Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1022/15. The contractual start date was in December 2012. The final report began editorial review in March 2017 and was accepted for publication in July 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Iain Pretty is involved with the delivery of referral management services to NHS England, for which he receives financial reward. He was involved with the development of early pilot models in referral management at NHS Trafford. He was involved in the evaluation of the Index of Sedation Need (IOSN) tool. Paul Coulthard chaired the Oral Surgery and Oral Medicine Working group that developed the Guide for Commissioning Oral Surgery and Oral Medicine. This guide advocated the use of referral management systems in pathway management. He was involved in the development of the IOSN tool.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Goldthorpe et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Structure of the research and this report
This research project comprised two distinct projects. The first was a diagnostic test accuracy study and the second was an interrupted time study (ITS) that sought to examine the impact of the implementation of a referral management system with combined primary care oral surgery diversion.
The current chapter sets the context for the work from clinical, commissioner and patient perspectives, and provides the research questions to be addressed. Chapter 2 provides a brief literature review, highlighting the main evidence base for demand management and the issues identified in its implementation.
See Table 1 for a simple schematic of the study elements, with the relevant chapters highlighted.
| Components | Year | |||
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |
| Diagnostic test accuracy | ITS | |||
| Elements | Efficiency of remote clinical triage | Health needs assessment | Consultant triage with primary care | GDP triage and primary care |
| Baseline data collection | Implementation | Referral diversions and impact | ||
| Chapter(s) | Mixed methods – Chapter 2 | Mixed methods – Chapter 3 | Referral metrics and health economics – Chapter 4 | |
| Qualitative assessments – Chapter 5 | ||||
Chapter 3 describes the diagnostic test accuracy study. This was conducted under ethics approval gained from the NHS National Research Ethics Service, London Fulham Committee, approval number 12/LO/1912.
The ITS element of the work is described in Chapter 4 for the initial non-intervention year, and in Chapter 5 (post intervention). The study gained favourable ethics approval (NHS Research Ethics Committee Grampian number 13/NS/0141).
Chapter 6 presents a summary and implications arising from the work.
Oral surgery
The specialty of oral surgery deals with the diagnosis and management of pathology of the mouth and jaws that requires surgical intervention. Oral surgery involves the treatment of children, adolescents and adults, and the management of dentally anxious and medically complex patients. Oral surgery care is provided by oral surgeons and by oral and maxillofacial surgeons, as the clinical competencies of these two specialties overlap. Oral surgery is a recognised specialty of dentistry, whereas the UK General Medical Council recognises ‘Oral and Maxillofacial Surgery’ as a medical specialty. 1
NHS England’s Commissioning Guide for Oral Surgery and Oral Medicine1 describes the provision of oral surgery within the English NHS. The guidance describes three levels of case complexity, known as Levels 1, 2 and 3. 1 Oral surgery complexity is generally assessed based on both the type of procedure and patient factors. For example, a very simple surgical procedure can be complicated by a patient’s medical history or degree of anxiety. A full list of procedures and conditions that would be treated in each complexity Level can be found in Appendix 1.
In England, oral surgery is typically delivered in one of three settings and by three distinct groups of clinicians:
-
Primary care general dental practice – most surgical procedures are conducted in general practice by general dental practitioners (GDPs). The removal of simple teeth and roots is covered under the mandatory services section of the General Dental Service (GDS) contract. 2 The extraction of one or more teeth or roots in a single course of treatment attracts a band 2 charge for the patient and results in a ‘payment’ of 3 Units of Dental Activity (UDAs) for the dental practitioner (UDA prices vary between practices, but an average value of £25 is usually used). Patients will typically be free of systemic disease and will not require adjunct sedation, and the procedure will not be technically demanding. Such procedures are known as Level 1 procedures. There is an expectation that all Level 1 procedures will be undertaken in practice unless there are patient factors that complicate management. If a GDP does not feel able to undertake the procedure, they should look within the practice to see if another clinician can assist. Ultimately, it is the provider’s (GDS contract holder’s) responsibility to ensure that Level 1 procedures are undertaken in practice.
-
Intermediate services, dentists with a special interest (DwSpIs) – these services provide Level 2 care, and are typically delivered by a clinician with enhanced skills and experience who may or may not be on a specialist register. Indeed, such services could be provided by a consultant-grade clinician operating and remunerated as a Level 2 provider. It is expected that most Level 2 services will be provided in a primary care setting (where additional equipment may be required) under Any Qualified Provider (AQP), GDS or Personal Dental Service (PDS) contracts, in which case patient’s charges will be levied. Level 2 procedures may be delivered as part of continuing care or, as is most usual, by referral. The basis for the development of the DwSpI services was the 2004 framework document produced by the Department of Health (DH) and the Faculty of General Dental Practice, which was followed in 2006 by guidelines for commissioning such services. 3,4
-
Consultant or specialist care – the commissioning guidance describes Levels 3a and 3b but, for the purposes of this report, Level 3 providers are typically consultant-led services delivered in, and by, NHS hospital trusts under NHS standard contracts. Although Level 3 services are led by consultants, they will typically engage a wider workforce, including specialty and associate specialist-grade clinicians and those in formal training positions. Hospitals delivering oral surgery services at Level 3 include district general hospitals, larger training hospitals (foundation trusts) and dental hospitals that have the additional requirement to train dental undergraduates. 5
Health needs assessments
Commissioning of primary care services often takes place with little needs assessment or knowledge of where referrals come from and where populations receiving care are based. Detailed knowledge of the population, their needs and treatment preferences are essential to ensure that primary care services can be delivered effectively. 6
There is no defined methodology for determining the needs of a population for oral surgery services, in contrast to, for example, orthodontic services, where there is a clear and well-defined approach. 7 The Adult Dental Health Survey, of 2009,8 reported that 8% of dentate adults had one or more untreatable teeth (on average 2.2 teeth), but it is difficult to know when or if this need for an extraction is or will be expressed as demand. For example, many decayed roots will be asymptomatic. Data from the NHS Business Services Authority (BSA) may provide indications of activity in relation to band 2 course of treatment provision (which includes tooth extraction, but also includes fillings and root fillings) and the number of extractions provided in primary care, while Hospital Episodes Statistics (HES) can provide similar information for secondary care. None of these methodologies provides information on case complexity; coding and tariff charges in secondary care are not consistently applied and the use of general anaesthesia (GA) or sedation in both settings is poorly understood. 9,10
Referrals from primary care
In 2006, a new dental contract was introduced in England that replaced a fee-for-item service with a banded course of treatment approach. UDAs are awarded based on the type of care delivered, for example 1 UDA for a check-up with preventative care, 3 UDAs for any number of extractions (although most frequently one), any number of fillings or root filings plus any treatment included in band 1, and 12 UDAs for work requiring laboratory input, such as crowns and dentures, plus any treatment included in a band 1 or 2 course of treatment. Co-payments or patient charges are levied according to the three bandings: band 1, £19.70; band 2, £53.90; and band 3, £233.70. These charges apply to services provided under GDS and PDS contracts, but do not apply to services provided under hospital contracts. An anomaly in the contract required dentists to claim the UDA tariff for the procedures that they were referring for and collect the appropriate patient charge revenue. This created a perverse incentive to refer: dentists would be paid the same fee to refer a patient as to undertake the procedure. This resulted in the NHS paying twice for activity: once in primary care, and then again in secondary care. The contract incentive was, in part, responsible for the increase in referrals seen since 2006. Other factors contributing to the seeming relentless increase in referrals,11 which has been mirrored in medicine,12 include a lack of oral surgery experience at the undergraduate level among junior GDPs,13 and the increasing proportion of older patients retaining their teeth but presenting with complex medical histories and polypharmacy. Despite the 2006 contract being causally linked to the increase in referrals, it had been recognised for some time that the capacity in oral surgery services was under pressure. 3 Kendall, in an assessment of English oral surgery services, demonstrated that in a 3-year period from 2004, referrals doubled from a monthly average of 182 to 364. 14
Reasons for referral from primary to secondary care vary, but a questionnaire completed by dentists in Greater Manchester15 found the following:
-
anticipated surgical difficulty (69% of cases)
-
medical history issues (49% of cases)
-
require a second opinion (32% of cases)
-
practitioners do not undertake surgical procedures (29% of cases)
-
practitioners lack appropriate facilities or staff (28% of cases)
-
patients require emergency management of pain, swelling or haemorrhage (11% of cases).
Reasons for referral were not mutually exclusive.
The costs of providing oral surgery in secondary care are substantial. In 2009/10, in the north-west region alone, the total cost amounted to £53,864,857. In addition to the cost element, the increase in referrals has caused issues around workforce insufficiency and capacity, and has negatively impacted on 18-week referral to treatment targets. Although some trusts have welcomed the increased activity, others, especially those departments in district general hospitals (DGHs) staffed by oral maxillofacial surgery (OMFS) services, have found that the oral surgery referrals deflect activity from their core offering and that many are inappropriate.
Primary care (Level 2) services
As with many service developments in the NHS, formal evaluation and published reports on primary care oral surgery services are sparse. Kendall provided one of two such descriptions of how a Level 2 provider might work14 and this is described below, while Bell describes a retrospective audit of a primary care scheme designed to address issues in provision of services to remote areas. 16
Utilising two GDP practices in the Croydon area, combined with a simple referral management system, all non-urgent referrals for oral surgery procedures were captured and then subjected to a two-stage triage process. The first was an administrative check of the paper referral form and the second was a clinical assessment of a patient’s suitability for primary care treatment. The scheme reported no reduction in the total number of referrals received, but the offer of a primary care service did not appear to stimulate demand or increase Level 1 (work that should be performed by a GDP) referrals from GDPs. Of the 3117 non-urgent referrals, 36% were sent to secondary care and 59% to primary care (data were missing in 5% of cases). No referrals were returned to the GDP as being unsuitable – that is, at Level 1.
The removal of a substantial amount of activity from a single trust (nearly 60% of referrals) could cause concern over the stability of the service. Kendall states, however, that, rather than destabilising the unit, the reduction enabled a balance to be obtained, a reduction in waiting times and a re-focus on the core provision of oral maxillofacial procedures rather than oral surgery. 14
The service was revisited in both 201117 and 2012. 18 Kendall reported that, after 2.5 years of service, the background referral numbers continued to rise but the proportion of referrals directed to the primary care (Level 2) service had also increased, from 60% in 2004 to nearly 80% in 2010. With so many referrals being appropriate for Level 2 services, this suggests that much of this work was being undertaken in GDS and, with the provision of a service to deliver this, it is now being referred outwards. The number of Level 1 referrals remained low, at 1.1%. 17 Kendall reports a basic economic analysis with referral management costing around £7 per referral and a £600 saving per case seen in primary care. However, a system-wide economic appraisal was not undertaken and a formal health economic evaluation of costs and effects was not possible from the data available.
Referral management
The recognised increase in referrals from both GDPs and general medical practitioners (GPs) into hospital services has initiated several approaches to management of the problem. A Cochrane systematic review divided these approaches broadly into three main groups: (1) financial, (2) managerial or (3) professional education. 19 Each of the main groups involves varying degrees of active interruption to the referral process:
-
Professional education involves the production, dissemination and support of clear referral guidance, often using harmonised referrals forms to encourage collection of appropriate data, and often supported by targeted continuing professional development initiatives.
-
Managerial systems include the use of referral management services, clinical assessment services, clinical assessment and treatment services and as ‘in-house’ second opinions or peer review.
-
Financial approaches (at least those of relevance to the NHS) are based on fundholding by referrers and, hence, they incentivise care provided within the practice or referred to lower-priced primary care facilities.
The Cochrane review concluded that research into the management of referrals was limited. 19 Preliminary findings suggested that passive systems, such as the introduction of referral guidelines, were unlikely to change referral behaviours. The use of structured referral forms has some potential, but informatics support would be needed to make such forms useable in a practice environment (i.e. to force adherence to completion of mandatory fields). Financial methods risked the application of unselective reductions in referrals and negative impacts on patient care. 19 None of the studies examined a formal referral triage and capture service, such as that employed by Kendall. 14,17
The King’s Fund reviewed referral management systems,20 recognising that such systems can be as simple as a referral guideline through to active interventions in the referral pathway. It summarised that not all referrals were needed, but some patients who needed a referral did not receive one. The review found that the quality of referral letters was often poor, and appropriate primary care treatment or investigations had often not been undertaken prior to referral.
Focusing on capture and assessment referral solutions, the report found a range of strengths and weaknesses (including the filtering of inappropriate referrals, improving quality of referrals and providing commissioning intelligence), but also potentially increasing costs, delay to a patient’s journey and the creation of barriers between primary care and secondary care colleagues. 20 Of interest was the reported belief by primary care trusts (PCTs) that their referral management systems were reducing activity despite the fact that the data from acute trusts did not support this supposition.
A study by Cox et al. 21 highlights this anomaly. Using data from NHS Norfolk and using an active referral management centre (RMC) approach, Cox et al. 21 found that, in all cases, the use of the RMC approach increased referrals rather than decreased them. The authors concluded that the RMC approach, as the most expensive management option, was the least effective. 21 The authors’ retrospective time series design looked only at decreasing attendance, that is, reducing overall referrals, and there were no primary care redirection services. Their approach, therefore, would reduce only those referrals that evidence clearly showed were inappropriate. Referrals that were incomplete or poor quality, although initially returned, would be corrected and resent, thus increasing the number of referrals. These findings are consistent with those of Kendall’s work in dentistry, which revealed very low rates of Level 1 referrals – that is, those that might be considered inappropriate. 14
Two recent comprehensive reviews have examined demand management. 22,23 The key findings of these reviews provide the current context for our study, and, rather than duplicate the reviews in a formal literature review chapter, the key findings of these two large reviews are summarised here. The first, by Blank et al. ,22 sought to examine interventions related to referrals from primary care to specialist services. The work focused exclusively on referrals from GPs and excluded dentistry. The systems of referral were described as complex because of the interplay of local factors, such as waiting times, the directory of services and access to specialists. The review found stronger evidence to support interventions that involved peer review, improved the quality of referral information, offered specialist contact prior to referral, electronic referrals and the provision of community specialist services. 22 It found weaker and conflicting evidence over the use of gatekeeping systems and alterations in remuneration. The current work reported here addresses the issues raised in the review, apart from specialist contact prior to referral. By incorporating a standard referral form with mandatory fields, referral quality is improved, an electronic-only submission route can be implemented and a primary care service for the delivery of appropriate oral surgery procedures is introduced. The referral management and triage process can be considered a ‘gatekeeper’ with the potential to divert referrals and reject those considered ‘inappropriate’.
The second review, by Winpenny et al. ,23 focused on the effectiveness and efficiency of moving hospital services (outpatients) into primary care, and examined 184 studies, some of which included dental settings. They found that minor surgical procedures could be carried out in primary care safely and effectively, but that provision of such services could stimulate demand by addressing previously unmet need. The cost-effectiveness of these services was likely to depend on local contracting, and this also applied to general practitioner with a special interest (GPwSI) services, which also demonstrated evidence of supply-induced demand. 23 The review found that direct access to specialist services in some cases (such as audiology for hearing tests) offered obvious benefits, but that in other cases (such as musculoskeletal services) it risked generating a substantial increase in demand. The review considered referral management services as a substudy group and included a qualitative study element with individuals working, commissioning or implementing such services. The group identified four emerging themes from their interviews:
-
the lack of clarity relating the aims of functions of referral management services
-
the challenge of stakeholder adoption and buy-in
-
practical and administrative difficulties
-
the impact of perceived effectiveness of the aims and priorities of such services.
The group recommended that future schemes should have clarity of aims and defined indicators of success. In addition, the group identified a research need in the evaluation of clinical effectiveness and cost-effectiveness of RMCs.
Electronic referral management systems
The NHS ‘Choose and Book’ system, now known as the NHS e-Referral Service (eRS),24 is an example of a large, national electronic referral system. Choose and Book has reduced the administrative burden associated with appointment booking and may have reduced the non-attendance rate at secondary care clinics. 24,25 However, this system may not be appropriate for all specialties and in all contexts. Prior to and following the introduction of Choose and Book, independent electronic referral management systems were developed. For example, Maddison et al. 26 evaluated electronic referral management with central triage and an adjunct specialist primary care service for uncomplicated musculoskeletal conditions. They found that, although the number of referrals greatly increased following the introduction of referral management, waiting times fell. In addition, duplicate referrals disappeared and a high degree of patient satisfaction was reported. However, Kim et al. 27 found that, although electronic referral management improved access to care, there were some barriers to implementation. Some referring clinics reported that multistep login procedures and a lack of computer access and reliable internet connection contributed to electronic referrals taking longer to complete, which was associated with lower satisfaction with overall clinical care. Again, this finding highlights the importance of considering the context in which the referral management interventions are implemented.
Consultant triage
When GDPs are aware that their referrals are being scrutinised by a peer with a specialist training, their referral behaviours may alter around who and how they choose to refer to secondary care. Studies of peer-reviewed interventions, in which referral quality has been judged by consultants and fed back to GPs, have resulted in some improvement in the quality of referral information and a reduction in the number of overall referrals into secondary care,28–30 although it may not lead to permanent changes in practice. 31 In addition, electronic referrals directly from GPs to consultant triagers prior to making Choose and Book appointments were found to be associated with shorter waiting times for appointments than paper referrals. 25 There is some evidence to suggest that the consultant triage element may improve the quality and appropriateness of dental referrals; however, GDPs may feel that their clinical autonomy is compromised by examination of their referrals during the triage process.
Despite the apparent lack, or contradictory nature, of evidence to support active referral management systems, by 2009, 91% of PCTs had some form of referral management system in place for GPs. 21 These systems seek to influence either the decision to refer, the destination of the referral or the quality of the information provided in the referral. At the time of writing there are several referral management systems in place across NHS England Area Teams (ATs) for dentistry – largely resulting from the guidance issued in the Dental Commissioning Guides in which RMCs are central to the process of directing referrals into Level 2 services. 1
Quality of referrals from general dental practitioners
In addition to managing waiting lists, reducing costs and improving overall patient satisfaction, referral management has the potential to improve the quality of referrals from primary care, which may improve triage efficiency and the overall diagnostic accuracy of the content of referrals. 20 Qualitative work around quality and appropriateness of referrals from GPs assessed by senior NHS clinical and managerial staff in five PCT areas in England32 found that important attributes of appropriate referrals were:
-
Necessity – should the patient be referred based on clinical examination, National Institute for Health and Care Excellence (NICE) guidelines or their own medical history?
-
Destination – could and should the patient be treated in an intermediate setting rather than in secondary care?
-
Quality – is the information contained in the referral relevant and thorough, and have the necessary investigations taken place?
This is congruent with the NHS Quality, Innovation, Productivity and Prevention (QIPP) agenda around promoting quality while making efficiency savings, and offers evidence to suggest that referral management interventions do have the potential to be cost-effective while supporting improvements in quality. In 2011, a commentary on the implications of QIPP for dentistry identified the development of centralised assessment and triage services and establishment of primary care-based specialised services as innovations that could contribute to the QIPP agenda. 33
Many audits have assessed the quality of referrals from GDPs into all specialties. The results are usually poor, with ‘Dear Sir’ letters still being commonly employed, which contain little in the way of clinical detail, rationale for treatment, results of special investigations or the provision of radiographs. 34,35 Increasing the quality of referrals facilitates the provision of triage, informs commissioning (if data are appropriately captured) and increases the efficiencies of primary and secondary care services by enabling appointment scheduling and clinical staff allocation to be appropriate to complexity.
The King’s Fund describes the financial challenges facing the NHS, stating that difficult ‘trade-offs’ will be required. 36 Cost-saving measures in the NHS are rarely welcomed and often viewed as reducing quality and impacting on patient choice. However, beyond the clear need for dentistry to contribute to savings the NHS must make, there is the possibility that referral management allied to primary care diversion has much to offer in terms of quality enhancement, for example:
-
care closer to home
-
more convenient appointment times and extended opening hours
-
reduced waiting times (Kendall reports 6 weeks in primary care vs. 18 weeks in secondary care14)
-
single ‘see and treat’ appointments reducing opportunity costs for patients
-
greater productivity leading to increased capacity.
Concerns and consequences
Despite the apparent ‘easy win’ that centralised triage and primary care-based oral surgery services offer for patients and the NHS, concerns have been voiced. The removal of ‘simpler’ cases from secondary care is a potentially destabilising move, and the resultant shift of case mix to more complex patients is a perceived risk to the training of both undergraduates and specialist trainees. 13 Indeed, the use of a referral management system could, by reducing undergraduate training experiences, result in an increase in referrals from a population of graduates with no oral surgery skills. Hospital trusts may argue that the current tariff arrangements are based on the assumption that hospitals treat a wide range of cases, with payment for simpler procedures helping to generating revenue to offset the higher costs incurred in treating more complex cases that cannot be fully recovered from the tariffs. 22
Clinicians in secondary care have argued that, although care can be delivered in primary care, there is not always a compelling reason why it should. The reduced governance in primary care (for example, wrong site surgery reporting) combined with the single-handed nature of oral surgery provision in primary care, compared with a team approach in hospital, threatens, it is argued, the quality of the care provided. If patients experience complications, these will largely need to be managed by secondary care and, hence, savings are lost, patients experience poor outcomes and the system fails. 23
A further concern is that implementing primary care specialist services adds another service to the system without adequately managing the supply side, that is, without ensuring that there is corresponding downsizing of secondary care services. So instead of substitution, supplementation occurs, producing an overall increase in costs, which is a significant risk for a financially strapped NHS. A good example of possible pitfalls is described by Richardson et al. 37 in the context of developing skill mix by introducing nurse practitioners.
Aims and objectives
Considering the identified evidence gaps and the pressing need for the NHS to understand the quality and financial impact of referral management services, there is a need for a high-quality, contemporary evaluation of this change in service organisation and delivery. 22,23,38
This project aimed to evaluate the introduction of an electronic referral management system with consultant-level triage and the introduction of a new primary care service for oral surgery within a defined health-care system containing a diverse set of hospital providers. The study design used a mixed-methods approach with ITS design.
In addition, a diagnostic accuracy study of remote clinical triage was undertaken to assess the efficiency of this important stage in the referral management process. The research programme contains the necessary elements to address the research gaps identified by the previous systematic reviews,20,22,23 primarily the impact on quality of referrals, use of electronic referrals, the provision of community specialist services and the effect of gatekeeping systems.
The main research question to be addressed by this work was the following:
-
How does a robust online referral management and triage system, allied to provision of a specialist primary care service, impact on the costs and quality of oral surgery services provided by different providers in different settings in a defined health-care system?
At the highest level, we wanted to know if we can change the behaviour of referring GDPs without destabilising a complex, interdependent acute sector, to ensure that only those who need hospital care are managed in this setting. In order to fully answer this main research question, the following secondary research questions were formulated:
-
Chapter 2 , Efficiency of remote clinical triage
-
How do remote clinical triage outcomes conducted by an experienced consultant compare with outcomes of face-to-face examination (reference test) performed by the same consultant?
-
How do remote clinical triage outcomes performed by GDPs and different consultants compare with outcomes of face-to-face examination performed by an experienced consultant (reference test)?
-
What are the views of triagers on the benefits and problems of a remote clinical triage system and how can the system be improved based on their experiences?
-
-
Chapter 3 , Implementation and health needs assessment (phase 1)
-
What are the practical issues for the NHS in introducing an all-electronic referral system from scratch?
-
What is the effect of all-electronic referral system on
-
the total number of referrals
-
the quality of referrals including an assessment of compliance with national referral guidelines
-
the time taken to complete referrals?
-
-
What are the views of key stakeholders on the benefits and problems of the electronic referral system and how can the system be improved based on their experiences?
-
-
Chapter 4 , Active referral management with consultant and general dental practitioner triage: quantitative findings including economic evaluation (phases 2 and 3)
-
What are the differences in referral numbers, referral quality and the mean cost per referral between virtual management (phase 1) and consultant-led active management (phase 2)?
-
What are the differences in referral numbers, referral quality and mean cost per referral between the year of virtual management (phase 1) and GDP-led active management (phase 3)?
-
How do these findings (differences in referral numbers, referral quality and the mean cost per referral between study phases) differ by the provider of secondary care?
-
Does consultant-led triage offer improved costs over GDP self-determined provider choice (phase 2 vs. phase 3)?
-
How do the views and experiences of patients differ between those using primary and secondary care services?
-
-
Chapter 5 , Active referral management with consultant and general dental practitioner triage: qualitative findings (phases 2 and 3)
-
The use of the ITS methodology with robust adjunct and parallel qualitative components enables these issues to be addressed from both a metric and a narrative perspective.
-
What are the issues encountered when establishing a new primary care oral surgery service?
-
What are the views of stakeholders on the development and implementation of the primary care service?
-
What are the views of service users on the quality of service they received from the referral management and triage system?
-
Public and patient involvement
Public and patient involvement has been a key element of this work, from the design stage, in which consent and patient information sheets were reviewed and revised, through to the extensive involvement of patients (see Appendix 2) in the qualitative component of the research. Patients’ voices are heard and reflected strongly in the current work, as their views and experiences are key to meeting the aims of the research. Service redesign impacts multiple stakeholders and, although professional views are often heard, we have sought to ensure that those of service users in Sefton are recognised and reflected.
Chapter 2 Efficiency of remote clinical triage
Introduction
To manage demand, focus services on need and ensure that patients are seen in the correct setting, a gatekeeper function has been introduced by services within both oral surgery pathways and the wider NHS, for example in dermatology services. 17,39 Such gatekeeper services vary in their design and implementation in terms of what is assessed, and by whom, and how it is delivered, but all can be considered a form of clinical triage. The concept of primary care services underpinned by effective clinical triage has been advocated by NHS England in its commissioning advice to ATs, although there is little detail on how this might be achieved. 1,6
The provision of Level 2 services within primary care is predicated on the safe and efficient diversion of suitable patients to such services. This can be achieved in several ways, such as by:
-
undertaking a face-to-face clinical assessment of the patient
-
enabling referrers to select determine the case complexity
-
using machine learning or algorithms to classify the case complexity
-
clinical assessment of the referral – remote clinical triage by consultant staff.
There are advantages and disadvantages to each of these approaches. The use of face-to-face clinical assessments would be expensive, would require significant expansion of the clinical workforce, estate and support staff and would delay the patient journey by introducing an additional step. These factors seem at odds with the primary drivers for introducing Level 2 services and, hence, such an approach could not be recommended. 40
Referrer-based triage makes broad assumptions that the population of referring dentists can adequately assess case complexity, has a good knowledge of the various complicating factors that can affect patient care and understands the local directory of services available for individual procedures. However, such an approach is relatively inexpensive and ensures rapid referral to a provider without a delay to the patient journey. It preserves and enhances clinical autonomy, and it can be argued that dentists know their patients best, as they have had the benefit of making a full clinical examination. However, GDP decision-making may be biased and influenced by patient demands (e.g. for GA or sedation) or by a wish to continue to send patients to ‘known’ consultants or to support colleagues in primary care. Of course, the patient could be allocated to an inappropriate service, leading to either a failure to reduce the burden in secondary care or the need for an onward referral if inappropriately assigned to a primary care service. However, this approach (peer assessment) is endorsed by The King’s Fund20 and is explored in phase 3 of this study (see Chapters 4 and 5).
The use of artificial intelligence, or algorithmic triage, is in its infancy. A number of systems have been assessed in emergency medicine departments and for trauma management. 41 Such systems generally support clinical decision-making rather than taking full control over the process of triage. In dentistry there have been some studies that have examined machine learning for treatment planning. 42 The development of an algorithm that captured, via the referral process, key elements of the pathway would be a simple matter – that is, identify those ‘red flags’ that would indicate a Level 3 patient. However, GDPs may be become familiar with the process and seek to circumvent it to get their patient to their preferred provider. Automated triage does have several benefits, as it:
-
could almost instantly send a referral to the provider, ensuring no delay to a patient’s journey
-
would be workforce neutral and, hence, capacity to deliver triage is limitless
-
would be more economical as there are no costs associated with the number of referrals
-
can be audited and assessed by appropriate clinicians to determine accuracy and appropriateness.
In the current work, it was decided not to deploy an algorithmic solution. The use of primary care Level 2 providers was in its infancy at the start of the study, and it was felt that the evaluation of algorithms would be more appropriate with mature services for which data were available to help support the development and assessment of automated decision-making.
It has been proposed that a hybrid of these two systems can be adopted: a system that provides the governance, clinical leadership and independence of the face-to-face approach while mitigating the costs, time and estate requirements of it. Remote clinical triage involves the assessment of standardised referral forms and appropriate attachments (most frequently dental radiographs) to undertake a case complexity assessment. Triagers are asked not to recommend a treatment plan, direct to a specific service or otherwise assess the referral, but to assign a Level 1, 2 or 3 complexity score to each referral. Once scored, an algorithm is applied to the referral to send it to an appropriate provider, and in most systems this is determined by patient choice for secondary care and geographical proximity for primary care Level 2 services (usually based on home postcode).
Remote clinical triage has been utilised in several settings43 and for various clinical disciplines, but the efficiency of this approach for oral surgery referrals based on the described case complexity assignments has not been assessed. 44,45
The use of consultant-level triage was considered as a ‘reference standard’, and designating an experienced clinician to lead the service was thought, by many, to ensure safe and appropriate triage in the absence of established pathways. The use of consultant-led (if not actually delivered) triage is also recommended in the current NHS oral surgery commissioning guides. 1
Consultants involved in the triage process will be aware of appropriate clinical guidelines (e.g. NICE guidance on the removal of third molars35) and the type of procedure and anaesthetic requested. This guidance, along with further obligatory information, such as medical history, social demographic information and levels of anxiety, will be common factors driving decision-making. The referral trajectory, however, involves GDPs initially carrying out a consultation and examination with the patient face to face, deciding there is a need to refer the patient for specialist treatment, then entering the appropriate referral data. Consultants then interpret the referral data and decide on the appropriate level of specialist care.
There are a number interactions taking place among individuals and organisations that may be subject to other influences and drivers, additional to official guidance and system parameters. For example, ‘intuition’ of clinicians is frequently cited as a factor involved in triage decision-making;46 however, this is a phenomenon that is difficult to define. 47 Considine et al. 48 state that knowledge and experience influence triage nurses’ decision-making; the integration of factual knowledge (a series of facts relating to a patient), procedural knowledge (decision rules, clinical guidance) and conceptual knowledge (assimilation of prior knowledge and new information) result in a unified comprehension that is applicable to a range of situations. Clinician experience is defined as a combination of the passing of time and gaining skills and exposure to an event. Together, the combination of knowledge and experience may form the elusive ‘intuition’ that is observed in experienced consultants, particularly as focusing on a specialty affords more opportunity to develop conceptual knowledge through exposure to events in a specific area.
Clinicians undertaking triage may consider several factors, in addition to clinical information and guidelines, in assessing a referral. Most literature around triage decision-making is based in acute emergency settings when the patient is present and available for examination. 41,46,49 Edwards44 investigated decision-making using telephone triage in accident and emergency departments and concluded that experienced nurses considered several additional factors, such as contextual information and risk minimisation, in addition to purely medical information, when making decisions around treatment. In addition, lifestyle factors were found to be important in orthopaedics when deciding whether or not patients should be recommended for planned total joint replacement. 47,50 There is, however, a dearth of research examining the complexities of remote clinical decision-making in the absence of the patient for elective treatment.
Although many consultants in oral surgery would have ‘triaged’ their own referrals – for example, a desk-based exercise to prioritise referrals or determine staff allocation – there were no data on the efficiency of a formal triage process where decision-making was based on case complexity and the diversion of patients to primary care. This study was therefore undertaken to determine the use of such triage in a diagnostic test accuracy study.
Aims
The aim of this research was to undertake a diagnostic test accuracy study of the accuracy of remote clinical triage performed by both GDPs and consultants, compared with a reference standard of face-to-face clinical consultation performed by an experienced consultant.
Recognising that clinical decision-making is a complex area, and that agreement levels between and within clinicians will vary, a qualitative element of the study sought to understand the reasons for this by examining the impact of variation on the feasibility of such services, and suggesting how remote clinical triage may be improved or enhanced.
More specifically, we sought to answer the following research questions:
-
How do remote clinical triage outcomes conducted by an experienced consultant compare with outcomes of face-to-face examination (reference test) performed by the same consultant?
-
How do remote clinical triage outcomes performed by GDPs and different consultants compare with outcomes of face-to-face examination performed by an experienced consultant (reference test)?
-
What are the views of triagers on the benefits and problems of a remote clinical triage system and how can the system be improved based on their experiences?
Methods
Ethics approval was sought and gained from NHS National Research Ethics Service, London Fulham Committee, approval number 12/LO/1912. The research was divided into two main stages:
-
The first stage was an assessment of remote triage versus face-to-face clinical assessment.
-
The second stage examined the use of different examiners in the assessment and triage of referrals.
A qualitative component featured in both stages. Patients recruited to the study were > 18 years of age, able to consent and had been referred to a secondary care facility by their GDP for an oral surgery procedure. The setting where the study took place was Greater Manchester, as NHS Manchester had recently implemented remote clinical triage as part of a centralised referral management system.
Stage 1: assessment of remote triage versus face-to-face clinical assessment by a single consultant
A total of 282 referrals to the NHS Manchester referral system were assessed (based on the level of acceptable precision at a 95% confidence level, a minimum sample size of 279 participants was calculated) to investigate sensitivity and specificity of referrals triaged to secondary or primary care. It is important that there is high precision when comparing triage methods and that erroneous referrals should ideally to be sent to secondary care rather than to primary care, to ensure patient safety and service quality. Therefore, our sample size was calculated based on a sensitivity of 0.98 and a specificity of 0.88. 51
Sample size calculation
A total of 279 referrals were required, if taking the most conservative estimate, given a primary care prevalence of 30% and a sensitivity of 0.98 based on people referred to secondary care via assessment of standardised referral form only out of people referred to secondary care from face-to-face triage:
Process
A single consultant in oral surgery (PC) first examined all the referral forms. These were supplied on the agreed oral surgery pro forma that requires a minimum data set to be provided and adequate radiographs supplied. To reduce incorporation bias, all non-relevant patient-identifiable information, such as patient name and address, was removed from the e-referral form that incorporated the pro forma. A decision was rendered in each case from the following options:
-
suitable for secondary care consultant-led services (Level 3)
-
suitable for primary care advanced services, such as those offered by DwSpIs or those on the oral surgery specialist list (Level 2)
-
suitable for primary care – any competent GDP should be able to provide this treatment safely and effectively within general dental practice (Level 1)
-
rejected – sent back to original GDP as a result of incomplete form or missing radiographs.
