Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 15/15/09. The contractual start date was in November 2016. The final report began editorial review in September 2021 and was accepted for publication in June 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Perkins et al. This work was produced by Perkins et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Perkins et al.
Chapter 1 Introduction
Parts of this report have been reproduced from Eli et al. 1,2 These are Open Access articles distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Eli et al. 3 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 (CC BY-NC-ND 4.0) license, which permits others to copy and distribute this work, for non-commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Background and study rationale
This study evaluated the use of the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) process during the early implementation phase (first 2 years) in acute NHS trusts in England. ReSPECT is an emergency care and treatment plan (ECTP) designed to address the shortcomings of standalone do not attempt cardiopulmonary resuscitation (DNACPR) decisions.
Cardiopulmonary resuscitation (CPR) is a highly invasive medical treatment that is associated with potentially serious complications (e.g. rib fractures, sternal fractions, internal organ damage). 4 CPR attempts on someone with minimal comorbidities and a reversible cause of cardiac arrest can be life-saving. 5 Conversely, if CPR is attempted as someone approaches the end of their natural life, then it has little chance of success and deprives them of a dignified death. DNACPR decisions, introduced in the 1970s, provide a system through which CPR may be withheld in the event of cardiac arrest, which occurs as part of the process of natural death. 6 Current UK guidelines describe a DNACPR decision may be made:
-
at the request of a patient
-
if CPR has little chance of success
-
where the burdens of treatment outweigh the benefit.
Although DNACPR is a relatively straightforward concept, independent reviews7–10 identified the following substantial problems with the process of DNACPR decision-making and implementation:
-
A reluctance or fear in both patients and doctors to discuss CPR, leading to failures to involve patients in decision-making. 10–13
-
Poor communication with patients and people important to them (e.g. their family). 10,14–16
-
Variable levels of understanding of the incorporation of ethics issues in clinical decision-making. 10
-
CPR decisions being made in an ad hoc manner, with variation across different care settings, within similar care settings (e.g. hospitals, care homes, general practices) and among individual clinicians. 11,17
-
Unjustified DNACPR decisions being made for people with physical and mental disabilities. 8,18
-
Variation in the method of recording CPR decisions, and inconsistency in which methods of recording are accepted in different geographical regions and by different organisations within those regions, making good communication problematic. 19,20
-
People being subjected to CPR attempts that will be of no benefit or are contrary to their wishes. 7,10,15
-
Conflation of the term ‘DNACPR’ (which is meant only to apply to resuscitation) with limitations on other elements of care and treatment. 10,21,22
-
Evidence that patients with DNACPR decisions receive poorer care than patients with similar conditions and backgrounds without such decisions in place. 11,23,24
An ECTP is a patient-centred advance planning process for potential future emergency treatment situations. ECTPs seek to provide guidance on emergency treatments (including CPR) that should be considered in the event an emergency situation arises where the person does not have capacity to communicate their values and preferences or where there is insufficient time to consult. ECTP encompasses approaches variously described as limitation of treatment, limitation of care and treatment escalation plans (TEPs). Examples include the Universal Form of Treatment Options (UFTO), personal emergency plans and the Physician Orders for Life-Sustaining Treatment (POLST).
Evidence indicates that ECTPs may address care quality concerns associated with standalone DNACPR decisions. Evaluations of the POLST have shown that the system improved communication,25,26 implementation of end-of-life preferences and patient satisfaction. 27–31 In the UK, an evaluation of the UFTO found that UFTO was associated with a 23.3% [95% confidence interval (CI) 7.8% to 36.1%] reduction in harms (measured by the global trigger tool23) and that UFTO provided clarity of goals of care and reduced negative associations with resuscitation decisions. An internal evaluation of Gloucestershire Hospitals NHS Foundation Trust’s Unwell Patient escalation pathway found that the pathway reduced (from 17% to 5%) the proportion of resuscitation cases terminated for futility and increased (from 17% to 28%) overall cardiac arrest survival (David Gabbott, Gloucestershire Hospitals NHS Foundation Trust, 2015, personal communication).
In October 2014, a stakeholder meeting for patients, clinicians and policy-makers to discuss findings of the DNACPR decisions evidence synthesis project10 identified the need for a national ECTP as a priority. Patients, clinicians and policy-makers recommended early evaluation following criticism by the independent enquiry into the Liverpool Care Pathway32 concerning absence of evaluation early in the national adoption process. The 2015 Health Select Committee report echoed the urgent need for such work. 9
Evidence and stakeholder recommendations prompted the Resuscitation Council UK (RCUK) (London, UK) and the Royal College of Nursing (London, UK) to establish a National Working Group to develop a national ECTP process, building on previous work. The National Working Group had representation from patients, professional organisations, regulatory bodies, the Care Quality Commission (CQC) (London, UK), acute, community and ambulance service NHS organisations, and patient and public members. Through an iterative development and usability testing process,33 an ECTP (i.e. the ReSPECT process) was produced. The ReSPECT process was adopted by the first acute NHS trusts in late 2016 and early 2017, and more widely from February 2017. The RCUK and the National Working Group provide support for organisations adopting the ReSPECT process and monitor its use. The ReSPECT process was designed for use with all patients
As noted earlier, ECTPs have been found to improve communication. Clinicians engaging with their patients to make a ReSPECT plan is central to the ReSPECT process. 33 Sharing the process of making the recommendations made on the ReSPECT plan has similarities with shared decision-making, which has been receiving increased policy, practice and research interest. The NHS Long Term Plan34 commits to giving people more control over their own health and more personalised care. The delivery plan for that objective of universal personalised care describes how the comprehensive model for personalised care should reach 2.5 million people by 2023/24. 35 A central component of the comprehensive model is the use of shared decision-making.
The ReSPECT process is a process that leads to recommendations about future clinical decisions in case an emergency arises, but it is not in itself a treatment decision. The ReSPECT process is designed for patients and families to share in the process of making ReSPECT recommendations and to agree them with their clinician. The responsibility for the recommendation stays with the clinician and responsibility for the eventual treatment decisions lies with the clinician caring for the patient at the time the emergency or urgent care is needed.
Understanding how, when and where the ReSPECT process was used in practice early during its adoption in UK NHS acute hospitals (1) allowed assessment of how far the ReSPECT process was going to address concerns associated with standalone DNACPR processes and (2) provided useful information about how clinicians approach making shared recommendations for future clinical treatment. We anticipated that the ReSPECT process would be used for all patients in acute settings as it was designed to be. The primary focus of this study was to evaluate how and where the ReSPECT process was used to support the DNACPR process in the acute care setting and its impact on patients. A wider evaluation of the process of implementation of ReSPECT was beyond the scope of this study.
Overview of research design, aims and objectives
This study focused on how, when and why ReSPECT process recommendations are made and what effects they have on patient outcomes in early adopting acute NHS hospitals. The rationale for focusing on acute settings was that (1) adoption was likely to occur initially in hospital settings, (2) 78% of incidents and complaints relating to DNACPR occurred in the hospital setting (with 90% of those incidents and complaints associated with severe harm or death),10 and (3) UK literature reports problems with communication, decision-making and implementation of DNACPR decisions in this setting. 10
We included some evaluation of adoption in the communities our six sites served through (1) evaluating the frequency, process and ethics basis of decisions in patients presenting to hospital with an ECTP decision initiated in the community and (2) conducting focus groups with community clinicians.
Design
Our mixed-methods evaluation comprised four work packages. The evaluation investigates different areas of practice and service organisation that the introduction of the ReSPECT process aims to affect and provides a narrative summary of key findings across the work packages. The work packages are reported in detail in subsequent chapters, as follows.
Work package 1 (see Chapter 2)
The first work package is a qualitative study of ReSPECT decision-making processes, using observations of ReSPECT conversations and interviews with clinicians and patients/family members, and an analysis of the quality of ReSPECT form completion. These data are combined with interviews and focus groups with general practitioners (GPs) and other community staff regarding their experiences of the ReSPECT process (note that this was originally part of work package 4 but is reported with work package 1).
Work package 2 (see Chapter 3)
For work package 2, we carried out an interrupted time series (ITS) analysis using measures of process and survival outcomes for in-hospital cardiac arrests (IHCAs), using data from the National Cardiac Arrest Audit (NCAA), a survey and freedom of information request about use of DNACPR forms and other emergency planning approaches. The planned analysis covered 2 years before and 2 years after ReSPECT implementation.
Work package 3 (see Chapter 4)
Work package 3 was a retrospective observational study that comprised descriptive and regression analyses, using routinely collected data from adult acute patient medical records and the NHS Safety Thermometer audit.
Work package 4 (see Chapter 5)
The final work package (i.e. work package 4) provides a narrative summary of key findings from each previous work package (i.e. work packages 1–3).
Aim
We aimed to determine, in adults admitted to acute NHS hospitals, how, when and why ReSPECT plans are made, as well as what effects ReSPECT plans have on patient care.
Objectives
The overarching objectives of each work package were as follows.
Work package 1
-
To describe the clinician decision-making processes behind ReSPECT form completion, including how, when and why judgements are made, their ethics basis and patients’/families’ understanding and experiences of the process.
-
To explore the ethics basis and the experience of patients/families in the decision-making process.
-
To explore GPs’ experiences of the ReSPECT process, including uptake and attitudes to the ReSPECT process in the community, and how the ReSPECT process transfers across the acute/primary care boundary.
Work package 2
-
To quantify the effect of the introduction of the ReSPECT process on the frequency of, and outcomes from, in-hospital resuscitation attempts when compared with standalone DNACPR decisions.
Work package 3
-
To present a descriptive summary of patient characteristics according to ReSPECT treatment recommendation and to conduct an analysis of whether or not a DNACPR decision, made in the context of an overall treatment plan, is independently associated with risk of patient harm.
Work package 4
-
To synthesise the key findings from the study, to identify future research priorities from the patient, clinician and policy-maker perspective and to effectively disseminate findings, ensuring that key messages are integrated into future development work of the ReSPECT process.
A description of the context for implementation from regular meetings between sites, researchers and the ReSPECT National Working Group was planned as part of work package 4, on the recommendation of the Study Steering Committee. However, this work was discontinued because the ReSPECT National Working Group developed support and monitoring systems that would have duplicated this aspect of the study and this placed an undue burden on participants.
The ReSPECT process
The ReSPECT process involves discussion and is recorded on a two-sided form. During this study, versions 1 and 2 of the form were in use (see Report Supplementary Material 1). Both versions of the form were broadly similar, but with the second version clarifying how to record capacity and who was involved in the discussions during the process. The first page of the forms contains identifying information and relevant information about the patient’s medical history and condition, a section for recording patient preferences for care and treatment, a record of the focus of the clinicians’ recommendations for either life-sustaining or comfort care and then a space to record the individual clinical recommendations. The second page of the forms requires a record of the patient’s mental capacity, their own or their families’ involvement in making the plan and where in the medical records full details of the discussion are documented. When early adopting sites implemented the ReSPECT process, few supporting materials were available; however, these materials have been expanded during the course of the study and are available via the ReSPECT website [URL: www.resus.org.uk/respect (accessed 30 September 2022)].
Setting
Six acute NHS trusts and GPs from the areas of the trusts were purposefully selected for in-depth qualitative and quantitative evaluations. All acute hospital trusts that were participating in the NCAA were analysed in the ITS component.
Characteristics of sites
Of the six acute NHS trusts participating in work package 1, three implemented the ReSPECT process between December 2016 and December 2018. We used purposive sampling for diversity according to volume of admissions, performance according to CQC banding, social class and ethnic mix of populations served, and approach to ReSPECT implementation and its uptake.
Four sites were teaching hospitals with general and specialist regional and national services. One site comprised three district general hospitals. All sites provided some specialist services to national and international patients, although these services differed in number and specialties. The numbers of inpatient beds in participating hospitals ranged from 450 to 1300. Inpatient activity ranged from over 100,000 a year to over 200,000 inpatient and day case admissions. Trusts with more than one acute hospital chose which trust(s) would participate in the study. During the study, two of our sites merged to form one trust (but retained their different approaches to the ReSPECT process during the study) and one trust merged with another trust not participating in this study. Our participating trusts had CQC ratings of either ‘needing improvement’ or ‘good’ from inspections around the beginning of the project in 2016–17. One trust had recently improved from a CQC rating of ‘inadequate’.
Sites covered urban (n = 3), both rural and urban (n = 2) and mostly rural (n = 1) populations. Populations served by participating trusts ranged from approximately 500,000 to > 1,000,000 people. Two trusts served areas with a larger, than average, ethnic minority population. Two trusts served areas with a larger, than average, white population. One trust served a mixture of areas, with some areas having larger, than average, ethnic minority population and other areas having a larger, than average, white population. Based on the Index of Multiple Deprivation (IMD) figures,36 two trusts served areas in which the majority of the population was more affluent than the average in England, whereas four trusts served areas in which the populations were more deprived than average. Childhood poverty rates ranged from almost 15% to 33% in areas served by the different trusts. Compared with the average life expectancy in England, life expectancy was worse for some trusts’ populations, but better in other trusts’ populations.
We were unable to select sites according to type of ReSPECT implementation, as planned, because of the small number of early adopting sites from which to recruit at the time. An overall summary of the implementation approaches used by sites follows.
Three sites changed from using a standalone paper-based DNACPR system to a paper-based ReSPECT system, and one of these sites also developed an electronic version during the study. One of the previous DNACPR systems was area wide (i.e. covering local acute trusts, community health-care organisations and the ambulance service). Another site used an area-wide DNACPR form and recorded escalation plans separately in the patient record. One site had its own electronic ECTP and changed to using an electronic ReSPECT form. One site has been using its own electronic ECTP for several years prior to implementing the ReSPECT process. Here, additional sections from the ReSPECT from were added to the site’s own ECTP on the electronic system and the site was piloting the actual ReSPECT form (paper version) on two wards. Adoption of the ReSPECT process in general practices in the areas served by our sites varied. In the two sites that had an area-wide DNACPR system and one other site, general practices across the area also adopted the ReSPECT process, but later than the acute trusts. At another site, the Clinical Commissioning Group (CCG) adopted the ReSPECT process a considerable time after the acute trust. At two sites, there was no area-wide plan to adopt the ReSPECT process at the time of the study.
All sites had a ReSPECT implementation lead. The professions of the ReSPECT implementation leads varied from resuscitation officers to medical or palliative care consultants. Working groups supported the lead at all sites to varying degrees, particularly when it came to running implementation activities. Some working groups included representation from community health-care providers and the ambulance service, and most working groups involved a range of clinicians from different acute specialties.
Five sites implemented the ReSPECT form on 1 day. At the sixth site, the adaptation to the site’s own ECTP was implemented on 1 day, and the pilot of the full ReSPECT form was conducted on two wards. The working groups carried out awareness-raising activities and conducted staff education for between 2 and 6 months before the implementation date. Most sites reported using e-mail, banners on trust intranets and attending meetings and giving presentations to raise awareness.
Staff education about the ReSPECT process included presentations, information tailored to different professions and, in some cases, advanced communication training for staff who would conduct ReSPECT conversations. One site emphasised the differences between its existing ECTP and ReSPECT as a focus for its training. Not many educational materials were available to the early adopting sites from the National Working Group and some sites reported developing their own. Some sites developed their own patient information leaflets. Some sites also used reminders and prompts to help embed the ReSPECT process. Audits were used to monitor progress and provide feedback.
Sites developed their own policies for the ReSPECT process, including policies regarding who could conduct ReSPECT conversations and who should take responsibility for what was recorded on the form. At most sites, a consultant was the senior responsible clinician, but at several sites a senior specialist trainee could be too. At some sites, junior doctors and senior nurses could initiate ReSPECT conversations; however, senior doctors had to review the process and sign forms as the responsible clinician. In other sites, junior doctors could sign ReSPECT forms as long as they were reviewed by a senior doctor within a specified time frame.
Patient and public involvement
Grant application
We discussed and refined the study design and end points at a patient and public involvement (PPI) meeting. The PPI group felt that the overall design captured the key priorities from the October 2014 stakeholder meeting. The PPI group encouraged use of routinely available information. Observation of ReSPECT conversations was considered feasible provided that the process was handled sensitively. The team’s proposal to use patient experience questionnaires was rejected in favour of the richer perspectives that could be obtained from patient and relative interviews. The PPI group agreed to become the study’s PPI Advisory Group.
Strategic oversight
The Study Steering Committee had two PPI members. At their request, the PPI Advisory Group and the study team agreed that they could attend the PPI Advisory Group meetings throughout the study to facilitate communication between the groups and to contribute their insights and expertise to the PPI Advisory Group.
Management
Our funded PPI co-applicant’s contribution included development of the study proposal and subsequent protocol, discussion of consent processes, attendance at PPI Advisory Group meetings and review of patient information resources.
PPI Advisory Group
The PPI Advisory Group met approximately every 6 months or when there was a particular need for their advice. At all meetings, the study team updated the PPI Advisory Group on progress. Each meeting focused on areas where the study team needed PPI input. The first meeting involved a discussion of different consent models for different work packages that informed the Health Research Authority application for Research Ethics and Confidentiality Group approvals (details are reported in Report Supplementary Material 2).
Advice was sought on the direction of work package 1 qualitative data collection, based on early analysis of interview and observation data, to ensure that emerging issues of concern for PPI members would be explored in the remaining data collection. The group provided input for topics used in the GP focus groups. When the study was designed it was anticipated that the ReSPECT process would be used for a broad population; however, in practice, the ReSPECT process was used mostly with acutely unwell patients. The PPI group and the study team discussed their concerns about the difficulties in collecting interview data from patients and families/friends, and this discussion informed an amendment to include patients with a ReSPECT form who were not part of clinician observations (although this did not substantially increase patient recruitment) and to conduct informal observations on wards for further context. The PPI group advised that future research should consider how best to capture the patient voice (e.g. include interviews with patients when they are not so acutely ill).
The PPI group advised that our findings would be complex, covering difficult issues, and that we should use creative mediums and formats (e.g. plays, videos) that people could understand and respond to for dissemination.
Members of the PPI group commented on papers and provided input for the final report. Members of the PPI group have also advised on future research to evaluate the ReSPECT process in community settings.
We originally planned a meeting to present findings to stakeholders, including public and patient representation; however, owing to the COVID-19 pandemic, this event could not be held. Likewise, owing to the COVID-19 pandemic, we have had to modify our plans for a stakeholder meeting that would have included PPI representation. Instead we delivered a virtual dissemination event that included members of the PPI Advisory Group.
Members of the PPI Advisory Group and Study Steering Group were recruited through the University of Warwick’s (Coventry, UK) User Teaching and Research Action Partnership (UNTRAP) and co-applicants’ networks. UNTRAP provided initial advice and training for the study PPI members who needed it and Warwick Clinical Trials Unit (Coventry, UK) (WCTU) provided update training in 2019 for some members. All PPI study advisors were offered remuneration for their work.
Ethics approvals
We gained NHS ethics approval (reference 17/WM/0134) and Confidentiality Advisory Group (CAG) approvals (reference 17/CAG/0060) for the study. A summary table of the approvals, including amendments, is presented in Report Supplementary Material 2. The study sponsors were the University of Warwick (lead) and University Hospitals Birmingham NHS Foundation Trust (Birmingham, UK).
Ethics issues
The main ethics issues concerned consent and confidentiality. The degree of patient, relative and staff involvement and intrusiveness of the research varied between work packages. We gained approvals for different consent models that were proportionate, depending on what was being asked of research participants.
The research involved five main activities:
-
Interviewing clinicians, patients and families.
-
Observing clinicians engaged in ReSPECT conversations with patients and/or families.
-
Contextual observations and informal conversations about the ReSPECT process.
-
Accessing clinical records.
-
Use of anonymised data from the NCAA.
Interviewing clinicians, patients and families
We obtained written informed consent from clinician, patient and relative interview participants. Approaching patients and family members around the time a ReSPECT discussion occurred raised concerns about intrusion of privacy and causing further distress to patients and families who would already be anxious. The clinical team caring for the patient made the first approach and guided the researcher as to whether or not it was appropriate to approach the patient/family and, if it was appropriate, the timing of any approach. Interviews were tailored to individual patient and family member needs and could be brief. It was made clear that the interview could be stopped at any time if the participant wished to so.
To facilitate participation of people who did not speak English or who were deaf and able to use sign language, we made provision for a translator who was not a member of hospital staff.
Observation of clinicians engaged in making ReSPECT recommendations
We sought written informed consent from clinicians for observing their involvement in developing ReSPECT recommendations. The focus of the researcher’s observation was the clinician. However, the researcher was present when the clinician interacted with a patient or member of the patient’s family. At the start of any such interaction, the clinician introduced the researcher to the patient/family member and sought their permission for the researcher to remain, explaining that the researcher was there to observe the clinician. If the patient/family member did not want the researcher to be present, then the researcher would withdraw. The patient/family member could change their mind at any point without giving a reason and without prejudice. Verbal consent was sought from other staff present during observations.
For logistical reasons, it was not possible to obtain written consent from all patients and their families for the presence of a researcher conducting observations within a particular clinical area (e.g. hospital ward/emergency department). However, information about the study was displayed in these clinical areas and the researchers were clearly identified by their attire (i.e. a top with the word ‘researcher’ printed on the front and back).
Clinicians with whom the researcher had informal conversations regarding the ReSPECT process gave verbal consent. The researcher used pseudonyms to anonymise all participants in fieldnotes.
Accessing clinical records
The study required the research team to access relevant information from the patients’ clinical records and NHS Safety Thermometer audit data. Our approach sought to balance (1) respect for the patient’s right to information in their medical record being treated confidentially, (2) the risk to the validity and public interest in the research being harmed by a biased sample, and (3) consideration of practicable alternatives to obtaining consent.
This part of the data collection was the subject of our CAG approvals. CAG approvals allowed us to collect pseudoanonymised data on all eligible patients on participating wards from patient records without the patient’s consent. We provided study information leaflets that detailed how patients could inform study staff that they did not want their data collected or that they wanted their data removed after collection and before the end of the study data collection period. The rationale for CAG approvals is outlined in Report Supplementary Material 3.
Use of anonymised data from the National Cardiac Arrest Audit
Anonymous data from the NCAA were transferred in accordance with appropriate regulations and WCTU standard operation procedures on data security to the University of Warwick study team. The data were accessed by the study statisticians only and contained aggregated data with no individual patient-level data. The NCAA hold this information under CAG approval [reference ECC 2–06(n)/2009]. The NCAA Management Committee gave permission to access the data required for this study.
We planned repeated annual surveys to understand what systems were in place to record DNACPR decisions; however, after a poor response to the first survey, we gained additional approval to conduct freedom of information requests to NCAA participating sites. We needed a much higher response rate to conduct a robust analysis.
Outline of report content
In Chapters 2–4 we report each work package in more detail, and this is followed by a narrative synthesis of findings from all work packages in Chapter 5 and a discussion of overall findings, assessment of future research needs and conclusions in Chapter 6.
Chapter 2 Qualitative study of decision-making processes
Introduction
Although DNACPR processes have been widely used in hospital practice, increasing evidence shows that these processes are ethically fraught. In particular, audits and evaluations of DNACPR forms have shown that these forms are interpreted inconsistently by health-care staff, potentially carrying unintended consequences for patients, such as the denial of other types of treatment. 24,37–39 DNACPR decisions are often not accompanied by transparent documentation of decision-making processes and do not contextualise this decision within the patient’s preferences and wider treatment. 16,40,41 As DNACPR forms tend to be institution specific, the forms cannot be transferred across medical settings. 19,41 Historically, DNACPR decisions were often made without involving or informing patients and their families. 11,21,38 Following the Court of Appeal judgment in R (Tracey) versus Cambridge University Hospitals NHS Foundation Trust and others in 2014,42 it is a legal requirement in the UK for clinicians to consult with patients, or families of patients who lack capacity, about these DNACPR decisions. Few recent studies have investigated CPR discussions or decision-making post the Tracey judgment.
The ReSPECT process aims to place CPR recommendations within broader treatment considerations. 43 The goal of ReSPECT conversations are that patients and clinicians develop a shared understanding of the patient’s condition and preferences, agree on a direction of emergency care and treatment, and make shared recommendations about treatment options, including CPR. 44 Previous research on DNACPR and advance care planning (ACP) conversations found that patient involvement in decision-making is often inconsistent, with variations in the extent to which clinicians seek patient input or engage with patient values. 21,45 An integrative review noted that patients expect CPR-related conversations to elicit their values and preferences for shared understanding and decision-making. 46 However, a systematic review of ACP processes found that doctors use conversation scripts to overcome unpredictability and prompt their preferred medical decision. 45 Doctors hold differing views over whether or not patients should decide for themselves about resuscitation and treatment escalation, with decisions reliant on either patient preference or medical opinion,38 and this either/or approach runs counter to the ReSPECT process, which is designed for shared understanding. 43
Research suggests that ECTP forms facilitate conversations between clinicians and patients. 47 The ReSPECT process is supported by the ReSPECT form, which, in the community, is a patient-held document that is completed by clinicians. 43 The ReSPECT form is designed to prompt clinicians to discuss emergency treatment options with patients to (1) structure the documentation of decision-making for greater transparency and (2) be carried by patients across medical settings. 43 Through successive open-text boxes, the ReSPECT form facilitates a stepwise summary of discussions and decision-making. Taken together, the sections of the ReSPECT form are aimed at promoting the consistency, transparency and ethics justifiability of clinical decision-making.
Objectives
Our objectives were as follows:
-
To describe the decision-making process, including how, when and why judgements are made, their ethics basis and patients’/families’ understanding and experiences of the process, through a case study evaluation of ReSPECT decisions in clinical practice and a review of written records.
-
To establish uptake and attitudes to the ReSPECT process in the community through (1) focus groups with GPs, (2) collection of contextual data on ReSPECT implementation at sites, (3) a synthesis of findings and (4) identification of areas for improvement and further work.
For the case study evaluation, we sought to determine the following:
-
How, when and why are clinicians making ReSPECT decisions in the acute hospital setting?
-
What happens when a patient brings a ReSPECT form or a similar document from the community to hospital?
-
How is the ReSPECT system used within the process of decision-making?
-
To what extent is the patient, and where appropriate family members, involved in the decisions? (Note that by ‘decision’ we mean the decision to make a ReSPECT recommendation, and our focus is on patient/family involvement in the process of thinking through and making this recommendation.)
-
How do patients/family members experience the decision-making process and their subsequent care?
-
What influences the ReSPECT decision-making process, including considerations of ethics (or not), and why?
-
From the clinician perspective, what are the perceived effects of the ECTP process on clinical decision-making and patient care, including their ethics dimensions, and what changes are needed to improve ReSPECT decision-making?
-
From the perspective of clinicians working with acute admissions, what changes are needed to improve ReSPECT decision-making, including the ethics dimensions of the decisions?
Key findings from this work package have been previously published. 1,48,49
Methods
Sampling and recruitment
ReSPECT conversations were observed in hospitals within six acute NHS trusts. In each study site, observations were designed to include five ward areas (i.e. three medical areas, one surgical area and one orthopaedic area). Ward areas were selected by the local principal investigator in each of the study sites. The local site principal investigators connected the researcher with physicians or surgeons working in the selected ward areas. In two sites, the ReSPECT process had been digitised and incorporated into the hospital’s digital patient note system. In one site, doctors were prompted to issue patients with a ReSPECT form within 48 hours of admission, whereas in the other five sites ReSPECT forms were optional.
Data collection methods
Between August and December 2017, data collection took place in two hospitals. Cynthia Ochieng (a qualitative researcher with a PhD in public health) shadowed consultant clinicians during ward rounds to observe ReSPECT conversations. Through analysing these initial data, we recognised that ReSPECT conversations also took place outside ward rounds. We, therefore, reviewed recruitment processes and changed our approach to an expanded observation framework, which included ReSPECT conversations throughout the day, alongside contextual observations of ward practices and informal conversations with clinical staff about the ReSPECT process. Between April 2019 and January 2020, Karin Eli (a medical anthropologist experienced in fieldwork research with a focus on narrative and lived experience) used this expanded observation framework to collect data in the remaining four NHS trusts.
Observations and interviews took place between 10 and 28 months after implementation of the ReSPECT process at each hospital site. For both Cynthia Ochieng and Karin Eli, this was their first research study involving ReSPECT or other ACP processes. Cynthia Ochieng and Karin Eli worked as part of a wider research team [which included FG (a GP and medical sociologist), CH (a health services researcher with nursing background) and A-MS (a clinical ethicist with general practice background)] that designed the qualitative aspects of the study. Both Frances Griffiths and Anne-Marie Slowther had clinical experience of DNACPR and ACP, and Claire A Hawkes was involved in the development of the ReSPECT process. Anne-Marie Slowther, Frances Griffiths and Claire A Hawkes were also involved in a previous National Institute for Health and Care Research (NIHR)-funded research study on DNACPR. 38
Most clinicians were interviewed within 72 hours of the observation(s). Interviews explored clinicians’ reflections on ReSPECT conversations and on conversations they chose not to hold, and clinicians’ broader experiences with the ReSPECT process. When possible, Cynthia Ochieng and Karin Eli interviewed patients and/or their families. However, most patients who had ReSPECT conversations were elderly and acutely unwell, and this limited the number of interviews that could be conducted with patients and/or their families.
To contextualise the findings, Karin Eli interviewed ReSPECT implementation leads in five of the study sites (in the sixth site, the implementation lead was unavailable for interview, but earlier implementation data from a telephone interview were available to contextualise the findings). The interviews focused on local implementation processes, challenges, lessons learned and future directions.
Analysis
The analysis of the observations and interviews was adapted to each research question, as follows.
How, when and why are clinicians making ReSPECT decisions in the acute hospital setting?
Karin Eli extracted data from observed ReSPECT conversations, capturing categories relating to the site and ward area, the content and outcome of conversations, timing and setting of conversations, reasons for holding ReSPECT conversations, and patient and clinician characteristics. Karin Eli then used inductive thematic analysis to open-code 21 observed conversations. Based on this, Karin Eli developed codes that focused on how each actor (i.e. clinician, patient and/or relative) framed the ReSPECT conversation and contributed to the flow of the conversation. Karin Eli then reanalysed the conversations according to these codes. Using the coded conversations, Karin Eli, Claire A Hawkes, Frances Griffiths and Anne-Marie Slowther decided on a key set of attributes, according to which a ReSPECT conversation typology would be developed:
-
Central purpose: confirm ReSPECT recommendation, establish resuscitation and/or treatment escalation recommendation, deliver bad news, make palliative care decisions or establish consensus among colleagues about limitations of treatment.
-
Extent of detail: limited (i.e. focus on CPR and/or intensive care admission only) or detailed (i.e. discussion of additional treatment options and plans).
-
Outcomes: complete (i.e. leading to a ReSPECT form) or incomplete (i.e. ending inconclusively, or leading to an interim, partially completed ReSPECT form).
-
Directionality of conversation: closed ended (i.e. with the clinician employing persuasive or directive speech) or open ended (i.e. with the clinician opening the conversation to patient/relative wishes and preferences).
-
Conversation prompts: patient’s condition, hospital or ward initiative, patient’s or relative’s expressed wishes, or unstated/unclear. 1
Karin Eli used these key attributes to develop a set of conversation types, which Claire A Hawkes, Frances Griffiths and Anne-Marie Slowther reviewed. After agreeing on the conversation types, Karin Eli applied the typology to all observed conversations and analysed extracts of the clinician interviews that applied to these conversations to explore relationships between conversation types and the research question ‘why, when and how do secondary care clinicians enact the ReSPECT process?’.
What happens when a patient brings a ReSPECT form or a similar document from the community to hospital?
Interview excerpts where clinicians and patients reflected on their experiences with community ReSPECT forms or similar documents were extracted and analysed thematically.
How is the ReSPECT system used within the process of decision-making?
Observed ReSPECT conversations were analysed to ascertain whether or not the ReSPECT form was used in the conversation, and whether or not key patient-facing elements of the form (e.g. questions about patient preferences/wishes, clarifications of which treatments will and will not be provided) were mentioned in the conversations.
To what extent is the patient and, where appropriate, family members involved in the decisions?
Observed ReSPECT conversations were analysed to ascertain whether they were open ended (i.e. exploratory) or closed ended (i.e. persuasive). Clinician interviews were analysed thematically to ascertain attitudes towards patient and relative involvement.
How do patients/family members experience the decision-making process and their subsequent care?
Patient and relative interviews were analysed thematically to explore the patient’s/family member’s experiences of the ReSPECT conversation, including the decision-making process involved and their subsequent care.
What influences the ReSPECT decision-making process (ethics and clinician perspectives)
The clinician interviews were reanalysed thematically. The analysis investigated the potential role of ethics considerations in prompting ReSPECT conversations, the role of ethics dimensions (e.g. a weighing of burdens and benefits) in the making of ReSPECT decisions, and the extent to which patients’ wishes and preferences are included in the decision-making process. In addition, the analysis examined clinicians’ attitudes towards the ReSPECT process and form, with particular attention to how ReSPECT influences (or does not influence) decision-making compared with previous systems, the perceived flaws in the ReSPECT process and how clinicians would like these flaws to be addressed.
Ethics considerations
Patients and families provided verbal assent before each ReSPECT conversation was observed. Written informed consent was provided by clinicians who were formally observed and/or interviewed, by patients and families who were interviewed and by ward managers (in the last four sites) to state their agreement to contextual observations on their ward. Verbal consent was provided by clinicians who participated in informal conversations with the researcher during contextual observations. Families were interviewed if the patient lacked capacity, or with the patient’s consent if they did have capacity. All participant quotes presented in this report have been screened for identifying details. Participant identifications (IDs) indicate study site number and a random participant number, and cannot be traced to the participants.
Findings
As described in our publication,1 across the six study sites, 49 ReSPECT conversations were observed in 12 ward types (i.e. acute geriatrics, acute medicine, acute stroke, critical care, emergency medicine, gastroenterology and general medicine, geriatrics/gerontology, hepatobiliary surgery, orthogeriatric, orthopaedics, renal and respiratory). Most conversations (n = 30) were observed during ward rounds. Observations were also conducted in colorectal surgery, emergency surgical admissions, haematology and frailty assessment wards, but no ReSPECT conversations were observed in these wards.
Thirty-four doctors (consultant-level doctor, n = 22; middle grade-level doctor, n = 6; junior doctor, n = 6) conducted the conversations. Most (n = 26) doctors conducted one conversation, three doctors conducted two conversations, two doctors conducted three conversations, one doctor conducted four conversations and one doctor conducted five conversations. Although most patients (n = 32) were aged ≥ 80 years, the ages of patients ranged widely, with the youngest patient aged 22 years. Twenty-three conversations were held with the patient, 19 conversations were held with the patient and their relative(s), six conversations were held with the relative(s) and one conversation was a conversation between colleagues.
Interviews were conducted with 47 clinicians (including 31 clinicians who were observed conducting ReSPECT conversations), 13 patients and 19 family members (note that there were seven group interviews with families or with patients and families combined).
The findings are presented with respect to each of the research questions.
How, when and why are clinicians making ReSPECT decisions in the acute hospital setting?
Descriptive findings
Based on a thematic analysis of observed ReSPECT conversations, the following conversation typology was developed (adapted from Eli et al. 1):
-
Resuscitation and escalation (n = 31). Conversations in which the key aim is to record a recommendation about CPR and/or other elements of escalation of treatment [e.g. ventilation, intensive treatment unit (ITU) admission]. These conversations could be either open ended (i.e. exploratory; n = 13) or closed ended (i.e. persuasive; n = 18).
-
Confirmation of decision (n = 8). Conversations in which the key aim is to confirm with a patient and/or their family members whether they still agree with or would like to revise a previous ReSPECT or DNACPR recommendation.
-
Bad news (n = 4). Conversations focused on delivering devastating prognostic news. Although DNACPR and other escalation decisions are discussed, the prognosis is central.
-
Palliative/future care (n = 5). Conversations in which the focus is on decision-making regarding future hospital admissions, care in the community and transitioning to comfort care.
-
Clinical decision (n = 1). Conversations between colleagues, where only clinicians are involved.
Thematic findings
Working with the conversation types, we developed three themes corresponding to the research question ‘how, when and why are clinicians making ReSPECT decisions in the acute hospital setting?’:
-
why: planning for the possible and the inevitable
-
when: responding to hospital-based, clinical and patient/relative prompts
-
how: engaging with treatment options, patients and families.
The findings presented in this subsection have been adapted from Eli et al. 1 The adaptation retains the data and interpretations presented in the primary publication, but presents different illustrative participant quotes to avoid replication.
Why: planning for the possible and the inevitable
Depending on their key aim, as outlined in the conversation typology above, ReSPECT conversations implicated either a patient’s possible future deterioration or a response to a patient’s deterioration in the present.
Most resuscitation and escalation conversations were held with patients who were identified as at risk of imminent physiological deterioration. Most patients were elderly and suffered from multiple comorbidities. Doctors explained that these patients needed CPR decisions during the current admission both to prevent harm to the patients and to ensure that the medical team had a clearly documented plan in case of deterioration:
It’s making sure that the patient doesn’t have something that they shouldn’t have because it’s going to cause them harm. So it’s a benefit to them. And you also realise that the ward’s not going to be chaos.
Site 5, C01
To verify that patients agreed with a ReSPECT recommendation recorded when they had been acutely unwell, clinicians sometimes held confirmation of decision conversations with patients who had resuscitation and escalation conversations. These conversations also employed a possible future framework.
Bad news conversations responded to a clinically observed or diagnosed deterioration in a patient’s condition, and were concerned with present-tense changes:
The patient was deteriorating significantly . . . the aim of the discussion was to make quite sure that he was aware of the critical nature of the, of his wife’s illness . . . it was a fact-finding conversation as well to determine what the patient’s previously expressed wishes may have been.
Site 4, C02
Palliative care conversations also responded to deterioration in a patient’s condition; however, unlike bad news conversations, this deterioration was an expected part of a longer disease process, such that the ReSPECT conversation focused on planning for the patient’s end-of-life care, rather than providing information and ascertaining wishes about escalation of treatment.
When: responding to hospital-based, clinical and patient/relative prompts
Specific prompts guided clinicians in deciding when (during an admission and during the day) to hold a ReSPECT conversation.
Some conversations were prompted by a patient’s looming transfer to another ward, nursing home or hospice, which made treatment planning more urgent, and this was particularly the case for palliative care conversations. Hospital- or ward-based initiatives prompted some resuscitation and escalation conversations. In one hospital, a reminder to hold ReSPECT conversations appeared on all patients’ digitised notes, and doctors said that they incorporated the ReSPECT process into their ‘mental checklist’ (site 6, C02) during ward rounds. However, this meant that doctors prioritised CPR-related conversations to optimise their time and complete the task set by the digitised reminder.
Patients’ conditions prompted the majority of ReSPECT conversations. However, clinicians varied in their interpretation of which conditions necessitated the ReSPECT process. Some clinicians reserved these conversations for patients at risk for deterioration during the current admission or for patients who had experienced a substantial change during the admission:
. . . and now the situation changed and he, this person is very poorly . . . , we have to review it because now we know that ICU [intensive care unit] admission will not probably be appropriate for this person . . .
Site 4, C01
However, clinicians sometimes held ReSPECT conversations with patients who were not expected to deteriorate in the near future, but whose terminal diagnosis meant that they could benefit from a ReSPECT conversation.
In some cases, doctors conducted palliative care ReSPECT conversations when families requested that these conversations be held or after patients expressed their wishes to avoid or end life-saving treatment:
[My colleague] had seen him yesterday and it was reported to me that he said he was fed up; that he just wants to go home to die; so I wanted to explore that with him and make sure that was still his wish.
Site 3, C07
How: engaging with treatment options, and with patients and their families
Doctors varied in their engagement with treatment options beyond CPR, and in their engagement with patients’ and families’ wishes and questions during ReSPECT conversations.
Although some resuscitation and escalation conversations mentioned treatment options beyond CPR, many conversations were limited to CPR discussions, especially conversations conducted quickly during a ward round. Doctors explained that they did not want to ‘overwhelm’ (site 4, C03) patients with information about various treatment options when these options were likely irrelevant to their patients. In some cases, doctors felt that patients were not well informed enough to imagine treatment options beyond CPR:
. . . once you get down to the fine detail, ‘Would you want antibiotics if you had pneumonia? Would you want fluids if you weren’t able to swallow? . . . ‘ It’s, I just think that is really, really difficult to imagine being in that situation.
Site 3, C05
Doctors spoke about treatments beyond CPR and intensive care in all bad news and palliative care conversations. Doctors also did so in some confirmation conversations and in resuscitation and escalation conversations. In the palliative care context, detailed conversations focused on decision-making about comfort care and re-admission. In the resuscitation and escalation context, detailed conversations outlined which treatments the patient would and would not want (or be offered).
Most resuscitation and escalation conversations aimed at recording the treatment recommendation deemed most medically appropriate. Therefore, doctors often used persuasive language during these conversations. For example, one doctor (site 4, C06) asked an elderly patient for her views on CPR, but immediately explained that they had observed only one case in which CPR was successful and that the patient was aged 18 years.
Doctors sometimes took a persuasive stance in bad news conversations. In two observed conversations, doctors attempted to persuade the patient’s family that a DNACPR decision was essential.
In palliative care conversations, doctors emphasised the need to understand what a patient values and to plan accordingly:
And so, the process of ReSPECT is, is the all-important question: ‘what’s important to that patient right now?’.
Site 3, C07
Doctors also encouraged patients to express preferences and wishes in some resuscitation and escalation conversations and in some bad news conversations, in which doctors asked open-ended questions. This approach sometimes led doctors to recommend treatment plans that they had not considered before:
There’s been the odd one where having the conversation has changed what we’ve done. So even people who we thought were medically treatable but their priority was to get home. So we’ve compromised and got them home, because that’s what they wanted. And they were probably in the last year of life. There have been people who have found it quite empowering.
Site 2, C04
Thirteen conversations remained incomplete, leading to no or partial ReSPECT decisions, and this usually happened when there were disagreements between doctors and patients/families, or when patients felt that they needed more time to think about their treatment options. One doctor explained that they chose not to complete a digital ReSPECT form for an elderly patient who expressed conflicting CPR wishes:
. . . this is where maybe ReSPECT becomes tricky and where maybe it does fall down a bit. Because it’s, it is quite black or white, it, although there are sections where you can write free text and responses, the difficulty with him for example is you have to click on one of two things, is he for resuscitation or is he not for resuscitation? Now, at the moment he, kind of, is for resuscitation, but at the same time he’s also saying he doesn’t really think he wants to be or should be . . .
What happens when a patient brings a ReSPECT form or a similar document from the community to hospital?
Clinicians are most likely to see community-issued ReSPECT forms come in with elderly patients
Clinicians were aware that ReSPECT conversations often take place when people move into care homes. Clinicians said that many of their patients with a community-issued ReSPECT form were admitted to hospital from care homes, and these patients tended to be ‘elderly with comorbidities’ (site 4, C07) or with ‘severe disability or advanced dementia’ (site 3, C05). Community-issued ReSPECT forms ‘almost always’ (site 4, C09) recordeDNACPR decisions for these patients.
Community-issued ReSPECT forms are generally useful, but recommendations may be questioned
When a patient arrives on a ward with a pre-existing ReSPECT form, the clinician first checks that the form is appropriate and valid, and this often involves a short conversation with the patient or their family to confirm that they are happy with the existing recommendations. Some clinicians reported that they have ‘to confirm that it still applies, every time the patient comes in’ (site 3, C07). Knowing the date that the ReSPECT form was issued was considered important, as a patient’s health can deteriorate rapidly:
. . . it’s good to know when they were written . . . the situation might be completely different now.
Site 4, C09
Forms issued in community settings were generally considered useful. Knowing that the patient had already had a discussion about possible treatments and expressed their values and preferences was said to be particularly useful for patients admitted into critical care, where intervention could carry significant burdens. Clinicians also reported that they find it useful to have information about ‘treatment escalation decisions beyond resuscitation’ (site 3, C04) and reasons for certain treatment decisions.
