Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/136/79. The contractual start date was in April 2014. The final report began editorial review in October 2016 and was accepted for publication in March 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Alys Young sits on an expert reference group convened by the Royal College of Psychiatry and the charitable organisation SignHealth, in order to draw up guidelines for commissioners of primary mental health services for Deaf people. Katherine Rogers is chairperson of the British Society for Mental Health and Deafness. Steve Pilling is in receipt of funding from the National Horizon Scanning Centre to develop care pathways for the Improving Access to Psychological Therapies programme. Rachel Belk works part-time in a NHS clinical role as a genetics counsellor, where she occasionally works with Deaf patients. Claire Dodds works as a freelance British Sign Language/English interpreter, occasionally within health-care settings.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Young et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Introduction
This exploratory, mixed-methods study is focused on adults who are Deaf, who use British Sign Language (BSL) as their first, preferred or strongest language, and who experience anxiety and/or depression. Specifically it addresses the effectiveness and cost-effectiveness of the Improving Access to Psychological Therapies (IAPT) programme in the delivery of psychological therapies for Deaf BSL users. IAPT services deliver approved psychological interventions to address anxiety and depressive disorders. Services are delivered in primary care settings1 and follow the National Institute for Health and Care Excellence (NICE)-approved stepped care model, which includes low-intensity treatment at step 2 [e.g. cognitive–behavioural therapy (CBT) and guided self-help] and high-intensity treatment at step 3 (including CBT for individuals with an inadequate response to therapy at step 2, as well as those with more serious disorders). 1 This study is confined to step 2 and step 3 aspects of the IAPT service model. First, it compares the service delivery and clinical outcomes of two kinds of IAPT service accessed by Deaf BSL users: (1) the usual service that might be accessed via sign language interpreters and/or other reasonable adjustments, which is referred to in this study as ‘standard IAPT’; and (2) a bespoke adaptation of the IAPT service delivered in BSL by Deaf therapists to Deaf people that incorporates additional culturally orientated adaptations, referred to in this study as ‘BSL-IAPT’. Second, this study sets out to lay the groundwork required prior to considering any large-scale study, whether a randomised clinical trial or other controlled, prospective study design. This includes instrument design and adaptation, testing the feasibility of recruitment in sufficient numbers and engagement with the Deaf community.
British Sign Language and Deaf people
British Sign Language is a fully grammatical, living language, distinct from English,2 and its status as an indigenous minority language of the UK was recognised by the UK government in 2003. 3 In Scotland, in 2015, its legal position was further strengthened by the BSL (Scotland) Act. 4 Deaf people are, therefore, afforded the status of other minority groups whose access to services should not simply be protected, but actively promoted, under the provisions of the Public Sector Equality Duty 2011,5 following the Equality Act 2010. 6
In common with other language-using groups, distinct cultural norms, practices and traditions are associated with BSL users, who are thus regarded as constituting a minority cultural–linguistic community in the UK. 7 Deaf people who sign regard their language as a marker of positive cultural identity, not as a feature of failing to speak or having a hearing loss. 7 To be Deaf is not an audiologically determined definition but, rather, a culturally determined one. 8,9 This cultural–linguistic identity is conventionally marked by the use of upper-case ‘D’, as in Deaf, in the same way in which one might refer to French or Polish people. Lower-case ‘d’ (deaf) is usually reserved for those people with an acquired hearing loss or who prefer to communicate using spoken language. 10 We follow this convention throughout the report. Although some Deaf people may also use, to differing extents, the spoken language of the country in which they live, their signed language, such as BSL, is their first, preferred, strongest or, in some cases, only language. Literacy in the written word remains a challenge for many Deaf people, in part because of the phonological basis of learning to read. 11 It is erroneous to assume that information written down is accessible because it is not dependent on hearing. 10
Estimates of the Deaf population vary considerably as a result of how data are collected; in some cases there is a failure to distinguish between the ‘disability’ of deafness and cultural–linguistic identity, in others the question asked is too restrictive to permit viable extrapolations to be made. For example, the Ipsos MORI General Practitioner (GP) Patient Survey (2009/10) quotes a figure of 101,107 ‘Deaf Sign Language Users’ in England alone. 12,13 The Office for National Statistics (ONS) data release14 on languages records 22,000 sign language users in England and Wales, of whom 15,000 said specifically that their language was BSL. The Welsh Assembly Government estimates that BSL is the first or preferred language of 3000 people in Wales. 15 The Scottish Council on Deafness estimates that it is the first or preferred language of 6000 people in Scotland. 16 The Department for Communities in Northern Ireland suggests that there are 5000 sign language users, of whom 3500 use BSL and 1500 use Irish Sign Language. 17 Overall, conservative estimates indicate a UK population of Deaf BSL users of between 60,000 and 70,000.
Improving Access to Psychological Therapies
Improving Access to Psychological Therapies is a large-scale initiative within the NHS aimed at redressing long-standing imbalances between psychological therapy demand and supply. 1,18–20 The national IAPT census 201421 records 255 IAPT services, based on a 95% response rate. IAPT services deliver approved psychological interventions to address anxiety and depressive disorders in primary care settings. 1 IAPT services follow the NICE-approved stepped care model, which includes low-intensity treatment at step 2 (e.g. CBT and guided self-help) and high-intensity treatment at step 3 (including CBT for individuals with an inadequate response to therapy at step 2, as well as those with more serious disorders). 1 This study is confined to step 2 and step 3 aspects of the IAPT service model. IAPT practitioners are drawn from existing professionals, for example clinical psychologists, and, additionally, the IAPT initiative has included the training of a new workforce of psychological well-being practitioners (PWPs). 1
The adaptation of the IAPT service for Deaf people was provided by the health charity SignHealth under the title ‘BSL Healthy Minds’ and was supported by the British Society for Mental Health and Deafness. 22 It involved training Deaf people as PWPs in order to deliver therapy directly to Deaf clients who experienced anxiety and depression at step 2 and step 3 levels. 22 In other words, it was a linguistically and culturally matched service delivery model. We refer to this intervention model as BSL-IAPT throughout the report. However, during the course of the study, services other than BSL Healthy Minds started to offer specialist IAPT provision for Deaf people, a trend we explore in the course of this work in seeking to model ‘BSL-IAPT’ separately from its identity with an original sole provider (see Chapter 5). Elsewhere in England, Deaf people would routinely access IAPT through their usual local provider(s), although the kinds of adaptations that might be provided for such access and treatment were not known. We refer to this as standard IAPT throughout the report and explore the variations within its provision (see Chapter 5).
This naturally occurring experimental condition created a rare opportunity to compare the effectiveness and cost-effectiveness of two models of IAPT delivery for Deaf people with depression and/or anxiety without the requirement to withhold, replace or enhance an intervention, as both were a usual standard of care depending on where a Deaf person resided. However, the achievement of this overarching objective, to compare the effectiveness and cost-effectiveness of the two models of delivery, required considerable groundwork. We report here the development of a number of components that were prerequisites to any future trial or large-scale observational study, but which also have independent value and implications for future research, clinical services and available information for commissioners of IAPT services.
Deaf people and mental health
Deaf people experience significantly poorer mental health than the hearing population, with the prevalence of some common mental health problems, such as depression and anxiety, being up to twice as high. 23,24 In only a minority of cases are mental ill-health and deafness causally connected (i.e. where the aetiology of deafness is coincidental with organic origins of mental illness/neurological impairment). Of greater significance is how early childhood deafness interferes with the usual processes of language acquisition and psychosocial development. The incidence of mental health problems in deaf children/young people is around 1.5 times greater than among their hearing counterparts. 25 In adulthood, although the incidence of major psychoses is broadly consistent with that among hearing people, the prevalence of depressive disorders and anxiety is significantly higher (33% of the Deaf population vs. around 20% of the hearing population). 26
Studies have demonstrated the inaccessibility of health services to Deaf BSL users,27–30 including mental health services, resulting in late diagnoses and loss of benefit from early preventative interventions. 31 Poor access to information about health-related matters in BSL results in poor awareness among Deaf community members of mental health issues, including personal support strategies, help-seeking behaviours, routes of referral and treatment options. Often Deaf people use mental health services only when a difficulty has escalated to the point at which secondary/tertiary care intervention is required. 23,27,28 Poor treatment outcomes are related, in part, to late access to preventative and primary mental health services. 23
The Department of Health (DH) review of mental health services for Deaf people27 resulted in significant strategic investment in NHS specialist services to address this health inequality. The latest investment is in primary care: IAPT.
Improving Access to Psychological Therapies and Deaf people
BSL-IAPT was originally offered in two health authorities before being offered in five areas from April 2013. However, service accessibility has been declining since April 2014 as a result of new commissioning arrangements subsequent to the transformation from a primary care trust (PCT) structure in England to Clinical Commissioning Groups (CCGs) instead. 32
Moreover, in the course of this study it became apparent that a few service providers, other than BSL Healthy Minds, were starting to develop specialist provision for Deaf people, including using qualified Deaf PWPs. Provider and model of provision were no longer synonymous. We return to this issue in Chapter 5 where we explore key components of service models and provision and define the components of a BSL-IAPT intervention, independent of the original provider. However, at the start of the research project BSL-IAPT was distinguished by the following core components in its original form as delivered by BSL Healthy Minds:
-
standard assessment instruments [Patient Health Questionnaire-9 item (PHQ-9), Generalised Anxiety Disorder-7 (GAD-7) and the Work and Social Adjustment Scale (WSAS)] that are translated into BSL, and their internal reliability for use with Deaf people established by the applicants33
-
Deaf people trained as PWPs to deliver the IAPT programme in BSL
-
self-help guidance that is culturally adapted. 22
Where a BSL-IAPT service does not exist or is not commissioned, Deaf people access the usual IAPT provision in their locality, which we refer to in this report as standard IAPT. The range of adaptations, if any, made by standard IAPT services to meet the requirements of Deaf BSL users were not known at the start of the project, nor had their utility and effectiveness been previously explored. It is estimated that there are around 255 standard IAPT services in England,21 although at the start of the project it was not known how many Deaf people have used these services.
What is the problem and what is the opportunity?
It is not possible to determine whether or not the current investment in a core specialist service (BSL-IAPT as provided by BSL Healthy Minds) is justified and should be extended nationally. This is because it is not known if it confers any benefit for Deaf people over and above accessing standard IAPT services, particularly given the range of potential adaptations for Deaf people to the standard IAPT service, the effectiveness of which is also unknown. The cost-effectiveness of BSL-IAPT has not been investigated. A rigorous examination of effectiveness and cost-effectiveness is needed to guide decision-making about longer-term sustainability and appropriate targeted primary care intervention for this particularly hard-to-reach group.
Data from all IAPT patients, collected through universal key performance indicators (KPIs) and the IAPT minimum data set, are uploaded centrally, allowing for comparisons to be made by service provider and individual patient characteristics. This presents a major research opportunity because (1) internationally, most evidence concerning Deaf people’s mental health is drawn from hospital inpatient/outpatient population studies with very limited evidence from primary care; (2) although the internal reliability of the BSL-IAPT tools has been determined, validation of clinical cut-off points requires analysis based on a clinical sample; and (3) the effectiveness of BSL-IAPT depends on its culturally perceived acceptability, not just its linguistic accessibility, requiring investigation of the service delivery process.
This study will be the first step in determining whether or not BSL-IAPT is justified for Deaf people. Importantly, the study will provide valuable information to inform the need for and design of follow-on research to assess the effectiveness and cost-effectiveness questions. Although the proposed project concerns Deaf people specifically, it is an example of an important comparison relevant to many service sectors within the NHS. It asks what difference exists in terms of benefit, if any, between standard services made linguistically accessible to particular cultural–linguistic groups of patients, and adaptations of standard services designed specifically around the cultural identity and language preferences of specific groups.
Chapter 2 Overview of design and methods
Introduction
This exploratory, mixed-methods study has three objectives that deliver new evidence and outputs in their own right while laying the groundwork for any future larger-scale study, whether a randomised clinical trial or other controlled, prospective study design.
Objectives
-
To explore the following questions:
-
Is BSL-IAPT more effective than standard IAPT for Deaf people with anxiety and/or depression?
-
Is any additional benefit from BSL-IAPT worth any additional cost to provide it?
-
-
To establish relevant BSL versions of assessment tools and methods to answer research questions (a) and (b).
-
To gauge the feasibility of a larger-scale definitive study and inform its future design.
Methods
The component studies, the preparatory issue, they addressed and their individual objectives and methods are as follows.
Study 1: qualitative exploration of the acceptability of individual randomisation and development of trial-related terminology in British Sign Language (see Chapter 3)
Preparatory issues to be addressed
-
Deaf people are rarely provided with a service matched to their linguistic/cultural needs. The possibility of being randomised in to or out of a service perceived as specialist for Deaf people may be an impediment to adequate recruitment.
-
Deaf people have been routinely excluded from randomised controlled trials (RCTs). Terminology does not exist in common use for key concepts associated with trial participation that would support informed choice and recruitment to any future study.
Objectives
-
To investigate the acceptability of randomisation among Deaf service users.
-
To develop trial-related terminology in BSL to support informed choice and recruitment.
Method
-
Deaf-led focus groups in BSL with service users and members of the Deaf community.
Study 2: secondary data analysis of patient numbers and outcomes data (see Chapter 4)
Preparatory issues to be addressed
-
There are no valid outcome data on Deaf people who have used BSL-IAPT because the correct clinical cut-off points for the BSL assessment instruments used have not been established. Outcome data on Deaf users of standard IAPT have never been collected and analysed.
-
The comparability of the two populations of service users is unknown.
-
The feasibility of recruiting sufficient numbers to a large-scale study is yet to be established.
Objectives
-
To establish the clinical cut-off points for the BSL-IAPT assessment tools (PHQ-9 and GAD-7) for patients with anxiety and/or depression.
-
To explore the population characteristics of BSL-IAPT and Deaf users of standard IAPT services, including demographic characteristics, referral routes and adherence, and to compare clinical outcomes.
-
To map probable numbers of users of BSL-IAPT and Deaf users of standard IAPT who would be eligible for recruitment to a large-scale study.
-
To establish effect size and estimate recruitment targets should a full trial be indicated.
Method
-
Secondary data analysis of pre-existing clinical data.
Study 3: mixed-methods modelling of BSL-IAPT and standard Improving Access to Psychological Therapies as accessed by Deaf people (see Chapter 5)
Preparatory issues to be addressed
-
Although BSL-IAPT was initially synonymous with a single provider in specified regions, it became available in some other parts of England as a component of standard provision. Therefore, what constitutes BSL-IAPT required definition if it were to be operationalised in any future comparative study.
-
The range and nature of adaptations for Deaf people who accessed standard IAPT were unknown and, therefore, it could not yet adequately be modelled as an intervention if it were to be operationalised in any future comparative study.
Objectives
-
To produce a replicable description of ‘standard IAPT’ when implemented with BSL users.
-
To produce a replicable description of the core components of BSL-IAPT differentiated from its delivery by a single-service provider.
Methods
-
Online survey and individual interviews with a subsample of BSL-IAPT and standard IAPT providers.
Study 4: translation and validation of the EQ-5D-5L version in British Sign Language and exploratory analysis of appropriate utility weights (see Chapter 6)
Preparatory issues to be addressed
-
There is no BSL version of this common health outcome instrument routinely used in research and evaluation studies that has been validated. (There is no validated version in any signed language in the world.)
-
Pre-existing utility weights may not be suitable for this population.
Objectives
-
To translate and test the reliability of a BSL version of the EuroQol-5 Dimensions, five-level version (EQ-5D-5L).
-
To conduct further analyses of the BSL EQ-5D-5L data collected as part of this study (study 5), to inform future research with this population.
Methods
-
Translation via accepted protocols with adaptations for visual languages. Online data collection from users of the BSL version and analysis of psychometric properties.
-
Systematic literature review and secondary analysis of data collected in this project to establish appropriate utility weights.
Study 5: exploratory economic evaluation (see Chapter 7)
Preparatory issue to be addressed
-
An exploratory economic evaluation would be required prior to any future feasibility study or full trial.
Objectives
-
To explore the potential costs of health and social care, and the health benefit in terms of quality-adjusted life-years (QALYs) for Deaf users of BSL-IAPT and Deaf users accessing standard IAPT.
-
To estimate the net cost per QALY gained by BSL-IAPT.
The key research questions were:
-
Is BSL-IAPT potentially cost-effective compared with standard IAPT, when service-specific PHQ-9 and GAD-7 tools and cut-off points were used to identify people with depression/anxiety and to measure recovery?
-
Does the potential cost-effectiveness of BSL-IAPT vary if different assumptions are made about the probability, costs or QALYs of treatment events?
Methods
-
Systematic, focused economic literature review and secondary analysis of data collected in other studies within the project.
Patient and public involvement
Deaf service users and members of the general Deaf population were engaged throughout the study in a variety of different ways. Both the Project Advisory Group (PAG) and the Study Steering Committee (SSC) benefited from the input of several lay community members, some of whom had experience of mental health services. Minutes and meeting notes were made available in BSL before and after meetings, and alternative ways of contributing were explored with those who could, on occasion, not attend in person [e.g. video-conferencing, individual discussion and contribution via skype™ (Microsoft Corporation, Redmond, WA, USA), etc.].
Deaf BSL users were also the lead participants in the exploration of trial-related terminology in study 1 (see Chapter 3). Building on that work, a separate patient and public involvement (PPI) group was established, consisting entirely of Deaf community members, to further comment on the findings of study 1, and to co-develop the additional project output of the BSL glossary of terms commonly used in recruitment materials and trial-related information (see Appendices 1 and 2). Further to this, the PPI group developed an additional resource aimed at supporting active public involvement in NHS, public health and social care research. Aimed at professionals and Deaf people alike, the video allowed Deaf BSL users to share their experiences of PPI within this project and in other areas, including examples of good practice with relevance for future studies (see Appendix 3).
Ethics approval
Studies 1, 3 and 4 received ethics approval from the University of Manchester Research Ethics Committee (REC) (reference numbers: 14183, 150715 and 14183, respectively). Study 2 received ethics approval from the NHS REC – Proportionate Review Subcommittee of the National Research Ethics Service (NRES) Committee London – Camberwell St Giles (reference 14/LO/2234).
The University of Manchester and NHS protocols for data protection were adhered to.
Chapter 3 Qualitative exploration of the acceptability of individual randomisation and development of trial-related terminology in British Sign Language (study 1)
Some parts of this chapter have previously appeared in Young et al. 34 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The text below includes minor additions and formatting changes to the original text. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. When paragraphs are repeated here verbatim, they have been displayed as quotations with reference to the original paper.
Background
Failure to recruit adequate numbers is a common reason for trials not succeeding. 35–37 Among a range of factors that have been identified as underlying poor recruitment is whether or not randomisation is perceived as acceptable among the population(s) to be recruited. 38,39 Previous research identifies two main aspects of acceptability of randomisation to be considered: understanding for informed consent and treatment-specific preferences.
With regard to understanding, studies have demonstrated that some terms commonly used in trial recruitment (such as ‘randomisation’, ‘trial’, ‘placebo’, ‘arm’) may be unfamiliar to participants, but also that participants apply their understanding of terms gained from a familiar context to the unfamiliar one of trial participation, resulting in potential misunderstandings. 40–42 In addition, studies of language in trials have demonstrated ‘that there is a difference between understanding the mechanics of a process, such as randomisation (how it occurs), and participants’ comprehension of the purpose of that process (why it is necessary and its implications). 41,43 It is argued that both are required for informed consent and recall of one might hide misapprehension of the other’. 34
In the case of Deaf people’s understanding of key trial-related terminology, the situation is more complex. There are very low levels of awareness, even in lay terms, of such concepts as randomisation, trial and informed choice. In part this is because of a lack of history of Deaf people’s involvement in clinical research. RCTs routinely exclude them because of the confounding factors that their participation might bring, whether these are perceived in terms of disability (hearing loss) or in terms of language use. 34,44 Deafness also impacts on general knowledge. Deaf people commonly experience highly limited access to information on a wide range of everyday subjects because it is not available in a signed language. 8,45 Means of incidental learning, such as overhearing, accessing popular media or interactions with multiple peer groups, are also affected. Consequently, it is recognised that many Deaf people experience what has been termed a ‘low fund of information’. 46 Therefore, many Deaf people who are potential trial participants might not be even casually familiar with the terms and concepts used in participant information sheets or informed consent forms, even if these are presented in BSL. Furthermore, because of Deaf people’s lack of involvement in or incidental awareness of clinical trials, there is no pre-existing agreed or familiar lexicon for most of the terms that would be used in recruitment and information materials for potential participants to any future trial. This dearth of vocabulary, or usual means of expression, is not a result of any failure in the capacity of BSL. It is simply a result of a lack of contact with the context, which has meant that vocabulary has not been necessary and is yet to evolve. It is a situation similar to that in spoken languages prior to the digital age, where words did not exist for concepts such as ‘online’, ‘log on’ or ‘texting’ because they had not previously been required. Objective ii in the study reported here addresses the exploration and development of trial-related terminology in BSL. 34
The second aspect of the acceptability of randomisation concerns perceived preferences for a particular intervention. For example, as a systematic review of barriers to cancer trial participation has demonstrated, if there is a strong lay perception of one treatment being better than the other, or one not being regarded as appropriate or desirable, then this can act as a barrier to consent to randomisation and trial entry. 47 However, other studies have shown that, even if participants have a preference for one arm of a trial over another, or a belief that one is likely to be more effective than another, they may still consent to randomisation. In part this response may be attributed to participants perceiving that random allocation gives them a chance of treatment that they believe is superior to the alternative, and that they would not otherwise have been able to access. 48
With respect to Deaf people, perceived treatment preferences that may influence the acceptability of randomisation are likely to be fundamentally connected with language and culture. It is well evidenced that Deaf people experience significant health inequalities in terms of access to services and health outcomes in a range of domains. 23,31,49,50 In part this results from a failure to adequately provide sign-interpreted access to health care despite the requirements of the Public Sector Equality Duty5 and the NHS Accessible Information Standard. 51 Lack of cultural competence of health practitioners also plays a part in Deaf people’s less than optimum engagement with treatment. 45,52–54
In this context it is, therefore, very rare for any health service to be offered to Deaf people where the practitioner is Deaf themselves and shares a common culture, and where the treatment/intervention might be delivered directly without the requirement of an interpreter being present. The BSL-IAPT service that potentially formed one arm of a future trial was a rare exception to this situation in being directly delivered by Deaf people in BSL to other Deaf people. However, in its original form as BSL Healthy Minds, it was available in only a few regions of England. Consequently, there were four potential randomisation scenarios:
-
randomisation to BSL-IAPT and living in an area where BSL-IAPT is provided (= usual care)
-
randomisation to BSL-IAPT but living in an area where it is not provided (= access to a previously unavailable service)
-
randomisation to standard IAPT and living in an area where standard IAPT is usually provided (= usual care)
-
randomisation to standard IAPT and living in an area where usually BSL-IAPT is provided (= access to a service usually not available).
It was not known how these potential randomisation scenarios would be regarded in the context of the same service potentially delivered directly by a linguistically and culturally matched practitioner or via an interpreter from a hearing person. Objective i therefore sought to explore factors influencing the acceptability of randomisation from Deaf people’s cultural–linguistic perspective and is reported below.
Objectives
-
To investigate the acceptability of randomisation among Deaf service users.
-
To develop trial-related terminology in BSL to support informed choice and recruitment.
Methods
Design
The qualitative study was underpinned by a phenomenological approach, with data being collected by means of focus groups. Phenomenology55 suited the focus of this study, which was on both how key concepts are understood and the assumptions that might underpin the meaning participants bring and attribute to such issues as randomisation. 56 Focus groups were used because of their appropriateness in cultural terms as well as the exploratory nature of the research objectives. It has been remarked that Deaf culture is a particularly collective, rather than individualistic, culture,7,57 and Deaf people often prefer group discussion over individual interviews to explore new ideas or information because this is more culturally coherent,45 a trait observed in other cultural communities internationally such as Maori and First Nation peoples. 58
Inclusion criteria
A purposive sample was sought of Deaf people aged 18 years or over, who used BSL as their first or preferred language. Anyone currently receiving support through the IAPT programme was excluded because additional ethical permissions would be required for participants who were current patients of the National Health Service in England.
Young et al. 34
Recruitment
An explanation of the study in BSL was posted on the research group website and advertisements to participate in the focus groups were placed on a signed Facebook [Facebook, Inc., Menlo Park, CA, USA] site accessed by the Deaf community and through email, shared networks and word of mouth/word of hand.
Young et al. 34
Ethics
The study was approved by the University of Manchester Research Ethics Committee (Ref: 14183). Informed consent was obtained from all participants. Participant information sheets were made available in advance of the focus groups in BSL on a website as well as in plain English. Prior to the focus groups, the researchers clarified the information in BSL again, face to face, and participants had the opportunity to ask questions. All participants were provided with a pre-written, postage paid withdrawal form to facilitate easily withdrawal of consent for their data to be used subsequent to the focus groups.
Young et al. 34
Data collection
The focus groups were facilitated by two Deaf native BSL users who were part of the research team: one had a higher degree in research and was very experienced in focus group facilitation; the other was new to research but had worked for many years in the Deaf community in various social and support roles. Both facilitators were known to Deaf participants insofar as the Deaf community is small and it is not unusual to know or know of other Deaf people; however, neither had a personal or close professional relationship with any of the participants. Deaf facilitators ensured that data could be collected directly, without the more usual circumstance of an interpreter being required to facilitate discussion and, because Deaf participants and facilitators shared a common cultural background and identity, it was assumed that this would aid open and relaxed discussion. However, some participants remarked in the course of the focus groups that they perceived the facilitators to be ‘clever Deaf people’ and therefore different from themselves because the facilitators were more familiar with the kinds of issues that were being addressed in the groups.
At times, this meant that facilitators had to resist requests from participants to explain clearly what randomisation meant and why there might be an issue about acceptability. The notion of another Deaf person standing back and facilitating discussion that explored ideas rather than conveying face-to-face reliable information was difficult for some of the participants as it transgressed their expectations of Deaf people’s obligations to each other to support information access and understanding. As previous studies have documented,59 Deaf people experience a strong sense of collective obligation to each other to convey new information and knowledge when acquired in BSL because of the usual barriers that Deaf people experience to the acquisition of information that is mostly disseminated in English/spoken language.
The group sessions were in two parts, each lasting between 1.5 and 2 hours, with refreshments provided. In part 1, participants were introduced to the purpose of the study and clinical trials in general. They were introduced to the concept of randomisation and why researchers might want to do that. They were then invited to explore together what the implications of randomisation might be for someone who participated in a study about BSL-IAPT compared with standard IAPT, with adjustments for Deaf people’s access. In part 2, discussion focused more specifically on how to provide good information in BSL to support recruitment and informed consent. The specific terms that the group were asked to discuss were ‘randomisation’, ‘feasibility’, ‘informed choice’, ‘trial’, ‘consent’ and ‘experimental study’.
Three cameras were used to capture the discussions. These were time-coded enabling the later simultaneous display of all interactions and communication for purposes of analysis. PowerPoint [Microsoft Corporation, Redmond, W A, USA] was initially used as a prompt to different sections of the discussion. In some instances the prompts were visual diagrams, e.g. showing two arms of a trial and how it relates to initial recruitment of a sample; in others the prompts were specific words written in English that could be referred back to as prompts during the discussion.
Young et al. 34
Data analysis
All data were kept in their source language for purposes of analysis. The video files were uploaded to NVivo 10 [QSR International, Warrington, UK] which has the facility to tag and segment video data, in this case visual language data, for purposes of thematic coding without the need to transcribe data. This was important because if the data were transcribed this would equal translation in the case of BSL data, as BSL has no written form. This contrasts with many spoken languages where to transcribe data is only to change its modality (from spoken to written) and not to translate. 60–63
Young et al. 34
‘All data were watched and re-watched independently by two researchers (CD and CNG) with the aim of creating an initial coding framework’ (p. 5). 34 Two separate coding frameworks were developed from the same data. The first addressed the specific question of the acceptability of randomisation (objective i) and the second addressed terminology and ways of conveying key concepts associated with recruitment to RCTs (objective ii). The coding frameworks for each, including the themes and subthemes, are shown in Tables 1 and 2. Although the intention had been to code for each objective separately, inevitably when watching the same material, there was some overlap in tagging data segments for different purposes.
The two researchers carrying out the analysis brought different personal and professional biographies to the task: one is a native Deaf sign language user from a Deaf family who has worked for over 10 years in research roles; the other is a hearing researcher who learned BSL as an adult and who has been a qualified and registered sign language interpreter for 11 years, in addition to her research role. Their initial coding frameworks were compared and discussed with a third researcher (AY) who was overseeing the analysis (a hearing, late learner signer who has worked in the Deaf studies field for 25 years). Many of the same themes had been identified arising from specific examples in the data but were not clustered in exactly the same way in how they had been organised by the two researchers. Further discussion led to a framework consisting of the following four areas under which there were additional layers/sub-themes.
Young et al. 34
| Theme | Subtheme |
|---|---|
| Participation in research | Value for Deaf people |
| Obligation to the community now and in the future | |
| Choice | Who chooses? |
| Control of access and outcome | |
| Preferences | Language and communication |
| Cultural considerations | |
| Evidence | Shared cultural understanding |
| Deaf epistemology |
| Theme | Subtheme |
|---|---|
| Strengths and challenges arising from properties of a visual language | Acceptance of generality/specificity |
| Verb directionality | |
| Conceptual understandings/misunderstandings of common terms | Orientation towards avoidance of misunderstanding |
| Substitution of alternative words/expression | |
| Bilingualness and English influences on understanding and expression | Visual decoding of English words |
| Tests not discussion | |
| Power differentials in acquiring and generating new knowledge | Perceptions of class |
| Language-in-use |
Results: participants
Four focus groups were convened in various locations across England. All participants were aged ≥ 30 years, with three aged ≥ 61 years. Of the 19 participants, two were unemployed and four were retired. The rest were in employment, although the majority of these were in part-time employment. The entire sample had a self-declared strong Deaf identity. Table 3 shows distribution of numbers per group and characteristics.
| Group | Participants | Characteristic | ||||||
|---|---|---|---|---|---|---|---|---|
| Sex | Ethnicity | Deaf parents? | Age BSL acquired | Involvement in Deaf community | I feel I am culturally Deaf | Highest qualification | ||
| 1 | 1a | Male | White British | Yes | From birth | Often involved | Very much so | Postgraduate diploma |
| 1b | Male | White British | No | 4–7 years | Often involved | Very much so | Vocational qualification | |
| 1c | Female | White British | No | 12–16 years | Often involved | Quite so | School leaving certificate | |
| 1d | Female | Asian Indian British | No | ≥ 25 years | Very involved | Very much so | Vocational qualification | |
| 1e | Female | White British | No | Missing | Often involved | Quite so | Professional diploma | |
| 2 | 2a | Female | White British | No | 1–3 years | Missing | Very much so | On the job training |
| 2b | Female | White British | No | 4–7 years | Very involved | Very much so | Vocational qualification | |
| 2c | Female | White British | No | 4–7 years | Very involved | Quite so | Missing | |
| 2d | Female | White British | No | 4–7 years | Started age 40 years | Very much so | Vocational qualification | |
| 2e | Female | White British | Yes | From birth | Often involved | Very much so | Missing | |
| 3 | 3a | Male | Asian Indian British | Yes | ≥ 25 years | Often involved | Quite so | Missing |
| 3b | Female | White British | No | 1–3 years | Often involved | Very much so | Professional diploma | |
| 3c | Male | White British | No | From birth | Often involved | Quite so | Professional diploma | |
| 3d | Female | White British | No | 8–11 years | Often involved | Very much so | Postgraduate certificate | |
| 3e | Female | White Jewish | No | ≥ 25 years | Often involved | Somewhat | Professional diploma | |
| 4 | 4a | Female | White British | No | 4–7 years | Very involved | Very much so | University degree |
| 4b | Female | Jewish | No | 17–24 years | Often involved | Somewhat | Missing | |
| 4c | Female | White British | No | 17–24 years | Very involved | Very much so | Postgraduate certificate | |
| 4d | Female | White British | No | ≥ 25 years | Often involved | Quite so | Professional diploma | |
Results: the acceptability of randomisation
Introduction
Through the two-part focus group structure, participants had the opportunity first to gain an understanding of what a RCT would mean in practice; the underlying rationale for it, including the key concept of equipoise; whether or not participants were permitted to change their mind or drop out of a trial; and the crucial importance of informed consent. Therefore, the subsequent guided discussions about the acceptability of randomisation and participants’ views of participation in a RCT were based on this new knowledge and group reflections on it. The purpose of the study was not to reveal ignorance but, rather, having supplied information directly in participants’ preferred language and given them the opportunity to assimilate this through Deaf-led facilitated discussion, to see what views were revealed and what might underpin those. The main themes to emerge are discussed in turn.
Participation in research
Rather than addressing participation within a RCT directly, many group members addressed participation in research in general, seeing randomisation within one particular kind of research as a subset of the general issue about Deaf participation in research studies. Participation in research that was about Deaf people was seen overall as something that was very positive, primarily because it had the potential to improve services for Deaf people or make Deaf lives ‘easier’. In this respect, several participants discussed what they perceived as the general ignorance of service providers about their needs and the perceived lack of priority given to quality health and social care services for Deaf people. Therefore, if participation in any form of research might assist with improving services or lobbying for new support to address Deaf people’s needs, group members argued that it was to be welcomed.
Research and the evidence it might produce, therefore, was seen as form of leverage. To some extent, participation by Deaf people was perceived and talked about as a political act. However, it was also perceived as an altruistic act in that participation was about benefiting the needs of all Deaf people without necessarily accruing benefit for the individual who participates. This motivation was linked, by those group members who discussed it, with a sense of collective responsibility to assist in improving the lives of all Deaf people today, and for future generations.
From a cultural perspective, this response should be understood in terms of many Deaf people holding a strong sense of the value of what other Deaf people in prior generations did to enable a better future for the Deaf community. Examples often cited include the respect for elders who are seen as having kept BSL alive when it was disallowed or unrecognised within public, educational and political structures. 64 In addition, the cultural value given to heritage and the continuation of Deaf culture through social bonds and structures over hundreds of years65–67 is seen as part of the multigenerational legacy to which Deaf people today also contribute. This orientation towards the collective good is of particular importance where culture is not predominantly transmitted through family structures, as most Deaf people have hearing, non-signing families.
In terms of the acceptability of randomisation, this view of the value of research participation in terms of the whole community, not just the individual, prompted the response among some participants of ‘why not give it a go?’, ‘let’s just do it’ and ‘what is there to lose?’. This was particularly the case in two of the focus groups where there was a greater tendency to whole group agreement and the adoption of group views, rather than differences between individuals within the groups. A small minority of group members had a more specific response, which was, if such a research design had the potential to be definitive about what was the most effective means of delivering therapy for Deaf people then, on that basis, they would want to participate in the research. However, participation was still framed in terms of the collective good even though it was an individual decision.
In summary: The question of the acceptability of randomisation is subsumed under a perception of the value of research in general for future generations of Deaf people. The details of what randomisation might imply are of less importance than a perceived cultural obligation to participate if to do so will benefit Deaf people.
Choice
There was a great deal of discussion in all of the focus groups about choice. With respect to randomisation, the abstract idea that participants would be allocated to a group through a process of randomisation was more informally understood to imply that someone would choose into which group an individual might be put. Even though the facilitators explained what randomisation meant, using a range of metaphors and examples, it still prompted many questions about ‘who’ does the choosing rather than the method by which allocation might be done. For example, the commonly used explanation about randomisation being like tossing a coin with a chance of heads or tails still prompted the question ‘but who tosses the coin?’. The explanation of a computer being used for allocation still promoted enquiries about who controlled that computerised process. Some group members found it hard to get past the notion that even if random meant by chance, someone must still, somewhere along the process, exercise some choice about what the possibilities are for any given individual.
One potential explanation for this response is related to the cultural resonance for Deaf people that choices are usually made ‘for’ them, or denied to them, by hearing people who are not cultural kin. Therefore, what is perceived as an outcome over which they have no control (to which group they are allocated in a RCT), is easily equated with many examples in Deaf life of disempowerment where the choices available are restricted or controlled by others. 68 To some extent this attitude is historical in that the history of social welfare, particularly with respect to Deaf people, is one of dependency creation by hearing people who largely controlled the flow of information and the structures of Deaf people’s lives, including who Deaf people might marry, which jobs they might have and how and where they might meet. 69,70 Even as late as the 1980s, and before the establishment of sign language interpreting as a regulated and qualified profession, Deaf people had to be clients of social services to access any form of interpreting. 71 Today, some rules within public offices and structures still disallow fundamental expectations and rights of citizenship such as jury service. 72,73
The question of the acceptability of randomisation is influenced by experiences of restriction of choice and disempowerment that have a strong historical resonance for Deaf people today.
Perceptions of service delivery models
Of the total number of 19 people who participated in the focus groups, two had personal experience of having used standard IAPT, BSL-IAPT or both, and a further two had experience of both Deaf counsellors and hearing counsellors with an interpreter. The others had no similar experiences, but were well aware that there was a BSL-IAPT service that was delivered by Deaf, trained PWPs directly in BSL without an interpreter. It was clearly explained that ethically a RCT could not be undertaken unless there was no clear evidence that one treatment is more effective than another. Groups were invited to discuss their views on that position and whether or not they agreed that that a trial could be undertaken on that basis. As this was a new concept, there was a great deal of clarification required and checking of understanding prior to moving on to discussion of opinions about it. Nonetheless, all of the groups became far more engaged in discussing issues of preference for one approach to therapy or another and the relative merits of each rather than whether or not it was reasonable to proceed on the basis of no strong evidence of one being more effective than the other. The perceptions of service delivery models shared are enlightening for a range of issues that might influence a person’s willingness to be randomised in a trial comparing standard IAPT with adjustment for Deaf people with BSL-IAPT.
Preference-related issues included communication and language concerns. On the one hand, some group members expressed dissatisfaction with the prospect of engaging with an IAPT therapist through an interpreter. This was because the experience of indirect communication would, in their view, result in a less satisfactory relationship because it would be harder to express sensitive issues, make emotional responses clear, and participate in therapeutic discussion if the therapist were not directly engaged with them. In addition, a few participants expressed concerns about the interpreters, namely whether or not they would be familiar with the range of therapeutic concepts and vocabulary or whether or not, as a Deaf client, they would in fact also become a language resource for the interpreter, teaching the interpreter the appropriate terminology? The problem with this was the time it would take away from addressing their own problems and needs within the therapeutic session.
That said, not everyone who expressed concerns about an interpreted IAPT experience saw it as an absolute reason not to engage in a process of randomisation that might mean that they were randomised into standard IAPT. One group in particular spent time thinking about potential solutions. These included the possibility of any future trial ensuring that the interpreters likely to be used within the standard IAPT arm are given additional training prior to the trial starting, so that participants could be assured of a good experience if randomised into that arm. Part of that good experience was linked with taking away any potential stress or anxiety that might be caused by concerns about who the interpreter might be and if they were going to be experienced enough in this particular domain of work. Thus, from group members’ perspectives, trusting the skills and experience of the interpreter had the potential to render randomisation into a standard IAPT service acceptable. However, there was no perception that by implementing such measures one would actually be changing the ‘usual service’, which might be the comparator arm in any future trial design.
From a different perspective, a minority of group members were anxious about language and communication for an alternative reason. For them, the main concern would be that any future research would too easily assume that if an individual used BSL then she/he would automatically prefer BSL-IAPT because it would be a directly delivered therapeutic service from a Deaf professional. One group member in particular felt strongly that such an assumption was itself discriminatory and, in their experience, using spoken language directly with a therapist and lip-reading that therapist, or using an interpreter for receptive communication from a therapist but speaking for themselves within the session, was more satisfactory. For this person, as well as for many others in the groups, the issue of individual preference and individual comfort, whatever that might be, would trump all other considerations.
There were a range of other factors associated with preference that were not directly related to language/communication but more related to cultural perspectives and the nature of the Deaf community. For example, the Deaf PWPs who may be encountered in BSL-IAPT were by definition members of the Deaf community like the clients they served. They were therefore likely to be well known and also to have been encountered by clients in other social or professional settings. This phenomenon is not unusual for Deaf people, and the situational and individual ethical issues it may provoke have been written about previously in terms of small communities of practice. 58 Consequently, some participants expressed concerns about whether or not their confidentiality would be kept if they had a Deaf PWP. The point here was not so much that they did not trust the Deaf PWP, but rather that it would be a nagging consideration in the back of their mind, and for someone struggling with anxiety this could be an added burden. On the other hand, the idea of a hearing person with little or no understanding of Deaf culture or Deaf people being the therapist was also a concern. The main problems were perceived to be the need to explain about Deaf people and the Deaf way of life as they went along rather than trusting the therapist would just ‘get it’. In effect, clients would have to become their own cultural broker too, and group members were concerned that this could be potentially detrimental to the well-being of someone experiencing depression and/or anxiety, despite being part of an intervention designed to help them. A similar concern has been recorded in a small interview study of Deaf people with experience of BSL-IAPT. 74
Some group members also worried about the qualifications and skills of a Deaf person working as a PWP. Although, from a communication perspective, a hearing therapist with an interpreter was not ideal, the hearing professional in their view was likely to be more experienced and to understand more about the work they did than the Deaf professional. There were two roots to this point of view. The first was that Deaf PWPs were very new and there is not a long history of Deaf professionals’ involvement in mental health as therapists in the community; therefore, the range of experience they were likely to have built up was seen as less than the wider pool of hearing therapists. The other was an expression of a common perception, particularly among older Deaf people, that hearing people are likely to know best and be better qualified because they have more access to information, have a greater possibility of gaining professional experiences, and work in the mainstream of general society. This point of view has previously been analysed as one of internalised oppression akin to that recorded among cultural groups which have experienced colonisation. 7,75
The possibility of randomisation represented a threat to the expression of an individual’s linguistic and cultural preferences which were considered a key priority in engagement with therapeutic services. These preferences varied and it was not a foregone conclusion that everyone would prefer a Deaf, BSL-using PWP. The possibility of not having linguistic preferences and cultural needs met was seen as detrimental to mental well-being and therefore randomisation could be seen as detrimental to well-being for some people.
Evidence
In the course of facilitating the focus groups, the two Deaf researchers ensured that they too modelled equipoise. Throughout, they repeated and maintained a stance that there was currently no evidence that one service delivery model (BSL-IAPT or standard IAPT with reasonable adjustments such as an interpreter) was more or less effective than the other. However, in all of the groups, there were challenges to this position from group members, cast in terms of cultural collusion. For example, some group members suggested that the researchers ‘had to say’ that they believed that, but as Deaf people of course they could not. In another group, members said they would ‘go along’ with the assumption for sake of the discussion but everyone of course knew that the two service delivery models could not be ‘equivalent’. What was interesting about dialogue such as this was the lack of attention to the notion of objective research evidence, in terms of outcomes and recovery, and the greater priority given to shared cultural knowledge, experience and understanding. Group members were appealing to facilitators, who were Deaf like them, to acknowledge that Deaf people’s understanding about the superiority of an intervention delivered in one’s own language was self-evident, a view that they thought was bound to be shared.
Although other literature concerning lay understanding of randomisation has recorded the appeal to common-sense notions of what must be better or preferable,41,76 the discussions in this study were a little different. They were stressing the importance of cultural, collective understanding. This has more recently been debated in the literature in terms of Deaf epistemologies in acknowledgement of diversity within a cultural group. 77–80 It is argued that knowledge generated, owned and expressed by Deaf people, which is formed from within a Deaf world view and Deaf ontological experience of life, should not only be regarded as legitimate, but as having priority setting or directive worth. 81,82
This approach highlights a different form of evidence. It is one that is increasingly important in trial design, particularly in the feasibility and modelling phases of the Medical Research Council’s Framework for Complex Interventions,83,84 but one that generates a different standard of evidence than that for which RCTs are intended. Group members, however, appealed to it, in suggesting that perhaps any future research might be designed to give patients experience of both approaches to IAPT delivery and ask them which they preferred and why. Although it was acknowledged as helpful for researchers to be Deaf people, as in this project, the importance of lay Deaf people was also emphasised, as not all Deaf knowledge is the same because of the roles and positions Deaf people find themselves in. The researchers were identified as ‘clever Deaf’ people, for example, and were contrasted by group members with the alternative lives of many ordinary Deaf people who struggle with education, employment and literacy.
There is a strong appeal to cultural common sense that access to a service in one’s own language and that is culturally matched is preferable. Randomisation may be resisted for its failure to acknowledge Deaf epistemological positioning.
Conclusion
Evidence from this study highlights a confluence of factors affecting the acceptability of randomisation that are deeply embedded in Deaf people’s historical and contemporary experiences of society, as well as shared cultural characteristics. Although individual preferences, along with perceptions and misperceptions of what randomisation implies, have some influence, the culturally contextual nature of Deaf people’s thinking predominates. This does not mean, however, that a service delivered by a Deaf person in BSL is automatically to be preferred or perceived as more appropriate. The four main influences on Deaf people’s attitudes and conclusions about the acceptability of randomisation were:
-
Research involving randomisation is a subset of research in general, which, if it benefits Deaf people today and in the future, is perceived as acceptable.
-
Randomisation can be perceived as an example of forced choice without personal power, which is a common experience for Deaf people, and on that basis may be unacceptable.
-
If randomisation implies not having personal linguistic preferences and cultural needs met, then it is of itself a threat to personal well-being.
-
Randomisation may be resisted on grounds of its perceived denial of the value of Deaf people’s common sense, knowledge and belief in what is best for them, which happens often in Deaf people’s lives.
There was, therefore, no clear picture about the acceptability of randomisation and, in fact, some helpful suggestions arose in the course of discussion about how to allay fears and concerns that may be a barrier to participation in RCTs. There was not an absolute rejection of the possibility of participation in research involving randomisation. Instead there was a strong appeal to see its implications from a cultural not just a linguistic access or service model perspective.
The nature of the sample and small scale of the exploratory work is a limitation to these findings because the generalisability of these views across the diversity of the Deaf community is untested. Results tentatively suggest that there are grounds for moving towards a feasibility study as randomisation has not been rejected outright, provided that the implications of the culturally embedded perspectives expressed here are incorporated into how recruitment might be undertaken in the future. The second element of effective recruitment would involve language, terminology and the provision of information, which we address in the trial-related terminology in BSL study reported below.
Results: trial-related terminology in British Sign Language
This study has been published in Trials34 as an Open Access article distributed under the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0. The text below includes minor additions and formatting changes to the original text.
Results and implications
The principal results and conclusions (reproduced from the abstract of the original article) were:
Six necessary conditions for developing trial information to support comprehension were identified. These included:
developing appropriate expressions and terminology from a community basis, rather than testing out previously derived translations from a different language;
paying attention to language-specific features which support best means of expression (in the case of BSL expectations of specificity, verb directionality, handshape);
bilingual influences on comprehension;
deliberate orientation of information to avoid misunderstanding not just to promote accessibility;
sensitivity to barriers to discussion about intelligibility of information that are cultural and social in origin, rather than linguistic;
the importance of using contemporary language-in-use, rather than jargon free or plain language, to support meaningful understanding.
Young et al. 34
Additionally, the study identified six necessary conditions that need to be met when developing signed participant information for Deaf people so that it is acceptable, accessible, transmitted accurately and understood as intended. The authors conclude that these are relevant to all signed languages, not just BSL, and potentially apply to further development of written and spoken information for hearing participants for whom the majority language (English) is not their first or preferred language. The conditions identified were:
1. A community-participatory, exploratory approach to arriving at appropriate clinical trial terminology is highly effective in instances where languages, in this case BSL, have not yet had the contact with a topic that would mean a common vocabulary/preferred means of expression has developed.
2. Languages have properties associated with their form and grammar that naturally enable some approaches to explanation to support comprehension that others may not. In this case, verb directionality, expectations of specificity and simultaneous contextual, semantic layering within expressions enabled features of the underpinning trial design to be clarified and remain consistent.
3. It is important to take into consideration bilingual influences on comprehension even when information is presented monolingually; this is a decoding strategy for unfamiliar terms and concepts that is available to those who are bilingual and multi-lingual and can be a source of both strength and misunderstanding.
4. Orientation of information to avoid misunderstanding is an important axis to consider when creating new information for a cultural-linguistic group unfamiliar with the topic. It is subtly different from an orientation designed to support comprehension and may, as in the case of the sample in this study, be a preferred orientation.
5. The researcher should understand cultural, contextual or social barriers that participants might face in engaging in open, constructive discussions of the information materials and consent procedures, over and above those that might be created by language per se. In the case of Deaf people, these barriers might derive from negative historical experiences of the education system, and class differentials.
6. Clarity of expression, in the sense of plain language or avoidance of jargon, is not sufficient to promote comprehension. Attention to language-in-use in contemporary discussion is an important means of expression to effectively communicate complex concepts because it reflects common cultural usage.
Young et al. 34
The study reinforces the ethical imperative to ensure that trial participants who are Deaf are provided with optimum resources to understand the implications of participation and to make an informed choice. We include, as one of the products of this study, a glossary of terms and their alternatives in BSL for key concepts associated with trial participation and the production of recruitment and information materials in BSL (see Appendices 1 and 2).
Chapter 4 Secondary data analysis of patient numbers and outcomes data (study 2)
Some of this study has previously appeared in Belk et al. 85 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The text below includes minor additions and formatting changes to the original text. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. When paragraphs are repeated here verbatim, they have been displayed as quotations with reference to the original paper.
Background
Previous studies of primary mental health care with respect to Deaf populations have been hampered by small sample sizes because of the dispersed nature and minority status of Deaf people in the general population. Diagnostic uncertainty has also been a problem in drawing conclusions from studies that have relied either on patient self-report or on assessment by clinical personnel unused to working with Deaf sign language users. 33,86,87 Consequently, knowledge about the prevalence of anxiety and/or depression in Deaf populations has been limited both in the UK and internationally. 33,85 A well-cited study suggests a prevalence of 33% in the adult Deaf population. 26 Studies of anxiety and/or depression among Deaf people have been further hampered by the lack of clinical assessment tools in BSL (and in other signed languages) whose validity and reliability have been tested and established. 86,88
However, since 2011, the screening and assessment instruments used within the NHS IAPT programme have been available in BSL versions, whose psychometric properties have been investigated and found to be good. 33 These are the PHQ-9 BSL and GAD-7 BSL, both of which were translated in collaboration with the originators and validated on a population of Deaf people in the UK. 33 Furthermore, they have been used since 2011 by Deaf PWPs in the adaptation of the IAPT programme that was established for Deaf people that we refer to as BSL-IAPT. 22 Therefore, the possibility existed of analysing a data set of Deaf people with a certain diagnosis of anxiety and/or depression, who were screened at point of access to a service and whose progress was regularly monitored using tools known to be linguistically and clinically valid. In its own right, this would represent, as far as we are aware, the largest data set of its kind in primary mental health care with Deaf people anywhere in the world, from which a great deal of knowledge could be gained. More specifically, the analysis would permit several outcomes to be established that would be crucial to any further study, as well as being significant in their own right.
First among these was to establish the appropriate clinical cut-off points to be used for the BSL-IAPT assessment tools (PHQ-9 BSL and GAD-7 BSL). As is the case with any translated version of a standard instrument, the clinical cut-off point that is in use for one cultural–linguistic population may not be appropriate for another; it cannot be assumed to have the same sensitivity and specificity as for the population in which it was originally validated. 89 Field testing in the linguistic and cultural population in which the translated version is applied is required not only to measure operating characteristics of reliability and validity,90–92 but also to establish whether the clinical cut-off point is the same or different. Such testing has been carried out for many translations of GAD-7 and PHQ-9 into languages other than English,93 and also with respect to English versions used with populations with cultural differences or particular distinguishing characteristics (e.g. a group in another English-speaking country, one with a specific illness or one based in primary care). 85,94–97 No such field testing had yet been carried out with the BSL population. Furthermore, the analysis of a large data set of patients who had used BSL-IAPT in terms of referral rates, adherence and clinical outcomes would enable calculation of recruitment targets should a full trial be indicated.
