 66 and 67 (see Appendix 1) show the number and types of services received on the wards and as outpatient/day cases, respectively, for the 11 patients in the study. Two patients moved temporarily from the control ward to another ward in the same hospital (one for 3 weeks and the other for 4 weeks). The most commonly used service was occupational therapy. Patients received art and music therapy on the control ward only.
No patient in either the control or intervention wards was reported to have used any community-based services during their hospital stay.
Prescribed medication use
Care homes
The use of prescribed medications for anxiety and depression was reported for 27 residents from six care homes at baseline and for 23 residents from five care homes at follow-up (see Appendix 1, Table 68). Antipsychotic medication was reported to have been prescribed twice during the baseline and three times during the follow-up period. Hypnotics and antidepressants were prescribed 15 times at baseline and 13 times at follow-up. For the majority, the date on which the drug was first prescribed was provided, but the end date was not; this suggests that most were being taken on an ongoing basis rather than PRN. None was specifically stated as PRN.
Data were collected on the strength and dose of each drug prescribed, with the intention of applying a monetary value to drug use before and after LSW implementation. 143 However, given the overall low usage and minimal difference between the two data collection periods, drug use does not appear to have been a main driver of LSW-related costs in these care homes. Drug use for individual residents has, therefore, not been valued. These care homes may not, however, be typical of all homes.
Hospital wards
In the hospital wards, details about the use of medication were extracted from data on reported incidents. In the control wards, PRN medication for anxiety and depression was given 67 times over the total of 72 weeks the three patients stayed on the ward. In the intervention wards, PRN medication was prescribed 97 times over a total of 94 patient-weeks. PRN medication for anxiety and depression was therefore prescribed approximately once per patient week in both control and intervention wards. Antipsychotic medication was prescribed PRN more often in the control ward (see Appendix 1, Table 69). However, these data are based on very small numbers of patients and are not generalisable. Medication was also given on an ongoing basis (see Appendix 1, Table 70).
It is not clear from the data whether few patients were prescribed medication for anxiety and depression on a regular basis or whether these data were not reported consistently.
Care-home- and ward-level impact
Partial care-home-wide and ward-level data on staff sickness and turnover, prescribing and incidents were received from three care homes, the control ward and the three intervention wards.
In two care homes, staff sick leave over the 6-month period following LSW training was the equivalent of 200 days in one care home and 103 days in the other (assuming 7.5 hours worked per day). In the control ward over an equivalent 6-month period, staff were off sick for 285 days. The data for the three intervention wards were provided as the percentages of staff off sick over a 6-month period; these were 5.6%, 5.3% and 6.8%. Given the different sizes and staff make-up of the wards, it is not possible to translate these percentages into days or hours.
One care home provided data on staff turnover in the 6 months following LSW training; eight staff left and nine were appointed. In the control ward, four staff left and four were appointed. Only one intervention ward provided data on staff turnover where, in a full year, four staff left and eight were appointed.
One home, the control ward and three intervention wards provided data on falls and incidents. There were 51 reported incidents (including falls) in the care home. In the control ward, 31 incidents (including falls) resulted in patient injuries; a further 21 were attacks on staff or other patients. In the three intervention wards, there were 43, 49 and 27 falls, with six resulting in significant or serious injury.
Two care homes provided data on the number of residents prescribed antipsychotic drugs across the whole home. Two residents were prescribed antipsychotic drugs in one home and 12 were prescribed them in the other (a SCH). In the latter, this included one resident prescribed PRN; the remainder were prescribed on a regular basis.
No data were available from the control ward.
In the intervention wards, six antipsychotic drugs were prescribed to be taken on a regular basis at a cost of £269.29, £417.07 and £1332.69, respectively. By far the most costly regular medication was aripiprazole, at £214.36, £264.12 and £926.35, respectively. The relatively high cost of regularly prescribed antipsychotic drugs on the third ward may be related to its geographical location, which covers a number of SCHs. Staff attitudes may also play a role, according to the person providing the data, with staff on this ward more comfortable about using antipsychotic medication. Five antipsychotic drugs were prescribed to be taken orally, PRN, at a cost per ward of £28.52, £58.97 and £22.60, respectively.
The costs of prescribed medication
For the purposes of estimating the main drivers of costs in relation to medication, Table 71 (see Appendix 1) gives the costs of packs of drugs for the dosages taken by participants in this study and the associated daily costs. The most expensive drugs when costed per day were amisulpride, quetiapine and venlafaxine; these drugs were taken on a continuous basis by one study participant each in the care homes (out of a total of 30 residents for whom we had data on medication). From the care-home-wide data, three people in two care homes had been taking quetiapine for > 3 months. At a cost of £7.54 per day, this equates to almost £700 each. A reduction in the use of these drugs as a result of LSW could, therefore, result in substantial savings.
For hospital ward participants, the most commonly prescribed drug was lorazepam, which has minimal cost. However, the ward-level data from the intervention wards show aripiprazole to be the most costly overall, at between £200 and £900 per ward over 6 months.
Chapter 9 Doing life story work in care homes and hospitals: findings from qualitative interviews
Introduction
This chapter reports the findings of in-depth, qualitative research carried out at the end of the feasibility study with people with dementia, carers and staff in both study settings. The aim was to assess how acceptable people with dementia, carers and staff found the LSW intervention, its implementation and the processes involved in evaluating its outcomes.
Methods
People with dementia
We collected qualitative information from 10 participants with dementia already consented into the study: nine in care homes and one in a hospital setting. Each had a life story product compiled as part of the project, in many cases made for them by someone else, usually a member of staff. We explored people’s experiences of doing LSW and perceived outcomes and challenges, as well as their experiences of taking part in the research.
Sessions took place on the day of final follow-up. We held guided conversations, using the life story product as a starting point, supplemented by questions from a topic guide. We also took detailed field notes of the conversations and participants’ reactions. Conversations were not audio recorded and took between 10 and 30 minutes.
Carers
We interviewed 12 carers, eight whose family member was in a care home, and four whose family member was in intervention hospital wards. All had consented to take part in the study and their relatives had life story products compiled as part of the study. Carers were interviewed either in person (usually at the care home or hospital ward) or over the telephone, whichever they preferred. Interviews were audio recorded with the person’s consent and took around 30–45 minutes.
Staff
We conducted focus groups and interviews with staff in five of the six care homes, and all four hospital wards. Table 72 (see Appendix 1) shows the number of sessions and participants for each site. A total of 30 staff were involved in this stage of the research.
We needed managers’ permission to hold focus groups with staff, as they required the staff to be removed from their normal duties for the duration of the session. In some sites this was not possible, so we conducted individual interviews instead. In CH6, one key staff member was not available at the time of the focus group, so we conducted a separate interview with this participant.
Analysis
Interviews and focus groups with carers and staff members were audio recorded and transcribed. Transcriptions, together with notes from conversations with people with dementia, were managed and coded using the framework approach111 and analysed thematically.
Findings
People with dementia
Findings from people with dementia centre on their in-the-moment reactions to the life story product and its effectiveness as an aid to memory and interaction.
In-the-moment reactions to the life story product
Of the 10 people with dementia interviewed, only two recalled having any involvement in making the life story product, which may have contributed to a lack of a sense of ownership of the product. When asked to talk about his life story book, for example, one care home resident said ‘I didn’t do it, you’d better ask her [the member of staff who made it]’ (RC3P01), and this was a sentiment expressed by others: ‘it’s just something they did, you know’ (IH2P04). Some people gave a distinct sense of being underwhelmed – ‘I read it once and then put it away’ (RC3P01) – or said staff ‘shouldn’t have bothered’ to make it (RC1P08).
Some of the people with dementia had not seen their life story book before looking through it with the researcher. Most had no recollection of making it, and some found this disconcerting (recognising photographs, for example, but not knowing how these had come to be there). Others were confused by the format of the book, or why certain things had been included. One book opened using an unusual mechanism which the person struggled to operate alone, while another person was unsure why there were heart shapes stuck onto her photographs, and one memory box contained birthday cards, which caused the participant to say, ‘I didn’t think it was my birthday’ (RC3P06).
One person noted that the information in his book was wrong, and others felt that the book did not cover their whole lives, that there was more that they could have added: ‘Well you’ve only seen the gist of my life in it, you know, it takes in my early days a bit. I have more photographs at home’ (IH2P04).
However, several people with dementia did seem to enjoy looking at the life story product with us. For some, this was indicated non-verbally; for example, one woman who could not speak looked intently at each photograph for a long time while smiling broadly, and others expressed similar sentiments in different ways:
Resident was happy and chatting generally, hard to make out words. Sometimes seemed to be talking about something relevant, for example when I said ‘is this a picture of your dad?’ she said ‘he was the one . . .’ (but didn’t finish the sentence) and said ‘he was a lovely man’ and laughed. Seemed happy, laughing and smiling, and talking to me.
Field notes, RC1P06
Others were able to tell us how they felt: ‘Had a long chat with [person with dementia] about his life story, prompted by his folder but continuing long after he had put it down. He said he had enjoyed talking to us about his life story’ (field notes, RC4P03).
It is impossible to say to what extent this enjoyment was derived from the LSW itself, and how much from the opportunity for social interaction more generally. However, it was clear that the life story product did provide a hook for interaction.
The life story product as an aid to memory and interaction
The presence of a life story product in some cases prompted memories of places, people and events:
I remember them, yeah [referring to people in photographs].
Would you have remembered without the book, do you think?
No, I don’t think so.
When people did not recognise people or places at first, captions and writing proved useful. In some cases, people with dementia could read the captions themselves, which then prompted them to talk further about the pictures. In other cases, we as researchers could read the captions or writing, and engage the person in a more detailed conversation than was possible without them. Even when photographs did not have captions, people were able to talk about them in some way, commenting on the clothes or appearance of the people in them, for example.
However, participants had mixed feelings about remembering the events and people depicted in their life stories. Some expressed sadness at recalling people who had died, or who they had lost contact with, but people also found it pleasurable to look back and see pictures of friends and family looking happy.
One woman appeared to enjoy looking at her book at the time, but staff reported that she later became upset, saying that the more recent information in the book was not true. Here, the life story book, although acting as an effective memory aid, appeared to highlight conflicts between the person’s sense of reality and the memories recalled. Remembering, of itself, may not always be a positive outcome.
Overall
Overall, people with dementia had little recollection of involvement in making their life story products, and this perhaps led to a lack of a sense of ownership. Looking at life story books could prompt some sad memories, but the in-the-moment interactions tended to be positive, and in many cases there was much smiling and laughing during the course of looking at the books. Although some might have felt underwhelmed by their life story book, a physical product has an important role to play in facilitating interactions, particularly with people who do not know the person with dementia well. However, there is the potential for confusion or distress if, for example, unfamiliar objects are included, or information is wrong or contradicts a person’s understanding of their present reality.
Carers
Doing and using life story work
Carers expressed mixed feelings about doing LSW. In many ways, it was seen as a positive experience for families: it was pleasant to remember happy times, and gathering stories and memories could build bonds between family members. Some carers found sharing life story information with others to be a positive experience; one described the process of writing her husband’s life story after he was taken into hospital as ‘cathartic’, and how it gave her a sense of pride in his achievements:
I think it was because I realised how much I knew of him and . . . I’ve always sort of been really proud of him, because he’s achieved things, you know.
IH1C01
However, some carers also expressed grief or sadness at the person no longer being ‘the person we knew’, or realising a sense of their relative’s fragility.
Carers talked about the difficulty of involving their relatives in the process of doing LSW when the relatives could not talk, could not remember photographs or stories, or had no interest in looking back over their lives. Overall, however, carers seemed to be willing to be involved in the LSW process and pleased to be asked to be involved, as they considered it a worthwhile activity.
Outcomes of life story work
Carers observed a range of outcomes of doing LSW. One of the most important benefits identified was that LSW could help staff understand the person with dementia, including elements of their past and more up-to-date information (e.g. about their current likes and dislikes). Part of this was preserving the identity of the person with dementia:
You’re never past it, are you, I guess, because there should always be an element of trying to keep some of that history for him even though he can’t retain it himself; and still, I mean he’s still the same person he just can’t always tell us who he is.
RC4C03
Another benefit observed by carers was the power of LSW (both the collection of information and a physical product) to facilitate conversations with both staff and visitors. This was felt to be particularly valuable in hospital wards, where temporary staff had no previous knowledge of the person. In such cases a memory board on a wall provided a valuable starting point for a conversation. For hospital patients who had been discharged and were now living in care homes, carers felt that having a life story product had played an important role in passing on information about the person and helping new staff to get to know them:
I think that’s very good because it’s informative to them, you know, and it’s good that they can talk to [person with dementia] then a bit; but it’s not that she really understands, well none of us know how much she understands, you know, but at least they can talk to her about it and see if they get a response.
IH2C11
In care homes, staff turnover was lower, and residents stayed for longer, so there was less need for quick access to life story information. Instead, carers felt that life story products were mostly used to facilitate conversations with them, as well as with grandchildren or less frequent visitors:
There’s another lady that comes to visit mum now and again and she, likes to get the box out and look at the pictures with her, so, you know, it’s something else to do; ‘cos mum can’t speak any more, so I think people that don’t know what to do are at a loss.
RC4C06
One carer identified LSW as ‘something to keep [mum] occupied’ and several thought that their relative enjoyed looking through the life story product, and in some cases felt it even helped their relative to remember more: ‘I didn’t think mum got anything out of it, but as the days went on you would get names of people who she’d never mentioned before’ (RC1C04).
Although carers identified these elements of LSW as of benefit to staff and carers themselves, they could also have distinct indirect benefits for the person with dementia, in terms of increased interaction and understanding and, possibly, more personalised care.
Some carers were not convinced that LSW had had any positive outcomes for their relative. Some reflected that relatives did not remember people in the photographs, or did not have any interest in looking at them, and therefore the benefits of doing LSW for the person with dementia was limited, although there may have been positive outcomes for other people.
Challenges of using life story work
Some carers found it both time-consuming to find photographs and difficult to choose which pictures and stories to select. One said that receiving a list from a staff member including categories such as ‘pictures from childhood’ and ‘pictures from work’ had helped to narrow it down. Another carer, whose friend had dementia, found it particularly difficult to find information, as all of the person’s relatives had died, and so ‘there was nobody there to ask really’ (IH2C11). Several carers found it frustrating when their relative could not remember events and people in photographs. Some also felt that doing LSW might be ‘emotional’ for the person with dementia, although this had not actually happened to any of the participants when doing LSW, and was based only on carers’ past experiences of, for example, looking at family photographs.
Carers felt strongly that LSW should have been started much earlier. Depending on the person’s circumstances, this might have been when they were admitted to the care home, or even when they were first diagnosed with dementia. This might have allowed the person with dementia to play a bigger role in putting the life story together, and given carers more time to collect information.
Overall
Carers had mixed views about the benefits of LSW for people with dementia. Although some direct positive benefits were described, other carers felt that there was no benefit to people with dementia at all, as they could no longer recognise people in photographs.
However, positive benefits were identified for both family carers and staff working with people with dementia. Families enjoyed looking back at their photographs and memories, remembering positive things about their relatives’ lives and reaffirming their relatives’ identities. Carers felt that staff had benefited from knowing more about the lives of the people with dementia in their care, and could build relationships with them through doing and using LSW. Carers suggested the presence of a physical life story product both encouraged and facilitated interactions with both staff and visitors, particularly those not well known to the person with dementia, or who struggled to make conversation. This could lead to indirect benefits for the person with dementia themselves, through more interactions and perhaps more personalised care.
Staff
Doing life story work
The process of doing LSW differed between research settings, as discussed in Chapter 6. In both care homes and hospitals, some life story information was collected on the person’s arrival (usually using a template), or soon after if they were unwell or the family was distressed. In some sites, more LSW was done later.
Staff usually attempted to collect information from the person with dementia themselves first, but explained that this could be difficult as people were often unable to recall details about their lives. Family involvement was, therefore, seen as important, although this was not always forthcoming.
In most sites, templates were used for the initial collecting of information. Some staff saw these as a useful starting point and a way of collecting the same information from everyone. Others felt them to be restrictive, lacking space for photographs or asking questions that were not always applicable, for example about a person’s role during the war. In two care homes, activities co-ordinators set up a folder for each resident to enable all staff to collect life story information during their daily work. This was in addition to the use of templates.
Not all LSW in our care home and hospital sites resulted in the construction of a life story product. In some cases completed templates were considered to be a ‘life story product’; however, in other sites further LSW was done and another, more personalised, product was made. On the ward with the OTTIs, this usually took the form of both a book and a memory board. Books were A4 folders with typed information in plastic wallets, which could be added to if further information became available later. Memory boards were put on the walls in patients’ rooms. In care homes, life story products included photo albums with captions, memory boxes, folders with written information and photographs, scrapbooks and, in one case, a memory blanket.
Completed templates were usually stored in a person’s care records and, although theoretically people with dementia and their families could look at them, it was rare for anyone other than staff to do so. Where a more comprehensive life story product was developed, a staff member often kept this until it was ‘finished’, with families sometimes unaware that the product was being made. Once complete, it was then kept in the person’s room and more usually used by both residents and families, and sometimes by staff who looked at it with the person.
Outcomes of life story work
For people with dementia, staff described the emotional aspects of LSW, both good and bad. For some, LSW had provided an opportunity to ‘open up’ about aspects of their lives that they had previously been unable to talk about:
I think she knew she was coming towards the end of her life and I think she just wanted to offload and tell people that, look, you know, I’m not really this person, this is really what I am . . . she broke her heart, but afterwards she said thank you.
RC1FG1
Staff talked about people being proud of the achievements recorded in their life story books, and had observed people feeling valued because others were taking an interest in them.
Some staff also felt that doing LSW allowed them to tailor activities to residents’ preferences, although they pointed out that it was important not to assume that people would still want to do the same activities they had done in the past. LSW had also uncovered opportunities for new activities, for example gardening.
Staff reported using life story products primarily for getting to know people better, but also for calming people down, understanding behaviour and problem solving. In the hospital ward that had made memory boards for patients’ rooms, these were valued as communication aids for temporary staff in particular, giving them something to talk to the person about, which was seen as having value for the patient too:
We take that information from the life story book and put it in a simple form on the wall . . . and it’ll just have the patient’s name on, the wife, the daughter, maybe where they’ve worked, where they’re from, a little bit of information, so that when bank staff or someone who doesn’t know the patient very well . . . they’ve got that communication aid, which just helps them providing the care that the patient needs.
IH2FG2
Staff in intervention hospital wards also talked about the value of LSW for easing the transition to a new place after discharge from hospital.
Staff described how a physical life story product was beneficial for families as well as being an aid to concentration for people with dementia, as it provided something for them to look at together, to stimulate conversation or even just an activity for the carer if the person with dementia was not very responsive.
Staff noted that sometimes people with dementia could remember more when prompted with a visual life story product, and that families were sometimes surprised by what the person could remember. However, others felt that the main benefits had come from spending time with people, rather than creating a life story product as such:
I think he just enjoys the company more than anything. So I don’t know whether or not the life story, although it’s something you can talk to him about, it’s something he relates to, I think it’s the company he’s getting and the time you’re spending with him more than the life story.
RC1FG1
Some staff felt that knowing more about a person helped them to see that person as an individual. They had used LSW to help them to calm an agitated person, and found that knowing more about people made it easier to have conversations with them, and even provide better care or more appropriate activities. This helped staff to build relationships with the people with dementia in their care.
Challenges of life story work
Not everything about LSW was seen positively by staff. Some found it difficult to do LSW with people with dementia, when people were reluctant to give information or unable to remember things about their lives. Some staff mentioned the difficulty of getting at ‘the truth’ about a person’s history, and having to follow up information given by the person themselves by asking their family clarifying questions. Other staff members were happy to write down and use the information given by the person, but some noted that family members could be distressed if the information written in a life story product was wrong.
Doing LSW could be emotional for people with dementia, families and even staff, although this was not always considered to be a negative. Staff sometimes found it difficult to know who would respond well and who would not, and people with dementia responded differently at different times. Staff acknowledged that there was a degree of judgement in deciding who to do LSW with and when, and what to include in any written life story product.
Family involvement in LSW varied, and some staff found it challenging to involve families. Families were often asked to provide photographs, and also information about their relative’s life if the person with dementia could not provide this him- or herself. Some care home staff had struggled to engage families, and in some cases there was a sense of disappointment about this:
I think that it would be fair to say that I think the families could have a lot more responsibility in doing this . . . [S]ome have been fantastic, but I think the easy part for them is just bringing you some photographs, I do think they could spare some time during visiting to sit and help put these things together, they just don’t, it’s another task for the staff to do.
RC1FG1
Families were sometimes reluctant to get involved in LSW, for example because their relative was very ill or had been admitted to hospital in difficult circumstances, or if they felt that it was ‘too late’ for LSW to have any benefit for the person themselves. If the person with dementia was in hospital, families could feel too overwhelmed to fill in a template, or might fear that upsetting information would come out. There might also be conflict within families, which could make it difficult for staff to do LSW with them. Staff also raised the question of how to do LSW when a person has no family or known friends:
Sometimes we get people in we know nothing at all about, they’ve got no relatives alive, they’ve got no visitors visiting them, so the only thing you can do is find out what they’re interested in, and maybe centred around the football team that they like . . . show them the pictures, see if they prompt any memories of anything.
IH2FG2
A common observation from staff across all settings was that, although they did have time to collect information about residents’ lives (and some felt that they knew their residents very well), they did not have time to sit and make a life story product. LSW, in that sense, was more successful when one member of staff (or team, in the case of the OTTI team on the hospital ward) took responsibility for leading LSW, collating information (even if this was collected by other staff members) and creating a life story product. However, in several sites this had been done solely for the purpose of the research, and only one care home site planned to continue doing LSW in this way. This site had been involved in a project with the local school to collect life story information, and three members of staff were trained as dementia champions, each taking responsibility for a particular aspect of LSW in the home (memory blankets, memory boxes near residents’ doors and birthday celebrations). This concentration of effort and commitment from several staff members meant that there was confidence at this care home that LSW would continue after the research was over.
