Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/59/26. The contractual start date was in March 2015. The final report began editorial review in July 2017 and was accepted for publication in November 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Shaw et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Research context and relevant literature
In this chapter, we provide an overview of the National Institute for Health Research (NIHR) brief and how our research contributes to it, describe the NHS landscape as our research context and summarise the evidence base, generally in relation to alternatives to face-to-face consultations (e.g. e-mail and telephone consultations) and, specifically, on the use of virtual consultations.
There is a significant push from national-level decision-makers for the NHS to make better use of digital technologies, including virtual consultations. However, the current evidence on the development and use of virtual consultations is sparse. The few studies conducted to date have shown great potential for the use of virtual media, such as Skype™ (Microsoft Corporation, Redmond, WA, USA) and FaceTime (Apple Inc., Cupertino, CA, USA) for online communication between patients and clinicians. However, much of the literature uses experimental methods and classifies service models primarily by the nature of the technology and secondarily by the task supported by that technology. Although there are lessons to be learned about the potential of virtual consultations from this literature, we conclude that further work is needed to understand how and why individuals, teams and organisations do (and do not) adopt virtual consultations.
Introduction to the research
Health services face rising costs as a result of increasing disease prevalence, high ‘did not attend’ (DNA) rates and poor patient engagement, resulting in poor health outcomes and greater use of emergency care. 1,2 Most outpatient models fail to reliably provide responsive care when patients need intervention. Reducing hospital follow-up appointments is a priority in the NHS. Unless new ways of delivering care are found, chronic disease management will be unaffordable and undeliverable. Current policy places considerable faith in digital technologies and their potential to deliver more efficient, effective, patient-centric care in the community. 3–6 The UK’s National Information Board (see the glossary in Appendix 1 for a description of national organisations and initiatives) has argued that, in order to respond effectively to these demographic and epidemiological trends, we need a different kind of health service, in which the traditional outpatient consultation, for example, will become increasingly obsolete. 5 Technology-supported consulting is viewed as at least a partial solution to the current challenges of delivering health care.
Digital technology plays a significant (although varied) role in local plans across the NHS to reconfigure hospital services and transform the delivery of health services. 7 Attending regular clinics can be expensive, physically challenging and inconvenient for patients. Virtual consultations (using Skype or similar media) have the potential to fundamentally change the way in which patients interact with clinicians.
Following proof of concept work with NHS Choices, we were funded by the Health Foundation8,9 to explore the scope and feasibility of video outpatient consultations in the diabetes clinic in Newham. The Diabetes Appointments via Webcam in Newham (DAWN) project documented 62% acceptance rates across all ages, a reduction in DNA (from 40% to 23% at the end of year 1) and small efficiency savings of £63K. 8,9 Our subsequent project on Diabetes Review, Education And Management via Skype (DREAMS) was also funded by the Health Foundation (2012–14), and explored Skype-supported video consultations in ‘hard-to-reach’ patients with diabetes mellitus. 10 As well as improved clinical outcomes, DREAMS showed improved engagement and better self-management among regular users. 11
The online environment is known to produce subtle alterations in the dynamics of human interaction, with a potential risk that clinical clues will be missed or the clinician–patient dynamic will be altered adversely. 12 As a new service model, it also brings operational and cultural challenges, including training and supporting staff, as well as patients, in using digital technologies. For this reason, we sought to undertake further in-depth research.
Aims and objectives
As set out in our protocol published previously,13 the VOCAL (Virtual Online Consultations – Advantages and Limitations) study aimed to define good practice and inform its implementation in relation to clinician–patient consultations via Skype and similar media, addressing three key objectives:
-
at the macro level, to build relationships with key stakeholders nationally and identify from their perspective how to overcome policy and legal barriers to the introduction of remote consultations as a regular service option
-
at the meso level, to illuminate and explore the sociotechnical microsystem that supports the remote consultation, thereby identifying how organisations can best support the introduction and sustainability of this service model in areas where it proves to be acceptable and effective
-
at the micro level, to study the clinician–patient interaction in a maximum variety sample of 30–45 remote outpatient consultations in two clinical areas; in particular, to highlight examples of good communicative practice, to identify and characterise examples of suboptimal communicative practice and to propose approaches for minimising the latter.
The study addressed the following research questions:
-
At the macro level: what is the national-level context for the introduction of virtual consultations in NHS organisations and what measures might incentivise and make these easier?
-
At the meso level: how is a successful virtual consultation achieved in an organisation in which the processes and systems are mostly oriented to more traditional consultations?
-
At the micro level: what defines ‘quality’ in a virtual consultation and what are the barriers to achieving this?
In the following sections, we outline how our research contributes to the NIHR brief and describe the current evidence base relating to virtual consultations. The VOCAL study was designed as a multilevel study capturing macro-level barriers and incentives to, and facilitators of, supporting virtual consultations (objective 1), meso-level administrative and clinical processes that need to change to embed online consultations (objective 2) and micro-level details of the interactions in consultations (objective 3). As this included a significant research component focused on the national-level context, we set out the detail of the wider landscape in which virtual consultations are evolving in Chapter 3.
The National Institute for Health Research Health Services and Delivery Research commissioning brief
The VOCAL study was funded in response to a call from the NIHR Health Services and Delivery Research (HSDR) programme for ‘assessing alternatives to face-to-face contact with patients’ (HSDR call number 13/59). The call emphasised the rapid increase in new forms of interaction between patients and health professionals, including consultations by Skype, e-mail and webcam, and the potential that these new forms of contact hold for improving the quality and experience of patient care and securing cost-savings. The two themes were:
-
primary research evaluating the cost-effectiveness of non-face-to-face contact with health professionals
-
qualitative research on the impact of new forms on the clinician–patient dynamic, and appropriateness for hard-to-reach groups.
Our study responds directly to the second theme, which offered a unique opportunity to build on our previous work in setting up Skype consultations for the diabetes clinic at Newham. 8–11 Guided by the brief, we sought to examine in depth any changes in the dynamics of the clinician–patient interaction and communication in virtual consultations in three clinics spread across two clinical areas (the Adult/Young Adult Diabetes and antenatal Diabetes clinics in the Diabetes service, and the Hepatobiliary And Pancreatic Cancer Surgery clinic in Cancer Surgery, enabling comparison across different conditions, clinics and teams), the appropriateness and satisfaction of staff and different patient groups using virtual consultations (including young adults, older people and those from ethnic minority groups) and the ways in which wider organisational- and national-level environments shape virtual consultation services.
In the following sections, we review the current evidence generally on alternatives to face-to-face consultations, and specifically on virtual consultations, and provide an overview of the strengths and weaknesses of different methodological approaches.
The development of alternatives to face-to-face consultations
New technologies that support alternatives to face-to-face consulting are often seen by decision-makers as potentially providing more flexible and convenient ways for patients to interact with health professionals, while at the same time improving financial efficiency and the clinical effectiveness of services. 2,14,15 However, the use of alternatives to face-to-face contact with patients is a relatively new area of activity in health care, with limited evidence currently available to inform decisions about how best to develop and use a range of technologies. As well as video, these technologies include telephone, text messaging, e-mail consultations, online portals, telemedicine and telehealth. We summarise the evidence on each of these below.
Telephone
Telephone contact is used variably for assessment and triage of acute problems;16–33 general practice consultations;34–40 to offer health education;41,42 and to offer support for those with chronic illness43,44 or those in need of palliative care. 45 The literature on telephone consultations consists largely of small and heterogeneous primary studies, most of which had practical challenges or methodological flaws. Systematic reviews have tended to conclude that, although telephone contact may allow minor problems to be dealt with without a face-to-face visit (and sometimes with apparent cost-savings), it may miss rare but serious conditions and/or lead to higher rates of face-to-face visits in the days following. This is particularly the case when those responding to calls have limited training and are working largely to an algorithm, as, for instance, with NHS 111. 21 Telephone consulting, it seems, requires skill and judgement, perhaps because of the lack of visual cues. Detailed analyses of the clinician–patient interaction using conversation analysis have found that, compared with traditional face-to-face consulting, telephone consultations have a more linear format and tend to focus on a narrow range of preplanned themes, with fewer opportunities for the patient to raise ad hoc issues. 34,35 One study combined telephone consulting with video consultation to support patients receiving palliative care and reported that the combination offered both practical support and reassurance. 45
Text messaging and e-mail
There is a significant body of literature on text messaging as a means of, for instance, supporting people with chronic illness;46–48 facilitating adherence and/or attendance;49–52 conveying results of tests;53 or sending health promotion messages. 54–57 Systematic reviews have indicated that text messaging can be effective in facilitating short-term behaviour and medication adherence in particular. 51 However, the quality of studies is often poor, with research frequently conducted with population samples that may not be representative, and with limited understanding of long-term effectiveness and patient satisfaction. 52,58,59 Findings generally show that the text-messaging medium is popular with varied groups of patients, who use it both to send questions and to receive messages sent by health professionals and administrators. Similarly, systematic reviews of a large number of primary studies (mostly of weak methodological quality) have confirmed that it is technically possible to consult via e-mail, and that some patient groups value such contact. 60,61 Other studies have raised the possibility of increased inequality of access62–64 and professional uncertainty about safety, workload and remuneration, and about the ‘rules of engagement’ for online interaction. 64,65
Online portals
Studies of online portals (e.g. facilitating prescription ordering,66 appointment booking67,68 and patients’ access to their online record69) have demonstrated proof of concept. 70–72 However, such portals are often not widely used by patients beyond the research setting.
Telemedicine
Telemedicine involves the use of technology to deliver clinical care at a distance (including, potentially, video-based consultation), typically with one part of the health service, usually in primary care, linking remotely to another, usually in secondary care (e.g. teledermatology). There are many proof-of-concept studies73–77 and examples of up-and-running services, largely in remote regions (e.g. in rural Wales, UK78). However, the adoption, spread and sustainability of telemedicine tends to be disappointing, because of issues of cost, patient preferences and subtle but vital impacts on professional roles, interactions and work routines. 73,79,80
Telehealth
Telehealth (involving the exchange of data between a patient at home and their clinician, often via a remote monitoring centre, to inform diagnosis and monitoring) and telecare (involving the use of technologies, installed at home or attached to the person’s body, to allow remote monitoring of position or environment) are both the subject of considerable debate. Proof of concept (that the technology ‘works’) has been shown for many telehealth81–84 and telecare81,82,85–87 technologies, and some randomised trials have demonstrated improved outcomes, such as reduced hospital admission and mortality rates. 83 However, many trials have been criticised as being small, unrepresentative and methodologically flawed. To date, the largest trial achieved improvements in outcomes, but only at a significant cost that is out of reach within the NHS. 83
Combinations of different technologies
Combinations of different technologies (e.g. home-based and telemedicine services,84 or telephone and video consultation45) show that the efficacy, acceptability and costs of such services vary considerably.
Summary
In summary, studies examining the potential of new technologies to support alternatives to face-to-face consultations suggest that many of the mediums set out above (text messaging, e-mail consultations and so on) offer potential for patients, clinicians and the wider health system. However, many studies are of poor methodological quality and questions remain unanswered about the relative cost and effectiveness of individual technologies and their combinations. Overall, the literature suggests that different technologies (particularly telephone and text messaging) offer potential as alternatives to face-to-face consultations for different patients in different clinical settings. For the VOCAL study, this raised questions about the potential and appropriateness of video-based consultations, as well as the adoption and spread of technology-mediated services in health care. For instance, qualitative findings on telephone consultations raised questions about whether and how the addition of a visual medium would mirror the ethos and interaction of the face-to-face environment. Findings from studies of other technologies raised the possibility of increased inequality of access, a need to review the ‘rules of engagement’ for online interactions between clinicians and patients, and changes to work routines required to embed technologies in the everyday work of health care.
Evidence relating to the use of virtual consultations
The evidence base on virtual consultations (using Skype or similar technology) has been steadily accumulating. 88–98 A number of published studies focus broadly on video or remote consulting (e.g. exploring issues of usability and acceptability). 45,99–113 Many focus specifically on the clinical use of Skype,91,114–123 either on its own or in combination with other technologies [e.g. WhatsApp (WhatsApp Inc., Mountain View, CA, USA) messaging124 or FaceTime125,126]. A handful of papers examine the perceived ethical, legal or technical issues relating to virtual consultations. 127,128 Studies generally report positive benefits, particularly in terms of patient satisfaction and increased accessibility. However, most are brief descriptions of small, pilot-stage projects (some with as few as five patients), or randomised controlled trials (RCTs) offering one or more virtual consultations compared with traditional face-to-face contact, often with limited follow-up.
Below, we extend the literature review that we conducted at the start of the VOCAL study,13 by reviewing the higher-quality primary studies from a 2015 review88 of 27 published studies of the use of Skype, which reported largely positive benefits. We focus on studies from the review that are most relevant to the VOCAL study, along with some additional studies published since 2015. In doing so, we have adapted and extended the literature review that was previously published in our study protocol in BMJ Open. 13
A number of studies have focused on the use of virtual consultations for the treatment of chronic diseases. A study of family based behavioural support for adolescents with poorly controlled type 1 diabetes focused on the ‘working alliance’ (the strength of the relationships between patients, caregivers and health-care professionals). 129 Findings showed that 10 sessions via Skype were as effective at preserving the working alliance as 10 face-to-face sessions. 114 Adherence to treatment and glycaemic control were also similar. 91 However, losses to follow-up were high: of the 47 (out of 92) participants randomised to Skype sessions, follow-up data were available for only 32.
In our work in Newham, we introduced virtual consultations for Diabetes in 2011, with 480 remote consultations documented in 104 patients between 2011 and 2014. 10,11 Findings showed that virtual consultations were popular with both patients (especially young adults) and staff. In patients who chose to use the remote service, it appeared to be associated with increased engagement (overall DNA rates were 13% in patients accepting the Skype option and 28% in those who chose not to use this option, although denominator populations for these figures were self-selecting and hence not strictly comparable), improved glycaemic control (the average glycated haemoglobin level pre and post introduction of remote consulting was 70 mmol/l and 65 mmol/l, respectively, for those who used the service) and fewer accident and emergency (A&E) attendances than those not using the remote service (raw data on this were statistically significant, although numbers were small). These figures were encouraging; however, patients were not randomised and there were multiple potential confounders, and 45 patients who initially signed up to the remote service subsequently withdrew from it.
A recently published RCT130 showed similarly positive results for patients with type 2 diabetes who were not responding to usual care. A total of 102 participants (n = 165) were randomised to either monthly video conferences with a nurse via tablet computer over 32 weeks or usual clinic-based care. Allocation to the trial group required participants to regularly self-monitor blood glucose, blood pressure and weight, and to upload results so that these were available to both the nurse and patient during video consultations. Authors reported a significant improvement in glycaemic control in the virtual consultation arm compared with those receiving clinic-based care. However, these differences were no longer significant at 6 months, and authors were unable to tease out whether it was the video conference per se, the effect of immediate response to increased measurements, increased personal contact or a combination that led to the initial improvement.
In a study of the management of depression in older housebound adults, participants were randomised to receive in-person problem-solving therapy, Skype-delivered problem-solving therapy or a weekly telephone call with no therapeutic content. 92 Both the in-person and Skype-delivered therapy were effective at reducing depression scores and disability outcomes. However, at the 36-week follow-up, the participants in the Skype arm experienced significantly better outcomes than those receiving in-person therapy. The authors ventured that the more focused nature of the Skype sessions may be responsible for sustained benefits.
A number of studies have examined the use of virtual consultations for clinical follow-up, either as an alternative to or an addition to face-to-face consultations. A 2014 study reported on the use of Skype for orthopaedic follow-up. 94 The Skype service was offered to 78 patients, following total joint arthroplasty. Participants were invited to consult with their surgeon via Skype in addition to scheduled follow-up appointments at 1, 3, 4, 6 and 9 weeks. Just under half of the participants (n = 34) underwent at least one Skype consultation. The remainder (n = 44) did not have appropriate electronic devices or internet connection to use the Skype service. There was no significant difference in clinical outcomes for the users and non-users of this service (however, the study was probably underpowered). However, those participants followed up using the Skype service had fewer unscheduled in-clinic visits. Those using the Skype service rated their postoperative satisfaction as higher than those who were not using it. A key finding in a follow-on paper with 228 participants was that time spent on the consultation, and patient-borne costs, were lower in the Skype group. 96 A linked economic evaluation showed that service costs were also significantly lower in the Skype group. 95 Although no issues were missed in patients in the trial, a subsequent commentary queried whether or not remote assessment might be less safe. 97
Skype was used to deliver follow-up training for ‘pursed lips breathing’ (a technique used to manage breathlessness in chronic obstructive pulmonary disease). An initial study with 16 participants reported that those who received the follow-up sessions had better breathlessness management than those with basic training alone. 115 A subsequent small-scale trial confirmed these findings. 116
A small trial (n = 55) comparing remote ‘video visits’ during follow-up after prostate cancer surgery with usual care found video visits to be ‘equivalent in efficiency’ to conventional outpatient visits, as measured by the amount of time spent face to face, patient wait time and total time devoted to care. 99 There were no significant differences in patient perception of visit confidentiality, efficiency, education quality or overall satisfaction. Video visits incurred lower patient-borne costs and were associated with similar levels of urologist satisfaction to conventional outpatient visits. Other studies have shown similar levels of patient satisfaction, particularly in terms of time saved (as a result of not needing to travel to clinics) and costs saved. 101,104,107
In a randomised trial of Skype sessions versus standard home care in supporting families with premature infants, the nine families randomised to Skype sessions reported very positive experiences. All found the technology easy to use, noting that virtual consultations were better than telephone calls. 131 Tellingly, the authors commented that ‘The families readily embraced the use of ICT [information, communication and technology], whereas motivating some of the nurses to accept and use ICT was a major challenge’,131 raising questions about the ways in which virtual media might be embedded in clinical work.
Virtual clinics via Skype have also been used for counselling and mental health consultations. Skype proved to be an effective medium for supporting independence and self-confidence among those aged 12–18 years with spina bifida. 98 In a 15-minute consultation once per week, the nurse supported patients with continence care and self-care. Participants reported that they felt more confident talking about personal issues via Skype than face to face. They also valued the privacy that consultations via Skype allowed (e.g. enabling young people to speak about their care from a private space at home rather than in a face-to-face consultation with a parent or carer), and increased the accessibility of the service (particularly for those patients with complex physical needs).
Issues surrounding privacy, security and reimbursement for virtual consultation services are the topic of significant public and professional debate. Despite this, and often being mentioned in passing in discussion sections of studies,108 such issues have rarely been systematically explored. 127 Technical difficulties are also typically mentioned in passing, but are rarely explored in any depth. Studies beyond the medical literature have shown that Skype is often ‘laggy’ (e.g. audio and video data can become unsynchronised). However, in one study that looked at the effect of collaborative song-writing as therapy, some participants reported that this lag could be helpful, making them select words with care and focusing them more on the interaction. 117 There are times when Skype compresses the video, so that facial expressions are hard to interpret. 117 It may be that the quality of hardware or bandwidth is critical to some (although perhaps not all) kinds of clinical consultation. 103,128
In summary, the research literature on virtual consultations remains sparse. The contribution of virtual media to consultations in health care has been studied mainly by using experimental methods (especially RCTs), but with no adequately powered randomised trials and only a handful of controlled before-and-after studies conducted to date. These studies have generally focused on evaluating the outcomes of the technology. To date, there have been no rigorous and theoretically grounded qualitative or mixed-methods studies of the kind undertaken in the VOCAL study.
Overall, the literature suggests that there is great potential for the use of virtual media tools, such as Skype, for virtual communication between patients and clinicians. Although the studies reviewed are broadly positive, the small sample sizes, select nature of samples and high losses to follow-up call into question any unqualified conclusion that the technology is ‘effective’, and the lack of negative studies raises questions about potential publication bias. For the VOCAL study, current evidence raises questions about the relevance of video-based consultations for different clinical conditions and patients, the accessibility and acceptability of Skype and other virtual media to both patients and (clinical and non-clinical) staff, the ways in which practical and technical issues (e.g. the availability of smart technology, delays in data transfer) shape virtual consultations and how ethical, legal, regulatory and payment issues shape the adoption of virtual media. In addition, none of the studies reviewed examined the detail of interaction and what gets either added in or left out of consultations when they take place virtually, raising the question for the VOCAL study about what a good-quality interaction means in the context of a virtual consultation.
Although the RCT is widely viewed as a gold-standard design for testing the efficacy of an intervention experimentally, the trials that have been undertaken on remote consultations have provided few or no data on the organisational complexities of implementing a radically new technology-based service, and they cannot address the question of how video consultation services emerge and become embedded in a real-world setting (i.e. outside the specific confines of a randomised trial and with a view to long-term sustainability). To fill this gap in the literature, studies are needed to explore the emergence of video consultation services naturalistically (i.e. by capturing real-world quantitative and qualitative data on the emerging services and documenting the challenges faced).
Chapter 2 Methods
Study design
In contrast to much of the published research literature described in the previous chapter, which has tended to compare ‘technology on’ with ‘technology off’ in an experimental or quasi-experimental design, the design of our study was oriented to teasing out the (often subtle) social and material interactions occurring between patient, staff member and technology(ies). Although experimental studies have their place, technology-focused approaches are crude and deterministic. 81,132–136 In-depth qualitative studies can reveal how individual identity, experience, expectations and material skill might shape and alter these technology-mediated interactions and make them more (or less) efficient and effective. 137
We conducted a multilevel mixed-methods study of virtual consultations with macro-, meso- and micro-level components. At the macro level, we combined interviews with 12 national policy-makers and other key stakeholders with analysis of national-level policy documents in order to explore barriers and incentives to, and facilitators of, supporting virtual consultations. At the meso level, we mapped the administrative and clinical processes that needed to change to embed online consultations [e.g. changes to clinical pathways, changes to staff roles, rethinking the use of traditional outpatient space, updating information governance (IG)]. At the micro level, we studied interactional dynamics by generating a multimodal data set (audio transcript, video and computer screen capture) of 30 virtual consultations in Diabetes and Cancer Surgery, alongside a matched data set of 17 (audio-recorded) face-to-face consultations.
Changes to the study protocol
In our original study protocol, we proposed collecting 30–45 virtual consultations between patients and clinicians in Diabetes and Cancer Surgery (10–15 in Cancer Surgery and 20–30 in Diabetes) and then, using fine-tuned linguistic techniques, examining the detail of the interaction. As we began to analyse these micro-level data and examine the interactional dynamics, we quickly realised that it would be helpful to compare these with usual care (i.e. traditional face-to-face consultations) and examine if/where any interactional differences occur. We therefore adapted our study design and protocol to incorporate a comparable sample of face-to-face consultations in Diabetes and Cancer Surgery, audio-recorded to enable analysis of the type of talk that takes place. We used the Roter interaction analysis system (RIAS) to compare different categories of talk in face-to-face and virtual consultations. As we found few significant differences in communication practices (see Chapters 5 and 6), we limited our proposals to minimise suboptimal communicative practices (objective 3) in the guidance for patients and providers on using Skype and similar virtual media for remote consultations (see Practitioner Resources on the NIHR Journals Library website: www.journalslibrary.nihr.ac.uk/programmes/hsdr/135926/#/).
Theoretical approach
Our study drew on strong structuration theory (SST),138,139 which sees society (through rules, values and norms) as profoundly shaping human behaviour, and human behaviour (through peoples’ interpretations and choices, as well as technology-mediated actions), in turn, changing society.
As we have set out in previous work,67,139,140 structuration theory links the macro of the social environment (social structures) with the micro of human action (agency) and considers how the relationship between structure and agency changes over time. 141 The structure–agency link is mediated through ‘scripts’ (patterns of behaviour and interaction in social settings, including the adoption and adaptation of particular technologies), which gradually change over time. 137 Scripts link to organisational routines and, hence, to the potential for innovations to become embedded and routinised in everyday practice. 142
Strong structuration theory proposes that external social structures (social norms, rules and so on) are mediated largely through position-practices (defined as a social position and associated identity and practices), together with the network of social relations that recognise and support it (‘position-practice relations’, of which the clinician–patient relationship is a good example). It also sees human agency as crucial to engaging with technologies. 143 Within the VOCAL study, SST therefore offered the potential to theorise human characteristics, such as identity and social role (e.g. what it means to be a ‘clinician’, ‘carer’ or ‘patient’), interpersonal relationships (e.g. the clinician–patient relationship), situational knowledge (e.g. patient expectations of a consultation) and the capabilities needed to operate technology.
Four components of SST guided our thinking and analysis of virtual consultations in the VOCAL study: external structures, internal structures, actions and outcomes (Figure 1).
FIGURE 1.
Strong structuration theory, adapted to encompass a technology dimension. Reprinted from Social Science & Medicine, Volume 70, Issue 9, Greenhalgh T and Stones R, Theorising big IT programmes in healthcare: Strong structuration theory meets actor-network theory, 1285–1294, Copyright 2010, with permission from Elsevier. 139
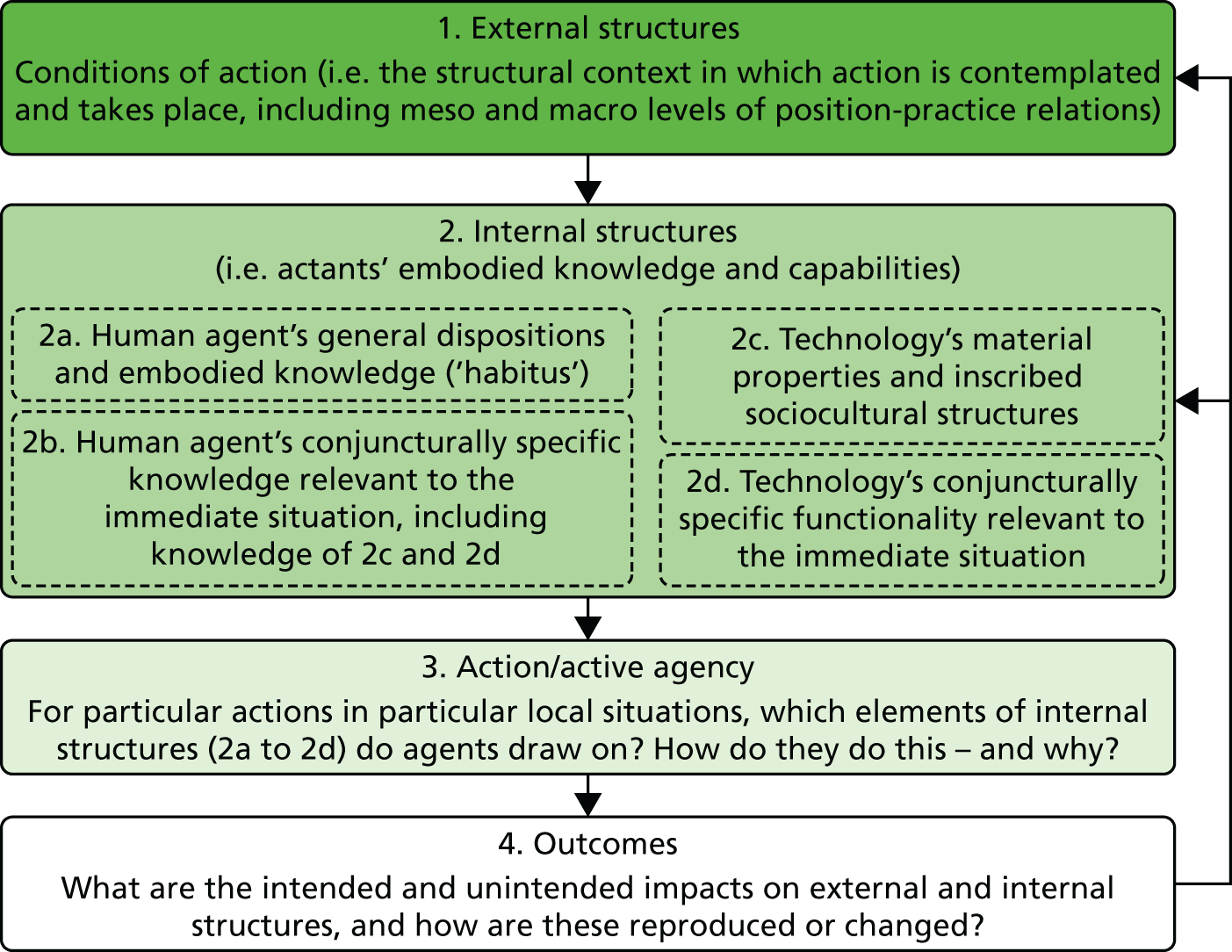
The first component of SST, ‘external structures’, refers to the position-practice relations that characterise the meso (organisational) and macro (national-level policy and decision-making) levels, and that change over time (e.g. the ways in which the medical profession is, arguably, less trusted in the face of media reporting about errors).
The second component of SST, ‘internal structures’, refers to the representations of society that we all have in our heads. They include general dispositions (e.g. discourses and world views, moral principles, attitudes, technical and other embodied skills and personal values – what Bourdieu called ‘habitus’144), as well as specific knowledge of an aspect of the world and how one is expected to act within it (e.g. a nurse’s understanding of what is involved in supporting patients with their self-management of diabetes).
The third component of SST is ‘activation/active agency’. We used ethnography to study specific examples of interactions – what SST calls ‘conjunctures’ (the medical consultation is a good example) – to capture how people play out their position-practice relations, behaving in a way that they believe is appropriate and responding in a moment-by-moment way to the other party(ies). To study the agency (i.e. human intention) behind these actions, SST incorporates theories from phenomenology (the study of people’s shifting fields and horizons of action arising from the focused activity at hand145), ethnomethodology (the study of how one person responds, moment by moment, to the talk and action of another146) and symbolic interactionism (the study of the subjective meaning and interpretation of human behaviour147).
The health-care setting is heavily institutionalised, and behaviour is often ritualised (i.e. we know, and play out, the roles expected of us as doctors, patients and so on). Behaviour in the consultation is strongly influenced by such things as regulations and other governance measures, norms, beliefs, professional and lay codes of practice and deeply held traditions (all of which are embodied and reproduced by human agents, including clinicians, administrators and patients), rather than exclusively by business concerns, such as efficiency and profit. A person’s knowledge of these institutional structures (in SST terms, the ‘strategic terrain’) may be more or less accurate and more or less adequate. A good example of this might be the older patient who retains the perception that it would be rude to offer suggestions to the doctor, whereas, in reality, the doctor is keen to promote shared decision-making.
The fourth component of SST is outcomes (see Figure 1). The outcome of human action in the consultation may be intended or unintended, and will feed back on external and internal structures – either preserving them or changing them as they are enacted. A good example of this in our study is whether or not a virtual consultation that is experienced positively will increase the likelihood that the patient will adhere to treatment and attend the next consultation (in person or virtually).
The clinical consultation is a social encounter shaped by social and institutional forces. For instance, clinicians resist technologies that (in their opinion) interfere with good clinical practice and the exercise of professional judgement,67 consulting patients will be more or less sick and have socioculturally shaped expectations of being cared for and comforted and their circumstances and/or illness may affect their ability to use the technology (e.g. those consulting virtually may be reliant on a relative or carer at home to access and use the technology). SST enabled us to focus on how bodily, emotional and cognitive functions interact with an individual’s disposition, symbolic interpretation and (imperfect) knowledge to affect how the consultation unfolds, and to consider the ways in which wider organisational, institutional and regulatory environments shape interactions in and around virtual consultations.
Action research
Our interests lay in studying the ways in which virtual consultations did (and did not) become embedded in the work of Diabetes and Cancer Surgery clinics. We were therefore keen to work with local managers and commissioners to understand the organisational change required to embed (and potentially spread) the virtual consultation option. Our study was therefore informed by the principles of action research. 148,149
Action research has been described as ‘a mutual learning process within which people work together to discover what the issues are, why they exist, and how they might be addressed’. 150 The idea is that practitioners and researchers work together to identify and seek to address issues as they arise in the context of research, and, in this case, in the development of a virtual consultation service. This meant that we keenly responded to requests for input (e.g. regarding issues with loading and updating Skype on clinic computers or plans to spread virtual consultations beyond Diabetes and Cancer Surgery clinics), and judiciously fed back emerging findings to local- and national-level decision-makers whose work was concerned with developing or spreading virtual consultations (e.g. relating to national payment systems).
Below, we summarise the main focus of our action research-related activities across the different levels of the study. Given that a virtual consultation service had already evolved in the Adult/Young Adult Diabetes clinic prior to the start of the study and the focus of Barts Health NHS Trust was on considering the potential for roll-out elsewhere within the organisation, much of our focus was at the organisational level, which appeared to be integral to the ongoing and measured development of virtual consultation services. Although all of our activities were broadly guided by the action research cycle (plan, act, observe, reflect148) and aimed to feed into service development, our contact with local and national stakeholders provided opportunities for increased insight and our extended fieldwork enabled insights into the complexities of relevant policies, organisational and decision-making processes that would not have been available to us through standard interviews or observations alone.
Macro level: national and wider social context
Our approach to interviewing national-level stakeholders (see Sampling: macro level) involved a two-stage process of an initial informal interview with all those identified, followed by in-depth interviews with a subsample of individuals. This provided an important opportunity, not only to collect data for the macro level of the study, but also to engage stakeholders and discuss emerging findings. Discussions typically related to the set-up of virtual consultation services (something that had taken place in the Adult/Young Adult Diabetes clinic prior to the VOCAL study), an overview of organisational activity and a discussion of overall approach and methodology. In several cases (with representatives from industry and NHS England), this led to repeated contact and ongoing discussion about the evolution of virtual consultation services.
The main focus of our work in this area related to national payment systems. In the first year of the study it became clear that there was interest, from within Barts Health NHS Trust and more widely, in extending the (local) spread and (national) scale-up of virtual consultation services. This was coupled with concerns over the lack of a nationally agreed tariff for virtual consultations (i.e. each service being required to negotiate locally with commissioners as to the cost of a virtual consultation). Although a small tariff existed for a telephone consultation, this was substantially different from that for a face-to-face follow-up, resulting in a significant disincentive for NHS trusts to explore this option. In other words, it made more financial sense to bring someone physically to the clinic for follow-up than to carry this out online and risk, for instance, being paid the equivalent of a telephone consultation.
To explore this further, we met with a representative from pricing development at NHS Improvement (then Monitor, see Appendix 1), and with colleagues from NHS England, to discuss potential ways forward. It quickly became clear that this was not an issue that we could resolve in the short term. However, we gained an appreciation of the ways in which a new tariff might be established, fed this back to colleagues at Barts Health NHS Trust and, given the limited in-house capacity, we jointly agreed to focus efforts elsewhere in the short term. We subsequently continued to raise the issue of the tariff in discussions with relevant decision-makers and, in partnership with a colleague from NHS England, have since incorporated the issue of national payment into further work (funded by the Health Foundation; see Chapter 6) that seeks to extend the spread and scale-up of virtual consultations.
Other activities involved meeting with a member of the NHS Chief Executive’s team to explore the role of virtual consultations in relation to the development of a new innovation and technology tariff, reviewing the Care Quality Commission’s inspection framework for digital health, and feeding into national guidance on IG requirements (see Meso level: organisational context).
Meso level: organisational context
With virtual consultations already set up in the Adult/Young Adult Diabetes clinic prior to the start of the VOCAL study, a significant amount of work needed to be done at the organisational level to begin working towards virtual consultations becoming ‘business as usual’ in the trust. In this respect, a significant amount of our action research-related activity focused on the following four areas.
First, following requests from all three clinic teams, we sought workarounds to organisational barriers to developing virtual consultations. For instance, early on in the study, it became apparent that those seeking to use Skype for virtual consultations were experiencing problems in both downloading and upgrading the software. In the Adult/Young Adult Diabetes clinic, team members were unable to perform regular upgrades (required by Skype) and required support from the ICT department, and in the Antenatal Diabetes clinic, the team was unable to gain agreement from the ICT department that they could have Skype on their computers. Formal requests from both teams via the generic ICT support e-mail hit a brick wall. Facilitated by the trust’s chief clinical information officer (CCIO), we engaged with the ICT department members directly to explore how their priorities might align with what the clinics were trying to do in providing virtual consultations. A number of issues came to light, including that there was no formal agreement within Barts Health NHS Trust for the use of Skype and, hence, no agreement with the ICT department to support Skype or to respond to related requests, as well as concerns over IG, network capacity to cope with demand for Skype and the potential impact of Skype-related requests on (already stretched) staff time and resources. Taking these concerns into account, we worked with the ICT department to find a workaround that would enable virtual consultations to run in a handful of clinics. This involved requests for Skype support going directly to a nominated ICT manager, who then passed them on to the relevant person within their team to resolve, and so enabling the development of virtual consultation services in the three clinics participating in the study.
Second, we supported the development of IG guidance. In an effort to address the ICT department members’ concerns about IG (see above), we worked with the trust’s IG department, which was aware that Skype was beginning to be used, but (at that stage) was unsure of how best to support it. Along with a colleague in one of the local Clinical Commissioning Groups (CCGs; with expertise in IG), we drafted IG guidance, with regular input and clarifications from the Barts Health NHS Trust IG department. The guidance was subsequently approved by Barts Health NHS Trust. In parallel, a member of the VOCAL study steering group connected us with the Information Governance Alliance (IGA; at NHS Digital, formerly the Health and Social Care Information Centre – see Appendix 1), which we worked with to pool materials, informing the IGA’s own guidance and gaining IGA approval for the Barts Health NHS Trust’s own guidance.
Third, we sought to develop a community of practice of those interested in, or actively developing, virtual consultations. This largely involved us in linking key individuals, clinical teams and departments within Barts Health NHS Trust, but, as the study progressed, increasingly involved us in linking with external partners (e.g. industry partners, other NHS providers) interested in either supporting or learning more about the work being undertaken at Barts Health NHS Trust. Within the trust, we also proactively set up two consolidating learning workshops involving staff from the Diabetes teams (i.e. Adult/Young Adult and Antenatal clinics) to gather feedback from all those involved in, or impacted by, the virtual consultation model. We chose not to undertake further workshops, as we were welcomed into mainstream governance structures and working groups (see below) and found it helpful to concentrate our efforts there.
Finally, and fourth, a significant proportion of our time was focused on facilitating or unblocking barriers to video conferencing within the three study clinics; however, as the study progressed and the trust became increasingly interested in virtual consultations, so our attention turned to rolling out the service to other departments. Initially, this led us to liaise with members of the trust’s senior management team to feed in emerging evidence from the study. We then sought to monitor and support plans to roll out virtual consultation services via two main activities:
-
Establishing an outpatient project strategy group to facilitate dialogue and co-ordinate efforts across different clinics (including endocrinology, haematology and neurology) and other departments involved in setting up and running virtual consultations. This included clinic representatives, ICT and IG and operations and business strategy. The group met monthly to discuss developments and was led by a senior member of the Barts Health NHS Trust operations and strategy department. Members of the VOCAL study team (SV, JM and JW) formed part of the advisory group and provided direct input on developments.
-
Developing guidance and protocol documents (drawing on findings from the VOCAL study) to guide roll-out, including standard operating procedures (SOPs), service set-up protocols and guidance templates (see Practitioner Resources on the NIHR Journals Library website). These materials were internally approved within the trust, and are routinely used as part of service development.
Micro level: virtual consultations
At the micro level, we were oriented to practical support for virtual consultations facilitated by the presence of a researcher (typically at the patient end) who was able to, for instance, help resolve technical issues with the equipment. Our contact with patients also provided helpful insights into perceptions (and the potential use) of virtual consultation services. We fed such insights back to clinic staff members, who, in turn, shaped and modified their own virtual consultation service accordingly. For instance, in Cancer Surgery, staff had initially assumed that patients needed to come into the clinic for a post-operative follow-up appointment that involved breaking ‘bad news’, and so had selectively invited patients for virtual consultation on the basis that they would receive only ‘good news’ virtually. Patients’ feedback indicated that people would prefer to receive bad news in their own home with their family/carer nearby and without the need for (sometimes extensive) travel before and after their appointment. This led to staff rethinking the basis on which they offered virtual consultations to patients.
Finally, prompted by discussions with the IG department (see Meso level: organisational context above) about security and privacy, we developed a leaflet summarising what patients can expect from a Skype consultations (see Practitioner Resources on the NIHR Journals Library website).
Project management and governance
The study was delivered by a core working group (TG, SV, JW, JM and SS), supported by a 6-monthly independent steering group and a patient advisory group (PAG; see Patient and public involvement). The steering group had a lay chairperson and cross-sector stakeholder representation, including patients, NHS stakeholders and national-level decision-makers (see Appendix 2).
The study received ethics approval from City Road and Hampstead NHS Research Ethics Committee on 9 December 2014 (reference number 14/LO/1883).
In line with changes to the VOCAL study protocol (see Changes to the study protocol), the following substantial amendments were sought and approved:
-
substantial amendment 1: audio-recording face-to-face consultations for comparison with Skype consultations; approved on 23 February 2016
-
substantial amendment 2: sharing selected video recordings (with patient consent) with technology developers to inform and improve the design of remote consulting technology; approved on 1 December 2016.
Patient and public involvement
Patients and their carers have been key to the VOCAL project and, in fact, the original impetus (in 2011) to use virtual consultations was initiated by service users (many from deprived backgrounds and/or minority ethnic groups) within the Diabetes clinic in Newham. At that time, we sought patient feedback as an integral part of both service development and ongoing evaluation (e.g. from focus groups, in-depth telephone surveys and online questionnaires, to refine the intervention in the Diabetes clinic10).