Two clinicians commented that community-issued ReSPECT forms are not useful. One clinician reported that only CPR decisions are useful and the other clinician said that they would ‘always have the discussion again’ (site 4, C04). Another clinician expressed concern that community-issued ReSPECT forms might include recommendations for treatment that they do not think clinically appropriate, which could create tension with patients’ expectations:
. . . as long as the form didn’t then ask me to give treatment that I didn’t think was going to be in their best interests, that’s my concern . . . I just would hate to have patient families’ expectations built even higher than they already are about having treatment that’s not likely to be in their best interests.
Site 3, C05
Clinicians said that they do not always adhere to the recommendations recorded on community-based ReSPECT forms. Clinicians said that they would question recommendations against certain treatments if they felt that these treatments would be beneficial:
. . . if it is actually going to benefit . . . and only will go on for a very short period of time then, yes, I would consider it.
Site 3, C06
ReSPECT decisions are not questioned if the patient was admitted to hospital because of the condition that the ReSPECT form addresses. DNACPR decisions are also not questioned:
. . . the resuscitation part, it is saying ‘do not resuscitate’, I would almost always appreciate that decision.
Site 3, C06
There are advantages to initiating the ReSPECT process in the community
Hospital doctors felt that GPs would be good at holding ReSPECT conversations, as GPs know their patients well and can ‘appreciate the [patient’s] medical comorbidity, the psychological support, the social infrastructure’ (site 6, C06). Some hospital doctors also thought that holding these conversations while patients were relatively well and comfortable [as opposed to in hospital when ‘they feel vulnerable’ (site 1, C03)] is better for patients. Other hospital doctors said that community-issued ReSPECT forms indicate ‘what is important for the . . . patient in terms of symptomatic versus curative intent’ (site 4, C02) and provided a prompt for discussions about ceilings of care:
. . . it won’t have detailed ceilings for all hospital treatments, but it will be enough to allow me to elaborate upon that . . .
Site 2, C04
However, one participant pointed out that, when people are healthy, they do not consider emergency situations:
. . . you don’t sit at home watching TV at night thinking, ‘You know, I only want to have resuscitation in such and such circumstances’. It’s not, it’s not what people think about.
Site 1, C02
There needs to be better sharing of ReSPECT recommendations across primary and secondary care
Participants agreed that all health-care professionals involved in treating a patient should have the same ReSPECT information. However, participants expressed confusion about whether or not community-issued forms apply when patients are admitted to hospital. The original format of the ReSPECT form (i.e. a hard copy held by patients) was criticised as being impracticable in emergencies, as ‘a lot of people don’t bring the ReSPECT form with them, they are in a rush to come to the hospital and they don’t remember’ (site 2, C01), and, likewise, for patients who frequently transition between primary and secondary care:
. . . we’ve got dialysis patients who’ve got ReSPECT forms in place. The recommendation is that they should carry that with them at all times. That’s not practical. What we need is something that is available to the community based health services and ambulance service, and the hospital.
Site 1, C07
Participants felt that a standardised electronic copy of the ReSPECT form that could be ‘attached to the patient’s electronic record and visible across all health care’ (site 1, C04) would more seamlessly transfer ReSPECT decisions.
How is the ReSPECT system used within the process of decision-making?
The ReSPECT form is rarely used during conversations with patients and/or families
A paper ReSPECT form was used to engage with patients/families in only six conversations. In one conversation, the doctor showed a relative a blank ReSPECT form on a smartphone screen. In the two sites where digitised ReSPECT forms were used, patients/families had no interaction with the ReSPECT form during the conversation. Several clinicians at these two sites mentioned this as a downside of the digitisation of the ReSPECT process.
Most ReSPECT conversations elicit patients’ views on cardiopulmonary resuscitation and/or other treatment options
In most ReSPECT conversations the clinician asked the patient/relative about the patient’s wishes and preferences for CPR and/or other treatment options, including intensive care escalation and re-admission. However, in eight conversations, clinicians did not ask about patients’ preferences and, instead, informed them about the decisions the clinicians had already made about CPR and/or intensive care escalation. Clinicians took this approach when they were certain that these interventions would be futile, as one clinician explained:
. . . it was pointless to have a discussion knowing that you would not be able to offer the patient the options they might want.
Fieldnotes, site 1, C09
When clinicians asked about the patient’s wishes and preferences, the approach taken was either persuasive or exploratory. In persuasive conversations, although clinicians asked patients or their families what they would want, clinicians would also voice their own recommendation, explaining that CPR and/or intensive care escalation would be futile, sometimes using emotionally evocative language (e.g. telling patients that CPR would be undignified or would distress their families). In exploratory conversations, clinicians explored patients’ and families’ wishes openly, allowing these wishes to guide the rest of the conversation and the development of treatment recommendations. For example, after breaking bad news to a patient’s partner, an intensive care consultant said ‘I’m sorry to have to warn you about this but in this circumstance we do ask you as the person closest to her if you would know what her wishes would be in this situation’ (fieldnotes, site 4, C02). The patient’s partner asked for resuscitation, but not at the expense of patient’s quality of life, and the consultant responded with ‘we will resuscitate her’, but ‘there is a possibility it would not be successful . . . after repeated attempts we will step back and allow things to take their course’ (fieldnotes, site 4, C02).
In several cases, exploratory conversations resulted in no recommendations, as patients found it difficult to engage in the conversation, expressed ambivalence or asked for more time. In these cases, clinicians explained that they would either revisit the conversation later or leave the conversation where it was, hoping that it would encourage the patient to consider treatment escalation and have future conversations about this in community settings or with their families.
During ReSPECT conversations, many clinicians explain what treatments would and would not be provided
Clinicians spoke about what treatments (other than CPR) would and would not be provided in more than half of the observed ReSPECT conversations. The level of detail, however, was variable. In conversations conducted during ward rounds, treatments were typically mentioned in the context of the patient’s general management, rather than directly linked to what clinicians conceptualised as the ReSPECT conversation, which focused on CPR and/or intensive care. In conversations conducted outside ward round contexts, treatments were typically mentioned in the context of the ReSPECT process. In these cases, clinicians employed a reassuring tone, explaining to patients that they will still be treated regardless of a DNACPR decision, and this could be framed broadly [e.g. ‘it’s doesn’t mean we’ll stop treating you’ (fieldnotes, site 4, C09)] or specifically {‘[the doctor] said they will give her i.v. [intravenous] antibiotics and fluids, and fluid resuscitation, but ‘won’t bring you down to ICU [intensive care unit]’ (fieldnotes, site 4, C08)}.
However, in many (n = 21) of the observed ReSPECT conversations, clinicians did not speak about treatments other than CPR and/or intensive care escalation.
To what extent is the patient, and where appropriate family members, involved in the decisions?
Patients and families are involved in ReSPECT conversations, but not always in decision-making
Of the 49 ReSPECT conversations observed, 48 conversations involved patients and/or their families and one conversation was a discussion between clinical colleagues for a patient who lacked capacity, had no next of kin and no friends, and for whom an independent mental capacity advocate could not be located. Conversations varied in the extent to which patients/families were involved in the decision-making process. Twenty conversations were open ended, with clinicians actively eliciting the patients’ wishes and preferences, and taking these into account in decision-making. However, in 20 other conversations, clinicians took a persuasive stance, using conversational scripts to sway the conversation towards a decision aligned with medical opinion or simply informing the patient/relative about a medical decision that had already been made. For example, a doctor was observed saying ‘should the situation worsen, we will not put [the patient] on a machine’ (site 4, C07) to a relative. The remaining conversations were confirmatory, with clinicians asking patients/families if they agreed with a previously issued ReSPECT decision or community DNACPR.
Clarity and uncertainty about patients’ trajectories affect whether or not patients/families are informed or involved in decision-making
As reported in our earlier publication,2 using clinician interview data, a clinician’s clarity or uncertainty about a patient’s trajectory often determined the extent to which the patient/family was included in ReSPECT conversations. When clinicians were uncertain about a patient’s trajectory, the ReSPECT conversation emphasised patient preferences to a greater extent:
. . . the greyer . . . the decision then the more and more you allow the patient’s own perspective to sort of sway the ultimate outcome.
Site 1, C09
Similarly, although clinicians were certain that palliative patients were nearing the end of their lives, ReSPECT conversations acknowledged clinicians’ uncertainty about how patients wished to spend their last weeks or months, thereby emphasising patient preferences in certain aspects of care:
. . . my only main aim was, to get out what she wants from the rest of her life, and how she wants to be treated and how she wants to be, like, managed in all her, including her end-of-life care and everything, so . . .
Site 6, C07
By contrast, when a patient’s illness and treatment trajectory seemed clear, then clinicians tended to take a persuasive approach to ReSPECT conversations:
What I don’t think’s particularly helpful is having a discussion with a patient where it’s very clear from a medical objective point of view that it would be futile to escalate treatment to give them the impression that you’re giving an option of escalating treatment. Because again, I don’t think that’s, that’s fair. So if it’s very clear then I think our job is to explain why we’re making these decisions carefully and sensitively.
Site 3, C05
Accordingly, some clinicians said that ReSPECT conversations were mainly focused on informing patients/families about what was possible medically, rather than seeking their involvement in decision-making. Several clinicians stated that it was important to clarify to patients and, in particular, families that clinicians were not asking them to make medical decisions:
. . . you don’t want the family to feel that they have decided . . . that’s the last thing you want, the last thing you want is for them to feel responsible for having made that decision.
Site 4, C10
Some clinicians advocated a middle ground approach. Although clinicians did not ask patients/families to participate in medical decision-making, clinicians used ReSPECT conversations to contextualise the eventual clinical decision:
It’s a shared decision . . . we give the medical information. We take on board the family’s values and preferences, and we issue a recommendation based on that. And I think that’s important rather than feeling, letting the family feel either that they’ve got to make the decision, and we’re washing our hands of it, or that we’re making the decision for them doesn’t matter what they think.
Site 5, C08
The ReSPECT decision-making process is shaped by the patient’s autonomy
Many of our patient and family interviewees expressed their preferences after their doctor had explained CPR to them, and believed that their doctor respected their wishes. One patient reported disagreeing with their doctor who suggested a particular treatment, and some family members felt that the doctor would have implemented their wishes, even if they disagreed with the clinical recommendations:
I think she would have listened to us, and done everything she could have to have implemented any other action that we insisted upon.
Site 6, F02
In contrast, other patients and families felt that their doctor simply informed them about the ReSPECT decision without discussion or explanation, as one patient said:
The doctor told me . . . ‘I hope you know we won’t, won’t resuscitate you’.
Site 2, P03
This patient went on to say that they agreed with the doctor’s decision, but also felt unable to disagree:
I’m quite prepared to go along with that. Well, I can’t do anything else, can I?
Site 2, P03
Several patients commented that they trusted the doctor to make the right decision on their behalf, as doctors are experienced, highly trained and will do whatever is in the patient’s best interests:
. . . to be honest, I always say, ‘I’ll leave it in your hands’. You know, they know best.
Site 1, P05
Many ReSPECT discussions were held while the patient’s family were present. Patients said that their family provided emotional support, but that the decision was theirs alone to make:
. . . my daughter . . . she says, ‘It’s your decision, mum. I’m here to support you, whatever you decide’.
Site 2, P06
One patient, who felt shaken by the ReSPECT discussion, said they did not want to make any decisions without their children, but was worried about upsetting them.
If a patient lacked capacity to make their own decisions, then their family was responsible for expressing their wishes. These family members said that the ReSPECT process should reflect the patient’s wishes:
. . . you do have to stop and think actually what that individual wants, not actually what you want.
Site 2, F02
A few patients had discussed their preferences with their family prior to their hospital admission, and this made the ReSPECT conversation easier for their families:
. . . my dad’s always, sort of, you know, very open about what happens, you know, when his time comes, . . . I know exactly what they want the end of their life, so, yeah, so, you know, we have talked about things like that.
Site 2, P02
How do patients/family members experience the decision-making process and their subsequent care?
Patients and families do not always recall or understand their ReSPECT conversation
Although some patients had good recall of the conversation, several patients could not clearly remember what was discussed. For example, one patient said there had been no discussion of resuscitation:
It hasn’t been spoken about. That word ‘resuscitation’ has never come into it.
Site 1, P01
Lack of recall could be due to the confusion of being in hospital, or being very ill or in pain at the time of the conversation [e.g. ‘I was in a bit of pain anyway, you know’ (site 1, P04)]. Family members too described having the conversation while feeling anxious and upset [e.g. ‘we were all a bit uptight, you know, because we’d . . . had the ambulance journey’ (site 6, F01)] or in the time of crisis:
. . . when you come in [to hospital] so much is going on, it’s something’s happened all of a sudden . . . you’re trying to focus on your [relative] . . . you’re trying to work out what’s going to happen to them.
Site 2, F02
Having ReSPECT conversations with ill patients or in an emergency was criticised by one person, who thought that this timing was inappropriate:
. . . when you’re really poorly, you know, it’s not a good time. ’Cause then you feel like giving up. So you need to be well for such conversations.
Site 2, P01
Some patients, and most families, felt they had understood the ReSPECT conversation, and that the purpose of ReSPECT had been clearly explained to them. There were some misunderstandings, however. One patient initially thought that the conversation was related to organ donation, then assumed that much of the conversation was to prevent litigation if the patient received treatment they did not want, and this patient’s doctor ‘made it clear that it wasn’t’ (site 1, P04).
Patients and families are unprepared for the conversation
Only one patient had expected to have a ReSPECT discussion during their hospital stay, after experiencing multiple previous conversations with doctors about resuscitation. Generally, however, patients and families were unprepared for this discussion. The unexpectedness of the conversation confused some people:
. . . my mind was kind of catching up with where he was going,’cause I didn’t, there was no real lead into it.
Site 6, P01
Some patients felt unable to think through their wishes or questions:
And now, looking back, now I’ve had time to think, there’s lots of things I would have asked, which I didn’t.
Site 2, P01
One person suggested that the ReSPECT process should be a two-stage process, with an initial conversation/leaflet signposting what the patient would need to think about:
. . . to have reasonable input from someone like me, I need to know we’re going to have that conversation, maybe even with a bullet list.
Site 6, P01
Another patient said that it was important to have time to discuss the philosophical aspects of life and death decisions with someone of faith.
People who were unprepared often felt upset after the conversation:
It shocked me a bit, actually. Very shocked and a bit frightened . . . I felt quite brave at the time and thought that I could cope with it, but as soon as the doctor went I wanted to cry.
Site 2, P01
The conversation left some patients/families concerned and confused as to their future trajectory. For example, one patient was told that they were having the conversation because of repeated hospital admissions that left them concerned that they were dying. Another patient reported that the conversation made them realise how quickly their health had deteriorated:
I never thought it would go downhill this fast.
Site 1, P03
Several patients and families said that, although upsetting, it was important to contemplate treatment planning, and one patient said that it was ‘marvellous’ (site 1, P03) tthat hey were able to express their preferences:
I know it’s an upsetting conversation and I did get upset, but it’s a conversation you need to have.
Site 3, F06
Participants mentioned that the transferability of the ReSPECT form was crucial so that everyone involved in a patient’s care (GPs, hospital staff, etc.) knew the patient’s wishes.
ReSPECT discussions focus on resuscitation
Many participants said that resuscitation was the focus of ReSPECT conversations. Patients and families recalled how doctors described the consequences or side effects of CPR:
I knew that if they had have done CPR, like, it probably would’ve broken her ribs and done a lot of damage, . . . And I just didn’t want it for my mum.
Site 2, F01
Although nearly all participants recalled discussing CPR, very few participants could recall the doctor talking them through other available treatments:
. . . no future treatment was talked about.
Site 1, P02
. . . we didn’t mention anything about intensive care or anything like that because I don’t think he had the time.
Site 2, F02
During the ReSPECT discussion, some patients sought reassurance of a peaceful, painless death:
You just hope it’s going to be peaceful but I was told that you wouldn’t suffer if they, you know, they wouldn’t resuscitate but, but I, I wouldn’t suffer. Well, which is what everybody wants to know, you know?
Site 2, P04
Concern for family shaped some patients’ views on resuscitation. One patient declined CPR because they did not want to place the responsibility for making resuscitation decisions on their son’s shoulders:
I didn’t want to put my closest people, you know, through any trouble . . . I didn’t want my son to have to go through it all, you know, just make a decision like that.
Site 2, P07
Several patients reported that they did not want to be resuscitated because they were elderly, saying that they could die at any time, did not want to burden their family and feared being left in worse health.
Family members described deciding not to attempt resuscitation as being in the patients’ best interests. The lack of quality of life a patient would experience after resuscitation influenced the decision to decline it:
I just think she would’ve just deteriorated and deteriorated and deteriorated, and I don’t think she would’ve ever come out of the bed, I think, after having that done, to be honest.
Site 2, F02
Families described how previous resuscitation decisions helped make the ReSPECT conversation easier, and these participants said that if they were aware that the patient would want to decline resuscitation then they felt obliged to ensure that decision was made, regardless of how hard it was for them:
I felt terrible saying it because it’s my mum and, you know, I don’t want her to go . . . I know that if she does go then she wouldn’t want to be brought back, and she’s already sort of, like, stated that she didn’t want to be resuscitated if anything happened. So I had to ask the question.
Site 2, F01
Families drew on previous experience when patients had repeated admissions. Conversations held on first admissions tended to be longer and more in-depth than follow-up conversations:
. . . we’d already made the decision ’cause I said to the [doctor] that [she had] already been in before, we’ve been through it again. So perhaps he didn’t feel like he needed to go through all that detail.
Site 2, F02
Doctors’ communication skills are both praised and criticised
Doctors were often praised by patients and families for their good communication skills. Participants felt able to ask the doctor questions and express their preferences:
. . . he listened, he didn’t sort of, like, talk over, he let us, sort of, like, say what we wanted to say . . . he made it, sort of, like, quite easy.
Site 2, F01
Doctors clarified what the current state of the patient’s health was, what might happen, and what treatment they would or would not receive if they deteriorated. In communicating about difficult medical decisions, doctors tended to speak clearly and honestly. Although participants appreciated this honesty, the honesty shocked participants who did not expect a resuscitation discussion:
. . . she told us straight which was her job to do. It’s no good beating about the bush if you’re doing, if you’re talking about life or death . . . it hits you hard, straight away when you get it straight in your face like that.
Site 6, F01
Other participants recalled that the doctor warned them that the conversation was going to be difficult, and they found this warning useful in preparing themselves.
Patients and families often praised doctors for being calm, kind, caring and compassionate:
. . . he was very sympathetic and very understanding, and he, sort of, put me at ease and everything.
Site 2, F01
Doctors also reassured families that they had made the right decision for the patient:
Doctor went over and said, ‘I think you’re making the right decision’, you know, just to give us, just to give me peace of mind.
Site 2, F02
Alongside this praise, participants acknowledged that these conversations were not easy for doctors:
I think it’s difficult for doctors. . . It is a horrible thing to have to tell someone.
Site 1, P03
However, not all participants were positive about their doctors’ communication skills. One person commented that doctors do not speak in patient-friendly language:
. . . doctors will talk doctor-talk.
Site 1, P01
Another patient felt that their doctor was too blunt in how they introduced the topic and ‘they could have been more subtle, couldn’t they, I think, not just come straight out with it’ (site 2, P03).
Patients and families commented that ReSPECT conversations could be improved by clinicians allowing more time. Several participants commented that their conversation was ‘short’ and their doctor was ‘a bit quick’ (site 1, P04). The lack of time meant that doctors did not discuss the different issues in detail. Some family members reported that they had to wait at the patient’s bedside until the doctors had time for a conversation.
Patients are unaware if or how the ReSPECT process affects their subsequent care
Patients did not discuss if or how the ReSPECT process affected the care they received. One patient was concerned that if they engaged with the ReSPECT process then they would receive different treatment, or no treatment:
I was just a little bit worried that if I sign up to this ReSPECT that I might not get the treatment that I need to keep me alive. Will it just be assumed that I’m going to die and just leave me. So that’s a little bit concerning . . . I’m getting the impression that there’s going to be different treatments for different people.
Site 2, P01
What influences the ReSPECT decision-making process, including considerations of ethics (or not), and why?
The following themes, and associated ethics values, are addressed in this subsection:
-
The patient’s condition is central to initiating the ReSPECT decision-making process.
-
Clinicians vary in their conceptualisation of ReSPECT as a shared decision-making process.
The patient’s condition is central to initiating the ReSPECT decision-making process
Most doctors said that they initiated ReSPECT conversations with patients who were at risk of deteriorating during their current hospital admission, and these conversations usually focused on making decisions about resuscitation:
I think when someone’s acutely unwell their main priority is, is discussing resuscitation and ceilings of, of treatment while they’re unwell and once they’re stabilised, that gives you time to have these further discussion to explore their wishes for their future care.
Site 3, C04
Accordingly, doctors often deferred ReSPECT conversations with patients who were acutely unwell, but deemed to be stable:
I didn’t think that she was someone who was likely to have a cardiac arrest that morning, the following day.
Site 2, C05
By contrast, an intensivist said that with ‘critically unwell’ patients the ReSPECT conversations were ‘repeated often on a daily basis . . . And if there’s a change . . . that particular ReSPECT form, the printed version is crossed out and, and is updated’ (site 4, C02).
Although ReSPECT conversations with patients who were deteriorating were often persuasive, uncertainty about a patient’s prognosis often led to ReSPECT conversations with a shared decision-making stance. For example, a consultant explained why a particular patient was asked about his intensive care preferences:
And he is one of those borderline patients that will sometimes be accepted by ITU and sometimes not. And my decision about whether to escalate him to ITU would be based very much on his preferences, so I had to ask.
Site 2, C04
Clinicians also initiated ReSPECT conversations with patients who had terminal illness, where the focus was not on acute deterioration, but rather on ascertaining the patients’ wishes for their end-of-life care:
. . . he’s got a terminal diagnosis, we’ve exhausted all the treatment options and all our focus now is on, is gonna be on his, on his symptom control. And so, the process of ReSPECT is, is the all-important question: ‘What’s important to that patient right now?’ . . . to make future care plans about whether a return to hospital is the right thing, what would be his preferred place of death . . .
Site 3, C07
The foci of ReSPECT conversations and decision-making differed according to the type of ward where conversations took place. In geriatric wards for longer-term patients, ReSPECT conversations tended to focus on broader aspects of treatment planning, involving patients and families in decision-making about palliation and re-admission. However, in acute geriatric wards (e.g. frailty-focused medical wards), ReSPECT conversations tended to focus on decision-making concerning CPR and/or intensive care. As an emergency medicine consultant explained, although the ReSPECT process was a shared decision-making process, during an acute admission, there was limited scope to explore patients’ wishes beyond resuscitation:
. . . is an acute situation the right time to have that [conversation] when they’re, they’ve got what’s almost certainly compromised mental capacity?
Site 5, C08
Focusing on limited conversations with acutely ill patients, as noted in our data, responds to the ethics duty to protect the patient from harm, for example from unsuccessful CPR or invasive interventions in intensive care unit (ICU), although possibly at the expense of articulating and recording recommended treatments that will benefit the patient. In the context of less acute patient conditions, ReSPECT conversations were more likely to be shaped by considerations of patient autonomy and wider consideration of benefits, with clinicians expressing a concern to elicit the views and wishes of the patient, particularly in situations of clinical uncertainty.
Clinicians vary in their conceptualisation of ReSPECT as a shared decision-making process
Differences between doctors’ approaches to shared decision-making reflected different ethics stances. Many doctors spoke of ReSPECT decisions as ultimately medical, saying that, although patients and families should be involved, the final decision is based on clinical judgement. A key reason for taking a persuasive or prescriptive approach to ReSPECT decision-making was to avoid patient harm. When doctors identified an intervention as futile, they limited discussion about it. For example, a respiratory consultant who supported shared decision-making in some ReSPECT conversations drew the line where futility was involved:
What I don’t think’s particularly helpful is having a discussion with a patient where it’s very clear from a medical objective point of view that it would be futile to escalate treatment to give them the impression that you’re giving an option of escalating treatment. Because again, I don’t think that’s, that’s fair.
Site 3, C05
To avoid situations where patients requested treatments that doctors deemed futile, doctors employed conversational strategies that limited patient involvement. A junior doctor working with a largely elderly patient population used a conversational script that positioned CPR as ineffective in elderly people before asking patients about their wishes. Without this script, the doctor explained, awkward situations arose:
But I have had conversations where I would say, ‘Have you had any thoughts about CPR?’. Sometimes. if I leave it open, I find their response would be, ‘Oh yeah, I’d, I’d like it, please’. And then he becomes . . . obviously it’s a little bit more difficult to walk it back and say that, ‘No, I don’t feel that that’s appropriate’.
Site 4, C08
Notions of futility were closely linked to weighing the harms and benefits of particular interventions. When harms were deemed to outweigh benefits, doctors informed patients and families about their decision, as opposed to asking patients and families to participate in decision-making. A consultant described using ReSPECT discussions to explain medical reasoning about harms and benefits:
. . . it’s when the risks and benefits and burdens outweigh the benefit then you shouldn’t give that treatment. And it has to be black and white like that for them to understand the decision-making that we’re trying to logically go through.
Site 5, C03
The balancing of harms and benefits was not limited to individual interventions and individual patients. Some doctors were concerned about the harms that a futile intervention might pose to the wider ward environment:
. . . it’s just trying to make sure ethically that we’re not doing things that are futile. Making sure that, you know, that we actually support and sometimes almost understand the impact of that decision not only for the patient or their family, but in the hospital environment actually how if there’s a horrible cardiac arrest how that impacts on the other patients, on the nursing staff, on the students . . .
Site 6, C06
Some doctors included the ReSPECT conversation itself in the balancing of harms and benefits, arguing that an incorrectly timed or framed conversation may burden patients.
The doctors who articulated a ‘harms and benefits’ perspective appeared to be guided by the ethics duty to protect patients from harm, characterised as ‘futile’ treatment, and to provide overall benefit (by balancing medical risks and benefits of possible treatments). The patient’s views and preferences were then sought in discussion of the pre-identified and selected options. However, if doctors were confident that one option was advisable, then patients were informed about the recommendation rather than included in decision-making. When patients’ and/or families’ wishes clashed with medical opinion, then most doctors chose the medical position, inferring limits on a patient’s autonomy, as one intensivist explained:
. . . if patients have unrealistic expectations we are not expected to provide that treatment just because the patients ask for it.
Site 4, C07
Some doctors described trying to achieve a compromise, whereby doctors denied futile treatment but explored with patients/families what could be done to respect the patients’/families’ values and preferences while not compromising the clinical duty to protect patients from harm. For example, a consultant described seeking consensus with patients from religious minority groups whose values did not necessarily match the values espoused by their doctors:
So there are some sections of the population who vehemently believe in preservation of life no matter what, at all costs, which is contrary to most of our views, but we have to acknowledge that and at least be seen to be doing everything we can to preserve life within what’s reasonable and acceptable.
Site 5, C03
A key aspect of negotiating between patient/family preferences and medical decisions was achieving a shared understanding to ensure that patients/families followed and agreed with medical logic. Most disagreements, doctors said, reflected misunderstandings:
. . . sometimes what happens is that the doctors, the nurses, the therapists understand the frailty and the futility of cardiac resuscitation, but actually the patient and the next of kin don’t.
Site 6, C06
To overcome misunderstandings, doctors checked patients’/families’ understanding and then provided an explanation to correct it. An acute medicine consultant said that when patients request CPR:
. . . I try to find out what is their understanding of resuscitation. Do they know what exactly we mean? Quite many times they think resuscitation means stopping treatment. So to clarify [to] them that we are not stopping any medical treatment.
Site 5, C04
Another acute medicine consultant spoke about considering patients’ backgrounds when explaining decisions:
. . . you’ve got to take that into account if you know that some patients will have different beliefs, different religious kind of backgrounds, and it’s about explaining to them that actually it’s not about withholding something and keeping it back but it’s about not giving the wrong treatment.
Site 5, C01
These doctors wanted to ensure that patients/families understood what was being recommended by the doctor and why. Doctors explicitly acknowledged patients’ values, wishes and concerns, and, in some cases, provided the possibility of modifying recommendations, therefore, respecting their autonomy, with the expectation or hope that patients/families would then agree with the recommendation.
There were some exceptions to doctors’ assertions that ReSPECT recommendations were ultimately medical. Doctors would respect a patient’s treatment refusal, although the doctors would sometimes try to convince a patient to reconsider, and this was not surprising given the legal requirement for a valid consent before treatment can be initiated. In palliative care contexts, the ReSPECT decision-making process focused more explicitly on patients’ wishes, preferences and values. A surgeon whose patient was diagnosed with inoperable stage IV cancer described the ‘main aim’ of the ReSPECT conversation as understanding ‘what she wants from the rest of her life, and how she wants to be treated’:
. . . as a doctor, it’s my duty to wish, to respect my patient decisions. Even if she comes to say to me she will like the full treatment, she wants the CPR, I, it’s my duty, I’m duty-bound, it’s, I’ll be happy to do it.
Site 6, C07
Similarly, in geriatrics wards, where there was substantial overlap with palliative care, doctors centred ReSPECT conversations on the patient’s wishes, framing the discussion through the lens of ‘What’s important to that patient right now?’ (site 3, C07), instead of limiting possibilities.
Doctors also said that they were more inclined to consider patients’/families’ wishes for treatment escalation in cases of uncertain prognosis or low likelihood of cardiac arrest. For example, this consultant contrasted futile and low-risk cases:
. . . if I had someone who was actively dying, we’re palliating, yet the family were adamant that he be resuscitated, I would be very firm in that situation that we were not resuscitating, that was my decision. For some, for a patient who’s otherwise well, is in for something minor and is going home tomorrow with no life limiting diagnoses, I would be more flexible.
Site 6, C02
Other doctors said that recording a ‘for CPR’ decision for patients unlikely to benefit from CPR was a form of showing goodwill to patients or their families. Speaking about an elderly patient who was undecided about his CPR wishes, a doctor said:
. . . but when it comes to CPR, to a certain extent, I think there’s a degree of showing that we’re doing what we can . . . so if it was his wish, and his wish was for us to try, I wouldn’t mind, you know, I wouldn’t not do it.
Site 4, C10
Some doctors talked about the importance of acknowledging the patient’s family’s emotional needs, particularly in the context of CPR recommendations.
You know, I have hundreds of patients over a year, they have one mum. And actually, if it’s important for them, I must, as [inaudible] part of the grieving process, it’s important for them to feel like everything had been done, even if maybe it wasn’t appropriate.
Site 3, C08
This acknowledgement was sometimes linked to concerns about future complaints or litigation. For example, a consultant described recording a ‘for CPR’ recommendation to avoid distressing the family and leading to complaints.
. . . what we don’t [want] is to leave behind people who are bitter and unhappy and very distressed that nobody was listening to them. Because it ultimately, it’s not the end of it, they usually start complaining to different institutions, to ombudsman, to the hospital, it lasts a long time and it brings no closure for them.
Site 4, C01
From the clinician perspective, what are the perceived effects of the emergency care and treatment plan process on clinical decision-making and patient care, including their ethics dimensions, and what changes are needed to improve ReSPECT decision-making?
The findings presented in this subsection address the perceived effects of the ECTP process on clinical decision-making. The question about changes needed to improve ReSPECT decision-making is addressed in the next subsection, which responds to a similar question.
The following themes are addressed in this section:
-
Clinicians perceive the ReSPECT form as bringing patients’ wishes to the foreground.
-
Clinicians perceive the ReSPECT process as influencing treatment planning, although not all clinicians agree on how to use the form in practice.
-
Clinicians perceive the ReSPECT form as improving communication through structured and detailed documentation.
-
The ReSPECT process promotes quality and continuity of care in the hospital and across settings.
Clinicians perceive the ReSPECT form as bringing patients’ wishes to the foreground
Although most clinicians prioritised the medical perspective in the decision-making process, clinicians also perceived the ReSPECT process and form as foregrounding patients’ wishes, describing this as a key benefit. Some clinicians found the paper-based ReSPECT form helpful when engaging patients/families in discussions. For example, one clinician said that they used the form with patients whose prognosis was uncertain to involve them in decision-making, and this process proved useful even when patients did not have a definite preference to record:
But it, it allows, it’s to open the door to a, to a further conversation and allows them to go away and think about it and discuss with their family and to, and to talk about what they would like to do.
Site 2, C05
According to one clinician, the ReSPECT process allowed clinicians to facilitate patient autonomy by encouraging patients to think about what might be important to them in a future scenario.
Although most clinicians did not use the ReSPECT form during conversations with patients, several clinicians cited the form as helpful in prompting, guiding and structuring conversations with patients, expanding their remit beyond CPR decisions. This was especially the case for less experienced doctors, as one early-career doctor explained:
I think previously I, I didn’t know about ReSPECT forms, so it was always about resuscitation and ward-based ceiling of care.
Site 3, C03
Expanding conversations to include various treatment options, one clinician explained, allowed for a greater consideration of patients’ wishes:
. . . by having a ReSPECT conversation, we can better gauge what a patient would deem acceptable versus what they would say, ‘No, I don’t want this’.
Site 6, C06
Moreover, several clinicians said that the ReSPECT process, through eliciting patients’ wishes, enabled alternative understandings of quality of life, and that this led to changes in treatment recommendations.
Clinicians perceive the ReSPECT process as influencing treatment planning, although not all agree clinicians on how to use it in practice
Numerous clinicians said that the ReSPECT process broadened their thinking about treatment planning, prompting them to think about treatments other than CPR. This allowed clinicians to acknowledge patients’ complex needs:
. . . the DNACPR form didn’t say, didn’t have anything in between, if you like. So it was either not for resuscitation or for resuscitation, there was nothing else in between . . . but the ReSPECT form allows you still to choose something in the middle. It doesn’t have to be all for treatment or none for treatment.
Site 2, C03
Another consultant explained that this change in mindset led clinicians to construct treatment planning as provision, rather than denial:
And also I think it helps clinicians to understand that it’s not just a negative thing about what we don’t do. It’s a little bit about what we will do as well.
Site 5, C08
For some clinicians, the broadening of thinking about treatment planning translated into more detailed conversations with patients/families:
. . . the difference that ReSPECT has made from resuscitation forms is that I think we have, I have a lot more open discussions now regarding [what] people would and wouldn’t want . . . You know, so, coming into hospital or, you know, i.v. [intravenous] antibiotics, i.v. fluids, that sort of thing, all the way up to, you know, resuscitation, intubation, and things like that.
Site 4, C10
A change in mindset about the scope of treatment planning was closely linked with a change in clinicians’ understandings of patient/family involvement in treatment planning conversations. One consultant explained the contrast with DNACPR, which recorded a medical decision, sometimes without patient involvement:
. . . we’ve realised that actually that decision is ultimately ours, and we’re accountable for it, but it is wise and sensitive and probably appropriate to engage the family in that decision, and at least making that decision with their agreement. And then possibly, more recently, the, you know, the patient’s cultural views and the ways that they would want to be treated do now feed into that as well.
Site 5, C03
Although this consultant did not cite the ReSPECT form directly as leading to this change of practice, other doctors said that the form improved the quality of discussions:
But knowing that I’ve got to think through bits on the form, or needing, be needing to, to complete the form, I do try to, to broaden my approach, rather than just a simple question usually. Even if it’s only to ask in general terms, or, what people’s expectations would be if they got less well.
Site 6, C05
This suggests that the ReSPECT process encourages clinicians to consider the patient as a person, rather than focusing on a specific condition or event, emphasising benefit to the patient rather than avoiding harm from treatments.
Although some clinicians perceived the ReSPECT process as expanding the scope of their treatment planning conversations and recommendations, other clinicians described the ReSPECT process as similar to DNACPR:
But ReSPECT is, despite the good intentions, is just a different word for DNACPR . . . If I mention that I’m going to have a ReSPECT discussion for a patient who is having some elective operation, like a hernia operation, people will go, ‘Are you mad?’.
Site 5, C09
Many clinicians said that the ReSPECT process did not work as a universal form, and some clinicians avoided completing the form for patients who were for full active treatment. Without a ReSPECT form in place, the default understanding was that the patient was for all treatment:
. . . if the person is for a full active treatment . . . then we wouldn’t have a ReSPECT form in place.
Site 6, C01
In part, this reification of CPR decision-making reflected the form’s design. One middle grade-level doctor, who identified as an advocate of the ReSPECT process, said that:
. . . the ReSPECT form currently that we have is a, as I say, a black or white answer, it’s for or not for resuscitation. And so having that conversation becomes quite pivotal to the, to the rest of that conversation on the ReSPECT form.
Site 4, C10
Along similar lines, another clinician said:
But either for or not for resuscitation, that’s the only real decision that that form prompts me to do.
Site 2, C02
This conceptualisation of the ReSPECT form as DNACPR was shared across medical teams. One consultant explained that nurses equated the ReSPECT form with a DNACPR decision:
. . . sometimes the nurses were [inaudible], said, ‘Oh, a patient’s deteriorated, they don’t have a ReSPECT form’, because the ReSPECT form has replaced our resuscitation form.
Site 1, C06
Clinicians perceive the ReSPECT form as improving communication through structured and detailed documentation
Doctors noted that the ReSPECT form provides space to document the patient’s future care plan (as opposed to DNACPR forms):
. . . because planning for the future is a big part of the ReSPECT process, it’s not only about do not resuscitate decision, it’s about the, the planning for the future. It gives us the opportunity to, to discuss it with the families. And the, the place to document this discussion.
Site 4, C01
This form structure was especially important for palliative patients or those who required multiple treatment decisions. As one geriatrician explained, when speaking about a patient who asked to die at home:
I was able to write a very specific future care plan, which was ‘Avoid, relieve breathlessness, try and avoid coming back to hospital, make’’ you know, ‘slightly relax control of [condition]’, and those, those types of things.
Site 3, C07
In another case, a doctor explained that, although they used the ReSPECT form as a DNACPR and ceilings of treatment form in hospital, they also used the ReSPECT form to prompt ACP discussions between GPs and outpatients:
In outpatients I have used ReSPECT conversation as a trigger for advanced care planning, I don’t usually complete the advanced care planning myself in outpatients but I will prompt GPs and patients to have the conversation, or district nurses.
Site 2, C04
Several clinicians emphasised that the ReSPECT form did not change their conversational practices. In some cases, clinicians explained that this was because they already practised patient-centred communication:
I think as a geriatrician we have always done these and we’ve always done them well.
Site 6, C06
Other clinicians perceived the ReSPECT form as providing a new structure for documentation, without affecting communication practices:
I suppose that I would tend to fill out the form after having the discussions and more use it as a documentation process rather than having the form in front of me I suppose.
Site 6, C01
In some cases, clinicians said that the ReSPECT form has not changed their documentation practices, asserting that they saw no material difference between documenting the discussion in the notes or on the ReSPECT form:
. . . it’s always part of the plan for me, it’s always part of the plan. It was red form in [the] other hospital and previously we just used to write it in the notes, so it’s always part of the plan.
Site 2, C06
The ReSPECT process promotes quality and continuity of care in the hospital and across settings
Many clinicians noted that the ReSPECT process led to improvements in quality of care. For example, one consultant explained that the ReSPECT process reduced the harms associated with do not attempt resuscitation (DNAR) forms, particularly the mistaken withdrawal of treatment:
. . . so when I was a junior doctor and we had DNAR forms, one thing that always upset me was that if we had a patient on a DNAR form, some doctors assumed that meant do not treat, so they treat them with nothing . . . The ReSPECT form is much clearer, and the ReSPECT process is much clearer about this is not just . . . I think it, it has eased the confusion that it’s not just about CPR.
Site 5, C08
Another consultant said that, before the implementation of the ReSPECT form, treatment recommendations, even when recorded in detail, were not easily accessible, leading to harm in emergency situations:
. . . before we just used to write it all in the notes. But then there’s a risk of it being missed, you know. Beautiful two pages of prose written in the notes a week ago, then when the patient arrests no one necessarily knows that it’s there, or can’t find it. But having it as a ReSPECT form in the front of the notes, easily recognisable, easily found, and also on [the hospital’s digitised notes] there on every handover, that, that’s transformed it.
Site 4, C02
The benefits of recording decisions on the ReSPECT form extend beyond current admissions. One clinician explained that, when patients are re-admitted, the ReSPECT form allows for continuity of care:
. . . by having an instant look at it it can present with a good picture of the patient and the management if it’s done sensibly and properly. Then for the next admission, especially if they are recurrent patients, the same patients presenting again and again, then it’s such a timesaver for the next time for anybody else or ourselves.
Site 3, C01
With the ReSPECT form transferable across settings, several clinicians noted that the form promotes continuity of care between the hospital, ambulance crews and care or nursing homes. These clinicians include detailed instructions with other settings in mind:
. . . and that’s where ReSPECT comes in really helpfully, because then, the ambulance crew that, that responds to that 3 a.m. call can look at that and say, ‘Well, actually, this was the, this was the objective from that discussion’, and it would help their decision-making at the point . . .
Site 3, C07
Overall, clinicians perceived the ReSPECT form as supporting a more holistic approach to anticipatory decision-making that is inclusive of patients’ wishes and clinical needs.
From the perspective of clinicians working with acute admissions, what changes are needed to improve ReSPECT decision-making, including ethics dimensions of the decisions?
The following themes are addressed in this subsection:
-
Additional time and resources are needed to ensure that ReSPECT conversations are had with every patient who could benefit from them.
-
Improvements in the ReSPECT form, clinician education and transfer across settings are needed to facilitate higher-quality conversations and decision-making.
-
ReSPECT form digitisation should be improved.
-
The ReSPECT process needs to engage more carefully with patients’ lived realities.
Additional time and resources are needed to ensure that ReSPECT conversations are had with every patient who could benefit from them
Doctors cited time limitations as the main barrier to ReSPECT conversations. Compared with more urgent patient care, the ReSPECT process was said to be frequently deprioritised. Therefore, although doctors acknowledged the importance of having ReSPECT conversations, it is clear that doctors do not have ReSPECT conversations with every patient who could benefit from them. According to one geriatrician:
I don’t think this type of discussion takes place anywhere near enough, we’re working in a struggling health system that hasn’t got the resources to spend time having these discussions.
Site 3, C04
As a result, doctors tend to hold ReSPECT conversations with patients at risk of deterioration. The exception is one trust where doctors are prompted to have ReSPECT conversations with all patients, although doctors often resort to CPR-focused discussions. According to one, ‘[o]n a busy post-take round . . . it could be quite difficult to just go through absolutely every possible occurrence’ (site 6, C05). The other participating trusts do not have similar prompts and, as one junior doctor explained, ‘it’s just not really required and it’s quite a busy job so we just don’t have time’ (site 4, C09). Time limitations are inextricable from staff shortages, and some doctors explained that the ReSPECT vision cannot be realised with current staffing levels:
[It’s] a great idea, but it still has to be delivered by, you know, a limited number of people.
Site 5, C09
Owing to time limitations, doctors noted that the ReSPECT form cannot be used as a universal form, as one emergency medicine consultant explained:
I don’t think that we should do that for every patient in the emergency department because . . . it would be impractical. It would ground us, grind us to a halt if, if we had a resuscitation discussion with every patient.
Site 5, C08
Doctors’ reasons for holding ReSPECT conversations selectively rather than universally were not only practical, but also ethical. For example, a geriatrician explained why ReSPECT conversations are held with only a minority of patients:
. . . [i]f I have too much workload on any particular day I won’t be feeling comfortable to fill in ReSPECT form unless I know them pretty well. Because then I feel that I’m not doing it honestly or, or adequately if they are just very new patient and I don’t know much about them.
Site 3, C01
For this doctor, to have a hurried conversation shows lack of respect for the person whose treatment and care will be affected by the recommendations, and a hurried conversation could also lead to poorer care if considerations of treatment options are not adequately discussed.