Creating a product not only was considered to be time-consuming, but in some cases also provoked anxiety. Reasons for this included finding it difficult to connect with the person they were working with (and so being unable to collect information about their life) and worrying specifically about making a product: it not being ‘good enough’, their handwriting being unreadable or their being unable to use a computer:
You two [other staff in focus group] don’t like computers but I’ve got awful handwriting and I think it’d just be easier for somebody to see it and read it, if it was like typed up, it’d probably last longer as well.
IH1FG1
Both staff literacy and skill levels and the availability of technology such as computers and scanners were influential here. Care homes, in particular, had few available computers, and in some cases staff used their own computers at home (in their own time) to make the life story products.
Overall
Staff were mostly enthusiastic about doing LSW and positive about the benefits it could bring, particularly for their own practice but also for carers and people with dementia. However, there was little time allocated to do LSW, and staff sometimes felt unable to do it in addition to their normal duties. In hospitals, where there were many temporary workers and a more regular turnover of patients, a physical product was considered valuable to facilitate staff interactions with people with dementia and help them to manage behaviour that might otherwise be challenging. In care homes, many staff members felt that they already knew the people they worked with well and some questioned the need for a physical product.
Acceptability of the research
The people with dementia we interviewed told us that they enjoyed talking to us and ‘didn’t mind’ answering our questions. However, as we interviewed only those who were happy to talk to us, this is not surprising. People with dementia sometimes conflated doing LSW with being involved in the research; for example, they might respond to questions about the process with answers about the photographs. This was perhaps understandable, as the LSW and research processes had been running concurrently, and the difference was not always clear.
Most carers explained that they were happy to take part in the research, that it did not take up much time and that, in many cases, they visited their relatives regularly anyway, and so meeting us did not cause an extra burden. Some carers felt that, although the research might not help their relative, it might provide useful information for others in the future and they were, therefore, happy to take part. There were also, however, comments that were more negative. For example, one carer noted the time and expense spent on the research, and predicted that little would be implemented as a result, and another noted how difficult it was to describe his family situation.
Carers described a range of ways in which they felt that the research had an impact on their relatives. Some noted that their relatives might not understand the premise of the research, but would be pleased that it was being done. In a small number of cases, however, carers felt that the person might have felt some anxiety, possibly as a result of feeling that they had said something wrong:
I don’t think it wasn’t that he wasn’t happy to talk to you but I think afterwards . . . he sort of gave me the impression that he felt, because he hadn’t been expecting it, but I don’t know that he would ever expect it even if you’d warned him, that he’d said things on the spur of the moment that perhaps if he’d had chance to think about it he wouldn’t have said.
RC4C03
If I didn’t do it [sit with the person while we went through the measures] she would be very worried if you were asking her all these questions, and she worries when you write things down because she thinks you’re recording everything.
RC2C07
As described in Chapter 6, some carers expressed difficulty or dissatisfaction with the QoL measures. They found it particularly hard to fill in the proxy measures which ask how the person with dementia is feeling. There were a variety of reasons given for this: their relative’s condition was deteriorating, for example, or it stayed the same and so the answers to the questions also stayed the same each time. Carers found it difficult to know how their relative felt, and therefore felt that they were just guessing at answers. Others noted that their relative’s mood was so changeable that it was impossible to say how they had been feeling in the past week.
The research appeared to have more of an impact on staff, and some described how they felt pressure to have achieved something in terms of LSW by the end of the study, or felt that they were doing us a ‘disservice’ by not doing LSW as planned. Several mentioned that they found it hard to take time out of their work to fill in the questionnaires or to take part in the focus groups, and there was a suggestion that staff should be given extra time or support to do this. This also applied to doing the LSW that was planned as part of the study:
It’s great they [care home provider] get involved in these kind of studies but I do think that they need to offer support to the staff. If we’re going to be doing this study as we should, as we’d wanted to do it, and as we should, there should have been staffing arrangements made to free up time for people to do it properly.
RC1FG1
Hospital staff, in particular, noted that it had been difficult to find the time to ask carers for consent for the research team to contact them (see Chapter 6) and suggested that a dedicated member of staff to do this would have been helpful.
Staff found questionnaires repetitive and vague, found the tick-box nature of the measures constraining and suggested that the answers had nothing to do with LSW.
As explained in Chapter 7, we did not persist with the QoL measures with people with dementia who found them distressing, and several carers and members of staff either pulled out of the study or simply did not fill in the measures at all time points.
Chapter 10 Discussion and conclusions
Discussion of findings
Stage 1: literature review and qualitative work
-
Both elements of stage 1 showed that LSW is not simple conceptually, nor is it easy to pin down its potential benefits. Personal, temporal and organisational challenges may prevent positive outcomes being achieved, and an individually tailored approach is essential to ensuring maximum benefit for different people at different times.
-
The different models of LSW identified in the review and the theories of change that emerged echoed the different purposes of LSW identified in the qualitative work. Is LSW mainly about people preserving their own memories or is it to help staff learn about the person they are working with? Is its aim to improve QoL by reaffirming identity, or by personalising care and responding better to behaviour that challenges?
-
We saw these tensions played out in care settings in the survey and in the feasibility study, where the focus was on LSW as a tool for care and for managing behaviour. This does not necessarily make LSW in those settings any less valuable, but it may narrow the scope for benefit. It also raises the question of whether or not the potential personal benefits might be better achieved earlier in the dementia journey, when people with dementia themselves may have more control over the process and final product.
-
The experiences of people with dementia, family carers and professionals about good practice in LSW were consistent with messages from the literature review and, together, suggested a set of learning points for good practice (see Conclusions).
Stage 2: surveys
The survey of services suggests that LSW has spread relatively widely, particularly in hospital assessment settings, albeit to a lesser extent in care homes.
We found wide variation between different services in the type of LSW they did, and in its overall objectives, including involvement of the person with dementia, whether it was past or forward looking and how it was used in the care setting. We saw throughout that these differences may reflect the different places on the dementia care pathway at which the services were located. Settings with an assessment and care planning focus tended to produce life story products that were less dynamic and sometimes designed specifically to capture information to pass on to other care settings. Care homes were more likely to be capturing information to inform everyday care and interactions with the person with dementia.
Across the board, however, the actual use of the life story product was not as common as might be hoped for. Doing LSW is one thing; using it to inform and improve care is clearly another.
The service survey emphasised the role of carers in doing LSW, and the survey of carers gave further detail. Although carers played an important part in services’ LSW, they were unlikely to be trained to do it beforehand. Carers were likely to report heavy involvement and, in some cases, had led the LSW. Again, however, the actual use of the life story by care staff, and even by the person with dementia and carers, was lower than might be expected.
Different models of LSW in the carers’ accounts echoed those found in the review, the qualitative work and the services survey, suggesting again two different types and uses of LSW.
Stage 2: feasibility study process
Our overall conclusion from this stage is that formal evaluation of LSW would be possible only with substantial staffing. Enabling people with dementia (and, to some extent, their family carers) to participate in a meaningful way meant that we used essentially qualitative methods to collect quantitative data. Working with people with dementia requires patience, and there will always be a high risk that data cannot be collected on a given day.
However, working in care homes and hospital wards is, of itself, labour intensive and runs the risk of ‘wasted’ researcher time. Contacting family members and other consultees relies on the goodwill of staff, and carers themselves often have busy/stressful lives and other priorities. Embedding researchers in the care settings is probably the best way to deal with these types of problems.
Staff turnover and the differing priorities of care settings also mean that the best-laid plans for data collection can fail. Continuity in management commitment to the intervention itself and to the research is clearly an issue, as others have also found. 140
Overall, our work means that we now have a clear idea of the challenges and benefits of attempting to establish evaluation of this complex intervention in care settings that are themselves complex and often complicated.
Stage 2: feasibility study outcomes
Even after successful recruitment of people to the study, gathering data was challenging. Completion rates for outcome measures were mixed, being best overall for family carers in care homes and worst for people with dementia in hospital wards. Completion of measures by staff in care homes was particularly disappointing, given the commitment of the care home provider to the study.
However, we learned much of use for future research.
First, we observed fatigue effects, both immediate (for people with dementia) and over time (for staff and carers). To deal with the first issue, future research should randomise the order in which measures are presented to people with dementia. To deal with the second issue, two follow-up points after baseline, rather than three, might be better. We saw a considerable reduction in completion in all groups at 6 months after baseline. A shorter follow-up period would certainly have benefits in relation to the participation of people with dementia and carers. However, we think that follow-up for staff should be at longer intervals. This would allow for the ‘bedding in’ of the intervention into the culture of the care setting but also help to avoid any learning of the ‘right’ answers caused by repeating measurement at short intervals.
Completion was not always a function of capacity for people with dementia. Local or embedded research teams could be more flexible in response to the priorities of the care settings and needs of residents or patients, and allow data to be gathered at a time and pace to suit both.
We felt strongly that the QoL measures both missed and were influenced by ‘in-the-moment’ benefits for people with dementia. Different methods – whether qualitative (such as observation, photovoice or video ethnography) or quantitative (such as measurement of QoL ‘in the moment’ with subsequent aggregation) – are needed to catch these more fleeting benefits. Exploring and developing different methods is essential for any future research if it is properly to include the views of people with dementia themselves, rather than those of their proxies. Our observations also have implications for the way in which QoL measures are used with people with dementia in care settings, where many different activities may take place across each day and week.
The measures also missed how LSW was used, in particular the use of LSW for de-escalation of behaviour that challenges in hospital settings. Formal observational techniques at selected times of the day, in care homes and hospitals, would be useful for future research, but have substantial resource implications.
We did observe some change in our outcome measures from baseline to follow-up and these were significant for staff attitudes towards dementia in care homes, for self-reported QoL (using DEMQOL) for people with dementia in care homes between baseline and final follow-up, and for the experiences of carers.
The first change we think could be an effect of LSW, as we saw evidence of it in both measures of staff attitudes. Whether the change was due to the training associated with implementing LSW or to LSW itself is not clear. Neither is it clear whether the change can be maintained over time or whether it alters staff behaviour. However, we believe that this apparent effect is worth exploring in future research.
The second effect was measured only for the 12 people with dementia able to complete DEMQOL; they may thus have been less cognitively impaired than others in the study. However, the pattern was consistent over time (QoL improved further at each follow-up) and was also evident when we reran the analysis for only those who completed DEMQOL at all three follow-up points.
We saw deterioration in carers’ experience scores in the care homes and an improvement in the hospital setting. We are not sure that either effect is related to LSW. People with dementia in the care homes were often approaching the end of the dementia journey, as we saw from the number of deaths in our sample. It is perhaps unsurprising that carers were less able to engage in their usual activities, and so on, as time passed. For carers of people in hospital, by contrast, it was often the case that the person with dementia had been admitted in a crisis, but, during his or her stay, was stabilised and assessed and had his or her future care planned (in some cases meaning admission to long-term-care). Again, we can understand why carers might feel that restrictions in their lives might have lightened somewhat. These findings, however, do suggest that the CES is a good candidate measure for any future research looking at the experiences of carers of people with dementia.
Stage 2: collecting resource-use data
Staff collected resource-use data from care homes either alone or in conjunction with researchers. Data collection forms were filled out more consistently and completely if researchers were involved. Hospital staff collected data from hospital wards and this was equally time-consuming. In a full evaluation, either researchers would need to gain ethical approval and consent from study participants to extract data from their care/medical notes, or care home/ward staff would need to be appropriately trained in collecting the data and their time for doing so would have to be ring-fenced.
Reporting some data, for example on antipsychotic prescribing, was simple for the care homes, as their systems were already set up to run these queries. In the hospital intervention wards, the only way to provide an indication of the volume of prescribing was through the total cost per drug over a specified time period. In a full evaluation, this may be a useful reporting method for a ward-level intervention.
Stage 2: resource-use outcomes
The cost of delivering the LSW training in care homes ranged from £950 to £1581; these costs would change if different staff members attended training sessions. The average cost (based on salary only) of creating and using LSW products for a resident in the care homes was £37.42 spread over a 16-week period. These costs included staff working in conjunction with residents as well as working alone, making it difficult to categorise which were additional costs and which were part of routine care. If we assume all costs are additional, resource implications would be relatively small at an individual resident level but could be substantial if extrapolated to all residents.
Life story work was a part of routine care in the hospital intervention wards, so there were no initial training costs. The average cost (salary only) of creating and using LSW products was £68.21 per patient over a 3-week period. The more intensive activity here may be due to staff attempting to complete life story products before patients are discharged, or to OTTI staff having dedicated time for this activity.
The intention had been to calculate the monetary value of, and the potential savings from, the NHS and other resources, including prescribing. However, given the small number of data, we did not calculate these costs, as they would not be robust and might be misleading.
However, the main drivers of costs are usually the services used most frequently or that have the highest costs per use.
The most frequently used services in care homes were visits to the care home by the GP and the district nurse. Care home staff accompanied residents to these consultations on at least 25% of occasions, which would add to overall costs if this took staff away from other valuable duties. Visits by the GP showed some reduction at follow-up compared with baseline, but visits by the district nurse did not.
The resources with the highest monetary values per use were an inpatient stay on a general medical ward, an accident and emergency (A&E) attendance by ambulance, an outpatient appointment and a GP visit to a care home. Because of their relatively high costs, these events are more likely to affect total costs than, for example, visits to the care home by professionals allied to medicine. As an example, four residents taken to A&E by ambulance in the 3 months prior to baseline would have cost £920, plus the value of the time for care home staff to accompany them on two of these occasions. During the follow-up period, two residents attended A&E by ambulance with no accompanying staff, at a cost of £460. Over a larger number of residents in a full evaluation, any differences in the costs of this type of activity might be substantial.
In a full evaluation, then, the priority should be on collecting data on high-cost or high-volume services such as hospital inpatient admissions, outpatient attendances, A&E attendances, and visits to care homes by GPs and district nurses. The number of times care home staff accompany residents to such appointments should also be recorded, as these may have opportunity costs.
The use of prescribed medication for anxiety and depression by participants in the care homes was small, with no recorded PRNs. Care-home-wide data on antipsychotic prescribing were provided by two homes. In one, prescribing of antipsychotic medication was low; in the other (the SCH) 12 residents were prescribed antipsychotics, all but one on a continuous basis. Overall, however, for study participants in these care homes, the use of antipsychotic or other drugs was not a big driver of costs.
Owing to the small numbers of participants in the hospital settings, it is not possible to judge from individual patient data how extensively antipsychotic drugs were used. However, ward-level data suggest antipsychotic prescribing costs up to £1350 per ward over 6 months.
Some drugs might drive overall costs but the majority, especially those available in generalist form, are not expensive, even on an ongoing basis, in comparison with other costs such as A&E attendances or GP consultations. In a full evaluation, the daily costs of the most expensive drugs or the ones most likely to be affected by LSW would need to be calculated for each participant. From this study, these are amisulpride, quetiapine, venlafaxine and aripiprazole.
Each result shows little on its own, as we would expect from small numbers, but taken as a whole there is the suggestion of a decrease in service use and adverse events. Although these data were never intended to be robust enough to demonstrate change, they do suggest a possible reduction in service use and an indication of the main drivers of costs that might be collected in a full evaluation.
Stage 2: participants’ experiences of life story work as part of the research project
Carers, in particular, were unsure of the benefits of LSW for their relatives with dementia, particularly when the dementia had progressed and the person could no longer even recognise people in photographs. This sometimes led to carers’ reluctance to get involved in the LSW, feeling that it would have no effect. However, people with dementia in the study appeared to enjoy looking at their life story books, and staff were more certain that there was a positive effect, particularly in terms of facilitating interactions with both visiting family members and staff (particularly temporary staff), as well as encouraging staff to get to know the person. This suggests indirect benefits to LSW for the person with dementia, however far the dementia has progressed.
Staff were positive about collecting life story information, and many described how this was ‘already’ done, whether through use of a template on admission to the care setting or through the course of everyday interactions with the person. There was some scepticism about the need for a physical life story product, particularly as these were considered time-consuming to make. When products were made, staff usually led the process, often with some family involvement through, for example, providing photographs or stories. However, lack of time was a barrier, and some staff described how they spent time outside work making products. LSW was considered easier when one person or a small team took responsibility for it; where this had been implemented in sites, all staff members were encouraged to collect information, but did not have responsibility for making a product. This person or team could also take the lead in encouraging family members to be involved.
Although some aspects of LSW can be beneficial for people with dementia, it is unclear whether this is attributable to the presence of a physical life story product, or the act of spending time with someone, learning about their life. This may, of course, occur without LSW, but LSW can be a mechanism for this, and a physical life story product can have further benefits in facilitating interactions and therefore enhancing relationships with family members and staff.
Strengths and limitations
There are two main strengths to our work.
The first strength was the use of a mixed-methods design, which allowed us to identify strong commonalities across the existing literature about LSW and carry out new qualitative exploration and preliminary outcome assessment. This enabled us to identify hypothesised routes to efficacy for LSW and then to explore these in a small outcome study. The qualitative work produced in-depth understanding; the literature review allowed us to develop models of LSW and theories of change; the survey generated insights into the practice of LSW nationally; the feasibility study was completed despite substantial challenges to process and progress; we observed some effects; and we were able to ascribe costs and possible savings to LSW. We thus generated new knowledge about LSW itself while improving understanding about how to approach the next stage of evaluation.
The second strength was the involvement of people with dementia, family carers, organisations that advocate for the rights of both, and care providers. Their involvement was not only as participants but also as influential advisors at all stages of the work. This strengthened our research practice and our understanding about the benefits and challenges of being involved in research for people with dementia and their carers. This understanding is invaluable for planning our own future research and also, we hope, that of others.
The two main limitations of the research are what we were not able to do.
We had planned to use the literature review to estimate the size of outcomes achieved in LSW, but there was insufficient evidence to allow this.
We had also hoped to do some Markov chain modelling to inform decisions about whether or not to carry out future evaluation. Five main factors militated against this:
-
There was a dearth of outcome data in the existing literature.
-
There were very low levels of data return for people with dementia in the hospital settings.
-
The only detected effect for people with dementia (and only in care homes) was for a very small proportion of respondents, and they were probably not typical residents.
-
There were question marks about implementation of LSW in both hospital and care home settings.
-
The largest effect observed related to attitudes to dementia for staff in care homes, not for people with dementia.
Given these issues, we did not feel that modelling would provide a secure basis for future research.
Conclusions
Life story work has spread widely in health settings in England (although less so in social care settings), but our work has shown that what it is, how it is done and the outcomes it achieves vary substantially.
There are two predominant models of LSW.
First, there is LSW that is led by the person with dementia, usually at a relatively early stage of the dementia journey, and which serves to reinforce a sense of identity and support pride in the life led to date. This sort of LSW may be carried out over a long period and generate detailed and substantial life story products. This work is often narrative or at least biographical.
The second model, found more often in care settings (and thus at a later stage of the dementia journey), is less likely to involve the person with dementia (although there is no reason why it should not) and more likely to involve family carers. Although it is also about telling the story of a person’s life, it is more often directed to aspects of and contents about a person’s life that might aid communication with and increase staff understanding about the person. It may also be used to calm or soothe the person with dementia. This type of LSW is, thus, almost entirely care-focused, although there is no reason why a ‘type 1’ life story should not inform a ‘type 2′ life story.
The feasibility element of our project was more about the second type of LSW and found some evidence that it might improve care home staff attitudes about dementia, although it is not clear whether this change comes from the LSW training or from doing LSW itself. Care homes are important in the later stages of the dementia journey and the challenges of delivering person-centred care in these settings are widely acknowledged. We therefore feel that future LSW evaluative research could profitably focus on staff attitudes and whether or not changed attitudes lead to changed care practices. Overall, it does not seem to be expensive to implement this type of LSW, and there are some hints of areas of resource-use savings. Taken together, these suggest an agenda for future evaluation and one that can be carefully informed by the rich learning that came from our feasibility work.
Implications for health care
Stage 1 of our work was based on in-depth qualitative research and a systematic review of the literature. Although this work could not point to definite outcomes from LSW, it did find consistent messages about good practice in doing LSW. The survey of health and social care services showed that not all services follow these practices. We have, therefore, drawn together good practice learning points which are summarised below, and we will disseminate these widely to health and social care audiences.
Good practice learning points for life story work
-
Whether someone wants to take part in LSW is an individual thing. It should not be assumed that a person necessarily wants to make or share a life story and no one should be pushed into doing so.
-
A person’s life story is never finished and LSW needs to reflect this. To avoid setting people ‘in stone’, ensure that life story documents can be added to and updated.
-
LSW can be emotional and may raise sensitive issues. Some people will value the opportunity to talk about these issues, but staff require training to handle this and should not be expected to do so without support.
-
A person with dementia may have very different views from others about what their life story is for. Respect the person’s wishes about what goes into the life story and who will see it, now and in the future. If they do not have capacity to express their views, consult someone who knows them well.
-
Staff should consider making and sharing their own life stories. How does this feel? Who would they share them with?
-
Beginning the process early will enable people with dementia to take a more active role in producing their life story and communicate how they would like it to be used in the future. However, it is never too late to use LSW to improve care for a person and invoke a ‘nice feeling’.
-
Outcomes for better care will only come about if care staff take (and, indeed, are granted) the time to absorb life story information and the flexibility to use this to inform and improve the care they provide.
-
Short summaries might be useful for busy staff, helping them to achieve better care, but they cannot replace a life story owned, shared and added to by a person with dementia him- or herself.
-
The process of collecting life story information enables staff to connect and build relationships with people with dementia and their families. However, in order to have wider benefits it is also important to produce something that can be used and enjoyed by others.
Stage 2 was intentionally exploratory. Although we did observe effects in this stage of the work, particularly in relation to staff attitudes in care homes, it is clearly not right at this stage to draw out implications for health and social care providers.
Recommendations for research
The main point of stage 2 was to learn whether or not formal evaluation of LSW is possible and we have outlined above some of the detailed learning about how such evaluation might be designed and carried out. We will not repeat that detail here but confine ourselves to the larger research needs that have emerged. In order of priority, there is a need for:
-
Formal evaluation of LSW as a method of changing staff attitudes about dementia, and particularly in care homes. This should compare LSW, as such, against more general training input about dementia.