We set up a dedicated PAG in 2015. The main purpose of the PAG was to continue to incorporate patient feedback within our work and help to capture patients’ experiences of both the research process and the proposed virtual consultation services. The group was facilitated by Anna Collard, who has a background in community anthropology. The intention, set out in its terms of reference, was that the PAG would provide advice and feedback to the VOCAL research team and steering group. The intention was that the VOCAL research team and steering group would inform the PAG about research findings as they went along. The focus of the group was on the interactions between the clinician and the patient in Skype consultations, and not on any one particular condition (i.e. either diabetes or cancer). Patients from the PAG were also asked to review key documents, such as patient information leaflets.
Summary of patient advisory group meetings
The PAG was set to meet every 6 months (or four times over 2 years, 2015–17). In the event, the group met three times during the lifetime of the project (one meeting was cancelled, as a mutually convenient date and time could not be found). In place of the formal meeting, a number of members were contacted by the research nurse (DC-R) and asked to provide comments either by telephone or e-mail on a summary update of the VOCAL research that was circulated to them. Following completion of the project in July 2017, we also followed up with one volunteer member of the PAG to discuss key findings and provide tailored input to a lay summary of the study.
At first, patients were recruited directly by clinicians in the Adult/Young Adult Diabetes, Antenatal Diabetes and Hepatobiliary and Pancreatic Cancer Surgery clinics. After that, other approaches were also used to involve patients in the PAG (see Widening patient involvement).
A total of 12 patients and one spouse attended across the three PAG meetings, with attendance at each meeting ranging from three to nine members, plus facilitators. In one case, a patient with cancer was recruited by snowballing from his son, who had diabetes and had been recruited via the Diabetes clinic. Formal demographic data were not collected on the 12 PAG members, as this was considered intrusive. Participants represented a range of ethnic backgrounds, including South Asian, African Caribbean, sub-Saharan African, white Irish and white British, as well as a wide age range (from recent college leavers to one participant who described himself as being ‘in my 80s’). Their experiences as patients included having insulin-treated and tablet-treated diabetes, gestational diabetes and cancer.
One of the PAG meetings was attended by Professor Trisha Greenhalgh, the VOCAL study academic lead, and the final meeting by Joseph Wherton, the VOCAL Research Fellow. Both updated patients on the VOCAL study and findings to date, answered questions and reported back patient comments and/or queries to the steering group.
Focus of the patient advisory group meetings
In general, each PAG meeting focused on three key issues: (1) the VOCAL study itself, progress and feedback; (2) discussions on the general use of Skype, experiences, advantages and limitations; and (3) developing a wider virtual consultation service and evaluating its strengths and limitations.
In one of the PAG meetings, the group was shown (with the written consent of the patients involved) two video clip recordings of virtual consultations, one as part of a filmed VOCAL consultation and one from a different research study (also led by TG) as the basis for discussion. These two consultations were very different (e.g. one was for antenatal diabetes and one for heart failure; in one, the patient used a personal computer, and in the other, a mobile phone; one was with a doctor and one was with a nurse; and the clinician in each case had a different style).
Two representatives from a Newham-based international charity to address female genital mutilation (FGM) were invited by our patient participants to attend their group on one occasion. They shared their experiences of setting up and using a Skype service to provide remote counselling to women and girls who had experienced (or were at risk of) FGM. Common issues included the use of the Skype medium for discussion of sensitive issues, privacy and security concerns, and the technical and practical challenges of establishing and maintaining contact when the end-user may be unfamiliar with the technology. Overall, these experienced users of Skype for FGM support were positive about its benefits, reassuring about the discussion of sensitive topics and able to describe to our patient group how potential practical and technical challenges could be creatively overcome.
In the final PAG meeting, patients were asked to comment on a patient leaflet designed to introduce patients to Skype use for appointments.
Widening patient involvement
As reported, it proved to be difficult to sustain patient engagement in the PAG, in part, because of the reliance early on in the study on referrals to the PAG from clinicians. As a result of the difficulties, different approaches to engaging patients in discussions about the VOCAL study were explored in an effort to incorporate a wider set of views that went beyond ‘self-selecting’ patients. Approaches used included a visit to a prenatal diabetes education session, which nine mothers and one spouse attended. As part of the wider appeal, the PAG facilitators were also in touch with a number of other patient groups for feedback on the VOCAL study. These included one group promoting peer support for younger people with diabetes, and another working to prevent mothers with gestational diabetes developing type 2 diabetes. In addition, a voluntary sector group providing support to patients with cancer was contacted. The October 2016 PAG meeting was also publicised through the local Healthwatch newsletter.
In addition to the PAG, the VOCAL steering group had an independent lay chairperson and included one patient representative (see Appendix 2). The patient representative was not a member of the PAG.
Summary of comments from the patient advisory group
The PAG members had diverse views on many aspects of the study. Three areas of strong agreement among the PAG members were striking, however. The first was that Skype consultations were not, and should never be, a replacement for traditional face-to-face consultations. The second was that if Skype consultations were offered, they should be offered to all patients attending the clinic and not just to ‘selected’ ones. The PAG influenced our thinking in this regard: although clinicians felt that it was their duty and prerogative to ‘select’ patients to be offered the Skype option, the PAG was of the view that it was the patient’s ‘right’ to have the option of a Skype consultation. Patients did, however, consider that the potential benefits of virtual consultations were dependent on the type of consultation (i.e. what it is for), the level of familiarity between patient and clinician, and the link with test results (with receiving routine blood test results in particular being perceived to lend itself to online contact). The third was that there were few (if any) concerns about security and confidentiality, with virtual consultations assumed to be as confidential and secure as face-to-face and telephone consultations. Some patients also felt that they were a potential resource to support the evolution of virtual consultation services, by providing ‘Skype training’ to other patients who are not familiar with its use.
Setting and context
We have been working for several years with the front-line clinical team in the Diabetes clinic to develop virtual consulting as part of business as usual in Barts Health NHS Trust, the UK’s largest acute trust (formed in 2012 when three trusts in different boroughs merged).
We studied three clinics on different sites: Diabetes (Adult/Young Adult), based at Newham hospital and with a community outreach clinic in a local general practitioner (GP) surgery (Shrewsbury Road), the Antenatal Diabetes service based at Mile End Hospital and the Hepatobiliary and Pancreatic Cancer Surgery service at the Royal London Hospital. These sites are located across adjacent London boroughs (Newham and Tower Hamlets), both of which are characterised by a high level of socioeconomic deprivation, ethnic and linguistic diversity, and a high burden of disease. 151,152 Like many acute trusts, Barts Health NHS Trust is under pressure to deliver services more cost-effectively, while responding to rising need and demand. 153,154
At the time of our study, the national health-care landscape was characterised by significant financial pressure, with NHS organisations struggling in the face of constrained budgets and growing demand, and technology being seen as a logical route towards achieving cost-savings and increasing quality. This national picture was mirrored in Barts Health NHS Trust, where remote consultation services in the Diabetes clinic and Cancer Surgery evolved in the context of considerable financial, organisational and staff pressures. 153,155 Barts Health NHS Trust serves a population of around 2.5 million in east London, with around 2000 clinics across eight different locations, over 15,000 staff and an annual turnover of £1.4B. In 2015, Barts Health NHS Trust was rated as ‘inadequate’ by the Care Quality Commission (the independent regulator of health and social care in England; see Appendix 1), with significant concerns reported in safety, effectiveness and responsiveness, and with the leadership of the trust. 156 The trust was also put into ‘special measures’ (a set of measures applied to NHS bodies with a view to resetting expectations of financial discipline and performance) in September 2016, following substantial and mounting financial deficits. 157 It is against this background that Barts Health NHS Trust set out a significant programme of improvement, both within the trust and with the relevant health and social care agencies (commissioners and providers), called Transforming Services Together: Strategy and Investment Case (TST). 158 The focus of TST is on radically changing the way in which services are designed and delivered, and this has fed into subsequent sustainability and transformation plans (see Appendix 1 for an overview). This includes the redesign of outpatient pathways, enabling quicker access to specialist advice, both virtually and face to face. As part of this work, and in line with the national-level impetus for technology-enabled care, Barts Health NHS Trust established an outpatient project strategy group (see Action research) focused on the potential roll-out of virtual consultations beyond those Diabetes and Cancer Surgery clinics included within the VOCAL study.
Adult/Young Adult Diabetes Services
The Adult/Young Adult Diabetes service has a long tradition of applied research and quality improvement activity aimed at ensuring that services are accessible, culturally congruent and oriented to meeting the needs of the most vulnerable patients (e.g. limited English speakers with low health literacy). A key component of this work has been developing links with local GPs and deploying specialist nurses and bilingual health advocates in community outreach roles. Unusually, a high proportion of patients with diabetes in this catchment area are young. Newham has one of the youngest populations in the UK, and the UK’s highest prevalence of type 2 diabetes in the 16- to 25-year age group (0.57/1000), attributable to a combination of risk factors (e.g. poverty, ethnicity, diet).
Engagement with traditional health service models is typically low, with poor health outcomes (e.g. young adults with poorly controlled diabetes have an increased risk of sight-threatening retinopathy and adverse pregnancy outcomes) and increased use of unplanned care through the A&E department. At the time of our study, outpatient consultations via Skype for patients who choose this option were already an integral part of the service.
The Adult/Young Adult Diabetes service is an integrated community diabetes service, in which the consultants provide 6-monthly reviews of the patient’s condition, treatment and medication, with ongoing support from diabetes nurse specialists (from a partnering trust, the East London NHS Foundation Trust). The Adult/Young Adult Diabetes clinic is led by a diabetologist, who runs two weekly clinics on a Monday and Wednesday morning. The appointments are run for young adults (aged 16–26 years), adults and patients with insulin pumps. The diabetologist works closely with five other diabetes consultants running separate clinics, including Adult General Diabetes, a foot clinic and antenatal care. The lead diabetologist offers virtual consultations to all her adult and young adult patients as an alternative to follow-up appointments. She would typically conduct 40–50 follow-up appointments per month (i.e. virtual and face-to-face consultations), with each appointment lasting up to 30 minutes.
At each clinic, the consultants are supported by a nurse assistant who conducts the pre-appointment medical tests and checks (weight, blood pressure and recent eye test results), adds these to the patient’s clinic outcome form and provides this to the consultant (along with the patient’s hospital notes) to support the consultation. The nurse assistant also plays a key role in helping to co-ordinate the running of the clinic, by informing the consultant when the patient is ready to be called in for their consultation (by placing the patient’s medical notes and outcome form on the clinician’s desk after the pre-appointment checks) and bringing any remaining medical files for DNA appointments to the clinician at the end of the clinic.
There are six nurses in total: three running appointments with young adults and three with adults who also offer a diabetes pre-pregnancy service. The virtual consultation option is offered by the nurses supporting young adults. They work with the same patients, with one nurse specialising in supporting those with insulin pumps. The nurses provide diabetes management support, including adjustments to insulin doses, diet review/management and education on the ‘DAFNE’ (Dose Adjustment For Normal Eating) guidelines. The number of patients seen by the nursing team varies greatly depending on the availability of the nurses at the clinic and changes in the needs of their patients. Typically, there is at least one nurse at clinics running from Monday through to Thursday, with between 35 and 45 patients seen in total each month. The duration of nurse appointments (approximately 45 minutes) tends to be much longer than that of consultant appointments, as they involve more in-depth discussion about blood sugar readings, diet and diabetes management.
One receptionist manages the booking and checking in of patients for the 6-monthly scheduled appointments with the consultant. This includes scheduled face-to-face and Skype appointments. The receptionist checks the patient into their appointment using the Cerner (Cerner Corporation, North Kansas City, MO, USA) electronic patient record (EPR) on their arrival (indicating their arrival to the nurse assistant) and checks them out after the appointment. In most cases, the receptionist will book the patient in for their next follow-up appointment and print off the appointment letter at the reception desk. In addition to managing the appointment bookings and recording attendance, the receptionist is also responsible for ordering and preparing the patient medical folders. This involves reviewing the clinic schedule (approximately 2 weeks prior to clinic) and ordering (and often chasing up) hospital notes from central storage at the main hospital building. When the required hospital notes arrive, the receptionist is responsible for ensuring that they are organised and labelled for the appropriate clinic and clinician. Immediately prior to the clinic, the receptionist will also print a list of all patients to be seen (with basic personal information) for the nurse assistant and consultants. At the end of each clinic, the receptionist will record the DNA appointments in the EPR and box up the hospital notes for collection and central storage. Additional administrative support includes a service manager to manage the running of the clinic, including staff time and resources, working space and budget. The consultant also has a secretary, who is primarily responsible for dealing with the patient databases and the transcription, generation and postage of GP letters.
Antenatal Diabetes services
The Antenatal Diabetes team consists of three diabetes consultants, three obstetricians, two nurses (diabetes and endocrinology nurse specialists), one midwife, one service co-ordinator and an administrator. The service provides care to approximately 350 patients per year, nearly all with gestational diabetes. The weekly Antenatal Diabetes clinic runs on a Friday morning, with up to 50 patients per clinic. A Wednesday morning ‘spill over’ clinic is also conducted, which tends to be used for new patients.
Much of the medical information used to support the consultation is held within the patients’ maternity folder. Key medical information is replicated in the hospital records. However, day-to-day insulin doses and blood sugar readings, as well as appointment notes and recent medical tests (e.g. scans, blood tests), are stored in the patient-held maternity folder, and it is therefore a key artefact in the consultation. Although patients are assigned appointment slots, there is still much flexibility as to when patients are seen, and the diabetes consultants and midwife clinicians will often decide among themselves as to who will, and when to see, particular patients. In addition to the outpatient clinic consultations, the midwife conducts a weekly virtual (telephone) clinic to keep in touch with patients they wish to monitor more closely (e.g. patients struggling to manage their blood sugar levels). These patients are asked to call the midwife during a fixed time period, although it generally involves the midwife needing to initiate contact.
Like the Adult/Young Adult Diabetes clinic described above, the Antenatal Diabetes clinic requires pre-appointment tests and checks. This is supported by a team of 3 or 4 nurse assistants who call the patients’ names at the waiting room and take them into an examination room for pre-appointment check (weight, blood pressure, ketones), documenting these in the patient’s maternity folder. The outpatient clinic has one main reception desk (usually with two receptionists) to manage the flow of patients into the clinic. This involves booking patients in and out of the appointments on the Cerner EPR, but also tracking their order of arrival to ensure some consistency and fairness in waiting time. This allows greater flexibility for the clinicians to decide when to see patients and maintain a constant flow of appointments. This is an important task, given the large number of patients and multiple staff and appointment types involved. The receptionists also organise the hospital records prior to the clinic, so that these can be taken (along with the maternity folder) during the consultation.
Booking of subsequent appointments following the consultation is done by an antenatal diabetes administrator, who remains present at the outpatient clinic to obtain the clinic outcome forms and book the required appointment. The service co-ordinator remains in a separate office and leads on the overall management of the patient appointments, and is responsible for contacting patients to confirm or rearrange appointments when needed and for making sure that the hospital records are prepared and stored before/after the clinic.
Hepatobiliary and Pancreatic Cancer Surgery service
The Royal London Hepatobiliary and Pancreatic Cancer Surgery service is a tertiary service to which patients often have to travel long distances. It provides contrasting organisational, demographic and clinical challenges to the diabetes example, while also being nested, broadly speaking, in the same meso-level context. Patients with pancreatic and liver cancer have a very diverse demographic and may live up to 200 miles from the clinic. They have in common a life-threatening diagnosis, major surgery and a prolonged postoperative phase, in which they have to cope with multiple physical, emotional and practical challenges. Almost all patients have a direct and ongoing relationship with both the consultant surgeon (SB) and the specialist nurse (SR), sometimes going back several years. At the start of our study, the service had just begun to introduce virtual consultations in order to spare selected patients unnecessary travel.
The Hepatobiliary and Pancreatic Cancer Surgery clinic runs on Monday mornings, led by a consultant surgeon and supported by two specialist registrars and a hepatopancreatobiliary (HPB) clinical nurse specialist. Up to 25 patients can be seen during one clinic, with around 10–15% of these being related to postoperative cancer follow-up. The HPB nurse specialist leads on the planning and co-ordination of the clinic, preparing the lists and notes of patients to be seen, and allocating patients to the particular consultants, depending on their availability and the complexity of the patient’s condition or stage in their treatment. The HPB nurse specialist also takes a leading role in contacting, and being the contact point for, patients to address or follow-up on queries or issues related to their treatment. The HPB nurse also plays a key role in compiling relevant test results (e.g. from blood tests) needed for upcoming consultations.
The Hepatobiliary and Pancreatic Cancer Surgery clinic is run in a shared hospital space alongside other clinical services. The clinical team is supported by a team of nurse assistants based within this space, who support all of the clinic services running during the Monday morning clinic. The nurse assistants conduct required pre-appointment checks and inform the HPB nurse specialist when the patient is ready to be seen. The reception desk (with a team of up to four receptionists) check patients into their appointments on the Cerner EPR on arrival, and then books them out when leaving. As is the case in the Adult/Young Adult Diabetes clinic, the receptionist will book the patient into their next appointment (indicated on the clinic outcome form). However, the appointment letters are printed and posted to the patient via a centralised printing room. The GP letters are typed by the consultant or specialist registrars immediately after the appointment and sent on to the team secretary for printing and posting.
The team office space is spread across different parts of the main hospital building. However, much of the team members’ time outside the outpatient appointment is spent in theatre and on hospital walk-rounds.
Sampling
Sampling: macro level
To sample for the national-level interviews, we began with individuals charged with delivering IT strategy in NHS England. Alongside a review of policy documents (from 2000 onwards), we used a combination of purposive sampling (identifying a range of potential interviewees from policy documents and colleagues (e.g. steering group members) and snowball sampling (asking each interviewee to nominate a colleague) to ensure maximum variation in our sampling frame and enable us to build up a rich picture of the national context. We initially identified 45 potential stakeholders from across the government (e.g. NHS England, Care Quality Commission, NHS Improvement), professional organisations (e.g. the Royal College of Physicians, Medical Protection Society), patient groups (e.g. National Voices), industry (e.g. Microsoft) and charitable and third-sector organisations (e.g. the Health Foundation). We then invited a maximum variety sample of 39 of these stakeholders to talk informally with the study team. Of these, we spoke with 36, and three were uncontactable. We then undertook semistructured interviews with a purposive sample of 12 of these stakeholders, ensuring variation in the number of different institutions, groups and perspectives represented.
Sampling: meso level
The goal of sampling in the meso-level study was to map the people, interactions and organisational routines that support the virtual consultation, with a view to building a rich ‘ecological’ picture of the sociotechnical microsystem159 (and its wider embedding in the organisation) needed to make this model work as ‘business as usual’. We began from each of the three clinics where virtual consultations were held, mapped the individuals and technologies involved there and then moved outwards to include finance and clinical informatics departments (among others) in order to explore the organisational change required to embed online care within the NHS.
Sampling: micro level
The goal of sampling in the micro-level study was to capture the breadth of experience (of patients and staff) of the remote consultation. We therefore sought a purposive sample (i.e. based on the characteristics of the clinic population) of up to 30 consultations across the Adult/Young Adult and Antenatal Diabetes clinics, and up to 15 consultations in the Hepatobiliary and Pancreatic Cancer Surgery service. The lower number in Cancer Surgery was because we anticipated far greater practical and ethical challenges to gaining informed consent and avoiding harm, and we did not want to put excessive pressure on either the service as a whole or individual patients, clinicians or researchers. Within each subsample, we sought maximum variety in clinical, social, ethnic and personal circumstances, as well as in health and IT literacy.
In Diabetes, we extended a successful pilot study10 to a wider group and sought a maximum variety sample, including:
-
young people (aged 16–25 years) – many of whom are busy (e.g. studying or at work), not well engaged with secondary care, have high DNA rates and risk adverse outcome if lost to follow-up
-
older people – who may find it difficult to travel (e.g. because of comorbidity)
-
limited English speakers – some of whom find the health system difficult to navigate and require an interpreter
-
women who had recently had diabetes in pregnancy – many of whom may be busy with young children and/or have other duties, and struggle to engage with the service.
Our sample for Cancer Surgery was a tertiary care surgical centre in which each patient typically requires multiple contacts, some of which can require a (perhaps lengthy and inconvenient) trip. We sought to include the following kinds of interaction that might be suited to remote consultations:
-
preliminary orientation – following a first face-to-face consultation, a nurse might contact the patient remotely to explain what will happen during their hospital admission and deal with questions and concerns
-
postoperative follow-up – where clinically appropriate, a convalescing patient with cancer may potentially be seen remotely rather than attend in person
-
post-treatment surveillance – patients who have had tests at their local hospital and are transmitted to the tertiary centre may be contacted remotely to discuss the results.
Clinician participants included all consenting members of clinic teams (senior and junior doctors, specialist nurses) across both Diabetes clinics and the Cancer Surgery service.
As virtual consulting is a new medium, with potentially harmful effects for some patients, it was crucial (from a clinical and an ethical perspective) that clinicians were able to exercise judgement about which patients to invite to join the study. Patient participants were therefore selected for invitation on the judgement of the clinician, from the denominator population of all those attending participating outpatient clinics. Exclusion criteria were no 3G access at home, lack of familiarity (by patient or family carer) with the relevant technology, clinical inappropriateness (e.g. the need for direct physical examination), inability to give informed consent and comorbidity preventing participation (e.g. severe visual impairment).
The clinic populations included a high proportion of limited English speakers, whose inclusion was different in different services, reflecting current clinic ways of working. In the Adult/Young Adult Diabetes clinic, bilingual health advocates were available and trained in the use of remote consulting, so limited English was not an exclusion criterion there. In the Antenatal Diabetes clinic and the Cancer Surgery clinic, those who were comfortable with a family member interpreter were included, but a remote interpreting service was not available.
Someone not involved in the VOCAL study (e.g. a receptionist) made the initial approach to patients, providing them with a letter of invitation and consent forms as they arrived for their outpatient consultation. Those wishing to hear more were then contacted by a researcher, following a (minimum) 1-week reflection phase to give people time to think about the study before being contacted.
Training in the use of remote technology or technical support for its use at home were not offered.
Data collection
A summary of data collection and analysis across the different levels (macro, meso and micro) in the VOCAL study is presented in Table 1.
| Data source | Type and nature of data | First-order interpretation | Higher-order categories |
|---|---|---|---|
| Macro-level study of the wider context for introducing remote consulting |
|
|
External social structures, such as:
|
| Meso-level study of the sociotechnical microsystem in each setting |
|
|
External social structures, such as:Internal social structures (what actors ‘know’ and how they interpret the strategic terrain)‘Scripts’ held by patients and staff about how they should behave and how they change over time Assumptions built into the technology about: |
| Micro-level study of virtual consultations |
|
|
|
| Micro-level study of matched face-to-face consultations |
|
||
| Descriptive and demographic data in the remote consultation service in Diabetes and Cancer Surgery |
|
|
|
Data collection: macro level
Capturing the perspective of national decision-makers was key to our multilevel analysis of the contextual factors accounting for the success and potential transferability of this new service model. To achieve both these ends, we identified relevant policy documents from 2000 onwards, spoke informally with 36 national-level stakeholders and conducted 12 ‘executive-level’ semistructured interviews (see Table 1).
A topic guide was used in interviews (see Appendix 3) that focused on the key drivers and facilitators for remote outpatient consultations, operationalisation of (and potential blocks to) relevant policy, and key successes and disappointments.
Data collection: meso level
Our focus at meso level was on mapping the sociotechnical microsystem that supports remote consultations. To do this, we drew on a methodology for ‘mapping the sociotechnical healthcare ecosystem’159 that combines a sociotechnical approach (mapping the people and technologies involved) and a human ecology approach (placing particular emphasis on relationships and interdependencies).
Data collection focused on the work routines and processes required to accommodate and support the use of Skype for remote consulting. We captured this through:
-
ethnographic observation of the work involved in remote consulting, involving physically visiting the different departments and observing the clinical and administrative work that takes place
-
naturalistic interviews with clinicians, administrators and executives, involving asking people ‘on the job’ what they are doing and why they are doing it (as people often find it easier to talk about the detail of their job while they are actually doing it160); and
-
collecting key documentation (e.g. existing operating procedures, informal guides and notes made by staff to help them do their job, meeting minutes) and e-mail correspondence.
We originally planned to conduct consolidation workshops with service staff. However, as we engaged with clinics, we found that we were welcomed into each of the clinics and within mainstream governance structures and working groups (e.g. formal and informal meetings with representatives from ICT and the outpatient project strategy group). We therefore elected to focus our efforts and observations there.
Data collection: micro level
Our micro-level data set consisted of video-recordings of consultations (see Table 1), incorporating two video streams: what the clinician sees and does in the clinic, and what the patient sees and does at the remote site (typically their bedroom or living room at home, although sometimes via a handheld device elsewhere). We recorded consultations using a small digital camcorder with wide-angle lens and remote control (Sony Handycam DCR-SR72; Sony Corporation, Tokyo, Japan), mounted on a mini tripod and positioned unobtrusively (e.g. on a shelf). The camera’s field of view captured as much as possible of each individual and their orientation towards the screen (either on a computer or handheld device), as well as some contextual detail (e.g. the layout of the room). In 10 of the cases, the consultation was recorded at the clinic end but not at the patient end, either because the patient did not wish to be filmed in their home (but was happy to be filmed from the clinic) or because it was not practically possible to arrange for the recording to take place (e.g. for consultations that were agreed between the patient and consultant only a short time beforehand or if the patient could not predict where they would conduct the consultation remotely). We also captured clinician and patient interaction with the video-conferencing software and other tools used in the consultation. We used a commercially available screen-capture software tool (ACA Systems; ACA Systems, Washington, DC, USA) to record screen images showing on each party’s computer screen as a video file. This was run directly from a USB memory stick. The researcher (JW) was minimally involved in the virtual consultations, being present to start and stop the recordings, but then leaving the room during the consultation. In some cases, the patient or clinician sought advice or support from the researcher in setting up the virtual consultation (e.g. switching on the video). After the consultation, the researcher returned to the room and confirmed that both patient and clinician were still willing for the video material to be used as part of the VOCAL study. The software was run using an encrypted USB stick, and so could only operate on a PC or laptop. In many cases, the patient would use a mobile, tablet or Mac computer (Apple Inc., Cupertino, CA, USA), which could not run the encrypted device. In such cases, the researcher positioned a second digital camera to capture the screen.
Each end of the consultation resulted in two digital files: one screen capture and one video. We synchronised these into one file using video-editing software (Sony Movie Studio; Sony Corporation, Tokyo, Japan) – meaning that the video of the computer screen could be played exactly in parallel with a video of the patient looking at the screen – and then aligned the patient and clinician ‘ends’.
Care was taken to obtain and maintain informed consent. Information sheets and consent forms (see Appendices 4–9) incorporated guidance issued by the General Medical Council on the video-recording of consultations for research purposes, including an opportunity to withdraw consent after the consultation. 161 When recording remote consultations, the researcher arrived at the patient’s chosen venue (usually their home) at least 30 minutes before the booked time slot, so as to explain the procedure again, confirm consent and get it in writing, and informally discuss the patient’s hopes, fears and expectations for the consultation. We sought similar consent from the health professional at the clinic end of the consultation.
The face-to-face consultations were audio-recorded using a digital recorder. Patients were identified by the clinician before the appointment and invited to participate in the study. Participants were selected on the basis that the type of consultation was similar to those conducted via Skype (e.g. routine follow-up cancer appointments) and that the consultant would consider such cases suitable for a consultation via Skype. During the face-to-face consultations, the researcher (JW) sat to one side in the consultation room to audio-record the conversation and take field notes of the actions and interactions between the clinician and patient.
We transcribed all face-to-face and virtual consultations using ELAN (version 5; Max Plank Institute for Psycholinguistics, Nijmegen, the Netherlands), a specialised program for transcribing and analysing complex video and audio resources that allows researchers to capture the complexity of the data set, simultaneously follow video, audio and multiple ‘tiers’ of transcription (e.g. doctor, patient, carer) and record analytic memos and notes. This was particularly important for the multimodal data in our data set, the transcription of which requires judgements to be made about the level of detail to include162 and how to interpret and represent, for instance, non-verbal behaviour and body language. 163
In addition to the above, we made contemporaneous field notes when at each patient’s home (e.g. relating to the patient’s material circumstances and cultural factors affecting their self-management) and the clinic (e.g. relating to the physical circumstances in which the clinician makes the remote call, including the use of additional artefacts and technologies, such as paper or electronic records).
We collected a minimum data set (age, gender, ethnicity) on all patients seen in each clinic, as well as those participating in virtual consultations within the study. The way in which this was calculated in each clinic differed depending on the availability of the data. In Hepatobiliary and Pancreatic Cancer Surgery, the demographic data were drawn from a review of 12 months of clinic lists (July 2016 to June 2017). In Antenatal Diabetes, data were drawn from an audit conducted in 2015–16 (the most accurate available data in this setting). In Adult/Young Adult Diabetes, data were drawn from a 12-month review of records for nurse clinics (with young adults, from June 2015 to May 2016) and a 12-month review for consultant clinics (with adults and young adults, from August 2016 to July 2017). We used Pearson’s chi-squared test to compare categorical groups for gender, age and ethnicity.
Data analysis
Data analysis: macro level
Interviews with national stakeholders were initially analysed thematically to provide the wider context for understanding what is going on locally. In previous studies of small-scale encounters and organisational routines in health care, we have found that staff refer (more or less accurately) to such influences as ‘national policy’, ‘the law’ or ‘my Royal College’. We therefore compared data from (macro-level) interviews and documents in each of these themes with statements, actions and interpretations made by (meso-level) organisational actors, searching for tensions and ambiguities (e.g. the general push for remote consultations in the NHS by national-level stakeholders, alongside locally negotiated payment systems at the organisational level). Finally, guided by interpretive policy analysis,164,165 we extended our analysis to identify the key ‘storylines’166 shaping policy and debate around remote consultations, and to surface the ambiguities.
Data analysis: meso level
Our approach to mapping the sociotechnical health-care ecosystem159 provided detailed data about the logistical and technical barriers involved in introducing and running remote consultation services (in Diabetes and Cancer Surgery clinics, as well as the wider hospital, such as ICT and IG departments), and the tasks performed to overcome them. This included data about issues related to technology (e.g. installing Skype onto NHS computers, reconfiguring electronic clinic booking systems to identify ‘webcam’ appointments), clinic management (e.g. obtaining private office space for Skype appointments), administrative processes (e.g. setting up and recording ‘Skype appointments’ on clinic systems), patient enrolment (e.g. explaining the Skype service) and clinical reasoning with regard to a patient’s suitability for Skype (e.g. the need for physical examination, engagement with self-management).
We used both diagrams and narrative as synthesising devices to draw together a visual representation and linked verbal account of these human and technical interactions, and the interdependencies on which the successful execution of a virtual consultation depends (i.e. the service as a whole, as well as individual virtual consultations).
We also drew on the notion of ‘organisational routines’142,167 defined as ‘recognizable, repetitive patterns of interdependent action carried out by multiple actors’. 168 Routines are how organisational life is patterned, and, hence, studying these provides important insights into how innovations like remote consultations may (or may not) be assimilated in health care, and how that assimilation changes over time. In studying routines for remote consultations, we identified and compared artefacts, such as protocols (‘proxy routine’167); understandings held by staff of how this routine should be enacted (‘ostensive routine’167), and the range of ways in which the routine is actually enacted in an observed instance (‘performative routine’167). We were also interested in ‘routine dynamics’168 (i.e. the dynamics within and across routines), and so identified and examined the internal dynamics of (particularly) performative routines to understand how they contribute to both stability and change in virtual consultations and wider services.
We identified the work required (at clinic, departmental and executive levels) to make a repetitive pattern of action appear to be routine; examined the dynamics within and across different routines as they are put into practice, in an attempt to develop and deliver remote consultation services; and analysed the convergence and divergence between proxy, ostensive and performative routines to reveal the tension between current business as usual and the new ways of working implied by a remote consultation model.
Data analysis: micro level
Our initial analysis of the micro-level data involved repeated viewing of selected virtual consultations and discussion in interdisciplinary meetings (including representation from sociology, linguistics, human–computer interaction and medicine), alongside review of the interview data with patients and clinicians. This led us to identify a number of questions, including, for instance, the ways in which the context of the consultation (often involving patients in their home setting and the clinician at the clinic) shaped communication; if/how the usual format of the medical consultation (opening, history-taking, examination, diagnosis and review) might shift when conducted over Skype, how the talk about technology in consultations might reorient the interaction between patients and clinicians or how sensitive topics (such as breaking bad news) are avoided or addressed.
On the basis of these early emerging themes, we explored the literature to find a methodology to add depth and detail to our findings and identified the RIAS, a method for coding medical dialogue that has been widely used in Europe and the USA. 169
The RIAS is an established system for assessing medical interactions and, hence, offered a suitable analytical approach for detailed examination of the interactions between patients and clinicians in both virtual and face-to-face consultations. Broadly derived from social exchange theories related to interpersonal influence, problem-solving and reciprocity,170–172 RIAS offers a coding system that allows researchers to systematically quantify the occurrence of different types of talk that occur during medical encounters that reflect accepted patient and provider roles and obligations in a ‘meeting between experts’. 169 It thus offers a complementary perspective to other approaches to analysing interaction and communication (such as conversation analysis). It offers a predefined framework of what its authors consider to be ‘mutually exclusive and exhaustive categories’169 for codifying the contributions of patients and clinicians to remote consultations.
The RIAS coding draws a distinction between task-focused and socioemotional talk. For physicians, task-focused behaviours are defined as technically based skills used in problem-solving, which comprise the base of the ‘expertness’ acquired through professional medical education and for which a physician is consulted. From a communication perspective, physicians’ task-related talk includes talk related to the performance of medical functions, such as data gathering, tests and procedures, the physical examination and patient education and counselling. The socioemotional dimension of physician talk includes those exchanges with explicit affective content related to the building of social and emotional rapport, for instance, the use of social amenities, empathy, concern or reassurance. Patients’ communication is viewed similarly, with the task-focused talk reflected largely in patient question-asking and information-giving, and the socioemotional domain including the expression of concern, optimism, empathy, laughter and joking and social chit-chat.
Table 2 shows the high-level clusters and detailed categories used in the RIAS, with examples drawn from our data. The first three clusters (socioemotional, task focused and process) are drawn from Roter’s original work;170,173,174 the fourth is a new category relating to technology talk, initially introduced by others175 and adapted by us.
| Cluster/category | Codes | Description |
|---|---|---|
| Socioemotional talk and behaviour | ||
| Social behaviour | Personal remarks, social conversation | Greetings (e.g. ‘How are you today’?), conversation on a non-medical topic (e.g. weather, sport) |
| Laughs, jokes | Friendly jokes and laughing | |
| Compliments | Expression of approval of someone outside the clinic encounter (e.g. another doctor or nurse) | |
| Approval | Expression of approval or gratitude towards what the other person has said or done (e.g. ‘Thank you’, ‘Great, well done’) | |
| Verbal attentiveness | Agreement | Shows agreement or understanding of what the person has said (e.g. ‘Okay’, ‘Yes’) |
| ‘Back-channel’ talk (clinician only) | Indicators of sustained interest, attentive listening [e.g. ‘Right (go on)’, ‘Yep (I’m listening)’] | |
| Empathy | Recognising the emotional state of the other person (e.g. ‘The pain must be very upsetting for you’) | |
| Legitimising statement | Indicating that the other’s emotional situation, actions or thoughts are understandable or normal (e.g. ‘It is natural to feel that way’) | |
| Concerns/reassurance | Shows concern | Expression indicating that a condition or event is serious or worrisome (e.g. ‘I cannot seem to control my blood sugar levels well at all’) |
| Seeks reassurance | Questions of concern that convey the need or desire to be reassured or encouraged (e.g. ‘Do you think it’s serious?’) | |
| Gives reassurance/optimism | Statements indicating optimism, encouragement, relief of worry or reassurance (e.g. ‘These readings are so much better than before’) | |
| Partnership statement | Statements that convey the physician’s alliance with the patient (e.g. ‘But we can work together to find the best insulin dose for you’) | |
| Self-disclosure | Statements that describe the physician’s personal experiences in areas that have medical and/or emotional relevance for the patient (e.g. ‘I’ve worked with one other person with this type of condition before’) | |
| Negative talk | Disagree | Indication of disapproval, criticism, complaint, rejection of what the other person has said or done (e.g. ‘You shouldn’t skip your medication like that’) |
| Criticise | Indication of disapproval, complaint, rejection, coolness or disbelief directed towards another not involved in the exchange (e.g. a different hospital) | |
| Task-focused talk | ||
| Asking questions | Medical (closed/open) | Questions about medical condition, including closed (e.g. ‘Where is the tumour?’) and open (e.g. ‘Tell me about the pain you have been experiencing’) |
| Therapeutic regime (closed/open) | Questions about ongoing or future treatment plan, including closed (e.g. ‘When is our next appointment?’) and open (e.g. ‘What will the treatment involve?’) | |
| Lifestyle (closed/open) | Questions about lifestyle, diet and employment, including closed (e.g. ‘What time do you have breakfast?’) and open (e.g. ‘What sort of food should I be eating instead?’) | |
| Psychosocial (closed/open) | Questions about psychosocial concerns or problems, and social/family life (e.g. ‘Are you stressed about this?’) and open (e.g. ‘How are you feeling?’) | |
| Other (closed/open) | Questions that do not fall into the above categories, including closed (e.g. ‘What date is it today?’) and open (e.g. ‘Where do I go to get out of the hospital?’) | |
| Information giving | Medical | Fact/opinion relating to medical condition, such as symptoms, diagnosis, prognosis, test results (e.g. ‘You have gained 5 pounds since the last visit’) |
| Therapeutic regime | Fact/opinion relating to ongoing or future treatment plan (e.g. ‘We will see you in about 6 months’) | |
| Lifestyle | Fact/opinion relating to lifestyle, diet, employment (e.g. ‘I go for a walk every morning’) | |
| Psychosocial | Fact/opinion relating to psychosocial concerns and social/family life (e.g. ’I was feeling quite down about the whole thing’) | |
| Other | Facts/opinions that do not fall into the above categories (e.g. ‘Today’s date is the 14th of June’) | |
| Counselling (clinician only) | Medical/therapy | Statements to suggest resolution or action to be taken for medical problem, drug regimen, future appointments (e.g. ‘Increase your morning insulin by 2 units’) |
| Lifestyle/psychosocial | Statements to suggest resolution or action to be taken for lifestyle, family, activities of daily living (e.g. ‘Try to do more exercise during the day’) | |
| Requests | Asks for understanding | Mechanism by which the doctor or patient quickly checks with the other to see if information that was just said has been followed or understood (e.g. ‘Okay?’, ‘Does that make sense?) |
| Asks opinion | Asking for the patient’s opinion or perspective (e.g. ‘Do you think it would be good to keep the next appointment?’) | |
| Asks permission | Question that specifically asks for permission to give information or to proceed (e.g. ‘May I examine you?’) | |
| Requests service (patient only) | Patient-initiated requests for service or treatment (e.g. ‘Could you write a prescription for more testing strips’) | |
| Process talk | ||
| Direction | Orientation | Telling the other what is about to happen or serve to orient or guide them (e.g. ‘I am just checking the diary for you’, ‘please move your head to the side’) |
| Transition | Sentence fragments that indicate movement to another topic or placeholder (e.g. ‘Now let us take a look at your records’) | |
| Checks understanding | Paraphrase/checks | Mechanism for requesting repetition of the other’s previous statement (e.g. ‘I did not quite get that part’) |
| Bid for repetition | Requesting repetition of the other’s previous statement (e.g. ‘Could you say that again please?’) | |
| Technology-related talk and behaviour | ||
| Socioemotional | Any socioemotional category relating to technology | Includes social behaviour (e.g. laughter in response to a technical issue), Verbal attentiveness (e.g. agreement or understanding of technical issues expressed by the other person), concern/reassurance (e.g. seeking reassurance that they can be heard/seen by the other) |
| Task focused | Any task-focused category relating to technology | Asking questions (e.g. asking if their video is switched on), information-giving (e.g. ‘The volume is on maximum setting’) and counselling (e.g. informing the patient to message them on the system if they need to get in touch) |
| Process | Any process category relating to technology | Includes orientation (e.g. statements that indicate what they can see on the screen to guide consultation), transition (e.g. placeholders to deal with technical issues) and checks understanding (e.g. asking the person to repeat themselves as a result of technical problems) |
The RIAS has not been used extensively in the analysis of virtual consultations previously, although we identified one paper (a conference proceeding) that explored the theoretical potential of the RIAS in technology-mediated consultations,176 three small empirical studies in different clinical conditions,175,177,178 a narrative review of 10 studies of telehealth,179 including the three aforementioned studies that used the RIAS and seven more that used a less robust coding tool, and a validation study of the new RIAS codes for technology-related talk. 180 Given the technology-mediated nature of the virtual consultations that we were analysing, we added the fourth cluster (see Table 2) on technology-related talk to extend the technical cluster introduced by researchers who recently adapted the RIAS for the study of telehealth175 and adapt this to include categories of socioemotional, task-focused and process talk.