Another geriatrician characterised ReSPECT conversations as emotionally laborious, saying that these conversations could not be held quickly and consecutively:
. . . they’re not conversations that should feel rushed and they, they should feel personally and it’s exploring the, the patient’s wishes and, and their family’s wishes. That does take time, I think that clinicians are human and very heavy discussions about ceilings of care and, and future wishes are, are draining.
Site 3, C04
Doctors said that trust policies placed additional barriers on the ReSPECT process. In particular, the requirement that consultants sign or countersign ReSPECT forms means that nurses and junior doctors, who are often the health-care professionals closest to the patients, either cannot or do not complete ReSPECT forms. Speaking about a patient who did not have a ReSPECT form, a junior doctor said that ‘she should have some sort of ceiling of care written down in her notes. But this ward is, kind of run by very junior doctors and we’re not always allowed to make those decisions’ (site 4, C06). Another junior doctor noted that unclear trust policies about countersigning made the ReSPECT process more complicated:
. . . all these rules floated around that if an FY1 [foundation year 1 doctor] was to do it, it would last for 24 hours, if a registrar would do it, it would last for 4 days, if a consultant does it then it would last forever, kind of weird rules that different wards didn’t agree with and some didn’t believe . . .
Site 4, C08
To overcome this, some consultants suggested that limitations should be lifted and all qualified staff be allowed to complete ReSPECT forms, although others cautioned that junior members of staff may not have sufficient experience and training. Balancing expertise and experience against time limitations remains a difficult ethics challenge.
Many doctors suggested that patients would benefit if ReSPECT conversations were held in primary care or outpatient settings:
. . . the real big change that’s needed is with those conversations we had earlier and not in extremis, in acute admissions, but in outpatients and in general practice so that it is not done at the time when things are, people are already very vulnerable and scared and are ill.
Site 3, C08
Although doctors tended to idealise the GP–patient relationship, describing it as imbued with a trust that patients do not feel towards hospital clinicians, some also cautioned that ReSPECT conversations held in community settings might not adequately address acute care scenarios, and would need to be reviewed on admission to hospital.
Improvements in the ReSPECT form, clinician education and transfer across settings are needed to facilitate higher-quality conversations and decision-making
Many doctors noted that aspects of the ReSPECT process conflict with clinical practice. Some doctors critiqued the ReSPECT form’s level of detail (considering it either too detailed or not detailed enough), the number of signatures required and the form’s lack of sufficient space for treatment recommendations. For example, a consultant who prepared a ReSPECT form as part of a patient’s discharge plan said ‘I was, you know, really having to struggle to get on with my text into the box at the bottom’ (site 6, C01).
Some doctors expressed reluctance to use the ReSPECT form in place of existing forms. One consultant explained that their ward’s communication form is superior:
And I would hate for the ReSPECT form to replace our communication form, because I feel that the ReSPECT form doesn’t have enough space to really document the, to keep a narrative of what’s been discussed.
Site 1, C06
Going further, another doctor said that the ReSPECT form is ‘just paperwork’ (site 6, C03) and that discussions are still recorded in the notes.
In most cases, however, doctors complete ReSPECT forms following discussions with patients/families. However, doctors overwhelmingly complete the forms for patients who are not for CPR. and most doctors explained that this is because ‘the default position, unless it has been explicitly discussed or documented, is that everyone is for CPR’ (site 5, C03). Some doctors worried that completing a ReSPECT form for patients who were for CPR would put patients at risk because medical teams perceived the ReSPECT form as equivalent to a DNACPR. One acute medicine doctor explained that they documented ‘for CPR’ decisions in the notes, rather than in a ReSPECT form, to avoid a catastrophic scenario, and another doctor explained:
. . . unless we can identify very quickly which patients are for resuscitation and which patients are not for resuscitation, putting in a ReSPECT form is going to create a lot of confusion. And I don’t want to be, I don’t want to be the person who makes a mistake . . .
Site 2, C01
As a result of this practice, doctors sometimes have repeated ReSPECT conversations with patients who are for CPR and have no documentation of these conversations.
Doctors noted that ReSPECT forms are often inadequately completed. For example, one geriatrician said ‘we have seen very much poor quality ReSPECT forms being done’, with doctors completing these forms ‘in 2, 3 minutes without doing justice’, thereby leading to forms that ‘are so general, they don’t feel [like an] individual plan for any individual patient’ (site 3, C01). Another doctor explained that, owing to the poor quality of many completed forms, ‘if you see a ReSPECT form you do wonder, you know, what’s the conversation that’s been had before. Because it’s not filled in very well most of the time’ (site 1, C06).
To overcome shortcomings in form completion, some doctors suggested changes in design. One consultant suggested that the form should feature ‘a short list of major interventions, you know, critical care, CPR and others to be specified’ (site 1, C04). Two junior doctors working on the same ward said that the ReSPECT form should include checkboxes for escalation decisions, such as ‘non-invasive ventilation, invasive ventilation, those kind of things’ (site 4, C09), to prevent an exclusive focus on CPR and increase clarity about future treatment, and ‘then that way all the parameters are thought about’ (site 4, C08).
Another design change suggested by doctors is the inclusion of uncertainty. Several doctors noted that they do not complete ReSPECT forms if patients/families disagree with medical advice or if patients/families are undecided about the treatment they want. Where the ReSPECT form has been digitised, doctors cannot complete the form without clicking on the CPR box, meaning that some ReSPECT conversations that are held are not documented.
Doctors also said that training should be provided to improve the quality of ReSPECT form completion. A geriatrician noted that gaps between specialties meant that some doctors complete the ReSPECT form as intended, whereas others focuse exclusively on CPR because ‘not everybody works in a holistic way’ (site 6, C06), necessitating additional education for clinical staff. An intensivist (site 5, C03) said that ‘quite a lot of resourcing, education and developing skills in clinical staff’ are needed to ensure that doctors havedReSPECT conversations early in a patient’s admission:
So education of, not just patients and the public, but also staff as well, and the confidence and skills to actually think about these issues and raise them with patients, and not just leave it to the intensivist who might be providing the last bit of resuscitation and then post-resuscitation care.
Site 5, C03
Despite the intentions of its developers, the ReSPECT form frequently does not transfer well across settings. Nurses often forget to provide the form to patients on discharge or systematically keep the form in the medical notes, nursing home staff sometimes misplace the form, and patients sometimes forget to bring the form with them to hospital. In hospitals where the ReSPECT form is digitised, doctors often do not provide patients with a paper form to take home, and this increases miscommunication across community and hospital settings, as one consultant noted:
We’ve got difficulties, particularly around the, the intersections of different sectors of healthcare. Primary care to secondary care, from secondary care to care homes or community. And it’s at those junctions in care where the, the form should flow with the patient.
Site 6, C05
To overcome this, some doctors suggested that an electronic system should replace the paper form. For example, a consultant said that ReSPECT ‘would probably need to be electronic because of course, you know, when the patient dials 999 for an ambulance, the one thing the ambulance men won’t remember to bring is the ReSPECT form that’s lying around gathering dust somewhere’ (site 1, C04).
Other doctors said that a national registry shared across NHS trusts and community care settings would be ideal, if unlikely.
ReSPECT form digitisation should be improved
The ReSPECT form had been digitised in two participating trusts. Although some doctors cited this as beneficial for record-keeping, other doctors felt that digitisation detracted from the ReSPECT process. In one trust, doctors said that the digitised ReSPECT form is unwieldy, leading to duplication of records, lack of patient interaction with the form and the recording of resuscitation status only, rather than detailed treatment plan recommendations. One consultant said that digitisation means that emergency medicine doctors avoid completing the form:
I know lots of consultant colleagues who complained about not being able to make the thing go green and sign it off, and I think that’s, I think anecdotally, certainly, it’d stop people completing it when they’re seeing people, particularly in the ED [emergency department], so it puts people off doing it on admission.
Site 6, C02
This consultant also said that the digitised ReSPECT system prompts doctors to complete a new form with every admission, making it an untenable option for outpatients and, therefore, ‘having a paper form in front of their . . . dialysis folder is by far the easiest solution’ (site 6, C02).
In one trust, digitisation has affected the transferability of the ReSPECT form across settings. As the digitised form cannot be printed, when patients are discharged, doctors have to copy the information onto a paper form, leading to duplication and often to no forms being provided to patients:
If anything, I think it’s a barrier to us generating the forms. They should be able to be just printed off . . . But I think that form’s a barrier, because you have to find the form and you have to fill it in.
Site 6, C05
Doctors were also concerned that the digitised form has lost the visual impact and meaning of the original paper form, and this is particularly the case with the patient preference scale, which is translated into percentages. Doctors noted that this scale is ambiguous and difficult to interpret in practice, As one consultant explained:
Because, well, to say 10% comfort care, 90% curative, or 20–80, or whatever, you know, I don’t know how people will really practically interpret that. And, you know, people’s interpretation will vary from person to person, I think. There’s not a dial that you can set 20–80 on the patient, or on the monitor, or on the infusion pump, or . . . you know, it’s, what does that translate to?
Site 4, C02
The solution to this ambiguity, one junior doctor learned, is to ignore the patient preference scale:
. . . initially when I’m like, asking my seniors, ‘What do I put for numbers?’ and I think everyone is just like, ‘It doesn’t really matter’, almost . . . I think everyone sort of tends towards comfort, but the numbers don’t really . . . We’re not really sure how to use the numbers basically.
Site 4, C05
Digitisation also means that patients cannot interact with the form during ReSPECT conversations:
And I think also the form being on a computer screen that’s, doesn’t, you know, it’s not easy, it’s not an easy thing for patients to interact with either.
Site 6, C02
The ReSPECT process needs to engage more carefully with patients’ lived realities
Many doctors noted that the ReSPECT form is less useful in emergency and acute medicine. The form, they said, was designed for patients who are well enough to engage with it meaningfully and not for acutely ill patients. As a result, doctors often do not use the patient preference scale. One consultant explained:
A frail patient in pain who’s had an acute admission, I think it’s entirely inappropriate to ask them to put a cross, because it’s meaningless, you’ll get them to put it one day, they’ll put it in a completely different place the other day. And it’s just not valid.
Site 2, C02
This approach extended beyond the patient preferences scale to include the ReSPECT conversation more broadly. Often, doctors take a persuasive approach or focus on resuscitation alone to avoid overwhelming acutely ill patients:
I think the challenge is the very sick person at the front door who feels lousy and doesn’t really have the energy to engage with a detailed conversation, but medically we still need to make some decisions about ceilings of care. And we end up being perhaps a little bit more directive than ReSPECT was originally designed for.
Site 2, C04
Doctors also noted that, although the ReSPECT process is useful in outpatient settings, the discussions that the ReSPECT process are meant to elicit – about quality of life and future preferences – re untenable in an acute setting. As one emergency medicine consultant explained:
I don’t think that anyone can, anyone who’s sick enough to be in a resus room and having a discussion about their care has the mental capacity to be making those judgements because I couldn’t do it now.
Site 5, C08
To overcome mismatches between form design and acute contexts, several doctors said that ReSPECT forms should be completed in primary care or outpatient settings, where patients are better able to speak about quality of life. 50
An additional concern raised was that the ReSPECT process and form might imply that treatment is available when medically impossible. For example, a consultant said that asking patients about their wishes may introduce false hope:
And I tell my colleagues, ‘Why do you ask them what they wish if you are not going to offer that?’ ’Cause then if you ask them and they say, ‘Yes’, you are, they expect you to do it. But it might not be the, from a medical point of view it might not be the appropriate thing to do.
Site 4, C07
Doctors were also concerned that patients/families might not be informed enough to make the right decisions. Doctors frequently said that many patients have never considered CPR, escalation of care and other treatment planning options before being admitted to hospital and, therefore, ReSPECT discussions are often limited:
As most of them end up being quite one-sided, it, I found that it ends up being less of a discussion that I would like, but more of a . . . ’cause normally, I found that most patients don’t really have clear thoughts about what they’d want beyond DNACPR.
Site 4, C08
In other cases, doctors worried that patients might express wishes for active treatment without knowing what this treatment entails:
I still have some concerns that does the average patient understand enough about these treatments to be able to make those decisions? And are they inherently more likely to want treatments that actually aren’t likely to be beneficial and could be burdensome?
Site 3, C05
Doctors said that the risk of making uninformed decisions should be mitigated during the ReSPECT conversation, but that not all doctors provide patients and their families with enough information:
. . . a slight danger of ReSPECT would be people only having half the discussion and saying that the patient wishes, for everything, it should be for everything rather than what’s medically appropriate for their treatment options.
Site 3, C04
To pre-empt situations where patients/families express uninformed preferences, doctors suggested that patients, and the public more broadly, should be educated about the ReSPECT process and the implications of particular treatments.
Summary
Conducted during the early implementation of the ReSPECT process in six study sites, observations of hospital-based ReSPECT conversations showed that doctors use the ReSPECT process for a wide range of treatment planning. Although CPR decisions remain a focus of ReSPECT conversations, doctors use the ReSPECT process to contextualise these decisions within broader treatment options, and some doctors discuss treatments that would not be provided alongside treatments that would be provided. Still, some doctors conceptualise the ReSPECT process as a DNACPR replacement, and most doctors hold ReSPECT conversations with only patients who are considered likely to require invasive treatment in the near future, and this suggests that the intentions of ReSPECT’s developers have yet to be fully realised in practice.
Although the ReSPECT process emphasises patient/family engagement, some doctors involved patients/families in decision-making, whereas other doctors informed or persuaded patients/families about a medical decision. Doctors explained that paternalistic attitudes to ReSPECT discussions reflect concerns with minimising futile treatments and avoiding harm. However, some doctors also said that the ReSPECT process allowed them to view quality of life from a patient’s perspective, and even alter treatment plans accordingly. When patients and families were asked about their experiences of ReSPECT conversations, they mostly perceived these conversations as providing information about a medical decision, rather than as shared decision-making processes. However, the experiences of patients and families varied, with patients expressing more confusion and stress, and families expressing feelings of reassurance, and this suggests that ReSPECT conversations may engage patients and families differently. We also found that the ReSPECT form was used in only a small minority of conversations. As the ReSPECT form includes a section that elicits patients’ values and preferences, its absence may limit possibilities for patient/relative engagement, and this is particularly important in trusts where ReSPECT has been digitised. Finally, many observed conversations were incomplete because patients/families disagreed with doctors’ recommendations or because patients/families experienced indecision or distress, and theses incomplete conversations highlight a key challenge in the acute hospital-based ReSPECT process, that is if patients’ values and preferences should be involved in decision-making and, if so, how.
Review of written records
This qualitative analysis evaluates whether or not the decision-making processes recorded in hospital-issued ReSPECT forms fulfil the ReSPECT process’ ethics aims (i.e. consistency, transparency and ethics justifiability). This subsection has been adapted from Eli et al. 3 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The adaptation retains the data and interpretations presented in the primary manuscript.
Methods
Sampling and recruitment
The six hospitals involved in the observational study also participated in the records review. Working with a pilot sample of 20 completed ReSPECT forms, a sampling frame, categorising records by ward, admission type (i.e. elective or emergency) and patient age, was developed to maximise the collection of diverse records.
Data collection methods
In each site, patient records (i.e. completed ReSPECT forms and related notes, if available) were collected within the first 2 years following ReSPECT implementation. Hospital research staff followed the sampling frame for selection of records and any deviation from this was discussed with the research team (e.g. if it was difficult to identify forms for younger patients or forms where the patient was ‘for CPR’). The collected records included ReSPECT forms versions 1.0 and 2.0. Despite some differences, the two versions were largely similar and the completed forms could be analysed using the same analysis tool. Data collection took place between August 2017 and April 2020, covering ReSPECT forms completed between July 2017 and January 2020 (i.e. prior to the COVID-19 pandemic affecting UK health care).
Analysis
Following an accountability for reasonableness (AFR) framework, which focuses on ethics decision-making,51 a qualitative evaluation tool was developed for a structured analysis of the quality of completed ReSPECT forms. AFR is an ethics framework that was originally developed for resource allocation decision-making. AFR focuses on the process of decision-making rather than on specific ethics principles, stipulating that decision-making should be transparent, based on reasons agreed as justifiable by the relevant stakeholders and open to review. 51 The process should be consistently applied to justify the ethics principle of equity. The tool’s development was inspired by an evaluation tool designed for a study on ethics decision-making in critical care admissions. 52 The development process involved several sessions with Anne-Marie Slowther, Claire A Hawkes, Frances Griffiths, Karin Eli and Zoe Fritz. The team established assessment guidelines, and the tool underwent ongoing testing and refinement. The final version of the tool assessed ReSPECT forms for the following:
-
Consistency. Have the forms been completed to the standard indicated by ReSPECT form guidelines?53
-
Transparency. Do the ReSPECT forms and relevant sections of the patient notes contain complete information about patients’ preferences, diagnoses, reasons for treatment recommendations, assessments of capacity (where relevant) and who participated in the ReSPECT discussion?
-
Ethics justifiability. Do the reasons for treatment recommendations indicate that clinicians considered patients’ preferences and clinical conditions, as well as the benefits and burdens of specific treatments?
All patient records (i.e. forms and patient notes, where available) were analysed by Karin Eli, with additional analysis provided by Claire A Hawkes, Frances Griffiths and Anne-Marie Slowther (with each scoring about one-third of records). Following comparison and discussion of the findings, the team achieved consensus on the key findings.
Ethics considerations
Data were collected with CAG approval (without individual consent). Patient and clinician identifiers were redacted prior to transfer to the study team. NHS researchers sent the pseudoanonymous records to the ReSPECT Evaluation Study Team using an encrypted NHS platform. Records were stored in password-protected files on a secure University of Warwick server.
Findings
Of the 162 completed forms, the analysis included 141 forms (paper forms, n = 121; digitised, n = 20; version 1.0, n = 87; version 2.0, n = 54). Twenty-one forms were excluded because of duplication (n = 2) or incomparability with the rest of the sample due to one trust’s incorporation of the ReSPECT form within its overall patient record system (n = 19). Twenty-eight records did not include patient notes.
Consistency
All forms included a CPR recommendation. Most forms (n = 87, 61.7%) included a recommendation regarding a focus on either life-sustaining treatment or symptom control.
Most forms included free-text treatment recommendations (n = 119, 84.4%). However, the level of specificity and detail varied substantially across forms. Specific treatments (e.g. non-invasive ventilation) were mentioned in less than half of the forms (n = 65, 46.1%), whereas some forms (n = 54, 38.3%) recorded general instructions (e.g. ‘for ward-based care’), which could be misinterpreted as they were site-specific instructions and did not clarify what treatments were and were not available on the wards.
Most forms (n = 97, 68.8%) recorded who was involved in the ReSPECT discussion. Where patients lacked capacity, some forms (n = 31, 54.3%) included families’ names or roles, whereas others (n = 26, 45.6%) included no information about ReSPECT discussion participants or only the names of the doctors involved.
Transparency
Although acute diagnosis was recorded in a minority of forms (n = 61, 43.2%), lists of chronic conditions were recorded in most forms (n = 120, 85.1%). Few forms included reasons for treatment recommendations (n = 13, 9.2%) and only a small minority of these forms stated that treatment recommendations were informed by patient preferences.
In most cases, ReSPECT discussions were mentioned in the notes (n = 91, 64.5%), but only a few forms (n = 11, 7.8%) included guidance on where to find ReSPECT discussion records in the notes. At times, there were mismatches between information recorded on the form and in the notes, such as when notes detailed treatment planning recommendations not included in the form.
No formal capacity assessments were recorded in the available notes for patients without capacity. Some clinical notes (17/38, 44.7%) included references to patients’ capacity, but most did not.
Only a minority of forms (n = 49, 34.8%) included an appropriate senior responsible clinician signature in the correct place on the form, and this may be because of a design fault in the form that led to confusion about where the clinician completing the form should sign if they were also the senior responsible clinician.
Ethics justifiability
Of the forms that included reasons for treatment recommendations (n = 13, 9.2%), most referred to the futility of treatment only (e.g. ‘CPR likely futile’). The weighing of the burdens and benefits of specific treatments was mentioned in only one form. Very few forms recorded how patient preferences or values had informed the recommendations.
Most forms (n = 122, 86.5%) included information about the patient’s capacity. Although 65 patients were recorded as having capacity, their preferences were recorded in just over half of the forms [n = 34 (52.3%) on the patient preferences scale; n = 17 (26.2%) in the free-text box]. For the 57 patients who were recorded as not having capacity, just over half (n = 31, 54.4%) of the forms recorded that a person close to the patient had been involved in the ReSPECT conversation.
Summary
An evaluation of completed ReSPECT forms and relevant segments of patient notes showed that CPR recommendations were recorded on all forms, and that most forms mentioned other treatment recommendations. This finding signals a shift towards placing CPR decision-making within a wider context of clinical care. Nevertheless, forms varied substantially in the detail provided. Although specific treatment recommendations were documented in some forms {e.g. ‘for i.v. [intravenous] fluids’}, other forms included generalised statement, such as ‘for ward based care’. Many forms did not record patient wishes and preferences and it was not always clear who had been involved in the process. Because clinicians tended not to document their reasons for recommending particular treatments, and rarely recorded engaging with questions of burdens and benefits, it was difficult to assess the ethics justifiability of the recommendations made.
Focus groups with general practitioners
This section of the study aimed to explore GPs’ experiences of the ReSPECT process. Our aims were to:
-
establish uptake and attitudes to the ReSPECT process in the community
-
evaluate how the ReSPECT process transfers across the acute/primary care boundary.
Methods
Sampling and recruitment
We conducted focus groups with GPs, in areas served by five of the six hospitals that participated in the study’s other work packages. The sixth site’s focus group could not go ahead because of the COVID-19 pandemic.
To obtain a convenience sample, the study team sent information about the research to key contacts in areas served by the hospitals (including a GP partnership, a GP interest group, a health and care commissioning group, and a palliative care specialist with GP and other health-care professional contacts) that facilitated recruitment in their networks. Five focus groups of between 3 and 10 participants were conducted, with 27 GPs participating in total. Participants in three focus groups had used the ReSPECT process in their clinical practice (Table 1).
| Focus group (n) | Is ReSPECT used in participants’ general practices? | Number of months the ReSPECT process had been used by their local hospital at the time of the focus group |
|---|---|---|
| 1 (n = 10) | Yes | 27 |
| 2 (n = 3) | No | 23 |
| 3 (n = 5) | No | 23 |
| 4 (n = 4) | Yes | 27 |
| 5 (n = 5) | Yes | 27 |
As the study progressed, we learned that it would be valuable to include other community health-care professionals to advance our understanding of the implementation of ReSPECT in the community. We conducted two individual interviews, with a paramedic and a community-based palliative care doctor (group ID: Int1), representing one of the hospital areas. These participants were recruited by a palliative care specialist and both participants used the ReSPECT process in their clinical practice.
All participants were paid £150 and were offered Continuing Professional Development certificates for their participation.
Data collection methods
All focus groups were facilitated by Karin Eli, four focus groups were co-facilitated by Claire A Hawkes and one focus group was co-facilitated by Anne-Marie Slowther. In two focus groups, facilitators were joined by a palliative care specialist from the local hospital and the palliative care specialist responded to participants’ locally specific questions about the ReSPECT process. At the start of each group, facilitators circulated a ReSPECT form and described the ReSPECT process. Although working in areas served by hospitals using the ReSPECT form, some GPs had not encountered the ReSPECT form prior to the focus group and these GPs’ discussions were informed by their experience of other forms, such as DNACPR and specialised local forms (note that we use the term ‘ReSPECT-type conversations’ to refer to these broader experiences). The two interviews were conducted by Karin Eli over Skype™ (Microsoft Corporation, Redmond, WA, USA). Both interviewees had seen patients with ReSPECT forms, and the palliative care doctor had conducted ReSPECT conversations.
Both focus groups and interviews explored participants’ experiences of the ReSPECT form (e.g. completing it themselves and seeing patients discharged from hospital with ReSPECT forms), how participants initiated ReSPECT-type conversations and participants’ experiences of ReSPECT recommendations being communicated across the primary care–secondary care interface.
Focus groups were conducted between April and November 2019 and lasted between 60 and 105 minutes. Interviews were conducted in March 2020 and lasted between 50 and 70 minutes. All focus groups and interviews were audio-recorded. Recordings were transcribed verbatim.
Analysis
Transcripts were analysed using inductive thematic analysis. 55 Caroline J Huxley closely coded the transcripts at the semantic level and identified candidate themes. These candidate themes were discussed and refined within the research team (KE, FG, A-MS and CAH), resulting in five themes.
Ethics considerations
Written informed consent was obtained from participants before each focus group discussion or interview. In the report, we have removed identifying details and have assigned all participants a group ID that cannot be traced back to them.
Findings
An earlier version of this section has appeared in the study team’s publication on GPs’ experiences the of ReSPECT process. 54 This earlier version has been adapted for this report. The adaptation includes additional findings gleaned through interviews with health-care professionals, which have not been included in the preprint. However, the adaptation retains the interpretations and some of the data presented in the preprint publication.
The ReSPECT form is an end-of-life care document
Participants expressed an implicit assumption that the ReSPECT form is an end-of-life care document for patients who are frail, under palliative care or in the final stages of a chronic illness. ReSPECT-type conversations are predominantly initiated by the GPs themselves, and are typically triggered by a deterioration in the patient’s health:
So there’s, like, a point where a patient’s condition turns that you can identify and then you begin to have a discussion.
FG4
Participants felt that it is important to identify and record patients’ wishes while they have capacity. The ReSPECT process is also initiated as part of routine care home admissions, and our paramedic participant said that ambulance crews mainly see ReSPECT forms with care home residents.
Participants often had a ‘hunch’ or ‘just knew’ that the timing was right to have a ReSPECT-type conversation, and participants would use verbal cues from the patient (e.g. references to recent experiences in hospital) as an opening for the conservation. Less commonly, patients themselves initiate ReSPECT-type conversations to express their wishes to decline CPR in an emergency. These patients are often healthy, and our participants questioned the morality of completing a ReSPECT-type form in these cases:
. . . some patients will want a DNACPR in place when there’s really nothing wrong with them . . . they just don’t like the idea of going through resuscitation. Then, that’s a whole other minefield . . . am I really doing the right thing for this person when they could have a really positive outcome potentially with treatment?
FG2
The ReSPECT process is best carried out in the community
Participants agreed that ReSPECT-type conversations can be carried out well within primary care. Conversations are often planned in advance, and so patients are prepared to discuss end-of-life care. Some GPs have lengthy pre-existing relationships with their patients, and these relationships make the conversation easier:
. . . because I’ve known them for so long . . . you can easily just say ‘While you’re here? I know we, we haven’t talked about this before and I think it is time that we are going to talk what’s going to happen in the future’.
FG5
Participants described ReSPECT discussions as an ongoing process that takes time to complete. As patients are not usually at immediate risk, there is more time for ReSPECT discussions to unfold in primary care than in hospital. Furthermore, community palliative care allows even more time for ReSPECT discussions than primary care, and the palliative care doctor noted that they can develop rapport with the patient without rushing the process.
Both our paramedic and palliative care doctor observed that, although community settings are ideal for ReSPECT discussions, GPs do not issue ReSPECT forms for every patient who needs one. The GPs described time and resource constraints that prevent them from initiating ReSPECT-type conversations. GPs reported that they feel constrained by the 10-minute consultation slot and are aware of a busy waiting room outside:
I think as doctors we find it, we don’t talk about it because we, it’s an add on to our normal consultation in 10 minutes.
FG1
Our participants reported feeling reluctant to hold sensitive ReSPECT-type conversations with patients they have not met before:
So some people you know really well, and, and it’s easy to, to bring things up and, and to chat to them, and be frank with them, whereas sometimes you’re in a situation where actually, you’re being asked to do it, or you think it’s appropriate to do it, and then you, but you’ve never met them before, and then, then it’s a lot more tricky.
FG3
A lack of experience and confidence in end-of-life planning also prevents GPs from initiating ReSPECT-type conversations.
Several participants suggested that it would be beneficial for health-care professionals other than doctors to initiate or be involved in the ReSPECT process:
. . . how many district nurses, or nurses fill in ReSPECT forms? Because arguably they . . . know all the patients far better than we do.
FG1
The paramedic thought that ambulance crews might talk about CPR more accurately and honestly than GPs because they have witnessed the physical and psychological impacts of CPR. However, participants noted that ReSPECT conversations can be especially difficult when patients do not agree with clinical recommendations, and dealing with such situations requires specialised training, which most nurses and paramedics have not received:
I don’t think that necessarily precludes [them] from doing it at all. I just think there is probably a fair amount of training I suppose that would need to take place to be able to do it.
INT1
Although GPs reported barriers to completing the ReSPECT process in primary care, GPs ultimately thought that it is the appropriate place to hold such conversations. All participants were critical of the hospital-issued ReSPECT forms they had seen, and thought that forms are being completed by inexperienced junior doctors in busy environments.
The ReSPECT process is an emotional process
Participants gauged how emotionally prepared a patient is to have a ReSPECT-type conversation by assessing their reaction when the topic is raised. If the patient reacs with alarm or withdrawal, then the participants would delay the conversation:
. . . tentative early attempts at discussing prognosis and decisions to escalate treatment . . . were distressing for [the patient] and the family. And so, we sort of shelved it and ended up having to go back to it a few weeks later when it was much easier to then complete it.
INT1
Many GPs include the patient’s family in these conversations, for emotional support and to ensure that everyone understands the plan.
A few GPs reported that they are emotionally unaffected by ReSPECT-type conversations because of professional experience. More frequently, GPs find it hard to maintain an emotional distance, particularly when they know the patient well. Emotional reactions can be affected by the patient’s reaction. If the patient reacts positively, then GPs feel that they had ‘done a good thing’ (FG3); however, distressed patients often leave GPs feeling ‘quite emotional [having] gone through that with them’ (FG3).
Conversations are driven by cultural understandings of death
Participants held implicit views of what a ‘good death’ was. 54 A good death was described as involving no CPR or invasive treatment and occurring at home or in a hospice, as this is what patients usually wanted for themselves. These understandings often underpinned ReSPECT conversations and the medical recommendations GPs recorded. However, some participants acknowledged that, in some non-Western cultures, a ‘good death’ means maintaining life for as long as possible, rather than focusing on quality of life. Nevertheless, clinical recommendations are based on the doctor’s understandings of a ‘good death’, and these sometimes conflict with the patient’s wishes. Such disagreements tend to focus on resuscitation. When patients/relative want CPR attempted and GPs feel that this was inappropriate, our participants try to nudge them in the direction they think appropriate:
[I] start talking about how many times during resuscitation that you break ribs . . . And they, they buy that and then they, they hear it when I say it, because quite a lot of those patients have known me for so long.
FG5
The palliative care doctor said that he/she records the patient’s wishes even when the patient’s wishes conflict with medical advice:
I would record the decision but in the knowledge that it’s probably not going to change what actually happens in practice.
INT1
General practitioners noted that patients’ families often feel ‘scared’ by terms such as ‘death’ or ‘dying’. Likewise, families feel that ,by engaging in the conversation, they are ‘condemning’ their relative. A few participants were keen to break down taboos and normalise discussions about end-of-life care, and these participants suggested holding ReSPECT-type discussions earlier (e.g. on first diagnosis or as part of a routine check-up).
There can be difficulties translating the ReSPECT process across care settings
Participants described situations in which their ReSPECT recommendations translated into care, for example when paramedics used the ReSPECT process to decide whether or not to transport a patient to hospital. However, participants also described situations when their ReSPECT recommendations were not transferred into care, and often this involved patients being admitted to hospital, despite a recorded preference for remaining at home. Structural reasons sometimes accounted for this, including a lack of hospice, home care service availability, care home staffing or resources.
Several GPs were aware that their lack of knowledge of specialist interventions could make their ReSPECT forms less meaningful in hospital, as their forms focus on preferences around hospital admission and resuscitation, and on treating chronic or terminal illness, rather than emergencies.
Some GPs had not seen hospital-issued ReSPECT forms even though their patients’ discharge letters mentioned the ReSPECT process. All participants supported an electronic version of the form that would be transferable between settings:
. . . so that all the different people providing care for a particular patient have got the . . . same kind of document that they can resort to in terms of palliative care and patient’s wishes.
FG4
For paramedics, digital sharing would enable the implementation of ReSPECT recommendations even when patients misplace the paper form. Without a digital record, paramedics spend time looking for a ReSPECT form if it seems that a patient should have one (e.g. if they see strong analgesics or oxygen tubing):
. . . it’s very reliant on . . . our own investigatory skills.
INT1
Participants critiqued hospital-issued ReSPECT forms and felt that the forms had limited value in community settings. Medical jargon commonly used in hospital-issued forms, such as ‘for ward-based care’ or ‘level 2 ceiling of care’, is not informative for community practitioners. In addition, hospital-issued forms tend to focus on specific treatments available in hospital, or are used as replacement DNACPR forms:
I feel like sometimes it is literally just, it’s like the same as the old DNACPR form . . . the resuscitation bit is like the tiniest little bit at the bottom. And the rest of that has kind of been left.
FG1
To improve transferability, several participants suggested including prompts on the ReSPECT form as to what information was required.
Summary
Community health-care professionals had varied levels of exposure to the ReSPECT form. The ReSPECT form was conceptualised as an end-of-life planning document that is best completed in community care settings. Completing the ReSPECT form is an emotional process for patients and health-care professionals. ReSPECT conversations are shaped by what a ‘good death’ is thought to be, and health-care professionals often nudge patients in specific directions they consider best for the patient. ReSPECT recommendations are not always communicated or transferable across care settings. The focus on active treatments, or use of specific phrases and jargon, means that ReSPECT forms issued in a hospital are often of limited value in community settings. A digital version of ReSPECT form that is transferable between settings would enable better communication.
Placing findings in context: challenges to ReSPECT implementation in the study sites
Our interviews with implementation leads revealed three challenges that may have affected the success of implementing the ReSPECT process in the study sites.
Achieving culture change: from DNACPR to ECTP
Implementation leads noted that, during early implementation, clinicians continued to perceive the ReSPECT process as a replacement DNACPR, and the implementation leads suggested that this reflected (1) the short period for implementation planning/activities; (2) the lack of local policies to support the timely completion of ReSPECT forms for all patients; (3) the lack of mandatory ReSPECT training for clinicians; (4) the limited involvement of junior doctors and senior nurses in ReSPECT implementation; (5) change fatigue from one CPR form to another; (6) clinicians’ concerns over issuing ReSPECT forms to patients who were for CPR; and (7) time pressures that limit clinicians’ opportunities to participate in training and to conduct ReSPECT conversations.
Engaging community health-care settings
Not all CCGs adopted the ReSPECT process, and none adopted the ReSPECT process simultaneously with the acute trusts. Owing to the variation in community adoption of the ReSPECT process, acute trusts’ engagement ranged from co-ordinating plans for implementation to raising awareness of the ReSPECT process in individual health-care organisations. One site mentioned that plans to engage with the public during implementation had not been realised. Implementers were concerned that (1) GPs were not aware that patients had a ReSPECT form following hospital admission, (2) GPs did not know that the ReSPECT form was patient-held and (3) the terminology used in hospital-issued forms did not transfer well to primary care or ambulance services.
Digitising the ReSPECT form effectively
Two trusts digitised the ReSPECT form. Digitisation improved ReSPECT form transferability, prompting, revising and auditing within hospitals, but also affected the implementation time frame and transferability across settings. Implementers identified the following challenges: (1) ensuring that digitised ReSPECT forms could be printed and given to patients, (2) ensuring version control and (3) engaging patients in ReSPECT conversations in the absence of paper forms.
To overcome the above challenges, implementation leads identified the following as effective strategies: (1) regular audits to support ReSPECT form quality assessments, progress towards implementation goals and training development; (2) mandatory training; (3) repeated/refresher training; (4) ReSPECT reminders (via hospital computer systems); and (5) continued revision of digitised ReSPECT forms based on clinician feedback.
Chapter summary
This qualitative analysis of observations, interviews, focus groups and completed ReSPECT forms shows that, at this early stage of implementation, the ReSPECT process is used for different reasons, ranging from making decisions about CPR to making decisions about palliative care. Hospital doctors vary in the extent to which they seek patients’/families’ views, in the extent to which they view the ReSPECT process as a shared decision-making process, and in whether or not they speak about treatment options other than CPR. A limited view of the ReSPECT process as primarily for recording CPR recommendations for deteriorating patients reflects both the ongoing influence of DNACPR frameworks and persistent limitations on clinicians’ time to conduct these conversations. A paternalistic approach to ReSPECT decision-making is driven by ethics concerns with the harms and potential futility of treatment escalation, and by the lack of patients’ right to request treatments not in their best interest,2 with doctors wary of offering patients/families seemingly counterproductive choices in treatment planning. Hospital doctors also vary in their views of the ReSPECT process as beneficial or not, with some doctors asserting that the ReSPECT process has improved patient–doctor conversations about treatment planning and the documentation and transferability thereof, and other doctors saying that it has not. This is echoed in the focus groups and interviews with GPs and community health-care professionals, which also demonstrated mixed experiences with the ReSPECT process and, especially, with hospital-issued forms.
These findings gain further depth when contextualised through the analysis of completed ReSPECT forms. This analysis shows that the introduction of ReSPECT forms has had some positive effect, moving the focus away from DNACPR to include wider treatment recommendations. However, the quality of form completion suggests that clinicians only partially document the decision-making logic that the ReSPECT process promotes, with wide variability in the specificity of treatment recommendations and with reasoning for treatment recommendations infrequently recorded. This finding echoes previous research on decision-making records in critical care,52 suggesting that doctors do not articulate clinical decision-making reasoning.
Notably, despite the ReSPECT process’ emphasis on patient/family engagement, all hospital-based data (i.e. observations, clinician interviews, patient/relative interviews and completed ReSPECT forms) indicate that clinicians inconsistently involve and/or account for patients’/families’ preferences. These inconsistencies may reflect practices carried over from DNACPR processes. 11,21 Indeed, previous studies on doctor–patient communication in DNACPR and even ACP processes noted that patient/family engagement varied widely. 38,45 In their interviews, patients and families expressed that ReSPECT conversations informed them, rather than involved them in a shared decision-making process. Possibilities for patient/relative engagement were limited further by the infrequent use of the ReSPECT form in conversations. In addition, many observed conversations were incomplete because patients/families disagreed with doctors’ recommendations, or because patients/families found it difficult to engage with ReSPECT conversations because of indecision or distress.
Community health practitioners, GPs and many hospital doctors suggested that ReSPECT conversations should be held in primary care or outpatient settings because the conversations would (1) involve patients in decision-making before they became acutely ill, (2) be held in a more familiar environment and (3) be within the context of a potentially longer-term relationship between patient and clinician. However, as GPs noted, this idealisation of primary care environments ignores the time pressures that GPs experience and the difficulties associated with initiating ReSPECT conversations. This finding relates to doctors’ overarching concerns of how to involve patients and families meaningfully in ReSPECT conversations while also timing these conversations appropriately, fostering trust, managing emotional reactions and offering appropriate treatment options. 2 In addition, although GPs spoke of ReSPECT as an end-of-life document, hospital doctors spoke of ReSPECT as an emergency treatment planning document, suggesting possible mismatches between the ways in which ReSPECT forms are completed in primary and secondary care, which may affect the form’s transferability and utility across settings.
Taken together, our findings suggest that, although the ReSPECT process has led to improvements, an apparent gap persists between the intentions that underlie the ReSPECT process and its implementation in practice. Bridging this gap would require work to promote a shared understanding and valuing of the ReSPECT process’ emphasis on transparency, patient/relative involvement and a holistic approach to emergency care and treatment planning in the ongoing implementation of the ReSPECT process in practice. 29
Strengths and limitations
The inclusion of six NHS trusts is a particular strength, as each trust represents different implementation timelines, localities and procedures (although two trusts merged during the study). Nevertheless, despite recruiting hospitals and interview/focus group participants from diverse geographical areas, including urban centres and rural areas, we were limited to hospitals and primary care in England.
Our observations of ReSPECT conversations allowed us to compare interview and observation data. However, because the hospital principal investigators selected the participating wards, wards for acute patients (e.g. acute medical units) predominated in some sites and wards for longer-term patients (e.g. respiratory wards) predominated in others. In the first two sites, observations were limited to ward rounds, inadvertently privileging resuscitation and escalation conversations. Owing to the cross-sectional design, we could not follow up on incomplete ReSPECT conversations. Finally, we were not able to interview many patients and families because most patients were acutely unwell and, therefore, unable or unwilling to participate, many family members had limited time (or were absent) during visiting hours, and some families expressed emotional distress due to the patient’s illness.
A particular strength of evaluating ReSPECT documentation is that the written record has both legal and patient care ramifications, and may influence the development of the ReSPECT process and its ongoing implementation. However, as data were collected during early implementation, the salience of our findings may be limited in the longer term. In addition, most of our data were collected through paper ReSPECT forms, and the digitisation of the ReSPECT form may raise additional issues.
Not all GPs who took part in our focus groups used the ReSPECT from and their reflections were based on experience with similar forms. In addition, our focus group participants may have self-selected because of an interest in palliative care, which might have contributed to the end-of-life emphasis in the focus group discussions. Finally, owing to the COVID-19 pandemic, we could not conduct focus groups in one hospital area that had been included in work package 1.
Chapter 3 Interrupted time series analysis to evaluate association of ReSPECT recommendations on patient outcomes
Parts of this chapter are reproduced from Hawkes et al. 56 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 (CC BY-NC-ND 4.0) license, which permits others to copy and distribute this work, for non-commercial use, provided the original work is properly cited.
Introduction
A key concern of patients and families who contacted an end-of-life support line during our scoping review was that they would be subjected to resuscitation when it had little to no chance of success. 57 The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report identified that resuscitation decisions are often not considered in patients admitted to hospital,5 and a key reason for this is their binary nature (i.e. for resuscitation or DNACPR), which does not allow decisions to be contextualised with other treatments. This means that a large proportion of resuscitation attempts are undertaken in patients for whom the NCEPOD reviewers considered a DNACPR decision should have been made prior to the cardiac arrest. These findings are consistent with data from the NCAA (2015–16) that indicate that 6.5% of resuscitation attempts are terminated after arrival of the resuscitation team, as it is considered futile to continue. 58
We hypothesised that, if the ReSPECT process is successful in allowing resuscitation decisions to be contextualised to overall treatment plans, then the proportion of resuscitation attempts terminated by the resuscitation team as they consider resuscitation as futile will decline, the total number of resuscitation attempts will reduce and the proportion of patients in whom CPR is attempted who survive and go home from hospital (and their functional status) will increase.
Objective
Our aim was to quantify the effect of the introduction of the ReSPECT process on frequency of, and outcomes from, in-hospital resuscitation attempts.
Methods
Study design
We carried out a longitudinal observational study.
Recruitment
The study used anonymised data from the NCAA, which were aggregated monthly with information from individual hospitals. The information retrieved from hospitals was taken from the systems used for recording advance decisions for use in a medical emergency for adult patients. All adult acute hospitals that contributed to the NCAA during the study period were included.
Withdrawals and exclusions
We used routinely collected anonymised audit data from the NCAA. Use of anonymised information was approved by the Ethics Committee. Specialist hospitals were excluded.