-
Qualitative research that explores the motivation and ‘emotional intelligence’ of care staff, recognising that delivering person-centred care for people with dementia requires particular qualities of both.
-
Methodological development in assessing QoL for people with dementia ‘in the moment’. Existing measures of QoL do not capture the temporary pleasure that LSW (and other interventions) may give to people with dementia, even if the interventions do not have an effect that is measurable with existing instruments. The additive effect of episodes of temporary pleasure may well be worth having, but without ways of measuring it we will never be able to tell. Given the predominance of QoL measurement in health economics, and thereby its influencing on commissioning, we believe that this type of development is essential to the future of good-quality care for people with dementia. Such development would need to be multidisciplinary, involving cognitive psychologists and health economists as well as health service researchers.
Acknowledgements
First, our thanks must go to the people living with dementia, their families and friends, and staff working with them who volunteered to take part in this project when they had many other demands on their time and energy.
Our external partners gave support to the project from the start and acted as a steering group throughout, and without their dedication the research could not have gone ahead: Nada Savitch (Innovations in Dementia); Polly Kaiser (Pennine Care NHS Foundation Trust); and Jean Tottie (Life Story Network).
We would also like to thank our project advisory group, including our two networks of ‘virtual advisors’ (co-ordinated by Steve Milton of Innovations in Dementia and Joy Watkins of Uniting Carers), who provided invaluable comments and guidance throughout the study.
Professor Esme Moniz-Cook (Humber NHS Foundation Trust) acted as a specialist advisor to the project and advised on the selection of outcome measures. Victoria Allgar (Hull York Medical School) provided statistical advice to the project. Dr Linda Cusworth was involved in the design of the survey of carers, and carried out preliminary analysis of the data from that survey. Julie Glanville (York Health Economics Consortium) conducted specialist literature searches for the review. Lara Charlesworth (University of Leeds) contributed to the feasibility study fieldwork. We are grateful to all of them.
We are indebted to the authors of the outcome measures for allowing us to use these in our research: Professor Rebecca Logsdon (QoL-AD); Dr Nele Spruytte (QCPR); Professor Sube Banerjee (DEMQOL and DEMQOL-Proxy); Dr Hareth Al-Janabi (CES); Professor Bob Woods (ADQ); Dr Sarah Goldberg (Carer Satisfaction Questionnaire); Tage Søndergård Kristensen (CBI); and Dr Paulette Hunter (PDQ).
Anonymous referees and the NIHR editorial team provided helpful comments on the draft report which have improved this final version.
Finally, our thanks to Teresa Frank, who provided invaluable administrative support throughout the project and in the production of this report, and to Sarah Boatman, for hours of data entry.
Contributions of authors
Kate Gridley (Research Fellow, Social Policy Research Unit) was principal investigator until October 2014, designed the study, managed all aspects of the study, conducted fieldwork throughout, and drafted Chapters 3, 4 and 6 and elements of Chapter 7.
Dr Jenni Brooks (Research Fellow, Social Policy Research Unit) conducted fieldwork for the feasibility studies, conducted and analysed the interviews and focus groups for this stage of the research, and drafted Chapter 9.
Professor Yvonne Birks (Professor of Health and Social Care, Social Policy Research Unit) contributed to the feasibility study design, contributed to the review and provided advice throughout.
Dr Kate Baxter (Research Fellow, Social Policy Research Unit) contributed to the design of the section of the study about the costs of LSW, analysed the resource-use and costs data, and drafted Chapter 8.
Professor Gillian Parker (Professor of Social Policy Research, Social Policy Research Unit) was principal investigator after Kate Gridley went on maternity leave in October 2014. She also designed the study, carried out the systematic review, conducted and analysed the surveys, analysed the outcome measures, drafted Chapters 1, 2, 5, 7 and 10, and was responsible for editing the final report.
Publications
Gridley K. Understanding the Outcomes of Life Story Work. In Kaiser P, Eley R, editors. Life Story Work with People with Dementia. London: Jessica Kingsley Publishers; 2016. In press.
Data sharing statement
Data extraction tables from the review and data from the feasibility study can be accessed via the corresponding author, Professor Gillian Parker.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Quality Outcomes for People with Dementia: Building on the Work of the National Dementia Strategy. London: Department of Health; 2010.
- National Institute for Health and Care Excellence . Dementia Quality Standard 2010. www.nice.org.uk/guidance/qs1 (accessed May 2016).
- Kitwood T. The experience of dementia. Aging Ment Health 1997;1:13-22. http://dx.doi.org/10.1080/13607869757344.
- Cohene T, Baecker R, Marziali E. Designing Interactive Life Story Multimedia for a Family Affected by Alzheimer’s Disease: A Case Study n.d.:1300-3. http://dx.doi.org/10.1145/1056808.1056901.
- Ryan T, Walker R. Making Life Story Books. London: British Agencies for Adoption and Fostering; 1985.
- Hewitt H. A life story approach for people with profound learning disabilities. Br J Nurs 2000;9:90-5. http://dx.doi.org/10.12968/bjon.2000.9.2.6398.
- Clarke A, Hanson E, Ross H. Seeing the person behind the patient: enhancing the care of older people using a biographical approach. J Clin Nurs 2003;12:697-706. http://dx.doi.org/10.1046/j.1365-2702.2003.00784.x.
- Gibson F. The Lost Ones: Recovering the Past to Help their Present. Stirling: Dementia Services Development Centre; 1991.
- Murphy C. It Started With a Seashell: Life Story Work and People With Dementia. Stirling: Dementia Services Development Centre; 1994.
- Kellett U, Moyle W, McAllister M, King C, Gallagher F. Life stories and biography: a means of connecting family and staff to people with dementia. J Clin Nurs 2010;19:1707-15. http://dx.doi.org/10.1111/j.1365-2702.2009.03116.x.
- McKeown J, Clarke A, Repper J. Life story work in health and social care: systematic literature review. J Adv Nurs 2006;55:237-47. http://dx.doi.org/10.1111/j.1365-2648.2006.03897.x.
- Moos I, Bjorn A. Use of the life story in the institutional care of people with dementia: a review of intervention studies. Ageing Soc 2006;26:431-54. http://dx.doi.org/10.1017/S0144686X06004806.
- Russell C, Timmons S. Life story work and nursing home residents with dementia. Nurs Older People 2009;21:28-32. http://dx.doi.org/10.7748/nop2009.05.21.4.28.c7017.
- McKeown J, Clarke A, Ingleton C, Ryan T, Repper J. The use of life story work with people with dementia to enhance person-centred care. Int J Older People Nurs 2010;5:148-58. http://dx.doi.org/10.1111/j.1748-3743.2010.00219.x.
- Case for Change – Community-Based Services for People Living With Dementia. London: Department of Health; 2011.
- See Me, Not Just the Dementia: Understanding People’s Experiences of Living in a Care Home. London: Commission for Social Care Inspection; 2008.
- Woods B, Spector A, Jones C, Orrell M, Davies SP. Reminiscence therapy for dementia. Cochrane Database Syst Rev 2005;2. http://dx.doi.org/10.1002/14651858.cd001120.pub2.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: New Guidance. London: MRC; 2008.
- Guidance for Undertaking Reviews in Health Care. York: CRD; 2008.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Lancaster: Institute for Health Research; 2006.
- Pawson R. Evidence-based policy: the promise of ‘realist synthesis’. Evaluation 2002;8:340-58. http://dx.doi.org/10.1177/135638902401462448.
- Parker G, Bhakta P, Katbamna S, Lovett C, Paisley S, Parker S, et al. Best place of care for older people after acute and during subacute illness: a systematic review. J Health Serv Res Policy 2000;5:176-89.
- Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLOS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000097.
- Crete-Nishihata M, Baecker RM, Massimi M, Ptak D, Campigotto R, Kaufman LD, et al. Reconstructing the past: personal memory technologies are not just personal and not just for memory. Hum-Comput Interact 2012;27:92-123.
- van den Brandt-van Heek ME, Kenyon G, Bohlmeijer E, Randall WL. Storying Later Life. Oxford: Oxford University Press; 2011.
- Savitch N, Stokes V. We Can Do IT Too. Milton Keynes: Speechmark; 2011.
- Berman C. Older adults with dementia: the value of Life-story Work. Bold 2009;20:19-22.
- McCarthy B. Hearing the Person with Dementia: Person-Centred Approaches to Communication for Families and Caregivers. London: Jessica Kingsley; 2011.
- Do You See Me? Recognising, Understanding and Caring for People with Dementia, Depression and Delirium. London: Let’s Respect; 2011.
- Rose S. Video portraits: creating lasting records. JDC 2006;14:23-4.
- Hagens C, Beaman A. Reminiscing, poetry writing, and remembering boxes. Activ Adapt Ageing 2003;27:97-112. http://dx.doi.org/10.1300/j016v27n03_07.
- Caron W, Hepburn K, Luptak M, Grant L, Ostwald S, Keenan J. Expanding the discourse of care: family constructed biographies of nursing home residents including commentary by Hargrave TD. Fam Syst Health 1999;17:323-35. http://dx.doi.org/10.1037/h0089873.
- Hepburn K, Caron WA, Gaugier JE. Promoting Family Involvement in Long-Term Care Settings: A Guide to Programs that Work. Baltimore, MD: Health Professions Press; 2005.
- Hepburn KW, Caron W, Luptak M, Ostwald S, Grant L, Keenan JM. The family stories workshop: stories for those who cannot remember. Gerontologist 1997;37:827-32. http://dx.doi.org/10.1093/geront/37.6.827.
- Smith KL, Damaniakis T, Baecker RM, Marziali E. Crete-Nishihata . Multimedia biographies: a reminiscence and social stimulus tool for persons with cognitive impairment. J Technol Hum Serv 2009;27:287-306. http://dx.doi.org/10.1080/15228830903329831.
- Thompson R. Using life story work to enhance care. Nurs Older People 2011;23:16-21. http://dx.doi.org/10.7748/nop2011.10.23.8.16.c8713.
- Gibson F, Marshall M. Perspectives on Rehabilitation and Dementia. London: Jessica Kingsley; 2005.
- Batson P, Thorne K, Peak J. Life story work sees the person beyond the dementia. JDC 2002;10:15-7.
- Gibson F, Carson Y. Life story work in practice: aiming for enduring change. JDC 2010;18:20-2.
- Caratella A, Reed S. Collected short stories. JDC 2011;19:16-7.
- Remembering Together: Making a Life History Book. London: Alzheimer’s Society; 2001.
- Yasuda K, Kuwabara K, Kuwahara N, Abe S, Tetsutani N. Effectiveness of personalised reminiscence photo videos for individuals with dementia. Neuropsychol Rehabil 2009;19:603-19. http://dx.doi.org/10.1080/09602010802586216.
- Williams BR, Woodby LL, Goode PS, Blizard T, Burgio KL. Forever: feasibility of life review in early dementia: veterans’ experiences remembered. Gerontologist 2011;51.
- Kelson E, Chaudhury H. Sustaining personhood in dementia care: exploring staff perception of residents’ visual life stories. Gerontologist 2008;48.
- Mackenzie J. Working with lesbian and gay people with dementia. JDC 2009;17:17-9.
- Thwaites S, Sara A. Tailor-made cognitive stimulation. JDC 2010;18:19-20.
- Rainbow A. The Reminiscence Skills Training Handbook. Bicester: Speechmark; 2003.
- Price L. Creating an interactive toolbox for the person, family and staff. JDC 2010;18.
- Dementia Skills Starters: A Set of Six Workbooks Covering Key Areas of Dementia Care. Stirling: Dementia Services Development Centre, University of Stirling; 2010.
- Hopkins G. This Is Your Life 2002. www.communitycare.co.uk/articles/07/03/2002/35387/this-is-your-life.htm (accessed 17 January 2013).
- Archibald C. Activities II. Stirling: School of Human Sciences, University of Stirling; 1993.
- Thompson R. Realising the potential: developing life story work in practice. Found Nurs Stud Dissem Ser 2010;5:1-4.
- Archibald C. Activities. Stirling: School of Human Sciences, University of Stirling; 1990.
- Burgess R. Life story project lives on. JDC 2008;16:16-7.
- Cole A, Williams H. Life story work as an aid to well-being. Signpost 2004;9:14-7.
- Egan MY, Munroe S, Hubert C, Rossiter T, Gauthier A, Eisner M, et al. Caring for residents with dementia and aggressive behavior: impact of life history knowledge. J Gerontol Nurs 2007;33:24-30.
- Haight BK, Bachman DL, Hendrix S, Wagner MY, Meeks A, Johnson J. Life review: treating the dyadic family unit with dementia. Clin Psychol Psychother 2003;10:165-74. http://dx.doi.org/10.1002/cpp.367.
- Heathcote J. Life story work in practice: magic moments. JDC 2010;18:22-4.
- Murphy C. Crackin’ Lives: An Evaluation of a Life Story Book Project to Assist Patients from a Long-Stay Psychiatric Hospital in their Move to Community Care Situations. Stirling: Dementia Services Development Centre, University of Stirling; 2000.
- Gibson F, Haight B, Michel Y, Innes A, McCabe L. Evaluation in Dementia Care. London: Jessica Kingsley; 2006.
- Gibson F. The Lost Ones; Recovering the Past to Help their Present: Practice Example 3. Stirling: Dementia Services Development Centre, University of Stirling; 1991.
- Insights No. 4. Supporting those with Dementia: Reminiscence Therapy and Life Story Work. Glasgow: Institute for Research and Innovation in Social Services; 2010.
- Day MR, Wills Y. A biographical approach. Nurs Older People 2008;20:22-4.
- Cohen GD. Two new intergenerational interventions for Alzheimer’s disease patients and families. Am J Alzheimers Dis 2000;15:137-42. http://dx.doi.org/10.1177/153331750001500304.
- Flynn Z, Chapman B. Making animated films with people with dementia. JDC 2011;19:23-5.
- Haight BK, Gibson F, Michel Y. The Northern Ireland life review/life storybook project for people with dementia. Alzheimers Dement 2006;2:56-8. http://dx.doi.org/10.1016/j.jalz.2005.12.003.
- Damianakis T, Crete-Nishihata M, Smith KL, Baecker RM, Marziali E. The psychosocial impacts of multimedia biographies on persons with cognitive impairments. Gerontologist 2010;50:23-35. http://dx.doi.org/10.1093/geront/gnp104.
- Chapman SB, Weiner MF, Rackley A, Hynan LS, Zientz J. Effects of cognitive-communication stimulation for Alzheimer’s disease patients treated with donepezil. J Speech Lang Hear Res 2004;47:1149-63. http://dx.doi.org/10.1044/1092-4388(2004/085).
- Buron B. Life history collages: effects on nursing home staff caring for residents with dementia. J Gerontol Nurs 2010;36:38-4. http://dx.doi.org/10.3928/00989134-20100602-01.
- Chaudhury H. Place-biosketch as a tool in caring for residents with dementia. Alzheimers Care Q 2002;3:42-5.
- Anonymous . Making a life story book. Alzheimers Care Q 2000;1.
- State of the Art in Dementia Care. London: Centre for Policy on Ageing; 1997.
- Archibald C. Sharing activities. JDC 1999;7:20-2.
- Baker J. Life story books for the elderly mentally ill. Int J Lang Commun Disord 2001;36:185-7. http://dx.doi.org/10.3109/13682820109177881.
- Bryan K, Maxim J. Enabling care staff to relate to older communication disabled people. Int J Lang Commun Disord 1998;33:121-5. http://dx.doi.org/10.3109/13682829809179408.
- Buron B. Promoting Personhood Among Nursing Home Residents Living With Dementia 2009.
- Buron B. Exploring life history collage exposure on personhood and person centered nursing home dementia care. Alzheimers Dement 2011;1. http://dx.doi.org/10.1016/j.jalz.2011.05.1823.
- Clarke A, Hollands J, Smith J. Windows to a Damaged World. London: Counsel and Care; 1996.
- Damianakis T, Smith K, Baecker R, Marziali E. Crete-Nishitaka . Remembering my life: the production and evaluation of individuals with Alzheimer’s or mild cognitive impairment responses to digital life histories. Gerontologist 2008;48.
- Day MR, Wills T. Mind matters. World Ir Nurs 2007;15:35-6.
- Dodd K. Psychological and other non-pharmacological interventions in services for people with learning disabilities and dementia. AMHID 2010;4:28-35. http://dx.doi.org/10.5042/amhld.2010.0056.
- Bruce E, Scheitz P, Downs M, Bowers B. Excellence in Dementia Care. Maidenhead: Open University Press; 2008.
- Gibson F, Gibson F. The Past in the Present: Using Reminiscence in Health and Social Care. Baltimore, MD: Health Professions Press; 2004.
- Gibson F. Reminiscence and Life Story Work: A Practice Guide. London: Jessica Kingsley; 2011.
- Gilfoy K, Knocker S. Magic across the generations. JDC 2009;17:22-5.
- Heathcote J. Memories are Made of This: Reminiscence Activities for Person-Centred Care. London: Alzheimer’s Society; 2007.
- Ingersoll-Dayton B. The couples’ life story project: a dyadic approach to dementia care. Gerontologist 2011;51.
- Ingersoll-Dayton B, Spencer B. A couples’ life story approach to dementia care. Gerontologist 2010;50.
- Jones GMM, Jones G, Miesen B. Care-Giving in Dementia: Research and Applications. New York, NY: Tavistock/Routledge; 1992.
- Kikhia B, Bengtsson JE, Synnes K, Sani Z, ul H, Hallberg J, et al. ICOST 2010. Berlin: Springer-Verlag; 2010.
- Killick J. When your heart wants to remember. Elderly Care 1997;9:38-9.
- Kunz JA, Kunz JA, Soltys FG. Transformational Reminiscence: Life Story Work. New York, NY: Springer Publishing Co.; 2007.
- Lai CKY, Chi I, Kayser-Jones J. A randomized controlled trial of a specific reminiscence approach to promote the well-being of nursing home residents with dementia. Int Psychogeriatr 2004;16:33-49. http://dx.doi.org/10.1017/S1041610204000055.
- Lai KY. Improving the Quality of Life for Nursing Home Residents with Dementia: A Life Story Approach. Hong Kong: University of Hong Kong; 2004.
- Luyendyk K. Using life histories to enhance dementia caregiving. Can Nurs Home 2007;18:4-6.
- Magniant RCP, Magniant RCP. Art Therapy with Older Adults: A Sourcebook. Springfield, IL: Charles C Thomas Publisher; 2004.
- May H, Edwards P, Brooker D, May H, Edwards P, Brooker D. Enriched Care Planning for People with Dementia: A Good Practice Guide for Delivering Person-Centred Care. London: Jessica Kingsley Publishers; 2009.
- Mitchell R. Shooting into the past. Nurs Older People 2006;18:12-4.
- Ryan EB, Martin LS, Beaman A. Communication strategies to promote spiritual well-being among people with dementia. J Pastoral Care Counsel 2005;59:43-55. http://dx.doi.org/10.1177/154230500505900105.
- Shi L, Setchi R. User-oriented ontology-based clustering of stored memories. Expert Syst Appl 2012;39:9730-42. http://dx.doi.org/10.1016/j.eswa.2012.02.087.
- Woods RT, Portnoy S, Head D, Jones G, Gemma M, Jones M, et al. Care-Giving in Dementia: Research and Applications. New York, NY: Tavistock/Routledge; 1992.
- Petrukowicz MA, Johnson MMS. Using life histories to individualise nursing home staff attitudes towards residents. Gerontologist 1991;31:102-6. http://dx.doi.org/10.1093/geront/31.1.102.
- Pinquart M, Forstmeier S. Effects of reminiscence interventions on psychosocial outcomes: a meta-analysis. Aging Ment Health 2012;16:541-58. http://dx.doi.org/10.1080/13607863.2011.651434.
- Vasse E, Spijker A, Rikkert MO, Koopmans R. Vernooij-Dassen . A systematic review of communication strategies for people with dementia in residential and nursing homes. Int Psychogeriatr 2010;22:189-200. http://dx.doi.org/10.1017/S1041610209990615.
- Subramaniam P, Woods B. The impact of individual reminiscence therapy for people with dementia: systematic review. Expert Rev Neurother 2012;12:545-55. http://dx.doi.org/10.1586/ern.12.35.
- Gridley K, Brooks J, Birks Y, Baxter K, Parker G. Improving Care for People With Dementia: Development and Initial Feasibility Study for Evaluation of Life Story Work in Dementia Care (Research Protocol) n.d. www.nets.nihr.ac.uk/__data/assets/pdf_file/0005/81761/PRO-11-2000-11.pdf (accessed 9 August 2016).
- Trivedi D, Goodman C, Gage H, Baron N, Scheibl F, Iliffe S, et al. The effectiveness of inter-professional working for older people living in the community: a systematic review. Health Soc Care Community 2013;21:113-28. http://dx.doi.org/10.1111/j.1365-2524.2012.01067.x.
- Haywood KL. Patient-reported outcome I: measuring what matters in musculoskeletal care. Musculoskeletal Care 2006;4:187-203. http://dx.doi.org/10.1002/msc.94.
- Hewlett SA. Patients and clinicians have different perspectives on outcomes in arthritis. J Rheumatol 2003;30:877-9.
- Shumway M, Saunders T, Shern D, Pines E, Downs A, Burbine T, et al. Preferences for schizophrenia treatment outcomes among public policy makers, consumers, families, and providers. Psychiatr Serv 2003;54:1124-8. http://dx.doi.org/10.1176/appi.ps.54.8.1124.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- McAdams DP. The Stories we Live by: Personal Myths and the Making of the Self. New York, NY: William Morrow; 1993.
- Scherrer KS, Ingersoll-Dayton B, Spencer B. Constructing couples’ stories: narrative practice insights from a dyadic dementia intervention. Clin Soc Work J 2014;42:90-100. http://dx.doi.org/10.1007/s10615-013-0440-7.
- Butler RN. The life review: an interpretation of reminiscence in the aged. Psychiatry 1963;26:65-76.
- Morgan S, Woods RT. Life review with people with dementia in care homes: a preliminary randomized controlled trial. Non-Pharmacol Ther Dementia 2010;1:43-59.
