Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR128799. The contractual start date was in October 2020. The draft manuscript began editorial review in February 2023 and was accepted for publication in September 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Forbat et al. This work was produced by Forbat et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Forbat et al.
Chapter 1 Background
Context
Size and impact of the problem
Care homes (CHs) now operate as subacute units with high levels of morbidity and mortality. 1 Care homes will be the leading place of death by 2040, and mortality can be as high as 56% within a year of admission. 2 Consequently, there is an urgent need to find methods and approaches to optimise end-of-life care for this population.
Although some specialist palliative care (SPC) teams offer services to CH residents, recent surveys in England, Wales and Scotland3–5 demonstrate that referrals are usually reactive rather than anticipatory, but there is considerable goodwill from SPC to support residents in CH. 6 The National Audit of Care at the End of Life has prioritised systems and processes that support CH residents to receive personalised end-of-life care. 7
Some CH residents (hereafter ‘residents’) experience multiple admissions to hospital prior to their death,6 despite some admissions being preventable. 8 Hospital admissions are costly and may prompt futile or burdensome interventions that can cause distress to residents and family members. 9 Many residents will require SPC to enable CH staff to manage complex symptoms1 to avoid hospitalisation at end of life. Well-managed death and dying is contingent on high-quality interdisciplinary care,10 anticipatory care11,12 and resident-centred planning. 13
Care homes can be homely, warm and supportive environments. Supporting these establishments to improve the care they give at end of life can make them even better places for people to spend their final months and weeks of life, especially when compared with clinical settings like hospitals. CHs are an important location in the nexus of service provision for older people and are the de facto hospice. 14
Supporting residents to die in the care home
Care home staff wish to reduce preventable hospitalisations, yet often lack clear methods of doing so. 15 Palliative care interventions for residents in CHs report positive outcomes including reducing hospitalisations16 and improving advance/anticipatory care planning (ACP),17 while advocating for the role of specialist senior nursing practitioners. 18 Increasing anticipatory planning (including Advance Care Plans and anticipatory prescribing) improves the confidence of care staff to discuss goals of care with residents, their families and friends and supporting healthcare professionals and can lead to a reduction in hospitalisations. 19 Some studies issue caution on the impact on hospitalisations, but report improvements in preferred place of death. 20
Nurses in CHs who are supported to administer anticipatory medications can reduce hospital admissions and facilitate faster symptom management. 21 Provision of support to CH staff has been shown to improve end-of-life care for residents. 22 Needs Rounds have clear benefits for residents’ health outcomes: reducing admissions to acute care and improving quality of dying, and increasing workforce knowledge and confidence. 23–25
Telehealth is increasingly used to support CHs engage in early palliative care discussions and is acceptable to CH staff and relatives. 26 Such evidence supports changes to practice due to COVID-19,27 and telehealth has been used in Australian Needs Rounds adaptations, with positive outcomes reported. 28
Supporting the palliative care education of CH staff (despite it not being part of statutory training) needs to be seen as a priority to improve outcomes both for staff and for residents requiring a palliative approach. 29,30 Education in ACP, as part of palliative care provision, has led to increasing rates of completed plans and advance directives, improving consistency of clinical decision with resident preferences. 11,31 Advance care planning interventions mitigate distress and improve communication with relatives. 32 Yet, in a recent systematic review of 16 trials with a staff education component,33 many interventions did not result in improved quality of life, quality of death or reduced hospitalisations. Educational interventions can lack sufficient power to result in different clinical behaviour, programmes can be inconsistent and the necessary steps for sustainable change are often lacking. 29,34 Calls for standardisations in palliative care education in CHs may be helpful,35 yet this risks education not being tailored to specific contexts and circumstances. 36 Furthermore, the wider workforce context means there are inherent difficulties in providing coherent training and education where there is high turnover of staff. 35
Workforce issues continue to hamper many initiatives in improving palliative care in CHs,37 though some studies report that retention and burnout were not related, and indeed that burnout rates were unexpectedly low. 38 Maintaining few staffing vacancies is associated with greater likelihood of CHs being rated good or outstanding by the regulatory body. 39
Providing end-of-life support to CHs is an increasingly important area of service development. UK service delivery innovations such as ECHO,40 Gold Standards Framework (GSF),41 Macmillan’s education for carers ‘Foundations in Palliative Care’, Six Steps to Success,42 the EU funded PACE work43 and person-centred dementia care with the Namaste programme44 offer staff training and development, but rarely provide facilitation of evidence-based clinical input for people who are dying. Currently, only the PACE study has been fully tested in a randomised controlled trial across six European countries. The English Enhanced Health in Care Homes (EHCH) approach aims to improve links between CHs and primary care, yet it had patchy implementation due to multiple barriers such as communication, appropriate outcomes, trust and complexity. 44
Hospital prevention studies form an important backdrop to CH research. 45,46 Care Home Innovation Partnerships (CHIP) in Liverpool, for example, paired community matrons with CHs to review residents, develop ACP and treat minor ailments. The study reported a 15% reduction in emergency calls and a 19% reduction of hospital transfers. 47 Integrated care approaches, with health and social care working together, show promising impact on hospitalisations,48,49 alongside active management of long-term conditions. 50 Determining what constitutes an inappropriate admission, however, is not straightforward. 51
Advance care planning is an important tool in ensuring tailored and appropriate care. Studies suggest that while staff knowledge is important,52 their self-efficacy also plays an important role in engaging in ACP conversations. 53 However, training CH staff in conducting ACP conversations is a recognised deficit. 54 Involvement of family members can be important in ACP. 55 It is likely that ACP is one of several tools which need to be used to avoid unnecessary hospitalisations. 56
COVID-19 in care homes
Since commencing this study, publications on CH research have focused on responses to, and experiences of, the COVID-19 pandemic. In England, there were already 29,542 excess deaths in CHs by 7 August 2020. 57 In Scotland, estimates of years of life lost by CH residents were calculated at 5600 years. 58 Data from before COVID-19 suggest that relative risk of dying in CHs had already increased, with shorter intervals from admission to death. 59 Recommendations from a mixed-methods study on COVID-19 on CHs in England suggested a need for greater training and support for CH staff providing palliative care. 30 Evidence suggests an increase in ACP in CHs during the pandemic, which was helped by education/training for staff to promote their confidence and competence in having these conversations. 60,61 The increase in resident mortality alongside increased responsibility for end-of-life care took a considerable toll on staff mental health. 62 COVID-19 also brought about new practice developments63 and research examining ACP in the broader health and social care community, including the role of GPs64 and SPC teams. 65
Despite these studies, there is a need for greater understanding of the delivery of palliative care during the pandemic to CH residents. 66
National Health Service policy and practice
There is currently no statutory training requirement and no robust approach to delivering optimal palliative care to CH residents. NHS England wants to improve care in all settings and has committed to ‘explore improvements’ (p. 13)67 for residents in CHs but recognises that there are substantial difficulties in providing adequate care in these settings. The Care Quality Commission (CQC) articulates a requirement for ‘a clear focus on end of life care and applies in all services where end of life is delivered. The approach includes […] care homes’ (p. 21). 67 The CQC further states that there is more outstanding care by hospices than any other service, yet their data separate hospice care from nursing/CH care. This underlines a fundamental problem that CHs are not yet considered to be providing effective palliative care, despite the evident morbidity and mortality of residents.
Facilitating improved end-of-life care in CHs is an explicit driver for NHS England. 68 The ‘Ambitions Framework’ for palliative and end-of-life care has yet to be fully realised, but includes important elements such as fair access to care and staff/communities able to provide care and talk about death/dying. Clinical commissioning of palliative care clinical and education services across England is variable. 69
In the UK, while some SPC teams are based in hospitals and generalist palliative care is provided by primary care, it is the hospice teams who provide at-home support and care to people living in the community with advanced disease.
The Scottish Government’s 2015 Strategic Framework for Action on Palliative and End of Life Care sets out a vision of universal access to palliative care by 2021. This includes individuals, families and carers having timely, focused, conversations with appropriately skilled professionals to plan end-of-life care, in accordance with their needs and preferences. The vision sought to widen the range of health and social care staff providing palliative care, delivering appropriate training and supporting clinical and health economic evaluations of palliative and end-of-life care models. Furthermore, Healthcare Improvement Scotland commits to testing and implementing improvements to identify those who can benefit from palliative and end-of-life care,70 yet at present, there is no delivery model for this in CHs.
Wales set out a priority action in Health Boards providing access, support and education from SPC to CHs,71 but with no dominant model being offered beyond each community clinical nurse specialist linking with one or more CH. Northern Ireland guidelines recommend a designated nurse within the SPC team for CHs. 72
CH culture inevitably impacts working practices and resident care/experiences. 73 There is a need for high-quality leadership and facilitation alongside innovation41 and consideration of the nursing workforce and culture of education. 74 CH context, including the level of anticipatory and scheduled contact with primary care, is an important facet in effective healthcare in residential care, alongside joint working where residents’ needs are discussed, prioritised and responded to with a common purpose and shared values. 75
Understanding context and adjusting implementation in response to CH culture, including local priorities, readiness for change and facilitation champions are all important. 76 CH culture, and the culture change movement, has become a research focus seeking to identify characteristics which lead to care improvements. 77–80 Indeed, CHs which embrace culture change are more likely to provide better resident care. 81
The context in which CHs operate is complex, with stretched social care funding budgets from years of austerity, residents with complex needs and high levels of multiple morbidity, alongside suboptimal continuity of care within primary care services. 82 While approaches such as EHCH and My Health My Care My Home83 seek to address some of the multisector issues, this continues to be a complex space for providers, commissioners, service users and families. 84
Why is this research needed now?
Recognising the scale of people dying in CHs, the clinical risks associated with hospitalisation, and hence the drive to enable people to remain in their CHs with appropriate advance planning and support for staff, creates a context of urgent clinical innovation. Without a clear national model with robust evidence base, suboptimal care is a risk. However, there is a model of providing SPC in CHs in Australia which provided compelling data to improve care, called Palliative Care Needs Rounds (hereafter referred to as Needs Rounds). The definitive stepped-wedge trial of Needs Rounds85 provided robust evidence from 1700 residents that the new approach to care can substantially improve outcomes for residents, staff and the acute sector.
In order to deliver the Needs Rounds model in the UK, adaptation is required due to the different service organisation and delivery models and the need to engage with key stakeholders such as residents, carers, palliative care services, CHs and the acute care sector. 86
Needs Rounds: intervention description
Needs Rounds were developed and tested in Canberra. The Australian approach includes three components:
-
Monthly hour-long triage meetings focused on 8–10 residents in each CH who are at risk of dying without a plan in place. A checklist24 (see Report Supplementary Material 1) is used to identify the most appropriate residents to review. Needs Rounds are facilitated by a palliative care specialist where they discuss with CH staff, residents’ physiological, psychosocial and spiritual needs. The palliative care specialist provides education at each Needs Rounds based on the residents discussed, for example, on recognising deterioration/dying, medicine side effects or anatomy/physiology. Discussions instigate actions, which are always personalised for the individual, including medication reviews, and ACP.
-
Case conferences/family meetings to discuss resident goals of care and communication with family and wider multidisciplinary team (MDT).
-
Direct clinical work from the SPC clinician with the CH resident, focused on requirements identified in the Needs Round triage meeting.
Each component of Needs Rounds is usually delivered in the CH. However, some elements (e.g. 1 and 2) can be delivered using videoconferencing,28 either in situations of excessive distance or when required due to infection control measures.
Needs Rounds outcomes
The pilot Needs Rounds intervention outcomes in Australia support UK strategic priorities, such as decreasing length of hospitalisations [p < 0.01; confidence interval (CI) −5.05 to −1.41 days], improving rates of residents dying in their preferred place23 and enabling staff to normalise death and dying25 by adopting an outreach model of SPC. A further Australian stepped-wedge trial of Needs Rounds with 1700 CH residents achieved reduced acute length of stay (p = 0.048) and evidenced improvements in residents dying with dignity, compassion and comfort (p = 0.019) and improved workforce confidence (p = 0.09). 85
Goals of the elements essential to the intervention
Needs Rounds draw together requirements for looking after older people in care, including case management and specialist outreach services,87 increasing ACP88 and staff education. 49,89 Needs Rounds strengthen current models by widening the beneficiary beyond those with advanced dementia90 and meeting core strategic targets such as improving symptom management,91 increasing preferred place of death92 and providing a framework for person-centred care to residents. 93
Creating a basic organisational structure that promotes palliative care collaboration through monthly multidisciplinary meetings (both internal and external health and social care professionals) is an important first step to build a solid foundation to provide palliative care. Such a foundation helps to break the isolation of CHs and can promote greater sustainability of further initiatives.
The context of Australian and United Kingdom care homes using Needs Rounds
While Australian CHs and UK CHs vary, many of the practicalities are similar. Both countries face similar tensions in service delivery for example high turnover of staff and residents with complex multiple morbidities. Usual care in the area of Australia where the stepped-wedge trial was conducted had reactive provision of direct clinical care from the local SPC team. This is very similar to most UK provision. 3,4
The four core elements by which the two countries’ CH contexts differ are as follows:
-
The sites involved in the Australian study all employed a registered nurse, which is an important difference in adapting and implementing Needs Rounds for the UK. This may mean that UK Needs Rounds require greater links with primary care (not just SPC). In the UK, SPC will require primary care to facilitate prescribing and, in CHs with no on-site nurses, administering of medication. It may also mean that the Needs Round ‘case-based education’ component of the model will include greater emphasis on core information and skills.
-
Australian CHs tend to be larger than the average size in the UK (average Australian size in the stepped-wedge study was 90, whereas the average in England is 29.5 and 38 in Scotland). 94 This means that the delivery of Needs Rounds will be to fewer residents and smaller staff groups in the UK.
-
Australia has a larger proportion of adults over the age of 65 residing in CHs (5.2%)95 compared with England/Wales (3.2%). 96 It is not clear, however, whether the acuity of residents’ symptoms is comparable across countries.
-
Both countries operate CHs without mandatory training for their staff on palliative or end-of-life care. In Australia, however, CH staff are able to access a national education programme (PEPA – Programme of Experience in the Palliative Approach https://pepaeducation.com/) which enables CH staff to attend a workshop on palliative care, and some days shadowing staff from SPC (e.g. in an inpatient unit). By contrast, in the UK, education is provided via initiatives such as ECHO, Six Steps or the GSF.
Aims and objectives
The implementation objectives were to:
-
co-design a UK version of Needs Rounds, which is responsive to the different (macro, meso and micro) contextual characteristics of the UK CH sector (Phase 1)
-
implement the adapted model of care, assess feasibility, acceptability and effectiveness, and ultimately propose how the model of care can be further refined and adopted in the UK context to reap the benefits demonstrated in the Australian work (Phase 2).
The intervention objectives were to:
-
determine the transferability of the core elements of the Needs Rounds intervention in the UK context (Phase 1 and 2)
-
delineate the mechanisms of action (individual and group) that enable more effective palliative and end-of-life care practices to be realised in UK CHs (Phase 2)
-
identify the relationships between (1) the mechanisms of action embedded in Needs Rounds, (2) how these mechanisms function in different CH contexts and (3) the outcomes arising for different stakeholders and parts of the care system (Phase 2).
The process evaluation objectives were to:
-
document the outcomes of UK Needs Rounds on hospitalisations (including costs), quality of death/dying and staff capability (Phase 2)
-
assess and report the perspectives of CH residents, relatives, CH staff and palliative care staff on using UK Needs Rounds (Phase 2).
The primary aim was to improve palliative care, through developing the Needs Rounds approach for CH residents/staff to access SPC. The primary outcome was to understand what works for whom under which circumstance and why, when using the UK model of Needs Rounds.
Structure of the report
This report is formed of eight chapters.
Chapter 1, this background chapter, introduces the research. Chapter 2 outlines the study’s methodology. Chapter 3 reports the sample and ‘what works for whom under what circumstances’. Chapter 4 reports data on core quantitative outcome measures, specifically staff ability to adopt a palliative approach, the quality of death and dying of residents, and family perceptions of care. Chapter 5 reports the treatment effect and cost–benefit analysis. Chapter 6 outlines the patient and public involvement and engagement (PPIE) evaluation, and Chapter 7 reports research engagement by CH. Chapter 8 presents the discussion and conclusions.
Chapter 2 Methodology and methods
Research design
This pragmatic critical-realist implementation study used the integrated Promoting Action on Research Implementation in Health Services (i-PARIHS) framework in six case studies. Each case comprised a SPC team working with three to six CHs each.
Integrated Promoting Action on Research Implementation in Health Services represents an integrated approach, recognising that most implementation is complex, requiring attention to multiple factors simultaneously for an innovation to be successful. The development of theory is central to i-PARIHS to enable effective implementation of research evidence into everyday practice. Programme theories explaining micro changes and transactions, such as working hypotheses or local theories of change, are explored to elucidate core concepts. For this study, theory was generated regarding (1) influential components of the UK context and (2) the mechanisms of how to implement Needs Rounds in UK CHs to (3) deliver desired outcomes.
The study was designed prior to the COVID-19 pandemic. Changes required to the protocol and impacts on data collection are detailed in subsequent sections and summarised in Summary of changes to protocol.
The following guidelines have been drawn on in reporting the study: CHEERS (health economics),97 GRIP Longform (PPIE),98 RAMESES II (realist evaluations),99 TIDieR (intervention description and replication)100 and StaRI (implementation science) (see Report Supplementary Material 2–6). 101
The implementation strategy was to adjust the Australian model, based on feedback in Phase 1 and 2 (qualitative interviews and workshops) to create a UK adaptation.
Study phases
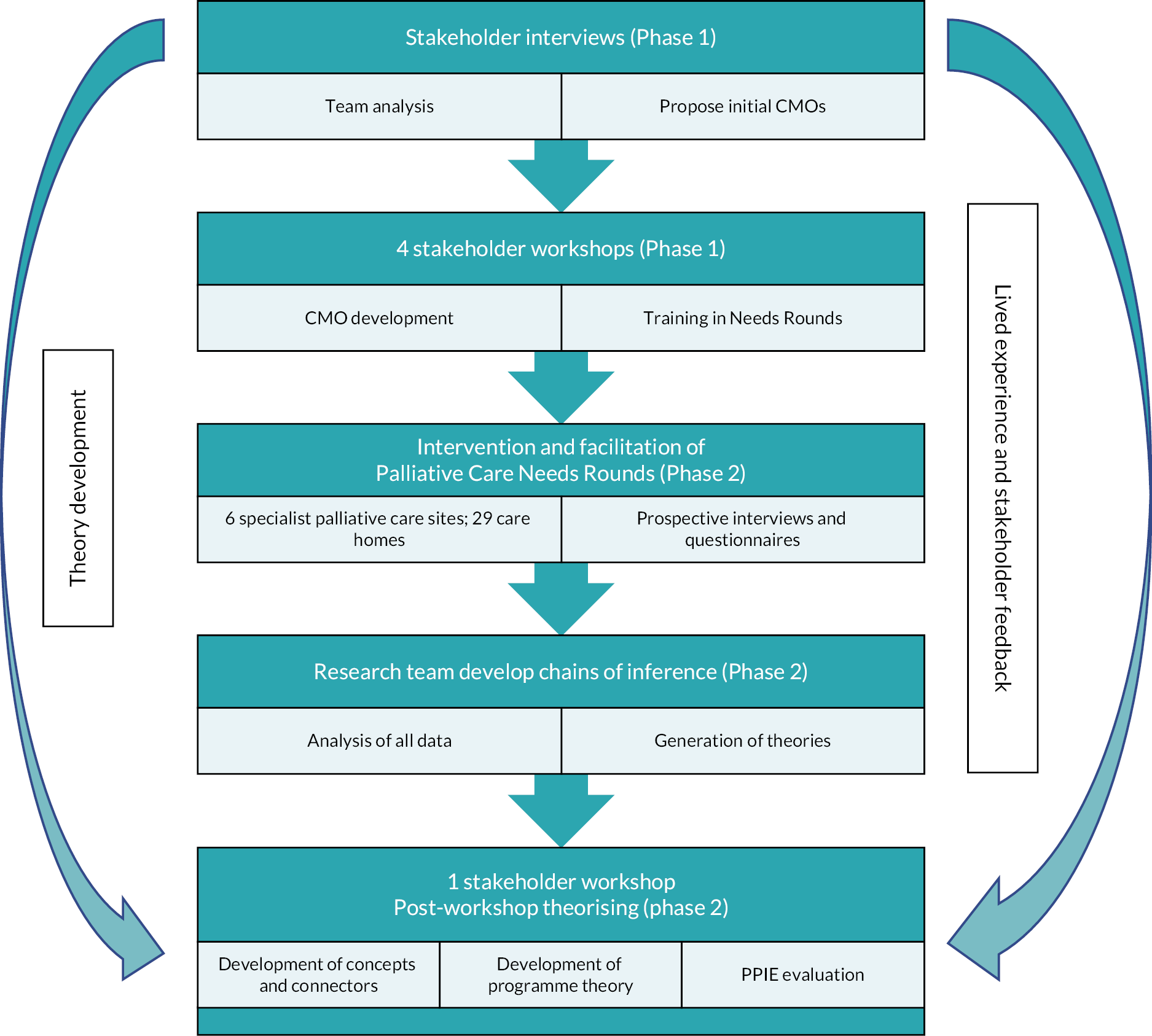
The study had two core phases. The phases and core activities are depicted in Figure 1.
FIGURE 1.
Co-design process in developing a candidate programme theory.
Overview of Phase 1
Purpose: Phase 1 sought to generate an initial programme theory of ‘what elements of Needs Rounds would work for whom in what circumstances and why, in the UK context’.
-
Qualitative interviews were conducted with key stakeholders to understand how Needs Rounds could be used.
-
The findings from the interviews were presented to participants during two online workshops. Workshop discussion focused on whether the data reflected participants’ experiences, any identified gaps and the anticipated mechanisms of change required for Needs Rounds to be successfully implemented.
-
Team analysis of interview and workshop data led to the development of five theories and an initial programme theory.
-
A third workshop was held to generate feedback on the initial programme theory and the context, mechanism outcome (CMO) configurations. The five theories’ CMOs were communicated within the workshop using fictionalised vignettes – to help illustrate the interconnections by describing example residents (see Report Supplementary Material 7–11 for vignettes). Discussions arising from the presentation of CMOs focused on overarching themes and connectors between the theories. Discussions were captured by the investigator team (including academics and PPIE).
-
A fourth Phase 1 workshop was run, focused on presenting the initial programme theory and providing training on the UK Needs Round approach.
Workshop participants included Phase 1 interviewees and a wider pool of stakeholders. The workshops created the collaborative space to co-design the UK approach to Needs Rounds. All workshop discussions were audio-recorded. Phase 1 ran for 6 months, from January 2021 to June 2021.
Overview of Phase 2
Purpose: to implement UK Needs Rounds and finalise the programme theory of ‘what works for whom under what circumstances and why’. Secondary aims were to generate data relating to cost–benefit of the intervention, determine the impact on resident quality of dying, family perceptions of care and evaluate the PPIE across the study.
-
Implementation of the UK Needs Rounds model was conducted with six SPC teams, each of whom were working with three to six CHs in their locality. Implementation ran for 12 months, from July 2021 to June 2022.
-
Implementation involved the three-part model described in Needs Rounds: intervention description, with a minor modification that sites could choose to integrate with local primary care services in ways that suited usual provision, including where there were GP retainers, EHCH or regular primary care rounds.
-
Throughout Phase 2, prospective interviews were conducted with SPC and CH staff using Needs Rounds to understand their reflections on the intervention.
-
In May 2022, towards the end of the implementation period, a workshop was held to refine the overarching programme theory based on the prospective interviews and views articulated during the workshop. The workshop sought to elicit further feedback on implementation and post-study implementation, confirm and agree preferred dissemination methods for stakeholders and discuss study dissemination. Discussion of the theories was aided by an artist providing an illustration of each of the theories, coupled with live illustrations of the unfolding workshop conversation. The illustration produced of the five theories is available in Report Supplementary Material 12; Chapter 3 contains the illustration of the final programme theory (see Figure 3).
Workshop participants in Phase 2 involved people involved in delivering the intervention, from the CHs and SPC services.
-
Phase 2 also included a qualitative evaluation of the PPIE process and outcomes for the study; data collection to determine cost–benefit analysis; impact on other outcomes of interest such as staff capability of adopting a palliative approach (CAPA), quality of resident dying and family perceptions of care.
Woven throughout, Phase 1 and Phase 2 were reflexive analytic research team meetings to discuss the chains of inference connecting the theories and the overarching programme theory. These team meetings provided space to reflect on how academic, clinical and lived experience impacted our interpretations.
Data sources
Recruitment to the study
Specialist palliative care sites were recruited to the study first. Existing networks of the principal investigator (PI) were approached with study materials outlining the aims, objectives and methods of the study. These sites were named in the protocol and hence agreed prior to funding. One hospice withdrew after the study was funded, and consequently, further recruitment activity took place to identify an additional site. This site was confirmed and in place prior to commencement of the study.
Subsequently, hospices that agreed to participate in the study identified local CHs to invite to participate.
Recruitment was augmented by ENRICH, a UK network focused on enabling research in CHs. ENRICH holds databases of CHs who have demonstrated an interest in participating in studies, and they contacted CHs in some of the case study areas to invite eligible homes to participate.
Interviewees were recruited through the collaborating CHs and SPC sites, using snowballing and personal networks to identify relevant stakeholders in the local communities.
Recruitment was sought across England and Scotland, with four sites in England (west Midlands, Midlands, East Anglia and South) and two in Scotland (central and northern). Purposive maximum variability sampling of SPC services focused on recruiting a heterogeneous and information-rich sample, including urban/rural, service size, deprivation, cultural demographics, use of ECHO or other SPC input models and funding models. CH recruitment sought diversity by being part of a national chain or independently run and size. These variables reflect the dominant contextual influences which were likely to impact how Needs Rounds are used in the UK.
Due to COVID-19 restrictions, recruitment was all conducted remotely, using e-mail, phone calls and video calls, rather than a combination of these approaches alongside in-person meetings.
Inclusion criteria
Stakeholders (for interviews in Phase 1 and workshop participants)
-
Work for SPC or a CH in one of the six cases, are a resident in one of the CHs, are a relative of a CH resident in one of the six cases or work in acute care impacted by hospitalised CH residents.
-
Willing to provide informed consent.
-
Have capacity to provide their own consent to participate.
-
Not engaged in any current safeguarding investigations.
Care homes (to use UK Needs Rounds)
-
Located within the service area of the SPC service.
-
Provide care to residents who have high clinical nursing/medical needs.
-
Willing to sign a memorandum of understanding with the research team, outlining provision of hospitalisation data, facilitate access to staff for interviews and engagement in delivering Needs Rounds.
-
A range of medium and large sizes (focusing primarily on larger CHs), sole traders and large corporate provider and with a range of funding models (social care and self-funded residents).
Residents who are discussed at Needs Rounds
-
Resident in a collaborating CH in one of the six case study locations.
-
An anticipated life expectancy of < 6 months or a deteriorating condition where they are at risk from dying without an adequate care plan in place.
-
Experiencing suboptimal biopsychosocial symptoms.
Relatives completing the CANHELP Lite (family’s perceptions of care) questionnaire
-
Relative of a resident who was discussed in Needs Rounds.
-
Able to provide their own informed consent.
Interviewees for the patient and public involvement and engagement evaluation
-
Coinvestigator or staff at one of the case study sites.
-
Able to provide their own informed consent.
Phase 1
Data were generated from two sources: (1) interviews and (2) a sequence of four workshop discussions.
Twenty-eight interviews (individual or paired) were conducted with participants from six case study sites. Interviews involved relatives (n = 2), clinicians/managers in CHs (n = 12), clinicians in SPC (n = 7) and their related acute/primary care staff (n = 5), allied health practitioners (n = 1) and one CH staff member who did not specify their role. Formal respondent checking of transcripts was not used, since the workshops provided opportunity to clarify, check accuracy and validate ideas/opinions with participants.
Staff participants were asked about their local context, such as services’ geography, policy, structure, funding and practice elements. Relatives were asked about their experiences of their family member’s care including symptom management, goals of care and ACP and communication and responsiveness.
These data were analysed to develop realist theories regarding how implementation would work in practice, what might influence implementation in each case study site, to identify CMOs. Interview data were collected between February 2021 and April 2021. Interviews ranged from 37 to 119 minutes, with an average of 56 minutes.
The analysis from these interviews was then presented to participants during two online workshops. Workshop discussion focused on whether the data reflected participants’ experiences, any identified gaps and the anticipated mechanisms of change required for Needs Rounds to be successfully implemented.
Team analysis of both the interview data and the two workshop discussions led to the development of five theories and an initial programme theory. These five theories and programme theory were then presented for discussion and examination at a third workshop, to generate feedback on (1) the initial programme theory, (2) the CMO configurations and (3) overarching themes and connectors between the theories.
A fourth workshop was then held to present the initial programme theory and use feedback from participants to make revisions to it. This fourth workshop also included training on the UK Needs Round approach for the CH staff and SPC staff who would be delivering the intervention.
Forty-three unique participants attended the workshops in Phase 1. These participants were from 23 organisations including CHs, SPC organisations, and people with PPIE experience. The workshops were conducted in April and June 2021 and lasted for approximately 3.5 hours each.
Throughout the four workshops, the research team, including PPIE members, made notes capturing key parts of the discussion. Transcripts of the workshop discussion were also used as data sources and hence were subject to analysis.
It was intended to conduct interviews and workshops face to face. However, due to ongoing COVID-19 restrictions, reduced willingness/ability to travel and greater familiarity with online platforms, all data collection was conducted online.
Phase 2
Staff accounts of the intervention
During the intervention phase, qualitative interviews with key stakeholders, in each case study site, were conducted to determine the mechanisms of change and examine the CMOs/theories that were generated in Phase 1. Interviews collected prospective data on acceptability, appropriateness, feasibility, implementation cost, coverage and sustainability. Further data on providers’ context were also examined alongside how the intervention was delivered in each site (mechanisms including resources and reasoning, such as preparedness of sites and agency to affect practice). In the final interviews, stakeholders were asked to reflect on mechanism to disseminate the findings.
Interview questions pertaining to the CH context were drawn from conceptual work by Estabrook et al. 102 to dynamically explore each CH’s culture. Interview topics covered, for example, leadership, culture, time/space, staff/resident turnover or introduction of new policies/procedures and prioritisation of the intervention in workload.
Audio-recorded interviews were conducted at:
-
four months (capturing early adoption, n = 19 interviews/21 participants; 4 nurses, 9 management, 1 carer, 6 SPC clinicians and 1 nurse and deputy manager)
-
eight months (mid-range, n = 21 interviews/22 participants; 12 management, 3 nursing, 6 SPC clinicians and 1 nurse and deputy manager)
-
eleven months (longer-term implementation, n = 14 interviews/15 participants; 6 management, 2 nursing, 6 SPC clinicians and 1 nurse/deputy manager).
The Australian Palliative Care Needs Rounds stepped-wedge trial showed that 6 months allows time for clinicians and services to become sufficiently familiar with the Needs Rounds model. The Australian study indicated month-on-month improvements in staff capability over time, and hence this 12-month time frame allowed analysis over the course of implementation.
Interview duration in Phase 2 reflected the clinical/care pressures within the CHs. Interviews ranged from 16 to 117 minutes, with an average of 35 minutes. Interviewees in Phase 2 had not been interviewed in Phase 1 since many were not in role until implementation commenced.
Data from these interviews were presented for discussion in a final workshop, held online in May 2022, in the penultimate month of the implementation period. The purpose of this final workshop was to refine the overarching programme theory (and by default also the five theories). The workshop sought to elicit further feedback on implementation, post-study implementation and develop a dissemination plan. Workshop discussion was aided by an artist who prepared an illustration of each of the five theories (available in the Report Supplementary Material 12). The artist also attended the workshop and produced further live illustrations of the unfolding conversation (which is presented in Chapter 3, showing the final programme theory).
Workshop participants in Phase 2 involved people who were delivering the intervention, from the CHs and SPC services.
Data were intended to be collected through a mixture of face-to-face and phone interviews, alongside in-person workshops. However, with ongoing COVID-19 restrictions in visiting CHs, all data collection was conducted online/via phone. Sample size was focused on theoretical sufficiency, which was achieved. Transcripts were not returned to interviewees, but participant checking was facilitated through the workshop discussions. These data are reported throughout Chapter 3 and in Qualitative appraisals of costs.
Resident data
A bespoke spreadsheet was developed to capture resident data. This included basic demographic information including age, ethnicity, first language, number of deaths and Eastern Cooperative Oncology Group (ECOG) performance scale. The ECOG describes an individual’s level of functioning in terms of their ability to care for themself, daily activity and physical ability. Scores ranged from 0 to 4, whereby lower scores represent higher levels of functioning and independence.
Preferred place of death (and actual place of death if they died during the study) and health service use during the 3-month data collection periods (name of hospital, duration of admission, speciality/ward of admission, mode of transport to hospital, gender, age and contact with primary care) were also requested.
Data were collected by CH staff. COVID-19 lockdowns precluded external researchers attending. Further, ethical approval permitted access to residents’ personal data only by routine members of the care team.
Training and support were provided to CH staff to increase the robustness of data collection and reporting. Videos were made to demonstrate data capture, and individualised phone calls, video calls and e-mails were used with each CH to support data reporting. The spreadsheet was revised and simplified during baseline data collection to aid reporting. The data collection tool was revised again during the follow-up period and formatted as a Word document to increase response rates.
Specialist palliative care clinicians were asked to report information regarding the assessments and interventions triggered by Needs Rounds. This included, for example, physical assessments, blood/urine tests or other clinical investigations, referrals to other NHS services, changes in pharmacotherapy and commencement of syringe drivers.
Data on resident demographics are reported in Chapter 3, Sample.
Economic evaluation
Economic evaluation planned to involve a cost–benefit analysis103 drawing on the following data (Tables 1 and 2).
| Cost type | Cost detail | Measurement of costs |
|---|---|---|
| Direct costs | Intervention costs on-site:
|
Included within the project budget and therefore directly recorded. Where appropriate additional detail was collected directly from the CHs |
| Additional NHS staff time attending CH Additional prescriptions |
Estimated in the SoECAT, with additional costs recorded by intervention staff as required | |
| Indirect costs | Wider additional costs incurred by the CH, including
|
These changes, and their associated costs, were collected from CHs in a proforma through the interviews |
| Intangible costs | Inconvenience to staff, residents, family and carers as a result of the intervention | Explored in the qualitative interviews in Phase 2 |
| Cost type | Cost detail | Measurement of costs |
|---|---|---|
| Direct costs | Costs of ambulance journeys | Estimated from the 2019/20 National Tariff Payment System105 |
| Hospital stay cost | Hospital-specific PLICs data for England106 and Scotland107 on stay costs by age and gender to estimate a day rate to use in the hospital costing | |
| Primary care usage | Explored in the qualitative interviews in Phase 2 | |
| Indirect costs | Wider additional costs incurred by the CH, in connection with resident hospital admissions, including staffing, travel, equipment or facilities | Explored in the qualitative interviews in Phase 2 |
| Intangible costs | Inconvenience to residents and their family/carers arising from hospitalisation | These were not measured directly but were explored in the qualitative interviews in Phase 2 |
Linked hospital data were not sought, as this would have required considerable additional resource (time and personnel) and result in reduced data of less robust quality for drawing generalisable conclusions. The reduced volume and robustness of data would occur because individual-level consent would be required to access such information, effectively reducing the pool of data to those without cognitive impairment. Since the average prevalence of dementia in CH residents is 69%,108 this presented an unacceptable reduction in sample size.
In a change to the protocol, the cost–benefit analysis was unable to be completed. This was caused by two main issues, both COVID-19-related.
First, challenges in the recruitment of CHs and paucity of CH data received from those who did participate affected both the sample size and the level of data available to the project for economic analysis. Estimation of the benefit (in reduced hospitalisation) was compromised both by sample size and the confounding effect of COVID-19 on the pre/post research design.
Second, the secondary outcome of cost–benefit was predicated on pre-COVID-19 clinical concerns about high rates of hospitalisation and transfer to/from hospital of CH residents. COVID-19 led to substantial changes to health service use and in particular reducing hospitalisations (including circumstances where hospitals have refused transfers from CH residents and vice versa). Consequently, the impact of our Needs Rounds intervention in reducing hospitalisations costs cannot be disaggregated from the impact of COVID-19 on health service use and its development during the study.
Data on economic analysis are reported in Chapter 5.
Staff capability
Care home staff CAPA was assessed on a nine-item validated self-report questionnaire (see Report Supplementary Material 13) (He, 2016, personal communication). Capability of adopting a palliative approach has a unidimensional scale; higher scores indicate greater capability. Internal consistency is very high with a Cronbach’s alpha of 0.95 and a split-half reliability coefficient of 0.93 (He, personal communication). Data were collected from a range of staff members, predominantly nurses, care assistants and managers, between July 2021 and July 2022. Although the aim was to collect data each month from those attending Needs Rounds, the average response rate from CHs was 3 months of data, not necessarily from the same staff members each time. Questionnaires were completed by CH staff, either hard copy or online depending on site preferences.
Data on staff capability are reported in Staff capability of adopting a palliative approach.
Quality of death and dying
The Quality of Death and Dying Index109 (QODDI) was requested to be completed by CH staff for each decedent resident prospectively at the time of death throughout the study (see Report Supplementary Material 13). This 17-item questionnaire examines four correlated but distinct domains: symptom control, preparation, connectedness and transcendence. The decedent’s experience is rated on a 0–10 scale, where higher scores indicate a better death. The Cronbach’s alpha for the QODDI total score is 0.89. Following correspondence with the scale’s originator confirming psychometric robustness of excluding items, one item on access to euthanasia was removed, as this is not legal in England or Scotland.
The QODDI was designed for completion by relatives; however, staff are more consistently likely to have seen the resident in the weeks prior to death (primarily due to COVID-19 visiting restrictions). Hence, staff completion resulted in more reliable and valid data. No suitable staff measure exists, and the questionnaire worked well in the Australian stepped-wedge trial. 85 Questionnaires were completed in either hard copy or online, depending on site preferences. Data were collected between July 2021 and June 2022.
Data on the QODDI are reported in Quality of death and dying.
CANHELP Lite: Families’ perceptions of care
Relative reports of care quality were focused on those where residents were discussed at Needs Rounds, using the CANHELP Lite (see Report Supplementary Material 13). 110 The second part of the questionnaire was used, which focuses on satisfaction with care. This involved 22 items collecting self-report data on family views of CH staff, illness management, communication, relationships with clinicians and relative involvement. The Cronbach’s alpha for the total score is 0.88–0.94. Questionnaires were completed either in hard copy or online, depending on family/site preferences. Relatives were only asked once to complete this measure, even if the resident was discussed at Needs Rounds more than once. Data were returned between August 2021 and May 2022.
Data on the CANHELP Lite are reported in Families’ perceptions: CANHELP Lite.
Audio recordings of monthly Needs Rounds
Sites were requested to record Needs Rounds discussions, to allow analysis of how monthly meetings proceeded, including the case-based learning and assessment of adaptations made by clinical teams for their local areas. Recordings were made from July 2021 to June 2022.
Data from the audio recordings were used to inform assessment of fidelity, which is reported in Fidelity.
Patient public involvement and engagement interviews
All research team members (including academics, clinicians and PPIE members) were invited to participate in a one-off interview focused on their experiences and process of PPIE throughout the study. One-to-one phone/video-conference interviews were conducted to examine the successes and opportunities of patient/public involvement in this study to enhance future PPIE work.
Data were collected and analysed by an independent researcher in October and November 2022. This component of the study was conducted by one female qualitative researcher completing her doctorate in the social sciences. Prior to the study, the independent researcher had no relationship to any of the PPIE members and only a limited relationship with three of the academics, who she knew on an informal basis through university networks. Interviews ranged from 23 to 72 minutes, with an average of 49 minutes. Interviews were recorded and transcribed. Transcripts were then anonymised; interviewees are referred to in this report via their role in the study (e.g. academic 1 or PPIE 1).
Data on the PPIE evaluation are reported in Chapter 6.
Care home survey
A third phase was suggested by the project Steering Group, to conduct a survey of CHs across the UK. The survey would gather feedback on the fit of the UK Needs Rounds approach for services not involved in the intervention study. This component was not integrated into the original funded protocol, but was part of the published intervention protocol. 104 Further discussions with study team and steering group identified that a national survey would not be possible within the time span of the study, and that ongoing workforce issues exacerbated by COVID-19 would likely result in a low response rate, precluding generalisability.
Modes of analysis/interpretation
Qualitative data
Transcripts of audio data and documentary evidence were stored and organised using Nvivo 11, 12 and 20.
Critical realism informed the thematic analysis used with all qualitative data, following the five-step process outlined by Braun and Clarke. 111 Stage 1 involved familiarisation with the data set through repeated rereadings. Stage 2 involved identifying an initial thematic framework, which was used in Stage 3 where data were indexed with reference to the thematic framework. In Stage 4, data were synthesised from across respondents into consolidated themes. Stage 5 focused on interpretation and finalisation of key themes generated from the data.
Within- and between-case analysis was conducted inductively (inferring from specific data to draw conclusions and develop theory), drawing on process tracing and constant comparative methods, respectively. Deductive analysis (testing the theories with reference to data) was also used to refine the CMO theories. Following realist approaches, data analysis also drew on a ‘retroductive’ approach, to move beyond induction and deduction to allow for ‘the identification of hidden causal forces that lie behind identified patterns or changes in those patterns’ (p. 1). 112 Retroduction describes the team’s interpretation of generative causation in identifying and naming contexts and mechanisms which lead to the intervention outcomes.
Phase 1 (pre-implementation) data were analysed to create an initial programme theory to be tested during implementation. Analysis focused on identifying the contexts (in which Needs Rounds would run), mechanisms of change and outcomes. Contexts were analysed as either inner/micro/meso context (individual or organisational level) or outer/macro (such as the wider policy/cultural context). Mechanisms of change were organised into categories to include facilitators (people), facilitation (process), resources and reasoning. Innovation focused on understandings of Needs Rounds, perceptions of value and degree of fit. CMO configurations and their chains of inference were generated for five theories from these data.
Qualitative data collected in Phase 2 (at months 4, 8 and 11 of implementation) were used to refine the programme theory. The coding was organised in relation to the five theories (see Theory 1: confidence and competence and Theory 5: supporting families), identifying CMOs. CMO configurations were updated based on what worked or did not work during implementation. Analysis was an iterative process, examining differences between the initial programme theories and Phase 2 implementation data.
Further coding was developed to allow analysis of engagement of sites in the data collection by CH staff. Tables were created identifying the main CMOs under each theory with illustrative data.
The PPIE evaluation analysis was conducted by the independent researcher to maintain the confidentiality of respondents. All other qualitative data were analysed by three experienced female qualitative researchers (all of whom hold PhDs) who had ongoing contact with staff at all study sites. Codes and themes were discussed between those three team members to develop consensus on data interpretation.
The guiding principle for analysis and sampling was theoretical sufficiency113 with triangulation used for all data sources to aid development of the theory.
Survey data
The quantitative analysis was conducted by social scientists with expertise in statistics, who were not involved in data collection. Therefore, the researchers responsible for analysing the survey data had no interaction with either CH staff or hospice staff. During the analysis, ID numbers were used (e.g. ST00335) in place of organisations’ names, creating a quasi-blinded state whereby the researchers analysing the survey data were not connecting results to specific CHs or case study identity during analysis.
Staff capability: CAPA
Scores for each of the nine CAPA items were coded one to five and summed to give an overall CAPA score (ranging from 9 to 45) whereby higher scores indicate greater capability.
Data were analysed using generalised least squares random-effects models with robust standard errors. This allowed adjustment for repeated observations from the minority of CH staff members that completed the survey more than once (16.4%). Regressions were conducted for overall CAPA scores and for each of the nine CAPA items individually. In each of the analyses, the main predictor variable was staff role, with variables to control for date of survey completion, size of CH, ownership of CH (private or voluntary, not for profit) and hospice. To determine size of the CH, the number of beds reported at each site was categorised as medium (11–49 beds) or large (50 + beds) based on categories defined by the CQC. 114 There were no CHs in the study categorised as small (1–10 beds).