Data collection
A national audit (2014) indicated that approximately 80% of acute NHS trusts were using a standalone DNACPR form (or a modified version) for making resuscitation decisions. 19 Although a new ReSPECT form (i.e. version 1.0) and supporting documentation was expected to be made available nationally in 2017, it would then have to be incorporated into local trust policies over the following months. Therefore, to establish baseline systems and time of change to the ReSPECT process, we planned to undertake an annual survey of NHS trusts. The survey (see Report Supplementary Material 4) was to be completed by a member of NHS staff responsible for the NCAA data (usually a resuscitation officer). The survey asked each NHS trust (1) what system was currently in use and for how long; (2) when training for the ReSPECT process started; (3) when the ReSPECT process was first implemented; (4) when the entire organisation had adopted the ReSPECT process; and (5) what was the proportion of patients who had a ReSPECT conversation and form. The first survey was sent to hospitals in November 2017, but the response rate was poor (66%) and the information received was often incomplete. Therefore, we abandoned the idea of undertaking annual surveys and, in January 2019, asked for the same information to be provided retrospectively via freedom of information requests (see Report Supplementary Material 5). Data obtained via the survey and freedom of information requests were then combined with data from the NCAA, which routinely collects data from participating hospitals on all individuals (excluding neonates) who sustain an IHCA and receive resuscitation by the hospital resuscitation team (or equivalent). Data are reported per 2222 call to the team and collated monthly. In addition to hospital and patient characteristics, the NCAA collect the following data:
-
total number of admissions to each hospital (including elective, non-elective and day cases, but excluding babies born in hospital and neonates)
-
total number of 2222 calls solely for cardiac arrest
-
team visit data
-
arrest data
-
outcome data.
A cardiac arrest is defined by the NCAA as any resuscitation event commencing in hospital, where an individual receives chest compression(s) and/or defibrillation and is attended by the hospital-based resuscitation team (or equivalent) in response to a 2222 call. A team visit is entered in the NCAA each time an individual (excluding neonates) receives chest compression(s) and/or defibrillation and is attended by the hospital-based resuscitation team (or equivalent) in response to the 2222 call. A team visit can end only when the individual achieves return of spontaneous circulation (ROSC) > 20 minutes or dies. Cardiac arrest data used in this analysis were status at team arrival [i.e. dead – resuscitation stopped, resuscitation ongoing, ROSC achieved before team arrival, deteriorating (not yet arrested), presenting/first documented rhythm, date/time resuscitation started, date/time resuscitation stopped, reason resuscitation stopped at end of team visit, status at discharge from hospital (alive or dead) and cerebral performance category (CPC) at discharge from hospital] (for definitions see Report Supplementary Material 3).
Standardised case identification methods, data definitions, and online and manual data validation ensures that consistent high-quality data are collected. 59,60 This study and access to data were approved by the NCAA Steering Committee.
Outcome measures
Primary outcome measure
-
The proportion of resuscitation attempts that are terminated because of futility (calculated as the number of resuscitation attempts for which the reason resuscitation was stopped was ‘Dead – futility’/number of team visits).
Secondary outcome measures
-
The number of IHCAs attended by the resuscitation team per 1000 admissions.
-
Patient status at team arrival [i.e. dead – resuscitation stopped, resuscitation ongoing, ROSC achieved before team arrival, deteriorating (not yet arrested)]. Calculated as the number in each category per number of team visits.
-
The proportion of resuscitation attempts that are terminated because of presence of a DNACPR recommendation (as this represents a failure of implementation). Calculated as the number of resuscitation attempts for which the reason resuscitation was stopped was ‘Dead – DNAR identified’ per number of team visits.
-
Vital status at hospital discharge (i.e. alive or dead). Calculated as the number alive per number of team visits.
-
The proportion of shockable arrhythmic cardiac arrests. Calculated as the number of patients with a shockable rhythm per number of team visits.
-
CPC at discharge. Calculated as the number in each CPC per number of team visits.
We had intended to also examine the proportion of cardiac arrests to total number of hospital deaths as a secondary outcome, but were unable to obtain the required data (as this information is not included in the routine audit data collected by the NCAA).
Data management
The survey to assess use of the ReSPECT process was conducted using an electronic survey tool (Qualtrics®, Provo, UT, USA), using the same hospital identifiers as the NCAA to allow data linkage. Completed data sets from Qualtrics were extracted by the trial statistician on completion, and combined with outcome data for analysis purposes.
Anonymised data (with each hospital identified by a unique numerical code) from the NCAA were transferred to the University of Warwick using a secure link, in accordance with WCTU standard operating procedures and a data-sharing agreement between the Intensive Care National Audit & Research Centre, NCAA and the University of Warwick.
Statistical analysis
Data on advance planning systems in use in hospitals during the study period and the dates they were implemented are presented using basic descriptive analyses. Primary and secondary outcomes were observed over a 5-year period and collated monthly. It was hoped that, following its launch in late 2016/early 2017, use of the ReSPECT process would lead to widespread adoption. The NCAA data should then have, therefore, included observations pre and post implementation of the ReSPECT process for the majority of hospitals and be suitable for ITS analysis.
Our plan was to fit a regression line to the pre-implementation data and another to the post-implementation data, and then compare the two linear models with regard to levels, trends and changes in trends between the pre- and post-implementation periods. To enhance the chances of detecting a step change that might be attributed to implementation of the ReSPECT process, we planned to exclude the first 3–6 months’ data post implementation (i.e. the bedding-in period).
We also anticipated that data from hospitals that did not adopt the process during the study period might be used as counterfactual information. However, uptake of the process was slower and less widespread than anticipated. Therefore, we modified our approach, deviating from the analysis plan in the protocol. First, to ensure eight data points (i.e. the minimum recommended for undertaking an ITS analysis) in both the pre- and post-intervention periods, data were aggregated monthly rather than quarterly. Second, it was not possible to identify and exclude a bedding-in period common to all hospitals. Data from all time points are, therefore, included in the analysis, which means that changes over time due to implementation of the ReSPECT process will be less pronounced.
Using information from the freedom of information requests, we created a series of indicator variables for each hospital, one per month, set to one if the hospital was using the ReSPECT process for advanced decisions that month and zero otherwise. Thus, over time, the proportion with an indicator variable set to 1 increases as more hospitals start using the ReSPECT process. This means that there is no true post-implementation period, but, instead, there is a period post first implementation of the process, during which the number of hospitals that have implemented the ReSPECT process increases over time. To account for this, the degree of implementation (i.e. the proportion of hospitals that were using the ReSPECT process) at each time point has been included as a covariate in the ITS models. Calendar month was also included as a covariate in the models to adjust for known seasonality in the outcome measures.
The primary analysis is a multiple group ITS, comparing the proportion of resuscitation attempts abandoned because of futility in hospitals that did and did not (ever) implement the ReSPECT process. For convenience, we denote hospitals that implemented the ReSPECT process at some point during the study period as ‘ReSPECT hospitals’ and hospitals that did not implement the ReSPECT process during the study period as ‘other hospitals’. The pre-intervention period was from January 2015 to December 2016 and the post-intervention period was the months from January 2017 (i.e. when hospitals first started to implement the process) to December 2019.
The proportion of ReSPECT hospitals that had implemented the process at each time point was calculated as the number of hospitals using the ReSPECT process divided by the total number of ReSPECT hospitals. The proportion of resuscitation attempts abandoned because of futility, in ReSPECT hospitals and in other hospitals separately, was calculated monthly as the total number of resuscitation attempts abandoned because of futility divided by the total number of IHCAs attended by the team.
The results of the ITS analysis are presented graphically, with the proportion of resuscitation attempts abandoned because of futility in each group plotted over time, as well as the predicted values from the models. Key estimates from the models are reported with 95% CIs and p-values [i.e. the slope (trend) in each group pre and pos timplementation, the difference in levels between the groups at the start of the study period, the difference in slopes between the groups in pre- and post-implementation periods and the difference in the change in slopes (pre and post implementation) between the groups]. As change in each group is measured relative to the pre-intervention period, the difference in the change in slopes (i.e. pre and post intervention) should be considered the best measure of the effect of implementation of the ReSPECT process. The same ITS analysis approach was used to investigate the association of the intervention with the proportion of resuscitation attempts that are terminated because of presence of a DNACPR recommendation, vital status at hospital discharge (i.e. per cent alive) and proportion of cardiac arrests with a shockable rhythm. All other secondary outcomes are presented graphically only.
The ITS analyses were performed using the itsa command within Stata® 16 (StataCorp LP, College Station, TX, USA). The Cumby–Huizinga statistic was used to test for autocorrelation and to determine the autocorrelation structure (i.e. identify the appropriate lag). Covariates (i.e. calendar month and the per cent of ReSPECT hospitals that had implemented the process each calendar month) were included in models to adjust for seasonality and differences between hospitals in the time from national launch of the ReSPECT process to implementation. The regression models were calculated with Newey–West standard errors to deal with the autocorrelation and possible heteroscedasticity.
Results
Data on patient demographics and resuscitation outcomes from the NCAA were obtained for 216 hospitals and information about usage of advanced care planning systems was obtained from 189 hospitals (Figure 1). After matching and excluding duplicates, 186 hospitals were available for analysis. The majority of these (131/186, 70%) hospitals contributed data to the NCAA for the full 60 months (see Table 1), although 15 (8%) hospitals contributed data for < 36 months.
FIGURE 1.
Combination of data to create the analysis data set. FOI, freedom of information.
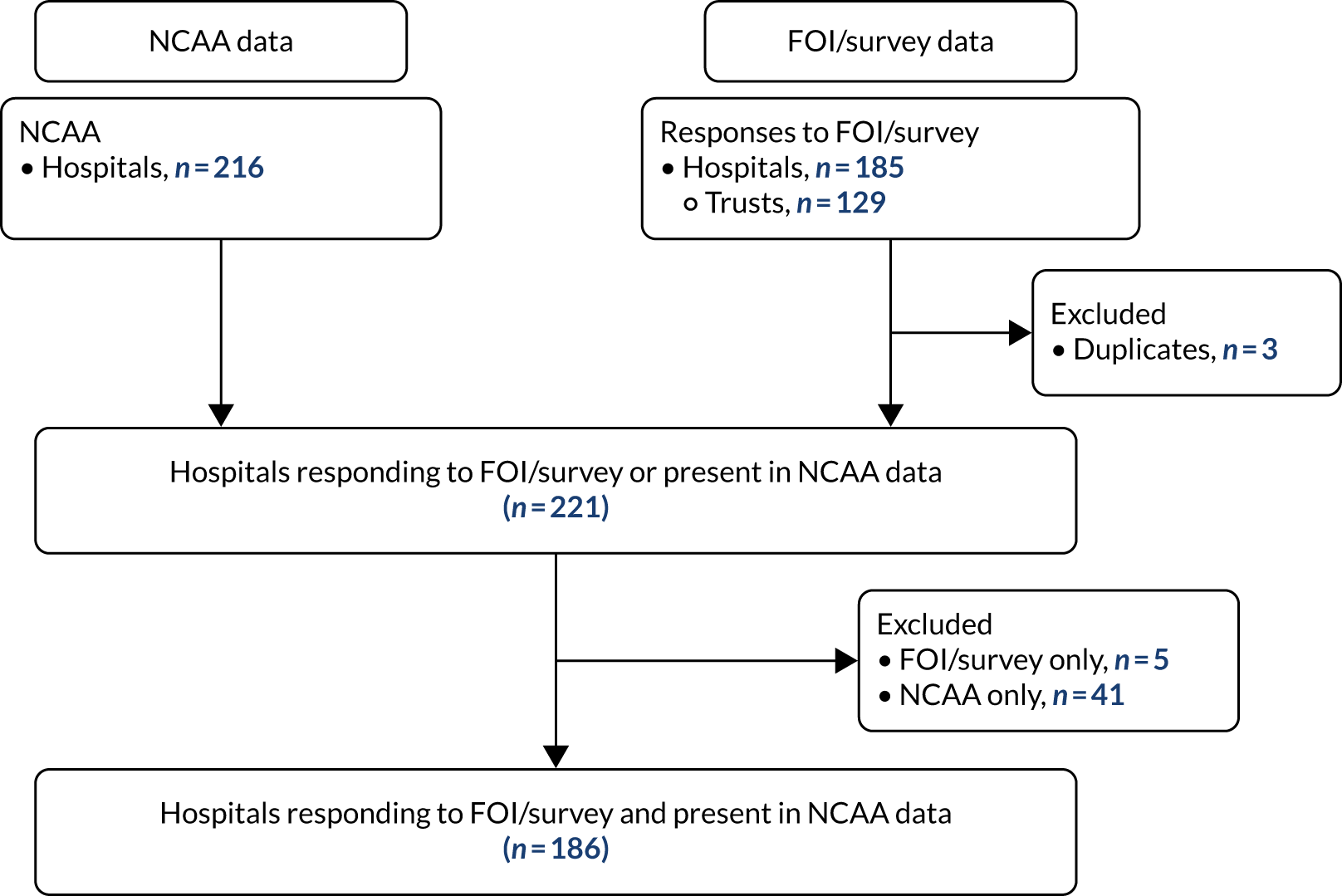
Implementation of the ReSPECT process
The number of hospitals using a standalone DNACPR form or the most common advanced planning systems (i.e. DNACPR plus a TEP, ReSPECT process or other ECTP) during each one-quarter year are shown in Figure 2. Advanced planning systems that did not clearly fit into the preceding categories were grouped together as ‘other’).
FIGURE 2.
Advance planning system usage at study hospitals (n = 186) during the period 2015–19. Q, quarter.
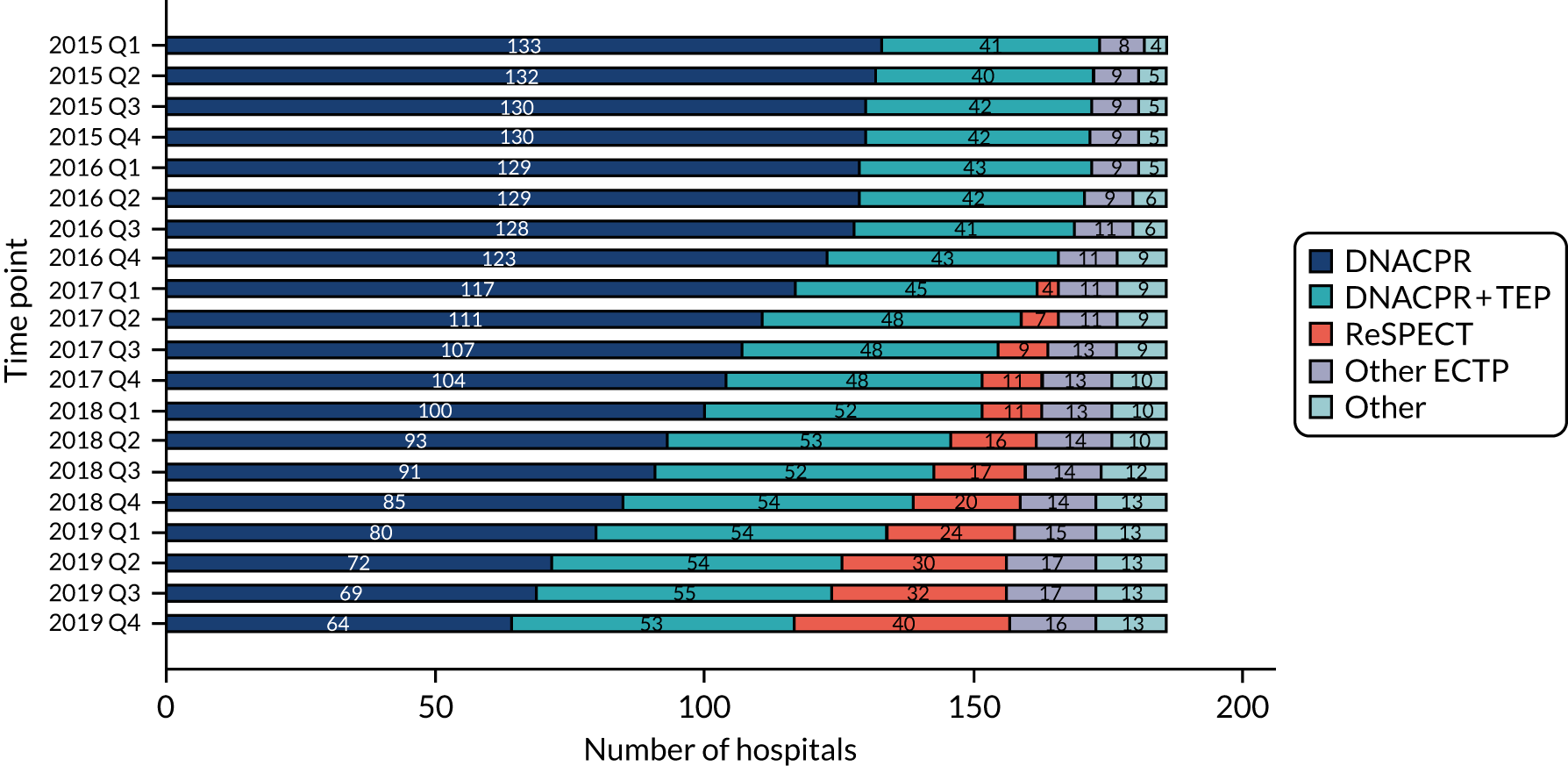
Between January 2015 and December 2019, use of DNACPR as a standalone form in acute hospitals had reduced from 72% (133/186) to 34% (64/186). Over the same period, use of advanced planning systems had increased, with the use of DNACPR plus a TEP increasing from 22% (41/186) to 28% (53/186), the use of another ECTP increasing from 4% (8/186) to 9% (16/186) and the use of a ReSPECT from increasing from 0% to 22% (with first use in December 2016). Uptake of the ReSPECT form has, therefore, increased more rapidly than alternative advanced planning systems and accounts for 60% (36/66) of the moves away from use of standalone DNACPR. The pace of change appeared to have slowed by the last year of the study, as 94% (62/66) of the moves away from standalone DNACPR occurred between the beginning of 2016 and end of 2018.
Resuscitation outcomes
The characteristics of patients from participating hospitals who sustained an IHCA, together with a summary of associated resuscitation activity and resuscitation outcomes, are presented in Table 2. The majority of the information relates to hospitals that did not adopt the ReSPECT process. Of the information available from ReSPECT hospitals, the majority relates to the pre-implementation period. The number of monthly admissions were markedly larger in hospitals that adopted the ReSPECT process, pre and post implementation, than in other hospitals. Otherwise, the groups appeared broadly comparable.
| Number of months contributing to the NCAA | Hospitals that implemented the ReSPECT process during the study period (N = 40), n (%) | Hospitals that did not implement the ReSPECT process during the study period (N = 146), n (%) | Total (N = 186), n (%) |
|---|---|---|---|
| 1–12 | 1 (2) | 6 (4) | 7 (4) |
| 13–24 | 1 (3) | 7 (5) | 8 (4) |
| 25–36 | 2 (5) | 12 (8) | 14 (8) |
| 37–48 | 6 (15) | 20 (14) | 26 (14) |
| 49–60 | 30 (75) | 101 (69) | 131 (70) |
Analysis of primary and secondary outcomes
Primary outcome
The proportion of resuscitation attempts abandoned because of futility is plotted by month, for ReSPECT hospitals and for other hospitals separately (Figure 3). The vertical line at December 2016 indicates the point at which hospitals first started implementing the ReSPECT process (see Figure 3). Prior to implementation of the process, the proportion of attempts abandoned because of futility was already falling rapidly, from approximately 9% in January 2015 to 4% in December 2016 in hospitals that went on to implement the ReSPECT process, and from 11% in January 2015 to 6% in December 2016 in other hospitals.
Post implementation, the proportion of CPR attempts abandoned because of futility fell a further 1% (to 3% in December 2019) in hospitals that implemented the ReSPECT process and by 2% (to 4% in December 2019) in other hospitals. Most of the reduction in proportion of CPR attempts abandoned because of futility observed during the entire study period (ReSPECT hospitals, 83%; other hospitals, 71%) occurred prior to the process being implemented. Predicted values from the ITS analyses models are also shown in Figure 3. Model fit appears reasonable but, nevertheless, there is considerable scatter about the regression line, with some relatively large differences between the predicted and actual values (e.g. at the start of the study in January 2015). For this reason, estimates of effect sizes from the ITS model (i.e. levels, slopes, differences in level and differences in slopes), reported in full in Table 3, may be unreliable.
FIGURE 3.
Interrupted time series analysis of the proportion of resuscitation attempts abandoned because of futility. Note that the vertical dotted line represents the date at which hospitals first implemented the ReSPECT process.
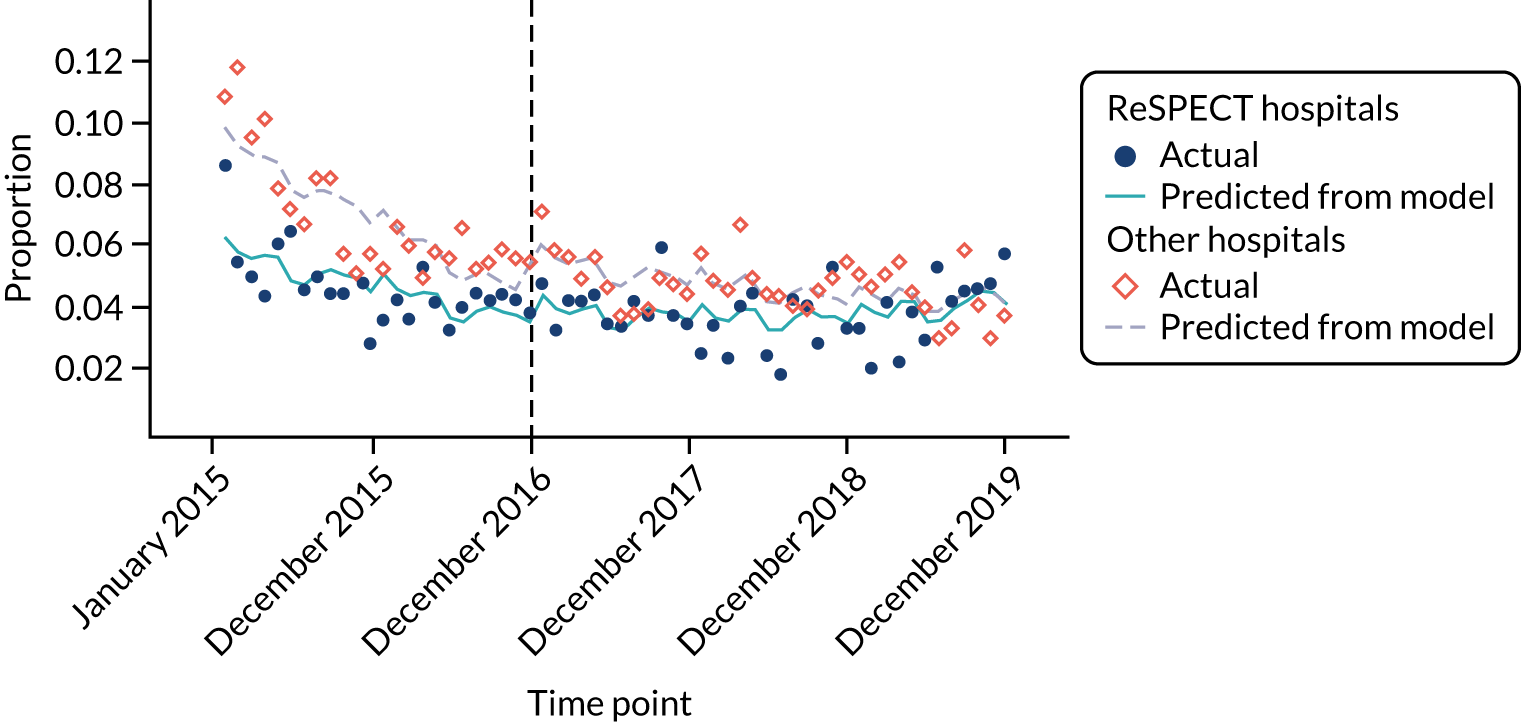
The difference in slope between the groups pre intervention was statistically significant (0.001, 95% CI 0.0002 to 0.0023; p = 0.02), but ReSPECT hospitals started from a lower level (on average, 0.04 per month less than in other hospitals), and this suggests that, prior to intervention, the two groups were not comparable. The proportion of resuscitation attempts abandoned because of futility did not change much in ReSPECT hospitals during the post-intervention period, but continued to fall, by 0.001 per month, in other hospitals. The difference in slope between the two groups post intervention was statistically significant (0.0005, 95% CI 0.0001 to 0.0009; p = 0.02), but there was no difference in the change in slope between the pre-and post-intervention periods in two groups (–0.0008, 95% CI –0.0019 to 0.0003; p = 0.17). Overall, therefore, there was no evidence that implementation of the ReSPECT process led to a reduction in the proportion of resuscitation attempts abandoned because of futility.
Secondary outcomes
Proportion of resuscitation attempts abandoned because of presence of a DNACPR recommendation
The proportion of resuscitation attempts abandoned because of presence of a DNACPR recommendation is plotted over time, along with predictions from the regression models, in Figure 4.
FIGURE 4.
Interrupted time series analysis of proportion of resuscitation attempts abandoned because of presence of a DNACPR recommendation. Note that the vertical dotted line represents the date at which hospitals first implemented the ReSPECT process.

The model fit is fairly poor (i.e. observed values do not follow the predicted line very closely and there is no clear pattern). There was no difference between the two groups at the start of the study (0.004, 95% CI –0.007 to 0.015; p = 0.48) and no discernible trend in either group over the pre-intervention period (Table 3). There was no difference in trend (pre intervention) between the two groups (–0.0005, 95% CI –0.001 to 0.0002; p = 0.14). Post intervention, there was no statistically significant trend in either group, but the difference in trend between the groups was statistically significant (0.004, 95% CI 0.001 to 0.007; p = 0.01). Given that the difference in trend is estimated from the model and model fit is poor, then this finding ought to be interpreted cautiously. The difference in trends between the groups pre and post intervention was also statistically significant (0.0009, 95% CI 0.0001 to 0.0017; p = 0.02), but, again, owing to the poor model fit, it would be unwise to draw any strong conclusions. In summary, we found no convincing evidence that implementation of the ReSPECT process had affected the proportion of resuscitation attempts abandoned because of presence of a DNACPR recommendation.
| Outcome | Prior to implementation of the ReSPECT process | Post implementation of the ReSPECT process | Difference in change in slope between the pre- and post-intervention periods | |||||
|---|---|---|---|---|---|---|---|---|
| Level at the start of the study (ReSPECT – other hospitals) (95% CI) | p-value | Slope prior to intervention (change per month) | p-value | Slope post intervention (change per month) | p-value | Difference in slope post intervention vs. pre intervention | p-value | |
| Primary | ||||||||
| Proportion of resuscitation attempts abandoned because of futility | ||||||||
| ReSPECT hospitalsa | –0.10 (–0.17 to –0.03) | 0.006 | –0.05 (–0.12 to 0.02) | 0.19 | ||||
| Other hospitalsb | –0.23 (–0.31 to –0.15) | < 0.001 | –0.10 (–0.17 to –0.02) | 0.001 | ||||
| Difference | –3.79 (–5.46 to –2.13) | < 0.001 | 0.13 (0.02 to 0.23) | 0.02 | 0.05 (0.01 to 0.09) | 0.02 | –0.08 (–0.19 to 0.03) | 0.17 |
| Secondary | ||||||||
| Proportion of resuscitation attempts abandoned because of presence of a DNACPR | ||||||||
| ReSPECT hospitalsa | –0.03 (–0.10 to 0.03) | 0.31 | 0.04 (–0.02 to 0.11) | 0.18 | ||||
| Other hospitalsb | 0.02 (–0.01 to 0.05) | 0.20 | 0.01 (–0.06 to 0.07) | 0.86 | ||||
| Difference | 0.40 (–0.72 to 1.52) | 0.48 | –0.05 (–0.12 to 0.02) | 0.14 | 0.04 (0.01 to 0.07) | 0.013 | 0.09 (0.01 to 0.17) | 0.02 |
| Vital status at hospital discharge (% alive) | ||||||||
| ReSPECT hospitalsa | –0.11 (–0.33 to 0.11) | 0.31 | 0.22 (0.01 to 0.44) | 0.04 | ||||
| Other hospitalsb | 0.01 (–0.14 to 0.15) | 0.90 | 0.25 (0.03 to 0.46) | 0.02 | ||||
| Difference | 0.25 (–2.77 to 3.28) | 0.87 | –0.12 (–0.38 to 0.14) | 0.35 | –0.03 (–0.14 to 0.09) | 0.66 | 0.10 (–0.19 to 0.38) | 0.50 |
| Proportion with a shockable rhythm | ||||||||
| ReSPECT hospitalsa | 0.05 (–0.10 to 0.20) | 0.52 | 0.11 (–0.09 to 0.31) | 0.27 | ||||
| Other hospitalsb | 0.08 (–0.03 to 0.19) | 0.17 | 0.14 (–0.05 to 0.34) | 0.16 | ||||
| Difference | 2.80 (–1.90 to 2.46) | 0.80 | 0.03 (–0.21 to 015) | 0.76 | –0.03 (–0.14 to 0.08) | 0.57 | –0.0026 (–0.21 to 0.21) | 0.98 |
Vital status at hospital discharge
The proportion of patients who sustained an IHCA who are alive at hospital discharge, in hospitals that did and did not adopt the ReSPECT process, is plotted over time in Figure 5. There is a strong seasonal effect (with better survival during the summer months) and a small but consistent upwards trend over the study period. Predicted values from the ITS models fit the data reasonably well (see Figure 5) and suggest that the proportion of resuscitation attempts where the patient was alive at discharge was fairly stable in both groups over the pre-intervention period and rose slowly (again in both groups) during the post-intervention period. There were no statistically significant differences between the groups (see Table 3). Therefore, there was no evidence that implementation of the ReSPECT process had affected the proportion of resuscitation attempts where the patient was alive at discharge.
FIGURE 5.
Interrupted time series analysis of vital status at hospital discharge. Note that the vertical dotted line represents the date at which hospitals first implemented the ReSPECT process.
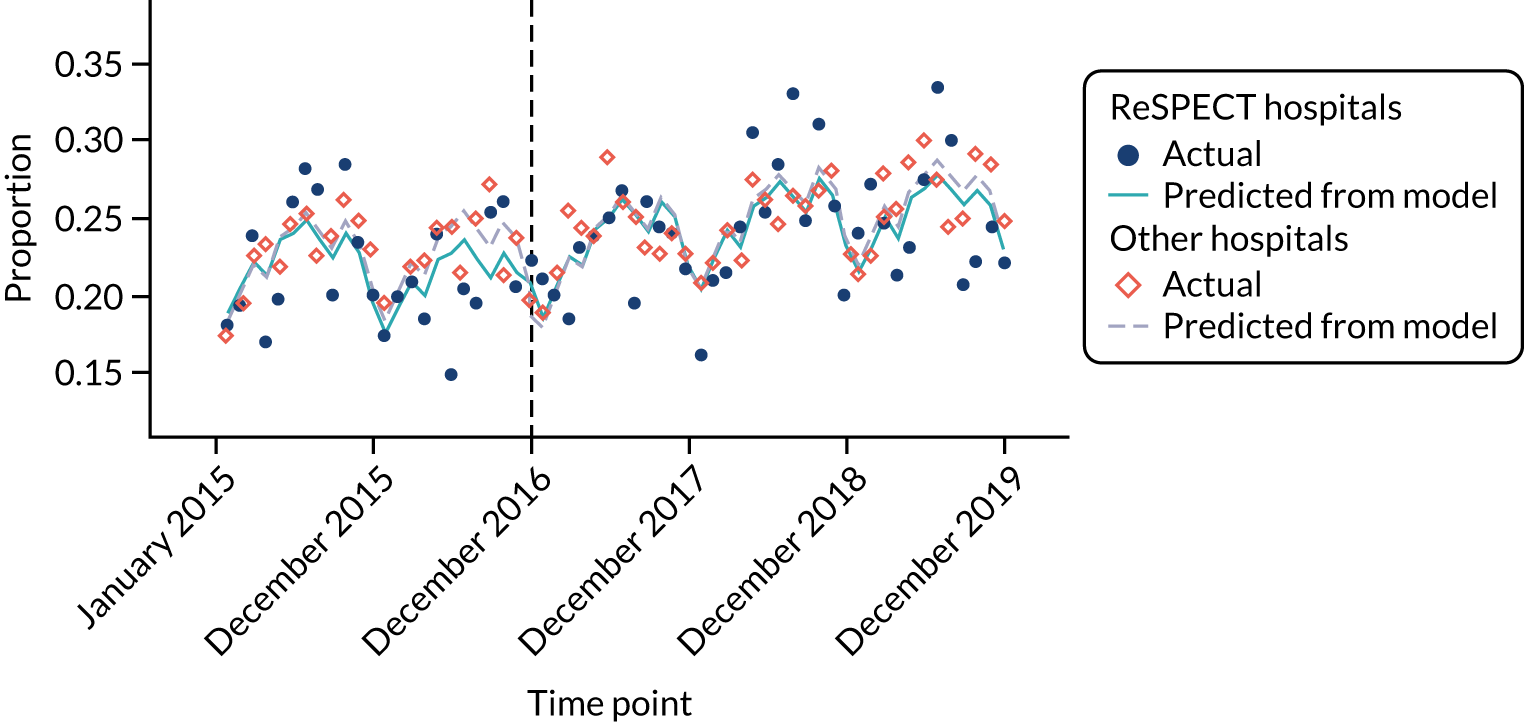
Proportion of in-hospital cardiac arrests with a shockable rhythm
The proportion of IHCAs that have a shockable rhythm is plotted over time, for ReSPECT hospitals and for other hospitals separately, in Figure 6. There is a seasonal effect and perhaps a slight upwards trend over time. Predicted values from the ITS models are also shown. Model fit is generally quite good, but a little poorer for ReSPECT hospitals in the post-implementation period compared with pre implementation. There is little visible difference between the models for the two groups of hospitals and ITS analysis found no statistically significant trends or differences (Table 4). There was no evidence that implementation of the ReSPECT process had affected the proportion of IHCAs with a shockable rhythm.
FIGURE 6.
Interrupted time series analysis of IHCAs proportion with a shockable rhythm. Note that the vertical dotted line represents the date at which hospitals first implemented the ReSPECT process.

| Variable | ReSPECT hospitalsa (N = 40) | Other hospitalsb (N = 146) | |
|---|---|---|---|
| Pre implementation | Post implementation | ||
| Mean number of months of NCAA data | 44 | 14 | 55 |
| Total hospital admissions per month, mean (SD) | 6760 (3946) | 6996 (3745) | 6063 (2872) |
| Number of 2222 calls for IHCA per month, mean (SD) | 10.3 (7.6) | 8.0 (5.8) | 10.3 (8.2) |
| Number of 2222 team visits per month | |||
| Mean (SD) | 7.6 (4.9) | 6.6 (4.9) | 7.4 (4.8) |
| Count | 13,032 | 3701 | 59,262 |
| Patient age (years), mean (SD) | 73.3 (6.5) | 71.7 (7.8) | 72.2 (7.3) |
| Patient sex, n (%) | |||
| Female | 5305 (41) | 1497 (40) | 23,817 (40) |
| Male | 7727 (59) | 2204 (60) | 35,401 (60) |
| Patient ethnicity, n (%) | |||
| White | 10,830 (83) | 3086 (83) | 47,549 (80) |
| Mixed | 51 (0) | 27 (1) | 381 (1) |
| Asian | 424 (3) | 230 (6) | 3622 (6) |
| Black | 96 (1) | 43 (1) | 1298 (2) |
| Other | 78 (1) | 49 (1) | 988 (2) |
| Not stated | 1553 (12) | 266 (7) | 5423 (9) |
| Patient type, n (%) | |||
| Obstetric | 19 (< 1) | 7 (< 1) | 136 (< 1) |
| Medical | 11,008 (84) | 3129 (85) | 49,475 (84) |
| Elective surgery | 567 (4) | 175 (5) | 3369 (6) |
| Emergency surgery | 830 (6) | 223 (6) | 3737 (6) |
| Staff | 7 (< 1) | 4 (< 1) | 38 (< 1) |
| Trauma | 419 (3) | 108 (3) | 1550 (3) |
| Outpatient | 152 (1) | 43 (1) | 745 (1) |
| Visitor | 30 (< 1) | 12 (< 1) | 169 (< 1) |
| Status at team arrival, n (%) | |||
| ROSC achieved | 1448 (11) | 439 (12) | 6114 (10) |
| Deteriorating | 680 (5) | 221 (6) | 3660 (6) |
| Resuscitation ongoing | 10,734 (83) | 3007 (81) | 48,936 (83) |
| Dead | 122 (1) | 33 (1) | 489 (1) |
| Location of arrest, n (%) | |||
| Cardiac catheter laboratory | 422 (11) | 171 (15) | 2673 (13) |
| Obstetrics area | 13 (< 1) | 4 (< 1) | 78 (< 1) |
| CCU | 1494 (39) | 480 (42) | 5825 (28) |
| PHDU | 0 (0) | 0 (0) | 2 (< 1) |
| Emergency department | 1189 (31) | 239 (21) | 5964 (29) |
| Imaging department | 222 (6) | 85 (7) | 979 (5) |
| ICU or ICU/HDU | 404 (10) | 130 (11) | 4436 (21) |
| Clinic | 54 (1) | 12 (1) | 257 (1) |
| Non-clinical area | 80 (2) | 26 (2) | 419 (2) |
| Other internal area | 14 (< 1) | 1 (< 1) | 66 (< 1) |
| PICU | 2 (< 1) | 0 (< 1) | 2 (< 1) |
| Specialist treatment area | 186 (2) | 65 (3) | 814 (2) |
| Theatre and recovery | 163 (2) | 42 (2) | 981 (3) |
| HDU | 141 (2) | 48 (2) | 877 (2) |
| Ward | 7557 (83) | 2069 (81) | 31,774 (82) |
| Emergency admissions unit | 1077 (12) | 325 (13) | 4008 (10) |
| Other intermediate care area | 14 (< 1) | 4 (< 1) | 78 (< 1) |
| Rhythm at arrival | |||
| Shockable, n (%) | |||
| Ventricular fibrillation | 1451 (11) | 439 (12) | 6924 (12) |
| Ventricular tachycardia | 690 (5) | 247 (7) | 3149 (5) |
| Unknown rhythm | 92 (1) | 17 (< 1) | 304 (1) |
| Non-shockable, n (%) | |||
| Asystole | 2622 (20) | 753 (20) | 12,074 (20) |
| Bradycardia | 25 (< 1) | 2 (< 1) | 98 (< 1) |
| Pulseless electrical activity | 6800 (52) | 1918 (52) | 31,164 (53) |
| Unknown rhythm | 313 (2) | 44 (1) | 937 (2) |
| Rhythm unknown | 332 (3) | 78 (2) | 1933 (3) |
| Rhythm never determined | 707 (5) | 203 (5) | 2679 (5) |
| Outcome, n (%) | |||
| Alive (ROSC > 20 minutes) | 6601 (51) | 1914 (52) | 30,902 (52) |
| Dead (ROSC < 20 minutes) | 787 (6) | 230 (6) | 3588 (6) |
| Dead (futility) | 505 (4) | 190 (5) | 3347 (6) |
| Dead (DNAR identified) | 298 (2) | 84 (2) | 1341 (2) |
| Dead (no ROSC) | 4841 (37) | 1283 (35) | 20,038 (34) |
| Time of IHCA, n (%) | |||
| Week day | 4906 (38) | 1415 (38) | 22,550 (38) |
| Week night | 4603 (35) | 1308 (35) | 20,412 (34) |
| Weekend day | 1724 (13) | 483 (13) | 8120 (14) |
| Weekend night | 1795 (14) | 495 (13) | 8178 (14) |
| Patient status at discharge, n (%) | |||
| Alive | 2833 (22) | 918 (25) | 13,754 (23) |
| Dead | 10,194 (78) | 2780 (75) | 45,346 (77) |
| CPC, n (%) | |||
| 1 (good) | 2298 (88) | 761 (92) | 10,295 (87) |
| 2 (moderate disability) | 241 (9) | 48 (6) | 1046 (9) |
| 3 (severe disability) | 62 (2) | 15 (2) | 409 (3) |
| 4 (comatose or vegetative state) | 7 (0) | 1 (0) | 56 (0) |
| CPC method of assessment, n (%) | |||
| Communication with clinical team | 447 (17) | 110 (13) | 1650 (15) |
| Direct patient assessment | 113 (4) | 36 (4) | 677 (6) |
| Inferred from notes | 2047 (79) | 679 (82) | 8708 (79) |
| Days from admission to resuscitation, mean (SD) | 5.5 (5.0) | 5.4 (6.0) | 6.0 (6.4) |
| Duration (minutes) of resuscitation, mean (SD) | 17.0 (23.2) | 17.9 (27.0) | 18.4 (29.1) |
| Time (minutes) from resuscitation to death, median (IQR) | 465.1 (1, 900.5) | 427.4 (2, 067.0) | 471.0 (2, 194.0) |
Number of in-hospital cardiac arrests per 1000 admissions
There was a very strong seasonal effect (with maximum numbers during winter months) and a small but consistent downwards trend in the number of IHCAs per 1000 hospital admissions in both groups over the study period (Figure 7). Prior to implementation of the ReSPECT process, the average number of IHCAs per 1000 admissions in ReSPECT hospitals fell from 1.54 in the first quarter of 2015 to 1.14 in the last quarter of 2016. In other hospitals, the average number of IHCAs per 1000 admissions fell from 1.71 in the first quarter of 2015 to 1.32 in the last quarter of 2016. Post implementation, the number of IHCAs per 1000 admissions continued to fall in both groups, to 0.93 in ReSPECT hospitals and to 1.01 in other hospitals, in the last quarter of 2019. The trajectory in ReSPECT hospitals was similar to that observed in the other hospitals, despite starting the study period at a lower level. There is no suggestion that implementation of the ReSPECT process has influenced the number of IHCAs per 1000 admissions.
FIGURE 7.
Number of IHCAs attended by the resuscitation team per 1000 admissions.
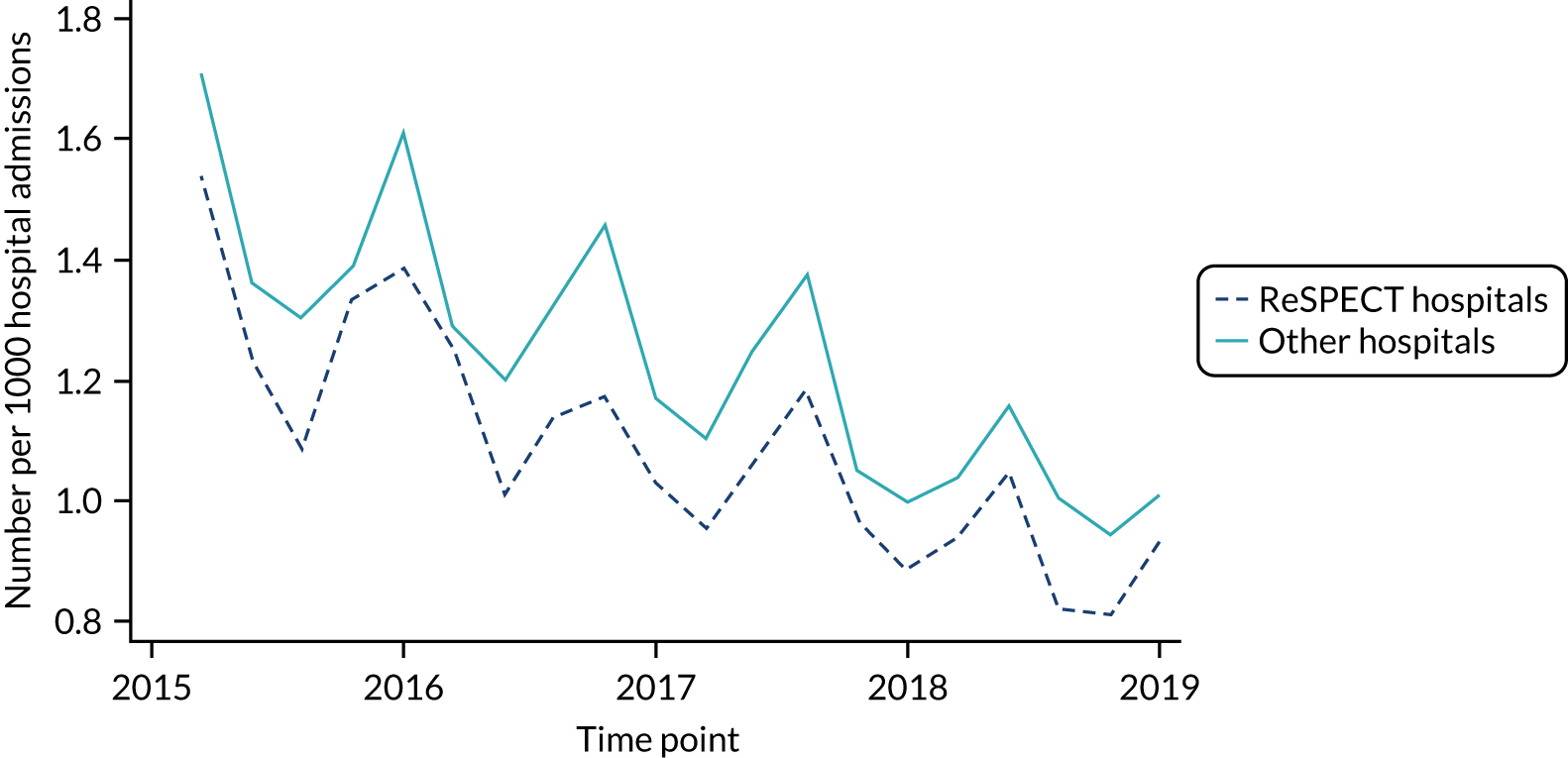
Patient status at team arrival
The proportion of patients who have an IHCA in each category (i.e. ROSC achieved, resuscitation ongoing, resuscitation stopped, deteriorating) at team arrival are plotted for ReSPECT hospitals and for other hospitals separately in Figure 8. In both groups, the proportions in the ‘deteriorating’ and ‘ROSC achieved’ categories appear to be rising very slowly over time and the proportion in the ‘resuscitation ongoing’ category falling. The proportion dead (i.e. resuscitation stopped) remained fairly constant and very small in both groups. Again, there is no suggestion that implementation of the ReSPECT process has affected this outcome.