- Kitwood T. Towards a theory of dementia care: the interpersonal process. Ageing Soc 1993;13:51-67. http://dx.doi.org/10.1017/S0144686X00000647.
- Kitwood T. Dementia Reconsidered: The Person Comes First. Buckinghamshire: Open University Press; 1997.
- Moniz-Cook E, Vermooij-Dassen M, Woods R, Verhey F, Chattat R, De Vugt M, et al. A European consensus on outcome measures for psychosocial intervention research in dementia care. Aging Ment Health 2008;12:14-29. http://dx.doi.org/10.1080/13607860801919850.
- Banerjee S, Samsi K, Petrie CD, Alvir J, Treglia M, Schwam EM, et al. What do we know about quality of life in dementia? A review of the emerging evidence on the predictive and explanatory value of disease specific measures of health related quality of life in people with dementia. Int J Geriatr Psychiatry 2009;24:15-24. http://dx.doi.org/10.1002/gps.2090.
- Smith SC, Lamping DL, Banerjee S, Harwood RH, Foley B, Smith P, et al. The development of a new measure of health related quality of life for people with dementia: DEMQOL. Psychol Med 2007;37:737-46. http://dx.doi.org/10.1017/S0033291706009469.
- Logsdon RG, Gibbons LE, McCurry SM, Logsdon RG, Gibbons LE, McCurry SM, et al. Assessing quality of life in older adults with cognitive impairment. Psychosom Med 2002;64:510-19. http://dx.doi.org/10.1097/00006842-200205000-00016.
- Bowling A, Rowe G, Adams S, Sands P, Samsi K, Crane M, et al. Quality of life in dementia: a systematically conducted narrative review of dementia-specific measurement scales. Aging Ment Health 2015;19:13-31. http://dx.doi.org/10.1080/13607863.2014.915923.
- Bouman AIE, Ettema TP, Wetzels RB, van Beek APA, de Lange J, Droes RM. Evaluation of QUALIDEM: a dementia-specific quality of life instrument for persons with dementia in residential settings; scalability and reliability in four Dutch field surveys. Int J Geriatr Psychiatry 2011;26:711-22. http://dx.doi.org/10.1002/gps.2585.
- Spruytte N, Van Audenhove C, Lammertyn F, Storms G. The quality of the caregiving relationship in informal care for older adults with dementia and chronic psychiatric patients. Psychol Psychother 2002;75:295-311. http://dx.doi.org/10.1348/147608302320365208.
- Kuhn MH, McPartland S. An empirical investigation of self-attitudes. Am Sociol Rev 1954;19:65-76. http://dx.doi.org/10.2307/2088175.
- Addis DR, Tippett LJ. Memory of myself: autobiographical memory and identity in Alzheimer’s disease. Memory 2004;12:56-74. http://dx.doi.org/10.1080/09658210244000423.
- Al-Janabi H, Flynn T, Coast J. Estimation of a preference-based carer experience scale. Med Decis Making 2011;31:458-68. http://dx.doi.org/10.1177/0272989X10381280.
- Goldberg SE, Bradshaw LE, Kearney FC, Russell C, Whittamore KH, Foster PER, et al. Care in a specialist medical and mental health unit compared with standard care for older people with cognitive impairment admitted to a general hospital: a randomised controlled trial (NIHR TEAM trial). BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f4132.
- Lintern T. Quality in Dementia Care: Evaluating Staff Attitudes and Behaviour 2001.
- Hunter P, Hadjistavropoulos T, Smythe W, Malloy D, Kaasalainen S, Williams J. The personhood in dementia questionnaire (PDQ): establishing an association between beliefs about personhood and health providers’ approaches to person-centred care. J Aging Stud 2013;27:276-87. http://dx.doi.org/10.1016/j.jaging.2013.05.003.
- Subramaniam P, Woods B, Whitaker C. Life review and life story books for people with mild to moderate dementia: a randomised controlled trial. Aging Ment Health 2014;18:363-75. http://dx.doi.org/10.1080/13607863.2013.837144.
- Maslach C, Jackson SE. Maslach Burnout Inventory Manual. Palo Alto, CA: Consulting Psychologists Press; 1986.
- Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress 2005;19:192-207. http://dx.doi.org/10.1080/02678370500297720.
- Brown CA, Lilford RJ. The stepped wedge trial design: a systematic review. BMC Med Res Methodol 2006;6. http://dx.doi.org/10.1186/1471-2288-6-54.
- Department of Health . Policy: Dementia n.d. www.gov.uk/government/policies/improving-care-for-people-with-dementia (accessed July 2014).
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98. http://dx.doi.org/10.1016/0022-3956(75)90026-6.
- Centre for Dementia Studies, Brighton and Sussex Medical School . DEMQOL and DEMQOL-Proxy – Interview Manual n.d. www.bsms.ac.uk/_pdf/cds/interviewer-manual.pdf (accessed 9 August 2016).
- Moyle W, Murfield JE, Griffiths SG, Venturato L. Assessing quality of life of older people with dementia: a comparison of quantitative self-report and proxy accounts. J Adv Nurs 2012;68:2237-46. http://dx.doi.org/10.1111/j.1365-2648.2011.05912.x.
- Fowler FJ. Improving Survey Questions: Design and Evaluation. Thousand Oaks, CA: Sage Publications; 1995.
- Davies SL, Goodman C, Manthorpe J, Smith A, Carrick N, Iliffe S. Enabling research in care homes: an evaluation of a national network of research ready care homes. BMC Med Res Methodol 2014;14. http://dx.doi.org/10.1186/1471-2288-14-47.
- Trigg R, Watts S, Jones R, Tod A. Predictors of quality of life ratings from persons with dementia: the role of insight. Int J Geriatr Psychiatry 2011;26:83-91. http://dx.doi.org/10.1002/gps.2494.
- Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: Personal Social Services Research Unit, University of Kent; 2011.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2015.
- Department of Health . Reference Costs 2012 to 2013. National Schedule of Reference Costs: The Main Schedule 2013. www.gov.uk/government/publications/nhs-reference-costs-2012-to-2013 (accessed 14 June 2016).
- Chisholm D, Knapp MRJ, Knudsen HC, Amaddeo F, Gaite L, Van Wijngaarden B, et al. Client socio-demographic and service receipt inventory – European Version: development of an instrument for international research. Br J Psychiatry Suppl 2000;177:s28-33. http://dx.doi.org/10.1192/bjp.177.39.s28.
- Moniz-Cook E, Woods R, Gardiner E, Silver M, Agar S. The challenging behaviour scale (CBS): development of a scale for staff caring for older people in residential and nursing homes. Br J Clin Psychol 2001;40:309-22. http://dx.doi.org/10.1348/014466501163715.
- Dritschel BH, Williams JMG, Baddeley AD, Nimmo-Smith I. Autobiographical fluency: a method for the study of personal memory. Mem Cognit 1992;20:133-40. http://dx.doi.org/10.3758/BF03197162.
Appendix 1 Tables
| Database | Interface |
|---|---|
| MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations | OvidSP |
| EMBASE | OvidSP |
| PsycINFO | OvidSP |
| Cumulative Index to Nursing and Allied Health Literature | EBSCOhost |
| Cochrane Database of Systematic Reviews | The Cochrane Library/Wiley Online Library |
| Cochrane Central Register of Controlled Trials | The Cochrane Library/Wiley Online Library |
| Database of Abstracts of Reviews of Effects | The Cochrane Library/Wiley Online Library |
| Health Technology Assessment database | The Cochrane Library/Wiley Online Library |
| Science Citation Index | Web of Science |
| Social Sciences Citation Index | Web of Science |
| Conference Proceedings Citation Index – Science | Web of Science |
| Conference Proceedings Citation Index: Social Science & Humanities | Web of Science |
| Social Policy and Practice | Ovid |
| Social Services Abstracts | ProQuest |
| Social Care Online | www.scie-socialcareonline.org.uk/ |
| Research Register for Social Care | www.researchregister.org.uk/ |
| Applied Social Sciences Index and Abstracts | ProQuest |
| ClinicalTrials.gov | www.clinicaltrials.gov |
| NHS Evidence | www.evidence.nhs.uk/ |
| OpenGrey | www.opengrey.eu/ |
| Resource | Number of records identified |
|---|---|
| MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations | 123 |
| EMBASE | 171 |
| PsycINFO | 177 |
| Social Policy and Practice | 165 |
| Cochrane Database of Systematic Reviews | 2 |
| Cochrane Central Register of Controlled Trials | 6 |
| Database of Abstracts of Reviews of Effects | 6 |
| Health Technology Assessment database | 1 |
| Science Citation Index Expanded, Social Sciences Citation Index, Conference Proceedings Citation Index – Science, Conference Proceedings Citation Index: Social Science & Humanities | 224 |
| Cumulative Index to Nursing and Allied Health Literature | 104 |
| Applied Social Sciences Index and Abstracts | 33 |
| Social Services Abstracts | 19 |
| Social Care Online | 113 |
| Research Register for Social Care | 0 |
| ClinicalTrials.gov | 2 |
| NHS Evidence | 53 |
| OpenGrey | 0 |
| Additional studies identified from reference lists of studies included for review | 19 |
| Total | 1218 |
| Total after deduplication | 657 |
| Primary study publication details | Further exclusion as not relevant | Excluded from both reviews | Good practice review | Theory of change review |
|---|---|---|---|---|
| Alzheimer’s Society. Remembering Together: Making a Life History Book. London: Alzheimer’s Society; 200141 | Y | Y | ||
| Anon. Making a life story book. Alzheimers Care Q 2000;1:4371 | X | Y | ||
| Archibald C. Activities II. Stirling: School of Human Sciences, University of Stirling; 199351 | X | Y | ||
| Archibald C. Activities. Stirling: School of Human Sciences, University of Stirling; 199053 | X | Y | ||
| Archibald C. Sharing activities. J Dement Care 1999;7:20–273 | X | |||
| Baker J. Life story books for the elderly mentally ill. Int J Lang Commun Disord 2001;36(Suppl.):185–774 | X | |||
| Batson P, Thorne K, Peak J. Life story work sees the person beyond the dementia. J Dement Care 2002;10:15–1738 | Y | Y | ||
| Berman C. Older adults with dementia: the value of Life-story Work. Bold 2009;20:19–2227 | Y | |||
| Bruce E, Scheitz P. Working with Life History. In Downs M, Bowers B., editors. Excellence in Dementia Care. Maidenhead: Open University Press; 2008. pp. 168–8582 | X | |||
| Bryan K, Maxim J. Enabling care staff to relate to older communication disabled people. Int J Lang Commun Disord 1998;33(Suppl.):121–575 | X | |||
| Burgess R. Life story project lives on. J Dement Care 2008;16:16–1754 | Y | |||
| Buron B. Exploring life history collage exposure on personhood and person centered nursing home dementia care. Alzheimers Dement 2011;1:S63777 | X | |||
| Buron B. Life history collages: effects on nursing home staff caring for residents with dementia. J Gerontol Nurs 2010;36:38–4869 | Y | |||
| Buron B. Promoting Personhood among Nursing Home Residents Living with Dementia. PhD thesis. Little Rock, AR: University of Arkansas; 200976 | X | |||
| Caratello A, Reed S. Collected short stories. J Dement Care 2011;19:16–1740 | Y | |||
| Caron W, Hepburn K, Luptak M, Grant L, Ostwald S, Keenan J. Expanding the discourse of care: family constructed biographies of nursing home residents including commentary by Hargrave TD. Families Systems Health 1999;17:323–3532 | Y | Y | ||
| Centre for Policy on Ageing. State of the Art in Dementia Care. London: Centre for Policy on Ageing; 199772 | X | |||
| Chapman SB, Weiner MF, Rackley A, Hynan LS, Zientz J. Effects of cognitive-communication stimulation for Alzheimer’s disease patients treated with donepezil. J Speech Lang Hearing Res 2004;47:1149–6368 | Y | |||
| Chaudhury H. Place-biosketch as a tool in caring for residents with dementia. Alzheimers Care Q 2002;3:42–570 | Y | |||
| Clarke A, Hanson EJ, Ross H. Seeing the person behind the patients: enhancing the care of older people using a biographical approach. J Clin Nurs 2003;12:697–7067 | Y | Y | ||
| Clarke A, Hollands J, Smith J. Windows to a Damaged World. London: Counsel and Care; 199678 | X | |||
| Cohen GD. Two new intergenerational interventions for Alzheimer’s disease patients and families. Am J Alzheimers Dis 2000;15:137–4264 | Y | |||
| Cole A, Williams H. Life story work as an aid to well-being. Signpost 2004;9:14–1755 | Y | |||
| Crete-Nishihata M, Baecker RM, Massimi M, Ptak D, Campigotto R, Kaufman LD, et al. Reconstructing the past: personal memory technologies are not just personal and not just for memory. Hum-Computer Interact 2012;27:92–12324 | Y | |||
| Damianakis T, Crete-Nishihata M, Smith KL, Baecker RM, Marziali E. The psychosocial impacts of multimedia biographies on persons with cognitive impairments. Gerontologist 2010:50:23–3567 | Y | |||
| Damianakis T, Crete-Nishitaka, Smith K, Baecker R, Marziali E. Remembering my life: the production and evaluation of individuals with Alzheimer’s or mild cognitive impairment responses to digital life histories. Gerontologist 2008:48(Special Issue III):32479 | X | |||
| Day MR, Wills T. Mind matters. World Irish Nurs Midwifery 2007;15:35–680 | X | |||
| Day MR, Wills Y. A biographical approach. Nurs Older People 2008;20:22–2463 | Y | |||
| Dodd K. Psychological and other non-pharmacological interventions in services for people with learning disabilities and dementia. Adv Ment Health Learning Disabilities 2010;4:28–3581 | X | |||
| Egan MY, Munroe S, Hubert C, Rossiter T, Gauthier A, Eisner M, et al. Caring for residents with dementia and aggressive behaviour: impact of life history knowledge. J Gerontol Nurs 2007;33:24–3056 | Y | Y | ||
| Flynn Z, Chapman B. Making animated films with people with dementia. J Dement Care 2011;19:23–565 | Y | |||
| Gibson F, Carson Y. Life story work in practice: aiming for enduring change. J Dement Care 2010;18:20–239 | Y | |||
| Gibson F, Haight B, Michel Y. Evaluating Long-Stay Care Settings: A Study of a Life Review and Life Story Book Project. In Innes A, McCabe L, editors. Evaluation in Dementia Care. London: Jessica Kingsley; 2006. pp. 124–4360 | Y | Y | ||
| Gibson F. Fit for Life: The Contribution of Life Story Work. In Marshall M, editor. Perspectives on Rehabilitation and Dementia. London: Jessica Kingsley Publishers; 2005. pp. 175–937 | Y | |||
| Gibson F. Reminiscence with People with Dementia and their Carers. In Gibson F, editor. Reminiscence and Life Story Work: A Practice Guide. London: Jessica Kingsley; 2011. pp. 187–21784 | X | |||
| Gibson F. The Lost Ones; Recovering the Past to Help their Present: Practice Example 3. Stirling: University of Stirling, Dementia Services Development Centre; 199161 | X | |||
| Gibson, F. Tangible Representations of Reminiscence. In Gibson F. The Past in the Present: Using Reminiscence in Health and Social Care. 2004, Baltimore, MD: Health Professions Press; 200483 | X | |||
| Gilfoy K, Knocker S. Magic across the generations. J Dement Care 2009;17:22–585 | X | |||
| Hagens C, Beaman A. Reminiscing, poetry writing, and remembering boxes. Activities Adaptation Ageing 2003;27:3–4, 97–11231 | Y | Y | ||
| Haight BK, Bachman DL, Hendrix S, Wagner MY, Meeks A, Johnson J. Life review: treating the dyadic family unit with dementia. Clin Psychol Psychother 2003;10:165–7457 | Y | Y | ||
| Haight BK, Gibson F, Michel Y. The Northern Ireland life review/life storybook project for people with dementia. Alzheimers Dement 2006;2:56–5866 | Y | |||
| Heathcote J. Life story work in practice: magic moments. J Dement Care 2010;18:22–2458 | Y | |||
| Heathcote J. Memories are Made of This: Reminiscence Activities for Person-Centred Care. London: Alzheimer’s Society; 200786 | X | |||
| Hepburn K, Caron WA. The Family Stories Workshop. In Gaugier J, editor. Promoting Family Involvement in Long-Term Care Settings: A Guide to Programs That Work. Baltimore, MD: Health Professions Press; 2005. pp. 143–6133 | Y | |||
| Hepburn KW, Caron W, Luptak M, Ostwald S, Grant L, Keenan JM. The family stories workshop: stories for those who cannot remember. Gerontologist 1997;37:827–3234 | Y | Y | ||
| Hopkins G. This is Your Life. Community Care; 2002. URL: www.communitycare.co.uk/articles/07/03/2002/35387/this-is-your-life.htm50 | Y | |||
| Ingersoll-Dayton B, Spencer B. A couples’ life story approach to dementia care. Gerontologist 2010;50(Suppl. 1):36888 | X | |||
| Ingersoll-Dayton, B. The couples’ life story project: a dyadic approach to dementia care. Gerontologist 2011;51(Suppl. 2):1487 | X | |||
| Institute for Research and Innovation in Social Services. Insights No. 4. Supporting those with Dementia: Reminiscence Therapy and Life Story Work. Glasgow: Institute for Research and Innovation in Social Services; 201062 | Y | |||
| Jones GMM. A Nursing Model for the Care of the Elderly. In Jones G, Miesen B. Care-Giving in Dementia: Research and Applications (Vol. 1). New York, NY: Tavistock/Routledge; 1992. pp. 100–1889 | X | |||
| Kellett U, Moyle W, McAllister M, King C, Gallagher F. Life stories and biography: a means of connecting family and staff to people with dementia. J Clin Nurs 2010;19:1707–1510 | Y | Y | ||
| Kelson E, Chaudhury H. Sustaining personhood in dementia care: exploring staff perception of residents’ visual life stories. Gerontologist 2008;48(Special Issue III):23744 | Y | |||
| Kikhia B, Bengtsson JE, Synnes K, Sani Z ul H, Hallberg J. Creating Digital Life Stories through Activity Recognition with Image Filtering, in Ageing Friendly Technology for Health and Independence. In Lee Y, et al., editors. ICOST 2010. Berlin: Springer-Verlag; 2010. pp. 203–1090 | X | |||
| Killick J. When your heart wants to remember. Elderly Care1997;9:38–991 | X | |||
| Kunz JA. Mental Health Applications of Reminiscence and Life Review. In Transformational Reminiscence: Life Story Work. New York, NY: Springer Publishing Co; 2007. pp. 155–8092 | X | |||
| Lai CKY, Chi I, Kayser-Jones J, A randomised controlled trial of a specific reminiscence approach to promote the well-being of nursing home residents with dementia. Int Psychogeriatr 2004;16:33–4993 | X | |||
| Lai KY. Improving the Quality of Life for Nursing Home Residents with Dementia: A Life Story Approach. PhD thesis. Hong Kong: University of Hong Kong; 200494 | X | |||
| Let’s Respect. Do You See Me? Recognising, Understanding and Caring for People with Dementia, Depression and Delirium. London: Let’s Respect; 201129 | Y | |||
| Luyendyk K. Using life histories to enhance dementia caregiving. Can Nurs Home 2007;18:4–695 | X | |||
| Mackenzie J. Working with lesbian and gay people with dementia. J Dement Care 2009;17:17–1945 | Y | |||
| Magniant RCP. Lifebooks with Older Adults: Making Memories Last. In Magniant RCP, editor. Art Therapy with Older Adults: A Source book. Springfield, IL: Charles C Thomas Publisher; 2004. pp. 53–6896 | X | |||
| May H, Edwards P, Brooker D. Life Story. In May H, Edwards P, Brooker D. Enriched Care Planning for People with Dementia: A Good Practice Guide for Delivering Person-Centred Care. London: Jessica Kingsley Publishers; 2009. pp. 23–3297 | X | |||
| McCarthy B. Hearing the Person with Dementia: Person-Centred Approaches to Communication for Families and Caregivers. London: Jessica Kingsley; 201128 | Y | |||
| McKeown J, Clarke A, Ingleton C, Ryan T, Repper J. The use of life story work with people with dementia to enhance person-centred care. Int J Older People Nurs 2010;5:148–5814 | Y | Y | ||
| Mitchell R. Shooting into the past. Nurs Older People 2006;18:12–1498 | X | |||
| Murphy C. ‘It Started with a Sea-Shell’: Life Story Work and People with Dementia. Stirling: University of Stirling, Dementia Services Development Centre; 19949 | Y | |||
| Murphy C. Crackin’ Lives: An Evaluation of a Life Story Book Project to Assist Patients from a Long-Stay Psychiatric Hospital in their Move to Community Care Situations. Stirling: University of Stirling, Dementia Services Development Centre; 200059 | Y | Y | ||
| Petrukowicz MA, Johnson MMS. Using life histories to individualise nursing home staff attitudes towards residents. Gerontologist 1991;31:102–6102 | X | |||
| Price L. Creating an interactive toolbox for the person, family and staff. J Dement Care 2010;18:1748 | Y | |||
| Rainbow A. The Reminiscence Skills Training Handbook. Bicester: Speechmark; 200347 | Y | |||
| Rose S. Video portraits: creating lasting records. J Dement Care 2006;14:23–430 | Y | |||
| Ryan EB, Martin LS, Beaman A. Communication strategies to promote spiritual well-being among people with dementia. J Pastoral Care Counseling 2005;59:43–5599 | X | |||
| Savitch N, Stokes V. We Can Do IT Too. Milton Keynes: Speechmark; 201126 | Y | |||
| Shi L, Setchi R. User-oriented ontology-based clustering of stored memories. Expert Syst Appl 2012;39:9730–42100 | X | |||
| Smith KL, Crete-Nishihata, Damaniakis T, Baecker RM, Marziali E. Multimedia biographies: a reminiscence and social stimulus tool for persons with cognitive impairment. J Technol Hum Serv 2009;27:287–30635 | Y | |||
| Thompson R. Realising the potential: developing life story work in practice. Foundation Nurs Stud 2010;5:1–452 | Y | |||
| Thompson R. Realising the Potential: Developing Life Story Work in Practice. Final Report. 2009 | Y | |||
| Thompson R. Using life story work to enhance care. Nurs Older People 2011;23:16–2136 | Y | |||
| Thwaites S, Sara A. Tailor-made cognitive stimulation. J Dement Care 2010;18:19–2046 | Y | |||
| University of Stirling Dementia Services Development Centre. Dementia Skills Starters: A Set of Six Workbooks Covering Key Areas of Dementia Care. Stirling: University of Stirling Dementia Services Development Centre; 201049 | Y | |||
| van den Brandt-van-Heek M-E. Asking the Right Questions: Enabling People with Dementia to Speak for Themselves. In Kenyon G, Bohlmeijer E, Randall WL, editors. Storying Later Life. Oxford: Oxford University Press; 2011. pp. 338–5325 | Y | |||
| Williams BR, Woodby LL, Goode PS, Blizard T, Burgio KL. Forever: feasibility of life review in early dementia: Veterans’ experiences remembered. Gerontologist 2011;51(Suppl. 2):56943 | Y | Y | ||
| Williams BR. Feasibility of Life Review in Early Dementia: Veterans’ Experiences Remembered. URL: www.hsrd.research.va.gov/research/abstracts.cfm?Project ID=2141700380#.UWV5qJPvsmM | ||||
| Woods RT, Portnoy S, Head D, Jones G. Reminiscence and Life Review with Persons with Dementia: Which Way Forward? In Jones GM, Meisen B. editors. Care-Giving in Dementia: Research and Applications. New York, NY; Tavistock/Routledge: 1992. pp. 137–61101 | X | |||
| Yasuda K, Kuwabara K, Kuwahara N, Abe S, Tetsutani N. Effectiveness of personalised reminiscence photo videos for individuals with dementia. Neuropsychol Rehabil 2009;19:603–1942 | Y | Y | ||
| n = 83 | 6 | 27 | 47 | 18 |
| Systematic reviews and meta-analyses | Good practice review | Theory of change review |
|---|---|---|
| McKeown J, Clarke A, Repper J. Life story work in health and social care: systematic literature review. J Adv Nurs 2006;55:237–4711 | Y | N |
| Moos I, Bjorn A. Use of the life story in the institutional care of people with dementia: a review of intervention studies. Ageing Soc 2006;26:431–54 | N | N |
| Pinquart M, Forstmeier S. Effects of reminiscence interventions on psychosocial outcomes: a meta-analysis. Ageing Ment Health 2012;16:541–58103 | N | N |