BSL-IAPT, however, was available in only a limited number of areas in England;32 this ranged from two to five PCTs over the life of the research project. Therefore, although it was assumed that Deaf people were accessing IAPT through standard services elsewhere in England, the number of patients was unknown. The minimum data set required of IAPT providers for monthly upload to the Health and Social Care Information Centre (HSCIC) does not include a requirement to identify the language of the patient, therefore it was not possible to readily identify BSL users. 98 Additionally, the disability field in the minimum data set that included ‘hearing’ did not differentiate spoken or signed language. 98 It was not clear if the barriers to health-care access and uptake experienced by Deaf people in other parts of the health service24 would also apply with respect to primary mental health care. In addition, the patient characteristics of those Deaf people accessing standard IAPT could be different from those accessing BSL-IAPT. For example, in an area where no service was available in BSL it might be the better-educated Deaf people who were assertive and confident enough to seek out a service where one was not readily available in their preferred language. In an area where a BSL service was available there might be a greater diversity of Deaf patients. However, all such potential variables were unknown at the start of the project and hypotheses untested. Should any future feasibility study or clinical trial be justified, then the comparability of the Deaf populations accessing standard IAPT and BSL-IAPT would require investigation. Finally, without analysis of the outcomes for patients who had used standard IAPT in comparison with those who had used BSL-IAPT, it would not be possible to estimate an effect size or whether or not any scaled-up study might be justified.
Objectives
-
To establish the clinical cut-off points for the BSL-IAPT assessment tools (PHQ-9 and GAD-7) for patients with anxiety and/or depression.
-
To explore the population characteristics of Deaf users of BSL-IAPT and standard IAPT services, including demographic characteristics, referral routes and adherence, and to compare clinical outcomes.
-
To map probable numbers of users of BSL-IAPT and Deaf users of standard IAPT who would be eligible for recruitment to a large-scale study.
-
To establish effect size and estimate recruitment targets should a full trial be indicated.
Each of the objectives will be addressed in turn in this chapter.
Objective i: to establish the clinical cut-off points for the BSL-IAPT assessment tools (PHQ-9 item and GAD-7) for patients with anxiety and/or depression
Methods
Study design
A secondary data analysis was used to establish the clinical cut-off points of PHQ-9 BSL and GAD-7 BSL, which involved two data sets: (1) data set 1 (n = 502) contains Deaf BSL users who had used the BSL-IAPT service defined by the single-service provider BSL Healthy Minds; and (2) data set 2 (n = 85) contains Deaf participants from the study by Rogers et al. 33 who reported that they had no mental health difficulties and had not used a mental health service in the past 12 months, at the time when that study was carried out. Both of the data sets contain the data of Deaf people who had completed the PHQ-9 BSL and GAD-7 BSL.
Parameter estimates, including the area under the curve (AUC) value, sensitivity, positive predicted value and negative predicted value, were used in the calculation of the clinical cut-off points of PHQ-9 BSL and GAD-7 BSL, which were reported in greater detail in Belk et al. 85
Setting
The BSL-IAPT clinical data set (data set 1) contains the data for those Deaf people who had used the BSL-IAPT service in a small number of areas in the UK between December 2011 and February 2015. Data set 2 from the Rogers et al. study33 was collected in 2011/12.
Participants
To meet the inclusion criteria for this study, a person in data set 1 needed to be ‘a Deaf sign language user, aged 16 years or over, had accessed BSL-IAPT services since December 2011, had received a step 2 or step 3 service and had attended a minimum of one therapist contact session’. 85 These inclusion criteria for data set 1 resulted in a total number of 502 (see figure 1 in Belk et al. 85).
Measurement
The data collected included the PHQ-9 BSL and GAD-7 BSL scores. The PHQ-9 BSL and GAD-7 BSL were translated from the original English versions:33
The originators of the instrument established a score of 10 as the clinical cut-off for moderate depression in the English version Kroenke et al. 99 measured against the ‘gold standard’ of an MHP interview. This score yielded a sensitivity of 88%, a specificity of 88% and a positive likelihood ratio of 7.1. GAD-7 is scored by a frequency scale from 0 to 3 for each item and is also most commonly totalled to give a score between 0 and 21. It was validated against other health measures and against an MHP interview. A clinical cut-off of 10 was identified against the MHP interview diagnosing generalised anxiety disorder (GAD) with a sensitivity of 89% and a specificity of 82%. 100 However, a later study101 evaluated GAD-7 as a broader instrument to test for any anxiety disorder and determined an acceptable AUC of 0.86. From this AUC, a lower cut-off of 8 for any anxiety disorder was recommended, which gave a sensitivity of 77%, a specificity of 82% and a positive likelihood ratio of 4.4. This lower cut-off was the one adopted by IAPT to sit alongside that for the PHQ-9. 102
We note that there are, to date, no published analyses of the operation of the clinical cut-off scores for both instruments with respect to the IAPT population in general. Patient characteristics in this population, in comparison with those on which the original cut-off scores for the English versions were originally derived, may indicate that a revision of the cut-off scores currently in use in IAPT services is required. However for the purposes of this study, we use the published IAPT-recommended cut-off scores.
Belk et al. 85
Sample size
Preparatory sample size calculations were carried out based on Gilbody et al. 97 a study which observed a sensitivity of 91.7% and specificity of 78.3% for PHQ-9 as a screening tool for depression in 93 patients. We assumed a prevalence rate of 33% for anxiety and/or depression in the Deaf population based on the well-cited Kvam et al. 26 study rather than more general estimates of mental health difficulties in the Deaf population. Following the same specificity and sensitivity as in the Gilbody et al. study97 we estimated that a 90% CI for an AUC to within +/–0.1 would require a sample size of at least 117 (39 depressed and 78 not-depressed patients). This calculation suggested that the numbers in the respective datasets would be sufficient.
Belk et al. 85
Results
The results of the study to establish the clinical cut-off points for the PHQ-9 BSL and GAD-7 BSL are reported in Belk et al. 85
The main findings, derived from the abstract of the article, are as follows:
The clinical cut-offs for PHQ-9 BSL and GAD-7 BSL are 8 and 6 respectively. This compares with the original English version cut-offs in the hearing population of 10 and 8 respectively. The three different statistical choices for calculating clinical cut-offs all showed a lower clinical cut-off for the Deaf population with respect to the PHQ-9 BSL and GAD-7 BSL with the exception of the Maximising criteria when used with the PHQ-9 BSL. Applying the new clinical cut-offs, the percentage of Deaf BSL-IAPT service users showing reliable recovery is 54.0% compared to 63.7% using the cut-offs scores used for English speaking hearing people. These compare favourably with national IAPT data for the general population.
Belk et al. 85
Further conclusions and implications of this work are:
Appropriate clinical cut-offs for these instruments are now established for Deaf BSL users. Assessment of the clinical effectiveness of BSL-IAPT, both for clinical practice and to allow accurate comparison with mainstream IAPT services, can now be made. Comparison is important in the national [English] monitoring of IAPT services through the mandatory data that flows upwards to the HSCIC.
Belk et al. 85
Objective ii: to explore the population characteristics of Deaf users of BSL-IAPT and standard Improving Access to Psychological Therapies
Methods
Study design
This was a secondary data analysis of routinely recorded client data obtained from standard IAPT services that had provided a service to Deaf individuals. Analyses of the characteristics of the clients and service-related factors, such as waiting times and clinical outcomes, were compared with the client data and outcomes from the cohort of Deaf people who had used BSL-IAPT reported under objective i and in Belk et al. 85
Ethics
Ethics permission was sought and approved by the Proportionate Review Subcommittee of NRES (reference 14/LO/2234) for transfer of the anonymised data to the research team at the University of Manchester for the purpose of secondary data analysis, subject to the required research and development (R&D) approvals being gained for each service.
Setting
Standard Improving Access to Psychological Therapies
It was not possible to identify overall numbers of Deaf clients who had used standard IAPT services from secondary data analysis of IAPT returns to the HSCIC, as language preference is not a field required in the minimum data set and, therefore, BSL would not be recorded. In addition, the disability field’s subsection ‘hearing’ would not discriminate between a sign language user and a spoken language user. Consequently, clients could be identified only if individual providers located and extracted individual service records. Following ethics approval and local R&D approval, services that had eligible clients were provided with a standard operating procedure (SOP) for the identification of clients who met the study inclusion criteria, recording of anonymised client data onto a standard pro-forma, and secure data transfer to the research team (see Appendix 4 for the SOP and Appendix 5 for the data recording template). The SOP also included suggested strategies for the identification of relevant client records in the absence of any standard system. These included using one or several of the following:
-
checking the subfield ‘hearing impaired’ within the disability field in the IAPT patient management system (note that this does not necessarily imply BSL users in all cases)
-
if present, checking a bespoke field about language use and/or interpreter booking that might identify BSL in a separate administration system used by the clinical site
-
ascertaining whether or not clients might be known to a member of staff who specialises in service provision to Deaf and/or other minority language groups
-
extraction of all clients who are recorded as deaf/hearing impaired through the disability field and then carrying out an individual review of these records for identification of language use.
Ethics approval for the study on the data of Deaf BSL users from standard IAPT services was granted on 30 July 2015. The date of approval for each local R&D varied across each service, with the earliest being granted in December 2015 and the latest being granted in July 2016. However, the date on which the SOP was signed ranges from a few days to several months after the date of R&D approval. The inclusion dates for services that returned data varied according to how individual services were able to identify Deaf BSL users who had used their service and how services recorded the data. For example, some services had accessible records covering 3 years, others only 6 months. The transfer of the data from standard IAPT services occurred between April and July 2016.
BSL-IAPT
The BSL-IAPT data set contained those who were referred to a BSL-IAPT service (which was defined for this study as a sole provider, BSL Healthy Minds) between December 2011 and February 2015. The process of data transfer is recorded in Belk et al. 85
Participants
The inclusion criteria for Deaf clients whether drawn from BSL-IAPT or standard IAPT within the secondary data analysis were that individuals were Deaf BSL users; were aged ≥ 16 years; had been referred to an IAPT service since January 2012 and had received a step 2 and/or step 3 service; had at least one appointment with a therapist; and had completed the PHQ-9/GAD-7 on at least one occasion.
Variables
Both data sets contained demographic information about the clients (e.g. year of birth, sex, ethnic group, national identity, religious belief, relationship status, sexual orientation and employment status), clinical characteristics (such as provisional diagnosis, whether the client had previously accessed either BSL-IAPT or standard IAPT service, and information on prescribed medication), date information (date of first referral, dates of appointments attended and date the care episode ended) and outcome scores for PHQ-9 and GAD-7. In some instances, information about waiting time as well as source of referral was available.
Measurement
In the case of the BSL-IAPT data set, the validated BSL versions of the PHQ-9 and GAD-7 (PHQ-9 BSL and GAD-7 BSL) were used,33 and the clinical cut-off points that had been established for the BSL versions in our study reported under objective i (see Belk et al. 85) applied. In the case of the standard IAPT data set of Deaf clients, the English-language versions of PHQ-9 and GAD-7 were used and the IAPT-recommended clinical cut-off points applied. 102 These are based on original studies with English-speaking populations of hearing people,99,101 but were used in standard IAPT services working with Deaf clients. The PHQ-9 BSL and GAD-7 BSL clinical cut-off scores used for the BSL versions were 8 and 6, respectively, whereas for the English versions completed by Deaf people in standard IAPT services, the cut-off points were 10 and 8, respectively.
Study size
The sample sizes were determined by the maximum numbers of eligible clients available in the two data sets to optimise precision in estimation.
Statistical methods
Characteristics and outcomes of clients were compared descriptively by IAPT group. Independent sample t-tests were used to compare mean scores for the PHQ-9 and GAD-7 by group. The prevalence of anxiety and/or depression, recovery and reliable recovery were compared by group using Pearson’s chi-squared test; reliable improvement was compared by group using the chi-squared test for trend. Because of their skewness, waiting times were compared by group using the Mann–Whitney U-test.
Results
Participants
BSL-IAPT data set
The BSL-IAPT data set contained data from a total of 502 clients. The participant flow diagram is shown in Figure 1. A total of 429 clients with first PHQ-9 score and/or first GAD-7 score were included in the secondary data analysis.
FIGURE 1.
Participant flow diagram for BSL-IAPT cohort (using BSL clinical cut-off points for caseness). Spec = Sens, specificity and sensitivity are equalised. Reproduced from Belk et al. 85 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited (http://creativecommons.org/licenses/by/4.0/).
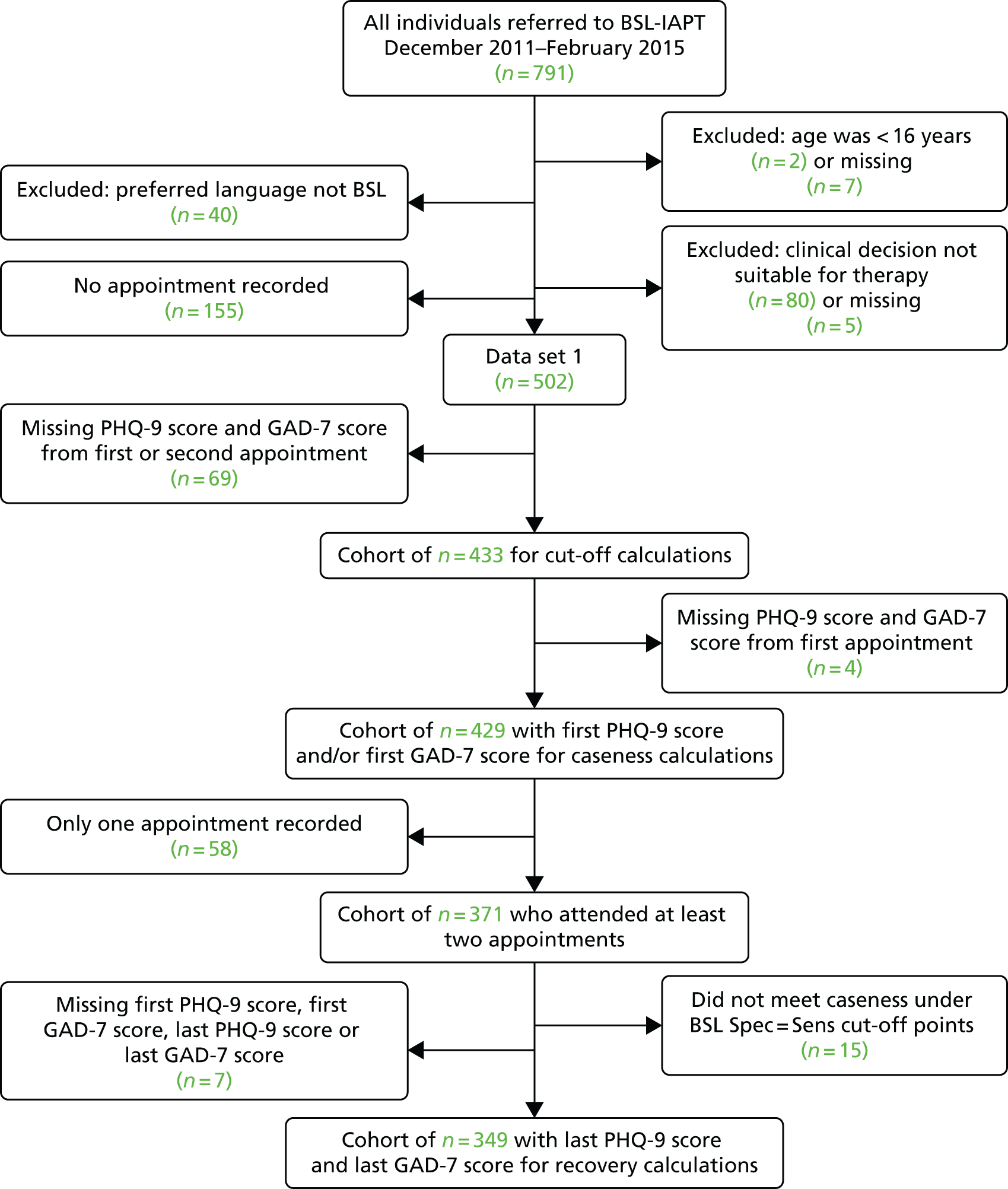
Standard Improving Access to Psychological Therapies data set
Initially, 22 NHS trusts and three non-NHS service providers granted approval and agreed to provide data from Deaf BSL users who had used their IAPT services (approvals covered 74 individual IAPT services in total, as some trusts covered several IAPT services). These approvals generated 24 separate data extractions. Some trusts provided separate extractions for each service under their authority; others provided a single extraction covering all services under their authority. Therefore, we are unable to say with any confidence exactly how many individual services are represented in our sample. Four NHS trusts and one non-NHS service provider were not included in the final analysis, as either the data they provided were not useable or contained no appointments data, or subsequent to approval they found themselves no longer able to meet the data extraction deadline. There were issues relating to how the data were recorded (or not recorded), despite the services being provided with the code key for each variable for the data transfer. Examples of the issues that some services expressed about the task of extracting data on Deaf BSL users included the following: the task proved too time-consuming for them; their recording system did not contain the information requested; there were difficulties in identifying the correct person to do the data extraction; and digital records did not cover the whole period requested.
Despite the issues with data extraction, service providers were able to identify which clients were Deaf and which were BSL users in different ways, including through mention of BSL in the client’s notes, through their interpreter booking system and through a service’s own bespoke label, which stated that a client was a BSL user. One standard IAPT service was able to identify which clients were Deaf BSL users because they had been working with a therapist who was Deaf and a BSL user. Another service provided data where clients were externally identified as Deaf BSL users via interpreter agency booking records. As shown in the participant flow diagram in Figure 2, data from a total of 116 Deaf BSL clients from standard IAPT services were included in the secondary data analysis.
FIGURE 2.
Participant flow diagram for standard IAPT cohort (using English cut-off points for caseness).
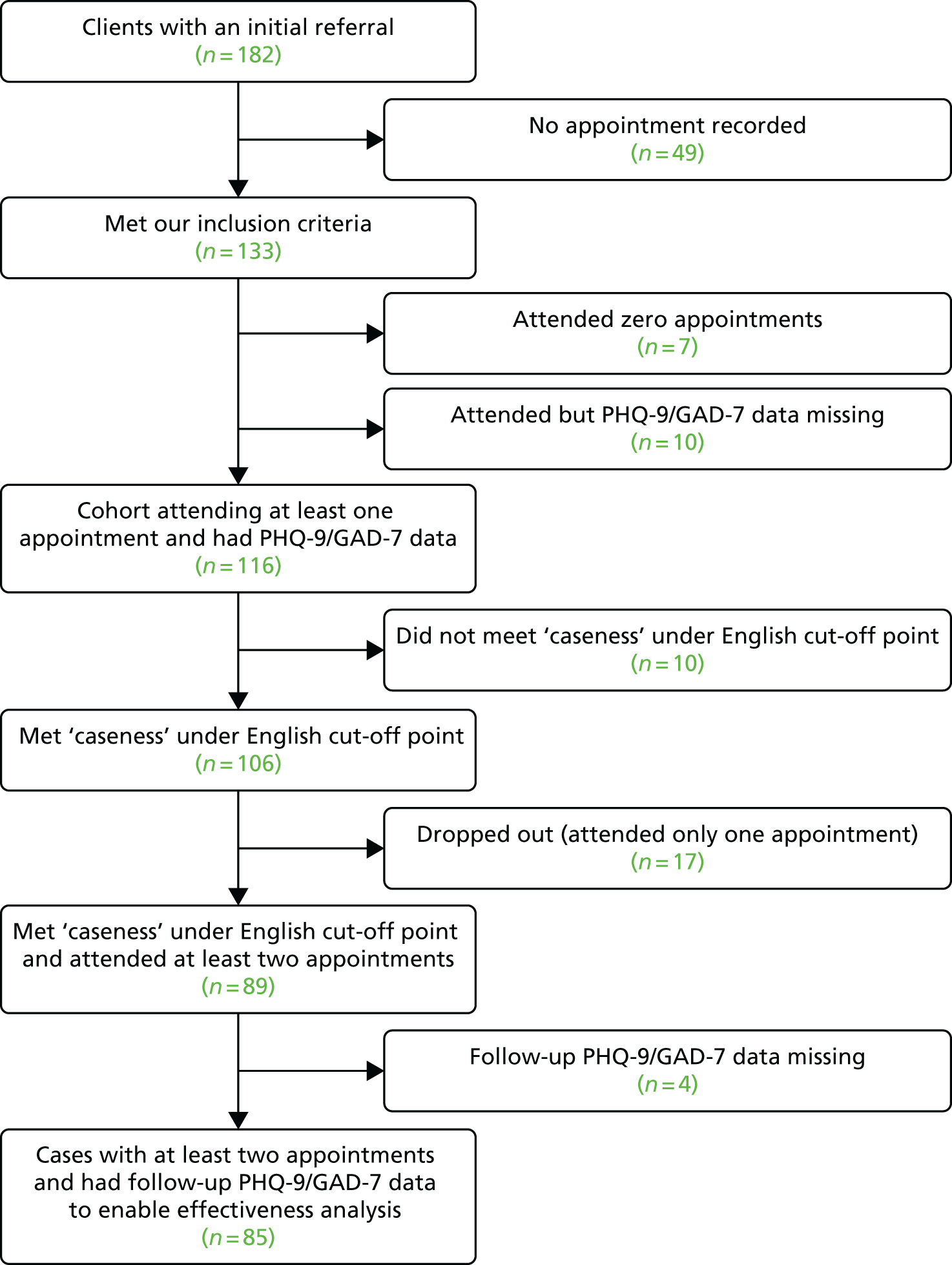
Characteristics of clients
Table 4 compares the age group, sex, sexual orientation and relationship status of Deaf standard IAPT and BSL-IAPT clients. Percentages in the different age groups were reasonably similar, as were the two means {standard IAPT 43.3 [standard deviation (SD) 14.5], BSL-IAPT 42.1 [SD 13.4]}. The two groups were similar in terms of sex, although many more of the standard IAPT clients were unwilling to disclose their sexuality (32.8% vs. 0.7%). There were discrepancies in the way relationship status was collected for the two IAPT groups. This information was unknown or missing for 43.1% of the standard IAPT group compared with 20.0% of the BSL-IAPT group, but the percentages of participants who were married or in a civil partnership, separated, single and widowed were similar.
| Variable | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 116) | BSL (N = 429) | |
| Age group (years) | ||
| 16–24 | 13 (11.2) | 36 (8.4) |
| 25–34 | 21 (18.1) | 104 (24.2) |
| 35–44 | 27 (23.3) | 113 (26.3) |
| 45–54 | 32 (27.6) | 102 (23.8) |
| 55–64 | 16 (13.8) | 46 (10.7) |
| 65–74 | 4 (3.4) | 20 (4.7) |
| ≥ 75 | 3 (2.6) | 8 (1.9) |
| Sex | ||
| Female | 73 (62.9) | 262 (61.1) |
| Male | 43 (37.1) | 167 (38.9) |
| Sexual orientation | ||
| Heterosexual | 52 (44.8) | 252 (58.7) |
| Gay/lesbian | 8 (6.9) | 38 (8.9) |
| Bisexual | 5 (1.2) | |
| Person asked and does not know or is not sure | 5 (1.2) | |
| Unknown | 38 (32.8) | 1 (0.2) |
| Unwilling to disclose | 16 (13.8) | 3 (0.7) |
| Missing data | 2 (1.7) | 125 (29.1) |
| Relationship status | ||
| Cohabiting | 26 (6.1) | |
| Divorced | 29 (6.8) | |
| Long-term relationship | 28 (6.5) | |
| Married/civil partnership | 20 (17.2) | 85 (19.8) |
| Separated | 3 (3.4) | 21 (4.9) |
| Single | 38 (32.8) | 143 (33.3) |
| Widowed | 4 (3.4) | 11 (2.6) |
| Unknown | 49 (42.2) | |
| Missing data | 1 (0.9) | 86 (20.0) |
The standard IAPT service providers did not record ethnicity or national identity in a consistent form, and there were differences with the way in which these variables were recorded for BSL-IAPT clients. Table 5 shows the categories that were recorded, highlighting that it was difficult to make direct comparisons between the groups. Ethnicity was not stated or missing for 21.6% of standard IAPT clients, compared with 9.1% of BSL-IAPT clients. National identity was not known or missing for 29.3% of standard IAPT clients, compared with 66.4% of BSL-IAPT clients. There was a similar problem with religious belief, with this being unknown or missing, or the client being unwilling to disclose the information, in more than half of each group (Table 6). More standard IAPT clients than BSL-IAPT clients were employed (31.0% vs. 25.4%), whereas fewer standard IAPT clients were unemployed and seeking work (33.6% vs. 40.3%) at the first care episode (see Table 6).
| Variable | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 116) | BSL (N = 429) | |
| Ethnic group | ||
| White: unspecified | 67 (57.8) | |
| White: British | 14 (12.1) | 334 (77.9) |
| White: other | 8 (1.9) | |
| Mixed: white and black Caribbean | 3 (0.7) | |
| Mixed: unspecified | 2 (1.7) | |
| Asian or Asian British: Indian | 7 (1.6) | |
| Asian or Asian British: Pakistani | 25 (5.8) | |
| Asian or Asian British: Bangladeshi | 2 (0.5) | |
| Asian or Asian British: any other Asian background | 3 (0.7) | |
| Asian or Asian British: unspecified | 5 (4.3) | |
| Caribbean | 2 (1.7) | 3 (0.7) |
| Black or black British: African | 2 (0.5) | |
| Black or black British: any other black background | 1 (0.2) | |
| Any other ethnic group | 1 (0.9) | 2 (0.5) |
| Not stated | 24 (20.7) | 2 (0.5) |
| Missing data | 1 (0.9) | 37 (8.6) |
| National identity | ||
| British | 58 (50.0) | |
| English | 18 (15.5) | 138 (32.2) |
| Scottish | 2 (0.5) | |
| Welsh | 2 (0.5) | |
| Irish | 2 (0.5) | |
| Other | 6 (5.2) | |
| Not known | 33 (28.4) | |
| Missing data | 1 (0.9) | 283 (66.4) |
| Variable | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 116) | BSL (N = 429) | |
| Religious belief | ||
| Christian | 30 (25.9) | 136 (31.7) |
| Hindu | 1 (0.9) | 1 (0.2) |
| Jewish | 1 (0.2) | |
| Muslim | 4 (3.4) | 27 (6.3) |
| Other | 1 (0.9) | |
| Unwilling to disclose | 13 (11.2) | |
| None or N/A | 21 (18.1) | 40 (9.3) |
| Unknown | 45 (38.8) | 5 (1.2) |
| Missing data | 1 (0.9) | 219 (50.0) |
| Initial employment status | ||
| Employed | 36 (31.0) | 109 (25.4) |
| Unemployed and seeking work | 39 (33.6) | 173 (40.3) |
| Students in full- (≥ 16 hours/week) or part-time (≤ 16 hours/week) education/training and not working/actively seeking work | 5 (4.3) | 25 (5.8) |
| Long-term sick/disabled, those who receive Incapacity Benefit, Income Support or both; or Employment/Support Allowance | 15 (12.9) | 53 (12.4) |
| Homemaker looking after the family or home and not working and not actively seeking work | 2 (1.7) | 20 (4.7) |
| Not receiving benefits and not working and not actively seeking work | 2 (0.5) | |
| Unpaid voluntary work and not working or actively seeking work | 13 (3.0) | |
| Retired | 7 (6.0) | 30 (7.0) |
| Declined to provide a response | 3 (0.7) | |
| Null | 8 (6.9) | |
| Missing/not recorded | 4 (3.4) | 1 (0.2) |
Table 7 shows a breakdown of region by IAPT group. Region for the standard IAPT group was the region of the service provider; five regions were not represented. The largest contributions came from Yorkshire and Humber (20.7%), London (16.4%), the South West (15.5%) and the South East (13.8%). In the BSL-IAPT group, most clients were from the North West (63.9%), with the next most common region being Yorkshire and Humber (14.0%).
| Variable | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 116) | BSL (N = 429) | |
| Region | ||
| North West | 9 (7.8) | 274 (63.9) |
| North East | 10 (8.6) | 7 (1.6) |
| East Midlands | 0 (0) | 23 (5.4) |
| West Midlands | 7 (6.0) | 0 (0) |
| East of England | 0 (0) | 3 (0.7) |
| London | 19 (16.4) | 0 (0) |
| South Central | 0 (0) | 42 (9.8) |
| South East Coast | 0 (0) | 18 (4.2) |
| South East | 16 (13.8) | 0 (0) |
| South West | 18 (15.5) | 1 (0.2) |
| Wales | 0 (0) | 1 (0.2) |
| Yorkshire and Humber | 24 (20.7) | 60 (14.0) |
| North East/Yorkshire and Humber | 13 (11.2) | 0 (0) |
Preferred language was recorded only for the standard IAPT group, the BSL-IAPT group all having a preference for BSL. BSL was the most common preferred language (58.6% of all clients, 86.1% of all those giving a preference) (Table 8). Clients in the standard IAPT group could also have had more than one care episode, although most (90.5%) had only one.
| Variable | Standard IAPT (N = 116), n (%) |
|---|---|
| Preferred language | |
| BSL | 68 (58.6) |
| English | 10 (8.6) |
| Other | 1 (0.9) |
| Unknown | 35 (30.2) |
| Missing data | 2 (1.7) |
| Care episodes | |
| 1 | 105 (90.5) |
| 2 | 8 (6.9) |
| 3 | 3 (2.6) |
There were differences in provisional diagnosis between the two IAPT groups, although it is not clear why this was the case (Table 9). The most common provisional diagnoses among standard IAPT clients were depressive episode (33.6%) and mixed anxiety and depressive disorder (14.7%); these were also the most common diagnoses among BSL-IAPT clients, but in reverse order (mixed anxiety and depressive disorder 47.8%, depressive episode 18.4%). It is important to note that a provisional diagnosis was unknown or missing for 40.5% of the standard IAPT clients and 5.4% of BSL-IAPT clients. Excluding clients with missing data, the most common provisional diagnoses were depressive episode (56.5%) and mixed anxiety and depressive disorder (24.6%) for standard IAPT clients and mixed anxiety and depressive disorder (50.5%) and depressive episode (19.5%) for BSL-IAPT clients. A higher anxiety component among BSL-IAPT clients was also evident in provisional diagnoses for generalised anxiety disorder (excluding missing data, standard IAPT 4.3% vs. BSL-IAPT 9.9%). The two groups appeared to be similar in terms of long-term conditions, although the information was more likely to be absent among standard IAPT clients (37.1%) than among BSL-IAPT clients (30.1%).
| Variable | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 116) | BSL (N = 429) | |
| Provisional diagnosis | ||
| Mental and behavioural disorders attributable to alcohol | 4 (0.9) | |
| Bipolar affective disorder | 2 (0.5) | |
| Depressive episode | 39 (33.6) | 79 (18.4) |
| Recurrent depressive disorder | 2 (1.7) | 36 (8.4) |
| Dysthymia | 1 (0.2) | |
| Agoraphobia (with or without history of panic disorder) | 3 (0.7) | |
| Social phobias | 1 (0.9) | 2 (0.5) |
| Specific (isolated) phobias | 2 (0.5) | |
| Panic disorder (episodic paroxysmal anxiety) | 9 (2.1) | |
| Generalised anxiety disorder | 3 (2.6) | 40 (9.3) |
| Mixed anxiety and depressive disorder | 17 (14.7) | 205 (47.8) |
| Obsessive–compulsive disorder | 1 (0.9) | 7 (1.6) |
| Post-traumatic stress disorder | 4 (3.4) | 14 (3.3) |
| Hypochondriacal disorder | 2 (0.5) | |
| Adjustment disorder | 1 (0.9) | |
| Disappearance and death of family member | 1 (0.9) | |
| Unknown/not specified | 17 (14.7) | |
| Missing data | 30 (25.9) | 23 (5.4) |
| Any long-term conditions | ||
| No | 47 (40.5) | 224 (52.2) |
| Yes | 26 (22.4) | 76 (17.7) |
| Unknown | 30 (25.9) | 35 (8.2) |
| Unwilling to disclose | 12 (10.3) | 20 (4.7) |
| Missing data | 1 (0.9) | 74 (17.2) |
Source of referral was another variable more likely to be missing among standard IAPT clients (13.8%) (Table 10). By far the most common sources of referral among standard IAPT clients were a general medical practitioner (44.0%) and self (30.2%). This was also true among BSL-IAPT clients, but with the order reversed [more were self-referred (40.6%) than referred by a general medical practitioner (25.4%)]. Previously accessing another type of service was missing or not applicable for 44.0% of standard IAPT clients, and only 6.0% were known to have previously accessed specialist Deaf services. By comparison, 49.2% of BSL-IAPT clients had previously accessed mainstream services, although it was not clear if this was related to mainstream mental health services or specifically standard IAPT services.
| Variable | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 116) | BSL (N = 429) | |
| Referral source | ||
| General medical practitioner | 51 (44.0) | 109 (25.4) |
| Other primary health care | 1 (0.9) | 54 (12.6) |
| Self | 35 (30.2) | 174 (40.6) |
| Social services | 2 (1.7) | 50 (11.7) |
| Education service | 7 (1.6) | |
| Other independent sector mental health services | 2 (0.5) | |
| Voluntary sector | 2 (1.7) | 4 (0.9) |
| Accident and emergency department | 1 (0.2) | |
| Community Mental Health Team (adult mental health) | 1 (0.9) | 9 (2.1) |
| Jobcentre Plus | 1 (0.2) | |
| Other service or agency | 1 (0.9) | 18 (4.2) |
| PMHS | 2 (1.7) | |
| Sign Language Service | 1 (0.9) | |
| Other | 4 (3.4) | |
| Missing data | 16 (13.8) | |
| Previously accessed other type of service | ||
| Yes | 7 (6.0) | 211 (49.2) |
| No | 58 (50.0) | 218 (50.8) |
| Unknown | 7 (6.0) | |
| N/A | 27 (23.3) | |
| Missing data | 17 (14.7) | |
The proportion of clients for whom information on the prescription of psychotropic medication was unknown, not stated, missing or not applicable was higher in the standard IAPT group (30.2%) than in the BSL-IAPT group (1.2%) (Table 11). After removing the missing responses, 13.6% of standard IAPT clients reported that they had been prescribed psychotropic medication but did not indicate whether or not they were taking the medication; no BSL-IAPT clients fell into this category. Again, allowing for missing responses, similar percentages in the two groups had not been prescribed such medication (standard IAPT 55.6% vs. BSL-IAPT 57.3%). The number of appointments booked was similar in the two IAPT groups [standard IAPT: mean 9.8 appointments booked (SD 12.5 appointments booked), median 7 appointments booked; BSL-IAPT: mean 8.7 appointments booked (SD 6.3 appointments booked), median 8 appointments booked]. The same was true of the number of appointments attended [standard IAPT: mean 7.3 appointments attended (SD 8.7 appointments attended), median 5 appointments attended; BSL-IAPT: mean 6.2 appointments attended (SD 4.9 appointments attended), median 5 appointments attended]. The most common number category of booked and attended appointments in each IAPT group was three to nine (see Table 11). One standard IAPT client had booked 111 appointments and had attended 68; one BSL-IAPT client had booked 43 and attended 39.
| Variable | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 116) | BSL (N = 429) | |
| Prescribed psychotropic medication | ||
| Prescribed (not stated if taking or not) | 11 (9.5) | |
| Prescribed but not taking | 4 (3.4) | 34 (7.9) |
| Prescribed and taking | 21 (18.1) | 139 (32.4) |
| Not prescribed | 45 (38.8) | 232 (54.1) |
| Unknown | 1 (0.9) | 19 (4.4) |
| Not stated (declined) | 3 (2.6) | 5 (1.2) |
| Missing data or N/A | 24 (20.7) | |
| Missing data | 7 (6.0) | |
| Number of appointments booked | ||
| 1 | 8 (6.9) | 19 (4.4) |
| 2 | 8 (6.9) | 22 (5.1) |
| 3–9 | 60 (51.7) | 243 (56.6) |
| 10–19 | 31 (26.7) | 118 (27.5) |
| 20–29 | 5 (4.3) | 19 (4.4) |
| 30–49 | 2 (1.7) | 8 (1.9) |
| 50–99 | 1 (0.9) | |
| ≥ 100 | 1 (0.9) | |
| Number of appointments attended | ||
| 0 | 1 (0.2) | |
| 1 | 17 (14.7) | 57 (13.3) |
| 2 | 18 (15.5) | 36 (8.4) |
| 3–9 | 53 (46.9) | 281 (65.5) |
| 10–19 | 22 (19.0) | 41 (9.6) |
| 20–29 | 2 (1.7) | 10 (2.3) |
| 30–49 | 3 (2.6) | 3 (0.7) |
| 50–99 | 1 (0.9) | |
| ≥ 100 | 0 (0) | |
Outcomes data
Table 12 shows PHQ-9 and GAD-7 scores for the first care episode for standard IAPT and BSL-IAPT clients. None of the comparisons by IAPT group was significant except for the last PHQ-9 score, which was higher for standard IAPT clients than for BSL-IAPT clients [mean 9.24 vs. 7.66, 95% confidence interval (CI) for difference in means 0.07 to 3.10; p = 0.041]. This difference in means represents a small effect size (Cohen’s d = 0.25, r = 0.12).
| IAPT group | t-test | df | p-value | ||||
|---|---|---|---|---|---|---|---|
| Standard | BSL | ||||||
| n | Mean score (SD) | n | Mean score (SD) | ||||
| PHQ-9 | |||||||
| First | 116 | 14.98 (5.53) | 429 | 14.57 (5.97) | 0.68 | 543 | 0.499 |
| Last | 98 | 9.24 (6.89) | 366 | 7.66 (6.24) | 2.06 | 142.4 | 0.041 |
| Change | 98 | –5.68 (6.39) | 366 | –6.81 (6.94) | 1.45 | 462 | 0.149 |
| GAD-7 | |||||||
| First | 116 | 12.77 (5.48) | 428 | 12.46 (4.96) | 0.57 | 542 | 0.567 |
| Last | 98 | 7.97 (5.83) | 366 | 7.00 (5.50) | 1.53 | 462 | 0.126 |
| Change | 98 | –4.70 (5.19) | 365 | –5.45 (6.15) | 1.11 | 461 | 0.269 |
The standard IAPT data also contained information on subsequent care episodes. Table 13 shows scores for the PHQ-9 and GAD-7 for the first three care episodes. Data for the second and third episodes were sparse: only nine clients had first and last scores for care episode 2 and only one had first and last scores for care episode 3 (and these took the same values). Across all clients, mean scores were higher for care episode 2 than for care episode 1. For clients with data for both care episodes, PHQ-9 scores increased slightly, whereas GAD-7 scores decreased slightly, but none of the differences was significant (data not shown).
| Care episode | ||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||
| n | Mean score (SD) | n | Mean score (SD) | n | Mean score (SD) | |
| PHQ-9 | ||||||
| First | 116 | 14.98 (5.53) | 11 | 15.45 (6.24) | 3 | 17.33 (7.23) |
| Last | 98 | 9.24 (6.89) | 9 | 10.00 (8.17) | 1 | 22.00 (N/A) |
| Change | 98 | –5.68 (6.39) | 9 | –7.22 (8.18) | 1 | 0.00 (N/A) |
| GAD-7 | ||||||
| First | 116 | 12.77 (5.48) | 11 | 14.27 (5.12) | 3 | 11.33 (7.37) |
| Last | 98 | 7.97 (5.83) | 9 | 8.78 (7.33) | 1 | 17.00 (N/A) |
| Change | 98 | –4.70 (5.19) | 9 | –7.33 (5.45) | 1 | 0.00 (N/A) |
Depression and/or anxiety
Table 14 shows the numbers of clients who were initially identified as having depression and/or anxiety based on English cut-off points for the standard IAPT clients and on BSL cut-off points for BSL-IAPT clients. Most clients in both groups had depression and anxiety (75.9% for standard IAPT, 81.6% for BSL-IAPT). Ten standard IAPT clients (6.9%) did not meet caseness, compared with 18 BSL-IAPT clients (4.2%). Depressive scores above the cut-off points were similar in the two groups (standard IAPT clients 84.5%, BSL-IAPT 86.4%) but more in the BSL-IAPT group had higher anxiety scores (standard IAPT clients 82.8%, BSL-IAPT 91.1%). The difference between the two IAPT groups marginally failed to be statistically significant [χ2(3) = 7.05; p = 0.070]. Had the standard IAPT clients been assessed on the lower BSL cut-off points of 8 and 6 for the PHQ-9 and GAD-7, respectively, the numbers and percentages would have changed slightly in favour of caseness: 94 (81.0%) with both depression and anxiety, seven (6.0%) with depression, eight (6.9%) with anxiety and seven (6.0%) not meeting caseness.
| Diagnosis | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 116) | BSL (N = 428) | |
| Depression and anxiety | 88 (75.9) | 350 (81.6) |
| Depression | 10 (8.6) | 20 (4.7) |
| Anxiety | 8 (6.9) | 40 (9.3) |
| Did not meet caseness | 10 (8.6) | 18 (4.2) |
Recovery, reliable improvement and reliable recovery
For the calculations of recovery, reliable improvement and reliable recovery, the IAPT guidelines are followed (IAPT 2014). 103 According to these, ‘caseness’ pertains to entry into the service: an individual is defined as having reached ‘caseness’ if their score on the PHQ-9 and/or GAD-7 at assessment is equal to or higher than the cut-off value. ‘Recovery’ is said to have been reached when a client’s PHQ-9 and GAD-7 scores both fall below the clinical cut-off point and they were at ‘caseness’ at intake. ‘Reliable recovery’ is defined as the combination of ‘recovery’ and ‘reliable improvement’. ‘Reliable improvement’ is calculated using the ‘reliable change index’. The reliable change index enables the quantification of ‘reliable improvement’ and ‘reliable deterioration’ (i.e. a score change larger than the reliable change index signals a clinically significant change). This measure, when combined with ‘recovery’, enables the identification of those individuals who have ‘reliably recovered’ (i.e. shown both ‘recovery’ and ‘reliable improvement’, and who have completed therapy). Unfortunately, data on completion of therapy were not consistently recorded by standard IAPT providers, so we could not reproduce the calculations of recovery, reliable improvement and reliable recovery in Belk et al. 85 for standard IAPT clients. For the analyses here, the IAPT definition of ‘completed therapy’ was followed, which is defined as having attended a minimum of two treatment appointments104 (Table 15).
| Criterion | IAPT group, n (%) | |
|---|---|---|
| Standard (under English cut-off points) (N = 116) | BSL (under BSL cut-off points) (N = 429) | |
| Meeting caseness | 106 (91.4) | 411 (95.8) |
| Had at least two appointments | 99 (85.3) | 371 (86.5) |
| Meeting caseness and had at least two appointments | 89 (76.7) | 356 (83.0) |
The numbers of clients showing recovery, reliable improvement and reliable recovery are shown in Table 16.
| Measurement of recovery | IAPT group, n (%) | |
|---|---|---|
| Standard (English cut-off points) (N = 89) | BSL (BSL cut-off points) (N = 349) | |
| Recovery | ||
| Recovered | 35 (41.2) | 150 (43.0) |
| Did not recover | 50 (58.8) | 199 (57.0) |
| N/A: no follow-up data | 4 | 7 |
| Reliable improvement | ||
| Reliably improved | 54 (63.5) | 233 (66.8) |
| No reliable change | 28 (32.9) | 95 (27.2) |
| Reliably deteriorated | 3 (3.5) | 21 (6.0) |
| N/A: no follow-up data | 4 | 7 |
| Reliable recovery | ||
| Reliably recovered | 34 (40.0) | 141 (40.4) |
| Did not reliably recover | 51 (60.0) | 208 (59.6) |
| N/A: no follow-up data | 4 | 7 |
The association between the type of IAPT service (standard or BSL) and the recovery outcome was not significant [χ2(1) = 0.09, 95% CI for difference between percentage recovered –13.0% to 10.0%; p = 0.763]. Non-significant results were also found for the association between the type of IAPT service and reliable improvement [χ2trend(1) = 0.01, 95% CI for difference between percentage reliably improved –14.9% to 7.5%; p = 0.917], and between the type of IAPT service and reliable recovery [χ2(1) = 0.01, 95% CI for difference between percentage reliably recovered –11.5% to 11.4%; p = 0.946]. Although the three CIs contained 0 (consistent with the non-significant test results), they were all relatively wide.
Figures 3 and 4 show rates for reliable improvement and reliable recovery, respectively, for the standard IAPT services compared with the BSL-IAPT service. The numbers of clients with caseness and at least two therapeutic appointments for each service are shown. For most standard IAPT services, this was three or fewer, so a number of the rates are either 0% or 100%. For standard IAPT services with five or more clients in the analysis, the reliable improvement rate was similar to that of the BSL-IAPT service as a whole, whereas the reliable recovery rate for these standard IAPT services showed more variation than the BSL-IAPT service rate.
FIGURE 3.
Reliable improvement for standard IAPT providers compared with BSL-IAPT data.
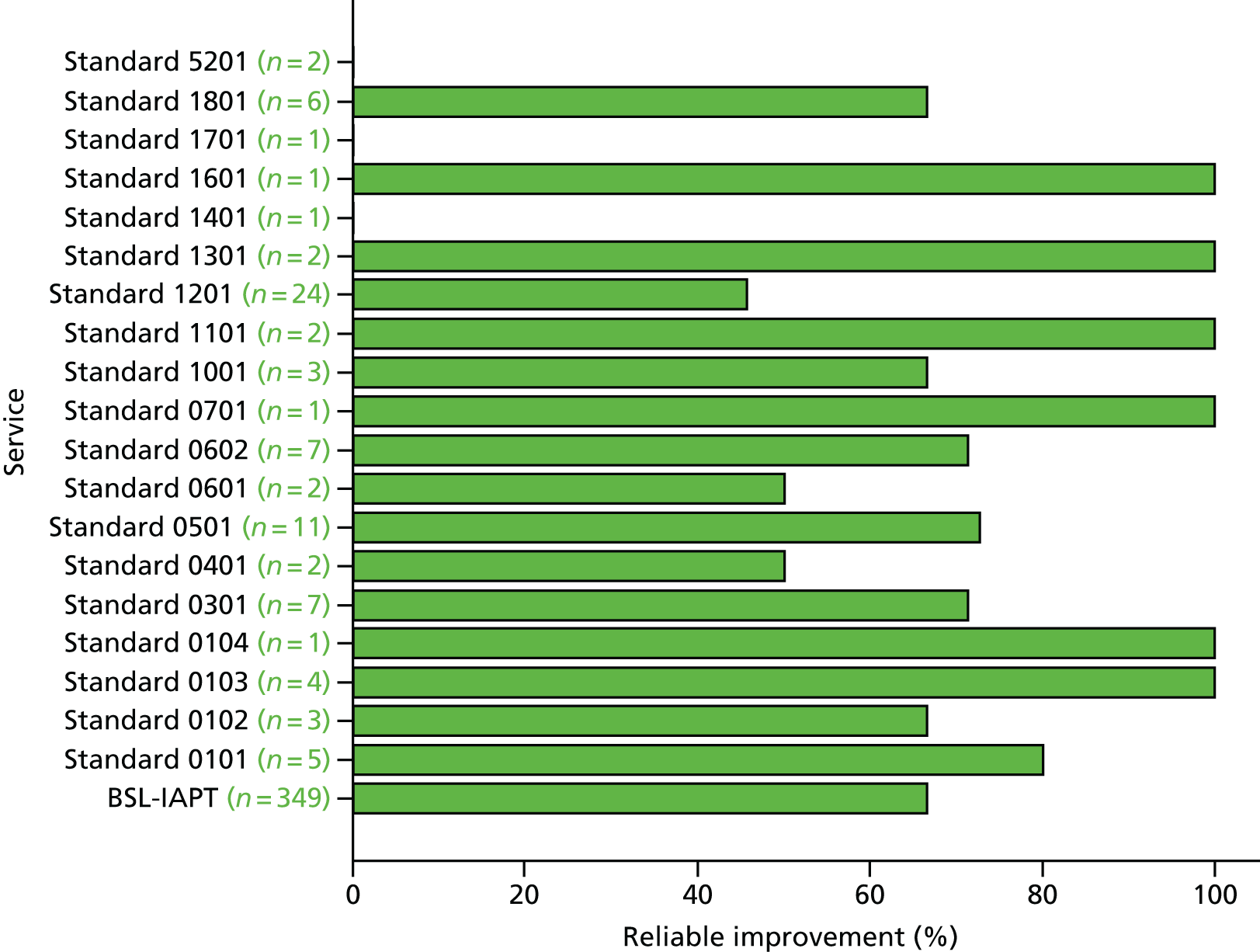
FIGURE 4.
Reliable recovery for standard IAPT providers compared with BSL-IAPT data.
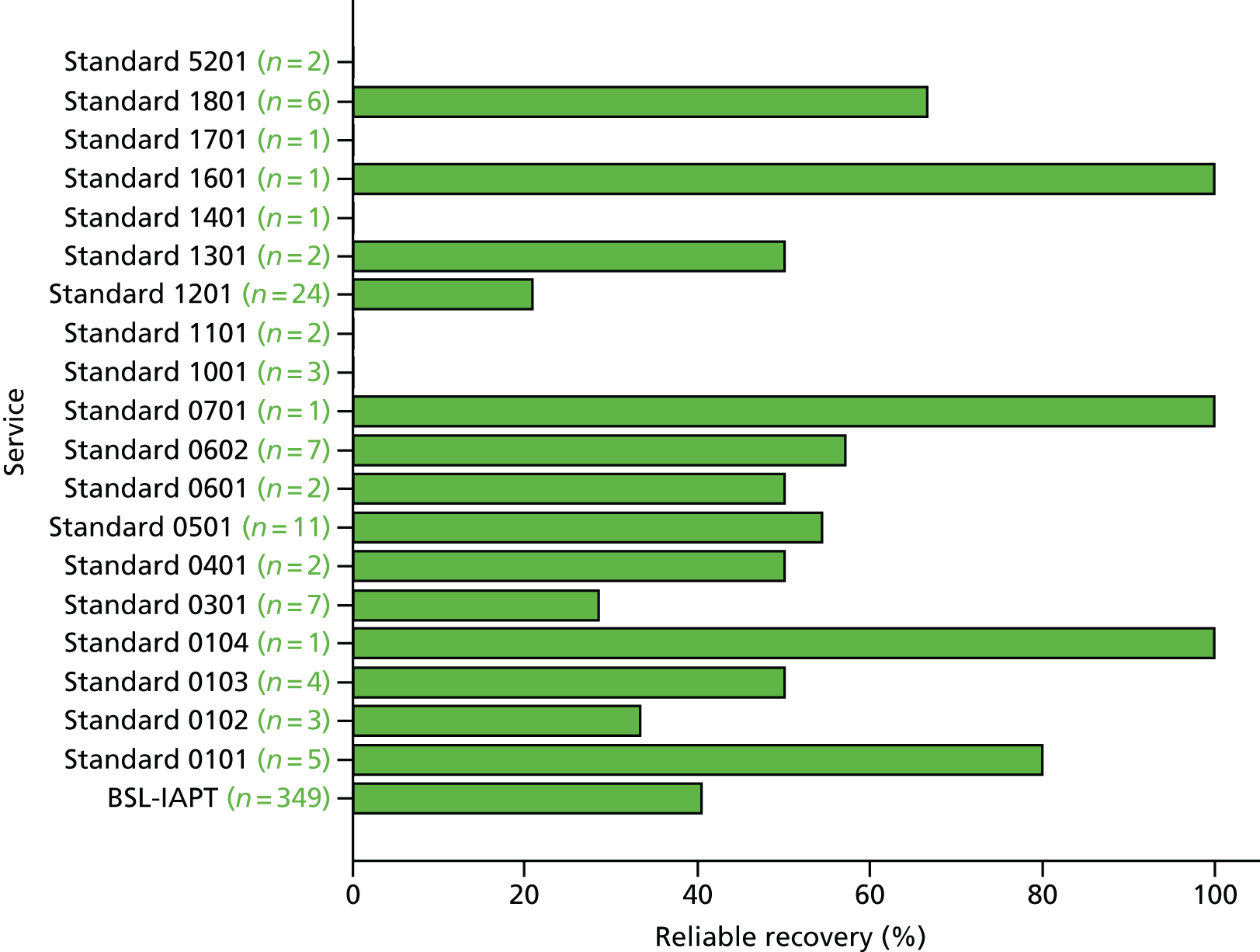
Waiting times
Waiting times were calculated in number of days from date of referral to first appointment. The waiting times for standard IAPT ranged from 0 to 382 days (six clients had missing data, 11 had a waiting time of 0 days) and for BSL-IAPT the waiting times ranged from 3 to 306 days; both groups showed a positively skewed distribution (Table 17 and Figures 5 and 6). The median waiting time in the standard IAPT group was shorter than that for the BSL-IAPT group (21.5 days vs. 27.0 days) and the difference in distribution between groups was significant (Mann–Whitney U-test = 19439.5, z = –2.85; p = 0.004). It is not clear whether or not the 11 zeros for standard IAPT clients were observed values, which seems unlikely in a busy service. When the analysis was repeated without these clients, the median waiting times were not significantly different (26.0 days vs. 27.0 days, Mann–Whitney U-test = 19439.5, z = –1.31; p = 0.189).
| Measure | IAPT group | |
|---|---|---|
| Standard (n = 110) | BSL (n = 429) | |
| Mean (SD) | 32.35 (45.27) | 36.91 (33.70) |
| Median | 21.50 | 27.00 |
| Range | 0–382 | 3–306 |
| Mode | 0 | 14 |
FIGURE 5.