Following a washout period of at least 3 weeks, the same consultant (PC) clinically examined the same patients ‘face to face’ (blinded to his previous remote triage decision) to determine a reference standard clinical triage. At the face-to-face assessment, decisions were made and noted regarding the most suitable hypothetical setting for treatment (although all patients in the study were ultimately treated in hospital). Study triage examinations took place as part of standard initial consultation prior to oral surgery procedures.
For the qualitative element of stage 1, an experienced qualitative researcher carried out detailed observations of a purposive sample (n = 30) of the consultant’s clinical (face-to-face) sessions. Cases were selected to be representative of types of clinical diagnoses, medical complexity and patient demographics, such as gender and age. During paper-based decision-making, the consultant was asked to articulate decision-making processes in real time (thinking aloud). Both procedures were audio recorded and transcribed prior to analysis and data were scrutinised to consider key factors that simplify or complicate decision-making. This approach was utilised to illuminate the processes of clinical decision-making.
Stage 2: examining the use of different examiners in the assessment and triage of referrals
In the second stage of the diagnostic accuracy and ‘workability’ test, the paper referrals of the cases that had been assessed face to face were provided to four other clinicians (one further consultant in oral surgery, one consultant in OMFS and two GDPs with experience in oral surgery). Each was asked to undertake a triage with the same options as described above. The decisions from these groups were compared with the reference decision (face to face) performed by a single consultant in oral surgery (PC). Although it was intended that this study would utilise consultant-led triage, we felt that it was important to explore if there are any major discrepancies between consultants and other dental professionals in where they believe certain cases should be referred to.
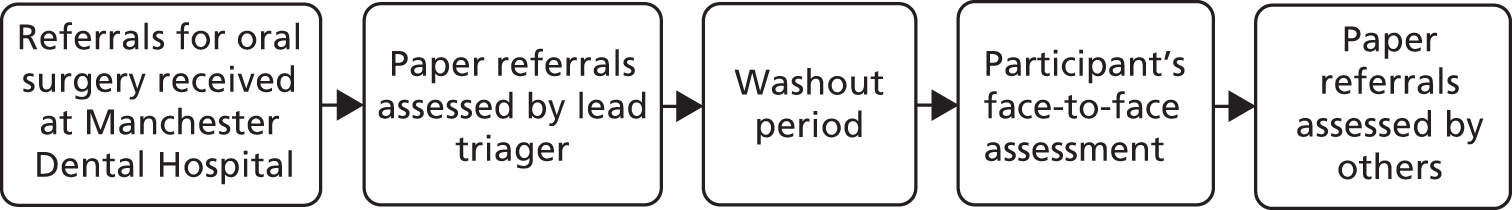
The sensitivity and specificity of the clinicians’ decisions were tested against the original consultant’s face-to-face examination decision. Additionally, tests for paired sensitivities were undertaken to determine the equality between the additional examiners using the median sensitivity score. The participant flow diagram is shown in Figure 1.
FIGURE 1.
Participant flow in the diagnostic test accuracy study.
For the qualitative element, where discrepancies in the decision-making between examiners were identified, referrals were selected for case presentations to be discussed in two focus groups. For the composition of the focus groups, see Table 2.
| Focus group | Anonymised code for transcript | |
|---|---|---|
| 1 | 2 | |
| Facilitator 1 | Facilitator 2 | F1/F2 |
| Consultant oral surgeon (reference standard clinician) | Consultant oral surgeon (reference standard clinician) | C1 |
| Consultant oral surgeon | Consultant oral surgeon | C2 |
| GDP (> 25 years’ experience) | GDP (> 25 years’ experience) | GDP |
| Dentist with specialist oral surgery contract | Dentist with specialist oral surgery contract | SPD |
| Research team project manager | Newly qualified dentist (3 years) | NQD1 |
| Newly qualified dentist (2 years) | NQD2 | |
-
Cases were selected if there was a discrepancies existed between decision-making following the reference standard face-to-face examinations and the reference consultant’s (PC) decision-making following examination of the corresponding paper referral.
-
Cases were selected based on referrals resulting in differences in decision-making between different clinicians (GDPs/consultants).
Qualitative data analysis
Observations and the consultant’s narration for the triage process in stage 1 and the discussion of the focus groups in stage 2 were digitally recorded and transcribed. All transcripts were anonymised and checked for accuracy. Analysis drew upon some common techniques of grounded theory approaches (after Glaser and Strauss52), including the technique of constant comparison, whereby analysis was carried out concurrently with data collection so that emerging issues could be explored iteratively. Stages of coding consistent with a grounded theory approach, comprising initial coding of text segments, followed by recoding and memo writing to generate conceptual themes, were carried out. Themes were constantly compared within and across cases, paying attention to negative cases and possible reasons for differences. The data were organised with the aid of qualitative data software package NVivo 11 (QSR International, Melbourne, VIC, Australia). Two researchers discussed emerging themes regularly to enable refinement of conceptual categories and to identify common threads or differences across the different respondent groups. The team ensured that an audit trail of all stages of the analysis, to maximise credibility, dependability, confirmability and transferability,53,54 was made available.
Results
A total of 551 eligible referrals were considered, of which 460 were booked into study clinics and, following consent, accounting for non-attendance and clinic cancellations, a total of 282 participants were recruited to the study. All participants required an oral surgery procedure. The mean age of participants was 42 years (± 10.2 years) and 53% were female. No adverse events arising from the face-to-face assessments were reported.
Stage 1: assessment of remote triage versus face-to-face clinical assessment by a single consultant
Quantitative results
The decisions made by the reference triager (experienced oral surgery consultant – PC) are shown in Table 3. Table 4 demonstrates these decisions based on their efficiency. For example, if a Level 2 case is directed to Level 3, it is considered efficient as care can be provided (although there is potential loss to primary care and any associated savings). A Level 3 case sent to Level 2 is considered as inefficient, as this will require an onwards referral to secondary care and this impacts on the patient’s journey and may incur charges in both settings.
| Face-to-face decision | Remote triage decision | Total (%) | ||
|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | ||
| Level 1 | 1 | 0 | 0 | 1 (1) |
| Level 2 | 3 | 173 | 26 | 202 (71) |
| Level 3 | 0 | 40 | 39 | 79 (28) |
| Total (%) | 4 (1) | 213 (76) | 65 (23) | 282 (100) |
| Decision type | Frequency | Per cent | Total per cent |
|---|---|---|---|
| Equal | 213 | 75.5 | 75.5 |
| Efficient triage error | 33 | 11.7 | 87.2 |
| Inefficient triage error | 36 | 12.8 | 100.0 |
| Total | 282 | 100.0 |
Data collected on the benefit of face-to-face assessment showed that there was a consistent collection of metrics that contributed to the change in decision. For those Level 3 cases sent to Level 2, this was a result of the treatment plan being different from that originally indicated on the referral (13 cases), additional radiography demonstrating increased case complexity (13 cases), discrepancies in the medical history (six cases) and the patient’s anxiety being higher than expected (four cases).
For sensitivity and specificity assessment, the decisions were dichotomised. Given the very small numbers of Level 1 referrals, these were combined with Level 2 referrals to provide an indication of primary care, and Level 3 referrals became the positive diagnosis. Therefore, a test with high specificity (88%) in this example will correctly identify those cases suitable for Level 2 care, but will send some Level 2 cases into Level 3, hence efficient triage error. High specificity was seen throughout the experiment.
Stage 2: examining the use of different examiners in the assessment and triage of referrals
Table 5 demonstrates the comparison of the primary examiner’s (PC) remote and face-to-face triage sensitivity and specificity results, and then demonstrates the results from additional examiners. The results of a comparative analysis show that there were no differences in the specificity scores of any examiner, although the primary examiner had consistently and significantly higher sensitivities than the other examiners.
| Examiner | Prevalence of Level 3 referrals | |
|---|---|---|
| Referrals, % (N = 238) | 95% CI | |
| Primary examiner | ||
| Sensitivity | 51.5 | 38.9 to 64.0 |
| Specificity | 88.4 | 82.6 to 92.8 |
| Oral surgery consultant II | ||
| Sensitivity | 18.2 | 9.7 to 29.6 |
| Specificity | 94.8 | 90.3 to 97.6 |
| OMFS consultant | ||
| Sensitivity | 12.1 | 5.3 to 22.5 |
| Specificity | 94.8 | 90.3 to 98.7 |
| GDP 1 | ||
| Sensitivity | 19.7 | 10.9 to 31.3 |
| Specificity | 95.9 | 91.8 to 98.3 |
| GDP 2 | ||
| Sensitivity | 10.6 | 4.3 to 20.6 |
| Specificity | 92.4 | 87.4 to 95.9 |
Qualitative results
The participant codes are shown in Table 2. The qualitative results of stage 1 [observation and think aloud by the reference triager (PC)] and stage 2 (focus groups) are presented together because of the complementary nature of the outputs. Focus groups revealed several processes involved in triage decision-making. Where the discrepancy between remote triage and face-to-face consultation decisions resulted in the face-to-face patient being ‘diverted’ to secondary care, there was often missing or inaccurate information on the referral form or the radiograph was inadequate. Patients also disclosed additional clinical details at their face-to-face consultation, often around sensitive but relevant subjects, such as alcohol intake and mental health. The main themes that arose from the data were as follows:
-
Quality of information: quality of referral information was discussed frequently in the focus groups, where issues were raised around the minimum data set needed to carry out remote triage accurately. Some pragmatic suggestions were made for minor alterations to the online pro forma.
-
Holistic view of patient: clinicians habitually attempted to construct a narrative and context for the patient in the referral in the absence of the individual, resulting in attempts to form a holistic view of the patient. At times, it was reminiscent of the treatment planning process rather than the simple assessment of case complexity.
-
Organisational context: treatment decision-making must be made pragmatically, in the context of available resources. This is especially relevant when considering the capacity for primary care to deliver certain information about patients, such as sedation assessments, and availability of panoramic radiographs.
-
Quality of information: accurate information surrounding diagnoses and medical history of the patient is vital for case complexity assessment, both for remote triage and during face-to-face consultations. When the patient is present, questions can be asked, an examination can be carried out and the patient can influence the consultation by expressing preferences and fears. However, to decide on case complexity based on referral information given by a GDP in the absence of the patient, it is essential that the clinical detail and information relating to medical history is thorough and accurate. In addition, good-quality radiographs are an important element in the assessment of case complexity, especially in relation to more complex tooth extractions.
A combination of an inadequately completed medical history and either no or a poor-quality radiograph can result in a referral that is difficult to triage. The following describes a case in which a consultant had triaged the patient to primary care based on the information on the referral form. However, following examination of a good-quality radiograph, he was sure the patient should be treated in hospital because of the position of the inferior alveolar nerve in relation to the tooth (with an attendant risk of postoperative paraesthesia):
. . . we’re saying that he needed the X-ray to make a decision and that showed [after] he did get an X-ray but I changed this because it’s close to the nerve . . .
C1 (focus group 2)
When information is missing or inaccurate, an inappropriate referral decision can be made. The example below describes a patient who was correctly reported as having epilepsy. However, during consultation it was found that the epilepsy was controlled to a much lower extent than reported in the referral information and it was decided the patient should be treated in a hospital. This resulted in an adjustment to the previous decision that the case was suitable to be seen in primary care:
But added to it but probably the main thing was the fact that his epilepsy was not controlled . . .
C1
Aha, because the difference [evidence in the transcript of the consultation] . . . consultant has changed his mind from primary to secondary because the epilepsy was not reported accurately.
C1 (focus group 1)
Supplementary information contained on the forms, such as the Index of Sedation Need (IOSN), also influenced decision-making for triage, as the patient needs to be diverted to the provider with the facilities to administer the appropriate adjunct sedation. 9,10,55 For example, simple surgery may be Level 1, but a request for sedation and supporting information to justify that sedation is required may move a referral to Level 2:
So I have assessed to the primary care specialist because it’s multiple surgicals, more than a GDP could handle. In terms of additional information, the patient is anxious and needs sedation, but again it could be primary care, but it would have to be primary care with sedation service – that wasn’t clear from the referral letter – the box hadn’t been ticked to indicate either way and again there is no IOSN or mention of anxiety.
C1 (C1 decision-making transcript)
Holistic view of the patient
Clinicians attempted to construct a narrative and context for the patient, looking for cues that might indicate an individual’s lifestyle and social circumstances, and using this to create a holistic view of the patient upon which they based their decision-making. Experienced clinicians described attempting to go beyond descriptive clinical information to form a holistic view of the patient behind the referral. One consultant describes this succinctly as:
The difference between treating the picture in the X-ray and the patient.
C2 (focus group 1)
The following triager described an attempt to form a holistic picture of the patient from the information provided on the referral form. It appears that he appraised the information available to attribute causes for the patient’s carious teeth. In the absence of this information, he exercised caution and selected secondary care treatment for this patient:
Incomplete information, because it doesn’t tell us whether they want that [IV sedation] or not. It just said, ‘difficult extraction’, great. There’s no selected choice for sedation and no indication of sedation needs or the patient’s anxiety . . . But how come they have got to that state, why have they got multiple teeth that are like, grossly carious and requiring surgical extraction? It could be, anxiety could be a reason, it could be economic reasons or education. You don’t know. But again, we haven’t got enough information to make a decision, so again I was moving up [to secondary care] rather than down [ to primary care] because I wasn’t sure.
C1 (focus group 1)
The process of decision-making when information regarding patients’ lifestyle, behaviours and anxiety levels was absent or ambiguous appears difficult for consultants who may be used to a shared approach. The process was articulated well in the discussion below around two key factors: the clinical information from the referral and the hypothetical patient. Again, when in doubt, the default approach was to refer to secondary care:
You have, it’s got here, GA justification for access medical.
But, they’re case complexities but what I think I’m hearing is . . .
It’s patient complexity.
. . . it’s very difficult to disassociated these two things and that you can’t just . . . because that case complexity is level one isn’t it?
. . . complexity of procedure is one, but the whole patient.
But, the information you do have, they’ve had a bad experience at the dentist before it may be better to have someone that’s a bit slicker when they go to hospital . . .
Organisational context
Organisational considerations, such as costs, resources and efficiencies for both patients and health services, influenced treatment decision-making. Clinicians making triage decisions had local knowledge regarding the services and estate available with different providers and wanted to minimise the need for multiple appointments. Cost and time implications for patients were considered, even if clinical indications suggested that a procedure could be carried out in primary care. For example, if it is likely that a detailed (panoramic) radiograph will be needed, and possibly a general anaesthetic because the patient is anxious, a clinician may be more likely to refer to secondary care, where these services are available, thus reducing the potential number of appointments needed. In addition, where medical history indicates potential complications, it may be not only safer, but also more efficient, for the patient to be referred to secondary care because of access to other services and specialties:
Patient is on warfarin has a history of alcoholism and problems with his liver. I think that’s high risk to do that. I wouldn’t even want to do restorative with IV block on somebody who has got…I wouldn’t want an IV block you could end up killing them . . .
So, again I’m basing it on the inconvenience to the patient.
And, how to get rid of that inconvenience, where they could just go to hospital have the test, the next day have the tooth out . . .
Yes, inconvenience, also cost effectiveness, you know, going to the doctor, getting the blood test. They have got to take the blood, send the blood to the hospital. Get the hospital or lab, get the blood results back . . .
So, what’s actually driving this here, is not necessarily the case complexity around surgery again, it’s the facilities that are available in the hospital.
Clinicians argued that good-quality radiographs are vital for accurate triage, and this was an issue highlighted consistently in the discourse. However, since the introduction of the 2006 dental contract removed the financial incentive for investing in panoramic imaging machines (there is no longer a specific fee for item for these larger, more expensive radiographs) there has been a reduction in the number of primary care practices offering this radiographic service. This type of radiograph is particularly helpful for diagnosing third molar (wisdom teeth) problems, particularly the shape of the root and the proximity to the inferior alveolar nerve (damage to which is a common risk factor for such surgery). Radiographs that are of poor quality or otherwise inadequate could affect decision-making, as triagers were instructed to take a default position of referring to the higher level of care when in doubt:
. . . Just as R’s saying, because there’s no decent X-ray you can’t actually make the decision. So whatever you write is right and wrong, isn’t it? So we just don’t know. We’re just guessing.
So it needs a referral just from an imaging point of view.
There were more DPT [dental panoramic tomography] machines around and now there are fewer than ever.
Often, GDP practices have access only to bitewing and periapical radiographs, which show only the first six teeth of each quadrant. This is insufficient to make some diagnoses, as demonstrated by the following observations from a hospital consultation:
We’ll need to get another X-ray today as well – they knew that when they sent you, just with those ones in your mouth there is a limit to how far back you can hold that, but we need to see the whole tooth to see the shape of the root – we’ve just got the very front of it on the X-ray. So we do a different sort that’s from outside your mouth so you haven’t got that problem of holding it steady
C1 (C1 P1 98–115)
The following extract from focus group 2 highlights how the issue of access to high-quality radiographs has been a long-standing problem. Clinicians have considered the situation to be problematic to the extent that possible solutions were debated:
There is a common theme here that, especially for the last ones. For the vast majority of wisdom teeth actually the imaging is inadequate and actually . . . so you wonder whether a default would be, you know, if you haven’t got a DTP [dental panoramic tomography] in your . . . you know, that should be a reason for referral because the general consensus that the vast majority of imaging is pretty rubbish and then you . . .
I think . . . and we also . . . I mean we, at the [name of] practice, take local practices’ referrals for DTPs [dental panoramic tomographs] . . .
It’s tricky, isn’t it, because what the ideal is the NHS to be supporting general practice and us to all have DPT machine so they can send that image digitally so you can make the right decision, but that would be very expensive. Your way would be cheaper but would a dentist want to do that? So the patient might come to your place and say, oh this is impressive, because you’ve got this machine, why has my dentist not got this machine, and they start coming here.
Local practices may be unable to provide radiographs of adequate quality to support triage if they do not have the appropriate equipment, and this can affect triage decisions. Sometimes a pragmatic decision needed to be made around convenience and cost for the patient:
See the trouble I have at the moment is I don’t have a practice. I don’t have an OPG machine in the practice. Now I can do . . . being a DwSpI I can do the surgery but because I don’t have an OPG machine means I’m having to refer them to [a district general hospital]. Do I then muck around and get the patient to go into [a district general hospital], do an OPG and then come back to me for the treatment or do I . . . ? I might as well just make the referral, get their OPG done and have it done there.
I know. It’s not as slick as it should be.
No.
It’s messing the patients around at the moment, isn’t it, because it’s not easy to image.
Currently, records held by GDPs are not linked to other NHS records, such as those held by GP practices. Therefore, obtaining accurate information for the referral form is reliant on patients disclosing accurate information, particularly about their medical history. The following discussion related to a consultant describing a discrepancy between a decision made during paper triage (decision to refer to specialist primary care) and following a face-to-face consultation, during which the patient disclosed a higher quantity of alcohol consumption:
. . . So, again, that’s . . . it’s often the case there, I guess sometimes that happens between a consultation thing I’ll have something like [alcohol consumption] and the patient might deny something. Then they go through to see the nurse for a pre-op assessment for a GA or something and they confess to lots more because they’ve had a few minutes to think about it. So it could be that they do deny it to the general dentist and then somebody asks the same questions and they start thinking, oh well maybe there is something I need to tell them.
C1 (focus group 2)
A possible driver for an initial referral to specialist or secondary care from general dental practice may be the time and effort taken to carry out a procedure versus remuneration available in primary care. The following quotation is from a GDP who described possible reasons for a referral for a procedure that he felt was uncomplicated:
One of the drivers for multiple quadrants being referred out and the situation for even cons [fillings] for sedation is the fact that GDPs can only claim three UDAs for it. So, that’s the driver from the primary care side. But, if you look at each, what you can see on the radiograph, if it was just that tooth in isolation, it’s not technically difficult to take that out.
GDP (focus group 1)
Clinician specialty and experience
Clinician experience is defined as a combination of the passing of time and gaining skills and exposure to an event. Focusing on a medical specialty, such as oral surgery, affords more opportunity to develop conceptual knowledge and increases exposure to events specific to this area of expertise. 48 Where differences were found in the decision-making of GDPs and consultants, GDPs tended to focus on the clinical information, whereas consultants tended to try to form a holistic view of the patient. It seems that their experience had taught them to focus on the severity and management of existing illnesses and to not assume that existing conditions are necessarily well controlled.
Although experienced GDPs undertaking triage of referrals might consider themselves to be more than capable of carrying out certain procedures, newly qualified GDPs and consultants were more likely to triage referrals to a specialty or secondary care service:
I think that if I was a patient that sore and someone brushed me off and sent me for a referral waiting 8/12 weeks . . . I’d be annoyed. But what if you fractured it and it was very sub gingival and you haven’t got the surgical [skill]? You’re then having to refer to have the rest of it retrieved out.
I think you’ve got to start off knowing that it is going to be surgical.
. . . Clinical experience is something that is accumulative isn’t it? As your decision-making evolves, your ability to carry out procedures evolves?
Consultants were more likely to consider the patient’s medical history and draw on their experience of complications that can result during surgery:
And, if you look at them, I mean you can’t really see what’s on the right, but if you look at the molar, what does that look like? It doesn’t look like it’s going to be a particularly traumatic extraction . . .
But, I would argue even if it is someone with more experience it’s risky to do that in practice. Just like people don’t get caught out very often, but sometimes they do, they end up sending them to A&E [accident and emergency] because the patient . . . or they don’t even know, because three days later the patient is still bleeding, goes to A&E and get transfused, and it happens. They get transfused and all sorts of problems.
I think where maybe in . . . sometimes the practice you get a biased view and that’s because of nine times out ten you don’t have a problem. But, we’ve also had a biased view, because we see the ones that don’t get away with it in our chequered history.
Discussion
Triage is described as:
The medical screening of patients to determine their priority for treatment; the separation of a large number of casualties, in military or civilian disaster medical care, into three groups: those who cannot be expected to survive even with treatment, those who will recover without treatment, and the priority group of those who need treatment in order to survive.
Stedman’s Medical Dictionary 56
This definition of triage still permeates the medical literature today (with findings of variation not dissimilar to those reported here), with examples from emergency medicine and military field operations. 57 However, the picture is changing, with the implementation of telephone triage on helplines such as 11144 and remote dermatology services. 39,58 Triage is not merely the selection of those who need care to survive but is becoming a tool by which the complex map of medical services can be navigated to ensure that patients receive the right type of care, in the right setting, delivered by the most appropriate clinical team with the most efficient use of resources.
This mixed-methods element of the project assessed the efficiency of remote clinical triage compared with a reference standard of face-to-face clinical assessment by an experienced oral surgery consultant. The qualitative results from the reference examiner (stage 1) suggest that consultants are willing to triage referrals to primary care, and the quantitative findings suggest the proportion of Level 2 cases is similar to that seen in the work of Kendall14 – around 70% for both remote (76%) and face-to-face (71%) assessment. The specificity of remote triage was high, and those cases that are suitable for primary care were identified as such. The rates of efficient and inefficient triage error were broadly similar, at 11.7% and 12.8%, respectively. The lead consultant (reference triager) had superior triage outcomes to the other examiners (with respect to sensitivity). However, as they had responsibility for face-to-face assessments this afforded a clear continuation of clinical decision-making processes, which was not available to other examiners. The results showed that there were no appreciable differences between the decisions of the other examiners.
The rate of inefficient triage calls is higher than that reported from the Croydon service, where the proportion of patients initially triaged to primary care (Level 2) who were subesquently referred to secondary care (Level 3) was reported to 0.5%, much lower than the 11% rate we report. However, it is important to note that the reference assessment of these patients took place in a secondary care rather than a primary care setting. It may be that an environmental impact facilitated an increase in the assessed complexity of these patients. For example, during an assessment in a primary care, treatment under GA would rarely be discussed, as it cannot be provided. Without the option of GA, the patient may elect for sedation or even treatment under local anaesthetic. 9 However, when offered the possibility of GA in a hospital they may request this option and, hence, create a demand-led uplift to their case complexity.
The rate of Level 1 cases is consistent with that in Croydon: 1% in both settings. This suggests that the majority of referrals from GDPs are appropriate. 17 This suggests that anecdotal explanations for the increase in referrals, for example that it is the result of financial incentives, are incorrect; rather, it may suggest that the increasing age and complexity of dentate patients could be a more important driver. Despite this, it should also be recognised that many GDPs are capable of delivering, and frequently deliver, Level 2 procedures, and the availability of a service may encourage such clinicians to refer rather than treat in practice. Another possibility is the presence of a structure-centralised referral system has changed GDP behaviour and resulted in a reduction in inappropriate (Level 1) referrals. This issue will be discussed in later chapters.
It is appropriate to consider the triage decisions in the context of the likely commissioning framework. It would be unusual to remove 70% of activity from an acute trust provider without causing significant destabilisation. In Greater Manchester it was the stated ambition of commissioners to reduce oral surgery flows into secondary care by 30–40%. A reduction of this size not only creates a stable system in the hospitals but also permits a range of Level 2 referrals to be seen in Level 3 environments, where they can be used for training purposes, and provides the possibility of reducing costs for the local commissioners. The costs of Level 2 care are borne by the primary care budget and not by the local commissioners’ hospital budget. If the triage service is directed to reduce inefficient triage errors (i.e. the incorrect assignment of Level 3 cases to Level 2) at the expense of efficient triage errors (the assignment of Level 2 cases to Level 3), then patient safety, service stability and training opportunities are maximised. The thresholds for such a triage service can be adjusted over time to ensure that there is a balance between capacity in each service area and that all stakeholders’ interests are recognised. The adage of caution first is appropriate, and if in doubt referrals should be ‘moved up’ to the next tier of care.
Given the complexities of patients, their presentation and the fact that a referral form is merely a summary and snapshot of a complex picture, it is not surprising that remote triage is associated with some inefficiencies. However, it should be recognised59 that treatment planning variation is seen across medical disciplines even when clinicians can physically examine patients, and it is not a phenomenon purely of remote assessment. Bader and Shugars60 said of dentists’ clinical decision-making:
Even when differences in patients are controlled, variation in dentists’ clinical decisions is ubiquitous. While its consequences remain undetermined, the variation in basic clinical decisions such as caries diagnosis signals the need to consider the extent to which the appropriateness of care is affected.
Bader and Shugars60
The qualitative assessment sheds useful light on the process of identifying elements that are either intrinsic to clinical behaviour or can be changed and improved to enhance the triage system’s performance. There is a clear recognition that triage can only be as good as the information provided by the referrer, and the clinicians involved in the study were often frustrated by the lack of information or, when information was provided, its quality. Ambiguous terms such as ‘bleeding problems’ or poor social histories caused the triagers to send more cases to secondary care based on lack of confidence rather than a firm decision. Although not optimising the system for identification of all Level 2 cases, the results of the study support the safe operation of a triage service and places patients’ interests first. Given the potential high percentage of cases that are available for diversion, it seems reasonable that some marginal Level 2/3 cases are sent to Level 3 – if only to support training.
The qualitative data make it clear that radiographs, accurate clinical data and medical history are vital to accurate decision-making. The findings highlight potential issues with patients not disclosing sensitive information to GDPs, for example around alcohol and mental health, or GDPs not asking for fear of alienating patients. Patients attending the face-to-face assessment in a hospital environment may have disclosed these issues more readily – or it could simply be they are seeing a new clinician, and one they do not have an enduring and continuing relationship with. Evidence suggests that clinicians vary in their ability to get full disclosure from patients. 61 Consideration should be given to GDPs having access (with appropriate permission to view) to GP summary care records for the purposes of medical and drug history confirmation. Triagers found the IOSN to be helpful in their decision-making process. The IOSN combines medical, treatment and patient factors into a single, consistent one-page referral form. When completed correctly, the IOSN has been shown to be predictive of patients’ needs for sedation. 62
Individual differences in triagers’ experience, training and setting inevitably impact on triage decision-making. Although the variances are not surprising, the underlying reasons behind them seem easier to address for triage than those for full treatment-planning variances. The triager’s role is to assess case complexity, not to design a treatment plan for the patient. The desire for a holistic evaluation of the patient is to be commended, but may also undermine the triage process as clinicians try to second guess the patient’s likely presentation following triage. It is also clear that, although many hospital staff will undertake internal triage, this form of case assessment is different. Consideration should be given to calibration of triagers and the formation of triage groups that can be internally benchmarked and externally audited. The use of triage guidelines and case examples would be helpful.
It should also be noted that these referrals were all seen and accepted by secondary care (to ensure a consistent face-to-face reference assessment was undertaken by PC). There was, therefore, no opportunity for the triage assessors to reject the referral requesting further information or clarification. The use of such a system, where additional information can easily be requested and added, would seem to address many of the concerns expressed by the triagers who felt that their accuracy in decision-making might have benefited from opportunities to ask further questions of the referrer.
Summary of main findings
In this section of the project, we posed three research questions:
-
How do remote clinical triage outcomes conducted by an experienced consultant compare with outcomes of face-to-face examination (reference test) performed by the same consultant?
There was substantial variance between triage decisions and face-to-face examination decisions. The default position was to refer to secondary care if there was a query or uncertainty over a referral.
-
How do remote clinical triage outcomes performed by GDPs and different consultants compare with outcomes of face-to-face examination performed by an experienced consultant (reference test)?
The performance of the various clinicians was very similar, and differed from the reference triager. Experienced GDPs would be more likely to refer to primary care (Level 2) than consultants.
-
What are the views of triagers on the benefits and problems of a remote clinical triage system and how can the system be improved based on their experiences?
The qualitative work highlighted the complexity of the decision-making process important of providing complete information in the referral forms and high-quality radiographs to aid decision-making. The availability of specialised equipment in primary care was an impediment to referral to Level 2 services. Experienced consultants and newly qualified GDPs were more likely than an experienced GDP to err on the side of caution and select secondary care as an appropriate treatment destination. Clinicians seemed to find it difficult to make objective decisions solely on the information provided without attempting to create a holistic picture of the patient. Suggested improvements to the system based on the findings are set out below.
Conclusions and implications
The clinical triage system is imperfect but fit for purpose, recognising that a pragmatic clinical decision-making process is utilised. Although consultants and experienced GDPs performed at a similar level, the use of consultants to triage ensures that there is an acceptable level of governance in the approach, especially in embryonic schemes if there has not been sufficient time or experience to develop cohesive guidelines and to refine and reflect on processes to ensure that they are delivering the objectives of the system. There is a clear emphasis on patient safety embedded within the approach.
This part of the project identified several elements that were incorporated into the electronic referral system. The learning from this part of the project may help to inform the development and design of any oral surgery referral service. Key elements are described below.
The use of an electronic referral form enables a number of issues to be addressed. For example, forms cannot be submitted until mandatory elements are completed. Although it would be impossible to assess the value or accuracy of the submitted information, it does prevent the ‘blank box’ issue described by the triagers. Electronic referrals can also be quickly rejected by triagers and returned to the referring dentist for correction, amendment or the addition of further information. Such two-way, rapid communication between triagers and referrers could also promote the provision of clinical advice, which may be of value when interpreting the impact of medical and drug history on a patient’s outcomes. The increase in patients on polypharmacy makes such a system important for the future. Electronic referral forms enable conditional input to be facilitated, ensuring that referrers enter only information relevant to their patient. Electronic referral systems also lend themselves to aggregation of the information in electronic referral forms into databases to provide a health needs assessment tool for commissioners to understand the needs of the population referred for care.
The provision of high-quality and diagnostic radiographs should be a mandatory part of the referral process. Such images not only facilitate triage, but should also be deployed in the treatment-planning process. The accurate assessment of treatment complexity increases efficiencies of services by enabling ‘see and treat’ appointments. High-quality radiographs provided at referral stage reduce the need for repeat imaging in referral treatment centres, sustainably decreasing appointment times and complying with radiology guidelines. 63
The incorporation of the IOSN tool into referrals seems to add benefit. Although the IOSN tool is not designed to either restrict or promote access to sedation, the data provided were viewed as useful not only by triagers but also by treating clinicians. 62 The IOSN enables assessors to determine if the drive for sedation is based purely on patient anxiety or if it is a combination of medical complexities or treatment burden. 55 This promotes the concept that sedation is not simply for those who are anxious, but may add quality to a service if a procedure is time-consuming or unpleasant. 9
Referral management systems typically end at the disposal of the referral to the indicated provider. Perhaps the inclusion of whole-journey monitoring would assist in refining the triage process – that is, the provider could provide outcomes on the quality of the referral, the accuracy of the triage and whether or not additional information (and of what type) may have helped achieve better care. Such data could inform the development of referral forms and guidance, monitor the performance of individual triagers and identify individual practices or practitioners from which or from whom poor-quality referrals are frequently sent.
Chapter 3 describes how these recommendations have been implemented in an all-electronic referral management system for oral surgery referrals for a defined population.
Chapter 3 Implementation and health needs assessment (phase 1)
Introduction
This first stage of the study took place in the calendar year 2014 (1 January through to 31 December 2014). It involved the establishment and provision of an electronic referral management system with no active triage – that is, referrals were simply captured by the system and then passed straight on to the provider of choice of the referring dentist. This phase of the study is identified in the study overview diagram in Table 1.
This phase of the research was conducted in the geographical region previously covered by Sefton PCT. This site was selected for the research as it offered the following:
-
no current referral management system of any kind for GDPs
-
no current primary care oral surgery service
-
patient access to three hospital types –
-
hospital A – a busy DGH with oral surgery and maxillofacial services
-
hospital B – a large regional foundation trust offering extensive dental services including tertiary referrals for oral surgery and maxillofacial services
-
hospital C – a dental school hosted by a foundation trust providing both service and educational elements
-
-
support from local commissioners to adopt and host the study as well as commitment to undertaking a procurement of a primary care service in years 2 and 3.