| Subramaniam P, Woods B. The impact of individual reminiscence therapy for people with dementia: systematic review. Expert Rev Neurother 2012;12:545–5570 | Y | N |
| Vasse E, Vernooij-Dassen, Spijker A, Rikkert MO, Koopmans R. A systematic review of communication strategies for people with dementia in residential and nursing homes. Int Psychogeriatr 2010;22:189–200104 | N | N |
| Woods B, Spector AE, Jones CA, Orrell M, Davies SP. Reminiscence therapy for dementia. Cochrane Database Syst Rev 2005;18:CD00112017 | N | N |
| n = 6 | 2 | 0 |
| First author and date | Country | Type of publication or study | Setting | n involved | Methods used, if research | Who delivered LSW? |
|---|---|---|---|---|---|---|
| Alzheimer’s Society 200141 | UK | Guide to practice | – | – | – | – |
| Archibald 199051 | UK | Guide to practice | – | – | – | – |
| Archibald 199353 | UK | Guide to practice | – | – | – | – |
| Batson 200238 | UK | Evaluation of LSW | Home/care home | 9 | Semistructured interviews | Health-care professionals |
| Berman 200927 | Malta | Theoretical | – | – | – | – |
| Burgess 200854 | UK | Description of LSW project | Day club | 20 | – | Facilitator and care staff |
| Buron 201069 | USA | Evaluation of LSW | Nursing home | Five people with dementia, 36 staff | Pre-test, post-test staff individualised care measure | Nursing care staff |
| Caron 199932 | USA | Description of LSW project | Nursing home | At least 12 ‘biography groups’ of family carers | – | Not entirely clear but probably care staff and a facilitator |
| Catarella 201140 | UK | Description of LSW project | Care home | Staff and 20 family members | – | Social enterprise specialising in life story products |
| Chapman 200468 | USA | Evaluation of LSW when in combination with Donepezil | Own home | 54 with mild to moderate Alzheimer’s Disease | RCT (creation of life story book plus drug vs. drug + placebo condition) | Speech and language therapists/students |
| Chaudhury 200270 | USA | Evaluation of LSW | Nursing home | 12 people with dementia and their family carers, plus 12 professional and care staff | ‘Short survey’ n.o.s. | Not clear but probably the author |
| Clarke 20037 | UK | Evaluation of LSW project | Transitional care unit in NHS trust and nursing home | Qualitative before and after design, with focus groups with staff in both settings and semistructured interviews with people with dementia and family members | Support workers in care settings | |
| Cohen 200064 | USA | Description and underpinning rational for LSW, early evaluation also | Not clear but evaluation appears to be in a long-term care setting | 40 people with dementia in evaluation | Not clear but appears to be pre-test, post-test | Not entirely clear but seems to involve college students as volunteers and family members of people with dementia |
| Cole 200455 | UK | Description of LSW project and how to do it advice | Mobile community day service | Not stated | – | Not clear – care staff? |
| Crete-Nishihata 201224 | Canada | Evaluation of LSW | Not clear but perhaps own home and long-term care settings | 12 people with dementia and their family members | Semistructured interviews with family members | Family members with support from research assistants |
| Damianakis 201067 | Canada | Evaluation of LSW (related to R23) | 10 in own home, two in long-term care setting | 12 family members of people with dementia (six with diagnosed AD and six with diagnosed MCI) | Observation and in-depth interviews | Family members supported by ‘multi-media biographers and social workers’ |
| Day 200863 | UK | Guide to practice | – | – | – | – |
| Egan 200756 | Canada | Evaluation of LSW | Long-term care settings | Four people with dementia and all staff who worked with them | Single subject, repeated measures design logging aggressive behaviours, plus interviews with staff | Research assistants |
| Flynn 201165 | UK | Description of LSW | Varied care and housing settings | Not reported | – | Authors |
| Gibson 199161 | UK | Guide to practice | – | – | – | – |
| Gibson 200537 | n/a | Description of LSW | – | – | – | – |
| Gibson 200660 | UK | Evaluation of LSW | Residential care setting | 30 people with dementia, 14 care staff | Pilot study using pre-test, post-test design and control group. Range of standardised measures | Not entirely clear. One part of chapter mentions family members (p. 128), but rest of chapter is about care staff |
| Gibson 201039 | UK | Description of LSW project | NHS trust settings | 30 staff from 15 ‘facilities’ | – | NHS staff n.o.s. |
| Hagens 200331 | Canada | Evaluation of LSW project | Nursing home | Five people with confirmed cognitive impairment | Participant observation and interviews with two residents | Authors |
| Haight 200357 | USA | Evaluation of LSW when done with and without family carer | Not clear but appears to be in own home | 22 pairs of people with dementia and family carers | Pre-test, post-test comparing LSW with and without involvement of family carer, and a control condition | Not entirely clear but seems that authors worked with people with dementia and carers |
| Haight 200666 | UK | Evaluation of LSW | Long-term care settings | 30 people with dementia and 15 care staff | Pilot study of 15 intervention and 15 controls | Care staff and people with dementia, with family input |
| Heathcote 201058 | UK | Guide to practice | – | – | – | – |
| Hepburn 199734 | USA | Description and ‘field testing’ of LSW | Nursing homes | – | – | Professional facilitator and family members |
| Hepburn 200533 | USA | As above | As above | – | – | As above |
| Hopkins 200250 | UK | Description of LSW project | Residential care setting | Two staff in each of two ‘care communities’ | – | Care staff |
| IRISS 201062 | UK | Description of LSW | – | – | – | – |
| Kellett 201010 | Australia | Evaluation of LSW | Residential care | Seven family members, seven care staff | Qualitative pilot study using focus groups with participants | Family members and care staff facilitated by researcher |
| Kelson 200844 | Canada | Evaluation of LSW | Long-term care settings | Not reported | Qualitative study using focus groups with care staff | Not reported, possibly one of the authors |
| Let’s Respect 201129 | UK | Guide to practice | – | – | – | – |
| Mackenzie 200945 | UK | Guide to practice | – | – | – | – |
| McCarthy 201128 | UK | Guide to practice | – | – | – | – |
| McKeown 201014 | UK | Evaluation of LSW | NHS inpatient and day care settings | Four people with dementia, their family carers and care staff | Multiple case study design. Semistructured interviews, observation and conversation | Author facilitated |
| Murphy 19949 | UK | Evaluation of LSW project | Nursing homes | 34 care and nursing staff in two homes, seven family friends/carers, four people with dementia | Individual interviews – not clear if structured or unstructured | Not clear – perhaps advocacy service that funded project |
| Murphy 200059 | UK | Description of LSW and guide to practice | – | – | – | – |
| Price 201048 | UK | Description of LSW project | Specialist ward in NHS trust | – | – | Care staff |
| Rainbow 200347 | UK | Guide to practice | – | – | – | – |
| Rose 200630 | UK | Description of LSW | Range of settings | – | – | Author who is a film-maker works with people with dementia and family members |
| Savitch 201126 | UK | Guide to practice | – | – | – | – |
| Smith 200935 | Canada | Description of LSW project (related to studies 25 and 72) | See 25 and 72 | See 25 and 72 | See 25 and 72 | See 25 and 72 |
| Thompson 201052 | UK | Evaluation of LSW project | Seven older adult mental health service wards in two NHS trusts | Various | Mixed methods design, including before and after test of staff attitudes and staff questionnaire, reflection, and feedback from family members | Admiral Nurses worked with staff to facilitate use of LSW |
| Thompson 201136 | UK | Guide to practice | – | – | – | – |
| Thwaites 201046 | UK | Description of LSW project | Inpatient setting in NHS trust | – | – | Care staff |
| USDSDC 201149 | UK | Guide to practice | – | – | – | – |
| van den Brandt-van-Heek 201125 | The Netherlands | Guide to practice | – | – | – | – |
| Williams 201143 | USA | Evaluation of feasibility and acceptability of LSW | Veterans’ health service settings or own home | 12 veterans with diagnosed early-stage dementia | Observational checklist and short interview survey of people with dementia | Not clear, possibly author |
| Yasuda 200942 | Japan | Evaluation of LSW | Memory clinic | 15 memory clinic outpatients with probable diagnosis of AD | Experimental ABCA design, with TV programmes as control conditions | Authors |
1: increases understanding of person in family and intergenerational context.
1.1: which provides knowledge of personal identity and meaning.
1.1.1: which enables personalised nursing care.
2: increases (staff) knowledge of person with dementia.
2.1: which increases staff respect for people with dementia.
2.1.1: which improves ability to provide personalised care.
2.2: which increases tolerance, understanding and empathy of care staff.
2.3: which changes view of person’s adaptability, goal setting and interaction skills.
2.3.1: which prompts more meaningful interaction.
2.3.1.1: which provides more positive staff attitudes and job satisfaction.
2.3.1.1.1: which improves QoL for people with dementia.
3: facilitates meaningful conversation with person.
3.1: which increases staff knowledge of and comfort with the person with dementia.
3.1.1: which enables staff to modify their behaviour to meet specific needs of people with dementia.
3.1.1.1: which leads care staff to respect and promote people with dementia’s remaining ‘competencies’.
4: can assist communication.
4.1: which aids development of positive relationship between people with dementia and others.
5: provides mechanism for increasing connection between staff and person with dementia.
6: promotes more individualised approaches to interaction with person.
6.1: which leads to more mutually satisfying communication between people with dementia and staff.
7: makes personhood of person with dementia more ‘accessible’ to others.
7.1: which restores the person’s history.
7.1.1: which helps to improve communication between people with dementia and staff in care environment.
8: provides foundation for interactions between staff and family.
8.1: which reinforces unique expertise and legitimacy of family’s knowledge and its importance in care context.
8.1.1: which balances out technical expertise of staff.
8.1.1.1: which alters power relationships in nursing home environment.
8.1.1.1.1: which promotes more equal and collaborative relationship between staff and family.
8.2: which gives staff information that captures unique narratives of the person with dementia.
8.2.1: which supplements ‘medical discourse’ usually predominant in nursing home care.
8.2.1.1: which provides basis for new modes of discourse and ways of thinking about people with dementia.
9: signifies that family/friend are trying to make work of staff more satisfying.
9.1: which shows that the family/close person values the work of staff.
9.1.1: which endorses a shared family/staff goal of person-centred care.
10: provides organisationally sanctioned role for family and friends in gathering and relaying the life story.
10.1: which assists care staff to personalise care for residents.
11: activity symbolises family members’ continuing loyalty to the person with dementia.
11.1: which reshapes carer/family member’s experiences of the illness of the person with dementia.
11.2: which allows families to experience themselves as a group.
11.2.1: which provides them with vital support.
11.2.1.1: which helps to ‘normalise’ experience of placing people with dementia in long-term care.
11.2.1.1.1: which helps remove stigma and shame.
12: signifies continued involvement of family/friends.
12.1: which endorses a shared family/staff goal of person-centred care.
13: allows family/friends to gain distance from immediate situation of person.
13.1: which thereby affirms the whole life of the people with dementia.
13.1.1: which helps families ‘heal from trauma and guild of nursing home placement’.
14: provides a new technique to assist family member.
14.1: which empowers family member by increasing sense that they can make a difference to how person with dementia is seen (in care environment).
14.1.1: which can help to alleviate family members’ sense of helplessness.
15: provides a legacy of memories and family history/captures things that would otherwise be lost.
15.1: whch provides an ‘exit gift’.
15.1.1: which is a legacy.
15.1.1.1: but also can help family members work through cognitive and eventual actual loss of person with dementia.
15.2: which becomes an external memory aid and communication resource.
15.2.1: which prompts interesting conversations with person with dementia.
16: allows family members to reacquaint themselves with person’s past and individuality.
16.1: which reactivates family pride in the person with dementia.
16.1.1: which helps elicit more meaningful, pleasurable interactions between family and person with dementia.
17: provides pleasurable or engaging moments/conversations for person and family member/carer.
17.1: which increases communication between them.
17.2: which supports identity, communication and well-being.
18: structures time in a satisfying and pleasant way.
18.1: which competes with time that might otherwise be filled with agitation.
18.1.1: which reduces discomfort of people with dementia.
18.1.2: which reduces burden on caregivers.
19: triggers predominantly positive emotions (and occasional moments of sadness).
19.1: which supports identity, communication and well-being.
20: provides a gateway to activities that memory makes possible.
20.1: which allows reviewing the past.
20.2: which allows connecting to family members.
21: emphasises what can be remembered rather than what cannot.
21.1: which can raise self-esteem and improve well-being of people with dementia.
22: stimulates/supports reminiscence of past events.
22.1: which supports identity, communication and well-being.
23: helps person to remember distant past.
23.1: which counters threats to personhood.
24: conveys texture and detail of the person’s life.
24.1: which may improve understanding of the person with dementia.
24.1.1: which may help to improve care.
25: reinforces personal identity.
25.1: which leads to preservation of personhood.
26: values past lives.
26.1: which helps people with dementia to value themselves.
26.1.1: which improves QoL for people with dementia.
Final outcomes are shown in bold.
1: family members involvement in LSW leads to greater involvement in life of care home.
1.1: leads to greater knowledge of the families of the person with dementia.
2: creates stronger bonds between (family) carers than conventional family involvement mechanisms.
2.1: which may lead to carers becoming a more autonomous interest group.
2.1.1: which means that their voice may be more strongly heard in the system.
2.1.1.1: which may affect the social climate of the care home.
3: leads to interactions with family members.
3.1: strengthened understanding of and relationship with family members.
4: leads to staff and family carers using knowledge of people with dementia in their ‘intergenerational context’.
4.1: leads to social stimulation for the resident.
4.1.1: leads to ‘benefits’ for residents.
4.2: empowered staff.
4.2.1: to provide individualised and ‘less pathologically oriented care’.
5: increases staff awareness of experience and meaning of caring for family member with dementia.
5.1: leads to engagement in more participatory approach.
5.1.1: which promotes insight into and appreciation of how to work with family carers.
5.1.1.1: which leads to more ‘inclusive delivery and planning of dementia care.
5.1.1.2: which improves care outcomes for residents.
6: is an enjoyable and a shared process.
6.1: which reduces concerns about behaviour of people with dementia.
6.1.1: which leads to reported improved mood and reduced problem behaviours for people with dementia.
7: means family carers are less bothered by problem behaviours.
7.1: which leads to reported improved mood and reduced problem behaviours for people with dementia.
8: provides family carers with a ‘sounding board’.
8.1: which helps them see people with dementia as ‘creating fewer problems.
8.1.1: leads to carers feeling more focused and able to plan for the future.
8.1.1.1: leads to lowered measured burden scores.
9: helps to recognise the (family) carers’ legitimate and unique contribution to care.
9.1: which leads to increased involvement in and connection to the place of care.
10: helps family carers feel more in charge.
10.1: which enables them to organise their caregiving ‘in a more efficient manner’.
10.1.1: which ‘strengthened them in their caregiving processes’.
11: empowers family members to contribute family knowledge.
11.1: knowledge is shared with, recognised and valued by staff.
11.1.1: which leads to increased sense of satisfaction for family carers.
12: facilitates intergenerational interaction by preserving family legacy.
12.1: which supports in the person with dementia the ‘generativity or desire to give of oneself to future generations’.
13: creates legacies for family members.
13.1: which preserves long-term memories before they are lost to advancing illness.
14: leads to sharing of life story with family members.
14.1: helps maintain ‘accurate memories of the self’.
15: enables family members to discover more about their family history.
15.1: which generates shared interest for family carers.
15.1.1: which helps family members to see more of the person ‘beyond the dementia’.
16: allows family/close people to break free of ‘disease saturated narrative’.
16.1: associated with fuller sense of meaning and accomplishments of life of people with dementia.
16.1.1: which helps family/close people deal with impact of dementia.
17: helps family members recall the person they knew prior to the onset of disease.
17.1: leads to family members re-engaging with people with dementia.
17.1.1: leads to enhanced personal coping for family members/carers.
17.2: leads to family members shifting perception of people with dementia.
17.2.1: leads to enhanced personal coping for family members/carers.
18: revives memories of the ‘whole person’.
18.1: enables family carers to step out of their everyday experience.
18.1.1: leads to them seeing beyond ‘disease saturated context’.
19: brings carers back in touch with pre-dementia memories.
19.1: which they then share with the other carers.
19.1.1: which enables them to see what has been lost but also what they have ‘refound’ which was previously obscured by ‘disease saturated narratives’.
19.1.1.1: which allows carers to connect with grieving processes.
20: allows family member to ‘show’ the person their relative was.
20.1: which helps to maintain ‘continuity’ of the person.
20.1.1: which leads to upholding personhood of people with dementia.
20.1.1.1: which enhances possibility of staff providing person-centred care.
21: enhances resident and care staff communication.
21.1: helps with staff job satisfaction.
21.1.1: which might have longer lasting effect on care environment.
22: enables staff to take an interest in the story of the person with dementia.
22.1: which engenders a sense of being valued and being interesting.
22.1.1: which can lead to people with dementia taking pride in themselves.
22.1.2: which values their lives.
23: increased recognition of people with dementia’s history, personhood and life experiences.
23.1: leads to self-affirmation for people with dementia.
23.2: leads to enhanced communication and social interaction between family members.
24: enables staff to gain fuller and more dynamic picture of people with dementia.
24.1: which increases their knowledge of the person.
24.1.1: which enables them to find out more about person’s needs and behaviour.
24.1.2: helps staff see person in context of whole life rather than in terms of their medical condition/physical needs.
24.1.3: which provides a talking point between staff and people with dementia.
24.1.3.1: which helps develop common bond between people with dementia and staff.
25: increases knowledge of former interests and tastes of people with dementia.
25.1: which is input into care planning.
25.1.1: which allows for provision of more meaningful activities for people with dementia.
26: increases knowledge of the ‘normal life’ of the person with dementia.
26.1: helps care staff to relate to individual as someone who is ‘knowable’.
26.1.1: which facilitates empathetic identification.
26.1.1.1: which helps to transcend the ‘job’ aspect of caregiving.
26.1.1.2: which helps staff to ‘approach the daily routine of work on a more humane level’.
27: increases knowledge of resident’s personal past.
27.1: leads to increased understanding of current actions or behaviour of people with dementia.
28: increases knowledge of care staff about people with dementia.
28.1: which may help staff to form more genuine and empathetic relationships with residents.
28.1.1: which may assist care staff to individualise their approach to the resident.
28.1.1.1: which may help to minimise residents’ aggression.
29: increases understanding of care staff about people with dementia.
29.1: leads to staff seeing person beyond being a patient.
29.1.1: leads to person-centred care.
30: increases staff knowledge about the person with dementia.
30.1: which helps to make the person ‘more real’.
30.1.1: which enables staff to see the person with dementia as an individual.
30.1.1.1: which helps them to deliver better care.
31: increases staff knowledge about people with dementia.
31.1: which enables a less ‘one dimensional’ perception of the person.
31.2: which enables more individualised conversation.
32: helps staff have greater knowledge of the person with dementia.
32.1: which enables them to see beyond the dementia.
32.1.1: which might enhance job satisfaction while working with challenging group.
33: improves attitudes of staff towards people in their care.
33.1: which increases staff awareness of positives of working with older people.
33.1.1: which enables family members to feel more satisfied with care that the residents received.
34: using outputs, reminds people with dementia, staff and family members of enduring capabilities of people with dementia.
34.1: which leads to enhanced interactions with and for people with dementia.
34.1.1: which leads to better solutions to behavioural issues being adopted.
34.1.1.1: which enables more satisfying interactions
34.1.1.2: which reduces anxiety, agitation or boredom.
34.2: which leads to improved communication.
35: creates something new which represents the uniqueness of the person with dementia.
35.1: which signals family loyalty.