Additionally, a paired t-test was carried out using the subset of CH staff members with multiple responses (n = 28). Most (60.7%) completed the CAPA survey only twice; however, for those with three or more responses, their first and last submitted CAPA scores were compared.
Quality of death and dying
As specified in Quality of death and dying, the item on euthanasia was removed, reducing the QODDI to 16 items. However, a large proportion of missing data was observed for some of the remaining items (see Quality of death and dying for further discussion on missing data), leaving only five complete QODDI responses using the 16-item survey. Thus, to optimise the sample size and facilitate analysis, subsets of the QODDI were calculated. Analysis was conducted using QODDI10, a subset of the QODDI questionnaire, which included 10 items. The QODDI10 was selected to preserve the largest proportion of the sample with complete responses (92.6%). Robustness checks were carried out by repeating the analysis with alternative subsets of the QODDI, including 12-item (QODDI12) and 14-item versions (QODDI14), which returned similar results. However, it is important to note that the validity of the QODDI as a shortened 10-item scale has not been rigorously tested, and thus, direct comparison should not be made with studies using the full version of the instrument. In Recommendations for future research, we recommend future research to validate shorter versions of the scales used in CH research to reduce burden on the staff. Scores for each of the QODDI items were coded from 0 to 10 and summed to give an overall QODDI score (ranging from 0 to 100 for the QODDI10), whereby higher scores indicate better quality of death. Data were analysed using linear regression models with robust standard errors. The outcome variable was total score on the QODDI10. Model 1 included only the main predictor variable, date of death; the relationship between date of death and QODDI score was important to examine to identify if deaths that occurred later in the Needs Rounds intervention were of better quality than those occurring early in the intervention period. In model 2, additional controls for size of CH and CH ownership were included to account for CH-related factors that might influence the quality of the decedent’s death. In the third model, staff role is controlled for to identify if certain staff groups were more likely to rate deaths as higher or lower quality, in addition to a variable which measured the time between the decedent’s death and when the QODDI survey was completed. Those who completed the QODDI survey closer to death may be more likely to accurately remember the details of the death, but there could be heightened psychological factors related to the reporting, whereas those reporting at a later date might have reduced accuracy in recalling the details. The final model included dummy variables created for five of the six hospices; 8A784 was dropped from the analyses as only one QODDI response was returned. The aim of this model was to identify any differences in quality of death between the hospice locations after accounting for all other relevant factors.
Family perceptions: CANHELP Lite
This questionnaire was analysed with descriptive statistics. Inferential analysis was not possible due to the low number of returns (n = 13).
Fidelity
Fidelity is concerned with the extent to which an intervention or programme is carried out in the way intended. It encapsulates the delivery, receipt and enactment of an innovation. 115 Various tools have been created to measure fidelity, focusing on both content and/or processes that impact implementation outcomes. Content focuses on the specific information to be conveyed, while process focuses on facilitation, including the skills of the practitioner, and the quality of delivery and engagement. 116 Given the centrality of i-PARIHS to this study, facilitation is reported in more detail (see Facilitation and facilitators).
Assessment of fidelity to the agreed approach to Needs Rounds was conducted based on the singular UK model developed and agreed in workshops. Fidelity was assessed against the published checklist,24 since Phase 1 determined that the UK approach would closely model the approach outlined in the checklist.
Fidelity was assessed through analysis of a random sample of 20% of all audio-recorded Needs Rounds. Fidelity is most often associated with positivist research paradigms; within this study, however, it was approached as a realist endeavour to map engagement with the agreed model. A three-tier scoring system, of 1 (high adherence), 2 (moderate) and 3 (low), was adopted. Operational definitions for these scores were developed to aid coding. For example, case-based learning is a core element of Needs Rounds meetings and was coded as high (relevant learning included for the majority of residents discussed), moderate (some relevant learning provided during the Needs Rounds, but not for most residents) and low (little or no relevant learning provided during the meeting). The fidelity schema was collaboratively developed by two researchers, with reference to the literature on fidelity, and coding was conducted by one researcher. The fidelity criteria are provided in Report Supplementary Material 14.
Estimating the treatment effect of the intervention on health service outcomes
Data on hospitalisations were requested from CHs across 5 months at baseline, between March and July 2021, and across a further 3 months at follow-up, from March to May 2022 (months 9–12 of the intervention).
At baseline, 11 CHs returned data for at least one of the months requested; however, there were a substantial number of missing and incomplete data. A minimum of 1 month’s complete data were obtained from nine of the 29 participating CHs; the average response rate was 3 months of data across those nine CHs, with only one site providing complete data for all five baseline months. At follow-up, six CHs returned at least 1 month of complete data; however, one had not provided adequate baseline data, and thus comparison could not be made.
Exposure was calculated by examining the reported data on the number of beds within each of the five CHs, the number of empty beds reported each month and the number of days of data that were reported (i.e. if data were returned for March and April, the number of baseline days equalled 61).
Using data reported from the CHs about the number of hospital admissions over the baseline period and the resulting number of nights spent in hospital, calculations were made to create ratios for admissions per 1000 exposure and nights in hospital per 1000 exposure for analysis.
Only five CHs returned data at both baseline and follow-up, which severely restricted the possibilities for analysis and interpretation. Our analysis therefore reports descriptive statistics in Chapter 5 for the estimated treatment effect on the two outcomes above (number of admissions and number of hospital days) for each of the CHs, as well as an average treatment effect. The sample size is too small to conduct an inferential test for statistical significance on the average treatment effect.
Care must be taken in interpreting both the site-specific treatment effects and the average treatment effect both due to the low power of the analysis and the confounding effect of COVID-19 on estimating a casual effect using a pre/post research design.
Estimating the cost effectiveness of the intervention on health service outcomes
A cost–benefit analysis of the intervention was planned from a health and social services perspective. The health economic analysis plan was described in the original funding bid. The intervention cost was to be derived from both direct and indirect costs to both NHS and CHs of delivering the intervention. Calculations were to include the change in NHS costs incurred following the intervention, including both primary and secondary care, by valuing the reduction in hospital stays, hospital days as a result of the intervention, ambulance usage, GP callouts and visits by specialists.
As described above, due to insufficient data, this analysis was not possible, both as a result of the small samples of data returned by CHs and the compromised validity of the primary treatment effect estimation due to COVID-19. There was insufficient detail in the data collected to accurately estimate the costs of hospitalisations or the wider health service costs. To augment the sparse quantitative data, in Chapter 5 we also provide qualitative data on costs gathered in the study.
Care home participation
To examine which, if any, factors related to the involved CHs were associated with greater participation in the study, analyses were conducted to examine different areas of participation.
Four binary variables were created: whether the CHs provided baseline data, whether the CHs provided follow-up data, whether the CHs returned any QODDI surveys and whether the CHs returned any CAPA surveys. These were scored as zero for no data returned and one for some data returned. A fifth overall participation score was calculated by summing four variables representing participation in different areas of the study (Table 3), including the number of QODDI and CAPA surveys returned and the number of months CHs returned data on hospitalisations and assessments and interventions triggered by Needs Rounds (see Resident data).
| Overall participation | Scoring (range) |
|---|---|
| Number of QODDI surveys returned | 0–15 |
| Number of CAPA surveys returned | 0–24 |
| Number of months of hospitalisations data returned | 0–8 |
| Number of months of assessments and interventions triggered by Needs Rounds data returned | 2–13 |
Descriptive data were compared for all aforementioned participation variables across the following predictor variables: CH size, ownership, country, location and types of care provided (see Descriptive analysis).
Some variables were derived using data that CHs provided. For example, CHs were categorised as either medium or large based on the number of beds they reported against CQC categories (see Staff capability: CAPA), and each site reported their ownership as either private or not for profit. The CHs were located either in England or Scotland, so a simple binary variable was created to reflect this and draw comparison between the two countries.
To determine whether location impacted CH participation, a binary rural–urban variable was created. Using the Office for National Statistics postcode directory,117 the postcode for each CH was used to find the 2011 output area (OA11) code. For the English CHs, the OA11 codes were cross-referenced in the Department for Environment, Food and Rural Affairs, 2011 Rural–Urban Classification lookup tables for small area geographies118 to determine which CHs were in rural areas and which were urban. This process differed slightly for the Scottish CHs, in that the OA11 codes were used to obtain sixfold urban or rural codes from the Scottish Postcode Directory Files. 119 The sixfold codes were collapsed into the twofold (binary) rural urban classification using the Scottish Government Urban Rural Classification. 120
Finally, using the carehome.co.uk profile for each site, data were collected on the types of care provided at each home. Types of care included nursing, residential, convalescent, respite, day or lunch clubs, specialist care, dementia care and care to adults under 65 years.
A binary logistic regression was conducted to model participation, by means of completing baseline data, as a function of potential predictors of participation. The same models were applied in a linear regression analysis with overall participation score as the outcome. In model 1, location variables were included to identify how participation varied in England compared to Scotland and in urban versus rural CHs. In model 2, factors relating to the CH such as the size and the ownership were added. Ownership was dropped from this model for the baseline data analysis because, as shown in Descriptive analysis, 100% of the voluntary, not-for-profit CHs in the sample provided baseline data. In model 3, we controlled for the type of care provided. Residential was selected as it is one of the two main types of CH (i.e. CH with nursing – referred to in this section as nursing, or CH without nursing – referred to in this section as residential). When considering types of care provided, 24 (82.8%) provided some form of nursing care and 11 provided residential care (37.95). All CHs that provided nursing care also provided residential care, but not all CHs that provided residential care also provided nursing care (Table 4). Therefore, by including a dichotomous variable for the provision of residential care, we are comparing CHs that provide residential or residential and nursing care with those that solely provide nursing care. Due to small cell counts, it was not possible to include all care type variables in the analyses.
| Provides residential care | Provides nursing care | |||
|---|---|---|---|---|
| No | Yes | |||
| n | % | n | % | |
| No | 0 | 0.0 | 18 | 100.0 |
| Yes | 5 | 45.5 | 6 | 54.5 |
| Total | 5 | 17.2 | 24 | 82.8 |
Patient and public involvement and engagement
This is described more fully in Chapter 6 and in Equality, diversity and inclusion. However, in brief, the PPIE approach was informed by the National Standards and INVOLVE guidelines (49) and aimed to ensure the study was focused on improving services for residents and families. Terms of reference were developed to guide involvement and engagement (see Report Supplementary Material 15).
Lived experience is central to decision-making121 and has led to a proliferation of more collaborative approaches. 122,123 As a reflection of this position, research methodologies that privilege engagement with the communities or populations studied are increasingly used. 122,123 The language of coproduction and co-design has become more commonplace and adopted as an ethical approach to research. 124,125
The study had three PPIE members, defined as people who could speak about their lived experience of CHs/palliative care, or as a community member who might use a CH. One PPIE had an uncle living in a CH (not one of the study sites), who died towards the end of the implementation phase. A second PPIE member had undertaken lay inspections in CHs. The third PPIE member did not have direct experience of CHs and spoke from the position of a community member.
Patient and public involvement and engagement representatives were involved from the outset as co-applicants to ensure the research questions and aims were informed by people with non-academic/non-clinical experiences of CHs. Patient and public involvement and engagement members informed the choice of family outcome measures (focusing on a measure which would be least burdensome and most meaningful to relatives), devised interview questions, participated in recruitment of the research fellow (RF), contributed to ethical approval documentation and attended the research ethics committee (REC) meeting.
Patient and public involvement and engagement members attended monthly investigator meetings and provided advice on all aspects of the study. After each monthly meeting, they were invited to a debrief where further thoughts, reflections and questions could be raised with a member of the academic team. Patient and public involvement and engagement members participated in the workshops to coproduce UK Palliative Care Needs Rounds, data collection and data analysis.
As noted in Patient public involvement and engagement interviews, the PPIE work was evaluated via one-to-one interviews with a researcher external to the core Needs Rounds team. The interviews focused on all members of the teams’ experiences and reflections on PPIE. Furthermore, throughout the study, data were collected on PPIE resources/costs and evidence of impact.
It was intended to combine face-to-face involvement with online working. However, due to ongoing COVID-19 restrictions, ability to travel and greater familiarity with online platforms, all PPIE was conducted online.
Facilitators
Facilitation and facilitators are critical for successful implementation and a core element of i-PARIHS. Facilitators are agents of change who lead or champion an innovation. Facilitators for each site were identified during Phase 1 data collection.
A role description and person specification were developed, to ensure core skills, experiences and expertise of these facilitators. Although being a registered nurse (RN) was not a prerequisite, all six clinicians were RNs. The person specification listed the following:
-
registered health practitioner
-
minimum 3 years of postgraduate experience in palliative care
-
demonstrated advanced clinical knowledge, skills, experience and practice in the clinical assessment, diagnosis, investigation, treatment and referral as well as follow-up care of patients requiring SPC
-
understanding of multiple morbidities of CH population
-
demonstrated high-level communication, liaison, interpersonal and negotiation skills and an ability to form relationships with internal and external stakeholders
-
proven ability to prioritise and undertake timely comprehensive assessments of patients using evidence-based practice
-
proven ability to work within a risk management framework to ensure a high standard of safe clinical practice.
Specialist palliative care staff facilitating Needs Rounds should therefore be experienced clinicians. Core skills include diagnosing deterioration/dying, understanding of anatomy and physiology associated with ageing, frailty and life-limiting conditions, knowledge of medicines and equipment frequently used in palliative care contexts (such as syringe drivers), ability to communicate effectively with patients, family members and members of a broad MDT.
Training and skills of people facilitating Needs Rounds
Training was provided on Needs Round for all CH staff and hospice staff who would be delivering the intervention located in six geographically disparate areas.
The fourth videoconference-based workshop session in Phase 1 encompassed several facilitated examples of a Needs Round case discussion with some participants taking the role of SPC clinician and others in the role of CH staff. Other clinicians adopted the role of observer, with a task of reflecting on key learning regarding how to participate in Needs Rounds and actions they would need to undertake to be ready at their site for implementation. Observers therefore had the opportunity to act as a reflecting team to identify strengths and areas for development.
The Needs Round simulation exercise made use of the videoconference platform’s ‘chat’ function, allowing the verbal exchanges in the Needs Round to be accompanied by synchronous written commentary on the techniques used. Supplying this written commentary within the chat facility allowed the trainers to demonstrate links between theory and practice without the need to stop the simulation.
The platform’s breakout room structure was then used to form small groups to discuss the learning and run further bespoke simulations to allow participants to change roles and engage as both observers and active members. These smaller groups enabled deepening relationships between participants who would be delivering the intervention in each of the case study sites.
Action learning sets
To aid the SPC facilitators and gain coherence around the process of facilitation, action learning sets126 were adopted for monthly discussions with the SPC nurses delivering the Needs Rounds. The action learning sets offered a regular time for online video meetings of peer-to-peer learning, to share difficulties and solutions, in a collaborative relationship, facilitated by a member of the research team. Action learning sets provided opportunity to reflect on issues prospectively and develop learning and insights into the implementation across Scotland and England and enabled SPC staff to:
-
focus on their role within the Needs Round project
-
provide an opportunity to discuss emergent issues with each other and engage in problem-solving
-
give space for each SPC clinician to describe their situation and learning
-
provide a context which values being open, reflexive, practical and shared
-
not be overly structured, to allow for maximum scope of issues and topics to be within the remit of the action learning set
-
be non-hierarchical
-
be attentive to individuals’ contexts and hence complementary to the importance of context in implementation science.
Reflections within these monthly meetings fed into development of the programme theory. Due to the geographic spread of the sites, these action learning sets were always anticipated to run online. However, due to pandemic restrictions, the SPC clinicians did not get the opportunity to augment their online relationships with face-to-face meetings at workshops.
Ethical considerations
Ethical approval was granted by Frenchay REC [287447] for the study.
Participants were provided with a participant information sheet (PIS). Easy read PIS and posters summarising the study were used to inform residents of the research and encourage participation in the Phase 1 interviews/workshops.
Informed consent was taken for participation in interviews, questionnaires and Needs Rounds recordings. Informed consent was not required for resident data as this was summary data to ensure anonymity, collated by routine care staff. A ‘no surprises’ approach was adopted, whereby posters were displayed within CHs to ensure that residents, relatives and staff members would be aware of the study and data being collected.
All resident demographic data were captured at CH level, not individual level, to ensure that data were anonymous and could not be traced to any individual. ID numbers are used throughout this report in place of organisations’ names.
All PISs, interview topic guides and questionnaires were examined by our PPIE representatives for appropriateness, and amendments made where requested.
Changes to data collection procedures (with researchers not involved in collecting demographic data), noted in the modified protocol, were introduced to minimise risk to CH staff and residents, as well as the research team. CHs were excluded if their size would preclude anonymity of residents.
Study management and sponsorship
A project steering group oversaw the study. It was chaired by an academic with expertise in CH research and had membership from individuals with expertise in implementation science, health economics, healthcare commissioning, palliative care and lay members providing the perspective of patients/public. The steering group was only able to meet online, due to ongoing COVID-19 restrictions and increased familiarity and desire to use video conferencing platforms. The research sponsor was the University of Stirling.
Summary of changes to protocol
Following study funding approval, several changes were made to the protocol:
-
CH data were collected and reported by routine care staff, rather than academic researchers. This was to minimise the potential for COVID-19 spreading and to ensure that only routine care staff had access to identifiable personal data.
-
The funded protocol had proposed using the Charlson Comorbidity Index (CCI) as a proxy for the health status for CH residents. In its place, the ECOG (Eastern Cooperative Oncology Group performance scale) was used, which is simpler than the CCI. This change was made following piloting of the CCI in the spring of 2021; CH staff reported that it was too complex. The ECOG, while described as an oncology tool, solely describes performance status and is not diagnosis-specific. Hence, it was an appropriate alternative to the CCI.
-
Cost data were scheduled for collection at baseline and follow-up from CH, for example, staff costs and non-staff expenditure; however, due to very low data returns, and feedback from both CH staff and the study steering group, these data were omitted from data requests. The removal of these data prompts was to increase completion rates by focusing on data which was easily gathered and reported by CH staff.
-
With the paucity of data reported by CH on health service use, it was not possible to conduct the planned cost–benefit analysis.
At the time of publishing the study protocol,104 an additional phase had been planned involving surveying UK CHs on the final model, which was not in the funded protocol. This additional data collection was subsequently determined to be beyond the scope of the study and problematic to conduct, while COVID-19 was still impacting data returns and hence not conducted at time of writing.
Chapter 3 Implementation of palliative care Needs Rounds
Some of the text within this chapter has been previously published in Open Access articles:
Sample
Thirty-four CHs agreed to participate in this intervention study. Twenty-nine CHs completed the intervention, with four CHs withdrawing at month 5. Those who withdrew had not provided baseline data. We report on the 29 retained CHs (Table 5).
| n | %a | ||
|---|---|---|---|
| Ownership | Privately owned | 25 | 86.2 |
| Voluntary/not for profit | 4 | 13.8 | |
| Country | England | 19 | 65.5 |
| Scotland | 10 | 34.5 | |
| Rural–urban | Rural | 6 | 20.7 |
| Urban | 23 | 79.3 | |
| Region | Central Scotland | 4 | 13.8 |
| East England | 7 | 24.1 | |
| East Midlands | 2 | 6.9 | |
| Highlands and Islands (Scotland) | 6 | 20.7 | |
| London | 1 | 3.4 | |
| South East England | 5 | 17.2 | |
| West Midlands | 4 | 13.8 | |
| Local authority | Cambridgeshire | 4 | 13.8 |
| Clackmannanshire | 3 | 10.3 | |
| Derbyshire | 2 | 6.9 | |
| Essex | 3 | 10.3 | |
| Falkirk | 1 | 3.4 | |
| Highland | 6 | 20.7 | |
| Kingston upon Thames | 1 | 3.4 | |
| Staffordshire | 4 | 13.8 | |
| Surrey | 5 | 17.2 | |
| Type of care | Nursing | 24 | 82.8 |
| Residential | 11 | 37.9 | |
| Palliative | 23 | 79.3 | |
| Convalescent | 17 | 58.6 | |
| Respite | 24 | 82.8 | |
| Day care and lunch clubs | 6 | 20.7 | |
| Dementia care | 22 | 75.9 | |
| Independent living/sheltered housing | 4 | 13.8 | |
| Age of service users | Older adults aged 65 + | 29 | 100.0 |
| Adults aged under 65 | 18 | 62.1 | |
| Specialist services | Specialist care | 25 | 86.2 |
| Specialist dementia unit | 6 | 20.7 | |
| Physiotherapy | 8 | 27.6 |
Of these, 24 homes had registered nurses employed by the home to provide 24-hour care (i.e. CHs with nursing), and 5 were CHs without registered nursing staff onsite (i.e. CHs without nursing). The type of care provided by the homes is presented in Figure 2. Any homes dual registered as providing services with and without nursing are recorded as nursing homes.
FIGURE 2.
Bar chart: types of care provided by the CHs in the sample.
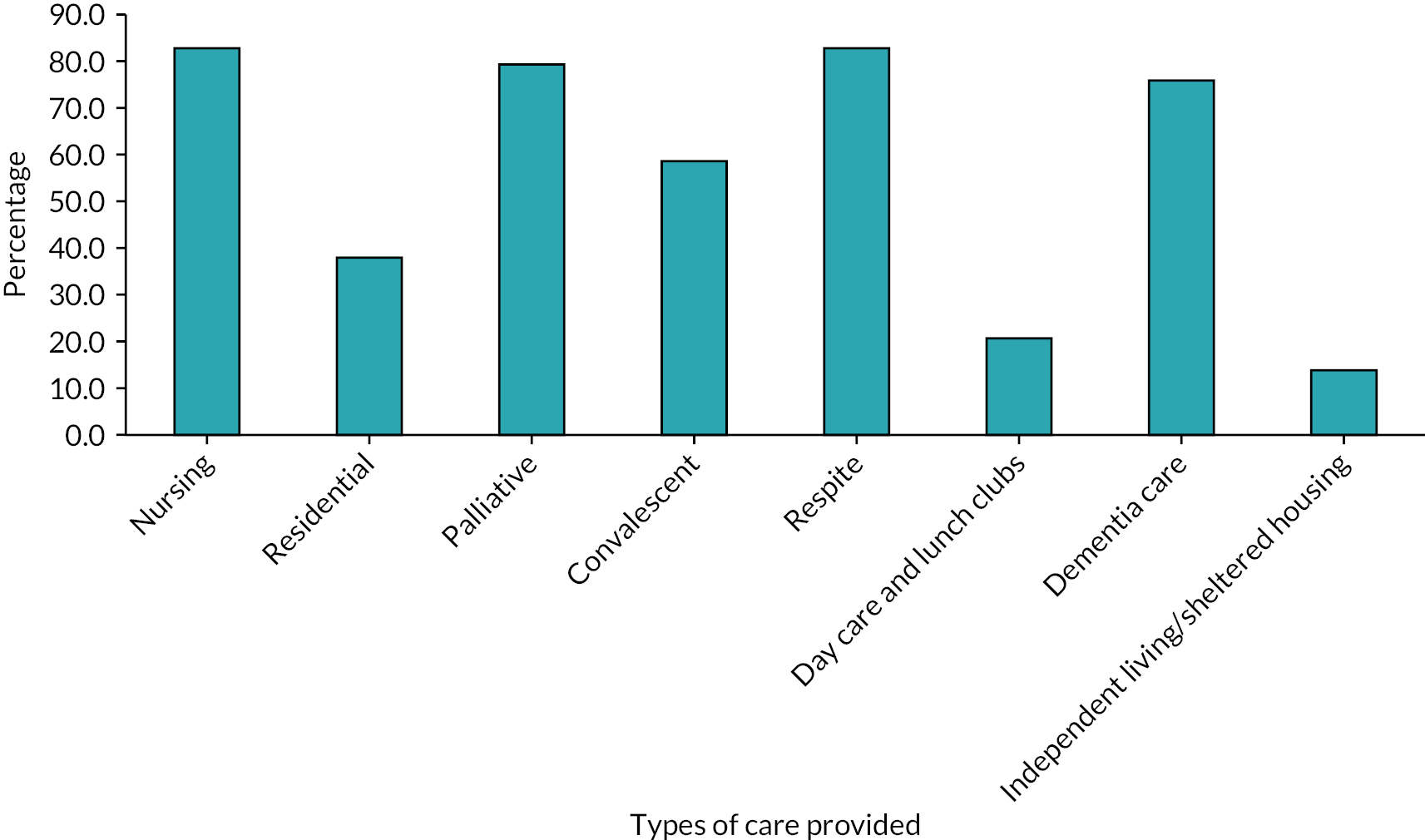
Thirteen CHs provided baseline data about their residents (Table 6). Across those 13 CHs, in March 2021, 540 residents were reported, 63.9% female and 36.1% male. Most residents (76.1%) were aged 80 years or older, with 6.5% under the age of 65 and only 2.2% (n = 12) under the age of 50. Residents were predominantly (98.7%) White British, with only small percentages of residents of African ethnicity (0.2%), mixed or multiple ethnic backgrounds (0.6%) or any other ethnic group (0.6%).
| CH ID | ST00 335 |
ST00 453 |
ST00 340 |
ST00 341 |
ST00 467 |
ST00 313 |
ST00 348 |
ST00 327 |
ST00 329 |
ST00 402 |
ST00 497 |
ST00 419 |
ST00 492 |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of service usersa | 63 | 55 | 27 | 41 | 36 | 52 | 46 | 15 | 32 | 35 | 68 | 38 | 27 | |
| Status | New (this month) | 0 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 2 | 0 |
| In the home | 63 | 46 | 24 | 41 | 26 | 50 | 32 | 15 | 32 | 26 | 68 | 35 | 26 | |
| Deceased | 0 | 4 | 3 | 0 | 10 | 2 | 12 | 0 | 0 | 5 | 0 | 1 | 1 | |
| Discharged | 0 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | |
| Sex | Female | 40 | 37 | 20 | 25 | 22 | 36 | 25 | 14 | 12 | 24 | 44 | 25 | 21 |
| Male | 23 | 23 | 7 | 16 | 14 | 16 | 21 | 1 | 20 | 11 | 24 | 13 | 6 | |
| Age | < 50 years | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 3 | 0 | 7 |
| 50–59 years | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 7 | |
| 60–64 years | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 4 | |
| 65–69 years | 2 | 3 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 4 | |
| 70–74 years | 3 | 6 | 3 | 5 | 1 | 1 | 0 | 0 | 0 | 0 | 7 | 2 | 3 | |
| 75–79 years | 5 | 6 | 0 | 7 | 5 | 4 | 1 | 0 | 2 | 4 | 11 | 4 | 1 | |
| 80–84 years | 17 | 13 | 5 | 7 | 10 | 4 | 5 | 3 | 10 | 9 | 18 | 11 | 0 | |
| 85–89 years | 17 | 13 | 6 | 9 | 11 | 10 | 11 | 5 | 5 | 12 | 10 | 9 | 1 | |
| 90–94 years | 14 | 10 | 8 | 8 | 6 | 9 | 14 | 3 | 13 | 5 | 12 | 7 | 0 | |
| ≥ 95 years | 5 | 7 | 5 | 2 | 2 | 22 | 15 | 4 | 2 | 3 | 2 | 2 | 0 | |
| Ethnicity | White British | 60 | 57 | 27 | 41 | 36 | 52 | 46 | 15 | 32 | 35 | 67 | 38 | 27 |
| Other mixed/multiple ethnic background | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | |
| African | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Other ethnic group | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| ECOG score | 0 | 10 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| 1 | 7 | 0 | 3 | 0 | 0 | 0 | 1 | 5 | 24 | 1 | 19 | 0 | 0 | |
| 2 | 19 | 0 | 0 | 9 | 5 | 0 | 7 | 3 | 2 | 3 | 9 | 1 | 0 | |
| 3 | 17 | 2 | 13 | 11 | 16 | 0 | 28 | 4 | 1 | 20 | 16 | 15 | 9 | |
| 4 | 10 | 58 | 10 | 21 | 15 | 0 | 9 | 2 | 5 | 11 | 24 | 22 | 19 | |
Of the 540 residents reported at baseline, ECOG scores were recorded for 488 (90.4%). The majority of residents were categorised as grade four (42.0%, n = 205) ‘completely disabled, confined to bed or chair and unable to carry out any self-care’ or grade three (31.3%, n = 152) ‘capable of only limited self-care, confined to bed or chair for more than 50% of waking hours’ with only 2.7% (n = 13) categorised as grade zero ‘fully active, able to carry out tasks without restriction’.
Fidelity
Implementation proceeded with only minor modifications from the Australian model described in Needs Rounds: intervention description. Sites wished to have flexibility in linking the intervention with primary care provision in their area, and this was agreed at commencement of Phase 2.
Recordings were provided by the palliative care clinicians for 73 of the 223 Needs Rounds undertaken (33%). The variation in provision of these data is explained by one SPC site not recording any discussions, citing concerns about jeopardising trust and development of the relationship with CHs. Another site recorded every Needs Round. A further 21 Needs Rounds recordings were unavailable because confidential material (such as a resident’s name) had been used and hence were deleted rather than forwarded to the research team. It is possible that non-recordings reflect hesitancy in being assessed as not following the agreed approach.
Fidelity was assessed for 20% of the recorded Needs Rounds, thus on 14 meetings. Overall, sites scored low on fidelity. There were some marked differences between different SPC clinicians, with some achieving medium and high scores on many variables (notably checklist, developing an action plan and keeping to time). The most consistent success was in discussing resident biopsychosocial concerns, with physical symptoms taking precedence at the start of most discussions. See Table 7 for fidelity scores of this 20% sample.
| Site ID → | 8CL93 | 8CL93 | 8CL93 | 8CL93 | 8CL93 | 8CL93 | 8JD12 |
|---|---|---|---|---|---|---|---|
| Fidelity variables ↓ | |||||||
| Site ID → | 8JD12 | 8JD12 | 8JD12 | 8C928 | S25614 | S25614 | S25614 |
| Fidelity variables ↓ | |||||||
| Keeping to time | High | High | High | High | Low | Low | Low |
| n. residents discussed | Moderate | Moderate | Low | Low | Low | Moderate | Low |
| Checklist | High | High | High | Moderate | Low | Low | High |
| Biopsychosocial | High | High | High | High | Low | High | High |
| Action plan | High | Low | Low | Low | Low | Low | High |
| Case-based education | High | High | High | High | Low | Low | Low |
| Case conferences | Low | Low | Low | Low | Low | Low | Low |
| Clinical intervention | Low | Low | Low | Low | Low | Low | Low |
| Keeping to time | High | Low | Low | Low | Moderate | Moderate | High |
| n. residents discussed | Low | Low | Low | Low | Moderate | Low | Low |
| Checklist | Moderate | Low | Low | Low | Moderate | Low | High |
| Biopsychosocial | Moderate | Low | Moderate | Low | Low | Moderate | High |
| Action plan | Moderate | Low | Low | Low | Low | Low | High |
| Case-based education | Moderate | Low | Low | Low | Moderate | Low | High |
| Case conferences | Low | Low | Low | Low | Low | Low | Low |
| Clinical intervention | Low | Low | Low | Low | Low | Low | Low |
The number of residents discussed was lower than in the Australian model.
All sampled recordings scored ‘low’ on case conferences and provided clinical interventions. However, from numerical data collected on all Needs Rounds conducted, 158 clinical interventions from SPC clinicians were triggered; these interventions were reflected in Needs Rounds audio recordings despite not occurring during the 20% random sample for fidelity analysis.
Use of the checklist24 was apparent in some of the opening prompts from the SPC clinician: ‘So, what would you say are your kind of main priorities in terms of his care or any concerns that you have around it …?’ (SPC 8A784). While the triggers for discussing residents in the checklist were sometimes explicitly oriented to, often conversation focused solely on residents in their last few days of life. This indicated that CH staff felt that Needs Rounds (and palliative care) was focused only on those last few days of life. ‘We only have two residents that are end of life’ (CH staff, 8JD12).
Provision of education or learning within Needs Rounds was variable. While recordings showed that education was provided, it was often very brief and difficult to discern what new knowledge was being developed. Some SPC clinicians provided resident-based education thoroughly and systematically throughout Needs Rounds though, combining Socratic questions (asking questions which elicit CH staff current knowledges and encourage them to extend their understandings by engaging in dialogue to stimulate their learning) and gentle challenges where the CH staff responses indicated a growth of knowledge and reflexivity:
SPC clinician: What are some of the clues that you look for when you’re thinking about prognosis? What other things?
CH staff, 8JD12: Probably when she’s not really eating anymore, no food anymore. And it’s like she’s … you can think that she’s really given up because even fluid she’s not taking, medications she won’t take anymore. And I think that’s the thing now that, oh, she’s really giving up, I think this is what she (overlapping conversation).
Thus, while some elements of the UK Needs Rounds model were delivered consistently (discussion of resident physical symptoms and concerns), other components were less predictably addressed (such as focusing on residents beyond those in the last few days of life) or not covered (case conferences). In practice, none of the sites made formalised links with primary care, so the Needs Rounds approach was delivered in a similar manner to Australia. Each of these aspects of implementation is described more fully in Programme theory: what works for whom under which circumstances in the description of the programme theory.
Facilitation and facilitators
Facilitation is a key component of successful implementation. The core i-PARIHS notions of ‘flexible and responsive’128 facilitation informed coding and analysis of recorded Needs Rounds, workshop discussions, interview data and reflections within the learning sets. This section presents the facilitation process, strategies and actions and some of the important roles that facilitators took on to fire the mechanisms that made Needs Rounds work. Reflections on what did not work are also highlighted at the end of this section.
Facilitation style was apparent through the development of rapport and relationship building. The relationship then became important in enabling the facilitation strategies to take place. Rapport was visible through informal interactions such as joking or teasing, as well as empathic exchanges around the very challenging nature of the work, supporting people in their last months, weeks and days of life as well as supporting grieving residents:
SPC clinician: So how are you as the staff? Because obviously, you know, you get quite attached to your residents, how do you manage that kind of situation either two people going quite quickly or people who have been here a while? Do you have a time to be able to kind of reflect on it or do you just get on with it?
CH staff: I mean, we’re really upset because (overlapping conversation)
SPC clinician: Yeah, yeah.
CH staff, 9CL93, Recorded Needs Round: But even residents were upset because they can see they’re not on the dining room and some of them would visit as well.
Rapport was also visible within Needs Rounds meetings. For example, the ease with which staff were able to acknowledge the limits to their understanding and be open to learn from each other, one SPC clinician said in a Needs Round:
I’ve come across a lot of things just lately that I’ve learned myself in regard to the guardianship issues, and things like that. I mean, the other day I didn’t realize was, we had the lady pass [die] in the hospital, that guardianship finished as soon as they passed. And I wasn’t aware of that. And her family didn’t want any involvement. They never visited, or anything like that. And I’m like, ‘so who’s responsible for this lady after [death]?’
SPC clinician, S25614, Recorded Needs Round
Similar admissions of not-knowing were used by CH staff: ‘I was a bit nervous and hesitant. I told the nurse yesterday I’m not doing it she will have to do it and she did do it because I was not really sure of … (CH staff, 8CL93). Needs Rounds participants were able to highlight the differences and intersection of their knowledge, which enabled them to challenge any institutional hierarchies. As the following quotation from a Needs Round demonstrates, these exchanges were managed with considerable finesse and attention to each other’s expertise:
SPS clinician: Would it help if I came in, you know, like we have a meeting, would it help if I came in and we had like a, I don’t know, like a question and answers …?
CH staff: Yeah. Anything …
SPS clinician: … scenario so they can, they can ask me, you know …
CH staff: They can approach you. You know what it means, sometimes.
SPC clinician: What would you do? What would, you know?
(Overlapping talk)
CH staff: Yeah. Because you’ve got the experience. I am, yes, Registered Care Manager, but I haven’t got as much experience for you in that, in that line of, you know, tunnel vision to end of life. Whereas you can probably, they’ll ask you questions and you’ll just roll off the tongue because that’s your, your, your, you know, your forte.
SPC clinician, 8C928, Recorded Needs Round: And they may bring some patients to me that they’re concerned about.
SPC clinicians also routinely provided positive feedback to the CH staff, reinforcing and reflecting the confidence and competence of the workforce:
… and that’s where palliative care nurse can be useful in terms of having those discussions. But I certainly wouldn’t put down your contribution because you know the resident very well. And you are recognising all the right things.
SPC clinician, 8JD12, Recorded Needs Round
As the quotation above illustrates, SPC clinicians were able to reinforce both CH staff knowledge of the residents as well as their clinical skills and knowledge. Rapport was visible through some of these brief, but important, exchanges: ‘Wow, you guys are magic here. (Laughter)’ (SPC clinician, 8CL93).
Education and learning were intended to be core components of each monthly Needs Round meeting. While not all SPC clinicians integrated this routinely into discussion of residents, where it was covered, the approach was consistently one of elegantly weaving the learning into the evolving discussions. Consequently, the facilitation strategies were hinged on introducing relevant topics and building on CH staff knowledge. This often resulted in careful exchanges and negotiations to determine each other’s level of understanding, to assess what new learning could be brought to the discussion:
SPC clinician: In terms of that skin integrity and the, kind of, more rapid breakdown, is that something that you’ve seen before in quite elderly, frail residence?
CH staff: The gangrene … the gangrene is not something that we’ve seen very often. It’s not to do with him being bed-ridden. It’s just no circulation. There’s no circulation. They’ve got a doctor in hospital. And there’s no circulation in that foot. So it’s not to do with poor care or anything.
SPC clinician: Oh no, no, no, I wasn’t suggesting at all, no.
CH staff: It’s just literally there’s no blood there.
SPC clinician: Yeah, yeah, yeah. Because I mean, it is something that does happen particularly with people who are very restricted in terms of their mobility and being nursed in bed. They reach to the point at which with their nutritional status being really low.
CH staff: Yes.
SPC clinician, 8JD12, Recorded Needs Round: And very poor circulation. Probably due to an element of the heart not working quite so well anyway. Whether or not they have any heart conditions on top. That you will get very rapid skin breakdown. And, you know, you can, kind of, take that almost as a sign of the nearness of end of life. Because the body is deteriorating quite a lot, kind of, physiologically, it is not the same as it was when that person was younger. So, although it isn’t a sign of dying as such, it is a sign of, you know, quite rapid, clinical, deterioration in terms that person’s physiological state. Is there anything you’ve noticed about him that you would think that means that maybe end-of-life isn’t too far away?’
At the start of meetings, deciding which residents to discuss was a further enactment of the facilitation process, where both SPC clinicians and CH staff would suggest their ideas and collaboratively determine who to focus on:
CH staff: Yes. We can talk about [resident’s initials]?
SPC clinician 1: Last time you had a gentleman. He was 95. [different resident’s initials]. I think you said his code was gonna be. He had mixed vascular dementia. Some AF [atrial fibrillation] Pneumonia. He had been unwell recently and been taken off his Digoxin. Because his heart rate had dropped a lot.
CH staff: Yeah. Yeah. He’s got a heart rate. Yeah. Yeah.
SPC clinician 1: Not that one?
CH staff: No.
SPC clinician 1: No? Okay. Do you want to discuss that gentleman? Or somebody different?
SPC clinician 2, 8CL93, Recorded Needs Round: We can review him and maybe somebody else.
Negotiating when to meet was also a frequent component of the end of Needs Rounds discussions. SPC clinicians being flexible and responsive to CH routines and practices was an important mechanism to help ensure that Needs Rounds took place. SPC clinicians scheduled these for quieter periods of the day and offered remote options to accommodate local lockdowns:
She [SPC clinician] books meetings very much in advance. So, till the end of the year. Now until December, it was booked, so I know exactly, so I put myself on shift and if I’m off, I know I have to come in at this time. So, I have to just get through my medication and everything. Not quickly, but usually 11:00 is a time that we usually finish the medications rounds and things like that.
Registered nurse, ST00316, Phase 2
Managers’ involvement was key to facilitation. This impacted the likelihood of staff members benefiting from protected time to reflect on residents’ holistic needs. Managers who were committed to Needs Rounds were more likely to schedule time off for staff to attend, and provide motivation and encouragement. Staffing capacity also impacted scheduling and some people attended on their days off or at the end of their shift. One CH manager reflected on the staffing challenges they were facing:
I don’t see [staffing shortages] improving for quite a long time. Right now, I have got 99 hours a week vacancy for registered nurses and 370 odd hours vacancy for carers. So, it is our recruiting problem that we’ve got. The job for that is okay, but you’re just not getting anybody turning up for interview. The staff that we do have, you know, they are working extra hours, that kind of thing, to try and keep our staffing levels safe … They’re just busy firefighting.
CH manager, ST00419, Phase 2
During the initial programme theory development workshops, it was emphasised that successful implementation would require engagement of different types of staff members, particularly care staff. While the above demonstrates how managers played an important role in deciding which staff would attend, sector-wide workforce issues affected both the numbers and types of staff members who were able to participate. Managers, clinical leads and nursing staff were more likely to participate than care staff: ‘It’s difficult with carers because it’s busy and if I will take one … everyone is behind’ (CH manager, ST00402, Phase 2).
Integrated Promoting Action on Research Implementation in Health Services attends to the various people who shape and are shaped by implementation. The recipients’ tenet focuses on factors related to the people involved in innovations, including their motivations, values and beliefs. Participants decided to take part for a variety of reasons including a general commitment to quality improvement/research and development, an interest in improving palliative and end-of-life care, previous experience of using GSF, a desire to fill a gap in existing provision and to create a direct link to the hospice. Engagement levels varied, and sometimes managers were more involved than nursing and care staff. Where managers were committed, Needs Rounds were perceived to run more effectively:
I think the ones that dropped out, interestingly, I think the managers were less engaged … the ones where the managers really wanted them, they’ve happened more reliably. So, for example, this morning, the manager puts it in the diary and expects it to happen … so she accepts it on their behalf and diaries it. That’s worked well, actually, because there’s an expectation that it’s important and valuable.
SPC clinician, 8A784, Phase 2
During early implementation, there was a lack of understanding and awareness about what Needs Rounds involved, reflecting a lack of engagement with the study communication materials. Although a significant amount of information was shared (meetings with research team and SPC clinicians, memorandum of understandings, implementation packs, workshop training and site posters), not all of these resources were necessarily read or understood or shared across the wider CH team. In one of the sites where the SPC clinicians changed, some CHs still did not fully understand what Needs Rounds were, four months into the process:
Bear in mind I joined at four months in. So, I came to do my first meeting with them when they were like, well, what is this? So, you know, and then I mean trying to do a quick kind of roll through the project, they’ve just been told they were to do these meetings.
SPC clinician, S25614, Phase 2
Clarity of understanding is a key aspect of the innovation component within i-PARIHS. Clarity was impacted by staff turnover, with knowledge being lost when members of staff left, low rates of attendance at the training workshops and the quantity and format of the communication materials. As one SPC clinician noted:
I think there’s a lot of information they had, which I think clearly none of them have read really, but I think it’s … does take going through it with them and trying to summarize it for them … [it] has been an ongoing process and … it’s been really hard to get them up to speed.
SPC clinician, 8A784, Phase 2
Poorer understanding of Needs Rounds highlights that inadequate information-sharing processes were in place, and that a different facilitation mechanism is required to ensure clarity.
Programme theory: what works for whom under which circumstances
This section describes what works, for whom, under what circumstances and why with UK Needs Rounds.
We present the overarching programme theory, generated from interview and workshop data during Phase 1 (initial mapping of CMOs) and Phase 2 (implementation). The programme theory (Figure 3 and Box 1) is depicted with five colours, each of which represents one of the five theories (generated in Phase 1) which are combined within the final programme theory.
FIGURE 3.
Illustrated programme theory. © 2022 Cassandra Harrison Art. All rights reserved. Reproduced with permission.