Sefton is in the north-west of England within the Merseyside region and was formed by the merger of Bootle and Southport in the mid-1970s. Sefton has a population of approximately 270,000 with a mean deprivation score of 25.7 (England’s best score = 5.7 and worst score = 42.0). 64 The health and lifestyles of adults in Sefton are generally better than the regional (north-west) average and similar to England’s average. Adult oral health for England is described in the 2009 Adult Dental Health Survey;8 however, data were not provided at the PCT/local authority level. The picture of oral health for the north-west region shows that the number of people with no teeth is decreasing but around one-third of all adults have decayed, untreated teeth. 8
Dental services in Sefton reflect the national picture of primary, community and secondary care services. A total of 34 dental practices in Sefton hold a NHS contract for either GDS or PDS provision. Those with PDS provision are typically orthodontic practices. A few practices have small NHS contracts and offer most of their adult services privately but may see children under the NHS (so called child-only contracts). Community dental services provide special care dentistry to adults and specialised paediatric services to children.
Aim
In this phase of research, the aim was to establish a passive electronic referral system (without deflection or presence of a Level 2 provider) and evaluate the impact on oral surgery services and key stakeholder groups in Sefton. We sought to answer the following research questions:
-
What are the practical issues for the NHS in introducing an all-electronic referral system from scratch?
-
What is the effect of an all-electronic referral system on –
-
the total number of referrals?
-
the quality of referrals including an assessment of compliance with national referral guidelines?
-
the time taken to complete referrals?
-
-
What are the views of key stakeholders on the benefits and problems of the electronic referral system and how can the system be improved based on their experiences?
Data from this first phase of implementation were used to undertake a health needs assessment of referrals from the Sefton area to inform commissioning for the introduction of a primary care (Level 2) service in phase 2 of implementation (reported in Chapter 4).
Description of the electronic referral system
The intervention in phase 1 of a complete centralised referral management system for Sefton was the provision of an electronic referral management system to capture oral surgery referrals from primary care dentists. Early in the design phase it was decided to include oral medicine and oral maxillofacial referrals in the referral system to make the system more attractive to users (a one-stop shop), but these referrals did not form part of the study data set.
The referral system was a zero footprint (no software needed to be downloaded) solution that was developed at NHS Trafford during the pilot phase of this work. The application runs in the Microsoft.NET Framework and was accessed via a secure URL (uniform resource locator). To ensure that patient data were protected, and to meet the governance guidelines for such services, the application was hosted by an approved N3 hosting service and access required the users to enter a username, strong password and then a second one-time password (OTP). The OTP was delivered by text message or voice call. The OTP system provides an additional level of security, as passwords cannot be lost, disclosed to others or hacked.
The application could be accessed by any modern browser and the end users needed only a computer and broadband connection to use the system. Dental radiographs and other files could simply be uploaded and attached to the referral information. Once completed, referrals were transformed into a PDF (portable document format) package with all the relevant information. These could then be viewed and assessed by designated triagers (who accessed the same system) and then sent onwards to providers using NHS NET e-mail.
The system provided a range of administrative functions for both referrers and triagers, and each referral could be tracked using the unique reference number (URN) produced when a referral was submitted. This tracking system was available to both patients and referrers.
The system provided a referral view page that enabled a referrer to view a range of elements related to their referral, including the status and any comments made by the triagers (case notes system). Such comments could be replied to, referral information could be quickly edited and the referral could be resubmitted for further assessment.
Once a referral was assessed as completed, the provider was sent a NHS NET e-mail that contained the PDF wrapper, individual files (for example original images) as well as, within the body of the e-mail, the referrer’s details and the nature of the treatment requested. The software, database and installation instructions are also available for NHS users under an open-source licence.
The referral form reflected the learning from the diagnostic test study described in Chapter 2. We ensured that an IOSN form accompanied any referrals for which sedation was indicated, enabled the uploading of high-quality radiographs (we supplied radiograph scanners to those practices that did not have digital radiographs) and ensured that fields with mandatory information had to be completed prior to submission. The medical history form was comprehensive and sought to identify those elements that would be important for both case complexity assessment and treatment provision. A copy of the referral form is shown in Appendix 3.
All dentists were asked to use the referral management system from 1 January 2014 for all oral surgery, oral medicine and oral maxillofacial referrals.
Methods
The study used a mixed-methods approach using quantitative data collected by the system and contemporary HES data. The qualitative element collected data using multiple methods from representatives of key stakeholder groups.
All NHS dental practices operating in the study area, plus the community dental service, were approached (n = 34) and invited to provide feedback on implementation of the system. All practices were offered the system and provided with login details, but the following were excluded from the analysis:
-
one emergency dental service that did not refer patients onwards
-
five private practices that used a private oral surgeon and did not refer to NHS services
-
one orthodontic practice that did not refer directly to oral surgery.
Therefore, the total number of practices available to contribute to the study was 27.
Quantitative methods
Each referral entered onto the system was automatically recorded and data were collected prior to being sent to the secondary care provider of choice. No diversion, rejection or other communication was employed during stage 1 of the study. Each referral was passively triaged (assessment made but no deflection of referral made) by a consultant in either oral surgery or oral maxillofacial surgery. In total, four consultants were involved in the triage provision over the duration of the study. Consultants provided one of the following triage decisions (although these were recorded, they were not enacted):
-
Level 1 referral – suitable for GDP – potentially inappropriate.
-
Level 2 referral – suitable for DwSpI service in primary care.
-
Level 3 referral – suitable for consultant-led care in hospital.
-
Level 1 referral with sedation – suitable for DwSpI service in primary care.
-
Level 2 referral with sedation – suitable for DwSpI service in primary care.
-
Level 3 referral with sedation – suitable for consultant-led care in hospital.
-
Rejected referral as radiographs not provided or not diagnostic.
-
Rejected as outside scope of referral system.
-
Rejected for another reason.
Referrals were also assessed to obtain the following metrics regarding complexity: American Society of Anesthesiologists (ASA) status, Office of Population Censuses and Surveys (OPCS) code likely to apply for the procedure described, smoking status, alcohol status and the number of teeth to be extracted or treated.
The impact of the electronic referral system on referral number and quality of referrals was undertaken by comparing the assessment of 2809 referrals sent to secondary care in 2013 from Sefton GDPs prior to the introduction of the new system in 2014. These referrals were sourced from secondary care providers and were restricted to Sefton GDP referrals. Variables collected for the quality assessment were:
-
type of referral – generic letter or referral pro forma
-
the inclusion of radiographs
-
presence of a medical history and GP details
-
the presence of a diagnosis
-
an indication of the need for either sedation or GA.
These metrics reflected the elements that caused concern among the triagers in the diagnostic test accuracy study. The number of referrals was compared using HES data for 2013 and 2014, for a defined set of OPCS oral surgery codes (those with a F prefix: F09.1, F09.3, F09.5, F10.4, F10.8 and F12.1). The 2014 HES data for number of oral surgery referrals were compared with the number of referrals captured by the new system.
Qualitative methods
Data were collected using three main mechanisms:
-
Feedback from GDS and PDS practices, community dental services, triagers and patients was collected pragmatically, with troubleshooting activity often taking place in response to problems encountered by referring dentists, triagers and/or patients. Participants informed the research team of any problems in an ad hoc manner as they arose (through either e-mail or telephone call), and this contact was recorded and placed in an electronic folder.
-
Observational data were taken in note form during site visits to dental practices. Site visits involved a member of the research team delivering instruction on system use to dentists and managers and explaining more about participation in the research project.
-
Participants from stakeholder groups were invited to take part in qualitative interviews, which were recorded, transcribed and analysed. Interviews were semistructured, with interviewers using topic guides as prompts, but allowing for exploration of participant-generated issues in a patient-centred approach to data generation. Open-ended questions were used to encourage participants to elaborate on relevant topics, and lines of interest were explored as they arose during the interviews. Interviews were carried out over the telephone or face to face in the participant’s workplace. See the table of all participants in Appendix 2, and later chapters focusing on qualitative work for more details of sampling strategy and recruitment within Chapter 5.
Thematic analysis65 was used to identify emerging issues and themes from the data using an inductive approach. This is a flexible way of analysing qualitative data that can be used to answer several research questions across a range of theoretical approaches. Use of the constant comparative method66 helped to ensure that the analysis was consistent and based on evidence from the data. Categories and memos were coded into a series of documents that were continually refined and elaborated. Coding and analysis of data were carried out in parallel with the completion of interviews. Data were organised with the aid of qualitative data software package NVivo. Categories were collapsed and widened as new data emerged, with the researcher returning to texts to compare incidents for each theme. Analysis was completed when no further themes emerged from the data (data saturation was reached).
Analysis drew on established theories of organisational change, specifically normalisation process theory (NPT), which has been developed to study implementation and adoption of (as well as barriers to) new work practices and technological interventions within health system contexts. 67,68 The aim of NPT is to understand the numerous processes involved in changing new practices into those established and embedded in routine. 67 By taking a factorial but integrated approach, NPT can offer a flexible and pragmatic theoretical approach that can help us understand the factors that affect routine incorporation of a complex system into everyday practice, while generating findings that may have resonance for other complex interventions in different settings and contexts. A strength of NPT in the context of this study is that it allows for an integrated whole-systems approach to implementation to take place, considering the various perspectives taken by numerous individuals and groups of stakeholders.
An audit trail of all stages of the analysis, to maximise credibility, dependability, confirmability and transferability,54,68 was created. To ensure reliability, interpretation of the data was discussed and refined by three researchers (JG, IAP and CS) throughout the analytic process. Further reliability was established through triangulating findings with observational work, study documents and qualitative data.
Results
Results are provided for 2014 (phase 1) only. Chapter 4 provides comparative results across all three phases of the implementation of the centralised referral system following the ITS design.
Quantitative results
Referral metrics
In 2014, a total of 112 oral medicine, 80 maxillofacial and 670 oral surgery referrals were received from dental practices in Sefton. The remainder of this section considers only the 670 oral surgery referrals.
Of the referrals received, 2.5% were considered by the triagers as Level 1 procedures, 67.2% as Level 2 and 22.8% as Level 3. A rejection rate of 7.5% would have been applied (if the system had been active), and these were all cases in which radiographs had either not been supplied or were of insufficient quality to enable triage. The average number of referrals per practice was 19, ranging from 0 to 73 referrals. Only 3 of the 27 practices failed to submit any referrals, two of which belonged to the same corporate group.
Patient factors
The mean age of the patients referred was 43.9 years [standard deviation (SD) 18.35 years] and 55% were female. In total, 57% of patients had an ASA rating of 1, 31% a rating of 2 and 10% a rating of 3. The mean Index of Multiple Deprivation (2015 data)69 was 21.13 (SD 15.9). Smoking was reported in only 13% of cases and alcohol intake at any level in 20%.
A total of 247 comorbidities were reported, representing a 37% rate within the referred population. The most common comorbidities are shown in Table 6.
| Description and code of comorbidity | Patients (n) |
|---|---|
| J459 = asthma | 40 |
| I10X = hypertension | 36 |
| Other NOS | 17 |
| Z921 = anticoagulant therapy | 16 |
| E349 = endocrine disorder | 15 |
| F99X = mental health problems | 15 |
| E119 = type 2 diabetes | 12 |
| K769 = chronic liver disease | 11 |
| Z922 = bisphosphonate therapy | 11 |
| I259 = ischaemic heart disease | 10 |
| K929 = disease of digestive system | 9 |
| G409 = epilepsy | 7 |
| J449 = COPD/COAD | 7 |
| Z859 = history of malignant disease | 6 |
| E109 = type 1 diabetes | 4 |
The clinical activity based on the referring dentist’s choice on the referral form is shown in Table 7.
| Procedure type | Patients, n (%) |
|---|---|
| Complex impaction | 37 (5.52) |
| Difficult extraction | 209 (31.19) |
| Other oral surgery procedure or opinion | 109 (16.27) |
| Buried or fractured roots | 108 (16.12) |
| Simple impactions | 88 (13.13) |
| Routine extractions | 79 (11.79) |
| Surgical endodontics | 40 (5.97) |
| Total | 670 (100) |
The total number of oral surgery referrals in 2014 captured by the electronic referral system was 670. During the same year, the number of referrals identified via the HES system was 723 (based on the identified OPCS codes). Comparison with HES data in 2013 (the year before the introduction of the electronic referral system) and 2014 showed an 11% drop in oral surgery referrals in Sefton, from 810 in 2013 to 723 in 2014.
The quality of referral data is shown in Table 8. It should be noted these baseline data merely reflect whether or not the information was provided and do not reflect the quality or accuracy of that information.
| Metric | Data (%) | |
|---|---|---|
| Baseline, 2013 (n = 2809) | Online referral, 2014 (n = 670) | |
| Radiographs supplied | 19 | 92.5 |
| GP details supplied | 47 | 100 |
| Medical history completed | 38 | 100 |
| Pro forma used | 17 | 100 |
| Letter only | 83 | 0 |
| Diagnosis present | 73 | 100 |
| Anaesthetic requested or none required indicated | 42 | 100 |
Provider factors
The referrals were dispersed to providers as shown in Table 9. This shows the total number of referrals to each site, and then the proportion of those referrals classified by the triagers as Level 1, 2 or 3. The remainder of the referrals (n = 6) were sent to hospitals outside the Mersey area, mainly to hospitals in Cheshire.
| Level | Hospital (%) | ||
|---|---|---|---|
| A | B | C | |
| 1 | 2.8 | 5.0 | 0.0 |
| 2 | 80.0 | 55.2 | 71.7 |
| 3 | 17.2 | 49.0 | 28.3 |
| Total (n) | 386 | 123 | 155 |
Qualitative results
Three key areas were found to be important to implementation processes:
-
understanding the intervention aims
-
readiness for change
-
demonstrative feedback.
These emergent themes mapped closely on to the NPT constructs of coherence, cognitive participation, collective action and reflexive feedback. NPT therefore provided a useful theory for understanding the processes of implementing the electronic referral management system. 70 These three themes will now be discussed in greater detail and be illustrated by quotations from interview transcripts and correspondence with participants.
Understanding intervention aims
The NPT construct of coherence refers to the ways in which participants make sense of operationalising new ways of working. 68 A strong understanding of the underpinning philosophy behind the work people are carrying out can give meaning to specific tasks and responsibilities. Two components of the coherence construct, communal and individual specification, relate to the sense-making work done by individuals and groups to understand the aims and objectives of sets of tasks. This framework relates closely to the issues around understanding the aims of this new referral system reported by dental practice staff.
Effective communication, cascading from commissioners down to patients via general dental practices and secondary care oral surgery clinics, was vital to develop an understanding of the purpose of the electronic referral system.
The following pathways of communication were particularly important:
-
communication from commissioners to primary and secondary care services about aims of the pilot, timelines and resources and subsequent feedback from practices
-
quality of referral information from primary to specialist and secondary care services
-
general dental practices to patients regarding the new tier 2 specialist service starting in the second phase of the study.
Initial correspondence introducing the referral management system and evaluation was sent in the form of e-mails and letters to dental practices from the commissioning and research teams. For information to reach all members of the practice, the recipient needed to acknowledge the significance of the correspondence, then effectively cascade the information among colleagues.
This worked best when the practice manager or some other senior staff member formally disseminated the information. When this process broke down, colleagues in the same practice could have differing information regarding the changes to the current oral surgery service. In the community dental service, where colleagues regularly worked different hours, in different clinics and at outreach centres, there was no centralised dissemination of information. Some individuals could be competently using electronic referral management in a community clinic where their colleagues had no knowledge of the initiative, which could lead to misunderstanding around its purpose and importance for future practice:
I passed that information on to some of our other dentists . . . one of the dentists that works here, I explained it to him and he said he’s not using this system, he’s just sending letters to the consultant. So I thought ‘Oh, perhaps that pilot has come to an end and we can just do letters like we used to’.
CS12
Similarly, some clinicians used existing, more general, knowledge around administrative aims of the NHS when trying to understand the aims of the new electronic system, and assumed it to be part of a wider initiative for a paper-free NHS:
I thought it was just really, to make things paper free.
CS7
A number of introductory and update meetings were set up by the research and commissioning teams to introduce the new referral management system and the accompanying research project and, later, to present information about key milestones for the project, such as commissioning the new specialist (Level 2) service. These were held at various times and venues to maximise attendance, which was generally good. Many practices that had a member of staff attend the information meetings implemented the system without problems and could transfer knowledge about the use and purpose of referral management throughout their practices.
Although attendance at these meetings was cited by many practitioners as being the main source of information regarding setting up and getting started with the new system, a small number of clinicians seemed to misunderstand the division between the research piece (such as participating in interviews), which was voluntary, and actual use of the system to refer patients to oral surgery, which was a NHS commissioning initiative intended for adoption by all eligible practices. This resulted in a small number of practices assuming that they could ‘opt out’ of using electronic referral management in much the same way that they did not have to give consent to be involved in the research and, consequently, these practices continued to write referral letters to secondary care consultants.
An understanding of the need to provide comprehensive referral information, vital for consultant triagers to decide where a patient would best be treated, could be a barrier to GDPs adopting the system, as their time is limited or they are simply unused to accessing and reporting referral information to such a high level of detail. This could represent a change in the perceived responsibilities of the GDP, who had perhaps previously considered this level of taking information from patients to be the role of the secondary care practitioner at the patient’s consultation appointment. Some participants did not understand that they were providing information for the triage decision-making process and saw electronic referral management as simply more work:
Some of the information, you feel like maybe that’s the job of the clinician at the hospital . . . there was a section on IV sedation and about the patient’s anxiety and stuff and there was a section they had to fill the responses to. Well, we wouldn’t normally have them in the surgery because it takes too long.
CS7
Readiness for change
Readiness for change relates to the NPT constructs of cognitive participation and collective action, which describe the relational and operational works needed to complete and embed a new intervention in routine practice. Cognitive participation refers to the importance of ‘legitimation’ to reflect the importance for individuals to believe that they should be involved in doing the work associated with the new intervention. This, then, has implications for collectively working within organisational settings to enable the initiation and sustainability of new work. The collective action construct refers to the practical actions within organisational settings. This is useful in conceptualising issues arising from using the technology that may entail changes to practices and ways of interacting, or new skill sets. Skill set workability is an additional component of collective action that clarifies divisions of labour and who assumes what tasks when a set of new processes is put into operation. 70 Features of these two constructs were related in the data and analysis referred to within this theme below.
Not all practices had the necessary technological infrastructure required to act to implement the system. Restricted access to a computer or appropriate software could be a barrier to using electronic referrals for some practices or individual members of staff. For example, one practice was using Microsoft Windows software that was too old to be compatible with the system. Online referring could involve a walk to, and possibly a wait for, a computer located elsewhere in the building. In another practice, internet access was restricted to one computer situated in reception (apparently to restrict employees’ personal internet use).
Some clinicians preferred to enter referral details directly after seeing a patient, while the consultation was fresh in their minds. However, access to a computer connected to the internet was not always available in their surgeries, and they had to wait to access a communal computer. In addition, one practice had no computer on site, and so the practice manager’s laptop was used to make referrals. This became problematic when she was away from the office or on holiday, as her computer contained personal data and she was reluctant to reveal passwords. As a solution, the practice eventually bought a PC; however, this was not a purchase that had been anticipated:
I need to have a desktop, then it’s easier because once they’re up and running and trained I don’t need to come in specifically and I don’t need to worry about it when I’m away. But, yeah, it does mean I’ve got to purchase . . . it’s not been budgeted for.
CS4
There were some issues during the early virtual implementation period regarding access to OTP codes, which are sent to a pre-registered telephone as part of the login procedure, and are valid only for a set period of time of around 3 minutes. Occasionally a private or inaccessible telephone number had been registered in error, which meant that staff could not access their OTP codes within the timeout period. However, troubleshooting issues around OTP codes depended on individuals feeding back problems arising within the practice to the research team that could change factors, such as the timeout period. Practitioners who did not access solutions could become frustrated and withdraw from using the system:
The PIN [personal identification number] code expiry result can delay logging in. Because it expires after 90 seconds. I’ll have to go back to her and see what the errors were, but she says she’s just gone back to paper for the time being, because she’s tried it a few times and it didn’t work.
CS11
Radiographs were sent electronically with the referrals as a key element to support the triage process. Issues tended to arise because the type and quality of radiographic equipment varied from practice to practice. In the case of those practices without digital radiographic facilities, the research team provided scanners free of charge, which enabled smaller, intraoral radiographs taken using X-ray film be converted to a JPEG (Joint Photographic Experts Group) file and uploaded as an attachment to the referral. There were some initial queries regarding uploading the software needed for the radiograph scanners, but feedback suggested that thescanners were easy to use and images could be successfully attached to referrals.
Within the collective action element of the NPT framework, relational integration is a concept that relates to the process of building confidence in one’s ability to work in new ways and in colleagues’ abilities to interact usefully with new procedures. 67 If this trust-building process helps to shape and normalise new ways of working, the intervention is more likely to be implemented successfully. The necessary relational integration work could break down when individuals lack skills or motivation to interact productively with technology. 71
The level of technological complexity adopted by a practice did not dictate the referral behaviour of all staff. Although most participants found the system helpful and easy to use, some members of staff (both clinical and administrative) lacked basic computer skills, particularly those who entered the workplace some time ago. Within a single practice, some individuals could be referring patients for oral surgery procedures online, while others continued to write or type referral letters. This is reflected in the fact that lack of computer skills was cited as the reason for continued use of letter writing:
There’s a few technophobes . . . you know, they find it hard enough to check their e-mails, let alone manage a system like this.
CS10
There has been an increased use of information technology (IT) within the NHS dental contract and, from 2017, all practices will need to submit claims for payment online. However, much of the IT activity has been administrative work that may be devolved to others in the practice, whereas a referral requires clinical input, hence the need to expose clinicians to IT, even if they may have previously been shielded from the need to use IT. 72
There was an assumption among interview participants that as colleagues used the system they would become more familiar with the processes and would improve their IT skills; however, if the number of oral surgery referrals were low, fewer opportunities to form habitual use of the online system existed:
There was no chance to get into using the system.
CS8
Motivation to acquire the basic skills needed to enter referrals online could be minimal, particularly among older participants, who could be ‘set in their ways’:
If I was staying longer, I would get used to computers, but I’m going to retire anyway, it doesn’t seem worth it.
CS15
Lack of motivation to acquire relevant skills could be exacerbated by an assumption that use of the online system could be circumnavigated by continuing to write referral letters directly to a named consultant or hospital department. Conversely, impetus to change ways of working could be brought about by an understanding that using the referral system was a ‘compulsory’ commissioning initiative that would eventually be implemented more widely:
. . . I was told that if I send them out by post they would be rejected and then you can’t even copy it again so I thought I might as well just learn this from now and I won’t be having that problem.
CS1
Established use of a technology could, however, prove to be both a facilitator of and a barrier to using the online referral system. Many users from practices where electronic records and booking systems were already established had become accustomed to using their own system, and were reluctant to incorporate supplementary systems into their practice. Although many users cited the ease with which they were able to copy and paste patient details, such as medical histories, from their records onto the referral system, others were unused to moving information between different types of systems, and strongly expressed a wish for the systems to be integrated, with information being automatically transferred:
I have to say the online referral system has failed to take off at the practice. Dentists have tried but still prefer paper referrals as they didn’t like the password process or the need to cut and paste details . . . they find writing the referrals or creating them through [existing system] much quicker.
CS11
Some smaller practices, and those with paper-based record systems, did manage to effectively navigate barriers to implementation by delegating oral surgery referrals to a computer-literate individual. This appeared to work best when a mutually convenient and consistent procedure could be agreed with referring clinicians on how to check patient information to be entered:
I’ve crossed off half an hour every week to go through them with him . . . because I input all the data, so I can input the date, address, he doesn’t have to sit through that boring bit . . . just the clinical. Even the medical history I do but I take him through all that to make sure it is accurate, but I input all that . . . it’s 5 minutes for one.
CS4
The way dental practices were structured and managed affected their readiness to change. Within the collective action construct, the contextual integration component relates to the ways in which the power to distribute resources and influence new ways of working is used in practice. Successful implementation was more likely to take place where there was a figurehead, with commitment to working with the system, who had sufficient (formal or informal) power within the organisation to influence other members of staff. Initially, this was around the operation of the new system (how to log in and input data). However, for the impetus and motivation to sustain use and fully incorporate online referrals into a practice, there was a need to convey an understanding that online referral was important and helpful, for example to access the new primary care service and to prepare for a roll-out of referral management to other dental specialties.
Members of staff who could lead on implementation would typically be a principal dentist, but could also be a practice manager, nurse or receptionist with leadership skills and the motivation and remit to convey key messages around implementing a new system within their practice.
The size of a practice did not appear to impact on ability to make changes to the referral behaviours of staff. Smaller practices may have more challenges to overcome regarding infrastructure and computer literacy of staff, but could be flexible and found various ways to problem solve. For example, in one practice, referral tasks were shared and appropriately delegated; a computer-literate member of staff took responsibility for inputting electronic referrals, whereas another staff member typed letters to dental specialties for which online referral was not available.
Interestingly, practices belonging to a dental corporate body were, disproportionately, among the small number of those who did not effectively implement electronic referral management. These practices received on-site training and information sessions from the research team; however, practice managers at each site stated that their attempts to adopt the service within their organisations had been unsuccessful.
In all cases the corporate practices had undergone at least one change in practice manager or had been bought by a larger chain during the early implementation period. This disruption may mean that changes to oral surgery referrals were low on management agendas for these practices. In addition, the practice manager’s role in these organisations was primarily managing business-related tasks, such as finance and estates, with a dentist taking the clinical lead. These corporate practice managers could also be responsible for up to three other practices in the locality, so were subject to extra demands on their time. As such, there seemed to be no overall lead with a legitimate influence on the referring behaviours of dentists at the practice; therefore, electronic referral was adopted inconsistently, depending on the motivation of individuals in each practice.
Conversely, where an individual had considerable influence on the organisation of the practice, such as the practice principal (PP) or contract holder, and was resistant to use of electronic referral management, implementation of the system could be completely blocked, despite intervention from commissioners. One practice was offered IT support 3 months into the evaluation. The practice receptionist told the research team that the practice owner had no intention of securing internet access at the practice as he felt it was ‘too inconvenient’. Thus, this practice continued to use paper-based referrals for the duration of the study and their patients had no access to the specialist primary care service.
Demonstrative feedback
Demonstrative feedback refers to the benefits or frustrations felt in practice by individuals and organisations as a result of using the system, in addition to verbal comments from patients and colleagues. Positive feedback was important to sustaining and embedding changes in practice brought about by the referral system, whereas negative experiences could result in disengagement. Reflexive monitoring is a relevant NPT construct that refers to the appraisal work participants carry out to evaluate the ways that new methods of working affect them and others involved. Two of the four components of reflexive monitoring are described as communal and individual appraisal, and refer to the ways in which individuals and groups collectively decide whether or not and how a new system is working. If this appraisal is negative or if sufficient time for feedback to take place is not given, successful implementation is less likely.
Many interview participants perceived the online referral management system as having several benefits for both patients and their practices. A belief that change would be beneficial was needed to provide motivation to acquire the skills needed to operate the system and to then make changes needed within a practice to facilitate implementation. Once this process had taken place at an individual level, opinions could then be shared among practice members and a group appraisal could be facilitated. As online referral management became embedded in the practice, the perceived advantages could be demonstrated, resulting in sustained use and established change in the way referrals were made.
Initially, completing online referrals could be more time consuming than writing letters, because of the amount of time needed to complete the pro forma in an accurate and detailed way (estimated by some participants at around 5 minutes). However, once the data had been entered, referrals were processed and received by the appropriate service provider demonstrably quicker than with the previous system:
I think the patients get through the system quicker, it’s only a few days and they’ve been triaged and sent to the hospitals . . . Sometimes [a referral letter] could sit on the desk for 2 days before somebody thinks to throw it in the post box . . . then of course you’re reliant on somebody at the other end opening it.
CS16
Many practitioners completing the referrals felt that the information required by the system, although slightly more time-consuming to provide, would be of better quality in terms of amount and detail of content, which would benefit the quality of the service offered to patients:
Ultimately, once the dentist gets used to it, it seems fine because you can track the referral . . . I can see a definite advantage at the oral surgery end, I think you’re getting so much more information from the referrer.
CS12
The system provides each referral with a URN, which can be used by patients and practitioners to track referrals online. Individuals can enter a reference number on the appropriate page of the website and the system will indicate where the referral is in the pathway. This was perceived as being advantageous to patients in terms of having improved access to information and autonomy over tracking their own referrals, but also as helpful to practices, as staff could see at a glance where their patients were in the referral process. They also gained reassurance that their referrals had been received and were being dealt with:
I know I’ve got that [tracking] option and if you have a patient who particularly asks ‘how long?’ we can tell them with certainty, it keeps them off your case and they can chase it themselves.
CS14
When this feedback did not take place at both the individual and collective levels, implementation within a practice did not take place, or was limited to a lone practitioner or a small number of practitioners who were successfully engaging with the system. There was a view that those who were not engaging with the system needed to have the potential benefits pointed out to them, in the absence of personal experience:
So, I think, yeah, it’s like anything – if they’re not giving themselves chance to find out, if they have a sit down presentation and more background, I think people [will be] more receptive probably.
CS11
Table 10 shows the impact the findings had on the timing of implementation. Practices could be categorised into standard, late, rogue and non-adopters of the system (see Table 10 for definitions). For standard adopters, equipment and skills were up to date, and perceived benefits for patients and communication acted as drivers for change. A key staff member with the ability to execute change initiatives took the lead on implementation. These items all acted as facilitators. For late adopters, these changes came later in response to resolving initial barriers associated with equipment and skills, or as key staff became aware of the potential benefits and commissioning plans around referral management and took the lead on implementation. Resistance to implementing the system from the PP or contract holder was the cause of, and key barrier to, non-adoption, even if other facilitators were in place.
| Theme (NPT construct) | Adopters | |||
|---|---|---|---|---|
| Standarda | Lateb | Roguec | Nond | |
| Understanding system aims (coherence) | Facilitator: at least one key member of staff attended information and training meetings or accessed website information and training, and disseminated effectively. Staff understand aim to improve efficiency and waiting time for patients referred for oral surgery | Barrier: had not attended information meetings, received or acted on initial correspondence or received details after system implemented, thus had poor understanding of aims | Barrier: had not attended information meetings, received or acted on initial correspondence or received details after system implemented, thus had poor understanding of aims | Barrier: PP/contract holder resistant to implementation. Implementation blocked |
| Readiness for change (collective action) | Facilitator: computer present in the practice, software was up to date, at least one key member of staff had basic IT skills | Barrier: initial software issues, basic IT training needs identified, login problem-solving needed | Barrier: some IT skill gaps remaining, resistance from some individuals to learn/practise skills required | N/A |
| Facilitator: at least one key member of staff with motivation and recognised authority, remit and responsibility for implementation | Facilitator: key staff member taking lead on implementation as a response to IT troubleshooting or communication with good dissemination of knowledge | Barrier: no key member of staff taking lead on implementation, either through lack of motivation or authority. Corporate-owned practice with no management remit for influencing clinical practice. Poor dissemination of knowledge | ||
| Demonstrative feedback (reflexive monitoring) | Facilitator: implementation sustained as a result of positive feedback from patients and colleagues. Greater efficiencies such as shorter wait for primary care service and less snail mail recognised | Facilitator: became gradually aware of primary care service and associated reduced waiting time because of feedback, which acted as motivator to implement | N/A | N/A |
Discussion
This first stage of the referral project saw the implementation of a passive referral management system that sought to capture all oral surgery referrals from dental practices in the Sefton area. The data suggest that the implementation was a success, with only three practices within the included cohort failing to refer in that period, two of which were practices owned by corporate bodies. It is not clear how oral surgery cases were handled by these practices. They could have been referred internally, referred privately or referred by letter to circumvent the system, or a referral could have been delayed.
Implementation of the new system
In addition to producing data to support population health needs assessment, the outputs from phase 1 provide information about the impact of the implementation of a new, all-electronic system within NHS GDP practices, without triage or deflection to the most appropriate service. At this stage, it is worth reflecting on the differences between GPs and GDPs. Dentistry is a largely surgical discipline, with the patient usually sitting in a dental chair in a dental surgery, and the activity is focused on assessing or treating the oral cavity. 73 A computer, if present in surgery, will be (if only for infection control purposes) some distance from the dentist and the patient and will be used to record the treatment provided. 74 Many dentists do not have clinical dental software systems, but may have a simple appointment system in place at the front desk. 75 GDPs are required to meet the costs of installing and running IT systems from their general NHS contract and, unlike GPs, they do not have access to specific funds for IT systems. GDPs were not included in the roll-out of the NHS intranet, N3, and do not have access to NHS databases such as the Personal Demographics Service. GPs will typically consider their computer as a major clinical tool, perhaps in the same way a dentist may view their drill. 76,77 GPs have access to a range of clinical databases beyond the electronic health record held on their practice systems and even the issuance of prescriptions is largely performed on a computer. 78
A strength of phase 1 of the study is that it identified key barriers and facilitators at an early phase in the process of implementation of an electronic referral system within dental practices, and could offer practical troubleshooting solutions. We collected qualitative data throughout the duration of the study. This enabled us to track developments around implementation over time and compare these earlier findings with later phases in the project as part of an evolving process. Several data sources (interviews, observations and feedback via telephone and e-mail) were used to triangulate and strengthen our results. In addition, our findings incorporate NPT, which is an established theory of implementation evaluation. 67 This can help strengthen and add coherence to the findings. 79 The evaluation research, incorporating a time series analysis with a qualitative element, was progressed in harmony with the implementation of the electronic referral management system through a close working relationship with commissioners. This is in contrast to other studies whose design has impeded implementation of new systems in real-life settings. 80,81
One of the attractions of the system we implemented is that practice staff needed only basic computer skills to use the system, for example to have previously accessed e-mails or made an online purchase. Despite early reports of individuals lacking the necessary skills, most participating practices had at least one member of staff who initially had the computer literacy to take responsibility for inputting referral data, and who could potentially transfer basic skills to other staff members, if they had the leadership skills and remit to do so. The main driver of successful implementation in the context of this study appeared to be the presence of an individual(s) in each practice with the authority to implement change and who was adequately informed about the new processes and motivated enough to relay to their team the benefits of adopting the new way of working. Barriers to implementation arose when there were disparate working hours and locations (e.g. in the community dental service), and where those taking responsible for change management were not seen to have the authority or jurisdiction to implement the changes (e.g. as observed in corporate body-owned practices). An important factor for both initial engagement and sustained implementation was that practices, of whatever size, were structured in a way that facilitates information sharing and communication around invoking new initiatives. Our findings resonate with the findings of research concerning the broader implementation of technology in health-care systems. Interventions that have been successfully introduced on a larger scale have appointed ‘champions’: individuals (often GPs) with a specific remit to assist in operationalising new technologies and adjunct ways of working. 82 Although there may be opportunities for a similarly formal position in rolling out electronic referral management systems, more work needs to be done around the effective qualities of a successful ‘champion’ in the context of dentistry.