35.2: which is a concrete representation of family expertise.
36: leads to focus on preserved abilities rather than areas of weakness.
36.1: people with dementia may continue to stay involved in their environment.
36.1.1: which may lead to longer-term maintenance of abilities and slowed rate of decline in discourse, functional ability, emotional well-being and global functioning.
37: offsets negative feelings associated with dementia for the person with dementia.
37.1: which may enhance well-being of people with dementia.
38: offers people with dementia opportunity to share significant or important facts with staff.
38.1: which gives opportunity of reciprocity – ‘giving something back’.
38.1.1: which redresses imbalance of power between people with dementia and staff.
39: provides information which can provide common ground for conversation between staff and residents.
39.1: leads to increased understanding and appreciation of the resident.
39.1.1: which helps staff see person with dementia as an individual.
40: leads to engagement in meaningful conversations.
40.1: person with dementia continues to stay involved in their environment.
40.1.1: leads to longer-term maintenance of abilities and slowed rate of decline in discourse, functional ability, emotional well-being and global functioning.
41: allows voice of person with dementia to be heard.
41.1: which enhances possibility of staff providing person-centred care.
42: increased sense of being listened to for people with dementia.
42.1: which increases the sense of control for the person with dementia in relation to interactions with others.
43: via a ‘therapeutic listener’ elicits troubling memories.
43.1: which allows people with dementia to work through these memories or integrate them into their lives.
43.1.1: which leads to resolution of long-standing emotional issues.
44: provides a ‘listening tool’.
44.1: which enables staff to identify and understand individual needs of people with dementia.
44.1.1: which leads to more person-centred care.
44.2: which provides way of passing information about people with dementia between care settings.
44.2.1: which leads to more person-centred care.
45: mode of display (video) catches attention of people with dementia.
45.1: which allows them to focus their attention for substantial periods of time.
45.1.1: which leads to improved psychological stability.
45.1.2: which leads to reduced (family) carer burden.
46: [concrete nature of LSW product] enables knowledge about the person with dementia to circulate round the care home.
46.1: which has an impact on the entire social environment of the home.
47: [nature of LSW product] provides easy access to information about lives of people with dementia.
47.1: which increases staff knowledge about residents.
47.1.1: which might, but does not always, lead to change in staff behaviour.
47.1.2: which might, but does not always, lead to changes in care outcomes for residents.
Final outcomes are shown in bold.
| Group | Date focus group held | Type of group | Location | Experience of LSW | Participants (female/male split) |
|---|---|---|---|---|---|
| DF1 | January 2013 | Voluntary sector day service | South of England | Minimal (we introduced the idea using props) | 10 (six female, four male) |
| DF2 | January 2013 | Voluntary sector reminiscence group | South of England | Some (participants were all members of a reminiscence group so were familiar with the concept) | Five (four female, one male) |
| DF3 | February 2013 | User-led support and campaigning group | North-west of England | Considerable (five participants had been supported to do LSW through the NHS) | Seven (three female, four male) |
| DF4 | February 2013 | Support group held in a church | North-east of England | Minimal (we introduced the idea using props) | Three (two female, one male) |
| Total | 25 participants with dementia (15 female, 10 male) | ||||
| Group | Date focus group held | Location | Participants (female/male split) | Current/former carers | Relationships to people with dementia |
|---|---|---|---|---|---|
| CF 1 | January 2013 | London | Six (three female, three male) | Five current/one former | Three daughters, one son, one son-in-law and one husband |
| CF2 | February 2013 | London | Seven (six female, one male) | Seven current | Two daughters, one son, one granddaughter, three wives |
| CF3 | February 2013 | York | Eight (seven female, one male) | Five current/three former | Three daughters, one daughter-in-law, one niece, two wives, one husband |
| Total | 21 carer participants (16 female, 5 male) | ||||
| Group | Date focus group held | Location | Participants (female/male split) | Roles | Settings (where LSW had been used) |
|---|---|---|---|---|---|
| PF 1 | February 2013 | London | Nine (eight female, one male) | OTs, nurse, day centre managers, housing association officer, library worker, self-employed | Acute mental health wards, early diagnosis unit, day services, community (with families), supported housing, hospital library, care homes |
| PF2 | February 2013 | York | Eight (eight female, none male) | Arts and health practitioner, assistant psychologists, OT, care worker, support worker, volunteer co-ordinator, voluntary sector manager | Care homes, inpatient assessment unit, MAS, older adults’ mental health service, retirement villages and nursing homes, community, day services |
| PF3 | February 2013 | York | 10 (10 female, none male) | Speech and language therapists, OTs, OT technical instructor, research nurse, care home managers, social work manager | Community mental health teams, assessment and treatment community service, general hospital, specialist dementia residential care, day services, reablement |
| Total | 27 professional participants (26 female, 1 male) | ||||
| Category of service | Source of information | Number of potential organisations identified | Issues with source | Filtering/sampling of numbers | Number of services/settings after filtering/sampling | Sampling proportion (%) | Final sample size |
|---|---|---|---|---|---|---|---|
| Memory clinics/services | Royal College of Psychiatrists website | 146 | Most have physical address but no e-mail or contact name | Contacted all and asked for e-mail contact. Some services no longer in existence and some were found that were not on original list | 114 | 100 | 114 |
| SCHs | CQC database – care homes (with or without nursing) which specify dementia as their sole specialism | 134 | Most have name of registered manager and telephone number | Contact with these to check nature of service provision and identify e-mail contact to generate final sample | 134 | 100 | 122 |
| IPAs | Mental health NHS trusts in CQC database of registered health and social care providers. Then checked against the NHS Choices website | 66 trusts clearly identified as providing mental health services | Trusts listed as providers of one or more dementia specialist services, but not clear what these services are | Contacted trusts and also a clinical psychologists’ network. Identified wards in trusts identified as providing inpatient assessment services | 89 | 100 | 89 |
| CDSs | CQC database – registered social care or health-care organisations (not care homes) registered for care of people with dementia and providing relevant service typea | 4907 social care 204 NHS 42 independent health care |
Physical address provided but not always e-mail contact name | Random 3% sample of 5153 identified organisations. Contact with all of these to check nature of service provision and identify e-mail contact to generate final sample | 150 | 3, with further direct contact | 101 |
| Generalist long-term care homes | CQC database – care homes (with or without nursing) that do not specify dementia as their sole specialism but that are registered for care of people over the age of 65 years and for dementia care | 3051 | Most have name of registered manager and telephone number | Random 5% sample of 3051 care homes. Contact with these to check nature of service provision and identify e-mail contact to generate final sample | 150 | 5, with further direct contact | 139 |
| Total | 8550 | 637 | 565 |
| Service category | Number of survey links distributed | Number of services found to be ‘out of scope’a | Number of services ‘in scope’ | Number of returned questionnaires | % response rate of in scope |
|---|---|---|---|---|---|
| Memory clinics/services | 114 | 1 | 113 | 72 | 64 |
| SCHs | 122 | 0 | 122 | 75 | 61 |
| IPAs | 89 | 2 | 87 | 61 | 70 |
| CDSs | 101 | 1 | 100 | 52 | 52 |
| Generalist long-term care homes | 139 | 0 | 139 | 44 | 32 |
| Not classifiable | – | – | – | 3 | < 0.1 |
| Total | 565 | 4 | 561 | 307 | 58 |
| Service category | % of services or settings that responded (a) | % of responding services that carried it out or referred to other services for LSW (b) | Sampling proportion (%) | Population size (c) | Estimated % of all services carrying out LSW currently or refer to another service for LSW (d = b/100*a) | Estimate of number of services/settings where LSW is currently carried out (d/100*c) |
|---|---|---|---|---|---|---|
| Memory clinics/services | 64 | 44.4 | 100 | 146 | 28.4 | 41 |
| Dementia specialist care homes | 61 | 78.7 | 100 | 134 | 48.0 | 64 |
| IPAs | 70 | 88.5 | 100 | 89 | 62.0 | 55 |
| CDSs | 52 | 26.9 | 3 | 5153 | 14.0 | 721 |
| Generalist care homes | 32 | 70.5 | 5 | 3051 | 22.6 | 689 |
| Type of record included in life story | % of service using specified type of record | |||||
|---|---|---|---|---|---|---|
| Memory assessment | SCH | Inpatient assessment | CDS provider | Generalist care home | All | |
| Photo album | 36 | 33 | 37 | 43 | 35 | 36 |
| Photo album with text/stories | 76 | 32 | 53 | 21 | 41 | 45 |
| Book with mix of photos and text | 72 | 47 | 45 | 36 | 45 | 49 |
| Written summary | 44 | 72 | 78 | 57 | 83 | 70 |
| Box or other container with important objects/memories | 56 | 40 | 37 | 36 | 31 | 40 |
| Collage or display for wall/door | 24 | 22 | 24 | 14 | 24 | 22 |
| DVD or film | 16 | 0 | 4 | 0 | 10 | 5 |
| Poem | 4 | 2 | 6 | 7 | 7 | 6 |
| n (100%)a | 25 | 60 | 51 | 14 | 29 | 179 |
| Uses of life story | % of respondents selecting | % of respondents choosing this option who then said it was the most important | Type of service that most often chose this option as the most important (% choosing) | Type of service that least often chose this option as the most important (% choosing) |
|---|---|---|---|---|
| Help person remember important parts of their lives | 89 | 14 | SCHs (20) and community care providers (20) | Inpatient assessment (4) |
| To give pleasure to person when they look at it | 82 | 10 | MAS (25) | Generalist care home (0) |
| To help soothe or calm person | 81 | 3 | Inpatient assessment (7) | Generalist care home (0) and community care provider (0) |
| To help staff see person behind the dementia | 98 | 55 | Generalist home care (75) | MAS (38) |
| As something for person and staff to enjoy looking at together | 81 | 10 | SCH (13) | MAS (0) |
| As something for person and family member/close person to enjoy looking at together | 84 | 7 | MAS (21) | SCH (2) |
| So that health/social care workers elsewhere can provider better care | 72 | 10 | Inpatient assessment (17) | Community care provider (0) |
| n (100%) | 181a | 179b | 179b |
| Type of information | Always included (%) | Sometimes included (%) | Never included/not answered (%) | n (100%) | Comparison of services/settings |
|---|---|---|---|---|---|
| Names | 78 | 16 | 5 | 189 | χ2 = 31.25, df = 8; p < 0.0001 |
| Details/descriptions | 46 | 42 | 12 | 189 | χ2 = 33.65, df = 8; p < 0.0001 |
| Reactions to and meanings of this person | 20 | 44 | 36 | 189 | χ2 = 19.18, df = 8; p = 0.014 |
| Type of information | Always included (%) | Sometimes included (%) | Never included/not answered (%) | n (100%) | Comparison of services/settings |
|---|---|---|---|---|---|
| List of important events, dates, places, stage of life | 62 | 24 | 13 | 189 | χ2 = 11.73, df = 8; p = 0.163 |
| Details about the above | 67 | 22 | 11 | 189 | χ2 = 15.26, df = 8; p = 0.054 |
| Feelings about the above | 42 | 40 | 19 | 189 | χ2 = 10.11, df = 8; p = 0.257 |
| Type of information | Always included (%) | Sometimes included (%) | Never included/not answered (%) | n (100%) | Comparison of services/settings |
|---|---|---|---|---|---|
| What they like to eat | 73 | 12 | 15 | 189 | χ2 = 25.59, df = 8; p = 0.003 |
| What they like to wear | 66 | 19 | 15 | 189 | χ2 = 25.17, df = 8; p = 0.001 |
| What they like doing | 82 | 8 | 11 | 189 | χ2 = 25.91, df = 8; p = 0.001 |
| What they like to talk about | 68 | 18 | 14 | 189 | χ2 = 19.66, df = 8; p = 0.012 |
| What they prefer not to talk about | 53 | 28 | 19 | 189 | χ2 = 17.49, df = 8; p = 0.025 |
| Type of information | Always included (%) | Sometimes included (%) | Never included/not answered (%) | n (100%) | Comparison of services/settings |
|---|---|---|---|---|---|
| Medical or care needs | 30 | 27 | 44 | 189 | χ2 = 23.83, df = 8; p = 0.002 |
| Spiritual or cultural needs | 59 | 28 | 13 | 189 | χ2 = 24.99, df = 8; p = 0.002 |
| Type of life story | % of services or settings | Comparison of services/settings | |||||
|---|---|---|---|---|---|---|---|
| Memory service | SCH | Inpatient assessment | Community care provider | Generalist care home | All | ||
| One-off, nothing added | 11 | 13 | 26 | 20 | 3 | 15 | χ2 = 8.61, df = 4; p = 0.072 |
| Things about the past added along the way | 57 | 64 | 62 | 60 | 70 | 63 | χ2 = 1.156, df = 4; p = 0.885 |
| Things about recent events added as they happen | 21 | 53 | 26 | 47 | 53 | 40 | χ2 = 15.35, df = 4; p = 0.004 |
| n (100%) | 28 | 61 | 55 | 15 | 30 | 189 | |
| Who can look at the life story? | % of services or settings | Comparison of services/settings | |||||
|---|---|---|---|---|---|---|---|
| Memory service | SCH | Inpatient assessment | Community care provider | Generalist care home | All | ||
| The person with dementia | 96 | 91 | 96 | 93 | 96 | 94 | χ2 = 1.575, df = 4; p = 0.813 |
| Family members and close people | 100 | 93 | 98 | 100 | 89 | 95 | χ2 = 6.13, df = 4; p = 0.189 |
| Selected staff who work here | 50 | 23 | 28 | 47 | 39 | 32 | χ2 = 7.68, df = 4; p = 0.104 |
| Any staff who work here | 5 | 5 | 69 | 7 | 0 | 24 | χ2 = 82.70, df = 4; p < 0.0001 |
| Staff elsewhere | 5 | 5 | 18 | 13 | 0 | 15 | χ2 = 9.17, df = 4; p = 0.06 |
| n (100%) | 28 | 61 | 55 | 15 | 30 | 189 | |
| Does the person with dementia give permission? | % of services and settings | |||||
|---|---|---|---|---|---|---|
| Memory services | SCH | Inpatient assessment | Community care provider | Generalist care home | All | |
| Always | 82 | 63 | 35 | 87 | 73 | 61 |
| Sometimes | 5 | 23 | 57 | 7 | 27 | 30 |
| Never or not known | 14 | 14 | 8 | 7 | 0 | 9 |
| n (100%) | 22 | 56 | 51 | 15 | 26 | 170 |
| Where life story is usually kept | % of services and settingsa | Comparison of services/settings | |||||
|---|---|---|---|---|---|---|---|
| Memory services | SCH | Inpatient assessment | Community care provider | Generalist care home | All | ||
| Person with dementia keeps it | 100 | 29 | 43 | 47 | 31 | 44 | χ2 = 35.30, df = 4; p< 0.0001 |
| Family member keeps it | 0 | 0 | 0 | 7 | 0 | < 1 | χ2 = 10.39, df = 4; p = 0.34 |
| In office or other secure place | 0 | 27 | 4 | 33 | 23 | 17 | χ2 = 18.43, df = 4; p = 0.001 |
| In person’s care record | 14 | 66 | 65 | 60 | 85 | 61 | χ2 = 27.79, df = 4; p< 0.0001 |
| On display | 5 | 14 | 16 | 0 | 4 | 11 | χ2 = 6.08, df = 4; p = 0.193 |
| n (100%) | 22 | 56 | 51 | 15 | 26 | 170 | |
| Policy or practice | % of services having this policy or practice | N (100%) | Comparison of services/settings | |||||
|---|---|---|---|---|---|---|---|---|
| Memory services | SCH | Inpatient assessment | Community care provider | Generalist care home | All | |||
| Responsiveness to individual need | ||||||||
| Offer LSW to everyone regardless of stage of dementia | 43 | 86 | 90 | 92 | 86 | 82 | 156 | χ2 = 25.73, df = 4; p < 0.0001 |
| People with dementia with a visual impairment are offered opportunity to do LSW | 91 | 98 | 96 | 100 | 95 | 96 | 153 | χ2 = 2.84, df = 4; p = 0.586 |
| How LSW is done is adjusted, depending on the needs and strengths of the person with dementia | 96 | 89 | 92 | 100 | 87 | 91 | 159 | χ2 = 2.78, df = 4; p = 0.596 |
| Use a template to guide LSW throughout | 81 | 77 | 88 | 46 | 52 | 75 | 158 | χ2 = 16.76, df = 4; p = 0.002 |
| Decisions about format and look of life story made mainly by staff/volunteers who do LSW | 33 | 44 | 69 | 23 | 33 | 47 | 152 | χ2 = 16.18, df = 4; p = 0.003 |
| Training and supervision of those carrying out LSW | ||||||||
| Staff/volunteers do own LSW before working with service users | 14 | 10 | 6 | 43 | 5 | 11 | 156 | χ2 = 16.13, df = 4; p = 0.003 |
| Staff learn how to do LSW ‘on the job’ rather than through training | 62 | 73 | 52 | 62 | 76 | 64 | 154 | χ2 = 6.02, df = 4; p = 0.198 |
| Staff doing LSW get regular supervision from senior or more experienced staff | 62 | 73 | 94 | 100 | 86 | 82 | 153 | χ2 = 16.49, df = 4; p = 0.002 |
| We train family members/close people before they do LSW | 33 | 22 | 19 | 46 | 25 | 25 | 152 | χ2 = 5.12, df = 4; p = 0.275 |
| Knowledge of LSW and use across service/setting | ||||||||
| Everyone who works/volunteers here knows what LSW is | 52 | 80 | 69 | 85 | 74 | 72 | 152 | χ2 = 7.14, df = 4; p = 0.129 |
| Everyone who works/volunteers here knows how to use a life story to improve care of person with dementia | 33 | 80 | 61 | 85 | 67 | 66 | 153 | χ2 = 15.53, df = 4; p = 0.002 |
| Institutional policies to support LSW and whether or not these varied by services and settings | ||||||||
| LSW is done in spare moments in care routine | 32 | 38 | 55 | 43 | 52 | 45 | 158 | χ2 = 5.06, df = 4; p = 0.281 |
| LSW done in dedicated and protected time | 48 | 67 | 37 | 62 | 52 | 52 | 157 | χ2 = 9.61, df = 4; p = 0.048 |
| Senior staff are fully committed to LSW being done | 67 | 96 | 83 | 100 | 91 | 88 | 156 | χ2 = 15.01, df = 4; p = 0.005 |
| Any staff wanting to do LSW will have time freed up from other duties | 38 | 87 | 51 | 77 | 83 | 68 | 158 | χ2 = 25.94, df = 4; p < 0.0001 |
| Uses of life story | Number of carers reporting this use | Number of carers reporting this as the most important use |
|---|---|---|
| Help person remember important parts of their lives | 31 | 14 |
| To give pleasure to person when they look at it | 26 | 12 |
| To help soothe or calm person | 12 | 9 |
| To help carer remember the person | 18 | 7 |
| As something for carer and person to enjoy looking at together | 25 | 8 |
| Something to share with family members/close people | 24 | 7 |
| So that health/social care workers can provide better care | 25 | 17 |
| Total (n) | 38 | 38 |
| Type of information | Number of carers reporting this is included in the life story |
|---|---|
| Names of family and close people | 31 |
| Details/descriptions of family and close people | 21 |
| Reactions to family and close people | 13 |
| List of important events, dates, places, stage of life | 24 |
| Details about the above | 29 |
| Feelings about the above | 12 |
| What likes to eat | 19 |
| What likes to wear | 12 |
| What likes doing | 26 |
| What likes to talk about | 20 |
| What prefers not to talk about | 5 |
| Medical or care needs | 12 |
| Spiritual or cultural needs | 14 |
| Total (n) | 38 |
| Temporal orientation of the life story | Number of carers reporting that the life story included this |
|---|---|
| Memories and information about the past | 37 |
| Current information | 22 |
| Hopes and views about the future | 5 |
| Total (n) | 38 |
| Location of the life story | Number of carers reporting this |
|---|---|
| In the home of the person with dementia | 19 |
| In the carer’s home | 5 |