Waiting time (days) for standard IAPT group.
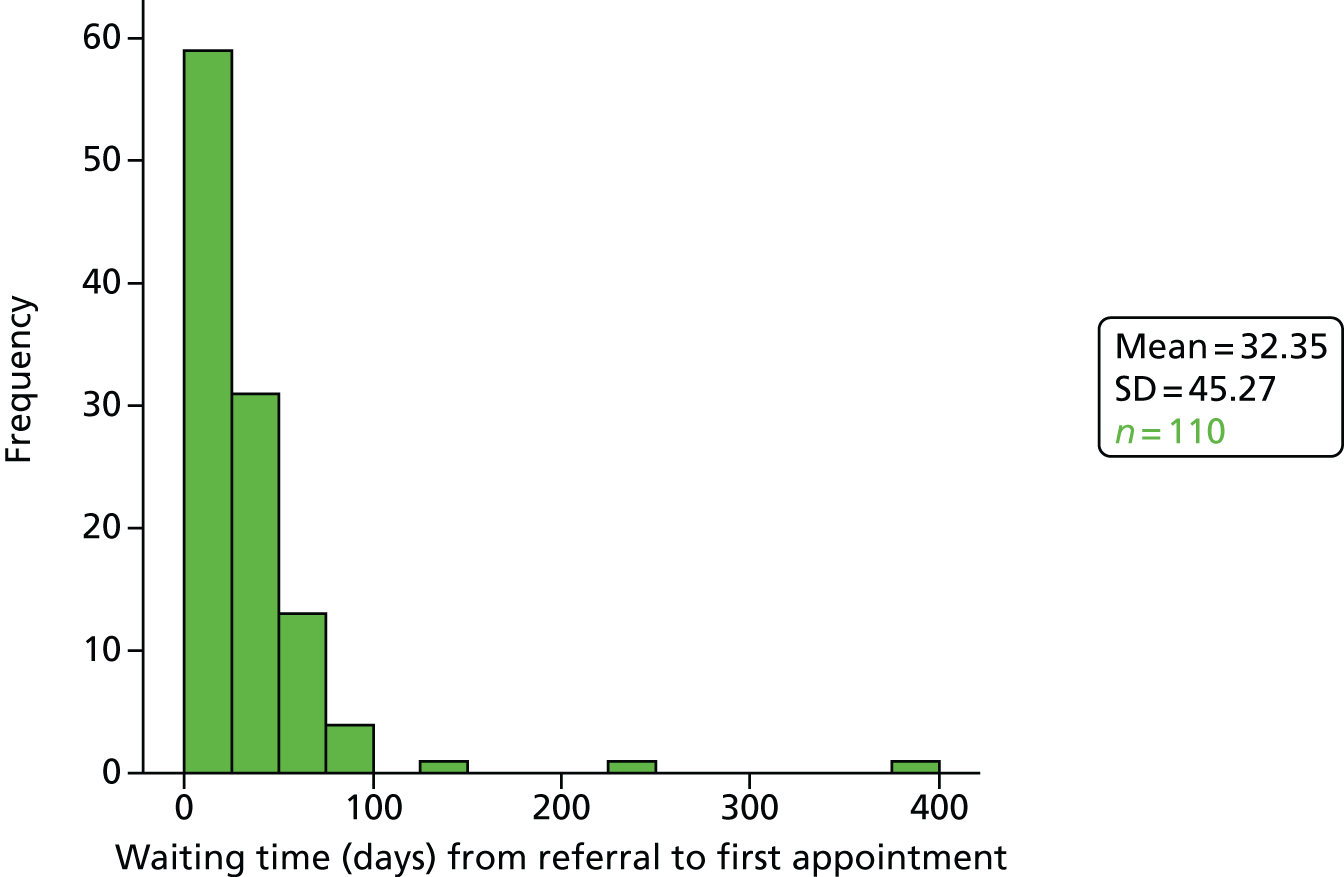
FIGURE 6.
Waiting time (days) for BSL-IAPT group.
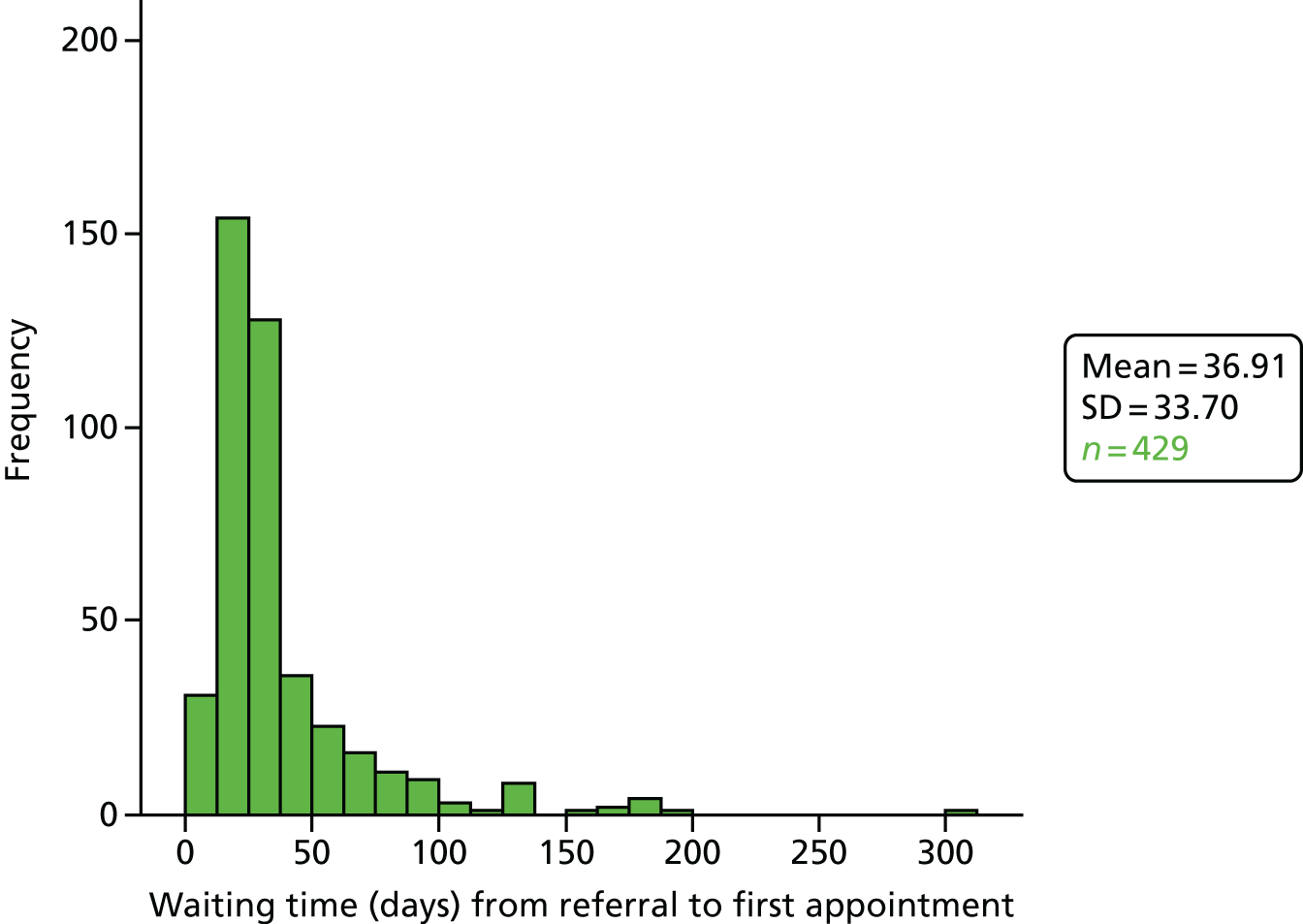
The IAPT guide states the goal that ‘. . . by March 2016, 75% of people referred to the IAPT programme begin treatment within 6 weeks of referral, and 95% begin treatment within 18 weeks of referral’ (p. 5). 103 Six weeks is equivalent to 42 days, and 18 weeks to 126 days. Both standard IAPT and BSL-IAPT met these targets (Table 18).
| Criterion | IAPT group, n (%) | |
|---|---|---|
| Standard (N = 110) | BSL (N = 429) | |
| Within 6 weeks of referral | 86 (78.2%) | 328 (76.5%) |
| Within 18 weeks of referral | 107 (97.3%) | 414 (96.5%) |
It was not possible to report difference in waiting time against quarter-years for standard IAPT because it was not possible to extract the information needed from the number of days between first referral and date of first appointment alone. However, the comparison for the waiting time for each quarter-year has been examined for the BSL-IAPT data set (Figures 7 and 8). It was found that the mean for waiting time started high (mean = 61 days for first quarter in 2011), which is probably accounted for by the set-up time and BSL-IAPT service lead-in (including the incremental training of Deaf people as PWPs), and then dropped to 25–30 days as the service bedded in. The marked rise in waiting times in 2014 onwards could be a consequence of changes from PCT local commissioning to CCG commissioning arrangements from April 2013, which affected the number and location of BSL-IAPT outlets and saw a change in funding arrangements from largely block commissioning arrangements to greater use of individual funding requests (IFRs) (see Chapter 5).
FIGURE 7.
The mean waiting time (days) for BSL-IAPT for each quarter from 2011 to 2015. Q, quarter.
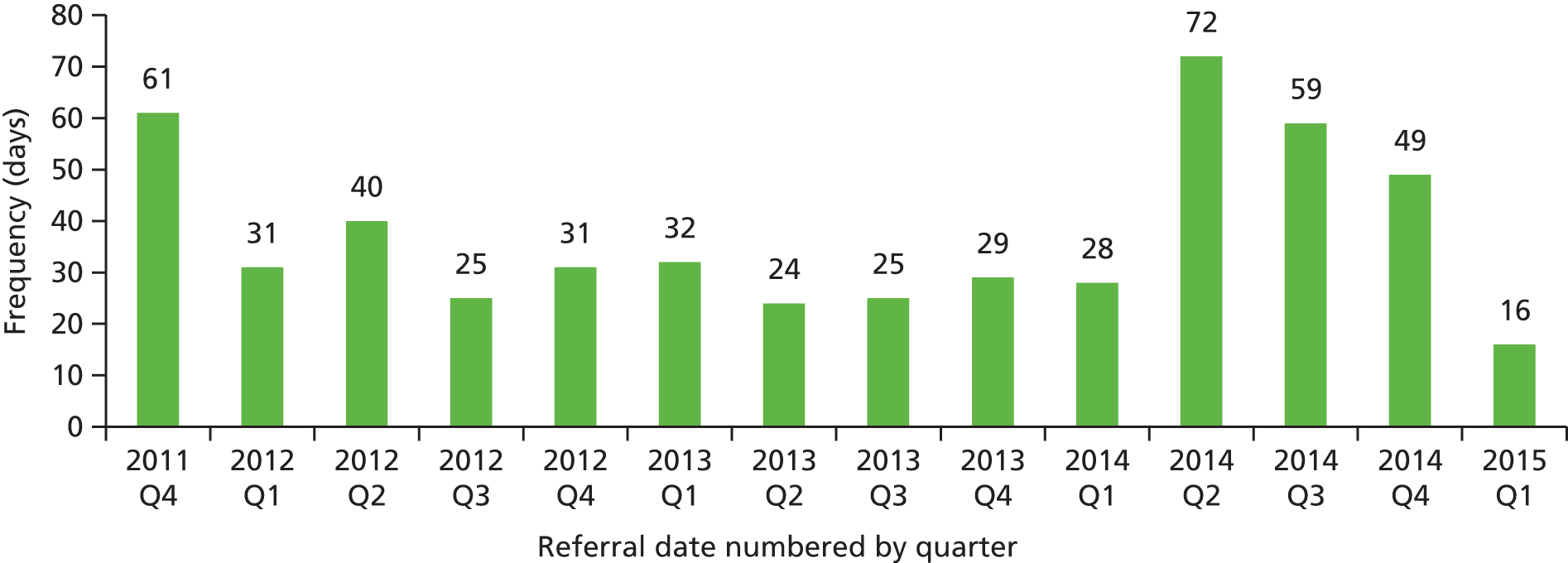
FIGURE 8.
Waiting times (days) for BSL-IAPT per quarter. Q, quarter.

Discussion
The numbers of Deaf service users of standard IAPT on which these analyses have been run are not representative of the complete national picture. Data are drawn from only 19 trusts and two private providers, across no more than 74 services. We opened discussions with 30 other standard IAPT services that reported having seen at least one Deaf client but that were unable to arrange approval and complete the data extraction required in the time permitted. There are at least 255 IAPT services in England as a whole, and within these there may be many more Deaf clients of whom we remain unaware. Therefore, it is unknown how representative the data on Deaf clients in standard IAPT services are in comparison with the national picture. That said, it has not been possible previously to identify any Deaf users of standard IAPT or to explore their characteristics and outcomes. This is the first study that has done so.
Our concern that Deaf users of standard IAPT may have different demographic, educational and employment characteristics from the population of users of BSL-IAPT was not upheld, based on the available data. The two populations are largely comparable. With regard to patterns of service delivery and adherence, the numbers of appointments booked and attended by clients, whether standard IAPT or BSL-IAPT, were also comparable. Calculations using the available data showed that the median waiting time was shorter for clients of standard IAPT services than for clients of BSL-IAPT services (21.5 days vs. 27.0 days; p = 0.004).
Clinical characteristics at point of entry into therapy were difficult to compare by IAPT group because of differences in recording and missing data. A provisional diagnosis was not available for well over one-third of standard IAPT clients, compared with 1 in 20 BSL-IAPT clients. Interestingly, among those for whom a provisional diagnosis was present, there was a marked difference between the IAPT groups. More than half of standard IAPT clients had been given a provisional diagnosis of a depressive episode, whereas one-quarter had been provisionally diagnosed as having a mixed anxiety and depressive disorder. More than half of BSL-IAPT clients had been given a provisional diagnosis of mixed anxiety and depressive disorder, whereas one in five were provisionally diagnosed as having a depressive episode. Long-term conditions, on the other hand, were similar in the two groups.
In terms of clinical outcomes, the prevalence of depression and/or anxiety in the two IAPT groups from initial PHQ-9/GAD-7 scores marginally failed to show a significant difference (p = 0.070). Slightly more clients attending BSL-IAPT services had GAD-7 scores indicating anxiety (91.1% vs. 82.2%), whereas the two groups had similar percentages with PHQ-9 scores indicating depression. The significant difference found when comparing the final PHQ-9 score between the two IAPT groups is that Deaf clients from the standard IAPT service were more likely to be depressed than the Deaf clients from the BSL-IAPT service. That is to say that, at the start of the treatment, there are no differences in the depression score, as measured by PHQ-9, between the two IAPT groups, but on comparing the final PHQ-9 scores available from Deaf clients, the scores are significantly different. Completion of treatment was not consistently recorded across standard IAPT providers, so we had to use a definition based on attending two appointments. Using this definition, rates for recovery, reliable improvement and reliable recovery were very similar in the two IAPT groups.
The recent methodological announcement by the HSCIC105 clarifies that, from July 2016, calculation of rates of reliable recovery and reliable improvement should be based on those who have ‘finished the course of treatment’, as defined by a valid endcode in the client data upload, rather than those who have ‘completed’ treatment, defined in the IAPT KPIs as having had a minimum of two therapeutic appointments. 104 In our original calculations of reliable recovery (and reliable improvement) based on the BSL-IAPT data set, we were able to use this strict definition of ‘finished the course of therapy’ as endcodes were available for 226 clients. 85 The broader definition of ‘completed’ was available for 349 clients, and was used in our comparative analyses of Deaf users of standard IAPT and of BSL-IAPT, as endcodes were not consistently available in the standard IAPT data transfer we had received.
Given these caveats, we found no significant difference between Deaf clients of standard IAPT and BSL-IAPT in reliable improvement (63.5% vs. 66.8%; p = 0.917) and no significant difference in reliable recovery (40.0% vs. 40.4%; p = 0.946), based on attending a minimum of two therapeutic appointments as the definition of completing treatment. However, given the very small numbers of Deaf clients seen by most of the standard IAPT services in comparison with the large numbers seen by the BSL-IAPT service, comparative data on the outcomes of Deaf clients seen in standard IAPT services and those in the BSL-IAPT service should be treated with caution. It seems unlikely that those standard IAPT services who have achieved high rates of reliable recovery and reliable improvement based on, in some cases, one or two clients only, would maintain these given a larger and potentially more diverse pool of Deaf clients. It should be noted that, compared with the standard IAPT services, the BSL-IAPT service has seen a larger number, and possibly more clinically diverse population, of Deaf clients and their consistency in achieving reliable recovery and reliable improvement rates has been tested with greater experience and larger numbers, leading to more precise estimates.
Belk et al. ,85 using the tighter definition of completed therapy for 226 patients receiving BSL-IAPT, found that 76.5% of Deaf clients attending BSL-IAPT services achieved reliable improvement, whereas only 54.0% achieved reliable recovery. Gyani et al. 106 reported that, across all IAPT services (general population) between October 2008 and September 2009, 63.7% of service users achieved reliable improvement and 40.3% reliable recovery. Based on data collected in March 2015, the HSCIC107 reported a reliable improvement rate of 61.5% and a reliable recovery rate of 43.1%. All of these figures were based on a recorded endcode indicating that treatment had been finished. BSL-IAPT outcomes are better than those recorded for the general population.
The comparative analyses carried out also reveal concerns about the consistency of data recording and the reliability of some of the data. This was true both for basic demographic characteristics and for more complex issues, such as waiting time. For example, for 11 standard IAPT clients, the number of days between first referral and first appointment is recorded as zero. This may be because these individuals were seen immediately, but that is unlikely in busy services; or it may be because the client was discharged as the waiting time exceeded IAPT minimum standards but was then re-referred to be seen immediately to avoid the service having to report failure to meet minimum targets. Alternatively, it may simply be an error of recording. It is not possible to be sure, but if the 11 zeros are excluded from the analysis, there is no difference in waiting times between the IAPT groups (26.0 days vs. 27.0 days; p = 0.189).
Objective iii: to map probable numbers of users of BSL-IAPT and Deaf users of standard Improving Access to Psychological Therapies who would be eligible for recruitment to a large-scale study
Method
Although language preference is not a required field in the minimum data set upload from IAPT services to the HSCIC, it is an optional code on the two most common data management systems in use by IAPT services at the time of data collection: iaptus and Patient Case Management Information System. Using this route, it would therefore be possible to gain a national picture of the number of BSL users accessing standard IAPT services within a given time frame. We first established with the operating managers of the two data management systems whether or not, in theory, it would be possible to run a data extraction from the records they held on behalf of IAPT services, which would identify how many BSL users had been seen by how many IAPT services. This was feasible. Furthermore, it would be possible to compare the numbers of Deaf BSL users seen against the total number of all clients seen by service. Establishing a common time frame for these client figures would be more difficult, as different IAPT services had started using the two data management systems at different times and some had stopped using them; therefore, it would be possible to obtain aggregate figures by service only up to a common cut-off date (e.g. 31 May 2015); to go beyond this date would require considerably more investment of time by the data management system providers. BSL-IAPT data reported earlier as data set 1 (n = 502)85 were used to calculate numbers of first appointments per quarter between 1 December 2011 and 31 March 2015.
Potential numbers of users of the BSL-IAPT service in the 10 regions where it was originally established were estimated by SignHealth, the provider of BSL-IAPT. Their figures are based on the prevalence of depression in the Deaf population, assuming that 50% of the Deaf population will access mental health services and, of these, 15% should access IAPT services based on the DH’s own target for IAPT uptake.
Ethics
This process of identifying numbers of clients overall and numbers of clients who were BSL users did not require any individualised client records being transferred to the research team, nor any client attributes or clinical information other than whether or not the client was a BSL user. Nonetheless, the NRES committee from which we had gained original approval for the study overall advised that we could not acquire these aggregated data unless each individual standard IAPT service gave permission for inclusion in the data extraction that the two data management systems would run. Every IAPT service in England was written to on an individual basis and a simple online consent form enabling ‘opt in’ was set up.
Results
Permissions requested and consents obtained are shown in Figure 9.
FIGURE 9.
Permissions to obtain numbers of BSL clients from data management systems. PCMIS, Patient Case Management Information System.
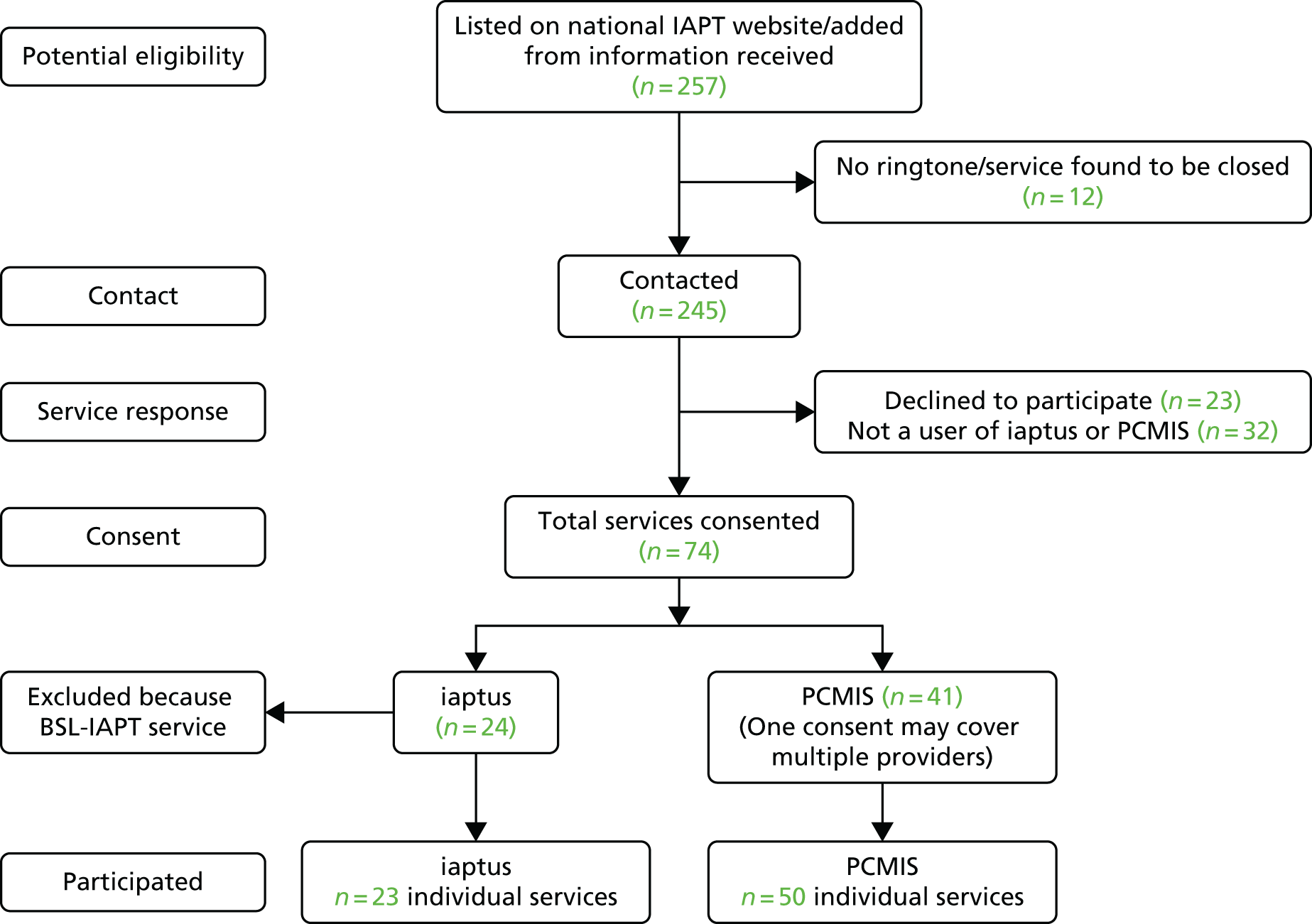
Results from iaptus
Having excluded the data from the BSL-IAPT service, the 23 iaptus services that gave permission are 24.5% of the total number (n = 94) of standard IAPT services where data management system records were available. In the 23 services who had seen Deaf clients who were BSL users (n = 14), they accounted for 0.02% (n = 109) of the total number of clients seen (n = 636,150) and 0.01% (n = 109) of the total number of clients (n = 811,229) of all services that gave permission for their data to be included. Of those services that had seen Deaf clients who were BSL users, the mean number of clients was 7.8 (range 1–24 clients, median = 4 and mode = 2).
Results from the Patient Case Management Information System
Forty-one services that used the Patient Case Management Information System consented for their data to be included. Of those 41 services, the data management system recorded that 11 services had seen BSL users, which accounts for 0.01% (n = 22) of the total number of clients seen in those 11 services (n = 161,899). When the total number of clients of all 41 services are included (n = 358,938), BSL clients accounts for 0.006%. Of those services that had seen Deaf clients who were BSL users, the mean number of clients was 2 (range 1–4 clients, median = 2 and mode = 2).
It is not possible to be sure why Deaf BSL clients as a percentage of the total clients seen in one data management system is almost double that in another. It may be that the iaptus system makes it easier to record this client characteristic or it may simply be an artefact of which services use which system and the number of Deaf clients they attract for reasons unconnected with the data management system. Finally, as not all users of both systems gave permission for their data to be included, it is not possible to comment on how representative these figures are of the total number of BSL users who are seen by standard IAPT services.
Results from BSL-IAPT
Five hundred and two clients who met the study inclusion/exclusion criteria were seen with a first appointment between 1 December 2011 and 31 March 2015. These were mapped by quarter-years to show patterns of likely throughput for estimating patterns of potential recruitment to any future study. The mean number of clients per quarter was 35.8, but there were wide variations (range 3–82), which reflected the initial start-up period and embedding of the service and changes in capacity experienced by BSL-IAPT over the study period as new funding arrangements were put in place following the transition from PCTs to CCGs (Figure 10). The number of clients who met the study eligibility criteria and were seen by the service was 119 in 2012, 158 in 2013 and 194 in 2014. Figures are not available in this study for 2015 and 2016, but discussions with the service provider suggest that they are less than previously reported, although this is not necessarily a reflection of reduced demand; it is also influenced by capacity to provide a service and funding arrangements (see Chapter 5).
FIGURE 10.
First appointment date for BSL-IAPT numbered by quarter. Q, quarter.
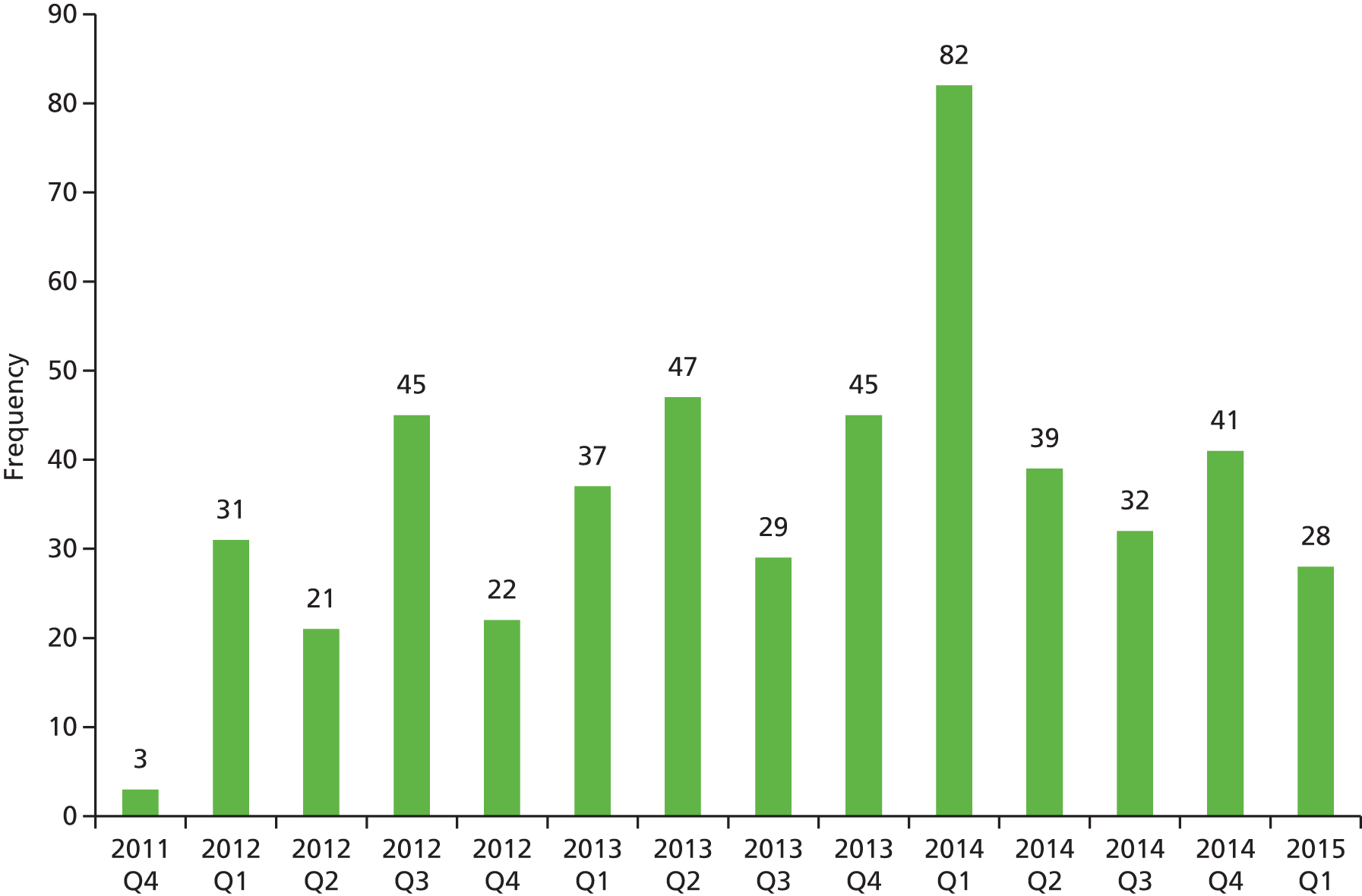
BSL-IAPT’s own predictions of the true numbers of potential clients requiring their service by region are presented in Table 19. These estimates are based on whole population figures per region, not on time periods of access to the service.
| BSL-IAPT region of activity/potential activity | Estimated numbers of Deaf clients requiring a service |
|---|---|
| North West | 955 |
| South Central | 433 |
| South East Coast | 400 |
| East Midlands | 627 |
| Yorkshire and Humber | 726 |
| East of England | 680 |
| London | 2106 |
| South West | 524 |
| West Midlands | 832 |
| North East | 309 |
| Total | 7592 |
Discussion
Despite the considerable challenges in acquiring data on Deaf users of standard IAPT services and the limited numbers of services that gave permission for the secondary analysis of data uploaded to the data management systems, these are the first available data on numbers of Deaf users of standard IAPT services. It is reasonable to assume that Deaf BSL users are likely to make up < 1% of clients that standard IAPT providers will see. However, as the modelling work reported in Chapter 5 illustrates, Deaf people face considerable barriers to accessing a standard IAPT service and being able to use it effectively; some of these barriers derive from the lack of awareness and training of staff within those services. Therefore, this estimate of Deaf users of a standard IAPT service should be placed in the context of less than optimal service access from a client’s point of view and, therefore, is probably a considerable underestimate of potential users given the heightened prevalence of depression/anxiety in the Deaf population (see Chapter 1). The estimated figures from SignHealth, the BSL-IAPT provider, are based on population estimates of Deaf people in each region that are not verified.
The BSL-IAPT service was originally offered in an area covered by two PCTs, which increased to five, followed by a reduction to three CCGs during the life of the data collection. Therefore, estimates of probable users of the service are strongly influenced by its availability geographically but also by funding arrangements. Consequently, extrapolations of probable numbers of service users in the future cannot be made other than to say it attracts high numbers of clients for a service that is commissioned currently in only three areas; access otherwise is subject to individual funding arrangements.
Objective iv: to establish effect size and estimate recruitment targets should a full trial be indicated
Background
Analysis of available data suggests an annual throughput of Deaf clients in BSL-IAPT of < 200 per year, but estimates of potential service uptake of considerably more. Limited figures drawn from a small sample of all standard IAPT providers suggests that Deaf people make up 0.01% or less of all clients seen. However, these figures are likely to be a considerable underestimate of potential demand because of service delivery factors affecting how services respond to Deaf people in terms of access and availability; this is discussed in depth in Chapter 5. In addition, the small number of standard IAPT services that participated, and incomplete and inconsistent service data recording, all raise concerns about the validity of any estimates of total numbers of Deaf people accessing IAPT nationally. Consequently, the effect size calculations and estimates of recruitment numbers for any future large-scale study, outlined in Method, are based on weak evidence. Two potential target recruitment scenarios are modelled assuming (1) a fully powered individual RCT and (2) a prospective observational study of factors associated with reliable improvement and reliable recovery in Deaf clients.
Method
In both potential study designs, the measures to be used as the primary outcomes will be reliable improvement and reliable recovery, as these take into account measurement error103,106 and are the IAPT methodological standard for outcome reporting. 105
Randomised controlled trial
We found little difference between standard IAPT clients and BSL-IAPT clients in reliable improvements (63.5% vs. 66.8%; p = 0.917) and no difference in reliable recovery (40.0% vs. 40.4%; p = 0.946), based on attending two treatments as a definition of completing treatment. However, this analysis was based on the comparison of a single service (BSL-IAPT) with multiple standard IAPT services, the majority of which had seen very few Deaf clients. Unlike the BSL-IAPT service, these services were yet to encounter large numbers and potentially a wide diversity of Deaf clients in terms of clinical presentation, communication and language. The comparisons made therefore entail a high degree of statistical uncertainty.
We calculate, for example, that if a reliable recovery rate of 40% is expected, at least 369 Deaf clients of standard IAPT are required in total, 40% of whom have reliably recovered, to have a 95% CI for the estimate with a precision (margin of error) of ± 5%. For a reliable improvement rate of 64%, at least 355 Deaf clients of standard IAPT are required. Our sample of Deaf clients of standard IAPT used for recovery calculations (n = 89) fell far short of this number. Furthermore, in the comparative analyses it should be noted that BSL-IAPT is a single-service provider with the same personnel (regardless of delivery location), whereas standard IAPT is made up a number of different services with variable degrees of experience of Deaf people, ranging from 1 to 24 clients. To reduce uncertainty in the comparative analyses of clinical outcomes, a far greater number of Deaf clients per standard IAPT service would be required.
Consequently, the original objective to compare the clinical effectiveness of BSL-IAPT with standard IAPT for Deaf people remains, as it is yet to be satisfactorily answered. An individual RCT design could be justified, taking into consideration the results from this study with respect to data recording, fidelity to intervention in light of the modelling of service delivery components (see Chapter 5), and with reliable measurements of clinical progress and health state now in place.
For the RCT, effect sizes for reliable improvement and reliable recovery were taken from Belk et al. ,85 who compared these in Deaf clients using the BSL-IAPT and non-Deaf clients using standard IAPT services. Their definitions of reliable improvement and reliable recovery were based on completion of treatment actually being recorded, rather than having attended two appointments, but we will assume that the differences in percentages between the two groups will be similar when translated to the definition based on having attended two appointments. Potential sample sizes were calculated using the software accompanying Machin et al. 108 In a randomised study with no confounding, the sample size calculation to compare the percentage of reliable recovery in two independent groups is based on a chi-squared test. Sample sizes were calculated for a range of effects (differences between rates of reliable improvement and reliable recovery in the two arms).
Prospective observational study
This study would determine what factors are associated with reliable improvement and reliable recovery for Deaf clients based on current practice. Gyani et al. 106 provided such an analysis in their paper, but the proposed study would focus on Deaf clients only and the findings of the proposed study would be compared against those of Gyani et al. 106 to see if there were any differences in Deaf clients. This would inform service providers of factors positively or negatively related to reliable improvement and reliable recovery in Deaf clients, which would alert them to potential facilitators and barriers and may enable them to tailor their treatment accordingly. Reliable improvement and reliable recovery would be calculated using the clinical cut-off points appropriate to the versions of the PHQ-9 and GAD-7 used by the IAPT service to measure scores of depression and anxiety.
This would be a prospective observational study with data collected over the first care episode for a client by all providers following a standard protocol. Type of service (standard IAPT or BSL-IAPT) would be an important variable to see whether or not this had any effect when adjusted for other factors. This could also include variables expected to be related to the outcomes that are not currently collected by all providers for Deaf clients, and also collect data on satisfaction with the service.
For this proposed study, the main analysis is multiple logistic regression, with reliable recovery (yes or no) as the dependent variable, and factors expected to be related to this in Deaf clients as the independent variables (as in Gyani et al. 106). Potential sample sizes were calculated from a rule-of-thumb proposed by Peduzzi et al. 109 for logistic regression, who showed that, for reliable estimation of model parameters, at least 10 participants were needed for each independent variable for each of the two outcome categories (yes or no). This approach requires an estimate of the percentages showing reliable improvement and reliable recovery with reported treatment completion, and these were taken from Belk et al. 85 as 76.5% and 54.0%, respectively. These rates applied to BSL-IAPT clients in that study. Although we could estimate rates for reliable improvement and reliable recovery only for Deaf clients with at least two therapeutic appointments for standard IAPT and BSL-IAPT clients in objective ii, these were similar, and it is reasonable to assume that rates with treatment completion for Deaf standard IAPT clients will be similar to those observed for BSL-IAPT clients in Belk et al. 85
Reliable improvement and reliable recovery would be based on treatment as recorded as having been completed. In Belk et al. ,85 only 226 of 349 BSL-IAPT clients (just under two-thirds) had an endcode indicating that this had happened, and the sample size for the study will need to be multiplied up by 349/226 to make an allowance for participants not completing their treatment within the time frame of the study.
Results
Randomised controlled trial
Table 20 shows the number of participants needed for an individually randomised controlled trial comparing reliable improvement in Deaf clients randomised to either the BSL-IAPT service or a standard IAPT service. Table 21 shows the number needed for an individually randomised trial comparing reliable recovery. Sample sizes for a range of differences in reliable improvement and reliable recovery rates were compared with the rates estimated by Belk et al. ,85 which were 76.5% and 54.0%, respectively.
| Reliable improvement for BSL-IAPT (%) | Reliable improvement for standard IAPT (%) | Effect (%) | Number needed per arm for analysis | Total number needed for analysis | Total number to be recruited for treatment to be completeda |
|---|---|---|---|---|---|
| 76.5 | 71.5 | 5.0 | 1207 | 2414 | 3728 |
| 76.5 | 69.0 | 7.5 | 553 | 1106 | 1708 |
| 76.5 | 66.5 | 10.0 | 319 | 638 | 986 |
| 76.5 | 64.0 | 12.5 | 209 | 418 | 646 |
| 76.5 | 61.5 | 15.0 | 149 | 298 | 462 |
| 76.5 | 59.0 | 17.5 | 111 | 222 | 344 |
| 76.5 | 56.5 | 20.0 | 87 | 174 | 270 |
| Reliable improvement for BSL-IAPT (%) | Reliable improvement for standard IAPT (%) | Effect (%) | Number needed per arm for analysis | Total number needed for analysis | Total number to be recruited for treatment to be completeda |
|---|---|---|---|---|---|
| 54.0 | 49.0 | 5.0 | 1568 | 3136 | 4844 |
| 54.0 | 46.5 | 7.5 | 697 | 1394 | 2154 |
| 54.0 | 44.0 | 10.0 | 392 | 784 | 1212 |
| 54.0 | 41.5 | 12.5 | 250 | 500 | 774 |
| 54.0 | 39.0 | 15.0 | 173 | 346 | 536 |
| 54.0 | 36.5 | 17.5 | 126 | 252 | 390 |
| 54.0 | 34.0 | 20.0 | 96 | 192 | 298 |
The total number of participants needed to be recruited for an individually randomised RCT to compare reliable improvement or reliable recovery in Deaf clients between the BSL-IAPT service and standard IAPT services is very high when the expected difference between the two is small. The total number becomes more manageable when the difference is large. At the moment there is a lack of evidence on which to base any judgement of whether the expected difference will be small or large without further research.
Prospective observational study
Table 22 shows the number of participants needed for the prospective observational study of factors associated with reliable improvement or reliable recovery for 6–20 factors. The sample size calculations depend on the percentage showing reliable improvement and reliable recovery, which, from Belk et al. ,85 were taken to be 76.5% and 54.0%.
| Number of factors | Reliable improvement | Reliable recovery | ||
|---|---|---|---|---|
| Total number needed for analysis | Total number to be recruited for treatment to be completeda | Total number needed for analysis | Total number to be recruited for treatment to be completeda | |
| 6 | 256 | 396 | 131 | 203 |
| 8 | 341 | 527 | 174 | 274 |
| 10 | 426 | 658 | 218 | 337 |
| 12 | 511 | 790 | 261 | 404 |
| 14 | 596 | 921 | 305 | 471 |
| 16 | 681 | 1052 | 348 | 538 |
| 18 | 766 | 1183 | 392 | 606 |
| 20 | 852 | 1316 | 435 | 672 |
Reliable improvement and reliable recovery could be modelled in the same study by fitting two logistic regression models with different outcome variables. Numbers needed for analysis are larger for a model for reliable improvement (this is because the prevalence of reliable improvement is further away from 50%, when sample size is minimised). Even for reliable recovery, the number of participants needed is relatively high when there are 12 or more factors in the model, which is usual in such studies. For instance, a model for reliable recovery with 12 factors would require at least 261 participants with data for analysis and 404 to be recruited if the proportion not reaching treatment completion is similar to that seen in Belk et al. 85 Relevant factors would be chosen before the start of the study, chosen to be non-overlapping, representing different domains. Nominal variables such as provisional diagnosis must be converted into sets of binary (yes or no) dummy variables for analysis and also for the sample size calculation. As this will increase the number of independent variables and the required sample size, it may be necessary to group similar categories together in the dummy variables.
Discussion
There is a lack of evidence on which to calculate potential sample sizes required for any future study, whether a RCT or another design, and estimates of effect size remain uncertain. This is because the comparative analyses of clinical outcome data undertaken are based on a small number of participants, which in the case of standard IAPT services are a small proportion of all standard IAPT services, being those that self-selected to participate. Statistical uncertainty arises from a comparison of clinical outcomes from a single-service provider with those from multiple providers, many of whom have seen only one or two Deaf clients. The total number of Deaf users of IAPT cannot currently be ascertained, nor can the potential numbers of clients in this population be reliably extrapolated from secondary data. The study has also revealed deficits in accurate recording of clinical data. Therefore, although potential sample sizes for two different study designs have been estimated, it is not possible to judge how realistic recruitment to them might be without further research to enable greater precision.
Chapter 5 Mixed-methods modelling of BSL-IAPT and standard IAPT as accessed by Deaf people (study 3)
Background
As a national (England) programme, IAPT has an established protocol for referral, assessment and therapy, and standardised approaches to training/qualification of therapists and standards of service delivery. 18,19,103 When Deaf people use standard IAPT, a range of potential variables come into play despite this standardisation to enable access and to support therapy. However, the variation in these, how common they might be and their effectiveness were unknown. Although the provision of a sign language interpreter is the most obvious potential adaptation, it is not the only possibility, and gateways into a standard IAPT service might also present barriers to access, based on previous work about the accessibility of primary care services in general for Deaf people. 28,29,52 Understanding the current landscape of provision and adaptations is an important component in defining the broader context in which to understand the effectiveness and cost-effectiveness of current standard IAPT provision for Deaf people.
At the start of the project, the specialist version of IAPT designed for Deaf people in BSL had been developed by a sole provider, BSL Healthy Minds, under the auspices of a Deaf health charity, SignHealth. 22 A considerable investment had been made in the recruitment and training of Deaf people as qualified PWPs in order to deliver IAPT with and for Deaf people, and initially we referred to this intervention as BSL-IAPT. In the course of the project it became apparent that provider and model of provision were no longer necessarily synonymous. This was because a small number of the trained Deaf PWPs were working for other IAPT providers and also some providers of IAPT had chosen to invest in a specialist service for Deaf people, particularly in parts of England where historically there had been a high density of Deaf people living. Since the changes in commissioning arrangements, with the move from PCTs to CCGs that happened during the life of the project,110 access to BSL-IAPT through BSL Healthy Minds has declined, with block commissioning arrangements being increasingly replaced by the use of IFRs instead. 32 This is also apparent in the waiting time data reported in Chapter 4. The originating BSL-IAPT service provider submitted an application to the DH for National Specialist Commissioning status in 2015, but this was rejected.
Given these changes and uncertainties, the intervention (BSL-IAPT) and the service provider are now potentially divisible for definitional purposes. Consequently, BSL-IAPT, its components and its potential variations, also require modelling for potential use in any future larger-scale trial or observational study.
Objectives
-
To produce a replicable description of ‘standard IAPT’ when implemented with BSL users.
-
To produce a replicable description of the core components of BSL-IAPT differentiated from its delivery by a single-service provider.
Methods
Design
A sequential mixed-methods study design111 was used, consisting first of a survey of IAPT practitioners with closed and open questions in order to capture a broad range of views and experiences. This was followed by semistructured individual interviews of a subgroup of IAPT practitioners to explore in greater depth those topics identified from the survey responses that warranted further enquiry.
Survey inclusion criteria
All current practitioners delivering therapy at steps 2 and 3 under the IAPT umbrella to adults in England were eligible to take part. The definition of practitioner is not confined to PWPs, as other mental health professionals are also IAPT practitioners. Practitioners may be directly employed by the NHS, or may be subcontracted to provide IAPT treatments under an ‘any qualified provider’ arrangement, which operates in some areas. They may also be employed by private providers to the NHS. The IAPT workforce survey 2014112 reports that IAPT employs a 6307-strong whole-time equivalent workforce (including trainees) across IAPT in England; however, this includes non-IAPT-qualified counsellors and therapists as well as supervisors who do not treat clients, and employment support workers.
Interview inclusion criteria
For practitioners working in any service other than that provided by BSL Healthy Minds, the inclusion criteria were:
-
are currently working as an IAPT practitioner
-
AND have completed an initial survey
-
AND have indicated that they are willing to be contacted for a follow-up semistructured interview
-
OR have contacted the research team directly to indicate willingness to be interviewed regardless of having completed a survey.
For practitioners working in the BSL Healthy Minds service (the main provider of BSL-IAPT intervention), the inclusion criterion was:
-
all practitioners and other staff currently involved in the development and maintenance of the specialist service.
Ethics approval
Ethics approval for the study was granted through the University of Manchester REC (reference ethics/150715). For NHS provider services, R&D approval was also required from each individual trust prior to directly inviting individual participation; this included participation in the initial survey.
Recruitment to the survey
Recruitment route 1
-
Following R&D approval, an invitation to complete the survey was sent to a key contact within each service via e-mail, asking them to circulate to practitioners. A reminder was sent 2 weeks after the initial invitation.
Recruitment route 2
-
Practitioners were also alerted to the study and how to take part via a number of indirect routes. These included:
-
a personal e-mail invitation to participate distributed to British Association of Behavioural & Cognitive Psychotherapists members who categorised themselves as PWPs, high-intensity therapists or IAPT trainees (approximately 500, although the numbers of those who were actively working within IAPT services at that time was unknown)
-
contact with service/team managers of 23 private providers of IAPT services to the NHS, asking them to circulate the invitation to practitioners within their service (total number of practitioners who meet the inclusion criteria unknown)
-
contact with 39 IAPT training providers, asking them to circulate the invitation to their students (total number of practitioners who meet the inclusion criteria unknown)
-
260 flyers placed in conference packs for two IAPT provider events
-
eight advertisements in online forums and on websites associated with IAPT networks, which are accessed by IAPT practitioners, including a banner on the iaptus homepage (software management system for psychological therapies used by IAPT services)
-
a small advert on the British Association of Counselling & Psychotherapy noticeboard
-
repeat calls in the North West Psychological Professions Network newsletter.
-
Recruitment to the interview
A theoretical sampling approach was taken to deciding who to invite for interview based on the widest diversity of representation possible according to the criteria: (a) experience, including those who had direct experience of IAPT with a Deaf person and those who did not; (b) service context (NHS, contracted provider, private); (c) professional background of IAPT practitioner (PWP, psychologist, counsellor, etc.); and (d) a role in an IAPT service provider (e.g. service manager, individual practitioner, specialist practitioner).
Additionally, all staff involved in the delivery of the BSL Healthy Minds service, which had been the originator of a BSL-IAPT service, were invited to participate in a semistructured interview, regardless of whether or not they had completed a survey. This was because they had crucial knowledge about and experience of the operation and rationale behind a specialist IAPT provision for Deaf people, which was central to being able to model the intervention.
Data collection
The survey was hosted online using the software SelectSurvey.NET™ (version 4; ClassApps.com, Kansas City, MO, USA) and contained open and closed questions (see Appendix 6). A paper-based version was available instead on request. It invited practitioners to respond to questions outlining a range of variables associated with the delivery of IAPT to Deaf people. Practitioners were asked either to respond according to their own experience, if they had had a client who was Deaf, or to respond according to what they would do within their service if a client who was Deaf was referred to them. The survey also established basic information about the practitioners’ professional background and experience as well as the context and structure of the service in which they worked.
The semistructured interview was generated, in part, from findings from the survey responses that required further investigation about the range of adaptations and variations in the delivery of standard IAPT for Deaf people and pre-existing questions associated with modelling the BSL-IAPT intervention and potential axes of variation in its delivery (see Appendix 7).
Analysis
Survey data were analysed using descriptive statistics supported by IBM® SPSS Statistics® version 22 (IBM Corporation, Armonk, NY, USA). The approach to analysis of the qualitative data from both standard IAPT practitioners and BSL-IAPT practitioners was informed by realist synthesis113 and the practices of realist evaluation. 114 Realist evaluation is underpinned by a philosophical orientation that acknowledges the material reality of the social world and its structures, but also acknowledges that how it is known results from individual or collective interpretation filtered through language, culture and historical experience. Different individuals in varied social, linguistic and cultural settings will respond differently to the same set of circumstances, experiences, events, actions and available resources. 114 Consequently, realist evaluation is fundamentally concerned with a context-embedded approach to understanding outcomes that seeks to identify the mechanisms that may lead to particular outcomes for individuals in given circumstances. This is conventionally summarised as investigating what works, for whom, in which circumstances and why. 115 We employed this orientation to understand the data that practitioners had shared about access to and the practice of IAPT, to identify key variables in adaptations that may or may not be made and their consequences for Deaf people using standard IAPT.
In the case of interviews with practitioners drawn from standard IAPT, data were transcribed into written English by a registered research transcribing service and then read and reread by two researchers who independently identified thematic areas of interest. When consensus was reached on what these themes should be, the data were reread and under each theme area, the variations in practice and their interpretation by participants were mapped against a grid divided into three:
-
context (defined as the action or event or practice that occurred in the given context of the individual’s knowledge/experience, e.g. self-referral, therapeutic alliance)
-
mechanism (defined both as means of effect and resource that might underpin or be required for the effect, e.g. assessments in BSL, the provision of an interpreter, an IAPT practitioner experienced in the given problem)
-
outcome (the consequences and their variation of the context plus mechanism, e.g. ease with which Deaf people can access the service, level of satisfaction with the therapy).
Scrutiny of the table then led to the generation of context, mechanism, outcome propositions, which were tested out for their validity and variation by rereading the transcripts of the interview data as a whole, to judge the credibility of the propositions generated – did they explain the variations noted in how standard IAPT may be adapted for Deaf people and the probable results of those adaptations? These form the structure of the presentation of the interview findings.
In the case of the BSL-IAPT interview data, the same procedure was followed with the addition of the BSL interviews being translated into English by a qualified and registered BSL interpreter prior to transcription.
Results: standard Improving Access to Psychological Therapies practitioners
The following combines relevant survey results with the interview analysis.
Survey respondents
Given the means of distribution of the survey, it is not possible to know the total number of potential respondents. Of the 118 useable responses, none was from a Deaf BSL user, and none was from someone who worked for the BSL Healthy Minds service. Therefore, the views expressed are exclusively from hearing practitioners operating within service structures we refer to as standard IAPT (i.e. not exclusively set up as a specialist IAPT service provider). That said, 61 respondents (51.7%) stated that their service had Deaf BSL users as clients and 35 respondents (29.7%) had personally provided therapy to Deaf clients who were BSL users. In addition, 11 respondents (9.3%) reported that there was at least one Deaf BSL user working as a therapist within their service, although this does not necessarily equate to 11 services with Deaf therapists because multiple respondents may be drawn from the same service.