The RIAS has a record of good reliability and demonstrated predictive validity, as well as sensitivity to varying medical contexts. 169 Following a 3-day training course delivered by a senior researcher and tutor from RIASworks (January 2017), VOCAL study researchers were able to immediately and systematically code virtual consultations, applying meaningful codes to the small segments of speech (what the RIAS calls ‘verbal utterances’) of patients and providers. The process of coding took approximately 4 minutes for each minute of video or audio data.
The RIAS analysis was undertaken on a subset of the data in which remote consultations were matched with the closest equivalent face-to-face one. A total of 34 recordings were coded to explore how the use of Skype for virtual consultations affects the interaction and dialogue of the medical encounter. This subsample included 12 Antenatal Diabetes consultations (six conducted remotely via Skype and six conducted face to face), 12 Adult/Young Adult Diabetes consultations (six remote and six face-to-face consultations) and 10 Cancer Surgery appointments (five remote and five face-to-face consultations). The consultations were all follow-up appointments after the patient had met the clinician at least once. In the Antenatal Diabetes context, the appointment took place approximately 1 week beforehand to establish a schedule for insulin dosing. In Adult/Young Adult Diabetes, the consultation formed part of a routine 6-monthly review to discuss the patient’s condition, recent test results and treatment plan. For Cancer Surgery, the consultation formed part of the follow-up assessment of the patient’s postoperative recovery and review of medical tests [blood tests, computed tomography (CT) scans] and symptoms (the follow-up interval varied from 3 to 6 months). Virtual and face-to-face consultations in the data set for each clinic all involved the same clinician (i.e. a consultant diabetologist specialising in the care of pregnant women in the antenatal context, a different consultant diabetologist in the adult diabetes context and a surgeon and a nurse specialist combined in the cancer surgery context). The face-to-face comparisons were selected based on the similarity of the consultation (stage of treatment, purpose of appointment) and the clinician’s judgement that they would also have been suitable for the virtual consultation option.
All consultations were coded using bespoke RIAS software, in accordance with the clusters and categories in Table 2 (and, in some cases, further subcategories). To assess and address any inconsistencies, three coders conducted a preliminary analysis on two video files to form agreement on the RIAS category definitions. Discrepancies in coding were discussed and resolved, with the definition of each code recorded to inform further analysis. This phase informed the adaption of the RIAS categories to distinguish between ‘technology talk’ and existing coding categories from the RIAS manual. To assure coding reliability, two coders then independently coded eight recordings (five remote consultations and three face-to-face consultations). We used Pearson’s r correlation to assess inter-rater reliability across each code. This resulted in acceptable reliability ranging from 0.72 to 0.98 across all categories of patient and clinician talk.
Descriptive statistics were used to present proportions of talk across the sample, and for the three different clinical contexts. It had initially been planned to undertake parametric analysis, but the assumptions for normal distribution of the data were not accepted (the Shapiro–Wilk normality test showed significant results at a p-value of < 0.05). Therefore, the Mann–Whitney U-tests (non-parametric) were used to compare interactions for virtual and face-to-face consultations.
Data summary and synthesis of micro-, meso- and macro-level data
Table 3 summarises the final macro-, meso- and micro-level data sets for the VOCAL study.
| Level | ||
|---|---|---|
| Macro (national context) | Meso (organisational context) | Micro (remote consultation) |
|
36 informal, scene-setting interviews:12 formal semistructured interviews drawn from across these groups 5 observations of events/meetings oriented to national-level development of digital health 50 national-level documents, especially the Five Year Forward View,2 the Wachter review of NHS IT4 and the Accelerated Access Review15 Minutes of the VOCAL steering group meetings (including feedback from national policy, industry and patient members on emerging findings) |
Field notes from approximately 100 hours of ethnographic observation, 15 semistructured, naturalistic interviews and two workshops with:16 documents/systems, including:Meeting minutes and e-mail correspondences (e.g. from IG, ICT, the business and operations strategy department) Quantitative data, e.g. the number invited and recruited, access (appointments and DNA rates) and consultation length Minutes from three PAG meetings (12 patients and one spouse) |
30 Skype consultations from remote clinics, videotaped at both the clinic and the patient’s home:
|
The synthesis of the data sets summarised in Table 3 was guided by the following questions, informed by the SST framework (see Theoretical approach):
-
How does the dynamic relationship between the macro (external social structures), meso (organisational routines and logics) and micro (individual understandings, dispositions and front-line actions) contexts explain how a real-time video consultation unfolds in the contrasting clinical settings of routine diabetes care and preoperative and postoperative cancer care?
-
How do the outcomes of remote video consultations feed back in the short term to change (positively or negatively) the position-practice relations of the patient and the clinician, and in the longer term, the ability of the organisation and the health-care system to accommodate and sustain this service model?
In Chapters 3–5, we present the macro-, meso- and micro-level findings addressing these questions.
Chapter 3 The national and wider social context shaping virtual consultation services (macro level)
The macro element of the study was geared towards identifying the national-level drivers for virtual consultations, as well as potential blocks to development and implementation. Analysis of our data set indicated a significant policy push for technology-supported new service models between 2009 and 2017, including virtual consultations in both secondary and primary care. This has been matched by interest from industry and (to some extent) from professional organisations. However, as our detailed analysis below shows, national-level support for rolling out virtual consultations to the wider NHS has met significant challenges, especially in relation to reimbursement through the national tariff system.
The following themes were evident in our macro-level data.
National policy on the digitisation of health and social care
The context for technological innovation in the UK public sector is currently extremely challenging. Analysis of our macro-level data set highlighted a significant policy push to develop the UK’s digital economy181–185 and digital government,186–189 as well as digital health. 4,5,15,182,190–196 However, constraints imposed by ongoing financial austerity have meant that there has been little slack to support either technological innovation or the piloting, organisational learning and extensive groundwork that is often needed to routinise new technologies or practices within the NHS and the wider public sector.
In health care, spending plans for the NHS set out an average real-terms increase per year of 0.75% above inflation between 2017–18 and 2020–21. 197 However, with costs and demand for health care rising faster than funding (as a result of treatments becoming more expensive, and people living longer and hence needing additional care),198 there are already significant overspending problems for the vast majority of NHS hospitals. 199 As set out in Figure 2, this means that there is a significant projected gap (£12B by 2022–23) between existing spending plans and the funding required to keep up with the rate of increase in NHS costs and demand, and little slack in the system to enable technological innovation.
FIGURE 2.
NHS spending scenarios. 199 Reproduced with permission from Appleby J and Gainsbury S. NHS Funding Choices and the 2017 General Election. London: Nuffield Trust; 2017.
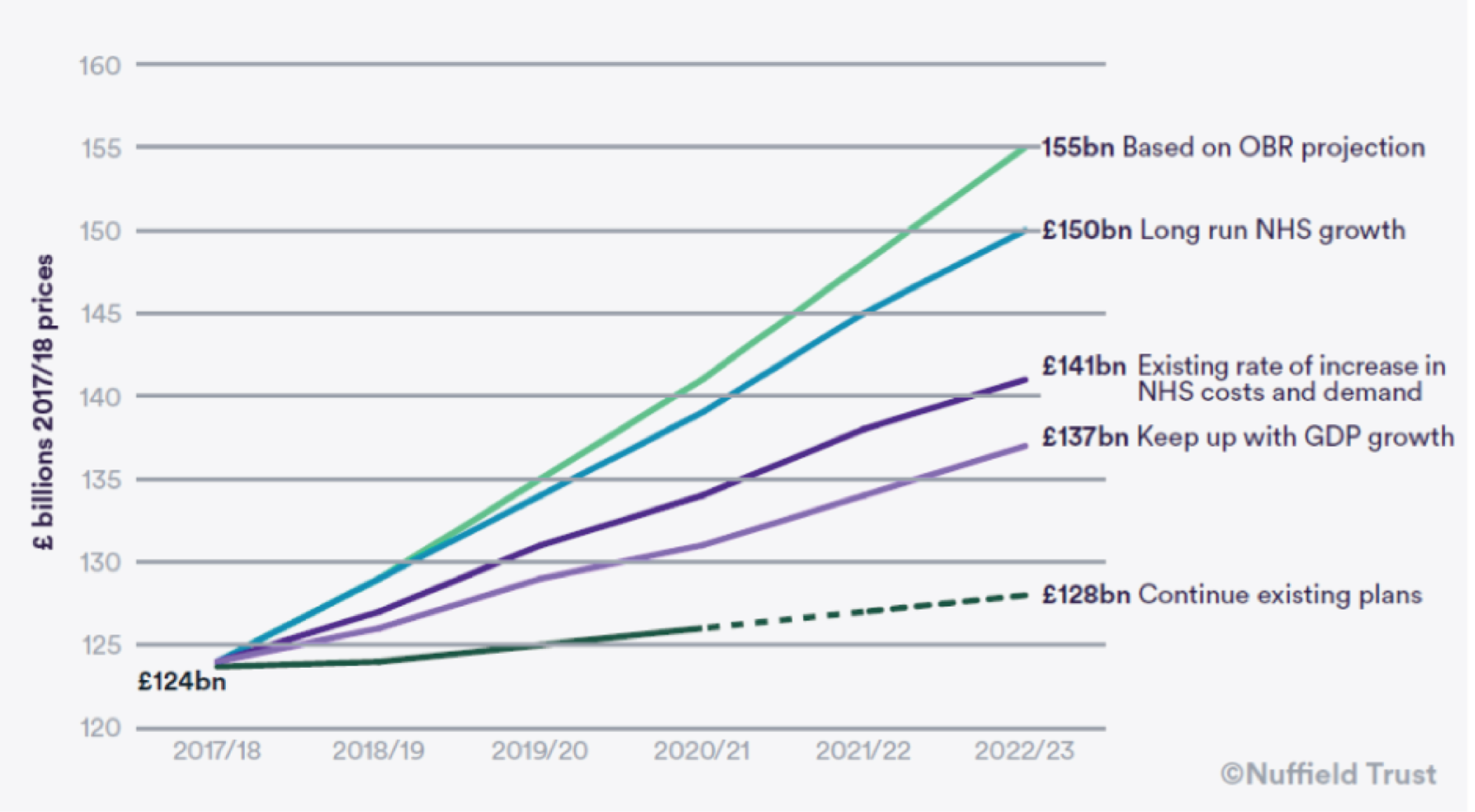
At the time of writing, shortly after the general election in June 2017, and in the wake of the UK’s referendum decision in June 2016 to leave the European Union, there is significant uncertainty about the future direction of public spending. Spending plans indicate a decreasing share of gross domestic product (GDP) being devoted to the NHS (from around 7.3% in 2016–17 to 6.9% by 2022–23199), representing the largest sustained fall in NHS spending as a share of GDP in any period since 1951. 200 Compared with other countries, the UK is a relatively low spender on health care, and has already slipped into the bottom half of the Organisation for Economic Co-operation and Development’s health spending league198 and may well slip further. 201 Based on manifesto pledges ahead of the election, it seems likely that the projected decline in health spending as a proportion of GDP is set to continue. 199
Our analysis suggests that the low growth in NHS spending combined with sustained increases in demand are taking their toll on providers. 202 NHS trusts face significant challenges in meeting financial and performance targets (as evidenced, for instance, by the rising number of trusts missing the 4-hour target in A&E and the downgrading of the 18-week referral to treatment standard203). NHS finance directors are sceptical about the chances of the NHS delivering the required productivity gains over the next 5 years. 200
Against a background of worsening austerity, both the Five Year Forward View2 and the General Practice Forward View204 encouraged local health and social care economies to develop novel ways of working to deliver efficient, person-centred, cross-sector care. This was also a major focus of the Wachter Review,4 which centred specifically on the implementation of information systems across the NHS and social care, with particular attention given to the use of electronic health records and the ways in which digital health tools might support an (implicitly more efficient) ‘paperless’ NHS. Of the 10 recommendations made by Wachter, several addressed the need to train a national cohort of CCIOs in both primary and secondary care, who would have a dual role in supporting the digitisation of records and services and supporting the development of local improvement plans linked to new information systems. The Wachter review called for ‘new national funding to help Trusts go digital and achieve maximum benefit from digitisation’ (contains public sector information licensed under the Open Government Licence v3.0). 4 This led to the appointment of 12 NHS hospital trusts as ‘digital exemplars’,205 each receiving up to £10M to enable the use of digital technology to drive improvements in the care of patients (e.g. using real-time video links between ambulances and emergency departments to support better care during journeys to hospital).
The overall strategic terrain is thus characterised, on the one hand, by intense and worsening financial pressure, but on the other hand, by a ring-fenced funding stream for developing new structures and cross-sector linkages supported by information and communication technologies. In this context, technology appears to be seen as a logical route towards achieving cost-savings (e.g. by reducing staff time, supporting caring for people at home) and increasing quality (e.g. through monitoring care), and industry is depicted as an important partner in achieving this. Our data suggest that the stance taken by government and industry assumes that the digitisation of health and care services is the de facto option that needs to be engaged with across the public sector. As one GP involved in national-level debate about digital health put it, ‘The assumption is that if you don’t [engage with technology], you jolly well should.’ Although there was widespread acknowledgement of the need to train staff, few documents or informants mentioned the limited access, skills or motivation of the target patient population, 21% of whom (and a disproportionate number of poor, sick and elderly people) cannot use the web and 14% of whom are estimated to have no access to the Internet. 182,187,206
Despite the drive to digitise the NHS, we could find no formal national policy documents and limited guidance that explicitly related to virtual consultations. Guidance appeared to be restricted to a two-page guide on the use of remote consultations in the NHS produced by the Health and Social Care Information Centre (now NHS Digital; see Appendix 1), and focusing largely on issues of IG.
As indicated by the following extract from an interview in May 2016 with a senior decision-maker in NHS England, the push for virtual consultations was linked to the overarching theme of ‘telehealth’ and has come through a range of announcements and initiatives:
Would you say that there’s a coherent picture of what [telehealth] might look like?
No, there isn’t, not that I’ve seen. And I’m quite actively involved in this space. There might be some small documents floating around.
The policy of digitising health appears to be folded into other programmes – for instance, the ‘New Models of Care’ programme stemming from the Five Year Forward View2 that commenced in January 2015 and included the NHS ‘vanguards’, 50 local innovative services focused on delivering the ‘New Models of Care’ programme and supported by a dedicated tranche of innovation funding. 207 Although it is arguably commendable that policy has been programme focused and not technology focused, it has meant that virtual consultations (and/or the infrastructure, staff training and organisational development underpinning them) have not been actively commissioned or funded centrally. Rather, when technology-based new service models have emerged, they have arisen through local initiatives.
As the senior decision-maker quoted above went on to say: ‘There are pockets of success, and there are certain vanguards exploring it, there’s bits and bobs. But there’s not actively a digital fund for telehealth’. At the time of our fieldwork, this looks set to change, with a new NHS Digital Academy under development following the recommendations of the Wachter review. 4 The aim of the Academy is to develop a workforce of trained ‘clinician-informaticists’ in NHS trusts, give them appropriate resources and authority, and improve both capacity and capability in the health and care system. The Wachter review4 called for approximately £42M (1% of the £4.2B to be spent on digitising the NHS) to support workforce development and deployment. However, no confirmation has yet been given on the amount to be invested in the Digital Academy or the wider NHS.
Transformation, telehealth and innovation
Since the early 2000s, there has been a strong policy emphasis on the need for the ‘transformation’ of health and social care provision in response to the problems faced by the rising incidence of chronic illness and with growing pressures on services. 2,191,208–210 Telehealth (i.e. remote transfer of data and/or communication between a patient at home and a health-care provider) has been promoted as a key part of this ‘transformation’ agenda. There is strong policy support for ‘disruptive innovation’ (i.e. services transformed rapidly and radically through technology), on the assumption that change that is sufficiently radical to be experienced as uncomfortable in the short term is more likely to achieve the long-term goals of improved efficiency and effectiveness than more incremental approaches.
As described in National policy on the digitisation of health and social care, there is significant scepticism that transforming services and outcomes can be achieved in the context of current/planned NHS spending. Documents and interviews in our macro-level data set indicate that the NHS will struggle to meet the requirement, set by the Five Year Forward View,2 to save £22B by 2020. In an effort to address this, the government’s sustainability and transformation fund includes additional funding (£1.8B in 2016–17, accessible subject to meeting specific financial controls) for NHS trusts, to help reduce reported deficits. However, if some or all of those funds are used to plug the deficit year on year, there will be little in the way of funding (or the organisational ‘slack’ that tends to go with it) for the service change and new models of care that are thought to be required to modernise and reshape NHS services.
In the documents we reviewed, telehealth generally tended to be associated with the goals of personalisation, integration and collaboration, and is typically presented in deterministic terms (in other words, that simply having access to particular technologies would lead to desired outcomes such as improved health status, more personalised care and reduced costs):
[We have an] unexploited opportunity to combine different technologies and changed ways of working in order to transform care delivery. For example, equipping house-bound elderly patients who suffer from congestive heart failure with new biosensor technology that can be remotely monitored can enable community nursing teams to improve outcomes and reduce hospitalisations.
Five Year Forward View (p. 34). 2
As one GP with a role in national-level discussions about telehealth told us:
It seems to be that they will take less time and be cheaper than face to face. And the very, very subsidiary thing that it might be more convenient for patients . . . hasn’t been presented as a major factor.
These findings resonate with a previous study by our team of earlier policy documents on telehealth. 81
A prominent focus of recent policy has been to smooth, standardise and speed up the innovation process in order for NHS patients to more quickly access medicines, medical technologies, diagnostics and digital products, and make life sciences a more attractive prospect for the UK economy. Our analysis highlighted naïve assumptions underpinning recent policy about the innovation process, which is often situated as a linear pathway involving identification of ‘gaps in the technology pipeline’ that might be addressed simply by articulating to innovators ‘the technology requirements that would best support [NHS] needs’ (Accelerated Access Review, p. 18; contains public sector information licensed under the Open Government Licence v3.0),15 and so smooth the innovation process from ‘discovery to adoption and spread into clinical practice’ (Personalised Health and Care 2020, p. 43; contains public sector information licensed under the Open Government Licence v3.0). 5 This approach emphasises supply-side innovation, with little attention given to how demand might be mobilised, and the kinds of recognition and rewards that might stimulate adoption. 211–213 Although meaningful dialogue with patients is emphasised in documents recommending accelerated access,15 this tends to focus on developing a shared understanding of what matters to users (e.g. through horizon scanning and evaluation). Shared understanding is important, but is not sufficient; technological advances need to be underpinned by a user-centred approach to design and delivery. 214
In documents, interviews and field notes in our macro-level data set, telehealth was widely considered to have a role in delivering changes ‘at scale’ and ‘at pace’. Our analysis indicated limited recognition that virtual consultations and similar technology-supported service innovations may not be adopted at all by front-line staff (or may later be abandoned by them). Furthermore, the potential time lag between the adoption of technology and any realisation of productivity gains was rarely acknowledged either by interviewees or in policy documents.
It is widely acknowledged that it is very difficult to innovate in the NHS and that ‘transformative’ and ‘disruptive’ innovation in a cash-limited, public sector setting is significantly harder than incremental change (see, for example, a recent book, by Fitzgerald and McDermott, summarising key empirical studies and theoretical perspectives215). As Fitzgerald and McDermott215 point out, a crucial precondition for organisational innovation is the ability to capture emerging knowledge and feed it into organisational learning. Our macro-level findings suggested important sectoral differences in attitudes towards such knowledge capture. Industry interviewees expressed confidence in the standard commercial ‘fail early, fail often’ approach of iterating software design to optimise the use of a technology in a particular setting. In contrast, clinicians and policy-makers’ responses reflected what might be called the ‘does it already work?’ culture of UK public-sector health care (a prevailing expectation for RCT evidence generated elsewhere, but assumed to be transferable to the current setting). Senior national-level decision-makers from different departments in NHS England clearly acknowledged that ‘the evidence is still very limited when it comes to digital offering’ and that there is a need ‘for us to be producing some evidence that things are progressing well to keep the people at the political end happy’.
Interviewees from regulators, industry and professional organisations similarly talked about the limited evidence available and the need to know more about, for instance, ‘what makes a good-quality remote consultation?’. However, the emphasis in policy was very much on generating an evidence base focused on ‘expand[ing] NHS operational research, RCT capability and other methods to promote more rigorous ways of answering high impact questions in health services redesign’ (Five Year Forward View, p. 34; contains public sector information licensed under the Open Government Licence v3.0). 2 This approach to generating knowledge has characterised a number of government-funded initiatives designed to improve the evidence base and adoption of telehealth. The most widely cited is the Whole System Demonstrator (WSD) programme, established by the Department of Health to ‘provide a clear evidence base to support important investment decisions and show how the technology supports people to live independently, take control and be responsible for their own health and care’ (p. 1) (contains public sector information licensed under the Open Government Licence v3.0). 216 The WSD study involved a large RCT of telehealth and telecare, involving 6191 patients and 238 GP practices across three sites. The resulting evidence was viewed as ‘disappointing’, with further evidence required on cost-effectiveness, as well as mechanisms for reimbursement, and clinical buy-in, to support adoption of health care. 193
Other approaches (e.g. use of ‘test-bed’ sites – such as ‘NHS Innovation Test Beds’217 or ‘Healthy New Towns’;218 see Appendix 1 for an overview – bringing together new technologies, new staffing models and payment for outcomes) have been promoted. However, our findings suggest that public sector knowledge capture continues to be dominated by trial design, is a poor fit with the ongoing adaptation of digital technologies and is at odds with the commercial approach. As one interviewee from industry put it:
it’s a block to innovation . . . because everyone wants someone to prove they have done it before in exactly the same sort of customer as they are. Well, how does anyone ever start then! You know, someone at some point has to give someone a break. And that’s the thing that people find really hard: to get a break into the NHS.
Challenges for industry
In the documents we reviewed, the technology industry is depicted as the innovator and producer of transformative technologies15 that can change the lives of NHS patients; policy is concerned with speeding up access to such innovations and boosting the UK economy. In relation to virtual consultation technologies, it is assumed that if developed and implemented at scale by a thriving and innovation-driven technology industry, these will generate change and thereby (at least partly) solve the uncomfortable problem of how to address increasing pressures on the NHS (particularly with regard to the growing ‘burden’ of chronically ill and dependent citizens), while also saving money and creating ‘a virtuous circle of economic growth for the UK’ (p. 44) (contains public sector information licensed under the Open Government Licence v3.0). 5
Interviews and documents painted a picture of industry as a diverse group of companies, with some (typically larger ones) pursuing a strategy of offering a narrow range of products at scale and seeking to stifle competition across those ranges, and others [typically small and medium-sized enterprises (SMEs)] being more focused on identifying clinical or care issues in partnership with the NHS or social care, as well as users, and working to develop technologies that can help to address these issues. As one senior decision-maker said, ‘what we are seeing is a lot of telehealth organisations – small SMEs but also large-scale providers – working with large organisations, corporates, also some NHS organisations, to offer telehealth services’.
While a thriving technology industry that generates innovations is a key component of the policy vision for a more efficient health-care sector, the relationship between the technology industry and the public sector is complex and sometimes awkward, and makes health and social care a challenging market to enter and survive in. For example, procurement processes are typically long and complex; the market is known to have limited and shrinking resources; and block contracts often favour larger providers, making health care a challenging market to enter and survive in. There was clear recognition of these challenges within interviews and policy documents, for instance:
[Industry] largely recognise that a state-funded health care system such as the NHS must take issues of affordability seriously but find the approach to innovation, the slow track to reimbursement, and low prices without generating wider diffusion and volumes, all make the UK a challenging market.
Accelerated Access Review: Final Report Review of Innovative Medicines and Medical Technologies (p. 8). 15
Part of why progress has not been as fast as it should have been is that the NHS has oscillated between two opposite approaches to information technology adoption – neither of which now makes sense. At times we have tried highly centralised national procurements and implementations. When they have failed due to lack of local engagement and lack of sensitivity to local circumstances, we have veered to the opposite extreme of ‘letting a thousand flowers bloom’.
Five Year Forward View (p. 31). 2
The extension of NHS contracts to a wider range of providers, including SMEs, marks a pronounced shift from the National Programme for IT (2007–11), in which the strategy was ‘ruthless standardisation’ and potentially highly lucrative contracts were restricted to a very small number of preferred providers. 219 Our findings suggest that the balance is still not right, and that a focus on centralised versus decentralised approaches to technology adoption does not address the whole picture. As one senior representative from industry put it when we interviewed them in April 2016:
They’re all negotiating locally . . . So, I agree that the National Programme [for IT] was wrong. But where we are now is wrong. We have gone far too far the other way. Because you do still have to think about the whole-system cost, don’t you, and the whole-system benefit. And there are some things where it just makes sense, it just makes sense.
Some larger companies (e.g. Microsoft) appear to have an evolving process of technology development and supply that (at least on the surface) acknowledges and works with health-care organisations and individuals, as well as patients and carers, in order to develop more nuanced and marketable products (though as noted above, this is not necessarily oriented to the kinds of technologies that might facilitate virtual consultations). This is, however, a resource-intensive process with no guarantee of meeting shareholder or executive expectations at the end of it. The same companies appear to be less concerned with technologies that might facilitate virtual consultations (e.g. Skype, FaceTime) and more with the ‘wellness and wearables markets’ (senior executive, industry). This is perhaps as a result of their awareness that adoption will be slow for complex institutional reasons and, hence, virtual consultation technologies offer limited potential for profit. Companies are also aware of the potential for reputational risk associated with profiting from virtual consultations in the NHS, whereas the wellness and wearables market is (or could be) effectively ‘direct to consumer’.
Our data suggest that both larger and smaller firms sometimes (although not always) struggle to engage with health-care organisations and systems. Take the following extract from a senior executive working in one multinational technology supplier:
I would like to have more of an influence, I think . . . Its very difficult for, not just for [our company], for the large suppliers, to engage with the NHS. This is one of my, this is the problem . . . because there’s a kind of a disconnect between industry and the NHS, people are working in the NHS on the test beds, on the vanguards, on these pilots, but they’re working within the boundaries of what they know and actually they have no idea what is possible or what is already mainstream. So they think that they’re coming up with like this ground-breaking stuff and it’s just like [cringes] . . . if only we could talk, if only we could find a mechanism to increase awareness about what can we do.
Our analysis suggests that the NHS does not have the ‘slack’ to receive industry in a way that could build the necessary engagement to support development of virtual consultations. This resonates with the wider literature that characterises the NHS as inherently complex and sees no simple solution for technological innovation. 215 Interviewees (both within and outside industry) suggested that the Department of Health and NHS England might do more to ease the process of working with NHS providers and commissioners. Interviews with NHS decision-makers indicated that significant work already occurs to engage with suppliers and to ‘realistically manage expectations’ about NHS procurement processes and time frames. However, this did not appear to have made a significant difference to suppliers who spoke to us about slow time frames, ‘decision-making by committee’, ‘so much duplication’, ‘consultation about everything’ and the ‘need for everyone [i.e. all NHS providers/commissioners] to go out and evaluate every single thing’. The emphasis on one-off procurement contracts for particular technologies ran contrary to the desire on the part of industry stakeholders that we spoke with to develop mature NHS–industry partnerships, in which the latter is committed to supporting an evolving service via an evolving package of technology and support.
Interviewees (from industry and the NHS) spoke positively about some national-level initiatives (e.g. NHS Innovation Test Beds), which they felt may prove helpful in facilitating partnerships and working patterns, and so enable a less technology-centric way of working. However, most felt that it is currently unclear whether or not such initiatives can facilitate the capacity-building and articulation work (i.e. all of the tasks involved in assembling, scheduling, monitoring and co-ordinating all of the steps necessary to complete a task220) needed to enable a more iterative approach.
Both SMEs and larger companies often appeared to adopt a ‘plug-and-play’ model of technology. Such a model might appeal to health-care organisations seeking ‘easy solutions’ to the challenge of rising costs and expanding need, but as our meso-level data illustrate (see Chapter 4), a business model that rests on ‘off-the-shelf’ technologies that can be bought, installed and made to work, while ignoring the ongoing work required to embed, routinise and sustain them, may achieve short-term sales at the expense of longer-term problems.
The above findings suggest that providing technological solutions to the NHS will not be easy either for small, ‘niche’ software companies (SMEs) or for the larger providers with which the NHS has traditionally contracted. Our contact with representatives from the third-sector organisations also suggested that, although there is significant interest in engaging with discussion about technological innovation in health care, there is currently little capacity to do so.
Rolling out remote consultations
As noted at the start of Chapter 3, interviewees from both policy and industry acknowledged a general policy push for virtual consultations to spread across the NHS. However, we documented numerous concerns, particularly from participants drawn from the NHS and professional organisations, that delivering changes ‘at scale’ would be far from straightforward, as roll-out in any locality would be influenced by (among other things) differences in organisational culture, infrastructure, the nature and causes of professional resistance, IG challenges and the logistics of payment.
A key issue repeatedly raised by interviewees, but rarely evident in published documents, was how reimbursement for virtual consultations would be implemented. Our wider data set showed that, in localities that have introduced virtual consultations (including, but not limited to, Barts Health NHS Trust), payment has been negotiated with local commissioners on a site-by-site basis. However, establishing virtual consultations as business-as-usual across the entire NHS would require a more systematic plan for reimbursement that does not yet exist (and which some interviewees indicated would be problematic to implement). As one senior decision-maker in NHS England told us:
We have a drug tariff that does prescriptions very well, but we don’t have anything for digital. And I personally believe that telehealth falls under that space because the service that could be commissioned or could be reimbursed for but we don’t have the route to do that yet.
Our analysis highlighted several strands of work being undertaken by NHS Improvement (previously Monitor) and NHS England (see Appendix 1) to review payment and pricing, and indicated significant awareness within these organisations that there are specific challenges relating to reimbursement of virtual consultations. The development of an innovation and technology tariff has gone some way to addressing this, by removing the need for multiple local price negotiations (instead guaranteeing automatic reimbursement when an approved innovation is used), but is currently limited to six medical devices or apps (and does not currently include the use of virtual consultation technologies). Our analysis suggests that the current need for individual provider organisations to negotiate payment with local CCGs will continue to present a significant barrier to the national roll-out of virtual consultations, and might also compromise the long-term sustainability of existing virtual consultation services.
Some of our interviewees suggested that, in the longer term, the proposed shift away from activity-based funding and towards the introduction of capitated payments might facilitate roll-out. Capitated payments have been put forward as a long-term vision for health reform, for instance:
We are interested in learning from commissioners and providers that are implementing alternative payment approaches to enhance system-wide incentives . . . for example . . . to focus . . . on integrated care. Alternative payment approaches might include pathway, capitation or outcomes-based payments.
At their most radical, PACS [primary and acute care systems] would take accountability for the whole health needs of a registered list of patients, under a delegated capitated budget – similar to the Accountable Care Organisations that are emerging in Spain, the United States, Singapore, and a number of other countries.
Five Year Forward View (p. 21). 2
In this model, a lump-sum payment to a provider (or group of providers) could cover the majority of care for a group of patients across different settings and, in theory, enable funds to be spent however is thought best locally (in negotiation within/across providers and CCGs). It seems likely that moves to develop a more effective payment strategy within the NHS will combine different mechanisms, and be complemented by other levers for influencing quality and efficiency. 222 Even if capitated payments are pursued at scale, our analysis suggests that redesign of the payment system will take time and any impact would probably not be felt for several years.
Our meso-level data indicated that IG was a significant concern when setting up virtual consultations (see Chapter 4). This concern was not mirrored in our meso-level data set, with interviews or documents situating IG as something that can be sensibly addressed and dealt with (ensuring appropriate privacy and security of data), rather than as a potential block to further roll-out. As one GP involved in national-level discussions about telehealth told us: ‘I think it has to be looked at but I don’t really see it as a major obstacle . . . the main issue is the IT connection which is a security issue, not an IG issue’.
Digital participation
Our macro-level data suggested a widespread assumption that digital literacy among the general population and NHS clinicians and staff would develop in pace with technological advances. Interviews indicated that, for instance, NHS England and NHS Digital not only wanted to engage with this agenda (e.g. by supporting people from disadvantaged backgrounds, and in particular ethnic minorities, to improve their digital literacy182,183), but are also taking action to do so. As one senior decision-maker in NHS Digital told us:
Quite an interesting part of the move to NHS Digital is not just what we do with the public . . . but being a bit of a kind of moral compass and challenge . . . so as NHS Digital develops its products and services – things like patient online, online bookings, those kind of things – challenging the organisation a bit to remember digital inclusion and the challenge of leaving people behind.
There remained an assumption across many (but not all) interviews and documents that people need to engage with the digitisation of health and social care, and there is little or no option for doing otherwise in the future. As one interviewee neatly put it, ‘we are perhaps not getting as far as we could with this’.
Initiatives such as the government’s ‘digital strategy’ (Cabinet Office 2012)223 aim for digital services to be the default option for public sector services, including health and social care. Our analysis indicates that the focus of much work to date has been on redesigning digital services to make them accessible and straightforward to use, as well as offering ‘assisted digital support’ for those who have never accessed the internet (estimated at 10% of the UK population224). In line with the increasing consumerisation of technology and raised expectations about access to digital services, the approach to developing digital health services appears to be shifting. The above interviewee described less of an emphasis on digital skills and support and more on making digital health an attractive option for potential users:
What we learned through the programme is that there is a digital skills problem still but that’s probably not the biggest barrier because people are just becoming more adept in their everyday lives, technology’s becoming easier to use . . . What we found was that, actually, when people had a motivation and a perceived benefit they would make the minimal effort to develop the skills. What was more a problem [was] that we were not making a compelling digital offer that people wanted to do . . . that people are not viewing digital information offers, digital products, digital means of engaging with the health-care system with sufficient enthusiasm for them to make the effort . . .
Despite this shift, our analysis of policy documents and interviews with policy-makers, regulators and industry representatives indicated that the approach to developing telehealth tends to assume that digital is the de facto option that needs to be ‘engaged with’ (and which forms the starting point for a project or programme). This contrasted with those from patient organisations who advocated the language of ‘digital inclusion’ and emphasised digital health as one option among many.
The framing of digital literacy and digital connectivity as ‘deficits’ in disadvantaged populations that can be made good through training and support contrasts with approaches to health inequalities taken by some third-sector and patient organisations. The latter typically frame the challenge in social terms (e.g. poverty or loneliness) rather than technological ones. A technological framing tends to hone in on the provision of particular technologies, whereas a social (or sociotechnical) framing is more likely to produce a more broad-based solution that includes an assessment of the user experience, patient and carer needs and the use of co-design methodologies.
Chapter 4 The organisational context shaping virtual consultation services (meso level)
In this chapter, we focus on the implementation and use of virtual consultations via Skype within participating services, including Adult/Young Adult Diabetes, Antenatal Diabetes and Hepatobiliary Pancreatic Cancer Surgery services. We also briefly cover the planned roll-out of virtual consultations in other clinics and settings in Barts Health NHS Trust (as part of a wider strategy of mainstreaming this service model within the trust, linked latterly to the local sustainability and transformation plan).
This section should be read in conjunction with the description of Barts Health NHS Trust and the historical background of introducing virtual consultations in the Diabetes service, which began in 2009 (see Chapter 2).
Overview of virtual consultations in Diabetes and Cancer Surgery services
Virtual consultations in the Adult/Young Adult Diabetes service
The Diabetes service at Barts Health NHS Trust runs an outpatient clinic for adults and a separate clinic for ‘young adults’ aged 15–25 years (Monday through Thursday each week). Because diabetes is a lifelong condition, most patients are well known to all regular clinicians (both doctors and nurses). During the study period (March 2015 to July 2017), virtual consultations were offered to patients considered suitable (in practice, most of them), as an alternative option to face-to-face clinic attendance. This ‘mainstreamed’ approach, in which virtual consultations are used flexibly in conjunction with face-to-face appointments depending on the choice and support needs of the patient, is the result of several years’ piloting and embedding work by the Diabetes team from 2009 (see Chapter 2, Setting and context). Typically, patients see the consultant and diabetes specialist nurse every 4 months (but may be invited to attend more frequently if clinically indicated). Virtual consultations via Skype are conducted alongside the outpatient clinic service, within the same clinic space.
Over the study period, only 3.6% of consultations were formally logged on the trust’s system in the Adult/Young Adult Diabetes service as being undertaken virtually. These ‘official’ figures are widely considered to be a significant underestimate, and give limited insight into the level and complexity of activity that has actually been taking place in the clinic throughout the time of the study or the ways in which clinic staff and patients have repurposed the technology for a more subtle adaptation of the virtual consultation service. As we describe in Clinic management and administration, the administrative processes involved in scheduling and rebooking appointments in all three clinics require varied tasks involving different people (e.g. the clinician making a note of the next appointment on the required form and taking this to the receptionist, who then made a booking with the patient on the electronic system). Repurposing this process for virtual consultations was, at first, fairly straightforward. By the end of the study period, the video option had become a stable (although not yet fully embedded) service in the Adult/Young Adult Diabetes Clinic (see Figures 3 and 4), but had evolved in a different way from the original plan. Alongside scheduled Skype consultations, the consultant and clinic nurses had begun to conduct ad hoc clinician-led ‘extra’ appointments (e.g. to quickly check on a patient after an adjustment in treatment) and/or ad hoc patient-initiated encounters (‘seeing’ the doctor or nurse as present online and requesting a ‘quick Skype’ to discuss an immediate concern).
As the lead clinician for the service told us, ‘this has increased patient engagement hugely’. This comment should be interpreted in the context of a diabetes service focused (unusually) predominantly on young adults, the majority of whom are from deprived and/or minority ethnic backgrounds. Maintaining patient engagement is one of the key challenges (a major trigger for introducing virtual consultations was a DNA rate of around 50%, and a significant minority of patients whose glycaemic control was abysmal and whose records evidenced long-term lack of engagement with the service). Patient-initiated virtual consultations sometimes came from this ‘hard core’ of non-engaged or minimally engaged patients – who were at high risk of hospital admission for acute metabolic problems and of long-term kidney, eye, foot and cardiovascular complications, and who otherwise had not contacted the service in months nor responded to invitations.
Ad hoc and patient-initiated consultations were not easily recorded on the system. One reason for this is that part way through the study, the diabetes specialist nurses began to shift over to using the ‘EMIS Health’ electronic record system (a system widely used in primary care). In contrast to the Cerner electronic records used traditionally in the diabetes clinic, there is no straightforward way for staff to record a ‘webcam’ consultation as codified (and hence searchable and aggregable) data. Hence, what feels like an onerous administrative process takes much-needed time away from clinical care. Another issue is that many ad hoc and patient-initiated consultations are extremely short (perhaps a brief exchange of messages or a 1- or 2-minute video follow-up after a longer consultation, to confirm that all is well following a change in therapy). Recording of such consultations tends to happen reliably only when there is a significant change in a patient’s care or treatment (a new drug for instance).
Other ad hoc instances of virtual consultations are not now formally recorded and are simply embedded in the ebb and flow of patient care and clinic routines. For patients who, for instance, have comorbidities or experience significant life events (e.g. a first pregnancy with gestational diabetes), these ad hoc virtual consultations appear to have become an inseparable part of the diabetes service, offering a means of engaging with a named clinician at times when they are in need of clinical advice (e.g. about very high blood sugar levels or titration) and/or emotional support. It is at the point when such patients are seen in the clinic (usually every few months) that the activity gets formally recorded in a letter to the patient’s GP, informing them about the regular Skype contact.
Hence, while only 3.6% of pre-booked outpatient appointments for the consultant diabetologist were formally coded on the electronic record as having occurred via Skype, the actual proportion was estimated to be around 20% (as a result of ad hoc consultations not being scheduled through the EPR booking system and, hence, not being visible in clinic audits). For the Young Adult Diabetes nurse appointments, all clinical encounters were documented on a separate diabetes management system (Diamond; Hicom Technology, Brookwood, UK). In the first year of the study, 8% of all pre-booked consultations were undertaken via Skype. During the same period, the DNA rate for virtual consultations was zero (compared with 39% for face-to-face consultations).
Those patients taking up the virtual consultation option in both nurse- and consultant-led clinics within the service were similar in terms of gender, with a slightly higher (but non-significant) proportion of white British/European patients (Table 4). There was a significant difference in the age of patients for consultant-led appointments [χ2(3, N = 307) = 11.7; p = 0.01], with a higher proportion of patients in the younger age category (aged 16–34 years) taking up the virtual consultation option, and no patients aged > 55 years.
| Characteristic | Value |
|---|---|
| Consultant-led appointments (remote) | |
| Age (years), range (median) | 17–50 (23) |
| Gender (%) | |
| Male | 50 |
| Female | 50 |
| Ethnicity (%) | |
| White British/European | 50 |
| Black Caribbean | 11 |
| Asian | 39 |
| Consultant-led appointments (overall) | |
| Age (years), range (median) | 17–94 (45) |
| Gender (%) | |
| Male | 50 |
| Female | 50 |
| Ethnicity (%) | |
| White British/European | 35 |
| Black African | 3 |
| Black Caribbean | 12 |
| Asian | 46 |
| Other | 4 |
| Nurse-led appointments (remote) | |
| Age (years), range (median) | 18–26 (22) |
| Gender (%) | |
| Male | 44 |
| Female | 56 |
| Ethnicity (%) | |
| White British/European | 60 |
| Black African | 13 |
| Black Caribbean | 7 |
| Asian | 20 |
| Nurse-led appointments (overall) | |
| Age (years), range (median) | 17–26 (22) |
| Gender (%) | |
| Male | 51 |
| Female | 49 |
| Ethnicity (%) | |
| White British/European | 36 |
| Black African | 11 |
| Black Caribbean | 9 |
| Asian | 44 |
The Diabetes Pre-Pregnancy Clinic at Barts Health NHS Trust (part of the Adult Diabetes service) supports women with diabetes who are planning to conceive in the near future, on the grounds that the outlook for the fetus is best if tight diabetes control is achieved 3 months before conception. In contrast to the other two diabetes clinics described above, this service does not have designated clinic or office space, and so a major challenge was setting up and managing virtual consultations across multiple spaces in the hospital – a complex logistical challenge not anticipated in the documents or interviews in our macro-level data set. Notwithstanding these logistical issues, virtual consultations continue to be viewed as a potentially useful means of helping to achieve tighter diabetes control in young women who are often highly motivated, but who do not yet have the additional risk or metabolic volatility of a current pregnancy. Implementation of virtual consultations in this service continues as part of a wider restructuring of the service (including staff roles and treatment programmes).