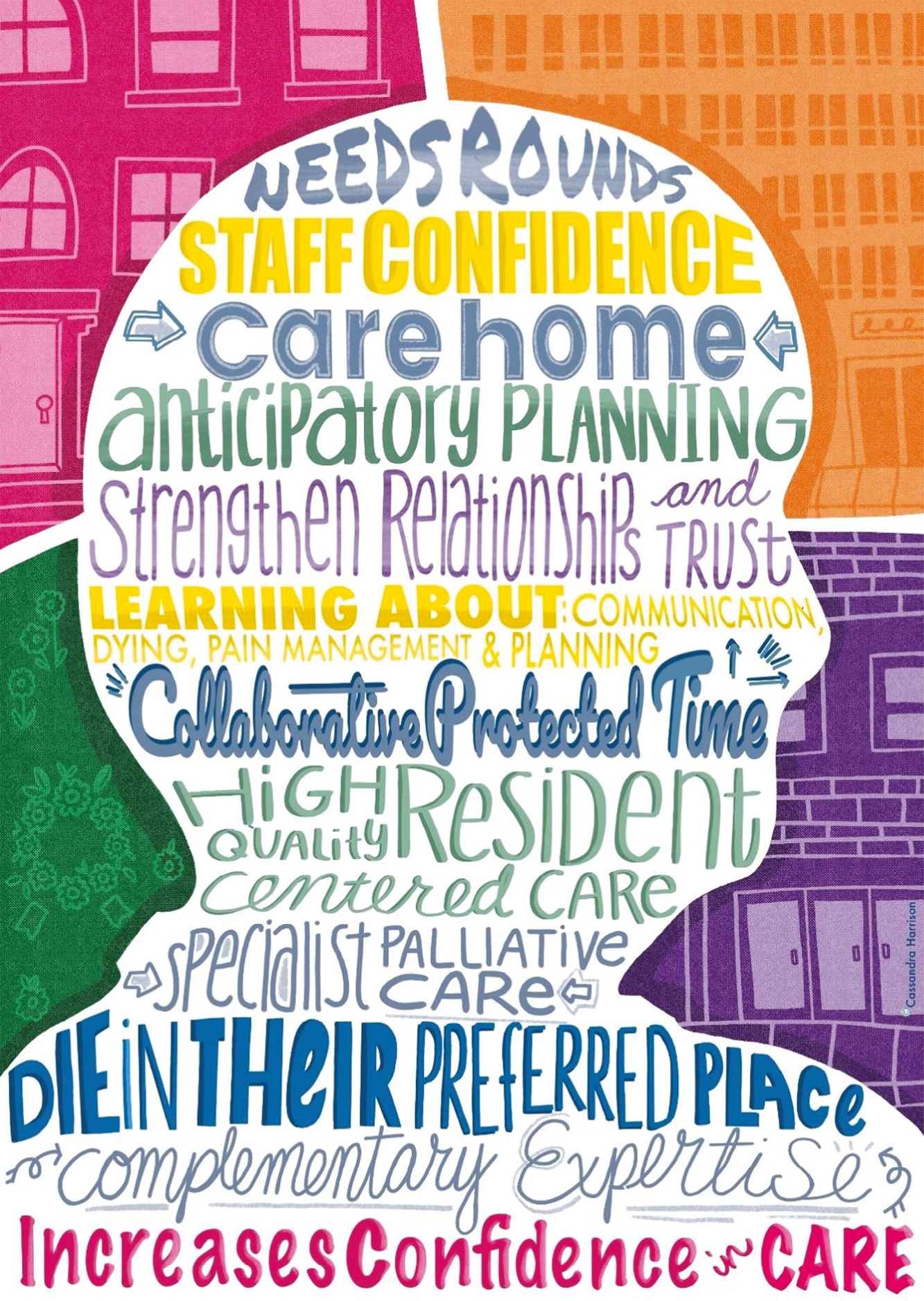
The five theories centre on (1) staff confidence and competence, (2) place of care, (3) collaboration and interagency working, (4) better-quality lives and deaths and (5) communicating with families.
Appendix 1 provides further detail on the data and analysis leading to the initial theories and initial programme theory (developed at the end of Phase 1) to illustrate the evolution of the theories throughout the course of the whole study. Appendix 1 also provides CMO maps to illustrate the complex intersections and interactions between CMOs for each of the theories (see Appendix 1, Tables 22–31 and Figures 8–12).
While CHs experience workforce challenges, such as high turnover and recruitment, difficulties, exacerbated by poor pay and conditions, staff having variable skills and confidence and sometimes having insufficient support within the wider health system, Needs Rounds can provide CH staff and specialist palliative care staff with the opportunity to collaborate during a protected time, to plan for residents’ last months and weeks of life. Flexibly arranging Needs Rounds to suit CH needs, having manager buy-in, and building collaborative relationships can help to encourage time to be protected. Needs Rounds augment existing practice by building CH staff confidence for those who attend and prompt anticipatory planning and care. A facilitation approach that is responsive to the difficult context in which CHs operate can improve collaboration. Needs Rounds can strengthen relationships and trust and shift power dynamics between CH and hospice services by harnessing complementary expertise. Integrating learning into Needs Rounds strengthens understandings of the dying process, symptom and pain management, advance/anticipatory care planning and communication mechanisms between CH staff, families, specialist palliative care staff and primary care. This leads to high-quality resident-centred care, enabling residents to be cared for and die in their preferred place. This also benefits relatives by increasing their confidence in care quality and CH staff by providing timely expert input.
KeyFacilitation/facilitators
Theory 1: confidence and competence
Theory 2: place of care
Theory 3: collaboration and interagency working
Theory 4: better-quality lives and deaths
Theory 5: supporting families
Five theories
The five theories are presented denoting contexts (c), mechanisms (m) and outcomes (o), with key tenets of i-PARIHS implicit within the descriptions. The theories show:
-
the inner (micro/meso) and outer (macro) context
-
facilitation mechanisms (also described in Facilitation and facilitators)
-
key recipients – CH staff, SPC clinicians, residents, relatives and GPs – and how they impact implementation, motivations for participation, skills and knowledge, collaboration, power and authority and existing networks
-
innovation focused on understandings of Needs Rounds reported in Facilitation and facilitators above and degree of fit with existing practice.
After describing the five theories, the key themes that connect them are detailed, as well as presenting cases of what did not work during implementation.
Theory 1: confidence and competence
This theory is provided in Box 2.
Providing support and learning through discussions about residents’ needs in a tailored responsive way and building on existing skills (m) for CHs with high staff turnover (c) improves staff confidence and competence to provide high-quality palliative and end-of-life care to CH residents (o).
The skills and knowledge of people involved in implementation is a key micro (inner) contextual factor and a focus of the recipients’ category within i-PARIHS. 128 Participants identified a need for better understanding of death and dying in CHs without registered nursing staff and for staff members who lacked experience of caring for people who are dying:
She [SPC clinician] gave the staff more confidence really. Because some of them haven’t dealt with death and then when they did, they thought people were choking when they weren’t choking, and to realise how it happened and stuff that’s just give them confidence.
CH manager, ST00329, Phase 2
Confidence was gained through the Needs Rounds, which helped to provide a better understanding of how various individual components must be attended to and integrated for good end-of-life care to happen:
They know that some person, some residents are dying, but they didn’t have this bigger picture, what it takes to deliver the best care at the time, they didn’t know what the nurses need to do, what the GP needs to do, how you need to approach the family, how you need to approach the residents. And it was all discussed, everyone has a like, you know, there was an open atmosphere that everyone could ask questions, there was no, you know, stupid questions, and they saw a huge value in this.
CH deputy clinical manager, ST00348, Phase 2
Although there were gaps in knowledge and practice, many CH staff believed they were already delivering high-quality care, and this view was echoed by SPC clinicians. Many had previous experience of innovation and change, including GSF, ECHO and regular contact with primary care, which meant that good practice was often in place on ACP and identifying if residents needed a palliative approach: ‘We already followed the Gold Standards Framework. So, that was already embedded in the culture in the home, and the surgeries, and all the other professionals’ (CH manager, ST00395, Phase 2). This highlights how there is a good degree of fit between Needs Rounds and existing practice, a key facet of the innovation component within i-PARIHS.
SPC clinicians provided positive feedback to CH staff when they were doing well and having the validation of an expert helped to build confidence:
Because they knew I had many years of hospice experience and stuff like that, so you could genuinely say, yeah, well, you’ve got a handle on that, well done, that kind of thing. So, I would hope that that was a good kind of sort of confidence boost.
SPC, S25614, Phase 2
Needs Rounds helped CH staff feel supported. Instead of making decisions in isolation, CH staff valued having an extra person to discuss residents with, especially given that staff in CHs lacked face-to-face support from outside health services for extended periods of time during COVID-19. 129 This was reinforced by one CH manager:
I think it gave the nurses a bit of confidence that someone is there … the way we felt during the past years is like you’re on your own, you’re locked in here, you’re on your own … And you sort of feel like you’re left on you own so you have to make very important decisions in regard to someone’s life, which you’re not a specialist in, but having [hospice] involvement has, you know, you’ve got that peace of mind, you’re not left on your own.
CH manager, ST00348, Phase 2
Participants who attended Needs Rounds highlighted the positive impact that discussions had on their knowledge and confidence in supporting CH residents, specifically on disease trajectories and the dying process, symptom management and communicating with families and other professionals:
So, certain factors that normally may not get picked up. It kind of comes up [in the Needs Rounds] in terms of the families, the contact points, whether we covered certain emotional as well as certain sort of care documents that we need to look at. So, these kind of things really help going into detail of someone’s pain management and also, in terms of their hopes and concerns which are sometimes difficult things to discuss with family but with the discussions we have as a group discussion, it helps our senior nurses and end-of-life champions to go back and then answer the questions asked and then at the end, it overall helps us and the family.
CH staff, ST00403, Phase 2
However, there were concerns raised about the extent to which information was disseminated across wider teams. Although some staff in CHs described how information was shared during handovers and meetings, for others, this was limited to those participating in the Needs Rounds discussions:
What I doubt would happen as that that disseminates beyond the four walls of that room. So, in terms of, you know, oh well I learned this today about how to approach this situation, let’s share this with staff because this is not something—these are not conversations that we routinely have or think about having. So yeah, that would be my guess that they’ve benefitted but how wide that goes.
SPC, S25614, Phase 2
Some SPC clinicians offered separate education sessions outside of Needs Rounds to meet CH staff needs, and while this was not part of the protocol, Needs Rounds acted as a catalyst for this. These sessions focused on the dying process, verification of death and ACP.
Some SPC clinicians provided direct clinical support to CHs, and this helped to build confidence. While this was part of the original intended model of care, adherence to this varied across the sites. There were multiple reasons for this: (1) the ability to provide direct clinical input was restricted by COVID-19, (2) some CH staff were unaware that this was an option and (3) some SPC clinicians stated that they had offered to do direct clinical work but that this had been declined. Yet when it did happen, clinical work was perceived as valuable in developing knowledge and understanding. This included support with pain management, as one SPC clinician explained:
I was able to assess her swallow and give her a little drink and realised that there’s no way she could take medication and she definitely needed to be on a syringe pump and then talk that through with the staff, and that was I think really helpful for them and just understanding syringe pumps and understand the situation.
SPC, S55997, Phase 2
Integrated Promoting Action on Research Implementation in Health Services emphasises the importance of facilitation, and the approach adopted by the SPC clinicians helped to build confidence. Adopting a collaborative, non-judgemental partnership approach, grounded in trust, helped CH staff to feel at ease and confident to participate in the Needs Rounds sessions.
Theory 2: place of care
This theory is provided in Box 3.
Proactive ACP by confident and competent CH staff (m) builds on good practice (c) and reassures families and GPs about care quality, so that care is aligned with resident preferences, including hospitalisations (o).
The context of residents’ place of death has shifted significantly due to COVID-19. Participants talked about how hospital transfers had reduced because of the pandemic, highlighting the overwhelming pressure on hospitals, residents and families not wanting to risk infection and CH staff only transferring residents in an emergency. COVID-19 resulted in ACP becoming embedded in CH practice:
I think COVID pushed them into having to know exactly what would a person’s wishes be because they were having so many deaths … it’s just almost standard that they’ve got all these things in place.
SPC S25614, Phase 2
After COVID, it did change because we did have a period where everybody was in isolation, the ambulances were not coming out, so we had to have those conversation with the families about the DNAR, about the preferred place to care, for care. So, we are pretty good at discussing the preferred place to.
CH manager, ST00322, Phase 1
By the start of implementation (July 2021), proactive discussion and documentation of resident and family wishes as part of admissions and review processes were already happening in many of the CHs. Alongside COVID-19, this was shaped by previous experience of innovation and change, including use of the GSF and regular GP rounds, and using tools such as ReSPECT (ACP documentation) and National Early Warning Score (NEWS2, a standardised assessment and response to acute illness tool to document wishes and assess residents’ needs): ‘We normally, from that admission, we’ll plan whether they need a resuscitation, or they want to go to hospital, their preferred place of last days, so things like that, we will plan anyway’ (CH manager/registered nurse, ST00335, Phase 2).
This again reinforces a good degree of fit between Needs Rounds processes and existing practices and procedures within CHs, which maps onto the innovation component of i-PARIHS.
Consequently, many CH staff already knew the wishes of their residents, and for most, their preferred place of death was the CH: ‘The majority of the time unless it’s an acute occurrence then they, their families, tend to want them to stay with us anyway, particularly around the end of life’ (CH manager, ST00435, Phase 2).
Despite the macro context altering practice on ACP, there were examples within the data of Needs Rounds instigating a proactive approach and contributing to residents dying in their preferred place. SPC clinicians discussed the nuances surrounding ACP, including what residents understood by preferences for active treatment, reasons for and against acute care and what outcomes residents and families would be hoping to achieve through hospitalisations. One SPC clinician reflected on the role of Needs Rounds in prompting these discussions:
I think there’s far more clarity about what you have to go to hospital for, and I can probably think of a number of discussions that we’ve had about residents who’ve not been sure about whether to go or not in one month and then they had the discussions and they’ve made the choices. And by the time we review them at the next Needs Round, they’ve made their choice about not going. So, I don’t know statistically but I would, I get the sense that yeah, there will have been avoided hospitalisations.
SPC, 8CL93, Phase 2
There was a perceived need amongst some participants that CHs without onsite nurses required more support to make decisions about hospitalisations. One GP, for example, noted: ‘They’ve got a lower threshold for contacting me. Whereas the one with the nursing, that’s just not necessary. They can handle a lot more’ (GP, 8JD12, Phase 1).
Key contextual factors influencing this, highlighted within the interviews, included there being fewer deaths in CHs without nurses, fear around making the wrong decisions, staff not having the same level of training due to an absence of in-house nurses and poor pay and conditions. These factors interact to shape confidence and competence around the referral of residents to hospital teams. Participants from a CH without onsite nursing reflected on the benefits of having support from a specialist with a nursing background to help improve their knowledge:
Yeah. It’s good speaking to [hospice nurse] and getting a different approach to things really because obviously she’s got a nursing background that helps us as well really into areas that we probably don’t know a lot about.
Deputy CH manager, ST00327, Phase 2
One SPC clinician talked about the lack of support from GPs and the progress they had made through case-based education:
I do think the residential homes need more support from a GP. Whereas now at the minute, a GP will say to send them into hospital. So, I think it’s quite difficult for them to make that call whether to send them or not. But I’ve seen a reduction in that home where they’re not blue lightening them, willy-nilly if you like because they was … I still think it must be scary for them to make that call.
SPC, 8C928, Phase 2
Low confidence was discussed by a CH participant without onsite nursing who said that their practice around hospital transfers had not changed because they did not want to take responsibility for decision-making about hospitalisation. Power, responsibility and clinical hierarchies are visible here (discussed further in Theory 3: collaboration and interagency working) as well as evident gaps in learning, with a need to build confidence on decision-making about hospital transfers:
We’re calling the ambulance because, obviously, it’s not down to us, obviously. So, we call the ambulance and they’ll ring us back … But that’ll go back on them then because they have been called. It’s not our responsibility, then, if anything happens.
CH manager, ST00329, Phase 2
The fear of being viewed as negligent by families was also perceived as impacting hospitalisations: ‘I think, it’s around that fear of the fact that if they didn’t do something [sending to hospital], they might be seen as being negligent’ (SPC 8JD12, Phase 1).
One of the key areas where Needs Rounds were able to add value was in relation to communication. Providing education on communicating with families was integral to the discussions, including discussion of hospitalisation. One SPC clinician reflected on how they incorporated this into the Needs Rounds:
I just gently tried to challenge that a little bit around what is going to be achieved by hospitalisation in a 95-year-old with Alzheimer’s. And sometimes rather than phrasing the question ‘do you want hospitalisation?’ it’s talking about is it going to change outcomes? Is it going to change what happens? Is it going to increase distress? So just started to really push that a little bit in terms of trying to give them confidence.
SPC, 8JD12, Phase 2
Although CH staff were having conversations about hospitalisation prior to implementation, the learning provided through Needs Rounds helped to improve the depth, content and approach towards the discussion so that families and residents could think through the implications of their choices. This helped build CH staff competence to provide high-quality proactive anticipatory care, as well as their confidence in communicating this with families, so that families felt at ease for their loved ones to be cared for in the home. This was reinforced by one participant who said:
I think this has given us the confidence to give education to support the next of kin of the families; that we can provide a certain level of care here in the care home. So, again, it gave myself and the staff a bit of encouragement to say, well, you don’t necessarily need to go to the hospital. And we haven’t, the residents that we have discussed, we have managed to nurse them here and the families, I believe, have got that confidence that we can do it here.
CH manager, ST00418, Phase 2
The learning component of Needs Rounds also helped to improve communication between some CH staff and GPs. Care home staff became more assertive with GPs in communicating their assessments of resident needs, to prevent a transfer to hospital. As one SPC clinician said:
She phoned up and she said she’s really anxious about this resident, she wants someone to come see them now and the GP has said, ‘If you need someone to see them now, you need to call 999’. And she said, ‘But I didn’t need to call 999, I know I didn’t need to call 999’. She’s great. And then she said, ‘So [the GP]’s coming in 45 minutes’.
SPC, S55997, Phase 2
Theory 3: collaboration and interagency working
This theory is provided in Box 4.
An approach based on communication, collaboration and reciprocity that shifts power dynamics and builds trust between CHs and hospices and harnesses complementary expertise (m), for CHs impacted by workforce issues and negative attitudes towards CH staff (c), leads to improved relationships and better resident care (o).
Needs Rounds supported interagency working by improving communication skills and confidence. Needs Rounds strengthened relationships between SPC and CH staff, which required reciprocity and a sharing of different but complementary expertise.
Relationships between care homes and specialist palliative care
Participants were cognisant of the difficult context within which CH staff worked, and, as will be demonstrated later in this section, this impacted SPC clinicians’ facilitation styles with CH staff. Residents with complex needs, poor support within the wider health system, inadequate pay and conditions and high staff turnover are some of the contextual factors highlighted as impacting CHs:
It is particularly challenging and complex work to be working within the care home sector. I think the type of work that care home staff do is not well acknowledged and appreciated within society. I think rates of pay are poor, I think opportunities for promotion and development can sometimes be limited, and for these reasons people will- are more likely to move on to other jobs.
GP, S25614, Phase 1
SPC praised the work that CH staff do, despite these negative micro, macro, and meso issues:
They’re really up against it. I mean, they don’t have the luxury of medical staff to hand, and often, not nursing staff. So, they’ve got a huge responsibility for not a wonderful period, and most of them are just so dedicated. There’s a high turnover of staff in a lot of the care homes, so they get people that are trained-up to do the job and are caring for the patient—resident, sorry. And then, they are offered another position somewhere with a higher grade of pay.
SPC, 55997, Phase 2
The wider community context was cited as being of importance in building relationships between organisations. Hospice staff were eager to support CH staff and counter prevailing negative perceptions of CHs: ‘Care home staff can feel very got at sometimes that people are very punitive, you did that wrong, you should’ve done that’ (Education lead, 8C928, Phase 1).
The view that CH staff are less capable can result in a lack of responsiveness to their requests as their decision-making abilities are questioned; this erodes confidence and negatively impacts on the quality of resident care. The need for a collaborative, reciprocal partnership between CHs and SPC was identified during Phase 1 to counter negative attitudes and ensure that CHs felt supported: ‘we don’t want to be going in and telling people what they need to know. It’s about relationships and partnerships’ (Education lead, S25614, Phase 1).
Relationship building is fundamental for successful implementation of Needs Rounds. How power is exercised is central to relationships, and managing power dynamics is a key facilitation mechanism required to create equality, mutuality and reciprocity. Power and authority are also central to the facilitation and recipient components within i-PARIHS.
Rapport building helped staff in CHs to feel at ease to discuss residents in the sessions:
Allowing a bit of just chat beforehand and using humour as well within the discussion so that you know it doesn’t seem like a serious kind of, you know, triage proper clinical meeting … it’s that just trying to get them to relax into being able to just talk about what their concerns are about the resident as opposed to trying to keep it very clinical and use all the right terminology.
SPC, 8CL93, Phase 2
SPC clinicians adopted a supportive and non-judgemental approach, seeking to build trust:
I think it’s about knowing that I’m supportive, knowing that I’m not gonna judge them if they have one person they want to talk about, or if they’ve got eight or even on the several occasions when they’ve just not been prepared at all is that I’m not going to judge, and I’m there to understand what they are up against.
SPC, 8A784, Phase 2
Care home staff valued this approach and contrasted it with receiving negative feedback from other professionals where there were evident power differentials: ‘Because sometimes when other professionals are coming today will say, oh you’re doing this wrong, you’re doing that wrong, whereas she will ask questions, but she will not judge you’ (CH staff, ST00402, Phase 2).
Conversely, clinicians used positive feedback and reassurance when CH staff demonstrated good practice to build their confidence and recognise their expertise. In doing so, this helped to forge a sense of equality and mutuality and flatten power hierarchies:
Obviously [SPC8CL93], she’s very confident about us as well. We have everything in place that we need for our residents, like power of attorney wise, advanced care plans, the ReSPECT forms, DNAR, the anticipatory medicines – we already have them in place, on board and she saw that. She said, ‘You really are doing very well you know’.
Registered nurse clinical lead, ST00403, Phase 2
Another SPC clinician altered power dynamics and contributed towards a reciprocal relationship by praising the strengths of the CH staff and sharing their own knowledge gaps so that the dynamic was focused on doing together, with both parties learning, rather than creating an expert/recipient dichotomy:
I’m not going in there to tell them what to do or to teach their granny how to suck eggs. It’s working collaboratively together … like you know you go into a care home and they’re really really good at wound care. No, it’s not my forte … and so it’s sharing. You know my weaknesses as well, and looking at their strengths and my strengths, their weaknesses, and mine and their weaknesses, and sharing them so we’re on a par.
SPC, 8C928, Phase 2
For some SPC clinicians, however, there was a lack of reciprocity. Some felt that they were putting significant effort into the Needs Rounds, and this was often met with low levels of engagement among CH staff. One SPC clinician, for example, noted that Needs Rounds were cancelled yet did not receive any communications from the CH regarding this: ‘You can be supportive, but actually there’s got to be a bit of reciprocity there as well, hasn’t there? … but I just needed to flag up that my time is precious’ (SPC, 8A784, Phase 2).
One CH manager reflected on the asymmetrical nature of their relationship with their SPC clinician, noting that the SPC clinician put in significantly more work: ‘It was more her that bent backwards rather than us.’ (CH manager and nurse, ST00395, Phase 2). For another site, a lack of reciprocity resulted in the SPC clinicians feeling apprehensive about doing the Needs Rounds: ‘There was times when I was thinking well, I’ve got to go into such and such … Not dreaded it, but [we] weren’t really looking forward to it’ (SPC 9C928, Phase 2).
While poor engagement was challenging for the SPC clinicians, wider contextual factors were at play. As mentioned in theory 1, workforce challenges restricted the numbers of staff that were able to attend Needs Rounds. COVID-19 significantly amplified CH workforce issues, with staff leaving the sector and isolating, and additional pressures from testing and monitoring:
The increased requirements for care homes around the pandemic has been really difficult, expectations of PPE and then of course at the beginning, the movement of patients from hospital and coping with outbreaks, managing residents who are, don’t have access to their families. I think it’s extremely challenging. And then they had a lot of sickness and the recruiting is challenging.
GP, 8A784, Phase 1
One SPC clinician explained how they navigated these wider contextual barriers to facilitate engagement:
You recognise that staff are stressed, they’re short-staffed, there’s people off sick at last minute … you can read people and you can tell that there were staff who were a bit stressed … I mean, if you’ve got something you need to do, well, I’ll come with you and we’ll chat as you go. And that way, I got to see the residents as well, which was wonderful.
SPC, S55997, Phase 2
By being responsive to the CH staff’s needs, the SPC clinician was able to fit alongside the CH workload and restrictions on staff time.
Building trust was also an important relationship mechanism identified by both the SPC clinicians and the CH staff. Trust was generated by building rapport, and this was aided by continuity of staff attending the Needs Rounds. Trust also intersected with issues of power. Reducing power hierarchies and bridging boundaries was perceived by the SPC clinicians as being central to building trust: ‘It’s really important to build their trust, gain their trust … So yeah, I think you just have to be able to relate to people and definitely don’t want to seem like you come from your ivory tower’ (SPC, S25614, Phase 2).
Where there was a lack of trust, the Needs Rounds did not work. This was made clear by one SPC clinician who said:
I think she [care home manager] perhaps feels, you know, vulnerable, maybe that’s a strong word, but you know, letting somebody into a, her home … She does very much see me as from [name of hospice]. I think she is nervous about that.
SPC, 8JD12, Phase 2
A lack of trust and unequal power dynamics impeded Needs Rounds. The manager’s perception that the SPC clinician was there to scrutinise and judge their practice, rather than provide support and guidance, was perceived to restrict discussions and block access to residents to undertake clinical work. This mistrust is situated in the wider context of deeply ingrained negative attitudes towards care staff and care work, resulting in perceptions of defensiveness.
The fragility of organisations’ sense of worth and value underpins the importance of relationship work which requires a delicate balancing of sharing expertise. SPC clinicians frequently praised the expertise of CH staff and the excellent work being undertaken in those settings. However, in flattening hierarchies, a by-product was that SPCs sometimes failed to recognise the value they brought to the collaboration:
It’s not until now that I look back and I think, ‘Do you know what? This Needs Rounds really worked because I can see the improvements in some of the homes.’ At the time, when you’re going through, I was like, ‘I don’t really know if I’m making a difference.’ I have made a difference, I know that now, but it was hard to see that at times.
SPC, 8C928, Phase 2
For Needs Rounds to work, there must be recognition of the expertise that both CH staff and SPC clinicians hold, weaving these in a collaborative way. Action learning sets were held monthly throughout the implementation period to support the SPC clinicians. However, it was not until month 5 of implementation that SPC clinicians started to report positive feedback from CH staff, and SPC clinicians talked about challenges in facilitating a partnership approach while also using their expertise to direct discussions. To strengthen collaborations, a feedback mechanism is required to enable parties to identify and describe how their involvement is generating a positive impact on the others.
Wider relationships in the health system
The nature of existing networks is a component within the recipients i-PARIHS characteristic. Despite there being various other interventions to support CH staff (see Theory 1) including EHCHs and primary care rounds via retainer, clear gaps in the existing system were evident. SPC clinicians reflected that much of the work they undertook was generalist in nature: ‘Most patients I’ve seen are not desperately specialist. It is generic palliative care stuff’ (SPC, 8A784). This led some to believe that generalist rather than specialist support is required, and that greater links need to be forged with primary care:
It has to be integrated with other parts of end of life care … put it with the GP and to have a combined round where a palliative care nurse goes in, they’ve got legitimacy, they’re part of the process. And then liaising with the GP, they’re talking face-to-face with the care home staff, you’ve got everybody in the same room, that probably is the most helpful thing.
SPC, 8JD12, Phase 2
This again highlights issues of power and expertise, with the SPC clinician underlining the legitimacy, or the power, of the GP. The need for integration with primary care was implicit within the initial programme theory and was emphasised by GPs:
I think we’re crucial. (Laughter) I think it’s our bread and butter … I think I’d feel really my nose out of joint if I wasn’t involved. We’ve got to be part of the team haven’t we, there? So, yeah. I mean it would be ideal really, yeah kind of, I guess joining for a monthly ward round.
GP, 8JD12, Phase 1
It was envisaged that Needs Rounds would help to create better joined up working between CH staff and other professionals. However, this did not work during the implementation phase, largely because the MDT meeting component of the intervention did not happen. Challenges in co-ordinating diaries prevented Needs Rounds from aligning with existing MDTs and primary care and thereby limiting contact between SPC and other agencies, which reduced the potential for change.
Despite not formally including GPs in Needs Round meetings, the approach still enhanced communication with GPs and other primary care clinicians. The interviews in both Phases 1 and 2 showed that there was significant variation between the quality of relationships, with lack of response from primary care being a particular issue. As was noted by one CH interviewee: ‘Sometimes you find you’ve got to phone two and three times before you get the appropriate response that you’re looking for or you get a call back’ (registered nurse, ST00325, Phase 1). Paramedics also highlighted challenges in communicating with primary care, especially out-of-hours GPs:
Early hours of the morning or on a Sunday night for example, three in the morning and we try to contact the out of hours GP because the patient’s deteriorated. We call the out of hours GP and they say, I don’t want to interfere in this patient because I don’t know them […] they might say, I’ll tell you what, see how they go and maybe they can contact their own GP first thing in the morning but that’s all very well. But if the patients on this trajectory, they’re uncomfortable and they’re struggling to breath and they’re anxious waiting to contact their GP. I mean that can be a real frustration.
Paramedic, Phase 1
A lack of responsiveness was exacerbated by COVID-19, as GPs and other agencies withdrew face-to-face contact, instead relying on communications via e-mail, Zoom and phone:
It was very time-consuming to get hold of GPs because most of the time we need to ring the GP surgery, you have to hold for 15, 20 minutes. Nobody was working in offices, everyone was working at home, so when you try and get a specialist nurse, they were not working. They’re working from home, so there’s no direct telephone you can contact them. Everything is through e-mail.
CH manager and nurse, ST00395, Phase 2
During Phase 1, CH staff reported that they often struggled to get a timely response from GPs, and this negatively impacted resident assessments and anticipatory prescribing:
Sometimes it’s very difficult to get certain medication and especially for end of life, and sometimes it’s not the fact that the GP will not help, but I think it’s whoever answers the phone, whoever passes all the messages, or whoever checks the prescriptions, sometimes they are not trained and they don’t know why we are keep asking for Midazolam and Morphine, ‘We gave you something two days ago, why do you want it again’?.
CH manager and nurse, ST00322, Phase 1
Learning through Needs Rounds enabled CH staff to build their confidence and communication skills. Understandings of deterioration, dying and death were used alongside their knowledge of their residents to detect changes and recognise when they were approaching the end of life. CH staff communicated residents’ needs with assertiveness with GPs to ensure that anticipatory medications were in place:
They [staff member] were then able to phone the GP and have the discussion with them of no I want, ‘just in case’ meds put in. Because if this person does go really downhill over the weekend, I don’t want to be trying to get out of hours GPs. I don’t want them in pain while I’m waiting four hours for NHS 24 to answer the phone, you know … I think just the staff having the confidence to … I wouldn’t say argue with them but debate and have the conversations and ask them to explain their decisions.
CH manager, ST00340, Phase 2
CH staff also used their connections with the hospice to improve GP responsiveness. This was made clear by one interviewee who talked about their experience of organising pain medications:
We were struggling with the GP prescribing lots of oral pain relief, codeine, and things like that, and she was like, ‘No, I recommend the patch with oramorph on the side, as a top-up.’ So I got in contact with a GP, explained that I’ve been advised this by a specialist and they prescribed it straightaway no questions asked.
CH nurse, ST00435, Phase 2
Needs Rounds provided a direct link to hospice expertise, which helped care to be more responsive, and this sometimes negated the need for external referral:
Beforehand, if we had any concerns, we would have to ring the nearby hospice or the GP and get someone to talk to but this was more of an ongoing review for … you could directly speak to the person and get an advice from them directly. And that we’re able to make sure everything was in place and if there’s any gaps identified … we could do the corrections then and there.
Registered nurse, ST00335, Phase 2
Although using the expert status of the hospice does not change power dynamics between CH and GPs (the mechanism is utilising the power of the hospice), it did help to improve communication and responsiveness.
Theory 4: better-quality lives and deaths
This theory is provided in Box 5.
For the CH workforce impacted by sector-wide inequitable pay and conditions and high staff turnover (c), Needs Rounds augment existing good practice by focusing on residents’ holistic needs, enhance communication with GPs, improve symptom management and provide tailored learning (m), improving the lives and deaths of CH residents (o).
SPC clinicians praised the high-quality care being practised pre implementation, and Needs Rounds focused on augmenting this. CH staff had strong relationships with their residents: ‘Because they [CH staff] just know the residents so well, they care so much … I know it’s cliché but they are … staff are their family’ (SPC, S25614, Phase 2).
Knowing residents well enables CH staff to identify subtle changes that may not be detected by other professionals:
Senior NHS manager, Phase 1, workshop 3: ‘[CH staff] are the specialists actually because the nuances they know can make such a difference. They might not know the actual [...] clinical terms, but the amount of detail that they know can make such a difference to somebody’s life and the noticing that goes on that we don’t actually capture’.
Needs Rounds sought to triage residents to ensure that the most appropriate people were discussed. Triggers included those who were at the end of life, conflict, deterioration and residents who were difficult to manage. While residents who were perceived as being closer to death were frequently selected, the SPC clinicians encouraged CH staff to think more broadly about anyone who was in the last 12 months of life:
We [usually] pick a resident at quite late stage, really the last month maybe of their life. But last time [SPC clinician] was so really good, she was suggesting that we might talk about somebody who is not actually imminent, he’s not coming towards the very end.
Registered nurse, ST00348, Phase 2
Care home staff were thus informally learning that SPC could be appropriate to people with a life-limiting illness even if they were not in the final weeks or days of life. The SPC clinicians highlighted the need for CH staff to have more confidence in their knowledge of residents and identifying deterioration and dying:
I think the issue … around their confidence around perhaps that I think they … I said, ‘Do you think you recognise dying? Do the people here recognise dying?’ They said that, in the main, they feel that they do. But I think it’s perhaps having the confidence then to go with what their gut instinct is.
SPC, 8JD12, Phase 2
Drawing on ‘gut instinct’, or their knowledge of residents and their assessment skills, alongside additional support, case-based learning about signs of deterioration and being able to communicate this to other professionals, is integral to high-quality care provision.
One of the key areas that Needs Rounds aided was symptom management. One CH interviewee reflected that their approach to assessing, documenting and treating pain had changed because of Needs Rounds: ‘We are getting better at utilising [PRN medication], documenting it, putting stress and distress care plans in, and having pain management care plans now of what we’re doing to try and manage pain’ (CH manager, ST00419, Phase 2).
Staff were more proactive in their pain management, but also able to expand their approach, considering the last 12 months of life rather than the last few days. Having these plans in place also enabled CH staff to be more assertive about the needs of residents who experienced fluctuating levels of pain that was undetected by external health professionals:
The CPNs are very much looking for hard evidence rather than anecdotal evidence … I understand that, you know. I don’t want every resident within the care home sedated, you know. That’s not what we’re looking for. But we are wanting every resident in the care home to have the best quality of life for their last six months, a year, whatever, you know, or even weeks that they’ve got.
CH manager, ST00419, Phase 2
As identified in theory 3, relationship building between CH staff and SPC clinicians is a vital mechanism in improving palliative and end-of-life care. When SPC clinicians recognise and value the knowledge that CH staff have of residents, listen to their concerns and collectively create action plans; this helps to improve resident care, making sure that residents’ wishes are met and that their pain is managed so they have a comfortable peaceful death:
Other professionals aren’t always keen on the uptake to do anything different or hugely different, but since doing the Needs Rounds, we have been able to titrate her medication up and it’s been of huge benefit to this particular resident in managing her pain … I think that’s because this lady has been listened to and the staff have been listened to.
CH nursing manager, ST00418, Phase 2
As mentioned in theories 1, 2 and 3, Needs Rounds also helped to develop CH staff confidence in communicating with primary care clinicians, with requests being met and more timely actions being carried out. This timeliness was identified as being particularly important when a resident is at end of life.
Direct clinical work also assisted CH staff to recognise dying earlier in the process and ensure that anticipatory medications were in place so that resident pain was managed. As mentioned in theory 1, clinical work did not always take place because of COVID-19 restrictions and managers not wishing for this to happen; however, when it did happen, it worked well:
[The SPC clinician] really assisted, and that death was a lot easier than what it could’ve been, if that hadn’t got the [medication] patch sorted and things like that and [the resident] was probably a lot more comfortable having that on.
CH nurse manager, ST00435, Phase 2
Having time to reflect and proactively plan for death enabled CH staff to ensure that care was resident and family focused; symptoms were also well-managed, and residents and families were prepared:
[Needs Rounds] contributed because … everything was in place … and just to stop a minute and think of the resident’s experience … He did not suffer, the family was aware. He was ready. He got a little bit more religious towards the end, and it was just so peaceful.
Deputy CH manager, ST00327, Phase 2
The above example highlights the importance of spiritual care. While medical components such as pain and symptom management are integral to a peaceful death, so too are meeting residents’ psychosocial and spiritual needs. During the action learning sets, SPC clinicians reflected that there was often a lack of attention to residents’ non-medical requirements, so these gaps were focused on in the subsequent Needs Rounds. SPC clinicians, for example, asked questions about religion during the discussions: ‘I also asked the [hospice] chaplain to go in and see her … So I used [the hospice]’s resources to go into that nursing home and support that family and the patient and the staff as well’ (SPC, 8JD12, Phase 2).
Other services such as complementary therapy were also used to improve the quality of residents’ lives.
She [complementary therapist] came out with me to quite a few of the care homes on one of the Needs Rounds. I was able to talk to the activities coordinators, and was teaching them just touch massage. We use non-verbal communication and things like that … It was really worthwhile.
SPC, S55997, Phase 2
Thus, although the CH was often already providing excellent care, Needs Rounds identified gaps and helped CH staff to build on their existing practice to ensure that a holistic range of needs were met to improve quality of life and death for residents.
Theory 5: supporting families
This theory is provided in Box 6.
Variable skills, confidence and frequency of support from CH staff to families (c) are addressed by Needs Rounds providing time and space to reflect and plan how to talk with families about care and future resident needs (m) resulting in staff reporting that families feeling more involved, informed and confident in the care provided to their relatives (o).
With limited primary data from family members, the theory on families is derived from what CH staff and SPC clinicians told us about what worked or did not work with families, rather than being based on their direct feedback.
Some CH teams were confident in communicating with and supporting families prior to Needs Rounds being delivered. Such sites already had good processes in place for this, for example ascertaining resident and family wishes at point of admission. During Phase 1, a family member reflected on the CH support they had received pre implementation:
I’ve tried to have my moments at home but there was a few times where I was distressed, and there was a couple of times where the senior nurse in the, in the building said, ‘come in and have a chat, we’re worried about you’.
Family member, S55997, Phase 1
During implementation, where CH staff were effectively supporting families; praise, support and positive reassurance were used to enhance confidence (see Theories 1 and 3).
In contrast, some CH staff felt nervous, found it difficult to talk about death and dying with relatives and did not always have the time to support them. As demonstrated in theory 1, Needs Rounds helped to develop CH staff confidence, including the confidence to talk to families about death and dying and how palliative and end-of-life care is managed, including care planning, symptom control and anticipatory medication. When CH staff recognise that residents are dying, they are better able to plan and care for residents, ensuring that the family are fully informed and involved in decisions about care, anticipate what care and treatment will be required to keep residents comfortable and work with other health professionals to ensure these are in place. Needs Rounds prompt action earlier in the process:
[Before Needs Rounds] we would wait for something to go wrong rather than being proactive and say to the family that this person is possibly in the last days of their life and we need to consider plans for them ahead. So, I think that’s the major change, so we are able to recognise that [dying process] in a much better way and able to communicate that with the GP and the family and make plans for them well ahead of time, yeah.
CH Registered nurse, ST00335, Phase 2
Being proactive and recognising deterioration, combined with timely communication and support, helps to prepare families so that they can process and plan for their relative dying:
What has helped us, is actually doing anticipatory care and preparing families for that. And, you know, and then being able to accommodate families for them to be better prepared for those last days and having that time to come in, and, you know, make peace with their families and that kind of thing.
CH manager, ST00419, Phase 2
During the Needs Rounds, the SPC clinicians assisted CH staff by talking through strategies for how best to communicate, what terminology to use and when to approach families. Sometimes, the SPC clinicians spoke directly with families, but the CH staff were also encouraged to do this themselves and use the Needs Rounds sessions for reflexive practice:
[The CH has] almost practiced the conversation before they’ve had it with them [the family] … they’ve kind of taken that, ‘give it a go and we’ll talk about it at the Round and see you know whether there’s anything that was really hard to do and we’ll kind of unpick that a bit and reflect on it’.
SPC, 8CL93, Phase 2
Having more confident and competent staff improves the quality of residents’ lives and deaths (see Theory 4), and this can build family confidence in the care being provided. CH staff communicated with families to aid understanding of what care can be offered as an alternative to hospitalisation. Having an extra layer of specialist support from the hospice was viewed positively:
They chose here, and we were able to provide this man a dignified death and he was able to, be able to have the syringe driver, his pain was managed well, we didn’t need to transfer him to hospital … so we were able to give them [family] the confidence … [Needs Rounds] had given myself and the staff the confidence to put our abilities out there.
Deputy CH manager, ST00418, Phase 2
Strong communication skills can also be used to resolve conflict. On the Needs Rounds checklist, family conflict is a trigger to discuss residents. Often conflict or disagreements with or within families relates to different perspectives on care and treatment decisions: ‘You can appreciate when residents’ conditions are declining and really, it’s not in their best interest for them continuing to go back and forth to hospital. We can explain that. We can’t really enforce it’ (Clinical lead, ST00333, Phase 1).
Families can find it difficult to accept that their relative is dying and seek burdensome and futile treatments which can cause tensions with CH staff. Care home staff talked about forming close relationships with residents and wanting them to have a peaceful death in the home surrounded by people who care about them. CH teams developed confidence through Needs Rounds to have conversations with families about the potential risks of hospitalisation:
The family, one son in particular was in denial … he talked about having [a treatment] giving her hope, and I’d said, you know, I can probably understand that and who wouldn’t want hope. I said but what they did explain to you was … it’s a terminal condition she’s got and we have to think of what is best for her at this moment in time and for her comfort and for her pain levels.
CH manager, ST00340, Phase 2
In the above example, the CH staff communicated to the family that their mother might not survive if transferred to hospital. Despite being advised of the potential risks, the family decided to proceed with a hospital admission, where their mother died. Although the CH staff’s communications did not prevent hospitalisation, they delivered the required information to allow the family to make an informed decision.
Tensions can also arise due to CH staff not listening to family concerns. In one site, a daughter had recognised changes in her mother and believed that she was dying. Although the CH staff did not share this view, the SPC clinician was able to identify signs of dying and arrange necessary end-of-life medications. Through direct clinical input (assessment and medication management), the resident’s symptoms were managed so that they were comfortable in their final days. Support was also provided to the daughter who had been distressed by witnessing her mother in such anguish:
I’ve never seen somebody so distressed with dementia, and she was, nobody wanted to diagnose that she was dying in this home … I’ve never seen that level of distress and her poor daughter was beside herself. And within … we got her really settled with just five milligrams of midazolam. So we just put a tiny amount in and supporting that daughter who’d been through a very traumatic experience, I think, it was very traumatic seeing mum like that for days on end.
SPC, 8A784, Phase 2
The SPC clinicians also supported CH staff to resolve conflict within families. In one site, a son was strongly advocating for his mother to have active treatment in hospital, despite his mother having capacity and not wanting to go. The SPC clinician offered to attend a family meeting, and although the CH felt confident enough to manage the communications themselves, they took advice about how best to approach this:
[The CH] said, ‘it went really, really well, I spoke to them [the family], used what you said you’d do, and it went well, and the son was fine’. So, yeah, I just think they’d rather ask me but then do it themselves.
SPC, 8C928, Phase 2
An approach based on doing alongside, with advice and support from the SPC clinician about how to communicate the potential risks and distress from hospitalisation, and not doing directly for, is important in enabling the CH team to build their confidence and have the skills to continue supporting families’ post implementation. This reflects the centrality of honing the facilitation approach, as advocated by i-PARIHS.