FIGURE 8.
Patient status at team arrival. (a) ReSPECT hospitals; and (b) other hospitals.

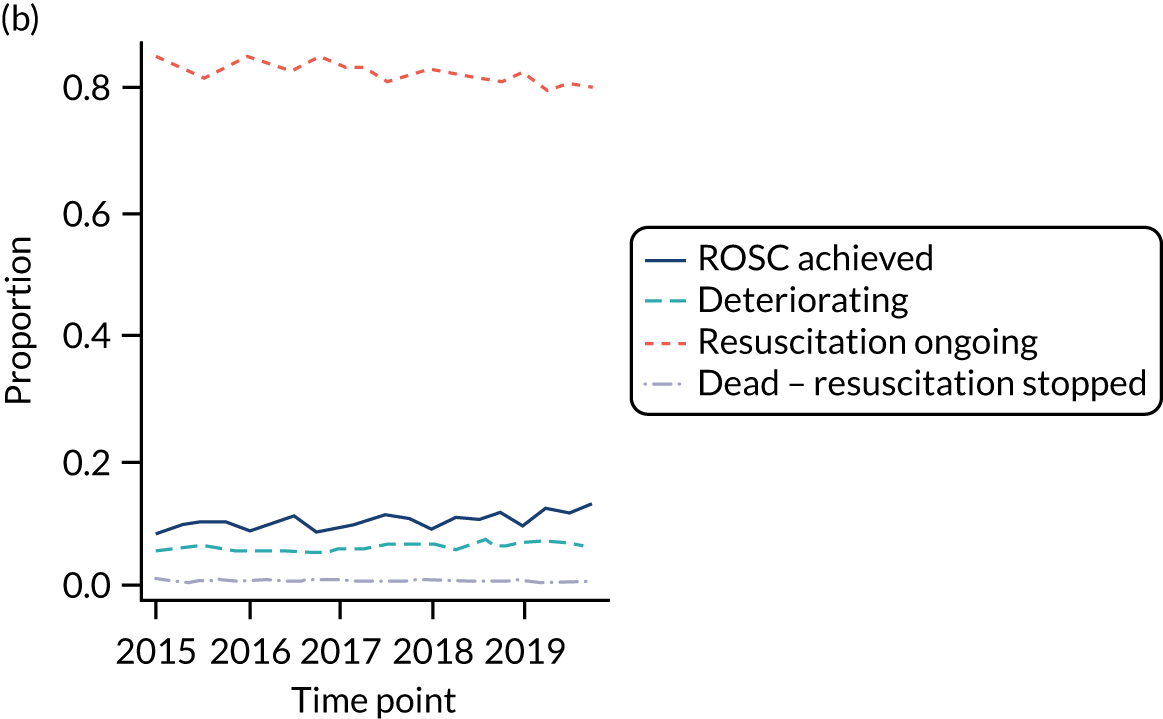
Cerebral performance category at discharge
The proportion of patients who sustained an IHCA in each CPC at discharge is presented in Figure 9. Over time, the proportion of patients with good cerebral performance (i.e. CPC 1) was increasing in both groups and there appeared to be a corresponding reduction in the proportion of patients with moderate disability (i.e. CPC 2). There was no suggestion that implementation of the ReSPECT process had affected cerebral performance at discharge.
FIGURE 9.
Cerebral performance category at discharge. (a) ReSPECT hospitals; and (b) other hospitals.
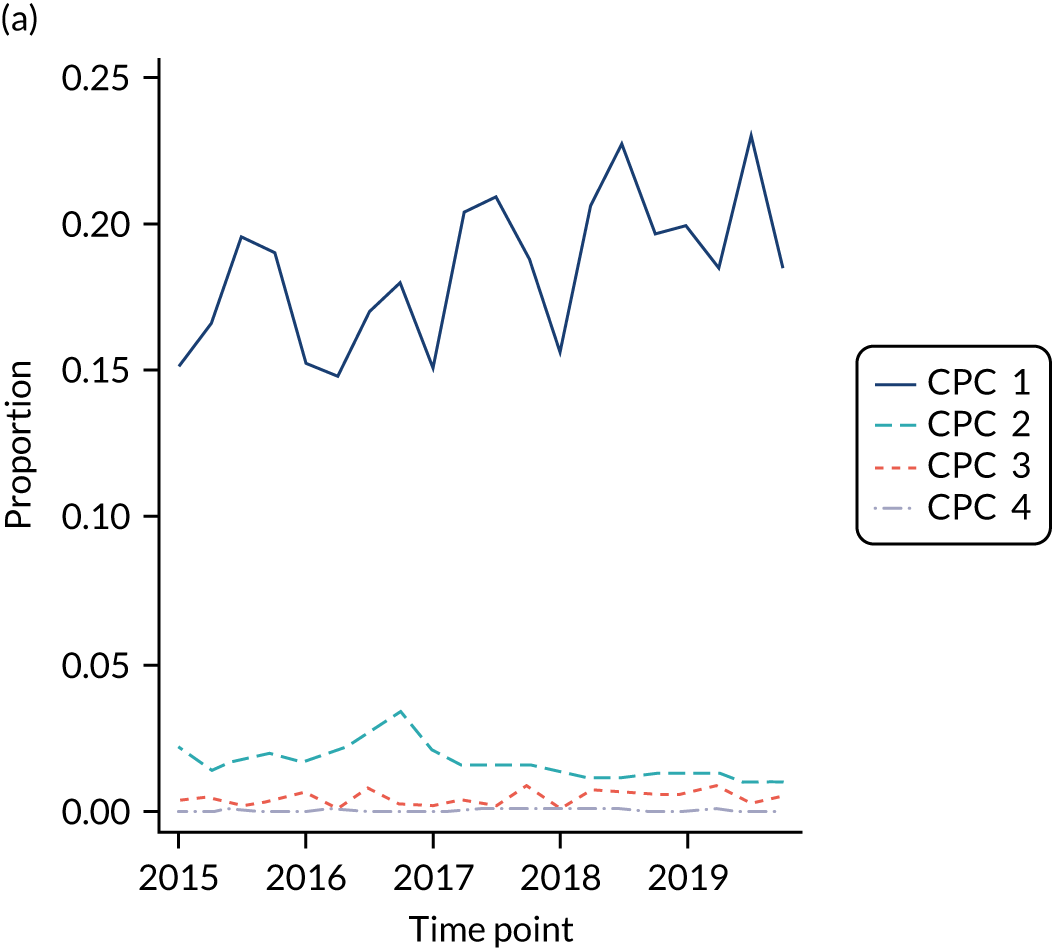
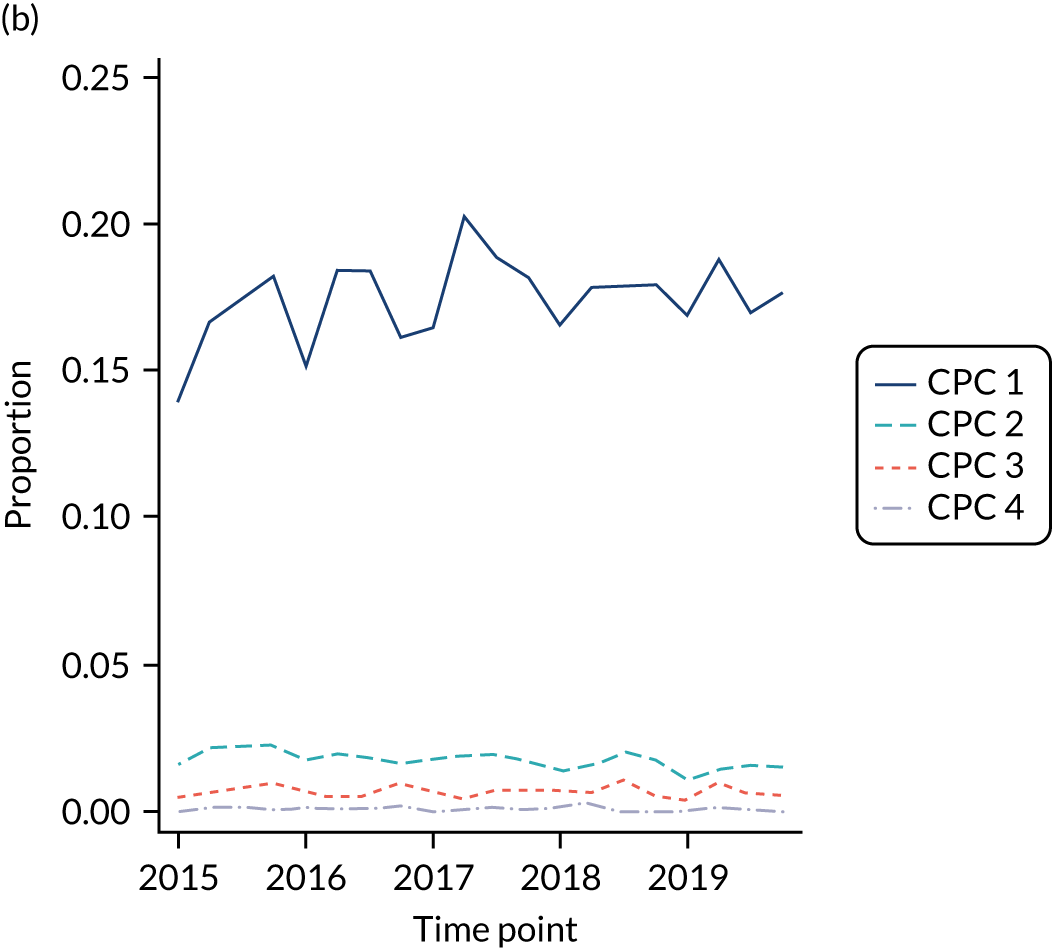
Summary
Between January 2015 and December 2019, use of a DNACPR as a standalone form in acute adult hospitals reduced from 72% to 34%. Over the same period, use of advanced planning systems increased, with the use of DNACPR plus a TEP increasing from 22% to 28% (53/186), the use of another ECTP increasing from 4% to 9% and the use of a ReSPECT from increasing from 0% to 22% (with first use in December 2016). Since its launch, use of the ReSPECT process has increased more rapidly than alternative advanced planning systems. Most (62/66) of the moves away from standalone DNACPR systems occurred between the beginning of 2016 and end of 2018, and adoption of the ReSPECT process accounted for nearly 60% (36/66) of these moves. Prior to implementation of the ReSPECT process, the proportion of CPR attempts abandoned because of futility was already falling rapidly from 9% in January 2015 to 4% in December 2016 in hospitals that went on to implement the ReSPECT process and from 11% in January 2015 to 6% in December 2016 in other hospitals. Post implementation, the proportion of CPR attempts abandoned because of futility fell a further 1% (to 3% in December 2019) in hospitals that implemented the ReSPECT process and by 2% (to 4% in December 2019) in other hospitals. Most of the reduction in proportion of CPR attempts abandoned because of futility observed during the study period (ReSPECT hospitals, 83%; other hospitals, 71%) occurred prior to the ReSPECT process being implemented. We found no evidence that implementation of the ReSPECT process had any effect on resuscitation outcomes.
Strengths and limitations
We obtained information about the implementation of the ReSPECT process from the majority of potential hospitals. Approximately 70% of the 186 hospitals included in the analysis contributed outcome data to the NCAA for the full 60-month study period. However, only 22% of hospitals implemented the ReSPECT process during the study period, with each, on average, contributing data to the NCAA for just 14 months post implementation (range 2–35 months). Formal power calculations were not possible for our ITS analyses (as that would have required complex statistical modelling and plausible estimates of key parameters, which were not available). Nevertheless, it is clear that, as implementation of the ReSPECT process occurred in fewer hospitals, sometimes fairly late in the study period, and we were unable to exclude a bedding-in period, the impact of the ReSPECT process has been made harder to detect (i.e. the ITS analysis is less powerful than we hoped, despite utilising all the available national resuscitation outcome data). Furthermore, having to aggregate the outcome data for the ITS analysis monthly, rather than quarterly, meant that the data (when plotted over time) were less smooth, which adversely affected model fit. It should also be noted that whether or not a CPR attempt is abandoned because of futility is a subjective judgement.
Chapter 4 Patient characteristics and outcomes associated with the ReSPECT process
Introduction
Do not attempt cardiopulmonary resuscitation decisions are used for patients at risk of deterioration and who would not benefit from a resuscitation attempt. The ReSPECT process, in contrast, was designed for use with all patients and in all settings, although guidance suggests that the ReSPECT process will have increasing relevance for people who have complex health needs, people who are likely to be nearing the end of their lives and people who are at risk of sudden deterioration or cardiac arrest. 44 Discussions relating to DNACPR and ECTPs are difficult for all involved. The ReSPECT process was designed to support a change in culture in which discussion of emergency care and treatment could become a more normal part of clinical practice. 43 DNACPR decisions that concern withholding one specific clinical treatment at the end of life have also been criticised for being conflated with a patient’s wider care and treatment, leading to an increased risk of patient harm from withholding care and treatment that the patient would continue to benefit from. 38 By placing resuscitation decisions within broader emergency and care treatment planning, the ReSPECT process may have the potential to reduce the risk of patient harms associated with standalone DNACPR decisions. Therefore, assessment of (1) the ReSPECT process’ association with patient outcomes, (2) the characteristics of patients with whom the ReSPECT process is used, (3) the types of recommendations made and (4) how ReSPECT process use is associated with patient outcomes is needed, and is addressed in this part of the study.
Objectives
Our objectives were to (1) provide a descriptive summary of patient characteristics according to ReSPECT treatment choice and (2) evaluate whether or not a DNACPR decision made in the context of an overall treatment plan is independently associated with risk of patient harm.
This work package sought to answer the following five research questions:
-
What combinations of ECTPs are recorded on the ReSPECT form, and how are ECTPs related to patient characteristics and overall outcomes of patients?
-
Which patient characteristics predict assignment to the ReSPECT process or other emergency care plans?
-
Which patient characteristics predict assignment to a DNACPR?
-
Do particular patient preferences and emergency care and treatment recommendations predict a DNACPR decision?
-
Is a DNACPR decision an independent predictor of patient harm?
Methods
Design
We carried out a retrospective observational study of routinely collected data from patient records and the NHS Safety Thermometer programme. 61 Participants were recruited from six acute hospitals that were using the ReSPECT process. To facilitate synthesis of findings, these were the same hospitals that participated in work package 1. Wards were selected by the research team, following discussion with participating hospital research teams, to ensure adequate numbers and coverage of the range of commonly found wards and clinical specialties found in district general hospitals.
Adult inpatients were included in the study unless they informed the research team they did not want their data used. Paediatric and neonatal patients, and adult day case admissions were excluded. The recruitment target was 3000 patients (i.e. at least 500 patients per site). Recruitment was co-ordinated to occur simultaneously with the routine monthly NHS Safety Thermometer audits. Five sites chose to collect data on a few wards each month and one site collected data on all participating wards on 1 day. Harm-free care was defined, in accordance with NHS Classic Safety Thermometer guidance:61
. . . the proportion of patients without any documented evidence of a new pressure ulcer category II–IV (developed at least 72 hours after admission to the site), harm from a fall in care in the last 72 hours, a new urinary infection (in patients with a urethral urinary catheter, which has developed since admission to this organisation) or new VTE [venous thromboembolism] (developed since admission to this organisation).
Patients whose care was not harm free per the above definitions were deemed to have experienced harm. We were unable to obtain any information regarding harms from medication (as proposed in the initial protocol), as this information is not routinely collected in all hospitals.
Participant’s opportunity to dissent from their records being used for research before and after data collection (opt-out and withdrawals)
As the intention was to assess all inpatients in selected wards at participating hospital sites on a single day, timed to coincide with each hospital’s NHS Safety Thermometer audit, we had permission from the CAG to collect data without obtaining individual informed consent, which was not feasible and would have introduced bias into the sample. Instead, leaflets were distributed to patients on the relevant wards in the days preceding data collection. The leaflets explained the study and gave details of how patients could dissent from data in their medical records being used for this research before data collection (referred to as opt-out from now on) or request withdrawal of their data from the study subsequently.
Data collection
Data were obtained through a combination of retrospective case note review and routine data collection (via the NHS Safety Thermometer). Research nurses at local sites used a case report form (see Report Supplementary Material 6) to collect the following: (1) demographics (i.e. age, sex, ethnicity and abbreviated home postcode as a proxy for socioeconomic status using the IMD36); (2) reason for admission; (3) comorbidities, including cognitive impairment (e.g. dementia, learning difficulties), Charlson Comorbidity Index score (which is a weighted index to predict 10-year survival in people with multiple comorbidities), GO-FAR (Good Outcome Following Attempted Resuscitation) score62 (which predicts chance of surviving IHCA with good outcome) and assessment of whether or not the condition is likely to be fatal (measured by the McCabe Scale);63 (4) ReSPECT information (i.e. patient preference, emergency care treatment recommendations, resuscitation status, capacity, who was involved in the discussions, when, where and by whom was the decision made); (5) NHS Safety Thermometer audit data; and (6) length of hospital stay, survival to discharge and discharge location. NHS Safety Thermometer data were collected through the hospital standard audit process or by the study research nurses. All data were entered by the site research staff and stored on a secure database maintained by WCTU.
Two sites used electronic ReSPECT forms, rather than paper forms. At one of these sites, in accordance with local policy, the digitised process involved screening all patients to determine whether or not the discussion with the patient involved the clinician recommending them for all treatments and CPR, and this was recorded on the screening question section of the electronic record. We have denoted this group as ‘screening’ and included them in the analyses, where possible. As information on ‘involvement in making the plan’ was not available for these patients, then this group could not be included in some of the regression models. At the other site, a pre-existing electronic ECTP form was modified to add in any missing sections from the ReSPECT form. The default position for patients who did not have a ReSPECT form would be that the patient is for CPR and full escalation of treatment, unless limits to escalation were recorded in the patient’s medical records.
Statistical analysis
Overall approach
Our five research questions (listed in Objectives) were answered using a combination of basic descriptive statistics and regression analyses. Data on recruitment, completeness and content of ReSPECT forms, patient characteristics, harms and outcomes are presented using standard descriptive methods (see Objectives, research questions 1 and 5). To identify and quantify which patient characteristics and emergency care and treatment recommendations predict assignment to a clinician recommendation or DNACPR decision, or predict risk of harm, multiple regression techniques were used (see Objectives, research questions 2–5). Odds ratios (ORs) and risk ratios (as appropriate) and 95% CIs from basic (adjusted by recruitment site) and fully adjusted (multivariable) regression models are reported, with the former quantifying the effect of each characteristic on the outcome separately and the latter quantifying the independent effect (after adjusting for the other variables in the model). Clinician recommendation has four categories (i.e. ‘focus on symptom control’, ‘focus on life sustaining treatment’, ‘unclear’ and ‘not completed’). Therefore, for models to predict clinician recommendation, a multinomial regression was required (see Objectives, research question 2). Multinomial regression fits a series of pairwise models (subject to some overarching constraints) to the data, allowing comparison of each group to the reference category (‘focus on symptom control’ in this case). Clinicians would consider various patient characteristics to inform recommendations on the ReSPECT form. The choice of covariates for statistical modelling was based on these patient characteristics and the established knowledge of their likely effect on our selected outcomes. Variables considered for inclusion in the multivariable model were age at admission, sex, ethnicity, socioeconomic status, admission type, patient type, cognitive impairment, GO-FAR score,62 Charlson Comorbidity Index score64 (grouped by quartiles), McCabe Scale and involvement in making the plan. 63 We had planned to explore the effect of patient preference (i.e. section 3 of the ReSPECT form) on DNACPR and clinician recommendation; however, owing to this item being very poorly completed, patient involvement was used instead. Owing to collinearity between GO-FAR score, Charlson Comorbidity Index and McCabe Scale (because they are inter-related), only Charlson Comorbidity Index, which appeared to be the strongest predictor, was included in the multivariable models. Similarly, logistic regression with DNACPR (yes/no) as the dependent (y) variable was used to identify and quantify which patient characteristics predict assignment to DNACPR (see Objectives, research question 3), as well as estimate the effect of emergency care and treatment recommendations and involvement in making the plan on DNACPR decisions (see Objectives, research question 4). Patients were categorised as experiencing harm if they experienced at least one of the new harms (i.e. acquired during admission) listed in the NHS Safety Thermometer definition. Logistic regression with harm (yes/no) as the dependent (y) variable was, therefore, used to assess the effect of DNACPR decision on risk of harm (see Objectives, research question 5), while accounting for patient characteristics. Finally, as an ad hoc analysis, we use logistic regression with ReSPECT form (yes/no) as the dependent (y) variable to investigate whether or not patient characteristics, resuscitation status [DNACPR (yes/no)] and clinician recommendation influence chance of having a ReSPECT form. All regression models included recruitment site as a fixed effect (to adjust for any unobserved differences between hospitals) (see Appendix 1 for details of derived variables).
Statistical policies
Continuous variables that follow an approximately normal (or symmetric) distribution are summarised using means and standard deviations (SDs), and variables that were skewed are summarised using median and interquartile ranges (IQRs). Categorical data were summarised using frequencies and percentages. Distributional assumptions were assessed using the appropriate graphical methods (e.g. histograms and box plots). The significance level was set at 5%, with p-values of between 0.05 and 0.10 considered as weak evidence of an effect. There was no adjustment for multiple testing. The value of including categorical variables in the regression models was assessed using a linear test of trend (if ordinal) and a likelihood ratio test otherwise.
Sample size justification
For generalisability, we needed to ensure a reasonable spread of patients/decisions, and to model risk of harm we needed sufficient number of harmful events to have occurred. Based on data from one site’s experience with a similar ECTP, we expected 70% of patients to have had a ReSPECT decision, of whom 20% would have a DNACPR decision. Some 20–30% of patients were expected to have a no DNACPR decision, which, by default, means that they would receive resuscitation in the event of cardiac arrest. Assuming a ‘harm rate’ of 6.5% (based on 2014 NHS Safety Thermometer data61), enrolment of 3000 participants was expected to provide 200 incidences of harm for the risk modelling. The recruitment target for each site was, therefore, a minimum of 500 patients.
Results
Recruitment
Recruitment began at the first site (i.e. site A) in October 2017 and was completed in April 2020. Data collection at the final site (i.e. site F) was cut short by the COVID-19 pandemic and so its recruitment total is less than the planned 500 patients. The numbers of participants eligible and recruited, by site, are given in Table 5. Data collection commenced between 8 and 11 months after initiation of the ReSPECT process at each site, and lasted 1–2 months (two sites) or 7–12 months (four sites).
| Eligibility/recruitment | Site, n (%) | ||||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | All | |
| Eligible | 878 (25a) | 476 (14a) | 665 (19a) | 681 (19a) | 645 (18a) | 183 (5a) | 3518 (100) |
| Opted outb | 5 (0.6) | 0 (0) | 51 (8) | 0 (0) | 21 (3) | 0 (0) | 67 (2) |
| Withdrewc | 1 (0.1) | 1 (0.2) | 10 (2) | 0 (0) | 0 (0) | 0 (0) | 12 (0.3) |
| Recruited | 872 (99) | 475 (100) | 604 (91) | 681 (100) | 624 (97) | 183 (100) | 3439 (98) |
The numbers of participants recruited by site, ward type and whether or not a ReSPECT form (full or screening) was in the patient notes are given in Table 6. Most (53%) participants were recruited from medical wards. The proportion of participants with a ReSPECT form ranged from 6% to 41% for full ReSPECT forms and from 6% to 88% for any ReSPECT forms.
| Site, n (%) | |||||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | All | |
| Type of warda | |||||||
| Surgery | 186 (21) | 68 (14) | 116 (19) | 202 (30) | 107 (17) | 33 (18) | 712 (21) |
| Trauma and orthopaedic | 78 (9) | 27 (6) | 25 (4) | 0 (0) | 67 (11) | 25 (14) | 222 (6) |
| Medicine | 465 (53) | 282 (59) | 332 (55) | 401 (59) | 252 (40) | 79 (43) | 1811 (53) |
| Critical careb | 43 (5) | 25 (5) | 42 (7) | 78 (11) | 39 (6) | 18 (10) | 245 (7) |
| Older person medicine | 54 (6) | 65 (14) | 89 (15) | 0 (0) | 134 (21) | 27 (15) | 369 (11) |
| Medicine/critical care | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 25 (4) | 0 (0) | 25 (1) |
| Gynaecology | 9 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 9 (< 1) |
| Not completed | 37 (4) | 8 (2) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 46 (1) |
| ReSPECT form | |||||||
| Full | 212 (24) | 90 (19) | 118 (20) | 42 (6) | 169 (27) | 75 (41) | 706 (20) |
| Screeningc | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 86 (47) | 86 (3) |
| None | 660 (76) | 385 (81) | 486 (80) | 639 (94) | 455 (73) | 22 (12) | 2647 (77) |
| Total | 872 | 475 | 604 | 681 | 624 | 183 | 3439 |
Most (539/655, 82%) ReSPECT forms were completed after hospital admission. Among those forms completed after hospital admission, the majority (280/655, 43%) were completed within the first 48 hours of hospital admission (Figure 10). There was a very long tail, reflecting the fact that a small number of patients had been admitted for a long time before a ReSPECT recommendation was recorded.
FIGURE 10.
Histogram of time that ReSPECT recommendation was recorded following hospital admission.

What combinations of emergency care and treatment plans are recorded on the ReSPECT form?
Most hospitals (4/6) used paper ReSPECT forms, which, once completed, were stored in the patient’s physical medical records for the duration of their stay. In two hospitals (i.e. sites C and F), ReSPECT forms were electronic and were stored in the patient’s electronic record. Overall, 35% (279/792) of ReSPECT forms were electronic, 69% (193/279) of which were full ReSPECT forms and 31% (86/279) were screening ReSPECT forms. The number of patients recruited by ward type, whether or not they had a ReSPECT form (full or screening) and the care group are given in Table 7. Only 21% (380/1811) of patients on a medical ward had a ReSPECT form compared with 15% (110/712) of patients on a surgical ward and 52% (192/369) of patients on older person medical wards. A large minority of patients (284/653, 43%) with ReSPECT forms for whom DNACPR was recommended had no clinician recommendation recorded.
| Type of warda | ReSPECT form (N = 792), n (%) | No ReSPECT form (N = 2647), n (%) | All (N = 3439), n (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CPR recommended | DNACPR recommended | Total with ReSPECT forms | |||||||
| Focus on sustaining life | Focus on comfort care | No clinician recommendation | Focus on sustaining life | Focus on comfort care | No clinician recommendation | ||||
| Surgery | 22 (19) | 0 (0) | 7 (29) | 18 (20) | 40 (14) | 23 (8) | 110 (14) | 602 (23) | 712 (21) |
| Trauma and orthopaedic | 23 (20) | 0 (0) | 0 (0) | 8 (9) | 10 (4) | 14 (5) | 55 (7) | 167 (6) | 222 (6) |
| Medicine | 45 (40) | 2 (67) | 9 (38) | 35 (38) | 150 (55) | 139 (49) | 380 (48) | 1431 (54) | 1811 (53) |
| Critical careb | 17 (15) | 0 (0) | 1 (4) | 5 (5) | 8 (3) | 12 (4) | 43 (5) | 202 (8) | 245 (7) |
| Older person medicine | 4 (4) | 1 (33) | 7 (29) | 25 (27) | 63 (23) | 92 (32) | 192 (24) | 177 (7) | 369 (11) |
| Medicine/critical care | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (1) | 1 (< 1) | 3 (< 1) | 22 (1) | 25 (1) |
| Gynaecology | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) | 1 (< 1) | 8 (< 1) | 9 (< 1) |
| Not completed | 1 (0) | 0 (0) | 0 (0) | 1 (1) | 4 (1) | 2 (1) | 8 (1) | 38 (1) | 46 (1) |
| Total | 112 (100) | 3 (100) | 24 (100) | 92 (100) | 277 (100) | 284 (100) | 792 (100) | 2647 (100) | 3439 (100) |
The content and completeness of ReSPECT forms are summarised in Table 8. Many items in full ReSPECT forms were poorly completed. The optional personal preference scale was completed by only 30% (213/706) of patients and personal preference group by only 34% (241/706) of patients. Thirty-seven per cent (260/706) of patients had no record concerning whether or not the patient had a legal proxy. The clinician recommendation was not completed for 29% (208/706) of forms. Other sections of full ReSPECT forms were better completed. There was no CPR decision recorded in only 2% (11/706) of forms and no record of the patient’s mental capacity recorded in 13% (95/706) of forms. CPR was not recommended in 92% of the full ReSPECT forms and 45% of the forms stated that the patient did not have sufficient capacity to make decisions. Seventy-three per cent (513/706) of forms had been completed in consultation with the patient or family, but 16% (114/706) of forms recorded there had been no consultation and for 11% of forms this section had not been completed. Hospital policies varied as to what professions and grades of staff could undertake a ReSPECT discussion and be the first signatory on the form, but most often the first signatory was a consultant (40%) or SPR ST3 (specialty registrar speciality trainee year 3) (32%). The senior clinician signature was not present on 22% of full ReSPECT forms, but for 41% of these forms the first signatory was a consultant (i.e. the omission was to avoid repetition). Screening ReSPECT forms collected far more limited information (e.g. clinician recommendation and CPR decision), but this information was fully complete (as by default all were for ‘focus on life-sustaining treatment’ and CPR) and for many (63/86, 73%) we were able to obtain grade of the clinician who electronically signed the form from hospital records. Overall, of the 792 patients with a ReSPECT form (full or screening), 204 (26%) had ‘focus on life-sustaining treatment’ recommended by the clinician and 284 (36%) had ‘focus on symptom control’ recommended. For 96 (12%) patients, the position was unclear and 208 (26%) patients had no recommendation. CPR was recommended for 128 (16%) patients with a ReSPECT form (full or screening) and not recommended for 653 (82%) patients. The CPR recommendation had not been completed for 11 (1%) patients with a ReSPECT form.
| Item on ReSPECT form | Full forms (N = 706), n (%) | Screening forms (N = 86), n (%) |
|---|---|---|
| Personal preference scale | ||
| Completed | 213 (30) | N/A |
| Not completed | 493 (70) | |
| Personal preference group | ||
| Prioritise sustaining life | 25 (4) | N/A |
| Prioritise comfort | 163 (23) | |
| Equal balance | 53 (7) | |
| Not completed | 465 (66) | |
| Clinician recommendation | ||
| Focus on life-sustaining treatment | 118 (17) | 86 (100) |
| Focus on symptom control | 284 (40) | 0 (0) |
| Unclear position | 96 (14) | 0 (0) |
| Not completed | 208 (29) | 0 (0) |
| Clinical guidance on interventions | N/A | |
| CPR status | ||
| Recommended | 42 (6) | 86 (100) |
| Not recommended | 653 (92) | 0 (0) |
| Not completed | 11 (2) | 0 (0) |
| Sufficient capacity | ||
| No | 315 (45) | N/A |
| Yes | 296 (42) | |
| Not completed | 95 (13) | |
| Legal proxy | ||
| Yes | 140 (20) | N/A |
| No | 33 (5) | |
| Unknown | 155 (22) | |
| Not completed | 260 (36) | |
| Not applicable | 118 (17) | |
| Involvement in making the plan | ||
| Patient | 293 (42) | N/A |
| Relative | 220 (31) | |
| No consultation | 114 (16) | |
| Not completed | 79 (11) | |
| Grade of first clinician signing the form | ||
| Foundation year 1 | 17 (2) | 1 (1) |
| Foundation year 2 | 32 (5) | 9 (10) |
| Specialty trainee years 1 and 2 | 50 (7) | 0 (0) |
| Specialty registrar | 227 (32) | 48 (56) |
| GP specialty trainee | 9 (1) | 0 (0) |
| Consultant | 283 (40) | 5 (6) |
| GP | 5 (1) | 0 (0) |
| Nurse/allied health professional | 3 (< 1) | 0 (0) |
| Not completed | 80 (11) | 23 (27) |
| First clinician signature presenta | ||
| Yes | 656 (93) | N/A |
| No | 50 (7) | |
| Senior clinician signature present | ||
| Yes | 432 (61) | N/A |
| No | 156 (22) | |
| Not applicable | 118 (17) | |
Clinicians’ specific treatment recommendations from full ReSPECT forms are summarised in Table 9, cross-tabulated by McCabe Scale, a measure of morbidity which classifies each patient’s condition as non-fatal, ultimately fatal and rapidly fatal. Notably, decisions regarding ‘referral to intensive care unit’ and ‘ward-based care only’ were recorded more often than other aspects (for 48% and 47% of patients, respectively). Referral to ICU was not recommended for 44% (310/704) of patients and this did not appear to depend on McCabe Scale category. Ward-based care only was recommended in 45% of patients, with greater proportions in the ultimately (48%) and rapidly fatal (50%) groups. The recommendations that a patient was not for full escalation were also more common in the ultimately (32%) and rapidly fatal (38%) groups than in the non-fatal group (14%). Although few patients had a recommendation made about re-admission to hospital, there was a difference between McCabe Scale groups. Nine per cent of patients in the rapidly fatal group were not recommended future hospital admission compared with 2% of patients in the non-fatal group and 3% of patients in the ultimately fatal group. Recommendations regarding non-invasive and invasive ventilation were fairly common (being recorded for 26% and 32% of patients, respectively).
| Variable | McCabe Scale | All | ||
|---|---|---|---|---|
| Non-fatal (N = 402), n (%) | Ultimately fatal (N = 704),a n (%) | Rapidly fatal (N = 80), n (%) | (N = 704),a n (%) | |
| Referral to ICU | ||||
| No | 172 (43) | 101 (46) | 37 (46) | 310 (44) |
| Yes | 22 (5) | 10 (5) | 2 (3) | 34 (5) |
| Not recorded | 208 (52) | 111 (50) | 41 (50) | 362 (51) |
| Referral to HDU | ||||
| No | 87 (21) | 62 (28) | 21 (26) | 170 (24) |
| Yes | 21 (5) | 14 (6) | 0 (0) | 35 (5) |
| Not recorded | 294 (73) | 146 (66) | 59 (74) | 501 (71) |
| For full escalation | ||||
| No | 96 (14) | 70 (32) | 30 (38) | 196 (28) |
| Yes | 10 (2) | 5 (2) | 2 (3) | 17 (2) |
| Not recorded | 296 (74) | 147 (66) | 48 (60) | 493 (70) |
| Ward-based care only | ||||
| No | 16 (4) | 8 (4) | 2 (3) | 26 (4) |
| Yes | 172 (43) | 106 (48) | 40 (50) | 319 (45) |
| Not recorded | 214 (53) | 108 (49) | 38 (48) | (51) |
| Invasive ventilation | ||||
| No | 113 (28) | 73 (33) | 24 (30) | 210 (30) |
| Yes | 10 (2) | 5 (2) | 0 (0) | 15 (2) |
| Not recorded | 279 (70) | 144 (65) | 56 (70) | 481 (68) |
| Non-invasive ventilation | ||||
| No | 65 (16) | 47 (21) | 14 (18) | 126 (18) |
| Yes | 32 (8) | 22 (10) | 5 (6) | 59 (8) |
| Not recorded | 305 (76) | 153 (69) | 61 (76) | 521 (74) |
| Inotropic support/vasoactive drugs | ||||
| No | 65 (16) | 36 (16) | 14 (18) | 115 (16) |
| Yes | 16 (4) | 8 (4) | 3 (4) | 27 (4) |
| Not recorded | 321 (80) | 178 (80) | 63 (79) | 564 (80) |
| Renal replacement therapy | ||||
| No | 75 (19) | 41 (18) | 14 (18) | 130 (18) |
| Yes | 8 (2) | 5 (2) | 0 (0) | 13 (2) |
| Not recorded | 319 (79) | 176 (79) | 66 (82) | 563 (80) |
| Antibiotics | ||||
| No | 9 (2) | 5 (2) | 3 (4) | 17 (2) |
| Yes | 41 (10) | 30 (14) | 11 (14) | 82 (12) |
| Not recorded | 352 (88) | 187 (84) | 66 (82) | 607 (86) |
| NG/NJ/PEJ/PN feeding | ||||
| No | 32 (8) | 17 (8) | 3 (4) | 52 (7) |
| Yes | 7 (2) | 5 (2) | 0 (0) | 12 (2) |
| Not recorded | 363 (90) | 200 (90) | 77 (96) | 642 (91) |
| Observations/MEWS | ||||
| No | 11 (3) | 5 (2) | 2 (3) | 18 (3) |
| Yes | 18 (4) | 11 (5) | 1 (1) | 30 (4) |
| Not recorded | 373 (93) | 206 (93) | 77 (96) | 658 (93) |
| Clinical hydration | ||||
| No | 8 (2) | 5 (2) | 2 (3) | 15 (2) |
| Yes | 38 (9) | 22 (10) | 8 (10) | 68 (10) |
| Not recorded | 356 (89) | 195 (88) | 70 (87) | 623 (88) |
| Cardioversion | ||||
| No | 60 (15) | 27 (12) | 12 (15) | 99 (14) |
| Yes | 5 (1) | 5 (2) | 1 (1) | 11 (2) |
| Not recorded | 337 (84) | 190 (86) | 67 (84) | 596 (84) |
| Palliative or comfort care | ||||
| No | 10 (2) | 13 (6) | 3 (4) | 26 (4) |
| Yes | 24 (6) | 22 (10) | 11 (14) | 57 (8) |
| Not recorded | 368 (92) | 187 (84) | 66 (83) | 623 (88) |
| Not for hospital re-admission | ||||
| No | 15 (4) | 10 (5) | 2 (3) | 27 (4) |
| Yes | 7 (2) | 7 (3) | 7 (9) | 21 (3) |
| Not recorded | 380 (95) | 205 (92) | 71 (88) | 658 (93) |
How are combinations of emergency care and treatment plans related to patient characteristics and overall outcomes of patients?