Motivation to implement the electronic referral management system could be assisted in the early stages by practices having a clear understanding of the aims of the initiative and, later in the process, of its benefits. Sustained use was reported when these benefits were demonstrated pragmatically and through feedback from patients and colleagues. Benefits to patients included faster pathways to specialist care and shorter waiting times for treatment, which were facilitated by quicker processing of electronic referrals rather than the previously used postal system. Comprehensive, clinically relevant, information captured by the referral forms aided faster triage, both within the system itself and upon receipt of the referral request by secondary care providers. Both primary care practitioners and patients could also benefit from the online referral tracking system, which displayed the status of the referral and the name of the selected provider. This replaced the previous necessity to call hospitals to trace referrals, which had proved time-consuming and sometimes required a resubmission of the referral. Other research around the introduction of new electronic systems, including telehealth, has emphasised the social and reflexive processes involved in the adoption of new technology. 83,84 For a new system to become fully integrated into everyday practice in health services, a process of feedback and subsequent reflexive monitoring may be necessary.
One barrier to the implementation of the new system may have been the lack of dental practices and patients realising the full benefit from day 1 of inception. There was initial scepticism about whether or not the additional effort required in primary care would provide tangible benefits. The primary care oral surgery service was not operational in this first phase while data were collected to inform commissioning and to assess the impact of implementing the system without active deflection. The proposed benefits of faster care closer to home and within primary care were, therefore, not realised in this initial roll out.
Effective communication between the commissioning team (and, if applicable, the referral management service provider) and general dental practices is important. Good lines of communication can highlight key timelines for implementation, highlight the aims and objectives of the new system and create impetus for change through an emphasis on the benefits to patients and practitioners and the plans for continued roll out of the service (such as the introduction of the Level 2 primary care service). Practices that understood the likelihood that they will ultimately be expected by local commissioners to refer online to multiple specialties located in several geographic areas were more likely to implement the system effectively. Group meetings were effective ways of sharing information around the research project and commissioning plans for the service; however, the success of these information-sharing meetings relied on practitioners receiving timely details of these events.
Currently, effective information sharing relies on individuals within a practice recognising the importance of information they receive and circulating this effectively with colleagues. Information sharing in this way sometimes broke down, resulting in some practitioners receiving inconsistent messages. Introducing and managing change is a human process and there will always be gaps in how individuals receive, internalise and act on communications. However, participants suggested that communication could be improved through addressing correspondence to named individual dentists, rather than to practices. A detailed referral, including medical history and radiograph, is essential for consultant triagers and hospitals to make informed decisions about where, and by whom, patients should ultimately be treated. This can be emphasised through training and feedback to practices by consultants and the dental RMC.
These key messages relating to the introduction and sustained use of an online referral management and triage system for oral surgery are specific to this project, and lessons learned for implementation of this system in primary care dentistry are described in the following sections. However, the overarching themes may have resonance with many interventions and change management initiatives across different health specialties and organisations.
Impact on referral numbers
The total number of referrals for oral surgery was 670 in the 12-month period, as captured by the electronic referral system. It is difficult to ascertain if the number of referrals changed directly because of introducing the electronic referral system. Establishing a baseline referral rate was problematic, as data on referrals are not routinely collected by the NHS BSA (although there is a FP17R form, it is rarely completed) and hospital data will generally code on the patient’s GP details, rather than GDP. We did, however, acquire HES data for key OPCS codes (those codes with an F prefix: F09.1, F09.3, F09.5, F10.4, F10.8, and F12.1) for all three hospitals included within the study footprint, and identified those codes that were likely to be related to oral surgery (vs., for example, maxillofacial or oral medicine procedures) to provide likely referral numbers in 2013 and allow like-for-like comparisons for 2013 and 2014 (before and after the introduction of the electronic referral system).
In 2013, the total number of referrals from patients with a Sefton GP was 810. In 2014, using the same method of measurement (HES data), it was 723. This suggests a decrease in referral number of about 11% (810 vs. 723) associated with the implementation of the referral management system, but significant caution should be applied in interpreting this apparent reduction. The study design was an ITS and we did not have a control population to compare changes. The reduction could be a secular change, but the depression in referrals was marked and was not seen in other parts of the north-west (this is expanded upon in Chapter 5).
The disparity between the 2014 HES numbers and the electronic referral system numbers (723 vs. 670) demonstrates the difficulties in relying on HES data to provide an accurate figure for referral numbers. It is also important to remember that not all NHS oral surgery referrals came through the new referral system; accepting the figure of 670 referrals through the electronic referral system at face value assumes that no GP referrals were made and all Sefton residents attended Sefton GDPs for their dental care. The difference suggests that about 50 referrals came from non-system users, GPs or another source, such as private dentists or NHS dentists outside the Sefton area. It can be hypothesised that the introduction of a referral management system alone (without triage and demand management) could reduce demand and increase referral quality. In the current work, the results of phase 1 suggest that there was an effect, given that an 11% fall in referrals during the implementation period was seen (the effect could have been larger given the 50 or so referrals that did not go through the system).
A fall in referral number could be attributed to problems identified in the qualitative work with implementation, and the system acting as a potential disincentive to refer simple cases. During the phase 1 implementation year there was no evidence that the new system stimulated demand; however, this was not anticipated as no new services (Level 2) were offered in phase 1. It can be argued that the introduction of a referral system alone will decrease the number of referrals, given the increased scrutiny on practices inherent in the process. This argument assumes that many referrals, driven by the unintended consequences of incentives to increase referrals in the 2006 contract, would be Level 1 – and, hence, are ‘inappropriate’ for secondary care. This predicted pattern of referral was not seen in the electronic referral data of the current study. One would not expect, nor want, a referral management system to reduce the number of Level 2 or 3 referrals from primary care. The fall in referrals we detected is more likely to be a result of the inconveniences inherent in adopting a new system acting as a disincentive to refer, which seems to be supported by our qualitative findings.
Impact on referral quality
One of our research questions considers the impact of the new system on the quality of referrals submitted to secondary care. The assessment of over 2000 referrals submitted in 2013 (pre implementation of the new system) demonstrates the limited information content of referrals and the relatively poor quality of referral prior to the introduction of referral capture. Less than 20% of referrals were provided using an approved pro forma (although they existed and were promoted by NHS commissioners) and the remaining referrals relied on a letter. One of the reasons for this finding may be found in the qualitative work – practitioners liked to use the internal referral letter feature of their practice software – rather than completing a form that required a minimum data set.
The failure of referring dentists to provide GP details, and the fact that less than half of referrals had a completed medical history, demonstrate the value that electronic referral handling can provide. By making fields mandatory, failure to complete them prevents a referral from being submitted. For this reason, the online system increased the provision of important patient metrics to 100% in all cases, except for radiographs. Radiographs were not a mandatory requirement of this process, and, hence, a referral could be submitted without them. It must be remembered that some oral surgery procedures, for example those involving soft tissues, would not require any imaging. In total, 7.5% of referrals in the phase 1 period were rejected for failure to supply a radiograph when one was required.
By insisting on the completion of the referral pro forma online, the use of conditional formatting and mandatory fields clearly improved the completion of the referral forms. We are unable, at this stage, to determine if this has improved the overall quality of referrals. For example, a dentist could provide minimal or incorrect information in any field. However, the diagnostic test study in Chapter 2, in which we assessed the accuracy of the triage process, provided complementary information on the quality of referrals and how to improve this key element of the process.
Electronic referral systems for health needs assessment
The patients referred for oral surgery procedures were mainly in their mid-forties, with slightly more females than males. This is representative of the general population described in the 2011 census data; the average age of a Sefton resident is 43 years and approximately are 52% females. The reported smoking rate was low, at 13%, which is consistent with Sefton’s overall reported smoking prevalence of 19.6% (which rises to 23% in the most deprived areas). Reported alcohol consumption was low, with only 20% reporting any, irrespective of amount, and only 17 individuals (2.6%) consuming over 14 units per week. Sefton’s reported alcohol consumption suggests that 20% of men and 10% of women drink more than the weekly recommended amount. 85
Patients referred into services were generally fit and well at presentation, with the clear majority being rated as one would expect from primary care referrals, that is, ASA grade 1 or 2. The presence of comorbidities in these patients was determined by assessing information provided on the referral form against the list of mandatory NHS comorbidities to be recorded by secondary care, and was a source of further additional information for providers. The proportion of individuals on anticoagulant therapies or bisphosphonates, at 2% and 1.6%, respectively, is surprisingly low given that these drugs are often cited by GDPs as reason for referral to secondary care. 86,87
By undertaking a passive triage process, we determined the proportion of cases that could have been seen in primary care, and the type of procedure and patient referred. Of all the referrals assessed, only 2.5% were considered by the consultant triagers to be Level 1 referrals. These referrals were from a range of practices, and there was not a clear indication that a small number of ‘frequent flyer’ providers or performers were outliers in their contribution to Level 1 referrals. This small proportion of cases that should be managed in general dental practice is consistent with that reported by Kendall from the Croydon project. 17 This finding suggests that the elimination of Level 1 referrals is unlikely to lead to substantial increases in secondary care capacity or cost savings. It also undermines the suggestion that the introduction of a referral management service alone (without diversion services) is unlikely to achieve a significant reduction in referral numbers. This is consistent with finding from the GP literature, in which the simple introduction of referral centres as ‘gatekeepers’ had no impact on the numbers of referrals being received by secondary care. 21
The number of cases that could be diverted to specialist practice in primary care (Level 2) was 67.2% – again, consistent with the data reported by Kendall. 14 We also learnt about the clinical nature of these referrals, with over one-third being described by the referring dentist as a ‘difficult extraction’. Simple and complex impactions were also considerable contributors to the cases deemed suitable for referral to specialist practices, but surgical endodontics (or apicectomies) represented only 6% of the total referral number. These data can help inform commissioning of primary care services by determining likely numbers (and, hence, the number of sites required to meet the needs of referrals and budget planning), and inform the development of service specifications for primary care-based services. Well-defined service specifications facilitate efficient procurement. 6 For example, the number of impactions suggests that, for this population, a panoramic radiograph facility would be essential; however, a service specification that called for a surgical microscope to undertake apicectomies would produce an overspecification and, hence, the risk of a higher bid price. Health needs assessments for complex conditions or procedures, such as those managed by oral surgery services, can be supported, in part, by referral management systems. It must be noted that the data produced by these systems represent expressed need (patients who have attended the dentist and been referred). However, given the nature of oral surgery presentations, typically un-restorable teeth that are symptomatic, it is likely that expressed demand is very close to population need. The findings of phase 1 informed the procurement of the Level 2 service implemented in phase 2 of the study.
The referral management system could provide data on:
-
the number of total referrals to oral surgery from a defined practice base
-
the complexity of these referrals, as assessed by consultant triage of referrals
-
the treatments and procedures requested by the referring dentist in these referrals
-
the patient-related factors likely to influence care or drive referrals
-
the geographic location of patients
-
their current preference in terms of hospitals.
Phase 2 of implementation was active deflection of referrals. Data from phase 1 (passive) referrals enabled the research team and commissioners to estimate the impact of active defection on the three hospitals receiving referrals from Sefton primary care dentists. When the study was being proposed and initially mobilised, each trust was contacted and engaged with the research. Hospital A readily took part and a directorate manager stated that they saw very few Level 2 referrals and, consequently, the new system would have little impact on their services. The commissioners also stated that they felt that, overall, very little oral surgery activity was referred to hospital A. It was therefore surprising to see the data presented in Table 9, which show not only that the majority of Sefton’s oral surgery referrals were sent to this hospital, but that 80% of this activity was Level 2 in nature.
This is an important finding, and demonstrates the value of undertaking health needs assessments in combination with system-level assessments. The interpretation of HES data and other acute trust data is complex, often based on registered GP inputs rather than GDP inputs. 88 Furthermore, the validity of HES data is based on the ability of coding staff to interpret clinical records accurately. The simple nature of the referral management system data – where referrals are captured and then sent to named providers – enables commissioners to understand referral flows and service utilisation. Had the primary care diversion service been introduced without any system evaluation, this could have destabilised hospital A. An evaluation of the system based on referral data enables the best alternative services to be commissioned – for example, a primary care centre close to hospital A could be a preferred location for this type of service.
Summary of main findings
Implementation of triage without deflection enabled us to evaluate the effects of a mandatory electronic data capture of referrals alone. It also enabled us to explore some of the barriers to, and facilitators of, successful early implementation and adoption of the new system. In this section of the project, we posed a number of research questions:
-
What are the practical issues for the NHS in introducing an all-electronic referral system from scratch?
This phase of the project showed that, with the full backing of commissioners and senior consultants in acute trusts, an electronic referral system can be successfully established within a short time period. Clear communication is the most important factor, along with a clear message that there is a universal, mandatory requirement to use the new system. Timely, pragmatic support for dental practices is also important; for example the provision of, and support in using, radiograph scanners.
-
What is the effect of an all-electronic referral system on the total number of referrals?
The introduction of the new system seemed to be associated with a fall in the total number of referrals, probably because of the greater inconvenience of providing more detailed clinical information. This fall could have resulted from a reduction in Level 1 referrals (although without comparable baseline data it is not possible to verify this). The introduction of an electronic referral system alone (without deflection) does not produce the efficiencies wanted by commissioners. The majority of referrals were for Level 2 cases and ≈80% in hospitals A and C, but for some reason only ≈50% in hospital B.
-
What is the quality of referrals including an assessment of compliance with national referral guidelines?
The completeness of clinical information and the quality of the information content of referrals were markedly improved by the introduction of the referral system, particularly as it was a mandatory requirement to complete all fields of the standardised referral form. A very small proportion of referrals were Level 1 (inappropriate) referrals.
-
How much time was taken to complete referrals?
Clinicians reported that, once they were familiar with the system, each referral took about 5 minutes.
-
What are the views of key stakeholders on the benefits and problems of the electronic referral system, and how can the system be improved based on their experiences?
Lack of computer literacy, financial implications of computerisation and corporate priorities were significant barriers to implementation. The most important factor that supported uptake and sustained use was having a designated person(s) in each practice who had a clear understanding of the reasons for introducing the new system with the authority to implement the change. Clear communication was also critical in explaining the processes involved, the reasons for introducing the system and the benefits it would bring.
Conclusion
This phase of the study showed that rapid implementation of an electronic referral system for a defined population is possible with the full commitment of commissioners. Most practices quickly adopted the system, often employing their own pragmatic solutions to support implementation within the specific context of their workplace. The system produced an immediate improvement in quality of referrals, provided valuable information to support health needs assessment and may have suppressed inappropriate referrals to some degree, but a casual relationship between implementation and a fall in the number of referrals was difficult to demonstrate.
This qualitative analysis has identified several barriers to, and facilitators of, early implementation of an electronic referral management system. The findings offer pragmatic guidance in the early implementation of similar systems in general dental practices. Although this analysis focuses on one specific area of implementation, the findings from several discrete qualitative studies at each phase of the study can be used to carry out a normalisation process evaluation that encompasses a more holistic theory of implementation.
In Chapter 4, we explore the impact of the introduction of the primary care service, the active direction of referrals into primary care and the resultant impact on services and costs.
Chapter 4 Active referral management with consultant and general dental practitioner triage: quantitative findings including economic evaluation (phases 2 and 3)
Introduction
The second and third phases of the study took place in calendar years 2015 and 2016. Following an appraisal of the health needs assessment, the local commissioning team proceeded with an AQP procurement for a primary care (Level 2) oral surgery service to cover the Sefton geographical footprint. An AQP procurement is a threshold process that enables providers to demonstrate that they meet the requirements of a service specification produced by the service commissioner, and, hence, are awarded a contract, usually at a set price per procedure and without any guarantee of minimum activity. The service specification for the procurement was informed by the health needs assessment in terms of likely clinical activity, likely numbers of patients and the geographical location of patients. Following this process, a single provider met the criteria and two physical locations were identified in Sefton to cover the geographical spread of referrals.
In phase 2 (2015), referrals were actively triaged by consultants in oral surgery and OMFS, and in phase 3 (2016) GDPs could select their own preferred providers (i.e. self-triage). In phase 2, referrals that were deemed to be Level 1 were sent to the new (AQP) Level 2 provider. There was no change in the services offered by the three secondary care services. The primary care (AQP) provider offered the full range of Level 2 services, except for apicectomies (surgical endodontics) and soft-tissue surgery requiring pathology services.
In phases 2 and 3, we undertook an economic evaluation, looking at case-by-case costs for patient management in appropriate settings compared with phase 1 (no deflection). The purpose of the evaluation was to examine if there are cost savings from ‘active’ triage of referrals for minor oral surgery. The NHS has developed tier 2 services in many specialties with the aim of improving care and reducing costs, usually without an evaluation of the costs and effects of the new service. The danger is that a new Level 2 service may improve the service but may also increase costs substantially by introducing a new service and failing to recover resources from secondary care. In this study we had the opportunity to undertake a robust health economic analysis to assess the impact of both consultant-led (phase 2) and GDP-led active triage.
Changes to intervention in phases 2 and 3
Using the same electronic referral system as phase 1, the final two phases of the study used ‘active’ triage to divert non-Level 3 activity to a single primary care (Level 2) service in the Sefton area. The new service started taking referrals from the electronic referral system at the start of phase 2. The same consultant-led triage team was utilised in phase 2. During phase 3, the referral form was modified to enable the referring GDPs in Sefton to select either a primary or secondary care destination for their referral. The decision to add GDP assessment of referral direction was based on The King’s Fund recommendation for peer assessment and the need to reflect local capacity for consultant triaging. 20 Each referral was also assessed by the consultant triage team as an audit of the GDPs’ decisions but the GDPs’ referral decisions were respected, except for those referrals deemed to be suitable for a 2-week wait appointment.
Aims
The overarching aim of this part of the study was to measure the number of referrals, referral quality and costs of an electronic referral management and triage system, allied to provision of a specialist primary care service. More specifically, the following research questions were addressed:
-
What are the differences in the number of referrals, referral quality and the mean cost per referral between virtual management (phase 1) and consultant-led active management (phase 2)?
-
What are the differences in the number of referrals, referral quality and mean cost per referral between the year of virtual management (phase 1) and GDP-led active management (phase 3)?
-
How do these findings (differences in the number of referrals, referral quality and the mean cost per referral between study phases) differ by the provider of secondary care?
-
Does consultant-led triage offer reduced costs over GDP self-determined provider choice (phase 2 vs. phase 3)?
-
How do the views, and experiences, of patients differ between those using primary and secondary care services?
Methods
In phase 2, each referral entered into the system was triaged by a member of the consultant team to either Level 1, 2 or 3, using the same decisions as those described in Chapter 3. In phase 3, GDPs used the electronic system to decide if their patient should be referred to either to either a Level 2 or 3 service. Further assessment of referrals to determine ASA status, OCPS code and the number of teeth to be extracted was also undertaken.
Consultant triager decisions were dichotomised as primary care (Level 1 or 2) or secondary care (Level 3). Descriptive statistics were generated to describe measures of central tendency and location (mean and SD or median and interquartile range). For each phase of diversion, comparative analyses of referrals to primary and secondary care were undertaken. Categorical data were analysed using the chi-squared test and risk difference, as appropriate; continuous data were analysed using t-tests.
The ITS for phases 2 and 3 were assessed using referral data aggregated monthly for 24 months, with an outcome measure of referrals to primary care as a proportion of all referrals. We were unable to include referrals for phase 1, as all Level 1 and 2 referrals went to primary care, with perfect prediction of the outcome. The ITS model therefore reflects referrals for phase 2 (2015) and phase 3 (2016).
A segmented regression analysis was undertaken, using a heteroscedasticity- and autocorrelation-consistent variance estimate (Newey–West) with a lag of 5. The initial 12 months (phase 2) reported referrals from the consultant-led diversion, and the following 12 months (phase 3) referrals from the GDP-led diversion. Accordingly, the ‘intervention’ indicated the change from consultant- to GDP-led referrals at 12 months. Covariates in the model were the main effects of study month, intervention and an interaction term of study month and intervention.
Patients attending for procedures in each setting were consented to receive a paper questionnaire following their surgery to collect data on patient outcomes, experiences and costs. Patients not returning their questionnaires after 6 weeks were sent up to two reminders at approximately 4-week intervals and were given the option to complete the questionnaire over the telephone with the assistance of a researcher. A £10 gift voucher was offered to those completing and returning the questionnaire. Additional consent was obtained to interview patients for the qualitative component of the study, which is reported in Chapter 5, and again to view their dental records for an assessment of complications following treatment.
Health economics
Setting and location
The economic evaluation included all patients processed through the referral management system and treated in hospital A (DGH), hospital B (large foundation trust hospital), hospital C (a dental hospital) or local (Level 2) primary care oral surgery services in Sefton.
Unit costs
For the economic evaluation, we first sought to identify the costs for each oral surgery procedure in each of the three hospitals. This was undertaken using Secondary Uses Service data covering the period 2013–16. The costing profile demonstrated considerable differences between each hospital based on its allocation of the treatment to outpatient care, day case are or inpatient care. Using a standardised tariff scoring approach, procedures were categorised into those predicted to be outpatient, day case or elective (inpatient procedures). This allocation of treatment procedures was then compared with the actual claims and tariffs charged (Table 11). It is clear from these data that there is a difference in the way that similar procedures were being coded in each hospital. For example, in hospital A, many procedures were universally coded as day case and, hence, attracted a significantly higher tariff than in hospital C that made very little use of the day case tariff and much greater use of the outpatient tariff.
| Hospital code and type | Procedure description | Tariff (£) | ||||
|---|---|---|---|---|---|---|
| OP claimed | OP predicted | DC claimed | DC predicted | Elective | ||
| Hospital A – district general | Surgical removal of wisdom tooth NEC | 0 | 445 | 444 | 0 | 1 |
| Surgical removal of retained root of tooth | 0 | 434 | 430 | 0 | 4 | |
| Unspecified simple extraction of tooth | 8 | 268 | 259 | 0 | 1 | |
| Apicectomy of tooth | 0 | 206 | 206 | 0 | 0 | |
| Surgical removal of tooth NEC | 0 | 201 | 200 | 0 | 1 | |
| Hospital B – foundation trust | Unspecified simple extraction of tooth | 1054 | 1154 | 94 | 1 | 3 |
| Biopsy of lesion of mouth NEC | 781 | 834 | 42 | 1 | 12 | |
| Excision of lesion of mouth NEC | 479 | 533 | 44 | 0 | 10 | |
| Surgical removal of retained root of tooth | 385 | 487 | 87 | 2 | 16 | |
| Surgical removal of wisdom tooth NEC | 326 | 1178 | 777 | 8 | 57 | |
| Hospital C – dental hospital | Unspecified simple extraction of tooth | 742 | 767 | 25 | 0 | 0 |
| Surgical removal of tooth NEC | 162 | 177 | 15 | 0 | 0 | |
| Surgical removal of wisdom tooth NEC | 111 | 140 | 29 | 0 | 0 | |
| Surgical removal of impacted wisdom tooth | 72 | 97 | 25 | 0 | 0 | |
| Surgical removal of retained root of tooth | 67 | 71 | 4 | 0 | 0 | |
We therefore coded the cost for each referral based on the 2015 tariff, as applied by each of the hospitals using a median charge base. The cost of treating patients in primary care was at a fixed tariff of £150 (based on a band II treatment (3 UDAs) attracting an enhanced UDA rate of £50).
When assessing the cost of the referral management programme, a cost per referral of £8.22 was used. This covers the cost of the referral management infrastructure and the cost per case of clinical triage based on consultant-level staff.
This figure was obtained from the financial envelope provided for two recent dental referral management procurements. The cost for referral management in phase 3 was fixed at £4.00 per referral, with the reduction reflecting the lack of consultant costs. The total cost of the management service over 2 years is added to the (fixed) cost of treating redirected referrals in specialist primary dental care to produce the additional cost per referral avoided.
Information on the number and type of treatment failures that had arisen during a 1-month period post treatment was recorded in questionnaires completed by the patient, the referrer and the provider in the referral management programme. The mean complication cost (treatments provided 1 month post oral surgery episode) per referral by provider [primary care (Level 2) oral surgery service, hospitals A, B and C] was added to the provider’s (fixed) cost of treating a referral.
Societal costs
In addition to the cost to the NHS, we estimated costs from a societal perspective, which is the preferred perspective for economic evaluations. This was based on an approach that imputes the costs associated with time travelling to and from an appointment and the personal costs of travel. Costs to patients and patient carers (i.e. accompanying persons to the appointment) were calculated from data collected in a patient questionnaire on the costs incurred in travelling to and from an appointment, and waiting and being treated at treatment facilities. Details of these costs can be seen in Table 12.
| Indirect cost | Cost (£) | Reference for price of indirect cost |
|---|---|---|
| Travel cost – car | 0.45 per mile | HMRC tax rates per business mile (first 10,000 miles)a |
| Travel cost – motorbike | 0.24 per mile | HMRC tax rates per business mile (first 10,000 miles)a |
| Travel cost – cycle | 0.20 per mile | HMRC tax rates per business mile (first 10,000 miles)a |
| Travel cost – train | 0.30 per mile | Based on a single trip from Macclesfield to Manchester |
| Travel cost – taxi | 1 mile: 3.90 | Manchester local government authorityb |
| 3 miles: 7.50 | ||
| 5 miles: 11.20 | ||
| 7 miles: 15.00 | ||
| 9 miles: 18.60 | ||
| 10 miles: 20.40 | ||
| Travel cost – bus | 0.45 per mile | Average (in sample) ticket price |
| Travel cost – walk | – | – |
| Parking tickets and other ticketed travel expenditures | Reported by the patient | Average (in sample) ticket price |
| Cost of travel time to and from an appointment | 15.73 per hour | Office for National Statisticsc |
| NHS prescription items (as a result of complications) | 8.40 per item | NHS Choices websited |
These costs included both the cost of lost time as well as out-of-pocket costs for public or private transport and parking, etc. Time costs were estimated using the general average wage for the UK working population,89 following standard practice in health economic evaluations. A final personal cost was the number of NHS prescription items (painkillers or antibiotics) recorded on either the patient, referrer or provider questionnaires.
Table 11 provides an outline of the unit costs we used to calculate indirect costs. To establish the societal costs incurred in treating a referral, the average indirect cost per referral by provider (specialist primary care or each of the secondary care providers) was added to costs incurred by each provider for treating each referral. Secondary care provider treatments tariffs, UDA band treatment costs and societal unit costs were based on 2015/16 prices.
Comparators and outcomes of the economic evaluation
The cost analysis was designed to evaluate the impact of a change in service by comparing the overall cost of minor oral surgery services in different phases of ‘active’ implementation of the referral management programme with the service cost in virtual management. Virtual management was chosen as the main comparator to ‘active management’ because no referral destination data prior to the introduction of the referral management programme were available. The time horizon over which costs were compared was 2 years (virtual management and active management). No discount rates were applied to costs because there was no extrapolation of costs to years when the referral management programme was not in place. A 2-year time horizon was appropriate because each year of ‘active management’ was compared with ‘virtual management’ (in a separate analysis) to distinguish the cost consequences of consultant-led active management from GDP-led active management.
The mean cost per referral was chosen as the decision criterion because the referral management programme aimed to establish a reduction in costs among clinically equivalent strategies, treatment in secondary care or at a primary care oral surgery service. The premise of the economic model is that there is clinical equivalence in these settings, which is difficult to examine and is not proven.
Outcome heterogeneity is explored by examining findings among the different providers of secondary care. SEs of mean cost differences show the level of uncertainty in the model estimates. To test the effects of these cost differences on the results, the difference in the mean cost per referral (between the year of virtual management and year of consultant-led active management, and between virtual management and GDP-led active management-years) is calculated using the secondary care unit costs (treatment tariffs) of a single hospital for all secondary care providers.
Results
It should be remembered that this was a mixed-methods study with qualitative data collected in parallel with (and informed by) the quantitative data. The quantitative results are presented and discussed in Number of referrals, Referral quality metrics and Health economics, and the qualitative element of the study is described in Chapter 5.
Number of referrals
Table 13 provides an overview of trends in number of referrals for each year from 2013 to 2016 using HES data and data from the electronic referral system. HES data are presented for Sefton and two north-west PCTs for reference. The Sefton HES data show an 11% decrease in referrals following the introduction of the electronic referral system.
| Year (including phase) | Location | |||||||
|---|---|---|---|---|---|---|---|---|
| Sefton – RMa | Sefton – HESb | PCT 1 – HESb | PCT 1 – HESb | |||||
| Number of referrals | ± % | Number of referrals | ± % | Number of referrals | ± % | Number of referrals | ± % | |
| 2013 | – | – | 810 | – | 1480 | – | 1154 | – |
| Phase 1 – 2014 | 670 | –17 | 723 | –11 | 1467 | –1 | 1322 | +15 |
| Phase 2 – 2015 | 643 | –20 | 702 | –14 | 1665 | +13 | 1497 | +30 |
| Phase 3 – 2016 | 861 | +6 | 874 | +8 | 1862 | +26 | 2089 | +81 |
Looking at the data produced by the electronic referral system, there was a decrease in the total number of referrals between phase 1 (passive triage) and phase 2, with a corresponding reduction in the HES data. The total number of referrals increased greatly between phase 2 (consultant led) and phase 3 (GDP led), and, again, this rise was mirrored in the HES data.
Comparative HES data from the two other former PCT areas over the same time show year-on-year increases in referrals in one PCT by 81% between 2015 and 2016. In contrast, there seems to have been a modest increase in Sefton referrals, which is much smaller than the trends exhibited in the other PCTs.
It appears from these data that, although there has been a modest increase in Sefton referrals, this reflects a general pattern of increasing number of referrals generally and the referral management system appears to have a suppressive effect.
The number of referrals and their final provider destination are shown in Table 14, which includes phase 1 (no active deflection) data for comparison purposes. In phase 1, although there were no actual referrals to primary care, the same consultant-led team used in phase 2 was making triage decisions. When comparing phase 2 with phase 3, there was an overall 25% increase in the number of referrals (i.e. 643 vs. 861), and the GDP referred more cases to secondary care than the consultants. Figure 2 presents the weighted proportion of referrals to primary care over the 24-month period.
| Type of referral | Phase (year), triage type | |
|---|---|---|
| 2 (2015) | 3 (2016) | |
| Consultant, n (%) | GDP, n (%) | |
| Level 1 | 15 (2.3) | |
| Level 2 | 287 (44.7) | 369 (42.9) |
| Level 3 | 341 (53.0) | 492 (57.1) |
| Total | 643 (100) | 861 (100) |
FIGURE 2.
The proportion of referrals to primary care over phases 2 and 3.
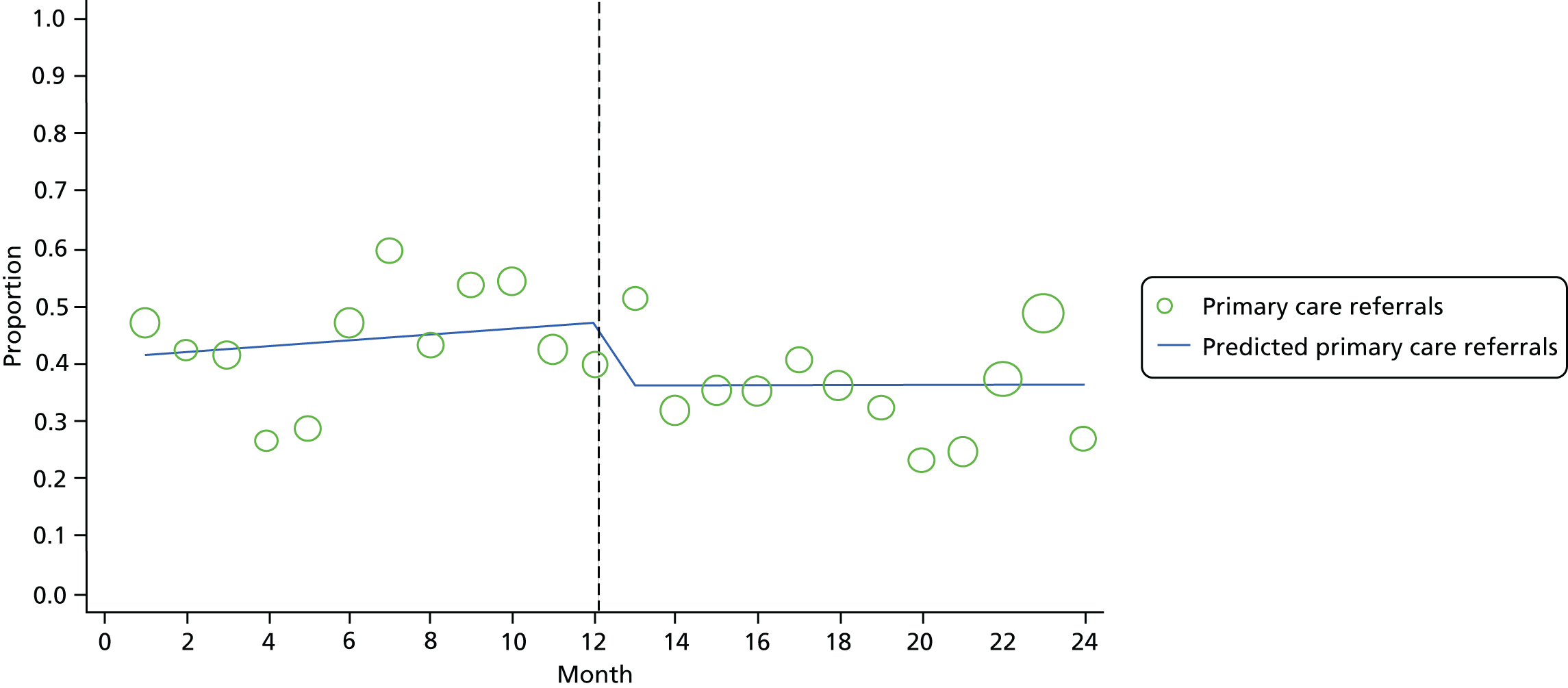
Figure 2 shows the proportion of referrals to primary care over phases 2 and 3. Referrals in months 0–12 are the result of consultant-led triage, and thereafter of GDP-led triage. The y-axis represents the proportion of referrals to primary care. The size of the circles is proportional to the total number of referrals. The dashed line at 12 months indicates the change from consultant-led referral to GDP-led referral at the end of the month.