Key connectors and examples of what did not work
The following presents the generative connectors that link the five theories. This section also details the factors that enable successful implementation of Needs Rounds. While the focus is on what works for whom under what circumstances, we also use the data to reflect on what has not worked. This informed the development from the initial programme theory to the final overarching programme theory.
Time
Time was a key connector within the theories and is also central to the ‘recipients’ characteristic in i-PARIHS. Needs Rounds are intended to provide protected time to discuss residents’ holistic needs, and while they did sometimes, they were not always prioritised or were cut short. Available time was impacted by wider macro workforce issues, including high turnover and unfilled vacancies; COVID-19 exacerbated these problems. If CH managers are unable to allow their staff time to attend Needs Rounds, then they do not benefit from the improved outcomes that the approach can engender.
Having protected time to discuss residents resulted in more proactive care, with Needs Rounds prompting proactive management of resident needs to manage symptoms more effectively. Staff having time to continue learning about recognising deterioration and the dying process, and how to communicate with families, improves the quality of residents’ lives and deaths and prepares family members for their relative dying.
Time also shaped which residents were discussed, with triggers predominantly focusing on those closer to dying. Specialist palliative care clinicians did encourage CH staff to discuss residents at an earlier stage, to improve their quality of life.
Effectively planning Needs Rounds around CH routines so that they occurred at a quieter time of the day was helpful in enabling CH staff to attend the sessions. However, a lack of time was detrimental to implementation in several ways. First, it restricted who could attend the sessions, which impacted the overall scale of change. Carers who were identified in Phase 1 as being integral to the success of Needs Rounds were often excluded because there was no time or availability to participate. Second, time acted as a barrier to management and wider staff members engaging with materials about what Needs Rounds are, which disrupted the early implementation period. Third, time prevented MDT meetings from happening as aligning schedules between busy professionals was too difficult.
Relationships
Pervasive public discourses regarding CH staff being less skilled than other healthcare professionals were recognised and challenged during the Phase 1 interviews and workshops. Valuing the important work of CH staff, using their skills and knowledge of their residents, and adopting a facilitation approach that fostered these assets was integral to the programme theory. It was anticipated that a collaborative, partnership approach was needed where SPC and CHs learn together, to enable CH staff to provide high-quality palliative and end-of-life care beyond the duration of the project. It was evident that this had been achieved in many of the sites, with a non-judgemental partnership approach underpinned by trust.
Demonstrable shifts in power were evident in Phase 2 interviews, with clear acknowledgement of each party holding expertise. Care home staff were celebrated for providing excellent care, for knowing their residents, anticipating their needs and undertaking proactive care planning to facilitate good deaths. Indeed, rather than being viewed as inferior, CH staff were conceived as experts in the provision of palliative and end-of-life care and respected for working in an extremely challenging context.
Specialist palliative care clinicians were also praised for their skills and knowledge, being supportive and being present. However, for some, respect had to be earned rather than given by virtue of their role as senior nurses from specialist services. This occurred against a backdrop of COVID-19, where many CHs were left with little face-to-face external support, resulting in feelings of abandonment. One way for SPC staff to build trust was to demonstrate skills and knowledge by combining case-based learning with direct clinical work to enhance the value that they offered. This was part of the original implementation plan, though did not happen consistently in the sites. This was due to a combination of COVID-19 visiting restrictions, a lack of a perceived need and direct clinical intervention not being offered by the sites.
Some SPC clinicians had not readily identified their added value and expertise due to the existing high-quality work being conducted by the CH teams’ pre implementation. However, this does not accord with the feedback from CH staff who valued the support they had received, particularly in building staff confidence and improving communications with families and GPs. While the initial programme theory focused on developing the confidence of the CH staff, the final programme theory has been broadened out to include a feedback loop so that SPC clinicians also know what value they contribute. This feedback loop creates a more equal relationship where different expertise is acknowledged and collectively harnessed to improve resident and family care and support.
Despite there being a shift in power between the CHs and SPC, Needs Rounds did not address power dynamics in the wider health and social care context. Externally, it was evident that SPC clinicians were still conceived as experts and CH staff used this status to influence their interactions with GPs so that their requests were met with responsiveness. While this helped to improve communication, it was often by referring to the SPC clinicians’ recommendations that actions were carried out swiftly.
During the Phase 1 interviews and workshops it was made clear that for Needs Rounds to be effective, a range of staff members should attend the monthly meetings, including care staff. Care staff spend a significant amount of time with residents, resulting in the development of knowledge about their needs, which enables the detection of changes that may signal deterioration and death. However, the wider macro context impacted care staff attendance, with workforce issues restricting the ability of carers to participate, which often resulted in knowledge generated within the Needs Round being held by nursing and management staff. There is a lack of consensus in the data about the extent to which learning from the Needs Rounds was disseminated to staff not attending; therefore, the programme theory reflects that the benefits arise for those who participate in the Needs Rounds sessions.
Communication
Communication is a key theme that connects the five theories. The Phase 2 interview data demonstrate that improved communication was one of the main outcomes resulting from Needs Rounds. Needs Rounds provided a direct communication mechanism between CHs and SPC, in some cases circumventing the need for referral through the GP.
Needs Rounds also helped CH teams to improve their confidence and assertiveness when communicating resident needs to GPs. This augmented existing good practice on documenting, communicating, directly providing and working with GPs to ensure medications are in place to enable residents to die in the CH. Enhanced communication contributes to better-quality dying, with residents’ wishes regarding place of death being fulfilled.
CH staff also improved their communication with families. While for many of the CHs, there was already excellent practice around ACP, the SPC clinicians supported CH staff to improve both the content and process of communication to prepare families for their loved one dying and to resolve conflict between and within CHs and families. This included discussing staff skills to bolster family confidence in their ability to provide high-quality palliative and end-of-life care.
Despite this, three communication gaps were also evident. First, the full understanding what Needs Rounds are and how they function was missing for some participants. While information was provided through meetings with the research team, e-mail correspondence, an implementation pack, a memorandum of understanding and workshops, it was evident that these were often not fully engaged with. Furthermore, understanding and knowledge were also lost through staff changes. This resulted in gaps in understanding amongst CH staff members who lacked clarity about Needs Rounds.
Second, there was a lack of awareness amongst SPC clinicians about their value and how they were positively perceived by the CH staff. The action learning sets with the six SPC clinicians were an important peer support mechanism which enabled discussions and reflections on their learning and problem-solving, including this absence of a feedback loop. However, an additional feedback mechanism is required to aid communication between CHs and SPC clinicians.
Finally, the multidisciplinary team and family meetings did not happen in practice, largely due to COVID-19. These were intended to act as formal mechanisms to improve communication between CHs, external agencies and families.
Contextual changes and harms
COVID-19 was ongoing throughout the study, and this formed the major contextual issues for the study. National and local lockdowns were announced and removed during Phase 1, with Phase 2 impacted only by local lockdowns and outbreaks.
No harms were reported within the study. When COVID-19 outbreaks occurred and when staff had capacity, Needs Rounds were conducted online to manage infection control.
Chapter 4 Outcomes in adopting palliative approach, family perceptions of care and quality of dying/death
Staff capability of adopting a palliative approach
A total of 171 CH staff members completed the CAPA survey. Nurses were the largest single group of respondents (42.9%) followed by care assistants (20.1%). For analysis, data were grouped into four categories: managerial (26.0%, including managers and deputy managers); care (21.5%, including care assistants and senior carers); nursing and clinical (46.1%, including nurses, student and associate nurses, and clinical leads); and other (6.4% including administrative staff, activity and lifestyle co-ordinators and health and well-being specialists). Twenty-eight (16.4%) provided multiple responses at different time points.
Examination of overall CAPA scores suggests that two groups, care and other staff, had lower levels of capability than managerial staff (Table 8). Working in a larger CH (50 + beds) compared to a medium CH (11–49 beds) was associated with lower CAPA scores. Conversely, factors that had a positive impact on staff capability included working in not-for-profit homes (compared to privately owned). The organisations’ definitions used in this section are drawn from carehome.co.uk. Staff who completed the CAPA survey later into the Needs Rounds intervention period achieved significantly higher CAPA scores than those completing the survey earlier in the intervention. This suggests that engagement with the Needs Rounds approach may have had a positive impact on staff ability to adopt a palliative approach over time.
| Coefficient (std err) | |
|---|---|
| Staff group (ref. managerial) | |
| Care staff | −7.4 (1.8)* |
| Nursing and clinical staff | −1.4 (1.2) |
| Other staff | −6.1 (2.5)** |
| Date of survey completion | 0.4 (0.2)** |
| Size of home (ref. medium) | |
| Large | −4.8 (1.4)*** |
| Ownership of home (ref. private) | |
| Voluntary, not for profit | 3.9 (1.5)** |
| Hospice (ref. 8JD12) | |
| S55997 | −4.2 (2.5) |
| 8A784 | 1.5 (3.7) |
| 8CL93 | −0.7 (2.2) |
| 8C928 | −6.5 (2.6)** |
| S25614 | −1.6 (2.4) |
| Constant | 32.5 (2.5)* |
| n observations | 201 |
| n groups | 155 |
| Wald Chi2 | 51.5 |
| R square | 0.27 |
Variations across the nine capability of adopting a palliative approach items
Staff capability scores were higher in the not-for-profit CHs compared to privately owned. But no significant differences were observed for the items ‘identifying the needs of people with life-limiting illness’, ‘identifying required interventions’ and ‘discussing end-of-life issues’ (Table 9). Date of survey completion was positively associated with most CAPA items, apart from ‘discussing end-of-life issues’, ‘implementing required interventions’ and ‘discussing the needs of those with life-limiting illnesses with palliative care specialists’. This suggests that, for these three items, perceived capability in these components of palliative care did not differ, depending on the stage of the Needs Rounds intervention.
| Identify needs | Identify intervention | Discuss end of life | Implement intervention | Assess needs | Personal coping | Discuss needs | Refer to specialist | Culturally centred care | |
|---|---|---|---|---|---|---|---|---|---|
| Coefficient (standard error) | |||||||||
| Staff group (ref. managerial) | |||||||||
| Care staff | −0.7 (0.2)* | −0.8 (0.2)** | −0.9 (0.2)** | −1.0 (0.2)** | −0.8 (0.2)** | −0.8 (0.2)** | −0.9 (0.2)** | −1.0 (0.2)** | −0.8 (0.2)** |
| Nursing and clinical staff | −0.2 (0.1) | −0.2 (0.1) | −0.3 (0.2) | −0.2 (0.1) | −0.1 (0.1) | −0.2 (0.1) | −0.1 (0.2) | −0.1 (0.1) | −0.2 (0.1) |
| Other staff | −0.5 (0.3) | −0.6 (0.3) | −0.8 (0.3) | −1.0 (0.4)* | −0.7 (0.4)*** | −0.6 (0.3) | −0.7 (0.3)*** | −0.8 (0.3)*** | −0.5 (0.4) |
| Date of survey completion | 0.1 (0.0)** | 0.1 (0.0)* | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0)*** | 0.1 (0.0)* | 0.0 (0.0) | 0.1 (0.0)*** | 0.1 (0.0)*** |
| Size of home (ref. medium) | |||||||||
| Large | −0.5 (0.2)* | −0.4 (0.2)*** | −0.5 (0.2)* | −0.6 (0.2)** | −0.5 (0.2)* | −0.4 (0.2)*** | −0.7 (0.2)** | −0.8 (0.2)** | −0.5 (0.2)*** |
| Ownership of home (ref. private) | |||||||||
| Voluntary, not for profit | 0.2 (0.2) | 0.3 (0.2) | 0.3 (0.2) | 0.5 (0.2)* | 0.5 (0.2)*** | 0.4 (0.2)*** | 0.5 (0.2)* | 0.5 (0.2)*** | 0.7 (0.2)** |
| Hospice (ref. 8JD12) | |||||||||
| 8A784 | 0.3 (0.5) | 0.3 (0.5) | 0.2 (0.5) | 0.2 (0.4) | 0.3 (0.5) | 0.1 (0.5) | 0.3 (0.5) | 0.1 (0.4) | −0.2 (0.6) |
| S55997 | −0.6 (0.3) | −0.6 (0.3)*** | −0.4 (0.3) | −0.6 (0.3)*** | −0.4 (0.3) | −0.4 (0.3) | −0.3 (0.3) | −0.6 (0.3) | −0.6 (0.3) |
| 8CL93 | −0.2 (0.3) | −0.2 (0.3) | 0.1 (0.3) | −0.2 (0.3) | −0.1 (0.3) | −0.2 (0.2) | 0.1 (0.3) | 0.0 (0.3) | −0.3 (0.3) |
| S25614 | −0.4 (0.3) | −0.4 (0.3) | −0.2 (0.4) | −0.3 (0.3) | −0.1 (0.3) | −0.2 (0.3) | 0.1 (0.3) | −0.0 (0.3) | −0.5 (0.3) |
| 8C928 | −1.0 (0.6) | −0.8 (0.6) | −1.0 (0.3)* | −0.6 (0.4) | −0.7 (0.3)*** | −0.7 (0.3)*** | −0.2 (0.3) | −0.7 (0.4) | −0.9 (0.4) |
| Constant | 3.9 (0.3) | 3.6 (0.3) | 3.6 (0.3) | 3.7 (0.3) | 3.5 (0.3) | 3.5 (0.3) | 3.7 (0.3) | 3.7 (0.3) | 3.4 (0.3) |
| n observations | 204 | 204 | 205 | 203 | 204 | 204 | 204 | 204 | 204 |
| n groups | 157 | 157 | 158 | 157 | 158 | 158 | 157 | 157 | 157 |
| Wald χ2 | 37.3 | 42.2 | 71.1 | 63.0 | 50.0 | 37.5 | 60.7 | 57.5 | 38.2 |
| R2 | 0.20 | 0.19 | 0.22 | 0.29 | 0.22 | 0.21 | 0.25 | 0.30 | 0.21 |
Some variation between hospices was observed for both overall CAPA scores and the individual components. However, there was a substantial difference in response rates across hospices; the lowest response rate, returning only three CAPA surveys, was 8C928, representing 1.4% of the total sample. In comparison, 8CL93 returned 99 surveys, representing 44.2% of the total respondents. Therefore, it is important to note that some of the results are reflective of only a small number of staff members and cannot be generalised across the site as a whole.
Care staff reported lower perceived capability across each of the nine CAPA items compared to managerial staff.
Paired t-test
Of the 28 staff members who completed CAPA more than once, 57.1% were nursing and clinical staff, 25.0% managerial staff, 7.1% care staff and 10.7% were other staff members. Responses were submitted from 13 CHs across three of the hospices. Time between the survey responses varied from 1 day to several months. Overall CAPA scores ranged from 9 to 45, with higher scores indicating higher capability. The mean score for the first round of CAPA surveys was 32.3 compared to 34.8 in the final round, showing an average improvement of 2.6 points.
A paired samples t-test was performed to compare CAPA responses between staff members’ first completion and final completion of the survey. The results (Table 10) indicate a statistically significant but small difference between first CAPA score (mean = 32.3, standard deviation = 7.5) and final CAPA score (mean = 34.8; standard deviation = 7.5), t(27) = 2.8, p = 0.01.
| Variable | Observations | Mean | Std err. | Std dev. | 95% CI | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| First CAPA survey | 28 | 32.3 | 1.4 | 7.5 | 29.3 | 35.2 |
| Final CAPA survey | 28 | 34.8 | 1.4 | 7.5 | 31.9 | 37.7 |
| Difference | 28 | 2.6 | 0.9 | 4.9 | 0.7 | 4.5 |
| t | 2.75 | |||||
| df | 27 | |||||
| Sig. two-tailed | 0.010 | |||||
The average time between first and final completion of the CAPA surveys was 4 months (range: 1 day to 11 months). However, it should be noted that responses to the CAPA surveys were submitted throughout the 12-month intervention period (Table 11), so these findings do not necessarily reflect a before-and-after comparison. The significant increase in CAPA scores suggests that, as time in the intervention progresses, staff grow more confident in their ability to adopt a palliative approach.
| Date of completion | Number of responses |
|---|---|
| July 2021 | 6 |
| August 2021 | 9 |
| September 2021 | 4 |
| October 2021 | 4 |
| December 2021 | 4 |
| January 2022 | 9 |
| February 2022 | 9 |
| March 2022 | 2 |
| April 2022 | 3 |
| May 2022 | 2 |
| June 2022 | 3 |
| July 2022 | 1 |
Quality of death and dying
A total of 81 (QODDI) responses were returned across the six sites. The highest response rate, consistent with other survey data across the project, was from site 8CL93 (n = 29, 35.8%), and the lowest response rate was from site 8A784 (n = 1, 1.2%). Of the 29 CHs, 18 provided one or more responses to the QODDI, representing 62.1% of the CHs. Date of death was provided for 96.3% of the sample, and decedents reported in the surveys died between March 2021 and June 2022. On average, the QODDI survey was completed 46 days following the death of the decedent, and completion date ranged from the same day as the decedent’s death to 319 days (approx. 10.5 months) later.
The level of missing (or not applicable) data varied by response items. Four items had no missing data (‘pain control’, ‘having control of surroundings’, ‘bladder control’ and ‘breathing comfortably.’), whereas for one item (‘use of a mechanical ventilator or kidney dialysis’) data were missing for almost all responses (91.4%). Six items had missing responses for more than 10% of the sample: ‘funeral arrangements in order prior to death’ (11.1%), ‘healthcare costs taken care of’ (12.3%), ‘being hugged or touched by loved ones’ (17.3%), ‘saying goodbye to loved ones’ (24.7%), ‘visits from religious or spiritual advisors’ (76.5%) and ‘use of a ventilator or dialysis to prolong life’ (91.4%).
Excluding the item with 91.4% missing data (for ‘use of a ventilator’), the percentage of respondents scoring 10 (almost perfect) ranged from 6.2% for ‘having control of their bladder and bowels’ to 56.8% for ‘funeral arrangements in order prior to death’. The percentage of respondents scoring 0 (terrible) ranged from 0.0% for ‘being hugged or touched’ and ‘breathing comfortably’ to 14.8% for ‘having bladder and bowel control’. Only two items had more than 10.0% of respondents scoring 0, ‘bladder control’ as mentioned previously and ‘worrying about the strain on loved ones’ (12.4%).
Due to the single response from 8A784, this case was dropped from the analyses to promote anonymity, leaving 80 remaining QODDI responses across five SPCs and 17 CHs. In accordance with the volume of missing data, it was essential to determine subsets of the QODDI (see Table 12). QODDI16 represents the full QODDI, with only five complete responses (6.3%) to all 16 items. QODDI14 represents the QODDI with the ‘visits from religious or spiritual advisors’ and ‘use of a ventilator or dialysis to prolong life’ items removed, and a total of 45 (56.3%) complete responses were available. QODDI12 represents the QODDI after all items with ≥ 15.0% missing responses removed, that is QODDI14 minus ‘being hugged or touched by loved ones’ and ‘saying goodbye to loved ones’; 57 complete responses (71.3%) were recorded for QODDI12. And finally, QODDI10 represents the QODDI after all items with ≥ 10.0% missing responses (see previous paragraph) removed. The sample size of complete responses for QODDI10 was 74, representing 92.5% of the full sample.
| n | Scoring range | Minimum score | Maximum score | Mean score | |
|---|---|---|---|---|---|
| QODDI16 | 5 | 0–160 | 108 | 159 | 133.8 |
| QODDI14 | 45 | 0–140 | 67 | 139 | 113.2 |
| QODDI12 | 57 | 0–120 | 51 | 119 | 92.9 |
| QODDI10 | 74 | 0–100 | 28 | 99 | 73.5 |
Figure 4 shows the distribution of QODDI10 responses by SPC site, and (in purple) for all sites. They range from 28 to 99 points, with a mean score of 73.5 (Table 12). Higher QODDI scores indicate better quality of death. The distribution plot (total) shows a slight left skew/tail, with fewer low-scoring responses compared to higher-scoring responses. Examining the distributions more closely comparing by site, it is evident that 8JD12 and S55997 provide mostly higher scoring responses, suggesting higher quality deaths, whereas 8C928 provides more below-average responses, indicating poorer quality deaths.
FIGURE 4.
Distribution graphs of QODDI10 responses by hospice and overall.
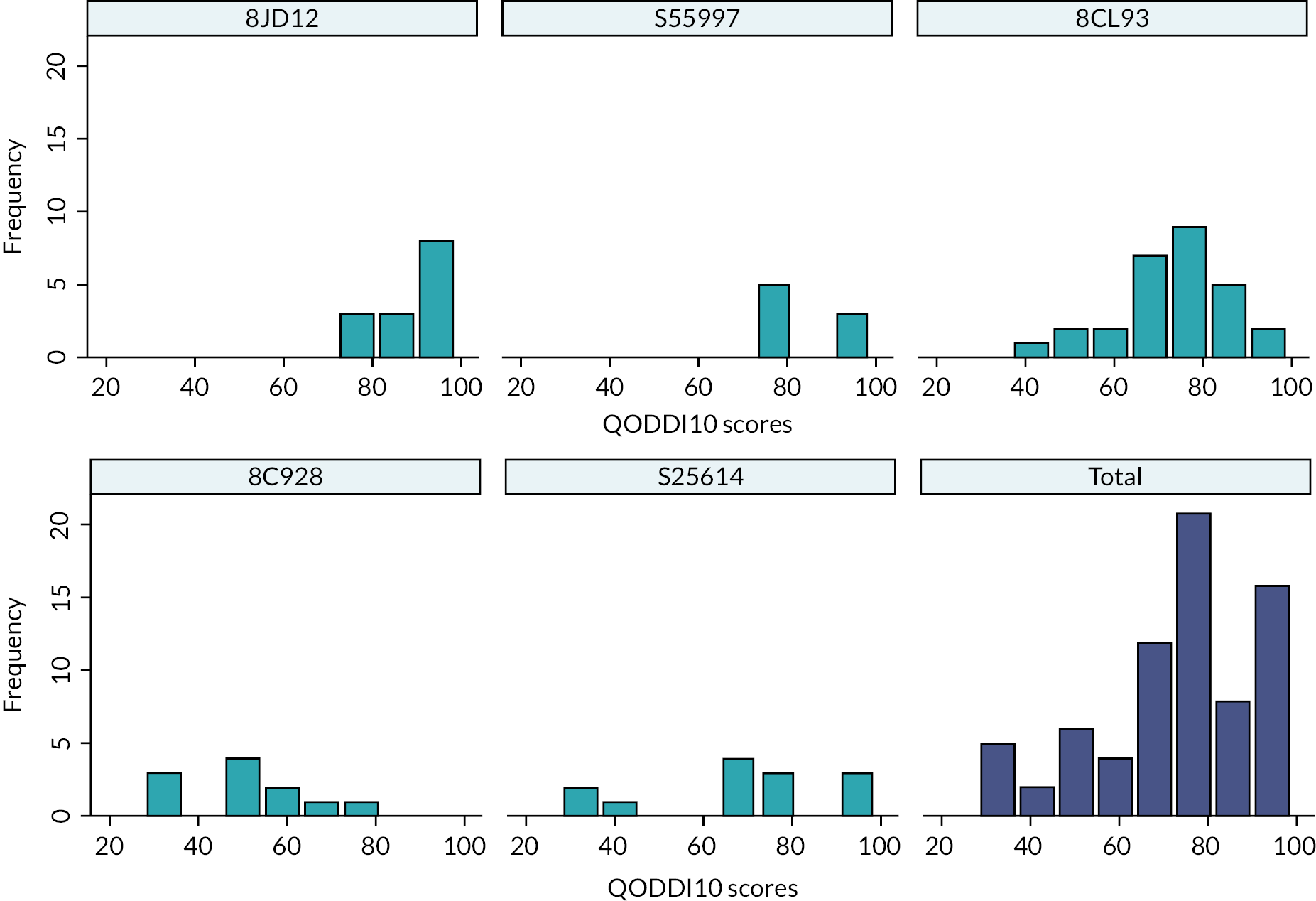
The QODDI10 was predominantly completed by managerial staff (n = 42, 56.8%), who were the majority respondents across four of the five sites (Figure 5). Managers across sites were closely involved in care delivery and be able to confidently complete the questionnaire. In site 8C928, most QODDI surveys were completed by ‘other’ staff members including care assistants, team leaders and assistant practitioners. In two cases (8JD12 n = 1, 8CL93 n = 1), data on the staff role were missing.
FIGURE 5.
Bar chart: number of QODDI10 responses by staff role and hospice.
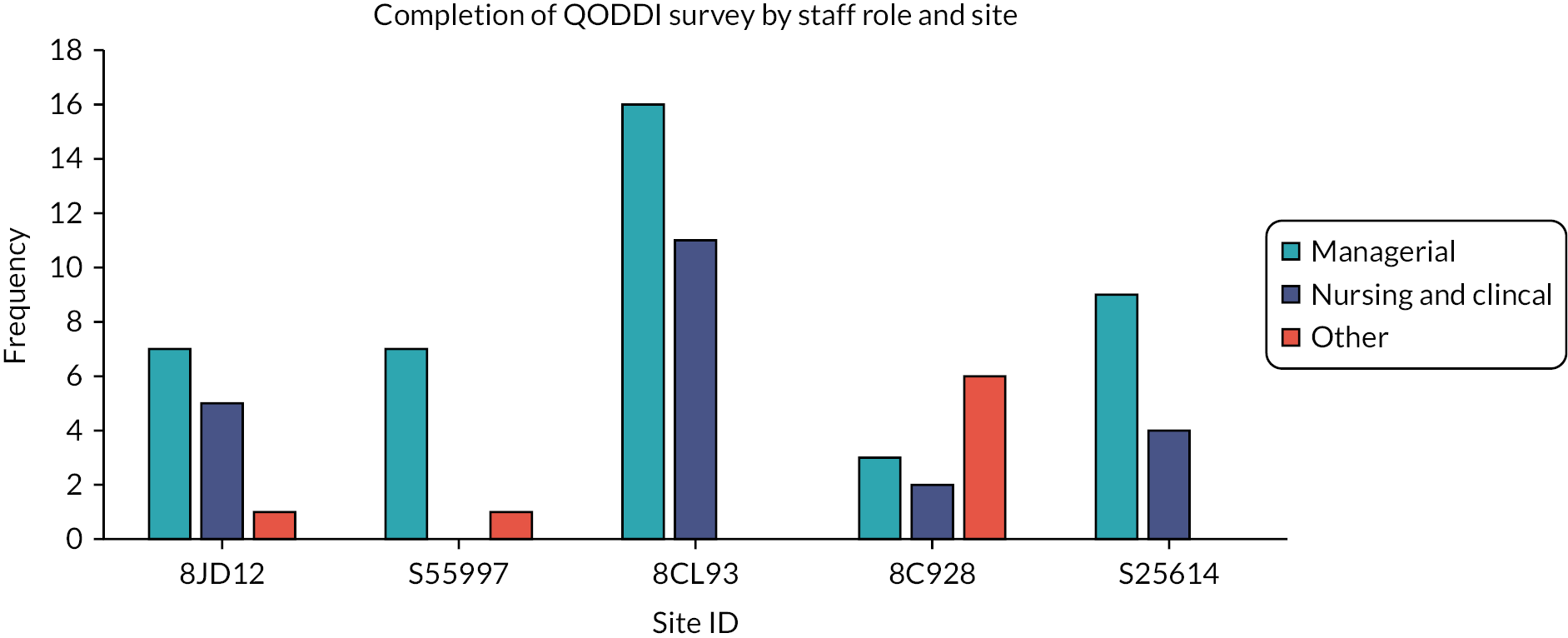
Date of death was significantly positively associated with QODDI10 scores (r = 0.34, p = 0.003) in the bivariate analysis, suggesting that deaths occurring later into the Needs Rounds intervention were rated more positively than those towards the start. This was consistent in the regression analysis (Table 13), whereby date of death was significantly positively associated with QODDI10 score until the inclusion of staff role and time between death and survey completion in model 3. This suggests a positive association between Needs Rounds and improved quality of death and dying.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Coefficient (standard error) | ||||
| Date of death | 0.1 (0.0)* | 0.1 (0.0)* | 0.0 (0.0) | 0.0 (0.0) |
| Size (ref. medium) | ||||
| Large (50 + beds) | −3.6 (5.4) | −9.3 (4.4)** | −14.5 (6.6)** | |
| Ownership (ref. private) | ||||
| Voluntary, not for profit | −6.0 (4.1) | −8.8 (4.3)** | −9.6 (4.6)** | |
| Staff role (ref. managerial) | ||||
| Nursing staff Other staff |
−1.7 (5.4) −17.3 (8.0)** |
−0.3 (5.0) −5.9 (6.1) |
||
| Time between death and QODDI completion | −0.1 (0.1)** | −0.1 (0.1) | ||
| Hospice (ref. 8JD12) | ||||
| S55997 | −11.0 (8.2) | |||
| 8C928 | −41.9 (11.0)*** | |||
| 8CL93 | −12.6 (3.5)* | |||
| S25614 | −22.0 (6.2)* | |||
| Constant | −1277.33 (422.8)* | −1484.6 (482.3)* | −143.4 (686.6) | −401.8 (629.9) |
| n observations | 71 | 71 | 71 | 71 |
| F | (1,69) = 10.2 | (3,67) = 4.8 | (6,64) = 5.5 | (10,60) = 9.4 |
| Prob > F | 0.002 | 0.004 | 0.001 | 0.000 |
| R 2 | 0.1179 | 0.1433 | 0.2764 | 0.4963 |
In the final model, significant predictors of QODDI10 score included the size of the CH, whereby large CHs scored on average 14.5 points lower than medium CHs; this indicates that individuals living in medium CHs (11–49 beds) experienced higher-quality deaths than those in CHs with 50 or more beds. Furthermore, ownership was negatively associated with QODDI10 scores, whereby not-for-profit homes scored on average 9.6 points lower than private CHs. Individuals living in private CHs experienced higher-quality deaths than those in not-for-profit CHs. Hospices 8CL93, 8C928 and S25614 all reported lower QODDI10 scores (poorer quality of deaths) in comparison to 8JD12 after controlling for all other relevant variables.
Families’ perceptions: CANHELP Lite
Thirteen family members (85% of whom were adult children) of residents from seven CHs across four of the sites provided responses to the CANHELP Lite.
Family members were largely satisfied with the care provided to their relatives. When asked whether care staff were compassionate and supportive towards their relative, family members were ‘somewhat satisfied’ (7.7%), ‘very satisfied’ (38.5%) or ‘completely satisfied’ (53.8%). Moreover, 38.5% of family members were ‘very satisfied’ and 53.8% were ‘completely satisfied’ that their relative received help with personal care when needed.
Other aspects of care that scored particularly well included care staff working together as a team, listening to what family members say and being able to discuss options with staff about transfers to hospital, use of life-sustaining technology and offering palliative care.
Aspects of care that family members were less satisfied with
Family members were more likely to be satisfied that their relatives’ physical symptoms, such as pain, were being adequately assessed and controlled in comparison to their emotional problems, such as anxiety. A larger number (23.1%) indicated they were not sure about their satisfaction regarding their relatives’ emotional needs being met, and a small percentage (7.7%) indicated they were ‘not very satisfied’ (Figure 6).
FIGURE 6.
Bar chart: family member’s satisfaction that their relatives’ physical symptoms and emotional problems are being adequately assessed and controlled.
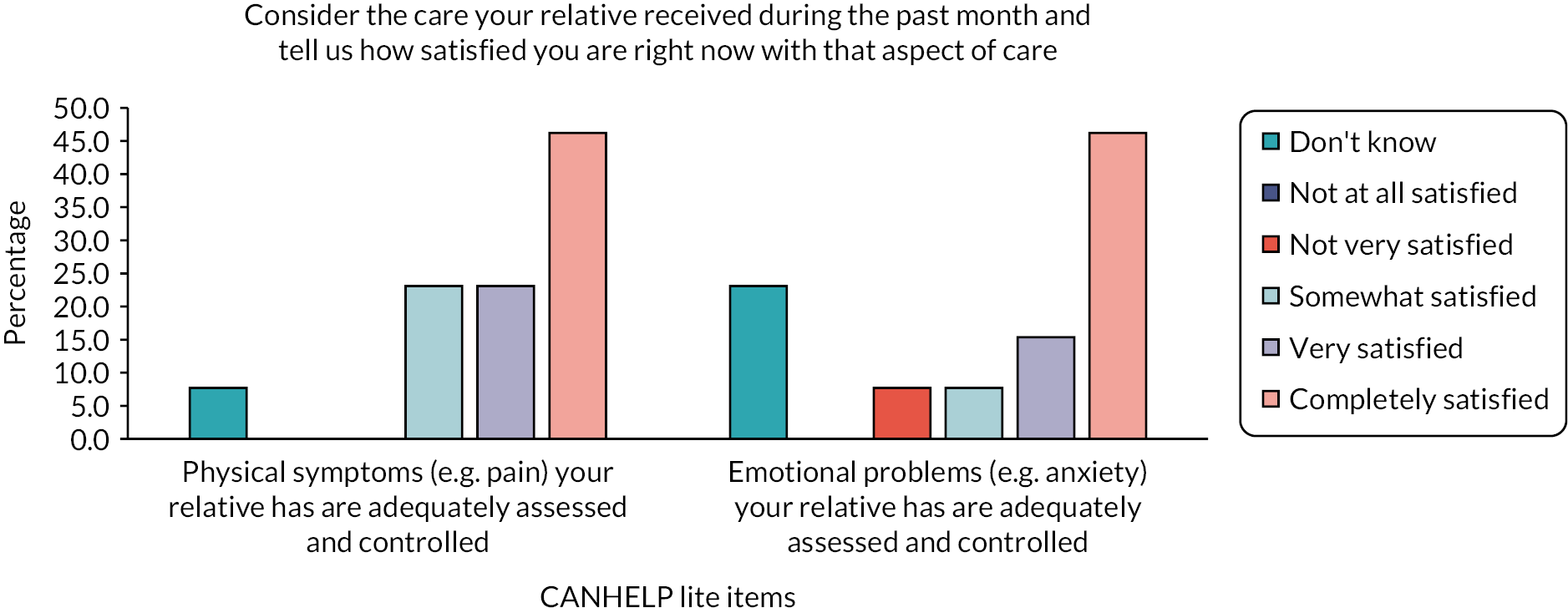
The lowest levels of satisfaction were observed for the questions regarding doctors (Figure 7), though the questionnaire does not elicit feedback on which doctors this relates to (e.g. primary or secondary care). While most family members indicated some level of satisfaction, there were higher percentages of people indicating they were ‘not at all satisfied’ or ‘not very satisfied’ than for other questions in the survey.
FIGURE 7.
Bar chart: family members’ satisfaction with doctors taking an interest in their relatives, being available when needed and having trust and confidence in those doctors.
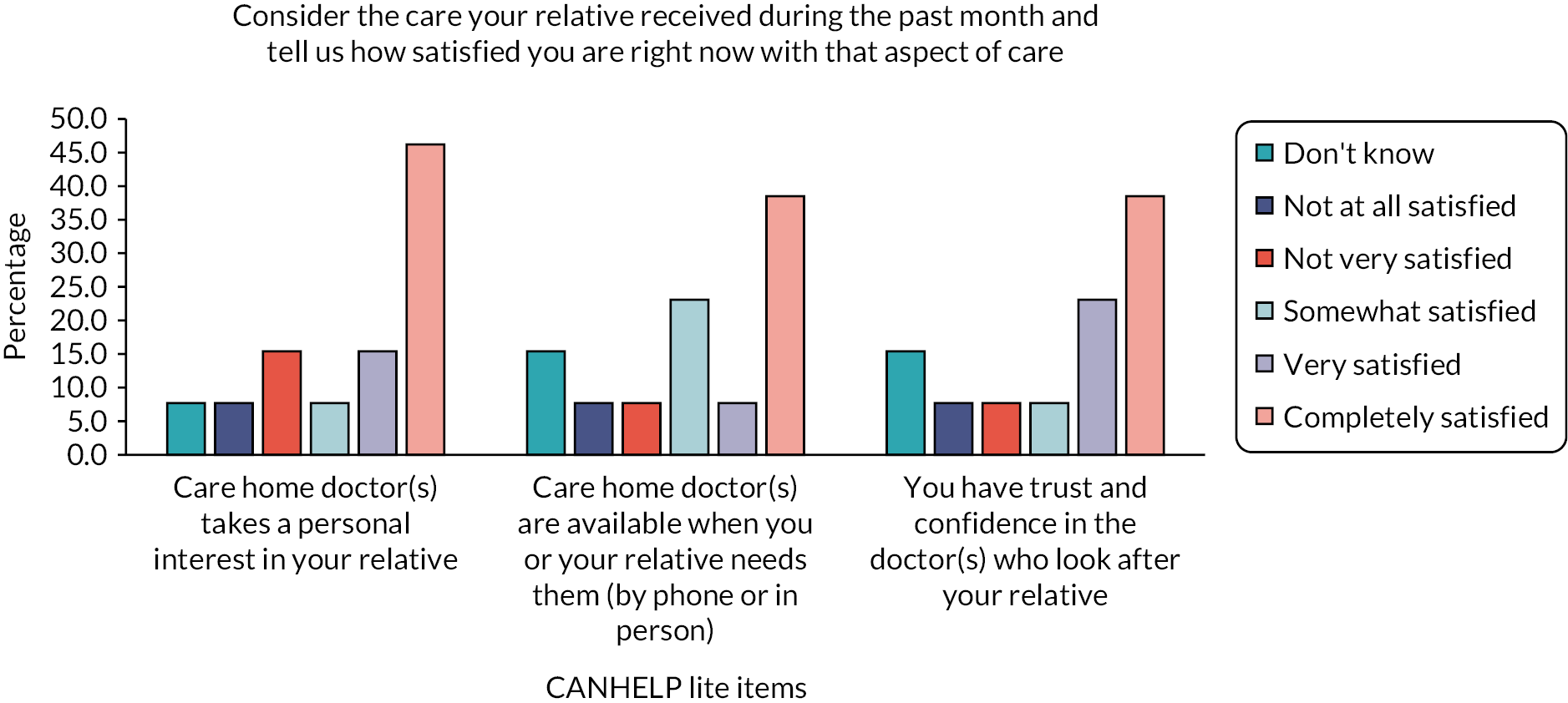
Improving family members’ perception of care
Communication appears to be a key area to improve family members’ perception of their relatives’ care. A minority of family members indicated they were ‘not very satisfied’ with the consistency with which they received information (15.4%) or that staff were explaining things to them in an honest or straightforward manner (7.7%). Family members want to understand their relatives’ condition and receive regular updates. Finally, only 46.2% of family members were ‘completely satisfied’ that their relatives’ care environment was calm and restful, indicating that most family members saw room for improvement in this area.
Overall, findings suggest that family members are mostly satisfied with aspects of their relatives’ care. They considered relationships with doctors to be the least satisfactory, and areas for improvement were identified for communication, supporting residents’ emotional well-being and providing a calm care environment.
Chapter 5 Treatment effect and cost–benefit analysis
In this chapter, we describe the quantitative analysis of the treatment effect for hospital admissions and hospital stays. We also describe findings from both the quantitative and qualitative cost–benefit analysis.
As noted in Chapter 2 (Ethical considerations), the study proceeded with data collection on CHs and resident demographics on a ‘no surprises’ basis. Posters were placed in CHs with residents/relatives advised of the project, enabling them to opt out of being included. This resulted in 17 residents opting out (with no data returned to the research team) from four CHs. Five residents opted out at the baseline data collection (March 2021), 12 at follow-up (March/April 2022).
Estimating the treatment effect
Baseline data were received for 11 (38%) CHs, only 9 of which provided complete data for a minimum of 1 month. While six supplied follow-up data, one of those had not supplied baseline data. Consequently, only five (17%) have data for both pre and post periods. The analysis represents 17% (n = 250) of the beds in the study. The paucity of data returned to the research team reflects the ongoing and substantial impact of COVID-19 on CH staff and data collection procedures.
Due to the resulting small sample size (n = 5) and corresponding low power, statistical analysis of the data was limited. Descriptive analysis was conducted of the two outcome measures: number of hospital admissions and number of hospital days.
The two rightmost columns of Table 14 show the number of admissions per 1000 CH bed-days and the number of hospital days per 1000 CH bed-days, respectively. The upper panel presents the baseline data, and the lower panel the follow-up data. Two CHs showed a reduction in one or both of the outcome measures at follow-up compared to the baseline, while three CHs show a worsening of the outcome measures. Combining data from the five CHs shows an overall increase in both admissions and nights in hospital from baseline to follow-up. Admissions increased from 1.6 per 1000 CH bed-days to 2.2, and nights in hospital per 1000 CH bed-days increased from 9.9 to 14.9.
| Baseline | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Care home ID | Number of beds | Baseline days | Empty beds | Bed-daysa | Exposure | Hospital admissions | Nights in hospital | Admission per 1000 exposures | Nights per 1000 exposures |
| Follow-up | |||||||||
| ST00335 | 66 | 153 | 560 | 10,098 | 9538 | 17 | 116 | 1.8 | 12.2 |
| ST00453 | 54 | 91 | 178 | 4914 | 4736 | 9 | 60 | 1.9 | 12.7 |
| ST00327 | 26 | 122 | 809 | 3172 | 2363 | 1 | 0 | 0.4 | 0.0 |
| ST00402 | 46 | 122 | 0 | 5612 | 5612 | 11 | 63 | 2.0 | 11.2 |
| ST00419 | 58 | 92 | 1525 | 5336 | 3811 | 4 | 18 | 1.0 | 4.7 |
| Total | 250 | 580 | 3072 | 29,132 | 26,060 | 42 | 257 | 1.6 | 9.9 |
| ST00335 | 66 | 92 | 215 | 6072 | 5857 | 8 | 16 | 1.4 | 2.7 |
| ST00453 | 54 | 31 | 68 | 1674 | 1606 | 3 | 7 | 1.9 | 4.4 |
| ST00327 | 26 | 61 | 472 | 1586 | 1114 | 2 | 9 | 1.8 | 8.1 |
| ST00402 | 46 | 92 | 84 | 4232 | 4148 | 15 | 90 | 3.6 | 21.7 |
| ST00419 | 58 | 92 | 230 | 5336 | 5106 | 12 | 143 | 2.4 | 28.0 |
| Total | 250 | 368 | 1069 | 18,900 | 17,831 | 40 | 265 | 2.2 | 14.9 |
The sample size of n = 5 is too small to be able to conduct a meaningful inferential test for statistical significance of the treatment effect. Care must also be taken in interpreting the estimated treatment effect as the impact of COVID-19 on patterns of hospitalisation between the two time points confound estimation of the treatment effect using a pre and post research design.
Cost–benefit analysis
The quantitative cost–benefit analysis was intended to compare a valuation of the benefits (costed reduction in hospital admission days) with the intervention costs. We have not been able to compute this for three reasons. First, our average treatment effect estimate is negative, so there is not an estimated benefit. Second, low power from the reduced sample and the confounding effect of COVID-19 mean that there is still a lot of uncertainty in our estimate of the treatment effect. Finally, sparse data collection from CHs on the estimates of their costs (due at least in part to the pressure of the pandemic) mean that we do not have good estimates of additional costs beyond the project itself. While some cost-related data were received in CH returns, both the quality and quantity were too low to produce meaningful summaries of their costs.
Our approach to the economic evaluation followed the CHEERS checklist. 97 However, in practice, many of the checklist elements were not possible to complete. We do not report a time horizon or discount rate, as no calculation was carried out. Outcomes were to be valued by costing avoided hospital admissions, and this was not done as the treatment effect on avoiding admissions was not reliable. Without appropriate data, we did not conduct the planned modelling or analytics, beyond describing the sample available. The sample size was insufficient to explore any distributional effects of a varying treatment effect across sites, and we were not able to do any exploration of the uncertainty around our estimates.
Direct costs of the intervention included SPC staff time. Sites were allocated 0.4FTE staffing to run the intervention, encompassing clinical (i.e. running Needs Rounds meetings, all related liaison with CH staff and other services, attending learning sets) and research tasks (including uploading completed questionnaires and recordings). This budget also covered time to attend the training provided in workshops. The total annual SPC staffing cost was £137,148.
We report below (see Qualitative appraisals of costs) qualitative data collected about costs during the study.