| At a day centre | 1 |
| At the care home where the person with dementia lives | 20 |
| Total (n) | 38 |
| Who looks? | How often this person looks or looked at the life story | Total (N) | ||||
|---|---|---|---|---|---|---|
| Every week | Every month | Less than every month | Never | Do not know | ||
| Carer | 13 | 10 | 9 | 2 | 3 | 37 |
| Person with dementia | 13 | 7 | 8 | 4 | 5 | 37 |
| Care professionals/staff | 7 | 3 | 6 | 7 | 10 | 33 |
| Care home ID | Number of rooms | Proportion with dementia or dementia like symptoms (%) | Percentage self-funders (%) | Manager | Original site? |
|---|---|---|---|---|---|
| CH1 | 39 | 67 | 38 | Remained | Replacement |
| CH2 | 41 | 37 | 34 | Changed | Original |
| CH3 | 35 | 50 | 63 | Remained | Original |
| CH4 | 40 | 35 | 90 | Remained | Original |
| CH5 | 40 | 74 | 31 | Changed | Original |
| CH6 | 38 | 100 (SCH) | 66 | Remained | Replacement |
| Ward ID | Beds | Intake | Ward manager | LSW |
|---|---|---|---|---|
| IW1 | 12 | Mixed ward (some functional, some organic) | Remained | Established |
| IW2 | 10 | Organic | Changed | Established |
| IW3 | 11 | Organic | Remained | Established |
| CW | 18 | Mixed ward (some functional, some dementia) | Remained | None |
| Care home ID | Staff trained | Staff recruited | Conditions for recruitment |
|---|---|---|---|
| CH1 | 12 | 11 (92%) | Dedicated room, staff met the researchers individually or in small groups |
| CH2 | Missinga | 4 (% not known) plus 1 for focus group | No dedicated space or time. Staff usually engaged in another task when they met researchers. Most asked to take the information away with them. Activities co-ordinator did not do training but was involved in delivery of LSW so was invited to the focus group at final follow-up |
| CH3 | 11 | 10 (91%) | Dedicated room, staff met the researchers individually or in small groups. Manager led by example |
| CH4 | 14 | 7 (50%) | Communal lounge, staff met the researchers individually or in small groups |
| CH5 | 6 | 3 (50%) | Dedicated room, but only three members of staff available to meet researchers |
| CH6 | 15 | 15 (100%) | Dedicated room, staff met with the researchers as a single (large) group |
| Total recruited | 51 | ||
| Ward ID | Staff team | n (%) staff completed measures TP1 | n (%) staff completed measures TP2 | n (%) staff completed measures TP3 | Total N completed measures | Conditions for recruitment |
|---|---|---|---|---|---|---|
| IW1 | Morning: 4 Afternoon: 4 1 manager (Total 9) |
8 (89) | 8 (89) | 8 (89) | 24 | Dedicated room; all staff aware of researcher’s presence |
| IW2 | Morning: 5 Afternoon: 5 1 manager 3 part-time OT technicians (WTE 1.4) (Total 14) |
7 (58) | 8 (65) | 5 (40) | 20 | Dedicated room, but staff ‘extremely busy’ at TP3 |
| IW3 | Morning: 4 Afternoon: 4 1 manager (Total 9) |
7 (78) | 8 (89) | 6 (67) | 21 | Dedicated room, but staff seemed unaware of researcher’s presence for some of TP3 |
| CW | Morning: 6 Afternoon: 6 1 manager 1 OT (Total 14) |
7 (50) | 6 (43) | 6 (43) | 19 | No dedicated room at TP2; researchers approached staff while they were working on the ward |
| Overall | 47 | 30 (64) | 30 (64) | 25 (53) | – |
| Care home ID | Originally selected | Excluded after selection | Reselected | Total approached (directly or via consultee) |
|---|---|---|---|---|
| CH1 | 10 | 1 | 2a | 11 |
| CH2 | 10 | 0 | 0 | 10 |
| CH3 | 10 | 0 | 0 | 10 |
| CH4 | 10 | 0 | 0 | 10 |
| CH5 | 10 | 4 | 2b | 8 |
| CH6 | 10 | 0 | 0 | 10 |
| Total | 60 | 5 | 4 | 59 |
| Care home ID | PWD with capacity (n = 16) | PWD without capacity (n = 43) | Total | Total recruited | |||
|---|---|---|---|---|---|---|---|
| Consented (self) | Refused (self) | Advised to include (consultee) | Advised not to include (consultee) | Refused consent to contact/did not respond (potential consultee) | |||
| CH1 | 3 | 0 | 5 | 1 | 2 | 11 | 8 |
| CH2 | 5 | 1 | 2 | 2 | 0 | 10 | 7 |
| CH3 | 3 | 0 | 5 | 1 | 1 | 10 | 8 |
| CH4 | 0 | 1 | 6 | 0 | 3 | 10 | 6 |
| CH5 | 2 | 0 | 3 | 1 | 2 | 8 | 5 |
| CH6 | 1 | 0 | 4 | 2 | 3 | 10 | 5 |
| Total | 14 | 2 | 25 | 7 | 11 | 59 | 39 |
| Care home ID | People with dementia recruited | Family carers recruited | Reasons for difference in numbers |
|---|---|---|---|
| CH1 | 8 | 6 | No family carers identified for two participants |
| CH2 | 7 | 5 | Unable to make contact with one carer and another took the information but did not respond |
| CH3 | 8 | 6 | One person with dementia had no family carer. One family member refused |
| CH4 | 6 | 6 | N/A |
| CH5 | 5 | 5 | N/A |
| CH6 | 5 | 3 | One family member refused and another did not respond |
| Total | 39 | 31 | Three people with dementia had no family carer Four carers refused/did not respond One carer was unable to be contacted |
| Recruitment process | IW1 | IW2 | IW3 | CW | Total |
|---|---|---|---|---|---|
| New admissions flagged to research team as potentially eligible | 9 | 13 | 20 | 8 | 50 |
| Of these | |||||
| Excluded because staff concerned about causing distress to family | 0 | 0 | 3 | 0 | 3 |
| Excluded owing to doubt over dementia diagnosis | 1 | 1 | 0 | 2 | 4 |
| Eligible patients identified | 8 | 12 | 17 | 6 | 43 |
| Of these | |||||
| Patients transferred, discharged or died before staff approached potential consultees | 5 | 1 | 4 | 0 | 10 |
| Potential consultees not approached two months after admission: excluded | 0 | 0 | 2 | 0 | 2 |
| Potential consultee not approached one month after recruitment period finished: excluded | 0 | 1 | 3 | 0 | 4 |
| Potential consultees approached by staff | 3 | 10 | 8 | 6 | 27 |
| Of these | |||||
| Consultee refused consent to contact/did not respond to staff | 1 | 4 | 1 | 1 | 7 |
| Consultee advised not to include/did not respond to researcher | 0 | 1 | 3 | 2 | 6 |
| Patient excluded after consultee approached (e.g. fell ill) | 0 | 0 | 2 | 0 | 2 |
| Consultee advised to include the person with dementia | 2 | 5 | 2 | 3 | 12 |
| Ward ID | People with dementia recruited | Family carers recruited | Reasons for difference in numbers |
|---|---|---|---|
| IW1 | 2 | 1 | One carer did not want to be included as spends all day filling in forms already |
| IW2 | 5 | 5 | N/A |
| IW3 | 2 | 1 | One carer did not want to be included as husband is deteriorating and did not want to answer questions about his QoL |
| CW | 3 | 3 | N/A |
| Totals | 12 | 10 |
| Care home ID | PWD | Numbers of study participants who actually ‘did’ LSW | Staff undertaking LSW | Approach to LSW | Organisational context |
|---|---|---|---|---|---|
| CH1 | 8 | 8 (100%) | Activities co-ordinator (some info collected by care staff) | Tailored to the individual | Consistent management, activities co-ordinator allocated dedicated time |
| CH2 | 7 | 2 (29%) | Staff who undertook training were allocated to work with named residents | ‘Some important things’ template | Two changes in management, activities co-ordinator did not receive training |
| CH3 | 8 | 4 (50%) | Single member of staff undertook all LSW | Tailored to the individual | Consistent management, but activities co-ordinator left early on |
| CH4 | 6 | 3 (50%) | Activities co-ordinator | Tailored to the individual | Consistent management |
| CH5 | 5 | 1 (20%) | Staff who undertook training were allocated to work with named residents | Tailored to individual, done by volunteer | Two changes in management, activities co-ordinator did not receive training, staff suffering project fatigue |
| CH6 | 5 | 5 (100%) | Activities co-ordinator (some information collected by care staff) | Tailored to the individual, group activities | Consistent management, activities co-ordinator and care staff allocated dedicated time. SCH |
| Ward ID | Approach to collecting LSW | Use of LSW information |
|---|---|---|
| IW1 | Ward staff give a template to carers to collect life story information | Information is compiled into hand-written booklets kept in the main office |
| IW2 | Ward staff give a template to carers to collect life story information. Three OTTIs collect information from patients one to one and during activities | The OTTIs compile electronic life story books. Multiple copies can be printed so that both staff and patients have a copy. Life story information is posted on bedroom walls and used by staff in de-escalation |
| IW3 | Ward staff give a template to carers to collect life story information | Any information returned is kept in care records |
| CW | LSW not yet implemented | LSW not yet implemented |
| Care home ID | n recruited | n withdrawn (self) | n withdrawn (consultee) | n died | n remaining at 6-month follow-up |
|---|---|---|---|---|---|
| CH1 | 8 | 0 | 1 | 2 | 5 |
| CH2 | 7 | 0 | 0 | 0 | 7 |
| CH3 | 8 | 1 | 1 | 0 | 6 |
| CH4 | 6 | 0 | 0 | 0 | 6 |
| CH5 | 5 | 0 | 0 | 0 | 5 |
| CH6 | 5 | 0 | 0 | 0 | 5 |
| Total | 39 | 1 | 2 | 2 | 34 (87%) |
The ‘I am’ fluency task was administered separately to only a small number of the study participants, and is discussed in Appendix 7.
| Measure | n recruited | n (%) completed measures at | |||
|---|---|---|---|---|---|
| Baseline | Baseline and 1 month | Baseline and 2 month | Baseline and 6 months | ||
| QoL-AD | 39 | 25 (64) | 23 (59) | 23 (59) | 18 (46) |
| DEMQOL | 39 | 12 (31) | 12 (31) | 12 (31) | 12 (31) |
| QCPR | 39 | 13 (33) | 7 (18) | 5 (13) | 4 (10) |
| Ward ID | n recruited | n withdrawn (self) | n withdrawn (consultee) | n died | n remaining at 6-month follow-up |
|---|---|---|---|---|---|
| IW1 | 2 | 0 | 0 | 0 | 2 |
| IW2 | 5 | 0 | 0 | 0 | 5 |
| IW3 | 2 | 0 | 0 | 0 | 2 |
| CW1 | 3 | 0 | 1 | 0 | 2 |
| Total | 12 | 0 | 1 | 0 | 11 (92%) |
| Measure | n recruited | n completed measures at | ||
|---|---|---|---|---|
| Baseline | Baseline and first follow-up (1–2 months) | Baseline and 6 month follow-up | ||
| QoL-AD | 12 | 2 | 0 | 0 |
| DEMQOL | 12 | 1 | 0 | 0 |
| QCPR | 12 | 1 | 1 | 0 |
| Care home | n recruited | n withdrawn | n remaining at 6-month follow-up |
|---|---|---|---|
| CH1 | 6 | 2 | 4 |
| CH2 | 5 | 0 | 5 |
| CH3 | 6 | 2 | 4 |
| CH4 | 6 | 1 | 5 |
| CH5 | 5 | 0 | 5 |
| CH6 | 3 | 1 | 2 |
| Total | 31 | 6 | 25 (80%) |
| Measure | n recruited | n (%) completed measures at | |||
|---|---|---|---|---|---|
| Baseline | Baseline and 1 month | Baseline and 2 months | Baseline and 6 months | ||
| CES | 31 | 27 (87) | 23 (74) | 19 (61) | 14 (45) |
| QCPR | 31 | 30 (97) | 22 (71) | 18 (58) | 18 (58) |
| QoL-AD – proxy | 31 | 30 (97) | 23 (74) | 21 (68) | 19 (61) |
| DEMQOL proxy | 31 | 23 (74) | 18 (58) | 17 (55) | 13 (42) |
| Ward ID | n recruited | n withdrawn | n remaining at 6-month follow-up |
|---|---|---|---|
| IW1 | 1 | 0 | 1 |
| IW2 | 5 | 1 | 4 |
| IW3 | 1 | 0 | 1 |
| CW1 | 3 | 2 | 1 |
| Total | 10 | 3 | 7 |
| Measure | n recruited | n completed measures at | ||
|---|---|---|---|---|
| Baseline | Baseline and second follow-up (1–2 months) | Baseline and 6 months | ||
| CES | 10 | 10 | 8 | 7 |
| QCPRa | 10 | 6 | 6 | 5 |
| CSQ | 10 | N/A | N/A | 6 at discharge of person with dementia only |
| QoL-AD – proxyb | 10 | 7 | 7 | 6 |
| DEMQOL proxyb | 10 | 8 | 5 | 6 |
| Care home ID | n recruited | n withdrawn | n remaining at 6-month follow-up |
|---|---|---|---|
| CH1 | 11 | 0 | 11 |
| CH2 | 4 | 1 | 3 |
| CH3 | 10 | 3 | 7 |
| CH4 | 7 | 0 | 7 |
| CH5 | 3 | 0 | 3 |
| CH6 | 15 | 1 | 14 |
| Total | 50 | 5 | 45 (90%) |
| Measure | n recruited | n (%) completed measures | |||
|---|---|---|---|---|---|
| Baseline | Baseline and 1-month follow-up | Baseline and 2-month follow-up | Baseline and 6-month follow-up | ||
| ADQ | 50 | 46 (92) | 27 (54) | 17 (34) | 18 (36) |
| PDQ | 50 | 46 (92) | 21 (42) | 16 (32) | 16 (32) |
| CBI | 50 | 48 (96) | 26 (52) | 17 (34) | 15 (30) |
| Task | Time (hours) | Trainer costs | |||
|---|---|---|---|---|---|
| Assuming consultant annual salary (£53,000 p.a.)a | Assuming dementia training team hourly salary (£26 per hour)a | Assuming dementia training team annual salary (£38,000 p.a.)a | Assuming senior social worker hourly cost (£51 per hour)b | ||
| Course development | 7.5 | £294 | £218 | £211 | £383 |
| Course arrangements | 7.5 | £294 | £218 | £211 | £383 |
| Total | 15 | £588 | £437 | £421 | £765 |
| Type of staff member | Care home | ||||
|---|---|---|---|---|---|
| 1 | 3 | 4 | 5 | 6 | |
| Care assistant (no NVQ/qualification data missing) | 4 | 4 | 7 | 3 | 4 |
| Care assistant (NVQ) | 5 | 1 | 4 | 2 | 5 |
| Team leader | 3 | 1 | 1 | 1 | |
| Activities co-ordinator | 1 | 1 | 1 | 1 | |
| Bank/contract care assistant | 2 | ||||
| Laundry assistant | 1 | 1 | |||
| Night-time care assistant | 1 | ||||
| Care manager | 1 | ||||
| Night-time care leader | 1 | ||||
| Chef manager | 1 | ||||
| Housekeeper | 1 | ||||
| Actual salaries (assuming consultant annual salary £53,000 p.a.) | Actual salaries (assuming dementia training team annual salary £38,000 p.a.) | All hourly costs estimated (from Curtis142) | |
|---|---|---|---|
| Average | £1065 | £895 | £1449 |
| Range | £950 to £1145 | £784 to £979 | £1235 to £1581 |
| Number of incidents reported | 3 months prior to baseline | 3 months prior to follow-up |
|---|---|---|
| Number of participants with three or more incidents | 9 | 7 |
| Number of participants with two incidents | 8 | 2 |
| Number of participants with one incident | 7 | 4 |
| Number of participants with no incidents | 14 | 24 |
| Missing | 0 | 1 |
| Control ward | Intervention wards | |
|---|---|---|
| Number of patients for whom data were reported | 3 | 8 |
| Mean (range) length of stay (weeks) | 24 (22–26) | 12 (3–23) |
| Mean number of total incidents reported | 84 | 75 |
| Mean number of incidents reported per week | 3.5 | 6.3 |
| Maximum number of incidents reported per patient | 98 over 26 weeks | 255 over 16 weeks |
| Service | 3 months to baseline | 3 months to follow-up | ||
|---|---|---|---|---|
| Number of admissions | Total number of inpatient-days | Number of admissions | Total number of inpatient-days | |
| Acute psychiatric unit | 0 | 0 | 0 | 0 |
| General medical ward | 3 | 5 | 0 | 0 |
| Service | 3 months to baseline | 3 months to follow-up | ||
|---|---|---|---|---|
| Number of attendances | Number of times staff accompanied resident | Number of attendances | Number of times staff accompanied resident | |
| Psychiatric outpatient visit | 1 | 0 | 0 | 0 |
| Other hospital outpatient visit | 4 | 0 | 1 | 1 |
| Day hospital (e.g. for minor procedure) | 0 | 0 | 0 | 0 |
| Other (fracture clinic, radiography department) | 3 | 1 | 0 | 0 |
| A&E attendance (taken by ambulance) | 4 | 2 | 2 | 0 |
| A&E attendance (taken by family/friend) | 0 | 0 | 0 | 0 |
| Telephone calls for specialist advice | 3 months to baseline | 3 months to follow-up | ||
|---|---|---|---|---|
| Number of calls | Attended by staff | Number of calls | Attended by staff | |
| Call to GP for advice | 8 | 0 | 9 | 1 |
| Call to NHS 111 service | 1 | 0 | 0 | 0 |
| Professional visiting the care home | 3 months to baseline | 3 months to follow-up | ||
|---|---|---|---|---|
| Number of appointments | Number of times staff accompanied resident | Number of appointments | Number of times staff accompanied resident | |
| GP | 74 | 28 | 42 | 11 |
| District nurse | 67 | 15 | 65 | 13 |
| Podiatrist | 10 | 8 | 5 | 3 |
| Community psychiatric nurse | 7 | 5 | 2 | 0 |
| Continence nurse | 7 | 4 | 1 | 0 |
| Physiotherapist | 4 | 1 | 2 | 1 |
| OT | 4 | 3 | 1 | 0 |
| Dietitian | 2 | 2 | 3 | 2 |
| Specialist nurse (e.g. diabetes mellitus) | 2 | 1 | 2 | 0 |
| Speech and language therapist | 2 | 1 | 1 | 1 |
| Social worker | 1 | 0 | 0 | 0 |
| Psychiatrist | 0 | 0 | 0 | 0 |
| Psychologist | 0 | 0 | 0 | 0 |
| Befriender | 0 | 0 | 0 | 0 |
| Other (chiropodist, optician, mental health team, phlebotomist, dentist) | 35 | 18 | 4 | 4 |
| Type of service | 3 months to baseline | 3 months to follow-up | ||
|---|---|---|---|---|
| Number of appointments | Number of times staff accompanied resident | Number of appointments | Number of times staff accompanied resident | |
| Visits to GP at the surgery | 6 | 4 | 3 | 0 |
| Trips out with family or friends | 84 | 1 | 134 | 1 |
| Other (nurse, podiatrist, dentist, church, singing, coffee morning) | 20 | 1 | 6 | 0 |
| Type of service | Number of contacts | |
|---|---|---|
| Control ward, N = 3 patients (total inpatient-weeks = 72) | Intervention ward, N = 8 patients (total inpatient-weeks = 94) | |
| Occupational therapy | 53 | 168 |
| Physiotherapy | 37 | 2 |
| Duty doctor | 25 | |
| Consultant/SHO (ward rounds) | 69 | |
| Doctor review on ward (physical examination) | 21 | |
| Medical assessment | 1 | |
| Art therapy | 17 | |
| Music therapy | 12 | |
| Nursing one to one | 5 | |
| Social worker | 5 | |
| Speech and language therapy | 2 | 1 |
| Podiatrist | 1 | 1 |
| Pharmacist | 1 | |
| Dietitian | 1 | |
| Type of service | Number of contacts | |
|---|---|---|
| Control ward, N = 3 patients (total inpatient-weeks = 72) | Intervention ward, N = 8 patients (total inpatient-weeks = 94) | |
| A&E | 1 | 3 |
| CT scan | 1 | |
| Radiography | 1 | |
| Colorectal appointment | 3 | |
| Urology | 1 | |
| Endoscopy | 1 | |
| Hospital appointment | 1 | |
| Mammogram | 1 | |
| Opticians | 1 | |
| Chiropodist | 1 | |
| Name of medication | 3 months to baseline | 3 months to follow-up |
|---|---|---|
| Antipsychotics | ||
| Amisulpride | 0 | 1 |
| Olanzapine | 1 | 1 |
| Risperidone | 1 | 1 |
| Hypnotics and antidepressants | ||
| Citalopram | 2 | 3 |
| Diazepam | 1 | 1 |
| Fluoxetine | 1 | 1 |
| Mirtazapine | 3 | 3 |
| Sertraline | 2 | 1 |
| Trazodone | 1 | 0 |
| Venlafaxine | 1 | 1 |
| Zopiclone | 4 | 3 |
| Name of medication | Control ward, N = 3 patients (total inpatient-weeks = 72) | Intervention ward, N = 8 patients (total inpatient-weeks = 94) |
|---|---|---|
| Antipsychotics | ||
| Haloperidol (intramuscular injection) PRN | 5 | 0 |
| Risperidone PRN | 0 | 1 |
| Hypnotics and antidepressants | ||
| Diazepam PRN | 0 | 4 |
| Lorazepam (oral) PRN | 37 | 63 |
| Lorazepam (intramuscular injection) PRN | 2 | 5 |
| Promethazine PRN | 1 | 11 |
| Zopiclone PRN | 2 | 10 |
| Un-named PRN medication | 20 | 3 |
| Name of medication | Control ward, N = 3 patients (total inpatient-weeks = 72) | Intervention ward, N = 8 patients (total inpatient-weeks = 94) |
|---|---|---|
| Antipsychotics | ||
| Quetiapine | 1 | 0 |
| Risperidone | 2 | 1 |
| Hypnotics and antidepressants | ||
| Diazepam | 1 | 2 |
| Lorazepam | 0 | 1 |
| Name of medication | Pack cost (generic unless stated)a | Daily cost (£) |
|---|---|---|
| Antipsychotics | ||
| Amisulpride | 15 mg, 28 tablets, £96.04 | 3.43 |
| Haloperidol (intramuscular injection) | £0.36 | 0.36 |
| Quetiapine | 4 × 100 mg, 60 tablets, £113.10 (brand only @ 100 mg) | 7.54 |
| Olanzapine | 2.5 mg, 28 tablets, £21.85 (brand only @ 2.5 mg) | 0.78 |
| Risperidone | 1 mg, 20 tablets, £1.01 (brand £8.36) | 0.05–0.42 |
| Hypnotics and antidepressants | ||
| Citalopram | 10 mg, 28 tablets, £1.04 | 0.04 |
| Diazepam | 2 mg, 28 tablets, £0.96 | 0.03 |
| Fluoxetine | 20 mg, 30 tablets, £1.09 | 0.04 |
| Lorazepam (oral) | 1 mg, 28 tablets, £0.96 | 0.03 |
| Lorazepam (intramuscular injection) | £0.35 | 0.35 |
| Mirtazapine | 45 mg, 28 tablets, £2.24 | 0.08 |
| Promethazine | 2 × 10 mg, 28 tablets, £2.96 | 0.11 |
| Sertraline | 50 mg, 28 tablets, £1.75 (brand £17.82) | 0.06–0.64 |
| Trazodone | 50 mg, 84 tablets, £27.14 | 0.32 |
| Venlafaxine | 2 × 75 mg, 28 tablets, £22.08 (brand only @ 75 mg) | 1.58 |
| Zopiclone | 7.5 mg, 28 tablets, £1.43 | 0.05 |
| Site | CH1 | CH2 | CH3 | CH4 | CH5 | CH6 | IW1 | IW2 | IW3 | CW | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Staff in focus groups | 3 | 0 | 4 | 0 | 0 | 2 | 7 | 5 | 2 | 3 | 26 |
| Interviews | 0 | 2 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 4 |
| Total number of staff | 3 | 2 | 4 | 0 | 1 | 3 | 7 | 5 | 2 | 3 | 30 |
Appendix 2 Search strategies
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R)
Interface/URL: OvidSP.