Before the intervention (the switch from consultant to GDP), there was a non-significant increase [odds ratio (OR) 1.02 per month, 95% confidence interval (CI) 0.98 to 1.06, secular trend, per month]. After the intervention, there was an increase in consultant-led to GDP-led referrals (OR 0.98 per month, 95% CI 0.93 to 1.03, gradual effect, per month), although this finding was not statistically significant. There was, however, an immediate effect of the intervention (OR 0.62, 95% CI 0.42 to 0.93). The odds of referral to primary care following the intervention are about 38% lower than the before the intervention.
Referral quality metrics
Post referral redirections from primary care to secondary care (representing inefficient triage) were small. A total of 12 cases (4%) in phase 2 and 15 (4%) cases in phase 3 were sent by the primary care provider onwards for hospital care. The reasons for the onwards referrals are shown in Table 15.
| Reason for onwards direction | Phase (year), number of referrals | |
|---|---|---|
| 2 (2015) | 3 (2016) | |
| Patient preference factors | ||
| Patient wanted GA | 4 | 6 |
| Patient refused treatment in primary care | 3 | 4 |
| Referral process | ||
| Procedure more complex than anticipated | 3 | 2 |
| Medical history inaccurate | 2 | 3 |
| Total | 12 (4%) | 15 (4%) |
There was a significant difference in the ASA score between primary and secondary care settings for both phases. Table 16 provides a cross-tabulation of the ASA scores for referrals by phase 2 and 3. In phase 2, for an ASA score of 1, 52% went to primary and 48% went to secondary care; for an ASA score of 2, 53% went to primary care and 47% to secondary care; for an ASA score of 3, only 23% went to primary care and 77% went to secondary acre; and the one patient who had an ASA score of 4 went to secondary care. In phase 3, for each ASA score, higher proportions went to secondary care (an ASA score of 1, 57%; an ASA score of 2, 59%; and an ASA score of 3, 84%). Thus, it would seem that GDPs were referring more patients across the board to secondary care irrespective of their ASA status.
| ASA score | Phase (year), number of patients | |||
|---|---|---|---|---|
| 2 (2015) | 3 (2016) | |||
| Primary | Secondary | Primary | Secondary | |
| 1 | 177 | 166 | 177 | 236 |
| 2 | 87 | 76 | 100 | 142 |
| 3 | 17 | 56 | 12 | 62 |
| 4 | 0 | 1 | 0 | 1 |
| Total | 281 | 299 | 289 | 441 |
There was no difference in age (2015 results: t = 1.3, degrees of freedom = 641; p = 0.18; 2016 results: t = 0.75, degrees of freedom = 865; p = 0.46), smoking status [2015 results: Pearson’s χ2(3) = 1.9; p = 0.59; 2016 results: Pearson’s χ2(3) = 7.5100; p = 0.06] or alcohol consumption [2015 results: Pearson’s χ2(3) = 2.9; p = 0.41; 2016 results: Pearson’s χ2(3) = 3.1; p = 0.38] in either setting in each phase of the study. There was a significant difference in the mean number of teeth indicated for extraction in primary and secondary referrals at both time points. In 2015, the mean number of teeth indicated for extraction was lower in those attending primary care (n = 281, mean = 1.22, SD = 0.59) than in those attending secondary care (n = 288, mean = 1.78, SD = 1.69), a difference in means of 0.56 teeth (95% CI 0.35 to 0.77; p < 0.0001). In 2016, the mean number of teeth indicated for extraction was lower in those attending primary care (n = 289, mean = 1.22, SD = 0.72) than in those attending secondary care (n = 440, mean = 1.70, SD = 2.11), a difference in means of 0.48 teeth (95% CI 0.22 to 0.73; p < 0.0005).
Health economics
The difference in referral costs for each hospital in each phase of the study is shown in Table 17. The mean cost saving per referral from consultant-led triage (phase 1 vs. phase 2) was £108.23 (NHS cost perspective) and £103.92 (societal cost perspective). The mean cost saving per referral from GDP-led triage (phase 1 vs. phase 3) was smaller, £84.13 (NHS cost perspective) or £80.28 (societal cost perspective). All four results were statistically significant (p < 0.01).
| Hospital provider | Perspective, cost (£) difference (SE); p-value | |
|---|---|---|
| NHS | Societal | |
| Phase 1 vs. phase 2 | ||
| Cost centre | ||
| All secondary care | –108.23 (11.59); p = 4.31 × 10–20 | –103.92 (11.57); p = 9.53 × 10–19 |
| Hospital A only | –157.85 (12.07); p = 2.50 × 10–35 | –153.28 (11.91); p = 2.29 × 10–34 |
| Hospital B only | –126.71 (31.63); p = 8.17 × 10–5 | –125.88 (31.61); p = 8.97 × 10–5 |
| Hospital C only | 0.84 (6.70); p = 9.00 × 10–1 (i.e. p = 0.90) | 9.32 (6.78); p = 1.70 × 10–1 (i.e. p = 0.17) |
| Phase 1 vs. phase 3 | ||
| Cost centre | ||
| All secondary care | –84.13 (11.56); p = 5.62 × 10–13 | –80.28 (11.55); p = 5.55 × 10–12 |
| Hospital A only | –144.04 (12.28); p = 1.95 × 10–29 | –139.84 (12.14); p = 1.61 × 10–28 |
| Hospital B only | –87.53 (29.73); p = 3.46 × 10–3 (i.e. p = 0.003) | –87.17 (29.71); p = 3.57 × 10–3 (i.e. p = 0.004) |
| Hospital C only | 11.22 (6.24); p = 7.33 × 10–2 (i.e. p = 0.07) | 13.33 (6.36); p = p = 5.71 × 10–2 (i.e. p = 0.06) |
When considering the differences between GDP and consultant triage, the actual decisions taken by the GDPs were compared with the audit decisions taken by the consultants. Several decisions made by the consultants were not available to the GDPs (for example, Level 1 referrals and rejections) and, hence, Table 18 reports the distribution of referrals together with the relative management costs for those referrals where there was a listed decision by both groups.
| Triage type | Care setting, number of decisions | Triage cost (£) | |
|---|---|---|---|
| Primary (Level 2) | Secondary (Level 3) | ||
| GDP | 251 | 581 | 4.00 × 832 = 3328 |
| Consultant | 384 | 412 | 8.22 × 796 = 6543 |
These were then applied to mean costs in secondary care with the resultant cost differences shown in Table 19.
| Triage type | Care setting, number of decisions | Costs (£) | ||||
|---|---|---|---|---|---|---|
| Primary (Level 2) | Secondary (Level 3) | Primary | Secondary | Triage | Total | |
| GDP | 251 | 581 | 179.74 × 251 = 45,115 | 401.81 × 581 = 233,452 | 4.00 × 832 = 3328 | 45,115 + 233,452 + 3328 = 281,895 |
| Consultant | 384 | 412 | 179.74 × 384 = 69,020 | 401.81 × 412 = 165,546 | 8.22 × 796 = 6543 | 69,020 + 165,546 + 6543 = 241,109 |
| Difference | 40,189 | |||||
When societal costs were included, the savings resulting from the use of consultant triage amounted to £40,189. The societal costs are provided in Table 20.
| Cost component | Care setting, average cost (£) per referral (SD) | |
|---|---|---|
| Primary | Secondary | |
| NHS cost component: cost of treating a complication incurred after oral surgery treatment | 0.62 (2.05) | 3.28 (12.21) |
| Societal cost component: cost of travelling to appointment | 11.58 (19.45) | 9.43 (17.68) |
| Societal cost component: time travelling to appointment | 31.71 (26.14) | 25.22 (21.34) |
| Societal cost component: patient out-of-pocket expenditures (prescriptions) | 0.70 (2.42) | 0.65 (4.03) |
| Mean societal cost | 44.60 (20.74) | 38.58 (22.13) |
Table 21 shows the mean cost saving per referral from active triage (consultant and GDP led) if all secondary care providers adopted the same tariff allocations, that is, if the tariff behaviour of hospital A is applied to all hospitals.
| Tariff model applied | Perspective, cost difference (SE); p-value | |
|---|---|---|
| NHS | Societal | |
| Phase 1 vs. phase 2 | ||
| Hospital A | –144.04 (9.31); p = 4.11 × 10–20 | –139.72 (9.21); p = 3.54 × 10–19 |
| Hospital B | –66.76 (13.09); p = 3.32 × 10–20 | –62.45 (13.05); p = 4.21 × 10–19 |
| Hospital C | 21.54 (2.39); p = 2.66 × 10–20 | 25.88 (2.52); p = 5.87 × 10–19 |
| Phase 1 vs. phase 3 | ||
| Hospital A | –116.21 (9.16); p = 3.23 × 10–20 | –112.36 (9.09); p = 2.56 × 10–19 |
| Hospital B | –64.76 (12.84); p = 6.75 × 10–20 | –60.90 (12.82); p = 4.34 × 10–19 |
| Hospital C | 17.39 (1.98); p = 7.53 × 10–20 | 21.26 (2.04); p = 3.32 × 10–19 |
Patient questionnaire
All patients referred through the system in phases 2 and 3 were approached to see if they would consent to complete a questionnaire to provide their views of the service. Questionnaires were sent to a total of 402 patients (28.2% of the 1427 patients approached), and 214 (53.2%) completed questionnaires were received. A range of metrics and free-text comments were received. Here we present aggregated data for participants referred in phases 2 and 3. These data were not used to compare patient responses for phases 2 and 3 because of the relatively small numbers, the possibility of non-response bias and the very high satisfaction scores. Metric results are shown in Table 22.
| Question and care setting | Response (%) | ||||
|---|---|---|---|---|---|
| No | Yes | Do not mind | Not sure | p-value | |
| Was this the surgery/hospital you wanted? | |||||
| Primary | 9 | 39 | 53 | – | p = 0.011a |
| Secondary | 4 | 60 | 36 | – | |
| Was this the surgery/hospital you wanted? | |||||
| Primary | 4 | 95 | – | 1 | p = 0.477 |
| Secondary | 5 | 92 | – | 3 | |
| Did the surgery resolve/fix your dental problem? | |||||
| Primary | 5 | 85 | – | 10 | p = 0.0001b |
| Secondary | 16 | 57 | – | 27 | |
| Would you recommend treatment at the same place to someone with a similar dental complaint? | |||||
| Primary | 5 | 82 | – | 13 | p = 0.065 |
| Secondary | 3 | 93 | – | 4 | |
| Have you had to return to the surgeon or your own dentist for any complications because of your procedure? | |||||
| Primary | 84 | 16 | – | – | p = 0.448 |
| Secondary | 79 | 21 | – | – | |
In addition to these questions, patients were also asked how satisfied they were with both the estate (setting of care) and the surgeon who performed their procedure. These data are shown in Table 23, and no significant differences between the primary and secondary care services were detected for either satisfaction score.
| Question | Level of satisfaction | Care setting (%) | |
|---|---|---|---|
| Primary | Secondary | ||
| Overall, how satisfied were you with the surgeon? | Very satisfied | 71 | 73 |
| Satisfied | 20 | 20 | |
| Neutral | 6 | 3 | |
| Dissatisfied | 3 | 1 | |
| Very dissatisfied | 1 | 1 | |
| Overall, how satisfied were you with the clinic? | Very satisfied | 64 | 66 |
| Satisfied | 21 | 28 | |
| Neutral | 8 | 4 | |
| Dissatisfied | 4 | 1 | |
| Very dissatisfied | 2 | 1 | |
Discussion
The final two phases of the programme saw the introduction of the AQP primary care service in Sefton with active deflection, procured based on the health needs assessment data provided by phase 1 of the study. In phase 2, referrals were triaged by the same consultants, in either oral surgery or oral maxillofacial surgery, who triaged in phase 1 (no deflection), and in phase 3 the referring GDP could select either primary or secondary care at the end of the electronic referral form.
Number of referrals
Unusually in ITSs, the intervention was, by design, going to result in a greater than zero change. The proportion of referrals in phase 2 identified as Level 1 remained low, at less than 3% of the total. Although the HES data suggest (see Table 13) that introduction of a centralised referral and triage system supressed the number of referrals, we cannot be sure what proportion of this decrease was Level 1 (inappropriate) referrals. This is important for commissioners who may believe that reduction of Level 1 referrals present a significant opportunity for cost savings. The low figures are also an issue for undergraduate teaching purposes, as there are few referrals that can be diverted from primary care into dental schools.
Although there are differences between the HES and referral management system data because of referrals from sources other than GDPs, most typically either GPs or internal referrals (e.g. between orthodontics and oral surgeons), it still appears from these data that, although there has been a modest increase in Sefton referrals, this is seen against a pattern of increasing referrals. Therefore, the referral management system appears to have a suppressive effect on the number of referrals; however, our ability to draw firm causal inferences is limited by the study design and the lack of a robust control population.
The number of Level 2 referrals into the primary care service was below that of phase 1, at 45% and 42% in phases 2 and 3, respectively. There was an immediate decrease in the proportion of referrals into primary care compared with that of the previous year. This could be a because of lack of confidence by GDPs to refer to Level 2, a lack of understanding in relation to the services offered by Level 2 or a possible greater influence from patients themselves exerted at the time of referral (when the destination was selected) for a hospital appointment. The system does, however, result in a significant redirection of care from the secondary care setting to the primary care (Level 2) service.
There was an increase in the total number of referrals seen between phases 2 and 3, when GDPs made the referral decisions.
Quality of referrals
Patients attending primary care presented with lower ASA scores, fewer comorbidities and fewer teeth requiring extraction, as expected. One concern over the use of primary care services is that of quality; do patients receive a service that is inferior to that of a hospital? The patient-reported data do not support this hypothesis, with the NHS Friends and Family Test and level of complications being the same between each setting (see Tables 22 and 23). Perhaps a reflection of the simpler procedures seen in primary care, primary care patients reported a significantly higher level of symptom resolution than those in secondary care. Those attending a hospital setting stated that they received the location they wanted, whereas those attending primary care were less concerned about this. The satisfaction scores presented in Table 23 demonstrate that both primary and secondary care settings were accepted by patients and provided satisfactory facilities and treatments.
Impact on costs
Although there are obvious improvements to be made in terms of referral quality (the requirement to meet the minimum data set prior to referral submission), and increases in governance as referrals are sent and received using secure and approved methods, there is no avoiding the need for the NHS to save money and use resources more efficiently.
Perhaps the most surprising element of the economic evaluation was the baseline assessment of hospital costs and the variances seen between each. Hospital A, the district general, appeared to use the day case tariff almost exclusively; for example, out of 286 cases of ‘simple tooth extraction’, 259 (90.5%) were coded as a day cases and only eight were coded as outpatient procedures. For surgical extractions of wisdom teeth, all 444 cases were claimed as day cases. This presents a difference in price of £129 for the outpatient tariff and £628 for the day case tariff. The outpatient tariff would also attract a new patient consultation fee, but the difference in cost was nonetheless substantial. In hospital A, the top five most common procedures were all, with the exception of eight outpatient procedures, coded as day cases.
These tariff applications should be contrasted with those used by hospital C, the local dental hospital (hosted by a foundation trust and run in close collaboration with a university). This institution’s coding behaviour was also at odds with what would be expected, with almost all activity falling under outpatient charges. Of the top five procedures, none was claimed as a day case tariff. This is unusual, as the facility provided treatment under general anaesthetic, which would usually attract a day case charge. The hospital does attract additional funding via the dental service increment for training pathway, but it would be unlikely that these procedures would be performed by undergraduates.
Hospital B (a large foundation trust) appeared to be coding at, or close to, expectations. A broad range of tariffs were used, including outpatients, day case and elective care. However, the differences in costs between the hospitals impact on the cost-saving potential of the referral management system. It could be argued that the simplest way to save costs would be to refer all patients to hospital C. However, pragmatically, this approach would be impossible to implement. Not only would capacity issues arise, but patient choice would also be adversely affected and it would appear that the hospital is coding incorrectly. A simple adjustment to its coding practices would result in a loss of savings for commissioners and damaging knock-on consequences for the wider hospital system.
Secondary care costs and tariffs are complex, subject to local negotiation and uplift, and often tied to other services, Commissioning for Quality and Innovation agenda requirements and commissioner agreements. 90 Nonetheless, these data demonstrate the importance of understanding the tariff landscape prior to embarking on implementation of a referral management system, if cost savings are to be sustainable and meaningful. The savings realised by diverting referrals from hospital A may be considerable and, hence, interpreted as a positive impact of referral management, and yet they are the result of a high, and possibly inappropriate, tariff being applied, and any changes could destabilise the trust. Such a Pyrrhic victory should be avoided by extensive and robust evaluation of the local tariff costs.
Having considered these issues, the referral management programme secured savings in both phase 2 and phase 3 when the total costs of the referral management system, the (Level 2) primary care service and all hospitals are considered. The savings are higher when hospital A is considered alone, and, when considering hospital C, the average cost of referrals increases (although only modestly). Hospital B appeared to be coding patients using a wide range of tariffs and was perhaps the best indicator of the potential savings per referral. The striking difference in findings from hospital C compared with hospital A and hospital B implies that cost savings are far from certain if the referral management programme was introduced in other hospitals, underlining the importance of a comprehensive understanding of the local context before commissioning decisions are taken.
The societal costs were not significantly different between the two care settings (Level 2 and Level 3). However, primary care sites should offer a wider choice, and generally be closer to home, and, hence, the location of the Level 2 service in this study may not have been geographically optimal as the travel component of the costs is slightly higher than that in secondary care. Attention should be given to the location of patients, referral flows and transport links when commissioning such services to ensure that maximum benefit is derived.
Limitations of the health economic evaluation
The economic evaluation was limited to a comparison of ‘active’ referral management with virtual management, where the programme was in place but no redirection took place. The correct comparator in any economic evaluation is usual care, in this case no referral management programme. Treating data in the year of virtual management as a proxy for referral behaviour under no referral management may introduce bias if there is a Hawthorne effect. 91 For example, there may have been fewer GDP referrals in the first year of the programme because GDPs were aware that their referral forms would be more closely scrutinised under the referral management system. A further limitation is that the economic evaluation considers only costs. The evaluation would benefit from a comparison of cost changes under the referral management programme with changes that may have occurred in quality of health-care service delivery received by patients. Ideally, this would be a measure of the oral health gains from treatment, but this was beyond the scope of the current study.
Summary of main findings
In phase 2, we could evaluate the effect of a fully working centralised referral management system coupled to a newly commissioned primary care (Level 2) service. In phase 3, we could compare the costs and effects of triage performed remotely by consultants or by the GDPs completing the referral form for their patients. A patient questionnaire enabled us to collect data on patients’ views and experiences. This quantitative data were designed to complement a deeper qualitative assessment of patients’ views, which will be reported in Chapter 5.
In this chapter, we posed a number of research questions:
-
What are the differences in the number of referrals, referral mix, referral quality and the mean cost per referral between virtual management (phase 1) and consultant-led active management (phase 2)?
The number of referrals fell slightly between phases 1 and 2, perhaps because of a delay in referral as GDPs familiarised themselves with the new service. The mean cost saving, per referral, from consultant-led triage (phase 1 vs. phase 2) was £108.23 (NHS cost perspective) or £103.92 (societal cost perspective), which in both cases is statistically significant.
-
What are the differences in the number of referrals, referral mix, referral quality and mean cost per referral between the year of virtual management (phase 1) and GDP-led active management (phase 3)?
The total number of referrals increased significantly when GDPs performed the triage, and a significantly larger proportion of referrals were sent to Level 3 providers. The mean cost saving per referral from GDP-led triage (phase 1 vs. phase 3) was smaller than that from the consultant-led service [£84.13 (NHS cost perspective) or £80.28 (societal cost perspective)] and in both cases the difference is statistically significant.
-
How do these findings (differences in the number of referrals, referral quality and the mean cost per referral between study phases) differ by the provider of secondary care?
There were large differences in cost savings between the hospitals, primarily because of the different approaches to activity coding in each trust. This key finding demonstrated the importance of a comprehensive understanding of the local context before commissioning a referral management service.
-
Does consultant-led triage offer improved costs over GDP self-determined provider choice (phase 2 vs. phase 3)?
Yes, but these differences are small in comparison with the effect that trust activity coding has over costs.
-
How do the views and experiences of patients differ between those using primary and secondary care services?
Patients demonstrated high satisfaction levels with the service and the metrics used, such as the NHS Friends and Family Test, and the level of complications were the same for each setting.
Conclusion
Primary care oral surgery services, when underpinned by a referral management service, offer suitable alternatives to secondary care for Level 2 procedures. The use of consultant-level triagers produces significantly higher levels of diversions to primary care than GDP-level triagers. Patients appear satisfied with the provision of surgery in primary care settings, and there was no difference in reported complication rates.
There are potential cost savings to be realised using primary care services, but these need to be balanced and understood against the tariff and coding behaviour of the area’s acute trusts. A thorough understanding of the patient flows, charges and procedures can be provided by a referral management service but, without commissioner input and challenge to secondary care, savings will not be realistic and could be inflated by overcharging in the acute sector.
Chapter 5 Active referral management with consultant and general dental practitioner triage qualitative findings (phases 2 and 3)
Introduction
This chapter describes three discrete elements assessed as part of the mixed-methods approach:
-
a further exploration of implementation in the primary care service as the system incorporates live diversion to specialist primary care, including a case study of the primary care oral surgery provider
-
the views of secondary care providers and commissioners on the development and implementation of the intervention, and implications for further roll-out across the local area
-
views of service users.
Each contributes to the wider understanding of implementing the intervention and its impact. Findings from each of the stakeholders (primary care, specialist service, secondary care and commissioners) are incorporated into a whole-systems NPT analysis, which can be found in Appendix 4. This synthesises data from each source to produce an applied model of implementation.
Aims
The aim of this study was to explore the implementation of this specialist oral surgery service in Sefton and to examine issues around acceptability and workability of the new service. This part of the study used qualitative methods conducted in parallel and designed to be complementary to the quantitative methods described in Chapter 4. Three broad research questions were posed:
-
What are the issues encountered when establishing a new primary care oral surgery service?
-
What are the views of stakeholders on the development and implementation of the primary care service?
-
What are the views of service users on the quality of service they received from the referral management and triage system?
Methods
Nested case study
A nested case study was conducted as part of a larger piece of mixed-methods research evaluating the referral system. It focused on implementation and acceptability of the specialist primary care service over 16 months. A case study research strategy aims to understand the dynamics present within a single organisational setting. 92 This was a holistic93 case study, in that it looked at only one unit of analysis: setting up and implementing the specialist primary care service in Sefton. It was also intrinsic in design, in that it aimed to gain a better understanding of this specific service rather than of a wider phenomenon. 94
Data collection
Qualitative interviews were conducted with several relevant stakeholders during the first year of live implementation to address the boarder research questions. These included the surgeon holding the specialist contract, commissioners, secondary care staff and service users (see Appendix 2 for details of participants, and Methods and Data analysis in Other stakeholders: secondary care providers and commissioners for more detail regarding sampling and topic guides). Interviews were carried out by an experienced researcher, either over the telephone, face to face or in the staff member’s dental practice or office. Topics for discussion were identified through reviewing relevant literature and discussion with the research team, and were informed by NPT. 67,95 All transcripts were anonymous and checked for accuracy against the audio record.
Data analysis
Qualitative interviews
The analytic process drew upon some common techniques of grounded theory approaches,66 including the technique of constant comparison, whereby analysis will be carried out concurrently with data collection so that emerging issues can be explored iteratively. Stages of coding comprised initial coding of text segments, followed by recoding and memo writing to generate conceptual themes. Themes were constantly compared within and across cases, paying attention to negative cases and possible reasons for differences. Data were organised with the aid of the qualitative data software package NVivo. Emerging themes were discussed by authors to enable refinement of conceptual categories and to discuss common threads or differences across the different respondent groups.
Analysis drew on established theories of organisational change, particularly NPT, which has been developed to study implementation and adoption of (as well as barriers to) new work practices and technological interventions within health system contexts,67,95 The aim of NPT is to understand the numerous processes involved in changing new practices into those established and embedded in routine. 67 By taking a factorial but integrated approach, NPT can offer a flexible and pragmatic theoretical approach that can help us understand the factors that affect routine incorporation of a complex system into everyday practice, while generating findings that may have resonance for other complex interventions in different settings and contexts. A strength of NPT, in the context of this study, is that it allowed an integrated whole-systems approach to implementation to take place, considering the various perspectives taken by numerous individuals and groups of stakeholders.
An audit trail of all stages of the analysis, to maximise credibility, dependability, confirmability and transferability, was created. 54,68 To ensure reliability, interpretation of the data was discussed and refined by three researchers (JG, CS and IAP) throughout the analytic process. Further reliability was established through triangulating findings with observational work, study documents and quantitative data.
Results
An inductive analysis of the data revealed themes congruent with three out of the four NPT domains – (1) coherence, (2) collective action and (3) reflexive monitoring – which informed an understanding of the sense-making, operational work and appraisal participants undertook when engaging with the specialist primary care service. 68 Understanding new treatment pathways and understanding clinical relevance drew on the construct of coherence, collective action between providers and clinical governance drew from the collective action construct and comparison with other treatment experience was informed by reflexive monitoring.
Understanding new treatment pathways
A barrier to coherence about the new services was a lack of information given to patients about their possible treatment destination. During the first year of implementation, patients expected to be treated by their GDP in their regular practice or in a hospital setting according to traditional treatment pathways. As the evaluation moved into its third active year, with GDP decision-making being introduced, patients reported less confusion around their referral and subsequent treatment setting. In phase 2, as the decision on treatment setting was made by a consultant, the referring GDP was unable, at the time of referral, to indicate where the patient would be seen.
Differentiation between sets of working practices (e.g. paper letters to consultants and electronic referral management) is important for developing a coherent understanding of complex interventions. 95 Particularly in the early months of the service, patients were not well informed about the new treatment pathways and would often carry out investigative work to chase their referral and subsequently check on the authenticity of the new specialist service. This was carried out within the context of several drivers to see treatment completed in a timely manner, combined with lack of information about pathways and ultimate treatment provider. The following description by a patient of undertaking a number of processes in order to obtain information about their referral was an experience that was not uncommon in the early days of the specialist service becoming active:
I think I waited about 3 months, and nothing came through. So I went back to the dentist and they said, ‘oh we’ll check up on it’. In the meantime, I rang the dental hospital and they had no knowledge of me. So they said, try the [district general] hospital . . . They had no knowledge of me. So I went back to my dentist and told them this . . . And then all of a sudden, out of the blue, I got a phone call from [specialist service], asking me to go through there the following day . . . I was happy at first, and then I thought, oh hang on a minute, you know because I just didn’t expect it . . . So I went to my [referring] dentist and I said to them, this all seems to be sorted out. And they said, oh, we’ve never heard of this place . . . then they said to me, ‘oh, I wouldn’t go if I was you, because it’s one of these things, they get your phone number, they ring you up, you get there and then they charge you’. So anyway, the girl rang back for something and I checked with her, and said, ‘is it NHS?’ She explained everything and said it was. It was a way of getting the waiting list down and that.
Patient 1440
General dental practitioners felt that they had not been provided with information about the new service in a sufficiently timely way, despite the commissioning team sending letters and holding information meetings prior to implementation. Staff from referring practices tended to blame the commissioning team for failing to communicate adequately. It took a number of months for staff within the referring practices, the patients, the specialist service and the evaluation team to feed back to each other before a shared understanding around the service and its aims could begin to develop:
It’s 5 minutes down the road, the guy that did it [DwSpI], which is great. But it was just, we weren’t told he was there and then it got us into a tricky situation. So in terms of the Department of Health, I’ve no real faith in them or NHS Mersey, I’ve no real faith in them getting us the information on time.
CS4
My dentist spoke to me about it. He said, ‘Oh, yes, I’ve heard of these. They are doing this.’ And he seemed to know about it. But none of the receptionists did.
Patient 1140
Understanding clinical relevance
A lack of coherence around understanding new treatment pathways led to confusion around where treatment would take place. In addition, patients lacked an understanding of the clinical reasons for referral and why they were chosen to be treated by a specific provider in a particular setting. This suggests that patients may not take an active role in the referral process at GDP appointments. Discovering that they have been referred to a new service may, however, prompt patients to ask new questions about the type of treatment they can expect:
I didn’t know if the referral clinic where I was sent to was going to just give me the same injection and try to get it out again. So I rang up and I said will I be sedated, or anything like that? Because I didn’t know what was going to happen to me after having this referral, you see.
Patient 2220
In the following case, a patient had been diverted to the specialist primary care service, then referred on to hospital because of an underlying complication. By the time the interview took place she had seen three clinicians in relation to her treatment (GDP, specialist oral surgeon and consultant oral surgeon); however, she remained unsure of why she had not been treated by her regular GDP. Adding to the confusion, it transpired that she had mistaken her appointment at the specialist service for an orthodontist appointment:
But when I got to the orthodontist, he basically just said, ‘I know it’s a waste of your time, but you had to come and see me, face to face, for me to tell you, your dentist is right. And then I refer you on to the hospital’ . . . I thought it was a strange place to go . . . That wasn’t really explained.
Patient 1138
A lack of coherence around the early implementation of the specialist service was apparent, particularly in the early months of the service. This seemed to affect patients’ overall impression of the quality of the service offered, but it did not appear to be a barrier to their attendance at appointments and completion of treatment. However, a lack of understanding regarding the aims of the whole oral surgery pathway (electronic referrals combined with specialist primary care diversion) could be a barrier to GDPs’ awareness of the service. The specialist oral surgeon providing Level 2 service felt that this subsequently affected the numbers of referrals received. This is particularly relevant to the final year of the evaluation, when GDPs made autonomous decisions about patient treatment destinations (in contrast to the previous year, when treatment destination was decided remotely by consultant triage):
So all the initial hard work has been done, setting up the practice and everything and all these things . . . On the other hand, now I’m not having enough patients to do that. I need more patients. More patients, but the system from my side, it’s great, it is working well.
CS25
Collective action between providers
Some of the issues around developing a shared sense of coherence between GDPs and patients were attributed to a lack of initial operational work to inform and facilitate referrals from general dental practice. Often, information regarding the aims of the new service was absent or was not cascaded within general practice teams. The surgeon working in the new service had concerns regarding the integration of referral management (and subsequent primary care diversion) into everyday practice. He felt that information and training of new associates in the referral management system was insufficient, resulting in some GDPs, particularly new staff members, bypassing the referral management system and referring directly to secondary care consultants:
But what happens is most of the big practices, they have more dentists changing, the new dentists come. Those people, they don’t understand the referral system, unless the practice principal sits with them and explains to them. So more and more new dentists come, more and more come. But more understanding, more teaching for the dentists, ‘this is how the system is going to work, and it’s a quick service and you have a lot of advantages’ and everything needs to be explained.
CS25L
The need for effective communication is important throughout the whole of the oral surgery pathway system. Demand management is a complex process that requires strong clinical leadership against a backdrop of risk recognition and patient safety and experience. Commissioners have highlighted that clinical governance is crucial, and it is important that Level 2 providers have access to a recognised and experienced consultant providing clinical supervision:
I think some lessons learnt there about being absolutely clear who is providing that service, and if it is a dentist with enhanced skills, and it may well be, that we have them linked into consultants or specialists for clinical supervision.
CS22
Relational integration refers to the knowledge work carried out in order to build accountability and maintain confidence in a new set of practices and with other participants as a new intervention develops. 95 Communication between and within the skill set involved in making the referral management system work is vital to ensure that cost reduction or containment is balanced with clinical quality, service experience and benefits to the broader NHS network. For example, consultant triagers need to feel that they have enough information about the primary care provider to select and divert appropriate patients out of the hospital system, according to the provider’s skill set. A meeting involving triagers and the primary care service provider that took place during the first year of operation of the new service was found to be useful in facilitating communication between both parties to identify any clinical and safety issues, refining boundaries for referrals and encouraging two-way communication between consultant triagers and the specialist primary care service:
It can’t be faceless, to be quite honest. I mean, just from the initial meeting we had with the current Level two provider, you got the impression there were certain things he’d be happy doing and certain things he wouldn’t, and without that meeting you wouldn’t know. And then you’re wasting everybody’s time then, because if you send something that’s too complex the patient’s wasting time, they’re going for an additional consultation, they’re disappointed.
CS18
Comparison with other treatment experiences
Although patients could be initially confused about their treatment pathways, most patients found the prospect of being treated in a primary care setting acceptable. Typically, their focus tended to be on having symptoms alleviated in a timely manner, and they were indifferent whether their treatment took place in hospital or in a local setting, particularly when they had little prior experience of referrals to hospital for dental treatment. They had confidence in the ability of the NHS to provide safe and appropriate treatment in a general sense and were unconcerned about how it was provided.
No it doesn’t bother me, because the setting was just the same. The one in the hospital it’s perhaps a bigger room, but it’s still the same, obviously, you’re only sat in a dentist’s chair aren’t you?
Patient 1081
When patients had previous experience of dental treatment in a hospital setting, a comparative experience upon which to base what May et al. 95 refer to as an individual appraisal was present. These patients had certain expectations based on previous history of hospital treatment upon which to draw their appraisal of the new service. Some patients were concerned by the lack of artefacts and clinical surroundings associated with a hospital setting, such as dedicated car parking and an apparently sterile environment. The patient quoted below had previous experience of being treated in a hospital setting:
I have to say the professional care was absolutely fine . . . it was just that the general surroundings . . . I didn’t know where to park my car because it’s on a main road. There was a pub across the road but I didn’t like the look of that so I just parked up a side street. But the treatment was absolutely fine. The dentist was lovely, the dental assistants were nice and all the rest of it.