Virtual consultations in the Antenatal Diabetes service
Barts Health NHS Trust offers an Antenatal Diabetes Clinic that supports women with diabetes throughout their pregnancy. Although virtual consultations with non-pregnant adults with diabetes were already business as usual, the combination of diabetes and pregnancy raised additional challenges. Many (although not all) women in this group are recently diagnosed and have no pre-existing relationship with the diabetes doctor or nurse. Diabetes in pregnancy must be tightly controlled to avoid damage to the developing fetus, but, for metabolic reasons, is sometimes very difficult to control. Diabetes during pregnancy usually requires frequent adjustments of medication that need reviewing after only a few days. The Antenatal Diabetes Clinic provides ongoing assessment and support for patients with pre-existing diabetes and for those women who have developed gestational diabetes since becoming pregnant. To create space for some follow-ups to be undertaken remotely, a virtual clinic was created for Tuesday afternoons (a time when the lead consultant had confidential office space available).
An early observation was that this clinic was by far the busiest of the three settings within the diabetes services, with a very high throughput of patients [a clinician typically saw 30–35 women per clinic, in appointments lasting an average of 8 minutes and with no personal lists (i.e. each clinician tended to call the next patient in the queue rather than a patient they had seen previously)]. During the study period, virtual consultations were offered to highly selected patients as an alternative to visiting the hospital for follow-up appointments 3–4 days after a clinic visit (see discussion on this in the next section, Virtual consultations in the Hepatobiliary and Pancreatic Cancer Surgery service). When an initial pilot showed that only around 1 in 50 eligible women was being offered virtual consultations, the option was discontinued in this setting (see the discussion on this in Evolution of virtual consultation services over the study period). In total, of the 6562 Antenatal Diabetes follow-up consultations conducted during the pilot period (July to November 2015), approximately 1320 were undertaken by the consultant offering the remote option and 24 (around 2% for this consultant) were done virtually. However, it is worth noting that, although 1320 patients were logged onto the EPR system as having their consultations undertaken by this consultant, the way in which the clinic team works (often seeing the next patient rather than sticking to their own personal list) means that some of those patients will have been seen by other members of the clinical team and that the overall proportion of virtual consultations is likely to be slightly higher for that consultant.
The profile of patients taking up the option of the virtual consultation service in the Antenatal Diabetes clinic was very similar in terms of ethnicity, compared with those in face-to-face appointments (Table 5). Patients taking up the option of the virtual consultation service were slightly more likely to be white British/European and tended to be in a narrower age range than those attending only face-to-face consultations. These differences were not statistically significant.
| Characteristic | Value |
|---|---|
| Diabetes Antenatal (remote) | |
| Age (years), range (median) | 30–37 (34) |
| Ethnicity (%) | |
| White British/European | 20 |
| Black Caribbean | 10 |
| Asian | 60 |
| Other | 10 |
| Diabetes Antenatal (overall) | |
| Age (years), range (median) | 20–45 (31–35)a |
| Ethnicity (%) | |
| White British/European | 11 |
| Black African | 16 |
| Black Caribbean | 4 |
| Asian | 68 |
| Other | 1 |
Virtual consultations in the Hepatobiliary and Pancreatic Cancer Surgery service
The Hepatobiliary and Pancreatic Cancer Surgery service at Barts Health NHS Trust is a tertiary referral service that takes patients living up to 200 miles away. The patient typically sees both the consultant and specialist nurse during their appointment. However, this is often decided during the running of the clinic, with the nurse on some occasions leading a consultation alone (e.g. with a routine follow-up appointment), but the consultant being available at the clinic to address complex clinical issues and concerns.
Virtual consultations were introduced in 2015 for selected patients who had undergone surgery for pancreatic or liver cancer, primarily to save the patient a long and arduous journey in the period following major surgery. Virtual consultations were initially offered within a designated time slot (Monday afternoon), and conducted with both the consultant surgeon and the nurse specialist together (because cancer care is by nature interprofessional and often requires a dialogue between surgeon, nurse and patient). In all cases, patients were selected for virtual consultation based on the consultant’s assessment that they would not require a physical examination at that appointment. The Monday afternoon slot was initially chosen for practical reasons (the surgeon and nurse were often in theatre, running clinics or on ward rounds), and so a specific time had to be established. However, over the course of the study, the consultant and the nurse decided to incorporate the use of Skype within their usual face-to-face clinical work, in order to maximise the scope and frequency of appointments. For instance, this allowed the nurse to initiate and progress the consultation, with the consultant available to join or support the consultation when needed (as in a usual face-to-face clinic), as opposed to both the consultant and the nurse being present for the full duration of the appointment.
During the study period (November 2015 to July 2017), 12 virtual consultations were undertaken in the Hepatobiliary and Pancreatic Cancer Surgery service, out of 161 total consultations (i.e. 7%). However, it is worth noting that the proportion has been steadily rising and, towards the end of the study, it was 20% of all consultations. Those taking up the option of the virtual consultation service were somewhat more likely to be female and white British/European than those attending face-to-face consultations only, but these differences were not statistically significant (Table 6).
| Characteristic | Value |
|---|---|
| Cancer Surgery follow-up (remote) | |
| Age (years), range (median) | 55–84 (70) |
| Gender (%) | |
| Male | 42 |
| Female | 58 |
| Ethnicity (%) | |
| White British/European | 70 |
| Black Caribbean | 7 |
| Asian | 21 |
| Other | 2 |
| Cancer Surgery follow-up (overall) | |
| Age (years), range (median) | 28–84 (68) |
| Gender (%) | |
| Male | 51 |
| Female | 48 |
| Ethnicity (%) | |
| White British/European | 62 |
| Black African | 2 |
| Black Caribbean | 15 |
| Asian | 21 |
Evolution of virtual consultation services over the study period
In each of the three clinics, virtual consultations have been introduced slowly and adaptively. Prompted by initial enthusiasm from clinical leads and a desire to provide technology-enabled care (often as a means of increasing access for patients and/or easing demand within the service), each clinic typically began by piloting a virtual consultation service outside their usual clinic routines, and with a small number of carefully selected patients (selection being based on clinical judgement about the condition of the patient). This pilot period lasted a minimum of 6 months and allowed clinical and administrative staff protective time and space to learn about the technology and how best to link it with routine clinical care. It was only once this process of experiential learning had taken place and staff felt confident in the use of the technology that they felt able to adopt and embed it within the usual clinic routines or, as in the case of Antenatal Diabetes, make a decision not to adopt the technology at that time.
In the Adult/Young Adult Diabetes clinic, the virtual consultation service was already established when the study began. The service was initially offered in 2011 by the lead consultant, before gaining positive feedback from patients, evaluating the service and then extending it to other clinicians. As the service became more embedded in routine care, so it evolved to embrace both clinician-initiated contacts (via formal Skype appointments) and patient-initiated contacts (via the Skype messaging service). The former were planned and scheduled, whereas the latter were (largely) ad hoc, depending on the needs of the patient and the availability of the clinician. This evolution of the service was informed by patients’ and clinicians’ expectations of the service, having gained experience of using Skype in the context of their clinical care. However, by the end of the VOCAL study, it was noteworthy that some doctors and nurses did not offer the option of virtual consultation, and the virtual consultation service remained limited to certain clinics, suggesting that, despite the enthusiasm of some clinicians, the service is not yet fully embedded, even in the service that originally introduced it.
To date, the evolution of the service – particularly its adaptation over time to include more patient-initiated contact – has informed the development of wider organisational support for virtual consultations in Barts Health NHS Trust. For instance, knowledge of clinician-initiated and patient-initiated contacts informed the SOPs for virtual consultations that were later adopted within Barts Health NHS Trust (including guidance about patient and clinician expectations about responsiveness to patient-initiated contacts).
In the Hepatobiliary and Pancreatic Cancer Surgery, the initial set-up of virtual consultations was limited to the surgeon’s office and established outside usual clinic hours. The focus was on creating a safe space (physically and logistically) that allowed the clinic to test out virtual consultations with a small group of selected patients at specific times and away from the usual clinics. Patients were invited for virtual consultation on the basis that they were receiving good news during a postoperative follow-up (the assumption being that bad news had to be imparted face to face in the clinic), and with no requirement for a physical examination. A total of 12 virtual consultations were undertaken over 18 months, allowing familiarisation with the technology, consideration of logistical issues (primarily around interfacing with established clinics and the use of shared office space) and reflection on the selection of patients to be invited into the service. Over the course of our fieldwork, a decision was made to extend the use of virtual consultations beyond cancer follow-up to include other appointments within the Hepatobiliary and Pancreatic Cancer Surgery service, to integrate the virtual consultation option within the usual morning clinic and (having now gained good experience of the technology and its use with patients in a clinical context) for the nurse to take a lead on virtual consultations (with the consultant available if needed). This work is under way as part of the wider roll-out of virtual consultations at the trust.
As set out above (see Virtual consultations in the Antenatal Diabetes service), virtual consultations were initially thought to be a good idea for the Antenatal Diabetes service, which is a busy clinic, requiring frequent patient contact and average appointment times of 8 minutes. As with the Hepatobiliary and Pancreatic Cancer Surgery clinic, the nurse consultant initially invited follow-up patients to virtual consultations outside the usual clinic time of Friday morning and, instead, during a dedicated session on Tuesday afternoons. In part this was to allow a dedicated time to test out virtual consultations, but was also the only time when the clinician’s shared office was known to be empty. The consultant saw around 10 patients between one and three times each (a total of 24 virtual consultations) over a 6-month period. As reported above, given the low proportion of virtual consultations after this time, it was felt that additional time should not be invested, and the service was discontinued.
The initial piloting work of virtual consultation services outlined above was (at least in part) facilitated by a locally agreed tariff for virtual consultations that was equivalent to a face-to-face consultation, thereby enabling some slack within the system to support potential innovation in service delivery. However, as Barts Health NHS Trust has sought to scale up virtual consultation services beyond the clinics included within the study, commissioners have become interested in revisiting the local tariff.
Trust policy and service-level agreements
The implementation and sustained use of virtual consultations in participating services at Barts Health NHS Trust required the development of technical support and IG protocols. This was attributable to the impact of the use of (in this case) Skype software on the trust’s technical infrastructure and the legal, regulatory and local policy issues relating to the protection of patient data, privacy and consent. A major challenge has been to address the lack of consensus on these issues (both locally and nationally).
In relation to technical support, and in line with local policy in most NHS trusts, Barts Health NHS Trust policy states that new software downloads must be performed by ICT staff and requested through the IT helpdesk as standard procedure. During project setup, however, and despite the VOCAL study including both the CCIO and the estates and facilities manager as co-signatories, we found that ICT staff simply did not respond to such requests when they related to the installation of Skype (which was not routinely provided on trust computers). This was attributable to the absence of trust policy and service-level agreements in relation to supporting Skype on NHS computers (and, thus, a mismatch between what had been offered in the research bid and what was de facto supported on the ground). The original piloting of Skype in the diabetes service had been achieved through ‘informal’ requests to install Skype on a handful of computers in a single clinic.
Following considerable negotiation from the research team and clinicians in participating services, a ‘bespoke’ agreement was established, in which requests to install Skype on additional computers were to be made directly to a designated ICT manager, who would then arrange for the downloads to be completed. The implementation of this arrangement took 2 months. The need for what might be called a workaround at such an early stage in the project was perhaps telling, and almost certainly reflects the extreme pressure under which the ICT department was operating at the time. Our interviews with local ICT staff and managers strongly suggest that, although they were comfortable with virtual consultations being undertaken via Skype as a small ‘demonstration’ project by a clinician with whom they were on first-name terms, they feared that extending the option to download Skype (or similar media) on any trust computer would ‘open the floodgates’ to requests for technical support at a time when they were only just managing to meet existing demand.
The action research component of the VOCAL study sought to establish how technical support for virtual consultations could be provided across Barts Health NHS Trust in the long term. Notwithstanding the short-term workaround described above, a mainstream trust policy on virtual consultations using Skype needed to be established in collaboration with the IG and ICT departments. Working with service managers and the Barts Health IG Manager, the research team produced an internal policy document, covering issues relevant to IG in relation to virtual consultations and SOPs on technical support. The draft document, which was based on the setting up and running of the Skype service within the diabetes clinic and took 2 months to develop, was then reviewed by representatives across key departments, took 9 months to gain formal approval and become trust policy, and has since been continually adapted. Establishing formal agreements with the ICT department, and the views of their staff on the impact of virtual media, such as Skype, on the service infrastructure proved to be key to both setting up the virtual consultations in our participating services and subsequently addressing wider roll-out across the trust. The approved document was subsequently made available to all departments via the trust intranet.
At the outset of this study, the need for a formal, written agreement with the ICT department and a formal Barts Health NHS Trust policy on virtual consultations more generally was not anticipated to be a rate-limiting step, either by the research team or by participating clinical teams. In retrospect, however, this document can be seen as what Latour would call an ‘immutable mobile’225 – that is, an artefact describing ‘the way things are’ that is accepted by all key actors, and which serves to stabilise what would otherwise be a highly unstable arrangement of people and technologies. 226 Immutable mobiles include maps, diagrams, graphs and lists of agreed procedures that move within a network and its nodal points of passage, but which retain the same essential properties in different contexts, thereby allowing relations to be performed in the same way in a variety of different settings and locations.
In relation to IG, local implementation was held back by both local and national concerns about the security of virtual consultations in general, and Skype consultations in particular. This concern relates to the security of data streams (the hypothetical risk of someone eavesdropping on calls or accessing messages sent through Skype) and account security (access to information saved on computers). As part of the action research element of this study, the research team worked with participating clinical services and IG teams at Barts Health NHS Trust, with the support of an IG specialist within the local CCG, to identify models of best practice and establish IG policy on the use of Skype within the trust.
As part of the collaborative work with the IG team, we undertook a review of Skype security, which found that the encryption meets the minimum NHS network requirements. Many other virtual media applications (e.g. FaceTime) also meet such criteria. However, it is important to highlight that alternative voice-over-internet protocol (VoIP) systems (a group of technologies for the delivery of voice communications over the internet), some of which are currently being considered by Barts Health NHS Trust and other NHS trusts as alternatives to Skype, would need to undergo similar reviews on their data security.
In relation to account security, our ethnographic fieldwork informed the development of a guiding document for clinic staff to minimise risk to patient privacy and confidentiality. That guidance has been included in the internal SOP document. In addition, we have produced a summary document for wider dissemination to other NHS trusts. This has been reviewed and endorsed by the UK IGA, which used it as the starting point for developing national policy guidelines on the use of Skype and FaceTime across the NHS.
New clinical roles and practices: triage, technical support and direct access
It was evident from our interviews and ethnographic observations that clinicians involved in virtual consultations took on new roles and practices in relation to patient triage (judging a patient’s suitability for virtual consultation), patient setup (ensuring that the technology worked, and supporting patients with its use) and medical documentation (changing how electronic and paper documents and other artefacts were used in consultations).
In relation to patient triage, there were no formal criteria in any specialty on how to assess patient suitability for virtual consultations. It was clear that such decisions were made by the clinician on a case-by-case basis, informed by a range of factors that varied across the different clinical contexts. Within the Adult/Young Adult Diabetes clinic, such decisions were discussed and mutually agreed between the clinician and patient, depending on the patient’s support needs and wishes. The reality was that most patients (although not necessarily most appointments) were considered eligible for the virtual option.
Within the Antenatal Diabetes Clinic, offering virtual consultations was thought to be considerably more risky, and there were two patients (mother and fetus) to consider. Although moderate perturbations in blood glucose levels would likely cause little harm to the mother, serious complications (e.g. congenital abnormalities, intrauterine death) were possible in the fetus. Furthermore, resistance to insulin tends to increase as pregnancy progresses, necessitating up-titration of the insulin dose, sometimes on a daily basis. Owing to the complexity and risk involved in this clinical context, the option for a virtual consultation was offered only to patients considered to have relatively stable blood sugar readings and the capacity to self-manage effectively. Furthermore, because the clinical picture can change on an almost daily basis, close familiarity with the patient’s history and background appeared to be crucial, especially since the virtual encounter was undertaken in the absence of a full medical record (since the patient held that record). This is illustrated by the following quotation from the consultant:
I always find when I have a patient who I haven’t really got under the skin of. So let’s say it’s a lady who has gestational diabetes, diagnosed at 28 weeks and I’ve met her at 32 weeks for literally less than 5 minutes, and I might have thought well sugars are all fine: ‘We’ll see you for a scan in 4 weeks, why don’t you Skype at 2 weeks?’ I’ve had a few of those because I think they’re all fine. That Skype appointment to me is terrifying because I then get my orange bit of paper. There’s not much information on it because at the time I wasn’t very worried and I’ve lost that opportunity to go through it again. I think as clinicians, if you can’t remember the patient, then you’re duty bound to go back and check in your mind that you have got all the information you need. As soon as you don’t have the notes, if you can’t remember the patient, you might have this orange piece of paper saying all seems fine, why not Skype in 2 weeks. But actually you’re just a bit worried. Whereas someone like [patient X, known to consultant], who I’m Skyping three times a week, I mean, I totally get her.
In the Hepatobiliary and Pancreatic Cancer Surgery clinic, virtual consultations were offered to patients for postoperative follow-up if the consultant was confident of the treatment outcome, based on the details of the operation performed and the postoperative CT scan result.
Another aspect of patient triage was confirming that the patient had access to Skype (on a computer or a mobile device) and that they or a family member knew how to use it, since these were prerequisites for inclusion in the study and the trust does not offer technical support for patient-owned technologies. Patients seeking to use the virtual consultation option must establish contact with the clinician’s Skype account before a consultation can take place.
As part of the action research for this study, the research team collaborated with clinicians, the IG department and local CCG IG managers to produce a patient leaflet containing information about using Skype and written details of the clinic Skype username/ID (identification). Although patients found this material useful, additional support was often provided by the clinician as part of the setup phase. For instance, prior to a first virtual consultation, the clinician typically contacted the patient (via e-mail or telephone) to confirm their account details, check that they had registered and confirm that a contact invitation had been received. Clinicians sometimes also conducted ‘test calls’ with patients before their consultation, so that the patient could familiarise themselves with the technology or check that the video and audio worked.
Patients and clinicians often shared documents (e.g. paper medical record) and similar artefacts (such as lists of blood sugar readings) as part of their consultation. The ease (or not) with which such material exchanges happened was of course influenced by whether the consultation was face to face or virtual; these data are discussed in more detail below in the section on the micro-level findings (see Chapter 5).
In relation to the organisational processes associated with material artefacts (e.g. creating or editing them), the introduction of Skype has had little impact within the Adult/Young Adult Diabetes and Hepatobiliary and Pancreatic Cancer Surgery clinics, as all key documents are stored and accessed electronically.
In the Antenatal Diabetes Clinic, however, a paper patient-held maternity record (on which all members of the multidisciplinary team entered data) was used. This was readily shared across the desk in the face-to-face setting, but impossible to share easily in the virtual setting – a restriction that had a considerable impact on how the clinical consultation unfolded, and strongly influenced the triage decision on who was ‘suitable’ for a virtual consultation. The consultant’s perception of risk was also influenced by the fact that the antenatal outpatient clinic was set up to generate additional medical information (collected by additional ancillary staff) to support their clinical assessment. For example, patients’ weight, blood pressure and urinary ketone levels are taken on arrival at the clinic, and these data are made available to the clinician along with the hospital and patient-held maternity record. In comparison, the virtual consultation with an antenatal patient was invariably data sparse.
In the Adult/Young Adult Diabetes clinic, the use of virtual consultations facilitated patients’ direct access to the clinician, because patients could send a short message service (SMS) message via Skype and/or contact a clinician informally for an ad hoc consultation (this process usually involved the consultant indicating on Skype that they were online and ‘not busy’, the patient messaging them to ask if they were free and then together arranging a time shortly after to connect). Although it had been known at the outset that this option was technically possible, neither the clinicians nor the research team had anticipated how this function would be repurposed by patients to bypass the appointment system and establish a direct communication channel with their doctor or nurse. This ad hoc part of the service was used by some patients to contact the clinician between their scheduled appointments to ask questions or raise concerns. This ‘open access’ aspect of the service was welcomed by the Diabetes team because it aligned with the clinic’s goals to enhance patient self-management and engagement (as noted in Virtual consultations in the Adult/Young Adult Diabetes service, the virtual consultation service had originally been established to solve the problem of a high DNA rate in patients who were typically from socioeconomically deprived and/or minority ethnic groups). Dealing with such messages and the ad hoc requests for an unscheduled Skype call appeared to be practically manageable, because the virtual consultations ran alongside the diabetes outpatient clinic. In contrast, clinicians’ access to Skype within the Antenatal Diabetes and Hepatobiliary and Pancreatic Cancer Surgery settings was restricted to specific times (and a narrow time window), which limited their capacity to respond in the same way.
The repurposing of Skype technology to contact clinicians outside scheduled appointments raised challenges in relation to managing patients’ expectations (e.g. about when and for what purposes a consultant can be contacted). We noted occasional examples of patients using the Skype messaging service to contact the consultant outside usual hours for non-medical and non-urgent matters, with an apparent expectation of ‘24/7’ service). This also has implications for clinician workload, reimbursement (see Chapter 3, Rolling out remote consultations) and medicolegal issues.
Clinic management and administration
Embedding virtual consultations in clinic routines was a complex and difficult process that took many months and which was strongly influenced by physical space and the material properties of technologies and artefacts. Our ethnographic data highlight how work practices and the often subtle, but important, social, professional and material contexts in which such work takes place have a bearing on the capacity to embed the technology in routine practice.
This process of embedding virtual consultations is presented in Figures 3–8, which map out the human and technical interactions and interdependencies on which the execution of both face-to-face and Skype consultations depended in the Adult/Young Adult Diabetes clinic (see Figures 3 and 4), the Antenatal Diabetes Clinic (see Figures 5 and 6), and the Hepatobiliary and Pancreatic Cancer Surgery clinic (see Figures 7 and 8). Drawing on Feldman’s notion of ‘organisational routine’142,167 – defined as ‘a repetitive, recognizable pattern of interdependent actions, involving multiple actors’159 – we explored how face-to-face and virtual consultations were enacted, purposefully capturing the complex (and very different) actions involved in trying to make face-to-face and virtual consultations happen in different clinical and material contexts. In contrast to the protocols (‘proxy routines’167) and descriptions of staff (‘ostensive routine’167) across Barts Health NHS Trust, these observed instances of consultations (referred to by Feldman as ‘performative routines’167) enabled us to identify the social and organisational factors shaping the ways in which clinics sought to embed the Skype technology and virtual consultation services over time. It also allowed us to tease out the logistical and practical aspects of clinic work, and the technologies and artefacts supporting it, that facilitated the use (or non-use) of the technology within particular clinical contexts.
FIGURE 3.
The routine for a face-to-face consultation in the Adult/Young Adult Diabetes clinic.
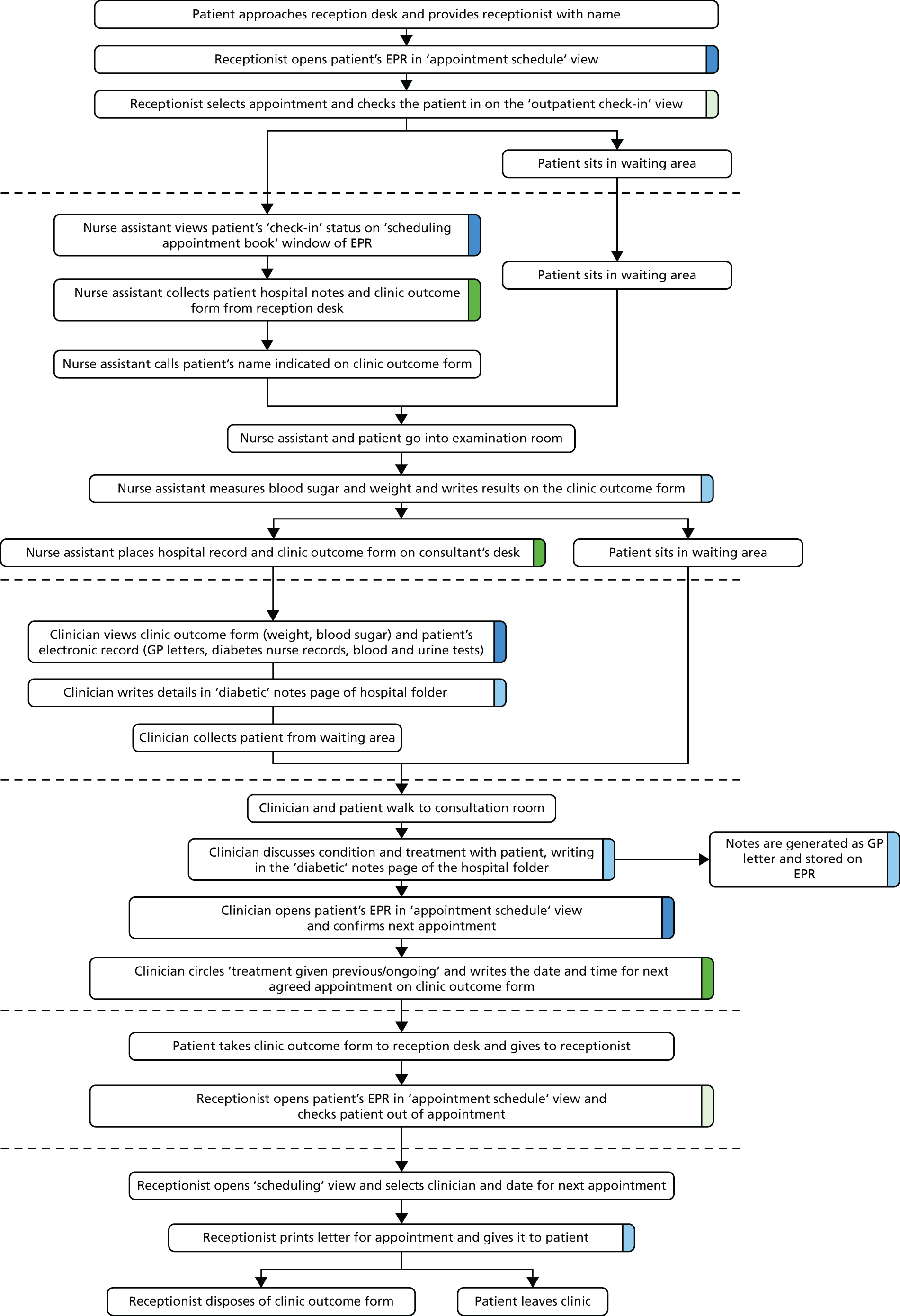
FIGURE 4.
The routine for a virtual consultation in the Adult/Young Adult Diabetes clinic. ID, identification.
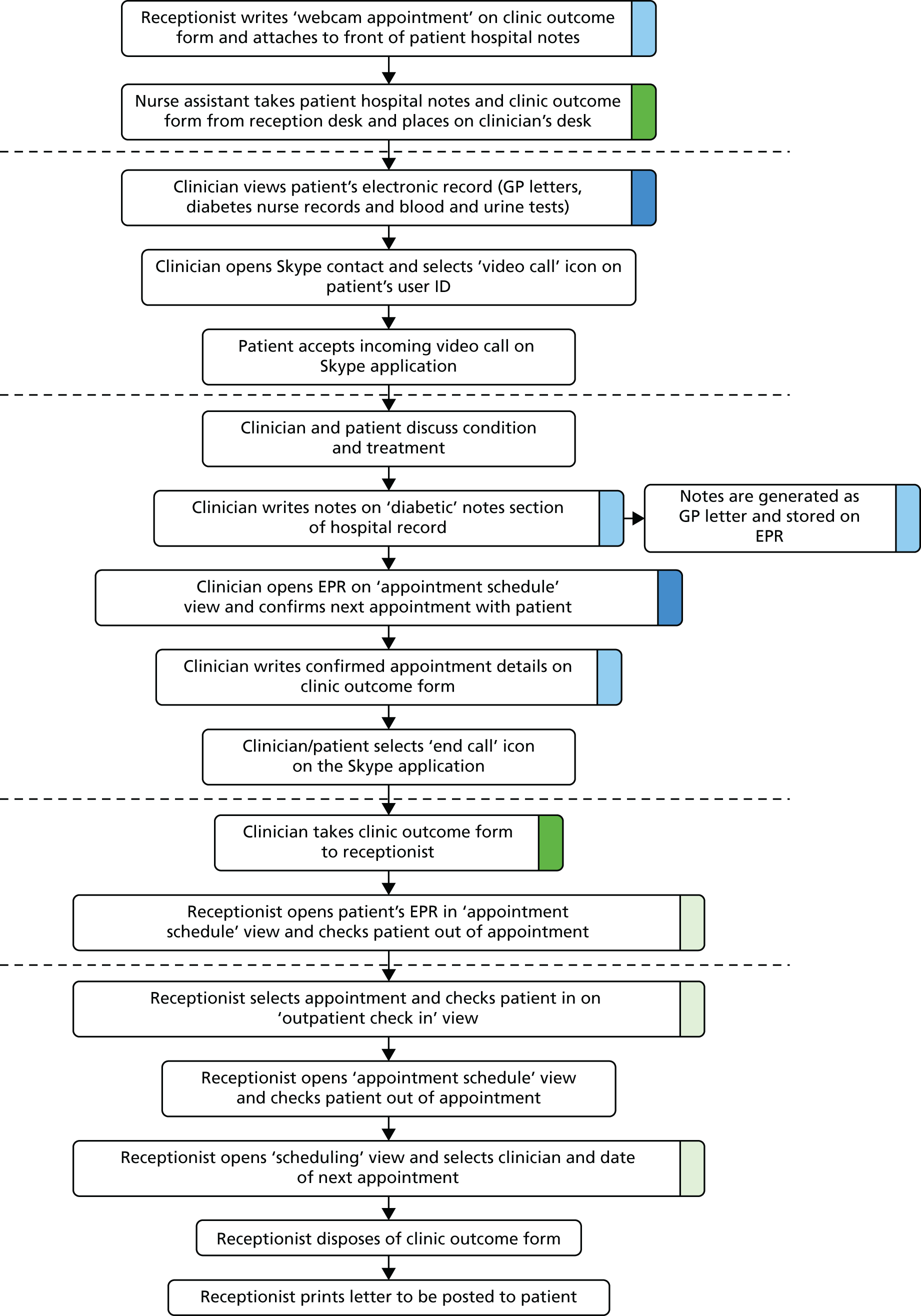
FIGURE 5.
The routine for a face-to-face consultation in the Antenatal Diabetes Clinic. ID, identification.

FIGURE 6.
The routine for a virtual consultation in the Antenatal Diabetes Clinic. ID, identification.

FIGURE 7.
The routine for a face-to-face consultation in the Cancer Surgery clinic.

FIGURE 8.
The routine for a virtual consultation in the Cancer Surgery clinic. ID, identification.

The work involved in embedding face-to-face and virtual consultations in clinic work broadly related to four key processes or subroutines: generating data/information (highlighted in light blue in Figures 3–8), enabling access to data/information (highlighted in blue), facilitating patient access through the clinic (highlighted in green), and tracking the patient through the clinic/care pathway (highlighted pale green). Crucially, as we come on to discuss below, each of these processes was supported by technical and material artefacts, the movement of artefacts across the (virtual and physical) spaces of the clinic/hospital and the role of multiple clinical and non-clinical actors.
As is visible in Figures 3–8, the introduction of virtual consultations significantly affected the ways in which consultations were undertaken across the three clinics. The physical presence of the patient within the clinic setting was fundamental to existing ways of identifying, scheduling, conducting, rebooking and monitoring patient appointments. For instance, in Figure 7 the physical presence of the patient at reception prompts ‘check in’ and generation of the clinic outcome form; this enables the nurse assistant to identify the patient, conduct the relevant tests and record the results on the form, which in turn enables the remainder of the consultation to take place. Embedding virtual consultations within existing services involved significant reworking of those processes in ways that accounted for the ‘virtual’ presence of the patient. The extent to which existing face-to-face consultation routines needed to be reoriented, and the ways in which this was managed by staff varied across the three clinic settings depending on the people, technologies, material artefacts, physical and spatial arrangements, clinical pathways and assessment procedures already in place. As we set out in the remainder of this section, this meant great variation in how the Skype technology and virtual consultation service were (and were not) embedded in clinics.
Work routines across the three clinics were adapted to align the Skype technology and virtual consultation service with existing roles, processes and structures. This included processes and structures related to EPR management, appointment scheduling and recording attendance. These routines and structures vary across different clinics, and so staff have collectively evolved their own roles and workarounds within their local settings.
At the outset of the study, the Cerner EPR system was used across the Barts Health NHS Trust clinic as a shared scheduling tool to book appointments and indicate when the patient had arrived at the clinic and attended their appointment. The EPR system continued to be used throughout the study in both the Antenatal Diabetes and Hepatobiliary and Pancreatic Cancer Surgery clinics, providing a facility for auditing, service management and acting as a commissioning resource. It therefore needs to accurately reflect staff time and activity (including appointment type, frequency and durations).
In the Antenatal Diabetes clinic, the EPR was used to access medical information (stage of pregnancy, type of diabetes, blood results) and confirm upcoming appointments. However, in this context, the majority of clinic data were documented and reviewed using the maternity folder held by the patient. In the Cancer Surgery context, the EPR was used to review blood test results and CT scans as part of the patient’s cancer treatment review, and to review previous GP letters generated and stored through the system.
Within the Adult/Young Adult Diabetes service, the Cerner EPR system was used at the outset of the study to review previous appointments with the consultant (via GP letters generated and stored through the system), blood/urine results (for annual review) and clinical outcomes from other clinical departments. This was used in conjunction with the Diamond diabetes management system (used by the diabetes nurse specialists to document blood sugar readings and free-text documentation of the consultation discussion), hospital notes (with past medical history not documented electronically) and pre-appointment weight and blood pressure measurements (obtained on arrival at the clinic). Towards the end of the study, a new system (EMIS) was introduced for recording nurse consultations, leading to subtle but important disruption to the virtual consultation routine – and, in particular, to difficulties in recording (in the form of coded data) that a virtual consultation had taken place (see Overview of virtual consultations in Diabetes and Cancer Surgery services above). A key challenge to the introduction of virtual consultations at Barts Health NHS Trust was the reconfiguration of the EPR system to allow the booking of ‘webcam follow-up’ appointments on the clinic appointment schedules. Each consultant has an EPR ‘profile’ through which appointments are booked by the administration teams. The available appointment types and time slots that can be booked are configured according to their existing clinic schedule. The introduction of the ‘webcam appointments’ in any clinical service involved a lengthy process of form filling, enquiries (by e-mail/telephone) and discussions and agreements among senior service managers. Prior to the VOCAL study, EPR configurations were implemented by the administrative teams within the particular clinical service. However, changes in organisational structures meant that the EPR had become managed centrally by the trust’s ICT department. Consequently, the reconfiguration of EPR for the implementation of Skype required new formal procedures, forms and authorisations that had not previously been required when EPR was managed within the clinics (where clinical and EPR management staff knew and routinely worked with each other and had a culture of collaborative troubleshooting and mutual support).
The designation of virtual consultation appointment slots needed to be aligned with existing appointment schedules, clinician availability, and clinic and office space. As noted above, these routines and structures varied across the different clinics, and so staff developed their own scheduling times and processes for virtual consultations. Within the Adult/Young Adult Diabetes service, virtual consultations were conducted alongside the outpatient clinic. This was possible because the clinic and administrative staff within the service occupied their own office and clinic space, enabling them to access Skype during the usual clinic hours. The virtual consultation service became embedded in the work of the clinic, so staff and patients repurposed the technology to enable a more flexible approach that involved more ad hoc consultations that did not require formal booking. In contrast, the outpatient clinic spaces for Antenatal Diabetes and Hepatobiliary and Pancreatic Cancer Surgery were shared with other departments and located separately from the clinicians’ offices. This meant that specific times and locations had to be established for Skype appointments. In addition, in the Hepatobiliary and Pancreatic Cancer Surgery, the booking of patient appointments required a high level of flexibility, as so much depended on postoperative recovery of individual patients and test results (e.g. from CT scans or blood tests). It was crucial to maintain this flexibility with the introduction of the virtual consultation service; hence, the nurse booked patients into face-to-face appointments (via the routine set out in Figure 7) and then offered the Skype option by telephone when the test results had been received. This created an additional layer of work, requiring the nurse to schedule both a face-to-face and a virtual consultation, and then cancel the face-to-face appointment once the virtual consultation had taken place.
It was necessary to change the process of documenting appointment attendance to accommodate virtual consultations. In face-to-face consultations in the Adult/Young Adult Diabetes clinic (see Figure 3), patient attendance to the outpatient clinic was routinely recorded by the receptionist at the clinic entrance when the patient physically appeared, which, in turn, prompted the nurse assistant to obtain the patient’s hospital record and clinic outcome form for pre-appointment medical checks – events that did not happen in virtual consultations. Instead, the ‘usual’ receptionist role was effectively bypassed (see Figure 4), and clinicians took on the role of ensuring that attendance was accurately documented; the consultant walked to the reception desk after the clinic to report on who had ‘attended’, providing the clinic outcome form (which is usually completed by hand by the consultant to indicate the next appointment and handed in to reception by the patient on their departure, i.e. exactly the same information as required for a face-to-face consultation by a different routine) for the receptionist to input onto the patient’s records and book future appointments. In the virtual consultation service, the receptionist effectively checks the patient ‘in’ and ‘out’ in the same step as booking the next appointment. This routine was additionally supported by a new role for the nurse assistant, who collated the hospital records of the patients scheduled for a Skype consultation and simply placed them on the clinician’s desk at the start of each clinic, with a handwritten note on the top saying ‘Webcam’.
In the Antenatal Diabetes clinic, the receptionist role of checking the patient in and directing them through to the first of several pre-appointment checks (see Figure 5) was similarly bypassed. Instead, the consultant contacted the service administrator by telephone following the virtual consultation so that the administrator could record the patient’s attendance (see Figure 6). In the Hepatobiliary and Pancreatic Cancer Surgery clinic, the nurse accessed the EPR system directly after the Skype consultation in order to check the patient in and immediately out again (see Figure 8), before the consultant then sent relevant documentation to administrative staff via e-mail. In all cases, recording attendance in the face-to-face clinic was considerably easier and quicker than doing so in the virtual clinic. However, there was more parallel work at the time of face-to-face consultations to generate, exchange and physically move patient data and material artefacts (the clinic outcome form, the EPR and so on) in ways that enabled the legitimate transfer of the patient from one place to the next.
A major concern when seeking to embed virtual consultations in administrative and clinical routines was the absence of recent and accurate medical information, obtained through the pre-appointment checks and the comprehensive maternity notes used across the other clinical departments treating the patient. Take the following example from a consultant in the Antenatal Diabetes clinic:
So I feel much more vulnerable, in terms of not having all their records there. Not picking up on things that may have happened to the patient . . . You can see [on the patient-held maternity record] if they have seen another professional. OK you can ask someone on Skype, but, what I have discovered is that people will not tell you, which is reasonable, something they think you are not interested in.
In face-to-face consultations in the Antenatal Diabetes clinic, the consultation is dependent upon the patient-held maternity folder, which records, for instance, blood sugar readings, insulin doses and pre-appointment checks, such as blood pressure, weight or urine ketones. This information is not routinely replicated in the hospital or EPRs. Hence, virtual consultations take place in the absence of a full medical record, and were a particular challenge when the clinician did not have an established relationship with the patient (as, for instance, with many of the patients being seen for gestational diabetes). As one of the Antenatal Diabetes consultants neatly put it:
I think the problem is, whereas with most diabetes clinics you get to know the patients fairly well, often the name and when you see the notes, you recollect them. The antenatal patient is different. They may see me once. It would be a brief, superficial appointment, rather than someone seen for the last 10 years. Because we see so many patients, I don’t have that confidence that I know the patient prior to seeing them on the Skype screen . . . And its affected by patients being so huge number, and some will only be under our care for about 6 weeks.