Qualitative appraisals of costs
The most prevalent cost spoken about by both CH staff and SPC clinicians was that of time, predominantly staff time. However, the concept of time was multifaceted, including unambiguous explicit and implicit costs, but also broader matters of time management. Table 15 summarises the key themes derived from the qualitative interviews, organised by explicit (direct financial costs) and implicit costs (including opportunity costs and intangible costs).
| Superordinate theme | Subtheme | Explicit cost | Implicit costs |
|---|---|---|---|
| Time | Priorities and floor time | Staff wages – financial cost to organisations | No immediate benefit to resident |
| Opportunity costs | Clinical opportunity costs | ||
| Staff wages | Use of staff leisure time | ||
| Travel | Fuel and time | Staff wages – financial cost to organisations Financial cost to organisations and individuals |
Opportunity costs |
| NHS costs | Medication | Financial cost to the NHS | Moral cost of discarding unused medications |
| Purchases | Printing and postage | Financial cost to organisations and individuals | |
| Additional interventions and equipment | Financial cost to organisations |
Priorities and floor time
Interviewees highlighted competing priorities as a significant factor impacting upon their availability to participate in Needs Rounds, often describing the challenge of finding time to complete the research tasks associated with the Needs Rounds study. For implementation, however, the primary concern was how Needs Rounds competed with clinically urgent priorities on the ‘floor’.
I feel the nurse should be in [the Needs Round] because she knows the resident well … So, I need a nurse to be present on that day and that’s very important. And sometimes […] there is GP rounds or there could be three admissions that day, and it’s just one nurse on one floor. So, it’s very difficult for the nurse to pick out that time […] she really needs at least an hour of time.
CH Nurse Manager, CHNM_ST00456, mid-implementation
The choices made to prioritise tasks, often those related to immediate benefit to patient care, meant that Needs Rounds were positioned as a lower clinical priority. The intention to use Needs Rounds to anticipate care needs and reduce unplanned admissions takes a backseat to urgent care. While no cost is attached to this element, there are opportunity costs in how staff use their time.
Organising efficient use of staff time to ensure optimal staff engagement with the monthly Needs Rounds was seen as possible, even if not always managed effectively:
I think these things are all doable with … it’s … they take, you know, it takes a chunk out of your time […] they’ve got that organised. So, it’s part of that nursing day to factor that in. So, yeah, that would put a pressure on resources if it was to be done … if they could do it in that proper way. But I think it really just depends on, you know, how proactive they are about that.
SPC clinician SPCS25614, mid implementation
Another interviewee described feeling that they were able to provide additional resources and opportunities by planning ahead and organising their caseload/workload in advance: ‘I think that’s what’s allowed me to get up these extra things like with the complimentary therapist and with health and wellbeing and with working with [Training Staff] to look at education, and things like that’ (SPC clinician, SPC8JD12, early implementation).
There are also costs associated with SPC clinician time. For this study, SPC staff worked 2 days per week, supporting the research tasks as well as the monthly clinical meetings. SPC clinicians reported that it would be feasible to complete 10 Needs Rounds per week if working on a full-time basis, though one noted that up to 20 meetings per week would be possible. Thus, the SPC staff costs could be distributed across a greater number of CHs.
Opportunity costs, particularly with last-minute cancellations of Needs Rounds, were noted. Such changes resulted in wasted time, notably if a Needs Round was cancelled after the SPC clinician had already travelled to the CH. In addition to the time/travel costs (described further below), there is a subsequent implicit cost in CH staff and residents not benefitting from the Needs Rounds embedded education and guidance.
Staff wages
Interviewees highlighted that a strategy to balance urgent resident care with attending Needs Rounds was staff using their own time to attend the meetings:
We are quite a busy care home. Even in the meetings, normally we’re trying to do them as quick as possible and then back on the floor. […] I used to have the meetings when I wasn’t on duty so I was coming on my day off, and that was the best thing.
CH Nurse Manager, ST00402, late implementation
Several CH staff describe financial costs incurred in paying staff to work additional hours to cover Needs Rounds, as well as the opportunity costs of staff being unable to attend to direct patient care during the Needs Rounds. Other data suggest that Needs Rounds might increase wage costs, but have longer-term positive impacts on the sector:
People are coming in on their off days. They’re having to squeeze things around last minute to make sure that care delivery isn’t affected and so you know while people can carry on for so long and they have done for the past kind of two years [during the COVID-19 pandemic], there will still be a point at which individually people won’t be able to and I think you know you’re going to start seeing people leaving jobs, changing jobs, just not being to carry on. Maybe the main aim of Needs Rounds wasn’t supporting staff’s well-being. I think where it has been able to do that hopefully that’s given some people enough support that they’ve considered that it’s worth carrying on doing the job that they are doing.
SPC Clinician, 83L93, late implementation
The use of overtime has both explicit and implicit cost implications. Paid overtime has more apparent financial costs to the organisation paying staff. However, both paid and unpaid overtime holds cost in terms of staff missing out on their free time and leisure activities.
Travel costs
Travel time was a cost incurred by SPC clinicians as they travelled to and from different CH locations. Journey times varied from as little as 5 minutes to as much as 3.5 hours each way. Most involved car journeys between 20 and 60 minutes each way, but some CHs were reached by foot or cycling. Opportunity costs were also incurred in travel time; to mitigate this, one CH located 3.5-hour drive from the hospice agreed to meet online some months to increase efficiencies.
Some SPC clinicians spoke about organising their diaries to manage combining journeys efficiently, as one said ‘If you’re organized, you can see, you can do a Round and see three or four people on the same day’ (SPC clinician 8A784, early implementation).
Travel time also has both explicit and implicit cost implications. Explicit implications are largely associated with the cost of staff wages (for organisations) and fuel costs:
I think just mileage is a huge one. Obviously for us as I put in my mileage sheet for the first month and then I can’t remember like a couple of hundred pounds or something because I had to ‘cause I was driving so far, but so that is a big one. Also, yeah, travel time.
SPC, ST00339, early implementation
Participants described a work culture of not claiming mileage costs for shorter distances. This therefore operates as displacing costs from service provider to SPC clinician:
Petrol […] I think I think the pay is good, so I wouldn’t say … ‘Actually I think we need to claim this back’. ‘cause I think the pay is good for the hours that I do. There’s a couple of times where I went to a nursing home which is quite away from me and [the manager] wasn’t there again. That was my fault. Should have double checked. I do that now I’ll ring on the day. ‘I’m just leaving. Are you still there?’ ‘Yeah, I’m fine’, but I did do it twice.
SPC, 8C928, early implementation
Medications
Forty-seven medicines across all six sites were recorded as having been deprescribed during the intervention period. One interviewee raised a financial cost to the NHS through the disposal of unused medications, specifically unused ‘Just In Case’ (JIC) medications:
The cost obviously to the health service having all these medications supplied and sometimes that person passed away and the medication must be destroyed, they are not cost directly to us but these are costs to the NHS because with COVID, we were not allowed to send any medication back to the pharmacy so we had lots of medications that had to be disposed of.
CH nurse, ST00403, mid implementation
In this case, the CH staff describe that the palliative care team made recommendations for all JIC medications to be in place, rather than seeking new prescriptions once symptoms have already escalated. While these are needed in some circumstances, in cases where they remain unused, the medication is wasted. One interviewee said: ‘The whole scale of the medication that would have been necessary should things having to turn to the worse, and if that person dies, suddenly all that would just had to be destroyed’ (CH staff, ST00403, mid implementation).
Care home staff explain that while this type of waste occurred prior to the intervention, it has increased with the pre-emptive approach of Needs Rounds. JIC medicines are considered good practice in the community, so standard practice (CH residents with complex symptoms not having JIC prescribed) is problematic, despite the cost. However, a SPC clinician described using a considered approach which bases these anticipatory prescription decisions upon assessment and individualised care:
There is a strong argument, of course, for Just in Case medications, which is why we have them. But equally that what the care home was saying is that often they’re not used and there is there is an economic cost to that that perhaps we I think is something that could be looked at. You know, Just in Case medications I think need to be arranged in a timely way. […] it is about individualised care … I think assessment is key in this situation. You’ve made a decision that you don’t want to prescribe Just in Case medications. You need to be assessing this resident for pain, agitation, secretions so that these medications can be got in a timely way. They had a good relationship with the pharmacy and I did point out coming up to a weekend and out of hours, these things are difficult. So I think it is I think it is a balance, but they were thinking about that. I suspect there probably is a cost in terms of just in case medications, but I think that that’s broader actually than just the Needs Round.
SPC, 8JD12, mid implementation
Emergency legislation introduced in the UK lockdowns to facilitate reuse of dispensed medicines was noted as an enabler of higher quality, anticipatory care in Phase 1 interviews:
[CHs] don’t really have stock but they can use the ‘medication reuse’ national policy. And ours have not needed to use that but we have seen that being used over [area] during the COVID pandemic, so if somebody dies, they consented for the medications to be used by somebody else so it’s that rather than a stock. […] that’s enabled access to timely anticipatory medication’.
GP, 8A784, Phase 1
The financial savings are implicit both in terms of the costs of medicines as well as dispensing time from pharmacies and the symptom burden of the resident.
Office costs
There were financial costs to CHs, SPCs and individuals in relation to practical and administrative elements of the study. These costs were research-related (e.g. printing and postage of questionnaires, and photocopying of posters) and hence reflect the study context rather than wider implementation. One SPC clinician (site 8A784, early implementation) said ‘I photocopy things at work […] I think if I didn’t photocopy the posters and bring them, I don’t think they’d be up on the walls’. Another said:
One cost is that some of the care homes do quite value some of the hard copies of information so you know printing costs. It’s small, but, you know, if you, so I’m working mainly from home. So printing costs. And you know if you are giving an envelope, a family questionnaire in an envelope, put a stamp on it, these are small costs, but that’s the only thing I’ve really come across.
SPC Clinician, 8JD12, mid implementation
A further SPC clinician noted her desire to purchase additional office supplies (files) to aid her admin processes. Such costs may endure with implementation.
Additional interventions and equipment
Two interviewees referred to occasions where referrals were made for complementary therapy for residents which would not ordinarily have occured. There were also explicit costs in relation to the purchase of items recommended by SPC clinicians:
The way she helps is coming up with some new ideas, things we don’t think about like for [a resident] she came up with the idea about having a red blanket in his room in case the cancer burst and there’d be a lot of blood. So like the red blanket and the family will not be too alarmed seeing a lot of blood […] So that was the thing that we put in plan and that was very helpful.
CH Nurse, ST00404, mid implementation
In this instance, the staff were able to source the blankets without purchasing externally. However, the CH staff explained that the manager had agreed to purchase any further items deemed necessary.
Summary
Qualitative data suggest the major cost of the Needs Rounds intervention was staff time. This had explicit costs of staff wages (existing working hours, overtime, and travel time) and implicit costs including opportunity costs, primarily due to the late cancellation of Needs Rounds. However, when CH staff cancel Needs Rounds due to competing priorities, they inadvertently create an implicit cost in that neither the staff nor the residents’ benefit from the intervention. Time-related issues such as prioritising floor time over engaging in Needs Rounds pose a dilemma which is not easily resolvable without a changed funding model for staffing.
While some of the costs highlighted by interviewees were spoken about within the context of specific situations, given the detail provided, it is reasonable to accept that many of the economic costs highlighted could apply to other individuals and organisations within the study. However, if Needs Rounds are implemented in practice, costs associated with the research element of the study would be avoidable, particularly the time required to fulfil the quantitative data requirements of the study.
Chapter 6 Patient and public involvement and engagement evaluation
Introduction
This chapter summarises the roles, training and support of PPIE in the study. The impact of PPIE is then described, before moving to present the qualitative interview data from the study team describing feedback on the PPIE process.
Patient and public involvement and engagement roles and activities
Opportunities were offered to all three PPIE coinvestigators throughout the study, starting from proposal development, based on their interests and time. They were invited to speak from their lay experience, of having a relative in a CH, being lay inspector of CHs, or imagining their futures in a CH as residents themselves. As autonomous members, they drew on these positions flexibly throughout the study.
The PPIE budget was available to these three coinvestigators to use as they wished; they advised that this was a novel, empowering experience which demonstrated trust. The consequence was that PPIE members controlled how much input they had and choose activities which fit their interests and skill sets best.
As fully integrated team members, they were invited to, and often attended, monthly team meetings. Indeed, at least two PPIE members attended all monthly investigator meetings, and two attended quarterly steering group meetings.
Patient and public involvement and engagement members were on interview panels for the appointment of a RF and assisted in preparing interview questions for the recruitment process. PPIE members were also actively involved in co-constructing interview topic guides for Phase 1 and 2, reading a sample of transcripts and discussing data analysis. All PPIE members contributed to development of ethical approval paperwork, with one attending the REC meeting. Patient and public involvement and engagement members contributed to study outputs and were coauthors on draft funder reports, journal articles104,127 and conference abstracts.
One PPIE member expressed an interest in conducting research interviews. They were supported to learn about this data collection method, by shadowing an academic research team member. However, the short time frame in which interviews were arranged and conducted, and PPIE availability, meant that they were unable to lead any interview data collection during the study.
Patient and public involvement and engagement members all acted as advocates and champions of the research, for example through promoting the study via their networks (e.g. Twitter, LinkedIn). Early in the study’s timeline, PPIE members made a video talking about themselves and their role in the study, which was distributed to all research sites, to underline the importance of their role in the study.
Patient and public involvement and engagement had opportunities to build new relationships, which have led to invitations to join other research teams and grant applications about CHs.
Patient and public involvement and engagement training and support
Informal, prospective training was provided on a range of topics and processes. At the start of the study, sessions were held on implementation science and study design. As the study progressed, training and support changed to focus on topics relevant to the stage of the research. For example, all investigator meetings included lay descriptions of research processes, and informal training/education was woven into project meetings and communications throughout on key elements of methodology, methods, outcomes and dissemination.
Technical support in using online platforms was offered, for example, a trial Zoom session where PPIE members could test their use of breakout rooms, recording discussions and editing their names. This training and support were provided prior to the study’s Phase 1 workshops to increase PPIE members’ confidence in their role within the workshops, such as recording and monitoring discussions. This adaptation was required to accommodate ongoing travel and infection control procedures due to COVID-19. PPIE members received editorial support for writing outputs such as blogs, poems and newsletter articles.
Prior to the ethics panel meeting, there was a discussion and briefing on likely process and content of ethics meeting, and the PPIE member was advised not to prepare materials as the PI would respond to research questions; the PPIE member was asked to be ready to speak from an ‘expert by experience’ position. A post-meeting debrief was held, attending to the content and process of the ethics committee meeting.
Support was also provided by way of written instructions and synchronous ‘screen share’ sessions when required. These were used, for example, when completing Conflict of Interest forms for NIHR or ensuring NETSCC profiles were fully completed online.
Following monthly investigator meetings, PPIE members were invited to debrief sessions with one member of the academic team, where further discussion of the meeting took place to digest and explore any areas they wished. Patient and public involvement and engagement members were also encouraged to send further thoughts/queries via e-mail, to which they receive a prompt response, with feedback on how their views would be integrated.
Indeed, when PPIE contributed by providing feedback on, inter alia, interview topic guides and draft funder reports, the academic research team would respond to such input by indicating the ways in which the feedback had been used, or explaining why it was not possible to include all elements. This feedback loop was used more at the start of the project, with less being communicated as the project entered year 3.
The study’s RFs were described by PPIE members as pivotal in enabling PPIE members to contribute. The RFs ran the monthly debrief sessions and acted (alongside the PI) as a core contact point for all PPIE members. Thus, PPIE members had frequent contact and regular updates from the study team.
Impact of patient and public involvement and engagement
Patient and public involvement and engagement members chose the measure used with families for secondary outcomes, informed the approach to consent/ethics within the study (including adjustments to paperwork approved by the ethics committee) and ensured the language and pitching of the study was tailored to non-academic audiences (including a substantial re-framing for workshop three to ensure all participants were able to understand and contribute fully). Patient and public involvement and engagement members also contributed ideas for information to collate during baseline data collection.
Drawing on their varied experiences as lay members of the public, people with friends/relatives in CHs, and with an interest in public services has ensured that the needs of CH residents and their families were discussed at every investigator meeting. This was also demonstrated within steering group meetings, where their lay experiences were given time and space to feed into wider discussions regarding the importance of integrating palliative care into CHs. Patient and public involvement and engagement members’ involvement in investigator meetings and steering group meetings also led to asking clarifying questions, which were helpful for all present. Steering group preparatory activities were also altered and improved through PPIE feedback, for example using non-technical imagery to communicate the study’s progress and stages of theory development.
Patient and public involvement and engagement members engaged in analytic discussions of interview data, which increased their familiarity with the data. While no additional codes were developed because of their input, the impact was related to more meaningful engagement in discussions of theory development. They worked closely with one academic member of the team who, after their analysis meetings, invited PPIE members to collaborate on other studies. Hence, the impact extends beyond this study into other CH-related research.
Patient and public involvement and engagement influenced study dissemination; their involvement in writing blogs, poems and newsletter articles meant that PPIE was clearly articulated and hence visible to stakeholders. Patient and public involvement and engagement members also suggested that the study team write to members of Parliament in constituencies where the study was being conducted to alert them to the study and raise its profile.
Patient and public involvement and engagement members were actively engaged in the workshop preparation and delivery. Their role led to a non-technical approach to describing the developing theory, simplification of the technology platforms used to host the workshop discussions and adoption of a ‘guardian angel’ approach (as a way of giving status and permission to challenge any language which was too technical).
Patient and public involvement and engagement evaluation interviews
This section presents the themes derived from the interviews with members of the research team. It first lays out the expectations of the team and the role ascribed to the PPIE members in the study, before focusing on how PPIE members influenced the language academics used, the positioning PPIE and academics drew on, how the team worked together and the professional learning/development for PPIE members.
Eleven interviewees took part. Two eligible people did not participate: one did not reply to the initial request or follow-up e-mail, and one did not have time to take part. The sample for this substudy focused on the evaluation of PPIE was therefore eight academics (some of whom also hold clinical roles) and three PPIE members.
The six themes presented in the subsequent findings section all encompass a variety of subthemes (see Table 16 for the coding tree).
| 1. PPIE integral to the team | Expectations of tokenism and prior experiences of PPIE |
| Commitment of PPIE to the Needs Round Study | |
| Involved from the start | |
| Intensity of involvement | |
| Cutting-edge PPIE | |
| 2. Language in the team – ‘bearing the audience in mind’ | Bearing the audience in mind |
| The ‘guardian angel’ concept | |
| Accessible for audiences | |
| Jargon | |
| Receiving feedback from PPIE | |
| 3. Relationship-centred research team | The PI |
| Relationships in the team | |
| Post-meeting debrief sessions | |
| Good communication | |
| 4. Porous positions | Lived experience of academics and PPIE |
| Blurring boundaries | |
| Equal footing | |
| PPIE member’s familiarity with research | |
| 5. Negotiations | Payment negotiations |
| Agenda of meetings | |
| Not patronising | |
| Remit of academics and PPI | |
| Epistemological concerns | |
| 6. Professional development and learning | Opportunity of more PPIE experience |
| New skills | |
| Things explained by the team | |
| Having PI involved more in future | |
| Underpinning values | |
| Understanding PPIE in general |
Patient and public involvement and engagement was integral to the team
Patient and public involvement and engagement members were explicitly positioned as core to the team and described as ‘co-facilitators’ and ‘co-applicant’ (academic 9 and PPIE 3, respectively). Indeed, PPIE members were ‘involved from the word go’ and considered a ‘key part’ of the team (PPIE member 1 and academic 7, respectively). Another PPIE member stated:
We are members of the steering group that had oversaw the project, but also part of the operational group that met once a month just to double check how things were ticking on along. So it wasn’t like ‘go to PPIE when you want to do an easy read version of the leaflet’. I mean, that’s easy, isn’t it? It was more of, you know, we are there when they were talking about the funding, how much the funding was going to be, you know, what people’s roles are, what will the research look like, how often we would meet, what next, what next, what next, we’re looking at the phase of the project, what it would include, the model, the theory, the engagement part, like the workshops. All of it.
PPIE 3
Similarly, PPIE 2 stated that the study’s user involvement and engagement was ‘cutting edge’, stating that her involvement at the Needs Rounds Study had ‘exceeded [her] expectations’. The notion that this was ‘top level PPIE’ was related to the ‘complete autonomy’ that had been extended to PPIE, as well the responsibility she was allowed to assume in the project. Patient and public involvement and engagement members, for example, had control over the activities they were involved in and in shaping how the PPIE budget was spent. Further, she described the significance of being involved in an interview panel and the importance of her involvement in this given how the researcher being appointed ‘was pivotal for the project’.
Both academics and PPIE members described how the dedication of most PPIE members was consistent throughout the study. Patient and public involvement and engagement members were ‘involved from the outset’ (academic 1), which was in distinct contrast to some academic interviewees’ prior experiences of PPIE being ‘tacked on at the end’ (academic 1) and being treated as ‘tokenistic’ (academic; 1, 4, 5 and 9). Given her past experience, academic 5 describes her expectation of PPIE in the Needs Round study:
When I came into the study, because of my previous experience with PPIEs, I thought, ‘Yes, they would be there and contribute a bit.’ But I thought they would be in the background, but they’ve been very much more in the foreground of the study.
Academic 5
Patient and public involvement and engagement members were described as ‘active voices’ in discussions regarding research, funding and impact (academic 2). Patient and public involvement and engagement members' central roles in the research meant that the language used by the team shifted to facilitate their inclusion.
Language in the team – ‘bearing the audience in mind’
Patient and public involvement and engagement members framed part of their role as posing questions for academics to consider in relation to their research and dissemination practices:
The thing is, [academics] get a bit too professionalized sometimes and then you sort of forget about basic questions that might get asked and I know there was one time, you know, when you think you sort of covered everything. There’s always something that you’ve forgotten about.
PPIE 1
Patient and public involvement and engagement members described how they asked questions to clarify what academics shared in public. Patient and public involvement and engagement members were asked to act in the capacity of ‘guardian angels’ to ‘watch out for language becoming too technical’ (PPIE 2) in workshops which involved practitioners and members of the public. This was designed to make the workshops more accessible to participants, thereby encouraging greater participation.
Overall, academic interviewees considered the questions and comments from PPIE regarding language and the content of the study to be helpful and constructive. Several academics made note of how the research was communicated:
[It is] always valuable to get feedback when you’re presenting results, and particularly not just a sense check, but also, if people don’t understand it, then I’m not explaining it clearly enough. And it’s easy for me to start using jargon or make assumptions.
Academic 2
Others described adapting how they communicated findings. In this way, PPIE influenced the study’s engagement with practitioners and the public, foregrounding accessibility. Hence, the questions asked by PPIE members ‘just grounds people a bit more’ and ‘challenge[d] [academics] to be better at articulating what [they] want to achieve from the projects, in ways that make sense beyond academic circles’ (academic 6).
Academics described how the presence of the PPIE members provided them a helpful reminder to modify their communication; they were more likely to ‘bear the audience in mind’ or ‘pay […] attention to language’ when PPIE members were present (academic 6 and 9, respectively):
I’ve just enjoyed it more than meeting with sort of academics all the time. It’s made me think a lot about communicating to non-academic audiences […] I’m thinking about okay how am I going to make this easier to understand for somebody who isn’t a [area of expertise] researcher.
Academic 3
Relationship-centred research team
Patient and public involvement and engagement members appreciated the relational investment from the academics in the team. Monthly meetings, post-meeting debriefs, regular e-mail exchanges and staff availability meant that there were considerable points of contact in place. One PPIE continually referred to different moments in which a member of the team had taken time to explain something to her. This kind of support was described as both significant and continual: ‘[Team meetings] were every month and so and, you know, every step of the way it was explained what was going on and if you needed help, you know, there’s always a call afterwards’ (PPIE 1).
Patient and public involvement and engagement members held their relationship to the academics in high regard and described how ‘patient’ and ‘accommodating’ some members of the team were with them to foster a sense of partnership:
She’s very good teaching, training skills. […] Even if it was not of any real like, you know, oh isn’t the answer obvious, kind of thing, never showed that. I didn’t even consider that. I don’t know why I didn’t think of that, let’s just hold on to that, she’d says oh really, just ‘really good’, it really just always made me think. ‘Oh, right, okay, I said something that was … that took me ages to say and I said it’ and she’s, you know, she’s heard it. […] she’s really good.
PPIE 3
Other PPIE members also provided examples of times when they had felt supported. This was particularly important given the emotive topic of death and dying:
I knew I had support there that if I got upset by anything that was said, I think it came out [in the study data] that one young carer said that she had a fear around meeting death for the first time with a resident. And I found that very moving, you know, because it was how I felt when I was meeting death for the first time with my grandmother. So, I think I had lots of empathy.
PPIE 2
It is noteworthy that this was the only example of a PPIE member reporting an emotional response regarding the study’s focus.
Academics made a concerted effort to build and maintain relationships:
The team at Stirling responds really quickly to emails from them, and I think that’s again a kind of support thing, [….] So to be really responsive and quick, we don’t let emails from [PPIE members] sit in our inboxes, whereas we might with other emails. And I think again that’s relationship building and respect, and just making it clear that they’re valued.
Academic 6
The PPIE debrief sessions held after monthly team meetings were also mentioned as a core supportive mechanism. Academic interviewees described how the debrief sessions provided a space where PPIE members could ‘express their opinion’ or ‘unpick’ anything they did not understand (academic 7 and 6, respectively). PPIE 3 described this in the interviews:
We developed these hourly meetings or half-hour meetings after the main meeting, just to decipher in plain English that we knew what was going on. And that was a really good idea. So, I think we’re always well looked after.
PPIE 3
The debrief sessions were credited with strengthening the relationships in the team, making them feel valued and cared for. Academic 1 said ‘It’s also just having a chat, getting to know each other, and I think that’s where the kind of informal building up relationships happens’, while a PPIE member noted:
It’s just nice to have a chat if somebody was there and sort of find out a little bit about them as well, because I think it’s the human face, isn’t it? And, you know, sort of being able to relate to somebody.
PPIE 1
The ‘informal’ tone of the monthly research meeting was also important in building reciprocal relationships and enabled the team to get to know each other. All participants reflected on the ‘good ethos’ and ‘really good dynamic’ within the team (academic 9 and 1, respectively). Patient and public involvement and engagement members described feeling at ease within the team:
It’s quite a nice group, quite a relaxed group of people. And there always was there’s all humour in the group, […] There’s always a bit of a joke. And that does help, so the chairing – it’s quite a relaxed atmosphere. It was good. You’re encouraged to speak.
PPIE 3
Likewise, several academics felt that the team provided a ‘safe space’, engendering the ‘feeling [of being] able to talk’ (academic 3 and 1, respectively). This dynamic furthermore appeared to be intertwined with the lack of ‘a hard and fast distinction between academics and PPIE members’ (academic 6), as well as the notion that the PPIE members and academics involved in the study were on equal footing: ‘My feeling is that in this project, having people treated as being more equal members and making less of a distinction, was probably more, yeah, contributed to its success’ (academic 2).
Porous positions
The lack of a distinction was mentioned by five of the eight academics interviewed for this evaluation. Academics, like PPIE members, could also draw on their own lived experiences of CHs and palliative care:
There’s kind of weird insider–outsider sort of business, and that’s what I’ve mentioned before about these kind of blurred boundaries with–within this project. Like, you know, [academic colleague]’s parents who are in the care home just now and she supports them and that’s lived experience. So having these kinds of boxes of what is your … You have lived experience; you have academic experience. […] It’s blurred. It’s not neatly cut.
Academic 1
The quote illustrates how both academics and PPIE members can straddle multiple positions and speak from various standpoints. With team members occupying multiple identities and knowledges, there is a porous membrane between having academic knowledge and lived experience.
There was an acknowledgement that PPIE members’ perspectives, and their corresponding role, could change over the course of the project. Academic 6 emphasised that ‘personal experiences might shift as time goes on’. A PPIE member reflected this idea regarding how her input changed when someone close to her, who lived in a CH, died: ‘I was giving [the PI] quite a lot of detail in that because it was the exact sort of resident who should be taken to a Needs Rounds’ (PPIE 2).
PPIE 2 draws attention to her multivocality, as she speaks from a variety of different perspectives. She, furthermore, described her familiarity of the research processes in the study and her ability ‘to spot things on the research side of things’, ‘I’ve been doing [PPIE] for 15 years, so it’s very gradual. You do pick up the research terminology and you kind of know the research processes’ (PPIE 2).
Although a ‘lack of distinction’ and the ‘notion of equality’ were consistent across most of the interviews, some academic interviewees perceived the role and input from PPIE members to be focused on personal experience, whereas academics would focus on other elements:
There’d be some members of the PPIE team that might be more likely to be able to draw on past experience of being in PPIE work or in practice, or […] they might be talking about their own personal experiences of loss and death and draw on those side of things. Whereas you might have a senior academic who might talk more about or be able to contribute more in terms of theories and knowledge and expertise. […] So, it kind of creates a more rounded circle.
Academic 4
PPIE 1 emphasised that her lack of familiarity with research was something that was an asset and markedly distinctive to the academics: ‘Sometimes it’s good to not have some idea of what’s going on, but, you know, if you know too much, it’s just like when you’re a researcher, aren’t you, really?’ (PPIE 1). PPIE’s 1 positionality as ‘newcomer’ was also discussed by PPIE 2, who felt that her perspective was helpful and ‘novel’.
This focus on complementary inputs showcased that while team members could draw on and speak from multiple standpoints, they still held primarily different roles. The subsequent theme will discuss these roles further, illustrating how academic interviewees understood and negotiated their respective remit when working alongside PPIE members.
Negotiations
Negotiations refers to how academic team members held and negotiated their remit alongside PPIE members. Several academics drew attention to the clarity of remit extended to them in the context of the monthly meetings:
[The PI] knows what she’s wanting so she’s very clear and not wishy-washy about what it is that she needs and the roles that everybody has and what they need to deliver within that. So [the PI] very much makes a good chair of a meeting because she was in there, like this is the agenda with a lighter one, okay whose responsibility was it to do x, y and z […] I think that helps, you know, just structure the meetings that people were clear and knowing, I guess, sort of … that there wasn’t any sort of faff […] It was an hour meeting it meant that we got … the agenda was always got through.
Academic 7
The above interview extract foregrounds the discussion of the tasks involved in the research projects. It, moreover, exemplifies the responsibilities assumed by the PI, which include managing the meeting’s schedule, structure, time management as well as the contributions made by PPIE members. Some interviewees described how, on occasion, the contributions of PPIE made in the monthly meetings could be tangential requiring management by the chair. Academic 6, for example, considered the time spent in meetings explaining aspects of the study to PPIE:
I think sometimes [PPIE] comment on things which are more within I think the academic methodological clinical sphere, and they’ll ask questions which demonstrate that they’re kind of maybe moving beyond where their role sits. So they’ll say, ‘Oh, I don’t understand this term,’ and it would be [referring to] a methodology paper. And they’ll have been included for information and then they’ll say, ‘Oh this doesn’t make sense,’ and it’s actually for an academic journal, and PPIE people aren’t the audience for this output […] The purpose of this communication isn’t that everybody understands, this is that it fits with this journal. So I think there’s a bit of blurring sometimes about what’s meant to be for everybody to understand, and what are certain outputs for certain people. […] you don’t need to understand all of everything. And that’s I guess part of how I think about teams, is that we all bring different strengths, so, as long as we understand how we’re contributing, then that should be okay.
Academic 6
Two academics suggested that the role of the PPIE members would differ if the project was exclusively quantitative:
I think it’s a more challenging relationship for the quantitative elements because so much of what we do does have to be more rigid, and particularly in a sort of health study where you have to pre-register your hypotheses and how you’re going to analyse it. And a lot of that is kind of determined, there’s not as much choice. So, the value comes later, I guess, when you’re then trying to understand the findings or think through the implications, and that doesn’t work so well with the idea of being involved throughout, I guess. Now, I suppose one encounters that by having people involved really early on at the start when you’re conceptualizing the project, and actually writing the funding application, because there, I suppose, you’re deciding what the hypotheses are, and what the primary outcome should be. But there’s that kind of bit in the middle where there’s not a lot of scope for input. And I guess, that doesn’t sit as well, with the idea of kind of being involved, I suppose, throughout […] If the analysis you’re doing is quite statistically complex, then it’s quite a big ask for people to be up to speed with that, and we don’t necessarily expect the other academic members of the research team to understand all the ins and outs of the models that we’re using or whatever.
Academic 2
The remit of the PPIE members shifted throughout the study. The study had a lot of ‘moving parts, with various tasks to be involved with’ (PPIE 3) and that, as a result, their ‘input changed a lot’. Patient and public involvement and engagement members were involved in coding transcripts, the coproduction of interview schedules, co-authoring of reports and facilitation of workshops. Consequently, the negotiation of tasks, time frames and skills was ongoing throughout the study.
PPIE 3 explained that the time invested in explaining various aspects of the study made her feel like her contributions were ‘valuable’. Thus, the work done by academics could be considered an important part of PPIE’s involvement in the study. It, nonetheless, was something that academics had to attend to and negotiate in the monthly team meetings.
Academics and PPIE members were considered on an equal footing, despite also holding specific roles, but which required explicit work to signpost appropriate elements for PPIE members to contribute meaningfully to the study.
Professional development and learning
All interviewees were asked if the study had generated any transferable learning for them regarding the PPIE. Several academics answered by referring to the central and integral part PPIE members played and how this would inform other research projects: ‘The PPIE element had been tokenistic [in past research projects] and now it’s made me think we need to have this much more in the realms of people actually on the project with us’ (academic 5).
Academics reflected on the underpinning values of the study, for example:
I think that that whole thing about paying attention to the kind of values base to begin with. Paying attention to, you know, the integration. Paying attention to language, really actively working on that the whole way through. That whole business of checking out and checking in. And just not taking … so make not taking it for granted. Make it really explicit without being patronizing. You know, that actually work with our colleagues. So really building that kind of relationship-based work.
Academic 9
The quote underlines the need for active engagement in values, and ‘continual checking in and checking out’ throughout the study. Another academic described how the project used terms of reference (see Report Supplementary Material 15) to explicitly outline how the team would position themselves ‘in relation to the power and authority’ (academic 6).
Academics thus reflected on how this experience of PPIE would be used by them in future studies, and the underpinning ethics and processes, PPIE members named specific skills they developed over the course of the study. For example, sitting on a recruitment interview panel:
That very first [interview] was with [the PI] and it was a valuable opportunity because it led to other [research projects in which PPIE was required]. Once I knew how to do it and then develop the skill, then other people started asking me would I sit on the interview panel. And because I’d already done it with [the PI], it made the whole thing easier.
PPIE 2
PPIE 2 also had the opportunity to attend the NHS ethics committee meeting, though was disappointed by their lack of involvement at the meeting:
I was so looking forward to it. I helped with the ethics application, obviously, and on the day, we attended the ethics committee virtually, but it wasn’t a positive experience for me. It was positive in that we did get ethics approval, but I wasn’t included in that meeting at all (by the REC). I wasn’t acknowledged. And there was another PPI member on that Ethics committee, and you could easily identify who he was, and I thought he might have asked me a question about the PPI, but he didn’t speak to me at all […] I know that the tone of it was very business-like, but it was quite unfriendly.
PPIE 2
High levels of support in advance of the REC from the team were contrasted with poor engagement experienced at the ethics committee meeting. The PPIE member noted that ‘We had a pre-meeting, you know, [researcher and PI], and I saw that I was very well prepared and then it was just as if nothing, just that was it’. Despite being involved in drafting the ethics application and attending the meeting, there was no acknowledgement of the PPIE member during this, nor were any questions directed at her. So, although the intention was to enhance the PPIE member’s development in relation to ethical governance, processes and structures external to the team hindered this being fully realised.
Another PPIE participant focused on the ‘insights’ and ‘little glimpses’ she gained throughout her involvement of the Needs Round study:
I have learned quite a lot about what goes on and, you know, it could, you know, go towards other projects because I think things are changing all the time with technology and virtual wards and things […] I’m always open to new things, but I think I hadn’t realized how complex it was. And I have got a better understanding now.
PPIE 1
What she learnt related both to the study’s content as well as to the research processes that academics drew on and could be applied to other studies.
Summary
Patient and public involvement and engagement members were considered a key part and partners with academics. Specifically, their feedback regarding the language used when communicating with non-academic audiences was considered helpful. In addition, they represented a sitting reminder to academics to be accessible in their communication.
The data highlighted the role of relationship-building and the debrief sessions in supporting PPIE members. The constant communication and dynamics were equally considered an important feature in ensuring that the PPIE members felt valued. Indeed, there appeared to be a space in the team for members to speak from multiple perspectives. The complexity of tasks, inputs and contributions had to be negotiated by academics.
Interviewees described a range of learning and professional development, which related to both the process and value of having PPIE members as partners, as well as the underpinning values which contributed to the team’s dynamics. PPIE members highlighted how the study provided them the opportunity to develop more skills, learn and be involved in further research projects.
Chapter 7 Research engagement by care homes
Introduction
As noted in prior chapters, engagement from CH staff in the research elements of the study was inconsistent and at times very weak. In this chapter, we summarise their participation, and withdrawals, before presenting data on how CHs engaged with data collection and return.
In addition to quantitative data collected on participation, during Phase 2 interviews (conducted in month 9 implementation, and month 11/12 of implementation), respondents from CHs were asked to reflect on the difficulties they had encountered in engaging in the research tasks. The data presented here reflect the complexity of the COVID-19 context of the study and highlight learning for future CH studies.
Core difficulties included pressure on staff time and prioritisation (including those exacerbated by COVID-19), suboptimal administrative procedures and record keeping within CHs and difficulties using excel.
Care home participation
Withdrawals from the study
Forty-five CHs were recruited over the entire study period, 16 of which withdrew (11 prior to implementation commencing and 5 withdrew during implementation). All six hospices had at least one home withdraw from the study (Table 17). Of the CHs that withdrew, the majority (94%) were for-profit/privately owned and provided nursing care (81%). Half were in Scotland and half in England, mostly located in central Scotland (38%) or East England (38%). The average number of beds across the 16 CHs was 53, the smallest providing care for up to 26 residents and the largest up to 123 residents. When divided into categories, nine were classified as medium-sized homes (11–49 beds) and seven large (50 + beds). All homes provided care to older adults over the age of 65 years, but 50% of the withdrawals also provided care to adults younger than 65, two of which accepted residents from the age of 18 years.
| Hospice | Participating CHs | Withdrawn |
|---|---|---|
| S55997 | 6 | 2 |
| 8CL93 | 6 | 1 |
| 8C928 | 6 | 1 |
| S25614 | 4 | 6 |
| 8JD12 | 4 | 3 |
| 8A784 | 3 | 3 |
| Total | 29 | 16 |
Descriptive analysis
Examining the survey data, the highest rate of participation was observed for the CAPA surveys, and 23 CHs (79.3%) returned one or more CAPA survey. Eighteen CHs (62.1%) returned one or more QODDI survey. In comparison to the survey data (CAPA and QODDI), lower levels of participation were observed for the return of baseline (n = 14, 48.3%) and follow-up data. Baseline data were collected on people residing in study CHs in March 2021, and included data such as the status of residents, sociodemographic characteristics, staffing costs and interactions with healthcare professionals. The follow-up data were collected from March to May 2022 and included a repeat of the sociodemographic questions about CH residents. Data on staffing costs and interactions with healthcare professionals were not requested at follow-up, due to feedback from CH staff and the steering group. Only 12 of the CHs (41.4%) provided follow-up data, of which 9 (75.0%) had provided baseline data.
Table 18 shows the descriptive characteristics of the CHs participating in different aspects of the study. Percentages shown in the table represent the response rate for each factor, for example 50% of large CHs in the sample provided baseline data. Participation in the family perceptions survey (CANHELP Lite) was not included when calculating participation, since so few were returned to the team, and reporting on these data would risk maintaining site anonymity. A descriptive overview is included in Families’ perceptions: CANHELP Lite.
| Provided baseline data | Provided follow-up data | Returned one or more QODDI | Returned one or more CAPA | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n = 14 | n = 12 | n = 18 | n = 23 | ||||||
| n | % | n | % | n | % | n | % | ||
| Size of CH | Medium (11–49 beds) | 7 | 46.7 | 8 | 53.3 | 8 | 53.3 | 11 | 73.3 |
| Large (50 + beds) | 7 | 50.0 | 4 | 28.6 | 10 | 71.4 | 12 | 85.7 | |
| Ownership | Private | 10 | 40.0 | 10 | 40.0 | 14 | 56.0 | 20 | 80.0 |
| Voluntary, not for profit | 4 | 100.0 | 2 | 50.0 | 4 | 100.0 | 3 | 75.0 | |
| Country | England | 9 | 47.4 | 8 | 42.1 | 11 | 57.9 | 13 | 68.4 |
| Scotland | 5 | 50.0 | 4 | 40.0 | 7 | 70.0 | 10 | 100.0 | |
| Location | Urban | 10 | 43.5 | 7 | 30.4 | 16 | 69.6 | 18 | 78.3 |
| Rural | 4 | 66.7 | 5 | 83.3 | 2 | 33.3 | 5 | 83.3 | |
| Types of care provided by the CHs | Nursing care | 12 | 50.0 | 11 | 45.8 | 16 | 66.7 | 20 | 83.3 |
| Residential care | 4 | 36.4 | 4 | 36.4 | 4 | 36.4 | 6 | 54.6 | |
| Convalescent | 9 | 52.9 | 9 | 52.9 | 9 | 52.9 | 13 | 76.5 | |
| Respite care | 11 | 45.8 | 10 | 41.7 | 13 | 54.2 | 19 | 79.2 | |
| Day or lunch clubs | 3 | 50.0 | 3 | 50.0 | 4 | 66.7 | 5 | 83.3 | |
| Specialist care | 13 | 52.0 | 11 | 44.0 | 15 | 60.0 | 19 | 76.0 | |
| Dementia care | 13 | 59.1 | 10 | 45.5 | 14 | 63.6 | 17 | 77.3 | |
| Under 65 years | 9 | 50.0 | 8 | 44.4 | 13 | 72.2 | 13 | 72.2 | |
Overall participation scores (as described in Care home participation) ranged from 3 to 48 whereby a higher score indicated greater engagement and participation in different aspects of the study. Mean participation scores (Table 19) were higher in large CHs compared to medium and in voluntary compared to privately owned homes. Smaller differences were observed between the location variables, whereby CHs in Scotland had higher average participation scores than in England and CHs in urban areas scored higher than rural.
| Overall participation scores | |||
|---|---|---|---|
| n | Mean | ||
| Size of CH | Medium (11–49 beds) | 15 | 14.9 |
| Large (50 + beds) | 14 | 23.1 | |
| Ownership | Private | 25 | 17.0 |
| Voluntary, not for profit | 4 | 30.5 | |
| Country | England | 19 | 18.6 |
| Scotland | 10 | 19.4 | |
| Location | Urban | 23 | 19.4 |
| Rural | 6 | 16.8 | |
| Nursing care | No | 5 | 7.8 |
| Yes | 24 | 21.2 | |
| Residential care | No | 18 | 22.9 |
| Yes | 11 | 12.2 | |
| Convalescent care | No | 12 | 20.5 |
| Yes | 17 | 17.7 | |
| Respite care | No | 5 | 17.0 |
| Yes | 24 | 19.3 | |
| Day or lunch clubs | No | 23 | 18.9 |
| Yes | 6 | 18.7 | |
| Specialist care | No | 4 | 17.5 |
| Yes | 25 | 19.1 | |
| Dementia care | No | 7 | 13.7 |
| Yes | 22 | 20.5 | |
| Care to under 65s | No | 11 | 16.9 |
| Yes | 18 | 20.1 | |
Regression analyses
None of the included predictor variables were statistically significant in predicting participation at baseline (Table 20). However, the provision of residential care was significantly negatively associated with overall participation score (Table 21), suggesting that those describing themselves as nursing-only homes had higher levels of engagement with the study overall, compared to residential-only or combined nursing and residential homes. The lack of statistically significant results is likely partially attributable to the small sample size (n = 29); thus, the patterns and directions of non-significant coefficients are still important to discuss.
| Model 1 | Model 2 | Model 3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | Sig. | 95% CI | OR | sig. | 95% CI | OR | Sig. | 95% CI | ||||
| LCI | UCI | LCI | UCI | LCI | UCI | |||||||
| Country (ref. England) | ||||||||||||
| Scotland | 0.97 | 0.972 | 0.20 | 4.74 | 1.00 | 0.999 | 0.20 | 4.92 | 0.94 | 0.944 | 0.18 | 4.89 |
| Location (ref. urban) | ||||||||||||
| Rural | 2.61 | 0.325 | 0.39 | 17.71 | 3.12 | 0.273 | 0.41 | 23.96 | 4.53 | 0.187 | 0.48 | 42.71 |
| Size of home (ref. medium) | ||||||||||||
| Large | 1.55 | 0.589 | 0.32 | 7.61 | 0.96 | 0.968 | 0.16 | 5.87 | ||||
| Care type (ref. nursing only) | ||||||||||||
| Residential care | 0.28 | 0.205 | 0.04 | 2.00 | ||||||||
| Constant | 0.78 | 0.602 | 0.30 | 2.02 | 0.60 | 0.457 | 0.15 | 2.31 | 1.14 | 0.881 | 0.21 | 6.15 |
| n | 29 | 29 | 29 | |||||||||
| Pseudo R² | 0.026 | 0.033 | 0.077 | |||||||||
| Log Likelihood | −19.56 | −19.42 | −18.53 | |||||||||
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | Robust std. err. | Sig. | Coefficient | Robust std. err. | Sig. | Coefficient | Robust std. err. | Sig. | |
| Country (ref. England) | |||||||||
| Scotland | 1.22 | 3.66 | 0.742 | 2.45 | 3.30 | 0.465 | 1.99 | 3.16 | 0.536 |
| Location (ref. urban) | |||||||||
| Rural | −2.80 | 3.50 | 0.432 | −0.90 | 2.79 | 0.750 | 0.98 | 3.16 | 0.758 |
| Size (ref. medium) | |||||||||
| Large | 6.44 | 3.91 | 0.112 | 2.91 | 3.19 | 0.371 | |||
| Ownership (ref. voluntary, not for profit) | |||||||||
| Private | −11.82 | 8.06 | 0.155 | −11.45 | 8.20 | 0.176 | |||
| Care type (ref. nursing only) | |||||||||
| Residential care | −8.79 | 2.86 | 0.005** | ||||||
| Constant | 19.02 | 3.47 | 0.000*** | 25.29 | 8.54 | 0.007*** | 29.77 | 8.85 | 0.003 |
| n | 29 | 29 | 29 | ||||||
| R² | 0.011** | 0.257 | 0.364 | ||||||
| F | (2,26) = 0.46 | (4,24) = 1.51 | (5,23) = 2.27 | ||||||
When examining the results predicting participation at baseline and overall participation score, there are several discrepancies. For example, the results suggested that Scottish CHs are less likely to participate at baseline compared to English homes, but the coefficient for overall participation is positive, which would imply Scottish CHs have a higher level of engagement when participating in different aspects of the study. A total of 18 Scottish CHs were recruited into the study, 44.4% (n = 8) of which withdrew. However, in England, 27 CHs were recruited into the study, 29.6% (n = 8) of which withdrew. As such, there were fewer Scottish CHs participating in the study (n = 10) compared to English (n = 19). Additionally, some CHs were recruited onto the project later than others. Since baseline data were collected retrospectively (i.e. data on residents were collected in relation to March 2021), many CHs completed this at a much later date, potentially impacting their ability to provide accurate baseline data. Thus, CHs joining later may have been less likely to provide baseline data if they did not have this readily available. Descriptively, although a higher number of English CHs provided baseline data, the response rate when examined by country (see Table 18) was higher in Scotland (50.0%) than in England (47.4%) which does not align with the trend suggested in the regression analysis.