Given the small number of services and respondents who took part in comparison with the IAPT workforce overall, these figures suggest that there is a response bias in the survey to those services and practitioners with some experience of Deaf people. Indeed, 21 respondents (17.8%) reported some BSL skills, ranging from basic communication to Level 3 (five people), which corresponds to a reasonable proficiency but below full fluency. Nonetheless, four people said that they had provided therapy to a Deaf person one to one in BSL without an interpreter. From a cultural awareness and cultural competency perspective, of the 21 who said that they had some degree of BSL skills, only four reported frequent involvement in the Deaf community. Sixteen said that they had been on training specifically about how to work with Deaf clients.
The sample was biased towards highly experienced IAPT practitioners, with 56 respondents (47.5%) having over 4 years’ IAPT experience and only 15 (8.7%) having less than 1 year’s experience. The majority of respondents were female (n = 99, 83.9%). The sample was heavily biased towards white British respondents (n = 92, 78%).
Of the 117 participants who supplied information about their role/job title, 28 had senior status (e.g. service manager, service lead PWP, senior psychologist) and six were trainees (e.g. assistant psychologist, PWP trainees). The rest were therapists, either PWPs or other professionals trained as IAPT practitioners, 13 of whom were high-intensity therapists, with a further three being high-intensity therapy trainees.
Interview participants
A total of 32 individual IAPT practitioners who completed the survey indicated that they would be willing to participate in a follow-up interview; of these, 20 were contacted and 14 took part. Two additional interviews were conducted with Deaf practitioners working within standard IAPT settings, who contacted us directly to indicate that they would be willing to be interviewed, but who chose not to complete the survey. Sixteen people were interviewed in total from standard IAPT services, 13 of whom were women. Twelve participants had over 3 years’ experience working in IAPT, nine of whom had over 4 years’ experience. All but one worked in a direct clinical role seeing clients.
Flexibility in the delivery of services
Overall, service providers described a range of axes of flexibility in the delivery of services including:
-
location (e.g. in prison, community centres, libraries, GP surgeries)
-
services for designated groups only (e.g. women, veterans)
-
practitioners who specialised in particular conditions (e.g. trauma, long-term physical health conditions, sexual assault survivors, older adults)
-
partnership working with other organisations, including the possibility of referral to any qualified provider.
The general rationale for such flexibility included familiarity of location; increasing access and comfort in provision; meeting specialist needs when required; shorter waiting lists; and supporting patient choice. However, these characteristics of structure and components of advantage did not operate in the same way for Deaf clients.
For example, flexibility in location of services (e.g. in the community) did not generally take into consideration the fact that, for reasons of cultural familiarity, Deaf people’s community, and the spaces associated with it, may not be same as those of a hearing person. Therefore, the rationale of increasing comfort and access may not operate in the same way and, furthermore, may not be recognised as operating differently. Where there was a specialist service for Deaf people operating within a mainstream service, there tended to be only one practitioner – thus reducing the possibility of choice of therapist for the client. The categories of ‘Deaf’ and ‘BSL user’ could funnel a client to a single Deaf specialist practitioner rather than to a specialist in their particular problem (e.g. trauma, coping with a long-term health condition). On the other hand, if a Deaf client was seen by a practitioner with a specialism within a specific condition/symptom cluster, that person may have little or no previous experience of working with a Deaf person.
The survey asked respondents to consider their service’s capacity in meeting Deaf clients’ preferences with regard to a therapist of the same sex, hearing status and direct versus interpreted therapy. Although sex posed few difficulties, and delivery of therapy to Deaf people through an interpreter was relatively easily met, direct therapeutic encounters without mediation were clearly problematic in terms of meeting client preference (Figure 11).
FIGURE 11.
Meeting Deaf clients’ preferences for therapist. Would Deaf BSL users be given the opportunity to choose any of the following options with regard to their allocated worker?
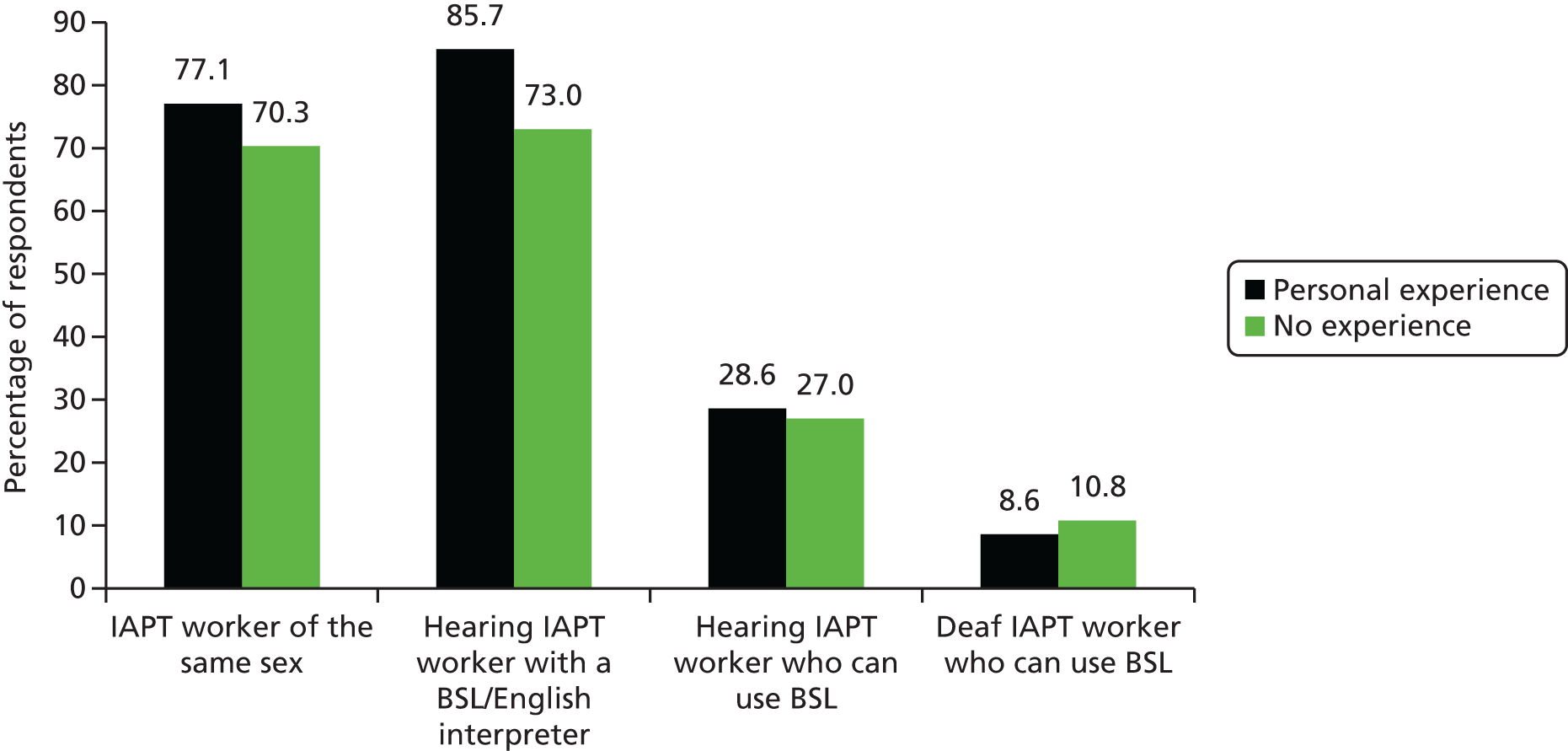
Results are presented below and throughout this chapter differentiated by those respondents who said that they had delivered an IAPT service to Deaf clients themselves (whether with or without an interpreter), which we term ‘personal experience’, and those who had no personal experience of service delivery to a Deaf client.
Some solutions regarding more limited flexibility of provision for Deaf people were offered as possibilities, for example referral to a qualified provider in a location/service that Deaf people may be familiar with (e.g. a Deaf women’s health project); being prepared to wait to be seen in order to be able to access a Deaf specialist therapist; or referral by a local IAPT service to a specialist practitioner/provider outside its immediate area of operation dependent on money, availability and arrangements in place.
These adaptations and special arrangements had compromises and potential risks too. For example, the Deaf person may have to choose between seeing someone who is experienced in their particular area of concern or seeing someone who is Deaf/Deaf experienced. Referral on may mean that the Deaf person waits longer to be seen and thus that their difficulties have escalated. Where no consideration is given to the cultural and linguistic suitability of a model of provision for a Deaf client, this may result in an unsatisfactory or less effective experience. It raises the question of who might be a ‘qualified provider’ in the case of a Deaf client. These variations can be represented diagrammatically (Figure 12).
FIGURE 12.
Impact of service structure flexibility on Deaf clients.

Pathways for Deaf clients within standard Improving Access to Psychological Therapies structures
Some mainstream IAPT services had invested in specialist provision or a specialist pathway for Deaf clients. They were in the minority. Of 17 practitioners interviewed, six described their own specialist provision or their specialist pathway drawn from four services. The majority had never thought about it before, but many appreciated our contact with them because it prompted them to do so. Several remained in touch with the project and requested that we send them information and resources as they became available.
We consider in detail what the components and characteristics might be of a specialist BSL-IAPT service within a standard IAPT provider when considering BSL-IAPT later in this chapter (see Results: interviews with BSL-IAPT practitioners). At this point, we address only the issues raised by standard IAPT services with respect to pathways to provision for Deaf people. Broadly speaking, there were three main approaches.
Pathway model 1: divert to external Deaf specialist service provider
In this approach, a standard IAPT practitioner would be unlikely to encounter a Deaf client at all because the CCG has an arrangement to buy in a specialist BSL-IAPT provider service (such as BSL Healthy Minds), and so Deaf clients are usually diverted to this service either directly by the referrer, via self-referral or by the IAPT service at first contact. This is usually a block commissioning arrangement in the given area. However, such arrangements are rare, and more usually standard IAPT services made individual requests to their local CCG for a Deaf client who was referred to them to be seen by a specialist provider. This might be a BSL-IAPT provider or it might be another specialist Deaf mental health service if the patient was deemed to need greater levels of care and intervention than appropriate to primary care provision. Whether or not referral to an outside specialist provider occurred was usually dependent on cost and CCG policies, a point we return to later (see Pathways of self-referral to Improving Access to Psychological Therapies).
Therefore, it was more usual for a standard IAPT practitioner whose service had this divert to specialist provider pathway in place to encounter a Deaf client only if they had chosen not to use the specialist BSL-IAPT service/external specialist provider on offer. This issue of choice is interesting because during the research study we met Deaf clients who had tried BSL-IAPT and as a result decided that they wished to use a mainstream provision instead, clients who had never realised that they might have had a choice in the first place and others for whom the notion of choice seemed irrelevant if there was a specialist BSL-IAPT provision available in their own language and delivered by a culturally competent practitioner. We return to the issue of client choice later when considering therapeutic effectiveness.
This variety of specialist pathways, in which a Deaf client is diverted to a specialist BSL-IAPT service or provider for Deaf people that sits outside standard provision in their locality, is rare. It was block commissioned only in five locations when our study began, and by the end of the study in only two. Furthermore, standard IAPT services attempting to achieve a specialist pathway for Deaf clients through dependence on IFRs103 reported difficulties and/or long delays in organising, which was not ideal from a client’s point of view. More often than not, the reluctance to block commission or agree to IFRs was associated with perceived cost. On the face of it, the standard service plus interpreters was cheaper than commissioning specialist provision despite there being no evidence of cost-effectiveness or clinical effectiveness that would indicate that one was preferable to the other, which was the starting point of this whole project. This uncertainty is now reflected in the Royal College of Psychiatry guidance for commissioners of primary mental health-care services for Deaf people,116 which used evidence from this project.
Pathway model 2: a designated specialist pathway for Deaf clients within the service structure
In this approach, the standard IAPT service has in place a specialist practitioner or provider, whether as part of its service or as part of its usual partnership arrangements with local qualified providers. This person may be Deaf or hearing. In some instances this person is regarded as the specialist because they have had prior experience of working with Deaf clients, although this does not necessarily mean that they are able to communicate directly with a Deaf client without an interpreter. In other cases the specialist partner provider is Deaf, and this constitutes the most important factor in their specialist status (additional to their qualifications and training).
The difficulties identified in this model included the fact that the individual within the specialist pathway could easily become overwhelmed with referrals. In part, this was because it was common for Deaf clients to require a longer than average engagement with the IAPT service (a point we return to later in the section on readiness of Deaf clients to engage with therapy; see The therapeutic encounter). The type of therapy that a Deaf client might be offered could also be influenced by the type of therapy that the specialist practitioner delivered (e.g. if the specialist practitioner was trained in offering only counselling or CBT). A client assessed as requiring a different kind of therapy from that which the specialist practitioner could offer would then move within the service to a hearing clinician with an interpreter. The step level of service with which a Deaf client might engage could also be influenced by the level at which the specialist provider sat (e.g. in order to have a Deaf therapist a client might need to engage with the service at step 3 because that is where the Deaf therapist was located when in reality they might require step 2 only). The reverse was also true in the case of a Deaf person requiring therapy at a higher step level or needing a different type of therapy than the specialist therapist was qualified to give. A client may then be referred on to BSL-IAPT (pathway model 1) or stepped up within the service to a clinician who may have little or no experience of working with a Deaf client plus interpreter provision (pathway model 3). It was rare for standard IAPT services that included a specialist practitioner or a referral pathway to a specialist local partner/provider to offer a Deaf client a choice of more than one therapist. The resulting long waiting times meant that some Deaf clients compromised, and were unable to see their first choice of practioner, in order to be seen sooner.
Pathway model 3: the same pathway as for any client, with the addition of an interpreter
This pathway consists of the same arrangements that would be made for any referred client to standard IAPT, but with the addition of sign language interpreters. Of the 35 survey respondents who said that they had personal experience of providing therapy to a Deaf client, 27 had achieved this with a sign language interpreter. In most cases, the therapist did not have experience of Deaf clients, but was chosen for their knowledge and relevant experience of other aspects of the client’s presentation (e.g. chronic obstructive pulmonary disease). In some instances, the therapist was chosen not because of their knowledge/experience of Deaf clients or of the client’s specific condition, but simply because they were available and willing to work with an interpreter. Although what makes this a specialist pathway may seem minimal at first glance, we have included it as a specialist pathway within standard IAPT structures because some services had thought about it and had deliberately executed this option; in comparison, the vast majority, who were yet to encounter a Deaf client, remained unaware of the alternatives and had not considered other possibilities in any depth. The additional issues associated with interpreted therapeutic provision are considered in a later section (see The therapeutic encounter).
These variations in pathway are represented diagrammatically in Figure 13.
FIGURE 13.
Pathways diagram (standard IAPT services).
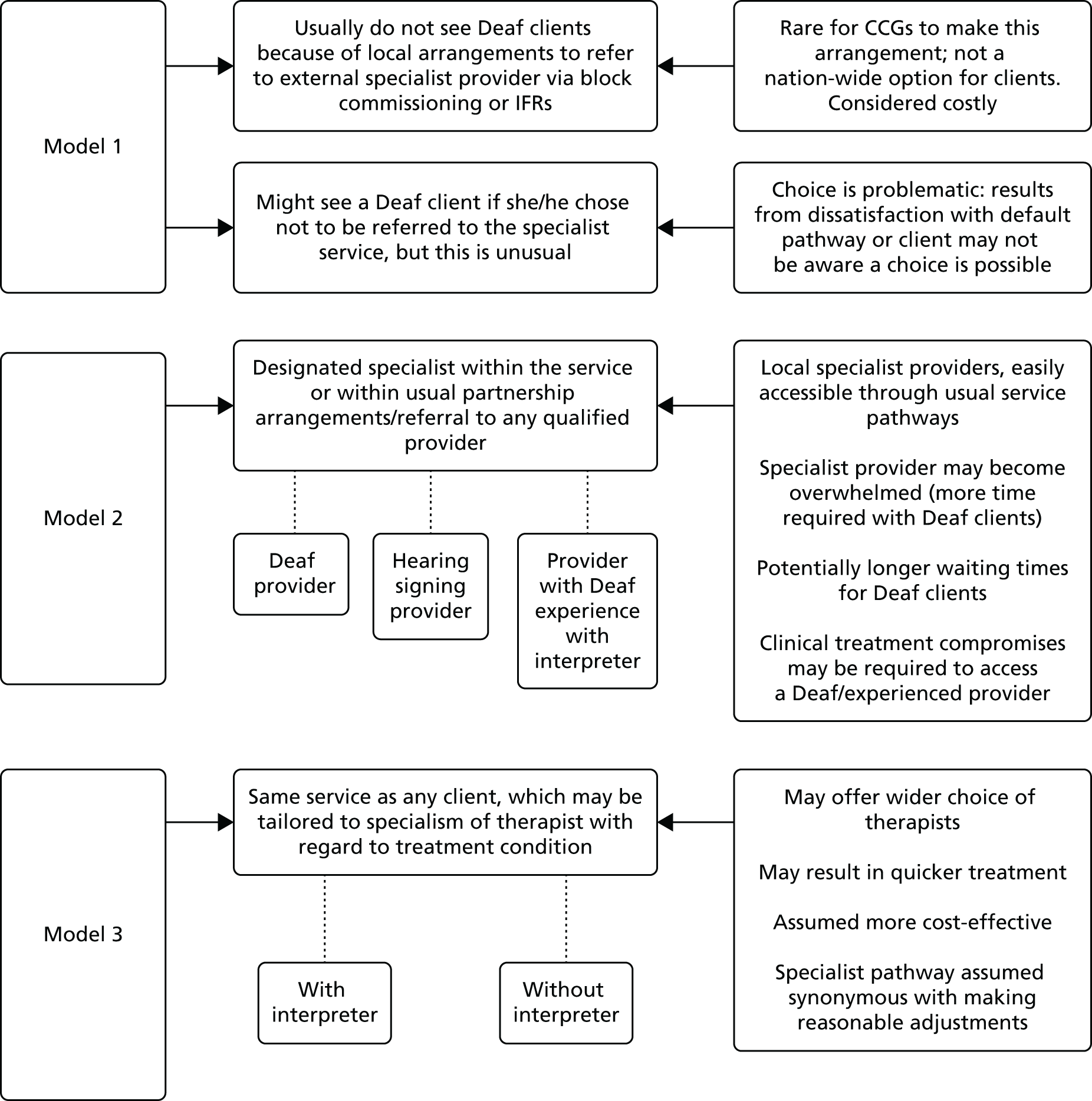
Pipeline into the service
I’m not aware we’ve ever excluded anyone at all from the service based on the fact that they don’t speak English well enough to arrange an initial appointment.
Standard IAPT practitioner
Overall referral pathway trends
Respondents were asked who was the source of referral of Deaf clients to their service, regardless of whether or not the respondent had worked with these clients personally. Three said that no Deaf person had ever been referred to their service and a further 45 did not know if this had ever happened. Therefore, only 70 respondents were able to provide a picture of referral sources based on knowledge and/or experience. Of these, 59 had knowledge of referrals via a GP and 33 of self-referrals. Seven were aware of instances of referral from a statutory agency and six from a third sector agency.
The process of engaging with the study prompted some standard IAPT providers who were interviewed to consider whether or not there were any blockages in the pipeline into IAPT services for Deaf people. Participants with no experience of Deaf clients and no specialist pathway reflected on how their usual processes of raising awareness of IAPT provision and managing referrals might work (or not) for potential clients who were Deaf. Among the minority from standard IAPT services who considered that they had a specialist pathway, there was nonetheless recognition that getting into the service in the first place might be problematic for Deaf people. In this section we consider the various potential hurdles for Deaf clients reaching an IAPT service. In later sections we address issues in the use of that service.
Promotion, advertising and awareness raising about Improving Access to Psychological Therapies services
Many of the services we spoke with and that replied to the survey actively undertook promotion, outreach, advertising and awareness-raising activity about IAPT in their local communities. Views on the accessibility for Deaf people of information about their service were mixed with no strong tendency to assume that information was inaccessible (Figure 14).
FIGURE 14.
Views on the accessibility of information for Deaf BSL users.
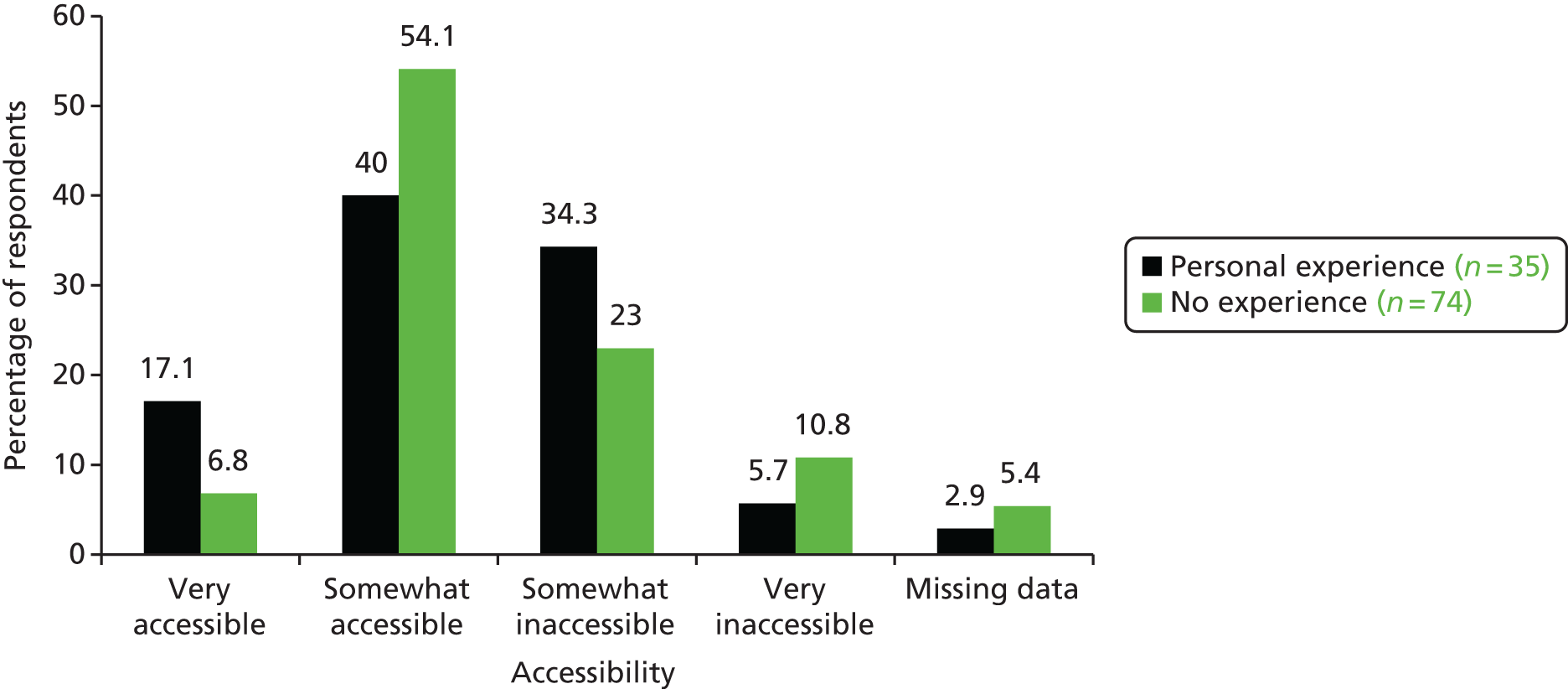
Improving Access to Psychological Therapies services readily accept self-referrals as well as referrals from health or social care agencies; therefore, promoting the service to potential service users was considered important. In addition, some services said that they undertook active monitoring of ‘under-represented’ groups. A list of activities undertaken was generated from the responses received, but not all of those services that engaged in the study appreciated the problematic nature of some of these activities from the perspective of Deaf clients; our interpretation reflects our knowledge of the barriers these might pose rather than necessarily the services’ own knowledge (Table 23).
| Strategy/action | Implications | Consequences |
|---|---|---|
| IAPT providers seek to promote their services and raise awareness by producing information about the service in a variety of spoken languages and in some cases easy-read versions (but not in a signed language) | Assumes Deaf people could read information even if it was not in BSL and fully understand it. But this is not the case for many Deaf people, who struggle with literacy in the written word | Harder for Deaf people to be aware that the service exists |
| Ignores the issue of language preference and language rights to have accessible information in own language | Unaware services make the false assumption that there are no barriers to Deaf clients’ awareness of the service and their potential self-referral | |
| Does not consider the duty imposed by the NHS Accessible Information Standard 2015 with respect to Deaf people and others with specific communication requirements | ||
| Service is advertised on the radio because it is a cheap approach that has been shown to be effective | Inaccessible for Deaf people | Although not all means of advertising and promotion necessarily have to be accessible to all groups, there was minimal consideration given to how this approach might be exclusionary |
| ‘Word of mouth’ is a useful means of raising awareness of the service and encouraging self-referral | Deaf people’s communities and social groups are different and so word of mouth does not operate in the same way in terms of creating communities of informal knowledge. Where Deaf people have contact with other groups/settings/contexts where word of mouth about IAPT may be operating they will face barriers to accessing that conversation in the first place | Levels of awareness among Deaf people as to who might benefit from an IAPT service in a given locality remain low |
| Word of mouth could operate well from Deaf person to Deaf person, but without initial experience of IAPT in a local provision this is unlikely | ||
| IAPT reporting mechanisms, as well as locally imposed standards in some cases, will monitor under-represented groups | Reporting would only be effective in highlighting the under-representation of Deaf people in the service if Deaf BSL users were a monitored category. Although locally some services did record Deaf BSL users, it is not a minimum data set requirement for formal reporting purposes. In the usual standard IAPT reporting requirements Deaf people are not distinguished by language category (e.g. BSL), only by disability (hearing) which would not identify BSL users | Deaf BSL users are a hidden group |
| Scale of potential need remains unknown | ||
| Not clear whether or not they are under-represented in any given service | ||
| Service will not target their awareness raising and promotion to an under-represented group if the group is not identified in the first place | ||
| In services with stretched resources, targeting awareness raising at specific under-represented groups may be a luxury that cannot be afforded | Awareness-raising strategies are generic | Resource constraints further compound the invisibility of the under-represented group by not being identified as being in need of greater concentration of awareness raising |
| Services run community drop-in sessions to raise awareness in particular communities and groups of people | Does not recognise that ‘community’ may be differently understood by Deaf people; therefore, their community locations are not likely to be the same as those targeted by IAPT services | IAPT services do not encounter Deaf people in their outreach activities and therefore erroneously assume that there is a lack of need for information and knowledge |
The impacts for Deaf people on reaching the service in the first place with respect to promotion, advertising and awareness raising can be represented diagrammatically (Figure 15).
FIGURE 15.
Impact of ineffective service promotion and awareness raising.
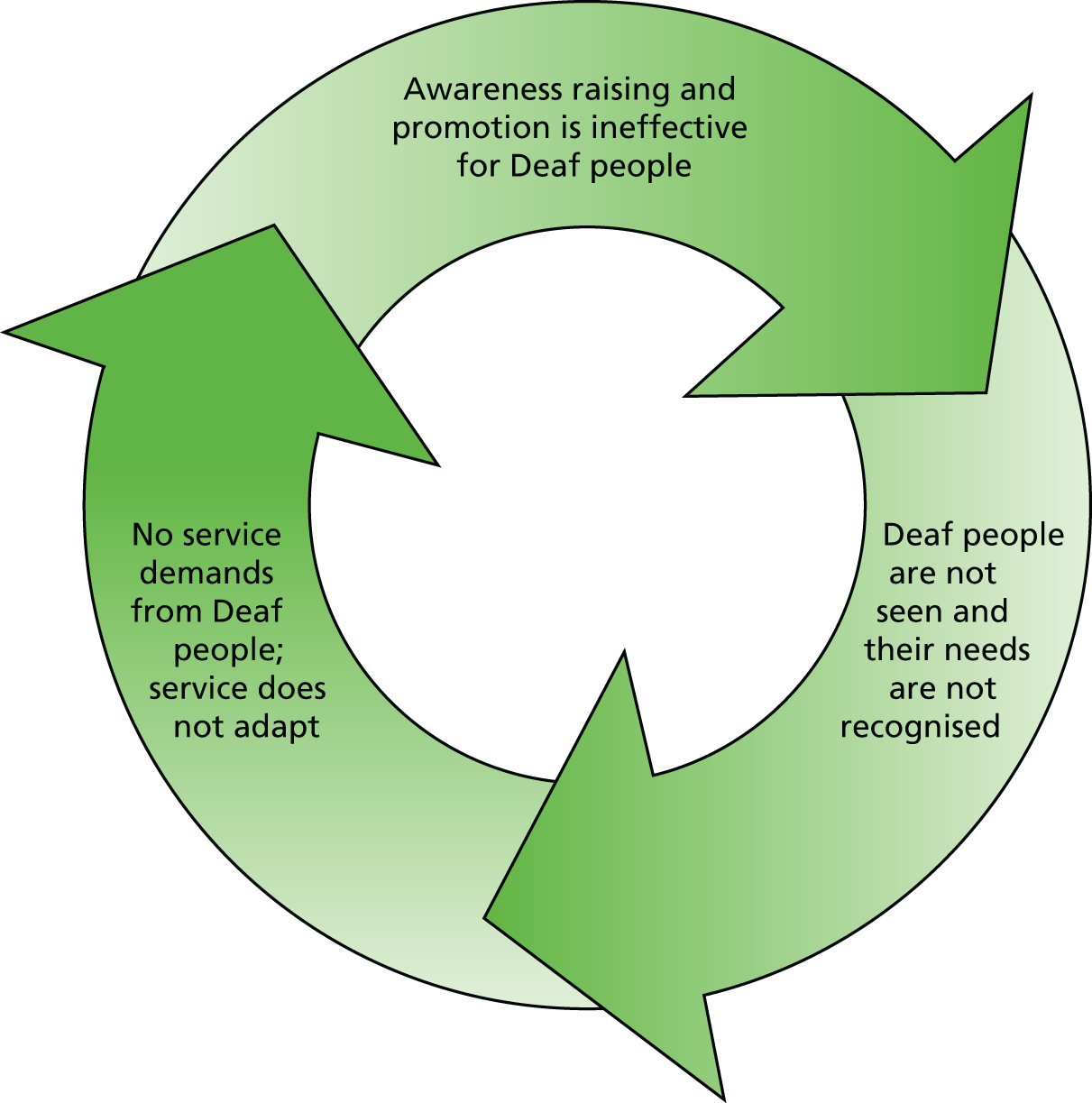
Six practitioners (from four services) participated in detailed interviews and described a specialist treatment pathway within a standard IAPT structure and the associated awareness-raising and information concerns. They were very aware of the difficulties associated with service promotion and information, discussed previously, which could pose barriers to Deaf people being aware of and accessing a local IAPT service. Three of the standard IAPT services from which participants were drawn had a specialist practitioner available and reported that she/he also had a remit to raise awareness and promote the service to Deaf communities in their area. However, as this usually fell to one individual, the activity was fragile and at greater risk of being reduced or lost due to internal and external pressures (e.g. worker diverted to other service priorities; choosing to undertake study, thereby reducing hours; maternity/sick leave; promotion or relocation). One respondent reported a high proportion of self-referrals, which they attributed to Deaf people locally being aware of their specialist provision. Another described in detail the fact that they deliberately target Deaf people through community-relevant means, thus creating a ‘word of hand’. Examples included posting information on online sites in BSL that Deaf people access; sharing information with local Deaf charities or sensory services; attending in person Deaf community interest groups to talk about the service; establishing well-being groups locally within the Deaf community run by the therapist; and linking up with local ‘Deaf Health Champions’, a time-limited initiative in some regions to campaign for better access to health information and raise Deaf people’s awareness of health issues. 117 These examples demonstrate that it is possible for standard IAPT provision successfully to reach Deaf people’s awareness and influence their knowledge given enough cultural competence and understanding of the Deaf community.
Pathways of self-referral to Improving Access to Psychological Therapies
The survey asked respondents to consider how common it was for Deaf people to self-refer; one respondent said that their service did not accept self-referrals, but 66 out of the 107 who replied (62%) said they did not know, five that it had never happened and a further five that it happened on only one occasion. Self-referral therefore was not usual. Nonetheless, respondents were asked to consider how easy it might be for Deaf clients to self-refer into their service. The results presented in Figure 16 are differentiated by those who had personal experience of having delivered a service to at least one Deaf person and those who had no personal experience.
FIGURE 16.
Assumed ease of self-referral. How easy is it for Deaf people to self-refer?
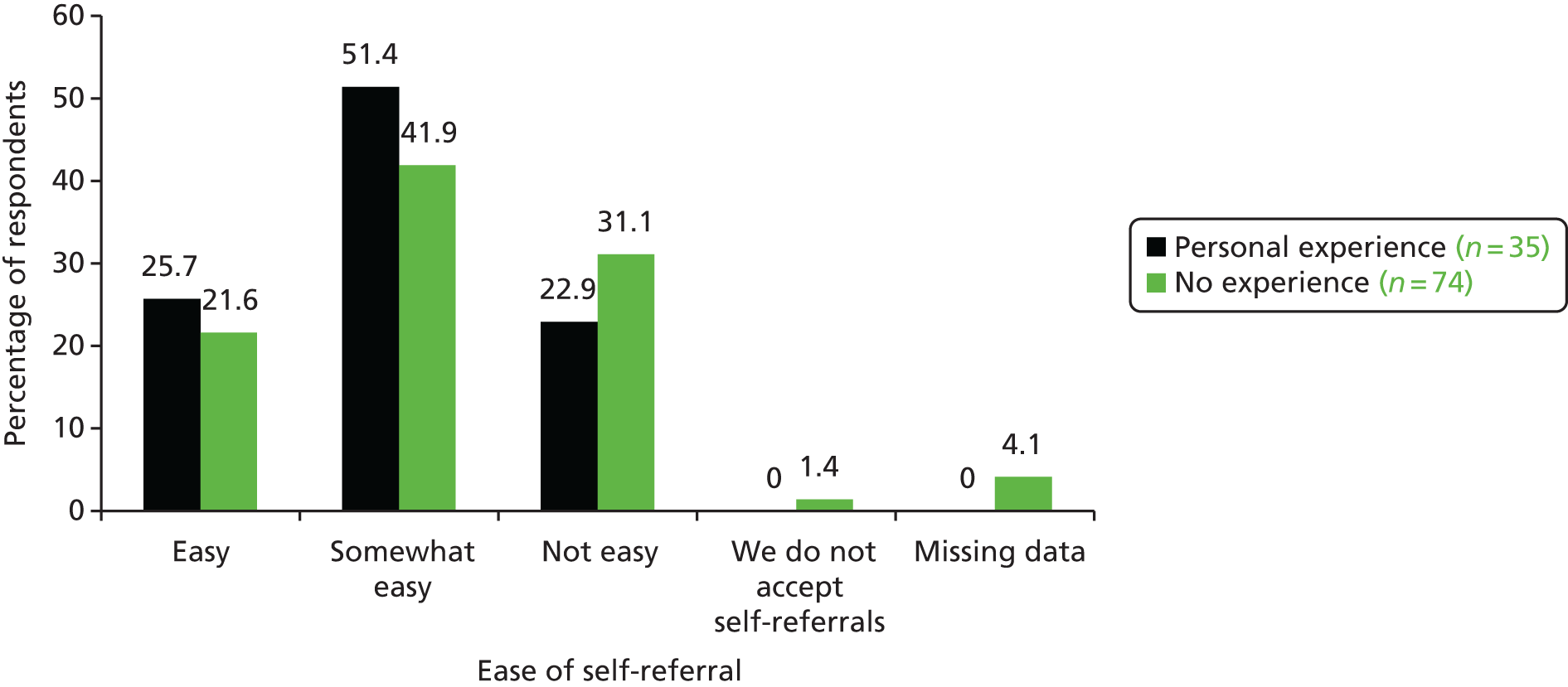
Overall, the picture is optimistic about ease of self-referral; however, analysis of the interview data reveals some complex, hidden or unacknowledged considerations that might mean that in reality the picture is less positive. In some instances, it was not appreciated how apparently inclusive practices might nonetheless create barriers for Deaf people. In others, the adjustments offered or made to usual practices had indirect consequences that were undesirable. Both perspectives could result in insufficient change to promote equality of access, in this case with respect to self-referral. To illustrate these issues we draw out some of the most common myths and assumptions, multiple examples of which were provided in the individual interviews and through the survey, and set them in the context of their potential effects for a Deaf client.
Changing the medium of contact does not necessarily make contact accessible
The survey asked respondents about how Deaf people would contact their service if they wished to self-refer and also how the service would respond. The picture is clearly one of written contact, whether by text, e-mail or letter rather than in BSL or through the medium of an interpreter (Table 24). This is highly problematic, given the low levels of literacy among Deaf people previously discussed (see Chapter 1). In addition, from a language rights perspective, it does not involve any adjustment to meet the language requirements of a potential client at the point of first contact. It is akin to a user of a spoken language other than English (e.g. Gujarati) being required to make initial contact and be responded to in English only. The potential barriers that this might create are more apparent for spoken language users. However, for Deaf users of a signed language, it is a common assumption that, by changing the medium (written rather than spoken), one can make contact accessible because it does not rely on hearing. The deafness rather than the language use is recognised and predominates.
| Survey question | ‘Yes’ response | n (%) |
|---|---|---|
| A Deaf BSL user would make a self-referral to your service via: | We do not accept self-referrals | 1 (0.8) |
| By SMS/text message | 13 (11) | |
| By NGT service (Text Relay, TextDirect or Typetalk) | 8 (6.8) | |
| By letter | 70 (59.3) | |
| Online (e.g. e-mail, message through webpage) | 83 (70.3) | |
| By video call [e.g. Skype, FaceTime (Apple Inc., Cupertino, CA, USA), Glide (www.glide.me)] | 2 (1.7) | |
| A self-referral from a Deaf BSL user would be responded to via: | We do not accept self-referrals | 1 (0.8) |
| By SMS/text message | 28 (23.7) | |
| By NGT service (Text Relay, TextDirect or Typetalk) | 7 (5.9) | |
| By letter | 89 (75.4) | |
| Online (e.g. e-mail, message through webpage) | 67 (56.8) | |
| By video call (e.g. Skype, FaceTime, Glide) | 2 (1.7) |
These issues were elaborated further in the interview data. Several services had means of initial contact and self-referral that were online via an electronic referral form, or by direct e-mail, or by letter. In some cases, online contact and online forms were the only means of initial contact or self-referral. This initial contact could include requesting clients to complete initial assessments online such as the PHQ-9 and GAD-7 in English as a form of triage. Some services viewed this standard online accessibility as helpful for Deaf clients because it does not require the use of a telephone and does not rely on spoken language. The possibility that standard assessments in English as a form of triage for service access might be unreliable for Deaf people was not considered because of lack of awareness that it was, in effect, a test of Deaf people’s literacy rather than a reliable psychological screening instrument for clients whose first language is not English. First contact in written English might also pose a psychological or emotional barrier for Deaf people, many of whom have school experiences of being taught in a language other than a signed language and for whom completing forms in a written language that is not their own evokes distressing memories. Changing the medium of contact to avoid sound and hearing does not necessarily address the issue of language preference and access.
Reasonable adjustments may not be that reasonable
Some services were aware of text telephones, text relay and next-generation text services118 and advertised that they could be contacted this way. However, this advertised adjustment assumed that Deaf people have text telephones or are happy to use TextDirect. This is not the case for some Deaf people, who prefer not to use English-based communication. For this adjustment to contact to work, it also requires that those within the service know what a call via text telephone is or to be experienced with text relay and able to use it. A workable system requires adjustment by both parties, and this was not always true for service providers, even those who promoted this form of access.
In contrast, in one service that provided a specialist pathway for Deaf people, the introduction of a short message service (SMS) self-referral process had proved very successful, but the key was the agile responsiveness of the service itself to that initial contact to progress a referral forward. This, in turn, increased clients’ confidence that the service understood their needs and would meet them. Text-based contact, however, still relies on a degree of literacy in English, although it has become a culturally acceptable form of quick contact among Deaf BSL users for convenience.
Universal gateways do not have universal effects
Where initial contact and self-referral was either exclusively by telephone or via online completion of forms, the onus lay with the potential client to find a means of accessing the universal gateway offered by the service. One service pointed out that it did not discriminate or change its practices according to the client group, but applied universal standards. It did not consider that these common standards might have differential effects for different clients. In the case of Deaf clients, the main problem lies in the lack of autonomy in contacting a service that this might pose. For example, to access by telephone would require an interpreter or even a family member or friend to make the call or interpret the conversation on their behalf. Some practitioners suggested this as a logical solution to not being able to use a telephone, and said their services would be happy to accept referrals in this way. Others explained that they would not accept such a referral because it was not the client themselves who was giving the information but a third party; this was particularly the case when the client was required to opt in to therapy (regardless of the fact that client may not be able to use the telephone anyway). One respondent described it might be problematic by saying, ‘we have to have explicit permission, and that could be a bit difficult if somebody’s language was completely absent’. In another example, a paper-based form was available only on request by telephone; therefore, even if the Deaf client could independently complete the self-referral form they would need to involve a third party in order to request that form in the first place.
Completion of a form that is in English could again mean that a client had to work with a translator/interpreter or a friend or family member to assist them. Given the probable nature of the self-referrals involved, all of these options that might require third party involvement disallow autonomous action by the individual, may involve a lack of confidentiality (if a qualified interpreter bound by their code of ethics is not used) or just be too sensitive or distressing for the Deaf person to contemplate. This imposed lack of autonomy, given the conditions of access available, could itself pose an additional barrier, albeit indirectly, to self-referral.
The barriers to self-referral are summarised in Figure 17.
FIGURE 17.
Summary of barriers to self-referral despite assumptions of adjustments having been made.
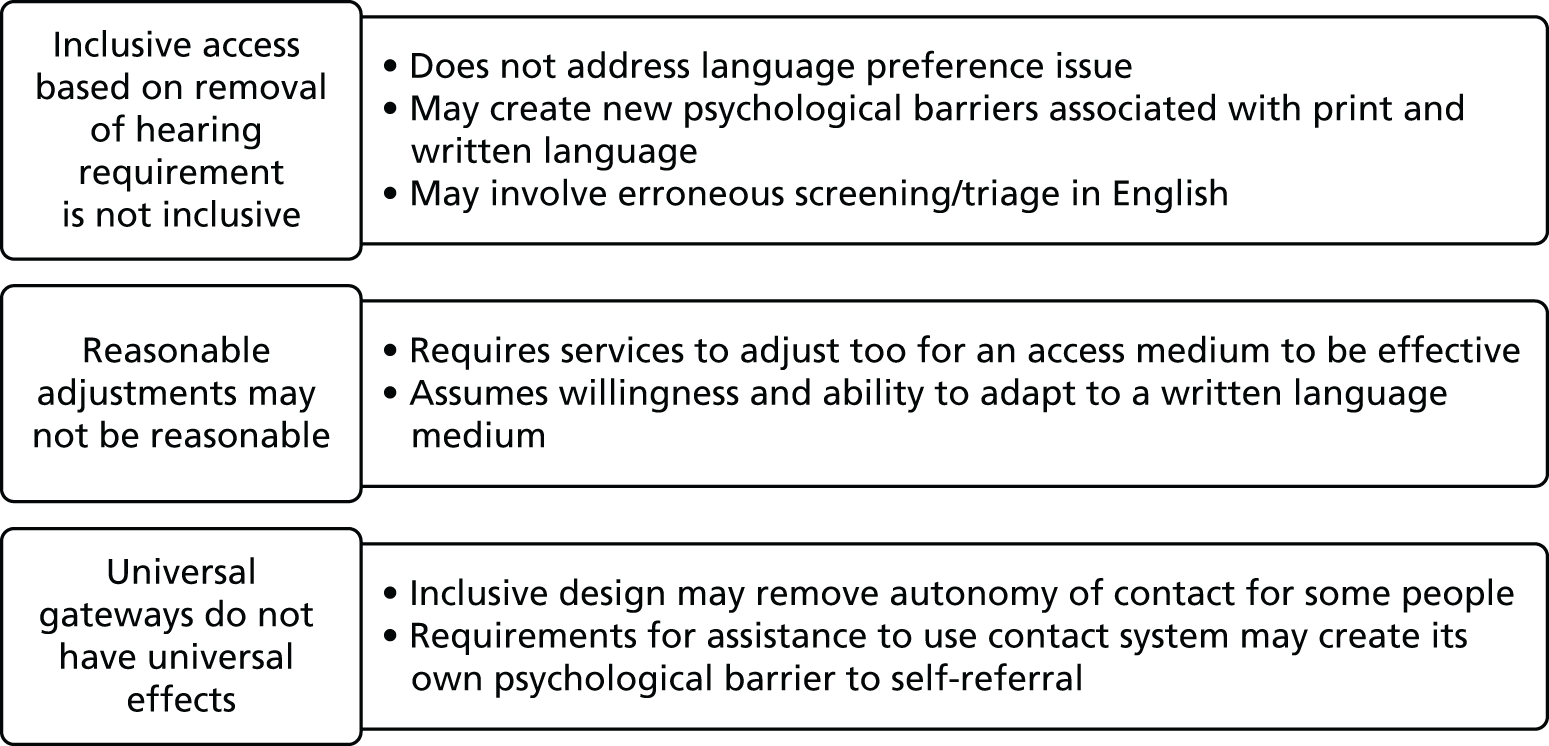
Referral via a general practitioner or other professional
Although IAPT services permit and in some instances actively promote self-referral, it is also common for GPs or other health or social care professionals to make referrals. Although the standard IAPT services with a specialist pathway appreciated the potential difficulties that this could pose for Deaf clients, the majority of services had not considered before that there might be additional barriers created in comparison with hearing people’s access via GP/professional referral routes.
A key problem is Deaf people’s engagement with health and social care services in the first place. When this is ineffective, the potential pathway to referral to IAPT via this route is also ineffective. Previous research in the UK has demonstrated that Deaf people wait longer than average before going to see their GP, meaning that a condition might have escalated before treatment is sought. 52 Primary care services do not consistently meet Deaf people’s communication and language requirements for a consultation, and, therefore, subsequent treatment is often not optimally effective. 119 Confidence that communication with a GP will be smooth and that the professional understands the influence of linguistic and cultural identity on a Deaf person’s presentation of symptoms and engagement with treatment is crucial. 120 The new NHS England Accessible Information Standard: Specification51 and the draft Principles for High Quality Interpreting and Translation Services in Primary Care121 are both designed to address these concerns and raise standards of care for Deaf people (as well as other language-using groups). However, the effectiveness of this guidance remains untested.
Additionally, primary care referral routes via GPs are constrained by the local arrangements for funding and service provision. In the majority of cases referral to standard IAPT services is the usual response with few standard IAPT services having special arrangements in place for Deaf people. In a minority of cases there is a block commissioning arrangement in place for Deaf people to be referred to a specialist IAPT provider. Where this is not the case, and the standard IAPT service is not considered appropriate for a Deaf client, then an IFR could be made through the GP, but this is dependent on the GP recognising that the standard service available does not meet a client’s needs. It also takes time and competes for priority in comparison with other demands on available funds.
Consequently, primary care referral routes into IAPT may:
-
not be effective for Deaf people who do not use them to access help in the first place
-
fail to meet Deaf people’s linguistic requirements during consultation
-
not be aware of Deaf people’s specialist needs in terms of psychological support and treatment
-
not be aware that specialist IAPT services for Deaf people are available
-
take additional time in cases where an IFR is made and block commissioning arrangements are not in place.
These influences are summarised in Figure 18.
FIGURE 18.
Influences on referral into IAPT via GP.
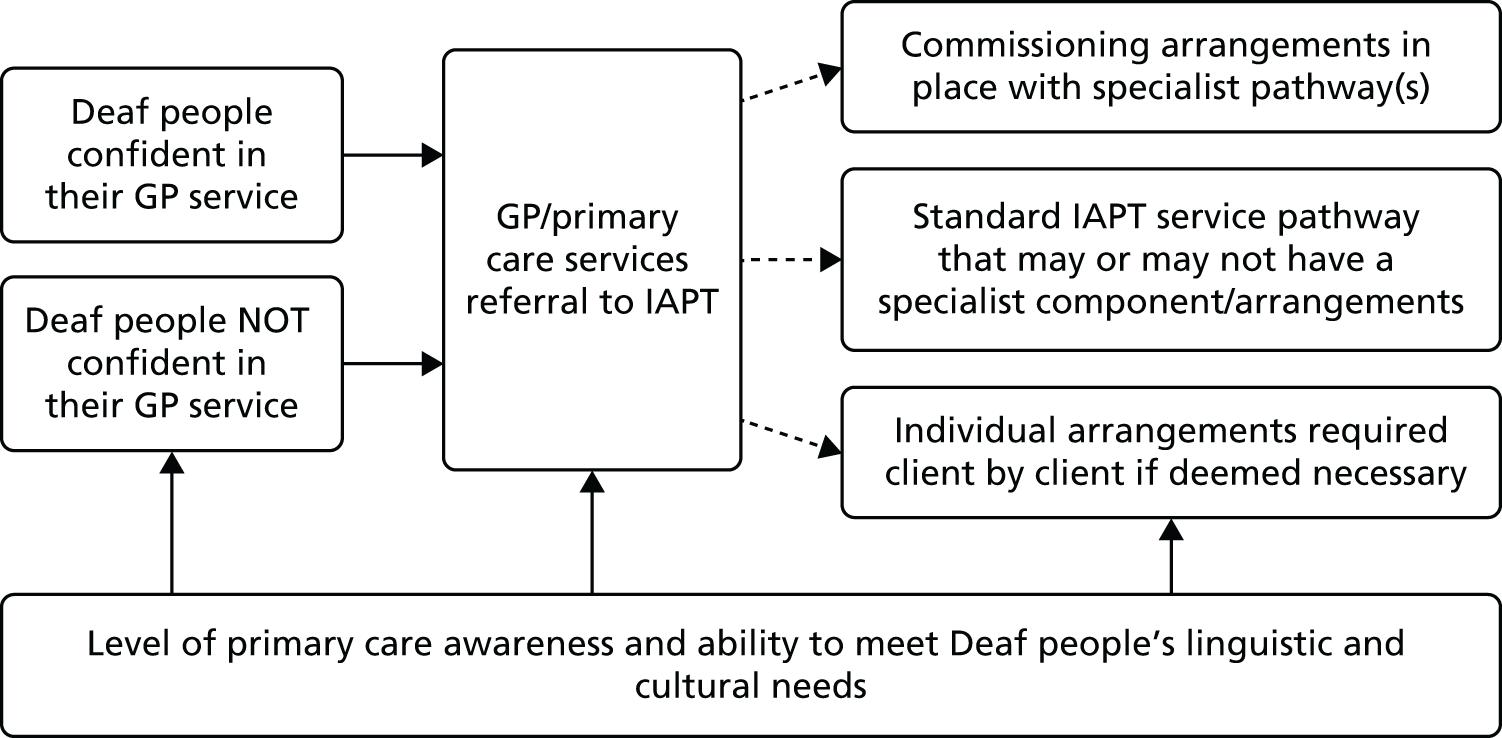
The therapeutic encounter
Within standard IAPT, a Deaf client may be allocated to a Deaf therapist, a hearing therapist who is a fluent sign language user, a therapist who might know a little bit of sign language and/or have met a Deaf patient before, or a therapist who has never encountered a Deaf person and has no fluency in sign language at all. Given this diversity, participants identified a number of key issues that may require consideration when working with Deaf people within IAPT. There was varied awareness of their implications or potential significance among practitioners, largely dependent on whether or not the service or individual therapists had experience of working with Deaf clients. Where this experience and specialist knowledge was lacking, these issues tended not to be recognised. However, even if these factors were understood, constraints on service delivery associated with time and cost could militate against their significance being taken into consideration in the course of service delivery.
Deaf clients may not be used to therapeutic practice
For the standard IAPT services that had a specialist practitioner within them (usually a Deaf or hearing fluent signer), it was commented that, in the practitioner’s experience, many Deaf people were unaware of and unused to what a therapeutic relationship entailed. They therefore generally allocated an additional introductory session to cover such issues as boundaries, confidentiality and expectations of communication in therapy. Some also delivered information sessions within community settings to raise general awareness of therapy, mental health and well-being. These actions were especially important when the therapist was part of the cultural Deaf community themselves and, therefore, the client might encounter them in other roles and contexts. It was seen as a vital part of trust building, transparency and also empowerment for the client, who could, armed with new knowledge, seek a different route to support if they wished. This good practice was, however, very rare and services unused to Deaf people or without a specialist practitioner did not comment on the provision of such requirements.