As the detailed maps of organisational routines in Figures 4, 6 and 8 highlight, staff developed workarounds and performed ‘hidden work’ to support the safe delivery of clinical care in the remote environment and ensure that all key aspects of the interaction were adequately recorded. They found pragmatic solutions to practical problems, such as generating their own ‘temporary notes’ (as with the handwritten ‘Webcam’ note referred to above) and assuming responsibility for aligning these with the main EPR, as described here:
So what I have been doing with Skype patients is writing myself brief notes on this and holding them here, with view to file in the hospital notes when pregnancy has concluded. This becomes part of hospital records.
Antenatal Diabetes Consultant
This development of knowledge and practice required ongoing adaptation and resolution. For instance, considerable additional time and effort was involved in reconfiguring technical systems to accommodate ‘webcam’ appointments. In the Antenatal Diabetes clinic, in particular, the lack of ‘organisational slack’ – limited resources, fixed protocols and distributed roles and responsibilities – was a major barrier to the collaborative and adaptive efforts needed to embed virtual consultations as business as usual.
Resourcing and managing the roll-out of virtual consultations
Following the insights from our meso-level ethnography and interviews, a trust-wide decision was made to establish a cross-departmental working group to assist with overcoming the numerous practical, technical and operational barriers to the smooth and efficient use of Skype for virtual consultations. This came on the back of the publication of TST,158 which set out a significant programme of improvement within Barts Health NHS Trust and with relevant health and social care agencies (see Chapter 2, Setting and context). TST is concerned with radically redesigning services, including outpatient pathways, and includes plans to speed up access to specialist advice via traditional face-to-face services, as well as the roll-out of virtual consultations. The VOCAL study came at a time when senior management at the trust was turning its attention to roll-out beyond a handful of clinics. This senior level buy-in was crucial to moving that work forward, and to establishing an outpatient project strategy group (chaired by the chief medical officer) focused on the roll-out of remote consultations beyond those Diabetes and Cancer Surgery clinics included in the VOCAL study:
And [the director of operations] was saying to me, ‘Look, we’ve got buy-in from the chief medical officer, and from the director of strategy. They want to see this happen.’ And so we sort of talked about who are the kind of key people who we need to involve. And came up with a cast list of individuals that we need to get on board with this. So really it was ICT, who are really important, finance, outpatients – as in the core service – and then each of the sites. So we, we wanted to have kind of a senior lead from each of, each of the sites, to actually drive it forward.
Programme Lead
The outpatient project strategy group (see Action research) was initially focused on supporting the three services in the study, but later extended its remit to include the wider roll-out of virtual consultations across outpatient services. Initially, the roll-out focused on developing virtual consultation services in neurology, rheumatology, haematology and endocrinology, with plans in place to extend this to include cardiology (inherited arrhythmia), urology, lipid clinics and diabetes community services. The work undertaken in the diabetes service since 2011 has been crucial in highlighting the complex challenges of embedding virtual consultation services within routine practice at Barts Health NHS Trust. Ongoing input from the diabetes consultant and programme lead, arguably ‘telehealth champions’,227 also played a role in promoting and legitimating virtual consultations as ‘business as usual’ within the trust and building key relationships.
Collaboration across clinics and staff at Barts Health NHS Trust and the sharing of knowledge and practices have been critical to the development of virtual consultation services to date. Local teams worked collaboratively with one another (e.g. in working through business cases, SOPs and clinical pathways, as they sought to pilot and then embed virtual consultation services, or in identifying unused space that might be used for private Skype clinics), taking account of the need to ensure patient safety and clinical appropriateness, co-evolve the introduction of new technologies and the development of new team roles and processes, and address IG issues and concerns.
The roll-out has also needed to accommodate competing policy priorities locally and nationally, working with national policy-makers, regulators and industry partners to find workable ways forward through close dialogue and practical problem-solving. In practice, this has required cross-departmental collaborations with a number of external partners, including the IGA and NHS England (IG), CCGs (local tariff and outpatient process) and Microsoft UK (providers of technology). For instance, as part of the action research in the VOCAL study, Barts Health NHS Trust has also been working closely with Microsoft to test various options for virtual consultations, while providing the technology provider with the information required to produce more patient- and health-care-friendly tools.
Other departments in the trust have now commenced virtual consultations with apparent success. Progress has been varied, with some ‘moving faster than others’, often driven along by ‘clinicians who are really passionate, and driving it, and they want to see it happen’ [programme lead]. Formal evaluation of this wider roll-out is soon to commence.
Chapter 5 Virtual consultations (micro level)
This chapter focuses on our analysis of the clinician–patient interactions. We present our initial analysis of virtual consultations via Skype within the Adult/Young Adult Diabetes, Antenatal Diabetes, and Hepatobiliary and Pancreatic Cancer Surgery services at Barts Health NHS Trust. We then present a detailed, micro-level analysis of those virtual consultations and comparator face-to-face consultations.
This chapter should be read in conjunction with the methods section on micro-level analysis and use of the RIAS in Chapter 2.
Description of the data set
Obtaining video and audio-recordings of both ends of a virtual consultation raised substantial logistical, technical and ethics challenges. Two researchers were often needed – one to record in the clinic and the other to attend the patient’s home (perhaps many miles away). Patients (and staff) were usually, but not always, happy to have a researcher set up the video camera and then leave the room while the consultation took place. Whereas the pilot phase consultations were relatively easy to set up to include data collection for research (because they were undertaken outside regular clinic hours), once video consultations became ‘business as usual’, it was much harder for staff to find sufficient time to recruit potential research participants and alert the research team to a planned video consultation. In addition, as noted in Evolution of virtual consultation services over the study period, a significant proportion of video consultations in the Adult/Young Adult Diabetes clinic were ad hoc (undertaken spontaneously when the patient sent a SMS Skype message when they saw the clinician was online, or fitted in informally by the clinician as a ‘quick follow-up’); these were impossible to schedule in advance for video recording.
Our target had been to obtain at least 30 high-quality recordings of complete virtual consultations (20 in Diabetes, including Antenatal, and 10 in Cancer Surgery); we also sought to collect a sample of comparator face-to-face consultations. At the end of the study, in July 2017, we had collected recordings of a total of 30 remote and 17 face-to-face consultations (Table 7).
| Clinical service/type of consultation | Value |
|---|---|
| Adult/Young Adult Diabetes (remote) | |
| Total recorded (n) | 12 |
| Male/female (n) | 5/7 |
| Age (years), range (median) | 21–50 (23) |
| Ethnicity (n) | |
| White British | 5 |
| White other | 2 |
| Black Caribbean | 1 |
| Asian Bangladeshi | 1 |
| Asian Indian | 3 |
| Adult/Young Adult Diabetes (face to face) | |
| Total recorded (n) | 6 |
| Male/female (n) | 3/3 |
| Age (years), range (median) | 21–58 (26) |
| Ethnicity (n) | |
| White British | 2 |
| Black Caribbean | 1 |
| Asian Bangladeshi | 2 |
| Asian other | 1 |
| Antenatal Diabetes (remote) | |
| Total recorded (n) | 6 |
| Male/female (n) | 6 F |
| Age (years), range (median) | 30–37 (34) |
| Ethnicity (n) | |
| White British | 1 |
| Asian Bangladeshi | 1 |
| Asian other | 3 |
| Black Caribbean | 1 |
| Antenatal Diabetes (face to face) | |
| Total recorded (n) | 6 |
| Male/female (n) | 6 F |
| Age (years), range (median) | 26–36 (33) |
| Ethnicity (n) | |
| White British | 0 |
| Asian Bangladeshi | 3 |
| Asian other | 1 |
| Asian Indian | 1 |
| Black Caribbean | 1 |
| Cancer Surgery (remote) | |
| Total recorded (n) | 12 |
| Male/female (n) | 4/8 |
| Age (years), range (median) | 55–85 (74) |
| Ethnicity (n) | |
| White British | 9 |
| White other | 1 |
| Asian (Indian) | 1 |
| Black Caribbean | 1 |
| Cancer Surgery (face to face) | |
| Total recorded (n) | 5 |
| Male/female (n) | 3/2 |
| Age (years), range (median) | 45–75 (69) |
| Ethnicity (n) | |
| White British | 2 |
| Asian other | 1 |
| Black Caribbean | 2 |
As detailed in Chapter 2, the RIAS analysis was undertaken on a subset of the data set in which virtual and face-to-face consultations were matched as closely as possible for clinical content and (in all cases) for clinician; the subsample consisted of 12 Antenatal Diabetes consultations (six conducted remotely via Skype and six conducted face to face), 12 Adult/Young Adult Diabetes consultations (six remote and six face to face) and 10 Cancer Surgery appointments (five remote and five face to face). Patients for virtual consultations had been purposefully selected and recruited by the clinician involved, based on their assessment that a virtual consultation would be safe and appropriate. As summarised in Table 7, patients having virtual consultations within the study were more likely to be of white British ethnicity (the same ethnicity as the clinician), but were of a similar age to those having face-to-face consultations. The ethnic differences probably reflected the fact that some Diabetes and Antenatal Diabetes patients were limited English speakers, which was considered to be too risky at this early stage in the evaluation of virtual consultations.
Our initial analysis of the virtual consultation data, based on repeated watching of the merged audio and video streams (which could be viewed in parallel on screen), identified the following five overarching themes (we explore these in more detail below).
Technical set-up and preparation
Virtual consultations usually required a technical set-up phase immediately before the consultation could begin, on both the patient’s and the clinician’s computers, to resolve audio/video issues, connectivity and accessing the application. This often (but not always) involved collaborative interactions to work around unanticipated problems (e.g. ensuring that both parties could see and hear each other) and resolve technical issues (e.g. regarding broadband connection). Sometimes, the technical set-up phase included informal and ad hoc technical assistance from the clinician to the patient (and, in several cases, from the researcher during set-up of the consultation). Technical problems were always either resolved or worked around, with none of the virtual consultations recorded within the study failing or being abandoned as a result of technical issues.
Materiality work
Face-to-face consultations were characterised by shared physical space and material objects; patients and clinicians typically engaged together with numerous physical artefacts as consultations unfolded. For example, in a diabetes consultation, the patient would typically bring a paper diary (or smartphone) with blood glucose readings and share it across the corner of the consulting desk; the clinician might share the paper record with the patient to discuss a test result, or draw a diagram on a scrap of paper to help explain a medical issue. Antenatal patients carried a patient-held paper record.
In remote consultations, patients and clinicians interacted with various artefacts and resources to support dialogue, clinical reasoning and documentation, and in an attempt to overcome a lack of physical co-presence. For instance, our data set included frequent reference to existing electronic and paper records (at both the patient end and the clinician end), interaction with medical devices (e.g. insulin pump), paper or electronic diaries (to schedule or confirm upcoming appointments) and note-taking (e.g. to record an agreed change in insulin dose). Patients and clinicians together developed strategies to overcome the absence of shared physical objects and spaces (e.g. patients read aloud their insulin dosages and blood glucose readings, while the clinician wrote them down on the paper record).
Different kinds of talk
Both face-to-face and remote consultations involved different kinds of talk (see Table 2 in Chapter 2 for a full list of how the RIAS classifies these). For example, we distinguished between task-focused clinical talk (such as exchanging information about the condition and its investigation and treatment, educating the patient) and socioemotional talk (e.g. social conversation, showing concern or reassurance). Our interviews with both patients and clinicians had identified a widespread perception that virtual consultations involved less social ‘chit-chat’ and more task-focused clinical talk than face-to-face consultations, and that this was (in their view) why virtual consultations were typically shorter.
Shared knowledge and common ground
It was clear from our initial analysis of virtual consultations that some flowed better than others and that a small fraction of consultations in our data set appeared to be awkward and disjointed, with parties frequently misunderstanding one another and/or needing to seek clarification. This was an important finding, given the concerns raised by some clinicians and patients that a remote consultation would never (or rarely) achieve the quality of interaction possible in a face-to-face consultation (described by some participants as ‘high bandwidth’). The content and flow of most virtual consultations in our data set appeared to be of high quality, and these features appeared to be related to the degree of shared knowledge and common ground between the patient and clinician. Effective communication seemed to follow from an existing, positive interpersonal relationship.
Interruptions and repair work
Virtual consultations presented new possibilities for interruption during the consultation. This included disruptions related to the technology (e.g. loss of audio quality, an incoming call on the mobile device being used for the consultation), as well as non-technological interruptions in the domestic environment (e.g. visitors or family encroaching on the consultation).
We explored these initial five themes in more depth by focusing on a subset of virtual consultations that were selected because they all focused on the same clinical issue (follow-up of the antenatal patient with diabetes), and comparing these with a sample of face-to-face consultations (also in Antenatal Diabetes). The rationale for selection was that such consultations tended to involve young people with few or no comorbidities, and they followed a standard pattern and did not involve a physical examination. Hence, any differences (in talk and interaction) between face-to-face and virtual consultations were more likely to be attributable to technical and material factors rather than clinical confounders. We later extended the same detailed analysis to the other consultations in our data set.
The hypothesis-driven questions we derived from our initial analysis of Antenatal Diabetes consultations were as follows:
-
Question 1: are virtual consultations (which are perceived by clinicians and patients to be shorter and more ‘to the point’) actually shorter and more task oriented?
-
Question 2: how do virtual consultations differ from face-to-face ones in the kind of talk that occurs (apart from technology-related talk)? To what extent can these differences be explained by technical and material influences?
-
Question 3: what kinds of technology-related talk occur in virtual consultations?
-
Question 4: do remote consultations contain more breaches in conversation (e.g. requiring checking of understanding, repairs and so on) than face-to-face ones? What characterises those consultations that have a high proportion of such breaches? To what extent do ‘shared knowledge and common ground’ protect against such breaches?
-
Question 5: how do interruptions (technical, domestic) impact on the flow of conversation in virtual consultations?
To address these questions, we then applied the RIAS, as described in the micro-level analysis section in Chapter 2.
Findings from our analysis using the Roter interaction analysis system
In the VOCAL study, we found that the RIAS proved to be useful in highlighting the different kinds of talk in virtual consultations and exploring how the technology influenced, and was influenced by, the interactions and dynamics between patients and clinicians.
In order to interpret the RIAS analysis, a broad understanding of the categories is needed (see Table 2 for a detailed breakdown). In summary, guided by the RIAS and additional work applying the coding framework to telemedicine,175 all talk and behaviour in virtual consultations in the VOCAL study were classified according to the following categories:
-
socioemotional (broadly capturing talk related to social etiquette, indicating interest or understanding, concerns or attempts to reassure and negative talk)
-
task focused (broadly capturing talk to instruct or guide, question-asking, information-giving, checking for understanding, requests and counselling in the form of giving instruction or advice to the patient)
-
process oriented (relating to verbal interactions aimed at supporting the flow and direction of the conversation)
-
technology related (any of the above, but relating specifically to the technology and/or its use).
The results presented below are based on a detailed micro-level analysis of 34 consultations in three different clinical contexts to explore how the use of Skype for virtual consultations affects the interaction and dialogue of the medical encounter. This includes 12 Antenatal Diabetes consultations (six conducted remotely via Skype and six conducted face to face), 12 Adult/Young Adult Diabetes consultations (six remote and six face to face) and 10 Cancer Surgery appointments (five remote and five face to face). The consultations were all follow-up appointments after the patient had met the clinician at least once. In the Antenatal Diabetes context, that appointment took place approximately 1 week beforehand to establish a schedule for insulin dosing. In the Adult/Young Adult Diabetes clinic, the consultation formed part of a routine 6-monthly review to discuss the patient’s condition, recent test results and treatment plan. For the Cancer Surgery, the consultation formed part of the follow-up assessment of the patient’s postoperative recovery and review of medical tests (blood tests, CT scans) and symptoms (the follow-up interval varied from 3 to 6 months). Virtual and face-to-face consultations in the data set for each clinic all involved the same clinician (i.e. a consultant diabetologist specialising in the care of pregnant women in the antenatal context, a different consultant diabetologist in the adult diabetes context, and a surgeon and a nurse specialist combined in the Cancer Surgery context).
As detailed in Chapter 2, patients for virtual consultations had been purposefully selected and recruited by the clinician involved, based on their assessment that a virtual consultation would be safe and appropriate. The face-to-face comparisons were selected based on the similarity of the consultation (stage of treatment, purpose of appointment) and the clinician’s judgement that they would also have been suitable for the remote consultation option. As summarised in Table 7, patients having virtual consultations were more likely to be of white British ethnicity (the same ethnicity as the clinician), but were of a similar age to those having face-to-face consultations. The ethnic differences probably reflected the fact that some Diabetes and Antenatal Diabetes patients were limited English speakers, which was considered too risky at this early stage in the evaluation of virtual consultations.
Question 1: are virtual consultations shorter and more ‘to the point’ than face-to-face ones?
Consultation length (defined by the RIAS as frequency of utterances) was shorter for virtual consultations than face-to-face consultations across all three clinical settings. There was a small difference in consultation length in the Adult/Young Adult Diabetes service, with virtual consultations being slightly shorter in terms of the number of utterances for virtual consultations [median = 337, interquartile range (IQR) = 112.5] than face-to-face consultations (median = 366, IQR = 93.8), and in terms of duration (19:40 minutes vs. 20:10 minutes). These differences were not statistically significant for length (U = 10.0; p = 0.20) or duration (U = 18.0; p = 0.10). In the antenatal setting, there was little difference in the length of virtual consultations (median = 167, IQR = 125.5) and face-to-face consultations (median = 168, IQR = 76.3). The duration of consultations measured in minutes showed virtual consultations to be slightly shorter (7:38 minutes) than face-to-face consultations (8:13 minutes), although this difference did not reach statistical significance (U = 15.0; p = 0.63). In the Cancer Surgery clinic, virtual consultations were non-significantly shorter in duration (11:50 minutes for remote consultations vs. 19:40 minutes for face-to-face consultations, U = 6.0; p = 0.23) and had a (non-significantly) lower number of utterances (median = 192, IQR = 69.5) than face-to-face consultations (median = 217, IQR = 142.5, U = 9.0; p = 0.47).
A consultation that is ‘to the point’ would focus predominantly (although certainly not exclusively) on task-oriented clinical talk. Figures 9–11 show the overall proportion of types of talk for virtual and face-to-face consultations across the three clinics, according to the coded RIAS clusters. Taken together, they show that, aside from a small proportion of time spent on technology-related matters in virtual consultations, the proportions of talk were very similar across both kinds of consultation – although this may be partly attributable to the fact that the patient samples for virtual and face-to-face consultations were closely matched for type of condition and type of appointment. As noted above, the ad hoc consultations (which addressed a very different patient group – ‘hard to reach’, with unstable or complex needs, and/or seeking urgent input from the clinician) were not captured in our micro-level data set.
FIGURE 9.
Types of talk in the Adult/Young Adult Diabetes clinic. (a) Virtual consultations; and (b) face-to-face consultations.

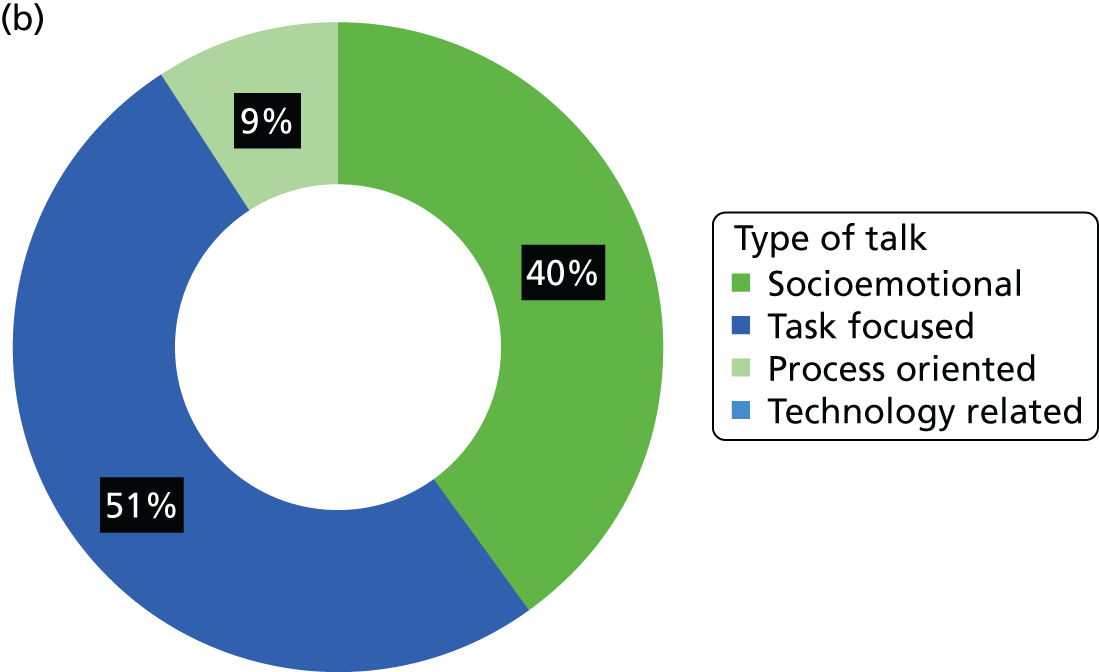
FIGURE 10.
Types of talk in Antenatal Diabetes. (a) Virtual consultations; and (b) face-to-face consultations.
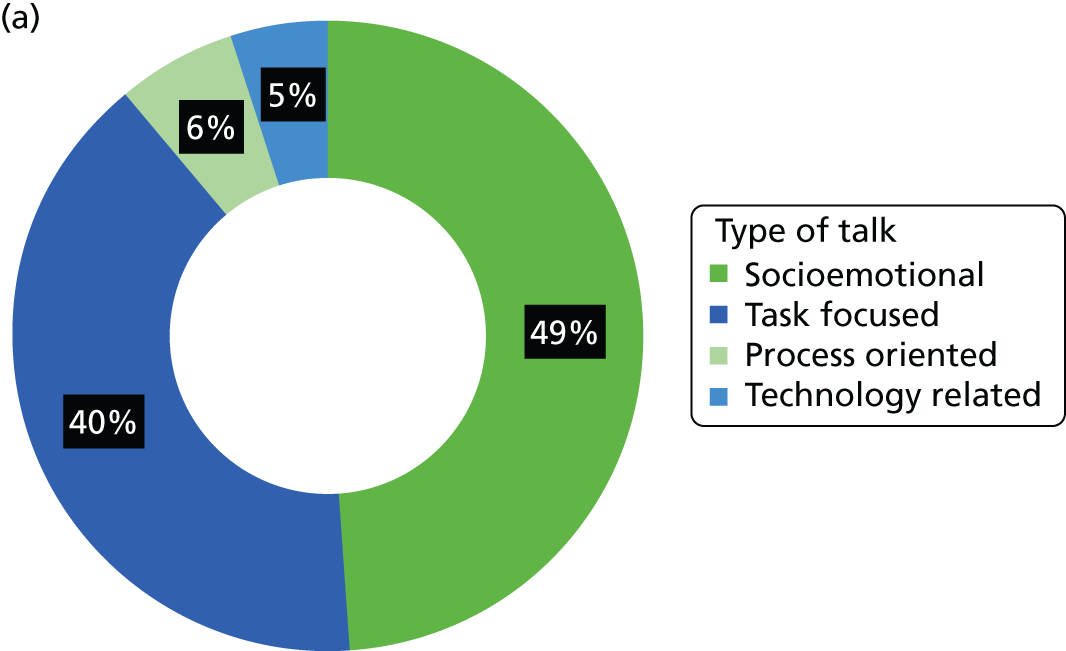
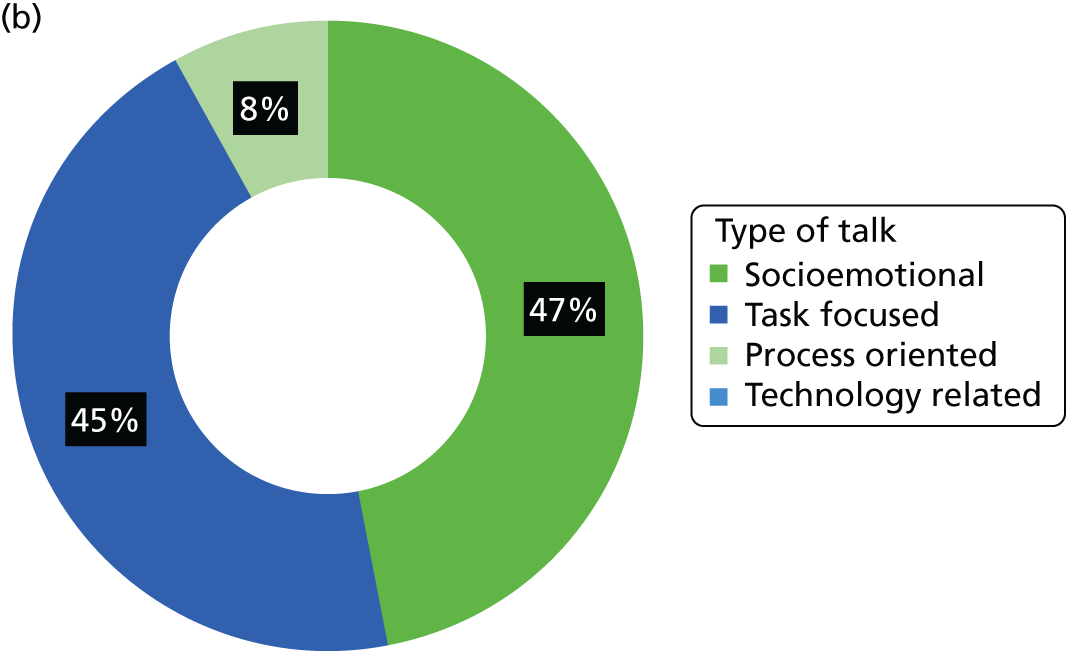
FIGURE 11.
Types of talk in Cancer Surgery. (a) Virtual consultations; and (b) face-to-face consultations.
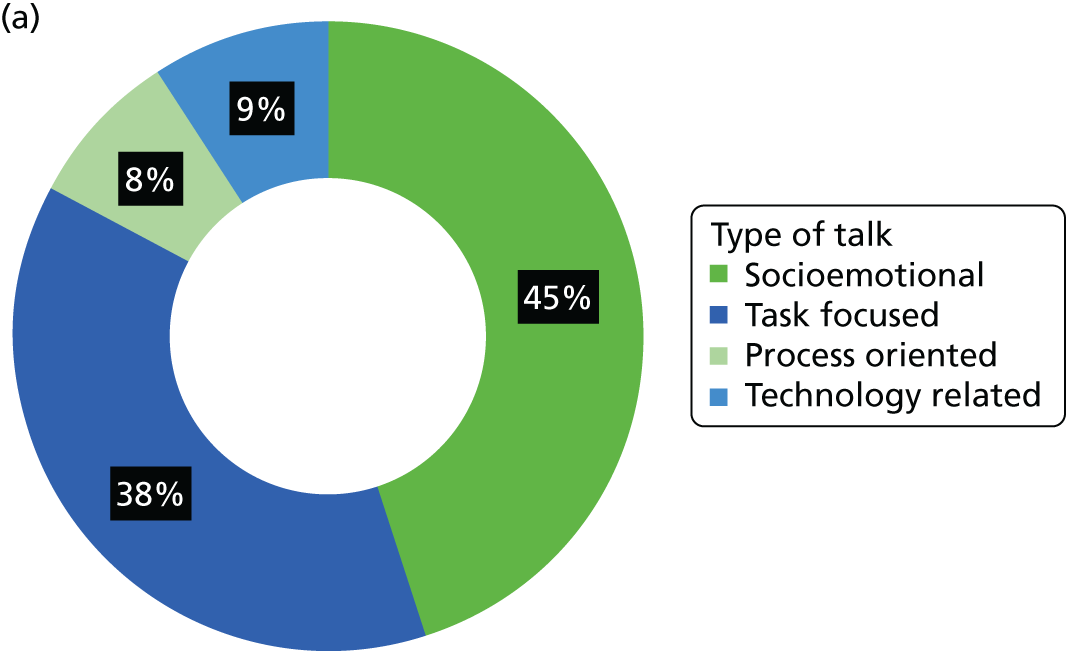

These proportions are illustrated in more detail for the three clinics in Tables 8–10, which compare the frequencies of socioemotional talk, task-focused clinical talk, process talk and technology-related talk in virtual and face-to-face consultations.
| RIAS categories | Talk in each type of consultation, median (IQR) | |||||
|---|---|---|---|---|---|---|
| Remote | Face to face | |||||
| Clinician talk | Patient talk | Total | Clinician talk | Patient talk | Total | |
| Socioemotional | 72 (26.5) | 55 (34.0) | 120 (51.5) | 54 (30.0) | 88 (71.8) | 117 (71.0) |
| Social behaviour | 15 (12.8) | 11 (8.8) | 26 (22.0) | 19 (14.0) | 18 (24.5) | 36 (37.3) |
| Verbal attentiveness | 25 (16.0) | 27 (8.3) | 50 (20.0) | 21 (9.3) | 49 (26.0) | 65 (44.3) |
| Concern/reassurance | 22 (8.8) | 18 (29.8) | 39 (35.5) | 19 (20.0) | 8 (13.5) | 31 (24.0) |
| Negative talk | 0 (1.3) | 0 (0.3) | 0 (1.5) | 0 (2.5) | 2 (6.5) | 2 (8.3) |
| Task focused | 82 (38.8) | 82 (49.8) | 170 (53.5) | 122 (24.5) | 74 (34.3) | 206 (4.5) |
| Asking questions | 24 (23.5) | 1 (4.0) | 25 (20.5) | 30 (22.3) | 1 (2.0) | 33 (22.5) |
| Information-giving | 44 (21.0) | 80 (49.5) | 129 (59.0) | 66 (15.3) | 68 (54.3) | 141 (44.8) |
| Counselling | 5 (4.0) | N/A | 5 (4.0) | 13 (7.8) | – | 13 (7.8) |
| Requests | 12 (13.0) | 0 | 12 (13.0) | 15 (7.0) | 1 (2.3) | 15 (7.0) |
| Process oriented | 31 (21.5) | 3 (4.0) | 35 (21.5) | 29 (8.3) | 7 (9.5) | 35 (11.8) |
| Direction | 12 (8.5) | 1 (3.5) | 12 (7.5) | 10 (11.8) | 2 (2.8) | 12 (11.5) |
| Check understanding | 18 (13.5) | 2 (3.3) | 22 (13.3) | 18 (7.3) | 5 (6.8) | 23 (9.0) |
| Technology related | 1 (6.0) | 1 (2.8) | 2 (8.8) | – | – | – |
| Socioemotional | 0 (1.5) | 0 (1.0) | 0 (2.5) | – | – | – |
| Task focused | 0 (0.5) | 0 (0.3) | 0 (0.8) | – | – | – |
| Process oriented | 1 (3.0) | 0 (1.8) | 2 (4.0) | – | – | – |
| Total | 181 (42.3) | 143 (84.3) | 337 (112.5) | 204 (38.8) | 173 (82.5) | 366 (93.8) |
| RIAS categories | Talk in each type of consultation, median (IQR) | |||||
|---|---|---|---|---|---|---|
| Remote | Face to face | |||||
| Clinician talk | Patient talk | Total | Clinician talk | Patient talk | Total | |
| Socioemotional | 35 (44.5) | 38 (39.0) | 74 (80.8) | 43 (24.8) | 36 (26.0) | 83 (38.0) |
| Social behaviour | 7 (4.8) | 5 (3.3) | 12 (8.3) | 7 (2.3) | 4 (3.3) | 12 (4.5) |
| Verbal attentiveness | 21 (25.3) | 25 (5.0) | 46 (57.0) | 17 (16.8) | 26 (19.5) | 34 (49.3) |
| Concern/reassurance | 10 (9.8) | 8 (13.0) | 20 (16.0) | 18 (9.5) | 6 (5.8) | 27 (14.5) |
| Negative talk | 0 (0.3) | 0 (0.8) | 0 (1.0) | 0 | 0 | 0 |
| Task focused | 37 (27.5) | 29 (19.0) | 66 (48.5) | 42 (22.3) | 23 (24.2) | 73 (30.2) |
| Asking questions | 7 (7.3) | 3 (2.5) | 11 (5.8) | 10 (3.8) | 3 (1.8) | 12 (4.8) |
| Information-giving | 16 (20.3) | 21 (19.5) | 42 (26.0) | 20 (12.3) | 18 (13.8) | 40 (34.8) |
| Counselling | 5 (3.5) | – | 5 (3.5) | 5 (6.0) | – | 5 (6.0) |
| Requests | 6 (5.0) | 0 | 6 (5.0) | 11 (7.5) | 1 (1.8) | 13 (7.5) |
| Process oriented | 6 (8.0) | 2 (2.5) | 8 (10.3) | 11 (12.8) | 1 (2.8) | 14 (13.3) |
| Direction | 2 (1.5) | 1 (2.0) | 3 (3.0) | 8 (8.8) | 0 (0.3) | 8 (8.0) |
| Check understanding | 5 (6.3) | 2 (4.0) | 7 (10.3) | 4 (3.5) | 1 (2.5) | 6 (6.3) |
| Technology related | 5 (6.3) | 3 (3.5) | 7 (9.0) | – | – | – |
| Socioemotional | 2 (3.3) | 2 (3.0) | 4 (3.3) | – | – | – |
| Task focused | 1 (3.3) | 0 (1.0) | 1 (4.0) | – | – | – |
| Process oriented | 2 (1.3) | 1 (1.3) | 3 (2.5) | – | – | – |
| Total | 89 (66) | 77 (59.5) | 167 (125.5) | 103 (38.8) | 69 (51.3) | 168 (76.3) |
| RIAS categories | Talk in each type of consultation, median (IQR) | |||||
|---|---|---|---|---|---|---|
| Remote | Face to face | |||||
| Clinician talk | Patient talk | Total | Clinician talk | Patient talk | Total | |
| Socioemotional | 23 (46.5) | 35 (34.5) | 77 (35.0) | 31 (39.0) | 49 (38.0) | 71 (72.5) |
| Social behaviour | 6 (12.0) | 10 (16.0) | 13 (26.0) | 7 (14.0) | 7 (24.0) | 12 (36.0) |
| Verbal attentiveness | 12 (27.5) | 19 (20.0) | 46 (19.0) | 15 (17.0) | 23 (14.5) | 39 (21.5) |
| Concern/reassurance | 7 (7.0) | 9 (6.0) | 12 (11.0) | 5 (11.5) | 6 (11.5) | 9 (21.5) |
| Negative talk | 0 | 0 (0.5) | 0 (0.5) | 0 (0.5) | 1 (2.5) | 2 (2.5) |
| Task focused | 42 (40.5) | 33 (26.5) | 73 (39.0) | 70 (38.5) | 35 (44.5) | 114 (63.0) |
| Asking questions | 9 (6.5) | 2 (9.5) | 13 (12) | 17 (10.0) | 2 (11.0) | 28 |
| Information-giving | 23 (29.5) | 17 (28.5) | 56 (32.5) | 39 (29.5) | 36 (46.0) | 75 (45.0) |
| Counselling | 0 (1) | – | 1 | 1 (10.0) | – | 1 |
| Requests | 4 (6.5) | 0 (1.0) | 4 (7.5) | 4 (8.5) | 0 (0.5) | 4 (9.0) |
| Process oriented | 9 (14.5) | 5 (6.5) | 15 (20.5) | 19 (16.5) | 4 (5.5) | 23 (21.0) |
| Direction | 8 (12.5) | 2 (3.0) | 10 (15.5) | 8 (9.5) | 1 (2.5) | 9 (9.5) |
| Check understanding | 2 (2.5) | 3 (4.0) | 5 (5.0) | 8 (10.5) | 3 (5.0) | 10 (14.0) |
| Technology related | 8 (8.5) | 4 (13.5) | 12 (22.0) | – | – | – |
| Socioemotional | 3 (4.0) | 3 (9.0) | 6 (13) | – | – | – |
| Task focused | 1 (3.0) | 1 (1%) | 2 (5.5) | – | – | – |
| Process oriented | 3 (4.5) | 1 (2.5) | 3 (6.0) | – | – | – |
| Total | 108 (48.5) | 84 (21.0) | 192 (69.5) | 137 (62.5) | 72 (57.5) | 217 (142.5) |
Across the three clinics, the most common kinds of talk for clinicians and patients in both face-to-face and virtual consultations were verbal attentiveness and information-giving.
Clinicians exhibited more socioemotional talk in virtual consultations than face-to-face consultations, which challenges the hypothesis that virtual consultations are perhaps more ‘to the point’.
The dominance of talk (i.e. who spoke more) was calculated by dividing the number of utterances for clinician talk by the number of utterances for patient talk. In the Adult/Young Adult Diabetes consultations, clinician dominance was the same in face-to-face (median = 1.2, IQR = 0.7) and virtual consultations (median = 1.2, IQR = 0.6). In the Antenatal Diabetes clinic, consultations were slightly clinician-dominated, but less so for virtual consultations (median = 1.2, IQR = 0.3) than face-to-face consultations (median = 1.7, IQR = 0.5) – a difference that was statistically significant (U = 3.5; p = 0.018). The Hepatobiliary and Pancreatic Cancer Surgery clinic showed a greater level of clinician dominance for face-to-face consultations (median = 1.4, IQR = 0.5) than for virtual consultations (median = 1.3, IQR = 1.8), but this was not statistically significant (U = 10.0; p = 0.59). The one difference that was statistically significant was probably attributable to the fact that patients in virtual Antenatal Diabetes consultations spent some time reading out their blood glucose results to the clinician.
There was no significant difference between virtual and face-to-face consultations in ‘directedness’ (what the RIAS calls the ratio of clinician-to-patient ‘control’ over the consultation, and which was calculated by dividing the patient’s biomedical questions and biomedical information from the clinician by the clinician’s closed questions, directions and biomedical information from the patient). The average directedness score was 0.82 for face-to-face consultations and 0.83 for virtual consultations in the Antenatal Diabetes setting, 0.5 for face-to-face consultations and 0.7 for virtual consultations in the Adult/Young Adult setting, and 0.9 for face-to-face consultations and 1.0 for virtual consultations in the Cancer Surgery follow-up setting (none of these differences was statistically significant). These figures suggest that differences in directedness between clinical conditions (and linked to a particular clinician’s style of consulting) appear to be far greater than any differences associated with the virtual technology.
Question 2: how do virtual consultations differ from face-to-face ones in the kind of non-technology talk that occurs?
The main finding from our RIAS analysis was that broadly similar kinds of talk occurred in similar proportions in virtual and face-to-face consultations. To explore that in finer detail, we removed ‘technology talk’ from the analysis and compared a broader range of categories of talk across patient and clinician talk in virtual and face-to-face consultations. The findings are presented in Figure 12.
FIGURE 12.
Total patient and clinician talk, with technology talk removed from remote consultations. (a) Remote consultations; and (b) face-to-face consultations.
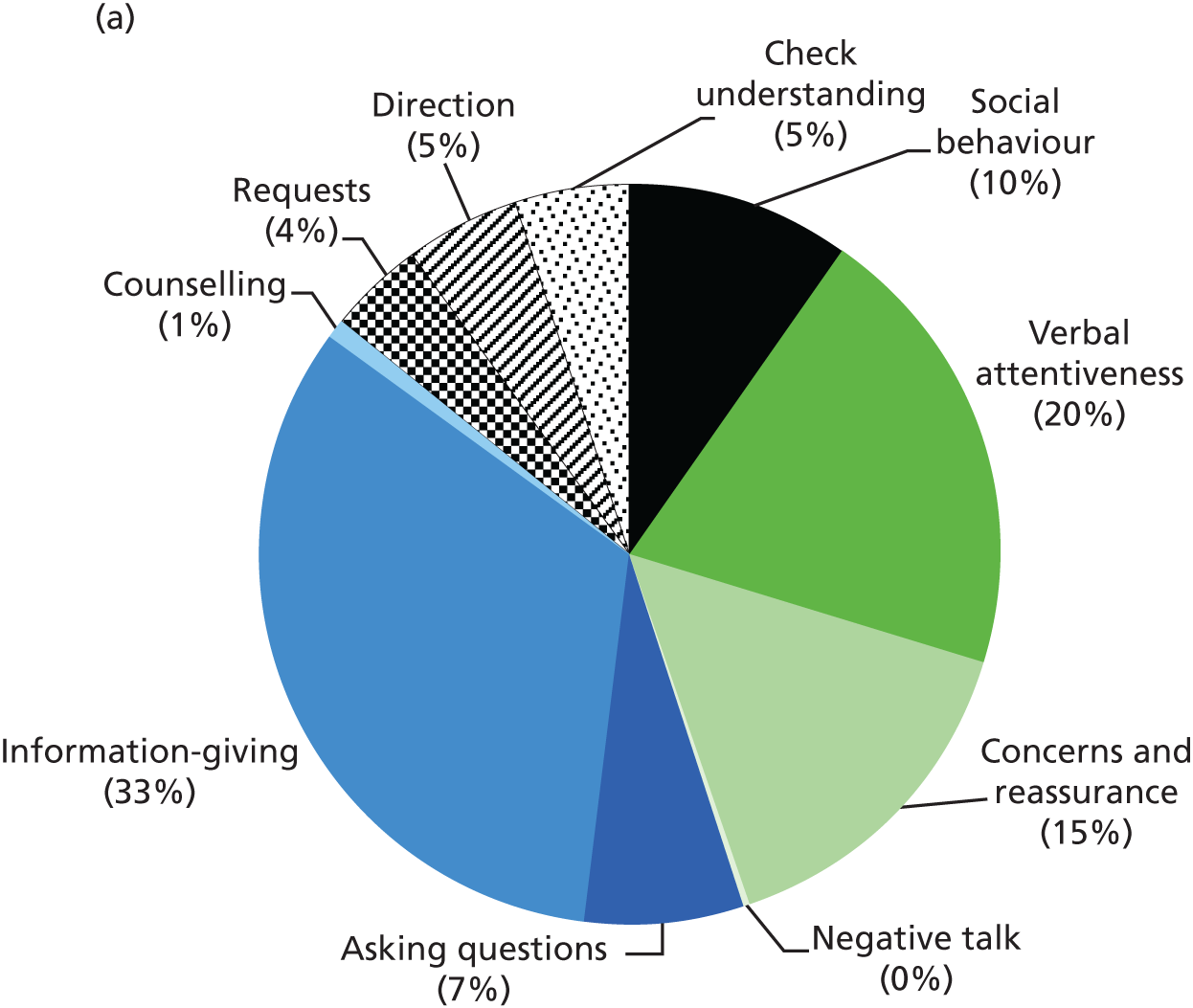

Notwithstanding the small sample size (which could have concealed real differences between the two modes of consulting) and excluding technology-related talk, the only significant differences that emerged related to the following areas: ‘personal talk’ (constituent category for ‘social behaviour’); ‘verbal attentiveness’ (a subcategory of socioemotional talk); direction and orientation (subcategories of process talk); counselling, requests and exchanging and sharing information (subcategories of clinical task-oriented talk); pauses and silence; and achieving closure. We consider these in turn.