Large CHs were also found to be less likely to participate at baseline but had higher participation scores. Descriptive analysis revealed that participation scores for staff in large CHs were, on average, 8.2 points higher than in medium CHs (see Table 19). One interpretation of this might be that the number of staff is likely to be higher in large compared to medium homes; therefore, for research activities like the CAPA which were completed by different members of staff, larger CHs have the potential for higher participation scores simply because of a larger staff pool. Future analysis should look to equivalise the overall participation scores based on the CH size to avoid potential skews in the data.
In contrast, the direction of the results for both rural CHs and residential CHs aligned for baseline and overall participation. The CH being in a rural location compared to urban was positively associated with baseline and overall participation and residential care provision was negatively associated with both participation outcomes.
The lack of statistically significant results makes it difficult to draw any substantial conclusions about the factors that predict participation in palliative care research among CHs.
Routine collection of data
Care home managers were typically responsible for collating the data for the study pertaining to CH residents and health service use. Most CH managers were also identified as responsible for distributing the family questionnaires, with RNs or care staff focused on the quality of death and CAPA measures.
Dispatching researchers to conduct data collection to reduce CH burden was not feasible in this study due to COVID-19 restricting access and subsequently increasing CH workload:
That’s all because of COVID and the staffing levels that we’ve got in that, you know. So, it was difficult to time-manage and to get [DCHM, ST00419] to … she ended up coming in on her days off and that kind of thing to get the spreadsheet up to date and all that.
CH manager, ST00419, Phase 2
Inadequate time prevented CH staff from collecting resident data. Data collection was perceived as a substantial piece of work that required sufficient time that many CH staff could not spare. Care home staff described that they were already overloaded with paperwork and did not have the time or resource for additional work for the study, a key issue exacerbated by COVID-19. Thus, despite renumeration being available to CHs to provide data, this was not possible in most CHs due to lack of workforce.
Relatedly, usability impacted participation levels. Confusion over aspects such as how to record empty beds and ECOG scores, a lack of skills in using spreadsheets and an absence of administrative support reduced data returns: ‘It was me [that filled in the spreadsheet]. That’s me, but I’m no good on spreadsheets and stuff like that.’ (CH manager, ST00329, Phase 2).
Some staff felt that the difficulty emanated from the breadth of information requested and CH data being spread across different formats and systems. This was despite the efforts of the research team to engage with CH managers, and health economists, prior to implementation to understand what data points would be easily obtained. One CH manager indicated that data on hospital admissions were not usually collected by CH staff, and hence, the project’s request for this information triggered a whole system change. The manager highlighted that the new spreadsheet for capturing these data would be integrated into routine admin:
I think, we’ve got lesson learned that the biggest thing was register. So what we did, we implemented this [spreadsheet] now and we’ve got a register for admission, hospital admissions for infections, for wounds, general admissions to the care home, and we’ve got like big spreadsheet with everything. […]
CH nurse manager, ST00402, Phase 2
Yeah, do you think you’ll carry on doing that then after the end of the project?
Interviewer
Yes, yes, yes, definitely. [previously] I couldn’t find all information I needed. So then it is like jigsaw, now it’s all in place but I have like space, you know, cells missing from my spreadsheet. So, it’s like I had date of birth but I didn’t have a discharge date and, so, I compared this one with CQC hospital notifications and death notifications, and then I compare this one with CD book (laughs) to see who else was here. And I compare this one also with diary and communication book and old MARs (chuckles).
CH nurse manager, ST00402, Phase 2
Challenges were experienced by staff because they were asked to provide information on data points that were not routinely collected by them. One CH nurse, for example, talked about the difficulties in reporting resident ethnicity as this was not usually recorded. Staff lacked confidence in how to approach these conversations:
The difficult part [of completing the spreadsheet] […] the things that we’re asking, is the ethnicity. I mean, mostly they are British but it’s not the usual questions that the residents answer in terms of their demographics. […] one of the first questions is like, it just, it’s hard to think, well, how do I answer that if I’ve not actually [got information on resident ethnicity]. […] because mostly will be British, I would say if I’m going to ask my staff they will be mostly British but we don’t have an evidence for them unless we ask the family, but not all families will be keen to discuss these things.
CH RN, ST00339, Phase 2
The lack of attention to these characteristics indicated that race and ethnicity are often rendered invisible within the CH; this in turn suggests that there may be a lack of attentiveness to how cultural practices intersect with dying and death.
Participants demonstrated a lack of understanding as to the salience of some of the data being collected, and this impacted on engagement and participation levels. This included cost data, which some of the CH managers were perplexed by.
The economic evaluation approach taken, cost–benefit analysis, does have a high requirement for data. This meant that it was necessary to ask for a lot of detail from CHs on costs. For a future study, alternative approaches to economic evaluation, such as social return on investment (SROI), which have a lower data burden than a cost–benefit analysis, could be considered. But the need to accurately account for costs will remain with any approach, and so strategies and support to mitigate the difficulties experienced by CHs will be required.
Questionnaire completions and returns
COVID-19 was offered as an explanation by CH staff for low rates of promotion of the family questionnaire:
What has been really difficult, we haven’t managed to do yet, is the family perception ones […] there’s questionnaires that get sent out from various other things, various other people and they don’t bother because they don’t have to … And to be honest, because they haven’t had as much involvement with the Needs Rounds that we hoped, they probably don’t remember half of that because there’s so much that’s been going out over the months with COVID.
CH manager, ST00340, Phase 2
Due to local lockdowns and COVID-19 outbreaks, some CH staff did not wish to canvas the views of relatives. Concerns about relatives being unhappy overrode prompts from the research team to distribute questionnaires:
It’s really wrong time to send the sheets back to family because they were not happy with that, that we’re in lockdown. ‘oh, you know, you haven’t seen your mum for months but could you tell us about end-of-life’ […] So I just thought, you know what, I’ll put that on hold for now […] I wasn’t brave enough to ask relatives.
CH nurse manager, ST00402, Phase 2
When residents who were very close to death were discussed at Needs Rounds, staff were reluctant to request families to complete questionnaires. The timing was viewed as insensitive, and this prevented CH staff from asking them at that time:
Actually, we had only that person who was in the last [Needs Round], and [the SPC nurse] met him and the next two days he passed away […] So, that didn’t seem appropriate [to send the family a care questionnaire] because the family were really, really very close.
CH nurse manager, ST00456, Phase 2
Completing the QODDI also presented difficulties in finding time:
We really don’t get the time to do that. [SPC clinician] has been telling me to do the ones who … the two residents who passed away, but I, to date, am not getting the time to do that. We are bombarded with so much other work that they’re completely running out of time to do this extra work. That’s the problem that I’m facing. If it is paper, and if I do it then and there with [SPC clinician], but then it’s fine. But otherwise, I really don’t get that time to catch up later on. That’s my problem.
CH nurse manager, ST00316, Phase 2
The CAPA questionnaire received the highest level of return of all measures. Typically, this was completed at the start of each Needs Round and was prompted by the SPC clinician. This strategy was effective, though the clinical pressures of delivering care sometimes disrupted 100% response rates: ‘There were a couple of times, all hands up, where we got into the Needs Rounds at the last minute because something has happened on the floor and we completely forgot about it’ (CH manager, ST00340, Phase 2).
Preferences for paper format were aided by the SPC clinicians taking them to the monthly Needs Rounds. These clinicians then uploaded these to the research team securely via SharePoint. Another site provided their phone for the CH staff to use:
I’ve got the CAPA on my phone … you don’t [want to] be a nag. It’s been about forming relationships and yet, there’s a lot of that. There are things for them to do. It’s not without things for them to do.
SPC, 8A784, Phase 2
It was not always clear whether CH staff had identified a specific person to complete and return data to the research team. This was presented as a humorous element of CH task management, but represented a challenge as identifying a responsible individual was not always possible:
I’ve delegated that job to [deputy manager] because [deputy manager] loves a good spreadsheet. So … but it was difficult. […] she ended up coming in on her days off and that kind of thing to get the spreadsheet up to date and all that.
CH manager, ST00419, Phase 2
Others indicated that the role had been delegated, but with staff absences, this was not always effective:
CH manager, ST00434, Phase 2: we just don’t have the time. That’s the only thing.
Interviewer: So, time is essentially that …?
CH manager, ST00434, Phase 2: I do have an admin but she’s actually acting up as deputy at the moment because my deputy is off sick with [serious illness] herself.
Data collection procedures
Some CH staff found Excel to be difficult to work with and reported having blank cells despite completing sheets. To address this problem, the research team changed the format in which the data were requested and developed a Word document, as this was perceived by CH staff as being more user friendly:
Interviewer: So, is using Excel particularly difficult?
CH nurse manager, ST00456, Phase 2: Yeah. Because I did put in all the data the first time and I did try sending it, but then it- some of the boxes were not working.
As a response to this feedback, CH staff were sent the option of Word document versions to complete; of the 25 follow-up responses over the 3 months, 19 (76%) were returned via Word document rather than Excel.
CH managers reported that completing information on vacant bed-days was too complex: ‘It was confusing about what rooms were vacant, like what days they were vacant and that kind of thing.’ (Deputy CH manager, ST00327, P2).
Some CH staff found the amount of data collection onerous, while others reported it being manageable:
Like anybody, we were the same, we have a lot of paperwork to do here for work itself and then when you get another paperwork, you will think, oh my God, not more paperwork but I mean it wasn’t that time-consuming.
Mental Health and Disability Nurse, ST00403, Phase 2
SPC clinicians each played a role in encouraging CH staff to complete and return data to the research team. This added to their workload, with regular reminders and prompts: ‘It feels like that that gentle persistence has paid off because they’ve […] kept it on their back burner, but they have now started to [return] the spreadsheets’ (SPC, 8JD12, Phase 2).
Limited data collection was intended to be led by SPC teams, focused on audio recording Needs Rounds to allow for analysis of their content and process. Often, concerns about meetings meant that such recordings did not happen. Specialist palliative care clinicians explained their reluctance with reference to how seeking permission to record and the unfamiliarity of the process would interfere with relationship development between CH and hospice. However, as noted in Chapter 3, some CHs managed both high levels of data return and positive relationship development. Consequently, the two could be managed, but relied on the SPC facilitator to be confident at managing the different process.
Summary
A range of factors impacted CH staff ability and desire to return data to the research team. Conducting complex data collection while CHs were in intermittent lockdowns, experiencing extreme staffing shortages and being asked to complete bespoke tools all acted as barriers to high levels of data collection.
Chapter 8 Discussion and conclusions
Summary of findings
The programme theory summarises the core finding – of what works for whom under which circumstances and why. The programme theory drew on all the evidence gathered in the two phases via stakeholder interviews, workshops and questionnaires, to understand the micro, meso and macro contexts in which Needs Rounds ran, alongside the mechanisms that enabled implementation and outcomes to be achieved. Development of the programme theory drew on both data regarding what works and what did not work.
What works for whom, under what circumstances and why?
What works? Monthly Palliative Care Needs Rounds can provide CH staff and SPC staff with protected time and the opportunity to collaborate to plan for residents’ last months and weeks of life. Fidelity to the Needs Rounds checklist24 was low for case conferences and providing clinical interventions. However, 158 clinical interventions from SPC clinicians were triggered. Implementation showed that additional family meetings/multidisciplinary meetings did not work as the third of the three-component model. Both direct clinical work and family/MDT meetings were hampered by COVID-19 restrictions. Specialist palliative care was welcomed, but some input was generalist palliative care delivered by the SPC clinicians.
For whom? Qualitative data showed that Palliative Care Needs Rounds work for CH staff (greater understandings of palliative care, improving collaborations and trust), and SPC staff (improving collaborations and strengthening relationships and trust). Palliative Care Needs Rounds benefit CH residents (better informed staff, improved quality of dying). Palliative Care Needs Rounds also benefit relatives (giving greater confidence in the quality of care). There was insufficient evidence to demonstrate impact on healthcare systems, notably health economic impact.
Under what circumstances? The study was conducted during COVID-19 restrictions, and hence Palliative Care Needs Rounds were implemented and assessed during extreme workforce challenges, including high turnover and recruitment difficulties, exacerbated by poor pay and conditions. COVID-19 also meant that core parts of the model were not tested, such as family meetings.
Beyond COVID-19, CH staff have variable skills and confidence and sometimes have insufficient support within the wider health system. Flexibly arranging Needs Rounds to suit CH needs, having manager buy-in and building collaborative relationships can help to encourage time to be protected for the monthly meetings. Facilitation by SPC staff which is responsive to the complexities of CH context helps build collaborative relationships.
Why? Palliative Care Needs Rounds can provide timely expert input to CH staff and residents. The learning/educational component of Needs Rounds can strengthen understandings of ACP, the dying process, symptom and pain management, and communication mechanisms between CH staff, families, SPC staff and primary care. Needs Rounds can offer protected time and collaborations. Needs Rounds can shift power dynamics between CH and hospice services by harnessing complementary expertise. For relatives, Needs Rounds can work well because they increase confidence in quality care. Needs Rounds can augment existing practice by building CH staff confidence for those who attend.
Facilitation and facilitators are important mechanisms for successful implementation. Facilitation styles that worked included developing positive relationships, demonstrated through jokes, compliments and referring to what they had learnt from each other. Facilitative approaches were collaborative and involved gentle work in determining people’s current knowledge and areas for extending insights as well as which residents were appropriate to discuss. Managers needed to be key facilitators to enable staff to attend Needs Rounds, through rotas or overtime.
The programme theory is as follows:
While CHs experience workforce challenges, like high turnover and recruitment difficulties, exacerbated by poor pay and conditions, staff have variable skills and confidence and sometimes having insufficient support within the wider healthcare system. Needs Rounds can provide CH staff and SPC staff with the opportunity to collaborate during a protected time, to plan for residents’ last months and weeks of life. Flexibly arranging Needs Rounds to suit CH needs, having manager buy-in and building collaborative relationships can help to encourage time to be protected. Needs Rounds augment existing practice by building CH staff confidence for those who attend and prompting anticipatory planning and care. A facilitation approach that is responsive to the difficult context in which CHs operate can improve collaboration. In addition, Needs Rounds can strengthen relationships and trust and shift power dynamics between CH and hospice services by harnessing complementary expertise. Integrating learning into Needs Rounds strengthens understandings of the dying process, symptom and pain management, ACP and communication mechanisms between CH staff, families, SPC staff and primary care. This leads to higher-quality resident-centred care, enabling residents to be cared for and die in their preferred place. Needs Rounds also benefit relatives by increasing their confidence in care quality and CH staff by providing timely expert input.
The implementation of Needs Rounds was grounded in flexible facilitation to respond to CH contexts. Integrated Promoting Action on Research Implementation in Health Services underpinned the development of the model and approach to implementation. The innovation construct within i-PARIHS128 recognises that evidence is often adapted in line with recipients’ underlying knowledge sources, including their contexts, motivations and perceptions regarding the innovation. This innovation construct was explicitly harnessed within the study in the coproduction approach used to elucidate a range of stakeholder views, understand how Needs Rounds fit with existing CH organisational processes and explicate how these intertwine with external systems. Consequently, the intervention was designed to enable Needs Rounds to be responsive to wider contexts to improve the chance of successful uptake into practice.
Specialist palliative care staff were aware of the difficult context that CHs work within and tailored their facilitation approach around this. Building and engaging in reciprocal relationships, where collective expertise is acknowledged and harnessed, helped to build trust and improved interagency working. Needs Rounds enhanced communication mechanisms with primary care through learning about how best to communicate with GPs and using the expert status of the SPC clinicians, resulting in more responsiveness to requests to meet residents’ wishes and preferences, so that they could receive end-of-life care in their preferred place.
Over the 12-month intervention period, we found statistically significant increase in CAPA scores, indicating that CH staff grew more confident in their ability to adopt a palliative approach. This was a clinically important difference, as reflected in the qualitative interview data.
Deaths occurring later into the intervention were rated more positively than those at the beginning of the implementation period. Thus, Needs Rounds appear to improve the quality of death/dying for CH residents. Family members are mostly satisfied with their relatives’ care. However, since limited data were available for analysis, it is not possible to conclude the scale of this or impact of Needs Rounds on family perceptions of care.
Direct costs attributed to running Needs Rounds include staff time, from both CHs and SPC, alongside expenses such as equipment, medications and travel. The sample size of health service use data was too small to be able to conduct a meaningful inferential test for statistical significance of the treatment effect. The limited data available indicated a slight rise in hospitalisation rates.
The PPIE evaluation concluded that involvement and engagement were woven throughout the study, with three PPIE people included as full team members engaging in a wide range of activities. The impact of their engagement was varied and included adjustments to study measures, recruitment of research staff and being invited to participate in other research studies.
Analysis of patterns of data returns indicated that CH staff struggled to engage with some of the research processes, notably returning quantitative data. The conduct of the study during COVID-19 national lockdowns and ongoing impact on workforce resulted in more difficulties than typical in this already challenging environment. Fidelity to the coproduced UK model of Needs Rounds was variable, and in assessing a random selection, many sites achieved low scores despite qualitative interviews providing evidence of managing to achieve important outcomes.
Sitting these findings alongside outcomes from the prior Australian work enables a holistic assessment of ‘what works for whom under what circumstances and why’. The Australian evidence base is drawn out in subsequent subsections around palliative care in CHs, building interagency relationships and hospital transfers.
Palliative care in care homes
The study identified that Needs Rounds can be implemented in CHs, improving access to and provision of palliative care for residents, benefiting them, the staff and relatives. The Needs Rounds approach includes components that are recognised as necessary for integrating palliative care into CHs, namely facilitation, education/learning, alongside internal and external engagement. 130
The Needs Rounds study helps to address micro and meso needs identified in the European Association of Palliative Care’s (EAPC) white paper on palliative care in long-term care facilities,131 while also indicating the intervention is congruent with the macro context. The EAPC’s proposed futures include, at meso level, a focus on identifying facilitators and raising awareness, while developing a shared palliative care vision. Greater team working and support for managers introducing change are also noted at meso level. At micro level, EAPC identifies the creation of a culture of learning or development, delivering palliative care education/training and building confidence as requirements. Embedding palliative care into delivery, encouraging reflexivity among staff and planning for sustainability are also core elements of the micro level context advocated for by EAPC and addressed by Needs Rounds.
Provision of responsive education, tailored to staff needs, is woven throughout each monthly Needs Rounds meeting. A recent review of literature on palliative and end-of-life care education programmes demonstrates the need for such flexibility in addressing CHs’ needs and organisational context,35 alongside implementation frameworks. Thus, Needs Rounds help address this recommendation, and the strengthened relationships between CHs and SPC means CHs are better placed to draw on wider hospice education programmes, beyond the learning provided in Needs Rounds meetings. Education, while clearly a priority,30 remains a challenging area, given the precarity in workforce retention. This study augments evidence on Needs Rounds from Australia where it was demonstrated to provide education and support to CHs leading to more confident/competent staff25 and better-quality deaths for residents. 85
Strengthened relationships and interagency working
At a meso level, Needs Rounds showed improvements in interagency working between hospices and CHs. Collaborative facilitation and partnership working flattened the hierarchies that frequently permeate multidisciplinary team working with CHs. 132 Although models of improving healthcare for older people in CHs often point to primary care as a core partner, including EHCH in England,133 realist reviews challenge this perspective. General practitioners are rarely perceived as being central for delivering improvement in CHs,134 and there is insufficient evidence to support the belief that linking GP practices to CHs improves resident outcomes. 75 Being present and responsive is more important than having a named primary care provider, particularly when staff training was focused on areas of their interest and need. 75
Nevertheless, interagency working with primary care may continue to have an important place in policy initiatives and practice developments for aligning CHs and primary care. In England, the EHCH programme was introduced to standardise some aspects of healthcare for CH residents, and as an extension to the core GP contract, it promotes the provision of a clinical lead for each CH, weekly home rounds and identification of residents for MDT review, holistic assessment, development of care plans and prioritisation of residents for structured medication reviews. EHCH thus looks well positioned to dovetail with Needs Rounds. However, EHCH implementation started in 2020 and is due for completion by 2024 with patchy uptake to date. None of the English sites in this study had operational EHCH. In Scotland, the approach to palliative care in CHs has prioritised holistic assessment, MDTs, ACP and prompt access to generalist and specialist input. 83 The key implication lies in the integration with current practice in both countries. This would involve primary care integration with CHs being complemented by the SPC input from the Needs Rounds model.
Needs Rounds demonstrate relative advantage over other innovations designed to enhance interagency working between CHs and SPC. Palliative Care Needs Rounds provide a structure to be present and responsive, with case-based education focused on emergent and pressing topics. Thus, Needs Rounds create a mechanism where staff felt they had a common purpose for change to occur. Needs Rounds also improved communications with primary care, which resulted in increased responsiveness to CH staff requests for support.
The outcome of improved interagency working and associated mechanisms stand counter to studies which report ongoing hierarchical structures, and dichotomies between health and social care, reported in Canada. 135
The Needs Rounds facilitation approach was based on fostering mutuality and reciprocity to enable CH staff and SPC clinicians to learn together, and thereby disrupts and reformulates negative attitudes towards care work. 136 These negative stereotypes are exacerbated by unequal hierarchies that exist between MDT working in the social care sector, with care staff often being viewed as inferior. 132 Needs Rounds counter such stereotypes by adopting an approach that acknowledges CH expertise and champions the vital role of CH staff. The important role of communication in establishing and enhancing interagency and interprofessional relationships meshes with evidence from Australia on core mechanisms that enable Needs Rounds to work. 137
Hospital transfers
Although in this study Needs Rounds did not reduce hospitalisation rates, there is evidence that they have improved processes. That is, CH residents were able to be cared for and die in their preferred place, which is predominantly in the CH rather than hospital. The Needs Rounds evidence base for reducing hospitalisations and length of stay was established in two Australian studies. 23,138
Decision-making around hospital transfers is complex. 139 Hospital transfers, which are not clinically indicated, should be reduced to improve patient care and increase opportunities for people to die in their preferred place. Practices around hospitalisation have been significantly impacted by COVID-19. A realist review into ACP through COVID-19 found that residents and relatives opted against hospitalisations due to higher risks of infection and fears of having a lonely death. 60 However, ACPs risk not being sufficiently robust to enable preferences is to be fully understood and honoured. 140 A relative advantage of Needs Rounds is that learning is tailored to take account of these contextual factors and support decision-making and actions around hospital transfers. This tailored learning also increases the confidence and competence of CH staff to facilitate better-quality lives and deaths and have timely conversations to increase family confidence in the ability of CHs to meet their relatives’ need.
COVID-19
Needs Rounds took place in the context of COVID-19, with the study commencing 6 months after the initial UK lockdown. When the intervention started, CH staff had accrued considerably more experience in caring for dying residents and improved the use of ACP reinforcing the need to engage in such conversations rather than solely produce a document reflecting resuscitation preferences. 141 Needs Rounds augmented this improvement through discussions about residents’ symptoms and needs.
COVID-19 also led to depleted support from primary care, while increasing workload on the CH staff. COVID-19’s impact on the CH workforce significantly reduced available resources including personnel to attend from both within the CH and to host the visiting SPC clinician. Use of online video platforms, to accommodate local lockdowns during the implementation phase, enabled Needs Rounds to continue, which reflects Needs Rounds use in Australia. 27,28
Engaging care homes in research
Structural challenges such as limited time to complete research tasks were reflected in our data, despite offers to reimburse CHs for their time collating data. Difficulties of conducting research in CHs have been documented including the limitations on staff time to complete data returns. 130,142 Other core challenges and solutions include management engagement, ensuring research processes work for CH staff, managing ethical hurdles and structural challenges to collecting research data in CHs. 143 While the research team’s relationship with each site was very positive, feedback from some CH staff indicated variable understanding about what data were requested and the rationale.
Analysis returned limited significant results regarding the prediction of CH participation across the study. Comparison with the wider literature is difficult; previous studies focus mainly on the recruitment of CHs, rather than participation levels. 144 Overall, most CH managers were found to have little experience of research,145 which is also likely to impact participation, not just recruitment into research. Largely, the factors examined in relation to recruitment were administrative, such as staff time and turnover146 or linked to processes within the CH such as lack of understanding, compliance and gate keeping. 147 Moreover, in some cases, it was believed that certain research areas, for example, death and dying, could result in unfavourable publicity for the home,145 highlighting a lack of education or awareness on the importance of such research and potential stigmas which researchers may not be aware of. A substantial gap in previous literature was identified for studies that examined CH specific factors, such as size or type of care provided, in relation to the home’s participation in research activities.
The SPC clinicians were asked to audio-record each Needs Round meeting, yet only 33% of meetings were recorded. Hesitancy was explained in part due to the impact it might have on relationship building between CH and SPC. This points to learning regarding the kind of data which might be reasonably expected to be returned from such sites, where clinical practice/knowledge and skills are being displayed and where the need for trust development is a greater priority for the clinicians than producing research data. This may be particularly pertinent in studies which involve new relationships, rather than interventions delivered within existing and established professional networks. The research team encouraged recordings to take place, but also did not wish to jeopardise relationships, and hence the intervention and determining the primary outcome. Consequently, where one SPC clinician who was adamant that recording would be detrimental to the clinical relationship, the research team prioritised the intervention over data collection.
The data demands from CHs to conduct a full cost–benefit analysis were quite intense, and this may have impacted participation in monthly data returns. While an economic evaluation is important in contributing to the UK evidence for Needs Rounds, the burden of data collection on CHs does need to be considered.
Methodology
Conceptualising and reporting fidelity has been identified as an area for further development in palliative care interventions in CHs. 130 This study offers an outline of conceptualising fidelity in critical realist domains and how fidelity articulates with the development of programme theories. Critical realism challenges the ‘epistemic fallacy,’148 which occurs when the real and the known are conflated. It is based on ontological pluralism and seeks to avoid reductionism. 149 Acknowledging the inherent limitations of the knowledge production process, this study aimed to move beyond a partial account based on participant recollections or experiences. Thus, fidelity was assessed using both semistructured interviews and transcripts of the Needs Rounds recordings. The analysis was based on how participants reported the facilitation happening, as well as observations of the interactions between CH staff and SPC clinicians within the Needs Rounds. Attention was also paid to social, cultural and temporal dimensions which are often marginalised within fidelity analysis. 150
Alternative economic evaluation approaches (such as Social Return on Investment) could be considered that would balance the robustness of economic evidence against the impact on CHs providing data. But the need to accurately account for costs will remain with any approach, and so strategies and support to mitigate the difficulties experienced by CHs will be required. These could include streamlined data collection instruments, additional training and support for data collection by CHs or where possible researchers onsite to help gather the data.
Conclusions
Implementation objectives
Across Phase 1 and 2, we co-designed and built a programme theory for a UK version of Needs Rounds, which is responsive to the different (macro, meso and micro) contextual characteristics of the UK CH sector.
In Phase 2, we implemented the UK model of care. We determined that Needs Rounds were feasible to run in the UK and acceptable to both CHs and SPC staff. We were unable to determine all the anticipated outcomes, due to the paucity of data impacting economic analysis and analysis of family perceptions of care. However, the qualitative interview data indicated that Needs Rounds can improve the provision of palliative and end-of-life care in CHs.
Intervention objectives
We determined the transferability of the core elements of the Needs Rounds intervention in a UK context in Phase 1 and 2. For example, the model was adapted to adjust to primary care relationships with UK CHs and attended to the UK CH workforce configuration.
The programme theory delineated the mechanisms that enabled Needs Rounds to be used, such as providing the time and space to engage in proactive ACP, augmenting existing good practice and skills and developing communication, collaboration and reciprocity, alongside adjusted power dynamics and interagency trust.
The programme theory depicts the mechanisms common across sites. Individual differences were observed in CHs pertaining to regularity and accessibility of primary care staff, yet sites reported benefits of Needs Rounds despite this important variable. The outcomes of interest to stakeholders and observed in the data were stronger connections between CHs and hospices, improved trust and better connections between CHs and other services. Needs Rounds can improve communications between CH staff and GPs and CH staff and families.
Process evaluation objectives
Due to insufficient data, we were unable to determine whether UK Needs Rounds impacted hospitalisations including any cost implications. Quality of death and dying improved, with analysis indicating that deaths occurring later into the Needs Rounds intervention were rated more positively than those towards the start. We determined that the size of the CH also impacted quality of death and dying, with large CHs scoring lower than medium CHs. Not-for-profit homes scored on average lower than private CHs. We determined that CH staff grew more confident in their ability to adopt a palliative approach.
While there were insufficient cost data to conduct the planned cost–benefit analysis, the qualitative data highlighted the wider staff costs within the CH required to support Needs Rounds beyond the direct intervention costs. A fuller economic evaluation would be required to balance both these direct and indirect staff costs against the benefits of the intervention.
The potential for improving care
Needs Rounds can improve the provision of palliative and end-of-life care in CHs. The relative advantage of Needs Rounds has three dimensions: (1) has no direct cost to CHs, (2) provides direct clinical work and (3) focuses on specialist (rather than primary) palliative care. These features distinguish it from other approaches, such as the GSF. 151
Needs Rounds can help to develop stronger connections between CHs and hospices, improve trust and increase better connections between CHs and other services. Needs Rounds improve communications between CH staff and GPs, and CH staff and families.
Care home staff were widely praised by SPC clinicians for their expertise, insights and ability to provide high-quality care. With this strong foundation, Needs Rounds still had clear additional value and CH staff readily identified the usefulness of input from SPC clinicians. However, improved communication mechanisms are required to ensure that SPC can identify their added value. Despite precarious workforce arrangements,152 CHs enabled staff to have time away from their routine duties to attend Needs Rounds, though the numbers attending were often limited by staffing capacity.
Implications for commissioning and service delivery
Needs Rounds can provide a protected time where there can be increased collaboration between CH and SPC teams, focused on improving CH staff confidence, resident quality of living and dying and augment approaches to ACP. It is incumbent upon commissioners and service providers to ensure that CH residents with complex needs receive equitable care, when compared to older people living in their own homes. Needs Rounds can be one such approach and could contribute as one of the range of ways that CH residents gain the support they need to live and die well.
Future work could therefore focus on the sustainability of Needs Rounds, engaging with commissioners and policy-makers to secure funding to integrate and embed Needs Rounds into CH and hospice practice across the UK. This is needed over and above links with primary care to ensure access to specialist support and input, especially while primary care is so overwhelmed with work. Further establishing how Needs Rounds could work alongside primary care would be an important development for commissioning and delivery.
Interagency working between CHs and SPC should be routine elements of service level agreements. Using the Needs Rounds checklist to identify residents to discuss and provide biopsychosocial support, provide learning and develop clinical action plans will improve resident care, staff competence and relative satisfaction. Needs Rounds may not be required every month (e.g. depending on acuity of residents and size of CH) and could be linked with primary care rounds where they exist.
Provision of learning is beneficial, particularly given the increase in CAPA scores observed and qualitative feedback. CH managers should seek to ensure care staff can attend to benefit from the Needs Rounds meetings, and managers of larger homes should ensure rotation of staff attending to address the lower CAPA scores observed in CHs with more residents.
Needs Rounds can also be used to meet regulation requirements. While the CQC in England153 and Care Inspectorate in Scotland154 do not provide an inspection rating on end-of-life care, CHs should have a strategy in place to show how personalised support is provided to CH residents who are dying. Needs Rounds provide a formal mechanism to achieve this and align with several of the key CQC/Care Inspectorate aims, including enabling the person to express their preferences, reducing preventable hospital admissions, maximising quality of life, including through symptom and pain management, and supporting carers. Needs Rounds address 32 recommendations of the Scottish 'Healthcare framework for adults living in care homes'. 155
Scalability and sustainability will be dependent upon resources available for staffing Needs Rounds. This may require redeployment of existing resource to CHs, rather than an expectation of additional funding, particularly given the context of austerity in the UK. Both scalability and sustainability will also be related to how Needs Rounds articulate with primary care services. For scale, since primary care extends across the UK and since all UK residents should have access to general practice, there are key opportunities to wrap Needs Rounds into GP contacts. This approach would extend the building and maintenance of multidisciplinary working and trust, rather than SPC.
Implications for care home research
Despite the prevalence of CHs as a site of death, palliative care remains a marginalised focus of work, often receiving only a passing mention. 156 Future research needs to increase the evidence regarding living well and dying well in CHs across the UK in order to address issues of equity in access to specialist care and support.
Lower CAPA scores for CH staff than managers indicate that this is an urgent area for development. While Needs Rounds can support care staff learning and development, longer-term follow-up will be needed to determine how much knowledge and learning are retained and applied by those attending Needs Rounds.
Given the importance of relationships and facilitation to successful implementation of interventions, a discourse analysis of the Needs Rounds recordings data set could be conducted to further understand relationships dynamics and how the facilitation approach shapes delivery.
The project highlighted several common factors in working with CHs. The minimal engagement with study materials may reflect the lack of capacity staff have to read and retain information given the other pressures on their role. While this may be explained with reference to the pandemic, it is also possible that different strategies (beyond e-mails, phone calls and videos) are needed to communicate with CHs. Future studies conducting research in CHs may consider using fewer data collection tools or varying the methods of data collection, that is, some on-site researchers, to reduce the burden on staff completing surveys. Validating shorter versions of the questionnaires, if possible, would also mean that surveys with fewer items are easier to administer and complete by CH staff and should yield less missing and incomplete data.
Care home manager buy-in was essential to recruitment and retention of sites. While national CH research networks (such as ENRICH) have potential to support managers understand the importance of research, this remains suboptimal. Strategies to resource engagement in research may go some way to providing incentives for managers to prioritise this as a core function. Providing finance to backfill managers’ time may not be sufficient, given the lack of quantitative data returned to the team despite such resource.
Systemic workforce issues also hamper research, particularly studies such as this which run over several years, including 12 months of intervention time. The high turnover of CH staff means that many were only present for some of the study, and many others will have moved in the post-study dissemination period. As noted above, minimal engagement in study information is further complicated by staff moving in and out of CHs during the study. The task-oriented and busy shifts of care staff do not allow time for reading and reflecting on research materials. Evidence of this was seen across the sites, whereby different staff members were responsible for the completion of the data elements. For example, many sites’ data were completed by managers. Many CH managers may find they do not have the capacity to engage fully in the research activities due to other responsibilities within their role; however, the research tasks may fall to them by default. Reimbursing CH staff for their time attending Needs Rounds interventions (as a parallel to the reimbursement of SPC clinicians’ employers) may also be necessary in future research to promote engagement.
Limitations
COVID-19
The study was conducted when UK health and social care systems were impacted by COVID-19. The project commenced between the first and second national lockdowns. The impact of COVID-19 was more long-lasting and consequential within the social care sector than almost any other part of UK society.
Multiple adaptations to the study’s data collection and implementation were made to accommodate COVID-19. This included moving all data collection online, developing new strategies to develop and strengthen relationships between the research team and sites by use of Teams, bespoke videos, e-mails and phone calls. All workshops (including training in delivering Needs Rounds and co-design of the programme theory) were redesigned to allow for delivery via Zoom, and the steering group only met online.
While restrictions lifted in different domains at different times as the project progressed, the perseverance of impact in CHs was marked. Care homes often remained closed to external visitors, including any clinician who was not routine care staff or attending in an emergency capacity. The consequence of this was that the SPC nurses were unable to attend Needs Rounds in person for some of the study timeline. Academic researchers were unable to attend sites to build relationships or gather qualitative data. Families and friends of residents were unable to visit and support residents, meaning that the care tasks they would routinely conduct were added to the responsibilities of paid care staff.
With the use of barrier nursing, increased staff illness due to infection with COVID-19 and increased resident acuity due both directly to COVID-19 and indirectly as hospital services sought to reduce admissions, the impact on CHs was considerable.
The COVID-19 context of the study meant that CH staff had considerable pressures on their time, which impacted their ability to fully engage in the study. This included reduced ability to complete CH data returns (with consequent impact on the amount and quality of data available for analysis), reduced desire to distribute and follow-up questionnaires for families, lower numbers of staff attending monthly Needs Rounds meetings and shorter/fewer interviews with CH staff during Phase 2.
Doubtless, COVID-19 also impacted both recruitment and retention of CHs to the study. Recruitment was all conducted online or via phone, eradicating the ability to build relationships more fluidly through personal contact. The extreme levels of CH staff sickness, staff distress and increased workload meant that engaging in a research study was unable to be a priority.
Data returns
Throughout the quantitative analysis, the small sample sizes are identified as a limitation, and in many cases, these restricted the possible analyses with the data. Particularly, the CANHELP Lite survey asking about family members’ perceptions of care was only completed by 13 family members, and this limited sample size meant that only descriptive analysis could be conducted and, to avoid identification, responses could not be compared across sites. Future research might consider supporting CHs to recruit family members, providing promotional materials and information about the benefits of participating in research or offering incentives to participate.
The CAPA survey had the highest response rate across the survey data, with 171 individual responses, allowing for working samples of 155–158 across the different regression analyses. The main limitation with the CAPA survey was that only 28 staff members completed the survey on multiple occasions; thus, pre–post comparison before and after intervention was limited. Researchers might consider administering the CAPA at the start of the project and then again to the same staff members at the end, rather than leaving it open throughout.
Eighty-one responses were received for the QODDI survey; however, only 5 completed all 16 items. As discussed in Quality of death and dying, this required the analysis to be conducted with a subset of the items, limiting the validity of the findings. Due to the missing demographic data at follow-up, as many of the sites did not return data on the status or characteristics of service users, it is not possible to calculate how many service users died over the period of Needs Rounds to determine a response rate for the QODDI. During the monthly check-ins further prompts to CH staff to complete QODDI surveys and would give more complete data on the service users within the homes across the whole intervention period. As noted elsewhere, the limited demographic and health service use data meant that it has not been possible to conduct a cost–benefit or other form of health economic analysis. Further, CHs reported demographic data that indicated a bias towards White British residents, meaning that the theories derived from the data are not based on a representative sample of the UK.
It was not possible to analyse fully what happened within each Needs Round. All SPC clinicians were asked to record Needs Rounds and provide that recording to the research team. Specialist palliative cares reported that this was fraught, with several barriers to providing these recordings.
Specialist palliative cares were concerned that recording would disrupt relationship development and trust with CH staff. For one site, this meant that no recordings were undertaken. Other sites were variable in their ability to record and then share the audio file. Specialist palliative care staff reported that their priority was on building trust in order to provide a clinical service.
Further, many of the recordings included use of residents’ names. Due to the ethical approvals requiring no identifiable details to be shared with the research team, this meant that some recordings were unable to be shared with the researchers. One site’s SPC clinician would routinely record organic Needs Rounds discussions and then redact any names used. Other sites asked CH staff not to use resident names at the start of the Needs Rounds but found it hard to adhere to this atypical manner of speaking.
The study was also limited by the lack of involvement of CH residents and relatives. Throughout Phase 1 and 2 interviews and workshops, attempts to recruit people residing in CHs were not successful. Consequently, the theory was developed without direct insight from service users. Recruitment of relatives (both to interview in Phase 1 and to complete questionnaires in Phase 2) was also suboptimal.
Three lay members were part of the team, despite extensive work to recruit more people with direct experience of CHs, including people residing in CHs. As described in COVID-19, the PPIE input was therefore focused on lay members or people with a relative living in a CH for older people. Input from people with lived experience of CHs was similarly restricted in Phase 1 (interviews with key stakeholders). The study was therefore impaired by the paucity of first-hand experiences of residing in residential care as a context, their preferences for outcomes or gaining their insights into mechanism which might assist in changing care practices. Difficulties in recruiting a wider sample of PPIE members are likely related to COVID-19 and gatekeeper access to residents in CHs that would be willing and able to consent to such involvement.
Realist methodology
Focusing on ‘what works for whom under what circumstances’ allows a thorough analysis and representation of effective components of the intervention. However, this risks underreporting of negative findings, including when elements did not work or where outcomes were counterproductive. Reporting this study, we manage this tension in producing an ethically sound programme theory by way of inverting elements which did not work. Thus, if data showed communication was poor because managers lacked time to engage with them, then this was reframed as time being required for managers to engage with the materials. Therefore, examples of what did not work were formulated as what could work. Key connectors and examples of what did not work describes what did not work and how this shaped the development of the programme theory.
Equality, diversity and inclusion
The study set no specific sampling parameters around protected characteristics, but purposefully sought geographically dispersed sites with ethnically diverse populations, which would reflect rural and urban areas in Scotland and England.