Therapists may not be used to Deaf people
A Deaf client may be a therapist’s first encounter with a culturally Deaf person, with sign language or with a sign language interpreter. Consequently, there is also much for the therapist to adjust to in this therapeutic relationship. Some commented on how the Deaf client had educated them and made them more aware, which they valued. However, the implications for the Deaf person of having to do this, which is a common life experience for Deaf people in many contexts, were not always considered. For example, could this experience of always having to explain oneself and educate the hearing world to Deaf cultural norms actually have been a factor in some Deaf people’s experience of anxiety or depression? If so, a therapeutic relationship that also involved this dynamic may have been unhelpful, a view we return to later when considering models of BSL-IAPT.
More time is needed
Some therapists who used an interpreter always allocated additional time for the session in recognition of the fact that communication was indirect and could take longer than direct communication. However, explicit permission was usually required from a senior clinician and it might be withheld for resource reasons (time, client load, cost in interpreter payments or therapist time). The decision to request additional time for clients was not entirely a therapeutic one, with some therapists reluctant to request it because of how particular services operated or what they anticipated would be a negative response. Other participants in the study did not recognise that additional time might be an issue at all. Our analysis of average duration of therapy for Deaf clients using standard IAPT services demonstrates the longer time required in therapy, an analysis of which the respondents were unaware at the time of the interview (see Chapter 4). Some participants did indeed comment on the longer time that might be required for Deaf client within their service in comparison with a hearing client. They felt that this might be because the Deaf person came to the service at a later stage in the progression of their problems in comparison with the average hearing client. However, those making this observation did not always appreciate the barriers to self-referral or referral through primary care.
Using interpreters
The survey asked respondents to consider ease of booking a sign language interpreter for sessions with clients. The majority of those with prior personal experience of working with a Deaf client and those without thought it easy or quite easy to book an interpreter. However, those without personal experience were more likely to see it as difficult and a third without personal experience simply did not know (Figure 19).
FIGURE 19.
Views on ease of booking a BSL/English interpreter.

Some participants in the interviews who had personal experience of delivering therapy to a Deaf client through an interpreter had no prior experience of delivering therapy through an interpreter (whether spoken or signed language interpreter) and had received no training or support to do so. Others who were experienced in working with spoken language interpreters did not necessarily consider that there might be any differences in working with a sign language interpreter. These were often those staff who were allocated Deaf clients because of assumed insight into the differences involved in indirect therapeutic communication. Some therapists who were new to using a sign language interpreter had nonetheless also learned some basic BSL themselves such as ‘hello’, ‘how are you’ and ‘thank you’, as they felt it built trust with the Deaf client.
We also came across examples of it being decided that an interpreter was not necessary, but it was unclear on what basis such a decision had been reached and whether or not the therapist and client were able to adequately communicate with each other in reaching that decision. Examples included using spoken language on the assumption that the Deaf client had lip-reading skills, and writing things down on paper during therapy to enable dialogue. In the survey data, of the 35 therapists who responded and said they had personal experience of providing therapy to a Deaf client who was a BSL user, eight had done so on the basis of the client lip-reading the therapist and four on the basis of using pen and paper within one-to-one sessions. However, the ability of a therapist who was unused to communicating with Deaf people to monitor the quality and effectiveness of such communication has to be questioned. These questions remain valid even when a client may deliberately seek a therapist with no connection with the Deaf community and/or deliberately choose not have an interpreter because of their concerns about confidentiality or trust within their own cultural community.
In those standard IAPT services that included a specialist pathway for Deaf people but whose specialist practitioner was not a fluent signer, there was a strong awareness that was it was important not only to book an interpreter but also that the choice of interpreter was often important. It was important in terms of trust, particularly with respect to confidentiality and when there might be conflict of interest if the interpreter worked with the Deaf person in a different role in their life. Preference was also important to the Deaf person in terms of confidence that the interpreter would represent them well in the therapeutic encounter. Consistency of interpreter was also highly valued (e.g. the same interpreter being booked for each of the sessions). However, therapists also reflected that these ideal conditions might not always be met because of practical issues of timing and booking.
The survey asked respondents to consider the likelihood of using the same sign language interpreter throughout the course of the sessions with the same client. Only 60% of those with personal experience of delivering therapy to a Deaf person said that this always occurred despite best intentions to do so, indicating that it was problematic even when recognised as important (Figure 20).
FIGURE 20.
Likelihood of the use of the same sign language interpreter throughout the course of the sessions.
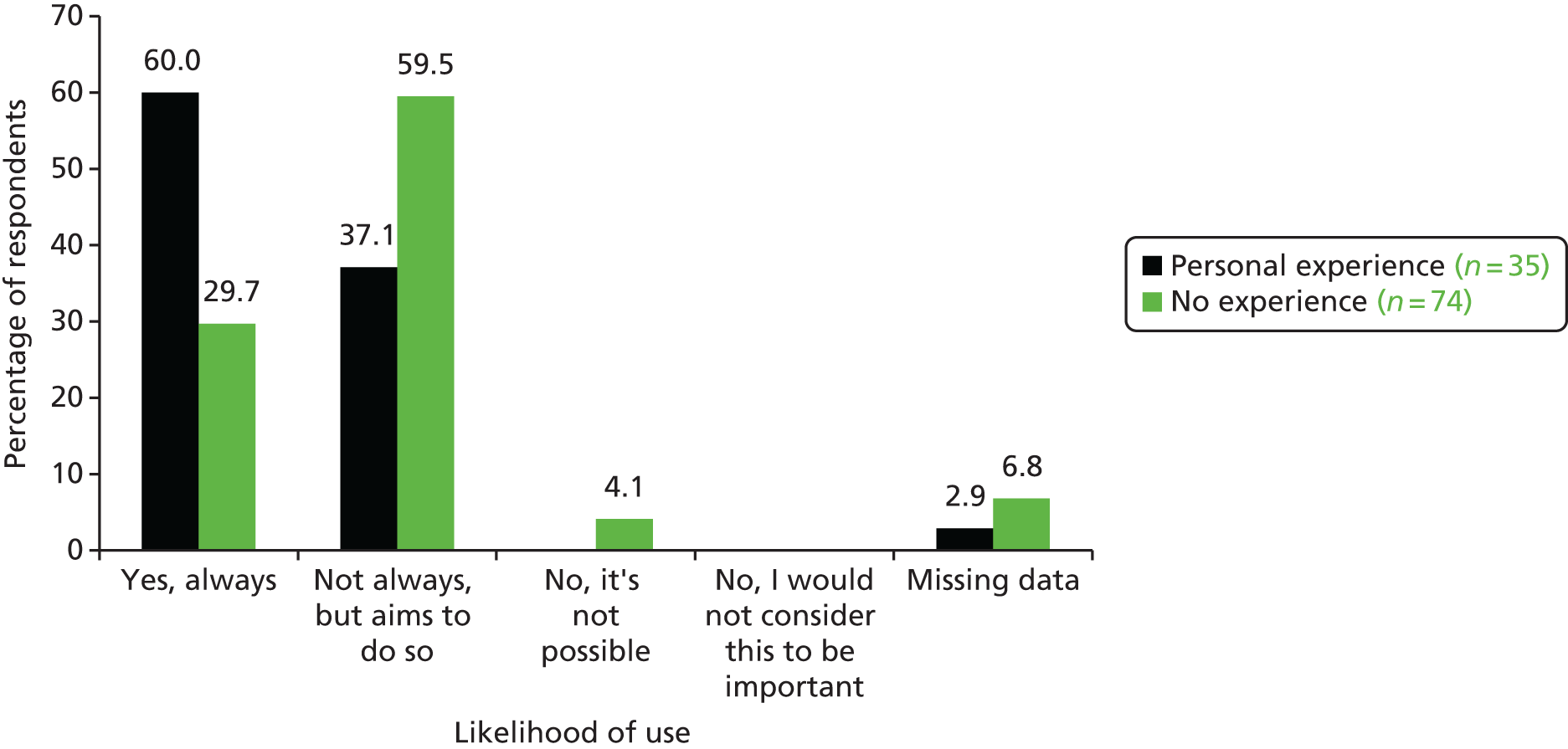
From the interview data it was clear that when the therapist or the service was less Deaf aware, the identity of interpreter, client choice and consistency were not thought about and/or not given priority.
It is also the case that therapists had encountered some Deaf people who were unused to using interpreters and were not sure how best to work with them within a therapeutic encounter. This was especially problematic if the therapist too was inexperienced in working with sign language interpreters. Finally, there were examples of the Deaf client teaching the therapist how to use an interpreter, best practice and how best to facilitate the indirect interpreted encounter. This is added pressure on clients, who are seeking a service from a professional and should not be expected to have to educate that professional in order to receive the service. Given that many clients who use IAPT are experiencing anxiety, this additional role could also be unhelpful in building trust with their therapist.
Assessment, monitoring and outcome measures
The survey asked respondents about their confidence in identifying mental health problems among Deaf people and identifying when Deaf people might have problems in managing their anxiety or depression (Figures 21 and 22). Those with personal experience of having delivered therapy to a Deaf person (even if it were only one Deaf person), expressed greater confidence with respect to both questions, but only 40% were very confident/quite confident about identifying mental health problems and only 37.1% were very confident/quite confident of spotting difficulties in coping. Among the group with no personal experience, the degree of confidence overall was much less. These figures suggest that there are training needs for therapists in standard IAPT about how mental health problems such as depression and or anxiety might be manifest in BSL users, regardless of whether or not the therapist has any prior personal experience of working with a Deaf client.
FIGURE 21.
Confidence in identifying mental health problems in Deaf BSL users.
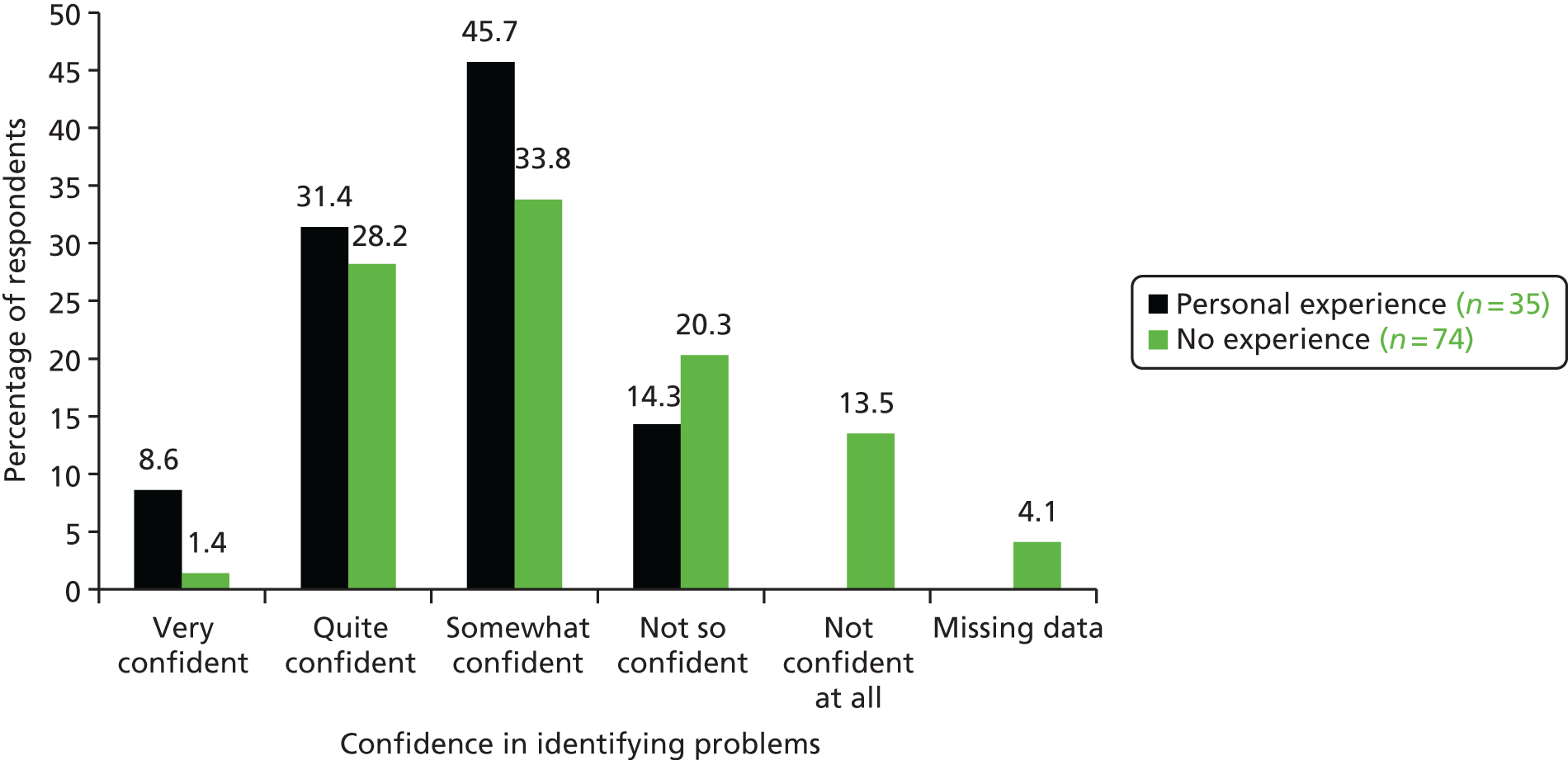
FIGURE 22.
Confidence in identifying Deaf BSL users’ difficulties with coping with depression and/or anxiety.
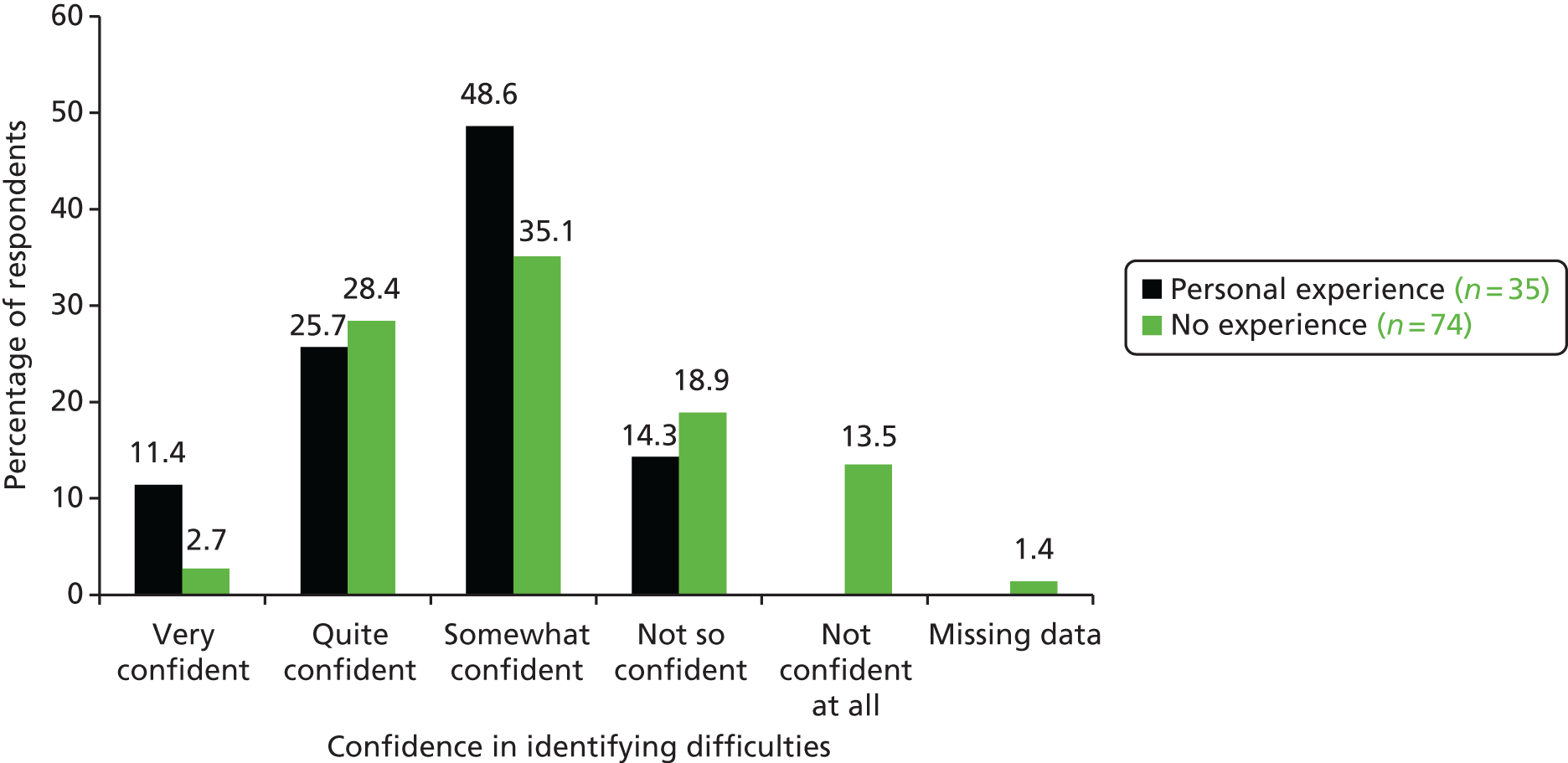
The survey asked respondents about how they have used or would use the IAPT standard assessments (GAD-7, PHQ-9, WSAS) with Deaf people who used BSL (Figure 23). Although some had sought to ensure that the assessments were carried out in BSL rather than in English, only a minority had used the reliability tested BSL versions, rather than ad hoc interpretation or fixed translated versions, the reliability of which was untested. Most said they had used or would use the English version with a Deaf person who was a BSL user, either in written, online or spoken form. This approach ignores the common difficulties most Deaf people have with literacy in English and assumes a high level of lip-reading and/or auditory skills. This is despite the fact that over half of lip-reading skills are attributable to guesswork through experience122 and the highly heterogeneous nature of speech recognition ability among Deaf people.
FIGURE 23.
The use of PHQ-9, GAD-7 or WSAS with Deaf BSL users.
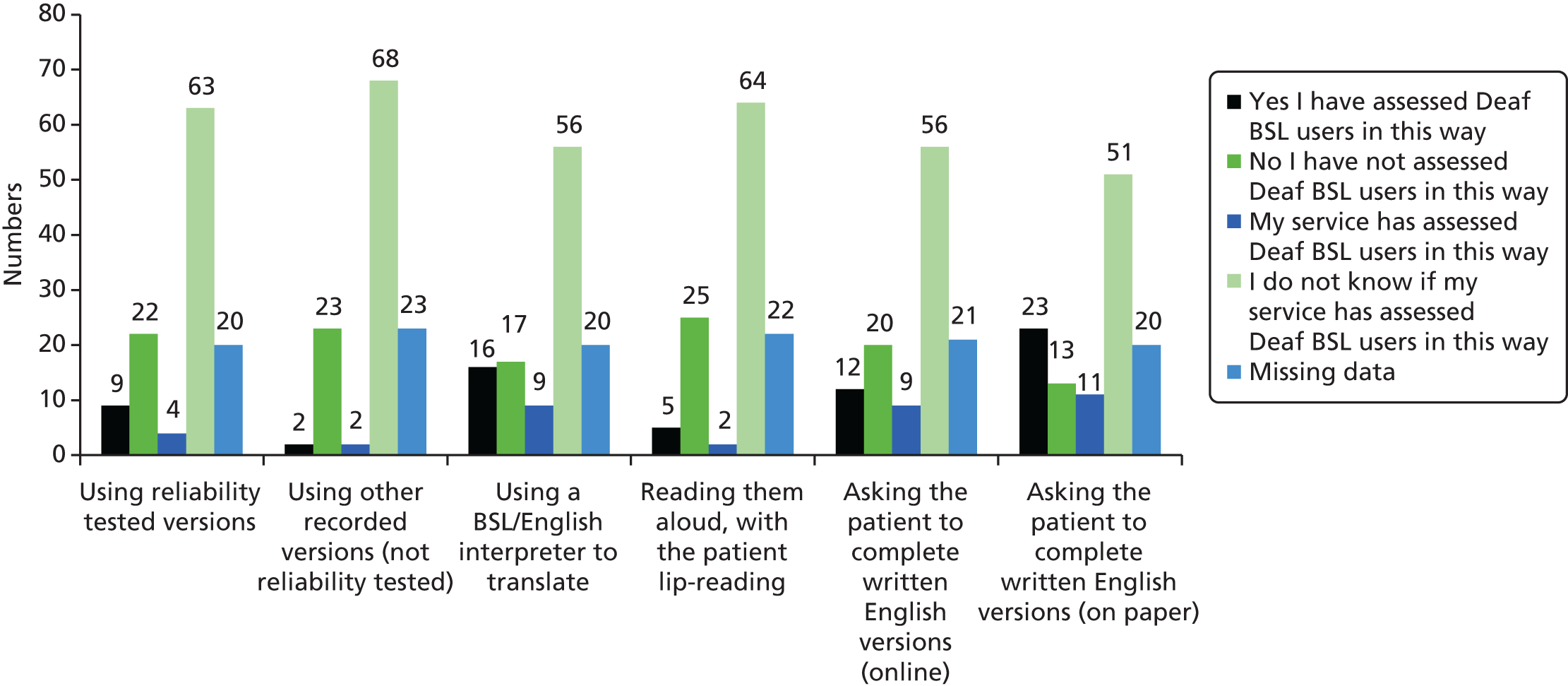
In our interview sample, only one participant used the BSL versions of the IAPT assessment and monitoring tools (GAD-7 BSL, PHQ-9 BSL and WSAS BSL). There was very low awareness that these even existed, but two interviewees who participated in this study subsequently requested copies of them. Several services used the paper versions in English of the standard tools with an interpreter translating them ‘live’ to the client. However, there was no way to know if they were being interpreted in the same way each time, particularly if interpreters varied between sessions. In addition, the validity of the interpretation could not be assured as, unlike in the validated versions, the interpreter may not have the knowledge of the original intent in the English version to produce the most accurate translation. Therapists varied in how comfortable they were with this practice. Some who did not have experience of working with a Deaf client had not considered the implications of using a ‘live’ interpreted assessment each time.
The English versions of the assessment tools were also being used without interpreters for Deaf people on the false assumption that a Deaf person did not require hearing to understand the written word and, therefore, that they were accessible. Only a small minority of participants were aware that standard assessments would need to be not only correctly translated/validated, but also normed against specific populations to establish the correct clinical cut-off points for their use in their translated versions. Assessment and monitoring practices, therefore, which are associated with patient recovery in the case of Deaf people, were highly variable, raising questions about their accuracy even within accepted margins of error for the use of such measures.
Services with a specialist pathway for Deaf clients did attempt to seek feedback from Deaf clients in order to improve their services. In the vast majority of cases there were no arrangements to ensure that standard means of feedback from clients for service improvement would be Deaf-accessible.
The various axes of variability identified in the therapeutic encounter are summarised in Figure 24.
FIGURE 24.
Axes of variability in the therapeutic encounter.
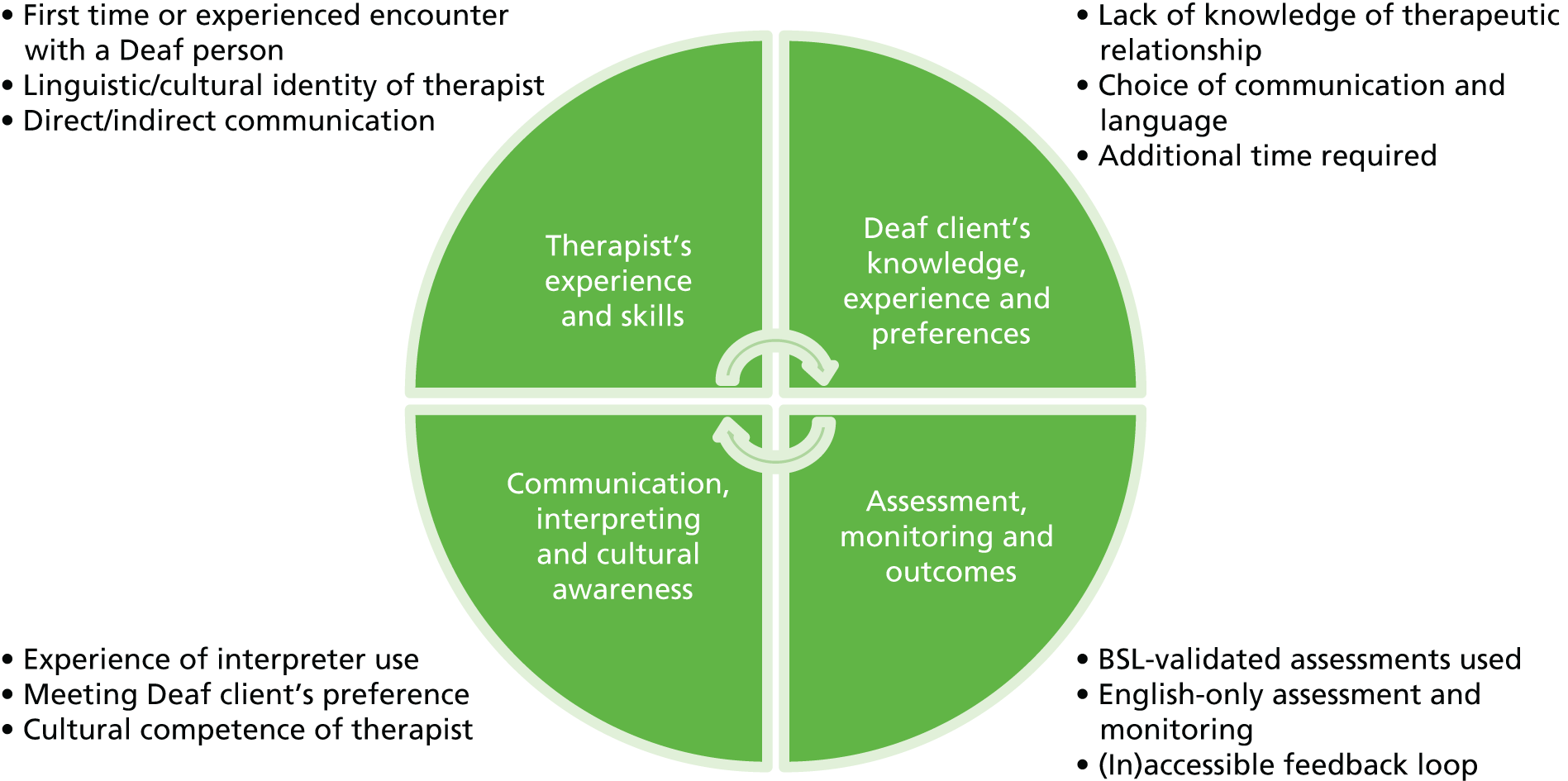
Results: interviews with BSL-IAPT practitioners
Participants
In exploring the parameters and characteristics of a BSL-IAPT service, we draw exclusively on interviews with personnel from the single originating service provider (BSL Healthy Minds). Of the 14 potential participants, 12 agreed to be interviewed. Seven were Deaf staff who declared either that they grew up using BSL as native first language or that they use BSL as their main and preferred language. The five hearing people interviewed also all signed; the two with advanced qualifications in BSL had managerial and lead roles in the delivery of the service. Of the seven Deaf staff interviewed, six were clinical practitioners or senior practitioners and only one hearing staff member interviewed worked in a direct clinical role with Deaf clients. Of the 12 interviewees, 11 had worked for the service for at least 3 years, five of whom had worked for the service for over 4 years.
Small communities of practice
Client choice
From participants’ perspectives, the advantages for a Deaf client of having a Deaf therapist who shared the same language and culture were unquestionable, yet there was recognition too of some disadvantages that arose from the small and interconnected nature of the Deaf community. It was not unusual for a client to know the therapist, for example through shared school experiences, volunteer and committee work within the Deaf community, or more remotely as a well-known figure in the local/regional/national Deaf community. Although such experiences of multiple roles and knowledge of an individual in a variety of contexts is very common in the Deaf community, as it is in many other small communities of practice,123–125 for some clients it was a barrier to engagement in therapy and an alternative therapist might be requested. From BSL-IAPT’s perspective, the fact that they had a pool of Deaf therapists on which to draw to meet a client’s request for an alternative therapist was a key strength of their service model. Participants pointed out that, by contrast, in standard IAPT services where a single Deaf person may be employed, they were usually the only choice available for a Deaf client.
However, this strength of multiple therapists being available had its limitations. For example, currently there is only one person in the BSL-IAPT service who is able to deliver step 4 intervention and only one clinical psychologist within the service. There may not always be capacity within the team to transfer a client to a different therapist because of the workload overall, or because of the geographical location of the client. In rare cases, a client requesting a different Deaf therapist has had to be referred instead to a standard IAPT service because their request could not be met. In addition, step 3 BSL-IAPT therapists are not available in all localities where the service operates.
Therapist/client boundaries
For Deaf therapists, the consequences of a small and strongly interconnected Deaf community could be a challenge also. This was not just because meeting a client outside therapy might be a common occurrence. It was also because many clients had little experience of a therapeutic relationship or therapist/client boundaries because access to mental health services has been limited in the past for Deaf people, and the use of mental health provision in primary care remains uncommon in the Deaf community. Consequently, BSL-IAPT has innovated a number of professional practices designed to offset this lack of experience and prevent difficulties with boundary crossing between therapist and client outside of the therapy session.
These include using a contract with the client when they first enter therapy so they understand not just the structure of the therapy but also the expectations of them and their engagement. This involves explanation and agreement about not contacting the therapist outside sessions unless this is planned (e.g. to support guided self-help) and, conversely, that a therapist will not necessarily acknowledge that they know a client when they meet in a different role/context unless that has been agreed as acceptable. Moreover, therapists are not permitted to add a client to their Facebook page as a ‘friend’. Deaf people utilise Facebook and social media a great deal to facilitate many social activities given the inaccessibility of the telephone and the limited communication of SMS by contrast. Therefore, this restriction is substantial.
Participants also pointed out culturally normative aspects of rapport between Deaf people that could be a challenge in establishing and maintaining appropriate therapeutic boundaries. For example, it is quite usual for Deaf people to establish rapport with each other by seeking information to position the other person within the Deaf historical, familial and social landscape, a phenomenon well recorded previously. 59,126 Therefore, it was not seen as unusual or intrusive for a Deaf client to ask a therapist about their background, education, family, and so forth. However, this contravened more usual therapeutic practices of therapist distance. Therefore, working out how to respect cultural expectations yet maintain appropriate detachment was identified by participants as particularly challenging.
Pathways into the service
Awareness raising
BSL-IAPT has placed a high priority on awareness-raising events in the Deaf community. These are not just restricted to disseminating knowledge about the service, they are more fundamentally focused on raising awareness of what depression and anxiety mean and their consequences, and combating stigma about mental ill health. This task is seen as an ongoing challenge despite nearly 5 years of operation so far. As one participant said, ‘currently it is not so much that the Deaf community is buying into the service but that the service is buying into the Deaf community’. From their perspective, this balance needs to be reversed if awareness raising is to be considered to have truly succeeded.
Self-referral
From BSL-IAPT’s perspective, self-referral is predicated on flexible and appropriate communication that poses no barriers to Deaf people, but also permits the exercise of choice in how a potential client might want to contact the service. This includes contact by text and e-mail but additionally those in the service receiving these messages are aware of what might be typical in Deaf people’s use of English and equipped with skills in plain English in knowing how to respond. Contact in BSL is also possible via Skype and other platforms and messages can be posted to the service in BSL on a secure Facebook page. The service seeks to remove as many hurdles as possible in making initial contact.
However, as many participants explained, some structural conditions outside the control of BSL-IAPT can hinder this no-barriers approach. Some areas in which BSL-IAPT delivers a service do not permit clients to self-refer. In addition, many potential clients are referred via their GP. Participants who discussed this felt that for some Deaf people this places an additional barrier in their way. For example, they may be put off going to their GP in the first place because of concerns about how they would communicate with their GP (e.g. whether or not an interpreter be available), or a lack of confidence that their GP would be aware of Deaf people’s needs. These concerns are consistent with previous research28,29,52 and participants pointed out how much worse they were likely to be if someone were experiencing anxiety or depression.
An additional barrier to acting on self-referrals was funding arrangements. In those cases in which a block-commissioning contract from the CCG did not exist, the alternative was to make an application via an IFR, but that has to come from the GP practice. Although participants with financial and managerial responsibility pointed out that BSL-IAPT will work with a GP practice on behalf of a client who has self-referred to achieve this end, it can take considerable time to arrange, in their experience between 6 weeks and 1 year.
Responding to referrals
The principal reason for delay in responding to a referral was identified as financial rather than an issue of capacity within the service. In the absence of a block-commissioning contract in the area, in order to provide a service, every referral, whether from a GP or self-referral, required individual financial arrangements to be agreed. In addition, many commissioners were of the view that the higher cost of BSL-IAPT in comparison with the standard IAPT service with the addition of interpreters, was not justified. The time taken to negotiate the funding arrangements where referral to BSL-IAPT was accepted meant that the service regularly fails to meet the IAPT waiting time target set as ‘. . . by March 2016, 75% of people referred to the IAPT programme begin treatment within 6 weeks of referral, and 95% begin treatment within 18 weeks of referral’ (p. 5). 127 There are no reliable data on how many clients, when faced with this waiting time, choose to seek referral to standard IAPT instead, are referred there regardless of personal preference, or whether they are aware that there is an alternative. Data reported in Chapter 4 demonstrate how waiting times for BSL-IAPT substantially increased from the time that the new CCG structure was put in place in April 2013 in comparison with previous service performance.
BSL-IAPT service-specific adaptations
Length of therapy
Participants who commented on length of therapy had the impression that it was common for clients to have more sessions than the IAPT national average. At step 2, they estimated that the usual number of sessions would be 10 and at step 3 it would be 20. These compare with official IAPT data of an average of seven face-to-face sessions at step 2 and 12 face-to-face sessions at step 3. 128 From the data now available about Deaf people accessing standard IAPT services, it is possible to put the figures for BSL-IAPT into a broader context and show that, even though more sessions were needed for Deaf people in BSL-IAPT, it was still far fewer than those reported for Deaf people accessing standard IAPT (see Chapter 4). This comparison was unknown at the time of participants’ engagement with this study.
A number of reasons were offered for the greater number of sessions required for Deaf people in BSL-IAPT. These included more time to explain what therapy is to some clients because of poor levels of prior knowledge and understanding (see Chapter 3 for further discussion of this issue). In addition, the requirement to build up familiarity with concepts and practices used in therapy meant that it could take longer for therapy to be effective. The range of what was offered during the course of therapy was also quite extensive, with some of the guided self-help tasks taking longer because of the degree of support that a client might require to grasp them and complete them.
Use of British Sign Language assessments
Participants described consistent use of the PHQ-9 and GAD-7 in their BSL versions and were enthusiastic and supportive of their use with Deaf people both because they respect an individual’s linguistic identity and because of their utility in therapy. However, participants also discussed how the BSL assessments could be challenging for some clients and in some cases take more time. Some clients had never had any kind of assessment before and could find the concept and practice challenging until they got used to it. For some, a much slower pace was required in viewing each item in the assessments. For some with minimal or low-level BSL skills, the language within them was difficult to understand and required further and repeated explanations. Low-level or minimal language sign language users, referred to in the USA as low-functioning Deaf people,129 commonly have ineffective access to any language (whether spoken, signed or written) in childhood. For such clients, assessments in English are not an option either, as their skills in written/spoken language are even more minimal. In a few cases, participants described how they had to re-sign in a different way the assessment questions before they were understood. One participant reported that at least once it was necessary to conduct a single assessment over two sessions.
Issues of presentation that were an artefact of the technology were also identified as problematic in some cases. For example, each question was presented by a single BSL clip on a single screen. Therefore, it was not possible, as in the English written version, to scan quickly through the questions. Each clip took time to watch and consider. The different degrees of self-assessment response were available as a reminder in BSL, but did not pop up after each question. This could be cognitively challenging for individuals who found it hard to hold them in their head or did not find the English shorthand buttons on screen, to register a response, helpful. Participants described alternative ways in which they recorded client responses, including pen and paper completed by the client autonomously, or the therapist doing this on behalf of the client. Later these responses were transferred to a computerised record, but the technology that would do this automatically and that was linked to the BSL versions of the assessments was not in use in the service.
Additional materials
The BSL-IAPT service had innovated adaptations of a range of IAPT materials so that they were appropriate for Deaf people. For example, 14 self-help guides are now available in BSL with some further changes to support better access and understanding. The guides were also used within face-to-face therapy sessions as a means of engaging with clients, some of whom may struggle to understand the meaning of some basic concepts such as ‘depression’ or ‘anxiety’.
Direct engagement
Direct engagement in BSL without the use of an interpreter was seen as a key advantage of the service. It avoided a layer of complexity introduced by indirect communication through an interpreter. This complexity included a therapist not being able to ‘read’ the body language and non-verbal expressions of a client if the spoken language message through the interpreter was not in sync with the client’s communication because of the time lag inherent in interpreting. It also included the avoidance of misunderstandings that might arise because of the translation choices made in the interpreting process. Participants expressed concern that not all interpreters booked in standard IAPT services would necessarily have mental health experience or be able to understand and appropriately convey a client’s communication if affected by their mental health needs (e.g. appropriately representing slow or hesitant signing in slow and hesitant speech, rather than tidying up the communication for the sake of clarity of semantic content). Some participants reported that they knew of clients who developed more of a therapeutic relationship with the interpreter than with the therapist because they felt a closer bond with an interpreter who could communicate in their language and understood their cultural milieu.
Cultural competence is the other key factor identified by participants as an advantage of direct engagement, over and above communication. Participants argued that the client can feel confident that the therapist understands their culture, the kinds of life experiences they may have gone through with regard to education, employment, family relations and day-to-day discriminations. Therefore, there is no need within a session for a client to have to explain ‘about’ himself/herself, leaving more room for direct work on presenting difficulties. The trust engendered by a client believing that the therapist would understand their life experiences and the issues they face attendant on being Deaf was seen as positive for building rapport, empathy and an effective therapeutic relationship.
Participants also described the advantages of a Deaf therapist being able to normalise mental ill health as something that happens to hearing people as well as Deaf people based on their professional knowledge, which clients recognised as valid. Deaf therapists also acted indirectly as role models for Deaf clients in terms of envisaging potential recovery.
Other value-added features of the BSL-IAPT service delivery structure
Participants drew attention to the benefits deriving from the structure of the service, which supports service quality and therefore indirectly has a positive impact on clients. These were possible only because of the larger numbers of Deaf therapists and hearing people who signed well within a single-service provider. For example, there was a peer group of Deaf therapists who could be drawn on by individual therapists for support and to reduce isolation. Group supervision enabled the sharing of ideas, information and resources as well as best practices in adapting to the range of Deaf client needs. There was a shared understanding of the requirements and challenges of Deaf clients without having to explain these to people who might be linguistically and culturally unaware. Remote supervision in BSL without the requirement of an interpreter was also possible. All of these features were felt to add to the safety of therapists as well as acting as quality assurance mechanisms in the delivery of the service.
Conclusion
The key elements of the BSL-IAPT service and their perceived advantages and limitations can be summarised diagrammatically (Figure 25).
FIGURE 25.
Perceived advantages and limitations of the BSL-IAPT service.
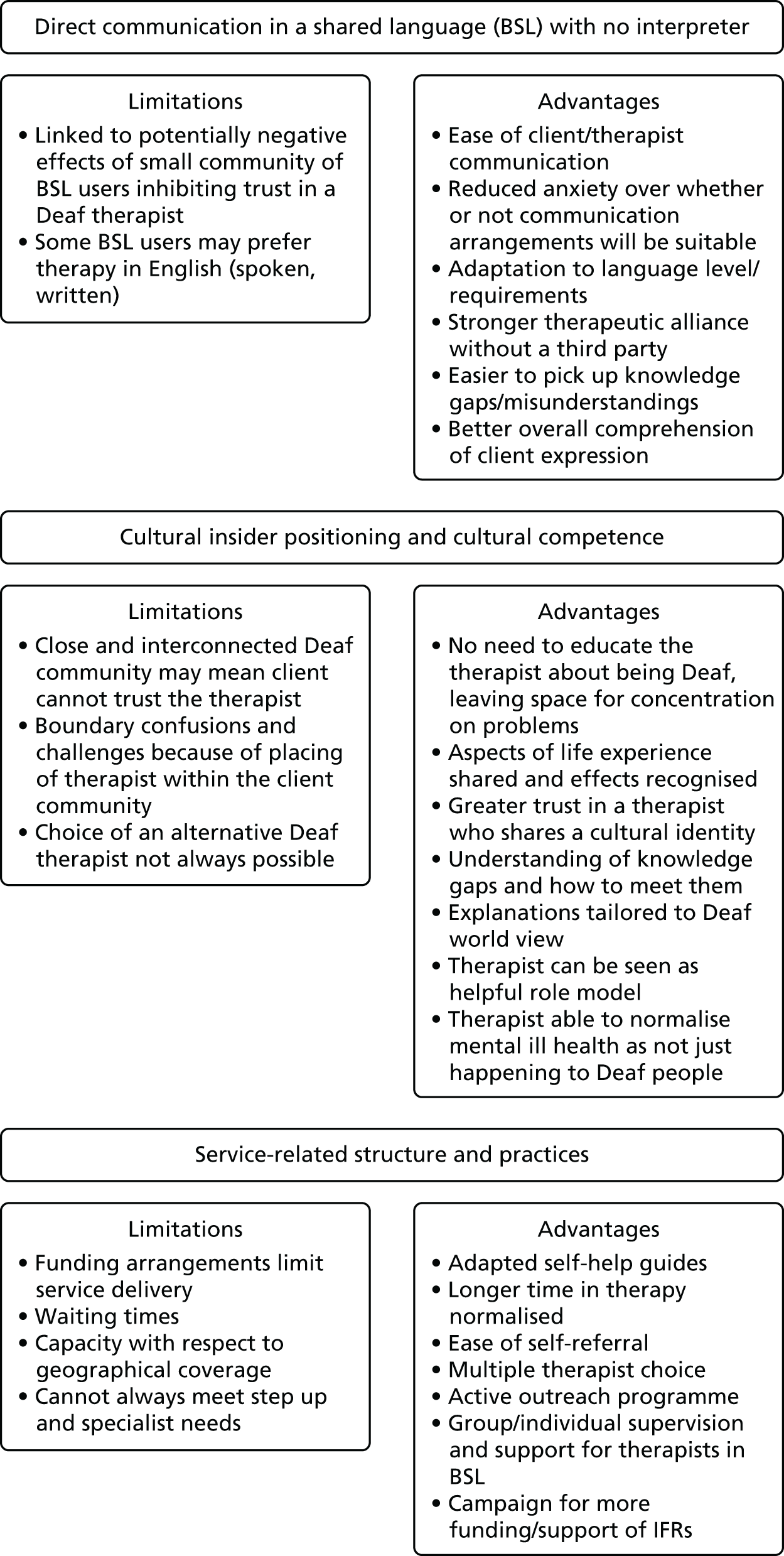
Chapter 6 Translation and validation of the EQ-5D-5L version in British Sign Language (study 4)
Some of this study has previously appeared in Rogers et al. 130 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The text below includes minor additions and formatting changes to the original. When paragraphs are repeated here verbatim, they have been displayed as quotations with reference to the original paper.
Background
Before this study, there was no validated BSL version of the common health outcome instruments that are routinely used in research and evaluation studies. Previous studies on the health status of Deaf populations demonstrated that they experience inequality in positive health-related outcomes. 52,131
A measure of health outcomes can be obtained by using a standardised tool developed by EuroQol, namely the EuroQol-5 Dimensions (EQ-5D). 132 The EQ-5D can be used to measure a wide range of health conditions and can be used in economic evaluation studies to estimate health benefits in terms of QALYs. The QALY is a measure that weights years lived by the time spent in different health states. One QALY is equivalent to 1 year spent in full health. The QALY is recommended by NICE for economic evaluations. 133 The EQ-5D can be used to estimate the weights to use in calculating QALYs. There are currently two versions of the EQ-5D. The first has three levels (no problems, some problems and severe/extreme problems) for each aspect or domain of health (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). The second, more recent, version uses the same health domains but has five possible levels for each domain (no problems, slight problems, moderate problems, severe problems and extreme problems).
There was no validated version of any of the versions of the EQ-5D in BSL or indeed in any signed language. We undertook in this study to produce a BSL version of the EQ-5D-5L and to establish its psychometric properties and validity. This is a necessary prerequisite for estimating the cost-effectiveness of BSL-IAPT and standard IAPT accessed by Deaf people in the UK. The BSL EQ-5D-5L can be used in future research studies with this population. This formed objective i below.
Objectives
-
To translate and test the reliability of a BSL version of the EQ-5D-5L.
-
To conduct further analyses of the BSL EQ-5D-5L data collected as part of this study (study 5), to inform future research with this population.
Methods: objective i
Translating EQ-5D-5L version into British Sign Language
The technique used in the translation and reliability testing of standard instruments builds on our previous work [see Rogers et al. 33 for PHQ-9 BSL, GAD-7 BSL and WSAS BSL; and Rogers et al. 134 for Clinical Outcomes in Routine Evaluation – Outcome Measure (CORE-OM) BSL]. The translation procedure for the EQ-5D-5L BSL followed international standards, as required by the EuroQol group; this consisted of five stages (Figure 26). As BSL is a visual, non-written language, additional amendments were required; these amendments were approved by EuroQol. Additional amendments were necessary in order to ensure an operationally equivalent version was achieved; this is not a written/print version. The aim of this procedure is to ensure that the BSL version will be as semantically equivalent as possible to the English version.
FIGURE 26.
Flow chart illustrating translation of the EQ-5D-5L into BSL.

Two translation teams were established for this translation procedure: the forward translation team [two experienced translators who are Deaf native BSL users, fluent in written English (one is a registered interpreter)]; and the back translation team (one Deaf and one hearing, both registered interpreters, who are bilingual in BSL and English).
In detail:
Forward translation: The two forward translators independently translated the EQ-5D-5L into BSL (first draft). A key problem identified concerned the repetition of the level descriptors; in the English version, these are distinguished by slight changes in the adjective used in each sentence e.g. ‘I have no problems in walking about; I have slight problems in walking about; I have moderate problems in walking about, etc.’. In a written language, this format works because someone reading the questionnaire is able to scan between the level descriptors, which are all on the same page, make comparisons and reach a decision; there is simultaneous presentation of available choices. In a visual language, where the ‘text’ of the questionnaire is presented on screen via an online interface, repeating the level descriptors one after another is a sequential experience for the ‘viewer’. To compare the different options would require flicking between five different videos, separately presented on screen, which is not an equivalent cognitive task to seeing a written version where there is simultaneous access to the range of responses from which to choose. After discussion with the forward translators and the representatives from the EuroQol Group, a change in the format of presentation of the potential responses was permitted. The five level descriptors are, for each domain, presented by a single signed phrase in the form of: ‘the health domain (e.g. mobility difficulties) followed by none; slight; moderate; severe; unable/can’t’. The grammar of BSL permits intensity to be marked in increasing degrees, having established the core subject first, through inflecting facial expression, handshape, movement and, in some instances, location of signing. 87 The viewer is able to see all possible choices of response simultaneously (as a reader of written text might) and come to their decision. Those taking the assessment give their response by clicking on one of the available choices represented on screen by corresponding English words and a BSL reference translation is given at the start and is available to be seen again throughout if required.
Back translation: The two back translators independently translated the BSL version (second draft) back into English, compared the back translations with the original version and produced a report on the back translation process to the project manager. This resulted in the third draft.
Respondent testing: the third draft was tested using a sample of eight lay Deaf respondents (five men, three women), aged between 33 to 58, with varying educational backgrounds. They included both healthy people and patients, as outlined by the EuroQol group. The ‘patients’ were those who reported that they were currently experiencing health difficulties in response to general descriptive questions about their health and any current treatment. They were asked to complete the EQ-5D-5L BSL, not having had previous access to or experience of the assessment in English, and then they took part in a structured interview. Additionally, they completed a rating exercise (on a scale of 0–100) to establish their response for each health dimension, which confirmed that the severity descriptors for each dimension were appropriate. Feedback resulted in some additional changes to the translation, including clarification of the acronym EQ-5D, a clearer distinction between pain and/or discomfort and a greater emphasis on ‘today’ to be conveyed for each dimension as it was signed.
Testing with bilingual Deaf people: To explore agreement between the English and BSL versions of EQ-5D, 11 bilingual Deaf people completed both versions. Cohen’s kappa (k) statistic was used to assess the level of agreement between the English and BSL versions. Although the sample was small, it was found that the level of agreement between the two versions was very high. Statistical agreement (Cohen’s kappa) between the BSL and English versions of each dimension of EQ-5D-5L was high: mobility, k = 1 (p < 0.001); usual activities, k = 1 (p < 0.001); pain/discomfort, k = 0.81 (p < 0.001); anxiety/depression, k = 1 (p < 0.001). For self-care, all respondents used only one category of the five levels for the English and BSL versions; thus it was not possible to estimate Cohen’s kappa. The analyses above demonstrate that the content of each item in the BSL version of EQ-5D-5L was equivalent to the English items in the original version.
Fourth draft: This took into account comments from the respondent testing and the EuroQol translation review team and was the version then used for reliability testing. Examples of the amendments made include: (i) Emphasising more strongly that the question is asking about the severity of problems for today only; (ii) making it clearer that the mobility domain refers to the ability to walk rather than barriers to mobility including communication barriers; and (iii) making the distinction between pain and discomfort clearer.
Rogers et al. 130
Although the findings from the respondent testing stage resulted in further changes to the EQ-5D-5L BSL, how Deaf people conceptualised the key words varied across the group. For example, in the case of ‘mobility’, some thought that it related simply to the use of the legs (i.e. being able to walk), whereas others also associated it with the use of arms (e.g. being able to pick up glasses). A couple of people also thought that it related to getting to places, and that because of communication barriers, it would be difficult to use a taxi or bus. This is related to how Deaf people view the world and how everyday life experiences influence how they conceptualise.
Testing the reliability and validation of the EQ-5D-5L version British Sign Language
Materials
Deaf people who use BSL completed a short demographic survey, the BSL versions of EQ-5D-5L, Clinical Outcomes in Routine Evaluation – 10-item version (CORE-10) BSL and Clinical Outcomes in Routine Evaluation – 6-item version (CORE-6D) BSL, through an online platform. SelectSurvey was used as a tool for the online data collection, where the EQ-5D-5L BSL, as well as other questionnaires, were uploaded. Deaf people were asked to take part in the retest of the EQ-5D-5L BSL approximately 1 week later.
Sample size
A sample size of 51 allows a 95% CI for an intraclass correlation coefficient of 0.75 to be estimated to within ± 0.1. Previous studies demonstrated that this sample size was entirely feasible. 33,134
Analysis
The psychometric properties of the EQ-5D-5L BSL were examined. The analyses included content validity (assessed by interviewing a small sample of Deaf people); internal consistency of the items and test–retest were assessed for its reliability (using Cronbach’s alpha values and weighted kappa scores); and convergent validity was assessed by determining how well EQ-5D-5L BSL correlates with CORE-10 BSL and CORE-6D BSL (using Kendall’s tau coefficient).
Findings: objective i
The study with respect to objective i, the translations and validation of the EQ-5D-5L in BSL, has been published as open access in Quality of Life Research journal. 130
The principal results and conclusions (reproduced from the abstract) were as follows.
The psychometric properties of the EQ-5D-5L BSL are good, indicating that it can be used to measure health status in the Deaf signing population in the UK. Convergent validity between EQ-5D-5L BSL and CORE-10 BSL and CORE-6D BSL is consistent, demonstrating that the BSL version of EQ-5D-5L is a good measure of the health status of an individual. The test-retest reliability of EQ-5D-5L BSL, for each dimension of health, was shown to have Cohen’s kappa values of 0.47 to 0.61; these were in the range of moderate to good, and were therefore acceptable. This is the first time EQ-5D-5L has been translated into a signed language for use with Deaf people and is a significant step forward towards conducting studies of health status and cost-effectiveness in this population.
Rogers et al. 130
Methods: objective ii
The data from the members of the signing Deaf population who completed the EQ-5D-5L BSL in the translation and validation study were explored in more detail to calculate utility values for the sampled population and to compare these to the published population norms to allow us to consider the impact of being Deaf on utility.
Specific research questions were:
-
What are the EQ-5D utility values for the sampled Deaf population?
-
How do the EQ-5D scores and utility values from the Deaf participants compare with published population norms for the general population?