Social behaviour and personal talk
Across all clinical settings, the number of utterances related to the social behaviour category was slightly higher for virtual consultations (median = 17, IQR = 15.5) than face-to-face consultation settings (median = 14, IQR = 31.5), but there was no significant difference across the 34 cases (U = 138.5; p = 0.84.) Analysis of the subcategories within this cluster revealed a significantly higher proportion of utterances for ‘personal talk’ (e.g. ‘hello’, ‘how are you’?) during virtual consultations (median = 9, IQR = 4.0) than during face-to-face consultations (median = 4, IQR = 5.8) in the antenatal setting only (U = 4.0, p = 0.02). This difference may be partly explained by the fact that the initial interaction between the patient and the clinician in face-to-face encounters is done in the waiting area and during the walk to the consultation room (in other words, the difference was probably spurious). There was very little ‘chit-chat’ in either virtual consultations or face-to-face consultations in this context of Antenatal Diabetes follow-up. This may have been because of high patient numbers – a clinician typically saw 30–35 patients per clinic – and to the likely absence of an established or prolonged relationship (since most patients had recently diagnosed gestational diabetes). Personal talk in this context largely consisted of social gestures and niceties (e.g. ‘how are you?’, ‘bye’, ‘see you soon’), rather than social conversation. For instance, establishing a Skype connection (and ‘popping up’ on each other’s computer screens) would sometimes lead to laughter, greetings and waving.
Verbal attentiveness
Across the three clinics, clinicians presented more verbal attentiveness talk (in the form of agreement and back-channelling) for virtual consultations (median = 24, IQR = 20.5) than for face-to-face consultations (median = 17, IQR = 14.0), but this difference was not statistically significant (U = 115.0; p = 0.31). Conversely, patients presented more verbal attentiveness in face-to-face consultations (median = 37, IQR = 26.0) than in virtual consultations (median = 26, IQR = 14.0), which was statistically significant (U = 87.5; p = 0.02). The change in proportion of verbal attentiveness may be an artefact of the difference in talk dominance (see the discussion in Question 1: are virtual consultations shorter and more ‘to the point’ than face-to-face ones?) and also indicates (through the higher proportion of clinician back-channel talk) that the patient is more likely to take the floor and lead on information provision when communicating virtually.
Direction and orientation
Clinicians gave more direction talk during face-to-face consultations (median = 8, IQR = 9.0) than during remote consultations (median = 6, IQR = 11.5), but this difference was not found to be significant (U = 98.0; p = 0.11). However, analysis of the different clinic settings showed that the clinician in the antenatal setting did present significantly more direction talk during face-to-face consultations (median = 8, IQR = 8.8) than during virtual consultations (median = 2, IQR = 1.5, U = 0.05; p = 0.01). Analysis of the subcategories showed that this difference was attributable to a significantly higher occurrence of ‘transition’ statements by the clinician during face-to-face consultations in the Antenatal Diabetes setting (median = 7, IQR = 2.8) than that in remote consultations (median = 1, IQR = 1.8, U = 0.5; p = 0.01). For example, during face-to-face consultations, the clinician played a more active role using placeholder statements (e.g. ‘Right, let’s take a look [at your maternity folder]’, ‘Hang on, I’m just going to get the nurse to take a look at your rash’). These differences were unsurprising, and probably relate to the different physical environments, material artefacts and staff availability in the different types of consultation.
During face-to-face consultations in the Antenatal Diabetes clinic, patients did not use any talk that could be coded as giving direction, orientation or instruction. In contrast, in some virtual consultations, the patient did give direction or instruction. Much of this talk related to the patient’s role in communicating their blood glucose readings to the clinician over Skype and writing the details in their maternity folder (e.g. referring to their own notes or getting a pen to write things down). However, this difference in ‘direction’ talk was not statistically significant (U = 11; p = 0.18).
Counselling
Although not statistically significant (U = 108.0; p = 0.22), the proportion of ‘counselling talk’ from clinicians was greater during face-to-face consultations (median = 5, IQR = 11.0) than during virtual consultations (median = 4, IQR = 5.5), across all clinical settings. The reasons for this difference varied depending on the clinical context. In the diabetes setting, the clinician often had direct access to the patient’s notes on blood sugar readings and their insulin pumps, which may have facilitated a dialogue on managing their condition. During some of the Cancer Surgery clinics, the clinician conducted a physical examination of the patient if they reported any pain or symptoms, which may explain the higher levels of education and counselling talk in that setting.
Requests
In the Antenatal Diabetes setting, requests (asking for something) were significantly more frequent during face-to-face consultations (median = 13, IQR = 7.5) than during virtual ones (median = 6, IQR = 5.0, U = 4.0; p = 0.02). This difference was accounted for almost entirely by a higher rate of the clinician asking the patient to confirm their understanding in face-to-face consultations (median = 8, IQR = 3.0) than that in virtual consultations (median = 2, IQR = 4.5), which was found to be statistically significant (U = 2.0; p = 0.01). The majority of this talk was characterised by an inflected word or phrase (e.g. ‘Okay?) that invited the patient to indicate their understanding following an ‘information-giving’ or ‘counselling’ statement. Some face-to-face consultations involved the patient requesting a prescription (note that unless the patient and clinician were co-located, it would not be possible for the patient to obtain a printed and signed prescription, and electronic prescriptions were not in use in this setting).
Asking questions
The proportion of question-asking from clinicians in each of the clinics was similar for virtual and face-to-face consultations. However, in the Antenatal Diabetes setting, there were significant differences with regard to open versus closed medical questions. Closed questions included direct questions seeking specific information, whereby short responses are generally the only response options (e.g. ‘Are you just taking one tablet of the metformin?’). Open questions were characterised by their non-specificity and/or probing intent (e.g. ‘How was the scan?’). Most clinician questions in virtual consultations were open ended (median = 2, IQR = 3.8) as opposed to closed (median = 1, IQR = 3.0). In face-to-face consultations, the opposite was the case; the median number of open-ended questions was 2 (IQR = 1.3), and the median number of closed questions was 4 (IQR = 2.5). The higher occurrence of closed medical questions in virtual consultations was statistically significant (U = 5.5; p = 0.04). These differences in the occurrence of open and closed questions appeared to be largely attributable to the differences in the spatial and material aspects of consultations. In particular, the maternity folder could be shared and viewed by the clinicians during face-to-face appointments, whereas virtual consultations relied on the patient to verbally represent and summarise this information – often in response to questions from the clinician.
Sharing information
Tables 11–13 show a breakdown of the information shared between patients and clinicians in virtual and face-to-face consultations across the three clinical settings. In the RIAS, medical information relates to statements of fact or opinion relating to the medical condition, symptoms, diagnosis, prognosis, past tests, test results and medical background of the patient. Therapy information relates to statements of fact or opinion regarding the ongoing or future (beginning with this visit) treatment plan, such as information relating to medications used or drug regimen. Lifestyle information relates to statements of fact or opinion relating to lifestyle (smoking, diet, sleep, alcohol and exercise habits), family and home situations, work or employment, health habits and self-care issues. Psychosocial information relates to concerns or problems such as stress, feelings and emotions, values and beliefs. Other information relates to talk that does not fall into the other categories, and includes neutral statements about the consultation (e.g. ‘today’s date is . . .’).
| Information | Type of consultation | |
|---|---|---|
| Virtual | Face to face | |
| Medical condition | ||
| Clinician | 9 (10.0) | 16 (16.0) |
| Patient | 26 (27.0) | 31 (23.0) |
| Therapy | ||
| Clinician | 24 (17.8) | 39 (10.0) |
| Patient | 18 (14.5) | 26 (15.0) |
| Lifestyle | ||
| Clinician | 0 (1.25) | 1 (2.3) |
| Patient | 10 (20.3) | 8 (7.0) |
| Psychosocial | ||
| Clinician | 0 1 (1.5) | 1 (2.0) |
| Patient | 5 (17.3) | 5 (7.0) |
| Other | ||
| Clinician | 1 (4.8) | 5 (6.0) |
| Patient | 6 (8.5) | 6 (14.5) |
| Information | Type of consultation | |
|---|---|---|
| Virtual | Face to face | |
| Medical condition | ||
| Clinician | 5 (1.8) | 4 (6.8) |
| Patient | 16 (16) | 12 (8.8) |
| Therapy | ||
| Clinician | 15 (19.0) | 11 (11.3) |
| Patient | 2 (4.0) | 4 (3.5) |
| Lifestyle | ||
| Clinician | 1 (2.3) | 1 (2.0) |
| Patient | 1 (2.3) | 3 (9.5) |
| Psychosocial | ||
| Clinician | 1 (1.3) | 1 (1.0) |
| Patient | 1 (1.3) | 0 (1.0) |
| Other | ||
| Clinician | 1 (2.5) | 0 (2.0) |
| Patient | 1 (2.3) | 0 (1.3) |
| Information | Type of consultation | |
|---|---|---|
| Virtual | Face to face | |
| Medical condition | ||
| Clinician | 11 (14.0) | 12 (11.5) |
| Patient | 8 (21.5) | 13 (19.5) |
| Therapy | ||
| Clinician | 12 (19.5) | 21 (22.5) |
| Patient | 6 (13.5) | 7 (12.5) |
| Lifestyle | ||
| Clinician | 0 | 0 (1) |
| Patient | 1 (2.5) | 2 (6.5) |
| Psychosocial | ||
| Clinician | 0 (0.5) | 1 (3.0) |
| Patient | 2 (5.0) | 1 (3.5) |
| Other | ||
| Clinician | 0 | 2 (4.0) |
| Patient | 1 (1.5) | 2 (6.0) |
Although there was much information shared in virtual and face-to-face consultations, the kinds of information shared differed across clinics. In the Antenatal Diabetes service, there was a higher proportion of information-giving talk from the clinician in virtual consultations (88%) versus face-to-face consultations (65%) about therapeutic regime – perhaps because instructions and advice that could remain implicit in a face-to-face interaction were made explicit (or explained in more detail or repeated) in the virtual interaction. A far smaller proportion of clinician information-giving related to lifestyle (4% compared with 0.3%) or psychosocial issues (4% compared with 0.2%) in virtual consultations. This may have been a result of the clinician having direct access to the patient’s medical information (blood glucose readings, insulin doses) and being able to direct questions to broader health-related issues in face-to-face consultations. In contrast, virtual consultations often required the verbal exchange of medical information, with the patient providing more information about their medical condition.
Patients took on a greater role in providing medical information during virtual consultations, mainly in order to convey the data they had collected to the clinician. The verbalisation of patient-generated data resulted in a greater level of affective talk on the part of the patient (e.g. optimism or concern about their blood glucose readings) in the virtual setting than in the face-to-face setting, although the differences did not reach statistical significance.
These differences in the types of talk across the different clinical settings were not statistically significant.
Examples of differences in information-sharing are given in Tables 14 (for a face-to-face consultation) and 15 (for a virtual consultation). In the exchange in Table 14, the clinician views the patient’s blood glucose results and insulin dosages (which are not verbalised by either party), as well as the result of an ultrasound scan. Her talk is mostly focused on commenting on these results and suggesting a change in treatment. In contrast, much of the talk in the virtual consultation (see Table 15) consists of the patient reading out both her blood glucose results and her (varying) insulin dosages from her own record and expressing concern about the former, while the clinician records the patient’s readings on paper in the clinic before commenting and suggesting a change in treatment.
| Speaker | Questioning/information-sharing |
|---|---|
| Clinician and patient sit together with the maternity folder open on the clinician’s desk, including written blood glucose readings and insulin levels | |
| Doctor | Great, so . . . So we’ve met before |
| And you are, 30 weeks? | |
| Patient | Yes, 30 weeks |
| Doctor | Great |
| And you are taking insulin and metformin? | |
| Patient | Yes |
| [0.19] | |
| And you had a scan 2 weeks ago? | |
| Patient | Yes, 2 weeks |
| Doctor | It looks good |
| Patient | Yes, this month |
| Doctor | Fine |
| [0.16] | |
| Brilliant. How have the sugars been? | |
| Patient | Sometimes controlled, sometimes a little bit up |
| Doctor | Ok, all right |
| Patient | I increased, a little bit, my insulin |
| Doctor | Perfect. In fact I wonder if you can go up just a little bit more |
| I wonder about 8. How would you feel? Or even 9 | |
| Speaker | Questioning/information-sharing |
|---|---|
| Doctor | Now how have your sugars been since I saw you on Friday? |
| Patient | Not great to be honest |
| Doctor | OK |
| Patient | So, what was Friday’s date, it was 14th wasn’t it |
| And you [. . .] | |
| To be fair, after I left you we had Chinese and we had dim sum and I thought we made some fairly OK choices but apparently not because my sugars was 11.9 | |
| Doctor | Yep |
| Patient | And then after dinner it was 10.4 |
| Doctor | Yep |
| Patient | Erm, and then |
| The following day, it was 28 | |
| So the insulin I took was 28, 2834, 34 | |
| Doctor | Yep |
| Patient | And I misread the . . . It was supposed to be 30 after dinner, or 32 after dinner, and I misread it as 34 so I just took that |
| OK | |
| And my numbers were 7.2, 7.2, 8.3 and 6.9 | |
| Doctor | Lovely, OK |
| Yep | |
| Patient | And then the following day |
| I took 28, 30, 30, 34 | |
| Doctor | Yep |
| Patient | And my numbers were 6.8 |
| Doctor | Yep |
| Patient | 8.4, 7.8 and 8.5 |
| Doctor | Yep |
| Patient | So again, not ideal |
Pauses and silence
There were significantly more pauses (a silence of 2 seconds or more) during face-to-face consultations (median = 3, IQR = 4.5) than during virtual consultations (median = 0.0, IQR = 1.0, U = 58.5; p = 0.002). The reasons for this were not immediately apparent. However, it is noteworthy that many of the pause events involved the clinician interacting with paper materials (e.g. reading and writing clinical notes) and interacting with the computer (e.g. accessing the EPR, checking appointment schedules). It is possible that the shared physical presence in face-to-face consultations allows such activities to be implicitly understood and made aware of (e.g. a patient may stop talking if the clinician turns to the computer). In virtual consultations, in contrast, it appears that the clinician may need to indicate their action through transition talk (e.g. ‘I will just check your appointment time on the computer’) or the patient may continue to talk while the clinician views the information on their screen.
Closing the consultation
The closing phase of virtual consultations was usually clearly defined and always marked the end of the appointment. In contrast, in face-to-face consultations, the clinician often directed the patient to the reception desk or asked them to wait for one of the nurses (e.g. to address additional clinical concerns). Hence, the end of a face-to-face appointment was often less clearly defined and ‘closing’ comments or social gestures were less appropriate.
Because the virtual Antenatal Diabetes service was still at a pilot stage during this research, the closing phase typically also included making a new appointment, as illustrated in Table 16. Such interactions (which contrasted with appointment-booking in the main diabetes clinic) illustrate how the remote service was not fully embedded in the ‘business as usual’ of the Antenatal Diabetes clinic.
| Speaker | Discussion |
|---|---|
| Doctor | I’ll tell you what, do you want – cause I’m away next week would you like to Skype again on Friday? |
| Before I go away | |
| Patient | On Friday? OK. Yep |
| What – | |
| Doctor | Would you be free on Friday afternoon by any chance? |
| Patient | That’s fine, what time? |
| Doctor | Do you have a preference? |
| Patient | I don’t |
| Doctor | Um, OK well I’ll be doing clinic in the morning |
| I’m just checking my diary | |
| Patient | OK |
| Doctor | Um |
| [0.7] | |
| So what I could do is aim to Skype you at maybe 2 o’clock, or something?2 o’clock, OK | |
| Does does that sound reasonable? And if I have a problem with that I’ll message you on Skype | |
| Patient | OK. Alright, that sounds good |
Question 3: what kinds of technology-related talk occur in virtual consultations?
Technology-related talk was talk that related to patients’ or clinicians’ use of the virtual consultation technology and service. As with other categories (see Table 2), technology talk was extracted for analysis using the RIAS coding method, and clustered according to the three clusters:
-
socioemotional technology talk, related to the affective or emotional aspects of using the technology
-
task-focused talk, information exchange in relation to the technology
-
process-oriented talk, to support the use of the technology.
In the Antenatal Diabetes setting, technology-related talk constituted 4% of the overall talk in virtual consultations (seven utterances per consultation). Almost all of the technology talk in this setting occurred during the initial opening phase of each consultation and was process oriented rather than task oriented (i.e. it related to establishing connectivity, visibility and audibility, or resolution of any technical barriers to effective communication). In the Adult/Young Adult Diabetes setting, technology talk constituted, on average, only 1% of the overall talk in virtual consultations (five utterances) and also involved process talk around the start of the consultation. In this setting, the use of Skype for virtual consultations was more embedded within the day-to-day running of the service, meaning that the format was familiar to patients and clinicians. In the Hepatobiliary and Pancreatic Cancer Surgery setting, technology-related talk constituted, on average, 9% of a virtual consultation. Technology-related talk in this setting included process-oriented talk, as well as the socioemotional dimension of using the technology. The latter related to concerns around use, reassurance and optimism when it was working, and friendly jokes and laughter when using it, or when technical issues arose.
Most technology-related talk (92%) fell into the following categories:
-
orientation (40% of technology-related talk) – saying ‘hi’ or ‘hello’ to indicate connection, or telling the other party about technical issues (e.g. ‘my camera is slipping a little bit’)
-
reassurance/optimism (22% of technology talk) – positive or reassuring statements in relation to the technology (e.g. ‘I can see you perfectly’, ‘We’re there’)
-
seeking reassurance (14%) – checking call quality or connectivity (e.g. ‘Can you hear me?’; ‘I hope you can see me okay’)
-
laughs/jokes (8%) in relation to the technology
-
transition (8%) indicating an action or movement in relation to the technology, such as addressing audio/visual issues (e.g. ‘hang on a minute’, ‘let me just turn on the camera so I can see you’).
The remaining 8% of technology talk consisted of:
-
giving information – a patient explaining to the clinician that Skype was not working on their laptop
-
agreement – indicating understanding in relation to the technology (e.g. in response to a patient explaining a technical issue)
-
personal – apologising if the technology is not working properly or a setting needs to be adjusted
-
bid for repetition – if a person asks the speaker to repeat what they said because the audio cut out
-
concern – statements expressing concern about the technology
-
checks understanding – paraphrasing and checking what the other person said in relation to the technology.
Table 17 gives an example of technology-oriented process talk at the beginning of a virtual Antenatal Diabetes consultation and Table 18 gives the opening exchange of a face-to-face consultation. The virtual interaction is very different from that in the face-to-face exchange. It illustrates that until a connection is established, neither clinician nor patient adopts the traditional role expected of them (both are focused on trying to get the technology to work, and neither is treating this as a formal part of the consultation). As soon as the connection is established, they adopt the usual social conventions of a doctor–patient consultation (at this point, but not before, the virtual exchange in Table 17 begins to mirror the face-to-face consultation in Table 18).
| Speaker | Opening exchange |
|---|---|
| Patient | Ah! |
| Doctor | Ah hello! |
| [0.53] | |
| Patient | Can’t hear anything |
| [0.5] | |
| Hold on | |
| [1.26] | |
| Uh | |
| [2.26] | |
| One minute, can’t hear you | |
| [0.18] | |
| Doctor | Are you all right, can you hear me now? |
| [0.04] | |
| Researcher | Can you hear us? |
| Doctor | I can hear you |
| Patient | Is it this one? |
| [0.11] | |
| No, no | |
| [1.29] | |
| Volume, this one | |
| Doctor | Hello? |
| Patient | There it is |
| Hold on | |
| [0.47] | |
| OK, can you hear me? | |
| Doctor | I can hear you, can you hear me |
| Patient | Ah, brilliant, yeah |
| Doctor | We’re on! Great |
| How are you? | |
| Patient | I’m fine |
| Um | |
| (0.27) | |
| OK | |
| Um | |
| (0.27) | |
| OK | |
| Doctor | Great. Alright |
| Now, just looking at what I wrote down at our last meeting, we’d started you on some insulin | |
| Patient | Yep |
| Doctor | (0.04) |
| How’s that been going? |
| Speaker | Opening exchange |
|---|---|
| Clinician brings patient from the waiting room to the consultation room and reads through the patient’s maternity folder | |
| Clinician | Right, so we met last time, we’ve met a few times |
| Patient | Mhm |
| Clinician | So, |
| You’ve had a scan today | |
| Patient | Yes |
| Clinician | How was the scan? |
| Patient | The scan was good! |
| Clinician | Was it? |
| Patient | Yeah |
| Clinician | Brilliant, and you’ve seen the baby doctors, what did they say, were they happy? |
| Patient | Yes, they’re happy, everything is OK, nice growing |
| Clinician | Fantastic |
| Patient | And they’re preparing for my caesarean |
| (2.10) | |
| Clinician | So C section booked for the sixteenth of January! |
Question 4: what kinds of breaches occur in virtual consultations and why?
Technical breaches included instances where the flow or continuation of the consultation was disrupted by technical or usability problems. As detailed above, the extent of technology talk varied across the different clinical settings. Over the 16 virtual consultations analysed using the RIAS, 12 breaches occurred in total, across eight cases (50%). The majority of these breaches (83%) occurred during the opening stage of the consultation.
Close to half (49%) of the technology-related talk that occurred during the virtual consultations was linked to technology breaches. Over half of this breach-related technology talk (51%) consisted of process talk – mainly orientation to inform and guide the actions of the other person in attempting to resolve the breach (31%); transition talk as a placeholder to inform the other person to wait while they attempted to resolve an issue (11%); and paraphrasing or bids for repetition, owing to impaired/loss of audio (4%). Socioemotional technology talk constituted 42% of the talk during the breaches. This included seeking reassurance (16%; e.g. ‘Are you there?’) and providing reassurance when managing the breach (e.g. ‘Don’t worry, I can still hear you’) or in response to the breach being resolved (e.g. ‘Ah, good, you’re back now’). Although breaches were overlaid with some concern and the need to seek reassurance, such events also included social responses in the form of jokes and laughter (4%; Table 19).
| Speaker | Exchange |
|---|---|
| Clinician | Sorry – your your uh, the picture has frozen |
| Patient | Right (( )) |
| Clinician | We can hear you very well, |
| but the | |
| I can see you moving, (( )) that’s fine | |
| Yeah but (( )) your picture has frozen | |
| But a uh – at a very happy expression so we don’t mind | |
| Patient | Yes [Laugh] |
| Clinician | [Laugh] |
| Um | |
| (0.39) | |
| So we will see you again, or | |
| touch touch ba- +base – oh yeah you are moving again, now, | |
| Nurse | That’s better |
| Patient | Right |
| Clinician | We we’ll make contact again in |
| November or December, after you’ve had another CT scan and another set of blood tests |
Some information-seeking and information-sharing was conducted during the breaches (7%). This mainly involved asking and telling the other person about the quality of the image/audio on their settings and their opinion about how to proceed (e.g. ‘Do you think it would be better to stay talking on the phone and just use the video?’).
The breaches in the consultations in our data set resulted from a number of different technical issues, with different approaches and strategies adopted to resolve them. These included the following:
-
Connectivity (one instance), whereby the start of the consultation was disrupted, because the patient was unable to access the Skype application on their computer. This type of breach required both parties to make contact via an alternative means of communication (i.e. mobile phone or house/office telephone) to understand the problem (i.e. letting the other person know that they could not access Skype or had attempted to initiate contact) and devise and agree on a solution. In this case, the patient decided to use Skype on an alternative device (mobile phone), instead of their laptop.
-
In two further cases, patients experienced problems accessing Skype on their devices, but were able to resolve this issue before the consultation commenced (these were not classed as breaches in the analysis).
-
-
Establishing audio (three instances), whereby there was disruption caused by problems in hearing the other person (once on the patient end, once on the clinician end and once undetermined). In one of these instances, the issue was quickly resolved through a change to the patient’s audio settings (see Table 17) during the opening stage of the call. In the second instance, the sound could not be established, despite efforts by the clinician and patient to identify the problem, and so it was decided (through discussion with the patient over the telephone) to conduct the consultation using a mobile phone on speaker phone (for audio), while continuing to run the video display on the computer. In the third, the audio was received at a low level on the patient end; hence, both patient and clinician decided to move closer to the computer (microphone) and speak more loudly throughout the consultation. One challenge to establishing audio in such circumstances was the difficulty in establishing the source of the problem (e.g. microphone, speakers, computers or device settings) and which end the problem was arising from. Navigating these issues in the absence of immediate verbal communication on both sides of the call presented significant challenges and required some other means of verbal communication (e.g. telephone, messaging, texting), some existing knowledge of the other person and knowledge of the technology and common issues related to its use.
-
Activating the video display (one instance), whereby the start of the consultation was disrupted by the absence of the patient’s video display. In contrast to the difficulties with audio, this issue was quickly resolved with the consultant informing the patient of the need to activate their video display.
-
Sound-quality issues (two instances), whereby the consultation involved persistent sound-quality problems, causing pauses and bids for repetition during the consultation. In both cases, the interference was caused by a feedback sound loop from a voice dictation device (for clinical letters and reports) attached to the clinician’s computer.
-
Temporary loss of audio/video (two instances), whereby the conversation was affected by a temporary loss of audio or video quality as a result of poor internet connectivity. In one case, the listener identified the loss of sound and requested that the other person repeated what they had missed. In the second case, the call was disrupted on two separate occasions, as a result of loss of video, which distracted the users and prompted them to confirm that they could still hear each other.
Non-technical breaches in conversation (e.g. misunderstandings requiring one party to repeat themselves or seek clarification) were uncommon, and the RIAS analysis did not surface subtle examples of this. A further analysis using conversation analysis is under way, and will be reported separately.
Question 5: what kinds of interruptions occur in virtual consultations and what is the impact of these?
Interruptions included disruption to the flow or continuity of the consultation (Table 20). Across the 16 consultations, there were only two interruptions (in two separate remote consultations) related to the use of Skype within the home setting. In both settings, family members were visible and this led to a change of topic in conversation.
| Speaker | Exchange |
|---|---|
| Virtual consultation with the patient outside his house (on mobile phone), as he is locked out of the house | |
| Patient | With exercise benig cut out of every day really, kind of messes with the . . . |
| Oh [0.3] my family has just arrived | |
| Clinician | [Laughs] |
| Do you want to | |
| Oh hello [child comes up to screen] | |
| Is that the daughter? | |
| Hello [clinician waves] | |
| Patient | That’s Dr [name] |
| Clinician | Hello [waving] |
| Patient | Say hi [to daughter] |
| Clinician | Is that the other one at the back? |
| Hello [waving] | |
| [Laughs] | |
| Patient | This is [son’s name] |
| Clinician | Hello |
| Have they been to the park? | |
| Patient | That’s everybody here |
| Yeah | |
| I’ll stay here with you | |
| Clinician | Do you want to go in [patient’s name] |
| Or do you want to stay outside? | |
| Patient | No I’m going to cool down outside |
| I’ll just keep on talk, so | |
| No so, tell me | |
| Clinician | What’s the issue with the pump at the moment |
It is likely that such interruptions were relatively few in number because efforts were made by the clinicians and patients to find appropriate times and private spaces that would minimise the possibilities for interruption.
Events also occurred within clinics that could have potentially disrupted the flow of the consultation, including the telephone ringing (three instances) and staff knocking on the door (one instance). As clinicians did not actively respond to these interferences, they were not coded as an interruption to the consultation within our analysis.
Finally, interruptions in the flow were sometimes caused by the clinician’s use of Skype on the same computer that they used to access the EPR at certain points of the consultation. This use of the computer for the dual purpose of remote consultation and information access presented possibilities for interruption. In two cases, the clinician used transition talk as a placeholder, as they attempted to return to the video view (e.g. ‘Let’s go back, sorry’). The flow of conversation appeared to quickly resume.
Summary
In summary, and based on a small subsample of consultations analysed in depth, virtual consultations appeared to be slightly shorter and slightly less clinician dominated than, but as equally clinician controlled as, face-to-face consultations. Apart from technology-related utterances, the kinds of talk were broadly similar in the two settings, but some subtle differences in certain categories of talk were evident.
Our analysis suggests that the main differences emerging between face-to-face and virtual consultations were a consequence of social, physical and material differences between the two settings (e.g. the absence of shared maternity notes had an impact on the direction of questioning and information-sharing in Antenatal Diabetes consultations). The physical setting of the clinic also provided social and physical arrangements that shaped interaction. Differences in patient–clinician interaction were rarely attributable to video-mediated interaction per se, but rather to contextual differences beyond the video link (e.g. whether or not a nurse was at hand, whether or not the clinician could see the patient’s blood glucose readings). The higher proportion of pauses and mutual silence during face-to-face consultations is one area that requires further investigation. Such moments in a clinical encounter may play an important role in opening up opportunities for the patient to raise concerns.
Chapter 6 Discussion and concluding remarks
To our knowledge, this is the first research study in any clinical field to have taken an in-depth, mixed-methods and multilevel approach to the study of remote video consultations. Building on earlier work with the diabetes service at Barts Health NHS Trust, and taking account of the national context (especially the perspectives of policy-makers and those in industry), we followed three clinic teams (in Diabetes, Antenatal Diabetes and Hepatobiliary and Pancreatic Cancer Surgery) for 2 years as they strove to mainstream the service and measure the impact on staff and patients. A significant component of our work was action research – working with front-line teams and also with national policy-makers to identify and address the multiple interacting barriers to the smooth embedding of the service.
We identified five key cross-cutting themes that spanned the micro, meso and macro levels of our data set. Table 21 summarises the main links identified, based on the combined analysis of consultations (micro), organisational ethnography (meso) and national-level stakeholder interviews and document analysis (macro). Below, we highlight how the themes are framed and addressed somewhat differently by different stakeholders at different levels. This analysis draws on the SST approach outlined in Chapter 2; for each stakeholder, we consider how they view the strategic terrain, which perspectives are salient to them as they consider key decisions, what they believe other actors think and how all this shapes and constrains the actions they take (or choose not to take) in particular situations.
| Theme | Level | ||
|---|---|---|---|
| Macro | Meso | Micro | |
| Embedding remote consultations in a clinical service | Logistical challenges rarely acknowledged or considered; some interviewees revealed a ‘plug and play’ mindset | Much time and effort needed to achieve alignment with existing structures, processes and systems | N/A |
| Selecting/inviting patients for remote consultations | Detail not considered; remote service assumed to be applicable to most or all patients in a specialty | Clinicians sought to make the service more accessible and reduce the travel burden for their patients | Not all patients were offered the option of remote consultations, because clinicians judged these to be unsafe. In some specialties, the majority of patients were deemed ‘unsuitable’ |
| Doing a remote consultation | Detail not considered, but assumed to be ‘equivalent’ to face to face | Major mismatches in organisational routines between remote and face-to-face consultations required considerable set-up effort and ‘hidden work’ | Remote consultations included much ‘technical talk’ before the clinical interaction could begin. They were less clinician dominated than face-to-face consultations |
| Privacy and security | Policy-makers and industry placed high priority on avoiding breaches of legal or regulatory standards | Working through IG issues locally was time-consuming, but essential; developing common SOPs helped to bring a focus on these issues | Patients were relatively unconcerned about privacy or security when consulting with a known and trusted clinician; clinicians sometimes used workarounds to deliver care effectively |
| Roll-out and scale-up | Assumed to occur rapidly and largely unproblematically once proof of concept was established | Numerous practical, logistical and technical challenges at a local level are likely to recur in each new setting | Consultations reveal how local contingencies require ongoing adaptation by front-line staff |
After discussing the cross-cutting themes, we consider the strengths and limitations of the study, before offering some conclusions and suggestions for further research.
Theme 1: embedding virtual consultations in a clinical service
It is often stated that new technologies need to be ‘embedded’ in organisational infrastructures and routines. Despite this wide acknowledgement of the need for embedding, our macro-level data suggested that little consideration had been given to this issue by either policy-makers or those in industry. Rather, the use of Skype for virtual consulting was assumed to be a straightforward matter of downloading the software onto the relevant computers – an illustration, perhaps, of the ‘plug and play’ mindset we have described previously in telehealth discourses. 81
A significant storyline in our macro-level data was the financial pressures faced by the public sector and the resulting pressures within the health-care sector to work with fewer resources. Technology was often depicted as a logical route towards achieving cost-savings (e.g. by reducing staff time, supporting caring for people at home) and increasing quality (e.g. through improved access). This powerful overarching narrative (evident in both industry and policy discourses) rarely acknowledged the need for technologies to become embedded within existing organisational structures, processes and routines (and the corresponding need to allocate time and resources to this early phase), nor did they acknowledge that once embedded, technologies can and must continually evolve and adapt over time.
In contrast, it was evident from our meso-level data that the introduction and use of Skype technology for virtual consulting required much time and effort, and many resources (and, in some cases, interpersonal or interdepartmental conflict) to achieve alignment with existing management and administrative structures, processes and systems. This is described in detail in Chapter 4, and included addressing the concerns of the ICT department about IG and workload, reconfiguring the EPR (e.g. to create new appointment slots that would indicate that they were ‘webcam’ appointments), and aligning with the routines of appointment scheduling and recording attendance.
Embedding of the technology within existing work routines and practices required high-level commitment across the team and mutual awareness of what other collaborators were doing in order to provide a context for each party’s own activity. 228 Strong clinical leadership and ‘championing’ the new technology and mode of service delivery appeared to be key to overcoming the multiple and interacting barriers on both a small and larger scale. Clinical leaders offered a meso-level ‘organising vision’229 for the introduction and roll-out of the remote approach that provided a shared rationale for why Skype technology should be adopted/used and activated, and co-ordinated stakeholders to promote adoption and diffusion. At the clinic level, in particular, this input helped to ensure that the team functioned collaboratively and effectively towards the shared goal of making virtual consultation services business as usual. Our data illustrated starkly that a high workload and lack of organisational slack (time, space, people, expertise) severely limited front-line teams’ capacity to initiate and successfully maintain the embedding of virtual consultations in clinic work.
Theme 2: selecting/inviting patients to use the virtual consultation service
At the macro level, the prevailing policy assumption was that once a virtual service was established as business as usual, it would be a viable, affordable (indeed, cost-saving) option for a high proportion of patients in any given service. For example, the National Information Board stated that:
Better use of data and technology has the power to improve health, transforming the quality and reducing the cost of health and care services.
National Information Board (p. 3). 5
This was also the case for industry strategists. For example, in an interview with a leading IT provider, the focus was largely on particular products and their potential to be bought into the NHS:
And for, you know, videoconference and instant message functionality generally you think, ‘oh my goodness, it would be so easy to do’. And everyone would be on the same system so it would work. Instantly. There would be no interoperability issues.
The above quotations illustrate that, for national-level stakeholders, the strategic terrain (i.e. the different aspects of the external world as viewed by these actors) was shaped by what we have described elsewhere81 as a ‘modernist’ organising vision for technology-enabled care delivery. A modernist vision has the following features: technological innovations are rational solutions to the challenges facing the health service (especially rising rates of non-communicable diseases and escalating patient demand) and they will help to achieve efficiency and cost-effectiveness of services, and have the potential to ‘empower’ both clinicians and patients.
The quotations above – and a modernist vision for technology-enabled care more generally – implies three assumptions that appear to be relatively unexamined by both national policy-makers and industry providers. First, that new technologies (specifically in this case study, virtual consulting) are an effective way of driving new and more efficient models of care into practice at scale, thereby reducing the high and rising burden of outpatient appointments. Second, that when planning the provision of a technology-supported service in a particular condition, the clinical condition can be considered in broad-brush terms (i.e. as a textbook ideal type, as in ‘patients with diabetes in pregnancy’). Third, that the patient population can generally be treated as more or less homogeneous in terms of their wider characteristics (or, perhaps, that any differences can be construed as ‘gaps’ – such as digital literacy – that can be ‘filled’ by education).
At the meso level, the original introduction of virtual appointments for diabetes at Barts Health NHS Trust back in 2009 was not unrelated to the growing pressures on outpatient services and the year-on-year reduction in budgets. But it was driven more immediately by the high DNA rate among young adults (around 50%), and by a belief of the lead consultant and diabetes specialist nurse that large numbers of young adults were becoming disengaged from the service and defaulting from follow-up. In particular, a virtual service was considered to be a potential way to retain ‘harder to reach’ patients, such as black and minority ethnic and lower socioeconomic groups (who were, for example, less likely to be allowed paid time off work for appointments, and who struggled to meet the cost of transport to hospital). The clinicians’ view was that the use of technology would make the service more accessible to a group of patients whom they viewed as particularly vulnerable. For example, and as part of a general strategy of making the service more accessible to patients who were reluctant to engage, they encouraged patients to message them on Skype and spent time responding to these messages; the virtual service included a growing proportion of patient-initiated consultations, in which patients would see that the doctor or nurse was online and send a Skype message asking for a non-booked consultation. Earlier publications on the virtual diabetes service at Barts Health NHS Trust emphasised how a ‘disengaged’ clinic subpopulation had been successfully re-engaged by offering the service and making it possible for such patients to contact the doctor or nurse at their convenience, whenever and wherever they sought advice or support. 9,11
The extension of the virtual consulting model to Antenatal Diabetes services was driven partly by the need to address steadily rising patient numbers in the Antenatal Diabetes outpatient clinic (the incidence of gestational diabetes is increasing in parallel with growing levels of obesity, for example). However, clinicians were also motivated to try to reduce the burden on pregnant women of making frequent visits to a busy hospital clinic, perhaps with toddlers in tow. Gestational diabetes can be labile and need daily adjustments in insulin dose, and hence become burdensome and potentially difficult for the (otherwise well) pregnant woman. In keeping with the idea that pregnancy is a normal physiological state, not an illness, both midwives and doctors seek to avoid ‘medicalising’ the condition if at all possible.
Similarly, the clinical lead of the Hepatobiliary and Pancreatic Cancer Surgery service was keen to reduce the burden on his patients of making long journeys for a clinic check-up in the postoperative period. As long as there was no clinical reason for the patient to be seen face to face, it was viewed as clinically more appropriate for the patient to stay at home and be seen remotely.
Thus, when making the (meso-level) decision to introduce a virtual consultation service, clinical leads saw the strategic terrain at least partly in terms of improving the quality and accessibility of the service for patients, for whom a journey to the hospital was – variously – unnecessary, inconvenient, unaffordable or clinically inadvisable. Such drivers were rarely mentioned by national-level stakeholders (whose economic models did not generally include patient-borne costs or patient time).
Although the doctors (and to some extent, nurses and midwives too) in participating clinical teams viewed the virtual consultation service as improving accessibility and increasing choice for patients in general, they did not view this service as automatically available to all clinic patients. Rather, and in every particular case without exception, a clinical judgement was made on the ‘suitability’ and ‘appropriateness’ of the patient for the virtual services.
Decisions around suitability were made on a case-by-case basis and informed by a range of factors that varied across the different clinical contexts, and were discussed and mutually agreed with the patient. Such decisions appeared to be difficult to anticipate in advance and to require three things: (1) clinical experience in the relevant specialty, (2) tacit knowledge about how virtual consultations play out in this particular condition (e.g. content to be discussed, materials/resources needed, likelihood or not that a physical examination will be needed) and (3) personal knowledge of the patient. The last of these appeared to involve a subjective assessment of the patient’s health literacy (in general, and specifically, in relation to the clinical condition), IT literacy, the ability to communicate (e.g. across a language barrier) and confidence. The main question driving the decision appeared to be ‘would a virtual consultation be clinically safe for this patient, with this condition, at this time, for this aspect of their care?’ (see the quotation in Chapter 4, New clinical roles and practices: triage, technical support and direct access).