Date range: 1946 to present.
Search date: 28 August 2012.
Retrieved records: 123.
Search strategy
-
dementia/ or alzheimer disease/ or aphasia, primary progressive/ (87,566)
-
(dementia or demented or confused).ti,ab. (69,187)
-
alzheimer$1.ti,ab,jw. (80,263)
-
or/1-3 (140,560)
-
(life adj4 story$).ti,ab. (471)
-
(life adj4 stories).ti,ab. (279)
-
(life adj4 review).ti,ab. (1831)
-
(life adj4 history).ti,ab. (9320)
-
(life adj4 histories).ti,ab. (1457)
-
(life adj4 narrative$1).ti,ab. (280)
-
or/5-10 (12,965)
-
4 and 11 (146)
-
animals/ not humans/ (3,678,892)
-
(rat or rats or mouse or mice or murine or rodent or rodents or hamster or hamsters or pig or pigs or porcine or rabbit or rabbits or dogs or dog or cat or cats or cow or cows or bovine or sheep or ovine or monkey or monkeys or horse or horses).ti. (1,686,732)
-
12 not (13 or 14) (145)
-
limit 15 to english language (123)
EMBASE
Interface/URL: OvidSP.
Date range: 1974 to week 34, 2012.
Search date: 28 August 2012.
Retrieved records: 171.
Search strategy
Bottom of form
-
dementia/ or alzheimer disease/ or primary progressive aphasia/ (154,081)
-
(dementia or demented or confused).ti,ab. (91,546)
-
alzheimer$1.ti,ab,jw. (101,856)
-
or/1-3 (197,184)
-
(life adj4 story$).ti,ab. (615)
-
(life adj4 stories).ti,ab. (340)
-
(life adj4 review).ti,ab. (2359)
-
(life adj4 history).ti,ab. (9774)
-
(life adj4 histories).ti,ab. (1506)
-
(life adj4 narrative$1).ti,ab. (337)
-
or/5-10 (14,207)
-
4 and 11 (212)
-
(Animal/ or Animal Experiment/ or Nonhuman/) not (exp Human/ or Human Experiment/) (4,807,439)
-
(rat or rats or mouse or mice or murine or rodent or rodents or hamster or hamsters or pig or pigs or porcine or rabbit or rabbits or dogs or dog or cat or cats or cow or cows or bovine or sheep or ovine or monkey or monkeys or horse or horses).ti. (1,926,871)
-
12 not (13 or 14) (207)
-
limit 15 to english language (171)
PsycINFO
Interface/URL: OvidSP.
Date range: 1806 to August week 3, 2012.
Search date: 30 August 2012.
Retrieved records: 177.
Search strategy
-
dementia/ or alzheimer’s disease/ or Aphasia/ (49,550)
-
(dementia or demented or confused).ti,ab,id. (43,618)
-
alzheimer$1.ti,ab,jw,id. (35,455)
-
or/1-3 (69,379)
-
(life adj4 story$).ti,ab,id. (1485)
-
(life adj4 stories).ti,ab,id. (1457)
-
(life adj4 review).ti,ab,id. (1716)
-
(life adj4 history).ti,ab,id. (4725)
-
(life adj4 histories).ti,ab,id. (1315)
-
(life adj4 narrative$1).ti,ab,id. (1192)
-
or/5-10 (10,587)
-
4 and 11 (194)
-
limit 12 to english language (177)
Social Policy and Practice July 2012
Interface/URL: OvidSP.
Search date: 28 August 2012.
Retrieved records: 165.
Search strategy
-
(dementia$ or alzheimer$ or aphasia or demented or confused).af. (11,546)
-
(life adj4 story$).af. (975)
-
(life adj4 stories).af. (180)
-
(life adj4 review).af. (227)
-
(life adj4 history).af. (250)
-
(life adj4 histories).af. (112)
-
(life adj4 narrative$1).af. (77)
-
or/2-7 (1638)
-
1 and 8 (165)
Cochrane Database of Systematic Reviews/Cochrane Central Register of Controlled Trials
Interface/URL: The Cochrane Library/Wiley Online Library. Issue 8 of 12 August 2012.
Search date: 29 August 2012.
Retrieved records:
Cochrane Database of Systematic Reviews: 2.
Cochrane Central Register of Controlled Trials: 6.
Search strategy
| #1 | MeSH descriptor Dementia, this term only | 1103 |
| #2 | MeSH descriptor Alzheimer Disease, this term only | 1905 |
| #3 | MeSH descriptor Aphasia, Primary Progressive, this term only | 5 |
| #4 | (dementia or demented or confused):ti,ab | 4075 |
| #5 | alzheimer*:ti,ab,so | 4044 |
| #6 | (#1 OR #2 OR #3 OR #4 OR #5) | 6965 |
| #7 | (life near/4 story*):ti,ab | 6 |
| #8 | (life near/4 stories):ti,ab | 8 |
| #9 | (life near/4 review):ti,ab | 121 |
| #10 | (life near/4 history):ti,ab | 27 |
| #11 | (life near/4 histories):ti,ab | 27 |
| #12 | (life near/4 narrative*):ti,ab | 1 |
| #13 | (#7 OR #8 OR #9 OR #10 OR #11 OR #12) | 153 |
| #14 | (#6 AND #13) | 9 |
Database of Abstracts of Reviews of Effects/Health Technology Assessment database
Interface/URL: The Cochrane Library/Wiley Online Library. Issue 8 of 12 August 2012.
Search date: 29 August 2012.
Retrieved records:
Database of Abstracts of Reviews of Effects: 6.
Health Technology Assessment: 1.
Search strategy
| #1 | MeSH descriptor Dementia, this term only | 1103 |
| #2 | MeSH descriptor Alzheimer Disease, this term only | 1905 |
| #3 | MeSH descriptor Aphasia, Primary Progressive, this term only | 5 |
| #4 | (dementia or demented or confused) | 9481 |
| #5 | alzheimer* | 4564 |
| #6 | (#1 OR #2 OR #3 OR #4 OR #5) | 10565 |
| #7 | (life near/4 story*) | 8 |
| #8 | (life near/4 stories) | 10 |
| #9 | (life near/4 review) | 505 |
| #10 | (life near/4 history) | 96 |
| #11 | (life near/4 histories) | 96 |
| #12 | (life near/4 narrative*) | 20 |
| #13 | (#7 OR #8 OR #9 OR #10 OR #11 OR #12) | 619 |
| #14 | (#6 AND #13) | 62 |
Science Citation Index Expanded, Social Sciences Citation Index, Conference Proceedings Citation Index – Science, Conference Proceedings Citation Index: Social Science & Humanities
Interface/URL: Web of Science.
Search date: 29 August 2012.
Retrieved records: 224.
Search strategy
Lemmatization=Off
Timespan=All Years
# 11 224
(#3 and #10) AND Language=(English)
# 10 49,751
(#4 or #5 or #6 or #7 or #8 or #9) AND Language=(English)
# 9 859
(TS=(life near/4 narrative*)) AND Language=(English)
# 8 5387
(TS=(life near/4 histories)) AND Language=(English)
# 7 41,397
(TS=(life near/4 history)) AND Language=(English)
# 6 2639
(TS=(life near/4 review)) AND Language=(English)
# 5 1030
(TS=(life near/4 stories)) AND Language=(English)
# 4 1162
(TS=(life near/4 story*)) AND Language=(English)
# 3 178,943
(#1 or #2) AND Language=(English)
# 2 2826
(SO=alzheimer*) AND Language=(English)
# 1 178,555
(TS=(dementia or alzheimer* or “primary progressive aphasia” or demented or confused)) AND Language=(English)
Cumulative Index to Nursing and Allied Health Literature
Interface/URL: EBSCOhost.
Search date: 30 August 2012.
Retrieved records: 104.
Search strategy
S11 (S1 or S2 or S3) and S10 104
S10 S4 OR S5 or S6 or S7 or S8 or S9 2318
S9 TI (life N4 narrative*) or AB (life N4 narrative*) 226
S8 TI (life N4 histories) or AB (life N4 histories) 162
S7 TI (life N4 history) or AB (life N4 history) 662
S6 TI (life N4 review) or AB (life N4 review) 792
S5 TI (life N4 stories*) or AB (life N4 stories*) 292
S4 TI (life N4 story*) or AB (life N4 story*) 406
S3 TI alzheimer* or AB alzheimer* or SO alzheimer* 11,354
S2 TI (dementia or demented or confused) or AB (dementia or demented or confused) 18,798
S1 MH (dementia+ or Alzheimer’s disease or aphasia+) 32,272
Applied Social Sciences Index and Abstracts
Interface/URL: ProQuest.
Search date: 30 August 2012.
Retrieved records: 33.
Search strategy
S15 S4 and S14 • 33*
S14 S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 • 1950*
S13 SU(“Life narratives”) • 63*
S12 SU(“Life histories”) • 214*
S11 SU(“Life stories”) • 117*
S10 TI,AB(life NEAR/4 narrative*) • 261*
S9 TI,AB(life NEAR/4 histories) • 800*
S8 TI,AB(life NEAR/4 history) • 800*
S7 TI,AB(life NEAR/4 review) • 422*
S6 TI,AB(life NEAR/4 stories) • 493*
S5 TI,AB(life NEAR/4 story*) •273*
S4 S1 or S2 or S3 • 6842*
S3 TI,AB,PUB(alzheimer*) • 2821*
S2 TI,AB(dementia OR demented OR confused) • 4884*
S1 SU.EXPLODE(“Alcoholic dementia” OR “Alzheimer’s disease” OR “Dementia” OR “Lewy body dementia” OR “Multi-infarct dementia” OR “Presenile Alzheimer’s disease” OR “Presenile dementia” OR “Semantic dementia” OR “Senile dementia” OR “Subcortical dementia” OR “Vascular dementia” OR “Agraphia” OR “Anomic aphasia” OR “Aphasia” OR “Conduction aphasia” OR “Developmental dyscalculia” OR “Dyscalculia” OR “Peripheral agraphia”) • 4550*
*Approximate result count without duplicates.
Social Services Abstracts
Interface/URL: ProQuest.
Search date: 30 August 2012.
Retrieved records: 19.
Search strategy
S14 S4 and S12Limits applied 19*
S13 S4 and S12 • 21*
S12 S5 or S6 or S7 or S8 or S9 or S10 or S11 • 876*
S11 SU(“Life History”) • 144*
S10 TI,AB(life NEAR/4 narrative*) • 138*
S9 TI,AB(life NEAR/4 histories) • 336*
S8 TI,AB(life NEAR/4 history) • 336*
S7 TI,AB(life NEAR/4 review) • 169*
S6 TI,AB(life NEAR/4 stories) • 253*
S5 TI,AB(life NEAR/4 story*) • 126*
S4 S1 or S2 or S3 • 2294*
S3 TI,AB,PUB(alzheimer*) •868*
S2 TI,AB(dementia or demented or confused) • 1703*
S1 SU(“Senility” or “Alzheimer’s disease” or “Aphasia”) • 1211*
*Approximate result count without duplicates.
Social Care Online
Interface/URL: www.scie-socialcareonline.org.uk/.
Search date: 31 August 2012.
Retrieved records: 113.
Search strategy
(freetext=“dementia*” or freetext=“alzheimer*” or freetext=“aphasia” or freetext=“demented” or freetext=“confused”) and (freetext=“life stor*” or freetext=“life review” or freetext=“life histor*” or freetext=“life narrativ*”)
Research Register for Social Care
Interface/URL: www.scie.org.uk/publications/researchresources/research-register-for-social-care (closed April 2014).
Search date: 31 August 2012.
Retrieved records: 0.
Search strategy
Free-text searches on following:
life stor*
life history*
life narrative*
life review*
ClinicalTrials.gov
Interface/URL: www.clinicaltrials.gov/.
Search date: 31 August 2012.
Retrieved records: 2.
Search strategy
(dementia OR alzheimer OR aphasia) AND (“life story” OR “life stories” OR “life review” OR “life history” OR “life histories” OR “life narrative” OR “life narratives”)
NHS Evidence
Interface/URL: www.evidence.nhs.uk/.
Search date: 31 August 2012.
Retrieved records: 53.
Search strategy
dementia* OR alzheimer* OR aphasia) AND (“life story” OR “life stories” OR “life review” OR “life history” OR “life histories” OR “life narrative” OR “life narratives”) = 53
[Search strategy limited by: Type of information: grey literature]
OpenGrey
Interface/URL: www.opengrey.eu/.
Search date: 31 August 2012.
Retrieved records: 0.
Search strategy
(dementia* OR alzheimer* OR aphasia) AND (“life story” OR “life stories” OR “life review” OR “life history” OR “life histories” OR “life narrative” OR “life narratives”)
Appendix 3 Algorithm for selection for relevance
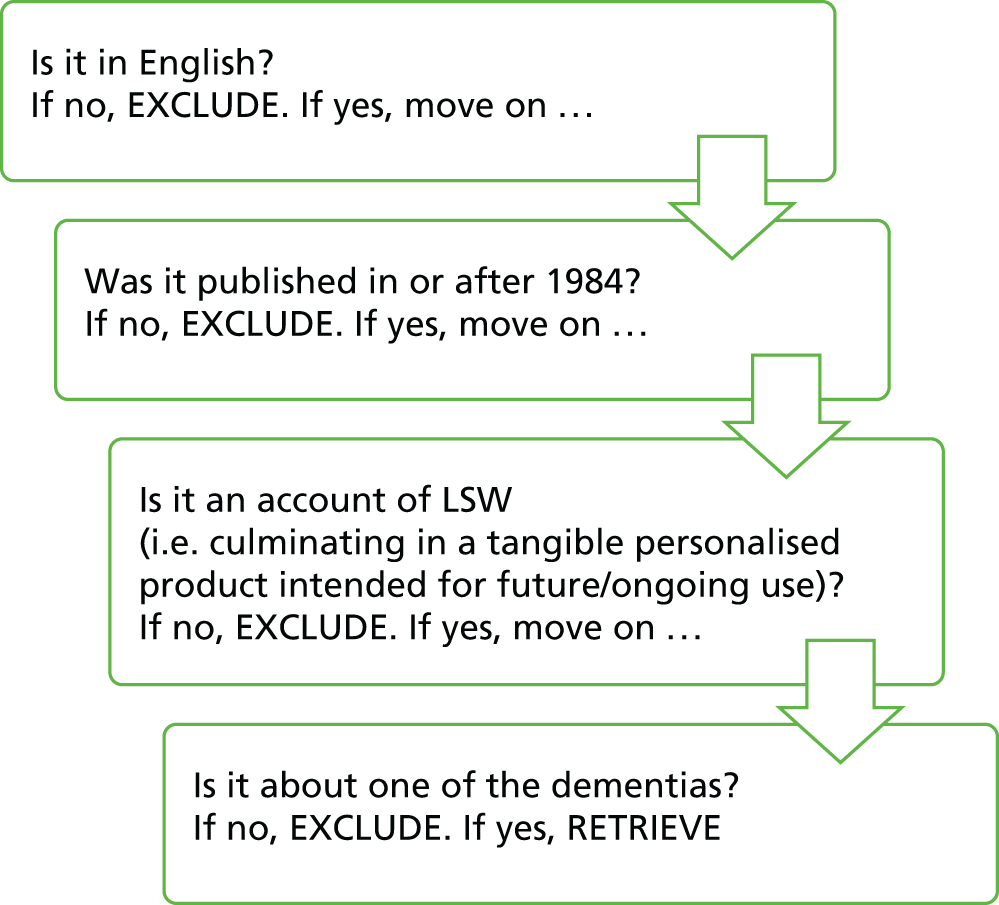
Notes for reviewers
-
Be inclusive – if you are unsure at any stage, mark with a query and opt to retrieve. A decision can then be made based on a full reading.
-
Data will be extracted only from written records – videos and podcasts should therefore be excluded.
-
Exclude single case studies.
Appendix 4 Instructions for selection for inclusion
Appendix 5 Paperwork for focus groups
Information sheets
Focus groups with people with dementia
Focus groups with family carers
Focus groups with professionals
Consent forms
People with dementia
Carers
Professionals
Summary of findings
Appendix 6 Topic guides for focus groups with carers/people with dementia/professionals
Topic Guides
Focus groups with people with dementia
Focus groups with family cares
Focus groups with professionals
Appendix 7 ‘I Am’ Fluency Task
The feasibility of using the ‘I Am’ Fluency Task with people with dementia living in care homes
The ‘I Am’ Fluency Task is an adapted version of the Twenty Statements Task125 that was developed to examine the accessibility of self-concept statements (e.g. I am generous, I am a mother, I am a psychologist). The original Twenty Statements Task asks participants to describe their sense of self by responding open endedly to the question ‘Who am I?’. This task was modified such that participants were given 2 minutes to generate as many statements as possible beginning with the phrase I am, the assumption being that the ability to generate statements in a given time reflects accessibility to self-concept.
Fourteen people with dementia living in care homes were approached to complete the ‘I Am’ Fluency Task. Of these 14 participants, 11 were able to generate self-concept statements that described aspects of their identity, with the number of ‘I am’ statements generated in 2 minutes ranging from 2 to 10. Of the remaining three participants, two presented with language difficulties consistent with anomic aphasia and were therefore unable to generate any statements in response to the task instructions, and one participant, whose spoken language was consistent with Wernicke’s aphasia, gave responses that were inconsistent with the task. Overall, those without language deficits were able to complete the task. Some individuals commented that they were not used to thinking about themselves in such a way, and others tended to talk in detail about their statements, and this prevented them from generating many in the given time frame. Such observations might explain the small number of statements generated by some participants, as correlational analysis demonstrates that an inability to generate many statements in the allotted time is not attributable to a general fluency deficit.
It was anticipated that people with dementia would find it difficult to complete the ‘I Am’ Fluency Task and so the ‘Me/Not Me’ task was also designed for the purposes of this research. The ‘Me/Not Me’ task presents participants with a list of 30 words (e.g. grandmother, loving, retired) and asks participants to rate each for self-descriptiveness. This is done by selecting one of three responses: ‘me’, ‘not me’ or ‘sometimes me’. All 11 participants who completed the ‘I Am’ Fluency Task were able to complete this task, and most of them completed it with ease. However, a couple of the participants did not engage with the forced choice element of the task; they would speak for several minutes regarding their answer and would then have to be guided by the experimenter towards selecting the most appropriate of the three responses (e.g. when given the statement ‘happy’ one participant spoke in depth about being happy most days but also feeling down on occasions; this participant was subsequently guided to give the response ‘sometimes me’). This tendency to give an embellished response to each item is reflected in the finding that it took participants an average of 7 minutes and 48 seconds to respond to all 30 items in the ‘Me/Not Me’ task.
Aphasic participants were also able to respond to some items on the ‘Me/Not Me’ task. Ability on this task varied for those with aphasia; the most extremely aphasic participant responded to 13 of the 30 statements, for instance in response to being asked if she was a driver she responded ‘no I don’t drive’. The second participant who presented with anomic aphasia responded to most items (27/30) despite very limited language ability. The participant who presented with language consistent with Wernicke’s aphasia responded to all items, yet it was not clear that she responded appropriately to all items; for instance, in response to being asked if she was a good listener she replied ‘yes, I like to know everything’ and yet when asked if she was an aunt, she replied ‘they are all right’.
In an attempt to examine the accessibility of autobiographical memory, the Autobiographical Fluency Task147 was administered to participants. This task examines the ability of participants to generate both personal semantic (names of people known to them) and personal incident (personally experienced events) memories for three lifetime periods: childhood, early adult life and recent life. Participants were given 2 minutes to generate as much information as possible for each of the six components of this task. Nine of the 14 participants who were approached to take part in this research were able to complete this task; two withdrew from taking part at this stage and the task was not attempted with the three aphasic participants.
Overall, most participants were able to generate names and events from across the lifespan, with events from early adulthood and names from childhood being most accessible. When asking about recent times a number of participants were disorientated to time and generated event memories from more than 5 years ago (e.g. finishing the army in 1947). These memories were not included in the analysis.
The pattern of findings from the autobiographical fluency task replicates that of Addis and Tippett,126 who also found that individuals with Alzheimer’s disease were impaired on both personal semantic and personal incident memory relative to a control group of aged matched individuals without dementia. Suggesting that the findings from individuals in the present research likely indicates impaired autobiographical memory. Indeed, it was clear from administering this task that participants found it difficult to recall information from across their lifespan, yet the data that were collected suggest that, nevertheless, they engaged with the task and understood the task instructions.
Appendix 8 Text version of provider survey
Appendix 9 Paperwork for carer survey
Appendix 10 Paperwork for feasibility study
Information sheets
Care homes: people with dementia
Comparison hospital: people with dementia
Care homes: family carers
Comparison hospital: family carers
Care homes: consultees
Comparison hospital: consultees
Care homes: staff
Comparison hospital: staff
Consent forms
People with dementia
Carers
Consultees
Staff
List of abbreviations
- A&E
- accident and emergency
- ADQ
- Approaches to Dementia Questionnaire
- CBI
- Copenhagen Burnout Inventory
- CDS
- community dementia support service
- CES
- Carer Experience Scale
- CIC
- community interest company
- DVD
- digital versatile disc
- GP
- general practitioner
- IPA
- inpatient dementia assessment service
- IW
- intervention ward
- LSW
- life story work
- MAS
- memory assessment service
- MeSH
- medical subject heading
- MRC
- Medical Research Council
- OT
- occupational therapist
- OTTI
- occupational therapy technical instructor
- PDQ
- Personhood in Dementia Questionnaire
- PRN
- pro re nata (‘as required’)
- QCPR
- Scale for the Quality of the Current Relationship in Caregiving
- QoL
- quality of life
- QoL-AD
- Quality of Life – Alzheimer’s Disease
- SCH
- dementia-specialist long-term care home
- SCREC
- Social Care Research Ethics Committee