Data were collected on resident sex, age and ethnicity (reported in Chapter 3). At baseline, most residents were female (63.9%) and over the age of 80 (76.1%). There was little ethnic diversity, with 98.7% of the sample of CH residents being White British, compared with 18% of the UK population being black, Asian, mixed or other ethnicity. 157 Care home residents are typically older women, with around 2.8 more women than men and 59.2% of residents being over 85. 158
Since the study was focused on people living in CHs, the research explicitly focused on older adults. Hence, the study addressed important equality and equity issues, pertaining to age as a protected characteristic under the Equality Act (2010).
Equality, diversity and inclusion data were not collected on CH staff engaged in the intervention, which may reflect how gender is often rendered invisible within palliative care research. 159 However, the CH workforce is widely recognised to be predominantly women. 160
Care home residents were not directly recruited, but nevertheless participant information materials including posters used in CHs were designed to use large font, high readability scores and attractive layout to promote greater understanding of the study among residents and staff. This approach was adopted as part of the ‘no surprises’ ethics framework, but also to embed principles of inclusion in the study.
The research team included people with a range of gender and ages, but all identify as White British or white and African (Egyptian). The team explicitly included people with lived experience of palliative care and/or CHs; this PPIE is explained in greater detail in Chapter 6 and in Patient and public involvement and engagement.
Patient and public involvement and engagement
Patient and public involvement and engagement members
Three PPIE coinvestigators participated in core activity throughout, commencing with proposal development. For example, PPIE members contributed to ethics paperwork, attended monthly team meetings and co-facilitated the co-design workshops. They drew on their personal experiences of CHs and social care.
Patient and public involvement and engagement and the wider literature
The PPIE in this study exceeded the expectations laid out in the National Standards. 161 The evaluation of PPIE indicated that integrating people with lived experience and lay members into the study team was valued by all parties and was an ‘invited space’ curated by academics and inhabited by people with personal experience as well as clinical/academic expertise to create ‘new solidarities’ (p. 452). 162 The independent evaluation of PPIE offered prospective insights into the CMOs of involvement.
Commencing involvement and engagement during the development of the protocol is a common feature of PPIE,163 and in this study, early involvement allowed time to develop relationships, which became a core mechanism for ongoing engagement. 164 Recognising the porous nature of people’s identities and experiences meant that academics/clinicians were also able to speak about their lived experiences, without invalidating PPIE members’ contributions. 127 The explicit values165 of the research team ensured that PPIE members’ views were respected, alongside expertise brought by academic/clinical members of the team. Thus, PPIE involved both the hardware (methods, approaches, guidelines) and software (values, relationships)166 of involvement expected in NIHR studies.
The epistemological traditions of research projects can interlink with, and bear implications for, the role of PPIE members. Questions of how technicalities or methodological expertise sit alongside PPIE involvement have been foregrounded by others. 167 Evaluation interviews regarding whether PPIE would be as engaged in the quantitative data as qualitative rest on assumptions about the ease of articulating underpinning epistemology and methodology. As other authors have noted,168 simplifying some of the language may provide enough of a bridge to allow people without technical knowledge enough insights to inform the process and focus of a range of methodologies within palliative care research. Simplifying language was embedded throughout the current study, including research team meetings and all workshops with diverse stakeholders.
Interviewees in the PPIE evaluation offered only one reflection on the emotional content of a study focused on CHs, dying and death. This absence may reflect the level of support offered to PPIE members (see Patient and public involvement and engagement training and support) or indeed that talking about death/dying/care was manageable without being burdensome. Consequently, there were no barriers to full and extensive engagement of PPIE members in this study focused on palliative care, which has historically been constructed as a sensitive topic. Providing support and debriefs are likely to have mitigated any potential difficulties, which are reported in other PPIE palliative care studies. 169,170 In describing the supports provided to PPIE, this report seeks to render visible the otherwise imperceptible activities undertaken by academic research team members to enable PPIE to flourish. 171
The study achieved success criteria of increased knowledge, agency and confidence of PPIE and academic/clinician team members developing inclusive practices, extended reach of PPIE in research and changes to how the project proceeded. 172
Recommendations for future research
Several recommendations arise from this study, addressing the data deficits and novel research to extend understandings. As a priority, enhancing the UK evidence for Needs Rounds would involve calculating the cost–benefit analysis and treatment effect. However, consideration should be given to the data burden placed on CHs by conducting a full cost–benefit analysis, and future research could balance this against the economic evidence required, perhaps considering approaches such as SROI.
Conducting research at a time of national lockdowns and considerable risk and overwork for staff indicates that other methods for CH data collection need to be developed. It is not sufficient to reimburse staff to take on additional hours to provide data, since this approach did not yield adequate data in this study. Since local restrictions on access have been a feature of CHs for a long time, historically due to other infectious conditions such as norovirus, different approaches should be developed. Establishing minimum data sets routinely collected by CHs173 will aid this, but further innovations in methodology may also be required. Furthermore, additional research might consider testing and validating shorter versions of the surveys in a range of populations, for example, the QODDI10 analysed in this report, as shorter surveys will further reduce burden on CH staff when participating in research.
Future research could examine how Needs Rounds can and should be run alongside primary care. There are two potential areas of research. First, we noted considerable variation in this study, within and between sites, in prior relationships with primary care providers. Further research would include examining the mechanisms and outcomes of closer working and approaches to combining primary care rounds with palliative care Needs Rounds. Second, the implementation of Needs Rounds will require alignment with existing policy and primary care practice. In England, the changes driven by the EHCH strategy offer a ready structure to host Needs Rounds. However, modifying or extending a recently introduced programme will pose challenges at every level, from national decision-makers to local teams. Research that draws on implementation science thinking and organisational theory may be particularly useful to guide this next step for Needs Rounds.
Further research is also required to understand relationship dynamics between CH staff and wider health professionals involved in the provision of palliative and end-of-life care, including, for example, paramedics and pharmacists.
Little data were collected on family perceptions of care, and understanding the impact on such views will be important to gain insight into how Needs Rounds and care quality are understood by relatives. Further, the perceptions and experiences of CH residents will also be important data to inform understanding the outcomes of Needs Rounds. Consequently, semistructured interviews exploring families’ and residents’ perspectives of UK Needs Rounds would provide a fully rounded account of the impact of the approach to care, which was not possible given the limitations of COVID-19 during this study.
A discourse analysis of the Needs Rounds recordings data set would help increase understandings of the relationship dynamics and how the facilitation approach shapes delivery. Such a study would build on the recognised importance of facilitation and facilitators in delivering interventions. The use of discourse analysis would allow examination of naturally occurring data (rather than data created for the purposes of a research study) and hence understand how relationships are managed in situ, and the characteristics of facilitation which help or hinder interprofessional collaboration.
A follow-up study evaluating how much knowledge and learning is retained and applied by those attending Needs Rounds would provide evidence regarding the long-term impact on staff, including those moving to different CH providers. Consequently, this would support building a wider evidence base of knowledge retention by staff in the context of a fluid workforce.
Additional information
Contributions of authors
Liz Forbat (https://orcid.org/0000-0002-7218-5775) (Professor of Ageing and Palliative Care) conceptualised the project, developed the methodology, acquired funding, conducted project administration, provided staff supervision, led management of resources, conducted the research including formal analysis of data, performed validation of the research and contributed to writing original drafts as well as reviewing and editing.
Aisha Macgregor (https://orcid.org/0000-0001-5812-9323) (Research Fellow of Qualitative Research) was involved in project administration, conducting the research including leading formal analysis of data, validation of the research and contributed to writing original drafts as well as reviewing and editing.
Karen Spilsbury (https://orcid.org/0000-0002-6908-0032) (Professor of Care Homes) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research and contributed to writing original drafts as well as reviewing and editing.
Brendan McCormack (https://orcid.org/0000-0001-8525-8905) (Professor of Implementation Science) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research and contributed to writing original drafts as well as reviewing and editing.
Alasdair Rutherford (https://orcid.org/0000-0003-2530-1195) (Professor of Health Economics and Social Statistics) conducted cost–benefit analysis, supervised the statistics analysis, was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research and contributed to writing original drafts as well as reviewing and editing.
Barbara Hanratty (https://orcid.org/0000-0002-3122-7190) (Professor of General Practice) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research and contributed to writing original drafts as well as reviewing and editing.
Jo Hockley (https://orcid.org/0000-0001-5445-0515) (Research Fellow of Care Homes) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research and contributed to writing original drafts as well as reviewing and editing.
Lisa Davison (https://orcid.org/0000-0002-9874-7713) (Research Fellow of Statistics) conducted analysis of questionnaires, was involved in formal analysis of quantitative data, validation of the research and contributed to writing original drafts as well as reviewing and editing.
Margaret Ogden (https://orcid.org/0000-0002-7644-2310) (Patient/Public Involvement and Engagement) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research and contributed to reviewing and editing drafts.
Irene Soulsby (Patient/Public Involvement and Engagement) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research and contributed to reviewing and editing drafts.
Maisie McKenzie (Patient/Public Involvement and Engagement) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research and contributed to reviewing and editing drafts.
The team wish to acknowledge and thank the peer reviewers who provided thoughtful feedback on this report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/KRWQ5829.
Primary conflicts of interest: Liz Forbat received funding via her institution from the NIHR to conduct this study. Karen Spilsbury received funding for membership of REF subpanel 3; and payment to her institution for NIHR research collaboration. She was a member of the NIHR funding committee from 2014 to 2018 and NIHR PRP core committee member (from 2022). Brendan McCormack received funding for membership of REF subpanel 3; was a member of the NIHR HS&DR Research Committee from 2016 to 2020; was a member of the Novo Nordisk Foundation (Denmark) Nursing Research Funding Committee from 2020 to 2022 and received an honorarium; he was a non-executive director of Age Scotland from 2014 to 2022; and holds Director appointment of a private consultancy for person-centred healthcare; and is Director, International Community of Practice for Person-centred Practice – not-for-profit global network registered as a CIC in Scotland. Margaret Ogden received personal funding for patient and public involvement and engagement activity related to care home and palliative care studies for University of Central Lancashire and All Ireland Institute of Hospice and Palliative Care.
Data-sharing statement
Data sharing will be facilitated through appropriate ethics and consent approvals.
Fully anonymised data will be shared with researchers providing full ethical approvals. Metadata in the form of limited demographic information (when captured) will also be available. The rationale for the limit on providing demographic information is to preserve anonymity of respondents. We recognise, though, that researchers may have specific research questions (e.g. pertaining to gender) in which case such limited demographic metadata will be provided if their protocol explicitly requires this information.
Data access and storage will be managed using The University of Stirling’s cloud-based SharePoint.
Publications and other outputs from the study will clearly indicate how to access primary data. Requests for access to the data should be addressed to the corresponding author or to the data custodian.
Ethics statement
Needs Rounds were adopted by CHs as the new standard of care, with CH managers confirming involvement. Bespoke Memoranda of Understanding were written and circulated for all CHs to confirm their role and all expectations and responsibilities. All resident data were collected by routine care staff to preclude the necessity of additional people needing access to the CH. This was adopted for two reasons, first as a COVID-19 containment strategy to minimise visitors in the CH; second, due to the difficulties in securing individual informed consent/proxy consent for all CH residents across all sites throughout the year of intervention and additional baseline data collection period. If data had been collected only on those residents who are able to provide their own consent or who had an appropriate welfare guardian/personal consultee, and where all decedents during the baseline period were excluded, then the sample size would have shrunk considerably, undermining the robustness of the study.
Primary care providers for each CH were advised that the research was being conducted. The correspondence indicated that the CH had agreed to participate, rather than individual residents.
Our No Surprises approach, and discussion with PPIE members, reassured us that this approach was both compliant legally with GDPR and the Common Law Duty of Confidentiality and was acceptable to PPIE. NHS Ethics approval was gained from the South West Frenchay REC on 15-Dec-2020 (20/SW/0152).
Information governance statement
The project steering group met five times during the course of the study, with further support between meetings from specific members. Investigators met monthly throughout with ongoing contact as required between meetings.
All data were handled in line with the Data Protection Act (2018) and General Data Protection Regulation (EU GDPR) 2016/679. University of Stirling is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. A data management plan was developed and adhered to.
Under the Data Protection legislation University of Stirling is the Data Processor; University of Stirling is the Data Controller, and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for The University of Stirling’s Data Protection Officer via: data.protection@stir.ac.uk
The University provides researchers with access to ‘SharePoint’ to safely and securely store research data. SharePoint is Tier D-compliant. This includes the following standards: ISO 27001, ISO 27018, SSAE16 SOC 1 and SOC 2, HIPAA and EU Model Clauses (EUMC). This is a cloud storage solution in Office 365. SharePoint enforces two-factor authentication, single sign-on through Active Directory and encryption of data in transit and at rest. Files are stored in SharePoint and are backed by SharePoint encryption.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Macgregor A, Rutherford A, McCormack B, Hockley J, Ogden M, Soulsby I, et al. Palliative and end-of-life care in care homes: protocol for codesigning and implementing an appropriate scalable model of Needs Rounds in the UK. BMJ Open 2021;11:e049486. https://doi.org/10.1136/bmjopen-2021-049486
Macgregor A, McCormack B, Spilsbury K, Hockley J, Rutherford A, Ogden M, et al. Supporting care home residents in the last year of life through ‘Needs Rounds’: development of a pre-implementation programme theory through a rapid collaborative online approach. Front Health Serv 2023;2:1019602. https://doi.org/10.3389/frhs.2022.1019602
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Kelley AS, Morrison RS. Palliative care for the seriously ill. N Engl J Med 2015;373:747-55.
- Bone AE, Gomes B, Etkind SN, Verne J, Murtagh FEM, Evans CJ, et al. What is the impact of population ageing on the future provision of end-of-life care? Population-based projections of place of death. Palliat Med 2018;32:329-36.
- Newman A. Results of a National Survey of Support to Adult Care Homes in England: A Specialist Palliative Care Provider Perspective. Cardiff: The National Council for Palliative Care; 2017.
- Newman A, Allnatt G, Nelson A, Byrne A. Results of a Survey of Support to Adult Care Homes in Wales: A Specialist Palliative Care Provider Perspective. Cardiff: Marie Curie Palliative Care Research Centre; 2018.
- Scottish C. Supporting Solace: Palliative and End of Life Care Data Report. Edinburgh: Scottish Care; 2017.
- Wilson DM, Shen Y, Birch S. New evidence on end-of-life hospital utilization for enhanced health policy and services planning. J Palliat Med 2017;20:752-8.
- NHS Benchmarking Network . National Audit of Care at the End of Life: First Round of the Audit (2018 19) Report 2019.
- Xing J, Mukamel DB, Temkin-Greener H. Hospitalizations of nursing home residents in the last year of life: nursing home characteristics and variation in potentially avoidable hospitalizations. J Am Geriatr Soc 2013;61:1900-8.
- Ouslander JG, Lamb G, Perloe M, Givens JH, Kluge L, Rutland T, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs. J Am Geriatr Soc 2010;58:627-35.
- Hanson LC, Henderson M, Menon M. As individual as death itself: a focus group study of terminal care in nursing homes. J Palliat Med 2002;5:117-25.
- Martin RS, Hayes B, Gregorevic K, Lim WK. The effects of advance care planning interventions on nursing home residents: a systematic review. J Am Med Dir Assoc 2016;17:284-93.
- Vandervoort A, Houttekier D, Vander Stichele R, van der Steen JT, Van den Block L. Quality of dying in nursing home residents dying with dementia: does advanced care planning matter? A nationwide postmortem study. PLOS ONE 2014;9.
- Vig EK, Davenport NA, Pearlman RA. Good deaths, bad deaths, and preferences for the end of life: a qualitative study of geriatric outpatients. J Am Geriatr Soc 2002;50:1541-8.
- Connolly MJ, Broad JB, Boyd M, Kerse N, Gott M. Residential aged care: the de facto hospice for New Zealand’s older people. Australas J Ageing 2014;33:114-20.
- Cohen AB, Knobf MT, Fried TR. Avoiding hospitalizations from nursing homes for potentially burdensome care: results of a qualitative study. JAMA Inter Med 2017;177:137-9.
- Chu C-P, Huang C-Y, Kuo C-J, Chen Y-Y, Chen C-T, Yang T-W, et al. Palliative care for nursing home patients with dementia: service evaluation and risk factors of mortality. BMC Palliat Care 2020;19.
- Walther W, Müller-Mundt G, Wiese B, Schneider N, Stiel S. Providing palliative care for residents in LTC facilities: an analysis of routine data of LTC facilities in Lower Saxony, Germany. BMC Palliat Care 2022;21.
- Vellani S, Boscart V, Escrig-Pinol A, Cumal A, Krassikova A, Sidani S, et al. Complexity of nurse practitioners’ role in facilitating a dignified death for long-term care home residents during the COVID-19 pandemic. J Pers Med 2021;11.
- Caplan GA, Meller A, Squires B, Chan S, Willett W. Advance care planning and hospital in the nursing home. Age Ageing 2006;35:581-5.
- Garden G, Usman A, Readman D, Storey L, Wilkinson L, Wilson G, et al. Advance care plans in UK care home residents: a service evaluation using a stepped wedge design. Age Ageing 2022;51.
- Wilson E, Morbey H, Brown J, Payne S, Seale C, Seymour J. Administering anticipatory medications in end-of-life care: a qualitative study of nursing practice in the community and in nursing homes. Palliat Med 2015;29:60-7.
- Seymour J, Kumar A, Froggatt K. Do nursing homes for older people have the support they need to provide end-of-life care? A mixed methods enquiry in England. Palliat Med 2011;25:125-38.
- Chapman MD, Johnston N, Lovell C, Forbat L, Liu WM. Avoiding costly hospitalisation at end of life: findings from a specialist palliative care pilot in residential care for older adults. BMJ Support Pallat Care 2018;8:102-9.
- Forbat L, Chapman M, Lovell C, Liu WM, Johnston N. Improving specialist palliative care in residential care for older people: a checklist to guide practice. BMJ Support Palliat Care 2018;8:347-53.
- Johnston N, Lovell C, Liu WM, Chapman MD, Forbat L. Normalising and planning for death in residential care: findings from a qualitative focus group study of a specialist palliative care intervention. BMJ Support Palliat Care 2019;9:e12-e12.
- Perri G-A, Abdel-Malek N, Bandali A, Grosbein H, Gardner S. Early integration of palliative care in a long-term care home: a telemedicine feasibility pilot study. Palliat Support Care 2020;18:460-7.
- Chapman M, Russell B, Philip J. Systems of care in crisis: the changing nature of palliative care during COVID-19. J Bioeth Inq 2020;17:761-5.
- Rainsford S, Hall Dykgraaf S, Phillips C. Effectiveness of telehealth palliative care Needs Rounds in rural residential aged care during the COVID-19 pandemic: a hybrid effectiveness-implementation study. Aust J Rural Health 2022;30:108-14.
- Nolan M, Davies S, Brown J, Wilkinson A, Warnes T, McKee K, et al. The role of education and training in achieving change in care homes: a literature review. J Res Nurs 2008;13:411-33.
- Sleeman KE, Bradshaw A, Ostler S, Tunnard I, Bone AE, Goodman C, et al. Strengthening Palliative and End-of-life Care in Care Homes: An Action Plan to Meet Current and Future Needs. Policy Recommendations from the CovPall Care Homes Study. London: Kings College London; 2022.
- Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med 2014;28:1000-25.
- Chan HY, Pang SM. Let me talk – an advance care planning programme for frail nursing home residents. J Clin Nurs 2010;19:3073-84.
- Lamppu PJ, Pitkala KH. Staff training interventions to improve end-of-life care of nursing home residents: a systematic review. J Am Med Dir Assoc 2021;22:268-78.
- Anstey S, Powell T, Coles B, Hale R, Gould D. Education and training to enhance end-of-life care for nursing home staff: a systematic literature review. BMJ Support Palliat Care 2016;6:353-61.
- Iida K, Ryan A, Hasson F, Payne S, McIlfatrick S. Palliative and end-of-life educational interventions for staff working in long-term care facilities: an integrative review of the literature. Int J Older People Nurs 2021;16.
- Frey R, Balmer D, Robinson J, Boyd M, Gott M. What factors predict the confidence of palliative care delivery in long-term care staff? A mixed-methods study. Int J Older People Nurs 2020;15.
- Hunter PV, McCleary L, Akhtar-Danesh N, Goodridge D, Hadjistavropoulos T, Kaasalainen S, et al. Mind the gap: is the Canadian long-term care workforce ready for a palliative care mandate?. Ageing Soc 2020;40:1223-43.
- Costello H, Cooper C, Marston L, Livingston G. Burnout in UK care home staff and its effect on staff turnover: MARQUE English national care home longitudinal survey. Age Ageing 2019;49:74-81.
- Allan S, Vadean F. The association between staff retention and English care home quality. J Aging Soc Policy 2021;33:708-24.
- White C, McIlfatrick S, Dunwoody L, Watson M. Supporting and improving community health services – a prospective evaluation of ECHO technology in community palliative care nursing teams. BMJ Support Palliat Care 2015;9:202-8.
- Kinley J, Stone L, Dewey M, Levy J, Stewart R, McCrone P, et al. The effect of using high facilitation when implementing the Gold Standards Framework in Care Homes programme. Palliat Med 2014;28:1099-109.
- Smets T, Onwuteaka-Philipsen BBD, Miranda R, Pivodic L, Tanghe M, van Hout H, et al. PACE trial group . Integrating palliative care in long-term care facilities across Europe (PACE): protocol of a cluster randomized controlled trial of the ‘PACE Steps to Success’ intervention in seven countries. BMC Palliat Care 2018;17.
- Stacpoole M, Hockley J, Thompsell A, Simard J, Volicer L. Implementing the Namaste Care Program for residents with advanced dementia: exploring the perceptions of families and staff in UK care homes. Annals Palliat Med 2017;6:327-39.
- Stocker R, Bamford C, Brittain K, Duncan R, Moffatt S, Robinson L, et al. Care home services at the vanguard: a qualitative study exploring stakeholder views on the development and evaluation of novel, integrated approaches to enhancing healthcare in care homes. BMJ Open 2018;8.
- Gardner RL, Pelland K, Youssef R, Morphis B, Calandra K, Hollands L, et al. Reducing hospital readmissions through a skilled nursing facility discharge intervention: a pragmatic trial. J Am Med Dir Assoc 2020;21:508-12.
- Hullick CJ, Hall AE, Conway JF, Hewitt JM, Darcy LF, Barker RT, et al. Reducing hospital transfers from aged care facilities: a large-scale stepped wedge evaluation. J Am Geriatr Soc 2021;69:201-9.
- Giebel C, Harvey D, Akpan A, Chamberlain P. Reducing hospital admissions in older care home residents: a 4-year evaluation of the Care Home Innovation Programme (CHIP). BMC Health Serv Res 2020;20.
- Morciano M, Checkland K, Billings J, Coleman A, Stokes J, Tallack C, et al. New integrated care models in England associated with small reduction in hospital admissions in longer-term: a difference-in-differences analysis. Health Policy 2020;124:826-33.
- Kinley J, Hockley J, Stone L, Dewey M, Hansford P, Stewart R, et al. The provision of care for residents dying in UK nursing care homes. Age Ageing 2014;43:375-9.
- Bowman CE, Elford J, Dovey J, Campbell S, Barrowclough H. Acute hospital admissions from nursing homes: some may be avoidable. Postgrad Med J 2001;77:40-2.
- Harrison JK, McKay IK, Grant P, Hannah J, Quinn TJ. Appropriateness of unscheduled hospital admissions from care homes. Clin Med (London, England) 2016;16:103-8.
- Stone L, Kinley J, Hockley J. Advance care planning in care homes: the experience of staff, residents, and family members. Int J Palliat Nurs 2013;19:550-7.
- Gilissen J, Pivodic L, Wendrich-van Dael A, Cools W, Vander Stichele R, Van den Block L, et al. Nurses’ self-efficacy, rather than their knowledge, is associated with their engagement in advance care planning in nursing homes: a survey study. Palliat Med 2020;34:917-24.
- Spacey A, Scammell J, Board M, Porter S. A critical realist evaluation of advance care planning in care homes. J Adv Nurs 2021;77:2774-84.
- Harrison Dening K, Sampson EL, De Vries K. Advance care planning in dementia: recommendations for healthcare professionals. Palliat Care 2019;12.
- Searle B, Barker RO, Stow D, Spiers GF, Pearson F, Hanratty B. Which interventions are effective at decreasing or increasing emergency department attendances or hospital admissions from long-term care facilities? A systematic review. BMJ Open 2023;13.
- Morciano M, Stokes J, Kontopantelis E, Hall I, Turner AJ. Excess mortality for care home residents during the first 23 weeks of the COVID-19 pandemic in England: a national cohort study. BMC Med 2021;19.
- Burton JK, Reid M, Gribben C, Caldwell D, Clark DN, Hanlon P, et al. Impact of COVID-19 on care-home mortality and life expectancy in Scotland. Age Ageing 2021;50:1029-37.
- Espuny Pujol F, Hancock R, Morciano M. Trends in survival of older care home residents in England: a 10-year multi-cohort study. Soc Sci Med 2021;282.
- Spacey A, Porter S. Understanding advance care planning in care homes throughout the COVID-19 pandemic: a critical realist review and synthesis. Palliat Med 2022;37:663-76.
- Cousins E, Preston N, Doherty J, Varey S, Harding A, McCann A, et al. Implementing and evaluating online advance care planning training in UK nursing homes during COVID-19: findings from the Necessary Discussions multi-site case study project. BMC Geriatr 2022;22.
- Spacey A, Porter S, Board M, Scammell J. Impact of the COVID-19 pandemic on end of life care delivery in care homes: a mixed method systematic review. Palliat Med 2021;35:1468-79.
- Harding A, Preston N, Doherty J, Cousins E, Varey S, McCann A, et al. Developing and evaluating online COVID-centric advance care planning training and information resources for nursing staff and family members in nursing homes: the necessary discussions study protocol. BMC Geriatr 2021;21.
- Dujardin J, Schuurmans J, Westerduin D, Wichmann AB, Engels Y. The COVID-19 pandemic: a tipping point for advance care planning? Experiences of general practitioners. Palliat Med 2021;35:1238-48.
- Bradshaw A, Dunleavy L, Walshe C, Preston N, Cripps RL, Hocaoglu M, et al. CovPall study team . Understanding and addressing challenges for advance care planning in the COVID-19 pandemic: an analysis of the UK CovPall survey data from specialist palliative care services. Palliat Med 2021;35:1225-37.
- Bolt SR, van der Steen JT, Mujezinović I, Janssen DJA, Schols JMGA, Zwakhalen SMG, et al. Practical nursing recommendations for palliative care for people with dementia living in long-term care facilities during the COVID-19 pandemic: a rapid scoping review. Int J Nurs Stud 2021;113.
- Department of Health . Our Commitment to You for End of Life Care The Government Response to the Review of Choice in End of Life Care. NHS Finance and Operations NHS Group NHSCS 17189 2016.
- Department of Health . Government Response to the House of Commons Health Select Committee Report on End of Life Care (Fifth Report of Session 2014–15) 2015.
- Lancaster H, Finlay I, Downman M, Dumas J. Commissioning of specialist palliative care services in England. BMJ Support Palliat Care 2018;8:93-101.
- Healthcare Improvement Scotland . Palliative and End of Life Care Programme 2022. www.healthcareimprovementscotland.org/our_work/person-centred_care/palliative_care.aspx (accessed 13 January 2023).
- Llywodraeth Cymru Welsh Government, GIG Cymru NHS Wales . Palliative and End of Life Care Delivery. Plan 2017.
- Guidelines and Audit Implementation Network . Guidelines for Palliative and End of Life Care in Nursing Homes and Residential Care Homes 2013.
- Killett A, Burns D, Kelly F, Brooker D, Bowes A, La Fontaine J, et al. Digging deep: how organisational culture affects care home residents’ experiences. Ageing Soc 2016;36:160-88.
- Spilsbury K, Hanratty B, McCaughan D. Supporting Nursing in Care Homes. Project Report for the RCN Foundation. York: University of York; 2015.
- Goodman C, Dening T, Gordon AL, Davies SL, Meyer J, Martin FC, et al. Effective health care for older people living and dying in care homes: a realist review. BMC Health Serv Res 2016;16.
- Goodman C, Sharpe R, Russell C, Meyer J, Gordon A, Dening T, et al. Care Home Readiness: A Rapid Review and Consensus Workshops on How Organisational Context Affects Care Home Engagement with Health Care Innovation. UK: NHS England; 2017.
- Rahman AN, Schnelle JF. The nursing home culture-change movement: recent past, present, and future directions for research. Gerontologist 2008;48:142-8.
- Culture Change in Longterm Care. Binghamton, NY: Haworth Press; 2004.
- Wild D, Kydd A. Culture change in care homes: a literature review. Nurs Older People 2016;28:35-9.
- Shier V, Khodyakov D, Cohen LW, Zimmerman S, Saliba D. What does the evidence really say about culture change in nursing homes?. Gerontologist 2014;54:S6-S16.
- Grabowski DC, O’Malley AJ, Afendulis CC, Caudry DJ, Elliot A, Zimmerman S. Culture change and nursing home quality of care. Gerontologist 2014;54:S35-45.
- Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data. BMJ 2017;356.
- Scottish Government . Healthcare Framework for Adults in Care Homes My Health My Care My Home 2022.
- Kinley J, Hockley J, Stone L, Brazil K. Family perceptions of care at the end of life in UK nursing care homes. J Res Nurs 2018;23:203-17.
- Liu WM, Koerner J, Lam L, Johnston N, Samara J, Chapman M, et al. Improved quality of death and dying in care homes: a palliative care stepped wedge randomised control trial. J Am Geriatr Soc 2019;68:305-12.
- Bone AE, Morgan M, Maddocks M, Sleeman KE, Wright J, Taherzadeh S, et al. Developing a model of short-term integrated palliative and supportive care for frail older people in community settings: perspectives of older people, carers and other key stakeholders. Age Ageing 2016;45:863-73.
- Luckett T, Phillips J, Agar M, Virdun C, Green M, Davidson P. Elements of effective palliative care models: a rapid review. BMC Health Serv Res 2014;14.
- Finucane A, Stevenson B, Moyes R, Oxenham D, Murray S. Improving end-of-life care in nursing homes: implementation and evaluation of an intervention to sustain quality of care. Palliat Med 2013;27:772-8.
- Arora S, Smith T, Snead J, Zalud-Cerrato S, Marr L, Watson M, et al. Project ECHO: an effective means of increasing palliative care capacity. Am J Manag Care 2017;23:SP267-71.
- Moore KJ, Candy B, Davis S, Gola A, Harrington J, Kupeli N, et al. Implementing the compassion intervention, a model for integrated care for people with advanced dementia towards the end of life in nursing homes: a naturalistic feasibility study. BMJ Open 2017;7.
- Cimino NM, McPherson ML. Evaluating the impact of palliative or hospice care provided in nursing homes. J Gerontol Nurs 2014;40:10-4.
- Rosenwax AJ. Who receives specialist palliative care in Western Australia – and who misses out. Palliat Med 2006;20:439-45.
- NHS Scotland . Personalising Realistic Medicine: Chief Medical Officer for Scotland’s Annual Report 2017–2018 2019.
- Assets . SO 343 Care Home Analysis 2020.
- Australian Bureau of Statistics . Disability, Ageing and Carers 2015. www.abs.gov.au/ausstats/abs@.nsf/Lookup/4430.0main+features302015#:~:text=Most%20older%20Australians%20(94.8%25),homes%20and%20aged%20care%20hostels.2015 (accessed 31 July 2023).
- Office for National Statistics . Changes in the Older Resident Care Home Population Between 2001 and 2011 2014.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. CHEERS Task Force . Consolidated health economic evaluation reporting standards (CHEERS) statement. BMJ 2013;346.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348.
- Pinnock H, Barwick M, Carpenter C, Eldridge S, Grandes G, Griffiths C, et al. Standards for reporting implementation studies (StaRI) statement. BMJ 2017;356.
- Estabrooks CA, Squires JE, Cummings GG, Birdsell JM, Norton PG. Development and assessment of the Alberta Context Tool. BMC Health Serv Res 2009;9.
- Hoomans T, Severens JL. Economic evaluation of implementation strategies in health care. Implement Sci 2014;9.
- Macgregor A, Rutherford A, McCormack B, Hockley J, Ogden M, Soulsby I, et al. Palliative and end-of-life care in care homes: protocol for codesigning and implementing an appropriate scalable model of Needs Rounds in the UK. BMJ Open 2021;11.
- NHS Improvement . National Tarrifs n.d. https://improvement.nhs.uk/resources/national-tariff/2019 (accessed 31 July 2023).
- NHS Digital . National Tarrifs. https://digital.nhs.uk/data-and-information/publications/statistical/acute-patient-level-activity-and-costing (accessed 31 July 2023).
- NHS Scotland . Scottish National Tarrif 2022. www.isdscotland.org/Tariff/ (accessed 13 January 2023).
- Prince M, Knapp M, Guerchet M, McCrone P, Prina M, Comas-Herrera A, et al. Dementia UK: Update. London: King’s College London and the London School of Economics; 2014.
- Curtis JR, Patrick DL, Engelberg RA, Norris K, Asp C, Byock I. A measure of the quality of dying and death Initial validation using after-death interviews with family members. J Pain Symptom Manage 2002;24:17-31.
- Nadin S, Miandad MA, Kelly ML, Marcella J, Heyland DK. Measuring family members’ satisfaction with end-of-life care in long-term care: adaptation of the CANHELP lite questionnaire. Biomed Res Int 2017. https://doi.org/10.1155/2017/4621592.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Gilmore B, McAuliffe E, Power J, Vallières F. Data analysis and synthesis within a realist evaluation: toward more transparent methodological approaches. Int J Qual Methods 2019;18.
- LaDonna KA, Artino AR, Balmer DF. Beyond the guise of saturation: rigor and qualitative interview data. J Grad Med Educ 2021;13:607-11.
- Care Quality Commission . The State of Adult Social Care Services 2014 to 2017 2017. www.cqc.org.uk/sites/default/files/20170703_ASC_end_of_programme_FINAL2.pdf (accessed 31 July 2023).
- Borrelli B, Sepinwall D, Ernst D, Bellg AJ, Czajkowski S, Breger R, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J Consult Clin Psychol 2005;73:852-60.
- Feely M, Seay KD, Lanier P, Auslander W, Kohl PL. Measuring fidelity in research studies: a field guide to developing a comprehensive fidelity measurement system. Child Adolesc Soc Work J 2018;35:139-52.
- Office for National Statistics . ONS Postcode Directory 2022. https://geoportal.statistics.gov.uk/datasets/ons::ons-postcode-directory-august-2022-1/about (accessed 13 January 2023).
- Department for Environment Food and Rural Affairs . Rural Urban Classification 2011 Lookup Tables for Small Area Geographies 2021. www.gov.uk/government/statistics/2011-rural-urban-classification-lookup-tables-for-all-geographies (accessed 13 January 2023).
- National Records of Scotland . Scottish Postcode Directory Files 2023. www.nrscotland.gov.uk/statistics-and-data/geography/our-products/scottish-postcode-directory/2022-2 (accessed 13 January 2023).
- Scottish Government . Scottish Government Urban Rural Classification 2020 2022. www.gov.scot/binaries/content/documents/govscot/publications/advice-and-guidance/2022/05/scottish-government-urban-rural-classification-2020/documents/scottish-government-urban-rural-classification-2020/scottish-government-urban-rural-classificat (accessed 13 January 2023).
- Daly Lynn J, Washbrook M, Ryan A, McCormack B, Martin S. Partnering with older people as peer researchers. Health Expect 2021;24:1879-89.
- Green G. Power to the people: to what extent has public involvement in applied health research achieved this?. Res Involv Engagem 2016;2.
- Bennett H, Brunner R. Nurturing the buffer zone: conducting collaborative action research in contemporary contexts. Qual Res 2022;22:74-92.
- Lignou S, Capitao L, Hamer-Hunt JM, Singh I. Co-production:an ethical model for mental health research?. Am J Bioethics 2019;19:49-51.
- Willis P, Almack K, Hafford-Letchfield T, Simpson P, Billings B, Mall N. Turning the co-production corner: methodological reflections from an action research project to promote LGBT inclusion in care homes for older people. Int J Environ Res Public Health 2018;15.
- Gifford J. Action Learning: Principles and Issues in Practice. Brighton, UK: Institute for employment studies; 2005.
- Macgregor A, McCormack B, Spilsbury K, Hockley J, Rutherford A, Ogden M, et al. Supporting care home residents in the last year of life through ‘Needs Rounds’: Development of a pre-implementation programme theory through a rapid collaborative online approach. Front Health Serv 2023;2. https://doi.org/10.3389/frhs.2022.1019602.
- Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci 2016;11.
- Department of Health and Social Care . Technical Report on the COVID-19 Pandemic in the UK 2022.
- Collingridge Moore D, Payne S, Van den Block L, Ling J, Froggatt K, Gatsolaeva Y, et al. Strategies for the implementation of palliative care education and organizational interventions in long-term care facilities: a scoping review. Palliat Med 2020;34:558-70.
- Froggatt KA, Moore DC, Van den Block L, Ling J, Payne SA, Van den Block L, et al. Palliative care implementation in long-term care facilities: European association for palliative care white paper. J Am Med Dir Assoc 2020;21:1051-7.
- Manthorpe J, Vandrevala T, Abrams R, Samsi K. Working with colleagues and other professionals when caring for people with dementia at the end of life: home care workers’ experiences. Int J Care Caring 2019;3:567-83.
- NHS England and NHS Improvement . The Framework for Enhanced Health in Care Homes [Internet] 2020. www.england.nhs.uk/wp-content/uploads/2020/03/the-framework-for-enhanced-health-in-care-homes-v2-0.pdf (accessed 13 January 2023).
- Chadborn NH, Devi R, Goodman C, Williams CD, Sartain K, Gordon AL. General practitioners’ role in improving health care in care homes: a realist review. Fam Pract 2022;40:119-27.
- Sutherland N. Structures, tensions, and processes shaping long-term care home staff’s role in end of life decision-making for residents with dementia. J Aging Stud 2020;54.
- Algoso M, Peters K, Ramjan L, East L. Exploring undergraduate nursing students’ perceptions of working in aged care settings: a review of the literature. Nurse Educ Today 2016;36:275-80.
- Koerner J, Johnston N, Samara J, Liu W-M, Chapman M, Forbat L. Context and mechanisms that enable implementation of specialist palliative care Needs Rounds in care homes: results from a qualitative interview study. BMC Palliat Care 2021;20.
- Forbat L, Liu WM, Koerner J, Lam L, Samara J, Chapman M, et al. Reducing time in acute hospitals: a stepped wedge randomised control trial of a specialist palliative care intervention in residential care homes. Palliat Med 2020;34:571-9.
- Harrad-Hyde F, Armstrong N, Williams CD. ‘Weighing up risks’: a model of care home staff decision-making about potential resident hospital transfers. Age Ageing 2022;51.
- Jones CW, Taylor L, Clement-Rees A. COVID-19 deaths in care homes: primary care management study. BMJ Support Palliat Care 2022.
- Hopkins SA, Lovick R, Polak L, Bowers B, Morgan T, Kelly MP, et al. Reassessing advance care planning in the light of covid-19. BMJ 2020;369.
- Lam HR, Chow S, Taylor K, Chow R, Lam H, Bonin K, et al. Challenges of conducting research in long-term care facilities: a systematic review. BMC Geriatr 2018;18.
- Law E, Ashworth R. Facilitators and barriers to research participation in care homes: thematic analysis of interviews with researchers, staff, residents and residents’ families. J Long-Term Care 2022:49-60.
- Shepherd V, Nuttall J, Hood K, Butler CC. Setting up a clinical trial in care homes: challenges encountered and recommendations for future research practice. BMC Res Notes 2015;8:1-4.
- Goodman C, Baron NL, Machen I, Stevenson E, Evans C, Davies SL, et al. Culture, consent, costs and care homes: enabling older people with dementia to participate in research. Aging Ment Health 2011;15:475-81.
- Davies SL, Goodman C, Manthorpe J, Smith A, Carrick N, Iliffe S. Enabling research in care homes: an evaluation of a national network of research ready care homes. BMC Med Res Methodol 2014;14:1-8.
- Hall S, Longhurst S, Higginson IJ. Challenges to conducting research with older people living in nursing homes. BMC Geriatr 2009;9:1-8.
- Bhaskar R. The Possibility of Naturalism. Brighton: Harvester; 1979.
- Bhaskar R, Danermark B. Metatheory, interdisciplinarity and disability research: a critical realist perspective. Scand J Disabil Res 2006;8:278-97.
- Masterson-Algar P, Burton CR, Rycroft-Malone J, Sackley CM, Walker MF. Towards a programme theory for fidelity in the evaluation of complex interventions. J Eval Clin Pract 2014;20:445-52.
- International. G . The Gold Standards Framework (GSF) Care Homes Training Programme 2019. www.gsfinternational.org.uk/_files/ugd/3f4876_333d9049be54409f85b65593218243b8.pdf (accessed 13 January 2023).
- UK Government . Adult Social Care Workforce Survey: December 2021 Report 2021 n.d. www.gov.uk/government/statistics/adult-social-care-workforce-survey-december-2021/adult-social-care-workforce-survey-december-2021-report (accessed 13 January 2023).
- Social Care Institute for Excellence . Person Centred Care for Older People in Care Homes Egham, UK 2017. www.scie.org.uk/person-centred-care/older-people-care-homes/end-of-life-care#:~:text=In%202015%2C%20CQC%20developed%20with%20other%20organisations%20a,CQC%20inspectors%20always%20ask%20a%20question%20about%20it (accessed 13 January 2023).
- Care Inspectorate . Palliative and End of Life Care Policy – Policy Context Dundee; Care Inspectorate 2017. www.careinspectorate.com/images/documents/4185/HWT%20policy%20cover%20palliative%20and%20end%20of%20life%20care%20MASTER.pdf (accessed 13 January 2023).
- Scottish Government . My Health, My Care, My Home – Healthcare Framework for Adults Living in Care Homes 2022.
- Hasson F, Nicholson E, Muldrew D, Bamidele O, Payne S, McIlfatrick S. International palliative care research priorities: a systematic review. BMC Palliat Care 2020;19.
- UK Government . Ethnicity Facts and Figures 2021 n.d. www.ethnicity-facts-figures.service.gov.uk/ (accessed 25 May 2023).
- Office for National Statistics . Changes in the Older Resident Care Home Population Between 2001 and 2011 2014.
- Gott M, Morgan T, Williams L. Gender and palliative care: a call to arms. Palliat Care Soc Pract 2020;14.
- Skills for C . The State of the Adult Social Care Sector and Workforce in England 2022. www.skillsforcare.org.uk/adult-social-care-workforce-data/Workforce-intelligence/publications/national-information/The-state-of-the-adult-social-care-sector-and-workforce-in-England.aspx:Workforceintelligence (accessed 13 January 2023).
- NIHR . National Standards for Public Involvement in Research 2018.
- Mosse D. Can the experience of participatory development help think critically about ‘patient and public involvement’ in UK healthcare?. Sociol Res Online 2019;24:444-61.
- Hoffmann K, Helle Schou L, Karin P, Jarden M. Current trends in patient and public involvement in cancer research: a systematic review. Health Expect 2019;22:3-20.
- Pearce C. The complexities of developing equal relationships in patient and public involvement in health research. Soc Theory Health 2021;19:362-79.
- Chambers E, Gardiner C, Thompson J, Seymour J. Patient and carer involvement in palliative care research: an integrative qualitative evidence synthesis review. Palliat Med 2019;33:969-84.
- Wilsdon J, Wynne B, Stilgoe J. The Public Value of Science: Or How to Ensure That Science Really Matters. Demos; 2005.
- Boaz A, Chambers M, Stuttaford M. Public participation: more than a method? Comment on ‘Harnessing the potential to quantify public preferences for healthcare priorities through citizens’ juries’. Int J Health Policy Manag 2014;3:291-3.
- Johnson H, Davies J, Leniz J, Chukwusa E, Markham S, Sleeman K. Opportunities for public involvement in big data research in palliative and end-of-life care. Palliat Med 2021;35:1724-6.
- Perkins P, Barclay S, Booth S. What are patients’ priorities for palliative care research? Focus group study. Palliat Med 2007;21:219-25.