Patient 1975
However, as alluded to in the example above, patients tended to be satisfied with their treatment, and many patients made positive comparisons with the hospital service. Patients were particularly positive about shorter waiting times for treatment and having a choice of out-of-hours appointment times at the primary care site. Although some patients had arrived at their first appointment at the specialist primary care service expecting to have an initial consultation followed by a different appointment for treatment (as per the conventional hospital pathway), they generally preferred consultation and treatment to be provided at the same appointment.
When I went in to see this guy in [primary care site], he said to me, they could speed up things so you don’t have so long to wait and do it in one go. Certainly, when I phoned the hospital they had said there’s at least a 3-month waiting list and that’s just for a consultation.
Patient 1975
Discussion
Staff at the primary care service coped well with the cases diverted to their service, and were working slightly below available capacity (this is reflected in the projected diversions identified in phase 1 vs. the actual diversion rate realised in phases 2 and 3). The primary care service kindly allowed us to have access to its service audit data, which had been collected anonymously over the course of the service. Most referrals were diverted appropriately, with a small number of patients attending for a consultation with no treatment. The main reason for not requiring treatment was that symptoms had resolved over time and treatment was no longer deemed necessary. The numbers of patients referred on for other treatment (e.g. for inaccurate information present on original referral, or for lower wisdom teeth being closely associated with the inferior alveolar nerves) were small (see Chapter 4 – 4% in both years), suggesting that diversion to the service was operating efficiently. Indeed, the onwards referral rates to secondary care were lower than those suggested by the diagnostic test accuracy study.
Initially, some staff from general practices and patients were unaware of the specialist primary care service, and lacked a coherent understanding of its objectives. On some occasions, patients chased their own referrals, contacting practices and hospitals before discovering details of the primary care service in a serendipitous manner. This was attributed by GDPs to a lack of information disseminated in a timely and effective way by commissioning teams. The Level 2 service surgeon felt that new staff members coming into new positions were not updated with details of his service or local service reorganisation. In particular, dentists moving from an area where referral management is not in place would not be familiar with the service pathway for oral surgery in Sefton.
In addition to setting up information networks between dental practices and the primary care service, it is important that communication pathways are in place between primary and secondary care oral surgery services. This can ensure that specialist primary care services can access clinical supervision and that clear clinical boundaries are decided with regard to responsibility for borderline Level 2 and 3 procedures. This is essential for ensuring efficiency of services for patients (that they are not making unnecessary visits to different service providers) and that those clinical governance requirements are satisfied.
The Level 2 service was acceptable to patients, who expected to be treated in hospital only if they if they had previous experience of referral. Patients preferred the shorter waiting times for appointments; they were generally happy with the staff and their clinical skills and they liked the convenience of being treated locally.
Other stakeholders: secondary care providers and commissioners
Introduction
The diversion of patients to primary care services is a potential threat to secondary care providers. The removal of activity can potentially destabilise essential services, alter case mix dramatically, affect training opportunities or place existing services at risk. 96,97 It is essential that secondary care services are preserved to deliver the care required at Level 3 for those patients who need it. The referral management intervention was introduced in the context of increasing difficulties for local trusts to meet government directives for 18-week waiting list targets and the demands of operating in a NHS subject to increasing cuts and efficiency drives. This reflects the benefits to secondary care of referral management: the ability to manage demand in their services and understand processes involved in adjustment to new ways of working.
The electronic referral management system did not directly impact on secondary care until primary care service came online in phases 2 and 3 of the study. Perceived issues for trusts in this study were around impact on staff jobs and training through the loss of less complex cases and, to a lesser extent, a possible increase in the administrative burden. Consideration also needs to be given to the acceptability of service reorganisation, whereby some procedures previously carried out in hospital outpatient clinics are delegated to less qualified staff, to be carried out within primary care settings.
Prevailing theories of professionalism in health care assumes that members of existing professions are drawn to more specialised and prestigious work. Furthermore, those in esteemed roles are considered content to delegate the simpler or less satisfying procedures to those in less revered positions, while retaining the option to take back these simpler tasks, should demand dictate it necessary to protect their profession or individual role. 98 These issues were relevant to this study in two ways: first, in the diversion of less complex tasks to the specialist primary care service, now led by a GDP with specialist training rather than a consultant-seconded role; and, second, in the final year, when consultants deferred their triage role to GDPs, who took responsibility for triaging patient’s needs and decision-making on ultimate treatment destination. Concerns may exist around clinical competence, patients’ safety and protection of roles within the current climate of waiting list targets, budget cuts and scarce resources within the NHS.
Methods
Semistructured interviews were conducted by experienced qualitative researchers, using topic guides as prompts that were modified and refined according to responses from participants. Topics for discussion were identified through discussion with the study steering group and research team, and informed by NPT. 67 Subjects of interest were explored further as they arose during the interviews, and open-ended questions were used to encourage participants to elaborate on relevant topics.
Topics covered in the guide included:
-
understanding of why the electronic system and Level 2 diversion had been introduced and knowledge of the intervention under study (coherence)
-
opinions on the likely impact of the intervention on the trust and individual roles (cognitive participation)
-
descriptions of what has happened in the trust to enable implementation and effects on workload and daily tasks (collective action)
-
appraisal of benefits, costs and impact (reflexive monitoring).
Interviews were carried out either face to face in a quiet office in the hospital or over the telephone. Decisions on how the interviews would take place were based on pragmatic reasons. Interviews lasted between 12 and 47 minutes, and were audio recorded and transcribed verbatim as soon as possible after the interview had taken place. Purposive sampling was used to identify appropriate members of trust staff undertaking various relevant roles from all three hospitals. These included directorate managers, administrative staff and nurses.
Focus group
Two members of the research team attended a focus group, which was based around a topic guide developed from gaps in data around triage processes, discerned from previous interviews. Iain A Pretty was the facilitator and Joanna Goldthorpe was the scribe. The facilitator endeavoured to ensure that each participant had the chance to speak and that all views were respected. For example, if a participant had not contributed to the discussion for a period, the facilitator would ask a question directed to them.
Participants were from the following clinical backgrounds:
-
Primary care: two principal dentists (one female, one male, GDS) and an associate dentist (female).
-
Secondary care: one maxillofacial consultant (female) and one consultant oral surgeon (male) who had been involved in triage activities for the study.
Topics covered in the topic guide included:
-
key drivers for triage decision-making
-
advantages and concerns regarding each provider
-
characteristics of a good provider
-
patients’ priorities for treatment.
The discussion took place in a conference room at a neutral location convenient to all participants. The discussion was audio recorded and transcribed using intelligent verbatim style and lasted 105 minutes.
Data analysis
Thematic analysis65 was used to identify emerging issues and themes from the data using an inductive approach. This is a flexible way of analysing qualitative data that can be used to answer several research questions across a range of theoretical approaches. Use of the constant comparative method66 helped to ensure that the analysis was consistent and based on evidence from the data. Coding and analysing the data were carried out by one person (JG) to ensure consistency, in parallel with completion of interviews. Themes were refined through discussion with other authors (IAP and CS), of those who contributed, who had read selected transcripts or quotations. Analysis was completed when no further themes emerged from the data (i.e. data saturation was reached). The data were organised using NVivo and Microsoft Word (Microsoft Corporation, Redmond, WA, USA) software.
Participants
All participants were adult (aged 18 years or older) UK NHS trust staff from participating hospitals or commissioners employed by NHS England or Public Health England.
Secondary care
Seven secondary care staff took part in 11 interviews and two members of staff took part in a focus group alongside staff from primary care (see Appendix 2 for full description of clinical participants). Four participants were female and three were male.
Commissioners
Two participants took part in four interviews. Both participants were female.
Results
Themes emerging from the data were as follows: integrating new systems into existing processes; changing relationships and skill mix; reviewing costs and benefits over time; wider implementation; and rolling out the intervention (NPT construct of cognitive participation and collective action). Changing relationships and skill mix refers to the challenges of adapting to new ways of interacting with primary care practitioners and new models of care (NPT construct of cognitive participation). Reviewing costs and benefits over time encompasses participant concerns and predictions of impact at the start of implementation, which may or may not have occurred or been assuaged (NPT construct of reflexive monitoring).
Integrating new systems into existing processes
Integrating new systems into existing processes describes a process of attempting to integrate the new system into existing practices and procedures at the trusts, within the context of restricted opportunities and resources. This set of findings relates to the NPT constructs of cognitive participation and collective action. Cognitive participation describes the relational work individuals and groups of people do to build an association with a new technology or complex intervention, and collective action describes how practices are enacted and put into operation. Specifically, the component of initiation is relevant in understanding whether or not staff ‘bought in’ to the intervention.
Primary care dental practices often had to adjust their day-to-day methods of working with respect to administration and IT systems; however, this was not the case in secondary care. Hospital managers were asked to create a dedicated, secure e-mail address to receive referrals. Once referrals had arrived, hospital booking staff or consultants’ secretaries printed out paper versions, which were then scanned and integrated into the existing hospital bookings and records system. The process is similar for traditional paper-based referrals, the only real change being in the way referrals are delivered to the hospital. Consequently, little impact was felt on hospital administration systems and associated staff workload. However, this meant that staff who thought that electronic referral management would have the potential to enhance existing trust systems might be disappointed.
Prior to engagement with electronic referral management, one trust manager welcomed what was viewed as a small step towards modernising existing hospital systems. She expressed an ambition to ultimately upgrade and integrate all hospital systems, with the aim of becoming paper free and improving efficiency through better data management and monitoring. There was also an expectation that the quality and content of referrals would improve, which had historically been a source of frustration:
We have repeatedly worked with GDPs on the quality of the referral both in terms of sending information out to them. You’re sending referrals back. It’s time consuming. It’s laborious. It has less progress than you would like . . . So the theory of it is that it could improve the quality of referrals . . . And leave people here to do things, which are more added value for the services that we are providing.
CS3
In practice, expectations of improvement were realised to the extent that referral content was seen to be much improved. Referral information was reported as having improved in terms of quality and amount of detail provided. This improvement appeared to take place within the context of the referral management technology as the system allowed consultants to give electronic feedback to GDPs and ask for more detail as part of the triage process. This feedback encouraged a virtual dialogue between consultants and practices, which reinforced the need for a complete set of referral information:
The fact that its sources are better and include an X-ray now makes a big difference, we can refer it back if they have not completed all the information quite quickly, whereas, in the past you’d be sending a letter to them asking them for more information or just ending up seeing the patient without the information that you would ideally need. So I think it’s improved the quality, potentially, because, you know, the practitioner referring learns quicker that we need detail, all the information to triage.
CS24
As mentioned in the quotation above, a benefit was that all referrals had to be sent with an accompanying radiograph to be accepted for triage, which aided diagnostic decision-making and was of benefit to consultants undertaking triage activities. However, X-ray attachments often did not transfer to the hospital setting in a way that was helpful or usable. Radiographs were frequently not transferred to hospital record systems when sent as attachments to referrals, or consultants reported that image quality was compromised by electronic copies being printed and scanned into hospital systems. This resulted in hospital radiography departments taking additional radiographs and patients undergoing repeat radiography.
The thing that I haven’t got clear as to how those X-rays come to us at the clinic. X-rays don’t come through or are so blurred I can’t use them.
CS21
To maximise the use of radiographs and other imaging sent to referral management services, consideration must be given to the integration of images into the hospital picture archiving and communication system (PACS) services. There are good examples of image sharing between organisations, such as the NHS North West PACS Portal. 99
Changing relationships and skill mix
Changing relationships and skill mix refers to the challenges of adapting to new ways of interacting with new models of care and the diversion of less complex cases to practitioners with varying skills and experience. Collective action relates the operational work people carry out to facilitating an intervention. Collective action components of relational integration and skill set workability are relevant to this set of findings. Relational integration refers to tasks undertaken to build accountability and maintain confidence in a set of practices and in each other as they use them, such as consultants adjusting to new methods of communicating with GDPs. Skill set workability refers to allocation of work and the division of labour that is built up around a set of practices. This related directly to the changing opportunities for practitioners with a variety of skills to undertake less complex work traditionally carried out by consultants.
The introduction of the electronic referral management system altered the way in which GDPs communicated with consultants. Previously, referral letters were often written directly to a named, preferred consultant. These relationships could be established over time and a dialogue was able to develop over treatment plans and individual cases. One consultant highlighted the move away from this relationship and towards a more remote centralised model as a potential threat to service efficiency and convenience of patients if consistent information was not given and received. He felt that it was important to ensure that GDPs and consultant triagers understood the best treatment destination in ambiguous cases, particularly patients on bisphosphonates. Potential implications included the referral of patients from specialist primary care to a second appointment at hospital because of lack of skills or resources to complete procedures or failure to identify opportunities to divert referrals from hospital care:
Overall it’s a good system but that is the thing that concerns me, you know, because traditionally dentists would just pick up the phone to us and say, ‘oh, I’m worried about such and such what should I do’ and you go, ‘all right just send it up’, but if they have to send it through that process now I’m then going to be potentially contradicted . . . it may be that I’m talking rubbish, it may be that when they triage them, anybody who is on bisphosphonates, they agree that they should be done in the hospital, I do not know, but I’m not sure what the guidelines are.
CS20
Similarly, another consultant was concerned advice and feedback given electronically during the triage process had not been acted on, because no immediate feedback was received from the GDP. In this case, a referral was rejected as it was considered appropriate for a 2-week hospital waiting list (possible cancer). A notification would have automatically been sent by e-mail to the practice and the option to follow up the e-mail with a telephone call remained; however, this concern highlights possible difficulties in adjustment from a one-to-one dialogue with primary care practitioners:
You know, if it’s says,’ I think this is a suspicious lesion’, I would say, ‘don’t send on this because it’s not a 2-week wait’. Make sure you send this patient on a 2-week wait referral if you’re concerned and then I ping it back and there’s my . . . sort of in my brain I’m thinking, well, does this dentist actually pick this up and does the 2-week referral come through in the appropriate format?
CS21
Prior to the introduction of the specialist primary care service, trusts had been triaging referral letters and arranging clinic lists for treatment with clinicians with differing skill levels, depending on needs of the patient. Pressures within the oral surgery service around meeting 18-week waiting list targets led to the implementation of a number of initiatives in the trusts, including running clinics on Saturdays and employing staff-grade oral surgeons to undertake less complex procedures. Therefore, consultants were accustomed to delegating some procedures to less qualified staff.
Introducing the specialist primary care service, however, meant a greater loss of control from trusts, in that the service operated outside the hospital setting and was not directly overseen by a consultant. Most consultants felt that this change was necessary because of pressures on resources caused by increasing numbers of patients referred for minor oral surgery procedures. There was a degree of inevitability felt as a result of costs involved in consultant-led treatment, which echoed the stance of commissioners:
The time has come really that we can’t afford for maxillofacial surgeons to be doing tooth extractions.
CS23
Clinical staff mostly trusted the procurement process to ensure that levels of compliance and clinical safety were adhered to by the primary care service. However, some concerns were raised regarding clinical supervision and protection against litigation, in the context of the specialist service being led by a primary care practitioner:
Most GDPs run businesses and the last thing they want is things going wrong in the business . . . we’ve got a litigation department who’ll deal with it and, yes, it’s happened but we’re OK, we will carry on. But if somebody walks out [of primary care service] and says ‘I got butchered by the doctor’, it doesn’t take long for your business to be fairly well wrecked.
CS18
As a result of these concerns being raised, a meeting was set up to review clinical governance for the primary care service, with the outcome being that communication pathways were enhanced with a named consultant providing formal clinical supervision for the specialist primary care surgeon. The debate over who is best placed to provide specialist service for minor cases, however, remains. An alternative model suggested by commissioners at the start of the procurement process offered consultants the opportunity to carry out minor oral surgery services under a primary care contract.
Some discussions took place early in the process with interested parties; however, ultimately, no proposals of this nature were received. The consultant quoted above remained an advocate for this model because of concerns around the potential for litigations and a view that patients would receive better care from a consultant-led service:
So in the end your level of expertise is always going to be higher in [hospitals] and I think the only way you can level that playing field is by having your expertise outside . . . personally, I’m in favour of that, in the long term, in the contracts that have us doing some days outside, because that’s how you will get the best care.
CS18
One commissioner thought that the reason for the demonstrated lack of interest in a consultant model of service provision might have been the fact that the contract covered a limited time period and operated in a small geographical area, and there was not sufficiently lucrative enough to attract serious proposals:
I was a little bit disappointed . . . it’s quite a small contract so I think we were always going to be looking for somebody local who could provide it . . . it wasn’t a big enough contract to attract interest from a new provider.
CS22
Triaging of referrals had been subject to some deliberation prior to implementation, with a team of consultants from a pilot area (Greater Manchester) earmarked to carry out triage of referrals during the early study period. This had been met with some resistance from local Sefton consultants, who felt that they were better placed to understand capacity and need in their area. Ultimately, triage work was provided by local consultants, and in phase 3, by GDPs. The commissioning team expressed a preference for consultant-led triage over GDP autonomous triage; however, the commissioning team did not concur that it was necessary for triagers to be familiar with local services:
If you get the actual [primary care] providers doing it would depend on their capability, and there is quite a range of capability and there is an almost perverse incentive which . . . they are creating their own workload. I prefer it with secondary care clinicians, local ones, fine. I’m not precious about who they are really.
CS23
Perceived and actual costs and benefits over time
Reviewing costs and benefits over time encompasses participant concerns and predictions of impact at the start of implementation in relation to whether or not these have been realised. The NPT construct of reflexive monitoring clarifies these findings within the larger implementation landscape. Reflexive monitoring is the appraisal work that people do to assess and comprehend changes to the processes that underpin their work. All four components are relevant to these findings. Systemisation describes the processes involved in determining how effective and useful changes are; individual and communal appraisal relates to experiential experiences that help to determine the worth of the intervention; and reconfiguration is appraisal work that may help to redefine or alter practices or components of a new intervention.
Data taken from the RMC showed that, of the three trusts, the greatest reduction in numbers of referrals was in those for hospital A (the district general). Sefton referrals made up a small part of the overall referrals to the foundation trust (hospital B) and dental hospital (hospital C) (reflecting that both served a much larger geographical footprint). Therefore, the impact of primary care diversion was lower for hospitals B and C, and this was reflected in data collected from interviews with trust staff. Although data from the RMC suggested that a larger impact would be felt by the DGH (hospital A), views were inconsistent across the study period. Fears and assumptions around the introduction of referral management were not generally borne out by experience within the parameters of this study, although concerns for the future remained.
In line with the wider commissioning agenda, potential benefits of referral management for all trusts included fewer cases of low complexity being treated in hospital outpatient clinics, meaning shorter waiting lists for patients. Thus, pressure on trust staff was reduced because their workload was more manageable and there was no need for waiting list initiatives. Consultants, particularly those working at the foundation trust hospital, felt that their enhanced skills would be used more efficiently in treating patients with more complex medical issues. The benefits for patients were presumed to be shorter waiting times and treatment in convenient locations:
I think it will improve waiting times more than anything else . . . I think that [referral management] will bring back the number of patients that we need to see to a reasonable level so we don’t need to run additional sessions . . . bring it back to something that’s manageable.
CS24
Although the anticipated benefits of referral management were shared among hospital staff and commissioners, predicted costs varied slightly between trusts. The foundation trust felt that, ultimately, it might lose or need to redeploy staff-grade surgeons employed to carry out less complex procedures as part of waiting list initiatives. The dental hospital shared its concern about loss of lower-grade surgical staff; however, it focused on fears that it would experience a shortage of cases suitable for student teaching, as less complex cases were diverted to Level 2 primary care services. In many cases, predictions and assumptions made by staff were not realised because of the low numbers of overall referrals coming from general practices in the relevant area:
I can say I see no difference whatsoever . . . the numbers it probably only represents 3% or 4% or our actual referrals.
CS18
Fears regarding teaching cases can be assuaged to a certain extent, as the referral management system allows a certain number of Level 1 and 2 cases to be diverted to hospitals, based on need. For this to happen in the future, a formal needs assessment would be needed to produce a plan for numbers and types of cases required. However, the smal number of Level 1 cases seen within the system reflects an ongoing issue with oral surgery case provision in dental schools. An additional layer of complexity to this potential solution is the desire of commissioners and consultants that decisions around retaining less complex cases remain independent of the providers:
So long as you are keeping separate the people that are triaging from the end user in effect, then that’s OK.
CS24
Staff from the DGH shared concerns about the loss of lower-grade surgical staff and had concerns that newly qualified dental nurses would have reduced exposure to simpler procedures, narrowing their scope of experience and reducing their options for future employment in primary care. Although data from the referral management service indicated a considerable reduction in Level 2 referrals, there was some contradiction between responses received in phases 2 and 3 regarding the impact felt by clinic staff.
During phase 2, several comments from staff suggested that the number of less complex clinical cases coming into outpatient oral surgery clinics had reduced, certainly during the mid-year period (the time period after the waiting lists had been cleared):
Clinics are getting smaller, nurses are falling on their training, that’s the only thing I can tell you from what I’ve seen . . . I would say probably in the last 3 months.
CS19
Similarly, the lead consultant felt that the mix of case complexity he was seeing in patients attending his clinics had altered in this period, to the extent that he felt that diversion of simpler cases may have gone too far:
There has been a reduction in dental alveolar minor role surgery referrals, there has definitely been a reduction . . . I just wonder if its gone a wee bit too much the other way.
CS20
However, just over 12 months later this sentiment was no longer being reported. Despite referral management data showing only a slight increase in the number of referrals to the DGHs, the same consultant reported a new increase in less complex cases in the final year (phase 3) of the study:
I was expecting [the reduction] to be about 30% or 40%, but I’m still seeing loads . . . it’s just my gut feeling and the figures will tell but I see some of them and I think, ‘well that is a Level 2’, but it’s still coming to us.
CS20
This change in perception of impact was attributed to an increase in the number of referrals from local areas currently without referral management, rather than a failure of the intervention. It was also the case that phase 3 did see a reduction in the total number of referrals sent to primary care and, hence, this, combined with an overall increase in referral numbers, may have given the impression of increasing levels of simpler cases. It was felt that the scope of referral management would need to be increased to impact on many practices referring into the area before potential benefits could be realised:
A load of them come through [local town] which isn’t actually in Sefton. So we certainly still seem to see a fair number of those types of cases.
CS20
The view that referrals were increasing experientially outside the study area and across dental specialties was shared by the commissioning team, who did not have an explanation for this pattern:
There’s been an increase in GDP referrals across a number of specialties, it’s not just oral surgery so I’m trying to understand how that is.
CS23
A sense that impact would be felt more keenly as the footprint of referral management grew was widely shared. Concerns expressed at the start of the implementation period, although largely not realised within the parameters of this study, remained regarding any future plans to roll out the intervention in the wider geographical area:
The concerns we’ve got in the long term is that if the information from this project ends up being extrapolated across the whole region, we may find there’s a huge effect . . . the numbers involved are too small to make any difference to us at the moment.
CS18
Discussion
The introduction of the referral management system for oral surgery had minimum impact on existing administration practices in secondary care trusts. It was felt that quality of referrals improved. The transfer of radiographs from the referral management system to hospital systems proved problematic, and communication pathways between consultants and GDPs needed reconsideration.
The transfer of less complex cases to a primary care provider was mostly acceptable to secondary care staff, with some reservations expressed around clinical supervision and protection from litigation. Consultant-led primary care provision appears to be acceptable as an option for other models of tier 2 oral surgery diversion, despite the lack of interest shown for the contract offered as part of this study. The commissioning team had some reservations about GDP autonomy in triaging, and felt that the experience and knowledge held by consultants made a consultant-led triage model more appropriate. However, GDP autonomous decision-making was acceptable to consultants, provided there was the option for GDPs to defer responsibility in cases of uncertainty. Consultants did not express views indicative of a protectionist stance towards their profession, and seemed comfortable with the staff skill mix within oral surgery services.
This acceptance may be influenced by the resource-limited context in which the referral management intervention was introduced, and priorities for service redesign aligned with those of the commissioning team. This supports Nancarrow and Borthwick’s98 observation that modern climates for workforce change tend to be consensual, rather than combative.
Hospital staff expected that the introduction of diversion of less complex cases to primary care to have a greater impact at the start of the implementation period than was perceived to be the case at the end of the study. Commissioners and consultants attributed this to the increase of oral surgery referrals in the wider geographical area, and to the study pilot area not being large enough to have the significant impact that may be brought about by extending the footprint of referral management implementation.
Feedback given in these interviews led to a number of changes being made to the system and the way it was implemented, for example improvements in electronic communication between GDPs and consultants, specific, guidelines being produced on referring patients with certain medical histories, tailored to the local context of service provision; the development of a model to divert training cases back to teaching hospitals; and the creation of a cloud-based storage system for radiographs. The intervention, therefore, shows flexibility and the ability to respond and adapt to local concerns and organisational idiosyncrasies.
Themes arising from these data mapped onto three of the four NPT constructs readily. The use of NPT as a framework for understanding implementation processes is helpful, and will aid integration of all findings into a holistic theory of implementation. A weakness of this research may be the small number of secondary care practitioners and commissioners participating in the interviews. However, this reflects the small number of those working in the secondary care trusts who were aware enough of the referral management intervention to feel able to contribute in a meaningful way. This reflects the low levels of impact on administration systems and usual ways of working.
Reflections on quality: a qualitative exploration of patients’ views of oral surgery services
Patients are essential stakeholders in oral surgery care pathways. Refusal to accept primary care provision, failure to attend appointments or reluctance to accept care from non-hospital staff could undermine the approach investigated here. Reports from the preliminary work in Greater Manchester suggested that patients responded well to diversion to primary care. Primary care providers can usually offer a wide range of flexible appointment times, often in extended hours, and practices are often intentionally accessible on transport routes and within reach of easy parking. The work in Greater Manchester suggested that, out of some 600 diverted patients, only seven refused treatment at the selected provider, and in each case this was related to travel distance rather than to any objection to the care setting. Providers report that patients want to be seen quickly, and this tends to override any other consideration in terms of provider choice. However, patient choice is only one area of interest. Secondary care providers have raised concern about the quality of service offered in primary care, and many feel that patients will ultimately return to secondary care, possibly with complications from the initial treatment.
Following the Darzi review on quality within the NHS,100 there has been a recent focus on quality within health services. Research has tended to concentrate on quality in primary care and other medical services; however, the literature on quality specifically regarding dental services is sparse. 101 There are several possible issues separating dentistry from other health services, which could impact on perceptions of quality. These include the traditional view of dentistry as surgical treatment, often with aesthetically focused outcomes. Dental care in the UK is delivered in a combination of ways, with the most common being a co-payment arrangement on a varied scale according to the provider (private or NHS) and the type of treatment carried out. 102 Some dental patients’ notions of quality might therefore be more closely be aligned to those of the private sector ‘consumer’ rather than the NHS ‘patient’.
Consumers’ views of quality, as reported in business and marketing literature, are assumed to be organised hierarchically, with identification with a brand as representing ‘quality’ being firstly associated with basic satisfaction with the service or product provided. When a value added element of ‘surprise and delight’ is introduced (such as a free gift), positive views associated with that service or product are enhanced and can be further assimilated into the consumer consciousness, often resulting in the establishment of an emotional attachment or brand loyalty. 103,104
However, dental care is often associated with pain and anxiety, and how this is managed will be at the forefront of patients’ views on the quality of the service provided. 102 Recognising the dearth of research around what constitutes quality in dentistry, Tickle et al. 105 investigated and identified priorities for dental care patients, the top 11 of which are (in hierarchical order of importance) availability of appointments; quality of treatment; professionalism of staff; hygiene/cleanliness; attitude of staff; painless treatment; cost-effectiveness or value for money; staff priorities; putting patients at ease; quality of advice; and convenience. These priorities appear to map comfortably onto the three encompassing domains of quality within the NHS identified by the Darzi review:100 patient safety, clinical effectiveness and patient experience priorities. Therefore, dental patients’ views of quality may also have resonance with those of the wider NHS patient population.
Patient experience priorities106 described above (e.g. attitude of staff, putting patients at ease) are also described interchangeably within health research literature as ‘patient centeredness’, and the social and communication skills of health care professionals are often labelled as patient-centred attributes. Good patient-centred care has been found to have a positive effect on a number of objective and self-reported quality outcomes in primary care. 107 Although important, patient-centeredness may be of lower priority than technical quality of care and continuity. 108,109 Although patients’ views of their relationships with health-care professionals are important components of a holistic impression of quality, positive appraisal of individuals may, conversely, skew overall impressions of the services in which they work. This is known in the literature as the ‘halo error’106 or ‘halo effect’. 110 The nature of interpersonal relationships with staff can, therefore, greatly influence patients’ overall impressions of quality.
Furthermore, relationships that may have been formed between patients and GDPs, and/or patients and hospital-based oral surgeons could be disturbed through a new oral surgery referral process. Existing research describes continuity of care, particularly regarding interpersonal relationships with a named clinician or familiar care team, as being important to patient satisfaction levels and notions of quality. 109,111,112 Referral management may prevent GDPs referring directly to a named consultant who may have treated the patient previously. This disruption to continuity of care may thus impact on notions of quality.
Quality of care is a major concern when introducing cost-saving initiatives and, therefore, there was a need to explore patient’s views on this service, considering the altered pathways within the oral surgery service brought about by referral management and triage system. Furthermore, the importance of integrating service users in health services research is widely recognised and has potential benefits for policy-making, research, practice, improved implementation, better care and better health. 113
The aim of this part of the study was, therefore, to explore patients’ views around what represents satisfaction or quality of care in both the primary and secondary care oral surgery services operating within the geographical and organisational parameters of the pilot study.
Methods
Participants
All participants were adult (aged 18 years or older) UK NHS dental patients who had been referred by their GDP for oral surgery within the geographical area of the study and provided informed consent to take part in a recorded interview. In total, 30 participants were interviewed. One recording proved to be unintelligible and the recorder failed during one interview, leaving a total of 28 interview transcriptions in the analysis. Fourteen participants were female and 14 were male. The average age of participants was 60 years and 3 months. Nine participants were treated at the specialist primary care service, four at the foundation trust hospital, three at the dental hospital and 12 at the DGH. Initially, purposive sampling was used to identify patients of various ages and demographics; however, as the study progressed it became increasingly clear that most participants had attended the specialist primary care service or the DGH. Accordingly, our sampling strategy changed with the aim of including more participants who had attended the foundation trust (hospital B) and dental hospital (hospital C). A description of service users who participated in interviews is given in Appendix 2.
Interviews
Semistructured interviews were conducted by experienced qualitative researchers using topic guides as prompts, but allowing for exploration of participant-generated issues. Topics for discussion were identified through reviewing relevant literature and discussion with the research team. Subjects of interest were explored further as they arose during the interviews and open-ended questions were used to encourage participants to elaborate on relevant topics.
Topics covered in the guide included:
-
initial GDP consultation (understanding reasons for referral, the examination)
-
whole experience across settings (comparisons with other NHS settings, what could be done better)
-
the oral surgery treatment procedure (feelings around consultation and treatment).
All interviews were carried out over the telephone and typically lasted 30 minutes. They were audio recorded and transcribed verbatim as soon as possible after the interview had taken place.
Data analysis
Thematic analysis65 was used to identify emerging issues and themes from the data using an inductive approach. This is a flexible way of analysing qualitative data that can be used to answer many research questions across a range of theoretical approaches. Use of the constant comparative method66 helped to ensure that the analysis was consistent and based on evidence from the data. The data were analysed and coded by one individual to ensure consistency, in parallel with completion of interviews. The topic guide changed slightly to reflect emerging findings; for example, in the later version, participants were asked to reflect on expectations compared with experience and to give specific examples of good or bad features of the service. Themes were refined through discussion between three authors (JG, CS and IAP) who had read the selected transcripts or quotations. Analysis was completed when no further themes emerged from the data (data saturation was reached). The data were organised using NVivo and Microsoft Word software. An audit trail was kept of all stages of the analysis to maximise credibility, dependability, conformability and transferability. 53,54
Results
Patients had been assessed and treated in the various settings included in the study. They had been treated at one of the specialist primary care sites or at one of the three hospital settings included in the study (dental hospital, district general or foundation trust). Findings were similar for participants attending services at all sites included in the study; therefore, a comparison-based focus was not appropriate.
Patients had a good general understanding of the clinical reasons for their treatment and why they were being referred. They generally reported that their GDPs offered concise, easy-to-understand diagnoses, good explanations of procedures referred for and any reasons for interim treatments such as antibiotics. Very few complications during or after surgery were reported, and participants appeared satisfied overall with treatment and levels of clinical safety and expertise in both primary and secondary care. The following is a typical comment:
They told me everything briefly but very concisely . . . why they needed to do it this particular way.
1123
Themes emerging from the data included the following: understanding service organisation and patient pathways, managing expectations and patient-centred care. Understanding service organisation and patient pathways described patients’ understanding of the oral surgery service and their journey from primary care, specifically with regard to the service this study evaluated. Managing expectations explored patients’ general assumptions regarding waiting lists and continuity of care within NHS settings, and how expectations can impact on notions of quality within specific services. Patient-centred care described how relationships with staff and personalised care affected participants’ perceptions of quality. Themes were explored further and illustrated with quotations from participants displaying identification numbers, sex, age and treatment setting.
Understanding service organisation and patient pathways
Although participants understood clinical reasons for being referred, levels of understanding of patient pathways and the organisation of the oral surgery service were low. Participants tended to be indifferent to treatment taking place at the specialist primary care or secondary care setting. In the minority of cases where a specific preference for primary or secondary care was stated (n = 2), it was framed as idiosyncratic and not related to the service itself (e.g. ‘I just don’t like hospitals’). Some participants would have preferred to be treated by their GDP for reasons of convenience, and felt that they were unnecessarily referred for what were perceived as minor procedures. The following participant had experience of treatment in both hospital and specialist primary care settings; however, in both instances the participant would have accepted treatment at their general dental practice:
It was very similar to the [hospital] experience . . . he actually told me that the reason I had been referred [to specialist primary care] was because of the angle of the root or something. But on both occasions they seemed to take the tooth out very easily. Both times I have walked away and gone, ‘why wasn’t that done at the dentist?