Patient characteristics and survival outcomes of all participants, by whether or not they had a ReSPECT form, are given in Table 10. The same information is presented, further cross-tabulated by care group, in Appendix 5. Patients with full ReSPECT forms were generally older than patients with screening or no ReSPECT form (mean age of patients: full ReSPECT form, 80.6 years; screening ReSPECT form, 61.8 years; no ReSPECT form, 65.4 years). There was little difference in sex or ethnicity between the groups, but patients with screening ReSPECT forms were less deprived than patients with full or no ReSPECT forms. (This is likely to reflect higher socioeconomic status at the single site where such forms were used.) The majority (74%) of patients were emergency admissions (via a GP or emergency department), with the proportion being greatest (90%) in patients with full ReSPECT forms. Patients with full ReSPECT forms (42%) were also more likely to have a fatal condition than patients with screening ReSPECT forms (7%) and patients with no ReSPECT forms (24%), have a longer hospital stay (median length of stay: full ReSPECT form, 28 days; screening ReSPECT form, 21 days; no ReSPECT form, 16 days) and be discharged to a place other than home (full ReSPECT form, 66%; screening ReSPECT form, 82%; no ReSPECT form, 84%). Patients with full ReSPECT forms were also less likely to be alive at hospital discharge (full ReSPECT form, 83%; screening ReSPECT form, 85%; no ReSPECT form, 94%). Overall, 29% of patients had cognitive impairment, but this was far more common in patients with full ReSPECT forms (52%) than in patients with no ReSPECT form (23%). Impairment was largely due to either dementia (43%) or acute confusional state (38%). Overall, it seems that full ReSPECT forms were used predominantly for medical emergency patients, older patients and in patients who are most unwell.
| Variable | Full ReSPECT form (N = 706) | Screening ReSPECT form (N = 86) | No ReSPECT form (N = 2647) | Total (N = 3439) |
|---|---|---|---|---|
| Age (years) at admission, mean (SD) | 80.6 (12) | 61.8 (17) | 65.4 (19) | 68.5 (19) |
| Sex, n (%) | ||||
| Female | 384 (54) | 41 (48) | 1304 (49) | 1729 (50) |
| Male | 321 (46) | 44 (51) | 1341 (51) | 1706 (50) |
| Not completed | 1 (< 1) | 1 (1) | 2 (< 1) | 4 (< 1) |
| Ethnicity, n (%) | ||||
| White | 601 (85) | 67 (78) | 2,124 (80) | 2792 (81) |
| Mixed | 4 (1) | 1 (1) | 17 (1) | 22 (1) |
| Asian | 35 (5) | 4 (5) | 190 (7) | 229 (7) |
| Black | 13 (2) | 3 (3) | 101 (4) | 117 (3) |
| Other | 4 (1) | 0 (0) | 45 (2) | 49 (1) |
| Not completed | 49 (7) | 11 (13) | 170 (6) | |
| Socioeconomic status,a n (%) | ||||
| Tertile 1 (most deprived) | 212 (30) | 6 (7) | 989 (37) | 1207 (35) |
| Tertile 2 | 238 (34) | 20 (23) | 987 (37) | 1245 (36) |
| Tertile 3 (least deprived) | 252 (36) | 60 (70) | 621 (23) | 933 (27) |
| Not completed | 4 (1) | 0 (0) | 50 (2) | 54 (2) |
| Patient admission category, n (%) | ||||
| Transferred from another hospital | 25 (4) | 12 (14) | 205 (8) | 242 (7) |
| Planned admission | 14 (2) | 14 (16) | 396 (15) | 424 (12) |
| Referral from GP | 14 (2) | 0 (0) | 57 (2) | 71 (2) |
| Emergency (via GP) | 69 (10) | 7 (8) | 159 (6) | 235 (7) |
| Emergency (via emergency department) | 562 (80) | 42 (49) | 1713 (65) | 2317 (67) |
| Outpatients | 14 (2) | 7 (8) | 73 (3) | 94 (3) |
| Other | 1 (< 1) | 0 (0) | 10 (1) | 11 (< 1) |
| Not completed | 7 (1) | 4 (5) | 24 (1) | 45 (1) |
| Patient type, n (%) | ||||
| Medical: emergency | 605 (86) | 49 (57) | 1719 (65) | 2373 (69) |
| Medical: elective | 14 (2) | 14 (16) | 165 (6) | 193 (6) |
| Surgery: emergency | 78 (11) | 19 (22) | 447 (17) | 544 (16) |
| Surgery: elective | 9 (1) | 4 (5) | 316 (12) | 329 (10) |
| Primary reason for admission, n (%) | ||||
| Cancer/neoplasm | 38 (5) | 13 (15) | 211 (8) | 262 (8) |
| Fall/injury/musculoskeletal | 185 (26) | 22 (26) | 546 (21) | 753 (22) |
| Gastrointestinal conditions | 64 (9) | 18 (21) | 422 (16) | 504 (15) |
| Respiratory conditions | 64 (9) | 18 (21) | 422 (16) | 504 (15) |
| Cardiac conditions | 46 (7) | 1 (1) | 246 (9) | 293 (9) |
| ENT conditions | 2 (< 1) | 1 (1) | 49 (2) | 52 (2) |
| Urological conditions | 47 (6) | 6 (7) | 160 (6) | 213 (6) |
| Central nervous system conditions | 54 (8) | 6 (7) | 216 (8) | 276 (8) |
| Infectious disease | 20 (3) | 3 (3) | 46 (2) | 69 (2) |
| Poisoning | 2 (< 1) | 0 (0) | 14 (1) | 16 (< 1) |
| Gynaecological/obstetric conditions | 1 (< 1) | 0 (0) | 19 (1) | 20 (1) |
| Mental health conditions | 4 (1) | 0 (0) | 20 (1) | 24 (1) |
| Blood/organs disease | 4 (1) | 0 (0) | 14 (1) | 18 (1) |
| Endocrine disorders | 6 (1) | 2 (2) | 14 (1) | 22 (1) |
| Eye diseases | 0 (0) | 0 (0) | 2 (< 1) | 2 (< 1) |
| Circulatory diseases | 0 (0) | 2 (2) | 44 (2) | 46 (1) |
| Skin | 2 (< 1) | 0 (0) | 10 (< 1) | 12 (< 1) |
| Renal | 3 (< 1) | 0 (0) | 29 (1) | 32 (1) |
| Infection (excluding respiratory) | 20 (3) | 1 (1) | 94 (4) | 115 (3) |
| Acute confusional state | 8 (1) | 0 (0) | 22 (1) | 30 (1) |
| Dental | 0 (0) | 0 (0) | 1 (< 1) | 1 (< 1) |
| Other | 4 (1) | 0 (0) | 14 (1) | 18 (1) |
| Not completed | 38 (5) | 13 (15) | 211 (8) | 262 (8) |
| Cognitive impairment, n (%) | ||||
| No | 336 (48) | 58 (67) | 2034 (77) | 2428 (71) |
| Yes | 370 (52) | 28 (33) | 613 (23) | 1011 (29) |
| If yes, which cause (multiple possible), n (%) | ||||
| Dementia | 203 (55) | 1 (4) | 216 (37) | 420 (43) |
| Learning difficulty | 7 (2) | 3 (10) | 51 (9) | 61 (6) |
| CVA/head injury | 56 (15) | 6 (21) | 123 (21) | 185 (19) |
| Acute confusional state | 124 (34) | 11 (39) | 242 (41) | 377 (38) |
| Cause not recorded | 41 (11) | 1 (4) | 63 (10) | 105 (11) |
| Brain tumour or condition | 8 (2) | 0 (0) | 15 (2) | 23 (2) |
| Mental health condition | 6 (2) | 1 (4) | 16 (3) | 23 (2) |
| Other | 64 (18) | 10 (70) | 104 (18) | 187 (19) |
| GO-FAR score, mean (SD) | 10.66 (9.5) | 13.95 (7.8) | 6.65 (9.1) | 7.64 (9.4) |
| GO-FAR category, n (%) | ||||
| Very low (> 24) | 55 (8) | 7 (8) | 73 (3) | 135 (4) |
| Low (14–23) | 210 (30) | 35 (41) | 481 (18) | 726 (21) |
| Average (–5 to 13) | 377 (53) | 35 (41) | 1717 (65) | 2129 (62) |
| Above average (–15 to –6) | 30 (4) | 0 (0) | 260 (10) | 290 (8) |
| Not completed | 34 (5) | 9 (11) | 116 (4) | 159 (5) |
| Charlson Comorbidity Index, mean (SD) | 6.68 (3.0) | 4.43 (3.0) | 4.56 (3.0) | 4.99 (3.1) |
| McCabe Scale, n (%) | ||||
| Non-fatal | 402 (57) | 77 (90) | 2022 (76) | 2501 (73) |
| Ultimately fatal | 222 (31) | 5 (6) | 467 (18) | 694 (20) |
| Rapidly fatal | 80 (11) | 1 (1) | 153 (6) | 234 (7) |
| Not completed | 2 (< 1) | 3 (3) | 5 (< 1) | 10 (< 1) |
| Length of stay (days), median (IQR) | 28 (14–52) | 21 (9–47) | 16 (8–37) | 19 (9–40) |
| Patient status at discharge, n (%) | ||||
| Alive | 584 (83) | 73 (85) | 2491 (94) | 3148 (92) |
| Dead | 119 (17) | 6 (7) | 153 (6) | 278 (8) |
| Not completed | 3 (< 1) | 7 (8) | 3 (< 1) | 13 (< 1) |
| Discharge location, if alive, n (%) | ||||
| Home | 386 (66) | 60 (82) | 2090 (84) | 2536 (81) |
| Inpatient rehabilitation unit | 15 (3) | 1 (1) | 38 (2) | 54 (2) |
| Nursing/residential home | 118 (20) | 7 (10) | 141 (6) | 266 (8) |
| Another hospital | 9 (2) | 3 (4) | 66 (3) | 78 (2) |
| Hospice | 12 (2) | 0 (0) | 8 (< 1) | 20 (1) |
| Other | 44 (8) | 0 (0) | 146 (6) | 190 (6) |
Which patient characteristics predict assignment to ReSPECT or other emergency care plans?
Clinician recommendation has four groups (i.e. ‘focus on symptom control’, ‘focus on life-sustaining treatment’, ‘unclear’ and ‘not completed’). Our main interest is in comparison of the ‘focus on life-sustaining treatment’ with the ‘focus on symptom control’ groups because these are the two options clinicians should have used on the versions of the ReSPECT form (i.e. versions 1.0 and 2.0) in this study. The relative risk ratios (RRRs) and 95% CIs from multinomial regression models to identify and quantify predictors of assignment to the ‘focus on sustaining life’ group compared with the ‘focus on symptom control’ (baseline) group only (i.e. only one of the three possible pairwise comparisons with baseline) are presented in Table 11.
| Variable | Count (n) | Adjusted by recruitment site only (basic models) | Fully adjusted (multivariable model)a (n = 635) | ||
|---|---|---|---|---|---|
| RRRb (95% CI) | p-value | RRRb (95% CI) | p-value | ||
| Age (years) at admission | 706 | 0.96 (0.94 to 0.98) | < 0.001 | 0.98 (0.95 to 1.01) | 0.118 |
| Sex | |||||
| Male | 321 | 1.00 | 0.275 | 1.00 | 0.929 |
| Female | 384 | 0.92 (0.53 to 1.60) | 0.97 (0.52 to 1.82) | ||
| Ethnicity | |||||
| White | 601 | 1.00 | 0.778 | 1.00 | 0.501 |
| Ethnic minorities | 56 | 1.94 (0.79 to 4.77) | 1.44 (0.50 to 4.15) | ||
| Socioeconomic status | |||||
| Tertile 1 (most deprived) | 212 | 1.00 | 0.541c | 1.00 | 0.353c |
| Tertile 2 | 238 | 1.35 (0.63 to 2.91) | 1.78 (0.74 to 4.30) | ||
| Tertile 3 (least deprived) | 252 | 1.17 (0.48 to 2.85) | 1.29 (0.44 to 3.72) | ||
| Admission type | |||||
| Elective | 23 | 1.00 | 0.184 | 1.00 | 0.883 |
| Emergency | 683 | 0.45 (0.14 to 1.46) | 0.90 (0.23 to 3.53) | ||
| Patient type | |||||
| Medical | 619 | 1.00 | 0.525 | 1.00 | 0.721 |
| Surgical | 87 | 1.27 (0.61 to 2.61) | 1.17 (0.49 to 2.82) | ||
| Cognitively impaired | |||||
| No | 336 | 1.00 | 0.069 | 1.00 | 0.837 |
| Yes | 370 | 1.68 (0.96 to 2.92) | 0.93 (0.46 to 1.89) | ||
| GO-FAR score | |||||
| Very low (> 24) | 55 | 0.67 (0.20 to 2.25) | 0.404c | ||
| Low (14–23) | 210 | 0.43 (0.21 to 0.88) | |||
| Average (–5 to 13) | 378 | 1.00 | |||
| Above average (–15 to –6) | 30 | 1.40 (0.37 to 5.31) | |||
| Charlson Comorbidity Index (points) | |||||
| 0–3 | 53 | 1.00 | < 0.001c | 1.00 | 0.040c |
| 4–5 | 238 | 0.24 (0.09 to 0.62) | 0.43 (0.12 to 1.53) | ||
| 6–7 | 185 | 0.30 (0.11 to 0.81) | 0.60 (0.16 to 2.30) | ||
| 8–25 | 211 | 0.12 (0.04 to 0.33) | 0.21 (0.05 to 0.80) | ||
| McCabe Scale | |||||
| Non-fatal | 402 | 1.00 | 0.017d | 11 | |
| Ultimately fatal | 223 | 0.55 (0.29 to 1.06) | |||
| Rapidly fatal | 80 | 0.36 (0.13 to 1.05) | |||
| Involvement in making the plan | |||||
| Patient | 293 | 1.00 | 0.248d | 1.00 | 0.220d |
| Relative | 220 | 0.46 (0.24 to 0.89) | 0.42 (0.18 to 0.98) | ||
| No consultation | 114 | 0.37 (0.13 to 1.09) | 0.30 (0.08 to 1.14) | ||
| Not completed | 79 | 1.99 (0.86 to 4.60) | 1.84 (0.71 to 4.78) | ||
After adjusting for recruitment site only, age, socioeconomic status, Charlson Comorbidity Index, McCabe Scale and involvement in making the plan, all appeared to influence clinician recommendation.
After adjusting for recruitment site (basic model), patient characteristics and involvement in making the plan (multivariable model), however, only Charlson Comorbidity Index was statistically significant in the model (i.e. found to be an independent predictor of assignment to the ‘focus on life sustaining-treatment’ group). Compared with patients with the greatest chance of surviving 10 years (i.e. 0–3 points per Charlson Comorbidity Index), patients with 4–5 points were 57% less likely to be in the ‘focus on life-sustaining treatment’ group (RRR 0.43, 95% CI 0.12 to 1.53), patients with 6–7 points were 40% less likely to be in the ‘focus on life-sustaining treatment’ group (OR 0.60, 95% CI 0.16 to 2.30) and patients with 8–25 points were 79% less likely to be in the ‘focus on life-sustaining treatment’ group (OR 0.21, 95% CI 0.05 to 0.80; p = 0.04) (test of linear trend).
Which patient characteristics predict assignment to a DNACPR? Do particular patient preferences and emergency care and treatment recommendations predict a DNACPR decision?
We were unable to assess the effect of patient preference on DNACPR decisions because it was very poorly completed (65% not completed). As an alternative, we explored the effect of involvement in making the plan on DNACPR decisions. The ORs and 95% CIs from logistic regression models to assess the effect of patient characteristics, involvement in making the plan and clinician recommendation on DNACPR decisions are given in Tables 12, 14 and 15.
| Variable | Adjusted by recruitment site only (basic models) | Fully adjusted (multivariable model)a (N = 624) | |||
|---|---|---|---|---|---|
| n | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age at admission | 695 | 1.06 (1.04 to 1.09) | < 0.001 | 1.02 (0.98 to 1.06) | 0.237 |
| Sex | |||||
| Male | 313 | 1.00 | 0.109 | 1.00 | 0.577 |
| Female | 381 | 1.67 (0.89 to 3.15) | 1.28 (0.54 to 3.06) | ||
| Ethnicity | |||||
| White | 591 | 1.00 | < 0.001 | 1.00 | 0.299 |
| Ethnic minorities | 55 | 0.24 (0.11 to 0.52) | 0.49 (0.12 to 1.89) | ||
| Socioeconomic status | |||||
| Tertile 1 (most deprived) | 210 | 1.00 | 0.431b | 1.00 | 0.286b |
| Tertile 2 | 233 | 1.12 (0.53 to 2.34) | 0.61 (0.19 to 1.98) | ||
| Tertile 3 (least deprived) | 248 | 1.51 (0.69 to 3.31) | 0.49 (0.13 to 1.89) | ||
| Admission type | |||||
| Elective | 23 | 1.00 | 0.590 | 1.00 | 0.202 |
| Emergency | 672 | 1.50 (0.34 to 6.64) | 0.17 (0.01 to 2.58) | ||
| Patient type | |||||
| Medical | 609 | 1.00 | 0.386 | 1.00 | 0.159 |
| Surgical | 86 | 0.69 (0.30 to 1.60) | 0.40 (0.11 to 1.43) | ||
| Cognitively Impaired | |||||
| No | 332 | 1.00 | 0.062 | 1.00 | 0.712 |
| Yes | 363 | 1.85 (0.97 to 3.45) | 1.20 (0.46 to 3.13) | ||
| GO-FAR score | |||||
| Very low (> 24) | 54 | 1.98 (0.46 to 8.60) | 0.957b | ||
| Low (14–23) | 210 | 1.70 (0.78 to 3.71) | |||
| Average (–5 to 13) | 367 | 1.00 | |||
| Above average (–15 to –6) | 30 | 2.21 (0.29 to –16.89) | |||
| Charlson Comorbidity Index (points) | |||||
| 0–3 | 53 | 1.00 | < 0.001b | 1.00 | 0.048b |
| 4–5 | 235 | 5.55 (2.40 to 12.85) | 2.74 (0.70 to 10.75) | ||
| 6–7 | 182 | 8.13 (3.05 to 21.67) | 5.92 (1.10 to 31.89) | ||
| 8–25 | 206 | 9.24 (3.47 to 24.61) | 4.01 (0.87 to 18.58) | ||
| McCabe Scale | |||||
| Non-fatal | 396 | 1.00 | 0.354a | ||
| Ultimately fatal | 218 | 1.11 (0.56 to 2.20) | |||
| Rapidly fatal | 79 | 1.78 (0.53 to 6.03) | |||
| Clinician recommendation | |||||
| Focus on life-sustaining treatment | 118 | 1.00 | < 0.001a | 1.00 | < 0.001a |
| Focus on symptom control | 280 | 26.09 (7.72 to 88.22) | 69.84 (14.40 to 338.68) | ||
| Unclear position | 93 | 4.10 (1.61 to 10.44) | 5.82 (1.54 to 21.96) | ||
| Not completed | 204 | 7.95 (3.33 to 19.00) | 23.10 (6.23 to 85.65) | ||
| Involvement in making the plan | |||||
| Patient | 291 | 1.00 | 0.193a | 1.00 | 0.058a |
| Relative | 215 | 4.10 (1.39 to 12.13) | 6.42 (1.30 to 31.85) | ||
| No consultation | 113 | 2.85 (0.83 to 9.76) | 1.96 (0.39 to 9.87) | ||
| Not completed | 76 | 0.34 (0.17 to 0.72) | 0.30 (0.09 to 0.95) | ||
| Variable | McCabe Scale, n (%) | All (N = 3439), n (%) | |||
|---|---|---|---|---|---|
| Non-fatal (N = 2501), n (%) | Ultimately fatal (N = 694), n (%) | Rapidly fatal (N = 234), n (%) | Not complete (N = 10), n (%) | ||
| New pressure ulcer | |||||
| None | 2174 (87) | 590 (85) | 206 (88) | 8 (80) | 2978 (87) |
| Grade 2 | 39 (2) | 17 (2) | 6 (3) | 0 (0) | 62 (2) |
| Grade 3 | 8 (< 1) | 1 (< 1) | 1 (< 1) | 0 (0) | 10 (< 1) |
| Grade 4 | 0 (0) | 1 (< 1) | 0 (0) | 0 (0) | 1 (< 1) |
| Upgradeable | 7 (< 1) | 8 (1) | 1 (< 1) | 0 (0) | 16 (< 1) |
| Not completed | 273 (11) | 77 (11) | 20 (9) | 2 (20) | 372 (11) |
| Falls | |||||
| No fall | 1997 (80) | 554 (80) | 208 (88) | 6 (60) | 2764 (80) |
| No harm | 64 (3) | 15 (2) | 4 (2) | 0 (0) | 83 (2) |
| Low | 70 (3) | 22 (3) | 2 (1) | 2 (20) | 96 (3) |
| Moderate | 81 (3) | 23 (3) | 4 (2) | 0 (0) | 108 (3) |
| Severe | 49 (2) | 19 (3) | 1 (< 1) | 0 (0) | 69 (2) |
| Death | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Not completed | 240 (9) | 61 (9) | 16 (7) | 2 (20) | 319 (9) |
| UTI | |||||
| No UTI | 2111 (84) | 591 (85) | 212 (91) | 8 (80) | 2922 (85) |
| Old UTI | 61 (3) | 15 (2) | 2 (1) | 0 (0) | 78 (2) |
| New UTI | 84 (3) | 16 (2) | 4 (2) | 0 (0) | 104 (3) |
| Not completed | 245 (10) | 72 (11) | 16 (6) | 2 (20) | 335 (10) |
| Urinary catheter in situ | |||||
| No catheter | 1753 (70) | 447 (65) | 139 (59) | 6 (60) | 2345 (68) |
| 1–28 days | 430 (17) | 140 (20) | 62 (27) | 2 (20) | 634 (18) |
| > 28 days | 54 (2) | 30 (4) | 5 (2) | 0 (0) | 89 (3) |
| Days unknown | 37 (2) | 14 (2) | 11 (5) | 0 (0) | 62 (2) |
| Not completed | 227 (9) | 110 (16) | 17 (7) | 2 (20) | 309 (9) |
| VTE risk assessment | |||||
| Yes | 2067 (83) | 583 (84) | 218 (93) | 8 (80) | 2876 (84) |
| No | 177 (7) | 45 (7) | 5 (2) | 0 (0) | 227 (7) |
| Not applicable | 5 (< 1) | 4 (< 1) | 0 (0) | 0 (0) | 9 (< 1) |
| Not completed | 252 (10) | 62 (9) | 11 (5) | 2 (20) | 327 (10) |
| VTE prophylaxis | |||||
| Yes | 1613 (64) | 441 (64) | 168 (72) | 6 (60) | 2228 (65) |
| No | 359 (15) | 100 (14) | 29 (12) | 0 (0) | 488 (14) |
| Not applicable | 241 (10) | 75 (11) | 26 (11) | 2 (20) | 344 (10) |
| Not completed | 252 (11) | 78 (11) | 11 (4) | 2 (20) | 519 (11) |
| VTE treated | |||||
| None | 1979 (79) | 548 (79) | 190 (81) | 8 (80) | 2725 (79) |
| Old DVT | 29 (1) | 11 (2) | 1 (< 1) | 0 (0) | 41 (1) |
| Old PE | 13 (1) | 5 (1) | 1 (< 1) | 0 (0) | 19 (1) |
| Old other | 47 (2) | 8 (1) | 1 (< 1) | 0 (0) | 56 (2) |
| New DVT | 20 (1) | 4 (1) | 3 (1) | 0 (0) | 27 (1) |
| New PE | 6 (< 1) | 3 (< 1) | 1 (< 1) | 0 (0) | 10 (< 1) |
| New other | 20 (1) | 8 (1) | 1 (< 1) | 0 (0) | 29 (1) |
| Not completed | 387 (15) | 107 (15) | 36 (15) | 2 (20) | 532 (15) |
| Harm-free carea | |||||
| Yes | 2017 (81) | 548 (79) | 208 (89) | 6 (60) | 2779 (81) |
| No | 302 (12) | 99 (14) | 18 (8) | 2 (20) | 421 (12) |
| Not completed | 182 (7) | 47 (7) | 8 (3) | 2 (20) | 239 (7) |
| Variable | Adjusted by recruitment site only (basic models) |
Fully adjusted (multivariable model)a (N = 2855) |
|||
|---|---|---|---|---|---|
| Count (n) | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age at admission | 3439 | 1.01 (1.01 – 1.02) | < 0.001 | 1.01 (1.00 – 1.02) | 0.005 |
| Sex | |||||
| Male | 1706 | 1.00 | 0.841 | 1.00 | 0.897 |
| Female | 1729 | 1.02 (0.83 to 1.25) | 1.02 (0.80 to 1.29) | ||
| Ethnicity | |||||
| White | 2792 | 1.00 | 0.579 | 1.00 | 0.804 |
| Ethnic minorities | 417 | 1.09 (0.80 to 1.48) | 1.05 (0.73 to 1.51) | ||
| Socioeconomic status | |||||
| Tertile 1 (most deprived) | 1207 | 1.00 | 0.007b | 1.00 | 0.381b |
| Tertile 2 | 1245 | 0.75 (0.59 to 0.96) | 0.96 (0.70 to 1.31) | ||
| Tertile 3 (least deprived) | 933 | 0.74 (0.57 to 0.96) | 0.78 (0.51 to 1.18) | ||
| Admission type | |||||
| Elective | 522 | 1.00 | < 0.001 | 1.00 | < 0.001 |
| Emergency | 2917 | 1.69 (1.21 to 2.34) | 2.58 (1.73 to 3.85) | ||
| Patient type | |||||
| Medical | 2566 | 1.00 | 0.817 | 1.00 | 0.302 |
| Surgical | 873 | 0.97 (0.77 to 1.23) | 1.17 (0.87 to 1.56) | ||
| Cognitively impaired? | |||||
| No | 2428 | 1.00 | 0.014 | 1.00 | 0.070 |
| Yes | 1011 | 1.32 (1.05 to 1.64) | 1.28 (0.98 to 1.67) | ||
| GO-FAR score | |||||
| Very low (> 24) | 135 | 1.38 (1.01 to 1.89) | 0.764b | ||
| Low (14–23) | 726 | 0.83 (0.65 to 1.05) | |||
| Average (–5 to 13) | 2129 | 1.00 | |||
| Above average (–15 to –6) | 290 | 1.38 (1.01 to 1.89) | |||
| Charlson Comorbidity Index (quartile) | |||||
| 1 | 1048 | 1.00 | 0.002b | 1.00 | 0.102b |
| 2 | 1041 | 1.45 (1.09 to 1.92) | 1.05 (0.71 to 1.56) | ||
| 3 | 646 | 1.97 (1.46 to 2.66) | 1.53 (1.00 to 2.34) | ||
| 4 | 603 | 1.69 (1.24 o 2.31) | 1.29 (0.83 to 2.01) | ||
| McCabe Scale | |||||
| Non-fatal | 2501 | 1.00 | 0.099c | ||
| Ultimately fatal | 694 | 1.41 (1.13 to 1.75) | |||
| Rapidly fatal | 234 | 0.71 (0.47 to 1.07) | |||
| CPR status | |||||
| Recommended | 2786 | 1.00 | 0.761 | 1.00 | 0.350 |
| Not recommended | 653 | 1.04 (0.80 to 1.35) | 0.86 (0.62 to 1.19) | ||
| Variable | Count (n) | Univariable | Multivariable (N = 3073) | ||
|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| Age at admission (years) | 3439 | 1.07 (1.06 to 1.08) | < 0.001 | 1.05 (1.04 to 1.06) | < 0.001 |
| Sex | |||||
| Male | 1706 | 1.00 | 0.014 | 1.00 | 0.943 |
| Female | 1729 | 1.23 (1.04 to 1.45) | 1.01 (0.82 to 1.23) | ||
| Ethnicity | |||||
| White | 2792 | 1.00 | < 0.001 | 1.00 | 0.740 |
| Ethnic minorities | 417 | 0.57 (0.42 to 0.76) | 0.94 (0.67 to 1.33) | ||
| Socioeconomic status | |||||
| Tertile 1 (most deprived) | 1207 | 1.00 | < 0.001 | 1.00 | 0.758 |
| Tertile 2 | 1245 | 1.11 (0.90 to 1.36) | 0.96 (0.73 to 1.26) | ||
| Tertile 3 (least deprived) | 933 | 1.74 (1.41 to 2.14) | 0.96 (0.70 to 1.31) | ||
| Admission type | |||||
| Elective | 522 | 1.00 | < 0.001 | 1.00 | < 0.001 |
| Emergency | 2917 | 6.63 (4.33 to 10.17) | 2.68 (1.64 to 4.36) | ||
| Patient type | |||||
| Medical | 2566 | 1.00 | < 0.001 | 1.00 | < 0.001 |
| Surgical | 873 | 0.35 (0.27 to 0.44) | 0.57 (0.43 to 0.76) | ||
| Cognitively impaired? | |||||
| No | 2428 | 1.00 | < 0.001 | 1.00 | < 0.001 |
| Yes | 1011 | 3.57 (3.03 to 4.35) | 2.17 (1.79 to 2.63) | ||
| Charlson Comorbidity Index (points) | |||||
| 0–3 | 1048 | 1.00 | < 0.001a | 1.00 | < 0.001a |
| 4–5 | 1041 | 5.56 (4.07 to 7.60) | 1.38 (0.93 to 2.06) | ||
| 6–7 | 646 | 7.53 (5.44 to 10.42) | 1.49 (0.97 to 2.27) | ||
| 8–25 | 603 | 10.11 (7.32 to 13.96) | 2.46 (1.62 to 3.73) | ||
From the models adjusting for site only (basic models), it appears that age at admission, ethnicity, cognitive impairment, Charlson Comorbidity Index and clinician recommendation influence the chance of having a DNACPR decision. After further adjusting for patient characteristics (multivariable model), only Charlson Comorbidity Index, clinician recommendation and involvement in making the plan were statistically significant (i.e. found to be independent predictors of having a DNACPR decision), but there is considerable uncertainty regarding the magnitude of these effects because of the sparsity of the data (as 92% of the patients with full ReSPECT forms had a DNACPR decision, there was little information about patients with full ReSPECT forms who were for CPR). The multivariable model suggests that patients scoring 4–5 points per Charlson Comorbidity Index were nearly three times more likely than patients scoring 0–3 points to have a DNACPR decision (OR 2.74, 95% CI 0.70 to 10.75). Similarly, patients scoring 6–7 points were nearly six times more likely to have a DNACPR decision than patients scoring 0–3 points (OR 5.92, 95% CI 1.10 to 31.89). Patients scoring 8–25 points were four times more likely patients scoring 0–3 points to have a DNACPR decision (OR 4.01, 95% CI 0.87 to 18.58; p = 0.048). Patients in the ‘focus on symptom control’ group were 70 times more likely to have a DNACPR decision than patients in the ‘focus on life-sustaining treatment’ group (OR 69.84, 95% CI 14.40 to 338.68). Patients for whom the position was unclear were four times more likely to have a DNACPR decision (OR 5.82, 95% CI 1.54 to 21.96; p < 0.001). Compared with patients who were involved in making the plan, patients who had a relative involved were over six times more likely to have a DNACPR decision (OR 6.42, 95% CI 1.30 to 31.85). Where there was no consultation regarding the plan, the risk of having a DNACPR decision almost doubled compared with when the patient was involved (OR 1.96, 95% CI 0.39 to 9.87). For patients for whom the ‘involvement in making the plan’ section of the full ReSPECT form had not been completed, the chance of having a DNACPR decision was 70% less than when the patient was involved (OR 0.30, 95% CI 0.09 to 0.95; p = 0.058).
Is a DNACPR decision an independent predictor of patient harm?
Table 13 presents the proportions of patients with harms and harm-free care in each McCabe Scale group and the whole sample combined. Most patients (81%) had harm-free care, but patients in the rapidly fatal group had harm-free care more often than patients in the other groups. Although patients who had an underlying rapidly fatal condition had a similar proportion of new pressure ulcers, they had proportionately fewer harms from a fall, fewer urinary tract infections in spite of more having a catheter in situ, had a higher proportion of venous thromboembolism (VTE) assessments and VTE prophylactic treatment, but proportionally no more treated VTEs that the other groups.
See Table 19 for the ORs and 95% CIs from the logistic regression models to assess the effect of patient characteristics and CPR decision on risk of harm are given in Table 20. In the models adjusting for site only (basic models), age at admission, socioeconomic status, admission type, being cognitively impaired and Charlson Comorbidity Index appeared to influence risk of harms. The effect of age at admission, admission type and being cognitively impaired on risk of harms remained when differences in patient characteristics were taken into account (multivariable model). The relative risk of harm iancreased 1% per year of age (OR 1.01, 95 CI 1.00 to 1.02; p = 0.005) and cognitive impairment was associated with approximately 30% greater risk (OR 1.28, 95% CI 0.98 to 1.67; p = 0.07). The estimate of the OR associated with emergency admissions, however, increased from 1.69 to 2.58 (95% CI 1.73 to 3.85; p < 0.001).
Summary
-
The optional personal preference section was completed in 30% of full ReSPECT forms.
-
The clinician recommendation was ‘focus on life-sustaining treatment’ for only 17% of patients with a full ReSPECT form. The clinician recommendation was ‘focus on symptom control’ for 40% of patients with a full ReSPECT form.
-
CPR was not recommended for the majority (92%) of patients with full ReSPECT forms.
-
Charlson Comorbidity Index was the only independent predictor of clinician recommendation. Increasing number of points per Charlson Comorbidity Index (i.e. decreasing the chance of surviving 10 years) made it more likely that the clinician would recommend ‘focus on symptom control’.
-
Charlson Comorbidity Index, clinician recommendation and involvement in making the plan were independent predictors of having a DNACPR decision, but there was considerable uncertainty about the magnitude of the ORs. Increasing the number of points per Charlson Comorbidity Index (i.e. decreasing the chance of surviving 10 years), having the clinician recommend ‘focus on symptom control’ and having a relative (or no one) consulted when making the plan increased the chance of having a DNACPR decision.
-
Most (81%) patients experienced harm-free care. Age at admission, admission type and having cognitive impairment were independent predictors of harm. Increasing age at admission, emergency admission and cognitive impairment were associated with greater risk of harm.
-
We found no evidence that patients not recommended for CPR attempts (i.e. DNACPR) were at greater risk of serious harm than patients for whom CPR was recommended, but the CI was fairly wide and up to a 19% greater relative risk could not be excluded.
-
Age at admission, admission type, patient type, having cognitive impairment and Charlson Comorbidity Index were independent predictors of having a full ReSPECT form (authorised or adapted). Increasing age at admission, emergency admission, cognitive impairment and increasing number of points per Charlson Comorbidity Index (i.e. decreasing the chance of surviving 10 years) were associated with increased chance of having a full ReSPECT form. Being a surgical patient reduced the chance of having a ReSPECT form.
Strengths and limitations
To the best of our knowledge, this is the first analysis of the use of the ReSPECT process and its effect on patient outcomes in early adopting English NHS hospitals. Therefore, the analysis will provide useful information for organisations involved in the study, as well for organisations considering adoption of the ReSPECT process in the future.
Inclusion of six NHS acute trusts from different areas of England, serving different populations, means that we have a wide range of adult inpatients represented in our data. Data were collected from patients in a range of inpatient wards commonly found in acute NHS hospitals. By including different clinical specialties and general wards, we are confident that our data were collected from a good cross-section of the inpatient population. We covered medical, older person medical, surgical, critical care, trauma and orthopaedic wards. Although one site contributed data below the site target of 500 cases, owing to the COVID-19 pandemic, overall, we recruited over our target of 3000 patients across all six sites. We included data from 98% of eligible adult inpatients in the study, increasing confidence that we have a representative sample of the adult acute inpatient population. Unfortunately, although we had a roughly proportionate number of patients from ethnic minority backgrounds, compared with available census data, there were insufficient numbers to allow each ethnic subgroup to be included separately.
Our descriptive analyses are based on good-quality data, and this means that we are able to present a clear picture of how the ReSPECT forms were being used. In addition, we have been able to identify aspects of form completion that require improvement.
Our understanding, at the design stage of the study, was that the ReSPECT process would be implemented for use with all hospital inpatients; however, this did not turn out to be the case and our sample of patients with a full or screening ReSPECT form was 23% (792/3439), rather than the originally anticipated 70%. This was because the ReSPECT process was mostly used for the group of patients requiring a DNACPR decision, rather than all patients, and this considerably reduced the numbers available for statistical analyses that required information from the ReSPECT form. The proportion of patients with ReSPECT forms recommending CPR attempts was also far less than anticipated (6% vs. 20%), and this led to unstable models when we were investigating the effect of clinician recommendation on the chance of not being recommended for CPR (i.e. DNACPR). It also should be noted that the national NHS Safety Thermometer audit was stopped because of data quality concerns a few months after we completed data collection.
Chapter 5 Summary of findings
Our key findings and messages seek to address the overarching objective of the study, that is to describe how, when and why ECTPs are made, and what implications this has for patients. Work package teams identified key findings relating to their work package aims and objectives, and these were presented to, and discussed among, the study investigators, Study Steering Committee and our PPI group. Our original plans to present the work to a larger stakeholder group was not possible because of the COVID-19 pandemic and will now occur after publication of this report. Related findings from the various work packages are presented in the following themes, addressing how the ReSPECT process has been adopted, how the ReSPECT process is used in clinical practice in acute NHS hospitals, the association between the ReSPECT process and health outcomes, and initial insights into the role of the ReSPECT process in the community.
Adoption of the ReSPECT process
There has been progress towards the goal of moving away from standalone DNACPR in acute hospitals, where use has reduced from 72% (in 2015) to 34% (in 2019). There remains variation in the systems used to record resuscitation decisions, emergency care and TEPs. Use of the ReSPECT process has increased more rapidly than alternative emergency care and treatment planning systems, and has accounted for nearly 60% of moves away from standalone DNACPR. By the end of 2019, the ReSPECT process was being used in 22% of the 189 acute trusts surveyed. Data supplied by the RCUK (2020) indicate that roll-out has continued and the ReSPECT process has been adopted across 70% of England hospitals. 65
Six acute hospital trusts that were identified as early adopters of the ReSPECT process took part in the qualitative and retrospective observational parts of the present study. Adoption of the ReSPECT process into community health settings varied. In two sites that had an area-wide DNACPR system and in one other site, general practices across the area also adopted the ReSPECT process, but later than the acute trusts. At another site, the CCG adopted the ReSPECT process a considerable time after the acute trust. At two sites, there was no area-wide plan to adopt the ReSPECT process at the time of the study.
There was some variation in the approach to implementation across the six trusts. Local policies were developed on who could initiate ReSPECT conversations and who was regarded as the senior responsible clinician. Clinician guidance in five of the six trusts was that a ReSPECT conversation should take place for patients considered at risk of deterioration. One trust recommended that a ReSPECT plan is made for all patients. Four hospital sites used the paper-based ReSPECT form, whereas two sites developed their own electronic record based on the ReSPECT form. One of these sites developed an additional shortened screening electronic ReSPECT form for use where the decision was for full escalation of treatment. One site used the paper form during data collection for work package 3, but has since developed its own electronic ReSPECT record.
Characteristics of those involved in the ReSPECT process
The evaluation of 3439 clinical records identified that full ReSPECT forms were completed for, on average, one in five (20%, range 6–41%) inpatients. Characteristics associated with ReSPECT form completion were older age, emergency admission, admission for medical (rather than surgical) problems, increasing comorbidities and cognitive impairment. We did not find associations with ethnicity, socioeconomic status or the presence of learning disabilities. Patients with a ReSPECT form were less likely to survive to hospital discharge (83% vs. 94%) and were more likely to be discharged to a nursing home (20% vs. 8%) than patients without a ReSPECT form.
The majority (82%) of ReSPECT forms were completed following admission to hospital. Among these forms, 42% were completed within the first 48 hours of admission and the remainder were spread across the duration of hospital stay.
Consultants were involved in 84% of ReSPECT decisions. Other grades of clinical staff involved were foundation doctors (8%), middle grade doctors (43%) and nurses/allied health professionals (1%). Patients and families were recorded as participating in making recommendations in 41% and 30% of ReSPECT forms, respectively.
Clinicians told us that they prioritised conversations with patients whom they identified as terminally ill or anticipated were at imminent risk of deterioration. Conversations were usually prompted by the patient’s condition, when a poor diagnosis/prognosis became known, when patients or families expressed treatment or planning requests, or if the patient was going to be transferred to a different setting. ReSPECT conversations were often constrained by time limitations, busy ward environments and the urgency of the situation. Clinicians told us that ReSPECT conversations take time to do well, meaning that clinicians often held conversations with fewer patients than they would have liked to.
Mental capacity and involvement in decision-making
The patient’s mental capacity was recorded in 86% of records, and half of these patients were assessed as having sufficient mental capacity to be involved in making the plan and the other half did not. One in five forms noted the presence of a legal proxy (e.g. lasting power of attorney).
Two-thirds of patients who were recorded as having mental capacity indicated a preference in relation to their priorities for care, for example prioritise life-sustaining treatment (10%), comfort (71%) or an equal balance (17%).
Section six of the ReSPECT form contains a section where clinicians can record who was involved in making the ReSPECT plan. The patient was most frequently recorded as being involved in the plan (40%), followed by relatives (31%). At the time of data collection, the ReSPECT form recorded that one in six (16%) recommendations were made without involvement of patients or families, and in approximately 1 in 10 forms (11%) this section was not completed. The study did not examine whether or not conversations were held subsequently or recorded elsewhere in the medical records.
ReSPECT conversations
Observations of ReSPECT conversations conducted in acute hospitals, and interviews with clinicians, patients and families about their experiences of ReSPECT conversations, provided insights into why, when and how ReSPECT conversations are conducted in hospital settings.
Clinicians conducted ReSPECT conversations to address a range of treatment planning needs, ranging from resuscitation to palliative care. Some clinicians took an open-ended approach to ReSPECT conversations and other clinicians took a persuasive approach. The choice of approach may have been influenced by the focus of the conversation (e.g. deciding on a discharge plan for a palliative care patient vs. recording a CPR decision for an acutely unwell patient with multiple comorbidities on the current admission), as well as by clinician training, understandings of the aims of the ReSPECT process and time limitations. Although some ReSPECT conversations included broader treatment considerations, CPR recommendations remained a focus in most conversations.
On the relatively rare occasions where patients had thought in advance about resuscitation and discussed this with their family, patients said that ReSPECT conversations were easier and less stressful than did patients who had not previously thought about this. Knowing the patient’s wishes also made families feel more confident in situations where families were required to share information on the patient’s behalf. In a few cases, patients expressed wishes for modified or no treatment and families asked for clarity about the treatment plan. Clinicians responded to these prompts by initiating a ReSPECT conversation. However, patients and families did not specially ask for a ‘ReSPECT conversation’. Clinicians said that ReSPECT conversations sometimes had to be delayed or broken into multiple conversations if patients/families had not thought about their wishes in advance, were not emotionally ready for the conversation or were ambivalent about their preferences. Conversations were often incomplete because patients/families disagreed with doctors’ recommendations or because patients/families found it difficult to engage with ReSPECT conversations because of indecision or distress.
ReSPECT conversations were complex and required sufficient time and highly developed clinical communication skills (Box 1). Developing rapport with the patient/family required understanding of the emotional burden demanded of both patients/families and clinicians, as well as the clinician being able to understand and interpret patients’ and families’ reactions, patients’ and families’ individual circumstances, the stages of acceptance of the patient’s health condition, and how much patients and families can cope with during each interaction.
-
ReSPECT conversations take time for clinicians to do well. Managing time for ReSPECT conversations presented different challenges in different specialties. Finding time was accomplished more easily in specialties that were used to taking time to plan care and treatment with patients with complex needs (e.g. palliative care, care of older people).
-
Patients being acutely unwell affects ReSPECT conversations. Being acutely ill meant that for many patients and their families the immediate health concerns were paramount in their minds, making it difficult to comprehend and discuss uncertain future possibilities. In addition, a patient’s disease trajectory and trajectory on the acute admission will affect the nature and focus of conversations.
-
Good recommendations were characterised by building rapport and trust, which takes time and has particular challenges in acute settings.
-
Considering the challenges involved when time is lacking and having no or minimal previous interactions with the patient/family in the acute setting, the focus is on immediate treatment needs.
-
Creating a shared understanding involves clinicians soliciting patients’ views about their values and preferences before making assumptions that patients will understand their clinical perspectives and values.
-
Clinician and patient/family values should be taken into account when making treatment recommendations, ensuring that patients assumptions/understandings are explored by talking patients through the rationale for the clinical recommendations.
-
Ensuring that recommendations are presented well, considering the patients values, concerns and clinical situation, and taking time to have a conversation, on more than one occasion if necessary, is required to ensure that clinicians recommendations are understood.
-
Clinicians should consider and record how they weigh harms and benefits associated with particular treatment options in conversations.
Clinicians did not use the ReSPECT supporting materials (i.e. leaflets) during conversations with patients/families. Likewise, the paper ReSPECT form was infrequently used by clinicians during conversations with patients/families. In conversations where the paper ReSPECT form was used during the conversation, clinicians said that the form facilitated engagement with conversations and better understanding of treatment options. In trusts that digitised the recording of ReSPECT decisions, the form was not used in conversations with patients/families, and some doctors said that this formed a barrier to engagement.
Patients/families could mainly recall discussing resuscitation, rather than a range of treatments. In most conversations, patients/families were invited to ask questions to check their understanding of the clinical recommendation and to, occasionally, express their concerns. A few patients/families openly expressed disagreement with clinical recommendations. When making treatment recommendations, some clinicians took patient/family preferences into consideration; however, ReSPECT recommendations ultimately reflected medical decision-making, and forms often lacked sufficient detail about the rationale for the treatment recommendations.
Shared understanding or shared decision-making?
Most – but not all – resuscitation and escalation conversations and bad news conversations aimed primarily at recording the treatment recommendation that the clinician considered most medically appropriate. When clinicians were uncertain about a patient’s trajectory, then ReSPECT conversations would explore patient preferences to a greater extent (suggestive of a shared decision-making process). By contrast, when a patient’s illness and treatment trajectory seemed clear, then clinicians tended to take a persuasive approach to ReSPECT conversations, which suggests that these conversations were aimed at ensuring that patients/families have an understanding of the clinical recommendation, rather than engaging patients/families in making a shared statement of treatment recommendations.
A key reason given by clinicians for taking a persuasive or prescriptive approach to ReSPECT conversations was to avoid patient harm from invasive treatments that would not be successful. Although often adopting a persuasive approach, clinicians still saw their recommendations as having been agreed between themselves and the patients/families, rather than being solely their clinical recommendation. Clinicians were reluctant to make a recommendation that the patient or their family disagreed with, usually deferring further conversation and completion of the form. Out of the 49 observed conversations, 13 (26.5%) were incomplete, either because of disagreement between the patient/family and the doctor, or because the patient did not appear to be emotionally ready for the conversation. Therefore, all recommendations were seen as shared with the patient/family in some way, but the shared agreement manifest in the recorded recommendations was, in most cases, a passive process (i.e. the patient or their family did not object), rather than a true shared decision-making process.
In contrast, in palliative care conversations, doctors emphasised the importance of understanding what patients valued and planned future treatment recommendations according to these values, an approach that seems to be much more aligned to a shared decision-making process model. This model was also described by GPs who conducted ReSPECT conversations in a community setting when they (and community palliative care services) had time and opportunity to plan conversations because of the less urgent nature of the situation.