- Johnson H, Ogden M, Brighton L, Etkind S, Oluyase A, Chukwusa E, et al. Patient and public involvement in palliative care research: what works, and why? A qualitative evaluation. Palliat Med 2021;35:151-60.
- Mathie E, Smeeton N, Munday D, Rhodes G, Wythe H, Jones J. The role of patient and public involvement leads in facilitating feedback: ‘invisible work’. Res Involv Engagem 2020;6.
- Holmes L, Cresswell K, Williams S, Parsons S, Keane A, Wilson C, et al. Innovating public engagement and patient involvement through strategic collaboration and practice. Res Involv Engagem 2019;5.
- Burton JK, Wolters AT, Towers A-M, Jones L, Meyer J, Gordon AL, et al. Developing a minimum data set for older adult care homes in the UK: exploring the concept and defining early core principles. Lancet Healthy Longev 2022;3:e186-93.
Appendix 1 Evolution of initial theories and context, mechanism, outcome maps
The maps depict the complexity of the interactions between the contexts, mechanisms and outcomes. The distinction between contexts and mechanisms can become blurred, with some contexts becoming mechanisms, and mechanisms changing the context.
For each of the CMO maps, contexts are depicted in blue, mechanisms in purple and outcomes in orange. The resulting theory is furthest right in grey.
Theory 1: confidence and competence
FIGURE 8.
Context, mechanism and outcome mapping of theory 1. PEOLC, Palliative and End of Life Care.
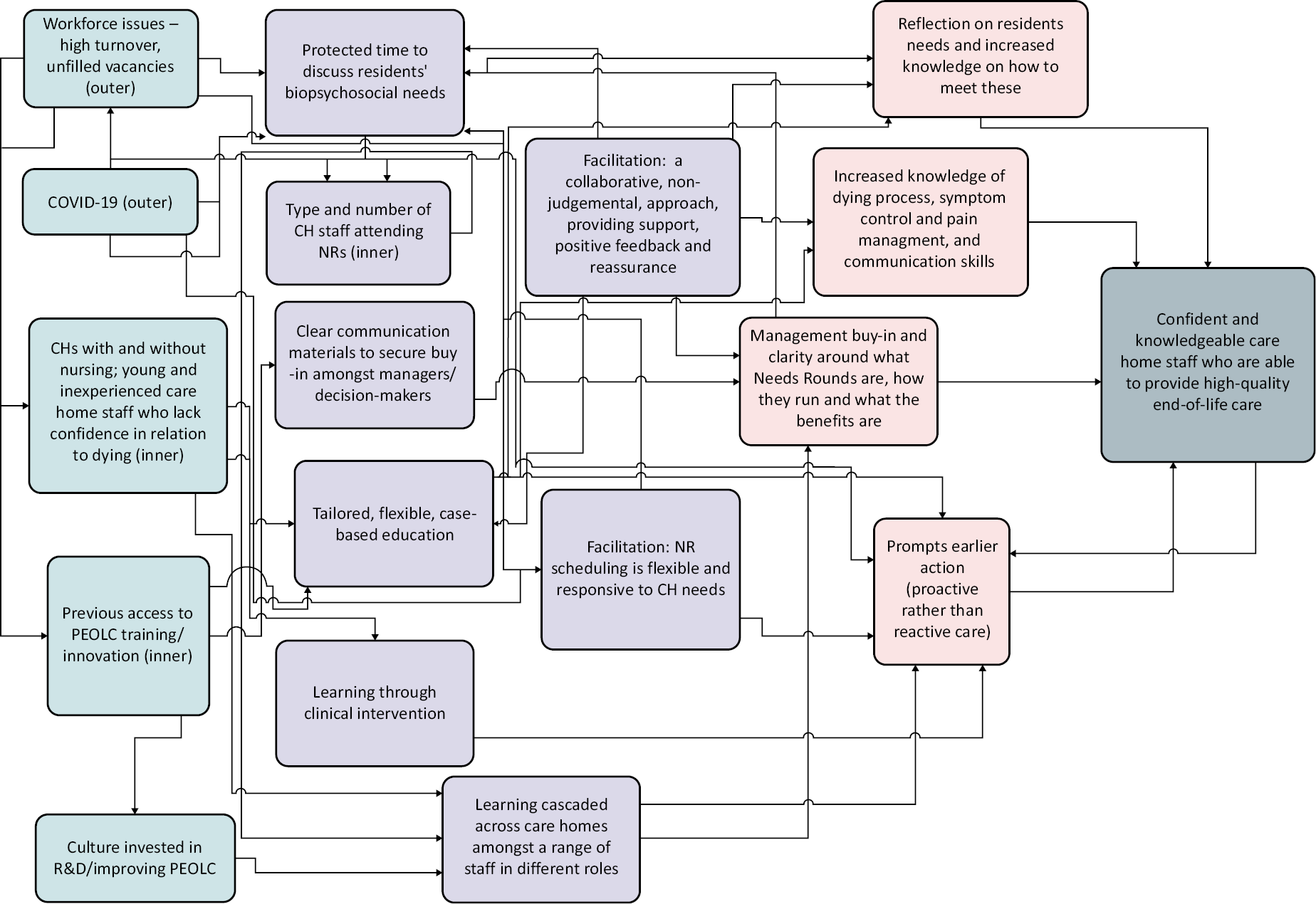
| Original | Providing case-based education (m) in a tailored way to suit staff needs (c) might improve staff confidence and competence to provide high-quality palliative and end-of-life care to CH residents |
| Revised | Providing support and learning through discussions about residents’ needs (m) in a tailored responsive way (c) improves staff confidence and competence for those who attend to provide high-quality palliative and end-of-life care to CH residents (o) |
| Code | Mechanisms | Context | Outcomes |
|---|---|---|---|
| O | Tailored case-based education provided by SPC clinicians to meet the needs of residents discussed at Needs Rounds, addressing staff knowledge/skills deficiencies (literature)1 | For people with a lack of knowledge, skills and confidence in relation to ACP, recognising deterioration, symptom and pain management, and communicating with professionals, residents and relatives (inner – local) |
Staff may be more confident and skilled to provide high-quality end-of-life care, leading to a wider perception of CHs as experts in the provision of palliative and end of life care (literature)2 |
| R | Tailored case-based education provided by SPC clinicians to meet the needs of residents discussed at Needs Rounds, addressing staff knowledge/skills deficiencies (literature)3 (confirmed) |
For high turnover within the sector, particularly amongst care staff, exacerbating the numbers of younger and inexperienced staff members who are uncomfortable with death and dying (outer) (amended) |
Improves knowledge and confidence in relation to illness trajectories, recognising and understanding different stages of dying, symptom management and communication with families and other health professionals (amended) |
| O | Management to rota in a range of different staff members to ensure that learning is cascaded amongst the organisation, including both newer and older members of staff, and a variety of job roles | For CHs impacted by macro workforce issues, with a transient workforce, to share knowledge/learning amongst more and less experienced members of staff, and for a range of staff roles (nursing, management, unit leads, carers, housekeepers, chefs etc.) (outer) |
Staff may feel confident and skilled to provide high-quality end-of-life care, including ACP, recognising deterioration, symptom and pain management, and communicating with professionals, residents and relatives |
| R | Protected staff time to discuss residents’ physical, psychosocial and spiritual needs, with management scheduling cover in rotas for staff to attend the Needs Round sessions, and people coming in on days off (amended) |
For CHs affected by macro workforce challenges (outer). Staffing issues restricted the ability of some homes to allow staff time off the floor to attend. This impacted the type of staff attending NRs, with clinical leads, nursing staff and management being more likely to attend compared to care staff. This also often resulted in low numbers of staff attending the NRs (inner – local). Staffing issues have been exacerbated by COVID-19 (outer) (amended) |
When staff were scheduled to attend, this led to improved knowledge and confidence in relation to illness trajectories, recognising and understanding different stages of dying, symptom management and communication with families and other health professionals. However, the scale of this was restricted as a result of low numbers of people being able to attend due to wider workforce issues |
| O | Clear communication materials on the benefits of Needs Rounds to secure buy-in amongst management and those in leadership positions within wider chains/organisations | For local managers and managers in CH chains to build on a culture/ethos of investment in training, learning and development (inner – organisational) |
Management may be more engaged and more likely to allocate time for staff to attend Needs Rounds |
| R | Clear communication materials on the benefits of Needs Rounds and time to secure buy-in amongst management and those in leadership positions within wider chains/organisations (amended) |
For local managers and managers in CH chains to build on a culture/ethos of investment in training, learning and development (inner – organisational) Macro workforce issues shape staffing levels (outer) (amended) |
Management more engaged and more likely to allocate time for staff to attend Needs Rounds where workforce capacity allows (amended) |
| O | Targeted education for CH staff on palliative and end-of-life care (literature) | Access to appropriate expertise (outer) (literature) across home types (residential vs. nursing) Culture of leadership in valuing education (inner) (literature) |
Staff are more confident talking about palliative and end-of-life care with residents, relatives and MDT (literature)4 CHs able to provide palliative care (literature)5 |
| R | Targeted education for CH staff on palliative and end-of-life care (literature) (confirmed) |
Access to appropriate expertise (outer) (literature) across home types (residential vs. nursing) Culture of leadership in valuing education (inner) (literature) (confirmed) |
Staff are more confident talking about palliative and end-of-life care with residents, relatives and MDT (literature)6 CHs able to provide palliative care (literature)7 (confirmed) |
| O | Proactive approach to residents’ needs can be delivered through comfort care rounds (literature) | Culture of the CH allows proactive rather than reactive care (inner/micro) (literature) | Increases in staff knowledge, practice and confidence8 |
| R | Proactive approach to residents’ needs with Needs Rounds prompting earlier action (amended) |
Culture of the CH allows proactive rather than reactive care (inner/micro) (confirmed) |
Improves knowledge and confidence in relation to illness trajectories, recognising and understanding different stages of dying, symptom management and communication with families and other health professionals (amended) |
| A | Information and access to training, services and resources outwith Needs Rounds | For people who lack access to training on palliative and end-of-life care, which has been exacerbated by COVID-19 (outer) |
Improves knowledge and confidence in relation to illness trajectories, recognising and understanding different stages of dying, symptom management and communication with families and other health professionals. |
| A | Clarity on what Needs Rounds are and how they work (innovation) | For a range of different staff members (in CHs and SPC) to ensure information is not held by few staff members, and to prevent it from being lost when staff leave (inner – organisational) |
Better engagement with Needs Rounds |
| A | Learning from NRs cascaded amongst a variety of CH staff through handovers and meetings | To ensure information is disseminated beyond those attending NRs (inner – organisational), the numbers of which have been limited by wider workforce capacity (outer) | Contradictory evidence on the extent to which this has resulted in more confident, knowledgeable staff. Care homes say this is disseminated beyond those attending NRs; however, there is a lack of knowledge about what NRs are. Some SPC are also sceptical about the extent to which this is shared beyond those attending |
| A | Planning of the NRs sessions is flexible and responsive to CH needs (when delivered and format of delivery) | To meet the needs of CHs’ established routines in a context of COVID-19 where breakouts restricted access and staff capacity reduced due to additional testing, reporting, and higher turnover (outer) | Staff enabled to engage with and attend NR sessions |
| A | Facilitation focused on relationship building – based on collaboration, partnership and a non-judgemental approach | For CH staff attending Needs Rounds who lack confidence (inner – individual) to enable full engagement with, and participate in, Needs Rounds | Improves knowledge and confidence in relation to illness trajectories, recognising and understanding different stages of dying, symptom management and communication with families and other health professionals |
| A | Needs Rounds clinical support | Provides a direct link to SPC without having to go to the GP for referral (additional resource and specialist expertise) (inner – organisational) |
Improves knowledge and confidence in relation to illness trajectories, recognising and understanding different stages of dying, symptom management and communication with families and other health professionals |
| A | Triaging residents, discussing holistic needs and tailored case-based education | Builds on CH previous experience of innovation and change (especially GSF) (inner – individual) For those who lack understanding about differences between palliative and end-of-life care (inner – individual) |
Improves knowledge and confidence in relation to illness trajectories, recognising and understanding different stages of dying, symptom management and communication with families and other health professionals |
| A | Regular feedback for SPC clinicians from CHs about their views and experiences of using NRs | For SPC who lack confidence that NR is adding value for CHs (inner – individual) |
SPC feel confident that they are providing a valuable service and feel fulfilled in their role. Building stronger relationships where support is responsive to CH staff need |
Theory 2: place of care
FIGURE 9.
Context, mechanism and outcome mapping of theory 2.
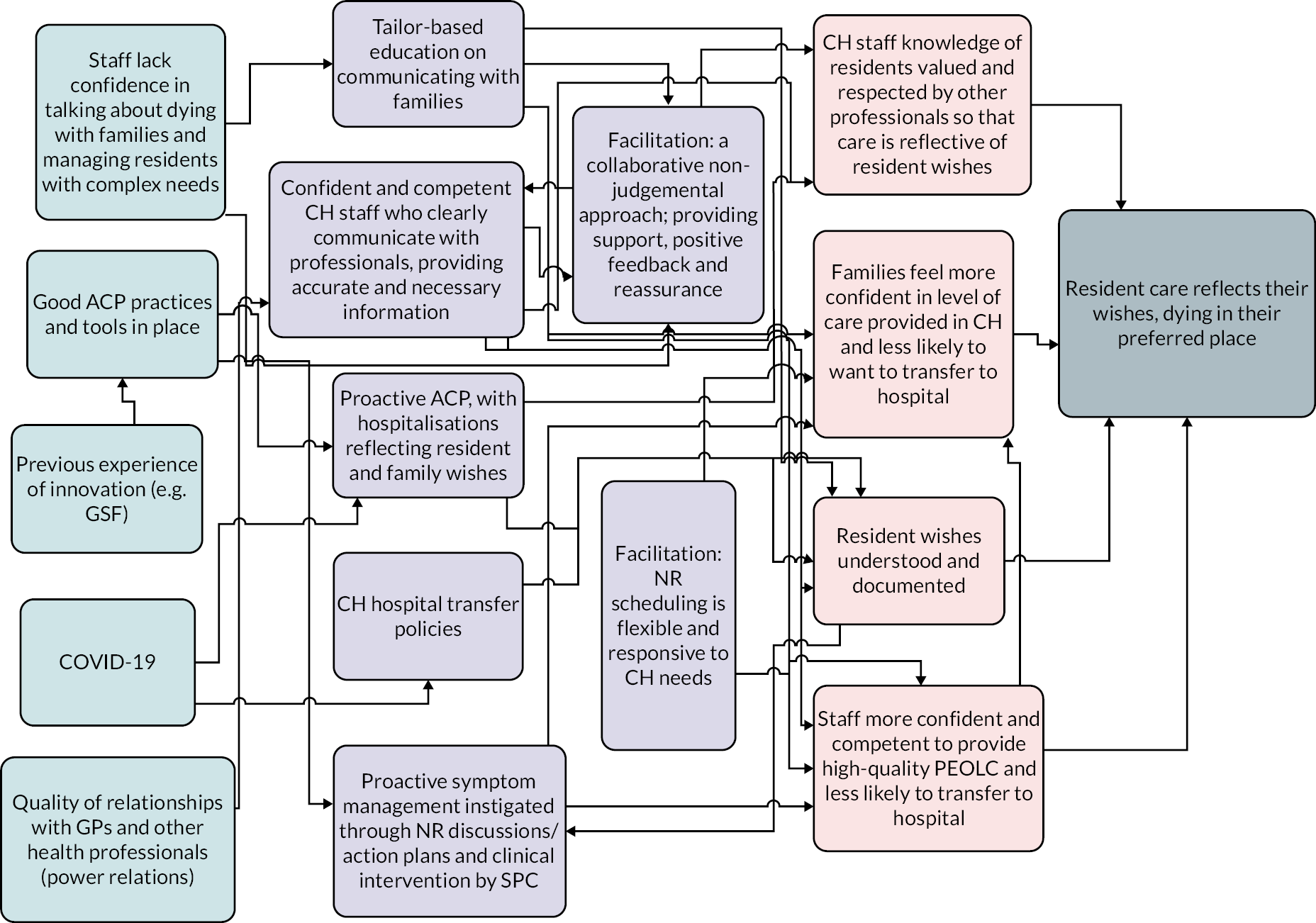
| Original | Proactive ACP (m) that is well documented, stored and shared (c) might lead to a reduction in hospitalisations and care aligned with resident preferences |
| Revised | Proactive ACP by confident and competent CH staff (m) builds on good practice (c) and reassures families and GPs about care quality, so that care is aligned with resident preferences (o) |
| Code | Mechanisms | Context | Outcomes |
|---|---|---|---|
| O | Proactive ACP facilitated by the SPC clinician, and involvement from CH staff, families, residents (where they have capacity), the GP and other relevant professionals | For residents at risk of dying without a plan in place (inner – local) and aligned with existing proactive care planning mechanisms including weekly rounds (EHCHF) and GSF meetings (outer) | May lead to better understanding of resident wishes and preferences which may reduce inappropriate hospitalisations, reduce burdensome interventions, and distress to the resident and their families, by allowing residents to receive palliative and end-of-life care and die in their preferred place. This may also lead to cost savings to the health service6 |
| R | Proactive ACP, with hospitalisation being used in accordance with resident and family wishes (amended) |
For residents at risk of dying without a plan in place (inner – local) and aligned with existing proactive care planning mechanisms, including weekly rounds (EHCHF) and GSF meetings, (outer) and using tools such as ReSPECT and NEWS2 to document wishes and assess resident needs Advance care planning practices impacted by COVID-19 (outer) (amended) |
Building on existing practice, increasing staff confidence to reduce avoidable hospital transfers, by allowing residents to receive palliative and end-of-life care and die in their preferred place. Quants data – vs. small sample (N = 5), and overall an increase from 1.6 to 2.2/1000; stay increased from 9.5 to 14.9 |
| O | Advance/anticipatory care plans and care records documented, communicated and stored using the preferred local information sharing system in a timely way. (deleted) |
For CH staff to ensure knowledge of resident is recorded and shared internally (inner – local) and shared with external professionals involved in making assessments around hospitalisations (e.g. paramedics, GPs, hospices) (inner – organisational) (deleted) |
Staff may be more confident to use best practice tools to ensure that resident preferences are documented, enabling their wishes to be respected, including around preferred place of care/death and, e.g. DNACPR. (deleted) Reason: Information on how care records talk about format – e.g. electronic and paper; some say that information not shared and others say that existing systems are used to share info (e.g. SystemOne, My Care Choices Register/Single Point). Cannot attribute this to being from NRs though, so I have deleted this from the CMO |
| O | Confident and competent CH staff clearly communicating with professionals, providing accurate and necessary information (confirmed) |
For GPs, ambulance staff and hospices involved in assessing whether hospitalisation is necessary (meso – organisational) For CHs with and without nursing to have competence to care for people with complex needs without referral out (micro – inner) (confirmed) |
Care home staff knowledge of residents valued and respected to ensure that care is responsive to needs and is in accordance with resident wishes. (confirmed) |
| O | Changes to CH hospital transfer policy to ensure this only happens when appropriate and in line with resident and family preferences (deleted) |
To guide CH staff around best practice/required processes to be followed, especially those who lack confidence and experience in ACP. (micro – inner) (deleted) |
Understanding of resident wishes and preferences which may reduce inappropriate hospitalisations, burdensome interventions, and distress to the resident and their families, by allowing residents to receive palliative and end-of-life care and die in their preferred place. (deleted: on the whole this was already in place so no change to policy happened) |
| O | Symptom management by SPC staff within CHs | Variation in access to SPC, particularly for those in remote communities | SPC decreases hospitalisations and number of deaths in hospitals9 (literature) |
| R | Proactive symptom management instigated through NR discussions/action plans and clinical intervention by SPC (amended) |
For CHs with and without nursing who may lack confidence (inner – individual) and have variable access to external palliative care support (outer) (amended) |
Staff more confident and competent to provide high-quality end-of-life care and less likely to transfer to hospital (amended) |
| O | Provide support to CH managers around palliative and end-of-life care (literature) Deleted |
Level of buy-in amongst manager and culture of open communication within CHs Inner – organisational (literature) Deleted |
More open culture of death literacy across the organisation. Decreased hospitalisation of CH residents (literature)10 Deleted Reason: data focused on providing support to a range of staff. Focus on getting management buy-in to enable people to attend, rather than showing that this results in a more open communication culture |
| A | Tailored case-based education on communicating with families | For those who lack confidence in talking to families about dying process | Families feel more confident in level of care provided and more likely to want care to be provided in the CH rather than hospital |
Theory 3: collaboration
FIGURE 10.
Context, mechanism and outcome mapping of theory 3.
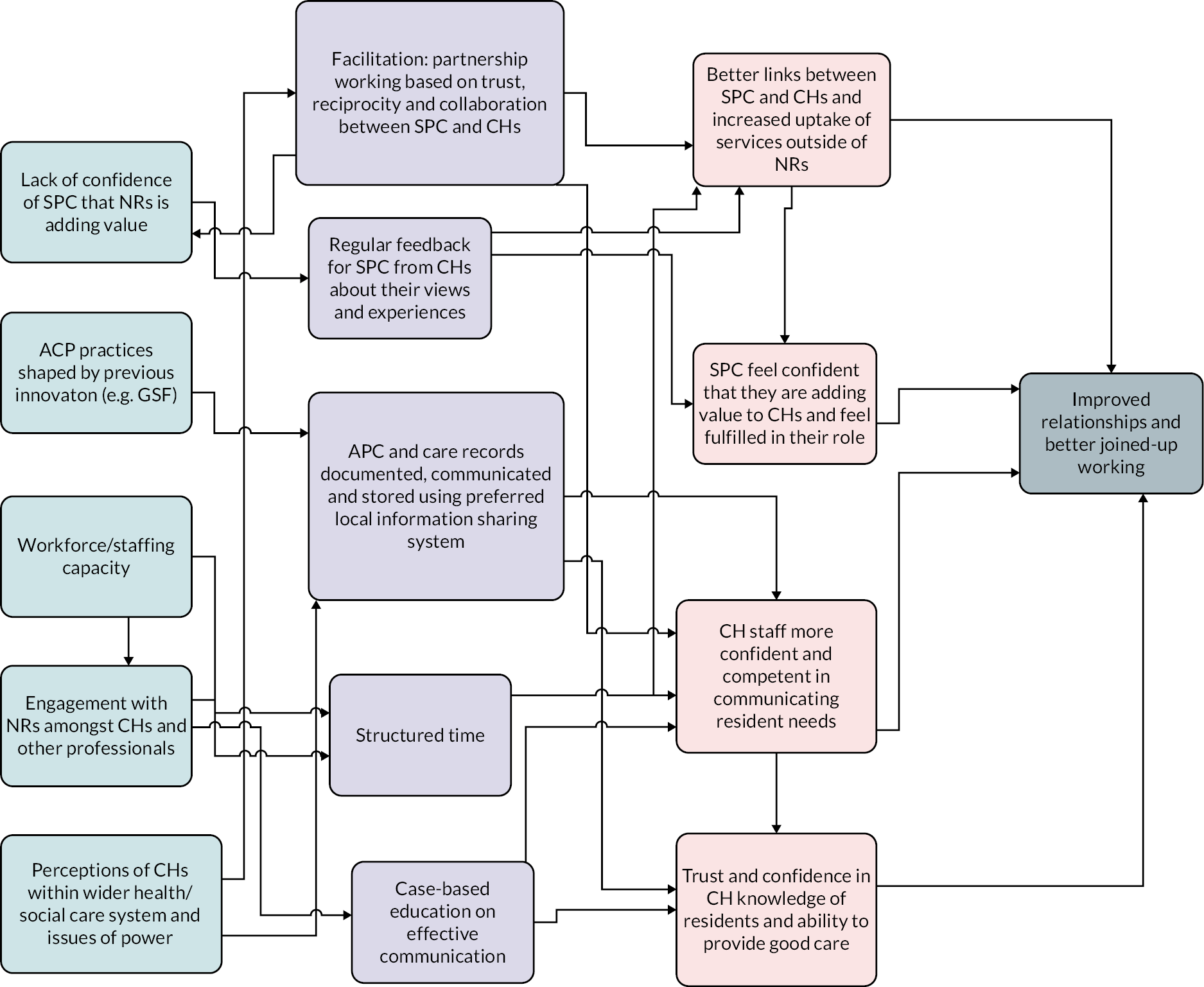
| Original | An approach based on collaboration, empowerment and partnership (m) that challenges unequal power dynamics and builds trust (c) may lead to improved relationships and better joined up working |
| Revised | An approach based on communication, collaboration and reciprocity (m) that shifts power dynamics and builds trust between CHs and SPC (c) leads to improved relationships and better resident care |
| Code | Mechanisms | Context | Outcomes |
|---|---|---|---|
| O | Partnership working, based on reciprocity and collaboration, between SPC clinicians and CHs | To build trusting relationships based on an equal partnership, where the knowledge and expertise of partners are valued and respected and to expand existing links to meet the growing number of people dying within a year of admission to hospital (literature) (inner – organisational) |
This may strengthen relationships and improve mutual understanding between hospices and CHs, leading to better engagement by CH staff in Needs Rounds and improved uptake of wider SPC out with Needs Rounds |
| R | Facilitation: partnership working, based on trust, reciprocity and collaboration, between SPC clinicians and CHs (amended) |
For CHs and SPC to build trusting relationships based on an equal partnership, where the knowledge and expertise of partners are valued and respected and to expand existing links to meet the growing number of people dying within a year of admission to hospital (literature) (inner – organisational) |
Strengthened relationships and improved mutual understanding between hospices and CHs and improved uptake of wider SPC outwith Needs Rounds (amended) |
| O | Care homes feel a sense of ownership over Needs Rounds, with support through shared facilitation and expertise (deleted) |
To empower CH workers who feel undervalued and unappreciated11 (inner – local) deleted |
Care home staff feel engaged and motivated to deliver Needs Rounds and drive forward change Deleted (reason: very difficult to engage with some of the CHs, issues with retention, issues in allowing multiple people off the floor, issues with cancellations. Although facilitation approach has been based on partnership and collaboration, it is not possible to claim that CHs felt an ownership over NRs as they were very much driven by SPC clinicians) |
| O | Structured time to develop relationships | For SPC and CHs (inner – organisational) (and others if aligned with EHCHF/GSF meetings) through proactive, monthly Needs Rounds discussions (outer) | Better knowledge amongst staff of professional roles and expertise, and boundary management, may lead to more appropriate referrals and the development of better knowledge of residents and their needs |
| R | Structured time to develop relationships (confirmed) |
For SPC and CHs (inner – organisational) through proactive, monthly Needs Rounds discussions (outer) Time restrictions due to workforce challenges (outer) (amended) |
Better links between CH and SPC and improved uptake of wider SPC out with Needs Rounds. Lack of evidence that relationships in wider system have improved. Lack of alignment with other MDTs in practice (amended) |
| O | Multidisciplinary team meetings for ACP following Needs Rounds discussions, based on a collaborative approach (deleted) |
For CH staff, the SPC clinician(s), relatives/residents (where have capacity), GPs and other relevant professionals (e.g. psychiatrists, pharmacy, geriatrician) to address challenges created through high turnover/poor continuity of CH workers, and negative attitudes towards CH staff (inner – organisational) (deleted) |
This may improve the quality of advance care plans, ensuring these reflect resident and relative preferences, and lead to better access to anticipatory medications, to prevent reactive decision-making and unnecessary hospitalisations. This may also improve joint working/the development of relationships through better communication, trust and sharing expertise, preventing duplication, and professionals taking ownership for their clinical area of care (deleted: reason – MDTs did not happen. Issues with trying to co-ordinate diaries and SPC only being hired for 2 days/week. Lack of alignment with existing provision) |
| O | Case-based education on effective communication with professionals | For CH staff with low confidence in communicating with professionals and for CHs with workforce issues (high turnover, shortages, use of agency staff), leading to blockages in communication | Improved communication, based on the provision of accurate, relevant, up-to-date information |
| R | Case-based education on effective communication with professionals, especially GPs (amended) |
Variation in quality of relationships/interagency working Power issues between CHs and other professionals (links with attitudes towards CHs) (amended) |
CH staff more confident and competent in communications, providing information based on their knowledge of their residents. Being supported by palliative and end-of-life care expert improves confidence and trust in CHs’ ability to provide high-quality care (amended) |
| O | Advance/anticipatory care plans and care records documented, communicated and stored using the preferred local information sharing system in a timely way | For CHs, acute care, primary care, hospices and other relevant professionals and aligning with existing mechanisms for ACP/reviews (EHCHs, GSF) | Up-to-date and accurate understanding of resident’s history and care wishes may enable care to be delivered in a way that reflects their preferences. This may also help to build trust and improve interdisciplinary relationships |
| R | ACP and care records documented and stored using the preferred local information sharing system in a timely way, and CH staff confidently communicating this to others (amended) |
Building on existing ACP systems already in place. Variation in systems used to document and store ACPs and care records (both paper and electronic). But issues around a lack of information sharing across different professional boundaries. A few examples of information sharing – System One used to order medications, My Care Choices Register to share care plan with different agencies. BUT issue with attributing this to NRs (amended) |
CHs know their residents wishes and communicate with relevant professionals to ensure these are met to provide good-quality lives and deaths (amended) |
| O | Formal systems for collaborative working between CHs and other services | Clarity around roles and responsibilities12 and limited infrastructure to support multidisciplinary working13 (inner – organisational) | Reduced isolation for CH staff supporting residents with complex needs Improved ACPs (literature)14 better interagency working (literature)15 |
| R | Direct link for CHs to specialist care (amended) |
For CHs who lack support from specialist and generalist services (amended) |
Stronger relationships and more responsive support for CH staff (amended) |
| A | Support from SPC through case-based education sessions, building in positive feedback and reassurance, and direct clinical work | For CHs who lacked direct face-to-face support through COVID-19 | Stronger relationships and staff feel more supported and confident to provide high-quality PEOLC |
| A | Regular feedback for SPC from CHs about their views and experiences of using NRs | For SPC who lack confidence that NRs is adding value for CHs | SPC feel confident that they are providing a valuable service and feel fulfilled in their role. Building stronger relationships where support is responsive to CH staff need |
Theory 4: better-quality lives and deaths
FIGURE 11.
Context, mechanism and outcome mapping of theory 4.

| Original | Needs Rounds (m) focused on addressing poor interdisciplinary working, suboptimal symptom management and minimal education (c) may improve palliative and end-of-life care for CH residents (o) |
| Revised | Needs Rounds (m) augment existing practice by focusing on holistic needs, improve communication deficiencies with GPs, suboptimal symptom management and minimal education (c) to improve palliative and end of life care for CH residents (o) |
| Code | Mechanisms | Context | Outcomes |
|---|---|---|---|
| O | Applied learning about palliative/end-of-life care in Needs Rounds (literature) | Suboptimal symptom management + hospitalisations are common. Staff education of symptom management typically minimal (literature) (inner – local and outer) |
May lead to improved symptom management and a reduction in hospitalisations |
| R | Applied learning through case-based education and clinical support from SPC to assess residents and manage symptoms (amended) |
Staff education of symptom management typically minimal (literature) (inner – local and outer) Impacted by COVID-19 restrictions (outer) Clinical work shaped by facilitation approach and perceived value (inner – organisational and local) (amended) |
Better relationships developed between SPC and CHs. Better symptom management and better-quality deaths for residents |
| O | Optimal death/dying is contingent on high-quality interdisciplinary care involving anticipatory and resident centred care planning (including documentation and sharing, medication reviews and physical assessments, and symptom management) (literature)15 | To engage CHs, SPC, GPs, residents, relatives, pharmacists and any other relevant professionals to work collaboratively to address unplanned and reactionary decision-making, leading to inappropriate hospitalisations16 (inner – organisational) | This may lead to well-managed death and dying. This may also result in better CQC/Care inspectorate reports as a result of improved care standards and documentation |
| R | High-quality interdisciplinary care (see T3) involving anticipatory and resident-centred care planning (including documentation and sharing, medication reviews and physical assessments, and symptom management) (confirmed) |
Variable relationships between CHs and general palliative care providers; unequal power dynamics a barrier to MDT working. COVID-19 restricted face-to-face contact but improved ACP and reduced hospitalisations. Building on good ACP practices already in place (amended) |
CHs more assertive in communication with GPs and other health/social care professionals, enabling care to be reflective of resident and family wishes (amended) |
| O | Triaging residents using the Needs Rounds checklist to prioritise who to discuss | For those most at risk of dying without a plan in place, in CHs with a lack of proactive resident-centred (inner – micro) | This may lead to those most at risk of dying have an ACP in place |
| R | Triaging residents using the Needs Rounds checklist to prioritise who to discuss (confirmed) |
For those most at risk of dying without a plan in place and building on good practice on proactive ACP (CH policies, GSF etc.) (inner – local) (amended) |
Those most at risk of dying have an ACP in place (confirmed) |
| O | Discussing physical, psychosocial and spiritual needs | For residents without a high-quality ACP in place Service availability impacted by local commissioning priorities, often centralising a medical model approach (outer) |
Residents’ end-of-life care may be more tailored to their needs and reflective of their wishes and preferences17 |
| R | Discussing physical, psychosocial and spiritual needs (confirmed) |
For CHs focused primarily on medical aspects of care such as pain and symptom management (amended) |
Care homes linked in with holistic services (e.g. complementary therapies) Residents’ end-of-life care is more tailored to their needs and reflective of their wishes and preferences (amended) |
| O | Good-quality ACP | Care home culture of completing and accessibly storing high-quality ACPs (inner – organisational) |
SPC improves the quality of life and death of CH residents18,19 and avoids futile/burdensome treatments20 (literature) |
| R | Good-quality ACP (confirmed) |
Building on CH culture of completing and accessibly storing high-quality ACPs (inner – organisational) Care home past experience of innovation (e.g. GSF and EHCHF) (inner – local) (amended) |
Good deaths reflecting resident and family wishes (amended) |
| O | Proactive symptom management and anticipatory medication management by SPC staff within CHs | Confidence and competence in symptom management amongst CH staff (inner – local) and legislation regulating anticipatory medication stock (outer) | SPC decreases hospitalisations and number of deaths in hospitals21 and avoids futile treatments 22R |
| R | Proactive care (NR prompt earlier action) (amended) |
To address reactive decision-making in CHs for those who lack confidence and competence (inner – local) (amended) |
Staff more confident and competent in pain and symptom management, leading to better-quality deaths (amended) |
| A | Clinical support from SPC to assess residents and manage symptoms | Variation in extent to which this happened. Impacted by COVID-19 restrictions (outer), but also not always offered by SPC, and not always a perceived need by CHs (inner – organisational) |
Better relationships developed between SPC and CHs. Better symptom management and better-quality deaths for residents |
Theory 5: supporting families
FIGURE 12.
Context, mechanism and outcome mapping of theory 5.
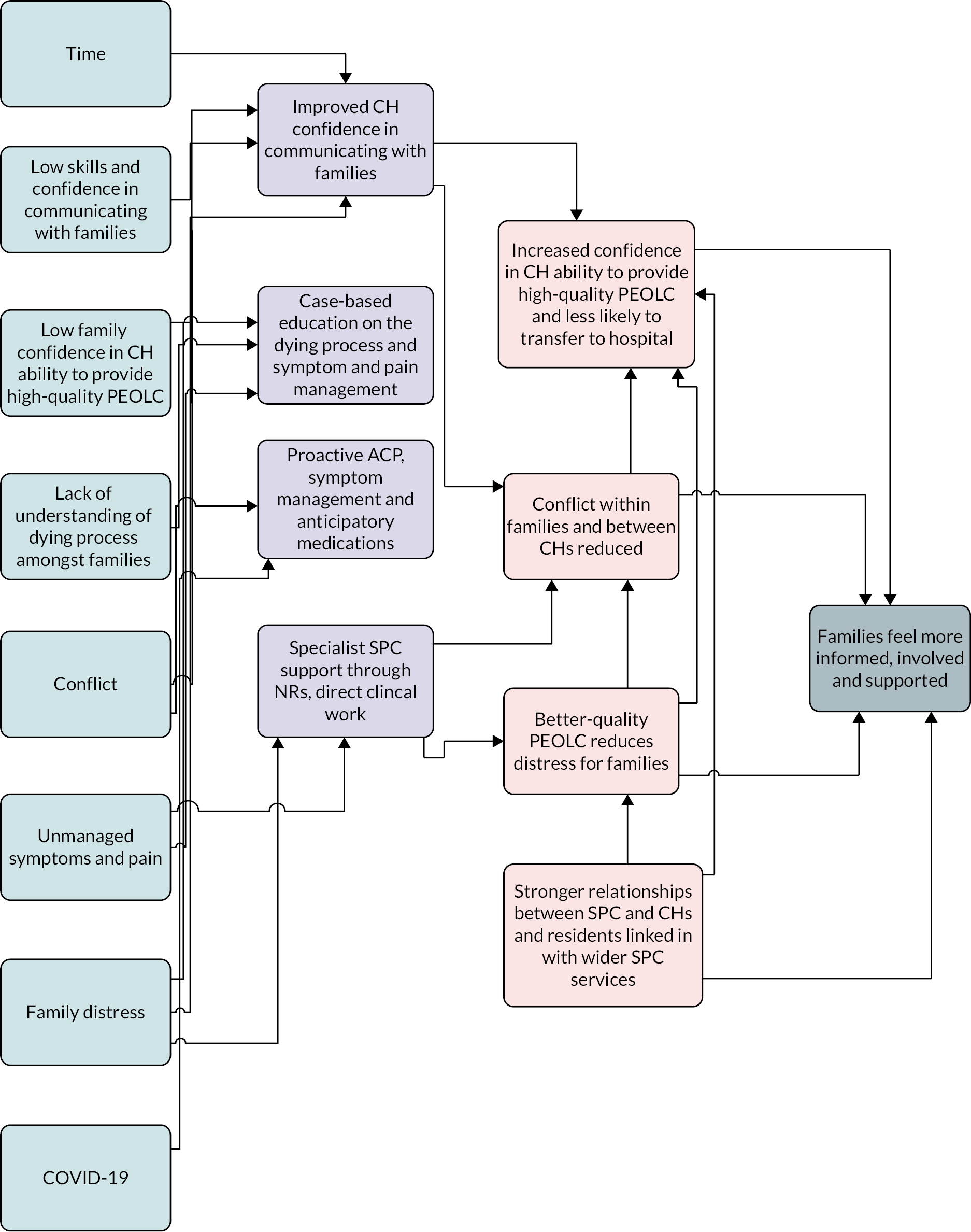
| Original | Better education for CH staff (m) to address conflict amongst families and between CHs (c) may result in families feeling more involved, informed and supported (o) |
| Revised | Better education for CH staff (m) to improve communication between CHs and families (c) results in families feeling more involved, informed and confident in the care provided to their loved one (o) |
| Code | Mechanisms | Context | Outcomes |
|---|---|---|---|
| O | Checklist including family conflict as a trigger for discussion at Needs | For CHs and family members who disagree over the desired course of care and treatment | Less conflict between family members and CH staff |
| R | Checklist including family conflict as a trigger for discussion at Needs (confirmed) |
For CHs and family members who disagree over the desired course of care and treatment (inner – individual) (confirmed) |
Care homes feel more supported in dealing with families (amended – this is about the checklist, as opposed to direct SPC support) |
| O | Case conferences delivered flexibly using face-to-face and remote options, to answer family questions around symptoms and deterioration, set goals of care and trigger LPOA process (deleted) |
For CHs in remote areas who have adapted to COVID-19 restrictions by using remote options to facilitate MDT meetings (outer). For families who lack knowledge around deterioration and dying to prevent inappropriate hospitalisations at the end of life21 (inner – micro) (deleted) |
Increased MDT meetings. Improved understanding of illness trajectory may reduce conflict with CH staff and families (deleted: reason – these have not been happening, largely due to COVID-19, so it was not possible to test these out) |
| O | Improved CH staff confidence and skills in the delivery of holistic resident-centred care | For families with negative perceptions of CHs22 (inner – micro) |
Improving the quality of care, delivered in a tailored way to meet resident wishes may improve family perceptions about CHs |
| R | Improved CH staff confidence to talk to families about dying, communicating about the high-quality care being provided (amended) |
For CHs who lack time, confidence and skills to proactively talk to families and for families with low confidence in the ability of CHs to provide high-quality PEOLC (inner – local) (amended) |
Families more confident in the quality of care being provided to their loved ones and less likely to transfer to hospital. Families feel more informed and involved (amended) |
| O | Case-based education on communicating with families and SPC having discussions with families | For CH staff who lack confidence in communicating with families, who are fearful of saying the wrong thing or being blamed and who find communicating with families emotionally challenging. SPC clinicians skilled in having conversations around end-of-life care (inner – micro) |
Staff more confident and able to have conversations with families and equipped with tools to manage emotional impact of work. SPC instigating conversations, leading to improved confidence in the CH |
| R | Case-based education on communicating with families and the dying process (amended) |
For staff members to communicate with families who do not understand the dying process and who are conflicted about care choices, and for families and CH staff who disagree over care choices, including hospitalisation. For families who have low confidence in the ability of CHs to provide high-quality PEOLC (amended) |
Resolving conflict amongst families, or between families and CHs, leading to better-quality relationships (amended) |
| O | Clear accurate and timely communication around death and dying, changes in illness trajectory and ACP | To address a lack of formal information-sharing mechanisms/consistent liaison between CHs and families,23 which is exacerbated by workforce issues including low staff ratios and high staff turnover, which restricts deep knowledge about resident needs, wishes and preferences (inner – micro and outer) |
Families may feel more informed, involved and supported. Families may be less likely to disagree with each other and disagree with staff around the best course of action |
| R | Clear accurate and timely communication around death and dying, changes in illness trajectory and ACP (confirmed) |
For CH staff who lack confidence in communicating with families For staff who lack time, which is exacerbated by workforce issues including low staff ratios and high staff turnover, which restricts deep knowledge about resident needs, wishes and preferences (inner – micro and outer) |
Families may feel more informed, involved and supported. Families may be less likely to disagree with each other and disagree with staff around the best course of action (confirmed) |
| O | Prioritising the delivery personalised (rather than service/policy-oriented) care (literature) (deleted) |
Flexible adoption and use of care and decision-making protocols (such as transfer to hospital) (literature) (deleted) |
Family no longer required to adopt a care co-ordinator role; greater confidence in the CH24 (literature) (deleted) (no direct feedback from family and this has not come out of interviews with CHs and SPC) |
| O | Proactive symptom management by SPC staff within CHs | Variation in access to SPC, particularly for those in remote communities | SPC decreases hospitalisations and number of deaths in hospitals (literature) and increases family confidence in the care provided25 |
| R | Specialist support for CH staff from SPC through NRs and direct clinical work, including proactive symptom management, and better links with hospice (amended) |
For residents experiencing pain and other symptoms. For families who lack confidence in CH ability to provide high-quality care and who experience distress seeing their loved one in pain. (inner – local) Variation in access to SPC, particularly for those in remote communities (outer) (amended) |
Residents linked in with wider hospice services (e.g. complementary therapies). Increased family confidence in care provided resulting in reduced distress for families (amended) |
List of abbreviations
- ACP
- advance/anticipatory care planning
- CAPA
- capability of adopting a palliative approach (questionnaire)
- CCI
- Charlson Comorbidity Index
- CH
- care home (including with and without nursing care)
- CMO
- context, mechanism, outcome
- EAPC
- European Association of Palliative Care
- ECOG
- Eastern Cooperative Oncology Group (a measure of patient functioning)
- EHCH
- Enhanced Health in Care Homes
- GP
- general practitioner
- GSF
- Gold Standards Framework
- i-PARIHS
- integrated Promoting Action on Research Implementation in Health Services (methodology)
- JIC
- Just In Case medicines
- MDT
- multidisciplinary team
- NEWS
- National Early Warning Score
- PI
- principal investigator
- PIS
- participant information sheet
- PPIE
- patient and public involvement and engagement
- QODDI
- Quality of Death and Dying Index (questionnaire)
- REC
- research ethics committee
- RF
- research fellow
- SPC
- specialist palliative care
- SROI
- social return on investment
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/KRWQ5829).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