1166
Despite not having a strong preference for treatment setting, participants did prefer to know in advance where their procedure would take place. GDPs often did not inform participants about the new primary care provision, and, consequently, some patients did not understand that their treatment might ultimately take place outside a hospital setting. Participants frequently reported having to make several telephone calls to chase appointments, with referring dental practices unable to inform them where their referral had been sent. This could prove to be frustrating and anxiety inducing:
The worst thing was having to wait for the appointment and then having to chase everything myself. I seemed to be coming up against brick walls all the time. And the fact that the dentists didn’t know, the receptionist didn’t know . . . the right hand didn’t seem to know what the left hand was doing.
1140
Patients who were treated at the specialist service could have little understanding of why they had been sent there rather than to hospital. For example, one participant thought that she had been sent to an orthodontist, rather than to an oral surgeon. Another participant had become worried after being told that the new service was private and she would have to pay for treatment:
I was happy at first, because [specialist primary care service] could see me the following day and then I thought, ‘hang on a minute’ because I just didn’t expect it. So I went to the dentist and they said, ‘we’ve never heard of this place. I wouldn’t go if I were you it’s one of those things, you get there and they charge you’ . . . I went back and she explained everything, that it was NHS and it was a way of getting the waiting lists down and that.
2224
Expectations
Although discussed in the context of the oral surgery service, aspects of service quality, such as receiving treatment in a timely manner, were conceptualised as being part of the NHS as a whole. Some participants had expectations, mostly shaped by previous experience of other health services, which did not match the reality of NHS service delivery in the present day. However, many patients accepted that compromises such as longer waiting times were necessary to receive health care free at the point of delivery:
You have to understand, you’re one of many, but then everyone wants hospitals and doctors these days. Nothing happens overnight no matter what it is.
1328
A short waiting time was reported as important to participants, in terms of both time from referral to appointment and time to see a clinician at the treatment setting. Most frustration was expressed around waiting for appointments of up to 16 weeks. The NHS has set acute trusts maximum waiting times from referral to treatment of 2 weeks for urgent suspected cancer cases and 18 weeks for all other elective procedures (considered non-urgent), something that was poorly communicated to patients. Waiting for appointments, however, was more acceptable when participants’ expectations were managed; they appeared to be willing to wait short periods of time provided they knew approximately how long they would be waiting and the reasons behind the wait. Often patients thought that their referrals had been lost in the system. Participants frequently reported chasing appointments themselves, which could add to their sense of frustration:
Just having an idea of what is expected and what is reasonable . . . helps. Everyone’s concern ultimately is, ‘have they forgotten about me?’. I only got an appointment a couple of days ago when I phoned up to see what happened . . . you begin to think, ‘maybe there has been a little mistake’.
1211
Although many patients did understand that they might have to wait months for NHS treatment, those in pain or discomfort reported much more desperation and frustration with the appointments system. These patients tended to appreciate the shorter waiting times offered by the primary care service and placed much more emphasis on expedience of treatment as a priority:
I was happy to just have it dealt with because it was really beginning to bug me . . . If it was giving me as much pain I’d be quite happy to go back to [specialist primary care service] rather than wait 2 months to be seen . . .
1975
Participants could be unaware of NHS policy regarding waiting time, and mistakenly believe they had been referred as an ‘urgent’ case due to pain or discomfort. They tended to overestimate how much influence GDPs have over the time that a patient referred to secondary care waits for an appointment. Participants reported that GDPs had noted ‘urgent’ on some referrals, but in practice they have little ability to influence waiting times outside NHS parameters for urgent suspected cancer cases. This could result in unrealistic expectations, which would impact particularly on secondary care patients:
I remember people saying . . . with having toothache you wouldn’t think they’d leave you that long, but it must have been about 2 weeks [until specialist primary care service appointment].
2224
Patients reported coming to appointments with expectations that they would have to wait around half an hour past their appointment time to be seen by a clinician, and most reported waiting an acceptable amount of time to be seen. Once patients had arrived at a hospital setting for consultation and treatment, waiting times to see the clinician could be managed in an acceptable way by giving information to the patient and encouraging patients to move between waiting areas (this, however, is likely to prove more difficult in smaller dental practices):
They told me exactly how to get around to X-ray . . . they have a system where if you’re going from one area, the first waiting room to a waiting room nearer the consultants, which gives the impression of things happening, but you’re just moving from one seat to another, I don’t think I was in any one place for more than 5 minutes.
1138
Continuity of care was reported as important to participants and mentioned most often in relation to primary care and a preference for seeing the same dentist for check-ups and treatment. For secondary care, consistency was conceptualised as either seeing and being treated by the same clinician or, more frequently, being treated within the same team, under a named consultant who had access to the patients’ records or knew their medical history. Patients with complex medical histories who were undergoing several procedures preferred consistency of care and anxieties around how dental treatment could become exacerbated by change. The following patient had several pre-existing health conditions and was undergoing a series of dental procedures. She was exercised to find out, first, that her previous consultant was no longer carrying out minor oral surgery and second, that she was assessed and treated by a more junior member of staff rather than the replacement consultant:
I did have my faith in him and I wanted to see him because he did my last one and I didn’t know he wasn’t there any more . . . I don’t really want to see someone who doesn’t know my full history . . . and he [replacement consultant] wasn’t there and I’m faceless, I’m nameless.
1925
Other patients viewed consistency of care as a component of efficiency, with concerns around increased waiting time as a result of taking repeated medical histories from patients and unnecessary communication between clinicians. Treatment by different clinicians could be acceptable if they were part of the same care team and this was communicated effectively to the patient:
If you saw consultant A on a Monday and consultant B on a Wednesday . . . then they’re asking you the same questions just to catch up it feels like it’s being passed around. On the other hand I’m thinking about communication. If a registrar says, ‘I’m the registrar, I’m following up your case and this will be sent to the consultant who looks at my work’, then you know this is part of the same team.
1172
Participants who had undergone previous treatment in a secondary care setting often had their expectations shaped by the experience. Older patients were more likely to have been treated in hospital, often using GA, and could be unaware of changes in NHS practices over the years in respect of routine oral surgery treatment. Discovering that GA was now used only exceptionally could be difficult for highly anxious patients, who were likely to put pressure on their GDPs to refer them for GA; however, participants were able to understand the risks attached to being unconscious during treatment and accepted that this was a universal change in practice across the NHS. The following patient, for example, accepted that GA was no longer deemed appropriate for her treatment and had looked to her GP to manage anxiety around the procedure:
The only thing that frightened me was that it was done under a local anaesthetic where the other one had been done under a general. I just got the impression it was better for the patient in some respects you’re not under [general] anaesthetic as it can be a bit dodgy sometimes can’t it? . . . I had a couple of Valium from my doctor instead.
1147
Patient-centred care
Participants placed high value on patient-centred components of care. Positive interpersonal skills of health-care professionals were important, particularly to anxious patients, who reported feeling soothed by individuals who displayed a caring attitude. Participants appreciated having their anxiety acknowledged and accepted by staff and described distraction techniques, such as making jokes and general conversation, as effective in putting them at ease:
To be honest, I was quite surprised that I actually wasn’t nervous. They all made me feel dead comfortable. There were two nurses and a surgeon and they were all having a bit of a laugh and a joke, to put me at ease. So I thought that was nice, that they weren’t just sitting there in silence.
1138
In addition to the way clinical staff interacted with patients, the content of communication was important. Participants wanted staff to provide information about their own clinical treatment and appreciated the opportunity to ask questions in a non-judgemental environment. Anxious patients liked to know what would happen at their appointments in some detail; it was important that they knew what to expect about both staffing and their treatment plan:
I couldn’t work out what the dental nurses were doing . . . I need to know what people are doing . . . The clinician was very good, he explained everything and every question that I asked, he didn’t look at me like I was stupid.
1140
Furthermore, participants (again, particularly those who experienced anxiety around dental treatment) greatly appreciated staff giving specific reassurances around efficiency of their treatment: that it would be pain free and they would receive necessary anaesthetic, and that the surgeon was sufficiently experienced and technically skilled to carry out the procedure:
[Dental nurse] must work with the dentist who took my tooth out, they seemed as though they knew each other very well. Now she was absolutely marvellous, she reassured me and I felt much better after speaking to her . . . she was saying, ‘if anybody can sort it out for you, he can’.
.2224
Participants could have expectations around what would happen at their appointments, which did not match their actual treatment plans, and this tended to be attributed to insufficient communication by staff to patients. This issue is particularly relevant given the difference in the treatment plans for specialist primary care and secondary care patients within this service; hospital patients attending their first appointment were surprised to be sent for radiography and be given an appointment for treatment at a future date, or specialist primary care patients sometimes arrived unprepared to be treated on the same day. Misunderstanding around treatment plans may undermine patient confidence and could possibly become a safety issue for patients with comorbidities, who may, for example, need to plan mealtimes:
I was slightly unnerved because I hadn’t gone prepared to have an extraction and I’d have eaten more beforehand knowing then that I wouldn’t be able to eat after, things like that . . . it was fine for me, I’m fit and healthy. I think if you were a bit more old and vulnerable it wouldn’t have been satisfactory.
1213
Discussion
By taking a focused, in-depth approach to analysing participants’ experiences, this work expands on and complements the patient satisfaction survey described in Chapter 4. In addition, this work adds to dearth of research around the meaning of quality in dental services, particularly oral surgery, and encompasses experiences of both primary and secondary care treatment.
Initially, purposive sampling was intended to identify participants from a variety of age groups and backgrounds. This strategy was amended, as eligible patients referred to the dental hospital or the foundation trust hospital were under-represented in our sample and we felt that it was more appropriate to concentrate on gaining a sample able to explore experiences across all relevant treatment settings. Possibly because of this amended approach, findings disproportionately represent the experiences of older participants.
Participants were generally happy with clinical aspects of their treatment, and only minor complications during or following surgery were occasionally reported. Findings highlighted the importance of GDPs communicating details regarding the referral pathway and triage procedure to patients, including possible treatment destinations and the introduction of the new specialist primary care service. This could help alleviate frustration and confusion felt in patients trying to locate and chase errant referrals, thus offering a better overall patient experience.
In addition, precise communication from referring GDPs to patients around elements of service delivery, such as possible waiting times, appropriateness of anaesthetic and skill levels of treating surgeons, can help manage expectations of patients, particularly those who may have conflicting past experiences of dental care, oral surgery or other hospital treatment. Care should be taken to ensure that patients, especially those experiencing pain or anxiety, understand NHS procedures regarding waiting list targets and limitations of GDPs to influence waiting times at the point of referral.
We asked participants in this research to discuss aspects of quality relating specifically to the oral surgery service they were treated in, rather than general notions or interpretations of quality. However, features relating to ‘patient experience’ priorities described in the Darzi review have resonance with findings of this study in the sections discussing expectations and patient-centred care. Similarly, these emerging themes map closely on many of the findings of Tickle et al. 6 around the priorities of dental patients, namely availability of appointments, professionalism of staff, staff priorities and putting patients at ease. Overall, the findings suggest that the inevitable interruption of the GDP–patient relationship, initiated by the referral and triage pathways, can be negated through good communication, managing expectations around treatment within the oral surgery service and practising patient-centred care.
Summary of main findings
The three elements of this qualitative part of the mixed-methods design sought to address the three broad research questions that we were posed:
-
What are the issues encountered when establishing a new primary care oral surgery service?
The establishment of the service appeared to go very smoothly. After some initial minor problems because of communication deficits and a lack of understanding of the objectives of the service, the referrals received were appropriate. The need for ongoing communication about the aims of the service were highlighted. Similarly, a good relationship with secondary care and local consultants was essential to provide support and smooth operation of the system. The new service was well accepted by patients, who appreciated the convenience in terms of a local service and short waits for appointments.
-
What are the views of stakeholders on the development and implementation of the primary care service?
The foundation trust and dental hospital secondary care services felt that the new service has little impact on their workload because their catchment area was much larger than Sefton. The service was felt to have a more pronounced effect on the DGH, although this was reduced when consultant triage was replaced with GDP triage. There seemed to be a view among consultants and hospital managers that, because of the financial pressures on the NHS and the demand pressures on its services, the introduction of Level 2 services was inevitable and it was, in general, supported.
-
What are the views of service users on the quality of service they received from the referral management and triage system?
Patients accepted the services and appreciated the timeliness of appointments and the local accessibility of the service. The main requirement of patients was that their problem was dealt with quickly and effectively; the setting and who did it were secondary considerations. Patients expected clear communication about the process and viewed patient-centred care as a key indicator of the quality of the service.
Conclusions
Primary care service changes can be implemented, but timely and effective communication is important. This communication needs to continue and involve all levels of service provision for the system to work effectively. There is a need to recognise that staff turnover may require a regular updating of the directory of services available to primary care referrers.
For a referral management system to have a significant effect on large trusts with large catchment areas, the referral management needs often operate on a footprint that mirrors that of the catchment areas. Provision of timely and rapid alleviation of a patient’s problem was more highly valued than the location of the service and, hence, when commissioning primary care services, an emphasis should be placed on the provider’s ability to deliver care promptly.
Concerns regarding the acceptability of Level 2 services seem unfounded, with patients reporting high levels of satisfaction, with patient-centred care and good communication being cited as important and desirable features.
Chapter 6 Conclusions
Summary of main findings
Remote triage
The evidence suggests that the use of remote clinical triage is an acceptable way of identifying cases that might be suitable for primary care services. Where error exists, it occurs on the side of caution, with patients who may have been appropriate for Level 2 being sent to secondary care. Although this approach may reduce the cost savings available, it is efficient and safe for patients. Such reduction in the identification of all Level 2 cases should be considered against the context of what proportion of all cases could be removed from secondary care without destabilisation, and the need to preserve appropriate cases for training. When assessed in phases 2 and 3 of the current work, only 4% of patients sent to the primary care provider required onwards referral to secondary care, largely because information was missing from the referral form.
Electronic referral management
Findings from the research indicate that an electronic-only referral pathway for primary care-based GDPs is feasible, and can be implemented with appropriate engagement and communication. The use of an electronic system enables a minimum data set for referrals to be mandated, preventing submission of referrals if information is absent. The system does not, however, control for the quality of the information submitted, instead relying on the triage process to assess this. The results suggest that such an implementation will significantly improve the quality of referrals into care pathways. The use of a simple, secure, web-based system with appropriate information governance enabled referral data to be used to inform commissioning and provide health needs and case complexity assessments. There is sufficient IT infrastructure within primary care dental practices to support the introduction of an electronic referral system, although consideration should be given to rural or other areas where access to broadband facilities may be restricted.
Primary care Level 2 services
The evidence clearly suggests that, to realise cost savings and reduce demand in secondary care, at alternative clinical services are required. 21 The development of such services should be informed by prior health needs assessments, which inform commissioning not only of the Level 2 services, but also of the likely impact on Level 3 services. Implementation of such services should be accompanied by effective, and ongoing, communication to referrers and service users. Our study shows that patients will readily accept treatment in Level 2 services and report similar levels of satisfaction to those seen in hospitals, and there is no increase in complication rates. Patients reported their main priority as being seen promptly (especially those in pain or who were anxious) rather than the location of care.
Costs and savings
The combination of a referral management system and Level 2 primary care oral surgery service offers the ability to save significant costs to the NHS without any increase in societal expenditure. These cost savings should also be considered alongside the quality improvement seen in referrals, the management of demand of stretched secondary care services and the speed with which primary care can appoint and treat patients. The degree of cost saving will be dependent on the application of the tariff by the served secondary care organisations. Larger savings produced by referral management may suggest that inappropriate tariff charging is taking place. Referral management systems in areas where secondary care costs are not fully understood may produce erroneous savings.
Overall strengths and limitations
The study has a number of strengths. The use of a real-world setting, with a ‘virgin’ territory in which no formal referral management or Level 2 provision had been employed, enables stronger causation assessments to be made. The availability of three hospitals serving Sefton helps generalisability to other areas. The partnership working with commissioners to enable not only the referral management system but also the incremental development of the Level 2 service ensured that the ITS approach was meaningful. The mixed-methods approach facilitates a deeper understanding of the underlying issues and impacts of service implementation and change and, when combined with the high levels of general practice engagement, provides a whole-system view. The use of hospital-specific tariff applications in the health economic evaluation permitted a more sophisticated understanding of the impacts of referral diversions than could have been achieved with the use of average costs or tariff guidance costs.
The small geographical footprint is a limitation of the study – the referral flows were largely into hospital A and, hence, the impact on the two other trusts was minor and prevented a full exploration of the potential issues for these organisations. Further research should take place on footprints that represent the capture area of those trusts studied. The use of commonly collected NHS data was problematic, and this lack of a robust counterfactual limits the casual inferences that can be made regarding systemic changes in referral behaviour. Our follow-up period could also have been extended to view the impact of staff turnover in all clinical care settings.
As with all research projects that extend over a number of years, there have been temporal changes within the dental landscape. The establishment of local professional networks (LPNs) in dentistry, aligned with managed clinical networks (MCNs), has sought to drive improvement in care pathways. There was no MCN in the Sefton area during the study, although, in the future, such networks and groups will probably be the driving force for implementing any referral system, and for supporting those GDPs requiring additional training.
What have we added to the evidence base?
This work addresses evidence gaps highlighted by recent reviews22,23 and supports findings from other dental14 and non-dental21 studies. There is a clear need for a diversion service to be introduced alongside referral management if costs savings are to be achieved – referral management alone is likely to be costly and ineffective – as found by Cox et al. 21 However, a period of non-diversion should be considered as part of a staged implementation to ensure that any additional services are commissioned using locally derived data of demand and needs. The current work provides evidence that health needs assessments can be informed by the capture and assessment of referrals in such a model.
Referral management is not a panacea – its introduction requires careful planning, communication and engagement. 38 Consideration must be made of the local secondary care environment, the tariff costs, the workforce and the needs for training.
Implications
The continuing financial pressures facing the NHS require new ways of working, and demand management plays an important role. Commissioning policy in dentistry advocates for strengthening the Level 2 provision across all dental specialties, with referral management systems ensuring that diversion to such services is safe and efficient. 1 Yet, the policy documents say little about how such services should be designed and implemented. The lack of NHS IT infrastructure in dentistry prohibits the use of the national eRS and, hence, NHS ATs must consider alternatives. When doing so, they need to have sight of the local context, the clinical leadership required to make change and the workforce to deliver it.
Further research
Research recommendation 1: whole-system approaches
The use of referral management with linked diversion services requires further exploration across the health-care economy. The relatively small footprint of the Sefton study has suggested benefits, but can these be industrialised or applied to different disciplines? Earlier studies have concentrated on the use of referral management systems as ‘gatekeepers’ only, aiming to reduce the overall referral volume out of primary care. Such systems have largely failed to deliver such decreases, suggesting that primary care practitioners are recognising a patient need for referral, or their inability to provide what is required. It is this second point that also warrants further investigation from a qualitative perspective, as this involves not only issues of practitioner competency and training but also potential legal and regulatory issues.
Both the General Medical Council and the General Dental Council have clear statements on referring patients:
You should refer patients on if the treatment required is outside your scope of practice or competence. You should be clear about the procedure for doing this.
General Dental Council114
Practitioners may, therefore, feel compelled to refer even if such procedures or treatments should fall within their competency. Such issues require careful consideration and interplay between undergraduate health education, postgraduate training, the regulatory bodies and commissioners. The NHS commissioning guides for dentistry make clear what they expect a primary care practitioner to deliver, and contracting bodies have stated that, in order to comply with the General Dental Council’s regulations they would expect the individual to refer within the contract – that is, to a colleague within the practice with the relevant experience – and to seek and acquire the skills necessary to perform Level 1 procedures. A further complexity to this issue is that the redirection of referrals into primary care may, if not carefully managed, result in a decrease in appropriate training cases for students at both the undergraduate and postgraduate level, resulting in further decreases in competency and, hence, a driver for referring.
The development of LPNs and aligned MCNs is now under way within the dental commissioning landscape. MCNs in oral surgery may well lead on referral management issues, and their involvement in any future research will be key to understanding the role of the profession and their local leadership in changing practice.
We therefore recommend that further research is undertaken on this complex area to ensure that demand management systems are fully integrated into the health ecosystem.
Research recommendation 2: other specialties within dentistry
This research has examined the referring of oral surgery cases from primary to secondary care. This specialty was selected as the referrals are both common and costly, combined with a clear specification for primary care Level 2 services. The relative differences in potential costs between the primary and secondary care provision also facilitated an assessment of cost benefit. However, referral management need not be focused on cost saving alone, but may seek to manage demand for smaller services, ensuring that those who would gain the most benefit are prioritised. It may be used to increase the quality of referrals by mandating a minimum data set and thus provide a highly granular intelligence to inform commissioning decisions.
We would recommend that other dental specialties are considered for further research using the established methodology described within this report. Examples of areas where referral management might be considered include:
-
Extraction of teeth under general anaesthetic for young children. Such services are often under pressure to deliver against 18-week targets, and, in some areas, waiting times are long, with adverse consequences for children. 115,116 The use of referral and triage systems may help identify those patients who could be seen safely in primary care under local anaesthetic and help preserve the hospital services for those requiring general anaesthetic.
-
Orthodontic referrals. Orthodontic treatment is provided, mainly, within primary care specialist practices, but complex cases and patients are seen within secondary care. 11 There are often long waiting lists at primary care providers, which encourages early and, often, inappropriate referrals. There is a potential for referral management to help identify cases suitable for each care setting and to help map need against capacity. 117
Both specialties have high costs associated with them, enabling a health economic evaluation to be undertaken in addition to the important health outcomes for patients.
Research recommendation 3: additional health-care systems
In addition to dental referrals there are a range of other areas that could be considered. For example, referrals from primary care optometry services are under-researched and may provide an opportunity for Level 2 services. The contractor status of optometry is not dissimilar to that of dentistry and has a similar primary care landscape of smaller independent contractors alongside larger corporate providers. The differences in referral patterns between these, and the appropriateness of them, would be of interest to commissioners and the broader NHS.
Like dental services, secondary care dermatology services are often under pressure, and in some cases images of skin lesions, analogous to dental radiographs, are needed to asses case complexity. Research suggests that many outpatient appointments are for inappropriate cases that could have been managed in primary care. 118 Although teledermatology has been utilised for many years, its application in reducing demand for secondary care outpatient services and diversions to established GPwSI services has not been formally explored. 119
Summary
The NHS has a need to manage demand, focus on identifying need and protect scarce resources for the benefit of patients. Referral management systems present one means by which this may be achieved, although it must be recognised that such systems cannot stand alone, and are part of a more complex health economy in which several drivers are in play. Further research should recognise this, adopting a mixed-methods approach to investigating their wider use.
Acknowledgements
Grant holders and steering group
The following individuals were grant holders on the project and provided invaluable assistance to the delivery of this project.
Dr Colette Bridgman – provided strategic leadership and NHS liaison throughout the project. Dr Bridgman was instrumental the design and implementation of the Greater Manchester dental referrals system that informed much of the thinking behind the Sefton project.
Stephanie Neil (lay member) – Ms Neil provided a valued contribution to the steering group by providing information on the user and patient perspective, including the design and analysis of the patient qualitative component.
Gina Lawrence – Ms Lawrence was responsible for the commissioning of the NHS Trafford electronic referral system that was used in the current work.
Sam Illingworth – provided strategic leadership from NHS England national perspective during the study period.
External commissioners
Ben Squires and Lindsey Bowes – Mr Squires and Ms Bowes were both key to the development of the Greater Manchester referral system that provided the referrals for the diagnostic test accuracy study and were instrumental in the implementation of the system across a large geographical area. Their commissioning knowledge and support was key in the development of the service specification for the Sefton Minor Oral Surgery service. Further to the completion of this work, both were responsible for securing funding for a cloud-based PACS system, a feature recommended within the current work to optimise radiograph quality.
Diagnostic test accuracy
Each of the following individuals spent considerable time examining, assessing and commenting on referrals. Their contribution to many hours of individual and focus groups discussions is gratefully recognised.
-
Julian Yates.
-
Stuart Clarke.
-
Ravi Singh.
-
Tina Liu.
-
Oral surgery nurses at Manchester Dental Hospital.
Triage team
The following individuals were responsible for triaging all the Sefton referrals that were submitted electronically. In addition to this, each provided invaluable clinical direction and suggestion during the study, including the incorporation of NHS numbers to the referral forms, escalation to 2-week wait and the effective use of supplemental triage for audit purposes.
-
Anne Begley.
-
Patrick Magennis.
-
Rob Laycock.
-
Mark Boyle.
-
Tim Lord.
Research nurses
-
Zena Haslam.
-
Moira Morrison.
Commissioning team
Ms Roger and Dr Gough were responsible for the implementation of the system in Sefton and the commissioning of the primary care service, and attended numerous engagement events and research meetings. Their willingness to host the study, commit to a long-term programme of work and facilitate the linkages between primary and secondary care was crucial to the success of the work.
-
Jean Rogers – NHS Cheshire & Merseyside.
-
Lesley Gough – Public Health England.
Oversight group
Professor Brunton chaired the Oversight Group and he, and the group, provided important strategic direction and advice to the steering group to ensure the success of the project.
-
Matt Sutton.
-
Margaret Ogden.
-
James Darcey.
-
Helen Worthington.
-
Anne-Marie Glenny.
Contributions of authors
Joanna Goldthorpe (Research Fellow, Qualitative Research) undertook the qualitative analysis and reporting.
Tanya Walsh (Reader, Biostatistics) undertook the quantitative analysis for both the diagnostic test accuracy and ITS components.
Martin Tickle (Professor, Dental Public Health) wrote the collated report and undertook the provision of the referral management solution and NHS interface.
Stephen Birch (Professor, Health Economics) conducted the economic evaluation and prepared the relevant sections of the report.
Harry Hill (Research Fellow, Health Economics) conducted the economic evaluation and prepared the relevant sections of the report.
Caroline Sanders (Senior Lecturer) undertook the qualitative analysis and reporting.
Paul Coulthard (Professor, Oral Surgery) undertook the triage activities for the diagnostic test accuracy and provided clinical leadership for the surgical components of the work.
Iain A Pretty (Professor, Dental Public Health) wrote the collated report and undertook the provision of the referral management solution and NHS interface.
Data sharing statement
We shall make data available to the scientific community with as few restrictions as feasible, while retaining exclusive use until the publication of major outputs. Anonymised data will be available from the corresponding author on request.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data is used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Chief Dental Officer . Guide for Commissioning Oral Surgery and Oral Medicine 2015. www.england.nhs.uk/commissioning/primary-care/dental/dental-specialities/ (accessed 29 January 2018).
- Department of Health . Standard General Dental Services Contract and Personal Dental Services Agreement – Publications n.d. www.gov.uk/government/publications/standard-general-dental-services-contract-and-personal-dental-services-agreement (accessed 15 November 2017).
- Thomas D, Walker R, Smith A, Shepherd J. The provision of oral surgery services in England and Wales 1984-1991. Br Dent J 1994;176:215-19. https://doi.org/10.1038/sj.bdj.4808417.
- Department of Health, Faculty of General Dental Practice (FDGP) . Guidelines for the Appointment of Dentists With Special Interests (DwSIs) in Minor Oral Surgery 2006. http://webarchive.nationalarchives.gov.uk/20101110164246tf_/http://www.dh.gov.uk/en/PublicationsPolicyAndGuidance/DH_4133855 (accessed 15 November 2017).
- Wilson N. Oral surgery services and training. Br Dent J 2011;210. https://doi.org/10.1038/sj.bdj.2011.52.
- NHS England . Securing Excellence in Commissioning NHS Dental Services 2013. www.england.nhs.uk/2013/02/dental/ (accessed 15 November 2017).
- Waldman HB, Perlman SP. Dental needs assessment and access to care for adolescents. Dent Clin North Am 2006;50:1-16. https://doi.org/10.1016/j.cden.2005.09.002.
- NHS Digital . Adult Dental Health Survey 2009. http://digital.nhs.uk/catalogue/PUB01086 (accessed 15 November 2017).
- Liu T, Pretty IA, Goodwin M. Estimating the need for dental sedation: evaluating the threshold of the IOSN tool in an adult population. Br Dent J 2013;214. https://doi.org/10.1038/sj.bdj.2013.427.
- Pretty IA, Goodwin M, Coulthard P, Bridgman CM, Gough L, Jenner T, et al. Estimating the need for dental sedation. 2. Using IOSN as a health needs assessment tool. Br Dent J 2011;211. https://doi.org/10.1038/sj.bdj.2011.726.
- Morris AJ, Burke FJ. Primary and secondary dental care: how ideal is the interface?. Br Dent J 2001;191:666-70. https://doi.org/10.1038/sj.bdj.4801263a.
- Evidence Adoption Centre . Effectiveness and Cost Effectiveness of Targeted Interventions to Reduce Unnecessary Referrals and Improve the Quality of Referrals from Primary Care to Secondary Care. Report 2010. http://commissioning.libraryservices.nhs.uk/wp-content/uploads/2013/06/ReferralManagementSchemes-Review.pdf (accessed 15 November 2017).
- Dental Programme Board . Review of Oral Surgery Services and Training 2010. www.baos.org.uk/resources/MEEOSreview.pdf (accessed 15 November 2017).
- Kendall N. Improving access to oral surgery services in primary care. Prim Dent Care 2009;16:137-42. https://doi.org/10.1308/135576109789389540.
- Coulthard P, Kazakou I, Koron R, Worthington HV. Referral patterns and the referral system for oral surgery care. Part 1: general dental practitioner referral patterns. Br Dent J 2000;188:142-5. https://doi.org/10.1038/sj.bdj.4800415.
- Bell G. An audit of 600 referrals to a primary care based oral surgery service. Br Dent J 2007;203. https://doi.org/10.1038/bdj.2007.571.
- Kendall N. Development of oral surgery services in primary care. Oral Surg 2011;4:57-64. https://doi.org/10.1111/j.1752-248X.2011.01117.x.
- O’Neill E, Gallagher JE, Kendall N. A baseline audit of referral and treatment delivered to patients in the intermediate minor oral surgery service in Croydon PCT. Prim Dent Care 2012;19:23-8. https://doi.org/10.1308/135576112798990728.
- Akbari A, Mayhew A, Al-Alawi M, Grimshaw J, Winkens R, Glidewell E, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev 2005;20. https://doi.org/10.1002/14651858.CD005471.
- Imison C, Naylor C. Referral Management: Lessons for Success. London: The King’s Fund; 2010.
- Cox JMS, Steel N, Clark AB, Kumaravel B, Bachmann MO. Do referral-management schemes reduce hospital outpatient attendances? Time-series evaluation of primary care referral management. Br J Gen Pract 2013;63:e386-92. https://doi.org/10.3399/bjgp13X668177.
- Blank L, Baxter S, Woods HB, Goyder E, Lee A, Payne N, et al. What is the evidence on interventions to manage referral from primary to specialist non-emergency care? A systematic review and logic model synthesis. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03240.
- Winpenny E, Miani C, Pitchforth E, Ball S, Nolte E, King S, et al. Outpatient services and primary care: scoping review, substudies and international comparisons. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04150.
- Walford S. Choose and book. Clin Med 2006;6:473-6. https://doi.org/10.7861/clinmedicine.6-5-473.
- Dennison J, Eisen S, Towers M, Ingham Clark C. An effective electronic surgical referral system. Ann R Coll Surg Engl 2006;88:554-6. https://doi.org/10.1308/003588406X130642.
- Maddison P, Jones J, Breslin A, Barton C, Fleur J, Lewis R, et al. Improved access and targeting of musculoskeletal services in northwest Wales: targeted early access to musculoskeletal services (TEAMS) programme. BMJ 2004;329:1325-7. https://doi.org/10.1136/bmj.329.7478.1325.
- Kim Y, Chen AH, Keith E, Yee HF, Kushel MB. Not perfect, but better: primary care providers’ experiences with electronic referrals in a safety net health system. J Gen Intern Med 2009;24:614-9. https://doi.org/10.1007/s11606-009-0955-3.
- Evans E, Aiking H, Edwards A. Reducing variation in general practitioner referral rates through clinical engagement and peer review of referrals: a service improvement project. Qual Prim Care 2011;19:263-72.
- Evans E. The Torfaen referral evaluation project. Qual Prim Care 2009;17:423-9.
- Patterson V, Humphreys J, Chua R. Email triage of new neurological outpatient referrals from general practice. J Neurol Neurosurg Psychiatr 2004;75:617-20. https://doi.org/10.1136/jnnp.2003.024489.
- Jiwa M, Walters S, Mathers N. Referral letters to colorectal surgeons: the impact of peer-mediated feedback. Br J Gen Pract 2004;54:123-6.
- Blundell N, Clarke A, Mays N. Interpretations of referral appropriateness by senior health managers in five PCT areas in England: a qualitative investigation. Qual Saf Health Care 2010;19:182-6. https://doi.org/10.1136/qshc.2007.025684.
- Brocklehurst P, Jones C, Tickle M. QIPP: cutting budgets or working smarter?. Br Dent J 2011;210:369-73. https://doi.org/10.1038/sj.bdj.2011.286.
- Shaffie N, Cheng L. Improving the quality of oral surgery referrals. Br Dent J 2012;213:411-13. https://doi.org/10.1038/sj.bdj.2012.929.
- Kim DS, Lopes J, Higgins A, Lopes V. Influence of NICE guidelines on removal of third molars in a region of the UK. Br J Oral Maxillofac Surg 2006;44:504-6. https://doi.org/10.1016/j.bjoms.2005.10.011.
- Quarterly Monitoring Report 22, March 2017. London: The King’s Fund; 2017.
- Richardson G, Maynard A, Cullum N, Kindig D. Skill mix changes: substitution or service development?. Health Policy 1998;45:119-32. https://doi.org/10.1016/S0168-8510(98)00038-4.
- Davies M, Elwyn G. Referral management centres: promising innovations or Trojan horses?. BMJ 2006;332:844-6. https://doi.org/10.1136/bmj.332.7545.844.
- Barbieri JS, Nelson CA, James WD, Margolis DJ, Littman-Quinn R, Kovarik CL, et al. The reliability of teledermatology to triage inpatient dermatology consultations. JAMA Dermatol 2014;150:419-24. https://doi.org/10.1001/jamadermatol.2013.9517.
- Dixon J, Holland P, Mays N. Primary care: core values developing primary care: gatekeeping, commissioning, and managed care. BMJ 1998;317:125-8. https://doi.org/10.1136/bmj.317.7151.125.