-
What participant characteristics are associated with utility values and does the EQ-5D utility value vary between Deaf people with and without depression?
-
Do the utility values derived from the EQ-5D-5L vary between the published value sets available?
-
To what extent do utility values derived from the EQ-5D-5L and CORE-6D BSL vary?
Calculating utility values
Utility values were calculated from the EQ-5D-5L BSL for all participants who completed the measure in the translation and validation study, at the first time point, using the published crosswalk system. The crosswalk system directly maps between the three- and five-level versions of the EQ-5D. It has been used since 2012 to calculate utility values from EQ-5D-5L data. 135
More recently, Devlin et al. 136 published a new value set for the EQ-5D-5L which, over time, is intended to replace the crosswalk system. This new value set was collected at a different time and on a different sample to the value set used for the EuroQol-5 Dimensions, three-level version (EQ-5D-3L). This means that there may be differences in utility estimates and QALYs estimated using the crosswalk system and the new value set that reflect differences resulting from design rather than underlying preferences and/or changes in preferences over time. Compared with the crosswalk method of calculating utility values, the new value set has fewer states ‘worse than death’ and the minimum utility value is higher (–0.281 vs. –0.594). This means that overall utilities may be higher using the new value set than those from the crosswalk system for the EQ-5D-5L or the original EQ-5D-3L.
Thus, we used the crosswalk method to generate our utility values for most analyses to facilitate comparison between utility values estimated using the older three-level version of the EQ-5D and the more recent five-level version. The new value set published by Devlin et al. 136 was compared with the crosswalk system in the analysis to address research question 4.
To compare the EQ-5D utility values to those derived from the CORE-6D BSL data derived from study 4, we used the methods reported in a published paper. 137 This included collapsing the five-level CORE-6D BSL data down into three levels and using a regression model to calculate utilities. 137
Analysis
Descriptive statistics were used to summarise the responses of Deaf people to the population norms for the EQ-5D domains (per cent reporting no problems) and EQ-5D utility weights (mean, SD), and to compare these with population norms. Deaf participants’ EQ-5D-5L scores and utility values were compared with published norms from the hearing population, identified via the EuroQoL website.
Linear regression was used to determine if participants’ sociodemographic characteristics were associated with Deaf participants’ health and EQ-5D-5L utility weights. The analysis was also used, with descriptive statistics, to assess whether or not utility values differed between people with and without depression. In line with clinical cut-off points from the hearing population, a CORE-10 score of ≥ 13 was used to identify participants with depression (note that cut-off values specific to the Deaf population are not available). 138 The CORE-6D utility values were included in this analysis to assess whether or not the CORE-6D, which is based on a subset of the CORE items, differed between the groups. Moreover, the comparison provides additional information with which to descriptively assess the differences in EQ-5D utility values between people with and without depression.
The data were analysed using Stata version 13.1 (StataCorp LP, College Station, TX, USA).
Results
Participants’ demographic and health-related characteristics used in the analyses are provided in the published report on the translation and validation of the EQ-5D-5L BSL. 130
Table 25 reports the percentage of people reporting no problems on each of the EQ-5D domains for the Deaf participants and the published population norms. Overall, compared with the published norms (which we would expect to be made up of predominantly hearing participants), fewer Deaf respondents selected ‘no problems’ for each of the domains. Exceptions to this were for the 18–24 years and ≥ 65 years age groups, who reported fewer problems than the population norm sample. However, there were only seven Deaf respondents in these age groups. In total, over 73% of Deaf participants reported some (slight to severe) problems on one or more of the EQ-5D-5L domains. The results for the group as a whole are presented in the paper by Rogers et al. , on the translation and validation of the EQ-5D-5L. 130
| Sample | EQ-5D domains (%) | ||||
|---|---|---|---|---|---|
| Mobility | Self-care | Usual activities | Pain/discomfort | Anxiety/depression | |
| Aged 18–24 years | |||||
| Deaf participants (n = 4) | 50 | 100 | 50 | 50 | 100 |
| Population norms (n = 304) | 95 | 99 | 95 | 83 | 88 |
| Aged 25–34 years | |||||
| Deaf participants (n = 14) | 64 | 86 | 57 | 57 | 36 |
| Population norms (n = 753) | 94 | 99 | 92 | 84 | 84 |
| Aged 35–44 years | |||||
| Deaf participants (n = 15) | 65 | 82 | 59 | 53 | 53 |
| Population norms (n = 561) | 92 | 98 | 93 | 78 | 83 |
| Aged 45–54 years | |||||
| Deaf participants (n = 26) | 69 | 85 | 54 | 46 | 31 |
| Population norms (n = 488) | 85 | 94 | 84 | 66 | 78 |
| Aged 55–64 years | |||||
| Deaf participants (n = 13) | 64 | 79 | 71 | 50 | 57 |
| Population norms (n = 484) | 75 | 94 | 76 | 53 | 71 |
| Aged 65–74 years | |||||
| Deaf participants (n = 3) | 100 | 100 | 100 | 67 | 100 |
| Population norms (n = 488) | 65 | 93 | 74 | 50 | 74 |
Table 26 shows the estimated EQ-5D-5L values according to age group and sex for the Deaf participants and general population norms. The overall mean utility value of the Deaf participants was 0.78 (SD 0.24), compared with 0.87 (SD 0.50) for the general populations norms. The majority of Deaf participants have lower utilities than the norms for their age group and sex. However, it was not possible to test whether these differences are statistically significant or attributable to chance.
| Population | Age group (years) | |||||
|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | |
| Female | ||||||
| Deaf participants (n = 53) | 0.86 (0.16) | 0.77 (0.25) | 0.76 (0.30) | 0.76 (0.23) | 0.82 (0.17) | 0.92 (0.12) |
| Population norms (n = 1926) | 0.94 | 0.93 | 0.91 | 0.85 | 0.82 | 0.78 |
| Male | ||||||
| Deaf participants (n = 22) | No data | 0.80 (0.19) | 0.90 (0.11) | 0.56 (0.38) | 0.87 (0.10) | 1 |
| Population norms (n = 1469) | 0.94 | 0.93 | 0.91 | 0.85 | 0.78 | 0.78 |
| Total female and male | ||||||
| Deaf participants (n = 75) | 0.86 (0.16) | 0.79 (0.212) | 0.82 (0.25) | 0.71 (0.28) | 0.84 (0.15) | 0.95 (0.09) |
| Population norms (n = 3395) | 0.94 | 0.93 | 0.91 | 0.85 | 0.80 | 0.78 |
Figure 27 plots the participants’ actual EQ-5D-5L values against the published norms for their sex and age group. The values calculated from the Deaf BSL sampled population are shown in light green, with the expected population norms for their age and sex in dark green. This demonstrates that, overall, participants’ EQ-5D-5L values are lower than the norms, which is demonstrated by the trend lines in Figure 27. Figure 27 also shows that a number of participants in the BSL sample had a score of 1 (indicating that they had no problems on any EQ-5D-5L domain). However, there were three participants who had negative utility scores (indicating a health state worse than death), showing a wide variation in the group. Overall, there was more variation in the observed EQ-5D utility values for the Deaf participants. However, this may reflect the relatively small number of Deaf participants with complete data for age, sex and the EQ-5D (n = 75), compared with the sample used to estimate population norms (n = 3395).
FIGURE 27.
Utility scores (calculated participants EQ-5D-5L values vs. expected general population using norms).
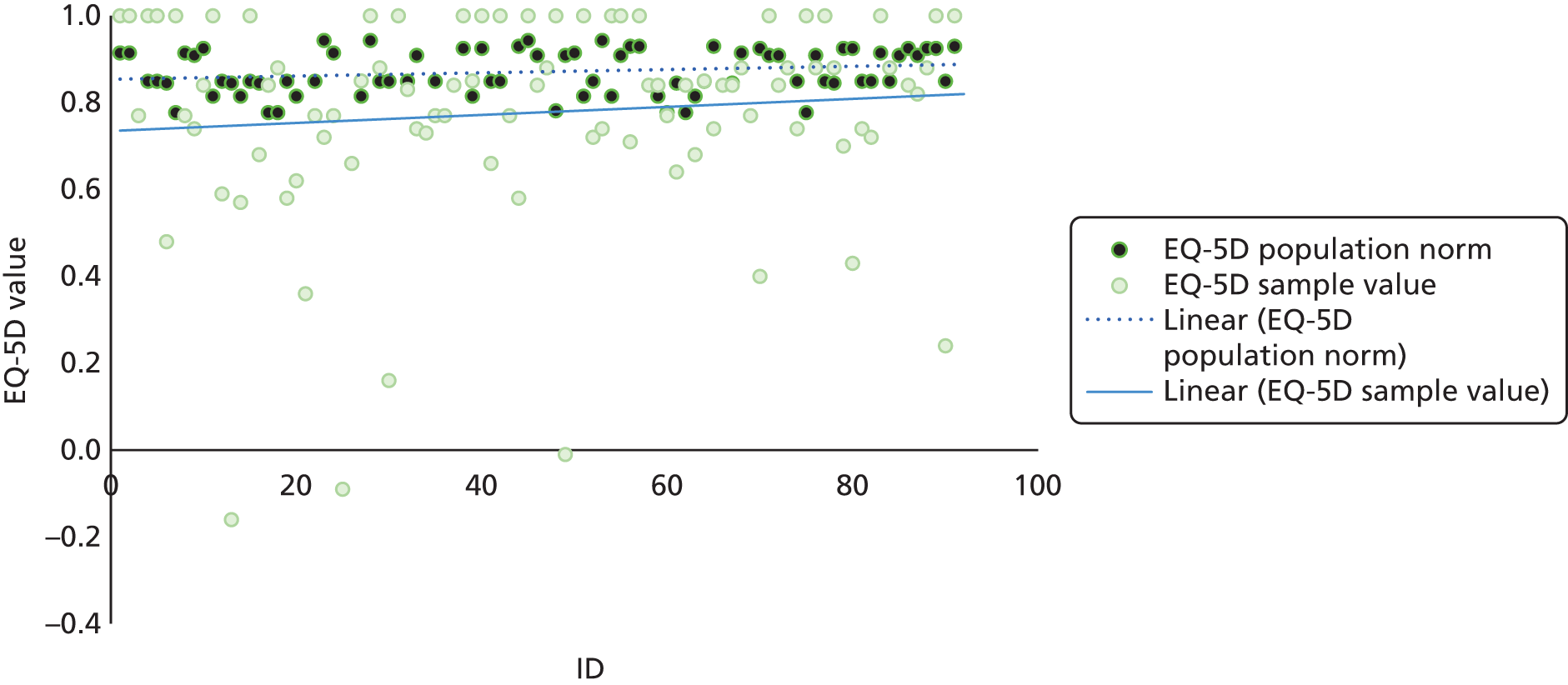
Table 27 summarises the results of the regression analysis to assess whether or not there was an association between Deaf participants’ sociodemographic and health characteristics and their EQ-5D utility weight. There was no evidence of an association between the utility value and participants’ demographic characteristics. As might be expected, measures of health were associated with the EQ-5D utility value. Higher CORE-6D total scores reflect worse mental health and were associated with lower EQ-5D-5L utility values, showing that, as symptoms of depression/anxiety increase, EQ-5D-5L utility values fall. In addition, having other health difficulties was associated with lower utility, as would be expected. It is worth noting that the analysis includes only the 64 Deaf participants for whom data on each of the variables were available.
| EQ-5D-5L utility value | Coefficient | Standard error | p-value | 95% CI |
|---|---|---|---|---|
| Age | 0.001 | 0.002 | 0.670 | 0.003 to 0.004 |
| Male (vs. female) | –0.010 | 0.047 | 0.830 | –0.104 to 0.084 |
| Not white British (vs. white British) | 0.030 | 0.053 | 0.571 | –0.075 to 0.135 |
| Productively active (vs. not) | –0.039 | 0.062 | 0.531 | –0.163 to 0.085 |
| Long-standing physical illness (vs. physically well) | –0.217 | 0.070 | 0.003 | –0.357 to –0.076 |
| Disability (vs. physically well) | –0.341 | 0.077 | < 0.001 | –0.495 to –0.187 |
| CORE-10 scaled clinical score | –0.009 | 0.004 | 0.043 | –0.017 to 0.000 |
| Constant | 0.921 | 0.095 | < 0.001 | 0.731 to 1.111 |
A second regression analysis explored whether utility was likely to vary between Deaf participants who had met the clinical threshold for depression and those who did not. This analysis included participants’ sociodemographic characteristics, but excluded the other health measures associated with the presence or absence of depression (p < 0.07; logistic regression, results reported in the Rogers et al. study130). The results indicate that those people who did not have depression had a higher utility value than those who did (coefficient 0.11, 95% CI 0.01 to 0.21; p = 0.029; n = 66).
Table 28 summarises the utility values estimated using the different value sets for the EQ-5D and using the CORE-6D measure and value set. The data indicate that the utility values vary by measure and value set. As might be expected, all the measures and value sets indicate differences in utility values between participants with and without depression. The results also indicate that the EQ-5D-5L utility scores using the new value set are similar to those of the CORE-6D overall and for people with and without depression. Accordingly, the utility values from the different measures are used in sensitivity analyses in the exploratory economic evaluation reported in the next chapter (see Chapter 7).
| Study sample | EQ-5D-5L BSL utility | CORE-6D, mean (SD)137 | |
|---|---|---|---|
| Crosswalk value set, mean (SD)135 | New value set, mean (SD)136 | ||
| All Deaf participants (n = 82) | 0.77 (0.03) | 0.83 (0.02) | 0.81 (0.02) |
| Deaf participants with depression | 0.67 (0.05) | 0.74 (0.05) | 0.71 (0.02) |
| Deaf participants without depression | 0.84 (0.03) | 0.90 (0.02) | 0.88 (0.01) |
Discussion: objective ii
The results of this study indicate that health status and associated utility values published for the general population may not be generalisable to the Deaf population. The mean utility in this group was nearly 10% lower than the general population published norms. In addition, depression and anxiety are shown to be more prevalent in this group. Statistical analysis indicated that, as may be expected, utility values for people with depression may be lower than for people without.
Over half (56.2%) of participants reported some problems with depression/anxiety on the relevant EQ-5D-5L domain. Applying the CORE-10 cut-off points for depression indicated that 43% of the sample had depression, although this should be interpreted with caution as there are no Deaf/BSL-specific cut-off points for this measure. The prevalence of depression/mental distress in the Deaf population has previously been reported as 33.8% (n = 431), using the Hopkins Symptom Checklist 3. 26 Figures for the UK (based on General Health Questionnaire responses) suggest that around one-fifth of the population experience symptoms of depression or anxiety. 139 This suggests that depression is more common in the Deaf BSL population than in the general UK population.
Dividing the group according to the CORE-10 cut-off points for depression indicated a statistically significant lower utility value for the Deaf participants with depression than those without depression, as would be expected. However, previous work suggests that the CORE-10 thresholds for depression may not be relevant to the Deaf BSL population. This may mean that the utilities for this group are inaccurate. If further studies were conducted to assess the impact of being Deaf on specific health issues, researchers would need to consider if measures with cut-off points for the general population only would be relevant for use in the Deaf population. In addition, it would be helpful to collect data on other commonly used measures of depression (e.g. PHQ-9 and GAD-7), as this would help to compare against published data for the general population with depression.
One study of the UK population reported a mean EQ-5D-3L utility value of 0.64 (SD 0.30) for a sample of 250 people with depression,135 which is similar to the estimate in our study using the EQ-5D-5L and crosswalk system to calculate utility. In contrast, a recent clinical trial reported baseline utility values of 0.464 (SD 0.313) (n = 305) and 0.504 (SD 0.288) (n = 276), according to assigned intervention group. 140 Another large study of people with diabetes or coronary heart disease and comorbid depression reported baseline EQ-5D-5L values of 0.476 (SD 0.281) (n = 145) and 0.433 (SD 0.296) (n = 156). 141 These much larger studies indicate that utility values in people with depression with and without physical comorbidities may be lower than in the Deaf BSL participants in our study with depression. This may suggest that, although depression is more common in the Deaf population, it is milder. However, our sample size is small, especially when considering the participants meeting the depression criteria (n = 36) and fact that the range of EQ-5D-5L values is large (–0.16 to 1). In addition, the clinical trials included people who were actively seeking treatment, which may be a group with more severe depression. Furthermore, the examples given applied different clinical measures to measure depression symptoms (PHQ-9 and GAD-7); therefore, it is hard to draw strong conclusions from these comparisons.
Ideally, we would have a sample of the Deaf population with scores using the Deaf versions of these symptom questionnaires (PHQ-9 BSL and GAD-7 BSL) to compare against. This would also help us to more accurately identify the Deaf population with depression, as these measures have cut-off points that are specific to the Deaf population (rather than relying on the CORE-10 hearing population cut-off points). Further work is ongoing to identify a larger range of published utility values for the population with depression, via a systematic review, which will be compared with our sampled Deaf population data in more detail and prepared as a paper for a submission to a peer-reviewed journal.
Our results provide EQ-5D-5L utility values relevant to a Deaf population, which have previously been unavailable. However, there are some limitations. In particular, the study sample (n = 92) is too small to draw strong conclusions. A larger prospective cohort study would help to inform which sociodemographic and clinical characteristics are key influencers of utility, which would allow us to more fully investigate utility in the Deaf BSL population. Additionally, the data collected were not designed to inform utility values for different samples; a larger follow-up study could assess the impact of being Deaf on people with mental health and physical health conditions.
Chapter 7 Exploratory economic evaluation (study 5)
Background
Economic evaluation compares the costs and health benefits (such as symptoms cured, life-years gained, improvements in overall health) of different care or treatments. The aim is to help patients, practitioners and commissioners choose care that offers value for money. A key concept is that care should be selected to give the most health benefit within the budget available. This is often translated to giving the most health benefit for the lowest cost. It is not known whether or not BSL-IAPT confers any benefit for Deaf people over and above accessing standard IAPT services. Similarly, the cost-effectiveness of BSL-IAPT has not been investigated. Rigorous examination of effectiveness and cost-effectiveness is needed to guide decision-making about longer-term sustainability and appropriate targeted primary care intervention for this hard-to-reach group.
Objectives
There were two key objectives of the economic evaluation:
-
to explore the potential costs of health and social care, and the health benefit in terms of QALYs for Deaf users of BSL-IAPT and Deaf users accessing standard IAPT
-
to estimate the net cost per QALY gained by BSL-IAPT.
The key research questions were:
-
The primary analysis addressed the question of whether or not BSL-IAPT was potentially cost-effective compared with standard IAPT, when service-specific PHQ-9 and GAD-7 tools and cut-off points were used to identify people with depression/anxiety and measure recovery.
-
Does the potential cost-effectiveness of BSL-IAPT vary if different assumptions are made about the probability, costs or QALYs of events?
Methods
Approach
The economic evaluation aimed to explore whether or not BSL-IAPT is cost-effective compared with standard IAPT services for the treatment of depression and/or anxiety in the Deaf BSL population in the UK. The overall perspective or decision-maker viewpoint used to determine the range of costs is that of health and social care providers. However, data constraints limited the perspective for the initial 6-month time horizon, when people are receiving IAPT treatment, to the providers of IAPT services. The costs of other health care and social care are not included. However, the costs of relapse/recurrence and recovery after the first 6 months do include a broader range of costs.
In the absence of a head-to-head trial of standard IAPT and BSL-IAPT for Deaf BSL users, it was recognised that a decision-analytic model to combine or synthesise available data was needed. The economic model focuses on Deaf BSL adults who are referred to IAPT for a low- (defined by NICE as step 2)142 or high-intensity (defined by NICE as step 3)142 intervention for the treatment of depression and/or anxiety. The key intervention is the BSL-IAPT specialist service, as provided by BSL Healthy Minds. This service was designed to meet the cultural and linguistic needs of the Deaf BSL population. IAPT interventions are delivered by health-care workers fluent in BSL, the majority of whom are Deaf. This is compared with the standard IAPT service, which the Deaf BSL population may access, usually through a sign language interpreter. Standard IAPT represents routine care for most Deaf BSL users.
The economic model estimates the costs and QALYs for 1 year after a person’s first contact with the service (i.e. the time horizon is 1 year), for the main or primary analysis. Depression and anxiety are long-term conditions, so the economic model also explored the costs and QALYs over longer time periods. However, these longer-term analyses are likely to be more uncertain, as the many of the data available for the model were collected over the short term.
The costs and outcomes for the long-term time horizons are discounted at a 3.5% rate per year, in line with UK recommendations. Discounting takes account of the fact that we prefer to take benefits now and delay costs to the future. Discounting is not needed for analyses using time frames of ≤ 1 year. 133 The price year is 2015 and costs are presented in UK pounds sterling (£).
The population, intervention, control, outcome and time frame statement
-
The target population for the economic model was Deaf BSL users with depression and/or anxiety. Although service users may have only one of these conditions, it is common to suffer from both. 143–146 This was demonstrated in the IAPT data sets, in which 75.9% (standard IAPT) and 81.6% (BSL-IAPT) of participants had mixed depression and anxiety at the point of entry into the IAPT service (see Table 14).
-
The intervention was the BSL-IAPT service, a specialist version of the IAPT service, with fluent BSL users delivering IAPT interventions.
-
The comparator was standard IAPT. In situations in which a Deaf BSL user is referred to a standard IAPT service, they are most likely to receive this intervention through the use of an interpreter.
-
The primary outcome of the economic analysis was the incremental cost-effectiveness ratio (ICER). This was estimated as the net cost of the intervention divided by the net health benefit. The measure of health benefit for the primary analysis was the QALY.
-
The primary time horizon for primary analysis was 1 year from entry into the decision model.
Model overview
In reality, depression and anxiety are complex conditions with varied and diverse treatment pathways. However, models are a simplification of real life. The economic model presents a simplification of the pathway of care for Deaf BSL users accessing IAPT services to capture the key costs and health benefits associated with IAPT treatment.
A review of the literature (see Appendix 8) indicated that there were no existing published economic evaluations of the BSL-IAPT service. Accordingly, a new decision-analytic model was developed to estimate the cost-effectiveness of BSL-IAPT. The model structure was agreed with the project team, including the PPI group, and the SSC, which included a health economics representative.
Model structure
The economic model structure includes two distinct parts: a decision tree and a Markov model.
The decision tree used the IAPT pathway18 and the stepped care pathway recommended by NICE142 to model the treatment events for depression and/or anxiety within the IAPT service. A diagram of the decision tree is shown in Figure 28. The decision tree illustrates the pathway of events that a person could experience during treatment. A number of events may happen at the same time in the decision tree; the pathway reflects the combination of events that a person could experience, but not necessarily the sequence they occur in.
FIGURE 28.
Decision tree.
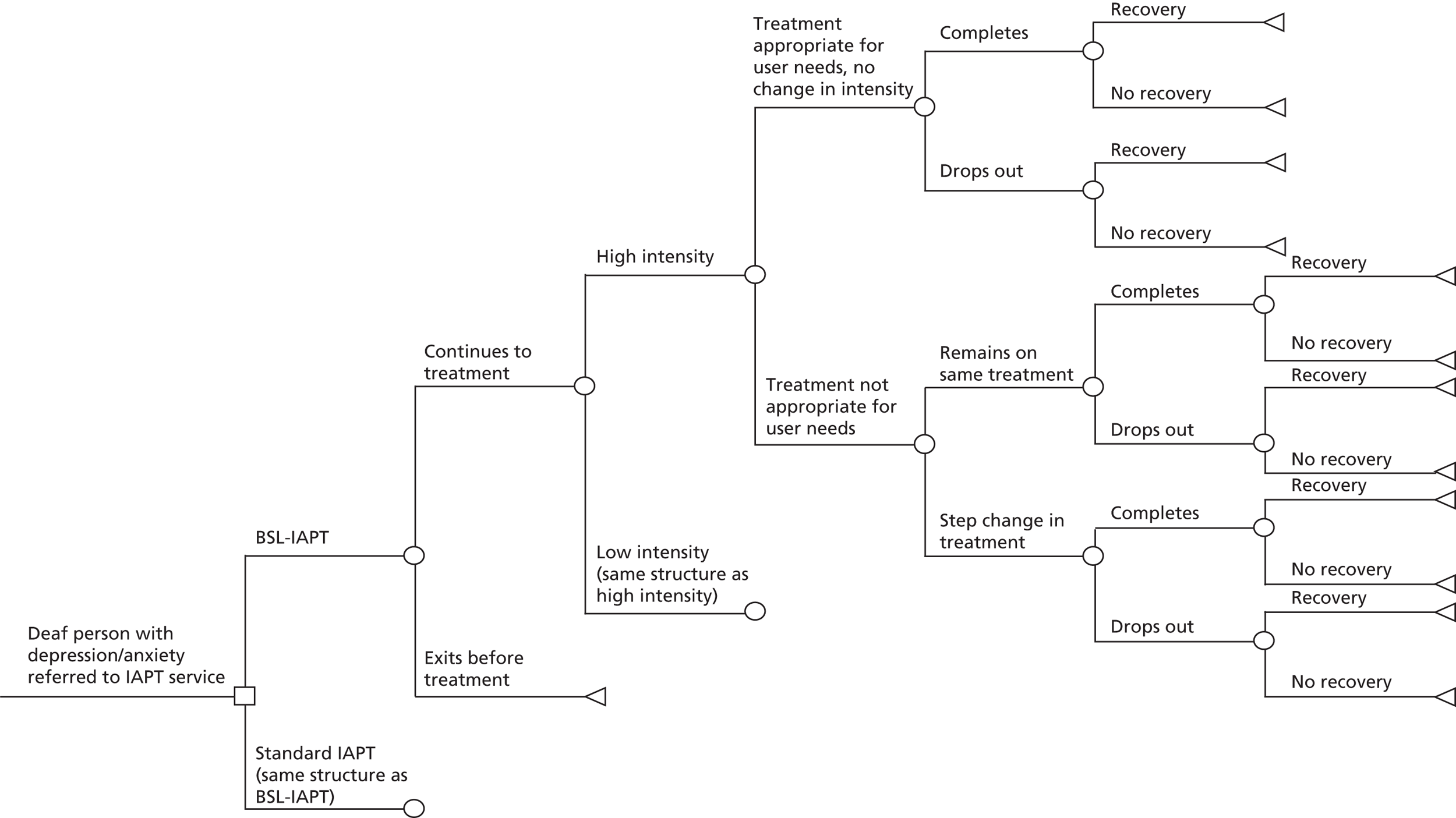
The decision tree begins with a Deaf BSL user referred (or who self-refers) to an IAPT service and models the events that may occur in the first 6 months from referral. This is represented in Figure 28 by a square node. Standard IAPT and BSL-IAPT pathways follow the same decision tree structure, although the probabilities, costs and benefits of different events may vary between the two interventions.
It is possible that people will exit the pathway before treatment. This may be for various reasons (e.g. their symptoms changed during the wait, which means that they are now no longer suitable for IAPT treatment, or they received another intervention during the wait and now no longer need the IAPT service). For people starting treatment, there are two possible options: low- or high-intensity treatment (step 2 and step 3 in the NICE guidelines). 142 The decision to refer to low- or high-intensity treatment will depend on patient characteristics/symptoms and treatment availability. Low- and high-intensity referrals have the same model structure in the decision tree, but have different probabilities and costs.
The model recognises that the intensity level may or may not be appropriate for the user’s needs. Service users may remain on the same treatment intensity throughout their IAPT therapy course (if appropriate), or they may need to change from low- to high-intensity or from high- to low-intensity services during treatment if the initial treatment is not appropriate. It is plausible that the BSL-IAPT service may be more able to appropriately refer users to low- or high-intensity intervention if it can assess symptoms more accurately (e.g. through more fluent and direct communication or using the BSL versions of the PHQ-9 and GAD-7 or more appropriate clinical cut-off points). Alternatively, services may be similar in terms of whether or not patients are appropriately referred, but BSL-IAPT may be better at identifying when a patient needs to change the intensity of treatment. Increasing the service’s ability to identify appropriate changes in treatment intensity effectively gives another chance of having a treatment benefit in the model. For the 6 months covered by the decision tree it is assumed that users will have multiple IAPT interventions only if the intensity of treatment is changed.
Service users may complete treatment or disengage and drop out, with these groups having different chances of benefiting from treatment. The benefit of treatment includes two potential outcomes: full recovery or partial recovery. It is assumed that those people who do not recover following treatment are either referred to other services or have no further treatment. The treatment pathways following a course of IAPT therapy are variable and complex and so further treatments are not explicitly included in the decision tree. However, they are included in the costs and outcomes of events in the Markov section of the economic model.
The Markov section of the model was used to capture longer time horizons and that depression and anxiety can be cyclical with recovery followed by relapse (return of symptoms before full recovery) or recurrence (recurrence of depression/anxiety symptoms following full recovery). It includes three possible states: partial or full recovery from depression/anxiety, relapse/recurrence and death. The Markov model is presented in Figure 29. Which health state people enter the Markov section of the model in is determined by the end points of the decision tree. For the decision tree pathways that end in recovery, the Markov model starts with a state of recovery (which is split into two substates for full recovery and partial recovery). Users can only move into the partial response state during the decision tree (i.e. following the modelled treatment). In the Markov model these users will either remain in this state or move out of it (into the recovery substate of full recovery, relapse or death). For the decision tree pathways that end in no recovery, the Markov model starts with a state of active depression/anxiety symptoms, which is termed as relapse/recurrence for subsequent cycles of the model. The Markov model allows transitions to occur between 3-month cycles, a half-cycle correction was applied.
FIGURE 29.
Markov model. a, Recovery consists of two substates: full and partial recovery. Users can only move into the partial recovery substate on entry to the Markov model, in the Markov they can remain or transition (move) to another state. There are no data available to model users moving into this state following the decision tree. b, Relapse is defined as the return of symptoms before full recovery and recurrence is defined as the recurrence of depression/anxiety symptoms following full recovery.
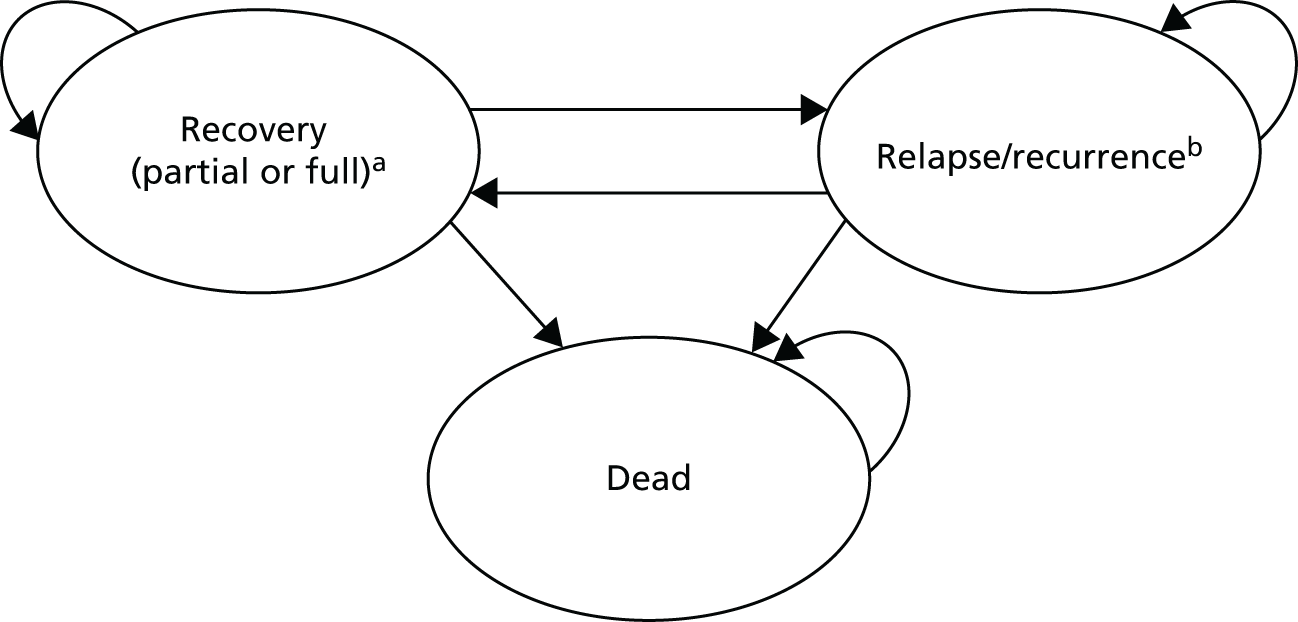
The economic model was constructed in Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA).
Users can move between health states (depicted by the arrows moving between states) and can remain in those states over a number of cycles (shown by the arrow looping back into the health state. Death is an absorbing state; people will remain in this state (shown by the single arrow looping back into ‘dead’).
Model parameters and data sources
Overview
The data for the model included the following categories: probabilities of events, outcomes, utilities, resource use and costs. Tables of the data estimates and sources used in the model are presented in Appendix 9.
The economic model synthesised data from a number of studies across the programme of work, as well as data from the wider literature. Data on outcomes and resource use (number of appointments and treatment intensity/step level) were estimated from the IAPT data sets analysed in study 2 (see Chapter 4). These data sets allowed us to make a comparison between the service options in terms of treatment effectiveness and the resource use and costs associated with IAPT intervention. The translation and validation of the BSL EQ-5D-5L (study 5; see Chapter 6), provided a sample of data to estimate utility values for Deaf BSL users.
These data were supplemented with data from the literature to estimate the probabilities, costs and outcomes over the longer term. This included the long-term rates of relapse/recurrence and recovery, costs of depression and/or anxiety, and mortality rates. Literature was identified through targeted searches of The Cochrane Library, NHS Evidence and MEDLINE database. Owing to a lack of evidence, which was specific to the Deaf population, data from the wider population had to be used to estimate some model parameters; this is discussed in Limitations. The choice of inputs in these cases was based on the availability of the best-quality (according to the hierarchy of evidence) and most relevant data. Given the probable mixed depression/anxiety diagnosis, the model used data relevant to the mixed diagnosis when possible. When these were not available, data that were either relevant to depression or anxiety were used, prioritising the best-quality sources of data.
Likelihood of treatment events
Probabilities of treatment events in the decision tree were estimated using the data from the BSL-IAPT and standard IAPT data sets described in Chapter 4. This assumes that the participants included in these two data sets are representative of the target population for the economic study. Parameter values used in the model are provided in Appendix 10, Tables 33 and 34.
After referral, the probability of whether a person continues to treatment or leaves the service before treatment was estimated from the total number of clients as the proportion of people with recorded appointments and the proportion of people with no recorded appointments, respectively. The probability a person had low- or high-intensity treatment was estimated as the proportion of service users with one or more attended appointments starting at each intensity level. Data about whether or not treatment was appropriate for a person’s needs were not available from the IAPT data sets. The probability that treatment was appropriate for a person’s needs was estimated by assuming that service users within the data sets were referred to an appropriate treatment if they did not experience a step change.
If the treatment given was appropriate for a person’s needs, then it was assumed that there would be no planned change in treatment. There is then the probability that a person completes treatment or not. The IAPT literature classifies service users with two or more attended appointments as having completed a treatment episode. 147 Accordingly, the probability of completing treatment was calculated as the proportion of users attending two or more appointments.
If the treatment given was not appropriate for a person’s needs, then there is the chance that they continue with that treatment or change the intensity of treatment. Data about whether people would remain on treatment or experience a switch was not available from the IAPT databases. Therefore, it was assumed that, if treatment was not appropriate, treatment intensity would be changed (i.e. patients on low-intensity treatment would experience a ‘step up’ to high-intensity treatment and vice versa).
The likelihood of treatment effect (full recovery or partial recovery) for use in the decision tree was also estimated using the IAPT data sets (BSL-IAPT or standard IAPT) described above. For the economic model, ‘recovery rate’ was derived from the BSL study’s clinical effectiveness analysis and additionally broken down by treatment intensity. Therefore, unlike the main clinical effectiveness, it was based on complete case analysis within these intensity subgroups. Full recovery was defined as the IAPT measure of reliable recovery (treatment was completed and PHQ-9 and GAD-7 scores are below the clinical cut-off point for depression/anxiety106), and the probability was estimated as the proportion of users within a data set who experienced reliable recovery. Unlike the main clinical effectiveness analysis, the economic model also took account of ‘partial recovery rate’. Partial recovery was defined as the IAPT measure of reliable improvement (treatment was completed and PHQ-9 and GAD-7 scores are lower than at referral but not below the clinical cut-off point for depression/anxiety106), and the probability was calculated as the users experiencing a reliable improvement but without reliable recovery.
Treatment effect rates for users who leave the service before starting treatment, or who drop out of treatment, could not be calculated as there are no follow-up data available in the IAPT data sets. In the primary analysis, these users are assumed to have no chance of recovery or partial recovery. It is possible that these people left the service because their symptoms improved or resolved. Accordingly, this assumption was tested in the sensitivity analysis.
The longer-term probabilities of relapse/recurrence and recovery were sourced from the published literature. The probabilities and published sources used are shown in Appendix 10, Table 35.
Mortality was not included in the decision tree section of the model for two reasons:
-
On referral to IAPT, initial assessment checks for warning signs for self-harm or suicide would be carried out and service users exhibiting these warning signs would be referred to services for complex and severe depression or alternative services and so leave the IAPT service. 142
-
Data from study 2 (see Chapter 4) identified no mortality cases during the IAPT intervention period.
Background all-cause mortality is included in the Markov model and is applied to the recovery health state, based on national UK life tables. 148 Individuals who are in the relapse/recurrence health state of the Markov model are at an increased risk of death. The estimate used was from a large case–control observational study of anxiety and depression as predictors of mortality,149 which found a hazard ratio of 1.32 (95% CI1.14 to 1.54) associated with anxiety and depression.
Baseline user characteristics are included in the Markov section of the model as these have an impact on the mortality rates used; a mean age of 42 (SD 13.4) years is used, with 61% of the hypothetical cohort being female (see Chapter 4).
It is important to note that adverse events were not considered in the model for practical reasons. There are difficulties in defining what is an adverse event of psychological therapy and what is an unrelated deterioration in a patient’s health. 150 Adverse events in psychological therapy are not well recorded or reported in clinical evaluations. 150 In addition, adverse event data were not captured in the IAPT data sets used in this study or in the IAPT data sets that are required for reporting to the HSCIC. 151
Utility values
The EQ-5D is the measure of health-related quality of life in adults preferred by NICE. 133 The EQ-5D-5L was translated into BSL and validated (see Chapter 6); this study concluded that it is a reliable measure of health status in the Deaf signing population in the UK. 130 The utility values used are reported in Chapter 6. The data from the translation and validation study were used to calculate EQ-5D utility values for the depression and remission health states included in the model. The values were calculated by separating the data into two groups based on the CORE-10 thresholds for anxiety and depression using the published English clinical cut-off points. 138 The published CORE-10 cut-off points are not specific to the Deaf population but were the only cut-off points that could be applied with the measures collected in this data set.
The utility value for partial recovery could not be identified from the data collected as part of the translation and validation of the EQ-5D-5L BSL (see Chapter 6). To fill this gap, the value was identified from recent work undertaken for NICE guidelines. 142,152 For one of the sensitivity analyses, utility values were estimated using the new value set for England136 rather than the crosswalk system. In this case the average of the utility estimates for full recovery and relapse/recurrence states is used as the utility rate for partial remission.
Resource use and costs
Costs include the following:
-
costs associated with IAPT appointments
-
costs associated with BSL-IAPT set up (BSL-IAPT arm only)
-
translation costs (standard IAPT arm only)
-
longer-term health and social care costs associated with depression/anxiety after the first 6 months.
The detailed service use and cost data are shown in Appendix 10, Tables 36 and 37.
The mean number of appointments for a person completing treatment was calculated from the relevant data set (BSL-IAPT or standard IAPT data). This included attended appointments and appointments where the user did not attend (i.e. the user did not cancel, but did not arrive for the appointment), as these appointments could not have been given to other users at short notice and hence the service will still incur the cost.
The unit costs for standard IAPT appointments and an interpreter cost were estimated from published sources. 153,154 There is currently no unit cost of an appointment for a national BSL-IAPT service. Accordingly, the unit cost from a published BSL Healthy Minds report was used as the average unit cost. 153,155 To inform the cost distribution and recognising that other service configurations may offer BSL-IAPT, the lower quartile cost of standard IAPT was used as the lower bound, with an upper bound set to the upper quartile cost of standard IAPT plus the cost of an interpreter.
The wider costs of relapse/recurrence were estimated from published sources. 156,157 A systematic review of studies assessing the cost of illness of depression found that the excess costs of treating depression were about one-third of total health-care costs for people without depression. 157 Data could not be found to inform the health-care costs of people recovered from depression; we assumed that costs would be two-thirds of the depression costs reported in the McCrone et al. paper. 156 Service users experiencing a partial recovery were assumed to have an average of the cost of relapse/recurrence and full recovery states as data could not be found to inform this.
Costs that were taken from older sources were updated to 2014/15 prices using the Hospital and Community Health Service index. 158
Primary analysis
The primary analysis addressed the question of whether or not BSL-IAPT was potentially cost-effective compared with standard IAPT when service-specific PHQ-9 and GAD-7 tools and cut-off points were used to identify people with depression/anxiety and measure recovery. The model estimated the net costs and QALYs of BSL-IAPT compared with standard IAPT. Monte Carlo simulation was used to take account of the fact that there is uncertainty and variation in the data used in the model. To do this, all the data inputs were assigned distributions. The Monte Carlo simulation samples from the distribution of possible values for each data input in the decision model. Probabilities and utilities were assigned beta distributions, and costs were assigned triangular distributions. Odds ratios and resource use were assigned normal distributions. Estimates of the mean and SD were used. This meant that mean costs and QALYs, as well as measures of variance (SD and 95% CI), could be estimated to assess the level of uncertainty in the results due to the data inputs.
The Monte Carlo simulation produced 10,000 pairs of net cost and net outcomes. These were then used to generate cost-effectiveness acceptability curves and the probability that the BSL-IAPT service is cost-effective compared with standard IAPT for Deaf BSL users, as recommended by NICE for health technology appraisals. 133 This approach revalues benefits (e.g. QALYs gained) in monetary terms. However, there is no universally agreed monetary value to attach to QALYs. Therefore, the simulated net QALYs were revalued using a range of willingness-to-pay values that a decision-maker may be willing to pay to gain 1 QALY, ranging from £0 to £30,000. This was based on the range of willingness-to-pay values historically used in NICE decisions. 159,160 This approach takes into account uncertainty about the amount that decision would be willing to pay to gain 1 additional QALY from BSL-IAPT.
Sensitivity analysis
Sensitivity analyses were conducted to assess whether or not variations in the model structure, time horizons, cost, utilities or outcome probabilities would alter the conclusions of the primary analysis. The costs, effects, ICERs and probability of cost-effectiveness at each threshold were re-estimated for each sensitivity analysis. An overview of the sensitivity analysis (assumptions tested) is provided in Appendix 11.
Results
The results of the primary and sensitivity analyses are presented below, along with estimates of uncertainty attributable to variation in the data used. The results are based on the limited data available. In particular, the model relied on service use and clinical data from the BSL-IAPT and standard IAPT data sets. Accordingly, it may well be that there is additional uncertainty due to the quality of the data and any differences between the demographic and clinical characteristics of the participants in the two types of IAPT service.
Primary analysis
The results of the primary analysis are shown in Table 29, when BSL-IAPT is compared with standard IAPT using the service-/language-specific PHQ-9 and GAD-7 scales and cut-off points for depression/anxiety. This indicates that BSL-IAPT is associated with a net saving of £240 per patient (SD £832 per patient; 95th percentiles –£2303 to £935).
| Outputs | IAPT group | Incremental difference | |
|---|---|---|---|
| BSL | Standard | ||
| Costs (£) | |||
| Mean | 2977 | 3218 | –240 |
| SD | 462 | 855 | 832 |
| 95th percentiles | 2108 to 3921 | 2003 to 5323 | –2303 to 935 |
| QALYs | |||
| Mean | 0.719 | 0.717 | 0.001 |
| SD | 0.033 | 0.034 | 0.006 |
| 95th percentiles | 0.653 to 0.780 | 0.648 to 0.781 | –0.009 to 0.013 |
| ICER | Dominant | ||
| Mean net monetary benefit per patient (if willing to pay £0 for an additional QALY) | £240 | ||
| Mean net monetary benefit per patient (if willing to pay £20,000 for an additional QALY) | £264 | ||
| Mean net monetary benefit per patient (if willing to pay £30,000 for an additional QALY) | £276 | ||
| Probability BSL-IAPT is cost-effective (if willing to pay £0 for an additional QALY) | 55% | ||
| Probability BSL-IAPT is cost-effective (if willing to pay £20,000 for an additional QALY) | 56.7% | ||
| Probability BSL-IAPT is cost-effective (if willing to pay £30,000 for an additional QALY) | 57.7% | ||
However, the 95th percentiles cross zero, indicating uncertainty about whether BSL-IAPT is associated with a net saving or net cost. The model predicts that BSL IAPT services are associated with a very small gain of 0.001 QALYs. Again, the 95th percentiles cross zero, indicating uncertainty about whether BSL-IAPT is associated with a QALY gain or loss. The cost-effectiveness plane in Figure 30 illustrates this uncertainty. Each dot represents a net cost–QALY pair from the Monte Carlo simulation. The figure shows that most of the points lie below zero, suggesting a net saving and that more of the points are towards the right, suggesting a net gain in QALYs.
FIGURE 30.
Cost-effectiveness plane: distribution of net costs and QALY pairs. WTPT, willingness-to-pay threshold.

The incremental cost-effectiveness acceptability analysis suggests that there is a 57% probability that BSL-IAPT is cost-effective if decision-makers are willing to pay £20,000 to gain 1 QALY; this increases slightly to 58% if decision-makers are willing to pay £30,000 per QALY gain. The cost-effectiveness acceptability curve in Figure 31 demonstrates that the probability that BSL-IAPT is cost-effective changes as the amount that decision-makers are willing to pay to gain 1 QALY changes.
FIGURE 31.
Cost-effectiveness acceptability plane. WTPT, willingness-to-pay threshold.
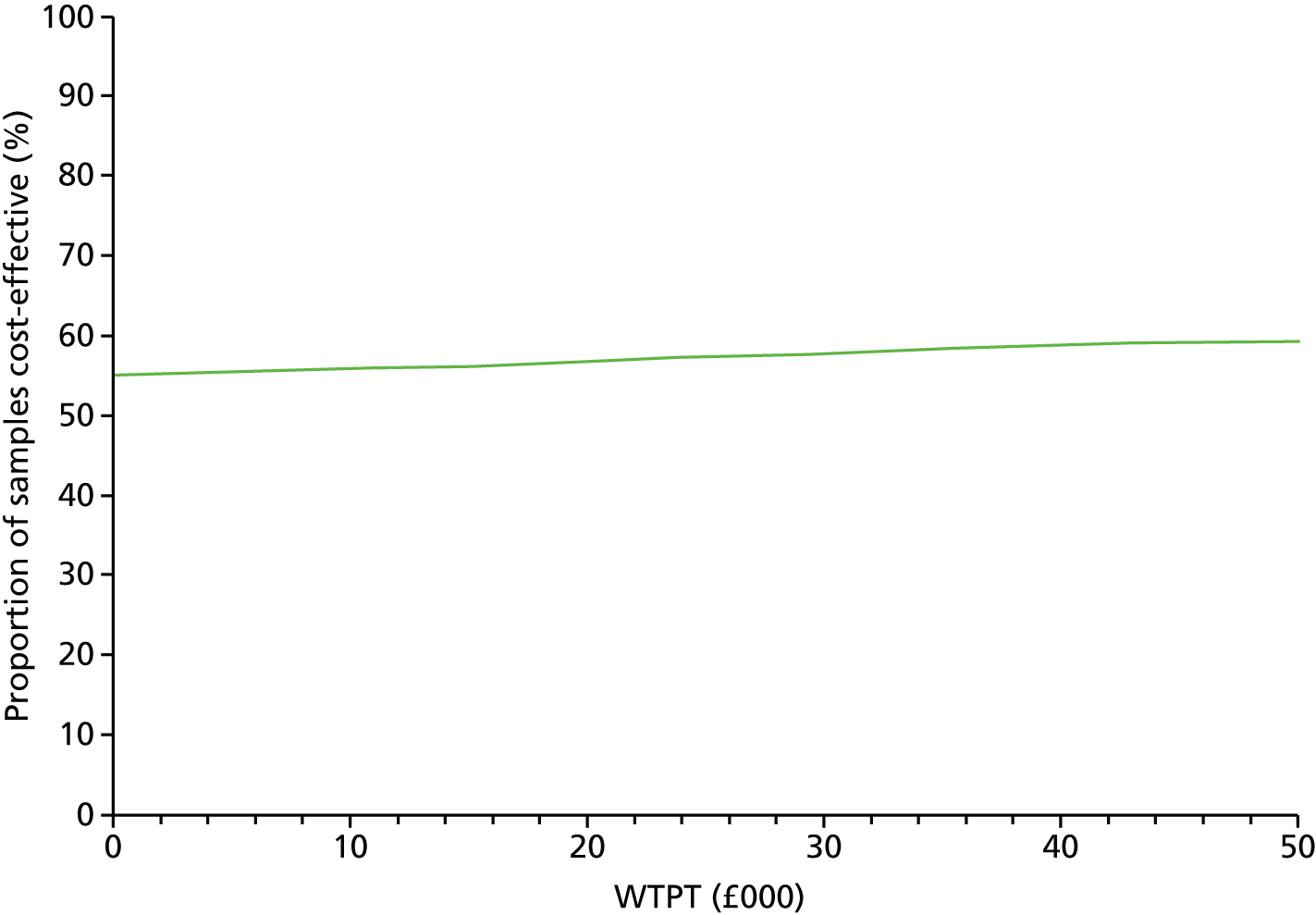
Sensitivity analysis
The full results of the sensitivity analyses are reported in Appendix 12, Table 39. Most of the sensitivity analyses indicated that BSL-IAPT was likely to be cost-effective even if decision-makers were not willing to pay anything to gain 1 additional QALY (probability of being cost-effective was > 50%). There were some exceptions to this. First, if the costs of an interpreter were excluded from the costs of the standard IAPT service, there was a net cost associated with BSL-IAPT of £307 (95th percentiles –£751 to £1155). The net gain in QALYs remained the same as for the primary analysis. The net cost per QALY gained was £256,224, with a 22–26% likelihood that BSL-IAPT could be cost-effective.
Second, the BSL-IAPT service was constrained to providing primarily low-intensity services, whereas standard IAPT services had more capacity to provide high- and low-intensity service. We performed a sensitivity analysis to explore the extent to which the cost-effectiveness of BSL-IAPT may change if it was possible to offer low-intensity services to more people. This increases the costs of BSL-IAPT and reduces the probability that BSL-IAPT is cost-effective to < 50%. It is important to note that this is a very exploratory analysis. What both of the sensitivity analyses demonstrate is that the costs of interpreters for standard IAPT and whether or not BSL-IAPT is able to provide high-intensity care are potentially important factors to consider in future service development and research.
Discussion
Summary of findings
The primary analysis indicated that BSL-IAPT may be more cost-effective than standard IAPT. However, there is uncertainty within the estimates and so this result is not conclusive. As noted in the previous section, limited data and reliance on the IAPT data also mean that the robustness of the results is uncertain. Even if decision-makers are not willing to pay an additional cost to gain 1 QALY, BSL is > 50% likely to be cost-effective. This is when the BSL version of the PHQ-9 and GAD-7 and BSL cut-off points are applied to the BSL-IAPT service to define whether or not a person has depression, reliable recovery and reliable improvement, and the English versions are applied to the standard IAPT service. The sensitivity analysis indicated that applying the same language and cut-off points for these measures to each service did not substantially change the conclusion.
Most of the sensitivity analyses indicated that BSL-IAPT was likely to be cost-effective even if decision-makers were not willing to pay anything to gain 1 additional QALY, with a probability of being cost-effective of > 50%. There were some exceptions to this. First, if the costs of an interpreter were excluded from the costs of the standard IAPT service, the net cost per QALY gained by BSL-IAPT was £256,224, with a 22–26% likelihood that BSL-IAPT could be cost-effective. Second, if the BSL-IAPT was able to offer high-intensity services to more people, the costs of BSL-IAPT increase, reducing the probability that BSL-IAPT is cost-effective to < 50%.
Nevertheless, there were limited data available with which to estimate the different variables in the model, so that there is a high level of variance and uncertainty in the estimates of the costs and QALYs associated with the two services. In addition, although in principle a 50% probability of cost-effectiveness may be interpreted as BSL-IAPT being cost-effective, or similar to standard IAPT, the uncertainty in the data means that the results are best treated as equivocal.