Ethics basis for recommendations
Two key ethics principles informed clinicians’ approaches to and reflections on the ReSPECT process: (1) respect for patient autonomy and (2) the duty to protect the patient from harm. Depending on the clinical context and the clinician’s perception of the process, respect for autonomy was conceptualised and enacted in different ways, including, in a few cases, actively involving the patient in formulating the recommendations; exploring a patient’s wishes, preferences and values, either directly or through their family, to shape the clinical decision-making process; or, at a minimal level, ensuring that the patient and/or their family understand the recommendations and rationale for them affording an opportunity for dissent. A wider concept of respect for persons was reflected in the views of several clinicians who believed the ReSPECT process prompted a more holistic consideration of patient treatment recommendations, moving the focus away from solely CPR decisions. However, our analysis of ReSPECT forms suggests that for many clinicians the main focus of ReSPECT form remains the CPR recommendation. The concern of clinicians to protect their patients from harm influenced both the decision to initiate a ReSPECT conversation (avoiding further distress in a very sick patient) and the conversation itself (avoiding discussion of treatments considered futile or likely to cause significant harm to the patient). Some clinicians also expressed the need to mitigate the psychological distress to families that could occur around these conversations, and how these ethics principles of respect for autonomy and protecting from harm were balanced was shaped by the context of the ReSPECT conversation, including urgency of the situation, level of uncertainty and external organisational pressures.
Recorded recommendations
Among 3439 patients, 706 had a full ReSPECT form and 86 had screening forms. Almost all full ReSPECT forms included recommendations relating to CPR (6% of forms recommended CPR, 92% of forms did not recommend CPR and this was not recorded in 2% of forms). The ReSPECT process extended emergency care planning from standalone DNACPR decisions to contextualising a CPR recommendation within other emergency care and treatment recommendations. Broader treatment goals, with a focus on life-sustaining treatment (17%) or symptom control (40%), were present in the majority of records. One or more specific clinical recommendations, in addition to recommendations relating to CPR, were recorded in 78% of records. The most common recommendations were about location of care [e.g. 49% of records had a recommendation about ICU (either for or not for treatment in that location) and 49% of records had a recommendation for ward-based care]. Recommendations relating to specific treatments focused on critical care interventions, for example invasive ventilation (32%), non-invasive ventilation (26%), vasopressor support (20%) and renal replacement therapy (20%). Other recommendations related to the use of antibiotics (14%), palliative care (12%), hydration (12%), feeding (9%) and appropriateness of re-admission to hospital (7%).
The qualitative evaluation of 141 completed ReSPECT forms and relevant segments of patient notes showed that CPR recommendations were recorded on all forms, and that most forms mentioned other treatment recommendations in addition. This finding signals a shift towards placing CPR decision-making within a wider context of clinical care. Nevertheless, as reported in the hospital wide review, forms varied substantially in the detail provided. The ethics justification, whereby clinicians weigh up the benefits and burdens of treatment with patient preferences and goals, was rarely recorded in sufficient detail to enable others to follow the decision-making process.
Association of a do not attempt resuscitation decision on risk of harm
Analysis of data from the NHS Safety Thermometer programme showed that most (81%) patients experienced harm-free care. Increasing age at admission, emergency admission and cognitive impairment were associated with greater risk of harm. We did not find evidence that the presence of a recommendation that CPR should not be attempted was associated with a greater risk of harm. The qualitative evaluation found that many clinicians reported that the ReSPECT process led to improvements in quality of care, including reducing the harms associated with DNACPR, in particular the mistaken withdrawal of treatment.
Association of a ReSPECT recommendation on resuscitation outcomes
Analysis of the NCAA showed that the proportion of resuscitation attempts abandoned because of futility was already falling quite rapidly prior to the launch of the ReSPECT process (from 11.2% in 2014 to 6.5% in 2016). Following the national launch of the ReSPECT process, the proportion of resuscitation attempts abandoned because of futility continued to fall. The ITS analysis did not find evidence that the rate of change was different at sites that had adopted the ReSPECT process compared with sites that did not. Similarly, no changes were identified in the frequency of IHCAs or outcomes following resuscitation.
These findings may be limited by the fact that only a small proportion (22%) of hospitals adopted the ReSPECT process, on average, 14 months after national roll-out. There was also variability between sites in the frequency with which each site reported futile resuscitation attempts, with some sites reporting no cases for long periods of time.
Insights about ReSPECT form completion in the community
Hospital clinicians were most likely to see community-issued ReSPECT forms brought in by elderly patients. Hospital clinicians viewed community-issued ReSPECT forms as generally useful for understanding patients’ preferences and would routinely review their recommendations at admission. However, specific treatment recommendations did not always transfer well between acute and community settings because the focus of ReSPECT conversations tended to differ between these settings. Community-issued ReSPECT forms usually focused on patients’ preferences about community-based care, hospital admission and place of death, whereas hospital-issued ReSPECT forms usually focused on interventions relevant to the current admission. As a result, community health-care professionals said that hospital-issued forms had limited value, although the forms could serve as prompts for additional ReSPECT conversations in the community.
Community health-care professionals and hospital doctors said that ReSPECT forms held by patients in the community were not always readily available to health professionals (e.g. paramedics or at hospital admission).
Summary
NHS acute hospitals are moving away from systems that record DNACPR decisions in isolation to systems that integrate DNACPR decisions within broader ECTPs. At the time of the research, the ReSPECT process was being used in one-fifth of acute hospitals. The approach to ReSPECT discussions and what is included on the ReSPECT form differs between hospitals and community settings. When ReSPECT forms cross this boundary with the patient, the forms provide information for the clinician and act as a prompt to review the recommendations for the patient’s new context.
Hospital clinicians prioritised ReSPECT conversations with patients whom they identified as terminally ill or anticipated were at imminent risk of deterioration. A move towards a more holistic approach in terms of treatment recommendations and conversations was observed, but there remains a focus on decisions relating to resuscitation as a central component of conversations.
Patients (and/or those close to the patient) were involved in making most, but not all, ECTPs. Involvement of patients focused usually on asking patients about their preferences for specific treatments or explaining recommendations. It was rare for patients’ values and preferences to be sought and for these to influence recommendations. The ReSPECT supporting materials were rarely used during decision-making. Two key ethics principles informed clinicians’ approaches to and reflections on the ReSPECT process: (1) respect for patient autonomy and (2) the duty to protect the patient from harm. Emergency care and treatment planning conversations are often complex and need to draw together patients’ preferences and values within a framework of clinical judgement. Patient and family support and preparation could facilitate conversations.
Chapter 6 Discussion
National adoption of the ReSPECT process
Previous research identified wide variation across health-care settings in the systems used to record DNACPR decisions, creating difficulty in transferring decisions, particularly between the community and hospital setting. 19,20,38 A stakeholder group from our previous research38 on DNACPR decisions identified the development of a unified national approach to recording decisions as one of five key priorities, and these findings were presented as written evidence to Health Select Committee’s fifth report into end of life care, which recommended standardising recording mechanisms for the NHS in England. 66 In response, the English government stated its intention to move towards widespread implementation of the ReSPECT process following initial pilot work. The present study identified that there remains a significant gap between the adoption of a single system across the NHS, with (at the time of the research) only 22% of trusts having adopted the ReSPECT process. The level of co-ordination of adoption by the different providers within a local health economy varies. The lack of a consistent approach was also identified by the CQC in its report Protect, Respect, Connect – Decisions About Living and Dying Well During COVID-19. 67 The lack of homogeneity in approach may lead to difficulties for patients, as different health-care organisations may discount or undervalue decisions recorded in forms other than its own preferred system. There has been no national mandate for a single system in England and Scotland; however, a national DNACPR policy has been implemented in Wales. 68 Although the RCUK report progress in the adoption of ReSPECT since our evaluation, there remains some way to go before the NHS can say that it has a unified national system for resuscitation and emergency care decisions.
Integration of DNACPR into overall treatment plans
Evidence from systematic reviews, conducted as part of our previous programme of work,11,69 identified that linking DNACPR decisions to discussions about overall treatment plans provided greater clarity about goals of care, aided communication between clinicians and reduced harms. [A key recommendation from our previous stakeholder group was to integrate DNACPR decisions within overall treatment plans. 38] These findings were supported by the Health Select Committee who recommended that ‘the Government review the use of DNACPR orders in acute care settings, including whether resuscitation decisions should be considered in the context of overall treatment plans’ (contains Parliamentary information licensed under the Open Parliament Licence v3.0). 70 The findings from this research shows that there has been partial success in meeting the aspiration of moving away from standalone DNACPR decisions, as rates have fallen from 72% to 34%.
One of the key aims of the ReSPECT process is to contextualise resuscitation decisions within overall treatment plans. 61,71 The current research found that just over 70% of patients had an overall treatment goal (to focus on life-sustaining treatment/symptom control) recorded by the clinician completing the form. Improving recording of this goal has since been addressed by the national ReSPECT team, with the addition of a middle option (i.e. a mixture of life-sustaining treatment and comfort care) in the latest version of the ReSPECT form (version 3.0). 72
Four out of five ReSPECT forms had at least one treatment recommendation (other than a CPR recommendation). Locations of care, particularly ICU and ward, appeared to be used to indicate what treatments were recommended for patients. Greater clarity could be given to the clinicians treating a patient in an emergency by specifying treatments that are or are not recommended (e.g. for non-invasive ventilation but not for invasive ventilation). Recommendations were largely relevant for acute care. More consideration needs to be given to the relevance of recommendations when patients were transferring between care settings.
When and why did discussions about emergency care and treatment plans take place
Guidance varies as to when to initiate a conversation about ECTPs. The NCEPOD’s ‘Time to Intervene’ recommended that CPR status must be considered and recorded for all acute admissions. 7 Joint guidance from the British Medical Association, RCUK and Royal College of Nursing suggests making specific anticipatory decisions about whether or not to attempt CPR for any person who is approaching the end of life and/or is at risk of cardiorespiratory arrest. Guidance from the ReSPECT group suggests that CPR can be for anyone, but will have increasing relevance for people who have complex health needs, people who are likely to be nearing the end of their lives and people who are at risk of sudden deterioration or cardiac arrest. 71 Across the six hospitals evaluated in this study, five recommended that a ReSPECT conversation should take place with patients who are at risk of deterioration. Similar to our findings in our previous scoping review of DNACPR decision,10 both the quantitative and qualitative analyses in this study indicate that clinicians prioritised conversations with patients whom they identified as terminally ill or anticipated were at imminent risk of deterioration. Clinicians often cited the lack of capacity/time to expand discussions to patients who are less acutely unwell. The approach adopted by the sixth hospital (i.e. use of an abbreviated ReSPECT form for patients without treatment limitations) seemed to facilitate conversations with a greater proportion of patients, and may be worth consideration if the aspiration set by NCEPOD is to be realised.
Involving patients and families when making recommendations
Compliance with the Human Rights Act73 requires that a patient is involved in the decision-making process in relation to their treatment and care. The Mental Capacity Act74 and Adults with Incapacity (Scotland) Act75 specify the requirement that for a person who lacks capacity, people close to the person must be consulted when decisions are made about what is in the person’s best interests. These legal principles were specifically applied to DNACPR decisions in the Court of Appeal judgement in R (Tracey) versus Cambridge University Hospitals NHS Foundation Trust in 201576 and was reiterated in the High Court hearing of Winspear versus City Hospitals Sunderland in 2015. 77
The quantitative evaluation highlights a significant gap between policy and practice, with only four out of five decisions containing documented evidence of involvement of the patient or people close to the patient. These concerning findings are similar to those reported by the Royal College of Physicians audit78 and in audits of electronic DNACPR records. 79,80 Whether the apparent gaps in involvement represents a failure to record, difficulty in contacting people close to the patient or a failure to involve in decision-making is uncertain. In the qualitative evaluation, we observed only one case of a resuscitation decision being completed without family involvement. In this case, despite significant effort, the clinician was unable to identify a suitable person to consult.
Ethics basis for decisions
The development of the ReSPECT process and documentation was largely driven by an ethics concern that the existing model of decision-making around future emergency treatments (i.e. DNACPR orders) did not sufficiently respect patient autonomy and could result in harm to the patient through a negative affect on other aspects of treatment and care. 81 Our study has shown that implementation of the ReSPECT process has initiated a shift in practice that goes some way to mitigating these ethics concerns. Clinicians appear to be acknowledging patients’ preferences and values in the decision-making process, albeit to varying extents, and treatments other than CPR are included in the recommendations for future emergency treatment plans, suggesting a more explicit awareness of the importance of respect for persons and their autonomy. However, meaningful involvement of the patient or their family in discussions leading to recommendations for future treatment requires time and engagement from the patient and their family, and this is often constrained by practical organisational pressures and also concerns of the clinician that either delaying decisions or initiating these discussions will cause harm to the patient. Consequently, the ReSPECT conversations observed in our study still tend to focus on CPR, with the rationale for more holistic treatment recommendations and inclusion of patient preferences somewhat underdeveloped. The literature82,83 on a similar intervention to support ECTPs in the USA identifies similar concerns by clinicians about potential harms to the patient of these conversations. Further work is needed to support clinicians to routinely involve patients and families in the decision-making process leading to recommendations about anticipated future treatment decisions, and to support patients and families to engage with these discussions in a way that benefits, rather than potentially harms, them.
Despite professional bodies’ expectations that decisions are made in a way that is transparent, fair and justifiable, and that attention is paid to recording the detail of decisions and the reasons for them,84 the ethics basis for emergency care treatment decisions were rarely specifically recorded. 48 This finding is not unique and has been observed in a previous study of decision-making relating to critical care admission52 and during the development of a tool to assess clinical ethics consultation records. 85 This finding also goes against the aim of the ReSPECT form, which was designed to facilitate the articulation of the ethics basis of recommendations with a specific prompt to provide reasons for the recommendations being made. Further research may help to identify the barriers to and facilitators of more transparent articulation and recording of the basis for emergency care treatment recommendations.
Shared decisions
The NHS Long Term Plan34 commits to giving people more control over their own health and more personalised care. The delivery plan for that objective of universal personalised care describes how the comprehensive model for personalised care should reach 2.5 million people by 2023/24. 35 A central component of the comprehensive model is the use of shared decision-making.
In considering the extent to which the ReSPECT decision-making we observed is shared-decision-making and whether or not this could be improved, it is worth reminding ourselves of the nature of these decisions. ReSPECT decision-making is a process that leads to a recommendation about future clinical decisions in case an emergency arises, and ReSPECT decision-making is not in itself a treatment decision. Patients and families can and should share in the process of decision-making about ReSPECT recommendations; however, responsibility for the recommendation stays with the clinician and responsibility for the eventual treatment decisions lies with the clinician caring for the patient at the time the emergency or urgent care is needed. Although the literature on shared decision-making focusses on the process of making real-time decisions about treatment with a patient who has capacity and, therefore, is not directly applicable to ReSPECT conversations, it is possible that insights from this literature may be helpful when considering how to improve meaningful patient and family involvement in these conversations and recommendations.
There is a large body of evidence on shared decision-making for what are known as preference-sensitive decisions. That is where the best strategy for an individual is unclear. This may arise when there is insufficient evidence to draw conclusions about the ratio of benefit or harm, or where the assessment is affected by the patient’s values. The best choice for the individual patient depends on their perspective of the known risks and benefits in the context of the scientific uncertainties. 86
In our study, we observed some ReSPECT conversations where clinicians were unclear about the patient trajectory (i.e. the first type of preference-sensitive decision referred to in Chapter 1). 86
In our study, we observed ReSPECT conversations where the clinicians appeared to be confident about the ratio of benefits and harms of particular treatments, in particular confidence around the likelihood of CPR or invasive ventilation being successful if attempted with little scope for the patient’s values to influence the best choice, and this suggests that there is little scope for shared decision-making. However, for any decision or recommendation about treatment, the clinician needs to reflect on their confidence in the decision, that is to what extent is the decision based on evidence and to what extent is the decision influenced by clinician’s own values. If the confidence is based on robust evidence and the influence of the clinician’s own values minimised, through discussion with the patient and colleagues, then it might be appropriate for the clinician to incline towards a persuasive approach. In a situation where the clinician believes that an intervention is likely to be ineffective or harmful, then a conversation may focus on ensuring that the patient/family member understands the reason for the recommendations, rather than actively seeking their input. However, even in these situations, understanding the patient’s values and preferences may shape the final recommendation, for example in the timing of treatment/non-treatment.
A shared decision-making process or model may be helpful in approaching all ReSPECT conversations, while also acknowledging that the final recommendation is made by the clinician. One such model is the three talk model of shared-decision-making in clinical practice. 87 This includes describing the choices, asking about goals, discussing alternatives, actively listening and working together with the patient/family to think carefully about options and reach informed preferences. This appears to reflect closely the ReSPECT process as envisaged by its developers. Finding, allocating and preserving the time for this process is difficult, and it is those setting priorities for our health system who need to grapple with this challenge, rather than the individual clinician. 88
Guidance from the National Institute for Health and Care Excellence (NICE) aimed to make shared decision-making part of everyday care in all health-care settings. 89 The themes identified in our research are similar to those based on the qualitative synthesis of available evidence used by NICE, notably time limitations, clinicians’ attitudes and skills, the patient’s capability/willingness to participate in shared decision-making, clinicians adopting a paternalistic approach, reluctance when there are high-stake decisions and the patient’s mental capacity preventing participation.
NICE has identified low to high certainty evidence supporting the use of patient decision aids. 90 The ReSPECT process is supported by several decision support tools and information leaflets, but it was rare to see these used in practice in the present study. Similarly, low uptake was observed in a UK study52,91 of a decision support tool for intensive care admission, suggesting that the acute care setting may present unique challenges.
Association between ReSPECT recommendations and resuscitation outcomes
We hypothesised that the introduction of the ReSPECT process would have a favourable effect on resuscitation outcomes, principally by facilitating shared decisions with patients and their families, therefore, reducing attempts at resuscitation where resuscitation would not lead to overall benefit for the patient. Instead, we observed an overall decline in resuscitation attempts discontinuing because of perceived futility, which pre-dated the national roll-out of the ReSPECT process. A similar pattern was observed in a separate analysis covering the 5-year period preceding this study. 92 Likewise, the overall incidence of cardiac arrest per 1000 admissions has also been declining before and through the time of the conduct of this study,58 and this could be explained by better detection of critical illness and decision-making prior to cardiac arrest occurring. Together, these data suggest that overall system changes to resuscitation practice were already occurring and have continued to do so.
Association of ReSPECT recommendations on harm to patients
A central theme from our previous evaluation of DNACPR decisions in the NHS was concern among clinicians in relation to the unintended consequences of a DNACPR, through withholding other aspects of care and treatment beyond solely resuscitation. 38 Studies from UK12,24,39,48,93,94 and international setting49,69,95–97 reported similar findings, whereby a DNACPR decision was associated with reduced medical, nursing and basic care. Contextualising resuscitation decisions within overall treatment plans appears to reduce this risk through providing greater clarity about treatment goals and reducing negative associations with resuscitation decisions. 41,48 The present research used the NHS Safety Thermometer92 to look for evidence of harm associated with the presence of a DNACPR recommendation recorded as part of the ReSPECT process. The majority (81%) of patients experienced harm-free care. Multivariate analysis identified that increased age and emergency admission were associated with an increased risk of harm, whereas we found no evidence that the presence of a DNACPR decision was associated with increased harm. These findings, although consistent with other studies that contextualise resuscitation within overall treatment plans,41,48 should, nevertheless, be interpreted within the context of the limitations described below.
Strengths and limitations
A strength of this study was the purposive sampling of six NHS hospitals that were selected to capture the range of NHS clinical services, socioeconomic status and ethnic diversity, urban and rural settings, university and local hospital types and geographical spread. The research took place early after the adoption of the ReSPECT process, which enabled the research team to provide feedback to the national ReSPECT working group early after implementation; however, although this ensured timely feedback following the deployment of the ReSPECT process, it reduced insights into longer-term changes to culture facilitated by the ReSPECT process.
Through the direct observation of ReSPECT conversations, we were able to compare interview and observation data to inform the thematic analysis. However, the settings observed were selected by the hospital lead investigators and sampling was limited to staff and patients/families who were able and willing to be observed and/or interviewed. Consequently, this may have provided a lens on those more comfortable/familiar with the ReSPECT process than may be seen across health-care settings. Time constraints limited our ability to return to see the conclusion of discussions, where initial conversations and decisions were left incomplete.
The ReSPECT conversation policies are decided locally, and in the participating trusts this meant that our observations and interviews focused on doctors. This limited exploration of experience of other health and social care professionals’ involvement in conducting ReSPECT conversations, which may be part of ReSPECT policies in other settings.
The ITS analyses relating to resuscitation outcomes were strengthened through the use of a large volume of routinely collected data from 186 hospitals. However, the adoption of the ReSPECT process was less than anticipated (only 22% of hospitals) and the time period for adoption (2–35 months) was longer than expected, and this reduced the power of the analyses to determine any change in outcomes.
The NHS Safety Thermometer was launched in 2010 and is used as part of the Commissioning for Quality and Innovation scheme. 98 The NHS Safety Thermometer focuses on harms relating to pressure ulcers, falls, catheters and urine infection, and VTE. An advantage of the tool’s use was that it was already embedded in NHS practice, thereby reducing the burden of data collection. Limitations include ambiguities about definitions, subjectivity of measurement and the potential for gaming, given the link to financial incentives. The relatively narrow focus of harms assessed by the NHS Safety Thermometer, compared with other harm evaluation instruments used in other studies (e.g. the global trigger tool), does not rule out the potential of an association with harm.
The focus of this evaluation was the use of ReSPECT in the acute hospital setting. By design, this limited insights into the use of the ReSPECT process in the community. During the conduct of focus groups with GPs, it became clear that not all GPs had used the ReSPECT form and, therefore, some of the GPs’ reflections were based on experience with similar forms. It is also possible that those interviewees who participated had self-selected because of an interest in palliative care, which might have contributed to the end-of-life emphasis in the focus group discussions.
Future research priorities
Although our research found that acute hospitals were moving away from using standalone DNACPR decisions for recording recommendations relating to CPR, there remains variation in approaches to making ECTPs. Hospital doctors and GPs differed in the types of patients they saw the ReSPECT process being most relevant for. Hospital doctors tended to prioritise patients most at risk of imminent deterioration following an acute admission. GPs conceptualise the ReSPECT form as an end-of-life planning document, which is best completed in primary care. The types of recommendations recorded tended to vary, with hospital doctors focusing on specific interventions/treatments (e.g. critical care admission) and GPs recording preferences around hospital admission and resuscitation, and on treating chronic or terminal illness rather than emergencies. These differences may limit the transferability of decisions between health-care settings. Based on these findings, we suggest that future research should explore the following:
-
Developing a programme theory to identify the hypothesised mechanisms through which the intervention is intended to work.
-
What are the advantages and disadvantages to the adoption of a single national system for emergency care and treatment planning?
-
What is the most effective approach to implementation?
-
What are the advantages and disadvantages of digital ReSPECT forms?
-
What interventions are effective for increasing participation in ECTPs following acute hospital admission?
-
How can the different professions (e.g. medicine, nursing, allied health professionals) best deliver a multiprofessional approach to shared decision-making for emergency care and treatment planning?
-
How, when and why are ReSPECT conversations undertaken in the community, and what influence do they have on patient and health service outcomes?
We identified that respect for patient autonomy and duty to protect from harm informed clinicians’ approach to varying degrees, depending on the clinical situation and the clinicians’ views of the ReSPECT process as a shared decision-making process. The types of conversations with patients and/or their families varied and included both exploratory and persuasive conversations. Clinicians rarely documented their weighing of potential burdens and benefits of treatments on the ReSPECT forms. Based on these findings, we suggest future research should explore the following:
-
How effective are structured communication approaches at enhancing shared decision-making relating to emergency care and treatment?
-
What decision support aids exist and how effective are the aids at enhancing shared decision-making relating to emergency care and treatment recommendations?
-
What are the training needs of those involved in making ECTPs?
-
What are the barriers to and facilitators of improving the transparency and ethics basis for emergency care treatment recommendations?
Dissemination
The dissemination strategy was affected by the COVID-19 pandemic, which occurred through the analysis, reporting and dissemination components of the work. Our dissemination activities are targeted towards our different audiences (i.e. patients, health-care professionals and those responsible for health-care policy). Our stakeholder event is aimed at all groups.
Stakeholder event for patients, health-care providers and health-care policy-makers
We held an online rather than a face-to-face dissemination meeting because of the ongoing effects of COVID-19. The event took place with the patient group Compassion in Dying and the Resuscitation Council UK in September 2021. The event was attended by 107 delegates. Over half of the participants were health-care professionals (61.6%) or health-care/social care managers (14.7%). Video-recordings of the event are available at the project website (https://warwick.ac.uk/fac/sci/med/research/ctu/trials/respect/).
During the meeting, a survey was undertaken that identified that:
-
Most participants (86.3%) agreed or strongly agreed that ReSPECT is the right process for emergency care and treatment planning in the UK.
-
There was strong support for mandating the use of ReSPECT in UK health-care and social care organisations, which would improve its transferability across organisations (85.3%).
The attendees at the meeting supported further research, addressing:
-
How can we support communication and decision-making in emergency care and treatment planning?
-
What are the training needs of staff from different professional backgrounds involved in making emergency care and treatment plans?
-
How can health-care organisations support doctors to participate in emergency care and treatment planning?
-
What are the most effective strategies for engaging people from different communities to participate in emergency care and treatment planning?
-
How effective are structured communication approaches at enhancing shared decision-making related to emergency care and treatment planning?
-
How can we improve the transparency of ethics reasoning and justification within the ReSPECT process?
The full results of the event survey are available in Report Supplementary Material 7.
Patients and the public
We have contributed content to the existing Wikipedia Do Not Resuscitate page [URL: https://en.wikipedia.org/wiki/Do_not_resuscitate (accessed 10 October 2022)], where we have discussed our findings relating to the contextualisation of resuscitation decisions, and we have referenced our published papers. We have also created a Wikipedia page dedicated to the ReSPECT process, where we describe what the ReSPECT process is and how widely it is used, which was available before we reported key findings from our evaluation.
Health-care providers
We have produced a number of papers from our research (Boxes 2–6).
To examine secondary care consultant clinicians’ experiences of conducting conversations about treatment escalation with patients and their relatives, using the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) process.
Design
Semistructured interviews following ward round observations.
Setting
Two NHS hospitals in England.
Participants
Fifteen medical and surgical consultants from 10 specialties, observed in 14 wards.
Analysis
Interview transcripts were analysed using thematic analysis.
Results
Three themes were developed: (1) determining when and with whom to conduct a ReSPECT conversation; (2) framing the ReSPECT conversation to manage emotions and relationships and (3) reaching ReSPECT decisions. The results showed that when timing ReSPECT conversations, consultant clinicians rely on their predictions of a patient’s short-term prognosis; when framing ReSPECT conversations, consultant clinicians seek to minimise distress and maximise rapport and when involving a patient or a patient’s relatives in decision-making discussions, consultant clinicians are guided by their level of certainty about the patient’s illness trajectory.
Conclusions
The management of uncertainty about prognoses and about patients’ emotional reactions is central to secondary care consultant clinicians’ experiences of timing and conducting ReSPECT conversations.
Reproduced with permission from Eli et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The box includes minor additions and formatting changes to the original box.
The Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) is an emergency care and treatment planning (ECTP) process, developed to offer a patient-centred approach to deciding about and recording treatment recommendations. Conversations between clinicians and patients or their representatives are central to the ReSPECT process. This study aims to understand why, when, and how ReSPECT conversations unfold in practice.
Methods
ReSPECT conversations were observed in hospitals within six acute National Health Service (NHS) trusts in England; the clinicians who conducted these conversations were interviewed. Following observation-based thematic analysis, five ReSPECT conversation types were identified: resuscitation and escalation; confirmation of decision; bad news; palliative care; and clinical decision. Interview-based thematic analysis examined the reasons and prompts for each conversation type, and the level of detail and patient engagement in these different conversations.
Results
Whereas resuscitation and escalation conversations concerned possible futures, palliative care and bad news conversations responded to present-tense changes. Conversations were timed to respond to organisational, clinical, and patient/relative prompts. While bad news and palliative care conversations included detailed discussions of treatment options beyond CPR, this varied in other conversation types. ReSPECT conversations varied in doctors’ engagement with patient/relative preferences, with only palliative care conversations consistently including an open-ended approach.
Conclusions
While ReSPECT supports holistic, person-centred, anticipatory decision-making in some situations, a gap remains between the ReSPECT’s aims and their implementation in practice. Promoting an understanding and valuing of the aims of ReSPECT among clinicians, supported by appropriate training and structural support, will enhance ReSPECT conversations.
Reproduced with permission from Eli et al. 1 © 2021 Elsevier.
The Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) form, which supports the ReSPECT process, is designed to prompt clinicians to discuss wider emergency treatment options with patients and to structure the documentation of decision-making for greater transparency.
Methods
Following an AFR framework, we analysed 141 completed ReSPECT forms (versions 1.0 and 2.0), collected from six NHS trusts in England during the early adoption of ReSPECT. Structured through an evaluation tool developed for this study, the analysis assessed the extent to which the records reflected consistency, transparency, and ethical justification of decision-making.
Results
Recommendations relating to CPR were consistently recorded on all forms and were contextualised within other treatment recommendations in most forms. The level of detail provided about treatment recommendations varied widely and reasons for treatment recommendations were rarely documented. Patient capacity, patient priorities and preferences, and the involvement of patients/relatives in ReSPECT conversations were recorded in some, but not all, forms. Clinicians almost never documented their weighing of potential burdens and benefits of treatments on the ReSPECT forms.
Conclusion
In most ReSPECT forms, CPR recommendations were captured alongside other treatment recommendations. However, ReSPECT form design and associated training should be modified to address inconsistencies in form completion. These modifications should emphasise the recording of patient values and preferences, assessment of patient capacity, and clinical reasoning processes, thereby putting patient/family involvement at the core of good clinical practice. Version 3.0 of ReSPECT responds to these issues.
Reproduced with permission from Eli et al. 3 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC-ND) license, which permits others to distribute this work, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ECTPs are recommended for all primary care patients in the United Kingdom who are expected to experience deterioration of their health. The Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) was developed to integrate resuscitation decisions with discussions about wider goals of care. It summarises treatment recommendations discussed and agreed between patients and their clinicians for a future emergency situation and was designed to meet the needs of different care settings. Our aim is to explore GPs’ experiences of using ReSPECT and how it transfers across the primary care and secondary care interface.
Methods
We conducted five focus groups with GPs in areas being served by hospitals in England that have implemented ReSPECT. Participants were asked about their experience of ReSPECT, how they initiate ReSPECT-type conversations, and their experiences of ReSPECT-type recommendations being communicated across primary and secondary care. Focus groups were transcribed and analysed using Thematic Analysis.
Results
GPs conceptualise ReSPECT as an end of life planning document, which is best completed in primary care. As an end of life care document, completing ReSPECT is an emotional process and conversations are shaped by what a ‘good death’ is thought to be. ReSPECT recommendations are not always communicated or transferable across care settings. A focus on the patient’s preferences around death, and GPs’ lack of specialist knowledge, could be a barrier to completion of ReSPECT that is transferable to acute settings.
Conclusion
Conceptualising ReSPECT as an end of life care document suggests a difference in how GPs understand ReSPECT from its designers. This impacts on the transferability of ReSPECT recommendations to the hospital setting.
Reproduced with permission from Huxley et al. 54 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The box includes minor additions and formatting changes to the original box.
Despite increasing emphasis on integrating emergency care and treatment planning (ECTP) into routine medical practice, clinicians continue to delay or avoid ECTP conversations with patients. However, little is known about the clinical logics underlying barriers to ECTP conversations.
Objective
This study aims to develop an ethnographic account of how and why clinicians defer and avoid ECTP conversations, and how they rationalise these decisions as they happen.
Design
A multisited ethnographic study.
Setting
Medical, orthopaedic, and surgical wards in five hospitals within four NHS trusts in England.
Participants
Thirty-four doctors were formally observed and 32 formally interviewed. Following an ethnographic case study approach, six cases were selected for in-depth analysis.
Analysis
Fieldnote data were combined with interview data, to develop a ‘thick description’ of each case. Using a conceptual framework of care, the analysis highlighted the clinical logics underlying these cases.
Results
The deferral or avoidance of ECTP conversations was driven by concerns over caring well, with clinicians attempting to optimise both medical and bedside practice. Conducting an ECTP conversation carefully meant attending to patients’ and relatives’ emotions and committing sufficient time for an in-depth discussion. However, conversation plans were often disrupted by issues related to timing and time constraints, leading doctors to defer these conversations, sometimes indefinitely. Additionally, whereas surgeons and geriatricians deferred conversations because they did not have the time to offer detailed discussions, emergency and acute medicine clinicians deferred conversations because the high-turnover ward environment, combined with patients’ acute conditions, meant triaging conversations to those most in need.
Conclusion
Overcoming barriers to ECTP conversations is not simply a matter of enhancing training or hospital policies, but of promoting good conversational practices that take into account the affordances of hospital time and space, as well as clinicians’ understandings of caring well.
Reproduced with permission from Eli et al. 50 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The box includes minor additions and formatting changes to the original box.
Resuscitation Council UK ReSPECT committee
Representatives from the RCUK have attended Study Steering Committee meetings throughout the duration of the project to keep up to date with the study’s progression and findings. Representatives of the RCUK have co-authored papers reporting the findings of the project. 1,3,33,43 Members of our research team sit on the ReSPECT Committee and disseminate findings through this group.
Those responsible for health-care policy
We contributed to the scope of the NICE consultation on shared decision-making (2019) to ensure the inclusion of ACP within the shared decision-making process. 89,90 We subsequently contributed to the draft guidance produced by the NICE consultation on shared decision-making (2020), particularly feeding back the need for shared decisions to be transferable between settings.
We contributed knowledge gained from the project to the CQC review of DNACPR decisions made during the COVID-19 pandemic,67 specifically in relation to DNACPR decisions being contextualised within the context of wider treatment discussions.
Acknowledgements
Non-author contributors
We thank Scott Regan (Senior Project Manager), Emma Skilton (Trial Manager) and Chloe Norman (Trial Manager), and the wider PPI group members, for their time and effort involved in the ReSPECT evaluation study.
In addition we would like to thank the NIHR anonymous reviewers for their comments to strengthen this final report.
Contribution of authors
Gavin D Perkins (https://orcid.org/0000-0003-3027-7548) (Professor, Critical Care Medicine) conceived the study, obtained funding, supervised the research, and drafted and approved the final report.
Claire A Hawkes (https://orcid.org/0000-0001-8236-3558) (Senior Research Fellow, Emergency care) conceived the study, obtained funding, analysed qualitative work, led work package 3, and drafted and approved the final report.
Karin Eli (https://orcid.org/0000-0001-9132-8404) (Senior Research Fellow, Health sciences) collected and analysed qualitative data for work package 1, and provided feedback on and approved the final report.
James Griffin (https://orcid.org/0000-0002-6364-0414) (Research Fellow, Statistics) designed and carried out statistical analyses, and drafted and approved the final report.
Claire Jacques (https://orcid.org/0000-0001-9842-7640) (Trial Manager, Clinical trials) was responsible for project co-ordination and collecting data for work package 2.
Caroline J Huxley (https://orcid.org/0000-0001-9755-6096) (Senior Research Fellow, Health Sciences) led and analysed GP focus groups.
Keith Couper (https://orcid.org/0000-0003-2123-2022) (Assistant Professor, Emergency Care) was the principal investigator at Birmingham Heartlands Hospital, Good Hope Hospital and Solihull Hospital, obtained funding, collected data for work packages 1 and 3, and provided feedback on and approved the final report.
Cynthia Ochieng (https://orcid.org/0000-0002-5574-6059) (Research Fellow, Health Sciences) collected and analysed qualitative data for work package 1, and provided feedback on and approved the final report.
Jonathan Fuld (https://orcid.org/0000-0003-1847-184X) (Consultant, Acute Medicine) conceived the study, obtained funding, and provided feedback on and approved the final report.
Zoe Fritz (https://orcid.org/0000-0001-9403-409X) (Consultant, Acute Medicine) was the principal investigator at Cambridge University Hospitals NHS Foundation Trust, conceived the study, obtained funding, collected data for work packages 1 and 3, and provided feedback on and approved the final report.
Rob George (Professor, Palliative care) conceived the study, obtained funding, and provided feedback on and approved the final report.
Doug Gould (https://orcid.org/0000-0003-4148-3312) (Senior Researcher, Health Sciences) provided data for work package 2, and provided feedback on and approved the final report.
Richard Lilford (https://orcid.org/0000-0002-0634-984X) (Professor, Health Sciences) conceived the study, obtained funding, and provided feedback on and approved the final report.
Martin Underwood (https://orcid.org/0000-0002-0309-1708) (Professor, Health Sciences) conceived the study, obtained funding, and provided feedback on and approved the final report.
Catherine Baldock (https://orcid.org/0000-0001-7180-3482) (Resuscitation Officer, Resuscitation) was co-principal investigator at the University Hospitals of Coventry and Warwickshire NHS Trust, collected data for work packages 1 and 3, and provided feedback on and approved the final report.
Chris Bassford (https://orcid.org/0000-0003-0305-834X) (Consultant, Intensive Care) was co-principal investigator at University Hospitals of Coventry and Warwickshire NHS Trust, collected data for work packages 1 and 3, and provided feedback on and approved the final report.
Peter-Marc Fortune (https://orcid.org/0000-0001-7033-002X) (Associate Medical Director) was the principal investigator at Manchester University NHS Foundation Trust, collected data for work packages 1 and 3, and provided feedback on and approved the final report.
John Speakman (Consultant, Palliative Care) was the principal investigator at Queen Elizabeth Hospital, collected data for work packages 1 and 3, and provided feedback on and approved the final report.
Anna Wilkinson (Consultant, Palliative Care) was the principal investigator at Hampshire Hospitals NHS Foundation Trust, collected data for work packages 1 and 3, and provided feedback on and approved the final report.
Bob Ewings (https://orcid.org/0000-0003-0185-7981) (PPI representative) was involved in the development of the study proposal and subsequent protocol, contributed to discussion of consent processes, attended PPI Advisory Group meetings and reviewed patient information resources.
Jane Warwick (https://orcid.org/0000-0002-7320-6603) (Professor, Statistics) conceived the study, obtained funding, designed and undertook statistical analyses, and drafted and approved the final report.
Frances Griffiths (https://orcid.org/0000-0002-4173-1438) (Professor, Health Sciences) conceived the study, obtained funding, supervised the qualitative work packages, and drafted and approved the final report.
Anne-Marie Slowther (https://orcid.org/0000-0002-3338-8457) (Professor, Health Sciences) conceived the study, obtained funding, supervised the qualitative work packages, and drafted and approved the final report.
Publications
Fritz Z, Slowther AM. Resuscitation policy should focus on the patient, not the decision. BMJ 2017;356:j813.
Perkins GD, Fritz Z. Time to change from do-not-resuscitate orders to emergency care treatment plans. JAMA Netw Open 2019;2:e1951770.
Eli K, Ochieng C, Hawkes C, Perkins GD, Couper K, Griffiths F, Slowther AM. Secondary care consultant clinicians’ experiences of conducting emergency care and treatment planning conversations in England: an interview-based analysis. BMJ Open 2020;10:e031633.
Eli K, Hawkes CA, Fritz Z, Griffin J, Huxley CJ, Perkins GD, et al. Assessing the quality of ReSPECT documentation using an accountability for reasonableness framework. Resusc Plus 2021;7:100145.
Eli K, Hawkes CA, Ochieng C, Huxley CJ, Baldock C, Fortune PM, et al. Why, when and how do secondary-care clinicians have emergency care and treatment planning conversations? Qualitative findings from the ReSPECT Evaluation study. Resuscitation 2021;162:343–50.
Huxley CJ, Eli K, Hawkes CA, Perkins GD, George R, Griffiths F, Slowther AM. General practitioners’ experiences of emergency care and treatment planning in England: a focus group study. BMC Fam Pract 2021;22:128.
Eli K, Hawkes C, Perkins GD, Slowther M, Griffiths F. Caring in the silences: why physicians and surgeons do not discuss emergency care and treatment planning with their patients – an analysis of hospital-based ethnographic case studies in England. BMJ Open 2022;12:e046189.
Eli K, Huxley CJ, Hawkes CA, Perkins GD, Slowther AM, Griffiths F. Why are some ReSPECT conversations left incomplete? A qualitative case study analysis. Resusc Plus 2022;10:100255.
Hawkes CA, Griffin J, Eli K, Griffiths F, Slowther AM, et al. Implementation of ReSPECT in acute hospitals: a retrospective observational study. Resuscitation 2022;178:26–35.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Eli K, Hawkes CA, Ochieng C, Huxley CJ, Baldock C, Fortune PM, et al. Why, when and how do secondary-care clinicians have emergency care and treatment planning conversations? Qualitative findings from the ReSPECT Evaluation study. Resuscitation 2021;162:343-50. https://doi.org/10.1016/j.resuscitation.2021.01.013.
- Eli K, Ochieng C, Hawkes C, Perkins GD, Couper K, Griffiths F, et al. Secondary care consultant clinicians’ experiences of conducting emergency care and treatment planning conversations in England: an interview-based analysis. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-031633.
- Eli K, Hawkes C, Fritz Z, Griffin J, Huxley C, Perkins GD, et al. Assessing the quality of ReSPECT documentation using an accountability for reasonableness framework. Resusc Plus 2021;7. https://doi.org/10.1016/j.resplu.2021.100145.
- Hoke RS, Chamberlain D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation 2004;63:327-38. https://doi.org/10.1016/j.resuscitation.2004.05.019.
- Nolan JP, Soar J, Smith GB, Gwinnutt C, Parrott F, Power S, et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation 2014;85:987-92. https://doi.org/10.1016/j.resuscitation.2014.04.002.
- Rabkin MT, Gillerman G, Rice NR. Orders not to resuscitate. New Engl J Med 1976;295:364-6. https://doi.org/10.1056/NEJM197608122950705.
- Findley GP, Shotton H, Kelly K, Mason M. Time to Intervene? A Review of Patients Who Underwent Cardiopulmonary Resuscitation As a Result of an In-Hospital Cardiorespiratory Arrest: A Report by the National Confidential Enquiry into Patient Outcome and Death. 2012.
- Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The confidential inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 2014;383:889-95. https://doi.org/10.1016/S0140-6736(13)62026-7.
- House of Commons Health Committee . End of Life Care: Fifth Report of Session 2014–15 2015.
- Perkins GD, Griffiths F, Slowther AM, George R, Fritz Z, Satherley P, et al. Do-not-attempt-cardiopulmonary-resuscitation decisions: an evidence synthesis. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04110.
- Mockford C, Fritz Z, George R, Court R, Grove A, Clarke B, et al. Do not attempt cardiopulmonary resuscitation (DNACPR) orders: a systematic review of the barriers and facilitators of decision-making and implementation. Resuscitation 2015;88:99-113. https://doi.org/10.1016/j.resuscitation.2014.11.016.
- Myint PK, Rivas CA, Bowker LK. In-hospital cardiopulmonary resuscitation: trainees’ worst and most memorable experiences. QJM 2010;103:865-73. https://doi.org/10.1093/qjmed/hcq129.
- Myint PK, Miles S, Halliday DA, Bowker LK. Experiences and views of specialist registrars in geriatric medicine on ‘do not attempt resuscitation’ decisions: a sea of uncertainty?. QJM 2006;99:691-700. https://doi.org/10.1093/qjmed/hcl096.
- Field RA, Soar J, Nolan JP, Perkins GD. Epidemiology and outcome of cardiac arrests reported in the lay-press: an observational study. J R Soc Med 2011;104:525-31. https://doi.org/10.1258/jrsm.2011.110228.
- Beed M, de Beer T, Brindley PG. Two decades of British newspaper coverage regarding do not attempt cardiopulmonary resuscitation decisions: lessons for clinicians. Resuscitation 2015;86:31-7. https://doi.org/10.1016/j.resuscitation.2014.10.002.
- Fritz Z, Cork N, Dodd A, Malyon A. DNACPR decisions: challenging and changing practice in the wake of the Tracey judgment. Clin Med 2014;14:571-6. https://doi.org/10.7861/clinmedicine.14-6-571.