- Reilly BM, Evans AT, Schaider JJ, Wang Y. Triage of patients with chest pain in the emergency department: a comparative study of physicians’ decisions. Am J Med 2002;112:95-103. https://doi.org/10.1016/S0002-9343(01)01054-3.
- Jung S-K, Kim T-W. New approach for the diagnosis of extractions with neural network machine learning. Am J Orthod Dentofac Orthop 2016;149:127-33. https://doi.org/10.1016/j.ajodo.2015.07.030.
- Estai M, Kruger E, Tennant M. Role of telemedicine and mid-level dental providers in expanding dental-care access: potential application in rural Australia. Int Dent J 2016;66:195-200. https://doi.org/10.1111/idj.12217.
- Edwards B. Telephone triage: how experienced nurses reach decisions. J Adv Nurs 1994;19:717-24. https://doi.org/10.1111/j.1365-2648.1994.tb01143.x.
- Bunn F, Byrne G, Kendall S. The effects of telephone consultation and triage on healthcare use and patient satisfaction: a systematic review. Br J Gen Pract 2005;55:956-61.
- Gerdtz MF, Bucknall TK. Why we do the things we do: applying clinical decision-making frameworks to triage practice. Accid Emerg Nurs 1999;7:50-7. https://doi.org/10.1016/S0965-2302(99)80103-9.
- Gooberman-Hill R, Sansom A, Sanders CM, Dieppe PA, Horwood J, Learmonth ID, et al. Unstated factors in orthopaedic decision-making: a qualitative study. BMC Musculoskelet Disord 2010;11. https://doi.org/10.1186/1471-2474-11-213.
- Considine J, Botti M, Thomas S. Do knowledge and experience have specific roles in triage decision-making?. Acad Emerg Med 2007;14:722-6. https://doi.org/10.1111/j.1553-2712.2007.tb01869.x.
- Chauveau P, Mazet-Guillaume B, Baron C, Roy PM, Tanguy M, Fanello S. Impact of the referral letter on triage decisions in adult patients admitted to the emergency department. Sante Publique 2013;25:441-51. https://doi.org/10.3917/spub.134.0441.
- Sansom A, Donovan J, Sanders C, Dieppe P, Horwood J, Learmonth I, et al. Routes to total joint replacement surgery: patients’ and clinicians’ perceptions of need. Arthritis Care Res 2010;62:1252-7. https://doi.org/10.1002/acr.20218.
- Malhotra RK, Indrayan A. A simple nomogram for sample size for estimating sensitivity and specificity of medical tests. Indian J Ophthalmol 2010;58:519-22. https://doi.org/10.4103/0301-4738.71699.
- Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine Publishing Co.; 1967.
- Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ 2000;320:50-2. https://doi.org/10.1136/bmj.320.7226.50.
- Lincoln YS. Emerging Criteria for Quality in Qualitative and Interpretive Research 1995;Vol. 1:275-89. https://doi.org/10.1177/107780049500100301.
- Coulthard P, Bridgman CM, Gough L, Longman L, Pretty IA, Jenner T. Estimating the need for dental sedation. 1. The Indicator of Sedation Need (IOSN) - a novel assessment tool. Br Dent J 2011;211. https://doi.org/10.1038/sj.bdj.2011.725.
- Stedman TL. Stedman’s Medical Dictionary. Cincinnati, OH: Anderson Co.; 1976.
- Wuerz R, Fernandes CM, Alarcon J. Inconsistency of emergency department triage. Emergency Department Operations Research Working Group. Ann Emerg Med 1998;32:431-5. https://doi.org/10.1016/S0196-0644(98)70171-4.
- Shapiro M, James WD, Kessler R, Lazorik FC, Katz KA, Tam J, et al. Comparison of skin biopsy triage decisions in 49 patients with pigmented lesions and skin neoplasms: store-and-forward teledermatology vs face-to-face dermatology. Arch Dermatol 2004;140:525-8. https://doi.org/10.1001/archderm.140.5.525.
- Bader JD, Shugars DA. Understanding dentists’ restorative treatment decisions. J Public Health Dent 1992;52:102-10. https://doi.org/10.1111/j.1752-7325.1992.tb02251.x.
- Bader JD, Shugars DA. Variation in dentists’ clinical decisions. J Public Health Dent 1995;55:181-8. https://doi.org/10.1111/j.1752-7325.1995.tb02364.x.
- Roter DL, Hall JA. Physician’s interviewing styles and medical information obtained from patients. J Gen Intern Med 1987;2:325-9. https://doi.org/10.1007/BF02596168.
- Goodwin M, Coulthard P, Pretty IA, Bridgman C, Gough L, Sharif MO. Estimating the need for dental sedation. 4. Using IOSN as a referral tool. Br Dent J 2012;212. https://doi.org/10.1038/sj.bdj.2012.183.
- The use of dental radiographs: update and recommendations . J Am Dent Assoc 2006;137:1304-12. https://doi.org/10.14219/jada.archive.2006.0393.
- Public Health England . Sefton Health Profile 2016 2016. http://fingertipsreports.phe.org.uk/health-profiles/2016/e08000014.pdf (accessed 15 November 2017).
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Glaser BG. The constant comparative method of qualitative analysis. Social Problems 1965;12:436-45. https://doi.org/10.2307/798843.
- May CR, Finch T, Ballini L, MacFarlane A, Mair F, Murray E, et al. Evaluating complex interventions and health technologies using normalization process theory: development of a simplified approach and web-enabled toolkit. BMC Health Serv Res 2011;11:1-11. https://doi.org/10.1186/1472-6963-11-245.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Department for Communities and Local Government . English Indices of Deprivation 2015 2015. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 12 February 2018).
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- Scantlebury A, Sheard L, Watt I, Cairns P, Wright J, Adamson J. Exploring the implementation of an electronic record into a maternity unit: a qualitative study using Normalisation Process Theory. BMC Med Inform Decis Mak 2017;17. https://doi.org/10.1186/s12911-016-0406-0.
- May CR, Johnson M, Finch T. Implementation, context and complexity. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0506-3.
- Miller RH, Sim I. Physicians’ use of electronic medical records: barriers and solutions. Health Aff 2004;23:116-26. https://doi.org/10.1377/hlthaff.23.2.116.
- Department of Health . Decontamination Health Technical Memorandum 01-05: Decontamination in Primary Care Dental Practices 2013. www.gov.uk/government/publications/decontamination-in-primary-care-dental-practices (accessed 29 January 2018).
- John JH, Thomas D, Richards D. Questionnaire survey on the use of computerisation in dental practices across the Thames Valley Region. Br Dent J 2003;195:585-90. https://doi.org/10.1038/sj.bdj.4810734.
- Mitchell E, Sullivan F. Information in practice: a descriptive feast but an evaluative famine: systematic review of published articles on primary care computing during 1980-97. BMJ 2001;322:279-82. https://doi.org/10.1136/bmj.322.7281.279.
- Benson T. Why general practitioners use computers and hospital doctors do not – part 2: scalability. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7372.1090.
- Charlton R. General practice. Clin Med 2010;10:600-4. https://doi.org/10.7861/clinmedicine.10-6-600.
- Morden A, Ong BN, Brooks L, Jinks C, Porcheret M, Edwards JJ, et al. Introducing evidence through research ‘push’: using theory and qualitative methods. Qual Health Res 2015;25:1560-75. https://doi.org/10.1177/1049732315570120.
- Bird L, Arthur A, Cox K. ‘Did the trial kill the intervention?’ experiences from the development, implementation and evaluation of a complex intervention. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-24.
- Hendy J, Chrysanthaki T, Barlow J, Knapp M, Rogers A, Sanders C, et al. An organisational analysis of the implementation of telecare and telehealth: the whole systems demonstrator. BMC Health Serv Res 2012;12:1-10. https://doi.org/10.1186/1472-6963-12-403.
- Shea CM, Belden CM, King J, Patel V, Furukawa M, Adler-Milstein J, et al. What is the extent of research on the characteristics, behaviors, and impacts of health information technology champions? A scoping review. BMC Med Inform Decis Mak 2015;16. https://doi.org/10.1186/s12911-016-0240-4.
- Blechar J, Knutsen L, Damsgaard J. Designing Ubiquitous Information Environments: Socio-Technical Issues and Challenges. New York, NY: Springer-Verlag; 2005.
- Webster A. Innovative health technologies and the social: redefining health, medicine and the body. Curr Sociol 2002;50:443-57. https://doi.org/10.1177/0011392102050003009.
- Kerr WC, Stockwell T. Understanding standard drinks and drinking guidelines. Drug Alcohol Rev 2012;31:200-5. https://doi.org/10.1111/j.1465-3362.2011.00374.x.
- Polymeri AA, Kodovazenitis GJ, Polymeris AD, Komboli M. Bisphosphonates: clinical applications and adverse events in dentistry. Oral Health Prev Dent 2015;13:289-99. https://doi.org/10.3290/j.ohpd.a34370.
- Curto A, Albaladejo A, Alvarado A. Dental management of patients taking novel oral anticoagulants (NOAs): Dabigatran. J Clin Exp Dent 2017;9:e289-e293. https://doi.org/10.4317/jced.53219.
- Street A, Gutacker N, Bojke C, Devlin N, Daidone S. Variations in outcome and costs among NHS providers for common surgical procedures: econometric analyses of routinely collected data. Health Serv Deliv Res 2014;2.
- Earnings and Working Hours 2015/16. 2016.
- Williams JG, Carpenter I. Hospital episode statistics: time for radical change. Clin Med 2012;12:23-4. https://doi.org/10.7861/clinmedicine.12-1-23.
- McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol 2014;67:267-77. https://doi.org/10.1016/j.jclinepi.2013.08.015.
- Eisenhardt KM. Building theories from case study research. Acad Manag Rev 1989;14:532-50.
- Casey D, Houghton C. Clarifying case study research: examples from practice. Nurse Res 2010;17:41-5. https://doi.org/10.7748/nr2010.04.17.3.41.c7745.
- Baxter P, Jack S. Qualitative case study methodology: study design and implementation for novice researchers. Qual Rep 2008;13:544-59.
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-29.
- Gilbert R, Franks G, Watkin S. The proportion of general practitioner referrals to a hospital respiratory medicine clinic suitable to be seen in a GPwSI respiratory clinic. Prim Care Respir J 2005;14:314-9. https://doi.org/10.1016/j.pcrj.2005.04.006.
- Smith HE, Wade J, Frew AJ. What proportion of adult allergy referrals to secondary care could be dealt with in primary care by a GP with special interest?. Clin Transl Allergy 2015;6. https://doi.org/10.1186/s13601-016-0091-1.
- Nancarrow SA, Borthwick AM. Dynamic professional boundaries in the healthcare workforce. Sociol Health Illn 2005;27:897-919. https://doi.org/10.1111/j.1467-9566.2005.00463.x.
- Singh S, Gulati A, Harrison BD, Curtin JJ, Seaton D. Picture archiving and communications system (PACS): the benefits and problems of digital imaging in the NHS. Clin Med 2007;7:202-3. https://doi.org/10.7861/clinmedicine.7-2-202.
- Darzi A. High quality care for all: NHS Next Stage Review final report. London Dep Heal 2008;92:16-9.
- Campbell S, Tickle M. How do we improve quality in primary dental care?. Br Dent J 2013;215:239-43. https://doi.org/10.1038/sj.bdj.2013.831.
- Campbell S, Tickle M. What is quality primary dental care?. Br Dent J 2013;215:135-9. https://doi.org/10.1038/sj.bdj.2013.740.
- Oliver RL, Rust RT, Varki S. Customer delight: foundations, findings, and managerial insight. J Retail 1997;73:311-36. https://doi.org/10.1016/S0022-4359(97)90021-X.
- Lemke F, Clark M, Wilson H. Customer experience quality: an exploration in business and consumer contexts using repertory grid technique. J Acad Mark Sci 2011;39:846-69. https://doi.org/10.1007/s11747-010-0219-0.
- Tickle M, O’ Malley L, Brocklehurst P, Glenny AM, Walsh T, Campbell S. A national survey of the public’s views on quality in dental care. Br Dent J 2015;219. https://doi.org/10.1038/sj.bdj.2015.595.
- Murphy K, Jako AR, Anhalt RL. Nature and consequences of halo error: a critical analysis. J Appl Psychol 1993;78:218-55. https://doi.org/10.1037/0021-9010.78.2.218.
- Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. J Fam Pract 2000;49:796-804.
- Cheraghi-Sohi S, Hole AR, Mead N, McDonald R, Whalley D, Bower P, et al. What patients want from primary care consultations: a discrete choice experiment to identify patients’ priorities. Ann Fam Med 2008;6:107-15. https://doi.org/10.1370/afm.816.
- Rhodes P, Campbell S, Sanders C. Trust, temporality and systems: how do patients understand patient safety in primary care? A qualitative study. Health Expect 2016;19:253-63. https://doi.org/10.1111/hex.12342.
- Phillips KA, Johnson FR, Maddala T. Measuring what people value: a comparison of ‘attitude’ and ‘preference’ surveys. Health Serv Res 2002;37:1659-79. https://doi.org/10.1111/1475-6773.01116.
- Saultz JW, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med 2004;2:445-51. https://doi.org/10.1370/afm.91.
- Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ 2003;327:1219-21. https://doi.org/10.1136/bmj.327.7425.1219.
- Nilsen ES, Myrhaug HT, Johansen M, Oliver S, Oxman AD. Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database Syst Rev 2006;3. https://doi.org/10.1002/14651858.CD004563.pub2.
- General Dental Council . Standards for the Dental Team 2013. www.gdc-uk.org/professionals/standards/team (accessed 15 November 2017).
- Goodwin M, Sanders C, Pretty IA. A study of the provision of hospital based dental general anaesthetic services for children in the northwest of England: part 1 – a comparison of service delivery between six hospitals. BMC Oral Health 2015;15. https://doi.org/10.1186/s12903-015-0028-4.
- Goodwin M, Sanders C, Davies G, Walsh T, Pretty IA. Issues arising following a referral and subsequent wait for extraction under general anaesthetic: impact on children. BMC Oral Health 2015;15. https://doi.org/10.1186/1472-6831-15-3.
- Lewis BRK, Plunkett DJ, Hickman J, Sandham JS. Re-shaping NHS orthodontic provision - the North Wales experience. Br Dent J 2017;222:803-8. https://doi.org/10.1038/sj.bdj.2017.458.
- Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: A scoping review. J Telemed Telecare 2016;22:504-12. https://doi.org/10.1177/1357633X16670495.
- Landow SM, Mateus A, Korgavkar K, Nightingale D, Weinstock MA. Teledermatology: key factors associated with reducing face-to-face dermatology visits. J Am Acad Dermatol 2014;71:570-6. https://doi.org/10.1016/j.jaad.2014.02.021.
Appendix 1 Oral surgery complexity levels
These complexity levels are taken from, and described in, the Guide for Commissioning Oral Surgery and Oral Medicine. 1 They are not exhaustive and ATs will generally revise and update these lists in combination with their Oral Surgery MCN. For each level, an assessment of the medical status of the patient is required; for example, a patient with a Level 1 procedure but with a complex medical history may be classified as Level 3.
Level 1 procedures/conditions
-
Extraction of erupted tooth/teeth including erupted uncomplicated third molars.
-
Effective management, including assessment for referral unerupted, impacted, ectopic and supernumerary teeth.
-
Extraction, as appropriate, of buried roots (whether fractured during extraction or retained root fragments).
-
Understanding and assistance in the investigation, diagnosis and effective management of oral mucosal disease.
-
Early referral of patients (using 2-week pathway) with possible premalignant or malignant lesions.
-
Management of dental trauma, including reimplantation of avulsed tooth/teeth.
-
Management of haemorrhage following tooth/teeth extraction.
-
Diagnosis and treatment of localised odontogenic infections and post-operative surgical complications with appropriate therapeutic agents.
-
Diagnosis and referral patients of with major odontogenic infections with the appropriate degree of urgency.
-
Recognition of disorders in patients with craniofacial pain including initial management of temporomandibular disorders and identification of those patients who require specialised management.
Level 2 procedures/conditions
-
Surgical removal of uncomplicated third molars involving bone removal.
-
Surgical removal of buried roots and fractured or residual root fragments.
-
Management and surgical removal of uncomplicated ectopic teeth (including supernumerary teeth).
-
Management and surgical exposure of teeth to include bonding of orthodontic bracket or chain.
-
Surgical endodontics.
-
Minor soft-tissue surgery to remove apparent non-suspicious lesions with appropriate histopathological assessment and diagnosis.
Level 3 procedures/conditions
-
Procedures involving soft/hard tissues where there is an increased risk of complications (such as nerve damage, displacement of fragments into the maxillary antrum and fracture of the mandible).
-
Management and/or treatment of salivary gland disease.
-
Surgical removal of tooth/teeth/root(s) that may involve access into the maxillary antrum.
-
Management of temporomandibular disorders and craniofacial pain that have not responded to initial therapy.
-
Treatment of cysts.
-
Management of suspicious/non-suspicious oral lesions.
-
The placement of dental implants requiring complicated additional procedures such as bone grafting, sinus lifts, etc.
-
Treatment of complex dentoalveolar injuries.
-
Management of spreading infections and incision of abscesses (or abscess) requiring an extra-oral approach to drain.
Appendix 2 Qualitative interview participants
| Participant number | Role | Practice level of engagement | Organisation type | Number of interviews | Focus group | Sex |
|---|---|---|---|---|---|---|
| CS1 | Associate dentist | High | Primary care | 2 | N | F |
| CS2 | Consultant’s secretary | N/A | NHS trust | 1 | N | F |
| CS3 | Associate directorate | N/A | NHS trust | 1 | N | F |
| CS4 | Practice manager | High | Primary care | 3 | N | F |
| CS5 | Practice manager | High | Primary care | 1 | N | F |
| CS6 | Practice manager | High | Primary care | 2 | N | F |
| CS7 | Principal dentist | High | Primary care | 2 | N | M |
| CS8 | Associate dentist | High | Primary care | 1 | N | F |
| CS9 | Principal dentist | High | Primary care | 1 | N | M |
| CS10 | Principal dentist | Medium | Primary care | 1 | N | M |
| CS11 | Practice manager | Low | Primary care | 2 | N | M |
| CS12 | Community dentist | Low | Primary care | 1 | N | F |
| CS13 | Principal dentist | High | Primary care | 2 | Y | M |
| CS14 | Nurse | Medium | Primary care | 2 | N | F |
| CS15 | Nurse | Medium | Primary care | 2 | N | F |
| CS16 | Administrator | High | Primary care | 1 | N | F |
| CS17 | Principal dentist | High | Primary care | 3 | Y | F |
| CS18 | Consultant | N/A | NHS trust | 2 | Y | M |
| CS19 | Deputy clinical director | N/A | NHS trust | 1 | N | F |
| CS20 | Consultant | N/A | NHS trust | 2 | N | M |
| CS21 | Consultant | N/A | NHS trust | 2 | Y | F |
| CS22 | Commissioner | N/A | PHE | 2 | N | M |
| CS21 | Commissioner | N/A | PHE | 2 | N | F |
| CS24 | Consultant | N/A | NHS trust | 1 | N | F |
| CS25 | DwSpI | N/A | Primary care | 1 | N | M |
| CS26 | Associate dentist | High | Primary care | 1 | Y | F |
| CS27 | Principal dentist | High | Primary care | 1 | N | F |
| CS28 | Principal dentist | High | Primary care | 1 | N | M |
| Participant ID | Sex | Age | Treatment setting |
|---|---|---|---|
| 1034 | F | 69 | PCS |
| 1081 | F | 43 | DGH |
| 1109 | F | 65 | DGH |
| 1138 | F | 28 | DGH |
| 1140 | F | 61 | DGH |
| 1147 | F | 65 | DGH |
| 1151 | M | 66 | DGH |
| 1166 | M | 42 | PCS |
| 1172 | M | 64 | DGH |
| 1175 | F | 51 | DGH |
| 1176 | F | 67 | DGH |
| 1189 | M | 80 | DGH |
| 1211 | M | 69 | PCS |
| 1213 | F | 46 | PCS |
| 1240 | M | 72 | PCS |
| 1279 | M | 57 | FTH |
| 1328 | M | 71 | FTH |
| 1403 | M | 71 | DGH |
| 1445 | M | 64 | PCS |
| 1921 | M | 62 | DH |
| 1925 | F | 70 | FTH |
| 1928 | F | 65 | DH |
| 1975 | F | 71 | PCS |
| 2084 | M | 51 | FTH |
| 2197 | M | 59 | PCS |
| 2224 | F | 80 | PCS |
| 2324 | F | 23 | DGH |
| 2398 | M | 58 | DH |
Appendix 3 Oral surgery referral form
This is a ‘paper’ version of the form. All referrals in the project were submitted online – this version demonstrates the fields that were required for the form, the medical history and the IOSN if sedation was requested.
Referral form
Medical history form
Index of Sedation Need form
Appendix 4 Normalisation process theory framework
An integrated model of implementation using NPT to synthesise findings from all stakeholders.
| NPT construct/component | Relevance | Stakeholder | Evidence | Recommendation | Stage of implementation |
|---|---|---|---|---|---|
| Coherence | |||||
| Communal specification | |||||
| Collective sense-making |
|
|
|
|
Early |
|
|
|
|
Early | |
| Individual specification | |||||
| Personal sense-making |
|
|
|
|
Early |
| Cognitive participation | |||||
| Initiation | |||||
| Understanding how key components motivate people to carry on engaging with new sets of practices |
|
|
|
|
Early |
| Collective action | |||||
| Interactional workability | |||||
| How new sets of practices are operationalised |
|
|
|
|
Early |
| Skill set workability | |||||
| The division of labour that underpins task allocation |
|
|
|
|
Early |
|
|
|
|
Early | |
|
|
|
|
Early | |
| Collective action | |||||
| Relational integration | |||||
| The process of building confidence and accountability into new ways of working |
|
|
|
|
Early |
|
|
|
|
Early and ongoing | |
|
|
|
|
Early and ongoing | |
| Reflexive monitoring Communal appraisal: collective evaluation of a set of new practices |
|
|
|
|
Early and ongoing |
| Reflexive monitoring Individual appraisal: individual evaluation of a set of new practices in relation to their existing workload and personal contexts |
|
|
|
|
Early and ongoing, informing plans for future roll out |
|
|
|
|
Early and ongoing, informing plans for future roll-out | |
Appendix 5 Patient questionnaire
Appendix 6 Reflexive statement
The qualitative interviews and analysis was led by author Joanna Goldthorpe, who has completed the following reflexive statement which relates to the context of this study only.
Prior assumptions and experience:
Having worked as a researcher in dentistry, but not as a practitioner, I felt my experience was more aligned to that of the patients, rather than the NHS staff and commissioners. I had some prior experience of working with maxillofacial surgeons in the context of pain research, but had little prior knowledge of any professional allegiances or dental care pathways from primary to secondary care. In addition, having never been referred to secondary care dentistry and little experience beyond childhood of secondary care NHS services in general, most of my assumptions and experience was based on being an adult patient in primary care dental surgeries, and anecdotes received from friends relating to dental care and dental anxiety. I am not an anxious patient myself and have never had an adverse experience at the dentist (I find it neutral experience), however I was expecting fear of the dentist to be mentioned more often in interviews than was realised.
Awareness of social setting and the social ‘distance’ between the researcher and the researched
Patients
I and the other interviewer (RM) explained to patients prior to interviews that I was a researcher (as opposed to a clinician) to try to put them at ease and reduce the effect of desirability bias. All patients opted to have interviews take place over the telephone, which may have enabled them to feel more relaxed and have ownership over the setting and pace of the interview. On the other hand, not having a face-to-face conversation may have reduced any connection with the interviewer and inhibited some responses. Myself and my colleague interviewer endeavoured to make some small talk at the start of the interview to try to build rapport with telephone respondents.
Practitioners
Most interviews with practitioners took place face to face, at their place of work. These interviews therefore took part in a familiar space and possibly allowed the respondents to feel in control of the process. All practitioners were made aware that interviewers had non-clinical backgrounds, which hopefully encouraged them to explain their answers in more detail and to not take for granted shared assumptions.
Awareness of wider social and political context
The researchers conducting interviews did not experience attempts to ‘hijack’ the research to elaborate on professional or personal agendas. However, when issues arose that were outside the parameters of the interview, perhaps raising clinical issues or those around service delivery (such as those around clinical guidelines for bisphosphonates), researchers fed back information to the study PI [principal investigator] who then arranged stakeholder meetings to address issues raised. This process appeared to be effective and allowed for iterative development of the intervention and service being researched.
Glossary
This glossary contains definitions provided in the Commissioning Guide for Oral Surgery and Oral Medicine [Chief Dental Officer. Guide for Commissioning Oral Surgery and Oral Medicine. 2015. URL: www.england.nhs.uk/commissioning/primary-care/dental/dental-specialities/ (accessed 29 January 2018). Contains public sector information licensed under the Open Government Licence v3.0].
- Any Qualified Provider contract
- A NHS contract that uses a threshold mechanism for procurement, typically has a fixed price and does not have a guaranteed contract volume.
- Bisphosphonates
- A class of drugs used in the treatment of osteoporosis and metastatic bone cancers. Patients on such medication may be at increased risk of bone necrosis following extractions.
- Care Quality Commission
- The independent regulator of health and social care in England. It is responsible for monitoring, inspecting and regulating services to make sure that the services meet fundamental standards of quality and safety, and it publishes findings, including performance ratings, to help people choose care.
- Clinical Commissioning Group
- A NHS organisation set up by the Health and Social Care Act 2012 [www.legislation.gov.uk/ukpga/2012/7/contents/enacted (accessed 29 January 2018)] to organise the delivery of NHS services in England. They replaced the primary care commissioning functions of primary care trusts.
- Commissioning
- Defined by the Department of Health as the means to secure the best-value health care for the local population and tax payers [Chief Dental Officer. Guide for Commissioning Oral Surgery and Oral Medicine. 2015. URL: www.england.nhs.uk/commissioning/primary-care/dental/dental-specialities/ (accessed 29 January 2018)].
- Commissioning for Quality and Innovation framework
- A payment framework that enables commissioners to reward excellence by linking a proportion of English health-care providers’ income to the achievement of local quality improvement goals.
- Continuing professional development
- Any activity that contributes to an individual health-care professional’s professional development and is relevant to their practice or intended practice.
- Corporate (dental) bodies
- Any corporate body authorised to carry out the business of dentistry and compete for NHS dental contracts from commissioners. To do so, the body must satisfy the conditions of board membership set out in the Dentists Act [www.legislation.gov.uk/ukpga/1984/24 (accessed 29 January 2018)]. One requirement is that a majority of the directors of a dental corporate body must be registered dentists or registered dental care professionals, or a combination of dentists and dental care professionals.
- Dentist with a special interest
- A general dental practitioner with additional training and/or experience in a specific clinical area who takes referrals for patients who may otherwise have been sent directly to a secondary care consultant, or one who provides an enhanced service for specific conditions or patient groups. Dentists with a special interest work as an intermediate between primary and secondary care – some trusts refer to it as a tier 2 service. Dentists with a special interest may provide their services under General Dental Service, Personal Dental Service or Any Qualified Provider contracts.
- FP17 form
- To claim payment for NHS activity under General Dental Service and Personal Dental Service contracts, providers submit FP17 forms detailing dental activity data. The data recorded on the FP17 show the patient charge collected, the number of units of activity performed and treatment banding information.
- General Dental Service contract
- The most widespread of the two main contract types for primary care dentistry. General Dental Service contracts are usually not time limited and contract holders are required to provide the full range of services described as ‘mandatory’. Patient charge revenue is collected and the Unit of Dental Activity is the currency of the contract.
- Health Education England
- A Special Health Authority of the Department of Health whose function is to provide national leadership and co-ordination for the education and training within the health and public health workforce within England.
- High-street dentists
- Also known as general dental practitioners, these are the only clinicians who can contract directly with the NHS. In England, general dental practitioners are provided with a target for their clinical activity, known as the annual contract value. NHS courses of dental treatment in England are categorised into three bands based treatment activity provided (bands 1, 2 and 3) to reflect differing degrees of treatment complexity. Band 1 relates to examinations and preventative treatments, whereas bands 2 and 3 relate to invasive and irreversible dental procedures. Band 1 attracts one Unit of Dental Activity, whereas bands 2 and 3 attract 3 and 12 Units of Dental Activity, respectively. The annual contract value is the annual target of Units of Dental Activity that a dental team must provide.
- Higher Education Academy
- The national body for enhancing learning and teaching in higher education.
- Higher Education Funding Council for England
- The body that promotes and funds high-quality, cost-effective teaching and research, meeting the diverse needs of students, the economy and society.
- Hospital Episodes Statistics
- A data warehouse that contains details of all admissions to NHS hospitals and all NHS outpatient appointments in England.
- International Statistical Classification of Diseases and Related Health Problems
- A medical classification list used by the World Health Organization. It contains codes for diseases, signs and symptoms, abnormal findings, complaints, social circumstances and external causes of injury or diseases. Currently, the International Classification of Diseases, 10th Edition, is in use.
- Local Professional Network
- Networks hosted and supported by NHS England’s regional teams. They are part of a family of clinical networks across the commissioning and provider services that are working with NHS England as a catalyst for positive change in the NHS.
- Managed Clinical Network
- Linked groups of health professionals and organisations from primary, secondary and tertiary care working in a co-ordinated manner, unconstrained by existing professional and organisational boundaries, to ensure equitable provision of a high-quality, clinically effective service.
- NHS Business Services Authority – Dental Services
- The body that remunerates dentists based on FP17 claims submitted and provides dental statistics and key information to national, regional and local NHS organisations.
- Office of Population Censuses and Surveys codes
- A published procedural classification and coding of operations, procedures and interventions. This is a four-character code system. The first character is always a letter and the other three are numbers. All codes beginning with ‘F’ are related to the mouth.
- Oral and maxillofacial surgery
- A surgical specialty whose practitioners treat and manage conditions and diseases affecting the face and neck, as well as the mouth and jaws.
- Patient charge revenue
- Revenue generated by the fees charged for dental treatment at bands 1, 2 and 3. This is a co-payment scheme and certain individuals are exempt from paying based on their age or benefit status.
- Patient-reported experience measure
- A rolling programme of experience gathering that reports regularly to demonstrate experience trends and can be used to inform service development and improvement. This is usually completed through questionnaires such as the NHS Friends and Family Test.
- Patient-reported outcome measure
- A quality-of-life measure. By measuring the quality of life before and after a treatment or intervention, then again a fixed amount of time afterwards, patient-reported outcome measures give insight into the impact of a treatment or intervention on a patient’s life.
- Payment by Results
- The mechanism that NHS secondary care providers use to finance their service by reporting elements of care provided.
- Performer
- A qualified clinician who is contracted to perform the service and is registered on the national performer list.
- Personal Dental Service
- One of the two main contract types for primary care dentistry. Personal dental service contracts are generally time limited and may be restricted to the provision of discrete service elements. Patient charge revenue is collected and Units of Dental Activity remain the currency of the contract in the same way as the General Dental Service contract.
- Provider
- The contract holder to provide a service. In dentistry, this may be an individual, a legal partnership or, increasingly, a corporate body.
- Secondary Uses Service
- Secondary Uses Service data provide patient-level information regarding service provision. This information can be used for health-care planning, commissioning services, Payment by Results and developing and enhancing national policy.
- Service Level Agreement Monitoring
- Service Level Agreement Monitoring data, sometimes called trading data, are routinely sent from NHS trusts to commissioning organisations as per provisions of the information schedule in the standard contract. Almost all acute trusts send trading data, but there is no standardised way of sharing the same information. Trading data are effectively a monthly invoice, aggregated and at patient level, sent as per the national timetable of reconciliation and post-reconciliation dates.
- Specialty and associate specialist-grade clinicians
- The specialty and associate specialist grade includes associate specialists, specialty doctors, staff grades, clinical assistants, general medical practitioners, general dental practitioners and hospital practitioners. Specialty and associate specialist clinicians provide experienced, specialist care, often within a multidisciplinary team. They are responsible for the delivery of a significant proportion of oral surgery service. Specialty and associate specialist doctors/dentists are non-training roles in which the doctor/dentist has at least 4 years of postgraduate experience, two of those being in a relevant specialty. Although staff grade and associate specialists are among the grades included as specialty and associate specialist doctors, these grades are now closed to new entrants. New recruits are named ‘specialty’ doctors or dentists.
- Unit of Dental Activity
- The contract currency for General Dental Service and Personal Dental Service contracts in England. Each dental procedure has been classified into a banding structure, which determines what patients pay in NHS dental charges and the number of Units of Dental Activity a dentist receives. Band 1 attracts 1 Unit of Dental Activity, whereas bands 2 and 3 attract 3 and 12 Units of Dental Activity, respectively. The annual contract value is the annual target of Units of Dental Activity that a dental contract must provide. The national average price for a Unit of Dental Activity is approximately £25, but the Unit of Dental Activity value is determined individually for each contract; therefore, dental practices in the same locality, serving similar populations, are likely to have different Unit of Dental Activity values.
List of abbreviations
- AQP
- Any Qualified Provider
- ASA
- American Society of Anesthesiologists
- AT
- Area Team
- CI
- confidence interval
- DGH
- district general hospital
- DH
- Department of Health
- DwSpI
- dentist with a special interest
- eRS
- e-Referral Service
- GA
- general anaesthesia
- GDP
- general dental practitioner
- GDS
- General Dental Service
- GP
- general medical practitioner
- GPwSI
- general practitioner with a special interest
- HES
- Hospital Episodes Statistics
- IOSN
- Index of Sedation Need
- IT
- information technology
- ITS
- interrupted time study
- LPN
- local professional network
- MCN
- managed clinical network
- NHS BSA
- NHS Business Services Authority
- NICE
- National Institute for Health and Care Excellence
- NPT
- normalisation process theory
- OMFS
- oral and maxillofacial surgery
- OPCS
- Office of Population Censuses and Surveys
- OR
- odds ratio
- OTP
- one-time password
- PACS
- picture archiving and communication system
- PCT
- primary care trust
- portable document format
- PDS
- Personal Dental Service
- PP
- practice principal
- QIPP
- Quality, Innovation, Productivity and Prevention
- RMC
- referral management centre
- SD
- standard deviation
- SE
- standard error
- UDA
- Unit of Dental Activity
- URL
- uniform resource locator
- URN
- unique reference number