Limitations
Scope and model structure
The objective of this study was to identify whether or not BSL-IAPT is potentially cost-effective compared with standard IAPT services accessed by Deaf people with reasonable adjustments. It does not consider a potential third option (a specialist service for Deaf people with the standard IAPT service on which there are limited data; see Chapter 5). In addition, it does not compare the cost-effectiveness of IAPT services against alternative service configurations and designs.
A number of assumptions were made, and constraints placed on the scope of the analysis, to deal with limited data availability. These increase uncertainty about the robustness of the results. The time horizon was limited to 12 months for the primary analysis, which is relatively short for evaluations of interventions for depression, which is often a long-term condition. The short time frame increases uncertainty about the potential cost-effectiveness of BSL-IAPT. However, the sensitivity analyses, using longer time horizons of up to 10 years, indicate broadly similar results.
The costs and consequences associated with adverse events linked with psychological therapy were not explicitly included in the decision tree part of the model. These data were not included in the IAPT data sets used to estimate variable values for the decision tree. A recent national survey of people who had received psychological therapy found that 5% of people reported lasting bad effects. 161 These included the worsening of existing symptoms and the onset of new symptoms. It may be that the costs and consequences of these types of effects are included in the model indirectly through the probability that service users experience partial or full recovery, and the subsequent costs and QALYs associated with that.
Difficult experiences and therapist effects while receiving therapy may also contribute to services users stopping or dropping out of therapy. 161,162 Again, these effects are not directly included in the model, which may overestimate the benefits of treatment and underestimate the costs. However, whether either the long-lasting or shorter-term bad effects differ between the BSL and standard IAPT services is unknown. The national survey data161 indicate that the rate of lasting bad effects was similar across all types of psychological therapy, including IAPT services.
The decision section of the model was restricted to treatment provided by IAPT and excludes the cost and QALY consequences of referral to other services in the first 6 months following referral. The BSL and standard IAPT data sets and the wider literature did not include sufficient data about the number and type of referrals to include these in the model. If the rate of referrals to other services differs between BSL and standard IAPT, then this will affect the relative cost-effectiveness of BSL-IAPT. The model also excluded the use of other primary care- and community-based health and social care services, as well as the use of secondary care services. This restricts the scope of the analysis and will underestimate the total costs of each service. However, whether or not excluding these costs from the model will affect the relative difference in the costs of the two services is unclear. There is evidence from evaluations of IAPT service that service users access other primary, community and hospital services. 163,164 However, whether or not there are differences between standard and BSL IAPT in the use of these services by Deaf people with depression/anxiety is unknown.
The impact of any differences in waiting times between referral and the start of treatment was not included in the economic model. There were no statistically significant differences in waiting times between the BSL and standard IAPT in the data sets used for our analysis. In this instance the constraint is unlikely to affect the results and conclusions drawn from the analysis. However, waiting times may be important for future analyses if delays affect the probability of reliable recovery or improvement following treatment or the intensity and duration of treatment required. There is a limit to how many BSL-fluent health-care workers are available (whether Deaf or hearing). If tailoring services to meet the needs of Deaf people by employing BSL-fluent workers is cost-effective, then such workers will be in demand. It is plausible that demand will outstrip supply, especially if the services considered are not solely limited to IAPT. This may lengthen waiting times for treatment.
Additionally, in the long term, health-care workers may need to be educated in Deaf awareness and be trained to a fluent level in BSL and/or additional Deaf, BSL-fluent individuals will need to be trained as PWPs, to cope with demand. This would incur additional costs (both time and money), over and above those included in the economic model. Future work may need to consider including the longer-term costs associated with training.
It is possible that having a specialist service for Deaf BSL users will raise awareness of the IAPT service, especially in a group faced with communication barriers in standard services. This raised awareness of the service may increase demand for and attendance at the services, which would lead to greater costs but also the potential for increased health benefits at a population level. It was beyond the scope of this study to incorporate future changes in the demand for and supply of IAPT services in the economic model.
Data
The validity and robustness of the results of this economic evaluation are dependent on the quality and completeness of the data included in the two IAPT data sets. A number of limitations and issues about the data are discussed in Chapter 4. Additional limitations in the range of data used for the economic model are discussed in this section.
The search used to identify existing economic and clinical evidence to inform the economic model was focused and systematic, and pre-specified inclusion and exclusion criteria were applied to identified studies. Time and resource constraints meant that it was not feasible to conduct a comprehensive search of the literature or to have two independent reviewers screen and extract data, and quality appraise each of the articles selected. However, as the objective of this review was to inform the modelling approach and fill in gaps in the data available from the IAPT data sets, rather than to inform full quantitative or qualitative comparison of the literature, this method was judged to be sufficient for purpose.
There is a paucity of available literature on health-care use by the Deaf BSL population. In some instances, evidence for the hearing (or not specified) population had to be used. This increases uncertainty about the longer-term costs and QALYs estimated for both BSL and standard IAPT. Even when data from the general population were used, there were limitations in the data available to estimate some parameters. For example, only one study that reported total health-care costs for people with depression at a national level (not restricted to patients receiving certain treatments) was identified.
The economic model estimates the costs and QALYs for 1 year after a person’s first contact with the service (i.e. the time horizon is 1 year), for the primary analysis. This is because the majority of the data used to inform the model are from short-term studies (in particular the IAPT data which we rely on for key parameters), which means that the analyses of longer time horizons are associated with greater uncertainty. Trials for interventions for depression tend to have shorter time frames, with few studies with a follow-up of > 12 months. 165 This may be why past economic evaluation modelling studies have focused on shorter time frames. 166
The target population for the economic model was Deaf BSL users with depression and/or anxiety. Originally, it was planned to analyse the diagnosis groups separately (e.g. for people who had depression only). However, the majority of the participants in the data sets had both anxiety and depression (75.9% in standard IAPT and 81.6% in BSL-IAPT). Having both diagnoses is recognised as being common in the literature. 143–146 Breaking down the data to estimate parameters for these subgroup analyses would mean relying on data from very small groups. Given that the data were already limited by sample size, we focused on the group as a whole.
There have been wide variations reported in the percentage of people recorded as having experienced a recovery following IAPT treatment across England (18.8–69.4%). 147 Variation is likely to be even more marked in the standard IAPT data. Within standard IAPT, Deaf BSL users may see therapists who have a varying knowledge/awareness of the Deaf community and BSL. Our data come from a limited sample (in particular the data for Deaf BSL users accessing standard IAPT services). It is not clear whether this over- or understates the variability of treatment provided and recovery that would be found nationally.
The intensity or step level of service with which a Deaf client might engage could also be influenced by the availability of a specialist provider (e.g. in order to have a Deaf therapist a client might need to engage with the service at step 3 because that is where the Deaf therapist was located when in reality they might require only step 2). It is not possible to identify whether intensity level was determined by availability rather than need in the IAPT data sets used in this study.
The economic modelling work relied heavily on data from Chapter 4 (study 2); these are the only data available for Deaf BSL users accessing either IAPT service. Within the model we have compared the service options and we have tried to make best use of the data we had available to us, assuming that these groups are comparable. However, the results must be interpreted with caution because we cannot fully assess how similar the two populations were at baseline owing to inconsistent data reporting between services. Thus, the results may have been influenced by different population characteristics rather than the service interventions. It is important to note that this limits the robustness of the economic evaluation.
There are also some questions about how comparable the data on the two service options are. For instance, BSL-IAPT is reliant on low-intensity interventions, with few services offering high-intensity treatment. This means that service users for whom high-intensity treatment may be more suitable are restricted to low-intensity treatment. This affects the duration and costs of treatment in the short term and could affect the probability of recovery. The reliance of BSL-IAPT on low-intensity treatment also restricts the possibility that a patient can be moved to a higher-intensity treatment that is appropriate for their needs. In addition, we know little about which treatments were offered within each of the services, and some of the variation in outcomes may be explained by this.
What this study adds to the evidence base
This is the first study to use an economic model to synthesise data from different sources and explore the potential cost-effectiveness of a service that has been specifically adapted to meet the cultural and linguistic needs of the Deaf BSL population in the UK. Although there are several limitations to the structure of the economic model used and the available data, the analysis provides an initial indication of the costs and QALYs of BSL and standard IAPT. The primary analysis indicates that BSL-IAPT may be more cost-effective than standard IAPT. Much of the sensitivity analysis to explore the impact of assumptions and data limitations appears to support this conclusion. The sensitivity analyses identified two key variables that affected the costs of each service and probable cost-effectiveness of BSL-IAPT. The first was the costs of interpreter services to facilitate access to standard IAPT care for Deaf BSL users. The second factor was the intensity of services provided by BSL-IAPT. If BSL-IAPT services are not constrained to providing primarily low-intensity services, in the future this could increase the costs of treatment and may improve the recovery rates above what was found in this study.
Key findings
-
A new cost-effectiveness model, evaluating the potential cost-effectiveness of BSL-IAPT in comparison with standard IAPT for Deaf BSL users, has been developed.
-
The costs of BSL-IAPT over 1 year were estimated to be £2977 compared with £3218 for standard IAPT. This indicated a net saving for BSL-IAPT of £240 (95th percentiles –£2303 to £935). However, the 95th percentiles cross zero, suggesting that the difference in costs may have occurred by chance.
-
The QALYs associated with BSL and standard IAPT were very similar, at 0.719 and 0.717, respectively. Again, the 95th percentiles overlapped, indicating that this small difference may have occurred by chance. The simulation and cost-effectiveness acceptability analysis indicated that, overall, there was a > 50% chance that BSL was cost-effective. Key factors that could change the cost-effectiveness of BSL-IAPT are the costs of interpreter services for standard IAPT and the range of services provided by BSL-IAPT.
-
The model structure and variable estimates were limited by the range and quality of data available. This means that the results are preliminary and uncertain.
Chapter 8 Discussion and conclusions
Introduction
The two overarching research questions underpinning this study are:
-
Is BSL-IAPT more effective than standard IAPT for Deaf people with anxiety and/or depression?
-
Is any additional benefit from BSL-IAPT worth any additional cost to provide it?
These questions originally were prompted by an unexpected, naturally occurring experimental condition. It resulted from the establishment of a specialist IAPT service designed to meet the needs of Deaf people who signed and available in a limited number of regions in England at the same time as Deaf people elsewhere were accessing the standard IAPT service with various adaptations to meet their linguistic needs. Our original intention was to use this natural experiment to design a RCT to address these core questions. However, it rapidly became apparent that a great deal of groundwork was required prior to considering any large-scale study, whether a randomised clinical trial or other controlled, prospective study design. This was because of the complexity of the research context and lack of some key components to carry out research in this field successfully. The various elements of the study reported here were designed to address these deficits, gauge the feasibility of a larger-scale study and inform its future design. Each of the studies reported here has also resulted in stand-alone products that contribute to future health research with Deaf people in general. Collectively, the results enable a nuanced assessment of the probable direction and feasibility of future research in this specific topic, as well as extending the current evidence base in this under-researched area of practice.
Establishing British Sign Language versions of assessment tools and methods
EQ-5D-5L version British Sign Language
This study has produced the first validated translation into a signed language of any of the suite of EQ-5D assessments. Its psychometric properties were demonstrated to be good, indicating that it can be used to measure the health status of Deaf individuals in the UK who use BSL. Its test–retest reliability for each dimension of health was in the range of moderate to good, and was, therefore, acceptable. This, with the previously validated BSL version of the CORE-OM,134 provide new validated tools to assess the overall and mental health status of Deaf individuals, whether from a clinical or research perspective. Both measures provide preference weights that can be used to estimate QALYs and compare the costs and health benefits of intervention within specific conditions and across conditions. 133
The EQ-5D-5L BSL opens up the possibility of a new era of research, testing out the effectiveness of health and lifestyle interventions, whether targeted specifically at Deaf BSL users or through the inclusion of this population in general health research. Previously, Deaf people were excluded from health research because of the lack of availability of a common assessment tool that is validated for this population. This is a significant step forward for a population who are known to experience poorer physical and mental health than the general population and where research effort to remedy this situation has been hampered by a lack of means of reliable measurement of health status and change.
The EQ-5D-5L BSL has been accepted by EuroQol, which will be made available for future use without restriction. It has also opened up the possibility of other countries seeking a validated and reliability tested version of the instrument in their own sign language and therefore is of international significance in the field. The protocol for translation of the instrument into a signed language and the results of the investigation into the psychometric properties of the EQ-5D-5L BSL are published. 130
The results of this study indicate that health status and associated utility values published for the general population may not be generalisable to the Deaf population. The mean utility in this group was nearly 10% lower than the general population published norms. In addition, depression and anxiety are shown to be more prevalent in this group. Statistical analysis indicated that, as may be expected, utility values for people with depression may be lower than for people without.
Our results provide EQ-5D-5L utility values relevant to a Deaf population, which have previously been unavailable. However, there are some limitations. In particular, the study sample (n = 92) is too small to draw strong conclusions. The sample of bilingual Deaf people who assessed agreement between the English and BSL versions of the EQ-5D-5L was small (n = 11). However, the 11 participants’ responses agreed perfectly on four of the five domains of the EQ-5D-5L. The only domain that showed any disagreement was the pain/discomfort scale, where one participant reported no pain or discomfort when using the BSL version, but slight pain or discomfort using the English version. Nevertheless, it is possible that a larger sample would show less agreement between the versions. The estimated weighted kappa scores used to assess test–retest reliability of the BSL EQ-5D-5L version were between 0.47 and 0.61. The kappa scores were in the moderate range (0.41–0.60) for three of the five domains and in the good range (0.61–0.80) for the other two. However, the 95% CIs for the scores were wide and the lower limits of the 95% CIs extended well into the fair and poor ranges for anxiety/depression and self-care respectively. This suggests some uncertainty about the test–retest reliability of the BSL EQ-5D-5L.
Added to these factors, the sample of participants were recruited online, which may limit how representative this sample is of the wider Deaf population. Nearly 9% of Deaf participants in this study stated they did not know if they had health difficulties. The limited interview data from this study indicate that Deaf people’s responses to the EQ-5D-5L may be mediated by their experiences of communication barriers and their experiences of accessibility of services in BSL rather than only the severity of symptoms. Combined with the small sample of Deaf participants, this indicates that further work is needed to establish norms for the EQ-5D and associated utility weights for the Deaf population. These issues also indicate the need for further work before we can assess and compare the impact of mental and physical health conditions on health and utility.
Calculating the clinical cut-off points for the PHQ-9 item British Sign Language and GAD-7 British Sign Language
Our previous studies33,88 produced the validated and reliability tested BSL versions of the PHQ-9 and GAD-7 that were adopted by IAPT for use with Deaf BSL users. A short guide on the availability of the BSL assessments and how they might be used in clinical practice has been produced by the current study as a new resource (see Appendix 9). Extending our work, we have now also established the appropriate clinical cut-off points for these instruments for use with the Deaf population in the UK. This has increased the validity of their use in clinical practice, which is an ongoing legacy of the study. It has also enhanced their validity for research purposes in ensuring the more accurate identification of caseness and evaluation of clinical outcomes.
We have demonstrated that clinical cut-off points for PHQ-9 BSL and GAD-7 BSL are 8 and 6, respectively. This compares with the original English version cut-off points in the hearing population of 10 and 8, respectively. The three different statistical choices for calculating clinical cut-off points (equalising, maximising and prioritising false-negative to false-positive ratio ≈1 : 2) all showed a lower clinical cut-off point for the Deaf population with respect to the PHQ-9 BSL and GAD-7 BSL, with the exception of the maximising criteria, when used with the PHQ-9 BSL. 85
Whether Deaf people are treated by a BSL-IAPT service or by a standard IAPT service, establishing the correct clinical cut-off points for the BSL instruments will ensure first the appropriate identification of caseness. This is important because of the long-standing history of Deaf people in mental health services being subject to both under- and overdiagnosis because of the complexity of assessment in signed languages and/or the absence of such assessment in the patient’s first language. The lower cut-off scores will avoid Deaf people in need of support being turned away from treatment, notwithstanding the fact that entry into treatment is in part a clinical judgement, not just a result of score alone. The correct cut-off scores will also contribute to more accurate assessment of recovery and/or requirement for further treatment, thus preventing the early discharge of Deaf people when further treatment is necessary. Finally, the application of the appropriate clinical cut-off scores will enhance the reliability of the mandatory data flow from IAPT services to the HSCIC, with respect to Deaf people in terms of meeting caseness, reliable recovery, reliable improvement and deterioration.
The primary limitation of this study was that the cut-off scores were not able to be verified through psychiatric interviews, which is the gold standard for this kind of clinical research. Instead, the methodology used discrimination between a group defined as having a mental health problem and a group who self-reported as not having a mental health problem. Although we consider that the choice of methodology was robust, it is different from that used by the originators of PHQ-9 and GAD-7. The inclusion of a clinical interview would be required in order to validate further the clinical cut-off points for PHQ-9 BSL and GAD-7 BSL. In addition, the well group comparator was derived from an anonymous data set of a pre-existing study. This meant that further information about the sample could not be collected with which to judge their comparability with the clinical data set sample.
Feasibility considerations
Acceptability of randomisation
Deaf people have few opportunities to access a health service available directly, without the requirement for a sign language interpreter, that is, delivered by Deaf practitioners and culturally matched to client needs. The gold standard of single study designs to evaluate effectiveness, safety and cost-effectiveness is the well-designed randomised clinical trial. A key component of the decision whether or not a RCT is feasible and acceptable is if randomisation is acceptable to Deaf people. In the published literature, there was no prior study of the acceptability of randomisation among Deaf people. Furthermore, Deaf people have historically been routinely excluded from RCTs. This means that there was little pre-existing knowledge or understanding among Deaf people about the meaning of randomisation, its implications, the potential benefits of participation in such studies and the basis on which informed choices about participation might be made. Our study with a small sample of people drawn from the Deaf community first equipped participants with knowledge and understanding about RCTs and key terminology and its meaning before exploring participants’ views, considerations and conclusions about the acceptability of randomisation.
The study demonstrated the strong influence of culturally rooted considerations from a whole community (rather than individual) perspective on the acceptability of randomisation. The four main influences on Deaf people’s attitudes and conclusions about the acceptability of randomisation were:
-
Research involving randomisation is perceived as a subset of research in general, which, provided it benefits Deaf people both currently and in the future, is considered acceptable.
-
Randomisation can be perceived as an example of forced choice without the individual exercise of agency, which is a common experience for Deaf people and on that basis may be unacceptable.
-
If randomisation implies not having personal linguistic preferences and cultural needs met, then it is of itself seen as a potential threat to personal well-being.
-
Randomisation may be resisted on grounds of its perceived denial of the value of Deaf people’s common sense, knowledge and belief of what is best for them, which happens often in Deaf people’s lives.
These results do not rule out the possibility that randomisation would be acceptable in future trials. They do highlight the need to attune future research to those aspects of culture, value and experience that would be important to take into consideration when deciding how potential Deaf participants should be informed about such a study. However, before this can happen, the findings of this first, small, study need to be further investigated with a larger sample of Deaf community members to ascertain the extent to which they are recognised as valid. This would help lay the groundwork required to develop appropriate participant information and recruitment strategies for specific trials. 167
In itself, this study adds to the small body of pre-existing work that has considered cultural influences on attitudes to randomisation. It highlights the importance of considering the influence of previous experiences of lack of control in decision-making that are rooted in power imbalances between populations of different social status. They include the historical denial of the legitimacy or primacy of cultural identity. In this case our findings bridge the concerns of post-colonial perspectives on the Deaf community7 and acceptability of randomisation and the work conducted by others to understand recruitment challenges in the hearing population,167 in a novel way. The principal limitation of the study was the small number of participants, who may not have been representative of the full diversity of Deaf people.
Trial-related terminology
Parts of this section have previously appeared in Young et al. 34 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The text below includes minor additions and formatting changes to the original text. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. When paragraphs are repeated here verbatim, they have been displayed as quotations with reference to the original paper.
A key barrier to Deaf people’s participation in any future study based on a trial design has been the lack of appropriate terminology, means of expression and general understanding of key concepts used in study information and recruitment materials. Although the general literature is replete with studies of a range of aspects of (in)accessible information and its consequences for participant recruitment, there has been no similar study undertaken with respect to a signed language in general, or BSL in particular. Our study explored the strengths and capacities of a signed language to aid understanding and prevent misunderstanding about key concepts such as ‘trial’, ‘informed choice’, ‘randomisation’ and ‘consent’. The focus was not on the translation of key terms. Rather it was on how to support understanding to permit informed choice about participation in randomised trials. Key to this were the characteristics of the particular language concerned – BSL – and the low levels of background knowledge among many Deaf people on which they might draw in reaching a personal decision whether or not to participate in a clinical trial. This study has been published in Trials34 and provides an evidence-based means of refining study recruitment materials in research involving Deaf people. It lays the groundwork for confident production of recruitment materials in any future study we may undertake about the effectiveness and cost-effectiveness of BSL-IAPT. Additionally, we have produced an online glossary and resource in BSL (and English) for other researchers considering undertaking work in this field. This is being made freely available as an additional output of this study.
The six principles we developed for accessible, acceptable, accurate, culturally attuned information production for recruitment are not just of specific relevance to studies involving signed languages other than BSL. They also apply to the further development of written and spoken information for hearing participants for whom the majority language (English) is not their first or preferred language. They are reproduced verbatim:34
1. A community-participatory, exploratory approach to arriving at appropriate clinical trial terminology is highly effective in instances where languages, in this case BSL, have not yet had the contact with a topic that would mean a common vocabulary/preferred means of expression has developed
2. Languages have properties associated with their form and grammar that naturally enable some approaches to explanation to support comprehension that others may not. In this case, verb directionality, expectations of specificity and simultaneous contextual, semantic layering within expressions enabled features of the underpinning trial design to be clarified and remain consistent
3. It is important to take into consideration bilingual influences on comprehension even when information is presented monolingually; this is a decoding strategy for unfamiliar terms and concepts that is available to those who are bilingual and multi-lingual and can be a source of both strength and misunderstanding
4. Orientation of information to avoid misunderstanding is an important axis to consider when creating new information for a cultural linguistic group unfamiliar with the topic. It is subtly different from an orientation designed to support comprehension and may, as in the case of the sample in this study, be a preferred orientation
5. The researcher should understand cultural, contextual or social barriers that participants might face in engaging in open, constructive discussions of the information materials and consent procedures, over and above those that might be created by language per se. In the case of Deaf people, these barriers might derive from negative historical experiences of the education system, and class differentials
6. Clarity of expression, in the sense of plain language or avoidance of jargon, is not sufficient to promote comprehension. Attention to language-in-use in contemporary discussion is an important means of expression to effectively communicate complex concepts because it reflects common cultural usage. Simple, straightforward language may still seem alien if it not recognisable as something shared and used within a given community.
Young et al. 34
The principal limitations of this study are that those who participated are not necessarily representative of the diversity of people in the Deaf community. They engaged with data collection on only two occasions, and with more time and exposure to the new ideas presented they may have made a greater and more diverse contribution.
Population identification
During the course of this study, the full extent of the difficulties in identifying Deaf users of IAPT services has become clear, and considerable inconsistencies in the recording of client information were identified. Both factors will affect decision-making about the type and design of any future study.
The biggest barrier to efficient secondary data analysis of Deaf client records is that there is no preferred language field requirement in the minimum data set upload from IAPT to the HSCIC; therefore, BSL users are not easily identifiable. The disability field ‘hearing’ will also not distinguish BSL use. The alternative means of identifying whether or not a service had seen a Deaf client proved possible but resource intensive and of limited value for the research question. This was to mine the records of the data management systems that IAPT services use because those contain an optional field for language use and we demonstrated that this could be used to identify anonymised patient records for potential transfer for secondary analysis purposes. However, the requirement for individual service providers to give individual consent for a query to be run about BSL clients through the data management system storage central files meant that this approach was highly time-consuming and impracticable. We would hope that the transition to the Health Research Authority system and the wider debate that is currently taking place on secondary use of NHS patient records without individual consent would assist such work in the future, but this remains unsure. Therefore, we conclude that any future study involving Deaf patients of IAPT services would have to prospectively identify Deaf patients using enhanced versions of the current IAPT service records to ensure consistency and saliency with the research questions under investigation. Retrospective records will not be sufficiently reliable.
Our success in identifying 116 Deaf users of standard IAPT services, despite the challenges of transfer of secondary data for analysis, has enabled some comparative analysis of client characteristics and clinical outcomes of Deaf users of standard IAPT and of BSL-IAPT. However, it has not enabled us to estimate with any accuracy the numbers of Deaf people who might be using standard IAPT services now and, therefore, to predict potential throughput in the future and assess the feasibility of recruitment to a fully powered trial or a prospective observational study.
The sample of Deaf users of BSL-IAPT (n = 502) and Deaf users of standard IAPT (n = 116) nonetheless represents, to the best of our knowledge, the largest sample recorded in the research literature of Deaf users of primary mental health-care services anywhere in the world. These data and the analyses we have performed on them represent in themselves a significant contribution to knowledge in this under-researched field.
Clinical effectiveness
Service delivery
During the course of this study, the initial demarcation of BSL-IAPT (delivered by a sole specialist provider) from standard IAPT (that Deaf people might access) became increasingly untenable. This was because a few standard IAPT services had started to gain experience and chosen to invest in provision for Deaf people. Models of service and provider identity were no longer entirely synonymous with respect to BSL-IAPT. Therefore, we undertook a study, underpinned by a realist inquiry method, to model the components and key variations in delivery of both BSL-IAPT and standard IAPT accessed by Deaf people.
It is commonly acknowledged that there is a wide variation in how different IAPT programmes nationally deliver services while adhering to a common set of requirements specified by IAPT. This can be regarded as a strength because it enables a degree of flexibility in service delivery to be responsive to conditions of specific geographical, client or service context. Therefore, with respect to standard IAPT, we expected to see a range of approaches to meeting the requirements of Deaf clients. Our sample of participating services and IAPT practitioners was skewed to those who had some experience of Deaf people as clients and largely consisted of services that were already interested in this client group. It was not nationally representative. Two of the practitioners who responded worked in standard IAPT services which had set up a specialist pathway for Deaf clients which employed therapists who were either Deaf or good sign language users. However, with regard to the rest, the overall picture that emerged of poor, and to some extent discriminatory, practice was even more remarkable given the positive bias of the sample to those with interest and experience.
Key issues we identified include the following.
-
Awareness of the implications of using written forms of communication and information for the accessibility of the service for Deaf people in terms of initial (self-) referral, ongoing engagement, assessment and self-guided support is highly limited.
-
Understanding of the relationship between ineffective means of service promotion to Deaf people and limited numbers of Deaf clients using the service is poor; consequently, the service has to make few adaptations to meet their needs.
-
The choice of therapist for Deaf clients is very limited.
-
Therapists have little experience and understanding of how to use an interpreter and the implications of interpreter use for therapeutic work.
-
Poor or non-existent understanding of the additional barriers faced by Deaf people that may arise as indirect consequences of structural practices insisted on by services (e.g. referral through a GP, completion of an English-based written form at first triage, only direct communication by client rather than through a third party if self-referring).
-
Lack of understanding of the inaccuracies inherent in using the English forms of clinical assessment (whether or not with an interpreter) for accurate assessment of illness and recovery of Deaf clients.
-
Services display poor background understanding of the knowledge needs, rather than simply the linguistic needs, of Deaf people using an IAPT service arising from life-long deficits in information access and little prior experience of mental health services. Consequently, adaptations to the therapeutic experience other than interpreter provision are rare.
-
Service providers show very limited cultural competence, combined with a limited awareness that this might be missing in their approach to working with Deaf people because connections are not readily made between deafness and cultural identity, rather than disability.
-
No robust systems of equality impact assessment within routine monitoring of service delivery.
That said, engagement with the project itself served as a catalyst for some services to reflect on their current practices. Overall, there was an enthusiasm and willingness to provide the best service possible for Deaf clients, but services struggled to do this in the face of a lack of guidance, training and resources.
With regard to BSL-IAPT, in this case defined in terms of the original sole provider, three key components of the specialist practice and service were identified: (1) direct communication between therapist and client in a shared language (BSL) with no interpreter; (2) cultural insider positioning and cultural competence; and (3) service-related structures and practices. Each had advantages and limitations. Advantages included scope to tailor an intervention based on an in-depth understanding of clients’ background knowledge requirements, linguistic range/variation and cultural preferences. These were central to the ease of the therapeutic encounter, empathy and trust building. However, shared experiences, whether historical or contemporary, and the consequences for being known in multiple roles within small communities of practice could be disadvantageous to both client and therapist. Although specialist structures of service delivery ensured that therapists had a Deaf peer group, that ready specialist supervision was available and that there was understanding of how to ensure the service at point of referral could be accessible, the disadvantages included limited capacity and funding, a concentration of services at low-intensity therapy and a perception of long waiting times.
The principal limitations to this study consist of the small number of services and individual therapists who participated from standard IAPT and their bias towards positive interest in Deaf people, which meant that the sample was not representative. The focus on BSL-IAPT defined as one specialist service provider also had its limitations in the definition of service model components because of a lack of comparison with other BSL-IAPT services. Although through the modelling work we have undertaken we are in a position to produce a replicable description of standard IAPT for Deaf people and BSL-IAPT that could be operationalised in any future large-scale comparative intervention study, we acknowledge that this would need to be undertaken with care with appropriate fidelity checks. The boundary between these two apparently different interventions cannot be demarcated by specialist versus non-specialist service provider alone. Characteristics of the two approaches to psychological therapies for Deaf people under IAPT would have to be both defined and controlled, independent of service provider context, for a meaningful effectiveness study to be carried out.
Comparative clinical outcome data
Secondary analysis of available client outcome data demonstrated no significant difference between Deaf clients of standard IAPT and BSL-IAPT in terms of reliable improvement (63.5% vs. 66.8%; p = 0.917) and no difference in terms of reliable recovery (40.0% vs. 40.4%; p = 0.946). This analysis was based on defining completed treatment as attending a minimum of two therapeutic appointments. This is in line with the IAPT KPI definition of completion. 104 This excludes those people who needed only one appointment. It includes, as completed therapy, people whose treatment is ongoing. Using the tighter definition of completed therapy and using a verified endcode to identify patients whose treatment had finished, we found that reliable improvement was achieved in 76.5% of the 226 Deaf clients attending BSL-IAPT services while reliable recovery was achieved in 54.0%. That endcode was not included in the standard IAPT data we received for Deaf patients. Based on data collected across all IAPT services (general population) between October 2008 and September 2009,106 reliable improvement was reported in 64% of service users and reliable recovery in 40%. For data collected in March 2015, the HSCIC reported reliable improvement as 61.5% and reliable recovery as 43.1%. These figures were based on a recorded endcode that treatment had been finished. Rates of reliable improvement and reliable recovery from both sets of data based on a less rigorous definition of completion are comparable to those recorded for the general population of users of standard IAPT services based on early and current IAPT outcome data. However, these results should be treated with considerable caution.
First, although we are confident that the sample of Deaf clients from standard IAPT is Deaf people who use BSL, rather than the broader definition of deaf people/hearing impaired who use spoken language, it is drawn from a very small proportion of standard IAPT services nationally: 19 trusts and two private providers. Furthermore, this was a self-selecting sample of service providers. Therefore, the extent to which the sample is representative of the national picture is unknown, in terms of numbers of clients or clinical outcomes.
Second, the mean number of Deaf clients seen by standard IAPT services is two. Therefore, the combined reliable recovery and reliable improvement calculations for standard IAPT services are based on services with very little experience of Deaf clients in terms of number or clinical diversity. Consequently, the extent to which reliable recovery and reliable improvement rates would be maintained when faced with larger numbers and increased diversity of clients is untested. By contrast, the rates of reliable recovery and reliable improvement reported by BSL-IAPT are based on an experience by a single service of 349 clients.
Third, it was not possible with the data available to comprehensively look at deterioration and whether or not this differed between services. Adequate data on those clients who dropped out of therapy or who were referred out of the service were not available. Chapter 4 indicates that 3.5% of Deaf people in standard IAPT had reliable deterioration, compared with 6% in BSL-IAPT. This raises the question of whether this is a result of differences in samples and sample sizes, differences in types of service provided (e.g. only low-intensity services are mostly available in BSL-IAPT), or something else. Further investigation is required.
For a more robust comparison of clinical outcome data for Deaf users of standard IAPT and those of BSL-IAPT, an increase in both the quantity and the quality of the available data would be required. We calculate, for example, that if we are expecting a reliable recovery rate of 40%, we need at least 369 Deaf clients of standard IAPT in total, 40% of whom reliably recovered, to have a 95% CI of ± 5%. For a reliable improvement rate of 64%, we need at least 355 Deaf clients of standard IAPT. Our sample of Deaf clients of standard IAPT used for recovery calculations (n = 89) fell far short of this number. Furthermore, in the comparative analyses it should be noted that BSL-IAPT is a single-service provider with the same personnel (regardless of delivery location), whereas standard IAPT is made up of a number of different services with variable degrees of experience of Deaf people ranging from 1 client to 24 clients. This, combined with growing evidence about therapist effects on participant engagement and negative outcomes,162,168 increases uncertainty about the robustness and transferability of our comparisons of outcomes. To reduce uncertainty in the comparative analyses of clinical outcomes, a far greater number of Deaf clients would be required per standard IAPT service, whether a single service or a combined standard IAPT service.
The BSL-IAPT service was constrained to provide primarily low-intensity (step 2) care, with 93% assigned to low-intensity treatments, compared with 38% in the standard IAPT services. The figure for BSL-IAPT is nearly twice the rate of referral to low-intensity care found in the evaluation of the IAPT demonstration sites (48%). 168 This may indicate that some clients were not treated appropriately, but the available data make this difficult to assess. These differences in the intensity of care received by participants with similar clinical characteristics reduce the comparability of reliable improvement and reliable recovery outcomes.
Economic model
This is the first study to assess the potential cost-effectiveness of a service specifically adapted to meet the cultural and linguistic needs of the Deaf BSL population in the UK. Although there are several limitations to the structure of the economic model used and the available data, the analysis provides an initial indication of the costs and QALYs of BSL-IAPT and standard IAPT accessed by Deaf people. The primary analysis indicates that BSL-IAPT may be more cost-effective than standard IAPT for Deaf people. Much of the sensitivity to explore the impact of assumptions and data limitations support this conclusion. The sensitivity analyses identified two key variables that affected the costs of each service and probable cost-effectiveness of BSL-IAPT. The first was the costs of interpreter services to facilitate access to standard IAPT care for Deaf BSL users. The second factor was the intensity of services provided by BSL-IAPT. If BSL-IAPT services are not constrained to providing primarily low-intensity services, in the future this could increase the costs of treatment and may improve the recovery rates above what was found in this study.
The results from the economic evaluation are in many ways preliminary and exploratory. The evaluation was constrained by limited evidence in the published literature about the cost-effectiveness of IAPT and psychological therapy for people with depression/anxiety in the general population. Added to this were the limitations discussed in the previous section about the scope and quality of the data sets for Deaf people using either BSL-IAPT or standard IAPT. These data limitations constrained the range of events included in the economic evaluation and meant that a number of simplifying assumptions were required.
The economic evaluation considered only one model of BSL-IAPT. As noted in Chapter 5, a few standard IAPT services are developing specialist services for Deaf people within the standard IAPT service. This type of service could reduce the costs of IAPT service provision for Deaf people by reducing the costs of interpreter services. It could also mean that Deaf people are able, more readily, to access high-intensity services. These are the two variables highlighted by the sensitivity analyses to be important issues in whether or not BSL-IAPT was cost-effective.
Data limitations meant that the costs and consequences of adverse events (worsening of existing symptoms and emergence of new symptoms) and of service users stopping or dropping out of therapy161,162 were not explicitly included in the decision tree part of the model. In the longer term, the costs and consequences of these events are modelled indirectly through the probability that service users do not experience partial or full recovery and the subsequent costs and QALYs associated with relapse/recurrence.
The decision section of the model was restricted to treatment provided by IAPT and excludes the cost and QALY consequences of referral to other services in the first 6 months following referral. The BSL-IAPT and standard IAPT data sets and the wider literature did not include sufficient data about the number and type of referrals to include these in the model. The model also excluded the use of other primary- and community-based health and social care services, as well as the use of secondary care services. However, whether or not excluding these costs from the model will affect the relative difference in the costs of the two services is unclear.
There is the potential that having a specialist service for Deaf BSL users raises awareness of the IAPT service, especially in a group who are faced with communication barriers in standard services. This raised awareness of the service may increase demand and attendance for the services, which would lead to greater costs but also the potential for increased health benefits at a population level. It was beyond the scope of this study to incorporate future changes in the demand for and supply of IAPT services in the economic model.
Future research and study design
The two overarching research questions that have driven this study remain relevant. We have progressed towards their answer with the development of new instrumentation, opening pathways for identification of potential participants and accelerated recruitment. We have modelled the variability of components of service delivery and contextualised their impact on service access, therapeutic experience and clinical outcomes, and developed a viable economic model for assessing the cost-effectiveness of intervention. We have assembled the largest sample to date of Deaf users of primary mental health-care services, including client characteristics and clinical outcomes. Nevertheless, the robustness and validity of the data and analysis of comparative clinical outcomes of Deaf users of standard IAPT services and BSL-IAPT is weak.
Key reasons are the small number of Deaf clients seen by a small and highly variable sample of standard IAPT services in terms of their models of delivery; differences in the range of services provided by BSL-IAPT (primarily low-intensity services from a single-service provider) and standard IAPT (mix of high- and low-intensity services); and the limited scope of secondary data collected for other reasons. Therefore, although the analysis concluded that there was no statistically significant difference between clinical outcomes (reliable recovery and reliable improvement) for Deaf people using BSL-IAPT or standard IAPT, and that both compared favourably with national IAPT outcome data, these results are not definitive and to some degree misleading. Consequently, the initial question to compare the effectiveness of BSL-IAPT and standard IAPT for Deaf people remains inadequately answered. Evidence is also weak for the number of current Deaf users of IAPT, whether standard IAPT or BSL-IAPT. It is not possible to conclude whether or not the estimates of numbers required for a clinical trial or another prospective study design are realistic because the probable effect size cannot be estimated with any precision based on current analyses and available data.
Although this study has made significant strides in establishing the prerequisites for clinical outcome research in this specialist field, further work is required prior to proposing any large-scale definitive study. We see this as consisting of six elements.
Defining the intervention
We now understand the axes of variability in how standard IAPT approaches work with Deaf clients. In addition, we have demonstrated how BSL-IAPT may be defined by elements, which, in theory, could be reproduced in other contexts, including among standard IAPT providers. In saying this, we are not suggesting that the effects would necessarily be the same (that is, unknown), only that the elements that define BSL-IAPT are not necessarily confined to a single specialist provider. Therefore, although any future study may still be cast in terms of a comparison of BSL-IAPT with standard IAPT accessed by Deaf people, these would be closely defined in terms of elements of the intervention, rather than of the setting or provider. Fidelity to BSL-IAPT as a model of intervention that has been carefully defined (in its standards and practices) would be a key factor to control in any prospective study. Given the scale and diversity of contexts in which IAPT operates, such control and fidelity checks may prove challenging to operationalise.
Developing the context
Poor access to secondary data about Deaf users of IAPT has severely hampered this study, as have inconsistent clinical recording practices. This is in addition to the challenges in using secondary data sources that were typically not designed to address the research question of interest. Literature from which extrapolations can be made of population characteristics in general is also sparse. There is poor epidemiological evidence. Moving forward, therefore, we suggest the need for a well-executed mental health clinical observatory with respect to Deaf people to be established. This would:
-
draw down clinical data from a variety of sources on a national scale and maintain a database of information sources relevant to Deaf people with mental/physical health problems
-
review and summarise available evidence with a particular focus on Deaf people’s health profiles and unmet needs, inequalities and need for reasonable adjustments
-
identify key NHS and social care data gaps and gaps in the evidence base to inform future research priorities.
The observatory would support the design and implementation of health studies with this underserved population, who in legislative terms are a population with ‘protected characteristics’. Better baseline data, whether of health and social care needs, what is provided and what is known to be (cost-)effective, as well as central accumulation of current clinical data, would improve all studies undertaken in this field.
Determinants of recovery, service use and quality-adjusted life-years
Our studies thus far have revealed the scale of variability in service delivery and its effects on access and availability of service, as well as elements of good clinical practice. However, which elements make a difference, in terms of service model, therapeutic practice and/or client characteristics, is unknown. We therefore propose that there is value in a well-controlled prospective observational study from which it will be able to examine the relative influence of a range of participant demographic, socioeconomic and clinical characteristics, as well as service and therapist factors. We can then compare this with current knowledge of determinants of reliable recovery, reliable improvement and reliable deterioration in the general population of IAPT users. The results would enable better targeting of resources to specific elements of IAPT practice with and for the Deaf community.
The study would allow prospective measurement of service use and health status data to help address the data limitations faced in developing and analysing economic models of the cost-effectiveness of health-care interventions for Deaf people. In making this suggestion we are aware of the considerable challenges faced in this current study in accessing, transferring and verifying clinical and service data. However, the strategies and mechanisms established will support a scaled-up study.
Service user involvement
Service users have contributed significantly to the success of the study reported here. In terms of research participation, their consistent reminders of the significance of cultural meaning, not just linguistic accessibility, in decision-making, preference and attitude to elements of future research designs has been invaluable. However, missing from the work thus far has been any extensive exploration with Deaf users of IAPT of their experiences, perspectives, preferences and expectations. Such qualitative work would enhance the proposed study of determinants of recovery as well as the definition of interventions in future work. It would support the co-design of relevant and appropriate recruitment methods and participant materials. The PPI work undertaken alongside the current study has made its own distinct contribution to what counts as effective involvement in health research by Deaf BSL users and how to ensure this. It is an aspect of user-led contribution that could be developed much further because Deaf people’s involvement is often alongside that of other (hearing) stakeholders and this study has shown the benefit of Deaf-led and Deaf-only user involvement too.
Further instrumentation design and testing
Our results provide EQ-5D-5L utility values relevant to a Deaf population, which have previously been unavailable. However, the study sample (n = 92) is too small to draw strong conclusions. A larger prospective cohort study is needed to confirm our initial results and identify which sociodemographic and clinical characteristics (presence of physical and mental health conditions) are key influencers of health status and utility. Such a study should include BSL versions of depression and anxiety measures (CORE-OM BSL, PHQ-9-BSL and GAD-7-BSL) to accurately identify people with these conditions. This would allow an assessment of differences in health status and utility between Deaf people with and without depression/anxiety. Including hearing participants would support comparisons of health status and utility to assess the extent to which the health status and utility of Deaf participants differs to that of hearing participants and establish appropriate norms.
Further work is ongoing to identify a larger range of published utility values for the population with depression, via a systematic review, which will be compared with our sampled Deaf population data in more detail. This will help inform the design of the larger prospective study.
Economic evaluation considerations
Little is known about the long-term impact of IAPT on service users’ health status and use of health and social care services, in the Deaf or hearing populations.
Pathways for care and possible outcomes in depression and anxiety are complex and inter-related. A more complex modelling methodology such as a discrete event simulation may be able to more accurately model pathways for depression and anxiety, as more data become available.
Analysis of linked secondary data sources over longer time horizons (e.g. 12 months and 5 years) could be used to assess the range and intensity of services used. This could also help to fill in the gaps about health and social care services used at the same time as IAPT. Current data sets available include, via NHS Digital (HHSCIC), ONS mortality data; Hospital Episode Statistics; the Mental Health Minimum Data Set, which includes data on specialist secondary mental health service use; and the IAPT data set. Other sources include linked data via the Clinical Practice Research Datalink. This requires that Deaf BSL users can be identified in at least one of the secondary data sets to be linked. Currently not all HSCIC records/minimum data set requirements include language. It is important to note that data linkage and secondary analysis of these data is, however, complex and time-consuming.
Under the NHS Accessible Information Standard, NHS services in England should ask Deaf people if they have information or communication needs and find out how to meet their needs. 51,154 This may include offering an interpreter or advocate. QALYs measure preferences for different levels of health; however, they do not measure preferences for different types of care. Stated preference techniques would allow researchers to quantitatively assess Deaf BSL users’ preferences for different aspects of health care (e.g. the assistance of an interpreter or a specially designed BSL service), and to see how they trade these off against other health (e.g. recovery, health status) and process characteristics (e.g. waiting time, distance to travel).
Conclusion
The various components of this study have significantly moved forward the field of health/mental health research involving Deaf BSL users. Its legacy is new assessment and measurement tools that will enable Deaf people’s inclusion for the first time in a range of clinical and health research in the future; the largest data set of secondary primary mental health-care data on Deaf people available in the UK; and greater awareness among the Deaf community of participation in RCTs and the basis of better information in BSL to enable choices to participate. We have advanced knowledge with respect to the core questions with which this study began and in doing so revealed the weaknesses of available evidence from which to be able to draw definitive conclusions. We have also revealed the fragility of current systems’ abilities to appropriately identify and verify clinical data and to account for variability in provision with respect to Deaf BSL users, which is a potential impediment to the development of further robust evidence. We offer potential solutions to barriers that prevent us being able confidently to judge the effectiveness and cost-effectiveness of BSL-IAPT compared with standard IAPT accessed by Deaf people. These questions remain valid and important for the improvement of the mental health of a population of service users who experience higher rates of anxiety and/or depression than the general population and, therefore, for the attendant impacts on family life, economic well-being and wider contribution to society.
Acknowledgements
The authors would like to take this opportunity to thank everyone who supported this project, including (but not limited to) the following.
Project Advisory Group
We would like to thank our PAG members for their helpful advice and guidance throughout. We benefited from a diverse group of Deaf and hearing professionals, academics and service users: Jacqui Bond, Mary Griggs, Brenda Hamlin, Roger Hewitt, Deirdre Maguire, Robert Pollard and Merfyn Williams.
Study Steering Committee
We wish to extend our gratitude to our SSC members, for their invaluable input: Peter Bower, Alison Bryan, Chris Evans, Deborah Innes, Neil Pritchard, Eldon Spackman and Robert West.
Patient and public involvement group
We express our special thanks to those in our PPI group, all of whom are Deaf BSL users: Golda Dahan, Lulu Friedli, Brenda Hamlin, Janet Huntington, Peter Mowat, Merfyn Williams and Shelagh Whiteside.
Translators
Jim Cromwell, Jen Dodds, Rosemary Oram and Nicholas Padden.
National Institute for Health Research Clinical Research Network
The research team acknowledges the support of the National Institute for Health Research Clinical Research Network.
Contributions of authors
Our study team combines a diversity of methodological, disciplinary and professional backgrounds and includes Deaf and hearing academics.
Professor Alys Young (Professor of Social Work Education and Research, chief investigator) specialises in social research with deaf/Deaf people and social work. She led the overall study design and oversaw the management of all aspects. She led the analysis of studies 1 and 3, and contributed to the analysis of study 2, drafted Chapters 1–3, 5 and 8, and oversaw the production of the final report.
Dr Katherine Rogers (Research Fellow and Trial Manager, co-investigator) specialises in health services research with Deaf people. She co-designed the original study and was the trial manager (apart from October 2014–October 2015). She co-led study 2 and led on the translation and validation work in study 4, contributing to the data analysis of these studies and aspects of study 3. She led the drafting of Chapter 4 and part of Chapter 6. She contributed to the final editing of the report.
Professor Linda Davies (Professor of Health Economics, co-investigator) specialises in the economic evaluation of health care for mental health and complex conditions. She co-designed the original study, led study 5 (the economic evaluation model), and contributed to the writing of Chapters 6 and 8, and co-led the writing of Chapter 7. She contributed to the final editing of the report.
Dr Mark Pilling (Research Statistician, co-investigator) specialises in statistical methodology and analysis relating to complex interventions. He contributed to the design of the original study, led on the statistical analysis in study 2 and contributed to writing Chapter 4.
Professor Karina Lovell (Professor of Mental Health, co-investigator) specialises in developing and evaluating complex interventions. She co-designed the original study and contributed to the final editing of the report.
Professor Steve Pilling (Professor of Clinical Psychology and Clinical Effectiveness, co-investigator) specialises in clinical psychology research. He co-designed the original study and contributed to the final editing of the report.
Ms Rachel Belk (Research Associate and trial manager cover) specialises in genetic counselling, with an interest in Deaf people. She covered for the trial manager’s absence between October 2014 and October 2015. She led on the data management for study 2 and co-wrote Chapter 4. She oversaw the recruitment to studies 2 and 3, and related governance. She contributed to the final editing of the report.
Ms Gemma Shields (Research Fellow, Health Economics) specialises in economic evaluations of health care for mental health and complex conditions. She led on the utility weight exploratory analysis in study 4 and co-wrote the corresponding part of Chapter 6. She co-led the development of the economic model in study 5 and co-led the writing of Chapter 7.
Ms Claire Dodds (Research Assistant) specialises in social research with Deaf BSL users and interpreting. She contributed to the recruitment to studies 2 and 3, and to the analysis in studies 1 and 3. She also contributed to writing aspects of Chapters 3 and 5, produced the BSL glossary and contributed to the editing of the final report.
Dr Malcolm Campbell (Lecturer in Statistics) specialises in statistical support for non-statisticians. He provided additional statistical analysis for study 2 and co-wrote Chapter 4.
Ms Catherine Nassimi-Green (Research Assistant) specialises in social research with Deaf BSL users. She collected data for studies 1 and 4 and led on aspects of PPI. She contributed to writing aspects of Chapter 3.
Dr Deborah Buck (Research Associate, Health Economics) specialises in methodology, data management and data analysis. She contributed to the construction of some of the data sets, analysis of studies 2 and 5, and contributed to the writing of Chapter 6.
Ms Rosemary Oram (Research Assistant) specialises in social work. She collected data for study 1 and contributed to writing aspects of Chapter 3.
Publications
Young A, Oram R, Dodds C, Nassimi-Green C, Belk R, Rogers K, et al. A qualitative exploration of trial-related terminology in a study involving Deaf British Sign Language users. BMC Trials 2016;17:1–12.
Rogers K, Pilling M, Davies L, Belk R, Nassimi-Green C, Young A. Translation, validity and reliability of the British Sign Language (BSL) version of the EQ-5D-5L. Qual Life Res 2016;25:1825–34.
Belk R, Pilling M, Rogers K, Lovell K, Young A. The theoretical and practical determination of clinical cut-offs for the British Sign Language versions of PHQ-9 and GAD-7. BMC Psychiatry 2016;16:372–83.
Data sharing statement
Anonymised data sets pertaining to Deaf clients of BSL-IAPT and standard IAPT may be shared only with permission from the original trusts that have provided these as they are bespoke data extractions. It is not possible to anonymise data from Deaf people in BSL because of the visual nature of the language; therefore, these data sets could not be made available unless translated. Initial inquiries should be made via the chief investigator, Professor Alys Young.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Talking Therapies: A Four-Year Plan of Action. A Supporting Document to No Health Without Mental Health: A Cross-government Mental Health Outcomes Strategy for People of All Ages. London: DH; 2011.
- Sutton-Spence R, Woll B. The Linguistics of British Sign Language. Cambridge: Cambridge University Press; 1999.
- Smith A. Written Ministerial Statement on British Sign Language. London: Hansard; 2003.
- British Sign Language (Scotland) Act 2015. Norwich: The Stationery Office; 2015.
- Equality Act 2010 (Specific Duties). London: HMSO; 2011.
- Equality Act 2010. London: HMSO; 2010.
- Ladd P. Understanding Deaf Culture: In Search of Deafhood. Clevedon: Multilingual Matters; 2003.
- Young A, Ferguson-Coleman E, Keady J. Understanding the personhood of Deaf people with dementia: methodological issues. J Aging Stud 2014;31:62-9. https://doi.org/10.1016/j.jaging.2014.08.006.
- Young A, Ferguson-Coleman E, Keady J. Understanding dementia: effective information access from the Deaf community’s perspective. Health Soc Care Community 2016;24:39-47. http://dx.doi.org/10.1111/hsc.12181.
- Young A, Hunt R. Research With d/Deaf People. London: NIHR School for Social Care Research; 2011.
- Mayer C. What really matters in the early literacy development of deaf children. J Deaf Stud Deaf Educ 2007;12:411-31. https://doi.org/10.1093/deafed/enm020.
- Commentary Report for the GP Patient Survey: 2009/10 Annual Report. Ipsos MORI; 2010.
- Hulme C, Powell S. Working With People Who Are Deaf British Sign Language (BSL) Users, Oral Deaf, Deafened, Deafblind and Hard of Hearing. 2016. www.nwppn.nhs.uk/index.php/our-work/supporting-clinical-excellence/mental-health-deafness (accessed 28 February 2017).
- 2011 Census: Quick Statistics for England and Wales, March 2011. Newport: ONS; 2013.