Applying SST to the decision of whether or not to offer the option of virtual consulting to a particular patient, the strategic terrain looks somewhat different from what it looked like for the macro- and meso-level stakeholders. At this micro level, and notwithstanding that this was an experimental service that had not yet been fully tested or incorporated into business as usual, the over-riding influence was a professional norm: primum non nocere (first, do no harm). Our interviews with doctors in particular highlighted the strong sense of clinical responsibility for the patient, along with a sense that they would be held accountable (both professionally and legally) if harm resulted from a virtual consultation. This theme, which was very strong in our micro-level data, was not in evidence in the meso- or macro-level data sets.
Expressed in the language of SST, our data support the conclusion that the clinicians’ general dispositions (based on education, experience, professional norms, values and so on) were oriented to providing a virtual service that they saw as accessible and convenient for patients, and which may also save money and help to ease the pressures on the outpatient clinic. But these general dispositions were often (and in the case of Antenatal Diabetes patients, almost always) over-ridden by the clinician’s conjuncturally specific assessment of whether or not a virtual consultation was appropriate for this patient in this situation, given these contingencies. Furthermore, it was only when the service had been introduced on a pilot basis and the clinicians began to make these fine-grained decisions that the non-suitability of virtual consulting for many patients became apparent.
The high barrier in some specialties to offering the virtual consulting option contrasted starkly with the view of our patient advisory panel that all patients should be offered the virtual option so that the service was available to all patients who chose to use it. This view was strongly and universally held by those participating in discussions on the topic. Implicit in this view was the assumption that it was the patient, not the clinician, who was best placed to make the judgement about the trade-offs between clinical safety and convenience of access. One patient made the point that, although the clinical grounds for ‘suitability’ may be best assessed by the clinician, there were many wider influences (such as the impossibility of getting time off work or the need to collect children from school) that were best assessed by the patient and/or carers.
Using SST, we can say that the strategic terrain for the patient is characterised by a host of practical, material and sociocultural influences, along with various commitments and accountabilities (to employers, other family members and so on). For the patient, the care of the clinical condition cannot be considered in isolation from the wider landscape of things at stake.
Theme 3: doing a remote consultation
‘Doing’ a remote consultation involved three phases: first, establishing connection (technical); second, the actual encounter (clinical); and third, arranging follow-up (administrative). Our macro-level data suggest that neither policy-makers nor industry stakeholders paid much attention to the detail of the virtual consultation. Apart from recognising the obvious fact that certain aspects of the physical examination would be impossible in the remote encounter, they appeared to assume that the latter would be unproblematic and unfold in a more or less similar way, once a successful technical connection had been established; the policy-makers we interviewed did not consider how the clinical encounter would link with the administrative task of booking the next appointment.
Our industry participants were keen to ensure that the technology was appropriately designed and adapted to support a high-quality connection, and that its functionality supported the nuanced affordances that were likely to be needed clinically. For example, they showed interest in reviewing (with consent) selected video-recorded consultations, better understanding how different clinicians and patients use virtual consultations and adapting the Skype software for different health-care settings and clinical contexts (e.g. improved video quality, the use of multiple screens, developing ‘virtual waiting rooms’). Their main focus, however, was on advanced design and functionality.
At the meso level, ‘doing’ a virtual consultation was far from straightforward. As noted in Chapter 4, ‘getting the patient set up’ for such a consultation involved considerable ‘hidden work’ around practical issues, especially providing flexible (and unofficial) IT support, undertaking ‘test calls’ with patients (in which no clinical discussion was held), following-up on ‘contact requests’ (in which the patient had sent a Skype message asking for a contact) and messaging the patient to inform them of their appointment time (or confirm or amend such an appointment). As Figures 3–8 illustrate, even when the virtual consultation service was relatively well routinised (as in the Young Adult Diabetes Clinic), much of this hidden work fell to the clinician.
Our micro-level analysis of the use of Skype to support actual consultations (described in detail in Chapter 5) revealed that consultations unfolded smoothly only when – and to the extent that – both parties engaged both in the technical set-up phase and in an ongoing process of adaptive troubleshooting to ensure that the technology ‘worked’ and the encounter mirrored, as far as possible, the conventional clinical encounter in that specialty. In the VOCAL study, the clinician was the main (and usually the only) staff member involved in the technical set-up phase before the consultation could begin. His or her role included fiddling with equipment and making adjustments to technology settings in order to resolve problems as and when they arose. Often, clinician and patient worked together to troubleshoot and perform one-off workarounds for unique technical and/or logistical problems.
The introduction of virtual consulting in this particular organisation137 (i.e. this does not necessarily mean that it must happen this way in other organisations) thus required a significant element of ‘reskilling’ and development of know-how among clinical staff to resolve unique technical problems and improvise in new situations. Our ethnographic observations affirmed the previous observation of Brown and Duguid230 that such knowledge is typically exchanged among staff on the clinical team through social interaction, and, in particular, via the exchange of stories (sometimes with humour when describing a technical difficulty and efforts to resolve it).
Arguably, the extension of the clinician role need not necessarily be a prerequisite for delivering virtual consulting (private-sector virtual consulting services, for example, appear to be characterised by a dedicated administrative and technical team who take responsibility for the initial technical set-up phase and ongoing technical/logistical support, while the clinician sticks to a more traditional clinical role231). As Barley137 observed, technology introduced into health-care settings is ‘an occasion for structuring’ – that is, it offers the opportunity for developing new roles and competences, but because of its inherent interpretive flexibility (i.e. technology can be used differently by different agents), it does not produce these new roles in a deterministic way. Whether the tacit knowledge for technical set-up and support is developed by clinicians, administrators or both, it is clear from our findings that organisations should consider how to create the conditions for social interaction that will cultivate and support the sharing of such tacit knowledge and know-how.
The patient was also required to develop and apply a set of technical skills, including the ability to troubleshoot in real time and interact with the clinician to deal with problems as they emerged. Different patients were more or less willing and more or less able to do this. As well as general IT literacy and specific experience and understanding of the Skype technology, factors influencing their capacity to consult remotely included the material properties of their hardware and software and people available to help out with set-up and troubleshooting.
In relation to the clinical aspects of virtual consultations, our study demonstrated that the interpersonal interactions and dynamics had subtle, but potentially important, differences when undertaken remotely compared with face to face (see Chapter 5). Although our sample was small and the findings provisional, it appears that for equivalent clinical interactions, virtual consultations are generally shorter, somewhat less clinician dominated (i.e. the patient had a higher proportion of talk time) and include considerably more technology-related interaction. But these differences were likely to be explained largely, if not entirely, by the physical and material differences between remote and face-to-face consultations, which necessitated the verbalisation of certain aspects of communication in the former, but not the latter. In addition, of course, some consultations (requiring a physical examination) cannot take place virtually.
The clinical aspects of the virtual consultation could not be separated cleanly from the technical and practical aspects. During the virtual consultation, for example, both clinician and patient made extensive use of other artefacts (including paper and electronic records) to support their own input to the interaction and make the other party aware of information that would have been more readily evident in a face-to-face encounter. Workarounds (often invisible or subtle) were frequently needed to adapt roles and processes to the contingent detail of an unfolding consultation. As detailed in Chapter 4, considerable ‘articulation work’ (i.e. the ability to co-ordinate resources, actions and people) was sometimes needed to deal with local contingencies and unanticipated situations.
We also found that an existing relationship and ‘common ground’ between the patient and clinician appeared to be a positive precondition (although perhaps not an absolute requirement) for effective virtual communication. An awareness of these social dimensions of video-mediated communication helped practitioners to evolve their approach to service delivery and relationship formation (e.g. utilising Skype for routine follow-up, developing an initial rapport with patients face to face, inviting patients to message them with questions).
Finally, as described in Chapter 5, the third phase of the virtual consultation – booking a follow-up slot – appeared to depend on the clinician’s willingness to engage with this administrative task, their familiarity and skill with the booking system and their ability and confidence to judge between a face-to-face encounter, a Skype video consultation and a Skype message interaction.
Theme 4: privacy and security
At the macro level, national-level stakeholders from government and industry were concerned about IG only insomuch as they recognised the need to ensure that regulatory requirements were fully met and that public perceptions of data security and privacy were positive. These concerns were generally expressed at a generic level (all digital health initiatives were viewed as raising similar IG challenges) and policy-makers did not appear to be aware of the detail of the specific privacy and security issues around remote video consulting. The national-level policy-makers in our steering group were keen to work with us in producing IG guidance on this topic, with a view to ensuring that the introduction of virtual consulting in other NHS organisations followed a more or less standardised and approved process.
At the meso level, one of the major barriers to the implementation of virtual consulting services within the trust was strong concerns around IG, particularly from the IT department. These concerns appeared to be driven by a perception of strict regulatory and legal pressures, and reinforced by a lack of national consensus on the appropriateness of Skype (and similar virtual media) for use within the NHS. As set out in Chapter 4, this barrier formed a significant part of the action research component of our study, in which we sought to address the prevailing lack of consensus through the creation of guidance and protocol documents (both local and national).
These documents appeared to act in some sense as ‘immutable mobiles’228 or ‘boundary objects’232 that served to support dialogue and co-operation across clinic and administrative departments (and between local teams and national policy-makers). Indeed, the way in which the documents (and the writing of them) brought people together for further discussion was at least as important as the actual list of procedures to be followed. Indeed, although protocols and SOPs certainly provided guidance that staff found helpful, it was also widely believed to be necessary to ‘work around’ official procedure when in the best interests of the patient.
Interestingly, our micro-level analysis showed that although patients and their carers were aware of IG issues at some level, they were generally relaxed about these and rarely, if ever, cited such issues as a reason not to consult remotely. This finding resonated strongly with our previous work on patient concerns about the summary care record, which showed that patients considered the trade-off between potential security breaches (a theoretical possibility, but in practice unlikely) and accessibility and quality of clinical care (potentially enhanced through the use of the new technology), and if they trusted the clinician, they tended to trust the clinician’s use of the technology. 233 Indeed, our interviews with patients revealed that some placed high value on the fact that a trusted clinician was ‘visiting’ their home and sometimes took time to show the clinician aspects of their home (such as posters on a bedroom wall) as a way of developing the established relationship further.
From the clinician’s perspective, the data security aspects of the consultation were taken very seriously. Clinicians were aware of procedures to maintain patient privacy and confidentiality; they applied these flexibly – and sometimes used workarounds in a way that prioritised the patient’s best interests (e.g. using the researcher’s login to ensure access in the face of technical problems).
Theme 5: roll-out and scale-up
Our macro-level analysis of policy documents and interviews with policy-makers (described in detail in Chapter 3) showed that, since at least the early 2000s, there has been a strong policy emphasis on the need for ‘transformation’ of health and social care provision. In these policy narratives, virtual consultations are depicted as having a role in delivering this transformation ‘at scale’ and ‘at pace’. The implication is thus that following an initial set of pilot studies and demonstration projects, the introduction of virtual consultations will gather speed rapidly. In reality, the literature on national roll-outs of ‘transformational’ IT projects in health care suggests that this assumption may be overoptimistic. 69 Indeed, just because a technological innovation has been successfully implemented and embedded in one locality, each new setting will continue to face significant implementation challenges, and there may be a considerable time lag between the adoption of technology and the realisation of any productivity gains.
Interviews with industry representatives from both large and smaller companies indicated a similar conviction in the potential of virtual consultations to deliver transformation at scale and pace. However, although industry representatives welcomed the shift away from the centralised procurement characteristic of the National Programme for IT (2007–11) and the extension of NHS contracts to a wider range of providers, they continued to struggle to engage with health-care organisations and systems. The relationship between the technology industry and the public sector was repeatedly cited as complex, with procurement processes in particular presenting challenges to potential scale-up. Interviewees talked about investment in industry–NHS partnerships as a means of working together to develop and adopt technologies, but recognised this a resource-intensive process with little guarantee of significant (i.e. national) roll-out in the short term.
At the meso level, much of our ethnographic fieldwork and action research consisted of observing and supporting the trust as they strove to overcome the many barriers to mainstreaming virtual consultation services. This initiative was explicitly driven by a strategic focus on transforming care and, as such, had the support of senior executive teams and dedicated resources and staff.
Specifically, the virtual consultation service that had initially developed as an ad hoc project led by interested clinicians within the Diabetes service was aligned with TST, a trust-wide initiative aimed at reducing the number of face-to-face consultations across all clinical services as appropriate. The TST initiative was associated with a significant shift in logistical and technical support, from bespoke support to the innovator department (Adult/Young Adult Diabetes) and two ‘early adopter’ departments (Antenatal Diabetes and Hepatobiliary and Pancreatic Cancer Surgery) to a service that now cuts across (at the time of writing) four local departments and with another four planned. As described in Chapter 4, Trust policy and service-level agreements, the provision of SOPs and central support undoubtedly helped to ‘oil the wheels’ for departments seeking to introduce and embed the new service. However, these central initiatives and resources inevitably also meant a shift towards the centralisation of control, which could potentially conflict with the ‘bottom-up’ and grounded approach we observed in the early adopter departments.
At the micro level, and as described in detail in Chapter 5, our in-depth analysis of virtual consultations has illuminated the numerous context-specific interactions and local contingencies that are integral to providing a successful technology-supported remote consulting service. The implication of these micro-level data are that imposing a centrally driven, standardised solution for implementation and embedding as part of the wider roll-out is unlikely to go smoothly. Indeed, we have recently shown, in using different types of technology as an example, that ‘scale-up’ and ‘roll-out’ should be considered to be social practices (i.e. the uptake of the technology should be studied in the context of what human actors find salient, meaningful, ethical, legal, materially possible and professionally or culturally appropriate in particular clinical or social situations). 136
Conclusions
One clear conclusion from this study is that setting up a virtual consultation service is no bowl of cherries. ‘Embedding’ Skype (or comparable technologies) at the meso level into organisational infrastructure and routines is likely to require not only substantial set-up resources, but also ongoing human effort, as well as time and resources. The lack of recognition of the magnitude of this challenge at the macro level by policy-makers (and, to a lesser extent, industry representatives) is one of the main findings of this study.
A second conclusion is that the adoption, implementation and day-to-day use of virtual consulting is necessarily both adaptive and contingent, involving what are often complex clinical decisions and with a strong over-riding framework of (for the clinician) clinical safety and (for the patient) practicality and personal accountability. In the Young Adult Diabetes service, in particular (which had been running remote consultations for several years when this study was commenced), clinicians had used their autonomy to ‘repurpose’ the Skype technology to facilitate access to care in a way that had not been anticipated at the national level. This adaptive and selective use of Skype at a local level aligns with the classic work by DeSanctis and Poole234 on adaptive structuration theory; it challenges the assumptions (particularly at the government and industry levels) that a ‘digital innovation’ is a fixed and clearly definable option, used in a particular way, that needs to be ‘engaged with’ in a standardised way across the public sector.
Our third conclusion is that the model–reality gap for ‘doing’ a virtual consultation is wide. The virtual consultation was depicted at the policy level as a straightforward and unproblematic task using a reliable ‘plug and play’ technology. The logistical reality of such consultations at the level of the organisation or clinical team (meso) and at the level of the actual interaction (micro) told a different story; clinical work tended to unfold in a unique and messy way, with multiple subtle contingencies (both clinical and technical). Dealing with these contingencies required work and interaction from both clinician and patient (only some of whom had the inclination and capacity to engage with this).
Fourth, although the governance and regulation of virtual consulting is widely perceived as something that can be ‘fixed’ through the development of standards and guidance (and while we ourselves contributed to the development of such guidance as part of this study), our findings suggest that ‘articulation’ (including unofficial workarounds) is part of the reality of virtual consulting. Goorman and Berg235 define articulation as follows:
All tasks involved in assembling, scheduling, monitoring and co-ordinating all of the steps necessary to complete a production task (patient trajectory). This means carrying through a course of action despite local contingencies, unanticipated glitches, incommensurable opinions and beliefs or inadequate knowledge of local circumstances. Every real world system is an open system . . . No formal description of a system (or plan for its work) can thus be complete . . . every real world system thus requires articulation to deal with the unanticipated contingencies that arise. Articulation resolves these inconsistencies by packaging a compromise that ‘gets the job done’ that is, that closes the system locally and temporally so that the work can go on.
What this means is that the generation, endorsement and dissemination of SOPs (a tangible achievement of this study) will not, in and of itself, make virtual consultations happen. Attention also needs to be paid to the messy reality of implementing these standards, in particular, in ‘imperfect’ real-world settings. To help with this, we have provided a set of practitioner resources alongside this report that have been informed by emerging findings, been actively used and refined as part of our action research and are intended to support service providers, professional bodies, policy-makers and patients and carers who are interested in or actively pursuing the development of virtual consultation services.
In relation to the prospects for extending the virtual consultation model to other clinical specialties and other NHS organisations – and notwithstanding the powerful prevailing policy discourse on ‘scale-up’ and ‘roll-out’, which is assumed to be achievable rapidly and ‘at scale’ – our findings indicate that mainstreaming virtual consulting across multiple departments in multiple organisations will be neither smooth nor quick. The clinical and logistical realities will play out differently for different clinical specialties and different hospital departments (not to mention primary care). On the basis of empirical data from the three departments we have studied in detail, our brief exposure to four further departments in the same trust and contact with various groups across Barts Health NHS Trust involved in virtual consultations (e.g. the outpatient project strategy group), as well as on the theoretical literature cited above, we anticipate that each and every department in every organisation that seeks to embed virtual consulting will need to take a sociotechnical systems approach236 to organisational change. Specifically, they will need to emphasise ‘minimal critical specification’ (no more specified than absolutely essential), the ‘sociotechnical criterion’ (problems should be resolved by groups that directly experience them) and ‘incompletion’ (the need for continual revision of objectives and structures). 236
Strengths and limitations of this study
The main strength of this study is that it is, to our knowledge, the first major study of remote video consultations from a sociomaterial perspective that has attempted to link different levels of data collection and analysis across the macro level (the historical and current policy drivers and wider sociocultural, technological and economic context), the meso level (the practicalities of organisational and service change) and the micro level (the fine-grained detail of the actual consultation). In contrast to trials of virtual consultations, which have provided little insight into the organisational complexities of implementing a new technology-enabled service or how such services evolve and (may or may not) become embedded in health-care settings, the naturalistic, mixed-methods and multilevel design of the VOCAL study has enabled the study of the emergence of video consultation services and the challenges faced in this process.
We succeeded in our goal of collecting rich qualitative data that allowed us to go beyond the more usual approach of making simplistic ‘technology on versus technology off’ comparisons with narrow, predefined outcome measures. In short, and notwithstanding the impressive features of the technology that allowed a clear video link to be set up with the patient at home, our ethnographic approach exposed the ‘messy reality’ of establishing a virtual consultation service and illuminated the pros and cons of using this medium for clinical interaction in different settings.
Another advantage of our study design was the prominent action research component. This operated most obviously at the meso level, allowing (indeed, requiring) the research team to work collaboratively with the clinical teams, as well as the trust managers and the ICT department, to help align (for example) the service development, technological development and IG aspects of the ‘embedding’ of Skype consultations. In addition, one member of our steering group was a member of NHS England’s Digital Health team; along with other key informants in our macro-level interviews, he was able to help us to establish a policy dialogue at the national level – particularly in relation to a possible national tariff for virtual consultations. Finally, our key informant interviews with industry representatives also fed back into discussions both locally and nationally about how the industry–NHS partnership over virtual consultations could be strengthened.
The main limitation of the study is its focus on a single NHS organisation, and the sample size for the detailed analysis of virtual consultations was small. In some ways, Barts Health NHS Trust faced a similar set of issues and challenges as any other acute hospital trust during the study period. In other ways, it was unique – or at least, an ‘outlier’ – in that it faced more severe financial pressures than most comparable organisations (as reported in Chapter 2, it was put on ‘special measures’ by the Care Quality Commission part way through our fieldwork). Thus, despite having many cutting-edge technologies and a state-of-the-art electronic record system in use (Barts Health NHS Trust won the ‘Digital Trust of the Year’ award in 2014), the reality on the ground was that there was zero ‘organisational slack’ to support new projects.
As organisational slack is a prerequisite for innovation in any organisation,237 it is likely that organisations under less tight financial and staffing pressures would have found it easier to introduce a remote consulting service. On the other hand, Barts Health NHS Trust was an innovator organisation in introducing such a service on a pilot basis back in 2009, and the innovator clinician (SV) was a co-applicant on this study and a passionate champion across Barts Health NHS Trust for the use of virtual consultations to reduce health inequalities. Organisations lacking ‘innovators’ and ‘champions’ are generally less likely to succeed in complex change projects,237 so it cannot be assumed that our own case study represented the most challenging context.
Although virtual consultations are relatively new to health care, a number of VoIP products have been available for years, and their numbers continue to grow. Our study focused on Skype as the VoIP product of choice within our case study site, as a result of its popularity (many people attached the idea of calling via the internet to Skype) and a good level of familiarity with Skype on the parts of patients and their families. As we set out in our findings chapters, the use of Skype led to accommodations in the social structure and processes of each of the clinical services and the wider trust. However, as Skype is one of a number of services that can support virtual consultations (others including, for example, FaceTime or GoogleTalk™; Google LLC, Mountain View, CA, USA.), it is possible that some of our conclusions are a product of Skype usage, rather than being common to all VoIP applications. It is also worth noting that a researcher was present in either the clinic or the patient’s home when each Skype consultation was set up (primarily to video-record the consultation as data for the study, but simultaneously being viewed by some patients and clinicians as a source of advice and support when seeking to set up a virtual consultation), which may have influenced the set up and progress of that consultation.
Some critics will view it as a limitation of the study that we did not set out to generate an ‘effect size’ or a cost-effectiveness analysis on the use of virtual consultations. This was deliberate. As we believe our findings have demonstrated, virtual consultations cannot be treated like a drug or even as a complex behavioural intervention to be tested ‘on’ patients. Rather, they are the result of a hugely complex sociotechnical system, in which ‘successful’ virtual consulting is contingent on multiple factors at multiple levels. If we appear to have produced ambiguous findings, this is perhaps because ambiguity and tension are inherent to complex sociotechnical systems. To questions such as ‘do virtual consultations work?’, ‘are virtual consultations safe?’ and ‘are virtual consultations cost effective?’, we suggest that the answer will always be ‘it depends’.
Use of findings from this research
The VOCAL study deliberately adopted an action research approach that involved working with national and local stakeholders, helping to identify and address potential blocks (e.g. developing new ways of working to enable Skype to be loaded onto clinic computers), develop processes (e.g. SOPs for those seeking to develop virtual consultation services) and feed into ongoing discussion (e.g. regarding the potential roll-out of virtual consultations via the outpatient project strategy group). This ‘action’ part of the study has generated a number of materials that are already in use within Barts Health NHS Trust and, in some cases, more widely. We have included relevant documents on the NIHR Journals Library website to support those thinking about or setting out to develop virtual consultation services. These resources are evidence based (in terms of both having been developed from research evidence in this study and, where relevant, drawing on documented best practice elsewhere).
The Diabetes service in Newham began conducting virtual consultations in 2011 and has generated considerable experience in developing the service (and related organisational routines) in the years since, as well as working with patients and carers to evaluate and evolve that service. Following publication9–11 and presentations across the UK about the service, the team in Newham have received over fifty requests for further information (often accompanied by requests for visits and assistance) from trusts across the UK. With a focus on making the best use of the accumulated experience at Barts Health NHS Trust, and being keen to ensure the application of our findings in practice, we have secured an Economic and Social Research Council Impact Acceleration Award and a Health Foundation Scaling Up Improvement grant to help us to extend and apply the research that we have undertaken in the VOCAL study. The grant is an important outcome of the VOCAL project, as it will help to ensure that our findings have the best chance of having an impact on practice by continuing to support and evaluate the wider roll-out of virtual consulting services across Barts Health NHS Trust, adapting and extending this roll-out and evaluation to two other NHS trusts, and collaboratively creating online resources to support the introduction and sustained use of virtual media tools for virtual consulting nationally.
Building on the relationships established as part of the VOCAL study, we are also currently exploring opportunities to work with Microsoft to develop more patient- and health-care-friendly tools via Skype (and related) technology.
Suggestions for further research
There is much scope for pursuing further the basic study design and methodological approaches used in this research to add depth and contrast to the findings presented here. The policy context is changing rapidly and (at the time of writing) the UK is entering a period of unprecedented environmental turbulence in terms of the economic, technological and regulatory context for innovation in the public sector. Notwithstanding a prevailing squeeze on finances and uncertainty about regulatory structures, there is much policy interest in digital ‘solutions’ and there is likely to be money available for pilot projects. We hope that those who draw on such funding to pilot and mainstream the use of virtual consultations will use a similar methodology to that described in this report to evaluate and document the multiple interacting influences on ‘success’. As Flyvbjerg238 has noted, ‘[A] scientific discipline without a large number of thoroughly executed case studies is a discipline without systematic production of exemplars, and . . . a discipline without exemplars is an ineffective one’.
There is currently significant interest (from policy-makers, industry representatives and those working in NHS management, as well as patients and carers) in the potential roll-out of digital ‘solutions’ across the NHS. Previous studies have highlighted how digital technologies, including Skype and similar virtual media, often succeed on a small scale, but fail to achieve widespread use (scale-up) or become routine practice in other settings (spread). 136 Given the current impetus from national policy for NHS organisations to rapidly adopt such technologies (i.e. at scale and pace), combined with the level of work involved in implementing them, both spread and scale-up are potentially fruitful areas for further study. This includes understanding professional and organisational drivers for adopting (and not adopting) digital technologies, such as Skype and other virtual media, into routine patient care; supporting decision-makers in designing policies that can support spread and scale-up and NHS organisations already attempting to incorporate digital technologies; and evaluating the impact of virtual consultations on NHS organisations, as well as patients and professionals. Current research in this field tends to undertheorise the process of scale-up and spread. A potentially fruitful theoretical approach would be to consider the adoption and use of technologies as social practices. 136
Our study has focused exclusively on Skype as the virtual media platform supporting virtual consultations. There is significant scope for exploring the use of other similar media (e.g. FaceTime) both in the public and private sectors, and the interaction with other digital technologies (e.g. virtual waiting rooms). The VOCAL study has focused largely on mediated consultations using a computer, with some sessions being reliant on other devices (mobile phones and tablets). This raises the question of whether or not there are any differences in interaction and perceived success as a function of the device (or combination of devices) being used.
Only a handful of previous studies (and none from the UK) have attempted to apply the RIAS (or a similar) analytic approach to the study of remote video consultations. As noted in Chapter 5, our sample size was too small to draw confident conclusions about the differences in the kinds of talk that occurred in the remote environment compared with the face-to-face environment. We did demonstrate that differences between clinical specialties were more significant than differences between remote and face-to-face consultations within a particular specialty and that many, if not all, differences in the latter were readily explained by practical and material factors. Much additional research could be done, however, to extend the empirical data set on talk in virtual consultations, generate further hypothesis-driven questions that could be addressed using the RIAS or a similar approach focused on categorising different kinds of talk across different genres of consultation and inform the development of guidance on any suboptimal communicative practices.
The micro-analysis of consultations could also take a more qualitative approach from the perspective of sociolinguistics (e.g. using conversation analysis or discourse analysis). For instance, as noted in Chapter 5, the higher proportion of pauses and mutual silence during face-to-face consultations is one area that requires further investigation. A detailed description of, and rationale for, such an approach is beyond the scope of this report (see The Handbook of Conversation Analysis239 for an introduction), but, briefly, this technique sees communication as a dynamic interaction that emerges moment by moment and allows a deeper and perhaps more sociologically critical analysis of the power dynamics of a consultation than is made possible through the RIAS approach. Such an approach would allow for a finer-grained analysis of spoken interaction that could yield original and important findings about the communication strategies that make up a ‘good’ remote consultation. We have applied for further funding to undertake a detailed interactional analysis of our data set and would be keen to collaborate with other researchers to pool empirical data and develop a common analytic approach.
Finally, our findings suggest that there is much further research to be done that looks at the interactions between the macro, meso and micro levels in the regulation and governance of virtual consultations. For example, our own team is currently undertaking a theory-driven, multilevel analysis of the tensions between risk, governance and patient-centred care, focusing on how institutional regulations impact everyday work practice and interaction with patients, using a theoretical model developed previously by Hillman et al. 240 There is much scope to apply such a framework to different kinds of virtual and technology-supported consultation.
Acknowledgements
Our thanks go to Barts Health NHS Trust and all of the staff, patients and carers who have given up their time to support and/or participate in the VOCAL study. Without them, the research study would not have been possible. We thank the members of our external steering group, especially Mrs Jenni Bowley, who chaired the group, and the members of our PAG.
Thanks also to Charles Gutteridge (CCIO at Barts Health NHS Trust) and Emma Byrne (previously at Queen Mary University of London), who helped to shape the initial proposal and the early stages of the project, and to Susan Larson from RIASworks for providing training in the RIAS approach to data analysis.
Contributions of authors
Sara Shaw (Senior Researcher, Sociology/Policy) was involved in the project design and led on the macro element of the study. She was also involved in the wider data collection, analysis, dissemination and publication. She led on co-ordinating the final report to NIHR.
Joseph Wherton (Senior Researcher, Health Psychology) was the lead researcher for the project, led on the ethics approval for the overall project and on the micro- and meso-level data collection and analysis, and was involved in the project design, analysis and write-up.
Shanti Vijayaraghavan (Consultant, Diabetes and Endocrinology) had the initial idea for studying the feasibility of virtual consulting in an outpatient setting and developed the idea into a research protocol (with TG). She led on establishing clinic processes for remote consultations in Diabetes and contributed to similar processes more widely in Barts Health NHS Trust, facilitated data collection and contributed to the dissemination, report writing and publications.
Joanne Morris (Research Manager) was the project manager for the study, and contributed to setting up virtual consultations in the Diabetes and Cancer Surgery clinics and to similar processes more widely in Barts Health NHS Trust, was involved in the project design, facilitated data collection and contributed to the dissemination, report writing and publications.
Satya Bhattacharya (Consultant in Hepatobiliary and Pancreatic Cancer Surgery) was involved in the project design and led on establishing clinic processes for virtual consultations in Pancreatic/Liver Cancer at the Royal London Hospital. He facilitated data collection and contributed to the dissemination, report writing and publications.
Philippa Hanson (Consultant, Endocrinology) was involved in the project design and setting up virtual consultations in Diabetes at Newham University Hospital and Mile End Hospital, facilitated data collection, and also contributed to the wider dissemination and publication from the study.
Desirée Campbell-Richards (Research Nurse) was involved in the project design and setting up virtual consultations in Diabetes at Newham University Hospital and Mile End Hospital, and also contributed to the PAG and the wider dissemination and publication from the study.
Seendy Ramoutar (Cancer Research Nurse) was involved in the project design and setting up virtual consultations in Pancreatic/Liver Cancer at the Royal London Hospital, facilitated data collection, and contributed to the wider dissemination and publication from the study.
Anna Collard (Freelance Researcher, Anthropology) was involved in the project design and led on the setting up and running of the PAG. She was also involved in the wider dissemination and publication.
Isabel Hodkinson (GP Principal/CCG Clinical Lead) acted as the lead contact with local CCGs, fed into the project design and data collection (particularly for the macro and meso levels of the study) and contributed to the report writing and publications.
Trisha Greenhalgh (Professor, Primary Care) was the chief investigator of the VOCAL study and (as such) its guarantor. She acted as the University of Oxford lead and was responsible for the overall project co-ordination and management, project design and supervision of the researchers and administrative staff. She was also involved in data collection, analysis and dissemination events, co-ordinating the study steering group, report writing and publications.
Publications
Greenhalgh T, Vijayaraghavan S, Wherton J, Shaw SE, Byrne E, Campbell-Richards D, et al. Protocol: the virtual online consultations – advantages and limitations (VOCAL) study. BMJ Open 2016;6:e009388.
Greenhalgh T, Shaw SE, Wherton J, Vijayaraghavan S, Morris J, Bhattacharya S, et al. Video outpatient consultations: a case study of real-world implementation at macro, meso and micro level. J Med Internet Res 2018;20:e150.
Data sharing statement
All data requests should be submitted to the corresponding author for consideration in the first instance. Data relating to establishing and monitoring virtual consultation services within Barts Health NHS Trust may be available from the trust, but cannot be distributed via the study team. Access to anonymised data drawn from consultations, interviews and observations with patients, staff and wider stakeholders may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Fischer EOD, Cooke O’Dowd N, Dorning H, Keeble E, Kossarova L. Quality at a Cost. QualityWatch Annual Statement. London: Health Foundation/Nuffield Trust; 2016.
- Five Year Forward View. London: NHS England; 2014.
- Honeyman M, Dunn P, McKenna H. A Digital NHS? An Introduction to the Digital Agenda and Plans for Implementation. London: The King’s Fund; 2014.
- Wachter R. Making IT Work: Harnessing the Power of Health Information Technology to Improve Care in England. Report to the National Advisory Group on Health Information Technology in England. London: The Stationery Office; 2016.
- Personalised Health and Care 2020: Using Data and Technology to Transform Outcomes for Patients and Citizens. London: The Stationery Office; 2014.
- Digital Strategy: Leading the Culture Change in Health and Care. London: Department of Health; 2012.
- Ham CA, Alderwick H, Dunn P, McKenna H. Delivering Sustainability and Transformation Plans: From Ambitious Proposals to Credible Plans. London: The King’s Fund; 2017.
- Diabetes Appointments via Webcam in Newham: Final Report for Shine 2011 Award Holder Teams. London: Health Foundation; 2012.
- Vijayaraghavan S, Campbell-Richards D, Sudra R, Morris J, Byrne E, Greenhalgh T. Diabetes appointments via webcam in Newham. Br J Diabetes Vasc Dis 2015;15:123-6. http://dx.doi.org/10.15277/bjdvd.2015.032.
- Vijayaraghavan S, Wherton J, Senn S, Byrne E, Greenhalgh T. Web-based Consultations in Diabetes – A Useful Tool for Supporting Patient Self-management? Final Report of DREAMS (Diabetes Review, Education and Management by Skype) Study to Health Foundation. Newham: Barts Health Trust; 2014.
- Morris J, Campbell-Richards D, Wherton J, Sudra R, Vijayaraghavan S, Greenhalgh T, et al. Webcam consultations for diabetes: findings from four years of experience in Newham. Pract Diab 2017;34:45-50. https://doi.org/10.1002/pdi.2078.
- Arminen I, Licoppe C, Spagnolli A. Respecifying mediated interaction. Res Lang Soc Interact 2016;49. https://doi.org/10.1080/08351813.2016.1234614.
- Greenhalgh T, Vijayaraghavan S, Wherton J, Shaw S, Byrne E, Campbell-Richards D, et al. Virtual online consultations: advantages and limitations (VOCAL) study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009388.
- Innovation Health and Wealth: Accelerating Adoption and Diffusion in the NHS. London: The Stationery Office; 2011.
- Taylor H. Accelerated Access Review: Final Report. Review of Innovative Medicines and Medical Technologies. London: Department of Health; 2016.
- Bunn F, Byrne G, Kendall S. The effects of telephone consultation and triage on healthcare use and patient satisfaction: a systematic review. Br J Gen Pract 2005;55:956-61.
- Leibowitz R, Day S, Dunt D. A systematic review of the effect of different models of after-hours primary medical care services on clinical outcome, medical workload, and patient and GP satisfaction. Fam Pract 2003;20:311-17. https://doi.org/10.1093/fampra/cmg313.
- Car J, Sheikh A. Telephone consultations. BMJ 2003;326:966-9. https://doi.org/10.1136/bmj.326.7396.966.
- Blank L, Coster J, O’Cathain A, Knowles E, Tosh J, Turner J, et al. The appropriateness of, and compliance with, telephone triage decisions: a systematic review and narrative synthesis. J Adv Nurs 2012;68:2610-21. https://doi.org/10.1111/j.1365-2648.2012.06052.x.
- Huibers L, Smits M, Renaud V, Giesen P, Wensing M. Safety of telephone triage in out-of-hours care: a systematic review. Scand J Prim Health Care 2011;29:198-209. https://doi.org/10.3109/02813432.2011.629150.
- Turner J, O’Cathain A, Knowles E, Nicholl J. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003451.
- Hanlon G, Strangleman T, Goode J, Luff D, O’Cathain A, Greatbatch D. Knowledge, technology and nursing: the case of NHS Direct. Hum Relations 2005;58:147-71. https://doi.org/10.1177/0018726705052179.
- Turnbull J, Prichard J, Halford S, Pope C, Salisbury C. Reconfiguring the emergency and urgent care workforce: mixed methods study of skills and the everyday work of non-clinical call-handlers in the NHS. J Health Serv Res Policy 2012;17:233-40. https://doi.org/10.1258/jhsrp.2012.011141.
- Munro J, Nicholl J, O’Cathain A, Knowles E. Impact of NHS direct on demand for immediate care: observational study. BMJ 2000;321:150-3. https://doi.org/10.1136/bmj.321.7254.150.
- Munro J, Sampson F, Nicholl J. The impact of NHS Direct on the demand for out-of-hours primary and emergency care. Br J Gen Pract 2005;55:790-2.
- Shah SM, Cook DG. Socio-economic determinants of casualty and NHS Direct use. J Public Health 2008;30:75-81. https://doi.org/10.1093/pubmed/fdn001.
- Pooler J. Technology and Talk in Calls to NHS Direct 2010.
- Giesen P, Moll van Charante E, Mokkink H, Bindels P, van den Bosch W, Grol R. Patients evaluate accessibility and nurse telephone consultations in out-of-hours GP care: determinants of a negative evaluation. Patient Educ Couns 2007;65:131-6. https://doi.org/10.1016/j.pec.2006.06.021.
- Turner J, Ginn C, Knowles E, O’Cathain A, Irwin C, Blank L, et al. Evaluation of NHS 111 Pilot Sites. Sheffield: University of Sheffield; 2011.
- Gamst-Jensen H, Lippert FK, Egerod I. Under-triage in telephone consultation is related to non-normative symptom description and interpersonal communication: a mixed methods study. Scand J Trauma Resusc Emerg Med 2017;25. https://doi.org/10.1186/s13049-017-0390-0.
- Akobeng AK, O’Leary N, Vail A, Brown N, Widiatmoko D, Fagbemi A, et al. Telephone consultation as a substitute for routine out-patient face-to-face consultation for children with inflammatory bowel disease: randomised controlled trial and economic evaluation. EBioMedicine 2015;2:1251-6. https://doi.org/10.1016/j.ebiom.2015.08.011.
- Kondo S, Shiba S, Udagawa R, Ryushima Y, Yano M, Uehara T, et al. Assessment of adverse events via a telephone consultation service for cancer patients receiving ambulatory chemotherapy. BMC Res Notes 2015;8. https://doi.org/10.1186/s13104-015-1292-8.
- Kaur R, Kajal KS, Kaur A, Singh P. Telephonic consultation and follow-up in diabetics: impact on metabolic profile, quality of life, and patient compliance. N Am J Med Sci 2015;7:199-207. https://doi.org/10.4103/1947-2714.157483.
- McKinstry B, Watson P, Pinnock H, Heaney D, Sheikh A. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. Br J Gen Pract 2009;59:e209-18. https://doi.org/10.3399/bjgp09X420941.
- Hewitt H, Gafaranga J, McKinstry B. Comparison of face-to-face and telephone consultations in primary care: qualitative analysis. Br J Gen Pract 2010;60:e201-12. https://doi.org/10.3399/bjgp10X501831.
- McKinstry B, Hammersley V, Burton C, Pinnock H, Elton R, Dowell J, et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010;19:298-303. https://doi.org/10.1136/qshc.2008.027763.
- Downes MJ, Mervin MC, Byrnes JM, Scuffham PA. Telephone consultations for general practice: a systematic review. Syst Rev 2017;6. https://doi.org/10.1186/s13643-017-0529-0.
- Reuter PG, Desmettre T, Guinemer S, Ducros O, Begey S, Ricard-Hibon A, et al. Effectiveness and cost-effectiveness of telephone consultations for fever or gastroenteritis using a formalised procedure in general practice: study protocol of a cluster randomised controlled trial. Trials 2016;17. https://doi.org/10.1186/s13063-016-1585-9.
- Calitri R, Warren FC, Wheeler B, Chaplin K, Fletcher E, Murdoch J, et al. Distance from practice moderates the relationship between patient management involving nurse telephone triage consulting and patient satisfaction with care. Health Place 2015;34:92-6. https://doi.org/10.1016/j.healthplace.2015.04.002.
- Campbell JL, Fletcher E, Britten N, Green C, Holt T, Lattimer V, et al. The clinical effectiveness and cost-effectiveness of telephone triage for managing same-day consultation requests in general practice: a cluster randomised controlled trial comparing general practitioner-led and nurse-led management systems with usual care (the ESTEEM trial). Health Technol Assess 2015;19. https://doi.org/10.3310/hta19130.
- Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: a systematic review. Am J Prev Med 2007;32:419-34. https://doi.org/10.1016/j.amepre.2007.01.004.
- Sobanko JF, Da Silva D, Chiesa Fuxench ZC, Modi B, Shin TM, Etzkorn JR, et al. Preoperative telephone consultation does not decrease patient anxiety before Mohs micrographic surgery. J Am Acad Dermatol 2017;76:519-26. http://dx.doi.org/10.1016/j.jaad.2016.09.027.
- Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 2007;334. https://doi.org/10.1136/bmj.39156.536968.55.
- Ikemoto K, Yamagata Y, Ikemoto T, Kawai T, Aono S, Arai YC. Telephone consultation partially based on a cognitive-behavioral approach decreases pain and improves quality of life in patients with chronic pain. Anesth Pain Med 2015;5. https://doi.org/10.5812/aapm.32140.