- Holland CL, Bowker LK, Myint PK. Barriers to involving older people in their resuscitation decisions: the primary–secondary care mismatch highlights the potential role of general practitioners. Int J Clin Pract 2013;67:379-84. https://doi.org/10.1111/ijcp.12067.
- Chakraborty N, Creaney WJ. ‘Do not resuscitate’ decisions in continuing care psychiatric patients: what influences decisions?. Psychiatr Bull 2006;30:376-8. https://doi.org/10.1192/pb.30.10.376.
- Freeman K, Field R, Perkins G. Variation in local trust do not attempt cardiopulmonary resuscitation (DNACPR) policies: a review of 48 English healthcare trusts. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006517.
- Clements M, Fuld J, Fritz Z. Documentation of resuscitation decision-making: a survey of practice in the United Kingdom. Resuscitation 2014;85:606-11. https://doi.org/10.1016/j.resuscitation.2014.02.005.
- Cohn S, Fritz ZBM, Frankau JM, Laroche CM, Fuld JP. Do not attempt cardiopulmonary resuscitation orders in acute medical settings: a qualitative study. QJM 2013;106:165-77. https://doi.org/10.1093/qjmed/hcs222.
- McAdam C, Barton A, Bull P, Rai G. An audit of nurses’ views on DNR decisions in 1989 and 2003. Br J Nurs 2005;14:1061-2. https://doi.org/10.12968/bjon.2005.14.20.20047.
- Fritz Z, Malyon A, Frankau JM, Parker RA, Cohn S, Laroche CM, et al. The Universal Form of Treatment Options (UFTO) as an alternative to do not attempt cardiopulmonary resuscitation (DNACPR) orders: a mixed methods evaluation of the effects on clinical practice and patient care. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0070977.
- Fritz Z, Fuld J, Haydock S, Palmer C. Interpretation and intent: a study of the (mis)understanding of DNAR orders in a teaching hospital. Resuscitation 2010;81:1138-41. https://doi.org/10.1016/j.resuscitation.2010.05.014.
- Hickman SE, Nelson CA, Perrin NA, Moss AH, Hammes BJ, Tolle SW. A comparison of methods to communicate treatment preferences in nursing facilities: traditional practices versus the physician orders for life-sustaining treatment program. J Am Geriatr Soc 2010;58:1241-8. https://doi.org/10.1111/j.1532-5415.2010.02955.x.
- Schmidt TA, Hickman SE, Tolle SW, Brooks HS. The physician orders for life-sustaining treatment program: Oregon emergency medical technicians’ practical experiences and attitudes. J Am Geriatr Soc 2004;52:1430-4. https://doi.org/10.1111/j.1532-5415.2004.52403.x.
- Fromme EK, Zive D, Schmidt TA, Cook JN, Tolle SW. Association between physician orders for life-sustaining treatment for scope of treatment and in-hospital death in Oregon. J Am Geriatr Soc 2014;62:1246-51. https://doi.org/10.1111/jgs.12889.
- Tolle SW, Tilden VP, Nelson CA, Dunn PM. A prospective study of the efficacy of the physician order form for life-sustaining treatment. J Am Geriatr Soc 1998;46:1097-102. https://doi.org/10.1111/j.1532-5415.1998.tb06647.x.
- Hickman SE, Nelson CA, Moss AH, Hammes BJ, Terwilliger A, Jackson A, et al. Use of the physician orders for life-sustaining treatment (POLST) paradigm program in the hospice setting. J Palliat Med 2009;12:133-41. https://doi.org/10.1089/jpm.2008.0196.
- Lee MA, Brummel-Smith K, Meyer J, Drew N, London MR. Physician orders for life-sustaining treatment (POLST): outcomes in a PACE program. Program of all-inclusive care for the elderly. J Am Geriatr Soc 2000;48:1219-25. https://doi.org/10.1111/j.1532-5415.2000.tb02594.x.
- Jesus JE, Geiderman JM, Venkat A, Limehouse WE, Derse AR, Larkin GL, et al. ACEP Ethics Committee . Physician orders for life-sustaining treatment and emergency medicine: ethical considerations, legal issues, and emerging trends. Ann Emerg Med 2014;64:140-4. https://doi.org/10.1016/j.annemergmed.2014.03.014.
- Neuberger J, Guthrie C, Aaronovitch D, Hameed K, Bonser T, Charlesworth-Smith D, et al. More Care, Less Pathway. A Review Of The Liverpool Care Pathway. London: Department of Health and Social Care; 2013.
- Hawkes CA, Fritz Z, Deas G, Ahmedzai SH, Richardson A, Pitcher D, et al. Development of the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT). Resuscitation 2020;148:98-107. https://doi.org/10.1016/j.resuscitation.2020.01.003.
- NHS . NHS Long Term Plan n.d. www.longtermplan.nhs.uk/ (accessed 11 October 2022).
- Personalised Care Group . Universal Personalised Care: Implementing the Comprehensive Model 2019.
- GOV . UK. English Indices of Deprivation 2019 n.d. www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed 10 October 2022).
- Stewart M, Baldry C. The over-interpretation of DNAR. Clin Gov 2011;16:119-28. https://doi.org/10.1108/14777271111124473.
- Perkins G, Griffiths F, Slowther A, George R, Fritz Z, Satherley P, et al. Do not attempt cardiopulmonary resuscitation (DNACPR) decisions: evidence synthesis. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04110.
- Moffat S, Skinner J, Fritz Z. Does resuscitation status affect decision making in a deteriorating patient? Results from a randomised vignette study. J Eval Clin Pract 2016;22:917-23. https://doi.org/10.1111/jep.12559.
- Harris D, Davies R. An audit of ‘do not attempt resuscitation’ decisions in two district general hospitals: do current guidelines need changing?. Postgrad Med J 2007;83:137-40. https://doi.org/10.1136/pgmj.2006.050260.
- Fritz Z, Malyon A, Frankau J, . The Universal Form of Treatment Options (UFTO) as an alternative to do not attempt cardiopulmonary resuscitation (DNACPR) orders: a mixed methods evaluation of the effects on clinical practice and patient care. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0070977.
- R (Tracey) Vs Cambridge University NHS Foundation Trust &Amp; Ors 2014. www.39essex.com/cop_cases/r-tracey-v-cambridge-university-hospitals-nhs-foundation-trust-ors/ (accessed 11 October 2022).
- Hawkes C, Fritz Z, Deas G, Ahmedzai SH, Richardson A, Pitcher D, et al. Development of the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT). Resuscitation 2020;148:98-107. https://doi.org/10.1016/j.resuscitation.2020.01.003.
- Resuscitation Council UK. ReSPECT for Healthcare Professionals. 2020. www.resus.org.uk/respect/health-and-care-professionals/?p=2 (accessed 11 October 2022).
- Lund S, Richardson A, May C. Barriers to advance care planning at the end of life: an explanatory systematic review of implementation studies. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0116629.
- Hall CC, Lugton J, Spiller JA, Carduff E. CPR decision-making conversations in the UK: an integrative review. BMJ Support Palliat Care 2019;9:1-11. https://doi.org/10.1136/bmjspcare-2018-001526.
- Hickman SE, Keevern E, Hammes BJ. Use of the physician orders for life-sustaining treatment program in the clinical setting: a systematic review of the literature. J Am Geriatr Soc 2015;63:341-50. https://doi.org/10.1111/jgs.13248.
- Lightbody CJ, Campbell JN, Herbison GP, Osborne HK, Radley A, Taylor DR. Impact of a treatment escalation/limitation plan on non-beneficial interventions and harms in patients during their last admission before in-hospital death, using the structured judgment review method. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-024264.
- Egelund GB, Jensen AV, Petersen PT, Andersen SB, Lindhardt BØ, Rohde G, et al. Do-not-resuscitate orders in patients with community-acquired pneumonia: a retrospective study. BMC Pulm Med 2020;20. https://doi.org/10.1186/s12890-020-01236-1.
- Eli K, Hawkes C, Perkins G, Slowther A, Griffiths F. Caring in the silences: why physicians and surgeons do not discuss emergency care and treatment planning with their patients — an analysis of hospital-based ethnographic case studies in England. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2020-046189.
- Martin DK, Giacomini M, Singer PA. Fairness, accountability for reasonableness, and the views of priority setting decision-makers. Health Policy 2002;61:279-90. https://doi.org/10.1016/S0168-8510(01)00237-8.
- Bassford C, Griffiths F, Svantesson M, Ryan M, Krucien N, Dale J, et al. Developing an intervention around referral and admissions to intensive care: a mixed-methods study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07390.
- Resuscitation Council UK. How to Complete a ReSPECT Form: Quick Guide for Clinicians n.d. https://derbyshire.eolcare.uk/content/documents/uploads/toolkit-docs/2-ReSPECT-Clinicians-Guide.pdf (accessed 11 October 2022).
- Huxley CJ, Eli K, Hawkes CA, Perkins GD, George R, Griffiths F, et al. General practitioners’ experiences of emergency care and treatment planning in England: a focus group study. BMC Fam Pract 2021;22. https://doi.org/10.1186/s12875-021-01486-w.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Hawkes CA, Griffin J, Eli K, Griffiths F, Slowther AM, . Implementation of ReSPECT in acute hospitals: a retrospective observational study. Resuscitation 2022;178:26-35. https://doi.org/10.1016/j.resuscitation.2022.06.020.
- Shotton HR, Findlay GP. Time to intervene: patients who had an in-hospital cardiorespiratory arrest. Br J Hosp Med 2012;73:546-7. https://doi.org/10.12968/hmed.2012.73.10.546.
- Intensive Care National Audit & Research Centre . Key Statistics From the National Cardiac Arrest Audit 2015 16 2016. www.icnarc.org/Our-Audit/Audits/Ncaa/Reports/Key-Statistics (accessed 11 October 2022).
- Intensive Care National Audit & Research Centre . NCAA Data Collection Manual n.d. www.icnarc.org/Our-Audit/Audits/Ncaa/Resources (accessed 11 October 2022).
- Intensive Care National Audit & Research Centre . NCAA Data Collection &Amp; Validation Advice Guide n.d. www.icnarc.org/Our-Audit/Audits/Ncaa/Resources/2015/07/02/Update-To-The-Ncaa-Data-Collection-Validation-Advice-Guide (accessed 11 October 2022).
- NHS Digital . NHS Safety Thermometer Report n.d. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-safety-thermometer-report (accessed 20 November 2022).
- Ebell MH, Jang W, Shen Y, Geocadin RG. Get With the Guidelines–Resuscitation Investigators. Development and validation of the Good Outcome Following Attempted Resuscitation (GO-FAR) score to predict neurologically intact survival after in-hospital cardiopulmonary resuscitation. JAMA Intern Med 2013;173:1872-8. https://doi.org/10.1001/jamainternmed.2013.10037.
- McCabe WR, Jackson GG. Gram-negative bacteremia: I. etiology and ecology. Arch Intern Med 1962;110:847-55. https://doi.org/10.1001/archinte.1962.03620240029006.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. https://doi.org/10.1016/0021-9681(87)90171-8.
- Resuscitation Council UK . Resuscitation Council UK Introduces Version 3 of ReSPECT Form 2020. www.resus.org.uk/about-us/news-and-events/resuscitation-council-uk-introduces-version-3-respect-form (accessed 20 November 2022).
- End of life care. Nurs Stand 2015;30. https://doi.org/10.7748/ns.30.2.17.s20.
- Care Quality Commission . Protect, Respect, Connect – Decisions About Living and Dying Well During COVID-19 2021. www.cqc.org.uk/sites/default/files/20210318_dnacpr_printer-version.pdf (accessed 11 October 2022).
- NHS Wales . Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) Policy 2016.
- Scarborough JE, Pappas TN, Bennett KM, Lagoo-Deenadayalan S. Failure-to-pursue rescue: explaining excess mortality in elderly emergency general surgical patients with preexisting ‘do-not-resuscitate’ orders. Ann Surg 2012;256:453-61. https://doi.org/10.1097/SLA.0b013e31826578fb.
- The Health Committee . Health – Fifth Report. End of Life Care 2015. https://publications.parliament.uk/pa/cm201415/cmselect/cmhealth/805/80502.htm (accessed 11 October 2022).
- Resuscitation Council UK . ReSPECT Resources n.d. www.resus.org.uk/respect/respect-resources (accessed 20 November 2022).
- ReSPECT . Recommended Summary Plan for Emergency Care and Treatment n.d. www.resus.org.uk/sites/default/files/2020-09/ReSPECT%20v3-1-formSPECIMENFINAL_0.pdf (accessed 20 November 2022).
- Great Britain . Human Rights Act 1998 1998.
- Great Britain . Mental Capacity Act 2005 2005.
- Scottish Parliament . Adults With Incapacity (Scotland) Act 2000 2000.
- Royal Courts of Justice . Tracey V Cambridge University Hospitals n.d. www.judiciary.uk/wp-content/uploads/2014/06/tracey-approved.pdf (accessed 11 October 2022).
- BAILII . England and Wales High Court (Queen’s Bench Division) Decisions n.d. www.bailii.org/ew/cases/EWHC/QB/2015/3250.html (accessed 20 November 2022).
- Royal College of Physicians . End of Life Care Audit – Dying in Hospital: National Report for England 2016 2016.
- Harrington L, Price K, Edmonds P. From paper to paperless: do electronic systems ensure safe and effective communication and documentation of DNACPR decisions?. Clin Med 2020;20. https://doi.org/10.7861/clinmed.2019-0450.
- Coleman JJ, Botkai A, Marson EJ, Evison F, Atia J, Wang J, et al. Bringing into focus treatment limitation and DNACPR decisions: how COVID-19 has changed practice. Resuscitation 2020;155:172-9. https://doi.org/10.1016/j.resuscitation.2020.08.006.
- Fritz Z, Slowther AM, Perkins GD. Resuscitation policy should focus on the patient, not the decision. BMJ 2017;356. https://doi.org/10.1136/bmj.j813.
- An HJ, Jeon HJ, Chun SH, Jung HA, Ahn HK, Lee KH, et al. Feasibility study of physician orders for life-sustaining treatment for patients with terminal cancer. Cancer Res Treat 2019;51:1632-8. https://doi.org/10.4143/crt.2019.009.
- Mack DS, Dosa D. Improving advanced care planning through physician orders for life-sustaining treatment (POLST) expansion across the United States: lessons learned from state-based developments. Am J Hosp Palliat Care 2020;37:19-26. https://doi.org/10.1177/1049909119851511.
- General Medical Council . Treatment and Care Towards the End of Life: Good Practice in Decision Making 2010.
- Pearlman SA, Zern SC, Blackson T, Ciarlo JA, Mackley AB, Locke RG. Use of neonatal simulation models to assess competency in bag-mask ventilation. J Perinatol 2016;36:242-6. https://doi.org/10.1038/jp.2015.175.
- Stiggelbout AM, Van der Weijden T, De Wit MP, Frosch D, Légaré F, Montori VM, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ 2012;344. https://doi.org/10.1136/bmj.e256.
- Elwyn G, Durand MA, Song J, Aarts J, Barr PJ, Berger Z, et al. A three-talk model for shared decision making: multistage consultation process. BMJ 2017;359. https://doi.org/10.1136/bmj.j4891.
- Pieterse AH, Stiggelbout AM, Montori VM. Shared decision making and the importance of time. JAMA 2019;322:25-6. https://doi.org/10.1001/jama.2019.3785.
- National Institute for Health and Care Excellence . Shared Decision Making. NICE Guideline [NG197] 2021. www.nice.org.uk/guidance/NG197 (accessed 11 October 2022).
- National Institute for Health and Care Excellence (NICE) . Shared Decision Making: Evidence Review for Decision Aids for People Facing Health Treatment or Screening Decisions 2020.
- Rees S, Bassford C, Dale J, Fritz Z, Griffiths F, Parsons H, et al. Implementing an intervention to improve decision making around referral and admission to intensive care: Results of feasibility testing in three NHS hospitals. J Eval Clin Pract 2020;26:56-65. https://doi.org/10.1111/jep.13167.
- Zenasni Z, Reynolds EC, Harrison DA, Rowan KM, Nolan JP, Soar J, et al. The impact of the Tracey judgment on the rates and outcomes of in-hospital cardiac arrests in UK hospitals participating in the National Cardiac Arrest Audit. Clin Med 2020;20:319-23. https://doi.org/10.7861/clinmed.2019-0454.
- Cohn S, Fritz ZB, Frankau JM, Laroche CM, Fuld JP. Do not attempt cardiopulmonary resuscitation orders in acute medical settings: a qualitative study. QJM 2013;106:165-77. https://doi.org/10.1093/qjmed/hcs222.
- Fritz Z, Malyon A, Frankau JM, Parker RA, Cohn S, Laroche CM, et al. The Universal Form of Treatment Options (UFTO) as an alternative to do not attempt cardiopulmonary resuscitation (DNACPR) orders: a mixed methods evaluation of the effects on clinical practice and patient care. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0070977.
- Brovman EY, Pisansky AJ, Beverly A, Bader AM, Urman RD. Do-not-resuscitate status as an independent risk factor for patients undergoing surgery for hip fracture. World J Orthop 2017;8:902-12. https://doi.org/10.5312/wjo.v8.i12.902.
- Sarkari NN, Perman SM, Ginde AA. Impact of early do-not-attempt-resuscitation orders on procedures and outcomes of severe sepsis. J Crit Care 2016;36:134-9. https://doi.org/10.1016/j.jcrc.2016.06.030.
- Maron DJ, Hochman JS, O’Brien SM, Reynolds HR, Boden WE, Stone GW, et al. International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial: rationale and design. Am Heart J 2018;201:124-35. https://doi.org/10.1016/j.ahj.2018.04.011.
- Power M, Stewart K, Brotherton A. What is the NHS Safety Thermometer?. Clin Risk 2012;18:163-9. https://doi.org/10.1258/cr.2012.012038.
Appendix 1 Derived variables and synthesis of information from ReSPECT forms
Socioeconomic status for each participant was estimated from their abbreviated postcode using the mapping tool provided with IMD 2019. 36 For calculation of IMD 2019, all neighbourhoods in England (n = 32,884) are ranked from least to most deprived and then grouped into deciles [from most deprived (decile 1) to least deprived (decile 10)]. Participants were assigned the IMD 2019 score (decile) for their neighbourhood based on their abbreviated postcode. For ease of presentation, deciles 1–3, 4–6 and 7–10 were combined and labelled ‘most deprived’, ‘average’ and ‘least deprived’, respectively.
Charlson Comorbidity Index (Table A.3) is used to predict 10-year survival in patients with one or more comorbidities. Each comorbid condition included in the index is given a score based on the associated average risk of dying. Scores are then added to provide an overall measure, which ranges from 0 (lowest risk of death) to 37 (greatest risk of death). Further details of the comorbidities included and scores for each are given in Appendix 6. The overall scores may then be converted into probabilities of surviving 10 years using the following formula:
where CCI is Charlson Comorbidity Index. For inclusion in regression models, the overall scores were categorised by splitting into quartiles (i.e. 0–3 points, 4–5 points, 6–7 points, 8–25 points). The smaller the score, then the better the chance of surviving 10 years.
A GO-FAR score (see Appendix 7) predicts survival to discharge with good outcome following IHCA [URL: www.mdcalc.com/go-far-good-outcome-following-attempted-resuscitation-score (accessed 10 October 2022)]. Details of how GO-FAR scores are calculated in Appendix 7. Patients are allocated to one of four risk categories (i.e. very low, low, average or above average). Patients in the ‘very low’, ‘low’, ‘average’ and ‘above average’ categories have < 1%, 1–3%, 3–15% and > 15% chance, respectively, of surviving to discharge with good outcome following IHCA.
The way in which patients’ personal preference was recorded on ReSPECT forms depended on the type used. In the authorised full version form, patients were given the opportunity to indicate how they would balance the priorities for their care by marking on a scale that had ‘prioritise sustaining life, even at the expense of some comfort’ written at one end and ‘prioritise comfort, even at the expense of sustaining life’ at the other end. Patients could also write their preference in words in the box below the scale. To quantify personal preference, therefore, ‘prioritise sustaining life’ was assigned the value 0 and ‘prioritise comfort’ was assigned the value 1. For intermediate points, the distance along the line to the point where they had marked was divided by the length of the line to give a preference score between 0 and 1. Patients who had not completed the scale but had clearly indicated a preference for either ‘prioritise sustaining life’ or ‘prioritise comfort care’ by writing in the box were assigned personal preference scores of 0 and 1, respectively. Personal preference scores were then categorised by assuming that scores 0–0.4 meant ‘prioritise sustaining life’, scores > 0.6 meant ‘prioritise comfort care’ and scores 0.4–0.6 meant an ‘Equal balance’ between the two. In the adjusted full version of the form, patients selected one of five categories (i.e. ‘care should prioritise medical intervention and sustaining life vs. ensuring my comfort’, ‘care should include life-sustaining intervention but being comfortable is also important to me’, ‘care should be equally balanced between sustaining life and providing comfort’, ‘care should be directed more towards comfort than sustaining life’ and ‘care should be providing comfort as a priority rather than sustaining life’). The first two categories were assumed to mean ‘prioritise sustaining life’, the latter two categories were assumed to mean ‘prioritise comfort care’ and the middle category was assumed to mean an ‘equal balance’ between the two.
Clinical recommendations for emergency care and treatment were codified by local staff. Patients were only allocated to the ‘focus on life-sustaining treatment’ and ‘focus on comfort care’ categories when the clinician’s recommendation was clear. Where information was provided on the ReSPECT form but it was not possible to determine which category was meant, the recommendation was coded as ‘unclear position’. If this section of the ReSPECT form had been left blank, then the recommendation was coded as missing. Patients with screening ReSPECT forms were assumed to be in the ‘focus on life sustaining’ group.
Clinicians recorded (free hand) what specific emergency care treatments they recommended in section 4 of the ReSPECT form. To capture these treatments we listed the most commonly noted recommendations (identified using a combination of clinical and review of options from other emergency care and treatment plans) in the case report form together with an ‘other please specify’ option. For regression analysis, patients were assumed to be for CPR unless they had a ReSPECT form where ‘CPR attempts not recommended’ had been clearly indicated.
Involvement in making the plan was recorded on all full ReSPECT forms using a series of boxes, which asked, in turn, who was consulted (i.e. patient, relative or no one). Where the neither patient nor relative boxes were ticked, and it was not clear that no personal representative had been involved, the information was assumed to be missing. As these boxes were not mutually exclusive, to assign patients to one category only we assumed that where both the patient and relative boxes were ticked the patient box should dominate (therefore, in our data the ‘relative’ category means that the relative alone was consulted).
Care groups were derived by combining whether or not the patient is recommended for CPR with the clinician recommendation. There are six categories: (1) DNACPR plus focus on life-sustaining treatment, (2) DNACPR plus focus on symptom control, (3) DNACPR and no clinician recommendation, (4) for CPR plus focus on symptom control, (5) for CPR plus focus on life-sustaining treatment and (6) for CPR and no clinician recommendation.
For the purposes of regression analyses, owing to small numbers, ethnicity was entered into models as a binary variable with the mixed, Asian, back and other groups combined (i.e. white/ethnic minorities).
Appendix 2 Ward types where ReSPECT conversations were observed
| Ward type | Number of sites where ward type was selected | Number of sites where ReSPECT conversations were observed, by ward type | Number of ReSPECT conversations observed, by ward type (across sites) | Number of doctors observed conducting ReSPECT conversations, by ward type (across sites) |
|---|---|---|---|---|
| Acute geriatrics | 1 | 1 | 2 | 2 |
| Acute medicine | 5 | 4 | 5 | 4 |
| Acute stroke | 1 | 1 | 2 | 2 |
| Colorectal surgery | 1 | 0 | 0 | 0 |
| Critical care | 3 | 2 | 3 | 5 |
| Emergency medicine | 2 | 1 | 1 | 1 |
| Emergency surgical admissions | 1 | 0 | 0 | 0 |
| Frailty assessment | 1 | 0 | 0 | 0 |
| Gastroenterology and general medicine | 1 | 1 | 1 | 1 |
| General surgery | 1 | 0 | 0 | 0 |
| Geriatrics/gerontology | 3 | 2 | 7 | 6 |
| Haematology | 1 | 0 | 0 | 0 |
| Hepatobiliary surgery | 2 | 1 | 1 | 1 |
| Orthogeriatrics | 1 | 1 | 5 | 1 |
| Trauma and orthopaedics | 3 | 3 | 11 | 6 |
| Renal | 3 | 2 | 4 | 2 |
| Respiratory | 4 | 3 | 7 | 3 |
| Total | 34 | 22 | 49 | 34 |
Appendix 3 Numbers of patients and families approached for consent, and reasons for not approaching and for consent being declined
| Numbers approached for consent and reasons for decline | Total (n) | Patients (n) | Family members (n) | Patient and relative groups (n)a |
|---|---|---|---|---|
| Number of people approached for consent | 58 | 32 | 26 | 9 |
| Number of people not approached for consent | 62 | 49 | 13 | 4 |
| Reasons for not approaching patients and families | ||||
| Patient confused/lacked capacity/could not recall conversation | 25 | 25 | 0 | 0 |
| Too upset | 12 | 2 | 10 | 3 |
| Patient too ill | 6 | 6 | 0 | 0 |
| Patient died | 3 | 2 | 1 | 0 |
| Hospital/logistical | 7 | 7 | 0 | 0 |
| Not interested in talking to researcher | 5 | 5 | 0 | 0 |
| Other | 4 | 2 | 2 | 1 |
| Number of people consented to participate | 32 | 13 | 19 | 7 |
| Number of people declined to consent | 26 | 19 | 7 | 2 |
| Reasons patients and families declined to participate | ||||
| Patient confused/lacked capacity/could not recall conversation | 2 | 2 | 0 | 0 |
| Too upset | 2 | 1 | 1 | 0 |
| Patient too ill | 6 | 5 | 1 | 0 |
| Hospital/logistical | 1 | 1 | 0 | 0 |
| Not interested in research | 7 | 6 | 1 | 0 |
| Other | 8 | 4 | 4 | 2 |
Appendix 4 Screening data ward classification
| Type of ward | Examples of wards listed in screening data that are included |
|---|---|
| Surgery | Cardiac surgery, elective surgery, general surgery, hepatobiliary, transplant, vascular |
| Trauma and orthopaedic | Elective orthopaedic, trauma, trauma orthopaedic |
| Medicine | Acute medicine unit, CDU, diabetes, gastroenterology, general, haematology, infectious disease, neurology, oncology, renal, stroke |
| Critical care | HDU, CCU, ICU, ITU, stepdown care |
| Older person medicine | Elderly care, elderly rehabilitation, frailty, medicine for elderly |
| Medicine/critical care | CCU/general medicine |
| Gynaecology | Gynae, EPAU |
Appendix 5 Participant characteristics and survival outcomes of participants by whether or not they had a ReSPECT form and care group
| Variable | Focus on sustaining life/CPR (N = 112), n (%) | Focus on comfort care/CPR (N = 3), n (%) | CPR only (N = 24), n (%) | Focus on sustaining life/DNACPR (N = 92), n (%) | Focus on comfort care/DNACPR (N = 277), n (%) | DNACPR only (N = 284), n (%) | No care group (N = 2647), n (%) |
|---|---|---|---|---|---|---|---|
| Age (years) at admission, mean (SD) | 61.9 (18.1) | 84.1 (5.2) | 77.1 (17.8) | 80.1 (10.9) | 81.8 (10.7) | 81.6 (11.8) | 65.4 (18.7) |
| Sex, n (%) | |||||||
| Female | 52 (46) | 2 (67) | 8 (33) | 47 (51) | 153 (55) | 163 (57) | 1304 (49) |
| Male | 59 (53) | 1 (33) | 16 (66) | 45 (49) | 123 (44) | 121 (43) | 1341 (51) |
| Not completed | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) | 0 (0) | 2 (< 1) |
| Ethnicity, n (%) | |||||||
| White | 83 (74) | 3 (100) | 21 (88) | 82 (89) | 239 (86) | 240 (85) | 2124 (80) |
| Mixed | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3 (1) | 17 (1) |
| Asian | 9 (8) | 0 (0) | 3 (13) | 1 (1) | 19 (7) | 7 (2) | 190 (7) |
| Black | 4 (4) | 0 (0) | 0 (0) | 0 (0) | 4 (1) | 8 (3) | 101 (4) |
| Other | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3 (1) | 45 (2) |
| Not completed | 13 (12) | 0 (0) | 0 (0) | 9 (10) | 15 (5) | 23 (8) | 170 (6) |
| Socioeconomic status, n (%) | |||||||
| Tertile 1 (most deprived) | 15 (13) | 0 (0) | 8 (33) | 9 (10) | 101 (36) | 85 (30) | 989 (37) |
| Tertile 2 | 32 (29) | 1 (33) | 7 (29) | 21 (23) | 83 (30) | 114 (40) | 987 (37) |
| Tertile 3 (least deprived) | 65 (58) | 2 (67) | 9 (38) | 61 (66) | 93 (34) | 82 (29) | 621 (23) |
| Not completed | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 3 (1) | 50 (2) |
| Patient admission category, n (%) | |||||||
| Transferred from another hospital | 13 (12) | 0 (0) | 0 (0) | 3 (3) | 12 (4) | 9 (3) | 205 (8) |
| Planned admission | 16 (14) | 0 (0) | 0 (0) | 3 (3) | 7 (3) | 2 (1) | 396 (15) |
| Referral from GP | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 9 (3) | 5 (2) | 57 (2) |
| Emergency (via GP) | 8 (7) | 0 (0) | 4 (17) | 15 (16) | 21 (8) | 28 (10) | 159 (6) |
| Emergency (via emergency department) | 62 (55) | 2 (67) | 19 (79) | 68 (74) | 222 (80) | 231 (81) | 1713 (65) |
| Outpatients | 9 (8) | 1 (33) | 1 (4) | 3 (3) | 3 (1) | 4 (1) | 73 (3) |
| Other | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) | 0 (0) | 8 (< 1) |
| Not completed | 4 (4) | 0 (0) | 0 (0) | 0 (0) | 2 (1) | 5 (2) | 34 (1) |
| Patient type, n (%) | |||||||
| Medical: elective | 67 (60) | 3 (100) | 23 (96) | 77 (84) | 225 (81) | 259 (91) | 1,719 (65) |
| Medical: emergency | 15 (14) | 0 (0) | 0 (0) | 3 (3) | 7 (3) | 3 (1) | 165 (6) |
| Surgery: elective | 25 (22) | 0 (0) | 1 (4) | 9 (10) | 42 (15) | 20 (7) | 447 (17) |
| Surgery: emergency | 5 (5) | 0 (0) | 0 (0) | 3 (3) | 3 (1) | 2 (1) | 316 (12) |
| Primary reason for admission, n (%) | |||||||
| Cancer/neoplasm | 15 (13) | 0 (0) | 3 (13) | 3 (3) | 21 (8) | 9 (3) | 211 (8) |
| Fall/injury/musculoskeletal | 29 (26) | 2 (67) | 3 (13) | 28 (30) | 82 (30) | 63 (22) | 546 (21) |
| Gastrointestinal conditions | 20 (18) | 0 (0) | 1 (4) | 5 (5) | 37 (13) | 19 (7) | 422 (16) |
| Respiratory conditions | 14 (13) | 0 (0) | 3 (13) | 18 (20) | 58 (21) | 80 (28) | 299 (11) |
| Cardiac conditions | 3 (3) | 1 (33) | 0 (0) | 5 (5) | 15 (5) | 23 (8) | 246 (9) |
| ENT conditions | 1 (1) | 0 (0) | 0 (0) | 1 (1) | 1 (< 1) | 0 (0) | 49 (2) |
| Urological conditions | 7 (6) | 0 (0) | 8 (33) | 9 (10) | 15 (5) | 14 (5) | 160 (6) |
| Central nervous system conditions | 8 (7) | 0 (0) | 4 (17) | 7 (8) | 19 (7) | 22 (8) | 216 (8) |
| Infectious disease | 5 (4) | 0 (0) | 1 (4) | 2 (2) | 6 (2) | 9 (3) | 46 (2) |
| Poisoning | 1 (1) | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 14 (1) |
| Gynaecological/obstetric conditions | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) | 0 (0) | 19 (1) |
| Mental health conditions | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (1) | 2 (1) | 20 (1) |
| Blood/organs disease | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3 (1) | 14 (1) |
| Endocrine disorders | 2 (2) | 0 (0) | 0 (0) | 4 (4) | 0 (0) | 2 (1) | 14 (1) |
| Eye diseases | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (< 1) |
| Circulatory diseases | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 44 (2) |
| Skin | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) | 1 (< 1) | 10 (< 1) |
| Renal | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3 (1) | 29 (1) |
| Infection (excluding respiratory) | 1 (1) | 0 (0) | 0 (0) | 3 (3) | 5 (2) | 12 (4) | 94 (4) |
| Acute confusional state | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) | 7 (2) | 22 (1) |
| Dental | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) |
| Other | 3 (3) | 0 (0) | 1 (4) | 6 (7) | 13 (5) | 15 (5) | 169 (6) |
| Cognitive impairment, n (%) | |||||||
| No | 74 (66) | 1 (33) | 13 (54) | 46 (50) | 122 (44) | 138 (49) | 2034 (77) |
| Yes | 38 (34) | 2 (67) | 11 (46) | 46 (50) | 155 (56) | 146 (51) | 613 (23) |
| If yes, which cause (multiple possible) | |||||||
| Dementia | 1 (3) | 1 (50) | 6 (55) | 20 (43) | 97 (63) | 79 (55) | 216 (8) |
| Learning difficulty | 4 (11) | 0 (0) | 0 (0) | 1 (2) | 3 (2) | 2 (1) | 51 (2) |
| CVA/head injury | 8 (21) | 0 (0) | 2 (18) | 5 (11) | 25 (16) | 22 (15) | 123 (5) |
| Acute confusional state | 15 (39) | 1 (50) | 4 (36) | 22 (48) | 43 (28) | 50 (35) | 242 (9) |
| Cause unknown | 3 (8) | 1 (50) | 1 (9) | 2 (4) | 19 (12) | 16 (11) | 63 (2) |
| Brain tumour or condition | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 6 (4) | 2 (1) | 15 (1) |
| Mental health condition | 1 (3) | 0 (0) | 0 (0) | 1 (2) | 2 (1) | 3 (2) | 16 (1) |
| Other | 24 (65) | 0 (0) | 1 (9) | 14 (30) | 23 (15) | 21 (15) | 104 (4) |
| GO-FAR score, mean (SD) | 12.88 (8.2) | 8 (10) | 9.26 (8.9) | 10.72 (9.4) | 10.43 (9.2) | 11.14 (10.2) | 6.65 (9.1) |
| GO-FAR category, n (%) | |||||||
| Very low (> 24) | 8 (75) | 0 (0) | 2 (8) | 7 (8) | 17 (6) | 28 (10) | 73 (3) |
| Low (14–23) | 39 (35) | 1 (33) | 4 (17) | 31 (34) | 87 (31) | 83 (29) | 481 (18) |
| Average (–5 to 13) | 52 (46) | 2 (67) | 17 (71) | 48 (52) | 159 (58) | 134 (47) | 1717 (65) |
| Above average (–15 to –6) | 1 (1) | 0 (0) | 0 (0) | 3 (3) | 12 (4) | 14 (5) | 260 (10) |
| Not completed | 12 (11) | 0 (0) | 1 (4) | 3 (3) | 2 (1) | 25 (9) | 116 (4) |
| Charlson Comorbidity Index, mean (SD) | 4.40 (4.0) | 6 (1) | 7.35 (3.7) | 6.60 (2.7) | 6.87 (2.9) | 6.70 (3.0) | 4.56 (3.0) |
| McCabe Scale, n (%) | |||||||
| Non-fatal | 95 (85) | 2 (67) | 12 (50) | 72 (78) | 139 (50) | 159 (56) | 2022 (76) |
| Ultimately fatal | 13 (12) | 0 (0) | 9 (38) | 13 (14) | 94 (34) | 98 (35) | 467 (18) |
| Rapidly fatal | 1 (1) | 1 (33) | 3 (12) | 5 (5) | 44 (16) | 27 (10) | 153 (6) |
| Not completed | 3 (3) | 0 (0) | 0 (0) | 2 (2) | 0 (0) | 0 (0) | 5 (< 1) |
| Length of stay (days), median (IQR) | 32 (9–47) | 3 (14–44) | 34 (14–55) | 40 (12–50) | 38 (13–46) | 40 (15–55) | 30 (8–37) |
| Mortality, n (%) | |||||||
| Alive | 96 (86) | 2 (66) | 20 (83) | 80 (87) | 229 (83) | 230 (81) | 2491 (94) |
| Dead | 9 (8) | 1 (33) | 4 (17) | 9 (10) | 48 (17) | 54 (19) | 153 (6) |
| Not completed | 7 (6) | 0 (0) | 0 (0) | 3 (3) | 0 (0) | 0 (0) | 3 (< 1) |
| Discharge location, if alive, n (%) | |||||||
| Home | 78 (81) | 1 (50) | 19 (95) | 54 (68) | 155 (68) | 139 (60) | 2090 (84) |
| Inpatient rehabilitation unit | 2 (2) | 0 (0) | 0 (0) | 1 (1) | 5 (2) | 8 (3) | 38 (2) |
| Nursing/residential home | 7 (7) | 0 (0) | 1 (5) | 21 (26) | 47 (21) | 49 (21) | 141 (6) |
| Another hospital | 6 (6) | 0 (0) | 0 (0) | 1 (1) | 1 (< 1) | 4 (2) | 66 (3) |
| Hospice | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 5 (2) | 6 (3) | 8 (< 1) |
| Other | 1 (1) | 1 (50) | 0 (0) | 2 (3) | 16 (7) | 24 (10) | 146 (6) |
| Sufficient capacity?, n (%) | |||||||
| No | 4 (4) | 3 (100) | 5 (21) | 33 (36) | 153 (55) | 117 (41) | |
| Yes | 13 (12) | 0 (0) | 13 (54) | 58 (63) | 95 (34) | 117 (41) | |
| Not completed | 9 (8) | 0 (0) | 6 (25) | 1 (1) | 29 (10) | 50 (18) | |
| Involvement in making the plan, n (%) | |||||||
| Patient involved | 11 (10) | 1 (33) | 11 (46) | 59 (64) | 94 (34) | 117 (41) | |
| Relative involved | 3 (3) | 1 (33) | 5 (21) | 28 (30) | 108 (39) | 75 (26) | |
| No consultation | 1 (1) | 1 (33) | 2 (8) | 4 (4) | 52 (19) | 54 (19) | |
| Not completed | 11 (10) | 0 (0) | 6 (25) | 1 (1) | 23 (8) | 28 (13) | |
| Grade of first clinician signing the form, n (%) | |||||||
| FY1 | 1 (1) | 0 (0) | 0 (0) | 3 (3) | 4 (1) | 9 (3) | |
| FY2 | 0 (0) | 0 (0) | 2 (8) | 3 (3) | 13 (5) | 14 (5) | |
| ST1 ST2 | 0 (0) | 0 (0) | 0 (0) | 5 (5) | 26 (9) | 19 (7) | |
| SPR ST3 | 10 (9) | 2 (67) | 8 (33) | 43 (47) | 89 (32) | 75 (26) | |
| GPST | 0 (0) | 0 (0) | 1 (4) | 1 (1) | 4 (1) | 3 (1) | |
| Consultant | 6 (5) | 1 (33) | 9 (39) | 33 (36) | 117 (42) | 117 (41) | |
| GP | 1 (1) | 0 (0) | 0 (0) | 1 (1) | 2 (1) | 1 (< 1) | |
| Nurse/allied health practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (< 1) | 2 (1) | |
| Not completed | 8 (7) | 0 (0) | 4 (17) | 3 (3) | 21 (8) | 44 (15) | |
Appendix 6 Calculation of the Charlson Comorbidity Index score
| Item | Level | Points |
|---|---|---|
| Age | < 50 years | 0 |
| 50–59 years | +1 | |
| 60–69 years | +2 | |
| 70–79 years | +3 | |
| ≥ 80 years | +4 | |
| Myocardial infarction | No | 0 |
| Yes | +1 | |
| Congestive heart failure | No | 0 |
| Yes | +1 | |
| Peripheral vascular disease | No | 0 |
| Yes | +1 | |
| Cerebrovascular accident or transient ischaemic attack | No | 0 |
| Yes | +1 | |
| Dementia | No | 0 |
| Yes | +1 | |
| Chronic obstructive pulmonary disorder | No | 0 |
| Yes | +1 | |
| Connective tissue disease | No | 0 |
| Yes | +1 | |
| Peptic ulcer disease | No | 0 |
| Yes | +1 | |
| Liver disease | None | 0 |
| Mild | +1 | |
| Moderate to severe | +3 | |
| Diabetes mellitus | None or diet-controlled | 0 |
| Uncomplicated | +1 | |
| End-organ damage | +3 | |
| Hemiplegia | No | 0 |
| Yes | +2 | |
| Moderate to severe chronic kidney disease | No | 0 |
| Yes | +2 | |
| Solid tumour | None | 0 |
| Localised | +2 | |
| Metastatic | +6 | |
| Leukaemia | No | 0 |
| Yes | +2 | |
| AIDS | No | 0 |
| Yes | +6 |
Appendix 7 Calculation of Good Outcome Following Attempted Resuscitation score
| Variable | Points |
|---|---|
| Age | |
| < 70 years | 0 |
| 70–74 years | +2 |
| 75–79 years | +5 |
| 80–84 years | +6 |
| ≥ 85 years | +11 |
| Neurologically intact or with minimal deficits at admission | –15 |
| Major trauma | +10 |
| Acute stroke | +8 |
| Metastatic or hematologic cancer | +7 |
| Septicaemia | +7 |
| Medical non-cardiac diagnosis on admission | +7 |
| Hepatic insufficiency | +6 |
| Admit from skilled nursing facility | +6 |
| Hypotension or hypoperfusion within 4 hours prior to arrest | +5 |
| Renal insufficiency or dialysis | +4 |
| Respiratory insufficiency within 4 hours of arrest | +4 |
| Pneumonia | +1 |
List of abbreviations
- ACP
- advance care planning
- AFR
- accountability for reasonableness
- CAG
- Confidentiality Advisory Group
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CPC
- cerebral performance category
- CPR
- cardiopulmonary resuscitation
- CQC
- Care Quality Commission
- DNACPR
- do not attempt cardiopulmonary resuscitation
- DNAR
- do not attempt resuscitation
- ECTP
- emergency care and treatment plan
- GO-FAR
- Good Outcome Following Attempted Resuscitation
- GP
- general practitioner
- ICU
- intensive care unit
- ID
- identification
- IHCA
- in-hospital cardiac arrest
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- ITS
- interrupted time series
- ITU
- intensive treatment unit
- NCAA
- National Cardiac Arrest Audit
- NCEPOD
- National Confidential Enquiry into Patient Outcome and Death
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- OR
- odds ratio
- POLST
- Physician Orders for Life-Sustaining Treatment
- PPI
- patient and public involvement
- RCUK
- Resuscitation Council UK
- ReSPECT
- Recommended Summary Plan for Emergency Care and Treatment
- ROSC
- return of spontaneous circulation
- RRR
- relative risk ratio
- SD
- standard deviation
- TEP
- treatment escalation plan
- UFTO
- Universal Form of Treatment Options
- UNTRAP
- User Teaching and Research Action Partnership
- VTE
- venous thromboembolism
- WCTU
- Warwick Clinical Trials Unit
Notes
-
ReSPECT forms (versions 1.1 and 2.0)
-
Health Research Authority application for Research Ethics and Confidentiality Group approvals, with amendment table
-
ReSPECT study case report forms
-
Results from the voting questions from the ReSPECT dissemination event (28/09/21)
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/LFPE3627).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