- Llywodraeth Cymru/Welsh Government . British Sign Language (BSL) 2010. http://gov.wales/topics/people-and-communities/equality-diversity/rightsequality/language/BSL/?lang=en (accessed 28 February 2017).
- Scottish Council on Deafness . Statistics: Incidences of Deafness 2016. www.scod.org.uk/faqs/statistics/ (accessed 28 February 2017).
- Sign Language. Belfast: Department for Communities; 2016.
- Clark DM. Implementing NICE guidelines for the psychological treatment of depression and anxiety disorders: the IAPT experience. Int Rev Psychiatry 2011;23:318-27. https://doi.org/10.3109/09540261.2011.606803.
- Improving Access to Psychological Therapies Implementation Plan: National Guidelines for Regional Delivery. London: DH; 2008.
- Parry G, Barkham M, Brazier J, Dent-Brown K, Hardy G, Kendrick T, et al. An Evaluation of a New Service Model: Improving Access to Psychological Therapies Demonstration Sites 2006–2009. Final Report. NIHR Service Delivery and Organisation Programme. London: NIHR; 2011.
- NHS England . 2014 Adult IAPT Workforce Census Report 2015. www.ewin.nhs.uk/tools_and_resources/2014-adult-iapt-workforce-census-report (accessed 28 February 2017).
- Flynn H. Best practice: healthy minds for Deaf people. Health Couns Psychother J 2012;12:34-9.
- Fellinger J, Holzinger D, Pollard R. Mental health of deaf people. Lancet 2012;379:1037-44. https://doi.org/10.1016/S0140-6736(11)61143-4.
- Alexander A, Ladd P, Powell S. Deafness might damage your health. Lancet 2012;379:979-81. https://doi.org/10.1016/S0140-6736(11)61670-X.
- Hindley PA, Hill PD, McGuigan S, Kitson N. Psychiatric disorder in deaf and hearing impaired children and young people: a prevalence study. J Child Psychol Psychiatry 1994;35:917-34. https://doi.org/10.1111/j.1469-7610.1994.tb02302.x.
- Kvam MH, Loeb M, Tambs K. Mental health in deaf adults: symptoms of anxiety and depression among hearing and deaf individuals. J Deaf Stud Deaf Educ 2007;12:1-7. https://doi.org/10.1093/deafed/enl015.
- A Sign of the Times: Modernising Mental Health Services for People Who are Deaf. London: DH; 2002.
- Why Do You Keep Missing Me? A Report into Deaf People’s Access to Primary Health Care. London: SignHealth; 2008.
- Why Are You Still Missing Me? A Report Following the Publication of the GP Patient Survey 2009. London: SignHealth; 2009.
- Emond A, Ridd M, Sutherland H, Allsop L, Alexander A, Kyle J. The current health of the signing Deaf community in the UK compared with the general population: a cross-sectional study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006668.
- Kuenburg A, Fellinger P, Fellinger J. Health care access among Deaf people. J Deaf Stud Deaf Educ 2016;21:1-10. https://doi.org/10.1093/deafed/env042.
- Hulme C. Can a Deaf charity develop an effective relationship with over 200 CCGs?. Br J Healthc Manag 2015;21:452-5. http://dx.doi.org/doi:10.12968/bjhc.2015.21.10.452.
- Rogers KD, Young A, Lovell K, Campbell M, Scott PR, Kendal S. The British Sign Language versions of the patient health questionnaire, the generalized anxiety disorder 7-item scale, and the work and social adjustment scale. J Deaf Stud Deaf Educ 2013;18:110-22. http://dx.doi.org/10.1093/deafed/ens040.
- Young A, Oram R, Dodds C, Nassimi-Green C, Belk R, Rogers K, et al. A qualitative exploration of trial-related terminology in a study involving Deaf British Sign Language users. Trials 2016;17. https://doi.org/10.1186/s13063-016-1349-6.
- Easterbrook PJ, Matthews DR. Fate of research studies. J R Soc Med 1992;85:71-6.
- Cullati S, Courvoisier DS, Gayet-Ageron A, Haller G, Irion O, Agoritsas T, et al. Patient enrollment and logistical problems top the list of difficulties in clinical research: a cross-sectional survey. BMC Med Res Methodol 2016;16. https://doi.org/10.1186/s12874-016-0151-1.
- Ross S, Grant A, Counsell C, Gillespie W, Russell I, Prescott R. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol 1999;52:1143-56. https://doi.org/10.1016/S0895-4356(99)00141-9.
- Hon YK, Narayanan P, Goh PP. Extended discussion of information for informed consent for participation in clinical trials. Cochrane Database Syst Rev 2012;5. http://dx.doi.org/10.1002/14651858.CD009835.
- Kerr C, Robinson E, Stevens A, Braunholtz D, Edwards S, Lilford R. Randomisation in trials: do potential trial participants understand it and find it acceptable?. J Med Ethics 2004;30:80-4. https://doi.org/10.1136/jme.2002.001123.
- Featherstone K, Donovan JL. Random allocation or allocation at random? Patients’ perspectives of participation in a randomised controlled trial. Br Med J 1998;317:1177-80. http://dx.doi.org/10.1136/bmj.317.7167.1177.
- Featherstone K, Donovan JL. ‘Why don’t they just tell me straight, why allocate it?’ The struggle to make sense of participating in a randomised controlled trial. Soc Sci Med 2002;55:709-19. https://doi.org/10.1016/S0277-9536(01)00197-6.
- Stead M, Eadie D, Gordon D, Angus K. ‘Hello, hello – it’s English I speak!’: a qualitative exploration of patients’ understanding of the science of clinical trials. J Med Ethics 2005;31:664-9. https://doi.org/10.1136/jme.2004.011064.
- Ndebele P, Wassenaar D, Masiye F, Munalula-Nkandu E. Trial participants’ understanding of randomization, double-blinding, and placebo use in low literacy populations: findings from a study conducted within a microbicide trial in Malawi. J Empir Res Hum Res Ethics 2014;9:2-10. http://dx.doi.org/10.1177/1556264614540592.
- Young A, Temple B, Young A, Temple B. Approaches to Social Research: The Case of Deaf Studies. New York, NY: Oxford University Press; 2014.
- Ferguson-Coleman E, Keady J, Young A. Dementia and the Deaf community: knowledge and service access. Aging Ment Health 2014;18:674-82. https://doi.org/10.1080/13607863.2014.880405.
- Pollard RQ, Marschark M, Clark MD. Psychological Perspectives on Deafness. Mahwah, NJ: Lawrence Erlbaum; 1998.
- Fayter D, McDaid C, Eastwood A. A systematic review highlights threats to validity in studies of barriers to cancer trial participation. J Clin Epidemiol 2007;60:990-1001. https://doi.org/10.1016/j.jclinepi.2006.12.013.
- Krieger JL, Palmer-Wackerly A, Dailey PM, Krok-Schoen JL, Schoenberg NE, Paskett ED. Comprehension of randomization and uncertainty in cancer clinical trials decision making among rural, appalachian patients. J Cancer Educ 2015;30:743-8. http://dx.doi.org/10.1007/s13187-015-0789-0.
- Harmer L. Health care delivery and deaf people: practice, problems, and recommendations for change. J Deaf Stud Deaf Educ 1999;4:73-110. https://doi.org/10.1093/deafed/4.2.73.
- Steinberg AG, Wiggins EA, Barmada CH, Sullivan VJ. Deaf women: experiences and perceptions of healthcare system access. J Womens Health 2002;11:729-41. https://doi.org/10.1089/15409990260363689.
- Accessible Information Standard: Specification. London: NHS England; 2015.
- Sick of It Report. London: SignHealth; 2014.
- Pereira PC, Fortes PA. Communication and information barriers to health assistance for deaf patients. Am Ann Deaf 2010;155:31-7. https://doi.org/10.1353/aad.0.0128.
- Iezzoni LI, O’Day BL, Killeen M, Harker H. Communicating about health care: observations from persons who are deaf or hard of hearing. Ann Intern Med 2004;140:356-62. https://doi.org/10.7326/0003-4819-140-5-200403020-00011.
- Giorgi A, Smith JA, Harré R, Van Langenhove L. Rethinking Psychology. London: Sage; 1995.
- Cohen MZ, Kahn DL, Steeves RH. Hermeneutic Phenomenological Research: A Practical Guide for Nurse Researchers. London: Sage; 2000.
- Mindess A. Reading Between the Signs – Intercultural Communication for Sign Language Interpreters. Boston, MA: Intercultural Press; 2006.
- Young A, Temple B, Young A, Temple B. Approaches to Social Research: The Case of Deaf Studies. New York, NY: Oxford University Press; 2014.
- Ferguson-Coleman E. Deaf With Dementia: A Narrative 2016.
- Temple B, Young A. Qualitative research and translation dilemmas. Qual Res 2004;4:161-78. http://dx.doi.org/10.1177/1468794104044430.
- Young A, Temple B. Approaches to Social Research: The Case of Deaf Studies. New York, NY: Oxford University Press; 2014.
- Stone C, West D. Translation, representation and the Deaf ‘voice’. Qual Res 2012;12:645-65. http://dx.doi.org/10.1177/1468794111433087.
- Sutton-Spence R, West D. Negotiating the legacy of hearingness. Qual Inq 2011;17:422-32. http://dx.doi.org/10.1177/1077800411405428.
- Canadian Association of the Deaf . Deaf Seniors: Position Statement 2015. http://cad.ca/issues-positions/seniors/ (accessed 28 February 2017).
- British Deaf Association . SHARE: The Deaf Visual Archive 2015. www.historypin.org/en/share-the-deaf-visual-archive/geo/51.451768,-0.113656,4/bounds/20.341258,-26.832406,70.06436,26.605094 (accessed 28 February 2017).
- Davis LJ. Enforcing Normalcy: Disability, Deafness and the Body. London: Verso; 1995.
- Lane H, Pillard RC, Hedberg U. The People of the Eye: Deaf Ethnicity and Ancestry (Perspectives on Deafness). New York, NY: Oxford University Press; 2011.
- Dimmock AF. Cruel Legacy: Introduction to the Record of Deaf People in History. Edinburgh: Scottish Workshop Publications; 1993.
- Griggs M. Deafness and Mental Health: Perceptions of Health Within the Deaf Community 1998.
- Lewis H. Deaf Liberation Theology (Explorations in Practical, Pastoral and Empirical Theology. Aldershot: Ashgate Publishing Ltd; 2007.
- Hynes D. Social Work With Deaf People 1988.
- Emery SD. Citizenship and the Deaf Community. Nijmegen: Ishara Press; 2011.
- Napier J, McEwin A. Do deaf people have the right to serve as jurors in Australia?. Altern Law J 2015;40:23-7.
- Hulme C. A Phenomenological Study into the British Sign Language Users’ Experiences of Psychological Therapies 2016.
- Lane H. The Mask of Benevolence: Disabling the Deaf Community. San Diego, CA: Dawn Sign Press; 1999.
- Robinson EJ, Kerr C, Stevens A, Lilford R, Braunholtz D, Edwards S. Lay conceptions of the ethical and scientific justifications for random allocation in clinical trials. Soc Sci Med 2004;58:811-24. https://doi.org/10.1016/S0277-9536(03)00255-7.
- De Clerck GAM. Deaf epistemologies as a critique and alternative to the practice of science: an anthropological perspective. Am Ann Deaf 2010;154:435-46. https://doi.org/10.1353/aad.0.0121.
- De Clerck GAM, Paul P, Moores D. Deaf Epistemologies: Multiple Perspectives on the Acquisition of Knowledge. Washington, DC: Gallaudet University Press; 2012.
- Young A, Ackerman J. Reflections on validity and epistemology in a study of working relations between deaf and hearing professionals. Qual Health Res 2001;11:179-89. https://doi.org/10.1177/104973230101100204.
- Young A, Temple B, Young A, Temple B. Approaches to Social Research: The Case of Deaf Studies. New York, NY: Oxford University Press; 2014.
- Bauman H-DL, Murray JJ. Deaf Gain: Raising the Stakes for Human Diversity. Minneapolis, MN: University of Minnesota Press; 2014.
- Bahan B, Bauman H-DL. Open Your Eyes: Deaf Studies Talking. Minneapolis, MN: University of Minnesota Press; 2008.
- A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health. London: Medical Research Council; 2000.
- Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2006.
- Belk RA, Pilling M, Rogers KD, Lovell K, Young A. The theoretical and practical determination of clinical cut-offs for the British Sign Language versions of PHQ-9 and GAD-7. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1078-0.
- Samady W, Sadler GR, Nakaji M, Malcarne VL. Translation of the multidimensional health locus of control scales for users of American sign language. Public Health Nurs 2008;25:480-9. https://doi.org/10.1111/j.1525-1446.2008.00732.x.
- Rogers KD, Young A, Lovell K, Evans C. The challenges of translating the clinical outcomes in Routine Evaluation-Outcome Measure (CORE-OM) into British Sign Language. J Deaf Stud Deaf Educ 2013;18:287-98. https://doi.org/10.1093/deafed/ent002.
- Rogers KD. Deaf People and Mental Well-being: Exploring and Measuring Mental Well-being in British Sign Language. Manchester: University of Manchester; 2013.
- Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ 2012;184:E191-6. https://doi.org/10.1503/cmaj.110829.
- Diez-Quevedo CMD, Rangil TMBM, Sanchez-Planell LMD, Kroenke KMD, Spitzer RLMD. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med 2001;63:679-86. https://doi.org/10.1097/00006842-200107000-00021.
- Donnelly PL. The use of the Patient Health Questionnaire – 9 Korean Version (PHQ-9K) to screen for depressive disorders among Korean Americans. J Transcult Nurs 2007;18:324-30. https://doi.org/10.1177/1043659607305191.
- García-Campayo J, Zamorano E, Ruiz MA, Pardo A, Pérez-Páramo M, López-Gómez V, et al. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes 2010;8. https://doi.org/10.1186/1477-7525-8-8.
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA 1999;282:1737-44. https://doi.org/10.1001/jama.282.18.1737.
- Crane PK, Gibbons LE, Willig JH, Mugavero MJ, Lawrence ST, Schumacher JE, et al. Measuring depression levels in HIV-infected patients as part of routine clinical care using the nine-item Patient Health Questionnaire (PHQ-9). AIDS Care 2010;22:874-85. https://doi.org/10.1080/09540120903483034.
- Dbouk N, Arguedas MR, Sheikh A. Assessment of the PHQ-9 as a screening tool for depression in patients with chronic hepatitis C. Dig Dis Sci 2008;53:1100-6. https://doi.org/10.1007/s10620-007-9985-z.
- Garlow SJ, Rosenberg J, Moore JD, Haas AP, Koestner B, Hendin H, et al. Depression, desperation, and suicidal ideation in college students: results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress Anxiety 2008;25:482-8. http://dx.doi.org/10.1002/da.20321.
- Gilbody S, Richards D, Barkham M. Diagnosing depression in primary care using self-completed instruments: UK validation of PHQ-9 and CORE-OM. Br J Gen Pract 2007;57:650-2.
- NHS Digital . Improving Access to Psychological Therapies Data Set 2016. http://content.digital.nhs.uk/iapt (accessed 28 February 2017).
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. https://doi.org/10.1001/archinte.166.10.1092.
- Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 2007;146:317-25. https://doi.org/10.7326/0003-4819-146-5-200703060-00004.
- The IAPT Data Handbook: Guidance on Recording and Monitoring Outcomes to Support Local Evidence-Based Practice. Version 2.0. London: IAPT; 2011.
- Improving Access to Psychological Therapies: Measuring Improvement and Recovery – Adult Services. Version 2.0. London: IAPT and NHS England; 2014.
- IAPT . IAPT Key Performance Indicator (KPI). Technical Guidance for Adult IAPT Services 2012 13. Version 2.0. 2012. file://nask.man.ac.uk/home$/IAPT_KPI_Technical_Guidance_2012-13_v2.0.pdf (accessed 24 April 2017).
- HSCIC . Announcement of Methodological Change: Improving Access to Psychological Therapies (IAPT) Monthly Reports Version 1.0 2016. http://content.digital.nhs.uk/media/21711/Methodological-Change-Paper--IAPT-monthly-reports--Jul-2016/pdf/Announcement_of_methodological_change_-_Monthly_IAPT_reports_July_2016.pdf (accessed 28 February 2017).
- Gyani A, Shafran R, Layard R, Clark DM. Enhancing recovery rates: lessons from year one of IAPT. Behav Res Ther 2013;51:597-606. https://doi.org/10.1016/j.brat.2013.06.004.
- Improving Access to Psychological Therapies (IAPT) Executive Summary. London; 2015.
- Machin D, Campbell MJ, Tan SB, Tan SH. Sample Size Tables for Clinical Studies (Third Edition). Chichester: Wiley-Blackwell; 2009.
- Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996;49:1373-9. https://doi.org/10.1016/S0895-4356(96)00236-3.
- ONS . English Health Geography 2016. http://webarchive.nationalarchives.gov.uk/20160105160709/http:/www.ons.gov.uk/ons/guide-method/geography/beginner-s-guide/health/english-health-geography/index.html (accessed 28 February 2017).
- Creswell JW. Qualitative, Quantitative and Mixed Methods Approaches. London: Sage; 2003.
- NHS England . 2015 Adult IAPT Workforce Census Report 2015. www.england.nhs.uk/mentalhealth/wp-content/uploads/sites/29/2016/09/adult-iapt-workforce-census-report-15.pdf (accessed 28 February 2017).
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction 2004. www.betterevaluation.org/sites/default/files/RMPmethods2.pdf (accessed 24 April 2017).
- Greenhalgh T, Wong G, Jagosh J, Greenhalgh J, Manzano A, Westhorp G, et al. Protocol – the RAMESES II study: developing guidance and reporting standards for realist evaluation. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008567.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Guidance for Commissioners of Primary Care Mental Health Services for Deaf People: Practical Mental Health Commissioning. London: Royal College of Psychiatrists; 2017.
- SignHealth . Deaf Health Champions 2015. www.signhealth.org.uk/annual-review-20142015-deaf-health-champions-in-bsl/ (accessed 24 April 2017).
- Next Generation Text Service . Welcome to the Next Generation Text Service 2016. http://ngts.org.uk/ (accessed 28 February 2017).
- Action on Hearing Loss . Access All Areas? A Report on the Experiences of People With Hearing Loss When Accessing Health Care 2013. www.actiononhearingloss.org.uk/accessallareas.aspx (accessed 28 February 2017).
- McKee MM, Paasche-Orlow MK, Winters PC, Fiscella K, Zazove P, Sen A, et al. Assessing health literacy in deaf American sign language users. J Health Commun 2015;20:92-100. https://doi.org/10.1080/10810730.2015.1066468.
- NHS England . Principles for High Quality Interpreting and Translation Services in Primary Care (Version 1.19) 2016. www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/03/it_principles.pdf (accessed 28 February 2017).
- Unknown . Speechreading, Part I: ‘Read My (Unreadable) Lips’ 2012. http://deaffriendly.com/articles/speechreading-part-i-read-my-unreadable-lips/ (accessed 28 February 2017).
- Guthmann DS, Sandberg K, Lazarus A, Zur O. Dual Relationships and Psychotherapy. New York, NY: Springer; 2002.
- Pugh R. Dual relationships: personal and professional boundaries in rural social work. Br J Soc Work 2007;37:1405-23. http://dx.doi.org/10.1093/bjsw/bcl088.
- Schank JA, Helbok, CM, Haldeman DC, Gallardo ME. Challenges and benefits of ethical small-community practice. Prof Psychol Res Pract 2010;41:502-10. http://dx.doi.org/10.1037/a0021689.
- Jones L, Pullen G. Cultural differences: deaf and hearing researchers working together. Disabil Society 1992;7:189-96. https://doi.org/10.1080/02674649266780211.
- Improving Access to Psychological Therapies (IAPT) Waiting Times Guidance and FAQ’s. London: NHS; 2015.
- Care Services Improvement Partnership . IAPT Outline Service Specification 2011. www.uea.ac.uk/documents/246046/11991919/iapt-pathfinder-outline-service-specification.pdf/9fc11891-ecc5-48e4-a974-9bbc8ab0c690 (accessed 28 February 2017).
- Bowe FG. Transition for Deaf and hard-of-hearing students: a blueprint for change. J Deaf Stud Deaf Educ 2003;8:485-93. https://doi.org/10.1093/deafed/eng024.
- Rogers KD, Pilling M, Davies L, Belk R, Nassimi-Green C, Young A. Translation, validity and reliability of the British Sign Language (BSL) version of the EQ-5D-5L. Qual Life Res 2016;25:1825-34. https://doi.org/10.1007/s11136-016-1235-4.
- Barnett S, Klein JD, Pollard RQ, Samar V, Schlehofer D, Starr M, et al. Community participatory research with deaf sign language users to identify health inequities. Am J Public Health 2011;101:2235-8. https://doi.org/10.2105/AJPH.2011.300247.
- EuroQol . EQ-5D Products 2017. www.euroqol.org/eq-5d-products.html (accessed 28 February 2017).
- NICE . Guide to the Methods of Technology Appraisal 2013. Process and Methods [PMG9] 2013. www.nice.org.uk/article/pmg9/chapter/foreword (accessed 28 February 2017).
- Rogers K, Evans C, Campbell M, Young A, Lovell K. The reliability of British Sign Language and English versions of the clinical outcomes in routine evaluation – outcome measure with d/Deaf populations in the UK: an initial study. Health Soc Care Community 2013;22:278-89. https://doi.org/10.1111/hsc.12078.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Devlin N, Shah K, Feng Y, Mulhern B, Van Hout B. Valuing Health-Related Quality of Life: An EQ-5D-5L Value Set for England 2016. www.ohe.org/publications/valuing-health-related-quality-life-eq-5d-5l-value-set-england#sthash.tDThhs9x.dpuf (accessed 28 February 2017).
- Mavranezouli I, Brazier J, Rowen D, Barkham M. Estimating a preference-based index from the Clinical Outcomes in Routine Evaluation-Outcome Measure (CORE-OM): valuation of CORE-6D. Med Decis Making 2013;33:381-95. http://dx.doi.org/10.1177/0272989X12464431.
- Barkham M, Bewick B, Mullin T, Gilbody S, Connell J, Cahill J, et al. The CORE-10: a short measure of psychological distress for routine use in the psychological therapies. Couns Psychother Res 2013;13:3-13. http://dx.doi.org/10.1080/14733145.2012.729069.
- ONS . Measuring National Well-Being: Life in the UK, 2015 2015. http://webarchive.nationalarchives.gov.uk/20160105160709/http://www.ons.gov.uk/ons/dcp171766_398059.pdf (accessed 28 February 2017).
- Green C, Richards DA, Hill JJ, Gask L, Lovell K, Chew-Graham C, et al. Cost-effectiveness of collaborative care for depression in UK primary care: economic evaluation of a randomised controlled trial (CADET). PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0104225.
- Camacho E, Ntais D, Coventry P, Bower P, Lovell K, Chew-Graham C, et al. Long-term cost-effectiveness of collaborative care (versus usual care) for people with depression and comorbid diabetes or cardiovascular disease: a Markov model informed by the COINCIDE randomised controlled trial. BMJ Open 2016;6. http://dx.doi.org/10.1136/bmjopen-2016-012514.
- NICE . Depression in Adults: Recognition and Management. Appendix 15 Economic Review 2013. www.nice.org.uk/guidance/cg90/evidence/full-guidance-appendix-15-243833294 (accessed 28 February 2017).
- Pini S, Cassano GB, Simonini E, Savino M, Russo A, Montgomery SA. Prevalence of anxiety disorders comorbidity in bipolar depression, unipolar depression and dysthymia. J Affect Disord 1997;42:145-53. http://dx.doi.org/10.1016/S0165-0327(96)01405-X.
- Maier W, Falkai P. The epidemiology of comorbidity between depression, anxiety disorders and somatic diseases. Int Clin Psychopharmacol 1999;14:1-6.
- Tyrer P. The case for cothymia: mixed anxiety and depression as a single diagnosis. Br J Psychiatry 2001;179:191-3. https://doi.org/10.1192/bjp.179.3.191.
- Levinson DF. The genetics of depression: a review. Biol Psychiatry 2006;60:84-92. https://doi.org/10.1016/j.biopsych.2005.08.024.
- HSCIC . Psychological Therapies: Annual Report on the Use of IAPT Services. England, 2014 15 2015. www.hscic.gov.uk/catalogue/PUB19098/psyc-ther-ann-rep-2014-15.pdf (accessed 28 February 2017).
- ONS . Interim Life Tables: England &Amp; Wales, 2010–2012 2014. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/bulletins/interimlifetables/englandandwales20102012 (accessed 28 February 2017).
- Mykletun A, Bjerkeset O, Overland S, Prince M, Dewey M, Stewart R. Levels of anxiety and depression as predictors of mortality: the HUNT study. Br J Psychiatry 2009;195:118-25. https://doi.org/10.1192/bjp.bp.108.054866.
- Duggan C, Parry G, McMurran M, Davidson K, Dennis J. The recording of adverse events from psychological treatments in clinical trials: evidence from a review of NIHR-funded trials. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-335.
- HSCIC . Technical Output Specification. Improving Access to Psychological Therapies Data Set v1.5 2014. http://content.digital.nhs.uk/media/13514/IAPT-v15-Technical-Output-Specification/xls/IAPT_Data_Set_v1.5_Technical_Output_Specification.xls (accessed 28 February 2017).
- Sapin C, Fantino B, Nowicki ML, Kind P. Usefulness of EQ-5D in assessing health status in primary care patients with major depressive disorder. Health Qual Life Outcomes 2004;2. https://doi.org/10.1186/1477-7525-2-20.
- DH . NHS Reference Costs 2014–15 2014. www.gov.uk/government/publications/nhs-reference-costs-2014-to-2015 (accessed 28 February 2017).
- NHS England . Accessible Information Standard: Resources: Notes on Meeting The Cost of Meeting Individuals’ Needs 2016. www.england.nhs.uk/ourwork/accessibleinfo/resources/cost-ind-needs/ (accessed 28 February 2017).
- BSL Healthy Minds . North West BSL Healthy Minds Evaluation Report October 2011 – November 2013 2014. www.uea.ac.uk/documents/246046/11991919/BSL+for+deaf+people+evaluation+report+.pdf/6815332a-72b8-46a9-b636-e67252fd894a (accessed 28 February 2017).
- McCrone P, Dhanasiri S, Patel A, Martin K, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026 2008. www.kingsfund.org.uk/sites/files/kf/Paying-the-Price-the-cost-of-mental-health-care-England-2026-McCrone-Dhanasiri-Patel-Knapp-Lawton-Smith-Kings-Fund-May-2008_0.pdf (accessed 28 February 2017).
- Luppa M, Heinrich S, Angermeyer MC, König HH, Riedel-Heller SG. Cost-of-illness studies of depression: a systematic review. J Affect Disord 2007;98:29-43. https://doi.org/10.1016/j.jad.2006.07.017.
- Personal Social Services Research Unit . Unit Costs of Health and Social Care 2015 2015. www.pssru.ac.uk/project-pages/unit-costs/2015/ (accessed 28 February 2017).
- Rawlins MD, Culyer AJ. National Institute for Clinical Excellence and its value judgments. BMJ 2004;329:224-7. https://doi.org/10.1136/bmj.329.7459.224.
- McCabe C, Claxton K, Culyer AJ. The NICE cost-effectiveness threshold: what it is and what that means. Pharmacoeconomics 2008;26:733-44. https://doi.org/10.2165/00019053-200826090-00004.
- Crawford MJ, Thana L, Farquharson L, Palmer L, Hancock E, Bassett P, et al. Patient experience of negative effects of psychological treatment: results of a national survey. Br J Psychiatry 2016;208:260-5. http://dx.doi.org/10.1192/bjp.bp.114.162628.
- Saxon D, Barkham M, Foster A, Parry G. The contribution of therapist effects to patient dropout and deterioration in the psychological therapies. Clin Psychol Psychother 2017;24:575-88. https://doi.org/10.1002/cpp.2028.
- Mukuria C, Brazier J, Barkham M, Connell J, Hardy G, Hutten R, et al. Cost-effectiveness of an improving access to psychological therapies service. Br J Psychiatry 2013;202:220-7. https://doi.org/10.1192/bjp.bp.111.107888.
- Tosh J, Kearns B, Brennan A, Parry G, Ricketts T, Saxon D, et al. Innovation in health economic modelling of service improvements for longer-term depression: demonstration in a local health community. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-150.
- NICE . Depression in Adults: Recognition and Management Clinical Guideline [CG90] 2009. www.nice.org.uk/guidance/cg90/resources/depression-in-adults-recognition-and-management-975742636741 (accessed 28 February 2017).
- Zimovetz EA, Wolowacz SE, Classi PM, Birt J. Methodologies used in cost-effectiveness models for evaluating treatments in major depressive disorder: a systematic review. Cost Eff Resour Alloc 2012;10. https://doi.org/10.1186/1478-7547-10-1.
- Donovan JL, Rooshenas L, Jepson M, Elliott D, Wade J, Avery K, et al. Optimising recruitment and informed consent in randomised controlled trials: the development and implementation of the Quintet Recruitment Intervention (QRI). Trials 2016;17. http://dx.doi.org/10.1186/s13063-016-1391-4.
- Di Bona L, Saxon D, Barham M, Dent-Brown K, Parry G. Predictors of patient non-attendance at Improving Access to Psychological Therapy services demonstration sites. J Affect Disord 2014;169:157-64. https://doi.org/10.1016/j.jad.2014.08.005.
- Richards D, Suckling R. Improving access to psychological therapies: phase IV prospective cohort study. Br J Clin Psychol 2009;48:377-96. https://doi.org/10.1348/014466509X405178.
- Glover G, Webb M, Evison F. Improving Access to Psychological Therapies: A Review of the Progress Made by Sites in the First Roll-Out Year 2010. http://webarchive.nationalarchives.gov.uk/20160302154833/http://www.iapt.nhs.uk/silo/files/iapt-a-review-of-the-progress-made-by-sites-in-the-first-roll8208-out-year.pdf (accessed 28 February 2017).
- Richards DA, Borglin G. Implementation of psychological therapies for anxiety and depression in routine practice: two year prospective cohort study. J Affect Disord 2011;133:51-60. https://doi.org/10.1016/j.jad.2011.03.024.
- Clark DM, Layard R, Smithies R, Richards DA, Suckling R, Wright B. Improving access to psychological therapy: initial evaluation of two UK demonstration sites. Behav Res Ther 2009;47:910-20. http://dx.doi.org/10.1016/j.brat.2009.07.010.
- Griffiths CA, Griffiths LJ. Recovery and reliable change rates for patients scoring severe on depression, anxiety or impaired functioning in a psychological therapies service: IAPT. Ment Health Rev J 2015;20:28-35. http://dx.doi.org/10.1108/MHRJ-06-2014-0022.
- Pintor L, Gastó C, Navarro V, Torres X, Fañanas L. Relapse of major depression after complete and partial remission during a 2-year follow-up. J Affect Disord 2003;73:237-44. https://doi.org/10.1016/S0165-0327(01)00480-3.
- Whiteford HA, Harris MG, McKeon G, Baxter A, Pennell C, Barendregt JJ, et al. Estimating remission from untreated major depression: a systematic review and meta-analysis. Psychol Med 2013;43:1569-85. http://dx.doi.org/10.1017/S0033291712001717.
- Curtis AB. PSSRU – Unit Costs of Health and Social Care 2015 2015. www.pssru.ac.uk/project-pages/unit-costs/2015/ (accessed 12 February 2016).
- Scott J, Palmer S, Paykel E, Teasdale J, Hayhurst H. Use of cognitive therapy for relapse prevention in chronic depression. Cost-effectiveness study. Br J Psychiatry 2003;182:221-7. https://doi.org/10.1192/bjp.182.3.221.
Appendix 1 Glossary of British Sign Language terms associated with trial-related information materials
Appendix 2 Glossary of terms associated with trial-related information materials (accompanying British Sign Language commentary)
This material is provided separately in BSL in digital video format (see Report Supplementary Material 1).
Appendix 3 Patient and public involvement film
This material is in BSL and spoken English and is provided separately in digital video format (see Report Supplementary Material 2).
Appendix 4 Study 3 data transfer standard operating procedure
Appendix 5 Data extraction template for clients who are Deaf British Sign Language users
Appendix 6 Questionnaire description IAPT services
Appendix 7 Guide for follow-up interview with questionnaire participants (standard IAPT)
Appendix 8 Literature search methods and results
A structured literature search was conducted to identify any existing economic evaluations of IAPT interventions and to identify the current clinical evidence base for IAPT. The combination of existing economic and clinical evidence helped to inform the structure of the model, in particular key outcomes for inclusion. The search was then adapted to identify studies to inform parameters in the Markov model.
Methods
To identify published literature, MEDLINE and The Cochrane Library (including the Health Technology Assessment database and NHS Economic Evaluation Database) were searched. Grey literature was identified through the NHS Evidence and IAPT websites. Across the database searches, search terms varied but included IAPT-specific terms (e.g. ‘improving access to psychological therapies’), economic evaluation terms (e.g. ‘cost-effectiveness’) and clinical study terms (e.g. ‘trial’ and ‘study’). When searching for evidence to inform the Markov model parameters, IAPT-specific terms were replaced with terms related to depression (e.g. ‘depression’). All identified citations were manually screened against a set of explicit eligibility criteria to assess their potential relevance to the literature review.
Inclusion criteria
Searches were structured to identify economic evaluations and/or clinical studies of IAPT intervention in the population with depression/anxiety treatment in primary/community care. Full economic evaluations were eligible for inclusion and had to compare at least two interventions (at least one of which being IAPT) in terms of cost-effectiveness. Clinical studies had to focus on the effectiveness of IAPT and could include trial and observational studies; case studies were excluded. Searches were restricted to identify studies published from 2006 onwards (the introduction of IAPT) and in English. When searches were adapted to identify evidence to inform the Markov model parameters, the inclusion criteria no longer restricted to IAPT studies and increased to include studies published within the last 15 years. Full-published papers or reports had to be accessible for inclusion, conference abstracts, letters and editorials were excluded. Table 30 details the full inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Population | |
|
|
| Interventions | |
|
|
| Comparator | |
|
|
| Clinical study criteria | |
|
|
| Economic evaluation criteria | |
|
|
| Time | |
|
|
| Other criteria | |
|
|
Final searches completed in July 2015 identified 434 papers/reports and other sources. Of these, nine effectiveness evaluations/data sources and two economic evaluations were included in the review; three papers were used to inform model parameters. Key data were extracted.
A number of clinical studies were identified, presented in Table 31. In addition to the identified published studies, the NHS annual reports for IAPT and IAPT guidance were reviewed. This review highlighted key pathways and outcomes to consider for inclusion in the economic model. No evidence specific to the use of IAPT in the Deaf population was found. Evidence to inform the Markov model parameters within the model is also outlined in Appendix 10 for completeness.
| Author | Study type and follow-up | Population | Headline results |
|---|---|---|---|
| IAPT clinical studies | |||
| NHS England103 |
|
|
|
| Richards and Suckling169 |
|
|
|
| Glover et al.170 |
|
|
|
| Richards and Borglin171 |
|
|
|
| Gyani et al.106 |
|
|
|
| Di Bona et al.168 |
|
|
|
| Griffiths and Griffiths173 |
|
|
|
| Additional studies used to inform model parametersa | |||
| Pintor et al.174 |
|
|
|
| Whiteford et al.175 |
|
|
|
| Mykletun et al.149 |
|
|
|
Two full economic evaluations were identified; both studies were conducted in the general population accessing IAPT (not specific to the Deaf population). One of the identified studies was a trial-based evaluation and so could not inform the development of the structure of an economic model, with the exception of providing detail on potential key outcomes. 149 The other compared alternative service configurations, using a discrete event simulation model, to estimate longer-term outcomes in depression. 164 This study noted some significant evidence gaps, which would be further increased in our study as data for the Deaf population is limited. We would not have had the evidence to inform a full range of parameters needed for this approach, and, as such, the resulting model would not have been robust. Further information on the identified economic evaluations is included in Table 32.
| Author | Study overview | Headline results |
|---|---|---|
| Mukuria et al.163 |
|
|
| Tosh et al.164 |
|
|
Appendix 9 Guide to using the Patient Health Questionnaire-9 item British Sign Language and Generalised Anxiety Disorder-7 British Sign Language
Appendix 10 Model inputs
| Parameter | IAPT group | |||||
|---|---|---|---|---|---|---|
| BSL | Standard | |||||
| Proportion (n) | Standard error | 95% CI | Proportion (n) | Standard error | 95% CI | |
| Initial referral | ||||||
| Exit pre-treatment | 0.265 (155) | 0.018 | 0.231 to 0.303 | 0.297 (49) | 0.357 | 0.232 to 0.371 |
| Referral to low intensity | 0.932 (383) | 0.012 | 0.910 to 0.953 | 0.376 (14) | 0.048 | 0.287 to 0.475 |
| Appropriate treatment | ||||||
| Low-intensity treatmenta | 0.893 (410) | 0.015 | 0.861 to 0.921 | 0.901 (87) | 0.032 | 0.831 to 0.954 |
| High-intensity treatmenta | 0.998 (367) | 0.002 | 0.992 to 1.000 | 0.861 (91) | 0.036 | 0.783 to 0.924 |
| Step change if treatment not appropriateb | 1 | N/A | N/A | 1 | N/A | N/A |
| Drop-out ratesc | ||||||
| Drop-out rate: low intensity | 0.139 (47) | 0.019 | 0.106 to 0.180 | 0.107 (3) | 0.060 | 0.034 to 0.290 |
| Drop-out rate: high intensity | 0.269 (7) | 0.089 | 0.130 to 0.475 | 0.204 (10) | 0.058 | 0.112 to 0.344 |
| Parameter | IAPT group | |||||
|---|---|---|---|---|---|---|
| BSL | Standard | |||||
| Proportion (n) | Standard error | 95% CI | Proportion (n) | Standard error | 95% CI | |
| Treatment effect | ||||||
| Full course of treatment (appropriate treatment, low intensity) | ||||||
| Recovery rate | 0.431 (124) | 0.029 | 0.374 to 0.489 | 0.636 (14) | 0.105 | 0.418 to 0.810 |
| Partial recovery rate | 0.249 (68) | 0.026 | 0.201 to 0.304 | 0.136 (3) | 0.075 | 0.043 to 0.356 |
| Full course of treatment (appropriate treatment, high intensity) | ||||||
| Recovery rate | 0.105 (2) | 0.072 | 0.025 to 0.354 | 0.308 (12) | 0.075 | 0.180 to 0.473 |
| Partial recovery rate | 0.500 (7) | 0.139 | 0.247 to 0.753 | 0.222 (8) | 0.070 | 0.112 to 0.393 |
| Full course of treatment after a step change (initial treatment not appropriate, initiate low-intensity step up to high intensity) | ||||||
| Recovery rate | 0.333 (14) | 0.074 | 0.205 to 0.493 | 0.500 (5) | 0.167 | 0.208 to 0.792 |
| Partial recovery rate | 0.439 (18) | 0.078 | 0.292 to 0.597 | 0.100 (1) | 0.012 | 0.012 to 0.509 |
| Full course of treatment after a step change (initial treatment not appropriate, initiate high-intensity step down to low intensity) | ||||||
| Recovery rate | 1.000 (1) | N/A | N/A | 0.214 (3) | 0.113 | 0.060 to 0.538 |
| Partial recovery rate | 0.000 | N/A | N/A | 0.571 (8) | 0.014 | 0.286 to 0.816 |
| Parameter | Source | Proportion (n) |
|---|---|---|
| Relapse (following recovery) at 24 months | Observational follow-up study of relapse of major depression after complete and partial remission (Pintor et al.174) | 15% (112)175 |
| Relapse (following partial recovery) at 24 months | Observational follow-up study of relapse of major depression after complete and partial remission (Pintor et al.174) | 68% (71)176 |
| Remission at 12 months | A systematic review and meta-analysis of spontaneous remission in patients with depression (Whiteford et al.175) | 53% (749)177 |
| Mortality hazard ratio depression/anxiety | Observational case–control study of anxiety and depression (Mykletun et al.149) | 1.32152 (61,349) |
| Number of appointments per service | Units per complete treatment (SD) | Units per incomplete treatment (SD) | Units prior to step change (SD) | Units following step change (SD) |
|---|---|---|---|---|
| BSL-IAPT | ||||
| Low intensity | 6.24 (2.63) | 1.51 (0.78) | 5.81 (3.53) | 8.95 (6.81) |
| High intensity | 11.37 (5.85) | 1.43 (0.79) | 1.00 (N/A) | 7.00 (N/A) |
| Standard IAPT | ||||
| Low intensity | 11.08 (8.60) | 2.00 (0.10) | 4.60 (8.28) | 5.30 (3.09) |
| High intensity | 6.95 (7.14) | 1.90 (1.10) | 2.93 (2.43) | 4.93 (3.22) |
| IAPT costs | Source | Applied | Cost (£) | Lower and upper bound (£) |
|---|---|---|---|---|
| BSL-IAPT appointmenta | E-mail feedback from SignHealth, lower and upper bounds in line with lower bound of standard IAPT and upper bound of standard IAPT plus an interpreter cost | Per appointment | 195 | 82.78 to 235.41 |
| Standard IAPT appointment | NHS reference costs. DH, 2014153 | Per appointment | 94.01156 | 82.78 to 115.41 |
| Translation cost (standard IAPT only) | NHS England, 2016154 | Per appointment | 120157 | 0 to 180 |
| Other health service costs | ||||
| Remission state | A systematic review of cost-of-illness studies of depression (Luppa et al.157)b | Monthly | 132.10160 | 66.05 to 198.16 |
| Partial response state | Assumption made due to lack of datac | Monthly | 165.13c | 82.56 to 247.69 |
| Relapse state | Cost-of-illness study on depression/anxiety in the UK (McCrone et al.156) | Monthly | 198.16 | 99.08 to 297.23 |
Appendix 11 Key sensitivity analysis
| Key | Rationale |
|---|---|
| Interpreter costs | Communication with a university employee who arranges translation services gave a range of £0 up to £300. A BSL Healthy Minds report refers to the cost of using an interpreter with specialist mental health training (£230).155 To give two extremes, we tested two scenarios: one in which no interpreter costs are paid and another in which the interpreter cost is the £230 included in the Healthy Minds report, with lower and upper bounds taken from communication with someone who arranges translation services |
| BSL-IAPT set-up costs | Set-up costs for BSL-IAPT were sourced from correspondence with SignHealth employees (who deliver the BSL Healthy Minds service). Costs were divided by the estimated number of users treated annually (which were varied by 50% to provide a range of costs in this scenario), and were annuitised over 10 years which gave a mean cost of £31.59 per patient. These were excluded from the primary analysis for two reasons: the standard IAPT service also incurs set-up costs, and these are unknown, and whether a set-up cost will be incurred/how large it will be depends on how BSL-IAPT is delivered |
| Choice of clinical cut-off points | In the primary analysis, we calculated parameters from the BSL-IAPT and standard IAPT data using the cut-off points most applicable to each group (i.e. the BSL-IAPT group had BSL cut-off points applied and the standard IAPT group had English cut-off points applied). This scenario tests the impact of this choice of cut-off points. We present the results using the parameters informed by the English cut-off points applied to the whole sample and the results using the parameters informed by the BSL cut-off points applied to the whole sample |
| Utilities | To give an alternative set of utility values, CORE-6D BSL data derived from study 4 were used. The CORE-6D is a measure of psychological distress. We followed methods reported in a published paper to generate time-trade-off utility values from the CORE-6D BSL data (Mavranezouli et al.137). There has also been a new value set released for England, which can be used to provide another estimate of EQ-5D values. To test the impact of changing the source of utility values we reran the model with these different utility values |
| Time horizons | Longer time frames are associated with greater uncertainty, though if a service is effective it will accrue benefits in the long term. Hence, we have produced results for a range of time horizons. Two sources were identified for relapse/remission rates in patients with a partial remission.177 Pintor et al.174 was chosen for the primary analysis, as it was a cohort study and so may be more likely to reflect routine care. However, it was a Spanish study, and so the study by Scott et al.177 a UK RCT, was used to provide an alternative |
| Outcome rates for drop outs | The primary analysis in the model assumes that service users who do not complete a course of treatment within an IAPT service do not experience any treatment effect. To test the impact of this assumption we ran the model with different levels of treatment effect for these patients |
| Appropriate referral and step change | The model recognises that referral to an intensity level may be appropriate for user needs or may not be appropriate. Service users may remain on their entry treatment intensity throughout their IAPT therapy course (if appropriate), or they may require a step change (from low to high, or high to low) during treatment Our data from the services include step change data, hence the primary model analysis includes this. However, the data for step changes is very limited. For the BSL-IAPT arm it is limited due to service availability, whereas in the standard IAPT arm it is limited due to lower patient numbers. Hence, one of our analyses assumes all users are appropriately referred and do not experience a step change In the data we have from the BSL-IAPT service step changes were limited by the reduced availability of step 3/high-intensity interventions. We test the impact of assuming BSL-IAPT has the same service availability as standard IAPT and subsequently has the same proportions of treatment events (referral to low or high intensity, step change and dropout) |
Appendix 12 Detailed results
| Analysis | Net cost (£) (95% CI) | Net QALY (95% CI) | ICER | Probability (%) cost-effective if WTPT = | ||
|---|---|---|---|---|---|---|
| £0/QALY gained | £20,000/QALY gained | £30,000/QALY gained | ||||
| Primary analysis | –240 (–2303 to 935) | 0.001 (–0.009 to 0.013) | Dominant | 55.0 | 56.7 | 57.7 |
| Interpreter costs | ||||||
| £0 (no interpreter fees incurred in any scenario) | 307 (–751 to 1155) | 0.00 (–0.009 to 0.013) | £256,224 | 21.9 | 24 | 25.7 |
| £230 (£0 to £300) | –646 (–3566 to 806) | 0.001 (–0.009 to 0.013) | Dominant | 69.0 | 70.4 | 70.9 |
| BSL-IAPT set-up costs | ||||||
| £31.59 (£21.06 to £63.18) | –198 (–2217 to 954) | 0.001 (–0.009 to 0.014) | Dominant | 51.9 | 54.3 | 55.3 |
| Costs of recovery | ||||||
| Cost of full recovery state set to £0 | –234 (–2270 to 944) | 0.001 (–0.009 to 0.013) | Dominant | 54.6 | 56.5 | 57.2 |
| Cost of full and partial recovery states set to £0 | –289 (–2320 to 893) | 0.001 (–0.009 to 0.013) | Dominant | 58.5 | 60.4 | 61.3 |
| Choice of clinical cut-off points | ||||||
| English clinical cut-off points applied to whole sample | –221 (–2280 to 947) | 0.006 (–0.004 to 0.020) | Dominant | 54.3 | 62.5 | 66.3 |
| BSL clinical cut-off points applied to whole sample | –239 (–2405 to 940) | 0.005 (–0.005 to 0.017) | Dominant | 53.8 | 60.3 | 63.2 |
| Utilities | ||||||
| Use of utility values derived from the CORE-6D data from study 4 | –233 (–2329 to 946) | 0.000 (–0.010 to 0.012) | Dominant | 54.4 | 54.9 | 55.1 |
| Use of utility values derived using the new value set for England | –232 (–2324 to 941) | 0.002 (–0.008 to 0.014) | Dominant | 54.2 | 57.4 | 59.3 |
| Time horizon (using rates from Pintor et al.174) | ||||||
| 6 months | –223 (–2336 to 944) | 0.001 (–0.003 to 0.005) | Dominant | 53.7 | 54.6 | 54.9 |
| 18 months | –229 (–2313 to 934) | 0.001 (–0.013 to 0.018) | Dominant | 54.5 | 56.3 | 57.3 |
| 5 years | –202 (–2221 to 968) | –0.002 (–0.025 to 0.020) | £82,988 south-west quadrant | 53.3 | 51.6 | 51.2 |
| 10 years | –214 (–2290 to 950) | –0.003 (–0.027 to 0.020) | £73,292 south-west quadrant | 53.3 | 50.9 | 50.0 |
| Lifetime | –202 (–2278 to 948) | –0.003 (0.027 to 0.020) | £71,687 south-west quadrant | 52.8 | 50.8 | 50.0 |
| Time horizon (using rates from Scott et al.177) | ||||||
| 6 months | –229 (–2344 to 952) | 0.001 (–0.003 to 0.005) | Dominant | 54.1 | 55.0 | 55.5 |
| 1 year | –231 (–2257 to 950) | 0.001 (–0.009 to 0.014) | Dominant | 54.2 | 56.6 | 57.7 |
| 18 months | –232 (–2277 to 945) | 0.002 (–0.013 to 0.018) | Dominant | 54.4 | 57.3 | 58.6 |
| 5 years | –228 (–2249 to 951) | 0.001 (–0.021 to 0.025) | Dominant | 54.2 | 56.3 | 56.8 |
| 10 years | –231 (–2317 to 926) | 0.001 (–0.021 to 0.027) | Dominant | 54.4 | 57.5 | 58.3 |
| Lifetime | –215 (–2243 to 937) | 0.002 (–0.022 to 0.027) | Dominant | 53.8 | 57.0 | 58.0 |
| Treatment effect for users who do not complete treatment/drop out | ||||||
| Treatment effect equal to 50% of the rates for users who complete treatment (i.e. users who drop out have half the recovery rate of a completer) | –235 (–2256 to 910) | 0.001 (–0.009 to 0.013) | Dominant | 55.3 | 56.6 | 57.7 |
| Treatment effect equal the rates for users who complete treatment (i.e. users who drop out have the same recovery rate of a completer) | –233 (–2349 to 944) | 0.001 (–0.009 to 0.013) | Dominant | 53.9 | 55.6 | 56.8 |
| Appropriate referral and step change | ||||||
| Assume all patients are appropriately referred and there are no step changes | –342 (–2643 to 925) | 0.001 (–0.010 to 0.014) | Dominant | 58.6 | 60.4 | 61.3 |
Glossary
- BSL Healthy Minds
- The service that originated BSL-IAPT and under which it is delivered by the organisation SignHealth.
- BSL-IAPT
- The term used in this study to refer to a specialised version of Improving Access to Psychological Therapies that is delivered in British Sign Language for Deaf people.
- deaf
- When written with a lower-case ‘d’, the word deaf usually refers to deaf people who use spoken language and do not affiliate with the Deaf community.
- Deaf
- When written with an upper-case ‘D’, the word Deaf refers to the cultural linguistic minority of Deaf people who use a signed language such as British Sign Language.
- iaptus
- Software management system for psychological therapies used by Improving Access to Psychological Therapies services (see www.iaptus.co.uk/).
- SignHealth
- A third-sector organisation that promotes the right of Deaf people to access health services and is also a service provider.
- Standard Improving Access to Psychological Therapies
- The term this report uses to indicate Improving Access to Psychological Therapies services that are not BSL-IAPT, but that may still be accessed by Deaf people.
- Stepped care model
- The stepped care programme is set out in the National Institute for Health and Care Excellence guidelines and implemented within the Improving Access to Psychological Therapies programme (Clark DM. Implementing NICE guidelines for the psychological treatment of depression and anxiety disorders: the IAPT experience. Int Rev Psychiatry 2011;23:318–27). Step 2 encompasses low-intensity interventions such as guided self-help and encouragement from a psychological well-being practitioner and step 3 is defined as high-intensity interventions such as weekly one-to-one therapy sessions.
The British Sign Language glossary of terms used in recruitment materials and trial-related information is available in English form (see Appendix 1) and in British Sign Language (see Appendix 2).
List of abbreviations
- AUC
- area under the curve
- BSL
- British Sign Language
- CBT
- cognitive–behavioural therapy
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CORE-10
- Clinical Outcomes in Routine Evaluation – 10-item version
- CORE-6D
- Clinical Outcomes in Routine Evaluation – 6-item version
- CORE-OM
- Clinical Outcomes in Routine Evaluation – Outcome Measure
- DH
- Department of Health
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GAD-7
- Generalised Anxiety Disorder-7
- GP
- general practitioner
- HSCIC
- Health and Social Care Information Centre
- IAPT
- Improving Access to Psychological Therapies
- ICER
- incremental cost-effectiveness ratio
- IFR
- individual funding request
- KPI
- key performance indicator
- NICE
- National Institute for Health and Care Excellence
- NRES
- National Research Ethics Service
- ONS
- Office for National Statistics
- PAG
- Project Advisory Group
- PCT
- primary care trust
- PHQ-9
- Patient Health Questionnaire-9 item
- PPI
- patient and public involvement
- PWP
- psychological well-being practitioner
- R&D
- research and development
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SD
- standard deviation
- SMS
- short message service
- SOP
- standard operating procedure
- SSC
- Study Steering Committee
- QALY
- quality-adjusted life-year
- WSAS
- Work and Social Adjustment Scale