- Middleton-Green L, Gadoud A, Norris B, Sargeant A, Nair S, Wilson L, et al. ‘A Friend in the Corner’: supporting people at home in the last year of life via telephone and video consultation-an evaluation. BMJ Support Palliat Care 2016. https://doi.org/10.1136/bmjspcare-2015-001016.
- Franklin VL, Greene A, Waller A, Greene SA, Pagliari C. Patients’ engagement with ‘Sweet Talk’ – a text messaging support system for young people with diabetes. J Med Internet Res 2008;10. https://doi.org/10.2196/jmir.962.
- Nelson LA, Mayberry LS, Wallston K, Kripalani S, Bergner EM, Osborn CY. Development and usability of REACH: a tailored theory-based text messaging intervention for disadvantaged adults with type 2 diabetes. JMIR Hum Factors 2016;3. https://doi.org/10.2196/humanfactors.6029.
- Keating SR, McCurry MK. Systematic review of text messaging as an intervention for adolescent obesity. J Am Assoc Nurse Pract 2015;27:714-20. https://doi.org/10.1002/2327-6924.12264.
- King E, Kinvig K, Steif J, Qiu AQ, Maan EJ, Albert AY, et al. Mobile text messaging to improve medication adherence and viral load in a vulnerable Canadian population living with human immunodeficiency virus: a repeated measures study. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.6631.
- Lin CL, Mistry N, Boneh J, Li H, Lazebnik R. Text message reminders increase appointment adherence in a pediatric clinic: a randomized controlled trial. Int J Pediatr 2016;2016. https://doi.org/10.1155/2016/8487378.
- Ershad Sarabi R, Sadoughi F, Jamshidi Orak R, Bahaadinbeigy K. The effectiveness of mobile phone text messaging in improving medication adherence for patients with chronic diseases: a systematic review. Iran Red Crescent Med J 2016;18. https://doi.org/10.5812/ircmj.25183.
- DeKoekkoek T, Given B, Given CW, Ridenour K, Schueller M, Spoelstra SL. mHealth SMS text messaging interventions and to promote medication adherence: an integrative review. J Clin Nurs 2015;24:2722-35. https://doi.org/10.1111/jocn.12918.
- Lim MS, Hocking JS, Hellard ME, Aitken CK. SMS STI: a review of the uses of mobile phone text messaging in sexual health. Int J STD AIDS 2008;19:287-90. https://doi.org/10.1258/ijsa.2007.007264.
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56-69. https://doi.org/10.1093/epirev/mxq004.
- Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control 2005;14:255-61. https://doi.org/10.1136/tc.2005.011577.
- Armanasco AA, Miller YD, Fjeldsoe BS, Marshall AL. Preventive health behavior change text message interventions: a meta-analysis. Am J Prev Med 2017;52:391-402. https://doi.org/10.1016/j.amepre.2016.10.042.
- Hofstetter AM, DuRivage N, Vargas CY, Camargo S, Vawdrey DK, Fisher A, et al. Text message reminders for timely routine MMR vaccination: a randomized controlled trial. Vaccine 2015;33:5741-6. https://doi.org/10.1016/j.vaccine.2015.09.042.
- Watson T, Simpson S, Hughes C. Text messaging interventions for individuals with mental health disorders including substance use: a systematic review. Psychiatry Res 2016;243:255-62. https://doi.org/10.1016/j.psychres.2016.06.050.
- Hall AK, Cole-Lewis H, Bernhardt JM. Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health 2015;36:393-415. https://doi.org/10.1146/annurev-publhealth-031914-122855.
- Vimalananda VG, Gupte G, Seraj SM, Orlander J, Berlowitz D, Fincke BG, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare 2015;21:323-30. https://doi.org/10.1177/1357633X15582108.
- Liddy C, Drosinis P, Keely E. Electronic consultation systems: worldwide prevalence and their impact on patient care-a systematic review. Fam Pract 2016;33:274-85. https://doi.org/10.1093/fampra/cmw024.
- Car J, Sheikh A. Email consultations in health care: 2 – acceptability and safe application. BMJ 2004;329:439-42. https://doi.org/10.1136/bmj.329.7463.439.
- Car J, Sheikh A. Email consultations in health care: 1 – scope and effectiveness. BMJ 2004;329:435-8. https://doi.org/10.1136/bmj.329.7463.435.
- Atherton H, Pappas Y, Heneghan C, Murray E. Experiences of using email for general practice consultations: a qualitative study. Br J Gen Pract 2013;63:e760-7. https://doi.org/10.3399/bjgp13X674440.
- Mayor S. GPs in England and Scotland are reluctant to use email consultations, survey finds. BMJ 2016;354. http://dx.doi.org/10.1136/bmj.i3690.
- Swinglehurst D, Greenhalgh T, Russell J, Myall M. Receptionist input to quality and safety in repeat prescribing in UK general practice: ethnographic case study. BMJ 2011;343. https://doi.org/10.1136/bmj.d6788.
- Greenhalgh T, Stones R, Swinglehurst D. Choose and Book: a sociological analysis of ‘resistance’ to an expert system. Soc Sci Med 2014;104:210-19. https://doi.org/10.1016/j.socscimed.2013.12.014.
- Dixon A, Robertson R, Bal R. The experience of implementing choice at point of referral: a comparison of the Netherlands and England. Health Econ Policy Law 2010;5:295-317. https://doi.org/10.1017/S1744133110000058.
- Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. BMJ 2010;341. https://doi.org/10.1136/bmj.c5814.
- Hattink B, Droes RM, Sikkes S, Oostra E, Lemstra AW. Evaluation of the Digital Alzheimer Center: testing usability and usefulness of an online portal for patients with dementia and their carers. JMIR Res Protoc 2016;5. https://doi.org/10.2196/resprot.5040.
- Tieu L, Sarkar U, Schillinger D, Ralston JD, Ratanawongsa N, Pasick R, et al. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4847.
- Ammerlaan JJ, Scholtus LW, Drossaert CH, van Os-Medendorp H, Prakken B, Kruize AA, et al. Feasibility of a website and a hospital-based online portal for young adults with juvenile idiopathic arthritis: views and experiences of patients. JMIR Res Protoc 2015;4. https://doi.org/10.2196/resprot.3952.
- May C, Harrison R, Finch T, MacFarlane A, Mair F, Wallace P. Telemedicine Adoption Study Group . Understanding the normalization of telemedicine services through qualitative evaluation. J Am Med Inform Assoc 2003;10:596-604. https://doi.org/10.1197/jamia.M1145.
- Nicolini D. Zooming in and out: studying practices by switching theoretical lenses and trailing connections. Organ Stud 2009;30:1391-418. https://doi.org/10.1177/0170840609349875.
- Nicolini D. Medical innovation as a process of translation: a case from the field of telemedicine. Brit J Manag 2010;21:1011-26. https://doi.org/10.1111/j.1467-8551.2008.00627.x.
- Ekeland AG, Bowes A, Flottorp S. Methodologies for assessing telemedicine: a systematic review of reviews. Int J Med Inform 2012;81:1-11. https://doi.org/10.1016/j.ijmedinf.2011.10.009.
- May C, Mort M, Williams T, Mair F, Gask L. Health technology assessment in its local contexts: studies of telehealthcare. Soc Sci Med 2003;57:697-710. https://doi.org/10.1016/S0277-9536(02)00419-7.
- Temple M, Dytham L, Bristow H. Action learning at the Future Hospital development sites. Future Hosp J 2016;3:13-5.
- Greenhalgh T, Robert G, Bate P, Kyriakidou O, Macfarlane F. Diffusion of Innovations in Health Service Organisations: A Systematic Literature Review. Oxford: Blackwells; 2005.
- Valikodath NG, Leveque TK, Wang SY, Lee PP, Newman-Casey PA, Hansen SO, et al. Patient attitudes toward telemedicine for diabetic retinopathy. Telemed J E Health 2017;23:205-12. https://doi.org/10.1089/tmj.2016.0108.
- Greenhalgh T, Procter R, Wherton J, Sugarhood P, Shaw S. The organising vision for telehealth and telecare: discourse analysis. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2012-001574.
- Greenhalgh T, Wherton J, Sugarhood P, Hinder S, Procter R, Stones R. What matters to older people with assisted living needs? A phenomenological analysis of the use and non-use of telehealth and telecare. Soc Sci Med 2013;93:86-94. https://doi.org/10.1016/j.socscimed.2013.05.036.
- Steventon A, Bardsley M, Billings J, Dixon J, Doll H, Hirani S, et al. Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial. BMJ 2012;344. https://doi.org/10.1136/bmj.e3874.
- Wade VA, Karnon J, Elshaug AG, Hiller JE. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-233.
- Oudshoorn N. How places matter: telecare technologies and the changing spatial dimensions of healthcare. Soc Stud Sci 2012;42:121-42. https://doi.org/10.1177/0306312711431817.
- Ethical Frameworks for Telecare Technologies for Older People at Home. Project 217787. Lancaster: University of Lancaster; n.d.
- Oudshoorn N. Who Cares? Telecare Technologies and the Transformation of Healthcare. London: Routledge; 2010.
- Armfield NR, Bradford M, Bradford NK. The clinical use of Skype – for which patients, with which problems and in which settings? A snapshot review of the literature. Int J Med Inform 2015;84:737-42. https://doi.org/10.1016/j.ijmedinf.2015.06.006.
- Armfield NR, Gray LC, Smith AC. Clinical use of Skype: a review of the evidence base. J Telemed Telecare 2012;18:125-7. https://doi.org/10.1258/jtt.2012.SFT101.
- Gentles SJ, Lokker C, McKibbon KA. Health information technology to facilitate communication involving health care providers, caregivers, and pediatric patients: a scoping review. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1390.
- Harris MA, Freeman KA, Duke DC. Seeing is believing: using Skype to improve diabetes outcomes in youth. Diabetes Care 2015;38:1427-34. https://doi.org/10.2337/dc14-2469.
- Choi NG, Hegel MT, Marti CN, Marinucci ML, Sirrianni L, Bruce ML. Telehealth problem-solving therapy for depressed low-income homebound older adults. Am J Geriatr Psychiatry 2014;22:263-71. https://doi.org/10.1016/j.jagp.2013.01.037.
- Jimison HB, Klein K, Marcoe JL. A Socialization Intervention in Remote Health Coaching for Older Adults in the Home 2013:7025-8. https://doi.org/10.1109/EMBC.2013.6611175.
- Sharareh B, Schwarzkopf R. Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty 2014;29:918-22.e1. https://doi.org/10.1016/j.arth.2013.09.019.
- Marsh J, Hoch JS, Bryant D, MacDonald SJ, Naudie D, McCalden R, et al. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Joint Surg Am 2014;96:1910-16. https://doi.org/10.2106/JBJS.M.01558.
- Marsh JD, Bryant DM, MacDonald SJ, Naudie DD, McCalden RW, Howard JL, et al. Feasibility, effectiveness and costs associated with a web-based follow-up assessment following total joint arthroplasty. J Arthroplasty 2014;29:1723-8. https://doi.org/10.1016/j.arth.2014.04.003.
- van Eck CF. Web-based follow-up after total joint arthroplasty proves to be cost-effective, but is it safe?. J Bone Joint Surg Br 2014;96. https://doi.org/10.2106/JBJS.N.00829.
- Levy S, Henderson L, McAlpine C. Growing up with confidence: using telehealth to support continence self-care deficits amongst young people with complex needs. J Innov Health Inform 2014;21:113-17. https://doi.org/10.14236/jhi.v21i3.58.
- Viers BR, Lightner DJ, Rivera ME, Tollefson MK, Boorjian SA, Karnes RJ, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol 2015;68:729-35. https://doi.org/10.1016/j.eururo.2015.04.002.
- Katz IJ, Pirabhahar S, Williamson P, Raghunath V, Brennan F, O’Sullivan A, et al. iConnect CKD – virtual medical consulting: a web-based chronic kidney disease, hypertension and diabetes integrated care program [published online ahead of print May 4 2017]. Nephrology 2017. https://doi.org/10.1111/nep.13070.
- Host BK, Turner AW, Muir J. Real-time teleophthalmology video consultation: an analysis of patient satisfaction in rural Western Australia [published online ahead of print April 23 2017]. Clin Exp Optom 2017. https://doi.org/10.1111/cxo.12535.
- Hansen CR, Perrild H, Koefoed BG, Zander M. Video consultations as add-on to standard care among patients with type 2 diabetes not responding to standard regimens: a randomized controlled trial. Eur J Endocrinol 2017;176:727-36. http://dx.doi.org/10.1530/eje-16-0811.
- Fang JL, Collura CA, Johnson RV, Asay GF, Carey WA, Derleth DP, et al. Emergency video telemedicine consultation for newborn resuscitations: the Mayo Clinic experience. Mayo Clin Proc 2016;91:1735-43. https://doi.org/10.1016/j.mayocp.2016.08.006.
- Dang S, Gomez-Orozco CA, van Zuilen MH, Levis S. Providing dementia consultations to veterans using clinical video telehealth: results from a clinical demonstration project [published online ahead of print July 7 2017]. Telemed J E Health 2017. https://doi.org/10.1089/tmj.2017.0089.
- Leng S, MacDougall M, McKinstry B. The acceptability to patients of video-consulting in general practice: semi-structured interviews in three diverse general practices. J Innov Health Inform 2016;23. https://doi.org/10.14236/jhi.v23i2.141.
- Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1717-7.
- Müller KI, Alstadhaug KB, Bekkelund SI. Acceptability, feasibility, and cost of telemedicine for nonacute headaches: a randomized study comparing video and traditional consultations. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5221.
- Seckeler MD, Gordon BM, Williams DA, Goldstein BH. Use of smart technology for remote consultation in the pediatric cardiac catheterization laboratory. Congenit Heart Dis 2015;10:E288-94. https://doi.org/10.1111/chd.12308.
- Robinson MD, Branham AR, Locklear A, Robertson S, Gridley T. Measuring satisfaction and usability of facetime for virtual visits in patients with uncontrolled diabetes [published online ahead of print August 21 2015]. Telemed J E Health 2015. https://doi.org/10.1089/tmj.2014.0238.
- Orlandoni P, Jukic Peladic N, Spazzafumo L, Venturini C, Cola C, Sparvoli D, et al. Utility of video consultation to improve the outcomes of home enteral nutrition in a population of frail older patients. Geriatr Gerontol Int 2016;16:762-7. https://doi.org/10.1111/ggi.12551.
- Westra I, Niessen FB. Implementing real-time video consultation in plastic surgery. Aesthetic Plast Surg 2015;39:783-90. https://doi.org/10.1007/s00266-015-0526-4.
- Kampik T, Larsen F, Bellika JG. Internet-based remote consultations – general practitioner experience and attitudes in Norway and Germany. Stud Health Technol Inform 2015;210:452-4.
- McGrath P. Technology-based patient consultations: research findings from haematology patients in regional, rural and remote Queensland. Patient 2015;8:199-206. https://doi.org/10.1007/s40271-014-0074-z.
- Freeman KA, Duke DC, Harris MA. Behavioral health care for adolescents with poorly controlled diabetes via Skype: does working alliance remain intact?. J Diabetes Sci Technol 2013;7:727-35. https://doi.org/10.1177/193229681300700318.
- Nield M, Hoo GW. Real-time telehealth for COPD self-management using Skype™. COPD 2012;9:611-19. https://doi.org/10.3109/15412555.2012.708067.
- Mark DD, Ikehara C, Matsuura C, Hara K, Li D. Validating the impact of teaching pursed-lips breathing with Skype: a pilot study. J Hosp Palliat Nurs 2013;15:424-32. https://doi.org/10.1097/NJH.0000000000000015.
- Krout RE, Baker FA, Muhlberger R. Designing, piloting, and evaluating an on-line collaborative songwriting environment and protocol using Skype telecommunication technology: perceptions of music therapy student participants. Music Ther Perspect 2010;28:79-85. https://doi.org/10.1093/mtp/28.1.79.
- Ahola Kohut S, Stinson JN, Ruskin D, Forgeron P, Harris L, van Wyk M, et al. iPeer2Peer program: a pilot feasibility study in adolescents with chronic pain. Pain 2016;157:1146-55. https://doi.org/10.1097/j.pain.0000000000000496.
- Chavooshi B, Mohammadkhani P, Dolatshahi B. A randomized double-blind controlled trial comparing Davanloo intensive short-term dynamic psychotherapy as internet-delivered vs treatment as usual for medically unexplained pain: a 6-month pilot study. Psychosomatics 2016;57:292-300. https://doi.org/10.1016/j.psym.2016.01.001.
- Castanho TC, Amorim L, Moreira PS, Mariz J, Palha JA, Sousa N, et al. Assessing cognitive function in older adults using a videoconference approach. EBioMedicine 2016;11:278-84. https://doi.org/10.1016/j.ebiom.2016.08.001.
- Gerlach UA, Vrakas G, Holdaway L, O’Connor M, Macedo R, Reddy S, et al. Skype clinics after intestinal transplantation – follow-up beyond post codes. Clin Transplant 2016;30:760-6. https://doi.org/10.1111/ctr.12745.
- Somers TJ, Kelleher SA, Westbrook KW, Kimmick GG, Shelby RA, Abernethy AP, et al. A small randomized controlled pilot trial comparing mobile and traditional pain coping skills training protocols for cancer patients with pain. Pain Res Treat 2016;2016. https://doi.org/10.1155/2016/2473629.
- Bennell KL, Nelligan R, Dobson F, Rini C, Keefe F, Kasza J, et al. Effectiveness of an internet-delivered exercise and pain-coping skills training intervention for persons with chronic knee pain: a randomized trial. Ann Intern Med 2017;166:453-62. https://doi.org/10.7326/M16-1714.
- Gur M, Nir V, Teleshov A, Bar-Yoseph R, Manor E, Diab G, et al. The use of telehealth (text messaging and video communications) in patients with cystic fibrosis: a pilot study. J Telemed Telecare 2017;23:489-93. https://doi.org/10.1177/1357633X16649532.
- Epstein EG, Sherman J, Blackman A, Sinkin RA. Testing the feasibility of Skype and FaceTime updates with parents in the neonatal intensive care unit. Am J Crit Care 2015;24:290-6. https://doi.org/10.4037/ajcc2015828.
- Fairweather GC, Lincoln MA, Ramsden R. Speech-language pathology teletherapy in rural and remote educational settings: decreasing service inequities. Int J Speech Lang Pathol 2016;18:592-60. https://doi.org/10.3109/17549507.2016.1143973.
- Baker DC, Bufka LF. Preparing for the telehealth world: navigating legal, regulatory, reimbursement, and ethical issues in an electronic age. Prof Psychol Res Pr 2011;42. https://doi.org/10.1037/a0025037.
- Caffery LJ, Smith AC. Investigating the quality of video consultations performed using fourth generation (4G) mobile telecommunications. J Telemed Telecare 2015;21:348-54. https://doi.org/10.1177/1357633X15577311.
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. J Couns Psychol 1989;36. https://doi.org/10.1037/0022-0167.36.2.223.
- Hansen CR, Perrild H, Koefoed BG, Zander M. Video consultations as add-on to standard care among patients with type 2 diabetes not responding to standard regimens: a randomized controlled trial. Eur J Endocrinol 2017;176:727-36. https://doi.org/10.1530/EJE-16-0811.
- Gund A, Sjöqvist BA, Wigert H, Hentz E, Lindecrantz K, Bry K. A randomized controlled study about the use of eHealth in the home health care of premature infants. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-22.
- Greenhalgh T, Russell J. Why do evaluations of eHealth programs fail? An alternative set of guiding principles. PLOS Med 2010;7. https://doi.org/10.1371/journal.pmed.1000360.
- Greenhalgh T, Potts HW, Wong G, Bark P, Swinglehurst D. Tensions and paradoxes in electronic patient record research: a systematic literature review using the meta-narrative method. Milbank Q 2009;87:729-88. https://doi.org/10.1111/j.1468-0009.2009.00578.x.
- Bratan T, Stramer K, Greenhalgh T. ‘Never heard of it’– understanding the public’s lack of awareness of a new electronic patient record. Health Expect 2010;13:379-91. https://doi.org/10.1111/j.1369-7625.2010.00608.x.
- Greenhalgh T, Swinglehurst D. Studying technology use as social practice: the untapped potential of ethnography. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-45.
- Shaw J, Shaw S, Wherton J, Hughes G, Greenhalgh T. Studying scale-up and spread as social practice: theoretical introduction and empirical case study. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.7482.
- Barley SR. Technology as an occasion for structuring: evidence from observations of CT scanners and the social order of radiology departments. Adm Sci Q 1986;31:78-108. https://doi.org/10.2307/2392767.
- Stones R. Structuration Theory. Basingstoke: Palgrave-Macmillan; 2005.
- Greenhalgh T, Stones R. Theorising big IT programmes in healthcare: strong structuration theory meets actor-network theory. Soc Sci Med 2010;70:1285-94. https://doi.org/10.1016/j.socscimed.2009.12.034.
- Greenhalgh T, Stones R, Swinglehurst D. Rethinking ‘resistance’ to big IT: a sociological study of why and when healthcare staff do not use nationally mandated information and communication technologies. Health Serv Deliv Res 2014;2.
- Giddens A. The Constitution of Society. Berkeley, CA: University of California Press; 1984.
- Feldman MS, Pentland BT. Reconceptualizing organizational routines as a source of flexibility and change. Adm Sci Q 2003;48:94-118. https://doi.org/10.2307/3556620.
- Orlikowski WJ, Yates J, Okamura K, Fujimoto M. Shaping electronic communication – the metastructuring of technology in the context of use. Organ Sci 1995;6:423-44. http://dx.doi.org/10.1287/orsc.6.4.423.
- Bourdieu P, Richardson JG. Handbook for Theory and Research for the Sociology of Education. Slough: Greenwood Press; 1986.
- Habermas J. The Theory of Communicative Action. Boston, MA: Beacon; 1987.
- Garfinkel H. Studies in Ethnomethodology. Englewood Cliffs, NJ: Prentice-Hall; 1967.
- Goffman E. The Presentation of Self in Everyday Life. New York, NY: Penguin; 1969.
- Waterman H, Tillen D, Dickson R, de Koning K. Action research: a systematic review and guidance for assessment. Health Technol Assess 2001;5. https://doi.org/10.3310/hta5230.
- Hart EB, Bond M, Gomm R, Davies C. Using Evidence in Health and Social Care. London: Sage; 2000.
- Bate P. Synthesizing research and practice: using the action research approach in health care settings. Soc Policy Adm 2000;34:478-93. https://doi.org/10.1111/1467-9515.00205.
- Joint Strategic Needs Assessment (2017–2019). London: Newham Council; 2016.
- Life and Health in Tower Hamlets: Joint Strategic Needs Assessment Summary Document. London: Tower Hamlets Council; 2015.
- Barts Health Clinical and Organisational Strategy: 2017–2021. London: Barts Health NHS Trust; 2016.
- The State of the NHS Provider Sector. London: NHS Providers; 2017.
- Quality Accounts and Annual Report 2015/2016. London: Barts Health NHS Trust; 2015.
- Barts Health NHS Trust: Quality Report. London: Care Quality Commission; 2015.
- NHS Improvement . Financial Improvement Notice to Barts Health NHS Trust 2016. http://bartsandtheLondon.nhs.uk/media/345491/financial_improvement_notice.pdf (accessed 29 June 2017).
- Transforming Services Together: Strategy and Investment Case. London: Barts Health NHS Trust; 2014.
- Brown MJ, Shaw NT, Mador RL. Mapping the sociotechnical healthcare ecosystem: expanding the horizons of sociotechnical inquiry. AMIA Annu Symp Proc 2008:1233-5.
- Barley SR, Kunda G. Bringing work back in. Organ Sci 2001;12:76-95. https://doi.org/10.1287/orsc.12.1.76.10122.
- Making and Using Visual and Audio Recordings of Patients – Guidance for Doctors. London: GMC; 2002.
- Bailey J. First steps in qualitative data analysis: transcribing. Fam Pract 2008;25:127-31. https://doi.org/10.1093/fampra/cmn003.
- Bezemer J, Norris S, Maier CDN. Text, Images and Interaction: A Reader in Multimodality. Boston, MA: Mouton de Gruyter; 2012.
- Wagenaar H. Meaning in Action. Interpretation and Dialogue in Policy Analysis. New York, NY: ME Sharpe; 2011.
- Yanow D. How Does a Policy Mean? Interpreting Policy and Organisational Actions. Washington, DC: Georgetown University Press; 1996.
- Hajer MA, Van der Brink M, Metze T. Words Matter in Policy and Planning: Discourse Theory and Method in the Social Sciences. Utrecht: Netherlands Graduate School of Urban and Regional Research; 2006.
- Feldman MS. A performative perspective on stability and change in organizational routines. Industrial and Corporate Change 2003;12:727-52. https://doi.org/10.1093/icc/12.4.727.
- Feldman MS, Pentland BT, D’Adderio L, Lazaric N. Beyond routines as things: introduction to the special issue on routine dynamics. Organ Sci 2016;27:505-13. https://doi.org/10.1287/orsc.2016.1070.
- Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns 2002;46:243-51. https://doi.org/10.1016/S0738-3991(02)00012-5.
- Roter DL, Hall JA. Doctors Talking with Patients/Patients Talking with Doctors: Improving Communication in Medical Visits. Westport, CT: Auburn House; 1992.
- Bales RF. Interaction Process Analysis. Cambridge: Addison-Wesley; 1950.
- Emerson RM. Social exchange theory. Annu Rev Sociology 1976;2:335-62. https://doi.org/10.1146/annurev.so.02.080176.002003.
- Roter D. An exploration of health education’s responsibility for a partnership model of client–provider relations. Patient Educ Couns 1987;9:25-31. https://doi.org/10.1016/0738-3991(87)90106-6.
- Roter D, Hall J. Studies of doctor–patient interaction. Ann Rev Public Health 1989;10:163-80. https://doi.org/10.1146/annurev.pu.10.050189.001115.
- Nelson EL, Spaulding R. Adapting the Roter interaction analysis system for telemedicine: lessons from four specialty clinics. J Telemed Telecare 2005;11:105-7. https://doi.org/10.1258/1357633054462010.
- Cloud-Buckner J, Gallimore JJ, Scott R. Theoretical discussion of CAMOCS and RIAS communication models to support healthcare information technology development. Proc Hum Factors Ergon Soc Ann Meet 2010;54:517-21. https://doi.org/10.1177/154193121005400505.
- Wakefield BJ, Bylund CL, Holman JE, Ray A, Scherubel M, Kienzle MG, et al. Nurse and patient communication profiles in a home-based telehealth intervention for heart failure management. Patient Educ Couns 2008;71:285-92. https://doi.org/10.1016/j.pec.2008.01.006.
- Agha Z, Roter DL, Schapira RM. An evaluation of patient-physician communication style during telemedicine consultations. J Med Internet Res 2009;11. https://doi.org/10.2196/jmir.1193.
- Miller EA. The continuing need to investigate the nature and content of teleconsultation communication using interaction analysis techniques. J Telemed Telecare 2011;17:55-64. https://doi.org/10.1258/jtt.2010.100203.
- Nelson EL, Miller EA, Larson K. Reliability associated with the Roter interaction analysis system (RIAS) adapted for the telemedicine context. Patient Educ Couns 2010;78:72-8. https://doi.org/10.1016/j.pec.2009.04.003.
- Information Economy Strategy 2013. London: Department for Business, Innovation and Skills; 2013.
- Digital Inclusion Strategy. London: Cabinet Office; 2014.
- Digital Inclusion Charter. London: Cabinet Office; 2014.
- Digital Economy Bill. London: The Stationery Office; 2016.
- Department for Digital, Culture, Media and Sport . Government’s First Director General for Digital and Media to Help Turn Britain into World-Leading Digital Economy 2016.
- Fox ML. Directgov 2010 and Beyond: Revolution not Evolution. London: Cabinet Office, Efficiency and Reform Group, and Government Digital Service; 2010.
- Digital Landscape Research. London: Cabinet Office; 2012.
- Cabinet Office . Government Digital Service Opens for Business 2011.
- Government Transformation Strategy 2017 to 2020. London: Cabinet Office; 2017.
- The Use of New Medical Technologies within the NHS. London: The Stationery Office; 2005.
- High Quality Care for All. London: NHS England; 2008.
- Civil Service Reform Plan. London: Civil Service; 2012.
- Digital Health in the UK: An Industry Study for the Office of Life Sciences. London: Office of Life Sciences; 2015.
- A Guide to Navigating the Innovation Pathway in England. London: Office of Life Sciences; 2016.
- NHS England . Medtech Devices and Apps to Join Fast Track Payment Scheme for Innovation 2016.
- Securing Excellence in GPIT: Operating Model 2016–18. London: NHS England; 2016.
- Spending Review and Autumn Statement 2015. London: UK Government; 2015.
- Fiscal Sustainability of Health Systems – Bridging Health and Finance Perspectives. Paris: OECD; 2015.
- Gainsbury S, Appleby J. NHS Funding Choices and the 2017 General Election. London: Nuffield Trust; 2017.
- Appleby J. NHS Spending: Squeezed as Never Before. London: The King’s Fund; 2015.
- Appleby J. How does NHS Spending Compare with Health Spending Nationally?. London: The King’s Fund; 2016.
- Murray RJ, Jabbal J, Thompson J. Sicker Patients the Main Reason for A&E Winter Pressures. London: The King’s Fund; 2017.
- Murray R, Jabbal J, Thompson J, Baird B, Maguire D. Half of NHS Areas Planning to Cancel or Delay Spending because of Financial Pressures. London: The King’s Fund; 2017.
- General Practice Forward View. London: NHS England; 2016.
- NHS England . 12 NHS Hospital Trusts to Trail Blaze NHS’s Digital Revolution 2016.
- Media Literacy: Understanding Digital Capabilities Follow-up. London: BBC; 2014.
- New Care Models: Vanguards – Developing a Blueprint for the Future of NHS and Care Services. London: NHS; 2016.
- The NHS Plan. London: Department of Health; 2000.
- Our Health, Our Care, Our Say: A New Direction for Community Services. London: Department of Health; 2006.
- Liberating the NHS: An Information Revolution. London: The Stationery Office; 2010.
- Albury D. Myths and Mechanisms a Brief Note on Findings from Research on Scaling and Diffusion. London: Innovation Unit; 2015.
- Lehoux P, Miller FA, Daudelin G, Denis JL. Providing value to new health technology: the early contribution of entrepreneurs, investors, and regulatory agencies. Int J Health Policy Manag 2017;6:509-18. https://doi.org/10.15171/ijhpm.2017.11.
- Greenhalgh T, Fahy N, Shaw SE. The bright elusive butterfly of value in health technology development; comment on ‘Providing value to new health technology: the early contribution of entrepreneurs, investors, and regulatory agencies’. Int J Health Policy Manag 2017;7:81-5. http://dx.doi.org/doi:10.15171/ijhpm.2017.65.
- Greenhalgh T, Procter R, Wherton J, Sugarhood P, Hinder S, Rouncefield M. What is quality in assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Med 2015;13. https://doi.org/10.1186/s12916-015-0279-6.
- Fitzgerald L, McDermott A. Challenging Perspectives on Organizational Change In Health Care. New York, NY: Routledge; 2017.
- Whole System Demonstrator Programme – Headline Findings. London: Department of Health; 2011.
- NHS England . Test Beds 2016. www.england.nhs.uk/ourwork/innovation/test-beds/ (accessed 29 June 2017).
- NHS England . Healthy New Towns 2017 n.d. www.england.nhs.uk/ourwork/innovation/healthy-new-towns/ (accessed 29 June 2017).
- Greenhalgh T, Stramer K, Bratan T, Byrne E, Russell J, Hinder S, et al. The Devil’s in the Detail: Final Report of the Independent Evaluation of the Summary Care Record and HealthSpace programmes. London: University College London; 2010.
- Gerson EM, Star SL. Analysing due process in the workplace. ACM Trans Office Info Syst 1986;4:257-70. https://doi.org/10.1145/214427.214431.
- National Tariff Payment System 2014/15. London: Monitor, NHS England; 2013.
- Charlesworth A, Hawkins L, Marshall L. NHS Payment Reform: Lessons from the Past and Directions for the Future. London: Nuffield Trust; 2014.
- Government Digital Strategy. London: Cabinet Office; 2012.
- GOV.UK . Digital Inclusion n.d. www.gov.uk/performance/digital-inclusion (accessed 8 July 2017).
- Latour B. Science in Action: How to Follow Scientists and Engineers Through Society. Cambridge, MA: Harvard University Press; 1987.
- Lynch M, Woolgar S. Representations in Scientific Practice. Cambridge, MA: MIT Press; 1990.
- Wade V, Eliott J. The role of the champion in telehealth service development: a qualitative analysis. J Telemed Telecare 2012;18:490-2. https://doi.org/10.1258/jtt.2012.GTH115.
- Pratt W, Reddy MC, McDonald DW, Tarczy-Hornoch P, Gennari JH. Incorporating ideas from computer-supported cooperative work. J Biomed Inform 2004;37:128-37. https://doi.org/10.1016/j.jbi.2004.04.001.
- Swanson EB, Ramiller NC. The organizing vision in information systems innovation. Organ Sci 1997;8. https://doi.org/10.1287/orsc.8.5.458.
- Brown JS, Duguid P. Knowledge and organization: a social practice perspective. Organ Sci 2001;12:198-213. https://doi.org/10.1287/orsc.12.2.198.10116.
- Lewis T. The doctor will see you now… on your smartphone. Guardian 2016.
- Star SL, Easterbrook SM. CSCW: Cooperation or Conflict?. London: Springer-Verlag; 1993.
- Greenhalgh T, Wood GW, Bratan T, Stramer K, Hinder S. Patients’ attitudes to the summary care record and HealthSpace: qualitative study. BMJ 2008;336:1290-5. https://doi.org/10.1136/bmj.a114.
- DeSanctis G, Poole MS. Capturing the complexity in advanced technology use: adaptive structuration theory. Organ Sci 1994;5:121-47. https://doi.org/10.1287/orsc.5.2.121.
- Goorman E, Berg M. Modelling nursing activities: electronic patient records and their discontents. Nurs Inq 2000;7:3-9. https://doi.org/10.1046/j.1440-1800.2000.00053.x.
- Cherns A. Principles of sociotechnical design revisited. Hum Relations 1987;40:153-61. http://dx.doi.org/10.1177/001872678704000303.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Flyvbjerg B. Five misunderstandings about case-study research. Qual Inq 2006;12:219-45. https://doi.org/10.1177/1077800405284363.
- Sidnell J, Stivers T. The Handbook of Conversation Analysis. Hoboken, NJ: John Wiley & Sons; 2012.
- Hillman A, Tadd W, Calnan S, Calnan M, Bayer A, Read S. Risk, governance and the experience of care. Sociol Health Illn 2013;35:939-55. https://doi.org/10.1111/1467-9566.12017.
Appendix 1 Glossary of national-level organisations, reports and initiatives
Accelerated Access Review15 A report published in October 2016 that was commissioned by the government and led by an independent chairperson, Sir Hugh Taylor, to examine ways of speeding up access to innovative health care and technologies. The review set out recommendations to the government, including the creation of a new accelerated access partnership to speed up and simplify the process for getting the most promising new treatments and diagnostics safely from preclinical development to patients.
Care Quality Commission The independent regulator of health and adult social care in England that monitors, inspects and regulates services to ensure that they meet quality and safety standards, and which publishes performance ratings in order to help people to choose their health care.
Five Year Forward View2 A report published in October 2014 by NHS England that set out a new vision for the future of the NHS based around five new models of care.
Health and Social Care Information Centre See NHS Digital.
Health Education England An organisation responsible for education, training and workforce development in the health sector in England.
Healthy New Towns An initiative announced in 2016, involving NHS England working with housing developments to rethink how health and social care services are provided to communities. Linked to the Five Year Forward View. 2
Innovation and Technology Tariff Introduced in 2017 to incentivise the adoption and spread of innovations in the NHS.
National Information Board Responsible for developing strategic priorities for data and technology in health care.
National Institute for Health and Care Excellence Established in 1999 as the National Institute for Clinical Excellence, the National Institute for Health and Care Excellence provides guidance, advice, quality standards and information services for health, public health and social care.
NHS Improvement Established on 1 April 2016 and responsible for overseeing the provision of NHS-funded care by foundation trusts, NHS trusts and independent providers. NHS Improvement brought together previous organisations, including Monitor and the NHS Trust Development Authority.
NHS Digital Established in 2013 (when it was known as the Health and Social Care Information Centre), NHS Digital is responsible for providing information, data and IT systems for commissioners, analysts and clinicians in health and social care across England.
NHS England Leads the NHS in England, including setting priorities and the overall direction of the NHS, overseeing commissioning within the NHS and holding the contracts for GPs and NHS dentists.
NHS Innovation Test Beds Announced in 2016, involving a series of projects focused on harnessing technology to address complex issues facing patients and the health service. Linked to the Five Year Forward View. 2
Monitor Responsible for authorising, monitoring and regulating NHS foundation trusts; part of NHS Improvement since 1 April 2016.
New models of care New approaches to designing and delivering care that were announced in the Five Year Forward View in 2014,2 the delivery of which is part of a vision for the future of the NHS. Models include integrated primary and acute care systems (focused on joining up GP, hospital, community and mental health services); multispecialty community providers (focused on moving specialist care out of hospitals into the community); enhanced health in care homes (focused on delivering improved health, care and rehabilitation services to older people); urgent and emergency care (focused on improving the co-ordination of services and reducing the pressure on A&E departments); and acute care collaborations (focused on linking hospitals together to improve services).
Public Health England Established in 2013 with the aim of protecting and improving the nation’s health and well-being, and reducing health inequalities.
Sustainability and transformation partnerships Collaborations between the NHS and local authorities in 44 geographical ‘footprints’ (with an average population size of 1.2 million people) across England, focused on improving health and care, and supporting the implementation of the Five Year Forward View. 2
Sustainability and transformation plans Five-year ‘place-based plans’ developed by sustainability and transformation partnerships, built around the needs of the whole population in each area and covering all aspects of NHS spending in England.
Vanguards Fifty sites from across health care in England, all of which were selected in 2015 to lead (with national support) on developing new care models in their local area. They are intended to inspire the rest of the health and care system to radically redesign the way in which it plans and delivers services.
Wachter review4 A report of an independent review, led by Robert Wachter, and published in September 2016, which includes recommendations to inform the approach to the further implementation of IT in health and care systems in England.
Appendix 2 The VOCAL study steering committee
| Name | Affiliation |
|---|---|
| Satya Bhattacharya | Consultant Surgeon, Barts Health NHS Trust |
| Jenni Bowley (chairperson) | Citizen/lay representative |
| Emma Byrne | Researcher in Health Technology, Queen Mary University of London |
| Desirée Campbell-Richards | Research Nurse, Barts Health NHS Trust |
| Anna Collard | Social Anthropologist, Independent Consultant |
| Trisha Greenhalgh | Professor of Primary Health Care, University of Oxford |
| Charles Gutteridge | CCIO, Barts Health NHS Trust |
| Philippa Hanson | Consultant Physician, Barts Health NHS Trust |
| Isabel Hodkinson | GP Principal; Clinical Lead, Tower Hamlets CCG |
| Geraint Lewis | Chief Data Officer, NHS England |
| Joanne Morris | Research Manager, Barts Health NHS Trust |
| Seendy Ramoutar | Clinical Nurse Specialist, Barts Health NHS Trust |
| Sara Shaw | Senior Researcher, University of Oxford |
| John Taylor | Citizen/lay representative |
| Shanti Vijayaraghavan | Consultant Physician with special interest in Diabetes, Barts Health NHS Trust |
| Helen Wenseley | Divisional Manager of Medicine, Barts Health NHS Trust |
| Joe Wherton | Senior Researcher, University of Oxford |
Appendix 3 Topic guide for interviews with national stakeholders
Appendix 4 Example patient information sheet (virtual consultations)
Appendix 5 Example patient information sheet (face-to-face consultations)
Appendix 6 Information sheet for service staff
Appendix 7 Patient consent form (virtual consultations)
Appendix 8 Patient consent form (face-to-face consultations)
Appendix 9 Clinician consent form
List of abbreviations
- A&E
- accident and emergency
- CCG
- Clinical Commissioning Group
- CCIO
- chief clinical information officer
- CT
- computed tomography
- DNA
- did not attend
- DREAMS
- Diabetes Review, Education And Management by Skype
- EPR
- electronic patient record
- FGM
- female genital mutilation
- GDP
- gross domestic product
- GP
- general practitioner
- HPB
- hepatopancreatobiliary
- HSDR
- Health Services and Delivery Research
- ICT
- information, communication and technology
- IG
- information governance
- IGA
- Information Governance Alliance
- IQR
- interquartile range
- NIHR
- National Institute for Health Research
- PAG
- patient advisory group
- RCT
- randomised controlled trial
- RIAS
- Roter interaction analysis system
- SME
- small and medium-sized enterprise
- SMS
- short message service
- SOP
- standard operating procedure
- SST
- strong structuration theory
- TST
- Transforming Services Together: Strategy and Investment Case
- VOCAL
- Virtual Online Consultations – Advantages and Limitations
- VoIP
- voice-over-internet protocol
- WSD
- Whole System Demonstrator
